User login
Post-birth hospitalizations dropped with Medicaid expansion
Women living in states that expanded Medicaid over the past decade were nearly 20% less likely to be hospitalized within 2 months of giving birth, according to a first-of-its-kind study published in Health Affairs.
Researchers analyzed patient records from eight states – four that expanded Medicaid insurance to include a broader swath of residents following the implementation of the Affordable Care Act, and four states that did not.
Hospitalizations in the 60 days after a woman gave birth fell by 17% in states that expanded Medicaid. The analysis also revealed an 8% drop in hospitalizations between 61 days and 6 months post partum.
“This is a very meaningful decline in hospitalization rates,” said Laura Wherry, PhD, a professor of economics and public service at New York University and a co-author of the study.
Women in states that chose not to expand Medicaid experienced a 7% increase in postpartum hospitalizations during that same time frame, the researchers report.
Many states raised income eligibility thresholds to 138% of the federal poverty level in 2014 with the implementation of the Affordable Care Act, which resulted in more coverage for low-income expectant mothers. To date, a dozen states have not implemented Medicaid expansion.
Dr. Wherry and her colleague wanted to take a closer look at outcomes for pregnant women during the postpartum period, both before and after states chose to expand Medicaid.
“A lot of prior work looking at the Medicaid program examined huge expansions to cover pregnant women during pregnancy, but often other periods of a woman’s life have been overlooked,” Dr. Wherry said. “What we were interested in is how that changed with the Affordable Care Act. You no longer needed to be pregnant to qualify.”
The researchers analyzed hospital discharge data between 2010 and 2017 before and after expansion in Iowa, Maryland, New Mexico, and Washington, which expanded coverage under Medicaid, and Florida, Georgia, Mississippi, and Utah, which did not do so.
Prior to 2014, fewer than 2% of births resulted in a postpartum hospitalization during the 60-day period in Medicaid expansion states. But in states that expanded Medicaid, hospitalizations decreased by 0.289 percentage points (P = .052), or 17% during the 60-day post-birth period.
Approximately 75% of the decline was attributed to diagnoses related to complications in pregnancy, childbirth, and the postpartum period.
Dr. Wherry said a variety of factors possibly drove down hospitalizations for new mothers who were able to obtain Medicaid coverage, including access to robust prenatal care, preconception counseling, and improved management of postpartum conditions outside the hospital.
The study provides a strategy for tackling the rising rate of maternal mortality in the United States, an increase largely attributed to postpartum deaths, said Lindsay Admon, MD, an ob.gyn. at the University of Michigan Medical School in Ann Arbor.
“This is one of the first studies showing or suggesting that Medicaid expansion not only led to improvements in Medicaid insurance but health outcomes as well,” said Dr. Admon, who is also researching maternal health and expanded Medicaid coverage.
Federal law has long required states to provide coverage for pregnant women up to 60 days post partum.
The 2021 American Rescue Act allowed states to extend coverage for pregnant women beyond the federal requirement to a year. More than half of states have chosen to do so. Since the study indicates that Medicaid expansion improves outcomes for these enrollees, Dr. Wherry and Dr. Admon said they hope state officials will consider the new findings during discussions to utilize the Rescue Act Coverage for pregnant women.
Dr. Wherry received support for the study from the Robert Wood Johnson Foundation Policies for Action Program and grant funding from the National Institute on Aging and the National Institute of Child Health and Human Development. Another author received grants from the Agency for Healthcare Research and Quality and the National Institute of Child Health and Human Development.
A version of this article first appeared on Medscape.com.
Women living in states that expanded Medicaid over the past decade were nearly 20% less likely to be hospitalized within 2 months of giving birth, according to a first-of-its-kind study published in Health Affairs.
Researchers analyzed patient records from eight states – four that expanded Medicaid insurance to include a broader swath of residents following the implementation of the Affordable Care Act, and four states that did not.
Hospitalizations in the 60 days after a woman gave birth fell by 17% in states that expanded Medicaid. The analysis also revealed an 8% drop in hospitalizations between 61 days and 6 months post partum.
“This is a very meaningful decline in hospitalization rates,” said Laura Wherry, PhD, a professor of economics and public service at New York University and a co-author of the study.
Women in states that chose not to expand Medicaid experienced a 7% increase in postpartum hospitalizations during that same time frame, the researchers report.
Many states raised income eligibility thresholds to 138% of the federal poverty level in 2014 with the implementation of the Affordable Care Act, which resulted in more coverage for low-income expectant mothers. To date, a dozen states have not implemented Medicaid expansion.
Dr. Wherry and her colleague wanted to take a closer look at outcomes for pregnant women during the postpartum period, both before and after states chose to expand Medicaid.
“A lot of prior work looking at the Medicaid program examined huge expansions to cover pregnant women during pregnancy, but often other periods of a woman’s life have been overlooked,” Dr. Wherry said. “What we were interested in is how that changed with the Affordable Care Act. You no longer needed to be pregnant to qualify.”
The researchers analyzed hospital discharge data between 2010 and 2017 before and after expansion in Iowa, Maryland, New Mexico, and Washington, which expanded coverage under Medicaid, and Florida, Georgia, Mississippi, and Utah, which did not do so.
Prior to 2014, fewer than 2% of births resulted in a postpartum hospitalization during the 60-day period in Medicaid expansion states. But in states that expanded Medicaid, hospitalizations decreased by 0.289 percentage points (P = .052), or 17% during the 60-day post-birth period.
Approximately 75% of the decline was attributed to diagnoses related to complications in pregnancy, childbirth, and the postpartum period.
Dr. Wherry said a variety of factors possibly drove down hospitalizations for new mothers who were able to obtain Medicaid coverage, including access to robust prenatal care, preconception counseling, and improved management of postpartum conditions outside the hospital.
The study provides a strategy for tackling the rising rate of maternal mortality in the United States, an increase largely attributed to postpartum deaths, said Lindsay Admon, MD, an ob.gyn. at the University of Michigan Medical School in Ann Arbor.
“This is one of the first studies showing or suggesting that Medicaid expansion not only led to improvements in Medicaid insurance but health outcomes as well,” said Dr. Admon, who is also researching maternal health and expanded Medicaid coverage.
Federal law has long required states to provide coverage for pregnant women up to 60 days post partum.
The 2021 American Rescue Act allowed states to extend coverage for pregnant women beyond the federal requirement to a year. More than half of states have chosen to do so. Since the study indicates that Medicaid expansion improves outcomes for these enrollees, Dr. Wherry and Dr. Admon said they hope state officials will consider the new findings during discussions to utilize the Rescue Act Coverage for pregnant women.
Dr. Wherry received support for the study from the Robert Wood Johnson Foundation Policies for Action Program and grant funding from the National Institute on Aging and the National Institute of Child Health and Human Development. Another author received grants from the Agency for Healthcare Research and Quality and the National Institute of Child Health and Human Development.
A version of this article first appeared on Medscape.com.
Women living in states that expanded Medicaid over the past decade were nearly 20% less likely to be hospitalized within 2 months of giving birth, according to a first-of-its-kind study published in Health Affairs.
Researchers analyzed patient records from eight states – four that expanded Medicaid insurance to include a broader swath of residents following the implementation of the Affordable Care Act, and four states that did not.
Hospitalizations in the 60 days after a woman gave birth fell by 17% in states that expanded Medicaid. The analysis also revealed an 8% drop in hospitalizations between 61 days and 6 months post partum.
“This is a very meaningful decline in hospitalization rates,” said Laura Wherry, PhD, a professor of economics and public service at New York University and a co-author of the study.
Women in states that chose not to expand Medicaid experienced a 7% increase in postpartum hospitalizations during that same time frame, the researchers report.
Many states raised income eligibility thresholds to 138% of the federal poverty level in 2014 with the implementation of the Affordable Care Act, which resulted in more coverage for low-income expectant mothers. To date, a dozen states have not implemented Medicaid expansion.
Dr. Wherry and her colleague wanted to take a closer look at outcomes for pregnant women during the postpartum period, both before and after states chose to expand Medicaid.
“A lot of prior work looking at the Medicaid program examined huge expansions to cover pregnant women during pregnancy, but often other periods of a woman’s life have been overlooked,” Dr. Wherry said. “What we were interested in is how that changed with the Affordable Care Act. You no longer needed to be pregnant to qualify.”
The researchers analyzed hospital discharge data between 2010 and 2017 before and after expansion in Iowa, Maryland, New Mexico, and Washington, which expanded coverage under Medicaid, and Florida, Georgia, Mississippi, and Utah, which did not do so.
Prior to 2014, fewer than 2% of births resulted in a postpartum hospitalization during the 60-day period in Medicaid expansion states. But in states that expanded Medicaid, hospitalizations decreased by 0.289 percentage points (P = .052), or 17% during the 60-day post-birth period.
Approximately 75% of the decline was attributed to diagnoses related to complications in pregnancy, childbirth, and the postpartum period.
Dr. Wherry said a variety of factors possibly drove down hospitalizations for new mothers who were able to obtain Medicaid coverage, including access to robust prenatal care, preconception counseling, and improved management of postpartum conditions outside the hospital.
The study provides a strategy for tackling the rising rate of maternal mortality in the United States, an increase largely attributed to postpartum deaths, said Lindsay Admon, MD, an ob.gyn. at the University of Michigan Medical School in Ann Arbor.
“This is one of the first studies showing or suggesting that Medicaid expansion not only led to improvements in Medicaid insurance but health outcomes as well,” said Dr. Admon, who is also researching maternal health and expanded Medicaid coverage.
Federal law has long required states to provide coverage for pregnant women up to 60 days post partum.
The 2021 American Rescue Act allowed states to extend coverage for pregnant women beyond the federal requirement to a year. More than half of states have chosen to do so. Since the study indicates that Medicaid expansion improves outcomes for these enrollees, Dr. Wherry and Dr. Admon said they hope state officials will consider the new findings during discussions to utilize the Rescue Act Coverage for pregnant women.
Dr. Wherry received support for the study from the Robert Wood Johnson Foundation Policies for Action Program and grant funding from the National Institute on Aging and the National Institute of Child Health and Human Development. Another author received grants from the Agency for Healthcare Research and Quality and the National Institute of Child Health and Human Development.
A version of this article first appeared on Medscape.com.
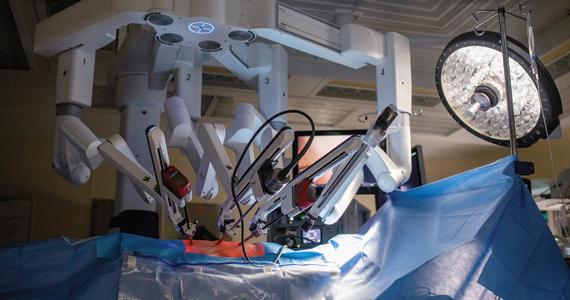
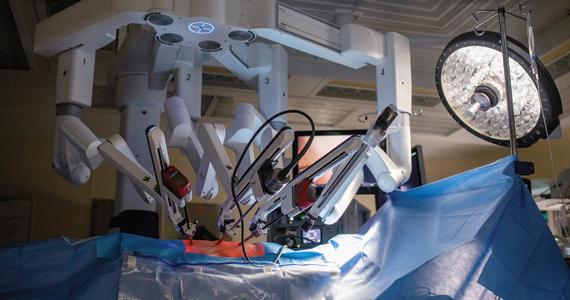
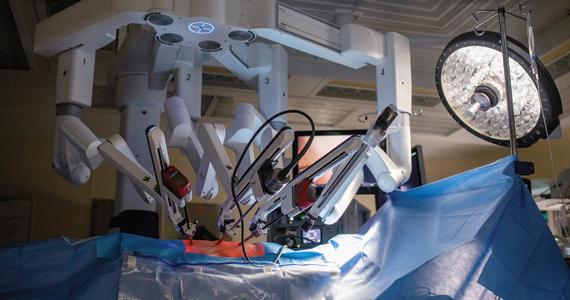
Liability in robotic gyn surgery
The approach to hysterectomy has been debated, with the need for individualization case by case stressed, and the expertise of the operating surgeon considered.
CASE Was surgeon experience a factor in case complications?
VM is a 46-year-old woman (G5 P4014) reporting persistent uterine bleeding that is refractory to medical therapy. The patient has uterine fibroids, 6 weeks in size on examination, with “mild” prolapse noted. Additional medical diagnoses included vulvitis, ovarian cyst in the past, cystic mastopathy, and prior evidence of pelvic adhesion, noted at the time of ovarian cystectomy. Prior surgical records were not obtained by the operating surgeon, although her obstetric history includes 2 prior vaginal deliveries and 2 cesarean deliveries (CDs). The patient had an umbilical herniorraphy a number of years ago. Her medications include hormonal therapy, for presumed menopause, and medication for depression (she reported “doing well” on medication). She reported smoking 1 PPD and had a prior tubal ligation.
VM was previously evaluated for Lynch Syndrome and informed of the potential for increased risks of colon, endometrial, and several other cancers. She did not have cancer as of the time of planned surgery.
The patient underwent robotic-assisted total laparoscopic hysterectomy and bilateral salpingo-oophorectomy. The operating surgeon did not have a lot of experience with robotic hysterectomies but told the patient preoperatively “I have done a few.” Perioperatively, blood loss was minimal, urine output was recorded as 25 mL, and according to the operative report there were extensive pelvic adhesions and no complications. The “ureters were identified” when the broad ligament was opened at the time of skeletonization of the uterine vessels and documented accordingly. The intraoperative Foley was discontinued at the end of the procedure. The pathology report noted diffuse adenomyosis and uterine fibroids; the uterus weighed 250 g. In addition, a “large hemorrhagic corpus luteum cyst” was noted on the right ovary.
The patient presented for a postoperative visit reporting “leaking” serosanguinous fluid that began 2.5 weeks postoperatively and required her to wear 3 to 4 “Depends” every day. She also reported constipation since beginning her prescribed pain medication. She requested a copy of her medical records and said she was dissatisfied with the care she had received related to the hysterectomy; she was “seeking a second opinion from a urologist.” The urologist suggested evaluation of the “leaking,” and a Foley catheter was placed. When she stood up, however, there was leaking around the catheter, and she reported a “yellowish-green,” foul smelling discharge. She called the urologist’s office, stating, “I think I have a bowel obstruction.” The patient was instructed to proceed to the emergency department at her local hospital. She was released with a diagnosis of constipation. Upon follow-up urologic evaluation, a vulvovaginal fistula was noted. Management was a “simple fistula repair,” and the patient did well subsequently.
The patient brought suit against the hospital and operating gynecologist. In part the hospital records noted, “relatively inexperienced robotic surgeon.” The hospital was taken to task for granting privileges to an individual that had prior privilege “problems.”
Continue to: Medical opinion...
Medical opinion
This case demonstrates a number of issues. (We will discuss the credentials for the surgeon and hospital privileges in the legal considerations section.) From the medical perspective, the rate of urologic injury associated with all hysterectomies is 0.87%.1 Robotic hysterectomy has been reported at 0.92% in a series published from Henry Ford Hospital.1 The lowest rate of urologic injury is associated with vaginal hysterectomy, reported at 0.2%.2 Reported rates of urologic injury by approach to hysterectomy are1:
- robotic, 0.92%
- laparoscopic, 0.90%
- vaginal, 0.33%
- abdominal, 0.96%.
Complications by surgeon type also have been addressed, and the percent of total urologic complications are reported as1:
- ObGyn, 47%
- gyn oncologist, 47%
- urogynecologist, 6%.
Intraoperative conversion to laparotomy from initial robotic approach has been addressed in a retrospective study over a 2-year period, with operative times ranging from 1 hr, 50 min to 9 hrs of surgical time.1 The vast majority of intraoperative complications in a series reported from Finland were managed “within minutes,” and in the series of 83 patients, 5 (6%) required conversion to laparotomy.2 Intraoperative complications reported include failed entry, vascular injury, nerve injury, visceral injury, solid organ injury, tumor fragmentation, and anesthetic-related complications.3 Of note, the vascular injuries included inferior vena cava, common iliac, and external iliac.
Mortality rates in association with benign laparoscopic and robotic procedures have been addressed and noted to be 1:6,456 cases based upon a meta-analysis.4 The analysis included 124,216 patients. Laparoscopic versus robotic mortality rates were not statistically different. Mortality was more common among cases of undiagnosed rare colorectal injury. This mortality is on par with complications from Roux-en-Y gastric bypass procedures. Procedures such as sacrocolpopexy are equated with higher mortality (1:1,246) in comparison with benign hysterectomy.5
Infectious complications following either laparoscopic or robotic hysterectomy were reported at less than 1% and not statistically different for either approach.6 The series authored by Marra et al evaluated 176,016 patients.
Overall, robotic-assisted gynecologic complications are rare. One series was focused on gynecological oncologic cases.7 Specific categories of complications included7:
- patient positioning and pneumoperitoneum
- injury to surrounding organs
- bowel injury
- port site metastasis
- surgical emphysema
- vaginal cuff dehiscence
- anesthesia-related problems.
The authors concluded, “robotic assisted surgery in gynecological oncology is safe and the incidence of complications is low.”7 The major cause of death related to robotic surgery is vascular injury–related. The authors emphasized the importance of knowledge of anatomy, basic principles of “traction and counter-traction” and proper dissection along tissue planes as key to minimizing complications. Consider placement of stents for ureter identification, as appropriate. Barbed-suturing does not prevent dehiscence.
Continue to: Legal considerations...
Legal considerations
Robotic surgery presents many legal issues and promises to raise many more in the future. The law must control new technology while encouraging productive uses, and provide new remedies for harms while respecting traditional legal principles.8 There is no shortage of good ideas about controlling surgical robots,9 automated devices more generally,10 and artificial intelligence.11 Those issues will be important, and watching them unfold will be intriguing.
In the meantime, physicians and other health care professionals, health care facilities, technology companies, and patients must work within current legal structures in implementing and using robotic surgery. These are extraordinarily complex issues, so it is possible only to review the current landscape and speculate what the near future may hold.
Regulating surgical robots
The US Food and Drug Administration (FDA) is the primary regulator of robots used in medicine.12 It has the authority to regulate surgical devices, including surgical robots—which it refers to as “robotically-assisted surgical devices,” or RASD. In 2000, it approved Intuitive Surgical’s daVinci system for use in surgery. In 2017, the FDA expanded its clearance to include the Senhance System of TransEnterix Surgical Inc. for minimally invasive gynecologic surgery.13 In 2021, the FDA cleared the Hominis Surgical System for transvaginal hysterectomy “in certain patients.” However, the FDA emphasized that this clearance is for benign hysterectomy with salpingo-oophorectomy.14 (The FDA has cleared various robotic devices for several other areas of surgical practice, including neurosurgery, orthopedics, and urology.)
The use of robots in cancer surgery is limited. The FDA approved specific RASDs in some “surgical procedures commonly performed in patients with cancer, such as hysterectomy, prostatectomy, and colectomy.”15 However, it cautioned that this clearance was based only on a 30-day patient follow up. More specifically, the FDA “has not evaluated the safety or effectiveness of RASD devices for the prevention or treatment of cancer, based on cancer-related outcomes such as overall survival, recurrence, and disease-free survival.”15
The FDA has clearly warned physicians and patients that the agency has not granted the use of RASDs “for any cancer-related surgery marketing authorization, and therefore the survival benefits to patients compared to traditional surgery have not been established.”15 (This did not apply to the hysterectomy surgery as noted above. More specifically, that clearance did not apply to anything other than 30-day results, nor to the efficacy related to cancer survival.)
States also have some authority to regulate medical practice within their borders.9 When the FDA has approved a device as safe and effective, however, there are limits on what states can do to regulate or impose liability on the approved product. The Supreme Court held that the FDA approval “pre-empted” some state action regarding approved devices.16
Hospitals, of course, regulate what is allowed within the hospital. For example, it may require training before a physician is permitted to use equipment, limit the conditions for which the equipment may be used, or decline to obtain equipment for use in the hospitals.17 In the case of RASDs, however, the high cost of equipment may provide an incentive for hospitals to urge the wide use of the latest robotic acquisition.18
Regulation aims primarily to protect patients, usually from injury or inadequate treatment. Some robotic surgery is likely to be more expensive than the same surgery without robotic assistance. The cost to the patient is not usually part of the FDA’s consideration. Insurance companies (including Medicare and Medicaid), however, do care about costs and will set or negotiate how much the reimbursement will be for a procedure. Third-party payers may decline to cover the additional cost when there is no apparent benefit from using the robot.19 For some institutions, the public perception that it offers “the most modern technology” is an important public message and a strong incentive to have the equipment.20
There are inconsistent studies about the advantages and disadvantages of RADS in gynecologic procedures, although there are few randomized studies.21 The demonstrated advantages are generally identified as somewhat shorter recovery time.22 The ultimate goal will be to minimize risks while maximizing the many potential benefits of robotic surgery.23
Continue to: Liability...
