User login
Guideline stresses new strategies for hypoglycemia management
The Endocrine Society has issued an updated clinical practice guideline on the prevention and management of hypoglycemia in patients with diabetes who are at high risk, addressing the wide variety of treatment advances, such as insulin pumps and continuous glucose monitoring (CGM) systems, that have appeared since the publication of the society’s last guideline on hypoglycemia, in 2009.
“CGM and insulin pumps have been much more commonly used in the last decade among people with diabetes, including children, and there are new forms of glucagon available,” said Anthony L. McCall, MD, PhD, chair of the panel that wrote the guideline.
“We had to update our guideline to match these developments in the diabetes field,” noted Dr. McCall, University of Virginia, Charlottesville, in a press statement.
The new guideline, developed by a multidisciplinary panel of clinical experts and published in the Journal of Clinical Endocrinology and Metabolism, addresses 10 key clinical questions regarding current issues relevant to hypoglycemia prevention and treatment in adult or pediatric patients with either type 1 or type 2 diabetes in the outpatient or inpatient setting.
Key guideline recommendations
The recommendations are based on factors including critical outcomes, implementation feasibility, and patient preferences.
Key guideline recommendations that are considered “strong,” based on evidence, include:
- The use of CGM rather than self-monitoring of blood glucose by fingerstick for patients with type 1 diabetes receiving multiple daily injections. The panel underscored that “comprehensive patient education on how to use and troubleshoot CGM devices and interpret these data is critically important for maximum benefit and successful outcomes.”
The use of a structured program for patient education versus unstructured advice for adult and pediatric outpatients with type 1 diabetes or type 2 diabetes receiving insulin therapy.
- Structured education on how to avoid repeated hypoglycemia is critical, and this education should be performed by experienced diabetes clinicians,” the panel asserts. “Moreover, insurance coverage for education should be available for all insulin-using patients.”
- The use of glucagon preparations that do not have to be reconstituted, as opposed to those that do (that is, available as a powder and diluent) in the treatment of outpatients with severe hypoglycemia.
Guideline recommendations that received conditional recommendations include:
- Use of real-time CGM and algorithm-driven insulin pumps in people with type 1 diabetes.
- Use of CGM for outpatients with type 2 diabetes at high risk for hypoglycemia.
- Use of long-acting and rapid-acting insulin analogs for patients at high risk for hypoglycemia.
Noting that there is “moderate-certainty” evidence for severe hypoglycemia reduction as an outcome in those using long-acting analog insulins versus human neutral protamine Hagedorn (NPH) insulin, the panel cautions that “most studies of long-acting analog insulins do not assess for significant adverse effects, including cardiovascular outcomes, and that many studies were designed to demonstrate noninferiority of analog insulin, compared with human NPH insulin.”
- Initiation of and continuation of CGM for select inpatient populations at high risk for hypoglycemia.
Hypoglycemia: One of top three preventable adverse drug reactions
The updated guidelines are especially important considering the common incidence of hypoglycemia, which the U.S. Department of Health and Human Services has determined to be one of the top 3 preventable adverse drug reactions, the panel says.
They note that between January 2007 and December 2011, emergency department visits for therapy-associated hypoglycemia among Medicare beneficiaries resulted in more than $600 million in spending.
Meanwhile, many people with type 1 or 2 diabetes may not experience or recognize the symptoms of hypoglycemia, which, in severe cases, can lead to unconsciousness or seizures, in addition to affecting quality of life, social life, work productivity, and ability to drive safely.
The key to accurate diagnosis of those patients is assessment of the three levels of hypoglycemia, described in a 2018 consensus statement:
- Level 1: Glucose less than 70 mg/dL (3.9 mmol/L) and greater than or equal to 54 mg/dL (3.0 mmol/L). This level of hypoglycemia should alert patients that they may need to ingest carbohydrate to prevent progressive hypoglycemia.
- Level 2: Glucose less than 54 mg/dL (3.0 mmol/L). This level of hypoglycemia is associated with increased risk for cognitive dysfunction and mortality.
- Level 3: A severe event characterized by altered mental and/or physical status requiring assistance. This level of hypoglycemia is life-threatening and requires emergent treatment, typically with glucagon.
Ultimately, “new technology and medications will help reduce hypoglycemia, and [clinicians] can better treat patients now with new, easier glucagons,” Dr. McCall told this news organization.
“People with diabetes, their caregivers, and diabetes specialists will all benefit from our guideline with a better understanding of best practices and interventions,” the panel notes.
Disparities still exist in access to insulin pumps
Separately, new research shows that while use of insulin pumps to manage type 1 diabetes has grown over 20 years, there has been no improvement in racial, ethnic, and socioeconomic disparities in their use in the United States. The findings are reported in Diabetes Technology & Therapeutics.
Using data from the SEARCH for Diabetes Youth Study across four time periods between 2001 and 2019, the researchers show that by the end of the period studied, insulin pump use was 67% among non-Hispanic White people, 41% among Hispanic people, 29% among Black people, and 46% among other racial and ethnic groups.
In addition, 70% of people with bachelor’s degrees or higher used the pumps, compared with 56% among those with some college, 40% among holders of high school degrees, and 18% among those with no high school education. By income level, 74% of those with household incomes of $75,000 or more, 66% with $50,000-$74,999, 51% with $25,000-$49,999, and 41% with less than $25,000 used the pumps.
“Diabetes technology has numerous benefits for patients with type 1 diabetes, but the problem is that there is a huge divide in who actually has access to these technologies,” said study lead Estelle Everett, MD, assistant professor of medicine in the division of endocrinology, diabetes & metabolism at the University of California, Los Angeles.
A version of this article first appeared on Medscape.com.
The Endocrine Society has issued an updated clinical practice guideline on the prevention and management of hypoglycemia in patients with diabetes who are at high risk, addressing the wide variety of treatment advances, such as insulin pumps and continuous glucose monitoring (CGM) systems, that have appeared since the publication of the society’s last guideline on hypoglycemia, in 2009.
“CGM and insulin pumps have been much more commonly used in the last decade among people with diabetes, including children, and there are new forms of glucagon available,” said Anthony L. McCall, MD, PhD, chair of the panel that wrote the guideline.
“We had to update our guideline to match these developments in the diabetes field,” noted Dr. McCall, University of Virginia, Charlottesville, in a press statement.
The new guideline, developed by a multidisciplinary panel of clinical experts and published in the Journal of Clinical Endocrinology and Metabolism, addresses 10 key clinical questions regarding current issues relevant to hypoglycemia prevention and treatment in adult or pediatric patients with either type 1 or type 2 diabetes in the outpatient or inpatient setting.
Key guideline recommendations
The recommendations are based on factors including critical outcomes, implementation feasibility, and patient preferences.
Key guideline recommendations that are considered “strong,” based on evidence, include:
- The use of CGM rather than self-monitoring of blood glucose by fingerstick for patients with type 1 diabetes receiving multiple daily injections. The panel underscored that “comprehensive patient education on how to use and troubleshoot CGM devices and interpret these data is critically important for maximum benefit and successful outcomes.”
The use of a structured program for patient education versus unstructured advice for adult and pediatric outpatients with type 1 diabetes or type 2 diabetes receiving insulin therapy.
- Structured education on how to avoid repeated hypoglycemia is critical, and this education should be performed by experienced diabetes clinicians,” the panel asserts. “Moreover, insurance coverage for education should be available for all insulin-using patients.”
- The use of glucagon preparations that do not have to be reconstituted, as opposed to those that do (that is, available as a powder and diluent) in the treatment of outpatients with severe hypoglycemia.
Guideline recommendations that received conditional recommendations include:
- Use of real-time CGM and algorithm-driven insulin pumps in people with type 1 diabetes.
- Use of CGM for outpatients with type 2 diabetes at high risk for hypoglycemia.
- Use of long-acting and rapid-acting insulin analogs for patients at high risk for hypoglycemia.
Noting that there is “moderate-certainty” evidence for severe hypoglycemia reduction as an outcome in those using long-acting analog insulins versus human neutral protamine Hagedorn (NPH) insulin, the panel cautions that “most studies of long-acting analog insulins do not assess for significant adverse effects, including cardiovascular outcomes, and that many studies were designed to demonstrate noninferiority of analog insulin, compared with human NPH insulin.”
- Initiation of and continuation of CGM for select inpatient populations at high risk for hypoglycemia.
Hypoglycemia: One of top three preventable adverse drug reactions
The updated guidelines are especially important considering the common incidence of hypoglycemia, which the U.S. Department of Health and Human Services has determined to be one of the top 3 preventable adverse drug reactions, the panel says.
They note that between January 2007 and December 2011, emergency department visits for therapy-associated hypoglycemia among Medicare beneficiaries resulted in more than $600 million in spending.
Meanwhile, many people with type 1 or 2 diabetes may not experience or recognize the symptoms of hypoglycemia, which, in severe cases, can lead to unconsciousness or seizures, in addition to affecting quality of life, social life, work productivity, and ability to drive safely.
The key to accurate diagnosis of those patients is assessment of the three levels of hypoglycemia, described in a 2018 consensus statement:
- Level 1: Glucose less than 70 mg/dL (3.9 mmol/L) and greater than or equal to 54 mg/dL (3.0 mmol/L). This level of hypoglycemia should alert patients that they may need to ingest carbohydrate to prevent progressive hypoglycemia.
- Level 2: Glucose less than 54 mg/dL (3.0 mmol/L). This level of hypoglycemia is associated with increased risk for cognitive dysfunction and mortality.
- Level 3: A severe event characterized by altered mental and/or physical status requiring assistance. This level of hypoglycemia is life-threatening and requires emergent treatment, typically with glucagon.
Ultimately, “new technology and medications will help reduce hypoglycemia, and [clinicians] can better treat patients now with new, easier glucagons,” Dr. McCall told this news organization.
“People with diabetes, their caregivers, and diabetes specialists will all benefit from our guideline with a better understanding of best practices and interventions,” the panel notes.
Disparities still exist in access to insulin pumps
Separately, new research shows that while use of insulin pumps to manage type 1 diabetes has grown over 20 years, there has been no improvement in racial, ethnic, and socioeconomic disparities in their use in the United States. The findings are reported in Diabetes Technology & Therapeutics.
Using data from the SEARCH for Diabetes Youth Study across four time periods between 2001 and 2019, the researchers show that by the end of the period studied, insulin pump use was 67% among non-Hispanic White people, 41% among Hispanic people, 29% among Black people, and 46% among other racial and ethnic groups.
In addition, 70% of people with bachelor’s degrees or higher used the pumps, compared with 56% among those with some college, 40% among holders of high school degrees, and 18% among those with no high school education. By income level, 74% of those with household incomes of $75,000 or more, 66% with $50,000-$74,999, 51% with $25,000-$49,999, and 41% with less than $25,000 used the pumps.
“Diabetes technology has numerous benefits for patients with type 1 diabetes, but the problem is that there is a huge divide in who actually has access to these technologies,” said study lead Estelle Everett, MD, assistant professor of medicine in the division of endocrinology, diabetes & metabolism at the University of California, Los Angeles.
A version of this article first appeared on Medscape.com.
The Endocrine Society has issued an updated clinical practice guideline on the prevention and management of hypoglycemia in patients with diabetes who are at high risk, addressing the wide variety of treatment advances, such as insulin pumps and continuous glucose monitoring (CGM) systems, that have appeared since the publication of the society’s last guideline on hypoglycemia, in 2009.
“CGM and insulin pumps have been much more commonly used in the last decade among people with diabetes, including children, and there are new forms of glucagon available,” said Anthony L. McCall, MD, PhD, chair of the panel that wrote the guideline.
“We had to update our guideline to match these developments in the diabetes field,” noted Dr. McCall, University of Virginia, Charlottesville, in a press statement.
The new guideline, developed by a multidisciplinary panel of clinical experts and published in the Journal of Clinical Endocrinology and Metabolism, addresses 10 key clinical questions regarding current issues relevant to hypoglycemia prevention and treatment in adult or pediatric patients with either type 1 or type 2 diabetes in the outpatient or inpatient setting.
Key guideline recommendations
The recommendations are based on factors including critical outcomes, implementation feasibility, and patient preferences.
Key guideline recommendations that are considered “strong,” based on evidence, include:
- The use of CGM rather than self-monitoring of blood glucose by fingerstick for patients with type 1 diabetes receiving multiple daily injections. The panel underscored that “comprehensive patient education on how to use and troubleshoot CGM devices and interpret these data is critically important for maximum benefit and successful outcomes.”
The use of a structured program for patient education versus unstructured advice for adult and pediatric outpatients with type 1 diabetes or type 2 diabetes receiving insulin therapy.
- Structured education on how to avoid repeated hypoglycemia is critical, and this education should be performed by experienced diabetes clinicians,” the panel asserts. “Moreover, insurance coverage for education should be available for all insulin-using patients.”
- The use of glucagon preparations that do not have to be reconstituted, as opposed to those that do (that is, available as a powder and diluent) in the treatment of outpatients with severe hypoglycemia.
Guideline recommendations that received conditional recommendations include:
- Use of real-time CGM and algorithm-driven insulin pumps in people with type 1 diabetes.
- Use of CGM for outpatients with type 2 diabetes at high risk for hypoglycemia.
- Use of long-acting and rapid-acting insulin analogs for patients at high risk for hypoglycemia.
Noting that there is “moderate-certainty” evidence for severe hypoglycemia reduction as an outcome in those using long-acting analog insulins versus human neutral protamine Hagedorn (NPH) insulin, the panel cautions that “most studies of long-acting analog insulins do not assess for significant adverse effects, including cardiovascular outcomes, and that many studies were designed to demonstrate noninferiority of analog insulin, compared with human NPH insulin.”
- Initiation of and continuation of CGM for select inpatient populations at high risk for hypoglycemia.
Hypoglycemia: One of top three preventable adverse drug reactions
The updated guidelines are especially important considering the common incidence of hypoglycemia, which the U.S. Department of Health and Human Services has determined to be one of the top 3 preventable adverse drug reactions, the panel says.
They note that between January 2007 and December 2011, emergency department visits for therapy-associated hypoglycemia among Medicare beneficiaries resulted in more than $600 million in spending.
Meanwhile, many people with type 1 or 2 diabetes may not experience or recognize the symptoms of hypoglycemia, which, in severe cases, can lead to unconsciousness or seizures, in addition to affecting quality of life, social life, work productivity, and ability to drive safely.
The key to accurate diagnosis of those patients is assessment of the three levels of hypoglycemia, described in a 2018 consensus statement:
- Level 1: Glucose less than 70 mg/dL (3.9 mmol/L) and greater than or equal to 54 mg/dL (3.0 mmol/L). This level of hypoglycemia should alert patients that they may need to ingest carbohydrate to prevent progressive hypoglycemia.
- Level 2: Glucose less than 54 mg/dL (3.0 mmol/L). This level of hypoglycemia is associated with increased risk for cognitive dysfunction and mortality.
- Level 3: A severe event characterized by altered mental and/or physical status requiring assistance. This level of hypoglycemia is life-threatening and requires emergent treatment, typically with glucagon.
Ultimately, “new technology and medications will help reduce hypoglycemia, and [clinicians] can better treat patients now with new, easier glucagons,” Dr. McCall told this news organization.
“People with diabetes, their caregivers, and diabetes specialists will all benefit from our guideline with a better understanding of best practices and interventions,” the panel notes.
Disparities still exist in access to insulin pumps
Separately, new research shows that while use of insulin pumps to manage type 1 diabetes has grown over 20 years, there has been no improvement in racial, ethnic, and socioeconomic disparities in their use in the United States. The findings are reported in Diabetes Technology & Therapeutics.
Using data from the SEARCH for Diabetes Youth Study across four time periods between 2001 and 2019, the researchers show that by the end of the period studied, insulin pump use was 67% among non-Hispanic White people, 41% among Hispanic people, 29% among Black people, and 46% among other racial and ethnic groups.
In addition, 70% of people with bachelor’s degrees or higher used the pumps, compared with 56% among those with some college, 40% among holders of high school degrees, and 18% among those with no high school education. By income level, 74% of those with household incomes of $75,000 or more, 66% with $50,000-$74,999, 51% with $25,000-$49,999, and 41% with less than $25,000 used the pumps.
“Diabetes technology has numerous benefits for patients with type 1 diabetes, but the problem is that there is a huge divide in who actually has access to these technologies,” said study lead Estelle Everett, MD, assistant professor of medicine in the division of endocrinology, diabetes & metabolism at the University of California, Los Angeles.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY AND METABOLISM
Multidrug-resistant gram-negative infections treatable with newer antibiotics, but guidance is needed
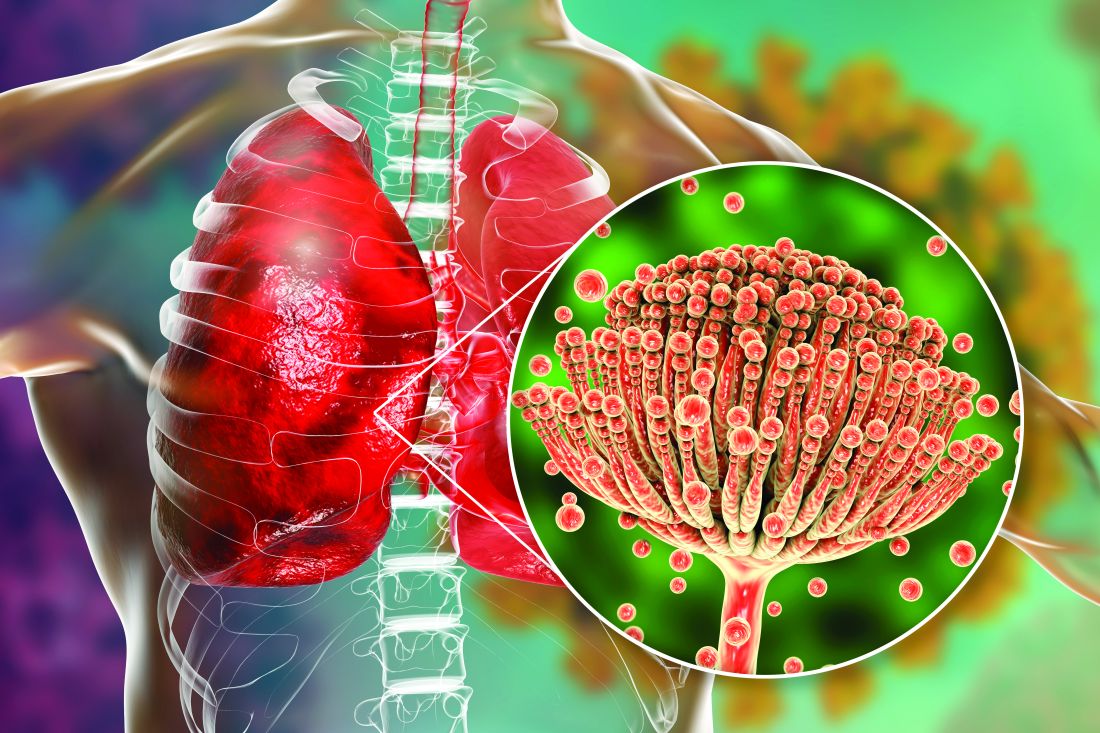
Multidrug-resistant gram-negative infections (MDRGNIs) are an emerging and deadly threat worldwide. Some of these infections are now resistant to nearly all antibiotics, and very few treatment options exist. Some of the remaining antibiotics for these MDRGNIs can cause acute kidney injury and have other toxic effects and can worsen antibiotic resistance. When deciding which drugs to use, clinicians need to juggle the possible lethality of the infection with the dangers of its treatment.
Samuel Windham, MD, and Marin H. Kollef, MD, authors of a recent article in Current Opinion in Infectious Diseases, express this urgency. They offer recommendations based on current guidelines and recently published research for treating MDRGNIs with some of the newer antibiotics.
Dr. Kollef, professor of pulmonary and critical care medicine at Washington University in St. Louis, said in an email, “Our recommendations differ in that they offer an approach that is based on disease severity, local resistance prevalence in MDRGNIs, and patient risk factors for infection with MDRGNIs. For patients with severe infection and risk factors for infection with MDRGNIs, we suggest empiric coverage for MDRGNIs until susceptibility data are available or based on rapid molecular testing. Selection of antibiotic therapy would be based on which MDRGNIs predominate locally.”
In their article, the authors discuss how to best utilize the newer antibiotics of ceftazidime-avibactam (CZA), cefiderocol, ceftolozane-tazobactam (C/T), meropenem-vaborbactam (MVB), imipenem-relebactam (I-R), aztreonam-avibactam (ATM-AVI), eravacycline, and plazomicin.
The scope of the problem
Bacterial infections are deadly and are becoming less treatable. The Centers for Disease Control and Prevention reported in 2022 that the COVID-19 pandemic has reversed years of decreases in health care–associated infections. Much of the increase has been caused by multidrug-resistant organisms.
In November 2022, authors of an article published in The Lancet estimated worldwide deaths from 33 bacterial genera across 11 infectious syndromes. They found that these infections were the second leading cause of death worldwide in 2019 (ischemic heart disease was the first). Furthermore, they discovered that 54.9% of these deaths were attributable to just five pathogens – Staphylococcus aureus, Escherichia coli, Streptococcus pneumoniae, Klebsiella pneumoniae, and Pseudomonas aeruginosa. Three of those five bacterial species – E. coli, K. pneumoniae, and P. aeruginosa – are gram-negative and are highly prone to drug resistance.
The CDC classified each of those three pathogens as an “urgent threat” in its 2019 Antibiotic Resistance Threats in the United States report. Of particular concern are gram-negative infections that have become resistant to carbapenems, a heavy-hitting class of antibiotics.
Regarding organisms that cause MDRGNIs, known as serine-beta-lactamases (OXA, KPC, and CTX-M) and metallo-beta-lactamases (NDM, VIM, and IMP). Carbapenem-resistant Pseudomonas aeruginosa and carbapenem-resistant Acinetobacter baumanii also produce carbapenemases, rendering them invulnerable to carbapenem antibiotics.
Traditionally, a common alternative used for carbapenem-resistant infections has been colistin, an older and very toxic antibiotic. The authors cite recent research demonstrating that CZA yields significantly better outcomes with regard to patient mortality and acute kidney injury than colistin and that CZA plus aztreonam can even decrease mortality and length of hospital stay for patients who have bloodstream infections with metallo-beta-lactamase-producing Enterobacterales, which are some of the hardest infections to treat.
