User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
AI-based software demonstrates accuracy in diagnosis of autism
A software program based on artificial intelligence (AI) is effective for distinguishing young children with autism spectrum disorder (ASD) from those with other conditions, according to results of a pivotal trial presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
The AI-based software, which will be submitted to regulatory approval as a device, employs an algorithm that assembles inputs from a caregiver questionnaire, a video, and a clinician questionnaire, according to Sharief Taraman, MD, a pediatric neurologist at CHOC, a pediatric health care system in Orange County, Calif.
Although the device could be employed in a variety of settings, it is envisioned for use by primary care physicians. This will circumvent the need for specialist evaluation except in challenging cases. Currently, nearly all children with ASD are diagnosed in specialty care, according to data cited by Dr. Taraman.
“The lack of diagnostic tools for ASD in primary care settings contributes to an average delay of 3 years between first parental concern and diagnosis and to long wait lists for specialty evaluation,” he reported at the virtual meeting, presented by MedscapeLive.
When used with clinical judgment and criteria from the American Psychiatric Association’s 5th edition of the Diagnostic and Statistical Manual (DSM-5), the data from the trial suggest the diagnostic tool in the hands of primary care physicians “could efficiently and accurately assess ASD in children 18 to 72 months old,” said Dr. Taraman, also an associate clinical professor of pediatrics at the University of California, Irvine.*
The AI-assisted software was evaluated in 425 children at 14 sites in 6 states. The study population was reflective of U.S. demographics. Although only 36% of the children were female, this is consistent with ASD prevalence. Only 60% of the subjects were White. Nearly 30% were Black or Latinx and other populations, such as those of Asian heritage, were represented.
Children between the ages of 18 and 72 months were eligible if both a caregiver and a health care professional were concerned that the child had ASD. About the same time that a caregiver completed a 20-item questionnaire and the primary care physician completed a 15-item questionnaire on a mobile device, the caregiver uploaded two videos of 1-2 minutes in length.
This information, along with a 33-item questionnaire completed by an analyst of the submitted videos, was then processed by the software algorithm. It provided a patient status of positive or negative for ASD, or it concluded that the status was indeterminate.
“To reduce the risk of false classifications, the indeterminate status was included as a safety feature,” Dr. Taraman explained. However, Dr. Taraman considers an indeterminate designation potentially actionable. Rather than a negative result, this status suggests a complex neurodevelopmental disorder and indicates the need for further evaluation.
The reference standard diagnosis, completed in all participants in this study, was a specialist evaluation completed independently by two experts. The presence or absence of ASD was confirmed if the experts agreed. If they did not, a third specialist made the final determination.
In comparison to the specialist determinations, all were correctly classified except for one child, in which the software was determined to have made a false-negative diagnosis. A diagnosis of ASD was reached in 29% of the study participants.
For those with a determinate designation, the sensitivity was 98.4% and the specificity was 78.9%. This translated into positive predictive and negative predictive values of 80.8% and 98.3%, respectively.
Of those identified as indeterminate by the AI-assisted algorithm, 91% were ultimately considered by specialist evaluation to have complex issues. In this group, ASD was part of the complex clinical picture in 20%. The others had non-ASD neurodevelopmental conditions, according to Dr. Taraman.
When the accuracy was evaluated across ages, ethnicity, and factors such as parent education or family income, the tool performed consistently, Dr. Taraman reported. This is important, he said, because the presence or absence of ASD is misdiagnosed in many underserved populations.
The focus on developing a methodology specific for use in primary care was based on evidence that the delay in the diagnosis of ASD is attributable to long wait times for specialty evaluations.
“There will never be enough specialists. There is a need for a way to streamline the diagnosis of ASD,” Dr. Taraman maintained. This is helpful not only to parents concerned about their children, he said, but also there are data to suggest that early intervention improves outcomes.
A specialist in ASD, Paul Carbone, MD, medical director of the child development program at the University of Utah, Salt Lake City, agreed. He said early diagnosis and intervention should be a goal.
“Reducing the age of ASD diagnosis is a priority because early entry into autism-specific interventions is a strong predictor of optimal developmental outcomes for children,” Dr. Carbone said.
Although he is not familiar with this experimental AI-assisted diagnostic program, he has published on the feasibility of ASD diagnosis at the primary care level. In his study, Dr. Carbone examined the Modified Checklist for Autism in Toddlers (M-CHAT) as one of several methodologies that might be considered.
Diagnosis of ASD “can be achieved through systematic processes within primary care that facilitate universal development surveillance and autism screening followed by prompt and timely diagnostic evaluations of at-risk children,” Dr. Carbone said.
MedscapeLive and this news organization are owned by the same parent company. Dr. Taraman reported a financial relationship with Cognoa, the company that is developing the ASD software for clinical use. Dr. Carbone reported that he has no conflicts of interest.
*Updated, 7/7/21
A software program based on artificial intelligence (AI) is effective for distinguishing young children with autism spectrum disorder (ASD) from those with other conditions, according to results of a pivotal trial presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
The AI-based software, which will be submitted to regulatory approval as a device, employs an algorithm that assembles inputs from a caregiver questionnaire, a video, and a clinician questionnaire, according to Sharief Taraman, MD, a pediatric neurologist at CHOC, a pediatric health care system in Orange County, Calif.
Although the device could be employed in a variety of settings, it is envisioned for use by primary care physicians. This will circumvent the need for specialist evaluation except in challenging cases. Currently, nearly all children with ASD are diagnosed in specialty care, according to data cited by Dr. Taraman.
“The lack of diagnostic tools for ASD in primary care settings contributes to an average delay of 3 years between first parental concern and diagnosis and to long wait lists for specialty evaluation,” he reported at the virtual meeting, presented by MedscapeLive.
When used with clinical judgment and criteria from the American Psychiatric Association’s 5th edition of the Diagnostic and Statistical Manual (DSM-5), the data from the trial suggest the diagnostic tool in the hands of primary care physicians “could efficiently and accurately assess ASD in children 18 to 72 months old,” said Dr. Taraman, also an associate clinical professor of pediatrics at the University of California, Irvine.*
The AI-assisted software was evaluated in 425 children at 14 sites in 6 states. The study population was reflective of U.S. demographics. Although only 36% of the children were female, this is consistent with ASD prevalence. Only 60% of the subjects were White. Nearly 30% were Black or Latinx and other populations, such as those of Asian heritage, were represented.
Children between the ages of 18 and 72 months were eligible if both a caregiver and a health care professional were concerned that the child had ASD. About the same time that a caregiver completed a 20-item questionnaire and the primary care physician completed a 15-item questionnaire on a mobile device, the caregiver uploaded two videos of 1-2 minutes in length.
This information, along with a 33-item questionnaire completed by an analyst of the submitted videos, was then processed by the software algorithm. It provided a patient status of positive or negative for ASD, or it concluded that the status was indeterminate.
“To reduce the risk of false classifications, the indeterminate status was included as a safety feature,” Dr. Taraman explained. However, Dr. Taraman considers an indeterminate designation potentially actionable. Rather than a negative result, this status suggests a complex neurodevelopmental disorder and indicates the need for further evaluation.
The reference standard diagnosis, completed in all participants in this study, was a specialist evaluation completed independently by two experts. The presence or absence of ASD was confirmed if the experts agreed. If they did not, a third specialist made the final determination.
In comparison to the specialist determinations, all were correctly classified except for one child, in which the software was determined to have made a false-negative diagnosis. A diagnosis of ASD was reached in 29% of the study participants.
For those with a determinate designation, the sensitivity was 98.4% and the specificity was 78.9%. This translated into positive predictive and negative predictive values of 80.8% and 98.3%, respectively.
Of those identified as indeterminate by the AI-assisted algorithm, 91% were ultimately considered by specialist evaluation to have complex issues. In this group, ASD was part of the complex clinical picture in 20%. The others had non-ASD neurodevelopmental conditions, according to Dr. Taraman.
When the accuracy was evaluated across ages, ethnicity, and factors such as parent education or family income, the tool performed consistently, Dr. Taraman reported. This is important, he said, because the presence or absence of ASD is misdiagnosed in many underserved populations.
The focus on developing a methodology specific for use in primary care was based on evidence that the delay in the diagnosis of ASD is attributable to long wait times for specialty evaluations.
“There will never be enough specialists. There is a need for a way to streamline the diagnosis of ASD,” Dr. Taraman maintained. This is helpful not only to parents concerned about their children, he said, but also there are data to suggest that early intervention improves outcomes.
A specialist in ASD, Paul Carbone, MD, medical director of the child development program at the University of Utah, Salt Lake City, agreed. He said early diagnosis and intervention should be a goal.
“Reducing the age of ASD diagnosis is a priority because early entry into autism-specific interventions is a strong predictor of optimal developmental outcomes for children,” Dr. Carbone said.
Although he is not familiar with this experimental AI-assisted diagnostic program, he has published on the feasibility of ASD diagnosis at the primary care level. In his study, Dr. Carbone examined the Modified Checklist for Autism in Toddlers (M-CHAT) as one of several methodologies that might be considered.
Diagnosis of ASD “can be achieved through systematic processes within primary care that facilitate universal development surveillance and autism screening followed by prompt and timely diagnostic evaluations of at-risk children,” Dr. Carbone said.
MedscapeLive and this news organization are owned by the same parent company. Dr. Taraman reported a financial relationship with Cognoa, the company that is developing the ASD software for clinical use. Dr. Carbone reported that he has no conflicts of interest.
*Updated, 7/7/21
A software program based on artificial intelligence (AI) is effective for distinguishing young children with autism spectrum disorder (ASD) from those with other conditions, according to results of a pivotal trial presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
The AI-based software, which will be submitted to regulatory approval as a device, employs an algorithm that assembles inputs from a caregiver questionnaire, a video, and a clinician questionnaire, according to Sharief Taraman, MD, a pediatric neurologist at CHOC, a pediatric health care system in Orange County, Calif.
Although the device could be employed in a variety of settings, it is envisioned for use by primary care physicians. This will circumvent the need for specialist evaluation except in challenging cases. Currently, nearly all children with ASD are diagnosed in specialty care, according to data cited by Dr. Taraman.
“The lack of diagnostic tools for ASD in primary care settings contributes to an average delay of 3 years between first parental concern and diagnosis and to long wait lists for specialty evaluation,” he reported at the virtual meeting, presented by MedscapeLive.
When used with clinical judgment and criteria from the American Psychiatric Association’s 5th edition of the Diagnostic and Statistical Manual (DSM-5), the data from the trial suggest the diagnostic tool in the hands of primary care physicians “could efficiently and accurately assess ASD in children 18 to 72 months old,” said Dr. Taraman, also an associate clinical professor of pediatrics at the University of California, Irvine.*
The AI-assisted software was evaluated in 425 children at 14 sites in 6 states. The study population was reflective of U.S. demographics. Although only 36% of the children were female, this is consistent with ASD prevalence. Only 60% of the subjects were White. Nearly 30% were Black or Latinx and other populations, such as those of Asian heritage, were represented.
Children between the ages of 18 and 72 months were eligible if both a caregiver and a health care professional were concerned that the child had ASD. About the same time that a caregiver completed a 20-item questionnaire and the primary care physician completed a 15-item questionnaire on a mobile device, the caregiver uploaded two videos of 1-2 minutes in length.
This information, along with a 33-item questionnaire completed by an analyst of the submitted videos, was then processed by the software algorithm. It provided a patient status of positive or negative for ASD, or it concluded that the status was indeterminate.
“To reduce the risk of false classifications, the indeterminate status was included as a safety feature,” Dr. Taraman explained. However, Dr. Taraman considers an indeterminate designation potentially actionable. Rather than a negative result, this status suggests a complex neurodevelopmental disorder and indicates the need for further evaluation.
The reference standard diagnosis, completed in all participants in this study, was a specialist evaluation completed independently by two experts. The presence or absence of ASD was confirmed if the experts agreed. If they did not, a third specialist made the final determination.
In comparison to the specialist determinations, all were correctly classified except for one child, in which the software was determined to have made a false-negative diagnosis. A diagnosis of ASD was reached in 29% of the study participants.
For those with a determinate designation, the sensitivity was 98.4% and the specificity was 78.9%. This translated into positive predictive and negative predictive values of 80.8% and 98.3%, respectively.
Of those identified as indeterminate by the AI-assisted algorithm, 91% were ultimately considered by specialist evaluation to have complex issues. In this group, ASD was part of the complex clinical picture in 20%. The others had non-ASD neurodevelopmental conditions, according to Dr. Taraman.
When the accuracy was evaluated across ages, ethnicity, and factors such as parent education or family income, the tool performed consistently, Dr. Taraman reported. This is important, he said, because the presence or absence of ASD is misdiagnosed in many underserved populations.
The focus on developing a methodology specific for use in primary care was based on evidence that the delay in the diagnosis of ASD is attributable to long wait times for specialty evaluations.
“There will never be enough specialists. There is a need for a way to streamline the diagnosis of ASD,” Dr. Taraman maintained. This is helpful not only to parents concerned about their children, he said, but also there are data to suggest that early intervention improves outcomes.
A specialist in ASD, Paul Carbone, MD, medical director of the child development program at the University of Utah, Salt Lake City, agreed. He said early diagnosis and intervention should be a goal.
“Reducing the age of ASD diagnosis is a priority because early entry into autism-specific interventions is a strong predictor of optimal developmental outcomes for children,” Dr. Carbone said.
Although he is not familiar with this experimental AI-assisted diagnostic program, he has published on the feasibility of ASD diagnosis at the primary care level. In his study, Dr. Carbone examined the Modified Checklist for Autism in Toddlers (M-CHAT) as one of several methodologies that might be considered.
Diagnosis of ASD “can be achieved through systematic processes within primary care that facilitate universal development surveillance and autism screening followed by prompt and timely diagnostic evaluations of at-risk children,” Dr. Carbone said.
MedscapeLive and this news organization are owned by the same parent company. Dr. Taraman reported a financial relationship with Cognoa, the company that is developing the ASD software for clinical use. Dr. Carbone reported that he has no conflicts of interest.
*Updated, 7/7/21
FROM CP/AACP PSYCHIATRY UPDATE
Few clinical guidelines exist for treating post-COVID symptoms
As doctors struggled through several surges of COVID-19 infections, most of what we learned was acquired through real-life experience. While many treatment options were promoted, most flat-out failed to be real therapeutics at all. Now that we have a safe and effective vaccine, we can prevent many infections from this virus. However, we are still left to manage the many post-COVID symptoms our patients continue to suffer with.
Symptoms following infection can last for months and range widely from “brain fog,” fatigue, dyspnea, chest pain, generalized weakness, depression, and a host of others. Patients may experience one or all of these symptoms, and there is currently no good way to predict who will go on to become a COVID “long hauler”.
Following the example of being educated by COVID as it happened, the same is true for managing post-COVID symptoms. The medical community still has a poor understanding of why some people develop it and there are few evidence-based studies to support any treatment modalities.
which they define as “new, recurring, or ongoing symptoms more than 4 weeks after infection, sometimes after initial symptom recovery.” It is important to note that these symptoms can occur in any degree of sickness during the acute infection, including in those who were asymptomatic. Even the actual name of this post-COVID syndrome is still being developed, with several other names being used for it as well.
While the guidelines are quite extensive, the actual clinical recommendations are still vague. For example, it is advised to let the patient know that post-COVID symptoms are still not well understood. While it is important to be transparent with patients, this does little to reassure them. Patients look to doctors, especially their primary care physicians, to guide them on the best treatment paths. Yet, we currently have none for post-COVID syndrome.
It is also advised to treat the patients’ symptoms and help improve functioning. For many diseases, doctors like to get to the root cause of the problem. Treating a symptom often masks an underlying condition. It may make the patient feel better and improve what they are capable of doing, which is important, but it also fails to unmask the real problem. It is also important to note that symptoms can be out of proportion to clinical findings and should not be dismissed: we just don’t have the answers yet.
One helpful recommendation is having a patient keep a diary of their symptoms. This will help both the patient and doctor learn what may be triggering factors. If it is, for example, exertion that induces breathlessness, perhaps the patient can gradually increase their level of activity to minimize symptoms. Additionally, a “comprehensive rehabilitation program” is also advised and this can greatly assist addressing all the issues a patient is experiencing, physically and medically.
It is also advised that management of underlying medical conditions be optimized. While this is very important, it is not something specific to post-COVID syndrome: All patients should have their underlying medical conditions well controlled. It might be that the patient is paying more attention to their overall health, which is a good thing. However, this does not necessarily reduce the current symptoms a patient is experiencing.
The CDC makes a good attempt to offer guidance in the frustrating management of post-COVID syndrome. However, their clinical guidelines fail to offer specific management tools specific to treating post-COVID patients. The recommendations offered are more helpful to health in general. The fact that more specific recommendations are lacking is simply caused by the lack of knowledge of this condition at present. As more research is conducted and more knowledge obtained, new guidelines should become more detailed.
Dr. Girgis practices family medicine in South River, N.J., and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, N.J. You can contact her at [email protected].
As doctors struggled through several surges of COVID-19 infections, most of what we learned was acquired through real-life experience. While many treatment options were promoted, most flat-out failed to be real therapeutics at all. Now that we have a safe and effective vaccine, we can prevent many infections from this virus. However, we are still left to manage the many post-COVID symptoms our patients continue to suffer with.
Symptoms following infection can last for months and range widely from “brain fog,” fatigue, dyspnea, chest pain, generalized weakness, depression, and a host of others. Patients may experience one or all of these symptoms, and there is currently no good way to predict who will go on to become a COVID “long hauler”.
Following the example of being educated by COVID as it happened, the same is true for managing post-COVID symptoms. The medical community still has a poor understanding of why some people develop it and there are few evidence-based studies to support any treatment modalities.
which they define as “new, recurring, or ongoing symptoms more than 4 weeks after infection, sometimes after initial symptom recovery.” It is important to note that these symptoms can occur in any degree of sickness during the acute infection, including in those who were asymptomatic. Even the actual name of this post-COVID syndrome is still being developed, with several other names being used for it as well.
While the guidelines are quite extensive, the actual clinical recommendations are still vague. For example, it is advised to let the patient know that post-COVID symptoms are still not well understood. While it is important to be transparent with patients, this does little to reassure them. Patients look to doctors, especially their primary care physicians, to guide them on the best treatment paths. Yet, we currently have none for post-COVID syndrome.