Liability
A recent study by De Ravin and colleagues of robotic surgery liability found a 250% increase in the total number of robotic surgery–related malpractice claims reported in 7 recent years (2014-2021), compared with the prior 7 (2006-2013).24 However, the number of cases varied considerably from year to year. ObGyn had the most significant gain (from 19% to 49% of all claims). During the same time, urology claims declined from 56% to 16%. (The limitations of the study’s data are discussed later in this article.)
De Ravin et al reported the legal bases for the claims, but the specific legal claim was unclear in many cases.24 For example, the vast majority were classified as “negligent surgery.” Many cases made more than 1 legal claim for liability, so the total percentages were greater than 100%. Of the specific claims, many appear unrelated to robotic surgery (misdiagnosis, delayed treatment, or infection). However, there were a significant number of cases that raised issues that were related to robotic surgery. The following are those claims that probably relate to the “robotic” surgery, along with the percentage of cases making such a claim as reported24:
- “Patient not a candidate for surgery performed” appeared in about 13% of the cases.24 Such claims could include that the surgeon should have performed the surgery with traditional laparoscopy or open technique, but instead using a robot led to the injury. Physicians may feel pressure from patients or hospitals, because of the equipment’s cost, to use robotic surgery as it seems to be the modern approach (and therefore better). Neither reason is sufficient for using robotic assistance unless it will benefit the patient.
- “Failure to calibrate or operate robot” was in 11% of the claims.24 Physicians must properly calibrate and otherwise ensure that surgical equipment is operating correctly. In addition, the hospitals supplying the equipment must ensure that the equipment is maintained correctly. Finally, the equipment manufacturer may be liable through “products liability” if the equipment is defective.25 The expanding use of artificial intelligence in medical equipment (including surgical robots) is increasing the complexity of determining what “defective” means.11
- “Training deficiencies or credentialing” liability is a common problem with new technology. Physicians using new technology should be thoroughly trained and, where appropriate, certified in the use of the new technology.26 Early adopters of the technology should be especially cautious because good training may be challenging to obtain. In the study, the claims of inadequate training were particularly high during the early 7 years (35%), but dropped during the later time (4%).24
- “Improper positioning” of the patient or device or patient was raised in 7% of the cases.24
- “Manufacturing problems” were claimed in a small number of cases—13% in 2006-2013, but 2% in 2014-2021.24 These cases raise the complex question of products liability for robotic surgery and artificial intelligence (AI). Products liability has been part of surgical practice for many years. There usually will be liability if there are “defects” in a product, whether or not resulting from negligence. What a “defect” in a computer program means is a complicated issue that will be significant in future liability cases.27
Several other cases reported in the De Ravin study were probably related to robotic surgery. For example, Informed Consent and Failure to Monitor each appeared in more than 30%, of 2014-2021 cases, and Failure to Refer in 16% of the cases.24,27
The outcomes of the reported cases were mostly verdicts (or trial-related settlements) for defendants (doctors and hospitals). The defense prevailed 69% of the time in the early period and 78% of the time in 2014-2021. However, there were substantial damages in some cases. The range of damages in 2006-2013 was $95,000 to $6 million (mean, $2.5 million); in 2014-2021, it was $10,000 to $5 million (mean, $1.3 million).24
An earlier study looked at reported cases against Intuitive Surgical, maker of the daVinci system, from 2000-2017.28 Of the 108 claims in the study, 62% were gynecologic surgeries. Of these claims, 35% were dismissed, but “no other information regarding settlements or trial outcomes was available.” The study did not report the basis for the lawsuits involving gynecologic surgeries.
We should exercise caution in reviewing these studies. Although the studies were of considerable value, the authors note significant limitations of the databases available. The database was Westlaw in the first study discussed (“Robotic surgery: the impact”24) and Bloomberg in the second (“Robotic urologic”28). For example, the “impact” study was based on “jury verdict reports” excluding settlements, and the latter excluded class actions and cases settled. Thus the studies undoubtedly understated the number of claims made (those that resulted in settlement before a lawsuit was filed), cases filed but abandoned, and settlements made before trial.
Despite these limitations, the studies provide valuable insights into current malpractice risks and future directions. It is worth remembering that these cases nearly all involved a single robot, the daVinci, produced by Intuitive Surgical. It is not a “smart” robot and is commonly referred to as a “master-slave” machine. With much more intelligent and independent machines, the future will raise more complex problems in the FDA approval process and malpractice and product liability claims when things go wrong.
Continue to: What’s the verdict?...
What’s the verdict?
The case of VM and operating surgeon Dr. G illustrates several important legal aspects of using surgical robots. It also demonstrates that the presence of the robot assist still requires the surgeon’s careful attention to issues of informed consent, adequate specific training, and thorough follow up. In the following discussion, we divide the case review into the elements of negligence-malpractice (duty and breach, causation, and damages) and conclude with a thought about how to proceed when things have gone wrong.
Dr. G’s statement, “I’ve done a few,” is indefinite, but it may suggest that Dr. G. had not received full, supervised training in the robotic assist he was planning to use. That problem was underlined by the conclusion that Dr. G was a “relatively inexperienced robotic surgeon.” If so, that failure could constitute a breach of the duty of care to the patient. In addition, if it is inaccurate or did not provide information VM reasonably needed in consenting to Dr. G proceeding with the surgery, there could be an issue of whether there was a partial failure of fully informed consent.
The hospital also may have potential liability. It was “taken to task for granting privileges to an individual that had prior privilege ‘problems,’” suggesting that it had not performed adequate review before granting hospital privileges. Furthermore, if Dr. G was not sufficiently practiced or supervised in robotic surgery, the hospital, which allowed Dr. G to proceed, might also be negligent.
VM had a series of problems postsurgery that ultimately resulted in additional care and “simple fistula repair.” Assuming that there was negligence, the next question is whether that failure caused the injury. Causation may be the most difficult part of the case for VM to prove. It would require expert testimony that the inadequate surgery (inappropriate use of robotic surgery or other error during surgery) and follow up resulted in the formation or increase in the likelihood of the fistula.
VM would also have to prove damages. Damages are those costs (the economic value) of injuries that would not have occurred but for negligence. Damages would include most of the cost of the follow-up medical care and any related additional future care required, plus costs that were a consequence of the negligence (such as lost work). In addition, damages would include pain and suffering that resulted from the negligence, subject to caps in some states.
When the patient was dissatisfied and reported a postsurgical problem, the hospital and Dr. G may have had an opportunity to avoid further dissatisfaction, complaints, and ultimately a lawsuit. Effective approaches for dealing with such dissatisfaction may serve the institution’s and physician’s values and financial best interests.
The jury verdict was in favor of the plaintiff. Jurors felt the operating surgeon should have conveyed his experience with robotic surgery more clearly as part of the informed consent process.
“Hey Siri! Perform a type 3 hysterectomy. Please watch out for the ureter!”29
Medicine is still at the frontier of surgical robots. Over future decades, the number and sophistication of these machines will increase substantially. They likely will become much more like robots, guided by AI, and make independent judgments. These have the potential for significant medical progress that improves the treatment of patients. At the same time, the last 20 years suggest that robotic innovation will challenge medicine, the FDA and other regulators, lawmakers, and courts. In the future, regulators and patients should embrace genuine advances in robotic surgery but not be dazzled by these new machines’ luster (or potential for considerable profits).30
The public may be wildly optimistic about the benefits without balancing the risks. The AI that runs them will be essentially invisible and constantly changing. Physicians and regulators must develop new techniques for assessing and controlling the software. Real surgical robots require rigorous testing, cautious promotion, disciplined use, and perpetual review. ●
- Petersen S, Doe S, Rubinfield I, et al. Rate of urologic injury with robotic hysterectomy. J Min Invasc Gynecol. 2018;25:867-871.
- Makinen J, Johansson J, Toma C, et al. Morbidity of 10,110 hysterectomies by type approach. Hum Reprod. 2001;16:1473-1478.
- Karasu A, Kran G, Sanlikan F. Intraoperative complications and conversion to laparotomy in gynecologic robotic surgery. J Investig Surg. 2022;35:912-915.
- Behbehani S, Suarez-Salvador E, Buras M, et al. Mortality rates in benign laparoscopic and robotic surgery: a systematic review and meta-analysis. J Min Invasc. 2020;27:603-612.
- Giurdano S, Victorzon M. Laparoscopic roux-en-Y gastric bypass in elderly patients (60 years or older): a meta-analysis of comparative studies. Scand J Surg. 2018;107:6-11.
- Marra A, Pulg-Asensio M, Edmond M, et al. Infectious complications of laparoscopic and robotic hysterectomy: a systematic literature review and meta-analysis. Int J Gynecol Cancer. 2019;29:518-530.
- Tse KY, Sheung H, Lim P. Robot-assisted gyneaecological cancer surgery-complications and prevention. Best Pract Res Clin Obstet Gynaecol. 2017;25:94-105.
- Hubbard FP. Sophisticated robots: balancing liability, regulation, and innovation. Fla Law Rev. 2014;66:1803-1872. https://scholarship.law.ufl.edu/cgi/viewcontent. cgi?article=1204&context=flr. Accessed December 20, 2022.
- Villanueva A. The legal battle with the future of autonomous surgical robotics. Ind Health Law Rev. 2020;17:367-392. https://journals.iupui.edu/index.php/ihlr/article /download/25051/23544. Accessed December 20, 2022.
- Lemley MA, Casey B. Remedies for robots. U Chi Law Rev. 2019;86:1311-1396. https://chicagounbound.uchicago.edu /cgi/viewcontent.cgi?article=6140&context=uclrev. Accessed December 20, 2022.
- Griffin F. Artificial intelligence and liability in health care. Health Matrix. 2021;31:65-106. https://scholarlycommons. law.case.edu/cgi/viewcontent.cgi?article=1659&context=hea lthmatrix. Accessed December 20, 2022.
- Britton D. Autonomous surgery: the law of autonomous surgical robots. J Law Tech Tex. 2017;1:152-189.
- US Food and Drug Administration. FDA clears new robotically-assisted surgical device for adult patients. October 13, 2017. https://www.fda.gov/news-events/press-announcements /fda-clears-new-robotically-assisted-surgical-device-adult -patients. Accessed December 20, 2022.
- US Food and Drug Administration. FDA authorizes first robotically-assisted surgical device for performing transvaginal hysterectomy. March 1, 2021. https://www.fda .gov/news-events/press-announcements/fda-authorizes -first-robotically-assisted-surgical-device-performing -transvaginal-hysterectomy. Accessed December 20, 2022.
- US Food and Drug Administration. Caution with robotically-assisted surgical devices in mastectomy: FDA Safety Communication, August 20, 2021. https://www.fda.gov/medical-devices/safety-communications/update-caution-robotically-assisted-surgical-devices-mastectomy-fda-safety-communication. Accessed December 22, 2022. Riegel v Medtronic, 552 US 312 (2008).
- Han ES, Advincula AP. Robotic surgery: advancements and inflection points in the field of gynecology. Obstet Gynecol Clin North Am. 2021;48:759-776.
- Witharm H. Robot-assisted surgery: an analysis of the legal and economic implications. Az J Interdisciplinary Studies. 2022;8:19-29. https://journals.librarypublishing.arizona.edu /azjis/article/id/5093/download/pdf/.
- Cameron S. Is daVinci robotic surgery a revolution or a rip-off? Healthline. August 10, 2016. https://www.healthline .com/health-news/is-da-vinci-robotic-surgery-revolution -or-ripoff-021215. Accessed December 20, 2022.
- Perez RE, Schwaitzberg SD. Robotic surgery: finding value in 2019 and beyond. Ann Laparosc Endosc Surg. 2019;4:1-7.
- Gitas G, Hanker L, Rody A, et al. Robotic surgery in gynecology: is the future already here? Minim Invasiv Therapy Allied Technol. 2022;4:1-0.
- Moon AS, Garofalo J, Koirala P, et al. Robotic surgery in gynecology. Surgical Clinics. 2020;100:445-460.
- Simshaw D, Terry N, Hauser K, et al. Regulating healthcare robots: maximizing opportunities while minimizing risks. Richmond J Law Tech. 2015;22:1-38. https://scholar works.iupui.edu/bitstream/handle/1805/11587/simshaw _2015_regulating.pdf?sequence=1&isAllowed=y. Accessed December 20, 2022.
- De Ravin E, Sell EA, Newman JG, et al. Medical malpractice in robotic surgery: a Westlaw database analysis. J Robotic Surg. 2022. https://doi.org/10.1007/s11701-022-01417-6. https:// link.springer.com/article/10.1007/s11701-022-014176#citeas. Accessed December 20, 2022.
- Beglinger C. A broken theory: the malfunction theory of strict products liability and the need for a new doctrine in the field of surgical robotics. Minnesotta Law Rev. 2019;104:1041-1093. . Accessed December 20, 2022.
- Azadi S, Green IC, Arnold A, et al. Robotic surgery: the impact of simulation and other innovative platforms on performance and training. J Minim Invasiv Gynecol. 2021;28:490-495.
- Koerner D. Doctor roboto: The no-man operation. U Tol L Rev. 2019;51:125-146.
- Nik-Ahd F, Souders CP, Zhao H, et al. Robotic urologic surgery: trends in litigation over the last decade. J Robotic Surg. 2019;13:729-734.
- Gültekin CalibriİB, Karabük E, Köse MF. “Hey Siri! Perform a type 3 hysterectomy. Please watch out for the ureter!” What is autonomous surgery and what are the latest developments? J Turk Ger Gynecol Assoc. 2021;22:58-70. https://www.ncbi .nlm.nih.gov/pmc/articles/PMC7944239/.
- Matsuzaki T. Ethical issues of artificial intelligence in medicine. California West Law Rev. 2018;55:255-273. https://scholarlycommons.law.cwsl.edu/cgi/viewcontent. cgi?article=1669&context=cwlr. Accessed December 20, 2022.
The approach to hysterectomy has been debated, with the need for individualization case by case stressed, and the expertise of the operating surgeon considered.
CASE Was surgeon experience a factor in case complications?
VM is a 46-year-old woman (G5 P4014) reporting persistent uterine bleeding that is refractory to medical therapy. The patient has uterine fibroids, 6 weeks in size on examination, with “mild” prolapse noted. Additional medical diagnoses included vulvitis, ovarian cyst in the past, cystic mastopathy, and prior evidence of pelvic adhesion, noted at the time of ovarian cystectomy. Prior surgical records were not obtained by the operating surgeon, although her obstetric history includes 2 prior vaginal deliveries and 2 cesarean deliveries (CDs). The patient had an umbilical herniorraphy a number of years ago. Her medications include hormonal therapy, for presumed menopause, and medication for depression (she reported “doing well” on medication). She reported smoking 1 PPD and had a prior tubal ligation.
VM was previously evaluated for Lynch Syndrome and informed of the potential for increased risks of colon, endometrial, and several other cancers. She did not have cancer as of the time of planned surgery.
The patient underwent robotic-assisted total laparoscopic hysterectomy and bilateral salpingo-oophorectomy. The operating surgeon did not have a lot of experience with robotic hysterectomies but told the patient preoperatively “I have done a few.” Perioperatively, blood loss was minimal, urine output was recorded as 25 mL, and according to the operative report there were extensive pelvic adhesions and no complications. The “ureters were identified” when the broad ligament was opened at the time of skeletonization of the uterine vessels and documented accordingly. The intraoperative Foley was discontinued at the end of the procedure. The pathology report noted diffuse adenomyosis and uterine fibroids; the uterus weighed 250 g. In addition, a “large hemorrhagic corpus luteum cyst” was noted on the right ovary.
The patient presented for a postoperative visit reporting “leaking” serosanguinous fluid that began 2.5 weeks postoperatively and required her to wear 3 to 4 “Depends” every day. She also reported constipation since beginning her prescribed pain medication. She requested a copy of her medical records and said she was dissatisfied with the care she had received related to the hysterectomy; she was “seeking a second opinion from a urologist.” The urologist suggested evaluation of the “leaking,” and a Foley catheter was placed. When she stood up, however, there was leaking around the catheter, and she reported a “yellowish-green,” foul smelling discharge. She called the urologist’s office, stating, “I think I have a bowel obstruction.” The patient was instructed to proceed to the emergency department at her local hospital. She was released with a diagnosis of constipation. Upon follow-up urologic evaluation, a vulvovaginal fistula was noted. Management was a “simple fistula repair,” and the patient did well subsequently.
The patient brought suit against the hospital and operating gynecologist. In part the hospital records noted, “relatively inexperienced robotic surgeon.” The hospital was taken to task for granting privileges to an individual that had prior privilege “problems.”
Continue to: Medical opinion...
Medical opinion
This case demonstrates a number of issues. (We will discuss the credentials for the surgeon and hospital privileges in the legal considerations section.) From the medical perspective, the rate of urologic injury associated with all hysterectomies is 0.87%.1 Robotic hysterectomy has been reported at 0.92% in a series published from Henry Ford Hospital.1 The lowest rate of urologic injury is associated with vaginal hysterectomy, reported at 0.2%.2 Reported rates of urologic injury by approach to hysterectomy are1:
- robotic, 0.92%
- laparoscopic, 0.90%
- vaginal, 0.33%
- abdominal, 0.96%.
Complications by surgeon type also have been addressed, and the percent of total urologic complications are reported as1:
- ObGyn, 47%
- gyn oncologist, 47%
- urogynecologist, 6%.
Intraoperative conversion to laparotomy from initial robotic approach has been addressed in a retrospective study over a 2-year period, with operative times ranging from 1 hr, 50 min to 9 hrs of surgical time.1 The vast majority of intraoperative complications in a series reported from Finland were managed “within minutes,” and in the series of 83 patients, 5 (6%) required conversion to laparotomy.2 Intraoperative complications reported include failed entry, vascular injury, nerve injury, visceral injury, solid organ injury, tumor fragmentation, and anesthetic-related complications.3 Of note, the vascular injuries included inferior vena cava, common iliac, and external iliac.
Mortality rates in association with benign laparoscopic and robotic procedures have been addressed and noted to be 1:6,456 cases based upon a meta-analysis.4 The analysis included 124,216 patients. Laparoscopic versus robotic mortality rates were not statistically different. Mortality was more common among cases of undiagnosed rare colorectal injury. This mortality is on par with complications from Roux-en-Y gastric bypass procedures. Procedures such as sacrocolpopexy are equated with higher mortality (1:1,246) in comparison with benign hysterectomy.5
Infectious complications following either laparoscopic or robotic hysterectomy were reported at less than 1% and not statistically different for either approach.6 The series authored by Marra et al evaluated 176,016 patients.
Overall, robotic-assisted gynecologic complications are rare. One series was focused on gynecological oncologic cases.7 Specific categories of complications included7:
- patient positioning and pneumoperitoneum
- injury to surrounding organs
- bowel injury
- port site metastasis
- surgical emphysema
- vaginal cuff dehiscence
- anesthesia-related problems.
The authors concluded, “robotic assisted surgery in gynecological oncology is safe and the incidence of complications is low.”7 The major cause of death related to robotic surgery is vascular injury–related. The authors emphasized the importance of knowledge of anatomy, basic principles of “traction and counter-traction” and proper dissection along tissue planes as key to minimizing complications. Consider placement of stents for ureter identification, as appropriate. Barbed-suturing does not prevent dehiscence.
Continue to: Legal considerations...
Legal considerations
Robotic surgery presents many legal issues and promises to raise many more in the future. The law must control new technology while encouraging productive uses, and provide new remedies for harms while respecting traditional legal principles.8 There is no shortage of good ideas about controlling surgical robots,9 automated devices more generally,10 and artificial intelligence.11 Those issues will be important, and watching them unfold will be intriguing.
In the meantime, physicians and other health care professionals, health care facilities, technology companies, and patients must work within current legal structures in implementing and using robotic surgery. These are extraordinarily complex issues, so it is possible only to review the current landscape and speculate what the near future may hold.
Regulating surgical robots
The US Food and Drug Administration (FDA) is the primary regulator of robots used in medicine.12 It has the authority to regulate surgical devices, including surgical robots—which it refers to as “robotically-assisted surgical devices,” or RASD. In 2000, it approved Intuitive Surgical’s daVinci system for use in surgery. In 2017, the FDA expanded its clearance to include the Senhance System of TransEnterix Surgical Inc. for minimally invasive gynecologic surgery.13 In 2021, the FDA cleared the Hominis Surgical System for transvaginal hysterectomy “in certain patients.” However, the FDA emphasized that this clearance is for benign hysterectomy with salpingo-oophorectomy.14 (The FDA has cleared various robotic devices for several other areas of surgical practice, including neurosurgery, orthopedics, and urology.)
