User login
Systemic racism: An editor’s note
This month’s editorial was jointly written by the editors of 10 prominent family medicine publications, including JFP, and is being published simultaneously in all 10 publications. In addition to this statement, each editor has developed action steps for their respective journals. At JFP, we plan to take the steps detailed here to help eliminate systemic racism. We will:
- continue to seek Black, Latino, and Native American physicians to serve on the JFP editorial advisory board.
- solicit manuscripts from these underrepresented groups of physicians.
- recruit peer reviewers from underrepresented communities.
- re-evaluate the thoroughness of manuscripts; where there are racial or ethnic differences in presentation of diseases or treatment outcomes, we will ensure that these differences are highlighted.
If you are interested in helping us to achieve these goals, I encourage you to contact me at [email protected].
We must all band together to eliminate disparities and biases in medical education and medical care so that all people receive the same high standard of respect and care that every human being deserves.
This month’s editorial was jointly written by the editors of 10 prominent family medicine publications, including JFP, and is being published simultaneously in all 10 publications. In addition to this statement, each editor has developed action steps for their respective journals. At JFP, we plan to take the steps detailed here to help eliminate systemic racism. We will:
- continue to seek Black, Latino, and Native American physicians to serve on the JFP editorial advisory board.
- solicit manuscripts from these underrepresented groups of physicians.
- recruit peer reviewers from underrepresented communities.
- re-evaluate the thoroughness of manuscripts; where there are racial or ethnic differences in presentation of diseases or treatment outcomes, we will ensure that these differences are highlighted.
If you are interested in helping us to achieve these goals, I encourage you to contact me at [email protected].
We must all band together to eliminate disparities and biases in medical education and medical care so that all people receive the same high standard of respect and care that every human being deserves.
This month’s editorial was jointly written by the editors of 10 prominent family medicine publications, including JFP, and is being published simultaneously in all 10 publications. In addition to this statement, each editor has developed action steps for their respective journals. At JFP, we plan to take the steps detailed here to help eliminate systemic racism. We will:
- continue to seek Black, Latino, and Native American physicians to serve on the JFP editorial advisory board.
- solicit manuscripts from these underrepresented groups of physicians.
- recruit peer reviewers from underrepresented communities.
- re-evaluate the thoroughness of manuscripts; where there are racial or ethnic differences in presentation of diseases or treatment outcomes, we will ensure that these differences are highlighted.
If you are interested in helping us to achieve these goals, I encourage you to contact me at [email protected].
We must all band together to eliminate disparities and biases in medical education and medical care so that all people receive the same high standard of respect and care that every human being deserves.
Advice for Applying to Dermatology as an Applicant of Color: Keep Going
As the dermatology admissions cycle restarts, I reflect back on my journey as a Black woman applying to dermatology. Before deciding, I internally questioned, “Is dermatology right for me?” There were not many faces that looked like mine within the field. After committing to dermatology, I asked dermatologists—almost any who would spare a few minutes to talk to me—how to get into this specialty and be successful when applying. I spoke to advisors and friends at my home department, emailed dermatologists far and wide, approached conference lecturers after their presentations, sought out advice from current residents, and asked prior applicants what they thought was important to match into dermatology. There had been too many unmatched students before me who had achieved good grades and aced US Medical Licensing Examination Step 1. The equation for success was missing a variable.
Mentorship
One weekend, I attended a conference for patients with skin of color. I talked to a student who had taken a year off (retroactively after not matching in prior years). She told me that the biggest key to matching was mentorship; forming a strong relationship with a clinician or investigator who had seen how well you perform in clinic or during research was paramount. Having a collaborator or instructor write you a letter of recommendation and make calls on your behalf could be the difference between matching or taking another year off. More often than any other aspect of the application, it is a lack of mentorship that many students of color do not have access to when pursuing a highly competitive specialty such as dermatology.1,2 In such a small field, applicants need someone to vouch for them—to speak on their behalf compassionately, invite them to collaborate on research projects, and inform them of conference opportunities to present their work.
Representation in Dermatology
We are told that you can accomplish anything with hard work and grit; however, without the platform to show how effectively you have worked, your efforts may never be seen. The diversity statistics for dermatology are clear and disheartening. Although 13% of Americans are Black, only 3% of all dermatologists are Black.2,3 Just over 4% of dermatologists are Hispanic compared with 16% of the general population. The Association of American Medical Colleges reported that the overall 2015 medical school acceptance rate was 41%.4 White (44%), Asian (42%), and Hispanic or Latino (42%) applicants all had similar acceptance rates; however, only one-third of Black applicants were accepted. At graduation in 2015, White individuals were 51% of matriculants. Medical graduates were only 6% Black.4 What percentage of these 6% Black graduates thought about applying into dermatology? How many had someone to encourage them to pursue the specialty or a mentor who they could ask about the nuances and strategy to be a competitive applicant?
In addition to discrimination, social psychologists have described stereotype threat, a risk for minorities that occurs when negative stereotypes associated with an individual’s group status become relevant after perceived cues.5 Therefore, some students of color might avoid competitive specialties such as dermatology because of this internalized lack of confidence in their own abilities and performance thinking, “I’ll never be good enough to match into dermatology.” I have seen this discouraging perception when classmates doubt their own talent and achievements, which is a variation of imposter syndrome—when an individual doubts their abilities and may have an internal fear of eventually being exposed as a fraud.
After several publications received press coverage on the lack of diversity in dermatology applicant selection,3,6,7 I looked around at my interview group composed of 25 to 40 interviewees and on average saw 2 to 3 Black applicants around the room. We always found a way during the packed interview day to find time to introduce ourselves. I almost always left with a new friend who shared feelings of anxiety, uncertainty, hope, and gratefulness from being the few Black people in the room. Bootstrapping might have helped us to make it into medical school, pass shelf examinations, and even get a great Step 1 score. However, the addition of mentorship—or better yet, sponsorship—helped to get us an interview in this competitive field. The impact of mentorship has been especially true for research, which has shown that students often gravitate toward mentors who look like them.8 However, the reality is that many Black and Hispanic students may be at a disadvantage for finding mentors in this way given that there are less than 10% of dermatologists who identify as individuals with skin of color. During the process of applying to dermatology, my greatest advocates were ethnically and racially diverse. The proverb is that it takes a village to raise a child; this reality extends to the medical student’s ability to thrive, not only in residency but also in the residency application process. My sponsors have been as different as their advice and perspectives, which helped me to think about the varied ways I viewed myself as an applicant and shaped what I looked for in residency.
Final Thoughts
Now that I have been a resident in the Department of Dermatology at the Warren Alpert Medical School of Brown University, I excitedly look for opportunities to mentor medical students and help create equity in the application process. Dermatology needs to increase the representation of minority applicants. Efforts to encourage minority medical students include joining the National Medical Association dermatology section through the Student National Medical Association, membership in the Skin of Color Society, getting involved with the Dermatology Interest Group at more medical schools, and awareness of medical student–friendly dermatology conferences. In addition, I was able to establish lifelong mentorship through the American Academy of Dermatology’s Minority Diversity Mentorship Program. One important component is an enhanced effort to increase the number of financial scholarships for away rotations (post–coronavirus disease 2019 pandemic) or application expenses geared to help underrepresented minorities. To truly increase diversity in dermatology, perhaps we need more physicians and residents willing to encourage students of color that dermatology is achievable.
- Brunsma DL, Embrick DG, Shin JH. Graduate students of color: race, racism, and mentoring in the white waters of academia. Sociology of Race and Ethnicity. 2017;3:1-13.
- Oyesanya T, Grossberg AL, Okoye GA. Increasing minority representation in the dermatology department: the Johns Hopkins experience. JAMA Dermatol. 2018;154:1133-1134.
- Pandya AG, Alexis AF, Berger TG, et al. Increasing racial and ethnic diversity in dermatology: a call to action. J Am Acad Dermatol. 2016;74:584-587.
- Current trends in medical education. American Association of Medical Colleges. Accessed January 20, 2021. http://www.aamcdiversityfactsandfigures2016.org/report-section/section-3/
- Spencer SJ, Logel C, Davies PG. Stereotype threat [published online September 10, 2015]. Annu Rev Psychol. 2016;67:415-437.
- Granstein RD, Cornelius L, Shinkai K. Diversity in dermatology—a call for action. JAMA Dermatol. 2017;153:499-500.
- Pritchett EN, Pandya AG, Ferguson NN, et al. Diversity in dermatology: roadmap for improvement. J Am Acad Dermatol. 2018;79:337-341.
- Blake-Beard S, Bayne ML, Crosby FJ, et al. Matching by race and gender in mentoring relationships: keeping our eyes on the prize. J Social Issues. 2011;67:622-643.
As the dermatology admissions cycle restarts, I reflect back on my journey as a Black woman applying to dermatology. Before deciding, I internally questioned, “Is dermatology right for me?” There were not many faces that looked like mine within the field. After committing to dermatology, I asked dermatologists—almost any who would spare a few minutes to talk to me—how to get into this specialty and be successful when applying. I spoke to advisors and friends at my home department, emailed dermatologists far and wide, approached conference lecturers after their presentations, sought out advice from current residents, and asked prior applicants what they thought was important to match into dermatology. There had been too many unmatched students before me who had achieved good grades and aced US Medical Licensing Examination Step 1. The equation for success was missing a variable.
Mentorship
One weekend, I attended a conference for patients with skin of color. I talked to a student who had taken a year off (retroactively after not matching in prior years). She told me that the biggest key to matching was mentorship; forming a strong relationship with a clinician or investigator who had seen how well you perform in clinic or during research was paramount. Having a collaborator or instructor write you a letter of recommendation and make calls on your behalf could be the difference between matching or taking another year off. More often than any other aspect of the application, it is a lack of mentorship that many students of color do not have access to when pursuing a highly competitive specialty such as dermatology.1,2 In such a small field, applicants need someone to vouch for them—to speak on their behalf compassionately, invite them to collaborate on research projects, and inform them of conference opportunities to present their work.
Representation in Dermatology
We are told that you can accomplish anything with hard work and grit; however, without the platform to show how effectively you have worked, your efforts may never be seen. The diversity statistics for dermatology are clear and disheartening. Although 13% of Americans are Black, only 3% of all dermatologists are Black.2,3 Just over 4% of dermatologists are Hispanic compared with 16% of the general population. The Association of American Medical Colleges reported that the overall 2015 medical school acceptance rate was 41%.4 White (44%), Asian (42%), and Hispanic or Latino (42%) applicants all had similar acceptance rates; however, only one-third of Black applicants were accepted. At graduation in 2015, White individuals were 51% of matriculants. Medical graduates were only 6% Black.4 What percentage of these 6% Black graduates thought about applying into dermatology? How many had someone to encourage them to pursue the specialty or a mentor who they could ask about the nuances and strategy to be a competitive applicant?
In addition to discrimination, social psychologists have described stereotype threat, a risk for minorities that occurs when negative stereotypes associated with an individual’s group status become relevant after perceived cues.5 Therefore, some students of color might avoid competitive specialties such as dermatology because of this internalized lack of confidence in their own abilities and performance thinking, “I’ll never be good enough to match into dermatology.” I have seen this discouraging perception when classmates doubt their own talent and achievements, which is a variation of imposter syndrome—when an individual doubts their abilities and may have an internal fear of eventually being exposed as a fraud.
After several publications received press coverage on the lack of diversity in dermatology applicant selection,3,6,7 I looked around at my interview group composed of 25 to 40 interviewees and on average saw 2 to 3 Black applicants around the room. We always found a way during the packed interview day to find time to introduce ourselves. I almost always left with a new friend who shared feelings of anxiety, uncertainty, hope, and gratefulness from being the few Black people in the room. Bootstrapping might have helped us to make it into medical school, pass shelf examinations, and even get a great Step 1 score. However, the addition of mentorship—or better yet, sponsorship—helped to get us an interview in this competitive field. The impact of mentorship has been especially true for research, which has shown that students often gravitate toward mentors who look like them.8 However, the reality is that many Black and Hispanic students may be at a disadvantage for finding mentors in this way given that there are less than 10% of dermatologists who identify as individuals with skin of color. During the process of applying to dermatology, my greatest advocates were ethnically and racially diverse. The proverb is that it takes a village to raise a child; this reality extends to the medical student’s ability to thrive, not only in residency but also in the residency application process. My sponsors have been as different as their advice and perspectives, which helped me to think about the varied ways I viewed myself as an applicant and shaped what I looked for in residency.
Final Thoughts
Now that I have been a resident in the Department of Dermatology at the Warren Alpert Medical School of Brown University, I excitedly look for opportunities to mentor medical students and help create equity in the application process. Dermatology needs to increase the representation of minority applicants. Efforts to encourage minority medical students include joining the National Medical Association dermatology section through the Student National Medical Association, membership in the Skin of Color Society, getting involved with the Dermatology Interest Group at more medical schools, and awareness of medical student–friendly dermatology conferences. In addition, I was able to establish lifelong mentorship through the American Academy of Dermatology’s Minority Diversity Mentorship Program. One important component is an enhanced effort to increase the number of financial scholarships for away rotations (post–coronavirus disease 2019 pandemic) or application expenses geared to help underrepresented minorities. To truly increase diversity in dermatology, perhaps we need more physicians and residents willing to encourage students of color that dermatology is achievable.
As the dermatology admissions cycle restarts, I reflect back on my journey as a Black woman applying to dermatology. Before deciding, I internally questioned, “Is dermatology right for me?” There were not many faces that looked like mine within the field. After committing to dermatology, I asked dermatologists—almost any who would spare a few minutes to talk to me—how to get into this specialty and be successful when applying. I spoke to advisors and friends at my home department, emailed dermatologists far and wide, approached conference lecturers after their presentations, sought out advice from current residents, and asked prior applicants what they thought was important to match into dermatology. There had been too many unmatched students before me who had achieved good grades and aced US Medical Licensing Examination Step 1. The equation for success was missing a variable.
Mentorship
One weekend, I attended a conference for patients with skin of color. I talked to a student who had taken a year off (retroactively after not matching in prior years). She told me that the biggest key to matching was mentorship; forming a strong relationship with a clinician or investigator who had seen how well you perform in clinic or during research was paramount. Having a collaborator or instructor write you a letter of recommendation and make calls on your behalf could be the difference between matching or taking another year off. More often than any other aspect of the application, it is a lack of mentorship that many students of color do not have access to when pursuing a highly competitive specialty such as dermatology.1,2 In such a small field, applicants need someone to vouch for them—to speak on their behalf compassionately, invite them to collaborate on research projects, and inform them of conference opportunities to present their work.
Representation in Dermatology
We are told that you can accomplish anything with hard work and grit; however, without the platform to show how effectively you have worked, your efforts may never be seen. The diversity statistics for dermatology are clear and disheartening. Although 13% of Americans are Black, only 3% of all dermatologists are Black.2,3 Just over 4% of dermatologists are Hispanic compared with 16% of the general population. The Association of American Medical Colleges reported that the overall 2015 medical school acceptance rate was 41%.4 White (44%), Asian (42%), and Hispanic or Latino (42%) applicants all had similar acceptance rates; however, only one-third of Black applicants were accepted. At graduation in 2015, White individuals were 51% of matriculants. Medical graduates were only 6% Black.4 What percentage of these 6% Black graduates thought about applying into dermatology? How many had someone to encourage them to pursue the specialty or a mentor who they could ask about the nuances and strategy to be a competitive applicant?
In addition to discrimination, social psychologists have described stereotype threat, a risk for minorities that occurs when negative stereotypes associated with an individual’s group status become relevant after perceived cues.5 Therefore, some students of color might avoid competitive specialties such as dermatology because of this internalized lack of confidence in their own abilities and performance thinking, “I’ll never be good enough to match into dermatology.” I have seen this discouraging perception when classmates doubt their own talent and achievements, which is a variation of imposter syndrome—when an individual doubts their abilities and may have an internal fear of eventually being exposed as a fraud.
After several publications received press coverage on the lack of diversity in dermatology applicant selection,3,6,7 I looked around at my interview group composed of 25 to 40 interviewees and on average saw 2 to 3 Black applicants around the room. We always found a way during the packed interview day to find time to introduce ourselves. I almost always left with a new friend who shared feelings of anxiety, uncertainty, hope, and gratefulness from being the few Black people in the room. Bootstrapping might have helped us to make it into medical school, pass shelf examinations, and even get a great Step 1 score. However, the addition of mentorship—or better yet, sponsorship—helped to get us an interview in this competitive field. The impact of mentorship has been especially true for research, which has shown that students often gravitate toward mentors who look like them.8 However, the reality is that many Black and Hispanic students may be at a disadvantage for finding mentors in this way given that there are less than 10% of dermatologists who identify as individuals with skin of color. During the process of applying to dermatology, my greatest advocates were ethnically and racially diverse. The proverb is that it takes a village to raise a child; this reality extends to the medical student’s ability to thrive, not only in residency but also in the residency application process. My sponsors have been as different as their advice and perspectives, which helped me to think about the varied ways I viewed myself as an applicant and shaped what I looked for in residency.
Final Thoughts
Now that I have been a resident in the Department of Dermatology at the Warren Alpert Medical School of Brown University, I excitedly look for opportunities to mentor medical students and help create equity in the application process. Dermatology needs to increase the representation of minority applicants. Efforts to encourage minority medical students include joining the National Medical Association dermatology section through the Student National Medical Association, membership in the Skin of Color Society, getting involved with the Dermatology Interest Group at more medical schools, and awareness of medical student–friendly dermatology conferences. In addition, I was able to establish lifelong mentorship through the American Academy of Dermatology’s Minority Diversity Mentorship Program. One important component is an enhanced effort to increase the number of financial scholarships for away rotations (post–coronavirus disease 2019 pandemic) or application expenses geared to help underrepresented minorities. To truly increase diversity in dermatology, perhaps we need more physicians and residents willing to encourage students of color that dermatology is achievable.
- Brunsma DL, Embrick DG, Shin JH. Graduate students of color: race, racism, and mentoring in the white waters of academia. Sociology of Race and Ethnicity. 2017;3:1-13.
- Oyesanya T, Grossberg AL, Okoye GA. Increasing minority representation in the dermatology department: the Johns Hopkins experience. JAMA Dermatol. 2018;154:1133-1134.
- Pandya AG, Alexis AF, Berger TG, et al. Increasing racial and ethnic diversity in dermatology: a call to action. J Am Acad Dermatol. 2016;74:584-587.
- Current trends in medical education. American Association of Medical Colleges. Accessed January 20, 2021. http://www.aamcdiversityfactsandfigures2016.org/report-section/section-3/
- Spencer SJ, Logel C, Davies PG. Stereotype threat [published online September 10, 2015]. Annu Rev Psychol. 2016;67:415-437.
- Granstein RD, Cornelius L, Shinkai K. Diversity in dermatology—a call for action. JAMA Dermatol. 2017;153:499-500.
- Pritchett EN, Pandya AG, Ferguson NN, et al. Diversity in dermatology: roadmap for improvement. J Am Acad Dermatol. 2018;79:337-341.
- Blake-Beard S, Bayne ML, Crosby FJ, et al. Matching by race and gender in mentoring relationships: keeping our eyes on the prize. J Social Issues. 2011;67:622-643.
- Brunsma DL, Embrick DG, Shin JH. Graduate students of color: race, racism, and mentoring in the white waters of academia. Sociology of Race and Ethnicity. 2017;3:1-13.
- Oyesanya T, Grossberg AL, Okoye GA. Increasing minority representation in the dermatology department: the Johns Hopkins experience. JAMA Dermatol. 2018;154:1133-1134.
- Pandya AG, Alexis AF, Berger TG, et al. Increasing racial and ethnic diversity in dermatology: a call to action. J Am Acad Dermatol. 2016;74:584-587.
- Current trends in medical education. American Association of Medical Colleges. Accessed January 20, 2021. http://www.aamcdiversityfactsandfigures2016.org/report-section/section-3/
- Spencer SJ, Logel C, Davies PG. Stereotype threat [published online September 10, 2015]. Annu Rev Psychol. 2016;67:415-437.
- Granstein RD, Cornelius L, Shinkai K. Diversity in dermatology—a call for action. JAMA Dermatol. 2017;153:499-500.
- Pritchett EN, Pandya AG, Ferguson NN, et al. Diversity in dermatology: roadmap for improvement. J Am Acad Dermatol. 2018;79:337-341.
- Blake-Beard S, Bayne ML, Crosby FJ, et al. Matching by race and gender in mentoring relationships: keeping our eyes on the prize. J Social Issues. 2011;67:622-643.
Resident Pearl
- Finding a strong mentor who can both advocate for and help guide a student of color through the admissions process is integral to matching into dermatology
Racial, social inequities persist in IBD
Although inflammatory bowel disease (IBD) affects primarily White patients, about one-quarter of cases are found in non-White racial and ethnic groups. Various factors have combined to lead to disparities in treatment and outcomes for non-Whites with IBD.
Ethnic and racial disparities, along with socioeconomic factors, were the subject of a presentation by Ruby Greywoode, MD, at the annual congress of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
“Historical and present-day realities of racial inequity and factors that contribute to socioeconomic status [include] educational and housing policies, employment practices, and generational wealth. Addressing health disparities requires acknowledging these systemic factors,” said Dr. Greywoode, who is with Montefiore Medical Center in New York.
An important concept in discussing health disparity is social determinants of health, which refers to nonbiological factors that affect health and health outcomes. These are “the conditions in which people live, work, learn, and play that affect their health and their quality of life,” said Dr. Greywoode.
Dr. Greywoode shared examples of social determinants that affect economic stability and financial worry. One study found that one in six IBD patients reported not taking their medications because of cost considerations. A survey of about 900 adults showed that 1 in 4 delayed medical care – half of those because of cost; patients who delayed care were 2.5 times more likely to report an IBD flare in the previous year.
Another important issue is food insecurity. Other presenters at the session emphasized the importance of high-quality nutrition in IBD, and Dr. Greywoode presented one survey showing that only 9% of patients who had both food security and social support reported cost-related medication nonadherence. Among those that had either food insecurity or poor social support, 12% reported cost-related medication nonadherence, but the proportion jumped to 57% among patients who had both food insecurity and lack of social support.
Session comoderator Kelly Issokson noted that socioeconomic factors often interfere with adoption of healthy diets. Whole foods and plant-based foods are expensive, and the financial pressures of the COVID-19 epidemic have made that worse. “Millions of people are slipping into poverty and food insecurity. This is one of the things she highlighted as factors in medication nonadherence,” said Ms. Issokson, who is the clinical nutritional coordinator at the digestive disease clinic at Cedars-Sinai Medical Center in Los Angeles.
Dr. Greywoode also described studies that looked at race, socioeconomic status, and IBD outcomes. A review from 2013 showed disparities among Whites, African Americans, and Hispanics with respect to undergoing ulcerative colitis–related colectomy and Crohn’s disease–related bowel resection. Ulcerative colitis patients on Medicaid had 230% greater in-patient mortality, compared with patients with private insurance, even after adjustment for multiple confounders.
But inequities are not static. “Since this publication, we have numerous other studies drawing conclusions that sometimes agree with and sometimes conflict with it. My belief is that health disparities in IBD will continue to be an active area of research. We know that it takes vigilance to identify, track, and address any disparities when they do arise,” said Dr. Greywoode.
Dr. Greywoode also noted that phenotypic differences based on race and ethnicity influence disparities. She showed results from a meta-analysis that found a difference in the frequency of perianal Crohn’s disease by race and ethnicity; the highest frequency occurred in Black patients (31%), followed by Asians (22%), Whites (14%), and Hispanics (13%). Another study showed that African American patients with Crohn’s disease were more likely to develop a new abscess (adjusted odds ratio, 2.27; 95% confidence interval, 1.31-3.93) or anal fissure (aOR, 1.76; 95% CI, 1.01-3.07), and were also more likely to be initiated on an anti–tumor necrosis factor drug (aOR, 1.85; 95% CI, 1.09-3.14).
Those differences underscore the need to recognize that IBD is not just a disease for White patients. “As we move forward in IBD research, we recognize that individuals of European ancestry are not the only ones who have IBD. There is a growing diverse racial and ethnic population with IBD,” said Dr. Greywoode.
She noted that, in the United States, it is estimated that about one in four adult patients are non-Hispanic African American, Hispanic, Asians, or other ethnicities. Nevertheless, Whites are overrepresented among participants in IBD clinical trials. Some trials are composed of as much as 95% White patients, and sometimes race isn’t even listed. “It’s unclear if [race/ethnicity data are] not collected or not deemed important, but we know that what is not collected is not measured, and what is not measured can’t be evaluated, either to praise or constructively criticize,” said Dr. Greywoode.
Fortunately, there are efforts in place to improve representation in clinical trials. There has been a mandate for almost 3 decades that federally funded research must include racial and ethnic minorities who have been traditionally underrepresented. The Food and Drug Administration has also provided guidance to industry to improve diversity in clinical trial participation, and industry groups have developed strategies, including improved representation among investigators and related early-career development programs. At the community and independent health care practice levels, clinical trial networks encourage patient participation with regulatory and data management support to bolster practices with insufficient resources.
Underrepresentation in clinical trials resonated with comoderator Tina Aswani Omprakash, who is a patient advocate and a master’s in public health student at the Icahn School of Medicine at Mount Sinai, New York. She called for greater awareness among physicians that IBD can occur among people of all backgrounds. “[Providers] would look at me and [say]: ‘There’s no way that, as a South Asian woman, you have that kind of disease.’ There’s that lack of believability,” said Ms. Aswani Omprakash.