It is also advised to treat the patients’ symptoms and help improve functioning. For many diseases, doctors like to get to the root cause of the problem. Treating a symptom often masks an underlying condition. It may make the patient feel better and improve what they are capable of doing, which is important, but it also fails to unmask the real problem. It is also important to note that symptoms can be out of proportion to clinical findings and should not be dismissed: we just don’t have the answers yet.
One helpful recommendation is having a patient keep a diary of their symptoms. This will help both the patient and doctor learn what may be triggering factors. If it is, for example, exertion that induces breathlessness, perhaps the patient can gradually increase their level of activity to minimize symptoms. Additionally, a “comprehensive rehabilitation program” is also advised and this can greatly assist addressing all the issues a patient is experiencing, physically and medically.
It is also advised that management of underlying medical conditions be optimized. While this is very important, it is not something specific to post-COVID syndrome: All patients should have their underlying medical conditions well controlled. It might be that the patient is paying more attention to their overall health, which is a good thing. However, this does not necessarily reduce the current symptoms a patient is experiencing.
The CDC makes a good attempt to offer guidance in the frustrating management of post-COVID syndrome. However, their clinical guidelines fail to offer specific management tools specific to treating post-COVID patients. The recommendations offered are more helpful to health in general. The fact that more specific recommendations are lacking is simply caused by the lack of knowledge of this condition at present. As more research is conducted and more knowledge obtained, new guidelines should become more detailed.
Dr. Girgis practices family medicine in South River, N.J., and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, N.J. You can contact her at [email protected].
As doctors struggled through several surges of COVID-19 infections, most of what we learned was acquired through real-life experience. While many treatment options were promoted, most flat-out failed to be real therapeutics at all. Now that we have a safe and effective vaccine, we can prevent many infections from this virus. However, we are still left to manage the many post-COVID symptoms our patients continue to suffer with.
Symptoms following infection can last for months and range widely from “brain fog,” fatigue, dyspnea, chest pain, generalized weakness, depression, and a host of others. Patients may experience one or all of these symptoms, and there is currently no good way to predict who will go on to become a COVID “long hauler”.
Following the example of being educated by COVID as it happened, the same is true for managing post-COVID symptoms. The medical community still has a poor understanding of why some people develop it and there are few evidence-based studies to support any treatment modalities.
which they define as “new, recurring, or ongoing symptoms more than 4 weeks after infection, sometimes after initial symptom recovery.” It is important to note that these symptoms can occur in any degree of sickness during the acute infection, including in those who were asymptomatic. Even the actual name of this post-COVID syndrome is still being developed, with several other names being used for it as well.
While the guidelines are quite extensive, the actual clinical recommendations are still vague. For example, it is advised to let the patient know that post-COVID symptoms are still not well understood. While it is important to be transparent with patients, this does little to reassure them. Patients look to doctors, especially their primary care physicians, to guide them on the best treatment paths. Yet, we currently have none for post-COVID syndrome.
It is also advised to treat the patients’ symptoms and help improve functioning. For many diseases, doctors like to get to the root cause of the problem. Treating a symptom often masks an underlying condition. It may make the patient feel better and improve what they are capable of doing, which is important, but it also fails to unmask the real problem. It is also important to note that symptoms can be out of proportion to clinical findings and should not be dismissed: we just don’t have the answers yet.
One helpful recommendation is having a patient keep a diary of their symptoms. This will help both the patient and doctor learn what may be triggering factors. If it is, for example, exertion that induces breathlessness, perhaps the patient can gradually increase their level of activity to minimize symptoms. Additionally, a “comprehensive rehabilitation program” is also advised and this can greatly assist addressing all the issues a patient is experiencing, physically and medically.
It is also advised that management of underlying medical conditions be optimized. While this is very important, it is not something specific to post-COVID syndrome: All patients should have their underlying medical conditions well controlled. It might be that the patient is paying more attention to their overall health, which is a good thing. However, this does not necessarily reduce the current symptoms a patient is experiencing.
The CDC makes a good attempt to offer guidance in the frustrating management of post-COVID syndrome. However, their clinical guidelines fail to offer specific management tools specific to treating post-COVID patients. The recommendations offered are more helpful to health in general. The fact that more specific recommendations are lacking is simply caused by the lack of knowledge of this condition at present. As more research is conducted and more knowledge obtained, new guidelines should become more detailed.
Dr. Girgis practices family medicine in South River, N.J., and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, N.J. You can contact her at [email protected].
Polypharmacy remains common for autism spectrum patients
Approximately one-third of individuals with autism spectrum disorder (ASD) are prescribed multiple medications to manage comorbidities and symptoms, according to data from a retrospective cohort study of more than 26,000 patients.
“Clinicians caring for patients with ASD are tasked with the challenges of managing the primary disease, as well as co-occurring medical conditions, and coordinating with educational and social service professionals to provide holistic care,” wrote Aliya G. Feroe of Harvard Medical School, Boston, and colleagues.
The medication classes used to treat individuals with ASD include ADHD medications, antipsychotics, antidepressants, mood stabilizers, benzodiazepines, anxiolytics, and hypnotics, but the prescription rates of these medications in ASD patients have not been examined in large studies, the researchers said.
In a study published in JAMA Pediatrics, the researchers identified 26,722 individuals with ASD using a United States health care database from Jan. 1, 2014, to Dec. 31, 2019. Data included records of inpatient and outpatient claims, and records of prescriptions filled through commercial pharmacies. Individuals received at least 1 of 24 of the most common medication groups for ASD or comorbidities. The average age of the study participants was 14 years, and 78% were male. Diagnostic codes for ASD were based on the International Classification of Diseases, Ninth Revision, and International Statistical Classification of Diseases and Related Health Problems, Tenth Revision.
Over the 6-year study period, approximately one-third of the participants were taking three or more medications at once, ranging from 28.6% to 31.5%. In any 1 year, approximately 41% of children were prescribed a single medication, 17% received two prescriptions, 7.9% received four, and 3.4% received five. Medication changes occurred more frequently within classes than between classes, and reasons for these changes may include patient preference, adverse effects, and cost, the researchers noted.
The overall number of children prescribed particular drugs remained consistent, the researchers noted. “For example, the total number of individuals prescribed methylphenidate shifted from 832 in 2014 to 850 in 2015, 899 in 2016, 863 in 2017, and 838 in 2018,” they wrote.
In 15 of the 24 medication groups included in the study, at least 15% of the individuals had unspecified anxiety disorder, anxiety neurosis, or major depressive disorder; in 11 of the medication groups, at least 15% had some form of ADHD. ADHD prevalence in patients taking stimulants varied based on ADHD type, the researchers said.
The most common comorbidities in patients taking antipsychotics were combined type ADHD (11.6%-17.8%) and anxiety disorder (13.1%-30.1%). The study findings suggest that many clinicians are incorporating medications into ASD management, the researchers said.
“Although there is no medical treatment for the core deficits of social communication and repetitive behavioral patterns in ASD, the American Academy of Pediatrics recommends that clinicians consider medications in the management of common comorbid conditions, including seizures, ADHD, anxiety disorders, mood disorders, and disruptive behavior disorders,” they said.
The findings were limited by several factors including the potential for inconsistent reporting of diagnoses and pharmacy claims, the researchers noted. Other limitations included a lack of direct clinical assessment to validate diagnoses and the absence of validated diagnostic instruments to screen for comorbidities, they added.
“Our findings suggest that clinicians may be increasingly using integrated approaches to treating patients with ASD and co-occurring conditions, and further work is necessary to determine the relative effects of pharmacotherapy vs. behavioral interventions on outcomes in patients with ASD,” the researchers concluded.
Many reasons for multiple medications
“The researchers put in a lot of effort to provide data on a large scale,” Herschel Lessin, MD, of Children’s Medical Group, Poughkeepsie, N.Y., said in an interview.
“The findings illustrate the reality that autistic children are prescribed a lot of medications for a lot of reasons, some of which are not entirely clear,” Dr. Lessin said. The study also reflects the chronic lack of behavioral health services for children, he noted. Many children with ASD are referred for services they are unable to access, he said. “As a result, they see doctors who can only prescribe medications to try to control behavior or symptoms for which the cause is unclear,” and which could be ASD or other comorbidities, he emphasized.
The large sample size strengthens the study findings, but some of the challenges include the use of claims data, which do not indicate how diagnoses were made, said Dr. Lessin. An additional limitation is the fact that many medications for children with autism are used off label, so the specific reason for their use may be unknown, he said.
The take-home message for clinicians is that children with ASD are getting a lot of medications, and pediatricians are not usually responsible for multiple medications,” Dr. Lessin said. Ultimately, the study is “a plea for more research,” to tease out details of what medications are indicated and helpful, he said.
The study received no outside funding. The researchers and Dr. Lessin had no financial conflicts to disclose. Dr. Lessin serves on the Pediatric News editorial advisory board.
Approximately one-third of individuals with autism spectrum disorder (ASD) are prescribed multiple medications to manage comorbidities and symptoms, according to data from a retrospective cohort study of more than 26,000 patients.
“Clinicians caring for patients with ASD are tasked with the challenges of managing the primary disease, as well as co-occurring medical conditions, and coordinating with educational and social service professionals to provide holistic care,” wrote Aliya G. Feroe of Harvard Medical School, Boston, and colleagues.
The medication classes used to treat individuals with ASD include ADHD medications, antipsychotics, antidepressants, mood stabilizers, benzodiazepines, anxiolytics, and hypnotics, but the prescription rates of these medications in ASD patients have not been examined in large studies, the researchers said.
In a study published in JAMA Pediatrics, the researchers identified 26,722 individuals with ASD using a United States health care database from Jan. 1, 2014, to Dec. 31, 2019. Data included records of inpatient and outpatient claims, and records of prescriptions filled through commercial pharmacies. Individuals received at least 1 of 24 of the most common medication groups for ASD or comorbidities. The average age of the study participants was 14 years, and 78% were male. Diagnostic codes for ASD were based on the International Classification of Diseases, Ninth Revision, and International Statistical Classification of Diseases and Related Health Problems, Tenth Revision.
Over the 6-year study period, approximately one-third of the participants were taking three or more medications at once, ranging from 28.6% to 31.5%. In any 1 year, approximately 41% of children were prescribed a single medication, 17% received two prescriptions, 7.9% received four, and 3.4% received five. Medication changes occurred more frequently within classes than between classes, and reasons for these changes may include patient preference, adverse effects, and cost, the researchers noted.
The overall number of children prescribed particular drugs remained consistent, the researchers noted. “For example, the total number of individuals prescribed methylphenidate shifted from 832 in 2014 to 850 in 2015, 899 in 2016, 863 in 2017, and 838 in 2018,” they wrote.
In 15 of the 24 medication groups included in the study, at least 15% of the individuals had unspecified anxiety disorder, anxiety neurosis, or major depressive disorder; in 11 of the medication groups, at least 15% had some form of ADHD. ADHD prevalence in patients taking stimulants varied based on ADHD type, the researchers said.
The most common comorbidities in patients taking antipsychotics were combined type ADHD (11.6%-17.8%) and anxiety disorder (13.1%-30.1%). The study findings suggest that many clinicians are incorporating medications into ASD management, the researchers said.
“Although there is no medical treatment for the core deficits of social communication and repetitive behavioral patterns in ASD, the American Academy of Pediatrics recommends that clinicians consider medications in the management of common comorbid conditions, including seizures, ADHD, anxiety disorders, mood disorders, and disruptive behavior disorders,” they said.
The findings were limited by several factors including the potential for inconsistent reporting of diagnoses and pharmacy claims, the researchers noted. Other limitations included a lack of direct clinical assessment to validate diagnoses and the absence of validated diagnostic instruments to screen for comorbidities, they added.
“Our findings suggest that clinicians may be increasingly using integrated approaches to treating patients with ASD and co-occurring conditions, and further work is necessary to determine the relative effects of pharmacotherapy vs. behavioral interventions on outcomes in patients with ASD,” the researchers concluded.
Many reasons for multiple medications
“The researchers put in a lot of effort to provide data on a large scale,” Herschel Lessin, MD, of Children’s Medical Group, Poughkeepsie, N.Y., said in an interview.
“The findings illustrate the reality that autistic children are prescribed a lot of medications for a lot of reasons, some of which are not entirely clear,” Dr. Lessin said. The study also reflects the chronic lack of behavioral health services for children, he noted. Many children with ASD are referred for services they are unable to access, he said. “As a result, they see doctors who can only prescribe medications to try to control behavior or symptoms for which the cause is unclear,” and which could be ASD or other comorbidities, he emphasized.
The large sample size strengthens the study findings, but some of the challenges include the use of claims data, which do not indicate how diagnoses were made, said Dr. Lessin. An additional limitation is the fact that many medications for children with autism are used off label, so the specific reason for their use may be unknown, he said.
The take-home message for clinicians is that children with ASD are getting a lot of medications, and pediatricians are not usually responsible for multiple medications,” Dr. Lessin said. Ultimately, the study is “a plea for more research,” to tease out details of what medications are indicated and helpful, he said.
The study received no outside funding. The researchers and Dr. Lessin had no financial conflicts to disclose. Dr. Lessin serves on the Pediatric News editorial advisory board.
Approximately one-third of individuals with autism spectrum disorder (ASD) are prescribed multiple medications to manage comorbidities and symptoms, according to data from a retrospective cohort study of more than 26,000 patients.
“Clinicians caring for patients with ASD are tasked with the challenges of managing the primary disease, as well as co-occurring medical conditions, and coordinating with educational and social service professionals to provide holistic care,” wrote Aliya G. Feroe of Harvard Medical School, Boston, and colleagues.
The medication classes used to treat individuals with ASD include ADHD medications, antipsychotics, antidepressants, mood stabilizers, benzodiazepines, anxiolytics, and hypnotics, but the prescription rates of these medications in ASD patients have not been examined in large studies, the researchers said.
In a study published in JAMA Pediatrics, the researchers identified 26,722 individuals with ASD using a United States health care database from Jan. 1, 2014, to Dec. 31, 2019. Data included records of inpatient and outpatient claims, and records of prescriptions filled through commercial pharmacies. Individuals received at least 1 of 24 of the most common medication groups for ASD or comorbidities. The average age of the study participants was 14 years, and 78% were male. Diagnostic codes for ASD were based on the International Classification of Diseases, Ninth Revision, and International Statistical Classification of Diseases and Related Health Problems, Tenth Revision.
Over the 6-year study period, approximately one-third of the participants were taking three or more medications at once, ranging from 28.6% to 31.5%. In any 1 year, approximately 41% of children were prescribed a single medication, 17% received two prescriptions, 7.9% received four, and 3.4% received five. Medication changes occurred more frequently within classes than between classes, and reasons for these changes may include patient preference, adverse effects, and cost, the researchers noted.
The overall number of children prescribed particular drugs remained consistent, the researchers noted. “For example, the total number of individuals prescribed methylphenidate shifted from 832 in 2014 to 850 in 2015, 899 in 2016, 863 in 2017, and 838 in 2018,” they wrote.
In 15 of the 24 medication groups included in the study, at least 15% of the individuals had unspecified anxiety disorder, anxiety neurosis, or major depressive disorder; in 11 of the medication groups, at least 15% had some form of ADHD. ADHD prevalence in patients taking stimulants varied based on ADHD type, the researchers said.
The most common comorbidities in patients taking antipsychotics were combined type ADHD (11.6%-17.8%) and anxiety disorder (13.1%-30.1%). The study findings suggest that many clinicians are incorporating medications into ASD management, the researchers said.
“Although there is no medical treatment for the core deficits of social communication and repetitive behavioral patterns in ASD, the American Academy of Pediatrics recommends that clinicians consider medications in the management of common comorbid conditions, including seizures, ADHD, anxiety disorders, mood disorders, and disruptive behavior disorders,” they said.
The findings were limited by several factors including the potential for inconsistent reporting of diagnoses and pharmacy claims, the researchers noted. Other limitations included a lack of direct clinical assessment to validate diagnoses and the absence of validated diagnostic instruments to screen for comorbidities, they added.
“Our findings suggest that clinicians may be increasingly using integrated approaches to treating patients with ASD and co-occurring conditions, and further work is necessary to determine the relative effects of pharmacotherapy vs. behavioral interventions on outcomes in patients with ASD,” the researchers concluded.
Many reasons for multiple medications
“The researchers put in a lot of effort to provide data on a large scale,” Herschel Lessin, MD, of Children’s Medical Group, Poughkeepsie, N.Y., said in an interview.
“The findings illustrate the reality that autistic children are prescribed a lot of medications for a lot of reasons, some of which are not entirely clear,” Dr. Lessin said. The study also reflects the chronic lack of behavioral health services for children, he noted. Many children with ASD are referred for services they are unable to access, he said. “As a result, they see doctors who can only prescribe medications to try to control behavior or symptoms for which the cause is unclear,” and which could be ASD or other comorbidities, he emphasized.
The large sample size strengthens the study findings, but some of the challenges include the use of claims data, which do not indicate how diagnoses were made, said Dr. Lessin. An additional limitation is the fact that many medications for children with autism are used off label, so the specific reason for their use may be unknown, he said.
The take-home message for clinicians is that children with ASD are getting a lot of medications, and pediatricians are not usually responsible for multiple medications,” Dr. Lessin said. Ultimately, the study is “a plea for more research,” to tease out details of what medications are indicated and helpful, he said.
The study received no outside funding. The researchers and Dr. Lessin had no financial conflicts to disclose. Dr. Lessin serves on the Pediatric News editorial advisory board.
