User login
Flu or strep? Rapid tests can mislead
A 62-year-old woman presented to our emergency department with fever, chills, hoarseness, pain on swallowing, and a painful neck. Her symptoms had begun 1 day earlier. Because acetaminophen brought no improvement, she went to an urgent care facility, where a nasal swab polymerase chain reaction test was positive for influenza A, and a throat swab rapid test was positive for group A streptococci. She was then referred to our emergency department.
She reported no pre-existing conditions predisposing her to infection. Her temperature was 99.9°F (37.7°C), pulse 112 beats per minute, and respiratory rate 24 breaths per minute. The physical examination was unremarkable except for bilateral anterior cervical adenopathy and bilateral anterior neck tenderness. Her pharynx was not injected, and no exudate, palatal edema, or petechiae were noted.
Results of initial laboratory testing were as follows:
- White blood cell count 20.5 × 109/L (reference range 3.9–11)
- Neutrophils 76% (42%–75%)
- Bands 15% (0%–5%)
- Lymphocytes 3% (21%–51%)
- Erythrocyte sedimentation rate 75 mm/h (< 20 mm/h)
- C-reactive protein 247.14 mg/L (≤ 3 mg/L)
- Serum aminotransferase levels were normal.
- Polymerase chain reaction testing of a nasal swab was negative for viral infection.
Throat swabs and blood samples were sent for culture.
She was started on ceftriaxone 1 g intravenously every 24 hours, with close observation in the medical intensive care unit, where she was admitted because of epiglottitis. On hospital day 3, the throat culture was reported as negative, but the blood culture was reported as positive for Haemophilus influenzae. Thus, the clinical diagnosis was acute epiglottitis due to H influenzae, not group A streptococci.
The patient completed 10 days of ceftriaxone therapy; her recovery was uneventful, and she was discharged on hospital day 10.
INFLUENZA: CHALLENGES TO PROMPT, ACCURATE DIAGNOSIS
During influenza season, emergency departments are inundated with adults with influenza A and other viral respiratory infections. This makes prompt, accurate diagnosis a challenge,1 given the broad differential diagnosis.2,3 Adults with influenza and its complications as well as unrelated conditions can present a special challenge.4
Our patient presented with acute-onset influenza A and was then found to have acute epiglottitis, an unexpected complication of influenza A.5 A positive rapid test for group A streptococci done at an urgent care facility led emergency department physicians to assume that the acute epiglottitis was due to group A streptococci. Unless correlated with clinical findings, results of rapid diagnostic tests may mislead the unwary practitioner. Accurate diagnosis should be based mainly on the history and physical findings. Results of rapid diagnostic tests can be helpful if interpreted in the clinical context.6–8
The rapid test for streptococci is appropriate for the diagnosis of pharyngitis due to group A streptococci in people under age 30 with acute-onset sore throat, fever, and bilateral acute cervical adenopathy, without fatigue or myalgias. However, the rapid test does not differentiate colonization from infection. Group A streptococci are common colonizers with viral pharyngitis. In 30% of cases of Epstein-Barr virus pharyngitis, there is colonization with group A streptococci. A positive rapid test in such cases can result in the wrong diagnosis, ie, pharyngitis due to group A streptococci rather than Epstein-Barr virus.
- Cunha BA. The clinical diagnosis of severe viral influenza A. Infection 2008; 36(1):92–93. doi:10.1007/s15010-007-7255-9
- Cunha BA, Klein NC, Strollo S, Syed U, Mickail N, Laguerre M. Legionnaires’ disease mimicking swine influenza (H1N1) pneumonia during the “herald wave” of the pandemic. Heart Lung 2010; 39(3):242–248. doi:10.1016/j.hrtlng.2009.10.009
- Cunha BA, Raza M. During influenza season: all influenza-like illnesses are not due to influenza: dengue mimicking influenza. J Emerg Med 2015; 48(5):e117–e120. doi:10.1016/j.jemermed.2014.12.051
- Cunha CB. Infectious disease differential diagnosis. In: Cunha CB, Cunha BA, eds. Antibiotic Essentials. Jaypee Brothers Medical Pub: New Delhi, India; 2017:493–526.
- Cunha BA. Pharyngitis. In: Cunha CB, Cunha BA, eds. Antibiotic Essentials. Jaypee Brothers Medical Pub: New Delhi, India; 2017:42–47.
- Cohen JF, Chalumeau M, Levy C, et al. Effect of clinical spectrum, inoculum size and physician characteristics on sensitivity of rapid antigen detection test for group A streptococcal pharyngitis. Eur J Clin Microbiol Infect Dis 2013; 32(6):787–793. doi:10.1007/s10096-012-1809-1
- Dimatteo LA, Lowenstein SR, Brimhall B, Reiquam W, Gonzales R. The relationship between the clinical features of pharyngitis and the sensitivity of a rapid antigen test: evidence of spectrum bias. Ann Emerg Med 2001; 38(6):648–652. doi:10.1067/mem.2001.119850
- Cunha BA. A positive rapid strep test in a young adult with acute pharyngitis: be careful what you wish for! IDCases 2017; 10:58–59. doi:10.1016/j.idcr.2017.08.012
A 62-year-old woman presented to our emergency department with fever, chills, hoarseness, pain on swallowing, and a painful neck. Her symptoms had begun 1 day earlier. Because acetaminophen brought no improvement, she went to an urgent care facility, where a nasal swab polymerase chain reaction test was positive for influenza A, and a throat swab rapid test was positive for group A streptococci. She was then referred to our emergency department.
She reported no pre-existing conditions predisposing her to infection. Her temperature was 99.9°F (37.7°C), pulse 112 beats per minute, and respiratory rate 24 breaths per minute. The physical examination was unremarkable except for bilateral anterior cervical adenopathy and bilateral anterior neck tenderness. Her pharynx was not injected, and no exudate, palatal edema, or petechiae were noted.
Results of initial laboratory testing were as follows:
- White blood cell count 20.5 × 109/L (reference range 3.9–11)
- Neutrophils 76% (42%–75%)
- Bands 15% (0%–5%)
- Lymphocytes 3% (21%–51%)
- Erythrocyte sedimentation rate 75 mm/h (< 20 mm/h)
- C-reactive protein 247.14 mg/L (≤ 3 mg/L)
- Serum aminotransferase levels were normal.
- Polymerase chain reaction testing of a nasal swab was negative for viral infection.
Throat swabs and blood samples were sent for culture.
She was started on ceftriaxone 1 g intravenously every 24 hours, with close observation in the medical intensive care unit, where she was admitted because of epiglottitis. On hospital day 3, the throat culture was reported as negative, but the blood culture was reported as positive for Haemophilus influenzae. Thus, the clinical diagnosis was acute epiglottitis due to H influenzae, not group A streptococci.
The patient completed 10 days of ceftriaxone therapy; her recovery was uneventful, and she was discharged on hospital day 10.
INFLUENZA: CHALLENGES TO PROMPT, ACCURATE DIAGNOSIS
During influenza season, emergency departments are inundated with adults with influenza A and other viral respiratory infections. This makes prompt, accurate diagnosis a challenge,1 given the broad differential diagnosis.2,3 Adults with influenza and its complications as well as unrelated conditions can present a special challenge.4
Our patient presented with acute-onset influenza A and was then found to have acute epiglottitis, an unexpected complication of influenza A.5 A positive rapid test for group A streptococci done at an urgent care facility led emergency department physicians to assume that the acute epiglottitis was due to group A streptococci. Unless correlated with clinical findings, results of rapid diagnostic tests may mislead the unwary practitioner. Accurate diagnosis should be based mainly on the history and physical findings. Results of rapid diagnostic tests can be helpful if interpreted in the clinical context.6–8
The rapid test for streptococci is appropriate for the diagnosis of pharyngitis due to group A streptococci in people under age 30 with acute-onset sore throat, fever, and bilateral acute cervical adenopathy, without fatigue or myalgias. However, the rapid test does not differentiate colonization from infection. Group A streptococci are common colonizers with viral pharyngitis. In 30% of cases of Epstein-Barr virus pharyngitis, there is colonization with group A streptococci. A positive rapid test in such cases can result in the wrong diagnosis, ie, pharyngitis due to group A streptococci rather than Epstein-Barr virus.
A 62-year-old woman presented to our emergency department with fever, chills, hoarseness, pain on swallowing, and a painful neck. Her symptoms had begun 1 day earlier. Because acetaminophen brought no improvement, she went to an urgent care facility, where a nasal swab polymerase chain reaction test was positive for influenza A, and a throat swab rapid test was positive for group A streptococci. She was then referred to our emergency department.
She reported no pre-existing conditions predisposing her to infection. Her temperature was 99.9°F (37.7°C), pulse 112 beats per minute, and respiratory rate 24 breaths per minute. The physical examination was unremarkable except for bilateral anterior cervical adenopathy and bilateral anterior neck tenderness. Her pharynx was not injected, and no exudate, palatal edema, or petechiae were noted.
Results of initial laboratory testing were as follows:
- White blood cell count 20.5 × 109/L (reference range 3.9–11)
- Neutrophils 76% (42%–75%)
- Bands 15% (0%–5%)
- Lymphocytes 3% (21%–51%)
- Erythrocyte sedimentation rate 75 mm/h (< 20 mm/h)
- C-reactive protein 247.14 mg/L (≤ 3 mg/L)
- Serum aminotransferase levels were normal.
- Polymerase chain reaction testing of a nasal swab was negative for viral infection.
Throat swabs and blood samples were sent for culture.
She was started on ceftriaxone 1 g intravenously every 24 hours, with close observation in the medical intensive care unit, where she was admitted because of epiglottitis. On hospital day 3, the throat culture was reported as negative, but the blood culture was reported as positive for Haemophilus influenzae. Thus, the clinical diagnosis was acute epiglottitis due to H influenzae, not group A streptococci.
The patient completed 10 days of ceftriaxone therapy; her recovery was uneventful, and she was discharged on hospital day 10.
INFLUENZA: CHALLENGES TO PROMPT, ACCURATE DIAGNOSIS
During influenza season, emergency departments are inundated with adults with influenza A and other viral respiratory infections. This makes prompt, accurate diagnosis a challenge,1 given the broad differential diagnosis.2,3 Adults with influenza and its complications as well as unrelated conditions can present a special challenge.4
Our patient presented with acute-onset influenza A and was then found to have acute epiglottitis, an unexpected complication of influenza A.5 A positive rapid test for group A streptococci done at an urgent care facility led emergency department physicians to assume that the acute epiglottitis was due to group A streptococci. Unless correlated with clinical findings, results of rapid diagnostic tests may mislead the unwary practitioner. Accurate diagnosis should be based mainly on the history and physical findings. Results of rapid diagnostic tests can be helpful if interpreted in the clinical context.6–8
The rapid test for streptococci is appropriate for the diagnosis of pharyngitis due to group A streptococci in people under age 30 with acute-onset sore throat, fever, and bilateral acute cervical adenopathy, without fatigue or myalgias. However, the rapid test does not differentiate colonization from infection. Group A streptococci are common colonizers with viral pharyngitis. In 30% of cases of Epstein-Barr virus pharyngitis, there is colonization with group A streptococci. A positive rapid test in such cases can result in the wrong diagnosis, ie, pharyngitis due to group A streptococci rather than Epstein-Barr virus.
- Cunha BA. The clinical diagnosis of severe viral influenza A. Infection 2008; 36(1):92–93. doi:10.1007/s15010-007-7255-9
- Cunha BA, Klein NC, Strollo S, Syed U, Mickail N, Laguerre M. Legionnaires’ disease mimicking swine influenza (H1N1) pneumonia during the “herald wave” of the pandemic. Heart Lung 2010; 39(3):242–248. doi:10.1016/j.hrtlng.2009.10.009
- Cunha BA, Raza M. During influenza season: all influenza-like illnesses are not due to influenza: dengue mimicking influenza. J Emerg Med 2015; 48(5):e117–e120. doi:10.1016/j.jemermed.2014.12.051
- Cunha CB. Infectious disease differential diagnosis. In: Cunha CB, Cunha BA, eds. Antibiotic Essentials. Jaypee Brothers Medical Pub: New Delhi, India; 2017:493–526.
