User login
Influenza update 2018–2019: 100 years after the great pandemic
This centennial year update focuses primarily on immunization, but also reviews epidemiology, transmission, and treatment.
EPIDEMIOLOGY
2017–2018 was a bad season
The 2017–2018 influenza epidemic was memorable, dominated by influenza A(H3N2) viruses with morbidity and mortality rates approaching pandemic numbers. It lasted 19 weeks, killed more people than any other epidemic since 2010, particularly children, and was associated with 30,453 hospitalizations—almost twice the previous season high in some parts of the United States.2
Regrettably, 171 unvaccinated children died during 2017–2018, accounting for almost 80% of deaths.2 The mean age of the children who died was 7.1 years; 51% had at least 1 underlying medical condition placing them at risk for influenza-related complications, and 57% died after hospitalization.2
Recent estimates of the incidence of symptomatic influenza among all ages ranged from 3% to 11%, which is slightly lower than historical estimates. The rates were higher for children under age 18 than for adults.3 Interestingly, influenza A(H3N2) accounted for 50% of cases of non-mumps viral parotitis during the 2014–2015 influenza season in the United States.4
Influenza C exists but is rare
Influenza A and B account for almost all influenza-related outpatient visits and hospitalizations. Surveillance data from May 2013 through December 2016 showed that influenza C accounts for 0.5% of influenza-related outpatient visits and hospitalizations, particularly affecting children ages 6 to 24 months. Medical comorbidities and copathogens were seen in all patients requiring intensive care and in most hospitalizations.5 Diagnostic tests for influenza C are not widely available.
Dogs and cats: Factories for new flu strains?
While pigs and birds are the major reservoirs of influenza viral genetic diversity from which infection is transmitted to humans, dogs and cats have recently emerged as possible sources of novel reassortant influenza A.6 With their frequent close contact with humans, our pets may prove to pose a significant threat.
Obesity a risk factor for influenza
Obesity emerged as a risk factor for severe influenza in the 2009 pandemic. Recent data also showed that obesity increases the duration of influenza A virus shedding, thus increasing duration of contagiousness.7
Influenza a cardiovascular risk factor
Previous data showed that influenza was a risk factor for cardiovascular events. Two recent epidemiologic studies from the United Kingdom showed that laboratory-confirmed influenza was associated with higher rates of myocardial infarction and stroke for up to 4 weeks.8,9
Which strain is the biggest threat?
Predicting which emerging influenza serotype may cause the next pandemic is difficult, but influenza A(H7N9), which had not infected humans until 2013 but has since infected about 1,600 people in China and killed 37% of them, appears to have the greatest potential.10
National influenza surveillance programs and influenza-related social media applications have been developed and may get a boost from technology. A smartphone equipped with a temperature sensor can instantly detect one’s temperature with great precision. A 2018 study suggested that a smartphone-driven thermometry application correlated well with national influenza-like illness activity and improved its forecast in real time and up to 3 weeks in advance.11
TRANSMISSION
Humidity may not block transmission
Animal studies have suggested that humidity in the air interferes with transmission of airborne influenza virus, partially from biologic inactivation. But when a recent study used humidity-controlled chambers to investigate the stability of the 2009 influenza A(H1N1) virus in suspended aerosols and stationary droplets, the virus remained infectious in aerosols across a wide range of relative humidities, challenging the common belief that humidity destabilizes respiratory viruses in aerosols.12
One sick passenger may not infect the whole plane
Transmission of respiratory viruses on airplane flights has long been considered a potential avenue for spreading influenza. However, a recent study that monitored movements of individuals on 10 transcontinental US flights and simulated inflight transmission based on these data showed a low probability of direct transmission, except for passengers seated in close proximity to an infectious passenger.13
WHAT’S IN THE NEW FLU SHOT?
The 2018–2019 quadrivalent vaccine for the Northern Hemisphere14 contains the following strains:
- A/Michigan/45/2015 A(H1N1)pdm09-like virus
- A/Singapore/INFIMH-16-0019/2016 (H3N2)-like virus
- B/Colorado/06/2017-like virus (Victoria lineage)
- B/Phuket/3073/2013-like virus (Yamagata lineage).
The A(H3N2) (Singapore) and B/Victoria lineage components are new this year. The A(H3N2) strain was the main cause of the 2018 influenza epidemic in the Southern Hemisphere.
The quadrivalent live-attenuated vaccine, which was not recommended during the 2016–2017 and 2017–2018 influenza seasons, has made a comeback and is recommended for the 2018–2019 season in people for whom it is appropriate based on age and comorbidities.15 Although it was effective against influenza B and A(H3N2) viruses, it was less effective against the influenza A(H1N1)pdm09-like viruses during the 2013–2014 and 2015–2016 seasons.
A/Slovenia/2903/2015, the new A(H1N1)pdm09-like virus included in the 2018–2019 quadrivalent live-attenuated vaccine, is significantly more immunogenic than its predecessor, A/Bolivia/559/2013, but its clinical effectiveness remains to be seen.
PROMOTING VACCINATION
How effective is it?
Influenza vaccine effectiveness in the 2017–2018 influenza season was 36% overall, 67% against A(H1N1), 42% against influenza B, and 25% against A(H3N2).16 It is estimated that influenza vaccine prevents 300 to 4,000 deaths annually in the United States alone.17
A 2018 Cochrane review17 concluded that vaccination reduced the incidence of influenza by about half, with 2.3% of the population contracting the flu without vaccination compared with 0.9% with vaccination (risk ratio 0.41, 95% confidence interval 0.36–0.47). The same review found that 71 healthy adults need to be vaccinated to prevent 1 from experiencing influenza, and 29 to prevent 1 influenza-like illness.
Several recent studies showed that influenza vaccine effectiveness varied based on age and influenza serotype, with higher effectiveness in people ages 5 to 17 and ages 18 to 64 than in those age 65 and older.18–20 A mathematical model of influenza transmission and vaccination in the United States determined that even relatively low-efficacy influenza vaccines can be very useful if optimally distributed across age groups.21
Vaccination rates are low, and ‘antivaxxers’ are on the rise
Although the influenza vaccine is recommended in the United States for all people age 6 months and older regardless of the state of their health, vaccination rates remain low. In 2016, only 37% of employed adults were vaccinated. The highest rate was for government employees (45%), followed by private employees (36%), followed by the self-employed (30%).22
A national goal is to immunize 80% of all Americans and 90% of at-risk populations (which include children and the elderly).23 The number of US hospitals that require their employees to be vaccinated increased from 37.1% in 2013 to 61.4% in 2017.24 Regrettably, as of March 2018, 14 lawsuits addressing religious objections to hospital influenza vaccination mandates have been filed.25
Despite hundreds of studies demonstrating the efficacy, safety, and cost savings of influenza vaccination, the antivaccine movement has been growing in the United States and worldwide.26 All US states except West Virginia, Mississippi, and California allow nonmedical exemptions from vaccination based on religious or personal belief.27 Several US metropolitan areas represent “hot spots” for these exemptions.28 This may render such areas vulnerable to vaccine-preventable diseases, including influenza.
Herd immunity: We’re all in this together
Some argue that the potential adverse effects and the cost of vaccination outweigh the benefits, but the protective benefits of herd immunity are significant for those with comorbidities or compromised immunity.
Educating the public about herd immunity and local influenza vaccination uptake increases people’s willingness to be vaccinated.29 A key educational point is that at least 70% of a community needs to be vaccinated to prevent community outbreaks; this protects everyone, including those who do not mount a protective antibody response to influenza vaccination and those who are not vaccinated.
DOES ANNUAL VACCINATION BLUNT ITS EFFECTIVENESS?
Some studies from the 1970s and 1980s raised concern over a possible negative effect of annual influenza vaccination on vaccine effectiveness. The “antigenic distance hypothesis” holds that vaccine effectiveness is influenced by antigenic similarity between the previous season’s vaccine serotypes and the epidemic serotypes, as well as the antigenic similarity between the serotypes of the current and previous seasons.
A meta-analysis of studies from 2010 through 2015 showed significant inconsistencies in repeat vaccination effects within and between seasons and serotypes. It also showed that vaccine effectiveness may be influenced by more than 1 previous season, particularly for influenza A(H3N2), in which repeated vaccination can blunt the hemagglutinin antibody response.30
A study from Japan showed that people who needed medical attention for influenza in the previous season were at lower risk of a similar event in the current season.31 Prior-season influenza vaccination reduced current-season vaccine effectiveness only in those who did not have medically attended influenza in the prior season. This suggests that infection is more immunogenic than vaccination, but only against the serotype causing the infection and not the other serotypes included in the vaccine.
An Australian study showed that annual influenza vaccination did not decrease vaccine effectiveness against influenza-associated hospitalization. Rather, effectiveness increased by about 15% in those vaccinated in both current and previous seasons compared with those vaccinated in either season alone.32
European investigators showed that repeated seasonal influenza vaccination in the elderly prevented the need for hospitalization due to influenza A(H3N2) and B, but not A(H1N1)pdm09.33
VACCINATION IN SPECIAL POPULATIONS
High-dose vaccine for older adults
The high-dose influenza vaccine has been licensed since 2009 for use in the United States for people ages 65 and older.
Recent studies confirmed that high-dose vaccine is more effective than standard-dose vaccine in veterans34 and US Medicare beneficiaries.35
The high-dose vaccine is rapidly becoming the primary vaccine given to people ages 65 and older in retail pharmacies, where vaccination begins earlier in the season than in providers’ offices.36 Some studies have shown that the standard-dose vaccine wanes in effectiveness toward the end of the influenza season (particularly if the season is long) if it is given very early. It remains to be seen whether the same applies to the high-dose influenza vaccine.
Some advocate twice-annual influenza vaccination, particularly for older adults living in tropical and subtropical areas, where influenza seasons are more prolonged. However, a recently published study observed reductions in influenza-specific hemagglutination inhibition and cell-mediated immunity after twice-annual vaccination.37
Vaccination is beneficial during pregnancy
Many studies have shown the value of influenza vaccination during pregnancy for both mothers and their infants.
One recently published study showed that 18% of infants who developed influenza required hospitalization.38 In that study, prenatal and postpartum maternal influenza vaccination decreased the odds of influenza in infants by 61% and 53%, respectively.
Another study showed that vaccine effectiveness did not vary by gestational age at vaccination.39
Some studies have shown that influenza virus infection can increase susceptibility to certain bacterial infections. A post hoc analysis of an influenza vaccination study in pregnant women suggested that the vaccine was also associated with decreased rates of pertussis in these women.40
Factors that make vaccination less effective
Several factors including age-related frailty and iatrogenic and disease-related immunosuppression can affect vaccine effectiveness.
Frailty. A recent study showed that vaccine effectiveness was 77.6% in nonfrail older adults but only 58.7% in frail older adults.41
Immunosuppression. Temporary discontinuation of methotrexate for 2 weeks after influenza vaccination in patients with rheumatoid arthritis improves vaccine immunogenicity without precipitating disease flare.42 Solid-organ and hematopoietic stem cell transplant recipients who received influenza vaccine were less likely to develop pneumonia and require intensive care unit admission.43
The high-dose influenza vaccine is more immunogenic than the standard-dose vaccine in solid-organ transplant recipients.44
Statins are widely prescribed and have recently been associated with reduced influenza vaccine effectiveness against medically attended acute respiratory illness, but their benefits in preventing cardiovascular events outweigh this risk.45
FUTURE VACCINE CONSIDERATIONS
Moving away from eggs
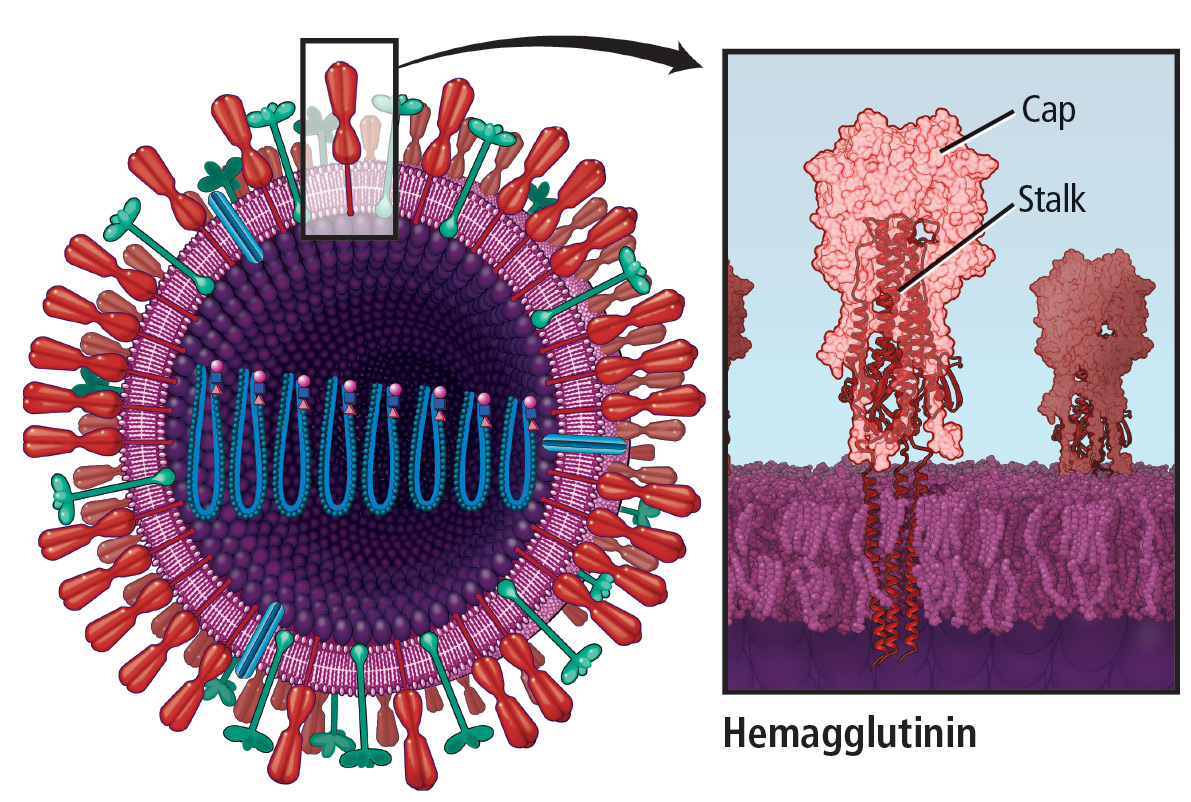
During the annual egg-based production process, which takes several months, the influenza vaccine acquires antigenic changes that allow replication in eggs, particularly in the hemagglutinin protein, which mediates receptor binding. This process of egg adaptation may cause antigenic changes that decrease vaccine effectiveness against circulating viruses.
The cell-based baculovirus influenza vaccine grown in dog kidney cells has higher antigenic content and is not subject to the limitations of egg-based vaccine, although it still requires annual updates. A recombinant influenza vaccine reduces the probability of influenza-like illness by 30% compared with the egg-based influenza vaccine, but also still requires annual updates.46 The market share of these non-egg-based vaccines is small, and thus their effectiveness has yet to be demonstrated.
The US Department of Defense administered the cell-based influenza vaccine to about one-third of Armed Forces personnel, their families, and retirees in the 2017–2018 influenza seasons, and data on its effectiveness are expected in the near future.47
A universal vaccine would be ideal
The quest continues for a universal influenza vaccine, one that remains protective for several years and does not require annual updates.48 Such a vaccine would protect against seasonal epidemic influenza drift variants and pandemic strains. More people could likely be persuaded to be vaccinated once rather than every year.
An ideal universal vaccine would be suitable for all age groups, at least 75% effective against symptomatic influenza virus infection, protective against all influenza A viruses (influenza A, not B, causes pandemics and seasonal epidemics), and durable through multiple influenza seasons.51
Research and production of such a vaccine are expected to require funding of about $1 billion over the next 5 years.
Boosting effectiveness
Estimates of influenza vaccine effectiveness range from 40% to 60% in years when the vaccine viruses closely match the circulating viruses, and variably lower when they do not match. The efficacy of most other vaccines given to prevent other infections is much higher.
New technologies to improve influenza vaccine effectiveness are needed, particularly for influenza A(H3N2) viruses, which are rapidly evolving and are highly susceptible to egg-adaptive mutations in the manufacturing process.
In one study, a nanoparticle vaccine formulated with a saponin-based adjuvant induced hemagglutination inhibition responses that were even greater than those induced by the high-dose vaccine.52
Immunoglobulin A (IgA) may be a more effective vaccine target than traditional influenza vaccines that target IgG, since different parts of IgA may engage the influenza virus simultaneously.53
Vaccines can be developed more quickly than in the past. The timeline from viral sequencing to human studies with deoxyribonucleic acid plasmid vaccines decreased from 20 months in 2003 for the severe acquired respiratory syndrome coronavirus to 11 months in 2006 for influenza A/Indonesia/2006 (H5), to 4 months in 2009 for influenza A/California/2009 (H1), to 3.5 months in 2016 for Zika virus.54 This is because it is possible today to sequence a virus and insert the genetic material into a vaccine platform without ever having to grow the virus.
TREATMENT
Numerous studies have found anti-influenza medications to be effective. Nevertheless, in an analysis of the 2011–2016 influenza seasons, only 15% of high-risk patients were prescribed anti-influenza medications within 2 days of symptom onset, including 37% in those with laboratory-confirmed influenza.55 Fever was associated with an increased rate of antiviral treatment, but 25% of high-risk outpatients were afebrile. Empiric treatment of 4 high-risk outpatients with acute respiratory illness was needed to treat 1 patient with influenza.55
Treatment with a neuraminidase inhibitor within 2 days of illness has recently been shown to improve survival and shorten duration of viral shedding in patients with avian influenza A(H7N9) infection.56 Antiviral treatment within 2 days of illness is associated with improved outcomes in transplant recipients57 and with a lower risk of otitis media in children.58
Appropriate anti-influenza treatment is as important as avoiding unnecessary antibiotics. Regrettably, as many as one-third of patients with laboratory-confirmed influenza are prescribed antibiotics.59
The US Food and Drug Administration warns against fraudulent unapproved over-the-counter influenza products.60
Baloxavir marboxil
Baloxavir marboxil is a new anti-influenza medication approved in Japan in February 2018 and anticipated to be available in the United States sometime in 2019.
This prodrug is hydrolyzed in vivo to the active metabolite, which selectively inhibits cap-dependent endonuclease enzyme, a key enzyme in initiation of messenger ribonucleic acid synthesis required for influenza viral replication.61
In a double-blind phase 3 trial, the median time to alleviation of influenza symptoms is 26.5 hours shorter with baloxavir marboxil than with placebo. One tablet was as effective as 5 days of the neuraminidase inhibitor oseltamivir and was associated with greater reduction in viral load 1 day after initiation, and similar side effects.62 Of concern is the emergence of nucleic acid substitutions conferring resistance to baloxavir; this occurred in 2.2% and 9.7% of baloxavir recipients in the phase 2 and 3 trials, respectively.
CLOSING THE GAPS
Several gaps in the management of influenza persist since the 1918 pandemic.1 These include gaps in epidemiology, prevention, diagnosis, treatment, and prognosis.
- Global networks wider than current ones are needed to address this global disease and to prioritize coordination efforts.
- Establishing and strengthening clinical capacity is needed in limited resource settings. New technologies are needed to expedite vaccine development and to achieve progress toward a universal vaccine.
- Current diagnostic tests do not distinguish between seasonal and novel influenza A viruses of zoonotic origin, which are expected to cause the next pandemic.
- Current antivirals have been shown to shorten duration of illness in outpatients with uncomplicated influenza, but the benefit in hospitalized patients has been less well established.
- In 2007, resistance of seasonal influenza A(H1N1) to oseltamivir became widespread. In 2009, pandemic influenza A(H1N1), which is highly susceptible to oseltamivir, replaced the seasonal virus and remains the predominantly circulating A(H1N1) strain.
- A small-molecule fragment, N-cyclohexyaltaurine, binds to the conserved hemagglutinin receptor-binding site in a manner that mimics the binding mode of the natural receptor sialic acid. This can serve as a template to guide the development of novel broad-spectrum small-molecule anti-influenza drugs.63
- Biomarkers that can accurately predict development of severe disease in patients with influenza are needed.
- Uyeki TM, Fowler RA, Fischer WA. Gaps in the clinical management of influenza: a century since the 1918 pandemic. JAMA 2018; 320(8):755–756. doi:10.1001/jama.2018.8113
- Garten R, Blanton L, Elal AI, et al. Update: influenza activity in the United States during the 2017–18 season and composition of the 2018–19 influenza vaccine. MMWR Morb Mortal Wkly Rep 2018; 67(22):634–642. doi:10.15585/mmwr.mm6722a4
- Tokars JI, Olsen SJ, Reed C. Seasonal incidence of symptomatic influenza in the United States. Clin Infect Dis 2018; 66(10):1511–1518. doi:10.1093/cid/cix1060
- Elbadawi LI, Talley P, Rolfes MA, et al. Non-mumps viral parotitis during the 2014–2015 influenza season in the United States. Clin Infect Dis 2018. Epub ahead of print. doi:10.1093/cid/ciy137
- Thielen BK, Friedlander H, Bistodeau S, et al. Detection of influenza C viruses among outpatients and patients hospitalized for severe acute respiratory infection, Minnesota, 2013–2016. Clin Infect Dis 2018; 66(7):1092–1098. doi:10.1093/cid/cix931
- Chena Y, Trovãob NS, Wang G, et al. Emergence and evolution of novel reassortant influenza A viruses in canines in southern China. MBio 2018; 9(3):e00909–e00918. doi:10.1128/mBio.00909-18
- Maier HE, Lopez R, Sanchez N, et al. Obesity increases the duration of influenza A virus shedding in adults. J Infect Dis 2018. Epub ahead of print. doi:10.1093/infdis/jiy370
- Warren-Gash C, Blackburn R, Whitaker H, McMenamin J, Hayward AC. Laboratory-confirmed respiratory infections as triggers for acute myocardial infarction and stroke: a self-controlled case series analysis of national linked datasets from Scotland. Eur Respir J 2018; 51(3):1701794. doi:10.1183/13993003.01794-2017
- Blackburn R, Zhao H, Pebody R, Hayward A, Warren-Gash C. Laboratory-confirmed respiratory infections as predictors of hospital admission for myocardial infarction and stroke: time-series analysis of English data for 2004–2015. Clin Infect Dis 2018; 67(1):8–17. doi:10.1093/cid/cix1144
- Newsweek; Andrew S. What is disease X? Deadly bird flu virus could be next pandemic. www.newsweek.com/disease-x-bird-flu-deaths-pandemic-what-h7n9-979723. Accessed October 3, 2018.
- Miller AC, Singh I, Koehler E, Polgreen PM. A smartphone-driven thermometer application for real-time population- and individual-level influenza surveillance. Clin Infect Dis 2018; 67(3):388–397. doi:10.1093/cid/ciy073
- Kormuth KA, Lin K, Prussin AJ 2nd, et al. Influenza virus infectivity is retained in aerosols and droplets independent of relative humidity, J Infect Dis 2018; 218(5):739–747. doi:10.1093/infdis/jiy221
- Hertzberg VS, Weiss H, Elon L, et. al. Behaviors, movements, and transmission of droplet-mediated respiratory diseases during transcontinental airline flights. Proc Natl Acad Sci U S A 2018; 115(14):3623–3627. doi:10.1073/pnas.1711611115
- Grohskopf LA, Sokolow LZ, Broder KR, Walter EB, Fry AM, Jernigan DB. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices—United States, 2018–19 influenza season. MMWR Recomm Rep 2018; 67(3):1–20. doi:10.15585/mmwr.rr6703a1
- Grohskopf LA, Sokolow LZ, Fry AM, Walter EB, Jernigan DB. Update: ACIP recommendations for the use of quadrivalent live attenuated influenza vaccine (LAIV4)—United States, 2018–19 influenza season. MMWR Morb Mortal Wkly Rep 2018; 67(22):643–645. doi:10.15585/mmwr.mm6722a5
- Flannery B, Chung JR, Belongia EA, et al. Interim estimates of 2017–18 seasonal influenza vaccine effectiveness—United States, February 2018. MMWR Morb Mortal Wkly Rep 2018; 67(6):180–185. doi:10.15585/mmwr.mm6706a2
- Demicheli V, Jefferson T, Ferroni E, Rivetti A, Di Pietrantonj C. Vaccines for preventing influenza in healthy adults. Cochrane Database Syst Rev 2018; 2:CD001269. doi:10.1002/14651858.CD001269.pub6
- Flannery B, Smith C, Garten RJ, et al. Influence of birth cohort on effectiveness of 2015–2016 influenza vaccine against medically attended illness due to 2009 pandemic influenza A(H1N1) virus in the United States. J Infect Dis 2018; 218(2):189–196. doi:10.1093/infdis/jix634
- Rondy M, El Omeiri N, Thompson MG, Leveque A, Moren A, Sullivan SG. Effectiveness of influenza vaccines in preventing severe influenza illness among adults: a systematic review and meta-analysis of test-negative design case-control studies. J Infect 2017; 75(5):381–394. doi:10.1016/j.jinf.2017.09.010
- Stein Y, Mandelboim M, Sefty H, et al; Israeli Influenza Surveillance Network (IISN). Seasonal influenza vaccine effectiveness in preventing laboratory-confirmed influenza in primary care in Israel, 2016–2017 season: insights into novel age-specific analysis. Clin Infect Dis 2018; 66(9):1383–1391. doi:10.1093/cid/cix1013
- Sah P, Medlock J, Fitzpatrick MC, Singer BH, Galvani AP. Optimizing the impact of low-efficacy influenza vaccines. Proc Natl Acad Sci U S A 2018; 115(20):5151–5156. doi:10.1073/pnas.1802479115
- QuickStats: percentage of currently employed adults aged ≥ 18 years who received influenza vaccine in the past 12 months, by employment category—national health interview survey, United States, 2012 and 2016. MMWR Morb Mortal Wkly Rep 2018; 67(16):480. doi:10.15585/mmwr.mm6716a8
- Healthy People.gov. Immunization and infectious diseases. IID-12. Increase the percentage of children and adults who are vaccinated annually against seasonal influenza. www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives. Accessed October 3, 2018.
- Greene MT, Fowler KE, Ratz D, Krein SL, Bradley SF, Saint S. Changes in influenza vaccination requirements for health care personnel in US hospitals. JAMA Network Open 2018; 1(2):e180143. doi:10.1001/jamanetworkopen.2018.0143
- Opel DJ, Sonne JA, Mello MM. Vaccination without litigation—addressing religious objections to hospital influenza-vaccination mandates. N Engl J Med 2018; 378(9):785–788. doi:10.1056/NEJMp1716147
- Horowitz J. Italy loosens vaccine law just as children return to school. New York Times Sept. 20, 2018. www.nytimes.com/2018/09/20/world/europe/italy-vaccines-five-star-movement.html.
- National Conference of State Legislature. States with religious and philosophical exemptions from school immunization requirements. www.ncsl.org/research/health/school-immunization-exemption-state-laws.aspx. Accessed October 3, 2018.
- Olive JK, Hotez PJ, Damania A, Nolan MS. The state of the antivaccine movement in the United States: a focused examination of nonmedical exemptions in states and counties. PLoS Med 2018; 15(6):e1002578. doi:10.1371/journal.pmed.1002578
- Logan J, Nederhoff D, Koch B, et al. ‘What have you HEARD about the HERD?’ Does education about local influenza vaccination coverage and herd immunity affect willingness to vaccinate? Vaccine 2018; 36(28):4118–4125. doi:10.1016/j.vaccine.2018.05.037
- Belongia EA, Skowronski DM, McLean HQ, Chambers C, Sundaram ME, De Serres G. Repeated annual influenza vaccination and vaccine effectiveness: review of evidence. Expert Rev Vaccines 2017; 16(7):1–14. doi:10.1080/14760584.2017.1334554
- Saito N, Komori K, Suzuki M, et al. Negative impact of prior influenza vaccination on current influenza vaccination among people infected and not infected in prior season: a test-negative case-control study in Japan. Vaccine 2017; 35(4):687–693. doi:10.1016/j.vaccine.2016.11.024
- Cheng AC, Macartney KK, Waterer GW, Kotsimbos T, Kelly PM, Blyth CC; Influenza Complications Alert Network (FluCAN) Investigators. Repeated vaccination does not appear to impact upon influenza vaccine effectiveness against hospitalization with confirmed influenza. Clin Infect Dis 2017; 64(11):1564–1572. doi:10.1093/cid/cix209
- Rondy M, Launay O, Castilla J, et al; InNHOVE/I-MOVE+working group. Repeated seasonal influenza vaccination among elderly in Europe: effects on laboratory confirmed hospitalised influenza. Vaccine 2017; 35(34):4298–4306. doi:10.1016/j.vaccine.2017.06.088
- Young-Xu Y, van Aalst R, Mahmud SM, et al. Relative vaccine effectiveness of high-dose versus standard-dose influenza vaccines among Veterans Health Administration patients. J Infect Dis 2018; 217(11):1718–1727. doi:10.1093/infdis/jiy088
- Shay DK, Chillarige Y, Kelman J, et al. Comparative effectiveness of high-dose versus standard-dose influenza vaccines among US Medicare beneficiaries in preventing postinfluenza deaths during 2012–2013 and 2013–2014. J Infect Dis 2017; 215(4):510–517. doi:10.1093/infdis/jiw641
- Madaras-Kelly K, Remington R, Hruza H, Xu D. Comparative effectiveness of high-dose versus standard-dose influenza vaccines in preventing postinfluenza deaths. J Infect Dis 2018; 218(2):336–337. doi:10.1093/infdis/jix645
- Tam YH, Valkenburg SA, Perera RAPM, et al. Immune responses to twice-annual influenza vaccination in older adults in Hong Kong. Clin Infect Dis 2018; 66(6):904–912. doi:10.1093/cid/cix900
- Ohfuji S, Deguchi M, Tachibana D, et al; Osaka Pregnant Women Influenza Study Group. Protective effect of maternal influenza vaccination on influenza in their infants: a prospective cohort study. J Infect Dis 2018; 217(6):878–886. doi:10.1093/infdis/jix629
- Katz J, Englund JA, Steinhoff MC, et al. Impact of timing of influenza vaccination in pregnancy on transplacental antibody transfer, influenza incidence, and birth outcomes: a randomized trial in rural Nepal. Clin Infect Dis 2018; 67(3):334–340. doi:10.1093/cid/ciy090
- Nunes MC, Cutland CL, Madhi SA. Influenza vaccination during pregnancy and protection against pertussis. N Engl J Med 2018; 378(13):1257–1258. doi:10.1056/NEJMc1705208
- Andrew MK, Shinde V, Ye L, et al; Serious Outcomes Surveillance Network of the Public Health Agency of Canada/Canadian Institutes of Health Research Influenza Research Network (PCIRN) and the Toronto Invasive Bacterial Diseases Network (TIBDN). The importance of frailty in the assessment of influenza vaccine effectiveness against influenza-related hospitalization in elderly people. J Infect Dis 2017; 216(4):405–414. doi:10.1093/infdis/jix282
- Park JK, Lee YJ, Shin K, et al. Impact of temporary methotrexate discontinuation for 2 weeks on immunogenicity of seasonal influenza vaccination in patients with rheumatoid arthritis: a randomised clinical trial. Ann Rheum Dis 2018; 77(6):898–904. doi:10.1136/annrheumdis-2018-213222
- Kumar D, Ferreira VH, Blumberg E, et al. A five-year prospective multi-center evaluation of influenza infection in transplant recipients. Clin Infect Dis 2018. Epub ahead of print. doi:10.1093/cid/ciy294
- Natori Y, Shiotsuka M, Slomovic J, et al. A double-blind, randomized trial of high-dose vs standard-dose influenza vaccine in adult solid-organ transplant recipients. Clin Infect Dis 2018; 66(11):1698–1704. doi:10.1093/cid/cix1082
- Omer SB, Phadke VK, Bednarczyk BA, Chamberlain AT, Brosseau JL, Orenstein WA. Impact of statins on influenza vaccine effectiveness against medically attended acute respiratory illness. J Infect Dis 2016; 213(8):1216–1223. doi:10.1093/infdis/jiv457
- Dunkle LM, Izikson R, Patriarca P, et al. Efficacy of recombinant influenza vaccine in adults 50 years of age or older. N Engl J Med 2017; 376(25):2427–2436. doi:10.1056/NEJMoa1608862
- STAT; Branswell H. How the US military might help answer a critical question about the flu vaccine. www.statnews.com/2018/03/02/flu-vaccine-egg-production-data. Accessed October 3, 2018.
- Paules CI, Sullivan SG, Subbarao K, Fauci AS. Chasing seasonal influenza—the need for a universal influenza vaccine. N Engl J Med 2018; 378(1):7–9. doi:10.1056/NEJMp1714916
- Jin XW, Mossad SB. Avian influenza: an emerging pandemic threat. Cleve Clin J Med 2005; 72:1129-1134. pmid:16392727
- Wei WI, Brunger AT, Skehel JJ, Wiley DC. Refinement of the influenza virus hemagglutinin by simulated annealing. J Mol Biol 1990; 212(4):737–761. doi:10.1016/0022-2836(90)90234-D
- Erbelding EJ, Post DJ, Stemmy EJ, et al. A universal influenza vaccine: the strategic plan for the National Institute of Allergy and Infectious Diseases, J Infect Dis 2018; 218(3):347–354. doi:10.1093/infdis/jiy103
- Shinde V, Fries L, Wu Y, et al. Improved titers against influenza drift variants with a nanoparticle vaccine. N Engl J Med 2018; 378(24):2346–2348. doi:10.1056/NEJMc1803554
- Maurer MA, Meyer L, Bianchi M, et al. Glycosylation of human IgA directly inhibits influenza A and other sialic-acid-binding viruses. Cell Rep 2018; 23(1):90–99. doi:10.1016/j.celrep.2018.03.027
- Graham BS, Mascola JR, Fauci AS. Novel vaccine technologies: essential components of an adequate response to emerging viral diseases. JAMA 2018; 319(14):1431–1432. doi:10.1001/jama.2018.0345
- Stewart RJ, Flannery B, Chung JR, et al. Influenza antiviral prescribing for outpatients with an acute respiratory illness and at high risk for influenza-associated complications during 5 influenza seasons—United States, 2011–2016. Clin Infect Dis 2018; 66(7):1035–1041. doi:10.1093/cid/cix922
- Zheng S, Tang L, Gao H, et al. Benefit of early initiation of neuraminidase inhibitor treatment to hospitalized patients with avian influenza A(H7N9) virus. Clin Infect Dis 2018; 66(7):1054–1060. doi:10.1093/cid/cix930
- Kumar D, Ferreira VH, Blumberg E, et al. A five-year prospective multi-center evaluation of influenza infection in transplant recipients. Clin Infect Dis 2018. Epub ahead of print. doi:10.1093/cid/ciy294
- Malosh RE, Martin ET, Heikkinen T, Brooks WA, Whitley RJ, Monto AS. Efficacy and safety of oseltamivir in children: systematic review and individual patient data meta-analysis of randomized controlled trials. Clin Infect Dis 2018; 66(10):1492–1500. doi:10.1093/cid/cix1040
- Havers FP, Hicks LA, Chung JR, et al. Outpatient antibiotic prescribing for acute respiratory infections during influenza seasons. JAMA Network Open 2018; 1(2):e180243. doi:10.1001/jamanetworkopen.2018.0243
- US Food and Drug Administration. FDA warns of fraudulent and unapproved flu products. www.fda.gov/newsevents/newsroom/pressannouncements/ucm599223.htm. Accessed October 3, 2018.
- Portsmouth S, Kawaguchi K, Arai M, Tsuchiya K, Uehara T. Cap-dependent endonuclease inhibitor S-033188 for the treatment of influenza: results from a phase 3, randomized, double-blind, placebo- and active-controlled study in otherwise healthy adolescents and adults with seasonal influenza. Open Forum Infect Dis 2017; 4(suppl 1):S734. doi:10.1093/ofid/ofx180.001
- Hayden FG, Sugaya N, Hirotsu N, et al; Baloxavir Marboxil Investigators Group. Baloxavir Marboxil for uncomplicated influenza in adults and adolescents. N Engl J Med 2018; 379(10):913–923. doi:10.1056/NEJMoa1716197
- Kadam RU, Wilson IA. A small-molecule fragment that emulates binding of receptor and broadly neutralizing antibodies to influenza A hemagglutinin. Proc Natl Acad Sci U S A 2018; 115(16):4240–4245. doi:10.1073/pnas.1801999115
This centennial year update focuses primarily on immunization, but also reviews epidemiology, transmission, and treatment.
EPIDEMIOLOGY
2017–2018 was a bad season
The 2017–2018 influenza epidemic was memorable, dominated by influenza A(H3N2) viruses with morbidity and mortality rates approaching pandemic numbers. It lasted 19 weeks, killed more people than any other epidemic since 2010, particularly children, and was associated with 30,453 hospitalizations—almost twice the previous season high in some parts of the United States.2
Regrettably, 171 unvaccinated children died during 2017–2018, accounting for almost 80% of deaths.2 The mean age of the children who died was 7.1 years; 51% had at least 1 underlying medical condition placing them at risk for influenza-related complications, and 57% died after hospitalization.2
Recent estimates of the incidence of symptomatic influenza among all ages ranged from 3% to 11%, which is slightly lower than historical estimates. The rates were higher for children under age 18 than for adults.3 Interestingly, influenza A(H3N2) accounted for 50% of cases of non-mumps viral parotitis during the 2014–2015 influenza season in the United States.4
Influenza C exists but is rare
Influenza A and B account for almost all influenza-related outpatient visits and hospitalizations. Surveillance data from May 2013 through December 2016 showed that influenza C accounts for 0.5% of influenza-related outpatient visits and hospitalizations, particularly affecting children ages 6 to 24 months. Medical comorbidities and copathogens were seen in all patients requiring intensive care and in most hospitalizations.5 Diagnostic tests for influenza C are not widely available.
Dogs and cats: Factories for new flu strains?
While pigs and birds are the major reservoirs of influenza viral genetic diversity from which infection is transmitted to humans, dogs and cats have recently emerged as possible sources of novel reassortant influenza A.6 With their frequent close contact with humans, our pets may prove to pose a significant threat.
Obesity a risk factor for influenza
Obesity emerged as a risk factor for severe influenza in the 2009 pandemic. Recent data also showed that obesity increases the duration of influenza A virus shedding, thus increasing duration of contagiousness.7
Influenza a cardiovascular risk factor
Previous data showed that influenza was a risk factor for cardiovascular events. Two recent epidemiologic studies from the United Kingdom showed that laboratory-confirmed influenza was associated with higher rates of myocardial infarction and stroke for up to 4 weeks.8,9
Which strain is the biggest threat?
Predicting which emerging influenza serotype may cause the next pandemic is difficult, but influenza A(H7N9), which had not infected humans until 2013 but has since infected about 1,600 people in China and killed 37% of them, appears to have the greatest potential.10
National influenza surveillance programs and influenza-related social media applications have been developed and may get a boost from technology. A smartphone equipped with a temperature sensor can instantly detect one’s temperature with great precision. A 2018 study suggested that a smartphone-driven thermometry application correlated well with national influenza-like illness activity and improved its forecast in real time and up to 3 weeks in advance.11
TRANSMISSION
Humidity may not block transmission
Animal studies have suggested that humidity in the air interferes with transmission of airborne influenza virus, partially from biologic inactivation. But when a recent study used humidity-controlled chambers to investigate the stability of the 2009 influenza A(H1N1) virus in suspended aerosols and stationary droplets, the virus remained infectious in aerosols across a wide range of relative humidities, challenging the common belief that humidity destabilizes respiratory viruses in aerosols.12
One sick passenger may not infect the whole plane
Transmission of respiratory viruses on airplane flights has long been considered a potential avenue for spreading influenza. However, a recent study that monitored movements of individuals on 10 transcontinental US flights and simulated inflight transmission based on these data showed a low probability of direct transmission, except for passengers seated in close proximity to an infectious passenger.13
WHAT’S IN THE NEW FLU SHOT?
The 2018–2019 quadrivalent vaccine for the Northern Hemisphere14 contains the following strains:
- A/Michigan/45/2015 A(H1N1)pdm09-like virus
- A/Singapore/INFIMH-16-0019/2016 (H3N2)-like virus
- B/Colorado/06/2017-like virus (Victoria lineage)
- B/Phuket/3073/2013-like virus (Yamagata lineage).
The A(H3N2) (Singapore) and B/Victoria lineage components are new this year. The A(H3N2) strain was the main cause of the 2018 influenza epidemic in the Southern Hemisphere.
The quadrivalent live-attenuated vaccine, which was not recommended during the 2016–2017 and 2017–2018 influenza seasons, has made a comeback and is recommended for the 2018–2019 season in people for whom it is appropriate based on age and comorbidities.15 Although it was effective against influenza B and A(H3N2) viruses, it was less effective against the influenza A(H1N1)pdm09-like viruses during the 2013–2014 and 2015–2016 seasons.
A/Slovenia/2903/2015, the new A(H1N1)pdm09-like virus included in the 2018–2019 quadrivalent live-attenuated vaccine, is significantly more immunogenic than its predecessor, A/Bolivia/559/2013, but its clinical effectiveness remains to be seen.
PROMOTING VACCINATION
How effective is it?