FROM JAMA PEDIATRICS
FDA to add myocarditis warning to mRNA COVID-19 vaccines
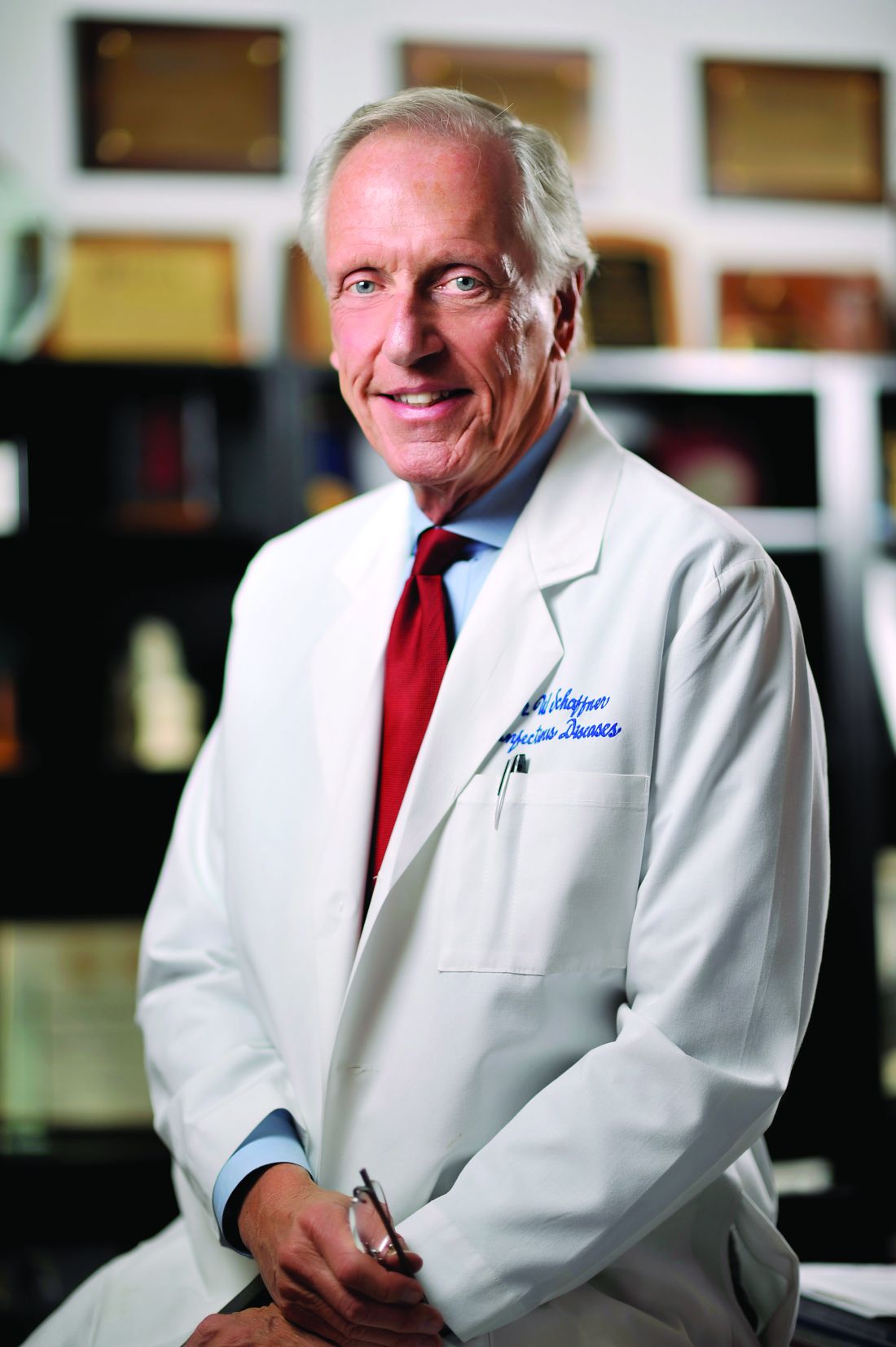
The Food and Drug Administration is adding a warning to mRNA COVID-19 vaccines’ fact sheets as medical experts continue to investigate cases of heart inflammation, which are rare but are more likely to occur in young men and teen boys.
Doran Fink, MD, PhD, deputy director of the FDA’s division of vaccines and related products applications, told a Centers for Disease Control and Prevention expert panel on June 23 that the FDA is finalizing language on a warning statement for health care providers, vaccine recipients, and parents or caregivers of teens.
The incidents are more likely to follow the second dose of the Pfizer or Moderna vaccine, with chest pain and other symptoms occurring within several days to a week, the warning will note.
“Based on limited follow-up, most cases appear to have been associated with resolution of symptoms, but limited information is available about potential long-term sequelae,” Dr. Fink said, describing the statement to the Advisory Committee on Immunization Practices, independent experts who advise the CDC.
“Symptoms suggestive of myocarditis or pericarditis should result in vaccine recipients seeking medical attention,” he said.
Benefits outweigh risks
Although no formal vote occurred after the meeting, the ACIP members delivered a strong endorsement for continuing to vaccinate 12- to 29-year-olds with the Pfizer and Moderna vaccines despite the warning.
“To me it’s clear, based on current information, that the benefits of vaccine clearly outweigh the risks,” said ACIP member Veronica McNally, president and CEO of the Franny Strong Foundation in Bloomfield, Mich., a sentiment echoed by other members.
As ACIP was meeting, leaders of the nation’s major physician, nurse, and public health associations issued a statement supporting continued vaccination: “The facts are clear: this is an extremely rare side effect, and only an exceedingly small number of people will experience it after vaccination.
“Importantly, for the young people who do, most cases are mild, and individuals recover often on their own or with minimal treatment. In addition, we know that myocarditis and pericarditis are much more common if you get COVID-19, and the risks to the heart from COVID-19 infection can be more severe.”
ACIP heard the evidence behind that claim. According to the Vaccine Safety Datalink, which contains data from more than 12 million medical records, myocarditis or pericarditis occurs in 12- to 39-year-olds at a rate of 8 per 1 million after the second Pfizer dose and 19.8 per 1 million after the second Moderna dose.
The CDC continues to investigate the link between the mRNA vaccines and heart inflammation, including any differences between the vaccines.
Most of the symptoms resolved quickly, said Tom Shimabukuro, deputy director of CDC’s Immunization Safety Office. Of 323 cases analyzed by the CDC, 309 were hospitalized, 295 were discharged, and 218, or 79%, had recovered from symptoms.
“Most postvaccine myocarditis has been responding to minimal treatment,” pediatric cardiologist Matthew Oster, MD, MPH, from Children’s Healthcare of Atlanta, told the panel.
COVID ‘risks are higher’
Overall, the CDC has reported 2,767 COVID-19 deaths among people aged 12-29 years, and there have been 4,018 reported cases of the COVID-linked inflammatory disorder MIS-C since the beginning of the pandemic.
That amounts to 1 MIS-C case in every 3,200 COVID infections – 36% of them among teens aged 12-20 years and 62% among children who are Hispanic or Black and non-Hispanic, according to a CDC presentation.
The CDC estimated that every 1 million second-dose COVID vaccines administered to 12- to 17-year-old boys could prevent 5,700 cases of COVID-19, 215 hospitalizations, 71 ICU admissions, and 2 deaths. There could also be 56-69 myocarditis cases.
The emergence of new variants in the United States and the skewed pattern of vaccination around the country also may increase the risk to unvaccinated young people, noted Grace Lee, MD, MPH, chair of the ACIP’s COVID-19 Vaccine Safety Technical Subgroup and a pediatric infectious disease physician at Stanford (Calif.) Children’s Health.
“If you’re in an area with low vaccination, the risks are higher,” she said. “The benefits [of the vaccine] are going to be far, far greater than any risk.”
Individuals, parents, and their clinicians should consider the full scope of risk when making decisions about vaccination, she said.
As the pandemic evolves, medical experts have to balance the known risks and benefits while they gather more information, said William Schaffner, MD, an infectious disease physician at Vanderbilt University, Nashville, Tenn., and medical director of the National Foundation for Infectious Diseases.
“The story is not over,” Dr. Schaffner said in an interview. “Clearly, we are still working in the face of a pandemic, so there’s urgency to continue vaccinating. But they would like to know more about the long-term consequences of the myocarditis.”
Booster possibilities
Meanwhile, ACIP began conversations on the parameters for a possible vaccine booster. For now, there are simply questions: Would a third vaccine help the immunocompromised gain protection? Should people get a different type of vaccine – mRNA versus adenovirus vector – for their booster? Most important, how long do antibodies last?
“Prior to going around giving everyone boosters, we really need to improve the overall vaccination coverage,” said Helen Keipp Talbot, MD, associate professor of medicine at Vanderbilt University. “That will protect everyone.”
A version of this article first appeared on Medscape.com.
The Food and Drug Administration is adding a warning to mRNA COVID-19 vaccines’ fact sheets as medical experts continue to investigate cases of heart inflammation, which are rare but are more likely to occur in young men and teen boys.
Doran Fink, MD, PhD, deputy director of the FDA’s division of vaccines and related products applications, told a Centers for Disease Control and Prevention expert panel on June 23 that the FDA is finalizing language on a warning statement for health care providers, vaccine recipients, and parents or caregivers of teens.
The incidents are more likely to follow the second dose of the Pfizer or Moderna vaccine, with chest pain and other symptoms occurring within several days to a week, the warning will note.
“Based on limited follow-up, most cases appear to have been associated with resolution of symptoms, but limited information is available about potential long-term sequelae,” Dr. Fink said, describing the statement to the Advisory Committee on Immunization Practices, independent experts who advise the CDC.
“Symptoms suggestive of myocarditis or pericarditis should result in vaccine recipients seeking medical attention,” he said.
Benefits outweigh risks
Although no formal vote occurred after the meeting, the ACIP members delivered a strong endorsement for continuing to vaccinate 12- to 29-year-olds with the Pfizer and Moderna vaccines despite the warning.
“To me it’s clear, based on current information, that the benefits of vaccine clearly outweigh the risks,” said ACIP member Veronica McNally, president and CEO of the Franny Strong Foundation in Bloomfield, Mich., a sentiment echoed by other members.
As ACIP was meeting, leaders of the nation’s major physician, nurse, and public health associations issued a statement supporting continued vaccination: “The facts are clear: this is an extremely rare side effect, and only an exceedingly small number of people will experience it after vaccination.
“Importantly, for the young people who do, most cases are mild, and individuals recover often on their own or with minimal treatment. In addition, we know that myocarditis and pericarditis are much more common if you get COVID-19, and the risks to the heart from COVID-19 infection can be more severe.”
ACIP heard the evidence behind that claim. According to the Vaccine Safety Datalink, which contains data from more than 12 million medical records, myocarditis or pericarditis occurs in 12- to 39-year-olds at a rate of 8 per 1 million after the second Pfizer dose and 19.8 per 1 million after the second Moderna dose.
The CDC continues to investigate the link between the mRNA vaccines and heart inflammation, including any differences between the vaccines.
Most of the symptoms resolved quickly, said Tom Shimabukuro, deputy director of CDC’s Immunization Safety Office. Of 323 cases analyzed by the CDC, 309 were hospitalized, 295 were discharged, and 218, or 79%, had recovered from symptoms.
“Most postvaccine myocarditis has been responding to minimal treatment,” pediatric cardiologist Matthew Oster, MD, MPH, from Children’s Healthcare of Atlanta, told the panel.
COVID ‘risks are higher’
Overall, the CDC has reported 2,767 COVID-19 deaths among people aged 12-29 years, and there have been 4,018 reported cases of the COVID-linked inflammatory disorder MIS-C since the beginning of the pandemic.
That amounts to 1 MIS-C case in every 3,200 COVID infections – 36% of them among teens aged 12-20 years and 62% among children who are Hispanic or Black and non-Hispanic, according to a CDC presentation.
The CDC estimated that every 1 million second-dose COVID vaccines administered to 12- to 17-year-old boys could prevent 5,700 cases of COVID-19, 215 hospitalizations, 71 ICU admissions, and 2 deaths. There could also be 56-69 myocarditis cases.
The emergence of new variants in the United States and the skewed pattern of vaccination around the country also may increase the risk to unvaccinated young people, noted Grace Lee, MD, MPH, chair of the ACIP’s COVID-19 Vaccine Safety Technical Subgroup and a pediatric infectious disease physician at Stanford (Calif.) Children’s Health.
“If you’re in an area with low vaccination, the risks are higher,” she said. “The benefits [of the vaccine] are going to be far, far greater than any risk.”
Individuals, parents, and their clinicians should consider the full scope of risk when making decisions about vaccination, she said.
As the pandemic evolves, medical experts have to balance the known risks and benefits while they gather more information, said William Schaffner, MD, an infectious disease physician at Vanderbilt University, Nashville, Tenn., and medical director of the National Foundation for Infectious Diseases.
“The story is not over,” Dr. Schaffner said in an interview. “Clearly, we are still working in the face of a pandemic, so there’s urgency to continue vaccinating. But they would like to know more about the long-term consequences of the myocarditis.”
Booster possibilities
Meanwhile, ACIP began conversations on the parameters for a possible vaccine booster. For now, there are simply questions: Would a third vaccine help the immunocompromised gain protection? Should people get a different type of vaccine – mRNA versus adenovirus vector – for their booster? Most important, how long do antibodies last?
“Prior to going around giving everyone boosters, we really need to improve the overall vaccination coverage,” said Helen Keipp Talbot, MD, associate professor of medicine at Vanderbilt University. “That will protect everyone.”
A version of this article first appeared on Medscape.com.
The Food and Drug Administration is adding a warning to mRNA COVID-19 vaccines’ fact sheets as medical experts continue to investigate cases of heart inflammation, which are rare but are more likely to occur in young men and teen boys.
Doran Fink, MD, PhD, deputy director of the FDA’s division of vaccines and related products applications, told a Centers for Disease Control and Prevention expert panel on June 23 that the FDA is finalizing language on a warning statement for health care providers, vaccine recipients, and parents or caregivers of teens.
The incidents are more likely to follow the second dose of the Pfizer or Moderna vaccine, with chest pain and other symptoms occurring within several days to a week, the warning will note.
“Based on limited follow-up, most cases appear to have been associated with resolution of symptoms, but limited information is available about potential long-term sequelae,” Dr. Fink said, describing the statement to the Advisory Committee on Immunization Practices, independent experts who advise the CDC.
“Symptoms suggestive of myocarditis or pericarditis should result in vaccine recipients seeking medical attention,” he said.
Benefits outweigh risks
Although no formal vote occurred after the meeting, the ACIP members delivered a strong endorsement for continuing to vaccinate 12- to 29-year-olds with the Pfizer and Moderna vaccines despite the warning.
“To me it’s clear, based on current information, that the benefits of vaccine clearly outweigh the risks,” said ACIP member Veronica McNally, president and CEO of the Franny Strong Foundation in Bloomfield, Mich., a sentiment echoed by other members.
As ACIP was meeting, leaders of the nation’s major physician, nurse, and public health associations issued a statement supporting continued vaccination: “The facts are clear: this is an extremely rare side effect, and only an exceedingly small number of people will experience it after vaccination.
“Importantly, for the young people who do, most cases are mild, and individuals recover often on their own or with minimal treatment. In addition, we know that myocarditis and pericarditis are much more common if you get COVID-19, and the risks to the heart from COVID-19 infection can be more severe.”
ACIP heard the evidence behind that claim. According to the Vaccine Safety Datalink, which contains data from more than 12 million medical records, myocarditis or pericarditis occurs in 12- to 39-year-olds at a rate of 8 per 1 million after the second Pfizer dose and 19.8 per 1 million after the second Moderna dose.
The CDC continues to investigate the link between the mRNA vaccines and heart inflammation, including any differences between the vaccines.
Most of the symptoms resolved quickly, said Tom Shimabukuro, deputy director of CDC’s Immunization Safety Office. Of 323 cases analyzed by the CDC, 309 were hospitalized, 295 were discharged, and 218, or 79%, had recovered from symptoms.
“Most postvaccine myocarditis has been responding to minimal treatment,” pediatric cardiologist Matthew Oster, MD, MPH, from Children’s Healthcare of Atlanta, told the panel.
COVID ‘risks are higher’
Overall, the CDC has reported 2,767 COVID-19 deaths among people aged 12-29 years, and there have been 4,018 reported cases of the COVID-linked inflammatory disorder MIS-C since the beginning of the pandemic.
That amounts to 1 MIS-C case in every 3,200 COVID infections – 36% of them among teens aged 12-20 years and 62% among children who are Hispanic or Black and non-Hispanic, according to a CDC presentation.
The CDC estimated that every 1 million second-dose COVID vaccines administered to 12- to 17-year-old boys could prevent 5,700 cases of COVID-19, 215 hospitalizations, 71 ICU admissions, and 2 deaths. There could also be 56-69 myocarditis cases.
The emergence of new variants in the United States and the skewed pattern of vaccination around the country also may increase the risk to unvaccinated young people, noted Grace Lee, MD, MPH, chair of the ACIP’s COVID-19 Vaccine Safety Technical Subgroup and a pediatric infectious disease physician at Stanford (Calif.) Children’s Health.
“If you’re in an area with low vaccination, the risks are higher,” she said. “The benefits [of the vaccine] are going to be far, far greater than any risk.”
Individuals, parents, and their clinicians should consider the full scope of risk when making decisions about vaccination, she said.
As the pandemic evolves, medical experts have to balance the known risks and benefits while they gather more information, said William Schaffner, MD, an infectious disease physician at Vanderbilt University, Nashville, Tenn., and medical director of the National Foundation for Infectious Diseases.
“The story is not over,” Dr. Schaffner said in an interview. “Clearly, we are still working in the face of a pandemic, so there’s urgency to continue vaccinating. But they would like to know more about the long-term consequences of the myocarditis.”
Booster possibilities
Meanwhile, ACIP began conversations on the parameters for a possible vaccine booster. For now, there are simply questions: Would a third vaccine help the immunocompromised gain protection? Should people get a different type of vaccine – mRNA versus adenovirus vector – for their booster? Most important, how long do antibodies last?
“Prior to going around giving everyone boosters, we really need to improve the overall vaccination coverage,” said Helen Keipp Talbot, MD, associate professor of medicine at Vanderbilt University. “That will protect everyone.”
A version of this article first appeared on Medscape.com.
Gray hair goes away and squids go to space
Goodbye stress, goodbye gray hair
Last year was a doozy, so it wouldn’t be too surprising if we all had a few new gray strands in our hair. But what if we told you that you don’t need to start dying them or plucking them out? What if they could magically go back to the way they were? Well, it may be possible, sans magic and sans stress.
Investigators recently discovered that the age-old belief that stress will permanently turn your hair gray may not be true after all. There’s a strong possibility that it could turn back to its original color once the stressful agent is eliminated.
“Understanding the mechanisms that allow ‘old’ gray hairs to return to their ‘young’ pigmented states could yield new clues about the malleability of human aging in general and how it is influenced by stress,” said senior author Martin Picard, PhD, of Columbia University, New York.
For the study, 14 volunteers were asked to keep a stress diary and review their levels of stress throughout the week. The researchers used a new method of viewing and capturing the images of tiny parts of the hairs to see how much graying took place in each part of the strand. And what they found – some strands naturally turning back to the original color – had never been documented before.
How did it happen? Our good friend the mitochondria. We haven’t really heard that word since eighth-grade biology, but it’s actually the key link between stress hormones and hair pigmentation. Think of them as little radars picking up all different kinds of signals in your body, like mental/emotional stress. They get a big enough alert and they’re going to react, thus gray hair.
