User login
COVID-19 will test medical supply stocks
In a JAMA Live Stream interview, in the United States.
Dr. Fauci got into the details of what is known, what is unknown, what is being done in laboratories, and what clinical elements are still not understood about this disease.
The next several weeks, he said, are likely to tell the tale of whether our health care system is up to the challenge of care for the most ill among those who will be affected by COVID-19.
“It shouldn’t panic or frighten us, but we have to know we’re dealing with a very serious problem that we have to address, and we have to deal with it in a very bold way,” said Dr. Fauci, director of the National Institute of Allergy and Infectious Diseases at the National Institutes of Health.
Speaking in an interview with JAMA Editor in Chief Howard Bauchner, MD, Dr. Fauci said the situation favors action over fear. “Let’s apply that energy to doing the things that we know can mitigate this.”
He added that he heard the message loud and clear from health care leaders in Italy and France during a World Health Organization coronavirus call earlier in the day. Officials in those countries, he said, were “almost pleading with the rest of the world to please take this very seriously, because it happens all of a sudden – very abruptly. ... The best time to mitigate is before that happens, because if you wait until after it happens you’re playing catch-up.”
Dr. Bauchner, noting that strict social distancing has been underway in many parts of the United States for several days, posited that, by early April, “We’ll really have a sense if we can manage in terms of serious illness.” Seattle, New York, Boston, and the San Francisco Bay Area may experience demand that outstrips ICU capacity at that point, but the rest of the country, he said, “is doing relatively well.”
Stress test on the health care system
Dr. Fauci agreed with this statement and added: “We’re going to know – for better or worse – whether we have enough of what it takes to be able to practice the kind of medicine that we optimally would want to practice.
In the matter of a week or 2 ... I think we’ll get a feel for whether or not we really have enough of the supplies that it takes.”
The well-publicized regional shortages in personal protective equipment (PPE) are forcing tough choices in some areas. As expedited – and even drive-through – testing begins, some of the demand for testing-related PPE may abate, especially if protocols include self-administration of nasal swabs, he noted.
Dr. Fauci added that the strategic national stockpile of medical supplies and equipment has not yet been tapped, “but you need to backfill that as quickly as you can once you start drawing from the strategic national stockpile.”
Returning to work after COVID-19 infection
Regarding the thorny question of when health care workers should be permitted to return to work after coronavirus infection, “it’s an evolving story,” said Dr. Fauci. Current guidance advises that health care providers stay away from work until two negative tests after resolution of fever and improvement of respiratory symptoms, or 3 fever-free days.
“We are approaching a point where you’re going to get enough people who are getting infected that we aren’t going to be able to do that,” he said. Depending on the stress to the health care system in a given locality, he said that facilities are going to have to “decide with good judgment” when health care workers go back on the job after coronavirus infection.
Asked how soon an individual would reliably test positive for COVID-19 after exposure, Dr. Fauci said, “We don’t know the answer to that. ... We can surmise it ...” He noted that it’s a median of about 5 days with a range of 2 to 14 days, before an infected individual becomes symptomatic. “I can say it’s not going to happen immediately,” he added, noting that he wouldn’t expect to see a positive test until about 2 days after exposure at the earliest. “When you get to the point where you are symptomatic, you’re almost certainly going to be positive then. ... This is just an extrapolation,” rather than conclusions drawn from solid data, he emphasized.
Higher risk reported in cardiac patients
Dr. Bauchner, who was relaying questions sent in from physicians during the live-streamed interview, asked about a newly issued joint statement from the American Heart Association, American College of Cardiology, and the Heart Failure Society of America, which on March 17 affirmed that individuals on ACE inhibitors and angiotensin receptor blockers (ARBs) continue that therapy if they should become ill with COVID-19. The European Society of Cardiology issued a similar recommendation a few days prior.
Despite these societies’ statements, Dr. Fauci pointed to population-level data in Italy as suggesting that the case isn’t yet closed. “We really need to get data, and we need to get data fast. There’s a mechanistic rationale for the concern. It’s there, and it’s firm,” he said. The theoretical concern is that ACE inhibitors can upregulate expression of the ACE-2 protein on cell membranes, which is the entry point for SARS-Cov-2 to enter cells.
He added that he remains concerned about the number of coronavirus fatalities of patients in Italy who had hypertension as their only, or primary, underlying health problem.“That to me was a bit of a red flag,” he said. “Patients with hypertension almost certainly had a physician, and the physician almost certainly treated that person with medication. Why should someone who has hypertension that was well controlled have a much greater chance of dying?” he asked, noting that “I look at a person with well-controlled hypertension as a relatively healthy person. I don’t know what the answer is, but somebody has to look very carefully,” ideally by means of a natural history study that identifies medications used by those who died from coronavirus.
Potential therapies
Regarding potential therapies for COVID-19, Dr. Fauci acknowledged the social media buzz and flurry of medical letters and case reports about the use of hydroxychloroquine (Plaquenil) to treat active infection. He said that he and other researchers are “in active discussion” about how best to study the efficacy and safety of hydroxychloroquine, but he also acknowledged that many treating clinicians will use hydroxychloroquine empirically in the absence of other treatments with proven efficacy.
Clinical trials underway in China for antiviral medication are facing some enrollment challenges currently “because people want to get the drug,” said Dr. Fauci. “They don’t want to be in the trial; they just want to get the drug.” Though each of two trials has targeted approximately 500 participants as the number needed for sufficient statistical power, Dr. Fauci urged Chinese data safety monitoring boards to “take a close look” at the data already accrued for the several hundred patients who have already enrolled for the studies “to see if there’s any hint of efficacy.”
In a JAMA Live Stream interview, in the United States.
Dr. Fauci got into the details of what is known, what is unknown, what is being done in laboratories, and what clinical elements are still not understood about this disease.
The next several weeks, he said, are likely to tell the tale of whether our health care system is up to the challenge of care for the most ill among those who will be affected by COVID-19.
“It shouldn’t panic or frighten us, but we have to know we’re dealing with a very serious problem that we have to address, and we have to deal with it in a very bold way,” said Dr. Fauci, director of the National Institute of Allergy and Infectious Diseases at the National Institutes of Health.
Speaking in an interview with JAMA Editor in Chief Howard Bauchner, MD, Dr. Fauci said the situation favors action over fear. “Let’s apply that energy to doing the things that we know can mitigate this.”
He added that he heard the message loud and clear from health care leaders in Italy and France during a World Health Organization coronavirus call earlier in the day. Officials in those countries, he said, were “almost pleading with the rest of the world to please take this very seriously, because it happens all of a sudden – very abruptly. ... The best time to mitigate is before that happens, because if you wait until after it happens you’re playing catch-up.”
Dr. Bauchner, noting that strict social distancing has been underway in many parts of the United States for several days, posited that, by early April, “We’ll really have a sense if we can manage in terms of serious illness.” Seattle, New York, Boston, and the San Francisco Bay Area may experience demand that outstrips ICU capacity at that point, but the rest of the country, he said, “is doing relatively well.”
Stress test on the health care system
Dr. Fauci agreed with this statement and added: “We’re going to know – for better or worse – whether we have enough of what it takes to be able to practice the kind of medicine that we optimally would want to practice.
In the matter of a week or 2 ... I think we’ll get a feel for whether or not we really have enough of the supplies that it takes.”
The well-publicized regional shortages in personal protective equipment (PPE) are forcing tough choices in some areas. As expedited – and even drive-through – testing begins, some of the demand for testing-related PPE may abate, especially if protocols include self-administration of nasal swabs, he noted.
Dr. Fauci added that the strategic national stockpile of medical supplies and equipment has not yet been tapped, “but you need to backfill that as quickly as you can once you start drawing from the strategic national stockpile.”
Returning to work after COVID-19 infection
Regarding the thorny question of when health care workers should be permitted to return to work after coronavirus infection, “it’s an evolving story,” said Dr. Fauci. Current guidance advises that health care providers stay away from work until two negative tests after resolution of fever and improvement of respiratory symptoms, or 3 fever-free days.
“We are approaching a point where you’re going to get enough people who are getting infected that we aren’t going to be able to do that,” he said. Depending on the stress to the health care system in a given locality, he said that facilities are going to have to “decide with good judgment” when health care workers go back on the job after coronavirus infection.
Asked how soon an individual would reliably test positive for COVID-19 after exposure, Dr. Fauci said, “We don’t know the answer to that. ... We can surmise it ...” He noted that it’s a median of about 5 days with a range of 2 to 14 days, before an infected individual becomes symptomatic. “I can say it’s not going to happen immediately,” he added, noting that he wouldn’t expect to see a positive test until about 2 days after exposure at the earliest. “When you get to the point where you are symptomatic, you’re almost certainly going to be positive then. ... This is just an extrapolation,” rather than conclusions drawn from solid data, he emphasized.
Higher risk reported in cardiac patients
Dr. Bauchner, who was relaying questions sent in from physicians during the live-streamed interview, asked about a newly issued joint statement from the American Heart Association, American College of Cardiology, and the Heart Failure Society of America, which on March 17 affirmed that individuals on ACE inhibitors and angiotensin receptor blockers (ARBs) continue that therapy if they should become ill with COVID-19. The European Society of Cardiology issued a similar recommendation a few days prior.
Despite these societies’ statements, Dr. Fauci pointed to population-level data in Italy as suggesting that the case isn’t yet closed. “We really need to get data, and we need to get data fast. There’s a mechanistic rationale for the concern. It’s there, and it’s firm,” he said. The theoretical concern is that ACE inhibitors can upregulate expression of the ACE-2 protein on cell membranes, which is the entry point for SARS-Cov-2 to enter cells.
He added that he remains concerned about the number of coronavirus fatalities of patients in Italy who had hypertension as their only, or primary, underlying health problem.“That to me was a bit of a red flag,” he said. “Patients with hypertension almost certainly had a physician, and the physician almost certainly treated that person with medication. Why should someone who has hypertension that was well controlled have a much greater chance of dying?” he asked, noting that “I look at a person with well-controlled hypertension as a relatively healthy person. I don’t know what the answer is, but somebody has to look very carefully,” ideally by means of a natural history study that identifies medications used by those who died from coronavirus.
Potential therapies
Regarding potential therapies for COVID-19, Dr. Fauci acknowledged the social media buzz and flurry of medical letters and case reports about the use of hydroxychloroquine (Plaquenil) to treat active infection. He said that he and other researchers are “in active discussion” about how best to study the efficacy and safety of hydroxychloroquine, but he also acknowledged that many treating clinicians will use hydroxychloroquine empirically in the absence of other treatments with proven efficacy.
Clinical trials underway in China for antiviral medication are facing some enrollment challenges currently “because people want to get the drug,” said Dr. Fauci. “They don’t want to be in the trial; they just want to get the drug.” Though each of two trials has targeted approximately 500 participants as the number needed for sufficient statistical power, Dr. Fauci urged Chinese data safety monitoring boards to “take a close look” at the data already accrued for the several hundred patients who have already enrolled for the studies “to see if there’s any hint of efficacy.”
In a JAMA Live Stream interview, in the United States.
Dr. Fauci got into the details of what is known, what is unknown, what is being done in laboratories, and what clinical elements are still not understood about this disease.
The next several weeks, he said, are likely to tell the tale of whether our health care system is up to the challenge of care for the most ill among those who will be affected by COVID-19.
“It shouldn’t panic or frighten us, but we have to know we’re dealing with a very serious problem that we have to address, and we have to deal with it in a very bold way,” said Dr. Fauci, director of the National Institute of Allergy and Infectious Diseases at the National Institutes of Health.
Speaking in an interview with JAMA Editor in Chief Howard Bauchner, MD, Dr. Fauci said the situation favors action over fear. “Let’s apply that energy to doing the things that we know can mitigate this.”
He added that he heard the message loud and clear from health care leaders in Italy and France during a World Health Organization coronavirus call earlier in the day. Officials in those countries, he said, were “almost pleading with the rest of the world to please take this very seriously, because it happens all of a sudden – very abruptly. ... The best time to mitigate is before that happens, because if you wait until after it happens you’re playing catch-up.”
Dr. Bauchner, noting that strict social distancing has been underway in many parts of the United States for several days, posited that, by early April, “We’ll really have a sense if we can manage in terms of serious illness.” Seattle, New York, Boston, and the San Francisco Bay Area may experience demand that outstrips ICU capacity at that point, but the rest of the country, he said, “is doing relatively well.”
Stress test on the health care system
Dr. Fauci agreed with this statement and added: “We’re going to know – for better or worse – whether we have enough of what it takes to be able to practice the kind of medicine that we optimally would want to practice.
In the matter of a week or 2 ... I think we’ll get a feel for whether or not we really have enough of the supplies that it takes.”
The well-publicized regional shortages in personal protective equipment (PPE) are forcing tough choices in some areas. As expedited – and even drive-through – testing begins, some of the demand for testing-related PPE may abate, especially if protocols include self-administration of nasal swabs, he noted.
Dr. Fauci added that the strategic national stockpile of medical supplies and equipment has not yet been tapped, “but you need to backfill that as quickly as you can once you start drawing from the strategic national stockpile.”
Returning to work after COVID-19 infection
Regarding the thorny question of when health care workers should be permitted to return to work after coronavirus infection, “it’s an evolving story,” said Dr. Fauci. Current guidance advises that health care providers stay away from work until two negative tests after resolution of fever and improvement of respiratory symptoms, or 3 fever-free days.
“We are approaching a point where you’re going to get enough people who are getting infected that we aren’t going to be able to do that,” he said. Depending on the stress to the health care system in a given locality, he said that facilities are going to have to “decide with good judgment” when health care workers go back on the job after coronavirus infection.
Asked how soon an individual would reliably test positive for COVID-19 after exposure, Dr. Fauci said, “We don’t know the answer to that. ... We can surmise it ...” He noted that it’s a median of about 5 days with a range of 2 to 14 days, before an infected individual becomes symptomatic. “I can say it’s not going to happen immediately,” he added, noting that he wouldn’t expect to see a positive test until about 2 days after exposure at the earliest. “When you get to the point where you are symptomatic, you’re almost certainly going to be positive then. ... This is just an extrapolation,” rather than conclusions drawn from solid data, he emphasized.
Higher risk reported in cardiac patients
Dr. Bauchner, who was relaying questions sent in from physicians during the live-streamed interview, asked about a newly issued joint statement from the American Heart Association, American College of Cardiology, and the Heart Failure Society of America, which on March 17 affirmed that individuals on ACE inhibitors and angiotensin receptor blockers (ARBs) continue that therapy if they should become ill with COVID-19. The European Society of Cardiology issued a similar recommendation a few days prior.
Despite these societies’ statements, Dr. Fauci pointed to population-level data in Italy as suggesting that the case isn’t yet closed. “We really need to get data, and we need to get data fast. There’s a mechanistic rationale for the concern. It’s there, and it’s firm,” he said. The theoretical concern is that ACE inhibitors can upregulate expression of the ACE-2 protein on cell membranes, which is the entry point for SARS-Cov-2 to enter cells.
He added that he remains concerned about the number of coronavirus fatalities of patients in Italy who had hypertension as their only, or primary, underlying health problem.“That to me was a bit of a red flag,” he said. “Patients with hypertension almost certainly had a physician, and the physician almost certainly treated that person with medication. Why should someone who has hypertension that was well controlled have a much greater chance of dying?” he asked, noting that “I look at a person with well-controlled hypertension as a relatively healthy person. I don’t know what the answer is, but somebody has to look very carefully,” ideally by means of a natural history study that identifies medications used by those who died from coronavirus.
Potential therapies
Regarding potential therapies for COVID-19, Dr. Fauci acknowledged the social media buzz and flurry of medical letters and case reports about the use of hydroxychloroquine (Plaquenil) to treat active infection. He said that he and other researchers are “in active discussion” about how best to study the efficacy and safety of hydroxychloroquine, but he also acknowledged that many treating clinicians will use hydroxychloroquine empirically in the absence of other treatments with proven efficacy.
Clinical trials underway in China for antiviral medication are facing some enrollment challenges currently “because people want to get the drug,” said Dr. Fauci. “They don’t want to be in the trial; they just want to get the drug.” Though each of two trials has targeted approximately 500 participants as the number needed for sufficient statistical power, Dr. Fauci urged Chinese data safety monitoring boards to “take a close look” at the data already accrued for the several hundred patients who have already enrolled for the studies “to see if there’s any hint of efficacy.”
REPORTING FROM JAMA LIVE STREAM
COVID-19 in China: Children have less severe disease, but are vulnerable
Clinical manifestations of COVID-19 infection among children in mainland China generally have been less severe than those among adults, but children of all ages – and infants in particular – are vulnerable to infection, according to a review of 2,143 cases.
Further, infection patterns in the nationwide series of all pediatric patients reported to the Chinese Center for Disease Control and Prevention from Jan. 16 to Feb. 8, 2020, provide strong evidence of human-to-human transmission, Yuanyuan Dong, MPH, a research assistant at Shanghai Children’s Medical Center, Shanghai Jiao Tong University, China, and colleagues reported in Pediatrics.
Of the 2,143 patients included in the review, 57% were boys and the median age was 7 years; 34% had laboratory-confirmed infection and 67% had suspected infection. More than 90% had asymptomatic, mild, or moderate disease (4%, 51%, and 39%, respectively), and 46% were from Hubei Province, where the first cases were reported, the investigators found.
The median time from illness onset to diagnosis was 2 days, and there was a trend of rapid increase of disease at the early stage of the epidemic – with rapid spread from Hubei Province to surrounding provinces – followed by a gradual and steady decrease, they noted.
“The total number of pediatric patients increased remarkably between mid-January and early February, peaked around February 1, and then declined since early February 2020,” they wrote. The proportion of severe and critical cases was 11% for infants under 1 year of age, compared with 7% for those aged 1-5 years; 4% for those aged 6-10 years; 4% for those 11-15 years; and 3% for those 16 years and older.