The use of robots in cancer surgery is limited. The FDA approved specific RASDs in some “surgical procedures commonly performed in patients with cancer, such as hysterectomy, prostatectomy, and colectomy.”15 However, it cautioned that this clearance was based only on a 30-day patient follow up. More specifically, the FDA “has not evaluated the safety or effectiveness of RASD devices for the prevention or treatment of cancer, based on cancer-related outcomes such as overall survival, recurrence, and disease-free survival.”15
The FDA has clearly warned physicians and patients that the agency has not granted the use of RASDs “for any cancer-related surgery marketing authorization, and therefore the survival benefits to patients compared to traditional surgery have not been established.”15 (This did not apply to the hysterectomy surgery as noted above. More specifically, that clearance did not apply to anything other than 30-day results, nor to the efficacy related to cancer survival.)
States also have some authority to regulate medical practice within their borders.9 When the FDA has approved a device as safe and effective, however, there are limits on what states can do to regulate or impose liability on the approved product. The Supreme Court held that the FDA approval “pre-empted” some state action regarding approved devices.16
Hospitals, of course, regulate what is allowed within the hospital. For example, it may require training before a physician is permitted to use equipment, limit the conditions for which the equipment may be used, or decline to obtain equipment for use in the hospitals.17 In the case of RASDs, however, the high cost of equipment may provide an incentive for hospitals to urge the wide use of the latest robotic acquisition.18
Regulation aims primarily to protect patients, usually from injury or inadequate treatment. Some robotic surgery is likely to be more expensive than the same surgery without robotic assistance. The cost to the patient is not usually part of the FDA’s consideration. Insurance companies (including Medicare and Medicaid), however, do care about costs and will set or negotiate how much the reimbursement will be for a procedure. Third-party payers may decline to cover the additional cost when there is no apparent benefit from using the robot.19 For some institutions, the public perception that it offers “the most modern technology” is an important public message and a strong incentive to have the equipment.20
There are inconsistent studies about the advantages and disadvantages of RADS in gynecologic procedures, although there are few randomized studies.21 The demonstrated advantages are generally identified as somewhat shorter recovery time.22 The ultimate goal will be to minimize risks while maximizing the many potential benefits of robotic surgery.23
Continue to: Liability...
Liability
A recent study by De Ravin and colleagues of robotic surgery liability found a 250% increase in the total number of robotic surgery–related malpractice claims reported in 7 recent years (2014-2021), compared with the prior 7 (2006-2013).24 However, the number of cases varied considerably from year to year. ObGyn had the most significant gain (from 19% to 49% of all claims). During the same time, urology claims declined from 56% to 16%. (The limitations of the study’s data are discussed later in this article.)
De Ravin et al reported the legal bases for the claims, but the specific legal claim was unclear in many cases.24 For example, the vast majority were classified as “negligent surgery.” Many cases made more than 1 legal claim for liability, so the total percentages were greater than 100%. Of the specific claims, many appear unrelated to robotic surgery (misdiagnosis, delayed treatment, or infection). However, there were a significant number of cases that raised issues that were related to robotic surgery. The following are those claims that probably relate to the “robotic” surgery, along with the percentage of cases making such a claim as reported24:
- “Patient not a candidate for surgery performed” appeared in about 13% of the cases.24 Such claims could include that the surgeon should have performed the surgery with traditional laparoscopy or open technique, but instead using a robot led to the injury. Physicians may feel pressure from patients or hospitals, because of the equipment’s cost, to use robotic surgery as it seems to be the modern approach (and therefore better). Neither reason is sufficient for using robotic assistance unless it will benefit the patient.
- “Failure to calibrate or operate robot” was in 11% of the claims.24 Physicians must properly calibrate and otherwise ensure that surgical equipment is operating correctly. In addition, the hospitals supplying the equipment must ensure that the equipment is maintained correctly. Finally, the equipment manufacturer may be liable through “products liability” if the equipment is defective.25 The expanding use of artificial intelligence in medical equipment (including surgical robots) is increasing the complexity of determining what “defective” means.11
- “Training deficiencies or credentialing” liability is a common problem with new technology. Physicians using new technology should be thoroughly trained and, where appropriate, certified in the use of the new technology.26 Early adopters of the technology should be especially cautious because good training may be challenging to obtain. In the study, the claims of inadequate training were particularly high during the early 7 years (35%), but dropped during the later time (4%).24
- “Improper positioning” of the patient or device or patient was raised in 7% of the cases.24
- “Manufacturing problems” were claimed in a small number of cases—13% in 2006-2013, but 2% in 2014-2021.24 These cases raise the complex question of products liability for robotic surgery and artificial intelligence (AI). Products liability has been part of surgical practice for many years. There usually will be liability if there are “defects” in a product, whether or not resulting from negligence. What a “defect” in a computer program means is a complicated issue that will be significant in future liability cases.27
Several other cases reported in the De Ravin study were probably related to robotic surgery. For example, Informed Consent and Failure to Monitor each appeared in more than 30%, of 2014-2021 cases, and Failure to Refer in 16% of the cases.24,27
The outcomes of the reported cases were mostly verdicts (or trial-related settlements) for defendants (doctors and hospitals). The defense prevailed 69% of the time in the early period and 78% of the time in 2014-2021. However, there were substantial damages in some cases. The range of damages in 2006-2013 was $95,000 to $6 million (mean, $2.5 million); in 2014-2021, it was $10,000 to $5 million (mean, $1.3 million).24
An earlier study looked at reported cases against Intuitive Surgical, maker of the daVinci system, from 2000-2017.28 Of the 108 claims in the study, 62% were gynecologic surgeries. Of these claims, 35% were dismissed, but “no other information regarding settlements or trial outcomes was available.” The study did not report the basis for the lawsuits involving gynecologic surgeries.
We should exercise caution in reviewing these studies. Although the studies were of considerable value, the authors note significant limitations of the databases available. The database was Westlaw in the first study discussed (“Robotic surgery: the impact”24) and Bloomberg in the second (“Robotic urologic”28). For example, the “impact” study was based on “jury verdict reports” excluding settlements, and the latter excluded class actions and cases settled. Thus the studies undoubtedly understated the number of claims made (those that resulted in settlement before a lawsuit was filed), cases filed but abandoned, and settlements made before trial.
Despite these limitations, the studies provide valuable insights into current malpractice risks and future directions. It is worth remembering that these cases nearly all involved a single robot, the daVinci, produced by Intuitive Surgical. It is not a “smart” robot and is commonly referred to as a “master-slave” machine. With much more intelligent and independent machines, the future will raise more complex problems in the FDA approval process and malpractice and product liability claims when things go wrong.
Continue to: What’s the verdict?...
What’s the verdict?
The case of VM and operating surgeon Dr. G illustrates several important legal aspects of using surgical robots. It also demonstrates that the presence of the robot assist still requires the surgeon’s careful attention to issues of informed consent, adequate specific training, and thorough follow up. In the following discussion, we divide the case review into the elements of negligence-malpractice (duty and breach, causation, and damages) and conclude with a thought about how to proceed when things have gone wrong.
Dr. G’s statement, “I’ve done a few,” is indefinite, but it may suggest that Dr. G. had not received full, supervised training in the robotic assist he was planning to use. That problem was underlined by the conclusion that Dr. G was a “relatively inexperienced robotic surgeon.” If so, that failure could constitute a breach of the duty of care to the patient. In addition, if it is inaccurate or did not provide information VM reasonably needed in consenting to Dr. G proceeding with the surgery, there could be an issue of whether there was a partial failure of fully informed consent.
The hospital also may have potential liability. It was “taken to task for granting privileges to an individual that had prior privilege ‘problems,’” suggesting that it had not performed adequate review before granting hospital privileges. Furthermore, if Dr. G was not sufficiently practiced or supervised in robotic surgery, the hospital, which allowed Dr. G to proceed, might also be negligent.
VM had a series of problems postsurgery that ultimately resulted in additional care and “simple fistula repair.” Assuming that there was negligence, the next question is whether that failure caused the injury. Causation may be the most difficult part of the case for VM to prove. It would require expert testimony that the inadequate surgery (inappropriate use of robotic surgery or other error during surgery) and follow up resulted in the formation or increase in the likelihood of the fistula.
VM would also have to prove damages. Damages are those costs (the economic value) of injuries that would not have occurred but for negligence. Damages would include most of the cost of the follow-up medical care and any related additional future care required, plus costs that were a consequence of the negligence (such as lost work). In addition, damages would include pain and suffering that resulted from the negligence, subject to caps in some states.
When the patient was dissatisfied and reported a postsurgical problem, the hospital and Dr. G may have had an opportunity to avoid further dissatisfaction, complaints, and ultimately a lawsuit. Effective approaches for dealing with such dissatisfaction may serve the institution’s and physician’s values and financial best interests.
The jury verdict was in favor of the plaintiff. Jurors felt the operating surgeon should have conveyed his experience with robotic surgery more clearly as part of the informed consent process.
“Hey Siri! Perform a type 3 hysterectomy. Please watch out for the ureter!”29
Medicine is still at the frontier of surgical robots. Over future decades, the number and sophistication of these machines will increase substantially. They likely will become much more like robots, guided by AI, and make independent judgments. These have the potential for significant medical progress that improves the treatment of patients. At the same time, the last 20 years suggest that robotic innovation will challenge medicine, the FDA and other regulators, lawmakers, and courts. In the future, regulators and patients should embrace genuine advances in robotic surgery but not be dazzled by these new machines’ luster (or potential for considerable profits).30
The public may be wildly optimistic about the benefits without balancing the risks. The AI that runs them will be essentially invisible and constantly changing. Physicians and regulators must develop new techniques for assessing and controlling the software. Real surgical robots require rigorous testing, cautious promotion, disciplined use, and perpetual review. ●
The approach to hysterectomy has been debated, with the need for individualization case by case stressed, and the expertise of the operating surgeon considered.
CASE Was surgeon experience a factor in case complications?
VM is a 46-year-old woman (G5 P4014) reporting persistent uterine bleeding that is refractory to medical therapy. The patient has uterine fibroids, 6 weeks in size on examination, with “mild” prolapse noted. Additional medical diagnoses included vulvitis, ovarian cyst in the past, cystic mastopathy, and prior evidence of pelvic adhesion, noted at the time of ovarian cystectomy. Prior surgical records were not obtained by the operating surgeon, although her obstetric history includes 2 prior vaginal deliveries and 2 cesarean deliveries (CDs). The patient had an umbilical herniorraphy a number of years ago. Her medications include hormonal therapy, for presumed menopause, and medication for depression (she reported “doing well” on medication). She reported smoking 1 PPD and had a prior tubal ligation.
VM was previously evaluated for Lynch Syndrome and informed of the potential for increased risks of colon, endometrial, and several other cancers. She did not have cancer as of the time of planned surgery.
The patient underwent robotic-assisted total laparoscopic hysterectomy and bilateral salpingo-oophorectomy. The operating surgeon did not have a lot of experience with robotic hysterectomies but told the patient preoperatively “I have done a few.” Perioperatively, blood loss was minimal, urine output was recorded as 25 mL, and according to the operative report there were extensive pelvic adhesions and no complications. The “ureters were identified” when the broad ligament was opened at the time of skeletonization of the uterine vessels and documented accordingly. The intraoperative Foley was discontinued at the end of the procedure. The pathology report noted diffuse adenomyosis and uterine fibroids; the uterus weighed 250 g. In addition, a “large hemorrhagic corpus luteum cyst” was noted on the right ovary.
The patient presented for a postoperative visit reporting “leaking” serosanguinous fluid that began 2.5 weeks postoperatively and required her to wear 3 to 4 “Depends” every day. She also reported constipation since beginning her prescribed pain medication. She requested a copy of her medical records and said she was dissatisfied with the care she had received related to the hysterectomy; she was “seeking a second opinion from a urologist.” The urologist suggested evaluation of the “leaking,” and a Foley catheter was placed. When she stood up, however, there was leaking around the catheter, and she reported a “yellowish-green,” foul smelling discharge. She called the urologist’s office, stating, “I think I have a bowel obstruction.” The patient was instructed to proceed to the emergency department at her local hospital. She was released with a diagnosis of constipation. Upon follow-up urologic evaluation, a vulvovaginal fistula was noted. Management was a “simple fistula repair,” and the patient did well subsequently.
The patient brought suit against the hospital and operating gynecologist. In part the hospital records noted, “relatively inexperienced robotic surgeon.” The hospital was taken to task for granting privileges to an individual that had prior privilege “problems.”
Continue to: Medical opinion...
Medical opinion
This case demonstrates a number of issues. (We will discuss the credentials for the surgeon and hospital privileges in the legal considerations section.) From the medical perspective, the rate of urologic injury associated with all hysterectomies is 0.87%.1 Robotic hysterectomy has been reported at 0.92% in a series published from Henry Ford Hospital.1 The lowest rate of urologic injury is associated with vaginal hysterectomy, reported at 0.2%.2 Reported rates of urologic injury by approach to hysterectomy are1:
- robotic, 0.92%
- laparoscopic, 0.90%
- vaginal, 0.33%
- abdominal, 0.96%.
Complications by surgeon type also have been addressed, and the percent of total urologic complications are reported as1:
- ObGyn, 47%
- gyn oncologist, 47%
- urogynecologist, 6%.
Intraoperative conversion to laparotomy from initial robotic approach has been addressed in a retrospective study over a 2-year period, with operative times ranging from 1 hr, 50 min to 9 hrs of surgical time.1 The vast majority of intraoperative complications in a series reported from Finland were managed “within minutes,” and in the series of 83 patients, 5 (6%) required conversion to laparotomy.2 Intraoperative complications reported include failed entry, vascular injury, nerve injury, visceral injury, solid organ injury, tumor fragmentation, and anesthetic-related complications.3 Of note, the vascular injuries included inferior vena cava, common iliac, and external iliac.
Mortality rates in association with benign laparoscopic and robotic procedures have been addressed and noted to be 1:6,456 cases based upon a meta-analysis.4 The analysis included 124,216 patients. Laparoscopic versus robotic mortality rates were not statistically different. Mortality was more common among cases of undiagnosed rare colorectal injury. This mortality is on par with complications from Roux-en-Y gastric bypass procedures. Procedures such as sacrocolpopexy are equated with higher mortality (1:1,246) in comparison with benign hysterectomy.5
Infectious complications following either laparoscopic or robotic hysterectomy were reported at less than 1% and not statistically different for either approach.6 The series authored by Marra et al evaluated 176,016 patients.
Overall, robotic-assisted gynecologic complications are rare. One series was focused on gynecological oncologic cases.7 Specific categories of complications included7:
- patient positioning and pneumoperitoneum
- injury to surrounding organs
- bowel injury
- port site metastasis
- surgical emphysema
- vaginal cuff dehiscence
- anesthesia-related problems.
The authors concluded, “robotic assisted surgery in gynecological oncology is safe and the incidence of complications is low.”7 The major cause of death related to robotic surgery is vascular injury–related. The authors emphasized the importance of knowledge of anatomy, basic principles of “traction and counter-traction” and proper dissection along tissue planes as key to minimizing complications. Consider placement of stents for ureter identification, as appropriate. Barbed-suturing does not prevent dehiscence.
Continue to: Legal considerations...
Legal considerations
Robotic surgery presents many legal issues and promises to raise many more in the future. The law must control new technology while encouraging productive uses, and provide new remedies for harms while respecting traditional legal principles.8 There is no shortage of good ideas about controlling surgical robots,9 automated devices more generally,10 and artificial intelligence.11 Those issues will be important, and watching them unfold will be intriguing.
In the meantime, physicians and other health care professionals, health care facilities, technology companies, and patients must work within current legal structures in implementing and using robotic surgery. These are extraordinarily complex issues, so it is possible only to review the current landscape and speculate what the near future may hold.
Regulating surgical robots
The US Food and Drug Administration (FDA) is the primary regulator of robots used in medicine.12 It has the authority to regulate surgical devices, including surgical robots—which it refers to as “robotically-assisted surgical devices,” or RASD. In 2000, it approved Intuitive Surgical’s daVinci system for use in surgery. In 2017, the FDA expanded its clearance to include the Senhance System of TransEnterix Surgical Inc. for minimally invasive gynecologic surgery.13 In 2021, the FDA cleared the Hominis Surgical System for transvaginal hysterectomy “in certain patients.” However, the FDA emphasized that this clearance is for benign hysterectomy with salpingo-oophorectomy.14 (The FDA has cleared various robotic devices for several other areas of surgical practice, including neurosurgery, orthopedics, and urology.)
The use of robots in cancer surgery is limited. The FDA approved specific RASDs in some “surgical procedures commonly performed in patients with cancer, such as hysterectomy, prostatectomy, and colectomy.”15 However, it cautioned that this clearance was based only on a 30-day patient follow up. More specifically, the FDA “has not evaluated the safety or effectiveness of RASD devices for the prevention or treatment of cancer, based on cancer-related outcomes such as overall survival, recurrence, and disease-free survival.”15
The FDA has clearly warned physicians and patients that the agency has not granted the use of RASDs “for any cancer-related surgery marketing authorization, and therefore the survival benefits to patients compared to traditional surgery have not been established.”15 (This did not apply to the hysterectomy surgery as noted above. More specifically, that clearance did not apply to anything other than 30-day results, nor to the efficacy related to cancer survival.)
States also have some authority to regulate medical practice within their borders.9 When the FDA has approved a device as safe and effective, however, there are limits on what states can do to regulate or impose liability on the approved product. The Supreme Court held that the FDA approval “pre-empted” some state action regarding approved devices.16
Hospitals, of course, regulate what is allowed within the hospital. For example, it may require training before a physician is permitted to use equipment, limit the conditions for which the equipment may be used, or decline to obtain equipment for use in the hospitals.17 In the case of RASDs, however, the high cost of equipment may provide an incentive for hospitals to urge the wide use of the latest robotic acquisition.18
Regulation aims primarily to protect patients, usually from injury or inadequate treatment. Some robotic surgery is likely to be more expensive than the same surgery without robotic assistance. The cost to the patient is not usually part of the FDA’s consideration. Insurance companies (including Medicare and Medicaid), however, do care about costs and will set or negotiate how much the reimbursement will be for a procedure. Third-party payers may decline to cover the additional cost when there is no apparent benefit from using the robot.19 For some institutions, the public perception that it offers “the most modern technology” is an important public message and a strong incentive to have the equipment.20
There are inconsistent studies about the advantages and disadvantages of RADS in gynecologic procedures, although there are few randomized studies.21 The demonstrated advantages are generally identified as somewhat shorter recovery time.22 The ultimate goal will be to minimize risks while maximizing the many potential benefits of robotic surgery.23
Continue to: Liability...
Liability
A recent study by De Ravin and colleagues of robotic surgery liability found a 250% increase in the total number of robotic surgery–related malpractice claims reported in 7 recent years (2014-2021), compared with the prior 7 (2006-2013).24 However, the number of cases varied considerably from year to year. ObGyn had the most significant gain (from 19% to 49% of all claims). During the same time, urology claims declined from 56% to 16%. (The limitations of the study’s data are discussed later in this article.)
De Ravin et al reported the legal bases for the claims, but the specific legal claim was unclear in many cases.24 For example, the vast majority were classified as “negligent surgery.” Many cases made more than 1 legal claim for liability, so the total percentages were greater than 100%. Of the specific claims, many appear unrelated to robotic surgery (misdiagnosis, delayed treatment, or infection). However, there were a significant number of cases that raised issues that were related to robotic surgery. The following are those claims that probably relate to the “robotic” surgery, along with the percentage of cases making such a claim as reported24:
- “Patient not a candidate for surgery performed” appeared in about 13% of the cases.24 Such claims could include that the surgeon should have performed the surgery with traditional laparoscopy or open technique, but instead using a robot led to the injury. Physicians may feel pressure from patients or hospitals, because of the equipment’s cost, to use robotic surgery as it seems to be the modern approach (and therefore better). Neither reason is sufficient for using robotic assistance unless it will benefit the patient.