- Cunha BA. Pharyngitis. In: Cunha CB, Cunha BA, eds. Antibiotic Essentials. Jaypee Brothers Medical Pub: New Delhi, India; 2017:42–47.
- Cohen JF, Chalumeau M, Levy C, et al. Effect of clinical spectrum, inoculum size and physician characteristics on sensitivity of rapid antigen detection test for group A streptococcal pharyngitis. Eur J Clin Microbiol Infect Dis 2013; 32(6):787–793. doi:10.1007/s10096-012-1809-1
- Dimatteo LA, Lowenstein SR, Brimhall B, Reiquam W, Gonzales R. The relationship between the clinical features of pharyngitis and the sensitivity of a rapid antigen test: evidence of spectrum bias. Ann Emerg Med 2001; 38(6):648–652. doi:10.1067/mem.2001.119850
- Cunha BA. A positive rapid strep test in a young adult with acute pharyngitis: be careful what you wish for! IDCases 2017; 10:58–59. doi:10.1016/j.idcr.2017.08.012
- Cunha BA. The clinical diagnosis of severe viral influenza A. Infection 2008; 36(1):92–93. doi:10.1007/s15010-007-7255-9
- Cunha BA, Klein NC, Strollo S, Syed U, Mickail N, Laguerre M. Legionnaires’ disease mimicking swine influenza (H1N1) pneumonia during the “herald wave” of the pandemic. Heart Lung 2010; 39(3):242–248. doi:10.1016/j.hrtlng.2009.10.009
- Cunha BA, Raza M. During influenza season: all influenza-like illnesses are not due to influenza: dengue mimicking influenza. J Emerg Med 2015; 48(5):e117–e120. doi:10.1016/j.jemermed.2014.12.051
- Cunha CB. Infectious disease differential diagnosis. In: Cunha CB, Cunha BA, eds. Antibiotic Essentials. Jaypee Brothers Medical Pub: New Delhi, India; 2017:493–526.
- Cunha BA. Pharyngitis. In: Cunha CB, Cunha BA, eds. Antibiotic Essentials. Jaypee Brothers Medical Pub: New Delhi, India; 2017:42–47.
- Cohen JF, Chalumeau M, Levy C, et al. Effect of clinical spectrum, inoculum size and physician characteristics on sensitivity of rapid antigen detection test for group A streptococcal pharyngitis. Eur J Clin Microbiol Infect Dis 2013; 32(6):787–793. doi:10.1007/s10096-012-1809-1
- Dimatteo LA, Lowenstein SR, Brimhall B, Reiquam W, Gonzales R. The relationship between the clinical features of pharyngitis and the sensitivity of a rapid antigen test: evidence of spectrum bias. Ann Emerg Med 2001; 38(6):648–652. doi:10.1067/mem.2001.119850
- Cunha BA. A positive rapid strep test in a young adult with acute pharyngitis: be careful what you wish for! IDCases 2017; 10:58–59. doi:10.1016/j.idcr.2017.08.012
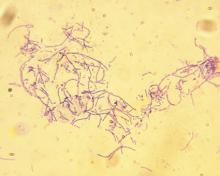
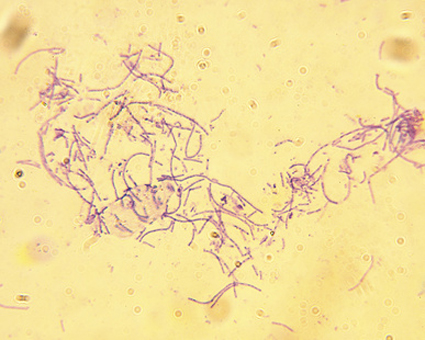
Norwegian scabies
DIAGNOSIS, TREATMENT, CONTROL
The differential diagnosis of Norwegian scabies includes psoriasis, eczema, contact dermatitis, insect bites, seborrheic dermatitis, lichen planus, systemic infection, palmoplantar keratoderma, and cutaneous lymphoma.2
Treatment involves eradicating the infestation with a topical ointment consisting of permethrin, crotamiton, lindane, benzyl benzoate, and sulfur, applied directly to the skin. However, topical treatments often cannot penetrate the crusted and thickened skin, leading to treatment failure. A dose of oral ivermectin 200 µg/kg on days 1, 2, and 8 is a safe, effective, first-line treatment for Norwegian scabies, rapidly reducing scabies symptoms.3 Adverse effects of oral ivermectin are rare and usually minor.
Norwegian scabies is extremely contagious, spread by close physical contact and sharing of contaminated items such as clothing, bedding, towels, and furniture. Scabies mites can survive off the skin for 48 to 72 hours at room temperature.4 Potentially contaminated items should be decontaminated by washing in hot water and drying in a drying machine or by dry cleaning. Body contact with other contaminated items should be avoided for at least 72 hours.
Outbreaks can spread among patients, visitors, and medical staff in institutions such as nursing homes, day care centers, long-term-care facilities, and hospitals.5 Early identification facilitates appropriate management and treatment, thereby preventing infection and community-wide scabies outbreaks.
Acknowledgment: The authors would like to sincerely thank Paul Williams for his editing of the article.
- Leone PA. Scabies and pediculosis pubis: an update of treatment regimens and general review. Clin Infect Dis 2007; 44(suppl 3):S153–S159. doi:10.1086/511428
- Siegfried EC, Hebert AA. Diagnosis of atopic dermatitis: mimics, overlaps, and complications. J Clin Med 2015; 4(5):884–917. doi:10.3390/jcm4050884
- Salavastru CM, Chosidow O, Boffa MJ, Janier M, Tiplica GS. European guideline for the management of scabies. J Eur Acad Dermatol Venereol 2017; 31(8):1248–1253. doi:10.1111/jdv.14351
- Khalil S, Abbas O, Kibbi AG, Kurban M. Scabies in the age of increasing drug resistance. PLoS Negl Trop Dis 2017; 11(11):e0005920. doi:10.1371/journal.pntd.0005920
- Anderson KL, Strowd LC. Epidemiology, diagnosis, and treatment of scabies in a dermatology office. J Am Board Fam Med 2017; 30(1):78–84. doi:10.3122/jabfm.2017.01.160190
DIAGNOSIS, TREATMENT, CONTROL
The differential diagnosis of Norwegian scabies includes psoriasis, eczema, contact dermatitis, insect bites, seborrheic dermatitis, lichen planus, systemic infection, palmoplantar keratoderma, and cutaneous lymphoma.2
Treatment involves eradicating the infestation with a topical ointment consisting of permethrin, crotamiton, lindane, benzyl benzoate, and sulfur, applied directly to the skin. However, topical treatments often cannot penetrate the crusted and thickened skin, leading to treatment failure. A dose of oral ivermectin 200 µg/kg on days 1, 2, and 8 is a safe, effective, first-line treatment for Norwegian scabies, rapidly reducing scabies symptoms.3 Adverse effects of oral ivermectin are rare and usually minor.
Norwegian scabies is extremely contagious, spread by close physical contact and sharing of contaminated items such as clothing, bedding, towels, and furniture. Scabies mites can survive off the skin for 48 to 72 hours at room temperature.4 Potentially contaminated items should be decontaminated by washing in hot water and drying in a drying machine or by dry cleaning. Body contact with other contaminated items should be avoided for at least 72 hours.
Outbreaks can spread among patients, visitors, and medical staff in institutions such as nursing homes, day care centers, long-term-care facilities, and hospitals.5 Early identification facilitates appropriate management and treatment, thereby preventing infection and community-wide scabies outbreaks.
Acknowledgment: The authors would like to sincerely thank Paul Williams for his editing of the article.
DIAGNOSIS, TREATMENT, CONTROL
The differential diagnosis of Norwegian scabies includes psoriasis, eczema, contact dermatitis, insect bites, seborrheic dermatitis, lichen planus, systemic infection, palmoplantar keratoderma, and cutaneous lymphoma.2
Treatment involves eradicating the infestation with a topical ointment consisting of permethrin, crotamiton, lindane, benzyl benzoate, and sulfur, applied directly to the skin. However, topical treatments often cannot penetrate the crusted and thickened skin, leading to treatment failure. A dose of oral ivermectin 200 µg/kg on days 1, 2, and 8 is a safe, effective, first-line treatment for Norwegian scabies, rapidly reducing scabies symptoms.3 Adverse effects of oral ivermectin are rare and usually minor.
Norwegian scabies is extremely contagious, spread by close physical contact and sharing of contaminated items such as clothing, bedding, towels, and furniture. Scabies mites can survive off the skin for 48 to 72 hours at room temperature.4 Potentially contaminated items should be decontaminated by washing in hot water and drying in a drying machine or by dry cleaning. Body contact with other contaminated items should be avoided for at least 72 hours.
Outbreaks can spread among patients, visitors, and medical staff in institutions such as nursing homes, day care centers, long-term-care facilities, and hospitals.5 Early identification facilitates appropriate management and treatment, thereby preventing infection and community-wide scabies outbreaks.
Acknowledgment: The authors would like to sincerely thank Paul Williams for his editing of the article.
- Leone PA. Scabies and pediculosis pubis: an update of treatment regimens and general review. Clin Infect Dis 2007; 44(suppl 3):S153–S159. doi:10.1086/511428
- Siegfried EC, Hebert AA. Diagnosis of atopic dermatitis: mimics, overlaps, and complications. J Clin Med 2015; 4(5):884–917. doi:10.3390/jcm4050884
- Salavastru CM, Chosidow O, Boffa MJ, Janier M, Tiplica GS. European guideline for the management of scabies. J Eur Acad Dermatol Venereol 2017; 31(8):1248–1253. doi:10.1111/jdv.14351
- Khalil S, Abbas O, Kibbi AG, Kurban M. Scabies in the age of increasing drug resistance. PLoS Negl Trop Dis 2017; 11(11):e0005920. doi:10.1371/journal.pntd.0005920
- Anderson KL, Strowd LC. Epidemiology, diagnosis, and treatment of scabies in a dermatology office. J Am Board Fam Med 2017; 30(1):78–84. doi:10.3122/jabfm.2017.01.160190
- Leone PA. Scabies and pediculosis pubis: an update of treatment regimens and general review. Clin Infect Dis 2007; 44(suppl 3):S153–S159. doi:10.1086/511428
- Siegfried EC, Hebert AA. Diagnosis of atopic dermatitis: mimics, overlaps, and complications. J Clin Med 2015; 4(5):884–917. doi:10.3390/jcm4050884
- Salavastru CM, Chosidow O, Boffa MJ, Janier M, Tiplica GS. European guideline for the management of scabies. J Eur Acad Dermatol Venereol 2017; 31(8):1248–1253. doi:10.1111/jdv.14351
- Khalil S, Abbas O, Kibbi AG, Kurban M. Scabies in the age of increasing drug resistance. PLoS Negl Trop Dis 2017; 11(11):e0005920. doi:10.1371/journal.pntd.0005920
- Anderson KL, Strowd LC. Epidemiology, diagnosis, and treatment of scabies in a dermatology office. J Am Board Fam Med 2017; 30(1):78–84. doi:10.3122/jabfm.2017.01.160190
Delaying antibiotics in elderly with UTI linked to higher sepsis, death rates
results of a large, population-based study suggest.
The risk of bloodstream infection was more than seven times greater in patients who did not receive antibiotics immediately after seeing a general practitioner for a UTI versus those who did, according to results of the study based on primary care records and other data for nearly 160,000 U.K. patients aged 65 years or older. Death rates and hospital admissions were significantly higher for these patients, according to the study published in The BMJ by Myriam Gharbi, PharmD, Phd, Imperial College London, and her colleagues.
The publication of these findings coincides with an increase in Escherichia coli bloodstream infections in England.
“Our study suggests the early initiation of antibiotics for UTI in older high risk adult populations (especially men aged [older than] 85 years) should be recommended to prevent serious complications,” Dr. Gharbi and her coauthors said in their report.
