User login
Improving Dermatologic Care for South Asian Patients: Understanding Religious and Cultural Practices
Traditional garments are particularly important in both Sikhism and Islam. Sikhs began wearing symbolic garments in the 16th century as markers of their identity during periods of religious persecution. Today, many Sikhs continue to maintain this tradition of wearing the Five Ks—kesh (uncut hair, often tied in a turban), kanga (wooden hair comb), kirpan (symbolic dagger), kachha (cotton underwear), and kara (steel bracelet).2 Similarly, Islamic traditions also provide guidance for clothing. Many Muslim women wear the hijab (headscarf), a garment that originated as protective headgear for nomadic desert cultures and has come to symbolize modest dress. Traditionally, the hijab is worn in the presence of all men who are not immediate relatives, although patients may make exceptions for medical care. Some Muslim men also may cover their heads with a skullcap and/or maintain long beards (occasionally dyed with henna pigment) as a way of keeping continuity with the tradition of the Prophet Muhammad and his companions.3
Certain styles of headwear can cause high tension on hair follicles and have been associated with traction alopecia.4 Persistent use of the same turban, hijab, or comb also may lead to seborrheic dermatitis or fungal scalp infections. Dermatologists should advise patients about these potential challenges and suggest modifications in accordance with the patient’s religious beliefs; for example, providers can suggest removing headwear at night, using prophylactic antifungal shampoos, and/or tying the hair in a ponytail or loosening the headgear to reduce traction.
Although Hinduism does not have a unifying garment or hair tradition in the vein of Sikhism or Islam, all 3 religions share a strong emphasis on bodily modesty, which may affect dermatologic examinations. Patients from all 3 religions may seek to expose as little skin as possible during a physical examination, and many patients may be uncomfortable with a physician of the opposite gender. Dermatologists may find the following practices to be helpful5:
• Talk through each aspect of the skin examination while it is being performed and expose the least amount of skin necessary during the process
• Offer the patient a chaperone or a same-gender provider, if possible
• Empower patients to assist in adjusting garments themselves to help the physician visualize all parts of the skin
Some Sikhs also may have specific concerns regarding cutting their hair. One aspect of kesh is that every hair is sacred, and thus, many Sikhs refrain from removing hair on any part of the body. As such, providers should carefully obtain the patient’s informed consent before performing any procedure or physical examination maneuvers (eg, hair pull test) that may result in loss of hair.2
Physicians of all disciplines can help address these challenges through increased outreach and cultural awareness; for example, dermatologists can create skin care pamphlets translated into various South Asian languages and distribute them at houses of worship or other community centers. This may help patients identify their skin needs and seek appropriate care. The onus must be on physicians to make these patients feel comfortable seeking care by creating nonjudgmental, culturally knowledgeable clinical environments. When asking about social history, the physician might consider asking an open-ended question such as, “What role does religion/spirituality play in your life?” They can then proceed to ask specific questions about practices that might affect the patient’s care.5
Given the current coronavirus disease 2019 pandemic, South Asian patients may be even further discouraged from seeking dermatologic care. By understanding religious traditions and taking steps to address biases, dermatologists can help mitigate health care disparities and provide culturally competent care to South Asian patients.
- Nadimpalli SB, Cleland CM, Hutchinson MK, et al. The association between discrimination and the health of Sikh Asian Indians. Health Psychol. 2016;35:351-355.
- The five Ks. BBC website. Updated September 29, 2009. Accessed February 4, 2021. https://www.bbc.co.uk/religion/religions/sikhism/customs/fiveks.shtml
- Islam. BBC website. Accessed February 2, 2021. https://www.bbc.co.uk/religion/religions/islam/
- James J, Saladi RN, Fox JL. Traction alopecia in Sikh male patients. J Am Board Fam Med. 2007;20:497-498.
- Hussain A. Recommendations for culturally competent dermatology care of Muslim patients. J Am Acad Dermatol. 2017;77:388-389.
Traditional garments are particularly important in both Sikhism and Islam. Sikhs began wearing symbolic garments in the 16th century as markers of their identity during periods of religious persecution. Today, many Sikhs continue to maintain this tradition of wearing the Five Ks—kesh (uncut hair, often tied in a turban), kanga (wooden hair comb), kirpan (symbolic dagger), kachha (cotton underwear), and kara (steel bracelet).2 Similarly, Islamic traditions also provide guidance for clothing. Many Muslim women wear the hijab (headscarf), a garment that originated as protective headgear for nomadic desert cultures and has come to symbolize modest dress. Traditionally, the hijab is worn in the presence of all men who are not immediate relatives, although patients may make exceptions for medical care. Some Muslim men also may cover their heads with a skullcap and/or maintain long beards (occasionally dyed with henna pigment) as a way of keeping continuity with the tradition of the Prophet Muhammad and his companions.3
Certain styles of headwear can cause high tension on hair follicles and have been associated with traction alopecia.4 Persistent use of the same turban, hijab, or comb also may lead to seborrheic dermatitis or fungal scalp infections. Dermatologists should advise patients about these potential challenges and suggest modifications in accordance with the patient’s religious beliefs; for example, providers can suggest removing headwear at night, using prophylactic antifungal shampoos, and/or tying the hair in a ponytail or loosening the headgear to reduce traction.
Although Hinduism does not have a unifying garment or hair tradition in the vein of Sikhism or Islam, all 3 religions share a strong emphasis on bodily modesty, which may affect dermatologic examinations. Patients from all 3 religions may seek to expose as little skin as possible during a physical examination, and many patients may be uncomfortable with a physician of the opposite gender. Dermatologists may find the following practices to be helpful5:
• Talk through each aspect of the skin examination while it is being performed and expose the least amount of skin necessary during the process
• Offer the patient a chaperone or a same-gender provider, if possible
• Empower patients to assist in adjusting garments themselves to help the physician visualize all parts of the skin
Some Sikhs also may have specific concerns regarding cutting their hair. One aspect of kesh is that every hair is sacred, and thus, many Sikhs refrain from removing hair on any part of the body. As such, providers should carefully obtain the patient’s informed consent before performing any procedure or physical examination maneuvers (eg, hair pull test) that may result in loss of hair.2
Physicians of all disciplines can help address these challenges through increased outreach and cultural awareness; for example, dermatologists can create skin care pamphlets translated into various South Asian languages and distribute them at houses of worship or other community centers. This may help patients identify their skin needs and seek appropriate care. The onus must be on physicians to make these patients feel comfortable seeking care by creating nonjudgmental, culturally knowledgeable clinical environments. When asking about social history, the physician might consider asking an open-ended question such as, “What role does religion/spirituality play in your life?” They can then proceed to ask specific questions about practices that might affect the patient’s care.5
Given the current coronavirus disease 2019 pandemic, South Asian patients may be even further discouraged from seeking dermatologic care. By understanding religious traditions and taking steps to address biases, dermatologists can help mitigate health care disparities and provide culturally competent care to South Asian patients.
Traditional garments are particularly important in both Sikhism and Islam. Sikhs began wearing symbolic garments in the 16th century as markers of their identity during periods of religious persecution. Today, many Sikhs continue to maintain this tradition of wearing the Five Ks—kesh (uncut hair, often tied in a turban), kanga (wooden hair comb), kirpan (symbolic dagger), kachha (cotton underwear), and kara (steel bracelet).2 Similarly, Islamic traditions also provide guidance for clothing. Many Muslim women wear the hijab (headscarf), a garment that originated as protective headgear for nomadic desert cultures and has come to symbolize modest dress. Traditionally, the hijab is worn in the presence of all men who are not immediate relatives, although patients may make exceptions for medical care. Some Muslim men also may cover their heads with a skullcap and/or maintain long beards (occasionally dyed with henna pigment) as a way of keeping continuity with the tradition of the Prophet Muhammad and his companions.3
Certain styles of headwear can cause high tension on hair follicles and have been associated with traction alopecia.4 Persistent use of the same turban, hijab, or comb also may lead to seborrheic dermatitis or fungal scalp infections. Dermatologists should advise patients about these potential challenges and suggest modifications in accordance with the patient’s religious beliefs; for example, providers can suggest removing headwear at night, using prophylactic antifungal shampoos, and/or tying the hair in a ponytail or loosening the headgear to reduce traction.
Although Hinduism does not have a unifying garment or hair tradition in the vein of Sikhism or Islam, all 3 religions share a strong emphasis on bodily modesty, which may affect dermatologic examinations. Patients from all 3 religions may seek to expose as little skin as possible during a physical examination, and many patients may be uncomfortable with a physician of the opposite gender. Dermatologists may find the following practices to be helpful5:
• Talk through each aspect of the skin examination while it is being performed and expose the least amount of skin necessary during the process
• Offer the patient a chaperone or a same-gender provider, if possible
• Empower patients to assist in adjusting garments themselves to help the physician visualize all parts of the skin
Some Sikhs also may have specific concerns regarding cutting their hair. One aspect of kesh is that every hair is sacred, and thus, many Sikhs refrain from removing hair on any part of the body. As such, providers should carefully obtain the patient’s informed consent before performing any procedure or physical examination maneuvers (eg, hair pull test) that may result in loss of hair.2
Physicians of all disciplines can help address these challenges through increased outreach and cultural awareness; for example, dermatologists can create skin care pamphlets translated into various South Asian languages and distribute them at houses of worship or other community centers. This may help patients identify their skin needs and seek appropriate care. The onus must be on physicians to make these patients feel comfortable seeking care by creating nonjudgmental, culturally knowledgeable clinical environments. When asking about social history, the physician might consider asking an open-ended question such as, “What role does religion/spirituality play in your life?” They can then proceed to ask specific questions about practices that might affect the patient’s care.5
Given the current coronavirus disease 2019 pandemic, South Asian patients may be even further discouraged from seeking dermatologic care. By understanding religious traditions and taking steps to address biases, dermatologists can help mitigate health care disparities and provide culturally competent care to South Asian patients.
- Nadimpalli SB, Cleland CM, Hutchinson MK, et al. The association between discrimination and the health of Sikh Asian Indians. Health Psychol. 2016;35:351-355.
- The five Ks. BBC website. Updated September 29, 2009. Accessed February 4, 2021. https://www.bbc.co.uk/religion/religions/sikhism/customs/fiveks.shtml
- Islam. BBC website. Accessed February 2, 2021. https://www.bbc.co.uk/religion/religions/islam/
- James J, Saladi RN, Fox JL. Traction alopecia in Sikh male patients. J Am Board Fam Med. 2007;20:497-498.
- Hussain A. Recommendations for culturally competent dermatology care of Muslim patients. J Am Acad Dermatol. 2017;77:388-389.
- Nadimpalli SB, Cleland CM, Hutchinson MK, et al. The association between discrimination and the health of Sikh Asian Indians. Health Psychol. 2016;35:351-355.
- The five Ks. BBC website. Updated September 29, 2009. Accessed February 4, 2021. https://www.bbc.co.uk/religion/religions/sikhism/customs/fiveks.shtml
- Islam. BBC website. Accessed February 2, 2021. https://www.bbc.co.uk/religion/religions/islam/
- James J, Saladi RN, Fox JL. Traction alopecia in Sikh male patients. J Am Board Fam Med. 2007;20:497-498.
- Hussain A. Recommendations for culturally competent dermatology care of Muslim patients. J Am Acad Dermatol. 2017;77:388-389.
Practice Points
- Providers should familiarize themselves with traditional garments of Sikhism and Islam, including head coverings and other symbolic items.
- Inform patients about health-conscious methods of wearing traditional headwear, such as removing certain headwear at night and tying hair in methods to avoid causing traction alopecia.
- Talk through each aspect of the skin examination while it is being performed and expose the least amount of skin necessary during the process. Offer the patient a chaperone or a same-gender provider, if possible.
- Empower patients to assist in adjusting garments themselves to help the physician visualize all parts of the skin.
Racial/ethnic disparities in cesarean rates increase with greater maternal education
While the likelihood of a cesarean delivery usually drops as maternal education level increases, the disparities seen in cesarean rates between White and Black or Hispanic women actually increase with more maternal education, according to findings from a new study presented at the Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
Typically, higher maternal education is associated with a lower likelihood of cesarean delivery, but this protective effect is much smaller for Black women and nonexistent for Hispanic women, leading to bigger gaps between these groups and White women, found Yael Eliner, MD, an ob.gyn. residency applicant at Boston University who conducted this research with her colleagues in the ob.gyn. department at Lenox Hill Hospital, New York, and Hofstra University, Hempstead, N.Y..
Researchers have previously identified racial and ethnic disparities in a wide range of maternal outcomes, including mortality, overall morbidity, preterm birth, low birth weight, fetal growth restriction, hypertensive disorders of pregnancy, diabetes, and cesarean deliveries. But the researchers wanted to know if the usual protective effects seen for cesarean deliveries existed in the racial and ethnic groups with these disparities. Past studies have already found that the protective effect of maternal education is greater for White women than Black women with infant mortality and overall self-rated health.
The researchers conducted a retrospective analysis of all low-risk nulliparous, term, singleton, vertex live births to U.S. residents from 2016 to 2019 by using the natality database of the Centers for Disease Control and Prevention. They looked only at women who were non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, and Hispanic women. They excluded women with pregestational and gestational diabetes, chronic hypertension, and hypertensive disorders of pregnancy.
Maternal education levels were stratified into those without a high school diploma, high school graduates (including those with some college credit), college graduates, and those with advanced degrees. The total population included 2,969,207 mothers with a 23.4% cesarean delivery rate.
Before considering education or other potential confounders, the cesarean delivery rate was 27.4% in Black women and 25.6% in Asian women, compared with 22.4% in White women and 23% in Hispanic women (P < .001).
Among those with less than a high school education, Black (20.9%), Asian (23.1%), and Hispanic (17.9% cesarean delivery prevalence was greater than that among White women (17.2%) (P < .001). The same was true among those with a high school education (with or without some college): 22% of White women in this group had cesarean deliveries compared with 26.3% of Black women, 26.3% of Asian women, and 22.5% of Hispanic women (P < .001).
At higher levels of education, the disparities not only persisted but actually increased.
The prevalence of cesarean deliveries was 23% in White college graduates, compared with 32.5% of Black college graduates, 26.3% of Asian college graduates, and 27.7% of Hispanic college graduates (P < .001). Similarly, in those with an advanced degree, the prevalence of cesarean deliveries in their population set was 23.6% of Whites, 36.3% of Blacks, 26.1% of Asians, and 30.1% of Hispanics (P < .001).
After adjusting for maternal education as well as age, prepregnancy body mass index, weight gain during pregnancy, insurance type, and neonatal birth weight, the researchers still found substantial disparities in cesarean delivery rates. Black women had 1.54 times greater odds of cesarean delivery than White women (P < .001). Similarly, the odds were 1.45 times greater for Asian women and 1.24 times greater for Hispanic women (P < .001).
Controlling for race, ethnicity, and the other confounders, women with less than a high school education or a high school diploma had similar likelihoods of cesarean delivery. The likelihood of a cesarean delivery was slightly reduced for women with a college degree (odds ratio, 0.93) or advanced degree (OR, 0.88). But this protective effect did not dampen racial/ethnic disparities. In fact, even greater disparities were seen at higher levels of education.
“At each level of education, all the racial/ethnic groups had significantly higher odds of a cesarean delivery than White women,” Dr. Eliner said. “Additionally, the racial/ethnic disparity in cesarean delivery rates increased with increasing level of education, and we specifically see a meaningful jump in the odds ratio at the college graduate level.”
She pointed out that the OR for cesarean delivery in Black women was 1.4 times greater than White women in the group with less than a high school education and 1.44 times greater in those with high school diplomas. Then it jumped to 1.69 in the college graduates group and 1.7 in the advanced degree group.
Higher maternal education was associated with a lower likelihood of cesarean delivery in White women and Asian women. White women with advanced degrees were 17% less likely to have a cesarean than White women with less than a high school education, and the respective reduction in risk was 19% for Asian women.
In Black women, however, education has a much smaller protective effect: An advanced degree reduced the odds of a cesarean delivery by only 7% and no significant difference showed up between high school graduates and college graduates, Dr. Eliner reported.
In Hispanic women, no protective effect showed up, and the odds of a cesarean delivery actually increased slightly in high school and college graduates above those with less than a high school education.
Dr. Eliner discussed a couple possible reasons for a less protective effect from maternal education in Black and Hispanic groups, including higher levels of chronic stress found in past research among racial/ethnic minorities with higher levels of education.
“The impact of racism as a chronic stressor and its association with adverse obstetric and prenatal outcomes is an emerging theme in health disparity research and is yet to be fully understood,” Dr. Eliner said in an interview. “Nonetheless, there is some evidence suggesting that racial/ethnic minorities with higher levels of education suffer from higher levels of stress.”
Implicit and explicit interpersonal bias and institutional racism may also play a role in the disparities, she said, and these factors may disproportionately affect the quality of care for more educated women. She also suggested that White women may be more comfortable advocating for their care.
“While less educated women from all racial/ethnic groups may lack the self-advocacy skills to discuss their labor course, educated White women may be more confident than women from educated minority groups,” Dr. Eliner told attendees. “They may therefore be better equipped to discuss the need for a cesarean delivery with their provider.”
Dr. Eliner elaborated on this: “Given the historical and current disparities of the health care system, women in racial/ethnic minorities may potentially be guarded in their interaction with medical professionals, with a reduced trust in the health care system, and may thus not feel empowered to advocate for themselves in this setting,” she said.
Allison Bryant Mantha, MD, MPH, vice chair for quality, equity, and safety in the ob.gyn. department at Massachusetts General Hospital, Boston, suggested that bias and racism may play a role in this self-advocacy as well.
“I’m wondering if it might not be equally plausible that the advocacy might be met differently by who’s delivering the message,” Dr. Bryant Mantha said. “I think from the story of Dr. Susan Moore and patients who advocate for themselves, I think that we know there is probably some differential by who’s delivering the message.”
Finally, even though education is usually highly correlated with income and frequently used as a proxy for it, but the effect of education on income varies by race/ethnicity.
Since education alone is not sufficient to reduce these disparities, potential interventions should focus on increasing awareness of the disparities and the role of implicit bias, improving patients’ trust in the medical system, and training more doctors from underrepresented groups, Dr. Eliner said.
“I was also wondering about the overall patient choice,” said Sarahn M. Wheeler, MD, an assistant professor of ob.gyn. at Duke University Medical Center in Durham, N.C., who comoderated the session with Dr. Bryant Mantha. “Did we have any understanding of differences in patient values systems that might go into some of these differences in findings as well? There are lots of interesting concepts to explore and that this abstract brings up.”
Dr. Eliner, Dr. Wheeler, and Dr. Bryant Mantha had no disclosures.
While the likelihood of a cesarean delivery usually drops as maternal education level increases, the disparities seen in cesarean rates between White and Black or Hispanic women actually increase with more maternal education, according to findings from a new study presented at the Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
Typically, higher maternal education is associated with a lower likelihood of cesarean delivery, but this protective effect is much smaller for Black women and nonexistent for Hispanic women, leading to bigger gaps between these groups and White women, found Yael Eliner, MD, an ob.gyn. residency applicant at Boston University who conducted this research with her colleagues in the ob.gyn. department at Lenox Hill Hospital, New York, and Hofstra University, Hempstead, N.Y..