Influenza vaccine effectiveness in the 2017–2018 influenza season was 36% overall, 67% against A(H1N1), 42% against influenza B, and 25% against A(H3N2).16 It is estimated that influenza vaccine prevents 300 to 4,000 deaths annually in the United States alone.17
A 2018 Cochrane review17 concluded that vaccination reduced the incidence of influenza by about half, with 2.3% of the population contracting the flu without vaccination compared with 0.9% with vaccination (risk ratio 0.41, 95% confidence interval 0.36–0.47). The same review found that 71 healthy adults need to be vaccinated to prevent 1 from experiencing influenza, and 29 to prevent 1 influenza-like illness.
Several recent studies showed that influenza vaccine effectiveness varied based on age and influenza serotype, with higher effectiveness in people ages 5 to 17 and ages 18 to 64 than in those age 65 and older.18–20 A mathematical model of influenza transmission and vaccination in the United States determined that even relatively low-efficacy influenza vaccines can be very useful if optimally distributed across age groups.21
Vaccination rates are low, and ‘antivaxxers’ are on the rise
Although the influenza vaccine is recommended in the United States for all people age 6 months and older regardless of the state of their health, vaccination rates remain low. In 2016, only 37% of employed adults were vaccinated. The highest rate was for government employees (45%), followed by private employees (36%), followed by the self-employed (30%).22
A national goal is to immunize 80% of all Americans and 90% of at-risk populations (which include children and the elderly).23 The number of US hospitals that require their employees to be vaccinated increased from 37.1% in 2013 to 61.4% in 2017.24 Regrettably, as of March 2018, 14 lawsuits addressing religious objections to hospital influenza vaccination mandates have been filed.25
Despite hundreds of studies demonstrating the efficacy, safety, and cost savings of influenza vaccination, the antivaccine movement has been growing in the United States and worldwide.26 All US states except West Virginia, Mississippi, and California allow nonmedical exemptions from vaccination based on religious or personal belief.27 Several US metropolitan areas represent “hot spots” for these exemptions.28 This may render such areas vulnerable to vaccine-preventable diseases, including influenza.
Herd immunity: We’re all in this together
Some argue that the potential adverse effects and the cost of vaccination outweigh the benefits, but the protective benefits of herd immunity are significant for those with comorbidities or compromised immunity.
Educating the public about herd immunity and local influenza vaccination uptake increases people’s willingness to be vaccinated.29 A key educational point is that at least 70% of a community needs to be vaccinated to prevent community outbreaks; this protects everyone, including those who do not mount a protective antibody response to influenza vaccination and those who are not vaccinated.
DOES ANNUAL VACCINATION BLUNT ITS EFFECTIVENESS?
Some studies from the 1970s and 1980s raised concern over a possible negative effect of annual influenza vaccination on vaccine effectiveness. The “antigenic distance hypothesis” holds that vaccine effectiveness is influenced by antigenic similarity between the previous season’s vaccine serotypes and the epidemic serotypes, as well as the antigenic similarity between the serotypes of the current and previous seasons.
A meta-analysis of studies from 2010 through 2015 showed significant inconsistencies in repeat vaccination effects within and between seasons and serotypes. It also showed that vaccine effectiveness may be influenced by more than 1 previous season, particularly for influenza A(H3N2), in which repeated vaccination can blunt the hemagglutinin antibody response.30
A study from Japan showed that people who needed medical attention for influenza in the previous season were at lower risk of a similar event in the current season.31 Prior-season influenza vaccination reduced current-season vaccine effectiveness only in those who did not have medically attended influenza in the prior season. This suggests that infection is more immunogenic than vaccination, but only against the serotype causing the infection and not the other serotypes included in the vaccine.
An Australian study showed that annual influenza vaccination did not decrease vaccine effectiveness against influenza-associated hospitalization. Rather, effectiveness increased by about 15% in those vaccinated in both current and previous seasons compared with those vaccinated in either season alone.32
European investigators showed that repeated seasonal influenza vaccination in the elderly prevented the need for hospitalization due to influenza A(H3N2) and B, but not A(H1N1)pdm09.33
VACCINATION IN SPECIAL POPULATIONS
High-dose vaccine for older adults
The high-dose influenza vaccine has been licensed since 2009 for use in the United States for people ages 65 and older.
Recent studies confirmed that high-dose vaccine is more effective than standard-dose vaccine in veterans34 and US Medicare beneficiaries.35
The high-dose vaccine is rapidly becoming the primary vaccine given to people ages 65 and older in retail pharmacies, where vaccination begins earlier in the season than in providers’ offices.36 Some studies have shown that the standard-dose vaccine wanes in effectiveness toward the end of the influenza season (particularly if the season is long) if it is given very early. It remains to be seen whether the same applies to the high-dose influenza vaccine.
Some advocate twice-annual influenza vaccination, particularly for older adults living in tropical and subtropical areas, where influenza seasons are more prolonged. However, a recently published study observed reductions in influenza-specific hemagglutination inhibition and cell-mediated immunity after twice-annual vaccination.37
Vaccination is beneficial during pregnancy
Many studies have shown the value of influenza vaccination during pregnancy for both mothers and their infants.
One recently published study showed that 18% of infants who developed influenza required hospitalization.38 In that study, prenatal and postpartum maternal influenza vaccination decreased the odds of influenza in infants by 61% and 53%, respectively.
Another study showed that vaccine effectiveness did not vary by gestational age at vaccination.39
Some studies have shown that influenza virus infection can increase susceptibility to certain bacterial infections. A post hoc analysis of an influenza vaccination study in pregnant women suggested that the vaccine was also associated with decreased rates of pertussis in these women.40
Factors that make vaccination less effective
Several factors including age-related frailty and iatrogenic and disease-related immunosuppression can affect vaccine effectiveness.
Frailty. A recent study showed that vaccine effectiveness was 77.6% in nonfrail older adults but only 58.7% in frail older adults.41
Immunosuppression. Temporary discontinuation of methotrexate for 2 weeks after influenza vaccination in patients with rheumatoid arthritis improves vaccine immunogenicity without precipitating disease flare.42 Solid-organ and hematopoietic stem cell transplant recipients who received influenza vaccine were less likely to develop pneumonia and require intensive care unit admission.43
The high-dose influenza vaccine is more immunogenic than the standard-dose vaccine in solid-organ transplant recipients.44
Statins are widely prescribed and have recently been associated with reduced influenza vaccine effectiveness against medically attended acute respiratory illness, but their benefits in preventing cardiovascular events outweigh this risk.45
FUTURE VACCINE CONSIDERATIONS
Moving away from eggs
During the annual egg-based production process, which takes several months, the influenza vaccine acquires antigenic changes that allow replication in eggs, particularly in the hemagglutinin protein, which mediates receptor binding. This process of egg adaptation may cause antigenic changes that decrease vaccine effectiveness against circulating viruses.
The cell-based baculovirus influenza vaccine grown in dog kidney cells has higher antigenic content and is not subject to the limitations of egg-based vaccine, although it still requires annual updates. A recombinant influenza vaccine reduces the probability of influenza-like illness by 30% compared with the egg-based influenza vaccine, but also still requires annual updates.46 The market share of these non-egg-based vaccines is small, and thus their effectiveness has yet to be demonstrated.
The US Department of Defense administered the cell-based influenza vaccine to about one-third of Armed Forces personnel, their families, and retirees in the 2017–2018 influenza seasons, and data on its effectiveness are expected in the near future.47
A universal vaccine would be ideal
The quest continues for a universal influenza vaccine, one that remains protective for several years and does not require annual updates.48 Such a vaccine would protect against seasonal epidemic influenza drift variants and pandemic strains. More people could likely be persuaded to be vaccinated once rather than every year.
An ideal universal vaccine would be suitable for all age groups, at least 75% effective against symptomatic influenza virus infection, protective against all influenza A viruses (influenza A, not B, causes pandemics and seasonal epidemics), and durable through multiple influenza seasons.51
Research and production of such a vaccine are expected to require funding of about $1 billion over the next 5 years.
Boosting effectiveness
Estimates of influenza vaccine effectiveness range from 40% to 60% in years when the vaccine viruses closely match the circulating viruses, and variably lower when they do not match. The efficacy of most other vaccines given to prevent other infections is much higher.
New technologies to improve influenza vaccine effectiveness are needed, particularly for influenza A(H3N2) viruses, which are rapidly evolving and are highly susceptible to egg-adaptive mutations in the manufacturing process.
In one study, a nanoparticle vaccine formulated with a saponin-based adjuvant induced hemagglutination inhibition responses that were even greater than those induced by the high-dose vaccine.52
Immunoglobulin A (IgA) may be a more effective vaccine target than traditional influenza vaccines that target IgG, since different parts of IgA may engage the influenza virus simultaneously.53
Vaccines can be developed more quickly than in the past. The timeline from viral sequencing to human studies with deoxyribonucleic acid plasmid vaccines decreased from 20 months in 2003 for the severe acquired respiratory syndrome coronavirus to 11 months in 2006 for influenza A/Indonesia/2006 (H5), to 4 months in 2009 for influenza A/California/2009 (H1), to 3.5 months in 2016 for Zika virus.54 This is because it is possible today to sequence a virus and insert the genetic material into a vaccine platform without ever having to grow the virus.
TREATMENT
Numerous studies have found anti-influenza medications to be effective. Nevertheless, in an analysis of the 2011–2016 influenza seasons, only 15% of high-risk patients were prescribed anti-influenza medications within 2 days of symptom onset, including 37% in those with laboratory-confirmed influenza.55 Fever was associated with an increased rate of antiviral treatment, but 25% of high-risk outpatients were afebrile. Empiric treatment of 4 high-risk outpatients with acute respiratory illness was needed to treat 1 patient with influenza.55
Treatment with a neuraminidase inhibitor within 2 days of illness has recently been shown to improve survival and shorten duration of viral shedding in patients with avian influenza A(H7N9) infection.56 Antiviral treatment within 2 days of illness is associated with improved outcomes in transplant recipients57 and with a lower risk of otitis media in children.58
Appropriate anti-influenza treatment is as important as avoiding unnecessary antibiotics. Regrettably, as many as one-third of patients with laboratory-confirmed influenza are prescribed antibiotics.59
The US Food and Drug Administration warns against fraudulent unapproved over-the-counter influenza products.60
Baloxavir marboxil
Baloxavir marboxil is a new anti-influenza medication approved in Japan in February 2018 and anticipated to be available in the United States sometime in 2019.
This prodrug is hydrolyzed in vivo to the active metabolite, which selectively inhibits cap-dependent endonuclease enzyme, a key enzyme in initiation of messenger ribonucleic acid synthesis required for influenza viral replication.61
In a double-blind phase 3 trial, the median time to alleviation of influenza symptoms is 26.5 hours shorter with baloxavir marboxil than with placebo. One tablet was as effective as 5 days of the neuraminidase inhibitor oseltamivir and was associated with greater reduction in viral load 1 day after initiation, and similar side effects.62 Of concern is the emergence of nucleic acid substitutions conferring resistance to baloxavir; this occurred in 2.2% and 9.7% of baloxavir recipients in the phase 2 and 3 trials, respectively.
CLOSING THE GAPS
Several gaps in the management of influenza persist since the 1918 pandemic.1 These include gaps in epidemiology, prevention, diagnosis, treatment, and prognosis.
- Global networks wider than current ones are needed to address this global disease and to prioritize coordination efforts.
- Establishing and strengthening clinical capacity is needed in limited resource settings. New technologies are needed to expedite vaccine development and to achieve progress toward a universal vaccine.
- Current diagnostic tests do not distinguish between seasonal and novel influenza A viruses of zoonotic origin, which are expected to cause the next pandemic.
- Current antivirals have been shown to shorten duration of illness in outpatients with uncomplicated influenza, but the benefit in hospitalized patients has been less well established.
- In 2007, resistance of seasonal influenza A(H1N1) to oseltamivir became widespread. In 2009, pandemic influenza A(H1N1), which is highly susceptible to oseltamivir, replaced the seasonal virus and remains the predominantly circulating A(H1N1) strain.
- A small-molecule fragment, N-cyclohexyaltaurine, binds to the conserved hemagglutinin receptor-binding site in a manner that mimics the binding mode of the natural receptor sialic acid. This can serve as a template to guide the development of novel broad-spectrum small-molecule anti-influenza drugs.63
- Biomarkers that can accurately predict development of severe disease in patients with influenza are needed.
This centennial year update focuses primarily on immunization, but also reviews epidemiology, transmission, and treatment.
EPIDEMIOLOGY
2017–2018 was a bad season
The 2017–2018 influenza epidemic was memorable, dominated by influenza A(H3N2) viruses with morbidity and mortality rates approaching pandemic numbers. It lasted 19 weeks, killed more people than any other epidemic since 2010, particularly children, and was associated with 30,453 hospitalizations—almost twice the previous season high in some parts of the United States.2
Regrettably, 171 unvaccinated children died during 2017–2018, accounting for almost 80% of deaths.2 The mean age of the children who died was 7.1 years; 51% had at least 1 underlying medical condition placing them at risk for influenza-related complications, and 57% died after hospitalization.2
Recent estimates of the incidence of symptomatic influenza among all ages ranged from 3% to 11%, which is slightly lower than historical estimates. The rates were higher for children under age 18 than for adults.3 Interestingly, influenza A(H3N2) accounted for 50% of cases of non-mumps viral parotitis during the 2014–2015 influenza season in the United States.4
Influenza C exists but is rare
Influenza A and B account for almost all influenza-related outpatient visits and hospitalizations. Surveillance data from May 2013 through December 2016 showed that influenza C accounts for 0.5% of influenza-related outpatient visits and hospitalizations, particularly affecting children ages 6 to 24 months. Medical comorbidities and copathogens were seen in all patients requiring intensive care and in most hospitalizations.5 Diagnostic tests for influenza C are not widely available.
Dogs and cats: Factories for new flu strains?
While pigs and birds are the major reservoirs of influenza viral genetic diversity from which infection is transmitted to humans, dogs and cats have recently emerged as possible sources of novel reassortant influenza A.6 With their frequent close contact with humans, our pets may prove to pose a significant threat.
Obesity a risk factor for influenza
Obesity emerged as a risk factor for severe influenza in the 2009 pandemic. Recent data also showed that obesity increases the duration of influenza A virus shedding, thus increasing duration of contagiousness.7
Influenza a cardiovascular risk factor
Previous data showed that influenza was a risk factor for cardiovascular events. Two recent epidemiologic studies from the United Kingdom showed that laboratory-confirmed influenza was associated with higher rates of myocardial infarction and stroke for up to 4 weeks.8,9
Which strain is the biggest threat?
Predicting which emerging influenza serotype may cause the next pandemic is difficult, but influenza A(H7N9), which had not infected humans until 2013 but has since infected about 1,600 people in China and killed 37% of them, appears to have the greatest potential.10
National influenza surveillance programs and influenza-related social media applications have been developed and may get a boost from technology. A smartphone equipped with a temperature sensor can instantly detect one’s temperature with great precision. A 2018 study suggested that a smartphone-driven thermometry application correlated well with national influenza-like illness activity and improved its forecast in real time and up to 3 weeks in advance.11
TRANSMISSION
Humidity may not block transmission
Animal studies have suggested that humidity in the air interferes with transmission of airborne influenza virus, partially from biologic inactivation. But when a recent study used humidity-controlled chambers to investigate the stability of the 2009 influenza A(H1N1) virus in suspended aerosols and stationary droplets, the virus remained infectious in aerosols across a wide range of relative humidities, challenging the common belief that humidity destabilizes respiratory viruses in aerosols.12
One sick passenger may not infect the whole plane
Transmission of respiratory viruses on airplane flights has long been considered a potential avenue for spreading influenza. However, a recent study that monitored movements of individuals on 10 transcontinental US flights and simulated inflight transmission based on these data showed a low probability of direct transmission, except for passengers seated in close proximity to an infectious passenger.13
WHAT’S IN THE NEW FLU SHOT?
The 2018–2019 quadrivalent vaccine for the Northern Hemisphere14 contains the following strains:
- A/Michigan/45/2015 A(H1N1)pdm09-like virus
- A/Singapore/INFIMH-16-0019/2016 (H3N2)-like virus
- B/Colorado/06/2017-like virus (Victoria lineage)
- B/Phuket/3073/2013-like virus (Yamagata lineage).
The A(H3N2) (Singapore) and B/Victoria lineage components are new this year. The A(H3N2) strain was the main cause of the 2018 influenza epidemic in the Southern Hemisphere.
The quadrivalent live-attenuated vaccine, which was not recommended during the 2016–2017 and 2017–2018 influenza seasons, has made a comeback and is recommended for the 2018–2019 season in people for whom it is appropriate based on age and comorbidities.15 Although it was effective against influenza B and A(H3N2) viruses, it was less effective against the influenza A(H1N1)pdm09-like viruses during the 2013–2014 and 2015–2016 seasons.
A/Slovenia/2903/2015, the new A(H1N1)pdm09-like virus included in the 2018–2019 quadrivalent live-attenuated vaccine, is significantly more immunogenic than its predecessor, A/Bolivia/559/2013, but its clinical effectiveness remains to be seen.
PROMOTING VACCINATION
How effective is it?
Influenza vaccine effectiveness in the 2017–2018 influenza season was 36% overall, 67% against A(H1N1), 42% against influenza B, and 25% against A(H3N2).16 It is estimated that influenza vaccine prevents 300 to 4,000 deaths annually in the United States alone.17
A 2018 Cochrane review17 concluded that vaccination reduced the incidence of influenza by about half, with 2.3% of the population contracting the flu without vaccination compared with 0.9% with vaccination (risk ratio 0.41, 95% confidence interval 0.36–0.47). The same review found that 71 healthy adults need to be vaccinated to prevent 1 from experiencing influenza, and 29 to prevent 1 influenza-like illness.
Several recent studies showed that influenza vaccine effectiveness varied based on age and influenza serotype, with higher effectiveness in people ages 5 to 17 and ages 18 to 64 than in those age 65 and older.18–20 A mathematical model of influenza transmission and vaccination in the United States determined that even relatively low-efficacy influenza vaccines can be very useful if optimally distributed across age groups.21
Vaccination rates are low, and ‘antivaxxers’ are on the rise
Although the influenza vaccine is recommended in the United States for all people age 6 months and older regardless of the state of their health, vaccination rates remain low. In 2016, only 37% of employed adults were vaccinated. The highest rate was for government employees (45%), followed by private employees (36%), followed by the self-employed (30%).22
A national goal is to immunize 80% of all Americans and 90% of at-risk populations (which include children and the elderly).23 The number of US hospitals that require their employees to be vaccinated increased from 37.1% in 2013 to 61.4% in 2017.24 Regrettably, as of March 2018, 14 lawsuits addressing religious objections to hospital influenza vaccination mandates have been filed.25
Despite hundreds of studies demonstrating the efficacy, safety, and cost savings of influenza vaccination, the antivaccine movement has been growing in the United States and worldwide.26 All US states except West Virginia, Mississippi, and California allow nonmedical exemptions from vaccination based on religious or personal belief.27 Several US metropolitan areas represent “hot spots” for these exemptions.28 This may render such areas vulnerable to vaccine-preventable diseases, including influenza.
Herd immunity: We’re all in this together
Some argue that the potential adverse effects and the cost of vaccination outweigh the benefits, but the protective benefits of herd immunity are significant for those with comorbidities or compromised immunity.
Educating the public about herd immunity and local influenza vaccination uptake increases people’s willingness to be vaccinated.29 A key educational point is that at least 70% of a community needs to be vaccinated to prevent community outbreaks; this protects everyone, including those who do not mount a protective antibody response to influenza vaccination and those who are not vaccinated.
DOES ANNUAL VACCINATION BLUNT ITS EFFECTIVENESS?
Some studies from the 1970s and 1980s raised concern over a possible negative effect of annual influenza vaccination on vaccine effectiveness. The “antigenic distance hypothesis” holds that vaccine effectiveness is influenced by antigenic similarity between the previous season’s vaccine serotypes and the epidemic serotypes, as well as the antigenic similarity between the serotypes of the current and previous seasons.
A meta-analysis of studies from 2010 through 2015 showed significant inconsistencies in repeat vaccination effects within and between seasons and serotypes. It also showed that vaccine effectiveness may be influenced by more than 1 previous season, particularly for influenza A(H3N2), in which repeated vaccination can blunt the hemagglutinin antibody response.30
A study from Japan showed that people who needed medical attention for influenza in the previous season were at lower risk of a similar event in the current season.31 Prior-season influenza vaccination reduced current-season vaccine effectiveness only in those who did not have medically attended influenza in the prior season. This suggests that infection is more immunogenic than vaccination, but only against the serotype causing the infection and not the other serotypes included in the vaccine.
An Australian study showed that annual influenza vaccination did not decrease vaccine effectiveness against influenza-associated hospitalization. Rather, effectiveness increased by about 15% in those vaccinated in both current and previous seasons compared with those vaccinated in either season alone.32
European investigators showed that repeated seasonal influenza vaccination in the elderly prevented the need for hospitalization due to influenza A(H3N2) and B, but not A(H1N1)pdm09.33
VACCINATION IN SPECIAL POPULATIONS
High-dose vaccine for older adults
The high-dose influenza vaccine has been licensed since 2009 for use in the United States for people ages 65 and older.
Recent studies confirmed that high-dose vaccine is more effective than standard-dose vaccine in veterans34 and US Medicare beneficiaries.35
The high-dose vaccine is rapidly becoming the primary vaccine given to people ages 65 and older in retail pharmacies, where vaccination begins earlier in the season than in providers’ offices.36 Some studies have shown that the standard-dose vaccine wanes in effectiveness toward the end of the influenza season (particularly if the season is long) if it is given very early. It remains to be seen whether the same applies to the high-dose influenza vaccine.
Some advocate twice-annual influenza vaccination, particularly for older adults living in tropical and subtropical areas, where influenza seasons are more prolonged. However, a recently published study observed reductions in influenza-specific hemagglutination inhibition and cell-mediated immunity after twice-annual vaccination.37
Vaccination is beneficial during pregnancy
Many studies have shown the value of influenza vaccination during pregnancy for both mothers and their infants.
One recently published study showed that 18% of infants who developed influenza required hospitalization.38 In that study, prenatal and postpartum maternal influenza vaccination decreased the odds of influenza in infants by 61% and 53%, respectively.
Another study showed that vaccine effectiveness did not vary by gestational age at vaccination.39
Some studies have shown that influenza virus infection can increase susceptibility to certain bacterial infections. A post hoc analysis of an influenza vaccination study in pregnant women suggested that the vaccine was also associated with decreased rates of pertussis in these women.40
Factors that make vaccination less effective
Several factors including age-related frailty and iatrogenic and disease-related immunosuppression can affect vaccine effectiveness.
Frailty. A recent study showed that vaccine effectiveness was 77.6% in nonfrail older adults but only 58.7% in frail older adults.41
Immunosuppression. Temporary discontinuation of methotrexate for 2 weeks after influenza vaccination in patients with rheumatoid arthritis improves vaccine immunogenicity without precipitating disease flare.42 Solid-organ and hematopoietic stem cell transplant recipients who received influenza vaccine were less likely to develop pneumonia and require intensive care unit admission.43
The high-dose influenza vaccine is more immunogenic than the standard-dose vaccine in solid-organ transplant recipients.44
Statins are widely prescribed and have recently been associated with reduced influenza vaccine effectiveness against medically attended acute respiratory illness, but their benefits in preventing cardiovascular events outweigh this risk.45
FUTURE VACCINE CONSIDERATIONS
Moving away from eggs
During the annual egg-based production process, which takes several months, the influenza vaccine acquires antigenic changes that allow replication in eggs, particularly in the hemagglutinin protein, which mediates receptor binding. This process of egg adaptation may cause antigenic changes that decrease vaccine effectiveness against circulating viruses.
The cell-based baculovirus influenza vaccine grown in dog kidney cells has higher antigenic content and is not subject to the limitations of egg-based vaccine, although it still requires annual updates. A recombinant influenza vaccine reduces the probability of influenza-like illness by 30% compared with the egg-based influenza vaccine, but also still requires annual updates.46 The market share of these non-egg-based vaccines is small, and thus their effectiveness has yet to be demonstrated.
The US Department of Defense administered the cell-based influenza vaccine to about one-third of Armed Forces personnel, their families, and retirees in the 2017–2018 influenza seasons, and data on its effectiveness are expected in the near future.47
A universal vaccine would be ideal
The quest continues for a universal influenza vaccine, one that remains protective for several years and does not require annual updates.48 Such a vaccine would protect against seasonal epidemic influenza drift variants and pandemic strains. More people could likely be persuaded to be vaccinated once rather than every year.
An ideal universal vaccine would be suitable for all age groups, at least 75% effective against symptomatic influenza virus infection, protective against all influenza A viruses (influenza A, not B, causes pandemics and seasonal epidemics), and durable through multiple influenza seasons.51
Research and production of such a vaccine are expected to require funding of about $1 billion over the next 5 years.
Boosting effectiveness
Estimates of influenza vaccine effectiveness range from 40% to 60% in years when the vaccine viruses closely match the circulating viruses, and variably lower when they do not match. The efficacy of most other vaccines given to prevent other infections is much higher.
New technologies to improve influenza vaccine effectiveness are needed, particularly for influenza A(H3N2) viruses, which are rapidly evolving and are highly susceptible to egg-adaptive mutations in the manufacturing process.
In one study, a nanoparticle vaccine formulated with a saponin-based adjuvant induced hemagglutination inhibition responses that were even greater than those induced by the high-dose vaccine.52
Immunoglobulin A (IgA) may be a more effective vaccine target than traditional influenza vaccines that target IgG, since different parts of IgA may engage the influenza virus simultaneously.53
Vaccines can be developed more quickly than in the past. The timeline from viral sequencing to human studies with deoxyribonucleic acid plasmid vaccines decreased from 20 months in 2003 for the severe acquired respiratory syndrome coronavirus to 11 months in 2006 for influenza A/Indonesia/2006 (H5), to 4 months in 2009 for influenza A/California/2009 (H1), to 3.5 months in 2016 for Zika virus.54 This is because it is possible today to sequence a virus and insert the genetic material into a vaccine platform without ever having to grow the virus.
TREATMENT
Numerous studies have found anti-influenza medications to be effective. Nevertheless, in an analysis of the 2011–2016 influenza seasons, only 15% of high-risk patients were prescribed anti-influenza medications within 2 days of symptom onset, including 37% in those with laboratory-confirmed influenza.55 Fever was associated with an increased rate of antiviral treatment, but 25% of high-risk outpatients were afebrile. Empiric treatment of 4 high-risk outpatients with acute respiratory illness was needed to treat 1 patient with influenza.55
Treatment with a neuraminidase inhibitor within 2 days of illness has recently been shown to improve survival and shorten duration of viral shedding in patients with avian influenza A(H7N9) infection.56 Antiviral treatment within 2 days of illness is associated with improved outcomes in transplant recipients57 and with a lower risk of otitis media in children.58
Appropriate anti-influenza treatment is as important as avoiding unnecessary antibiotics. Regrettably, as many as one-third of patients with laboratory-confirmed influenza are prescribed antibiotics.59
The US Food and Drug Administration warns against fraudulent unapproved over-the-counter influenza products.60
Baloxavir marboxil
Baloxavir marboxil is a new anti-influenza medication approved in Japan in February 2018 and anticipated to be available in the United States sometime in 2019.
This prodrug is hydrolyzed in vivo to the active metabolite, which selectively inhibits cap-dependent endonuclease enzyme, a key enzyme in initiation of messenger ribonucleic acid synthesis required for influenza viral replication.61
In a double-blind phase 3 trial, the median time to alleviation of influenza symptoms is 26.5 hours shorter with baloxavir marboxil than with placebo. One tablet was as effective as 5 days of the neuraminidase inhibitor oseltamivir and was associated with greater reduction in viral load 1 day after initiation, and similar side effects.62 Of concern is the emergence of nucleic acid substitutions conferring resistance to baloxavir; this occurred in 2.2% and 9.7% of baloxavir recipients in the phase 2 and 3 trials, respectively.
CLOSING THE GAPS
Several gaps in the management of influenza persist since the 1918 pandemic.1 These include gaps in epidemiology, prevention, diagnosis, treatment, and prognosis.
- Global networks wider than current ones are needed to address this global disease and to prioritize coordination efforts.
- Establishing and strengthening clinical capacity is needed in limited resource settings. New technologies are needed to expedite vaccine development and to achieve progress toward a universal vaccine.
- Current diagnostic tests do not distinguish between seasonal and novel influenza A viruses of zoonotic origin, which are expected to cause the next pandemic.
- Current antivirals have been shown to shorten duration of illness in outpatients with uncomplicated influenza, but the benefit in hospitalized patients has been less well established.
- In 2007, resistance of seasonal influenza A(H1N1) to oseltamivir became widespread. In 2009, pandemic influenza A(H1N1), which is highly susceptible to oseltamivir, replaced the seasonal virus and remains the predominantly circulating A(H1N1) strain.
- A small-molecule fragment, N-cyclohexyaltaurine, binds to the conserved hemagglutinin receptor-binding site in a manner that mimics the binding mode of the natural receptor sialic acid. This can serve as a template to guide the development of novel broad-spectrum small-molecule anti-influenza drugs.63
- Biomarkers that can accurately predict development of severe disease in patients with influenza are needed.
- Uyeki TM, Fowler RA, Fischer WA. Gaps in the clinical management of influenza: a century since the 1918 pandemic. JAMA 2018; 320(8):755–756. doi:10.1001/jama.2018.8113
- Garten R, Blanton L, Elal AI, et al. Update: influenza activity in the United States during the 2017–18 season and composition of the 2018–19 influenza vaccine. MMWR Morb Mortal Wkly Rep 2018; 67(22):634–642. doi:10.15585/mmwr.mm6722a4
- Tokars JI, Olsen SJ, Reed C. Seasonal incidence of symptomatic influenza in the United States. Clin Infect Dis 2018; 66(10):1511–1518. doi:10.1093/cid/cix1060
- Elbadawi LI, Talley P, Rolfes MA, et al. Non-mumps viral parotitis during the 2014–2015 influenza season in the United States. Clin Infect Dis 2018. Epub ahead of print. doi:10.1093/cid/ciy137
- Thielen BK, Friedlander H, Bistodeau S, et al. Detection of influenza C viruses among outpatients and patients hospitalized for severe acute respiratory infection, Minnesota, 2013–2016. Clin Infect Dis 2018; 66(7):1092–1098. doi:10.1093/cid/cix931
- Chena Y, Trovãob NS, Wang G, et al. Emergence and evolution of novel reassortant influenza A viruses in canines in southern China. MBio 2018; 9(3):e00909–e00918. doi:10.1128/mBio.00909-18
- Maier HE, Lopez R, Sanchez N, et al. Obesity increases the duration of influenza A virus shedding in adults. J Infect Dis 2018. Epub ahead of print. doi:10.1093/infdis/jiy370
- Warren-Gash C, Blackburn R, Whitaker H, McMenamin J, Hayward AC. Laboratory-confirmed respiratory infections as triggers for acute myocardial infarction and stroke: a self-controlled case series analysis of national linked datasets from Scotland. Eur Respir J 2018; 51(3):1701794. doi:10.1183/13993003.01794-2017
- Blackburn R, Zhao H, Pebody R, Hayward A, Warren-Gash C. Laboratory-confirmed respiratory infections as predictors of hospital admission for myocardial infarction and stroke: time-series analysis of English data for 2004–2015. Clin Infect Dis 2018; 67(1):8–17. doi:10.1093/cid/cix1144
- Newsweek; Andrew S. What is disease X? Deadly bird flu virus could be next pandemic. www.newsweek.com/disease-x-bird-flu-deaths-pandemic-what-h7n9-979723. Accessed October 3, 2018.
- Miller AC, Singh I, Koehler E, Polgreen PM. A smartphone-driven thermometer application for real-time population- and individual-level influenza surveillance. Clin Infect Dis 2018; 67(3):388–397. doi:10.1093/cid/ciy073
- Kormuth KA, Lin K, Prussin AJ 2nd, et al. Influenza virus infectivity is retained in aerosols and droplets independent of relative humidity, J Infect Dis 2018; 218(5):739–747. doi:10.1093/infdis/jiy221
- Hertzberg VS, Weiss H, Elon L, et. al. Behaviors, movements, and transmission of droplet-mediated respiratory diseases during transcontinental airline flights. Proc Natl Acad Sci U S A 2018; 115(14):3623–3627. doi:10.1073/pnas.1711611115
- Grohskopf LA, Sokolow LZ, Broder KR, Walter EB, Fry AM, Jernigan DB. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices—United States, 2018–19 influenza season. MMWR Recomm Rep 2018; 67(3):1–20. doi:10.15585/mmwr.rr6703a1
- Grohskopf LA, Sokolow LZ, Fry AM, Walter EB, Jernigan DB. Update: ACIP recommendations for the use of quadrivalent live attenuated influenza vaccine (LAIV4)—United States, 2018–19 influenza season. MMWR Morb Mortal Wkly Rep 2018; 67(22):643–645. doi:10.15585/mmwr.mm6722a5
- Flannery B, Chung JR, Belongia EA, et al. Interim estimates of 2017–18 seasonal influenza vaccine effectiveness—United States, February 2018. MMWR Morb Mortal Wkly Rep 2018; 67(6):180–185. doi:10.15585/mmwr.mm6706a2
- Demicheli V, Jefferson T, Ferroni E, Rivetti A, Di Pietrantonj C. Vaccines for preventing influenza in healthy adults. Cochrane Database Syst Rev 2018; 2:CD001269. doi:10.1002/14651858.CD001269.pub6
- Flannery B, Smith C, Garten RJ, et al. Influence of birth cohort on effectiveness of 2015–2016 influenza vaccine against medically attended illness due to 2009 pandemic influenza A(H1N1) virus in the United States. J Infect Dis 2018; 218(2):189–196. doi:10.1093/infdis/jix634
- Rondy M, El Omeiri N, Thompson MG, Leveque A, Moren A, Sullivan SG. Effectiveness of influenza vaccines in preventing severe influenza illness among adults: a systematic review and meta-analysis of test-negative design case-control studies. J Infect 2017; 75(5):381–394. doi:10.1016/j.jinf.2017.09.010
- Stein Y, Mandelboim M, Sefty H, et al; Israeli Influenza Surveillance Network (IISN). Seasonal influenza vaccine effectiveness in preventing laboratory-confirmed influenza in primary care in Israel, 2016–2017 season: insights into novel age-specific analysis. Clin Infect Dis 2018; 66(9):1383–1391. doi:10.1093/cid/cix1013
- Sah P, Medlock J, Fitzpatrick MC, Singer BH, Galvani AP. Optimizing the impact of low-efficacy influenza vaccines. Proc Natl Acad Sci U S A 2018; 115(20):5151–5156. doi:10.1073/pnas.1802479115
- QuickStats: percentage of currently employed adults aged ≥ 18 years who received influenza vaccine in the past 12 months, by employment category—national health interview survey, United States, 2012 and 2016. MMWR Morb Mortal Wkly Rep 2018; 67(16):480. doi:10.15585/mmwr.mm6716a8
- Healthy People.gov. Immunization and infectious diseases. IID-12. Increase the percentage of children and adults who are vaccinated annually against seasonal influenza. www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives. Accessed October 3, 2018.
- Greene MT, Fowler KE, Ratz D, Krein SL, Bradley SF, Saint S. Changes in influenza vaccination requirements for health care personnel in US hospitals. JAMA Network Open 2018; 1(2):e180143. doi:10.1001/jamanetworkopen.2018.0143
- Opel DJ, Sonne JA, Mello MM. Vaccination without litigation—addressing religious objections to hospital influenza-vaccination mandates. N Engl J Med 2018; 378(9):785–788. doi:10.1056/NEJMp1716147
- Horowitz J. Italy loosens vaccine law just as children return to school. New York Times Sept. 20, 2018. www.nytimes.com/2018/09/20/world/europe/italy-vaccines-five-star-movement.html.
- National Conference of State Legislature. States with religious and philosophical exemptions from school immunization requirements. www.ncsl.org/research/health/school-immunization-exemption-state-laws.aspx. Accessed October 3, 2018.
- Olive JK, Hotez PJ, Damania A, Nolan MS. The state of the antivaccine movement in the United States: a focused examination of nonmedical exemptions in states and counties. PLoS Med 2018; 15(6):e1002578. doi:10.1371/journal.pmed.1002578
- Logan J, Nederhoff D, Koch B, et al. ‘What have you HEARD about the HERD?’ Does education about local influenza vaccination coverage and herd immunity affect willingness to vaccinate? Vaccine 2018; 36(28):4118–4125. doi:10.1016/j.vaccine.2018.05.037
- Belongia EA, Skowronski DM, McLean HQ, Chambers C, Sundaram ME, De Serres G. Repeated annual influenza vaccination and vaccine effectiveness: review of evidence. Expert Rev Vaccines 2017; 16(7):1–14. doi:10.1080/14760584.2017.1334554
- Saito N, Komori K, Suzuki M, et al. Negative impact of prior influenza vaccination on current influenza vaccination among people infected and not infected in prior season: a test-negative case-control study in Japan. Vaccine 2017; 35(4):687–693. doi:10.1016/j.vaccine.2016.11.024
- Cheng AC, Macartney KK, Waterer GW, Kotsimbos T, Kelly PM, Blyth CC; Influenza Complications Alert Network (FluCAN) Investigators. Repeated vaccination does not appear to impact upon influenza vaccine effectiveness against hospitalization with confirmed influenza. Clin Infect Dis 2017; 64(11):1564–1572. doi:10.1093/cid/cix209
- Rondy M, Launay O, Castilla J, et al; InNHOVE/I-MOVE+working group. Repeated seasonal influenza vaccination among elderly in Europe: effects on laboratory confirmed hospitalised influenza. Vaccine 2017; 35(34):4298–4306. doi:10.1016/j.vaccine.2017.06.088
- Young-Xu Y, van Aalst R, Mahmud SM, et al. Relative vaccine effectiveness of high-dose versus standard-dose influenza vaccines among Veterans Health Administration patients. J Infect Dis 2018; 217(11):1718–1727. doi:10.1093/infdis/jiy088
- Shay DK, Chillarige Y, Kelman J, et al. Comparative effectiveness of high-dose versus standard-dose influenza vaccines among US Medicare beneficiaries in preventing postinfluenza deaths during 2012–2013 and 2013–2014. J Infect Dis 2017; 215(4):510–517. doi:10.1093/infdis/jiw641
- Madaras-Kelly K, Remington R, Hruza H, Xu D. Comparative effectiveness of high-dose versus standard-dose influenza vaccines in preventing postinfluenza deaths. J Infect Dis 2018; 218(2):336–337. doi:10.1093/infdis/jix645
- Tam YH, Valkenburg SA, Perera RAPM, et al. Immune responses to twice-annual influenza vaccination in older adults in Hong Kong. Clin Infect Dis 2018; 66(6):904–912. doi:10.1093/cid/cix900
- Ohfuji S, Deguchi M, Tachibana D, et al; Osaka Pregnant Women Influenza Study Group. Protective effect of maternal influenza vaccination on influenza in their infants: a prospective cohort study. J Infect Dis 2018; 217(6):878–886. doi:10.1093/infdis/jix629
- Katz J, Englund JA, Steinhoff MC, et al. Impact of timing of influenza vaccination in pregnancy on transplacental antibody transfer, influenza incidence, and birth outcomes: a randomized trial in rural Nepal. Clin Infect Dis 2018; 67(3):334–340. doi:10.1093/cid/ciy090
- Nunes MC, Cutland CL, Madhi SA. Influenza vaccination during pregnancy and protection against pertussis. N Engl J Med 2018; 378(13):1257–1258. doi:10.1056/NEJMc1705208
- Andrew MK, Shinde V, Ye L, et al; Serious Outcomes Surveillance Network of the Public Health Agency of Canada/Canadian Institutes of Health Research Influenza Research Network (PCIRN) and the Toronto Invasive Bacterial Diseases Network (TIBDN). The importance of frailty in the assessment of influenza vaccine effectiveness against influenza-related hospitalization in elderly people. J Infect Dis 2017; 216(4):405–414. doi:10.1093/infdis/jix282
- Park JK, Lee YJ, Shin K, et al. Impact of temporary methotrexate discontinuation for 2 weeks on immunogenicity of seasonal influenza vaccination in patients with rheumatoid arthritis: a randomised clinical trial. Ann Rheum Dis 2018; 77(6):898–904. doi:10.1136/annrheumdis-2018-213222
- Kumar D, Ferreira VH, Blumberg E, et al. A five-year prospective multi-center evaluation of influenza infection in transplant recipients. Clin Infect Dis 2018. Epub ahead of print. doi:10.1093/cid/ciy294
- Natori Y, Shiotsuka M, Slomovic J, et al. A double-blind, randomized trial of high-dose vs standard-dose influenza vaccine in adult solid-organ transplant recipients. Clin Infect Dis 2018; 66(11):1698–1704. doi:10.1093/cid/cix1082
- Omer SB, Phadke VK, Bednarczyk BA, Chamberlain AT, Brosseau JL, Orenstein WA. Impact of statins on influenza vaccine effectiveness against medically attended acute respiratory illness. J Infect Dis 2016; 213(8):1216–1223. doi:10.1093/infdis/jiv457
- Dunkle LM, Izikson R, Patriarca P, et al. Efficacy of recombinant influenza vaccine in adults 50 years of age or older. N Engl J Med 2017; 376(25):2427–2436. doi:10.1056/NEJMoa1608862
- STAT; Branswell H. How the US military might help answer a critical question about the flu vaccine. www.statnews.com/2018/03/02/flu-vaccine-egg-production-data. Accessed October 3, 2018.