So that’s all it takes? Cut the stress and a full head of gray can go back to brown? Not exactly. The researchers said there may be a “threshold because of biological age and other factors.” They believe middle age is near that threshold and it could easily be pushed over due to stress and could potentially go back. But if you’ve been rocking the salt and pepper or silver fox for a number of years and are looking for change, you might want to just eliminate the stress and pick up a bottle of dye.
One small step for squid
Space does a number on the human body. Forget the obvious like going for a walk outside without a spacesuit, or even the well-known risks like the degradation of bone in microgravity; there are numerous smaller but still important changes to the body during spaceflight, like the disruption of the symbiotic relationship between gut bacteria and the human body. This causes the immune system to lose the ability to recognize threats, and illnesses spread more easily.
Naturally, if astronauts are going to undertake years-long journeys to Mars and beyond, a thorough understanding of this disturbance is necessary, and that’s why NASA has sent a bunch of squid to the International Space Station.
When it comes to animal studies, squid aren’t the usual culprits, but there’s a reason NASA chose calamari over the alternatives: The Hawaiian bobtail squid has a symbiotic relationship with bacteria that regulate their bioluminescence in much the same way that we have a symbiotic relationship with our gut bacteria, but the squid is a much simpler animal. If the bioluminescence-regulating bacteria are disturbed during their time in space, it will be much easier to figure out what’s going wrong.
The experiment is ongoing, but we should salute the brave squid who have taken a giant leap for squidkind. Though if NASA didn’t send them up in a giant bubble, we’re going to be very disappointed.
Less plastic, more vanilla
Have you been racked by guilt over the number of plastic water bottles you use? What about the amount of ice cream you eat? Well, this one’s for you.
Plastic isn’t the first thing you think about when you open up a pint of vanilla ice cream and catch the sweet, spicy vanilla scent, or when you smell those fresh vanilla scones coming out of the oven at the coffee shop, but a new study shows that the flavor of vanilla can come from water bottles.
Here’s the deal. A compound called vanillin is responsible for the scent of vanilla, and it can come naturally from the bean or it can be made synthetically. Believe it or not, 85% of vanillin is made synthetically from fossil fuels!
We’ve definitely grown accustomed to our favorite vanilla scents, foods, and cosmetics. In 2018, the global demand for vanillin was about 40,800 tons and is expected to grow to 65,000 tons by 2025, which far exceeds the supply of natural vanilla.
So what can we do? Well, we can use genetically engineered bacteria to turn plastic water bottles into vanillin, according to a study published in the journal Green Chemistry.
The plastic can be broken down into terephthalic acid, which is very similar, chemically speaking, to vanillin. Similar enough that a bit of bioengineering produced Escherichia coli that could convert the acid into the tasty treat, according to researchers at the University of Edinburgh.
A perfect solution? Decreasing plastic waste while producing a valued food product? The thought of consuming plastic isn’t appetizing, so just eat your ice cream and try to forget about it.
No withdrawals from this bank
Into each life, some milestones must fall: High school graduation, birth of a child, first house, 50th wedding anniversary, COVID-19. One LOTME staffer got really excited – way too excited, actually – when his Nissan Sentra reached 300,000 miles.
Well, there are milestones, and then there are milestones. “1,000 Reasons for Hope” is a report celebrating the first 1,000 brains donated to the VA-BU-CLF Brain Bank. For those of you keeping score at home, that would be the Department of Veterans Affairs, Boston University, and the Concussion Legacy Foundation.
The Brain Bank, created in 2008 to study concussions and chronic traumatic encephalopathy, is the brainchild – yes, we went there – of Chris Nowinski, PhD, a former professional wrestler, and Ann McKee, MD, an expert on neurogenerative disease. “Our discoveries have already inspired changes to sports that will prevent many future cases of CTE in the next generation of athletes,” Dr. Nowinski, the CEO of CLF, said in a written statement.
Data from the first thousand brains show that 706 men, including 305 former NFL players, had football as their primary exposure to head impacts. Women were underrepresented, making up only 2.8% of brain donations, so recruiting females is a priority. Anyone interested in pledging can go to PledgeMyBrain.org or call 617-992-0615 for the 24-hour emergency donation pager.
LOTME wanted to help, so we called the Brain Bank to find out about donating. They asked a few questions and we told them what we do for a living. “Oh, you’re with LOTME? Yeah, we’ve … um, seen that before. It’s, um … funny. Can we put you on hold?” We’re starting to get a little sick of the on-hold music by now.
Goodbye stress, goodbye gray hair
Last year was a doozy, so it wouldn’t be too surprising if we all had a few new gray strands in our hair. But what if we told you that you don’t need to start dying them or plucking them out? What if they could magically go back to the way they were? Well, it may be possible, sans magic and sans stress.
Investigators recently discovered that the age-old belief that stress will permanently turn your hair gray may not be true after all. There’s a strong possibility that it could turn back to its original color once the stressful agent is eliminated.
“Understanding the mechanisms that allow ‘old’ gray hairs to return to their ‘young’ pigmented states could yield new clues about the malleability of human aging in general and how it is influenced by stress,” said senior author Martin Picard, PhD, of Columbia University, New York.
For the study, 14 volunteers were asked to keep a stress diary and review their levels of stress throughout the week. The researchers used a new method of viewing and capturing the images of tiny parts of the hairs to see how much graying took place in each part of the strand. And what they found – some strands naturally turning back to the original color – had never been documented before.
How did it happen? Our good friend the mitochondria. We haven’t really heard that word since eighth-grade biology, but it’s actually the key link between stress hormones and hair pigmentation. Think of them as little radars picking up all different kinds of signals in your body, like mental/emotional stress. They get a big enough alert and they’re going to react, thus gray hair.
So that’s all it takes? Cut the stress and a full head of gray can go back to brown? Not exactly. The researchers said there may be a “threshold because of biological age and other factors.” They believe middle age is near that threshold and it could easily be pushed over due to stress and could potentially go back. But if you’ve been rocking the salt and pepper or silver fox for a number of years and are looking for change, you might want to just eliminate the stress and pick up a bottle of dye.
One small step for squid
Space does a number on the human body. Forget the obvious like going for a walk outside without a spacesuit, or even the well-known risks like the degradation of bone in microgravity; there are numerous smaller but still important changes to the body during spaceflight, like the disruption of the symbiotic relationship between gut bacteria and the human body. This causes the immune system to lose the ability to recognize threats, and illnesses spread more easily.
Naturally, if astronauts are going to undertake years-long journeys to Mars and beyond, a thorough understanding of this disturbance is necessary, and that’s why NASA has sent a bunch of squid to the International Space Station.
When it comes to animal studies, squid aren’t the usual culprits, but there’s a reason NASA chose calamari over the alternatives: The Hawaiian bobtail squid has a symbiotic relationship with bacteria that regulate their bioluminescence in much the same way that we have a symbiotic relationship with our gut bacteria, but the squid is a much simpler animal. If the bioluminescence-regulating bacteria are disturbed during their time in space, it will be much easier to figure out what’s going wrong.
The experiment is ongoing, but we should salute the brave squid who have taken a giant leap for squidkind. Though if NASA didn’t send them up in a giant bubble, we’re going to be very disappointed.
Less plastic, more vanilla
Have you been racked by guilt over the number of plastic water bottles you use? What about the amount of ice cream you eat? Well, this one’s for you.
Plastic isn’t the first thing you think about when you open up a pint of vanilla ice cream and catch the sweet, spicy vanilla scent, or when you smell those fresh vanilla scones coming out of the oven at the coffee shop, but a new study shows that the flavor of vanilla can come from water bottles.
Here’s the deal. A compound called vanillin is responsible for the scent of vanilla, and it can come naturally from the bean or it can be made synthetically. Believe it or not, 85% of vanillin is made synthetically from fossil fuels!
We’ve definitely grown accustomed to our favorite vanilla scents, foods, and cosmetics. In 2018, the global demand for vanillin was about 40,800 tons and is expected to grow to 65,000 tons by 2025, which far exceeds the supply of natural vanilla.
So what can we do? Well, we can use genetically engineered bacteria to turn plastic water bottles into vanillin, according to a study published in the journal Green Chemistry.
The plastic can be broken down into terephthalic acid, which is very similar, chemically speaking, to vanillin. Similar enough that a bit of bioengineering produced Escherichia coli that could convert the acid into the tasty treat, according to researchers at the University of Edinburgh.
A perfect solution? Decreasing plastic waste while producing a valued food product? The thought of consuming plastic isn’t appetizing, so just eat your ice cream and try to forget about it.
No withdrawals from this bank
Into each life, some milestones must fall: High school graduation, birth of a child, first house, 50th wedding anniversary, COVID-19. One LOTME staffer got really excited – way too excited, actually – when his Nissan Sentra reached 300,000 miles.
Well, there are milestones, and then there are milestones. “1,000 Reasons for Hope” is a report celebrating the first 1,000 brains donated to the VA-BU-CLF Brain Bank. For those of you keeping score at home, that would be the Department of Veterans Affairs, Boston University, and the Concussion Legacy Foundation.
The Brain Bank, created in 2008 to study concussions and chronic traumatic encephalopathy, is the brainchild – yes, we went there – of Chris Nowinski, PhD, a former professional wrestler, and Ann McKee, MD, an expert on neurogenerative disease. “Our discoveries have already inspired changes to sports that will prevent many future cases of CTE in the next generation of athletes,” Dr. Nowinski, the CEO of CLF, said in a written statement.
Data from the first thousand brains show that 706 men, including 305 former NFL players, had football as their primary exposure to head impacts. Women were underrepresented, making up only 2.8% of brain donations, so recruiting females is a priority. Anyone interested in pledging can go to PledgeMyBrain.org or call 617-992-0615 for the 24-hour emergency donation pager.
LOTME wanted to help, so we called the Brain Bank to find out about donating. They asked a few questions and we told them what we do for a living. “Oh, you’re with LOTME? Yeah, we’ve … um, seen that before. It’s, um … funny. Can we put you on hold?” We’re starting to get a little sick of the on-hold music by now.
Goodbye stress, goodbye gray hair
Last year was a doozy, so it wouldn’t be too surprising if we all had a few new gray strands in our hair. But what if we told you that you don’t need to start dying them or plucking them out? What if they could magically go back to the way they were? Well, it may be possible, sans magic and sans stress.
Investigators recently discovered that the age-old belief that stress will permanently turn your hair gray may not be true after all. There’s a strong possibility that it could turn back to its original color once the stressful agent is eliminated.
“Understanding the mechanisms that allow ‘old’ gray hairs to return to their ‘young’ pigmented states could yield new clues about the malleability of human aging in general and how it is influenced by stress,” said senior author Martin Picard, PhD, of Columbia University, New York.
For the study, 14 volunteers were asked to keep a stress diary and review their levels of stress throughout the week. The researchers used a new method of viewing and capturing the images of tiny parts of the hairs to see how much graying took place in each part of the strand. And what they found – some strands naturally turning back to the original color – had never been documented before.
How did it happen? Our good friend the mitochondria. We haven’t really heard that word since eighth-grade biology, but it’s actually the key link between stress hormones and hair pigmentation. Think of them as little radars picking up all different kinds of signals in your body, like mental/emotional stress. They get a big enough alert and they’re going to react, thus gray hair.
So that’s all it takes? Cut the stress and a full head of gray can go back to brown? Not exactly. The researchers said there may be a “threshold because of biological age and other factors.” They believe middle age is near that threshold and it could easily be pushed over due to stress and could potentially go back. But if you’ve been rocking the salt and pepper or silver fox for a number of years and are looking for change, you might want to just eliminate the stress and pick up a bottle of dye.
One small step for squid
Space does a number on the human body. Forget the obvious like going for a walk outside without a spacesuit, or even the well-known risks like the degradation of bone in microgravity; there are numerous smaller but still important changes to the body during spaceflight, like the disruption of the symbiotic relationship between gut bacteria and the human body. This causes the immune system to lose the ability to recognize threats, and illnesses spread more easily.
Naturally, if astronauts are going to undertake years-long journeys to Mars and beyond, a thorough understanding of this disturbance is necessary, and that’s why NASA has sent a bunch of squid to the International Space Station.
When it comes to animal studies, squid aren’t the usual culprits, but there’s a reason NASA chose calamari over the alternatives: The Hawaiian bobtail squid has a symbiotic relationship with bacteria that regulate their bioluminescence in much the same way that we have a symbiotic relationship with our gut bacteria, but the squid is a much simpler animal. If the bioluminescence-regulating bacteria are disturbed during their time in space, it will be much easier to figure out what’s going wrong.
The experiment is ongoing, but we should salute the brave squid who have taken a giant leap for squidkind. Though if NASA didn’t send them up in a giant bubble, we’re going to be very disappointed.
Less plastic, more vanilla
Have you been racked by guilt over the number of plastic water bottles you use? What about the amount of ice cream you eat? Well, this one’s for you.
Plastic isn’t the first thing you think about when you open up a pint of vanilla ice cream and catch the sweet, spicy vanilla scent, or when you smell those fresh vanilla scones coming out of the oven at the coffee shop, but a new study shows that the flavor of vanilla can come from water bottles.
Here’s the deal. A compound called vanillin is responsible for the scent of vanilla, and it can come naturally from the bean or it can be made synthetically. Believe it or not, 85% of vanillin is made synthetically from fossil fuels!
We’ve definitely grown accustomed to our favorite vanilla scents, foods, and cosmetics. In 2018, the global demand for vanillin was about 40,800 tons and is expected to grow to 65,000 tons by 2025, which far exceeds the supply of natural vanilla.
So what can we do? Well, we can use genetically engineered bacteria to turn plastic water bottles into vanillin, according to a study published in the journal Green Chemistry.
The plastic can be broken down into terephthalic acid, which is very similar, chemically speaking, to vanillin. Similar enough that a bit of bioengineering produced Escherichia coli that could convert the acid into the tasty treat, according to researchers at the University of Edinburgh.
A perfect solution? Decreasing plastic waste while producing a valued food product? The thought of consuming plastic isn’t appetizing, so just eat your ice cream and try to forget about it.
No withdrawals from this bank
Into each life, some milestones must fall: High school graduation, birth of a child, first house, 50th wedding anniversary, COVID-19. One LOTME staffer got really excited – way too excited, actually – when his Nissan Sentra reached 300,000 miles.
Well, there are milestones, and then there are milestones. “1,000 Reasons for Hope” is a report celebrating the first 1,000 brains donated to the VA-BU-CLF Brain Bank. For those of you keeping score at home, that would be the Department of Veterans Affairs, Boston University, and the Concussion Legacy Foundation.
The Brain Bank, created in 2008 to study concussions and chronic traumatic encephalopathy, is the brainchild – yes, we went there – of Chris Nowinski, PhD, a former professional wrestler, and Ann McKee, MD, an expert on neurogenerative disease. “Our discoveries have already inspired changes to sports that will prevent many future cases of CTE in the next generation of athletes,” Dr. Nowinski, the CEO of CLF, said in a written statement.
Data from the first thousand brains show that 706 men, including 305 former NFL players, had football as their primary exposure to head impacts. Women were underrepresented, making up only 2.8% of brain donations, so recruiting females is a priority. Anyone interested in pledging can go to PledgeMyBrain.org or call 617-992-0615 for the 24-hour emergency donation pager.
LOTME wanted to help, so we called the Brain Bank to find out about donating. They asked a few questions and we told them what we do for a living. “Oh, you’re with LOTME? Yeah, we’ve … um, seen that before. It’s, um … funny. Can we put you on hold?” We’re starting to get a little sick of the on-hold music by now.
HMAs benefit children with relapsed/refractory AML
Hypomethylating agents are generally considered to be agents of choice for older adults with acute myeloid leukemia who cannot tolerate the rigors of more intensive therapies, but HMAs also can serve as a bridge to transplant for children and young adults with relapsed or refractory acute myeloid leukemia.
That’s according to Himalee S. Sabnis, MD, MSc and colleagues at Emory University and the Aflac Cancer and Blood Disorders Center at Children’s Healthcare of Atlanta.
In a scientific poster presented during the annual meeting of the American Society of Pediatric Hematology/Oncology, the investigators reported results of a retrospective study of HMA use in patients with relapsed or refractory pediatric AML treated in their center.
Curative intent and palliation
They identified 25 patients (15 boys) with a median age of 8.3 years (range 1.4 to 21 years) with relapsed/refractory AML who received HMAs for curative intent prior to hematopoietic stem cell transplant (HSCT), palliation, or in combination with donor leukocyte infusion (DLI).
Of the 21 patients with relapsed disease, 16 were in first relapse and 5 were in second relapse or greater. Four of the patients had primary refractory disease. The cytogenetic and molecular features were KMT2A rearrangements in six patients, monosomy 7/deletion 7 q in four patients, 8;21 translocation in three patients, and FLT3-ITD mutations in four patients.
The patients received a median of 5.3 HMA cycles each. Of the 133 total HMA cycles, 87 were with azacitidine, and 46 were with decitabine.
HMAs were used as monotherapy in 62% of cycles, and in combination with other therapies in 38%. Of the combinations, 16 were with donor leukocyte infusion, and 9 were gemtuzumab ozogamicin (Mylotarg).
Of the 13 patients for whom HMAs were used as part of treatment plan with curative intent, 5 proceeded to HSCT, and 8 did not. Of the 5 patients, 1 died from transplant-related causes, and 4 were alive post transplant. Of the 8 patients who did not undergo transplant, 1 had chimeric antigen receptor T- cell (CAR T) therapy, and 7 experienced disease progression.
The mean duration of palliative care was 144 days, with patients receiving from one to nine cycles with an HMA, and no treatment interruptions due to toxicity.
Of 5 patients who received donor leukocyte infusions, 3 reached minimal residual disease negativity; all 3 of these patients had late relapses but remained long-term survivors, the investigators reported.
They concluded that “hypomethylating agents can be used effectively as a bridge to transplantation in relapsed and refractory AML with gemtuzumab ozogamicin being the most common agent for combination therapy. Palliation with HMAs is associated with low toxicity and high tolerability in relapsed/refractory AML. Use of HMAs with DLI can induce sustained remissions in some patients.”
The authors propose prospective clinical trials using HMAs in the relapsed/refractory pediatric AML setting in combination with gemtuzumab ozogamicin, alternative targeted agents, and chemotherapy.