- “Failure to calibrate or operate robot” was in 11% of the claims.24 Physicians must properly calibrate and otherwise ensure that surgical equipment is operating correctly. In addition, the hospitals supplying the equipment must ensure that the equipment is maintained correctly. Finally, the equipment manufacturer may be liable through “products liability” if the equipment is defective.25 The expanding use of artificial intelligence in medical equipment (including surgical robots) is increasing the complexity of determining what “defective” means.11
- “Training deficiencies or credentialing” liability is a common problem with new technology. Physicians using new technology should be thoroughly trained and, where appropriate, certified in the use of the new technology.26 Early adopters of the technology should be especially cautious because good training may be challenging to obtain. In the study, the claims of inadequate training were particularly high during the early 7 years (35%), but dropped during the later time (4%).24
- “Improper positioning” of the patient or device or patient was raised in 7% of the cases.24
- “Manufacturing problems” were claimed in a small number of cases—13% in 2006-2013, but 2% in 2014-2021.24 These cases raise the complex question of products liability for robotic surgery and artificial intelligence (AI). Products liability has been part of surgical practice for many years. There usually will be liability if there are “defects” in a product, whether or not resulting from negligence. What a “defect” in a computer program means is a complicated issue that will be significant in future liability cases.27
Several other cases reported in the De Ravin study were probably related to robotic surgery. For example, Informed Consent and Failure to Monitor each appeared in more than 30%, of 2014-2021 cases, and Failure to Refer in 16% of the cases.24,27
The outcomes of the reported cases were mostly verdicts (or trial-related settlements) for defendants (doctors and hospitals). The defense prevailed 69% of the time in the early period and 78% of the time in 2014-2021. However, there were substantial damages in some cases. The range of damages in 2006-2013 was $95,000 to $6 million (mean, $2.5 million); in 2014-2021, it was $10,000 to $5 million (mean, $1.3 million).24
An earlier study looked at reported cases against Intuitive Surgical, maker of the daVinci system, from 2000-2017.28 Of the 108 claims in the study, 62% were gynecologic surgeries. Of these claims, 35% were dismissed, but “no other information regarding settlements or trial outcomes was available.” The study did not report the basis for the lawsuits involving gynecologic surgeries.
We should exercise caution in reviewing these studies. Although the studies were of considerable value, the authors note significant limitations of the databases available. The database was Westlaw in the first study discussed (“Robotic surgery: the impact”24) and Bloomberg in the second (“Robotic urologic”28). For example, the “impact” study was based on “jury verdict reports” excluding settlements, and the latter excluded class actions and cases settled. Thus the studies undoubtedly understated the number of claims made (those that resulted in settlement before a lawsuit was filed), cases filed but abandoned, and settlements made before trial.
Despite these limitations, the studies provide valuable insights into current malpractice risks and future directions. It is worth remembering that these cases nearly all involved a single robot, the daVinci, produced by Intuitive Surgical. It is not a “smart” robot and is commonly referred to as a “master-slave” machine. With much more intelligent and independent machines, the future will raise more complex problems in the FDA approval process and malpractice and product liability claims when things go wrong.
Continue to: What’s the verdict?...
What’s the verdict?
The case of VM and operating surgeon Dr. G illustrates several important legal aspects of using surgical robots. It also demonstrates that the presence of the robot assist still requires the surgeon’s careful attention to issues of informed consent, adequate specific training, and thorough follow up. In the following discussion, we divide the case review into the elements of negligence-malpractice (duty and breach, causation, and damages) and conclude with a thought about how to proceed when things have gone wrong.
Dr. G’s statement, “I’ve done a few,” is indefinite, but it may suggest that Dr. G. had not received full, supervised training in the robotic assist he was planning to use. That problem was underlined by the conclusion that Dr. G was a “relatively inexperienced robotic surgeon.” If so, that failure could constitute a breach of the duty of care to the patient. In addition, if it is inaccurate or did not provide information VM reasonably needed in consenting to Dr. G proceeding with the surgery, there could be an issue of whether there was a partial failure of fully informed consent.
The hospital also may have potential liability. It was “taken to task for granting privileges to an individual that had prior privilege ‘problems,’” suggesting that it had not performed adequate review before granting hospital privileges. Furthermore, if Dr. G was not sufficiently practiced or supervised in robotic surgery, the hospital, which allowed Dr. G to proceed, might also be negligent.
VM had a series of problems postsurgery that ultimately resulted in additional care and “simple fistula repair.” Assuming that there was negligence, the next question is whether that failure caused the injury. Causation may be the most difficult part of the case for VM to prove. It would require expert testimony that the inadequate surgery (inappropriate use of robotic surgery or other error during surgery) and follow up resulted in the formation or increase in the likelihood of the fistula.
VM would also have to prove damages. Damages are those costs (the economic value) of injuries that would not have occurred but for negligence. Damages would include most of the cost of the follow-up medical care and any related additional future care required, plus costs that were a consequence of the negligence (such as lost work). In addition, damages would include pain and suffering that resulted from the negligence, subject to caps in some states.
When the patient was dissatisfied and reported a postsurgical problem, the hospital and Dr. G may have had an opportunity to avoid further dissatisfaction, complaints, and ultimately a lawsuit. Effective approaches for dealing with such dissatisfaction may serve the institution’s and physician’s values and financial best interests.
The jury verdict was in favor of the plaintiff. Jurors felt the operating surgeon should have conveyed his experience with robotic surgery more clearly as part of the informed consent process.
“Hey Siri! Perform a type 3 hysterectomy. Please watch out for the ureter!”29
Medicine is still at the frontier of surgical robots. Over future decades, the number and sophistication of these machines will increase substantially. They likely will become much more like robots, guided by AI, and make independent judgments. These have the potential for significant medical progress that improves the treatment of patients. At the same time, the last 20 years suggest that robotic innovation will challenge medicine, the FDA and other regulators, lawmakers, and courts. In the future, regulators and patients should embrace genuine advances in robotic surgery but not be dazzled by these new machines’ luster (or potential for considerable profits).30
The public may be wildly optimistic about the benefits without balancing the risks. The AI that runs them will be essentially invisible and constantly changing. Physicians and regulators must develop new techniques for assessing and controlling the software. Real surgical robots require rigorous testing, cautious promotion, disciplined use, and perpetual review. ●
- Petersen S, Doe S, Rubinfield I, et al. Rate of urologic injury with robotic hysterectomy. J Min Invasc Gynecol. 2018;25:867-871.
- Makinen J, Johansson J, Toma C, et al. Morbidity of 10,110 hysterectomies by type approach. Hum Reprod. 2001;16:1473-1478.
- Karasu A, Kran G, Sanlikan F. Intraoperative complications and conversion to laparotomy in gynecologic robotic surgery. J Investig Surg. 2022;35:912-915.
- Behbehani S, Suarez-Salvador E, Buras M, et al. Mortality rates in benign laparoscopic and robotic surgery: a systematic review and meta-analysis. J Min Invasc. 2020;27:603-612.
- Giurdano S, Victorzon M. Laparoscopic roux-en-Y gastric bypass in elderly patients (60 years or older): a meta-analysis of comparative studies. Scand J Surg. 2018;107:6-11.
- Marra A, Pulg-Asensio M, Edmond M, et al. Infectious complications of laparoscopic and robotic hysterectomy: a systematic literature review and meta-analysis. Int J Gynecol Cancer. 2019;29:518-530.
- Tse KY, Sheung H, Lim P. Robot-assisted gyneaecological cancer surgery-complications and prevention. Best Pract Res Clin Obstet Gynaecol. 2017;25:94-105.
- Hubbard FP. Sophisticated robots: balancing liability, regulation, and innovation. Fla Law Rev. 2014;66:1803-1872. https://scholarship.law.ufl.edu/cgi/viewcontent. cgi?article=1204&context=flr. Accessed December 20, 2022.
- Villanueva A. The legal battle with the future of autonomous surgical robotics. Ind Health Law Rev. 2020;17:367-392. https://journals.iupui.edu/index.php/ihlr/article /download/25051/23544. Accessed December 20, 2022.
- Lemley MA, Casey B. Remedies for robots. U Chi Law Rev. 2019;86:1311-1396. https://chicagounbound.uchicago.edu /cgi/viewcontent.cgi?article=6140&context=uclrev. Accessed December 20, 2022.
- Griffin F. Artificial intelligence and liability in health care. Health Matrix. 2021;31:65-106. https://scholarlycommons. law.case.edu/cgi/viewcontent.cgi?article=1659&context=hea lthmatrix. Accessed December 20, 2022.
- Britton D. Autonomous surgery: the law of autonomous surgical robots. J Law Tech Tex. 2017;1:152-189.
- US Food and Drug Administration. FDA clears new robotically-assisted surgical device for adult patients. October 13, 2017. https://www.fda.gov/news-events/press-announcements /fda-clears-new-robotically-assisted-surgical-device-adult -patients. Accessed December 20, 2022.
- US Food and Drug Administration. FDA authorizes first robotically-assisted surgical device for performing transvaginal hysterectomy. March 1, 2021. https://www.fda .gov/news-events/press-announcements/fda-authorizes -first-robotically-assisted-surgical-device-performing -transvaginal-hysterectomy. Accessed December 20, 2022.
- US Food and Drug Administration. Caution with robotically-assisted surgical devices in mastectomy: FDA Safety Communication, August 20, 2021. https://www.fda.gov/medical-devices/safety-communications/update-caution-robotically-assisted-surgical-devices-mastectomy-fda-safety-communication. Accessed December 22, 2022. Riegel v Medtronic, 552 US 312 (2008).
- Han ES, Advincula AP. Robotic surgery: advancements and inflection points in the field of gynecology. Obstet Gynecol Clin North Am. 2021;48:759-776.
- Witharm H. Robot-assisted surgery: an analysis of the legal and economic implications. Az J Interdisciplinary Studies. 2022;8:19-29. https://journals.librarypublishing.arizona.edu /azjis/article/id/5093/download/pdf/.
- Cameron S. Is daVinci robotic surgery a revolution or a rip-off? Healthline. August 10, 2016. https://www.healthline .com/health-news/is-da-vinci-robotic-surgery-revolution -or-ripoff-021215. Accessed December 20, 2022.
- Perez RE, Schwaitzberg SD. Robotic surgery: finding value in 2019 and beyond. Ann Laparosc Endosc Surg. 2019;4:1-7.
- Gitas G, Hanker L, Rody A, et al. Robotic surgery in gynecology: is the future already here? Minim Invasiv Therapy Allied Technol. 2022;4:1-0.
- Moon AS, Garofalo J, Koirala P, et al. Robotic surgery in gynecology. Surgical Clinics. 2020;100:445-460.
- Simshaw D, Terry N, Hauser K, et al. Regulating healthcare robots: maximizing opportunities while minimizing risks. Richmond J Law Tech. 2015;22:1-38. https://scholar works.iupui.edu/bitstream/handle/1805/11587/simshaw _2015_regulating.pdf?sequence=1&isAllowed=y. Accessed December 20, 2022.
- De Ravin E, Sell EA, Newman JG, et al. Medical malpractice in robotic surgery: a Westlaw database analysis. J Robotic Surg. 2022. https://doi.org/10.1007/s11701-022-01417-6. https:// link.springer.com/article/10.1007/s11701-022-014176#citeas. Accessed December 20, 2022.
- Beglinger C. A broken theory: the malfunction theory of strict products liability and the need for a new doctrine in the field of surgical robotics. Minnesotta Law Rev. 2019;104:1041-1093. . Accessed December 20, 2022.
- Azadi S, Green IC, Arnold A, et al. Robotic surgery: the impact of simulation and other innovative platforms on performance and training. J Minim Invasiv Gynecol. 2021;28:490-495.
- Koerner D. Doctor roboto: The no-man operation. U Tol L Rev. 2019;51:125-146.
- Nik-Ahd F, Souders CP, Zhao H, et al. Robotic urologic surgery: trends in litigation over the last decade. J Robotic Surg. 2019;13:729-734.
- Gültekin CalibriİB, Karabük E, Köse MF. “Hey Siri! Perform a type 3 hysterectomy. Please watch out for the ureter!” What is autonomous surgery and what are the latest developments? J Turk Ger Gynecol Assoc. 2021;22:58-70. https://www.ncbi .nlm.nih.gov/pmc/articles/PMC7944239/.
- Matsuzaki T. Ethical issues of artificial intelligence in medicine. California West Law Rev. 2018;55:255-273. https://scholarlycommons.law.cwsl.edu/cgi/viewcontent. cgi?article=1669&context=cwlr. Accessed December 20, 2022.
- Petersen S, Doe S, Rubinfield I, et al. Rate of urologic injury with robotic hysterectomy. J Min Invasc Gynecol. 2018;25:867-871.
- Makinen J, Johansson J, Toma C, et al. Morbidity of 10,110 hysterectomies by type approach. Hum Reprod. 2001;16:1473-1478.
- Karasu A, Kran G, Sanlikan F. Intraoperative complications and conversion to laparotomy in gynecologic robotic surgery. J Investig Surg. 2022;35:912-915.
- Behbehani S, Suarez-Salvador E, Buras M, et al. Mortality rates in benign laparoscopic and robotic surgery: a systematic review and meta-analysis. J Min Invasc. 2020;27:603-612.
- Giurdano S, Victorzon M. Laparoscopic roux-en-Y gastric bypass in elderly patients (60 years or older): a meta-analysis of comparative studies. Scand J Surg. 2018;107:6-11.
- Marra A, Pulg-Asensio M, Edmond M, et al. Infectious complications of laparoscopic and robotic hysterectomy: a systematic literature review and meta-analysis. Int J Gynecol Cancer. 2019;29:518-530.
- Tse KY, Sheung H, Lim P. Robot-assisted gyneaecological cancer surgery-complications and prevention. Best Pract Res Clin Obstet Gynaecol. 2017;25:94-105.
- Hubbard FP. Sophisticated robots: balancing liability, regulation, and innovation. Fla Law Rev. 2014;66:1803-1872. https://scholarship.law.ufl.edu/cgi/viewcontent. cgi?article=1204&context=flr. Accessed December 20, 2022.
- Villanueva A. The legal battle with the future of autonomous surgical robotics. Ind Health Law Rev. 2020;17:367-392. https://journals.iupui.edu/index.php/ihlr/article /download/25051/23544. Accessed December 20, 2022.
- Lemley MA, Casey B. Remedies for robots. U Chi Law Rev. 2019;86:1311-1396. https://chicagounbound.uchicago.edu /cgi/viewcontent.cgi?article=6140&context=uclrev. Accessed December 20, 2022.
- Griffin F. Artificial intelligence and liability in health care. Health Matrix. 2021;31:65-106. https://scholarlycommons. law.case.edu/cgi/viewcontent.cgi?article=1659&context=hea lthmatrix. Accessed December 20, 2022.
- Britton D. Autonomous surgery: the law of autonomous surgical robots. J Law Tech Tex. 2017;1:152-189.
- US Food and Drug Administration. FDA clears new robotically-assisted surgical device for adult patients. October 13, 2017. https://www.fda.gov/news-events/press-announcements /fda-clears-new-robotically-assisted-surgical-device-adult -patients. Accessed December 20, 2022.
- US Food and Drug Administration. FDA authorizes first robotically-assisted surgical device for performing transvaginal hysterectomy. March 1, 2021. https://www.fda .gov/news-events/press-announcements/fda-authorizes -first-robotically-assisted-surgical-device-performing -transvaginal-hysterectomy. Accessed December 20, 2022.
- US Food and Drug Administration. Caution with robotically-assisted surgical devices in mastectomy: FDA Safety Communication, August 20, 2021. https://www.fda.gov/medical-devices/safety-communications/update-caution-robotically-assisted-surgical-devices-mastectomy-fda-safety-communication. Accessed December 22, 2022. Riegel v Medtronic, 552 US 312 (2008).
- Han ES, Advincula AP. Robotic surgery: advancements and inflection points in the field of gynecology. Obstet Gynecol Clin North Am. 2021;48:759-776.
- Witharm H. Robot-assisted surgery: an analysis of the legal and economic implications. Az J Interdisciplinary Studies. 2022;8:19-29. https://journals.librarypublishing.arizona.edu /azjis/article/id/5093/download/pdf/.
- Cameron S. Is daVinci robotic surgery a revolution or a rip-off? Healthline. August 10, 2016. https://www.healthline .com/health-news/is-da-vinci-robotic-surgery-revolution -or-ripoff-021215. Accessed December 20, 2022.
- Perez RE, Schwaitzberg SD. Robotic surgery: finding value in 2019 and beyond. Ann Laparosc Endosc Surg. 2019;4:1-7.
- Gitas G, Hanker L, Rody A, et al. Robotic surgery in gynecology: is the future already here? Minim Invasiv Therapy Allied Technol. 2022;4:1-0.
- Moon AS, Garofalo J, Koirala P, et al. Robotic surgery in gynecology. Surgical Clinics. 2020;100:445-460.
- Simshaw D, Terry N, Hauser K, et al. Regulating healthcare robots: maximizing opportunities while minimizing risks. Richmond J Law Tech. 2015;22:1-38. https://scholar works.iupui.edu/bitstream/handle/1805/11587/simshaw _2015_regulating.pdf?sequence=1&isAllowed=y. Accessed December 20, 2022.
- De Ravin E, Sell EA, Newman JG, et al. Medical malpractice in robotic surgery: a Westlaw database analysis. J Robotic Surg. 2022. https://doi.org/10.1007/s11701-022-01417-6. https:// link.springer.com/article/10.1007/s11701-022-014176#citeas. Accessed December 20, 2022.
- Beglinger C. A broken theory: the malfunction theory of strict products liability and the need for a new doctrine in the field of surgical robotics. Minnesotta Law Rev. 2019;104:1041-1093. . Accessed December 20, 2022.
- Azadi S, Green IC, Arnold A, et al. Robotic surgery: the impact of simulation and other innovative platforms on performance and training. J Minim Invasiv Gynecol. 2021;28:490-495.
- Koerner D. Doctor roboto: The no-man operation. U Tol L Rev. 2019;51:125-146.
- Nik-Ahd F, Souders CP, Zhao H, et al. Robotic urologic surgery: trends in litigation over the last decade. J Robotic Surg. 2019;13:729-734.
- Gültekin CalibriİB, Karabük E, Köse MF. “Hey Siri! Perform a type 3 hysterectomy. Please watch out for the ureter!” What is autonomous surgery and what are the latest developments? J Turk Ger Gynecol Assoc. 2021;22:58-70. https://www.ncbi .nlm.nih.gov/pmc/articles/PMC7944239/.
- Matsuzaki T. Ethical issues of artificial intelligence in medicine. California West Law Rev. 2018;55:255-273. https://scholarlycommons.law.cwsl.edu/cgi/viewcontent. cgi?article=1669&context=cwlr. Accessed December 20, 2022.
The loss of letters
My desk looks nothing like my grandfather’s. It stands about mid-abdomen high and has a small surface, perhaps just enough for the monitor and a mug. Yes, I can move it up and down (thank you 21st century), but it has no drawers. It is lean and immaculate, but it has no soul.
My grandfather sat at a large oak desk with three drawers on each side. Each was so heavy you had to be at least 6 years old to pull one open for exploring the contents inside. The desk surface was vast and although immobile, it had a greenish leather blotter for writing. Alongside his pile of correspondences was a treasure for those of us tall enough to get it: A heavy brass letter opener. It came, I believe, with a secretary who would open his letters and stack them neatly before placing this sometimes-pirate’s-sword far enough away from the edge for us to not reach it.
Upon my skinny, adaptable desk the other day sat a white envelope that was hand addressed to me. It was postmarked more than 2 weeks before as it had been waylaid in Endocrinology before being couriered to the rightful recipient. It had not been opened. Nor did I have any way to do so gracefully. I tore it apart with a fat finger while clicking through path reports that just arrived in my inbox.
Dear Dr. Benabio,
Pat
. She carefully looped her “y’s” and crossed her “t’s.” Not one cross out. She thought about each sentence before transcribing it. The paper once sat on her desk, touched her fingers and the envelope sealed with her saliva. It was not filled with trifling requests or complaints. It was not efficient, but it was more than just communication. She took the time to choose the words to capture her emotion and express her gratitude. It was respectful, dignified, decidedly nondigital. For a brief moment I thought I might write back, but quickly realized that was impractical. I knew I wouldn’t make the time to do so. I wish I had.
Having no drawers to save it, I held it up with just a corner of the page resting on my desk and scribbled in black ink “Reviewed. Please scan to media file. 12/8/22. JAB”
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
My desk looks nothing like my grandfather’s. It stands about mid-abdomen high and has a small surface, perhaps just enough for the monitor and a mug. Yes, I can move it up and down (thank you 21st century), but it has no drawers. It is lean and immaculate, but it has no soul.
My grandfather sat at a large oak desk with three drawers on each side. Each was so heavy you had to be at least 6 years old to pull one open for exploring the contents inside. The desk surface was vast and although immobile, it had a greenish leather blotter for writing. Alongside his pile of correspondences was a treasure for those of us tall enough to get it: A heavy brass letter opener. It came, I believe, with a secretary who would open his letters and stack them neatly before placing this sometimes-pirate’s-sword far enough away from the edge for us to not reach it.
Upon my skinny, adaptable desk the other day sat a white envelope that was hand addressed to me. It was postmarked more than 2 weeks before as it had been waylaid in Endocrinology before being couriered to the rightful recipient. It had not been opened. Nor did I have any way to do so gracefully. I tore it apart with a fat finger while clicking through path reports that just arrived in my inbox.