“CZA has been demonstrated to have excellent activity against MDR Pseudomonas aeruginosa and KPC Enterobacterales. It should be the preferred agent for use, compared with colistin, for the treatment of carbapenem-resistant gram-negative bacteria susceptible to CZA. Moreover, CZA combined with aztreonam has been shown to be an effective treatment for metallo-beta-lactamase MDRGNIs,” Dr. Kollef said.
Four key recommendations for treating MDRGNIs
The authors base their recommendations, in addition to the recent studies they cite concerning CZA, upon two major guidelines on the treatment of MDRGNIs: the European Society of Clinical Microbiology and Infectious Diseases’ Guidelines for the Treatment of Infections Caused by Multidrug-Resistant Gram-Negative Bacilli, and the Infectious Diseases Society of America’s (IDSA’s) Guidance on the Treatment of Antimicrobial Resistant Gram-Negative Infections (multiple documents, found here and here).
Dr. Windham and Dr. Kollef present a table showing the spectrum of activity of the newer antibiotics, as well as an algorithm for decision-making. They summarize their treatment recommendations, which are based upon the bacterial infection cultures or on historical risk (previous infection or colonization history). They encourage empiric treatment if there is an increased risk of death or the presence of shock. By pathogen, they recommend the following:
- For carbapenem-resistant Enterobacterales, clinicians should treat patients with cefiderocol, ceftazidime-avibactam, imipenem-cilastatin-relabactam, or meropenem-vaborbactam.
- For carbapenem-resistant Pseudomonas aeruginosa, clinicians should treat patients with cefiderocol, ceftazidime-avibactam, imipenem-cilastatin-relabactam, or ceftolozane-tazobactam.
- For carbapenem-resistant Acinetobacter baumanii, clinicians should treat patients with a cefiderocol backbone with or without the addition of plazomicin, eravacycline, or other older antibacterials.
- For metallo-beta-lactamase-producing organisms, clinicians should treat patients with cefiderocol, ceftazidime-avibactam, aztreonam, imipenem-cilastatin-relabactam, aztreonam, or aztreonam-avibactam. The authors acknowledge that evidence is limited on treating these infections.
“In general, ceftazidime-avibactam works pretty well in patients with MDRGNIs, and there is no evidence that any of the other new agents is conclusively better in treatment responses. CZA and ceftolozane-tazobactam were the first of the new antibiotics active against highly MDRGN to get approved, and they have been most widely used,” Cornelius “Neil” J. Clancy, MD, chief of the Infectious Diseases Section at the VA Pittsburgh Health Care System, explained. Dr. Clancy was not involved in the Windham-Kollef review article.
“As such, it is not surprising that resistance has emerged and that it has been reported more commonly than for some other agents. The issue of resistance will be considered again as IDSA puts together their update,” Dr. Clancy said.
“The IDSA guidelines are regularly updated. The next updated iteration will be online in early 2023,” said Dr. Clancy, who is also affiliated with IDSA. “Clinical and resistance data that have appeared since the last update in 2022 will be considered as the guidance is put together.”
In general, Dr. Kollef also recommends using a facility’s antibiogram. “They are useful in determining which MDRGN’s predominate locally,” he said.
Dr. Kollef is a consultant for Pfizer, Merck, and Shionogi. Dr. Clancy has received research funding from Merck and from the National Institutes of Health.
A version of this article first appeared on Medscape.com.
Multidrug-resistant gram-negative infections (MDRGNIs) are an emerging and deadly threat worldwide. Some of these infections are now resistant to nearly all antibiotics, and very few treatment options exist. Some of the remaining antibiotics for these MDRGNIs can cause acute kidney injury and have other toxic effects and can worsen antibiotic resistance. When deciding which drugs to use, clinicians need to juggle the possible lethality of the infection with the dangers of its treatment.
Samuel Windham, MD, and Marin H. Kollef, MD, authors of a recent article in Current Opinion in Infectious Diseases, express this urgency. They offer recommendations based on current guidelines and recently published research for treating MDRGNIs with some of the newer antibiotics.
Dr. Kollef, professor of pulmonary and critical care medicine at Washington University in St. Louis, said in an email, “Our recommendations differ in that they offer an approach that is based on disease severity, local resistance prevalence in MDRGNIs, and patient risk factors for infection with MDRGNIs. For patients with severe infection and risk factors for infection with MDRGNIs, we suggest empiric coverage for MDRGNIs until susceptibility data are available or based on rapid molecular testing. Selection of antibiotic therapy would be based on which MDRGNIs predominate locally.”
In their article, the authors discuss how to best utilize the newer antibiotics of ceftazidime-avibactam (CZA), cefiderocol, ceftolozane-tazobactam (C/T), meropenem-vaborbactam (MVB), imipenem-relebactam (I-R), aztreonam-avibactam (ATM-AVI), eravacycline, and plazomicin.
The scope of the problem
Bacterial infections are deadly and are becoming less treatable. The Centers for Disease Control and Prevention reported in 2022 that the COVID-19 pandemic has reversed years of decreases in health care–associated infections. Much of the increase has been caused by multidrug-resistant organisms.
In November 2022, authors of an article published in The Lancet estimated worldwide deaths from 33 bacterial genera across 11 infectious syndromes. They found that these infections were the second leading cause of death worldwide in 2019 (ischemic heart disease was the first). Furthermore, they discovered that 54.9% of these deaths were attributable to just five pathogens – Staphylococcus aureus, Escherichia coli, Streptococcus pneumoniae, Klebsiella pneumoniae, and Pseudomonas aeruginosa. Three of those five bacterial species – E. coli, K. pneumoniae, and P. aeruginosa – are gram-negative and are highly prone to drug resistance.
The CDC classified each of those three pathogens as an “urgent threat” in its 2019 Antibiotic Resistance Threats in the United States report. Of particular concern are gram-negative infections that have become resistant to carbapenems, a heavy-hitting class of antibiotics.
Regarding organisms that cause MDRGNIs, known as serine-beta-lactamases (OXA, KPC, and CTX-M) and metallo-beta-lactamases (NDM, VIM, and IMP). Carbapenem-resistant Pseudomonas aeruginosa and carbapenem-resistant Acinetobacter baumanii also produce carbapenemases, rendering them invulnerable to carbapenem antibiotics.
Traditionally, a common alternative used for carbapenem-resistant infections has been colistin, an older and very toxic antibiotic. The authors cite recent research demonstrating that CZA yields significantly better outcomes with regard to patient mortality and acute kidney injury than colistin and that CZA plus aztreonam can even decrease mortality and length of hospital stay for patients who have bloodstream infections with metallo-beta-lactamase-producing Enterobacterales, which are some of the hardest infections to treat.
“CZA has been demonstrated to have excellent activity against MDR Pseudomonas aeruginosa and KPC Enterobacterales. It should be the preferred agent for use, compared with colistin, for the treatment of carbapenem-resistant gram-negative bacteria susceptible to CZA. Moreover, CZA combined with aztreonam has been shown to be an effective treatment for metallo-beta-lactamase MDRGNIs,” Dr. Kollef said.
Four key recommendations for treating MDRGNIs
The authors base their recommendations, in addition to the recent studies they cite concerning CZA, upon two major guidelines on the treatment of MDRGNIs: the European Society of Clinical Microbiology and Infectious Diseases’ Guidelines for the Treatment of Infections Caused by Multidrug-Resistant Gram-Negative Bacilli, and the Infectious Diseases Society of America’s (IDSA’s) Guidance on the Treatment of Antimicrobial Resistant Gram-Negative Infections (multiple documents, found here and here).
Dr. Windham and Dr. Kollef present a table showing the spectrum of activity of the newer antibiotics, as well as an algorithm for decision-making. They summarize their treatment recommendations, which are based upon the bacterial infection cultures or on historical risk (previous infection or colonization history). They encourage empiric treatment if there is an increased risk of death or the presence of shock. By pathogen, they recommend the following:
- For carbapenem-resistant Enterobacterales, clinicians should treat patients with cefiderocol, ceftazidime-avibactam, imipenem-cilastatin-relabactam, or meropenem-vaborbactam.
- For carbapenem-resistant Pseudomonas aeruginosa, clinicians should treat patients with cefiderocol, ceftazidime-avibactam, imipenem-cilastatin-relabactam, or ceftolozane-tazobactam.
- For carbapenem-resistant Acinetobacter baumanii, clinicians should treat patients with a cefiderocol backbone with or without the addition of plazomicin, eravacycline, or other older antibacterials.
- For metallo-beta-lactamase-producing organisms, clinicians should treat patients with cefiderocol, ceftazidime-avibactam, aztreonam, imipenem-cilastatin-relabactam, aztreonam, or aztreonam-avibactam. The authors acknowledge that evidence is limited on treating these infections.
“In general, ceftazidime-avibactam works pretty well in patients with MDRGNIs, and there is no evidence that any of the other new agents is conclusively better in treatment responses. CZA and ceftolozane-tazobactam were the first of the new antibiotics active against highly MDRGN to get approved, and they have been most widely used,” Cornelius “Neil” J. Clancy, MD, chief of the Infectious Diseases Section at the VA Pittsburgh Health Care System, explained. Dr. Clancy was not involved in the Windham-Kollef review article.
“As such, it is not surprising that resistance has emerged and that it has been reported more commonly than for some other agents. The issue of resistance will be considered again as IDSA puts together their update,” Dr. Clancy said.
“The IDSA guidelines are regularly updated. The next updated iteration will be online in early 2023,” said Dr. Clancy, who is also affiliated with IDSA. “Clinical and resistance data that have appeared since the last update in 2022 will be considered as the guidance is put together.”
In general, Dr. Kollef also recommends using a facility’s antibiogram. “They are useful in determining which MDRGN’s predominate locally,” he said.
Dr. Kollef is a consultant for Pfizer, Merck, and Shionogi. Dr. Clancy has received research funding from Merck and from the National Institutes of Health.
A version of this article first appeared on Medscape.com.
Multidrug-resistant gram-negative infections (MDRGNIs) are an emerging and deadly threat worldwide. Some of these infections are now resistant to nearly all antibiotics, and very few treatment options exist. Some of the remaining antibiotics for these MDRGNIs can cause acute kidney injury and have other toxic effects and can worsen antibiotic resistance. When deciding which drugs to use, clinicians need to juggle the possible lethality of the infection with the dangers of its treatment.
Samuel Windham, MD, and Marin H. Kollef, MD, authors of a recent article in Current Opinion in Infectious Diseases, express this urgency. They offer recommendations based on current guidelines and recently published research for treating MDRGNIs with some of the newer antibiotics.
Dr. Kollef, professor of pulmonary and critical care medicine at Washington University in St. Louis, said in an email, “Our recommendations differ in that they offer an approach that is based on disease severity, local resistance prevalence in MDRGNIs, and patient risk factors for infection with MDRGNIs. For patients with severe infection and risk factors for infection with MDRGNIs, we suggest empiric coverage for MDRGNIs until susceptibility data are available or based on rapid molecular testing. Selection of antibiotic therapy would be based on which MDRGNIs predominate locally.”
In their article, the authors discuss how to best utilize the newer antibiotics of ceftazidime-avibactam (CZA), cefiderocol, ceftolozane-tazobactam (C/T), meropenem-vaborbactam (MVB), imipenem-relebactam (I-R), aztreonam-avibactam (ATM-AVI), eravacycline, and plazomicin.
The scope of the problem
Bacterial infections are deadly and are becoming less treatable. The Centers for Disease Control and Prevention reported in 2022 that the COVID-19 pandemic has reversed years of decreases in health care–associated infections. Much of the increase has been caused by multidrug-resistant organisms.
In November 2022, authors of an article published in The Lancet estimated worldwide deaths from 33 bacterial genera across 11 infectious syndromes. They found that these infections were the second leading cause of death worldwide in 2019 (ischemic heart disease was the first). Furthermore, they discovered that 54.9% of these deaths were attributable to just five pathogens – Staphylococcus aureus, Escherichia coli, Streptococcus pneumoniae, Klebsiella pneumoniae, and Pseudomonas aeruginosa. Three of those five bacterial species – E. coli, K. pneumoniae, and P. aeruginosa – are gram-negative and are highly prone to drug resistance.
The CDC classified each of those three pathogens as an “urgent threat” in its 2019 Antibiotic Resistance Threats in the United States report. Of particular concern are gram-negative infections that have become resistant to carbapenems, a heavy-hitting class of antibiotics.
Regarding organisms that cause MDRGNIs, known as serine-beta-lactamases (OXA, KPC, and CTX-M) and metallo-beta-lactamases (NDM, VIM, and IMP). Carbapenem-resistant Pseudomonas aeruginosa and carbapenem-resistant Acinetobacter baumanii also produce carbapenemases, rendering them invulnerable to carbapenem antibiotics.
Traditionally, a common alternative used for carbapenem-resistant infections has been colistin, an older and very toxic antibiotic. The authors cite recent research demonstrating that CZA yields significantly better outcomes with regard to patient mortality and acute kidney injury than colistin and that CZA plus aztreonam can even decrease mortality and length of hospital stay for patients who have bloodstream infections with metallo-beta-lactamase-producing Enterobacterales, which are some of the hardest infections to treat.
“CZA has been demonstrated to have excellent activity against MDR Pseudomonas aeruginosa and KPC Enterobacterales. It should be the preferred agent for use, compared with colistin, for the treatment of carbapenem-resistant gram-negative bacteria susceptible to CZA. Moreover, CZA combined with aztreonam has been shown to be an effective treatment for metallo-beta-lactamase MDRGNIs,” Dr. Kollef said.
Four key recommendations for treating MDRGNIs
The authors base their recommendations, in addition to the recent studies they cite concerning CZA, upon two major guidelines on the treatment of MDRGNIs: the European Society of Clinical Microbiology and Infectious Diseases’ Guidelines for the Treatment of Infections Caused by Multidrug-Resistant Gram-Negative Bacilli, and the Infectious Diseases Society of America’s (IDSA’s) Guidance on the Treatment of Antimicrobial Resistant Gram-Negative Infections (multiple documents, found here and here).
Dr. Windham and Dr. Kollef present a table showing the spectrum of activity of the newer antibiotics, as well as an algorithm for decision-making. They summarize their treatment recommendations, which are based upon the bacterial infection cultures or on historical risk (previous infection or colonization history). They encourage empiric treatment if there is an increased risk of death or the presence of shock. By pathogen, they recommend the following:
- For carbapenem-resistant Enterobacterales, clinicians should treat patients with cefiderocol, ceftazidime-avibactam, imipenem-cilastatin-relabactam, or meropenem-vaborbactam.
- For carbapenem-resistant Pseudomonas aeruginosa, clinicians should treat patients with cefiderocol, ceftazidime-avibactam, imipenem-cilastatin-relabactam, or ceftolozane-tazobactam.
- For carbapenem-resistant Acinetobacter baumanii, clinicians should treat patients with a cefiderocol backbone with or without the addition of plazomicin, eravacycline, or other older antibacterials.
- For metallo-beta-lactamase-producing organisms, clinicians should treat patients with cefiderocol, ceftazidime-avibactam, aztreonam, imipenem-cilastatin-relabactam, aztreonam, or aztreonam-avibactam. The authors acknowledge that evidence is limited on treating these infections.
“In general, ceftazidime-avibactam works pretty well in patients with MDRGNIs, and there is no evidence that any of the other new agents is conclusively better in treatment responses. CZA and ceftolozane-tazobactam were the first of the new antibiotics active against highly MDRGN to get approved, and they have been most widely used,” Cornelius “Neil” J. Clancy, MD, chief of the Infectious Diseases Section at the VA Pittsburgh Health Care System, explained. Dr. Clancy was not involved in the Windham-Kollef review article.
“As such, it is not surprising that resistance has emerged and that it has been reported more commonly than for some other agents. The issue of resistance will be considered again as IDSA puts together their update,” Dr. Clancy said.
“The IDSA guidelines are regularly updated. The next updated iteration will be online in early 2023,” said Dr. Clancy, who is also affiliated with IDSA. “Clinical and resistance data that have appeared since the last update in 2022 will be considered as the guidance is put together.”
In general, Dr. Kollef also recommends using a facility’s antibiogram. “They are useful in determining which MDRGN’s predominate locally,” he said.
Dr. Kollef is a consultant for Pfizer, Merck, and Shionogi. Dr. Clancy has received research funding from Merck and from the National Institutes of Health.
A version of this article first appeared on Medscape.com.
FROM CURRENT OPINION IN INFECTIOUS DISEASES
Parental atopic dermatitis, asthma linked to risk of AD in offspring
of life, an analysis of a large birth cohort found.
“The prevalence of AD in children has increased dramatically in recent years, and most studies reporting the impact of parental atopic history on AD are based on older data,” wrote the study authors, led by Cathal O’Connor, MD. “Given the recent interest in early intervention to prevent AD and other allergic diseases, enhanced early identification of infants at risk of AD is increasingly important.”
The detailed analysis of AD risk associated with parental atopy in early life “may help to risk stratify infants to optimize early interventions for prevention or early treatment of AD,” they wrote.
The study was published in Pediatric Dermatology.
For the analysis, Dr. O’Connor of the department of pediatrics and child health at University College Cork (Ireland) and colleagues conducted a secondary analysis of the Cork Babies After Scope: Evaluating the Longitudinal Impact Using Neurological and Nutritional Endpoints (BASELINE) Birth Cohort Study.
The study recruited 2,183 healthy first-born babies between August 2009 and October 2011 to examine the effects of environmental factors during pregnancy and infancy on childhood health and development. Skin barrier assessments were performed at birth, 2 months, 6 months, 12 months, and 24 months using a validated open chamber system to measure transepidermal water loss.
Parental atopy was self-reported at 2 months. Parents were asked at 2 months if the infant had an “itchy rash on the face or in the folds of the arms or legs,” as a screening question for AD. Experienced health care personnel used UK Working Party criteria to diagnose AD at 6, 12, and 24 months.
Complete data on AD status was available for 1,505 children in the cohort. Dr. O’Connor and colleagues calculated an overall AD prevalence of 18.6% at 6 months, 15.2% at 12 months, and 16.5% at 24 months.
Overall prevalence of AD was highest at 6 months. The study showed a similar or slightly higher impact of paternal atopy on offspring AD development, compared to maternal atopy.
Multivariable logistic regression analysis revealed that the odds of AD were 1.57 at 6 months and 1.66 at 12 months for maternal AD; 1.90 at 6 months and 1.85 at 24 months for paternal AD; 1.76 at 6 months and 1.75 at 12 months for maternal asthma; and 1.70 at 6 months, 1.86 at 12 months, and 1.99 at 24 months for paternal asthma.
“Parental allergic rhinitis was not associated with AD in offspring in the first 2 years, except for maternal rhinitis at 24 months [an adjusted odds ratio of 1.79],” the authors wrote. “The genetic predisposition to allergic rhinitis, given the key role of aeroallergen sensitization in its pathogenesis, may not be associated with early onset AD, but may have a greater impact in later onset or persistent AD.”
The authors acknowledged certain limitations of the study, including the fact that it was a secondary data analysis, and that parental AD, asthma, and rhinitis were self-reported, “which may reduce reliability and may contribute to the differences seen between the impact of maternal and paternal reported atopy on offspring,” they wrote. “Data on siblings were not captured, as participants in the study were first-born children. Filaggrin mutational analysis was not performed, which would have provided richer detail.”
Kelly M. Cordoro, MD, professor of dermatology and pediatrics at the University of California, San Francisco, who was asked to comment on the work, said that the study confirms the well-known association between parental atopy and the risk of atopy in offspring, which has been shown in several studies dating back decades.
“The authors try to parse risk based on maternal or paternal or biparental history of AD and/or asthma and/or rhinitis, but this type of nuanced analysis when diagnosis is based solely on parental report may be an over-reach,” she said.
“Given that this data supports the association between parental atopy and risk of AD in infants at various time points, the clinically relevant immediate next question is how can we leverage this knowledge to prevent onset of AD in infants at risk?” she said. “To date, interventions such as early introduction of emollients have been evaluated with mixed results.”
A recent Cochrane analysis concluded that, based on available data, skin care interventions such as emollient use during the first year of life in otherwise healthy infants is probably not effective for preventing eczema and may increase risk of skin infection.
“Effects of skin care interventions on risk of asthma are also uncertain,” said Dr. Cordoro, who is also chief of the division of pediatric dermatology at UCSF.
“In sum, this study offers additional data in support of the link between atopy in parents and offspring,” she said. “Understanding how to mitigate risk and prevent atopy requires unraveling of the complex interplay between genetic, environmental, immunologic, microbial and other factors. For now, dermatologists are unable to make broad evidence-based recommendations for otherwise healthy (i.e., with normal skin) but at-risk infants in terms of approaches to skin care that might prevent eczema and asthma.”
of life, an analysis of a large birth cohort found.
“The prevalence of AD in children has increased dramatically in recent years, and most studies reporting the impact of parental atopic history on AD are based on older data,” wrote the study authors, led by Cathal O’Connor, MD. “Given the recent interest in early intervention to prevent AD and other allergic diseases, enhanced early identification of infants at risk of AD is increasingly important.”
The detailed analysis of AD risk associated with parental atopy in early life “may help to risk stratify infants to optimize early interventions for prevention or early treatment of AD,” they wrote.
The study was published in Pediatric Dermatology.
For the analysis, Dr. O’Connor of the department of pediatrics and child health at University College Cork (Ireland) and colleagues conducted a secondary analysis of the Cork Babies After Scope: Evaluating the Longitudinal Impact Using Neurological and Nutritional Endpoints (BASELINE) Birth Cohort Study.
The study recruited 2,183 healthy first-born babies between August 2009 and October 2011 to examine the effects of environmental factors during pregnancy and infancy on childhood health and development. Skin barrier assessments were performed at birth, 2 months, 6 months, 12 months, and 24 months using a validated open chamber system to measure transepidermal water loss.
Parental atopy was self-reported at 2 months. Parents were asked at 2 months if the infant had an “itchy rash on the face or in the folds of the arms or legs,” as a screening question for AD. Experienced health care personnel used UK Working Party criteria to diagnose AD at 6, 12, and 24 months.