- Paules CI, Sullivan SG, Subbarao K, Fauci AS. Chasing seasonal influenza—the need for a universal influenza vaccine. N Engl J Med 2018; 378(1):7–9. doi:10.1056/NEJMp1714916
- Jin XW, Mossad SB. Avian influenza: an emerging pandemic threat. Cleve Clin J Med 2005; 72:1129-1134. pmid:16392727
- Wei WI, Brunger AT, Skehel JJ, Wiley DC. Refinement of the influenza virus hemagglutinin by simulated annealing. J Mol Biol 1990; 212(4):737–761. doi:10.1016/0022-2836(90)90234-D
- Erbelding EJ, Post DJ, Stemmy EJ, et al. A universal influenza vaccine: the strategic plan for the National Institute of Allergy and Infectious Diseases, J Infect Dis 2018; 218(3):347–354. doi:10.1093/infdis/jiy103
- Shinde V, Fries L, Wu Y, et al. Improved titers against influenza drift variants with a nanoparticle vaccine. N Engl J Med 2018; 378(24):2346–2348. doi:10.1056/NEJMc1803554
- Maurer MA, Meyer L, Bianchi M, et al. Glycosylation of human IgA directly inhibits influenza A and other sialic-acid-binding viruses. Cell Rep 2018; 23(1):90–99. doi:10.1016/j.celrep.2018.03.027
- Graham BS, Mascola JR, Fauci AS. Novel vaccine technologies: essential components of an adequate response to emerging viral diseases. JAMA 2018; 319(14):1431–1432. doi:10.1001/jama.2018.0345
- Stewart RJ, Flannery B, Chung JR, et al. Influenza antiviral prescribing for outpatients with an acute respiratory illness and at high risk for influenza-associated complications during 5 influenza seasons—United States, 2011–2016. Clin Infect Dis 2018; 66(7):1035–1041. doi:10.1093/cid/cix922
- Zheng S, Tang L, Gao H, et al. Benefit of early initiation of neuraminidase inhibitor treatment to hospitalized patients with avian influenza A(H7N9) virus. Clin Infect Dis 2018; 66(7):1054–1060. doi:10.1093/cid/cix930
- Kumar D, Ferreira VH, Blumberg E, et al. A five-year prospective multi-center evaluation of influenza infection in transplant recipients. Clin Infect Dis 2018. Epub ahead of print. doi:10.1093/cid/ciy294
- Malosh RE, Martin ET, Heikkinen T, Brooks WA, Whitley RJ, Monto AS. Efficacy and safety of oseltamivir in children: systematic review and individual patient data meta-analysis of randomized controlled trials. Clin Infect Dis 2018; 66(10):1492–1500. doi:10.1093/cid/cix1040
- Havers FP, Hicks LA, Chung JR, et al. Outpatient antibiotic prescribing for acute respiratory infections during influenza seasons. JAMA Network Open 2018; 1(2):e180243. doi:10.1001/jamanetworkopen.2018.0243
- US Food and Drug Administration. FDA warns of fraudulent and unapproved flu products. www.fda.gov/newsevents/newsroom/pressannouncements/ucm599223.htm. Accessed October 3, 2018.
- Portsmouth S, Kawaguchi K, Arai M, Tsuchiya K, Uehara T. Cap-dependent endonuclease inhibitor S-033188 for the treatment of influenza: results from a phase 3, randomized, double-blind, placebo- and active-controlled study in otherwise healthy adolescents and adults with seasonal influenza. Open Forum Infect Dis 2017; 4(suppl 1):S734. doi:10.1093/ofid/ofx180.001
- Hayden FG, Sugaya N, Hirotsu N, et al; Baloxavir Marboxil Investigators Group. Baloxavir Marboxil for uncomplicated influenza in adults and adolescents. N Engl J Med 2018; 379(10):913–923. doi:10.1056/NEJMoa1716197
- Kadam RU, Wilson IA. A small-molecule fragment that emulates binding of receptor and broadly neutralizing antibodies to influenza A hemagglutinin. Proc Natl Acad Sci U S A 2018; 115(16):4240–4245. doi:10.1073/pnas.1801999115
- Uyeki TM, Fowler RA, Fischer WA. Gaps in the clinical management of influenza: a century since the 1918 pandemic. JAMA 2018; 320(8):755–756. doi:10.1001/jama.2018.8113
- Garten R, Blanton L, Elal AI, et al. Update: influenza activity in the United States during the 2017–18 season and composition of the 2018–19 influenza vaccine. MMWR Morb Mortal Wkly Rep 2018; 67(22):634–642. doi:10.15585/mmwr.mm6722a4
- Tokars JI, Olsen SJ, Reed C. Seasonal incidence of symptomatic influenza in the United States. Clin Infect Dis 2018; 66(10):1511–1518. doi:10.1093/cid/cix1060
- Elbadawi LI, Talley P, Rolfes MA, et al. Non-mumps viral parotitis during the 2014–2015 influenza season in the United States. Clin Infect Dis 2018. Epub ahead of print. doi:10.1093/cid/ciy137
- Thielen BK, Friedlander H, Bistodeau S, et al. Detection of influenza C viruses among outpatients and patients hospitalized for severe acute respiratory infection, Minnesota, 2013–2016. Clin Infect Dis 2018; 66(7):1092–1098. doi:10.1093/cid/cix931
- Chena Y, Trovãob NS, Wang G, et al. Emergence and evolution of novel reassortant influenza A viruses in canines in southern China. MBio 2018; 9(3):e00909–e00918. doi:10.1128/mBio.00909-18
- Maier HE, Lopez R, Sanchez N, et al. Obesity increases the duration of influenza A virus shedding in adults. J Infect Dis 2018. Epub ahead of print. doi:10.1093/infdis/jiy370
- Warren-Gash C, Blackburn R, Whitaker H, McMenamin J, Hayward AC. Laboratory-confirmed respiratory infections as triggers for acute myocardial infarction and stroke: a self-controlled case series analysis of national linked datasets from Scotland. Eur Respir J 2018; 51(3):1701794. doi:10.1183/13993003.01794-2017
- Blackburn R, Zhao H, Pebody R, Hayward A, Warren-Gash C. Laboratory-confirmed respiratory infections as predictors of hospital admission for myocardial infarction and stroke: time-series analysis of English data for 2004–2015. Clin Infect Dis 2018; 67(1):8–17. doi:10.1093/cid/cix1144
- Newsweek; Andrew S. What is disease X? Deadly bird flu virus could be next pandemic. www.newsweek.com/disease-x-bird-flu-deaths-pandemic-what-h7n9-979723. Accessed October 3, 2018.
- Miller AC, Singh I, Koehler E, Polgreen PM. A smartphone-driven thermometer application for real-time population- and individual-level influenza surveillance. Clin Infect Dis 2018; 67(3):388–397. doi:10.1093/cid/ciy073
- Kormuth KA, Lin K, Prussin AJ 2nd, et al. Influenza virus infectivity is retained in aerosols and droplets independent of relative humidity, J Infect Dis 2018; 218(5):739–747. doi:10.1093/infdis/jiy221
- Hertzberg VS, Weiss H, Elon L, et. al. Behaviors, movements, and transmission of droplet-mediated respiratory diseases during transcontinental airline flights. Proc Natl Acad Sci U S A 2018; 115(14):3623–3627. doi:10.1073/pnas.1711611115
- Grohskopf LA, Sokolow LZ, Broder KR, Walter EB, Fry AM, Jernigan DB. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices—United States, 2018–19 influenza season. MMWR Recomm Rep 2018; 67(3):1–20. doi:10.15585/mmwr.rr6703a1
- Grohskopf LA, Sokolow LZ, Fry AM, Walter EB, Jernigan DB. Update: ACIP recommendations for the use of quadrivalent live attenuated influenza vaccine (LAIV4)—United States, 2018–19 influenza season. MMWR Morb Mortal Wkly Rep 2018; 67(22):643–645. doi:10.15585/mmwr.mm6722a5
- Flannery B, Chung JR, Belongia EA, et al. Interim estimates of 2017–18 seasonal influenza vaccine effectiveness—United States, February 2018. MMWR Morb Mortal Wkly Rep 2018; 67(6):180–185. doi:10.15585/mmwr.mm6706a2
- Demicheli V, Jefferson T, Ferroni E, Rivetti A, Di Pietrantonj C. Vaccines for preventing influenza in healthy adults. Cochrane Database Syst Rev 2018; 2:CD001269. doi:10.1002/14651858.CD001269.pub6
- Flannery B, Smith C, Garten RJ, et al. Influence of birth cohort on effectiveness of 2015–2016 influenza vaccine against medically attended illness due to 2009 pandemic influenza A(H1N1) virus in the United States. J Infect Dis 2018; 218(2):189–196. doi:10.1093/infdis/jix634
- Rondy M, El Omeiri N, Thompson MG, Leveque A, Moren A, Sullivan SG. Effectiveness of influenza vaccines in preventing severe influenza illness among adults: a systematic review and meta-analysis of test-negative design case-control studies. J Infect 2017; 75(5):381–394. doi:10.1016/j.jinf.2017.09.010
- Stein Y, Mandelboim M, Sefty H, et al; Israeli Influenza Surveillance Network (IISN). Seasonal influenza vaccine effectiveness in preventing laboratory-confirmed influenza in primary care in Israel, 2016–2017 season: insights into novel age-specific analysis. Clin Infect Dis 2018; 66(9):1383–1391. doi:10.1093/cid/cix1013
- Sah P, Medlock J, Fitzpatrick MC, Singer BH, Galvani AP. Optimizing the impact of low-efficacy influenza vaccines. Proc Natl Acad Sci U S A 2018; 115(20):5151–5156. doi:10.1073/pnas.1802479115
- QuickStats: percentage of currently employed adults aged ≥ 18 years who received influenza vaccine in the past 12 months, by employment category—national health interview survey, United States, 2012 and 2016. MMWR Morb Mortal Wkly Rep 2018; 67(16):480. doi:10.15585/mmwr.mm6716a8
- Healthy People.gov. Immunization and infectious diseases. IID-12. Increase the percentage of children and adults who are vaccinated annually against seasonal influenza. www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives. Accessed October 3, 2018.
- Greene MT, Fowler KE, Ratz D, Krein SL, Bradley SF, Saint S. Changes in influenza vaccination requirements for health care personnel in US hospitals. JAMA Network Open 2018; 1(2):e180143. doi:10.1001/jamanetworkopen.2018.0143
- Opel DJ, Sonne JA, Mello MM. Vaccination without litigation—addressing religious objections to hospital influenza-vaccination mandates. N Engl J Med 2018; 378(9):785–788. doi:10.1056/NEJMp1716147
- Horowitz J. Italy loosens vaccine law just as children return to school. New York Times Sept. 20, 2018. www.nytimes.com/2018/09/20/world/europe/italy-vaccines-five-star-movement.html.
- National Conference of State Legislature. States with religious and philosophical exemptions from school immunization requirements. www.ncsl.org/research/health/school-immunization-exemption-state-laws.aspx. Accessed October 3, 2018.
- Olive JK, Hotez PJ, Damania A, Nolan MS. The state of the antivaccine movement in the United States: a focused examination of nonmedical exemptions in states and counties. PLoS Med 2018; 15(6):e1002578. doi:10.1371/journal.pmed.1002578
- Logan J, Nederhoff D, Koch B, et al. ‘What have you HEARD about the HERD?’ Does education about local influenza vaccination coverage and herd immunity affect willingness to vaccinate? Vaccine 2018; 36(28):4118–4125. doi:10.1016/j.vaccine.2018.05.037
- Belongia EA, Skowronski DM, McLean HQ, Chambers C, Sundaram ME, De Serres G. Repeated annual influenza vaccination and vaccine effectiveness: review of evidence. Expert Rev Vaccines 2017; 16(7):1–14. doi:10.1080/14760584.2017.1334554
- Saito N, Komori K, Suzuki M, et al. Negative impact of prior influenza vaccination on current influenza vaccination among people infected and not infected in prior season: a test-negative case-control study in Japan. Vaccine 2017; 35(4):687–693. doi:10.1016/j.vaccine.2016.11.024
- Cheng AC, Macartney KK, Waterer GW, Kotsimbos T, Kelly PM, Blyth CC; Influenza Complications Alert Network (FluCAN) Investigators. Repeated vaccination does not appear to impact upon influenza vaccine effectiveness against hospitalization with confirmed influenza. Clin Infect Dis 2017; 64(11):1564–1572. doi:10.1093/cid/cix209
- Rondy M, Launay O, Castilla J, et al; InNHOVE/I-MOVE+working group. Repeated seasonal influenza vaccination among elderly in Europe: effects on laboratory confirmed hospitalised influenza. Vaccine 2017; 35(34):4298–4306. doi:10.1016/j.vaccine.2017.06.088
- Young-Xu Y, van Aalst R, Mahmud SM, et al. Relative vaccine effectiveness of high-dose versus standard-dose influenza vaccines among Veterans Health Administration patients. J Infect Dis 2018; 217(11):1718–1727. doi:10.1093/infdis/jiy088
- Shay DK, Chillarige Y, Kelman J, et al. Comparative effectiveness of high-dose versus standard-dose influenza vaccines among US Medicare beneficiaries in preventing postinfluenza deaths during 2012–2013 and 2013–2014. J Infect Dis 2017; 215(4):510–517. doi:10.1093/infdis/jiw641
- Madaras-Kelly K, Remington R, Hruza H, Xu D. Comparative effectiveness of high-dose versus standard-dose influenza vaccines in preventing postinfluenza deaths. J Infect Dis 2018; 218(2):336–337. doi:10.1093/infdis/jix645
- Tam YH, Valkenburg SA, Perera RAPM, et al. Immune responses to twice-annual influenza vaccination in older adults in Hong Kong. Clin Infect Dis 2018; 66(6):904–912. doi:10.1093/cid/cix900
- Ohfuji S, Deguchi M, Tachibana D, et al; Osaka Pregnant Women Influenza Study Group. Protective effect of maternal influenza vaccination on influenza in their infants: a prospective cohort study. J Infect Dis 2018; 217(6):878–886. doi:10.1093/infdis/jix629
- Katz J, Englund JA, Steinhoff MC, et al. Impact of timing of influenza vaccination in pregnancy on transplacental antibody transfer, influenza incidence, and birth outcomes: a randomized trial in rural Nepal. Clin Infect Dis 2018; 67(3):334–340. doi:10.1093/cid/ciy090
- Nunes MC, Cutland CL, Madhi SA. Influenza vaccination during pregnancy and protection against pertussis. N Engl J Med 2018; 378(13):1257–1258. doi:10.1056/NEJMc1705208
- Andrew MK, Shinde V, Ye L, et al; Serious Outcomes Surveillance Network of the Public Health Agency of Canada/Canadian Institutes of Health Research Influenza Research Network (PCIRN) and the Toronto Invasive Bacterial Diseases Network (TIBDN). The importance of frailty in the assessment of influenza vaccine effectiveness against influenza-related hospitalization in elderly people. J Infect Dis 2017; 216(4):405–414. doi:10.1093/infdis/jix282
- Park JK, Lee YJ, Shin K, et al. Impact of temporary methotrexate discontinuation for 2 weeks on immunogenicity of seasonal influenza vaccination in patients with rheumatoid arthritis: a randomised clinical trial. Ann Rheum Dis 2018; 77(6):898–904. doi:10.1136/annrheumdis-2018-213222
- Kumar D, Ferreira VH, Blumberg E, et al. A five-year prospective multi-center evaluation of influenza infection in transplant recipients. Clin Infect Dis 2018. Epub ahead of print. doi:10.1093/cid/ciy294
- Natori Y, Shiotsuka M, Slomovic J, et al. A double-blind, randomized trial of high-dose vs standard-dose influenza vaccine in adult solid-organ transplant recipients. Clin Infect Dis 2018; 66(11):1698–1704. doi:10.1093/cid/cix1082
- Omer SB, Phadke VK, Bednarczyk BA, Chamberlain AT, Brosseau JL, Orenstein WA. Impact of statins on influenza vaccine effectiveness against medically attended acute respiratory illness. J Infect Dis 2016; 213(8):1216–1223. doi:10.1093/infdis/jiv457
- Dunkle LM, Izikson R, Patriarca P, et al. Efficacy of recombinant influenza vaccine in adults 50 years of age or older. N Engl J Med 2017; 376(25):2427–2436. doi:10.1056/NEJMoa1608862
- STAT; Branswell H. How the US military might help answer a critical question about the flu vaccine. www.statnews.com/2018/03/02/flu-vaccine-egg-production-data. Accessed October 3, 2018.
- Paules CI, Sullivan SG, Subbarao K, Fauci AS. Chasing seasonal influenza—the need for a universal influenza vaccine. N Engl J Med 2018; 378(1):7–9. doi:10.1056/NEJMp1714916
- Jin XW, Mossad SB. Avian influenza: an emerging pandemic threat. Cleve Clin J Med 2005; 72:1129-1134. pmid:16392727
- Wei WI, Brunger AT, Skehel JJ, Wiley DC. Refinement of the influenza virus hemagglutinin by simulated annealing. J Mol Biol 1990; 212(4):737–761. doi:10.1016/0022-2836(90)90234-D
- Erbelding EJ, Post DJ, Stemmy EJ, et al. A universal influenza vaccine: the strategic plan for the National Institute of Allergy and Infectious Diseases, J Infect Dis 2018; 218(3):347–354. doi:10.1093/infdis/jiy103
- Shinde V, Fries L, Wu Y, et al. Improved titers against influenza drift variants with a nanoparticle vaccine. N Engl J Med 2018; 378(24):2346–2348. doi:10.1056/NEJMc1803554
- Maurer MA, Meyer L, Bianchi M, et al. Glycosylation of human IgA directly inhibits influenza A and other sialic-acid-binding viruses. Cell Rep 2018; 23(1):90–99. doi:10.1016/j.celrep.2018.03.027
- Graham BS, Mascola JR, Fauci AS. Novel vaccine technologies: essential components of an adequate response to emerging viral diseases. JAMA 2018; 319(14):1431–1432. doi:10.1001/jama.2018.0345
- Stewart RJ, Flannery B, Chung JR, et al. Influenza antiviral prescribing for outpatients with an acute respiratory illness and at high risk for influenza-associated complications during 5 influenza seasons—United States, 2011–2016. Clin Infect Dis 2018; 66(7):1035–1041. doi:10.1093/cid/cix922
- Zheng S, Tang L, Gao H, et al. Benefit of early initiation of neuraminidase inhibitor treatment to hospitalized patients with avian influenza A(H7N9) virus. Clin Infect Dis 2018; 66(7):1054–1060. doi:10.1093/cid/cix930
- Kumar D, Ferreira VH, Blumberg E, et al. A five-year prospective multi-center evaluation of influenza infection in transplant recipients. Clin Infect Dis 2018. Epub ahead of print. doi:10.1093/cid/ciy294
- Malosh RE, Martin ET, Heikkinen T, Brooks WA, Whitley RJ, Monto AS. Efficacy and safety of oseltamivir in children: systematic review and individual patient data meta-analysis of randomized controlled trials. Clin Infect Dis 2018; 66(10):1492–1500. doi:10.1093/cid/cix1040
- Havers FP, Hicks LA, Chung JR, et al. Outpatient antibiotic prescribing for acute respiratory infections during influenza seasons. JAMA Network Open 2018; 1(2):e180243. doi:10.1001/jamanetworkopen.2018.0243
- US Food and Drug Administration. FDA warns of fraudulent and unapproved flu products. www.fda.gov/newsevents/newsroom/pressannouncements/ucm599223.htm. Accessed October 3, 2018.
- Portsmouth S, Kawaguchi K, Arai M, Tsuchiya K, Uehara T. Cap-dependent endonuclease inhibitor S-033188 for the treatment of influenza: results from a phase 3, randomized, double-blind, placebo- and active-controlled study in otherwise healthy adolescents and adults with seasonal influenza. Open Forum Infect Dis 2017; 4(suppl 1):S734. doi:10.1093/ofid/ofx180.001
- Hayden FG, Sugaya N, Hirotsu N, et al; Baloxavir Marboxil Investigators Group. Baloxavir Marboxil for uncomplicated influenza in adults and adolescents. N Engl J Med 2018; 379(10):913–923. doi:10.1056/NEJMoa1716197
- Kadam RU, Wilson IA. A small-molecule fragment that emulates binding of receptor and broadly neutralizing antibodies to influenza A hemagglutinin. Proc Natl Acad Sci U S A 2018; 115(16):4240–4245. doi:10.1073/pnas.1801999115
KEY POINTS
- Influenza A(H7N9) is a prime candidate to cause the next influenza pandemic.
- Influenza vaccine prevents 300 to 4,000 deaths in the United States every year.
- The 2018–2019 quadrivalent influenza vaccine contains updated A(H3N2) and B/Victoria lineage components different from those in the 2017–2018 Northern Hemisphere vaccine.
- The live-attenuated influenza vaccine, which was not recommended during the 2016–2017 and 2017–2018 influenza seasons, is recommended for the 2018–2019 influenza season.
- Influenza vaccine is recommended any time during pregnancy and is associated with lower infant mortality rates.
- Overall influenza vaccination rates remain below the 80% target for all Americans and 90% for at-risk populations.
Crohn’s disease tied to anal canal high-risk HPV infection
Crohn’s disease was significantly associated with anal canal high-risk human papillomavirus (HPV) infection in a prospective, single-center study of patients undergoing colonoscopy for various indications.
High-risk HPV and HPV strain 16 were detected in 30% of patients with Crohn’s disease and 18% of patients without Crohn’s disease (P = .005), said Lucine Vuitton, MD, of University Hospital of Besançon (France) and her associates. “Increasing our knowledge of HPV infection of anal tissues could help physicians identify populations at risk and promote prophylaxis with vaccination and adequate screening,” the investigators wrote in the November issue of Clinical Gastroenterology and Hepatology.
Most anal cancers are squamous cell carcinomas, for which infection with high-risk HPV (especially high-risk HPV16) is a driving risk factor. Case studies and literature reviews have linked Crohn’s disease to increased rates of anal canal cancers, but population-based data were lacking, the researchers wrote. Therefore, they prospectively analyzed anal tissue samples from 467 consecutive patients undergoing colonoscopy at a tertiary care center in France. Median age was 54 years (interquartile range, 18-86 years), and 52% of patients were women. No patient had detectable macroscopic neoplastic lesions at the anal margin at baseline.
The researchers used the QIAamp DNA Blood minikit (Qiagen) for DNA extraction and the INNO-LiPA HPV Genotyping Extra kit (Fujirebio Diagnostics) for HPV DNA detection and genotyping. These methods identified HPV DNA in anal tissue samples from 34% of the patients and high-risk HPV DNA in 18% of patients. The most prevalent genotype was HPV16 (detected in 7% of samples), followed by HPV51, HPV52, and HPV39.
A total of 112 patients were receiving at least one immunosuppressive treatment for inflammatory bowel disease or another condition. Seventy patients had Crohn’s disease, and 29 patients had ulcerative colitis. The prevalence of anal canal high-risk HPV and HPV16 infection in patients with ulcerative colitis was similar to that seen in those without inflammatory bowel disease. However, patients with Crohn’s disease were more likely to have anal canal high-risk HPV infection (30%) and HPV16 infection (14%), compared with patients without Crohn’s disease (18% and 7%, respectively). Additionally, among 22 patients with Crohn’s disease and perianal involvement, 11 had HPV DNA in the anal canal versus 30% of other patients with inflammatory bowel disease.
Women were more likely to have anal canal high-risk HPV (23%) infection than were men (13%; P = .004). In a multivariable analysis of self-reported data and medical data, significant risk factors for high-risk HPV infection included female sex, a history of sexually transmitted infections, having more than 10 sexual partners over the life course, having at least one sexual partner during the past year, current smoking, and immunosuppressive therapy. The multivariable analysis also linked Crohn’s disease with anal canal high-risk HPV16 infection (odds ratio, 3.8), but the association did not reach statistical significance (95% confidence interval, 0.9-16.9).
Most patients with Crohn’s disease were on immunosuppressive therapy, “which markedly affected statistical power,” the researchers commented. Nonetheless, their findings support HPV vaccination for patients with Crohn’s disease, as well as efforts to target high-risk patients who could benefit from anal cancer screening, they said.
The work was funded by the APICHU research grant from Besançon (France) University Hospital and by the Région de Franche-Comté. Dr. Vuitton disclosed ties to AbbVie, Ferring, MSD, Hospira, Janssen, and Takeda. Three coinvestigators disclosed relationships with AbbVie, MSD, Hospira, Mayoli, and Roche.
SOURCE: Vuitton L et al. Clin Gastroenterol Hepatol. 2018 Nov. doi: 10.1016/j.cgh.2018.03.008.
Crohn’s disease was significantly associated with anal canal high-risk human papillomavirus (HPV) infection in a prospective, single-center study of patients undergoing colonoscopy for various indications.
High-risk HPV and HPV strain 16 were detected in 30% of patients with Crohn’s disease and 18% of patients without Crohn’s disease (P = .005), said Lucine Vuitton, MD, of University Hospital of Besançon (France) and her associates. “Increasing our knowledge of HPV infection of anal tissues could help physicians identify populations at risk and promote prophylaxis with vaccination and adequate screening,” the investigators wrote in the November issue of Clinical Gastroenterology and Hepatology.
Most anal cancers are squamous cell carcinomas, for which infection with high-risk HPV (especially high-risk HPV16) is a driving risk factor. Case studies and literature reviews have linked Crohn’s disease to increased rates of anal canal cancers, but population-based data were lacking, the researchers wrote. Therefore, they prospectively analyzed anal tissue samples from 467 consecutive patients undergoing colonoscopy at a tertiary care center in France. Median age was 54 years (interquartile range, 18-86 years), and 52% of patients were women. No patient had detectable macroscopic neoplastic lesions at the anal margin at baseline.
The researchers used the QIAamp DNA Blood minikit (Qiagen) for DNA extraction and the INNO-LiPA HPV Genotyping Extra kit (Fujirebio Diagnostics) for HPV DNA detection and genotyping. These methods identified HPV DNA in anal tissue samples from 34% of the patients and high-risk HPV DNA in 18% of patients. The most prevalent genotype was HPV16 (detected in 7% of samples), followed by HPV51, HPV52, and HPV39.
A total of 112 patients were receiving at least one immunosuppressive treatment for inflammatory bowel disease or another condition. Seventy patients had Crohn’s disease, and 29 patients had ulcerative colitis. The prevalence of anal canal high-risk HPV and HPV16 infection in patients with ulcerative colitis was similar to that seen in those without inflammatory bowel disease. However, patients with Crohn’s disease were more likely to have anal canal high-risk HPV infection (30%) and HPV16 infection (14%), compared with patients without Crohn’s disease (18% and 7%, respectively). Additionally, among 22 patients with Crohn’s disease and perianal involvement, 11 had HPV DNA in the anal canal versus 30% of other patients with inflammatory bowel disease.
Women were more likely to have anal canal high-risk HPV (23%) infection than were men (13%; P = .004). In a multivariable analysis of self-reported data and medical data, significant risk factors for high-risk HPV infection included female sex, a history of sexually transmitted infections, having more than 10 sexual partners over the life course, having at least one sexual partner during the past year, current smoking, and immunosuppressive therapy. The multivariable analysis also linked Crohn’s disease with anal canal high-risk HPV16 infection (odds ratio, 3.8), but the association did not reach statistical significance (95% confidence interval, 0.9-16.9).
Most patients with Crohn’s disease were on immunosuppressive therapy, “which markedly affected statistical power,” the researchers commented. Nonetheless, their findings support HPV vaccination for patients with Crohn’s disease, as well as efforts to target high-risk patients who could benefit from anal cancer screening, they said.
The work was funded by the APICHU research grant from Besançon (France) University Hospital and by the Région de Franche-Comté. Dr. Vuitton disclosed ties to AbbVie, Ferring, MSD, Hospira, Janssen, and Takeda. Three coinvestigators disclosed relationships with AbbVie, MSD, Hospira, Mayoli, and Roche.
SOURCE: Vuitton L et al. Clin Gastroenterol Hepatol. 2018 Nov. doi: 10.1016/j.cgh.2018.03.008.
Crohn’s disease was significantly associated with anal canal high-risk human papillomavirus (HPV) infection in a prospective, single-center study of patients undergoing colonoscopy for various indications.
High-risk HPV and HPV strain 16 were detected in 30% of patients with Crohn’s disease and 18% of patients without Crohn’s disease (P = .005), said Lucine Vuitton, MD, of University Hospital of Besançon (France) and her associates. “Increasing our knowledge of HPV infection of anal tissues could help physicians identify populations at risk and promote prophylaxis with vaccination and adequate screening,” the investigators wrote in the November issue of Clinical Gastroenterology and Hepatology.
Most anal cancers are squamous cell carcinomas, for which infection with high-risk HPV (especially high-risk HPV16) is a driving risk factor. Case studies and literature reviews have linked Crohn’s disease to increased rates of anal canal cancers, but population-based data were lacking, the researchers wrote. Therefore, they prospectively analyzed anal tissue samples from 467 consecutive patients undergoing colonoscopy at a tertiary care center in France. Median age was 54 years (interquartile range, 18-86 years), and 52% of patients were women. No patient had detectable macroscopic neoplastic lesions at the anal margin at baseline.
The researchers used the QIAamp DNA Blood minikit (Qiagen) for DNA extraction and the INNO-LiPA HPV Genotyping Extra kit (Fujirebio Diagnostics) for HPV DNA detection and genotyping. These methods identified HPV DNA in anal tissue samples from 34% of the patients and high-risk HPV DNA in 18% of patients. The most prevalent genotype was HPV16 (detected in 7% of samples), followed by HPV51, HPV52, and HPV39.
A total of 112 patients were receiving at least one immunosuppressive treatment for inflammatory bowel disease or another condition. Seventy patients had Crohn’s disease, and 29 patients had ulcerative colitis. The prevalence of anal canal high-risk HPV and HPV16 infection in patients with ulcerative colitis was similar to that seen in those without inflammatory bowel disease. However, patients with Crohn’s disease were more likely to have anal canal high-risk HPV infection (30%) and HPV16 infection (14%), compared with patients without Crohn’s disease (18% and 7%, respectively). Additionally, among 22 patients with Crohn’s disease and perianal involvement, 11 had HPV DNA in the anal canal versus 30% of other patients with inflammatory bowel disease.
Women were more likely to have anal canal high-risk HPV (23%) infection than were men (13%; P = .004). In a multivariable analysis of self-reported data and medical data, significant risk factors for high-risk HPV infection included female sex, a history of sexually transmitted infections, having more than 10 sexual partners over the life course, having at least one sexual partner during the past year, current smoking, and immunosuppressive therapy. The multivariable analysis also linked Crohn’s disease with anal canal high-risk HPV16 infection (odds ratio, 3.8), but the association did not reach statistical significance (95% confidence interval, 0.9-16.9).
Most patients with Crohn’s disease were on immunosuppressive therapy, “which markedly affected statistical power,” the researchers commented. Nonetheless, their findings support HPV vaccination for patients with Crohn’s disease, as well as efforts to target high-risk patients who could benefit from anal cancer screening, they said.
The work was funded by the APICHU research grant from Besançon (France) University Hospital and by the Région de Franche-Comté. Dr. Vuitton disclosed ties to AbbVie, Ferring, MSD, Hospira, Janssen, and Takeda. Three coinvestigators disclosed relationships with AbbVie, MSD, Hospira, Mayoli, and Roche.
SOURCE: Vuitton L et al. Clin Gastroenterol Hepatol. 2018 Nov. doi: 10.1016/j.cgh.2018.03.008.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Crohn’s disease was associated with high-risk human papillomavirus infection.
Major finding: High-risk HPV and HPV16 were detected in 30% of patients with Crohn’s disease versus 18% of those without Crohn’s disease (P = .005).
Study details: Analyses of anal tissue samples from 467 consecutive patients, including 70 with Crohn’s disease.
Disclosures: The work was funded by the APICHU research grant from Besançon (France) University Hospital and by the Région de Franche-Comté. Dr. Vuitton disclosed ties to AbbVie, Ferring, MSD, Hospira, Janssen, and Takeda. Three coinvestigators disclosed relationships with AbbVie, MSD, Hospira, Mayoli, and Roche.
Source: Vuitton L et al. Clin Gastroenterol Hepatol. 2018 Nov. doi: 10.1016/j.cgh.2018.03.008.
Click for Credit: Short-term NSAIDs; endometriosis; more
Here are 5 articles from the November issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Short-term NSAIDs appear safe for high-risk patients
To take the posttest, go to: https://bit.ly/2PgXKGx
Expires October 8, 2019
2. Chronic liver disease raises death risk in pneumonia patients
To take the posttest, go to: https://bit.ly/2NPSXXA
Expires October 8, 2019
3. Half of outpatient antibiotics prescribed with no infectious disease code
To take the posttest, go to: https://bit.ly/2pWEWxU
Expires October 6, 2019
4. Secondary fractures in older men spike soon after first, but exercise may help
To take the posttest, go to: https://bit.ly/2OCNl8A
Expires October 3, 2019
5. Consider ART for younger endometriosis patients
To take the posttest, go to: https://bit.ly/2NO1Sc4
Expires October 5, 2019
Here are 5 articles from the November issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Short-term NSAIDs appear safe for high-risk patients
To take the posttest, go to: https://bit.ly/2PgXKGx
Expires October 8, 2019
2. Chronic liver disease raises death risk in pneumonia patients
To take the posttest, go to: https://bit.ly/2NPSXXA
Expires October 8, 2019
3. Half of outpatient antibiotics prescribed with no infectious disease code
To take the posttest, go to: https://bit.ly/2pWEWxU
Expires October 6, 2019
4. Secondary fractures in older men spike soon after first, but exercise may help
To take the posttest, go to: https://bit.ly/2OCNl8A
Expires October 3, 2019
5. Consider ART for younger endometriosis patients
To take the posttest, go to: https://bit.ly/2NO1Sc4
Expires October 5, 2019
Here are 5 articles from the November issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Short-term NSAIDs appear safe for high-risk patients
To take the posttest, go to: https://bit.ly/2PgXKGx
Expires October 8, 2019
2. Chronic liver disease raises death risk in pneumonia patients
To take the posttest, go to: https://bit.ly/2NPSXXA
Expires October 8, 2019
3. Half of outpatient antibiotics prescribed with no infectious disease code
To take the posttest, go to: https://bit.ly/2pWEWxU
Expires October 6, 2019
4. Secondary fractures in older men spike soon after first, but exercise may help
To take the posttest, go to: https://bit.ly/2OCNl8A
Expires October 3, 2019
5. Consider ART for younger endometriosis patients
To take the posttest, go to: https://bit.ly/2NO1Sc4
Expires October 5, 2019
Health Care–Associated Urinary Tract Infections: Prevention and Management
From the University of Arizona College of Medicine, Tucson, AZ (Dr. Beatty), and the Baylor College of Medicine, Houston, TX (Dr. Mohajer).
Abstract
- Objective: To review management issues regarding health care–associated urinary tract infections (UTIs) commonly encountered by practicing clinicians.
- Methods: Review of the literature.
- Results: Because urinary catheter (UC) placement plays a major role in the development of catheter-associated UTIs (CA-UTI), clinicians should be aware of the appropriate and inappropriate uses of UCs and their association with CA-UTI development. Removal of a UC when no longer necessary is key to preventing CA-UTI. Treatment of asymptomatic bacteriuria is generally not indicated. Percutaneous nephrostomy and ureteral stenting need close monitoring, and early removal should be performed if infection is suspected. Candiduria rarely leads to symptoms unless it is related to an ascending process. Proper urine collection is crucial in determining whether contamination, colonization, or infection is present. Fluconazole is recommended in most cases of Candida UTI, while intravenous amphotericin B is recommended for fluconazole-resistant Candida species.
- Conclusion: Continued use of evidence-based strategies for preventing and managing health care–associated UTI should lead to further improvements in patient outcomes and overall decreased rates of infection.
Keywords: bacteriuria; catheter-associated UTI; catheterization; percutaneous nephrostomy; candiduria.
Health care–associated urinary tract infections (UTIs) are estimated to be the most common adverse infectious event in U.S. hospitals, occurring in 1 of 10 admitted patients.1-3 Approximately 32% of all health care–associated infections are UTIs.1 Furthermore, urinary catheters (UCs) are associated with 8% to 21% of health care–associated infections that occur in the intensive care unit.4 The most important predisposing factor for nosocomial UTI is urinary catheterization.5 Genitourinary manipulation and/or implementation also play a major role in the development of nosocomial UTIs.
In 2008, the U.S. Centers for Medicare & Medicaid Services instituted a new policy that reduced reimbursement rates for hospitalizations linked to health care–associated infections.6 Indwelling UCs are among the most overused health care devices in the hospital setting. They are placed in an estimated 15% to 25% of all hospitalized patients,7,8 and are often inserted in the emergency department (ED) without a physician order or appropriate indication.9 Intermittent straight catheterization, male or female condom catheterization, and/or placement of an indwelling UC are the most common causes of catheter-associated asymptomatic bacteriuria (CA-ASB) and catheter-associated UTIs (CA-UTI).5 Prevention and management of CA-ASB and CA-UTI can be challenging and require an evidence-based approach. Furthermore, guidelines for the management of UTIs in the setting of active percutaneous nephrostomy (PCN) drainage and/or ureteral stenting are not established.5 This may leave clinicians with little mainstream data to aid in management decisions.
In 2009 the Centers for Disease Control and Prevention provided a guideline for the appropriate and inappropriate use of indwelling UCs to help promote their proper use.10 In the time since the guideline’s initiatives were instituted around the United States, published data have shown some improvement in the use of UCs,11,12 but other recent reports indicate that rates of UC use have remained unchanged.13 This review discusses management issues regarding health care–associated UTIs that are commonly encountered by practicing clinicians, with a focus on current guidelines and evidence.
Catheter-Associated UTI
CA-UTI is defined as the presence of signs or symptoms of UTI with no other explainable infectious source along with ≥ 1000 colony-forming units (cfu) of ≥ 1 bacterial species per milliliter in a urine specimen from a catheter that has been changed within 48 hours of collection of the urine specimen.5 Signs and symptoms of CA-UTI include, but are not limited to: new-onset or worsening fever, chills, altered sensorium from baseline, lethargy, malaise, flank pain, pelvic pain, costovertebral angle tenderness, and acute hematuria.5 New-onset “foul-smelling” (odorous)urine and “cloudy” urine are neither sensitive nor specific when assessing for CA-UTI, and do not have significant clinical relevance when found alone.14,15 Patients who have removed or exchanged the UC during this event and then experience dysuria, increased frequency, urgency, or suprapubic pain are likely having symptoms of CA-UTI.5
What is the recommended method for collecting urine samples when CA-UTI is suspected?
In a patient with an indwelling catheter that has been in place for more than 2 weeks at the onset of a suspected CA-UTI, the catheter should be replaced (if still indicated) or removed to accelerate resolution of symptoms and to reduce the risk of subsequent catheter-associated bacteriuria and CA-UTI. The urine culture should be acquired from the freshly placed UC.5
When should a patient be empirically treated?
A patient presenting with evidence of sepsis should be empirically treated with antimicrobials. Empiric coverage should be based on risk factors for multidrug-resistant organisms and data pertaining to local antimicrobial resistance patterns. A urine specimen for urinalysis and possible culture should be sent prior to administering empiric antibiotics (if possible) in a symptomatic patient.5
What bacteria are commonly associated with CA-UTI?
The bacteria most commonly associated with CA-UTI are found in or around the gastrointestinal and genitourinary tracts and also are part of the normal skin flora. The introduction and/or facilitated ascension of these microorganisms is believed to occur during UC insertion.16,17 Two-thirds of all isolated uropathogens in those with indwelling UCs are extraluminally acquired (via ascension along the catheter-urethral mucosa interface), and one-third are believed to be intraluminally acquired.18
The most commonly isolated bacteria in CA-UTI are Enterobacteriaceae, which include Escherichia coli (most common), Klebsiella species (K. oxytoca, K. pneumoniae), Serratia species (S. marcescens), Citrobacter species (C. koseri), Enterobacter species (E. cloacae), and Proteus species; non-Enterobacteriaceae such as Pseudomonas species; and gram-positive cocci, which include coagulase-negative staphylococci (S. saprophyticus), Staphylococcus aureus, group B streptococci, and Enterococcus species (E. faecalis, E. faecium).19-21 Coagulase-negative staphylococci and Enterococcus species can lead to CA-UTI but are usually avirulent and more commonly isolated from asymptomatic individuals.19 Also, coagulase-negative staphylococci such as S. epidermidis and S. lugdunensis are usually the manifestation of contamination during the collection process and their presence should prompt a repeat sample collection under sterile techniques. Monomicrobial infection is usually seen in those with short-term catheter use and CA-UTI. In contrast, polymicrobial infection is more common in those with long-term indwelling UCs and CA-UTI.19 Providencia stuartii, Proteus mirabilis, S. aureus, and Morganella morganii have all been associated with CA-UTI in those with long-term indwelling UCs.
Growth of S. aureus in the urine should prompt further investigation with blood cultures to explore the possibility of hematogenous dissemination to the urinary tract. Organisms leading to bacteremia due to CA-UTI are most commonly gram-negative bacilli (E. coli, Klebsiella species, Pseudomonas aeruginosa) and E. faecalis.21
What is the difference between CA-ASB and CA-UTI?
