User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
‘Treat youth with gender dysphoria as individuals’
Young people with gender dysphoria should be considered as individuals rather than fall into an age-defined bracket when assessing their understanding to consent to hormone treatment, according to the Tavistock and Portman NHS Foundation Trust, as it awaits the verdict of its recent appeal in London against a High Court ruling.
The High Court ruling, made in December 2020 as reported by this news organization, stated that adolescents with gender dysphoria were unlikely to fully understand the consequences of hormone treatment for gender reassignment and was the result of a case brought by 24-year-old Keira Bell, who transitioned from female to male at the Gender Identity Development Service (GIDS), starting at the age of 16, but later “detransitioned.”
Along with changes made to rules around prescribing puberty blockers and cross-sex hormones to minors with gender dysphoria in countries such as Finland and Sweden, the English ruling signals a more cautious approach to any medical treatment for such children, as detailed in a feature published in April.
However, during the appeal, The Trust argued once more that puberty blockers give children time to “consider options” about their bodies and that the decision (the December ruling) was inconsistent with the law that “entitles children under the age of 16 to make decisions for themselves after being assessed as competent to do so by their doctor.”
Alongside other organizations, the United States–based Endocrine Society submitted written evidence in support of the Tavistock. “The High Court’s decision, if it is allowed to stand, would set a harmful precedent preventing physicians from providing transgender and gender diverse youth with high-quality medical care,” it noted in a statement.
Defending the High Court’s ruling, the lawyer for Ms. Bell said its conclusion was that puberty blockers for gender dysphoria are an “experimental” treatment with a very limited evidence base.
“The judgment of the [High Court] is entirely correct, and there is no proper basis for overturning it,” he asserted.
The 2-day appeal hearing ended on June 24, and a ruling will be made at a later date.
Do children understand the consequences of hormone treatment?
One central aspect of the overall case is the fact that Ms. Bell regrets her decision to transition at age 16, saying she only received three counseling sessions prior to endocrinology referral. And she consequently had a mastectomy at age 20, which she also bitterly regrets.
So a key concern is whether young people fully understand the consequences of taking puberty blockers and therapies that may follow, including cross-sex hormones.
Witness for the appeal Gary Butler, MD, consultant in pediatric and adolescent endocrinology at University College Hospital, London, where children are referred to from GIDS for hormone treatment, said the number of children who go on to cross-sex hormones from puberty blockers is “over 80%.”
But the actual number of children who are referred to endocrinology services (where puberty blockers are initiated) from GIDS is low, at approximately 16%, according to 2019-2020 data, said a GIDS spokesperson.
“Once at the endocrinology service, young people either participate in a group education session, or if under 15 years, an individualized session between the clinician and the patient and family members,” she added. The Trust also maintained that initiation of cross-sex hormones “is separate from the prescription of puberty blockers.”
Since the December ruling, The Trust has put in place multidisciplinary clinical reviews (MDCR) of cases, and in July, NHS England will start implementing an independent multidisciplinary professional review (MDPR) to check that the GIDS has followed due process with each case.
Slow the process down, give appropriate psychotherapy
Stella O’Malley is a psychotherapist who works with transitioners and detransitioners and is a founding member of the International Association of Therapists for Desisters and Detransitioners (IATDD).
Whatever the outcome of the appeal process, Ms. O’Malley said she would like to see the Tavistock slow down and take a broader approach to counseling children before referral to endocrinology services.
In discussing therapy prior to transition, Ms. O’Malley stated that her clients often say they did not explore their inner motivations or other possible reasons for their distress, and the therapy was focused more on when they transition, rather than being sure it was something they wanted to do.
“We need to learn from the mistakes made with people like Keira Bell. , especially when [children are] ... young and especially when they’re traumatized,” Ms. O’Malley said.
“Had they received a more conventional therapy, they might have thought about their decision from different perspectives and in the process acquired more self-awareness, which would have been more beneficial.”
“The ‘affirmative’ approach to gender therapy is too narrow; we need to look at the whole individual. Therapy in other areas would never disregard other, nongender issues such as attention deficit hyperactivity disorder or anxiety [which often co-exist with gender dysphoria] – issues bleed into each other,” Ms. O’Malley pointed out. “We need a more exploratory approach.”
“I’d also like to see other therapists all over the [U.K.] who are perfectly qualified and capable of working with gender actually start working with gender issues,” she said, noting that such an approach might also help reduce the long waiting list at the Tavistock.
The latter had been overwhelmed, and this led to a speeding up of the assessment process, which led to a number of professionals resigning from the service in recent years, saying children were being “fast-tracked” to medical transition.
Fertility and sexual function are complex issues for kids
Also asked to comment was Claire Graham, from Genspect, a group that describes itself as a voice for parents of gender-questioning kids.
She told this news organization that “parents are rightly concerned about their children’s ability to consent to treatments that may lead to infertility and issues surrounding sexual function.” She added that other countries in Europe were changing their approach. “Look to Sweden and Finland, who have both rowed back on puberty blockers and no longer recommend them.”
Ms. Graham, who has worked with children with differences in sexual development, added that it was very difficult for children and young people to understand the life-long implications of decisions made at an early age.
“How can children understand what it is to live with impaired sexual functioning if they have never had sex? Likewise, fertility is a complex issue. Most people do not want to become parents as teenagers, but we understand that this will often change as they grow,” said Ms. Graham.
“Many parents worry that their child is not being considered in the whole [and] that their child’s ability to consent to medical interventions for gender dysphoria is impacted by comorbidities, such as a diagnosis of autism or a history of mental health issues. These children are particularly vulnerable.”
“At Genspect, we hope that the decision from the ... court is upheld,” Ms. Graham concluded.
A version of this article first appeared on Medscape.com.
Young people with gender dysphoria should be considered as individuals rather than fall into an age-defined bracket when assessing their understanding to consent to hormone treatment, according to the Tavistock and Portman NHS Foundation Trust, as it awaits the verdict of its recent appeal in London against a High Court ruling.
The High Court ruling, made in December 2020 as reported by this news organization, stated that adolescents with gender dysphoria were unlikely to fully understand the consequences of hormone treatment for gender reassignment and was the result of a case brought by 24-year-old Keira Bell, who transitioned from female to male at the Gender Identity Development Service (GIDS), starting at the age of 16, but later “detransitioned.”
Along with changes made to rules around prescribing puberty blockers and cross-sex hormones to minors with gender dysphoria in countries such as Finland and Sweden, the English ruling signals a more cautious approach to any medical treatment for such children, as detailed in a feature published in April.
However, during the appeal, The Trust argued once more that puberty blockers give children time to “consider options” about their bodies and that the decision (the December ruling) was inconsistent with the law that “entitles children under the age of 16 to make decisions for themselves after being assessed as competent to do so by their doctor.”
Alongside other organizations, the United States–based Endocrine Society submitted written evidence in support of the Tavistock. “The High Court’s decision, if it is allowed to stand, would set a harmful precedent preventing physicians from providing transgender and gender diverse youth with high-quality medical care,” it noted in a statement.
Defending the High Court’s ruling, the lawyer for Ms. Bell said its conclusion was that puberty blockers for gender dysphoria are an “experimental” treatment with a very limited evidence base.
“The judgment of the [High Court] is entirely correct, and there is no proper basis for overturning it,” he asserted.
The 2-day appeal hearing ended on June 24, and a ruling will be made at a later date.
Do children understand the consequences of hormone treatment?
One central aspect of the overall case is the fact that Ms. Bell regrets her decision to transition at age 16, saying she only received three counseling sessions prior to endocrinology referral. And she consequently had a mastectomy at age 20, which she also bitterly regrets.
So a key concern is whether young people fully understand the consequences of taking puberty blockers and therapies that may follow, including cross-sex hormones.
Witness for the appeal Gary Butler, MD, consultant in pediatric and adolescent endocrinology at University College Hospital, London, where children are referred to from GIDS for hormone treatment, said the number of children who go on to cross-sex hormones from puberty blockers is “over 80%.”
But the actual number of children who are referred to endocrinology services (where puberty blockers are initiated) from GIDS is low, at approximately 16%, according to 2019-2020 data, said a GIDS spokesperson.
“Once at the endocrinology service, young people either participate in a group education session, or if under 15 years, an individualized session between the clinician and the patient and family members,” she added. The Trust also maintained that initiation of cross-sex hormones “is separate from the prescription of puberty blockers.”
Since the December ruling, The Trust has put in place multidisciplinary clinical reviews (MDCR) of cases, and in July, NHS England will start implementing an independent multidisciplinary professional review (MDPR) to check that the GIDS has followed due process with each case.
Slow the process down, give appropriate psychotherapy
Stella O’Malley is a psychotherapist who works with transitioners and detransitioners and is a founding member of the International Association of Therapists for Desisters and Detransitioners (IATDD).
Whatever the outcome of the appeal process, Ms. O’Malley said she would like to see the Tavistock slow down and take a broader approach to counseling children before referral to endocrinology services.
In discussing therapy prior to transition, Ms. O’Malley stated that her clients often say they did not explore their inner motivations or other possible reasons for their distress, and the therapy was focused more on when they transition, rather than being sure it was something they wanted to do.
“We need to learn from the mistakes made with people like Keira Bell. , especially when [children are] ... young and especially when they’re traumatized,” Ms. O’Malley said.
“Had they received a more conventional therapy, they might have thought about their decision from different perspectives and in the process acquired more self-awareness, which would have been more beneficial.”
“The ‘affirmative’ approach to gender therapy is too narrow; we need to look at the whole individual. Therapy in other areas would never disregard other, nongender issues such as attention deficit hyperactivity disorder or anxiety [which often co-exist with gender dysphoria] – issues bleed into each other,” Ms. O’Malley pointed out. “We need a more exploratory approach.”
“I’d also like to see other therapists all over the [U.K.] who are perfectly qualified and capable of working with gender actually start working with gender issues,” she said, noting that such an approach might also help reduce the long waiting list at the Tavistock.
The latter had been overwhelmed, and this led to a speeding up of the assessment process, which led to a number of professionals resigning from the service in recent years, saying children were being “fast-tracked” to medical transition.
Fertility and sexual function are complex issues for kids
Also asked to comment was Claire Graham, from Genspect, a group that describes itself as a voice for parents of gender-questioning kids.
She told this news organization that “parents are rightly concerned about their children’s ability to consent to treatments that may lead to infertility and issues surrounding sexual function.” She added that other countries in Europe were changing their approach. “Look to Sweden and Finland, who have both rowed back on puberty blockers and no longer recommend them.”
Ms. Graham, who has worked with children with differences in sexual development, added that it was very difficult for children and young people to understand the life-long implications of decisions made at an early age.
“How can children understand what it is to live with impaired sexual functioning if they have never had sex? Likewise, fertility is a complex issue. Most people do not want to become parents as teenagers, but we understand that this will often change as they grow,” said Ms. Graham.
“Many parents worry that their child is not being considered in the whole [and] that their child’s ability to consent to medical interventions for gender dysphoria is impacted by comorbidities, such as a diagnosis of autism or a history of mental health issues. These children are particularly vulnerable.”
“At Genspect, we hope that the decision from the ... court is upheld,” Ms. Graham concluded.
A version of this article first appeared on Medscape.com.
Young people with gender dysphoria should be considered as individuals rather than fall into an age-defined bracket when assessing their understanding to consent to hormone treatment, according to the Tavistock and Portman NHS Foundation Trust, as it awaits the verdict of its recent appeal in London against a High Court ruling.
The High Court ruling, made in December 2020 as reported by this news organization, stated that adolescents with gender dysphoria were unlikely to fully understand the consequences of hormone treatment for gender reassignment and was the result of a case brought by 24-year-old Keira Bell, who transitioned from female to male at the Gender Identity Development Service (GIDS), starting at the age of 16, but later “detransitioned.”
Along with changes made to rules around prescribing puberty blockers and cross-sex hormones to minors with gender dysphoria in countries such as Finland and Sweden, the English ruling signals a more cautious approach to any medical treatment for such children, as detailed in a feature published in April.
However, during the appeal, The Trust argued once more that puberty blockers give children time to “consider options” about their bodies and that the decision (the December ruling) was inconsistent with the law that “entitles children under the age of 16 to make decisions for themselves after being assessed as competent to do so by their doctor.”
Alongside other organizations, the United States–based Endocrine Society submitted written evidence in support of the Tavistock. “The High Court’s decision, if it is allowed to stand, would set a harmful precedent preventing physicians from providing transgender and gender diverse youth with high-quality medical care,” it noted in a statement.
Defending the High Court’s ruling, the lawyer for Ms. Bell said its conclusion was that puberty blockers for gender dysphoria are an “experimental” treatment with a very limited evidence base.
“The judgment of the [High Court] is entirely correct, and there is no proper basis for overturning it,” he asserted.
The 2-day appeal hearing ended on June 24, and a ruling will be made at a later date.
Do children understand the consequences of hormone treatment?
One central aspect of the overall case is the fact that Ms. Bell regrets her decision to transition at age 16, saying she only received three counseling sessions prior to endocrinology referral. And she consequently had a mastectomy at age 20, which she also bitterly regrets.
So a key concern is whether young people fully understand the consequences of taking puberty blockers and therapies that may follow, including cross-sex hormones.
Witness for the appeal Gary Butler, MD, consultant in pediatric and adolescent endocrinology at University College Hospital, London, where children are referred to from GIDS for hormone treatment, said the number of children who go on to cross-sex hormones from puberty blockers is “over 80%.”
But the actual number of children who are referred to endocrinology services (where puberty blockers are initiated) from GIDS is low, at approximately 16%, according to 2019-2020 data, said a GIDS spokesperson.
“Once at the endocrinology service, young people either participate in a group education session, or if under 15 years, an individualized session between the clinician and the patient and family members,” she added. The Trust also maintained that initiation of cross-sex hormones “is separate from the prescription of puberty blockers.”
Since the December ruling, The Trust has put in place multidisciplinary clinical reviews (MDCR) of cases, and in July, NHS England will start implementing an independent multidisciplinary professional review (MDPR) to check that the GIDS has followed due process with each case.
Slow the process down, give appropriate psychotherapy
Stella O’Malley is a psychotherapist who works with transitioners and detransitioners and is a founding member of the International Association of Therapists for Desisters and Detransitioners (IATDD).
Whatever the outcome of the appeal process, Ms. O’Malley said she would like to see the Tavistock slow down and take a broader approach to counseling children before referral to endocrinology services.
In discussing therapy prior to transition, Ms. O’Malley stated that her clients often say they did not explore their inner motivations or other possible reasons for their distress, and the therapy was focused more on when they transition, rather than being sure it was something they wanted to do.
“We need to learn from the mistakes made with people like Keira Bell. , especially when [children are] ... young and especially when they’re traumatized,” Ms. O’Malley said.
“Had they received a more conventional therapy, they might have thought about their decision from different perspectives and in the process acquired more self-awareness, which would have been more beneficial.”
“The ‘affirmative’ approach to gender therapy is too narrow; we need to look at the whole individual. Therapy in other areas would never disregard other, nongender issues such as attention deficit hyperactivity disorder or anxiety [which often co-exist with gender dysphoria] – issues bleed into each other,” Ms. O’Malley pointed out. “We need a more exploratory approach.”
“I’d also like to see other therapists all over the [U.K.] who are perfectly qualified and capable of working with gender actually start working with gender issues,” she said, noting that such an approach might also help reduce the long waiting list at the Tavistock.
The latter had been overwhelmed, and this led to a speeding up of the assessment process, which led to a number of professionals resigning from the service in recent years, saying children were being “fast-tracked” to medical transition.
Fertility and sexual function are complex issues for kids
Also asked to comment was Claire Graham, from Genspect, a group that describes itself as a voice for parents of gender-questioning kids.
She told this news organization that “parents are rightly concerned about their children’s ability to consent to treatments that may lead to infertility and issues surrounding sexual function.” She added that other countries in Europe were changing their approach. “Look to Sweden and Finland, who have both rowed back on puberty blockers and no longer recommend them.”
Ms. Graham, who has worked with children with differences in sexual development, added that it was very difficult for children and young people to understand the life-long implications of decisions made at an early age.
“How can children understand what it is to live with impaired sexual functioning if they have never had sex? Likewise, fertility is a complex issue. Most people do not want to become parents as teenagers, but we understand that this will often change as they grow,” said Ms. Graham.
“Many parents worry that their child is not being considered in the whole [and] that their child’s ability to consent to medical interventions for gender dysphoria is impacted by comorbidities, such as a diagnosis of autism or a history of mental health issues. These children are particularly vulnerable.”
“At Genspect, we hope that the decision from the ... court is upheld,” Ms. Graham concluded.
A version of this article first appeared on Medscape.com.
Even a pandemic can’t stop teens’ alcohol and marijuana use
Despite record-breaking decreases in perceived availability of alcohol and marijuana among 12th-grade students, their use of these substances did not change significantly during the COVID-19 pandemic, according to two surveys conducted in 2020.
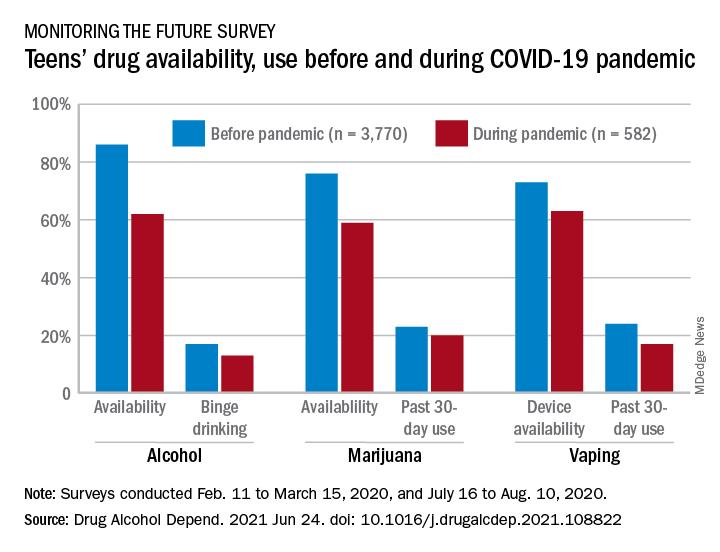
Vaping, however, did not show the same pattern. A decline in use over the previous 30 days was seen between the two surveys – conducted from Feb. 11 to March 15 and July 16 to Aug. 10 – along with a perceived reduction in the supply of vaping devices, Richard A. Miech, PhD, and associates said in Drug and Alcohol Dependence.
“Last year brought dramatic changes to adolescents’ lives, as many teens remained home with parents and other family members full time,” Nora D. Volkow, director of the National Institute on Drug Abuse, said in a separate written statement. “It is striking that, despite this monumental shift and teens’ perceived decreases in availability of marijuana and alcohol, usage rates held steady for these substances. This indicates that teens were able to obtain them despite barriers caused by the pandemic and despite not being of age to legally purchase them.”
In the first poll, conducted as part of the Monitoring the Future survey largely before the national emergency was declared, 86% of 12th-graders said that it was “fairly easy” or “very easy” to get alcohol, but that dropped to 62% in the second survey. For marijuana, prevalence of that level of availability was 76% before and 59% during the pandemic, Dr. Miech of the University of Michigan, Ann Arbor, and associates reported.
These results “indicate the largest decreases in substance use availability ever recorded in the 46 consecutive years it has been monitored by Monitoring the Future,” the investigators wrote.
The prevalence of marijuana use in the past 30 days declined from 23% before the pandemic to 20% during, with the respective figures for binge drinking in the past 2 weeks at 17% and 13%, and neither of those reductions reached significance, they noted.
“Adolescents may redouble their substance procurement efforts so that they can continue using substances at the levels at which they used in the past. In addition, adolescents may move to more solitary substance use. Social distancing policies might even increase substance use to the extent that they lead to feelings of isolation and loneliness that some adolescents address through increased substance use,” they suggested.
This hypothesis does not apply to vaping. The significant decline in availability – 73% before and 63% during – was accompanied by a significant drop in prevalence of past 30-day use from 24% to 17%, based on the survey data, which came from 3,770 responses to the first poll and 582 to the second.
In the case of vaping, the decline in use may have been caused by the decreased “exposure to substance-using peer networks ... and adults who provide opportunities for youth to initiate and continue use of substances,” Dr. Miech and associates said.