HMAs in treatment-related AML
Shilpa Shahani, MD, a pediatric oncologist and assistant clinical professor of pediatrics at City of Hope in Duarte, Calif., who was not involved in the study, has experience administering HMAs primarily in the adolescent and young adult population with AML.
“Azacitidine and decitabine are good for treatment-related leukemias,” she said in an interview. “They can be used otherwise for people who have relapsed disease and are trying to navigate other options.”
Although they are not standard first-line agents in younger patients, HMAs can play a useful role in therapy for relapsed or refractory disease, she said.
The authors and Dr. Shahani reported having no conflicts of interest to disclose.
Hypomethylating agents are generally considered to be agents of choice for older adults with acute myeloid leukemia who cannot tolerate the rigors of more intensive therapies, but HMAs also can serve as a bridge to transplant for children and young adults with relapsed or refractory acute myeloid leukemia.
That’s according to Himalee S. Sabnis, MD, MSc and colleagues at Emory University and the Aflac Cancer and Blood Disorders Center at Children’s Healthcare of Atlanta.
In a scientific poster presented during the annual meeting of the American Society of Pediatric Hematology/Oncology, the investigators reported results of a retrospective study of HMA use in patients with relapsed or refractory pediatric AML treated in their center.
Curative intent and palliation
They identified 25 patients (15 boys) with a median age of 8.3 years (range 1.4 to 21 years) with relapsed/refractory AML who received HMAs for curative intent prior to hematopoietic stem cell transplant (HSCT), palliation, or in combination with donor leukocyte infusion (DLI).
Of the 21 patients with relapsed disease, 16 were in first relapse and 5 were in second relapse or greater. Four of the patients had primary refractory disease. The cytogenetic and molecular features were KMT2A rearrangements in six patients, monosomy 7/deletion 7 q in four patients, 8;21 translocation in three patients, and FLT3-ITD mutations in four patients.
The patients received a median of 5.3 HMA cycles each. Of the 133 total HMA cycles, 87 were with azacitidine, and 46 were with decitabine.
HMAs were used as monotherapy in 62% of cycles, and in combination with other therapies in 38%. Of the combinations, 16 were with donor leukocyte infusion, and 9 were gemtuzumab ozogamicin (Mylotarg).
Of the 13 patients for whom HMAs were used as part of treatment plan with curative intent, 5 proceeded to HSCT, and 8 did not. Of the 5 patients, 1 died from transplant-related causes, and 4 were alive post transplant. Of the 8 patients who did not undergo transplant, 1 had chimeric antigen receptor T- cell (CAR T) therapy, and 7 experienced disease progression.
The mean duration of palliative care was 144 days, with patients receiving from one to nine cycles with an HMA, and no treatment interruptions due to toxicity.
Of 5 patients who received donor leukocyte infusions, 3 reached minimal residual disease negativity; all 3 of these patients had late relapses but remained long-term survivors, the investigators reported.
They concluded that “hypomethylating agents can be used effectively as a bridge to transplantation in relapsed and refractory AML with gemtuzumab ozogamicin being the most common agent for combination therapy. Palliation with HMAs is associated with low toxicity and high tolerability in relapsed/refractory AML. Use of HMAs with DLI can induce sustained remissions in some patients.”
The authors propose prospective clinical trials using HMAs in the relapsed/refractory pediatric AML setting in combination with gemtuzumab ozogamicin, alternative targeted agents, and chemotherapy.
HMAs in treatment-related AML
Shilpa Shahani, MD, a pediatric oncologist and assistant clinical professor of pediatrics at City of Hope in Duarte, Calif., who was not involved in the study, has experience administering HMAs primarily in the adolescent and young adult population with AML.
“Azacitidine and decitabine are good for treatment-related leukemias,” she said in an interview. “They can be used otherwise for people who have relapsed disease and are trying to navigate other options.”
Although they are not standard first-line agents in younger patients, HMAs can play a useful role in therapy for relapsed or refractory disease, she said.
The authors and Dr. Shahani reported having no conflicts of interest to disclose.
Hypomethylating agents are generally considered to be agents of choice for older adults with acute myeloid leukemia who cannot tolerate the rigors of more intensive therapies, but HMAs also can serve as a bridge to transplant for children and young adults with relapsed or refractory acute myeloid leukemia.
That’s according to Himalee S. Sabnis, MD, MSc and colleagues at Emory University and the Aflac Cancer and Blood Disorders Center at Children’s Healthcare of Atlanta.
In a scientific poster presented during the annual meeting of the American Society of Pediatric Hematology/Oncology, the investigators reported results of a retrospective study of HMA use in patients with relapsed or refractory pediatric AML treated in their center.
Curative intent and palliation
They identified 25 patients (15 boys) with a median age of 8.3 years (range 1.4 to 21 years) with relapsed/refractory AML who received HMAs for curative intent prior to hematopoietic stem cell transplant (HSCT), palliation, or in combination with donor leukocyte infusion (DLI).
Of the 21 patients with relapsed disease, 16 were in first relapse and 5 were in second relapse or greater. Four of the patients had primary refractory disease. The cytogenetic and molecular features were KMT2A rearrangements in six patients, monosomy 7/deletion 7 q in four patients, 8;21 translocation in three patients, and FLT3-ITD mutations in four patients.
The patients received a median of 5.3 HMA cycles each. Of the 133 total HMA cycles, 87 were with azacitidine, and 46 were with decitabine.
HMAs were used as monotherapy in 62% of cycles, and in combination with other therapies in 38%. Of the combinations, 16 were with donor leukocyte infusion, and 9 were gemtuzumab ozogamicin (Mylotarg).
Of the 13 patients for whom HMAs were used as part of treatment plan with curative intent, 5 proceeded to HSCT, and 8 did not. Of the 5 patients, 1 died from transplant-related causes, and 4 were alive post transplant. Of the 8 patients who did not undergo transplant, 1 had chimeric antigen receptor T- cell (CAR T) therapy, and 7 experienced disease progression.
The mean duration of palliative care was 144 days, with patients receiving from one to nine cycles with an HMA, and no treatment interruptions due to toxicity.
Of 5 patients who received donor leukocyte infusions, 3 reached minimal residual disease negativity; all 3 of these patients had late relapses but remained long-term survivors, the investigators reported.
They concluded that “hypomethylating agents can be used effectively as a bridge to transplantation in relapsed and refractory AML with gemtuzumab ozogamicin being the most common agent for combination therapy. Palliation with HMAs is associated with low toxicity and high tolerability in relapsed/refractory AML. Use of HMAs with DLI can induce sustained remissions in some patients.”
The authors propose prospective clinical trials using HMAs in the relapsed/refractory pediatric AML setting in combination with gemtuzumab ozogamicin, alternative targeted agents, and chemotherapy.
HMAs in treatment-related AML
Shilpa Shahani, MD, a pediatric oncologist and assistant clinical professor of pediatrics at City of Hope in Duarte, Calif., who was not involved in the study, has experience administering HMAs primarily in the adolescent and young adult population with AML.
“Azacitidine and decitabine are good for treatment-related leukemias,” she said in an interview. “They can be used otherwise for people who have relapsed disease and are trying to navigate other options.”
Although they are not standard first-line agents in younger patients, HMAs can play a useful role in therapy for relapsed or refractory disease, she said.
The authors and Dr. Shahani reported having no conflicts of interest to disclose.
FROM THE 2021 ASPHO CONFERENCE
‘Dreck’ to drama: How the media handled, and got handled by, COVID
For well over a year, the COVID-19 pandemic has been the biggest story in the world, costing millions of lives, impacting a presidential election, and quaking economies around the world.
But as vaccination rates increase and restrictions relax across the United States, relief is beginning to mix with reflection. Part of that contemplation means grappling with how the media depicted the crisis – in ways that were helpful, harmful, and somewhere in between.
“This story was so overwhelming, and the amount of journalism done about it was also overwhelming, and it’s going to be a while before we can do any kind of comprehensive overview of how journalism really performed,” said Maryn McKenna, an independent journalist and journalism professor at Emory University, Atlanta, who specializes in public and global health.
Some ‘heroically good’ reporting
The pandemic hit at a time when journalism was under a lot of pressure from external forces – undermined by politics, swimming through a sea of misinformation, and pressed by financial pressure to produce more stories more quickly, said Emily Bell, founding director of the Tow Center for Digital Journalism at Columbia University, New York.
The pandemic drove enormous audiences to news outlets, as people searched for reliable information, and increased the appreciation many people felt for the work of journalists, she said.
“I think there’s been some heroically good reporting and some really empathetic reporting as well,” said Ms. Bell. She cites The New York Times stories honoring the nearly 100,000 people lost to COVID-19 in May 2020 and The Atlantic’s COVID Tracking Project as exceptionally good examples.
Journalism is part of a complex, and evolving, information ecosystem characterized by “traditional” television, radio, and newspapers but also social media, search engine results, niche online news outlets, and clickbait sites.
On the one hand, social media provided a way for physicians, nurses, and scientists to speak directly to the world about their experiences and research. On the other hand, it’s challenging to elevate the really good work of traditional media over all of the bad or unhelpful signals, said Ms. Bell.
But, at the end of the day, much of journalism is a business. There are incentives in the market for tabloids to do sensational coverage and for outlets to push misleading, clickbait headlines, Ms. Bell said.
“Sometimes we’ll criticize journalists for ‘getting it wrong,’ but they might be getting it right in their business model but getting it wrong in terms of what it’s doing for society,” she said.
“We need to do a self-examination, when or if the dust from this ever settles, [on] how much of the past year was viewed as a business opportunity and did that get in the way of informing the public adequately,” Ms. McKenna said.
Digital platforms and journalists also need to reflect on how narratives build on one another, particularly online, said Ms. Bell. If you search for side effects of the Johnson & Johnson vaccine, for example, you will see a list of dozens of headlines that might give you the impression this is a major problem without the context that these effects are exceedingly rare, she notes.
There was also a personnel problem. Shrinking newsrooms over the last decade meant many outlets didn’t have dedicated science and health reporting, or very few staffers, if any. During the pandemic, suddenly general assignment and politics reporters had to be science and health reporters, too.
“You have a hard enough time with these issues if you’re a fairly seasoned science journalist,” said Gary Schwitzer, a former head of the health care news unit for CNN, journalism professor at the University of Minnesota, and founder of the watchdog site HealthNewsReview.org.
And outlets that had the staffing didn’t always put science reporters to full use, Ms. McKenna said. In March and April of 2020, major media outlets should have sent science reporters, not politics reporters, to President Donald Trump’s White House press briefings, which often included incorrect statements about COVID-19 science.
“I just don’t feel that the big outlets understood that that expertise would have made a difference,” she said.
New challenges, old problems
Some of the science journalism done during the pandemic has been some of the best ever seen in this country, said Mr. Schwitzer. But between the peaks of excellence, there is “the daily drumbeat coverage of dreck,” he added.
Many of the issues with this dreck coverage aren’t new or unique to the pandemic. For example, over the last year there have been far too many news stories based solely on weak information sources, like a drug company press release or a not-yet-peer-reviewed preprint article that hasn’t been put into proper context, said Mr. Schwitzer.
A quality science story should always include an independent perspective, he said, but many COVID-19 stories missed that perspective. This isn’t a new issue for science coverage – at Health News Review, Mr. Schwitzer and his colleagues saw stories without appropriate independent sources every day for 15 years.
It’s also challenging to write about uncertainty without over- or underselling what scientists know about a particular phenomenon. “We know that the media in general tends to portray science as more certain than it is,” said Dominique Brossard, PhD, professor and department chair at the University of Wisconsin–Madison and an expert on the intersection between science, media, and policy. This can lead to confusion when the science, and the advice based on that science, changes.
“The public has a really difficult time understanding what uncertainty means within science,” said Todd P. Newman, PhD, assistant professor at the University of Wisconsin–Madison who studies strategic communication within the context of science, technology, and the environment.
“I think the media generally has been good on the subject,” said Paul Offit, MD, director of the Vaccine Education Center, attending physician in the Division of Infectious Diseases at the Children’s Hospital of Philadelphia, and a prominent expert voice throughout the pandemic. “I think where they’ve been imperfect is they tend to be a little more dramatic in terms of how we’re doing.”
Dr. Offit isn’t the only expert to point to the drama of COVID-19 coverage. A study published in March 2021 by the National Bureau of Economic Research found 87% of stories by major U.S. media outlets leaned negative in the tone of their COVID-19 reporting, compared with 50% of stories from non-U.S. major outlets and 64% of articles in scientific journals. The negative emphasis persists even around positive developments, like vaccine trials and school re-openings.
John Whyte, MD, chief medical officer for WebMD, said he is very proud of the way WebMD and Medscape ramped up production of video series and other content to give health care providers the most up-to-date guidance on a rapidly evolving medical situation.
“But I think as [we] started to make progress – especially in the last 6 months – the coverage was never balanced enough; any positive news was immediately proceeded by negative,” he said.
“You want to be honest, but you also don’t want to be alarmist – and that’s where I think the challenge is at times in the media,” said Dr. Whyte. “We didn’t put enough optimism in at times, especially in recent months.”
“Any good coverage on vaccines immediately [was] covered by ‘[we] might need boosters in the fall.’ Why can’t [we] have an opportunity to breathe for a little while and see the good news?” he asked.
Variants or scariants?
Negativity and fear shaped much of the coverage around variants and vaccines earlier this year. In February 2021, Zeynep Tufekci, PhD, a sociologist at the University of North Carolina at Chapel Hill school of information and library science, wrote in The Atlantic about how much reporting has not reflected “the truly amazing reality of these vaccines,” and has instead highlighted “a chorus of relentless pessimism.”
This felt especially true earlier in 2021, when lots of coverage repeatedly emphasized what vaccinated people still could not do.
Eric Topol, MD, editor-in-chief of Medscape and executive vice president of Scripps Research in La Jolla, California, said New York Times editors told him earlier in the pandemic that he couldn’t use the word “scariant” in an opinion piece about the media’s overly fearful and sometimes inaccurate reporting around COVID-19 variants because they worried it would seem like the Times was coming after other media outlets.
“A variant is innocent until proven guilty,” said Dr. Topol. Had journalists approached the subject from that point of view, he said we would have seen “much more faithful reporting.”
Dr. Brossard and Dr. Newman worry that focusing on uncommon negative behavior, like people who break social distancing and mask rules by gathering at the beach or the bar, makes those actions seem more common than they actually are.
The evidence suggests that “if you show these kinds of things to people, you encourage them to do the same behavior,” said Dr. Brossard.
There have been other mistakes along the way, too. Early in the pandemic, many outlets pointed viewers to official government sources of information, some of which, like the White House press briefings in March and April of 2020, ended up being some of the most virulent spreaders of misinformation, said Ms. Bell.
Before that, a handful of journalists like Roxanne Khamsi were the few pushing back against the dominant media narrative in early 2020 that the novel coronavirus was less concerning than the seasonal flu.
“Science journalists have always been writing about studies that sometimes contradict each other, and what’s happened is that has only been condensed in time,” said Ms. Khamsi, a health care reporter for outlets like WIRED magazine and The New York Times and a former chief news editor for Nature Medicine.
Politics and misinformation
It’s impossible to talk about media coverage of COVID-19 without touching on politics and misinformation.
Coverage of the pandemic was politicized and polarized from the very beginning, said Sedona Chinn, PhD, an assistant professor at the University of Wisconsin–Madison who researches the prevalence and effects of scientific disagreements in media.
By looking at network news transcripts and articles from national outlets like the Washington Post and The New York Times, Dr. Chinn and her colleagues were able to determine politicization of coverage by counting the mentions of politicians versus scientists in COVID-19 coverage and polarization by looking at how different or similar the language was surrounding mentions of Republicans and Democrats.
If the two parties were working together or on the same page, they reasoned, the language would be similar.
From mid-March through May 2020, Dr. Chinn and fellow researchers found politicians were featured more often than scientists in newspaper coverage and as frequently as scientists in network news coverage. They also found polarized language around Republicans and Democrats, particularly in stories describing duels between the (at the time) Republican national government and Democratic state and local leaders.
It’s possible that polarization in news coverage helped contribute to polarized attitudes around the virus, the authors write in the study, which was published in August 2020 in the journal Science Communication.
The politicization and polarization of the issue is mirrored in our fractured media environment, where people tend to read, listen, and watch outlets that align with their political leanings. If that trusted outlet features misinformation, the people who follow it are more likely to accept that false information as truth, said Matt Motta, PhD, a political scientist at Oklahoma State University whose research includes public opinion and science communication.
This is true across the political spectrum, he said. When it comes to COVID-19, however, right-wing media outlets like Fox News and Breitbart are more likely to promote conspiratorial tropes and misinformation about the pandemic, according to Dr. Motta and his collaborator Dominik Stecula, PhD, a political scientist at Colorado State University who studies the news media environment and its effects on society.
Across the media ecosystem, reporting on the “infodemic” accompanying the pandemic – the rapid spread of misinformation and disinformation about the virus – has been a major challenge. Outlets may not be creating the misinformation, but they are the ones choosing to give it a platform, said Dr. Motta.
By repeating a false idea, even with the goal of debunking it, you can unintentionally cause the information to stick in people’s minds, said Dr. Brossard.
“Just because something is controversial doesn’t mean it’s worth covering,” said Dr. Motta. Using vaccines as an example, he said many reporters and scientists alike assume that if people have all the facts, they’ll land on the side of science.
“That is just fundamentally not how people think about the decision to get vaccinated,” he said. Instead, the choice is wrapped up with cultural factors, religious beliefs, political identity, and more.
The factors and challenges that shaped the media’s coverage of the pandemic aren’t going anywhere. Improving science and medical coverage in the future is a collective project for journalists, scientists, and everyone in between, said Dr. Newman.
“I call on scientists, too, to think really deeply about how they’re communicating – and especially how they’re communicating what they know and don’t know,” he said.
A version of this article first appeared on Medscape.com.
For well over a year, the COVID-19 pandemic has been the biggest story in the world, costing millions of lives, impacting a presidential election, and quaking economies around the world.
But as vaccination rates increase and restrictions relax across the United States, relief is beginning to mix with reflection. Part of that contemplation means grappling with how the media depicted the crisis – in ways that were helpful, harmful, and somewhere in between.
“This story was so overwhelming, and the amount of journalism done about it was also overwhelming, and it’s going to be a while before we can do any kind of comprehensive overview of how journalism really performed,” said Maryn McKenna, an independent journalist and journalism professor at Emory University, Atlanta, who specializes in public and global health.