CA-ASB is defined as the presence of ≥ 1 bacteria species growing on urine culture at ≥ 100,000 cfu/mL in a patient with a history of urinary catheterization and/or indwelling UC who lacks signs or symptoms of UTI. In a man with a condom catheter, CA-ASB is defined using the same criteria, but the urine sample is collected after a fresh condom catheter is applied.5 The difference between CA-ASB and CA-UTI is simply the presence or absence of signs and symptoms related to UTI. Currently, there is no standard definition for significant bacteriuria in a catheterized patient.5 Pyuria found on urinalysis is indicative of genitourinary inflammation and can be present in both CA-ASB and CA-UTI. The absence, presence, and/or degree of pyuria in catheterized patients does not accurately differentiate between CA-ASB and CA-UTI.5,22,23 On the other hand, the absence of pyuria in a symptomatic catheterized patient suggests an etiology other than CA-UTI.5
How can CA-UTI be prevented in patients with a short-term indwelling urinary catheter?
If a short-term UC is essential, the most important approach to preventing CA-UTI is limiting the duration of time it will be used. Strategies such as computer-based order entry and care maps with automated discontinuation of UCs have been shown to decrease catheter usage.19 Using closed-systems for UC collection with ports in the distal catheter for needle aspiration of urine has also been shown to decrease the incidence of CA-UTI.5 Securing the UC to avoid urethral trauma, aseptic techniques for insertion and repositioning, and placement of the tubing and collection bag below the level of the bladder to prevent reflux will likely also prevent CA-UTI, but these strategies have not been evaluated thoroughly.19
When should you screen for and treat CA-ASB?
The 2009 Infectious Diseases Society of America (IDSA) guidelines recommend that the only patients who should be screened and treated for CA-ASB are pregnant women and those who will undergo a potentially traumatic urologic procedure for which mucosal breaching may occur, causing bleeding. Routinely screening or treating patients for CA-ASB in not recommended in any other group of patients and will lead to unnecessary antibiotic use and antibiotic resistance.5
UTI Associated with Percutaneous Nephrostomy and Ureteral Stenting
Similar systemic symptoms of infection (fever, rigors, malaise, shock) are present in patients with and without percutaneous nephrostomy (PCN) and/or ureteral stent placement. Dysuria is not commonly present in those with PCN. The first signs of CA-UTI may be decreased urine output and pericatheter leakage due to an obstructive process resulting from the encrustation.24-27 The most common complaint among patients with either acute or chronic ureteral stenting is discomfort, which has been described as “urinary symptoms” and “body pain.”28 This discomfort can be related to ureteral hyperperistalsis after placement of the stent and is usually self-limiting. Ureteral stent migration, usually at the distal end, can also lead to discomfort, but is easily rectified with cystoscopy.25 Body pain and/or urinary symptoms in the setting of ureteral stenting are not indicative of infection alone.
What is urinary catheter and/or ureteral stent encrustation?
Encrustation is the formation of a conditioning film that develops on the surface of the UC or ureteral stent. The exact mechanism is not well understood, but it is believed to involve electrostatic interactions of urinary proteins that stimulate binding onto the stent or UC surface.25 Encrustation increases exponentially with the dwell time. Among patients with ureteral stents placed due to urolithiasis, encrustation occurred in 9.2% of stents removed prior to 6 weeks, 47.5% of stents removed at 6 weeks, and 76.3% of stents removed at 12 weeks.26 Encrustation is most common at the proximal and distal ends (pigtails) of the ureteral stent and usually spares or presents last within the lumen.29 Attempts have been made to prevent ureteral stent encrustation through the development of biodegradable, drug-eluting, and tissue-engineered substrates. These developments are promising, but currently there is limited observational data from large randomized trials to suggest that these new modalities decrease rates of encrustation.25 Encrustation is highly associated with certain microorganisms, especially those that create biofilms.30 Urease-producing bacteria, most commonly P. mirabilis, play a role in encrustation formation.31 Bacteria most commonly associated with encrustation include Proteus species (P. mirabilis is most common), P. aeruginosa, K. pneumoniae, Providencia species (P. stuartii is most common), and M. morganii.
Does ureteral stent bacterial colonization correlate with UTI?
Ureteral stent colonization with bacteria increases with dwell time and is found in 40% to 98.5% of stents placed.32-35 If UTI is suspected in a patient with an active indwelling ureteral stent, a sample of urine should be cultured while the stent is in place.25 Typically, genitourinary and normal skin flora pathogens are found when the ureteral stent is cultured. The top 3 organisms cultured from ureteral stents are S. aureus, P. aeruginosa, and E. faecalis.34 Urine culture usually does not correlate with stent culture results, which has brought up the debate of how bacterial colonization occurs. It has been postulated that colonization is actually a manifestation of contamination during the insertion procedure, but this has yet to be validated.25 In patients with symptoms of UTI in the setting of an indwelling ureteral stent, a positive culture has low sensitivity, with estimates between 21% and 40%.35 Therefore, a negative urine culture does not rule out UTI alone in a symptomatic patient. Multiple studies have suggested that colonization of the ureteral stent does not correlate strongly with developing a UTI.25,32-34
How can UTI be prevented in those receiving PCN or ureteral stent placement?
Antibiotic prophylaxis has been recommended to prevent UTI in patients who will undergo PCN or ureteral stent placement. The American Urological Association recommends empiric treatment even in the absence of signs and symptoms of UTI,36 but substantial evidence is lacking that this approach prevents infection.37 Ciprofloxacin or trimethoprim/sulfamethoxazole has been recommended by some for empiric coverage for enteric gram-negative bacilli and enterococcus in those undergoing genitourinary manipulation or instrumentation.32,38 Most patients who develop CA-UTI and pyelonephritis do so within the first 2 to 6 weeks after placement.37,39 Bacteriuria, candiduria, and/or pyuria are present in all patients approximately within 9 weeks even when sterile urine is confirmed prior to PCN placement.39 Data on the effectiveness of antibiotic prophylaxis to prevent CA-UTI in those with PCN or ureteral stenting is limited. Currently, there are no recommendations from the IDSA on how to prevent infection in these situations.5 Early or frequent stent removal or exchanges has been proven to reduce UTI in those with ureteral stenting.33 Patients with diabetes mellitus and chronic renal failure are at high-risk for UTI when ureteral stents are in place. This population should undergo close monitoring for UTI development and may warrant more frequent stent exchanges.27,40
What is the treatment of CA-UTI associated with PCN and/or ureteral stenting?
The IDSA guidelines do not apply to patients with PCN and/or ureteral stenting.5 There is no treatment protocol for UTI related to these processes. Generally speaking, they are considered “complicated UTI” by most experts. Broad-spectrum, empiric antibiotic administration along with prompt removal of the PCN and/or ureteral stent is the gold standard of therapy.27 The recommended duration of targeted antibiotic therapy is generally between 5 and 14 days.19 Most clinicians will treat this complicated UTI for at least 10 to 14 days. Antibiotic administration should be continued even after removal of the catheter and/or stent to complete the full course. Repeat urinalysis and culture is not indicated at the end of therapy if the patient is clinically improving or has remission of symptoms.
What is the exchange rate for those who require chronic PCN and/or ureteral stent use?
On average a PCN or ureteral stent should be exchanged every 2 to 3 months in patients who require chronic usage.24,27 Some patients with persistent complications may require more frequent exchanges (< 10 weeks).27 Encrustation and bacterial colonization become more prevalent the longer the devices are in place. This process is estimated to begin within the first 2 weeks after placement.27,33,34 A “forgotten stent” is one that has been left in place after the patient is lost to follow-up. This unfortunate event can lead to massive encrustation, UTI, stent fracturing, and complete ureteral obstruction.24 As noted, patients with diabetes mellitus, chronic renal failure, and frequent UTI may warrant more frequent exchanges, but this should be determined on a case-by-case basis.
Catheter-Associated UTI in Patients with Spinal Cord Injury
Spinal cord injury (SCI) at any level can cause neurogenic bladder. This process ultimately leads to urinary stasis and colonization of the bladder with bacteria. According to the IDSA, the acceptable indications for UC insertion are: clinically significant urinary retention (if medical therapy is not effective), urinary incontinence, accurate urine output monitoring required, and patient is unable and/or unwilling to collect urine (Table 1).5 Recently, further guidelines were published regarding appropriate and inappropriate indwelling UC placement in hospitalized medical patients (Table 2 and Table 3), expanding upon the earlier acceptable criteria provided by the IDSA.41 According to the IDSA and Ann Arbor Criteria for Appropriate Urinary Catheter Use, patients with SCI and subsequent neurogenic bladder without obstruction where intermittent bladder straight catheterization for the drainage of urine is not feasible will likely need an indwelling UC.41 SCI patients often experience decubitus ulcers, and an indwelling UC can be used if needed to help with wound healing if other urinary management alternatives have been attempted. Other such situations in which an indwelling UC can used before attempting alternative approaches would be in a patient who is actively dying and is pursuing comfort care and/or hospice.41
Which indwelling UCs should be used in patients with SCI?
Efforts to reduce the likelihood of infection in patients with SCI have led to several advances in the design and manufacturing of UCs. UCs are made of either latex, plastic, silicone, or polytetrafluoroethylene (Teflon). None of these substrates is free of complications, but of them latex UCs have been studied the most in regards to their associated complications. Aside from being allergenic in nature, latex UCs have an increased propensity to allow bacteria to adhere to their surface due to microscopic planes of unevenness.42 Silicone UCs are less frequently associated with infection but are more rigid, leading to increased discomfort.43,44 Hydrophilic and silver-hydrogel coatings are innovative methods that have been developed to increase comfort and reduce the likelihood of infection. Hydrophilic-coated UCs are associated with reduced microbial adherence, decreased encrustation, and better patient satisfaction.45,46 In SCI patients, these UCs have demonstrated lower complication rates, including UTI; fewer episodes of post-, intra-, and inter-catheterization bleeding; and decreased rates of antibiotic-resistant bacteria.45,46 Silver-hydrogel-coated UCs are less well studied but have also demonstrated reduced UTI rates in SCI patients; however, their efficacy over the long term has yet to be determined. Antibiotic-impregnated UCs are not currently recommended for either short- or long-term indwelling UC use.5
How can CA-UTI be prevented in a patient who will require a long-term indwelling catheter?
At this time, the data is insufficient to make a recommendation on routine UC exchange (eg, every 2 to 4 weeks) in patients who require long-term indwelling urethral or suprapubic catheters in an attempt to reduce the risk of CA-ASB or CA-UTI. This is also true for those who experience even repeated early catheter blockage from encrustation.5 Thus, the rate at which these exchanges occur can be controversial, but typically around every 4 weeks is a common approach. Some would argue that if the patient has repeated CA-UTI, an exchange rate of every 2 weeks might be needed, but data is currently lacking to support this practice.5 If intermittent urinary catheterization is feasible, it should be done at least every 6 hours and before bedtime. In general, when the volume of urine in the bladder reaches approximately 400 mL, the patient should undergo bladder catheterization to prevent stasis and infection.47 A closed drainage system is recommended in all patients who require long-term indwelling UC use.48,49 Placement of the collection bag above the catheter or above the level of the bladder and a breach in the closed drainage system have been shown to result in higher rates of catheter-associated bacteriuria.48,50 Proper hand hygiene and sterile and/or clean techniques should be used when placing or exchanging a UC. However, in one study there was no difference in bacteremia or UTIs when using sterile versus clean techniques.51
Asymptomatic bacteriuria should not be treated in patients with long-term indwelling UCs, and prophylactic antibiotics have led to the emergence of resistance.52 At this time it is not clear whether prophylactic weekly oral cyclic antibiotic administration can effectively reduce the frequency of CA-UTI in patients with SCI and chronic indwelling UC use.
What are the signs and symptoms of CA-UTI in a patient with SCI?
Subjective and objective findings may be limited when a patient with SCI presents with CA-UTI. These patients often lack the usual symptoms of UTI (dysuria, suprapubic discomfort, urgency, increased frequency) and pyelonephritis (flank pain, costovertebral angle tenderness). Caregivers and health care providers should be aware that nonspecific symptoms such as foul-smelling urine, pyuria, increased residual volume of urine in the bladder, change in voiding habits, worsening detrusor spasticity, and aggravation of autonomic dysreflexia can be the only initial presenting symptoms.53
What is the duration of therapy for CA-UTI in SCI, and how can antibiotic stewardship principles be applied in this patient population?
Antibiotic therapy is indicated for a duration of 7 days if there is prompt resolution of symptoms, or for a total of 10 to 14 days if the response is delayed, regardless of whether the patient remains with a UC.5 Antibiotic stewardship is very important to reduce the risk for developing drug resistance in this high-risk population. Methods such as prescriber education practices, institution protocols, guideline implementation, auditing and feedback, restriction and reauthorization practices, computer-assisted programs, de-escalation or streamlining, and antibiotic cycling or dosage optimization have all been shown to assist in antibiotic stewardship in UTIs.54
Candida UTI
What is the initial evaluation for a patient with candiduria?
The workup for candiduria hinges on determining whether the candiduria likely represents contamination, colonization, or infection; certain predisposing risk factors are associated with Candida UTI (Table 4).55-57 The most important aspect to candiduria is the patient’s clinical status and comorbid conditions.58 Among funguria, Candida species are the most common and represent 95% of organisms isolated on urine cultures (Table 5).59 Candiduria is usually present in those with significant comorbidities and rarely is associated with healthy individuals.59,60 Candiduria is increasing in prevalence among hospitalized patients, representing 22% to 40% of all nosocomial UTIs.59,60 Markers in the urine (leukocyte esterase, colony count of culture growth, presence or absence of Candida casts and pseudohyphae) cannot alone differentiate colonization from infection.55 When candiduria is discovered in a patient with symptoms related to UTI in the setting of predisposing risk factors, it should be considered a real infection until proven otherwise.
In a situation where an asymptomatic patient without an indwelling UC has Candida species isolated from a urine culture, a repeat culture (clean-catch midstream sample) should be performed to assess for a likely contaminated collection.55 If the patient has an indwelling UC then it should be exchanged and urine collected from the fresh catheter.61 When candiduria is found in healthy asymptomatic adults, it is most commonly associated with poor collection techniques or postcollection contamination.59 If candiduria persists in an asymptomatic patient, the patient should be assessed for predisposing factors. This includes checking hemoglobin A1C for developing diabetes and renal ultrasound looking for urolithiasis, renal abscess, hydronephrosis, and fungus ball. Postvoid residual urinary retention should also be ruled out with bladder ultrasound. Treatment of predisposing factors can lead to resolution of candiduria without antifungal treatment, and a urine culture should be repeated (1 to 2 weeks later).61 Asymptomatic patients lacking any predisposing factors can be observed with repeat urine cultures in 1 to 3 months.61
Candiduria may actually represent candidemia in those patients who have a predisposing risk factor for disseminated candidiasis. These risk factors include central venous catheters, administration of total parental nutrition, antibiotic use (especially broad spectrum), critical illness, recent surgical intervention (especially intra-abdominal), acute renal failure, nasogastric tube use, and active gastric acid suppression (ie, proton pump inhibitors).62,63 The hematogenous spread of Candida can lead to the detection of candiduria in 46% to 80% of persons who are experiencing candidemia.59 If the patient is at risk for candidemia, then blood fungal cultures should be drawn. It is not unreasonable to also order a serum-D-glucan assay if suspicions are high. A thorough skin assessment should be completed and ophthalmology consulted for a detailed eye exam in the event that the patient has candidemia. Candiduria is highly prevalent among those who are candidemic, but overall candidemia is encountered in less than 5% of patients in most intensive care units.59 Thus, most patients with candiduria do not have disseminated candidiasis.
Candiduria rarely leads to symptoms of UTI,58 unless the pathogenesis is related to an ascending process.56 Symptoms of Candida UTI are no different from those experienced from a bacterial etiology. Some patients may complain of pneumaturia and/or endorse seeing particulate matter in their urine.55 Patients showing signs of sepsis (fever, chills, flank pain) should be investigated for possible Candida pyelonephritis in the setting of candiduria.64
When should asymptomatic candiduria be treated?
In adult patients with asymptomatic candiduria, there are 2 situations in which antifungal therapy is recommended. A patient undergoing a traumatic urologic procedure would be treated to avoid the risk for candidemia caused by the procedure. Also, in neutropenic patients empiric antifungal therapy should be administered because there is a high likelihood that this candiduria may actually represent hematogenous spread from candidemia.61,65
What is the treatment for symptomatic Candida cystitis?
Empiric treatment with oral fluconazole 200 to 400 mg daily for a total of 2 weeks is recommended in patients with persisting candiduria and symptoms of cystitis.65 Identifying the species is a crucial step in the treatment of Candida UTI. Several species (C. glabrata, C. krusei) are known to be resistant to fluconazole. Species identification and antifungal sensitivities should be done and therapy directed after obtaining these results.55
What is the recommended treatment for Candida pyelonephritis?
Treatment for pyelonephritis caused by fluconazole-susceptible Candida species is oral fluconazole 200 to 400 mg (3-6 mg/kg) for a total of 2 weeks.65 A fluconazole-resistant organism should be suspected when a non-albicans Candida species is isolated, such as C. krusei or C. glabrata. In this circumstance, in vitro antifungal susceptibility testing should be done. Echinocandins are not a good option in this situation because they do not reach adequate urine concentration and treatment failure is well documented.66-68 Amphotericin B deoxycholate (AmB) 0.3 to 0.6 mg/kg daily for 1 to 7 days, with or without oral flucytosine (25 mg/kg) 4 times daily, is recommended by the IDSA for the treatment of fluconazole-resistant isolates of C. glabrata and C. krusei.65 Further imaging with ultrasound, CT, or magnetic resonance should be done to rule out urinary tract obstruction and/or “fungus ball” formation. Emphysematous pyelonephritis and necrosis can occur and usually require nephrectomy. Perinephric abscess will need drainage, which can be accomplished through interventional radiological techniques.55
If a “fungus ball” is suspected in the kidney, how does the management change in a patient with Candida pyelonephritis?
A fungus ball must be treated with both antifungals and surgical intervention. Antifungal therapy should be continued during the surgical removal process to avoid fungemia. Interventional radiology should be consulted and is usually the best option for removal. Fungus ball(s) can and often do cause urinary obstruction. Temporary nephrostomy tube placement may be warranted in these situations to relieve the obstruction.55,65 AmB can be infused through the nephrostomy tube to increase local concentrations. This route of administration is not known to be nephrotoxic.55 Fluconazole infusion through a nephrostomy tube has also been used in the successful treatment of a fungus ball.69
Summary
Health care–associated UTIs are the most common nosocomial infection in the United States. UC placement and genitourinary manipulation or instrumentation play a major role in the development of CA-UTI. Clinicians should be aware of the appropriate and inappropriate use of UCs and their association with CA-UTI development. Removal of a UC when no longer necessary is key in prevention of CA-UTI. Treatment of asymptomatic bacteriuria is generally not indicated. A multidisciplinary approach is essential when managing chronic indwelling UCs in SCI. PCN and ureteral stenting need close monitoring, and early removal should be performed if infection is suspected.
Candiduria is an emerging nosocomial source of UTI but rarely leads to symptoms unless related to an ascending process. Proper urine collection is crucial in determining whether you are dealing with contamination, colonization, or infection. If candiduria persists in an asymptomatic individual, then further investigations should be done in regards to possible predisposing risks factors. Fluconazole is recommended for treatment of most patients with Candida UTI, while intravenous AmB is the treatment of choice for fluconazole-resistant Candida species. As we continue to take an evidence-based approach to the prevention and management of health care-associated UTI, we will likely see continued improvement in patient outcomes and overall decreased rates of infection.
Corresponding author: Norman Beatty, MD, 1501 N. Campbell Ave., Tucson, AZ 85724; [email protected].
Financial disclosures: None.
1. Klevens RM, Edwards JR, Richards CL Jr. Estimating health care-associated infections and deaths in U.S. hospitals, 2002. Public Health Rep. 2007;122:160-166.
2. Burke JP. Infection control—a problem for patient safety. N Engl J Med. 2003;348:651-656.
3. Scott RD. The direct medical costs of healthcare-associated infections in U.S. hospitals and the benefits of prevention. Division of Healthcare Quality Promotion; National Center for Preparedness Detection and Control of Infectious Diseases; Coordinating Center for Infectious Diseases; Centers for Disease Control and Prevention. March 2009. Contract No.: CS200891-A. www.cdc.gov/HAI/pdfs/hai/Scott_CostPaper.pdf.
4. Eriksen HM, Iverson BG, Aavitsland P. Prevalence of nosocomial infections in hospitals in Norway, 2002 and 2003. J Hosp Infect. 2005;60:40-45.
5. Hooton TM, Bradley SF, Cardenas DD, et al. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis. 2010;50:625-663.
6. Mattie AS, Webster BL. Centers for Medicare and Medicaid Services’ “never events”: an analysis and recommendations to hospitals. Health Care Manag. 2008;27:338-349.
7. Warren JW. Catheter-associated urinary tract infections. Int J Antimicrob Agents. 2001;17:299-303.
8. Weinstein JW, Mazon D, Pantelick E, et al. A decade of prevalence surveys in a tertiary-care center: trends in nosocomial infection rates, device utilization, and patient acuity. Infect Control Hosp Epidemiol. 1999;20:543-548.
9. Fakih MG, Pena ME, Shemes S, et al. Effect of establishing guidelines on appropriate urinary catheter placement. Acad Emerg Med. 2010;17:337-340.
10. Gould CV, Umscheid CA, Agarwal RK, et al. Guideline for prevention of catheter-associated urinary tract infections 2009. Infect Control Hosp Epidemiol. 2010;31:319-326.
11. Fakih MG, Rey JE, Pena ME, et al. Sustained reductions in urinary catheter use over 5 years: bedside nurses view themselves responsible for evaluation of catheter necessity. Am J Infect Control. 2013;41:236-239.
12. Meddings J, Rogers MA, Krein SL, et al. Reducing unnecessary urinary catheter use and other strategies to prevent catheter-associated urinary tract infections: an integrative review. BMJ Qual Saf. 2014;23:277-289.
13. Gould C. Catheter-associated urinary tract infection: the national perspective. In: Essential Hospitals Engagement Network. Patient Harm Series II: new tools to prevent CAUTI webinar. April 16, 2014. http://bit.ly/1UWndRA.
14. Nicolle LE. Consequences of asymptomatic bacteriuria in the elderly. Int J Antimicrob Agents. 1994;4:107-111.
15. Nicolle LE. Urinary tract infections in long-term-care facilities. Infect Control Hosp Epidemiol. 2001;22:167-175
16. Cohen A. A microbiological comparison of a povidone-iodine lubricating gel and a control as catheter lubricants. J Hosp Infect. 1985;6(Suppl A):155-161.
17. Daifuku R, Stamm WE. Bacterial adherence to bladder uroepithelial cells in catheter-associated urinary tract infection. N Engl J Med. 1986;314:1208-1213.
18. Tambyah PA, Halvorson KT, Maki DG. A prospective study of pathogenesis of catheter-associated urinary tract infections. Mayo Clin Proc. 1999;74:131-136.
19. Nicolle LE. Catheter-related urinary tract infection. Drugs Aging. 2005;22:627-639.
20. Redder JD, Leth RA, Møller JK. Incidence rates of hospital-acquired urinary tract and bloodstream infections generated by automated compilation of electronically available healthcare data. J Hosp Infect. 2015;91:231-236.
21. Ortega M, Marco F, Soriano A, et al. Epidemiology and prognostic determinants of bacteraemic catheter-acquired urinary tract infection in a single institution from 1991 to 2010. J Infect. 2013;67:282-287.
22. Tambyah PA, Maki DG. The relationship between pyuria and infection in patients with indwelling urinary catheters: a prospective study of 761 patients. Arch Intern Med. 2000;160:673-677.
23. Musher DM, Thorsteinsson SB, Airola VM, II. Quantitative urinalysis:diagnosing urinary tract infection in men. JAMA. 1976;236:2069-2072.
24. Hausegger KA, Portugaller HR. Percutaneous nephrostomy and antegrade ureteral stenting: technique-indications-complications. Eur Radiol. 2006;16:2016-2030.
25. Lange D, Bidnur S, Hoag N, et al. Ureteral stent-associated complications--where we are and where we are going. Nat Rev Urol. 2015;12:17-25.
26. el-Faqih SR, Shamsuddin AB, Chakrabarti A, et al. Polyurethane internal ureteral stents in treatment of stone patients: morbidity related to indwelling times. J Urol. 1991;146:1487-1491.
27. Adamo R, Saad WE, Brown DB. Management of nephrostomy drains and ureteral stents. Tech Vasc Interv Radiol. 2009;12:193-204.
28. Joshi HB, Newns N, Stainthorpe A, et al. Ureteral Stent Symptom Questionnaire: development and validation of a multidimensional quality of life measure. J Urol. 2003;169:1060-1064.
29. Singh I, Gupta NP, Hemal AK, et al. Severely encrusted polyurethane ureteral stents: management and analysis of potential risk factors. Urology. 2001;58:526-531.
30. Saint S, Chenoweth CE. Biofilms and catheter-associated urinary tract infections. Infect Dis Clin North Am. 2003;17:411-432.
31. Mobley HL, Warren JW. Urease-positive bacteriuria and obstruction of long-term urinary catheters. J Clin Microbiol. 1987;25:2216-2217.
32. Kehinde EO, Rotimi VO, Al-Hunayan A, et al. Bacteriology of urinary tract infection associated with indwelling J ureteral stents. J Endourol. 2004;18:891-896.
33. Paick SH, Park HK, Oh SJ, Kim HH. Characteristics of bacterial colonization and urinary tract infection after indwelling of double-J ureteral stent. Urology. 2003;62:214-217.
34. Klis R, Korczak-Kozakiewicz E, Denys A, et al. Relationship between urinary tract infection and self-retaining double-J catheter colonization. J Endourol. 2009;23:1015-1019.
35. Farsi HM, Mosli HA, Al-Zemaity M, et al. Bacteriuria and colonization of double-pigtail ureteral stents: long-term experience with 237 patients. J Endourol. 1995;9:469-472.
36. Wolfe JS Jr, Bennet CJ, Dmochowski RR, et al. Best practice policy statement on urologic surgery antimicrobial prophylaxis. J Urol. 2008;179:1379-1390.
37. Bahu R, Chaftari AM, Hachem RY, et al. Nephrostomy tube related pyelonephritis in patients with cancer: epidemiology, infection rate and risk factors. J Urol. 2013;189:130-135.
38. Bratzler DW, Dellinger EP, Olsen KM, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Surg Infect (Larchmt). 2013;14:73-156.
39. Cronan JJ, Horn DL, Marcello A, et al: Antibiotics and nephrostomy tube care: preliminary observations. Part II. Bacteremia. Radiology. 1989;172(3 Pt 2):1043-1045.
40. Akay AF, Aflay U, Gedik A, et al. Risk factors for lower urinary tract infection and bacterial stent colonization in patients with a double J ureteral stent. Int Urol Nephrol. 2007;39:95-98.
41. Meddings J, Saint S, Fowler KE, et al. The Ann Arbor criteria for appropriate urinary catheter use in hospitalized medical patients: results obtained by using the RAND/ UCLA appropriateness method. Ann Intern Med. 2015;162(9 Suppl):S1-34.
42. Stickler D, Young R, Jones G, et al. Why are Foley catheters so vulnerable to encrustation and blockage by crystalline bacterial biofilm? Urol Res. 2003;31:306-311.
43. Denstedt J, Wollin T, Reid G. Biomaterials used in urology: current issues of biocompatibility, infection, and encrustation. J Endourol. 1998;12:493-500.
44. Morris N, Stickler D, Winters C. Which indwelling urethral catheters resist encrustation by Proteus mirabilis biofilms? Br J Urol. 1997;80:58-63.
45. Cardenas D, Moore K, Dannels-McClure A, et al. Intermittent catheterization with a hydrophilic-coated catheter delays urinary tract infections in acute spinal cord injury: a prospective, randomized, multicenter trial. PMR. 2011;3:408-417.
46. Spinu A, Onose G, Daia C, et al. Intermittent catheterization in the management of post spinal cord injury (SCI) neurogenic bladder using new hydrophilic, with lubrication in close circuit devices-our own preliminary results. J Med Life. 2012;5:21-28.
47. Shekelle P, Morton S, Clark K, et al. Systematic review of risk factors for urinary tract infection in adults with spinal cord dysfunction. J Spinal Cord Med. 1998;22:258-272.
48. Siddiq D, Darouiche R. New strategies to prevent catheter-associated urinary tract infections. Nat Rev Urol. 2012;9:305-314.
49. Gould C, Umscheid C, Agarwal R, et al. Guideline for prevention of catheter-associated urinary tract infections 2009. Infect Control Hosp Epidemiol. 2010;31:319-326.
50. Maki D, Tambyah P. Engineering out the risk for infection with urinary catheters. Emerg Infect Dis. 2001;7:342-347.
51. Munasinghe R, Yazdani H, Siddique M, et al. Appropriateness of use of indwelling urinary catheters in patients admitted to the medical service. Infect Control Hosp Epidemiol. 2001;22:647-649.
52. Nicolle L, Bradley S, Colgan R, et al; Infectious Diseases Society of America; American Society of Nephrology; American Geriatric Society. Infectious Diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clin Infect Dis. 2005;40: 643-654.
53. Linsenmeyer T, Oakley A. Accuracy of individuals with spinal cord injury at predicting urinary tract infections based on their symptoms. J Spinal Cord Med. 2002;26:352-357.
54. Abbo LM, Hooton TM. Antimicrobial stewardship and urinary tract infections. Antibiotics. 2014;3:174-192.
55. Kauffman CA. Diagnosis and management of fungal urinary tract infection. Infect Dis Clin North Am. 2014;28:61-74.
56. Alvarez-Lerma F, Nolla-Salas J, Leon C, et al. Candiduria in critically ill patients admitted to intensive care medical units. Intensive Care Med. 2003;29:1069-1076.
57. Colodner R, Nuri Y, Chazan B, et al. Community-acquired and hospital-acquired candiduria: comparison of prevalence and clinical characteristics. Eur J Clin Microbiol Infect Dis. 2008;27:301-305.
58. Kauffman CA, Vazquez JA, Sobel JD, et al. Prospective multicenter surveillance study of funguria in hospitalized patients. Clin Infect Dis. 2000;30:14-18.
59. Sobel JD, Fisher JF, Kauffman CA, et al. Candida urinary tract infections—epidemiology. Clin Infect Dis. 2011;52(suppl 6): S433-436.
60. Richards MJ, Edwards JR, Culver DH, et al. Nosocomial infections in combined medical-surgical intensive care units in the United States. Infect Control Hosp Epidemiol. 2000;21:510-515.
61. Fisher JF, Sobel JD, Kauffman CA, et al. Candida urinary tract infections—treatment. Clin Infect Dis. 2011;52(suppl 6):S457-466.
62. Blumberg HM, Jarvis WR, Soucie JM, et al. Risk factors for candidal bloodstream infections in surgical intensive care unit patients: the NEMIS prospective multicenter study. Clin Infect Dis. 2001;33:177-186.
63. Puzniak LP, Teutsch S, Powderly W, et al. Has the epidemiology of nosocomial candidemia changed? Infect Control Hosp Epidemiol. 2004;25:628-633.
64. Siddique MS, Gayed N, McGuire N, et al. Salient features of Candida pyelonephritis in adults. Infect Dis Clin Pract. 1992;1:239-245
65. Pappas PG, Kauffman CA, Andes DR, et al. Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;62:e1-e50.
66. Sobel JD, Bradshaw SK, Lipka CJ, et al. Caspofungin in the treatment of symptomatic candiduria. Clin Infect Dis. 2007;44:e46-9.
67. Malani AN. Failure of caspofungin for treatment of Candida glabrata candiduria. Case report and review of the literature. Infect Dis Clin Pract. 2010;18:271-272.
68. Schelenz S, Ross CN. Limitations of caspofugin in the treatment of obstructive pyelonephrosis due to Candida glabrata infection. BMC Infect Dis. 2006;56:126-130.
69. Chung BH, Chang SY, Kim SI, et al. Successfully treated renal fungal ball with continuous irrigation of fluconazole. J Urol. 2001;166:1835-1836.
From the University of Arizona College of Medicine, Tucson, AZ (Dr. Beatty), and the Baylor College of Medicine, Houston, TX (Dr. Mohajer).
Abstract
- Objective: To review management issues regarding health care–associated urinary tract infections (UTIs) commonly encountered by practicing clinicians.
- Methods: Review of the literature.
- Results: Because urinary catheter (UC) placement plays a major role in the development of catheter-associated UTIs (CA-UTI), clinicians should be aware of the appropriate and inappropriate uses of UCs and their association with CA-UTI development. Removal of a UC when no longer necessary is key to preventing CA-UTI. Treatment of asymptomatic bacteriuria is generally not indicated. Percutaneous nephrostomy and ureteral stenting need close monitoring, and early removal should be performed if infection is suspected. Candiduria rarely leads to symptoms unless it is related to an ascending process. Proper urine collection is crucial in determining whether contamination, colonization, or infection is present. Fluconazole is recommended in most cases of Candida UTI, while intravenous amphotericin B is recommended for fluconazole-resistant Candida species.
- Conclusion: Continued use of evidence-based strategies for preventing and managing health care–associated UTI should lead to further improvements in patient outcomes and overall decreased rates of infection.
Keywords: bacteriuria; catheter-associated UTI; catheterization; percutaneous nephrostomy; candiduria.
Health care–associated urinary tract infections (UTIs) are estimated to be the most common adverse infectious event in U.S. hospitals, occurring in 1 of 10 admitted patients.1-3 Approximately 32% of all health care–associated infections are UTIs.1 Furthermore, urinary catheters (UCs) are associated with 8% to 21% of health care–associated infections that occur in the intensive care unit.4 The most important predisposing factor for nosocomial UTI is urinary catheterization.5 Genitourinary manipulation and/or implementation also play a major role in the development of nosocomial UTIs.
In 2008, the U.S. Centers for Medicare & Medicaid Services instituted a new policy that reduced reimbursement rates for hospitalizations linked to health care–associated infections.6 Indwelling UCs are among the most overused health care devices in the hospital setting. They are placed in an estimated 15% to 25% of all hospitalized patients,7,8 and are often inserted in the emergency department (ED) without a physician order or appropriate indication.9 Intermittent straight catheterization, male or female condom catheterization, and/or placement of an indwelling UC are the most common causes of catheter-associated asymptomatic bacteriuria (CA-ASB) and catheter-associated UTIs (CA-UTI).5 Prevention and management of CA-ASB and CA-UTI can be challenging and require an evidence-based approach. Furthermore, guidelines for the management of UTIs in the setting of active percutaneous nephrostomy (PCN) drainage and/or ureteral stenting are not established.5 This may leave clinicians with little mainstream data to aid in management decisions.
In 2009 the Centers for Disease Control and Prevention provided a guideline for the appropriate and inappropriate use of indwelling UCs to help promote their proper use.10 In the time since the guideline’s initiatives were instituted around the United States, published data have shown some improvement in the use of UCs,11,12 but other recent reports indicate that rates of UC use have remained unchanged.13 This review discusses management issues regarding health care–associated UTIs that are commonly encountered by practicing clinicians, with a focus on current guidelines and evidence.
Catheter-Associated UTI
CA-UTI is defined as the presence of signs or symptoms of UTI with no other explainable infectious source along with ≥ 1000 colony-forming units (cfu) of ≥ 1 bacterial species per milliliter in a urine specimen from a catheter that has been changed within 48 hours of collection of the urine specimen.5 Signs and symptoms of CA-UTI include, but are not limited to: new-onset or worsening fever, chills, altered sensorium from baseline, lethargy, malaise, flank pain, pelvic pain, costovertebral angle tenderness, and acute hematuria.5 New-onset “foul-smelling” (odorous)urine and “cloudy” urine are neither sensitive nor specific when assessing for CA-UTI, and do not have significant clinical relevance when found alone.14,15 Patients who have removed or exchanged the UC during this event and then experience dysuria, increased frequency, urgency, or suprapubic pain are likely having symptoms of CA-UTI.5
What is the recommended method for collecting urine samples when CA-UTI is suspected?
In a patient with an indwelling catheter that has been in place for more than 2 weeks at the onset of a suspected CA-UTI, the catheter should be replaced (if still indicated) or removed to accelerate resolution of symptoms and to reduce the risk of subsequent catheter-associated bacteriuria and CA-UTI. The urine culture should be acquired from the freshly placed UC.5
When should a patient be empirically treated?
A patient presenting with evidence of sepsis should be empirically treated with antimicrobials. Empiric coverage should be based on risk factors for multidrug-resistant organisms and data pertaining to local antimicrobial resistance patterns. A urine specimen for urinalysis and possible culture should be sent prior to administering empiric antibiotics (if possible) in a symptomatic patient.5
What bacteria are commonly associated with CA-UTI?
The bacteria most commonly associated with CA-UTI are found in or around the gastrointestinal and genitourinary tracts and also are part of the normal skin flora. The introduction and/or facilitated ascension of these microorganisms is believed to occur during UC insertion.16,17 Two-thirds of all isolated uropathogens in those with indwelling UCs are extraluminally acquired (via ascension along the catheter-urethral mucosa interface), and one-third are believed to be intraluminally acquired.18
The most commonly isolated bacteria in CA-UTI are Enterobacteriaceae, which include Escherichia coli (most common), Klebsiella species (K. oxytoca, K. pneumoniae), Serratia species (S. marcescens), Citrobacter species (C. koseri), Enterobacter species (E. cloacae), and Proteus species; non-Enterobacteriaceae such as Pseudomonas species; and gram-positive cocci, which include coagulase-negative staphylococci (S. saprophyticus), Staphylococcus aureus, group B streptococci, and Enterococcus species (E. faecalis, E. faecium).19-21 Coagulase-negative staphylococci and Enterococcus species can lead to CA-UTI but are usually avirulent and more commonly isolated from asymptomatic individuals.19 Also, coagulase-negative staphylococci such as S. epidermidis and S. lugdunensis are usually the manifestation of contamination during the collection process and their presence should prompt a repeat sample collection under sterile techniques. Monomicrobial infection is usually seen in those with short-term catheter use and CA-UTI. In contrast, polymicrobial infection is more common in those with long-term indwelling UCs and CA-UTI.19 Providencia stuartii, Proteus mirabilis, S. aureus, and Morganella morganii have all been associated with CA-UTI in those with long-term indwelling UCs.
Growth of S. aureus in the urine should prompt further investigation with blood cultures to explore the possibility of hematogenous dissemination to the urinary tract. Organisms leading to bacteremia due to CA-UTI are most commonly gram-negative bacilli (E. coli, Klebsiella species, Pseudomonas aeruginosa) and E. faecalis.21
What is the difference between CA-ASB and CA-UTI?
CA-ASB is defined as the presence of ≥ 1 bacteria species growing on urine culture at ≥ 100,000 cfu/mL in a patient with a history of urinary catheterization and/or indwelling UC who lacks signs or symptoms of UTI. In a man with a condom catheter, CA-ASB is defined using the same criteria, but the urine sample is collected after a fresh condom catheter is applied.5 The difference between CA-ASB and CA-UTI is simply the presence or absence of signs and symptoms related to UTI. Currently, there is no standard definition for significant bacteriuria in a catheterized patient.5 Pyuria found on urinalysis is indicative of genitourinary inflammation and can be present in both CA-ASB and CA-UTI. The absence, presence, and/or degree of pyuria in catheterized patients does not accurately differentiate between CA-ASB and CA-UTI.5,22,23 On the other hand, the absence of pyuria in a symptomatic catheterized patient suggests an etiology other than CA-UTI.5
How can CA-UTI be prevented in patients with a short-term indwelling urinary catheter?
If a short-term UC is essential, the most important approach to preventing CA-UTI is limiting the duration of time it will be used. Strategies such as computer-based order entry and care maps with automated discontinuation of UCs have been shown to decrease catheter usage.19 Using closed-systems for UC collection with ports in the distal catheter for needle aspiration of urine has also been shown to decrease the incidence of CA-UTI.5 Securing the UC to avoid urethral trauma, aseptic techniques for insertion and repositioning, and placement of the tubing and collection bag below the level of the bladder to prevent reflux will likely also prevent CA-UTI, but these strategies have not been evaluated thoroughly.19
When should you screen for and treat CA-ASB?
The 2009 Infectious Diseases Society of America (IDSA) guidelines recommend that the only patients who should be screened and treated for CA-ASB are pregnant women and those who will undergo a potentially traumatic urologic procedure for which mucosal breaching may occur, causing bleeding. Routinely screening or treating patients for CA-ASB in not recommended in any other group of patients and will lead to unnecessary antibiotic use and antibiotic resistance.5
UTI Associated with Percutaneous Nephrostomy and Ureteral Stenting
Similar systemic symptoms of infection (fever, rigors, malaise, shock) are present in patients with and without percutaneous nephrostomy (PCN) and/or ureteral stent placement. Dysuria is not commonly present in those with PCN. The first signs of CA-UTI may be decreased urine output and pericatheter leakage due to an obstructive process resulting from the encrustation.24-27 The most common complaint among patients with either acute or chronic ureteral stenting is discomfort, which has been described as “urinary symptoms” and “body pain.”28 This discomfort can be related to ureteral hyperperistalsis after placement of the stent and is usually self-limiting. Ureteral stent migration, usually at the distal end, can also lead to discomfort, but is easily rectified with cystoscopy.25 Body pain and/or urinary symptoms in the setting of ureteral stenting are not indicative of infection alone.