As of Feb. 8, 2020, only one child in this group of study patients died and most cases of COVID-19 symptoms were mild. There were many fewer severe and critical cases among the children (6%), compared with those reported in adult patients in other studies (19%). “It suggests that, compared with adult patients, clinical manifestations of children’s COVID-19 may be less severe,” the investigators suggested.
“As most of these children were likely to expose themselves to family members and/or other children with COVID-19, it clearly indicates person-to-person transmission ” of novel coronavirus 2019, they said, adding that similar evidence of such transmission also has been reported from studies of adult patients.
The reasons for reduced severity in children versus adults remain unclear, but may be related to both exposure and host factors, Ms. Dong and associates said. “Children were usually well cared for at home and might have relatively [fewer] opportunities to expose themselves to pathogens and/or sick patients.”
The findings demonstrate a pediatric distribution that varied across time and space, with most cases concentrated in the Hubei province and surrounding areas. No significant gender-related difference in infection rates was observed, and although the median patient age was 7 years, the range was 1 day to 18 years, suggesting that “all ages at childhood were susceptible” to the virus, they added.
The declining number of cases over time further suggests that disease control measures implemented by the government were effective, and that cases will “continue to decline, and finally stop in the near future unless sustained human-to-human transmissions occur,” Ms. Dong and associates concluded.
In an accompanying editorial, Andrea T. Cruz, MD, of Baylor College of Medicine, Houston, and Steven L. Zeichner, MD, PhD, of the University of Virginia, Charlottesville, said the findings regarding reduced severity among children versus adults with novel coronavirus 2019 infection are consistent with data on non-COVID-19 coronavirus.
They pointed out that Ms. Dong and associates did find that 13% of virologically-confirmed cases had asymptomatic infection, “a rate that almost certainly understates the true rate of asymptomatic infection, since many asymptomatic children are unlikely to be tested.”
Of the symptomatic children, “5% had dyspnea or hypoxemia (a substantially lower percentage than what has been reported for adults) and 0.6% progressed to acute respiratory distress syndrome (ARDS) or multiorgan system dysfunction”; this also is at a lower rate than seen in adults, they said.
Very young children –infants or children in preschool – were more likely to have severe clinical manifestations than children who were older.
Thus, it appears that certain subpopulations of children are at increased risk for more significant COVID-19 illness: “younger age, underlying pulmonary pathology, and immunocompromising conditions,” Dr. Cruz and Dr. Zeichner suggested.
The two editorialists said the findings suggest children “may play a major role in community-based viral transmission.” Evidence suggests that children may have more upper respiratory tract involvement and that fecal shedding may occur for several weeks after diagnosis; this raises concerns about fecal-oral transmission, particularly for infants and children, and about viral replication in the gastrointestinal tract, they said. This has substantial implications for community spread in day care centers, schools, and in the home.
A great deal has been learned about COVID-19 in a short time, but there still is much to learn about the effect of the virus on children, the impact of children on viral spread, and about possible vertical transmission, they said.
“Widespread availability of testing will allow for us to more accurately describe the spectrum of illness and may result in adjustment of the apparent morbidity and mortality rate as fewer ill individuals are diagnosed,” Dr. Cruz and Dr. Zeichner wrote, adding that “rigorously gauging the impact of COVID-19 on children will be important to accurately model the pandemic and to ensure that appropriate resources are allocated to children requiring care.”
They noted that understanding differences in children versus adults with COVID-19 “can yield important insights into disease pathogenesis, informing management and the development of therapeutics.”
This study was partially supported by the Science and Technology Commission of Shanghai Municipality. The authors reported having no disclosures. Dr. Cruz and Dr. Zeichner are associate editors for Pediatrics. Dr. Cruz reported having no disclosures. Dr. Zeichner is an inventor of new technologies for the rapid production of vaccines, for which the University of Virginia has filed patent applications.
SOURCE: Dong Y et al. Pediatrics. 2020 Mar 16. doi: 10.1542/peds.2020-0702; Cruz A and Zeichner S. Pediatrics. 2020 Mar 16. doi: 10.1542/peds.2020-0834.
Clinical manifestations of COVID-19 infection among children in mainland China generally have been less severe than those among adults, but children of all ages – and infants in particular – are vulnerable to infection, according to a review of 2,143 cases.
Further, infection patterns in the nationwide series of all pediatric patients reported to the Chinese Center for Disease Control and Prevention from Jan. 16 to Feb. 8, 2020, provide strong evidence of human-to-human transmission, Yuanyuan Dong, MPH, a research assistant at Shanghai Children’s Medical Center, Shanghai Jiao Tong University, China, and colleagues reported in Pediatrics.
Of the 2,143 patients included in the review, 57% were boys and the median age was 7 years; 34% had laboratory-confirmed infection and 67% had suspected infection. More than 90% had asymptomatic, mild, or moderate disease (4%, 51%, and 39%, respectively), and 46% were from Hubei Province, where the first cases were reported, the investigators found.
The median time from illness onset to diagnosis was 2 days, and there was a trend of rapid increase of disease at the early stage of the epidemic – with rapid spread from Hubei Province to surrounding provinces – followed by a gradual and steady decrease, they noted.
“The total number of pediatric patients increased remarkably between mid-January and early February, peaked around February 1, and then declined since early February 2020,” they wrote. The proportion of severe and critical cases was 11% for infants under 1 year of age, compared with 7% for those aged 1-5 years; 4% for those aged 6-10 years; 4% for those 11-15 years; and 3% for those 16 years and older.
As of Feb. 8, 2020, only one child in this group of study patients died and most cases of COVID-19 symptoms were mild. There were many fewer severe and critical cases among the children (6%), compared with those reported in adult patients in other studies (19%). “It suggests that, compared with adult patients, clinical manifestations of children’s COVID-19 may be less severe,” the investigators suggested.
“As most of these children were likely to expose themselves to family members and/or other children with COVID-19, it clearly indicates person-to-person transmission ” of novel coronavirus 2019, they said, adding that similar evidence of such transmission also has been reported from studies of adult patients.
The reasons for reduced severity in children versus adults remain unclear, but may be related to both exposure and host factors, Ms. Dong and associates said. “Children were usually well cared for at home and might have relatively [fewer] opportunities to expose themselves to pathogens and/or sick patients.”
The findings demonstrate a pediatric distribution that varied across time and space, with most cases concentrated in the Hubei province and surrounding areas. No significant gender-related difference in infection rates was observed, and although the median patient age was 7 years, the range was 1 day to 18 years, suggesting that “all ages at childhood were susceptible” to the virus, they added.
The declining number of cases over time further suggests that disease control measures implemented by the government were effective, and that cases will “continue to decline, and finally stop in the near future unless sustained human-to-human transmissions occur,” Ms. Dong and associates concluded.
In an accompanying editorial, Andrea T. Cruz, MD, of Baylor College of Medicine, Houston, and Steven L. Zeichner, MD, PhD, of the University of Virginia, Charlottesville, said the findings regarding reduced severity among children versus adults with novel coronavirus 2019 infection are consistent with data on non-COVID-19 coronavirus.
They pointed out that Ms. Dong and associates did find that 13% of virologically-confirmed cases had asymptomatic infection, “a rate that almost certainly understates the true rate of asymptomatic infection, since many asymptomatic children are unlikely to be tested.”
Of the symptomatic children, “5% had dyspnea or hypoxemia (a substantially lower percentage than what has been reported for adults) and 0.6% progressed to acute respiratory distress syndrome (ARDS) or multiorgan system dysfunction”; this also is at a lower rate than seen in adults, they said.
Very young children –infants or children in preschool – were more likely to have severe clinical manifestations than children who were older.
Thus, it appears that certain subpopulations of children are at increased risk for more significant COVID-19 illness: “younger age, underlying pulmonary pathology, and immunocompromising conditions,” Dr. Cruz and Dr. Zeichner suggested.
The two editorialists said the findings suggest children “may play a major role in community-based viral transmission.” Evidence suggests that children may have more upper respiratory tract involvement and that fecal shedding may occur for several weeks after diagnosis; this raises concerns about fecal-oral transmission, particularly for infants and children, and about viral replication in the gastrointestinal tract, they said. This has substantial implications for community spread in day care centers, schools, and in the home.
A great deal has been learned about COVID-19 in a short time, but there still is much to learn about the effect of the virus on children, the impact of children on viral spread, and about possible vertical transmission, they said.
“Widespread availability of testing will allow for us to more accurately describe the spectrum of illness and may result in adjustment of the apparent morbidity and mortality rate as fewer ill individuals are diagnosed,” Dr. Cruz and Dr. Zeichner wrote, adding that “rigorously gauging the impact of COVID-19 on children will be important to accurately model the pandemic and to ensure that appropriate resources are allocated to children requiring care.”
They noted that understanding differences in children versus adults with COVID-19 “can yield important insights into disease pathogenesis, informing management and the development of therapeutics.”
This study was partially supported by the Science and Technology Commission of Shanghai Municipality. The authors reported having no disclosures. Dr. Cruz and Dr. Zeichner are associate editors for Pediatrics. Dr. Cruz reported having no disclosures. Dr. Zeichner is an inventor of new technologies for the rapid production of vaccines, for which the University of Virginia has filed patent applications.
SOURCE: Dong Y et al. Pediatrics. 2020 Mar 16. doi: 10.1542/peds.2020-0702; Cruz A and Zeichner S. Pediatrics. 2020 Mar 16. doi: 10.1542/peds.2020-0834.
Clinical manifestations of COVID-19 infection among children in mainland China generally have been less severe than those among adults, but children of all ages – and infants in particular – are vulnerable to infection, according to a review of 2,143 cases.
Further, infection patterns in the nationwide series of all pediatric patients reported to the Chinese Center for Disease Control and Prevention from Jan. 16 to Feb. 8, 2020, provide strong evidence of human-to-human transmission, Yuanyuan Dong, MPH, a research assistant at Shanghai Children’s Medical Center, Shanghai Jiao Tong University, China, and colleagues reported in Pediatrics.
Of the 2,143 patients included in the review, 57% were boys and the median age was 7 years; 34% had laboratory-confirmed infection and 67% had suspected infection. More than 90% had asymptomatic, mild, or moderate disease (4%, 51%, and 39%, respectively), and 46% were from Hubei Province, where the first cases were reported, the investigators found.
The median time from illness onset to diagnosis was 2 days, and there was a trend of rapid increase of disease at the early stage of the epidemic – with rapid spread from Hubei Province to surrounding provinces – followed by a gradual and steady decrease, they noted.
“The total number of pediatric patients increased remarkably between mid-January and early February, peaked around February 1, and then declined since early February 2020,” they wrote. The proportion of severe and critical cases was 11% for infants under 1 year of age, compared with 7% for those aged 1-5 years; 4% for those aged 6-10 years; 4% for those 11-15 years; and 3% for those 16 years and older.
As of Feb. 8, 2020, only one child in this group of study patients died and most cases of COVID-19 symptoms were mild. There were many fewer severe and critical cases among the children (6%), compared with those reported in adult patients in other studies (19%). “It suggests that, compared with adult patients, clinical manifestations of children’s COVID-19 may be less severe,” the investigators suggested.
“As most of these children were likely to expose themselves to family members and/or other children with COVID-19, it clearly indicates person-to-person transmission ” of novel coronavirus 2019, they said, adding that similar evidence of such transmission also has been reported from studies of adult patients.
The reasons for reduced severity in children versus adults remain unclear, but may be related to both exposure and host factors, Ms. Dong and associates said. “Children were usually well cared for at home and might have relatively [fewer] opportunities to expose themselves to pathogens and/or sick patients.”
The findings demonstrate a pediatric distribution that varied across time and space, with most cases concentrated in the Hubei province and surrounding areas. No significant gender-related difference in infection rates was observed, and although the median patient age was 7 years, the range was 1 day to 18 years, suggesting that “all ages at childhood were susceptible” to the virus, they added.
The declining number of cases over time further suggests that disease control measures implemented by the government were effective, and that cases will “continue to decline, and finally stop in the near future unless sustained human-to-human transmissions occur,” Ms. Dong and associates concluded.
In an accompanying editorial, Andrea T. Cruz, MD, of Baylor College of Medicine, Houston, and Steven L. Zeichner, MD, PhD, of the University of Virginia, Charlottesville, said the findings regarding reduced severity among children versus adults with novel coronavirus 2019 infection are consistent with data on non-COVID-19 coronavirus.
They pointed out that Ms. Dong and associates did find that 13% of virologically-confirmed cases had asymptomatic infection, “a rate that almost certainly understates the true rate of asymptomatic infection, since many asymptomatic children are unlikely to be tested.”
Of the symptomatic children, “5% had dyspnea or hypoxemia (a substantially lower percentage than what has been reported for adults) and 0.6% progressed to acute respiratory distress syndrome (ARDS) or multiorgan system dysfunction”; this also is at a lower rate than seen in adults, they said.
Very young children –infants or children in preschool – were more likely to have severe clinical manifestations than children who were older.
Thus, it appears that certain subpopulations of children are at increased risk for more significant COVID-19 illness: “younger age, underlying pulmonary pathology, and immunocompromising conditions,” Dr. Cruz and Dr. Zeichner suggested.
The two editorialists said the findings suggest children “may play a major role in community-based viral transmission.” Evidence suggests that children may have more upper respiratory tract involvement and that fecal shedding may occur for several weeks after diagnosis; this raises concerns about fecal-oral transmission, particularly for infants and children, and about viral replication in the gastrointestinal tract, they said. This has substantial implications for community spread in day care centers, schools, and in the home.
A great deal has been learned about COVID-19 in a short time, but there still is much to learn about the effect of the virus on children, the impact of children on viral spread, and about possible vertical transmission, they said.
“Widespread availability of testing will allow for us to more accurately describe the spectrum of illness and may result in adjustment of the apparent morbidity and mortality rate as fewer ill individuals are diagnosed,” Dr. Cruz and Dr. Zeichner wrote, adding that “rigorously gauging the impact of COVID-19 on children will be important to accurately model the pandemic and to ensure that appropriate resources are allocated to children requiring care.”
They noted that understanding differences in children versus adults with COVID-19 “can yield important insights into disease pathogenesis, informing management and the development of therapeutics.”
This study was partially supported by the Science and Technology Commission of Shanghai Municipality. The authors reported having no disclosures. Dr. Cruz and Dr. Zeichner are associate editors for Pediatrics. Dr. Cruz reported having no disclosures. Dr. Zeichner is an inventor of new technologies for the rapid production of vaccines, for which the University of Virginia has filed patent applications.
SOURCE: Dong Y et al. Pediatrics. 2020 Mar 16. doi: 10.1542/peds.2020-0702; Cruz A and Zeichner S. Pediatrics. 2020 Mar 16. doi: 10.1542/peds.2020-0834.
FROM PEDIATRICS
ACP outlines guide for COVID-19 telehealth coding, billing
and for handling clinician and staff absences due to illness or quarantine during the COVID-19 pandemic.
It strongly encourages practices to use telehealth, whenever possible, to mitigate exposure of patients who are sick or at risk because of other underlying conditions and to protect health care workers and the community from the spread of the disease.
The national organization of internists also recommends in the guidance that practices establish protocols and procedures for use by clinicians and all other staff in light of the pandemic.
The billing and coding tips are being offered to help practices deal with the rapidly changing situation surrounding the COVID-19 emergency, according to a statement from the ACP.
The coding-related guidance incorporates changes to a number of telehealth rules for Medicare beneficiaries, announced by the Centers for Medicare and Medicaid Services on March 17.
“Now in a full state of emergency, many Medicare restrictions related to telehealth have been lifted. Patients can be at home, and non-HIPAA compliant technology is allowed. There is no cost sharing for COVID-19 testing. In addition, to encourage use by patients, Medicare is allowing practices to waive cost sharing (copays and deductibles) for all telehealth services,” the organization said in the guidance. It notes, however, that the CMS does not currently reimburse for telephone calls.
The guidance includes details of the new ICD-10 codes, and stresses the importance of using the appropriate codes, given that some service cost-sharing has been waived for COVID-19 testing and treatment.
There is detailed coding guidance for virtual check-in, online evaluation and management, remote monitoring, originating site, and allowed technology and services.
In regard to clinician and staff absence due to illness or quarantine, the ACP says “practices may need to review emergency plans related to telework and to employee and clinician absence.” Among its recommendations are that practices and employers consider temporary adjustments to compensation formulas to accommodate those clinicians who experience a loss of income because they are paid based on production.
The organization emphasizes that, given the rapidly changing availability of testing for COVID-19, practices should contact their local health departments, hospitals, reference labs, or state health authorities to determine the status of their access to testing.
The full list of the ACP’s tips are available here.
Any new guidance for physicians will be posted on the ACP’s COVID-19 resource page.
and for handling clinician and staff absences due to illness or quarantine during the COVID-19 pandemic.
It strongly encourages practices to use telehealth, whenever possible, to mitigate exposure of patients who are sick or at risk because of other underlying conditions and to protect health care workers and the community from the spread of the disease.
The national organization of internists also recommends in the guidance that practices establish protocols and procedures for use by clinicians and all other staff in light of the pandemic.
The billing and coding tips are being offered to help practices deal with the rapidly changing situation surrounding the COVID-19 emergency, according to a statement from the ACP.
The coding-related guidance incorporates changes to a number of telehealth rules for Medicare beneficiaries, announced by the Centers for Medicare and Medicaid Services on March 17.
“Now in a full state of emergency, many Medicare restrictions related to telehealth have been lifted. Patients can be at home, and non-HIPAA compliant technology is allowed. There is no cost sharing for COVID-19 testing. In addition, to encourage use by patients, Medicare is allowing practices to waive cost sharing (copays and deductibles) for all telehealth services,” the organization said in the guidance. It notes, however, that the CMS does not currently reimburse for telephone calls.
The guidance includes details of the new ICD-10 codes, and stresses the importance of using the appropriate codes, given that some service cost-sharing has been waived for COVID-19 testing and treatment.
There is detailed coding guidance for virtual check-in, online evaluation and management, remote monitoring, originating site, and allowed technology and services.