Some ‘heroically good’ reporting
The pandemic hit at a time when journalism was under a lot of pressure from external forces – undermined by politics, swimming through a sea of misinformation, and pressed by financial pressure to produce more stories more quickly, said Emily Bell, founding director of the Tow Center for Digital Journalism at Columbia University, New York.
The pandemic drove enormous audiences to news outlets, as people searched for reliable information, and increased the appreciation many people felt for the work of journalists, she said.
“I think there’s been some heroically good reporting and some really empathetic reporting as well,” said Ms. Bell. She cites The New York Times stories honoring the nearly 100,000 people lost to COVID-19 in May 2020 and The Atlantic’s COVID Tracking Project as exceptionally good examples.
Journalism is part of a complex, and evolving, information ecosystem characterized by “traditional” television, radio, and newspapers but also social media, search engine results, niche online news outlets, and clickbait sites.
On the one hand, social media provided a way for physicians, nurses, and scientists to speak directly to the world about their experiences and research. On the other hand, it’s challenging to elevate the really good work of traditional media over all of the bad or unhelpful signals, said Ms. Bell.
But, at the end of the day, much of journalism is a business. There are incentives in the market for tabloids to do sensational coverage and for outlets to push misleading, clickbait headlines, Ms. Bell said.
“Sometimes we’ll criticize journalists for ‘getting it wrong,’ but they might be getting it right in their business model but getting it wrong in terms of what it’s doing for society,” she said.
“We need to do a self-examination, when or if the dust from this ever settles, [on] how much of the past year was viewed as a business opportunity and did that get in the way of informing the public adequately,” Ms. McKenna said.
Digital platforms and journalists also need to reflect on how narratives build on one another, particularly online, said Ms. Bell. If you search for side effects of the Johnson & Johnson vaccine, for example, you will see a list of dozens of headlines that might give you the impression this is a major problem without the context that these effects are exceedingly rare, she notes.
There was also a personnel problem. Shrinking newsrooms over the last decade meant many outlets didn’t have dedicated science and health reporting, or very few staffers, if any. During the pandemic, suddenly general assignment and politics reporters had to be science and health reporters, too.
“You have a hard enough time with these issues if you’re a fairly seasoned science journalist,” said Gary Schwitzer, a former head of the health care news unit for CNN, journalism professor at the University of Minnesota, and founder of the watchdog site HealthNewsReview.org.
And outlets that had the staffing didn’t always put science reporters to full use, Ms. McKenna said. In March and April of 2020, major media outlets should have sent science reporters, not politics reporters, to President Donald Trump’s White House press briefings, which often included incorrect statements about COVID-19 science.
“I just don’t feel that the big outlets understood that that expertise would have made a difference,” she said.
New challenges, old problems
Some of the science journalism done during the pandemic has been some of the best ever seen in this country, said Mr. Schwitzer. But between the peaks of excellence, there is “the daily drumbeat coverage of dreck,” he added.
Many of the issues with this dreck coverage aren’t new or unique to the pandemic. For example, over the last year there have been far too many news stories based solely on weak information sources, like a drug company press release or a not-yet-peer-reviewed preprint article that hasn’t been put into proper context, said Mr. Schwitzer.
A quality science story should always include an independent perspective, he said, but many COVID-19 stories missed that perspective. This isn’t a new issue for science coverage – at Health News Review, Mr. Schwitzer and his colleagues saw stories without appropriate independent sources every day for 15 years.
It’s also challenging to write about uncertainty without over- or underselling what scientists know about a particular phenomenon. “We know that the media in general tends to portray science as more certain than it is,” said Dominique Brossard, PhD, professor and department chair at the University of Wisconsin–Madison and an expert on the intersection between science, media, and policy. This can lead to confusion when the science, and the advice based on that science, changes.
“The public has a really difficult time understanding what uncertainty means within science,” said Todd P. Newman, PhD, assistant professor at the University of Wisconsin–Madison who studies strategic communication within the context of science, technology, and the environment.
“I think the media generally has been good on the subject,” said Paul Offit, MD, director of the Vaccine Education Center, attending physician in the Division of Infectious Diseases at the Children’s Hospital of Philadelphia, and a prominent expert voice throughout the pandemic. “I think where they’ve been imperfect is they tend to be a little more dramatic in terms of how we’re doing.”
Dr. Offit isn’t the only expert to point to the drama of COVID-19 coverage. A study published in March 2021 by the National Bureau of Economic Research found 87% of stories by major U.S. media outlets leaned negative in the tone of their COVID-19 reporting, compared with 50% of stories from non-U.S. major outlets and 64% of articles in scientific journals. The negative emphasis persists even around positive developments, like vaccine trials and school re-openings.
John Whyte, MD, chief medical officer for WebMD, said he is very proud of the way WebMD and Medscape ramped up production of video series and other content to give health care providers the most up-to-date guidance on a rapidly evolving medical situation.
“But I think as [we] started to make progress – especially in the last 6 months – the coverage was never balanced enough; any positive news was immediately proceeded by negative,” he said.
“You want to be honest, but you also don’t want to be alarmist – and that’s where I think the challenge is at times in the media,” said Dr. Whyte. “We didn’t put enough optimism in at times, especially in recent months.”
“Any good coverage on vaccines immediately [was] covered by ‘[we] might need boosters in the fall.’ Why can’t [we] have an opportunity to breathe for a little while and see the good news?” he asked.
Variants or scariants?
Negativity and fear shaped much of the coverage around variants and vaccines earlier this year. In February 2021, Zeynep Tufekci, PhD, a sociologist at the University of North Carolina at Chapel Hill school of information and library science, wrote in The Atlantic about how much reporting has not reflected “the truly amazing reality of these vaccines,” and has instead highlighted “a chorus of relentless pessimism.”
This felt especially true earlier in 2021, when lots of coverage repeatedly emphasized what vaccinated people still could not do.
Eric Topol, MD, editor-in-chief of Medscape and executive vice president of Scripps Research in La Jolla, California, said New York Times editors told him earlier in the pandemic that he couldn’t use the word “scariant” in an opinion piece about the media’s overly fearful and sometimes inaccurate reporting around COVID-19 variants because they worried it would seem like the Times was coming after other media outlets.
“A variant is innocent until proven guilty,” said Dr. Topol. Had journalists approached the subject from that point of view, he said we would have seen “much more faithful reporting.”
Dr. Brossard and Dr. Newman worry that focusing on uncommon negative behavior, like people who break social distancing and mask rules by gathering at the beach or the bar, makes those actions seem more common than they actually are.
The evidence suggests that “if you show these kinds of things to people, you encourage them to do the same behavior,” said Dr. Brossard.
There have been other mistakes along the way, too. Early in the pandemic, many outlets pointed viewers to official government sources of information, some of which, like the White House press briefings in March and April of 2020, ended up being some of the most virulent spreaders of misinformation, said Ms. Bell.
Before that, a handful of journalists like Roxanne Khamsi were the few pushing back against the dominant media narrative in early 2020 that the novel coronavirus was less concerning than the seasonal flu.
“Science journalists have always been writing about studies that sometimes contradict each other, and what’s happened is that has only been condensed in time,” said Ms. Khamsi, a health care reporter for outlets like WIRED magazine and The New York Times and a former chief news editor for Nature Medicine.
Politics and misinformation
It’s impossible to talk about media coverage of COVID-19 without touching on politics and misinformation.
Coverage of the pandemic was politicized and polarized from the very beginning, said Sedona Chinn, PhD, an assistant professor at the University of Wisconsin–Madison who researches the prevalence and effects of scientific disagreements in media.
By looking at network news transcripts and articles from national outlets like the Washington Post and The New York Times, Dr. Chinn and her colleagues were able to determine politicization of coverage by counting the mentions of politicians versus scientists in COVID-19 coverage and polarization by looking at how different or similar the language was surrounding mentions of Republicans and Democrats.
If the two parties were working together or on the same page, they reasoned, the language would be similar.
From mid-March through May 2020, Dr. Chinn and fellow researchers found politicians were featured more often than scientists in newspaper coverage and as frequently as scientists in network news coverage. They also found polarized language around Republicans and Democrats, particularly in stories describing duels between the (at the time) Republican national government and Democratic state and local leaders.
It’s possible that polarization in news coverage helped contribute to polarized attitudes around the virus, the authors write in the study, which was published in August 2020 in the journal Science Communication.
The politicization and polarization of the issue is mirrored in our fractured media environment, where people tend to read, listen, and watch outlets that align with their political leanings. If that trusted outlet features misinformation, the people who follow it are more likely to accept that false information as truth, said Matt Motta, PhD, a political scientist at Oklahoma State University whose research includes public opinion and science communication.
This is true across the political spectrum, he said. When it comes to COVID-19, however, right-wing media outlets like Fox News and Breitbart are more likely to promote conspiratorial tropes and misinformation about the pandemic, according to Dr. Motta and his collaborator Dominik Stecula, PhD, a political scientist at Colorado State University who studies the news media environment and its effects on society.
Across the media ecosystem, reporting on the “infodemic” accompanying the pandemic – the rapid spread of misinformation and disinformation about the virus – has been a major challenge. Outlets may not be creating the misinformation, but they are the ones choosing to give it a platform, said Dr. Motta.
By repeating a false idea, even with the goal of debunking it, you can unintentionally cause the information to stick in people’s minds, said Dr. Brossard.
“Just because something is controversial doesn’t mean it’s worth covering,” said Dr. Motta. Using vaccines as an example, he said many reporters and scientists alike assume that if people have all the facts, they’ll land on the side of science.
“That is just fundamentally not how people think about the decision to get vaccinated,” he said. Instead, the choice is wrapped up with cultural factors, religious beliefs, political identity, and more.
The factors and challenges that shaped the media’s coverage of the pandemic aren’t going anywhere. Improving science and medical coverage in the future is a collective project for journalists, scientists, and everyone in between, said Dr. Newman.
“I call on scientists, too, to think really deeply about how they’re communicating – and especially how they’re communicating what they know and don’t know,” he said.
A version of this article first appeared on Medscape.com.
For well over a year, the COVID-19 pandemic has been the biggest story in the world, costing millions of lives, impacting a presidential election, and quaking economies around the world.
But as vaccination rates increase and restrictions relax across the United States, relief is beginning to mix with reflection. Part of that contemplation means grappling with how the media depicted the crisis – in ways that were helpful, harmful, and somewhere in between.
“This story was so overwhelming, and the amount of journalism done about it was also overwhelming, and it’s going to be a while before we can do any kind of comprehensive overview of how journalism really performed,” said Maryn McKenna, an independent journalist and journalism professor at Emory University, Atlanta, who specializes in public and global health.
Some ‘heroically good’ reporting
The pandemic hit at a time when journalism was under a lot of pressure from external forces – undermined by politics, swimming through a sea of misinformation, and pressed by financial pressure to produce more stories more quickly, said Emily Bell, founding director of the Tow Center for Digital Journalism at Columbia University, New York.
The pandemic drove enormous audiences to news outlets, as people searched for reliable information, and increased the appreciation many people felt for the work of journalists, she said.
“I think there’s been some heroically good reporting and some really empathetic reporting as well,” said Ms. Bell. She cites The New York Times stories honoring the nearly 100,000 people lost to COVID-19 in May 2020 and The Atlantic’s COVID Tracking Project as exceptionally good examples.
Journalism is part of a complex, and evolving, information ecosystem characterized by “traditional” television, radio, and newspapers but also social media, search engine results, niche online news outlets, and clickbait sites.
On the one hand, social media provided a way for physicians, nurses, and scientists to speak directly to the world about their experiences and research. On the other hand, it’s challenging to elevate the really good work of traditional media over all of the bad or unhelpful signals, said Ms. Bell.
But, at the end of the day, much of journalism is a business. There are incentives in the market for tabloids to do sensational coverage and for outlets to push misleading, clickbait headlines, Ms. Bell said.
“Sometimes we’ll criticize journalists for ‘getting it wrong,’ but they might be getting it right in their business model but getting it wrong in terms of what it’s doing for society,” she said.
“We need to do a self-examination, when or if the dust from this ever settles, [on] how much of the past year was viewed as a business opportunity and did that get in the way of informing the public adequately,” Ms. McKenna said.
Digital platforms and journalists also need to reflect on how narratives build on one another, particularly online, said Ms. Bell. If you search for side effects of the Johnson & Johnson vaccine, for example, you will see a list of dozens of headlines that might give you the impression this is a major problem without the context that these effects are exceedingly rare, she notes.
There was also a personnel problem. Shrinking newsrooms over the last decade meant many outlets didn’t have dedicated science and health reporting, or very few staffers, if any. During the pandemic, suddenly general assignment and politics reporters had to be science and health reporters, too.
“You have a hard enough time with these issues if you’re a fairly seasoned science journalist,” said Gary Schwitzer, a former head of the health care news unit for CNN, journalism professor at the University of Minnesota, and founder of the watchdog site HealthNewsReview.org.
And outlets that had the staffing didn’t always put science reporters to full use, Ms. McKenna said. In March and April of 2020, major media outlets should have sent science reporters, not politics reporters, to President Donald Trump’s White House press briefings, which often included incorrect statements about COVID-19 science.
“I just don’t feel that the big outlets understood that that expertise would have made a difference,” she said.
New challenges, old problems
Some of the science journalism done during the pandemic has been some of the best ever seen in this country, said Mr. Schwitzer. But between the peaks of excellence, there is “the daily drumbeat coverage of dreck,” he added.
Many of the issues with this dreck coverage aren’t new or unique to the pandemic. For example, over the last year there have been far too many news stories based solely on weak information sources, like a drug company press release or a not-yet-peer-reviewed preprint article that hasn’t been put into proper context, said Mr. Schwitzer.
A quality science story should always include an independent perspective, he said, but many COVID-19 stories missed that perspective. This isn’t a new issue for science coverage – at Health News Review, Mr. Schwitzer and his colleagues saw stories without appropriate independent sources every day for 15 years.
It’s also challenging to write about uncertainty without over- or underselling what scientists know about a particular phenomenon. “We know that the media in general tends to portray science as more certain than it is,” said Dominique Brossard, PhD, professor and department chair at the University of Wisconsin–Madison and an expert on the intersection between science, media, and policy. This can lead to confusion when the science, and the advice based on that science, changes.
“The public has a really difficult time understanding what uncertainty means within science,” said Todd P. Newman, PhD, assistant professor at the University of Wisconsin–Madison who studies strategic communication within the context of science, technology, and the environment.
“I think the media generally has been good on the subject,” said Paul Offit, MD, director of the Vaccine Education Center, attending physician in the Division of Infectious Diseases at the Children’s Hospital of Philadelphia, and a prominent expert voice throughout the pandemic. “I think where they’ve been imperfect is they tend to be a little more dramatic in terms of how we’re doing.”
Dr. Offit isn’t the only expert to point to the drama of COVID-19 coverage. A study published in March 2021 by the National Bureau of Economic Research found 87% of stories by major U.S. media outlets leaned negative in the tone of their COVID-19 reporting, compared with 50% of stories from non-U.S. major outlets and 64% of articles in scientific journals. The negative emphasis persists even around positive developments, like vaccine trials and school re-openings.
John Whyte, MD, chief medical officer for WebMD, said he is very proud of the way WebMD and Medscape ramped up production of video series and other content to give health care providers the most up-to-date guidance on a rapidly evolving medical situation.
“But I think as [we] started to make progress – especially in the last 6 months – the coverage was never balanced enough; any positive news was immediately proceeded by negative,” he said.
“You want to be honest, but you also don’t want to be alarmist – and that’s where I think the challenge is at times in the media,” said Dr. Whyte. “We didn’t put enough optimism in at times, especially in recent months.”
“Any good coverage on vaccines immediately [was] covered by ‘[we] might need boosters in the fall.’ Why can’t [we] have an opportunity to breathe for a little while and see the good news?” he asked.
Variants or scariants?
Negativity and fear shaped much of the coverage around variants and vaccines earlier this year. In February 2021, Zeynep Tufekci, PhD, a sociologist at the University of North Carolina at Chapel Hill school of information and library science, wrote in The Atlantic about how much reporting has not reflected “the truly amazing reality of these vaccines,” and has instead highlighted “a chorus of relentless pessimism.”
This felt especially true earlier in 2021, when lots of coverage repeatedly emphasized what vaccinated people still could not do.
Eric Topol, MD, editor-in-chief of Medscape and executive vice president of Scripps Research in La Jolla, California, said New York Times editors told him earlier in the pandemic that he couldn’t use the word “scariant” in an opinion piece about the media’s overly fearful and sometimes inaccurate reporting around COVID-19 variants because they worried it would seem like the Times was coming after other media outlets.
“A variant is innocent until proven guilty,” said Dr. Topol. Had journalists approached the subject from that point of view, he said we would have seen “much more faithful reporting.”
Dr. Brossard and Dr. Newman worry that focusing on uncommon negative behavior, like people who break social distancing and mask rules by gathering at the beach or the bar, makes those actions seem more common than they actually are.
The evidence suggests that “if you show these kinds of things to people, you encourage them to do the same behavior,” said Dr. Brossard.
There have been other mistakes along the way, too. Early in the pandemic, many outlets pointed viewers to official government sources of information, some of which, like the White House press briefings in March and April of 2020, ended up being some of the most virulent spreaders of misinformation, said Ms. Bell.
Before that, a handful of journalists like Roxanne Khamsi were the few pushing back against the dominant media narrative in early 2020 that the novel coronavirus was less concerning than the seasonal flu.
“Science journalists have always been writing about studies that sometimes contradict each other, and what’s happened is that has only been condensed in time,” said Ms. Khamsi, a health care reporter for outlets like WIRED magazine and The New York Times and a former chief news editor for Nature Medicine.
Politics and misinformation
It’s impossible to talk about media coverage of COVID-19 without touching on politics and misinformation.
Coverage of the pandemic was politicized and polarized from the very beginning, said Sedona Chinn, PhD, an assistant professor at the University of Wisconsin–Madison who researches the prevalence and effects of scientific disagreements in media.
By looking at network news transcripts and articles from national outlets like the Washington Post and The New York Times, Dr. Chinn and her colleagues were able to determine politicization of coverage by counting the mentions of politicians versus scientists in COVID-19 coverage and polarization by looking at how different or similar the language was surrounding mentions of Republicans and Democrats.
If the two parties were working together or on the same page, they reasoned, the language would be similar.
From mid-March through May 2020, Dr. Chinn and fellow researchers found politicians were featured more often than scientists in newspaper coverage and as frequently as scientists in network news coverage. They also found polarized language around Republicans and Democrats, particularly in stories describing duels between the (at the time) Republican national government and Democratic state and local leaders.