Complete data on AD status was available for 1,505 children in the cohort. Dr. O’Connor and colleagues calculated an overall AD prevalence of 18.6% at 6 months, 15.2% at 12 months, and 16.5% at 24 months.
Overall prevalence of AD was highest at 6 months. The study showed a similar or slightly higher impact of paternal atopy on offspring AD development, compared to maternal atopy.
Multivariable logistic regression analysis revealed that the odds of AD were 1.57 at 6 months and 1.66 at 12 months for maternal AD; 1.90 at 6 months and 1.85 at 24 months for paternal AD; 1.76 at 6 months and 1.75 at 12 months for maternal asthma; and 1.70 at 6 months, 1.86 at 12 months, and 1.99 at 24 months for paternal asthma.
“Parental allergic rhinitis was not associated with AD in offspring in the first 2 years, except for maternal rhinitis at 24 months [an adjusted odds ratio of 1.79],” the authors wrote. “The genetic predisposition to allergic rhinitis, given the key role of aeroallergen sensitization in its pathogenesis, may not be associated with early onset AD, but may have a greater impact in later onset or persistent AD.”
The authors acknowledged certain limitations of the study, including the fact that it was a secondary data analysis, and that parental AD, asthma, and rhinitis were self-reported, “which may reduce reliability and may contribute to the differences seen between the impact of maternal and paternal reported atopy on offspring,” they wrote. “Data on siblings were not captured, as participants in the study were first-born children. Filaggrin mutational analysis was not performed, which would have provided richer detail.”
Kelly M. Cordoro, MD, professor of dermatology and pediatrics at the University of California, San Francisco, who was asked to comment on the work, said that the study confirms the well-known association between parental atopy and the risk of atopy in offspring, which has been shown in several studies dating back decades.
“The authors try to parse risk based on maternal or paternal or biparental history of AD and/or asthma and/or rhinitis, but this type of nuanced analysis when diagnosis is based solely on parental report may be an over-reach,” she said.
“Given that this data supports the association between parental atopy and risk of AD in infants at various time points, the clinically relevant immediate next question is how can we leverage this knowledge to prevent onset of AD in infants at risk?” she said. “To date, interventions such as early introduction of emollients have been evaluated with mixed results.”
A recent Cochrane analysis concluded that, based on available data, skin care interventions such as emollient use during the first year of life in otherwise healthy infants is probably not effective for preventing eczema and may increase risk of skin infection.
“Effects of skin care interventions on risk of asthma are also uncertain,” said Dr. Cordoro, who is also chief of the division of pediatric dermatology at UCSF.
“In sum, this study offers additional data in support of the link between atopy in parents and offspring,” she said. “Understanding how to mitigate risk and prevent atopy requires unraveling of the complex interplay between genetic, environmental, immunologic, microbial and other factors. For now, dermatologists are unable to make broad evidence-based recommendations for otherwise healthy (i.e., with normal skin) but at-risk infants in terms of approaches to skin care that might prevent eczema and asthma.”
of life, an analysis of a large birth cohort found.
“The prevalence of AD in children has increased dramatically in recent years, and most studies reporting the impact of parental atopic history on AD are based on older data,” wrote the study authors, led by Cathal O’Connor, MD. “Given the recent interest in early intervention to prevent AD and other allergic diseases, enhanced early identification of infants at risk of AD is increasingly important.”
The detailed analysis of AD risk associated with parental atopy in early life “may help to risk stratify infants to optimize early interventions for prevention or early treatment of AD,” they wrote.
The study was published in Pediatric Dermatology.
For the analysis, Dr. O’Connor of the department of pediatrics and child health at University College Cork (Ireland) and colleagues conducted a secondary analysis of the Cork Babies After Scope: Evaluating the Longitudinal Impact Using Neurological and Nutritional Endpoints (BASELINE) Birth Cohort Study.
The study recruited 2,183 healthy first-born babies between August 2009 and October 2011 to examine the effects of environmental factors during pregnancy and infancy on childhood health and development. Skin barrier assessments were performed at birth, 2 months, 6 months, 12 months, and 24 months using a validated open chamber system to measure transepidermal water loss.
Parental atopy was self-reported at 2 months. Parents were asked at 2 months if the infant had an “itchy rash on the face or in the folds of the arms or legs,” as a screening question for AD. Experienced health care personnel used UK Working Party criteria to diagnose AD at 6, 12, and 24 months.
Complete data on AD status was available for 1,505 children in the cohort. Dr. O’Connor and colleagues calculated an overall AD prevalence of 18.6% at 6 months, 15.2% at 12 months, and 16.5% at 24 months.
Overall prevalence of AD was highest at 6 months. The study showed a similar or slightly higher impact of paternal atopy on offspring AD development, compared to maternal atopy.
Multivariable logistic regression analysis revealed that the odds of AD were 1.57 at 6 months and 1.66 at 12 months for maternal AD; 1.90 at 6 months and 1.85 at 24 months for paternal AD; 1.76 at 6 months and 1.75 at 12 months for maternal asthma; and 1.70 at 6 months, 1.86 at 12 months, and 1.99 at 24 months for paternal asthma.
“Parental allergic rhinitis was not associated with AD in offspring in the first 2 years, except for maternal rhinitis at 24 months [an adjusted odds ratio of 1.79],” the authors wrote. “The genetic predisposition to allergic rhinitis, given the key role of aeroallergen sensitization in its pathogenesis, may not be associated with early onset AD, but may have a greater impact in later onset or persistent AD.”
The authors acknowledged certain limitations of the study, including the fact that it was a secondary data analysis, and that parental AD, asthma, and rhinitis were self-reported, “which may reduce reliability and may contribute to the differences seen between the impact of maternal and paternal reported atopy on offspring,” they wrote. “Data on siblings were not captured, as participants in the study were first-born children. Filaggrin mutational analysis was not performed, which would have provided richer detail.”
Kelly M. Cordoro, MD, professor of dermatology and pediatrics at the University of California, San Francisco, who was asked to comment on the work, said that the study confirms the well-known association between parental atopy and the risk of atopy in offspring, which has been shown in several studies dating back decades.
“The authors try to parse risk based on maternal or paternal or biparental history of AD and/or asthma and/or rhinitis, but this type of nuanced analysis when diagnosis is based solely on parental report may be an over-reach,” she said.
“Given that this data supports the association between parental atopy and risk of AD in infants at various time points, the clinically relevant immediate next question is how can we leverage this knowledge to prevent onset of AD in infants at risk?” she said. “To date, interventions such as early introduction of emollients have been evaluated with mixed results.”
A recent Cochrane analysis concluded that, based on available data, skin care interventions such as emollient use during the first year of life in otherwise healthy infants is probably not effective for preventing eczema and may increase risk of skin infection.
“Effects of skin care interventions on risk of asthma are also uncertain,” said Dr. Cordoro, who is also chief of the division of pediatric dermatology at UCSF.
“In sum, this study offers additional data in support of the link between atopy in parents and offspring,” she said. “Understanding how to mitigate risk and prevent atopy requires unraveling of the complex interplay between genetic, environmental, immunologic, microbial and other factors. For now, dermatologists are unable to make broad evidence-based recommendations for otherwise healthy (i.e., with normal skin) but at-risk infants in terms of approaches to skin care that might prevent eczema and asthma.”
FROM PEDIATRIC DERMATOLOGY
Poison centers fielding more calls about teen cannabis use
Poison control centers in the United States now receive more calls about adolescents abusing cannabis than alcohol or any other substance, according to a new study.
Many helpline calls about cannabis involve edible products, the researchers noted.
Over-the-counter medications – especially dextromethorphan-containing cough and cold medications and oral antihistamines, such as Benadryl – are other commonly abused substances.
But cannabis recently started topping the list.
“Since 2018, the most reported misused/abused substance involved exposure to marijuana,” according to the study, which was published online in Clinical Toxicology.
Adrienne Hughes, MD, assistant professor of emergency medicine at Oregon Health & Science University, Portland, and colleagues analyzed calls to United States poison control centers between 2000 and 2020. They focused on 338,000 calls about intentional substance abuse or misuse, including for the purpose of getting high, in individuals aged 6-18 years.
The calls were made to 55 certified helplines for health professionals, public health agencies, and members of the public seeking guidance about exposures to various substances.
Cannabis vs. alcohol
In 2000, alcohol was the substance involved in the largest number of cases (1,318, or 9.8% of all calls). Between 2000 and 2013, cases of alcohol abuse exceeded the number of cannabis cases each year.
But that changed in 2014, when cannabis overtook alcohol.
Over the 20-year study period, calls about exposure to cannabis increased 245%, from 510 in 2000 to 1,761 in 2020.
Edibles played a key role.
“Edible marijuana preparations accounted for the highest increase in call rates, compared with all other forms of marijuana,” the researchers reported.
Edible products are “often marketed in ways that are attractive to young people, and they are considered more discrete and convenient,” Dr. Hughes said. But they can have “unpredictable” effects.
“Compared to smoking cannabis, which typically results in an immediate high, intoxication from edible forms usually takes several hours, which may lead some individuals to consume greater amounts and experience unexpected and unpredictable highs,” she said.
For example, prior research has shown that edible cannabis consumption may lead to more acute psychiatric symptoms and cardiovascular events than does inhaled cannabis.
Trends in alcohol use may have held relatively steady, despite some minor declines in the poison center data, Dr. Hughes said.
“Anecdotally, there hasn’t been an obvious notable reduction in alcohol cases in the emergency department,” she said. “However, I wouldn’t expect a huge change given our data only found a slow mild decline in alcohol cases over the study period.”
The increase in cannabis-related calls coincides with more states legalizing or decriminalizing the drug for medical or recreational purposes. Currently, 21 states have approved recreational cannabis for adults who are at least 21 years old.
What are the risks?
Parents typically call a poison center about cannabis exposure after they see or suspect that their child has ingested loose cannabis leaves or edibles containing the substance, Dr. Hughes said.
“The poison center provides guidance to parents about whether or not their child can be watched at home or requires referral to a health care facility,” she said. “While marijuana carries a low risk for severe toxicity, it can be inebriating to the point of poor judgment, risk of falls or other injury, and occasionally a panic reaction in the novice user and unsuspecting children who accidentally ingest these products.”
Intentional misuse or abuse tends to occur in older children and teens.
Nonprescription drugs have a high potential for abuse because they are legal and may be perceived as safe, Dr. Hughes said.
If a child has a history of misusing or abusing substances or if a parent is worried that their child is at high risk for this behavior, they should consider securing medicines in a lock box, she advised.
That applies to cannabis too.
“I would recommend that parents also consider locking up their cannabis products,” she said.
The National Poison Data System relies on voluntary reporting, and the data are not expected to represent the actual number of intentional misuse and abuse exposures, the researchers noted.
Poison control centers in the United States are available for consultation about patients with known or suspected cannabis ingestion or other suspected poisonings (1-800-222-1222).
The researchers had no disclosures.
A version of this article first appeared on Medscape.com.
Poison control centers in the United States now receive more calls about adolescents abusing cannabis than alcohol or any other substance, according to a new study.
Many helpline calls about cannabis involve edible products, the researchers noted.
Over-the-counter medications – especially dextromethorphan-containing cough and cold medications and oral antihistamines, such as Benadryl – are other commonly abused substances.
But cannabis recently started topping the list.
“Since 2018, the most reported misused/abused substance involved exposure to marijuana,” according to the study, which was published online in Clinical Toxicology.
Adrienne Hughes, MD, assistant professor of emergency medicine at Oregon Health & Science University, Portland, and colleagues analyzed calls to United States poison control centers between 2000 and 2020. They focused on 338,000 calls about intentional substance abuse or misuse, including for the purpose of getting high, in individuals aged 6-18 years.
The calls were made to 55 certified helplines for health professionals, public health agencies, and members of the public seeking guidance about exposures to various substances.
Cannabis vs. alcohol
In 2000, alcohol was the substance involved in the largest number of cases (1,318, or 9.8% of all calls). Between 2000 and 2013, cases of alcohol abuse exceeded the number of cannabis cases each year.
But that changed in 2014, when cannabis overtook alcohol.
Over the 20-year study period, calls about exposure to cannabis increased 245%, from 510 in 2000 to 1,761 in 2020.
Edibles played a key role.
“Edible marijuana preparations accounted for the highest increase in call rates, compared with all other forms of marijuana,” the researchers reported.
Edible products are “often marketed in ways that are attractive to young people, and they are considered more discrete and convenient,” Dr. Hughes said. But they can have “unpredictable” effects.
“Compared to smoking cannabis, which typically results in an immediate high, intoxication from edible forms usually takes several hours, which may lead some individuals to consume greater amounts and experience unexpected and unpredictable highs,” she said.
For example, prior research has shown that edible cannabis consumption may lead to more acute psychiatric symptoms and cardiovascular events than does inhaled cannabis.
Trends in alcohol use may have held relatively steady, despite some minor declines in the poison center data, Dr. Hughes said.
“Anecdotally, there hasn’t been an obvious notable reduction in alcohol cases in the emergency department,” she said. “However, I wouldn’t expect a huge change given our data only found a slow mild decline in alcohol cases over the study period.”
The increase in cannabis-related calls coincides with more states legalizing or decriminalizing the drug for medical or recreational purposes. Currently, 21 states have approved recreational cannabis for adults who are at least 21 years old.
What are the risks?
Parents typically call a poison center about cannabis exposure after they see or suspect that their child has ingested loose cannabis leaves or edibles containing the substance, Dr. Hughes said.
“The poison center provides guidance to parents about whether or not their child can be watched at home or requires referral to a health care facility,” she said. “While marijuana carries a low risk for severe toxicity, it can be inebriating to the point of poor judgment, risk of falls or other injury, and occasionally a panic reaction in the novice user and unsuspecting children who accidentally ingest these products.”
Intentional misuse or abuse tends to occur in older children and teens.
Nonprescription drugs have a high potential for abuse because they are legal and may be perceived as safe, Dr. Hughes said.
If a child has a history of misusing or abusing substances or if a parent is worried that their child is at high risk for this behavior, they should consider securing medicines in a lock box, she advised.
That applies to cannabis too.
“I would recommend that parents also consider locking up their cannabis products,” she said.
The National Poison Data System relies on voluntary reporting, and the data are not expected to represent the actual number of intentional misuse and abuse exposures, the researchers noted.
Poison control centers in the United States are available for consultation about patients with known or suspected cannabis ingestion or other suspected poisonings (1-800-222-1222).
The researchers had no disclosures.
A version of this article first appeared on Medscape.com.
Poison control centers in the United States now receive more calls about adolescents abusing cannabis than alcohol or any other substance, according to a new study.
Many helpline calls about cannabis involve edible products, the researchers noted.
Over-the-counter medications – especially dextromethorphan-containing cough and cold medications and oral antihistamines, such as Benadryl – are other commonly abused substances.
But cannabis recently started topping the list.
“Since 2018, the most reported misused/abused substance involved exposure to marijuana,” according to the study, which was published online in Clinical Toxicology.
Adrienne Hughes, MD, assistant professor of emergency medicine at Oregon Health & Science University, Portland, and colleagues analyzed calls to United States poison control centers between 2000 and 2020. They focused on 338,000 calls about intentional substance abuse or misuse, including for the purpose of getting high, in individuals aged 6-18 years.
The calls were made to 55 certified helplines for health professionals, public health agencies, and members of the public seeking guidance about exposures to various substances.
Cannabis vs. alcohol
In 2000, alcohol was the substance involved in the largest number of cases (1,318, or 9.8% of all calls). Between 2000 and 2013, cases of alcohol abuse exceeded the number of cannabis cases each year.
But that changed in 2014, when cannabis overtook alcohol.
Over the 20-year study period, calls about exposure to cannabis increased 245%, from 510 in 2000 to 1,761 in 2020.
Edibles played a key role.
“Edible marijuana preparations accounted for the highest increase in call rates, compared with all other forms of marijuana,” the researchers reported.
Edible products are “often marketed in ways that are attractive to young people, and they are considered more discrete and convenient,” Dr. Hughes said. But they can have “unpredictable” effects.
“Compared to smoking cannabis, which typically results in an immediate high, intoxication from edible forms usually takes several hours, which may lead some individuals to consume greater amounts and experience unexpected and unpredictable highs,” she said.
For example, prior research has shown that edible cannabis consumption may lead to more acute psychiatric symptoms and cardiovascular events than does inhaled cannabis.
Trends in alcohol use may have held relatively steady, despite some minor declines in the poison center data, Dr. Hughes said.
“Anecdotally, there hasn’t been an obvious notable reduction in alcohol cases in the emergency department,” she said. “However, I wouldn’t expect a huge change given our data only found a slow mild decline in alcohol cases over the study period.”
The increase in cannabis-related calls coincides with more states legalizing or decriminalizing the drug for medical or recreational purposes. Currently, 21 states have approved recreational cannabis for adults who are at least 21 years old.
What are the risks?
Parents typically call a poison center about cannabis exposure after they see or suspect that their child has ingested loose cannabis leaves or edibles containing the substance, Dr. Hughes said.
“The poison center provides guidance to parents about whether or not their child can be watched at home or requires referral to a health care facility,” she said. “While marijuana carries a low risk for severe toxicity, it can be inebriating to the point of poor judgment, risk of falls or other injury, and occasionally a panic reaction in the novice user and unsuspecting children who accidentally ingest these products.”
Intentional misuse or abuse tends to occur in older children and teens.
Nonprescription drugs have a high potential for abuse because they are legal and may be perceived as safe, Dr. Hughes said.
If a child has a history of misusing or abusing substances or if a parent is worried that their child is at high risk for this behavior, they should consider securing medicines in a lock box, she advised.
That applies to cannabis too.
“I would recommend that parents also consider locking up their cannabis products,” she said.
The National Poison Data System relies on voluntary reporting, and the data are not expected to represent the actual number of intentional misuse and abuse exposures, the researchers noted.
Poison control centers in the United States are available for consultation about patients with known or suspected cannabis ingestion or other suspected poisonings (1-800-222-1222).
The researchers had no disclosures.
A version of this article first appeared on Medscape.com.
Postpartum hemorrhage rates and risk factors rising
The rate of postpartum hemorrhage for hospital deliveries in the United States increased significantly over a 20-year period, according to data from more than 76 million delivery hospitalizations from the National Inpatient Sample.
Postpartum hemorrhage remains the leading cause of maternal morbidity and mortality worldwide, and many clinical and patient-level risk factors appear to be on the rise, wrote Chiara M. Corbetta-Rastelli, MD, of the University of California, San Francisco, and colleagues.
Although practice changes have been introduced to reduce postpartum hemorrhage, recent trends in postpartum hemorrhage risk and outcomes in the context of such changes as hemorrhage safety bundles have not been examined, they said.
In a study published in Obstetrics & Gynecology, the researchers reviewed data from hospitalizations for females aged 15-54 years for deliveries between 2000 and 2019 using the National Inpatient Sample. They used a regression analysis to estimate average annual percentage changes (AAPC). Their objectives were to characterize trends and also to assess the association between risk factors and the occurrence of postpartum hemorrhage and related interventions. Demographics, clinical factors, and hospital characteristics were mainly similar between the group of patients with postpartum hemorrhage and those with no postpartum hemorrhage.
Approximately 3% (2.3 million) of 76.7 million hospitalizations for delivery were complicated by postpartum hemorrhage during the study period, and the annual rate increased from 2.7% to 4.3%.
Overall, 21.4% of individuals with delivery hospitalizations complicated by postpartum hemorrhage had one postpartum risk factor, and 1.4% had two or more risk factors. The number of individuals with at least one risk factor for postpartum hemorrhage increased significantly, from 18.6% to 26.9%, during the study period, with an annual percentage change of 1.9%.
Compared with deliveries in individuals without risk factors, individuals with one risk factor had slightly higher odds of postpartum hemorrhage (odds ratio, 1.14), but those with two or more risk factors were more than twice as likely to experience postpartum hemorrhage as those with no risk factors (OR, 2.31).
The researchers also examined the association of specific risk factors and interventions related to hemorrhage, notably blood transfusion and peripartum hysterectomy. Blood transfusions in individuals with postpartum hemorrhage increased from 5.4% to 16.7% between 2000 and 2011, (AAPC, 10.2%) then decreased from 16.7% to 12.6% from 2011 to 2019 (AAPC, –3.9%).
Peripartum hysterectomy in the study population increased from 1.4% to 2.4% from 2000 to 2009 (AAPC 5.0%), remained steady from 2009 to 2016, and then decreased from 2.1% to 0.9% from 2016 to 2019 (AAPC –27%).
Other risk factors associated with postpartum hemorrhage itself and with blood transfusion and hysterectomy in the setting of postpartum hemorrhage included prior cesarean delivery with placenta previa or accreta, placenta previa without prior cesarean delivery, and antepartum hemorrhage or placental abruption, the researchers noted.
“In addition to placental abnormalities, risk factors such as preeclampsia with severe features, polyhydramnios, and uterine leiomyomas demonstrated the highest rates of increase in our data,” they wrote in their discussion. These trends may lead to continuing increases in postpartum hemorrhage risk, which was not fully explained by the increase in risk factors seen in the current study, the researchers said.
The study findings were limited by several factors, including the use of billing codes that could lead to misclassification of diagnoses, as well as possible differences in the definition and coding for postpartum hemorrhage among hospitals, the researchers noted. Other limitations were the exclusion of cases of readmission for postpartum hemorrhage and lack of clinical details involving use of medications or nonoperative interventions, they said.
Notably, the study finding of stable to decreasing peripartum hysterectomy rates in hospitalized patients with postpartum hemorrhage conflicts with another recent study showing an increase in peripartum hysterectomy from 2009 to 2020, but this difference may reflect changes in billing, indications for hysterectomy, or study modeling, they said.
The current study was strengthened by the use of a large database to analyze population trends, a contemporary study period, and the inclusion of meaningful outcomes such as peripartum hysterectomy, the researchers wrote.
The shift in blood transfusion and peripartum hysterectomy may reflect the implementation of protocols to promote early intervention and identification of postpartum hemorrhage, they concluded.