The findings of this analysis “suggest that reducing adolescent substance use through attempts to restrict supply alone would be a difficult undertaking,” Dr. Miech said in the NIDA statement. “The best strategy is likely to be one that combines approaches to limit the supply of these substances with efforts to decrease demand, through educational and public health campaigns.”
The research was funded by a NIDA grant. The investigators did not declare any conflicts of interest.
Despite record-breaking decreases in perceived availability of alcohol and marijuana among 12th-grade students, their use of these substances did not change significantly during the COVID-19 pandemic, according to two surveys conducted in 2020.
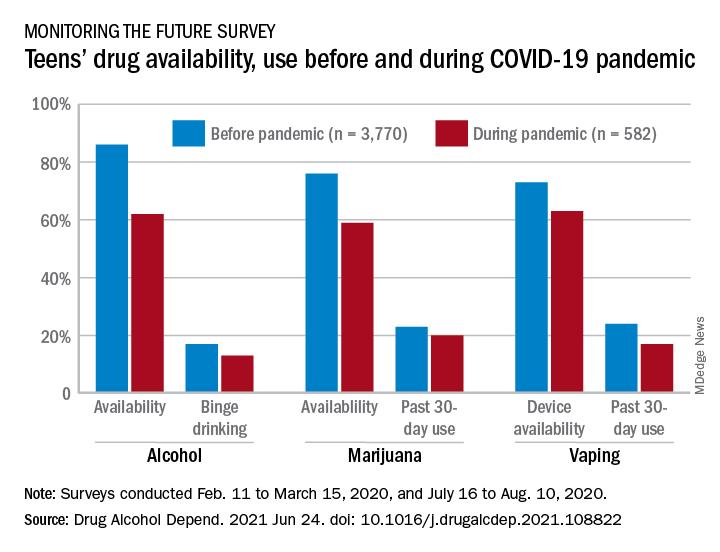
Vaping, however, did not show the same pattern. A decline in use over the previous 30 days was seen between the two surveys – conducted from Feb. 11 to March 15 and July 16 to Aug. 10 – along with a perceived reduction in the supply of vaping devices, Richard A. Miech, PhD, and associates said in Drug and Alcohol Dependence.
“Last year brought dramatic changes to adolescents’ lives, as many teens remained home with parents and other family members full time,” Nora D. Volkow, director of the National Institute on Drug Abuse, said in a separate written statement. “It is striking that, despite this monumental shift and teens’ perceived decreases in availability of marijuana and alcohol, usage rates held steady for these substances. This indicates that teens were able to obtain them despite barriers caused by the pandemic and despite not being of age to legally purchase them.”
In the first poll, conducted as part of the Monitoring the Future survey largely before the national emergency was declared, 86% of 12th-graders said that it was “fairly easy” or “very easy” to get alcohol, but that dropped to 62% in the second survey. For marijuana, prevalence of that level of availability was 76% before and 59% during the pandemic, Dr. Miech of the University of Michigan, Ann Arbor, and associates reported.
These results “indicate the largest decreases in substance use availability ever recorded in the 46 consecutive years it has been monitored by Monitoring the Future,” the investigators wrote.
The prevalence of marijuana use in the past 30 days declined from 23% before the pandemic to 20% during, with the respective figures for binge drinking in the past 2 weeks at 17% and 13%, and neither of those reductions reached significance, they noted.
“Adolescents may redouble their substance procurement efforts so that they can continue using substances at the levels at which they used in the past. In addition, adolescents may move to more solitary substance use. Social distancing policies might even increase substance use to the extent that they lead to feelings of isolation and loneliness that some adolescents address through increased substance use,” they suggested.
This hypothesis does not apply to vaping. The significant decline in availability – 73% before and 63% during – was accompanied by a significant drop in prevalence of past 30-day use from 24% to 17%, based on the survey data, which came from 3,770 responses to the first poll and 582 to the second.
In the case of vaping, the decline in use may have been caused by the decreased “exposure to substance-using peer networks ... and adults who provide opportunities for youth to initiate and continue use of substances,” Dr. Miech and associates said.
The findings of this analysis “suggest that reducing adolescent substance use through attempts to restrict supply alone would be a difficult undertaking,” Dr. Miech said in the NIDA statement. “The best strategy is likely to be one that combines approaches to limit the supply of these substances with efforts to decrease demand, through educational and public health campaigns.”
The research was funded by a NIDA grant. The investigators did not declare any conflicts of interest.
Despite record-breaking decreases in perceived availability of alcohol and marijuana among 12th-grade students, their use of these substances did not change significantly during the COVID-19 pandemic, according to two surveys conducted in 2020.
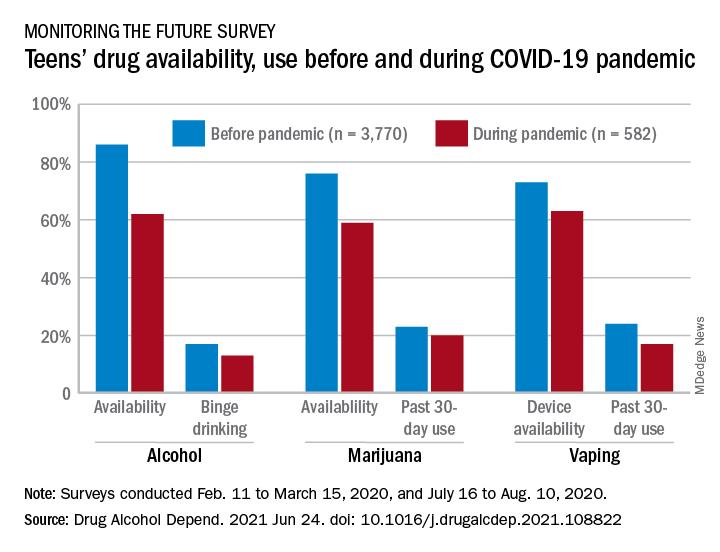
Vaping, however, did not show the same pattern. A decline in use over the previous 30 days was seen between the two surveys – conducted from Feb. 11 to March 15 and July 16 to Aug. 10 – along with a perceived reduction in the supply of vaping devices, Richard A. Miech, PhD, and associates said in Drug and Alcohol Dependence.
“Last year brought dramatic changes to adolescents’ lives, as many teens remained home with parents and other family members full time,” Nora D. Volkow, director of the National Institute on Drug Abuse, said in a separate written statement. “It is striking that, despite this monumental shift and teens’ perceived decreases in availability of marijuana and alcohol, usage rates held steady for these substances. This indicates that teens were able to obtain them despite barriers caused by the pandemic and despite not being of age to legally purchase them.”
In the first poll, conducted as part of the Monitoring the Future survey largely before the national emergency was declared, 86% of 12th-graders said that it was “fairly easy” or “very easy” to get alcohol, but that dropped to 62% in the second survey. For marijuana, prevalence of that level of availability was 76% before and 59% during the pandemic, Dr. Miech of the University of Michigan, Ann Arbor, and associates reported.
These results “indicate the largest decreases in substance use availability ever recorded in the 46 consecutive years it has been monitored by Monitoring the Future,” the investigators wrote.
The prevalence of marijuana use in the past 30 days declined from 23% before the pandemic to 20% during, with the respective figures for binge drinking in the past 2 weeks at 17% and 13%, and neither of those reductions reached significance, they noted.
“Adolescents may redouble their substance procurement efforts so that they can continue using substances at the levels at which they used in the past. In addition, adolescents may move to more solitary substance use. Social distancing policies might even increase substance use to the extent that they lead to feelings of isolation and loneliness that some adolescents address through increased substance use,” they suggested.
This hypothesis does not apply to vaping. The significant decline in availability – 73% before and 63% during – was accompanied by a significant drop in prevalence of past 30-day use from 24% to 17%, based on the survey data, which came from 3,770 responses to the first poll and 582 to the second.
In the case of vaping, the decline in use may have been caused by the decreased “exposure to substance-using peer networks ... and adults who provide opportunities for youth to initiate and continue use of substances,” Dr. Miech and associates said.
The findings of this analysis “suggest that reducing adolescent substance use through attempts to restrict supply alone would be a difficult undertaking,” Dr. Miech said in the NIDA statement. “The best strategy is likely to be one that combines approaches to limit the supply of these substances with efforts to decrease demand, through educational and public health campaigns.”
The research was funded by a NIDA grant. The investigators did not declare any conflicts of interest.
FROM DRUG AND ALCOHOL DEPENDENCE
Diversity of pediatric residents, fellows continues to lag
The proportion of underrepresented groups in pediatric fellowships decreased between 2007 and 2019, while those in pediatric residencies remained stagnant, new research revealed.
Researchers acknowledged that some of the factors contributing to the low proportion of minorities in the pediatric workforce may include educational disparities starting in primary or secondary school, such as underfunded schools and lack of educational resources.
“Something I really appreciated about the paper is that this goes beyond a student stepping into medical school, finding a mentor in pediatrics, and then eventually matriculating into a pediatric residency,” said Christle Nwora, MD, an internal medicine–pediatrics resident physician at Johns Hopkins Urban Health Residency Program in Baltimore, who was not involved in the study. “I like the idea of knowing that people aren’t going into the field and being very critical as to why.”
Prior studies, including a 2019 study published in JAMA Network Open, has found that minority students remain underrepresented in medical schools. However, this most recent study, published in Pediatrics, is one of the first to report trends in the race or ethnicity of pediatric residents and fellows.
“It’s been pretty well documented throughout the medical literature that the representation of underrepresented [groups] in medicine is low among all specialties,” study author Kimberly Montez, MD, MPH, FAAP, said in an interview. “This is one of the first studies that [show this trend] in pediatrics, [but] we were kind of expecting [these findings] knowing the rest of the literature out there.”
Dr. Montez and colleagues examined self-reported race and ethnicity data from 2007 to 2019 for pediatric residents and fellows from the GME Census reports. The annual number of pediatric trainees increased from 7,964 to 8,950 between 2007 and 2019. For pediatric subspecialty fellows, that number increased from 2,684 to 3,966.
The number of underrepresented pediatric trainees also increased over time, from 1,277 to 1,478 residents and 382 to 532 subspecialty fellows. However, researchers found that the trend in proportion of underrepresented in medicine (URiM) trainees was unchanged in pediatric residencies – 16% in 2007 to 16.5% in 2019 – and, overall, decreased for URiM subspecialty fellows from 14.2% in 2007 to 13.5% in 2019.
“I was shocked at the fact that there has been no significant increase either over the last 12 years,” said Joan Park, MD, a pediatric resident at Johns Hopkins Hospital, Baltimore, who was not involved in the study. “In the news, we’re seeing way more discussions in regards to racism and representation and the fact that that hasn’t really fueled or caught fire yet in medicine at all to really move that arrow is definitely really shocking.”
The recent study also pointed out that the percentage of underrepresented groups in pediatric residencies and fellowships is considerably lower in comparison with those groups’ representations in the U.S. population. For example, Black or African American people make up 13.4% of the U.S. population but just 5.6% of pediatric trainees. Meanwhile, American Indian or Alaskan Native people make up 1.3% of the U.S. population but make up 0.2% of pediatric trainees.
Dr. Montez hypothesized that the lack of underrepresented groups as pediatric trainees – or in the medical field, in general – may have to do with systemic barriers that span the entire educational continuum and affects them even before they reach medical school, including attendance at underfunded primary and secondary schools.
“Just think about all the barriers that exist for underrepresented minorities in medicine,” said Dr. Montez, assistant professor of pediatrics at Wake Forest University, Winston-Salem, N.C. “We know that underrepresented minorities are accepted and matriculate at lower rates than [those of] their nonminority counterparts. All of this occurs even just before getting into the field of pediatrics. So multiple barriers exist.”
Those barriers may also include racism, bias, and discrimination, which may play out unconsciously when members of an underrepresented group are applying for residencies or med school, such as “recognizing a name that may be from a different ethnic or racial background and then unconsciously biasing yourself against that applicant, for example,” Dr. Montez explained.
Dr. Montez said that although there has been progress, there is still a long way to go. She hopes the study will help academic institutions and professional organizations recognize the importance of diversity in pediatrics. She noted that pediatric trainees are more likely to experience microaggressions, which could potentially cause them to leave a program.
“I hope this will galvanize pediatric programs to really think a lot about the environment that they create for underrepresented minority trainees and also about their recruitment process in terms of making sure it’s standardized, using a holistic review,” Dr. Montez explained.
In 2016, the Association of American Medical Colleges published a diversity and inclusion strategic planning guide to improve training programs. Furthermore, in 2019, the Accreditation Council for Graduate Medical Education instituted a new common program requirement on diversity that requires programs to focus on systematic recruitment and retention of a diverse and inclusive workforce of residents and fellows.
“The same way pediatricians are aware of how the environment will shape the way a child grows up, we have to be mindful of the way an environment that surrounds the medical student will shape where they eventually end up as well,” said Dr. Nwora.
The experts disclosed no conflicts of interest.
The proportion of underrepresented groups in pediatric fellowships decreased between 2007 and 2019, while those in pediatric residencies remained stagnant, new research revealed.
Researchers acknowledged that some of the factors contributing to the low proportion of minorities in the pediatric workforce may include educational disparities starting in primary or secondary school, such as underfunded schools and lack of educational resources.
“Something I really appreciated about the paper is that this goes beyond a student stepping into medical school, finding a mentor in pediatrics, and then eventually matriculating into a pediatric residency,” said Christle Nwora, MD, an internal medicine–pediatrics resident physician at Johns Hopkins Urban Health Residency Program in Baltimore, who was not involved in the study. “I like the idea of knowing that people aren’t going into the field and being very critical as to why.”
Prior studies, including a 2019 study published in JAMA Network Open, has found that minority students remain underrepresented in medical schools. However, this most recent study, published in Pediatrics, is one of the first to report trends in the race or ethnicity of pediatric residents and fellows.
“It’s been pretty well documented throughout the medical literature that the representation of underrepresented [groups] in medicine is low among all specialties,” study author Kimberly Montez, MD, MPH, FAAP, said in an interview. “This is one of the first studies that [show this trend] in pediatrics, [but] we were kind of expecting [these findings] knowing the rest of the literature out there.”
Dr. Montez and colleagues examined self-reported race and ethnicity data from 2007 to 2019 for pediatric residents and fellows from the GME Census reports. The annual number of pediatric trainees increased from 7,964 to 8,950 between 2007 and 2019. For pediatric subspecialty fellows, that number increased from 2,684 to 3,966.
The number of underrepresented pediatric trainees also increased over time, from 1,277 to 1,478 residents and 382 to 532 subspecialty fellows. However, researchers found that the trend in proportion of underrepresented in medicine (URiM) trainees was unchanged in pediatric residencies – 16% in 2007 to 16.5% in 2019 – and, overall, decreased for URiM subspecialty fellows from 14.2% in 2007 to 13.5% in 2019.
“I was shocked at the fact that there has been no significant increase either over the last 12 years,” said Joan Park, MD, a pediatric resident at Johns Hopkins Hospital, Baltimore, who was not involved in the study. “In the news, we’re seeing way more discussions in regards to racism and representation and the fact that that hasn’t really fueled or caught fire yet in medicine at all to really move that arrow is definitely really shocking.”
The recent study also pointed out that the percentage of underrepresented groups in pediatric residencies and fellowships is considerably lower in comparison with those groups’ representations in the U.S. population. For example, Black or African American people make up 13.4% of the U.S. population but just 5.6% of pediatric trainees. Meanwhile, American Indian or Alaskan Native people make up 1.3% of the U.S. population but make up 0.2% of pediatric trainees.
Dr. Montez hypothesized that the lack of underrepresented groups as pediatric trainees – or in the medical field, in general – may have to do with systemic barriers that span the entire educational continuum and affects them even before they reach medical school, including attendance at underfunded primary and secondary schools.
“Just think about all the barriers that exist for underrepresented minorities in medicine,” said Dr. Montez, assistant professor of pediatrics at Wake Forest University, Winston-Salem, N.C. “We know that underrepresented minorities are accepted and matriculate at lower rates than [those of] their nonminority counterparts. All of this occurs even just before getting into the field of pediatrics. So multiple barriers exist.”
Those barriers may also include racism, bias, and discrimination, which may play out unconsciously when members of an underrepresented group are applying for residencies or med school, such as “recognizing a name that may be from a different ethnic or racial background and then unconsciously biasing yourself against that applicant, for example,” Dr. Montez explained.
Dr. Montez said that although there has been progress, there is still a long way to go. She hopes the study will help academic institutions and professional organizations recognize the importance of diversity in pediatrics. She noted that pediatric trainees are more likely to experience microaggressions, which could potentially cause them to leave a program.
“I hope this will galvanize pediatric programs to really think a lot about the environment that they create for underrepresented minority trainees and also about their recruitment process in terms of making sure it’s standardized, using a holistic review,” Dr. Montez explained.
In 2016, the Association of American Medical Colleges published a diversity and inclusion strategic planning guide to improve training programs. Furthermore, in 2019, the Accreditation Council for Graduate Medical Education instituted a new common program requirement on diversity that requires programs to focus on systematic recruitment and retention of a diverse and inclusive workforce of residents and fellows.
“The same way pediatricians are aware of how the environment will shape the way a child grows up, we have to be mindful of the way an environment that surrounds the medical student will shape where they eventually end up as well,” said Dr. Nwora.
The experts disclosed no conflicts of interest.
The proportion of underrepresented groups in pediatric fellowships decreased between 2007 and 2019, while those in pediatric residencies remained stagnant, new research revealed.
Researchers acknowledged that some of the factors contributing to the low proportion of minorities in the pediatric workforce may include educational disparities starting in primary or secondary school, such as underfunded schools and lack of educational resources.
“Something I really appreciated about the paper is that this goes beyond a student stepping into medical school, finding a mentor in pediatrics, and then eventually matriculating into a pediatric residency,” said Christle Nwora, MD, an internal medicine–pediatrics resident physician at Johns Hopkins Urban Health Residency Program in Baltimore, who was not involved in the study. “I like the idea of knowing that people aren’t going into the field and being very critical as to why.”
Prior studies, including a 2019 study published in JAMA Network Open, has found that minority students remain underrepresented in medical schools. However, this most recent study, published in Pediatrics, is one of the first to report trends in the race or ethnicity of pediatric residents and fellows.
“It’s been pretty well documented throughout the medical literature that the representation of underrepresented [groups] in medicine is low among all specialties,” study author Kimberly Montez, MD, MPH, FAAP, said in an interview. “This is one of the first studies that [show this trend] in pediatrics, [but] we were kind of expecting [these findings] knowing the rest of the literature out there.”
Dr. Montez and colleagues examined self-reported race and ethnicity data from 2007 to 2019 for pediatric residents and fellows from the GME Census reports. The annual number of pediatric trainees increased from 7,964 to 8,950 between 2007 and 2019. For pediatric subspecialty fellows, that number increased from 2,684 to 3,966.
The number of underrepresented pediatric trainees also increased over time, from 1,277 to 1,478 residents and 382 to 532 subspecialty fellows. However, researchers found that the trend in proportion of underrepresented in medicine (URiM) trainees was unchanged in pediatric residencies – 16% in 2007 to 16.5% in 2019 – and, overall, decreased for URiM subspecialty fellows from 14.2% in 2007 to 13.5% in 2019.
“I was shocked at the fact that there has been no significant increase either over the last 12 years,” said Joan Park, MD, a pediatric resident at Johns Hopkins Hospital, Baltimore, who was not involved in the study. “In the news, we’re seeing way more discussions in regards to racism and representation and the fact that that hasn’t really fueled or caught fire yet in medicine at all to really move that arrow is definitely really shocking.”
The recent study also pointed out that the percentage of underrepresented groups in pediatric residencies and fellowships is considerably lower in comparison with those groups’ representations in the U.S. population. For example, Black or African American people make up 13.4% of the U.S. population but just 5.6% of pediatric trainees. Meanwhile, American Indian or Alaskan Native people make up 1.3% of the U.S. population but make up 0.2% of pediatric trainees.
Dr. Montez hypothesized that the lack of underrepresented groups as pediatric trainees – or in the medical field, in general – may have to do with systemic barriers that span the entire educational continuum and affects them even before they reach medical school, including attendance at underfunded primary and secondary schools.