It’s possible that polarization in news coverage helped contribute to polarized attitudes around the virus, the authors write in the study, which was published in August 2020 in the journal Science Communication.
The politicization and polarization of the issue is mirrored in our fractured media environment, where people tend to read, listen, and watch outlets that align with their political leanings. If that trusted outlet features misinformation, the people who follow it are more likely to accept that false information as truth, said Matt Motta, PhD, a political scientist at Oklahoma State University whose research includes public opinion and science communication.
This is true across the political spectrum, he said. When it comes to COVID-19, however, right-wing media outlets like Fox News and Breitbart are more likely to promote conspiratorial tropes and misinformation about the pandemic, according to Dr. Motta and his collaborator Dominik Stecula, PhD, a political scientist at Colorado State University who studies the news media environment and its effects on society.
Across the media ecosystem, reporting on the “infodemic” accompanying the pandemic – the rapid spread of misinformation and disinformation about the virus – has been a major challenge. Outlets may not be creating the misinformation, but they are the ones choosing to give it a platform, said Dr. Motta.
By repeating a false idea, even with the goal of debunking it, you can unintentionally cause the information to stick in people’s minds, said Dr. Brossard.
“Just because something is controversial doesn’t mean it’s worth covering,” said Dr. Motta. Using vaccines as an example, he said many reporters and scientists alike assume that if people have all the facts, they’ll land on the side of science.
“That is just fundamentally not how people think about the decision to get vaccinated,” he said. Instead, the choice is wrapped up with cultural factors, religious beliefs, political identity, and more.
The factors and challenges that shaped the media’s coverage of the pandemic aren’t going anywhere. Improving science and medical coverage in the future is a collective project for journalists, scientists, and everyone in between, said Dr. Newman.
“I call on scientists, too, to think really deeply about how they’re communicating – and especially how they’re communicating what they know and don’t know,” he said.
A version of this article first appeared on Medscape.com.
Sotagliflozin use in T2D patients linked with posthospitalization benefits in analysis
The outcome measure –days alive and out of the hospital – may be a meaningful, patient-centered way of capturing disease burden, the researchers wrote in their paper, published in Annals of Internal Medicine.
“The question was: Can we keep patients alive and out of the hospital for any reason, accounting for the duration of each hospitalization?” author Michael Szarek, PhD, a visiting professor in the division of cardiology at the University of Colorado at Denver, Aurora, said in an interview.
“For every 100 days of follow-up, patients in the sotagliflozin group were alive and out of the hospital 3% more days in relative terms or 2.9 days in absolute terms than those in the placebo group (91.8 vs. 88.9 days),” the researchers reported in their analysis of data from the SOLOIST-WHF trial.
“If you translate that to over the course of a year, that’s more than 10 days,” said Dr. Szarek, who is also a faculty member of CPC Clinical Research, an academic research organization affiliated with the University of Colorado.
Most patients in both groups survived to the end of the study without hospitalization, according to the paper.
Sotagliflozin, a sodium-glucose cotransporter 1 and SGLT2 inhibitor, is not approved in the United States. In 2019, the Food and Drug Administration rejected sotagliflozin as an adjunct to insulin for the treatment of type 1 diabetes after members of an advisory committee expressed concerns about an increased risk for diabetic ketoacidosis with the drug.
Methods and results
To examine whether sotagliflozin increased days alive and out of the hospital in the SOLOIST-WHF trial, Dr. Szarek and colleagues analyzed data from this randomized, double-blind, placebo-controlled study. The trial’s primary results were published in the New England Journal of Medicine in January 2021. Researchers conducted SOLOIST-WHF at more than 300 sites in 32 countries. The trial included 1,222 patients with type 2 diabetes and reduced or preserved ejection fraction who were recently hospitalized for worsening heart failure.
In the new analysis the researchers looked at hospitalizations for any reason and the duration of hospital admissions after randomization. They analyzed days alive and out of the hospital using prespecified models.
Similar proportions of patients who received sotagliflozin and placebo were hospitalized at least once (38.5% vs. 41.4%) during a median follow-up of 9 months. Fewer patients who received sotagliflozin were hospitalized more than once (16.3% vs. 22.1%). In all, 64 patients in the sotagliflozin group and 76 patients in the placebo group died.
The reason for each hospitalization was unspecified, except for cases of heart failure, the authors noted. About 62% of hospitalizations during the trial were for reasons other than heart failure.
Outside expert cites similarities to initial trial
The results for days alive and out of the hospital are “not particularly surprising given the previous publication” of the trial’s primary results, but the new analysis provides a “different view of outcomes that might be clinically meaningful for patients,” commented Frank Brosius, MD, a professor of medicine at the University of Arizona, Tucson.
The SOLOIST-WHF trial indicated that doctors may be able to effectively treat patients with relatively new heart failure with sotagliflozin as long as patients are relatively stable, said Dr. Brosius, who coauthored an editorial in the New England Journal of Medicine that accompanied the initial results from the SOLOIST-WHF trial. It appears that previously reported benefits with regard to heart failure outcomes “showed up in these other indicators” in the secondary analysis.
Still, the effect sizes in the new analysis were relatively small and “probably more studies will be necessary” to examine these end points, he added.
SOLOIST-WHF was funded by Sanofi at initiation and by Lexicon Pharmaceuticals at completion. Dr. Szarek disclosed grants from Lexicon and grants and personal fees from Sanofi, as well as personal fees from other companies. His coauthors included employees of Lexicon and other researchers with financial ties to Lexicon and other pharmaceutical companies. Dr. Brosius disclosed personal fees from the American Diabetes Association and is a member of the Diabetic Kidney Disease Collaborative task force for the American Society of Nephrology that is broadly advocating the use of SGLT2 inhibitors by patients with diabetic kidney diseases. He also has participated in an advisory group for treatment of diabetic kidney disease for Gilead.
The outcome measure –days alive and out of the hospital – may be a meaningful, patient-centered way of capturing disease burden, the researchers wrote in their paper, published in Annals of Internal Medicine.
“The question was: Can we keep patients alive and out of the hospital for any reason, accounting for the duration of each hospitalization?” author Michael Szarek, PhD, a visiting professor in the division of cardiology at the University of Colorado at Denver, Aurora, said in an interview.
“For every 100 days of follow-up, patients in the sotagliflozin group were alive and out of the hospital 3% more days in relative terms or 2.9 days in absolute terms than those in the placebo group (91.8 vs. 88.9 days),” the researchers reported in their analysis of data from the SOLOIST-WHF trial.
“If you translate that to over the course of a year, that’s more than 10 days,” said Dr. Szarek, who is also a faculty member of CPC Clinical Research, an academic research organization affiliated with the University of Colorado.
Most patients in both groups survived to the end of the study without hospitalization, according to the paper.
Sotagliflozin, a sodium-glucose cotransporter 1 and SGLT2 inhibitor, is not approved in the United States. In 2019, the Food and Drug Administration rejected sotagliflozin as an adjunct to insulin for the treatment of type 1 diabetes after members of an advisory committee expressed concerns about an increased risk for diabetic ketoacidosis with the drug.
Methods and results
To examine whether sotagliflozin increased days alive and out of the hospital in the SOLOIST-WHF trial, Dr. Szarek and colleagues analyzed data from this randomized, double-blind, placebo-controlled study. The trial’s primary results were published in the New England Journal of Medicine in January 2021. Researchers conducted SOLOIST-WHF at more than 300 sites in 32 countries. The trial included 1,222 patients with type 2 diabetes and reduced or preserved ejection fraction who were recently hospitalized for worsening heart failure.
In the new analysis the researchers looked at hospitalizations for any reason and the duration of hospital admissions after randomization. They analyzed days alive and out of the hospital using prespecified models.
Similar proportions of patients who received sotagliflozin and placebo were hospitalized at least once (38.5% vs. 41.4%) during a median follow-up of 9 months. Fewer patients who received sotagliflozin were hospitalized more than once (16.3% vs. 22.1%). In all, 64 patients in the sotagliflozin group and 76 patients in the placebo group died.
The reason for each hospitalization was unspecified, except for cases of heart failure, the authors noted. About 62% of hospitalizations during the trial were for reasons other than heart failure.
Outside expert cites similarities to initial trial
The results for days alive and out of the hospital are “not particularly surprising given the previous publication” of the trial’s primary results, but the new analysis provides a “different view of outcomes that might be clinically meaningful for patients,” commented Frank Brosius, MD, a professor of medicine at the University of Arizona, Tucson.
The SOLOIST-WHF trial indicated that doctors may be able to effectively treat patients with relatively new heart failure with sotagliflozin as long as patients are relatively stable, said Dr. Brosius, who coauthored an editorial in the New England Journal of Medicine that accompanied the initial results from the SOLOIST-WHF trial. It appears that previously reported benefits with regard to heart failure outcomes “showed up in these other indicators” in the secondary analysis.
Still, the effect sizes in the new analysis were relatively small and “probably more studies will be necessary” to examine these end points, he added.
SOLOIST-WHF was funded by Sanofi at initiation and by Lexicon Pharmaceuticals at completion. Dr. Szarek disclosed grants from Lexicon and grants and personal fees from Sanofi, as well as personal fees from other companies. His coauthors included employees of Lexicon and other researchers with financial ties to Lexicon and other pharmaceutical companies. Dr. Brosius disclosed personal fees from the American Diabetes Association and is a member of the Diabetic Kidney Disease Collaborative task force for the American Society of Nephrology that is broadly advocating the use of SGLT2 inhibitors by patients with diabetic kidney diseases. He also has participated in an advisory group for treatment of diabetic kidney disease for Gilead.
The outcome measure –days alive and out of the hospital – may be a meaningful, patient-centered way of capturing disease burden, the researchers wrote in their paper, published in Annals of Internal Medicine.
“The question was: Can we keep patients alive and out of the hospital for any reason, accounting for the duration of each hospitalization?” author Michael Szarek, PhD, a visiting professor in the division of cardiology at the University of Colorado at Denver, Aurora, said in an interview.
“For every 100 days of follow-up, patients in the sotagliflozin group were alive and out of the hospital 3% more days in relative terms or 2.9 days in absolute terms than those in the placebo group (91.8 vs. 88.9 days),” the researchers reported in their analysis of data from the SOLOIST-WHF trial.
“If you translate that to over the course of a year, that’s more than 10 days,” said Dr. Szarek, who is also a faculty member of CPC Clinical Research, an academic research organization affiliated with the University of Colorado.
Most patients in both groups survived to the end of the study without hospitalization, according to the paper.
Sotagliflozin, a sodium-glucose cotransporter 1 and SGLT2 inhibitor, is not approved in the United States. In 2019, the Food and Drug Administration rejected sotagliflozin as an adjunct to insulin for the treatment of type 1 diabetes after members of an advisory committee expressed concerns about an increased risk for diabetic ketoacidosis with the drug.
Methods and results
To examine whether sotagliflozin increased days alive and out of the hospital in the SOLOIST-WHF trial, Dr. Szarek and colleagues analyzed data from this randomized, double-blind, placebo-controlled study. The trial’s primary results were published in the New England Journal of Medicine in January 2021. Researchers conducted SOLOIST-WHF at more than 300 sites in 32 countries. The trial included 1,222 patients with type 2 diabetes and reduced or preserved ejection fraction who were recently hospitalized for worsening heart failure.
In the new analysis the researchers looked at hospitalizations for any reason and the duration of hospital admissions after randomization. They analyzed days alive and out of the hospital using prespecified models.
Similar proportions of patients who received sotagliflozin and placebo were hospitalized at least once (38.5% vs. 41.4%) during a median follow-up of 9 months. Fewer patients who received sotagliflozin were hospitalized more than once (16.3% vs. 22.1%). In all, 64 patients in the sotagliflozin group and 76 patients in the placebo group died.
The reason for each hospitalization was unspecified, except for cases of heart failure, the authors noted. About 62% of hospitalizations during the trial were for reasons other than heart failure.
Outside expert cites similarities to initial trial
The results for days alive and out of the hospital are “not particularly surprising given the previous publication” of the trial’s primary results, but the new analysis provides a “different view of outcomes that might be clinically meaningful for patients,” commented Frank Brosius, MD, a professor of medicine at the University of Arizona, Tucson.
The SOLOIST-WHF trial indicated that doctors may be able to effectively treat patients with relatively new heart failure with sotagliflozin as long as patients are relatively stable, said Dr. Brosius, who coauthored an editorial in the New England Journal of Medicine that accompanied the initial results from the SOLOIST-WHF trial. It appears that previously reported benefits with regard to heart failure outcomes “showed up in these other indicators” in the secondary analysis.
Still, the effect sizes in the new analysis were relatively small and “probably more studies will be necessary” to examine these end points, he added.
SOLOIST-WHF was funded by Sanofi at initiation and by Lexicon Pharmaceuticals at completion. Dr. Szarek disclosed grants from Lexicon and grants and personal fees from Sanofi, as well as personal fees from other companies. His coauthors included employees of Lexicon and other researchers with financial ties to Lexicon and other pharmaceutical companies. Dr. Brosius disclosed personal fees from the American Diabetes Association and is a member of the Diabetic Kidney Disease Collaborative task force for the American Society of Nephrology that is broadly advocating the use of SGLT2 inhibitors by patients with diabetic kidney diseases. He also has participated in an advisory group for treatment of diabetic kidney disease for Gilead.
FROM ANNALS OF INTERNAL MEDICINE
Children and COVID: Vaccination trends beginning to diverge
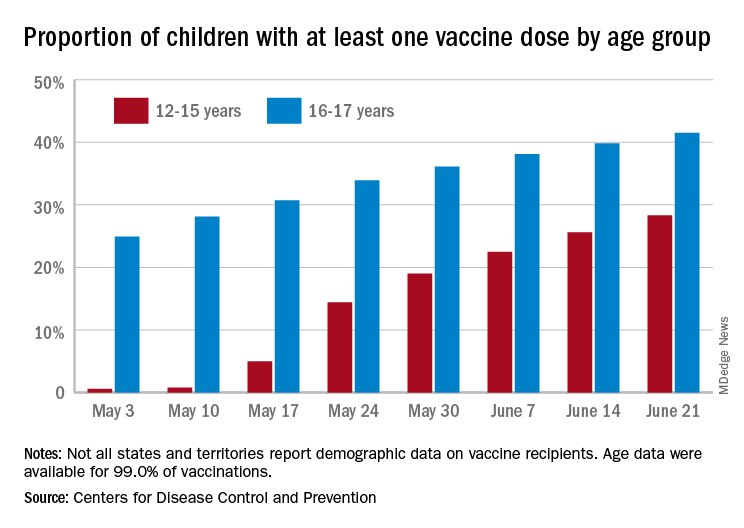
As more adolescents became eligible for a second dose of the Pfizer vaccine since it received approval from the Food and Drug Administration in mid-May, the share of 12- to 15-year-olds considered fully vaccinated rose from 11.4% on June 14 to 17.8% on June 28, an increase of 56%, the CDC’s COVID Data Tracker indicated June 22.
For children aged 16-17 years, who have been receiving the vaccine since early April, full vaccination rose by 9.6% in that same week, going from 29.1% on June 14 to 31.9% on June 21. The cumulative numbers for first vaccinations are higher, of course, but are rising more slowly in both age groups: 41.5% of those aged 16-17 had received at least one dose by June 21 (up by 4.3%), with the 12- to 15-year-olds at 28.3% (up by 10.5%), based on the CDC data.
Limiting the time frame to just the last 2 weeks, however, shows the opposite of rising among the younger children. During the 2 weeks ending June 7, 17.9% of those initiating a first dose were 12-15 years old, but that 2-week figure slipped to 17.1% as of June 14 and was down to 16.0% on June 21. The older group was slow but steady over that time: 4.8%, 4.7%, and 4.8%, the CDC said. To give those figures some context, those aged 25-39 years represented 23.7% of past-2-week initiations on June 7 and 24.3% on June 21.
Although no COVID-19 vaccine has been approved for children under 12 years, about 0.4% of that age group – just over 167,000 children – have received a first dose and almost 91,000 are fully vaccinated, according to CDC data.
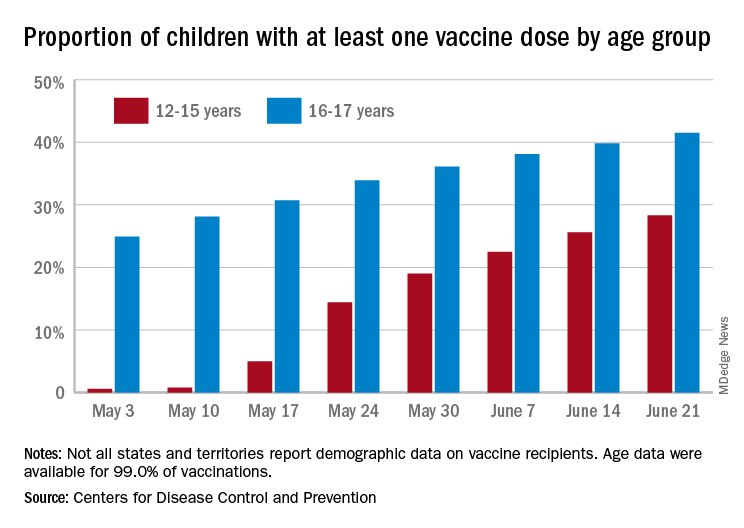
As more adolescents became eligible for a second dose of the Pfizer vaccine since it received approval from the Food and Drug Administration in mid-May, the share of 12- to 15-year-olds considered fully vaccinated rose from 11.4% on June 14 to 17.8% on June 28, an increase of 56%, the CDC’s COVID Data Tracker indicated June 22.
For children aged 16-17 years, who have been receiving the vaccine since early April, full vaccination rose by 9.6% in that same week, going from 29.1% on June 14 to 31.9% on June 21. The cumulative numbers for first vaccinations are higher, of course, but are rising more slowly in both age groups: 41.5% of those aged 16-17 had received at least one dose by June 21 (up by 4.3%), with the 12- to 15-year-olds at 28.3% (up by 10.5%), based on the CDC data.
Limiting the time frame to just the last 2 weeks, however, shows the opposite of rising among the younger children. During the 2 weeks ending June 7, 17.9% of those initiating a first dose were 12-15 years old, but that 2-week figure slipped to 17.1% as of June 14 and was down to 16.0% on June 21. The older group was slow but steady over that time: 4.8%, 4.7%, and 4.8%, the CDC said. To give those figures some context, those aged 25-39 years represented 23.7% of past-2-week initiations on June 7 and 24.3% on June 21.