Researchers have previously identified racial and ethnic disparities in a wide range of maternal outcomes, including mortality, overall morbidity, preterm birth, low birth weight, fetal growth restriction, hypertensive disorders of pregnancy, diabetes, and cesarean deliveries. But the researchers wanted to know if the usual protective effects seen for cesarean deliveries existed in the racial and ethnic groups with these disparities. Past studies have already found that the protective effect of maternal education is greater for White women than Black women with infant mortality and overall self-rated health.
The researchers conducted a retrospective analysis of all low-risk nulliparous, term, singleton, vertex live births to U.S. residents from 2016 to 2019 by using the natality database of the Centers for Disease Control and Prevention. They looked only at women who were non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, and Hispanic women. They excluded women with pregestational and gestational diabetes, chronic hypertension, and hypertensive disorders of pregnancy.
Maternal education levels were stratified into those without a high school diploma, high school graduates (including those with some college credit), college graduates, and those with advanced degrees. The total population included 2,969,207 mothers with a 23.4% cesarean delivery rate.
Before considering education or other potential confounders, the cesarean delivery rate was 27.4% in Black women and 25.6% in Asian women, compared with 22.4% in White women and 23% in Hispanic women (P < .001).
Among those with less than a high school education, Black (20.9%), Asian (23.1%), and Hispanic (17.9% cesarean delivery prevalence was greater than that among White women (17.2%) (P < .001). The same was true among those with a high school education (with or without some college): 22% of White women in this group had cesarean deliveries compared with 26.3% of Black women, 26.3% of Asian women, and 22.5% of Hispanic women (P < .001).
At higher levels of education, the disparities not only persisted but actually increased.
The prevalence of cesarean deliveries was 23% in White college graduates, compared with 32.5% of Black college graduates, 26.3% of Asian college graduates, and 27.7% of Hispanic college graduates (P < .001). Similarly, in those with an advanced degree, the prevalence of cesarean deliveries in their population set was 23.6% of Whites, 36.3% of Blacks, 26.1% of Asians, and 30.1% of Hispanics (P < .001).
After adjusting for maternal education as well as age, prepregnancy body mass index, weight gain during pregnancy, insurance type, and neonatal birth weight, the researchers still found substantial disparities in cesarean delivery rates. Black women had 1.54 times greater odds of cesarean delivery than White women (P < .001). Similarly, the odds were 1.45 times greater for Asian women and 1.24 times greater for Hispanic women (P < .001).
Controlling for race, ethnicity, and the other confounders, women with less than a high school education or a high school diploma had similar likelihoods of cesarean delivery. The likelihood of a cesarean delivery was slightly reduced for women with a college degree (odds ratio, 0.93) or advanced degree (OR, 0.88). But this protective effect did not dampen racial/ethnic disparities. In fact, even greater disparities were seen at higher levels of education.
“At each level of education, all the racial/ethnic groups had significantly higher odds of a cesarean delivery than White women,” Dr. Eliner said. “Additionally, the racial/ethnic disparity in cesarean delivery rates increased with increasing level of education, and we specifically see a meaningful jump in the odds ratio at the college graduate level.”
She pointed out that the OR for cesarean delivery in Black women was 1.4 times greater than White women in the group with less than a high school education and 1.44 times greater in those with high school diplomas. Then it jumped to 1.69 in the college graduates group and 1.7 in the advanced degree group.
Higher maternal education was associated with a lower likelihood of cesarean delivery in White women and Asian women. White women with advanced degrees were 17% less likely to have a cesarean than White women with less than a high school education, and the respective reduction in risk was 19% for Asian women.
In Black women, however, education has a much smaller protective effect: An advanced degree reduced the odds of a cesarean delivery by only 7% and no significant difference showed up between high school graduates and college graduates, Dr. Eliner reported.
In Hispanic women, no protective effect showed up, and the odds of a cesarean delivery actually increased slightly in high school and college graduates above those with less than a high school education.
Dr. Eliner discussed a couple possible reasons for a less protective effect from maternal education in Black and Hispanic groups, including higher levels of chronic stress found in past research among racial/ethnic minorities with higher levels of education.
“The impact of racism as a chronic stressor and its association with adverse obstetric and prenatal outcomes is an emerging theme in health disparity research and is yet to be fully understood,” Dr. Eliner said in an interview. “Nonetheless, there is some evidence suggesting that racial/ethnic minorities with higher levels of education suffer from higher levels of stress.”
Implicit and explicit interpersonal bias and institutional racism may also play a role in the disparities, she said, and these factors may disproportionately affect the quality of care for more educated women. She also suggested that White women may be more comfortable advocating for their care.
“While less educated women from all racial/ethnic groups may lack the self-advocacy skills to discuss their labor course, educated White women may be more confident than women from educated minority groups,” Dr. Eliner told attendees. “They may therefore be better equipped to discuss the need for a cesarean delivery with their provider.”
Dr. Eliner elaborated on this: “Given the historical and current disparities of the health care system, women in racial/ethnic minorities may potentially be guarded in their interaction with medical professionals, with a reduced trust in the health care system, and may thus not feel empowered to advocate for themselves in this setting,” she said.
Allison Bryant Mantha, MD, MPH, vice chair for quality, equity, and safety in the ob.gyn. department at Massachusetts General Hospital, Boston, suggested that bias and racism may play a role in this self-advocacy as well.
“I’m wondering if it might not be equally plausible that the advocacy might be met differently by who’s delivering the message,” Dr. Bryant Mantha said. “I think from the story of Dr. Susan Moore and patients who advocate for themselves, I think that we know there is probably some differential by who’s delivering the message.”
Finally, even though education is usually highly correlated with income and frequently used as a proxy for it, but the effect of education on income varies by race/ethnicity.
Since education alone is not sufficient to reduce these disparities, potential interventions should focus on increasing awareness of the disparities and the role of implicit bias, improving patients’ trust in the medical system, and training more doctors from underrepresented groups, Dr. Eliner said.
“I was also wondering about the overall patient choice,” said Sarahn M. Wheeler, MD, an assistant professor of ob.gyn. at Duke University Medical Center in Durham, N.C., who comoderated the session with Dr. Bryant Mantha. “Did we have any understanding of differences in patient values systems that might go into some of these differences in findings as well? There are lots of interesting concepts to explore and that this abstract brings up.”
Dr. Eliner, Dr. Wheeler, and Dr. Bryant Mantha had no disclosures.
While the likelihood of a cesarean delivery usually drops as maternal education level increases, the disparities seen in cesarean rates between White and Black or Hispanic women actually increase with more maternal education, according to findings from a new study presented at the Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
Typically, higher maternal education is associated with a lower likelihood of cesarean delivery, but this protective effect is much smaller for Black women and nonexistent for Hispanic women, leading to bigger gaps between these groups and White women, found Yael Eliner, MD, an ob.gyn. residency applicant at Boston University who conducted this research with her colleagues in the ob.gyn. department at Lenox Hill Hospital, New York, and Hofstra University, Hempstead, N.Y..
Researchers have previously identified racial and ethnic disparities in a wide range of maternal outcomes, including mortality, overall morbidity, preterm birth, low birth weight, fetal growth restriction, hypertensive disorders of pregnancy, diabetes, and cesarean deliveries. But the researchers wanted to know if the usual protective effects seen for cesarean deliveries existed in the racial and ethnic groups with these disparities. Past studies have already found that the protective effect of maternal education is greater for White women than Black women with infant mortality and overall self-rated health.
The researchers conducted a retrospective analysis of all low-risk nulliparous, term, singleton, vertex live births to U.S. residents from 2016 to 2019 by using the natality database of the Centers for Disease Control and Prevention. They looked only at women who were non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, and Hispanic women. They excluded women with pregestational and gestational diabetes, chronic hypertension, and hypertensive disorders of pregnancy.
Maternal education levels were stratified into those without a high school diploma, high school graduates (including those with some college credit), college graduates, and those with advanced degrees. The total population included 2,969,207 mothers with a 23.4% cesarean delivery rate.
Before considering education or other potential confounders, the cesarean delivery rate was 27.4% in Black women and 25.6% in Asian women, compared with 22.4% in White women and 23% in Hispanic women (P < .001).
Among those with less than a high school education, Black (20.9%), Asian (23.1%), and Hispanic (17.9% cesarean delivery prevalence was greater than that among White women (17.2%) (P < .001). The same was true among those with a high school education (with or without some college): 22% of White women in this group had cesarean deliveries compared with 26.3% of Black women, 26.3% of Asian women, and 22.5% of Hispanic women (P < .001).
At higher levels of education, the disparities not only persisted but actually increased.
The prevalence of cesarean deliveries was 23% in White college graduates, compared with 32.5% of Black college graduates, 26.3% of Asian college graduates, and 27.7% of Hispanic college graduates (P < .001). Similarly, in those with an advanced degree, the prevalence of cesarean deliveries in their population set was 23.6% of Whites, 36.3% of Blacks, 26.1% of Asians, and 30.1% of Hispanics (P < .001).
After adjusting for maternal education as well as age, prepregnancy body mass index, weight gain during pregnancy, insurance type, and neonatal birth weight, the researchers still found substantial disparities in cesarean delivery rates. Black women had 1.54 times greater odds of cesarean delivery than White women (P < .001). Similarly, the odds were 1.45 times greater for Asian women and 1.24 times greater for Hispanic women (P < .001).
Controlling for race, ethnicity, and the other confounders, women with less than a high school education or a high school diploma had similar likelihoods of cesarean delivery. The likelihood of a cesarean delivery was slightly reduced for women with a college degree (odds ratio, 0.93) or advanced degree (OR, 0.88). But this protective effect did not dampen racial/ethnic disparities. In fact, even greater disparities were seen at higher levels of education.
“At each level of education, all the racial/ethnic groups had significantly higher odds of a cesarean delivery than White women,” Dr. Eliner said. “Additionally, the racial/ethnic disparity in cesarean delivery rates increased with increasing level of education, and we specifically see a meaningful jump in the odds ratio at the college graduate level.”
She pointed out that the OR for cesarean delivery in Black women was 1.4 times greater than White women in the group with less than a high school education and 1.44 times greater in those with high school diplomas. Then it jumped to 1.69 in the college graduates group and 1.7 in the advanced degree group.
Higher maternal education was associated with a lower likelihood of cesarean delivery in White women and Asian women. White women with advanced degrees were 17% less likely to have a cesarean than White women with less than a high school education, and the respective reduction in risk was 19% for Asian women.
In Black women, however, education has a much smaller protective effect: An advanced degree reduced the odds of a cesarean delivery by only 7% and no significant difference showed up between high school graduates and college graduates, Dr. Eliner reported.
In Hispanic women, no protective effect showed up, and the odds of a cesarean delivery actually increased slightly in high school and college graduates above those with less than a high school education.
Dr. Eliner discussed a couple possible reasons for a less protective effect from maternal education in Black and Hispanic groups, including higher levels of chronic stress found in past research among racial/ethnic minorities with higher levels of education.
“The impact of racism as a chronic stressor and its association with adverse obstetric and prenatal outcomes is an emerging theme in health disparity research and is yet to be fully understood,” Dr. Eliner said in an interview. “Nonetheless, there is some evidence suggesting that racial/ethnic minorities with higher levels of education suffer from higher levels of stress.”
Implicit and explicit interpersonal bias and institutional racism may also play a role in the disparities, she said, and these factors may disproportionately affect the quality of care for more educated women. She also suggested that White women may be more comfortable advocating for their care.
“While less educated women from all racial/ethnic groups may lack the self-advocacy skills to discuss their labor course, educated White women may be more confident than women from educated minority groups,” Dr. Eliner told attendees. “They may therefore be better equipped to discuss the need for a cesarean delivery with their provider.”
Dr. Eliner elaborated on this: “Given the historical and current disparities of the health care system, women in racial/ethnic minorities may potentially be guarded in their interaction with medical professionals, with a reduced trust in the health care system, and may thus not feel empowered to advocate for themselves in this setting,” she said.
Allison Bryant Mantha, MD, MPH, vice chair for quality, equity, and safety in the ob.gyn. department at Massachusetts General Hospital, Boston, suggested that bias and racism may play a role in this self-advocacy as well.
“I’m wondering if it might not be equally plausible that the advocacy might be met differently by who’s delivering the message,” Dr. Bryant Mantha said. “I think from the story of Dr. Susan Moore and patients who advocate for themselves, I think that we know there is probably some differential by who’s delivering the message.”
Finally, even though education is usually highly correlated with income and frequently used as a proxy for it, but the effect of education on income varies by race/ethnicity.
Since education alone is not sufficient to reduce these disparities, potential interventions should focus on increasing awareness of the disparities and the role of implicit bias, improving patients’ trust in the medical system, and training more doctors from underrepresented groups, Dr. Eliner said.
“I was also wondering about the overall patient choice,” said Sarahn M. Wheeler, MD, an assistant professor of ob.gyn. at Duke University Medical Center in Durham, N.C., who comoderated the session with Dr. Bryant Mantha. “Did we have any understanding of differences in patient values systems that might go into some of these differences in findings as well? There are lots of interesting concepts to explore and that this abstract brings up.”
Dr. Eliner, Dr. Wheeler, and Dr. Bryant Mantha had no disclosures.
FROM THE PREGNANCY MEETING
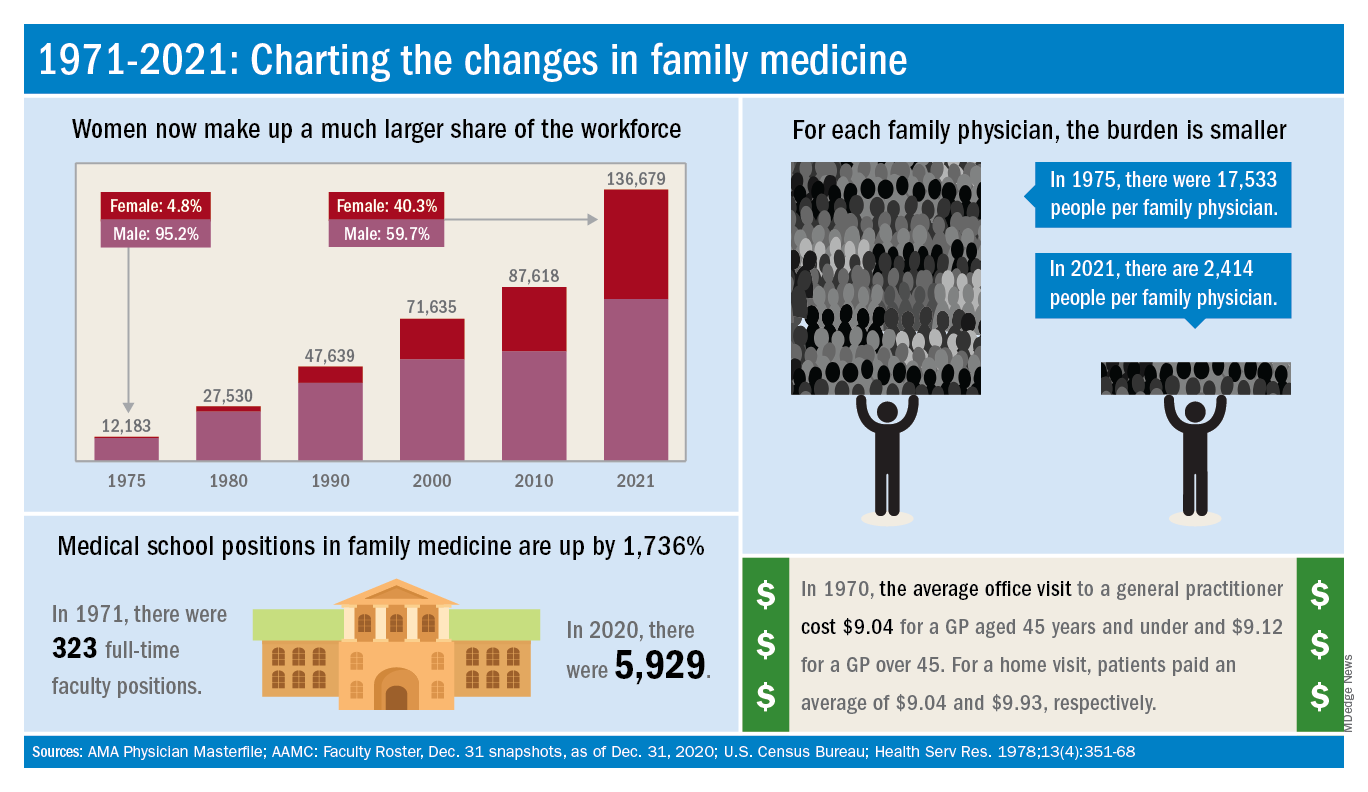
Family medicine has grown; its composition has evolved
and the men and women who practice it are no exception.
The family medicine workforce of 2021 is not the workforce of 1971. Not even close. Although we would like to give a huge shout-out to anyone who can claim to be a member of both.
Today’s FP workforce is, first of all, much larger than it was in 1971, although we can’t actually prove it because the American Medical Association’s data for that year are “only available in books that are locked away at the empty AMA headquarters,” according to a member of the AMA media relations staff who is, like so many people these days, working at home because of the pandemic.
The face of family medicine in 1975 vs. today
Today’s workforce is much larger than it was in 1975, when there were just over 12,000 family physicians in the United States. As of January 2021, the total was approaching 137,000, including all “physicians and residents in patient care, research, administration, teaching, retired, inactive, etc.,” the AMA explained.
Family physicians as a group are much more diverse than they were in 1975. That year, 8.3% of FPs were international medical graduates (IMGs). By 2010, IMGs made up almost 23% of the workforce, and in the 2020 resident match, 37% of the 4,662 available family medicine slots were filled by IMGs.
Women have made even greater inroads into the family physician ranks over the last 5 decades. In 1975, less than 5% of all FPs were females, but by 2021 the proportion of females in the specialty was just over 40%.
In the first 5 years of the family practice era, 1969-1973, only 12 women and 31 IMGs graduated from FP residency programs, those numbers representing 3.2% and 8.3%, respectively, of the total of 372, according to a 1996 study in JAMA. By 1990-1993, women made up 33% and IMGs 14% of the 9,400 graduates.
Another group that increased its presence in family medicine is doctors of osteopathy, who went from zero residency graduates in 1969-1973 to over 1,100 (11.8%) in 1990-1993, the JAMA report noted. By 2020, almost 1,400 osteopathic physicians entered family medicine residencies, filling 30% of all slots available, according to the National Resident Matching Program.
The medical schools producing all these new residents have raised their games since 1971: the number of full-time faculty in family medicine departments rose from 323 to 5,929 in 2020, based on data from the Association of American Medical Colleges (Faculty Roster, Dec. 31 snapshots, as of Dec. 31, 2020).
A shortage or a surplus of FPs?
It has been suggested, however, that all is not well in primary care land. A study conducted by the American Academy of Family Physicians in 2016 – a year after 2,463 graduates of MD- and DO-granting medical schools entered family medicine residencies – concluded “that the current medical school system is failing, collectively, to produce the primary care workforce that is needed to achieve optimal health.”
Warnings about physician shortages are nothing new, but how about the other side of the coin? The Jan. 15, 1981, issue of Family Practice News covered a somewhat controversial report from the Graduate Medical Education National Advisory Committee, which projected a surplus of 3,000 FPs, and as many as 70,000 physicians overall, by the year 1990.
