User login
New law will awaken employers to health care’s ‘transparency gap’
It has become increasingly apparent that our health care system is suffering from a severe case of “transparency gap.” There is a lack of transparency at every level of care in the system. Whether it is the hidden rebate/fee kickbacks from drug manufacturers to pharmacy benefit managers (PBMs), or the variability in pricing of imaging and procedures based on site of care, the need for transparency has become acute. The health insurance sector seems to specialize in opaqueness. The vertical integration of the three largest insurance companies with the three largest PBMs seems to have trapped the flow of money and services in one big black box. It can be difficult to decide if this transparency gap is a case of missing information, misinformation, or a deliberate hiding of information … or maybe a combination of all three.
Recently, I testified before a Wisconsin State Senate committee about the consequences and potential harm to patients and physician offices caused by mandated “white bagging,” which refers to the process whereby provider-administered drugs are shipped to the provider by a specialty pharmacy, as opposed to the provider buying the drug and billing the insurance company. I was very surprised to hear the large employers testifying against our position.
As I listened to the employer groups, it was clear that their protestations were predominantly focused on hospital billing, where markups on the administered medications can be 500% and upward. It made sense that if a business has a “self-funded” health plan, where the employer pays for the cost of care of the employees, those very high markups on the hospital administered medications would eventually become unsustainable. In addition to paying for the care of employees, employers also pay the health insurance company/PBMs to administer the plan. It is obvious that self-funded businesses are being overwhelmed by all these rising costs. What is not so clear is how much information employers get from their plan administrators on their policies and pricing.
An Employee Benefit Research Institute (ERBI) study examined the difference in prices of health care procedures, labs, and imaging based on site of care. It clearly shows that physicians’ offices are the least expensive overall for infusion therapy, even when compared with home infusion in most cases.
Here is where the missing information and the white-bagging issue intersect. When insurance administrators tell employers that letting the provider “buy and bill” costs an outrageous amount, they fail to tell the employers that physicians’ office prices are comparable, or, in some cases, less than what the employer would pay with white bagging. In addition, the possible harm to patients and to the physicians’ practices are never mentioned to the employer. Here is a list of some of the problems associated with white bagging:
- Delays in patient care when dosages or treatment plans are modified during the patient visit.
- Significant waste of drugs when patients’ treatments change or appointments are rescheduled.
- Unnecessary administrative burden for both the patient and physician, including inventory nightmares.
We see the transparency gap again when formularies are created with higher-priced, branded drugs in place of lower-priced generics and alternatives. How can a PBM explain that a formulary that prefers a $10,000 prostate cancer drug but excludes the $400 generic of that drug actually saves money? If the employer doesn’t know about the generic, no explanation is needed.
When physician offices attempt to override some of these harmful policies, the PBM or insurance company often points the finger at the employer as the culprit responsible for the policy. Often, the employers have no idea of the ramifications of the contracts that they have signed. As health care costs continue to rise, it is important that employers are educated on how they can save money and improve patient care by directly contracting with independent physician practices.
In addition, the Consolidated Appropriation Act of 2020-21 (CAA) “seeks to enforce good value from providers and vendors, and forbids hidden contracting terms that disfavor employers and their employees.” This year and next, the employers will become responsible for transparency reporting and demonstrating cost effectiveness of therapies for their employees. In theory, this should uncover many of the hidden policies that favor only the health plans and not the patients or their employers. Many employers are unaware of the CAA, and vendors are in no hurry to inform them of it.
Not only will the CAA help to eliminate much of the transparency gap in the system, but it may encourage employers to work directly with independent physicians’ offices to provide more cost effective and transparent services for their patients. The Coalition of State Rheumatology Organizations is working on a framework to enable practicing rheumatologists to do exactly this.
In the meantime, we must continue educating employers on white bagging and other policies that harm both their patients and their “bottom line.” This education is just one of the steps needed to rid the health care system of the transparency gap that leads to higher prices and poorer care for all patients.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is president of the CSRO, past chair of the Alliance for Safe Biologic Medicines, and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at [email protected].
It has become increasingly apparent that our health care system is suffering from a severe case of “transparency gap.” There is a lack of transparency at every level of care in the system. Whether it is the hidden rebate/fee kickbacks from drug manufacturers to pharmacy benefit managers (PBMs), or the variability in pricing of imaging and procedures based on site of care, the need for transparency has become acute. The health insurance sector seems to specialize in opaqueness. The vertical integration of the three largest insurance companies with the three largest PBMs seems to have trapped the flow of money and services in one big black box. It can be difficult to decide if this transparency gap is a case of missing information, misinformation, or a deliberate hiding of information … or maybe a combination of all three.
Recently, I testified before a Wisconsin State Senate committee about the consequences and potential harm to patients and physician offices caused by mandated “white bagging,” which refers to the process whereby provider-administered drugs are shipped to the provider by a specialty pharmacy, as opposed to the provider buying the drug and billing the insurance company. I was very surprised to hear the large employers testifying against our position.
As I listened to the employer groups, it was clear that their protestations were predominantly focused on hospital billing, where markups on the administered medications can be 500% and upward. It made sense that if a business has a “self-funded” health plan, where the employer pays for the cost of care of the employees, those very high markups on the hospital administered medications would eventually become unsustainable. In addition to paying for the care of employees, employers also pay the health insurance company/PBMs to administer the plan. It is obvious that self-funded businesses are being overwhelmed by all these rising costs. What is not so clear is how much information employers get from their plan administrators on their policies and pricing.
An Employee Benefit Research Institute (ERBI) study examined the difference in prices of health care procedures, labs, and imaging based on site of care. It clearly shows that physicians’ offices are the least expensive overall for infusion therapy, even when compared with home infusion in most cases.
Here is where the missing information and the white-bagging issue intersect. When insurance administrators tell employers that letting the provider “buy and bill” costs an outrageous amount, they fail to tell the employers that physicians’ office prices are comparable, or, in some cases, less than what the employer would pay with white bagging. In addition, the possible harm to patients and to the physicians’ practices are never mentioned to the employer. Here is a list of some of the problems associated with white bagging:
- Delays in patient care when dosages or treatment plans are modified during the patient visit.
- Significant waste of drugs when patients’ treatments change or appointments are rescheduled.
- Unnecessary administrative burden for both the patient and physician, including inventory nightmares.
We see the transparency gap again when formularies are created with higher-priced, branded drugs in place of lower-priced generics and alternatives. How can a PBM explain that a formulary that prefers a $10,000 prostate cancer drug but excludes the $400 generic of that drug actually saves money? If the employer doesn’t know about the generic, no explanation is needed.
When physician offices attempt to override some of these harmful policies, the PBM or insurance company often points the finger at the employer as the culprit responsible for the policy. Often, the employers have no idea of the ramifications of the contracts that they have signed. As health care costs continue to rise, it is important that employers are educated on how they can save money and improve patient care by directly contracting with independent physician practices.
In addition, the Consolidated Appropriation Act of 2020-21 (CAA) “seeks to enforce good value from providers and vendors, and forbids hidden contracting terms that disfavor employers and their employees.” This year and next, the employers will become responsible for transparency reporting and demonstrating cost effectiveness of therapies for their employees. In theory, this should uncover many of the hidden policies that favor only the health plans and not the patients or their employers. Many employers are unaware of the CAA, and vendors are in no hurry to inform them of it.
Not only will the CAA help to eliminate much of the transparency gap in the system, but it may encourage employers to work directly with independent physicians’ offices to provide more cost effective and transparent services for their patients. The Coalition of State Rheumatology Organizations is working on a framework to enable practicing rheumatologists to do exactly this.
In the meantime, we must continue educating employers on white bagging and other policies that harm both their patients and their “bottom line.” This education is just one of the steps needed to rid the health care system of the transparency gap that leads to higher prices and poorer care for all patients.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is president of the CSRO, past chair of the Alliance for Safe Biologic Medicines, and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at [email protected].
It has become increasingly apparent that our health care system is suffering from a severe case of “transparency gap.” There is a lack of transparency at every level of care in the system. Whether it is the hidden rebate/fee kickbacks from drug manufacturers to pharmacy benefit managers (PBMs), or the variability in pricing of imaging and procedures based on site of care, the need for transparency has become acute. The health insurance sector seems to specialize in opaqueness. The vertical integration of the three largest insurance companies with the three largest PBMs seems to have trapped the flow of money and services in one big black box. It can be difficult to decide if this transparency gap is a case of missing information, misinformation, or a deliberate hiding of information … or maybe a combination of all three.
Recently, I testified before a Wisconsin State Senate committee about the consequences and potential harm to patients and physician offices caused by mandated “white bagging,” which refers to the process whereby provider-administered drugs are shipped to the provider by a specialty pharmacy, as opposed to the provider buying the drug and billing the insurance company. I was very surprised to hear the large employers testifying against our position.
As I listened to the employer groups, it was clear that their protestations were predominantly focused on hospital billing, where markups on the administered medications can be 500% and upward. It made sense that if a business has a “self-funded” health plan, where the employer pays for the cost of care of the employees, those very high markups on the hospital administered medications would eventually become unsustainable. In addition to paying for the care of employees, employers also pay the health insurance company/PBMs to administer the plan. It is obvious that self-funded businesses are being overwhelmed by all these rising costs. What is not so clear is how much information employers get from their plan administrators on their policies and pricing.
An Employee Benefit Research Institute (ERBI) study examined the difference in prices of health care procedures, labs, and imaging based on site of care. It clearly shows that physicians’ offices are the least expensive overall for infusion therapy, even when compared with home infusion in most cases.
Here is where the missing information and the white-bagging issue intersect. When insurance administrators tell employers that letting the provider “buy and bill” costs an outrageous amount, they fail to tell the employers that physicians’ office prices are comparable, or, in some cases, less than what the employer would pay with white bagging. In addition, the possible harm to patients and to the physicians’ practices are never mentioned to the employer. Here is a list of some of the problems associated with white bagging:
- Delays in patient care when dosages or treatment plans are modified during the patient visit.
- Significant waste of drugs when patients’ treatments change or appointments are rescheduled.
- Unnecessary administrative burden for both the patient and physician, including inventory nightmares.
We see the transparency gap again when formularies are created with higher-priced, branded drugs in place of lower-priced generics and alternatives. How can a PBM explain that a formulary that prefers a $10,000 prostate cancer drug but excludes the $400 generic of that drug actually saves money? If the employer doesn’t know about the generic, no explanation is needed.
When physician offices attempt to override some of these harmful policies, the PBM or insurance company often points the finger at the employer as the culprit responsible for the policy. Often, the employers have no idea of the ramifications of the contracts that they have signed. As health care costs continue to rise, it is important that employers are educated on how they can save money and improve patient care by directly contracting with independent physician practices.
In addition, the Consolidated Appropriation Act of 2020-21 (CAA) “seeks to enforce good value from providers and vendors, and forbids hidden contracting terms that disfavor employers and their employees.” This year and next, the employers will become responsible for transparency reporting and demonstrating cost effectiveness of therapies for their employees. In theory, this should uncover many of the hidden policies that favor only the health plans and not the patients or their employers. Many employers are unaware of the CAA, and vendors are in no hurry to inform them of it.
Not only will the CAA help to eliminate much of the transparency gap in the system, but it may encourage employers to work directly with independent physicians’ offices to provide more cost effective and transparent services for their patients. The Coalition of State Rheumatology Organizations is working on a framework to enable practicing rheumatologists to do exactly this.
In the meantime, we must continue educating employers on white bagging and other policies that harm both their patients and their “bottom line.” This education is just one of the steps needed to rid the health care system of the transparency gap that leads to higher prices and poorer care for all patients.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is president of the CSRO, past chair of the Alliance for Safe Biologic Medicines, and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at [email protected].
Surveillance program highly predictive for early autism
A population-based developmental surveillance program showed high diagnostic accuracy in identifying autism in a community-based sample of infants, toddlers, and preschoolers, according to new data published online in JAMA Network Open.
Researchers, led by Josephine Barbaro, PhD, of Olga Tennison Autism Research Centre at La Trobe University, Bundoora, Australia, said their findings indicate the benefit of using early autism developmental surveillance from infancy to the preschool period rather than one-time screening.
For the study, maternal and child health nurses in Melbourne were trained to use the Social Attention and Communication Surveillance–Revised (SACS-R) and SACS-Preschool (SACS-PR) tools during well-child checkups at 11-30 months of age and at follow-up (42 months of age). Dr. Barbaro helped develop the SACS tools.
Children identified as being at high likelihood for autism (1-2 years of age: n = 327; 42 months of age: n = 168) and at low likelihood for autism plus concerns (42 months of age: n = 28) were referred by their nurse for diagnostic assessment by the researchers.
Diagnostic accuracy of the SACS-R and SACS-PR was determined by comparing likelihood for autism with children’s diagnostic outcome using clinical judgment based on standard autism assessments.
Researchers included 13,511 children ages 11 months to 42 months. Results indicated the SACS-R with SACS-PR (SACS-R+PR) had very high diagnostic accuracy for early autism detection.
According to the paper, SACS-R showed 83% positive predictive value (95% confidence interval, 0.77-0.87) and 99% estimated negative predictive value (95% CI, 0.01-0.02). Specificity (99.6%; 95% CI, 0.99-1.00) was high, with modest sensitivity (62%; 95% CI, 0.57-0.66). When the SACS-PR 42-month assessment was added, estimated sensitivity grew to 96% (95% CI, 0.94-0.98).
“Its greater accuracy, compared with psychometrics of commonly used autism screening tools when used in community-based samples, suggests that the SACS-R+PR can be used universally for the early identification of autism,” the authors wrote.
According to La Trobe University, the tool is used in 10 other countries around the world – among them China, Singapore, Poland, Japan, New Zealand, Nepal, and Bangladesh.
Early identification is crucial for children on the autism spectrum and their families because it facilitates early diagnosis and can help families get access to supports and services.
About 2% of the world’s population is on the autism spectrum. Some studies report prevalence of 4% or higher, the authors noted.
The authors called attention to a systematic review of universal autism screening in primary care, including the Infant-Toddler Checklist and the Modified Checklist for Autism in Toddlers and various versions. The authors of the review noted that few studies had enough participants to establish population sensitivity, specificity, and positive predictive value. Also, psychometric properties reported were modest and/or wide ranging, putting into question the diagnostic accuracy of the tools.
Dr. Barbaro and colleagues highlighted an advantage the current study offers. “A critical difference in this study was the use of a community-based sample rather than a clinical or high-likelihood sibling sample, which may not be representative of the general population of children on the autism spectrum because child outcomes, cognition, and autism prevalence vary by ascertainment strategy and multiplex or simplex status.”
The authors explained that, in the United States, The U.S. Preventive Services Task Force has said there is not enough evidence to recommend universal autism screening and instead recommends routine general developmental surveillance. The American Academy of Pediatrics recommends developmental surveillance between 9 and 30 months and autism-specific screening at 18 and 24 months because of the benefits of early supports and services.
Karen Pierce, PhD, codirector of the Autism Center of Excellence at University of California, San Diego, said in an interview that she was pleased to see that the researchers were able to identify a high percentage of children on the autism spectrum.
She said, however, that the system proposed in this paper involves a substantial amount of time for training the nurses.
The authors acknowledged that, saying, “there may be instances in which this could be impractical.”
Dr. Pierce said that, in the United States, parent questionnaires are combined with clinical judgment to decide which kids are at risk.
“It doesn’t take very much time to fill out these questionnaires,” she said. “That’s the sticking point. I’m not saying necessarily that it shouldn’t be adopted. It would be very hard, I think, to incorporate into current pediatric practice.”
She said a benefit of the SACS program is more hands-on observation of the child, beyond the parent report, which sometimes can reflect more emotionally how the parent is feeling about the child.
She pointed out it was impressive that the Australian team found virtually no false positives.
The researchers also identified an additional 168 children using the preschool version at 42 months who had actually passed at the earlier checkpoint, using the regular SACS-R.