“Just think about all the barriers that exist for underrepresented minorities in medicine,” said Dr. Montez, assistant professor of pediatrics at Wake Forest University, Winston-Salem, N.C. “We know that underrepresented minorities are accepted and matriculate at lower rates than [those of] their nonminority counterparts. All of this occurs even just before getting into the field of pediatrics. So multiple barriers exist.”
Those barriers may also include racism, bias, and discrimination, which may play out unconsciously when members of an underrepresented group are applying for residencies or med school, such as “recognizing a name that may be from a different ethnic or racial background and then unconsciously biasing yourself against that applicant, for example,” Dr. Montez explained.
Dr. Montez said that although there has been progress, there is still a long way to go. She hopes the study will help academic institutions and professional organizations recognize the importance of diversity in pediatrics. She noted that pediatric trainees are more likely to experience microaggressions, which could potentially cause them to leave a program.
“I hope this will galvanize pediatric programs to really think a lot about the environment that they create for underrepresented minority trainees and also about their recruitment process in terms of making sure it’s standardized, using a holistic review,” Dr. Montez explained.
In 2016, the Association of American Medical Colleges published a diversity and inclusion strategic planning guide to improve training programs. Furthermore, in 2019, the Accreditation Council for Graduate Medical Education instituted a new common program requirement on diversity that requires programs to focus on systematic recruitment and retention of a diverse and inclusive workforce of residents and fellows.
“The same way pediatricians are aware of how the environment will shape the way a child grows up, we have to be mindful of the way an environment that surrounds the medical student will shape where they eventually end up as well,” said Dr. Nwora.
The experts disclosed no conflicts of interest.
Cannabis use tied to increased risk for suicidal thoughts, actions
Young adults who use cannabis – either sporadically, daily, or those who have cannabis use disorder – have a significantly increased risk for suicidal thoughts and actions, according to U.S. national drug survey data.
The risks appear greater for women than men and remained regardless of whether the individual was depressed.
“We cannot establish that cannabis use caused increased suicidality,” Nora Volkow, MD, director, National Institute on Drug Abuse (NIDA), told this news organization.
“However, it is likely that these two factors influence one another bidirectionally, meaning people with suicidal thinking might be more vulnerable to cannabis use to self-medicate their distress, and cannabis use may trigger negative moods and suicidal thinking in some people,” said Dr. Volkow.
“It is also possible that these factors are not causally linked to one another at all but rather reflect the common and related risk factors underlying both suicidality and substance use. For instance, one’s genetics may put them at a higher risk for both suicide and for using marijuana,” she added.
The study was published online June 22 in JAMA Network Open.
Marked increase in use
Cannabis use among U.S. adults has increased markedly over the past 10 years, with a parallel increase in suicidality. However, the links between cannabis use and suicidality among young adults are poorly understood.
NIDA researchers sought to fill this gap. They examined data on 281,650 young men and women aged 18 to 34 years who participated in National Surveys on Drug Use and Health from 2008 to 2019.
Status regarding past-year cannabis use was categorized as past-year daily or near-daily use (greater than or equal to 300 days), non-daily use, and no cannabis use.
Although suicidality was associated with cannabis use, even young adults who did not use cannabis on a daily basis were more likely to have suicidal thoughts or actions than those who did not use the drug at all, the researchers found.
Among young adults without a major depressive episode, about 3% of those who did not use cannabis had suicidal ideation, compared with about 7% of non-daily cannabis users, about 9% of daily cannabis users, and 14% of those with a cannabis use disorder.
Among young adults with depression, the corresponding percentages were 35%, 44%, 53%, and 50%.
Similar trends existed for the associations between the different levels of cannabis use and suicide plan or attempt.
Women at greatest risk
Gender differences also emerged. than men with the same levels of cannabis use.
Among those without a major depressive episode, the prevalence of suicidal ideation for those with versus without a cannabis use disorder was around 14% versus 4.0% among women and 10% versus 3.0% among men.
Among young adults with both cannabis use disorder and major depressive episode, the prevalence of past-year suicide plan was 52% higher for women (24%) than for men (16%).
“Suicide is a leading cause of death among young adults in the United States, and the findings of this study offer important information that may help us reduce this risk,” lead author and NIDA researcher Beth Han, MD, PhD, MPH, said in a news release.
“Depression and cannabis use disorder are treatable conditions, and cannabis use can be modified. Through better understanding the associations of different risk factors for suicidality, we hope to offer new targets for prevention and intervention in individuals that we know may be at high risk. These findings also underscore the importance of tailoring interventions in a way that takes sex and gender into account,” said Dr. Han.
“Additional research is needed to better understand these complex associations, especially given the great burden of suicide on young adults,” said Dr. Volkow.
Gender difference ‘striking’
Commenting on the findings for this news organization, Charles B. Nemeroff, MD, PhD, professor and chair, department of psychiatry and behavioral sciences, Dell Medical School, University of Texas at Austin, said this study is “clearly of great interest; of course correlation and causality are completely distinct entities, and this study is all about correlation.
“This does not, of course, mean that cannabis use causes suicide but suggests that in individuals who use cannabis, suicidality in the broadest sense is increased in prevalence rate,” said Dr. Nemeroff, who serves as principal investigator of the Texas Child Trauma Network.
Dr. Nemeroff said “the most striking finding” was the larger effect in women than men – “striking because suicide is, in almost all cultures, higher in prevalence in men versus women.”
Dr. Nemeroff said he’d like to know more about other potential contributing factors, “which would include a history of child abuse and neglect, a major vulnerability factor for suicidality, comorbid alcohol and other substance abuse, [and] comorbid psychiatric diagnosis such as posttraumatic stress disorder.”
The study was sponsored by NIDA, of the National Institutes of Health. Dr. Volkow, Dr. Han, and Dr. Nemeroff have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Young adults who use cannabis – either sporadically, daily, or those who have cannabis use disorder – have a significantly increased risk for suicidal thoughts and actions, according to U.S. national drug survey data.
The risks appear greater for women than men and remained regardless of whether the individual was depressed.
“We cannot establish that cannabis use caused increased suicidality,” Nora Volkow, MD, director, National Institute on Drug Abuse (NIDA), told this news organization.
“However, it is likely that these two factors influence one another bidirectionally, meaning people with suicidal thinking might be more vulnerable to cannabis use to self-medicate their distress, and cannabis use may trigger negative moods and suicidal thinking in some people,” said Dr. Volkow.
“It is also possible that these factors are not causally linked to one another at all but rather reflect the common and related risk factors underlying both suicidality and substance use. For instance, one’s genetics may put them at a higher risk for both suicide and for using marijuana,” she added.
The study was published online June 22 in JAMA Network Open.
Marked increase in use
Cannabis use among U.S. adults has increased markedly over the past 10 years, with a parallel increase in suicidality. However, the links between cannabis use and suicidality among young adults are poorly understood.
NIDA researchers sought to fill this gap. They examined data on 281,650 young men and women aged 18 to 34 years who participated in National Surveys on Drug Use and Health from 2008 to 2019.
Status regarding past-year cannabis use was categorized as past-year daily or near-daily use (greater than or equal to 300 days), non-daily use, and no cannabis use.
Although suicidality was associated with cannabis use, even young adults who did not use cannabis on a daily basis were more likely to have suicidal thoughts or actions than those who did not use the drug at all, the researchers found.
Among young adults without a major depressive episode, about 3% of those who did not use cannabis had suicidal ideation, compared with about 7% of non-daily cannabis users, about 9% of daily cannabis users, and 14% of those with a cannabis use disorder.
Among young adults with depression, the corresponding percentages were 35%, 44%, 53%, and 50%.
Similar trends existed for the associations between the different levels of cannabis use and suicide plan or attempt.
Women at greatest risk
Gender differences also emerged. than men with the same levels of cannabis use.
Among those without a major depressive episode, the prevalence of suicidal ideation for those with versus without a cannabis use disorder was around 14% versus 4.0% among women and 10% versus 3.0% among men.
Among young adults with both cannabis use disorder and major depressive episode, the prevalence of past-year suicide plan was 52% higher for women (24%) than for men (16%).
“Suicide is a leading cause of death among young adults in the United States, and the findings of this study offer important information that may help us reduce this risk,” lead author and NIDA researcher Beth Han, MD, PhD, MPH, said in a news release.
“Depression and cannabis use disorder are treatable conditions, and cannabis use can be modified. Through better understanding the associations of different risk factors for suicidality, we hope to offer new targets for prevention and intervention in individuals that we know may be at high risk. These findings also underscore the importance of tailoring interventions in a way that takes sex and gender into account,” said Dr. Han.
“Additional research is needed to better understand these complex associations, especially given the great burden of suicide on young adults,” said Dr. Volkow.
Gender difference ‘striking’
Commenting on the findings for this news organization, Charles B. Nemeroff, MD, PhD, professor and chair, department of psychiatry and behavioral sciences, Dell Medical School, University of Texas at Austin, said this study is “clearly of great interest; of course correlation and causality are completely distinct entities, and this study is all about correlation.
“This does not, of course, mean that cannabis use causes suicide but suggests that in individuals who use cannabis, suicidality in the broadest sense is increased in prevalence rate,” said Dr. Nemeroff, who serves as principal investigator of the Texas Child Trauma Network.
Dr. Nemeroff said “the most striking finding” was the larger effect in women than men – “striking because suicide is, in almost all cultures, higher in prevalence in men versus women.”
Dr. Nemeroff said he’d like to know more about other potential contributing factors, “which would include a history of child abuse and neglect, a major vulnerability factor for suicidality, comorbid alcohol and other substance abuse, [and] comorbid psychiatric diagnosis such as posttraumatic stress disorder.”
The study was sponsored by NIDA, of the National Institutes of Health. Dr. Volkow, Dr. Han, and Dr. Nemeroff have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Young adults who use cannabis – either sporadically, daily, or those who have cannabis use disorder – have a significantly increased risk for suicidal thoughts and actions, according to U.S. national drug survey data.
The risks appear greater for women than men and remained regardless of whether the individual was depressed.
“We cannot establish that cannabis use caused increased suicidality,” Nora Volkow, MD, director, National Institute on Drug Abuse (NIDA), told this news organization.
“However, it is likely that these two factors influence one another bidirectionally, meaning people with suicidal thinking might be more vulnerable to cannabis use to self-medicate their distress, and cannabis use may trigger negative moods and suicidal thinking in some people,” said Dr. Volkow.
“It is also possible that these factors are not causally linked to one another at all but rather reflect the common and related risk factors underlying both suicidality and substance use. For instance, one’s genetics may put them at a higher risk for both suicide and for using marijuana,” she added.
The study was published online June 22 in JAMA Network Open.
Marked increase in use
Cannabis use among U.S. adults has increased markedly over the past 10 years, with a parallel increase in suicidality. However, the links between cannabis use and suicidality among young adults are poorly understood.
NIDA researchers sought to fill this gap. They examined data on 281,650 young men and women aged 18 to 34 years who participated in National Surveys on Drug Use and Health from 2008 to 2019.
Status regarding past-year cannabis use was categorized as past-year daily or near-daily use (greater than or equal to 300 days), non-daily use, and no cannabis use.
Although suicidality was associated with cannabis use, even young adults who did not use cannabis on a daily basis were more likely to have suicidal thoughts or actions than those who did not use the drug at all, the researchers found.
Among young adults without a major depressive episode, about 3% of those who did not use cannabis had suicidal ideation, compared with about 7% of non-daily cannabis users, about 9% of daily cannabis users, and 14% of those with a cannabis use disorder.
Among young adults with depression, the corresponding percentages were 35%, 44%, 53%, and 50%.
Similar trends existed for the associations between the different levels of cannabis use and suicide plan or attempt.
Women at greatest risk
Gender differences also emerged. than men with the same levels of cannabis use.
Among those without a major depressive episode, the prevalence of suicidal ideation for those with versus without a cannabis use disorder was around 14% versus 4.0% among women and 10% versus 3.0% among men.
Among young adults with both cannabis use disorder and major depressive episode, the prevalence of past-year suicide plan was 52% higher for women (24%) than for men (16%).
“Suicide is a leading cause of death among young adults in the United States, and the findings of this study offer important information that may help us reduce this risk,” lead author and NIDA researcher Beth Han, MD, PhD, MPH, said in a news release.
“Depression and cannabis use disorder are treatable conditions, and cannabis use can be modified. Through better understanding the associations of different risk factors for suicidality, we hope to offer new targets for prevention and intervention in individuals that we know may be at high risk. These findings also underscore the importance of tailoring interventions in a way that takes sex and gender into account,” said Dr. Han.
“Additional research is needed to better understand these complex associations, especially given the great burden of suicide on young adults,” said Dr. Volkow.
Gender difference ‘striking’
Commenting on the findings for this news organization, Charles B. Nemeroff, MD, PhD, professor and chair, department of psychiatry and behavioral sciences, Dell Medical School, University of Texas at Austin, said this study is “clearly of great interest; of course correlation and causality are completely distinct entities, and this study is all about correlation.
“This does not, of course, mean that cannabis use causes suicide but suggests that in individuals who use cannabis, suicidality in the broadest sense is increased in prevalence rate,” said Dr. Nemeroff, who serves as principal investigator of the Texas Child Trauma Network.
Dr. Nemeroff said “the most striking finding” was the larger effect in women than men – “striking because suicide is, in almost all cultures, higher in prevalence in men versus women.”
Dr. Nemeroff said he’d like to know more about other potential contributing factors, “which would include a history of child abuse and neglect, a major vulnerability factor for suicidality, comorbid alcohol and other substance abuse, [and] comorbid psychiatric diagnosis such as posttraumatic stress disorder.”
The study was sponsored by NIDA, of the National Institutes of Health. Dr. Volkow, Dr. Han, and Dr. Nemeroff have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Omnipod 5 ‘artificial pancreas’ shows benefit in type 1 diabetes
Insulet’s investigational Omnipod 5 automated insulin delivery system improves glycemic control in people with type 1 diabetes aged as young as 2 years, new data suggest.
The Omnipod 5 system combines a tubing-free insulin-filled delivery “Pod” with the Dexcom G6 continuous glucose monitor and an algorithm built into the Pod connecting the two devices via a smartphone app to semiautomate insulin delivery. It is currently under review by the Food and Drug Administration. The company expects to launch it in limited release during the second half of 2021.
Results from a pivotal trial of the system in children aged 2-5.9 years with type 1 diabetes were presented during the annual scientific sessions of the American Diabetes Association.
Follow-up data at 6 months were also presented for another pivotal study of 112 children aged 6-13.9 years and 129 adults aged 14-70 years. Those primary 3-month data were reported earlier this year at the Endocrine Society’s annual meeting and subsequently published online June 7, 2021, in Diabetes Care. Another study presented at ADA looked at quality of life in children using Omnipod 5 and their caregivers.
If approved by the FDA, the Omnipod 5 would be the third commercially available automated insulin delivery system – also called hybrid closed-loop or artificial pancreas systems – in the United States. It would be the second approved for children as young as 2 years of age and the first to deliver insulin subcutaneously without tubing.
‘No-tubing’ feature will be a draw for parents of young children
Asked to comment, pediatric endocrinologist Laura M. Jacobsen, MD, of the University of Florida, Gainesville, said in an interview: “I think the big advantage for the Omnipod 5 is that [if approved it will be] the only tubeless automated insulin delivery system in the U.S.”
“The automated delivery systems have just been wonderful for helping patients achieve time in range, especially overnight. And the fact that this goes down to such a young age where that can be very difficult is wonderful.”
Another difference between the Omnipod 5 and other systems is the ability to adjust glucose targets (from 110 to 150 mg/dL), although newer versions of the currently available hybrid closed-loop systems are expected to include that feature as well. “They’re all slightly different in the way the algorithms work, but I think the end result is similar,” Dr. Jacobsen said.
But, she said, the no-tubing feature might be particularly helpful for some very active young kids. “A lot of small kids do use the tubed pumps, and you can make it work with a lot of kids, but with some kids it just won’t ... the tubing gets caught. I think this really helps parents make the step. A lot of them don’t want to try the tubing whereas they see the Omnipod and might feel a little more confidence to try a pump.”
Overall, said Dr. Jacobsen, who has no financial disclosures with Insulet, Dexcom, or any of their competitors, “I think any addition to the technology field to improve quality of life for people with type 1 diabetes is important and people need choices.”
Pivotal data show benefit in ‘difficult-to-manage’ preschool children
Pivotal 3-month data for the Omnipod 5 in children aged 2-5.9 years with type 1 diabetes were presented on June 26 by pediatric endocrinologist Jennifer Sherr, MD, PhD, Yale University, New Haven, Conn.
“As a pediatric endocrinologist, I can attest to the difficulty of managing this age group, due to grazing eating patterns and erratic physical activity. Oftentimes, care providers may fear hypoglycemia as these youth can not verbalize or self-treat lows,” she remarked.
A total of 80 children were enrolled at 10 institutions across the United Sates. There was a single 14-day standard therapy phase (baseline), followed by 3 months of automated insulin delivery during which the children’s eating and exercise were unrestricted.
At 3 months, average hemoglobin A1c had fallen from 7.4% at baseline to 6.9%, a significant difference (P < .05). The proportions achieving the target A1c of less than 7% were 54% at 3 months versus 31% at baseline. The reduction was even greater among the 25 with baseline A1c of 8% or greater, although it was significant even among the 55 who started with a lower A1c (–1.06 vs. –0.31 percentage points; both P < .05).
Time in range rose from 57.2% at baseline to 68.1% at 3 months (P < .05).
“These youngsters are spending an average of 2.6 more hours/day in range,” Dr. Sherr commented, noting that the difference became apparent shortly after study start and was maintained during the 3 months.
Dr. Sherr noted that this 10.9% improvement in time in range with Omnipod 5 was similar to improvements in the previously reported pivotal study of older children and adults. Data from that study showed improvement in time in range from a gain of 15.6% for the 6 to 13.9 year olds to 8.0% for those aged 26-49 years. Interestingly, improvements in time in range were seen even in the oldest group, aged 50-70, who increased from an already high baseline of 69.9% to 79.1% with Omnipod 5 after 3 months.
In her current study, in the youngest age group, the improvement in time in range was achieved primarily by a reduction of time above range, from 2.4 fewer hours/day above 180 mg/dL, while time below 70 mg/dL was reduced by 4 minutes/day. Overnight time in range improved by 1.4 hours/night, with most of the improvements in reduction of hyperglycemia.
The proportions meeting the combined goals of less than 4% time below range and greater than 60% time in range rose from 29% to 65%.
There were no episodes of severe hypoglycemia or diabetic ketoacidosis during the 3-month study phase.
Another important related metric, sleep quality for parents/caregivers, also improved. The percentage reporting overall sleep quality of “very good” or “fairly good” increased from 65% at baseline to 90% with Omnipod 5, while “very bad” sleep quality fell from 8.8% to 0%.
All 80 patients completed the study and elected to continue in a 12-month extension phase.
Ongoing benefit seen in older children and adults
In a late-breaking poster presented on June 25, Anders L. Carlson, MD, medical director at the International Diabetes Center at Park Nicollet, Minneapolis, presented more follow-up data to the previously reported 3-month pivotal study, including 108 older children and 109 adults from the original study.
A1c remained lower after 6 months than at baseline for both children and adults (P < .001). In the children, A1c levels weren’t significantly different at the end of 6 versus 3 months, while in the adults there was an additional 0.1 percentage point decrease (P < .01).
There was one episode of diabetic ketoacidosis and no severe hypoglycemic episodes in the 3-month extension. “Sustained reduction of A1c indicates the potential long-term benefit of the Omnipod 5 System,” Dr. Carlson and colleagues concluded.
Reduced diabetes distress, don’t forget parents’ quality of life
Meanwhile, psychologist Korey K. Hood, PhD, of Stanford (Calif.) University, presented quality of life data at the meeting for 83 children aged 6-11.9 years and 42 teens aged 12-17.9 years using the Omnipod 5 from the larger study population and their parents.
Significant improvements were seen for both the youth and their caregivers in the Problem Areas in Diabetes score, a measure of diabetes-related emotional distress. Changes were less dramatic on the Hypoglycemic Confidence Scale, although improvements were significant for the caregivers of the younger children.
“We know this is a group that is really worried about hypoglycemia across a lot of situations, not just sleep but also school and outside of the home. So, to increase their confidence to this extent I think is a pretty important finding,” Dr. Hood commented.