Just a few months later, in the June 15, 1981, issue of FPN, an AAFP officer predicted that “the flood of new physicians in the next decade may affect family practice more than any other specialty.”
Mostly, though, the issue is shortages. In 2002, a status report on family practice from the Robert Graham Center acknowledged that “many centers of academic medicine continue to resist the development of family practice and primary care. ... Family medicine remains a true counterculture in these environments, and students may continue to face significant discouragement in response to interest they may express in becoming a family physician.”
and the men and women who practice it are no exception.
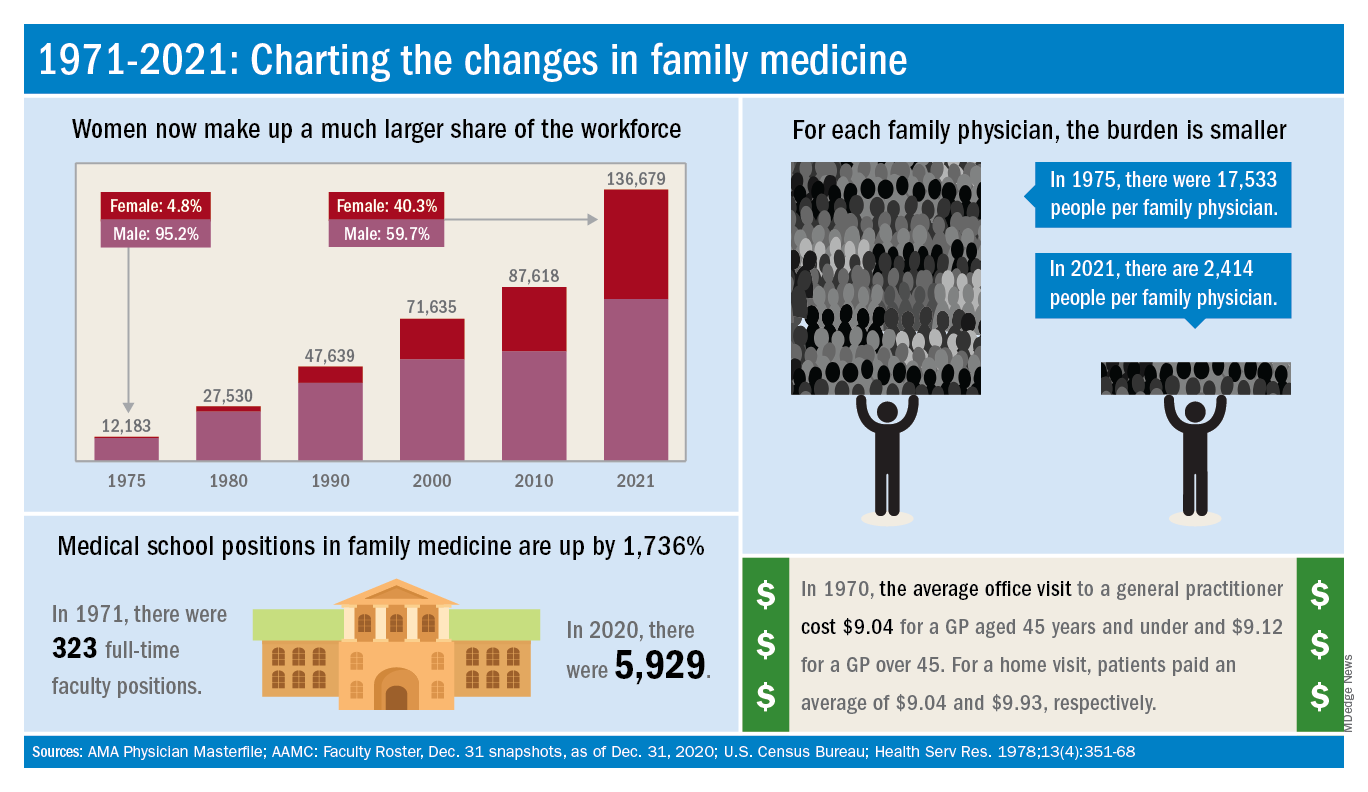
The family medicine workforce of 2021 is not the workforce of 1971. Not even close. Although we would like to give a huge shout-out to anyone who can claim to be a member of both.
Today’s FP workforce is, first of all, much larger than it was in 1971, although we can’t actually prove it because the American Medical Association’s data for that year are “only available in books that are locked away at the empty AMA headquarters,” according to a member of the AMA media relations staff who is, like so many people these days, working at home because of the pandemic.
The face of family medicine in 1975 vs. today
Today’s workforce is much larger than it was in 1975, when there were just over 12,000 family physicians in the United States. As of January 2021, the total was approaching 137,000, including all “physicians and residents in patient care, research, administration, teaching, retired, inactive, etc.,” the AMA explained.
Family physicians as a group are much more diverse than they were in 1975. That year, 8.3% of FPs were international medical graduates (IMGs). By 2010, IMGs made up almost 23% of the workforce, and in the 2020 resident match, 37% of the 4,662 available family medicine slots were filled by IMGs.
Women have made even greater inroads into the family physician ranks over the last 5 decades. In 1975, less than 5% of all FPs were females, but by 2021 the proportion of females in the specialty was just over 40%.
In the first 5 years of the family practice era, 1969-1973, only 12 women and 31 IMGs graduated from FP residency programs, those numbers representing 3.2% and 8.3%, respectively, of the total of 372, according to a 1996 study in JAMA. By 1990-1993, women made up 33% and IMGs 14% of the 9,400 graduates.
Another group that increased its presence in family medicine is doctors of osteopathy, who went from zero residency graduates in 1969-1973 to over 1,100 (11.8%) in 1990-1993, the JAMA report noted. By 2020, almost 1,400 osteopathic physicians entered family medicine residencies, filling 30% of all slots available, according to the National Resident Matching Program.
The medical schools producing all these new residents have raised their games since 1971: the number of full-time faculty in family medicine departments rose from 323 to 5,929 in 2020, based on data from the Association of American Medical Colleges (Faculty Roster, Dec. 31 snapshots, as of Dec. 31, 2020).
A shortage or a surplus of FPs?
It has been suggested, however, that all is not well in primary care land. A study conducted by the American Academy of Family Physicians in 2016 – a year after 2,463 graduates of MD- and DO-granting medical schools entered family medicine residencies – concluded “that the current medical school system is failing, collectively, to produce the primary care workforce that is needed to achieve optimal health.”
Warnings about physician shortages are nothing new, but how about the other side of the coin? The Jan. 15, 1981, issue of Family Practice News covered a somewhat controversial report from the Graduate Medical Education National Advisory Committee, which projected a surplus of 3,000 FPs, and as many as 70,000 physicians overall, by the year 1990.
Just a few months later, in the June 15, 1981, issue of FPN, an AAFP officer predicted that “the flood of new physicians in the next decade may affect family practice more than any other specialty.”
Mostly, though, the issue is shortages. In 2002, a status report on family practice from the Robert Graham Center acknowledged that “many centers of academic medicine continue to resist the development of family practice and primary care. ... Family medicine remains a true counterculture in these environments, and students may continue to face significant discouragement in response to interest they may express in becoming a family physician.”
and the men and women who practice it are no exception.
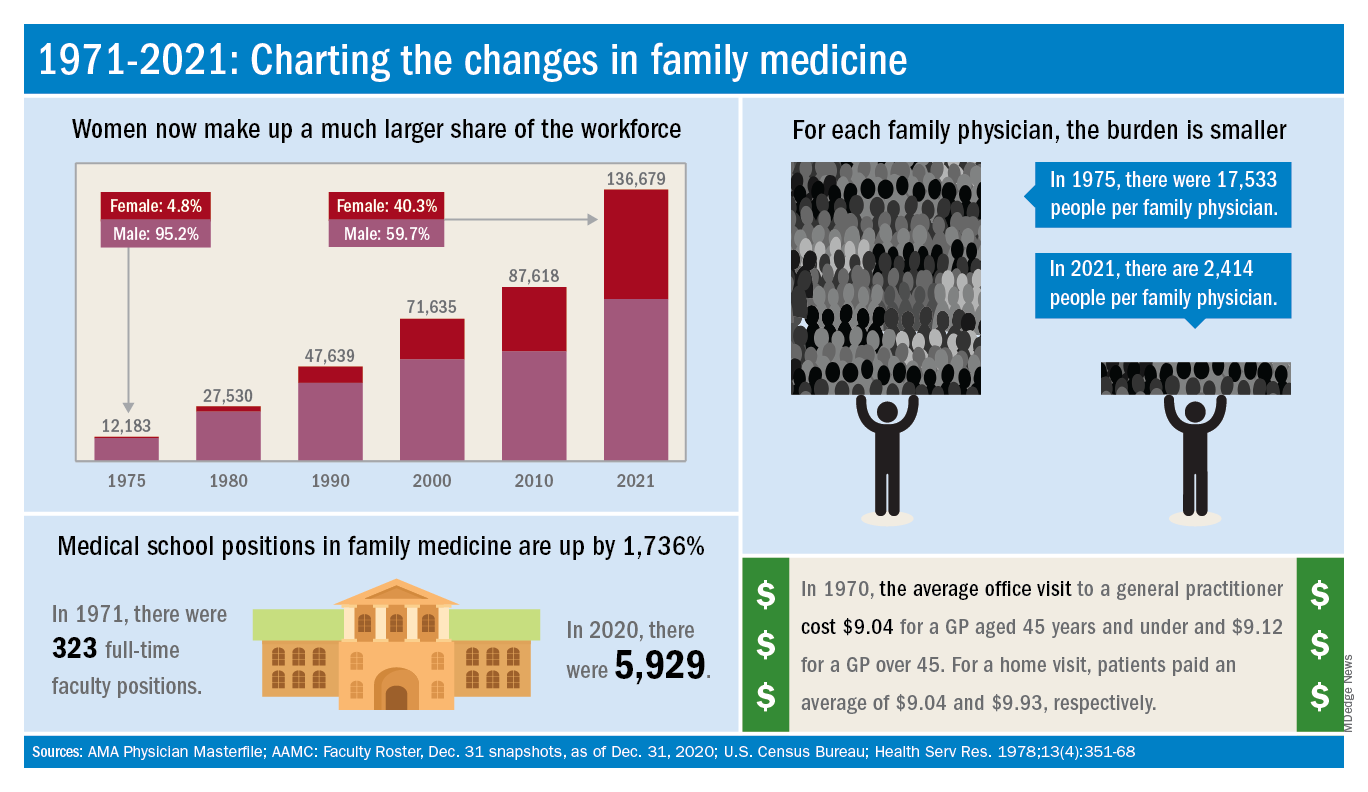
The family medicine workforce of 2021 is not the workforce of 1971. Not even close. Although we would like to give a huge shout-out to anyone who can claim to be a member of both.
Today’s FP workforce is, first of all, much larger than it was in 1971, although we can’t actually prove it because the American Medical Association’s data for that year are “only available in books that are locked away at the empty AMA headquarters,” according to a member of the AMA media relations staff who is, like so many people these days, working at home because of the pandemic.
The face of family medicine in 1975 vs. today
Today’s workforce is much larger than it was in 1975, when there were just over 12,000 family physicians in the United States. As of January 2021, the total was approaching 137,000, including all “physicians and residents in patient care, research, administration, teaching, retired, inactive, etc.,” the AMA explained.
Family physicians as a group are much more diverse than they were in 1975. That year, 8.3% of FPs were international medical graduates (IMGs). By 2010, IMGs made up almost 23% of the workforce, and in the 2020 resident match, 37% of the 4,662 available family medicine slots were filled by IMGs.
Women have made even greater inroads into the family physician ranks over the last 5 decades. In 1975, less than 5% of all FPs were females, but by 2021 the proportion of females in the specialty was just over 40%.
In the first 5 years of the family practice era, 1969-1973, only 12 women and 31 IMGs graduated from FP residency programs, those numbers representing 3.2% and 8.3%, respectively, of the total of 372, according to a 1996 study in JAMA. By 1990-1993, women made up 33% and IMGs 14% of the 9,400 graduates.
Another group that increased its presence in family medicine is doctors of osteopathy, who went from zero residency graduates in 1969-1973 to over 1,100 (11.8%) in 1990-1993, the JAMA report noted. By 2020, almost 1,400 osteopathic physicians entered family medicine residencies, filling 30% of all slots available, according to the National Resident Matching Program.
The medical schools producing all these new residents have raised their games since 1971: the number of full-time faculty in family medicine departments rose from 323 to 5,929 in 2020, based on data from the Association of American Medical Colleges (Faculty Roster, Dec. 31 snapshots, as of Dec. 31, 2020).
A shortage or a surplus of FPs?
It has been suggested, however, that all is not well in primary care land. A study conducted by the American Academy of Family Physicians in 2016 – a year after 2,463 graduates of MD- and DO-granting medical schools entered family medicine residencies – concluded “that the current medical school system is failing, collectively, to produce the primary care workforce that is needed to achieve optimal health.”
Warnings about physician shortages are nothing new, but how about the other side of the coin? The Jan. 15, 1981, issue of Family Practice News covered a somewhat controversial report from the Graduate Medical Education National Advisory Committee, which projected a surplus of 3,000 FPs, and as many as 70,000 physicians overall, by the year 1990.
Just a few months later, in the June 15, 1981, issue of FPN, an AAFP officer predicted that “the flood of new physicians in the next decade may affect family practice more than any other specialty.”
Mostly, though, the issue is shortages. In 2002, a status report on family practice from the Robert Graham Center acknowledged that “many centers of academic medicine continue to resist the development of family practice and primary care. ... Family medicine remains a true counterculture in these environments, and students may continue to face significant discouragement in response to interest they may express in becoming a family physician.”
Cardiovascular trials lose more women than men
A new analysis of 11 phase 3/4 cardiovascular clinical trials conducted by the Thrombolysis in Myocardial Infarction (TIMI) group shows that women are more likely than men to discontinue study medications, and to withdraw from trials. The differences could not be explained by different frequencies of reporting adverse events, or by baseline differences.
The findings are significant, since cardiovascular drugs are routinely prescribed to women based on clinical trials that are populated largely by men, according to lead study author Emily Lau, MD, who is an advanced cardiology fellow at Massachusetts General Hospital, Boston. “It highlights an important disparity in clinical research in cardiology, because if women are already not represented well in clinical trials, and if once in clinical trials they don’t complete the study, it’s very hard to extrapolate the clinical trial findings to our female population in an accurate way,” Dr. Lau said in an interview. She also noted that sex-specific and reproductive factors are increasingly recognized as being important in the development and progression of cardiovascular disease.
The study was published in the journal Circulation.
The study refutes previously advanced explanations for higher withdrawal among women, including sex difference and comorbidities, according to an accompanying editorial by Sofia Sederholm Lawesson, MD, PhD, Eva Swahn, MD, PhD, and Joakim Alfredsson, MD, PhD, of Linköping University, Sweden. They also pointed out that the study found a larger between-sex difference in failure to adhere to study drug in North America (odds ratio, 1.35; 95% confidence interval, 1.30-1.41), but a more moderate difference among participants in Europe/Middle East/Africa (OR, 1.13; 95% CI, 1.09-1.17) and Asia/Pacific (OR, 1.13; 95% CI, 1.03-1.23) regions. And there were no sex differences at all among South/Central American populations.
They noted that high rates of nonadherence increase the chances of a false negative finding and overestimation of drug safety. “We know the associations between nonadherence and clinical outcomes. The next step should be to better understand the underlying reasons for, as well as consistent reporting of, nonadherence, and discontinuation in RCTs,” the editorial authors wrote.
Dr. Lau suggested a simple method to better understand reasons for withdrawal: Addition of questions to the case report form that asks about reasons for drug discontinuation or study withdrawal. “Was it an adverse event? Was it because I’m a mother of three and I can’t get to the clinical trial site after work and also pick up my kids? Are there societal barriers for women, or was it the experience of the clinical trial that was maybe less favorable for women compared to men? Or maybe there are medical reasons we simply don’t know. Something as simple as asking those questions can help us better understand the barriers to female retention,” said Dr. Lau.
The analysis included data from 135,879 men (72%) and 51,812 women (28%) enrolled in the trials. After adjustment for baseline differences, women were more likely than were men to permanently discontinue study drug (adjusted odds ratio [aOR], 1.22: P < .001), which did not vary by study duration. The finding was consistent regardless of the type of drug studied, as well as across placebo and active study arms.
Women also were more likely to prematurely discontinue study drug (trial-adjusted OR, 1.18; P < .001). The rate of drug discontinuation due to adverse event was identical in both men and women, at 36%.
Women were more likely to withdraw consent than were men in a meta-analysis and when individual patient-level results were pooled (aOR, 1.26; P < .001 for both).
Dr. Lau received funding from the National Institutes of Health and has no relevant financial disclosures. The editorial authors had various disclosures, including lecture fees from Bayer, Pfizer, and Boehringer Ingelheim, and they served on advisory boards for AstraZeneca and MSD.
A new analysis of 11 phase 3/4 cardiovascular clinical trials conducted by the Thrombolysis in Myocardial Infarction (TIMI) group shows that women are more likely than men to discontinue study medications, and to withdraw from trials. The differences could not be explained by different frequencies of reporting adverse events, or by baseline differences.
The findings are significant, since cardiovascular drugs are routinely prescribed to women based on clinical trials that are populated largely by men, according to lead study author Emily Lau, MD, who is an advanced cardiology fellow at Massachusetts General Hospital, Boston. “It highlights an important disparity in clinical research in cardiology, because if women are already not represented well in clinical trials, and if once in clinical trials they don’t complete the study, it’s very hard to extrapolate the clinical trial findings to our female population in an accurate way,” Dr. Lau said in an interview. She also noted that sex-specific and reproductive factors are increasingly recognized as being important in the development and progression of cardiovascular disease.
The study was published in the journal Circulation.
The study refutes previously advanced explanations for higher withdrawal among women, including sex difference and comorbidities, according to an accompanying editorial by Sofia Sederholm Lawesson, MD, PhD, Eva Swahn, MD, PhD, and Joakim Alfredsson, MD, PhD, of Linköping University, Sweden. They also pointed out that the study found a larger between-sex difference in failure to adhere to study drug in North America (odds ratio, 1.35; 95% confidence interval, 1.30-1.41), but a more moderate difference among participants in Europe/Middle East/Africa (OR, 1.13; 95% CI, 1.09-1.17) and Asia/Pacific (OR, 1.13; 95% CI, 1.03-1.23) regions. And there were no sex differences at all among South/Central American populations.
They noted that high rates of nonadherence increase the chances of a false negative finding and overestimation of drug safety. “We know the associations between nonadherence and clinical outcomes. The next step should be to better understand the underlying reasons for, as well as consistent reporting of, nonadherence, and discontinuation in RCTs,” the editorial authors wrote.
Dr. Lau suggested a simple method to better understand reasons for withdrawal: Addition of questions to the case report form that asks about reasons for drug discontinuation or study withdrawal. “Was it an adverse event? Was it because I’m a mother of three and I can’t get to the clinical trial site after work and also pick up my kids? Are there societal barriers for women, or was it the experience of the clinical trial that was maybe less favorable for women compared to men? Or maybe there are medical reasons we simply don’t know. Something as simple as asking those questions can help us better understand the barriers to female retention,” said Dr. Lau.