Interventions can have an effect
“Hemorrhage remains a leading cause of maternal mortality in the United States and blood transfusion is the most common severe maternal morbidity,” Catherine M. Albright, MD, MS, associate professor of maternal-fetal medicine at the University of Washington, Seattle, said in an interview. “It is important to understand the current state, especially given that many hospitals have implemented policies and procedures to better identify and treat postpartum hemorrhage,” she said.
Dr. Albright said, “I was pleased to see that they did not just look at a diagnosis of postpartum hemorrhage but rather also looked at complications arising from postpartum hemorrhage, such as blood transfusion or hysterectomy.”
Postpartum hemorrhage is often a clinical diagnosis that uses estimated blood loss, a notoriously inaccurate measure, said Dr. Albright. “Additionally, the definitions of postpartum hemorrhage, as well as the ICD codes, changed during the time period of the study,” she noted. “These factors all could lead to both underreporting and overreporting of the true incidence of postpartum hemorrhage. Blood transfusion and hysterectomy are more objective outcomes and demonstrate true morbidity,” she said.
“Most of the risk factors that are listed in the article are not modifiable during that pregnancy,” said Dr. Albright. For example, a history of a prior cesarean or having a twin pregnancy is not something that can be changed, she said. “Many of the other risk factors or associated clinical factors, such as obesity, chronic hypertension, and pregestational diabetes, are modifiable, but before pregnancy. Universal and easy access to primary medical care prior to and between pregnancies may help to mitigate some of these factors,” she noted.
Looking ahead, “It would be helpful to ensure that these types of data are available at the state and hospital level; this will allow for local evaluation of programs that are in place to reduce postpartum hemorrhage risk and improve identification and treatment,” Dr. Albright said.
The study received no outside funding. Dr. Corbetta-Rastelli and Dr. Albright had no financial conflicts to disclose.
The rate of postpartum hemorrhage for hospital deliveries in the United States increased significantly over a 20-year period, according to data from more than 76 million delivery hospitalizations from the National Inpatient Sample.
Postpartum hemorrhage remains the leading cause of maternal morbidity and mortality worldwide, and many clinical and patient-level risk factors appear to be on the rise, wrote Chiara M. Corbetta-Rastelli, MD, of the University of California, San Francisco, and colleagues.
Although practice changes have been introduced to reduce postpartum hemorrhage, recent trends in postpartum hemorrhage risk and outcomes in the context of such changes as hemorrhage safety bundles have not been examined, they said.
In a study published in Obstetrics & Gynecology, the researchers reviewed data from hospitalizations for females aged 15-54 years for deliveries between 2000 and 2019 using the National Inpatient Sample. They used a regression analysis to estimate average annual percentage changes (AAPC). Their objectives were to characterize trends and also to assess the association between risk factors and the occurrence of postpartum hemorrhage and related interventions. Demographics, clinical factors, and hospital characteristics were mainly similar between the group of patients with postpartum hemorrhage and those with no postpartum hemorrhage.
Approximately 3% (2.3 million) of 76.7 million hospitalizations for delivery were complicated by postpartum hemorrhage during the study period, and the annual rate increased from 2.7% to 4.3%.
Overall, 21.4% of individuals with delivery hospitalizations complicated by postpartum hemorrhage had one postpartum risk factor, and 1.4% had two or more risk factors. The number of individuals with at least one risk factor for postpartum hemorrhage increased significantly, from 18.6% to 26.9%, during the study period, with an annual percentage change of 1.9%.
Compared with deliveries in individuals without risk factors, individuals with one risk factor had slightly higher odds of postpartum hemorrhage (odds ratio, 1.14), but those with two or more risk factors were more than twice as likely to experience postpartum hemorrhage as those with no risk factors (OR, 2.31).
The researchers also examined the association of specific risk factors and interventions related to hemorrhage, notably blood transfusion and peripartum hysterectomy. Blood transfusions in individuals with postpartum hemorrhage increased from 5.4% to 16.7% between 2000 and 2011, (AAPC, 10.2%) then decreased from 16.7% to 12.6% from 2011 to 2019 (AAPC, –3.9%).
Peripartum hysterectomy in the study population increased from 1.4% to 2.4% from 2000 to 2009 (AAPC 5.0%), remained steady from 2009 to 2016, and then decreased from 2.1% to 0.9% from 2016 to 2019 (AAPC –27%).
Other risk factors associated with postpartum hemorrhage itself and with blood transfusion and hysterectomy in the setting of postpartum hemorrhage included prior cesarean delivery with placenta previa or accreta, placenta previa without prior cesarean delivery, and antepartum hemorrhage or placental abruption, the researchers noted.
“In addition to placental abnormalities, risk factors such as preeclampsia with severe features, polyhydramnios, and uterine leiomyomas demonstrated the highest rates of increase in our data,” they wrote in their discussion. These trends may lead to continuing increases in postpartum hemorrhage risk, which was not fully explained by the increase in risk factors seen in the current study, the researchers said.
The study findings were limited by several factors, including the use of billing codes that could lead to misclassification of diagnoses, as well as possible differences in the definition and coding for postpartum hemorrhage among hospitals, the researchers noted. Other limitations were the exclusion of cases of readmission for postpartum hemorrhage and lack of clinical details involving use of medications or nonoperative interventions, they said.
Notably, the study finding of stable to decreasing peripartum hysterectomy rates in hospitalized patients with postpartum hemorrhage conflicts with another recent study showing an increase in peripartum hysterectomy from 2009 to 2020, but this difference may reflect changes in billing, indications for hysterectomy, or study modeling, they said.
The current study was strengthened by the use of a large database to analyze population trends, a contemporary study period, and the inclusion of meaningful outcomes such as peripartum hysterectomy, the researchers wrote.
The shift in blood transfusion and peripartum hysterectomy may reflect the implementation of protocols to promote early intervention and identification of postpartum hemorrhage, they concluded.
Interventions can have an effect
“Hemorrhage remains a leading cause of maternal mortality in the United States and blood transfusion is the most common severe maternal morbidity,” Catherine M. Albright, MD, MS, associate professor of maternal-fetal medicine at the University of Washington, Seattle, said in an interview. “It is important to understand the current state, especially given that many hospitals have implemented policies and procedures to better identify and treat postpartum hemorrhage,” she said.
Dr. Albright said, “I was pleased to see that they did not just look at a diagnosis of postpartum hemorrhage but rather also looked at complications arising from postpartum hemorrhage, such as blood transfusion or hysterectomy.”
Postpartum hemorrhage is often a clinical diagnosis that uses estimated blood loss, a notoriously inaccurate measure, said Dr. Albright. “Additionally, the definitions of postpartum hemorrhage, as well as the ICD codes, changed during the time period of the study,” she noted. “These factors all could lead to both underreporting and overreporting of the true incidence of postpartum hemorrhage. Blood transfusion and hysterectomy are more objective outcomes and demonstrate true morbidity,” she said.
“Most of the risk factors that are listed in the article are not modifiable during that pregnancy,” said Dr. Albright. For example, a history of a prior cesarean or having a twin pregnancy is not something that can be changed, she said. “Many of the other risk factors or associated clinical factors, such as obesity, chronic hypertension, and pregestational diabetes, are modifiable, but before pregnancy. Universal and easy access to primary medical care prior to and between pregnancies may help to mitigate some of these factors,” she noted.
Looking ahead, “It would be helpful to ensure that these types of data are available at the state and hospital level; this will allow for local evaluation of programs that are in place to reduce postpartum hemorrhage risk and improve identification and treatment,” Dr. Albright said.
The study received no outside funding. Dr. Corbetta-Rastelli and Dr. Albright had no financial conflicts to disclose.
The rate of postpartum hemorrhage for hospital deliveries in the United States increased significantly over a 20-year period, according to data from more than 76 million delivery hospitalizations from the National Inpatient Sample.
Postpartum hemorrhage remains the leading cause of maternal morbidity and mortality worldwide, and many clinical and patient-level risk factors appear to be on the rise, wrote Chiara M. Corbetta-Rastelli, MD, of the University of California, San Francisco, and colleagues.
Although practice changes have been introduced to reduce postpartum hemorrhage, recent trends in postpartum hemorrhage risk and outcomes in the context of such changes as hemorrhage safety bundles have not been examined, they said.
In a study published in Obstetrics & Gynecology, the researchers reviewed data from hospitalizations for females aged 15-54 years for deliveries between 2000 and 2019 using the National Inpatient Sample. They used a regression analysis to estimate average annual percentage changes (AAPC). Their objectives were to characterize trends and also to assess the association between risk factors and the occurrence of postpartum hemorrhage and related interventions. Demographics, clinical factors, and hospital characteristics were mainly similar between the group of patients with postpartum hemorrhage and those with no postpartum hemorrhage.
Approximately 3% (2.3 million) of 76.7 million hospitalizations for delivery were complicated by postpartum hemorrhage during the study period, and the annual rate increased from 2.7% to 4.3%.
Overall, 21.4% of individuals with delivery hospitalizations complicated by postpartum hemorrhage had one postpartum risk factor, and 1.4% had two or more risk factors. The number of individuals with at least one risk factor for postpartum hemorrhage increased significantly, from 18.6% to 26.9%, during the study period, with an annual percentage change of 1.9%.
Compared with deliveries in individuals without risk factors, individuals with one risk factor had slightly higher odds of postpartum hemorrhage (odds ratio, 1.14), but those with two or more risk factors were more than twice as likely to experience postpartum hemorrhage as those with no risk factors (OR, 2.31).
The researchers also examined the association of specific risk factors and interventions related to hemorrhage, notably blood transfusion and peripartum hysterectomy. Blood transfusions in individuals with postpartum hemorrhage increased from 5.4% to 16.7% between 2000 and 2011, (AAPC, 10.2%) then decreased from 16.7% to 12.6% from 2011 to 2019 (AAPC, –3.9%).
Peripartum hysterectomy in the study population increased from 1.4% to 2.4% from 2000 to 2009 (AAPC 5.0%), remained steady from 2009 to 2016, and then decreased from 2.1% to 0.9% from 2016 to 2019 (AAPC –27%).
Other risk factors associated with postpartum hemorrhage itself and with blood transfusion and hysterectomy in the setting of postpartum hemorrhage included prior cesarean delivery with placenta previa or accreta, placenta previa without prior cesarean delivery, and antepartum hemorrhage or placental abruption, the researchers noted.
“In addition to placental abnormalities, risk factors such as preeclampsia with severe features, polyhydramnios, and uterine leiomyomas demonstrated the highest rates of increase in our data,” they wrote in their discussion. These trends may lead to continuing increases in postpartum hemorrhage risk, which was not fully explained by the increase in risk factors seen in the current study, the researchers said.
The study findings were limited by several factors, including the use of billing codes that could lead to misclassification of diagnoses, as well as possible differences in the definition and coding for postpartum hemorrhage among hospitals, the researchers noted. Other limitations were the exclusion of cases of readmission for postpartum hemorrhage and lack of clinical details involving use of medications or nonoperative interventions, they said.
Notably, the study finding of stable to decreasing peripartum hysterectomy rates in hospitalized patients with postpartum hemorrhage conflicts with another recent study showing an increase in peripartum hysterectomy from 2009 to 2020, but this difference may reflect changes in billing, indications for hysterectomy, or study modeling, they said.
The current study was strengthened by the use of a large database to analyze population trends, a contemporary study period, and the inclusion of meaningful outcomes such as peripartum hysterectomy, the researchers wrote.
The shift in blood transfusion and peripartum hysterectomy may reflect the implementation of protocols to promote early intervention and identification of postpartum hemorrhage, they concluded.
Interventions can have an effect
“Hemorrhage remains a leading cause of maternal mortality in the United States and blood transfusion is the most common severe maternal morbidity,” Catherine M. Albright, MD, MS, associate professor of maternal-fetal medicine at the University of Washington, Seattle, said in an interview. “It is important to understand the current state, especially given that many hospitals have implemented policies and procedures to better identify and treat postpartum hemorrhage,” she said.
Dr. Albright said, “I was pleased to see that they did not just look at a diagnosis of postpartum hemorrhage but rather also looked at complications arising from postpartum hemorrhage, such as blood transfusion or hysterectomy.”
Postpartum hemorrhage is often a clinical diagnosis that uses estimated blood loss, a notoriously inaccurate measure, said Dr. Albright. “Additionally, the definitions of postpartum hemorrhage, as well as the ICD codes, changed during the time period of the study,” she noted. “These factors all could lead to both underreporting and overreporting of the true incidence of postpartum hemorrhage. Blood transfusion and hysterectomy are more objective outcomes and demonstrate true morbidity,” she said.
“Most of the risk factors that are listed in the article are not modifiable during that pregnancy,” said Dr. Albright. For example, a history of a prior cesarean or having a twin pregnancy is not something that can be changed, she said. “Many of the other risk factors or associated clinical factors, such as obesity, chronic hypertension, and pregestational diabetes, are modifiable, but before pregnancy. Universal and easy access to primary medical care prior to and between pregnancies may help to mitigate some of these factors,” she noted.
Looking ahead, “It would be helpful to ensure that these types of data are available at the state and hospital level; this will allow for local evaluation of programs that are in place to reduce postpartum hemorrhage risk and improve identification and treatment,” Dr. Albright said.
The study received no outside funding. Dr. Corbetta-Rastelli and Dr. Albright had no financial conflicts to disclose.
FROM OBSTETRICS & GYNECOLOGY
Study implicates myelin plasticity in absence seizures
NASHVILLE, TENN. – that seems to provoke dysregulation of the insulating layer surrounding nerve fibers, perpetuating a cycle of increasing nerve damage and more frequent seizures later on.
“This study was the first to demonstrate that, at least in some forms of epilepsy, myelin plasticity is part of the maladaptive plasticity response that underlines epilepsy progression,” Juliet Knowles, MD, PhD, assistant professor at Stanford (Calif.) University, said in an interview. She reported the findings at the 2022 annual meeting of the American Epilepsy Society.
Dr. Knowles and colleagues made their discovery using laboratory mice. They used an imaging technique known as qMTI – quantitative magnetization transfer in conjunction with diffusion MRI – to map changes in myelin sheath thickness, or myelin plasticity, in major white matter tracks of the brain.
“Over the last decade we’ve come to understand that myelin, which is the insulating substance that coats the projections of brain cells or neurons, is more dynamic than we used to think,” she said. “In fact, throughout life, myelin’s structure in some regions of the brain can be changed in response to neuro activity. It’s a newly appreciated form of brain plasticity.”
However, she said, myelin plasticity has mostly been studied in healthy brains; “We don’t know very much about what role myelin plasticity might play in disease states like epilepsy,” Dr. Knowles said. The study’s goal was to investigate myelin plasticity specifically in absence seizures.
“We hypothesized that maybe absence seizures prompt activity-dependent myelin plasticity, but that maybe seizure-induced myelin plasticity alters the way that brain networks act in a way that contributes to the disease process,” she said.
Maladaptive myelin plasticity
The researchers found that absence seizures were infrequent when they first started, but then they rapidly progressed. “Over a couple of weeks, they’ll go from having very few seizures to having many seizures per hour,” Dr. Knowles said.
Using qMTI, the researchers found increased myelin sheath thickness across the longitudinal extent of the anterior corpus callosum, but they found myelin sheath thickness unchanged in brain regions where absence seizures weren’t prominent.
They also found that genetically blocking activity-dependent myelination markedly decreased seizure progression and decreased ictal somatosensory electroencephalography (EEG) coherence. Conversely, blocking myelin plasticity had no effect on ictal EEG coherence between visual cortices connected by the posterior corpus callosum.
The next step for the researchers is to develop MRI methods to use in human studies, Dr. Knowles said.
“We are working on developing an imaging approach in these same animal models that we hope we can use also to study in a detailed way white matter plasticity in humans with epilepsy and we’re also continuing our studies in animal models to try to identify ways to target maladaptive myelin plasticity, which ultimately we hope will inform treatment of people with epilepsy,” Dr. Knowles said.
Of mice and men
Although this study used mice, Chris Dulla, PhD, associate professor and director of the neuroscience graduate program at Tufts University in Boston, said the finding is “probably pretty transferable” to humans.
“This is the first study that really showed it,” he said of the link between myelin changes and seizure frequency. “I think people have suspected it, but that’s why this is kind of a big deal because this is one of the first studies to show it conclusively.”
He offered suggestions for validating the findings in humans. “The first thing would be to do imaging studies in people where you can examine to see if those white matter tracks are altered in a similar way in people with epilepsy,” he said. “I think now this study gives us good reason to undertake the work that it would take to ask that question and answer it in the human brain.”
Dr. Knowles and Dr. Dulla have no relevant relationships to disclose.
NASHVILLE, TENN. – that seems to provoke dysregulation of the insulating layer surrounding nerve fibers, perpetuating a cycle of increasing nerve damage and more frequent seizures later on.
“This study was the first to demonstrate that, at least in some forms of epilepsy, myelin plasticity is part of the maladaptive plasticity response that underlines epilepsy progression,” Juliet Knowles, MD, PhD, assistant professor at Stanford (Calif.) University, said in an interview. She reported the findings at the 2022 annual meeting of the American Epilepsy Society.
Dr. Knowles and colleagues made their discovery using laboratory mice. They used an imaging technique known as qMTI – quantitative magnetization transfer in conjunction with diffusion MRI – to map changes in myelin sheath thickness, or myelin plasticity, in major white matter tracks of the brain.
“Over the last decade we’ve come to understand that myelin, which is the insulating substance that coats the projections of brain cells or neurons, is more dynamic than we used to think,” she said. “In fact, throughout life, myelin’s structure in some regions of the brain can be changed in response to neuro activity. It’s a newly appreciated form of brain plasticity.”
However, she said, myelin plasticity has mostly been studied in healthy brains; “We don’t know very much about what role myelin plasticity might play in disease states like epilepsy,” Dr. Knowles said. The study’s goal was to investigate myelin plasticity specifically in absence seizures.
“We hypothesized that maybe absence seizures prompt activity-dependent myelin plasticity, but that maybe seizure-induced myelin plasticity alters the way that brain networks act in a way that contributes to the disease process,” she said.
Maladaptive myelin plasticity
The researchers found that absence seizures were infrequent when they first started, but then they rapidly progressed. “Over a couple of weeks, they’ll go from having very few seizures to having many seizures per hour,” Dr. Knowles said.
Using qMTI, the researchers found increased myelin sheath thickness across the longitudinal extent of the anterior corpus callosum, but they found myelin sheath thickness unchanged in brain regions where absence seizures weren’t prominent.
They also found that genetically blocking activity-dependent myelination markedly decreased seizure progression and decreased ictal somatosensory electroencephalography (EEG) coherence. Conversely, blocking myelin plasticity had no effect on ictal EEG coherence between visual cortices connected by the posterior corpus callosum.
The next step for the researchers is to develop MRI methods to use in human studies, Dr. Knowles said.
“We are working on developing an imaging approach in these same animal models that we hope we can use also to study in a detailed way white matter plasticity in humans with epilepsy and we’re also continuing our studies in animal models to try to identify ways to target maladaptive myelin plasticity, which ultimately we hope will inform treatment of people with epilepsy,” Dr. Knowles said.
Of mice and men
Although this study used mice, Chris Dulla, PhD, associate professor and director of the neuroscience graduate program at Tufts University in Boston, said the finding is “probably pretty transferable” to humans.
“This is the first study that really showed it,” he said of the link between myelin changes and seizure frequency. “I think people have suspected it, but that’s why this is kind of a big deal because this is one of the first studies to show it conclusively.”
He offered suggestions for validating the findings in humans. “The first thing would be to do imaging studies in people where you can examine to see if those white matter tracks are altered in a similar way in people with epilepsy,” he said. “I think now this study gives us good reason to undertake the work that it would take to ask that question and answer it in the human brain.”
Dr. Knowles and Dr. Dulla have no relevant relationships to disclose.
NASHVILLE, TENN. – that seems to provoke dysregulation of the insulating layer surrounding nerve fibers, perpetuating a cycle of increasing nerve damage and more frequent seizures later on.
“This study was the first to demonstrate that, at least in some forms of epilepsy, myelin plasticity is part of the maladaptive plasticity response that underlines epilepsy progression,” Juliet Knowles, MD, PhD, assistant professor at Stanford (Calif.) University, said in an interview. She reported the findings at the 2022 annual meeting of the American Epilepsy Society.
Dr. Knowles and colleagues made their discovery using laboratory mice. They used an imaging technique known as qMTI – quantitative magnetization transfer in conjunction with diffusion MRI – to map changes in myelin sheath thickness, or myelin plasticity, in major white matter tracks of the brain.
“Over the last decade we’ve come to understand that myelin, which is the insulating substance that coats the projections of brain cells or neurons, is more dynamic than we used to think,” she said. “In fact, throughout life, myelin’s structure in some regions of the brain can be changed in response to neuro activity. It’s a newly appreciated form of brain plasticity.”
However, she said, myelin plasticity has mostly been studied in healthy brains; “We don’t know very much about what role myelin plasticity might play in disease states like epilepsy,” Dr. Knowles said. The study’s goal was to investigate myelin plasticity specifically in absence seizures.
“We hypothesized that maybe absence seizures prompt activity-dependent myelin plasticity, but that maybe seizure-induced myelin plasticity alters the way that brain networks act in a way that contributes to the disease process,” she said.
Maladaptive myelin plasticity
The researchers found that absence seizures were infrequent when they first started, but then they rapidly progressed. “Over a couple of weeks, they’ll go from having very few seizures to having many seizures per hour,” Dr. Knowles said.
Using qMTI, the researchers found increased myelin sheath thickness across the longitudinal extent of the anterior corpus callosum, but they found myelin sheath thickness unchanged in brain regions where absence seizures weren’t prominent.
They also found that genetically blocking activity-dependent myelination markedly decreased seizure progression and decreased ictal somatosensory electroencephalography (EEG) coherence. Conversely, blocking myelin plasticity had no effect on ictal EEG coherence between visual cortices connected by the posterior corpus callosum.
The next step for the researchers is to develop MRI methods to use in human studies, Dr. Knowles said.
“We are working on developing an imaging approach in these same animal models that we hope we can use also to study in a detailed way white matter plasticity in humans with epilepsy and we’re also continuing our studies in animal models to try to identify ways to target maladaptive myelin plasticity, which ultimately we hope will inform treatment of people with epilepsy,” Dr. Knowles said.