There were nonsignificant trends in improvement across groups on the Pittsburgh Sleep Quality Index, but overall sleep quality did significantly improve among parents of the younger children. And on the World Health Organization–5 quality of life survey, significant improvements again were seen among the caregivers of young children.
“Reduced diabetes distress and improved quality of life are key benefits of using the Omnipod 5 [automated insulin delivery] system that are complementary to the glycemic benefits achieved,” Dr. Hood said.
Dr. Jacobsen has reported no relevant financial relationships. Dr. Sherr has reported being an adviser for, consultant for, and/or grant recipient from Bigfoot Biomedical, Cecelia Health, Insulet, Medtronic Diabetes, Eli Lilly, Lexicon, Sanofi, and the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Hood has reported being a consultant for Cecelia Health, Havas, and Cercacor.
A version of this article first appeared on Medscape.com.
Insulet’s investigational Omnipod 5 automated insulin delivery system improves glycemic control in people with type 1 diabetes aged as young as 2 years, new data suggest.
The Omnipod 5 system combines a tubing-free insulin-filled delivery “Pod” with the Dexcom G6 continuous glucose monitor and an algorithm built into the Pod connecting the two devices via a smartphone app to semiautomate insulin delivery. It is currently under review by the Food and Drug Administration. The company expects to launch it in limited release during the second half of 2021.
Results from a pivotal trial of the system in children aged 2-5.9 years with type 1 diabetes were presented during the annual scientific sessions of the American Diabetes Association.
Follow-up data at 6 months were also presented for another pivotal study of 112 children aged 6-13.9 years and 129 adults aged 14-70 years. Those primary 3-month data were reported earlier this year at the Endocrine Society’s annual meeting and subsequently published online June 7, 2021, in Diabetes Care. Another study presented at ADA looked at quality of life in children using Omnipod 5 and their caregivers.
If approved by the FDA, the Omnipod 5 would be the third commercially available automated insulin delivery system – also called hybrid closed-loop or artificial pancreas systems – in the United States. It would be the second approved for children as young as 2 years of age and the first to deliver insulin subcutaneously without tubing.
‘No-tubing’ feature will be a draw for parents of young children
Asked to comment, pediatric endocrinologist Laura M. Jacobsen, MD, of the University of Florida, Gainesville, said in an interview: “I think the big advantage for the Omnipod 5 is that [if approved it will be] the only tubeless automated insulin delivery system in the U.S.”
“The automated delivery systems have just been wonderful for helping patients achieve time in range, especially overnight. And the fact that this goes down to such a young age where that can be very difficult is wonderful.”
Another difference between the Omnipod 5 and other systems is the ability to adjust glucose targets (from 110 to 150 mg/dL), although newer versions of the currently available hybrid closed-loop systems are expected to include that feature as well. “They’re all slightly different in the way the algorithms work, but I think the end result is similar,” Dr. Jacobsen said.
But, she said, the no-tubing feature might be particularly helpful for some very active young kids. “A lot of small kids do use the tubed pumps, and you can make it work with a lot of kids, but with some kids it just won’t ... the tubing gets caught. I think this really helps parents make the step. A lot of them don’t want to try the tubing whereas they see the Omnipod and might feel a little more confidence to try a pump.”
Overall, said Dr. Jacobsen, who has no financial disclosures with Insulet, Dexcom, or any of their competitors, “I think any addition to the technology field to improve quality of life for people with type 1 diabetes is important and people need choices.”
Pivotal data show benefit in ‘difficult-to-manage’ preschool children
Pivotal 3-month data for the Omnipod 5 in children aged 2-5.9 years with type 1 diabetes were presented on June 26 by pediatric endocrinologist Jennifer Sherr, MD, PhD, Yale University, New Haven, Conn.
“As a pediatric endocrinologist, I can attest to the difficulty of managing this age group, due to grazing eating patterns and erratic physical activity. Oftentimes, care providers may fear hypoglycemia as these youth can not verbalize or self-treat lows,” she remarked.
A total of 80 children were enrolled at 10 institutions across the United Sates. There was a single 14-day standard therapy phase (baseline), followed by 3 months of automated insulin delivery during which the children’s eating and exercise were unrestricted.
At 3 months, average hemoglobin A1c had fallen from 7.4% at baseline to 6.9%, a significant difference (P < .05). The proportions achieving the target A1c of less than 7% were 54% at 3 months versus 31% at baseline. The reduction was even greater among the 25 with baseline A1c of 8% or greater, although it was significant even among the 55 who started with a lower A1c (–1.06 vs. –0.31 percentage points; both P < .05).
Time in range rose from 57.2% at baseline to 68.1% at 3 months (P < .05).
“These youngsters are spending an average of 2.6 more hours/day in range,” Dr. Sherr commented, noting that the difference became apparent shortly after study start and was maintained during the 3 months.
Dr. Sherr noted that this 10.9% improvement in time in range with Omnipod 5 was similar to improvements in the previously reported pivotal study of older children and adults. Data from that study showed improvement in time in range from a gain of 15.6% for the 6 to 13.9 year olds to 8.0% for those aged 26-49 years. Interestingly, improvements in time in range were seen even in the oldest group, aged 50-70, who increased from an already high baseline of 69.9% to 79.1% with Omnipod 5 after 3 months.
In her current study, in the youngest age group, the improvement in time in range was achieved primarily by a reduction of time above range, from 2.4 fewer hours/day above 180 mg/dL, while time below 70 mg/dL was reduced by 4 minutes/day. Overnight time in range improved by 1.4 hours/night, with most of the improvements in reduction of hyperglycemia.
The proportions meeting the combined goals of less than 4% time below range and greater than 60% time in range rose from 29% to 65%.
There were no episodes of severe hypoglycemia or diabetic ketoacidosis during the 3-month study phase.
Another important related metric, sleep quality for parents/caregivers, also improved. The percentage reporting overall sleep quality of “very good” or “fairly good” increased from 65% at baseline to 90% with Omnipod 5, while “very bad” sleep quality fell from 8.8% to 0%.
All 80 patients completed the study and elected to continue in a 12-month extension phase.
Ongoing benefit seen in older children and adults
In a late-breaking poster presented on June 25, Anders L. Carlson, MD, medical director at the International Diabetes Center at Park Nicollet, Minneapolis, presented more follow-up data to the previously reported 3-month pivotal study, including 108 older children and 109 adults from the original study.
A1c remained lower after 6 months than at baseline for both children and adults (P < .001). In the children, A1c levels weren’t significantly different at the end of 6 versus 3 months, while in the adults there was an additional 0.1 percentage point decrease (P < .01).
There was one episode of diabetic ketoacidosis and no severe hypoglycemic episodes in the 3-month extension. “Sustained reduction of A1c indicates the potential long-term benefit of the Omnipod 5 System,” Dr. Carlson and colleagues concluded.
Reduced diabetes distress, don’t forget parents’ quality of life
Meanwhile, psychologist Korey K. Hood, PhD, of Stanford (Calif.) University, presented quality of life data at the meeting for 83 children aged 6-11.9 years and 42 teens aged 12-17.9 years using the Omnipod 5 from the larger study population and their parents.
Significant improvements were seen for both the youth and their caregivers in the Problem Areas in Diabetes score, a measure of diabetes-related emotional distress. Changes were less dramatic on the Hypoglycemic Confidence Scale, although improvements were significant for the caregivers of the younger children.
“We know this is a group that is really worried about hypoglycemia across a lot of situations, not just sleep but also school and outside of the home. So, to increase their confidence to this extent I think is a pretty important finding,” Dr. Hood commented.
There were nonsignificant trends in improvement across groups on the Pittsburgh Sleep Quality Index, but overall sleep quality did significantly improve among parents of the younger children. And on the World Health Organization–5 quality of life survey, significant improvements again were seen among the caregivers of young children.
“Reduced diabetes distress and improved quality of life are key benefits of using the Omnipod 5 [automated insulin delivery] system that are complementary to the glycemic benefits achieved,” Dr. Hood said.
Dr. Jacobsen has reported no relevant financial relationships. Dr. Sherr has reported being an adviser for, consultant for, and/or grant recipient from Bigfoot Biomedical, Cecelia Health, Insulet, Medtronic Diabetes, Eli Lilly, Lexicon, Sanofi, and the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Hood has reported being a consultant for Cecelia Health, Havas, and Cercacor.
A version of this article first appeared on Medscape.com.
Insulet’s investigational Omnipod 5 automated insulin delivery system improves glycemic control in people with type 1 diabetes aged as young as 2 years, new data suggest.
The Omnipod 5 system combines a tubing-free insulin-filled delivery “Pod” with the Dexcom G6 continuous glucose monitor and an algorithm built into the Pod connecting the two devices via a smartphone app to semiautomate insulin delivery. It is currently under review by the Food and Drug Administration. The company expects to launch it in limited release during the second half of 2021.
Results from a pivotal trial of the system in children aged 2-5.9 years with type 1 diabetes were presented during the annual scientific sessions of the American Diabetes Association.
Follow-up data at 6 months were also presented for another pivotal study of 112 children aged 6-13.9 years and 129 adults aged 14-70 years. Those primary 3-month data were reported earlier this year at the Endocrine Society’s annual meeting and subsequently published online June 7, 2021, in Diabetes Care. Another study presented at ADA looked at quality of life in children using Omnipod 5 and their caregivers.
If approved by the FDA, the Omnipod 5 would be the third commercially available automated insulin delivery system – also called hybrid closed-loop or artificial pancreas systems – in the United States. It would be the second approved for children as young as 2 years of age and the first to deliver insulin subcutaneously without tubing.
‘No-tubing’ feature will be a draw for parents of young children
Asked to comment, pediatric endocrinologist Laura M. Jacobsen, MD, of the University of Florida, Gainesville, said in an interview: “I think the big advantage for the Omnipod 5 is that [if approved it will be] the only tubeless automated insulin delivery system in the U.S.”
“The automated delivery systems have just been wonderful for helping patients achieve time in range, especially overnight. And the fact that this goes down to such a young age where that can be very difficult is wonderful.”
Another difference between the Omnipod 5 and other systems is the ability to adjust glucose targets (from 110 to 150 mg/dL), although newer versions of the currently available hybrid closed-loop systems are expected to include that feature as well. “They’re all slightly different in the way the algorithms work, but I think the end result is similar,” Dr. Jacobsen said.
But, she said, the no-tubing feature might be particularly helpful for some very active young kids. “A lot of small kids do use the tubed pumps, and you can make it work with a lot of kids, but with some kids it just won’t ... the tubing gets caught. I think this really helps parents make the step. A lot of them don’t want to try the tubing whereas they see the Omnipod and might feel a little more confidence to try a pump.”
Overall, said Dr. Jacobsen, who has no financial disclosures with Insulet, Dexcom, or any of their competitors, “I think any addition to the technology field to improve quality of life for people with type 1 diabetes is important and people need choices.”
Pivotal data show benefit in ‘difficult-to-manage’ preschool children
Pivotal 3-month data for the Omnipod 5 in children aged 2-5.9 years with type 1 diabetes were presented on June 26 by pediatric endocrinologist Jennifer Sherr, MD, PhD, Yale University, New Haven, Conn.
“As a pediatric endocrinologist, I can attest to the difficulty of managing this age group, due to grazing eating patterns and erratic physical activity. Oftentimes, care providers may fear hypoglycemia as these youth can not verbalize or self-treat lows,” she remarked.
A total of 80 children were enrolled at 10 institutions across the United Sates. There was a single 14-day standard therapy phase (baseline), followed by 3 months of automated insulin delivery during which the children’s eating and exercise were unrestricted.
At 3 months, average hemoglobin A1c had fallen from 7.4% at baseline to 6.9%, a significant difference (P < .05). The proportions achieving the target A1c of less than 7% were 54% at 3 months versus 31% at baseline. The reduction was even greater among the 25 with baseline A1c of 8% or greater, although it was significant even among the 55 who started with a lower A1c (–1.06 vs. –0.31 percentage points; both P < .05).
Time in range rose from 57.2% at baseline to 68.1% at 3 months (P < .05).
“These youngsters are spending an average of 2.6 more hours/day in range,” Dr. Sherr commented, noting that the difference became apparent shortly after study start and was maintained during the 3 months.
Dr. Sherr noted that this 10.9% improvement in time in range with Omnipod 5 was similar to improvements in the previously reported pivotal study of older children and adults. Data from that study showed improvement in time in range from a gain of 15.6% for the 6 to 13.9 year olds to 8.0% for those aged 26-49 years. Interestingly, improvements in time in range were seen even in the oldest group, aged 50-70, who increased from an already high baseline of 69.9% to 79.1% with Omnipod 5 after 3 months.
In her current study, in the youngest age group, the improvement in time in range was achieved primarily by a reduction of time above range, from 2.4 fewer hours/day above 180 mg/dL, while time below 70 mg/dL was reduced by 4 minutes/day. Overnight time in range improved by 1.4 hours/night, with most of the improvements in reduction of hyperglycemia.
The proportions meeting the combined goals of less than 4% time below range and greater than 60% time in range rose from 29% to 65%.
There were no episodes of severe hypoglycemia or diabetic ketoacidosis during the 3-month study phase.
Another important related metric, sleep quality for parents/caregivers, also improved. The percentage reporting overall sleep quality of “very good” or “fairly good” increased from 65% at baseline to 90% with Omnipod 5, while “very bad” sleep quality fell from 8.8% to 0%.
All 80 patients completed the study and elected to continue in a 12-month extension phase.
Ongoing benefit seen in older children and adults
In a late-breaking poster presented on June 25, Anders L. Carlson, MD, medical director at the International Diabetes Center at Park Nicollet, Minneapolis, presented more follow-up data to the previously reported 3-month pivotal study, including 108 older children and 109 adults from the original study.
A1c remained lower after 6 months than at baseline for both children and adults (P < .001). In the children, A1c levels weren’t significantly different at the end of 6 versus 3 months, while in the adults there was an additional 0.1 percentage point decrease (P < .01).
There was one episode of diabetic ketoacidosis and no severe hypoglycemic episodes in the 3-month extension. “Sustained reduction of A1c indicates the potential long-term benefit of the Omnipod 5 System,” Dr. Carlson and colleagues concluded.
Reduced diabetes distress, don’t forget parents’ quality of life
Meanwhile, psychologist Korey K. Hood, PhD, of Stanford (Calif.) University, presented quality of life data at the meeting for 83 children aged 6-11.9 years and 42 teens aged 12-17.9 years using the Omnipod 5 from the larger study population and their parents.
Significant improvements were seen for both the youth and their caregivers in the Problem Areas in Diabetes score, a measure of diabetes-related emotional distress. Changes were less dramatic on the Hypoglycemic Confidence Scale, although improvements were significant for the caregivers of the younger children.
“We know this is a group that is really worried about hypoglycemia across a lot of situations, not just sleep but also school and outside of the home. So, to increase their confidence to this extent I think is a pretty important finding,” Dr. Hood commented.
There were nonsignificant trends in improvement across groups on the Pittsburgh Sleep Quality Index, but overall sleep quality did significantly improve among parents of the younger children. And on the World Health Organization–5 quality of life survey, significant improvements again were seen among the caregivers of young children.
“Reduced diabetes distress and improved quality of life are key benefits of using the Omnipod 5 [automated insulin delivery] system that are complementary to the glycemic benefits achieved,” Dr. Hood said.
Dr. Jacobsen has reported no relevant financial relationships. Dr. Sherr has reported being an adviser for, consultant for, and/or grant recipient from Bigfoot Biomedical, Cecelia Health, Insulet, Medtronic Diabetes, Eli Lilly, Lexicon, Sanofi, and the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Hood has reported being a consultant for Cecelia Health, Havas, and Cercacor.
A version of this article first appeared on Medscape.com.
Intervention opens access to care for minority youths with type 1 diabetes
For racial or ethnic minority youths with type 1 diabetes, participating in an interventional program improves access to care, new research shows.
Youth categorized as Black, Indigenous, and other people of color (BIPOC) had significantly improved outpatient attendance during and after participating in Novel Interventions in Children’s Healthcare (NICH), a systems intervention for children with chronic health conditions and their families.
By comparison, no improvements in care access were observed among BIPOC children who were not able to access the program because of insurance or other reasons, David V. Wagner, PhD, Associate Professor and NICH research director at Oregon Health & Science University, Portland, reported at the annual scientific sessions of the American Diabetes Association.
The findings demonstrate a need for intensive, home-based services that aim to correct health inequities, said Dr. Wagner, who presented the findings along with Winniebhelle Cadiz, a scholar in the BUILD EXITO undergraduate research training program at Portland (Ore.) State University.
The NICH program hinges on trained interventionists who visit families at home, attend clinic visits, and work with schools and other contacts to help solve problems that keep children from following medical instructions, according to a program description.
“Families report having somebody by their side to help them navigate the system, address the transportation difficulties experienced, and help them and build that relationship with their health care provider seems to be hugely influential in terms of helping them navigate and access care,” Dr. Wagner said in a presentation of the study.
A NICH for youths with chronic health conditions
The NICH program differs from some other programs that have been developed in an attempt to improve health outcomes among youths in the community, according to Dr. Wagner.
“Many of the programs that exist out there are often piloted on, and seemingly built for, those who have more resources,” he said in his presentation. “Those who are in greatest need often have difficulty accessing and responding to the services.”
NICH doesn’t take the place of existing services, but is “an addition to the continuum of care” for youths and families who are struggling because of lack of resources or marginalization in the health care system, Dr. Wagner said.
While NICH is not specific to any one chronic health condition, several previous investigations have specifically looked at the impact of the NICH program on access to care in youths with type 1 diabetes.
Youths participating in the program for a year had fewer ED visits, including fewer visits with diabetic ketoacidosis (DKA), as well as fewer and shorter admissions as compared with the year prior to participating in the program, Dr. Wagner said.
In another study, youths had fewer admissions for diabetes or DKA and less frequent pediatric ICU contact during the NICH program, as compared with before the program.
Another study showed that, while NICH had no impact overall on access to care among youths with type 1 diabetes, BIPOC youths had an improvement in the mean number of outpatient visits as compared with preprogram levels. However, because none of those studies included a control group, Dr. Wagner said, it remained unclear whether this systems intervention might improve outpatient access among youths with type 1 diabetes as compared with those who did not participate.
Intervention linked to increased BIPOC care access
The latest study includes 144 youths with type 1 diabetes referred for the program. The mean age was 13.7 years, 58% were female, and 81% were non-Hispanic White. While 51 youths were able to participate in NICH, the remaining 93 were not served by the program because of insurance denial or nonresponse, according to investigators.
While participation in the program made no difference in access to care overall, results of this study suggest NICH reduced access disparities among BIPOC youths, the investigators said.
Those BIPOC youth, 28 in total, had significantly worse access to care prior to referral. However, BIPOC youth participation in NICH was associated with improved attendance at endocrinology appointments and outpatient attendance overall.
A mean change of 1.9 more appointments per year was seen among BIPOC youth who participated in NICH, compared with a mean decrease of 0.5 appointments per year among BIPOC youth not served by the program (P = .03), according to the study abstract.
Prior to NICH participation, outpatient attendance among BIPOC youths was about 2.5 visits per year, data presented by the investigators show.
Systemic changes needed
This study is representative of systemic changes that are needed to improve access to quality care for BIPOC youth, according Cynthia E. Muñoz, PhD, MPH, ADA’s president of health care and education.
“We know that there are increased risks for poor health outcomes for these children and youths, and we know that there is a risk for mental health and psychosocial challenges for youth from these communities,” said Dr. Muñoz, a bilingual licensed psychologist and assistant professor of clinical pediatrics at the University of Southern California, Los Angeles.
In his presentation, Dr. Wagner said lumping racial and ethnic minority participants under a single BIPOC header probably wasn’t ideal because of the diversity and differences among racial and ethnic minorities. However, it was necessary in this particular study because of limited sample size.
Dr. Wagner and coauthors disclosed no conflicts of interest related to the research, which was supported by the Leona M. and Harry B. Helmsley Charitable Trust.
For racial or ethnic minority youths with type 1 diabetes, participating in an interventional program improves access to care, new research shows.