In regard to clinician and staff absence due to illness or quarantine, the ACP says “practices may need to review emergency plans related to telework and to employee and clinician absence.” Among its recommendations are that practices and employers consider temporary adjustments to compensation formulas to accommodate those clinicians who experience a loss of income because they are paid based on production.
The organization emphasizes that, given the rapidly changing availability of testing for COVID-19, practices should contact their local health departments, hospitals, reference labs, or state health authorities to determine the status of their access to testing.
The full list of the ACP’s tips are available here.
Any new guidance for physicians will be posted on the ACP’s COVID-19 resource page.
and for handling clinician and staff absences due to illness or quarantine during the COVID-19 pandemic.
It strongly encourages practices to use telehealth, whenever possible, to mitigate exposure of patients who are sick or at risk because of other underlying conditions and to protect health care workers and the community from the spread of the disease.
The national organization of internists also recommends in the guidance that practices establish protocols and procedures for use by clinicians and all other staff in light of the pandemic.
The billing and coding tips are being offered to help practices deal with the rapidly changing situation surrounding the COVID-19 emergency, according to a statement from the ACP.
The coding-related guidance incorporates changes to a number of telehealth rules for Medicare beneficiaries, announced by the Centers for Medicare and Medicaid Services on March 17.
“Now in a full state of emergency, many Medicare restrictions related to telehealth have been lifted. Patients can be at home, and non-HIPAA compliant technology is allowed. There is no cost sharing for COVID-19 testing. In addition, to encourage use by patients, Medicare is allowing practices to waive cost sharing (copays and deductibles) for all telehealth services,” the organization said in the guidance. It notes, however, that the CMS does not currently reimburse for telephone calls.
The guidance includes details of the new ICD-10 codes, and stresses the importance of using the appropriate codes, given that some service cost-sharing has been waived for COVID-19 testing and treatment.
There is detailed coding guidance for virtual check-in, online evaluation and management, remote monitoring, originating site, and allowed technology and services.
In regard to clinician and staff absence due to illness or quarantine, the ACP says “practices may need to review emergency plans related to telework and to employee and clinician absence.” Among its recommendations are that practices and employers consider temporary adjustments to compensation formulas to accommodate those clinicians who experience a loss of income because they are paid based on production.
The organization emphasizes that, given the rapidly changing availability of testing for COVID-19, practices should contact their local health departments, hospitals, reference labs, or state health authorities to determine the status of their access to testing.
The full list of the ACP’s tips are available here.
Any new guidance for physicians will be posted on the ACP’s COVID-19 resource page.
Inactivated flu vaccine succeeds among autoimmune rheumatic disease patients
Use of the inactivated influenza vaccine by adults with autoimmune rheumatic diseases significantly reduced their risk of influenza-like illness, hospitalization for pneumonia and chronic obstructive pulmonary disease, and death from pneumonia, according to findings from an observational study of more than 30,000 patients in the U.K. Clinical Practice Research Datalink.
Although the inactivated vaccine has been recommended for patients with autoimmune rheumatic diseases (AIRDs), including rheumatoid arthritis and spondyloarthritis, the vaccine’s impact on patient outcomes including pneumonia, hospitalization, and death has not been well studied, wrote Georgina Nakafero, PhD, of the University of Nottingham, England, and colleagues.
In a study published in Rheumatology, the researchers identified 30,788 adults with AIRDs from the longitudinal Clinical Practice Research Datalink database in the United Kingdom. Of these, 66% were women, 76% had rheumatoid arthritis, and 61% had been prescribed methotrexate. The study included a total of 125,034 flu cycles between 2006 and 2009 and between 2010 and 2015.
Overall, vaccination with the inactivated influenza vaccine (IIV) reduced the risk of primary care consultation for influenza-like illness (adjusted odds ratio, 0.70), hospitalization for pneumonia (aOR, 0.61), exacerbation of chronic obstructive pulmonary disease (aOR, 0.67), and death caused by pneumonia (aOR, 0.48) in the study population. In a propensity score–adjusted analysis, only protection from influenza-like illness lost statistical significance.
In addition, vaccination was associated with a reduction in all-cause mortality among AIRDs patients, but restricting the outcomes to the active influenza periods may have confounded this result, the researchers said.
The study findings were limited by several factors including observational design, the use of a single vaccine efficacy estimate for each outcome, potential missed vaccination cycles, and potential confounding by indication and healthy user bias that could inflate the vaccine effectiveness, the researchers noted. However, the results were strengthened by the large sample size, including a range of AIRDs, and the use of both diagnostic and prescription codes, they said.
“The findings of this study, together with the results of our previous study demonstrating the safety of IIV in people with AIRDs, provides evidence to promote seasonal flu vaccination in this population,” they concluded. They still emphasized that randomized, controlled trials are needed for an assessment of vaccine efficacy.
The study was supported by Versus Arthritis and the National Institute of Health Research. Lead author Dr. Nakafero had no financial conflicts to disclose. Several coauthors disclosed relationships with companies, including AstraZeneca, Roche, and Pfizer.
SOURCE: Nakafero G et al. Rheumatology. 2020 Mar 11. doi: 10.1093/rheumatology/keaa078.
Use of the inactivated influenza vaccine by adults with autoimmune rheumatic diseases significantly reduced their risk of influenza-like illness, hospitalization for pneumonia and chronic obstructive pulmonary disease, and death from pneumonia, according to findings from an observational study of more than 30,000 patients in the U.K. Clinical Practice Research Datalink.
Although the inactivated vaccine has been recommended for patients with autoimmune rheumatic diseases (AIRDs), including rheumatoid arthritis and spondyloarthritis, the vaccine’s impact on patient outcomes including pneumonia, hospitalization, and death has not been well studied, wrote Georgina Nakafero, PhD, of the University of Nottingham, England, and colleagues.
In a study published in Rheumatology, the researchers identified 30,788 adults with AIRDs from the longitudinal Clinical Practice Research Datalink database in the United Kingdom. Of these, 66% were women, 76% had rheumatoid arthritis, and 61% had been prescribed methotrexate. The study included a total of 125,034 flu cycles between 2006 and 2009 and between 2010 and 2015.
Overall, vaccination with the inactivated influenza vaccine (IIV) reduced the risk of primary care consultation for influenza-like illness (adjusted odds ratio, 0.70), hospitalization for pneumonia (aOR, 0.61), exacerbation of chronic obstructive pulmonary disease (aOR, 0.67), and death caused by pneumonia (aOR, 0.48) in the study population. In a propensity score–adjusted analysis, only protection from influenza-like illness lost statistical significance.
In addition, vaccination was associated with a reduction in all-cause mortality among AIRDs patients, but restricting the outcomes to the active influenza periods may have confounded this result, the researchers said.
The study findings were limited by several factors including observational design, the use of a single vaccine efficacy estimate for each outcome, potential missed vaccination cycles, and potential confounding by indication and healthy user bias that could inflate the vaccine effectiveness, the researchers noted. However, the results were strengthened by the large sample size, including a range of AIRDs, and the use of both diagnostic and prescription codes, they said.
“The findings of this study, together with the results of our previous study demonstrating the safety of IIV in people with AIRDs, provides evidence to promote seasonal flu vaccination in this population,” they concluded. They still emphasized that randomized, controlled trials are needed for an assessment of vaccine efficacy.
The study was supported by Versus Arthritis and the National Institute of Health Research. Lead author Dr. Nakafero had no financial conflicts to disclose. Several coauthors disclosed relationships with companies, including AstraZeneca, Roche, and Pfizer.
SOURCE: Nakafero G et al. Rheumatology. 2020 Mar 11. doi: 10.1093/rheumatology/keaa078.
Use of the inactivated influenza vaccine by adults with autoimmune rheumatic diseases significantly reduced their risk of influenza-like illness, hospitalization for pneumonia and chronic obstructive pulmonary disease, and death from pneumonia, according to findings from an observational study of more than 30,000 patients in the U.K. Clinical Practice Research Datalink.
Although the inactivated vaccine has been recommended for patients with autoimmune rheumatic diseases (AIRDs), including rheumatoid arthritis and spondyloarthritis, the vaccine’s impact on patient outcomes including pneumonia, hospitalization, and death has not been well studied, wrote Georgina Nakafero, PhD, of the University of Nottingham, England, and colleagues.
In a study published in Rheumatology, the researchers identified 30,788 adults with AIRDs from the longitudinal Clinical Practice Research Datalink database in the United Kingdom. Of these, 66% were women, 76% had rheumatoid arthritis, and 61% had been prescribed methotrexate. The study included a total of 125,034 flu cycles between 2006 and 2009 and between 2010 and 2015.
Overall, vaccination with the inactivated influenza vaccine (IIV) reduced the risk of primary care consultation for influenza-like illness (adjusted odds ratio, 0.70), hospitalization for pneumonia (aOR, 0.61), exacerbation of chronic obstructive pulmonary disease (aOR, 0.67), and death caused by pneumonia (aOR, 0.48) in the study population. In a propensity score–adjusted analysis, only protection from influenza-like illness lost statistical significance.
In addition, vaccination was associated with a reduction in all-cause mortality among AIRDs patients, but restricting the outcomes to the active influenza periods may have confounded this result, the researchers said.
The study findings were limited by several factors including observational design, the use of a single vaccine efficacy estimate for each outcome, potential missed vaccination cycles, and potential confounding by indication and healthy user bias that could inflate the vaccine effectiveness, the researchers noted. However, the results were strengthened by the large sample size, including a range of AIRDs, and the use of both diagnostic and prescription codes, they said.
“The findings of this study, together with the results of our previous study demonstrating the safety of IIV in people with AIRDs, provides evidence to promote seasonal flu vaccination in this population,” they concluded. They still emphasized that randomized, controlled trials are needed for an assessment of vaccine efficacy.
The study was supported by Versus Arthritis and the National Institute of Health Research. Lead author Dr. Nakafero had no financial conflicts to disclose. Several coauthors disclosed relationships with companies, including AstraZeneca, Roche, and Pfizer.
SOURCE: Nakafero G et al. Rheumatology. 2020 Mar 11. doi: 10.1093/rheumatology/keaa078.
FROM RHEUMATOLOGY
Key clinical point: Adults with autoimmune rheumatic diseases who received the inactivated flu vaccine had lower rates of flu-like illness, hospitalization, and death than did those not vaccinated.
Major finding: Vaccination significantly reduced the risk of flu-like illness, hospitalization for pneumonia or COPD exacerbation, and death from pneumonia by 30%, 39%, 33%, and 52%, respectively.
Study details: The data come from 30,788 adults with AIRD and included 125,034 influenza cycles.
Disclosures: The study was supported by Versus Arthritis and the National Institute of Health Research. Lead author Dr. Nakafero had no financial conflicts to disclose. Several coauthors disclosed relationships with companies, including AstraZeneca, Roche, and Pfizer.
Source: Nakafero G et al. Rheumatology. 2020 Mar 11. doi: 10.1093/rheumatology/keaa078.
Clinicians petition government for national quarantine
Clinicians across the United States are petitioning the federal government to follow the lead of South Korea, China, and other nations by imposing an immediate nationwide quarantine to slow the inevitable spread of COVID-19. Without federal action, the creators say, their lives and the lives of their colleagues, patients, and families are being put at increased risk.
In addition to the quarantine, the petition, posted on the website Change.org, calls on U.S. leaders to institute emergency production and distribution of personal protective equipment for healthcare workers and to rapidly increase access to testing.
The petition – which garnered more than 40,000 signatures in just 12 hours and as of this writing was approaching 94,000 – was started by an apolitical Facebook group to focus attention on what members see as the most critical issues for clinicians: slowing the spread of the virus through a coast-to-coast quarantine, protection of medical personnel with adequate supplies of essential equipment, and widespread testing.
“We started this group last Friday out of the realization that clinicians needed information about the outbreak and weren’t getting it,” said coadministrator Jessica McIntyre, MD, a pediatric hospitalist at Elliot Hospital in Manchester, N.H.
“We wanted to get ahead of it and connect with people before we were in the trenches experiencing it and to see what other programs were doing. From a local perspective, it has been really hard to see what people are doing in other states, especially when the protocols in our own states are changing every single day as we collect more information,” she said in an interview.
The Horse Has Bolted
A family medicine physician in Illinois helped launch the Facebook group. She asked that her name not be used but said in an interview that earlier actions may have prevented or at least delayed the need for the more draconian measures that her group is recommending.
“Clearly South Korea is one of the superstars as far as response has gone, but the concern we have in the United States is that we’re well beyond that point – we needed to be testing people over a month ago, in the hope of preventing a quarantine,” she said in an interview.
According to National Public Radio, as of March 13, South Korea had conducted 3,600 tests per million population, compared with five per million in the United States.
“I think the most concerning part is to see where Italy is now and where we are in comparison. Our ICUs have not yet overflowed, but I think we’re definitely looking at that in the next few weeks – hopefully longer, but I suspect that it will happen shortly,” she continued.
She cited work by Harvard University biostatistician Xihong Lin, PhD, that shows that when health authorities in Wuhan, China – widely cited as the epicenter of the global pandemic – cordoned off the city, the infection rate dropped from one person infecting 3.8 others to one infecting 1.25, thereby significantly slowing the rate of transmission.
“This is absolutely what we need to be doing,” she said.
Real News
Within 3 days of its creation, the online group had accrued more than 80,000 members with advanced medical training, including MDs, DOs, physician assistants, nurse practitioners, and certified registered nurse anesthetists.
“A lot of us were already very busy with our day-to-day work outside of COVID-19, and I think a lot of us felt unsure about where to get the best information,” said coadministrator David Janssen, MD, a family medicine physician in group practice in Sioux Center, Iowa,
“If you turn on the TV, there’s a lot of politicizing of the issue, and there’s a lot of good information, but also a lot of bad information. When health care providers talk to other health care providers, that’s often how we get our information and how we learn,” he said in an interview.
The COVID-19 U.S. Physicians/APP Facebook group includes 20 volunteer moderators who handle hundreds of posts per hour from persons seeking information on the novel coronavirus, what to tell patients, and how to protect themselves.
“It’s been wonderful to see how providers have been helping other providers sort through issues. Teaching hospitals have their hands on the latest research, but a lot of people like myself are at small community hospitals, critical-access hospitals, where we may have a lot of questions but don’t necessarily have the answers readily available to us,” Dr. Janssen said.
Dr. Janssen said that his community of about 8,000 residents initially had only four COVID-19 testing kits, or one for every 2,000 people. The situation has since improved, and more tests are now available, he added.
Dr. McIntyre, Dr. Janssen, and the Illinois family physician have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Clinicians across the United States are petitioning the federal government to follow the lead of South Korea, China, and other nations by imposing an immediate nationwide quarantine to slow the inevitable spread of COVID-19. Without federal action, the creators say, their lives and the lives of their colleagues, patients, and families are being put at increased risk.
In addition to the quarantine, the petition, posted on the website Change.org, calls on U.S. leaders to institute emergency production and distribution of personal protective equipment for healthcare workers and to rapidly increase access to testing.
The petition – which garnered more than 40,000 signatures in just 12 hours and as of this writing was approaching 94,000 – was started by an apolitical Facebook group to focus attention on what members see as the most critical issues for clinicians: slowing the spread of the virus through a coast-to-coast quarantine, protection of medical personnel with adequate supplies of essential equipment, and widespread testing.
“We started this group last Friday out of the realization that clinicians needed information about the outbreak and weren’t getting it,” said coadministrator Jessica McIntyre, MD, a pediatric hospitalist at Elliot Hospital in Manchester, N.H.
“We wanted to get ahead of it and connect with people before we were in the trenches experiencing it and to see what other programs were doing. From a local perspective, it has been really hard to see what people are doing in other states, especially when the protocols in our own states are changing every single day as we collect more information,” she said in an interview.
The Horse Has Bolted
A family medicine physician in Illinois helped launch the Facebook group. She asked that her name not be used but said in an interview that earlier actions may have prevented or at least delayed the need for the more draconian measures that her group is recommending.
“Clearly South Korea is one of the superstars as far as response has gone, but the concern we have in the United States is that we’re well beyond that point – we needed to be testing people over a month ago, in the hope of preventing a quarantine,” she said in an interview.
According to National Public Radio, as of March 13, South Korea had conducted 3,600 tests per million population, compared with five per million in the United States.
“I think the most concerning part is to see where Italy is now and where we are in comparison. Our ICUs have not yet overflowed, but I think we’re definitely looking at that in the next few weeks – hopefully longer, but I suspect that it will happen shortly,” she continued.
She cited work by Harvard University biostatistician Xihong Lin, PhD, that shows that when health authorities in Wuhan, China – widely cited as the epicenter of the global pandemic – cordoned off the city, the infection rate dropped from one person infecting 3.8 others to one infecting 1.25, thereby significantly slowing the rate of transmission.
“This is absolutely what we need to be doing,” she said.
Real News
Within 3 days of its creation, the online group had accrued more than 80,000 members with advanced medical training, including MDs, DOs, physician assistants, nurse practitioners, and certified registered nurse anesthetists.
“A lot of us were already very busy with our day-to-day work outside of COVID-19, and I think a lot of us felt unsure about where to get the best information,” said coadministrator David Janssen, MD, a family medicine physician in group practice in Sioux Center, Iowa,
“If you turn on the TV, there’s a lot of politicizing of the issue, and there’s a lot of good information, but also a lot of bad information. When health care providers talk to other health care providers, that’s often how we get our information and how we learn,” he said in an interview.
The COVID-19 U.S. Physicians/APP Facebook group includes 20 volunteer moderators who handle hundreds of posts per hour from persons seeking information on the novel coronavirus, what to tell patients, and how to protect themselves.
“It’s been wonderful to see how providers have been helping other providers sort through issues. Teaching hospitals have their hands on the latest research, but a lot of people like myself are at small community hospitals, critical-access hospitals, where we may have a lot of questions but don’t necessarily have the answers readily available to us,” Dr. Janssen said.
Dr. Janssen said that his community of about 8,000 residents initially had only four COVID-19 testing kits, or one for every 2,000 people. The situation has since improved, and more tests are now available, he added.