“This underscores a supercritical point,” Dr. Pierce said. “Just because your child may have gotten screened at 12, 18, 24 months and they pass and everything’s looking great, it doesn’t necessarily mean at some point early in development around age 3 that there [wouldn’t] be some clearer signs of autism.”
She said in her own study, published in JAMA Pediatrics, 24% of their sample tested fine at first but were later identified as having autism.
“It underscores the need for repeat screening,” Dr. Pierce said. “That was a striking finding in this study.”
She also pointed out that the authors talk about the “false dichotomy” between screening and surveillance. “They are saying it doesn’t have to be that way. It can be a combined effort. We can have parents filling out screening tools and we can have more observational sessions with kids during checkups. It doesn’t have to be this rigid line between screening and surveillance. I would completely agree with that.”
Dr. Barbaro reported receiving grants from the Sir Robert Menzies Foundation and the Cooperative Research Centre for Living with Autism (Autism CRC) during the study. Funds are partially distributed to Dr. Barbaro for the background intellectual property. One coauthor reported grants from the Menzies Foundation and Autism CRC during the study. Another coauthor reported receiving salary from Autism CRC during the study. No other disclosures were reported. This work was supported by an Allied Health Sciences start-up grant from the Menzies Foundation and the Cooperative Research Centre for Living with Autism, established and supported under the Australian Government’s Cooperative Research Centres Program. Dr. Pierce reports no relevant financial relationships.
A population-based developmental surveillance program showed high diagnostic accuracy in identifying autism in a community-based sample of infants, toddlers, and preschoolers, according to new data published online in JAMA Network Open.
Researchers, led by Josephine Barbaro, PhD, of Olga Tennison Autism Research Centre at La Trobe University, Bundoora, Australia, said their findings indicate the benefit of using early autism developmental surveillance from infancy to the preschool period rather than one-time screening.
For the study, maternal and child health nurses in Melbourne were trained to use the Social Attention and Communication Surveillance–Revised (SACS-R) and SACS-Preschool (SACS-PR) tools during well-child checkups at 11-30 months of age and at follow-up (42 months of age). Dr. Barbaro helped develop the SACS tools.
Children identified as being at high likelihood for autism (1-2 years of age: n = 327; 42 months of age: n = 168) and at low likelihood for autism plus concerns (42 months of age: n = 28) were referred by their nurse for diagnostic assessment by the researchers.
Diagnostic accuracy of the SACS-R and SACS-PR was determined by comparing likelihood for autism with children’s diagnostic outcome using clinical judgment based on standard autism assessments.
Researchers included 13,511 children ages 11 months to 42 months. Results indicated the SACS-R with SACS-PR (SACS-R+PR) had very high diagnostic accuracy for early autism detection.
According to the paper, SACS-R showed 83% positive predictive value (95% confidence interval, 0.77-0.87) and 99% estimated negative predictive value (95% CI, 0.01-0.02). Specificity (99.6%; 95% CI, 0.99-1.00) was high, with modest sensitivity (62%; 95% CI, 0.57-0.66). When the SACS-PR 42-month assessment was added, estimated sensitivity grew to 96% (95% CI, 0.94-0.98).
“Its greater accuracy, compared with psychometrics of commonly used autism screening tools when used in community-based samples, suggests that the SACS-R+PR can be used universally for the early identification of autism,” the authors wrote.
According to La Trobe University, the tool is used in 10 other countries around the world – among them China, Singapore, Poland, Japan, New Zealand, Nepal, and Bangladesh.
Early identification is crucial for children on the autism spectrum and their families because it facilitates early diagnosis and can help families get access to supports and services.
About 2% of the world’s population is on the autism spectrum. Some studies report prevalence of 4% or higher, the authors noted.
The authors called attention to a systematic review of universal autism screening in primary care, including the Infant-Toddler Checklist and the Modified Checklist for Autism in Toddlers and various versions. The authors of the review noted that few studies had enough participants to establish population sensitivity, specificity, and positive predictive value. Also, psychometric properties reported were modest and/or wide ranging, putting into question the diagnostic accuracy of the tools.
Dr. Barbaro and colleagues highlighted an advantage the current study offers. “A critical difference in this study was the use of a community-based sample rather than a clinical or high-likelihood sibling sample, which may not be representative of the general population of children on the autism spectrum because child outcomes, cognition, and autism prevalence vary by ascertainment strategy and multiplex or simplex status.”
The authors explained that, in the United States, The U.S. Preventive Services Task Force has said there is not enough evidence to recommend universal autism screening and instead recommends routine general developmental surveillance. The American Academy of Pediatrics recommends developmental surveillance between 9 and 30 months and autism-specific screening at 18 and 24 months because of the benefits of early supports and services.
Karen Pierce, PhD, codirector of the Autism Center of Excellence at University of California, San Diego, said in an interview that she was pleased to see that the researchers were able to identify a high percentage of children on the autism spectrum.
She said, however, that the system proposed in this paper involves a substantial amount of time for training the nurses.
The authors acknowledged that, saying, “there may be instances in which this could be impractical.”
Dr. Pierce said that, in the United States, parent questionnaires are combined with clinical judgment to decide which kids are at risk.
“It doesn’t take very much time to fill out these questionnaires,” she said. “That’s the sticking point. I’m not saying necessarily that it shouldn’t be adopted. It would be very hard, I think, to incorporate into current pediatric practice.”
She said a benefit of the SACS program is more hands-on observation of the child, beyond the parent report, which sometimes can reflect more emotionally how the parent is feeling about the child.
She pointed out it was impressive that the Australian team found virtually no false positives.
The researchers also identified an additional 168 children using the preschool version at 42 months who had actually passed at the earlier checkpoint, using the regular SACS-R.
“This underscores a supercritical point,” Dr. Pierce said. “Just because your child may have gotten screened at 12, 18, 24 months and they pass and everything’s looking great, it doesn’t necessarily mean at some point early in development around age 3 that there [wouldn’t] be some clearer signs of autism.”
She said in her own study, published in JAMA Pediatrics, 24% of their sample tested fine at first but were later identified as having autism.
“It underscores the need for repeat screening,” Dr. Pierce said. “That was a striking finding in this study.”
She also pointed out that the authors talk about the “false dichotomy” between screening and surveillance. “They are saying it doesn’t have to be that way. It can be a combined effort. We can have parents filling out screening tools and we can have more observational sessions with kids during checkups. It doesn’t have to be this rigid line between screening and surveillance. I would completely agree with that.”
Dr. Barbaro reported receiving grants from the Sir Robert Menzies Foundation and the Cooperative Research Centre for Living with Autism (Autism CRC) during the study. Funds are partially distributed to Dr. Barbaro for the background intellectual property. One coauthor reported grants from the Menzies Foundation and Autism CRC during the study. Another coauthor reported receiving salary from Autism CRC during the study. No other disclosures were reported. This work was supported by an Allied Health Sciences start-up grant from the Menzies Foundation and the Cooperative Research Centre for Living with Autism, established and supported under the Australian Government’s Cooperative Research Centres Program. Dr. Pierce reports no relevant financial relationships.
A population-based developmental surveillance program showed high diagnostic accuracy in identifying autism in a community-based sample of infants, toddlers, and preschoolers, according to new data published online in JAMA Network Open.
Researchers, led by Josephine Barbaro, PhD, of Olga Tennison Autism Research Centre at La Trobe University, Bundoora, Australia, said their findings indicate the benefit of using early autism developmental surveillance from infancy to the preschool period rather than one-time screening.
For the study, maternal and child health nurses in Melbourne were trained to use the Social Attention and Communication Surveillance–Revised (SACS-R) and SACS-Preschool (SACS-PR) tools during well-child checkups at 11-30 months of age and at follow-up (42 months of age). Dr. Barbaro helped develop the SACS tools.
Children identified as being at high likelihood for autism (1-2 years of age: n = 327; 42 months of age: n = 168) and at low likelihood for autism plus concerns (42 months of age: n = 28) were referred by their nurse for diagnostic assessment by the researchers.
Diagnostic accuracy of the SACS-R and SACS-PR was determined by comparing likelihood for autism with children’s diagnostic outcome using clinical judgment based on standard autism assessments.
Researchers included 13,511 children ages 11 months to 42 months. Results indicated the SACS-R with SACS-PR (SACS-R+PR) had very high diagnostic accuracy for early autism detection.
According to the paper, SACS-R showed 83% positive predictive value (95% confidence interval, 0.77-0.87) and 99% estimated negative predictive value (95% CI, 0.01-0.02). Specificity (99.6%; 95% CI, 0.99-1.00) was high, with modest sensitivity (62%; 95% CI, 0.57-0.66). When the SACS-PR 42-month assessment was added, estimated sensitivity grew to 96% (95% CI, 0.94-0.98).
“Its greater accuracy, compared with psychometrics of commonly used autism screening tools when used in community-based samples, suggests that the SACS-R+PR can be used universally for the early identification of autism,” the authors wrote.
According to La Trobe University, the tool is used in 10 other countries around the world – among them China, Singapore, Poland, Japan, New Zealand, Nepal, and Bangladesh.
Early identification is crucial for children on the autism spectrum and their families because it facilitates early diagnosis and can help families get access to supports and services.
About 2% of the world’s population is on the autism spectrum. Some studies report prevalence of 4% or higher, the authors noted.
The authors called attention to a systematic review of universal autism screening in primary care, including the Infant-Toddler Checklist and the Modified Checklist for Autism in Toddlers and various versions. The authors of the review noted that few studies had enough participants to establish population sensitivity, specificity, and positive predictive value. Also, psychometric properties reported were modest and/or wide ranging, putting into question the diagnostic accuracy of the tools.
Dr. Barbaro and colleagues highlighted an advantage the current study offers. “A critical difference in this study was the use of a community-based sample rather than a clinical or high-likelihood sibling sample, which may not be representative of the general population of children on the autism spectrum because child outcomes, cognition, and autism prevalence vary by ascertainment strategy and multiplex or simplex status.”
The authors explained that, in the United States, The U.S. Preventive Services Task Force has said there is not enough evidence to recommend universal autism screening and instead recommends routine general developmental surveillance. The American Academy of Pediatrics recommends developmental surveillance between 9 and 30 months and autism-specific screening at 18 and 24 months because of the benefits of early supports and services.
Karen Pierce, PhD, codirector of the Autism Center of Excellence at University of California, San Diego, said in an interview that she was pleased to see that the researchers were able to identify a high percentage of children on the autism spectrum.
She said, however, that the system proposed in this paper involves a substantial amount of time for training the nurses.
The authors acknowledged that, saying, “there may be instances in which this could be impractical.”
Dr. Pierce said that, in the United States, parent questionnaires are combined with clinical judgment to decide which kids are at risk.
“It doesn’t take very much time to fill out these questionnaires,” she said. “That’s the sticking point. I’m not saying necessarily that it shouldn’t be adopted. It would be very hard, I think, to incorporate into current pediatric practice.”
She said a benefit of the SACS program is more hands-on observation of the child, beyond the parent report, which sometimes can reflect more emotionally how the parent is feeling about the child.
She pointed out it was impressive that the Australian team found virtually no false positives.
The researchers also identified an additional 168 children using the preschool version at 42 months who had actually passed at the earlier checkpoint, using the regular SACS-R.
“This underscores a supercritical point,” Dr. Pierce said. “Just because your child may have gotten screened at 12, 18, 24 months and they pass and everything’s looking great, it doesn’t necessarily mean at some point early in development around age 3 that there [wouldn’t] be some clearer signs of autism.”
She said in her own study, published in JAMA Pediatrics, 24% of their sample tested fine at first but were later identified as having autism.
“It underscores the need for repeat screening,” Dr. Pierce said. “That was a striking finding in this study.”
She also pointed out that the authors talk about the “false dichotomy” between screening and surveillance. “They are saying it doesn’t have to be that way. It can be a combined effort. We can have parents filling out screening tools and we can have more observational sessions with kids during checkups. It doesn’t have to be this rigid line between screening and surveillance. I would completely agree with that.”
Dr. Barbaro reported receiving grants from the Sir Robert Menzies Foundation and the Cooperative Research Centre for Living with Autism (Autism CRC) during the study. Funds are partially distributed to Dr. Barbaro for the background intellectual property. One coauthor reported grants from the Menzies Foundation and Autism CRC during the study. Another coauthor reported receiving salary from Autism CRC during the study. No other disclosures were reported. This work was supported by an Allied Health Sciences start-up grant from the Menzies Foundation and the Cooperative Research Centre for Living with Autism, established and supported under the Australian Government’s Cooperative Research Centres Program. Dr. Pierce reports no relevant financial relationships.
FROM JAMA NETWORK OPEN
Selling your practice
My previous column on practice valuation prompted a number of questions on the mechanics of selling a private practice. As usual, I cannot hope to cover this complex topic comprehensively in only 750 words, but here are the basics.
A generation ago, the sale of a medical practice was much like the sale of any other business: A retiring physician would sell his or her practice to a young doctor and the practice would continue on as before. Occasionally, that still happens, but changes in the business of medicine – most significantly the growth of managed care – have had a big impact on the way medical practices are bought and sold.
For one thing, there are far fewer solo practitioners these days, and polls indicate that most young physicians intend to continue that trend. .
For another, because the rules governing such sales have become so numbingly complex, the services of expert (and expensive) third parties are essential.
While these issues may complicate matters, there is still a market for the sale of medical practices. However, you must do everything possible to ensure you identify the best possible buyer and structure the best deal.
The first hurdle is the accurate valuation of your practice, which was covered in some detail in my last column. Briefly, for the protection of both parties, it is important that the appraisal be done by an experienced and neutral financial consultant, that all techniques used in the valuation be divulged and explained, and that documentation be supplied to support the conclusions reached.
Keep in mind that the valuation will not necessarily equal the purchase price; other factors may need to be considered before a final price can be agreed upon. Keep in mind, too, that there may be legal constraints on the purchase price. For example, if the buyer is a nonprofit corporation such as a hospital or HMO, by law it cannot pay in excess of fair market value for the practice – which may rule out any valuation of “good will.” In some states, the purchase of private practices by hospitals is prohibited altogether – so you might need to consider a long-term lease rather than a sale.
Once a value has been agreed upon, you must consider how the transaction will be structured. The most popular structures include purchase of assets, purchase of corporate stock, and merger.
Many buyers prefer to purchase assets, because it allows them to pick and choose only those items that have value to them. This can leave you with a bunch of “odd lot” assets to dispose of. But depending on the circumstances, an asset sale may still be to your advantage.
Sellers typically prefer to sell stock, because it allows them to sell their entire practice, which is often worth more than the sum of its parts, and often provides tax advantages.
The third option, merger, continues to grow in popularity and is a column subject in itself, and I will address it separately next month.
Tax issues must always be considered. Most private practices are corporations, and the sale of corporate stock will result in a long-term capital gain that will be taxed – currently at 15%-20%. As the saying goes, it’s not what you earn, it’s what you keep. So it may benefit you to accept a slightly lower price if the sale can be structured to provide significantly lower tax treatment. However, any gain that does not qualify as a long-term capital gain will be taxed as regular income – currently in the 32%-37% percent range – plus a Social Security tax of about 15%.
Payment in installments is a popular way to defer taxes, since they are incurred on each installment as it is paid; but such payments may be mistaken by the IRS for payments for referrals, which is illegal. And there is always the problem of making certain all payments are eventually made.
You may wish to continue working at the practice as an employee for an agreed-upon period of time, and this is often to the buyer’s advantage as well. Transitioning to new ownership in stages often maximizes the value of the business by improving patient retention, and allows patients to become accustomed to the transition. However, care must be taken, with the aid of good legal advice, to structure such an arrangement in a way that minimizes concerns of fraud and abuse.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
My previous column on practice valuation prompted a number of questions on the mechanics of selling a private practice. As usual, I cannot hope to cover this complex topic comprehensively in only 750 words, but here are the basics.