Youth categorized as Black, Indigenous, and other people of color (BIPOC) had significantly improved outpatient attendance during and after participating in Novel Interventions in Children’s Healthcare (NICH), a systems intervention for children with chronic health conditions and their families.
By comparison, no improvements in care access were observed among BIPOC children who were not able to access the program because of insurance or other reasons, David V. Wagner, PhD, Associate Professor and NICH research director at Oregon Health & Science University, Portland, reported at the annual scientific sessions of the American Diabetes Association.
The findings demonstrate a need for intensive, home-based services that aim to correct health inequities, said Dr. Wagner, who presented the findings along with Winniebhelle Cadiz, a scholar in the BUILD EXITO undergraduate research training program at Portland (Ore.) State University.
The NICH program hinges on trained interventionists who visit families at home, attend clinic visits, and work with schools and other contacts to help solve problems that keep children from following medical instructions, according to a program description.
“Families report having somebody by their side to help them navigate the system, address the transportation difficulties experienced, and help them and build that relationship with their health care provider seems to be hugely influential in terms of helping them navigate and access care,” Dr. Wagner said in a presentation of the study.
A NICH for youths with chronic health conditions
The NICH program differs from some other programs that have been developed in an attempt to improve health outcomes among youths in the community, according to Dr. Wagner.
“Many of the programs that exist out there are often piloted on, and seemingly built for, those who have more resources,” he said in his presentation. “Those who are in greatest need often have difficulty accessing and responding to the services.”
NICH doesn’t take the place of existing services, but is “an addition to the continuum of care” for youths and families who are struggling because of lack of resources or marginalization in the health care system, Dr. Wagner said.
While NICH is not specific to any one chronic health condition, several previous investigations have specifically looked at the impact of the NICH program on access to care in youths with type 1 diabetes.
Youths participating in the program for a year had fewer ED visits, including fewer visits with diabetic ketoacidosis (DKA), as well as fewer and shorter admissions as compared with the year prior to participating in the program, Dr. Wagner said.
In another study, youths had fewer admissions for diabetes or DKA and less frequent pediatric ICU contact during the NICH program, as compared with before the program.
Another study showed that, while NICH had no impact overall on access to care among youths with type 1 diabetes, BIPOC youths had an improvement in the mean number of outpatient visits as compared with preprogram levels. However, because none of those studies included a control group, Dr. Wagner said, it remained unclear whether this systems intervention might improve outpatient access among youths with type 1 diabetes as compared with those who did not participate.
Intervention linked to increased BIPOC care access
The latest study includes 144 youths with type 1 diabetes referred for the program. The mean age was 13.7 years, 58% were female, and 81% were non-Hispanic White. While 51 youths were able to participate in NICH, the remaining 93 were not served by the program because of insurance denial or nonresponse, according to investigators.
While participation in the program made no difference in access to care overall, results of this study suggest NICH reduced access disparities among BIPOC youths, the investigators said.
Those BIPOC youth, 28 in total, had significantly worse access to care prior to referral. However, BIPOC youth participation in NICH was associated with improved attendance at endocrinology appointments and outpatient attendance overall.
A mean change of 1.9 more appointments per year was seen among BIPOC youth who participated in NICH, compared with a mean decrease of 0.5 appointments per year among BIPOC youth not served by the program (P = .03), according to the study abstract.
Prior to NICH participation, outpatient attendance among BIPOC youths was about 2.5 visits per year, data presented by the investigators show.
Systemic changes needed
This study is representative of systemic changes that are needed to improve access to quality care for BIPOC youth, according Cynthia E. Muñoz, PhD, MPH, ADA’s president of health care and education.
“We know that there are increased risks for poor health outcomes for these children and youths, and we know that there is a risk for mental health and psychosocial challenges for youth from these communities,” said Dr. Muñoz, a bilingual licensed psychologist and assistant professor of clinical pediatrics at the University of Southern California, Los Angeles.
In his presentation, Dr. Wagner said lumping racial and ethnic minority participants under a single BIPOC header probably wasn’t ideal because of the diversity and differences among racial and ethnic minorities. However, it was necessary in this particular study because of limited sample size.
Dr. Wagner and coauthors disclosed no conflicts of interest related to the research, which was supported by the Leona M. and Harry B. Helmsley Charitable Trust.
For racial or ethnic minority youths with type 1 diabetes, participating in an interventional program improves access to care, new research shows.
Youth categorized as Black, Indigenous, and other people of color (BIPOC) had significantly improved outpatient attendance during and after participating in Novel Interventions in Children’s Healthcare (NICH), a systems intervention for children with chronic health conditions and their families.
By comparison, no improvements in care access were observed among BIPOC children who were not able to access the program because of insurance or other reasons, David V. Wagner, PhD, Associate Professor and NICH research director at Oregon Health & Science University, Portland, reported at the annual scientific sessions of the American Diabetes Association.
The findings demonstrate a need for intensive, home-based services that aim to correct health inequities, said Dr. Wagner, who presented the findings along with Winniebhelle Cadiz, a scholar in the BUILD EXITO undergraduate research training program at Portland (Ore.) State University.
The NICH program hinges on trained interventionists who visit families at home, attend clinic visits, and work with schools and other contacts to help solve problems that keep children from following medical instructions, according to a program description.
“Families report having somebody by their side to help them navigate the system, address the transportation difficulties experienced, and help them and build that relationship with their health care provider seems to be hugely influential in terms of helping them navigate and access care,” Dr. Wagner said in a presentation of the study.
A NICH for youths with chronic health conditions
The NICH program differs from some other programs that have been developed in an attempt to improve health outcomes among youths in the community, according to Dr. Wagner.
“Many of the programs that exist out there are often piloted on, and seemingly built for, those who have more resources,” he said in his presentation. “Those who are in greatest need often have difficulty accessing and responding to the services.”
NICH doesn’t take the place of existing services, but is “an addition to the continuum of care” for youths and families who are struggling because of lack of resources or marginalization in the health care system, Dr. Wagner said.
While NICH is not specific to any one chronic health condition, several previous investigations have specifically looked at the impact of the NICH program on access to care in youths with type 1 diabetes.
Youths participating in the program for a year had fewer ED visits, including fewer visits with diabetic ketoacidosis (DKA), as well as fewer and shorter admissions as compared with the year prior to participating in the program, Dr. Wagner said.
In another study, youths had fewer admissions for diabetes or DKA and less frequent pediatric ICU contact during the NICH program, as compared with before the program.
Another study showed that, while NICH had no impact overall on access to care among youths with type 1 diabetes, BIPOC youths had an improvement in the mean number of outpatient visits as compared with preprogram levels. However, because none of those studies included a control group, Dr. Wagner said, it remained unclear whether this systems intervention might improve outpatient access among youths with type 1 diabetes as compared with those who did not participate.
Intervention linked to increased BIPOC care access
The latest study includes 144 youths with type 1 diabetes referred for the program. The mean age was 13.7 years, 58% were female, and 81% were non-Hispanic White. While 51 youths were able to participate in NICH, the remaining 93 were not served by the program because of insurance denial or nonresponse, according to investigators.
While participation in the program made no difference in access to care overall, results of this study suggest NICH reduced access disparities among BIPOC youths, the investigators said.
Those BIPOC youth, 28 in total, had significantly worse access to care prior to referral. However, BIPOC youth participation in NICH was associated with improved attendance at endocrinology appointments and outpatient attendance overall.
A mean change of 1.9 more appointments per year was seen among BIPOC youth who participated in NICH, compared with a mean decrease of 0.5 appointments per year among BIPOC youth not served by the program (P = .03), according to the study abstract.
Prior to NICH participation, outpatient attendance among BIPOC youths was about 2.5 visits per year, data presented by the investigators show.
Systemic changes needed
This study is representative of systemic changes that are needed to improve access to quality care for BIPOC youth, according Cynthia E. Muñoz, PhD, MPH, ADA’s president of health care and education.
“We know that there are increased risks for poor health outcomes for these children and youths, and we know that there is a risk for mental health and psychosocial challenges for youth from these communities,” said Dr. Muñoz, a bilingual licensed psychologist and assistant professor of clinical pediatrics at the University of Southern California, Los Angeles.
In his presentation, Dr. Wagner said lumping racial and ethnic minority participants under a single BIPOC header probably wasn’t ideal because of the diversity and differences among racial and ethnic minorities. However, it was necessary in this particular study because of limited sample size.
Dr. Wagner and coauthors disclosed no conflicts of interest related to the research, which was supported by the Leona M. and Harry B. Helmsley Charitable Trust.
FROM ADA 2021
‘Staggering’ doubling of type 2 diabetes in children during pandemic
The incidence of type 2 diabetes in children appears to have doubled during the COVID-19 pandemic, data from two new U.S. studies suggest, with the lead investigator of one saying she was “surprised by the staggering increase in cases of type 2 diabetes ... and the increase in severity of presentation.”
Findings from the two separate retrospective chart reviews – one conducted in Washington, D.C., and the other in Baton Rouge, La. – were presented June 25 at the annual scientific sessions of the American Diabetes Association.
Although the two studies differed somewhat in the clinical parameters examined, both revealed a similar doubling of the rates of hospitalizations for type 2 diabetes among youth during 2020, compared with the same time period in 2019, as well as greater severity of metabolic disturbance.
And, as has been previously described with type 2 diabetes in youth, African American ethnicity predominated in both cohorts.
“Although we could not assess the cause of the increases in type 2 diabetes from our data, these disparities suggest that indirect effects of social distancing measures, including school closure and unemployment, are placing undue burden on underserved communities. Decreases in well-child care and fears of seeking medical care during the pandemic may have also contributed,” lead investigator of one of the studies, pediatric endocrinologist Brynn E. Marks, MD, Children’s National Hospital, Washington, said in an interview.
More hospitalizations, racial disparities aggravated by COVID-19
Lead author of the other study, Daniel S. Hsia, MD, Pennington Biomedical Research Center, Baton Rouge, said in an interview: “Since the pandemic, our data suggest that more children may be diagnosed with type 2 diabetes and may require hospitalization when they are diagnosed. Looking at both datasets, there appears to be a racial disparity in type 2 diabetes diagnoses that has only been exacerbated by the COVID-19 pandemic.”
Of concern, Dr. Hsia said, “The incidence rate of type 2 diabetes in children was already on the rise before the pandemic. While there may be a brief leveling off now that children are getting regular health care and going back to school in person, I believe these rates will continue to rise especially in light of the childhood obesity rates not improving.”
Their dataset captured all youth who were newly diagnosed with type 2 diabetes during the first full year of the COVID-19 pandemic, from March 11, 2020, to March 10, 2021, and compared those data with the time period from March 11, 2019, to March 10, 2020.
During the pandemic, the number of cases of type 2 diabetes increased by 182%, from 50 in 2019 to 141 in 2020. The average age at diagnosis was about 14 years in both time periods.
In the prepandemic period, 18 (36%) diagnosed with type 2 diabetes required inpatient admission, compared with 85 (60.3%) during the pandemic. At Children’s National, youth with suspected new-onset type 2 diabetes aren’t typically hospitalized unless they have severe hyperglycemia, ketosis, or are unable to schedule urgent outpatient follow-up, Dr. Marks noted.
The proportions of youth with new-onset type 2 diabetes who presented in diabetic ketoacidosis (DKA) rose from 2 (4%) prepandemic to 33 (23.4%) during the pandemic. Presentation with hyperosmolar DKA rose from 0 to 13 (9.2%).
However, during the pandemic only five youth were actively infected with SARS-CoV-2 at the time of type 2 diabetes diagnosis among the 90 tested.
Dr. Marks said: “We believe the increase in inpatient admissions was due to more severe presentation during the pandemic. ...We were surprised by the staggering increase in cases of type 2 diabetes ... and the increase in severity of presentation.”
Shift in diagnoses to type 2 diabetes
The pandemic also appears to have shifted the proportion of youth diagnosed with type 2 diabetes, compared with type 1 diabetes. Whereas 24% of youth with new-onset diabetes prepandemic had type 2 diabetes and the rest had type 1 diabetes, during pandemic the proportion with type 2 diabetes rose to 44%.
“Rates of type 2 diabetes rose steadily at a rate of 1.45 cases per month throughout the course of the pandemic, suggesting a cumulative effect of the indirect effects of social distancing measures,” Dr. Marks said.
Furthermore, she added, whereas 60% of youth diagnosed with type 2 diabetes before the pandemic were female, the rate fell to 40% during the pandemic. This trend might be because of activity levels in that, while male adolescents are typically more active, rates of exercise fell in both sexes during the pandemic but declined more sharply in males such that activity levels between the sexes became equal.
Although type 2 diabetes in youth has always been more common in ethnic minorities, the pandemic appears to have exacerbated these disparities.
While 58% of youth diagnosed with type 2 diabetes prepandemic identified as non-Hispanic Black, that proportion rose to 76.7% during the pandemic. Among Black youth with new-onset type 2 diabetes, 31 of 33 presented in DKA, and 12 of the 13 who presented in hyperosmolar DKA during the pandemic were Black.
“Strategies to promote health equity and address the undue burden of the COVID-19 pandemic on underserved communities must be developed to avoid worsening disparities and long-term health outcomes,” Dr. Marks said.
‘A microcosm’: Similar findings in a smaller population
Dr. Hsia and colleagues looked at a smaller number of patients in a shorter time period. In March–December 2019, the hospitalization rate for new-onset type 2 diabetes was 0.27% (8 out of 2,964 hospitalizations), compared with 0.62% (17 out of 2,729 hospitalizations) during the same period in 2020 (P < .048) – also more than a doubling. Age at admission, sex, and body mass index didn’t differ between the two groups.
Criteria for DKA were met by three children in 2019 versus eight in 2020, and hyperosmolar hyperglycemic syndrome in zero versus two, respectively. Mean hemoglobin A1c on admission was 12.4% in 2019 versus 13.1% in 2020 (P = .59), and mean serum glucose was 441 mg/dL versus 669 mg/dL (P = .14), respectively. Serum osmolality on admission was 314 mmol/kg in 2019 versus 335 mmol/kg in 2020 (P = .19).
“Clinically speaking the differences in the lab values were significant, but we did not have enough numbers ... to see a statistically significant difference. I think by looking at more centers, our site likely represents a microcosm of what is happening across the country,” Dr. Hsia said.
In 2019, 7 of the 8 children were African American, as were 16 of the 17 children in 2020. The other single child in each group was White.
Dr. Hsia said: “Larger studies that include more patients are needed to confirm our initial findings. More research is needed to understand why this increasing trend of type 2 diabetes diagnoses in children may be occurring [and] to better understand how stay-at-home orders and other restrictions due to COVID-19 have worsened risk factors for type 2 diabetes.”
“These include decreased physical activity, more screen time, disturbed sleep, and increased intake of processed foods, which can all lead to weight gain,” he concluded.
Dr. Marks reported receiving research support from Tandem, Dexcom, and the Cystic Fibrosis Foundation. Dr. Hsia reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The incidence of type 2 diabetes in children appears to have doubled during the COVID-19 pandemic, data from two new U.S. studies suggest, with the lead investigator of one saying she was “surprised by the staggering increase in cases of type 2 diabetes ... and the increase in severity of presentation.”
Findings from the two separate retrospective chart reviews – one conducted in Washington, D.C., and the other in Baton Rouge, La. – were presented June 25 at the annual scientific sessions of the American Diabetes Association.
Although the two studies differed somewhat in the clinical parameters examined, both revealed a similar doubling of the rates of hospitalizations for type 2 diabetes among youth during 2020, compared with the same time period in 2019, as well as greater severity of metabolic disturbance.
And, as has been previously described with type 2 diabetes in youth, African American ethnicity predominated in both cohorts.
“Although we could not assess the cause of the increases in type 2 diabetes from our data, these disparities suggest that indirect effects of social distancing measures, including school closure and unemployment, are placing undue burden on underserved communities. Decreases in well-child care and fears of seeking medical care during the pandemic may have also contributed,” lead investigator of one of the studies, pediatric endocrinologist Brynn E. Marks, MD, Children’s National Hospital, Washington, said in an interview.
More hospitalizations, racial disparities aggravated by COVID-19
Lead author of the other study, Daniel S. Hsia, MD, Pennington Biomedical Research Center, Baton Rouge, said in an interview: “Since the pandemic, our data suggest that more children may be diagnosed with type 2 diabetes and may require hospitalization when they are diagnosed. Looking at both datasets, there appears to be a racial disparity in type 2 diabetes diagnoses that has only been exacerbated by the COVID-19 pandemic.”
Of concern, Dr. Hsia said, “The incidence rate of type 2 diabetes in children was already on the rise before the pandemic. While there may be a brief leveling off now that children are getting regular health care and going back to school in person, I believe these rates will continue to rise especially in light of the childhood obesity rates not improving.”
Their dataset captured all youth who were newly diagnosed with type 2 diabetes during the first full year of the COVID-19 pandemic, from March 11, 2020, to March 10, 2021, and compared those data with the time period from March 11, 2019, to March 10, 2020.
During the pandemic, the number of cases of type 2 diabetes increased by 182%, from 50 in 2019 to 141 in 2020. The average age at diagnosis was about 14 years in both time periods.
In the prepandemic period, 18 (36%) diagnosed with type 2 diabetes required inpatient admission, compared with 85 (60.3%) during the pandemic. At Children’s National, youth with suspected new-onset type 2 diabetes aren’t typically hospitalized unless they have severe hyperglycemia, ketosis, or are unable to schedule urgent outpatient follow-up, Dr. Marks noted.
The proportions of youth with new-onset type 2 diabetes who presented in diabetic ketoacidosis (DKA) rose from 2 (4%) prepandemic to 33 (23.4%) during the pandemic. Presentation with hyperosmolar DKA rose from 0 to 13 (9.2%).
However, during the pandemic only five youth were actively infected with SARS-CoV-2 at the time of type 2 diabetes diagnosis among the 90 tested.
Dr. Marks said: “We believe the increase in inpatient admissions was due to more severe presentation during the pandemic. ...We were surprised by the staggering increase in cases of type 2 diabetes ... and the increase in severity of presentation.”
Shift in diagnoses to type 2 diabetes
The pandemic also appears to have shifted the proportion of youth diagnosed with type 2 diabetes, compared with type 1 diabetes. Whereas 24% of youth with new-onset diabetes prepandemic had type 2 diabetes and the rest had type 1 diabetes, during pandemic the proportion with type 2 diabetes rose to 44%.
“Rates of type 2 diabetes rose steadily at a rate of 1.45 cases per month throughout the course of the pandemic, suggesting a cumulative effect of the indirect effects of social distancing measures,” Dr. Marks said.
Furthermore, she added, whereas 60% of youth diagnosed with type 2 diabetes before the pandemic were female, the rate fell to 40% during the pandemic. This trend might be because of activity levels in that, while male adolescents are typically more active, rates of exercise fell in both sexes during the pandemic but declined more sharply in males such that activity levels between the sexes became equal.
Although type 2 diabetes in youth has always been more common in ethnic minorities, the pandemic appears to have exacerbated these disparities.
While 58% of youth diagnosed with type 2 diabetes prepandemic identified as non-Hispanic Black, that proportion rose to 76.7% during the pandemic. Among Black youth with new-onset type 2 diabetes, 31 of 33 presented in DKA, and 12 of the 13 who presented in hyperosmolar DKA during the pandemic were Black.
“Strategies to promote health equity and address the undue burden of the COVID-19 pandemic on underserved communities must be developed to avoid worsening disparities and long-term health outcomes,” Dr. Marks said.
‘A microcosm’: Similar findings in a smaller population
Dr. Hsia and colleagues looked at a smaller number of patients in a shorter time period. In March–December 2019, the hospitalization rate for new-onset type 2 diabetes was 0.27% (8 out of 2,964 hospitalizations), compared with 0.62% (17 out of 2,729 hospitalizations) during the same period in 2020 (P < .048) – also more than a doubling. Age at admission, sex, and body mass index didn’t differ between the two groups.
Criteria for DKA were met by three children in 2019 versus eight in 2020, and hyperosmolar hyperglycemic syndrome in zero versus two, respectively. Mean hemoglobin A1c on admission was 12.4% in 2019 versus 13.1% in 2020 (P = .59), and mean serum glucose was 441 mg/dL versus 669 mg/dL (P = .14), respectively. Serum osmolality on admission was 314 mmol/kg in 2019 versus 335 mmol/kg in 2020 (P = .19).