What is urinary catheter and/or ureteral stent encrustation?
Encrustation is the formation of a conditioning film that develops on the surface of the UC or ureteral stent. The exact mechanism is not well understood, but it is believed to involve electrostatic interactions of urinary proteins that stimulate binding onto the stent or UC surface.25 Encrustation increases exponentially with the dwell time. Among patients with ureteral stents placed due to urolithiasis, encrustation occurred in 9.2% of stents removed prior to 6 weeks, 47.5% of stents removed at 6 weeks, and 76.3% of stents removed at 12 weeks.26 Encrustation is most common at the proximal and distal ends (pigtails) of the ureteral stent and usually spares or presents last within the lumen.29 Attempts have been made to prevent ureteral stent encrustation through the development of biodegradable, drug-eluting, and tissue-engineered substrates. These developments are promising, but currently there is limited observational data from large randomized trials to suggest that these new modalities decrease rates of encrustation.25 Encrustation is highly associated with certain microorganisms, especially those that create biofilms.30 Urease-producing bacteria, most commonly P. mirabilis, play a role in encrustation formation.31 Bacteria most commonly associated with encrustation include Proteus species (P. mirabilis is most common), P. aeruginosa, K. pneumoniae, Providencia species (P. stuartii is most common), and M. morganii.
Does ureteral stent bacterial colonization correlate with UTI?
Ureteral stent colonization with bacteria increases with dwell time and is found in 40% to 98.5% of stents placed.32-35 If UTI is suspected in a patient with an active indwelling ureteral stent, a sample of urine should be cultured while the stent is in place.25 Typically, genitourinary and normal skin flora pathogens are found when the ureteral stent is cultured. The top 3 organisms cultured from ureteral stents are S. aureus, P. aeruginosa, and E. faecalis.34 Urine culture usually does not correlate with stent culture results, which has brought up the debate of how bacterial colonization occurs. It has been postulated that colonization is actually a manifestation of contamination during the insertion procedure, but this has yet to be validated.25 In patients with symptoms of UTI in the setting of an indwelling ureteral stent, a positive culture has low sensitivity, with estimates between 21% and 40%.35 Therefore, a negative urine culture does not rule out UTI alone in a symptomatic patient. Multiple studies have suggested that colonization of the ureteral stent does not correlate strongly with developing a UTI.25,32-34
How can UTI be prevented in those receiving PCN or ureteral stent placement?
Antibiotic prophylaxis has been recommended to prevent UTI in patients who will undergo PCN or ureteral stent placement. The American Urological Association recommends empiric treatment even in the absence of signs and symptoms of UTI,36 but substantial evidence is lacking that this approach prevents infection.37 Ciprofloxacin or trimethoprim/sulfamethoxazole has been recommended by some for empiric coverage for enteric gram-negative bacilli and enterococcus in those undergoing genitourinary manipulation or instrumentation.32,38 Most patients who develop CA-UTI and pyelonephritis do so within the first 2 to 6 weeks after placement.37,39 Bacteriuria, candiduria, and/or pyuria are present in all patients approximately within 9 weeks even when sterile urine is confirmed prior to PCN placement.39 Data on the effectiveness of antibiotic prophylaxis to prevent CA-UTI in those with PCN or ureteral stenting is limited. Currently, there are no recommendations from the IDSA on how to prevent infection in these situations.5 Early or frequent stent removal or exchanges has been proven to reduce UTI in those with ureteral stenting.33 Patients with diabetes mellitus and chronic renal failure are at high-risk for UTI when ureteral stents are in place. This population should undergo close monitoring for UTI development and may warrant more frequent stent exchanges.27,40
What is the treatment of CA-UTI associated with PCN and/or ureteral stenting?
The IDSA guidelines do not apply to patients with PCN and/or ureteral stenting.5 There is no treatment protocol for UTI related to these processes. Generally speaking, they are considered “complicated UTI” by most experts. Broad-spectrum, empiric antibiotic administration along with prompt removal of the PCN and/or ureteral stent is the gold standard of therapy.27 The recommended duration of targeted antibiotic therapy is generally between 5 and 14 days.19 Most clinicians will treat this complicated UTI for at least 10 to 14 days. Antibiotic administration should be continued even after removal of the catheter and/or stent to complete the full course. Repeat urinalysis and culture is not indicated at the end of therapy if the patient is clinically improving or has remission of symptoms.
What is the exchange rate for those who require chronic PCN and/or ureteral stent use?
On average a PCN or ureteral stent should be exchanged every 2 to 3 months in patients who require chronic usage.24,27 Some patients with persistent complications may require more frequent exchanges (< 10 weeks).27 Encrustation and bacterial colonization become more prevalent the longer the devices are in place. This process is estimated to begin within the first 2 weeks after placement.27,33,34 A “forgotten stent” is one that has been left in place after the patient is lost to follow-up. This unfortunate event can lead to massive encrustation, UTI, stent fracturing, and complete ureteral obstruction.24 As noted, patients with diabetes mellitus, chronic renal failure, and frequent UTI may warrant more frequent exchanges, but this should be determined on a case-by-case basis.
Catheter-Associated UTI in Patients with Spinal Cord Injury
Spinal cord injury (SCI) at any level can cause neurogenic bladder. This process ultimately leads to urinary stasis and colonization of the bladder with bacteria. According to the IDSA, the acceptable indications for UC insertion are: clinically significant urinary retention (if medical therapy is not effective), urinary incontinence, accurate urine output monitoring required, and patient is unable and/or unwilling to collect urine (Table 1).5 Recently, further guidelines were published regarding appropriate and inappropriate indwelling UC placement in hospitalized medical patients (Table 2 and Table 3), expanding upon the earlier acceptable criteria provided by the IDSA.41 According to the IDSA and Ann Arbor Criteria for Appropriate Urinary Catheter Use, patients with SCI and subsequent neurogenic bladder without obstruction where intermittent bladder straight catheterization for the drainage of urine is not feasible will likely need an indwelling UC.41 SCI patients often experience decubitus ulcers, and an indwelling UC can be used if needed to help with wound healing if other urinary management alternatives have been attempted. Other such situations in which an indwelling UC can used before attempting alternative approaches would be in a patient who is actively dying and is pursuing comfort care and/or hospice.41
Which indwelling UCs should be used in patients with SCI?
Efforts to reduce the likelihood of infection in patients with SCI have led to several advances in the design and manufacturing of UCs. UCs are made of either latex, plastic, silicone, or polytetrafluoroethylene (Teflon). None of these substrates is free of complications, but of them latex UCs have been studied the most in regards to their associated complications. Aside from being allergenic in nature, latex UCs have an increased propensity to allow bacteria to adhere to their surface due to microscopic planes of unevenness.42 Silicone UCs are less frequently associated with infection but are more rigid, leading to increased discomfort.43,44 Hydrophilic and silver-hydrogel coatings are innovative methods that have been developed to increase comfort and reduce the likelihood of infection. Hydrophilic-coated UCs are associated with reduced microbial adherence, decreased encrustation, and better patient satisfaction.45,46 In SCI patients, these UCs have demonstrated lower complication rates, including UTI; fewer episodes of post-, intra-, and inter-catheterization bleeding; and decreased rates of antibiotic-resistant bacteria.45,46 Silver-hydrogel-coated UCs are less well studied but have also demonstrated reduced UTI rates in SCI patients; however, their efficacy over the long term has yet to be determined. Antibiotic-impregnated UCs are not currently recommended for either short- or long-term indwelling UC use.5
How can CA-UTI be prevented in a patient who will require a long-term indwelling catheter?
At this time, the data is insufficient to make a recommendation on routine UC exchange (eg, every 2 to 4 weeks) in patients who require long-term indwelling urethral or suprapubic catheters in an attempt to reduce the risk of CA-ASB or CA-UTI. This is also true for those who experience even repeated early catheter blockage from encrustation.5 Thus, the rate at which these exchanges occur can be controversial, but typically around every 4 weeks is a common approach. Some would argue that if the patient has repeated CA-UTI, an exchange rate of every 2 weeks might be needed, but data is currently lacking to support this practice.5 If intermittent urinary catheterization is feasible, it should be done at least every 6 hours and before bedtime. In general, when the volume of urine in the bladder reaches approximately 400 mL, the patient should undergo bladder catheterization to prevent stasis and infection.47 A closed drainage system is recommended in all patients who require long-term indwelling UC use.48,49 Placement of the collection bag above the catheter or above the level of the bladder and a breach in the closed drainage system have been shown to result in higher rates of catheter-associated bacteriuria.48,50 Proper hand hygiene and sterile and/or clean techniques should be used when placing or exchanging a UC. However, in one study there was no difference in bacteremia or UTIs when using sterile versus clean techniques.51
Asymptomatic bacteriuria should not be treated in patients with long-term indwelling UCs, and prophylactic antibiotics have led to the emergence of resistance.52 At this time it is not clear whether prophylactic weekly oral cyclic antibiotic administration can effectively reduce the frequency of CA-UTI in patients with SCI and chronic indwelling UC use.
What are the signs and symptoms of CA-UTI in a patient with SCI?
Subjective and objective findings may be limited when a patient with SCI presents with CA-UTI. These patients often lack the usual symptoms of UTI (dysuria, suprapubic discomfort, urgency, increased frequency) and pyelonephritis (flank pain, costovertebral angle tenderness). Caregivers and health care providers should be aware that nonspecific symptoms such as foul-smelling urine, pyuria, increased residual volume of urine in the bladder, change in voiding habits, worsening detrusor spasticity, and aggravation of autonomic dysreflexia can be the only initial presenting symptoms.53
What is the duration of therapy for CA-UTI in SCI, and how can antibiotic stewardship principles be applied in this patient population?
Antibiotic therapy is indicated for a duration of 7 days if there is prompt resolution of symptoms, or for a total of 10 to 14 days if the response is delayed, regardless of whether the patient remains with a UC.5 Antibiotic stewardship is very important to reduce the risk for developing drug resistance in this high-risk population. Methods such as prescriber education practices, institution protocols, guideline implementation, auditing and feedback, restriction and reauthorization practices, computer-assisted programs, de-escalation or streamlining, and antibiotic cycling or dosage optimization have all been shown to assist in antibiotic stewardship in UTIs.54
Candida UTI
What is the initial evaluation for a patient with candiduria?
The workup for candiduria hinges on determining whether the candiduria likely represents contamination, colonization, or infection; certain predisposing risk factors are associated with Candida UTI (Table 4).55-57 The most important aspect to candiduria is the patient’s clinical status and comorbid conditions.58 Among funguria, Candida species are the most common and represent 95% of organisms isolated on urine cultures (Table 5).59 Candiduria is usually present in those with significant comorbidities and rarely is associated with healthy individuals.59,60 Candiduria is increasing in prevalence among hospitalized patients, representing 22% to 40% of all nosocomial UTIs.59,60 Markers in the urine (leukocyte esterase, colony count of culture growth, presence or absence of Candida casts and pseudohyphae) cannot alone differentiate colonization from infection.55 When candiduria is discovered in a patient with symptoms related to UTI in the setting of predisposing risk factors, it should be considered a real infection until proven otherwise.
In a situation where an asymptomatic patient without an indwelling UC has Candida species isolated from a urine culture, a repeat culture (clean-catch midstream sample) should be performed to assess for a likely contaminated collection.55 If the patient has an indwelling UC then it should be exchanged and urine collected from the fresh catheter.61 When candiduria is found in healthy asymptomatic adults, it is most commonly associated with poor collection techniques or postcollection contamination.59 If candiduria persists in an asymptomatic patient, the patient should be assessed for predisposing factors. This includes checking hemoglobin A1C for developing diabetes and renal ultrasound looking for urolithiasis, renal abscess, hydronephrosis, and fungus ball. Postvoid residual urinary retention should also be ruled out with bladder ultrasound. Treatment of predisposing factors can lead to resolution of candiduria without antifungal treatment, and a urine culture should be repeated (1 to 2 weeks later).61 Asymptomatic patients lacking any predisposing factors can be observed with repeat urine cultures in 1 to 3 months.61
Candiduria may actually represent candidemia in those patients who have a predisposing risk factor for disseminated candidiasis. These risk factors include central venous catheters, administration of total parental nutrition, antibiotic use (especially broad spectrum), critical illness, recent surgical intervention (especially intra-abdominal), acute renal failure, nasogastric tube use, and active gastric acid suppression (ie, proton pump inhibitors).62,63 The hematogenous spread of Candida can lead to the detection of candiduria in 46% to 80% of persons who are experiencing candidemia.59 If the patient is at risk for candidemia, then blood fungal cultures should be drawn. It is not unreasonable to also order a serum-D-glucan assay if suspicions are high. A thorough skin assessment should be completed and ophthalmology consulted for a detailed eye exam in the event that the patient has candidemia. Candiduria is highly prevalent among those who are candidemic, but overall candidemia is encountered in less than 5% of patients in most intensive care units.59 Thus, most patients with candiduria do not have disseminated candidiasis.
Candiduria rarely leads to symptoms of UTI,58 unless the pathogenesis is related to an ascending process.56 Symptoms of Candida UTI are no different from those experienced from a bacterial etiology. Some patients may complain of pneumaturia and/or endorse seeing particulate matter in their urine.55 Patients showing signs of sepsis (fever, chills, flank pain) should be investigated for possible Candida pyelonephritis in the setting of candiduria.64
When should asymptomatic candiduria be treated?
In adult patients with asymptomatic candiduria, there are 2 situations in which antifungal therapy is recommended. A patient undergoing a traumatic urologic procedure would be treated to avoid the risk for candidemia caused by the procedure. Also, in neutropenic patients empiric antifungal therapy should be administered because there is a high likelihood that this candiduria may actually represent hematogenous spread from candidemia.61,65
What is the treatment for symptomatic Candida cystitis?
Empiric treatment with oral fluconazole 200 to 400 mg daily for a total of 2 weeks is recommended in patients with persisting candiduria and symptoms of cystitis.65 Identifying the species is a crucial step in the treatment of Candida UTI. Several species (C. glabrata, C. krusei) are known to be resistant to fluconazole. Species identification and antifungal sensitivities should be done and therapy directed after obtaining these results.55
What is the recommended treatment for Candida pyelonephritis?
Treatment for pyelonephritis caused by fluconazole-susceptible Candida species is oral fluconazole 200 to 400 mg (3-6 mg/kg) for a total of 2 weeks.65 A fluconazole-resistant organism should be suspected when a non-albicans Candida species is isolated, such as C. krusei or C. glabrata. In this circumstance, in vitro antifungal susceptibility testing should be done. Echinocandins are not a good option in this situation because they do not reach adequate urine concentration and treatment failure is well documented.66-68 Amphotericin B deoxycholate (AmB) 0.3 to 0.6 mg/kg daily for 1 to 7 days, with or without oral flucytosine (25 mg/kg) 4 times daily, is recommended by the IDSA for the treatment of fluconazole-resistant isolates of C. glabrata and C. krusei.65 Further imaging with ultrasound, CT, or magnetic resonance should be done to rule out urinary tract obstruction and/or “fungus ball” formation. Emphysematous pyelonephritis and necrosis can occur and usually require nephrectomy. Perinephric abscess will need drainage, which can be accomplished through interventional radiological techniques.55
If a “fungus ball” is suspected in the kidney, how does the management change in a patient with Candida pyelonephritis?
A fungus ball must be treated with both antifungals and surgical intervention. Antifungal therapy should be continued during the surgical removal process to avoid fungemia. Interventional radiology should be consulted and is usually the best option for removal. Fungus ball(s) can and often do cause urinary obstruction. Temporary nephrostomy tube placement may be warranted in these situations to relieve the obstruction.55,65 AmB can be infused through the nephrostomy tube to increase local concentrations. This route of administration is not known to be nephrotoxic.55 Fluconazole infusion through a nephrostomy tube has also been used in the successful treatment of a fungus ball.69
Summary
Health care–associated UTIs are the most common nosocomial infection in the United States. UC placement and genitourinary manipulation or instrumentation play a major role in the development of CA-UTI. Clinicians should be aware of the appropriate and inappropriate use of UCs and their association with CA-UTI development. Removal of a UC when no longer necessary is key in prevention of CA-UTI. Treatment of asymptomatic bacteriuria is generally not indicated. A multidisciplinary approach is essential when managing chronic indwelling UCs in SCI. PCN and ureteral stenting need close monitoring, and early removal should be performed if infection is suspected.
Candiduria is an emerging nosocomial source of UTI but rarely leads to symptoms unless related to an ascending process. Proper urine collection is crucial in determining whether you are dealing with contamination, colonization, or infection. If candiduria persists in an asymptomatic individual, then further investigations should be done in regards to possible predisposing risks factors. Fluconazole is recommended for treatment of most patients with Candida UTI, while intravenous AmB is the treatment of choice for fluconazole-resistant Candida species. As we continue to take an evidence-based approach to the prevention and management of health care-associated UTI, we will likely see continued improvement in patient outcomes and overall decreased rates of infection.
Corresponding author: Norman Beatty, MD, 1501 N. Campbell Ave., Tucson, AZ 85724; [email protected].
Financial disclosures: None.
From the University of Arizona College of Medicine, Tucson, AZ (Dr. Beatty), and the Baylor College of Medicine, Houston, TX (Dr. Mohajer).
Abstract
- Objective: To review management issues regarding health care–associated urinary tract infections (UTIs) commonly encountered by practicing clinicians.
- Methods: Review of the literature.
- Results: Because urinary catheter (UC) placement plays a major role in the development of catheter-associated UTIs (CA-UTI), clinicians should be aware of the appropriate and inappropriate uses of UCs and their association with CA-UTI development. Removal of a UC when no longer necessary is key to preventing CA-UTI. Treatment of asymptomatic bacteriuria is generally not indicated. Percutaneous nephrostomy and ureteral stenting need close monitoring, and early removal should be performed if infection is suspected. Candiduria rarely leads to symptoms unless it is related to an ascending process. Proper urine collection is crucial in determining whether contamination, colonization, or infection is present. Fluconazole is recommended in most cases of Candida UTI, while intravenous amphotericin B is recommended for fluconazole-resistant Candida species.
- Conclusion: Continued use of evidence-based strategies for preventing and managing health care–associated UTI should lead to further improvements in patient outcomes and overall decreased rates of infection.
Keywords: bacteriuria; catheter-associated UTI; catheterization; percutaneous nephrostomy; candiduria.
Health care–associated urinary tract infections (UTIs) are estimated to be the most common adverse infectious event in U.S. hospitals, occurring in 1 of 10 admitted patients.1-3 Approximately 32% of all health care–associated infections are UTIs.1 Furthermore, urinary catheters (UCs) are associated with 8% to 21% of health care–associated infections that occur in the intensive care unit.4 The most important predisposing factor for nosocomial UTI is urinary catheterization.5 Genitourinary manipulation and/or implementation also play a major role in the development of nosocomial UTIs.
In 2008, the U.S. Centers for Medicare & Medicaid Services instituted a new policy that reduced reimbursement rates for hospitalizations linked to health care–associated infections.6 Indwelling UCs are among the most overused health care devices in the hospital setting. They are placed in an estimated 15% to 25% of all hospitalized patients,7,8 and are often inserted in the emergency department (ED) without a physician order or appropriate indication.9 Intermittent straight catheterization, male or female condom catheterization, and/or placement of an indwelling UC are the most common causes of catheter-associated asymptomatic bacteriuria (CA-ASB) and catheter-associated UTIs (CA-UTI).5 Prevention and management of CA-ASB and CA-UTI can be challenging and require an evidence-based approach. Furthermore, guidelines for the management of UTIs in the setting of active percutaneous nephrostomy (PCN) drainage and/or ureteral stenting are not established.5 This may leave clinicians with little mainstream data to aid in management decisions.
In 2009 the Centers for Disease Control and Prevention provided a guideline for the appropriate and inappropriate use of indwelling UCs to help promote their proper use.10 In the time since the guideline’s initiatives were instituted around the United States, published data have shown some improvement in the use of UCs,11,12 but other recent reports indicate that rates of UC use have remained unchanged.13 This review discusses management issues regarding health care–associated UTIs that are commonly encountered by practicing clinicians, with a focus on current guidelines and evidence.
Catheter-Associated UTI
CA-UTI is defined as the presence of signs or symptoms of UTI with no other explainable infectious source along with ≥ 1000 colony-forming units (cfu) of ≥ 1 bacterial species per milliliter in a urine specimen from a catheter that has been changed within 48 hours of collection of the urine specimen.5 Signs and symptoms of CA-UTI include, but are not limited to: new-onset or worsening fever, chills, altered sensorium from baseline, lethargy, malaise, flank pain, pelvic pain, costovertebral angle tenderness, and acute hematuria.5 New-onset “foul-smelling” (odorous)urine and “cloudy” urine are neither sensitive nor specific when assessing for CA-UTI, and do not have significant clinical relevance when found alone.14,15 Patients who have removed or exchanged the UC during this event and then experience dysuria, increased frequency, urgency, or suprapubic pain are likely having symptoms of CA-UTI.5
What is the recommended method for collecting urine samples when CA-UTI is suspected?
In a patient with an indwelling catheter that has been in place for more than 2 weeks at the onset of a suspected CA-UTI, the catheter should be replaced (if still indicated) or removed to accelerate resolution of symptoms and to reduce the risk of subsequent catheter-associated bacteriuria and CA-UTI. The urine culture should be acquired from the freshly placed UC.5
When should a patient be empirically treated?
A patient presenting with evidence of sepsis should be empirically treated with antimicrobials. Empiric coverage should be based on risk factors for multidrug-resistant organisms and data pertaining to local antimicrobial resistance patterns. A urine specimen for urinalysis and possible culture should be sent prior to administering empiric antibiotics (if possible) in a symptomatic patient.5
What bacteria are commonly associated with CA-UTI?
The bacteria most commonly associated with CA-UTI are found in or around the gastrointestinal and genitourinary tracts and also are part of the normal skin flora. The introduction and/or facilitated ascension of these microorganisms is believed to occur during UC insertion.16,17 Two-thirds of all isolated uropathogens in those with indwelling UCs are extraluminally acquired (via ascension along the catheter-urethral mucosa interface), and one-third are believed to be intraluminally acquired.18
The most commonly isolated bacteria in CA-UTI are Enterobacteriaceae, which include Escherichia coli (most common), Klebsiella species (K. oxytoca, K. pneumoniae), Serratia species (S. marcescens), Citrobacter species (C. koseri), Enterobacter species (E. cloacae), and Proteus species; non-Enterobacteriaceae such as Pseudomonas species; and gram-positive cocci, which include coagulase-negative staphylococci (S. saprophyticus), Staphylococcus aureus, group B streptococci, and Enterococcus species (E. faecalis, E. faecium).19-21 Coagulase-negative staphylococci and Enterococcus species can lead to CA-UTI but are usually avirulent and more commonly isolated from asymptomatic individuals.19 Also, coagulase-negative staphylococci such as S. epidermidis and S. lugdunensis are usually the manifestation of contamination during the collection process and their presence should prompt a repeat sample collection under sterile techniques. Monomicrobial infection is usually seen in those with short-term catheter use and CA-UTI. In contrast, polymicrobial infection is more common in those with long-term indwelling UCs and CA-UTI.19 Providencia stuartii, Proteus mirabilis, S. aureus, and Morganella morganii have all been associated with CA-UTI in those with long-term indwelling UCs.
Growth of S. aureus in the urine should prompt further investigation with blood cultures to explore the possibility of hematogenous dissemination to the urinary tract. Organisms leading to bacteremia due to CA-UTI are most commonly gram-negative bacilli (E. coli, Klebsiella species, Pseudomonas aeruginosa) and E. faecalis.21
What is the difference between CA-ASB and CA-UTI?
CA-ASB is defined as the presence of ≥ 1 bacteria species growing on urine culture at ≥ 100,000 cfu/mL in a patient with a history of urinary catheterization and/or indwelling UC who lacks signs or symptoms of UTI. In a man with a condom catheter, CA-ASB is defined using the same criteria, but the urine sample is collected after a fresh condom catheter is applied.5 The difference between CA-ASB and CA-UTI is simply the presence or absence of signs and symptoms related to UTI. Currently, there is no standard definition for significant bacteriuria in a catheterized patient.5 Pyuria found on urinalysis is indicative of genitourinary inflammation and can be present in both CA-ASB and CA-UTI. The absence, presence, and/or degree of pyuria in catheterized patients does not accurately differentiate between CA-ASB and CA-UTI.5,22,23 On the other hand, the absence of pyuria in a symptomatic catheterized patient suggests an etiology other than CA-UTI.5
How can CA-UTI be prevented in patients with a short-term indwelling urinary catheter?
If a short-term UC is essential, the most important approach to preventing CA-UTI is limiting the duration of time it will be used. Strategies such as computer-based order entry and care maps with automated discontinuation of UCs have been shown to decrease catheter usage.19 Using closed-systems for UC collection with ports in the distal catheter for needle aspiration of urine has also been shown to decrease the incidence of CA-UTI.5 Securing the UC to avoid urethral trauma, aseptic techniques for insertion and repositioning, and placement of the tubing and collection bag below the level of the bladder to prevent reflux will likely also prevent CA-UTI, but these strategies have not been evaluated thoroughly.19
When should you screen for and treat CA-ASB?
The 2009 Infectious Diseases Society of America (IDSA) guidelines recommend that the only patients who should be screened and treated for CA-ASB are pregnant women and those who will undergo a potentially traumatic urologic procedure for which mucosal breaching may occur, causing bleeding. Routinely screening or treating patients for CA-ASB in not recommended in any other group of patients and will lead to unnecessary antibiotic use and antibiotic resistance.5
UTI Associated with Percutaneous Nephrostomy and Ureteral Stenting
Similar systemic symptoms of infection (fever, rigors, malaise, shock) are present in patients with and without percutaneous nephrostomy (PCN) and/or ureteral stent placement. Dysuria is not commonly present in those with PCN. The first signs of CA-UTI may be decreased urine output and pericatheter leakage due to an obstructive process resulting from the encrustation.24-27 The most common complaint among patients with either acute or chronic ureteral stenting is discomfort, which has been described as “urinary symptoms” and “body pain.”28 This discomfort can be related to ureteral hyperperistalsis after placement of the stent and is usually self-limiting. Ureteral stent migration, usually at the distal end, can also lead to discomfort, but is easily rectified with cystoscopy.25 Body pain and/or urinary symptoms in the setting of ureteral stenting are not indicative of infection alone.
What is urinary catheter and/or ureteral stent encrustation?
Encrustation is the formation of a conditioning film that develops on the surface of the UC or ureteral stent. The exact mechanism is not well understood, but it is believed to involve electrostatic interactions of urinary proteins that stimulate binding onto the stent or UC surface.25 Encrustation increases exponentially with the dwell time. Among patients with ureteral stents placed due to urolithiasis, encrustation occurred in 9.2% of stents removed prior to 6 weeks, 47.5% of stents removed at 6 weeks, and 76.3% of stents removed at 12 weeks.26 Encrustation is most common at the proximal and distal ends (pigtails) of the ureteral stent and usually spares or presents last within the lumen.29 Attempts have been made to prevent ureteral stent encrustation through the development of biodegradable, drug-eluting, and tissue-engineered substrates. These developments are promising, but currently there is limited observational data from large randomized trials to suggest that these new modalities decrease rates of encrustation.25 Encrustation is highly associated with certain microorganisms, especially those that create biofilms.30 Urease-producing bacteria, most commonly P. mirabilis, play a role in encrustation formation.31 Bacteria most commonly associated with encrustation include Proteus species (P. mirabilis is most common), P. aeruginosa, K. pneumoniae, Providencia species (P. stuartii is most common), and M. morganii.
Does ureteral stent bacterial colonization correlate with UTI?
Ureteral stent colonization with bacteria increases with dwell time and is found in 40% to 98.5% of stents placed.32-35 If UTI is suspected in a patient with an active indwelling ureteral stent, a sample of urine should be cultured while the stent is in place.25 Typically, genitourinary and normal skin flora pathogens are found when the ureteral stent is cultured. The top 3 organisms cultured from ureteral stents are S. aureus, P. aeruginosa, and E. faecalis.34 Urine culture usually does not correlate with stent culture results, which has brought up the debate of how bacterial colonization occurs. It has been postulated that colonization is actually a manifestation of contamination during the insertion procedure, but this has yet to be validated.25 In patients with symptoms of UTI in the setting of an indwelling ureteral stent, a positive culture has low sensitivity, with estimates between 21% and 40%.35 Therefore, a negative urine culture does not rule out UTI alone in a symptomatic patient. Multiple studies have suggested that colonization of the ureteral stent does not correlate strongly with developing a UTI.25,32-34
How can UTI be prevented in those receiving PCN or ureteral stent placement?
Antibiotic prophylaxis has been recommended to prevent UTI in patients who will undergo PCN or ureteral stent placement. The American Urological Association recommends empiric treatment even in the absence of signs and symptoms of UTI,36 but substantial evidence is lacking that this approach prevents infection.37 Ciprofloxacin or trimethoprim/sulfamethoxazole has been recommended by some for empiric coverage for enteric gram-negative bacilli and enterococcus in those undergoing genitourinary manipulation or instrumentation.32,38 Most patients who develop CA-UTI and pyelonephritis do so within the first 2 to 6 weeks after placement.37,39 Bacteriuria, candiduria, and/or pyuria are present in all patients approximately within 9 weeks even when sterile urine is confirmed prior to PCN placement.39 Data on the effectiveness of antibiotic prophylaxis to prevent CA-UTI in those with PCN or ureteral stenting is limited. Currently, there are no recommendations from the IDSA on how to prevent infection in these situations.5 Early or frequent stent removal or exchanges has been proven to reduce UTI in those with ureteral stenting.33 Patients with diabetes mellitus and chronic renal failure are at high-risk for UTI when ureteral stents are in place. This population should undergo close monitoring for UTI development and may warrant more frequent stent exchanges.27,40
What is the treatment of CA-UTI associated with PCN and/or ureteral stenting?
The IDSA guidelines do not apply to patients with PCN and/or ureteral stenting.5 There is no treatment protocol for UTI related to these processes. Generally speaking, they are considered “complicated UTI” by most experts. Broad-spectrum, empiric antibiotic administration along with prompt removal of the PCN and/or ureteral stent is the gold standard of therapy.27 The recommended duration of targeted antibiotic therapy is generally between 5 and 14 days.19 Most clinicians will treat this complicated UTI for at least 10 to 14 days. Antibiotic administration should be continued even after removal of the catheter and/or stent to complete the full course. Repeat urinalysis and culture is not indicated at the end of therapy if the patient is clinically improving or has remission of symptoms.
What is the exchange rate for those who require chronic PCN and/or ureteral stent use?
On average a PCN or ureteral stent should be exchanged every 2 to 3 months in patients who require chronic usage.24,27 Some patients with persistent complications may require more frequent exchanges (< 10 weeks).27 Encrustation and bacterial colonization become more prevalent the longer the devices are in place. This process is estimated to begin within the first 2 weeks after placement.27,33,34 A “forgotten stent” is one that has been left in place after the patient is lost to follow-up. This unfortunate event can lead to massive encrustation, UTI, stent fracturing, and complete ureteral obstruction.24 As noted, patients with diabetes mellitus, chronic renal failure, and frequent UTI may warrant more frequent exchanges, but this should be determined on a case-by-case basis.
Catheter-Associated UTI in Patients with Spinal Cord Injury
Spinal cord injury (SCI) at any level can cause neurogenic bladder. This process ultimately leads to urinary stasis and colonization of the bladder with bacteria. According to the IDSA, the acceptable indications for UC insertion are: clinically significant urinary retention (if medical therapy is not effective), urinary incontinence, accurate urine output monitoring required, and patient is unable and/or unwilling to collect urine (Table 1).5 Recently, further guidelines were published regarding appropriate and inappropriate indwelling UC placement in hospitalized medical patients (Table 2 and Table 3), expanding upon the earlier acceptable criteria provided by the IDSA.41 According to the IDSA and Ann Arbor Criteria for Appropriate Urinary Catheter Use, patients with SCI and subsequent neurogenic bladder without obstruction where intermittent bladder straight catheterization for the drainage of urine is not feasible will likely need an indwelling UC.41 SCI patients often experience decubitus ulcers, and an indwelling UC can be used if needed to help with wound healing if other urinary management alternatives have been attempted. Other such situations in which an indwelling UC can used before attempting alternative approaches would be in a patient who is actively dying and is pursuing comfort care and/or hospice.41
Which indwelling UCs should be used in patients with SCI?
Efforts to reduce the likelihood of infection in patients with SCI have led to several advances in the design and manufacturing of UCs. UCs are made of either latex, plastic, silicone, or polytetrafluoroethylene (Teflon). None of these substrates is free of complications, but of them latex UCs have been studied the most in regards to their associated complications. Aside from being allergenic in nature, latex UCs have an increased propensity to allow bacteria to adhere to their surface due to microscopic planes of unevenness.42 Silicone UCs are less frequently associated with infection but are more rigid, leading to increased discomfort.43,44 Hydrophilic and silver-hydrogel coatings are innovative methods that have been developed to increase comfort and reduce the likelihood of infection. Hydrophilic-coated UCs are associated with reduced microbial adherence, decreased encrustation, and better patient satisfaction.45,46 In SCI patients, these UCs have demonstrated lower complication rates, including UTI; fewer episodes of post-, intra-, and inter-catheterization bleeding; and decreased rates of antibiotic-resistant bacteria.45,46 Silver-hydrogel-coated UCs are less well studied but have also demonstrated reduced UTI rates in SCI patients; however, their efficacy over the long term has yet to be determined. Antibiotic-impregnated UCs are not currently recommended for either short- or long-term indwelling UC use.5
How can CA-UTI be prevented in a patient who will require a long-term indwelling catheter?
At this time, the data is insufficient to make a recommendation on routine UC exchange (eg, every 2 to 4 weeks) in patients who require long-term indwelling urethral or suprapubic catheters in an attempt to reduce the risk of CA-ASB or CA-UTI. This is also true for those who experience even repeated early catheter blockage from encrustation.5 Thus, the rate at which these exchanges occur can be controversial, but typically around every 4 weeks is a common approach. Some would argue that if the patient has repeated CA-UTI, an exchange rate of every 2 weeks might be needed, but data is currently lacking to support this practice.5 If intermittent urinary catheterization is feasible, it should be done at least every 6 hours and before bedtime. In general, when the volume of urine in the bladder reaches approximately 400 mL, the patient should undergo bladder catheterization to prevent stasis and infection.47 A closed drainage system is recommended in all patients who require long-term indwelling UC use.48,49 Placement of the collection bag above the catheter or above the level of the bladder and a breach in the closed drainage system have been shown to result in higher rates of catheter-associated bacteriuria.48,50 Proper hand hygiene and sterile and/or clean techniques should be used when placing or exchanging a UC. However, in one study there was no difference in bacteremia or UTIs when using sterile versus clean techniques.51
Asymptomatic bacteriuria should not be treated in patients with long-term indwelling UCs, and prophylactic antibiotics have led to the emergence of resistance.52 At this time it is not clear whether prophylactic weekly oral cyclic antibiotic administration can effectively reduce the frequency of CA-UTI in patients with SCI and chronic indwelling UC use.
What are the signs and symptoms of CA-UTI in a patient with SCI?
Subjective and objective findings may be limited when a patient with SCI presents with CA-UTI. These patients often lack the usual symptoms of UTI (dysuria, suprapubic discomfort, urgency, increased frequency) and pyelonephritis (flank pain, costovertebral angle tenderness). Caregivers and health care providers should be aware that nonspecific symptoms such as foul-smelling urine, pyuria, increased residual volume of urine in the bladder, change in voiding habits, worsening detrusor spasticity, and aggravation of autonomic dysreflexia can be the only initial presenting symptoms.53
What is the duration of therapy for CA-UTI in SCI, and how can antibiotic stewardship principles be applied in this patient population?
Antibiotic therapy is indicated for a duration of 7 days if there is prompt resolution of symptoms, or for a total of 10 to 14 days if the response is delayed, regardless of whether the patient remains with a UC.5 Antibiotic stewardship is very important to reduce the risk for developing drug resistance in this high-risk population. Methods such as prescriber education practices, institution protocols, guideline implementation, auditing and feedback, restriction and reauthorization practices, computer-assisted programs, de-escalation or streamlining, and antibiotic cycling or dosage optimization have all been shown to assist in antibiotic stewardship in UTIs.54
Candida UTI
What is the initial evaluation for a patient with candiduria?
The workup for candiduria hinges on determining whether the candiduria likely represents contamination, colonization, or infection; certain predisposing risk factors are associated with Candida UTI (Table 4).55-57 The most important aspect to candiduria is the patient’s clinical status and comorbid conditions.58 Among funguria, Candida species are the most common and represent 95% of organisms isolated on urine cultures (Table 5).59 Candiduria is usually present in those with significant comorbidities and rarely is associated with healthy individuals.59,60 Candiduria is increasing in prevalence among hospitalized patients, representing 22% to 40% of all nosocomial UTIs.59,60 Markers in the urine (leukocyte esterase, colony count of culture growth, presence or absence of Candida casts and pseudohyphae) cannot alone differentiate colonization from infection.55 When candiduria is discovered in a patient with symptoms related to UTI in the setting of predisposing risk factors, it should be considered a real infection until proven otherwise.
In a situation where an asymptomatic patient without an indwelling UC has Candida species isolated from a urine culture, a repeat culture (clean-catch midstream sample) should be performed to assess for a likely contaminated collection.55 If the patient has an indwelling UC then it should be exchanged and urine collected from the fresh catheter.61 When candiduria is found in healthy asymptomatic adults, it is most commonly associated with poor collection techniques or postcollection contamination.59 If candiduria persists in an asymptomatic patient, the patient should be assessed for predisposing factors. This includes checking hemoglobin A1C for developing diabetes and renal ultrasound looking for urolithiasis, renal abscess, hydronephrosis, and fungus ball. Postvoid residual urinary retention should also be ruled out with bladder ultrasound. Treatment of predisposing factors can lead to resolution of candiduria without antifungal treatment, and a urine culture should be repeated (1 to 2 weeks later).61 Asymptomatic patients lacking any predisposing factors can be observed with repeat urine cultures in 1 to 3 months.61
Candiduria may actually represent candidemia in those patients who have a predisposing risk factor for disseminated candidiasis. These risk factors include central venous catheters, administration of total parental nutrition, antibiotic use (especially broad spectrum), critical illness, recent surgical intervention (especially intra-abdominal), acute renal failure, nasogastric tube use, and active gastric acid suppression (ie, proton pump inhibitors).62,63 The hematogenous spread of Candida can lead to the detection of candiduria in 46% to 80% of persons who are experiencing candidemia.59 If the patient is at risk for candidemia, then blood fungal cultures should be drawn. It is not unreasonable to also order a serum-D-glucan assay if suspicions are high. A thorough skin assessment should be completed and ophthalmology consulted for a detailed eye exam in the event that the patient has candidemia. Candiduria is highly prevalent among those who are candidemic, but overall candidemia is encountered in less than 5% of patients in most intensive care units.59 Thus, most patients with candiduria do not have disseminated candidiasis.
Candiduria rarely leads to symptoms of UTI,58 unless the pathogenesis is related to an ascending process.56 Symptoms of Candida UTI are no different from those experienced from a bacterial etiology. Some patients may complain of pneumaturia and/or endorse seeing particulate matter in their urine.55 Patients showing signs of sepsis (fever, chills, flank pain) should be investigated for possible Candida pyelonephritis in the setting of candiduria.64
When should asymptomatic candiduria be treated?
In adult patients with asymptomatic candiduria, there are 2 situations in which antifungal therapy is recommended. A patient undergoing a traumatic urologic procedure would be treated to avoid the risk for candidemia caused by the procedure. Also, in neutropenic patients empiric antifungal therapy should be administered because there is a high likelihood that this candiduria may actually represent hematogenous spread from candidemia.61,65
What is the treatment for symptomatic Candida cystitis?
Empiric treatment with oral fluconazole 200 to 400 mg daily for a total of 2 weeks is recommended in patients with persisting candiduria and symptoms of cystitis.65 Identifying the species is a crucial step in the treatment of Candida UTI. Several species (C. glabrata, C. krusei) are known to be resistant to fluconazole. Species identification and antifungal sensitivities should be done and therapy directed after obtaining these results.55
What is the recommended treatment for Candida pyelonephritis?
Treatment for pyelonephritis caused by fluconazole-susceptible Candida species is oral fluconazole 200 to 400 mg (3-6 mg/kg) for a total of 2 weeks.65 A fluconazole-resistant organism should be suspected when a non-albicans Candida species is isolated, such as C. krusei or C. glabrata. In this circumstance, in vitro antifungal susceptibility testing should be done. Echinocandins are not a good option in this situation because they do not reach adequate urine concentration and treatment failure is well documented.66-68 Amphotericin B deoxycholate (AmB) 0.3 to 0.6 mg/kg daily for 1 to 7 days, with or without oral flucytosine (25 mg/kg) 4 times daily, is recommended by the IDSA for the treatment of fluconazole-resistant isolates of C. glabrata and C. krusei.65 Further imaging with ultrasound, CT, or magnetic resonance should be done to rule out urinary tract obstruction and/or “fungus ball” formation. Emphysematous pyelonephritis and necrosis can occur and usually require nephrectomy. Perinephric abscess will need drainage, which can be accomplished through interventional radiological techniques.55
If a “fungus ball” is suspected in the kidney, how does the management change in a patient with Candida pyelonephritis?