A generation ago, the sale of a medical practice was much like the sale of any other business: A retiring physician would sell his or her practice to a young doctor and the practice would continue on as before. Occasionally, that still happens, but changes in the business of medicine – most significantly the growth of managed care – have had a big impact on the way medical practices are bought and sold.
For one thing, there are far fewer solo practitioners these days, and polls indicate that most young physicians intend to continue that trend. .
For another, because the rules governing such sales have become so numbingly complex, the services of expert (and expensive) third parties are essential.
While these issues may complicate matters, there is still a market for the sale of medical practices. However, you must do everything possible to ensure you identify the best possible buyer and structure the best deal.
The first hurdle is the accurate valuation of your practice, which was covered in some detail in my last column. Briefly, for the protection of both parties, it is important that the appraisal be done by an experienced and neutral financial consultant, that all techniques used in the valuation be divulged and explained, and that documentation be supplied to support the conclusions reached.
Keep in mind that the valuation will not necessarily equal the purchase price; other factors may need to be considered before a final price can be agreed upon. Keep in mind, too, that there may be legal constraints on the purchase price. For example, if the buyer is a nonprofit corporation such as a hospital or HMO, by law it cannot pay in excess of fair market value for the practice – which may rule out any valuation of “good will.” In some states, the purchase of private practices by hospitals is prohibited altogether – so you might need to consider a long-term lease rather than a sale.
Once a value has been agreed upon, you must consider how the transaction will be structured. The most popular structures include purchase of assets, purchase of corporate stock, and merger.
Many buyers prefer to purchase assets, because it allows them to pick and choose only those items that have value to them. This can leave you with a bunch of “odd lot” assets to dispose of. But depending on the circumstances, an asset sale may still be to your advantage.
Sellers typically prefer to sell stock, because it allows them to sell their entire practice, which is often worth more than the sum of its parts, and often provides tax advantages.
The third option, merger, continues to grow in popularity and is a column subject in itself, and I will address it separately next month.
Tax issues must always be considered. Most private practices are corporations, and the sale of corporate stock will result in a long-term capital gain that will be taxed – currently at 15%-20%. As the saying goes, it’s not what you earn, it’s what you keep. So it may benefit you to accept a slightly lower price if the sale can be structured to provide significantly lower tax treatment. However, any gain that does not qualify as a long-term capital gain will be taxed as regular income – currently in the 32%-37% percent range – plus a Social Security tax of about 15%.
Payment in installments is a popular way to defer taxes, since they are incurred on each installment as it is paid; but such payments may be mistaken by the IRS for payments for referrals, which is illegal. And there is always the problem of making certain all payments are eventually made.
You may wish to continue working at the practice as an employee for an agreed-upon period of time, and this is often to the buyer’s advantage as well. Transitioning to new ownership in stages often maximizes the value of the business by improving patient retention, and allows patients to become accustomed to the transition. However, care must be taken, with the aid of good legal advice, to structure such an arrangement in a way that minimizes concerns of fraud and abuse.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
My previous column on practice valuation prompted a number of questions on the mechanics of selling a private practice. As usual, I cannot hope to cover this complex topic comprehensively in only 750 words, but here are the basics.
A generation ago, the sale of a medical practice was much like the sale of any other business: A retiring physician would sell his or her practice to a young doctor and the practice would continue on as before. Occasionally, that still happens, but changes in the business of medicine – most significantly the growth of managed care – have had a big impact on the way medical practices are bought and sold.
For one thing, there are far fewer solo practitioners these days, and polls indicate that most young physicians intend to continue that trend. .
For another, because the rules governing such sales have become so numbingly complex, the services of expert (and expensive) third parties are essential.
While these issues may complicate matters, there is still a market for the sale of medical practices. However, you must do everything possible to ensure you identify the best possible buyer and structure the best deal.
The first hurdle is the accurate valuation of your practice, which was covered in some detail in my last column. Briefly, for the protection of both parties, it is important that the appraisal be done by an experienced and neutral financial consultant, that all techniques used in the valuation be divulged and explained, and that documentation be supplied to support the conclusions reached.
Keep in mind that the valuation will not necessarily equal the purchase price; other factors may need to be considered before a final price can be agreed upon. Keep in mind, too, that there may be legal constraints on the purchase price. For example, if the buyer is a nonprofit corporation such as a hospital or HMO, by law it cannot pay in excess of fair market value for the practice – which may rule out any valuation of “good will.” In some states, the purchase of private practices by hospitals is prohibited altogether – so you might need to consider a long-term lease rather than a sale.
Once a value has been agreed upon, you must consider how the transaction will be structured. The most popular structures include purchase of assets, purchase of corporate stock, and merger.
Many buyers prefer to purchase assets, because it allows them to pick and choose only those items that have value to them. This can leave you with a bunch of “odd lot” assets to dispose of. But depending on the circumstances, an asset sale may still be to your advantage.
Sellers typically prefer to sell stock, because it allows them to sell their entire practice, which is often worth more than the sum of its parts, and often provides tax advantages.
The third option, merger, continues to grow in popularity and is a column subject in itself, and I will address it separately next month.
Tax issues must always be considered. Most private practices are corporations, and the sale of corporate stock will result in a long-term capital gain that will be taxed – currently at 15%-20%. As the saying goes, it’s not what you earn, it’s what you keep. So it may benefit you to accept a slightly lower price if the sale can be structured to provide significantly lower tax treatment. However, any gain that does not qualify as a long-term capital gain will be taxed as regular income – currently in the 32%-37% percent range – plus a Social Security tax of about 15%.
Payment in installments is a popular way to defer taxes, since they are incurred on each installment as it is paid; but such payments may be mistaken by the IRS for payments for referrals, which is illegal. And there is always the problem of making certain all payments are eventually made.
You may wish to continue working at the practice as an employee for an agreed-upon period of time, and this is often to the buyer’s advantage as well. Transitioning to new ownership in stages often maximizes the value of the business by improving patient retention, and allows patients to become accustomed to the transition. However, care must be taken, with the aid of good legal advice, to structure such an arrangement in a way that minimizes concerns of fraud and abuse.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Registry data support lowering CRC screening age to 45
Approximately one-third of people between 45 and 49 years of age who undergo colonoscopies have neoplastic colorectal pathology, according to a retrospective analysis.
According to the researchers, led by Parth Trivedi, MD, of the Icahn School of Medicine at Mount Sinai, New York, there has progressively been a “disturbing” rise in early-onset colorectal cancer (CRC) in the United States, which has prompted guidelines from the American Cancer Society to the U.S. Preventive Services Task Force to recommend lowering the CRC screening starting age to 45 years old for average-risk individuals. Despite these recommendations, little research to date has fully characterized the prevalence of colorectal neoplasia in individuals younger than the currently recommended CRC onset screening age of 50 years.
Dr. Trivedi and colleagues, who published their study findings in Gastroenterology, retrospectively reviewed colonoscopy data recorded in the Gastrointestinal Quality Improvement Consortium Registry to address the current knowledge gaps on early-onset CRC. Collected data were for procedures conducted at 123 AMSURG ambulatory endoscopy centers across 29 states between January 2014 and February 2021. In total, 2,921,816 colonoscopies during the study period among patients aged 18-54 years were recorded by AMSURG-associated endoscopists; of these, 562,559 met inclusion criteria for high-quality screening or diagnostic colonoscopy procedures.
The researchers pooled a young-onset age group, including patients between the ages of 18 and 49 years old, in whom 145,998 procedures were performed, including 79,934 procedures in patients aged 45-49 years. A comparator group with 336,627 procedures in patients aged 50-54 years was also included in the study. The findings were categorized into CRC, advanced premalignant lesions (APL), and “any neoplasia,” the latter of which included all adenomas, sessile serrated polyps, and CRC.
Among patients aged 18-44 years, the most frequent indications were “diagnostic-other” (45.6%) as well as “diagnostic-bleeding” (39.4%). Among patients between 45 and 49 years of age, the most frequent indications were “screening” (41.4%) and “diagnostic-other” (30.7%). Nearly all (90%) procedures among those aged 50-54 years were for screening.
A multivariable logistic regression identified 5 variables predictive of either APL or CRC in patients between 18 and 49 years of age: increasing age (odds ratio, 1.08; 95% confidence interval, 1.07-1.08; P <0.01), male sex (OR = 1.67; 95% CI, 1.63-1.70; P <0.01), White race (vs. African American: OR = 0.76; 95% CI, 0.73-0.79, P <0.01; vs. Asian: OR = 0.89; 95% CI, 0.84-0.94, P <0.01), family history of CRC (OR = 1.21; 95% CI, 1.16-1.26; P <0.01) and polyps (OR = 1.33; 95% CI, 1.24-1.43; P <0.01), and examinations for bleeding (OR = 1.15; 95% CI, 1.12-1.18; P <0.01) or screening (OR = 1.20; 95% CI, 1.16-1.24; P <0.01).
The prevalence of neoplastic findings in the young-onset age-group increased with increasing age for the categories of any neoplasia, APLs, and CRC. Among patients aged 40-44, 26.59% had any neoplasia, 5.76% had APL, and 0.53% had CRC. In those aged 45-49 years, around 32% had any neoplasia, approximately 7.5% had APLs, and nearly 0.58% had CRC. In the 50- to 54-year-old group, the prevalences of any neoplasia, APL, and CRC were 37.72%, 9.48%, and 0.32%, respectively.
Across all age groups, a family history of CRC was associated with a higher prevalence of any neoplasia and APL. In addition, the rates of any APL and neoplasia in patients with a family history of CRC were comparable to patients who were 5 years older but had no family history of the disease. Across most young-onset age group, individuals with a positive family history had a lower CRC prevalence versus patients with no family history.
The researchers noted that their population data are derived from ambulatory endoscopy centers, which may introduce bias associated with insurance coverage or patient preference to attend specific endoscopic centers. Additionally, the investigators stated that many records on race and ethnicity were missing, further limiting the findings.
“The present analysis of neoplastic colorectal pathology among individuals younger than age 50 suggests that lowering the screening age to 45 for men and women of all races and ethnicities will likely detect important pathology rather frequently,” they concluded. In addition, the researchers noted that the study results “underscore the importance of early messaging to patients and providers in the years leading up to age 45.” Ultimately, improved “awareness of pathology prevalence in individuals younger than age 45 can help guide clinicians in the clinical management of CRC risk,” the researchers wrote.
Several of the researchers reported conflicts of interest with Exact Sciences Corp and Freenome. The study received no industry funding.
An alarming trend of increased colorectal cancer (CRC) incidence has been noted among individuals 20-49 years of age over the past 2 decades. This fact combined with the results of microsimulation studies have led all purveyors of CRC screening guidelines in the United States to lower their recommended age for the initiation of average-risk screening from 50 to 45. Despite this major shift in recommendations, relatively little is known about the rates of premalignant neoplasia in this population.
Future studies will need to document the actual effectiveness of CRC screening in persons aged 45-49 and examine the actual cost-benefit of lowering the recommended screening age.
Reid M. Ness, MD, MPH, AGAF is an associate professor in the division of gastroenterology, hepatology and nutrition, department of medicine, Vanderbilt University Medical Center, Nashville, Tenn., and at the VA Tennessee Valley Healthcare System, Nashville campus. He is also an investigator in the Vanderbilt-Ingram Cancer Center. Dr. Ness is a study investigator with Guardant Health.
An alarming trend of increased colorectal cancer (CRC) incidence has been noted among individuals 20-49 years of age over the past 2 decades. This fact combined with the results of microsimulation studies have led all purveyors of CRC screening guidelines in the United States to lower their recommended age for the initiation of average-risk screening from 50 to 45. Despite this major shift in recommendations, relatively little is known about the rates of premalignant neoplasia in this population.
Future studies will need to document the actual effectiveness of CRC screening in persons aged 45-49 and examine the actual cost-benefit of lowering the recommended screening age.
Reid M. Ness, MD, MPH, AGAF is an associate professor in the division of gastroenterology, hepatology and nutrition, department of medicine, Vanderbilt University Medical Center, Nashville, Tenn., and at the VA Tennessee Valley Healthcare System, Nashville campus. He is also an investigator in the Vanderbilt-Ingram Cancer Center. Dr. Ness is a study investigator with Guardant Health.
An alarming trend of increased colorectal cancer (CRC) incidence has been noted among individuals 20-49 years of age over the past 2 decades. This fact combined with the results of microsimulation studies have led all purveyors of CRC screening guidelines in the United States to lower their recommended age for the initiation of average-risk screening from 50 to 45. Despite this major shift in recommendations, relatively little is known about the rates of premalignant neoplasia in this population.
Future studies will need to document the actual effectiveness of CRC screening in persons aged 45-49 and examine the actual cost-benefit of lowering the recommended screening age.
Reid M. Ness, MD, MPH, AGAF is an associate professor in the division of gastroenterology, hepatology and nutrition, department of medicine, Vanderbilt University Medical Center, Nashville, Tenn., and at the VA Tennessee Valley Healthcare System, Nashville campus. He is also an investigator in the Vanderbilt-Ingram Cancer Center. Dr. Ness is a study investigator with Guardant Health.
Approximately one-third of people between 45 and 49 years of age who undergo colonoscopies have neoplastic colorectal pathology, according to a retrospective analysis.
According to the researchers, led by Parth Trivedi, MD, of the Icahn School of Medicine at Mount Sinai, New York, there has progressively been a “disturbing” rise in early-onset colorectal cancer (CRC) in the United States, which has prompted guidelines from the American Cancer Society to the U.S. Preventive Services Task Force to recommend lowering the CRC screening starting age to 45 years old for average-risk individuals. Despite these recommendations, little research to date has fully characterized the prevalence of colorectal neoplasia in individuals younger than the currently recommended CRC onset screening age of 50 years.
Dr. Trivedi and colleagues, who published their study findings in Gastroenterology, retrospectively reviewed colonoscopy data recorded in the Gastrointestinal Quality Improvement Consortium Registry to address the current knowledge gaps on early-onset CRC. Collected data were for procedures conducted at 123 AMSURG ambulatory endoscopy centers across 29 states between January 2014 and February 2021. In total, 2,921,816 colonoscopies during the study period among patients aged 18-54 years were recorded by AMSURG-associated endoscopists; of these, 562,559 met inclusion criteria for high-quality screening or diagnostic colonoscopy procedures.
The researchers pooled a young-onset age group, including patients between the ages of 18 and 49 years old, in whom 145,998 procedures were performed, including 79,934 procedures in patients aged 45-49 years. A comparator group with 336,627 procedures in patients aged 50-54 years was also included in the study. The findings were categorized into CRC, advanced premalignant lesions (APL), and “any neoplasia,” the latter of which included all adenomas, sessile serrated polyps, and CRC.
Among patients aged 18-44 years, the most frequent indications were “diagnostic-other” (45.6%) as well as “diagnostic-bleeding” (39.4%). Among patients between 45 and 49 years of age, the most frequent indications were “screening” (41.4%) and “diagnostic-other” (30.7%). Nearly all (90%) procedures among those aged 50-54 years were for screening.
A multivariable logistic regression identified 5 variables predictive of either APL or CRC in patients between 18 and 49 years of age: increasing age (odds ratio, 1.08; 95% confidence interval, 1.07-1.08; P <0.01), male sex (OR = 1.67; 95% CI, 1.63-1.70; P <0.01), White race (vs. African American: OR = 0.76; 95% CI, 0.73-0.79, P <0.01; vs. Asian: OR = 0.89; 95% CI, 0.84-0.94, P <0.01), family history of CRC (OR = 1.21; 95% CI, 1.16-1.26; P <0.01) and polyps (OR = 1.33; 95% CI, 1.24-1.43; P <0.01), and examinations for bleeding (OR = 1.15; 95% CI, 1.12-1.18; P <0.01) or screening (OR = 1.20; 95% CI, 1.16-1.24; P <0.01).