Of mice and men
Although this study used mice, Chris Dulla, PhD, associate professor and director of the neuroscience graduate program at Tufts University in Boston, said the finding is “probably pretty transferable” to humans.
“This is the first study that really showed it,” he said of the link between myelin changes and seizure frequency. “I think people have suspected it, but that’s why this is kind of a big deal because this is one of the first studies to show it conclusively.”
He offered suggestions for validating the findings in humans. “The first thing would be to do imaging studies in people where you can examine to see if those white matter tracks are altered in a similar way in people with epilepsy,” he said. “I think now this study gives us good reason to undertake the work that it would take to ask that question and answer it in the human brain.”
Dr. Knowles and Dr. Dulla have no relevant relationships to disclose.
AT AES 2022
Newer brand-name drugs fuel spending on antiseizure medications
NASHVILLE, TENN. – , pointing to a major shift to newer, costlier, brand-name drugs – a trend in spending that may not be sustainable, the lead author of a study of drug costs said.
The study, presented at the 2022 annual meeting of the American Epilepsy Society, evaluated claims data for prescriptions for common antiseizure medications in the Medicare Part D and Medicaid databases from 2012 to 2020. The study excluded gabapentin and pregabalin because they’re frequently prescribed for other indications in addition to epileptic seizures.
“We found that third-generation medications, even though they accounted for the smallest percentage of claims in 2020, took up the most astronomical portion of the money that was spent,” lead author Deepti Zutshi, MD, an associate professor of neurology at Wayne State University in Detroit, said in an interview.
The study found that Medicare Part D spending on antiseizure medications increased from $1.16 billion in 2012 to $2.68 billion in 2020. In Medicaid, spending followed a similar trend, increasing from $973 million in 2012 to $1.05 billion in 2020.
Analyzing Medicare/Medicaid claims data
The study categorized drugs two ways: by brand or generic; and by first, second, or third generation, Dr. Zutshi said. First-generation drugs include medications such as phenobarbital, phenytoin, valproate, and carbamazepine. Second-generation medications were released in the early 2000s and include medications such as lamotrigine and levetiracetam. Examples of third-generation drugs include lacosamide, vigabatrin, clobazam, and perampanel.
Prescribers shifted significantly to third-generation treatments, Dr. Zutshi said. In Medicare Part D, the total spent on third-generation antiseizure medications went from $124 million in 2012 to $1.08 billion in 2020, representing a quadrupling in percentage of costs, from 10.7% to 40.4%. The total number of claims for third-generation antiseizure medications was 240,000 in 2012 (1.3%) and 1.1 million in 2020 (4.4%).
When looking at brand versus generic, the total spent on brand-name antiseizure medications increased nearly threefold from $546 million in 2012 to $1.62 million in 2020, with the share of all funding spent on brand-name antiseizure medications jumping from 46.8% to 60.2%. However, the proportion of total claims for branded antiseizure medications actually dropped, from 9.24% in 2012 to 6.62% in 2020.
Medicaid trends followed a similar pattern. Third-generation antiseizure medications accounted for 1.7% of total claims in 2012 and 6% in 2020. Spending on third-generation antiseizure medications grew nearly eight times: from $147 million, or 15.1% of funding spent on antiseizure medications, in 2012 to $1.15 billion in 2020, a 56.1% share of costs. The total spend of branded antiseizure medications in Medicaid was $605 million in 2012 and $1.46 billion in 2020 – a jump in the share of total spending from 62.2% to 71.3%. As in Medicare Part D, the percentage of total claims for branded antiseizure medications in Medicaid also dropped from 2012 to 2020, from 12.1% to 6.8%.
Why the substantial increase in spending?
“The reason we are prescribing these more expensive medications may be that the third-generation medications have better side-effect profiles, improved safety and outcomes in pregnancy, or that they have less drug interactions with other medications,” Dr. Zutshi said.
That’s desirable for older patients on Medicare who are more likely to have comorbidities and be on other medications, or women of child-bearing age on Medicaid, Dr. Zutshi said. “But I don’t think people realize what the cost is to Medicare and Medicaid,” she said, “so this was a bit of a shocking finding in our paper when we looked at this. I wasn’t expecting to see the substantial increase of spending focusing on just a few medications.”
Neurologists and other providers have to be more aware of individual patients’ needs as well as cost when prescribing branded or third-generation antiseizure medications, Dr. Zutshi said. “We have to do what’s best for all of our patients, but it has to be sustainable. If not, we could start losing the ability to prescribe these medications in these vulnerable population groups, so we have to use them judiciously,” Dr. Zutshi said.
Controlling costs versus managing seizures
Timothy E. Welty, PharmD, a professor of pharmacy at Drake University in Des Moines, Iowa, noted some potential issues with the study’s methodology, namely that, while it excluded gabapentin and pregabalin, it did include other antiseizure medications that are used for other indications without accounting for them. Additionally, the pharmacy claims data the study used didn’t cross match with any diagnostic data.
Controlling drug costs is noteworthy, he said, but managing seizures is equally important. “You have to think not only in terms of preventing seizures and what impact that has on health care costs specifically, but what impact that has on overall costs to society,” Dr. Welty said. “Doing the best we can to get their seizures under control as quickly as possible has great benefits for the patient outside of health care costs.”
He added, “We just really need to educate pharmacists and decision makers within third-party payers, be it Medicare, Medicaid, private insurance, whatever, on the advances that are being made in the use of seizure medications to treat epilepsy and stop seizures, but it’s a far broader issue than just how many dollars are we spending on seizure medication.”
Dr. Zutshi and Dr. Welty have no relevant disclosures to report.
NASHVILLE, TENN. – , pointing to a major shift to newer, costlier, brand-name drugs – a trend in spending that may not be sustainable, the lead author of a study of drug costs said.
The study, presented at the 2022 annual meeting of the American Epilepsy Society, evaluated claims data for prescriptions for common antiseizure medications in the Medicare Part D and Medicaid databases from 2012 to 2020. The study excluded gabapentin and pregabalin because they’re frequently prescribed for other indications in addition to epileptic seizures.
“We found that third-generation medications, even though they accounted for the smallest percentage of claims in 2020, took up the most astronomical portion of the money that was spent,” lead author Deepti Zutshi, MD, an associate professor of neurology at Wayne State University in Detroit, said in an interview.
The study found that Medicare Part D spending on antiseizure medications increased from $1.16 billion in 2012 to $2.68 billion in 2020. In Medicaid, spending followed a similar trend, increasing from $973 million in 2012 to $1.05 billion in 2020.
Analyzing Medicare/Medicaid claims data
The study categorized drugs two ways: by brand or generic; and by first, second, or third generation, Dr. Zutshi said. First-generation drugs include medications such as phenobarbital, phenytoin, valproate, and carbamazepine. Second-generation medications were released in the early 2000s and include medications such as lamotrigine and levetiracetam. Examples of third-generation drugs include lacosamide, vigabatrin, clobazam, and perampanel.
Prescribers shifted significantly to third-generation treatments, Dr. Zutshi said. In Medicare Part D, the total spent on third-generation antiseizure medications went from $124 million in 2012 to $1.08 billion in 2020, representing a quadrupling in percentage of costs, from 10.7% to 40.4%. The total number of claims for third-generation antiseizure medications was 240,000 in 2012 (1.3%) and 1.1 million in 2020 (4.4%).
When looking at brand versus generic, the total spent on brand-name antiseizure medications increased nearly threefold from $546 million in 2012 to $1.62 million in 2020, with the share of all funding spent on brand-name antiseizure medications jumping from 46.8% to 60.2%. However, the proportion of total claims for branded antiseizure medications actually dropped, from 9.24% in 2012 to 6.62% in 2020.
Medicaid trends followed a similar pattern. Third-generation antiseizure medications accounted for 1.7% of total claims in 2012 and 6% in 2020. Spending on third-generation antiseizure medications grew nearly eight times: from $147 million, or 15.1% of funding spent on antiseizure medications, in 2012 to $1.15 billion in 2020, a 56.1% share of costs. The total spend of branded antiseizure medications in Medicaid was $605 million in 2012 and $1.46 billion in 2020 – a jump in the share of total spending from 62.2% to 71.3%. As in Medicare Part D, the percentage of total claims for branded antiseizure medications in Medicaid also dropped from 2012 to 2020, from 12.1% to 6.8%.
Why the substantial increase in spending?
“The reason we are prescribing these more expensive medications may be that the third-generation medications have better side-effect profiles, improved safety and outcomes in pregnancy, or that they have less drug interactions with other medications,” Dr. Zutshi said.
That’s desirable for older patients on Medicare who are more likely to have comorbidities and be on other medications, or women of child-bearing age on Medicaid, Dr. Zutshi said. “But I don’t think people realize what the cost is to Medicare and Medicaid,” she said, “so this was a bit of a shocking finding in our paper when we looked at this. I wasn’t expecting to see the substantial increase of spending focusing on just a few medications.”
Neurologists and other providers have to be more aware of individual patients’ needs as well as cost when prescribing branded or third-generation antiseizure medications, Dr. Zutshi said. “We have to do what’s best for all of our patients, but it has to be sustainable. If not, we could start losing the ability to prescribe these medications in these vulnerable population groups, so we have to use them judiciously,” Dr. Zutshi said.
Controlling costs versus managing seizures
Timothy E. Welty, PharmD, a professor of pharmacy at Drake University in Des Moines, Iowa, noted some potential issues with the study’s methodology, namely that, while it excluded gabapentin and pregabalin, it did include other antiseizure medications that are used for other indications without accounting for them. Additionally, the pharmacy claims data the study used didn’t cross match with any diagnostic data.
Controlling drug costs is noteworthy, he said, but managing seizures is equally important. “You have to think not only in terms of preventing seizures and what impact that has on health care costs specifically, but what impact that has on overall costs to society,” Dr. Welty said. “Doing the best we can to get their seizures under control as quickly as possible has great benefits for the patient outside of health care costs.”
He added, “We just really need to educate pharmacists and decision makers within third-party payers, be it Medicare, Medicaid, private insurance, whatever, on the advances that are being made in the use of seizure medications to treat epilepsy and stop seizures, but it’s a far broader issue than just how many dollars are we spending on seizure medication.”
Dr. Zutshi and Dr. Welty have no relevant disclosures to report.
NASHVILLE, TENN. – , pointing to a major shift to newer, costlier, brand-name drugs – a trend in spending that may not be sustainable, the lead author of a study of drug costs said.
The study, presented at the 2022 annual meeting of the American Epilepsy Society, evaluated claims data for prescriptions for common antiseizure medications in the Medicare Part D and Medicaid databases from 2012 to 2020. The study excluded gabapentin and pregabalin because they’re frequently prescribed for other indications in addition to epileptic seizures.
“We found that third-generation medications, even though they accounted for the smallest percentage of claims in 2020, took up the most astronomical portion of the money that was spent,” lead author Deepti Zutshi, MD, an associate professor of neurology at Wayne State University in Detroit, said in an interview.
The study found that Medicare Part D spending on antiseizure medications increased from $1.16 billion in 2012 to $2.68 billion in 2020. In Medicaid, spending followed a similar trend, increasing from $973 million in 2012 to $1.05 billion in 2020.
Analyzing Medicare/Medicaid claims data
The study categorized drugs two ways: by brand or generic; and by first, second, or third generation, Dr. Zutshi said. First-generation drugs include medications such as phenobarbital, phenytoin, valproate, and carbamazepine. Second-generation medications were released in the early 2000s and include medications such as lamotrigine and levetiracetam. Examples of third-generation drugs include lacosamide, vigabatrin, clobazam, and perampanel.
Prescribers shifted significantly to third-generation treatments, Dr. Zutshi said. In Medicare Part D, the total spent on third-generation antiseizure medications went from $124 million in 2012 to $1.08 billion in 2020, representing a quadrupling in percentage of costs, from 10.7% to 40.4%. The total number of claims for third-generation antiseizure medications was 240,000 in 2012 (1.3%) and 1.1 million in 2020 (4.4%).
When looking at brand versus generic, the total spent on brand-name antiseizure medications increased nearly threefold from $546 million in 2012 to $1.62 million in 2020, with the share of all funding spent on brand-name antiseizure medications jumping from 46.8% to 60.2%. However, the proportion of total claims for branded antiseizure medications actually dropped, from 9.24% in 2012 to 6.62% in 2020.
Medicaid trends followed a similar pattern. Third-generation antiseizure medications accounted for 1.7% of total claims in 2012 and 6% in 2020. Spending on third-generation antiseizure medications grew nearly eight times: from $147 million, or 15.1% of funding spent on antiseizure medications, in 2012 to $1.15 billion in 2020, a 56.1% share of costs. The total spend of branded antiseizure medications in Medicaid was $605 million in 2012 and $1.46 billion in 2020 – a jump in the share of total spending from 62.2% to 71.3%. As in Medicare Part D, the percentage of total claims for branded antiseizure medications in Medicaid also dropped from 2012 to 2020, from 12.1% to 6.8%.
Why the substantial increase in spending?
“The reason we are prescribing these more expensive medications may be that the third-generation medications have better side-effect profiles, improved safety and outcomes in pregnancy, or that they have less drug interactions with other medications,” Dr. Zutshi said.
That’s desirable for older patients on Medicare who are more likely to have comorbidities and be on other medications, or women of child-bearing age on Medicaid, Dr. Zutshi said. “But I don’t think people realize what the cost is to Medicare and Medicaid,” she said, “so this was a bit of a shocking finding in our paper when we looked at this. I wasn’t expecting to see the substantial increase of spending focusing on just a few medications.”
Neurologists and other providers have to be more aware of individual patients’ needs as well as cost when prescribing branded or third-generation antiseizure medications, Dr. Zutshi said. “We have to do what’s best for all of our patients, but it has to be sustainable. If not, we could start losing the ability to prescribe these medications in these vulnerable population groups, so we have to use them judiciously,” Dr. Zutshi said.
Controlling costs versus managing seizures
Timothy E. Welty, PharmD, a professor of pharmacy at Drake University in Des Moines, Iowa, noted some potential issues with the study’s methodology, namely that, while it excluded gabapentin and pregabalin, it did include other antiseizure medications that are used for other indications without accounting for them. Additionally, the pharmacy claims data the study used didn’t cross match with any diagnostic data.
Controlling drug costs is noteworthy, he said, but managing seizures is equally important. “You have to think not only in terms of preventing seizures and what impact that has on health care costs specifically, but what impact that has on overall costs to society,” Dr. Welty said. “Doing the best we can to get their seizures under control as quickly as possible has great benefits for the patient outside of health care costs.”
He added, “We just really need to educate pharmacists and decision makers within third-party payers, be it Medicare, Medicaid, private insurance, whatever, on the advances that are being made in the use of seizure medications to treat epilepsy and stop seizures, but it’s a far broader issue than just how many dollars are we spending on seizure medication.”
Dr. Zutshi and Dr. Welty have no relevant disclosures to report.
AT AES 2022
Teens’ undisclosed dieting may precede anorexia nervosa diagnosis
Adolescents later diagnosed with anorexia nervosa (AN) likely embark on the trajectory to AN with undisclosed dieting for weight loss at about age 14, a study of teens and parents found.
In the interview-based study, both adolescents and their parents described a similar prediagnosis sequence of behavioral changes occurring over roughly 1 year to 18 months, but parents lagged some 6 months behind in noticing their children’s disordered eating.
The findings suggest that even teens of normal weight should be asked about their eating habits and monitored more closely for contact with those who endorse these potentially harmful eating behaviors, according to Lisa M. Ranzenhofer, PhD, assistant professor of clinical psychology in psychiatry at Columbia University Medical Center in New York, and colleagues. Their report is in the Journal of Adolescent Health.
“We know that adolescents often have eating disorder behaviors long before they’re diagnosed, so we developed this interview as a tool to figure out how long a maladaptive behavior has been present,” Dr. Ranzenhofer said in an interview. “Most studies that report illness duration do so based on diagnosis, so this interview provides a more fine-grained assessment of the duration of problematic behavior, which may help improve understanding of the impact of duration on outcome, and hopefully facilitate better methods for early detection.” Since healthy adolescents are often seen once per year at an annual pediatrician visit, she added, teens engaging in significant dieting might benefit from more frequent monitoring since this behavior can evolve into an eating disorder over a relatively short time frame.
AN is associated with significant medical and psychiatric comorbidity and has a mortality rate among the highest of any psychiatric illness, the authors noted.
The study
The study cohort consisted of 71 girls ages 12-18 years participating in research from 2017 to 2021 at the Eating Disorders Research Unit of New York (N.Y.) State Psychiatric Institute. Patients had either the restricting or binge-eating/purging subtype of AN as diagnosed by the Eating Disorder Assessment–5 questionnaire. A semistructured 15-minute interview with the girls and their parents explored food restriction, dieting, loss of control/binge eating, purging, excessive/compulsive exercise, weight history, and amenorrhea.
Both parents and children were asked whether and when the children had been underweight or overweight, and whether and when primary amenorrhea (no menarche) or secondary amenorrhea (periods missed for 3 months) became evident. Dieting was defined as “deliberately changing eating patterns in any way to influence your shape or weight,” and restriction as “deliberately cutting down on the amount of food that you are eating, in order to change your shape or weight.” Loss-of-control eating was defined as “feeling unable to stop eating or control what or how much you are eating.”
In other characterizations, purging was defined as making yourself vomit on purpose, taking diuretics, or feeling driven to engage in these behaviors. Questions on exercise explored whether children might feel anxious when they do not exercise or inclined to exercise even if sick or injured, with excessive exercise defined as “Feeling like you must exercise, might continue exercising, sometimes in secret, if parents or doctors have told you to stop.”
Other questions focused on use of diuretics or laxatives and other strategies to compensate for calories consumed.
Responses revealed that restriction, underweight, dieting, and excessive exercise were present in most of the sample, while purging, loss-of-control eating, and overweight were reported by fewer than a third. With dieting typically emerging first around age 14, the other behaviors tended to manifest from age 14 to 14 and a half. The average age of formal diagnosis was just over 15 years. Parent-child dyads showed good agreement on the presence and timing of all behaviors except for dieting, for which children reported onset about 6 months earlier or longer duration compared with parents.
Although older age at the time of interview was associated with a lower body mass index percentile and higher eating disorder score, neither age of onset nor duration of disordered eating was associated with severity when researchers controlled for current age.
Telltale signs for parents
“For teens starting at a healthy weight, significant and intentional weight loss of more than 5-10 pounds can be a cause for concern,” Dr. Ranzenhofer said. Missed periods, refusing meals, skipping meals, fighting or arguing about eating, and withdrawal from normal activities and relationships are other signs of disordered eating. For overweight or obese teens, rapid weight loss and weight loss above and beyond that recommended are also concerning.
As for compulsive exercise, she said, “Altered exercise behavior might look like exercise that interferes with other activities, for example, being late to school or not doing homework in order to exercise.” Other red flags would be physical activity that varies considerably from that of peers, for instance, going running after a 2-hour sports practice and an inflexible routine that precludes being able to skip a day.
“All adolescents, male and female, should be screened regardless of weight trends – underweight, overweight, obese, or normal weight – regarding their body image and thoughts of dieting,” said Margaret E. Thew, DNP, FNP-BC, of the Medical College of Wisconsin, and medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee, commenting on the study but not involved in it. “Most adolescents make decisions to lose weight after trying to ‘eat healthy’ but may take an aggressive approach when they don’t see the weight loss they hope to see.”
According to Ms. Thew, the study findings support the benefit of giving medical caregivers and parents training on the red flags regarding eating disorders to foster early detection. “These include starting a new fad diet, eliminating foods, ‘healthy eating,’ over-exercising, skipping meals, or no longer eating foods they previously loved.”
She added that times of transition are key junctures to watch: The transition from grade school to middle school, middle to high school, and high school to college. “These tend to provoke eating disorder onset or relapse of eating disorder thoughts and behaviors after diagnosis,” Ms. Thew said. “It would benefit the patient to screen for concerns about disordered eating and provide resources, including consultation with a dietitian, as appropriate.”
This study was supported by grants from the National Institute of Mental Health and the Hilda and Preston Davis Foundation. Coauthor Joanna E. Steinglass, MD, disclosed receiving royalties from UpToDate. Ms. Thew disclosed no competing interests with regard to her comments.
Adolescents later diagnosed with anorexia nervosa (AN) likely embark on the trajectory to AN with undisclosed dieting for weight loss at about age 14, a study of teens and parents found.
In the interview-based study, both adolescents and their parents described a similar prediagnosis sequence of behavioral changes occurring over roughly 1 year to 18 months, but parents lagged some 6 months behind in noticing their children’s disordered eating.
The findings suggest that even teens of normal weight should be asked about their eating habits and monitored more closely for contact with those who endorse these potentially harmful eating behaviors, according to Lisa M. Ranzenhofer, PhD, assistant professor of clinical psychology in psychiatry at Columbia University Medical Center in New York, and colleagues. Their report is in the Journal of Adolescent Health.
“We know that adolescents often have eating disorder behaviors long before they’re diagnosed, so we developed this interview as a tool to figure out how long a maladaptive behavior has been present,” Dr. Ranzenhofer said in an interview. “Most studies that report illness duration do so based on diagnosis, so this interview provides a more fine-grained assessment of the duration of problematic behavior, which may help improve understanding of the impact of duration on outcome, and hopefully facilitate better methods for early detection.” Since healthy adolescents are often seen once per year at an annual pediatrician visit, she added, teens engaging in significant dieting might benefit from more frequent monitoring since this behavior can evolve into an eating disorder over a relatively short time frame.
AN is associated with significant medical and psychiatric comorbidity and has a mortality rate among the highest of any psychiatric illness, the authors noted.
The study
The study cohort consisted of 71 girls ages 12-18 years participating in research from 2017 to 2021 at the Eating Disorders Research Unit of New York (N.Y.) State Psychiatric Institute. Patients had either the restricting or binge-eating/purging subtype of AN as diagnosed by the Eating Disorder Assessment–5 questionnaire. A semistructured 15-minute interview with the girls and their parents explored food restriction, dieting, loss of control/binge eating, purging, excessive/compulsive exercise, weight history, and amenorrhea.