Dear Dr. Benabio,
Pat
. She carefully looped her “y’s” and crossed her “t’s.” Not one cross out. She thought about each sentence before transcribing it. The paper once sat on her desk, touched her fingers and the envelope sealed with her saliva. It was not filled with trifling requests or complaints. It was not efficient, but it was more than just communication. She took the time to choose the words to capture her emotion and express her gratitude. It was respectful, dignified, decidedly nondigital. For a brief moment I thought I might write back, but quickly realized that was impractical. I knew I wouldn’t make the time to do so. I wish I had.
Having no drawers to save it, I held it up with just a corner of the page resting on my desk and scribbled in black ink “Reviewed. Please scan to media file. 12/8/22. JAB”
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
My desk looks nothing like my grandfather’s. It stands about mid-abdomen high and has a small surface, perhaps just enough for the monitor and a mug. Yes, I can move it up and down (thank you 21st century), but it has no drawers. It is lean and immaculate, but it has no soul.
My grandfather sat at a large oak desk with three drawers on each side. Each was so heavy you had to be at least 6 years old to pull one open for exploring the contents inside. The desk surface was vast and although immobile, it had a greenish leather blotter for writing. Alongside his pile of correspondences was a treasure for those of us tall enough to get it: A heavy brass letter opener. It came, I believe, with a secretary who would open his letters and stack them neatly before placing this sometimes-pirate’s-sword far enough away from the edge for us to not reach it.
Upon my skinny, adaptable desk the other day sat a white envelope that was hand addressed to me. It was postmarked more than 2 weeks before as it had been waylaid in Endocrinology before being couriered to the rightful recipient. It had not been opened. Nor did I have any way to do so gracefully. I tore it apart with a fat finger while clicking through path reports that just arrived in my inbox.
Dear Dr. Benabio,
Pat
. She carefully looped her “y’s” and crossed her “t’s.” Not one cross out. She thought about each sentence before transcribing it. The paper once sat on her desk, touched her fingers and the envelope sealed with her saliva. It was not filled with trifling requests or complaints. It was not efficient, but it was more than just communication. She took the time to choose the words to capture her emotion and express her gratitude. It was respectful, dignified, decidedly nondigital. For a brief moment I thought I might write back, but quickly realized that was impractical. I knew I wouldn’t make the time to do so. I wish I had.
Having no drawers to save it, I held it up with just a corner of the page resting on my desk and scribbled in black ink “Reviewed. Please scan to media file. 12/8/22. JAB”
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Interval FITs could cut colonoscopies in those at above-average risk
In a new retrospective analysis of patients with above-average risk of colorectal cancer, multiple negative fecal immunohistochemical tests (FITs) were associated with a lower risk of advanced neoplasia. The findings suggest that multiple negative FITs could potentially identify individuals in high-risk surveillance who aren’t truly high risk, which could in turn ease the logjam of colonoscopies and free resources for truly high-risk individuals.
The study, conducted in Australia, was published online in Clinical Gastroenterology and Hepatology. It included patients who completed at least two FIT exams between surveillance colonoscopies and had no neoplasia or nonadvanced adenoma at prior colonoscopy. Above-average risk was defined as a family history or by findings at surveillance colonoscopy.
The study has some limitations. It is a retrospective analysis between the years 2008 and 2019, and colonoscopy guidelines in the United States have since changed, with a recommendation of surveillance colonoscopy at 7-10 years following 1-2 adenomas discovered at surveillance colonoscopy, and the current study includes follow-up colonoscopy at 5 years. “These data are informative for patients up to 5 years, but they’re not really informative afterwards. They just don’t have those data yet,” said Reed Ness, MD, who was asked to comment on the study.
The authors also don’t describe what they mean by a family history of colorectal cancer risk. “My take was that it’s an interesting result which would seem to support the possibility of returning some patients with a family history or adenoma history to a noncolonoscopy screening regimen after a negative surveillance colonoscopy. We’ll need to see where the data lead us in the future,” said Dr. Ness, who is an associate professor of medicine at Vanderbilt University Medical Center, Nashville, Tenn.
“We’re letting people go 10 years now, and some people are uncomfortable with allowing patients to go 10 years. So you could think of a scenario where you use FIT to try to find people that might have higher-risk lesions that need to come back for colonoscopy within that 10 years,” said Dr. Ness. That issue is particularly relevant given the wide range of adenoma detection rates among gastroenterologists, because FIT could detect a polyp that was missed during a colonoscopy.
The study included two groups with increased risk – those with a family history of colon cancer, and those with previously detected adenomas. The family history cohort may be useful for clinical practice, according to Priyanka Kanth, MD, who was also asked to comment on the study. “Some people may not need [a colonoscopy] at 5 years if they have no polyps found and negative FIT,” said Dr. Kanth, who is an associate professor of gastroenterology at Georgetown University, Washington.
She feels less certain about the group with previously detected adenomas, given the change in U.S. guidelines. “We have already changed that, so I don’t think we need to really do FIT intervals for that cohort,” said Dr. Kanth. “I think this is a good study that has a lot of information and also reassures us that we don’t need such frequent colonoscopy surveillance,” she added.
Steve Serrao, MD, PhD, who was also asked for comment, emphasized the importance of high-quality colonoscopies that reach the cecum 95% of the time, and achieving high adenoma-detection rates. The system can get overwhelmed conducting colonoscopies on patients with good insurance coverage who have already undergone high-quality colonoscopies. “That pushes out patients that haven’t necessarily had a colonoscopy or a FIT. People who don’t have access are kind of crowded out by these false-positive tests. The best modality is actually to do a high-quality colonoscopy and then to have a really well-directed strategy following that colonoscopy,” said Dr. Serrao, who is division chief of gastroenterology and hepatology at Riverside University Health System, Moreno Valley, Calif.
The researchers analyzed data from 4,021 surveillance intervals and 3,369 participants. A total of 1,436 had no neoplasia at the prior colonoscopy, 1,704 had nonadvanced adenoma, and 880 had advanced adenoma. Participants completed no or one to four FIT tests between colonoscopies, with the final colonoscopy performed within 2 years of FIT tests. The median age was 63.9 years; 53.6% were female; 71.1% had a prior adenoma; and 28.9% had a family history of colorectal cancer. A total of 29.4% of participants had one negative FIT; 6.9% had four negative FITs during the interval period; and 31.0% did not complete any FIT tests.
Of follow-up colonoscopies, 9.9% revealed advanced adenomas. Among the patients with no prior neoplasia, those with one negative FIT had a cumulative index function for advanced neoplasia at 5 years of 8.5% (95% confidence interval, 4.9%-13.3%). This was higher than for those with three negative FITs (4.5%; 95% CI, 2.0%-8.6%) or four negative FITs (1.9%; 95% CI, 0.5%-5.0%). The association held for individuals with prior nonadvanced adenoma but not those with advanced adenoma.
Over the 5-year interval, three or more negative FIT tests were associated with a 50%-70% reduction in advanced neoplasia risk at follow-up colonoscopy (P < .001). There was no significant association over a 3-year interval. Dr. Kanth, Dr. Serrao, and Dr. Ness have no relevant financial disclosures.
In a new retrospective analysis of patients with above-average risk of colorectal cancer, multiple negative fecal immunohistochemical tests (FITs) were associated with a lower risk of advanced neoplasia. The findings suggest that multiple negative FITs could potentially identify individuals in high-risk surveillance who aren’t truly high risk, which could in turn ease the logjam of colonoscopies and free resources for truly high-risk individuals.
The study, conducted in Australia, was published online in Clinical Gastroenterology and Hepatology. It included patients who completed at least two FIT exams between surveillance colonoscopies and had no neoplasia or nonadvanced adenoma at prior colonoscopy. Above-average risk was defined as a family history or by findings at surveillance colonoscopy.
The study has some limitations. It is a retrospective analysis between the years 2008 and 2019, and colonoscopy guidelines in the United States have since changed, with a recommendation of surveillance colonoscopy at 7-10 years following 1-2 adenomas discovered at surveillance colonoscopy, and the current study includes follow-up colonoscopy at 5 years. “These data are informative for patients up to 5 years, but they’re not really informative afterwards. They just don’t have those data yet,” said Reed Ness, MD, who was asked to comment on the study.
The authors also don’t describe what they mean by a family history of colorectal cancer risk. “My take was that it’s an interesting result which would seem to support the possibility of returning some patients with a family history or adenoma history to a noncolonoscopy screening regimen after a negative surveillance colonoscopy. We’ll need to see where the data lead us in the future,” said Dr. Ness, who is an associate professor of medicine at Vanderbilt University Medical Center, Nashville, Tenn.
“We’re letting people go 10 years now, and some people are uncomfortable with allowing patients to go 10 years. So you could think of a scenario where you use FIT to try to find people that might have higher-risk lesions that need to come back for colonoscopy within that 10 years,” said Dr. Ness. That issue is particularly relevant given the wide range of adenoma detection rates among gastroenterologists, because FIT could detect a polyp that was missed during a colonoscopy.
The study included two groups with increased risk – those with a family history of colon cancer, and those with previously detected adenomas. The family history cohort may be useful for clinical practice, according to Priyanka Kanth, MD, who was also asked to comment on the study. “Some people may not need [a colonoscopy] at 5 years if they have no polyps found and negative FIT,” said Dr. Kanth, who is an associate professor of gastroenterology at Georgetown University, Washington.
She feels less certain about the group with previously detected adenomas, given the change in U.S. guidelines. “We have already changed that, so I don’t think we need to really do FIT intervals for that cohort,” said Dr. Kanth. “I think this is a good study that has a lot of information and also reassures us that we don’t need such frequent colonoscopy surveillance,” she added.
Steve Serrao, MD, PhD, who was also asked for comment, emphasized the importance of high-quality colonoscopies that reach the cecum 95% of the time, and achieving high adenoma-detection rates. The system can get overwhelmed conducting colonoscopies on patients with good insurance coverage who have already undergone high-quality colonoscopies. “That pushes out patients that haven’t necessarily had a colonoscopy or a FIT. People who don’t have access are kind of crowded out by these false-positive tests. The best modality is actually to do a high-quality colonoscopy and then to have a really well-directed strategy following that colonoscopy,” said Dr. Serrao, who is division chief of gastroenterology and hepatology at Riverside University Health System, Moreno Valley, Calif.
The researchers analyzed data from 4,021 surveillance intervals and 3,369 participants. A total of 1,436 had no neoplasia at the prior colonoscopy, 1,704 had nonadvanced adenoma, and 880 had advanced adenoma. Participants completed no or one to four FIT tests between colonoscopies, with the final colonoscopy performed within 2 years of FIT tests. The median age was 63.9 years; 53.6% were female; 71.1% had a prior adenoma; and 28.9% had a family history of colorectal cancer. A total of 29.4% of participants had one negative FIT; 6.9% had four negative FITs during the interval period; and 31.0% did not complete any FIT tests.
Of follow-up colonoscopies, 9.9% revealed advanced adenomas. Among the patients with no prior neoplasia, those with one negative FIT had a cumulative index function for advanced neoplasia at 5 years of 8.5% (95% confidence interval, 4.9%-13.3%). This was higher than for those with three negative FITs (4.5%; 95% CI, 2.0%-8.6%) or four negative FITs (1.9%; 95% CI, 0.5%-5.0%). The association held for individuals with prior nonadvanced adenoma but not those with advanced adenoma.
Over the 5-year interval, three or more negative FIT tests were associated with a 50%-70% reduction in advanced neoplasia risk at follow-up colonoscopy (P < .001). There was no significant association over a 3-year interval. Dr. Kanth, Dr. Serrao, and Dr. Ness have no relevant financial disclosures.
In a new retrospective analysis of patients with above-average risk of colorectal cancer, multiple negative fecal immunohistochemical tests (FITs) were associated with a lower risk of advanced neoplasia. The findings suggest that multiple negative FITs could potentially identify individuals in high-risk surveillance who aren’t truly high risk, which could in turn ease the logjam of colonoscopies and free resources for truly high-risk individuals.
The study, conducted in Australia, was published online in Clinical Gastroenterology and Hepatology. It included patients who completed at least two FIT exams between surveillance colonoscopies and had no neoplasia or nonadvanced adenoma at prior colonoscopy. Above-average risk was defined as a family history or by findings at surveillance colonoscopy.
The study has some limitations. It is a retrospective analysis between the years 2008 and 2019, and colonoscopy guidelines in the United States have since changed, with a recommendation of surveillance colonoscopy at 7-10 years following 1-2 adenomas discovered at surveillance colonoscopy, and the current study includes follow-up colonoscopy at 5 years. “These data are informative for patients up to 5 years, but they’re not really informative afterwards. They just don’t have those data yet,” said Reed Ness, MD, who was asked to comment on the study.
The authors also don’t describe what they mean by a family history of colorectal cancer risk. “My take was that it’s an interesting result which would seem to support the possibility of returning some patients with a family history or adenoma history to a noncolonoscopy screening regimen after a negative surveillance colonoscopy. We’ll need to see where the data lead us in the future,” said Dr. Ness, who is an associate professor of medicine at Vanderbilt University Medical Center, Nashville, Tenn.
“We’re letting people go 10 years now, and some people are uncomfortable with allowing patients to go 10 years. So you could think of a scenario where you use FIT to try to find people that might have higher-risk lesions that need to come back for colonoscopy within that 10 years,” said Dr. Ness. That issue is particularly relevant given the wide range of adenoma detection rates among gastroenterologists, because FIT could detect a polyp that was missed during a colonoscopy.
The study included two groups with increased risk – those with a family history of colon cancer, and those with previously detected adenomas. The family history cohort may be useful for clinical practice, according to Priyanka Kanth, MD, who was also asked to comment on the study. “Some people may not need [a colonoscopy] at 5 years if they have no polyps found and negative FIT,” said Dr. Kanth, who is an associate professor of gastroenterology at Georgetown University, Washington.
She feels less certain about the group with previously detected adenomas, given the change in U.S. guidelines. “We have already changed that, so I don’t think we need to really do FIT intervals for that cohort,” said Dr. Kanth. “I think this is a good study that has a lot of information and also reassures us that we don’t need such frequent colonoscopy surveillance,” she added.
Steve Serrao, MD, PhD, who was also asked for comment, emphasized the importance of high-quality colonoscopies that reach the cecum 95% of the time, and achieving high adenoma-detection rates. The system can get overwhelmed conducting colonoscopies on patients with good insurance coverage who have already undergone high-quality colonoscopies. “That pushes out patients that haven’t necessarily had a colonoscopy or a FIT. People who don’t have access are kind of crowded out by these false-positive tests. The best modality is actually to do a high-quality colonoscopy and then to have a really well-directed strategy following that colonoscopy,” said Dr. Serrao, who is division chief of gastroenterology and hepatology at Riverside University Health System, Moreno Valley, Calif.
The researchers analyzed data from 4,021 surveillance intervals and 3,369 participants. A total of 1,436 had no neoplasia at the prior colonoscopy, 1,704 had nonadvanced adenoma, and 880 had advanced adenoma. Participants completed no or one to four FIT tests between colonoscopies, with the final colonoscopy performed within 2 years of FIT tests. The median age was 63.9 years; 53.6% were female; 71.1% had a prior adenoma; and 28.9% had a family history of colorectal cancer. A total of 29.4% of participants had one negative FIT; 6.9% had four negative FITs during the interval period; and 31.0% did not complete any FIT tests.
Of follow-up colonoscopies, 9.9% revealed advanced adenomas. Among the patients with no prior neoplasia, those with one negative FIT had a cumulative index function for advanced neoplasia at 5 years of 8.5% (95% confidence interval, 4.9%-13.3%). This was higher than for those with three negative FITs (4.5%; 95% CI, 2.0%-8.6%) or four negative FITs (1.9%; 95% CI, 0.5%-5.0%). The association held for individuals with prior nonadvanced adenoma but not those with advanced adenoma.
Over the 5-year interval, three or more negative FIT tests were associated with a 50%-70% reduction in advanced neoplasia risk at follow-up colonoscopy (P < .001). There was no significant association over a 3-year interval. Dr. Kanth, Dr. Serrao, and Dr. Ness have no relevant financial disclosures.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
It’s all about the brains: Guilt placebos, transplants, and negative feelings
Guilt reduction, now in deceptive and open-secret forms
Guilt plagues a lot of us, sometimes regularly. Maybe you felt bad about eating the leftovers that your partner was looking forward to eating at the end of the day. Or for not saving a seat for your friend who was running late to the movies. Maybe even hiding a secret that you know would hurt a person’s feelings. We’ve all felt it, and it doesn’t feel good.
But what if there was a pill that would make those feelings seem to hurt less? There’s already a pill for almost everything, right?
Well, researchers from the University of Basel are on the case and have conducted a study suggesting that a placebo might work. They asked participants to write down a time they felt super guilty about something, just to stir up those feelings again, then they were divided into three groups. One group was told they would receive real medication that was actually a placebo, one was told they would get a placebo, and one got nothing. The subjects’ guilty feelings were reduced in both the medication-that-was-really-a-placebo group and placebo-that-was-a-placebo group.
“Our study therefore supports the intriguing finding that placebos work even when they are administered openly, and that explanation of the treatment is key to its effectiveness,” lead author Dilan Sezer said in a written statement.
More research is needed, but the human mind is a very interesting place. It seems like we can convince ourselves of just about anything. Especially to feel less guilty.
It’s a mad, mad, mad, mad scientist’s world
Mad scientists. Life’s just more interesting with a few of them running around, but they’re mostly relegated to works of fiction. Real life is boring; we don’t actually have neurosurgeons going around claiming human brain transplant is technically feasible.
Best of all, this isn’t even Dr. Sergio Canavero’s first rodeo with mad science: In 2015 he claimed human head transplants were technically feasible, and in the past few years has claimed to have rehearsed head transplants on cadavers and successfully repaired spinal cord injuries in animals. Lots of claims in there, but precious little evidence. And contrary to what everyone at the head enhancement clinic says, people will notice if you start going around with a new head.
But let’s get back to brains. Ignoring the fact that brain transplant sounds like a zombie with a PhD nibbling on your skull, the article does appear in a peer-reviewed journal. So surely there’s some level of legitimacy. After all, it’s not like Dr. Canavero is an editor for this journal. [Editor’s note: By that we mean he is an editor for the journal.]
Man, he’s taking all the fun out of this.
Anyway, now that we’ve prefaced this with the mother of all caveats, what exactly is Dr. Canavero proposing with his brain transplant? It’s pretty simple: Just have a robot scoop out the first brain and place it into a fresh body, either a donated but moribund younger body or a cloned body. Reconnect all the nerves and vasculature and you’re good to go. Enjoy your wine and laugh in the face of death.
Naturally, such a … bold proposal is lacking in the details, but who cares about details, anyway? This is mad science, not respectable science. Professionals have standards. And if we hear that a human brain transplant was successfully completed on a non–dark and stormy night and the doctor didn’t cackle madly “It’s alive! It’s alive!” then honestly, what even was the point?
Ambivalence rules!
As the office’s unofficial Sith lord/Star Wars nerd, LOTME takes notice when science extols the benefits of unhappiness: “It’s good to be grumpy: Bad moods make us more detail-oriented, study shows.”
The investigators manipulated the emotions of participants by having them watch a clip from “Sophie’s Choice” or one from “Friends.” Then the subjects listened to short, emotionally neutral stories, some of which contained inconsistencies, with the text displayed on a computer screen. Sorry to say, gang at Central Perk, but round one went to the sad movie.
“When people are in a negative mood, they are more careful and analytical. They scrutinize what’s actually stated in a text, and they don’t just fall back on their default world knowledge,” lead author Vicky Lai, PhD, of the University of Arizona said in a statement from the school.
Negative mood. Careful and analytical. Grumpy is good.
You’ve fallen into Darth Science’s little trap, and we have you now.
A study conducted at the University of Geneva offers a slightly different conclusion. And by slightly different, we mean completely different. People over age 65 who watched a series of short TV clips depicting people in a state of emotional suffering experienced excessive modification of their neuronal connections, compared with those who watched emotionally neutral videos.
The brains of these subjects remained “frozen in a negative state by relating the suffering of others to their own emotional memories,” lead author Sebastian Baez Lugo said in a written release from the university.
Emotional suffering. Frozen brains. Grumpy is … not good?
So there you have it. Darth Science’s lesson for the day: A negative mood makes you careful and analytical, but negative thoughts are bad for your brain.
Guilt reduction, now in deceptive and open-secret forms
Guilt plagues a lot of us, sometimes regularly. Maybe you felt bad about eating the leftovers that your partner was looking forward to eating at the end of the day. Or for not saving a seat for your friend who was running late to the movies. Maybe even hiding a secret that you know would hurt a person’s feelings. We’ve all felt it, and it doesn’t feel good.
But what if there was a pill that would make those feelings seem to hurt less? There’s already a pill for almost everything, right?