The prevalence of neoplastic findings in the young-onset age-group increased with increasing age for the categories of any neoplasia, APLs, and CRC. Among patients aged 40-44, 26.59% had any neoplasia, 5.76% had APL, and 0.53% had CRC. In those aged 45-49 years, around 32% had any neoplasia, approximately 7.5% had APLs, and nearly 0.58% had CRC. In the 50- to 54-year-old group, the prevalences of any neoplasia, APL, and CRC were 37.72%, 9.48%, and 0.32%, respectively.
Across all age groups, a family history of CRC was associated with a higher prevalence of any neoplasia and APL. In addition, the rates of any APL and neoplasia in patients with a family history of CRC were comparable to patients who were 5 years older but had no family history of the disease. Across most young-onset age group, individuals with a positive family history had a lower CRC prevalence versus patients with no family history.
The researchers noted that their population data are derived from ambulatory endoscopy centers, which may introduce bias associated with insurance coverage or patient preference to attend specific endoscopic centers. Additionally, the investigators stated that many records on race and ethnicity were missing, further limiting the findings.
“The present analysis of neoplastic colorectal pathology among individuals younger than age 50 suggests that lowering the screening age to 45 for men and women of all races and ethnicities will likely detect important pathology rather frequently,” they concluded. In addition, the researchers noted that the study results “underscore the importance of early messaging to patients and providers in the years leading up to age 45.” Ultimately, improved “awareness of pathology prevalence in individuals younger than age 45 can help guide clinicians in the clinical management of CRC risk,” the researchers wrote.
Several of the researchers reported conflicts of interest with Exact Sciences Corp and Freenome. The study received no industry funding.
Approximately one-third of people between 45 and 49 years of age who undergo colonoscopies have neoplastic colorectal pathology, according to a retrospective analysis.
According to the researchers, led by Parth Trivedi, MD, of the Icahn School of Medicine at Mount Sinai, New York, there has progressively been a “disturbing” rise in early-onset colorectal cancer (CRC) in the United States, which has prompted guidelines from the American Cancer Society to the U.S. Preventive Services Task Force to recommend lowering the CRC screening starting age to 45 years old for average-risk individuals. Despite these recommendations, little research to date has fully characterized the prevalence of colorectal neoplasia in individuals younger than the currently recommended CRC onset screening age of 50 years.
Dr. Trivedi and colleagues, who published their study findings in Gastroenterology, retrospectively reviewed colonoscopy data recorded in the Gastrointestinal Quality Improvement Consortium Registry to address the current knowledge gaps on early-onset CRC. Collected data were for procedures conducted at 123 AMSURG ambulatory endoscopy centers across 29 states between January 2014 and February 2021. In total, 2,921,816 colonoscopies during the study period among patients aged 18-54 years were recorded by AMSURG-associated endoscopists; of these, 562,559 met inclusion criteria for high-quality screening or diagnostic colonoscopy procedures.
The researchers pooled a young-onset age group, including patients between the ages of 18 and 49 years old, in whom 145,998 procedures were performed, including 79,934 procedures in patients aged 45-49 years. A comparator group with 336,627 procedures in patients aged 50-54 years was also included in the study. The findings were categorized into CRC, advanced premalignant lesions (APL), and “any neoplasia,” the latter of which included all adenomas, sessile serrated polyps, and CRC.
Among patients aged 18-44 years, the most frequent indications were “diagnostic-other” (45.6%) as well as “diagnostic-bleeding” (39.4%). Among patients between 45 and 49 years of age, the most frequent indications were “screening” (41.4%) and “diagnostic-other” (30.7%). Nearly all (90%) procedures among those aged 50-54 years were for screening.
A multivariable logistic regression identified 5 variables predictive of either APL or CRC in patients between 18 and 49 years of age: increasing age (odds ratio, 1.08; 95% confidence interval, 1.07-1.08; P <0.01), male sex (OR = 1.67; 95% CI, 1.63-1.70; P <0.01), White race (vs. African American: OR = 0.76; 95% CI, 0.73-0.79, P <0.01; vs. Asian: OR = 0.89; 95% CI, 0.84-0.94, P <0.01), family history of CRC (OR = 1.21; 95% CI, 1.16-1.26; P <0.01) and polyps (OR = 1.33; 95% CI, 1.24-1.43; P <0.01), and examinations for bleeding (OR = 1.15; 95% CI, 1.12-1.18; P <0.01) or screening (OR = 1.20; 95% CI, 1.16-1.24; P <0.01).
The prevalence of neoplastic findings in the young-onset age-group increased with increasing age for the categories of any neoplasia, APLs, and CRC. Among patients aged 40-44, 26.59% had any neoplasia, 5.76% had APL, and 0.53% had CRC. In those aged 45-49 years, around 32% had any neoplasia, approximately 7.5% had APLs, and nearly 0.58% had CRC. In the 50- to 54-year-old group, the prevalences of any neoplasia, APL, and CRC were 37.72%, 9.48%, and 0.32%, respectively.
Across all age groups, a family history of CRC was associated with a higher prevalence of any neoplasia and APL. In addition, the rates of any APL and neoplasia in patients with a family history of CRC were comparable to patients who were 5 years older but had no family history of the disease. Across most young-onset age group, individuals with a positive family history had a lower CRC prevalence versus patients with no family history.
The researchers noted that their population data are derived from ambulatory endoscopy centers, which may introduce bias associated with insurance coverage or patient preference to attend specific endoscopic centers. Additionally, the investigators stated that many records on race and ethnicity were missing, further limiting the findings.
“The present analysis of neoplastic colorectal pathology among individuals younger than age 50 suggests that lowering the screening age to 45 for men and women of all races and ethnicities will likely detect important pathology rather frequently,” they concluded. In addition, the researchers noted that the study results “underscore the importance of early messaging to patients and providers in the years leading up to age 45.” Ultimately, improved “awareness of pathology prevalence in individuals younger than age 45 can help guide clinicians in the clinical management of CRC risk,” the researchers wrote.
Several of the researchers reported conflicts of interest with Exact Sciences Corp and Freenome. The study received no industry funding.
FROM GASTROENTEROLOGY
Cryoballoon ablation demonstrates long-term durability in BE
Similar to radiofrequency ablation, cryoballoon ablation (CBA) is a durable approach that can eradicate Barrett’s esophagus (BE) in treatment-naive patients with dysplastic BE, according to a single-center cohort study.
Endoscopic mucosal resection (EMR), radiofrequency ablation (RFA), and cryotherapy are established techniques used in endoscopic eradication therapy of BE, wrote study authors led by Mohamad Dbouk, MD, of Johns Hopkins Medical Institutions in Baltimore in Techniques and Innovations in Gastrointestinal Endoscopy. Unlike RFA which uses heat to induce tissue necrosis and reepithelialization of normal tissue, cryotherapy applies extreme cold in the treatment of BE. While cryotherapy as an endoscopic ablative technique has been studied over the past decade as an alternative treatment modality, Dr. Dbouk and researchers noted that long-term data on durability of and outcomes with this approach are lacking.
To gauge the durability of CBA for dysplastic BE, the researchers examined outcomes of 59 consecutive patients with BE and confirmed low-grade dysplasia (n = 22), high-grade dysplasia (n = 33), or intramucosal cancer (n = 4), all of whom were treated with CBA for the purposes of BE eradication. The single-center cohort comprised only treatment-naive patients who had a mean age of 66.8 (91.5% male). In the overall cohort, the mean length of the BE was 5 cm, although 23.7% of patients had BE ≥8 cm in length.
Following confirmation of dysplastic BE in biopsies and/or EMR specimens at baseline, patients underwent CBA applied to the gastric cardia as well as all visible BE with the cryoballoon focal ablation system and focal or pear-shaped cryoballoon. The investigators performed surveillance esophagogastroduodenoscopy (EGD) to assess the CBA response. Patients with high-grade dysplasia underwent EGD and biopsy every 3 months for the first year after completing CBA, every 6 months for the second year, and once per year thereafter. However, those with biopsies at baseline that showed low-grade dysplasia (LGD) underwent EGD and biopsy every 6 months during the first year after CBA and annually thereafter. Retreatment with ablation was allowed if recurrent dysplasia or intestinal metaplasia was found.
The study’s primary endpoints included short-term efficacy – defined as the rate of complete eradication of dysplasia (CE-D) and intestinal metaplasia (CE-IM) at 1-year follow-up – and durability – characterized by the proportion of patients with CE-D and CE-IM within 18 months and maintained at 2- and 3-year follow-up.
The median follow-up period for the patient cohort was 54.3 months. Approximately 95% of the 56 patients who were evaluable at 1 year achieved CE-D, while 75% achieved CE-IM. In an analysis that stratified patients by their baseline dysplasia grade, the rates of CE-D were each 96% in the LGD and HGD groups. At 1 year, the median number of CBA sessions used to achieve CE-IM was 3.
Throughout treatment and the follow-up period, none of the patients progressed beyond their dysplasia grade at baseline or developed esophageal cancer. All patients had maintained CE-D for years 2, 3, and 4. In addition, 98% of patients had CE-IM at 2 years, 98% had CE-IM at 3 years, and 97% of patients had CE-IM at 4 years. After stratification of patients by baseline grade of dysplasia, the researchers found no significant difference between groups in the rates of CE-D and CE-IM at each follow-up year.
In 48 patients who initially achieved CE-IM, 14.6% developed recurrent intestinal metaplasia (IM), including six in the esophagus and one in the GEJ, after a median of 20.7 months. Approximately 57% of patients who developed recurrent IM had baseline LGD, while 43% had HGD at baseline. The length of BE was not significantly associated with the risk of IM recurrence, according to a Cox proportional hazard analysis (hazard ratio, 1.02; 95% confidence interval, 0.86-1.2; P = .8).
Approximately 8.5% of patients had post-CBA strictures that required dilation during the study period. According to bivariate analysis, individuals with a BE length of ≥8 cm were significantly more likely to develop strictures, compared with patients without ultra-long BE (28.6% vs. 2.2%, respectively; P = .009). Strictures occurred during the first 4 months after the initial CBA. The median period from the first CBA treatment to stricture detection on follow-up EGD was 2 months. Around 1.7% of patients experienced postprocedural bleeding that required clipping for closure. These patients were on clopidogrel for atrial fibrillation during the first year of active treatment.
Limitations of the study included the small sample size as well as the inclusion of patients from a single center, which the researchers suggest may limit the generalizability of the results.
“More research is needed to confirm the long-term durability of CBA,” the authors concluded. “Randomized controlled trials comparing CBA with RFA are needed to assess the role of CBA as a first-line and rescue EET.”
Several of the researchers reported conflicts of interest with industry. The study received no industry funding.
Barrett’s endoscopic eradication therapy, resection of visible lesions, and ablation of remaining Barrett’s mucosa are the standard of care for dysplasia management. Radiofrequency ablation (RFA) is 91% successful in eliminating dysplasia and 78% in eliminating intestinal metaplasia (IM). Recurrence of dysplasia is rare, although recurrence of IM is 20%.
Given the impressive results of RFA, one might ask why alternative ablation therapies are needed. CbFAS equipment costs are lower than those of RFA, and discomfort after the procedure may be less. Failure of ablation is poorly understood, likely attributable to inadequate reflux suppression and maybe thicker areas of Barrett’s mucosa. The greater depth of injury with cryoablation may succeed in some cases of RFA failure. Complexity of this ablation procedure remains high, and excessive overlap of treatment sites probably explains the higher stricture rate. Where cryoballoon ablation fits in the Barrett’s ablation paradigm is not clear. The lower cost and availability may provide traction for this new technology in the established field of Barrett’s ablation.
Bruce D. Greenwald, MD, is a professor of medicine at the University of Maryland, Baltimore, and the Marlene and Stewart Greenebaum Comprehensive Cancer Center, Baltimore. He is a consultant for Steris Endoscopy.
Barrett’s endoscopic eradication therapy, resection of visible lesions, and ablation of remaining Barrett’s mucosa are the standard of care for dysplasia management. Radiofrequency ablation (RFA) is 91% successful in eliminating dysplasia and 78% in eliminating intestinal metaplasia (IM). Recurrence of dysplasia is rare, although recurrence of IM is 20%.
Given the impressive results of RFA, one might ask why alternative ablation therapies are needed. CbFAS equipment costs are lower than those of RFA, and discomfort after the procedure may be less. Failure of ablation is poorly understood, likely attributable to inadequate reflux suppression and maybe thicker areas of Barrett’s mucosa. The greater depth of injury with cryoablation may succeed in some cases of RFA failure. Complexity of this ablation procedure remains high, and excessive overlap of treatment sites probably explains the higher stricture rate. Where cryoballoon ablation fits in the Barrett’s ablation paradigm is not clear. The lower cost and availability may provide traction for this new technology in the established field of Barrett’s ablation.
Bruce D. Greenwald, MD, is a professor of medicine at the University of Maryland, Baltimore, and the Marlene and Stewart Greenebaum Comprehensive Cancer Center, Baltimore. He is a consultant for Steris Endoscopy.
Barrett’s endoscopic eradication therapy, resection of visible lesions, and ablation of remaining Barrett’s mucosa are the standard of care for dysplasia management. Radiofrequency ablation (RFA) is 91% successful in eliminating dysplasia and 78% in eliminating intestinal metaplasia (IM). Recurrence of dysplasia is rare, although recurrence of IM is 20%.
Given the impressive results of RFA, one might ask why alternative ablation therapies are needed. CbFAS equipment costs are lower than those of RFA, and discomfort after the procedure may be less. Failure of ablation is poorly understood, likely attributable to inadequate reflux suppression and maybe thicker areas of Barrett’s mucosa. The greater depth of injury with cryoablation may succeed in some cases of RFA failure. Complexity of this ablation procedure remains high, and excessive overlap of treatment sites probably explains the higher stricture rate. Where cryoballoon ablation fits in the Barrett’s ablation paradigm is not clear. The lower cost and availability may provide traction for this new technology in the established field of Barrett’s ablation.
Bruce D. Greenwald, MD, is a professor of medicine at the University of Maryland, Baltimore, and the Marlene and Stewart Greenebaum Comprehensive Cancer Center, Baltimore. He is a consultant for Steris Endoscopy.
Similar to radiofrequency ablation, cryoballoon ablation (CBA) is a durable approach that can eradicate Barrett’s esophagus (BE) in treatment-naive patients with dysplastic BE, according to a single-center cohort study.
Endoscopic mucosal resection (EMR), radiofrequency ablation (RFA), and cryotherapy are established techniques used in endoscopic eradication therapy of BE, wrote study authors led by Mohamad Dbouk, MD, of Johns Hopkins Medical Institutions in Baltimore in Techniques and Innovations in Gastrointestinal Endoscopy. Unlike RFA which uses heat to induce tissue necrosis and reepithelialization of normal tissue, cryotherapy applies extreme cold in the treatment of BE. While cryotherapy as an endoscopic ablative technique has been studied over the past decade as an alternative treatment modality, Dr. Dbouk and researchers noted that long-term data on durability of and outcomes with this approach are lacking.
To gauge the durability of CBA for dysplastic BE, the researchers examined outcomes of 59 consecutive patients with BE and confirmed low-grade dysplasia (n = 22), high-grade dysplasia (n = 33), or intramucosal cancer (n = 4), all of whom were treated with CBA for the purposes of BE eradication. The single-center cohort comprised only treatment-naive patients who had a mean age of 66.8 (91.5% male). In the overall cohort, the mean length of the BE was 5 cm, although 23.7% of patients had BE ≥8 cm in length.
Following confirmation of dysplastic BE in biopsies and/or EMR specimens at baseline, patients underwent CBA applied to the gastric cardia as well as all visible BE with the cryoballoon focal ablation system and focal or pear-shaped cryoballoon. The investigators performed surveillance esophagogastroduodenoscopy (EGD) to assess the CBA response. Patients with high-grade dysplasia underwent EGD and biopsy every 3 months for the first year after completing CBA, every 6 months for the second year, and once per year thereafter. However, those with biopsies at baseline that showed low-grade dysplasia (LGD) underwent EGD and biopsy every 6 months during the first year after CBA and annually thereafter. Retreatment with ablation was allowed if recurrent dysplasia or intestinal metaplasia was found.