Both parents and children were asked whether and when the children had been underweight or overweight, and whether and when primary amenorrhea (no menarche) or secondary amenorrhea (periods missed for 3 months) became evident. Dieting was defined as “deliberately changing eating patterns in any way to influence your shape or weight,” and restriction as “deliberately cutting down on the amount of food that you are eating, in order to change your shape or weight.” Loss-of-control eating was defined as “feeling unable to stop eating or control what or how much you are eating.”
In other characterizations, purging was defined as making yourself vomit on purpose, taking diuretics, or feeling driven to engage in these behaviors. Questions on exercise explored whether children might feel anxious when they do not exercise or inclined to exercise even if sick or injured, with excessive exercise defined as “Feeling like you must exercise, might continue exercising, sometimes in secret, if parents or doctors have told you to stop.”
Other questions focused on use of diuretics or laxatives and other strategies to compensate for calories consumed.
Responses revealed that restriction, underweight, dieting, and excessive exercise were present in most of the sample, while purging, loss-of-control eating, and overweight were reported by fewer than a third. With dieting typically emerging first around age 14, the other behaviors tended to manifest from age 14 to 14 and a half. The average age of formal diagnosis was just over 15 years. Parent-child dyads showed good agreement on the presence and timing of all behaviors except for dieting, for which children reported onset about 6 months earlier or longer duration compared with parents.
Although older age at the time of interview was associated with a lower body mass index percentile and higher eating disorder score, neither age of onset nor duration of disordered eating was associated with severity when researchers controlled for current age.
Telltale signs for parents
“For teens starting at a healthy weight, significant and intentional weight loss of more than 5-10 pounds can be a cause for concern,” Dr. Ranzenhofer said. Missed periods, refusing meals, skipping meals, fighting or arguing about eating, and withdrawal from normal activities and relationships are other signs of disordered eating. For overweight or obese teens, rapid weight loss and weight loss above and beyond that recommended are also concerning.
As for compulsive exercise, she said, “Altered exercise behavior might look like exercise that interferes with other activities, for example, being late to school or not doing homework in order to exercise.” Other red flags would be physical activity that varies considerably from that of peers, for instance, going running after a 2-hour sports practice and an inflexible routine that precludes being able to skip a day.
“All adolescents, male and female, should be screened regardless of weight trends – underweight, overweight, obese, or normal weight – regarding their body image and thoughts of dieting,” said Margaret E. Thew, DNP, FNP-BC, of the Medical College of Wisconsin, and medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee, commenting on the study but not involved in it. “Most adolescents make decisions to lose weight after trying to ‘eat healthy’ but may take an aggressive approach when they don’t see the weight loss they hope to see.”
According to Ms. Thew, the study findings support the benefit of giving medical caregivers and parents training on the red flags regarding eating disorders to foster early detection. “These include starting a new fad diet, eliminating foods, ‘healthy eating,’ over-exercising, skipping meals, or no longer eating foods they previously loved.”
She added that times of transition are key junctures to watch: The transition from grade school to middle school, middle to high school, and high school to college. “These tend to provoke eating disorder onset or relapse of eating disorder thoughts and behaviors after diagnosis,” Ms. Thew said. “It would benefit the patient to screen for concerns about disordered eating and provide resources, including consultation with a dietitian, as appropriate.”
This study was supported by grants from the National Institute of Mental Health and the Hilda and Preston Davis Foundation. Coauthor Joanna E. Steinglass, MD, disclosed receiving royalties from UpToDate. Ms. Thew disclosed no competing interests with regard to her comments.
Adolescents later diagnosed with anorexia nervosa (AN) likely embark on the trajectory to AN with undisclosed dieting for weight loss at about age 14, a study of teens and parents found.
In the interview-based study, both adolescents and their parents described a similar prediagnosis sequence of behavioral changes occurring over roughly 1 year to 18 months, but parents lagged some 6 months behind in noticing their children’s disordered eating.
The findings suggest that even teens of normal weight should be asked about their eating habits and monitored more closely for contact with those who endorse these potentially harmful eating behaviors, according to Lisa M. Ranzenhofer, PhD, assistant professor of clinical psychology in psychiatry at Columbia University Medical Center in New York, and colleagues. Their report is in the Journal of Adolescent Health.
“We know that adolescents often have eating disorder behaviors long before they’re diagnosed, so we developed this interview as a tool to figure out how long a maladaptive behavior has been present,” Dr. Ranzenhofer said in an interview. “Most studies that report illness duration do so based on diagnosis, so this interview provides a more fine-grained assessment of the duration of problematic behavior, which may help improve understanding of the impact of duration on outcome, and hopefully facilitate better methods for early detection.” Since healthy adolescents are often seen once per year at an annual pediatrician visit, she added, teens engaging in significant dieting might benefit from more frequent monitoring since this behavior can evolve into an eating disorder over a relatively short time frame.
AN is associated with significant medical and psychiatric comorbidity and has a mortality rate among the highest of any psychiatric illness, the authors noted.
The study
The study cohort consisted of 71 girls ages 12-18 years participating in research from 2017 to 2021 at the Eating Disorders Research Unit of New York (N.Y.) State Psychiatric Institute. Patients had either the restricting or binge-eating/purging subtype of AN as diagnosed by the Eating Disorder Assessment–5 questionnaire. A semistructured 15-minute interview with the girls and their parents explored food restriction, dieting, loss of control/binge eating, purging, excessive/compulsive exercise, weight history, and amenorrhea.
Both parents and children were asked whether and when the children had been underweight or overweight, and whether and when primary amenorrhea (no menarche) or secondary amenorrhea (periods missed for 3 months) became evident. Dieting was defined as “deliberately changing eating patterns in any way to influence your shape or weight,” and restriction as “deliberately cutting down on the amount of food that you are eating, in order to change your shape or weight.” Loss-of-control eating was defined as “feeling unable to stop eating or control what or how much you are eating.”
In other characterizations, purging was defined as making yourself vomit on purpose, taking diuretics, or feeling driven to engage in these behaviors. Questions on exercise explored whether children might feel anxious when they do not exercise or inclined to exercise even if sick or injured, with excessive exercise defined as “Feeling like you must exercise, might continue exercising, sometimes in secret, if parents or doctors have told you to stop.”
Other questions focused on use of diuretics or laxatives and other strategies to compensate for calories consumed.
Responses revealed that restriction, underweight, dieting, and excessive exercise were present in most of the sample, while purging, loss-of-control eating, and overweight were reported by fewer than a third. With dieting typically emerging first around age 14, the other behaviors tended to manifest from age 14 to 14 and a half. The average age of formal diagnosis was just over 15 years. Parent-child dyads showed good agreement on the presence and timing of all behaviors except for dieting, for which children reported onset about 6 months earlier or longer duration compared with parents.
Although older age at the time of interview was associated with a lower body mass index percentile and higher eating disorder score, neither age of onset nor duration of disordered eating was associated with severity when researchers controlled for current age.
Telltale signs for parents
“For teens starting at a healthy weight, significant and intentional weight loss of more than 5-10 pounds can be a cause for concern,” Dr. Ranzenhofer said. Missed periods, refusing meals, skipping meals, fighting or arguing about eating, and withdrawal from normal activities and relationships are other signs of disordered eating. For overweight or obese teens, rapid weight loss and weight loss above and beyond that recommended are also concerning.
As for compulsive exercise, she said, “Altered exercise behavior might look like exercise that interferes with other activities, for example, being late to school or not doing homework in order to exercise.” Other red flags would be physical activity that varies considerably from that of peers, for instance, going running after a 2-hour sports practice and an inflexible routine that precludes being able to skip a day.
“All adolescents, male and female, should be screened regardless of weight trends – underweight, overweight, obese, or normal weight – regarding their body image and thoughts of dieting,” said Margaret E. Thew, DNP, FNP-BC, of the Medical College of Wisconsin, and medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee, commenting on the study but not involved in it. “Most adolescents make decisions to lose weight after trying to ‘eat healthy’ but may take an aggressive approach when they don’t see the weight loss they hope to see.”
According to Ms. Thew, the study findings support the benefit of giving medical caregivers and parents training on the red flags regarding eating disorders to foster early detection. “These include starting a new fad diet, eliminating foods, ‘healthy eating,’ over-exercising, skipping meals, or no longer eating foods they previously loved.”
She added that times of transition are key junctures to watch: The transition from grade school to middle school, middle to high school, and high school to college. “These tend to provoke eating disorder onset or relapse of eating disorder thoughts and behaviors after diagnosis,” Ms. Thew said. “It would benefit the patient to screen for concerns about disordered eating and provide resources, including consultation with a dietitian, as appropriate.”
This study was supported by grants from the National Institute of Mental Health and the Hilda and Preston Davis Foundation. Coauthor Joanna E. Steinglass, MD, disclosed receiving royalties from UpToDate. Ms. Thew disclosed no competing interests with regard to her comments.
FROM JOURNAL OF ADOLESCENT HEALTH
Rise of the fungi: Pandemic tied to increasing fungal infections
COVID-19 has lifted the lid on the risks of secondary pulmonary fungal infections in patients with severe respiratory viral illness – even previously immunocompetent individuals – and highlighted the importance of vigilant investigation to achieve early diagnoses, leading experts say.
Most fungi are not under surveillance in the United States, leaving experts without a national picture of the true burden of infection through the pandemic. However, a collection of published case series, cohort studies, and reviews from Europe, the United States, and throughout the world – mainly pre-Omicron – show that fungal disease has affected a significant portion of critically ill patients with COVID-19, with concerning excess mortality, these experts say.
COVID-associated pulmonary aspergillosis (CAPA) has been the predominant fungal coinfection in the United States and internationally. But COVID-associated mucormycosis (CAM) – the infection that surged in India in early 2021 – has also affected some patients in the United States, published data show. So have Pneumocystitis pneumonia, cryptococcosis, histoplasmosis, and Candida infections (which mainly affect the bloodstream and abdomen), say the experts who were interviewed.
“We had predicted [a rise in] aspergillosis, but we saw more than we thought we’d see. Most fungal infections became more common with COVID-19,” said George Thompson, MD, professor of clinical medicine at the University of California, Davis, and cochair of the University of Alabama–based Mycoses Study Group Education Committee, a group of experts in medical mycology. Pneumocystitis, for instance, “has historically been associated with AIDS or different types of leukemia or lymphoma, and is not an infection we’ve typically seen in our otherwise healthy ICU patients,” he noted. “But we did see more of it [with COVID-19].”
More recently, with fewer patients during the Omicron phase in intensive care units with acute respiratory failure, the profile of fungal disease secondary to COVID-19 has changed. Increasing proportions of patients have traditional risk factors for aspergillosis, such as hematologic malignancies and longer-term, pre-COVID use of systemic corticosteroids – a change that makes the contribution of the viral illness harder to distinguish.
Moving forward, the lessons of the COVID era – the fungal risks to patients with serious viral infections and the persistence needed to diagnose aspergillosis and other pulmonary fungal infections using bronchoscopy and imperfect noninvasive tests – should be taken to heart, experts say.
“Fungal diseases are not rare. They’re just not diagnosed because no one thinks to look for them,” said Dr. Thompson, a contributor to a recently released World Health Organization report naming a “fungal priority pathogens” list.
“We’re going to continue to see [secondary fungal infections] with other respiratory viruses,” he said. And overall, given environmental and other changes, “we’re going to see more and more fungal disease in the patients we take care of.”
CAPA not a surprise
CAPA is “not an unfamiliar story” in the world of fungal disease, given a history of influenza-associated pulmonary aspergillosis (IAPA), said Kieren A. Marr, MD, MBA, adjunct professor of medicine and past director of the transplant and oncology infectious diseases program at Johns Hopkins University, Baltimore, who has long researched invasive fungal disease.
European researchers, she said, have led the way in describing a high incidence of IAPA in patients admitted to ICUs with influenza. In a retrospective multicenter cohort study reported in 2018 by the Dutch-Belgian Mycosis Study group, for instance, almost 20% of 432 influenza patients admitted to the ICU, including patients who were otherwise healthy and not immunocompromised, had the diagnosis a median of 3 days after ICU admission. (Across other cohort studies, rates of IAPA have ranged from 7% to 30%.)
Mortality was significant: 51% of patients with influenza and invasive pulmonary aspergillosis died within 90 days, compared with 28% of patients with influenza and no invasive pulmonary aspergillosis.
Reports from Europe early in the pandemic indicated that CAPA was a similarly serious problem, prompting establishment at Johns Hopkins University of an aggressive screening program utilizing biomarker-based testing of blood and bronchoalveolar lavage (BAL) fluid. Of 396 mechanically ventilated COVID-19 patients admitted to Johns Hopkins University hospitals between March and August 2020, 39 met the institution’s criteria for CAPA, Dr. Marr and her colleagues reported this year in what might be the largest U.S. cohort study of CAPA published to date.
“We now know definitively that people with severe influenza and with severe COVID also have high risks for both invasive and airway disease caused by airborne fungi, most commonly aspergilliosis,” Dr. Marr said.
More recent unpublished analyses of patients from the start of the pandemic to June 2021 show persistent risk, said Nitipong Permpalung, MD, MPH, assistant professor in transplant and oncology infectious diseases at Johns Hopkins University and lead author of the cohort study. Among 832 patients with COVID-19 who were mechanically ventilated in Johns Hopkins University hospitals, 11.8% had CAPA, he said. (Also, 3.2% had invasive candidiasis, and 1.1% had other invasive fungal infections.)
Other sources said in interviews that these CAPA prevalence rates generally mirror reports from Europe, though some investigators in Europe have reported CAPA rates more toward 15%.
(The Mycoses Study Group recently collected data from its consortium of U.S. medical centers on the prevalence of CAPA, with funding support from the CDC, but at press time the data had not yet been released. Dr. Thompson said he suspected the prevalence will be lower than earlier papers have suggested, “but still will reflect a significant burden of disease.”)
Patients in the published Johns Hopkins University study who had CAPA were more likely than those with COVID-19 but no CAPA to have underlying pulmonary disease, liver disease, coagulopathy, solid tumors, multiple myeloma, and COVID-19–directed corticosteroids. And they had uniformly worse outcomes with regards to severity of illness and length of intubation.
How much of CAPA is driven by the SARS-CoV-2 virus itself and how much is a consequence of COVID-19 treatments is a topic of active discussion and research. Martin Hoenigl, MD, of the University of Graz, Austria, a leading researcher in medical mycology, said research shows corticosteroids and anti–IL-6 treatments, such as tocilizumab, used to treat COVID-19–driven acute respiratory failure clearly have contributed to CAPA. But he contends that “a number of other mechanisms” are involved as well.
“The immunologic mechanisms are definitely different in these patients with viral illness than in other ICU patients [who develop aspergilliosis]. It’s not just the corticosteroids. The more we learn, we see the virus plays a role as well, suppressing the interferon pathway,” for example, said Dr. Hoenigl, associate professor in the division of infectious diseases and the European Confederation of Medical Mycology (ECMM) Center of Excellence at the university. The earliest reports of CAPA came “when ICUs weren’t using dexamethasone or tocilizumab,” he noted.
In a paper published recently in Lancet Respiratory Medicine that Dr. Hoenigl and others point to, Belgian researchers reported a “three-level breach” in innate antifungal immunity in both IAPA and CAPA, affecting the integrity of the epithelial barrier, the capacity to phagocytose and kill Aspergillus spores, and the ability to destroy Aspergillus hyphae, which is mainly mediated by neutrophils.
The researchers ran a host of genetic and protein analyses on lung samples (most collected via BAL) of 169 patients with influenza or COVID-19, with and without aspergillosis. They found that patients with CAPA had significantly lower neutrophil cell fractions than patients with COVID-19 only, and patients with IAPA or CAPA had reduced type II IFN signaling and increased concentrations of fibrosis-associated growth factors in the lower respiratory tracts (Lancet Respir Med. 2022 Aug 24).
Tom Chiller, MD, MPH, chief of the Center for Disease Control and Prevention’s Mycotic Disease Branch, said he’s watching such research with interest. For now, he said, it’s important to also consider that “data on COVID show that almost all patients going into the ICUs with pneumonia and COVID are getting broad-spectrum antibiotics” in addition to corticosteroids.
By wiping out good bacteria, the antibiotics could be “creating a perfect niche for fungi to grow,” he said.
Diagnostic challenges
Aspergillus that has invaded the lung tissue in patients with COVID-19 appears to grow there for some time – around 8-10 days, much longer than in IAPA – before becoming angioinvasive, said Dr. Hoenigl. Such a pathophysiology “implicates that we should try to diagnose it while it’s in the lung tissue, using the BAL fluid, and not yet in the blood,” he said.
Some multicenter studies, including one from Europe on Aspergillus test profiles in critically ill COVID-19 patients, have shown mortality rates of close to 90% in patients with CAPA who have positive serum biomarkers, despite appropriate antifungal therapy. “If diagnosed while confined to the lung, however, mortality rates are more like 40%-50% with antifungal therapy,” Dr. Hoenigl said. (Cohort studies published thus far have fairly consistently reported mortality rates in patients with CAPA greater than 40%, he said.)
Bronchoscopy isn’t always pragmatic or possible, however, and is variably used. Some patients with severe COVID-19 may be too unstable for any invasive procedure, said Dr. Permpalung.
Dr. Permpalung looks for CAPA using serum (1-3) beta-D-glucan (BDG, a generic fungal test not specific to Aspergillus), serum galactomannan (GM, specific for Aspergillus), and respiratory cultures (sputum or endotracheal aspirate if intubated) as initial screening tests in the ICU. If there are concerns for CAPA – based on these tests and/or the clinical picture – “a thoughtful risk-benefit discussion is required to determine if patients would benefit from a bronchoscopy or if we should just start them on empiric antifungal therapy.”
Unfortunately, the sensitivity of serum GM is relatively low in CAPA – lower than with classic invasive aspergillosis in the nonviral setting, sources said. BDG, on the other hand, can be falsely positive in the setting of antimicrobials and within the ICU. And the utility of imaging for CAPA is limited. Both the clinical picture and radiological findings of CAPA have resembled those of severe COVID – with the caveat of cavitary lung lesions visible on imaging.
“Cavities or nodules are a highly suspicious finding that could indicate possible fungal infection,” said pulmonologist Amir A. Zeki, MD, MAS, professor of medicine at the University of California, Davis, and codirector of the UC Davis Asthma Network Clinic, who has cared for patients with CAPA.
Cavitation has been described in only a proportion of patients with CAPA, however. So in patients not doing well, “your suspicion has to be raised if you’re not seeing cavities,” he said.
Early in the pandemic, when patients worsened or failed to progress on mechanical ventilation, clinicians at the University of California, Davis, quickly learned not to pin blame too quickly on COVID-19 alone. This remains good advice today, Dr. Zeki said.
“If you have a patient who’s not doing well on a ventilator, not getting better [over weeks], has to be reintubated, has infiltrates or lung nodules that are evolving, or certainly, if they have a cavity, you have to suspect fungal infection,” said Dr. Zeki, who also practices at the Veterans Affairs Medical Center in San Diego. “Think about it for those patients who just aren’t moving forward and are continuing to struggle. Have a high index of suspicion, and consult with your infectious disease colleagues.”
Empiric treatment is warranted in some cases if a patient is doing poorly and suspicion for fungal infection is high based on clinical, radiographic, and/or laboratory evidence, he said.
The CDC’s Dr. Chiller said that screening and diagnostic algorithms currently vary from institution to institution, and that diagnostic challenges likely dissuade clinicians from thinking about fungi. “Clinicians often don’t want to deal with fungi – they’re difficult to diagnose, the treatments are limited and can be toxic. But fungi get pushed back until it’s too late,” he said.
“Fungal diagnostics is an area we all need a lot more help with,” and new diagnostics are in the pipeline, he said. In the meantime, he said, “there are tools out there, and we just need to use them more, and improve how they’re used.”
While reported CAPA thus far has typically occurred in the setting of ICU care and mechanical ventilation, it’s not always the case, Dr. Permpalung said. Lung and other solid organ transplant (SOT) recipients with COVID-19 are developing CAPA and other invasive secondary invasive fungal infections despite not being intubated, he said.
Of 276 SOT recipients with COVID-19 who required inpatient treatment at Johns Hopkins University hospitals from the beginning of the pandemic to March 2022, 23 patients developed invasive fungal infections (13 CAPA). Only a fraction – 38 of the 276 – had been intubated, he said.
Mucormycosis resistance
After CAPA, candidiasis and COVID-19-associated mucormycosis (CAM) – most frequently, rhino-orbital-cerebral disease or pulmonary disease – have been the leading reported fungal coinfections in COVID-19, said Dr. Hoenigl, who described the incidence, timeline, risk factors, and pathogenesis of these infections in a review published this year in Nature Microbiology. .
In India, where there has long been high exposure to Mucorales spores and a greater burden of invasive fungal disease, the rate of mucormycosis doubled in 2021, with rhino-orbital-cerebral disease reported almost exclusively, he said. Pulmonary disease has occurred almost exclusively in the ICU setting and has been present in about 50% of cases outside of India, including Europe and the United States.
A preprint meta-analysis of CAM cases posted by the Lancet in July 2022, in which investigators analyzed individual data of 556 reported cases of COVID-19–associated CAM, shows diabetes and history of corticosteroid use present in most patients, and an overall mortality rate of 44.4%, most of which stems from cases of pulmonary or disseminated disease. Thirteen of the 556 reported cases were from the United States.
An important take-away from the analysis, Dr. Hoenigl said, is that Aspergillus coinfection was seen in 7% of patients and was associated with higher mortality. “It’s important to consider that coinfections [of Aspergillus and Mucorales] can exist,” Dr. Hoenigl said, noting that like CAPA, pulmonary CAM is likely underdiagnosed and underreported.
As with CAPA, the clinical and radiological features of pulmonary CAM largely overlap with those associated with COVID-19, and bronchoscopy plays a central role in definitive diagnosis. In the United States, a Mucorales PCR test for blood and BAL fluid is commercially available and used at some centers, Dr. Hoenigl said.
“Mucormycosis is always difficult to treat ... a lot of the treatments don’t work particularly well,” said Dr. Thompson. “With aspergillosis, we have better treatment options.”
Dr. Thompson worries, however, about treatment resistance becoming widespread. Resistance to azole antifungal agents “is already pretty widespread in northern Europe, particularly in the Netherlands and part of the U.K.” because of injudicious use of antifungals in agriculture, he said. “We’ve started to see a few cases [of azole-resistant aspergillosis in the United States] and know it will be more widespread soon.”