Although no COVID-19 vaccine has been approved for children under 12 years, about 0.4% of that age group – just over 167,000 children – have received a first dose and almost 91,000 are fully vaccinated, according to CDC data.
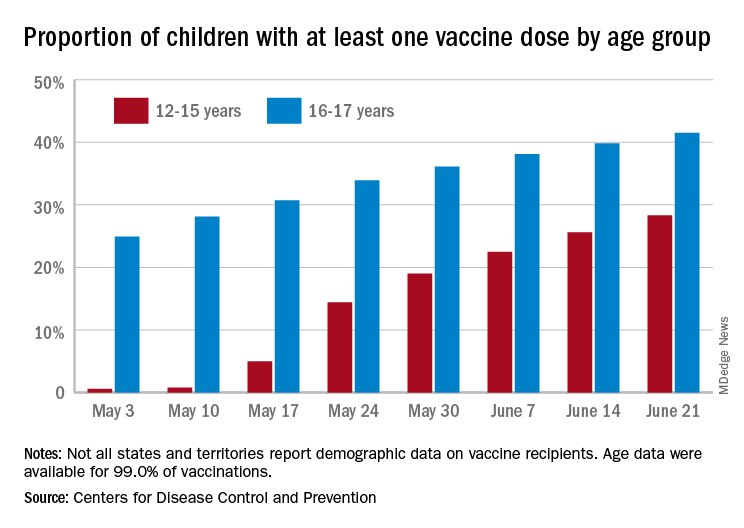
As more adolescents became eligible for a second dose of the Pfizer vaccine since it received approval from the Food and Drug Administration in mid-May, the share of 12- to 15-year-olds considered fully vaccinated rose from 11.4% on June 14 to 17.8% on June 28, an increase of 56%, the CDC’s COVID Data Tracker indicated June 22.
For children aged 16-17 years, who have been receiving the vaccine since early April, full vaccination rose by 9.6% in that same week, going from 29.1% on June 14 to 31.9% on June 21. The cumulative numbers for first vaccinations are higher, of course, but are rising more slowly in both age groups: 41.5% of those aged 16-17 had received at least one dose by June 21 (up by 4.3%), with the 12- to 15-year-olds at 28.3% (up by 10.5%), based on the CDC data.
Limiting the time frame to just the last 2 weeks, however, shows the opposite of rising among the younger children. During the 2 weeks ending June 7, 17.9% of those initiating a first dose were 12-15 years old, but that 2-week figure slipped to 17.1% as of June 14 and was down to 16.0% on June 21. The older group was slow but steady over that time: 4.8%, 4.7%, and 4.8%, the CDC said. To give those figures some context, those aged 25-39 years represented 23.7% of past-2-week initiations on June 7 and 24.3% on June 21.
Although no COVID-19 vaccine has been approved for children under 12 years, about 0.4% of that age group – just over 167,000 children – have received a first dose and almost 91,000 are fully vaccinated, according to CDC data.
AAP updates guidance for return to sports and physical activities
As pandemic restrictions ease and young athletes once again take to fields, courts, tracks, and rinks, doctors are sharing ways to help them get back to sports safely.
That means taking steps to prevent COVID-19.
It also means trying to avoid sports-related injuries, which may be more likely if young athletes didn’t move around so much during the pandemic.
For adolescents who are eligible, getting a COVID-19 vaccine may be the most important thing they can do, according to the American Academy of Pediatrics.
“The AAP encourages all people who are eligible to receive the COVID-19 vaccine as soon as it is available,” the organization wrote in updated guidance on returning to sports and physical activity.
“I don’t think it can be overemphasized how important these vaccines are, both for the individual and at the community level,” says Aaron L. Baggish, MD, an associate professor of medicine at Harvard Medical School, Boston, and director of the Cardiovascular Performance Program at Massachusetts General Hospital in Boston.
Dr. Baggish, team cardiologist for the New England Patriots, the Boston Bruins, the New England Revolution, U.S. Men’s and Women’s Soccer, and U.S. Rowing, as well as medical director for the Boston Marathon, has studied the effects of COVID-19 on the heart in college athletes and written return-to-play recommendations for athletes of high school age and older.
“Millions of people have received these vaccines from age 12 up,” Dr. Baggish says. “The efficacy continues to look very durable and near complete, and the risk associated with vaccination is incredibly low, to the point where the risk-benefit ratio across the age spectrum, whether you’re athletic or not, strongly favors getting vaccinated. There is really no reason to hold off at this point.”
While outdoor activities are lower-risk for spreading COVID-19 and many people have been vaccinated, masks still should be worn in certain settings, the AAP notes.
“Indoor spaces that are crowded are still high-risk for COVID-19 transmission. And we recognize that not everyone in these settings may be vaccinated,” says Susannah Briskin, MD, lead author of the AAP guidance.
“So for indoor sporting events with spectators, in locker rooms or other small spaces such as a training room, and during shared car rides or school transportation to and from events, individuals should continue to mask,” adds Dr. Briskin, a pediatrician in the Division of Sports Medicine and fellowship director for the Primary Care Sports Medicine program at University Hospitals Rainbow Babies & Children’s Hospital.
For outdoor sports, athletes who are not fully vaccinated should be encouraged to wear masks on the sidelines and during group training and competition when they are within 3 feet of others for sustained amounts of time, according to the AAP.
Get back into exercise gradually
In general, athletes who have not been active for more than a month should resume exercise gradually, Dr. Briskin says. Starting at 25% of normal volume and increasing slowly over time – with 10% increases each week – is one rule of thumb.
“Those who have taken a prolonged break from sports are at a higher risk of injury when they return,” she notes. “Families should also be aware of an increased risk for heat-related illness if they are not acclimated.”
Caitlyn Mooney, MD, a team doctor for the University of Texas, San Antonio, has heard reports of doctors seeing more injuries like stress fractures. Some cases may relate to people going from “months of doing nothing to all of a sudden going back to sports,” says Dr. Mooney, who is also a clinical assistant professor of pediatrics and orthopedics at UT Health San Antonio.
“The coaches, the parents, and the athletes themselves really need to keep in mind that it’s not like a regular season,” Dr. Mooney says. She suggests gradually ramping up activity and paying attention to any pain. “That’s a good indicator that maybe you’re going too fast,” she adds.
Athletes should be mindful of other symptoms too when restarting exercise, especially after illness.
It is “very important that any athlete with recent COVID-19 monitor for new symptoms when they return to exercise,” says Jonathan Drezner, MD, a professor of family medicine at the University of Washington, Seattle. “A little fatigue from detraining may be expected, but exertional chest pain deserves more evaluation.”
Dr. Drezner – editor-in-chief of the British Journal of Sports Medicine and team doctor for the Seattle Seahawks – along with Dr. Baggish and colleagues, found a low prevalence of cardiac involvement in a study of more than 3,000 college athletes with prior SARS-CoV-2 infection.
“Any athlete, despite their initial symptom course, who has cardiopulmonary symptoms on return to exercise, particularly chest pain, should see their physician for a comprehensive cardiac evaluation,” Dr. Drezner says. “Cardiac MRI should be reserved for athletes with abnormal testing or when clinical suspicion of myocardial involvement is high.”
If an athlete had COVID-19 with moderate symptoms (such as fever, chills, or a flu-like syndrome) or cardiopulmonary symptoms (such as chest pain or shortness of breath), cardiac testing should be considered, he notes.
These symptoms “were associated with a higher prevalence of cardiac involvement,” Dr. Drezner said in an email. “Testing may include an ECG, echocardiogram (ultrasound), and troponin (blood test).”
For kids who test positive for SARS-CoV-2 but do not have symptoms, or their symptoms last less than 4 days, a phone call or telemedicine visit with their doctor may be enough to clear them to play, says Dr. Briskin, who’s also an assistant professor of pediatrics at Case Western Reserve University, Cleveland.
“This will allow the physician an opportunity to screen for any concerning cardiac signs or symptoms, update the patient’s electronic medical record with the recent COVID-19 infection, and provide appropriate guidance back to exercise,” she adds.
Dr. Baggish, Dr. Briskin, Dr. Mooney, and Dr. Drezner had no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
As pandemic restrictions ease and young athletes once again take to fields, courts, tracks, and rinks, doctors are sharing ways to help them get back to sports safely.
That means taking steps to prevent COVID-19.
It also means trying to avoid sports-related injuries, which may be more likely if young athletes didn’t move around so much during the pandemic.
For adolescents who are eligible, getting a COVID-19 vaccine may be the most important thing they can do, according to the American Academy of Pediatrics.
“The AAP encourages all people who are eligible to receive the COVID-19 vaccine as soon as it is available,” the organization wrote in updated guidance on returning to sports and physical activity.
“I don’t think it can be overemphasized how important these vaccines are, both for the individual and at the community level,” says Aaron L. Baggish, MD, an associate professor of medicine at Harvard Medical School, Boston, and director of the Cardiovascular Performance Program at Massachusetts General Hospital in Boston.
Dr. Baggish, team cardiologist for the New England Patriots, the Boston Bruins, the New England Revolution, U.S. Men’s and Women’s Soccer, and U.S. Rowing, as well as medical director for the Boston Marathon, has studied the effects of COVID-19 on the heart in college athletes and written return-to-play recommendations for athletes of high school age and older.
“Millions of people have received these vaccines from age 12 up,” Dr. Baggish says. “The efficacy continues to look very durable and near complete, and the risk associated with vaccination is incredibly low, to the point where the risk-benefit ratio across the age spectrum, whether you’re athletic or not, strongly favors getting vaccinated. There is really no reason to hold off at this point.”
While outdoor activities are lower-risk for spreading COVID-19 and many people have been vaccinated, masks still should be worn in certain settings, the AAP notes.
“Indoor spaces that are crowded are still high-risk for COVID-19 transmission. And we recognize that not everyone in these settings may be vaccinated,” says Susannah Briskin, MD, lead author of the AAP guidance.
“So for indoor sporting events with spectators, in locker rooms or other small spaces such as a training room, and during shared car rides or school transportation to and from events, individuals should continue to mask,” adds Dr. Briskin, a pediatrician in the Division of Sports Medicine and fellowship director for the Primary Care Sports Medicine program at University Hospitals Rainbow Babies & Children’s Hospital.
For outdoor sports, athletes who are not fully vaccinated should be encouraged to wear masks on the sidelines and during group training and competition when they are within 3 feet of others for sustained amounts of time, according to the AAP.
Get back into exercise gradually
In general, athletes who have not been active for more than a month should resume exercise gradually, Dr. Briskin says. Starting at 25% of normal volume and increasing slowly over time – with 10% increases each week – is one rule of thumb.
“Those who have taken a prolonged break from sports are at a higher risk of injury when they return,” she notes. “Families should also be aware of an increased risk for heat-related illness if they are not acclimated.”
Caitlyn Mooney, MD, a team doctor for the University of Texas, San Antonio, has heard reports of doctors seeing more injuries like stress fractures. Some cases may relate to people going from “months of doing nothing to all of a sudden going back to sports,” says Dr. Mooney, who is also a clinical assistant professor of pediatrics and orthopedics at UT Health San Antonio.
“The coaches, the parents, and the athletes themselves really need to keep in mind that it’s not like a regular season,” Dr. Mooney says. She suggests gradually ramping up activity and paying attention to any pain. “That’s a good indicator that maybe you’re going too fast,” she adds.
Athletes should be mindful of other symptoms too when restarting exercise, especially after illness.
It is “very important that any athlete with recent COVID-19 monitor for new symptoms when they return to exercise,” says Jonathan Drezner, MD, a professor of family medicine at the University of Washington, Seattle. “A little fatigue from detraining may be expected, but exertional chest pain deserves more evaluation.”
Dr. Drezner – editor-in-chief of the British Journal of Sports Medicine and team doctor for the Seattle Seahawks – along with Dr. Baggish and colleagues, found a low prevalence of cardiac involvement in a study of more than 3,000 college athletes with prior SARS-CoV-2 infection.
“Any athlete, despite their initial symptom course, who has cardiopulmonary symptoms on return to exercise, particularly chest pain, should see their physician for a comprehensive cardiac evaluation,” Dr. Drezner says. “Cardiac MRI should be reserved for athletes with abnormal testing or when clinical suspicion of myocardial involvement is high.”
If an athlete had COVID-19 with moderate symptoms (such as fever, chills, or a flu-like syndrome) or cardiopulmonary symptoms (such as chest pain or shortness of breath), cardiac testing should be considered, he notes.
These symptoms “were associated with a higher prevalence of cardiac involvement,” Dr. Drezner said in an email. “Testing may include an ECG, echocardiogram (ultrasound), and troponin (blood test).”
For kids who test positive for SARS-CoV-2 but do not have symptoms, or their symptoms last less than 4 days, a phone call or telemedicine visit with their doctor may be enough to clear them to play, says Dr. Briskin, who’s also an assistant professor of pediatrics at Case Western Reserve University, Cleveland.
“This will allow the physician an opportunity to screen for any concerning cardiac signs or symptoms, update the patient’s electronic medical record with the recent COVID-19 infection, and provide appropriate guidance back to exercise,” she adds.
Dr. Baggish, Dr. Briskin, Dr. Mooney, and Dr. Drezner had no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
As pandemic restrictions ease and young athletes once again take to fields, courts, tracks, and rinks, doctors are sharing ways to help them get back to sports safely.
That means taking steps to prevent COVID-19.
It also means trying to avoid sports-related injuries, which may be more likely if young athletes didn’t move around so much during the pandemic.
For adolescents who are eligible, getting a COVID-19 vaccine may be the most important thing they can do, according to the American Academy of Pediatrics.
“The AAP encourages all people who are eligible to receive the COVID-19 vaccine as soon as it is available,” the organization wrote in updated guidance on returning to sports and physical activity.
“I don’t think it can be overemphasized how important these vaccines are, both for the individual and at the community level,” says Aaron L. Baggish, MD, an associate professor of medicine at Harvard Medical School, Boston, and director of the Cardiovascular Performance Program at Massachusetts General Hospital in Boston.
Dr. Baggish, team cardiologist for the New England Patriots, the Boston Bruins, the New England Revolution, U.S. Men’s and Women’s Soccer, and U.S. Rowing, as well as medical director for the Boston Marathon, has studied the effects of COVID-19 on the heart in college athletes and written return-to-play recommendations for athletes of high school age and older.
“Millions of people have received these vaccines from age 12 up,” Dr. Baggish says. “The efficacy continues to look very durable and near complete, and the risk associated with vaccination is incredibly low, to the point where the risk-benefit ratio across the age spectrum, whether you’re athletic or not, strongly favors getting vaccinated. There is really no reason to hold off at this point.”
While outdoor activities are lower-risk for spreading COVID-19 and many people have been vaccinated, masks still should be worn in certain settings, the AAP notes.
“Indoor spaces that are crowded are still high-risk for COVID-19 transmission. And we recognize that not everyone in these settings may be vaccinated,” says Susannah Briskin, MD, lead author of the AAP guidance.
“So for indoor sporting events with spectators, in locker rooms or other small spaces such as a training room, and during shared car rides or school transportation to and from events, individuals should continue to mask,” adds Dr. Briskin, a pediatrician in the Division of Sports Medicine and fellowship director for the Primary Care Sports Medicine program at University Hospitals Rainbow Babies & Children’s Hospital.
For outdoor sports, athletes who are not fully vaccinated should be encouraged to wear masks on the sidelines and during group training and competition when they are within 3 feet of others for sustained amounts of time, according to the AAP.
Get back into exercise gradually
In general, athletes who have not been active for more than a month should resume exercise gradually, Dr. Briskin says. Starting at 25% of normal volume and increasing slowly over time – with 10% increases each week – is one rule of thumb.
“Those who have taken a prolonged break from sports are at a higher risk of injury when they return,” she notes. “Families should also be aware of an increased risk for heat-related illness if they are not acclimated.”
Caitlyn Mooney, MD, a team doctor for the University of Texas, San Antonio, has heard reports of doctors seeing more injuries like stress fractures. Some cases may relate to people going from “months of doing nothing to all of a sudden going back to sports,” says Dr. Mooney, who is also a clinical assistant professor of pediatrics and orthopedics at UT Health San Antonio.
“The coaches, the parents, and the athletes themselves really need to keep in mind that it’s not like a regular season,” Dr. Mooney says. She suggests gradually ramping up activity and paying attention to any pain. “That’s a good indicator that maybe you’re going too fast,” she adds.
Athletes should be mindful of other symptoms too when restarting exercise, especially after illness.
It is “very important that any athlete with recent COVID-19 monitor for new symptoms when they return to exercise,” says Jonathan Drezner, MD, a professor of family medicine at the University of Washington, Seattle. “A little fatigue from detraining may be expected, but exertional chest pain deserves more evaluation.”
Dr. Drezner – editor-in-chief of the British Journal of Sports Medicine and team doctor for the Seattle Seahawks – along with Dr. Baggish and colleagues, found a low prevalence of cardiac involvement in a study of more than 3,000 college athletes with prior SARS-CoV-2 infection.
“Any athlete, despite their initial symptom course, who has cardiopulmonary symptoms on return to exercise, particularly chest pain, should see their physician for a comprehensive cardiac evaluation,” Dr. Drezner says. “Cardiac MRI should be reserved for athletes with abnormal testing or when clinical suspicion of myocardial involvement is high.”
If an athlete had COVID-19 with moderate symptoms (such as fever, chills, or a flu-like syndrome) or cardiopulmonary symptoms (such as chest pain or shortness of breath), cardiac testing should be considered, he notes.
These symptoms “were associated with a higher prevalence of cardiac involvement,” Dr. Drezner said in an email. “Testing may include an ECG, echocardiogram (ultrasound), and troponin (blood test).”
For kids who test positive for SARS-CoV-2 but do not have symptoms, or their symptoms last less than 4 days, a phone call or telemedicine visit with their doctor may be enough to clear them to play, says Dr. Briskin, who’s also an assistant professor of pediatrics at Case Western Reserve University, Cleveland.
“This will allow the physician an opportunity to screen for any concerning cardiac signs or symptoms, update the patient’s electronic medical record with the recent COVID-19 infection, and provide appropriate guidance back to exercise,” she adds.
Dr. Baggish, Dr. Briskin, Dr. Mooney, and Dr. Drezner had no relevant financial disclosures.
A version of this article first appeared on Medscape.com.