The study’s primary endpoints included short-term efficacy – defined as the rate of complete eradication of dysplasia (CE-D) and intestinal metaplasia (CE-IM) at 1-year follow-up – and durability – characterized by the proportion of patients with CE-D and CE-IM within 18 months and maintained at 2- and 3-year follow-up.
The median follow-up period for the patient cohort was 54.3 months. Approximately 95% of the 56 patients who were evaluable at 1 year achieved CE-D, while 75% achieved CE-IM. In an analysis that stratified patients by their baseline dysplasia grade, the rates of CE-D were each 96% in the LGD and HGD groups. At 1 year, the median number of CBA sessions used to achieve CE-IM was 3.
Throughout treatment and the follow-up period, none of the patients progressed beyond their dysplasia grade at baseline or developed esophageal cancer. All patients had maintained CE-D for years 2, 3, and 4. In addition, 98% of patients had CE-IM at 2 years, 98% had CE-IM at 3 years, and 97% of patients had CE-IM at 4 years. After stratification of patients by baseline grade of dysplasia, the researchers found no significant difference between groups in the rates of CE-D and CE-IM at each follow-up year.
In 48 patients who initially achieved CE-IM, 14.6% developed recurrent intestinal metaplasia (IM), including six in the esophagus and one in the GEJ, after a median of 20.7 months. Approximately 57% of patients who developed recurrent IM had baseline LGD, while 43% had HGD at baseline. The length of BE was not significantly associated with the risk of IM recurrence, according to a Cox proportional hazard analysis (hazard ratio, 1.02; 95% confidence interval, 0.86-1.2; P = .8).
Approximately 8.5% of patients had post-CBA strictures that required dilation during the study period. According to bivariate analysis, individuals with a BE length of ≥8 cm were significantly more likely to develop strictures, compared with patients without ultra-long BE (28.6% vs. 2.2%, respectively; P = .009). Strictures occurred during the first 4 months after the initial CBA. The median period from the first CBA treatment to stricture detection on follow-up EGD was 2 months. Around 1.7% of patients experienced postprocedural bleeding that required clipping for closure. These patients were on clopidogrel for atrial fibrillation during the first year of active treatment.
Limitations of the study included the small sample size as well as the inclusion of patients from a single center, which the researchers suggest may limit the generalizability of the results.
“More research is needed to confirm the long-term durability of CBA,” the authors concluded. “Randomized controlled trials comparing CBA with RFA are needed to assess the role of CBA as a first-line and rescue EET.”
Several of the researchers reported conflicts of interest with industry. The study received no industry funding.
Similar to radiofrequency ablation, cryoballoon ablation (CBA) is a durable approach that can eradicate Barrett’s esophagus (BE) in treatment-naive patients with dysplastic BE, according to a single-center cohort study.
Endoscopic mucosal resection (EMR), radiofrequency ablation (RFA), and cryotherapy are established techniques used in endoscopic eradication therapy of BE, wrote study authors led by Mohamad Dbouk, MD, of Johns Hopkins Medical Institutions in Baltimore in Techniques and Innovations in Gastrointestinal Endoscopy. Unlike RFA which uses heat to induce tissue necrosis and reepithelialization of normal tissue, cryotherapy applies extreme cold in the treatment of BE. While cryotherapy as an endoscopic ablative technique has been studied over the past decade as an alternative treatment modality, Dr. Dbouk and researchers noted that long-term data on durability of and outcomes with this approach are lacking.
To gauge the durability of CBA for dysplastic BE, the researchers examined outcomes of 59 consecutive patients with BE and confirmed low-grade dysplasia (n = 22), high-grade dysplasia (n = 33), or intramucosal cancer (n = 4), all of whom were treated with CBA for the purposes of BE eradication. The single-center cohort comprised only treatment-naive patients who had a mean age of 66.8 (91.5% male). In the overall cohort, the mean length of the BE was 5 cm, although 23.7% of patients had BE ≥8 cm in length.
Following confirmation of dysplastic BE in biopsies and/or EMR specimens at baseline, patients underwent CBA applied to the gastric cardia as well as all visible BE with the cryoballoon focal ablation system and focal or pear-shaped cryoballoon. The investigators performed surveillance esophagogastroduodenoscopy (EGD) to assess the CBA response. Patients with high-grade dysplasia underwent EGD and biopsy every 3 months for the first year after completing CBA, every 6 months for the second year, and once per year thereafter. However, those with biopsies at baseline that showed low-grade dysplasia (LGD) underwent EGD and biopsy every 6 months during the first year after CBA and annually thereafter. Retreatment with ablation was allowed if recurrent dysplasia or intestinal metaplasia was found.
The study’s primary endpoints included short-term efficacy – defined as the rate of complete eradication of dysplasia (CE-D) and intestinal metaplasia (CE-IM) at 1-year follow-up – and durability – characterized by the proportion of patients with CE-D and CE-IM within 18 months and maintained at 2- and 3-year follow-up.
The median follow-up period for the patient cohort was 54.3 months. Approximately 95% of the 56 patients who were evaluable at 1 year achieved CE-D, while 75% achieved CE-IM. In an analysis that stratified patients by their baseline dysplasia grade, the rates of CE-D were each 96% in the LGD and HGD groups. At 1 year, the median number of CBA sessions used to achieve CE-IM was 3.
Throughout treatment and the follow-up period, none of the patients progressed beyond their dysplasia grade at baseline or developed esophageal cancer. All patients had maintained CE-D for years 2, 3, and 4. In addition, 98% of patients had CE-IM at 2 years, 98% had CE-IM at 3 years, and 97% of patients had CE-IM at 4 years. After stratification of patients by baseline grade of dysplasia, the researchers found no significant difference between groups in the rates of CE-D and CE-IM at each follow-up year.
In 48 patients who initially achieved CE-IM, 14.6% developed recurrent intestinal metaplasia (IM), including six in the esophagus and one in the GEJ, after a median of 20.7 months. Approximately 57% of patients who developed recurrent IM had baseline LGD, while 43% had HGD at baseline. The length of BE was not significantly associated with the risk of IM recurrence, according to a Cox proportional hazard analysis (hazard ratio, 1.02; 95% confidence interval, 0.86-1.2; P = .8).
Approximately 8.5% of patients had post-CBA strictures that required dilation during the study period. According to bivariate analysis, individuals with a BE length of ≥8 cm were significantly more likely to develop strictures, compared with patients without ultra-long BE (28.6% vs. 2.2%, respectively; P = .009). Strictures occurred during the first 4 months after the initial CBA. The median period from the first CBA treatment to stricture detection on follow-up EGD was 2 months. Around 1.7% of patients experienced postprocedural bleeding that required clipping for closure. These patients were on clopidogrel for atrial fibrillation during the first year of active treatment.
Limitations of the study included the small sample size as well as the inclusion of patients from a single center, which the researchers suggest may limit the generalizability of the results.
“More research is needed to confirm the long-term durability of CBA,” the authors concluded. “Randomized controlled trials comparing CBA with RFA are needed to assess the role of CBA as a first-line and rescue EET.”
Several of the researchers reported conflicts of interest with industry. The study received no industry funding.
FROM TECHNIQUES AND INNOVATIONS IN GASTROINTESTINAL ENDOSCOPY
FDA approves first PARP inhibitor for early BRCA+ breast cancer
BRCA+ breast cancer
Specifically, the new approval is for the adjuvant treatment of adult patients with high-risk early-stage HER2-negative, BRCA-mutated breast cancer who have completed chemotherapy and local treatment.
The FDA also approved BRACAnalysis CDx (Myriad Genetics), a companion diagnostic test to identify patients who may benefit from olaparib.
The latest approval was based on phase 3 OlympiA trial results, which showed a 42% improvement in invasive and distant disease-free survival with olaparib in comparison with placebo. Data from OlympiaA and other clinical studies also confirm BRACAnalysis CDx as “an effective test for patients deciding on their best treatment options,” Myriad Genetics noted in a press release.
The OlympiA results, as reported by this news organization, were presented during the plenary session of the American Society of Clinical Oncology 2021 annual meeting and were published in the New England Journal of Medicine.
Those findings prompted an ASCO “rapid recommendation” updating of ASCO’s 2020 guidelines for the management of hereditary breast cancer.
The latest results from OlympiA show that olaparib reduced the risk of death by 32% (hazard ratio, 0.68) in comparison with placebo, according to a company press release announcing the approval. Overall survival data are slated for presentation at a European Society for Medical Oncology Virtual Plenary session on March 16, 2022.
A version of this article first appeared on Medscape.com.
Specifically, the new approval is for the adjuvant treatment of adult patients with high-risk early-stage HER2-negative, BRCA-mutated breast cancer who have completed chemotherapy and local treatment.
The FDA also approved BRACAnalysis CDx (Myriad Genetics), a companion diagnostic test to identify patients who may benefit from olaparib.
The latest approval was based on phase 3 OlympiA trial results, which showed a 42% improvement in invasive and distant disease-free survival with olaparib in comparison with placebo. Data from OlympiaA and other clinical studies also confirm BRACAnalysis CDx as “an effective test for patients deciding on their best treatment options,” Myriad Genetics noted in a press release.
The OlympiA results, as reported by this news organization, were presented during the plenary session of the American Society of Clinical Oncology 2021 annual meeting and were published in the New England Journal of Medicine.
Those findings prompted an ASCO “rapid recommendation” updating of ASCO’s 2020 guidelines for the management of hereditary breast cancer.
The latest results from OlympiA show that olaparib reduced the risk of death by 32% (hazard ratio, 0.68) in comparison with placebo, according to a company press release announcing the approval. Overall survival data are slated for presentation at a European Society for Medical Oncology Virtual Plenary session on March 16, 2022.
A version of this article first appeared on Medscape.com.
Specifically, the new approval is for the adjuvant treatment of adult patients with high-risk early-stage HER2-negative, BRCA-mutated breast cancer who have completed chemotherapy and local treatment.
The FDA also approved BRACAnalysis CDx (Myriad Genetics), a companion diagnostic test to identify patients who may benefit from olaparib.
The latest approval was based on phase 3 OlympiA trial results, which showed a 42% improvement in invasive and distant disease-free survival with olaparib in comparison with placebo. Data from OlympiaA and other clinical studies also confirm BRACAnalysis CDx as “an effective test for patients deciding on their best treatment options,” Myriad Genetics noted in a press release.
The OlympiA results, as reported by this news organization, were presented during the plenary session of the American Society of Clinical Oncology 2021 annual meeting and were published in the New England Journal of Medicine.
Those findings prompted an ASCO “rapid recommendation” updating of ASCO’s 2020 guidelines for the management of hereditary breast cancer.
The latest results from OlympiA show that olaparib reduced the risk of death by 32% (hazard ratio, 0.68) in comparison with placebo, according to a company press release announcing the approval. Overall survival data are slated for presentation at a European Society for Medical Oncology Virtual Plenary session on March 16, 2022.
A version of this article first appeared on Medscape.com.
BRCA+ breast cancer
BRCA+ breast cancer
Registry data support lowering CRC screening age to 45
Approximately one-third of people between 45 and 49 years of age who undergo colonoscopies have neoplastic colorectal pathology, according to a retrospective analysis.
According to the researchers, led by Parth Trivedi, MD, of the Icahn School of Medicine at Mount Sinai, New York, there has progressively been a “disturbing” rise in early-onset colorectal cancer (CRC) in the United States, which has prompted guidelines from the American Cancer Society to the U.S. Preventive Services Task Force to recommend lowering the CRC screening starting age to 45 years old for average-risk individuals. Despite these recommendations, little research to date has fully characterized the prevalence of colorectal neoplasia in individuals younger than the currently recommended CRC onset screening age of 50 years.
Dr. Trivedi and colleagues, who published their study findings in Gastroenterology, retrospectively reviewed colonoscopy data recorded in the Gastrointestinal Quality Improvement Consortium Registry to address the current knowledge gaps on early-onset CRC. Collected data were for procedures conducted at 123 AMSURG ambulatory endoscopy centers across 29 states between January 2014 and February 2021. In total, 2,921,816 colonoscopies during the study period among patients aged 18-54 years were recorded by AMSURG-associated endoscopists; of these, 562,559 met inclusion criteria for high-quality screening or diagnostic colonoscopy procedures.
The researchers pooled a young-onset age group, including patients between the ages of 18 and 49 years old, in whom 145,998 procedures were performed, including 79,934 procedures in patients aged 45-49 years. A comparator group with 336,627 procedures in patients aged 50-54 years was also included in the study. The findings were categorized into CRC, advanced premalignant lesions (APL), and “any neoplasia,” the latter of which included all adenomas, sessile serrated polyps, and CRC.
Among patients aged 18-44 years, the most frequent indications were “diagnostic-other” (45.6%) as well as “diagnostic-bleeding” (39.4%). Among patients between 45 and 49 years of age, the most frequent indications were “screening” (41.4%) and “diagnostic-other” (30.7%). Nearly all (90%) procedures among those aged 50-54 years were for screening.
A multivariable logistic regression identified 5 variables predictive of either APL or CRC in patients between 18 and 49 years of age: increasing age (odds ratio, 1.08; 95% confidence interval, 1.07-1.08; P <0.01), male sex (OR = 1.67; 95% CI, 1.63-1.70; P <0.01), White race (vs. African American: OR = 0.76; 95% CI, 0.73-0.79, P <0.01; vs. Asian: OR = 0.89; 95% CI, 0.84-0.94, P <0.01), family history of CRC (OR = 1.21; 95% CI, 1.16-1.26; P <0.01) and polyps (OR = 1.33; 95% CI, 1.24-1.43; P <0.01), and examinations for bleeding (OR = 1.15; 95% CI, 1.12-1.18; P <0.01) or screening (OR = 1.20; 95% CI, 1.16-1.24; P <0.01).
The prevalence of neoplastic findings in the young-onset age-group increased with increasing age for the categories of any neoplasia, APLs, and CRC. Among patients aged 40-44, 26.59% had any neoplasia, 5.76% had APL, and 0.53% had CRC. In those aged 45-49 years, around 32% had any neoplasia, approximately 7.5% had APLs, and nearly 0.58% had CRC. In the 50- to 54-year-old group, the prevalences of any neoplasia, APL, and CRC were 37.72%, 9.48%, and 0.32%, respectively.
Across all age groups, a family history of CRC was associated with a higher prevalence of any neoplasia and APL. In addition, the rates of any APL and neoplasia in patients with a family history of CRC were comparable to patients who were 5 years older but had no family history of the disease. Across most young-onset age group, individuals with a positive family history had a lower CRC prevalence versus patients with no family history.
The researchers noted that their population data are derived from ambulatory endoscopy centers, which may introduce bias associated with insurance coverage or patient preference to attend specific endoscopic centers. Additionally, the investigators stated that many records on race and ethnicity were missing, further limiting the findings.
“The present analysis of neoplastic colorectal pathology among individuals younger than age 50 suggests that lowering the screening age to 45 for men and women of all races and ethnicities will likely detect important pathology rather frequently,” they concluded. In addition, the researchers noted that the study results “underscore the importance of early messaging to patients and providers in the years leading up to age 45.” Ultimately, improved “awareness of pathology prevalence in individuals younger than age 45 can help guide clinicians in the clinical management of CRC risk,” the researchers wrote.
Several of the researchers reported conflicts of interest with Exact Sciences Corp and Freenome. The study received no industry funding.
Approximately one-third of people between 45 and 49 years of age who undergo colonoscopies have neoplastic colorectal pathology, according to a retrospective analysis.