Greater recognition of the diversity of patients, as well as the phenotypic differences found among ethnicities, could also inform clinical trial participation and, ultimately, more personalized medicine. “We have to look at these things, observe how they’re affecting populations differently, so that we can have proper medication solutions,” said Ms. Aswani Omprakash.
Dr. Greywoode and Ms. Issokson have no relevant financial disclosures. Ms. Aswani Omprakash has consulted for Genentech, AbbVie, Janssen, and Arena.
The AGA applauds researchers who are working to raise our awareness of health disparities in digestive diseases. The AGA is committed to addressing this important societal issue head on. Learn more about AGA’s commitment through the AGA Equity Project.
Updated Feb. 17, 2021.
Although inflammatory bowel disease (IBD) affects primarily White patients, about one-quarter of cases are found in non-White racial and ethnic groups. Various factors have combined to lead to disparities in treatment and outcomes for non-Whites with IBD.
Ethnic and racial disparities, along with socioeconomic factors, were the subject of a presentation by Ruby Greywoode, MD, at the annual congress of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
“Historical and present-day realities of racial inequity and factors that contribute to socioeconomic status [include] educational and housing policies, employment practices, and generational wealth. Addressing health disparities requires acknowledging these systemic factors,” said Dr. Greywoode, who is with Montefiore Medical Center in New York.
An important concept in discussing health disparity is social determinants of health, which refers to nonbiological factors that affect health and health outcomes. These are “the conditions in which people live, work, learn, and play that affect their health and their quality of life,” said Dr. Greywoode.
Dr. Greywoode shared examples of social determinants that affect economic stability and financial worry. One study found that one in six IBD patients reported not taking their medications because of cost considerations. A survey of about 900 adults showed that 1 in 4 delayed medical care – half of those because of cost; patients who delayed care were 2.5 times more likely to report an IBD flare in the previous year.
Another important issue is food insecurity. Other presenters at the session emphasized the importance of high-quality nutrition in IBD, and Dr. Greywoode presented one survey showing that only 9% of patients who had both food security and social support reported cost-related medication nonadherence. Among those that had either food insecurity or poor social support, 12% reported cost-related medication nonadherence, but the proportion jumped to 57% among patients who had both food insecurity and lack of social support.
Session comoderator Kelly Issokson noted that socioeconomic factors often interfere with adoption of healthy diets. Whole foods and plant-based foods are expensive, and the financial pressures of the COVID-19 epidemic have made that worse. “Millions of people are slipping into poverty and food insecurity. This is one of the things she highlighted as factors in medication nonadherence,” said Ms. Issokson, who is the clinical nutritional coordinator at the digestive disease clinic at Cedars-Sinai Medical Center in Los Angeles.
Dr. Greywoode also described studies that looked at race, socioeconomic status, and IBD outcomes. A review from 2013 showed disparities among Whites, African Americans, and Hispanics with respect to undergoing ulcerative colitis–related colectomy and Crohn’s disease–related bowel resection. Ulcerative colitis patients on Medicaid had 230% greater in-patient mortality, compared with patients with private insurance, even after adjustment for multiple confounders.
But inequities are not static. “Since this publication, we have numerous other studies drawing conclusions that sometimes agree with and sometimes conflict with it. My belief is that health disparities in IBD will continue to be an active area of research. We know that it takes vigilance to identify, track, and address any disparities when they do arise,” said Dr. Greywoode.
Dr. Greywoode also noted that phenotypic differences based on race and ethnicity influence disparities. She showed results from a meta-analysis that found a difference in the frequency of perianal Crohn’s disease by race and ethnicity; the highest frequency occurred in Black patients (31%), followed by Asians (22%), Whites (14%), and Hispanics (13%). Another study showed that African American patients with Crohn’s disease were more likely to develop a new abscess (adjusted odds ratio, 2.27; 95% confidence interval, 1.31-3.93) or anal fissure (aOR, 1.76; 95% CI, 1.01-3.07), and were also more likely to be initiated on an anti–tumor necrosis factor drug (aOR, 1.85; 95% CI, 1.09-3.14).
Those differences underscore the need to recognize that IBD is not just a disease for White patients. “As we move forward in IBD research, we recognize that individuals of European ancestry are not the only ones who have IBD. There is a growing diverse racial and ethnic population with IBD,” said Dr. Greywoode.
She noted that, in the United States, it is estimated that about one in four adult patients are non-Hispanic African American, Hispanic, Asians, or other ethnicities. Nevertheless, Whites are overrepresented among participants in IBD clinical trials. Some trials are composed of as much as 95% White patients, and sometimes race isn’t even listed. “It’s unclear if [race/ethnicity data are] not collected or not deemed important, but we know that what is not collected is not measured, and what is not measured can’t be evaluated, either to praise or constructively criticize,” said Dr. Greywoode.
Fortunately, there are efforts in place to improve representation in clinical trials. There has been a mandate for almost 3 decades that federally funded research must include racial and ethnic minorities who have been traditionally underrepresented. The Food and Drug Administration has also provided guidance to industry to improve diversity in clinical trial participation, and industry groups have developed strategies, including improved representation among investigators and related early-career development programs. At the community and independent health care practice levels, clinical trial networks encourage patient participation with regulatory and data management support to bolster practices with insufficient resources.
Underrepresentation in clinical trials resonated with comoderator Tina Aswani Omprakash, who is a patient advocate and a master’s in public health student at the Icahn School of Medicine at Mount Sinai, New York. She called for greater awareness among physicians that IBD can occur among people of all backgrounds. “[Providers] would look at me and [say]: ‘There’s no way that, as a South Asian woman, you have that kind of disease.’ There’s that lack of believability,” said Ms. Aswani Omprakash.
Greater recognition of the diversity of patients, as well as the phenotypic differences found among ethnicities, could also inform clinical trial participation and, ultimately, more personalized medicine. “We have to look at these things, observe how they’re affecting populations differently, so that we can have proper medication solutions,” said Ms. Aswani Omprakash.
Dr. Greywoode and Ms. Issokson have no relevant financial disclosures. Ms. Aswani Omprakash has consulted for Genentech, AbbVie, Janssen, and Arena.
The AGA applauds researchers who are working to raise our awareness of health disparities in digestive diseases. The AGA is committed to addressing this important societal issue head on. Learn more about AGA’s commitment through the AGA Equity Project.
Updated Feb. 17, 2021.
Although inflammatory bowel disease (IBD) affects primarily White patients, about one-quarter of cases are found in non-White racial and ethnic groups. Various factors have combined to lead to disparities in treatment and outcomes for non-Whites with IBD.
Ethnic and racial disparities, along with socioeconomic factors, were the subject of a presentation by Ruby Greywoode, MD, at the annual congress of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
“Historical and present-day realities of racial inequity and factors that contribute to socioeconomic status [include] educational and housing policies, employment practices, and generational wealth. Addressing health disparities requires acknowledging these systemic factors,” said Dr. Greywoode, who is with Montefiore Medical Center in New York.
An important concept in discussing health disparity is social determinants of health, which refers to nonbiological factors that affect health and health outcomes. These are “the conditions in which people live, work, learn, and play that affect their health and their quality of life,” said Dr. Greywoode.
Dr. Greywoode shared examples of social determinants that affect economic stability and financial worry. One study found that one in six IBD patients reported not taking their medications because of cost considerations. A survey of about 900 adults showed that 1 in 4 delayed medical care – half of those because of cost; patients who delayed care were 2.5 times more likely to report an IBD flare in the previous year.
Another important issue is food insecurity. Other presenters at the session emphasized the importance of high-quality nutrition in IBD, and Dr. Greywoode presented one survey showing that only 9% of patients who had both food security and social support reported cost-related medication nonadherence. Among those that had either food insecurity or poor social support, 12% reported cost-related medication nonadherence, but the proportion jumped to 57% among patients who had both food insecurity and lack of social support.
Session comoderator Kelly Issokson noted that socioeconomic factors often interfere with adoption of healthy diets. Whole foods and plant-based foods are expensive, and the financial pressures of the COVID-19 epidemic have made that worse. “Millions of people are slipping into poverty and food insecurity. This is one of the things she highlighted as factors in medication nonadherence,” said Ms. Issokson, who is the clinical nutritional coordinator at the digestive disease clinic at Cedars-Sinai Medical Center in Los Angeles.
Dr. Greywoode also described studies that looked at race, socioeconomic status, and IBD outcomes. A review from 2013 showed disparities among Whites, African Americans, and Hispanics with respect to undergoing ulcerative colitis–related colectomy and Crohn’s disease–related bowel resection. Ulcerative colitis patients on Medicaid had 230% greater in-patient mortality, compared with patients with private insurance, even after adjustment for multiple confounders.
But inequities are not static. “Since this publication, we have numerous other studies drawing conclusions that sometimes agree with and sometimes conflict with it. My belief is that health disparities in IBD will continue to be an active area of research. We know that it takes vigilance to identify, track, and address any disparities when they do arise,” said Dr. Greywoode.
Dr. Greywoode also noted that phenotypic differences based on race and ethnicity influence disparities. She showed results from a meta-analysis that found a difference in the frequency of perianal Crohn’s disease by race and ethnicity; the highest frequency occurred in Black patients (31%), followed by Asians (22%), Whites (14%), and Hispanics (13%). Another study showed that African American patients with Crohn’s disease were more likely to develop a new abscess (adjusted odds ratio, 2.27; 95% confidence interval, 1.31-3.93) or anal fissure (aOR, 1.76; 95% CI, 1.01-3.07), and were also more likely to be initiated on an anti–tumor necrosis factor drug (aOR, 1.85; 95% CI, 1.09-3.14).
Those differences underscore the need to recognize that IBD is not just a disease for White patients. “As we move forward in IBD research, we recognize that individuals of European ancestry are not the only ones who have IBD. There is a growing diverse racial and ethnic population with IBD,” said Dr. Greywoode.
She noted that, in the United States, it is estimated that about one in four adult patients are non-Hispanic African American, Hispanic, Asians, or other ethnicities. Nevertheless, Whites are overrepresented among participants in IBD clinical trials. Some trials are composed of as much as 95% White patients, and sometimes race isn’t even listed. “It’s unclear if [race/ethnicity data are] not collected or not deemed important, but we know that what is not collected is not measured, and what is not measured can’t be evaluated, either to praise or constructively criticize,” said Dr. Greywoode.
Fortunately, there are efforts in place to improve representation in clinical trials. There has been a mandate for almost 3 decades that federally funded research must include racial and ethnic minorities who have been traditionally underrepresented. The Food and Drug Administration has also provided guidance to industry to improve diversity in clinical trial participation, and industry groups have developed strategies, including improved representation among investigators and related early-career development programs. At the community and independent health care practice levels, clinical trial networks encourage patient participation with regulatory and data management support to bolster practices with insufficient resources.
Underrepresentation in clinical trials resonated with comoderator Tina Aswani Omprakash, who is a patient advocate and a master’s in public health student at the Icahn School of Medicine at Mount Sinai, New York. She called for greater awareness among physicians that IBD can occur among people of all backgrounds. “[Providers] would look at me and [say]: ‘There’s no way that, as a South Asian woman, you have that kind of disease.’ There’s that lack of believability,” said Ms. Aswani Omprakash.
Greater recognition of the diversity of patients, as well as the phenotypic differences found among ethnicities, could also inform clinical trial participation and, ultimately, more personalized medicine. “We have to look at these things, observe how they’re affecting populations differently, so that we can have proper medication solutions,” said Ms. Aswani Omprakash.
Dr. Greywoode and Ms. Issokson have no relevant financial disclosures. Ms. Aswani Omprakash has consulted for Genentech, AbbVie, Janssen, and Arena.
The AGA applauds researchers who are working to raise our awareness of health disparities in digestive diseases. The AGA is committed to addressing this important societal issue head on. Learn more about AGA’s commitment through the AGA Equity Project.
Updated Feb. 17, 2021.
FROM THE CROHN’S & COLITIS CONGRESS
APA apologizes for past support of racism in psychiatry
The American Psychiatric Association has issued a formal apology for its past support of structural racism in psychiatry.
The apology, issued Jan. 18, coincided with the federal holiday honoring the life and work of civil rights activist Dr. Martin Luther King Jr.
“We apologize for our role in perpetrating structural racism in this country, and we hope to begin to make amends for APA’s and psychiatry’s history of actions, intentional and not, that hurt Black, indigenous, and people of color,” APA President Jeffrey Geller, MD, MPH, said in a statement.
The apology was written and issued by the APA Board of Trustees. It acknowledges practices and events in psychiatry that contributed to racial inequality, and expresses the organization’s commitment to developing antiracist policies that promote equity in mental health for all.
“This apology is one important step we needed to take to move forward to a more equitable future. The board is issuing this document on Martin Luther King Jr. Day, because we hope that it honors his life’s work of reconciliation and equality. We do not take that legacy or his call to action lightly and will continue our important work,” said Dr. Geller.
One involved the Eastern State Hospital in Williamsburg, Va., the nation’s first psychiatric care facility, founded in 1773.
Eastern State, which for a time in the 1800s was called the Eastern Lunatic Asylum, was not segregated when founded. However, 70 years later, when the 13 founders of what is now the APA met to discuss improvements in mental health care delivery, the treatment system they created and the organization they founded aligned with that era’s racist social and political policies. In this system, Black patients received psychiatric care separately from White patients, the APA said.
The APA also acknowledged failing to act in Black Americans’ best interest at critical points in the United States’ sociopolitical evolution throughout the 19th and 20th centuries.
“This inactivity was notably evident while white supremacists lynched Black people during the Reconstruction Era as well as when Jim Crow segregation was in effect, which led to ‘separate but equal’ standards of care starting in 1896,” the APA said.
Later, the APA failed to declare support for Brown v. Board of Education of Topeka in 1954, along with further major civil rights legislation designed to improve social and psychological conditions for Black people, the organization admitted.
Throughout the decades that followed, psychiatric misdiagnosis among Black, indigenous, and people of color populations were also common, the APA acknowledged.
For example, late 20th century psychiatrists commonly attributed their minority patients’ frustrations to schizophrenia, while categorizing similar behaviors as “neuroticism” in White patients.
The APA pointed to one study which found that APA members diagnosed more Black than White patients with schizophrenia, even when both had otherwise identical clinical presentations.
“This reveals the basis for embedded discrimination within psychiatry that has contributed to reduced quality of care” for Black, indigenous, and people of color, and “perpetuation of dangerous stereotypes,” the APA said.
Saul Levin, MD, the APA’s medical director and CEO, said the Board of Trustees has taken “an important step in issuing this apology. The APA administration is committed to working toward inclusion, health equity, and fairness that everyone deserves.”
The APA Board of Trustees began drafting the apology late last year after it concluded that events and persistent inequities in health care and psychiatry had highlighted an organizational need for action.
The APA’s Presidential Task Force on Structural Racism is continuing with efforts to educate and engage members on the issue and implement changes within the organization.
A version of this article first appeared on Medscape.com.
The American Psychiatric Association has issued a formal apology for its past support of structural racism in psychiatry.
The apology, issued Jan. 18, coincided with the federal holiday honoring the life and work of civil rights activist Dr. Martin Luther King Jr.
“We apologize for our role in perpetrating structural racism in this country, and we hope to begin to make amends for APA’s and psychiatry’s history of actions, intentional and not, that hurt Black, indigenous, and people of color,” APA President Jeffrey Geller, MD, MPH, said in a statement.
The apology was written and issued by the APA Board of Trustees. It acknowledges practices and events in psychiatry that contributed to racial inequality, and expresses the organization’s commitment to developing antiracist policies that promote equity in mental health for all.
“This apology is one important step we needed to take to move forward to a more equitable future. The board is issuing this document on Martin Luther King Jr. Day, because we hope that it honors his life’s work of reconciliation and equality. We do not take that legacy or his call to action lightly and will continue our important work,” said Dr. Geller.
One involved the Eastern State Hospital in Williamsburg, Va., the nation’s first psychiatric care facility, founded in 1773.
Eastern State, which for a time in the 1800s was called the Eastern Lunatic Asylum, was not segregated when founded. However, 70 years later, when the 13 founders of what is now the APA met to discuss improvements in mental health care delivery, the treatment system they created and the organization they founded aligned with that era’s racist social and political policies. In this system, Black patients received psychiatric care separately from White patients, the APA said.
The APA also acknowledged failing to act in Black Americans’ best interest at critical points in the United States’ sociopolitical evolution throughout the 19th and 20th centuries.
“This inactivity was notably evident while white supremacists lynched Black people during the Reconstruction Era as well as when Jim Crow segregation was in effect, which led to ‘separate but equal’ standards of care starting in 1896,” the APA said.
Later, the APA failed to declare support for Brown v. Board of Education of Topeka in 1954, along with further major civil rights legislation designed to improve social and psychological conditions for Black people, the organization admitted.
Throughout the decades that followed, psychiatric misdiagnosis among Black, indigenous, and people of color populations were also common, the APA acknowledged.
For example, late 20th century psychiatrists commonly attributed their minority patients’ frustrations to schizophrenia, while categorizing similar behaviors as “neuroticism” in White patients.
The APA pointed to one study which found that APA members diagnosed more Black than White patients with schizophrenia, even when both had otherwise identical clinical presentations.
“This reveals the basis for embedded discrimination within psychiatry that has contributed to reduced quality of care” for Black, indigenous, and people of color, and “perpetuation of dangerous stereotypes,” the APA said.
Saul Levin, MD, the APA’s medical director and CEO, said the Board of Trustees has taken “an important step in issuing this apology. The APA administration is committed to working toward inclusion, health equity, and fairness that everyone deserves.”
The APA Board of Trustees began drafting the apology late last year after it concluded that events and persistent inequities in health care and psychiatry had highlighted an organizational need for action.
The APA’s Presidential Task Force on Structural Racism is continuing with efforts to educate and engage members on the issue and implement changes within the organization.
A version of this article first appeared on Medscape.com.
The American Psychiatric Association has issued a formal apology for its past support of structural racism in psychiatry.
The apology, issued Jan. 18, coincided with the federal holiday honoring the life and work of civil rights activist Dr. Martin Luther King Jr.
“We apologize for our role in perpetrating structural racism in this country, and we hope to begin to make amends for APA’s and psychiatry’s history of actions, intentional and not, that hurt Black, indigenous, and people of color,” APA President Jeffrey Geller, MD, MPH, said in a statement.
The apology was written and issued by the APA Board of Trustees. It acknowledges practices and events in psychiatry that contributed to racial inequality, and expresses the organization’s commitment to developing antiracist policies that promote equity in mental health for all.
“This apology is one important step we needed to take to move forward to a more equitable future. The board is issuing this document on Martin Luther King Jr. Day, because we hope that it honors his life’s work of reconciliation and equality. We do not take that legacy or his call to action lightly and will continue our important work,” said Dr. Geller.
One involved the Eastern State Hospital in Williamsburg, Va., the nation’s first psychiatric care facility, founded in 1773.
Eastern State, which for a time in the 1800s was called the Eastern Lunatic Asylum, was not segregated when founded. However, 70 years later, when the 13 founders of what is now the APA met to discuss improvements in mental health care delivery, the treatment system they created and the organization they founded aligned with that era’s racist social and political policies. In this system, Black patients received psychiatric care separately from White patients, the APA said.
The APA also acknowledged failing to act in Black Americans’ best interest at critical points in the United States’ sociopolitical evolution throughout the 19th and 20th centuries.
“This inactivity was notably evident while white supremacists lynched Black people during the Reconstruction Era as well as when Jim Crow segregation was in effect, which led to ‘separate but equal’ standards of care starting in 1896,” the APA said.
Later, the APA failed to declare support for Brown v. Board of Education of Topeka in 1954, along with further major civil rights legislation designed to improve social and psychological conditions for Black people, the organization admitted.
Throughout the decades that followed, psychiatric misdiagnosis among Black, indigenous, and people of color populations were also common, the APA acknowledged.
For example, late 20th century psychiatrists commonly attributed their minority patients’ frustrations to schizophrenia, while categorizing similar behaviors as “neuroticism” in White patients.
The APA pointed to one study which found that APA members diagnosed more Black than White patients with schizophrenia, even when both had otherwise identical clinical presentations.
“This reveals the basis for embedded discrimination within psychiatry that has contributed to reduced quality of care” for Black, indigenous, and people of color, and “perpetuation of dangerous stereotypes,” the APA said.
Saul Levin, MD, the APA’s medical director and CEO, said the Board of Trustees has taken “an important step in issuing this apology. The APA administration is committed to working toward inclusion, health equity, and fairness that everyone deserves.”
The APA Board of Trustees began drafting the apology late last year after it concluded that events and persistent inequities in health care and psychiatry had highlighted an organizational need for action.
The APA’s Presidential Task Force on Structural Racism is continuing with efforts to educate and engage members on the issue and implement changes within the organization.
A version of this article first appeared on Medscape.com.
Diversification of dermatology workforce takes shape
Stephanie Florez-Pollack, MD, a dermatology resident at the University of Pennsylvania, Philadelphia, began considering the field of dermatology when, as part of the Latino Medical Students Association, she was invited by Amit Pandya, MD, to a pizza party and dermatology discussion during her first year of medical school at the University of Texas Southwestern Medical Center, Dallas.
There, she met three Latinx residents who were part of the University of Texas Southwestern dermatology program. “I was so excited to hear their stories, where they came from, and how they ended up in dermatology,” she said. Dermatology had not been on her radar screen. Now there was a spark.
Volunteering at the free Agape dermatology clinic in Dallas later that year sharpened her interest. “For the first time, I really saw myself working in the field. Hearing patients’ stories and what they went through with what many people might think are very simple skin diseases made me realize there was potential to make a big impact in a person’s life,” said Dr. Florez-Pollack, who immigrated from Colombia with her family when she was 15.
– one that reflects the ethnic and racial make-up of the population. It’s a movement that involves early outreach to medical students, stepped-up mentorship and sponsorship, implicit bias training, and holistic review of residency applicants.
There is no published study of all the changes being made – of how many dermatology programs have new outreach programs, for instance, or new approaches to resident application reviews. However, participation in the American Academy of Dermatology Diversity Champions program increased significantly between 2019 and 2020, and a sizable body of articles and editorials on diversity have been published in the dermatology literature in recent years, including at least several on holistic review of resident applications. Five years ago, there were few publications, sources said.
“The conversation is happening now at multiple levels, including in our peer-reviewed literature, where people are looking objectively at ... how we can make changes for the better,” said Nada Elbuluk, MD, director of the dermatology diversity and inclusion program at the University of Southern California, Los Angeles.
Unpublished findings also indicate that the number of UIM dermatology residents is inching upward. “Residency selection may not be on everyone’s mind, but an understanding of how we select people into our specialty is something every derm should know about and care about,” said Kanade Shinkai, MD, PhD, professor of dermatology at the University of California, San Francisco, and editor in chief of JAMA Dermatology.
The wake-up calls
The impetus for current changes first came in 2015, when Bruce Wintroub, MD, professor and chair of dermatology at UCSF, and interim dean of the medical school at the time, delivered a passionate plenary lecture at the annual AAD meeting about the lack of equity, diversity and inclusion in the specialty and the role of unconscious bias. Moved in part by a “White Coats for Black Lives” die-in by medical students on his campus following the killing of unarmed Black men, Dr. Wintroub called on his colleagues to recruit more UIM physicians into the specialty and to make the field more inclusive.
In 2016, Dr. Wintroub joined Dr. Pandya and two other academic dermatologists in authoring a commentary, published in the Journal of the American Academy of Dermatology, about the need to step up efforts and make diversity a priority. Dermatology was among the least ethnically and racially diverse specialties, second only to orthopedics, they wrote, with black dermatologists making up only 3% of all dermatologists and Hispanics only 4.2% in the United States, compared with 12.8% and 16.3% in the U.S. population, respectively.
For the next year or so, they and others from six academic institutions formed an incubator of sorts, actively tracking and sharing actions they were taking to improve diversity and the practice environment. “We wanted to learn from each other, then disseminate information to other programs,” said Dr. Pandya, who chaired the AAD diversity task force and led the self-branded “diversity champions.” (Dr. Pandya maintains his appointment at UTSW but now practices at the Palo Alto Foundation Medical Group in Sunnyvale, Calif.)
In 2017, at a President’s Conference on Diversity in Dermatology called for by then-AAD president Henry Lim, MD, leaders of the Association of Professors of Dermatology, the Society for Investigative Dermatology, and other dermatology organizations agreed on key action items, which they described in JAAD in 2018: Helping to increase the pipeline of UIM students applying to medical school, increasing UIM medical students’ early exposure to dermatology, and increasing the number of UIM students recruited into dermatology residency programs.
Diversity in the physician workforce has been shown to improve outcomes for all patients, and is important for ameliorating health care disparities and improving satisfaction and care for all patients, the authors of the 2018 paper wrote. “Multiple studies,” they noted, “have shown that UIM physicians are more likely to practice in areas where health care disparities exist.”
For specific proposed actions, the leaders attending the diversity conference drew largely upon the “diversity champions’” experiences, and agreed to fund and officially develop a diversity champions program. They also decided to invest in “bioskills” workshops for undergraduates and medical students at historically black colleges and universities, and other institutions at historically black colleges and universities at medical schools through a partnership with Nth Dimension – an organization founded in 2004 to bring more women and underrepresented minorities into orthopedic surgery.