“Clinically speaking the differences in the lab values were significant, but we did not have enough numbers ... to see a statistically significant difference. I think by looking at more centers, our site likely represents a microcosm of what is happening across the country,” Dr. Hsia said.
In 2019, 7 of the 8 children were African American, as were 16 of the 17 children in 2020. The other single child in each group was White.
Dr. Hsia said: “Larger studies that include more patients are needed to confirm our initial findings. More research is needed to understand why this increasing trend of type 2 diabetes diagnoses in children may be occurring [and] to better understand how stay-at-home orders and other restrictions due to COVID-19 have worsened risk factors for type 2 diabetes.”
“These include decreased physical activity, more screen time, disturbed sleep, and increased intake of processed foods, which can all lead to weight gain,” he concluded.
Dr. Marks reported receiving research support from Tandem, Dexcom, and the Cystic Fibrosis Foundation. Dr. Hsia reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The incidence of type 2 diabetes in children appears to have doubled during the COVID-19 pandemic, data from two new U.S. studies suggest, with the lead investigator of one saying she was “surprised by the staggering increase in cases of type 2 diabetes ... and the increase in severity of presentation.”
Findings from the two separate retrospective chart reviews – one conducted in Washington, D.C., and the other in Baton Rouge, La. – were presented June 25 at the annual scientific sessions of the American Diabetes Association.
Although the two studies differed somewhat in the clinical parameters examined, both revealed a similar doubling of the rates of hospitalizations for type 2 diabetes among youth during 2020, compared with the same time period in 2019, as well as greater severity of metabolic disturbance.
And, as has been previously described with type 2 diabetes in youth, African American ethnicity predominated in both cohorts.
“Although we could not assess the cause of the increases in type 2 diabetes from our data, these disparities suggest that indirect effects of social distancing measures, including school closure and unemployment, are placing undue burden on underserved communities. Decreases in well-child care and fears of seeking medical care during the pandemic may have also contributed,” lead investigator of one of the studies, pediatric endocrinologist Brynn E. Marks, MD, Children’s National Hospital, Washington, said in an interview.
More hospitalizations, racial disparities aggravated by COVID-19
Lead author of the other study, Daniel S. Hsia, MD, Pennington Biomedical Research Center, Baton Rouge, said in an interview: “Since the pandemic, our data suggest that more children may be diagnosed with type 2 diabetes and may require hospitalization when they are diagnosed. Looking at both datasets, there appears to be a racial disparity in type 2 diabetes diagnoses that has only been exacerbated by the COVID-19 pandemic.”
Of concern, Dr. Hsia said, “The incidence rate of type 2 diabetes in children was already on the rise before the pandemic. While there may be a brief leveling off now that children are getting regular health care and going back to school in person, I believe these rates will continue to rise especially in light of the childhood obesity rates not improving.”
Their dataset captured all youth who were newly diagnosed with type 2 diabetes during the first full year of the COVID-19 pandemic, from March 11, 2020, to March 10, 2021, and compared those data with the time period from March 11, 2019, to March 10, 2020.
During the pandemic, the number of cases of type 2 diabetes increased by 182%, from 50 in 2019 to 141 in 2020. The average age at diagnosis was about 14 years in both time periods.
In the prepandemic period, 18 (36%) diagnosed with type 2 diabetes required inpatient admission, compared with 85 (60.3%) during the pandemic. At Children’s National, youth with suspected new-onset type 2 diabetes aren’t typically hospitalized unless they have severe hyperglycemia, ketosis, or are unable to schedule urgent outpatient follow-up, Dr. Marks noted.
The proportions of youth with new-onset type 2 diabetes who presented in diabetic ketoacidosis (DKA) rose from 2 (4%) prepandemic to 33 (23.4%) during the pandemic. Presentation with hyperosmolar DKA rose from 0 to 13 (9.2%).
However, during the pandemic only five youth were actively infected with SARS-CoV-2 at the time of type 2 diabetes diagnosis among the 90 tested.
Dr. Marks said: “We believe the increase in inpatient admissions was due to more severe presentation during the pandemic. ...We were surprised by the staggering increase in cases of type 2 diabetes ... and the increase in severity of presentation.”
Shift in diagnoses to type 2 diabetes
The pandemic also appears to have shifted the proportion of youth diagnosed with type 2 diabetes, compared with type 1 diabetes. Whereas 24% of youth with new-onset diabetes prepandemic had type 2 diabetes and the rest had type 1 diabetes, during pandemic the proportion with type 2 diabetes rose to 44%.
“Rates of type 2 diabetes rose steadily at a rate of 1.45 cases per month throughout the course of the pandemic, suggesting a cumulative effect of the indirect effects of social distancing measures,” Dr. Marks said.
Furthermore, she added, whereas 60% of youth diagnosed with type 2 diabetes before the pandemic were female, the rate fell to 40% during the pandemic. This trend might be because of activity levels in that, while male adolescents are typically more active, rates of exercise fell in both sexes during the pandemic but declined more sharply in males such that activity levels between the sexes became equal.
Although type 2 diabetes in youth has always been more common in ethnic minorities, the pandemic appears to have exacerbated these disparities.
While 58% of youth diagnosed with type 2 diabetes prepandemic identified as non-Hispanic Black, that proportion rose to 76.7% during the pandemic. Among Black youth with new-onset type 2 diabetes, 31 of 33 presented in DKA, and 12 of the 13 who presented in hyperosmolar DKA during the pandemic were Black.
“Strategies to promote health equity and address the undue burden of the COVID-19 pandemic on underserved communities must be developed to avoid worsening disparities and long-term health outcomes,” Dr. Marks said.
‘A microcosm’: Similar findings in a smaller population
Dr. Hsia and colleagues looked at a smaller number of patients in a shorter time period. In March–December 2019, the hospitalization rate for new-onset type 2 diabetes was 0.27% (8 out of 2,964 hospitalizations), compared with 0.62% (17 out of 2,729 hospitalizations) during the same period in 2020 (P < .048) – also more than a doubling. Age at admission, sex, and body mass index didn’t differ between the two groups.
Criteria for DKA were met by three children in 2019 versus eight in 2020, and hyperosmolar hyperglycemic syndrome in zero versus two, respectively. Mean hemoglobin A1c on admission was 12.4% in 2019 versus 13.1% in 2020 (P = .59), and mean serum glucose was 441 mg/dL versus 669 mg/dL (P = .14), respectively. Serum osmolality on admission was 314 mmol/kg in 2019 versus 335 mmol/kg in 2020 (P = .19).
“Clinically speaking the differences in the lab values were significant, but we did not have enough numbers ... to see a statistically significant difference. I think by looking at more centers, our site likely represents a microcosm of what is happening across the country,” Dr. Hsia said.
In 2019, 7 of the 8 children were African American, as were 16 of the 17 children in 2020. The other single child in each group was White.
Dr. Hsia said: “Larger studies that include more patients are needed to confirm our initial findings. More research is needed to understand why this increasing trend of type 2 diabetes diagnoses in children may be occurring [and] to better understand how stay-at-home orders and other restrictions due to COVID-19 have worsened risk factors for type 2 diabetes.”
“These include decreased physical activity, more screen time, disturbed sleep, and increased intake of processed foods, which can all lead to weight gain,” he concluded.
Dr. Marks reported receiving research support from Tandem, Dexcom, and the Cystic Fibrosis Foundation. Dr. Hsia reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Dose-dependent effect of ‘internet addiction’ and sleep problems
More evidence suggests the severity of internet addiction (IA) is directly related to the severity of sleep problems in youth.
Results from a study of more than 4,000 adolescent students show IA severity was linked to less sleep and to daytime sleepiness. In addition, boys aged 12-14 years who were addicted to computer games versus social media networking were the most affected.
Sleep issues could be “easily detectable manifestations of pathological internet addiction,” investigator Sergey Tereshchenko, PhD, Scientific Research Institute for Medical Problems of the North, Krasnoyask State Medical University, Russia, told this news organization.
These sleep problems require attention and correction, Dr. Tereshchenko added.
The findings were presented at the virtual Congress of the European Academy of Neurology 2021.
New phenomenon
IA is a relatively new psychological phenomenon and is most prevalent in “socially vulnerable groups,” such as adolescents, Dr. Tereshchenko said.
He cited numerous studies that have “convincingly demonstrated” IA is comorbid with a broad range of psychopathologic conditions, including depression, anxiety, and attention deficit hyperactivity disorder.
There is also growing evidence, including from systematic reviews in 2014 and 2019, that IA affects a wide range of sleep parameters.
However, most studies in adolescents have used only one psychometric tool to assess addiction, revealing only the “general IA pattern” and not the type of IA, Dr. Tereshchenko noted.
Adolescents may not be addicted to the internet itself but to certain behaviors like gaming or social networking, he said.
The “undoubted advantage” of his team’s research is the use of more than one tool, making it possible to “verify the predominant content of the addiction,” he added.
The investigators previously assessed general prevalence of IA in adolescents in Siberia and found about 6.8% of participants displayed pathological IA behavior – and that gaming addiction is more common in boys whereas addiction to social networking is more common in girls.
This prevalence rate is lower than in the Philippines (21.1%), Hong Kong (16.4%), Malaysia (14.1%), China (11%), and South Korea (9.7%), but slightly higher than in Japan (6.2%).
IA prevalence among adolescents in Europe ranges from 1% to 11%, with an average of 4.4%, said Dr. Tereshchenko.
Siberian students’ sleep
The current study included 4,344 students aged 12-18 years (average age, about 15 years) from 10 public schools in three large cities of Central Siberia (Krasnoyarsk, Abakan, and Kyzyl). There were slightly more girls than boys in the study sample.
Participants completed the Russian language version of the Chen Internet Addiction Scale (CIAS), which covers five symptomatic criteria for addictive behavior: withdrawal symptoms, signs of tolerance, compulsive use, psychological or physical problems, and difficulty managing time.
In this questionnaire, respondents rate several statements regarding the effect of internet use, each on a 4-point Likert scale: not at all (1 point), a little bit (2 points), moderately (3 points) and extremely (4). The total score ranges from 26 to 104.
A CIAS score of 26-42 indicates adaptive internet use, 43-64 indicates maladaptive internet use, and 65 and above indicates pathological internet use (PIU), which was classified as “internet-addicted.”
The researchers also used the nine-item Social Media Disorder Scale, as well as the Pittsburgh Sleep Quality Index to assess nighttime sleep.
Among other questions, teens were asked how long it usually took them to fall asleep and when they typically went to bed and woke up on school nights.
For daytime sleepiness, investigators used the targeted Pediatric Daytime Sleepiness Scale questionnaire, making them among the few research groups to use this psychometric instrument, Dr. Tereshchenko noted.
After parental consent was given, students completed the tests at the end of the day’s lessons. Total test time was about 45 minutes.
Sleep disturbance
Initial study results showed that compared with the other groups, adolescents with PIU tended to go to bed later, wake up later, take longer to fall asleep, sleep less at night, have more nighttime awakenings, and have more daytime sleepiness.
Sleep quality was the most impaired in boys aged 12-14 years who are addicted to internet computer games.
“In this group, 5 of the 6 sleep assessment parameters we studied were changed,” Dr. Tereshchenko reported.
Decreased total nighttime sleep was more common in older adolescents.
On average, boys and girls aged 15-18 years got less than the recommended 8 hours of sleep per night. Boys with IA got only about 6.4 hours per night and girls with IA got about 6.6 hours.
Interestingly, IA is generally more prevalent among teen girls than boys in Russia, which is not the case in Europe and North America, Dr. Tereshchenko noted.
Mechanisms linking IA and sleep disorders are not clear, but the relationship is probably multifactorial and perhaps interrelated, creating something of a “vicious circle,” he said.
“Sleep disturbances, which reflect psychosocial problems, depression, and anxiety-phobic disorders, can precede and contribute to IA. On the other hand, sleep disturbances such as insomnia can lead to increased use of the internet in the evening and at night, further exacerbating the problem,” said Dr. Tereshchenko.
Research is lacking on useful treatments for youth with IA, but these kids would likely benefit from behavioral therapy approaches, he added.
No escape?
Commenting on the study for this news organization, Maurice M. Ohayon, MD, DSc, PhD, director of the Stanford Sleep Epidemiology Research Center, Stanford University, California, said the topic of youth IA is “very important.”
Previous research in this field has shown a major impact from IA not only on sleep but also on mood – with irritability, depression, and even thoughts of suicide being possible red flags, said Dr. Ohayon, who was not involved in the current study.
Interestingly, his own research has also found that young teenage boys are most at risk for gaming addiction.
Although internet gaming has some positive effects, such as fostering leadership skills and relationships, it has become increasingly violent and isolating, with more adult professional gamers preying on younger players, Dr. Ohayon said.
“The major problem is that it’s putting children in a virtual world from which it’s difficult to escape,” he added.
Dr. Ohayon also noted concern about future developmental effects in kids who play video games for hours on end without coming out of their bedroom and with no physical contact with fellow players.
Parents should intervene before this situation occurs and limit the time their children spend on the gaming console, he said.
A version of this article first appeared on Medscape.com.
More evidence suggests the severity of internet addiction (IA) is directly related to the severity of sleep problems in youth.
Results from a study of more than 4,000 adolescent students show IA severity was linked to less sleep and to daytime sleepiness. In addition, boys aged 12-14 years who were addicted to computer games versus social media networking were the most affected.
Sleep issues could be “easily detectable manifestations of pathological internet addiction,” investigator Sergey Tereshchenko, PhD, Scientific Research Institute for Medical Problems of the North, Krasnoyask State Medical University, Russia, told this news organization.
These sleep problems require attention and correction, Dr. Tereshchenko added.
The findings were presented at the virtual Congress of the European Academy of Neurology 2021.
New phenomenon
IA is a relatively new psychological phenomenon and is most prevalent in “socially vulnerable groups,” such as adolescents, Dr. Tereshchenko said.
He cited numerous studies that have “convincingly demonstrated” IA is comorbid with a broad range of psychopathologic conditions, including depression, anxiety, and attention deficit hyperactivity disorder.
There is also growing evidence, including from systematic reviews in 2014 and 2019, that IA affects a wide range of sleep parameters.
However, most studies in adolescents have used only one psychometric tool to assess addiction, revealing only the “general IA pattern” and not the type of IA, Dr. Tereshchenko noted.
Adolescents may not be addicted to the internet itself but to certain behaviors like gaming or social networking, he said.
The “undoubted advantage” of his team’s research is the use of more than one tool, making it possible to “verify the predominant content of the addiction,” he added.
The investigators previously assessed general prevalence of IA in adolescents in Siberia and found about 6.8% of participants displayed pathological IA behavior – and that gaming addiction is more common in boys whereas addiction to social networking is more common in girls.
This prevalence rate is lower than in the Philippines (21.1%), Hong Kong (16.4%), Malaysia (14.1%), China (11%), and South Korea (9.7%), but slightly higher than in Japan (6.2%).
IA prevalence among adolescents in Europe ranges from 1% to 11%, with an average of 4.4%, said Dr. Tereshchenko.
Siberian students’ sleep
The current study included 4,344 students aged 12-18 years (average age, about 15 years) from 10 public schools in three large cities of Central Siberia (Krasnoyarsk, Abakan, and Kyzyl). There were slightly more girls than boys in the study sample.
Participants completed the Russian language version of the Chen Internet Addiction Scale (CIAS), which covers five symptomatic criteria for addictive behavior: withdrawal symptoms, signs of tolerance, compulsive use, psychological or physical problems, and difficulty managing time.
In this questionnaire, respondents rate several statements regarding the effect of internet use, each on a 4-point Likert scale: not at all (1 point), a little bit (2 points), moderately (3 points) and extremely (4). The total score ranges from 26 to 104.
A CIAS score of 26-42 indicates adaptive internet use, 43-64 indicates maladaptive internet use, and 65 and above indicates pathological internet use (PIU), which was classified as “internet-addicted.”
The researchers also used the nine-item Social Media Disorder Scale, as well as the Pittsburgh Sleep Quality Index to assess nighttime sleep.
Among other questions, teens were asked how long it usually took them to fall asleep and when they typically went to bed and woke up on school nights.
For daytime sleepiness, investigators used the targeted Pediatric Daytime Sleepiness Scale questionnaire, making them among the few research groups to use this psychometric instrument, Dr. Tereshchenko noted.
After parental consent was given, students completed the tests at the end of the day’s lessons. Total test time was about 45 minutes.
Sleep disturbance
Initial study results showed that compared with the other groups, adolescents with PIU tended to go to bed later, wake up later, take longer to fall asleep, sleep less at night, have more nighttime awakenings, and have more daytime sleepiness.
Sleep quality was the most impaired in boys aged 12-14 years who are addicted to internet computer games.
“In this group, 5 of the 6 sleep assessment parameters we studied were changed,” Dr. Tereshchenko reported.
Decreased total nighttime sleep was more common in older adolescents.
On average, boys and girls aged 15-18 years got less than the recommended 8 hours of sleep per night. Boys with IA got only about 6.4 hours per night and girls with IA got about 6.6 hours.
Interestingly, IA is generally more prevalent among teen girls than boys in Russia, which is not the case in Europe and North America, Dr. Tereshchenko noted.
Mechanisms linking IA and sleep disorders are not clear, but the relationship is probably multifactorial and perhaps interrelated, creating something of a “vicious circle,” he said.
“Sleep disturbances, which reflect psychosocial problems, depression, and anxiety-phobic disorders, can precede and contribute to IA. On the other hand, sleep disturbances such as insomnia can lead to increased use of the internet in the evening and at night, further exacerbating the problem,” said Dr. Tereshchenko.
Research is lacking on useful treatments for youth with IA, but these kids would likely benefit from behavioral therapy approaches, he added.
No escape?
Commenting on the study for this news organization, Maurice M. Ohayon, MD, DSc, PhD, director of the Stanford Sleep Epidemiology Research Center, Stanford University, California, said the topic of youth IA is “very important.”
Previous research in this field has shown a major impact from IA not only on sleep but also on mood – with irritability, depression, and even thoughts of suicide being possible red flags, said Dr. Ohayon, who was not involved in the current study.
Interestingly, his own research has also found that young teenage boys are most at risk for gaming addiction.
Although internet gaming has some positive effects, such as fostering leadership skills and relationships, it has become increasingly violent and isolating, with more adult professional gamers preying on younger players, Dr. Ohayon said.
“The major problem is that it’s putting children in a virtual world from which it’s difficult to escape,” he added.
Dr. Ohayon also noted concern about future developmental effects in kids who play video games for hours on end without coming out of their bedroom and with no physical contact with fellow players.
Parents should intervene before this situation occurs and limit the time their children spend on the gaming console, he said.
A version of this article first appeared on Medscape.com.
More evidence suggests the severity of internet addiction (IA) is directly related to the severity of sleep problems in youth.
Results from a study of more than 4,000 adolescent students show IA severity was linked to less sleep and to daytime sleepiness. In addition, boys aged 12-14 years who were addicted to computer games versus social media networking were the most affected.
Sleep issues could be “easily detectable manifestations of pathological internet addiction,” investigator Sergey Tereshchenko, PhD, Scientific Research Institute for Medical Problems of the North, Krasnoyask State Medical University, Russia, told this news organization.
These sleep problems require attention and correction, Dr. Tereshchenko added.
The findings were presented at the virtual Congress of the European Academy of Neurology 2021.
New phenomenon
IA is a relatively new psychological phenomenon and is most prevalent in “socially vulnerable groups,” such as adolescents, Dr. Tereshchenko said.
He cited numerous studies that have “convincingly demonstrated” IA is comorbid with a broad range of psychopathologic conditions, including depression, anxiety, and attention deficit hyperactivity disorder.
There is also growing evidence, including from systematic reviews in 2014 and 2019, that IA affects a wide range of sleep parameters.
However, most studies in adolescents have used only one psychometric tool to assess addiction, revealing only the “general IA pattern” and not the type of IA, Dr. Tereshchenko noted.
Adolescents may not be addicted to the internet itself but to certain behaviors like gaming or social networking, he said.
The “undoubted advantage” of his team’s research is the use of more than one tool, making it possible to “verify the predominant content of the addiction,” he added.
The investigators previously assessed general prevalence of IA in adolescents in Siberia and found about 6.8% of participants displayed pathological IA behavior – and that gaming addiction is more common in boys whereas addiction to social networking is more common in girls.