According to the researchers, led by Parth Trivedi, MD, of the Icahn School of Medicine at Mount Sinai, New York, there has progressively been a “disturbing” rise in early-onset colorectal cancer (CRC) in the United States, which has prompted guidelines from the American Cancer Society to the U.S. Preventive Services Task Force to recommend lowering the CRC screening starting age to 45 years old for average-risk individuals. Despite these recommendations, little research to date has fully characterized the prevalence of colorectal neoplasia in individuals younger than the currently recommended CRC onset screening age of 50 years.
Dr. Trivedi and colleagues, who published their study findings in Gastroenterology, retrospectively reviewed colonoscopy data recorded in the Gastrointestinal Quality Improvement Consortium Registry to address the current knowledge gaps on early-onset CRC. Collected data were for procedures conducted at 123 AMSURG ambulatory endoscopy centers across 29 states between January 2014 and February 2021. In total, 2,921,816 colonoscopies during the study period among patients aged 18-54 years were recorded by AMSURG-associated endoscopists; of these, 562,559 met inclusion criteria for high-quality screening or diagnostic colonoscopy procedures.
The researchers pooled a young-onset age group, including patients between the ages of 18 and 49 years old, in whom 145,998 procedures were performed, including 79,934 procedures in patients aged 45-49 years. A comparator group with 336,627 procedures in patients aged 50-54 years was also included in the study. The findings were categorized into CRC, advanced premalignant lesions (APL), and “any neoplasia,” the latter of which included all adenomas, sessile serrated polyps, and CRC.
Among patients aged 18-44 years, the most frequent indications were “diagnostic-other” (45.6%) as well as “diagnostic-bleeding” (39.4%). Among patients between 45 and 49 years of age, the most frequent indications were “screening” (41.4%) and “diagnostic-other” (30.7%). Nearly all (90%) procedures among those aged 50-54 years were for screening.
A multivariable logistic regression identified 5 variables predictive of either APL or CRC in patients between 18 and 49 years of age: increasing age (odds ratio, 1.08; 95% confidence interval, 1.07-1.08; P <0.01), male sex (OR = 1.67; 95% CI, 1.63-1.70; P <0.01), White race (vs. African American: OR = 0.76; 95% CI, 0.73-0.79, P <0.01; vs. Asian: OR = 0.89; 95% CI, 0.84-0.94, P <0.01), family history of CRC (OR = 1.21; 95% CI, 1.16-1.26; P <0.01) and polyps (OR = 1.33; 95% CI, 1.24-1.43; P <0.01), and examinations for bleeding (OR = 1.15; 95% CI, 1.12-1.18; P <0.01) or screening (OR = 1.20; 95% CI, 1.16-1.24; P <0.01).
The prevalence of neoplastic findings in the young-onset age-group increased with increasing age for the categories of any neoplasia, APLs, and CRC. Among patients aged 40-44, 26.59% had any neoplasia, 5.76% had APL, and 0.53% had CRC. In those aged 45-49 years, around 32% had any neoplasia, approximately 7.5% had APLs, and nearly 0.58% had CRC. In the 50- to 54-year-old group, the prevalences of any neoplasia, APL, and CRC were 37.72%, 9.48%, and 0.32%, respectively.
Across all age groups, a family history of CRC was associated with a higher prevalence of any neoplasia and APL. In addition, the rates of any APL and neoplasia in patients with a family history of CRC were comparable to patients who were 5 years older but had no family history of the disease. Across most young-onset age group, individuals with a positive family history had a lower CRC prevalence versus patients with no family history.
The researchers noted that their population data are derived from ambulatory endoscopy centers, which may introduce bias associated with insurance coverage or patient preference to attend specific endoscopic centers. Additionally, the investigators stated that many records on race and ethnicity were missing, further limiting the findings.
“The present analysis of neoplastic colorectal pathology among individuals younger than age 50 suggests that lowering the screening age to 45 for men and women of all races and ethnicities will likely detect important pathology rather frequently,” they concluded. In addition, the researchers noted that the study results “underscore the importance of early messaging to patients and providers in the years leading up to age 45.” Ultimately, improved “awareness of pathology prevalence in individuals younger than age 45 can help guide clinicians in the clinical management of CRC risk,” the researchers wrote.
Several of the researchers reported conflicts of interest with Exact Sciences Corp and Freenome. The study received no industry funding.
Approximately one-third of people between 45 and 49 years of age who undergo colonoscopies have neoplastic colorectal pathology, according to a retrospective analysis.
According to the researchers, led by Parth Trivedi, MD, of the Icahn School of Medicine at Mount Sinai, New York, there has progressively been a “disturbing” rise in early-onset colorectal cancer (CRC) in the United States, which has prompted guidelines from the American Cancer Society to the U.S. Preventive Services Task Force to recommend lowering the CRC screening starting age to 45 years old for average-risk individuals. Despite these recommendations, little research to date has fully characterized the prevalence of colorectal neoplasia in individuals younger than the currently recommended CRC onset screening age of 50 years.
Dr. Trivedi and colleagues, who published their study findings in Gastroenterology, retrospectively reviewed colonoscopy data recorded in the Gastrointestinal Quality Improvement Consortium Registry to address the current knowledge gaps on early-onset CRC. Collected data were for procedures conducted at 123 AMSURG ambulatory endoscopy centers across 29 states between January 2014 and February 2021. In total, 2,921,816 colonoscopies during the study period among patients aged 18-54 years were recorded by AMSURG-associated endoscopists; of these, 562,559 met inclusion criteria for high-quality screening or diagnostic colonoscopy procedures.
The researchers pooled a young-onset age group, including patients between the ages of 18 and 49 years old, in whom 145,998 procedures were performed, including 79,934 procedures in patients aged 45-49 years. A comparator group with 336,627 procedures in patients aged 50-54 years was also included in the study. The findings were categorized into CRC, advanced premalignant lesions (APL), and “any neoplasia,” the latter of which included all adenomas, sessile serrated polyps, and CRC.
Among patients aged 18-44 years, the most frequent indications were “diagnostic-other” (45.6%) as well as “diagnostic-bleeding” (39.4%). Among patients between 45 and 49 years of age, the most frequent indications were “screening” (41.4%) and “diagnostic-other” (30.7%). Nearly all (90%) procedures among those aged 50-54 years were for screening.
A multivariable logistic regression identified 5 variables predictive of either APL or CRC in patients between 18 and 49 years of age: increasing age (odds ratio, 1.08; 95% confidence interval, 1.07-1.08; P <0.01), male sex (OR = 1.67; 95% CI, 1.63-1.70; P <0.01), White race (vs. African American: OR = 0.76; 95% CI, 0.73-0.79, P <0.01; vs. Asian: OR = 0.89; 95% CI, 0.84-0.94, P <0.01), family history of CRC (OR = 1.21; 95% CI, 1.16-1.26; P <0.01) and polyps (OR = 1.33; 95% CI, 1.24-1.43; P <0.01), and examinations for bleeding (OR = 1.15; 95% CI, 1.12-1.18; P <0.01) or screening (OR = 1.20; 95% CI, 1.16-1.24; P <0.01).
The prevalence of neoplastic findings in the young-onset age-group increased with increasing age for the categories of any neoplasia, APLs, and CRC. Among patients aged 40-44, 26.59% had any neoplasia, 5.76% had APL, and 0.53% had CRC. In those aged 45-49 years, around 32% had any neoplasia, approximately 7.5% had APLs, and nearly 0.58% had CRC. In the 50- to 54-year-old group, the prevalences of any neoplasia, APL, and CRC were 37.72%, 9.48%, and 0.32%, respectively.
Across all age groups, a family history of CRC was associated with a higher prevalence of any neoplasia and APL. In addition, the rates of any APL and neoplasia in patients with a family history of CRC were comparable to patients who were 5 years older but had no family history of the disease. Across most young-onset age group, individuals with a positive family history had a lower CRC prevalence versus patients with no family history.
The researchers noted that their population data are derived from ambulatory endoscopy centers, which may introduce bias associated with insurance coverage or patient preference to attend specific endoscopic centers. Additionally, the investigators stated that many records on race and ethnicity were missing, further limiting the findings.
“The present analysis of neoplastic colorectal pathology among individuals younger than age 50 suggests that lowering the screening age to 45 for men and women of all races and ethnicities will likely detect important pathology rather frequently,” they concluded. In addition, the researchers noted that the study results “underscore the importance of early messaging to patients and providers in the years leading up to age 45.” Ultimately, improved “awareness of pathology prevalence in individuals younger than age 45 can help guide clinicians in the clinical management of CRC risk,” the researchers wrote.
Several of the researchers reported conflicts of interest with Exact Sciences Corp and Freenome. The study received no industry funding.
FROM GASTROENTEROLOGY
New HBV model may open door to more effective antivirals
A new mouse model that better represents chronic infection with hepatitis B virus (HBV) in humans may lead to more effective antiviral therapies for HBV, according to investigators.
During human infection, HBV genomes take the form of covalently closed circular DNA (cccDNA), a structure that has thwarted effective antiviral therapy and, until now, creation of an accurate mouse model, reported lead author Zaichao Xu, PhD, of Wuhan (China) University and colleagues.
“As the viral persistence reservoir plays a central role in HBV infection, HBV cccDNA is the key obstacle for a cure,” the investigators wrote in Cellular and Molecular Gastroenterology and Hepatology.
Although several previous mouse models have approximated this phenomenon with recombinant cccDNA-like molecules (rcccDNA), the present model is the first to achieve genuine cccDNA, which does not naturally occur in mice.
“Although rcccDNA supports persistent viral replication and antigen expression, the nature of rcccDNA may differ from authentic cccDNA, as additional sequences, like LoxP or attR, were inserted into the HBV genome,” the investigators noted.
The new model was created by first constructing an adeno-associated virus vector carrying a replication-deficient HBV1.04-fold genome (AAV-HBV1.04). When injected into mice, the vector led to cccDNA formation via ataxia-telangiectasia and Rad3-related protein (ATR)–mediated DNA damage response, a finding that was confirmed by blocking the same process with ATR inhibitors.
Immediately after injection, mice tested positive for both hepatitis B e antigen (HBeAg) and hepatitis B surface antigen (HBsAg), with peak concentrations after either 4 or 8 weeks depending on dose. HBV DNA was also detected in serum after injection, and 50% of hepatocytes exhibited HBsAg and hepatitis B core protein (HBc) after 1 week. At week 66, HBsAg, HBeAg, and HBc were still detectable in the liver.
“The expression of HBc could only be observed in the liver, but not in other organs or tissues, suggesting that the AAV-HBV1.04 only targeted the mouse liver,” the investigators wrote.
Further experimentation involving known cccDNA-binding proteins supported the similarity between cccDNA in the mouse model and natural infection.
“These results suggested that the chromatinization and transcriptional activation of cccDNA formed in this model dose not differ from wild-type cccDNA formed through infection.”
Next, Dr. Xu and colleagues demonstrated that the infected mice could serve as a reliable model for antiviral research. One week after injection with the vector, mice were treated with entecavir, polyinosinic-polycytidylic acid (poly[I:C]), or phosphate-buffered saline (PBS; control). As anticipated, entecavir suppressed circulating HBV DNA, but not HBsAg, HBeAg, or HBV cccDNA, whereas treatment with poly(I:C) reduced all HBV markers.
“This novel mouse model will provide a unique platform for studying HBV cccDNA and developing novel antivirals to achieve HBV cure,” the investigators concluded.
The study was supported by the National Natural Science Foundation of China, the Fundamental Research Funds for the Central Universities, Hubei Province’s Outstanding Medical Academic Leader Program, and others. The investigators reported no conflicts of interest.
On the heels of the wondrous development of curative antiviral agents for hepatitis C virus (HCV), renewed attention has been directed to efforts to bring about the cure of HBV. However, this task will hinge on successful elimination of covalently closed circular DNA (cccDNA), a highly stable form of viral DNA that is exceedingly difficult to eliminate. Efforts to develop successful curative strategies will in turn rely on development of small animal models that support HBV cccDNA formation and virus production, which has until recently proved elusive. In the past several years, several mouse HBV models supporting cccDNA formation have been constructed using adeno-associated vector (AAV)–mediated transduction of a linearized HBV genome. Both the AAV-HBV linear episome and cccDNA have been consistently replicated and detected in these models. While they recapitulate the key steps of the viral life cycle, these models do not, however, lend themselves to direct assessment of cccDNA, which have traditionally required detection of cccDNA in the liver.
Raymond T. Chung, MD, is a professor of medicine at Harvard Medical School and director of the Hepatology and Liver Center at Massachusetts General Hospital, both in Boston. He has no conflicts to disclose.
On the heels of the wondrous development of curative antiviral agents for hepatitis C virus (HCV), renewed attention has been directed to efforts to bring about the cure of HBV. However, this task will hinge on successful elimination of covalently closed circular DNA (cccDNA), a highly stable form of viral DNA that is exceedingly difficult to eliminate. Efforts to develop successful curative strategies will in turn rely on development of small animal models that support HBV cccDNA formation and virus production, which has until recently proved elusive. In the past several years, several mouse HBV models supporting cccDNA formation have been constructed using adeno-associated vector (AAV)–mediated transduction of a linearized HBV genome. Both the AAV-HBV linear episome and cccDNA have been consistently replicated and detected in these models. While they recapitulate the key steps of the viral life cycle, these models do not, however, lend themselves to direct assessment of cccDNA, which have traditionally required detection of cccDNA in the liver.
Raymond T. Chung, MD, is a professor of medicine at Harvard Medical School and director of the Hepatology and Liver Center at Massachusetts General Hospital, both in Boston. He has no conflicts to disclose.
On the heels of the wondrous development of curative antiviral agents for hepatitis C virus (HCV), renewed attention has been directed to efforts to bring about the cure of HBV. However, this task will hinge on successful elimination of covalently closed circular DNA (cccDNA), a highly stable form of viral DNA that is exceedingly difficult to eliminate. Efforts to develop successful curative strategies will in turn rely on development of small animal models that support HBV cccDNA formation and virus production, which has until recently proved elusive. In the past several years, several mouse HBV models supporting cccDNA formation have been constructed using adeno-associated vector (AAV)–mediated transduction of a linearized HBV genome. Both the AAV-HBV linear episome and cccDNA have been consistently replicated and detected in these models. While they recapitulate the key steps of the viral life cycle, these models do not, however, lend themselves to direct assessment of cccDNA, which have traditionally required detection of cccDNA in the liver.
Raymond T. Chung, MD, is a professor of medicine at Harvard Medical School and director of the Hepatology and Liver Center at Massachusetts General Hospital, both in Boston. He has no conflicts to disclose.
A new mouse model that better represents chronic infection with hepatitis B virus (HBV) in humans may lead to more effective antiviral therapies for HBV, according to investigators.
During human infection, HBV genomes take the form of covalently closed circular DNA (cccDNA), a structure that has thwarted effective antiviral therapy and, until now, creation of an accurate mouse model, reported lead author Zaichao Xu, PhD, of Wuhan (China) University and colleagues.
“As the viral persistence reservoir plays a central role in HBV infection, HBV cccDNA is the key obstacle for a cure,” the investigators wrote in Cellular and Molecular Gastroenterology and Hepatology.
Although several previous mouse models have approximated this phenomenon with recombinant cccDNA-like molecules (rcccDNA), the present model is the first to achieve genuine cccDNA, which does not naturally occur in mice.
“Although rcccDNA supports persistent viral replication and antigen expression, the nature of rcccDNA may differ from authentic cccDNA, as additional sequences, like LoxP or attR, were inserted into the HBV genome,” the investigators noted.
The new model was created by first constructing an adeno-associated virus vector carrying a replication-deficient HBV1.04-fold genome (AAV-HBV1.04). When injected into mice, the vector led to cccDNA formation via ataxia-telangiectasia and Rad3-related protein (ATR)–mediated DNA damage response, a finding that was confirmed by blocking the same process with ATR inhibitors.