Dr. McIntyre, Dr. Janssen, and the Illinois family physician have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Clinicians across the United States are petitioning the federal government to follow the lead of South Korea, China, and other nations by imposing an immediate nationwide quarantine to slow the inevitable spread of COVID-19. Without federal action, the creators say, their lives and the lives of their colleagues, patients, and families are being put at increased risk.
In addition to the quarantine, the petition, posted on the website Change.org, calls on U.S. leaders to institute emergency production and distribution of personal protective equipment for healthcare workers and to rapidly increase access to testing.
The petition – which garnered more than 40,000 signatures in just 12 hours and as of this writing was approaching 94,000 – was started by an apolitical Facebook group to focus attention on what members see as the most critical issues for clinicians: slowing the spread of the virus through a coast-to-coast quarantine, protection of medical personnel with adequate supplies of essential equipment, and widespread testing.
“We started this group last Friday out of the realization that clinicians needed information about the outbreak and weren’t getting it,” said coadministrator Jessica McIntyre, MD, a pediatric hospitalist at Elliot Hospital in Manchester, N.H.
“We wanted to get ahead of it and connect with people before we were in the trenches experiencing it and to see what other programs were doing. From a local perspective, it has been really hard to see what people are doing in other states, especially when the protocols in our own states are changing every single day as we collect more information,” she said in an interview.
The Horse Has Bolted
A family medicine physician in Illinois helped launch the Facebook group. She asked that her name not be used but said in an interview that earlier actions may have prevented or at least delayed the need for the more draconian measures that her group is recommending.
“Clearly South Korea is one of the superstars as far as response has gone, but the concern we have in the United States is that we’re well beyond that point – we needed to be testing people over a month ago, in the hope of preventing a quarantine,” she said in an interview.
According to National Public Radio, as of March 13, South Korea had conducted 3,600 tests per million population, compared with five per million in the United States.
“I think the most concerning part is to see where Italy is now and where we are in comparison. Our ICUs have not yet overflowed, but I think we’re definitely looking at that in the next few weeks – hopefully longer, but I suspect that it will happen shortly,” she continued.
She cited work by Harvard University biostatistician Xihong Lin, PhD, that shows that when health authorities in Wuhan, China – widely cited as the epicenter of the global pandemic – cordoned off the city, the infection rate dropped from one person infecting 3.8 others to one infecting 1.25, thereby significantly slowing the rate of transmission.
“This is absolutely what we need to be doing,” she said.
Real News
Within 3 days of its creation, the online group had accrued more than 80,000 members with advanced medical training, including MDs, DOs, physician assistants, nurse practitioners, and certified registered nurse anesthetists.
“A lot of us were already very busy with our day-to-day work outside of COVID-19, and I think a lot of us felt unsure about where to get the best information,” said coadministrator David Janssen, MD, a family medicine physician in group practice in Sioux Center, Iowa,
“If you turn on the TV, there’s a lot of politicizing of the issue, and there’s a lot of good information, but also a lot of bad information. When health care providers talk to other health care providers, that’s often how we get our information and how we learn,” he said in an interview.
The COVID-19 U.S. Physicians/APP Facebook group includes 20 volunteer moderators who handle hundreds of posts per hour from persons seeking information on the novel coronavirus, what to tell patients, and how to protect themselves.
“It’s been wonderful to see how providers have been helping other providers sort through issues. Teaching hospitals have their hands on the latest research, but a lot of people like myself are at small community hospitals, critical-access hospitals, where we may have a lot of questions but don’t necessarily have the answers readily available to us,” Dr. Janssen said.
Dr. Janssen said that his community of about 8,000 residents initially had only four COVID-19 testing kits, or one for every 2,000 people. The situation has since improved, and more tests are now available, he added.
Dr. McIntyre, Dr. Janssen, and the Illinois family physician have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
COVID-19 in pregnant women and the impact on newborns
Clinical question: How does infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in pregnant mothers affect their newborns?
Background: A novel coronavirus, now named SARS-CoV-2 by the World Health Organization (previously referred to as 2019-nCoV), is currently causing a worldwide pandemic. It is believed to have originated in Hubei province, China, but is now rapidly spreading in other countries. Although its effects are most severe in the elderly, SARS-CoV-2 has been infecting younger patients, including pregnant women. The effect of COVID-19, the disease caused by SARS-CoV-2, in pregnant women on their newborn children, is unknown, as is the nature of perinatal transmission of SARS-CoV-2.
Study design: Retrospective analysis.
Setting: Five hospitals in Hubei province, China.
Synopsis: Researchers retrospectively analyzed the clinical features and outcomes of 10 neonates (including two twins) born to nine mothers with confirmed SARS-CoV-2 infection in five hospitals in Hubei province, China, during Jan. 20–Feb. 5, 2020. The mothers were, on average, 30 years of age, but their prior state of health was not described. SARS-CoV-2 infection was confirmed in eight mothers by SARS-CoV-2 nucleic acid testing (NAT). The twins’ mother was diagnosed with COVID-19 based on chest CT scan showing viral interstitial pneumonia with other causes of fever and lung infection being “excluded,” despite a negative SARS-CoV-2 NAT test.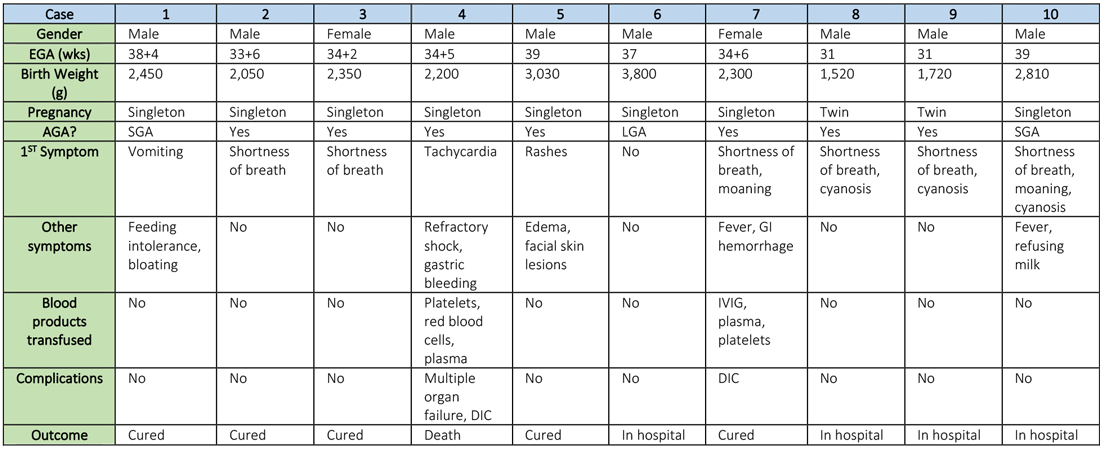
Symptoms occurred in the following:
- Before delivery in four mothers, three of whom were treated with oseltamivir (Tamiflu) after delivery.
- On the day of delivery in two mothers, one of whom was treated with oseltamivir and nebulized inhaled interferon after delivery.
- After delivery in three mothers.
Seven mothers delivered by cesarean section and two by vaginal delivery. Prenatal complications included intrauterine distress in six mothers, premature rupture of membranes in three (5-7 hours before onset of true labor), abnormal amniotic fluid in two, “abnormal” umbilical cord in two, and placenta previa in one.
The neonates born to these mothers included two females and eight males; four were full-term and six were premature (degree of prematurity not described). Symptoms first observed in these newborns included shortness of breath (six), fevers (two), tachycardia (one), and vomiting, feeding intolerance, “bloating,” refusing milk, and “gastric bleeding.” Chest radiographs were abnormal in seven newborns, including evidence of “infection” (four), neonatal respiratory distress syndrome (two), and pneumothorax (one). Two cases were described in detail:
- A neonate delivered at 34+5/7 weeks gestational age, was admitted due to shortness of breath and “moaning.” Eight days later, the neonate developed refractory shock, multiple organ failure, disseminated intravascular coagulation requiring transfusions of platelets, red blood cells, and plasma. He died on the ninth day.
- A neonate delivered at 34+6 weeks gestational age and was admitted 25 minutes after delivery due to shortness of breath and “moaning.” He required 2 days of noninvasive support/oxygen therapy and was observed to later develop “oxygen fluctuations” and thrombocytopenia at 3 days of life. The neonate was treated with “respiratory support,” intravenous immunoglobulin, transfusions of platelets and plasma, hydrocortisone (5 mg/kg per day for 6 days), low-dose heparin (2 units/kg per hr for 6 days), and low molecular weight heparin (2 units/kg per hr for 6 days). He was described to be “cured” 15 days later.
All nine neonates underwent pharyngeal swabs for SARS-CoV-2 NAT, and all were negative.
Bottom line: Although data are currently very limited, neonates born to mothers with COVID-19 appear to be at risk for adverse outcomes, including fetal distress, respiratory distress, thrombocytopenia associated with abnormal liver function, and death. There was no evidence of vertical transmission in this study.
Citation: Zhu H et al. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl Pediatr. 2020 Feb;9(1):51-60.
Dr. Chang is chief of pediatric hospital medicine at Baystate Children’s Hospital in Springfield, Mass., and associate professor of pediatrics at the University of Massachusetts, also in Springfield.
Clinical question: How does infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in pregnant mothers affect their newborns?
Background: A novel coronavirus, now named SARS-CoV-2 by the World Health Organization (previously referred to as 2019-nCoV), is currently causing a worldwide pandemic. It is believed to have originated in Hubei province, China, but is now rapidly spreading in other countries. Although its effects are most severe in the elderly, SARS-CoV-2 has been infecting younger patients, including pregnant women. The effect of COVID-19, the disease caused by SARS-CoV-2, in pregnant women on their newborn children, is unknown, as is the nature of perinatal transmission of SARS-CoV-2.
Study design: Retrospective analysis.
Setting: Five hospitals in Hubei province, China.
Synopsis: Researchers retrospectively analyzed the clinical features and outcomes of 10 neonates (including two twins) born to nine mothers with confirmed SARS-CoV-2 infection in five hospitals in Hubei province, China, during Jan. 20–Feb. 5, 2020. The mothers were, on average, 30 years of age, but their prior state of health was not described. SARS-CoV-2 infection was confirmed in eight mothers by SARS-CoV-2 nucleic acid testing (NAT). The twins’ mother was diagnosed with COVID-19 based on chest CT scan showing viral interstitial pneumonia with other causes of fever and lung infection being “excluded,” despite a negative SARS-CoV-2 NAT test.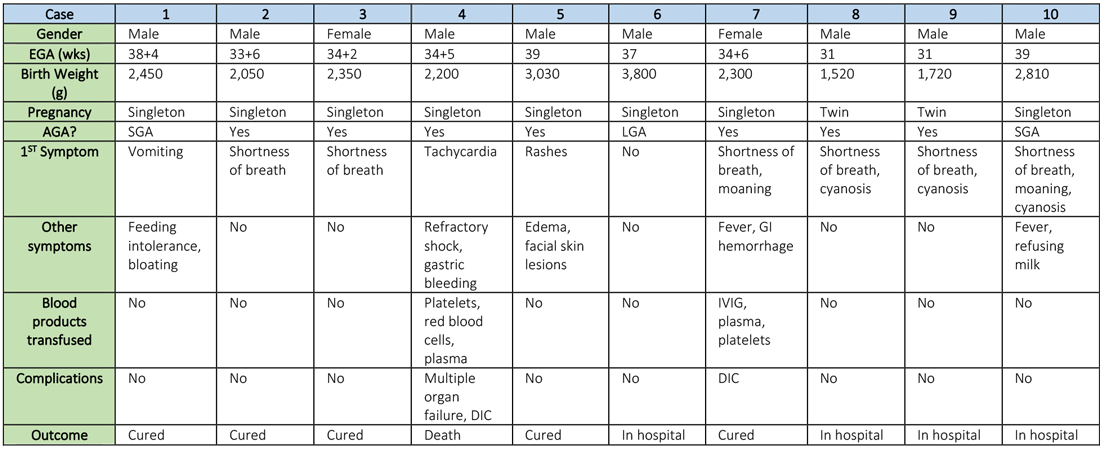
Symptoms occurred in the following:
- Before delivery in four mothers, three of whom were treated with oseltamivir (Tamiflu) after delivery.
- On the day of delivery in two mothers, one of whom was treated with oseltamivir and nebulized inhaled interferon after delivery.
- After delivery in three mothers.
Seven mothers delivered by cesarean section and two by vaginal delivery. Prenatal complications included intrauterine distress in six mothers, premature rupture of membranes in three (5-7 hours before onset of true labor), abnormal amniotic fluid in two, “abnormal” umbilical cord in two, and placenta previa in one.
The neonates born to these mothers included two females and eight males; four were full-term and six were premature (degree of prematurity not described). Symptoms first observed in these newborns included shortness of breath (six), fevers (two), tachycardia (one), and vomiting, feeding intolerance, “bloating,” refusing milk, and “gastric bleeding.” Chest radiographs were abnormal in seven newborns, including evidence of “infection” (four), neonatal respiratory distress syndrome (two), and pneumothorax (one). Two cases were described in detail:
- A neonate delivered at 34+5/7 weeks gestational age, was admitted due to shortness of breath and “moaning.” Eight days later, the neonate developed refractory shock, multiple organ failure, disseminated intravascular coagulation requiring transfusions of platelets, red blood cells, and plasma. He died on the ninth day.
- A neonate delivered at 34+6 weeks gestational age and was admitted 25 minutes after delivery due to shortness of breath and “moaning.” He required 2 days of noninvasive support/oxygen therapy and was observed to later develop “oxygen fluctuations” and thrombocytopenia at 3 days of life. The neonate was treated with “respiratory support,” intravenous immunoglobulin, transfusions of platelets and plasma, hydrocortisone (5 mg/kg per day for 6 days), low-dose heparin (2 units/kg per hr for 6 days), and low molecular weight heparin (2 units/kg per hr for 6 days). He was described to be “cured” 15 days later.
All nine neonates underwent pharyngeal swabs for SARS-CoV-2 NAT, and all were negative.
Bottom line: Although data are currently very limited, neonates born to mothers with COVID-19 appear to be at risk for adverse outcomes, including fetal distress, respiratory distress, thrombocytopenia associated with abnormal liver function, and death. There was no evidence of vertical transmission in this study.
Citation: Zhu H et al. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl Pediatr. 2020 Feb;9(1):51-60.
Dr. Chang is chief of pediatric hospital medicine at Baystate Children’s Hospital in Springfield, Mass., and associate professor of pediatrics at the University of Massachusetts, also in Springfield.
Clinical question: How does infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in pregnant mothers affect their newborns?
Background: A novel coronavirus, now named SARS-CoV-2 by the World Health Organization (previously referred to as 2019-nCoV), is currently causing a worldwide pandemic. It is believed to have originated in Hubei province, China, but is now rapidly spreading in other countries. Although its effects are most severe in the elderly, SARS-CoV-2 has been infecting younger patients, including pregnant women. The effect of COVID-19, the disease caused by SARS-CoV-2, in pregnant women on their newborn children, is unknown, as is the nature of perinatal transmission of SARS-CoV-2.
Study design: Retrospective analysis.
Setting: Five hospitals in Hubei province, China.
Synopsis: Researchers retrospectively analyzed the clinical features and outcomes of 10 neonates (including two twins) born to nine mothers with confirmed SARS-CoV-2 infection in five hospitals in Hubei province, China, during Jan. 20–Feb. 5, 2020. The mothers were, on average, 30 years of age, but their prior state of health was not described. SARS-CoV-2 infection was confirmed in eight mothers by SARS-CoV-2 nucleic acid testing (NAT). The twins’ mother was diagnosed with COVID-19 based on chest CT scan showing viral interstitial pneumonia with other causes of fever and lung infection being “excluded,” despite a negative SARS-CoV-2 NAT test.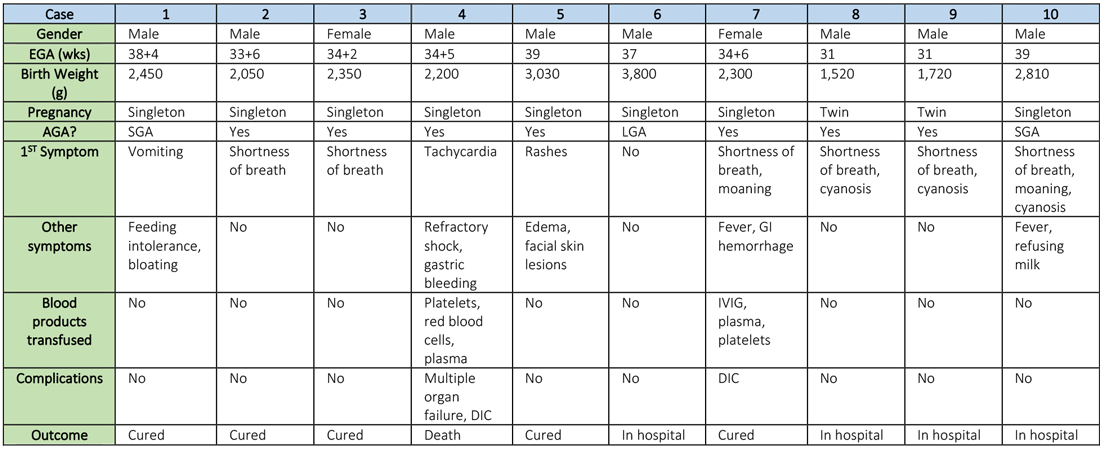
Symptoms occurred in the following:
- Before delivery in four mothers, three of whom were treated with oseltamivir (Tamiflu) after delivery.
- On the day of delivery in two mothers, one of whom was treated with oseltamivir and nebulized inhaled interferon after delivery.
- After delivery in three mothers.
Seven mothers delivered by cesarean section and two by vaginal delivery. Prenatal complications included intrauterine distress in six mothers, premature rupture of membranes in three (5-7 hours before onset of true labor), abnormal amniotic fluid in two, “abnormal” umbilical cord in two, and placenta previa in one.