Well, researchers from the University of Basel are on the case and have conducted a study suggesting that a placebo might work. They asked participants to write down a time they felt super guilty about something, just to stir up those feelings again, then they were divided into three groups. One group was told they would receive real medication that was actually a placebo, one was told they would get a placebo, and one got nothing. The subjects’ guilty feelings were reduced in both the medication-that-was-really-a-placebo group and placebo-that-was-a-placebo group.
“Our study therefore supports the intriguing finding that placebos work even when they are administered openly, and that explanation of the treatment is key to its effectiveness,” lead author Dilan Sezer said in a written statement.
More research is needed, but the human mind is a very interesting place. It seems like we can convince ourselves of just about anything. Especially to feel less guilty.
It’s a mad, mad, mad, mad scientist’s world
Mad scientists. Life’s just more interesting with a few of them running around, but they’re mostly relegated to works of fiction. Real life is boring; we don’t actually have neurosurgeons going around claiming human brain transplant is technically feasible.
Best of all, this isn’t even Dr. Sergio Canavero’s first rodeo with mad science: In 2015 he claimed human head transplants were technically feasible, and in the past few years has claimed to have rehearsed head transplants on cadavers and successfully repaired spinal cord injuries in animals. Lots of claims in there, but precious little evidence. And contrary to what everyone at the head enhancement clinic says, people will notice if you start going around with a new head.
But let’s get back to brains. Ignoring the fact that brain transplant sounds like a zombie with a PhD nibbling on your skull, the article does appear in a peer-reviewed journal. So surely there’s some level of legitimacy. After all, it’s not like Dr. Canavero is an editor for this journal. [Editor’s note: By that we mean he is an editor for the journal.]
Man, he’s taking all the fun out of this.
Anyway, now that we’ve prefaced this with the mother of all caveats, what exactly is Dr. Canavero proposing with his brain transplant? It’s pretty simple: Just have a robot scoop out the first brain and place it into a fresh body, either a donated but moribund younger body or a cloned body. Reconnect all the nerves and vasculature and you’re good to go. Enjoy your wine and laugh in the face of death.
Naturally, such a … bold proposal is lacking in the details, but who cares about details, anyway? This is mad science, not respectable science. Professionals have standards. And if we hear that a human brain transplant was successfully completed on a non–dark and stormy night and the doctor didn’t cackle madly “It’s alive! It’s alive!” then honestly, what even was the point?
Ambivalence rules!
As the office’s unofficial Sith lord/Star Wars nerd, LOTME takes notice when science extols the benefits of unhappiness: “It’s good to be grumpy: Bad moods make us more detail-oriented, study shows.”
The investigators manipulated the emotions of participants by having them watch a clip from “Sophie’s Choice” or one from “Friends.” Then the subjects listened to short, emotionally neutral stories, some of which contained inconsistencies, with the text displayed on a computer screen. Sorry to say, gang at Central Perk, but round one went to the sad movie.
“When people are in a negative mood, they are more careful and analytical. They scrutinize what’s actually stated in a text, and they don’t just fall back on their default world knowledge,” lead author Vicky Lai, PhD, of the University of Arizona said in a statement from the school.
Negative mood. Careful and analytical. Grumpy is good.
You’ve fallen into Darth Science’s little trap, and we have you now.
A study conducted at the University of Geneva offers a slightly different conclusion. And by slightly different, we mean completely different. People over age 65 who watched a series of short TV clips depicting people in a state of emotional suffering experienced excessive modification of their neuronal connections, compared with those who watched emotionally neutral videos.
The brains of these subjects remained “frozen in a negative state by relating the suffering of others to their own emotional memories,” lead author Sebastian Baez Lugo said in a written release from the university.
Emotional suffering. Frozen brains. Grumpy is … not good?
So there you have it. Darth Science’s lesson for the day: A negative mood makes you careful and analytical, but negative thoughts are bad for your brain.
Guilt reduction, now in deceptive and open-secret forms
Guilt plagues a lot of us, sometimes regularly. Maybe you felt bad about eating the leftovers that your partner was looking forward to eating at the end of the day. Or for not saving a seat for your friend who was running late to the movies. Maybe even hiding a secret that you know would hurt a person’s feelings. We’ve all felt it, and it doesn’t feel good.
But what if there was a pill that would make those feelings seem to hurt less? There’s already a pill for almost everything, right?
Well, researchers from the University of Basel are on the case and have conducted a study suggesting that a placebo might work. They asked participants to write down a time they felt super guilty about something, just to stir up those feelings again, then they were divided into three groups. One group was told they would receive real medication that was actually a placebo, one was told they would get a placebo, and one got nothing. The subjects’ guilty feelings were reduced in both the medication-that-was-really-a-placebo group and placebo-that-was-a-placebo group.
“Our study therefore supports the intriguing finding that placebos work even when they are administered openly, and that explanation of the treatment is key to its effectiveness,” lead author Dilan Sezer said in a written statement.
More research is needed, but the human mind is a very interesting place. It seems like we can convince ourselves of just about anything. Especially to feel less guilty.
It’s a mad, mad, mad, mad scientist’s world
Mad scientists. Life’s just more interesting with a few of them running around, but they’re mostly relegated to works of fiction. Real life is boring; we don’t actually have neurosurgeons going around claiming human brain transplant is technically feasible.
Best of all, this isn’t even Dr. Sergio Canavero’s first rodeo with mad science: In 2015 he claimed human head transplants were technically feasible, and in the past few years has claimed to have rehearsed head transplants on cadavers and successfully repaired spinal cord injuries in animals. Lots of claims in there, but precious little evidence. And contrary to what everyone at the head enhancement clinic says, people will notice if you start going around with a new head.
But let’s get back to brains. Ignoring the fact that brain transplant sounds like a zombie with a PhD nibbling on your skull, the article does appear in a peer-reviewed journal. So surely there’s some level of legitimacy. After all, it’s not like Dr. Canavero is an editor for this journal. [Editor’s note: By that we mean he is an editor for the journal.]
Man, he’s taking all the fun out of this.
Anyway, now that we’ve prefaced this with the mother of all caveats, what exactly is Dr. Canavero proposing with his brain transplant? It’s pretty simple: Just have a robot scoop out the first brain and place it into a fresh body, either a donated but moribund younger body or a cloned body. Reconnect all the nerves and vasculature and you’re good to go. Enjoy your wine and laugh in the face of death.
Naturally, such a … bold proposal is lacking in the details, but who cares about details, anyway? This is mad science, not respectable science. Professionals have standards. And if we hear that a human brain transplant was successfully completed on a non–dark and stormy night and the doctor didn’t cackle madly “It’s alive! It’s alive!” then honestly, what even was the point?
Ambivalence rules!
As the office’s unofficial Sith lord/Star Wars nerd, LOTME takes notice when science extols the benefits of unhappiness: “It’s good to be grumpy: Bad moods make us more detail-oriented, study shows.”
The investigators manipulated the emotions of participants by having them watch a clip from “Sophie’s Choice” or one from “Friends.” Then the subjects listened to short, emotionally neutral stories, some of which contained inconsistencies, with the text displayed on a computer screen. Sorry to say, gang at Central Perk, but round one went to the sad movie.
“When people are in a negative mood, they are more careful and analytical. They scrutinize what’s actually stated in a text, and they don’t just fall back on their default world knowledge,” lead author Vicky Lai, PhD, of the University of Arizona said in a statement from the school.
Negative mood. Careful and analytical. Grumpy is good.
You’ve fallen into Darth Science’s little trap, and we have you now.
A study conducted at the University of Geneva offers a slightly different conclusion. And by slightly different, we mean completely different. People over age 65 who watched a series of short TV clips depicting people in a state of emotional suffering experienced excessive modification of their neuronal connections, compared with those who watched emotionally neutral videos.
The brains of these subjects remained “frozen in a negative state by relating the suffering of others to their own emotional memories,” lead author Sebastian Baez Lugo said in a written release from the university.
Emotional suffering. Frozen brains. Grumpy is … not good?
So there you have it. Darth Science’s lesson for the day: A negative mood makes you careful and analytical, but negative thoughts are bad for your brain.
Mothers with disabilities less likely to start breastfeeding
Mothers with intellectual or developmental disabilities are less likely to initiate breastfeeding and to receive in-hospital breastfeeding support than are those without a disability, new data suggest.
In a population-based cohort study of more than 600,000 mothers, patients with an intellectual or developmental disability were about 18% less likely to have a chance to initiate breastfeeding during their hospital stay.
“Overall, we did see lower rates of breastfeeding practices and supports in people with intellectual and developmental disabilities, as well as those with multiple disabilities, compared to people without disabilities,” study author Hilary K. Brown, PhD, assistant professor of health and society at University of Toronto Scarborough in Ontario, told this news organization.
The study was published in The Lancet Public Health.
Disparities in breastfeeding
“There hasn’t been a lot of research on breastfeeding outcomes in people with disabilities,” said Dr. Brown, who noted that the study outcomes were based on the WHO-UNICEF Baby Friendly Hospital Initiative guidelines. “There have been a number of qualitative studies that have suggested that they do experience barriers accessing care related to breastfeeding and different challenges related to breastfeeding. But as far as quantitative outcomes, there has only been a handful of studies.”
To examine these outcomes, the investigators analyzed health administrative data from Ontario. They included in their analysis all birthing parents aged 15-49 years who had a single live birth between April 1, 2012, and March 31, 2018. Patients with a physical disability, sensory disability, intellectual or developmental disability, or two or more disabilities were identified via diagnostic algorithms and were compared with individuals without disabilities with respect to the opportunity to initiate breastfeeding, to engage in in-hospital breastfeeding, to engage in exclusive breastfeeding at hospital discharge, to have skin-to-skin contact, and to be provided with breastfeeding assistance.
The investigators considered a physical disability to encompass conditions such as congenital anomalies, musculoskeletal disorders, neurologic disorders, or permanent injuries. They defined sensory disability as hearing loss or vision loss. Intellectual or developmental disability was defined as having autism spectrum disorder, chromosomal anomaly, fetal alcohol spectrum disorder, or other intellectual disability. Patients with multiple disabilities had two or more of these conditions.
The study population included 634,111 birthing parents, of whom 54,476 (8.6%) had a physical disability, 19,227 (3.0%) had a sensory disability, 1,048 (0.2%) had an intellectual or developmental disability, 4,050 (0.6%) had multiple disabilities, and 555,310 (87.6%) had no disability.
The investigators found that patients with intellectual or developmental disabilities were less likely than were those without a disability to have an opportunity to initiate breastfeeding (adjusted relative risk [aRR], 0.82), to engage in any in-hospital breastfeeding (aRR, 0.85), to be breastfeeding exclusively at hospital discharge (aRR, 0.73), to have skin-to-skin contact (aRR, 0.90), and to receive breastfeeding assistance (aRR, 0.85) compared with patients without a disability.
They also found that individuals with multiple disabilities were less likely to have an opportunity to initiate breastfeeding (aRR, 0.93), to engage in any in-hospital breastfeeding (aRR, 0.93), to be exclusively breastfeeding at hospital discharge (aRR, 0.90), to have skin-to-skin contact (aRR, 0.93), and to receive breastfeeding assistance (aRR, 0.95) compared with patients without a disability.
An understudied population
Commenting on the study, Lori Feldman-Winter, MD, MPH, professor of pediatrics at Rowan University in Camden, N.J., said that one of its strengths is that it included patients who may be excluded from studies of breastfeeding practices. The finding of few differences in breastfeeding practices and supports for people with physical and sensory disabilities, compared with those without disabilities, was positive, she added.
“This is an understudied population, and it is important to call out that there may be practices related to breastfeeding care that suffer, due to implicit bias regarding persons with intellectual and multiple disabilities,” said Dr. Feldman-Winter. “The good news is that other disabilities did not show the same disparities. This study also shows how important it is to measure potential gaps in care across multiple sociodemographic and other variables, such as disabilities, to ensure equitable and inclusive care.”
Health care professionals need to be aware of disparities in breastfeeding care, she added. They need to be open to exploring potential biases when it comes to providing equitable care.
R. Douglas Wilson, MD, president of the Society of Obstetricians and Gynaecologists of Canada and professor emeritus of obstetrics and gynecology at the University of Calgary in Alberta, noted that the size of the cohort represents a strength of the study and that the findings suggest the possible need for closer follow-up of a new mother who is breastfeeding and who has an intellectual disability or multiple disabilities.
“You might keep that patient in hospital for an extra day, and then the home care nurse may look in on them more frequently than they would for someone who does not need that extra oversight,” said Dr. Wilson. When their patients are pregnant, obstetricians and gynecologists can find out whether their patients intend to breastfeed and put them in touch with nurses or lactation consultants to assist them, he added.
The study was funded by the National Institutes of Health and the Canada Research Chairs Program. Dr. Brown, Dr. Feldman-Winter, and Dr. Wilson reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Mothers with intellectual or developmental disabilities are less likely to initiate breastfeeding and to receive in-hospital breastfeeding support than are those without a disability, new data suggest.
In a population-based cohort study of more than 600,000 mothers, patients with an intellectual or developmental disability were about 18% less likely to have a chance to initiate breastfeeding during their hospital stay.
“Overall, we did see lower rates of breastfeeding practices and supports in people with intellectual and developmental disabilities, as well as those with multiple disabilities, compared to people without disabilities,” study author Hilary K. Brown, PhD, assistant professor of health and society at University of Toronto Scarborough in Ontario, told this news organization.
The study was published in The Lancet Public Health.
Disparities in breastfeeding
“There hasn’t been a lot of research on breastfeeding outcomes in people with disabilities,” said Dr. Brown, who noted that the study outcomes were based on the WHO-UNICEF Baby Friendly Hospital Initiative guidelines. “There have been a number of qualitative studies that have suggested that they do experience barriers accessing care related to breastfeeding and different challenges related to breastfeeding. But as far as quantitative outcomes, there has only been a handful of studies.”
To examine these outcomes, the investigators analyzed health administrative data from Ontario. They included in their analysis all birthing parents aged 15-49 years who had a single live birth between April 1, 2012, and March 31, 2018. Patients with a physical disability, sensory disability, intellectual or developmental disability, or two or more disabilities were identified via diagnostic algorithms and were compared with individuals without disabilities with respect to the opportunity to initiate breastfeeding, to engage in in-hospital breastfeeding, to engage in exclusive breastfeeding at hospital discharge, to have skin-to-skin contact, and to be provided with breastfeeding assistance.
The investigators considered a physical disability to encompass conditions such as congenital anomalies, musculoskeletal disorders, neurologic disorders, or permanent injuries. They defined sensory disability as hearing loss or vision loss. Intellectual or developmental disability was defined as having autism spectrum disorder, chromosomal anomaly, fetal alcohol spectrum disorder, or other intellectual disability. Patients with multiple disabilities had two or more of these conditions.
The study population included 634,111 birthing parents, of whom 54,476 (8.6%) had a physical disability, 19,227 (3.0%) had a sensory disability, 1,048 (0.2%) had an intellectual or developmental disability, 4,050 (0.6%) had multiple disabilities, and 555,310 (87.6%) had no disability.
The investigators found that patients with intellectual or developmental disabilities were less likely than were those without a disability to have an opportunity to initiate breastfeeding (adjusted relative risk [aRR], 0.82), to engage in any in-hospital breastfeeding (aRR, 0.85), to be breastfeeding exclusively at hospital discharge (aRR, 0.73), to have skin-to-skin contact (aRR, 0.90), and to receive breastfeeding assistance (aRR, 0.85) compared with patients without a disability.
They also found that individuals with multiple disabilities were less likely to have an opportunity to initiate breastfeeding (aRR, 0.93), to engage in any in-hospital breastfeeding (aRR, 0.93), to be exclusively breastfeeding at hospital discharge (aRR, 0.90), to have skin-to-skin contact (aRR, 0.93), and to receive breastfeeding assistance (aRR, 0.95) compared with patients without a disability.
An understudied population
Commenting on the study, Lori Feldman-Winter, MD, MPH, professor of pediatrics at Rowan University in Camden, N.J., said that one of its strengths is that it included patients who may be excluded from studies of breastfeeding practices. The finding of few differences in breastfeeding practices and supports for people with physical and sensory disabilities, compared with those without disabilities, was positive, she added.
“This is an understudied population, and it is important to call out that there may be practices related to breastfeeding care that suffer, due to implicit bias regarding persons with intellectual and multiple disabilities,” said Dr. Feldman-Winter. “The good news is that other disabilities did not show the same disparities. This study also shows how important it is to measure potential gaps in care across multiple sociodemographic and other variables, such as disabilities, to ensure equitable and inclusive care.”
Health care professionals need to be aware of disparities in breastfeeding care, she added. They need to be open to exploring potential biases when it comes to providing equitable care.
R. Douglas Wilson, MD, president of the Society of Obstetricians and Gynaecologists of Canada and professor emeritus of obstetrics and gynecology at the University of Calgary in Alberta, noted that the size of the cohort represents a strength of the study and that the findings suggest the possible need for closer follow-up of a new mother who is breastfeeding and who has an intellectual disability or multiple disabilities.
“You might keep that patient in hospital for an extra day, and then the home care nurse may look in on them more frequently than they would for someone who does not need that extra oversight,” said Dr. Wilson. When their patients are pregnant, obstetricians and gynecologists can find out whether their patients intend to breastfeed and put them in touch with nurses or lactation consultants to assist them, he added.
The study was funded by the National Institutes of Health and the Canada Research Chairs Program. Dr. Brown, Dr. Feldman-Winter, and Dr. Wilson reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Mothers with intellectual or developmental disabilities are less likely to initiate breastfeeding and to receive in-hospital breastfeeding support than are those without a disability, new data suggest.
In a population-based cohort study of more than 600,000 mothers, patients with an intellectual or developmental disability were about 18% less likely to have a chance to initiate breastfeeding during their hospital stay.
“Overall, we did see lower rates of breastfeeding practices and supports in people with intellectual and developmental disabilities, as well as those with multiple disabilities, compared to people without disabilities,” study author Hilary K. Brown, PhD, assistant professor of health and society at University of Toronto Scarborough in Ontario, told this news organization.
The study was published in The Lancet Public Health.
Disparities in breastfeeding
“There hasn’t been a lot of research on breastfeeding outcomes in people with disabilities,” said Dr. Brown, who noted that the study outcomes were based on the WHO-UNICEF Baby Friendly Hospital Initiative guidelines. “There have been a number of qualitative studies that have suggested that they do experience barriers accessing care related to breastfeeding and different challenges related to breastfeeding. But as far as quantitative outcomes, there has only been a handful of studies.”
To examine these outcomes, the investigators analyzed health administrative data from Ontario. They included in their analysis all birthing parents aged 15-49 years who had a single live birth between April 1, 2012, and March 31, 2018. Patients with a physical disability, sensory disability, intellectual or developmental disability, or two or more disabilities were identified via diagnostic algorithms and were compared with individuals without disabilities with respect to the opportunity to initiate breastfeeding, to engage in in-hospital breastfeeding, to engage in exclusive breastfeeding at hospital discharge, to have skin-to-skin contact, and to be provided with breastfeeding assistance.
The investigators considered a physical disability to encompass conditions such as congenital anomalies, musculoskeletal disorders, neurologic disorders, or permanent injuries. They defined sensory disability as hearing loss or vision loss. Intellectual or developmental disability was defined as having autism spectrum disorder, chromosomal anomaly, fetal alcohol spectrum disorder, or other intellectual disability. Patients with multiple disabilities had two or more of these conditions.
The study population included 634,111 birthing parents, of whom 54,476 (8.6%) had a physical disability, 19,227 (3.0%) had a sensory disability, 1,048 (0.2%) had an intellectual or developmental disability, 4,050 (0.6%) had multiple disabilities, and 555,310 (87.6%) had no disability.
The investigators found that patients with intellectual or developmental disabilities were less likely than were those without a disability to have an opportunity to initiate breastfeeding (adjusted relative risk [aRR], 0.82), to engage in any in-hospital breastfeeding (aRR, 0.85), to be breastfeeding exclusively at hospital discharge (aRR, 0.73), to have skin-to-skin contact (aRR, 0.90), and to receive breastfeeding assistance (aRR, 0.85) compared with patients without a disability.
They also found that individuals with multiple disabilities were less likely to have an opportunity to initiate breastfeeding (aRR, 0.93), to engage in any in-hospital breastfeeding (aRR, 0.93), to be exclusively breastfeeding at hospital discharge (aRR, 0.90), to have skin-to-skin contact (aRR, 0.93), and to receive breastfeeding assistance (aRR, 0.95) compared with patients without a disability.
An understudied population
Commenting on the study, Lori Feldman-Winter, MD, MPH, professor of pediatrics at Rowan University in Camden, N.J., said that one of its strengths is that it included patients who may be excluded from studies of breastfeeding practices. The finding of few differences in breastfeeding practices and supports for people with physical and sensory disabilities, compared with those without disabilities, was positive, she added.