Immediately after injection, mice tested positive for both hepatitis B e antigen (HBeAg) and hepatitis B surface antigen (HBsAg), with peak concentrations after either 4 or 8 weeks depending on dose. HBV DNA was also detected in serum after injection, and 50% of hepatocytes exhibited HBsAg and hepatitis B core protein (HBc) after 1 week. At week 66, HBsAg, HBeAg, and HBc were still detectable in the liver.
“The expression of HBc could only be observed in the liver, but not in other organs or tissues, suggesting that the AAV-HBV1.04 only targeted the mouse liver,” the investigators wrote.
Further experimentation involving known cccDNA-binding proteins supported the similarity between cccDNA in the mouse model and natural infection.
“These results suggested that the chromatinization and transcriptional activation of cccDNA formed in this model dose not differ from wild-type cccDNA formed through infection.”
Next, Dr. Xu and colleagues demonstrated that the infected mice could serve as a reliable model for antiviral research. One week after injection with the vector, mice were treated with entecavir, polyinosinic-polycytidylic acid (poly[I:C]), or phosphate-buffered saline (PBS; control). As anticipated, entecavir suppressed circulating HBV DNA, but not HBsAg, HBeAg, or HBV cccDNA, whereas treatment with poly(I:C) reduced all HBV markers.
“This novel mouse model will provide a unique platform for studying HBV cccDNA and developing novel antivirals to achieve HBV cure,” the investigators concluded.
The study was supported by the National Natural Science Foundation of China, the Fundamental Research Funds for the Central Universities, Hubei Province’s Outstanding Medical Academic Leader Program, and others. The investigators reported no conflicts of interest.
A new mouse model that better represents chronic infection with hepatitis B virus (HBV) in humans may lead to more effective antiviral therapies for HBV, according to investigators.
During human infection, HBV genomes take the form of covalently closed circular DNA (cccDNA), a structure that has thwarted effective antiviral therapy and, until now, creation of an accurate mouse model, reported lead author Zaichao Xu, PhD, of Wuhan (China) University and colleagues.
“As the viral persistence reservoir plays a central role in HBV infection, HBV cccDNA is the key obstacle for a cure,” the investigators wrote in Cellular and Molecular Gastroenterology and Hepatology.
Although several previous mouse models have approximated this phenomenon with recombinant cccDNA-like molecules (rcccDNA), the present model is the first to achieve genuine cccDNA, which does not naturally occur in mice.
“Although rcccDNA supports persistent viral replication and antigen expression, the nature of rcccDNA may differ from authentic cccDNA, as additional sequences, like LoxP or attR, were inserted into the HBV genome,” the investigators noted.
The new model was created by first constructing an adeno-associated virus vector carrying a replication-deficient HBV1.04-fold genome (AAV-HBV1.04). When injected into mice, the vector led to cccDNA formation via ataxia-telangiectasia and Rad3-related protein (ATR)–mediated DNA damage response, a finding that was confirmed by blocking the same process with ATR inhibitors.
Immediately after injection, mice tested positive for both hepatitis B e antigen (HBeAg) and hepatitis B surface antigen (HBsAg), with peak concentrations after either 4 or 8 weeks depending on dose. HBV DNA was also detected in serum after injection, and 50% of hepatocytes exhibited HBsAg and hepatitis B core protein (HBc) after 1 week. At week 66, HBsAg, HBeAg, and HBc were still detectable in the liver.
“The expression of HBc could only be observed in the liver, but not in other organs or tissues, suggesting that the AAV-HBV1.04 only targeted the mouse liver,” the investigators wrote.
Further experimentation involving known cccDNA-binding proteins supported the similarity between cccDNA in the mouse model and natural infection.
“These results suggested that the chromatinization and transcriptional activation of cccDNA formed in this model dose not differ from wild-type cccDNA formed through infection.”
Next, Dr. Xu and colleagues demonstrated that the infected mice could serve as a reliable model for antiviral research. One week after injection with the vector, mice were treated with entecavir, polyinosinic-polycytidylic acid (poly[I:C]), or phosphate-buffered saline (PBS; control). As anticipated, entecavir suppressed circulating HBV DNA, but not HBsAg, HBeAg, or HBV cccDNA, whereas treatment with poly(I:C) reduced all HBV markers.
“This novel mouse model will provide a unique platform for studying HBV cccDNA and developing novel antivirals to achieve HBV cure,” the investigators concluded.
The study was supported by the National Natural Science Foundation of China, the Fundamental Research Funds for the Central Universities, Hubei Province’s Outstanding Medical Academic Leader Program, and others. The investigators reported no conflicts of interest.
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
Bowel ultrasound may overtake colonoscopy in Crohn’s
Bowel ultrasound predicts the clinical course of Crohn’s disease for up to 1 year, according to results of a prospective trial involving 225 patients.
After additional confirmation in larger studies, ultrasound could serve as a noninvasive alternative to colonoscopy for monitoring and predicting disease course, reported lead author Mariangela Allocca, MD, PhD, of Humanitas University, Milan, and colleagues.
“Frequent colonoscopies are expensive, invasive, and not well tolerated by patients, thus noninvasive tools for assessment and monitoring are strongly needed,” the investigators wrote in Clinical Gastroenterology and Hepatology. “Bowel ultrasound accurately detects inflammatory bowel disease activity, extent, and complications, particularly in Crohn’s disease. Considering its low cost, minimal invasiveness ... and easy repeatability, bowel ultrasound may be a simple, readily available tool for assessing and monitoring Crohn’s disease.”
To test this hypothesis, Dr. Allocca and colleagues enrolled 225 consecutive patients with ileal and/or colonic Crohn’s disease diagnosed for at least 6 months and managed at a tertiary hospital in Italy. All patients underwent both colonoscopy and bowel ultrasound with no more than 3 months between each procedure.
Colonoscopy results were characterized by the Simplified Endoscopic Score for Crohn’s disease (SES-CD), whereas ultrasound was scored using a several parameters, including bowel wall pattern, bowel thickness, bowel wall flow, presence of complications (abscess, fistula, stricture), and characteristics of mesenteric lymph nodes and tissue. Ultrasound scores were considered high if they exceeded a cut-off of 3.52, which was determined by a receiver operating characteristic curve analysis.
Participants were followed for 12 months after baseline ultrasound. The primary objective was to determine the relationship between baseline ultrasound findings and negative disease course, defined by steroid usage, need for surgery, need for hospitalization, and/or change in therapy. The secondary objective was to understand the relationship between ultrasound findings and endoscopy activity.
Multivariable analysis revealed that ultrasound scores greater than 3.52 predicted a negative clinical disease course for up to one year (odds ratio, 6.97; 95% confidence interval, 2.87-16.93; P < .001), as did the presence of at least one disease complication at baseline (OR, 3.90; 95% CI, 1.21-12.53; P = 0.21). A worse clinical course at one-year was also predicted by a baseline fecal calprotectin value of at least 250 mcg/g (OR, 5.43; 95% CI, 2.25-13.11; P < .001) and male sex (OR, 2.60; 95% CI, 1.12-6.02; P = .025).
Investigators then assessed individual disease outcomes at 12 months and baseline results. For example, high ultrasound score and calprotectin at baseline each predicted the need for treatment escalation. In comparison, disease behavior (inflammatory, stricturing, penetrating) and C reactive protein predicted need for corticosteroids. The only significant predictor of hospitalization a year later was CRP.
“[B]owel ultrasound is able to predict disease course in Crohn’s disease patients,” they wrote. “It may identify patients at high risk of a negative course to adopt effective strategies to prevent any disease progression. Our data need to be confirmed and validated in further large studies.”
The investigators disclosed relationships with Janssen, AbbVie, Mundipharma, and others.
Patients with Crohn’s disease (CD) undergo multiple colonoscopies during their lifetime. Endoscopic assessment is often necessary to determine extent and severity of inflammation to guide choice of therapy, assess mucosal healing on current therapy, and for surveillance examination for colorectal dysplasia. Multiple colonoscopies over a lifetime present a significant financial burden for patients. The invasive nature of the procedure, along with the small but potential risk of perforation and patient discomfort make for an undesirable experience. Cross-sectional imaging offers the advantage of noninvasive modality to assess bowel wall and extraluminal complications related to CD. Bowel ultrasound, performed as point of care imaging by gastroenterologists, is an emerging imaging alternative to visualize the bowel.
In the study by Allocca et al., the authors developed a bowel ultrasound–based score incorporating bowel wall thickness, pattern, flow, and presence of extraluminal complications. The score was developed by comparing ultrasound parameters with colonoscopy findings for each segment of the colon and terminal ileum. In a cohort of 225 patients, a bowel ultrasound score of >3.52 along with at least one extraluminal complication, baseline fecal calprotectin of >250 mcg/g, and male gender were linked with adverse outcomes within 12 months (defined as need for steroids, change of therapy, hospitalization, or surgery).
While these observations need to be validated externally, this study further consolidates the role for bowel ultrasound as a viable imaging modality to monitor disease and response to therapy in CD. Prior studies have shown bowel ultrasound is a valid alternative to MR enterography – without the expense, limited availability, and need for gadolinium contrast. As the therapeutic targets in IBD move toward mucosa healing, bowel ultrasound offers the promise of a cost-effective, noninvasive, point-of care test that can be performed during an office consultation. The operator dependent nature of this modality may limit its uptake and utilization. The International Bowel Ultrasound Group (IBUS) has collaborated with the European Crohn’s and Colitis organization as well as the Canadian Association of Gastroenterology to establish training and research in bowel ultrasound. Soon, patients can expect a bowel ultrasound to become part of their routine assessment during an office consultation.
Manreet Kaur, MD, is medical director of the Inflammatory Bowel Disease Center and an associate professor in the division of gastroenterology and hepatology at Baylor College of Medicine, Houston. She has no relevant conflicts of interest.
Patients with Crohn’s disease (CD) undergo multiple colonoscopies during their lifetime. Endoscopic assessment is often necessary to determine extent and severity of inflammation to guide choice of therapy, assess mucosal healing on current therapy, and for surveillance examination for colorectal dysplasia. Multiple colonoscopies over a lifetime present a significant financial burden for patients. The invasive nature of the procedure, along with the small but potential risk of perforation and patient discomfort make for an undesirable experience. Cross-sectional imaging offers the advantage of noninvasive modality to assess bowel wall and extraluminal complications related to CD. Bowel ultrasound, performed as point of care imaging by gastroenterologists, is an emerging imaging alternative to visualize the bowel.
In the study by Allocca et al., the authors developed a bowel ultrasound–based score incorporating bowel wall thickness, pattern, flow, and presence of extraluminal complications. The score was developed by comparing ultrasound parameters with colonoscopy findings for each segment of the colon and terminal ileum. In a cohort of 225 patients, a bowel ultrasound score of >3.52 along with at least one extraluminal complication, baseline fecal calprotectin of >250 mcg/g, and male gender were linked with adverse outcomes within 12 months (defined as need for steroids, change of therapy, hospitalization, or surgery).
While these observations need to be validated externally, this study further consolidates the role for bowel ultrasound as a viable imaging modality to monitor disease and response to therapy in CD. Prior studies have shown bowel ultrasound is a valid alternative to MR enterography – without the expense, limited availability, and need for gadolinium contrast. As the therapeutic targets in IBD move toward mucosa healing, bowel ultrasound offers the promise of a cost-effective, noninvasive, point-of care test that can be performed during an office consultation. The operator dependent nature of this modality may limit its uptake and utilization. The International Bowel Ultrasound Group (IBUS) has collaborated with the European Crohn’s and Colitis organization as well as the Canadian Association of Gastroenterology to establish training and research in bowel ultrasound. Soon, patients can expect a bowel ultrasound to become part of their routine assessment during an office consultation.
Manreet Kaur, MD, is medical director of the Inflammatory Bowel Disease Center and an associate professor in the division of gastroenterology and hepatology at Baylor College of Medicine, Houston. She has no relevant conflicts of interest.
Patients with Crohn’s disease (CD) undergo multiple colonoscopies during their lifetime. Endoscopic assessment is often necessary to determine extent and severity of inflammation to guide choice of therapy, assess mucosal healing on current therapy, and for surveillance examination for colorectal dysplasia. Multiple colonoscopies over a lifetime present a significant financial burden for patients. The invasive nature of the procedure, along with the small but potential risk of perforation and patient discomfort make for an undesirable experience. Cross-sectional imaging offers the advantage of noninvasive modality to assess bowel wall and extraluminal complications related to CD. Bowel ultrasound, performed as point of care imaging by gastroenterologists, is an emerging imaging alternative to visualize the bowel.
In the study by Allocca et al., the authors developed a bowel ultrasound–based score incorporating bowel wall thickness, pattern, flow, and presence of extraluminal complications. The score was developed by comparing ultrasound parameters with colonoscopy findings for each segment of the colon and terminal ileum. In a cohort of 225 patients, a bowel ultrasound score of >3.52 along with at least one extraluminal complication, baseline fecal calprotectin of >250 mcg/g, and male gender were linked with adverse outcomes within 12 months (defined as need for steroids, change of therapy, hospitalization, or surgery).
While these observations need to be validated externally, this study further consolidates the role for bowel ultrasound as a viable imaging modality to monitor disease and response to therapy in CD. Prior studies have shown bowel ultrasound is a valid alternative to MR enterography – without the expense, limited availability, and need for gadolinium contrast. As the therapeutic targets in IBD move toward mucosa healing, bowel ultrasound offers the promise of a cost-effective, noninvasive, point-of care test that can be performed during an office consultation. The operator dependent nature of this modality may limit its uptake and utilization. The International Bowel Ultrasound Group (IBUS) has collaborated with the European Crohn’s and Colitis organization as well as the Canadian Association of Gastroenterology to establish training and research in bowel ultrasound. Soon, patients can expect a bowel ultrasound to become part of their routine assessment during an office consultation.
Manreet Kaur, MD, is medical director of the Inflammatory Bowel Disease Center and an associate professor in the division of gastroenterology and hepatology at Baylor College of Medicine, Houston. She has no relevant conflicts of interest.
Bowel ultrasound predicts the clinical course of Crohn’s disease for up to 1 year, according to results of a prospective trial involving 225 patients.
After additional confirmation in larger studies, ultrasound could serve as a noninvasive alternative to colonoscopy for monitoring and predicting disease course, reported lead author Mariangela Allocca, MD, PhD, of Humanitas University, Milan, and colleagues.
“Frequent colonoscopies are expensive, invasive, and not well tolerated by patients, thus noninvasive tools for assessment and monitoring are strongly needed,” the investigators wrote in Clinical Gastroenterology and Hepatology. “Bowel ultrasound accurately detects inflammatory bowel disease activity, extent, and complications, particularly in Crohn’s disease. Considering its low cost, minimal invasiveness ... and easy repeatability, bowel ultrasound may be a simple, readily available tool for assessing and monitoring Crohn’s disease.”
To test this hypothesis, Dr. Allocca and colleagues enrolled 225 consecutive patients with ileal and/or colonic Crohn’s disease diagnosed for at least 6 months and managed at a tertiary hospital in Italy. All patients underwent both colonoscopy and bowel ultrasound with no more than 3 months between each procedure.
Colonoscopy results were characterized by the Simplified Endoscopic Score for Crohn’s disease (SES-CD), whereas ultrasound was scored using a several parameters, including bowel wall pattern, bowel thickness, bowel wall flow, presence of complications (abscess, fistula, stricture), and characteristics of mesenteric lymph nodes and tissue. Ultrasound scores were considered high if they exceeded a cut-off of 3.52, which was determined by a receiver operating characteristic curve analysis.
Participants were followed for 12 months after baseline ultrasound. The primary objective was to determine the relationship between baseline ultrasound findings and negative disease course, defined by steroid usage, need for surgery, need for hospitalization, and/or change in therapy. The secondary objective was to understand the relationship between ultrasound findings and endoscopy activity.