The neonates born to these mothers included two females and eight males; four were full-term and six were premature (degree of prematurity not described). Symptoms first observed in these newborns included shortness of breath (six), fevers (two), tachycardia (one), and vomiting, feeding intolerance, “bloating,” refusing milk, and “gastric bleeding.” Chest radiographs were abnormal in seven newborns, including evidence of “infection” (four), neonatal respiratory distress syndrome (two), and pneumothorax (one). Two cases were described in detail:
- A neonate delivered at 34+5/7 weeks gestational age, was admitted due to shortness of breath and “moaning.” Eight days later, the neonate developed refractory shock, multiple organ failure, disseminated intravascular coagulation requiring transfusions of platelets, red blood cells, and plasma. He died on the ninth day.
- A neonate delivered at 34+6 weeks gestational age and was admitted 25 minutes after delivery due to shortness of breath and “moaning.” He required 2 days of noninvasive support/oxygen therapy and was observed to later develop “oxygen fluctuations” and thrombocytopenia at 3 days of life. The neonate was treated with “respiratory support,” intravenous immunoglobulin, transfusions of platelets and plasma, hydrocortisone (5 mg/kg per day for 6 days), low-dose heparin (2 units/kg per hr for 6 days), and low molecular weight heparin (2 units/kg per hr for 6 days). He was described to be “cured” 15 days later.
All nine neonates underwent pharyngeal swabs for SARS-CoV-2 NAT, and all were negative.
Bottom line: Although data are currently very limited, neonates born to mothers with COVID-19 appear to be at risk for adverse outcomes, including fetal distress, respiratory distress, thrombocytopenia associated with abnormal liver function, and death. There was no evidence of vertical transmission in this study.
Citation: Zhu H et al. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl Pediatr. 2020 Feb;9(1):51-60.
Dr. Chang is chief of pediatric hospital medicine at Baystate Children’s Hospital in Springfield, Mass., and associate professor of pediatrics at the University of Massachusetts, also in Springfield.
COVID-19: U.S. cardiology groups reaffirm continued use of RAAS-active drugs
Controversy continued over the potential effect of drugs that interfere with the renin-angiotensin-aldosterone system via the angiotensin-converting enzymes (ACE) may have on exacerbating infection with the SARS-CoV-2 virus that causes COVID-19.
A joint statement from the American Heart Association, American College of Cardiology, and the Heart Failure Society of America on March 17 gave full, unqualified support to maintaining patients on drugs that work this way, specifically the ACE inhibitors and angiotensin-receptor blockers (ARBs), which together form a long-standing cornerstone of treatment for hypertension, heart failure, and ischemic heart disease.
The three societies “recommend continuation” of ACE inhibitors or ARBs “for all patients already prescribed.” The statement went on to say that patients already diagnosed with a COVID-19 infection “should be fully evaluated before adding or removing any treatments, and any changes to their treatment should be based on the latest scientific evidence and shared decision making with their physician and health care team.”
“We understand the concern – as it has become clear that people with cardiovascular disease are at much higher risk of serious complications including death from COVID-19. However, we have reviewed the latest research – the evidence does not confirm the need to discontinue ACE inhibitors or ARBs, and we strongly recommend all physicians to consider the individual needs of each patient before making any changes to ACE-inhibitor or ARB treatment regimens,” said Robert A. Harrington, MD, president of the American Heart Association and professor and chair of medicine at Stanford (Calif.) University, in the statement.
“There are no experimental or clinical data demonstrating beneficial or adverse outcomes among COVID-19 patients using ACE-inhibitor or ARB medications,” added Richard J. Kovacs, MD, president of the American College of Cardiology and professor of cardiology at Indiana University in Indianapolis.
The “latest research” referred to in the statement likely focuses on a report that had appeared less than a week earlier in a British journal that hypothesized a possible increase in the susceptibility of human epithelial cells of the lungs, intestine, kidneys, and blood vessels exposed to these or certain other drugs, like the thiazolidinedione oral diabetes drugs or ibuprofen, because they cause up-regulation of the ACE2 protein in cell membranes, and ACE2 is the primary cell-surface receptor that allows the SARS-CoV-2 virus to enter.
“We therefore hypothesize that diabetes and hypertension treatment with ACE2-stimulating drugs increases the risk of developing severe and fatal COVID-19,” wrote Michael Roth, MD, and his associates in their recent article (Lancet Resp Med. 2020 Mar 11. doi: 10.1016/S2213-2600[20]30116-8). While the potential clinical impact of an increase in the number of ACE2 molecules in a cell’s surface membrane remains uninvestigated, the risk this phenomenon poses should mean that patients taking these drugs should receive heightened monitoring for COVID-19 disease, suggested Dr. Roth, a professor of biomedicine who specializes in studying inflammatory lung diseases including asthma, and associates.
However, others who have considered the impact that ACE inhibitors and ARBs might have on ACE2 and COVID-19 infections have noted that the picture is not simple. “Higher ACE2 expression following chronically medicating SARS‐CoV‐2 infected patients with AT1R [angiotensin receptor 1] blockers, while seemingly paradoxical, may protect them against acute lung injury rather than putting them at higher risk to develop SARS. This may be accounted for by two complementary mechanisms: blocking the excessive angiotensin‐mediated AT1R activation caused by the viral infection, as well as up-regulating ACE2, thereby reducing angiotensin production by ACE and increasing the production” of a vasodilating form of angiotensin, wrote David Gurwitz, PhD, in a recently published editorial (Drug Dev Res. 2020 Mar 4. doi: 10.1002/ddr.21656). A data-mining approach may allow researchers to determine whether patients who received drugs that interfere with angiotensin 1 function prior to being diagnosed with a COVID-19 infection had a better disease outcome, suggested Dr. Gurwitz, a molecular geneticist at Tel Aviv University in Jerusalem.
The statement from the three U.S. cardiology societies came a few days following a similar statement of support for ongoing use of ACE inhibitors and ARBs from the European Society of Cardiology’s Council on Hypertension.
Dr. Harrington, Dr. Kovacs, Dr. Roth, and Dr. Gurwitz had no relevant disclosures.
Controversy continued over the potential effect of drugs that interfere with the renin-angiotensin-aldosterone system via the angiotensin-converting enzymes (ACE) may have on exacerbating infection with the SARS-CoV-2 virus that causes COVID-19.
A joint statement from the American Heart Association, American College of Cardiology, and the Heart Failure Society of America on March 17 gave full, unqualified support to maintaining patients on drugs that work this way, specifically the ACE inhibitors and angiotensin-receptor blockers (ARBs), which together form a long-standing cornerstone of treatment for hypertension, heart failure, and ischemic heart disease.
The three societies “recommend continuation” of ACE inhibitors or ARBs “for all patients already prescribed.” The statement went on to say that patients already diagnosed with a COVID-19 infection “should be fully evaluated before adding or removing any treatments, and any changes to their treatment should be based on the latest scientific evidence and shared decision making with their physician and health care team.”
“We understand the concern – as it has become clear that people with cardiovascular disease are at much higher risk of serious complications including death from COVID-19. However, we have reviewed the latest research – the evidence does not confirm the need to discontinue ACE inhibitors or ARBs, and we strongly recommend all physicians to consider the individual needs of each patient before making any changes to ACE-inhibitor or ARB treatment regimens,” said Robert A. Harrington, MD, president of the American Heart Association and professor and chair of medicine at Stanford (Calif.) University, in the statement.
“There are no experimental or clinical data demonstrating beneficial or adverse outcomes among COVID-19 patients using ACE-inhibitor or ARB medications,” added Richard J. Kovacs, MD, president of the American College of Cardiology and professor of cardiology at Indiana University in Indianapolis.
The “latest research” referred to in the statement likely focuses on a report that had appeared less than a week earlier in a British journal that hypothesized a possible increase in the susceptibility of human epithelial cells of the lungs, intestine, kidneys, and blood vessels exposed to these or certain other drugs, like the thiazolidinedione oral diabetes drugs or ibuprofen, because they cause up-regulation of the ACE2 protein in cell membranes, and ACE2 is the primary cell-surface receptor that allows the SARS-CoV-2 virus to enter.
“We therefore hypothesize that diabetes and hypertension treatment with ACE2-stimulating drugs increases the risk of developing severe and fatal COVID-19,” wrote Michael Roth, MD, and his associates in their recent article (Lancet Resp Med. 2020 Mar 11. doi: 10.1016/S2213-2600[20]30116-8). While the potential clinical impact of an increase in the number of ACE2 molecules in a cell’s surface membrane remains uninvestigated, the risk this phenomenon poses should mean that patients taking these drugs should receive heightened monitoring for COVID-19 disease, suggested Dr. Roth, a professor of biomedicine who specializes in studying inflammatory lung diseases including asthma, and associates.
However, others who have considered the impact that ACE inhibitors and ARBs might have on ACE2 and COVID-19 infections have noted that the picture is not simple. “Higher ACE2 expression following chronically medicating SARS‐CoV‐2 infected patients with AT1R [angiotensin receptor 1] blockers, while seemingly paradoxical, may protect them against acute lung injury rather than putting them at higher risk to develop SARS. This may be accounted for by two complementary mechanisms: blocking the excessive angiotensin‐mediated AT1R activation caused by the viral infection, as well as up-regulating ACE2, thereby reducing angiotensin production by ACE and increasing the production” of a vasodilating form of angiotensin, wrote David Gurwitz, PhD, in a recently published editorial (Drug Dev Res. 2020 Mar 4. doi: 10.1002/ddr.21656). A data-mining approach may allow researchers to determine whether patients who received drugs that interfere with angiotensin 1 function prior to being diagnosed with a COVID-19 infection had a better disease outcome, suggested Dr. Gurwitz, a molecular geneticist at Tel Aviv University in Jerusalem.
The statement from the three U.S. cardiology societies came a few days following a similar statement of support for ongoing use of ACE inhibitors and ARBs from the European Society of Cardiology’s Council on Hypertension.
Dr. Harrington, Dr. Kovacs, Dr. Roth, and Dr. Gurwitz had no relevant disclosures.
Controversy continued over the potential effect of drugs that interfere with the renin-angiotensin-aldosterone system via the angiotensin-converting enzymes (ACE) may have on exacerbating infection with the SARS-CoV-2 virus that causes COVID-19.
A joint statement from the American Heart Association, American College of Cardiology, and the Heart Failure Society of America on March 17 gave full, unqualified support to maintaining patients on drugs that work this way, specifically the ACE inhibitors and angiotensin-receptor blockers (ARBs), which together form a long-standing cornerstone of treatment for hypertension, heart failure, and ischemic heart disease.
The three societies “recommend continuation” of ACE inhibitors or ARBs “for all patients already prescribed.” The statement went on to say that patients already diagnosed with a COVID-19 infection “should be fully evaluated before adding or removing any treatments, and any changes to their treatment should be based on the latest scientific evidence and shared decision making with their physician and health care team.”
“We understand the concern – as it has become clear that people with cardiovascular disease are at much higher risk of serious complications including death from COVID-19. However, we have reviewed the latest research – the evidence does not confirm the need to discontinue ACE inhibitors or ARBs, and we strongly recommend all physicians to consider the individual needs of each patient before making any changes to ACE-inhibitor or ARB treatment regimens,” said Robert A. Harrington, MD, president of the American Heart Association and professor and chair of medicine at Stanford (Calif.) University, in the statement.
“There are no experimental or clinical data demonstrating beneficial or adverse outcomes among COVID-19 patients using ACE-inhibitor or ARB medications,” added Richard J. Kovacs, MD, president of the American College of Cardiology and professor of cardiology at Indiana University in Indianapolis.
The “latest research” referred to in the statement likely focuses on a report that had appeared less than a week earlier in a British journal that hypothesized a possible increase in the susceptibility of human epithelial cells of the lungs, intestine, kidneys, and blood vessels exposed to these or certain other drugs, like the thiazolidinedione oral diabetes drugs or ibuprofen, because they cause up-regulation of the ACE2 protein in cell membranes, and ACE2 is the primary cell-surface receptor that allows the SARS-CoV-2 virus to enter.
“We therefore hypothesize that diabetes and hypertension treatment with ACE2-stimulating drugs increases the risk of developing severe and fatal COVID-19,” wrote Michael Roth, MD, and his associates in their recent article (Lancet Resp Med. 2020 Mar 11. doi: 10.1016/S2213-2600[20]30116-8). While the potential clinical impact of an increase in the number of ACE2 molecules in a cell’s surface membrane remains uninvestigated, the risk this phenomenon poses should mean that patients taking these drugs should receive heightened monitoring for COVID-19 disease, suggested Dr. Roth, a professor of biomedicine who specializes in studying inflammatory lung diseases including asthma, and associates.
However, others who have considered the impact that ACE inhibitors and ARBs might have on ACE2 and COVID-19 infections have noted that the picture is not simple. “Higher ACE2 expression following chronically medicating SARS‐CoV‐2 infected patients with AT1R [angiotensin receptor 1] blockers, while seemingly paradoxical, may protect them against acute lung injury rather than putting them at higher risk to develop SARS. This may be accounted for by two complementary mechanisms: blocking the excessive angiotensin‐mediated AT1R activation caused by the viral infection, as well as up-regulating ACE2, thereby reducing angiotensin production by ACE and increasing the production” of a vasodilating form of angiotensin, wrote David Gurwitz, PhD, in a recently published editorial (Drug Dev Res. 2020 Mar 4. doi: 10.1002/ddr.21656). A data-mining approach may allow researchers to determine whether patients who received drugs that interfere with angiotensin 1 function prior to being diagnosed with a COVID-19 infection had a better disease outcome, suggested Dr. Gurwitz, a molecular geneticist at Tel Aviv University in Jerusalem.
The statement from the three U.S. cardiology societies came a few days following a similar statement of support for ongoing use of ACE inhibitors and ARBs from the European Society of Cardiology’s Council on Hypertension.
Dr. Harrington, Dr. Kovacs, Dr. Roth, and Dr. Gurwitz had no relevant disclosures.
COVID-19 guidance for children’s health care providers
We are in uncharted waters with national and local states of emergency, schools and most activities being shut down, and rapidly evolving strategies on managing the COVID-19 outbreak. Everyone’s anxiety is appropriately high. As health care providers for children, you are facing changes in your personal life at home and in practice, likely including setting up televisits, trying to assess which patients to see, managing staffing challenges, and facing potential cash flow issues as expenses continue but revenue may fall short. And, of course, you will address a host of novel questions and concerns from the families you care for.
Your top priorities are to stay calm while offering clear recommendations on testing, quarantine, and treatment with guidance from our federal and local public health agencies. By providing clear guidance on the medical issues, you will offer substantial reassurance to families. But even with a medical plan in place, this remains a confusing and anxiety-provoking moment, one without much precedent in most people’s lives or in our national experience. Our aim is to complement that guidance by offering you some principles to help families manage the stress and anxiety that the disruptions and uncertainties that this public health emergency has created.
Offer clear, open, regular, and child-centered communication
If you have an email mailing list of your parents, you may want to summarize information you are gathering with a note they can expect at a specified time each day. You could request them to email you questions that then can be included as an FAQ (frequently asked questions).
Most children will have noticed people wearing face masks, or dramatic scenes on the news with hospital workers in full protective gear, breathlessly reporting growing numbers of the infected and the deceased. At a minimum, they are being commanded to wash hands and to not touch their faces (which is challenging enough for adults!), and are probably overhearing conversations about quarantines and contagion as well as family concerns about jobs and family finances. Many children are managing extended school closures and some are even managing the quarantine or serious illness of a loved one. When children overhear frightening news from distressed adults, they are going to become anxious and afraid themselves. Parents should remember to find out what their children have seen, heard, or understood about what is going on, and they should correct misinformation or misunderstandings with clear explanations. They also should find out what their children are curious about. “What has you wondering about that?” is a great response when children have questions, in order to make sure you get at any underlying worry.
It is fine to not have an answer to every question. It is difficult to offer clear explanations about something that we don’t yet fully understand, and it is fine to acknowledge what we don’t know. “That’s a great question. Let’s look together at the CDC [Centers for Disease Control and Prevention] website.” Offering to look for answers or information together can be a powerful way to model how to handle uncertainty. And always couch answers with appropriate (not false) reassurance: “Children and young adults appear to be very safe from this illness, but we want to take care to protect those that are older or already sick.”
Remember most children set their anxiety level based on their parent’s anxiety, and part of being child centered in your communication includes offering information in an age-appropriate manner. Preschool-aged children (up to 5 years) still have magical thinking. They are prone to finding masks and gowns scary and to assume that school stopping may be because they did something wrong. Tell them about the new illness, and about the doctors and officials working hard to keep people safe. Reassure them about all of the adults working hard together to understand the illness and take care of people who are sick. Their sense of time is less logical, so you may have to tell them more than once. Reassure them that children do not get very sick from this illness, but they can carry and spread it, like having paint on their hands, so they need to wash their hands often to take good care of other people.
School-age children (aged roughly 5-12 years) are better equipped cognitively to understand the seriousness of this outbreak. They are built to master new situations, but are prone to anxiety as they don’t yet have the emotional maturity to tolerate uncertainty or unfairness. Explain what is known without euphemisms, be truly curious about what their questions are, and look for answers together. Often what they need is to see you being calm in the face of uncertainty, bearing the strong feelings that may come, and preserving curiosity and compassion for others.
Adolescents also will need all of this support, and can be curious about more abstract implications (political, ethical, financial). Do not be surprised when they ask sophisticated questions, but still are focused on the personal disruptions or sacrifices (a canceled dance or sports meet, concerns about academic performance). Adolescence is a time of intense preoccupation with their emerging identity and relationships; it is normal for them to experience events in a way that may seem selfish, especially if it disrupts their time with friends. Remind parents to offer compassion and validation, while acknowledging that shared sacrifice and discomfort are a part of every individual’s experience when a society must respond to such a large challenge.