In the last 2 years, more than 450 UIM students have attended these bioskills workshops, getting a taste of basic dermatology procedures and interacting with dermatologists.
And in September 2020, 157 dermatologists representing 80 programs throughout the country attended the second AAD Diversity Champions conference, up from 84 attendees and 30 programs in 2019. On the agenda: Discussions of holistic application review, mentorship, recruitment of UIM faculty, and a 2-hour session on microaggressions. Similar programs are being led by other dermatology organizations.
(UIM was coined by the American Association of Medical Colleges to describe racial and ethnic populations that are underrepresented in medicine relative to their numbers in the general population.)
Achievement of racial/ethnic diversity “won’t happen unless the field actively encourages people to look at it – which is not what we were doing,” Dr. Wintroub said in an interview. “I think that’s been the major change. We’re opening the door and saying: ‘We want you and we welcome you.’ ”
Rethinking traditional mentorship
For Dr. Florez-Pollack, the door almost shut when she began to hear from fellow medical students that dermatology is “too competitive ... a field for only the top people in the class.” She felt doubt settling in.
“I had peers who were throwing a lot of money toward prep materials ... peers who had siblings in medicine and had started studying from day one [for the step 1 exam],” she said. “I thought, was it really worth the effort? Do I really want to be perfect to get into the field when other fields would be happy to have me as I am right now?”
Her immense enjoyment of an “Art of Observation” elective course helped renew her interest in the field; it reinforced her visual abilities as well as the potential for her to address implicit bias as a dermatologist. She sought Dr. Pandya’s guidance and sponsorship to help her grow connections, polish her resume, and present herself to other faculty.
Doors were opened, she said, for her to secure a 1-year research experience before her final year of medical school with UTSW faculty, and then a 1-month rotation/mentorship with William D. James, MD, professor of dermatology at the University of Pennsylvania, an institution with a history of diversity initiatives and a longstanding skin of color program.
Dr. Florez-Pollack sees her experience reflected in the findings of a recently published study – a thematic content analysis of telephone interviews with applicants to the UTSW dermatology residency program during the 2013-14 and 2014-15 application cycles. Of the 44 applicants who participated in the study, 13 were UIM applicants.
Six of the seven UIM applicants who matched were involved in a pipeline or enrichment program – and were exposed to the field early – compared with one or two of the six UIM applicants who did not match. Underrepresented applicants were more often discouraged from applying (54%) – told, for instance, that they could better serve their communities through other specialties – than were non-UIM applicants (13%). They also were affected more often by a lack of equitable resources, according to comments made by 70% of applicants (UIM and non-UIM).
Also notably, the investigators said, all of the UIM applicants who matched (and the majority of non-UIMs who matched) reported having a mentor during the process of applying, compared with 44% of those who didn’t match.
Rebecca Vasquez, MD, assistant professor of dermatology at UTSW, who led the study, was herself a mentee of Dr. Pandya. “He believed in me and gave me the courage to consider dermatology,” she said. (Dr. Vasquez was one of the Latinx women who inspired Dr. Florez-Pollack, in turn, when they met at Dr. Pandya’s pizza party. Dr. Florez-Pollack assisted with the research and was a coauthor of the study.)
Amy McMichael, MD, professor and chair of dermatology at Wake Forest University, Winston-Salem, N.C., said that dermatology as a field has traditionally been “very good at mentoring.” Many of the dermatology societies have long had mentorship programs, for instance, that guide medical students, and sometimes residents, through defined experiences or through periods of time.
But she advocates going deeper. “When it comes to sponsorship, we fall a little short,” she said. “Sponsorship is about promoting that person to the next level, making sure they achieve what they want to achieve ... putting them up for opportunities they may not have known existed. It’s continuous and focused.”
Olabola Awosika, MD, a fourth-year dermatology resident at Henry Ford Health System, Detroit, said her interest in dermatology was solidified during her participation in the AAD’s month-long mentorship program after her second year of medical school at Howard University, Washington. However, it wasn’t until her fourth year, when she did an away rotation at Wake Forest, that she realized that “gaining access to the field” takes years of mentorship, research opportunities, and networking. It was too late.
After initially not matching, she did a rotation at Johns Hopkins in dermatology during an internship year, followed by a 2-year research fellowship at George Washington University, Washington. As does Dr. Florez-Pollack, who now mentors medical students. She also serves on the Women’s Dermatologic Society diversity committee, which is now developing initiatives to help UIM dermatologists “become upwardly mobile in dermatology [after residency], so they have a seat at the table in various settings.”
Holistic review for residency
Dr. Vasquez, who grew up in South Texas in an uninsured family that received most of its medical care across the border in Mexico, believes that the “biggest stride being made today” with respect to diversity in the dermatology workforce – and in the larger physician workforce – is increased understanding of the role of social and cultural capital.
“We’d never really talked about this concept ... about how, if you don’t have the same upbringing, education, and resources, you’re already behind … and you may not do as well on standardized tests,” she said. “Now people are listening to it and understand it. That’s why more programs are looking at how to practice a more holistic approach to selecting applicants to interview.”
Some dermatology programs – at Wake Forest, UCSF, USC, Vanderbilt, and George Washington University for instance – have eliminated the use of U.S. Medical Licensing Examination step 1 scores and Alpha Omega Alpha Medical Honor Society status as filtering/screening metrics. Some also take a “second look” at UIM applicants.
Overall, those making changes are looking “at everything the applicant brings to the table – their story, their experiences,” said Dr. Elbuluk. “We want to understand the full picture of who they are and their journey to becoming a physician.”
Implicit bias training for members of residency review committees is becoming more common, as is such training across the board in dermatology departments. “We have to bring it to the forefront so that we can create more inclusive environments,” said Sharon E. Albers, MD, a dermatologist at Vanderbilt University Medical Center, Nashville, Tenn., who serves as the dermatology department’s diversity liaison to the medical school, and who, as a former faculty member of Meharry Medical College, remains engaged with the historically black institution.
One of her recent efforts, inspired by participation in the diversity champions program, has been developing pipeline programs to speak to middle and high school students about medicine and dermatology. For now, however, she credits a holistic review process for change. Last year, three of the five matched dermatology residents at Vanderbilt were UIM physicians – unprecedented for the institution, Dr. Albers said, and “evidence that holistic review works if you’re very intentional about it.”
Dr. Vasquez has analyzed data from the Accreditation Council of Graduate Medical Education and says that UIM dermatology residents comprised 8.0% of the total in 2019, marking an improvement over the prior 7 years. “We’ve introduced so many changes at the same time,” making it difficult to discern what’s most impactful, she said. “But something is working.”
(The AAMC, which has invested in pipeline programs for more than a decade and has championed holistic medical school admissions, states in its 2019 diversity data report that efforts to improve diversity in medicine have made “only marginal differences” – and that Black males in particular continue to be significantly underrepresented in medical schools. Persistent, structural racism was a common theme in the association’s 2015 report on Black males in medicine.)
Efforts to diversify the workforce – particularly holistic review – haven’t been without detractors. “It brings reaction,” Dr. Wintroub said. “Some people think you’re lowering quality in the field ... but that’s just not true.”
Diversity in the dermatology workforce is important not only for the care of patients from diverse backgrounds, but “perhaps more importantly, it brings new ideas and views and experiences into the field,” he said. “It pushes us to think in new directions ... that can only make our field better and richer.”
“We need to make sure our workforce is representative of the patients we serve – but also that all derms can manage patients of all skin types and demographics,” Dr. Shinkai said. “And we need more diversity in the leadership of our departments and dermatology organizations ... inclusivity needs to extend all the way to the highest reaches of our specialty.”
Adam Friedman, MD, professor and interim chair of dermatology at George Washington University and director of the department’s diversity, equity, and inclusion committee, agreed. “We need to both make sure our workforce mirrors the patients we serve, and said workforce is prepared to manage patients of all skin types and demographics. We need to cover the spectrum, from revamping medical education and mentorship opportunities to advancing diversity in the leadership of our departments, institutions, and societies. Addressing only part of the puzzle will not and can not be enough.”
Correction, 3/3/21: An earlier version of this article misstated Dr. Stephanie Florez-Pollack's name.
Stephanie Florez-Pollack, MD, a dermatology resident at the University of Pennsylvania, Philadelphia, began considering the field of dermatology when, as part of the Latino Medical Students Association, she was invited by Amit Pandya, MD, to a pizza party and dermatology discussion during her first year of medical school at the University of Texas Southwestern Medical Center, Dallas.
There, she met three Latinx residents who were part of the University of Texas Southwestern dermatology program. “I was so excited to hear their stories, where they came from, and how they ended up in dermatology,” she said. Dermatology had not been on her radar screen. Now there was a spark.
Volunteering at the free Agape dermatology clinic in Dallas later that year sharpened her interest. “For the first time, I really saw myself working in the field. Hearing patients’ stories and what they went through with what many people might think are very simple skin diseases made me realize there was potential to make a big impact in a person’s life,” said Dr. Florez-Pollack, who immigrated from Colombia with her family when she was 15.
– one that reflects the ethnic and racial make-up of the population. It’s a movement that involves early outreach to medical students, stepped-up mentorship and sponsorship, implicit bias training, and holistic review of residency applicants.
There is no published study of all the changes being made – of how many dermatology programs have new outreach programs, for instance, or new approaches to resident application reviews. However, participation in the American Academy of Dermatology Diversity Champions program increased significantly between 2019 and 2020, and a sizable body of articles and editorials on diversity have been published in the dermatology literature in recent years, including at least several on holistic review of resident applications. Five years ago, there were few publications, sources said.
“The conversation is happening now at multiple levels, including in our peer-reviewed literature, where people are looking objectively at ... how we can make changes for the better,” said Nada Elbuluk, MD, director of the dermatology diversity and inclusion program at the University of Southern California, Los Angeles.
Unpublished findings also indicate that the number of UIM dermatology residents is inching upward. “Residency selection may not be on everyone’s mind, but an understanding of how we select people into our specialty is something every derm should know about and care about,” said Kanade Shinkai, MD, PhD, professor of dermatology at the University of California, San Francisco, and editor in chief of JAMA Dermatology.
The wake-up calls
The impetus for current changes first came in 2015, when Bruce Wintroub, MD, professor and chair of dermatology at UCSF, and interim dean of the medical school at the time, delivered a passionate plenary lecture at the annual AAD meeting about the lack of equity, diversity and inclusion in the specialty and the role of unconscious bias. Moved in part by a “White Coats for Black Lives” die-in by medical students on his campus following the killing of unarmed Black men, Dr. Wintroub called on his colleagues to recruit more UIM physicians into the specialty and to make the field more inclusive.
In 2016, Dr. Wintroub joined Dr. Pandya and two other academic dermatologists in authoring a commentary, published in the Journal of the American Academy of Dermatology, about the need to step up efforts and make diversity a priority. Dermatology was among the least ethnically and racially diverse specialties, second only to orthopedics, they wrote, with black dermatologists making up only 3% of all dermatologists and Hispanics only 4.2% in the United States, compared with 12.8% and 16.3% in the U.S. population, respectively.
For the next year or so, they and others from six academic institutions formed an incubator of sorts, actively tracking and sharing actions they were taking to improve diversity and the practice environment. “We wanted to learn from each other, then disseminate information to other programs,” said Dr. Pandya, who chaired the AAD diversity task force and led the self-branded “diversity champions.” (Dr. Pandya maintains his appointment at UTSW but now practices at the Palo Alto Foundation Medical Group in Sunnyvale, Calif.)
In 2017, at a President’s Conference on Diversity in Dermatology called for by then-AAD president Henry Lim, MD, leaders of the Association of Professors of Dermatology, the Society for Investigative Dermatology, and other dermatology organizations agreed on key action items, which they described in JAAD in 2018: Helping to increase the pipeline of UIM students applying to medical school, increasing UIM medical students’ early exposure to dermatology, and increasing the number of UIM students recruited into dermatology residency programs.
Diversity in the physician workforce has been shown to improve outcomes for all patients, and is important for ameliorating health care disparities and improving satisfaction and care for all patients, the authors of the 2018 paper wrote. “Multiple studies,” they noted, “have shown that UIM physicians are more likely to practice in areas where health care disparities exist.”
For specific proposed actions, the leaders attending the diversity conference drew largely upon the “diversity champions’” experiences, and agreed to fund and officially develop a diversity champions program. They also decided to invest in “bioskills” workshops for undergraduates and medical students at historically black colleges and universities, and other institutions at historically black colleges and universities at medical schools through a partnership with Nth Dimension – an organization founded in 2004 to bring more women and underrepresented minorities into orthopedic surgery.
In the last 2 years, more than 450 UIM students have attended these bioskills workshops, getting a taste of basic dermatology procedures and interacting with dermatologists.
And in September 2020, 157 dermatologists representing 80 programs throughout the country attended the second AAD Diversity Champions conference, up from 84 attendees and 30 programs in 2019. On the agenda: Discussions of holistic application review, mentorship, recruitment of UIM faculty, and a 2-hour session on microaggressions. Similar programs are being led by other dermatology organizations.
(UIM was coined by the American Association of Medical Colleges to describe racial and ethnic populations that are underrepresented in medicine relative to their numbers in the general population.)
Achievement of racial/ethnic diversity “won’t happen unless the field actively encourages people to look at it – which is not what we were doing,” Dr. Wintroub said in an interview. “I think that’s been the major change. We’re opening the door and saying: ‘We want you and we welcome you.’ ”
Rethinking traditional mentorship
For Dr. Florez-Pollack, the door almost shut when she began to hear from fellow medical students that dermatology is “too competitive ... a field for only the top people in the class.” She felt doubt settling in.
“I had peers who were throwing a lot of money toward prep materials ... peers who had siblings in medicine and had started studying from day one [for the step 1 exam],” she said. “I thought, was it really worth the effort? Do I really want to be perfect to get into the field when other fields would be happy to have me as I am right now?”
Her immense enjoyment of an “Art of Observation” elective course helped renew her interest in the field; it reinforced her visual abilities as well as the potential for her to address implicit bias as a dermatologist. She sought Dr. Pandya’s guidance and sponsorship to help her grow connections, polish her resume, and present herself to other faculty.
Doors were opened, she said, for her to secure a 1-year research experience before her final year of medical school with UTSW faculty, and then a 1-month rotation/mentorship with William D. James, MD, professor of dermatology at the University of Pennsylvania, an institution with a history of diversity initiatives and a longstanding skin of color program.
Dr. Florez-Pollack sees her experience reflected in the findings of a recently published study – a thematic content analysis of telephone interviews with applicants to the UTSW dermatology residency program during the 2013-14 and 2014-15 application cycles. Of the 44 applicants who participated in the study, 13 were UIM applicants.
Six of the seven UIM applicants who matched were involved in a pipeline or enrichment program – and were exposed to the field early – compared with one or two of the six UIM applicants who did not match. Underrepresented applicants were more often discouraged from applying (54%) – told, for instance, that they could better serve their communities through other specialties – than were non-UIM applicants (13%). They also were affected more often by a lack of equitable resources, according to comments made by 70% of applicants (UIM and non-UIM).
Also notably, the investigators said, all of the UIM applicants who matched (and the majority of non-UIMs who matched) reported having a mentor during the process of applying, compared with 44% of those who didn’t match.
Rebecca Vasquez, MD, assistant professor of dermatology at UTSW, who led the study, was herself a mentee of Dr. Pandya. “He believed in me and gave me the courage to consider dermatology,” she said. (Dr. Vasquez was one of the Latinx women who inspired Dr. Florez-Pollack, in turn, when they met at Dr. Pandya’s pizza party. Dr. Florez-Pollack assisted with the research and was a coauthor of the study.)
Amy McMichael, MD, professor and chair of dermatology at Wake Forest University, Winston-Salem, N.C., said that dermatology as a field has traditionally been “very good at mentoring.” Many of the dermatology societies have long had mentorship programs, for instance, that guide medical students, and sometimes residents, through defined experiences or through periods of time.
But she advocates going deeper. “When it comes to sponsorship, we fall a little short,” she said. “Sponsorship is about promoting that person to the next level, making sure they achieve what they want to achieve ... putting them up for opportunities they may not have known existed. It’s continuous and focused.”
Olabola Awosika, MD, a fourth-year dermatology resident at Henry Ford Health System, Detroit, said her interest in dermatology was solidified during her participation in the AAD’s month-long mentorship program after her second year of medical school at Howard University, Washington. However, it wasn’t until her fourth year, when she did an away rotation at Wake Forest, that she realized that “gaining access to the field” takes years of mentorship, research opportunities, and networking. It was too late.
After initially not matching, she did a rotation at Johns Hopkins in dermatology during an internship year, followed by a 2-year research fellowship at George Washington University, Washington. As does Dr. Florez-Pollack, who now mentors medical students. She also serves on the Women’s Dermatologic Society diversity committee, which is now developing initiatives to help UIM dermatologists “become upwardly mobile in dermatology [after residency], so they have a seat at the table in various settings.”
Holistic review for residency
Dr. Vasquez, who grew up in South Texas in an uninsured family that received most of its medical care across the border in Mexico, believes that the “biggest stride being made today” with respect to diversity in the dermatology workforce – and in the larger physician workforce – is increased understanding of the role of social and cultural capital.
“We’d never really talked about this concept ... about how, if you don’t have the same upbringing, education, and resources, you’re already behind … and you may not do as well on standardized tests,” she said. “Now people are listening to it and understand it. That’s why more programs are looking at how to practice a more holistic approach to selecting applicants to interview.”
Some dermatology programs – at Wake Forest, UCSF, USC, Vanderbilt, and George Washington University for instance – have eliminated the use of U.S. Medical Licensing Examination step 1 scores and Alpha Omega Alpha Medical Honor Society status as filtering/screening metrics. Some also take a “second look” at UIM applicants.
Overall, those making changes are looking “at everything the applicant brings to the table – their story, their experiences,” said Dr. Elbuluk. “We want to understand the full picture of who they are and their journey to becoming a physician.”
Implicit bias training for members of residency review committees is becoming more common, as is such training across the board in dermatology departments. “We have to bring it to the forefront so that we can create more inclusive environments,” said Sharon E. Albers, MD, a dermatologist at Vanderbilt University Medical Center, Nashville, Tenn., who serves as the dermatology department’s diversity liaison to the medical school, and who, as a former faculty member of Meharry Medical College, remains engaged with the historically black institution.
One of her recent efforts, inspired by participation in the diversity champions program, has been developing pipeline programs to speak to middle and high school students about medicine and dermatology. For now, however, she credits a holistic review process for change. Last year, three of the five matched dermatology residents at Vanderbilt were UIM physicians – unprecedented for the institution, Dr. Albers said, and “evidence that holistic review works if you’re very intentional about it.”
Dr. Vasquez has analyzed data from the Accreditation Council of Graduate Medical Education and says that UIM dermatology residents comprised 8.0% of the total in 2019, marking an improvement over the prior 7 years. “We’ve introduced so many changes at the same time,” making it difficult to discern what’s most impactful, she said. “But something is working.”
(The AAMC, which has invested in pipeline programs for more than a decade and has championed holistic medical school admissions, states in its 2019 diversity data report that efforts to improve diversity in medicine have made “only marginal differences” – and that Black males in particular continue to be significantly underrepresented in medical schools. Persistent, structural racism was a common theme in the association’s 2015 report on Black males in medicine.)
Efforts to diversify the workforce – particularly holistic review – haven’t been without detractors. “It brings reaction,” Dr. Wintroub said. “Some people think you’re lowering quality in the field ... but that’s just not true.”
Diversity in the dermatology workforce is important not only for the care of patients from diverse backgrounds, but “perhaps more importantly, it brings new ideas and views and experiences into the field,” he said. “It pushes us to think in new directions ... that can only make our field better and richer.”
“We need to make sure our workforce is representative of the patients we serve – but also that all derms can manage patients of all skin types and demographics,” Dr. Shinkai said. “And we need more diversity in the leadership of our departments and dermatology organizations ... inclusivity needs to extend all the way to the highest reaches of our specialty.”
Adam Friedman, MD, professor and interim chair of dermatology at George Washington University and director of the department’s diversity, equity, and inclusion committee, agreed. “We need to both make sure our workforce mirrors the patients we serve, and said workforce is prepared to manage patients of all skin types and demographics. We need to cover the spectrum, from revamping medical education and mentorship opportunities to advancing diversity in the leadership of our departments, institutions, and societies. Addressing only part of the puzzle will not and can not be enough.”
Correction, 3/3/21: An earlier version of this article misstated Dr. Stephanie Florez-Pollack's name.
Stephanie Florez-Pollack, MD, a dermatology resident at the University of Pennsylvania, Philadelphia, began considering the field of dermatology when, as part of the Latino Medical Students Association, she was invited by Amit Pandya, MD, to a pizza party and dermatology discussion during her first year of medical school at the University of Texas Southwestern Medical Center, Dallas.
There, she met three Latinx residents who were part of the University of Texas Southwestern dermatology program. “I was so excited to hear their stories, where they came from, and how they ended up in dermatology,” she said. Dermatology had not been on her radar screen. Now there was a spark.
Volunteering at the free Agape dermatology clinic in Dallas later that year sharpened her interest. “For the first time, I really saw myself working in the field. Hearing patients’ stories and what they went through with what many people might think are very simple skin diseases made me realize there was potential to make a big impact in a person’s life,” said Dr. Florez-Pollack, who immigrated from Colombia with her family when she was 15.
– one that reflects the ethnic and racial make-up of the population. It’s a movement that involves early outreach to medical students, stepped-up mentorship and sponsorship, implicit bias training, and holistic review of residency applicants.
There is no published study of all the changes being made – of how many dermatology programs have new outreach programs, for instance, or new approaches to resident application reviews. However, participation in the American Academy of Dermatology Diversity Champions program increased significantly between 2019 and 2020, and a sizable body of articles and editorials on diversity have been published in the dermatology literature in recent years, including at least several on holistic review of resident applications. Five years ago, there were few publications, sources said.
“The conversation is happening now at multiple levels, including in our peer-reviewed literature, where people are looking objectively at ... how we can make changes for the better,” said Nada Elbuluk, MD, director of the dermatology diversity and inclusion program at the University of Southern California, Los Angeles.
Unpublished findings also indicate that the number of UIM dermatology residents is inching upward. “Residency selection may not be on everyone’s mind, but an understanding of how we select people into our specialty is something every derm should know about and care about,” said Kanade Shinkai, MD, PhD, professor of dermatology at the University of California, San Francisco, and editor in chief of JAMA Dermatology.
The wake-up calls
The impetus for current changes first came in 2015, when Bruce Wintroub, MD, professor and chair of dermatology at UCSF, and interim dean of the medical school at the time, delivered a passionate plenary lecture at the annual AAD meeting about the lack of equity, diversity and inclusion in the specialty and the role of unconscious bias. Moved in part by a “White Coats for Black Lives” die-in by medical students on his campus following the killing of unarmed Black men, Dr. Wintroub called on his colleagues to recruit more UIM physicians into the specialty and to make the field more inclusive.
In 2016, Dr. Wintroub joined Dr. Pandya and two other academic dermatologists in authoring a commentary, published in the Journal of the American Academy of Dermatology, about the need to step up efforts and make diversity a priority. Dermatology was among the least ethnically and racially diverse specialties, second only to orthopedics, they wrote, with black dermatologists making up only 3% of all dermatologists and Hispanics only 4.2% in the United States, compared with 12.8% and 16.3% in the U.S. population, respectively.
For the next year or so, they and others from six academic institutions formed an incubator of sorts, actively tracking and sharing actions they were taking to improve diversity and the practice environment. “We wanted to learn from each other, then disseminate information to other programs,” said Dr. Pandya, who chaired the AAD diversity task force and led the self-branded “diversity champions.” (Dr. Pandya maintains his appointment at UTSW but now practices at the Palo Alto Foundation Medical Group in Sunnyvale, Calif.)
In 2017, at a President’s Conference on Diversity in Dermatology called for by then-AAD president Henry Lim, MD, leaders of the Association of Professors of Dermatology, the Society for Investigative Dermatology, and other dermatology organizations agreed on key action items, which they described in JAAD in 2018: Helping to increase the pipeline of UIM students applying to medical school, increasing UIM medical students’ early exposure to dermatology, and increasing the number of UIM students recruited into dermatology residency programs.
Diversity in the physician workforce has been shown to improve outcomes for all patients, and is important for ameliorating health care disparities and improving satisfaction and care for all patients, the authors of the 2018 paper wrote. “Multiple studies,” they noted, “have shown that UIM physicians are more likely to practice in areas where health care disparities exist.”
For specific proposed actions, the leaders attending the diversity conference drew largely upon the “diversity champions’” experiences, and agreed to fund and officially develop a diversity champions program. They also decided to invest in “bioskills” workshops for undergraduates and medical students at historically black colleges and universities, and other institutions at historically black colleges and universities at medical schools through a partnership with Nth Dimension – an organization founded in 2004 to bring more women and underrepresented minorities into orthopedic surgery.
In the last 2 years, more than 450 UIM students have attended these bioskills workshops, getting a taste of basic dermatology procedures and interacting with dermatologists.