Multivariable analysis revealed that ultrasound scores greater than 3.52 predicted a negative clinical disease course for up to one year (odds ratio, 6.97; 95% confidence interval, 2.87-16.93; P < .001), as did the presence of at least one disease complication at baseline (OR, 3.90; 95% CI, 1.21-12.53; P = 0.21). A worse clinical course at one-year was also predicted by a baseline fecal calprotectin value of at least 250 mcg/g (OR, 5.43; 95% CI, 2.25-13.11; P < .001) and male sex (OR, 2.60; 95% CI, 1.12-6.02; P = .025).
Investigators then assessed individual disease outcomes at 12 months and baseline results. For example, high ultrasound score and calprotectin at baseline each predicted the need for treatment escalation. In comparison, disease behavior (inflammatory, stricturing, penetrating) and C reactive protein predicted need for corticosteroids. The only significant predictor of hospitalization a year later was CRP.
“[B]owel ultrasound is able to predict disease course in Crohn’s disease patients,” they wrote. “It may identify patients at high risk of a negative course to adopt effective strategies to prevent any disease progression. Our data need to be confirmed and validated in further large studies.”
The investigators disclosed relationships with Janssen, AbbVie, Mundipharma, and others.
Bowel ultrasound predicts the clinical course of Crohn’s disease for up to 1 year, according to results of a prospective trial involving 225 patients.
After additional confirmation in larger studies, ultrasound could serve as a noninvasive alternative to colonoscopy for monitoring and predicting disease course, reported lead author Mariangela Allocca, MD, PhD, of Humanitas University, Milan, and colleagues.
“Frequent colonoscopies are expensive, invasive, and not well tolerated by patients, thus noninvasive tools for assessment and monitoring are strongly needed,” the investigators wrote in Clinical Gastroenterology and Hepatology. “Bowel ultrasound accurately detects inflammatory bowel disease activity, extent, and complications, particularly in Crohn’s disease. Considering its low cost, minimal invasiveness ... and easy repeatability, bowel ultrasound may be a simple, readily available tool for assessing and monitoring Crohn’s disease.”
To test this hypothesis, Dr. Allocca and colleagues enrolled 225 consecutive patients with ileal and/or colonic Crohn’s disease diagnosed for at least 6 months and managed at a tertiary hospital in Italy. All patients underwent both colonoscopy and bowel ultrasound with no more than 3 months between each procedure.
Colonoscopy results were characterized by the Simplified Endoscopic Score for Crohn’s disease (SES-CD), whereas ultrasound was scored using a several parameters, including bowel wall pattern, bowel thickness, bowel wall flow, presence of complications (abscess, fistula, stricture), and characteristics of mesenteric lymph nodes and tissue. Ultrasound scores were considered high if they exceeded a cut-off of 3.52, which was determined by a receiver operating characteristic curve analysis.
Participants were followed for 12 months after baseline ultrasound. The primary objective was to determine the relationship between baseline ultrasound findings and negative disease course, defined by steroid usage, need for surgery, need for hospitalization, and/or change in therapy. The secondary objective was to understand the relationship between ultrasound findings and endoscopy activity.
Multivariable analysis revealed that ultrasound scores greater than 3.52 predicted a negative clinical disease course for up to one year (odds ratio, 6.97; 95% confidence interval, 2.87-16.93; P < .001), as did the presence of at least one disease complication at baseline (OR, 3.90; 95% CI, 1.21-12.53; P = 0.21). A worse clinical course at one-year was also predicted by a baseline fecal calprotectin value of at least 250 mcg/g (OR, 5.43; 95% CI, 2.25-13.11; P < .001) and male sex (OR, 2.60; 95% CI, 1.12-6.02; P = .025).
Investigators then assessed individual disease outcomes at 12 months and baseline results. For example, high ultrasound score and calprotectin at baseline each predicted the need for treatment escalation. In comparison, disease behavior (inflammatory, stricturing, penetrating) and C reactive protein predicted need for corticosteroids. The only significant predictor of hospitalization a year later was CRP.
“[B]owel ultrasound is able to predict disease course in Crohn’s disease patients,” they wrote. “It may identify patients at high risk of a negative course to adopt effective strategies to prevent any disease progression. Our data need to be confirmed and validated in further large studies.”
The investigators disclosed relationships with Janssen, AbbVie, Mundipharma, and others.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Children and COVID: Decline in new cases reaches 7th week
New cases of COVID-19 in U.S. children have fallen to their lowest level since the beginning of the Delta surge in July of 2021, according to the American Academy of Pediatrics and the Children’s Hospital Association.
. Over those 7 weeks, new cases dropped over 96% from the 1.15 million reported for Jan. 14-20, based on data collected by the AAP and CHA from state and territorial health departments.
The last time that the weekly count was below 42,000 was July 16-22, 2021, when almost 39,000 cases were reported in the midst of the Delta upsurge. That was shortly after cases had reached their lowest point, 8,447, since the early stages of the pandemic in 2020, the AAP/CHA data show.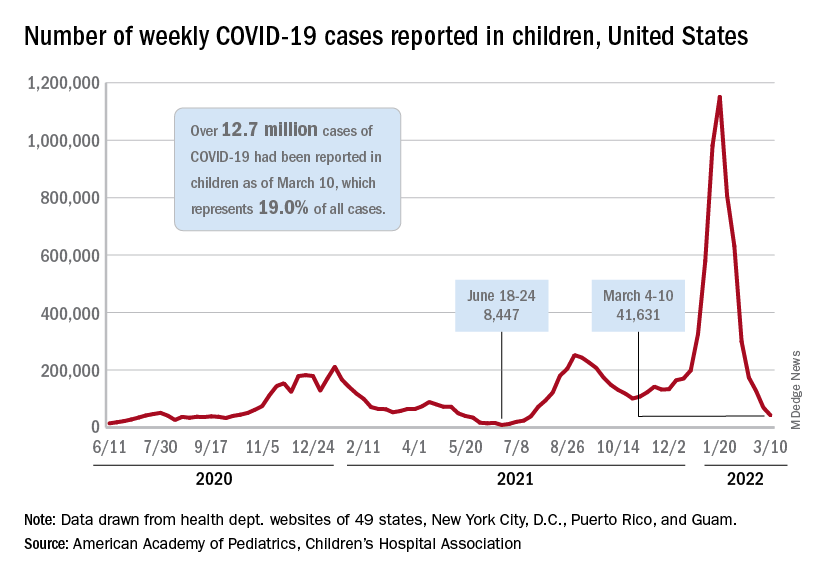
The cumulative number of pediatric cases is now up to 12.7 million, while the overall proportion of cases occurring in children held steady at 19.0% for the 4th week in a row, the AAP and CHA said in their weekly COVID-19 report. The Centers for Disease Control and Prevention, using an age range of 0-18 versus the states’ variety of ages, puts total cases at 11.7 million and deaths at 1,656 as of March 14.
Data from the CDC’s COVID-19–Associated Hospitalization Surveillance Network show that hospitalizations with laboratory-confirmed infection were down by 50% in children aged 0-4 years, by 63% among 5- to 11-year-olds, and by 58% in those aged 12-17 years for the week of Feb. 27 to March 5, compared with the week before.
The pace of vaccination continues to follow a similar trend, as the declines seen through February have continued into March. Cumulatively, 33.7% of children aged 5-11 have received at least one dose, and 26.8% are fully vaccinated, with corresponding numbers of 68.0% and 58.0% for children aged 12-17, the CDC reported on its COVID Data Tracker.
State-level data show that children aged 5-11 in Vermont, with a rate of 65%, are the most likely to have received at least one dose of COVID vaccine, while just 15% of 5- to 11-year-olds in Alabama, Louisiana, and Mississippi have gotten their first dose. Among children aged 12-17, that rate ranges from 40% in Wyoming to 94% in Hawaii, Massachusetts, and Rhode Island, the AAP said in a separate report based on CDC data.
In a recent report involving 1,364 children aged 5-15 years, two doses of the COVID-19 vaccine reduced the risk of infection from the Omicron variant by 31% in children aged 5-11 years and by 59% among children aged 12-15 years, said Ashley L. Fowlkes, ScD, of the CDC’s COVID-19 Emergency Response Team, and associates (MMWR 2022 Mar 11;71).
New cases of COVID-19 in U.S. children have fallen to their lowest level since the beginning of the Delta surge in July of 2021, according to the American Academy of Pediatrics and the Children’s Hospital Association.
. Over those 7 weeks, new cases dropped over 96% from the 1.15 million reported for Jan. 14-20, based on data collected by the AAP and CHA from state and territorial health departments.
The last time that the weekly count was below 42,000 was July 16-22, 2021, when almost 39,000 cases were reported in the midst of the Delta upsurge. That was shortly after cases had reached their lowest point, 8,447, since the early stages of the pandemic in 2020, the AAP/CHA data show.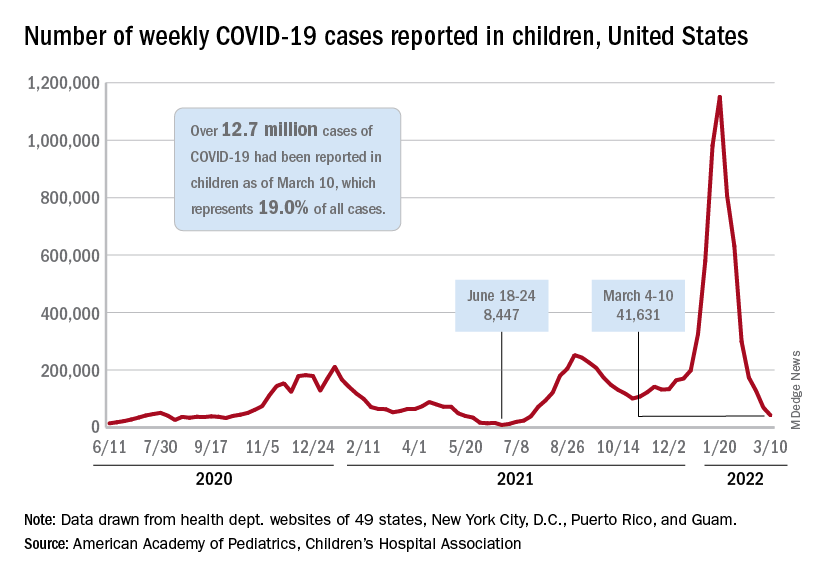
The cumulative number of pediatric cases is now up to 12.7 million, while the overall proportion of cases occurring in children held steady at 19.0% for the 4th week in a row, the AAP and CHA said in their weekly COVID-19 report. The Centers for Disease Control and Prevention, using an age range of 0-18 versus the states’ variety of ages, puts total cases at 11.7 million and deaths at 1,656 as of March 14.
Data from the CDC’s COVID-19–Associated Hospitalization Surveillance Network show that hospitalizations with laboratory-confirmed infection were down by 50% in children aged 0-4 years, by 63% among 5- to 11-year-olds, and by 58% in those aged 12-17 years for the week of Feb. 27 to March 5, compared with the week before.
The pace of vaccination continues to follow a similar trend, as the declines seen through February have continued into March. Cumulatively, 33.7% of children aged 5-11 have received at least one dose, and 26.8% are fully vaccinated, with corresponding numbers of 68.0% and 58.0% for children aged 12-17, the CDC reported on its COVID Data Tracker.
State-level data show that children aged 5-11 in Vermont, with a rate of 65%, are the most likely to have received at least one dose of COVID vaccine, while just 15% of 5- to 11-year-olds in Alabama, Louisiana, and Mississippi have gotten their first dose. Among children aged 12-17, that rate ranges from 40% in Wyoming to 94% in Hawaii, Massachusetts, and Rhode Island, the AAP said in a separate report based on CDC data.
In a recent report involving 1,364 children aged 5-15 years, two doses of the COVID-19 vaccine reduced the risk of infection from the Omicron variant by 31% in children aged 5-11 years and by 59% among children aged 12-15 years, said Ashley L. Fowlkes, ScD, of the CDC’s COVID-19 Emergency Response Team, and associates (MMWR 2022 Mar 11;71).
New cases of COVID-19 in U.S. children have fallen to their lowest level since the beginning of the Delta surge in July of 2021, according to the American Academy of Pediatrics and the Children’s Hospital Association.
. Over those 7 weeks, new cases dropped over 96% from the 1.15 million reported for Jan. 14-20, based on data collected by the AAP and CHA from state and territorial health departments.
The last time that the weekly count was below 42,000 was July 16-22, 2021, when almost 39,000 cases were reported in the midst of the Delta upsurge. That was shortly after cases had reached their lowest point, 8,447, since the early stages of the pandemic in 2020, the AAP/CHA data show.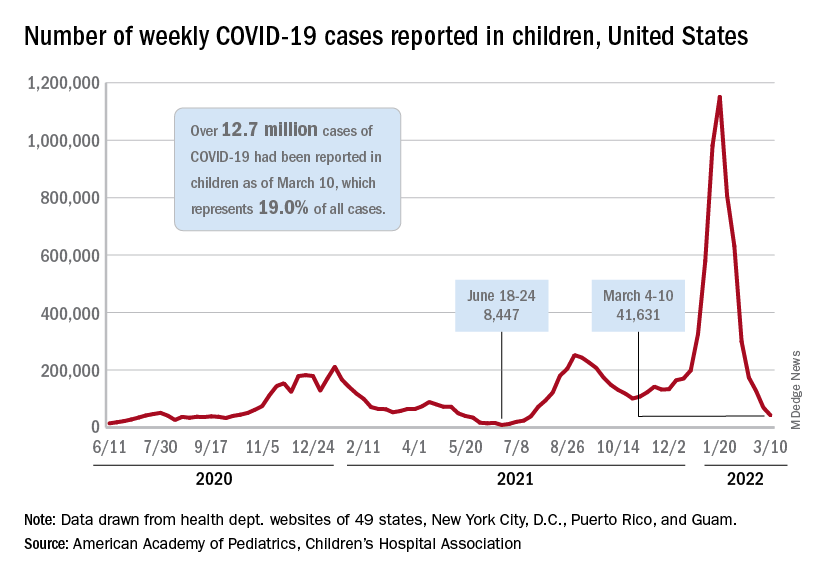
The cumulative number of pediatric cases is now up to 12.7 million, while the overall proportion of cases occurring in children held steady at 19.0% for the 4th week in a row, the AAP and CHA said in their weekly COVID-19 report. The Centers for Disease Control and Prevention, using an age range of 0-18 versus the states’ variety of ages, puts total cases at 11.7 million and deaths at 1,656 as of March 14.
Data from the CDC’s COVID-19–Associated Hospitalization Surveillance Network show that hospitalizations with laboratory-confirmed infection were down by 50% in children aged 0-4 years, by 63% among 5- to 11-year-olds, and by 58% in those aged 12-17 years for the week of Feb. 27 to March 5, compared with the week before.
The pace of vaccination continues to follow a similar trend, as the declines seen through February have continued into March. Cumulatively, 33.7% of children aged 5-11 have received at least one dose, and 26.8% are fully vaccinated, with corresponding numbers of 68.0% and 58.0% for children aged 12-17, the CDC reported on its COVID Data Tracker.
State-level data show that children aged 5-11 in Vermont, with a rate of 65%, are the most likely to have received at least one dose of COVID vaccine, while just 15% of 5- to 11-year-olds in Alabama, Louisiana, and Mississippi have gotten their first dose. Among children aged 12-17, that rate ranges from 40% in Wyoming to 94% in Hawaii, Massachusetts, and Rhode Island, the AAP said in a separate report based on CDC data.
In a recent report involving 1,364 children aged 5-15 years, two doses of the COVID-19 vaccine reduced the risk of infection from the Omicron variant by 31% in children aged 5-11 years and by 59% among children aged 12-15 years, said Ashley L. Fowlkes, ScD, of the CDC’s COVID-19 Emergency Response Team, and associates (MMWR 2022 Mar 11;71).