A fungus ball must be treated with both antifungals and surgical intervention. Antifungal therapy should be continued during the surgical removal process to avoid fungemia. Interventional radiology should be consulted and is usually the best option for removal. Fungus ball(s) can and often do cause urinary obstruction. Temporary nephrostomy tube placement may be warranted in these situations to relieve the obstruction.55,65 AmB can be infused through the nephrostomy tube to increase local concentrations. This route of administration is not known to be nephrotoxic.55 Fluconazole infusion through a nephrostomy tube has also been used in the successful treatment of a fungus ball.69
Summary
Health care–associated UTIs are the most common nosocomial infection in the United States. UC placement and genitourinary manipulation or instrumentation play a major role in the development of CA-UTI. Clinicians should be aware of the appropriate and inappropriate use of UCs and their association with CA-UTI development. Removal of a UC when no longer necessary is key in prevention of CA-UTI. Treatment of asymptomatic bacteriuria is generally not indicated. A multidisciplinary approach is essential when managing chronic indwelling UCs in SCI. PCN and ureteral stenting need close monitoring, and early removal should be performed if infection is suspected.
Candiduria is an emerging nosocomial source of UTI but rarely leads to symptoms unless related to an ascending process. Proper urine collection is crucial in determining whether you are dealing with contamination, colonization, or infection. If candiduria persists in an asymptomatic individual, then further investigations should be done in regards to possible predisposing risks factors. Fluconazole is recommended for treatment of most patients with Candida UTI, while intravenous AmB is the treatment of choice for fluconazole-resistant Candida species. As we continue to take an evidence-based approach to the prevention and management of health care-associated UTI, we will likely see continued improvement in patient outcomes and overall decreased rates of infection.
Corresponding author: Norman Beatty, MD, 1501 N. Campbell Ave., Tucson, AZ 85724; [email protected].
Financial disclosures: None.
1. Klevens RM, Edwards JR, Richards CL Jr. Estimating health care-associated infections and deaths in U.S. hospitals, 2002. Public Health Rep. 2007;122:160-166.
2. Burke JP. Infection control—a problem for patient safety. N Engl J Med. 2003;348:651-656.
3. Scott RD. The direct medical costs of healthcare-associated infections in U.S. hospitals and the benefits of prevention. Division of Healthcare Quality Promotion; National Center for Preparedness Detection and Control of Infectious Diseases; Coordinating Center for Infectious Diseases; Centers for Disease Control and Prevention. March 2009. Contract No.: CS200891-A. www.cdc.gov/HAI/pdfs/hai/Scott_CostPaper.pdf.
4. Eriksen HM, Iverson BG, Aavitsland P. Prevalence of nosocomial infections in hospitals in Norway, 2002 and 2003. J Hosp Infect. 2005;60:40-45.
5. Hooton TM, Bradley SF, Cardenas DD, et al. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis. 2010;50:625-663.
6. Mattie AS, Webster BL. Centers for Medicare and Medicaid Services’ “never events”: an analysis and recommendations to hospitals. Health Care Manag. 2008;27:338-349.
7. Warren JW. Catheter-associated urinary tract infections. Int J Antimicrob Agents. 2001;17:299-303.
8. Weinstein JW, Mazon D, Pantelick E, et al. A decade of prevalence surveys in a tertiary-care center: trends in nosocomial infection rates, device utilization, and patient acuity. Infect Control Hosp Epidemiol. 1999;20:543-548.
9. Fakih MG, Pena ME, Shemes S, et al. Effect of establishing guidelines on appropriate urinary catheter placement. Acad Emerg Med. 2010;17:337-340.
10. Gould CV, Umscheid CA, Agarwal RK, et al. Guideline for prevention of catheter-associated urinary tract infections 2009. Infect Control Hosp Epidemiol. 2010;31:319-326.
11. Fakih MG, Rey JE, Pena ME, et al. Sustained reductions in urinary catheter use over 5 years: bedside nurses view themselves responsible for evaluation of catheter necessity. Am J Infect Control. 2013;41:236-239.
12. Meddings J, Rogers MA, Krein SL, et al. Reducing unnecessary urinary catheter use and other strategies to prevent catheter-associated urinary tract infections: an integrative review. BMJ Qual Saf. 2014;23:277-289.
13. Gould C. Catheter-associated urinary tract infection: the national perspective. In: Essential Hospitals Engagement Network. Patient Harm Series II: new tools to prevent CAUTI webinar. April 16, 2014. http://bit.ly/1UWndRA.
14. Nicolle LE. Consequences of asymptomatic bacteriuria in the elderly. Int J Antimicrob Agents. 1994;4:107-111.
15. Nicolle LE. Urinary tract infections in long-term-care facilities. Infect Control Hosp Epidemiol. 2001;22:167-175
16. Cohen A. A microbiological comparison of a povidone-iodine lubricating gel and a control as catheter lubricants. J Hosp Infect. 1985;6(Suppl A):155-161.
17. Daifuku R, Stamm WE. Bacterial adherence to bladder uroepithelial cells in catheter-associated urinary tract infection. N Engl J Med. 1986;314:1208-1213.
18. Tambyah PA, Halvorson KT, Maki DG. A prospective study of pathogenesis of catheter-associated urinary tract infections. Mayo Clin Proc. 1999;74:131-136.
19. Nicolle LE. Catheter-related urinary tract infection. Drugs Aging. 2005;22:627-639.
20. Redder JD, Leth RA, Møller JK. Incidence rates of hospital-acquired urinary tract and bloodstream infections generated by automated compilation of electronically available healthcare data. J Hosp Infect. 2015;91:231-236.
21. Ortega M, Marco F, Soriano A, et al. Epidemiology and prognostic determinants of bacteraemic catheter-acquired urinary tract infection in a single institution from 1991 to 2010. J Infect. 2013;67:282-287.
22. Tambyah PA, Maki DG. The relationship between pyuria and infection in patients with indwelling urinary catheters: a prospective study of 761 patients. Arch Intern Med. 2000;160:673-677.
23. Musher DM, Thorsteinsson SB, Airola VM, II. Quantitative urinalysis:diagnosing urinary tract infection in men. JAMA. 1976;236:2069-2072.
24. Hausegger KA, Portugaller HR. Percutaneous nephrostomy and antegrade ureteral stenting: technique-indications-complications. Eur Radiol. 2006;16:2016-2030.
25. Lange D, Bidnur S, Hoag N, et al. Ureteral stent-associated complications--where we are and where we are going. Nat Rev Urol. 2015;12:17-25.
26. el-Faqih SR, Shamsuddin AB, Chakrabarti A, et al. Polyurethane internal ureteral stents in treatment of stone patients: morbidity related to indwelling times. J Urol. 1991;146:1487-1491.
27. Adamo R, Saad WE, Brown DB. Management of nephrostomy drains and ureteral stents. Tech Vasc Interv Radiol. 2009;12:193-204.
28. Joshi HB, Newns N, Stainthorpe A, et al. Ureteral Stent Symptom Questionnaire: development and validation of a multidimensional quality of life measure. J Urol. 2003;169:1060-1064.
29. Singh I, Gupta NP, Hemal AK, et al. Severely encrusted polyurethane ureteral stents: management and analysis of potential risk factors. Urology. 2001;58:526-531.
30. Saint S, Chenoweth CE. Biofilms and catheter-associated urinary tract infections. Infect Dis Clin North Am. 2003;17:411-432.
31. Mobley HL, Warren JW. Urease-positive bacteriuria and obstruction of long-term urinary catheters. J Clin Microbiol. 1987;25:2216-2217.
32. Kehinde EO, Rotimi VO, Al-Hunayan A, et al. Bacteriology of urinary tract infection associated with indwelling J ureteral stents. J Endourol. 2004;18:891-896.
33. Paick SH, Park HK, Oh SJ, Kim HH. Characteristics of bacterial colonization and urinary tract infection after indwelling of double-J ureteral stent. Urology. 2003;62:214-217.
34. Klis R, Korczak-Kozakiewicz E, Denys A, et al. Relationship between urinary tract infection and self-retaining double-J catheter colonization. J Endourol. 2009;23:1015-1019.
35. Farsi HM, Mosli HA, Al-Zemaity M, et al. Bacteriuria and colonization of double-pigtail ureteral stents: long-term experience with 237 patients. J Endourol. 1995;9:469-472.
36. Wolfe JS Jr, Bennet CJ, Dmochowski RR, et al. Best practice policy statement on urologic surgery antimicrobial prophylaxis. J Urol. 2008;179:1379-1390.
37. Bahu R, Chaftari AM, Hachem RY, et al. Nephrostomy tube related pyelonephritis in patients with cancer: epidemiology, infection rate and risk factors. J Urol. 2013;189:130-135.
38. Bratzler DW, Dellinger EP, Olsen KM, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Surg Infect (Larchmt). 2013;14:73-156.
39. Cronan JJ, Horn DL, Marcello A, et al: Antibiotics and nephrostomy tube care: preliminary observations. Part II. Bacteremia. Radiology. 1989;172(3 Pt 2):1043-1045.
40. Akay AF, Aflay U, Gedik A, et al. Risk factors for lower urinary tract infection and bacterial stent colonization in patients with a double J ureteral stent. Int Urol Nephrol. 2007;39:95-98.
41. Meddings J, Saint S, Fowler KE, et al. The Ann Arbor criteria for appropriate urinary catheter use in hospitalized medical patients: results obtained by using the RAND/ UCLA appropriateness method. Ann Intern Med. 2015;162(9 Suppl):S1-34.
42. Stickler D, Young R, Jones G, et al. Why are Foley catheters so vulnerable to encrustation and blockage by crystalline bacterial biofilm? Urol Res. 2003;31:306-311.
43. Denstedt J, Wollin T, Reid G. Biomaterials used in urology: current issues of biocompatibility, infection, and encrustation. J Endourol. 1998;12:493-500.
44. Morris N, Stickler D, Winters C. Which indwelling urethral catheters resist encrustation by Proteus mirabilis biofilms? Br J Urol. 1997;80:58-63.
45. Cardenas D, Moore K, Dannels-McClure A, et al. Intermittent catheterization with a hydrophilic-coated catheter delays urinary tract infections in acute spinal cord injury: a prospective, randomized, multicenter trial. PMR. 2011;3:408-417.
46. Spinu A, Onose G, Daia C, et al. Intermittent catheterization in the management of post spinal cord injury (SCI) neurogenic bladder using new hydrophilic, with lubrication in close circuit devices-our own preliminary results. J Med Life. 2012;5:21-28.
47. Shekelle P, Morton S, Clark K, et al. Systematic review of risk factors for urinary tract infection in adults with spinal cord dysfunction. J Spinal Cord Med. 1998;22:258-272.
48. Siddiq D, Darouiche R. New strategies to prevent catheter-associated urinary tract infections. Nat Rev Urol. 2012;9:305-314.
49. Gould C, Umscheid C, Agarwal R, et al. Guideline for prevention of catheter-associated urinary tract infections 2009. Infect Control Hosp Epidemiol. 2010;31:319-326.
50. Maki D, Tambyah P. Engineering out the risk for infection with urinary catheters. Emerg Infect Dis. 2001;7:342-347.
51. Munasinghe R, Yazdani H, Siddique M, et al. Appropriateness of use of indwelling urinary catheters in patients admitted to the medical service. Infect Control Hosp Epidemiol. 2001;22:647-649.
52. Nicolle L, Bradley S, Colgan R, et al; Infectious Diseases Society of America; American Society of Nephrology; American Geriatric Society. Infectious Diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clin Infect Dis. 2005;40: 643-654.
53. Linsenmeyer T, Oakley A. Accuracy of individuals with spinal cord injury at predicting urinary tract infections based on their symptoms. J Spinal Cord Med. 2002;26:352-357.
54. Abbo LM, Hooton TM. Antimicrobial stewardship and urinary tract infections. Antibiotics. 2014;3:174-192.
55. Kauffman CA. Diagnosis and management of fungal urinary tract infection. Infect Dis Clin North Am. 2014;28:61-74.
56. Alvarez-Lerma F, Nolla-Salas J, Leon C, et al. Candiduria in critically ill patients admitted to intensive care medical units. Intensive Care Med. 2003;29:1069-1076.
57. Colodner R, Nuri Y, Chazan B, et al. Community-acquired and hospital-acquired candiduria: comparison of prevalence and clinical characteristics. Eur J Clin Microbiol Infect Dis. 2008;27:301-305.
58. Kauffman CA, Vazquez JA, Sobel JD, et al. Prospective multicenter surveillance study of funguria in hospitalized patients. Clin Infect Dis. 2000;30:14-18.
59. Sobel JD, Fisher JF, Kauffman CA, et al. Candida urinary tract infections—epidemiology. Clin Infect Dis. 2011;52(suppl 6): S433-436.
60. Richards MJ, Edwards JR, Culver DH, et al. Nosocomial infections in combined medical-surgical intensive care units in the United States. Infect Control Hosp Epidemiol. 2000;21:510-515.
61. Fisher JF, Sobel JD, Kauffman CA, et al. Candida urinary tract infections—treatment. Clin Infect Dis. 2011;52(suppl 6):S457-466.
62. Blumberg HM, Jarvis WR, Soucie JM, et al. Risk factors for candidal bloodstream infections in surgical intensive care unit patients: the NEMIS prospective multicenter study. Clin Infect Dis. 2001;33:177-186.
63. Puzniak LP, Teutsch S, Powderly W, et al. Has the epidemiology of nosocomial candidemia changed? Infect Control Hosp Epidemiol. 2004;25:628-633.
64. Siddique MS, Gayed N, McGuire N, et al. Salient features of Candida pyelonephritis in adults. Infect Dis Clin Pract. 1992;1:239-245
65. Pappas PG, Kauffman CA, Andes DR, et al. Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;62:e1-e50.
66. Sobel JD, Bradshaw SK, Lipka CJ, et al. Caspofungin in the treatment of symptomatic candiduria. Clin Infect Dis. 2007;44:e46-9.
67. Malani AN. Failure of caspofungin for treatment of Candida glabrata candiduria. Case report and review of the literature. Infect Dis Clin Pract. 2010;18:271-272.
68. Schelenz S, Ross CN. Limitations of caspofugin in the treatment of obstructive pyelonephrosis due to Candida glabrata infection. BMC Infect Dis. 2006;56:126-130.
69. Chung BH, Chang SY, Kim SI, et al. Successfully treated renal fungal ball with continuous irrigation of fluconazole. J Urol. 2001;166:1835-1836.
1. Klevens RM, Edwards JR, Richards CL Jr. Estimating health care-associated infections and deaths in U.S. hospitals, 2002. Public Health Rep. 2007;122:160-166.
2. Burke JP. Infection control—a problem for patient safety. N Engl J Med. 2003;348:651-656.
3. Scott RD. The direct medical costs of healthcare-associated infections in U.S. hospitals and the benefits of prevention. Division of Healthcare Quality Promotion; National Center for Preparedness Detection and Control of Infectious Diseases; Coordinating Center for Infectious Diseases; Centers for Disease Control and Prevention. March 2009. Contract No.: CS200891-A. www.cdc.gov/HAI/pdfs/hai/Scott_CostPaper.pdf.
4. Eriksen HM, Iverson BG, Aavitsland P. Prevalence of nosocomial infections in hospitals in Norway, 2002 and 2003. J Hosp Infect. 2005;60:40-45.
5. Hooton TM, Bradley SF, Cardenas DD, et al. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis. 2010;50:625-663.
6. Mattie AS, Webster BL. Centers for Medicare and Medicaid Services’ “never events”: an analysis and recommendations to hospitals. Health Care Manag. 2008;27:338-349.
7. Warren JW. Catheter-associated urinary tract infections. Int J Antimicrob Agents. 2001;17:299-303.
8. Weinstein JW, Mazon D, Pantelick E, et al. A decade of prevalence surveys in a tertiary-care center: trends in nosocomial infection rates, device utilization, and patient acuity. Infect Control Hosp Epidemiol. 1999;20:543-548.
9. Fakih MG, Pena ME, Shemes S, et al. Effect of establishing guidelines on appropriate urinary catheter placement. Acad Emerg Med. 2010;17:337-340.
10. Gould CV, Umscheid CA, Agarwal RK, et al. Guideline for prevention of catheter-associated urinary tract infections 2009. Infect Control Hosp Epidemiol. 2010;31:319-326.
11. Fakih MG, Rey JE, Pena ME, et al. Sustained reductions in urinary catheter use over 5 years: bedside nurses view themselves responsible for evaluation of catheter necessity. Am J Infect Control. 2013;41:236-239.
12. Meddings J, Rogers MA, Krein SL, et al. Reducing unnecessary urinary catheter use and other strategies to prevent catheter-associated urinary tract infections: an integrative review. BMJ Qual Saf. 2014;23:277-289.
13. Gould C. Catheter-associated urinary tract infection: the national perspective. In: Essential Hospitals Engagement Network. Patient Harm Series II: new tools to prevent CAUTI webinar. April 16, 2014. http://bit.ly/1UWndRA.
14. Nicolle LE. Consequences of asymptomatic bacteriuria in the elderly. Int J Antimicrob Agents. 1994;4:107-111.
15. Nicolle LE. Urinary tract infections in long-term-care facilities. Infect Control Hosp Epidemiol. 2001;22:167-175
16. Cohen A. A microbiological comparison of a povidone-iodine lubricating gel and a control as catheter lubricants. J Hosp Infect. 1985;6(Suppl A):155-161.
17. Daifuku R, Stamm WE. Bacterial adherence to bladder uroepithelial cells in catheter-associated urinary tract infection. N Engl J Med. 1986;314:1208-1213.
18. Tambyah PA, Halvorson KT, Maki DG. A prospective study of pathogenesis of catheter-associated urinary tract infections. Mayo Clin Proc. 1999;74:131-136.
19. Nicolle LE. Catheter-related urinary tract infection. Drugs Aging. 2005;22:627-639.
20. Redder JD, Leth RA, Møller JK. Incidence rates of hospital-acquired urinary tract and bloodstream infections generated by automated compilation of electronically available healthcare data. J Hosp Infect. 2015;91:231-236.
21. Ortega M, Marco F, Soriano A, et al. Epidemiology and prognostic determinants of bacteraemic catheter-acquired urinary tract infection in a single institution from 1991 to 2010. J Infect. 2013;67:282-287.
22. Tambyah PA, Maki DG. The relationship between pyuria and infection in patients with indwelling urinary catheters: a prospective study of 761 patients. Arch Intern Med. 2000;160:673-677.
23. Musher DM, Thorsteinsson SB, Airola VM, II. Quantitative urinalysis:diagnosing urinary tract infection in men. JAMA. 1976;236:2069-2072.
24. Hausegger KA, Portugaller HR. Percutaneous nephrostomy and antegrade ureteral stenting: technique-indications-complications. Eur Radiol. 2006;16:2016-2030.
25. Lange D, Bidnur S, Hoag N, et al. Ureteral stent-associated complications--where we are and where we are going. Nat Rev Urol. 2015;12:17-25.
26. el-Faqih SR, Shamsuddin AB, Chakrabarti A, et al. Polyurethane internal ureteral stents in treatment of stone patients: morbidity related to indwelling times. J Urol. 1991;146:1487-1491.
27. Adamo R, Saad WE, Brown DB. Management of nephrostomy drains and ureteral stents. Tech Vasc Interv Radiol. 2009;12:193-204.
28. Joshi HB, Newns N, Stainthorpe A, et al. Ureteral Stent Symptom Questionnaire: development and validation of a multidimensional quality of life measure. J Urol. 2003;169:1060-1064.
29. Singh I, Gupta NP, Hemal AK, et al. Severely encrusted polyurethane ureteral stents: management and analysis of potential risk factors. Urology. 2001;58:526-531.
30. Saint S, Chenoweth CE. Biofilms and catheter-associated urinary tract infections. Infect Dis Clin North Am. 2003;17:411-432.
31. Mobley HL, Warren JW. Urease-positive bacteriuria and obstruction of long-term urinary catheters. J Clin Microbiol. 1987;25:2216-2217.
32. Kehinde EO, Rotimi VO, Al-Hunayan A, et al. Bacteriology of urinary tract infection associated with indwelling J ureteral stents. J Endourol. 2004;18:891-896.
33. Paick SH, Park HK, Oh SJ, Kim HH. Characteristics of bacterial colonization and urinary tract infection after indwelling of double-J ureteral stent. Urology. 2003;62:214-217.
34. Klis R, Korczak-Kozakiewicz E, Denys A, et al. Relationship between urinary tract infection and self-retaining double-J catheter colonization. J Endourol. 2009;23:1015-1019.
35. Farsi HM, Mosli HA, Al-Zemaity M, et al. Bacteriuria and colonization of double-pigtail ureteral stents: long-term experience with 237 patients. J Endourol. 1995;9:469-472.
36. Wolfe JS Jr, Bennet CJ, Dmochowski RR, et al. Best practice policy statement on urologic surgery antimicrobial prophylaxis. J Urol. 2008;179:1379-1390.
37. Bahu R, Chaftari AM, Hachem RY, et al. Nephrostomy tube related pyelonephritis in patients with cancer: epidemiology, infection rate and risk factors. J Urol. 2013;189:130-135.
38. Bratzler DW, Dellinger EP, Olsen KM, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Surg Infect (Larchmt). 2013;14:73-156.
39. Cronan JJ, Horn DL, Marcello A, et al: Antibiotics and nephrostomy tube care: preliminary observations. Part II. Bacteremia. Radiology. 1989;172(3 Pt 2):1043-1045.
40. Akay AF, Aflay U, Gedik A, et al. Risk factors for lower urinary tract infection and bacterial stent colonization in patients with a double J ureteral stent. Int Urol Nephrol. 2007;39:95-98.
41. Meddings J, Saint S, Fowler KE, et al. The Ann Arbor criteria for appropriate urinary catheter use in hospitalized medical patients: results obtained by using the RAND/ UCLA appropriateness method. Ann Intern Med. 2015;162(9 Suppl):S1-34.
42. Stickler D, Young R, Jones G, et al. Why are Foley catheters so vulnerable to encrustation and blockage by crystalline bacterial biofilm? Urol Res. 2003;31:306-311.
43. Denstedt J, Wollin T, Reid G. Biomaterials used in urology: current issues of biocompatibility, infection, and encrustation. J Endourol. 1998;12:493-500.
44. Morris N, Stickler D, Winters C. Which indwelling urethral catheters resist encrustation by Proteus mirabilis biofilms? Br J Urol. 1997;80:58-63.
45. Cardenas D, Moore K, Dannels-McClure A, et al. Intermittent catheterization with a hydrophilic-coated catheter delays urinary tract infections in acute spinal cord injury: a prospective, randomized, multicenter trial. PMR. 2011;3:408-417.
46. Spinu A, Onose G, Daia C, et al. Intermittent catheterization in the management of post spinal cord injury (SCI) neurogenic bladder using new hydrophilic, with lubrication in close circuit devices-our own preliminary results. J Med Life. 2012;5:21-28.
47. Shekelle P, Morton S, Clark K, et al. Systematic review of risk factors for urinary tract infection in adults with spinal cord dysfunction. J Spinal Cord Med. 1998;22:258-272.
48. Siddiq D, Darouiche R. New strategies to prevent catheter-associated urinary tract infections. Nat Rev Urol. 2012;9:305-314.
49. Gould C, Umscheid C, Agarwal R, et al. Guideline for prevention of catheter-associated urinary tract infections 2009. Infect Control Hosp Epidemiol. 2010;31:319-326.
50. Maki D, Tambyah P. Engineering out the risk for infection with urinary catheters. Emerg Infect Dis. 2001;7:342-347.
51. Munasinghe R, Yazdani H, Siddique M, et al. Appropriateness of use of indwelling urinary catheters in patients admitted to the medical service. Infect Control Hosp Epidemiol. 2001;22:647-649.
52. Nicolle L, Bradley S, Colgan R, et al; Infectious Diseases Society of America; American Society of Nephrology; American Geriatric Society. Infectious Diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clin Infect Dis. 2005;40: 643-654.
53. Linsenmeyer T, Oakley A. Accuracy of individuals with spinal cord injury at predicting urinary tract infections based on their symptoms. J Spinal Cord Med. 2002;26:352-357.
54. Abbo LM, Hooton TM. Antimicrobial stewardship and urinary tract infections. Antibiotics. 2014;3:174-192.
55. Kauffman CA. Diagnosis and management of fungal urinary tract infection. Infect Dis Clin North Am. 2014;28:61-74.
56. Alvarez-Lerma F, Nolla-Salas J, Leon C, et al. Candiduria in critically ill patients admitted to intensive care medical units. Intensive Care Med. 2003;29:1069-1076.
57. Colodner R, Nuri Y, Chazan B, et al. Community-acquired and hospital-acquired candiduria: comparison of prevalence and clinical characteristics. Eur J Clin Microbiol Infect Dis. 2008;27:301-305.
58. Kauffman CA, Vazquez JA, Sobel JD, et al. Prospective multicenter surveillance study of funguria in hospitalized patients. Clin Infect Dis. 2000;30:14-18.
59. Sobel JD, Fisher JF, Kauffman CA, et al. Candida urinary tract infections—epidemiology. Clin Infect Dis. 2011;52(suppl 6): S433-436.
60. Richards MJ, Edwards JR, Culver DH, et al. Nosocomial infections in combined medical-surgical intensive care units in the United States. Infect Control Hosp Epidemiol. 2000;21:510-515.
61. Fisher JF, Sobel JD, Kauffman CA, et al. Candida urinary tract infections—treatment. Clin Infect Dis. 2011;52(suppl 6):S457-466.
62. Blumberg HM, Jarvis WR, Soucie JM, et al. Risk factors for candidal bloodstream infections in surgical intensive care unit patients: the NEMIS prospective multicenter study. Clin Infect Dis. 2001;33:177-186.
63. Puzniak LP, Teutsch S, Powderly W, et al. Has the epidemiology of nosocomial candidemia changed? Infect Control Hosp Epidemiol. 2004;25:628-633.
64. Siddique MS, Gayed N, McGuire N, et al. Salient features of Candida pyelonephritis in adults. Infect Dis Clin Pract. 1992;1:239-245
65. Pappas PG, Kauffman CA, Andes DR, et al. Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;62:e1-e50.
66. Sobel JD, Bradshaw SK, Lipka CJ, et al. Caspofungin in the treatment of symptomatic candiduria. Clin Infect Dis. 2007;44:e46-9.
67. Malani AN. Failure of caspofungin for treatment of Candida glabrata candiduria. Case report and review of the literature. Infect Dis Clin Pract. 2010;18:271-272.
68. Schelenz S, Ross CN. Limitations of caspofugin in the treatment of obstructive pyelonephrosis due to Candida glabrata infection. BMC Infect Dis. 2006;56:126-130.
69. Chung BH, Chang SY, Kim SI, et al. Successfully treated renal fungal ball with continuous irrigation of fluconazole. J Urol. 2001;166:1835-1836.
H. pylori antibiotic resistance reaches ‘alarming levels’
Over the past decade, Helicobacter pylori strains have reached “alarming levels” of antimicrobial resistance worldwide, investigators reported in the November issue of Gastroenterology.
In a large meta-analysis spanning 2007-2017, H. pylori isolates showed a 15% or higher pooled prevalence of primary and secondary resistance to clarithromycin, metronidazole, and levofloxacin in almost all World Health Organization (WHO) regions. “Local surveillance networks are required to select appropriate eradication regimens for each region,” concluded Alessia Savoldi, MD, of the University of Tübingen (Germany) and her associates.
Typically, the threshold of antimicrobial resistance for choosing empiric regimens is 15%, Dr. Savoldi and her associates noted. Their systematic review and meta-analysis included 178 studies comprising 66,142 isolates from 65 countries. They defined H. pylori infection as a positive histology, serology, stool antigen, urea breath test, or rapid urease test. They excluded studies of fewer than 50 isolates, studies that only reported resistance as a percentage with no denominator, studies that failed to specify time frames or clustered data over more than 3 years, and data reported in guidelines, conference presentations, or letters without formal publication.
The prevalence of primary clarithromycin resistance exceeded 15% in the WHO European Region (18%; 95% confidence interval, 16%-20%), the Eastern Mediterranean Region (33%), and the Western Pacific Region (34%) and reached 10% in the Americas and the South East Asia region. Furthermore, primary resistance to metronidazole exceeded 15% in all WHO regions, ranging from 56% in the Eastern Mediterranean Region to 23% in the Americas. Resistance to levofloxacin was at least 15% in all WHO regions except the European region (11%).
In most regions, H. pylori also accrued substantially more antimicrobial resistance over time, the investigators said. Clarithromycin resistance rose from 13% during 2006 through 2008 to 21% during 2012 through 2016 (P less than .001). Levofloxacin resistance in the Western Pacific region increased from 12% to 31% during the same two time periods (P less than .001). Several other WHO regions showed less significant trends toward increasing resistance. Multidrug resistance also rose. Resistance to both clarithromycin and metronidazole increased markedly in all WHO areas with available data, reaching 14% in the Eastern Mediterranean and Western Pacific regions and 23% in the European region.
Secondary analyses linked resistance with dramatic increases in the odds of treatment failure. For example, clarithromycin resistance conferred a sevenfold increase in the odds of treatment failure for regimens containing clarithromycin (odds ratio, 7.0; 95% CI, 5.2 to 9.3; P less than .001). Corresponding ORs were 8.2 for levofloxacin resistance, 2.5 for metronidazole resistance, and 9.4 for dual clarithromycin-metronidazole resistance.
The investigators acknowledged several limitations. Of publications in this meta-analysis, 85% represented single-center studies with limited sample sizes, they wrote. Studies often excluded demographic and endoscopic details. Furthermore, only three studies provided prevalence data for the WHO Africa Region and these only provided overall estimates without stratifying by resistance type.
The German Center for Infection Research, Clinical Research Unit, and the WHO Priority List Pathogens project helped fund the work. One coinvestigator disclosed ties to RedHill Biopharma, BioGaia, and Takeda related to novel H. pylori therapies.
SOURCE: Savoldi A et al. Gastroenterology. 2018 Nov. doi: 10.1053/j.gastro.2018.07.007.
The first-line treatment of individuals with Helicobacter pylori infection using clarithromycin-based triple therapies or, if penicillin allergic, bismuth-based quadruple therapies is generally effective. However, reports of declining therapeutic efficacy have led to published guidelines to recommend confirmation of H. pylori eradication after completing a course of antibiotics. It is believed that increasing antibiotic use in agriculture and medicine around the globe have contributed to the increasing H. pylori antibiotic resistance and declining efficacy of standard H. pylori regimens.
Indeed, most H. pylori guidelines recommend antibiotic sensitivity testing after failing two courses of treatment; however, performing such testing successfully may require sending fresh gastric biopsy samples to an in-house H. pylori culture lab within 1 hour, which is generally not available to most clinicians. Clearly, the gap in knowledge of local antibiotic resistance could be addressed by having a readily accessible culture facility and the testing should be reimbursed by health insurance.
Single-center experiences with antibiotic sensitivity–guided salvage therapy in the United States, however, registered a lower efficacy rate of approximately 50%, which indicates that other host factors (such as gastric acidity pH less than 5.5 or body mass index greater than 30 kg/m2) may affect the minimum inhibitory concentration (MIC) of the antibiotics against H. pylori.
In order to better study the effects of these host factors relative to the effect of antibiotic resistance on therapeutic efficacy, it is critical that we practice precision medicine by determining the antibiotic sensitivity of the H. pylori strain prior to initiating the antibiotic treatment. It may be possible to achieve more than 90% therapeutic efficacy given known antibiotic sensitivities of the bacteria and optimized host factors to lower the MIC. In addition, with the increasing awareness of the importance of gut microbiota in health and disease, clinicians should strive to narrow the antibiotic coverage that will be possible if antibiotic sensitivity is known (for example, use high-dose amoxicillin and proton-pump inhibitor dual therapy).
John Y. Kao, MD, AGAF, is the current chair of the AGA Institute Council Esophageal, Gastric and Duodenal Disorders Section, a physician investigator in the University of Michigan Center for Gastrointestinal Research, and an associate professor in the department of medicine in the division of gastroenterology & hepatology and an associate program director of the GI Fellowship Program at Michigan Medicine at the University of Michigan, Ann Arbor. He has no conflicts.
The first-line treatment of individuals with Helicobacter pylori infection using clarithromycin-based triple therapies or, if penicillin allergic, bismuth-based quadruple therapies is generally effective. However, reports of declining therapeutic efficacy have led to published guidelines to recommend confirmation of H. pylori eradication after completing a course of antibiotics. It is believed that increasing antibiotic use in agriculture and medicine around the globe have contributed to the increasing H. pylori antibiotic resistance and declining efficacy of standard H. pylori regimens.
Indeed, most H. pylori guidelines recommend antibiotic sensitivity testing after failing two courses of treatment; however, performing such testing successfully may require sending fresh gastric biopsy samples to an in-house H. pylori culture lab within 1 hour, which is generally not available to most clinicians. Clearly, the gap in knowledge of local antibiotic resistance could be addressed by having a readily accessible culture facility and the testing should be reimbursed by health insurance.
Single-center experiences with antibiotic sensitivity–guided salvage therapy in the United States, however, registered a lower efficacy rate of approximately 50%, which indicates that other host factors (such as gastric acidity pH less than 5.5 or body mass index greater than 30 kg/m2) may affect the minimum inhibitory concentration (MIC) of the antibiotics against H. pylori.
In order to better study the effects of these host factors relative to the effect of antibiotic resistance on therapeutic efficacy, it is critical that we practice precision medicine by determining the antibiotic sensitivity of the H. pylori strain prior to initiating the antibiotic treatment. It may be possible to achieve more than 90% therapeutic efficacy given known antibiotic sensitivities of the bacteria and optimized host factors to lower the MIC. In addition, with the increasing awareness of the importance of gut microbiota in health and disease, clinicians should strive to narrow the antibiotic coverage that will be possible if antibiotic sensitivity is known (for example, use high-dose amoxicillin and proton-pump inhibitor dual therapy).
John Y. Kao, MD, AGAF, is the current chair of the AGA Institute Council Esophageal, Gastric and Duodenal Disorders Section, a physician investigator in the University of Michigan Center for Gastrointestinal Research, and an associate professor in the department of medicine in the division of gastroenterology & hepatology and an associate program director of the GI Fellowship Program at Michigan Medicine at the University of Michigan, Ann Arbor. He has no conflicts.
The first-line treatment of individuals with Helicobacter pylori infection using clarithromycin-based triple therapies or, if penicillin allergic, bismuth-based quadruple therapies is generally effective. However, reports of declining therapeutic efficacy have led to published guidelines to recommend confirmation of H. pylori eradication after completing a course of antibiotics. It is believed that increasing antibiotic use in agriculture and medicine around the globe have contributed to the increasing H. pylori antibiotic resistance and declining efficacy of standard H. pylori regimens.
Indeed, most H. pylori guidelines recommend antibiotic sensitivity testing after failing two courses of treatment; however, performing such testing successfully may require sending fresh gastric biopsy samples to an in-house H. pylori culture lab within 1 hour, which is generally not available to most clinicians. Clearly, the gap in knowledge of local antibiotic resistance could be addressed by having a readily accessible culture facility and the testing should be reimbursed by health insurance.
Single-center experiences with antibiotic sensitivity–guided salvage therapy in the United States, however, registered a lower efficacy rate of approximately 50%, which indicates that other host factors (such as gastric acidity pH less than 5.5 or body mass index greater than 30 kg/m2) may affect the minimum inhibitory concentration (MIC) of the antibiotics against H. pylori.
In order to better study the effects of these host factors relative to the effect of antibiotic resistance on therapeutic efficacy, it is critical that we practice precision medicine by determining the antibiotic sensitivity of the H. pylori strain prior to initiating the antibiotic treatment. It may be possible to achieve more than 90% therapeutic efficacy given known antibiotic sensitivities of the bacteria and optimized host factors to lower the MIC. In addition, with the increasing awareness of the importance of gut microbiota in health and disease, clinicians should strive to narrow the antibiotic coverage that will be possible if antibiotic sensitivity is known (for example, use high-dose amoxicillin and proton-pump inhibitor dual therapy).
John Y. Kao, MD, AGAF, is the current chair of the AGA Institute Council Esophageal, Gastric and Duodenal Disorders Section, a physician investigator in the University of Michigan Center for Gastrointestinal Research, and an associate professor in the department of medicine in the division of gastroenterology & hepatology and an associate program director of the GI Fellowship Program at Michigan Medicine at the University of Michigan, Ann Arbor. He has no conflicts.
Over the past decade, Helicobacter pylori strains have reached “alarming levels” of antimicrobial resistance worldwide, investigators reported in the November issue of Gastroenterology.
In a large meta-analysis spanning 2007-2017, H. pylori isolates showed a 15% or higher pooled prevalence of primary and secondary resistance to clarithromycin, metronidazole, and levofloxacin in almost all World Health Organization (WHO) regions. “Local surveillance networks are required to select appropriate eradication regimens for each region,” concluded Alessia Savoldi, MD, of the University of Tübingen (Germany) and her associates.
Typically, the threshold of antimicrobial resistance for choosing empiric regimens is 15%, Dr. Savoldi and her associates noted. Their systematic review and meta-analysis included 178 studies comprising 66,142 isolates from 65 countries. They defined H. pylori infection as a positive histology, serology, stool antigen, urea breath test, or rapid urease test. They excluded studies of fewer than 50 isolates, studies that only reported resistance as a percentage with no denominator, studies that failed to specify time frames or clustered data over more than 3 years, and data reported in guidelines, conference presentations, or letters without formal publication.
The prevalence of primary clarithromycin resistance exceeded 15% in the WHO European Region (18%; 95% confidence interval, 16%-20%), the Eastern Mediterranean Region (33%), and the Western Pacific Region (34%) and reached 10% in the Americas and the South East Asia region. Furthermore, primary resistance to metronidazole exceeded 15% in all WHO regions, ranging from 56% in the Eastern Mediterranean Region to 23% in the Americas. Resistance to levofloxacin was at least 15% in all WHO regions except the European region (11%).
In most regions, H. pylori also accrued substantially more antimicrobial resistance over time, the investigators said. Clarithromycin resistance rose from 13% during 2006 through 2008 to 21% during 2012 through 2016 (P less than .001). Levofloxacin resistance in the Western Pacific region increased from 12% to 31% during the same two time periods (P less than .001). Several other WHO regions showed less significant trends toward increasing resistance. Multidrug resistance also rose. Resistance to both clarithromycin and metronidazole increased markedly in all WHO areas with available data, reaching 14% in the Eastern Mediterranean and Western Pacific regions and 23% in the European region.
Secondary analyses linked resistance with dramatic increases in the odds of treatment failure. For example, clarithromycin resistance conferred a sevenfold increase in the odds of treatment failure for regimens containing clarithromycin (odds ratio, 7.0; 95% CI, 5.2 to 9.3; P less than .001). Corresponding ORs were 8.2 for levofloxacin resistance, 2.5 for metronidazole resistance, and 9.4 for dual clarithromycin-metronidazole resistance.
The investigators acknowledged several limitations. Of publications in this meta-analysis, 85% represented single-center studies with limited sample sizes, they wrote. Studies often excluded demographic and endoscopic details. Furthermore, only three studies provided prevalence data for the WHO Africa Region and these only provided overall estimates without stratifying by resistance type.
The German Center for Infection Research, Clinical Research Unit, and the WHO Priority List Pathogens project helped fund the work. One coinvestigator disclosed ties to RedHill Biopharma, BioGaia, and Takeda related to novel H. pylori therapies.
SOURCE: Savoldi A et al. Gastroenterology. 2018 Nov. doi: 10.1053/j.gastro.2018.07.007.
Over the past decade, Helicobacter pylori strains have reached “alarming levels” of antimicrobial resistance worldwide, investigators reported in the November issue of Gastroenterology.
In a large meta-analysis spanning 2007-2017, H. pylori isolates showed a 15% or higher pooled prevalence of primary and secondary resistance to clarithromycin, metronidazole, and levofloxacin in almost all World Health Organization (WHO) regions. “Local surveillance networks are required to select appropriate eradication regimens for each region,” concluded Alessia Savoldi, MD, of the University of Tübingen (Germany) and her associates.
Typically, the threshold of antimicrobial resistance for choosing empiric regimens is 15%, Dr. Savoldi and her associates noted. Their systematic review and meta-analysis included 178 studies comprising 66,142 isolates from 65 countries. They defined H. pylori infection as a positive histology, serology, stool antigen, urea breath test, or rapid urease test. They excluded studies of fewer than 50 isolates, studies that only reported resistance as a percentage with no denominator, studies that failed to specify time frames or clustered data over more than 3 years, and data reported in guidelines, conference presentations, or letters without formal publication.
The prevalence of primary clarithromycin resistance exceeded 15% in the WHO European Region (18%; 95% confidence interval, 16%-20%), the Eastern Mediterranean Region (33%), and the Western Pacific Region (34%) and reached 10% in the Americas and the South East Asia region. Furthermore, primary resistance to metronidazole exceeded 15% in all WHO regions, ranging from 56% in the Eastern Mediterranean Region to 23% in the Americas. Resistance to levofloxacin was at least 15% in all WHO regions except the European region (11%).