The analysis included data from 135,879 men (72%) and 51,812 women (28%) enrolled in the trials. After adjustment for baseline differences, women were more likely than were men to permanently discontinue study drug (adjusted odds ratio [aOR], 1.22: P < .001), which did not vary by study duration. The finding was consistent regardless of the type of drug studied, as well as across placebo and active study arms.
Women also were more likely to prematurely discontinue study drug (trial-adjusted OR, 1.18; P < .001). The rate of drug discontinuation due to adverse event was identical in both men and women, at 36%.
Women were more likely to withdraw consent than were men in a meta-analysis and when individual patient-level results were pooled (aOR, 1.26; P < .001 for both).
Dr. Lau received funding from the National Institutes of Health and has no relevant financial disclosures. The editorial authors had various disclosures, including lecture fees from Bayer, Pfizer, and Boehringer Ingelheim, and they served on advisory boards for AstraZeneca and MSD.
A new analysis of 11 phase 3/4 cardiovascular clinical trials conducted by the Thrombolysis in Myocardial Infarction (TIMI) group shows that women are more likely than men to discontinue study medications, and to withdraw from trials. The differences could not be explained by different frequencies of reporting adverse events, or by baseline differences.
The findings are significant, since cardiovascular drugs are routinely prescribed to women based on clinical trials that are populated largely by men, according to lead study author Emily Lau, MD, who is an advanced cardiology fellow at Massachusetts General Hospital, Boston. “It highlights an important disparity in clinical research in cardiology, because if women are already not represented well in clinical trials, and if once in clinical trials they don’t complete the study, it’s very hard to extrapolate the clinical trial findings to our female population in an accurate way,” Dr. Lau said in an interview. She also noted that sex-specific and reproductive factors are increasingly recognized as being important in the development and progression of cardiovascular disease.
The study was published in the journal Circulation.
The study refutes previously advanced explanations for higher withdrawal among women, including sex difference and comorbidities, according to an accompanying editorial by Sofia Sederholm Lawesson, MD, PhD, Eva Swahn, MD, PhD, and Joakim Alfredsson, MD, PhD, of Linköping University, Sweden. They also pointed out that the study found a larger between-sex difference in failure to adhere to study drug in North America (odds ratio, 1.35; 95% confidence interval, 1.30-1.41), but a more moderate difference among participants in Europe/Middle East/Africa (OR, 1.13; 95% CI, 1.09-1.17) and Asia/Pacific (OR, 1.13; 95% CI, 1.03-1.23) regions. And there were no sex differences at all among South/Central American populations.
They noted that high rates of nonadherence increase the chances of a false negative finding and overestimation of drug safety. “We know the associations between nonadherence and clinical outcomes. The next step should be to better understand the underlying reasons for, as well as consistent reporting of, nonadherence, and discontinuation in RCTs,” the editorial authors wrote.
Dr. Lau suggested a simple method to better understand reasons for withdrawal: Addition of questions to the case report form that asks about reasons for drug discontinuation or study withdrawal. “Was it an adverse event? Was it because I’m a mother of three and I can’t get to the clinical trial site after work and also pick up my kids? Are there societal barriers for women, or was it the experience of the clinical trial that was maybe less favorable for women compared to men? Or maybe there are medical reasons we simply don’t know. Something as simple as asking those questions can help us better understand the barriers to female retention,” said Dr. Lau.
The analysis included data from 135,879 men (72%) and 51,812 women (28%) enrolled in the trials. After adjustment for baseline differences, women were more likely than were men to permanently discontinue study drug (adjusted odds ratio [aOR], 1.22: P < .001), which did not vary by study duration. The finding was consistent regardless of the type of drug studied, as well as across placebo and active study arms.
Women also were more likely to prematurely discontinue study drug (trial-adjusted OR, 1.18; P < .001). The rate of drug discontinuation due to adverse event was identical in both men and women, at 36%.
Women were more likely to withdraw consent than were men in a meta-analysis and when individual patient-level results were pooled (aOR, 1.26; P < .001 for both).
Dr. Lau received funding from the National Institutes of Health and has no relevant financial disclosures. The editorial authors had various disclosures, including lecture fees from Bayer, Pfizer, and Boehringer Ingelheim, and they served on advisory boards for AstraZeneca and MSD.
FROM CIRCULATION
Seen or viewed: A black hematologist’s perspective
After a long day in hematology clinic, I skimmed the inpatient list to see if any of my patients had been admitted. Seeing Ms. Short’s name (changed for privacy), a delightful African American woman I met during my early days of fellowship, had me making the trek to the hospital. She was living with multiple myeloma complicated by extramedullary manifestations that had significantly impacted her quality of life.
During our first encounter, she showed me a growing left subscapular mass the size of an orange that was erythematous, hot, painful, and irritated. As an enthusiastic first-year fellow, I wanted to be aggressive in addressing her concerns in response to her obvious distress about this mass. Ultimately, she left clinic with antibiotics and an appointment with radiation oncology to see if they could use radiation to shrink the subscapular mass.
When I went back in to discuss the plan with her, she grabbed my hand, looked me in my eyes and said: “Thank you, I’ve been mentioning this for a while and you’re the first person to get something done about it.” In that moment I knew that she felt seen.
By the time I made it over to the hospital, she was getting settled in her room to start another cycle of cytoreductive chemotherapy.
“I told them I had a Black doctor!” she exclaimed as I walked into her hospital room. “I was looking for you today in clinic ... I kept telling them I had a Black doctor, but the nurses kept telling me no, that there were only Black nurse practitioners.” She had repeatedly told the staff that I, her “Black doctor,” did indeed exist, and she went on to describe me as “you know, the [heavy-chested] and short Black doctor I saw early this fall.” To this day, her description still makes me chuckle.
Though I laughed at her description, it hurt that I had worked in a clinic for 6 months yet was invisible. Initially disappointed, I left Ms. Short’s room with a smile on my face, energized and encouraged.
My time with Ms. Short prompted me to ruminate on my experience as a Black physician. To put it in perspective, 5% of all physicians are Black, 2% are Black women, and 2.3% are oncologists, even though African Americans make up 13% of the general U.S. population. I reside in a space where I am simultaneously scrutinized because I am one of the few (or the only) Black physicians in the building, and yet I am invisible because my colleagues and coworkers routinely ignore my presence.
Black physicians, let alone hematologists, are so rare that nurses often cannot fathom that a Black woman could be more than a nurse practitioner. Sadly, this is the tip of the iceberg of some of the negative experiences I, and other Black doctors, have had.
How I present myself must be carefully curated to make progress in my career. My peers and superiors seem to hear me better when my hair is straight and not in its naturally curly state. My introversion has been interpreted as being standoffish or disinterested. Any tone other than happy is interpreted as “aggressive” or “angry”. Talking “too much” to Black support staff was reported to my program, as it was viewed as suspicious, disruptive, and “appearances matter”.
I am also expected to be nurturing in ways that White physicians are not required to be. In my presence, White physicians have denigrated an entire patient population that is disproportionately Black by calling them “sicklers.” If there is an interpersonal conflict, I must think about the long-term consequences of voicing my perspective. My non-Black colleagues do not have to think about these things.
Imagine dealing with this at work, then on your commute home being worried about the reality that you may be pulled over and become the next name on the ever-growing list of Black women and men murdered at the hands of police. The cognitive and emotional impact of being invisible is immense and cumulative over the years.
My Blackness creates a bias of inferiority that cannot be overcome by respectability, compliance, professionalism, training, and expertise. This is glaringly apparent on both sides of the physician-patient relationship. Black patients’ concerns are routinely overlooked and dismissed, as seen with Ms. Short, and are reflected in the Black maternal death rate, pain control in Black versus White patients, and personal experience as a patient and an advocate for my family members.
Patients have looked me in the face and said, “all lives matter,” displaying their refusal to recognize that systematic racism and inequality exist. These facts and experiences are the antithesis of “primum non nocere.”
Sadly, my and Ms. Short’s experiences are not singular ones, and racial bias in medicine is a diagnosed, but untreated cancer. Like the malignancies I treat, ignoring the problem has not made it go away; therefore, it continues to fester and spread, causing more destruction. It is of great importance and concern that all physicians recognize, reflect, and correct their implicit biases not only toward their patients, but also colleagues and trainees.
It seems that health care professionals can talk the talk, as many statements have been made against racism and implicit bias in medicine, but can we take true and meaningful action to begin the journey to equity and justice?
I would like to thank Adrienne Glover, MD, MaKenzie Hodge, MD, Maranatha McLean, MD, and Darion Showell, MD, for our stimulating conversations that helped me put pen to paper. I’d also like to thank my family for being my editors.
Daphanie D. Taylor, MD, is a hematology/oncology fellow PGY-6 at Levine Cancer Institute, Charlotte, N.C.
References and further reading
Roy L. “‘It’s My Calling To Change The Statistics’: Why We Need More Black Female Physicians.” Forbes Magazine, 27 Feb. 2020.
“Diversity in Medicine: Facts and Figures 2019.” Association of American Medical Colleges, 2019.
“Facts & Figures: Diversity in Oncology.” American Society of Clinical Oncology. 2020 Jan 16.
After a long day in hematology clinic, I skimmed the inpatient list to see if any of my patients had been admitted. Seeing Ms. Short’s name (changed for privacy), a delightful African American woman I met during my early days of fellowship, had me making the trek to the hospital. She was living with multiple myeloma complicated by extramedullary manifestations that had significantly impacted her quality of life.
During our first encounter, she showed me a growing left subscapular mass the size of an orange that was erythematous, hot, painful, and irritated. As an enthusiastic first-year fellow, I wanted to be aggressive in addressing her concerns in response to her obvious distress about this mass. Ultimately, she left clinic with antibiotics and an appointment with radiation oncology to see if they could use radiation to shrink the subscapular mass.
When I went back in to discuss the plan with her, she grabbed my hand, looked me in my eyes and said: “Thank you, I’ve been mentioning this for a while and you’re the first person to get something done about it.” In that moment I knew that she felt seen.
By the time I made it over to the hospital, she was getting settled in her room to start another cycle of cytoreductive chemotherapy.
“I told them I had a Black doctor!” she exclaimed as I walked into her hospital room. “I was looking for you today in clinic ... I kept telling them I had a Black doctor, but the nurses kept telling me no, that there were only Black nurse practitioners.” She had repeatedly told the staff that I, her “Black doctor,” did indeed exist, and she went on to describe me as “you know, the [heavy-chested] and short Black doctor I saw early this fall.” To this day, her description still makes me chuckle.
Though I laughed at her description, it hurt that I had worked in a clinic for 6 months yet was invisible. Initially disappointed, I left Ms. Short’s room with a smile on my face, energized and encouraged.
My time with Ms. Short prompted me to ruminate on my experience as a Black physician. To put it in perspective, 5% of all physicians are Black, 2% are Black women, and 2.3% are oncologists, even though African Americans make up 13% of the general U.S. population. I reside in a space where I am simultaneously scrutinized because I am one of the few (or the only) Black physicians in the building, and yet I am invisible because my colleagues and coworkers routinely ignore my presence.
Black physicians, let alone hematologists, are so rare that nurses often cannot fathom that a Black woman could be more than a nurse practitioner. Sadly, this is the tip of the iceberg of some of the negative experiences I, and other Black doctors, have had.
How I present myself must be carefully curated to make progress in my career. My peers and superiors seem to hear me better when my hair is straight and not in its naturally curly state. My introversion has been interpreted as being standoffish or disinterested. Any tone other than happy is interpreted as “aggressive” or “angry”. Talking “too much” to Black support staff was reported to my program, as it was viewed as suspicious, disruptive, and “appearances matter”.
I am also expected to be nurturing in ways that White physicians are not required to be. In my presence, White physicians have denigrated an entire patient population that is disproportionately Black by calling them “sicklers.” If there is an interpersonal conflict, I must think about the long-term consequences of voicing my perspective. My non-Black colleagues do not have to think about these things.
Imagine dealing with this at work, then on your commute home being worried about the reality that you may be pulled over and become the next name on the ever-growing list of Black women and men murdered at the hands of police. The cognitive and emotional impact of being invisible is immense and cumulative over the years.
My Blackness creates a bias of inferiority that cannot be overcome by respectability, compliance, professionalism, training, and expertise. This is glaringly apparent on both sides of the physician-patient relationship. Black patients’ concerns are routinely overlooked and dismissed, as seen with Ms. Short, and are reflected in the Black maternal death rate, pain control in Black versus White patients, and personal experience as a patient and an advocate for my family members.
Patients have looked me in the face and said, “all lives matter,” displaying their refusal to recognize that systematic racism and inequality exist. These facts and experiences are the antithesis of “primum non nocere.”
Sadly, my and Ms. Short’s experiences are not singular ones, and racial bias in medicine is a diagnosed, but untreated cancer. Like the malignancies I treat, ignoring the problem has not made it go away; therefore, it continues to fester and spread, causing more destruction. It is of great importance and concern that all physicians recognize, reflect, and correct their implicit biases not only toward their patients, but also colleagues and trainees.
It seems that health care professionals can talk the talk, as many statements have been made against racism and implicit bias in medicine, but can we take true and meaningful action to begin the journey to equity and justice?
I would like to thank Adrienne Glover, MD, MaKenzie Hodge, MD, Maranatha McLean, MD, and Darion Showell, MD, for our stimulating conversations that helped me put pen to paper. I’d also like to thank my family for being my editors.
Daphanie D. Taylor, MD, is a hematology/oncology fellow PGY-6 at Levine Cancer Institute, Charlotte, N.C.
References and further reading
Roy L. “‘It’s My Calling To Change The Statistics’: Why We Need More Black Female Physicians.” Forbes Magazine, 27 Feb. 2020.
“Diversity in Medicine: Facts and Figures 2019.” Association of American Medical Colleges, 2019.
“Facts & Figures: Diversity in Oncology.” American Society of Clinical Oncology. 2020 Jan 16.
After a long day in hematology clinic, I skimmed the inpatient list to see if any of my patients had been admitted. Seeing Ms. Short’s name (changed for privacy), a delightful African American woman I met during my early days of fellowship, had me making the trek to the hospital. She was living with multiple myeloma complicated by extramedullary manifestations that had significantly impacted her quality of life.
During our first encounter, she showed me a growing left subscapular mass the size of an orange that was erythematous, hot, painful, and irritated. As an enthusiastic first-year fellow, I wanted to be aggressive in addressing her concerns in response to her obvious distress about this mass. Ultimately, she left clinic with antibiotics and an appointment with radiation oncology to see if they could use radiation to shrink the subscapular mass.
When I went back in to discuss the plan with her, she grabbed my hand, looked me in my eyes and said: “Thank you, I’ve been mentioning this for a while and you’re the first person to get something done about it.” In that moment I knew that she felt seen.
By the time I made it over to the hospital, she was getting settled in her room to start another cycle of cytoreductive chemotherapy.
“I told them I had a Black doctor!” she exclaimed as I walked into her hospital room. “I was looking for you today in clinic ... I kept telling them I had a Black doctor, but the nurses kept telling me no, that there were only Black nurse practitioners.” She had repeatedly told the staff that I, her “Black doctor,” did indeed exist, and she went on to describe me as “you know, the [heavy-chested] and short Black doctor I saw early this fall.” To this day, her description still makes me chuckle.
Though I laughed at her description, it hurt that I had worked in a clinic for 6 months yet was invisible. Initially disappointed, I left Ms. Short’s room with a smile on my face, energized and encouraged.
My time with Ms. Short prompted me to ruminate on my experience as a Black physician. To put it in perspective, 5% of all physicians are Black, 2% are Black women, and 2.3% are oncologists, even though African Americans make up 13% of the general U.S. population. I reside in a space where I am simultaneously scrutinized because I am one of the few (or the only) Black physicians in the building, and yet I am invisible because my colleagues and coworkers routinely ignore my presence.
Black physicians, let alone hematologists, are so rare that nurses often cannot fathom that a Black woman could be more than a nurse practitioner. Sadly, this is the tip of the iceberg of some of the negative experiences I, and other Black doctors, have had.
How I present myself must be carefully curated to make progress in my career. My peers and superiors seem to hear me better when my hair is straight and not in its naturally curly state. My introversion has been interpreted as being standoffish or disinterested. Any tone other than happy is interpreted as “aggressive” or “angry”. Talking “too much” to Black support staff was reported to my program, as it was viewed as suspicious, disruptive, and “appearances matter”.
I am also expected to be nurturing in ways that White physicians are not required to be. In my presence, White physicians have denigrated an entire patient population that is disproportionately Black by calling them “sicklers.” If there is an interpersonal conflict, I must think about the long-term consequences of voicing my perspective. My non-Black colleagues do not have to think about these things.
Imagine dealing with this at work, then on your commute home being worried about the reality that you may be pulled over and become the next name on the ever-growing list of Black women and men murdered at the hands of police. The cognitive and emotional impact of being invisible is immense and cumulative over the years.
My Blackness creates a bias of inferiority that cannot be overcome by respectability, compliance, professionalism, training, and expertise. This is glaringly apparent on both sides of the physician-patient relationship. Black patients’ concerns are routinely overlooked and dismissed, as seen with Ms. Short, and are reflected in the Black maternal death rate, pain control in Black versus White patients, and personal experience as a patient and an advocate for my family members.
Patients have looked me in the face and said, “all lives matter,” displaying their refusal to recognize that systematic racism and inequality exist. These facts and experiences are the antithesis of “primum non nocere.”
Sadly, my and Ms. Short’s experiences are not singular ones, and racial bias in medicine is a diagnosed, but untreated cancer. Like the malignancies I treat, ignoring the problem has not made it go away; therefore, it continues to fester and spread, causing more destruction. It is of great importance and concern that all physicians recognize, reflect, and correct their implicit biases not only toward their patients, but also colleagues and trainees.
It seems that health care professionals can talk the talk, as many statements have been made against racism and implicit bias in medicine, but can we take true and meaningful action to begin the journey to equity and justice?
I would like to thank Adrienne Glover, MD, MaKenzie Hodge, MD, Maranatha McLean, MD, and Darion Showell, MD, for our stimulating conversations that helped me put pen to paper. I’d also like to thank my family for being my editors.
Daphanie D. Taylor, MD, is a hematology/oncology fellow PGY-6 at Levine Cancer Institute, Charlotte, N.C.
References and further reading
Roy L. “‘It’s My Calling To Change The Statistics’: Why We Need More Black Female Physicians.” Forbes Magazine, 27 Feb. 2020.
“Diversity in Medicine: Facts and Figures 2019.” Association of American Medical Colleges, 2019.
“Facts & Figures: Diversity in Oncology.” American Society of Clinical Oncology. 2020 Jan 16.
AAD announces diversity initiatives
not only within the academy itself, but also in the profession of dermatology overall.
“Last year’s events surrounding social justice issues and the disproportionate impact of COVID-19 on minority communities underscored an urgent need for the academy to outline a strategy to address gaps in diversity, equity, and inclusion across the academy’s programs, provide better access to dermatologic care, and expand the pipeline for prospective dermatologists,” according to an AAD statement introducing the plan.
“The AAD has long recognized the importance of fostering diversity in the dermatology specialty and increasing dermatologic services to underserved populations as a key strategic goal,” Kanya Ferguson, MD, chair of the AAD’s diversity committee, said in an interview.