And in September 2020, 157 dermatologists representing 80 programs throughout the country attended the second AAD Diversity Champions conference, up from 84 attendees and 30 programs in 2019. On the agenda: Discussions of holistic application review, mentorship, recruitment of UIM faculty, and a 2-hour session on microaggressions. Similar programs are being led by other dermatology organizations.
(UIM was coined by the American Association of Medical Colleges to describe racial and ethnic populations that are underrepresented in medicine relative to their numbers in the general population.)
Achievement of racial/ethnic diversity “won’t happen unless the field actively encourages people to look at it – which is not what we were doing,” Dr. Wintroub said in an interview. “I think that’s been the major change. We’re opening the door and saying: ‘We want you and we welcome you.’ ”
Rethinking traditional mentorship
For Dr. Florez-Pollack, the door almost shut when she began to hear from fellow medical students that dermatology is “too competitive ... a field for only the top people in the class.” She felt doubt settling in.
“I had peers who were throwing a lot of money toward prep materials ... peers who had siblings in medicine and had started studying from day one [for the step 1 exam],” she said. “I thought, was it really worth the effort? Do I really want to be perfect to get into the field when other fields would be happy to have me as I am right now?”
Her immense enjoyment of an “Art of Observation” elective course helped renew her interest in the field; it reinforced her visual abilities as well as the potential for her to address implicit bias as a dermatologist. She sought Dr. Pandya’s guidance and sponsorship to help her grow connections, polish her resume, and present herself to other faculty.
Doors were opened, she said, for her to secure a 1-year research experience before her final year of medical school with UTSW faculty, and then a 1-month rotation/mentorship with William D. James, MD, professor of dermatology at the University of Pennsylvania, an institution with a history of diversity initiatives and a longstanding skin of color program.
Dr. Florez-Pollack sees her experience reflected in the findings of a recently published study – a thematic content analysis of telephone interviews with applicants to the UTSW dermatology residency program during the 2013-14 and 2014-15 application cycles. Of the 44 applicants who participated in the study, 13 were UIM applicants.
Six of the seven UIM applicants who matched were involved in a pipeline or enrichment program – and were exposed to the field early – compared with one or two of the six UIM applicants who did not match. Underrepresented applicants were more often discouraged from applying (54%) – told, for instance, that they could better serve their communities through other specialties – than were non-UIM applicants (13%). They also were affected more often by a lack of equitable resources, according to comments made by 70% of applicants (UIM and non-UIM).
Also notably, the investigators said, all of the UIM applicants who matched (and the majority of non-UIMs who matched) reported having a mentor during the process of applying, compared with 44% of those who didn’t match.
Rebecca Vasquez, MD, assistant professor of dermatology at UTSW, who led the study, was herself a mentee of Dr. Pandya. “He believed in me and gave me the courage to consider dermatology,” she said. (Dr. Vasquez was one of the Latinx women who inspired Dr. Florez-Pollack, in turn, when they met at Dr. Pandya’s pizza party. Dr. Florez-Pollack assisted with the research and was a coauthor of the study.)
Amy McMichael, MD, professor and chair of dermatology at Wake Forest University, Winston-Salem, N.C., said that dermatology as a field has traditionally been “very good at mentoring.” Many of the dermatology societies have long had mentorship programs, for instance, that guide medical students, and sometimes residents, through defined experiences or through periods of time.
But she advocates going deeper. “When it comes to sponsorship, we fall a little short,” she said. “Sponsorship is about promoting that person to the next level, making sure they achieve what they want to achieve ... putting them up for opportunities they may not have known existed. It’s continuous and focused.”
Olabola Awosika, MD, a fourth-year dermatology resident at Henry Ford Health System, Detroit, said her interest in dermatology was solidified during her participation in the AAD’s month-long mentorship program after her second year of medical school at Howard University, Washington. However, it wasn’t until her fourth year, when she did an away rotation at Wake Forest, that she realized that “gaining access to the field” takes years of mentorship, research opportunities, and networking. It was too late.
After initially not matching, she did a rotation at Johns Hopkins in dermatology during an internship year, followed by a 2-year research fellowship at George Washington University, Washington. As does Dr. Florez-Pollack, who now mentors medical students. She also serves on the Women’s Dermatologic Society diversity committee, which is now developing initiatives to help UIM dermatologists “become upwardly mobile in dermatology [after residency], so they have a seat at the table in various settings.”
Holistic review for residency
Dr. Vasquez, who grew up in South Texas in an uninsured family that received most of its medical care across the border in Mexico, believes that the “biggest stride being made today” with respect to diversity in the dermatology workforce – and in the larger physician workforce – is increased understanding of the role of social and cultural capital.
“We’d never really talked about this concept ... about how, if you don’t have the same upbringing, education, and resources, you’re already behind … and you may not do as well on standardized tests,” she said. “Now people are listening to it and understand it. That’s why more programs are looking at how to practice a more holistic approach to selecting applicants to interview.”
Some dermatology programs – at Wake Forest, UCSF, USC, Vanderbilt, and George Washington University for instance – have eliminated the use of U.S. Medical Licensing Examination step 1 scores and Alpha Omega Alpha Medical Honor Society status as filtering/screening metrics. Some also take a “second look” at UIM applicants.
Overall, those making changes are looking “at everything the applicant brings to the table – their story, their experiences,” said Dr. Elbuluk. “We want to understand the full picture of who they are and their journey to becoming a physician.”
Implicit bias training for members of residency review committees is becoming more common, as is such training across the board in dermatology departments. “We have to bring it to the forefront so that we can create more inclusive environments,” said Sharon E. Albers, MD, a dermatologist at Vanderbilt University Medical Center, Nashville, Tenn., who serves as the dermatology department’s diversity liaison to the medical school, and who, as a former faculty member of Meharry Medical College, remains engaged with the historically black institution.
One of her recent efforts, inspired by participation in the diversity champions program, has been developing pipeline programs to speak to middle and high school students about medicine and dermatology. For now, however, she credits a holistic review process for change. Last year, three of the five matched dermatology residents at Vanderbilt were UIM physicians – unprecedented for the institution, Dr. Albers said, and “evidence that holistic review works if you’re very intentional about it.”
Dr. Vasquez has analyzed data from the Accreditation Council of Graduate Medical Education and says that UIM dermatology residents comprised 8.0% of the total in 2019, marking an improvement over the prior 7 years. “We’ve introduced so many changes at the same time,” making it difficult to discern what’s most impactful, she said. “But something is working.”
(The AAMC, which has invested in pipeline programs for more than a decade and has championed holistic medical school admissions, states in its 2019 diversity data report that efforts to improve diversity in medicine have made “only marginal differences” – and that Black males in particular continue to be significantly underrepresented in medical schools. Persistent, structural racism was a common theme in the association’s 2015 report on Black males in medicine.)
Efforts to diversify the workforce – particularly holistic review – haven’t been without detractors. “It brings reaction,” Dr. Wintroub said. “Some people think you’re lowering quality in the field ... but that’s just not true.”
Diversity in the dermatology workforce is important not only for the care of patients from diverse backgrounds, but “perhaps more importantly, it brings new ideas and views and experiences into the field,” he said. “It pushes us to think in new directions ... that can only make our field better and richer.”
“We need to make sure our workforce is representative of the patients we serve – but also that all derms can manage patients of all skin types and demographics,” Dr. Shinkai said. “And we need more diversity in the leadership of our departments and dermatology organizations ... inclusivity needs to extend all the way to the highest reaches of our specialty.”
Adam Friedman, MD, professor and interim chair of dermatology at George Washington University and director of the department’s diversity, equity, and inclusion committee, agreed. “We need to both make sure our workforce mirrors the patients we serve, and said workforce is prepared to manage patients of all skin types and demographics. We need to cover the spectrum, from revamping medical education and mentorship opportunities to advancing diversity in the leadership of our departments, institutions, and societies. Addressing only part of the puzzle will not and can not be enough.”
Correction, 3/3/21: An earlier version of this article misstated Dr. Stephanie Florez-Pollack's name.
Black women show heightened risk for depression after early pregnancy loss
Black women are significantly more likely than non-Black women to develop major depression within a month of early pregnancy loss, based on data from a secondary analysis of 300 women.
Approximately 25% of women experience a pregnancy loss, and many of these women are at increased risk for psychological problems including major depression, wrote Jade M. Shorter, MD, of Stanford (Calif.) University, and colleagues.
Data from previous studies show that Black women experience higher rates of perinatal depression, compared with other racial groups, and that stress and adverse childhood experiences also are higher among Black individuals, they noted.
“Based on data showing higher rates of pregnancy loss, perinatal depression, and perceived stress in Black women, we hypothesized that the odds of having risk for major depression or high perceived stress 30 days after miscarriage treatment would be higher in Black participants when compared with non-Black participants,” they wrote.
In a study published in Obstetrics & Gynecology, the researchers conducted a secondary analysis of 300 women aged 18 years and older with nonviable intrauterine pregnancy between 5 and 12 weeks’ gestation who were part of a larger randomized trial conducted between May 2014 and April 2017. The women were randomized to medical treatment of either mifepristone 200 mg orally plus misoprostol 800 mcg vaginally after 24 hours or the usual treatment of misoprostol 800 mcg vaginally.
Depression was assessed using the Center for Epidemiological Studies–Depression scale, Perceived Stress Scale, and Adverse Childhood Experience scale. Adverse childhood experience data were collected at baseline; stress and depression data were collected at baseline and at 30 days after treatment.
A total of 120 participants self-identified as Black and 155 self-identified as non-Black.
Depression risk doubles in Black women
At 30 days after treatment for early pregnancy loss, 24% of women met criteria for major depression, including 57% of Black women and 43% of non-Black women. The odds of depression were twice as high among Black women, compared with non-Black women (odds ratio 2.02), and Black women were more likely to be younger, have lower levels of education, and have public insurance, compared with non-Black women.
The association between Black race and increased risk for depression at 30 days after treatment persisted after controlling for factors including parity, baseline depression, and adverse childhood experiences, the researchers noted.
The study findings were limited by several factors, including the potential for different depression risk in those from the original study who did and did not participate in the secondary analysis and by the use of the original Adverse Childhood Experience survey, which may not reflect the range of adversity faced by different demographic groups, the researchers noted. However, the results were strengthened by the collection of 30-day outcome data in the clinical setting and by the diverse study population.
“These findings should be not be used to stigmatize Black women; instead, it is important to consider the complex systemic factors, such as structural racism, that are the root causes of disparate health outcomes,” and to support appropriate mental health resources and interventions for all women who experience early pregnancy loss, the researchers emphasized.
Recognize risks, reduce barriers
“Early pregnancy loss is unfortunately a common event that affects 15%-20% of pregnancies,” Iris Krishna, MD, of Emory University, Atlanta, said in an interview.
However, “the mental health impact of early pregnancy loss is understudied, and as a result mental health disorders often go unnoticed and untreated,” she said.
Growing evidence shows that Black women in particular are at greater risk for chronic stressors that affect their overall health. “Black women are more likely to be exposed to trauma in their lifetime, such as physical and emotional abuse, neglect, and household instability, all of which predispose women to mental health disorders such as depression. Untreated maternal depression has an impact on future pregnancy outcomes such as increasing the risk of having a preterm delivery and/or delivering a low-birth-weight baby, outcomes where Black women are at disproportionately high risk in comparison to non-Black women,” Dr. Krishna said.
“This study found that the risk for depression after an early pregnancy loss is twice as high for Black women in comparison to non-Black women. The findings of this study further underscore the fact that Black women are at disproportionate high risk for poor maternal and pregnancy outcomes,” Dr. Krishna added.
“Structural racism is a major barrier to caring for the health of Black women. To care for the health of Black women we must overcome racial and ethnic disparities. Addressing disparities involves a multitiered approach, including identifying and addressing implicit bias in health care and improving access to health care for women of color,” she said.
“Additional research is needed in identifying at-risk women and mental health interventions that can improve the mental well-being of women after adverse pregnancy outcomes such as early pregnancy loss,” Dr. Krishna concluded.
The study was supported by the Society of Family Planning Research Fund. Lead author Dr. Shorter had no financial conflicts to disclose. Dr. Krishna had no financial conflicts to disclose.
SOURCE: Shorter JM et al. Obstet Gynecol. 2020 Dec 3. doi: 10.1097/AOG.0000000000004212.
Black women are significantly more likely than non-Black women to develop major depression within a month of early pregnancy loss, based on data from a secondary analysis of 300 women.
Approximately 25% of women experience a pregnancy loss, and many of these women are at increased risk for psychological problems including major depression, wrote Jade M. Shorter, MD, of Stanford (Calif.) University, and colleagues.
Data from previous studies show that Black women experience higher rates of perinatal depression, compared with other racial groups, and that stress and adverse childhood experiences also are higher among Black individuals, they noted.
“Based on data showing higher rates of pregnancy loss, perinatal depression, and perceived stress in Black women, we hypothesized that the odds of having risk for major depression or high perceived stress 30 days after miscarriage treatment would be higher in Black participants when compared with non-Black participants,” they wrote.
In a study published in Obstetrics & Gynecology, the researchers conducted a secondary analysis of 300 women aged 18 years and older with nonviable intrauterine pregnancy between 5 and 12 weeks’ gestation who were part of a larger randomized trial conducted between May 2014 and April 2017. The women were randomized to medical treatment of either mifepristone 200 mg orally plus misoprostol 800 mcg vaginally after 24 hours or the usual treatment of misoprostol 800 mcg vaginally.
Depression was assessed using the Center for Epidemiological Studies–Depression scale, Perceived Stress Scale, and Adverse Childhood Experience scale. Adverse childhood experience data were collected at baseline; stress and depression data were collected at baseline and at 30 days after treatment.
A total of 120 participants self-identified as Black and 155 self-identified as non-Black.
Depression risk doubles in Black women
At 30 days after treatment for early pregnancy loss, 24% of women met criteria for major depression, including 57% of Black women and 43% of non-Black women. The odds of depression were twice as high among Black women, compared with non-Black women (odds ratio 2.02), and Black women were more likely to be younger, have lower levels of education, and have public insurance, compared with non-Black women.
The association between Black race and increased risk for depression at 30 days after treatment persisted after controlling for factors including parity, baseline depression, and adverse childhood experiences, the researchers noted.
The study findings were limited by several factors, including the potential for different depression risk in those from the original study who did and did not participate in the secondary analysis and by the use of the original Adverse Childhood Experience survey, which may not reflect the range of adversity faced by different demographic groups, the researchers noted. However, the results were strengthened by the collection of 30-day outcome data in the clinical setting and by the diverse study population.
“These findings should be not be used to stigmatize Black women; instead, it is important to consider the complex systemic factors, such as structural racism, that are the root causes of disparate health outcomes,” and to support appropriate mental health resources and interventions for all women who experience early pregnancy loss, the researchers emphasized.
Recognize risks, reduce barriers
“Early pregnancy loss is unfortunately a common event that affects 15%-20% of pregnancies,” Iris Krishna, MD, of Emory University, Atlanta, said in an interview.
However, “the mental health impact of early pregnancy loss is understudied, and as a result mental health disorders often go unnoticed and untreated,” she said.
Growing evidence shows that Black women in particular are at greater risk for chronic stressors that affect their overall health. “Black women are more likely to be exposed to trauma in their lifetime, such as physical and emotional abuse, neglect, and household instability, all of which predispose women to mental health disorders such as depression. Untreated maternal depression has an impact on future pregnancy outcomes such as increasing the risk of having a preterm delivery and/or delivering a low-birth-weight baby, outcomes where Black women are at disproportionately high risk in comparison to non-Black women,” Dr. Krishna said.
“This study found that the risk for depression after an early pregnancy loss is twice as high for Black women in comparison to non-Black women. The findings of this study further underscore the fact that Black women are at disproportionate high risk for poor maternal and pregnancy outcomes,” Dr. Krishna added.
“Structural racism is a major barrier to caring for the health of Black women. To care for the health of Black women we must overcome racial and ethnic disparities. Addressing disparities involves a multitiered approach, including identifying and addressing implicit bias in health care and improving access to health care for women of color,” she said.
“Additional research is needed in identifying at-risk women and mental health interventions that can improve the mental well-being of women after adverse pregnancy outcomes such as early pregnancy loss,” Dr. Krishna concluded.
The study was supported by the Society of Family Planning Research Fund. Lead author Dr. Shorter had no financial conflicts to disclose. Dr. Krishna had no financial conflicts to disclose.
SOURCE: Shorter JM et al. Obstet Gynecol. 2020 Dec 3. doi: 10.1097/AOG.0000000000004212.
Black women are significantly more likely than non-Black women to develop major depression within a month of early pregnancy loss, based on data from a secondary analysis of 300 women.
Approximately 25% of women experience a pregnancy loss, and many of these women are at increased risk for psychological problems including major depression, wrote Jade M. Shorter, MD, of Stanford (Calif.) University, and colleagues.
Data from previous studies show that Black women experience higher rates of perinatal depression, compared with other racial groups, and that stress and adverse childhood experiences also are higher among Black individuals, they noted.
“Based on data showing higher rates of pregnancy loss, perinatal depression, and perceived stress in Black women, we hypothesized that the odds of having risk for major depression or high perceived stress 30 days after miscarriage treatment would be higher in Black participants when compared with non-Black participants,” they wrote.
In a study published in Obstetrics & Gynecology, the researchers conducted a secondary analysis of 300 women aged 18 years and older with nonviable intrauterine pregnancy between 5 and 12 weeks’ gestation who were part of a larger randomized trial conducted between May 2014 and April 2017. The women were randomized to medical treatment of either mifepristone 200 mg orally plus misoprostol 800 mcg vaginally after 24 hours or the usual treatment of misoprostol 800 mcg vaginally.
Depression was assessed using the Center for Epidemiological Studies–Depression scale, Perceived Stress Scale, and Adverse Childhood Experience scale. Adverse childhood experience data were collected at baseline; stress and depression data were collected at baseline and at 30 days after treatment.
A total of 120 participants self-identified as Black and 155 self-identified as non-Black.
Depression risk doubles in Black women
At 30 days after treatment for early pregnancy loss, 24% of women met criteria for major depression, including 57% of Black women and 43% of non-Black women. The odds of depression were twice as high among Black women, compared with non-Black women (odds ratio 2.02), and Black women were more likely to be younger, have lower levels of education, and have public insurance, compared with non-Black women.
The association between Black race and increased risk for depression at 30 days after treatment persisted after controlling for factors including parity, baseline depression, and adverse childhood experiences, the researchers noted.
The study findings were limited by several factors, including the potential for different depression risk in those from the original study who did and did not participate in the secondary analysis and by the use of the original Adverse Childhood Experience survey, which may not reflect the range of adversity faced by different demographic groups, the researchers noted. However, the results were strengthened by the collection of 30-day outcome data in the clinical setting and by the diverse study population.
“These findings should be not be used to stigmatize Black women; instead, it is important to consider the complex systemic factors, such as structural racism, that are the root causes of disparate health outcomes,” and to support appropriate mental health resources and interventions for all women who experience early pregnancy loss, the researchers emphasized.
Recognize risks, reduce barriers
“Early pregnancy loss is unfortunately a common event that affects 15%-20% of pregnancies,” Iris Krishna, MD, of Emory University, Atlanta, said in an interview.
However, “the mental health impact of early pregnancy loss is understudied, and as a result mental health disorders often go unnoticed and untreated,” she said.
Growing evidence shows that Black women in particular are at greater risk for chronic stressors that affect their overall health. “Black women are more likely to be exposed to trauma in their lifetime, such as physical and emotional abuse, neglect, and household instability, all of which predispose women to mental health disorders such as depression. Untreated maternal depression has an impact on future pregnancy outcomes such as increasing the risk of having a preterm delivery and/or delivering a low-birth-weight baby, outcomes where Black women are at disproportionately high risk in comparison to non-Black women,” Dr. Krishna said.
“This study found that the risk for depression after an early pregnancy loss is twice as high for Black women in comparison to non-Black women. The findings of this study further underscore the fact that Black women are at disproportionate high risk for poor maternal and pregnancy outcomes,” Dr. Krishna added.
“Structural racism is a major barrier to caring for the health of Black women. To care for the health of Black women we must overcome racial and ethnic disparities. Addressing disparities involves a multitiered approach, including identifying and addressing implicit bias in health care and improving access to health care for women of color,” she said.
“Additional research is needed in identifying at-risk women and mental health interventions that can improve the mental well-being of women after adverse pregnancy outcomes such as early pregnancy loss,” Dr. Krishna concluded.
The study was supported by the Society of Family Planning Research Fund. Lead author Dr. Shorter had no financial conflicts to disclose. Dr. Krishna had no financial conflicts to disclose.
SOURCE: Shorter JM et al. Obstet Gynecol. 2020 Dec 3. doi: 10.1097/AOG.0000000000004212.
FROM OBSTETRICS & GYNECOLOGY
Differences in right vs. left colon in Black vs. White individuals
The right colon appears to age faster in Black people than in White people, perhaps explaining the higher prevalence of right-side colon cancer among Black Americans, according to results from a biopsy study.
The findings were published online Dec. 30 in the Journal of the National Cancer Institute.
For the study, investigators analyzed colon biopsy specimens from 128 individuals who underwent routine colorectal screening.
The researchers compared DNA methylation levels in right and left colon biopsy samples from the same patient. They then assigned epigenetic ages to the tissue samples using the Hovarth clock, which estimates tissue age on the basis of DNA methylation.
DNA methylation is influenced by age and environmental exposures. Aberrant DNA methylation is a hallmark of colorectal cancer, the researchers explained.
The epigenetic age of the right colon of the 88 Black patients was 1.51 years ahead of their left colon; the right colon of the 44 White patients was epigenetically 1.93 years younger than their left colon.
The right colon was epigenetically older than the left colon in 60.2% of Black patients; it was younger in more than 70% of White patients.
A unique pattern of DNA hypermethylation was found in the right colon of Black patients.
“Our results provide biological plausibility for the observed relative preponderance of right colon cancer and younger age of onset in African Americans as compared to European Americans,” wrote the investigators, led by Matthew Devall, PhD, a research associate at the Center for Public Health Genomics at the University of Virginia, Charlottesville.
“Side-specific colonic epigenetic aging may be a promising marker to guide interventions to reduce CRC [colorectal cancer] burden,” they suggested.
If these findings are “corroborated in African Americans in future studies, these results could potentially explain racial differences in the site predilection of colorectal cancers,” Amit Joshi, MBBS, PhD, and Andrew Chan, MD, gastrointestinal molecular epidemiologists at Harvard Medical School, Boston, wrote in an accompanying editorial.
However, “it is not clear if the higher epigenetic aging measured using the Horvath clock ... directly translates to a higher risk of colorectal cancer,” they noted.
Some differences between the Black patients and the White patients in the study could explain the methylation differences, they pointed out. A higher proportion of Black patients smoked (37.5% vs. 15%), and Black patients were younger (median age, 55.5 years, vs. 61.7 years). In addition, the study included more Black women than White women (67% vs. 58%), and body mass indexes were higher for Black patients than White patients (31.36 kg/m2 vs 28.29 kg/m2).
“One or more of these factors, or others that were not measured, may be linked to differential methylation in the right compared with left colon,” the editorialists wrote.
Even so, among the Black patients, almost 70% of differentially methylated positions in the right colon were hypermethylated, compared to less than half in the left colon. These included positions previously associated with colorectal cancer, aging, and ancestry, “suggesting a role for genetic variation in contributing to DNA methylation differences in AA right colon,” the investigators said.
The work was supported the National Cancer Institute Cancer, the Case Comprehensive Cancer Center, and the University of Virginia Cancer Center. The authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The right colon appears to age faster in Black people than in White people, perhaps explaining the higher prevalence of right-side colon cancer among Black Americans, according to results from a biopsy study.
The findings were published online Dec. 30 in the Journal of the National Cancer Institute.
For the study, investigators analyzed colon biopsy specimens from 128 individuals who underwent routine colorectal screening.
The researchers compared DNA methylation levels in right and left colon biopsy samples from the same patient. They then assigned epigenetic ages to the tissue samples using the Hovarth clock, which estimates tissue age on the basis of DNA methylation.
DNA methylation is influenced by age and environmental exposures. Aberrant DNA methylation is a hallmark of colorectal cancer, the researchers explained.
The epigenetic age of the right colon of the 88 Black patients was 1.51 years ahead of their left colon; the right colon of the 44 White patients was epigenetically 1.93 years younger than their left colon.
The right colon was epigenetically older than the left colon in 60.2% of Black patients; it was younger in more than 70% of White patients.
A unique pattern of DNA hypermethylation was found in the right colon of Black patients.
“Our results provide biological plausibility for the observed relative preponderance of right colon cancer and younger age of onset in African Americans as compared to European Americans,” wrote the investigators, led by Matthew Devall, PhD, a research associate at the Center for Public Health Genomics at the University of Virginia, Charlottesville.
“Side-specific colonic epigenetic aging may be a promising marker to guide interventions to reduce CRC [colorectal cancer] burden,” they suggested.
If these findings are “corroborated in African Americans in future studies, these results could potentially explain racial differences in the site predilection of colorectal cancers,” Amit Joshi, MBBS, PhD, and Andrew Chan, MD, gastrointestinal molecular epidemiologists at Harvard Medical School, Boston, wrote in an accompanying editorial.