In most regions, H. pylori also accrued substantially more antimicrobial resistance over time, the investigators said. Clarithromycin resistance rose from 13% during 2006 through 2008 to 21% during 2012 through 2016 (P less than .001). Levofloxacin resistance in the Western Pacific region increased from 12% to 31% during the same two time periods (P less than .001). Several other WHO regions showed less significant trends toward increasing resistance. Multidrug resistance also rose. Resistance to both clarithromycin and metronidazole increased markedly in all WHO areas with available data, reaching 14% in the Eastern Mediterranean and Western Pacific regions and 23% in the European region.
Secondary analyses linked resistance with dramatic increases in the odds of treatment failure. For example, clarithromycin resistance conferred a sevenfold increase in the odds of treatment failure for regimens containing clarithromycin (odds ratio, 7.0; 95% CI, 5.2 to 9.3; P less than .001). Corresponding ORs were 8.2 for levofloxacin resistance, 2.5 for metronidazole resistance, and 9.4 for dual clarithromycin-metronidazole resistance.
The investigators acknowledged several limitations. Of publications in this meta-analysis, 85% represented single-center studies with limited sample sizes, they wrote. Studies often excluded demographic and endoscopic details. Furthermore, only three studies provided prevalence data for the WHO Africa Region and these only provided overall estimates without stratifying by resistance type.
The German Center for Infection Research, Clinical Research Unit, and the WHO Priority List Pathogens project helped fund the work. One coinvestigator disclosed ties to RedHill Biopharma, BioGaia, and Takeda related to novel H. pylori therapies.
SOURCE: Savoldi A et al. Gastroenterology. 2018 Nov. doi: 10.1053/j.gastro.2018.07.007.
FROM GASTROENTEROLOGY
Key clinical point: Helicobacter pylori now shows significant levels of antibiotic resistance worldwide, complicating choices of empiric therapy.
Major finding: Primary and secondary resistance to clarithromycin, metronidazole, and levofloxacin was 15% or more in all WHO regions except for primary clarithromycin resistance in the Americas (10%) and South East Asia (10%) and primary levofloxacin resistance in Europe (11%).
Study details: Meta-analysis of 178 studies comprising 66,142 isolates from 65 countries.
Disclosures: The German Center for Infection Research, Clinical Research Unit, and the WHO Priority List Pathogens project helped fund the work. One coinvestigator disclosed ties to RedHill Biopharma, BioGaia, and Takeda related to novel H. pylori therapies.
Source: Savoldi A et al. Gastroenterology. 2018 Nov. doi: 10.1053/j.gastro.2018.07.007
Thiopurines linked to zoster in IBD patients
For patients with inflammatory bowel disease (IBD), thiopurine exposure was associated with a significantly increased risk of herpes zoster, compared with 5-aminosalicylic acid (5-ASA) monotherapy, according to the results of two large retrospective cohort studies.
In the multivariable analysis, thiopurine monotherapy was linked to about a 47% increase in the risk of herpes zoster, compared with 5-ASA monotherapy (adjusted hazard ratio, 1.47; 95% confidence interval, 1.31-1.65; P less than .001). Combination therapy with thiopurines and tumor necrosis factor antagonists conferred about a 65% increase in zoster risk (aHR, 1.65; 95% CI, 1.22-2.23; P = .001). However, tumor necrosis factor–antagonist monotherapy did not appear to significantly increase the risk of zoster when compared with 5-ASA monotherapy, reported Nabeel Khan, MD, of the University of Pennsylvania in Philadelphia, and his associates.
“Compared to [patients without] IBD, ulcerative colitis (UC) and Crohn’s disease (CD) each were associated with significantly increased risk of herpes zoster infection,” the researchers wrote online in Clinical Gastroenterology and Hepatology. “With the approval of a new and potentially safer vaccine for herpes zoster, the effects of immunization of patients with IBD should be investigated.”
Past studies have linked IBD with a 1.2- to 1.8-fold increase in the risk of zoster, but these studies date to the prebiologic era or excluded patients who were in their midsixties or older, the researchers wrote. “Additionally, these prior studies have not assessed the validity of the codes used to identify herpes zoster and also did not account for the impact of vaccination,” they added. “They also did not take into consideration the severity of the disease or degree of steroid exposure.”
Therefore, the researchers conducted two retrospective cohort studies of patients in the United States Department of Veterans Affairs between 2000 and 2016. The first cohort study compared the incidence of herpes zoster among patients with IBD who received 5-ASA alone with matched patients without IBD. The second cohort study measured the incidence of herpes zoster in patients with IBD who received various medications and combination regimen. “The VA has a predominantly older population, which makes it an ideal cohort to study herpes zoster incidence in a high-risk population,” the investigators noted. “Unlike insurance databases, the VA database can be validated internally and vaccination records are documented.”
After adjusting for age, race, sex, geographic region, disease flare, corticosteroid use, and baseline comorbidities, the estimated hazard of developing herpes zoster was 1.81 (95% confidence interval, 1.56-2.11) among patients with ulcerative colitis and 1.56 (95% CI, 1.28-1.91) among patients with Crohn’s disease, as compared with patients without IBD. Regardless of their age or the medications they were receiving, patients with IBD had a higher incidence of zoster than the oldest group of patients without IBD (older than 60 years), regardless of age or medication. “The highest risk of herpes zoster was observed in patients with IBD who were less than 60 years of age and on combination therapy,” the investigators wrote. “Patients with IBD younger than 50 years who were on combination therapy had higher risk of herpes zoster, compared with patients with IBD older than 60 years of age who were not on immunosuppressive therapy.” Based on the findings, they recommended studying the efficacy of widespread use of the new herpes zoster vaccine in patients with IBD.
Pfizer provided unrestricted research funding but was not otherwise involved in the study. One coinvestigator disclosed ties to Pfizer and several other pharmaceutical companies. The remaining investigators reported having no conflicts of interest.
SOURCE: Khan N et al. Clin Gastroenterol Hepatol. 2018 Jan 5. doi: 10.1016/j.cgh.2017.12.052.
Patients with inflammatory bowel disease are thought to have altered immune regulation, which may increase the risk of systemic complications including infections like herpes zoster. Many of the prior studies assessing the risk of herpes zoster in IBD patients were done before the advent of biologics and excluded older patients, thereby limiting their utility. This study by Khan et al. aimed to better estimate the incidence and risk factors for development of herpes zoster and to determine the effect of immunosuppressant use on this risk. In two large, retrospective cohort studies they found that, compared with patients without IBD, patients with IBD had a significantly increased risk of developing herpes zoster. Furthermore, this risk was higher in those with recent or cumulative steroid use and in those treated with thiopurines (as monotherapy or in combination with anti-TNF agents). Interestingly, exposure to TNF antagonists alone was not associated with an increased risk of herpes zoster infection.
Richa Shukla, MD, assistant professor, section of gastroenterology and hepatology, Baylor College of Medicine, Houston.
Patients with inflammatory bowel disease are thought to have altered immune regulation, which may increase the risk of systemic complications including infections like herpes zoster. Many of the prior studies assessing the risk of herpes zoster in IBD patients were done before the advent of biologics and excluded older patients, thereby limiting their utility. This study by Khan et al. aimed to better estimate the incidence and risk factors for development of herpes zoster and to determine the effect of immunosuppressant use on this risk. In two large, retrospective cohort studies they found that, compared with patients without IBD, patients with IBD had a significantly increased risk of developing herpes zoster. Furthermore, this risk was higher in those with recent or cumulative steroid use and in those treated with thiopurines (as monotherapy or in combination with anti-TNF agents). Interestingly, exposure to TNF antagonists alone was not associated with an increased risk of herpes zoster infection.
Richa Shukla, MD, assistant professor, section of gastroenterology and hepatology, Baylor College of Medicine, Houston.
Patients with inflammatory bowel disease are thought to have altered immune regulation, which may increase the risk of systemic complications including infections like herpes zoster. Many of the prior studies assessing the risk of herpes zoster in IBD patients were done before the advent of biologics and excluded older patients, thereby limiting their utility. This study by Khan et al. aimed to better estimate the incidence and risk factors for development of herpes zoster and to determine the effect of immunosuppressant use on this risk. In two large, retrospective cohort studies they found that, compared with patients without IBD, patients with IBD had a significantly increased risk of developing herpes zoster. Furthermore, this risk was higher in those with recent or cumulative steroid use and in those treated with thiopurines (as monotherapy or in combination with anti-TNF agents). Interestingly, exposure to TNF antagonists alone was not associated with an increased risk of herpes zoster infection.
Richa Shukla, MD, assistant professor, section of gastroenterology and hepatology, Baylor College of Medicine, Houston.
For patients with inflammatory bowel disease (IBD), thiopurine exposure was associated with a significantly increased risk of herpes zoster, compared with 5-aminosalicylic acid (5-ASA) monotherapy, according to the results of two large retrospective cohort studies.
In the multivariable analysis, thiopurine monotherapy was linked to about a 47% increase in the risk of herpes zoster, compared with 5-ASA monotherapy (adjusted hazard ratio, 1.47; 95% confidence interval, 1.31-1.65; P less than .001). Combination therapy with thiopurines and tumor necrosis factor antagonists conferred about a 65% increase in zoster risk (aHR, 1.65; 95% CI, 1.22-2.23; P = .001). However, tumor necrosis factor–antagonist monotherapy did not appear to significantly increase the risk of zoster when compared with 5-ASA monotherapy, reported Nabeel Khan, MD, of the University of Pennsylvania in Philadelphia, and his associates.
“Compared to [patients without] IBD, ulcerative colitis (UC) and Crohn’s disease (CD) each were associated with significantly increased risk of herpes zoster infection,” the researchers wrote online in Clinical Gastroenterology and Hepatology. “With the approval of a new and potentially safer vaccine for herpes zoster, the effects of immunization of patients with IBD should be investigated.”
Past studies have linked IBD with a 1.2- to 1.8-fold increase in the risk of zoster, but these studies date to the prebiologic era or excluded patients who were in their midsixties or older, the researchers wrote. “Additionally, these prior studies have not assessed the validity of the codes used to identify herpes zoster and also did not account for the impact of vaccination,” they added. “They also did not take into consideration the severity of the disease or degree of steroid exposure.”
Therefore, the researchers conducted two retrospective cohort studies of patients in the United States Department of Veterans Affairs between 2000 and 2016. The first cohort study compared the incidence of herpes zoster among patients with IBD who received 5-ASA alone with matched patients without IBD. The second cohort study measured the incidence of herpes zoster in patients with IBD who received various medications and combination regimen. “The VA has a predominantly older population, which makes it an ideal cohort to study herpes zoster incidence in a high-risk population,” the investigators noted. “Unlike insurance databases, the VA database can be validated internally and vaccination records are documented.”
After adjusting for age, race, sex, geographic region, disease flare, corticosteroid use, and baseline comorbidities, the estimated hazard of developing herpes zoster was 1.81 (95% confidence interval, 1.56-2.11) among patients with ulcerative colitis and 1.56 (95% CI, 1.28-1.91) among patients with Crohn’s disease, as compared with patients without IBD. Regardless of their age or the medications they were receiving, patients with IBD had a higher incidence of zoster than the oldest group of patients without IBD (older than 60 years), regardless of age or medication. “The highest risk of herpes zoster was observed in patients with IBD who were less than 60 years of age and on combination therapy,” the investigators wrote. “Patients with IBD younger than 50 years who were on combination therapy had higher risk of herpes zoster, compared with patients with IBD older than 60 years of age who were not on immunosuppressive therapy.” Based on the findings, they recommended studying the efficacy of widespread use of the new herpes zoster vaccine in patients with IBD.
Pfizer provided unrestricted research funding but was not otherwise involved in the study. One coinvestigator disclosed ties to Pfizer and several other pharmaceutical companies. The remaining investigators reported having no conflicts of interest.
SOURCE: Khan N et al. Clin Gastroenterol Hepatol. 2018 Jan 5. doi: 10.1016/j.cgh.2017.12.052.
For patients with inflammatory bowel disease (IBD), thiopurine exposure was associated with a significantly increased risk of herpes zoster, compared with 5-aminosalicylic acid (5-ASA) monotherapy, according to the results of two large retrospective cohort studies.
In the multivariable analysis, thiopurine monotherapy was linked to about a 47% increase in the risk of herpes zoster, compared with 5-ASA monotherapy (adjusted hazard ratio, 1.47; 95% confidence interval, 1.31-1.65; P less than .001). Combination therapy with thiopurines and tumor necrosis factor antagonists conferred about a 65% increase in zoster risk (aHR, 1.65; 95% CI, 1.22-2.23; P = .001). However, tumor necrosis factor–antagonist monotherapy did not appear to significantly increase the risk of zoster when compared with 5-ASA monotherapy, reported Nabeel Khan, MD, of the University of Pennsylvania in Philadelphia, and his associates.
“Compared to [patients without] IBD, ulcerative colitis (UC) and Crohn’s disease (CD) each were associated with significantly increased risk of herpes zoster infection,” the researchers wrote online in Clinical Gastroenterology and Hepatology. “With the approval of a new and potentially safer vaccine for herpes zoster, the effects of immunization of patients with IBD should be investigated.”
Past studies have linked IBD with a 1.2- to 1.8-fold increase in the risk of zoster, but these studies date to the prebiologic era or excluded patients who were in their midsixties or older, the researchers wrote. “Additionally, these prior studies have not assessed the validity of the codes used to identify herpes zoster and also did not account for the impact of vaccination,” they added. “They also did not take into consideration the severity of the disease or degree of steroid exposure.”
Therefore, the researchers conducted two retrospective cohort studies of patients in the United States Department of Veterans Affairs between 2000 and 2016. The first cohort study compared the incidence of herpes zoster among patients with IBD who received 5-ASA alone with matched patients without IBD. The second cohort study measured the incidence of herpes zoster in patients with IBD who received various medications and combination regimen. “The VA has a predominantly older population, which makes it an ideal cohort to study herpes zoster incidence in a high-risk population,” the investigators noted. “Unlike insurance databases, the VA database can be validated internally and vaccination records are documented.”
After adjusting for age, race, sex, geographic region, disease flare, corticosteroid use, and baseline comorbidities, the estimated hazard of developing herpes zoster was 1.81 (95% confidence interval, 1.56-2.11) among patients with ulcerative colitis and 1.56 (95% CI, 1.28-1.91) among patients with Crohn’s disease, as compared with patients without IBD. Regardless of their age or the medications they were receiving, patients with IBD had a higher incidence of zoster than the oldest group of patients without IBD (older than 60 years), regardless of age or medication. “The highest risk of herpes zoster was observed in patients with IBD who were less than 60 years of age and on combination therapy,” the investigators wrote. “Patients with IBD younger than 50 years who were on combination therapy had higher risk of herpes zoster, compared with patients with IBD older than 60 years of age who were not on immunosuppressive therapy.” Based on the findings, they recommended studying the efficacy of widespread use of the new herpes zoster vaccine in patients with IBD.
Pfizer provided unrestricted research funding but was not otherwise involved in the study. One coinvestigator disclosed ties to Pfizer and several other pharmaceutical companies. The remaining investigators reported having no conflicts of interest.
SOURCE: Khan N et al. Clin Gastroenterol Hepatol. 2018 Jan 5. doi: 10.1016/j.cgh.2017.12.052.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: For patients with inflammatory bowel disease, thiopurine exposure was associated with a significantly increased risk of herpes zoster, compared with 5-aminosalicylic acid monotherapy.
Major finding: The adjusted hazard ratio was 1.47 (95% confidence interval, 1.31-1.65; P less than .001).
Study details: Two large retrospective cohort studies of veterans with and without inflammatory bowel disease.
Disclosures: Pfizer provided unrestricted research funding but was not otherwise involved in the study. One coinvestigator disclosed ties to Pfizer and several other pharmaceutical companies. The remaining investigators reported having no conflicts of interest.
Source: Khan N et al. Clin Gastroenterol Hepatol. 2018 Jan 5. doi: 10.1016/j.cgh.2017.12.052.
Hemorrhagic Crusted Papule on the Arm
The Diagnosis: Self-healing Langerhans Cell Histiocytosis
Histopathologic examination showed an infiltrate of mononuclear cells with indented nuclei admixed with a variable dermal inflammatory infiltrate. Immunohistochemistry demonstrated cells that were strongly positive for CD1a (Figure, A) and langerin (Figure, B) antigens as well as S-100 protein (Figure, C), which was consistent with Langerhans cell histiocytosis (LCH).
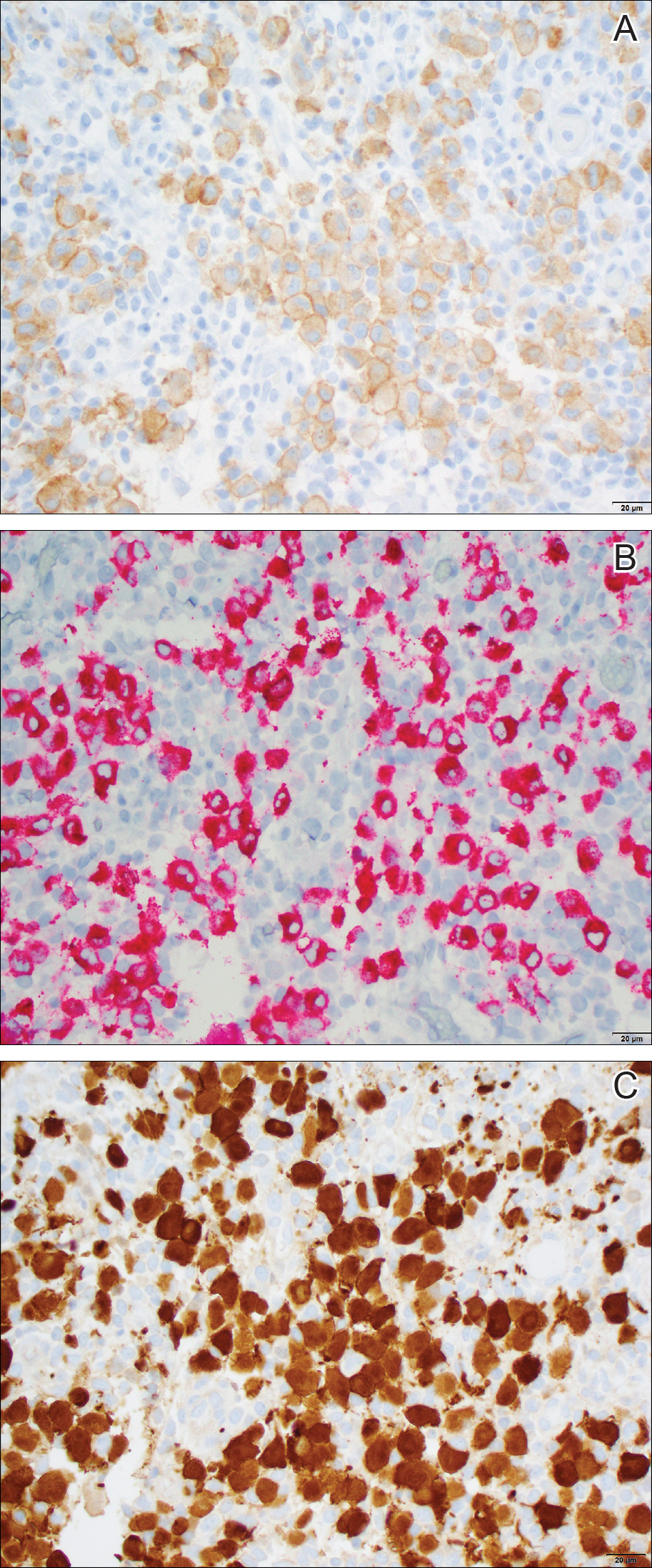
Histiocytoses are a heterogeneous group of disorders in which the infiltrating cells belong to the mononuclear phagocyte system.1,2 Langerhans cell histiocytosis is the most common dendritic cell-related histiocytosis, occurring in approximately 5 per 1 million children annually, giving it an incidence comparable to pediatric Hodgkin lymphoma and acute myeloid leukemia.1,2
Historically, there has been much debate about the pathogenesis of the disease.2 Until recently it was unknown whether LCH was primarily a neoplastic or an inflammatory disorder. Although the condition initially was thought to have a reactive etiology,1 more recent evidence suggests a clonal neoplastic process. Langerhans cell histiocytosis lesions are clonal and display malignancy-associated mechanisms such as immune evasion. Genome sequencing has revealed several mutations in precursor myeloid cells that result in the common downstream hyperactivation of the mitogen-activated protein kinase signaling pathway that regulates cell proliferation and differentiation.1
Langerhans cell histiocytosis displays a wide spectrum of clinical phenotypes, which historically were subclassified as eosinophilic granulomas (localized lesions in bone), Hand-Schüller-Christian disease (multiple organ involvement with the classic triad of skull defects, diabetes insipidus, and exophthalmos), and Letterer-Siwe disease (visceral lesions involving multiple organs).3 However, in 1997 the Reclassification Working Group of the Histiocyte Society redefined LCH as single-system single site (SS-s) LCH, single-system multisite LCH, and multisystem LCH.4
In SS-s LCH, the most common site is bone (82%), followed by the skin (12%).5 Skin SS-s LCH classically presents as multiple skin lesions at birth without systemic manifestations; the lesions spontaneously involute within a few months.6 Less commonly, skin SS-s LCH can present as a single lesion. Berger et al7 described 4 neonates with unilesional skin SS-s LCH. Since then, more than 30 cases have been reported in the literature,8 and we report herein another unilesional self-healing LCH.
The morphology of skin lesions in self-healing LCH is highly variable, with the most common being multiple erythematous crusted papules (50%), followed by eczematous scaly lesions resembling seborrheic dermatitis in intertriginous areas (37.5%).3,6 Unilesional self-healing LCH typically presents as an ulcerated or crusted nodule or papule on the trunk. This variability results in a large differential diagnosis. Self-healing LCH is easily mistaken for infectious processes including neonatal herpes simplex and varicella-zoster virus infection.9 Often, the dermatology department is consulted to rule out LCH when the asymptomatic neonate does not respond to parenteral acyclovir.
Less commonly, the magenta-colored papulonodules of self-healing LCH can mimic blueberry muffin rash and mandate a workup for intrauterine infections, especially cytomegalovirus, rubella, and blood dyscrasia.10 Other noninfectious processes in the differential of self-healing LCH include congenital infantile hemangioma, neonatal lupus erythematosus, seborrheic dermatitis (cradle cap), pyogenic granuloma, and psoriasis.3,10 Definitive diagnosis requires histopathology.
Because unilesional self-healing LCH has an excellent prognosis and usually resolves on its own, therapy is unnecessary.3,8 One large retrospective study (N=146) found that of all patients with skin lesions, 56% were managed with biopsy only.5 Other options include watchful waiting and topical corticosteroids. If the skin lesions are large, ulcerated, and/or painful, alkylating antitumor agents have been used. For extensive cutaneous disease, systemic corticosteroids combined with chemotherapy and psoralen plus UVA can be effective.6
The primary concern in the management of self-healing LCH is that the solitary skin lesion may be the harbinger of an aggressive disorder that can progress to systemic disease.5 Moreover, recurrent visceral or disseminated disease may occur months to years after resolution of solitary skin lesions.9 Studies have shown that localized and disseminated disease cannot be differentiated on the basis of clinical findings, histology, immunohistochemistry, or biomarkers.3,11 As a result, an evaluation for systemic disease should be performed at the time of diagnosis for cutaneous LCH.3,9 Minimum baseline studies recommended by the Writing Group of the Histiocyte Society include a complete blood cell count, liver function tests, coagulation studies, chest radiography, skeletal surveys, and urine osmolality testing.12 Periodic clinical follow-up is recommended for all variants of LCH.9
Our case was diagnosed as self-healing LCH based on histologic findings. No treatment was required, and at 3-month follow-up the infant was asymptomatic without recurrence and was meeting all developmental milestones.
- Berres ML, Merad M, Allen CE. Progress in understanding the pathogenesis of Langerhans cell histiocytosis: back to histiocytosis X? Br J Haematol. 2015;169:3-13.
- Jordan MB, Filipovich AH. Histiocytic disorders. In: Hoffman R, Benz EJ Jr, Silberstein LE, eds. Hematology: Basic Principles and Practice. 6th ed. Philadelphia, PA: Elsevier Saunders; 2013:686-700.
- Stein SL, Paller AS, Haut PR, et al. Langerhans cell histiocytosis presenting in the neonatal period: a retrospective case series. Arch Pediatr Adolesc Med. 2001;155:778-783.
- Favara BE, Feller AC, Pauli M, et al. Contemporary classification of histiocytic disorders. Pediatr Blood Cancer. 1997;29:157-166.
- Morimoto A, Ishida Y, Suzuki N, et al. Nationwide survey of single-system single site Langerhans cell histiocytosis in Japan. Pediatr Blood Cancer. 2010;54:98-102.
- Morren MA, Broecke KV, Vangeebergen L, et al. Diverse cutaneous presentations of Langerhans cell histiocytosis in children: a retrospective cohort study. Pediatr Blood Cancer. 2016;63:486-492.
- Berger TG, Lane AT, Headington JT, et al. A solitary variant of congenital self-healing reticulohistiocytosis: solitary Hashimoto-Pritzker disease. Pediatr Dermatol. 1986;3:230.
- Wheller L, Carman N, Butler G. Unilesional self-limited Langerhans cell histiocytosis: a case report and review of the literature. J Cutan Pathol. 2013;40:595-599.
- Battistella M, Fraitag S, Teillac DH, et al. Neonatal and early infantile cutaneous Langerhans cell histiocytosis: comparison of self-regressive and non-self-regressive forms. Arch Dermatol. 2010;146:149-156.
- Mehta V, Balachandran C, Lonikar V. Blueberry muffin baby: a pictoral differential diagnosis. Dermatol Online J. 2008;14:8.
- Kapur P, Erickson C, Rakheja D, et al. Congenital self-healing reticulohistiocytosis (Hashimoto-Pritzker disease): ten-year experience at Dallas Children's Medical Center. J Am Acad Dermatol. 2007;56:290-294.
- Writing Group of the Histiocyte Society. Histiocytosis syndromes in children. Lancet. 1987;24:208-209.
The Diagnosis: Self-healing Langerhans Cell Histiocytosis
Histopathologic examination showed an infiltrate of mononuclear cells with indented nuclei admixed with a variable dermal inflammatory infiltrate. Immunohistochemistry demonstrated cells that were strongly positive for CD1a (Figure, A) and langerin (Figure, B) antigens as well as S-100 protein (Figure, C), which was consistent with Langerhans cell histiocytosis (LCH).
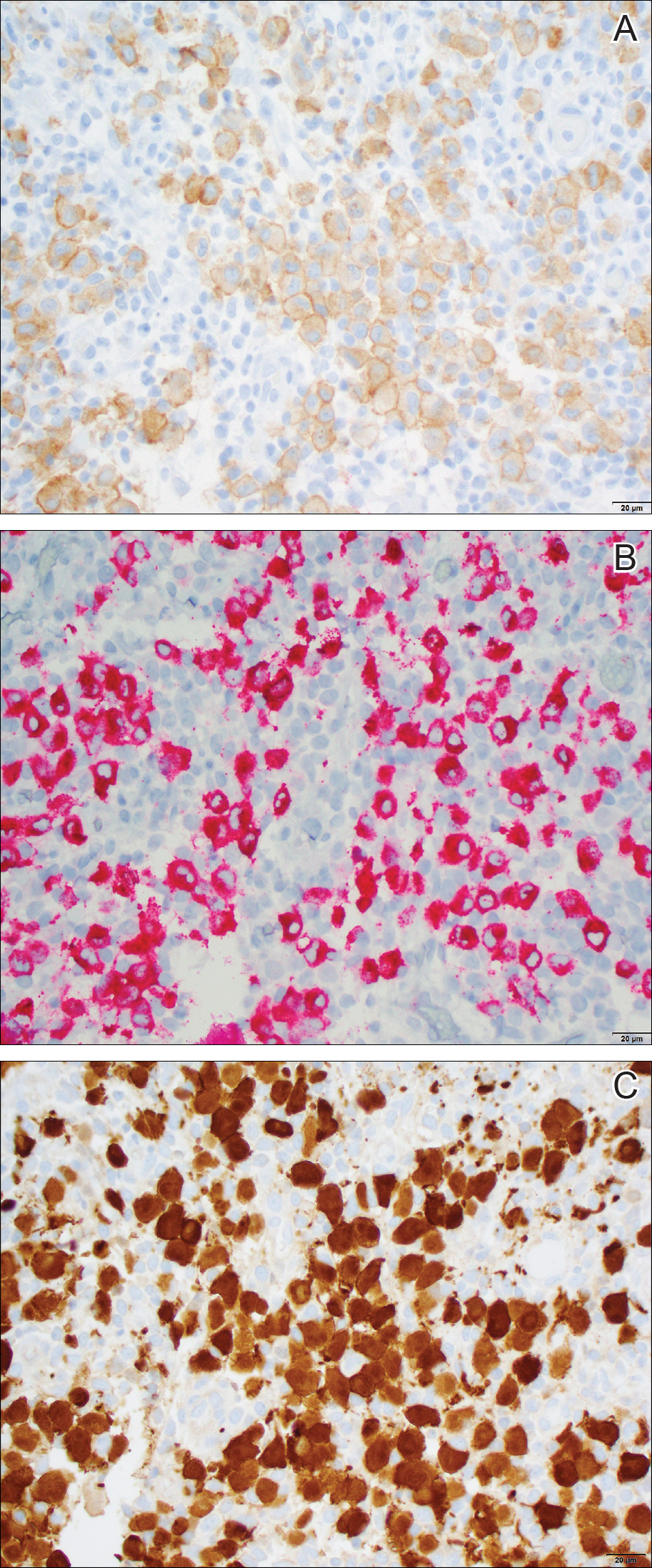
Histiocytoses are a heterogeneous group of disorders in which the infiltrating cells belong to the mononuclear phagocyte system.1,2 Langerhans cell histiocytosis is the most common dendritic cell-related histiocytosis, occurring in approximately 5 per 1 million children annually, giving it an incidence comparable to pediatric Hodgkin lymphoma and acute myeloid leukemia.1,2
Historically, there has been much debate about the pathogenesis of the disease.2 Until recently it was unknown whether LCH was primarily a neoplastic or an inflammatory disorder. Although the condition initially was thought to have a reactive etiology,1 more recent evidence suggests a clonal neoplastic process. Langerhans cell histiocytosis lesions are clonal and display malignancy-associated mechanisms such as immune evasion. Genome sequencing has revealed several mutations in precursor myeloid cells that result in the common downstream hyperactivation of the mitogen-activated protein kinase signaling pathway that regulates cell proliferation and differentiation.1
Langerhans cell histiocytosis displays a wide spectrum of clinical phenotypes, which historically were subclassified as eosinophilic granulomas (localized lesions in bone), Hand-Schüller-Christian disease (multiple organ involvement with the classic triad of skull defects, diabetes insipidus, and exophthalmos), and Letterer-Siwe disease (visceral lesions involving multiple organs).3 However, in 1997 the Reclassification Working Group of the Histiocyte Society redefined LCH as single-system single site (SS-s) LCH, single-system multisite LCH, and multisystem LCH.4
In SS-s LCH, the most common site is bone (82%), followed by the skin (12%).5 Skin SS-s LCH classically presents as multiple skin lesions at birth without systemic manifestations; the lesions spontaneously involute within a few months.6 Less commonly, skin SS-s LCH can present as a single lesion. Berger et al7 described 4 neonates with unilesional skin SS-s LCH. Since then, more than 30 cases have been reported in the literature,8 and we report herein another unilesional self-healing LCH.
The morphology of skin lesions in self-healing LCH is highly variable, with the most common being multiple erythematous crusted papules (50%), followed by eczematous scaly lesions resembling seborrheic dermatitis in intertriginous areas (37.5%).3,6 Unilesional self-healing LCH typically presents as an ulcerated or crusted nodule or papule on the trunk. This variability results in a large differential diagnosis. Self-healing LCH is easily mistaken for infectious processes including neonatal herpes simplex and varicella-zoster virus infection.9 Often, the dermatology department is consulted to rule out LCH when the asymptomatic neonate does not respond to parenteral acyclovir.
Less commonly, the magenta-colored papulonodules of self-healing LCH can mimic blueberry muffin rash and mandate a workup for intrauterine infections, especially cytomegalovirus, rubella, and blood dyscrasia.10 Other noninfectious processes in the differential of self-healing LCH include congenital infantile hemangioma, neonatal lupus erythematosus, seborrheic dermatitis (cradle cap), pyogenic granuloma, and psoriasis.3,10 Definitive diagnosis requires histopathology.
Because unilesional self-healing LCH has an excellent prognosis and usually resolves on its own, therapy is unnecessary.3,8 One large retrospective study (N=146) found that of all patients with skin lesions, 56% were managed with biopsy only.5 Other options include watchful waiting and topical corticosteroids. If the skin lesions are large, ulcerated, and/or painful, alkylating antitumor agents have been used. For extensive cutaneous disease, systemic corticosteroids combined with chemotherapy and psoralen plus UVA can be effective.6
The primary concern in the management of self-healing LCH is that the solitary skin lesion may be the harbinger of an aggressive disorder that can progress to systemic disease.5 Moreover, recurrent visceral or disseminated disease may occur months to years after resolution of solitary skin lesions.9 Studies have shown that localized and disseminated disease cannot be differentiated on the basis of clinical findings, histology, immunohistochemistry, or biomarkers.3,11 As a result, an evaluation for systemic disease should be performed at the time of diagnosis for cutaneous LCH.3,9 Minimum baseline studies recommended by the Writing Group of the Histiocyte Society include a complete blood cell count, liver function tests, coagulation studies, chest radiography, skeletal surveys, and urine osmolality testing.12 Periodic clinical follow-up is recommended for all variants of LCH.9
Our case was diagnosed as self-healing LCH based on histologic findings. No treatment was required, and at 3-month follow-up the infant was asymptomatic without recurrence and was meeting all developmental milestones.
The Diagnosis: Self-healing Langerhans Cell Histiocytosis
Histopathologic examination showed an infiltrate of mononuclear cells with indented nuclei admixed with a variable dermal inflammatory infiltrate. Immunohistochemistry demonstrated cells that were strongly positive for CD1a (Figure, A) and langerin (Figure, B) antigens as well as S-100 protein (Figure, C), which was consistent with Langerhans cell histiocytosis (LCH).
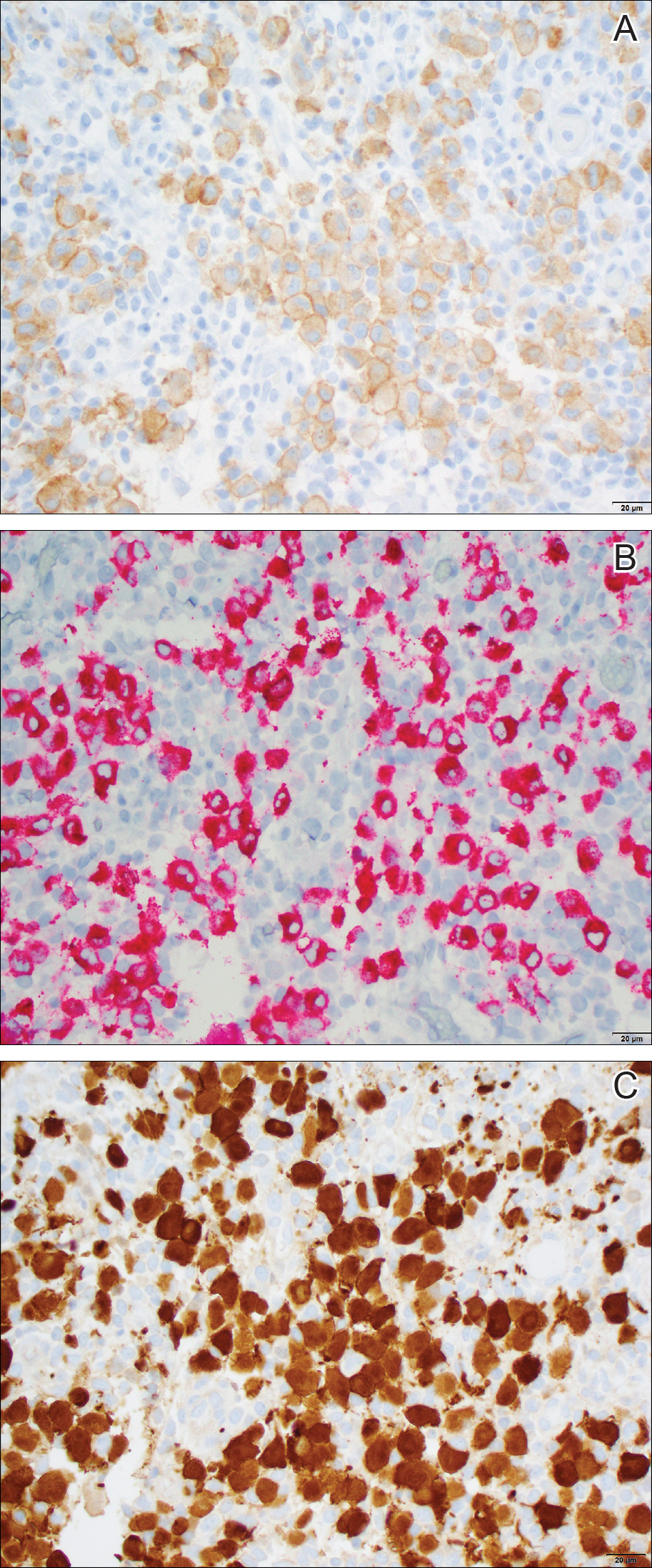
Histiocytoses are a heterogeneous group of disorders in which the infiltrating cells belong to the mononuclear phagocyte system.1,2 Langerhans cell histiocytosis is the most common dendritic cell-related histiocytosis, occurring in approximately 5 per 1 million children annually, giving it an incidence comparable to pediatric Hodgkin lymphoma and acute myeloid leukemia.1,2
Historically, there has been much debate about the pathogenesis of the disease.2 Until recently it was unknown whether LCH was primarily a neoplastic or an inflammatory disorder. Although the condition initially was thought to have a reactive etiology,1 more recent evidence suggests a clonal neoplastic process. Langerhans cell histiocytosis lesions are clonal and display malignancy-associated mechanisms such as immune evasion. Genome sequencing has revealed several mutations in precursor myeloid cells that result in the common downstream hyperactivation of the mitogen-activated protein kinase signaling pathway that regulates cell proliferation and differentiation.1
Langerhans cell histiocytosis displays a wide spectrum of clinical phenotypes, which historically were subclassified as eosinophilic granulomas (localized lesions in bone), Hand-Schüller-Christian disease (multiple organ involvement with the classic triad of skull defects, diabetes insipidus, and exophthalmos), and Letterer-Siwe disease (visceral lesions involving multiple organs).3 However, in 1997 the Reclassification Working Group of the Histiocyte Society redefined LCH as single-system single site (SS-s) LCH, single-system multisite LCH, and multisystem LCH.4
In SS-s LCH, the most common site is bone (82%), followed by the skin (12%).5 Skin SS-s LCH classically presents as multiple skin lesions at birth without systemic manifestations; the lesions spontaneously involute within a few months.6 Less commonly, skin SS-s LCH can present as a single lesion. Berger et al7 described 4 neonates with unilesional skin SS-s LCH. Since then, more than 30 cases have been reported in the literature,8 and we report herein another unilesional self-healing LCH.
The morphology of skin lesions in self-healing LCH is highly variable, with the most common being multiple erythematous crusted papules (50%), followed by eczematous scaly lesions resembling seborrheic dermatitis in intertriginous areas (37.5%).3,6 Unilesional self-healing LCH typically presents as an ulcerated or crusted nodule or papule on the trunk. This variability results in a large differential diagnosis. Self-healing LCH is easily mistaken for infectious processes including neonatal herpes simplex and varicella-zoster virus infection.9 Often, the dermatology department is consulted to rule out LCH when the asymptomatic neonate does not respond to parenteral acyclovir.
Less commonly, the magenta-colored papulonodules of self-healing LCH can mimic blueberry muffin rash and mandate a workup for intrauterine infections, especially cytomegalovirus, rubella, and blood dyscrasia.10 Other noninfectious processes in the differential of self-healing LCH include congenital infantile hemangioma, neonatal lupus erythematosus, seborrheic dermatitis (cradle cap), pyogenic granuloma, and psoriasis.3,10 Definitive diagnosis requires histopathology.
Because unilesional self-healing LCH has an excellent prognosis and usually resolves on its own, therapy is unnecessary.3,8 One large retrospective study (N=146) found that of all patients with skin lesions, 56% were managed with biopsy only.5 Other options include watchful waiting and topical corticosteroids. If the skin lesions are large, ulcerated, and/or painful, alkylating antitumor agents have been used. For extensive cutaneous disease, systemic corticosteroids combined with chemotherapy and psoralen plus UVA can be effective.6
The primary concern in the management of self-healing LCH is that the solitary skin lesion may be the harbinger of an aggressive disorder that can progress to systemic disease.5 Moreover, recurrent visceral or disseminated disease may occur months to years after resolution of solitary skin lesions.9 Studies have shown that localized and disseminated disease cannot be differentiated on the basis of clinical findings, histology, immunohistochemistry, or biomarkers.3,11 As a result, an evaluation for systemic disease should be performed at the time of diagnosis for cutaneous LCH.3,9 Minimum baseline studies recommended by the Writing Group of the Histiocyte Society include a complete blood cell count, liver function tests, coagulation studies, chest radiography, skeletal surveys, and urine osmolality testing.12 Periodic clinical follow-up is recommended for all variants of LCH.9
Our case was diagnosed as self-healing LCH based on histologic findings. No treatment was required, and at 3-month follow-up the infant was asymptomatic without recurrence and was meeting all developmental milestones.