“This is an understudied population, and it is important to call out that there may be practices related to breastfeeding care that suffer, due to implicit bias regarding persons with intellectual and multiple disabilities,” said Dr. Feldman-Winter. “The good news is that other disabilities did not show the same disparities. This study also shows how important it is to measure potential gaps in care across multiple sociodemographic and other variables, such as disabilities, to ensure equitable and inclusive care.”
Health care professionals need to be aware of disparities in breastfeeding care, she added. They need to be open to exploring potential biases when it comes to providing equitable care.
R. Douglas Wilson, MD, president of the Society of Obstetricians and Gynaecologists of Canada and professor emeritus of obstetrics and gynecology at the University of Calgary in Alberta, noted that the size of the cohort represents a strength of the study and that the findings suggest the possible need for closer follow-up of a new mother who is breastfeeding and who has an intellectual disability or multiple disabilities.
“You might keep that patient in hospital for an extra day, and then the home care nurse may look in on them more frequently than they would for someone who does not need that extra oversight,” said Dr. Wilson. When their patients are pregnant, obstetricians and gynecologists can find out whether their patients intend to breastfeed and put them in touch with nurses or lactation consultants to assist them, he added.
The study was funded by the National Institutes of Health and the Canada Research Chairs Program. Dr. Brown, Dr. Feldman-Winter, and Dr. Wilson reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE LANCET PUBLIC HEALTH
Congenital CMV linked to pediatric hyperdiploid ALL
Children with hyperdiploid acute lymphoblastic leukemia (ALL) are much more likely to also have congenital cytomegalovirus (CMV) infection, according to an analysis published in JAMA Network Open.
Although researchers found no association between ALL and congenital CMV infection overall, pediatric patients diagnosed with hyperdiploid ALL had sixfold greater odds of being positive for congenital CMV than cancer-free controls.
“These findings suggest mixed evidence for an association between congenital CMV infection and ALL” and that “a CMV-ALL association may be specific to hyperdiploid ALL,” said investigators, led by Jennifer Geris, PhD, a postdoctoral associate at Baylor College of Medicine, Houston.
A growing body of evidence suggests that CMV, a member of the herpesvirus family, may be a risk factor for ALL. Although the mechanism remains unclear, congenital CMV may encourage proliferation of CD34+ hematopoietic progenitor cells in bone marrow that are vulnerable to oncogenic transformation.
Two prior independent studies have suggested that prenatal CMV infection is associated with an increased risk of childhood ALL. However, given how common CMV infection is (more than 80% seropositivity worldwide) and the relatively rarity of pediatric ALL, Joseph Wiemels, PhD, argued in an accompanying editorial that CMV can’t be a direct cause of leukemia.
“Instead, CMV may play a supportive role” with infection in some infants altering immune function in a way that increases vulnerability to more direct causes of ALL, explained Dr. Wiemels, professor of population and public health sciences at the University of Southern California, Los Angeles. In other words, “exposure to CMV early rather than fulminant infection” at birth “may be the key epidemiologic feature.”
In the current study, Dr. Geris and colleagues tested dried newborn blood spots from 1189 children with ALL and 4,756 controls matched on age, sex, and mother’s race and ethnicity for the presence of cytomegalovirus at birth. Children were born in Michigan on or after Oct. 1, 1987.
Across the entire study population, congenital CMV was detected in 6 ALL cases (0.5%) and 21 controls (0.4%), with no difference in the odds of congenital CMV infection between the two groups. Among subjects positive for congenital CMV, it was not clear who had fulminant, clinically recognized disease and who did not.
Overall, 2 of 74 cases (2.7%) of hyperdiploid ALL were positive for congenital CMV. Compared with all controls in an unmatched analysis, those with hyperdiploid ALL were 6.26 times more likely to be CMV positive.
Overall, the investigators concluded that the current findings, in combination with previous evidence showing a similar connection, “strongly suggest CMV is associated specifically to hyperdiploid ALL.”
Although “the evidence supporting an association between CMV and ALL is tantalizing and mounting rapidly,” Dr. Wiemels noted that “much additional research attention is required to mechanistically describe pathways by which CMV may influence leukemia before the virus could be considered a potential target for prevention or clinical management of ALL.”
“We are still in the early chapters of the book describing the role of CMV and ALL,” but the virus might emerge as a clinical target “with much future promise for the health and well-being of our children,” he said.
The work was funded by the National Institutes of Health, the University of Minnesota, and the Department of Defense. The investigators and editorialist have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Children with hyperdiploid acute lymphoblastic leukemia (ALL) are much more likely to also have congenital cytomegalovirus (CMV) infection, according to an analysis published in JAMA Network Open.
Although researchers found no association between ALL and congenital CMV infection overall, pediatric patients diagnosed with hyperdiploid ALL had sixfold greater odds of being positive for congenital CMV than cancer-free controls.
“These findings suggest mixed evidence for an association between congenital CMV infection and ALL” and that “a CMV-ALL association may be specific to hyperdiploid ALL,” said investigators, led by Jennifer Geris, PhD, a postdoctoral associate at Baylor College of Medicine, Houston.
A growing body of evidence suggests that CMV, a member of the herpesvirus family, may be a risk factor for ALL. Although the mechanism remains unclear, congenital CMV may encourage proliferation of CD34+ hematopoietic progenitor cells in bone marrow that are vulnerable to oncogenic transformation.
Two prior independent studies have suggested that prenatal CMV infection is associated with an increased risk of childhood ALL. However, given how common CMV infection is (more than 80% seropositivity worldwide) and the relatively rarity of pediatric ALL, Joseph Wiemels, PhD, argued in an accompanying editorial that CMV can’t be a direct cause of leukemia.
“Instead, CMV may play a supportive role” with infection in some infants altering immune function in a way that increases vulnerability to more direct causes of ALL, explained Dr. Wiemels, professor of population and public health sciences at the University of Southern California, Los Angeles. In other words, “exposure to CMV early rather than fulminant infection” at birth “may be the key epidemiologic feature.”
In the current study, Dr. Geris and colleagues tested dried newborn blood spots from 1189 children with ALL and 4,756 controls matched on age, sex, and mother’s race and ethnicity for the presence of cytomegalovirus at birth. Children were born in Michigan on or after Oct. 1, 1987.
Across the entire study population, congenital CMV was detected in 6 ALL cases (0.5%) and 21 controls (0.4%), with no difference in the odds of congenital CMV infection between the two groups. Among subjects positive for congenital CMV, it was not clear who had fulminant, clinically recognized disease and who did not.
Overall, 2 of 74 cases (2.7%) of hyperdiploid ALL were positive for congenital CMV. Compared with all controls in an unmatched analysis, those with hyperdiploid ALL were 6.26 times more likely to be CMV positive.
Overall, the investigators concluded that the current findings, in combination with previous evidence showing a similar connection, “strongly suggest CMV is associated specifically to hyperdiploid ALL.”
Although “the evidence supporting an association between CMV and ALL is tantalizing and mounting rapidly,” Dr. Wiemels noted that “much additional research attention is required to mechanistically describe pathways by which CMV may influence leukemia before the virus could be considered a potential target for prevention or clinical management of ALL.”
“We are still in the early chapters of the book describing the role of CMV and ALL,” but the virus might emerge as a clinical target “with much future promise for the health and well-being of our children,” he said.
The work was funded by the National Institutes of Health, the University of Minnesota, and the Department of Defense. The investigators and editorialist have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Children with hyperdiploid acute lymphoblastic leukemia (ALL) are much more likely to also have congenital cytomegalovirus (CMV) infection, according to an analysis published in JAMA Network Open.
Although researchers found no association between ALL and congenital CMV infection overall, pediatric patients diagnosed with hyperdiploid ALL had sixfold greater odds of being positive for congenital CMV than cancer-free controls.
“These findings suggest mixed evidence for an association between congenital CMV infection and ALL” and that “a CMV-ALL association may be specific to hyperdiploid ALL,” said investigators, led by Jennifer Geris, PhD, a postdoctoral associate at Baylor College of Medicine, Houston.
A growing body of evidence suggests that CMV, a member of the herpesvirus family, may be a risk factor for ALL. Although the mechanism remains unclear, congenital CMV may encourage proliferation of CD34+ hematopoietic progenitor cells in bone marrow that are vulnerable to oncogenic transformation.
Two prior independent studies have suggested that prenatal CMV infection is associated with an increased risk of childhood ALL. However, given how common CMV infection is (more than 80% seropositivity worldwide) and the relatively rarity of pediatric ALL, Joseph Wiemels, PhD, argued in an accompanying editorial that CMV can’t be a direct cause of leukemia.
“Instead, CMV may play a supportive role” with infection in some infants altering immune function in a way that increases vulnerability to more direct causes of ALL, explained Dr. Wiemels, professor of population and public health sciences at the University of Southern California, Los Angeles. In other words, “exposure to CMV early rather than fulminant infection” at birth “may be the key epidemiologic feature.”
In the current study, Dr. Geris and colleagues tested dried newborn blood spots from 1189 children with ALL and 4,756 controls matched on age, sex, and mother’s race and ethnicity for the presence of cytomegalovirus at birth. Children were born in Michigan on or after Oct. 1, 1987.
Across the entire study population, congenital CMV was detected in 6 ALL cases (0.5%) and 21 controls (0.4%), with no difference in the odds of congenital CMV infection between the two groups. Among subjects positive for congenital CMV, it was not clear who had fulminant, clinically recognized disease and who did not.
Overall, 2 of 74 cases (2.7%) of hyperdiploid ALL were positive for congenital CMV. Compared with all controls in an unmatched analysis, those with hyperdiploid ALL were 6.26 times more likely to be CMV positive.
Overall, the investigators concluded that the current findings, in combination with previous evidence showing a similar connection, “strongly suggest CMV is associated specifically to hyperdiploid ALL.”
Although “the evidence supporting an association between CMV and ALL is tantalizing and mounting rapidly,” Dr. Wiemels noted that “much additional research attention is required to mechanistically describe pathways by which CMV may influence leukemia before the virus could be considered a potential target for prevention or clinical management of ALL.”
“We are still in the early chapters of the book describing the role of CMV and ALL,” but the virus might emerge as a clinical target “with much future promise for the health and well-being of our children,” he said.
The work was funded by the National Institutes of Health, the University of Minnesota, and the Department of Defense. The investigators and editorialist have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
How to talk with patients in ways that help them feel heard and understood
How do we become those professionals and make sure that we are doing a good job connecting and communicating with our patients?
Here are a few suggestions on how to do this.
Practice intent listening
When a patient shares their symptoms with you, show genuine curiosity and concern. Ask clarifying questions. Ask how the symptom or problem is affecting their day-to-day life. Avoid quick, rapid-fire questions back at the patient. Do not accept a patient self-diagnosis.
When a patient with a first-time headache says they are having a migraine headache, for example, ask many clarifying questions to make sure you can make a diagnosis of headache type, then use all the information you have gathered to educate the patient on what you believe they have.
It is easy to jump to treatment, but we always want to make sure we have the diagnosis correct first. By intently listening, it also makes it much easier to tell a patient you do not know what is causing their symptoms, but that you and the patient will be vigilant for any future clues that may lead to a diagnosis.
Use terminology that patients understand
Rachael Gotlieb, MD, and colleagues published an excellent study with eye-opening results on common phrases we use as health care providers and how often patients do not understand them.
Only 9% of patients understood what was meant when they were asked if they have been febrile. Only 2% understood what was meant by “I am concerned the patient has an occult infection.” Only 21% understood that “your xray findings were quite impressive” was bad news.
It is easy to avoid these medical language traps, we just have to check our doctor speak. Ask, “Do you have a fever?” Say, “I am concerned you may have an infection that is hard to find.”
Several other terms we use all the time in explaining things to patients that I have found most patients do not understand are the terms bilateral, systemic, and significant. Think carefully as you explain things to patients and check back to have them repeat to you what they think you said.
Be comfortable saying you don’t know
Many symptoms in medicine end up not being diagnosable. When a patient shares symptoms that do not fit a pattern of a disease, it is important to share with them why you think it is okay to wait and watch, even if you do not have a diagnosis.
Patients find it comforting that you are so honest with them. Doing this also has the benefit of gaining patients’ trust when you are sure about something, because it tells them you don’t have an answer for everything.
Ask your patients what they think is causing their symptoms
This way, you know what their big fear is. You can address what they are worried about, even if it isn’t something you are considering.
Patients are often fearful of a disease a close friend or relative has, so when they get new symptoms, they fear diseases that we might not think of. By knowing what they are fearful of, you can reassure when appropriate.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
How do we become those professionals and make sure that we are doing a good job connecting and communicating with our patients?
Here are a few suggestions on how to do this.
Practice intent listening
When a patient shares their symptoms with you, show genuine curiosity and concern. Ask clarifying questions. Ask how the symptom or problem is affecting their day-to-day life. Avoid quick, rapid-fire questions back at the patient. Do not accept a patient self-diagnosis.
When a patient with a first-time headache says they are having a migraine headache, for example, ask many clarifying questions to make sure you can make a diagnosis of headache type, then use all the information you have gathered to educate the patient on what you believe they have.
It is easy to jump to treatment, but we always want to make sure we have the diagnosis correct first. By intently listening, it also makes it much easier to tell a patient you do not know what is causing their symptoms, but that you and the patient will be vigilant for any future clues that may lead to a diagnosis.
Use terminology that patients understand
Rachael Gotlieb, MD, and colleagues published an excellent study with eye-opening results on common phrases we use as health care providers and how often patients do not understand them.
Only 9% of patients understood what was meant when they were asked if they have been febrile. Only 2% understood what was meant by “I am concerned the patient has an occult infection.” Only 21% understood that “your xray findings were quite impressive” was bad news.
It is easy to avoid these medical language traps, we just have to check our doctor speak. Ask, “Do you have a fever?” Say, “I am concerned you may have an infection that is hard to find.”
Several other terms we use all the time in explaining things to patients that I have found most patients do not understand are the terms bilateral, systemic, and significant. Think carefully as you explain things to patients and check back to have them repeat to you what they think you said.
Be comfortable saying you don’t know
Many symptoms in medicine end up not being diagnosable. When a patient shares symptoms that do not fit a pattern of a disease, it is important to share with them why you think it is okay to wait and watch, even if you do not have a diagnosis.
Patients find it comforting that you are so honest with them. Doing this also has the benefit of gaining patients’ trust when you are sure about something, because it tells them you don’t have an answer for everything.
Ask your patients what they think is causing their symptoms
This way, you know what their big fear is. You can address what they are worried about, even if it isn’t something you are considering.
Patients are often fearful of a disease a close friend or relative has, so when they get new symptoms, they fear diseases that we might not think of. By knowing what they are fearful of, you can reassure when appropriate.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
How do we become those professionals and make sure that we are doing a good job connecting and communicating with our patients?
Here are a few suggestions on how to do this.
Practice intent listening
When a patient shares their symptoms with you, show genuine curiosity and concern. Ask clarifying questions. Ask how the symptom or problem is affecting their day-to-day life. Avoid quick, rapid-fire questions back at the patient. Do not accept a patient self-diagnosis.
When a patient with a first-time headache says they are having a migraine headache, for example, ask many clarifying questions to make sure you can make a diagnosis of headache type, then use all the information you have gathered to educate the patient on what you believe they have.
It is easy to jump to treatment, but we always want to make sure we have the diagnosis correct first. By intently listening, it also makes it much easier to tell a patient you do not know what is causing their symptoms, but that you and the patient will be vigilant for any future clues that may lead to a diagnosis.
Use terminology that patients understand
Rachael Gotlieb, MD, and colleagues published an excellent study with eye-opening results on common phrases we use as health care providers and how often patients do not understand them.
Only 9% of patients understood what was meant when they were asked if they have been febrile. Only 2% understood what was meant by “I am concerned the patient has an occult infection.” Only 21% understood that “your xray findings were quite impressive” was bad news.
It is easy to avoid these medical language traps, we just have to check our doctor speak. Ask, “Do you have a fever?” Say, “I am concerned you may have an infection that is hard to find.”
Several other terms we use all the time in explaining things to patients that I have found most patients do not understand are the terms bilateral, systemic, and significant. Think carefully as you explain things to patients and check back to have them repeat to you what they think you said.
Be comfortable saying you don’t know
Many symptoms in medicine end up not being diagnosable. When a patient shares symptoms that do not fit a pattern of a disease, it is important to share with them why you think it is okay to wait and watch, even if you do not have a diagnosis.
Patients find it comforting that you are so honest with them. Doing this also has the benefit of gaining patients’ trust when you are sure about something, because it tells them you don’t have an answer for everything.
Ask your patients what they think is causing their symptoms
This way, you know what their big fear is. You can address what they are worried about, even if it isn’t something you are considering.
Patients are often fearful of a disease a close friend or relative has, so when they get new symptoms, they fear diseases that we might not think of. By knowing what they are fearful of, you can reassure when appropriate.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
Renowned stroke expert Ralph L. Sacco, MD, dies
Ralph L. Sacco, MD, the first neurologist to serve as president of the American Heart Association and the only physician to serve as president of both the AHA and the American Academy of Neurology, died Jan. 17 at the age of 65.
He died of a brain tumor at his home in Amagansett, N.Y., according to an obituary published in Neurology, Circulation, and Stroke.
“Ralph was one of a kind,” Nancy Brown, chief executive officer for the AHA and American Stroke Association, said in a statement. “His leadership was unparalleled, and his warm, generous heart and care transcended his research and clinic to every person fortunate to meet him and likely become a friend,” Ms. Brown said.
In a tweet, Natalia S. Rost, MD, professor of neurology at Harvard Medical School, Boston, called him, “a dear friend, an inspiring colleague, a generous mentor, an astute scientist, a consummate advocate for brain health worldwide.”
Dedicated to improving stroke care
Dr. Sacco was chair of the University of Miami Miller School of Medicine in the department of neurology; the Olemberg Family Chair in Neurological Disorders; professor of neurology, public health sciences, human genetics, and neurosurgery; executive director of the Evelyn F. McKnight Brain Institute; director and multi-principal investigator of the Miami Clinical and Translational Science Institute; and senior associate dean for clinical and translational science.
Dr. Sacco was a population-based researcher in the field of cerebrovascular diseases.
As founder of the Northern Manhattan Study, he paved the way for examining the differences in stroke risk related to race, ethnicity, sex, and neighborhood, and realizing the impact of modifiable lifestyle behaviors, such as alcohol consumption and physical activity, on stroke risk.
Dr. Sacco’s work led to more targeted stroke prevention programs and his “drive and dedication fueled changes that improved stroke research and fostered the development of targeted stroke care delivery, ultimately improving stroke recovery and post-stroke quality of life for many,” the AHA statement said.
Dr. Sacco was also founder and executive director of the Florida Stroke Registry, which consists of 167 Florida stroke centers. He was a member of the National Academy of Medicine.
In an obituary written by Orly Avitzur, MD, current president of the AAN, she notes that he “was the only physician to have become both the president of the AHA (2010-2011) and the AAN (2017-2019), positions that reflected the respect and admiration of professional colleagues earned over the years.”
During his tenure as AAN president, Dr. Sacco led an initiative to ensure that academic neurology, from department chairs to professors to students, knew about the abundance of academy resources available to them, the AAN noted in a statement.
Dr. Sacco was a “strong proponent of enlarging the neurology workforce through the academic pipeline and promoted the concept of the ‘newrologist’ to get people excited in careers in neurology, moving beyond just diagnosis and treatments to include interventions, preventative care, and the future of regenerative care,” the AAN said.
Dr. Sacco received numerous awards throughout his career, most recently the AHA 2022 Distinguished Scientist award. He also received the 2015 Gold Heart Award, the 2011 Distinguished National Leadership Award, and the 2006 William Feinberg Award.
In addition to his husband, Scott Dutcher, Dr. Sacco is survived by his father, Anthony P. Sacco, and his father’s wife, Rosemary; and his four siblings and their families, along with many nieces and nephews.
A version of this article first appeared on Medscape.com.
Ralph L. Sacco, MD, the first neurologist to serve as president of the American Heart Association and the only physician to serve as president of both the AHA and the American Academy of Neurology, died Jan. 17 at the age of 65.
He died of a brain tumor at his home in Amagansett, N.Y., according to an obituary published in Neurology, Circulation, and Stroke.
“Ralph was one of a kind,” Nancy Brown, chief executive officer for the AHA and American Stroke Association, said in a statement. “His leadership was unparalleled, and his warm, generous heart and care transcended his research and clinic to every person fortunate to meet him and likely become a friend,” Ms. Brown said.