“The importance and urgency of furthering these goals have been underscored by the social justice events of 2020 and the disproportionate impact that COVID-19 has had, specifically on Black and Latino communities,” added Dr. Ferguson, of the department of dermatology, at the University of Iowa, Iowa City. “The 3-year plan comprehensively expands current diversity, equity, and inclusion initiatives in an effort to accelerate the Academy’s progress toward its strategic goals.”
“Numerous barriers persist that contribute to the narrowing pipeline in medicine and ultimately in dermatology,” Dr. Ferguson noted. “The AAD’s diversity, equity, and inclusion initiatives, toolkits, and resources aim to address some of these barriers through early exposure, pipeline programming, and mentorship.”
As for the next steps, “the diversity committee will be working hard over the next few years to coordinate the integration and adoption of initiatives throughout the Academy’s activities,” she added. “This work will take a significant amount of collaboration and the committee is excited to move this forward in a meaningful and sustainable way.”
The AAD’s diversity committee headed the development of the plan, unanimously approved by the AAD’s board of directors, which outlines four key goals for the next 3 years, presented in the Diversity in Dermatology plan as follows:
“Promote and facilitate diversity, equity, and inclusion within the AAD.” Steps toward this goal include facilitating diverse representation on AAD committees, councils, and task forces, increasing representation of skin of color session speakers and lecture topics at Academy meetings, and ensuring equity in the selection process for awards including the Leadership Forum, Academic Dermatology Leadership Program, Advanced Leadership Forum, Journal of the AAD Editorial Mentorship Program, and other leadership activities.
- “Ensure dermatologic education and research encompasses health disparities and skin of color, and advocate for Black and Latino patient representation in research.” Steps toward this goal include increasing use of images reflecting the full spectrum of skin types, ensuring that skin of color populations receive information about dermatologic diseases, and supporting underrepresented minority (URM) dermatology physician scientists in leadership and professional development.
- “Expand Academy’s Advocacy Priorities to prioritize addressing health inequities.” Steps toward this goal include prioritizing issues that affect minority and marginalized populations, establishing relationships with relevant congressional leadership, and advocating for patient support groups for diseases that disproportionately impact skin of color patients.
- “Increase the number of practicing dermatologists who are underrepresented minorities and provide leadership and professional development programming.” Steps toward this goal include expanding the AAD mentorship program to include physician scientists, expanding diversity champion programs, expanding outreach to URM college students in STEM majors, and launching an AAD Summer Diversity & Inclusion camp for younger students to promote interest in a medical career.
The AAD diversity committee also has assembled a toolkit of resources designed to help its members learn how to talk about race, be an effective ally, and achieve cultural competency. Additional updated resources include guidelines on mentorship and outreach.
not only within the academy itself, but also in the profession of dermatology overall.
“Last year’s events surrounding social justice issues and the disproportionate impact of COVID-19 on minority communities underscored an urgent need for the academy to outline a strategy to address gaps in diversity, equity, and inclusion across the academy’s programs, provide better access to dermatologic care, and expand the pipeline for prospective dermatologists,” according to an AAD statement introducing the plan.
“The AAD has long recognized the importance of fostering diversity in the dermatology specialty and increasing dermatologic services to underserved populations as a key strategic goal,” Kanya Ferguson, MD, chair of the AAD’s diversity committee, said in an interview.
“The importance and urgency of furthering these goals have been underscored by the social justice events of 2020 and the disproportionate impact that COVID-19 has had, specifically on Black and Latino communities,” added Dr. Ferguson, of the department of dermatology, at the University of Iowa, Iowa City. “The 3-year plan comprehensively expands current diversity, equity, and inclusion initiatives in an effort to accelerate the Academy’s progress toward its strategic goals.”
“Numerous barriers persist that contribute to the narrowing pipeline in medicine and ultimately in dermatology,” Dr. Ferguson noted. “The AAD’s diversity, equity, and inclusion initiatives, toolkits, and resources aim to address some of these barriers through early exposure, pipeline programming, and mentorship.”
As for the next steps, “the diversity committee will be working hard over the next few years to coordinate the integration and adoption of initiatives throughout the Academy’s activities,” she added. “This work will take a significant amount of collaboration and the committee is excited to move this forward in a meaningful and sustainable way.”
The AAD’s diversity committee headed the development of the plan, unanimously approved by the AAD’s board of directors, which outlines four key goals for the next 3 years, presented in the Diversity in Dermatology plan as follows:
“Promote and facilitate diversity, equity, and inclusion within the AAD.” Steps toward this goal include facilitating diverse representation on AAD committees, councils, and task forces, increasing representation of skin of color session speakers and lecture topics at Academy meetings, and ensuring equity in the selection process for awards including the Leadership Forum, Academic Dermatology Leadership Program, Advanced Leadership Forum, Journal of the AAD Editorial Mentorship Program, and other leadership activities.
- “Ensure dermatologic education and research encompasses health disparities and skin of color, and advocate for Black and Latino patient representation in research.” Steps toward this goal include increasing use of images reflecting the full spectrum of skin types, ensuring that skin of color populations receive information about dermatologic diseases, and supporting underrepresented minority (URM) dermatology physician scientists in leadership and professional development.
- “Expand Academy’s Advocacy Priorities to prioritize addressing health inequities.” Steps toward this goal include prioritizing issues that affect minority and marginalized populations, establishing relationships with relevant congressional leadership, and advocating for patient support groups for diseases that disproportionately impact skin of color patients.
- “Increase the number of practicing dermatologists who are underrepresented minorities and provide leadership and professional development programming.” Steps toward this goal include expanding the AAD mentorship program to include physician scientists, expanding diversity champion programs, expanding outreach to URM college students in STEM majors, and launching an AAD Summer Diversity & Inclusion camp for younger students to promote interest in a medical career.
The AAD diversity committee also has assembled a toolkit of resources designed to help its members learn how to talk about race, be an effective ally, and achieve cultural competency. Additional updated resources include guidelines on mentorship and outreach.
not only within the academy itself, but also in the profession of dermatology overall.
“Last year’s events surrounding social justice issues and the disproportionate impact of COVID-19 on minority communities underscored an urgent need for the academy to outline a strategy to address gaps in diversity, equity, and inclusion across the academy’s programs, provide better access to dermatologic care, and expand the pipeline for prospective dermatologists,” according to an AAD statement introducing the plan.
“The AAD has long recognized the importance of fostering diversity in the dermatology specialty and increasing dermatologic services to underserved populations as a key strategic goal,” Kanya Ferguson, MD, chair of the AAD’s diversity committee, said in an interview.
“The importance and urgency of furthering these goals have been underscored by the social justice events of 2020 and the disproportionate impact that COVID-19 has had, specifically on Black and Latino communities,” added Dr. Ferguson, of the department of dermatology, at the University of Iowa, Iowa City. “The 3-year plan comprehensively expands current diversity, equity, and inclusion initiatives in an effort to accelerate the Academy’s progress toward its strategic goals.”
“Numerous barriers persist that contribute to the narrowing pipeline in medicine and ultimately in dermatology,” Dr. Ferguson noted. “The AAD’s diversity, equity, and inclusion initiatives, toolkits, and resources aim to address some of these barriers through early exposure, pipeline programming, and mentorship.”
As for the next steps, “the diversity committee will be working hard over the next few years to coordinate the integration and adoption of initiatives throughout the Academy’s activities,” she added. “This work will take a significant amount of collaboration and the committee is excited to move this forward in a meaningful and sustainable way.”
The AAD’s diversity committee headed the development of the plan, unanimously approved by the AAD’s board of directors, which outlines four key goals for the next 3 years, presented in the Diversity in Dermatology plan as follows:
“Promote and facilitate diversity, equity, and inclusion within the AAD.” Steps toward this goal include facilitating diverse representation on AAD committees, councils, and task forces, increasing representation of skin of color session speakers and lecture topics at Academy meetings, and ensuring equity in the selection process for awards including the Leadership Forum, Academic Dermatology Leadership Program, Advanced Leadership Forum, Journal of the AAD Editorial Mentorship Program, and other leadership activities.
- “Ensure dermatologic education and research encompasses health disparities and skin of color, and advocate for Black and Latino patient representation in research.” Steps toward this goal include increasing use of images reflecting the full spectrum of skin types, ensuring that skin of color populations receive information about dermatologic diseases, and supporting underrepresented minority (URM) dermatology physician scientists in leadership and professional development.
- “Expand Academy’s Advocacy Priorities to prioritize addressing health inequities.” Steps toward this goal include prioritizing issues that affect minority and marginalized populations, establishing relationships with relevant congressional leadership, and advocating for patient support groups for diseases that disproportionately impact skin of color patients.
- “Increase the number of practicing dermatologists who are underrepresented minorities and provide leadership and professional development programming.” Steps toward this goal include expanding the AAD mentorship program to include physician scientists, expanding diversity champion programs, expanding outreach to URM college students in STEM majors, and launching an AAD Summer Diversity & Inclusion camp for younger students to promote interest in a medical career.
The AAD diversity committee also has assembled a toolkit of resources designed to help its members learn how to talk about race, be an effective ally, and achieve cultural competency. Additional updated resources include guidelines on mentorship and outreach.
Neighborhood police complaints tied to Black preterm birth rates
The more complaints of excessive force by police reported by neighborhood residents, the more likely it is that Black pregnant people living in that neighborhood will deliver preterm, according to findings from a new study presented Jan. 28 at the virtual Society for Maternal-Fetal Medicine 2021 Annual Pregnancy Meeting.
“We know there are significant racial disparities in preterm birth which aren’t fully explained by traditional risk factors, like being older, having health problems like high blood pressure, or limited income,” Alexa Freedman, PhD, a postdoctoral fellow at NorthShore University HealthSystem and Northwestern University Institute for Policy Research, Evanston, Ill., told this news organization. “This has left many wondering if there are stressors unique to Black individuals that may be involved,” which has led to past research on the association of preterm birth with neighborhood segregation and historical “redlining” practices.
Black individuals have a substantially higher rate of preterm birth, compared with all other racial and ethnic groups in the US: 13.8% of Black infants born between 2016 and 2018 were preterm, compared with 11.6% among Native Americans – the next highest group – and 9.1% among White women.
“Studies have shown that psychosocial stress contributes to preterm birth disparities, potentially through several physiologic pathways that impact pregnancy outcomes,” Dr. Freedman told attendees. “Pregnant Black individuals have been reported to experience greater psychosocial stress regardless of socioeconomic status, possibly secondary to experiences of racism and discrimination.”
Though past research has examined neighborhood disadvantage and violence as stressors potentially contributing to preterm birth, little data exist on police–community relationships or police violence and pregnancy outcomes, despite being a “particularly salient stressor for Black individuals,” Dr. Freedman said. “Among pregnant Black individuals, prenatal depression has been correlated with concern about negative interactions between youth in their community and police.” To cite one example of the prevalence of racial bias in policing, she noted that “Chicago police are almost 10 times more likely to use force when interacting with a Black individual as compared [with] a White individual.”
The researchers therefore sought to determine whether a relationship existed between preterm birth rates and complaints regarding use of excessive force by police in the same neighborhood. They compiled records on all singleton live births from one Chicago hospital between March 2008 and March 2018, excluding those who lived outside Chicago, had a missing address, listed their race as “other,” or lacked data for specific other confounders.
Assessing police complaints within census blocks
The researchers obtained data on police complaints in Chicago from the Invisible Institute’s Citizen Police Data Project. They focused only on complaints of excessive use of force, “such as unnecessary physical contact and unnecessary display of a weapon,” Dr. Freedman said. They considered a person exposed in the neighborhood if a complaint was reported in her census block in the year leading up to birth. During their study period, more than 6,000 complaints of excessive force were reported across an estimated 70% of the blocks.
The study population had an average age of 31 and included 59.5% White, 12% Black, 20% Hispanic, and 8.5% Asian people. Just over half the pregnancies (55%) were first-time pregnancies, and 3.3% of the population had a history of preterm birth (before 37 weeks). The researchers also gathered data to adjust for the study population’s:
- Age
- Parity (number of times the woman has given birth).
- Population size of census block.
- Exposure to a homicide on the block in the year leading up to birth.
- Socioeconomic status by block (based on a composite of median home value, median income, percentage of a high school diploma, and percentage employed).
“Those who lived in a block with an excessive force complaint were more likely to be Black, more likely to deliver preterm, and more likely to be exposed to homicide,” Dr. Freedman told attendees.
The proportion of pregnant women exposed to police complaints was 15.8%, and 10.2% lived in neighborhoods where a homicide occurred in the year leading up to birth. Within the group exposed to a homicide, 16.5% lived in a neighborhood with an excessive force complaint and 9.1% did not.
Overall, 8.1% of the population gave birth preterm. When stratified by whether or not they lived in a block with an excessive force complaint, the researchers found the proportion of preterm births was higher among those who did than those who did not (9.3% vs. 7.8%).
Both before and after adjusting for confounders, Black people were the only racial/ethnic group who had a significantly increased risk of preterm birth if they lived on a block with a complaint. They were nearly 30% more likely to deliver preterm if an excessive force complaint had been reported nearby (odds ratio, 1.29). The odds of preterm birth were slightly elevated for White people and slightly reduced for Hispanic and Asian people, but none of those associations reached significance.
In a sensitivity analysis comparing 189 Black individuals to themselves, the researchers compared those who had one preterm birth and one term birth. They found that the preterm birth was 32% more likely to occur in a year when an excessive force complaint was filed after adjusting for age and birth order (OR, 1.32; 95% confidence interval, 0.82-2.13).
“Police violence reflects just one component of structural racism,” Dr. Freedman said in an interview. “Our findings highlight the need to more thoroughly consider how these systemic and structural factors contribute to disparities in maternal and fetal health.”
Clinical and policy implications
The clinical implications of these findings focus on the need for obstetric clinical teams to understand patients’ stressors and to provide support and resources, according to Dr. Freedman’s mentor, Ann Borders, MD, MSc, MPH, a maternal-fetal medicine physician at NorthShore and Evanston Hospital and a clinical associate professor at the University of Chicago Pritzker School of Medicine.
“Potential strategies include training on improved listening and respectful patient-centered care, such as provided by the CDC Hear Her campaign, and consideration of universal social determinants of health screening during obstetric care,” Dr. Borders told this news organization..
Though the study included a large sample size and allowed the researchers to control for individual and neighborhood characteristics, Dr. Freedman acknowledged that census blocks may or may not correlate with the way individuals define their own neighborhoods. They also didn’t have the data to assess the quality of prenatal care or the type of preterm birth, but they are developing a qualitative study to determine the best ways of measuring exposure to police violence.
In addition, the researchers’ reliance only on formal police complaints could have underestimated prevalence of excessive force, and the study did not take into account people’s direct experience with police violence; police violence that occurs within a person’s social network; or police violence widely covered in the news.
It wasn’t possible for the researchers to verify whether excessive force actually occurred or whether the force might have been justified, and it instead relied on the fact that someone lodged a complaint because he or she perceived the action as excessive.
Allison Bryant Mantha, MD, MPH, vice chair for Quality, Equity, and Safety at Massachusetts General Hospital in Boston and a board member of SMFM, said she was impressed with the adjustment of homicide exposure as a proxy for neighborhood crime.
“Many might assume that reports of police misconduct might be a marker for a ‘dangerous neighborhood,’ and it was thoughtful of the authors to adjust their analyses for exposure to crime to demonstrate that, even above and beyond crime, reports of police misconduct seem to be associated with adverse outcomes,” Dr. Bryant Mantha, who moderated the session, said in an interview.
Confronting this issue goes beyond what clinicians can do on their own, Dr. Bryant Mantha suggested.
“The greatest change will come with addressing the structural racism that underlies differential exposure to police misconduct in communities in the first place,” she said. “Concurrent with this, however, clinicians may consider adding in an assessment of neighborhood characteristics to include reports of police misconduct as they screen for other social determinants of health. While we do not have intervention studies to demonstrate efficacy, it is not a huge leap to imagine that recognition of this burden in individuals’ lives, plus offering ways to manage stress or seek redress, could be of benefit.”
The research was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institute on Minority Health and Health Disparities, and the Northwestern Medicine Enterprise Data Warehouse Pilot Data Program. Dr. Freedman, Dr. Borders, and Dr. Bryant Mantha have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The more complaints of excessive force by police reported by neighborhood residents, the more likely it is that Black pregnant people living in that neighborhood will deliver preterm, according to findings from a new study presented Jan. 28 at the virtual Society for Maternal-Fetal Medicine 2021 Annual Pregnancy Meeting.
“We know there are significant racial disparities in preterm birth which aren’t fully explained by traditional risk factors, like being older, having health problems like high blood pressure, or limited income,” Alexa Freedman, PhD, a postdoctoral fellow at NorthShore University HealthSystem and Northwestern University Institute for Policy Research, Evanston, Ill., told this news organization. “This has left many wondering if there are stressors unique to Black individuals that may be involved,” which has led to past research on the association of preterm birth with neighborhood segregation and historical “redlining” practices.
Black individuals have a substantially higher rate of preterm birth, compared with all other racial and ethnic groups in the US: 13.8% of Black infants born between 2016 and 2018 were preterm, compared with 11.6% among Native Americans – the next highest group – and 9.1% among White women.
“Studies have shown that psychosocial stress contributes to preterm birth disparities, potentially through several physiologic pathways that impact pregnancy outcomes,” Dr. Freedman told attendees. “Pregnant Black individuals have been reported to experience greater psychosocial stress regardless of socioeconomic status, possibly secondary to experiences of racism and discrimination.”
Though past research has examined neighborhood disadvantage and violence as stressors potentially contributing to preterm birth, little data exist on police–community relationships or police violence and pregnancy outcomes, despite being a “particularly salient stressor for Black individuals,” Dr. Freedman said. “Among pregnant Black individuals, prenatal depression has been correlated with concern about negative interactions between youth in their community and police.” To cite one example of the prevalence of racial bias in policing, she noted that “Chicago police are almost 10 times more likely to use force when interacting with a Black individual as compared [with] a White individual.”
The researchers therefore sought to determine whether a relationship existed between preterm birth rates and complaints regarding use of excessive force by police in the same neighborhood. They compiled records on all singleton live births from one Chicago hospital between March 2008 and March 2018, excluding those who lived outside Chicago, had a missing address, listed their race as “other,” or lacked data for specific other confounders.
Assessing police complaints within census blocks
The researchers obtained data on police complaints in Chicago from the Invisible Institute’s Citizen Police Data Project. They focused only on complaints of excessive use of force, “such as unnecessary physical contact and unnecessary display of a weapon,” Dr. Freedman said. They considered a person exposed in the neighborhood if a complaint was reported in her census block in the year leading up to birth. During their study period, more than 6,000 complaints of excessive force were reported across an estimated 70% of the blocks.
The study population had an average age of 31 and included 59.5% White, 12% Black, 20% Hispanic, and 8.5% Asian people. Just over half the pregnancies (55%) were first-time pregnancies, and 3.3% of the population had a history of preterm birth (before 37 weeks). The researchers also gathered data to adjust for the study population’s:
- Age
- Parity (number of times the woman has given birth).
- Population size of census block.
- Exposure to a homicide on the block in the year leading up to birth.
- Socioeconomic status by block (based on a composite of median home value, median income, percentage of a high school diploma, and percentage employed).