- Berres ML, Merad M, Allen CE. Progress in understanding the pathogenesis of Langerhans cell histiocytosis: back to histiocytosis X? Br J Haematol. 2015;169:3-13.
- Jordan MB, Filipovich AH. Histiocytic disorders. In: Hoffman R, Benz EJ Jr, Silberstein LE, eds. Hematology: Basic Principles and Practice. 6th ed. Philadelphia, PA: Elsevier Saunders; 2013:686-700.
- Stein SL, Paller AS, Haut PR, et al. Langerhans cell histiocytosis presenting in the neonatal period: a retrospective case series. Arch Pediatr Adolesc Med. 2001;155:778-783.
- Favara BE, Feller AC, Pauli M, et al. Contemporary classification of histiocytic disorders. Pediatr Blood Cancer. 1997;29:157-166.
- Morimoto A, Ishida Y, Suzuki N, et al. Nationwide survey of single-system single site Langerhans cell histiocytosis in Japan. Pediatr Blood Cancer. 2010;54:98-102.
- Morren MA, Broecke KV, Vangeebergen L, et al. Diverse cutaneous presentations of Langerhans cell histiocytosis in children: a retrospective cohort study. Pediatr Blood Cancer. 2016;63:486-492.
- Berger TG, Lane AT, Headington JT, et al. A solitary variant of congenital self-healing reticulohistiocytosis: solitary Hashimoto-Pritzker disease. Pediatr Dermatol. 1986;3:230.
- Wheller L, Carman N, Butler G. Unilesional self-limited Langerhans cell histiocytosis: a case report and review of the literature. J Cutan Pathol. 2013;40:595-599.
- Battistella M, Fraitag S, Teillac DH, et al. Neonatal and early infantile cutaneous Langerhans cell histiocytosis: comparison of self-regressive and non-self-regressive forms. Arch Dermatol. 2010;146:149-156.
- Mehta V, Balachandran C, Lonikar V. Blueberry muffin baby: a pictoral differential diagnosis. Dermatol Online J. 2008;14:8.
- Kapur P, Erickson C, Rakheja D, et al. Congenital self-healing reticulohistiocytosis (Hashimoto-Pritzker disease): ten-year experience at Dallas Children's Medical Center. J Am Acad Dermatol. 2007;56:290-294.
- Writing Group of the Histiocyte Society. Histiocytosis syndromes in children. Lancet. 1987;24:208-209.
- Berres ML, Merad M, Allen CE. Progress in understanding the pathogenesis of Langerhans cell histiocytosis: back to histiocytosis X? Br J Haematol. 2015;169:3-13.
- Jordan MB, Filipovich AH. Histiocytic disorders. In: Hoffman R, Benz EJ Jr, Silberstein LE, eds. Hematology: Basic Principles and Practice. 6th ed. Philadelphia, PA: Elsevier Saunders; 2013:686-700.
- Stein SL, Paller AS, Haut PR, et al. Langerhans cell histiocytosis presenting in the neonatal period: a retrospective case series. Arch Pediatr Adolesc Med. 2001;155:778-783.
- Favara BE, Feller AC, Pauli M, et al. Contemporary classification of histiocytic disorders. Pediatr Blood Cancer. 1997;29:157-166.
- Morimoto A, Ishida Y, Suzuki N, et al. Nationwide survey of single-system single site Langerhans cell histiocytosis in Japan. Pediatr Blood Cancer. 2010;54:98-102.
- Morren MA, Broecke KV, Vangeebergen L, et al. Diverse cutaneous presentations of Langerhans cell histiocytosis in children: a retrospective cohort study. Pediatr Blood Cancer. 2016;63:486-492.
- Berger TG, Lane AT, Headington JT, et al. A solitary variant of congenital self-healing reticulohistiocytosis: solitary Hashimoto-Pritzker disease. Pediatr Dermatol. 1986;3:230.
- Wheller L, Carman N, Butler G. Unilesional self-limited Langerhans cell histiocytosis: a case report and review of the literature. J Cutan Pathol. 2013;40:595-599.
- Battistella M, Fraitag S, Teillac DH, et al. Neonatal and early infantile cutaneous Langerhans cell histiocytosis: comparison of self-regressive and non-self-regressive forms. Arch Dermatol. 2010;146:149-156.
- Mehta V, Balachandran C, Lonikar V. Blueberry muffin baby: a pictoral differential diagnosis. Dermatol Online J. 2008;14:8.
- Kapur P, Erickson C, Rakheja D, et al. Congenital self-healing reticulohistiocytosis (Hashimoto-Pritzker disease): ten-year experience at Dallas Children's Medical Center. J Am Acad Dermatol. 2007;56:290-294.
- Writing Group of the Histiocyte Society. Histiocytosis syndromes in children. Lancet. 1987;24:208-209.

Dermatology consultation was called to the delivery room to evaluate a red, hemorrhagic, crusted, 5-mm papule on the right lateral upper arm of a preterm newborn. He appeared vigorous with an Apgar score of 7 at 1 minute and 8 at 5 minutes. Physical examination was otherwise normal. Of note, the mother presented late to prenatal care. Her herpes simplex and varicella-zoster virus status was unknown. A shave biopsy of the papule was performed at 3 days of age.
Medical exemptions spike after vaccine policy change
according to data from interviews with health officials and immunization staff after implementation of the policy.
In a study published in Pediatrics, Salini Mohanty, DrPH, of the University of Pennsylvania School of Nursing, Philadelphia, and her colleagues conducted semistructured phone interviews with 40 health officers and immunization staff who represented 35 of 61 California heath jurisdictions. The interviews occurred between August 2017 and September 2017, and participants discussed their experiences with medical exemption requests after the policy change.
Although the percentage of fully vaccinated kindergarten students in California increased from 93% in 2015-2016 to 95% in 2017-2018, and the rate of personal belief exemptions declined, overall medical exemption requests rose 250% from 0.2% in 2015-2016 to 0.7% 2017-2018, the researchers noted.
They identified four main issues based on participant responses: the role of stakeholders, the review of medical exemptions received by schools, the medical exemptions perceived as problematic, and the general frustration and concern over medical exemptions.
Based on the interviews, one concerning subtheme involved reports that some physicians wrote medical exemptions for vaccine-hesitant parents based on conditions such as allergies and autoimmune diseases.
“The Internet provides access to physicians who are willing to sign off on exemptions and to websites used to instruct parents on how to get physicians to approve medical exemptions,” the researchers said.
“Understanding how physicians interpret the law is important because they are writing the medical exemptions,” Dr. Mohanty and her associates noted, and they proposed increased outreach and education of physicians about the law to reduce problematic medical exemptions.
Many health officials expressed frustration with their inability to review medical exemptions submitted directly to schools. In fact, interviewees cited one California jurisdiction that was named in a lawsuit for attempting to track medical exemptions, “which had an impact on other jurisdictions decision to track,” they said.
Officials also expressed concern that parents’ use of medical exemptions to replace personal belief exemptions would reduce herd immunity. Overall, regions with high levels of personal belief exemptions showed the largest increases in medical exemptions after SB277, which could put these regions at increased risk for vaccine-preventable outbreaks, the researchers noted.
There also were reports of physicians “who advertised medical exemptions online for a fee.” Officials also reported “receiving medical exemptions signed by physicians who do not typically treat children (cardiologists, dermatologists, surgeons, and physicians at medical marijuana dispensaries) and by unauthorized nonphysician providers, including nurse practitioners,” Dr. Mohanty and her associates said.
The study findings were limited by several factors including small sample size and potential recall bias, the researchers noted. However, the study is the first to include perspectives of local health officials after a change in vaccine exemption policy.
The National Institutes of Health supported the study. Dr. Mohanty had no financial conflicts to disclose; one coauthor disclosed relationships with Merck, Pfizer, and Walgreens.
SOURCE: Mohanty S et al. Pediatrics. 2018. doi: 10.1542/peds.2018-1051.
Passage of SB277 has had a positive impact on the proportion of California kindergarteners who are fully vaccinated, Richard J. Pan, MD, MPH, and Dorit Rubinstein Reiss, LLB, PhD, wrote in an editorial.
“Vaccines are one of the greatest public health successes in history. Mandating vaccination for school is an effective strategy to prevent outbreaks,” they said. However, “this protection is undermined when unscrupulous physicians monetize their license and abuse the authority delegated to them from the state by granting unwarranted [medical exemptions (MEs)],” they said.
The editorialists emphasized that states have the authority to mandate vaccinations in the interest of public health, and that allowing physicians to grant medical exemptions is appropriate because doctors know their patients and know whether exemptions are needed.
“However, the lack of cooperation by patients’ families who desire unwarranted MEs makes disciplining physicians who are engaged in this unprofessional behavior difficult and costly because licensing boards need to subpoena patient records over families’ objections to obtain evidence. Similarly, professional standard-setting organizations, including professional associations and certification boards, have been reluctant to withdraw credentials or expel members who promote vaccine misinformation and grant unwarranted MEs,” they said. They proposed strategies including establishing a searchable database for MEs, allowing public health officials the option to review and invalidate MEs, and requiring parents to submit MEs to public health departments as well as to schools.
“Pediatricians can partner with public health advocates and proscience parents to pass laws that empower public health officers to protect our children and community. Every child needs community immunity,” they said.
Dr. Pan is a California State Senator, Sacramento, and Dr. Reiss is at the Hastings College of the Law, University of California, San Francisco. Their comments on the article by Mohanty et al. were published in Pediatrics (2018;142[5]:e20182009). Dr. Pan authored legislation (Senate Bill 277) to abolish nonmedical exemption. Dr. Reiss’s family owns regular stock in GlaxoSmithKline.
Passage of SB277 has had a positive impact on the proportion of California kindergarteners who are fully vaccinated, Richard J. Pan, MD, MPH, and Dorit Rubinstein Reiss, LLB, PhD, wrote in an editorial.
“Vaccines are one of the greatest public health successes in history. Mandating vaccination for school is an effective strategy to prevent outbreaks,” they said. However, “this protection is undermined when unscrupulous physicians monetize their license and abuse the authority delegated to them from the state by granting unwarranted [medical exemptions (MEs)],” they said.
The editorialists emphasized that states have the authority to mandate vaccinations in the interest of public health, and that allowing physicians to grant medical exemptions is appropriate because doctors know their patients and know whether exemptions are needed.
“However, the lack of cooperation by patients’ families who desire unwarranted MEs makes disciplining physicians who are engaged in this unprofessional behavior difficult and costly because licensing boards need to subpoena patient records over families’ objections to obtain evidence. Similarly, professional standard-setting organizations, including professional associations and certification boards, have been reluctant to withdraw credentials or expel members who promote vaccine misinformation and grant unwarranted MEs,” they said. They proposed strategies including establishing a searchable database for MEs, allowing public health officials the option to review and invalidate MEs, and requiring parents to submit MEs to public health departments as well as to schools.
“Pediatricians can partner with public health advocates and proscience parents to pass laws that empower public health officers to protect our children and community. Every child needs community immunity,” they said.
Dr. Pan is a California State Senator, Sacramento, and Dr. Reiss is at the Hastings College of the Law, University of California, San Francisco. Their comments on the article by Mohanty et al. were published in Pediatrics (2018;142[5]:e20182009). Dr. Pan authored legislation (Senate Bill 277) to abolish nonmedical exemption. Dr. Reiss’s family owns regular stock in GlaxoSmithKline.
Passage of SB277 has had a positive impact on the proportion of California kindergarteners who are fully vaccinated, Richard J. Pan, MD, MPH, and Dorit Rubinstein Reiss, LLB, PhD, wrote in an editorial.
“Vaccines are one of the greatest public health successes in history. Mandating vaccination for school is an effective strategy to prevent outbreaks,” they said. However, “this protection is undermined when unscrupulous physicians monetize their license and abuse the authority delegated to them from the state by granting unwarranted [medical exemptions (MEs)],” they said.
The editorialists emphasized that states have the authority to mandate vaccinations in the interest of public health, and that allowing physicians to grant medical exemptions is appropriate because doctors know their patients and know whether exemptions are needed.
“However, the lack of cooperation by patients’ families who desire unwarranted MEs makes disciplining physicians who are engaged in this unprofessional behavior difficult and costly because licensing boards need to subpoena patient records over families’ objections to obtain evidence. Similarly, professional standard-setting organizations, including professional associations and certification boards, have been reluctant to withdraw credentials or expel members who promote vaccine misinformation and grant unwarranted MEs,” they said. They proposed strategies including establishing a searchable database for MEs, allowing public health officials the option to review and invalidate MEs, and requiring parents to submit MEs to public health departments as well as to schools.
“Pediatricians can partner with public health advocates and proscience parents to pass laws that empower public health officers to protect our children and community. Every child needs community immunity,” they said.
Dr. Pan is a California State Senator, Sacramento, and Dr. Reiss is at the Hastings College of the Law, University of California, San Francisco. Their comments on the article by Mohanty et al. were published in Pediatrics (2018;142[5]:e20182009). Dr. Pan authored legislation (Senate Bill 277) to abolish nonmedical exemption. Dr. Reiss’s family owns regular stock in GlaxoSmithKline.
according to data from interviews with health officials and immunization staff after implementation of the policy.
In a study published in Pediatrics, Salini Mohanty, DrPH, of the University of Pennsylvania School of Nursing, Philadelphia, and her colleagues conducted semistructured phone interviews with 40 health officers and immunization staff who represented 35 of 61 California heath jurisdictions. The interviews occurred between August 2017 and September 2017, and participants discussed their experiences with medical exemption requests after the policy change.
Although the percentage of fully vaccinated kindergarten students in California increased from 93% in 2015-2016 to 95% in 2017-2018, and the rate of personal belief exemptions declined, overall medical exemption requests rose 250% from 0.2% in 2015-2016 to 0.7% 2017-2018, the researchers noted.
They identified four main issues based on participant responses: the role of stakeholders, the review of medical exemptions received by schools, the medical exemptions perceived as problematic, and the general frustration and concern over medical exemptions.
Based on the interviews, one concerning subtheme involved reports that some physicians wrote medical exemptions for vaccine-hesitant parents based on conditions such as allergies and autoimmune diseases.
“The Internet provides access to physicians who are willing to sign off on exemptions and to websites used to instruct parents on how to get physicians to approve medical exemptions,” the researchers said.
“Understanding how physicians interpret the law is important because they are writing the medical exemptions,” Dr. Mohanty and her associates noted, and they proposed increased outreach and education of physicians about the law to reduce problematic medical exemptions.
Many health officials expressed frustration with their inability to review medical exemptions submitted directly to schools. In fact, interviewees cited one California jurisdiction that was named in a lawsuit for attempting to track medical exemptions, “which had an impact on other jurisdictions decision to track,” they said.
Officials also expressed concern that parents’ use of medical exemptions to replace personal belief exemptions would reduce herd immunity. Overall, regions with high levels of personal belief exemptions showed the largest increases in medical exemptions after SB277, which could put these regions at increased risk for vaccine-preventable outbreaks, the researchers noted.
There also were reports of physicians “who advertised medical exemptions online for a fee.” Officials also reported “receiving medical exemptions signed by physicians who do not typically treat children (cardiologists, dermatologists, surgeons, and physicians at medical marijuana dispensaries) and by unauthorized nonphysician providers, including nurse practitioners,” Dr. Mohanty and her associates said.
The study findings were limited by several factors including small sample size and potential recall bias, the researchers noted. However, the study is the first to include perspectives of local health officials after a change in vaccine exemption policy.
The National Institutes of Health supported the study. Dr. Mohanty had no financial conflicts to disclose; one coauthor disclosed relationships with Merck, Pfizer, and Walgreens.
SOURCE: Mohanty S et al. Pediatrics. 2018. doi: 10.1542/peds.2018-1051.
according to data from interviews with health officials and immunization staff after implementation of the policy.
In a study published in Pediatrics, Salini Mohanty, DrPH, of the University of Pennsylvania School of Nursing, Philadelphia, and her colleagues conducted semistructured phone interviews with 40 health officers and immunization staff who represented 35 of 61 California heath jurisdictions. The interviews occurred between August 2017 and September 2017, and participants discussed their experiences with medical exemption requests after the policy change.
Although the percentage of fully vaccinated kindergarten students in California increased from 93% in 2015-2016 to 95% in 2017-2018, and the rate of personal belief exemptions declined, overall medical exemption requests rose 250% from 0.2% in 2015-2016 to 0.7% 2017-2018, the researchers noted.
They identified four main issues based on participant responses: the role of stakeholders, the review of medical exemptions received by schools, the medical exemptions perceived as problematic, and the general frustration and concern over medical exemptions.
Based on the interviews, one concerning subtheme involved reports that some physicians wrote medical exemptions for vaccine-hesitant parents based on conditions such as allergies and autoimmune diseases.
“The Internet provides access to physicians who are willing to sign off on exemptions and to websites used to instruct parents on how to get physicians to approve medical exemptions,” the researchers said.
“Understanding how physicians interpret the law is important because they are writing the medical exemptions,” Dr. Mohanty and her associates noted, and they proposed increased outreach and education of physicians about the law to reduce problematic medical exemptions.
Many health officials expressed frustration with their inability to review medical exemptions submitted directly to schools. In fact, interviewees cited one California jurisdiction that was named in a lawsuit for attempting to track medical exemptions, “which had an impact on other jurisdictions decision to track,” they said.
Officials also expressed concern that parents’ use of medical exemptions to replace personal belief exemptions would reduce herd immunity. Overall, regions with high levels of personal belief exemptions showed the largest increases in medical exemptions after SB277, which could put these regions at increased risk for vaccine-preventable outbreaks, the researchers noted.
There also were reports of physicians “who advertised medical exemptions online for a fee.” Officials also reported “receiving medical exemptions signed by physicians who do not typically treat children (cardiologists, dermatologists, surgeons, and physicians at medical marijuana dispensaries) and by unauthorized nonphysician providers, including nurse practitioners,” Dr. Mohanty and her associates said.
The study findings were limited by several factors including small sample size and potential recall bias, the researchers noted. However, the study is the first to include perspectives of local health officials after a change in vaccine exemption policy.
The National Institutes of Health supported the study. Dr. Mohanty had no financial conflicts to disclose; one coauthor disclosed relationships with Merck, Pfizer, and Walgreens.
SOURCE: Mohanty S et al. Pediatrics. 2018. doi: 10.1542/peds.2018-1051.
FROM PEDIATRICS
Key clinical point: Medical exemptions for childhood vaccinations in California increased after the implementation of Senate Bill 277 (SB277) eliminating nonmedical exemptions.
Major finding: Medical exemptions in California increased by 250% after the SB277 took effect.
Study details: The data come from 34 interviews with 40 health officers and immunization staff about their experiences with medical exemptions before and after the passage of SB277.
Disclosures: The National Institutes of Health supported the study. Dr. Mohanty had no financial conflicts to disclose; one coauthor disclosed relationships with Merck, Pfizer, and Walgreens.
Source: Mohanty S et al. Pediatrics. 2018. doi: 10.1542/peds.2018-1051.
Is respiratory compromise the new “sepsis”?
Hospitalists can play a key role in prevention
Clinicians and even the general public are aware of the dangers of sepsis, the life-threatening illness caused by a body’s response to an infection. Irrespective of one’s perception of pharmaceutical marketing materials or the evidence-based medicine used, awareness about sepsis has led to earlier diagnosis and interventions that have likely saved countless patients’ lives.
Moreover, hospitalists have played a key role in sepsis prevention. In their research, “Improving Survival from Sepsis in Noncritical Units: Role of Hospitalists and Sepsis Team in Early Detection and Initial Treatment of Septic Patients,” Adriana Ducci, MD, and her colleagues showed that a hospitalist-managed sepsis protocol improved sepsis case notifications and patient outcomes.
Although sepsis and respiratory compromise are clearly very different conditions, I believe that greater awareness about respiratory compromise will lead to earlier diagnosis and interventions, which will theoretically improve patient outcomes. Moreover, as with the sepsis awareness campaign, hospitalists can play a key role in recognizing respiratory compromise and in the implementation of appropriate interventions.
As defined by the Respiratory Compromise Institute, “respiratory compromise” is defined as a state in which there is a high likelihood of decompensation into respiratory failure and/or death, but, in which specific interventions – be it therapeutic and/or monitoring – might prevent or mitigate this decompensation.
A significant segment of patients who may be at risk for respiratory compromise are those receiving opioids. The cost of opioid-related adverse events, in terms of both human life and hospital expenses, remains at the forefront of the public eye. It has been estimated that yearly costs in the United States associated with opioid-related postoperative respiratory failure were estimated at $2 billion.
Thomas W. Frederickson MD, FACP, SFHM, MBA, the lead author of the Society of Hospital Medicine guide for Reducing Adverse Drug Events Related to Opioids (RADEO), emphasized in a podcast with the Physician-Patient Alliance for Health & Safety the need to identify patient conditions that pose a greater risk of respiratory compromise.
In particular, Dr. Frederickson pointed out the need to screen for obstructive sleep apnea (OSA): “Patients with obstructive sleep apnea are dependent upon their arousal mechanism in order to avoid respiratory depression and eventual respiratory failure. When these patients receive opioid medication, it decreases this ability for arousal. That puts them at risk for a sudden spiral that includes respiratory insufficiency and respiratory arrest. This can happen very quickly and part of the risk is that the traditional monitoring for sedation that we use in the hospital – that is on a periodic basis and depends upon nursing interventions and questioning – really becomes much less effective in this patient population that can have a respiratory arrest, because of failure to arouse, very quickly. So, a monitoring regimen that takes place every 60 minutes is likely to be ineffective.”
Patient conditions such as OSA should be considered, along with other comorbidities. As the RADEO Guide states: “Before starting opioid therapy, either in surgical or non-surgical settings, it is important to identify any real or potential risks of respiratory depression or other opioid-related adverse effects. Patient comorbidities such as OSA, neurologic disorders, organ impairment, substance abuse history, and other medication use are important aspects to consider.”
Although we have clearly recognized a significant increase in respiratory complications associated with opioid administration, there are other areas, which are non–opioid related, that can create respiratory compromise. We view many patients with stable or underlying respiratory conditions, whether it be COPD, sleep apnea, or preexisting pathophysiology, where either due to sedative agents, or an acute illness – like pneumonia – they can go from a stable condition to respiratory compromise and become at risk for respiratory failure.
A classic example of that in my world of anesthesia has been the well-recognized area of non–operating room anesthesia – in particular, in endoscopy suites where numerous endoscopy procedures are performed under the administration of propofol or other anxiolytic-like drugs. There has been a well-recognized incidence of sentinel events related to oxygenation and ventilation, including death.
Many clinicians see sedation as a benign introduction of relatively limited-effect drugs, which isn’t always true. So, therefore, it is essential that clinicians understand three things:
1. The drugs we employ as sedative agents can have variable effects on individuals depending on their tolerance and their underlying medical condition.
2. The dosages and particular combination of drugs employed may cause an adverse event – for example, the combination of opioids and benzodiazepines.
3. There are factors that can distract from the clinical assessment of routine vital signs, such as respiratory rate, heart rate, and blood pressure. For example, when pulse oximetry is administered with oxygen therapy, there can often be a delay in the recognition of hypoventilation. Consequently, that’s why more and more clinicians are beginning to utilize capnography, or CO2 monitoring, in the expired gas to earlier detect depressed respiratory rate and/or apnea, as well as signs of hypoventilation or inadequate ventilation.
There clearly are obstacles to continuous patient monitoring, such as the associated cost, familiarity with the utilization, the benefit, as well as the limitations of specific monitors in different clinical situations, which mandates an educational process to employ these. However, currently, patient monitoring provides the best early indicator of a patient’s deterioration and the possibility of respiratory compromise.
In my field, we have become very comfortable with capnography and patient monitoring, because for decades it’s been a standard of care for monitoring in the operating room. The role for utilization of capnography for patients who are receiving an opioid or sedative agent outside of the operating room needs to be further assessed. However, technology is not a silver bullet and should be used as an adjunct to clinical judgment in at-risk populations.
Simple recognition and greater awareness of respiratory compromise, just as with sepsis awareness campaigns, will mean more patients are diagnosed earlier, more appropriate interventions are made, and hopefully more adverse events and patient deaths are averted.
Dr. Vender is the emeritus Harris Family Foundation chairman of the department of anesthesiology at NorthShore University Health System in Evanston, Ill. He is clinical professor at the University of Chicago Pritzker School of Medicine and chairman, Clinical Advisory Committee, Respiratory Compromise Institute. Dr. Vender has consulted with Medtronic.
Hospitalists can play a key role in prevention
Hospitalists can play a key role in prevention
Clinicians and even the general public are aware of the dangers of sepsis, the life-threatening illness caused by a body’s response to an infection. Irrespective of one’s perception of pharmaceutical marketing materials or the evidence-based medicine used, awareness about sepsis has led to earlier diagnosis and interventions that have likely saved countless patients’ lives.
Moreover, hospitalists have played a key role in sepsis prevention. In their research, “Improving Survival from Sepsis in Noncritical Units: Role of Hospitalists and Sepsis Team in Early Detection and Initial Treatment of Septic Patients,” Adriana Ducci, MD, and her colleagues showed that a hospitalist-managed sepsis protocol improved sepsis case notifications and patient outcomes.
Although sepsis and respiratory compromise are clearly very different conditions, I believe that greater awareness about respiratory compromise will lead to earlier diagnosis and interventions, which will theoretically improve patient outcomes. Moreover, as with the sepsis awareness campaign, hospitalists can play a key role in recognizing respiratory compromise and in the implementation of appropriate interventions.
As defined by the Respiratory Compromise Institute, “respiratory compromise” is defined as a state in which there is a high likelihood of decompensation into respiratory failure and/or death, but, in which specific interventions – be it therapeutic and/or monitoring – might prevent or mitigate this decompensation.
A significant segment of patients who may be at risk for respiratory compromise are those receiving opioids. The cost of opioid-related adverse events, in terms of both human life and hospital expenses, remains at the forefront of the public eye. It has been estimated that yearly costs in the United States associated with opioid-related postoperative respiratory failure were estimated at $2 billion.
Thomas W. Frederickson MD, FACP, SFHM, MBA, the lead author of the Society of Hospital Medicine guide for Reducing Adverse Drug Events Related to Opioids (RADEO), emphasized in a podcast with the Physician-Patient Alliance for Health & Safety the need to identify patient conditions that pose a greater risk of respiratory compromise.
In particular, Dr. Frederickson pointed out the need to screen for obstructive sleep apnea (OSA): “Patients with obstructive sleep apnea are dependent upon their arousal mechanism in order to avoid respiratory depression and eventual respiratory failure. When these patients receive opioid medication, it decreases this ability for arousal. That puts them at risk for a sudden spiral that includes respiratory insufficiency and respiratory arrest. This can happen very quickly and part of the risk is that the traditional monitoring for sedation that we use in the hospital – that is on a periodic basis and depends upon nursing interventions and questioning – really becomes much less effective in this patient population that can have a respiratory arrest, because of failure to arouse, very quickly. So, a monitoring regimen that takes place every 60 minutes is likely to be ineffective.”
Patient conditions such as OSA should be considered, along with other comorbidities. As the RADEO Guide states: “Before starting opioid therapy, either in surgical or non-surgical settings, it is important to identify any real or potential risks of respiratory depression or other opioid-related adverse effects. Patient comorbidities such as OSA, neurologic disorders, organ impairment, substance abuse history, and other medication use are important aspects to consider.”
Although we have clearly recognized a significant increase in respiratory complications associated with opioid administration, there are other areas, which are non–opioid related, that can create respiratory compromise. We view many patients with stable or underlying respiratory conditions, whether it be COPD, sleep apnea, or preexisting pathophysiology, where either due to sedative agents, or an acute illness – like pneumonia – they can go from a stable condition to respiratory compromise and become at risk for respiratory failure.
A classic example of that in my world of anesthesia has been the well-recognized area of non–operating room anesthesia – in particular, in endoscopy suites where numerous endoscopy procedures are performed under the administration of propofol or other anxiolytic-like drugs. There has been a well-recognized incidence of sentinel events related to oxygenation and ventilation, including death.
Many clinicians see sedation as a benign introduction of relatively limited-effect drugs, which isn’t always true. So, therefore, it is essential that clinicians understand three things:
1. The drugs we employ as sedative agents can have variable effects on individuals depending on their tolerance and their underlying medical condition.
2. The dosages and particular combination of drugs employed may cause an adverse event – for example, the combination of opioids and benzodiazepines.
3. There are factors that can distract from the clinical assessment of routine vital signs, such as respiratory rate, heart rate, and blood pressure. For example, when pulse oximetry is administered with oxygen therapy, there can often be a delay in the recognition of hypoventilation. Consequently, that’s why more and more clinicians are beginning to utilize capnography, or CO2 monitoring, in the expired gas to earlier detect depressed respiratory rate and/or apnea, as well as signs of hypoventilation or inadequate ventilation.
There clearly are obstacles to continuous patient monitoring, such as the associated cost, familiarity with the utilization, the benefit, as well as the limitations of specific monitors in different clinical situations, which mandates an educational process to employ these. However, currently, patient monitoring provides the best early indicator of a patient’s deterioration and the possibility of respiratory compromise.
In my field, we have become very comfortable with capnography and patient monitoring, because for decades it’s been a standard of care for monitoring in the operating room. The role for utilization of capnography for patients who are receiving an opioid or sedative agent outside of the operating room needs to be further assessed. However, technology is not a silver bullet and should be used as an adjunct to clinical judgment in at-risk populations.
Simple recognition and greater awareness of respiratory compromise, just as with sepsis awareness campaigns, will mean more patients are diagnosed earlier, more appropriate interventions are made, and hopefully more adverse events and patient deaths are averted.
Dr. Vender is the emeritus Harris Family Foundation chairman of the department of anesthesiology at NorthShore University Health System in Evanston, Ill. He is clinical professor at the University of Chicago Pritzker School of Medicine and chairman, Clinical Advisory Committee, Respiratory Compromise Institute. Dr. Vender has consulted with Medtronic.
Clinicians and even the general public are aware of the dangers of sepsis, the life-threatening illness caused by a body’s response to an infection. Irrespective of one’s perception of pharmaceutical marketing materials or the evidence-based medicine used, awareness about sepsis has led to earlier diagnosis and interventions that have likely saved countless patients’ lives.
Moreover, hospitalists have played a key role in sepsis prevention. In their research, “Improving Survival from Sepsis in Noncritical Units: Role of Hospitalists and Sepsis Team in Early Detection and Initial Treatment of Septic Patients,” Adriana Ducci, MD, and her colleagues showed that a hospitalist-managed sepsis protocol improved sepsis case notifications and patient outcomes.
Although sepsis and respiratory compromise are clearly very different conditions, I believe that greater awareness about respiratory compromise will lead to earlier diagnosis and interventions, which will theoretically improve patient outcomes. Moreover, as with the sepsis awareness campaign, hospitalists can play a key role in recognizing respiratory compromise and in the implementation of appropriate interventions.
As defined by the Respiratory Compromise Institute, “respiratory compromise” is defined as a state in which there is a high likelihood of decompensation into respiratory failure and/or death, but, in which specific interventions – be it therapeutic and/or monitoring – might prevent or mitigate this decompensation.
A significant segment of patients who may be at risk for respiratory compromise are those receiving opioids. The cost of opioid-related adverse events, in terms of both human life and hospital expenses, remains at the forefront of the public eye. It has been estimated that yearly costs in the United States associated with opioid-related postoperative respiratory failure were estimated at $2 billion.
Thomas W. Frederickson MD, FACP, SFHM, MBA, the lead author of the Society of Hospital Medicine guide for Reducing Adverse Drug Events Related to Opioids (RADEO), emphasized in a podcast with the Physician-Patient Alliance for Health & Safety the need to identify patient conditions that pose a greater risk of respiratory compromise.
In particular, Dr. Frederickson pointed out the need to screen for obstructive sleep apnea (OSA): “Patients with obstructive sleep apnea are dependent upon their arousal mechanism in order to avoid respiratory depression and eventual respiratory failure. When these patients receive opioid medication, it decreases this ability for arousal. That puts them at risk for a sudden spiral that includes respiratory insufficiency and respiratory arrest. This can happen very quickly and part of the risk is that the traditional monitoring for sedation that we use in the hospital – that is on a periodic basis and depends upon nursing interventions and questioning – really becomes much less effective in this patient population that can have a respiratory arrest, because of failure to arouse, very quickly. So, a monitoring regimen that takes place every 60 minutes is likely to be ineffective.”
Patient conditions such as OSA should be considered, along with other comorbidities. As the RADEO Guide states: “Before starting opioid therapy, either in surgical or non-surgical settings, it is important to identify any real or potential risks of respiratory depression or other opioid-related adverse effects. Patient comorbidities such as OSA, neurologic disorders, organ impairment, substance abuse history, and other medication use are important aspects to consider.”
Although we have clearly recognized a significant increase in respiratory complications associated with opioid administration, there are other areas, which are non–opioid related, that can create respiratory compromise. We view many patients with stable or underlying respiratory conditions, whether it be COPD, sleep apnea, or preexisting pathophysiology, where either due to sedative agents, or an acute illness – like pneumonia – they can go from a stable condition to respiratory compromise and become at risk for respiratory failure.
A classic example of that in my world of anesthesia has been the well-recognized area of non–operating room anesthesia – in particular, in endoscopy suites where numerous endoscopy procedures are performed under the administration of propofol or other anxiolytic-like drugs. There has been a well-recognized incidence of sentinel events related to oxygenation and ventilation, including death.
Many clinicians see sedation as a benign introduction of relatively limited-effect drugs, which isn’t always true. So, therefore, it is essential that clinicians understand three things:
1. The drugs we employ as sedative agents can have variable effects on individuals depending on their tolerance and their underlying medical condition.
2. The dosages and particular combination of drugs employed may cause an adverse event – for example, the combination of opioids and benzodiazepines.
3. There are factors that can distract from the clinical assessment of routine vital signs, such as respiratory rate, heart rate, and blood pressure. For example, when pulse oximetry is administered with oxygen therapy, there can often be a delay in the recognition of hypoventilation. Consequently, that’s why more and more clinicians are beginning to utilize capnography, or CO2 monitoring, in the expired gas to earlier detect depressed respiratory rate and/or apnea, as well as signs of hypoventilation or inadequate ventilation.
There clearly are obstacles to continuous patient monitoring, such as the associated cost, familiarity with the utilization, the benefit, as well as the limitations of specific monitors in different clinical situations, which mandates an educational process to employ these. However, currently, patient monitoring provides the best early indicator of a patient’s deterioration and the possibility of respiratory compromise.
In my field, we have become very comfortable with capnography and patient monitoring, because for decades it’s been a standard of care for monitoring in the operating room. The role for utilization of capnography for patients who are receiving an opioid or sedative agent outside of the operating room needs to be further assessed. However, technology is not a silver bullet and should be used as an adjunct to clinical judgment in at-risk populations.
Simple recognition and greater awareness of respiratory compromise, just as with sepsis awareness campaigns, will mean more patients are diagnosed earlier, more appropriate interventions are made, and hopefully more adverse events and patient deaths are averted.
Dr. Vender is the emeritus Harris Family Foundation chairman of the department of anesthesiology at NorthShore University Health System in Evanston, Ill. He is clinical professor at the University of Chicago Pritzker School of Medicine and chairman, Clinical Advisory Committee, Respiratory Compromise Institute. Dr. Vender has consulted with Medtronic.
Full-dose quadrivalent flu vaccine shows increased efficacy in children
according to data from a randomized trial of nearly 2,000 children aged 6-35 months.
Data from previous studies have suggested that a full dose of vaccine may be more immunogenic in young children compared with a half dose, and Sanofi Pasteur has submitted a supplemental Biologics License Application to the Food and Drug Administration to allow use of the full 0.5-mL dose in children as young as 6 months, Monica Mercer, MD, of Sanofi Pasteur, said at a meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices in Atlanta.
Dr. Mercer presented findings from a phase IV randomized, observer-blinded study, in which the researchers assigned healthy children aged 6-35 months to receive Fluzone quadrivalent vaccine at a dose of 0.25 mL or 0.5 mL.
A total of 1,941 children (949 for the 0.25-mL dose and 992 for the 0.5-mL dose) were included in the safety analysis.
The most important safety outcome was to compare the rate of any fever, Dr. Mercer said at the meeting.
Overall, at 7 days after vaccination, the rate of fever was 11% for the half dose and 12% for the full dose, she said. The resulting difference of 0.84% met the criteria for noninferiority (less than 5%), she added.
In terms of safety, tenderness was the most frequently reported injection site reaction, noted in 47% of the half-dose group and 50% of the full-dose group. The rates of unsolicited adverse events were similar in both groups, the most common included diarrhea and cough, Dr. Mercer said.
No subjects in the full-dose group and three in the half-dose group discontinued the study because of adverse events. The only reported serious adverse event was one case of chronic urticaria in the half-dose group; no deaths were reported in either group.
As for efficacy, the full dose demonstrated noninferiority, compared with the half dose, against each of four strains: influenza A H1N1, influenza A H3N2, influenza B Victoria, and influenza B Yamagata. The geometric mean titers of the full and half doses for each of the four strains were, respectively, 310 and 214, 332 and 221, 348 and 261, and 349 and 243.
The potential action date for the supplemental Biologics License Application is January 2019, noted Dr. Mercer, who is employed by Sanofi Pasteur.
according to data from a randomized trial of nearly 2,000 children aged 6-35 months.
Data from previous studies have suggested that a full dose of vaccine may be more immunogenic in young children compared with a half dose, and Sanofi Pasteur has submitted a supplemental Biologics License Application to the Food and Drug Administration to allow use of the full 0.5-mL dose in children as young as 6 months, Monica Mercer, MD, of Sanofi Pasteur, said at a meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices in Atlanta.
Dr. Mercer presented findings from a phase IV randomized, observer-blinded study, in which the researchers assigned healthy children aged 6-35 months to receive Fluzone quadrivalent vaccine at a dose of 0.25 mL or 0.5 mL.
A total of 1,941 children (949 for the 0.25-mL dose and 992 for the 0.5-mL dose) were included in the safety analysis.
The most important safety outcome was to compare the rate of any fever, Dr. Mercer said at the meeting.
Overall, at 7 days after vaccination, the rate of fever was 11% for the half dose and 12% for the full dose, she said. The resulting difference of 0.84% met the criteria for noninferiority (less than 5%), she added.
In terms of safety, tenderness was the most frequently reported injection site reaction, noted in 47% of the half-dose group and 50% of the full-dose group. The rates of unsolicited adverse events were similar in both groups, the most common included diarrhea and cough, Dr. Mercer said.
No subjects in the full-dose group and three in the half-dose group discontinued the study because of adverse events. The only reported serious adverse event was one case of chronic urticaria in the half-dose group; no deaths were reported in either group.
As for efficacy, the full dose demonstrated noninferiority, compared with the half dose, against each of four strains: influenza A H1N1, influenza A H3N2, influenza B Victoria, and influenza B Yamagata. The geometric mean titers of the full and half doses for each of the four strains were, respectively, 310 and 214, 332 and 221, 348 and 261, and 349 and 243.
The potential action date for the supplemental Biologics License Application is January 2019, noted Dr. Mercer, who is employed by Sanofi Pasteur.
according to data from a randomized trial of nearly 2,000 children aged 6-35 months.
Data from previous studies have suggested that a full dose of vaccine may be more immunogenic in young children compared with a half dose, and Sanofi Pasteur has submitted a supplemental Biologics License Application to the Food and Drug Administration to allow use of the full 0.5-mL dose in children as young as 6 months, Monica Mercer, MD, of Sanofi Pasteur, said at a meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices in Atlanta.
Dr. Mercer presented findings from a phase IV randomized, observer-blinded study, in which the researchers assigned healthy children aged 6-35 months to receive Fluzone quadrivalent vaccine at a dose of 0.25 mL or 0.5 mL.
A total of 1,941 children (949 for the 0.25-mL dose and 992 for the 0.5-mL dose) were included in the safety analysis.
The most important safety outcome was to compare the rate of any fever, Dr. Mercer said at the meeting.
Overall, at 7 days after vaccination, the rate of fever was 11% for the half dose and 12% for the full dose, she said. The resulting difference of 0.84% met the criteria for noninferiority (less than 5%), she added.
In terms of safety, tenderness was the most frequently reported injection site reaction, noted in 47% of the half-dose group and 50% of the full-dose group. The rates of unsolicited adverse events were similar in both groups, the most common included diarrhea and cough, Dr. Mercer said.
No subjects in the full-dose group and three in the half-dose group discontinued the study because of adverse events. The only reported serious adverse event was one case of chronic urticaria in the half-dose group; no deaths were reported in either group.
As for efficacy, the full dose demonstrated noninferiority, compared with the half dose, against each of four strains: influenza A H1N1, influenza A H3N2, influenza B Victoria, and influenza B Yamagata. The geometric mean titers of the full and half doses for each of the four strains were, respectively, 310 and 214, 332 and 221, 348 and 261, and 349 and 243.
The potential action date for the supplemental Biologics License Application is January 2019, noted Dr. Mercer, who is employed by Sanofi Pasteur.
REPORTING FROM AN ACIP MEETING