The population-based cohort study comprised 157,264 adult primary care patients at least 65 years of age who had one or more suspected or confirmed lower UTIs from November 2007 to May 2015. The researchers found that health care providers had diagnosed a total of 312,896 UTI episodes in these patients during the period they studied. In 7.2% (22,534) of the UTI episodes, the researchers were unable to find records of the patients having been prescribed antibiotics by a general practitioner within 7 days of the UTI diagnosis. These 22,534 episodes included those that occurred in patients who had a complication before an antibiotic was prescribed. An additional 6.2% (19,292) of the episodes occurred in patients who were prescribed antibiotics, but not during their first UTI-related visit to a general practitioner or on the same day of such a visit. The researchers classified this group of patients as having been prescribed antibiotics on a deferred or delayed basis, as they were not prescribed such drugs within 7 days of their visit.
Overall, there were 1,539 cases (0.5% of the total number of UTIs) of bloodstream infection within 60 days of the initial urinary tract infection diagnosis, the researchers reported.
The bloodstream infection rate was 2.9% for patients who were not prescribed antibiotics ever or prior to an infection occurring, 2.2% in those who were prescribed antibiotics on a deferred basis, and 0.2% in those who were prescribed antibiotics immediately, meaning during their first visit to a general practitioner for a UTI or on the same day of such a visit (P less than .001). After adjustment for potential confounding variables such as age, sex, and region, the patients classified as having not been prescribed antibiotics or having been prescribed antibiotics on a deferred basis were significantly more likely to have a bloodstream infection within 60 days of their visit to a health care provider, compared with those who received antibiotics immediately, with odds ratios of 8.08 (95% confidence interval, 7.12-9.16) and 7.12 (95% CI, 6.22-8.14), respectively.
Hospital admissions after a UTI episode were nearly twice as high in the no- or deferred-antibiotics groups (27.0% and 26.8%, respectively), compared with the group that received antibiotics right away (14.8%), the investigators reported. The lengths of hospital stays were 12.1 days for the group classified as having not been prescribed antibiotics, 7.7 days for the group subject to delayed antibiotic prescribing, and 6.3 days for the group who received antibiotics immediately.
Deaths within 60 days of experiencing a urinary tract infection occurred in 5.4% of patients in the no-antibiotics group, 2.8% of the deferred-antibiotics group, and 1.6% of the immediate-antibiotics group. After adjustment for covariates, a regression analysis showed the risks for all-cause mortality were 1.16 and 2.18 times higher in the deferred-antibiotics group and the no-antibiotics group, respectively, according to the paper.
In the immediate-antibiotics group, those patients who received nitrofurantoin had a “small but significant increase” in 60-day survival versus those who received trimethoprim, the investigators noted in the discussion section of their report.
“This increase could reflect either higher levels of resistance to trimethoprim or a healthier population treated with nitrofurantoin, the latest being not recommended for patients with poor kidney function,” the researchers wrote.
This study was supported by the National Institute for Health Research and other U.K. sources. One study coauthor reported working as an epidemiologist with GSK in areas not related to the study.
SOURCE: Gharbi M et al. BMJ. 2019 Feb 27. doi: 10.1136/bmj.l525.
This study linking primary care prescribing to serious infections in elderly patients with urinary tract infections is timely, as rates of bloodstream infection and mortality are increasing in this age group, according to Alastair D. Hay, MB.ChB, a professor at University of Bristol, England.
“Prompt treatment should be offered to older patients, men (who are at higher risk than women), and those living in areas of greater socioeconomic deprivation who are at the highest risk of bloodstream infections,” Dr. Hay said in an editorial accompanying the report by Gharbi et al.
That said, the link between prescribing and infection in this particular study may not be causal: “The implications are likely to be more nuanced than primary care doctors risking the health of older adults to meet targets for antimicrobial stewardship,” Dr. Hay noted.
Doctors are cautious when managing infections in vulnerable groups, evidence shows, and the deferred prescribing reported in this study is likely not the same as the delayed prescribing seen in primary care, he explained.
“Most clinicians issue a prescription on the day of presentation, with verbal advice to delay treatment, rather than waiting for a patient to return or issuing a postdated prescription,” he said. “The group given immediate antibiotics in the study by Gharbi and colleagues likely contained some patients managed in this way.”
Patients who apparently had no prescription in this retrospective analysis may have had a same-day admission with a bloodstream infection; moreover, a number of bloodstream infections in older people are due to urinary tract bacteria, and so would not be prevented by treatment for urinary tract infection, Dr. Hay said.
“Further research is needed to establish whether treatment should be initiated with a broad or a narrow spectrum antibiotic and to identify those in whom delaying treatment (while awaiting investigation) is safe,” he concluded.
Dr. Hay is a professor in the Centre for Academic Primary Care, University of Bristol, England. His editorial appears in The BMJ (2019 Feb 27. doi: 10.1136/bmj.l780). Dr. Hay declared that he is a member of the managing common infections guideline committee for the National Institute for Health and Care Excellence (NICE).
This study linking primary care prescribing to serious infections in elderly patients with urinary tract infections is timely, as rates of bloodstream infection and mortality are increasing in this age group, according to Alastair D. Hay, MB.ChB, a professor at University of Bristol, England.
“Prompt treatment should be offered to older patients, men (who are at higher risk than women), and those living in areas of greater socioeconomic deprivation who are at the highest risk of bloodstream infections,” Dr. Hay said in an editorial accompanying the report by Gharbi et al.
That said, the link between prescribing and infection in this particular study may not be causal: “The implications are likely to be more nuanced than primary care doctors risking the health of older adults to meet targets for antimicrobial stewardship,” Dr. Hay noted.
Doctors are cautious when managing infections in vulnerable groups, evidence shows, and the deferred prescribing reported in this study is likely not the same as the delayed prescribing seen in primary care, he explained.
“Most clinicians issue a prescription on the day of presentation, with verbal advice to delay treatment, rather than waiting for a patient to return or issuing a postdated prescription,” he said. “The group given immediate antibiotics in the study by Gharbi and colleagues likely contained some patients managed in this way.”
Patients who apparently had no prescription in this retrospective analysis may have had a same-day admission with a bloodstream infection; moreover, a number of bloodstream infections in older people are due to urinary tract bacteria, and so would not be prevented by treatment for urinary tract infection, Dr. Hay said.
“Further research is needed to establish whether treatment should be initiated with a broad or a narrow spectrum antibiotic and to identify those in whom delaying treatment (while awaiting investigation) is safe,” he concluded.
Dr. Hay is a professor in the Centre for Academic Primary Care, University of Bristol, England. His editorial appears in The BMJ (2019 Feb 27. doi: 10.1136/bmj.l780). Dr. Hay declared that he is a member of the managing common infections guideline committee for the National Institute for Health and Care Excellence (NICE).
This study linking primary care prescribing to serious infections in elderly patients with urinary tract infections is timely, as rates of bloodstream infection and mortality are increasing in this age group, according to Alastair D. Hay, MB.ChB, a professor at University of Bristol, England.
“Prompt treatment should be offered to older patients, men (who are at higher risk than women), and those living in areas of greater socioeconomic deprivation who are at the highest risk of bloodstream infections,” Dr. Hay said in an editorial accompanying the report by Gharbi et al.
That said, the link between prescribing and infection in this particular study may not be causal: “The implications are likely to be more nuanced than primary care doctors risking the health of older adults to meet targets for antimicrobial stewardship,” Dr. Hay noted.
Doctors are cautious when managing infections in vulnerable groups, evidence shows, and the deferred prescribing reported in this study is likely not the same as the delayed prescribing seen in primary care, he explained.
“Most clinicians issue a prescription on the day of presentation, with verbal advice to delay treatment, rather than waiting for a patient to return or issuing a postdated prescription,” he said. “The group given immediate antibiotics in the study by Gharbi and colleagues likely contained some patients managed in this way.”
Patients who apparently had no prescription in this retrospective analysis may have had a same-day admission with a bloodstream infection; moreover, a number of bloodstream infections in older people are due to urinary tract bacteria, and so would not be prevented by treatment for urinary tract infection, Dr. Hay said.
“Further research is needed to establish whether treatment should be initiated with a broad or a narrow spectrum antibiotic and to identify those in whom delaying treatment (while awaiting investigation) is safe,” he concluded.
Dr. Hay is a professor in the Centre for Academic Primary Care, University of Bristol, England. His editorial appears in The BMJ (2019 Feb 27. doi: 10.1136/bmj.l780). Dr. Hay declared that he is a member of the managing common infections guideline committee for the National Institute for Health and Care Excellence (NICE).
results of a large, population-based study suggest.
The risk of bloodstream infection was more than seven times greater in patients who did not receive antibiotics immediately after seeing a general practitioner for a UTI versus those who did, according to results of the study based on primary care records and other data for nearly 160,000 U.K. patients aged 65 years or older. Death rates and hospital admissions were significantly higher for these patients, according to the study published in The BMJ by Myriam Gharbi, PharmD, Phd, Imperial College London, and her colleagues.
The publication of these findings coincides with an increase in Escherichia coli bloodstream infections in England.
“Our study suggests the early initiation of antibiotics for UTI in older high risk adult populations (especially men aged [older than] 85 years) should be recommended to prevent serious complications,” Dr. Gharbi and her coauthors said in their report.
The population-based cohort study comprised 157,264 adult primary care patients at least 65 years of age who had one or more suspected or confirmed lower UTIs from November 2007 to May 2015. The researchers found that health care providers had diagnosed a total of 312,896 UTI episodes in these patients during the period they studied. In 7.2% (22,534) of the UTI episodes, the researchers were unable to find records of the patients having been prescribed antibiotics by a general practitioner within 7 days of the UTI diagnosis. These 22,534 episodes included those that occurred in patients who had a complication before an antibiotic was prescribed. An additional 6.2% (19,292) of the episodes occurred in patients who were prescribed antibiotics, but not during their first UTI-related visit to a general practitioner or on the same day of such a visit. The researchers classified this group of patients as having been prescribed antibiotics on a deferred or delayed basis, as they were not prescribed such drugs within 7 days of their visit.
Overall, there were 1,539 cases (0.5% of the total number of UTIs) of bloodstream infection within 60 days of the initial urinary tract infection diagnosis, the researchers reported.
The bloodstream infection rate was 2.9% for patients who were not prescribed antibiotics ever or prior to an infection occurring, 2.2% in those who were prescribed antibiotics on a deferred basis, and 0.2% in those who were prescribed antibiotics immediately, meaning during their first visit to a general practitioner for a UTI or on the same day of such a visit (P less than .001). After adjustment for potential confounding variables such as age, sex, and region, the patients classified as having not been prescribed antibiotics or having been prescribed antibiotics on a deferred basis were significantly more likely to have a bloodstream infection within 60 days of their visit to a health care provider, compared with those who received antibiotics immediately, with odds ratios of 8.08 (95% confidence interval, 7.12-9.16) and 7.12 (95% CI, 6.22-8.14), respectively.
Hospital admissions after a UTI episode were nearly twice as high in the no- or deferred-antibiotics groups (27.0% and 26.8%, respectively), compared with the group that received antibiotics right away (14.8%), the investigators reported. The lengths of hospital stays were 12.1 days for the group classified as having not been prescribed antibiotics, 7.7 days for the group subject to delayed antibiotic prescribing, and 6.3 days for the group who received antibiotics immediately.
Deaths within 60 days of experiencing a urinary tract infection occurred in 5.4% of patients in the no-antibiotics group, 2.8% of the deferred-antibiotics group, and 1.6% of the immediate-antibiotics group. After adjustment for covariates, a regression analysis showed the risks for all-cause mortality were 1.16 and 2.18 times higher in the deferred-antibiotics group and the no-antibiotics group, respectively, according to the paper.
In the immediate-antibiotics group, those patients who received nitrofurantoin had a “small but significant increase” in 60-day survival versus those who received trimethoprim, the investigators noted in the discussion section of their report.
“This increase could reflect either higher levels of resistance to trimethoprim or a healthier population treated with nitrofurantoin, the latest being not recommended for patients with poor kidney function,” the researchers wrote.
This study was supported by the National Institute for Health Research and other U.K. sources. One study coauthor reported working as an epidemiologist with GSK in areas not related to the study.
SOURCE: Gharbi M et al. BMJ. 2019 Feb 27. doi: 10.1136/bmj.l525.
results of a large, population-based study suggest.