Be mindful of children’s vulnerabilities
Being child centered goes beyond thinking about their age and developmental stage. Parents are the experts on their children and will know about any particular vulnerabilities to the stresses of this serious outbreak. Children who are prone to anxiety or suffer from anxiety disorders may be more prone to silent worry. It is especially important to check in with them often, find out what they know and what they are worried about, and remind them to “never worry alone.” It also is important to continue with any recommended treatment, avoiding accommodation of their anxieties, except when it is required by public health protocols (i.e., staying home from school). Children with developmental disabilities may require additional support to change behaviors (hand washing) and may be more sensitive to changes in routine. And children with learning disabilities or special services in school may require additional support or structure during a prolonged period at home.
Preserve routines and structure
Routines and predictability are important to the sense of stability and well-being of most children (and adults). While disruptions are unavoidable, preserve what routines you can, and establish some new ones. For children who are out of school for several weeks, set up a consistent home routine, with a similar wake-up and bedtime, and a “school schedule.” There may be academic activities like reading or work sheets. If the parents’ work is disrupted, they can homeschool, shoring up weak academic areas or enhancing areas of interest. Be sure to preserve time for physical activity and social connections within this new framework. Social time does not require physical proximity, and can happen by screen or phone. Physical activity should be outside if at all possible. Predictability, preserved expectations (academic and otherwise), physical exercise, social connection, and consistent sleep will go a long way in protecting everyone’s ability to manage the disruptions of this epidemic.
Find opportunity in the disruption
Many families have been on a treadmill of work, school, and activities that have left little unscheduled time or spontaneity. Recommend looking at this disruption as a rare opportunity to slow down, spend time together, listen, learn more about one another, and even to have fun. Families could play board games, card games, watch movies together, or even read aloud. They might discover it is the time to try new hobbies (knitting, learning a new language or instrument), or to teach each other new skills. You might learn something new, or something new about your children. You also will offer a model of finding the opportunity in adversity, and even offer them some wonderful memories from a difficult time.
Take care of the vulnerable and ease others’ hardships
Without a doubt, this will be a difficult time for many people, medically, financially, and emotionally. One powerful strategy to build resilience in our children and strengthen our communities is to think with children about ways to help those who are most at risk or burdened by this challenge. Perhaps they want to make cards or FaceTime calls to older relatives who may be otherwise isolated. They may want to consider ways to support the work of first responders, even just with appreciation. They may want to reach out to elderly neighbors and offer to get groceries or other needed supplies for them. Balancing appropriate self-care with a focus on the needs of those who are more vulnerable or burdened than ourselves is a powerful way to show our children how communities pull together in a challenging time; enhance their feeling of connectedness; and build resilience in them, in our families, and in our communities.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected]
We are in uncharted waters with national and local states of emergency, schools and most activities being shut down, and rapidly evolving strategies on managing the COVID-19 outbreak. Everyone’s anxiety is appropriately high. As health care providers for children, you are facing changes in your personal life at home and in practice, likely including setting up televisits, trying to assess which patients to see, managing staffing challenges, and facing potential cash flow issues as expenses continue but revenue may fall short. And, of course, you will address a host of novel questions and concerns from the families you care for.
Your top priorities are to stay calm while offering clear recommendations on testing, quarantine, and treatment with guidance from our federal and local public health agencies. By providing clear guidance on the medical issues, you will offer substantial reassurance to families. But even with a medical plan in place, this remains a confusing and anxiety-provoking moment, one without much precedent in most people’s lives or in our national experience. Our aim is to complement that guidance by offering you some principles to help families manage the stress and anxiety that the disruptions and uncertainties that this public health emergency has created.
Offer clear, open, regular, and child-centered communication
If you have an email mailing list of your parents, you may want to summarize information you are gathering with a note they can expect at a specified time each day. You could request them to email you questions that then can be included as an FAQ (frequently asked questions).
Most children will have noticed people wearing face masks, or dramatic scenes on the news with hospital workers in full protective gear, breathlessly reporting growing numbers of the infected and the deceased. At a minimum, they are being commanded to wash hands and to not touch their faces (which is challenging enough for adults!), and are probably overhearing conversations about quarantines and contagion as well as family concerns about jobs and family finances. Many children are managing extended school closures and some are even managing the quarantine or serious illness of a loved one. When children overhear frightening news from distressed adults, they are going to become anxious and afraid themselves. Parents should remember to find out what their children have seen, heard, or understood about what is going on, and they should correct misinformation or misunderstandings with clear explanations. They also should find out what their children are curious about. “What has you wondering about that?” is a great response when children have questions, in order to make sure you get at any underlying worry.
It is fine to not have an answer to every question. It is difficult to offer clear explanations about something that we don’t yet fully understand, and it is fine to acknowledge what we don’t know. “That’s a great question. Let’s look together at the CDC [Centers for Disease Control and Prevention] website.” Offering to look for answers or information together can be a powerful way to model how to handle uncertainty. And always couch answers with appropriate (not false) reassurance: “Children and young adults appear to be very safe from this illness, but we want to take care to protect those that are older or already sick.”
Remember most children set their anxiety level based on their parent’s anxiety, and part of being child centered in your communication includes offering information in an age-appropriate manner. Preschool-aged children (up to 5 years) still have magical thinking. They are prone to finding masks and gowns scary and to assume that school stopping may be because they did something wrong. Tell them about the new illness, and about the doctors and officials working hard to keep people safe. Reassure them about all of the adults working hard together to understand the illness and take care of people who are sick. Their sense of time is less logical, so you may have to tell them more than once. Reassure them that children do not get very sick from this illness, but they can carry and spread it, like having paint on their hands, so they need to wash their hands often to take good care of other people.
School-age children (aged roughly 5-12 years) are better equipped cognitively to understand the seriousness of this outbreak. They are built to master new situations, but are prone to anxiety as they don’t yet have the emotional maturity to tolerate uncertainty or unfairness. Explain what is known without euphemisms, be truly curious about what their questions are, and look for answers together. Often what they need is to see you being calm in the face of uncertainty, bearing the strong feelings that may come, and preserving curiosity and compassion for others.
Adolescents also will need all of this support, and can be curious about more abstract implications (political, ethical, financial). Do not be surprised when they ask sophisticated questions, but still are focused on the personal disruptions or sacrifices (a canceled dance or sports meet, concerns about academic performance). Adolescence is a time of intense preoccupation with their emerging identity and relationships; it is normal for them to experience events in a way that may seem selfish, especially if it disrupts their time with friends. Remind parents to offer compassion and validation, while acknowledging that shared sacrifice and discomfort are a part of every individual’s experience when a society must respond to such a large challenge.
Be mindful of children’s vulnerabilities
Being child centered goes beyond thinking about their age and developmental stage. Parents are the experts on their children and will know about any particular vulnerabilities to the stresses of this serious outbreak. Children who are prone to anxiety or suffer from anxiety disorders may be more prone to silent worry. It is especially important to check in with them often, find out what they know and what they are worried about, and remind them to “never worry alone.” It also is important to continue with any recommended treatment, avoiding accommodation of their anxieties, except when it is required by public health protocols (i.e., staying home from school). Children with developmental disabilities may require additional support to change behaviors (hand washing) and may be more sensitive to changes in routine. And children with learning disabilities or special services in school may require additional support or structure during a prolonged period at home.
Preserve routines and structure
Routines and predictability are important to the sense of stability and well-being of most children (and adults). While disruptions are unavoidable, preserve what routines you can, and establish some new ones. For children who are out of school for several weeks, set up a consistent home routine, with a similar wake-up and bedtime, and a “school schedule.” There may be academic activities like reading or work sheets. If the parents’ work is disrupted, they can homeschool, shoring up weak academic areas or enhancing areas of interest. Be sure to preserve time for physical activity and social connections within this new framework. Social time does not require physical proximity, and can happen by screen or phone. Physical activity should be outside if at all possible. Predictability, preserved expectations (academic and otherwise), physical exercise, social connection, and consistent sleep will go a long way in protecting everyone’s ability to manage the disruptions of this epidemic.
Find opportunity in the disruption
Many families have been on a treadmill of work, school, and activities that have left little unscheduled time or spontaneity. Recommend looking at this disruption as a rare opportunity to slow down, spend time together, listen, learn more about one another, and even to have fun. Families could play board games, card games, watch movies together, or even read aloud. They might discover it is the time to try new hobbies (knitting, learning a new language or instrument), or to teach each other new skills. You might learn something new, or something new about your children. You also will offer a model of finding the opportunity in adversity, and even offer them some wonderful memories from a difficult time.
Take care of the vulnerable and ease others’ hardships
Without a doubt, this will be a difficult time for many people, medically, financially, and emotionally. One powerful strategy to build resilience in our children and strengthen our communities is to think with children about ways to help those who are most at risk or burdened by this challenge. Perhaps they want to make cards or FaceTime calls to older relatives who may be otherwise isolated. They may want to consider ways to support the work of first responders, even just with appreciation. They may want to reach out to elderly neighbors and offer to get groceries or other needed supplies for them. Balancing appropriate self-care with a focus on the needs of those who are more vulnerable or burdened than ourselves is a powerful way to show our children how communities pull together in a challenging time; enhance their feeling of connectedness; and build resilience in them, in our families, and in our communities.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected]
We are in uncharted waters with national and local states of emergency, schools and most activities being shut down, and rapidly evolving strategies on managing the COVID-19 outbreak. Everyone’s anxiety is appropriately high. As health care providers for children, you are facing changes in your personal life at home and in practice, likely including setting up televisits, trying to assess which patients to see, managing staffing challenges, and facing potential cash flow issues as expenses continue but revenue may fall short. And, of course, you will address a host of novel questions and concerns from the families you care for.
Your top priorities are to stay calm while offering clear recommendations on testing, quarantine, and treatment with guidance from our federal and local public health agencies. By providing clear guidance on the medical issues, you will offer substantial reassurance to families. But even with a medical plan in place, this remains a confusing and anxiety-provoking moment, one without much precedent in most people’s lives or in our national experience. Our aim is to complement that guidance by offering you some principles to help families manage the stress and anxiety that the disruptions and uncertainties that this public health emergency has created.
Offer clear, open, regular, and child-centered communication
If you have an email mailing list of your parents, you may want to summarize information you are gathering with a note they can expect at a specified time each day. You could request them to email you questions that then can be included as an FAQ (frequently asked questions).
Most children will have noticed people wearing face masks, or dramatic scenes on the news with hospital workers in full protective gear, breathlessly reporting growing numbers of the infected and the deceased. At a minimum, they are being commanded to wash hands and to not touch their faces (which is challenging enough for adults!), and are probably overhearing conversations about quarantines and contagion as well as family concerns about jobs and family finances. Many children are managing extended school closures and some are even managing the quarantine or serious illness of a loved one. When children overhear frightening news from distressed adults, they are going to become anxious and afraid themselves. Parents should remember to find out what their children have seen, heard, or understood about what is going on, and they should correct misinformation or misunderstandings with clear explanations. They also should find out what their children are curious about. “What has you wondering about that?” is a great response when children have questions, in order to make sure you get at any underlying worry.
It is fine to not have an answer to every question. It is difficult to offer clear explanations about something that we don’t yet fully understand, and it is fine to acknowledge what we don’t know. “That’s a great question. Let’s look together at the CDC [Centers for Disease Control and Prevention] website.” Offering to look for answers or information together can be a powerful way to model how to handle uncertainty. And always couch answers with appropriate (not false) reassurance: “Children and young adults appear to be very safe from this illness, but we want to take care to protect those that are older or already sick.”
Remember most children set their anxiety level based on their parent’s anxiety, and part of being child centered in your communication includes offering information in an age-appropriate manner. Preschool-aged children (up to 5 years) still have magical thinking. They are prone to finding masks and gowns scary and to assume that school stopping may be because they did something wrong. Tell them about the new illness, and about the doctors and officials working hard to keep people safe. Reassure them about all of the adults working hard together to understand the illness and take care of people who are sick. Their sense of time is less logical, so you may have to tell them more than once. Reassure them that children do not get very sick from this illness, but they can carry and spread it, like having paint on their hands, so they need to wash their hands often to take good care of other people.
School-age children (aged roughly 5-12 years) are better equipped cognitively to understand the seriousness of this outbreak. They are built to master new situations, but are prone to anxiety as they don’t yet have the emotional maturity to tolerate uncertainty or unfairness. Explain what is known without euphemisms, be truly curious about what their questions are, and look for answers together. Often what they need is to see you being calm in the face of uncertainty, bearing the strong feelings that may come, and preserving curiosity and compassion for others.
Adolescents also will need all of this support, and can be curious about more abstract implications (political, ethical, financial). Do not be surprised when they ask sophisticated questions, but still are focused on the personal disruptions or sacrifices (a canceled dance or sports meet, concerns about academic performance). Adolescence is a time of intense preoccupation with their emerging identity and relationships; it is normal for them to experience events in a way that may seem selfish, especially if it disrupts their time with friends. Remind parents to offer compassion and validation, while acknowledging that shared sacrifice and discomfort are a part of every individual’s experience when a society must respond to such a large challenge.
Be mindful of children’s vulnerabilities
Being child centered goes beyond thinking about their age and developmental stage. Parents are the experts on their children and will know about any particular vulnerabilities to the stresses of this serious outbreak. Children who are prone to anxiety or suffer from anxiety disorders may be more prone to silent worry. It is especially important to check in with them often, find out what they know and what they are worried about, and remind them to “never worry alone.” It also is important to continue with any recommended treatment, avoiding accommodation of their anxieties, except when it is required by public health protocols (i.e., staying home from school). Children with developmental disabilities may require additional support to change behaviors (hand washing) and may be more sensitive to changes in routine. And children with learning disabilities or special services in school may require additional support or structure during a prolonged period at home.
Preserve routines and structure
Routines and predictability are important to the sense of stability and well-being of most children (and adults). While disruptions are unavoidable, preserve what routines you can, and establish some new ones. For children who are out of school for several weeks, set up a consistent home routine, with a similar wake-up and bedtime, and a “school schedule.” There may be academic activities like reading or work sheets. If the parents’ work is disrupted, they can homeschool, shoring up weak academic areas or enhancing areas of interest. Be sure to preserve time for physical activity and social connections within this new framework. Social time does not require physical proximity, and can happen by screen or phone. Physical activity should be outside if at all possible. Predictability, preserved expectations (academic and otherwise), physical exercise, social connection, and consistent sleep will go a long way in protecting everyone’s ability to manage the disruptions of this epidemic.
Find opportunity in the disruption
Many families have been on a treadmill of work, school, and activities that have left little unscheduled time or spontaneity. Recommend looking at this disruption as a rare opportunity to slow down, spend time together, listen, learn more about one another, and even to have fun. Families could play board games, card games, watch movies together, or even read aloud. They might discover it is the time to try new hobbies (knitting, learning a new language or instrument), or to teach each other new skills. You might learn something new, or something new about your children. You also will offer a model of finding the opportunity in adversity, and even offer them some wonderful memories from a difficult time.
Take care of the vulnerable and ease others’ hardships
Without a doubt, this will be a difficult time for many people, medically, financially, and emotionally. One powerful strategy to build resilience in our children and strengthen our communities is to think with children about ways to help those who are most at risk or burdened by this challenge. Perhaps they want to make cards or FaceTime calls to older relatives who may be otherwise isolated. They may want to consider ways to support the work of first responders, even just with appreciation. They may want to reach out to elderly neighbors and offer to get groceries or other needed supplies for them. Balancing appropriate self-care with a focus on the needs of those who are more vulnerable or burdened than ourselves is a powerful way to show our children how communities pull together in a challenging time; enhance their feeling of connectedness; and build resilience in them, in our families, and in our communities.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected]
Physicians and health systems can reduce fear around COVID-19
A message from a Chief Wellness Officer
We are at a time, unfortunately, of significant public uncertainty and fear of “the coronavirus.” Mixed and inaccurate messages from national leaders in the setting of delayed testing availability have heightened fears and impeded a uniformity in responses, medical and preventive.
Despite this, physicians, nurses, and other health professionals across the country, and in many other countries, have been addressing the medical realities of this pandemic in a way that should make every one of us health professionals proud – from the Chinese doctors and nurses to the Italian intensivists and primary care physicians throughout many countries who have treated patients suffering from, or fearful of, a novel disease with uncertain transmission characteristics and unpredictable clinical outcomes.
It is now time for physicians and other health providers in the United States to step up to the plate and model appropriate transmission-reducing behavior for the general public. This will help reduce the overall morbidity and mortality associated with this pandemic and let us return to a more normal lifestyle as soon as possible. Physicians need to be reassuring but realistic, and there are concrete steps that we can take to demonstrate to the general public that there is a way forward.
First the basic facts. The United States does not have enough intensive care beds or ventilators to handle a major pandemic. We will also have insufficient physicians and nurses if many are quarantined. The tragic experience in Italy, where patients are dying from lack of ventilators, intensive care facilities, and staff, must not be repeated here.
Many health systems are canceling or reducing outpatient appointments and increasingly using video and other telehealth technologies, especially for assessing and triaging people who believe that they may have become infected and are relatively asymptomatic. While all of the disruptions may seem unsettling, they are actually good news for those of us in healthcare. Efforts to “flatten the curve” will slow the infection spread and help us better manage patients who become critical.
So, what can physicians do?
- Make sure you are getting good information about the situation. Access reliable information and data that are widely available through the Centers for Disease Control and Prevention, the National Institutes of Health, and the World Health Organization. Listen to professional news organizations, local and national. Pass this information to your patients and community.
- Obviously, when practicing clinically, follow all infection control protocols, which will inevitably change over time. Make it clear to your patients why you are following these protocols and procedures.
- Support and actively promote the public health responses to this pandemic. Systematic reviews of the evidence base have found that isolating ill persons, testing and tracing contacts, quarantining exposed persons, closing schools and workplaces, and avoiding crowding are more effective if implemented immediately, simultaneously (ie, school closures combined with teleworking for parents), and with high community compliance.
- Practice social distancing so that you remain as much in control as you can. This will make you feel psychologically better and safer, as well as reduce the risk for transmission. Take the essential precautionary measures that we are all being asked to take. Wash your hands. Do not shake hands. Clean shared items. Do not go to large public gatherings. Minimize large group travel as much as you can. Use video to see your patients or your own doctor.