Treatment resistance is a focus of the new WHO fungal priority pathogens list – the first such report from the organization. Of the 19 fungi on the list, 4 were ranked as critical: Cryptococcus neoformans, Candida auris, Aspergillus fumigatus, and Candida albicans. Like Dr. Thompson, Dr. Hoenigl contributed to the WHO report.
Dr. Hoenigl reported grant/research support from Astellas, Merck, F2G, Gilread, Pfizer, and Scynexis. Dr. Marr disclosed employment and equity in Pearl Diagnostics and Sfunga Therapeutics. Dr. Thompson, Dr. Permpalung, and Dr. Zeki reported that they have no relevant financial disclosures.
COVID-19 has lifted the lid on the risks of secondary pulmonary fungal infections in patients with severe respiratory viral illness – even previously immunocompetent individuals – and highlighted the importance of vigilant investigation to achieve early diagnoses, leading experts say.
Most fungi are not under surveillance in the United States, leaving experts without a national picture of the true burden of infection through the pandemic. However, a collection of published case series, cohort studies, and reviews from Europe, the United States, and throughout the world – mainly pre-Omicron – show that fungal disease has affected a significant portion of critically ill patients with COVID-19, with concerning excess mortality, these experts say.
COVID-associated pulmonary aspergillosis (CAPA) has been the predominant fungal coinfection in the United States and internationally. But COVID-associated mucormycosis (CAM) – the infection that surged in India in early 2021 – has also affected some patients in the United States, published data show. So have Pneumocystitis pneumonia, cryptococcosis, histoplasmosis, and Candida infections (which mainly affect the bloodstream and abdomen), say the experts who were interviewed.
“We had predicted [a rise in] aspergillosis, but we saw more than we thought we’d see. Most fungal infections became more common with COVID-19,” said George Thompson, MD, professor of clinical medicine at the University of California, Davis, and cochair of the University of Alabama–based Mycoses Study Group Education Committee, a group of experts in medical mycology. Pneumocystitis, for instance, “has historically been associated with AIDS or different types of leukemia or lymphoma, and is not an infection we’ve typically seen in our otherwise healthy ICU patients,” he noted. “But we did see more of it [with COVID-19].”
More recently, with fewer patients during the Omicron phase in intensive care units with acute respiratory failure, the profile of fungal disease secondary to COVID-19 has changed. Increasing proportions of patients have traditional risk factors for aspergillosis, such as hematologic malignancies and longer-term, pre-COVID use of systemic corticosteroids – a change that makes the contribution of the viral illness harder to distinguish.
Moving forward, the lessons of the COVID era – the fungal risks to patients with serious viral infections and the persistence needed to diagnose aspergillosis and other pulmonary fungal infections using bronchoscopy and imperfect noninvasive tests – should be taken to heart, experts say.
“Fungal diseases are not rare. They’re just not diagnosed because no one thinks to look for them,” said Dr. Thompson, a contributor to a recently released World Health Organization report naming a “fungal priority pathogens” list.
“We’re going to continue to see [secondary fungal infections] with other respiratory viruses,” he said. And overall, given environmental and other changes, “we’re going to see more and more fungal disease in the patients we take care of.”
CAPA not a surprise
CAPA is “not an unfamiliar story” in the world of fungal disease, given a history of influenza-associated pulmonary aspergillosis (IAPA), said Kieren A. Marr, MD, MBA, adjunct professor of medicine and past director of the transplant and oncology infectious diseases program at Johns Hopkins University, Baltimore, who has long researched invasive fungal disease.
European researchers, she said, have led the way in describing a high incidence of IAPA in patients admitted to ICUs with influenza. In a retrospective multicenter cohort study reported in 2018 by the Dutch-Belgian Mycosis Study group, for instance, almost 20% of 432 influenza patients admitted to the ICU, including patients who were otherwise healthy and not immunocompromised, had the diagnosis a median of 3 days after ICU admission. (Across other cohort studies, rates of IAPA have ranged from 7% to 30%.)
Mortality was significant: 51% of patients with influenza and invasive pulmonary aspergillosis died within 90 days, compared with 28% of patients with influenza and no invasive pulmonary aspergillosis.
Reports from Europe early in the pandemic indicated that CAPA was a similarly serious problem, prompting establishment at Johns Hopkins University of an aggressive screening program utilizing biomarker-based testing of blood and bronchoalveolar lavage (BAL) fluid. Of 396 mechanically ventilated COVID-19 patients admitted to Johns Hopkins University hospitals between March and August 2020, 39 met the institution’s criteria for CAPA, Dr. Marr and her colleagues reported this year in what might be the largest U.S. cohort study of CAPA published to date.
“We now know definitively that people with severe influenza and with severe COVID also have high risks for both invasive and airway disease caused by airborne fungi, most commonly aspergilliosis,” Dr. Marr said.
More recent unpublished analyses of patients from the start of the pandemic to June 2021 show persistent risk, said Nitipong Permpalung, MD, MPH, assistant professor in transplant and oncology infectious diseases at Johns Hopkins University and lead author of the cohort study. Among 832 patients with COVID-19 who were mechanically ventilated in Johns Hopkins University hospitals, 11.8% had CAPA, he said. (Also, 3.2% had invasive candidiasis, and 1.1% had other invasive fungal infections.)
Other sources said in interviews that these CAPA prevalence rates generally mirror reports from Europe, though some investigators in Europe have reported CAPA rates more toward 15%.
(The Mycoses Study Group recently collected data from its consortium of U.S. medical centers on the prevalence of CAPA, with funding support from the CDC, but at press time the data had not yet been released. Dr. Thompson said he suspected the prevalence will be lower than earlier papers have suggested, “but still will reflect a significant burden of disease.”)
Patients in the published Johns Hopkins University study who had CAPA were more likely than those with COVID-19 but no CAPA to have underlying pulmonary disease, liver disease, coagulopathy, solid tumors, multiple myeloma, and COVID-19–directed corticosteroids. And they had uniformly worse outcomes with regards to severity of illness and length of intubation.
How much of CAPA is driven by the SARS-CoV-2 virus itself and how much is a consequence of COVID-19 treatments is a topic of active discussion and research. Martin Hoenigl, MD, of the University of Graz, Austria, a leading researcher in medical mycology, said research shows corticosteroids and anti–IL-6 treatments, such as tocilizumab, used to treat COVID-19–driven acute respiratory failure clearly have contributed to CAPA. But he contends that “a number of other mechanisms” are involved as well.
“The immunologic mechanisms are definitely different in these patients with viral illness than in other ICU patients [who develop aspergilliosis]. It’s not just the corticosteroids. The more we learn, we see the virus plays a role as well, suppressing the interferon pathway,” for example, said Dr. Hoenigl, associate professor in the division of infectious diseases and the European Confederation of Medical Mycology (ECMM) Center of Excellence at the university. The earliest reports of CAPA came “when ICUs weren’t using dexamethasone or tocilizumab,” he noted.
In a paper published recently in Lancet Respiratory Medicine that Dr. Hoenigl and others point to, Belgian researchers reported a “three-level breach” in innate antifungal immunity in both IAPA and CAPA, affecting the integrity of the epithelial barrier, the capacity to phagocytose and kill Aspergillus spores, and the ability to destroy Aspergillus hyphae, which is mainly mediated by neutrophils.
The researchers ran a host of genetic and protein analyses on lung samples (most collected via BAL) of 169 patients with influenza or COVID-19, with and without aspergillosis. They found that patients with CAPA had significantly lower neutrophil cell fractions than patients with COVID-19 only, and patients with IAPA or CAPA had reduced type II IFN signaling and increased concentrations of fibrosis-associated growth factors in the lower respiratory tracts (Lancet Respir Med. 2022 Aug 24).
Tom Chiller, MD, MPH, chief of the Center for Disease Control and Prevention’s Mycotic Disease Branch, said he’s watching such research with interest. For now, he said, it’s important to also consider that “data on COVID show that almost all patients going into the ICUs with pneumonia and COVID are getting broad-spectrum antibiotics” in addition to corticosteroids.
By wiping out good bacteria, the antibiotics could be “creating a perfect niche for fungi to grow,” he said.
Diagnostic challenges
Aspergillus that has invaded the lung tissue in patients with COVID-19 appears to grow there for some time – around 8-10 days, much longer than in IAPA – before becoming angioinvasive, said Dr. Hoenigl. Such a pathophysiology “implicates that we should try to diagnose it while it’s in the lung tissue, using the BAL fluid, and not yet in the blood,” he said.
Some multicenter studies, including one from Europe on Aspergillus test profiles in critically ill COVID-19 patients, have shown mortality rates of close to 90% in patients with CAPA who have positive serum biomarkers, despite appropriate antifungal therapy. “If diagnosed while confined to the lung, however, mortality rates are more like 40%-50% with antifungal therapy,” Dr. Hoenigl said. (Cohort studies published thus far have fairly consistently reported mortality rates in patients with CAPA greater than 40%, he said.)
Bronchoscopy isn’t always pragmatic or possible, however, and is variably used. Some patients with severe COVID-19 may be too unstable for any invasive procedure, said Dr. Permpalung.
Dr. Permpalung looks for CAPA using serum (1-3) beta-D-glucan (BDG, a generic fungal test not specific to Aspergillus), serum galactomannan (GM, specific for Aspergillus), and respiratory cultures (sputum or endotracheal aspirate if intubated) as initial screening tests in the ICU. If there are concerns for CAPA – based on these tests and/or the clinical picture – “a thoughtful risk-benefit discussion is required to determine if patients would benefit from a bronchoscopy or if we should just start them on empiric antifungal therapy.”
Unfortunately, the sensitivity of serum GM is relatively low in CAPA – lower than with classic invasive aspergillosis in the nonviral setting, sources said. BDG, on the other hand, can be falsely positive in the setting of antimicrobials and within the ICU. And the utility of imaging for CAPA is limited. Both the clinical picture and radiological findings of CAPA have resembled those of severe COVID – with the caveat of cavitary lung lesions visible on imaging.
“Cavities or nodules are a highly suspicious finding that could indicate possible fungal infection,” said pulmonologist Amir A. Zeki, MD, MAS, professor of medicine at the University of California, Davis, and codirector of the UC Davis Asthma Network Clinic, who has cared for patients with CAPA.
Cavitation has been described in only a proportion of patients with CAPA, however. So in patients not doing well, “your suspicion has to be raised if you’re not seeing cavities,” he said.
Early in the pandemic, when patients worsened or failed to progress on mechanical ventilation, clinicians at the University of California, Davis, quickly learned not to pin blame too quickly on COVID-19 alone. This remains good advice today, Dr. Zeki said.
“If you have a patient who’s not doing well on a ventilator, not getting better [over weeks], has to be reintubated, has infiltrates or lung nodules that are evolving, or certainly, if they have a cavity, you have to suspect fungal infection,” said Dr. Zeki, who also practices at the Veterans Affairs Medical Center in San Diego. “Think about it for those patients who just aren’t moving forward and are continuing to struggle. Have a high index of suspicion, and consult with your infectious disease colleagues.”
Empiric treatment is warranted in some cases if a patient is doing poorly and suspicion for fungal infection is high based on clinical, radiographic, and/or laboratory evidence, he said.
The CDC’s Dr. Chiller said that screening and diagnostic algorithms currently vary from institution to institution, and that diagnostic challenges likely dissuade clinicians from thinking about fungi. “Clinicians often don’t want to deal with fungi – they’re difficult to diagnose, the treatments are limited and can be toxic. But fungi get pushed back until it’s too late,” he said.
“Fungal diagnostics is an area we all need a lot more help with,” and new diagnostics are in the pipeline, he said. In the meantime, he said, “there are tools out there, and we just need to use them more, and improve how they’re used.”
While reported CAPA thus far has typically occurred in the setting of ICU care and mechanical ventilation, it’s not always the case, Dr. Permpalung said. Lung and other solid organ transplant (SOT) recipients with COVID-19 are developing CAPA and other invasive secondary invasive fungal infections despite not being intubated, he said.
Of 276 SOT recipients with COVID-19 who required inpatient treatment at Johns Hopkins University hospitals from the beginning of the pandemic to March 2022, 23 patients developed invasive fungal infections (13 CAPA). Only a fraction – 38 of the 276 – had been intubated, he said.
Mucormycosis resistance
After CAPA, candidiasis and COVID-19-associated mucormycosis (CAM) – most frequently, rhino-orbital-cerebral disease or pulmonary disease – have been the leading reported fungal coinfections in COVID-19, said Dr. Hoenigl, who described the incidence, timeline, risk factors, and pathogenesis of these infections in a review published this year in Nature Microbiology. .
In India, where there has long been high exposure to Mucorales spores and a greater burden of invasive fungal disease, the rate of mucormycosis doubled in 2021, with rhino-orbital-cerebral disease reported almost exclusively, he said. Pulmonary disease has occurred almost exclusively in the ICU setting and has been present in about 50% of cases outside of India, including Europe and the United States.
A preprint meta-analysis of CAM cases posted by the Lancet in July 2022, in which investigators analyzed individual data of 556 reported cases of COVID-19–associated CAM, shows diabetes and history of corticosteroid use present in most patients, and an overall mortality rate of 44.4%, most of which stems from cases of pulmonary or disseminated disease. Thirteen of the 556 reported cases were from the United States.
An important take-away from the analysis, Dr. Hoenigl said, is that Aspergillus coinfection was seen in 7% of patients and was associated with higher mortality. “It’s important to consider that coinfections [of Aspergillus and Mucorales] can exist,” Dr. Hoenigl said, noting that like CAPA, pulmonary CAM is likely underdiagnosed and underreported.
As with CAPA, the clinical and radiological features of pulmonary CAM largely overlap with those associated with COVID-19, and bronchoscopy plays a central role in definitive diagnosis. In the United States, a Mucorales PCR test for blood and BAL fluid is commercially available and used at some centers, Dr. Hoenigl said.
“Mucormycosis is always difficult to treat ... a lot of the treatments don’t work particularly well,” said Dr. Thompson. “With aspergillosis, we have better treatment options.”
Dr. Thompson worries, however, about treatment resistance becoming widespread. Resistance to azole antifungal agents “is already pretty widespread in northern Europe, particularly in the Netherlands and part of the U.K.” because of injudicious use of antifungals in agriculture, he said. “We’ve started to see a few cases [of azole-resistant aspergillosis in the United States] and know it will be more widespread soon.”
Treatment resistance is a focus of the new WHO fungal priority pathogens list – the first such report from the organization. Of the 19 fungi on the list, 4 were ranked as critical: Cryptococcus neoformans, Candida auris, Aspergillus fumigatus, and Candida albicans. Like Dr. Thompson, Dr. Hoenigl contributed to the WHO report.
Dr. Hoenigl reported grant/research support from Astellas, Merck, F2G, Gilread, Pfizer, and Scynexis. Dr. Marr disclosed employment and equity in Pearl Diagnostics and Sfunga Therapeutics. Dr. Thompson, Dr. Permpalung, and Dr. Zeki reported that they have no relevant financial disclosures.
COVID-19 has lifted the lid on the risks of secondary pulmonary fungal infections in patients with severe respiratory viral illness – even previously immunocompetent individuals – and highlighted the importance of vigilant investigation to achieve early diagnoses, leading experts say.
Most fungi are not under surveillance in the United States, leaving experts without a national picture of the true burden of infection through the pandemic. However, a collection of published case series, cohort studies, and reviews from Europe, the United States, and throughout the world – mainly pre-Omicron – show that fungal disease has affected a significant portion of critically ill patients with COVID-19, with concerning excess mortality, these experts say.
COVID-associated pulmonary aspergillosis (CAPA) has been the predominant fungal coinfection in the United States and internationally. But COVID-associated mucormycosis (CAM) – the infection that surged in India in early 2021 – has also affected some patients in the United States, published data show. So have Pneumocystitis pneumonia, cryptococcosis, histoplasmosis, and Candida infections (which mainly affect the bloodstream and abdomen), say the experts who were interviewed.
“We had predicted [a rise in] aspergillosis, but we saw more than we thought we’d see. Most fungal infections became more common with COVID-19,” said George Thompson, MD, professor of clinical medicine at the University of California, Davis, and cochair of the University of Alabama–based Mycoses Study Group Education Committee, a group of experts in medical mycology. Pneumocystitis, for instance, “has historically been associated with AIDS or different types of leukemia or lymphoma, and is not an infection we’ve typically seen in our otherwise healthy ICU patients,” he noted. “But we did see more of it [with COVID-19].”
More recently, with fewer patients during the Omicron phase in intensive care units with acute respiratory failure, the profile of fungal disease secondary to COVID-19 has changed. Increasing proportions of patients have traditional risk factors for aspergillosis, such as hematologic malignancies and longer-term, pre-COVID use of systemic corticosteroids – a change that makes the contribution of the viral illness harder to distinguish.
Moving forward, the lessons of the COVID era – the fungal risks to patients with serious viral infections and the persistence needed to diagnose aspergillosis and other pulmonary fungal infections using bronchoscopy and imperfect noninvasive tests – should be taken to heart, experts say.
“Fungal diseases are not rare. They’re just not diagnosed because no one thinks to look for them,” said Dr. Thompson, a contributor to a recently released World Health Organization report naming a “fungal priority pathogens” list.
“We’re going to continue to see [secondary fungal infections] with other respiratory viruses,” he said. And overall, given environmental and other changes, “we’re going to see more and more fungal disease in the patients we take care of.”
CAPA not a surprise
CAPA is “not an unfamiliar story” in the world of fungal disease, given a history of influenza-associated pulmonary aspergillosis (IAPA), said Kieren A. Marr, MD, MBA, adjunct professor of medicine and past director of the transplant and oncology infectious diseases program at Johns Hopkins University, Baltimore, who has long researched invasive fungal disease.
European researchers, she said, have led the way in describing a high incidence of IAPA in patients admitted to ICUs with influenza. In a retrospective multicenter cohort study reported in 2018 by the Dutch-Belgian Mycosis Study group, for instance, almost 20% of 432 influenza patients admitted to the ICU, including patients who were otherwise healthy and not immunocompromised, had the diagnosis a median of 3 days after ICU admission. (Across other cohort studies, rates of IAPA have ranged from 7% to 30%.)
Mortality was significant: 51% of patients with influenza and invasive pulmonary aspergillosis died within 90 days, compared with 28% of patients with influenza and no invasive pulmonary aspergillosis.
Reports from Europe early in the pandemic indicated that CAPA was a similarly serious problem, prompting establishment at Johns Hopkins University of an aggressive screening program utilizing biomarker-based testing of blood and bronchoalveolar lavage (BAL) fluid. Of 396 mechanically ventilated COVID-19 patients admitted to Johns Hopkins University hospitals between March and August 2020, 39 met the institution’s criteria for CAPA, Dr. Marr and her colleagues reported this year in what might be the largest U.S. cohort study of CAPA published to date.
“We now know definitively that people with severe influenza and with severe COVID also have high risks for both invasive and airway disease caused by airborne fungi, most commonly aspergilliosis,” Dr. Marr said.
More recent unpublished analyses of patients from the start of the pandemic to June 2021 show persistent risk, said Nitipong Permpalung, MD, MPH, assistant professor in transplant and oncology infectious diseases at Johns Hopkins University and lead author of the cohort study. Among 832 patients with COVID-19 who were mechanically ventilated in Johns Hopkins University hospitals, 11.8% had CAPA, he said. (Also, 3.2% had invasive candidiasis, and 1.1% had other invasive fungal infections.)
Other sources said in interviews that these CAPA prevalence rates generally mirror reports from Europe, though some investigators in Europe have reported CAPA rates more toward 15%.
(The Mycoses Study Group recently collected data from its consortium of U.S. medical centers on the prevalence of CAPA, with funding support from the CDC, but at press time the data had not yet been released. Dr. Thompson said he suspected the prevalence will be lower than earlier papers have suggested, “but still will reflect a significant burden of disease.”)
Patients in the published Johns Hopkins University study who had CAPA were more likely than those with COVID-19 but no CAPA to have underlying pulmonary disease, liver disease, coagulopathy, solid tumors, multiple myeloma, and COVID-19–directed corticosteroids. And they had uniformly worse outcomes with regards to severity of illness and length of intubation.
How much of CAPA is driven by the SARS-CoV-2 virus itself and how much is a consequence of COVID-19 treatments is a topic of active discussion and research. Martin Hoenigl, MD, of the University of Graz, Austria, a leading researcher in medical mycology, said research shows corticosteroids and anti–IL-6 treatments, such as tocilizumab, used to treat COVID-19–driven acute respiratory failure clearly have contributed to CAPA. But he contends that “a number of other mechanisms” are involved as well.
“The immunologic mechanisms are definitely different in these patients with viral illness than in other ICU patients [who develop aspergilliosis]. It’s not just the corticosteroids. The more we learn, we see the virus plays a role as well, suppressing the interferon pathway,” for example, said Dr. Hoenigl, associate professor in the division of infectious diseases and the European Confederation of Medical Mycology (ECMM) Center of Excellence at the university. The earliest reports of CAPA came “when ICUs weren’t using dexamethasone or tocilizumab,” he noted.
In a paper published recently in Lancet Respiratory Medicine that Dr. Hoenigl and others point to, Belgian researchers reported a “three-level breach” in innate antifungal immunity in both IAPA and CAPA, affecting the integrity of the epithelial barrier, the capacity to phagocytose and kill Aspergillus spores, and the ability to destroy Aspergillus hyphae, which is mainly mediated by neutrophils.
The researchers ran a host of genetic and protein analyses on lung samples (most collected via BAL) of 169 patients with influenza or COVID-19, with and without aspergillosis. They found that patients with CAPA had significantly lower neutrophil cell fractions than patients with COVID-19 only, and patients with IAPA or CAPA had reduced type II IFN signaling and increased concentrations of fibrosis-associated growth factors in the lower respiratory tracts (Lancet Respir Med. 2022 Aug 24).
Tom Chiller, MD, MPH, chief of the Center for Disease Control and Prevention’s Mycotic Disease Branch, said he’s watching such research with interest. For now, he said, it’s important to also consider that “data on COVID show that almost all patients going into the ICUs with pneumonia and COVID are getting broad-spectrum antibiotics” in addition to corticosteroids.