The risk of bloodstream infection was more than seven times greater in patients who did not receive antibiotics immediately after seeing a general practitioner for a UTI versus those who did, according to results of the study based on primary care records and other data for nearly 160,000 U.K. patients aged 65 years or older. Death rates and hospital admissions were significantly higher for these patients, according to the study published in The BMJ by Myriam Gharbi, PharmD, Phd, Imperial College London, and her colleagues.
The publication of these findings coincides with an increase in Escherichia coli bloodstream infections in England.
“Our study suggests the early initiation of antibiotics for UTI in older high risk adult populations (especially men aged [older than] 85 years) should be recommended to prevent serious complications,” Dr. Gharbi and her coauthors said in their report.
The population-based cohort study comprised 157,264 adult primary care patients at least 65 years of age who had one or more suspected or confirmed lower UTIs from November 2007 to May 2015. The researchers found that health care providers had diagnosed a total of 312,896 UTI episodes in these patients during the period they studied. In 7.2% (22,534) of the UTI episodes, the researchers were unable to find records of the patients having been prescribed antibiotics by a general practitioner within 7 days of the UTI diagnosis. These 22,534 episodes included those that occurred in patients who had a complication before an antibiotic was prescribed. An additional 6.2% (19,292) of the episodes occurred in patients who were prescribed antibiotics, but not during their first UTI-related visit to a general practitioner or on the same day of such a visit. The researchers classified this group of patients as having been prescribed antibiotics on a deferred or delayed basis, as they were not prescribed such drugs within 7 days of their visit.
Overall, there were 1,539 cases (0.5% of the total number of UTIs) of bloodstream infection within 60 days of the initial urinary tract infection diagnosis, the researchers reported.
The bloodstream infection rate was 2.9% for patients who were not prescribed antibiotics ever or prior to an infection occurring, 2.2% in those who were prescribed antibiotics on a deferred basis, and 0.2% in those who were prescribed antibiotics immediately, meaning during their first visit to a general practitioner for a UTI or on the same day of such a visit (P less than .001). After adjustment for potential confounding variables such as age, sex, and region, the patients classified as having not been prescribed antibiotics or having been prescribed antibiotics on a deferred basis were significantly more likely to have a bloodstream infection within 60 days of their visit to a health care provider, compared with those who received antibiotics immediately, with odds ratios of 8.08 (95% confidence interval, 7.12-9.16) and 7.12 (95% CI, 6.22-8.14), respectively.
Hospital admissions after a UTI episode were nearly twice as high in the no- or deferred-antibiotics groups (27.0% and 26.8%, respectively), compared with the group that received antibiotics right away (14.8%), the investigators reported. The lengths of hospital stays were 12.1 days for the group classified as having not been prescribed antibiotics, 7.7 days for the group subject to delayed antibiotic prescribing, and 6.3 days for the group who received antibiotics immediately.
Deaths within 60 days of experiencing a urinary tract infection occurred in 5.4% of patients in the no-antibiotics group, 2.8% of the deferred-antibiotics group, and 1.6% of the immediate-antibiotics group. After adjustment for covariates, a regression analysis showed the risks for all-cause mortality were 1.16 and 2.18 times higher in the deferred-antibiotics group and the no-antibiotics group, respectively, according to the paper.
In the immediate-antibiotics group, those patients who received nitrofurantoin had a “small but significant increase” in 60-day survival versus those who received trimethoprim, the investigators noted in the discussion section of their report.
“This increase could reflect either higher levels of resistance to trimethoprim or a healthier population treated with nitrofurantoin, the latest being not recommended for patients with poor kidney function,” the researchers wrote.
This study was supported by the National Institute for Health Research and other U.K. sources. One study coauthor reported working as an epidemiologist with GSK in areas not related to the study.
SOURCE: Gharbi M et al. BMJ. 2019 Feb 27. doi: 10.1136/bmj.l525.
FROM THE BMJ
Anthrax booster expanded to 3 years for moderate-risk groups
A booster dose for pre-exposure prophylaxis with an anthrax vaccine may be given at 3 years after an initial series for individuals not currently at risk who wish to maintain protection, according to the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
In a unanimous 15-0 vote at the February meeting, ACIP committee members agreed on the recommendation after adjusting the wording to reflect a permissive, rather than mandated, guidance.
William Bower, MD, of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), presented data on Anthrax Vaccine Adsorbed (AVA) to support its protective effects over a longer booster dose interval.
The recommendations apply to persons aged 18 years or older who are not currently at high risk of exposure to Bacillus anthracis, but who might need to deploy to a high-risk area quickly, such as military personnel, Dr. Bower said.
In addition, data suggest that adults who have started, but not completed the pre-exposure priming series, can transition to the postexposure schedule prior to entering a high-risk area, he noted.
The previous pre-exposure anthrax vaccination schedule was a three-dose priming series at 0, 1, and 3 months, followed by a booster at 12 months and 18 months, then annually.
with “sustained immunological memory to at least month 42,” and suggested that even longer intervals between boosters may be possible, Dr. Bower said.
A dosing schedule of intramuscular injections at 0 and at 1 month and 6 months, with a booster at 42 months yielded survival estimates of approximately 84%-93%.
Dr. Bower noted that a new vaccine, AV7909, has demonstrated safety and effectiveness similar to AVA and could be used for pre-exposure prophylaxis if AVA is not available. AVA remains the preferred option, but ultimately will be replaced by AV7909, when the current AVA stockpile is exhausted.
Additional safety data on AV7909 will be reviewed by ACIP as they become available, and future guidance from the CDC will include statements on dosing for special populations including pregnant and breastfeeding women, said Dr. Bower.
“We anticipate that this [anthrax vaccine] work group will reconvene in 2021 to review data from pending studies” of AV7909, he said.
The ACIP members had no financial conflicts to disclose.
A booster dose for pre-exposure prophylaxis with an anthrax vaccine may be given at 3 years after an initial series for individuals not currently at risk who wish to maintain protection, according to the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
In a unanimous 15-0 vote at the February meeting, ACIP committee members agreed on the recommendation after adjusting the wording to reflect a permissive, rather than mandated, guidance.
William Bower, MD, of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), presented data on Anthrax Vaccine Adsorbed (AVA) to support its protective effects over a longer booster dose interval.
The recommendations apply to persons aged 18 years or older who are not currently at high risk of exposure to Bacillus anthracis, but who might need to deploy to a high-risk area quickly, such as military personnel, Dr. Bower said.
In addition, data suggest that adults who have started, but not completed the pre-exposure priming series, can transition to the postexposure schedule prior to entering a high-risk area, he noted.
The previous pre-exposure anthrax vaccination schedule was a three-dose priming series at 0, 1, and 3 months, followed by a booster at 12 months and 18 months, then annually.
with “sustained immunological memory to at least month 42,” and suggested that even longer intervals between boosters may be possible, Dr. Bower said.
A dosing schedule of intramuscular injections at 0 and at 1 month and 6 months, with a booster at 42 months yielded survival estimates of approximately 84%-93%.
Dr. Bower noted that a new vaccine, AV7909, has demonstrated safety and effectiveness similar to AVA and could be used for pre-exposure prophylaxis if AVA is not available. AVA remains the preferred option, but ultimately will be replaced by AV7909, when the current AVA stockpile is exhausted.
Additional safety data on AV7909 will be reviewed by ACIP as they become available, and future guidance from the CDC will include statements on dosing for special populations including pregnant and breastfeeding women, said Dr. Bower.
“We anticipate that this [anthrax vaccine] work group will reconvene in 2021 to review data from pending studies” of AV7909, he said.
The ACIP members had no financial conflicts to disclose.
A booster dose for pre-exposure prophylaxis with an anthrax vaccine may be given at 3 years after an initial series for individuals not currently at risk who wish to maintain protection, according to the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
In a unanimous 15-0 vote at the February meeting, ACIP committee members agreed on the recommendation after adjusting the wording to reflect a permissive, rather than mandated, guidance.
William Bower, MD, of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), presented data on Anthrax Vaccine Adsorbed (AVA) to support its protective effects over a longer booster dose interval.
The recommendations apply to persons aged 18 years or older who are not currently at high risk of exposure to Bacillus anthracis, but who might need to deploy to a high-risk area quickly, such as military personnel, Dr. Bower said.
In addition, data suggest that adults who have started, but not completed the pre-exposure priming series, can transition to the postexposure schedule prior to entering a high-risk area, he noted.
The previous pre-exposure anthrax vaccination schedule was a three-dose priming series at 0, 1, and 3 months, followed by a booster at 12 months and 18 months, then annually.
with “sustained immunological memory to at least month 42,” and suggested that even longer intervals between boosters may be possible, Dr. Bower said.
A dosing schedule of intramuscular injections at 0 and at 1 month and 6 months, with a booster at 42 months yielded survival estimates of approximately 84%-93%.
Dr. Bower noted that a new vaccine, AV7909, has demonstrated safety and effectiveness similar to AVA and could be used for pre-exposure prophylaxis if AVA is not available. AVA remains the preferred option, but ultimately will be replaced by AV7909, when the current AVA stockpile is exhausted.
Additional safety data on AV7909 will be reviewed by ACIP as they become available, and future guidance from the CDC will include statements on dosing for special populations including pregnant and breastfeeding women, said Dr. Bower.
“We anticipate that this [anthrax vaccine] work group will reconvene in 2021 to review data from pending studies” of AV7909, he said.
The ACIP members had no financial conflicts to disclose.
FROM AN ACIP MEETING
ACIP unanimously supports updates to Japanese encephalitis vaccination
according to a vote at a meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
Japanese encephalitis (JE) virus is a mosquito-borne flavivirus and those at risk for infection include travelers to countries where JE is endemic, as well as laboratory personnel who work with the virus.
The committee voted unanimously 15-0 in favor of the recommendations, which also advised vaccination for those whose travels in endemic areas are uncertain, but not for travelers with low-risk itineraries “such as shorter term travel limited to urban areas or travel that occurs outside of a well-defined JE virus transmission season.”
Susan Hills, MD, of the of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases, presented data in support of the recommendations.
A second unanimous vote confirmed recommendations for a primary series schedule for JE vaccination for adults aged 18-65 years as “two doses of vaccine administered on days 0 and 7-28.”
The third vote, also a unanimous 15-0, updated recommendations for a JE booster dose. The new recommendation is that adults and children receive a booster dose (a third dose) at least a year after completion of the primary JE vaccine series “if ongoing exposure or re-exposure to JE virus is expected.”
The currently available Japanese encephalitis vaccine in the United States is an inactivated Vero cell culture-derived vaccine marketed as IXIARO that was approved in March 2009 for individuals aged 17 years and older and approved in May 2013 for children aged 2 months through 16 years.
The ACIP members had no financial conflicts to disclose.
according to a vote at a meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
Japanese encephalitis (JE) virus is a mosquito-borne flavivirus and those at risk for infection include travelers to countries where JE is endemic, as well as laboratory personnel who work with the virus.
The committee voted unanimously 15-0 in favor of the recommendations, which also advised vaccination for those whose travels in endemic areas are uncertain, but not for travelers with low-risk itineraries “such as shorter term travel limited to urban areas or travel that occurs outside of a well-defined JE virus transmission season.”
Susan Hills, MD, of the of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases, presented data in support of the recommendations.
A second unanimous vote confirmed recommendations for a primary series schedule for JE vaccination for adults aged 18-65 years as “two doses of vaccine administered on days 0 and 7-28.”
The third vote, also a unanimous 15-0, updated recommendations for a JE booster dose. The new recommendation is that adults and children receive a booster dose (a third dose) at least a year after completion of the primary JE vaccine series “if ongoing exposure or re-exposure to JE virus is expected.”
The currently available Japanese encephalitis vaccine in the United States is an inactivated Vero cell culture-derived vaccine marketed as IXIARO that was approved in March 2009 for individuals aged 17 years and older and approved in May 2013 for children aged 2 months through 16 years.
The ACIP members had no financial conflicts to disclose.
according to a vote at a meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
Japanese encephalitis (JE) virus is a mosquito-borne flavivirus and those at risk for infection include travelers to countries where JE is endemic, as well as laboratory personnel who work with the virus.
The committee voted unanimously 15-0 in favor of the recommendations, which also advised vaccination for those whose travels in endemic areas are uncertain, but not for travelers with low-risk itineraries “such as shorter term travel limited to urban areas or travel that occurs outside of a well-defined JE virus transmission season.”