“Those who lived in a block with an excessive force complaint were more likely to be Black, more likely to deliver preterm, and more likely to be exposed to homicide,” Dr. Freedman told attendees.
The proportion of pregnant women exposed to police complaints was 15.8%, and 10.2% lived in neighborhoods where a homicide occurred in the year leading up to birth. Within the group exposed to a homicide, 16.5% lived in a neighborhood with an excessive force complaint and 9.1% did not.
Overall, 8.1% of the population gave birth preterm. When stratified by whether or not they lived in a block with an excessive force complaint, the researchers found the proportion of preterm births was higher among those who did than those who did not (9.3% vs. 7.8%).
Both before and after adjusting for confounders, Black people were the only racial/ethnic group who had a significantly increased risk of preterm birth if they lived on a block with a complaint. They were nearly 30% more likely to deliver preterm if an excessive force complaint had been reported nearby (odds ratio, 1.29). The odds of preterm birth were slightly elevated for White people and slightly reduced for Hispanic and Asian people, but none of those associations reached significance.
In a sensitivity analysis comparing 189 Black individuals to themselves, the researchers compared those who had one preterm birth and one term birth. They found that the preterm birth was 32% more likely to occur in a year when an excessive force complaint was filed after adjusting for age and birth order (OR, 1.32; 95% confidence interval, 0.82-2.13).
“Police violence reflects just one component of structural racism,” Dr. Freedman said in an interview. “Our findings highlight the need to more thoroughly consider how these systemic and structural factors contribute to disparities in maternal and fetal health.”
Clinical and policy implications
The clinical implications of these findings focus on the need for obstetric clinical teams to understand patients’ stressors and to provide support and resources, according to Dr. Freedman’s mentor, Ann Borders, MD, MSc, MPH, a maternal-fetal medicine physician at NorthShore and Evanston Hospital and a clinical associate professor at the University of Chicago Pritzker School of Medicine.
“Potential strategies include training on improved listening and respectful patient-centered care, such as provided by the CDC Hear Her campaign, and consideration of universal social determinants of health screening during obstetric care,” Dr. Borders told this news organization..
Though the study included a large sample size and allowed the researchers to control for individual and neighborhood characteristics, Dr. Freedman acknowledged that census blocks may or may not correlate with the way individuals define their own neighborhoods. They also didn’t have the data to assess the quality of prenatal care or the type of preterm birth, but they are developing a qualitative study to determine the best ways of measuring exposure to police violence.
In addition, the researchers’ reliance only on formal police complaints could have underestimated prevalence of excessive force, and the study did not take into account people’s direct experience with police violence; police violence that occurs within a person’s social network; or police violence widely covered in the news.
It wasn’t possible for the researchers to verify whether excessive force actually occurred or whether the force might have been justified, and it instead relied on the fact that someone lodged a complaint because he or she perceived the action as excessive.
Allison Bryant Mantha, MD, MPH, vice chair for Quality, Equity, and Safety at Massachusetts General Hospital in Boston and a board member of SMFM, said she was impressed with the adjustment of homicide exposure as a proxy for neighborhood crime.
“Many might assume that reports of police misconduct might be a marker for a ‘dangerous neighborhood,’ and it was thoughtful of the authors to adjust their analyses for exposure to crime to demonstrate that, even above and beyond crime, reports of police misconduct seem to be associated with adverse outcomes,” Dr. Bryant Mantha, who moderated the session, said in an interview.
Confronting this issue goes beyond what clinicians can do on their own, Dr. Bryant Mantha suggested.
“The greatest change will come with addressing the structural racism that underlies differential exposure to police misconduct in communities in the first place,” she said. “Concurrent with this, however, clinicians may consider adding in an assessment of neighborhood characteristics to include reports of police misconduct as they screen for other social determinants of health. While we do not have intervention studies to demonstrate efficacy, it is not a huge leap to imagine that recognition of this burden in individuals’ lives, plus offering ways to manage stress or seek redress, could be of benefit.”
The research was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institute on Minority Health and Health Disparities, and the Northwestern Medicine Enterprise Data Warehouse Pilot Data Program. Dr. Freedman, Dr. Borders, and Dr. Bryant Mantha have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The more complaints of excessive force by police reported by neighborhood residents, the more likely it is that Black pregnant people living in that neighborhood will deliver preterm, according to findings from a new study presented Jan. 28 at the virtual Society for Maternal-Fetal Medicine 2021 Annual Pregnancy Meeting.
“We know there are significant racial disparities in preterm birth which aren’t fully explained by traditional risk factors, like being older, having health problems like high blood pressure, or limited income,” Alexa Freedman, PhD, a postdoctoral fellow at NorthShore University HealthSystem and Northwestern University Institute for Policy Research, Evanston, Ill., told this news organization. “This has left many wondering if there are stressors unique to Black individuals that may be involved,” which has led to past research on the association of preterm birth with neighborhood segregation and historical “redlining” practices.
Black individuals have a substantially higher rate of preterm birth, compared with all other racial and ethnic groups in the US: 13.8% of Black infants born between 2016 and 2018 were preterm, compared with 11.6% among Native Americans – the next highest group – and 9.1% among White women.
“Studies have shown that psychosocial stress contributes to preterm birth disparities, potentially through several physiologic pathways that impact pregnancy outcomes,” Dr. Freedman told attendees. “Pregnant Black individuals have been reported to experience greater psychosocial stress regardless of socioeconomic status, possibly secondary to experiences of racism and discrimination.”
Though past research has examined neighborhood disadvantage and violence as stressors potentially contributing to preterm birth, little data exist on police–community relationships or police violence and pregnancy outcomes, despite being a “particularly salient stressor for Black individuals,” Dr. Freedman said. “Among pregnant Black individuals, prenatal depression has been correlated with concern about negative interactions between youth in their community and police.” To cite one example of the prevalence of racial bias in policing, she noted that “Chicago police are almost 10 times more likely to use force when interacting with a Black individual as compared [with] a White individual.”
The researchers therefore sought to determine whether a relationship existed between preterm birth rates and complaints regarding use of excessive force by police in the same neighborhood. They compiled records on all singleton live births from one Chicago hospital between March 2008 and March 2018, excluding those who lived outside Chicago, had a missing address, listed their race as “other,” or lacked data for specific other confounders.
Assessing police complaints within census blocks
The researchers obtained data on police complaints in Chicago from the Invisible Institute’s Citizen Police Data Project. They focused only on complaints of excessive use of force, “such as unnecessary physical contact and unnecessary display of a weapon,” Dr. Freedman said. They considered a person exposed in the neighborhood if a complaint was reported in her census block in the year leading up to birth. During their study period, more than 6,000 complaints of excessive force were reported across an estimated 70% of the blocks.
The study population had an average age of 31 and included 59.5% White, 12% Black, 20% Hispanic, and 8.5% Asian people. Just over half the pregnancies (55%) were first-time pregnancies, and 3.3% of the population had a history of preterm birth (before 37 weeks). The researchers also gathered data to adjust for the study population’s:
- Age
- Parity (number of times the woman has given birth).
- Population size of census block.
- Exposure to a homicide on the block in the year leading up to birth.
- Socioeconomic status by block (based on a composite of median home value, median income, percentage of a high school diploma, and percentage employed).
“Those who lived in a block with an excessive force complaint were more likely to be Black, more likely to deliver preterm, and more likely to be exposed to homicide,” Dr. Freedman told attendees.
The proportion of pregnant women exposed to police complaints was 15.8%, and 10.2% lived in neighborhoods where a homicide occurred in the year leading up to birth. Within the group exposed to a homicide, 16.5% lived in a neighborhood with an excessive force complaint and 9.1% did not.
Overall, 8.1% of the population gave birth preterm. When stratified by whether or not they lived in a block with an excessive force complaint, the researchers found the proportion of preterm births was higher among those who did than those who did not (9.3% vs. 7.8%).
Both before and after adjusting for confounders, Black people were the only racial/ethnic group who had a significantly increased risk of preterm birth if they lived on a block with a complaint. They were nearly 30% more likely to deliver preterm if an excessive force complaint had been reported nearby (odds ratio, 1.29). The odds of preterm birth were slightly elevated for White people and slightly reduced for Hispanic and Asian people, but none of those associations reached significance.
In a sensitivity analysis comparing 189 Black individuals to themselves, the researchers compared those who had one preterm birth and one term birth. They found that the preterm birth was 32% more likely to occur in a year when an excessive force complaint was filed after adjusting for age and birth order (OR, 1.32; 95% confidence interval, 0.82-2.13).
“Police violence reflects just one component of structural racism,” Dr. Freedman said in an interview. “Our findings highlight the need to more thoroughly consider how these systemic and structural factors contribute to disparities in maternal and fetal health.”
Clinical and policy implications
The clinical implications of these findings focus on the need for obstetric clinical teams to understand patients’ stressors and to provide support and resources, according to Dr. Freedman’s mentor, Ann Borders, MD, MSc, MPH, a maternal-fetal medicine physician at NorthShore and Evanston Hospital and a clinical associate professor at the University of Chicago Pritzker School of Medicine.
“Potential strategies include training on improved listening and respectful patient-centered care, such as provided by the CDC Hear Her campaign, and consideration of universal social determinants of health screening during obstetric care,” Dr. Borders told this news organization..
Though the study included a large sample size and allowed the researchers to control for individual and neighborhood characteristics, Dr. Freedman acknowledged that census blocks may or may not correlate with the way individuals define their own neighborhoods. They also didn’t have the data to assess the quality of prenatal care or the type of preterm birth, but they are developing a qualitative study to determine the best ways of measuring exposure to police violence.
In addition, the researchers’ reliance only on formal police complaints could have underestimated prevalence of excessive force, and the study did not take into account people’s direct experience with police violence; police violence that occurs within a person’s social network; or police violence widely covered in the news.
It wasn’t possible for the researchers to verify whether excessive force actually occurred or whether the force might have been justified, and it instead relied on the fact that someone lodged a complaint because he or she perceived the action as excessive.
Allison Bryant Mantha, MD, MPH, vice chair for Quality, Equity, and Safety at Massachusetts General Hospital in Boston and a board member of SMFM, said she was impressed with the adjustment of homicide exposure as a proxy for neighborhood crime.
“Many might assume that reports of police misconduct might be a marker for a ‘dangerous neighborhood,’ and it was thoughtful of the authors to adjust their analyses for exposure to crime to demonstrate that, even above and beyond crime, reports of police misconduct seem to be associated with adverse outcomes,” Dr. Bryant Mantha, who moderated the session, said in an interview.
Confronting this issue goes beyond what clinicians can do on their own, Dr. Bryant Mantha suggested.
“The greatest change will come with addressing the structural racism that underlies differential exposure to police misconduct in communities in the first place,” she said. “Concurrent with this, however, clinicians may consider adding in an assessment of neighborhood characteristics to include reports of police misconduct as they screen for other social determinants of health. While we do not have intervention studies to demonstrate efficacy, it is not a huge leap to imagine that recognition of this burden in individuals’ lives, plus offering ways to manage stress or seek redress, could be of benefit.”
The research was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institute on Minority Health and Health Disparities, and the Northwestern Medicine Enterprise Data Warehouse Pilot Data Program. Dr. Freedman, Dr. Borders, and Dr. Bryant Mantha have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Racial disparities in maternal morbidity persist even with equal access to care
An analysis of data from the U.S. military suggests that the maternal morbidity disparities between Black and White women cannot be attributed solely to differences in access to care and socioeconomics.
Even in the U.S. military health care system, where all service members have universal access to the same facilities and providers, researchers found substantial racial disparities in cesarean deliveries, maternal ICU admission, and overall severe maternal morbidity and mortality between Black patients and White patients, according to findings from a new study presented Jan. 28, 2021, at a meeting sponsored by the Society for Maternal-Fetal Medicine.
“This was surprising given some of the driving theories behind maternal race disparities encountered in this country, such as access to care and socioeconomic status, are controlled for in this health care system,” Capt. Jameaka Hamilton, MD, who presented the research, said in an interview. “Our findings indicate that there are likely additional factors at play which impact the obstetrical outcomes of women based upon their race, including systems-based barriers to accessing the military health care system which contribute to health care disparities, or in systemic or implicit biases which occur within our health care delivery.”
Plenty of recent research has documented the rise in maternal morbidity and mortality in the United States and the considerable racial disparities within those statistics. Black women are twice as likely to suffer morbidity and three to four times more likely to die in childbirth, compared with White women, Dr. Hamilton, an ob.gyn. from the San Antonio Uniformed Services Health Education Consortium at Ft. Sam Houston in San Antonio, Texas, reminded attendees. So far, much of this disparity has been attributed to social determinants of health.
Military retirees, active-duty personnel, and dependents, however, have equal access to federal health insurance and care at military health care facilities, or at covered civilian facilities where needed. Hence the researchers’ hypothesis that the military medical system would not show the same disparities by race that are seen in civilian populations.
The researchers analyzed maternal morbidity data from the Neonatal Perinatal Information Center from April 2018 to March 2019. The retrospective study included data from 13 military treatment facilities that had more than 1,000 deliveries per year. In addition to statistics on cesarean delivery and adult ICU admission, the researchers compared numbers on overall severe maternal morbidity based on the indicators defined by the Centers for Disease Control and Prevention.
The 15,305 deliveries included 23% Black patients and 77% White patients from the Air Force, Army, and Navy branches.
The cesarean delivery rate ranged from 19.4% to 35.5%. ICU admissions totaled 38 women, 190 women had postpartum hemorrhage, and 282 women experienced severe maternal morbidity. All three measures revealed racial disparities:
- Overall severe maternal morbidity occurred in 2.66% of Black women and 1.66% of White women (P =.0001).
- ICU admission occurred in 0.49% of Black women and 0.18% of White women (P =.0026).
- 31.68% of Black women had a cesarean delivery, compared with 23.58% of White women (P <.0001).
After excluding cases with blood transfusions, Black women were twice as likely to have severe maternal morbidity (0.64% vs. 0.32%). There were no significant differences in postpartum hemorrhage rates between Black and White women, but this analysis was limited by the small overall numbers of postpartum hemorrhage.
Among the study’s limitations were the inability to stratify patients by retiree, active duty, or dependent status, and the lack of data on preeclampsia rates, maternal age, obesity, or other preexisting conditions. In addition, the initial dataset included 61% of patients who reported their race as “other” than Black or White, limiting the number of patients whose data could be analyzed. Since low-volume hospitals were excluded, the outcomes could be skewed if lower-volume facilities are more likely to care for more complex cases, Dr. Hamilton added.
Allison Bryant Mantha, MD, MPH, vice chair for quality, equity, and safety in the ob.gyn. department at Massachusetts General Hospital, Boston, praised Dr. Hamilton’s work for revealing that differential access – though still problematic – cannot fully explain inequities between Black women and other women.
“The findings are not shocking given that what underlies some of these inequities – namely structural and institutional racism, and differential treatment within the system – are not exclusive to civilian health care settings,” Dr. Bryant Mantha, who moderated the session, said in an interview. “That said, doing the work to demonstrate this is extremely valuable.”
Although the causes of these disparities are systemic, Dr. Hamilton said individual providers can play a role in addressing them.
“There can certainly be more done to address this dangerous trend at the provider, hospital/institution, and national level,” she said. I think we as providers should continue to self-reflect and address our own biases. Hospitals and institutions should continue to develop policies that draw attention health care disparities.”
Completely removing these inequalities, however, will require confronting the racism embedded in U.S. health care at all levels, Dr. Bryant Mantha suggested.
“Ultimately, moving to an antiracist health care system – and criminal justice system, educational system, political system, etc. – and dismantling the existing structural racism in policies and practices will be needed to drive this change,” Dr. Bryant Mantha said. “Individual clinicians can use their voices to advocate for these changes in their health systems, communities, and states. Awareness of these inequities is critical, as is a sense of collective efficacy that we can, indeed, change the status quo.”
Dr. Hamilton and Dr. Bryant Mantha reported no disclosures.
An analysis of data from the U.S. military suggests that the maternal morbidity disparities between Black and White women cannot be attributed solely to differences in access to care and socioeconomics.
Even in the U.S. military health care system, where all service members have universal access to the same facilities and providers, researchers found substantial racial disparities in cesarean deliveries, maternal ICU admission, and overall severe maternal morbidity and mortality between Black patients and White patients, according to findings from a new study presented Jan. 28, 2021, at a meeting sponsored by the Society for Maternal-Fetal Medicine.
“This was surprising given some of the driving theories behind maternal race disparities encountered in this country, such as access to care and socioeconomic status, are controlled for in this health care system,” Capt. Jameaka Hamilton, MD, who presented the research, said in an interview. “Our findings indicate that there are likely additional factors at play which impact the obstetrical outcomes of women based upon their race, including systems-based barriers to accessing the military health care system which contribute to health care disparities, or in systemic or implicit biases which occur within our health care delivery.”
Plenty of recent research has documented the rise in maternal morbidity and mortality in the United States and the considerable racial disparities within those statistics. Black women are twice as likely to suffer morbidity and three to four times more likely to die in childbirth, compared with White women, Dr. Hamilton, an ob.gyn. from the San Antonio Uniformed Services Health Education Consortium at Ft. Sam Houston in San Antonio, Texas, reminded attendees. So far, much of this disparity has been attributed to social determinants of health.
Military retirees, active-duty personnel, and dependents, however, have equal access to federal health insurance and care at military health care facilities, or at covered civilian facilities where needed. Hence the researchers’ hypothesis that the military medical system would not show the same disparities by race that are seen in civilian populations.
The researchers analyzed maternal morbidity data from the Neonatal Perinatal Information Center from April 2018 to March 2019. The retrospective study included data from 13 military treatment facilities that had more than 1,000 deliveries per year. In addition to statistics on cesarean delivery and adult ICU admission, the researchers compared numbers on overall severe maternal morbidity based on the indicators defined by the Centers for Disease Control and Prevention.
The 15,305 deliveries included 23% Black patients and 77% White patients from the Air Force, Army, and Navy branches.
The cesarean delivery rate ranged from 19.4% to 35.5%. ICU admissions totaled 38 women, 190 women had postpartum hemorrhage, and 282 women experienced severe maternal morbidity. All three measures revealed racial disparities:
- Overall severe maternal morbidity occurred in 2.66% of Black women and 1.66% of White women (P =.0001).
- ICU admission occurred in 0.49% of Black women and 0.18% of White women (P =.0026).
- 31.68% of Black women had a cesarean delivery, compared with 23.58% of White women (P <.0001).
After excluding cases with blood transfusions, Black women were twice as likely to have severe maternal morbidity (0.64% vs. 0.32%). There were no significant differences in postpartum hemorrhage rates between Black and White women, but this analysis was limited by the small overall numbers of postpartum hemorrhage.
Among the study’s limitations were the inability to stratify patients by retiree, active duty, or dependent status, and the lack of data on preeclampsia rates, maternal age, obesity, or other preexisting conditions. In addition, the initial dataset included 61% of patients who reported their race as “other” than Black or White, limiting the number of patients whose data could be analyzed. Since low-volume hospitals were excluded, the outcomes could be skewed if lower-volume facilities are more likely to care for more complex cases, Dr. Hamilton added.