- Connect and reconnect with people you trust and love. See your family, your partner, your children, your friends. Speak to them on the phone and nourish those relationships. See how they feel and care for each other. They will be worried about you. Reassure them. Be in the moment with them and use the importance of these relationships to give yourself a chance not to overthink any fears you might have.
- Look after yourself physically. Physical fitness is good for your mental health. While White House guidelines suggest avoiding gyms, you can still enjoy long walks and outdoor activities. Take the weekend off and don’t work excessively. Sleep well – at least 7-8 hours. which has a series of really excellent meditation and relaxation tools.
- Do not panic. Uncertainty surrounding the pandemic makes all of us anxious and afraid. It is normal to become hypervigilant, especially with our nonstop media. It is normal to be concerned when we feel out of control and when we are hearing about a possible future catastrophe, especially when fed with differing sets of information from multiple sources and countries.
- Be careful with any large decisions you are making that may affect the lives of yourself and your loved ones. Think about your decisions and try to take the long view; and run them by your spouse, partner, or friends. This is not a time to be making sudden big decisions that may be driven unconsciously, in part at least, by fear and anxiety.
- Realize that all of these societal disruptions are actually good for us in health care, and they help your family and friends understand the importance of slowing the disease’s spread. That’s good for health care and good for everyone.
Finally, remember that “this is what we do,” to quote Doug Kirk, MD, chief medical officer of UC Davis Health. We must look after our patients. But we also have to look after ourselves so that we can look after our patients. We should all be proud of our work and our caring. And we should model our personal behavior to our patients and to our families and friends so that they will model it to their community networks. That way, more people will keep well, and we will have more chance of “flattening the curve” and reducing the morbidity and mortality associated with COVID-19.
Peter M. Yellowlees, MBBS, MD, is a professor in the Department of Psychiatry at the University of California, Davis. He is a longtime Medscape contributor.
This article first appeared on Medscape.com.
A message from a Chief Wellness Officer
We are at a time, unfortunately, of significant public uncertainty and fear of “the coronavirus.” Mixed and inaccurate messages from national leaders in the setting of delayed testing availability have heightened fears and impeded a uniformity in responses, medical and preventive.
Despite this, physicians, nurses, and other health professionals across the country, and in many other countries, have been addressing the medical realities of this pandemic in a way that should make every one of us health professionals proud – from the Chinese doctors and nurses to the Italian intensivists and primary care physicians throughout many countries who have treated patients suffering from, or fearful of, a novel disease with uncertain transmission characteristics and unpredictable clinical outcomes.
It is now time for physicians and other health providers in the United States to step up to the plate and model appropriate transmission-reducing behavior for the general public. This will help reduce the overall morbidity and mortality associated with this pandemic and let us return to a more normal lifestyle as soon as possible. Physicians need to be reassuring but realistic, and there are concrete steps that we can take to demonstrate to the general public that there is a way forward.
First the basic facts. The United States does not have enough intensive care beds or ventilators to handle a major pandemic. We will also have insufficient physicians and nurses if many are quarantined. The tragic experience in Italy, where patients are dying from lack of ventilators, intensive care facilities, and staff, must not be repeated here.
Many health systems are canceling or reducing outpatient appointments and increasingly using video and other telehealth technologies, especially for assessing and triaging people who believe that they may have become infected and are relatively asymptomatic. While all of the disruptions may seem unsettling, they are actually good news for those of us in healthcare. Efforts to “flatten the curve” will slow the infection spread and help us better manage patients who become critical.
So, what can physicians do?
- Make sure you are getting good information about the situation. Access reliable information and data that are widely available through the Centers for Disease Control and Prevention, the National Institutes of Health, and the World Health Organization. Listen to professional news organizations, local and national. Pass this information to your patients and community.
- Obviously, when practicing clinically, follow all infection control protocols, which will inevitably change over time. Make it clear to your patients why you are following these protocols and procedures.
- Support and actively promote the public health responses to this pandemic. Systematic reviews of the evidence base have found that isolating ill persons, testing and tracing contacts, quarantining exposed persons, closing schools and workplaces, and avoiding crowding are more effective if implemented immediately, simultaneously (ie, school closures combined with teleworking for parents), and with high community compliance.
- Practice social distancing so that you remain as much in control as you can. This will make you feel psychologically better and safer, as well as reduce the risk for transmission. Take the essential precautionary measures that we are all being asked to take. Wash your hands. Do not shake hands. Clean shared items. Do not go to large public gatherings. Minimize large group travel as much as you can. Use video to see your patients or your own doctor.
- Connect and reconnect with people you trust and love. See your family, your partner, your children, your friends. Speak to them on the phone and nourish those relationships. See how they feel and care for each other. They will be worried about you. Reassure them. Be in the moment with them and use the importance of these relationships to give yourself a chance not to overthink any fears you might have.
- Look after yourself physically. Physical fitness is good for your mental health. While White House guidelines suggest avoiding gyms, you can still enjoy long walks and outdoor activities. Take the weekend off and don’t work excessively. Sleep well – at least 7-8 hours. which has a series of really excellent meditation and relaxation tools.
- Do not panic. Uncertainty surrounding the pandemic makes all of us anxious and afraid. It is normal to become hypervigilant, especially with our nonstop media. It is normal to be concerned when we feel out of control and when we are hearing about a possible future catastrophe, especially when fed with differing sets of information from multiple sources and countries.
- Be careful with any large decisions you are making that may affect the lives of yourself and your loved ones. Think about your decisions and try to take the long view; and run them by your spouse, partner, or friends. This is not a time to be making sudden big decisions that may be driven unconsciously, in part at least, by fear and anxiety.
- Realize that all of these societal disruptions are actually good for us in health care, and they help your family and friends understand the importance of slowing the disease’s spread. That’s good for health care and good for everyone.
Finally, remember that “this is what we do,” to quote Doug Kirk, MD, chief medical officer of UC Davis Health. We must look after our patients. But we also have to look after ourselves so that we can look after our patients. We should all be proud of our work and our caring. And we should model our personal behavior to our patients and to our families and friends so that they will model it to their community networks. That way, more people will keep well, and we will have more chance of “flattening the curve” and reducing the morbidity and mortality associated with COVID-19.
Peter M. Yellowlees, MBBS, MD, is a professor in the Department of Psychiatry at the University of California, Davis. He is a longtime Medscape contributor.
This article first appeared on Medscape.com.
A message from a Chief Wellness Officer
We are at a time, unfortunately, of significant public uncertainty and fear of “the coronavirus.” Mixed and inaccurate messages from national leaders in the setting of delayed testing availability have heightened fears and impeded a uniformity in responses, medical and preventive.
Despite this, physicians, nurses, and other health professionals across the country, and in many other countries, have been addressing the medical realities of this pandemic in a way that should make every one of us health professionals proud – from the Chinese doctors and nurses to the Italian intensivists and primary care physicians throughout many countries who have treated patients suffering from, or fearful of, a novel disease with uncertain transmission characteristics and unpredictable clinical outcomes.
It is now time for physicians and other health providers in the United States to step up to the plate and model appropriate transmission-reducing behavior for the general public. This will help reduce the overall morbidity and mortality associated with this pandemic and let us return to a more normal lifestyle as soon as possible. Physicians need to be reassuring but realistic, and there are concrete steps that we can take to demonstrate to the general public that there is a way forward.
First the basic facts. The United States does not have enough intensive care beds or ventilators to handle a major pandemic. We will also have insufficient physicians and nurses if many are quarantined. The tragic experience in Italy, where patients are dying from lack of ventilators, intensive care facilities, and staff, must not be repeated here.
Many health systems are canceling or reducing outpatient appointments and increasingly using video and other telehealth technologies, especially for assessing and triaging people who believe that they may have become infected and are relatively asymptomatic. While all of the disruptions may seem unsettling, they are actually good news for those of us in healthcare. Efforts to “flatten the curve” will slow the infection spread and help us better manage patients who become critical.
So, what can physicians do?
- Make sure you are getting good information about the situation. Access reliable information and data that are widely available through the Centers for Disease Control and Prevention, the National Institutes of Health, and the World Health Organization. Listen to professional news organizations, local and national. Pass this information to your patients and community.
- Obviously, when practicing clinically, follow all infection control protocols, which will inevitably change over time. Make it clear to your patients why you are following these protocols and procedures.
- Support and actively promote the public health responses to this pandemic. Systematic reviews of the evidence base have found that isolating ill persons, testing and tracing contacts, quarantining exposed persons, closing schools and workplaces, and avoiding crowding are more effective if implemented immediately, simultaneously (ie, school closures combined with teleworking for parents), and with high community compliance.
- Practice social distancing so that you remain as much in control as you can. This will make you feel psychologically better and safer, as well as reduce the risk for transmission. Take the essential precautionary measures that we are all being asked to take. Wash your hands. Do not shake hands. Clean shared items. Do not go to large public gatherings. Minimize large group travel as much as you can. Use video to see your patients or your own doctor.
- Connect and reconnect with people you trust and love. See your family, your partner, your children, your friends. Speak to them on the phone and nourish those relationships. See how they feel and care for each other. They will be worried about you. Reassure them. Be in the moment with them and use the importance of these relationships to give yourself a chance not to overthink any fears you might have.
- Look after yourself physically. Physical fitness is good for your mental health. While White House guidelines suggest avoiding gyms, you can still enjoy long walks and outdoor activities. Take the weekend off and don’t work excessively. Sleep well – at least 7-8 hours. which has a series of really excellent meditation and relaxation tools.
- Do not panic. Uncertainty surrounding the pandemic makes all of us anxious and afraid. It is normal to become hypervigilant, especially with our nonstop media. It is normal to be concerned when we feel out of control and when we are hearing about a possible future catastrophe, especially when fed with differing sets of information from multiple sources and countries.
- Be careful with any large decisions you are making that may affect the lives of yourself and your loved ones. Think about your decisions and try to take the long view; and run them by your spouse, partner, or friends. This is not a time to be making sudden big decisions that may be driven unconsciously, in part at least, by fear and anxiety.
- Realize that all of these societal disruptions are actually good for us in health care, and they help your family and friends understand the importance of slowing the disease’s spread. That’s good for health care and good for everyone.
Finally, remember that “this is what we do,” to quote Doug Kirk, MD, chief medical officer of UC Davis Health. We must look after our patients. But we also have to look after ourselves so that we can look after our patients. We should all be proud of our work and our caring. And we should model our personal behavior to our patients and to our families and friends so that they will model it to their community networks. That way, more people will keep well, and we will have more chance of “flattening the curve” and reducing the morbidity and mortality associated with COVID-19.
Peter M. Yellowlees, MBBS, MD, is a professor in the Department of Psychiatry at the University of California, Davis. He is a longtime Medscape contributor.
This article first appeared on Medscape.com.
COVID-19 in pediatric patients: What the hospitalist needs to know
Coronavirus disease (COVID-19) was declared a pandemic by the World Health Organization on March 11. This rapidly spreading disease is caused by the novel coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The infection has spread to more than 140 countries, including the United States. As of March 16, more than 170,400 people had tested positive for SARS-CoV-2 and more than 6,619 people have died across the globe.
The number of new COVID-19 cases appears to be decreasing in China, but the number of cases are rapidly increasing worldwide. Based on available data, primarily from China, children (aged 0-19 years) account for only about 2% of all cases. Despite the probable low virulence and incidence of infection in children, they could act as potential vectors and transmit infection to more vulnerable populations. As of March 16, approximately 3,823 cases and more than 67 deaths had been reported in the United States with few pediatric patients testing positive for the disease.
SARS-CoV2 transmission mainly occurs via respiratory route through close contact with infected individuals and through fomites. The incubation period ranges from 2-14 days with an average of about 5 days. Adult patients present with cough and fever, which may progress to lower respiratory tract symptoms, including shortness of breath. Approximately 10% of all patients develop severe disease and acute respiratory distress syndrome (ARDS), requiring mechanical ventilation.
COVID-19 carries a mortality rate of up to 3%, but has been significantly higher in the elderly population, and those with chronic health conditions. Available data so far shows that children are at lower risk and the severity of the disease has been milder compared to adults. The reasons for this are not clear at this time. As of March 16, there were no reported COVID-19 related deaths in children under age 9 years.
The pediatric population: Disease patterns and transmission
The epidemiology and spectrum of disease for COVID-19 is poorly understood in pediatrics because of the low number of reported pediatric cases and limited data available from these patients. Small numbers of reported cases in children has led some to believe that children are relatively immune to the infection by SARS-CoV-2. However, Oifang et al. found that children are equally as likely as adults to be infected.1
Liu et al. found that of 366 children admitted to a hospital in Wuhan with respiratory infections in January 2020, 1.6% (six patients) cases were positive for SARS-CoV-2.2 These six children were aged 1-7 years and had all been previously healthy; all six presented with cough and fever of 102.2° F or greater. Four of the children also had vomiting. Laboratory findings were notable for lymphopenia (six of six), leukopenia (four of six), and neutropenia (3/6) with mild to moderate elevation in C-reactive protein (6.8-58.8 mg/L). Five of six children had chest CT scans. One child’s CT scan showed “bilateral ground-glass opacities” (similar to what is reported in adults), three showed “bilateral patchy shadows,” and one was normal. One child (aged 3 years) was admitted to the ICU. All of the children were treated with supportive measures, empiric antibiotics, and antivirals (six of six received oseltamivir and four of six received ribavirin). All six children recovered completely and their median hospital stay was 7.5 days with a range of 5-13 days.
Xia et al. reviewed 20 children (aged 1 day to 14 years) admitted to a hospital in Wuhan during Jan. 23–Feb. 8.3 The study reported that fever and cough were the most common presenting symptoms (approximately 65%). Less common symptoms included rhinorrhea (15%), diarrhea (15%), vomiting (10%), and sore throat (5%). WBC count was normal in majority of children (70%) with leukopenia in 20% and leukocytosis in 10%. Lymphopenia was noted to be 35%. Elevated procalcitonin was noted in 80% of children, although the degree of elevation is unclear. In this study, 8 of 20 children were coinfected with other respiratory pathogens such as influenza, respiratory syncytial virus, mycoplasma, and cytomegalovirus. All children had chest CT scans. Ten of 20 children had bilateral pulmonary lesions, 6 of 20 had unilateral pulmonary lesions, 12 of 20 had ground-glass opacities and 10 of 20 had lung consolidations with halo signs.
Wei et al., retrospective chart review of nine infants admitted for COVID-19 found that all nine had at least one infected family member.4 This study reported that seven of nine were female infants, four of nine had fever, two had mild upper respiratory infection symptoms, and one had no symptoms. The study did report that two infants did not have any information available related to symptoms. None of the infants developed severe symptoms or required ICU admission.
The youngest patient to be diagnosed with COVID-19 was a newborn of less than 24 hours old from England, whose mother also tested positive for SARS-CoV-2. However, Chen et al. found no evidence of vertical transmission of the virus from infected pregnant women to their newborns.5
Although the risk of infection in children has been reported to be low, the infection has been shown to be particularly severe in adults with compromised immune systems and chronic health conditions. Thus immunocompromised children and those with chronic health conditions are thought to be at a higher risk for contracting the infection, with the probability for increased morbidity and mortality. Some of these risk groups include premature infants, young infants, immunocompromised children, and children with chronic health conditions like asthma, diabetes, and others. It is essential that caregivers, healthy siblings, and other family members are protected from contracting the infection in order to protect these vulnerable children. Given the high infectivity of SARS-CoV-2, the implications of infected children attending schools and daycares may be far reaching if there is delayed identification of the infection. For these reasons, it is important to closely monitor and promptly test children living with infected adults to prevent the spread. It may become necessary to close schools to mitigate transmission.
Schools and daycares should work with their local health departments and physicians in case of infected individuals in their community. In China, authorities closed schools and allowed students to receive virtual education from home, which may be a reasonable choice depending on resources.
Current challenges
Given the aggressive transmission of COVID-19, these numbers seem to be increasing exponentially with a significant impact on the life of the entire country. Therefore, we must focus on containing the spread and mitigating the transmission with a multimodality approach.
Some of the initial challenges faced by physicians in the United States were related to difficulty in access to testing in persons under investigation (PUI), which in turn resulted in a delay in diagnosis and infection control. At this time, the need is to increase surge testing capabilities across the country through a variety of innovative approaches including public-private partnerships with commercial labs through Emergency Use Authorization (EUA) issued by the Centers for Disease Control and Prevention and the Department of Health and Human Services. To minimize exposure to health care professionals, telemedicine and telehealth capabilities should be exploited. This will minimize the exposure to infected patients and reduce the need for already limited personal protective equipment (PPE). As the number of cases rise, hospitals should expect and prepare for a surge in COVID-19–related hospitalizations and health care utilization.
Conclusion
Various theories are being proposed as to why children are not experiencing severe disease with COVID-19. Children may have cross-protective immunity from infection with other coronaviruses. Children may not have the same exposures from work, travel, and caregiving that adults experience as they are typically exposed by someone in their home. At this time, not enough is known about clinical presentations in children as the situation continues to evolve across the globe.
Respiratory infections in children pose unique infection control challenges with respect to compliant hand hygiene, cough etiquette, and the use of PPE when indicated. There is also concern for persistent fecal shedding of virus in infected pediatric patients, which could be another mode of transmission.6 Children could, however, be very efficient vectors of COVID-19, similar to flu, and potentially spread the pathogen to very vulnerable populations leading to high morbidity and mortality. School closures are an effective social distancing measure needed to flatten the curve and avoid overwhelming the health care structure of the United States.
Dr. Konanki is a board-certified pediatrician doing inpatient work at Wellspan Chambersburg Hospital and outpatient work at Keystone Pediatrics in Chambersburg, Pa. He also serves as the physician member of the hospital’s Code Blue Jr. committee and as a member of Quality Metrics committee at Keystone Health. Dr. Tirupathi is the medical director of Keystone Infectious Diseases/HIV in Chambersburg, Pa., and currently chair of infection prevention at Wellspan Chambersburg and Waynesboro (Pa.) Hospitals. He also is the lead physician for antibiotic stewardship at these hospitals. Dr. Palabindala is hospital medicine division chief at the University of Mississippi Medical Center, Jackson.