However, “it is not clear if the higher epigenetic aging measured using the Horvath clock ... directly translates to a higher risk of colorectal cancer,” they noted.
Some differences between the Black patients and the White patients in the study could explain the methylation differences, they pointed out. A higher proportion of Black patients smoked (37.5% vs. 15%), and Black patients were younger (median age, 55.5 years, vs. 61.7 years). In addition, the study included more Black women than White women (67% vs. 58%), and body mass indexes were higher for Black patients than White patients (31.36 kg/m2 vs 28.29 kg/m2).
“One or more of these factors, or others that were not measured, may be linked to differential methylation in the right compared with left colon,” the editorialists wrote.
Even so, among the Black patients, almost 70% of differentially methylated positions in the right colon were hypermethylated, compared to less than half in the left colon. These included positions previously associated with colorectal cancer, aging, and ancestry, “suggesting a role for genetic variation in contributing to DNA methylation differences in AA right colon,” the investigators said.
The work was supported the National Cancer Institute Cancer, the Case Comprehensive Cancer Center, and the University of Virginia Cancer Center. The authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The right colon appears to age faster in Black people than in White people, perhaps explaining the higher prevalence of right-side colon cancer among Black Americans, according to results from a biopsy study.
The findings were published online Dec. 30 in the Journal of the National Cancer Institute.
For the study, investigators analyzed colon biopsy specimens from 128 individuals who underwent routine colorectal screening.
The researchers compared DNA methylation levels in right and left colon biopsy samples from the same patient. They then assigned epigenetic ages to the tissue samples using the Hovarth clock, which estimates tissue age on the basis of DNA methylation.
DNA methylation is influenced by age and environmental exposures. Aberrant DNA methylation is a hallmark of colorectal cancer, the researchers explained.
The epigenetic age of the right colon of the 88 Black patients was 1.51 years ahead of their left colon; the right colon of the 44 White patients was epigenetically 1.93 years younger than their left colon.
The right colon was epigenetically older than the left colon in 60.2% of Black patients; it was younger in more than 70% of White patients.
A unique pattern of DNA hypermethylation was found in the right colon of Black patients.
“Our results provide biological plausibility for the observed relative preponderance of right colon cancer and younger age of onset in African Americans as compared to European Americans,” wrote the investigators, led by Matthew Devall, PhD, a research associate at the Center for Public Health Genomics at the University of Virginia, Charlottesville.
“Side-specific colonic epigenetic aging may be a promising marker to guide interventions to reduce CRC [colorectal cancer] burden,” they suggested.
If these findings are “corroborated in African Americans in future studies, these results could potentially explain racial differences in the site predilection of colorectal cancers,” Amit Joshi, MBBS, PhD, and Andrew Chan, MD, gastrointestinal molecular epidemiologists at Harvard Medical School, Boston, wrote in an accompanying editorial.
However, “it is not clear if the higher epigenetic aging measured using the Horvath clock ... directly translates to a higher risk of colorectal cancer,” they noted.
Some differences between the Black patients and the White patients in the study could explain the methylation differences, they pointed out. A higher proportion of Black patients smoked (37.5% vs. 15%), and Black patients were younger (median age, 55.5 years, vs. 61.7 years). In addition, the study included more Black women than White women (67% vs. 58%), and body mass indexes were higher for Black patients than White patients (31.36 kg/m2 vs 28.29 kg/m2).
“One or more of these factors, or others that were not measured, may be linked to differential methylation in the right compared with left colon,” the editorialists wrote.
Even so, among the Black patients, almost 70% of differentially methylated positions in the right colon were hypermethylated, compared to less than half in the left colon. These included positions previously associated with colorectal cancer, aging, and ancestry, “suggesting a role for genetic variation in contributing to DNA methylation differences in AA right colon,” the investigators said.
The work was supported the National Cancer Institute Cancer, the Case Comprehensive Cancer Center, and the University of Virginia Cancer Center. The authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Racial, ethnic disparities in maternal mortality, morbidity persist
Racial and ethnic disparities in maternal and infant outcomes persist in the United States, with Black women being 3-4 times more likely to die of pregnancy-related causes, compared with Latina and non-Latina white women, Elizabeth Howell, MD, said in a presentation at the 2020 virtual meeting of the American College of Obstetricians and Gynecologists.
Location matters, too, and ethnic disparities appear to transcend class, said Dr. Howell of Penn Medicine, Philadelphia. In New York City, for example, Black women are 8-12 times more likely to die than white women regardless of educational attainment.
Dr. Howell cited the definitions of health equity and health disparities as defined by Paula Braveman, MD, in 2014 in the journal Public Health Reports, as follows: “Health equity means social justice in health (i.e., no one is denied the possibility to be healthy for belonging to a group that has historically been economically/socially disadvantaged. Health disparities are the metric we use to measure progress toward achieving health equity.”
Structural racism and discrimination contribute to disparities in maternal and infant morbidity and mortality in several ways, she said. Patient factors include sociodemographics, age, education, poverty, insurance, marital status, language, and literacy. In addition, a patient’s knowledge, beliefs, and health behaviors, as well as stress and self-efficacy are involved. Community factors such as crime, poverty, and community support play a role.
“These factors contribute to the health status of a woman when she becomes pregnant,” Dr. Howell said. “These factors contribute as the woman goes through the health system.”
Then provider factors that impact maternal and infant morbidity and mortality include knowledge, experience, implicit bias, cultural humility, and communication; these factors affect the quality and delivery of neonatal care, and can impact outcomes, Dr. Howell said.
“It is really important to note that many of these pregnancy-related deaths are thought to be preventable,” she said. “They are often caused by delays in diagnosis, problems with communication, and other system failures. Site care has received a great deal of attention” in recent years, the ob.gyn. noted.
How hospital quality contributes to health disparities
Dr. Howell shared data from a pair of National Institutes of Health–funded parallel group studies she conducted at New York City hospitals to investigate the contribution of hospital quality to health disparities in severe maternal morbidity and very preterm birth (prior to 32 weeks).
The researchers used vital statistics linked with discharge abstracts for all New York City deliveries between 2011-2013 and 2010-2014. They conducted a logistic regression analysis and ranked hospitals based on metrics of severe maternal morbidity and very preterm birth, and assessed differences by race in each delivery location.
Overall, Black women were almost three times as likely and Latina women were almost twice as likely as White women to experience some type of severe maternal morbidity, with rates of 4.2%, 2.7%, and 1.5%, respectively.
The researchers also ranked hospitals, and found a wide variation; women delivering in the lowest-ranked hospitals had six times the rate of severe maternal morbidity. They also conducted a simulation/thought exercise and determined that the hospital of delivery accounted for approximately 48% of the disparity in severe maternal morbidity between Black and White women.
Results were similar in the parallel study of very preterm birth rates in New York City hospitals, which were 32%, 28%, and 23% for Black, Latina, and White women, respectively.
The researchers also conducted interviews with personnel including chief medical officers, neonatal ICU directors, nurses, and respiratory therapists. The final phase of the research, which is ongoing, is the dissemination of the information, said Dr. Howell.
Overall, the high-performing hospitals were more likely to focus on standards and standardized care, stronger nurse/physician communication, greater awareness of the potential impact of racism on care, and greater sharing of performance data.
Women who participated in focus groups reported a range of experiences, but women of color were likely to report poor communication, feeling traumatized, and not being heard.
Study implications
Dr. Howell discussed the implications of her study in a question and answer session. “It is incredibly important for us to think about all the levers that we have to address disparities.”
“It is a complex web of factors, but quality of care is one of those mechanisms, and it is something we can do something about,” she noted.
In response to a question about whether women should know the rates of adverse outcomes at various hospitals, she said, “I think we have a responsibility to come up with quality of care measures that are informative to the women we care for.”
Much of obstetric quality issues focus on overuse of resources, “but that doesn’t help us reduce disparities,” she said.
Dr. Howell had no financial conflicts to disclose.
Racial and ethnic disparities in maternal and infant outcomes persist in the United States, with Black women being 3-4 times more likely to die of pregnancy-related causes, compared with Latina and non-Latina white women, Elizabeth Howell, MD, said in a presentation at the 2020 virtual meeting of the American College of Obstetricians and Gynecologists.
Location matters, too, and ethnic disparities appear to transcend class, said Dr. Howell of Penn Medicine, Philadelphia. In New York City, for example, Black women are 8-12 times more likely to die than white women regardless of educational attainment.
Dr. Howell cited the definitions of health equity and health disparities as defined by Paula Braveman, MD, in 2014 in the journal Public Health Reports, as follows: “Health equity means social justice in health (i.e., no one is denied the possibility to be healthy for belonging to a group that has historically been economically/socially disadvantaged. Health disparities are the metric we use to measure progress toward achieving health equity.”
Structural racism and discrimination contribute to disparities in maternal and infant morbidity and mortality in several ways, she said. Patient factors include sociodemographics, age, education, poverty, insurance, marital status, language, and literacy. In addition, a patient’s knowledge, beliefs, and health behaviors, as well as stress and self-efficacy are involved. Community factors such as crime, poverty, and community support play a role.
“These factors contribute to the health status of a woman when she becomes pregnant,” Dr. Howell said. “These factors contribute as the woman goes through the health system.”
Then provider factors that impact maternal and infant morbidity and mortality include knowledge, experience, implicit bias, cultural humility, and communication; these factors affect the quality and delivery of neonatal care, and can impact outcomes, Dr. Howell said.
“It is really important to note that many of these pregnancy-related deaths are thought to be preventable,” she said. “They are often caused by delays in diagnosis, problems with communication, and other system failures. Site care has received a great deal of attention” in recent years, the ob.gyn. noted.
How hospital quality contributes to health disparities
Dr. Howell shared data from a pair of National Institutes of Health–funded parallel group studies she conducted at New York City hospitals to investigate the contribution of hospital quality to health disparities in severe maternal morbidity and very preterm birth (prior to 32 weeks).
The researchers used vital statistics linked with discharge abstracts for all New York City deliveries between 2011-2013 and 2010-2014. They conducted a logistic regression analysis and ranked hospitals based on metrics of severe maternal morbidity and very preterm birth, and assessed differences by race in each delivery location.
Overall, Black women were almost three times as likely and Latina women were almost twice as likely as White women to experience some type of severe maternal morbidity, with rates of 4.2%, 2.7%, and 1.5%, respectively.
The researchers also ranked hospitals, and found a wide variation; women delivering in the lowest-ranked hospitals had six times the rate of severe maternal morbidity. They also conducted a simulation/thought exercise and determined that the hospital of delivery accounted for approximately 48% of the disparity in severe maternal morbidity between Black and White women.
Results were similar in the parallel study of very preterm birth rates in New York City hospitals, which were 32%, 28%, and 23% for Black, Latina, and White women, respectively.
The researchers also conducted interviews with personnel including chief medical officers, neonatal ICU directors, nurses, and respiratory therapists. The final phase of the research, which is ongoing, is the dissemination of the information, said Dr. Howell.
Overall, the high-performing hospitals were more likely to focus on standards and standardized care, stronger nurse/physician communication, greater awareness of the potential impact of racism on care, and greater sharing of performance data.
Women who participated in focus groups reported a range of experiences, but women of color were likely to report poor communication, feeling traumatized, and not being heard.
Study implications
Dr. Howell discussed the implications of her study in a question and answer session. “It is incredibly important for us to think about all the levers that we have to address disparities.”
“It is a complex web of factors, but quality of care is one of those mechanisms, and it is something we can do something about,” she noted.
In response to a question about whether women should know the rates of adverse outcomes at various hospitals, she said, “I think we have a responsibility to come up with quality of care measures that are informative to the women we care for.”
Much of obstetric quality issues focus on overuse of resources, “but that doesn’t help us reduce disparities,” she said.
Dr. Howell had no financial conflicts to disclose.
Racial and ethnic disparities in maternal and infant outcomes persist in the United States, with Black women being 3-4 times more likely to die of pregnancy-related causes, compared with Latina and non-Latina white women, Elizabeth Howell, MD, said in a presentation at the 2020 virtual meeting of the American College of Obstetricians and Gynecologists.
Location matters, too, and ethnic disparities appear to transcend class, said Dr. Howell of Penn Medicine, Philadelphia. In New York City, for example, Black women are 8-12 times more likely to die than white women regardless of educational attainment.
Dr. Howell cited the definitions of health equity and health disparities as defined by Paula Braveman, MD, in 2014 in the journal Public Health Reports, as follows: “Health equity means social justice in health (i.e., no one is denied the possibility to be healthy for belonging to a group that has historically been economically/socially disadvantaged. Health disparities are the metric we use to measure progress toward achieving health equity.”
Structural racism and discrimination contribute to disparities in maternal and infant morbidity and mortality in several ways, she said. Patient factors include sociodemographics, age, education, poverty, insurance, marital status, language, and literacy. In addition, a patient’s knowledge, beliefs, and health behaviors, as well as stress and self-efficacy are involved. Community factors such as crime, poverty, and community support play a role.
“These factors contribute to the health status of a woman when she becomes pregnant,” Dr. Howell said. “These factors contribute as the woman goes through the health system.”
Then provider factors that impact maternal and infant morbidity and mortality include knowledge, experience, implicit bias, cultural humility, and communication; these factors affect the quality and delivery of neonatal care, and can impact outcomes, Dr. Howell said.
“It is really important to note that many of these pregnancy-related deaths are thought to be preventable,” she said. “They are often caused by delays in diagnosis, problems with communication, and other system failures. Site care has received a great deal of attention” in recent years, the ob.gyn. noted.
How hospital quality contributes to health disparities
Dr. Howell shared data from a pair of National Institutes of Health–funded parallel group studies she conducted at New York City hospitals to investigate the contribution of hospital quality to health disparities in severe maternal morbidity and very preterm birth (prior to 32 weeks).
The researchers used vital statistics linked with discharge abstracts for all New York City deliveries between 2011-2013 and 2010-2014. They conducted a logistic regression analysis and ranked hospitals based on metrics of severe maternal morbidity and very preterm birth, and assessed differences by race in each delivery location.
Overall, Black women were almost three times as likely and Latina women were almost twice as likely as White women to experience some type of severe maternal morbidity, with rates of 4.2%, 2.7%, and 1.5%, respectively.
The researchers also ranked hospitals, and found a wide variation; women delivering in the lowest-ranked hospitals had six times the rate of severe maternal morbidity. They also conducted a simulation/thought exercise and determined that the hospital of delivery accounted for approximately 48% of the disparity in severe maternal morbidity between Black and White women.
Results were similar in the parallel study of very preterm birth rates in New York City hospitals, which were 32%, 28%, and 23% for Black, Latina, and White women, respectively.
The researchers also conducted interviews with personnel including chief medical officers, neonatal ICU directors, nurses, and respiratory therapists. The final phase of the research, which is ongoing, is the dissemination of the information, said Dr. Howell.
Overall, the high-performing hospitals were more likely to focus on standards and standardized care, stronger nurse/physician communication, greater awareness of the potential impact of racism on care, and greater sharing of performance data.
Women who participated in focus groups reported a range of experiences, but women of color were likely to report poor communication, feeling traumatized, and not being heard.
Study implications
Dr. Howell discussed the implications of her study in a question and answer session. “It is incredibly important for us to think about all the levers that we have to address disparities.”
“It is a complex web of factors, but quality of care is one of those mechanisms, and it is something we can do something about,” she noted.
In response to a question about whether women should know the rates of adverse outcomes at various hospitals, she said, “I think we have a responsibility to come up with quality of care measures that are informative to the women we care for.”
Much of obstetric quality issues focus on overuse of resources, “but that doesn’t help us reduce disparities,” she said.
Dr. Howell had no financial conflicts to disclose.
FROM ACOG 2020
Rural Residency Curricula: Potential Target for Improved Access to Care?
To the Editor:
There is an irrefutable trend toward urban dermatology practice in the United States, leading to growing problems with rural access to care. The provision of rural clinical experiences and telehealth in dermatology residency training might increase the likelihood of trainees establishing a rural practice.
In 2017, the American Academy of Dermatology released an updated statement supporting direct patient access to board-certified dermatologists in an effort to reduce morbidity and mortality associated with skin disease.1 Twenty percent of the US population lives in a rural and medically underserved location, yet these areas remain largely underserved, in part because of an irrefutable trend toward urban dermatology practice.2-4 Successful approaches to improving rural access to dermatology care are poorly defined in the literature.
Several variables have been shown to influence a young physician’s decision to establish a clinical practice in geographically isolated areas, including rural upbringing, longitudinal rural clinical experiences during medical training, and family influences.5 Location of residency training is an additional variable that impacts practice location, though migration following dermatology residency is a complex phenomenon. However, training location does not guarantee retention of dermatology graduates in any particular geographic area.6 Practice incentives and stipends might encourage rural dermatology practice, yet these programs are underfunded. Last, telemedicine in dermatology (including teledermatology and teledermoscopy), though not always an ideal substitute for a live visit, can improve access to care in geographically isolated or underserved areas in general.7-9
Focused recruitment of medical students interested in rural dermatology practice to accredited dermatology residency programs aligned with this goal represents another approach to improve geographic diversity in the field of dermatology. Online access to this information would be useful for both applicants and their mentors.
We assessed viewable online curricula related to rural dermatology and telemedicine experiences at all Accreditation Council for Graduate Medical Education (ACGME)–accredited residency programs. Telemedicine experiences at Veterans Health Administration (VHA) health systems also were assessed.
Methods
This study was exempt from review by the institutional review board at the University of Minnesota (Minneapolis, Minnesota)(IRB #STUDY00004915) because no human subjects were involved. Online curricula of all ACGME-accredited dermatology residency programs in the United States and Puerto Rico were reviewed from November to December 2018. The following information was recorded: specialized “rural-track” training; optional elective time in rural settings; teledermatology training; and teledermoscopy training.
Additionally, population density at each program’s primary location was determined using US Census Bureau data and with consideration to communities contained within particular Metropolitan Statistical Areas (MSAs)(eTable). Data were obtained from the VHA system to assess teledermatology services at VHA locations affiliated with residency programs.
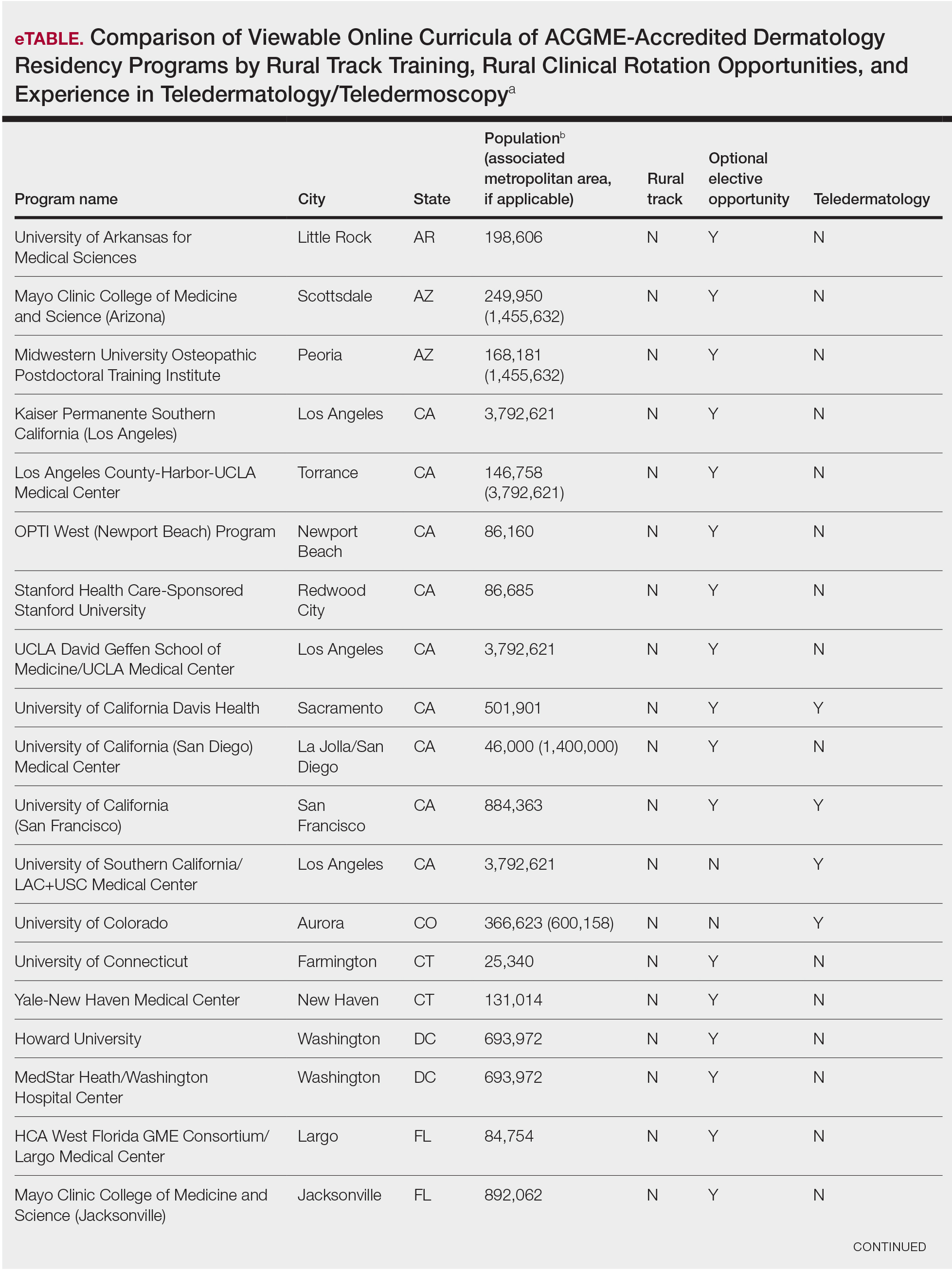
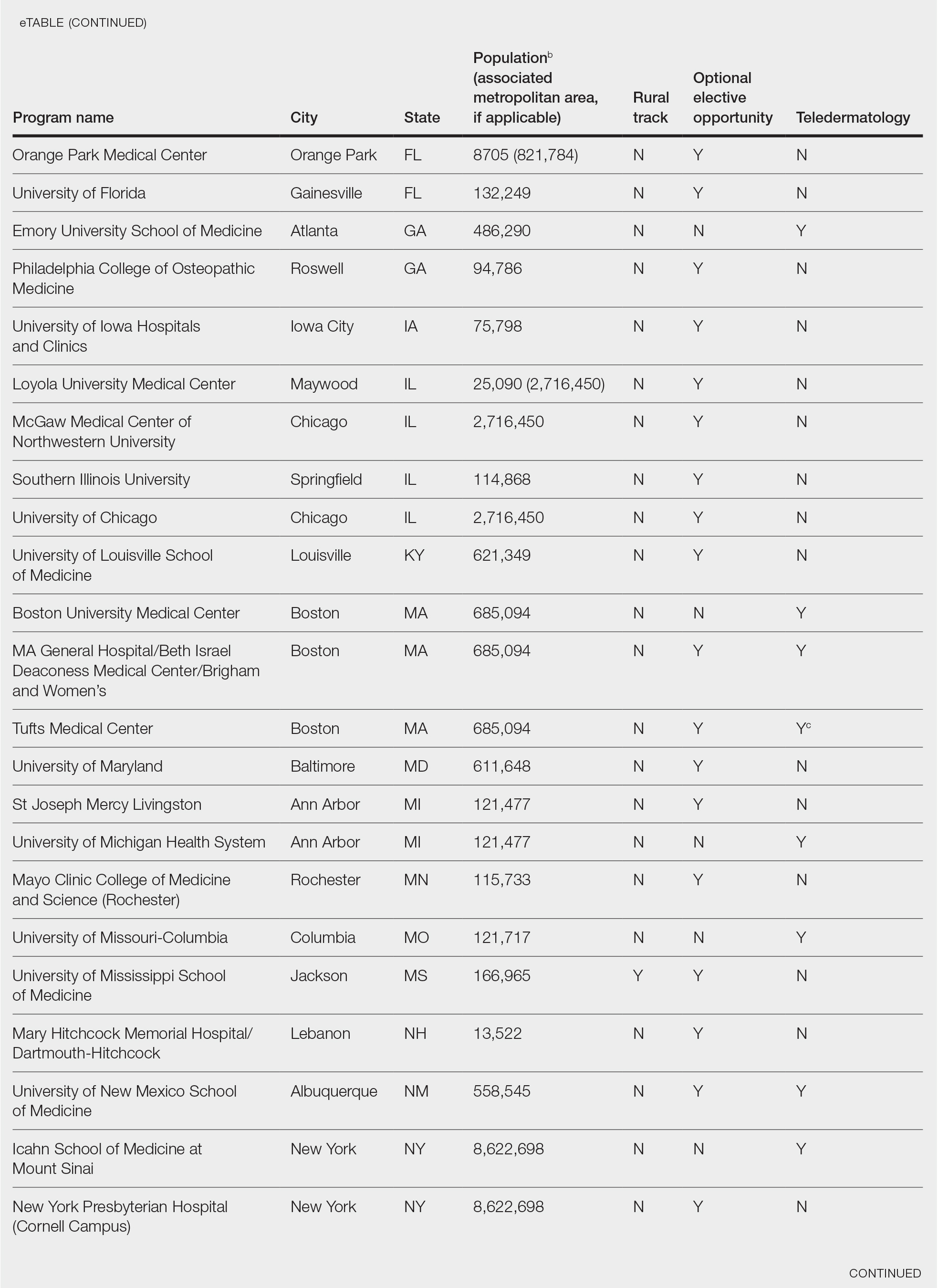
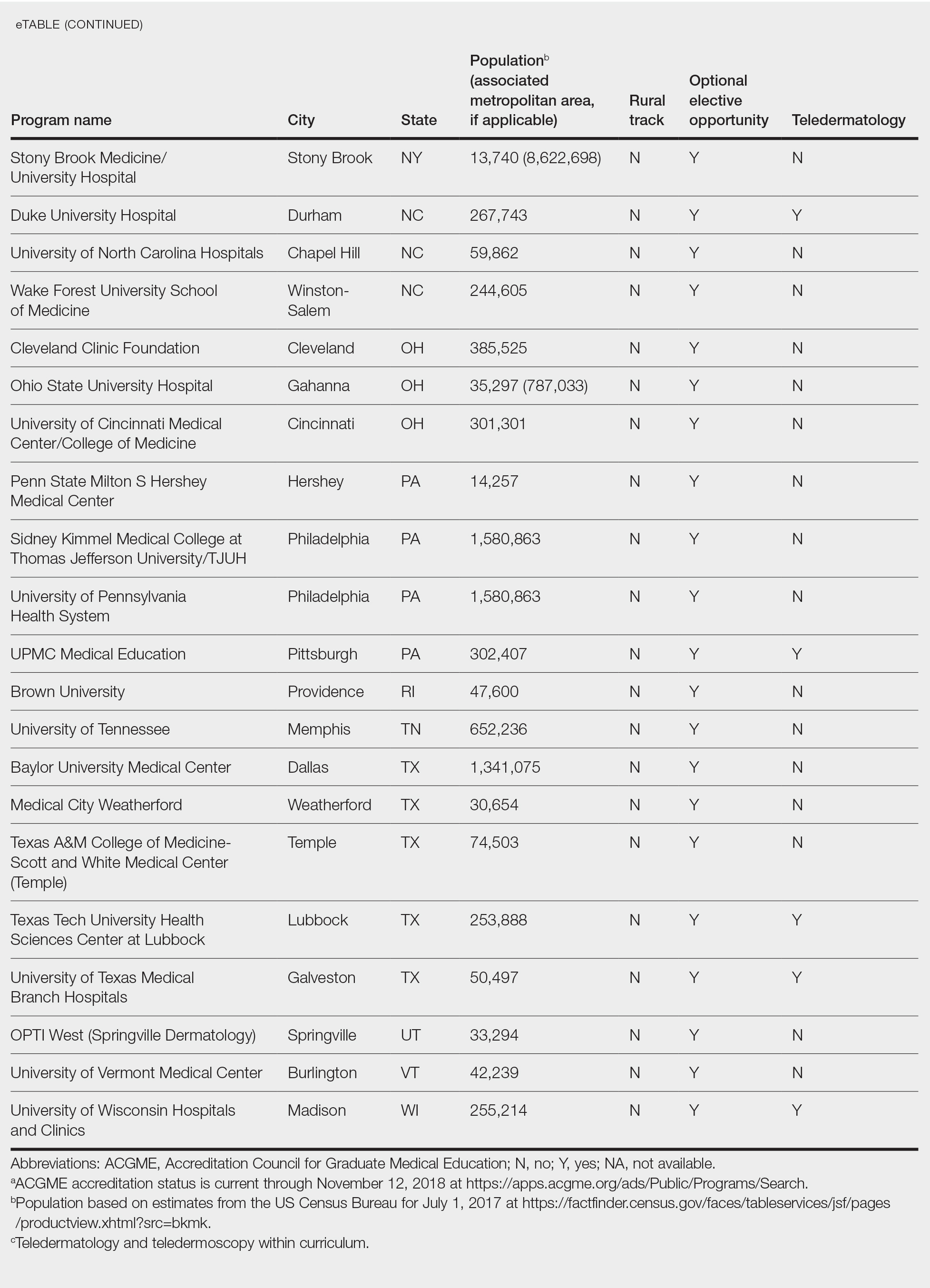
Results
Of 154 dermatology residency programs identified in the United States and Puerto Rico, 142 were accredited at the time of data collection. Fifteen (10%) were based in communities of 50,000 individuals or fewer that were not near a large metropolitan area. One program (<1%) offered a specific rural track. Fifty-six programs (39%) cited optional rotations or clinical electives, or both, that could be utilized for a rural experience. Eighteen (12%) offered teledermatology experiences and 1 (<1%) offered teledermoscopy during training. Fifty-three programs (37%) offered a rotation at a VHA hospital that had an active teledermatology service.