Allison Bryant Mantha, MD, MPH, vice chair for quality, equity, and safety in the ob.gyn. department at Massachusetts General Hospital, Boston, praised Dr. Hamilton’s work for revealing that differential access – though still problematic – cannot fully explain inequities between Black women and other women.
“The findings are not shocking given that what underlies some of these inequities – namely structural and institutional racism, and differential treatment within the system – are not exclusive to civilian health care settings,” Dr. Bryant Mantha, who moderated the session, said in an interview. “That said, doing the work to demonstrate this is extremely valuable.”
Although the causes of these disparities are systemic, Dr. Hamilton said individual providers can play a role in addressing them.
“There can certainly be more done to address this dangerous trend at the provider, hospital/institution, and national level,” she said. I think we as providers should continue to self-reflect and address our own biases. Hospitals and institutions should continue to develop policies that draw attention health care disparities.”
Completely removing these inequalities, however, will require confronting the racism embedded in U.S. health care at all levels, Dr. Bryant Mantha suggested.
“Ultimately, moving to an antiracist health care system – and criminal justice system, educational system, political system, etc. – and dismantling the existing structural racism in policies and practices will be needed to drive this change,” Dr. Bryant Mantha said. “Individual clinicians can use their voices to advocate for these changes in their health systems, communities, and states. Awareness of these inequities is critical, as is a sense of collective efficacy that we can, indeed, change the status quo.”
Dr. Hamilton and Dr. Bryant Mantha reported no disclosures.
An analysis of data from the U.S. military suggests that the maternal morbidity disparities between Black and White women cannot be attributed solely to differences in access to care and socioeconomics.
Even in the U.S. military health care system, where all service members have universal access to the same facilities and providers, researchers found substantial racial disparities in cesarean deliveries, maternal ICU admission, and overall severe maternal morbidity and mortality between Black patients and White patients, according to findings from a new study presented Jan. 28, 2021, at a meeting sponsored by the Society for Maternal-Fetal Medicine.
“This was surprising given some of the driving theories behind maternal race disparities encountered in this country, such as access to care and socioeconomic status, are controlled for in this health care system,” Capt. Jameaka Hamilton, MD, who presented the research, said in an interview. “Our findings indicate that there are likely additional factors at play which impact the obstetrical outcomes of women based upon their race, including systems-based barriers to accessing the military health care system which contribute to health care disparities, or in systemic or implicit biases which occur within our health care delivery.”
Plenty of recent research has documented the rise in maternal morbidity and mortality in the United States and the considerable racial disparities within those statistics. Black women are twice as likely to suffer morbidity and three to four times more likely to die in childbirth, compared with White women, Dr. Hamilton, an ob.gyn. from the San Antonio Uniformed Services Health Education Consortium at Ft. Sam Houston in San Antonio, Texas, reminded attendees. So far, much of this disparity has been attributed to social determinants of health.
Military retirees, active-duty personnel, and dependents, however, have equal access to federal health insurance and care at military health care facilities, or at covered civilian facilities where needed. Hence the researchers’ hypothesis that the military medical system would not show the same disparities by race that are seen in civilian populations.
The researchers analyzed maternal morbidity data from the Neonatal Perinatal Information Center from April 2018 to March 2019. The retrospective study included data from 13 military treatment facilities that had more than 1,000 deliveries per year. In addition to statistics on cesarean delivery and adult ICU admission, the researchers compared numbers on overall severe maternal morbidity based on the indicators defined by the Centers for Disease Control and Prevention.
The 15,305 deliveries included 23% Black patients and 77% White patients from the Air Force, Army, and Navy branches.
The cesarean delivery rate ranged from 19.4% to 35.5%. ICU admissions totaled 38 women, 190 women had postpartum hemorrhage, and 282 women experienced severe maternal morbidity. All three measures revealed racial disparities:
- Overall severe maternal morbidity occurred in 2.66% of Black women and 1.66% of White women (P =.0001).
- ICU admission occurred in 0.49% of Black women and 0.18% of White women (P =.0026).
- 31.68% of Black women had a cesarean delivery, compared with 23.58% of White women (P <.0001).
After excluding cases with blood transfusions, Black women were twice as likely to have severe maternal morbidity (0.64% vs. 0.32%). There were no significant differences in postpartum hemorrhage rates between Black and White women, but this analysis was limited by the small overall numbers of postpartum hemorrhage.
Among the study’s limitations were the inability to stratify patients by retiree, active duty, or dependent status, and the lack of data on preeclampsia rates, maternal age, obesity, or other preexisting conditions. In addition, the initial dataset included 61% of patients who reported their race as “other” than Black or White, limiting the number of patients whose data could be analyzed. Since low-volume hospitals were excluded, the outcomes could be skewed if lower-volume facilities are more likely to care for more complex cases, Dr. Hamilton added.
Allison Bryant Mantha, MD, MPH, vice chair for quality, equity, and safety in the ob.gyn. department at Massachusetts General Hospital, Boston, praised Dr. Hamilton’s work for revealing that differential access – though still problematic – cannot fully explain inequities between Black women and other women.
“The findings are not shocking given that what underlies some of these inequities – namely structural and institutional racism, and differential treatment within the system – are not exclusive to civilian health care settings,” Dr. Bryant Mantha, who moderated the session, said in an interview. “That said, doing the work to demonstrate this is extremely valuable.”
Although the causes of these disparities are systemic, Dr. Hamilton said individual providers can play a role in addressing them.
“There can certainly be more done to address this dangerous trend at the provider, hospital/institution, and national level,” she said. I think we as providers should continue to self-reflect and address our own biases. Hospitals and institutions should continue to develop policies that draw attention health care disparities.”
Completely removing these inequalities, however, will require confronting the racism embedded in U.S. health care at all levels, Dr. Bryant Mantha suggested.
“Ultimately, moving to an antiracist health care system – and criminal justice system, educational system, political system, etc. – and dismantling the existing structural racism in policies and practices will be needed to drive this change,” Dr. Bryant Mantha said. “Individual clinicians can use their voices to advocate for these changes in their health systems, communities, and states. Awareness of these inequities is critical, as is a sense of collective efficacy that we can, indeed, change the status quo.”
Dr. Hamilton and Dr. Bryant Mantha reported no disclosures.
FROM THE PREGNANCY MEETING
Model could reduce some disparities in lung cancer screening
New research suggests that proposed lung cancer screening guidelines could inadvertently increase racial and ethnic disparities, but adding in a risk prediction model could reduce some of these disparities by identifying people with high predicted benefit, regardless of race or ethnicity.
The draft United States Preventive Services Task Force (USPSTF) 2020 guidelines recommend annual lung cancer screening for individuals aged 50-80 who currently smoke or quit in the last 15 years, and who have a smoking history equivalent to at least one pack of cigarettes per day for 20 years or more.
This expands the age range and smoking history requirement compared to the 2013 USPSTF recommendations in an attempt to partially ameliorate racial disparities in screening eligibility. The 2013 guidelines recommend screening ever-smokers aged 55-80 with 30 or more pack-years and 15 or fewer quit-years.
However, neither the 2013 nor the 2020 USPSTF recommendations consider the higher risk of lung cancer and younger ages at diagnosis among African Americans, despite their smoking less than Whites, according to Rebecca Landy, PhD, of the National Cancer Institute in Bethesda, Md.
“For the same age and smoking history as Whites, minorities have substantially different lung cancer risk,” Dr. Landy said. “Incorporating individualized prediction models into USPSTF guidelines may reduce racial/ethnic disparities in lung cancer screening eligibility.”
Dr. Landy and colleagues set out to test that theory, and she presented the results at the 2020 World Congress on Lung Cancer (Abstract 3564), which was rescheduled for January 2021. The results were published in the Journal of the National Cancer Institute.
Study details
Dr. Landy and colleagues modeled the performance of National Lung Screening Trial–like screening (three annual CT screens, 5 years of follow-up) among three cohorts of ever-smokers aged 50-80 using the 2015 National Health Interview Survey.
One group was eligible by USPSTF 2013 guidelines, another by draft USPSTF 2020 guidelines, and yet another by augmenting the USPSTF 2020 guidelines using risk prediction to include individuals with 12 or more days of life gained according to the Life-Years From Screening–CT (LYFS-CT) model.
“Among each race/ethnicity, we calculated the number eligible for screening, proportion of preventable lung cancer deaths prevented, proportion of gainable life-years gained, and screening effectiveness, as well as the relative disparities in lung cancer deaths prevented and life-years gained,” Dr. Landy said.
Results
Under the 2013 guidelines, 8 million ever-smokers were eligible. The disparities in lung cancer death sensitivity, compared to Whites, were 15% for African Americans, 15% for Asian Americans, and 24% for Hispanic Americans. Disparities for life-year gained sensitivity were 15%, 13%, and 24%, respectively.
Under the 2020 draft guidelines, 14.5 million ever-smokers were eligible, but racial/ethnic disparities persisted. Disparities in lung cancer death sensitivity were 13% for African Americans, 19% for Asian Americans, and 27% for Hispanic Americans. Disparities for life-year gained sensitivity were 16%, 19%, and 27%, respectively.
Using the LYFS-CT predictive-risk model added an additional 3.5 million people and “nearly eliminated” disparities for African Americans, Dr. Landy noted. However, disparities persisted for Asian Americans and Hispanic Americans.
Disparities in lung cancer death sensitivity were 0% for African Americans, 19% for Asian Americans, and 23% for Hispanic Americans. Disparities for life-year gained sensitivity were 1%, 19%, and 24%, respectively.
More and widening disparity
The results showed that augmenting USPSTF criteria to include high-benefit people selected significantly more African Americans than Whites and could therefore reduce or even eliminate disparities between Whites and African Americans.
“The 2020 USPSTF draft recommendations would make 6.5 million more people eligible to be screened, in addition to the 8 million from the 2013 criteria,” said Gerard Silvestri, MD, of the Medical University of South Carolina, Charleston, who was not involved in this study.
“But there will be more White people than African American people added, and the disparity between them may widen. Using the risk prediction model outlined in this well-researched study could close the gap in disparity. It’s important to identify individual risk and life expectancy.”
Dr. Silvestri pointed out that, compared to Whites, African Americans develop lung cancer at an earlier age with fewer pack-years history of smoking and have worse outcomes.
“We can’t just focus on one aspect of disparity,” he said. “African Americans are much less likely to be insured or to identify a primary care provider for integrated care. We know that screening works. The 2020 USPSTF draft recommendations will enlarge the pool of eligible African Americans and reduce disparities if the other part of the equation holds; that is, they get access to care and screening.”
This study was funded by the National Institutes of Health/National Cancer Institute. Dr. Landy and Dr. Silvestri have no disclosures.
New research suggests that proposed lung cancer screening guidelines could inadvertently increase racial and ethnic disparities, but adding in a risk prediction model could reduce some of these disparities by identifying people with high predicted benefit, regardless of race or ethnicity.
The draft United States Preventive Services Task Force (USPSTF) 2020 guidelines recommend annual lung cancer screening for individuals aged 50-80 who currently smoke or quit in the last 15 years, and who have a smoking history equivalent to at least one pack of cigarettes per day for 20 years or more.
This expands the age range and smoking history requirement compared to the 2013 USPSTF recommendations in an attempt to partially ameliorate racial disparities in screening eligibility. The 2013 guidelines recommend screening ever-smokers aged 55-80 with 30 or more pack-years and 15 or fewer quit-years.
However, neither the 2013 nor the 2020 USPSTF recommendations consider the higher risk of lung cancer and younger ages at diagnosis among African Americans, despite their smoking less than Whites, according to Rebecca Landy, PhD, of the National Cancer Institute in Bethesda, Md.
“For the same age and smoking history as Whites, minorities have substantially different lung cancer risk,” Dr. Landy said. “Incorporating individualized prediction models into USPSTF guidelines may reduce racial/ethnic disparities in lung cancer screening eligibility.”
Dr. Landy and colleagues set out to test that theory, and she presented the results at the 2020 World Congress on Lung Cancer (Abstract 3564), which was rescheduled for January 2021. The results were published in the Journal of the National Cancer Institute.
Study details
Dr. Landy and colleagues modeled the performance of National Lung Screening Trial–like screening (three annual CT screens, 5 years of follow-up) among three cohorts of ever-smokers aged 50-80 using the 2015 National Health Interview Survey.
One group was eligible by USPSTF 2013 guidelines, another by draft USPSTF 2020 guidelines, and yet another by augmenting the USPSTF 2020 guidelines using risk prediction to include individuals with 12 or more days of life gained according to the Life-Years From Screening–CT (LYFS-CT) model.
“Among each race/ethnicity, we calculated the number eligible for screening, proportion of preventable lung cancer deaths prevented, proportion of gainable life-years gained, and screening effectiveness, as well as the relative disparities in lung cancer deaths prevented and life-years gained,” Dr. Landy said.
Results
Under the 2013 guidelines, 8 million ever-smokers were eligible. The disparities in lung cancer death sensitivity, compared to Whites, were 15% for African Americans, 15% for Asian Americans, and 24% for Hispanic Americans. Disparities for life-year gained sensitivity were 15%, 13%, and 24%, respectively.
Under the 2020 draft guidelines, 14.5 million ever-smokers were eligible, but racial/ethnic disparities persisted. Disparities in lung cancer death sensitivity were 13% for African Americans, 19% for Asian Americans, and 27% for Hispanic Americans. Disparities for life-year gained sensitivity were 16%, 19%, and 27%, respectively.
Using the LYFS-CT predictive-risk model added an additional 3.5 million people and “nearly eliminated” disparities for African Americans, Dr. Landy noted. However, disparities persisted for Asian Americans and Hispanic Americans.
Disparities in lung cancer death sensitivity were 0% for African Americans, 19% for Asian Americans, and 23% for Hispanic Americans. Disparities for life-year gained sensitivity were 1%, 19%, and 24%, respectively.
More and widening disparity
The results showed that augmenting USPSTF criteria to include high-benefit people selected significantly more African Americans than Whites and could therefore reduce or even eliminate disparities between Whites and African Americans.
“The 2020 USPSTF draft recommendations would make 6.5 million more people eligible to be screened, in addition to the 8 million from the 2013 criteria,” said Gerard Silvestri, MD, of the Medical University of South Carolina, Charleston, who was not involved in this study.
“But there will be more White people than African American people added, and the disparity between them may widen. Using the risk prediction model outlined in this well-researched study could close the gap in disparity. It’s important to identify individual risk and life expectancy.”
Dr. Silvestri pointed out that, compared to Whites, African Americans develop lung cancer at an earlier age with fewer pack-years history of smoking and have worse outcomes.
“We can’t just focus on one aspect of disparity,” he said. “African Americans are much less likely to be insured or to identify a primary care provider for integrated care. We know that screening works. The 2020 USPSTF draft recommendations will enlarge the pool of eligible African Americans and reduce disparities if the other part of the equation holds; that is, they get access to care and screening.”
This study was funded by the National Institutes of Health/National Cancer Institute. Dr. Landy and Dr. Silvestri have no disclosures.
New research suggests that proposed lung cancer screening guidelines could inadvertently increase racial and ethnic disparities, but adding in a risk prediction model could reduce some of these disparities by identifying people with high predicted benefit, regardless of race or ethnicity.
The draft United States Preventive Services Task Force (USPSTF) 2020 guidelines recommend annual lung cancer screening for individuals aged 50-80 who currently smoke or quit in the last 15 years, and who have a smoking history equivalent to at least one pack of cigarettes per day for 20 years or more.
This expands the age range and smoking history requirement compared to the 2013 USPSTF recommendations in an attempt to partially ameliorate racial disparities in screening eligibility. The 2013 guidelines recommend screening ever-smokers aged 55-80 with 30 or more pack-years and 15 or fewer quit-years.
However, neither the 2013 nor the 2020 USPSTF recommendations consider the higher risk of lung cancer and younger ages at diagnosis among African Americans, despite their smoking less than Whites, according to Rebecca Landy, PhD, of the National Cancer Institute in Bethesda, Md.
“For the same age and smoking history as Whites, minorities have substantially different lung cancer risk,” Dr. Landy said. “Incorporating individualized prediction models into USPSTF guidelines may reduce racial/ethnic disparities in lung cancer screening eligibility.”
Dr. Landy and colleagues set out to test that theory, and she presented the results at the 2020 World Congress on Lung Cancer (Abstract 3564), which was rescheduled for January 2021. The results were published in the Journal of the National Cancer Institute.
Study details
Dr. Landy and colleagues modeled the performance of National Lung Screening Trial–like screening (three annual CT screens, 5 years of follow-up) among three cohorts of ever-smokers aged 50-80 using the 2015 National Health Interview Survey.
One group was eligible by USPSTF 2013 guidelines, another by draft USPSTF 2020 guidelines, and yet another by augmenting the USPSTF 2020 guidelines using risk prediction to include individuals with 12 or more days of life gained according to the Life-Years From Screening–CT (LYFS-CT) model.
“Among each race/ethnicity, we calculated the number eligible for screening, proportion of preventable lung cancer deaths prevented, proportion of gainable life-years gained, and screening effectiveness, as well as the relative disparities in lung cancer deaths prevented and life-years gained,” Dr. Landy said.
Results
Under the 2013 guidelines, 8 million ever-smokers were eligible. The disparities in lung cancer death sensitivity, compared to Whites, were 15% for African Americans, 15% for Asian Americans, and 24% for Hispanic Americans. Disparities for life-year gained sensitivity were 15%, 13%, and 24%, respectively.
Under the 2020 draft guidelines, 14.5 million ever-smokers were eligible, but racial/ethnic disparities persisted. Disparities in lung cancer death sensitivity were 13% for African Americans, 19% for Asian Americans, and 27% for Hispanic Americans. Disparities for life-year gained sensitivity were 16%, 19%, and 27%, respectively.
Using the LYFS-CT predictive-risk model added an additional 3.5 million people and “nearly eliminated” disparities for African Americans, Dr. Landy noted. However, disparities persisted for Asian Americans and Hispanic Americans.
Disparities in lung cancer death sensitivity were 0% for African Americans, 19% for Asian Americans, and 23% for Hispanic Americans. Disparities for life-year gained sensitivity were 1%, 19%, and 24%, respectively.
More and widening disparity
The results showed that augmenting USPSTF criteria to include high-benefit people selected significantly more African Americans than Whites and could therefore reduce or even eliminate disparities between Whites and African Americans.
“The 2020 USPSTF draft recommendations would make 6.5 million more people eligible to be screened, in addition to the 8 million from the 2013 criteria,” said Gerard Silvestri, MD, of the Medical University of South Carolina, Charleston, who was not involved in this study.
“But there will be more White people than African American people added, and the disparity between them may widen. Using the risk prediction model outlined in this well-researched study could close the gap in disparity. It’s important to identify individual risk and life expectancy.”
Dr. Silvestri pointed out that, compared to Whites, African Americans develop lung cancer at an earlier age with fewer pack-years history of smoking and have worse outcomes.
“We can’t just focus on one aspect of disparity,” he said. “African Americans are much less likely to be insured or to identify a primary care provider for integrated care. We know that screening works. The 2020 USPSTF draft recommendations will enlarge the pool of eligible African Americans and reduce disparities if the other part of the equation holds; that is, they get access to care and screening.”
This study was funded by the National Institutes of Health/National Cancer Institute. Dr. Landy and Dr. Silvestri have no disclosures.