In a tweet, Natalia S. Rost, MD, professor of neurology at Harvard Medical School, Boston, called him, “a dear friend, an inspiring colleague, a generous mentor, an astute scientist, a consummate advocate for brain health worldwide.”
Dedicated to improving stroke care
Dr. Sacco was chair of the University of Miami Miller School of Medicine in the department of neurology; the Olemberg Family Chair in Neurological Disorders; professor of neurology, public health sciences, human genetics, and neurosurgery; executive director of the Evelyn F. McKnight Brain Institute; director and multi-principal investigator of the Miami Clinical and Translational Science Institute; and senior associate dean for clinical and translational science.
Dr. Sacco was a population-based researcher in the field of cerebrovascular diseases.
As founder of the Northern Manhattan Study, he paved the way for examining the differences in stroke risk related to race, ethnicity, sex, and neighborhood, and realizing the impact of modifiable lifestyle behaviors, such as alcohol consumption and physical activity, on stroke risk.
Dr. Sacco’s work led to more targeted stroke prevention programs and his “drive and dedication fueled changes that improved stroke research and fostered the development of targeted stroke care delivery, ultimately improving stroke recovery and post-stroke quality of life for many,” the AHA statement said.
Dr. Sacco was also founder and executive director of the Florida Stroke Registry, which consists of 167 Florida stroke centers. He was a member of the National Academy of Medicine.
In an obituary written by Orly Avitzur, MD, current president of the AAN, she notes that he “was the only physician to have become both the president of the AHA (2010-2011) and the AAN (2017-2019), positions that reflected the respect and admiration of professional colleagues earned over the years.”
During his tenure as AAN president, Dr. Sacco led an initiative to ensure that academic neurology, from department chairs to professors to students, knew about the abundance of academy resources available to them, the AAN noted in a statement.
Dr. Sacco was a “strong proponent of enlarging the neurology workforce through the academic pipeline and promoted the concept of the ‘newrologist’ to get people excited in careers in neurology, moving beyond just diagnosis and treatments to include interventions, preventative care, and the future of regenerative care,” the AAN said.
Dr. Sacco received numerous awards throughout his career, most recently the AHA 2022 Distinguished Scientist award. He also received the 2015 Gold Heart Award, the 2011 Distinguished National Leadership Award, and the 2006 William Feinberg Award.
In addition to his husband, Scott Dutcher, Dr. Sacco is survived by his father, Anthony P. Sacco, and his father’s wife, Rosemary; and his four siblings and their families, along with many nieces and nephews.
A version of this article first appeared on Medscape.com.
Ralph L. Sacco, MD, the first neurologist to serve as president of the American Heart Association and the only physician to serve as president of both the AHA and the American Academy of Neurology, died Jan. 17 at the age of 65.
He died of a brain tumor at his home in Amagansett, N.Y., according to an obituary published in Neurology, Circulation, and Stroke.
“Ralph was one of a kind,” Nancy Brown, chief executive officer for the AHA and American Stroke Association, said in a statement. “His leadership was unparalleled, and his warm, generous heart and care transcended his research and clinic to every person fortunate to meet him and likely become a friend,” Ms. Brown said.
In a tweet, Natalia S. Rost, MD, professor of neurology at Harvard Medical School, Boston, called him, “a dear friend, an inspiring colleague, a generous mentor, an astute scientist, a consummate advocate for brain health worldwide.”
Dedicated to improving stroke care
Dr. Sacco was chair of the University of Miami Miller School of Medicine in the department of neurology; the Olemberg Family Chair in Neurological Disorders; professor of neurology, public health sciences, human genetics, and neurosurgery; executive director of the Evelyn F. McKnight Brain Institute; director and multi-principal investigator of the Miami Clinical and Translational Science Institute; and senior associate dean for clinical and translational science.
Dr. Sacco was a population-based researcher in the field of cerebrovascular diseases.
As founder of the Northern Manhattan Study, he paved the way for examining the differences in stroke risk related to race, ethnicity, sex, and neighborhood, and realizing the impact of modifiable lifestyle behaviors, such as alcohol consumption and physical activity, on stroke risk.
Dr. Sacco’s work led to more targeted stroke prevention programs and his “drive and dedication fueled changes that improved stroke research and fostered the development of targeted stroke care delivery, ultimately improving stroke recovery and post-stroke quality of life for many,” the AHA statement said.
Dr. Sacco was also founder and executive director of the Florida Stroke Registry, which consists of 167 Florida stroke centers. He was a member of the National Academy of Medicine.
In an obituary written by Orly Avitzur, MD, current president of the AAN, she notes that he “was the only physician to have become both the president of the AHA (2010-2011) and the AAN (2017-2019), positions that reflected the respect and admiration of professional colleagues earned over the years.”
During his tenure as AAN president, Dr. Sacco led an initiative to ensure that academic neurology, from department chairs to professors to students, knew about the abundance of academy resources available to them, the AAN noted in a statement.
Dr. Sacco was a “strong proponent of enlarging the neurology workforce through the academic pipeline and promoted the concept of the ‘newrologist’ to get people excited in careers in neurology, moving beyond just diagnosis and treatments to include interventions, preventative care, and the future of regenerative care,” the AAN said.
Dr. Sacco received numerous awards throughout his career, most recently the AHA 2022 Distinguished Scientist award. He also received the 2015 Gold Heart Award, the 2011 Distinguished National Leadership Award, and the 2006 William Feinberg Award.
In addition to his husband, Scott Dutcher, Dr. Sacco is survived by his father, Anthony P. Sacco, and his father’s wife, Rosemary; and his four siblings and their families, along with many nieces and nephews.
A version of this article first appeared on Medscape.com.
Simulation-based training effective for transesophageal echo
Simulation-based teaching of transesophageal echocardiography (TEE) improved cardiology fellows’ knowledge, skills, and comfort with the procedure, compared with traditional training, a new study shows.
“TEE learning may be hampered by the lack of availability of teachers and equipment and by the need for esophageal intubation, which is semi-invasive,” Augustin Coisne, MD, PhD, of the Cardiovascular Research Foundation in New York, said in an interview. “In this setting, simulation emerges as a key educational tool, but we were lacking evidence supporting simulation-based educational programs.”
Fellows in the simulation group achieved higher theoretical test scores and practical test scores after the training than did those in the traditional group.
Furthermore, Dr. Coisne said, “the results of the subgroup analyses were surprising and unexpected. The effect of the simulation-based training was greater among fellows at the beginning of fellowship – i.e., 2 years or less of training – in both theoretical and practical tests and in women [versus men] for the theoretical test.”
Their results, from the randomized SIMULATOR study, were published online in JAMA Cardiology.
More ready, more confident
The researchers randomly assigned 324 cardiology fellows (mean age, 26.4 years; about 30% women) inexperienced in TEE from 42 French university centers to TEE training with or without simulation support. Both groups participated in traditional didactic training using e-learning with an online course that is compulsory for all cardiology fellows in France.
The simulation group also participated in two 2-hour teaching sessions using a TEE simulator.
Each fellow completed a theoretical and a practical test prior to training to assess their baseline TEE level and again 3 months after the end of the training program. A TEE simulator (U/S Mentor Simulator; 3D Systems Simbionix) was used for all tests, and 24 certified echocardiography teachers served as both trainers and raters.
The theoretical tests included 20 online video-based questions to evaluate recognition of standard TEE views, normal anatomy, and some pathological cases. Fellows had 90 seconds to choose the best answer for each question from five multiple-choice options.
For the practical tests, fellows had 3 minutes to familiarize themselves with the handling of the simulator, without specific training and before the probe introduction.
They were asked to show 10 basic views on the simulator and had a maximum of 1 minute for each view.
The coprimary outcomes were the scores in the final theoretical and practical tests. TEE duration and the fellows’ self-assessment of their proficiency were also evaluated.
At baseline, the theoretical and practical test scores were similar between the groups (33.0 for the simulator group vs. 32.5 for the traditional group, and 44.2 vs. 46.1, respectively).
After training, the fellows in the simulation group had higher theoretical and practical test scores than those in the traditional group (47.2% vs. 38.3% and 74.5% vs. 59.0%, respectively).
Score changes were consistently higher when the pretraining scores were lower, an association that was stronger in the simulation group.
Dr. Coisne noted that subgroup analyses showed that the effectiveness of the simulation training was greater when performed at the beginning of the fellowship. On the theoretical test, the point increase was 11.9 for the simulation group versus 4.25 points for the traditional training group; for the practical test, the increases were 24.0 points versus 10.1 points.
After training, it took significantly less time for the simulation group to complete a TEE than it did the traditional group (8.3 vs. 9.4 minutes).
Furthermore, simulation group fellows reported that they felt more ready (mean score, 3.0 vs. 1.7) and more confident (mean score, 3.3 vs. 2.4) about performing a TEE alone after training.
“The simulation approach is definitively scalable to every institution,” Dr. Coisne said. “However, a medico-economic analysis should be interesting because the cost of the simulator and its maintenance might be a limitation to spread simulation-based teaching. The possibility for smaller hospitals to pool their financial input to share a TEE simulator could be considered to increase its cost-effectiveness.”
Real-world outcomes required
Commenting on the study, S. Justin Szawlewicz, MD, chair of cardiovascular medicine at Deborah Heart and Lung Center in Brown Mills, N.J., pointed out that the authors indicated that the number of TEEs performed by the trainees was not collected.
“This would be useful information to determine if those who received simulator training sought out and performed more TEEs, and also to determine if cardiology trainees in France perform a similar number of TEEs as cardiology trainees in the United States.”
In addition, he said, “the 4 hours of simulator training in TEE is extra education and experience that the standard trainees didn’t get. Would 4 extra hours of standard training didactics also improve trainees’ scores?”
Noting that the fellows’ ability to perform TEE in real patients was not assessed, Dr. Szawlewicz said, “a study could be designed that evaluated TEE images from real patients to see if trainees receiving simulator training performed better, more comprehensive and efficient TEEs than standard training.”
Nevertheless, he concluded, “Four hours of simulator training appears to improve TEE knowledge and skills. This is something we would consider at our institution.”
Like Dr. Szawlewicz, Michael Spooner, MD, MBA, of Mercy One North Iowa Heart Center in Mason City, and Kathryn Bertlacher, MD, of the University of Pittsburgh Medical Center, noted in a related editorial, “data are not provided about change in the learner’s behavior or performance on an actual TEE after the course, nor are there data about clinical outcomes such as patient safety or completeness of subsequent TEEs.
“This limitation, which is a limitation of most of the existing TEE simulation literature, is a high bar to cross,” they concluded. “Reaching this bar will require studies such as this to provide foundational understanding.”
Twin-Medical provided the TEE simulators. No relevant conflicts of interest were disclosed.
A version of this article first appeared on Medscape.com.
Simulation-based teaching of transesophageal echocardiography (TEE) improved cardiology fellows’ knowledge, skills, and comfort with the procedure, compared with traditional training, a new study shows.
“TEE learning may be hampered by the lack of availability of teachers and equipment and by the need for esophageal intubation, which is semi-invasive,” Augustin Coisne, MD, PhD, of the Cardiovascular Research Foundation in New York, said in an interview. “In this setting, simulation emerges as a key educational tool, but we were lacking evidence supporting simulation-based educational programs.”
Fellows in the simulation group achieved higher theoretical test scores and practical test scores after the training than did those in the traditional group.
Furthermore, Dr. Coisne said, “the results of the subgroup analyses were surprising and unexpected. The effect of the simulation-based training was greater among fellows at the beginning of fellowship – i.e., 2 years or less of training – in both theoretical and practical tests and in women [versus men] for the theoretical test.”
Their results, from the randomized SIMULATOR study, were published online in JAMA Cardiology.
More ready, more confident
The researchers randomly assigned 324 cardiology fellows (mean age, 26.4 years; about 30% women) inexperienced in TEE from 42 French university centers to TEE training with or without simulation support. Both groups participated in traditional didactic training using e-learning with an online course that is compulsory for all cardiology fellows in France.
The simulation group also participated in two 2-hour teaching sessions using a TEE simulator.
Each fellow completed a theoretical and a practical test prior to training to assess their baseline TEE level and again 3 months after the end of the training program. A TEE simulator (U/S Mentor Simulator; 3D Systems Simbionix) was used for all tests, and 24 certified echocardiography teachers served as both trainers and raters.
The theoretical tests included 20 online video-based questions to evaluate recognition of standard TEE views, normal anatomy, and some pathological cases. Fellows had 90 seconds to choose the best answer for each question from five multiple-choice options.
For the practical tests, fellows had 3 minutes to familiarize themselves with the handling of the simulator, without specific training and before the probe introduction.
They were asked to show 10 basic views on the simulator and had a maximum of 1 minute for each view.
The coprimary outcomes were the scores in the final theoretical and practical tests. TEE duration and the fellows’ self-assessment of their proficiency were also evaluated.
At baseline, the theoretical and practical test scores were similar between the groups (33.0 for the simulator group vs. 32.5 for the traditional group, and 44.2 vs. 46.1, respectively).
After training, the fellows in the simulation group had higher theoretical and practical test scores than those in the traditional group (47.2% vs. 38.3% and 74.5% vs. 59.0%, respectively).
Score changes were consistently higher when the pretraining scores were lower, an association that was stronger in the simulation group.
Dr. Coisne noted that subgroup analyses showed that the effectiveness of the simulation training was greater when performed at the beginning of the fellowship. On the theoretical test, the point increase was 11.9 for the simulation group versus 4.25 points for the traditional training group; for the practical test, the increases were 24.0 points versus 10.1 points.
After training, it took significantly less time for the simulation group to complete a TEE than it did the traditional group (8.3 vs. 9.4 minutes).
Furthermore, simulation group fellows reported that they felt more ready (mean score, 3.0 vs. 1.7) and more confident (mean score, 3.3 vs. 2.4) about performing a TEE alone after training.
“The simulation approach is definitively scalable to every institution,” Dr. Coisne said. “However, a medico-economic analysis should be interesting because the cost of the simulator and its maintenance might be a limitation to spread simulation-based teaching. The possibility for smaller hospitals to pool their financial input to share a TEE simulator could be considered to increase its cost-effectiveness.”
Real-world outcomes required
Commenting on the study, S. Justin Szawlewicz, MD, chair of cardiovascular medicine at Deborah Heart and Lung Center in Brown Mills, N.J., pointed out that the authors indicated that the number of TEEs performed by the trainees was not collected.
“This would be useful information to determine if those who received simulator training sought out and performed more TEEs, and also to determine if cardiology trainees in France perform a similar number of TEEs as cardiology trainees in the United States.”
In addition, he said, “the 4 hours of simulator training in TEE is extra education and experience that the standard trainees didn’t get. Would 4 extra hours of standard training didactics also improve trainees’ scores?”
Noting that the fellows’ ability to perform TEE in real patients was not assessed, Dr. Szawlewicz said, “a study could be designed that evaluated TEE images from real patients to see if trainees receiving simulator training performed better, more comprehensive and efficient TEEs than standard training.”
Nevertheless, he concluded, “Four hours of simulator training appears to improve TEE knowledge and skills. This is something we would consider at our institution.”
Like Dr. Szawlewicz, Michael Spooner, MD, MBA, of Mercy One North Iowa Heart Center in Mason City, and Kathryn Bertlacher, MD, of the University of Pittsburgh Medical Center, noted in a related editorial, “data are not provided about change in the learner’s behavior or performance on an actual TEE after the course, nor are there data about clinical outcomes such as patient safety or completeness of subsequent TEEs.
“This limitation, which is a limitation of most of the existing TEE simulation literature, is a high bar to cross,” they concluded. “Reaching this bar will require studies such as this to provide foundational understanding.”
Twin-Medical provided the TEE simulators. No relevant conflicts of interest were disclosed.
A version of this article first appeared on Medscape.com.
Simulation-based teaching of transesophageal echocardiography (TEE) improved cardiology fellows’ knowledge, skills, and comfort with the procedure, compared with traditional training, a new study shows.
“TEE learning may be hampered by the lack of availability of teachers and equipment and by the need for esophageal intubation, which is semi-invasive,” Augustin Coisne, MD, PhD, of the Cardiovascular Research Foundation in New York, said in an interview. “In this setting, simulation emerges as a key educational tool, but we were lacking evidence supporting simulation-based educational programs.”
Fellows in the simulation group achieved higher theoretical test scores and practical test scores after the training than did those in the traditional group.
Furthermore, Dr. Coisne said, “the results of the subgroup analyses were surprising and unexpected. The effect of the simulation-based training was greater among fellows at the beginning of fellowship – i.e., 2 years or less of training – in both theoretical and practical tests and in women [versus men] for the theoretical test.”
Their results, from the randomized SIMULATOR study, were published online in JAMA Cardiology.
More ready, more confident
The researchers randomly assigned 324 cardiology fellows (mean age, 26.4 years; about 30% women) inexperienced in TEE from 42 French university centers to TEE training with or without simulation support. Both groups participated in traditional didactic training using e-learning with an online course that is compulsory for all cardiology fellows in France.
The simulation group also participated in two 2-hour teaching sessions using a TEE simulator.
Each fellow completed a theoretical and a practical test prior to training to assess their baseline TEE level and again 3 months after the end of the training program. A TEE simulator (U/S Mentor Simulator; 3D Systems Simbionix) was used for all tests, and 24 certified echocardiography teachers served as both trainers and raters.
The theoretical tests included 20 online video-based questions to evaluate recognition of standard TEE views, normal anatomy, and some pathological cases. Fellows had 90 seconds to choose the best answer for each question from five multiple-choice options.
For the practical tests, fellows had 3 minutes to familiarize themselves with the handling of the simulator, without specific training and before the probe introduction.
They were asked to show 10 basic views on the simulator and had a maximum of 1 minute for each view.
The coprimary outcomes were the scores in the final theoretical and practical tests. TEE duration and the fellows’ self-assessment of their proficiency were also evaluated.
At baseline, the theoretical and practical test scores were similar between the groups (33.0 for the simulator group vs. 32.5 for the traditional group, and 44.2 vs. 46.1, respectively).
After training, the fellows in the simulation group had higher theoretical and practical test scores than those in the traditional group (47.2% vs. 38.3% and 74.5% vs. 59.0%, respectively).
Score changes were consistently higher when the pretraining scores were lower, an association that was stronger in the simulation group.
Dr. Coisne noted that subgroup analyses showed that the effectiveness of the simulation training was greater when performed at the beginning of the fellowship. On the theoretical test, the point increase was 11.9 for the simulation group versus 4.25 points for the traditional training group; for the practical test, the increases were 24.0 points versus 10.1 points.
After training, it took significantly less time for the simulation group to complete a TEE than it did the traditional group (8.3 vs. 9.4 minutes).
Furthermore, simulation group fellows reported that they felt more ready (mean score, 3.0 vs. 1.7) and more confident (mean score, 3.3 vs. 2.4) about performing a TEE alone after training.
“The simulation approach is definitively scalable to every institution,” Dr. Coisne said. “However, a medico-economic analysis should be interesting because the cost of the simulator and its maintenance might be a limitation to spread simulation-based teaching. The possibility for smaller hospitals to pool their financial input to share a TEE simulator could be considered to increase its cost-effectiveness.”
Real-world outcomes required
Commenting on the study, S. Justin Szawlewicz, MD, chair of cardiovascular medicine at Deborah Heart and Lung Center in Brown Mills, N.J., pointed out that the authors indicated that the number of TEEs performed by the trainees was not collected.
“This would be useful information to determine if those who received simulator training sought out and performed more TEEs, and also to determine if cardiology trainees in France perform a similar number of TEEs as cardiology trainees in the United States.”
In addition, he said, “the 4 hours of simulator training in TEE is extra education and experience that the standard trainees didn’t get. Would 4 extra hours of standard training didactics also improve trainees’ scores?”
Noting that the fellows’ ability to perform TEE in real patients was not assessed, Dr. Szawlewicz said, “a study could be designed that evaluated TEE images from real patients to see if trainees receiving simulator training performed better, more comprehensive and efficient TEEs than standard training.”
Nevertheless, he concluded, “Four hours of simulator training appears to improve TEE knowledge and skills. This is something we would consider at our institution.”
Like Dr. Szawlewicz, Michael Spooner, MD, MBA, of Mercy One North Iowa Heart Center in Mason City, and Kathryn Bertlacher, MD, of the University of Pittsburgh Medical Center, noted in a related editorial, “data are not provided about change in the learner’s behavior or performance on an actual TEE after the course, nor are there data about clinical outcomes such as patient safety or completeness of subsequent TEEs.
“This limitation, which is a limitation of most of the existing TEE simulation literature, is a high bar to cross,” they concluded. “Reaching this bar will require studies such as this to provide foundational understanding.”
Twin-Medical provided the TEE simulators. No relevant conflicts of interest were disclosed.
A version of this article first appeared on Medscape.com.
FROM JAMA CARDIOLOGY