References
1. Bi Q et al. Epidemiology and transmission of COVID-19 in Shenzhen China: Analysis of 391 cases and 1,286 of their close contacts. medRxiv 2020.03.03.20028423.
2. Liu W et al. Detection of Covid-19 in children in early January 2020 in Wuhan, China. N Engl J Med. 2020 Mar 12. doi: 10.1056/NEJMc2003717.
3. Xia W et al. Clinical and CT features in pediatric patients with COVID‐19 infection: Different points from adults. Pediatr Pulmonol. 2020 Mar 5. doi: 10.1002/ppul.24718.
4. Wei M et al. Novel Coronavirus infection in hospitalized infants under 1 year of age in China. JAMA. 2020 Feb. 14. doi: 10.1001/jama.2020.2131.
5. Huijun C et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: A retrospective review of medical records. Lancet. 2020 Mar 7 395;10226:809-15.
6. Xu Y et al. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat Med. 2020 Mar 13. doi. org/10.1038/s41591-020-0817-4.
Coronavirus disease (COVID-19) was declared a pandemic by the World Health Organization on March 11. This rapidly spreading disease is caused by the novel coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The infection has spread to more than 140 countries, including the United States. As of March 16, more than 170,400 people had tested positive for SARS-CoV-2 and more than 6,619 people have died across the globe.
The number of new COVID-19 cases appears to be decreasing in China, but the number of cases are rapidly increasing worldwide. Based on available data, primarily from China, children (aged 0-19 years) account for only about 2% of all cases. Despite the probable low virulence and incidence of infection in children, they could act as potential vectors and transmit infection to more vulnerable populations. As of March 16, approximately 3,823 cases and more than 67 deaths had been reported in the United States with few pediatric patients testing positive for the disease.
SARS-CoV2 transmission mainly occurs via respiratory route through close contact with infected individuals and through fomites. The incubation period ranges from 2-14 days with an average of about 5 days. Adult patients present with cough and fever, which may progress to lower respiratory tract symptoms, including shortness of breath. Approximately 10% of all patients develop severe disease and acute respiratory distress syndrome (ARDS), requiring mechanical ventilation.
COVID-19 carries a mortality rate of up to 3%, but has been significantly higher in the elderly population, and those with chronic health conditions. Available data so far shows that children are at lower risk and the severity of the disease has been milder compared to adults. The reasons for this are not clear at this time. As of March 16, there were no reported COVID-19 related deaths in children under age 9 years.
The pediatric population: Disease patterns and transmission
The epidemiology and spectrum of disease for COVID-19 is poorly understood in pediatrics because of the low number of reported pediatric cases and limited data available from these patients. Small numbers of reported cases in children has led some to believe that children are relatively immune to the infection by SARS-CoV-2. However, Oifang et al. found that children are equally as likely as adults to be infected.1
Liu et al. found that of 366 children admitted to a hospital in Wuhan with respiratory infections in January 2020, 1.6% (six patients) cases were positive for SARS-CoV-2.2 These six children were aged 1-7 years and had all been previously healthy; all six presented with cough and fever of 102.2° F or greater. Four of the children also had vomiting. Laboratory findings were notable for lymphopenia (six of six), leukopenia (four of six), and neutropenia (3/6) with mild to moderate elevation in C-reactive protein (6.8-58.8 mg/L). Five of six children had chest CT scans. One child’s CT scan showed “bilateral ground-glass opacities” (similar to what is reported in adults), three showed “bilateral patchy shadows,” and one was normal. One child (aged 3 years) was admitted to the ICU. All of the children were treated with supportive measures, empiric antibiotics, and antivirals (six of six received oseltamivir and four of six received ribavirin). All six children recovered completely and their median hospital stay was 7.5 days with a range of 5-13 days.
Xia et al. reviewed 20 children (aged 1 day to 14 years) admitted to a hospital in Wuhan during Jan. 23–Feb. 8.3 The study reported that fever and cough were the most common presenting symptoms (approximately 65%). Less common symptoms included rhinorrhea (15%), diarrhea (15%), vomiting (10%), and sore throat (5%). WBC count was normal in majority of children (70%) with leukopenia in 20% and leukocytosis in 10%. Lymphopenia was noted to be 35%. Elevated procalcitonin was noted in 80% of children, although the degree of elevation is unclear. In this study, 8 of 20 children were coinfected with other respiratory pathogens such as influenza, respiratory syncytial virus, mycoplasma, and cytomegalovirus. All children had chest CT scans. Ten of 20 children had bilateral pulmonary lesions, 6 of 20 had unilateral pulmonary lesions, 12 of 20 had ground-glass opacities and 10 of 20 had lung consolidations with halo signs.
Wei et al., retrospective chart review of nine infants admitted for COVID-19 found that all nine had at least one infected family member.4 This study reported that seven of nine were female infants, four of nine had fever, two had mild upper respiratory infection symptoms, and one had no symptoms. The study did report that two infants did not have any information available related to symptoms. None of the infants developed severe symptoms or required ICU admission.
The youngest patient to be diagnosed with COVID-19 was a newborn of less than 24 hours old from England, whose mother also tested positive for SARS-CoV-2. However, Chen et al. found no evidence of vertical transmission of the virus from infected pregnant women to their newborns.5
Although the risk of infection in children has been reported to be low, the infection has been shown to be particularly severe in adults with compromised immune systems and chronic health conditions. Thus immunocompromised children and those with chronic health conditions are thought to be at a higher risk for contracting the infection, with the probability for increased morbidity and mortality. Some of these risk groups include premature infants, young infants, immunocompromised children, and children with chronic health conditions like asthma, diabetes, and others. It is essential that caregivers, healthy siblings, and other family members are protected from contracting the infection in order to protect these vulnerable children. Given the high infectivity of SARS-CoV-2, the implications of infected children attending schools and daycares may be far reaching if there is delayed identification of the infection. For these reasons, it is important to closely monitor and promptly test children living with infected adults to prevent the spread. It may become necessary to close schools to mitigate transmission.
Schools and daycares should work with their local health departments and physicians in case of infected individuals in their community. In China, authorities closed schools and allowed students to receive virtual education from home, which may be a reasonable choice depending on resources.
Current challenges
Given the aggressive transmission of COVID-19, these numbers seem to be increasing exponentially with a significant impact on the life of the entire country. Therefore, we must focus on containing the spread and mitigating the transmission with a multimodality approach.
Some of the initial challenges faced by physicians in the United States were related to difficulty in access to testing in persons under investigation (PUI), which in turn resulted in a delay in diagnosis and infection control. At this time, the need is to increase surge testing capabilities across the country through a variety of innovative approaches including public-private partnerships with commercial labs through Emergency Use Authorization (EUA) issued by the Centers for Disease Control and Prevention and the Department of Health and Human Services. To minimize exposure to health care professionals, telemedicine and telehealth capabilities should be exploited. This will minimize the exposure to infected patients and reduce the need for already limited personal protective equipment (PPE). As the number of cases rise, hospitals should expect and prepare for a surge in COVID-19–related hospitalizations and health care utilization.
Conclusion
Various theories are being proposed as to why children are not experiencing severe disease with COVID-19. Children may have cross-protective immunity from infection with other coronaviruses. Children may not have the same exposures from work, travel, and caregiving that adults experience as they are typically exposed by someone in their home. At this time, not enough is known about clinical presentations in children as the situation continues to evolve across the globe.
Respiratory infections in children pose unique infection control challenges with respect to compliant hand hygiene, cough etiquette, and the use of PPE when indicated. There is also concern for persistent fecal shedding of virus in infected pediatric patients, which could be another mode of transmission.6 Children could, however, be very efficient vectors of COVID-19, similar to flu, and potentially spread the pathogen to very vulnerable populations leading to high morbidity and mortality. School closures are an effective social distancing measure needed to flatten the curve and avoid overwhelming the health care structure of the United States.
Dr. Konanki is a board-certified pediatrician doing inpatient work at Wellspan Chambersburg Hospital and outpatient work at Keystone Pediatrics in Chambersburg, Pa. He also serves as the physician member of the hospital’s Code Blue Jr. committee and as a member of Quality Metrics committee at Keystone Health. Dr. Tirupathi is the medical director of Keystone Infectious Diseases/HIV in Chambersburg, Pa., and currently chair of infection prevention at Wellspan Chambersburg and Waynesboro (Pa.) Hospitals. He also is the lead physician for antibiotic stewardship at these hospitals. Dr. Palabindala is hospital medicine division chief at the University of Mississippi Medical Center, Jackson.
References
1. Bi Q et al. Epidemiology and transmission of COVID-19 in Shenzhen China: Analysis of 391 cases and 1,286 of their close contacts. medRxiv 2020.03.03.20028423.
2. Liu W et al. Detection of Covid-19 in children in early January 2020 in Wuhan, China. N Engl J Med. 2020 Mar 12. doi: 10.1056/NEJMc2003717.
3. Xia W et al. Clinical and CT features in pediatric patients with COVID‐19 infection: Different points from adults. Pediatr Pulmonol. 2020 Mar 5. doi: 10.1002/ppul.24718.
4. Wei M et al. Novel Coronavirus infection in hospitalized infants under 1 year of age in China. JAMA. 2020 Feb. 14. doi: 10.1001/jama.2020.2131.
5. Huijun C et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: A retrospective review of medical records. Lancet. 2020 Mar 7 395;10226:809-15.
6. Xu Y et al. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat Med. 2020 Mar 13. doi. org/10.1038/s41591-020-0817-4.
Coronavirus disease (COVID-19) was declared a pandemic by the World Health Organization on March 11. This rapidly spreading disease is caused by the novel coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The infection has spread to more than 140 countries, including the United States. As of March 16, more than 170,400 people had tested positive for SARS-CoV-2 and more than 6,619 people have died across the globe.
The number of new COVID-19 cases appears to be decreasing in China, but the number of cases are rapidly increasing worldwide. Based on available data, primarily from China, children (aged 0-19 years) account for only about 2% of all cases. Despite the probable low virulence and incidence of infection in children, they could act as potential vectors and transmit infection to more vulnerable populations. As of March 16, approximately 3,823 cases and more than 67 deaths had been reported in the United States with few pediatric patients testing positive for the disease.
SARS-CoV2 transmission mainly occurs via respiratory route through close contact with infected individuals and through fomites. The incubation period ranges from 2-14 days with an average of about 5 days. Adult patients present with cough and fever, which may progress to lower respiratory tract symptoms, including shortness of breath. Approximately 10% of all patients develop severe disease and acute respiratory distress syndrome (ARDS), requiring mechanical ventilation.
COVID-19 carries a mortality rate of up to 3%, but has been significantly higher in the elderly population, and those with chronic health conditions. Available data so far shows that children are at lower risk and the severity of the disease has been milder compared to adults. The reasons for this are not clear at this time. As of March 16, there were no reported COVID-19 related deaths in children under age 9 years.
The pediatric population: Disease patterns and transmission
The epidemiology and spectrum of disease for COVID-19 is poorly understood in pediatrics because of the low number of reported pediatric cases and limited data available from these patients. Small numbers of reported cases in children has led some to believe that children are relatively immune to the infection by SARS-CoV-2. However, Oifang et al. found that children are equally as likely as adults to be infected.1
Liu et al. found that of 366 children admitted to a hospital in Wuhan with respiratory infections in January 2020, 1.6% (six patients) cases were positive for SARS-CoV-2.2 These six children were aged 1-7 years and had all been previously healthy; all six presented with cough and fever of 102.2° F or greater. Four of the children also had vomiting. Laboratory findings were notable for lymphopenia (six of six), leukopenia (four of six), and neutropenia (3/6) with mild to moderate elevation in C-reactive protein (6.8-58.8 mg/L). Five of six children had chest CT scans. One child’s CT scan showed “bilateral ground-glass opacities” (similar to what is reported in adults), three showed “bilateral patchy shadows,” and one was normal. One child (aged 3 years) was admitted to the ICU. All of the children were treated with supportive measures, empiric antibiotics, and antivirals (six of six received oseltamivir and four of six received ribavirin). All six children recovered completely and their median hospital stay was 7.5 days with a range of 5-13 days.
Xia et al. reviewed 20 children (aged 1 day to 14 years) admitted to a hospital in Wuhan during Jan. 23–Feb. 8.3 The study reported that fever and cough were the most common presenting symptoms (approximately 65%). Less common symptoms included rhinorrhea (15%), diarrhea (15%), vomiting (10%), and sore throat (5%). WBC count was normal in majority of children (70%) with leukopenia in 20% and leukocytosis in 10%. Lymphopenia was noted to be 35%. Elevated procalcitonin was noted in 80% of children, although the degree of elevation is unclear. In this study, 8 of 20 children were coinfected with other respiratory pathogens such as influenza, respiratory syncytial virus, mycoplasma, and cytomegalovirus. All children had chest CT scans. Ten of 20 children had bilateral pulmonary lesions, 6 of 20 had unilateral pulmonary lesions, 12 of 20 had ground-glass opacities and 10 of 20 had lung consolidations with halo signs.
Wei et al., retrospective chart review of nine infants admitted for COVID-19 found that all nine had at least one infected family member.4 This study reported that seven of nine were female infants, four of nine had fever, two had mild upper respiratory infection symptoms, and one had no symptoms. The study did report that two infants did not have any information available related to symptoms. None of the infants developed severe symptoms or required ICU admission.
The youngest patient to be diagnosed with COVID-19 was a newborn of less than 24 hours old from England, whose mother also tested positive for SARS-CoV-2. However, Chen et al. found no evidence of vertical transmission of the virus from infected pregnant women to their newborns.5
Although the risk of infection in children has been reported to be low, the infection has been shown to be particularly severe in adults with compromised immune systems and chronic health conditions. Thus immunocompromised children and those with chronic health conditions are thought to be at a higher risk for contracting the infection, with the probability for increased morbidity and mortality. Some of these risk groups include premature infants, young infants, immunocompromised children, and children with chronic health conditions like asthma, diabetes, and others. It is essential that caregivers, healthy siblings, and other family members are protected from contracting the infection in order to protect these vulnerable children. Given the high infectivity of SARS-CoV-2, the implications of infected children attending schools and daycares may be far reaching if there is delayed identification of the infection. For these reasons, it is important to closely monitor and promptly test children living with infected adults to prevent the spread. It may become necessary to close schools to mitigate transmission.
Schools and daycares should work with their local health departments and physicians in case of infected individuals in their community. In China, authorities closed schools and allowed students to receive virtual education from home, which may be a reasonable choice depending on resources.
Current challenges
Given the aggressive transmission of COVID-19, these numbers seem to be increasing exponentially with a significant impact on the life of the entire country. Therefore, we must focus on containing the spread and mitigating the transmission with a multimodality approach.
Some of the initial challenges faced by physicians in the United States were related to difficulty in access to testing in persons under investigation (PUI), which in turn resulted in a delay in diagnosis and infection control. At this time, the need is to increase surge testing capabilities across the country through a variety of innovative approaches including public-private partnerships with commercial labs through Emergency Use Authorization (EUA) issued by the Centers for Disease Control and Prevention and the Department of Health and Human Services. To minimize exposure to health care professionals, telemedicine and telehealth capabilities should be exploited. This will minimize the exposure to infected patients and reduce the need for already limited personal protective equipment (PPE). As the number of cases rise, hospitals should expect and prepare for a surge in COVID-19–related hospitalizations and health care utilization.
Conclusion
Various theories are being proposed as to why children are not experiencing severe disease with COVID-19. Children may have cross-protective immunity from infection with other coronaviruses. Children may not have the same exposures from work, travel, and caregiving that adults experience as they are typically exposed by someone in their home. At this time, not enough is known about clinical presentations in children as the situation continues to evolve across the globe.
Respiratory infections in children pose unique infection control challenges with respect to compliant hand hygiene, cough etiquette, and the use of PPE when indicated. There is also concern for persistent fecal shedding of virus in infected pediatric patients, which could be another mode of transmission.6 Children could, however, be very efficient vectors of COVID-19, similar to flu, and potentially spread the pathogen to very vulnerable populations leading to high morbidity and mortality. School closures are an effective social distancing measure needed to flatten the curve and avoid overwhelming the health care structure of the United States.
Dr. Konanki is a board-certified pediatrician doing inpatient work at Wellspan Chambersburg Hospital and outpatient work at Keystone Pediatrics in Chambersburg, Pa. He also serves as the physician member of the hospital’s Code Blue Jr. committee and as a member of Quality Metrics committee at Keystone Health. Dr. Tirupathi is the medical director of Keystone Infectious Diseases/HIV in Chambersburg, Pa., and currently chair of infection prevention at Wellspan Chambersburg and Waynesboro (Pa.) Hospitals. He also is the lead physician for antibiotic stewardship at these hospitals. Dr. Palabindala is hospital medicine division chief at the University of Mississippi Medical Center, Jackson.
References
1. Bi Q et al. Epidemiology and transmission of COVID-19 in Shenzhen China: Analysis of 391 cases and 1,286 of their close contacts. medRxiv 2020.03.03.20028423.
2. Liu W et al. Detection of Covid-19 in children in early January 2020 in Wuhan, China. N Engl J Med. 2020 Mar 12. doi: 10.1056/NEJMc2003717.
3. Xia W et al. Clinical and CT features in pediatric patients with COVID‐19 infection: Different points from adults. Pediatr Pulmonol. 2020 Mar 5. doi: 10.1002/ppul.24718.
4. Wei M et al. Novel Coronavirus infection in hospitalized infants under 1 year of age in China. JAMA. 2020 Feb. 14. doi: 10.1001/jama.2020.2131.
5. Huijun C et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: A retrospective review of medical records. Lancet. 2020 Mar 7 395;10226:809-15.
6. Xu Y et al. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat Med. 2020 Mar 13. doi. org/10.1038/s41591-020-0817-4.