Comment
Program websites are a free and easily accessible means of acquiring relevant information. The paucity of readily available data on rural dermatology and teledermatology opportunities is unfortunate and a detriment to dermatology residency applicants interested in rural practice, which may result in a missed opportunity to foster a true passion for rural medicine. A brief comment on a website can be impactful, leading to a postgraduate year 4 dermatology elective rotation at a prospective fellowship training site or a rural dermatology experience.
The paucity of dermatologists working directly in rural areas has led to development of teledermatology initiatives to reach deeply into underserved regions. One of the largest providers of teledermatology is the VHA, which standardized its teledermatology efforts in 2012 and provides remarkable educational opportunities for dermatology residents. However, many residency program and VHA websites provide no information about the participation of dermatology residents in the provision of teledermatology services.
A limitation of this study is that it is based on online published curricula. Dermatology residency programs with excellent rural curricula that are not published online might exist.
Residency program directors with an interest in geographic diversity are encouraged to provide rural and teledermatology opportunities and to update these offerings on their websites, which is a simple modifiable strategy that can impact the rural dermatology care gap by recruiting students interested in filling this role. These efforts should be studied to determine whether this strategy impacts resident selection as well as whether focused rural and telemedicine exposure during training increases the likelihood of establishing a rural dermatology practice in the future.
- American Academy of Dermatology. Position statement on access to specialty care and direct access to dermatologic care. Revised May 20, 2017. Accessed December 13, 2020. https://server.aad.org/forms/Policies/Uploads/PS/PS-Access%20to%20Specialty%20Care%20and%20Direct%20Access%20to%20Dermatologic%20Care.pdf
- Dill MJ, Salsberg ES. The Complexities of Physician Supply and Demand: Projections Through 2025. Center for Workforce Studies, Association of American Medical Colleges (AAMC); November 2008. Accessed December 13, 2020. http://innovationlabs.com/pa_future/1/background_docs/AAMC%20Complexities%20of%20physician%20demand,%202008.pdf
- Glazer AM, Rigel DS. Analysis of trends in geographic distribution of US dermatology workforce density. JAMA Dermatol. 2017;153:472-473.
- Yoo JY, Rigel DS. Trends in dermatology: geographic density of US dermatologists. Arch Dermatol. 2010;146:779.
- Feng H, Berk-Krauss J, Feng PW, et al. Comparison of dermatologist density between urban and rural counties in the United States. JAMA Dermatol. 2018;154:1265-1271.
- Landow SM, Oh DH, Weinstock MA. Teledermatology within the Veterans Health Administration, 2002-2014. Telemed J E Health. 2015;21:769-773.
- Armstrong AW, Kwong MW, Ledo L, et al. Practice models and challenges in teledermatology: a study of collective experiences from teledermatologists. PloS One. 2011;6:e28687.
- Lewis H, Becevic M, Myers D, et al. Dermatology ECHO—an innovative solution to address limited access to dermatology expertise. Rural Remote Health. 2018;18:4415.
- Edison KE, Dyer JA, Whited JD, et al. Practice gaps. the barriers and the promise of teledermatology. JAMA Dermatol. 2012:148:650-651.
To the Editor:
There is an irrefutable trend toward urban dermatology practice in the United States, leading to growing problems with rural access to care. The provision of rural clinical experiences and telehealth in dermatology residency training might increase the likelihood of trainees establishing a rural practice.
In 2017, the American Academy of Dermatology released an updated statement supporting direct patient access to board-certified dermatologists in an effort to reduce morbidity and mortality associated with skin disease.1 Twenty percent of the US population lives in a rural and medically underserved location, yet these areas remain largely underserved, in part because of an irrefutable trend toward urban dermatology practice.2-4 Successful approaches to improving rural access to dermatology care are poorly defined in the literature.
Several variables have been shown to influence a young physician’s decision to establish a clinical practice in geographically isolated areas, including rural upbringing, longitudinal rural clinical experiences during medical training, and family influences.5 Location of residency training is an additional variable that impacts practice location, though migration following dermatology residency is a complex phenomenon. However, training location does not guarantee retention of dermatology graduates in any particular geographic area.6 Practice incentives and stipends might encourage rural dermatology practice, yet these programs are underfunded. Last, telemedicine in dermatology (including teledermatology and teledermoscopy), though not always an ideal substitute for a live visit, can improve access to care in geographically isolated or underserved areas in general.7-9
Focused recruitment of medical students interested in rural dermatology practice to accredited dermatology residency programs aligned with this goal represents another approach to improve geographic diversity in the field of dermatology. Online access to this information would be useful for both applicants and their mentors.
We assessed viewable online curricula related to rural dermatology and telemedicine experiences at all Accreditation Council for Graduate Medical Education (ACGME)–accredited residency programs. Telemedicine experiences at Veterans Health Administration (VHA) health systems also were assessed.
Methods
This study was exempt from review by the institutional review board at the University of Minnesota (Minneapolis, Minnesota)(IRB #STUDY00004915) because no human subjects were involved. Online curricula of all ACGME-accredited dermatology residency programs in the United States and Puerto Rico were reviewed from November to December 2018. The following information was recorded: specialized “rural-track” training; optional elective time in rural settings; teledermatology training; and teledermoscopy training.
Additionally, population density at each program’s primary location was determined using US Census Bureau data and with consideration to communities contained within particular Metropolitan Statistical Areas (MSAs)(eTable). Data were obtained from the VHA system to assess teledermatology services at VHA locations affiliated with residency programs.
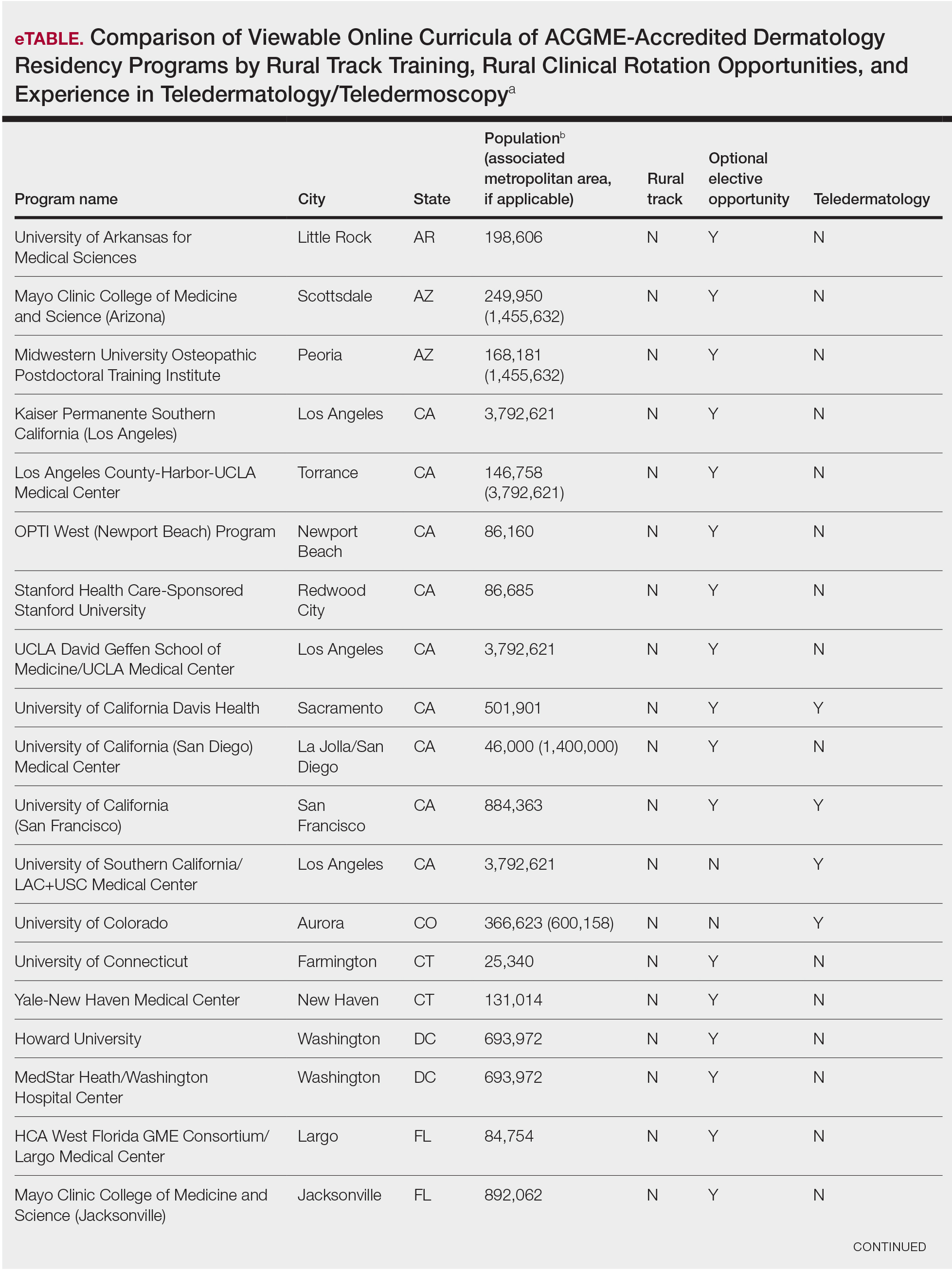
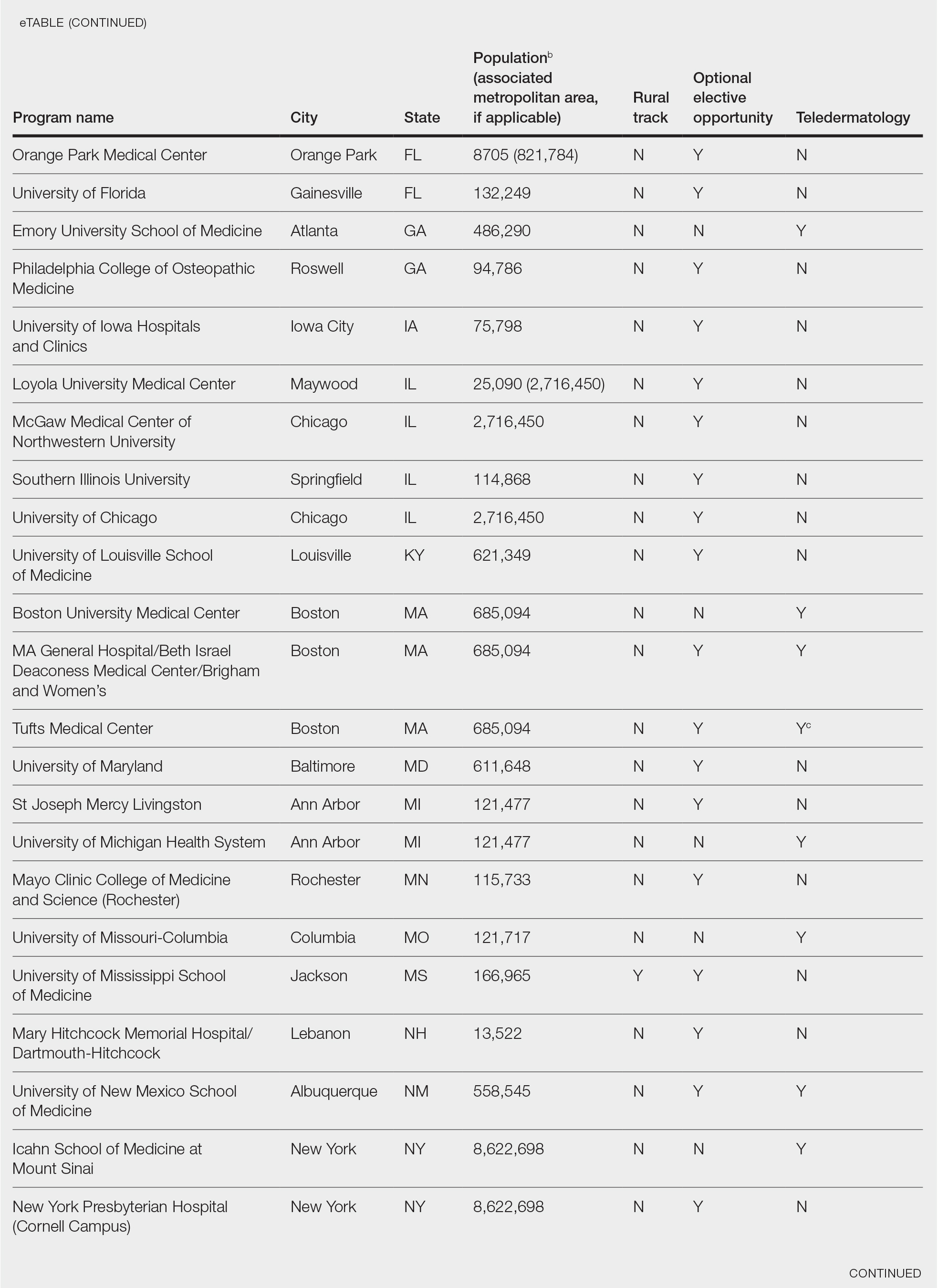
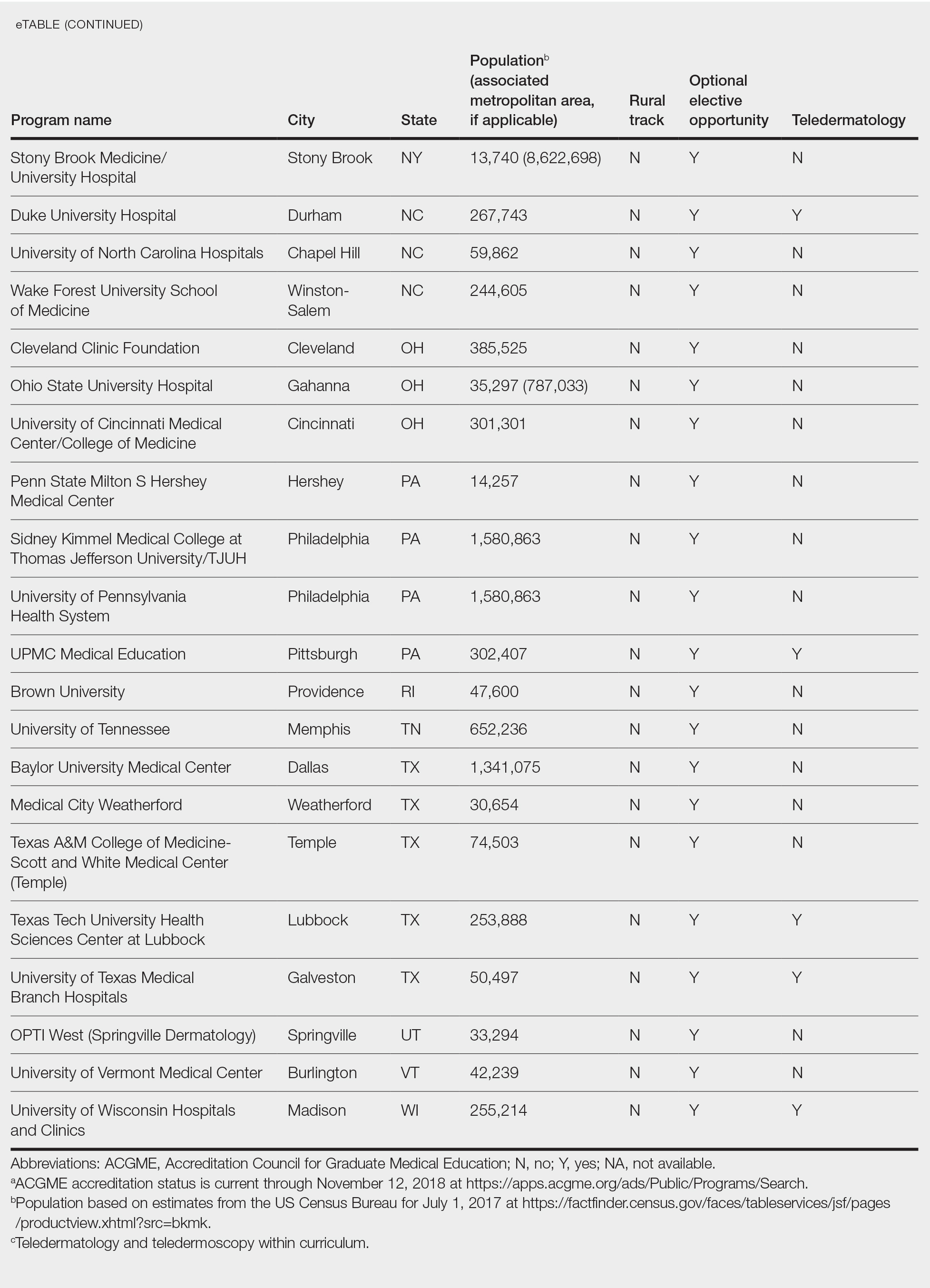
Results
Of 154 dermatology residency programs identified in the United States and Puerto Rico, 142 were accredited at the time of data collection. Fifteen (10%) were based in communities of 50,000 individuals or fewer that were not near a large metropolitan area. One program (<1%) offered a specific rural track. Fifty-six programs (39%) cited optional rotations or clinical electives, or both, that could be utilized for a rural experience. Eighteen (12%) offered teledermatology experiences and 1 (<1%) offered teledermoscopy during training. Fifty-three programs (37%) offered a rotation at a VHA hospital that had an active teledermatology service.
Comment
Program websites are a free and easily accessible means of acquiring relevant information. The paucity of readily available data on rural dermatology and teledermatology opportunities is unfortunate and a detriment to dermatology residency applicants interested in rural practice, which may result in a missed opportunity to foster a true passion for rural medicine. A brief comment on a website can be impactful, leading to a postgraduate year 4 dermatology elective rotation at a prospective fellowship training site or a rural dermatology experience.
The paucity of dermatologists working directly in rural areas has led to development of teledermatology initiatives to reach deeply into underserved regions. One of the largest providers of teledermatology is the VHA, which standardized its teledermatology efforts in 2012 and provides remarkable educational opportunities for dermatology residents. However, many residency program and VHA websites provide no information about the participation of dermatology residents in the provision of teledermatology services.
A limitation of this study is that it is based on online published curricula. Dermatology residency programs with excellent rural curricula that are not published online might exist.
Residency program directors with an interest in geographic diversity are encouraged to provide rural and teledermatology opportunities and to update these offerings on their websites, which is a simple modifiable strategy that can impact the rural dermatology care gap by recruiting students interested in filling this role. These efforts should be studied to determine whether this strategy impacts resident selection as well as whether focused rural and telemedicine exposure during training increases the likelihood of establishing a rural dermatology practice in the future.
To the Editor:
There is an irrefutable trend toward urban dermatology practice in the United States, leading to growing problems with rural access to care. The provision of rural clinical experiences and telehealth in dermatology residency training might increase the likelihood of trainees establishing a rural practice.
In 2017, the American Academy of Dermatology released an updated statement supporting direct patient access to board-certified dermatologists in an effort to reduce morbidity and mortality associated with skin disease.1 Twenty percent of the US population lives in a rural and medically underserved location, yet these areas remain largely underserved, in part because of an irrefutable trend toward urban dermatology practice.2-4 Successful approaches to improving rural access to dermatology care are poorly defined in the literature.
Several variables have been shown to influence a young physician’s decision to establish a clinical practice in geographically isolated areas, including rural upbringing, longitudinal rural clinical experiences during medical training, and family influences.5 Location of residency training is an additional variable that impacts practice location, though migration following dermatology residency is a complex phenomenon. However, training location does not guarantee retention of dermatology graduates in any particular geographic area.6 Practice incentives and stipends might encourage rural dermatology practice, yet these programs are underfunded. Last, telemedicine in dermatology (including teledermatology and teledermoscopy), though not always an ideal substitute for a live visit, can improve access to care in geographically isolated or underserved areas in general.7-9
Focused recruitment of medical students interested in rural dermatology practice to accredited dermatology residency programs aligned with this goal represents another approach to improve geographic diversity in the field of dermatology. Online access to this information would be useful for both applicants and their mentors.
We assessed viewable online curricula related to rural dermatology and telemedicine experiences at all Accreditation Council for Graduate Medical Education (ACGME)–accredited residency programs. Telemedicine experiences at Veterans Health Administration (VHA) health systems also were assessed.
Methods
This study was exempt from review by the institutional review board at the University of Minnesota (Minneapolis, Minnesota)(IRB #STUDY00004915) because no human subjects were involved. Online curricula of all ACGME-accredited dermatology residency programs in the United States and Puerto Rico were reviewed from November to December 2018. The following information was recorded: specialized “rural-track” training; optional elective time in rural settings; teledermatology training; and teledermoscopy training.
Additionally, population density at each program’s primary location was determined using US Census Bureau data and with consideration to communities contained within particular Metropolitan Statistical Areas (MSAs)(eTable). Data were obtained from the VHA system to assess teledermatology services at VHA locations affiliated with residency programs.