By wiping out good bacteria, the antibiotics could be “creating a perfect niche for fungi to grow,” he said.
Diagnostic challenges
Aspergillus that has invaded the lung tissue in patients with COVID-19 appears to grow there for some time – around 8-10 days, much longer than in IAPA – before becoming angioinvasive, said Dr. Hoenigl. Such a pathophysiology “implicates that we should try to diagnose it while it’s in the lung tissue, using the BAL fluid, and not yet in the blood,” he said.
Some multicenter studies, including one from Europe on Aspergillus test profiles in critically ill COVID-19 patients, have shown mortality rates of close to 90% in patients with CAPA who have positive serum biomarkers, despite appropriate antifungal therapy. “If diagnosed while confined to the lung, however, mortality rates are more like 40%-50% with antifungal therapy,” Dr. Hoenigl said. (Cohort studies published thus far have fairly consistently reported mortality rates in patients with CAPA greater than 40%, he said.)
Bronchoscopy isn’t always pragmatic or possible, however, and is variably used. Some patients with severe COVID-19 may be too unstable for any invasive procedure, said Dr. Permpalung.
Dr. Permpalung looks for CAPA using serum (1-3) beta-D-glucan (BDG, a generic fungal test not specific to Aspergillus), serum galactomannan (GM, specific for Aspergillus), and respiratory cultures (sputum or endotracheal aspirate if intubated) as initial screening tests in the ICU. If there are concerns for CAPA – based on these tests and/or the clinical picture – “a thoughtful risk-benefit discussion is required to determine if patients would benefit from a bronchoscopy or if we should just start them on empiric antifungal therapy.”
Unfortunately, the sensitivity of serum GM is relatively low in CAPA – lower than with classic invasive aspergillosis in the nonviral setting, sources said. BDG, on the other hand, can be falsely positive in the setting of antimicrobials and within the ICU. And the utility of imaging for CAPA is limited. Both the clinical picture and radiological findings of CAPA have resembled those of severe COVID – with the caveat of cavitary lung lesions visible on imaging.
“Cavities or nodules are a highly suspicious finding that could indicate possible fungal infection,” said pulmonologist Amir A. Zeki, MD, MAS, professor of medicine at the University of California, Davis, and codirector of the UC Davis Asthma Network Clinic, who has cared for patients with CAPA.
Cavitation has been described in only a proportion of patients with CAPA, however. So in patients not doing well, “your suspicion has to be raised if you’re not seeing cavities,” he said.
Early in the pandemic, when patients worsened or failed to progress on mechanical ventilation, clinicians at the University of California, Davis, quickly learned not to pin blame too quickly on COVID-19 alone. This remains good advice today, Dr. Zeki said.
“If you have a patient who’s not doing well on a ventilator, not getting better [over weeks], has to be reintubated, has infiltrates or lung nodules that are evolving, or certainly, if they have a cavity, you have to suspect fungal infection,” said Dr. Zeki, who also practices at the Veterans Affairs Medical Center in San Diego. “Think about it for those patients who just aren’t moving forward and are continuing to struggle. Have a high index of suspicion, and consult with your infectious disease colleagues.”
Empiric treatment is warranted in some cases if a patient is doing poorly and suspicion for fungal infection is high based on clinical, radiographic, and/or laboratory evidence, he said.
The CDC’s Dr. Chiller said that screening and diagnostic algorithms currently vary from institution to institution, and that diagnostic challenges likely dissuade clinicians from thinking about fungi. “Clinicians often don’t want to deal with fungi – they’re difficult to diagnose, the treatments are limited and can be toxic. But fungi get pushed back until it’s too late,” he said.
“Fungal diagnostics is an area we all need a lot more help with,” and new diagnostics are in the pipeline, he said. In the meantime, he said, “there are tools out there, and we just need to use them more, and improve how they’re used.”
While reported CAPA thus far has typically occurred in the setting of ICU care and mechanical ventilation, it’s not always the case, Dr. Permpalung said. Lung and other solid organ transplant (SOT) recipients with COVID-19 are developing CAPA and other invasive secondary invasive fungal infections despite not being intubated, he said.
Of 276 SOT recipients with COVID-19 who required inpatient treatment at Johns Hopkins University hospitals from the beginning of the pandemic to March 2022, 23 patients developed invasive fungal infections (13 CAPA). Only a fraction – 38 of the 276 – had been intubated, he said.
Mucormycosis resistance
After CAPA, candidiasis and COVID-19-associated mucormycosis (CAM) – most frequently, rhino-orbital-cerebral disease or pulmonary disease – have been the leading reported fungal coinfections in COVID-19, said Dr. Hoenigl, who described the incidence, timeline, risk factors, and pathogenesis of these infections in a review published this year in Nature Microbiology. .
In India, where there has long been high exposure to Mucorales spores and a greater burden of invasive fungal disease, the rate of mucormycosis doubled in 2021, with rhino-orbital-cerebral disease reported almost exclusively, he said. Pulmonary disease has occurred almost exclusively in the ICU setting and has been present in about 50% of cases outside of India, including Europe and the United States.
A preprint meta-analysis of CAM cases posted by the Lancet in July 2022, in which investigators analyzed individual data of 556 reported cases of COVID-19–associated CAM, shows diabetes and history of corticosteroid use present in most patients, and an overall mortality rate of 44.4%, most of which stems from cases of pulmonary or disseminated disease. Thirteen of the 556 reported cases were from the United States.
An important take-away from the analysis, Dr. Hoenigl said, is that Aspergillus coinfection was seen in 7% of patients and was associated with higher mortality. “It’s important to consider that coinfections [of Aspergillus and Mucorales] can exist,” Dr. Hoenigl said, noting that like CAPA, pulmonary CAM is likely underdiagnosed and underreported.
As with CAPA, the clinical and radiological features of pulmonary CAM largely overlap with those associated with COVID-19, and bronchoscopy plays a central role in definitive diagnosis. In the United States, a Mucorales PCR test for blood and BAL fluid is commercially available and used at some centers, Dr. Hoenigl said.
“Mucormycosis is always difficult to treat ... a lot of the treatments don’t work particularly well,” said Dr. Thompson. “With aspergillosis, we have better treatment options.”
Dr. Thompson worries, however, about treatment resistance becoming widespread. Resistance to azole antifungal agents “is already pretty widespread in northern Europe, particularly in the Netherlands and part of the U.K.” because of injudicious use of antifungals in agriculture, he said. “We’ve started to see a few cases [of azole-resistant aspergillosis in the United States] and know it will be more widespread soon.”
Treatment resistance is a focus of the new WHO fungal priority pathogens list – the first such report from the organization. Of the 19 fungi on the list, 4 were ranked as critical: Cryptococcus neoformans, Candida auris, Aspergillus fumigatus, and Candida albicans. Like Dr. Thompson, Dr. Hoenigl contributed to the WHO report.
Dr. Hoenigl reported grant/research support from Astellas, Merck, F2G, Gilread, Pfizer, and Scynexis. Dr. Marr disclosed employment and equity in Pearl Diagnostics and Sfunga Therapeutics. Dr. Thompson, Dr. Permpalung, and Dr. Zeki reported that they have no relevant financial disclosures.
Oral SERD camizestrant prolongs PFS vs. fulvestrant in breast cancer
SAN ANTONIO – compared with the first-generation SERD fulvestrant Faslodex, in the SERENA-2 trial, shows a study recently presented at the San Antonio Breast Cancer Symposium.
Among 180 postmenopausal women with ER+/HER2– breast cancers that had recurred or progressed following at least one line of endocrine therapy, the median progression-free survival (PFS) after a median follow-up of 16.6-17.4 months was 7.2 months for patients treated at a 75-mg dose of camizestrant and 7.7 months for those treated at a 150-mg dose, compared with 3.7 months for patients who received fulvestrant, reported Mafalda Oliveira, MD, PhD, from Vall d’Hebron University Hospital in Barcelona.
Oral agent
Camizestrant is a next-generation oral SERD and pure estrogen receptor antagonist that was shown in the SERENA-1 trial to be safe and to have clinical activity against ER+ breast cancers.
SERENA-2 pitted camizestrant at doses of 75 mg, 150 mg, or 300 mg against standard-dose fulvestrant, although the 300-mg dose was dropped in a protocol amendment after 20 patients had been assigned to that arm. (Currently planned studies with camizestrant will be conducted with the 75-mg dose.)
The investigators enrolled women with ER+/HER2– advanced breast cancer who had not previously received fulvestrant or an oral SERD. Eligible patients were limited to no more than one prior line of endocrine and one prior line of chemotherapy for advanced breast cancers. The study included patients with both measurable and unmeasurable disease.
The median patient age was about 60 years. Approximately 59% of patients in each arm had either lung or liver metastases. Patients with recurrence in bone only comprised 14.9%-19.4%.
Mutations in ESR1, a gene associated with hormonal resistance, were detectable in 29.7%-47.9% of patients.
Better PFS
As noted before, the primary endpoint of investigator-assessed median PFS favored camizestrant in both the 75-mg arm (7.2 months) and the 150-mg arm (7.7 months), with respective adjusted hazard ratios for progression versus fulvestrant of 0.58 (P = .0124) and 0.67 (P = .0161).
Camizestrant at the 75-mg dose was also superior to fulvestrant among patients who had previously received a cyclin-dependent kinase 4/6 inhibitor, with median PFS of 5.5 months and 3.8 months for the 75-mg and 150-mg doses, respectively, compared with 2.1 months.
The adjusted HR for progression with camizestrant with the 75-mg dose was 0.49, with a 90% confidence interval indicating significance. The 150-mg dose was not significantly superior to fulvestrant, however.
Both camizestrant doses were also superior for prolonging PFS versus fulvestrant among patients with lung and/or liver metastases, with median PFS of 7.2 months, 5.6 months, and 2.0 months, respectively.
The experimental SERD also outperformed fulvestrant in an analysis looking at PFS by ESR1 mutational status and ER-driven disease. Among patients with ESR1 wild type, however, median PFS rates with camizestrant 75 mg and fulvestrant were the same (7.2 months).
The 24-week objective response rates were 15.7% in the 75-mg camizestrant arm, 20% in the 150-mg arm, and 11.8% in the fulvestrant arm. The respective clinical benefit rates, including all patients with responses or stable disease, were 47.3%, 49.3%, and 38.4%. The camizestrant clinical benefit rates did not differ significantly from those with fulvestrant, however.
Treatment-related adverse events of grade 3 or greater occurred in only five patients, and only two patients, both in the 75-mg camizestrant arm, discontinued therapy because of adverse events. There were no treatment-related deaths.
Adverse events that occurred only with camizestrant included photopsia (flashing lights or floaters in the field of vision) and sinus bradycardia.
Promising, but early
Carlos Artega, MD, codirector of SABCS and director of the Simmons Comprehensive Cancer Center at UT Southwestern Medical Center, Dallas, who was not involved in the study, said the data look promising in comparison with fulvestrant.
“There is a clear suggestion that this might be better,” he said. “[Camizestrant] seems to be better at reducing the titer in plasma of the ESR1 mutation, and there is very strong basic science that supports that.”
He noted that the study numbers were relatively small, however.
Dr. Arteaga was speaking at a media briefing held immediately prior to the presentation of the data in an oral abstract session.
Fabrice Andre, MD, from Gustave Roussy in Villejuif, France, the invited discussant for the oral session, noted that, in patients with ESR1 wild type, where fulvestrant shows some efficacy, camizestrant appears to be equally effective, and that the latter agent may be more synergistic with targeted therapies than fulvestrant.
Given high patient dropout rates with currently available SERDs, there is a need for SERDs used in the adjuvant setting that are effective at minimally bioactive doses for patients who are predicted to poorly adherent, Dr. Andre said.
The study was funded by AstraZeneca. Dr. Oliveira has received personal funding from AstraZeneca, Guardant Health, Roche, Merck Sharp & Dohme, Pfizer, Seagen, iTeos Therapeutics, Eisai, Novartis, Relay Therapeutics, and Gilead. Dr. Arteaga is a scientific adviser to AstraZeneca and others, and has received grant support from Pfizer Lilly and Takeda. Dr. Andre disclosed fees to his hospital on his behalf from AstraZeneca, Daiichi Sankyo, Sanofi, Pfizer, Lilly, and Roche.
SAN ANTONIO – compared with the first-generation SERD fulvestrant Faslodex, in the SERENA-2 trial, shows a study recently presented at the San Antonio Breast Cancer Symposium.
Among 180 postmenopausal women with ER+/HER2– breast cancers that had recurred or progressed following at least one line of endocrine therapy, the median progression-free survival (PFS) after a median follow-up of 16.6-17.4 months was 7.2 months for patients treated at a 75-mg dose of camizestrant and 7.7 months for those treated at a 150-mg dose, compared with 3.7 months for patients who received fulvestrant, reported Mafalda Oliveira, MD, PhD, from Vall d’Hebron University Hospital in Barcelona.
Oral agent
Camizestrant is a next-generation oral SERD and pure estrogen receptor antagonist that was shown in the SERENA-1 trial to be safe and to have clinical activity against ER+ breast cancers.
SERENA-2 pitted camizestrant at doses of 75 mg, 150 mg, or 300 mg against standard-dose fulvestrant, although the 300-mg dose was dropped in a protocol amendment after 20 patients had been assigned to that arm. (Currently planned studies with camizestrant will be conducted with the 75-mg dose.)
The investigators enrolled women with ER+/HER2– advanced breast cancer who had not previously received fulvestrant or an oral SERD. Eligible patients were limited to no more than one prior line of endocrine and one prior line of chemotherapy for advanced breast cancers. The study included patients with both measurable and unmeasurable disease.
The median patient age was about 60 years. Approximately 59% of patients in each arm had either lung or liver metastases. Patients with recurrence in bone only comprised 14.9%-19.4%.
Mutations in ESR1, a gene associated with hormonal resistance, were detectable in 29.7%-47.9% of patients.
Better PFS
As noted before, the primary endpoint of investigator-assessed median PFS favored camizestrant in both the 75-mg arm (7.2 months) and the 150-mg arm (7.7 months), with respective adjusted hazard ratios for progression versus fulvestrant of 0.58 (P = .0124) and 0.67 (P = .0161).
Camizestrant at the 75-mg dose was also superior to fulvestrant among patients who had previously received a cyclin-dependent kinase 4/6 inhibitor, with median PFS of 5.5 months and 3.8 months for the 75-mg and 150-mg doses, respectively, compared with 2.1 months.
The adjusted HR for progression with camizestrant with the 75-mg dose was 0.49, with a 90% confidence interval indicating significance. The 150-mg dose was not significantly superior to fulvestrant, however.
Both camizestrant doses were also superior for prolonging PFS versus fulvestrant among patients with lung and/or liver metastases, with median PFS of 7.2 months, 5.6 months, and 2.0 months, respectively.
The experimental SERD also outperformed fulvestrant in an analysis looking at PFS by ESR1 mutational status and ER-driven disease. Among patients with ESR1 wild type, however, median PFS rates with camizestrant 75 mg and fulvestrant were the same (7.2 months).
The 24-week objective response rates were 15.7% in the 75-mg camizestrant arm, 20% in the 150-mg arm, and 11.8% in the fulvestrant arm. The respective clinical benefit rates, including all patients with responses or stable disease, were 47.3%, 49.3%, and 38.4%. The camizestrant clinical benefit rates did not differ significantly from those with fulvestrant, however.
Treatment-related adverse events of grade 3 or greater occurred in only five patients, and only two patients, both in the 75-mg camizestrant arm, discontinued therapy because of adverse events. There were no treatment-related deaths.
Adverse events that occurred only with camizestrant included photopsia (flashing lights or floaters in the field of vision) and sinus bradycardia.
Promising, but early
Carlos Artega, MD, codirector of SABCS and director of the Simmons Comprehensive Cancer Center at UT Southwestern Medical Center, Dallas, who was not involved in the study, said the data look promising in comparison with fulvestrant.
“There is a clear suggestion that this might be better,” he said. “[Camizestrant] seems to be better at reducing the titer in plasma of the ESR1 mutation, and there is very strong basic science that supports that.”
He noted that the study numbers were relatively small, however.
Dr. Arteaga was speaking at a media briefing held immediately prior to the presentation of the data in an oral abstract session.
Fabrice Andre, MD, from Gustave Roussy in Villejuif, France, the invited discussant for the oral session, noted that, in patients with ESR1 wild type, where fulvestrant shows some efficacy, camizestrant appears to be equally effective, and that the latter agent may be more synergistic with targeted therapies than fulvestrant.
Given high patient dropout rates with currently available SERDs, there is a need for SERDs used in the adjuvant setting that are effective at minimally bioactive doses for patients who are predicted to poorly adherent, Dr. Andre said.
The study was funded by AstraZeneca. Dr. Oliveira has received personal funding from AstraZeneca, Guardant Health, Roche, Merck Sharp & Dohme, Pfizer, Seagen, iTeos Therapeutics, Eisai, Novartis, Relay Therapeutics, and Gilead. Dr. Arteaga is a scientific adviser to AstraZeneca and others, and has received grant support from Pfizer Lilly and Takeda. Dr. Andre disclosed fees to his hospital on his behalf from AstraZeneca, Daiichi Sankyo, Sanofi, Pfizer, Lilly, and Roche.
SAN ANTONIO – compared with the first-generation SERD fulvestrant Faslodex, in the SERENA-2 trial, shows a study recently presented at the San Antonio Breast Cancer Symposium.
Among 180 postmenopausal women with ER+/HER2– breast cancers that had recurred or progressed following at least one line of endocrine therapy, the median progression-free survival (PFS) after a median follow-up of 16.6-17.4 months was 7.2 months for patients treated at a 75-mg dose of camizestrant and 7.7 months for those treated at a 150-mg dose, compared with 3.7 months for patients who received fulvestrant, reported Mafalda Oliveira, MD, PhD, from Vall d’Hebron University Hospital in Barcelona.
Oral agent
Camizestrant is a next-generation oral SERD and pure estrogen receptor antagonist that was shown in the SERENA-1 trial to be safe and to have clinical activity against ER+ breast cancers.
SERENA-2 pitted camizestrant at doses of 75 mg, 150 mg, or 300 mg against standard-dose fulvestrant, although the 300-mg dose was dropped in a protocol amendment after 20 patients had been assigned to that arm. (Currently planned studies with camizestrant will be conducted with the 75-mg dose.)
The investigators enrolled women with ER+/HER2– advanced breast cancer who had not previously received fulvestrant or an oral SERD. Eligible patients were limited to no more than one prior line of endocrine and one prior line of chemotherapy for advanced breast cancers. The study included patients with both measurable and unmeasurable disease.
The median patient age was about 60 years. Approximately 59% of patients in each arm had either lung or liver metastases. Patients with recurrence in bone only comprised 14.9%-19.4%.
Mutations in ESR1, a gene associated with hormonal resistance, were detectable in 29.7%-47.9% of patients.
Better PFS
As noted before, the primary endpoint of investigator-assessed median PFS favored camizestrant in both the 75-mg arm (7.2 months) and the 150-mg arm (7.7 months), with respective adjusted hazard ratios for progression versus fulvestrant of 0.58 (P = .0124) and 0.67 (P = .0161).
Camizestrant at the 75-mg dose was also superior to fulvestrant among patients who had previously received a cyclin-dependent kinase 4/6 inhibitor, with median PFS of 5.5 months and 3.8 months for the 75-mg and 150-mg doses, respectively, compared with 2.1 months.
The adjusted HR for progression with camizestrant with the 75-mg dose was 0.49, with a 90% confidence interval indicating significance. The 150-mg dose was not significantly superior to fulvestrant, however.
Both camizestrant doses were also superior for prolonging PFS versus fulvestrant among patients with lung and/or liver metastases, with median PFS of 7.2 months, 5.6 months, and 2.0 months, respectively.
The experimental SERD also outperformed fulvestrant in an analysis looking at PFS by ESR1 mutational status and ER-driven disease. Among patients with ESR1 wild type, however, median PFS rates with camizestrant 75 mg and fulvestrant were the same (7.2 months).
The 24-week objective response rates were 15.7% in the 75-mg camizestrant arm, 20% in the 150-mg arm, and 11.8% in the fulvestrant arm. The respective clinical benefit rates, including all patients with responses or stable disease, were 47.3%, 49.3%, and 38.4%. The camizestrant clinical benefit rates did not differ significantly from those with fulvestrant, however.
Treatment-related adverse events of grade 3 or greater occurred in only five patients, and only two patients, both in the 75-mg camizestrant arm, discontinued therapy because of adverse events. There were no treatment-related deaths.
Adverse events that occurred only with camizestrant included photopsia (flashing lights or floaters in the field of vision) and sinus bradycardia.
Promising, but early
Carlos Artega, MD, codirector of SABCS and director of the Simmons Comprehensive Cancer Center at UT Southwestern Medical Center, Dallas, who was not involved in the study, said the data look promising in comparison with fulvestrant.
“There is a clear suggestion that this might be better,” he said. “[Camizestrant] seems to be better at reducing the titer in plasma of the ESR1 mutation, and there is very strong basic science that supports that.”
He noted that the study numbers were relatively small, however.
Dr. Arteaga was speaking at a media briefing held immediately prior to the presentation of the data in an oral abstract session.
Fabrice Andre, MD, from Gustave Roussy in Villejuif, France, the invited discussant for the oral session, noted that, in patients with ESR1 wild type, where fulvestrant shows some efficacy, camizestrant appears to be equally effective, and that the latter agent may be more synergistic with targeted therapies than fulvestrant.
Given high patient dropout rates with currently available SERDs, there is a need for SERDs used in the adjuvant setting that are effective at minimally bioactive doses for patients who are predicted to poorly adherent, Dr. Andre said.
The study was funded by AstraZeneca. Dr. Oliveira has received personal funding from AstraZeneca, Guardant Health, Roche, Merck Sharp & Dohme, Pfizer, Seagen, iTeos Therapeutics, Eisai, Novartis, Relay Therapeutics, and Gilead. Dr. Arteaga is a scientific adviser to AstraZeneca and others, and has received grant support from Pfizer Lilly and Takeda. Dr. Andre disclosed fees to his hospital on his behalf from AstraZeneca, Daiichi Sankyo, Sanofi, Pfizer, Lilly, and Roche.
AT SABCS 2022