FROM WCLC 2020
Algorithm trims time to treatment of acute hypertension in pregnancy
Use of a semiautonomous algorithm to initiate treatment for hypertension emergencies in pregnancy significantly increased the number of individuals treated promptly, based on data from 959 obstetric patients.
Data show poor compliance with the current American College of Obstetricians and Gynecologists recommendations for treatment of acute severe hypertension with no more than 30-60 minutes’ delay; low compliance may be caused by “multiple factors including lack of intravenous access, inadequate health care practitioner or nursing availability, and implicit racial biases,” wrote Courtney Martin, DO, of Loma Linda (Calif.) University School of Medicine and colleagues.
Semiautomated treatment algorithms have been used to improve timely treatment of conditions including myocardial infarction, heart failure, acute stroke, and asthma, but their use in obstetrics to date has been limited, the researchers noted.
In a retrospective cohort study published in Obstetrics & Gynecology, the researchers identified pregnant and postpartum women treated for severe hypertension at a single center between January 2017 and March 2020. A semiautonomous treatment algorithm was implemented between May 2018 and March 2019. The algorithm included vital sign monitoring, blood pressure thresholds for diagnosis of severe hypertension, and automated order sets for recommended first-line antihypertensive therapy. The primary outcomes were treatment with antihypertensive therapy within 15, 30, and 60 minutes of diagnosis. “Severe hypertension was defined as systolic blood pressure 160 mm Hg or higher or diastolic blood pressure 110 mm Hg or higher,” the researchers said.
The study population was divided into three groups; a preimplementation group (373 patients) managed between January 2017 and April 2018, a during-implementation group (334 patients) managed between May 2018 and March 2019, and a postimplementation group (252 patients) managed between April 2019 and March 2020. Patient demographics were similar among all three groups.
Timely treatment improves with algorithm
Overall, treatment of severe hypertension within 15 minutes of diagnosis was 36.5% preimplementation, 45.8% during implementation, and 55.6% postimplementation. Severe hypertension treatment within 30 minutes of diagnosis was 65.9% preimplementation, 77.8% during implementation, and 79.0% post implementation. Differences were significant between pre- and post implementation for 15 minutes and 30 minutes, but no significant differences occurred in the patients treated within 60 minutes before and after implementation of the algorithm.
The study findings were limited by several factors, including the inability to separate peer-to-peer education and other training from the impact of the algorithm, as well as a lack of data on the effect of the algorithm on maternal or neonatal outcomes, the researchers noted.
However, the results support the potential of a semiautonomous algorithm to significantly improve adherence to the recommended treatment guidelines for severe hypertension in pregnancy and post partum, they said. Given the expected increase in hypertensive disorders in pregnancy because of the trends in older age and higher obesity rates in pregnant women, “Integration of semiautonomous treatment algorithms similar to ours into routine obstetric practices could help reduce the health care burden and improve clinical outcomes, especially in areas with limited health care resources,” they concluded.
Algorithm may reduce disparities
The overall rise in maternal mortality in the United States remains a concern, but “Even more concerning are the disturbing racial disparities that persist across socioeconomic strata,” wrote Alisse Hauspurg, MD, of the University of Pittsburgh in an accompanying editorial. “There is clear evidence that expeditious treatment of obstetric hypertensive emergency reduces the risk of severe morbidities including stroke, eclampsia, and maternal death,” she emphasized, but compliance with the ACOG recommendations to treat severe hypertension within 30-60 minutes of confirmation remains low, she said.
In this study, not only did use of the algorithm reduce time to antihypertensive therapy, but more than 50% of patients were treated for severe hypertension within 15 minutes, and more than 90% within 60 minutes, “which was sustained after the implementation phase,” and aligns with the ACOG recommendations, Dr. Hauspurg said. “Although Martin et al.’s algorithm was limited to the initial management of obstetric hypertensive emergency, it could readily be expanded to follow the full ACOG algorithm for management of hypertension in pregnancy,” she noted.
In addition, Black women are more frequently diagnosed with hypertensive disorders of pregnancy, including severe hypertension, and the algorithm might improve disparities, she said.
“It is plausible that widespread implementation of such a semiautonomous algorithm at hospitals across the country could reduce delays in treatment and prevent hypertension-related morbidities,” said Dr. Hauspurg. “The use of innovative approaches to management of severe hypertension and other obstetric emergencies has the potential to allow provision of more equitable care by overcoming health care practitioner and system biases, which could meaningfully reduce disparities in care and change the trajectory of maternal morbidity and mortality in the United States,” she emphasized.
Need to create culture of safety
“Maternal mortality in the United States is the highest among developed nations, and shocking disparities exist in outcomes for non-Hispanic Black and American Indian/Alaskan Native women,” said Lisa Hollier, MD, of Texas Children’s Health Plan in Bellaire. “In a California review of maternal deaths, the greatest quality improvement opportunities were missed diagnosis and ineffective treatment of preeclampsia and related diseases, which occurred in 65% of the cases where women died of preeclampsia/eclampsia,” she said.
The current study “is very timely as more and more states across the nation are participating in the AIM (Alliance for Innovation on Maternal Health) programs to prevent pregnancy-related mortality,” Dr. Hollier noted.
“This study demonstrated a significant association between implementation of the algorithm and an increased percentage of treatment of severe hypertension within 30 minutes,” Dr. Hollier said. “With the implementation of a comprehensive program that included treatment algorithms, the Illinois Perinatal Quality Collaborative improved timely treatment for women with severe high blood pressure, increasing the percentage of patients treated within 60 minutes from 41% at baseline to 79% in the first year of the project.”
The take-home message is that “implementation of the semiautonomous treatment algorithm can address important clinical variation, including delays in appropriate treatment of severe hypertension,” said Dr. Hollier. However, “One of the potential barriers [to use of an algorithm] is the need for accurate, real-time clinical assessment. Resources must be available to ensure appropriate monitoring,” Dr. Hollier noted. “Collaboration and support of implementation of these treatment algorithms must extend through the nursing staff, the physicians, and advanced-practice providers. Medical staff and administrative leaders are essential in creating a culture of safety and continuous process improvement,” she said.
In addition, “long-term follow-up on the implementation of broader quality improvement programs is essential,” Dr. Hollier said. “While implementation of an algorithm can, and did, result in process improvements, assessment of broader implementation of evidence-based bundles, combined with a systematic approach to redesign of multiple related processes needs to occur and include outcomes of severe maternal morbidity and mortality,” she explained.
The study received no outside funding. The researchers had no financial conflicts to disclose.
Neither Dr. Hauspurg nor Dr. Hollier had financial conflicts to disclose.
Use of a semiautonomous algorithm to initiate treatment for hypertension emergencies in pregnancy significantly increased the number of individuals treated promptly, based on data from 959 obstetric patients.
Data show poor compliance with the current American College of Obstetricians and Gynecologists recommendations for treatment of acute severe hypertension with no more than 30-60 minutes’ delay; low compliance may be caused by “multiple factors including lack of intravenous access, inadequate health care practitioner or nursing availability, and implicit racial biases,” wrote Courtney Martin, DO, of Loma Linda (Calif.) University School of Medicine and colleagues.
Semiautomated treatment algorithms have been used to improve timely treatment of conditions including myocardial infarction, heart failure, acute stroke, and asthma, but their use in obstetrics to date has been limited, the researchers noted.
In a retrospective cohort study published in Obstetrics & Gynecology, the researchers identified pregnant and postpartum women treated for severe hypertension at a single center between January 2017 and March 2020. A semiautonomous treatment algorithm was implemented between May 2018 and March 2019. The algorithm included vital sign monitoring, blood pressure thresholds for diagnosis of severe hypertension, and automated order sets for recommended first-line antihypertensive therapy. The primary outcomes were treatment with antihypertensive therapy within 15, 30, and 60 minutes of diagnosis. “Severe hypertension was defined as systolic blood pressure 160 mm Hg or higher or diastolic blood pressure 110 mm Hg or higher,” the researchers said.
The study population was divided into three groups; a preimplementation group (373 patients) managed between January 2017 and April 2018, a during-implementation group (334 patients) managed between May 2018 and March 2019, and a postimplementation group (252 patients) managed between April 2019 and March 2020. Patient demographics were similar among all three groups.
Timely treatment improves with algorithm
Overall, treatment of severe hypertension within 15 minutes of diagnosis was 36.5% preimplementation, 45.8% during implementation, and 55.6% postimplementation. Severe hypertension treatment within 30 minutes of diagnosis was 65.9% preimplementation, 77.8% during implementation, and 79.0% post implementation. Differences were significant between pre- and post implementation for 15 minutes and 30 minutes, but no significant differences occurred in the patients treated within 60 minutes before and after implementation of the algorithm.
The study findings were limited by several factors, including the inability to separate peer-to-peer education and other training from the impact of the algorithm, as well as a lack of data on the effect of the algorithm on maternal or neonatal outcomes, the researchers noted.
However, the results support the potential of a semiautonomous algorithm to significantly improve adherence to the recommended treatment guidelines for severe hypertension in pregnancy and post partum, they said. Given the expected increase in hypertensive disorders in pregnancy because of the trends in older age and higher obesity rates in pregnant women, “Integration of semiautonomous treatment algorithms similar to ours into routine obstetric practices could help reduce the health care burden and improve clinical outcomes, especially in areas with limited health care resources,” they concluded.
Algorithm may reduce disparities
The overall rise in maternal mortality in the United States remains a concern, but “Even more concerning are the disturbing racial disparities that persist across socioeconomic strata,” wrote Alisse Hauspurg, MD, of the University of Pittsburgh in an accompanying editorial. “There is clear evidence that expeditious treatment of obstetric hypertensive emergency reduces the risk of severe morbidities including stroke, eclampsia, and maternal death,” she emphasized, but compliance with the ACOG recommendations to treat severe hypertension within 30-60 minutes of confirmation remains low, she said.
In this study, not only did use of the algorithm reduce time to antihypertensive therapy, but more than 50% of patients were treated for severe hypertension within 15 minutes, and more than 90% within 60 minutes, “which was sustained after the implementation phase,” and aligns with the ACOG recommendations, Dr. Hauspurg said. “Although Martin et al.’s algorithm was limited to the initial management of obstetric hypertensive emergency, it could readily be expanded to follow the full ACOG algorithm for management of hypertension in pregnancy,” she noted.
In addition, Black women are more frequently diagnosed with hypertensive disorders of pregnancy, including severe hypertension, and the algorithm might improve disparities, she said.
“It is plausible that widespread implementation of such a semiautonomous algorithm at hospitals across the country could reduce delays in treatment and prevent hypertension-related morbidities,” said Dr. Hauspurg. “The use of innovative approaches to management of severe hypertension and other obstetric emergencies has the potential to allow provision of more equitable care by overcoming health care practitioner and system biases, which could meaningfully reduce disparities in care and change the trajectory of maternal morbidity and mortality in the United States,” she emphasized.
Need to create culture of safety
“Maternal mortality in the United States is the highest among developed nations, and shocking disparities exist in outcomes for non-Hispanic Black and American Indian/Alaskan Native women,” said Lisa Hollier, MD, of Texas Children’s Health Plan in Bellaire. “In a California review of maternal deaths, the greatest quality improvement opportunities were missed diagnosis and ineffective treatment of preeclampsia and related diseases, which occurred in 65% of the cases where women died of preeclampsia/eclampsia,” she said.
The current study “is very timely as more and more states across the nation are participating in the AIM (Alliance for Innovation on Maternal Health) programs to prevent pregnancy-related mortality,” Dr. Hollier noted.
“This study demonstrated a significant association between implementation of the algorithm and an increased percentage of treatment of severe hypertension within 30 minutes,” Dr. Hollier said. “With the implementation of a comprehensive program that included treatment algorithms, the Illinois Perinatal Quality Collaborative improved timely treatment for women with severe high blood pressure, increasing the percentage of patients treated within 60 minutes from 41% at baseline to 79% in the first year of the project.”
The take-home message is that “implementation of the semiautonomous treatment algorithm can address important clinical variation, including delays in appropriate treatment of severe hypertension,” said Dr. Hollier. However, “One of the potential barriers [to use of an algorithm] is the need for accurate, real-time clinical assessment. Resources must be available to ensure appropriate monitoring,” Dr. Hollier noted. “Collaboration and support of implementation of these treatment algorithms must extend through the nursing staff, the physicians, and advanced-practice providers. Medical staff and administrative leaders are essential in creating a culture of safety and continuous process improvement,” she said.
In addition, “long-term follow-up on the implementation of broader quality improvement programs is essential,” Dr. Hollier said. “While implementation of an algorithm can, and did, result in process improvements, assessment of broader implementation of evidence-based bundles, combined with a systematic approach to redesign of multiple related processes needs to occur and include outcomes of severe maternal morbidity and mortality,” she explained.
The study received no outside funding. The researchers had no financial conflicts to disclose.
Neither Dr. Hauspurg nor Dr. Hollier had financial conflicts to disclose.
Use of a semiautonomous algorithm to initiate treatment for hypertension emergencies in pregnancy significantly increased the number of individuals treated promptly, based on data from 959 obstetric patients.
Data show poor compliance with the current American College of Obstetricians and Gynecologists recommendations for treatment of acute severe hypertension with no more than 30-60 minutes’ delay; low compliance may be caused by “multiple factors including lack of intravenous access, inadequate health care practitioner or nursing availability, and implicit racial biases,” wrote Courtney Martin, DO, of Loma Linda (Calif.) University School of Medicine and colleagues.
Semiautomated treatment algorithms have been used to improve timely treatment of conditions including myocardial infarction, heart failure, acute stroke, and asthma, but their use in obstetrics to date has been limited, the researchers noted.
In a retrospective cohort study published in Obstetrics & Gynecology, the researchers identified pregnant and postpartum women treated for severe hypertension at a single center between January 2017 and March 2020. A semiautonomous treatment algorithm was implemented between May 2018 and March 2019. The algorithm included vital sign monitoring, blood pressure thresholds for diagnosis of severe hypertension, and automated order sets for recommended first-line antihypertensive therapy. The primary outcomes were treatment with antihypertensive therapy within 15, 30, and 60 minutes of diagnosis. “Severe hypertension was defined as systolic blood pressure 160 mm Hg or higher or diastolic blood pressure 110 mm Hg or higher,” the researchers said.
The study population was divided into three groups; a preimplementation group (373 patients) managed between January 2017 and April 2018, a during-implementation group (334 patients) managed between May 2018 and March 2019, and a postimplementation group (252 patients) managed between April 2019 and March 2020. Patient demographics were similar among all three groups.
Timely treatment improves with algorithm
Overall, treatment of severe hypertension within 15 minutes of diagnosis was 36.5% preimplementation, 45.8% during implementation, and 55.6% postimplementation. Severe hypertension treatment within 30 minutes of diagnosis was 65.9% preimplementation, 77.8% during implementation, and 79.0% post implementation. Differences were significant between pre- and post implementation for 15 minutes and 30 minutes, but no significant differences occurred in the patients treated within 60 minutes before and after implementation of the algorithm.
The study findings were limited by several factors, including the inability to separate peer-to-peer education and other training from the impact of the algorithm, as well as a lack of data on the effect of the algorithm on maternal or neonatal outcomes, the researchers noted.
However, the results support the potential of a semiautonomous algorithm to significantly improve adherence to the recommended treatment guidelines for severe hypertension in pregnancy and post partum, they said. Given the expected increase in hypertensive disorders in pregnancy because of the trends in older age and higher obesity rates in pregnant women, “Integration of semiautonomous treatment algorithms similar to ours into routine obstetric practices could help reduce the health care burden and improve clinical outcomes, especially in areas with limited health care resources,” they concluded.
Algorithm may reduce disparities
The overall rise in maternal mortality in the United States remains a concern, but “Even more concerning are the disturbing racial disparities that persist across socioeconomic strata,” wrote Alisse Hauspurg, MD, of the University of Pittsburgh in an accompanying editorial. “There is clear evidence that expeditious treatment of obstetric hypertensive emergency reduces the risk of severe morbidities including stroke, eclampsia, and maternal death,” she emphasized, but compliance with the ACOG recommendations to treat severe hypertension within 30-60 minutes of confirmation remains low, she said.
In this study, not only did use of the algorithm reduce time to antihypertensive therapy, but more than 50% of patients were treated for severe hypertension within 15 minutes, and more than 90% within 60 minutes, “which was sustained after the implementation phase,” and aligns with the ACOG recommendations, Dr. Hauspurg said. “Although Martin et al.’s algorithm was limited to the initial management of obstetric hypertensive emergency, it could readily be expanded to follow the full ACOG algorithm for management of hypertension in pregnancy,” she noted.
In addition, Black women are more frequently diagnosed with hypertensive disorders of pregnancy, including severe hypertension, and the algorithm might improve disparities, she said.
“It is plausible that widespread implementation of such a semiautonomous algorithm at hospitals across the country could reduce delays in treatment and prevent hypertension-related morbidities,” said Dr. Hauspurg. “The use of innovative approaches to management of severe hypertension and other obstetric emergencies has the potential to allow provision of more equitable care by overcoming health care practitioner and system biases, which could meaningfully reduce disparities in care and change the trajectory of maternal morbidity and mortality in the United States,” she emphasized.
Need to create culture of safety
“Maternal mortality in the United States is the highest among developed nations, and shocking disparities exist in outcomes for non-Hispanic Black and American Indian/Alaskan Native women,” said Lisa Hollier, MD, of Texas Children’s Health Plan in Bellaire. “In a California review of maternal deaths, the greatest quality improvement opportunities were missed diagnosis and ineffective treatment of preeclampsia and related diseases, which occurred in 65% of the cases where women died of preeclampsia/eclampsia,” she said.
The current study “is very timely as more and more states across the nation are participating in the AIM (Alliance for Innovation on Maternal Health) programs to prevent pregnancy-related mortality,” Dr. Hollier noted.
“This study demonstrated a significant association between implementation of the algorithm and an increased percentage of treatment of severe hypertension within 30 minutes,” Dr. Hollier said. “With the implementation of a comprehensive program that included treatment algorithms, the Illinois Perinatal Quality Collaborative improved timely treatment for women with severe high blood pressure, increasing the percentage of patients treated within 60 minutes from 41% at baseline to 79% in the first year of the project.”
The take-home message is that “implementation of the semiautonomous treatment algorithm can address important clinical variation, including delays in appropriate treatment of severe hypertension,” said Dr. Hollier. However, “One of the potential barriers [to use of an algorithm] is the need for accurate, real-time clinical assessment. Resources must be available to ensure appropriate monitoring,” Dr. Hollier noted. “Collaboration and support of implementation of these treatment algorithms must extend through the nursing staff, the physicians, and advanced-practice providers. Medical staff and administrative leaders are essential in creating a culture of safety and continuous process improvement,” she said.
In addition, “long-term follow-up on the implementation of broader quality improvement programs is essential,” Dr. Hollier said. “While implementation of an algorithm can, and did, result in process improvements, assessment of broader implementation of evidence-based bundles, combined with a systematic approach to redesign of multiple related processes needs to occur and include outcomes of severe maternal morbidity and mortality,” she explained.
The study received no outside funding. The researchers had no financial conflicts to disclose.
Neither Dr. Hauspurg nor Dr. Hollier had financial conflicts to disclose.
FROM OBSTETRICS & GYNECOLOGY