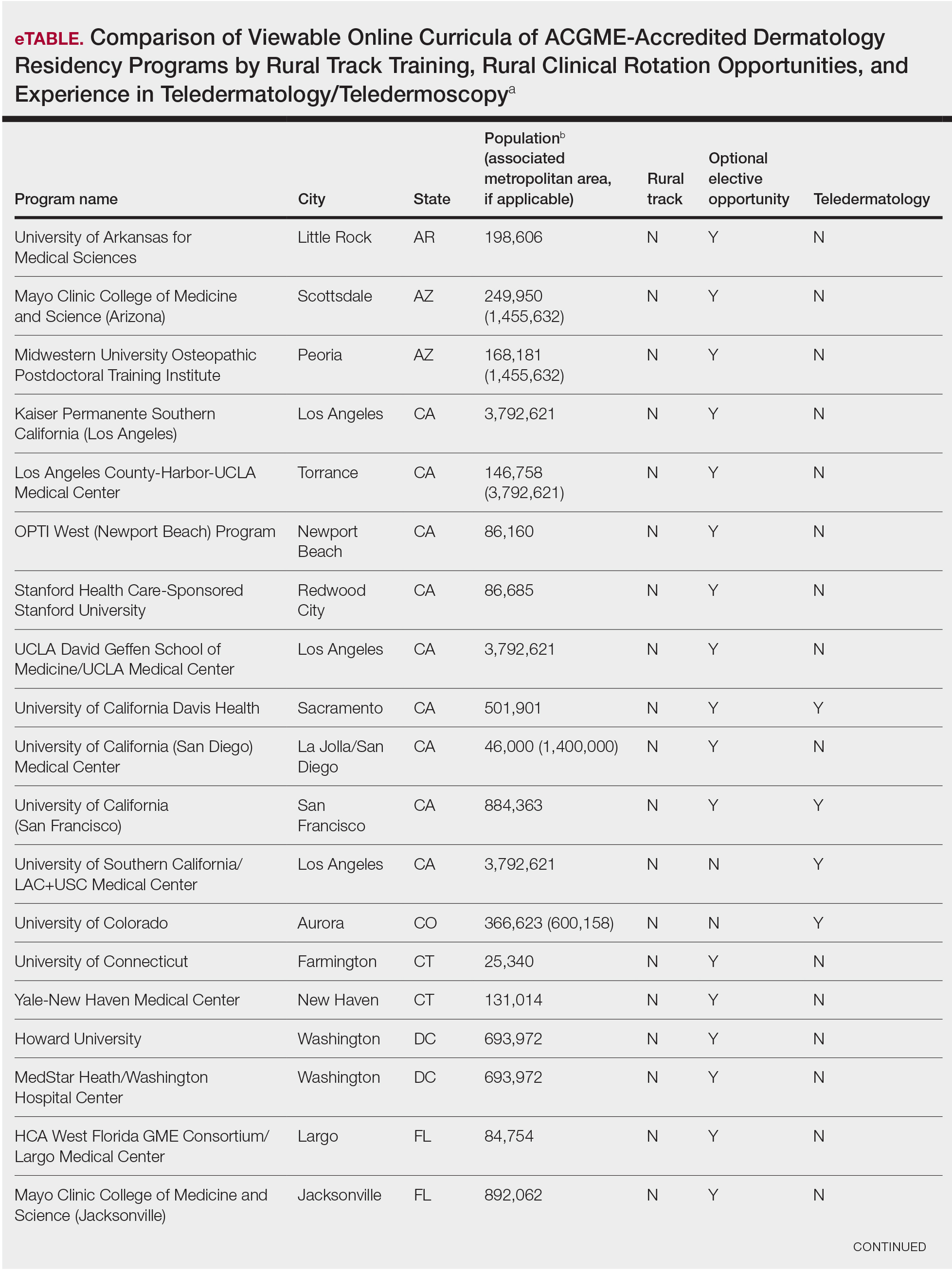
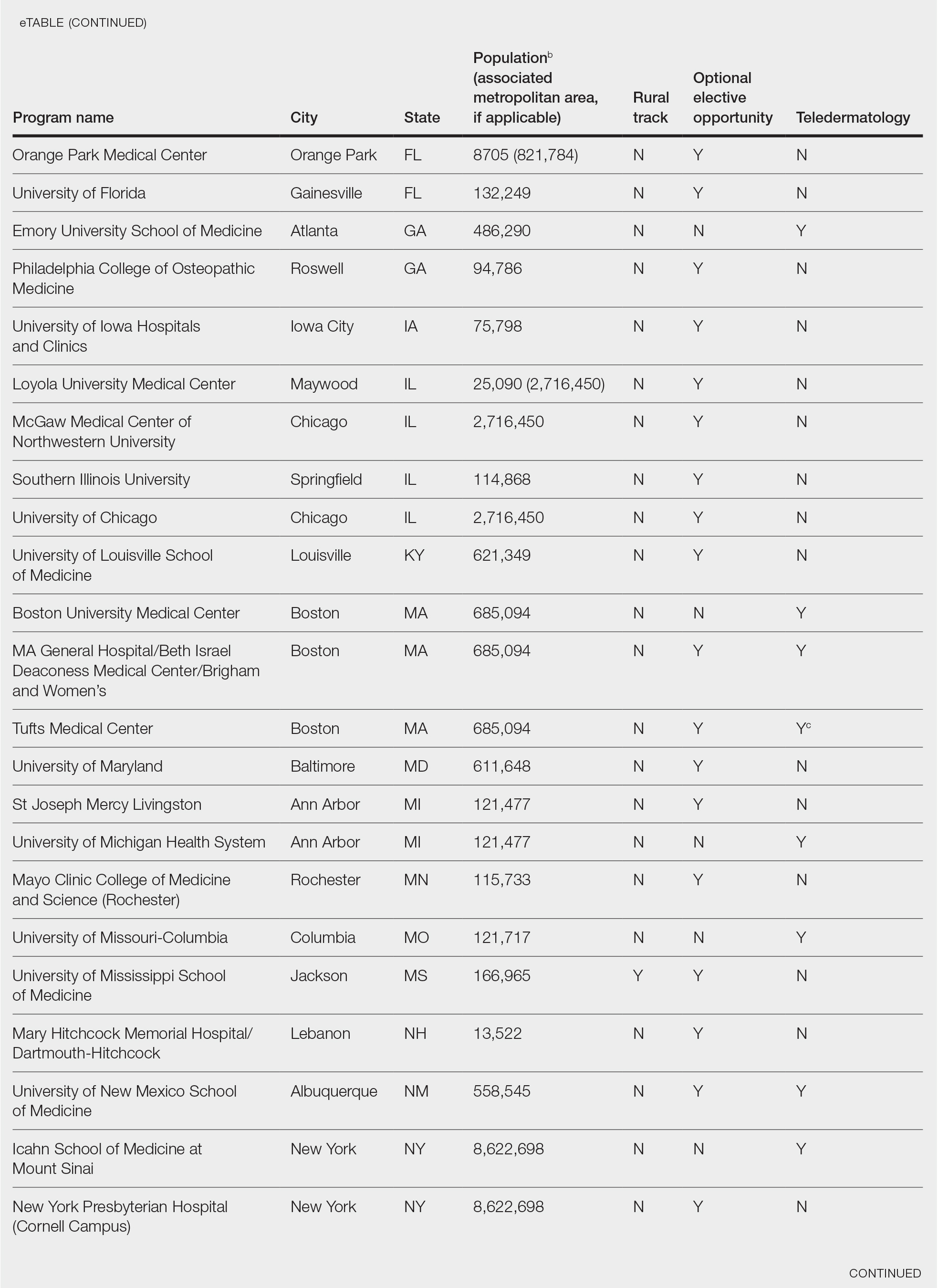
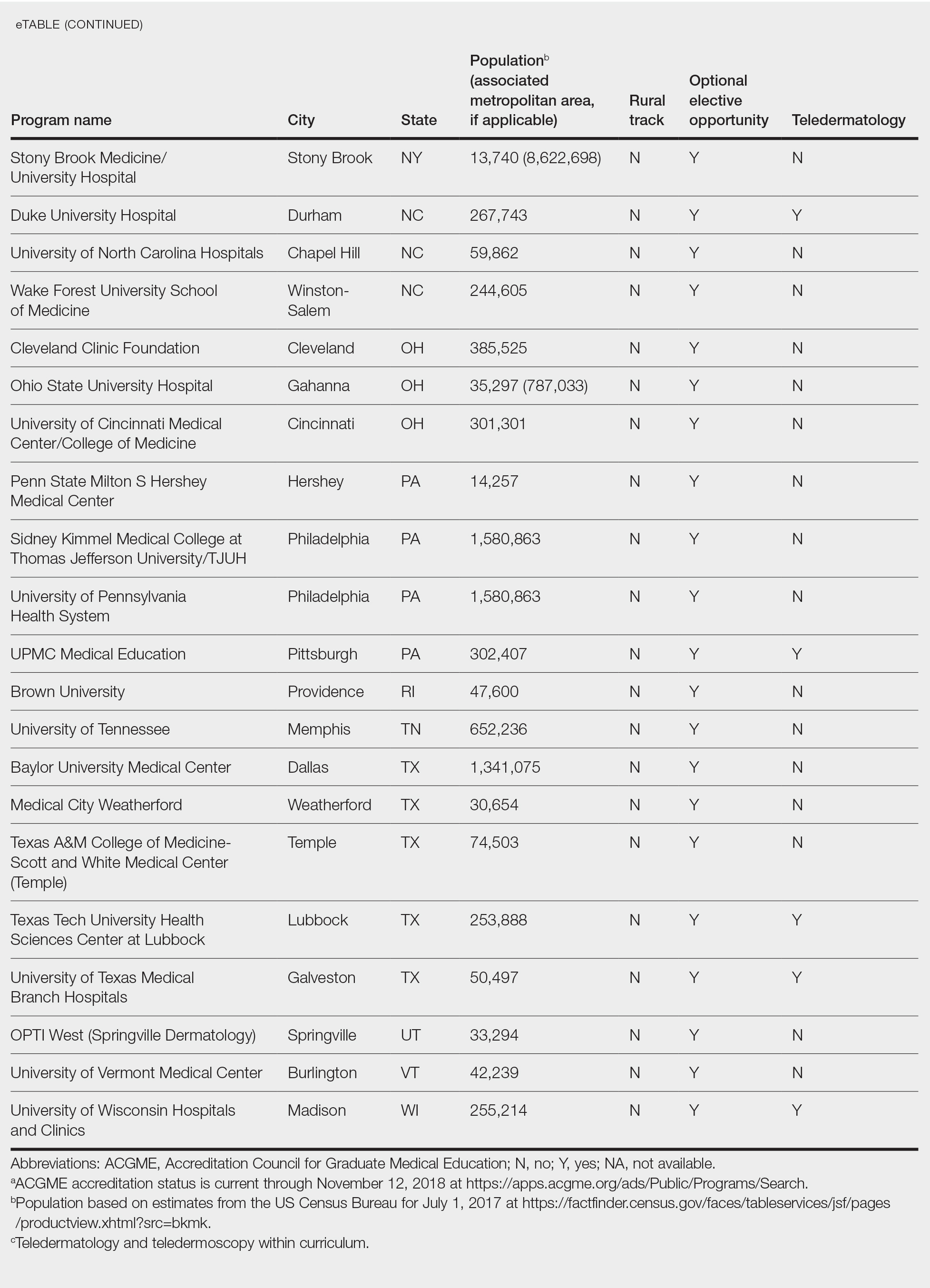
Results
Of 154 dermatology residency programs identified in the United States and Puerto Rico, 142 were accredited at the time of data collection. Fifteen (10%) were based in communities of 50,000 individuals or fewer that were not near a large metropolitan area. One program (<1%) offered a specific rural track. Fifty-six programs (39%) cited optional rotations or clinical electives, or both, that could be utilized for a rural experience. Eighteen (12%) offered teledermatology experiences and 1 (<1%) offered teledermoscopy during training. Fifty-three programs (37%) offered a rotation at a VHA hospital that had an active teledermatology service.
Comment
Program websites are a free and easily accessible means of acquiring relevant information. The paucity of readily available data on rural dermatology and teledermatology opportunities is unfortunate and a detriment to dermatology residency applicants interested in rural practice, which may result in a missed opportunity to foster a true passion for rural medicine. A brief comment on a website can be impactful, leading to a postgraduate year 4 dermatology elective rotation at a prospective fellowship training site or a rural dermatology experience.
The paucity of dermatologists working directly in rural areas has led to development of teledermatology initiatives to reach deeply into underserved regions. One of the largest providers of teledermatology is the VHA, which standardized its teledermatology efforts in 2012 and provides remarkable educational opportunities for dermatology residents. However, many residency program and VHA websites provide no information about the participation of dermatology residents in the provision of teledermatology services.
A limitation of this study is that it is based on online published curricula. Dermatology residency programs with excellent rural curricula that are not published online might exist.
Residency program directors with an interest in geographic diversity are encouraged to provide rural and teledermatology opportunities and to update these offerings on their websites, which is a simple modifiable strategy that can impact the rural dermatology care gap by recruiting students interested in filling this role. These efforts should be studied to determine whether this strategy impacts resident selection as well as whether focused rural and telemedicine exposure during training increases the likelihood of establishing a rural dermatology practice in the future.
- American Academy of Dermatology. Position statement on access to specialty care and direct access to dermatologic care. Revised May 20, 2017. Accessed December 13, 2020. https://server.aad.org/forms/Policies/Uploads/PS/PS-Access%20to%20Specialty%20Care%20and%20Direct%20Access%20to%20Dermatologic%20Care.pdf
- Dill MJ, Salsberg ES. The Complexities of Physician Supply and Demand: Projections Through 2025. Center for Workforce Studies, Association of American Medical Colleges (AAMC); November 2008. Accessed December 13, 2020. http://innovationlabs.com/pa_future/1/background_docs/AAMC%20Complexities%20of%20physician%20demand,%202008.pdf
- Glazer AM, Rigel DS. Analysis of trends in geographic distribution of US dermatology workforce density. JAMA Dermatol. 2017;153:472-473.
- Yoo JY, Rigel DS. Trends in dermatology: geographic density of US dermatologists. Arch Dermatol. 2010;146:779.
- Feng H, Berk-Krauss J, Feng PW, et al. Comparison of dermatologist density between urban and rural counties in the United States. JAMA Dermatol. 2018;154:1265-1271.
- Landow SM, Oh DH, Weinstock MA. Teledermatology within the Veterans Health Administration, 2002-2014. Telemed J E Health. 2015;21:769-773.
- Armstrong AW, Kwong MW, Ledo L, et al. Practice models and challenges in teledermatology: a study of collective experiences from teledermatologists. PloS One. 2011;6:e28687.
- Lewis H, Becevic M, Myers D, et al. Dermatology ECHO—an innovative solution to address limited access to dermatology expertise. Rural Remote Health. 2018;18:4415.
- Edison KE, Dyer JA, Whited JD, et al. Practice gaps. the barriers and the promise of teledermatology. JAMA Dermatol. 2012:148:650-651.
- American Academy of Dermatology. Position statement on access to specialty care and direct access to dermatologic care. Revised May 20, 2017. Accessed December 13, 2020. https://server.aad.org/forms/Policies/Uploads/PS/PS-Access%20to%20Specialty%20Care%20and%20Direct%20Access%20to%20Dermatologic%20Care.pdf
- Dill MJ, Salsberg ES. The Complexities of Physician Supply and Demand: Projections Through 2025. Center for Workforce Studies, Association of American Medical Colleges (AAMC); November 2008. Accessed December 13, 2020. http://innovationlabs.com/pa_future/1/background_docs/AAMC%20Complexities%20of%20physician%20demand,%202008.pdf
- Glazer AM, Rigel DS. Analysis of trends in geographic distribution of US dermatology workforce density. JAMA Dermatol. 2017;153:472-473.
- Yoo JY, Rigel DS. Trends in dermatology: geographic density of US dermatologists. Arch Dermatol. 2010;146:779.
- Feng H, Berk-Krauss J, Feng PW, et al. Comparison of dermatologist density between urban and rural counties in the United States. JAMA Dermatol. 2018;154:1265-1271.
- Landow SM, Oh DH, Weinstock MA. Teledermatology within the Veterans Health Administration, 2002-2014. Telemed J E Health. 2015;21:769-773.
- Armstrong AW, Kwong MW, Ledo L, et al. Practice models and challenges in teledermatology: a study of collective experiences from teledermatologists. PloS One. 2011;6:e28687.
- Lewis H, Becevic M, Myers D, et al. Dermatology ECHO—an innovative solution to address limited access to dermatology expertise. Rural Remote Health. 2018;18:4415.
- Edison KE, Dyer JA, Whited JD, et al. Practice gaps. the barriers and the promise of teledermatology. JAMA Dermatol. 2012:148:650-651.
Practice Points
- Access to dermatologic care in rural areas is a growing problem.
- Dermatology residency programs can influence medical students and resident dermatologists to provide care in rural and geographically isolated areas.
- Presenting detailed curricula that impact access to care on residency program websites could attract applicants with these career goals.
Racism in medicine: Implicit and explicit
With the shootings of Breonna Taylor, George Floyd, and other Black citizens setting off protests and unrest, race was at the forefront of national conversation in the United States – along with COVID-19 – over the past year.
“We’ve heard things like, ‘We’re in a post-racial society,’ but I think 2020 in particular has emphasized that we’re not,” said Gregory Johnson, MD, SFHM, chief medical officer of hospital medicine at Sound Physicians, a national physician practice. “Racism is very present in our lives, it’s very present in our world, and it is absolutely present in medicine.”
Yes, race is still an issue in the U.S. as we head into 2021, though this may have come as something of a surprise to people who do not live with racism daily.
“If you have a brain, you have bias, and that bias will likely apply to race as well,” Dr. Johnson said. “When we’re talking about institutional racism, the educational system and the media have led us to create presumptions and prejudices that we don’t necessarily recognize off the top because they’ve just been a part of the fabric of who we are as we’ve grown up.”
The term “racism” has extremely negative connotations because there’s character judgment attached to it, but to say someone is racist or racially insensitive does not equate them with being a Klansman, said Dr. Johnson. “I think we as people have to acknowledge that, yes, it’s possible for me to be racist and I might not be 100% aware of it. It’s being open to the possibility – or rather probability – that you are and then taking steps to figure out how you can address that, so you can limit it. And that requires constant self-evaluation and work,” he said.
Racism in the medical environment
Institutional racism is evident before students are even accepted into medical school, said Areeba Kara, MD, SFHM, associate professor of clinical medicine at Indiana University, Indianapolis, and a hospitalist at IU Health Physicians.
Mean MCAT scores are lower for applicants traditionally underrepresented in medicine (UIM) compared to the scores of well-represented groups.1 “Lower scores are associated with lower acceptance rates into medical school,” Dr. Kara said. “These differences reflect unequal educational opportunities rooted in centuries of legal discrimination.”
Racism is apparent in both the hidden medical education curriculum and in lessons implicitly taught to students, said Ndidi Unaka, MD, MEd, associate program director of the pediatric residency training program at Cincinnati Children’s Hospital.
“These lessons inform the way in which we as physicians see our patients, each other, and how we practice,” she said. “We reinforce race-based medicine and shape clinical decision making through flawed guidelines and practices, which exacerbates health inequities. We teach that race – rather than racism – is a risk factor for poor health outcomes. Our students and trainees watch as we assume the worst of our patients from marginalized communities of color.”
Terms describing patients of color, such as “difficult,” “non-compliant,” or “frequent flyer” are thrown around and sometimes, instead of finding out why, “we view these states of being as static, root causes for poor outcomes rather than symptoms of social conditions and obstacles that impact overall health and wellbeing,” Dr. Unaka said.
Leadership opportunities
Though hospital medicine is a growing field, Dr. Kara noted that the 2020 State of Hospital Medicine Report found that only 5.5% of hospital medical group leaders were Black, and just 2.2% were Hispanic/Latino.2 “I think these numbers speak for themselves,” she said.
Dr. Unaka said that the lack of UIM hospitalists and physician leaders creates fewer opportunities for “race-concordant mentorship relationships.” It also forces UIM physicians to shoulder more responsibilities – often obligations that do little to help them move forward in their careers – all in the name of diversity. And when UIM physicians are given leadership opportunities, Dr. Unaka said they are often unsure as to whether their appointments are genuine or just a hollow gesture made for the sake of diversity.
Dr. Johnson pointed out that Black and Latinx populations primarily get their care from hospital-based specialties, yet this is not reflected in the number of UIM practitioners in leadership roles. He said race and ethnicity, as well as gender, need to be factors when individuals are evaluated for leadership opportunities – for the individual’s sake, as well as for the community he or she is serving.
“When we can evaluate for unconscious bias and factor in that diverse groups tend to have better outcomes, whether it’s business or clinical outcomes, it’s one of the opportunities that we collectively have in the specialty to improve what we’re delivering for hospitals and, more importantly, for patients,” he said.
Relationships with colleagues and patients
Racism creeps into interactions and relationships with others as well, whether it’s between clinicians, clinician to patient, or patient to clinician. Sometimes it’s blatant; often it’s subtle.
A common, recurring example Dr. Unaka has experienced in the clinician to clinician relationship is being confused for other Black physicians, making her feel invisible. “The everyday verbal, nonverbal, and environmental slights, snubs, or insults from colleagues are frequent and contribute to feelings of exclusion, isolation, and exhaustion,” she said. Despite this, she is still expected to “address microaggressions and other forms of interpersonal racism and find ways to move through professional spaces in spite of the trauma, fear, and stress associated with my reality and lived experiences.” She said that clinicians who remain silent on the topic of racism participate in the violence and contribute to the disillusionment of UIM physicians.
Dr. Kara said that the discrimination from the health care team is the hardest to deal with. In the clinician to clinician relationship, there is a sense among UIM physicians that they’re being watched more closely and “have to prove themselves at every single turn.” Unfortunately, this comes from the environment, which tends to be adversarial rather than supportive and nurturing, she said.
“There are lots of opportunities for racism or racial insensitivity to crop up from clinician to clinician,” said Dr. Johnson. When he started his career as a physician after his training, Dr. Johnson was informed that his colleagues were watching him because they were not sure about his clinical skills. The fact that he was a former chief resident and board certified in two specialties did not seem to make any difference.
Patients refusing care from UIM physicians or expressing disapproval – both verbal and nonverbal – of such care, happens all too often. “It’s easier for me to excuse patients and their families as we often meet them on their worst days,” said Dr. Kara. Still, “understanding my oath to care for people and do no harm, but at the same time, recognizing that this is an individual that is rejecting my care without having any idea of who I am as a physician is frustrating,” Dr. Johnson acknowledged.
Then there’s the complex clinician to patient relationship, which research clearly shows contributes to health disparities.3 For one thing, the physician workforce does not reflect the patient population, Dr. Unaka said. “We cannot ignore the lack of race concordance between patients and clinicians, nor can the continued misplacement of blame for medical mistrust be at the feet of our patients,” she said.
Dr. Unaka feels that clinicians need to accept both that health inequities exist and that frontline physicians themselves contribute to the inequities. “Our diagnostic and therapeutic decisions are not immune to bias and are influenced by our deeply held beliefs about specific populations,” she said. “And the health care system that our patients navigate is no different than other systems, settings, and environments that are marred by racism in all its forms.”
Systemic racism greatly impacts patient care, said Dr. Kara. She pointed to several examples: Research showing that race concordance between patients and providers in an emergency department setting led to better pain control with fewer analgesics.4 The high maternal and infant mortality rates amongst Black women and children.5 Evidence of poorer outcomes in sepsis patients with limited English proficiency.6 “There are plenty more,” she said. “We need to be asking ourselves what we are going to do about it.”
Moving forward
That racial biases are steeped so thoroughly into our culture and consciousness means that moving beyond them is a continual, purposeful work in progress. But it is work that is critical for everyone, and certainly necessary for those who care for their fellow human beings when they are in a vulnerable state.
Health care systems need to move toward equity – giving everyone what they need to thrive – rather than focusing on equality – giving everyone the same thing, said Jenny Baenziger, MD, assistant professor of clinical medicine and pediatrics at Indiana University, Indianapolis, and associate director of education at IU Center for Global Health. “We know that minoritized patients are going to need more attention, more advocacy, more sensitivity, and more creative solutions in order to help them achieve health in a world that is often stacked against them,” she said.
“The unique needs of each patient, family unit, and/or population must be taken into consideration,” said Dr. Unaka. She said hospitalists need to embrace creative approaches that can better serve the specific needs of patients. Equitable practices should be the default, which means data transparency, thoroughly dissecting hospital processes to find existing inequities, giving stakeholders – especially patients and families of color – a voice, and tearing down oppressive systems that contribute to poor health outcomes and oppression, she said.
“It’s time for us to talk about racism openly,” said Dr. Kara. “Believe your colleagues when they share their fears and treat each other with respect. We should be actively learning about and celebrating our diversity.” She encourages finding out what your institution is doing on this front and getting involved.