This prevalence rate is lower than in the Philippines (21.1%), Hong Kong (16.4%), Malaysia (14.1%), China (11%), and South Korea (9.7%), but slightly higher than in Japan (6.2%).
IA prevalence among adolescents in Europe ranges from 1% to 11%, with an average of 4.4%, said Dr. Tereshchenko.
Siberian students’ sleep
The current study included 4,344 students aged 12-18 years (average age, about 15 years) from 10 public schools in three large cities of Central Siberia (Krasnoyarsk, Abakan, and Kyzyl). There were slightly more girls than boys in the study sample.
Participants completed the Russian language version of the Chen Internet Addiction Scale (CIAS), which covers five symptomatic criteria for addictive behavior: withdrawal symptoms, signs of tolerance, compulsive use, psychological or physical problems, and difficulty managing time.
In this questionnaire, respondents rate several statements regarding the effect of internet use, each on a 4-point Likert scale: not at all (1 point), a little bit (2 points), moderately (3 points) and extremely (4). The total score ranges from 26 to 104.
A CIAS score of 26-42 indicates adaptive internet use, 43-64 indicates maladaptive internet use, and 65 and above indicates pathological internet use (PIU), which was classified as “internet-addicted.”
The researchers also used the nine-item Social Media Disorder Scale, as well as the Pittsburgh Sleep Quality Index to assess nighttime sleep.
Among other questions, teens were asked how long it usually took them to fall asleep and when they typically went to bed and woke up on school nights.
For daytime sleepiness, investigators used the targeted Pediatric Daytime Sleepiness Scale questionnaire, making them among the few research groups to use this psychometric instrument, Dr. Tereshchenko noted.
After parental consent was given, students completed the tests at the end of the day’s lessons. Total test time was about 45 minutes.
Sleep disturbance
Initial study results showed that compared with the other groups, adolescents with PIU tended to go to bed later, wake up later, take longer to fall asleep, sleep less at night, have more nighttime awakenings, and have more daytime sleepiness.
Sleep quality was the most impaired in boys aged 12-14 years who are addicted to internet computer games.
“In this group, 5 of the 6 sleep assessment parameters we studied were changed,” Dr. Tereshchenko reported.
Decreased total nighttime sleep was more common in older adolescents.
On average, boys and girls aged 15-18 years got less than the recommended 8 hours of sleep per night. Boys with IA got only about 6.4 hours per night and girls with IA got about 6.6 hours.
Interestingly, IA is generally more prevalent among teen girls than boys in Russia, which is not the case in Europe and North America, Dr. Tereshchenko noted.
Mechanisms linking IA and sleep disorders are not clear, but the relationship is probably multifactorial and perhaps interrelated, creating something of a “vicious circle,” he said.
“Sleep disturbances, which reflect psychosocial problems, depression, and anxiety-phobic disorders, can precede and contribute to IA. On the other hand, sleep disturbances such as insomnia can lead to increased use of the internet in the evening and at night, further exacerbating the problem,” said Dr. Tereshchenko.
Research is lacking on useful treatments for youth with IA, but these kids would likely benefit from behavioral therapy approaches, he added.
No escape?
Commenting on the study for this news organization, Maurice M. Ohayon, MD, DSc, PhD, director of the Stanford Sleep Epidemiology Research Center, Stanford University, California, said the topic of youth IA is “very important.”
Previous research in this field has shown a major impact from IA not only on sleep but also on mood – with irritability, depression, and even thoughts of suicide being possible red flags, said Dr. Ohayon, who was not involved in the current study.
Interestingly, his own research has also found that young teenage boys are most at risk for gaming addiction.
Although internet gaming has some positive effects, such as fostering leadership skills and relationships, it has become increasingly violent and isolating, with more adult professional gamers preying on younger players, Dr. Ohayon said.
“The major problem is that it’s putting children in a virtual world from which it’s difficult to escape,” he added.
Dr. Ohayon also noted concern about future developmental effects in kids who play video games for hours on end without coming out of their bedroom and with no physical contact with fellow players.
Parents should intervene before this situation occurs and limit the time their children spend on the gaming console, he said.
A version of this article first appeared on Medscape.com.
MD jailed for road rage, career spirals downhill
It was a 95° F day in July 2015, and emergency physician Martin Maag, MD, was driving down Bee Ridge Road, a busy seven-lane thoroughfare in Sarasota, Fla., on his way home from a family dinner. To distance himself from a truck blowing black smoke, Dr. Maag says he had just passed some vehicles, when a motorcycle flew past him in the turning lane and the passenger flipped him off.
“I started laughing because I knew we were coming up to a red light,” said Dr. Maag. “When we pulled up to the light, I put my window down and said: ‘Hey, you ought to be a little more careful about who you’re flipping off! You never know who it might be and what they might do.’ ”
The female passenger cursed at Dr. Maag, and the two traded profanities. The male driver then told Dr. Maag: “Get out of the car, old man,” according to Dr. Maag. Fuming, Dr. Maag got out of his black Tesla, and the two men met in the middle of the street.
“As soon as I got close enough to see him, I could tell he really looked young,” Dr. Maag recalls. “I said: ‘You’re like 12 years old. I’m going to end up beating your ass and then I’m going to go to jail. Go get on your bike, and ride home to your mom.’ I don’t remember what he said to me, but I spun around and said: ‘If you want to act like a man, meet me up the street in a parking lot and let’s have at it like men.’ ”
The motorcyclist got back on his white Suzuki and sped off, and Dr. Maag followed. Both vehicles went racing down the road, swerving between cars, and reaching speeds of 100 miles per hour, Dr. Maag said. At one point, Dr. Maag says he drove in front of the motorcyclist to slow him down, and the motorcycle clipped the back of his car. No one was seriously hurt, but soon Dr. Maag was in the back of a police cruiser headed to jail.
Dr. Maag wishes he could take back his actions that summer day 6 years ago. Those few minutes of fury have had lasting effects on the doctor’s life. The incident resulted in criminal charges, a jail sentence, thousands of dollars in legal fees, and a 3-year departure from emergency medicine. Although Dr. Maag did not lose his medical license as a result of the incident, the physician’s Medicare billing privileges were suspended because of a federal provision that ties some felonies to enrollment revocations.
“Every doctor, every health professional needs to know that there are a lot of consequences that go with our actions outside of work,” he said. “In my situation, what happened had nothing to do with medicine, it had nothing to do with patients, it had nothing to do my professional demeanor. But yet it affected my entire career, and I lost the ability to practice emergency medicine for 3 years. Three years for any doctor is a long time. Three years for emergency medicine is a lifetime.”
The physician ends up in jail
After the collision, Dr. Maag pulled over in a parking lot and dialed 911. Several passing motorists did the same. It appeared the biker was trying to get away, and Dr. Maag was concerned about the damage to his Tesla, he said.
When police arrived, they heard very different accounts of what happened. The motorcyclist and his girlfriend claimed Dr. Maag was the aggressor during the altercation, and that he deliberately tried to hit them with his vehicle. Two witnesses at the scene said they had watched Dr. Maag pursue the motorcycle in his vehicle, and that they believed he crossed into their lane intentionally to strike the motorcycle, according to police reports.
“[The motorcyclist] stated that the vehicle struck his right foot when it hit the motorcycle and that he was able to keep his balance and not lay the bike down,” Sarasota County Deputy C. Moore wrote in his report. “The motorcycle was damaged on the right side near [his] foot, verifying his story. Both victims were adamant that the defendant actually and intentionally struck the motorcycle with his car due to the previous altercation.”
Dr. Maag told officers the motorcyclist had initiated the confrontation. He acknowledged racing after the biker, but said it was the motorcyclist who hit his vehicle. In an interview, Dr. Maag disputed the witnesses’ accounts, saying that one of the witnesses was without a car and made claims to police that were impossible from her distance.
In the end, the officer believed the motorcyclist, writing in his report that the damage to the Tesla was consistent with the biker’s version of events. Dr. Maag was handcuffed and taken to the Sarasota County Jail.
“I was in shock,” he said. “When we got to the jail, they got me booked in and fingerprinted. I sat down and said [to an officer]: ‘So, when do I get to bond out?’ The guy started laughing and said: ‘You’re not going anywhere. You’re spending the night in jail, my friend.’ He said: ‘Your charge is one step below murder.’”
‘I like to drive fast’
Aside from speeding tickets, Dr. Maag said he had never been in serious trouble with the law before.
The husband and father of two has practiced emergency medicine for more 15 years, and his license has remained in good standing. Florida Department of Health records show Dr. Maag’s medical license as clear and active with no discipline cases or public complaints on file.
“I did my best for every patient that came through that door,” he said. “There were a lot of people who didn’t like my personality. I’ve said many times: ‘I’m not here to be liked. I’m here to take care of people and provide the best care possible.’ ”
Sarasota County records show that Dr. Maag has received traffic citations in the past for careless driving, unlawful speed, and failure to stop at a red light, among others. He admits to having a “lead foot,” but says he had never before been involved in a road rage incident.
“I’m not going to lie, I like to drive fast,” he said. “I like that feeling. It just seems to slow everything down for me, the faster I’m going.”
After being booked into jail that July evening in 2015, Dr. Maag called his wife to explain what happened.
“She said, ‘I can’t believe you’ve done this. I’ve told you a million times, don’t worry about how other people drive. Keep your mouth shut,’” he recalled. “I asked her to call my work and let them know I wouldn’t be coming in the next day. Until that happened, I had never missed a day of work since becoming a physician.”
After an anxious night in his jail cell, Dr. Maag lined up with the other inmates the next morning for his bond hearing. His charges included felony, aggravated battery, and felony aggravated assault with a deadly weapon. A prosecutor recommended Dr. Maag’s bond be set at $1 million, which a judge lowered to $500,000.
Michael Fayard, a criminal defense attorney who represented Dr. Maag in the case, said even with the reduction, $500,000 was an outrageous bond for such a case.
“The prosecutor’s arguments to the judge were that he was a physician driving a Tesla,” Mr. Fayard said. “That was his exact argument for charging him a higher bond. It shouldn’t have been that high. I argued he was not a flight risk. He didn’t even have a passport.”
The Florida State Attorney’s Office did not return messages seeking comment about the case.
Dr. Maag spent 2 more nights in jail while he and his wife came up with $50,000 in cash, in accordance with the 10% bond rule. In the meantime, the government put a lien on their house. A circuit court judge later agreed the bond was excessive, according to Mr. Fayard, but by that time, the $50,000 was paid and Dr. Maag was released.
New evidence lowers charges
Dr. Maag ultimately accepted a plea deal from the prosecutor’s office and pled no contest to one count of felony criminal mischief and one count of misdemeanor reckless driving. In return, the state dropped the two more serious felonies. A no-contest plea is not considered an admission of guilt.
Mr. Fayard said his investigation into the road rage victim unearthed evidence that poked holes in the motorcyclist’s credibility, and that contributed to the plea offer.
“We found tons of evidence about the kid being a hot-rodding rider on his motorcycle, videos of him traveling 140 miles an hour, popping wheelies, and darting in and out of traffic,” he said. “There was a lot of mitigation that came up during the course of the investigation.”
The plea deal was a favorable result for Dr. Maag considering his original charges, Mr. Fayard said. He added that the criminal case could have ended much differently.
“Given the facts of this case and given the fact that there were no serious injuries, we supported the state’s decision to accept our mitigation and come out with the sentence that they did,” Mr. Fayard said. “If there would have been injuries, the outcome would have likely been much worse for Dr. Maag.”
With the plea agreement reached, Dr. Maag faced his next consequence – jail time. He was sentenced to 60 days in jail, a $1,000 fine, 12 months of probation, and 8 months of house arrest. Unlike his first jail stay, Dr. Maag said the second, longer stint behind bars was more relaxing.
“It was the first time since I had become an emergency physician that I remember my dreams,” he recalled. “I had nothing to worry about, nothing to do. All I had to do was get up and eat. Every now and then, I would mop the floors because I’m kind of a clean freak, and I would talk to guys and that was it. It wasn’t bad at all.”
Dr. Maag told no one that he was a doctor because he didn’t want to be treated differently. The anonymity led to interesting tidbits from other inmates about the best pill mills in the area for example, how to make crack cocaine, and selling items for drugs. On his last day in jail, the other inmates learned from his discharge paperwork that Dr. Maag was a physician.
“One of the corrections officers said: ‘You’re a doctor? We’ve never had a doctor in here before!’” Dr. Maag remembers. “He said: ‘What did a doctor do to get into jail?’ I said: ‘Do you really want to know?’ ”
About the time that Dr. Maag was released from jail, the Florida Board of Medicine learned of his charges and began reviewing his case. Mr. Fayard presented the same facts to the board and argued for Dr. Maag to keep his license, emphasizing the offenses in which he was convicted were significantly less severe than the original felonies charged. The board agreed to dismiss the case.
“The probable cause panel for the board of medicine considered the complaint that has been filed against your client in the above referenced case,” Peter Delia, then-assistant general counsel for the Florida Department of Health, wrote in a letter dated April 27, 2016. “After careful review of all information and evidence obtained in this case, the panel determined that probable cause of a violation does not exist and directed this case to be closed.”
A short-lived celebration
Once home, Dr. Maag was on house arrest, but he was granted permission to travel for work. He continued to practice emergency medicine. After several months, authorities dropped the house arrest, and a judge canceled his probation early. It appeared the road rage incident was finally behind him.
But a year later, in 2018, the doctor received a letter from the Centers for Medicare & Medicaid Services informing him that because of his charges, his Medicare number had been revoked in November 2015.
“It took them 3 years to find me and tell me, even though I never moved,” he said. “Medicare said because I never reported this, they were hitting me up with falsification of documentation because I had signed other Medicare paperwork saying I had never been barred from Medicare, because I didn’t know that I was.”
Dr. Maag hired a different attorney to help him fight the 3-year enrollment ban. He requested reconsideration from CMS, but a hearing officer in October 2017 upheld the revocation. Because his privileges had been revoked in 2015, Dr. Maag’s practice group had to return all money billed by Dr. Maag to Medicare over the 3-year period, which totaled about $190,000.
A CMS spokeswoman declined to comment about Dr. Maag’s case, referring a reporter for this news organization to an administrative law judge’s decision that summarizes the agency’s findings.
According to the summary, in separate reconsidered determinations, the CMS hearing officer concluded that the revocation was proper under section 424.535(a)(3). The regulation, enacted in 2011, allows CMS to revoke billing privileges if a provider was convicted of a federal or state felony within the preceding 10 years that the agency determines is detrimental to the Medicare program and its beneficiaries.
The hearing officer reasoned that Dr. Maag “had been convicted of a felony that is akin to assault and, even if it were not, his actions showed a reckless disregard for the safety of others.” She concluded also that CMS could appropriately revoke Dr. Maag’s Medicare enrollment because he did not report his felony conviction within 30 days as required.
Dr. Maag went through several phases of fighting the revocation, including an appeal to the Department of Health & Human Services Departmental Appeals Board. He argued that his plea was a no-contest plea, which is not considered an admission of guilt. Dr. Maag and his attorney provided CMS a 15-page paper about his background, education, career accomplishments, and patient care history. They emphasized that Dr. Maag had never harmed or threatened a patient, and that his offense had nothing to do with his practice.
In February 2021, Judge Carolyn Cozad Hughes, an administrative law judge with CMS, upheld the 3-year revocation. In her decision, she wrote that for purposes of revocation under CMS law, “convicted” means that a judgment of conviction has been entered by a federal, state, or local court regardless of whether the judgment of conviction has been expunged or otherwise removed. She disagreed with Dr. Maag’s contention that his was a crime against property and, therefore, not akin to any of the felony offenses enumerated under the revocation section, which are crimes against persons.
“Even disregarding the allegations contained in the probable cause affidavit, Petitioner cannot escape the undisputed fact, established by his conviction and his own admissions, that the ‘property’ he so ‘willfully and maliciously’ damaged was a motorcycle traveling at a high rate of speed, and, that two young people were sitting atop that motorcycle,” Judge Hughes wrote. “Moreover, as part of the same conduct, he was charged – and convicted – of misdemeanor reckless driving with ‘willful and wanton disregard for the safety of persons or property.’ Thus, even accepting Petitioner’s description of the events, he unquestionably showed no regard for the safety of the young people on that motorcycle.”
Judge Hughes noted that, although Dr. Maag’s crimes may not be among those specified in the regulation, CMS has broad authority to determine which felonies are detrimental to the best interests of the program and its beneficiaries.
A new career path
Unable to practice emergency medicine and beset with debt, Dr. Maag spiraled into a dark depression. His family had to start using retirement money that he was saving for the future care of his son, who has autism.
“I was suicidal,” he said. “There were two times that I came very close to going out to the woods by my house and hanging myself. All I wanted was to have everything go away. My wife saved my life.”
Slowly, Dr. Maag climbed out of the despondency and began considering new career options. After working and training briefly in hair restoration, Dr. Maag became a hair transplant specialist and opened his own hair restoration practice. It was a way to practice and help patients without having to accept Medicare. Today, he is the founder of Honest Hair Restoration in Bradenton, Fla.
Hair restoration is not the type of medicine that he “was designed to do,” Dr. Maag said, but he has embraced its advantages, such as learning about the business aspects of medicine and having a slower-paced work life. The business, which opened in 2019, is doing well and growing steadily.
Earlier this month, Dr. Maag learned CMS had reinstated his Medicare billing privileges. If an opportunity arises to go back into emergency medicine or urgent care, he is open to the possibilities, he said, but he plans to continue hair restoration for now. He hopes the lessons learned from his road rage incident may help others in similar circumstances.
“If I could go back to that very moment, I would’ve just kept my window up and I wouldn’t have said anything,” Dr. Maag said. “I would’ve kept my mouth shut and gone on about my day. Would I have loved it to have never happened? Yeah, and I’d probably be starting my retirement now. Am I stronger now? Well, I’m probably a hell of a lot wiser. But when all is said and done, I don’t want anybody feeling sorry for me. It was all my doing and I have to live with the consequences.”
Mr. Fayard, the attorney, says the case is a cautionary tale for doctors.
“No one is really above the law,” he said. “There aren’t two legal systems. You can’t just pay a little money and be done. At every level, serious charges have serious ramifications for everyone involved. Law enforcement and judges are not going to care of you’re a physician and you commit a crime. But physicians have a lot more on the line than many others. They can lose their ability to practice.”
A version of this article first appeared on Medscape.com.
It was a 95° F day in July 2015, and emergency physician Martin Maag, MD, was driving down Bee Ridge Road, a busy seven-lane thoroughfare in Sarasota, Fla., on his way home from a family dinner. To distance himself from a truck blowing black smoke, Dr. Maag says he had just passed some vehicles, when a motorcycle flew past him in the turning lane and the passenger flipped him off.
“I started laughing because I knew we were coming up to a red light,” said Dr. Maag. “When we pulled up to the light, I put my window down and said: ‘Hey, you ought to be a little more careful about who you’re flipping off! You never know who it might be and what they might do.’ ”
The female passenger cursed at Dr. Maag, and the two traded profanities. The male driver then told Dr. Maag: “Get out of the car, old man,” according to Dr. Maag. Fuming, Dr. Maag got out of his black Tesla, and the two men met in the middle of the street.
“As soon as I got close enough to see him, I could tell he really looked young,” Dr. Maag recalls. “I said: ‘You’re like 12 years old. I’m going to end up beating your ass and then I’m going to go to jail. Go get on your bike, and ride home to your mom.’ I don’t remember what he said to me, but I spun around and said: ‘If you want to act like a man, meet me up the street in a parking lot and let’s have at it like men.’ ”
The motorcyclist got back on his white Suzuki and sped off, and Dr. Maag followed. Both vehicles went racing down the road, swerving between cars, and reaching speeds of 100 miles per hour, Dr. Maag said. At one point, Dr. Maag says he drove in front of the motorcyclist to slow him down, and the motorcycle clipped the back of his car. No one was seriously hurt, but soon Dr. Maag was in the back of a police cruiser headed to jail.
Dr. Maag wishes he could take back his actions that summer day 6 years ago. Those few minutes of fury have had lasting effects on the doctor’s life. The incident resulted in criminal charges, a jail sentence, thousands of dollars in legal fees, and a 3-year departure from emergency medicine. Although Dr. Maag did not lose his medical license as a result of the incident, the physician’s Medicare billing privileges were suspended because of a federal provision that ties some felonies to enrollment revocations.