Susan Hills, MD, of the of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases, presented data in support of the recommendations.
A second unanimous vote confirmed recommendations for a primary series schedule for JE vaccination for adults aged 18-65 years as “two doses of vaccine administered on days 0 and 7-28.”
The third vote, also a unanimous 15-0, updated recommendations for a JE booster dose. The new recommendation is that adults and children receive a booster dose (a third dose) at least a year after completion of the primary JE vaccine series “if ongoing exposure or re-exposure to JE virus is expected.”
The currently available Japanese encephalitis vaccine in the United States is an inactivated Vero cell culture-derived vaccine marketed as IXIARO that was approved in March 2009 for individuals aged 17 years and older and approved in May 2013 for children aged 2 months through 16 years.
The ACIP members had no financial conflicts to disclose.
FROM AN ACIP MEETING
CDC: United States has hit a plateau with HIV
The annual number of new HIV infections has remained stable in recent years, and the Centers for Disease Control and Prevention says that’s not good – but solutions are at hand.
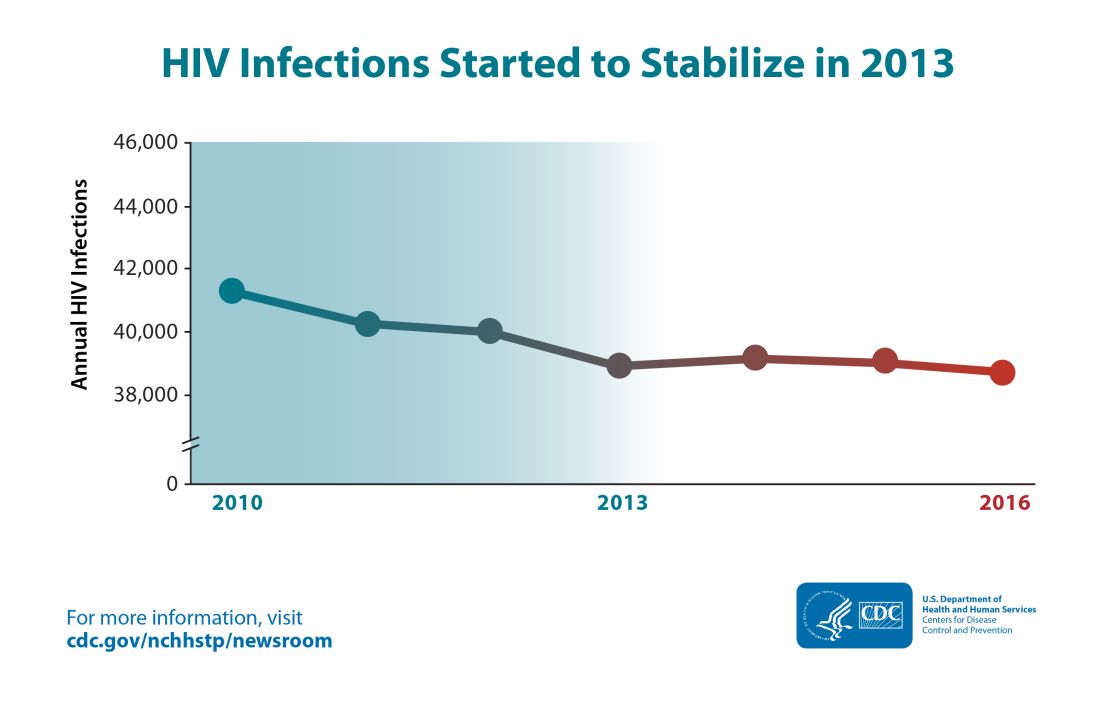
Though the estimated number of new HIV infections declined from just under 42,000 per year in 2010 to about 39,000 annually in 2013, that figure was essentially unchanged by 2016, with 38,700 new HIV infections seen that year.
“CDC estimates that the decline in HIV infections has plateaued because effective HIV prevention and treatment are not adequately reaching those who could most benefit from them. These gaps remain particularly troublesome in rural areas and in the South and among disproportionately affected populations like African Americans and Latinos,” said the CDC in a press release accompanying the report.
The report comes soon after President Trump’s State of the Union address, which announced a new multiagency initiative to eliminate the HIV epidemic in the United States, with the goal of reducing new HIV infections by 90% over the next 10 years. The multipronged initiative will implement geographically targeted HIV elimination teams in areas with high HIV prevalence, pulling together federal agencies, local and state governments, and community-level resources.
The initiative, called “Ending the Epidemic: A Plan for America” will combine an intensified approach to early diagnosis and treatment with efforts to boost uptake of pre-exposure prophylaxis for individuals at high risk for HIV infection.
The new CDC report used CD4 counts reported to the National HIV Surveillance System at the time of diagnosis to identify new (incident) cases and to track prevalence. Much of the report is devoted to finely detailed reporting of HIV incidence across sex, age, race/ethnicity, and transmission mode.
Though some groups, such as people who inject drugs, have seen a decrease of about 30% in the annual rate of new HIV cases, new cases have jumped for other groups. In particular, Latino gay and bisexual men saw new cases climb from 6,400 per year in 2010 to 8,300 in 2016. The incidence rate has stayed high and stable among African American gay and bisexual men, with 9,800 new cases reported in 2010; the same number was seen in 2016.
Among gay and bisexual men overall, the rate has also stayed stable, with about 26,000 new HIV infections reported at the beginning and end of the studied period. White heterosexual women saw about 1,000 new cases per year in 2010 and in 2016.
Some groups saw declines in new cases: African American and Latina heterosexual women each saw a falling incidence of new HIV cases. For the former group, new cases fell from 4,700 to 4,000, while the latter group of women saw new cases drop from 1,200 to 980 per year from 2010 to 2016.
Within these broad groups, HIV incidence also rose among some age groups and fell among others. Decreases were seen for younger African American gay and bisexual men (those aged 13-24 years), but rates increased by about two-thirds for men in this group aged 25-34 years. A similar increase was seen for Latino men in the 25-34 years age group, a change which drove the overall 30% increase in new infections for Latino gay and bisexual men.
White gay and bisexual men saw across-the-board decreases in new infections, though the overall decrease was less than 20%.
For heterosexual individuals as a group, new infections dropped by about 17%, from 10,900 to 9,100 annually. This change was driven mostly by decreases in women identifying as heterosexual.
“After a decades-long struggle, the path to eliminate America’s HIV epidemic is clear,” said Eugene McCray, MD, director of CDC’s Division of HIV/AIDS Prevention, in the press release. “Expanding efforts across the country will close gaps, overcome threats, and turn around troublesome trends.”
The press release cited local work in Washington and New York as evidence that targeted resources can make a difference in reducing new HIV cases. In these two areas, new infections dropped by 23% and 40% respectively from 2010 to 2016.
SOURCE: Centers for Disease Control. CDC Report: www.cdc.gov/hiv/library/reports/hiv-surveillance.html.
The annual number of new HIV infections has remained stable in recent years, and the Centers for Disease Control and Prevention says that’s not good – but solutions are at hand.
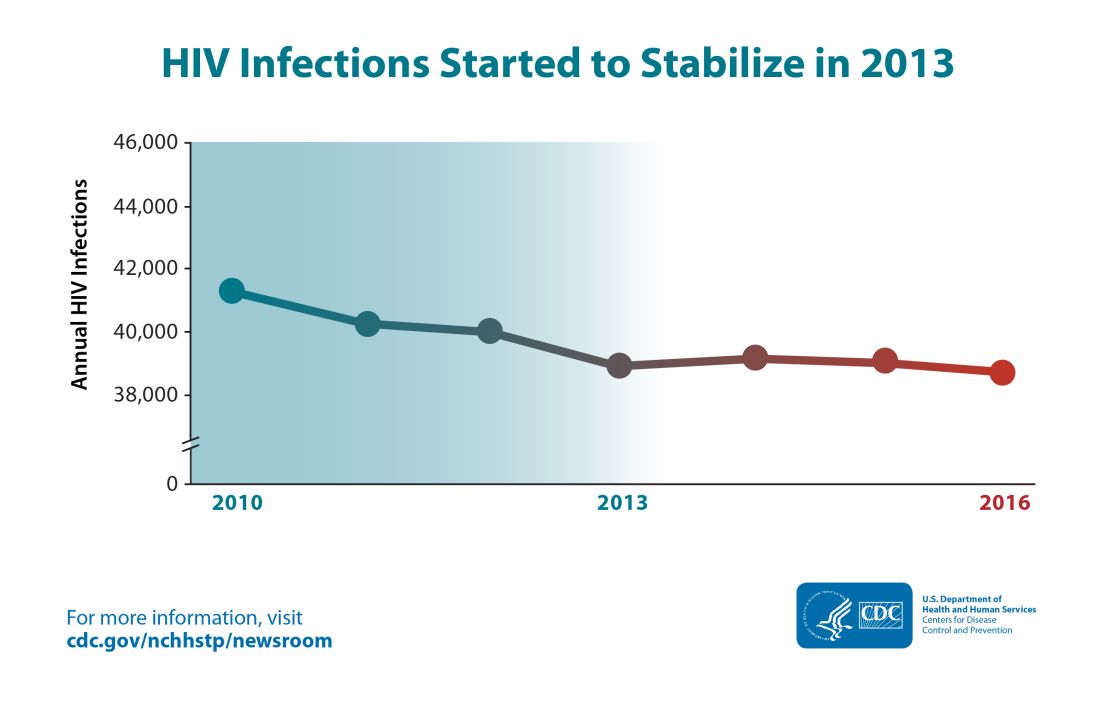
Though the estimated number of new HIV infections declined from just under 42,000 per year in 2010 to about 39,000 annually in 2013, that figure was essentially unchanged by 2016, with 38,700 new HIV infections seen that year.
“CDC estimates that the decline in HIV infections has plateaued because effective HIV prevention and treatment are not adequately reaching those who could most benefit from them. These gaps remain particularly troublesome in rural areas and in the South and among disproportionately affected populations like African Americans and Latinos,” said the CDC in a press release accompanying the report.
The report comes soon after President Trump’s State of the Union address, which announced a new multiagency initiative to eliminate the HIV epidemic in the United States, with the goal of reducing new HIV infections by 90% over the next 10 years. The multipronged initiative will implement geographically targeted HIV elimination teams in areas with high HIV prevalence, pulling together federal agencies, local and state governments, and community-level resources.
The initiative, called “Ending the Epidemic: A Plan for America” will combine an intensified approach to early diagnosis and treatment with efforts to boost uptake of pre-exposure prophylaxis for individuals at high risk for HIV infection.
The new CDC report used CD4 counts reported to the National HIV Surveillance System at the time of diagnosis to identify new (incident) cases and to track prevalence. Much of the report is devoted to finely detailed reporting of HIV incidence across sex, age, race/ethnicity, and transmission mode.
Though some groups, such as people who inject drugs, have seen a decrease of about 30% in the annual rate of new HIV cases, new cases have jumped for other groups. In particular, Latino gay and bisexual men saw new cases climb from 6,400 per year in 2010 to 8,300 in 2016. The incidence rate has stayed high and stable among African American gay and bisexual men, with 9,800 new cases reported in 2010; the same number was seen in 2016.
Among gay and bisexual men overall, the rate has also stayed stable, with about 26,000 new HIV infections reported at the beginning and end of the studied period. White heterosexual women saw about 1,000 new cases per year in 2010 and in 2016.
Some groups saw declines in new cases: African American and Latina heterosexual women each saw a falling incidence of new HIV cases. For the former group, new cases fell from 4,700 to 4,000, while the latter group of women saw new cases drop from 1,200 to 980 per year from 2010 to 2016.
Within these broad groups, HIV incidence also rose among some age groups and fell among others. Decreases were seen for younger African American gay and bisexual men (those aged 13-24 years), but rates increased by about two-thirds for men in this group aged 25-34 years. A similar increase was seen for Latino men in the 25-34 years age group, a change which drove the overall 30% increase in new infections for Latino gay and bisexual men.
White gay and bisexual men saw across-the-board decreases in new infections, though the overall decrease was less than 20%.
For heterosexual individuals as a group, new infections dropped by about 17%, from 10,900 to 9,100 annually. This change was driven mostly by decreases in women identifying as heterosexual.