Dr. Johnson believes that first and foremost, hospitalists need to be exposed to the data on health care disparities. “The next step is asking what we as hospitalists, or any other specialty, can do to intervene and improve in those areas,” he said. Focusing on unconscious bias training is important, he said, so clinicians can see what biases they might be bringing into the hospital and to the bedside. Maintaining a diverse workforce and bringing UIM physicians into leadership roles to encourage diversity of ideas and approaches are also critical to promoting equity, he said.
“You cannot fix what you cannot face,” said Dr. Unaka. Education on how racism impacts patients and colleagues is essential, she believes, as is advocacy for changing inequitable health system policies. She recommends expanding social and professional circles. “Diverse social groups allow us to consider the perspectives of others; diverse professional groups allow us to ask better research questions and practice better medicine.”
Start by developing the ability to question personal assumptions and pinpoint implicit biases, suggested Dr. Baenziger. “Asking for feedback can be scary and difficult, but we should take a deep breath and do it anyway,” she said. “Simply ask your team, ‘I’ve been thinking a lot about racial equity and disparities. How can I do better at my interactions with people of color? What are my blind spots?’” Dr. Baenziger said that “to help us remember how beautifully complicated and diverse people are,” all health care professionals need to watch Nigerian novelist Chimamanda Ngozi Adichie’s TED talk “The Danger of a Single Story.”
Dr. Baenziger also stressed the importance of conversations about “places where race is built into our clinical assessments, like eGFR,” as well as being aware that many of the research studies that are used to support everyday clinical decisions didn’t include people of color. She also encouraged clinicians to consider how and when they include race in their notes.7 “Is it really helpful to make sure people know right away that you are treating a ‘46-year-old Hispanic male’ or can the fact that he is Hispanic be saved for the social history section with other important details of his life such as being a father, veteran, and mechanic?” she asked.
“Racism is real and very much a part of our history. We can no longer be in denial regarding the racism that exists in medicine and the impact it has on our patients,” Dr. Unaka said. “As a profession, we cannot hide behind our espoused core values. We must live up to them.”
References
1. Lucey CR, Saguil, A. The Consequences of Structural Racism on MCAT Scores and Medical School Admissions: The Past Is Prologue. Acad Med. 2020 Mar;95(3):351-356. doi: 10.1097/ACM.0000000000002939.
2. Flores L. Increasing racial diversity in hospital medicine’s leadership ranks. The Hospitalist. 2020 Oct 21.
3. Smedley BD, et al, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Institute of Medicine Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Washington: National Academies Press; 2003.
4. Heins A, et al. Physician Race/Ethnicity Predicts Successful Emergency Department Analgesia. J Pain. 2010 July;11(7):692-697. doi: 10.1016/j.jpain.2009.10.017.
5. U.S. Department of Health and Human Serves, Office of Minority Health. Infant Mortality and African Americans. 2019 Nov 8. minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=23.
6. Jacobs ZG, et al. The Association between Limited English Proficiency and Sepsis Mortality. J Hosp Med. 2020;3;140-146. Published Online First 2019 Nov 20. doi:10.12788/jhm.3334.
7. Finucane TE. Mention of a Patient’s “Race” in Clinical Presentations. Virtual Mentor. 2014;16(6):423-427. doi: 10.1001/virtualmentor.2014.16.6.ecas1-1406.
With the shootings of Breonna Taylor, George Floyd, and other Black citizens setting off protests and unrest, race was at the forefront of national conversation in the United States – along with COVID-19 – over the past year.
“We’ve heard things like, ‘We’re in a post-racial society,’ but I think 2020 in particular has emphasized that we’re not,” said Gregory Johnson, MD, SFHM, chief medical officer of hospital medicine at Sound Physicians, a national physician practice. “Racism is very present in our lives, it’s very present in our world, and it is absolutely present in medicine.”
Yes, race is still an issue in the U.S. as we head into 2021, though this may have come as something of a surprise to people who do not live with racism daily.
“If you have a brain, you have bias, and that bias will likely apply to race as well,” Dr. Johnson said. “When we’re talking about institutional racism, the educational system and the media have led us to create presumptions and prejudices that we don’t necessarily recognize off the top because they’ve just been a part of the fabric of who we are as we’ve grown up.”
The term “racism” has extremely negative connotations because there’s character judgment attached to it, but to say someone is racist or racially insensitive does not equate them with being a Klansman, said Dr. Johnson. “I think we as people have to acknowledge that, yes, it’s possible for me to be racist and I might not be 100% aware of it. It’s being open to the possibility – or rather probability – that you are and then taking steps to figure out how you can address that, so you can limit it. And that requires constant self-evaluation and work,” he said.
Racism in the medical environment
Institutional racism is evident before students are even accepted into medical school, said Areeba Kara, MD, SFHM, associate professor of clinical medicine at Indiana University, Indianapolis, and a hospitalist at IU Health Physicians.
Mean MCAT scores are lower for applicants traditionally underrepresented in medicine (UIM) compared to the scores of well-represented groups.1 “Lower scores are associated with lower acceptance rates into medical school,” Dr. Kara said. “These differences reflect unequal educational opportunities rooted in centuries of legal discrimination.”
Racism is apparent in both the hidden medical education curriculum and in lessons implicitly taught to students, said Ndidi Unaka, MD, MEd, associate program director of the pediatric residency training program at Cincinnati Children’s Hospital.
“These lessons inform the way in which we as physicians see our patients, each other, and how we practice,” she said. “We reinforce race-based medicine and shape clinical decision making through flawed guidelines and practices, which exacerbates health inequities. We teach that race – rather than racism – is a risk factor for poor health outcomes. Our students and trainees watch as we assume the worst of our patients from marginalized communities of color.”
Terms describing patients of color, such as “difficult,” “non-compliant,” or “frequent flyer” are thrown around and sometimes, instead of finding out why, “we view these states of being as static, root causes for poor outcomes rather than symptoms of social conditions and obstacles that impact overall health and wellbeing,” Dr. Unaka said.
Leadership opportunities
Though hospital medicine is a growing field, Dr. Kara noted that the 2020 State of Hospital Medicine Report found that only 5.5% of hospital medical group leaders were Black, and just 2.2% were Hispanic/Latino.2 “I think these numbers speak for themselves,” she said.
Dr. Unaka said that the lack of UIM hospitalists and physician leaders creates fewer opportunities for “race-concordant mentorship relationships.” It also forces UIM physicians to shoulder more responsibilities – often obligations that do little to help them move forward in their careers – all in the name of diversity. And when UIM physicians are given leadership opportunities, Dr. Unaka said they are often unsure as to whether their appointments are genuine or just a hollow gesture made for the sake of diversity.
Dr. Johnson pointed out that Black and Latinx populations primarily get their care from hospital-based specialties, yet this is not reflected in the number of UIM practitioners in leadership roles. He said race and ethnicity, as well as gender, need to be factors when individuals are evaluated for leadership opportunities – for the individual’s sake, as well as for the community he or she is serving.
“When we can evaluate for unconscious bias and factor in that diverse groups tend to have better outcomes, whether it’s business or clinical outcomes, it’s one of the opportunities that we collectively have in the specialty to improve what we’re delivering for hospitals and, more importantly, for patients,” he said.
Relationships with colleagues and patients
Racism creeps into interactions and relationships with others as well, whether it’s between clinicians, clinician to patient, or patient to clinician. Sometimes it’s blatant; often it’s subtle.
A common, recurring example Dr. Unaka has experienced in the clinician to clinician relationship is being confused for other Black physicians, making her feel invisible. “The everyday verbal, nonverbal, and environmental slights, snubs, or insults from colleagues are frequent and contribute to feelings of exclusion, isolation, and exhaustion,” she said. Despite this, she is still expected to “address microaggressions and other forms of interpersonal racism and find ways to move through professional spaces in spite of the trauma, fear, and stress associated with my reality and lived experiences.” She said that clinicians who remain silent on the topic of racism participate in the violence and contribute to the disillusionment of UIM physicians.
Dr. Kara said that the discrimination from the health care team is the hardest to deal with. In the clinician to clinician relationship, there is a sense among UIM physicians that they’re being watched more closely and “have to prove themselves at every single turn.” Unfortunately, this comes from the environment, which tends to be adversarial rather than supportive and nurturing, she said.
“There are lots of opportunities for racism or racial insensitivity to crop up from clinician to clinician,” said Dr. Johnson. When he started his career as a physician after his training, Dr. Johnson was informed that his colleagues were watching him because they were not sure about his clinical skills. The fact that he was a former chief resident and board certified in two specialties did not seem to make any difference.
Patients refusing care from UIM physicians or expressing disapproval – both verbal and nonverbal – of such care, happens all too often. “It’s easier for me to excuse patients and their families as we often meet them on their worst days,” said Dr. Kara. Still, “understanding my oath to care for people and do no harm, but at the same time, recognizing that this is an individual that is rejecting my care without having any idea of who I am as a physician is frustrating,” Dr. Johnson acknowledged.
Then there’s the complex clinician to patient relationship, which research clearly shows contributes to health disparities.3 For one thing, the physician workforce does not reflect the patient population, Dr. Unaka said. “We cannot ignore the lack of race concordance between patients and clinicians, nor can the continued misplacement of blame for medical mistrust be at the feet of our patients,” she said.
Dr. Unaka feels that clinicians need to accept both that health inequities exist and that frontline physicians themselves contribute to the inequities. “Our diagnostic and therapeutic decisions are not immune to bias and are influenced by our deeply held beliefs about specific populations,” she said. “And the health care system that our patients navigate is no different than other systems, settings, and environments that are marred by racism in all its forms.”
Systemic racism greatly impacts patient care, said Dr. Kara. She pointed to several examples: Research showing that race concordance between patients and providers in an emergency department setting led to better pain control with fewer analgesics.4 The high maternal and infant mortality rates amongst Black women and children.5 Evidence of poorer outcomes in sepsis patients with limited English proficiency.6 “There are plenty more,” she said. “We need to be asking ourselves what we are going to do about it.”
Moving forward
That racial biases are steeped so thoroughly into our culture and consciousness means that moving beyond them is a continual, purposeful work in progress. But it is work that is critical for everyone, and certainly necessary for those who care for their fellow human beings when they are in a vulnerable state.
Health care systems need to move toward equity – giving everyone what they need to thrive – rather than focusing on equality – giving everyone the same thing, said Jenny Baenziger, MD, assistant professor of clinical medicine and pediatrics at Indiana University, Indianapolis, and associate director of education at IU Center for Global Health. “We know that minoritized patients are going to need more attention, more advocacy, more sensitivity, and more creative solutions in order to help them achieve health in a world that is often stacked against them,” she said.
“The unique needs of each patient, family unit, and/or population must be taken into consideration,” said Dr. Unaka. She said hospitalists need to embrace creative approaches that can better serve the specific needs of patients. Equitable practices should be the default, which means data transparency, thoroughly dissecting hospital processes to find existing inequities, giving stakeholders – especially patients and families of color – a voice, and tearing down oppressive systems that contribute to poor health outcomes and oppression, she said.
“It’s time for us to talk about racism openly,” said Dr. Kara. “Believe your colleagues when they share their fears and treat each other with respect. We should be actively learning about and celebrating our diversity.” She encourages finding out what your institution is doing on this front and getting involved.
Dr. Johnson believes that first and foremost, hospitalists need to be exposed to the data on health care disparities. “The next step is asking what we as hospitalists, or any other specialty, can do to intervene and improve in those areas,” he said. Focusing on unconscious bias training is important, he said, so clinicians can see what biases they might be bringing into the hospital and to the bedside. Maintaining a diverse workforce and bringing UIM physicians into leadership roles to encourage diversity of ideas and approaches are also critical to promoting equity, he said.
“You cannot fix what you cannot face,” said Dr. Unaka. Education on how racism impacts patients and colleagues is essential, she believes, as is advocacy for changing inequitable health system policies. She recommends expanding social and professional circles. “Diverse social groups allow us to consider the perspectives of others; diverse professional groups allow us to ask better research questions and practice better medicine.”
Start by developing the ability to question personal assumptions and pinpoint implicit biases, suggested Dr. Baenziger. “Asking for feedback can be scary and difficult, but we should take a deep breath and do it anyway,” she said. “Simply ask your team, ‘I’ve been thinking a lot about racial equity and disparities. How can I do better at my interactions with people of color? What are my blind spots?’” Dr. Baenziger said that “to help us remember how beautifully complicated and diverse people are,” all health care professionals need to watch Nigerian novelist Chimamanda Ngozi Adichie’s TED talk “The Danger of a Single Story.”
Dr. Baenziger also stressed the importance of conversations about “places where race is built into our clinical assessments, like eGFR,” as well as being aware that many of the research studies that are used to support everyday clinical decisions didn’t include people of color. She also encouraged clinicians to consider how and when they include race in their notes.7 “Is it really helpful to make sure people know right away that you are treating a ‘46-year-old Hispanic male’ or can the fact that he is Hispanic be saved for the social history section with other important details of his life such as being a father, veteran, and mechanic?” she asked.
“Racism is real and very much a part of our history. We can no longer be in denial regarding the racism that exists in medicine and the impact it has on our patients,” Dr. Unaka said. “As a profession, we cannot hide behind our espoused core values. We must live up to them.”
References
1. Lucey CR, Saguil, A. The Consequences of Structural Racism on MCAT Scores and Medical School Admissions: The Past Is Prologue. Acad Med. 2020 Mar;95(3):351-356. doi: 10.1097/ACM.0000000000002939.
2. Flores L. Increasing racial diversity in hospital medicine’s leadership ranks. The Hospitalist. 2020 Oct 21.
3. Smedley BD, et al, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Institute of Medicine Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Washington: National Academies Press; 2003.
4. Heins A, et al. Physician Race/Ethnicity Predicts Successful Emergency Department Analgesia. J Pain. 2010 July;11(7):692-697. doi: 10.1016/j.jpain.2009.10.017.
5. U.S. Department of Health and Human Serves, Office of Minority Health. Infant Mortality and African Americans. 2019 Nov 8. minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=23.
6. Jacobs ZG, et al. The Association between Limited English Proficiency and Sepsis Mortality. J Hosp Med. 2020;3;140-146. Published Online First 2019 Nov 20. doi:10.12788/jhm.3334.
7. Finucane TE. Mention of a Patient’s “Race” in Clinical Presentations. Virtual Mentor. 2014;16(6):423-427. doi: 10.1001/virtualmentor.2014.16.6.ecas1-1406.
With the shootings of Breonna Taylor, George Floyd, and other Black citizens setting off protests and unrest, race was at the forefront of national conversation in the United States – along with COVID-19 – over the past year.
“We’ve heard things like, ‘We’re in a post-racial society,’ but I think 2020 in particular has emphasized that we’re not,” said Gregory Johnson, MD, SFHM, chief medical officer of hospital medicine at Sound Physicians, a national physician practice. “Racism is very present in our lives, it’s very present in our world, and it is absolutely present in medicine.”
Yes, race is still an issue in the U.S. as we head into 2021, though this may have come as something of a surprise to people who do not live with racism daily.
“If you have a brain, you have bias, and that bias will likely apply to race as well,” Dr. Johnson said. “When we’re talking about institutional racism, the educational system and the media have led us to create presumptions and prejudices that we don’t necessarily recognize off the top because they’ve just been a part of the fabric of who we are as we’ve grown up.”
The term “racism” has extremely negative connotations because there’s character judgment attached to it, but to say someone is racist or racially insensitive does not equate them with being a Klansman, said Dr. Johnson. “I think we as people have to acknowledge that, yes, it’s possible for me to be racist and I might not be 100% aware of it. It’s being open to the possibility – or rather probability – that you are and then taking steps to figure out how you can address that, so you can limit it. And that requires constant self-evaluation and work,” he said.
Racism in the medical environment
Institutional racism is evident before students are even accepted into medical school, said Areeba Kara, MD, SFHM, associate professor of clinical medicine at Indiana University, Indianapolis, and a hospitalist at IU Health Physicians.
Mean MCAT scores are lower for applicants traditionally underrepresented in medicine (UIM) compared to the scores of well-represented groups.1 “Lower scores are associated with lower acceptance rates into medical school,” Dr. Kara said. “These differences reflect unequal educational opportunities rooted in centuries of legal discrimination.”
Racism is apparent in both the hidden medical education curriculum and in lessons implicitly taught to students, said Ndidi Unaka, MD, MEd, associate program director of the pediatric residency training program at Cincinnati Children’s Hospital.
“These lessons inform the way in which we as physicians see our patients, each other, and how we practice,” she said. “We reinforce race-based medicine and shape clinical decision making through flawed guidelines and practices, which exacerbates health inequities. We teach that race – rather than racism – is a risk factor for poor health outcomes. Our students and trainees watch as we assume the worst of our patients from marginalized communities of color.”
Terms describing patients of color, such as “difficult,” “non-compliant,” or “frequent flyer” are thrown around and sometimes, instead of finding out why, “we view these states of being as static, root causes for poor outcomes rather than symptoms of social conditions and obstacles that impact overall health and wellbeing,” Dr. Unaka said.
Leadership opportunities
Though hospital medicine is a growing field, Dr. Kara noted that the 2020 State of Hospital Medicine Report found that only 5.5% of hospital medical group leaders were Black, and just 2.2% were Hispanic/Latino.2 “I think these numbers speak for themselves,” she said.
Dr. Unaka said that the lack of UIM hospitalists and physician leaders creates fewer opportunities for “race-concordant mentorship relationships.” It also forces UIM physicians to shoulder more responsibilities – often obligations that do little to help them move forward in their careers – all in the name of diversity. And when UIM physicians are given leadership opportunities, Dr. Unaka said they are often unsure as to whether their appointments are genuine or just a hollow gesture made for the sake of diversity.
Dr. Johnson pointed out that Black and Latinx populations primarily get their care from hospital-based specialties, yet this is not reflected in the number of UIM practitioners in leadership roles. He said race and ethnicity, as well as gender, need to be factors when individuals are evaluated for leadership opportunities – for the individual’s sake, as well as for the community he or she is serving.
“When we can evaluate for unconscious bias and factor in that diverse groups tend to have better outcomes, whether it’s business or clinical outcomes, it’s one of the opportunities that we collectively have in the specialty to improve what we’re delivering for hospitals and, more importantly, for patients,” he said.
Relationships with colleagues and patients
Racism creeps into interactions and relationships with others as well, whether it’s between clinicians, clinician to patient, or patient to clinician. Sometimes it’s blatant; often it’s subtle.
A common, recurring example Dr. Unaka has experienced in the clinician to clinician relationship is being confused for other Black physicians, making her feel invisible. “The everyday verbal, nonverbal, and environmental slights, snubs, or insults from colleagues are frequent and contribute to feelings of exclusion, isolation, and exhaustion,” she said. Despite this, she is still expected to “address microaggressions and other forms of interpersonal racism and find ways to move through professional spaces in spite of the trauma, fear, and stress associated with my reality and lived experiences.” She said that clinicians who remain silent on the topic of racism participate in the violence and contribute to the disillusionment of UIM physicians.
Dr. Kara said that the discrimination from the health care team is the hardest to deal with. In the clinician to clinician relationship, there is a sense among UIM physicians that they’re being watched more closely and “have to prove themselves at every single turn.” Unfortunately, this comes from the environment, which tends to be adversarial rather than supportive and nurturing, she said.
“There are lots of opportunities for racism or racial insensitivity to crop up from clinician to clinician,” said Dr. Johnson. When he started his career as a physician after his training, Dr. Johnson was informed that his colleagues were watching him because they were not sure about his clinical skills. The fact that he was a former chief resident and board certified in two specialties did not seem to make any difference.
Patients refusing care from UIM physicians or expressing disapproval – both verbal and nonverbal – of such care, happens all too often. “It’s easier for me to excuse patients and their families as we often meet them on their worst days,” said Dr. Kara. Still, “understanding my oath to care for people and do no harm, but at the same time, recognizing that this is an individual that is rejecting my care without having any idea of who I am as a physician is frustrating,” Dr. Johnson acknowledged.
Then there’s the complex clinician to patient relationship, which research clearly shows contributes to health disparities.3 For one thing, the physician workforce does not reflect the patient population, Dr. Unaka said. “We cannot ignore the lack of race concordance between patients and clinicians, nor can the continued misplacement of blame for medical mistrust be at the feet of our patients,” she said.
Dr. Unaka feels that clinicians need to accept both that health inequities exist and that frontline physicians themselves contribute to the inequities. “Our diagnostic and therapeutic decisions are not immune to bias and are influenced by our deeply held beliefs about specific populations,” she said. “And the health care system that our patients navigate is no different than other systems, settings, and environments that are marred by racism in all its forms.”
Systemic racism greatly impacts patient care, said Dr. Kara. She pointed to several examples: Research showing that race concordance between patients and providers in an emergency department setting led to better pain control with fewer analgesics.4 The high maternal and infant mortality rates amongst Black women and children.5 Evidence of poorer outcomes in sepsis patients with limited English proficiency.6 “There are plenty more,” she said. “We need to be asking ourselves what we are going to do about it.”
Moving forward
That racial biases are steeped so thoroughly into our culture and consciousness means that moving beyond them is a continual, purposeful work in progress. But it is work that is critical for everyone, and certainly necessary for those who care for their fellow human beings when they are in a vulnerable state.
Health care systems need to move toward equity – giving everyone what they need to thrive – rather than focusing on equality – giving everyone the same thing, said Jenny Baenziger, MD, assistant professor of clinical medicine and pediatrics at Indiana University, Indianapolis, and associate director of education at IU Center for Global Health. “We know that minoritized patients are going to need more attention, more advocacy, more sensitivity, and more creative solutions in order to help them achieve health in a world that is often stacked against them,” she said.
“The unique needs of each patient, family unit, and/or population must be taken into consideration,” said Dr. Unaka. She said hospitalists need to embrace creative approaches that can better serve the specific needs of patients. Equitable practices should be the default, which means data transparency, thoroughly dissecting hospital processes to find existing inequities, giving stakeholders – especially patients and families of color – a voice, and tearing down oppressive systems that contribute to poor health outcomes and oppression, she said.
“It’s time for us to talk about racism openly,” said Dr. Kara. “Believe your colleagues when they share their fears and treat each other with respect. We should be actively learning about and celebrating our diversity.” She encourages finding out what your institution is doing on this front and getting involved.
Dr. Johnson believes that first and foremost, hospitalists need to be exposed to the data on health care disparities. “The next step is asking what we as hospitalists, or any other specialty, can do to intervene and improve in those areas,” he said. Focusing on unconscious bias training is important, he said, so clinicians can see what biases they might be bringing into the hospital and to the bedside. Maintaining a diverse workforce and bringing UIM physicians into leadership roles to encourage diversity of ideas and approaches are also critical to promoting equity, he said.
“You cannot fix what you cannot face,” said Dr. Unaka. Education on how racism impacts patients and colleagues is essential, she believes, as is advocacy for changing inequitable health system policies. She recommends expanding social and professional circles. “Diverse social groups allow us to consider the perspectives of others; diverse professional groups allow us to ask better research questions and practice better medicine.”
Start by developing the ability to question personal assumptions and pinpoint implicit biases, suggested Dr. Baenziger. “Asking for feedback can be scary and difficult, but we should take a deep breath and do it anyway,” she said. “Simply ask your team, ‘I’ve been thinking a lot about racial equity and disparities. How can I do better at my interactions with people of color? What are my blind spots?’” Dr. Baenziger said that “to help us remember how beautifully complicated and diverse people are,” all health care professionals need to watch Nigerian novelist Chimamanda Ngozi Adichie’s TED talk “The Danger of a Single Story.”
Dr. Baenziger also stressed the importance of conversations about “places where race is built into our clinical assessments, like eGFR,” as well as being aware that many of the research studies that are used to support everyday clinical decisions didn’t include people of color. She also encouraged clinicians to consider how and when they include race in their notes.7 “Is it really helpful to make sure people know right away that you are treating a ‘46-year-old Hispanic male’ or can the fact that he is Hispanic be saved for the social history section with other important details of his life such as being a father, veteran, and mechanic?” she asked.
“Racism is real and very much a part of our history. We can no longer be in denial regarding the racism that exists in medicine and the impact it has on our patients,” Dr. Unaka said. “As a profession, we cannot hide behind our espoused core values. We must live up to them.”
References
1. Lucey CR, Saguil, A. The Consequences of Structural Racism on MCAT Scores and Medical School Admissions: The Past Is Prologue. Acad Med. 2020 Mar;95(3):351-356. doi: 10.1097/ACM.0000000000002939.
2. Flores L. Increasing racial diversity in hospital medicine’s leadership ranks. The Hospitalist. 2020 Oct 21.
3. Smedley BD, et al, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Institute of Medicine Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Washington: National Academies Press; 2003.
4. Heins A, et al. Physician Race/Ethnicity Predicts Successful Emergency Department Analgesia. J Pain. 2010 July;11(7):692-697. doi: 10.1016/j.jpain.2009.10.017.
5. U.S. Department of Health and Human Serves, Office of Minority Health. Infant Mortality and African Americans. 2019 Nov 8. minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=23.
6. Jacobs ZG, et al. The Association between Limited English Proficiency and Sepsis Mortality. J Hosp Med. 2020;3;140-146. Published Online First 2019 Nov 20. doi:10.12788/jhm.3334.
7. Finucane TE. Mention of a Patient’s “Race” in Clinical Presentations. Virtual Mentor. 2014;16(6):423-427. doi: 10.1001/virtualmentor.2014.16.6.ecas1-1406.