“After a decades-long struggle, the path to eliminate America’s HIV epidemic is clear,” said Eugene McCray, MD, director of CDC’s Division of HIV/AIDS Prevention, in the press release. “Expanding efforts across the country will close gaps, overcome threats, and turn around troublesome trends.”
The press release cited local work in Washington and New York as evidence that targeted resources can make a difference in reducing new HIV cases. In these two areas, new infections dropped by 23% and 40% respectively from 2010 to 2016.
SOURCE: Centers for Disease Control. CDC Report: www.cdc.gov/hiv/library/reports/hiv-surveillance.html.
The annual number of new HIV infections has remained stable in recent years, and the Centers for Disease Control and Prevention says that’s not good – but solutions are at hand.
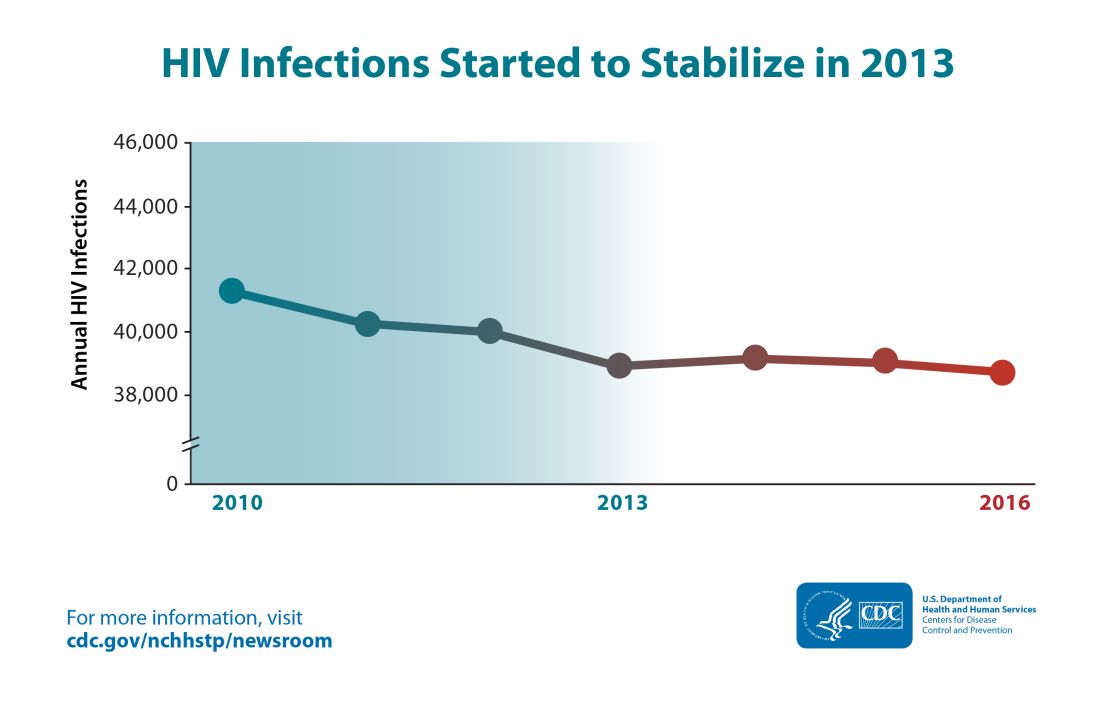
Though the estimated number of new HIV infections declined from just under 42,000 per year in 2010 to about 39,000 annually in 2013, that figure was essentially unchanged by 2016, with 38,700 new HIV infections seen that year.
“CDC estimates that the decline in HIV infections has plateaued because effective HIV prevention and treatment are not adequately reaching those who could most benefit from them. These gaps remain particularly troublesome in rural areas and in the South and among disproportionately affected populations like African Americans and Latinos,” said the CDC in a press release accompanying the report.
The report comes soon after President Trump’s State of the Union address, which announced a new multiagency initiative to eliminate the HIV epidemic in the United States, with the goal of reducing new HIV infections by 90% over the next 10 years. The multipronged initiative will implement geographically targeted HIV elimination teams in areas with high HIV prevalence, pulling together federal agencies, local and state governments, and community-level resources.
The initiative, called “Ending the Epidemic: A Plan for America” will combine an intensified approach to early diagnosis and treatment with efforts to boost uptake of pre-exposure prophylaxis for individuals at high risk for HIV infection.
The new CDC report used CD4 counts reported to the National HIV Surveillance System at the time of diagnosis to identify new (incident) cases and to track prevalence. Much of the report is devoted to finely detailed reporting of HIV incidence across sex, age, race/ethnicity, and transmission mode.
Though some groups, such as people who inject drugs, have seen a decrease of about 30% in the annual rate of new HIV cases, new cases have jumped for other groups. In particular, Latino gay and bisexual men saw new cases climb from 6,400 per year in 2010 to 8,300 in 2016. The incidence rate has stayed high and stable among African American gay and bisexual men, with 9,800 new cases reported in 2010; the same number was seen in 2016.
Among gay and bisexual men overall, the rate has also stayed stable, with about 26,000 new HIV infections reported at the beginning and end of the studied period. White heterosexual women saw about 1,000 new cases per year in 2010 and in 2016.
Some groups saw declines in new cases: African American and Latina heterosexual women each saw a falling incidence of new HIV cases. For the former group, new cases fell from 4,700 to 4,000, while the latter group of women saw new cases drop from 1,200 to 980 per year from 2010 to 2016.
Within these broad groups, HIV incidence also rose among some age groups and fell among others. Decreases were seen for younger African American gay and bisexual men (those aged 13-24 years), but rates increased by about two-thirds for men in this group aged 25-34 years. A similar increase was seen for Latino men in the 25-34 years age group, a change which drove the overall 30% increase in new infections for Latino gay and bisexual men.
White gay and bisexual men saw across-the-board decreases in new infections, though the overall decrease was less than 20%.
For heterosexual individuals as a group, new infections dropped by about 17%, from 10,900 to 9,100 annually. This change was driven mostly by decreases in women identifying as heterosexual.
“After a decades-long struggle, the path to eliminate America’s HIV epidemic is clear,” said Eugene McCray, MD, director of CDC’s Division of HIV/AIDS Prevention, in the press release. “Expanding efforts across the country will close gaps, overcome threats, and turn around troublesome trends.”
The press release cited local work in Washington and New York as evidence that targeted resources can make a difference in reducing new HIV cases. In these two areas, new infections dropped by 23% and 40% respectively from 2010 to 2016.
SOURCE: Centers for Disease Control. CDC Report: www.cdc.gov/hiv/library/reports/hiv-surveillance.html.
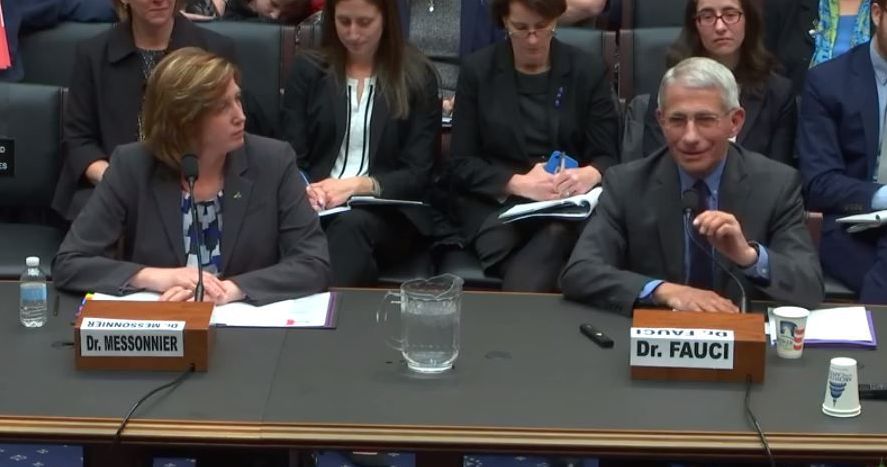
Fauci, Messonnier testify on measles outbreaks
Officials from the Centers for Disease Control and Prevention and the National Institute for Allergy and Infectious Diseases stressed the safety of measles vaccines and warned that misinformation is among the factors keeping more children from being vaccinated.
With nearly 160 cases of measles in 10 states during Jan. 1–Feb. 21, a disease once eradicated from the United States is resurfacing, with most cases affecting those who have not been vaccinated.
“Measles outbreaks have been and continue to be a constant threat to the health of the American people,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the CDC, testified at a Feb. 27 hearing of the Oversight and Investigations Subcommittee of the House Energy and Commerce Committee.
She noted that unvaccinated Americans traveling abroad are at risk for contracting the infection, and thus are at risk of spreading it when they return home. Foreigners coming to the country also carry the potential to spread the infection.
“Nationally, we enjoy high measles vaccination coverage,” Dr. Messonnier said.”There are pockets of people who are vaccine hesitant, who delay or even refuse to vaccinate themselves and their children. Outbreaks of measles occur when measles gets into these communities of unvaccinated people.”
She noted that those who eschew vaccination tend to live near one another and share common religious beliefs or racial or ethnic backgrounds.
She continued that vaccine hesitancy “is the result of the misunderstanding of the risk and seriousness of disease, combined with misinformation of the safety and effectiveness of vaccines. However, the specific issues fueling hesitancy varies by community.”
Strategies to increase vaccination need to be localized with national support from the CDC, Dr. Messonnier said, adding that rapid response is critical to control outbreaks.
Anthony Fauci, MD, director of the National Institute for Allergy and Infectious Diseases at NIH, agreed.
“I consider it really an irony that you have one of the most contagious viruses known to man juxtaposed against one of the most effective vaccines that we have and yet we don’t do and have not done what could be done, namely completely eliminate and eradicate this virus,” Dr. Fauci said.
Dr. Messonnier stressed that the only way to protect against measles is to get vaccinated.
“If they have questions, they should talk to their doctor,” she added. “Their doctor can provide them with more information about measles, answer their questions and reassure them so they go ahead and get vaccinated.”
Dr. Fauci concurred and added that “we should look upon it in two approaches. One, it’s for the safety of your own child. The other is a responsibility to the community. ... We all have a responsibility to be part of that umbrella of herd immunity and once it goes down below a certain percentage, then you have danger to the entire society.”
He stressed that the CDC is a good website to combat much of the misinformation that is floating around on the Internet.
The committee panel, while taking an interest in the recent outbreaks, did not hint at any specific legislative actions were being considered.
Officials from the Centers for Disease Control and Prevention and the National Institute for Allergy and Infectious Diseases stressed the safety of measles vaccines and warned that misinformation is among the factors keeping more children from being vaccinated.
With nearly 160 cases of measles in 10 states during Jan. 1–Feb. 21, a disease once eradicated from the United States is resurfacing, with most cases affecting those who have not been vaccinated.
“Measles outbreaks have been and continue to be a constant threat to the health of the American people,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the CDC, testified at a Feb. 27 hearing of the Oversight and Investigations Subcommittee of the House Energy and Commerce Committee.
She noted that unvaccinated Americans traveling abroad are at risk for contracting the infection, and thus are at risk of spreading it when they return home. Foreigners coming to the country also carry the potential to spread the infection.
“Nationally, we enjoy high measles vaccination coverage,” Dr. Messonnier said.”There are pockets of people who are vaccine hesitant, who delay or even refuse to vaccinate themselves and their children. Outbreaks of measles occur when measles gets into these communities of unvaccinated people.”
She noted that those who eschew vaccination tend to live near one another and share common religious beliefs or racial or ethnic backgrounds.
She continued that vaccine hesitancy “is the result of the misunderstanding of the risk and seriousness of disease, combined with misinformation of the safety and effectiveness of vaccines. However, the specific issues fueling hesitancy varies by community.”
Strategies to increase vaccination need to be localized with national support from the CDC, Dr. Messonnier said, adding that rapid response is critical to control outbreaks.
Anthony Fauci, MD, director of the National Institute for Allergy and Infectious Diseases at NIH, agreed.
“I consider it really an irony that you have one of the most contagious viruses known to man juxtaposed against one of the most effective vaccines that we have and yet we don’t do and have not done what could be done, namely completely eliminate and eradicate this virus,” Dr. Fauci said.
Dr. Messonnier stressed that the only way to protect against measles is to get vaccinated.
“If they have questions, they should talk to their doctor,” she added. “Their doctor can provide them with more information about measles, answer their questions and reassure them so they go ahead and get vaccinated.”
Dr. Fauci concurred and added that “we should look upon it in two approaches. One, it’s for the safety of your own child. The other is a responsibility to the community. ... We all have a responsibility to be part of that umbrella of herd immunity and once it goes down below a certain percentage, then you have danger to the entire society.”
He stressed that the CDC is a good website to combat much of the misinformation that is floating around on the Internet.
The committee panel, while taking an interest in the recent outbreaks, did not hint at any specific legislative actions were being considered.
Officials from the Centers for Disease Control and Prevention and the National Institute for Allergy and Infectious Diseases stressed the safety of measles vaccines and warned that misinformation is among the factors keeping more children from being vaccinated.
With nearly 160 cases of measles in 10 states during Jan. 1–Feb. 21, a disease once eradicated from the United States is resurfacing, with most cases affecting those who have not been vaccinated.
“Measles outbreaks have been and continue to be a constant threat to the health of the American people,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the CDC, testified at a Feb. 27 hearing of the Oversight and Investigations Subcommittee of the House Energy and Commerce Committee.
She noted that unvaccinated Americans traveling abroad are at risk for contracting the infection, and thus are at risk of spreading it when they return home. Foreigners coming to the country also carry the potential to spread the infection.
“Nationally, we enjoy high measles vaccination coverage,” Dr. Messonnier said.”There are pockets of people who are vaccine hesitant, who delay or even refuse to vaccinate themselves and their children. Outbreaks of measles occur when measles gets into these communities of unvaccinated people.”
She noted that those who eschew vaccination tend to live near one another and share common religious beliefs or racial or ethnic backgrounds.
She continued that vaccine hesitancy “is the result of the misunderstanding of the risk and seriousness of disease, combined with misinformation of the safety and effectiveness of vaccines. However, the specific issues fueling hesitancy varies by community.”
Strategies to increase vaccination need to be localized with national support from the CDC, Dr. Messonnier said, adding that rapid response is critical to control outbreaks.
Anthony Fauci, MD, director of the National Institute for Allergy and Infectious Diseases at NIH, agreed.
“I consider it really an irony that you have one of the most contagious viruses known to man juxtaposed against one of the most effective vaccines that we have and yet we don’t do and have not done what could be done, namely completely eliminate and eradicate this virus,” Dr. Fauci said.
Dr. Messonnier stressed that the only way to protect against measles is to get vaccinated.
“If they have questions, they should talk to their doctor,” she added. “Their doctor can provide them with more information about measles, answer their questions and reassure them so they go ahead and get vaccinated.”
Dr. Fauci concurred and added that “we should look upon it in two approaches. One, it’s for the safety of your own child. The other is a responsibility to the community. ... We all have a responsibility to be part of that umbrella of herd immunity and once it goes down below a certain percentage, then you have danger to the entire society.”
He stressed that the CDC is a good website to combat much of the misinformation that is floating around on the Internet.
The committee panel, while taking an interest in the recent outbreaks, did not hint at any specific legislative actions were being considered.
REPORTING FROM HOUSE COMMITTEE HEARING
Caring for aging HIV-infected patients requires close attention to unrelated diseases
A substantial proportion of non–AIDS-defining cancers, and other noninfectious comorbid diseases, could be prevented with interventions on traditional risk factors in HIV-infected patients, according to the results of large database analysis published online in The Lancet HIV.
The researchers analyzed traditional and HIV-related risk factors for four validated noncommunicable disease outcomes (non–AIDS-defining cancers, myocardial infarction, end-stage liver disease, and end-stage renal disease) among participants of the North American AIDS Cohort Collaboration on Research and Design (NA-ACCORD), according to Keri N. Althoff, PhD, of Johns Hopkins University, Baltimore, and her colleagues on behalf of the NA-ACCORD.
The study comprised individuals with the assessed disease conditions from among more than 180,000 adults (aged 18 years or older) with HIV from more than 200 sites who had at least two care visits within 12 months. The researchers used a population attributable fraction (PAF) approach to quantify the proportion of noncommunicable diseases that could be eliminated if particular risk factors were not present. According to the researchers, PAF can be used to inform prioritization of interventions.
Dr. Althoff and her colleagues found that, for non–AIDS-defining cancer, the significant preventable or modifiable risk factors were smoking, low CD4 cell count, detectable HIV RNA, a history of clinical AIDS diagnosis, and hepatitis B infection.
For myocardial infarction, the significant factors were smoking, elevated total cholesterol, hypertension, stage 4 chronic kidney disease, a low CD4 cell count, detectable HIV RNA, and hepatitis C infection.
For end-stage liver disease, the significant factors were low CD4 cell count, detectable HIV RNA, a history of a clinical AIDS diagnosis, and hepatitis B or C infection.
For end-stage renal disease, the significantly associated risk factors were elevated total cholesterol, hypertension, diabetes, low CD4 cell count, detectable HIV RNA, and a history of clinical AIDS diagnosis.
The most substantial PAF for each of the respective diseases was as follows: smoking for non–AIDS-related cancers (24%; 95% confidence interval, 13%-35%), elevated total cholesterol for myocardial infarction (44%; 95% CI, 30%-58%), and hepatitis C infection for end-stage liver disease (30%; 95% CI, 21%-39%). In addition, hypertension had the highest PAF for end-stage renal disease (39%; 95% CI, 26%-51%).
“Modifications to individual-level interventions and models of HIV care, and the implementation of structural and policy-level interventions that focus on prevention and modification of traditional risk factors are necessary to avoid noncommunicable diseases and preserve health among successfully antiretroviral-treated adults aging with HIV,” the researchers concluded.
The study was funded by the National Institutes of Health and the NA-ACCORD. Dr. Althoff reported having no relevant disclosures.
SOURCE: Althoff KN et al. The Lancet HIV. 2019 Jan 22. doi: 10.1016/S2352-3018(18)30295-9.
A substantial proportion of non–AIDS-defining cancers, and other noninfectious comorbid diseases, could be prevented with interventions on traditional risk factors in HIV-infected patients, according to the results of large database analysis published online in The Lancet HIV.
The researchers analyzed traditional and HIV-related risk factors for four validated noncommunicable disease outcomes (non–AIDS-defining cancers, myocardial infarction, end-stage liver disease, and end-stage renal disease) among participants of the North American AIDS Cohort Collaboration on Research and Design (NA-ACCORD), according to Keri N. Althoff, PhD, of Johns Hopkins University, Baltimore, and her colleagues on behalf of the NA-ACCORD.
The study comprised individuals with the assessed disease conditions from among more than 180,000 adults (aged 18 years or older) with HIV from more than 200 sites who had at least two care visits within 12 months. The researchers used a population attributable fraction (PAF) approach to quantify the proportion of noncommunicable diseases that could be eliminated if particular risk factors were not present. According to the researchers, PAF can be used to inform prioritization of interventions.
Dr. Althoff and her colleagues found that, for non–AIDS-defining cancer, the significant preventable or modifiable risk factors were smoking, low CD4 cell count, detectable HIV RNA, a history of clinical AIDS diagnosis, and hepatitis B infection.
For myocardial infarction, the significant factors were smoking, elevated total cholesterol, hypertension, stage 4 chronic kidney disease, a low CD4 cell count, detectable HIV RNA, and hepatitis C infection.
For end-stage liver disease, the significant factors were low CD4 cell count, detectable HIV RNA, a history of a clinical AIDS diagnosis, and hepatitis B or C infection.
For end-stage renal disease, the significantly associated risk factors were elevated total cholesterol, hypertension, diabetes, low CD4 cell count, detectable HIV RNA, and a history of clinical AIDS diagnosis.
The most substantial PAF for each of the respective diseases was as follows: smoking for non–AIDS-related cancers (24%; 95% confidence interval, 13%-35%), elevated total cholesterol for myocardial infarction (44%; 95% CI, 30%-58%), and hepatitis C infection for end-stage liver disease (30%; 95% CI, 21%-39%). In addition, hypertension had the highest PAF for end-stage renal disease (39%; 95% CI, 26%-51%).
“Modifications to individual-level interventions and models of HIV care, and the implementation of structural and policy-level interventions that focus on prevention and modification of traditional risk factors are necessary to avoid noncommunicable diseases and preserve health among successfully antiretroviral-treated adults aging with HIV,” the researchers concluded.
The study was funded by the National Institutes of Health and the NA-ACCORD. Dr. Althoff reported having no relevant disclosures.
SOURCE: Althoff KN et al. The Lancet HIV. 2019 Jan 22. doi: 10.1016/S2352-3018(18)30295-9.
A substantial proportion of non–AIDS-defining cancers, and other noninfectious comorbid diseases, could be prevented with interventions on traditional risk factors in HIV-infected patients, according to the results of large database analysis published online in The Lancet HIV.
The researchers analyzed traditional and HIV-related risk factors for four validated noncommunicable disease outcomes (non–AIDS-defining cancers, myocardial infarction, end-stage liver disease, and end-stage renal disease) among participants of the North American AIDS Cohort Collaboration on Research and Design (NA-ACCORD), according to Keri N. Althoff, PhD, of Johns Hopkins University, Baltimore, and her colleagues on behalf of the NA-ACCORD.
The study comprised individuals with the assessed disease conditions from among more than 180,000 adults (aged 18 years or older) with HIV from more than 200 sites who had at least two care visits within 12 months. The researchers used a population attributable fraction (PAF) approach to quantify the proportion of noncommunicable diseases that could be eliminated if particular risk factors were not present. According to the researchers, PAF can be used to inform prioritization of interventions.
Dr. Althoff and her colleagues found that, for non–AIDS-defining cancer, the significant preventable or modifiable risk factors were smoking, low CD4 cell count, detectable HIV RNA, a history of clinical AIDS diagnosis, and hepatitis B infection.
For myocardial infarction, the significant factors were smoking, elevated total cholesterol, hypertension, stage 4 chronic kidney disease, a low CD4 cell count, detectable HIV RNA, and hepatitis C infection.
For end-stage liver disease, the significant factors were low CD4 cell count, detectable HIV RNA, a history of a clinical AIDS diagnosis, and hepatitis B or C infection.
For end-stage renal disease, the significantly associated risk factors were elevated total cholesterol, hypertension, diabetes, low CD4 cell count, detectable HIV RNA, and a history of clinical AIDS diagnosis.
The most substantial PAF for each of the respective diseases was as follows: smoking for non–AIDS-related cancers (24%; 95% confidence interval, 13%-35%), elevated total cholesterol for myocardial infarction (44%; 95% CI, 30%-58%), and hepatitis C infection for end-stage liver disease (30%; 95% CI, 21%-39%). In addition, hypertension had the highest PAF for end-stage renal disease (39%; 95% CI, 26%-51%).
“Modifications to individual-level interventions and models of HIV care, and the implementation of structural and policy-level interventions that focus on prevention and modification of traditional risk factors are necessary to avoid noncommunicable diseases and preserve health among successfully antiretroviral-treated adults aging with HIV,” the researchers concluded.
The study was funded by the National Institutes of Health and the NA-ACCORD. Dr. Althoff reported having no relevant disclosures.
SOURCE: Althoff KN et al. The Lancet HIV. 2019 Jan 22. doi: 10.1016/S2352-3018(18)30295-9.
FROM THE LANCET HIV
Heart failure outcomes are worse in select HIV-infected individuals
People living with HIV (PLHIV) who have a low CD4 count or detectable viral load (VL) have an increased 30-day heart failure (HF) readmission rate as well as increased cardiovascular and all-cause mortality, compared with uninfected controls, according to Raza M. Alvi, MD, of Massachusetts General Hospital and Harvard Medical School, Boston, and his colleagues.
Overall, the 30-day HF hospital readmission rate was higher among PLHIV versus non-HIV–infected individuals (49% vs. 32%, P less than .001), according to the results of their cohort study of 2,308 individuals admitted to the hospital with decompensated HF.
PLHIV and the non-HIV control groups were both followed over 2 years with a median follow-up period of 19 months, the authors wrote in the American Heart Journal. Demographic make-up of the two groups was similar; in particular, there was no difference in blood pressure and heart rate between the PLHIV and non-HIV controls, suggesting that adherence with HF medications may be similar between groups. The cohorts differed primarily in that pulmonary artery systolic pressure was significantly higher (45 vs. 40 mm Hg; P less than .001) in the HIV group, as was cocaine use (36% vs. 19%; P less than .001) and hepatitis C virus (HCV) infection (13% vs. 7%; P less than .001).
The differing results between the two cohorts were primarily caused by the fact that, for PLHIV with HF, CD4 count and VL were risk factors for adverse outcomes among patients with all types of HF. (30-day HF readmission, cardiovascular [CV] mortality, and all-cause mortality), compared with those with CD4 count greater than or equal to 200 cells/mm3. In addition, a low CD4 count/high VL independently related to an increased 30-day HF readmission rate even after the researchers controlled for major traditional and nontraditional HF risk factors.
“Rates of 30-day HF readmission, CV mortality, and all-cause mortality are worse among individuals with a low CD4 count or nonsuppressed viral load,” the researchers concluded.
The National Institutes of Health sponsored the study. The authors reported that they had no conflicts.
SOURCE: Alvi RM et al. Am Heart J. 2019 Apr;210:39-48.
People living with HIV (PLHIV) who have a low CD4 count or detectable viral load (VL) have an increased 30-day heart failure (HF) readmission rate as well as increased cardiovascular and all-cause mortality, compared with uninfected controls, according to Raza M. Alvi, MD, of Massachusetts General Hospital and Harvard Medical School, Boston, and his colleagues.
Overall, the 30-day HF hospital readmission rate was higher among PLHIV versus non-HIV–infected individuals (49% vs. 32%, P less than .001), according to the results of their cohort study of 2,308 individuals admitted to the hospital with decompensated HF.
PLHIV and the non-HIV control groups were both followed over 2 years with a median follow-up period of 19 months, the authors wrote in the American Heart Journal. Demographic make-up of the two groups was similar; in particular, there was no difference in blood pressure and heart rate between the PLHIV and non-HIV controls, suggesting that adherence with HF medications may be similar between groups. The cohorts differed primarily in that pulmonary artery systolic pressure was significantly higher (45 vs. 40 mm Hg; P less than .001) in the HIV group, as was cocaine use (36% vs. 19%; P less than .001) and hepatitis C virus (HCV) infection (13% vs. 7%; P less than .001).
The differing results between the two cohorts were primarily caused by the fact that, for PLHIV with HF, CD4 count and VL were risk factors for adverse outcomes among patients with all types of HF. (30-day HF readmission, cardiovascular [CV] mortality, and all-cause mortality), compared with those with CD4 count greater than or equal to 200 cells/mm3. In addition, a low CD4 count/high VL independently related to an increased 30-day HF readmission rate even after the researchers controlled for major traditional and nontraditional HF risk factors.
“Rates of 30-day HF readmission, CV mortality, and all-cause mortality are worse among individuals with a low CD4 count or nonsuppressed viral load,” the researchers concluded.
The National Institutes of Health sponsored the study. The authors reported that they had no conflicts.
SOURCE: Alvi RM et al. Am Heart J. 2019 Apr;210:39-48.
People living with HIV (PLHIV) who have a low CD4 count or detectable viral load (VL) have an increased 30-day heart failure (HF) readmission rate as well as increased cardiovascular and all-cause mortality, compared with uninfected controls, according to Raza M. Alvi, MD, of Massachusetts General Hospital and Harvard Medical School, Boston, and his colleagues.
Overall, the 30-day HF hospital readmission rate was higher among PLHIV versus non-HIV–infected individuals (49% vs. 32%, P less than .001), according to the results of their cohort study of 2,308 individuals admitted to the hospital with decompensated HF.
PLHIV and the non-HIV control groups were both followed over 2 years with a median follow-up period of 19 months, the authors wrote in the American Heart Journal. Demographic make-up of the two groups was similar; in particular, there was no difference in blood pressure and heart rate between the PLHIV and non-HIV controls, suggesting that adherence with HF medications may be similar between groups. The cohorts differed primarily in that pulmonary artery systolic pressure was significantly higher (45 vs. 40 mm Hg; P less than .001) in the HIV group, as was cocaine use (36% vs. 19%; P less than .001) and hepatitis C virus (HCV) infection (13% vs. 7%; P less than .001).
The differing results between the two cohorts were primarily caused by the fact that, for PLHIV with HF, CD4 count and VL were risk factors for adverse outcomes among patients with all types of HF. (30-day HF readmission, cardiovascular [CV] mortality, and all-cause mortality), compared with those with CD4 count greater than or equal to 200 cells/mm3. In addition, a low CD4 count/high VL independently related to an increased 30-day HF readmission rate even after the researchers controlled for major traditional and nontraditional HF risk factors.
“Rates of 30-day HF readmission, CV mortality, and all-cause mortality are worse among individuals with a low CD4 count or nonsuppressed viral load,” the researchers concluded.
The National Institutes of Health sponsored the study. The authors reported that they had no conflicts.
SOURCE: Alvi RM et al. Am Heart J. 2019 Apr;210:39-48.
FROM THE AMERICAN HEART JOURNAL
Rhymin’ pediatric dermatologist provides Demodex tips
WAIKOLOA, HAWAII – Pediatric dermatologist Andrea L. Zaenglein, MD, has composed a whimsical couplet to help physicians broaden their differential diagnosis for acneiform rashes in children.
Pustules on noses: Think demodicosis!
The classic teaching has been that Demodex carriage and its pathologic clinical expression, demodicosis, are rare in children. Not so, Dr. Zaenglein asserted at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
“One of the things that we never used to see in kids but now I see all the time, probably because I’m looking for it, is Demodex. You’re not born with Demodex. Your carriage rate will increase over the years and by the time you’re elderly, 95% of us will have it – but not me. I just decided I’m not having these. I’m not looking for them, and I don’t want to know if they’re there,” she quipped, referring to the creepiness factor surrounding these facial parasitic mites invisible to the naked eye.
The mites live in pilosebaceous units. In animals, the disease is called mange. In humans, demodicosis is caused by two species of mites: Demodex folliculorum and D. brevis. The diagnosis is made by microscopic examination of mineral oil skin scrapings.
Primary demodicosis can take the form of pityriasis folliculorum, also known as spinulate demodicosis, papulopustular perioral, periauricular, or periorbital demodicosis, or a nodulocystic/conglobate version.
More commonly, however, .
“Demodicosis can be associated with immunosuppression. Kids with Langerhans cell histiocytosis seem to be prone to it. But you can see it in kids who don’t have any underlying immunosuppression, and I think there are more and more cases of that as we go looking for it,” said Dr. Zaenglein, professor of dermatology and pediatrics at Penn State University, Hershey, and immediate past president of the Society for Pediatric Dermatology.
Look for Demodex in children with somewhat atypical versions of common acneiform eruptions: for example, the ‘pustules on noses’ variant.
“Finding Demodex can alter your treatment and make it easier in these cases,” she said.
Metronidazole and ivermectin are the systemic treatment options for pediatric demodicosis.
“I tend to use topical permethrin, just because it’s easy to get. I’ll treat them once a week for 3 weeks in a row. But also make sure to treat the underlying primary inflammatory disorder,” the pediatric dermatologist advised.
Other topical options include ivermectin cream, crotamiton cream, metronidazole gel, and salicylic acid cream.
Dr. Zaenglein reported having financial relationships with Sun Pharmaceuticals, Allergan, and Ortho Dermatologics.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
WAIKOLOA, HAWAII – Pediatric dermatologist Andrea L. Zaenglein, MD, has composed a whimsical couplet to help physicians broaden their differential diagnosis for acneiform rashes in children.
Pustules on noses: Think demodicosis!
The classic teaching has been that Demodex carriage and its pathologic clinical expression, demodicosis, are rare in children. Not so, Dr. Zaenglein asserted at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
“One of the things that we never used to see in kids but now I see all the time, probably because I’m looking for it, is Demodex. You’re not born with Demodex. Your carriage rate will increase over the years and by the time you’re elderly, 95% of us will have it – but not me. I just decided I’m not having these. I’m not looking for them, and I don’t want to know if they’re there,” she quipped, referring to the creepiness factor surrounding these facial parasitic mites invisible to the naked eye.
The mites live in pilosebaceous units. In animals, the disease is called mange. In humans, demodicosis is caused by two species of mites: Demodex folliculorum and D. brevis. The diagnosis is made by microscopic examination of mineral oil skin scrapings.
Primary demodicosis can take the form of pityriasis folliculorum, also known as spinulate demodicosis, papulopustular perioral, periauricular, or periorbital demodicosis, or a nodulocystic/conglobate version.
More commonly, however, .
“Demodicosis can be associated with immunosuppression. Kids with Langerhans cell histiocytosis seem to be prone to it. But you can see it in kids who don’t have any underlying immunosuppression, and I think there are more and more cases of that as we go looking for it,” said Dr. Zaenglein, professor of dermatology and pediatrics at Penn State University, Hershey, and immediate past president of the Society for Pediatric Dermatology.
Look for Demodex in children with somewhat atypical versions of common acneiform eruptions: for example, the ‘pustules on noses’ variant.
“Finding Demodex can alter your treatment and make it easier in these cases,” she said.
Metronidazole and ivermectin are the systemic treatment options for pediatric demodicosis.
“I tend to use topical permethrin, just because it’s easy to get. I’ll treat them once a week for 3 weeks in a row. But also make sure to treat the underlying primary inflammatory disorder,” the pediatric dermatologist advised.
Other topical options include ivermectin cream, crotamiton cream, metronidazole gel, and salicylic acid cream.
Dr. Zaenglein reported having financial relationships with Sun Pharmaceuticals, Allergan, and Ortho Dermatologics.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
WAIKOLOA, HAWAII – Pediatric dermatologist Andrea L. Zaenglein, MD, has composed a whimsical couplet to help physicians broaden their differential diagnosis for acneiform rashes in children.
Pustules on noses: Think demodicosis!
The classic teaching has been that Demodex carriage and its pathologic clinical expression, demodicosis, are rare in children. Not so, Dr. Zaenglein asserted at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
“One of the things that we never used to see in kids but now I see all the time, probably because I’m looking for it, is Demodex. You’re not born with Demodex. Your carriage rate will increase over the years and by the time you’re elderly, 95% of us will have it – but not me. I just decided I’m not having these. I’m not looking for them, and I don’t want to know if they’re there,” she quipped, referring to the creepiness factor surrounding these facial parasitic mites invisible to the naked eye.
The mites live in pilosebaceous units. In animals, the disease is called mange. In humans, demodicosis is caused by two species of mites: Demodex folliculorum and D. brevis. The diagnosis is made by microscopic examination of mineral oil skin scrapings.
Primary demodicosis can take the form of pityriasis folliculorum, also known as spinulate demodicosis, papulopustular perioral, periauricular, or periorbital demodicosis, or a nodulocystic/conglobate version.
More commonly, however, .
“Demodicosis can be associated with immunosuppression. Kids with Langerhans cell histiocytosis seem to be prone to it. But you can see it in kids who don’t have any underlying immunosuppression, and I think there are more and more cases of that as we go looking for it,” said Dr. Zaenglein, professor of dermatology and pediatrics at Penn State University, Hershey, and immediate past president of the Society for Pediatric Dermatology.
Look for Demodex in children with somewhat atypical versions of common acneiform eruptions: for example, the ‘pustules on noses’ variant.
“Finding Demodex can alter your treatment and make it easier in these cases,” she said.
Metronidazole and ivermectin are the systemic treatment options for pediatric demodicosis.
“I tend to use topical permethrin, just because it’s easy to get. I’ll treat them once a week for 3 weeks in a row. But also make sure to treat the underlying primary inflammatory disorder,” the pediatric dermatologist advised.
Other topical options include ivermectin cream, crotamiton cream, metronidazole gel, and salicylic acid cream.
Dr. Zaenglein reported having financial relationships with Sun Pharmaceuticals, Allergan, and Ortho Dermatologics.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
REPORTING FROM SDEF HAWAII DERMATOLOGY SEMINAR