“Every doctor, every health professional needs to know that there are a lot of consequences that go with our actions outside of work,” he said. “In my situation, what happened had nothing to do with medicine, it had nothing to do with patients, it had nothing to do my professional demeanor. But yet it affected my entire career, and I lost the ability to practice emergency medicine for 3 years. Three years for any doctor is a long time. Three years for emergency medicine is a lifetime.”
The physician ends up in jail
After the collision, Dr. Maag pulled over in a parking lot and dialed 911. Several passing motorists did the same. It appeared the biker was trying to get away, and Dr. Maag was concerned about the damage to his Tesla, he said.
When police arrived, they heard very different accounts of what happened. The motorcyclist and his girlfriend claimed Dr. Maag was the aggressor during the altercation, and that he deliberately tried to hit them with his vehicle. Two witnesses at the scene said they had watched Dr. Maag pursue the motorcycle in his vehicle, and that they believed he crossed into their lane intentionally to strike the motorcycle, according to police reports.
“[The motorcyclist] stated that the vehicle struck his right foot when it hit the motorcycle and that he was able to keep his balance and not lay the bike down,” Sarasota County Deputy C. Moore wrote in his report. “The motorcycle was damaged on the right side near [his] foot, verifying his story. Both victims were adamant that the defendant actually and intentionally struck the motorcycle with his car due to the previous altercation.”
Dr. Maag told officers the motorcyclist had initiated the confrontation. He acknowledged racing after the biker, but said it was the motorcyclist who hit his vehicle. In an interview, Dr. Maag disputed the witnesses’ accounts, saying that one of the witnesses was without a car and made claims to police that were impossible from her distance.
In the end, the officer believed the motorcyclist, writing in his report that the damage to the Tesla was consistent with the biker’s version of events. Dr. Maag was handcuffed and taken to the Sarasota County Jail.
“I was in shock,” he said. “When we got to the jail, they got me booked in and fingerprinted. I sat down and said [to an officer]: ‘So, when do I get to bond out?’ The guy started laughing and said: ‘You’re not going anywhere. You’re spending the night in jail, my friend.’ He said: ‘Your charge is one step below murder.’”
‘I like to drive fast’
Aside from speeding tickets, Dr. Maag said he had never been in serious trouble with the law before.
The husband and father of two has practiced emergency medicine for more 15 years, and his license has remained in good standing. Florida Department of Health records show Dr. Maag’s medical license as clear and active with no discipline cases or public complaints on file.
“I did my best for every patient that came through that door,” he said. “There were a lot of people who didn’t like my personality. I’ve said many times: ‘I’m not here to be liked. I’m here to take care of people and provide the best care possible.’ ”
Sarasota County records show that Dr. Maag has received traffic citations in the past for careless driving, unlawful speed, and failure to stop at a red light, among others. He admits to having a “lead foot,” but says he had never before been involved in a road rage incident.
“I’m not going to lie, I like to drive fast,” he said. “I like that feeling. It just seems to slow everything down for me, the faster I’m going.”
After being booked into jail that July evening in 2015, Dr. Maag called his wife to explain what happened.
“She said, ‘I can’t believe you’ve done this. I’ve told you a million times, don’t worry about how other people drive. Keep your mouth shut,’” he recalled. “I asked her to call my work and let them know I wouldn’t be coming in the next day. Until that happened, I had never missed a day of work since becoming a physician.”
After an anxious night in his jail cell, Dr. Maag lined up with the other inmates the next morning for his bond hearing. His charges included felony, aggravated battery, and felony aggravated assault with a deadly weapon. A prosecutor recommended Dr. Maag’s bond be set at $1 million, which a judge lowered to $500,000.
Michael Fayard, a criminal defense attorney who represented Dr. Maag in the case, said even with the reduction, $500,000 was an outrageous bond for such a case.
“The prosecutor’s arguments to the judge were that he was a physician driving a Tesla,” Mr. Fayard said. “That was his exact argument for charging him a higher bond. It shouldn’t have been that high. I argued he was not a flight risk. He didn’t even have a passport.”
The Florida State Attorney’s Office did not return messages seeking comment about the case.
Dr. Maag spent 2 more nights in jail while he and his wife came up with $50,000 in cash, in accordance with the 10% bond rule. In the meantime, the government put a lien on their house. A circuit court judge later agreed the bond was excessive, according to Mr. Fayard, but by that time, the $50,000 was paid and Dr. Maag was released.
New evidence lowers charges
Dr. Maag ultimately accepted a plea deal from the prosecutor’s office and pled no contest to one count of felony criminal mischief and one count of misdemeanor reckless driving. In return, the state dropped the two more serious felonies. A no-contest plea is not considered an admission of guilt.
Mr. Fayard said his investigation into the road rage victim unearthed evidence that poked holes in the motorcyclist’s credibility, and that contributed to the plea offer.
“We found tons of evidence about the kid being a hot-rodding rider on his motorcycle, videos of him traveling 140 miles an hour, popping wheelies, and darting in and out of traffic,” he said. “There was a lot of mitigation that came up during the course of the investigation.”
The plea deal was a favorable result for Dr. Maag considering his original charges, Mr. Fayard said. He added that the criminal case could have ended much differently.
“Given the facts of this case and given the fact that there were no serious injuries, we supported the state’s decision to accept our mitigation and come out with the sentence that they did,” Mr. Fayard said. “If there would have been injuries, the outcome would have likely been much worse for Dr. Maag.”
With the plea agreement reached, Dr. Maag faced his next consequence – jail time. He was sentenced to 60 days in jail, a $1,000 fine, 12 months of probation, and 8 months of house arrest. Unlike his first jail stay, Dr. Maag said the second, longer stint behind bars was more relaxing.
“It was the first time since I had become an emergency physician that I remember my dreams,” he recalled. “I had nothing to worry about, nothing to do. All I had to do was get up and eat. Every now and then, I would mop the floors because I’m kind of a clean freak, and I would talk to guys and that was it. It wasn’t bad at all.”
Dr. Maag told no one that he was a doctor because he didn’t want to be treated differently. The anonymity led to interesting tidbits from other inmates about the best pill mills in the area for example, how to make crack cocaine, and selling items for drugs. On his last day in jail, the other inmates learned from his discharge paperwork that Dr. Maag was a physician.
“One of the corrections officers said: ‘You’re a doctor? We’ve never had a doctor in here before!’” Dr. Maag remembers. “He said: ‘What did a doctor do to get into jail?’ I said: ‘Do you really want to know?’ ”
About the time that Dr. Maag was released from jail, the Florida Board of Medicine learned of his charges and began reviewing his case. Mr. Fayard presented the same facts to the board and argued for Dr. Maag to keep his license, emphasizing the offenses in which he was convicted were significantly less severe than the original felonies charged. The board agreed to dismiss the case.
“The probable cause panel for the board of medicine considered the complaint that has been filed against your client in the above referenced case,” Peter Delia, then-assistant general counsel for the Florida Department of Health, wrote in a letter dated April 27, 2016. “After careful review of all information and evidence obtained in this case, the panel determined that probable cause of a violation does not exist and directed this case to be closed.”
A short-lived celebration
Once home, Dr. Maag was on house arrest, but he was granted permission to travel for work. He continued to practice emergency medicine. After several months, authorities dropped the house arrest, and a judge canceled his probation early. It appeared the road rage incident was finally behind him.
But a year later, in 2018, the doctor received a letter from the Centers for Medicare & Medicaid Services informing him that because of his charges, his Medicare number had been revoked in November 2015.
“It took them 3 years to find me and tell me, even though I never moved,” he said. “Medicare said because I never reported this, they were hitting me up with falsification of documentation because I had signed other Medicare paperwork saying I had never been barred from Medicare, because I didn’t know that I was.”
Dr. Maag hired a different attorney to help him fight the 3-year enrollment ban. He requested reconsideration from CMS, but a hearing officer in October 2017 upheld the revocation. Because his privileges had been revoked in 2015, Dr. Maag’s practice group had to return all money billed by Dr. Maag to Medicare over the 3-year period, which totaled about $190,000.
A CMS spokeswoman declined to comment about Dr. Maag’s case, referring a reporter for this news organization to an administrative law judge’s decision that summarizes the agency’s findings.
According to the summary, in separate reconsidered determinations, the CMS hearing officer concluded that the revocation was proper under section 424.535(a)(3). The regulation, enacted in 2011, allows CMS to revoke billing privileges if a provider was convicted of a federal or state felony within the preceding 10 years that the agency determines is detrimental to the Medicare program and its beneficiaries.
The hearing officer reasoned that Dr. Maag “had been convicted of a felony that is akin to assault and, even if it were not, his actions showed a reckless disregard for the safety of others.” She concluded also that CMS could appropriately revoke Dr. Maag’s Medicare enrollment because he did not report his felony conviction within 30 days as required.
Dr. Maag went through several phases of fighting the revocation, including an appeal to the Department of Health & Human Services Departmental Appeals Board. He argued that his plea was a no-contest plea, which is not considered an admission of guilt. Dr. Maag and his attorney provided CMS a 15-page paper about his background, education, career accomplishments, and patient care history. They emphasized that Dr. Maag had never harmed or threatened a patient, and that his offense had nothing to do with his practice.
In February 2021, Judge Carolyn Cozad Hughes, an administrative law judge with CMS, upheld the 3-year revocation. In her decision, she wrote that for purposes of revocation under CMS law, “convicted” means that a judgment of conviction has been entered by a federal, state, or local court regardless of whether the judgment of conviction has been expunged or otherwise removed. She disagreed with Dr. Maag’s contention that his was a crime against property and, therefore, not akin to any of the felony offenses enumerated under the revocation section, which are crimes against persons.
“Even disregarding the allegations contained in the probable cause affidavit, Petitioner cannot escape the undisputed fact, established by his conviction and his own admissions, that the ‘property’ he so ‘willfully and maliciously’ damaged was a motorcycle traveling at a high rate of speed, and, that two young people were sitting atop that motorcycle,” Judge Hughes wrote. “Moreover, as part of the same conduct, he was charged – and convicted – of misdemeanor reckless driving with ‘willful and wanton disregard for the safety of persons or property.’ Thus, even accepting Petitioner’s description of the events, he unquestionably showed no regard for the safety of the young people on that motorcycle.”
Judge Hughes noted that, although Dr. Maag’s crimes may not be among those specified in the regulation, CMS has broad authority to determine which felonies are detrimental to the best interests of the program and its beneficiaries.
A new career path
Unable to practice emergency medicine and beset with debt, Dr. Maag spiraled into a dark depression. His family had to start using retirement money that he was saving for the future care of his son, who has autism.
“I was suicidal,” he said. “There were two times that I came very close to going out to the woods by my house and hanging myself. All I wanted was to have everything go away. My wife saved my life.”
Slowly, Dr. Maag climbed out of the despondency and began considering new career options. After working and training briefly in hair restoration, Dr. Maag became a hair transplant specialist and opened his own hair restoration practice. It was a way to practice and help patients without having to accept Medicare. Today, he is the founder of Honest Hair Restoration in Bradenton, Fla.
Hair restoration is not the type of medicine that he “was designed to do,” Dr. Maag said, but he has embraced its advantages, such as learning about the business aspects of medicine and having a slower-paced work life. The business, which opened in 2019, is doing well and growing steadily.
Earlier this month, Dr. Maag learned CMS had reinstated his Medicare billing privileges. If an opportunity arises to go back into emergency medicine or urgent care, he is open to the possibilities, he said, but he plans to continue hair restoration for now. He hopes the lessons learned from his road rage incident may help others in similar circumstances.
“If I could go back to that very moment, I would’ve just kept my window up and I wouldn’t have said anything,” Dr. Maag said. “I would’ve kept my mouth shut and gone on about my day. Would I have loved it to have never happened? Yeah, and I’d probably be starting my retirement now. Am I stronger now? Well, I’m probably a hell of a lot wiser. But when all is said and done, I don’t want anybody feeling sorry for me. It was all my doing and I have to live with the consequences.”
Mr. Fayard, the attorney, says the case is a cautionary tale for doctors.
“No one is really above the law,” he said. “There aren’t two legal systems. You can’t just pay a little money and be done. At every level, serious charges have serious ramifications for everyone involved. Law enforcement and judges are not going to care of you’re a physician and you commit a crime. But physicians have a lot more on the line than many others. They can lose their ability to practice.”
A version of this article first appeared on Medscape.com.
It was a 95° F day in July 2015, and emergency physician Martin Maag, MD, was driving down Bee Ridge Road, a busy seven-lane thoroughfare in Sarasota, Fla., on his way home from a family dinner. To distance himself from a truck blowing black smoke, Dr. Maag says he had just passed some vehicles, when a motorcycle flew past him in the turning lane and the passenger flipped him off.
“I started laughing because I knew we were coming up to a red light,” said Dr. Maag. “When we pulled up to the light, I put my window down and said: ‘Hey, you ought to be a little more careful about who you’re flipping off! You never know who it might be and what they might do.’ ”
The female passenger cursed at Dr. Maag, and the two traded profanities. The male driver then told Dr. Maag: “Get out of the car, old man,” according to Dr. Maag. Fuming, Dr. Maag got out of his black Tesla, and the two men met in the middle of the street.
“As soon as I got close enough to see him, I could tell he really looked young,” Dr. Maag recalls. “I said: ‘You’re like 12 years old. I’m going to end up beating your ass and then I’m going to go to jail. Go get on your bike, and ride home to your mom.’ I don’t remember what he said to me, but I spun around and said: ‘If you want to act like a man, meet me up the street in a parking lot and let’s have at it like men.’ ”
The motorcyclist got back on his white Suzuki and sped off, and Dr. Maag followed. Both vehicles went racing down the road, swerving between cars, and reaching speeds of 100 miles per hour, Dr. Maag said. At one point, Dr. Maag says he drove in front of the motorcyclist to slow him down, and the motorcycle clipped the back of his car. No one was seriously hurt, but soon Dr. Maag was in the back of a police cruiser headed to jail.
Dr. Maag wishes he could take back his actions that summer day 6 years ago. Those few minutes of fury have had lasting effects on the doctor’s life. The incident resulted in criminal charges, a jail sentence, thousands of dollars in legal fees, and a 3-year departure from emergency medicine. Although Dr. Maag did not lose his medical license as a result of the incident, the physician’s Medicare billing privileges were suspended because of a federal provision that ties some felonies to enrollment revocations.
“Every doctor, every health professional needs to know that there are a lot of consequences that go with our actions outside of work,” he said. “In my situation, what happened had nothing to do with medicine, it had nothing to do with patients, it had nothing to do my professional demeanor. But yet it affected my entire career, and I lost the ability to practice emergency medicine for 3 years. Three years for any doctor is a long time. Three years for emergency medicine is a lifetime.”
The physician ends up in jail
After the collision, Dr. Maag pulled over in a parking lot and dialed 911. Several passing motorists did the same. It appeared the biker was trying to get away, and Dr. Maag was concerned about the damage to his Tesla, he said.
When police arrived, they heard very different accounts of what happened. The motorcyclist and his girlfriend claimed Dr. Maag was the aggressor during the altercation, and that he deliberately tried to hit them with his vehicle. Two witnesses at the scene said they had watched Dr. Maag pursue the motorcycle in his vehicle, and that they believed he crossed into their lane intentionally to strike the motorcycle, according to police reports.
“[The motorcyclist] stated that the vehicle struck his right foot when it hit the motorcycle and that he was able to keep his balance and not lay the bike down,” Sarasota County Deputy C. Moore wrote in his report. “The motorcycle was damaged on the right side near [his] foot, verifying his story. Both victims were adamant that the defendant actually and intentionally struck the motorcycle with his car due to the previous altercation.”
Dr. Maag told officers the motorcyclist had initiated the confrontation. He acknowledged racing after the biker, but said it was the motorcyclist who hit his vehicle. In an interview, Dr. Maag disputed the witnesses’ accounts, saying that one of the witnesses was without a car and made claims to police that were impossible from her distance.
In the end, the officer believed the motorcyclist, writing in his report that the damage to the Tesla was consistent with the biker’s version of events. Dr. Maag was handcuffed and taken to the Sarasota County Jail.
“I was in shock,” he said. “When we got to the jail, they got me booked in and fingerprinted. I sat down and said [to an officer]: ‘So, when do I get to bond out?’ The guy started laughing and said: ‘You’re not going anywhere. You’re spending the night in jail, my friend.’ He said: ‘Your charge is one step below murder.’”
‘I like to drive fast’
Aside from speeding tickets, Dr. Maag said he had never been in serious trouble with the law before.
The husband and father of two has practiced emergency medicine for more 15 years, and his license has remained in good standing. Florida Department of Health records show Dr. Maag’s medical license as clear and active with no discipline cases or public complaints on file.
“I did my best for every patient that came through that door,” he said. “There were a lot of people who didn’t like my personality. I’ve said many times: ‘I’m not here to be liked. I’m here to take care of people and provide the best care possible.’ ”
Sarasota County records show that Dr. Maag has received traffic citations in the past for careless driving, unlawful speed, and failure to stop at a red light, among others. He admits to having a “lead foot,” but says he had never before been involved in a road rage incident.
“I’m not going to lie, I like to drive fast,” he said. “I like that feeling. It just seems to slow everything down for me, the faster I’m going.”
After being booked into jail that July evening in 2015, Dr. Maag called his wife to explain what happened.
“She said, ‘I can’t believe you’ve done this. I’ve told you a million times, don’t worry about how other people drive. Keep your mouth shut,’” he recalled. “I asked her to call my work and let them know I wouldn’t be coming in the next day. Until that happened, I had never missed a day of work since becoming a physician.”
After an anxious night in his jail cell, Dr. Maag lined up with the other inmates the next morning for his bond hearing. His charges included felony, aggravated battery, and felony aggravated assault with a deadly weapon. A prosecutor recommended Dr. Maag’s bond be set at $1 million, which a judge lowered to $500,000.
Michael Fayard, a criminal defense attorney who represented Dr. Maag in the case, said even with the reduction, $500,000 was an outrageous bond for such a case.
“The prosecutor’s arguments to the judge were that he was a physician driving a Tesla,” Mr. Fayard said. “That was his exact argument for charging him a higher bond. It shouldn’t have been that high. I argued he was not a flight risk. He didn’t even have a passport.”
The Florida State Attorney’s Office did not return messages seeking comment about the case.
Dr. Maag spent 2 more nights in jail while he and his wife came up with $50,000 in cash, in accordance with the 10% bond rule. In the meantime, the government put a lien on their house. A circuit court judge later agreed the bond was excessive, according to Mr. Fayard, but by that time, the $50,000 was paid and Dr. Maag was released.
New evidence lowers charges
Dr. Maag ultimately accepted a plea deal from the prosecutor’s office and pled no contest to one count of felony criminal mischief and one count of misdemeanor reckless driving. In return, the state dropped the two more serious felonies. A no-contest plea is not considered an admission of guilt.
Mr. Fayard said his investigation into the road rage victim unearthed evidence that poked holes in the motorcyclist’s credibility, and that contributed to the plea offer.
“We found tons of evidence about the kid being a hot-rodding rider on his motorcycle, videos of him traveling 140 miles an hour, popping wheelies, and darting in and out of traffic,” he said. “There was a lot of mitigation that came up during the course of the investigation.”
The plea deal was a favorable result for Dr. Maag considering his original charges, Mr. Fayard said. He added that the criminal case could have ended much differently.
“Given the facts of this case and given the fact that there were no serious injuries, we supported the state’s decision to accept our mitigation and come out with the sentence that they did,” Mr. Fayard said. “If there would have been injuries, the outcome would have likely been much worse for Dr. Maag.”
With the plea agreement reached, Dr. Maag faced his next consequence – jail time. He was sentenced to 60 days in jail, a $1,000 fine, 12 months of probation, and 8 months of house arrest. Unlike his first jail stay, Dr. Maag said the second, longer stint behind bars was more relaxing.
“It was the first time since I had become an emergency physician that I remember my dreams,” he recalled. “I had nothing to worry about, nothing to do. All I had to do was get up and eat. Every now and then, I would mop the floors because I’m kind of a clean freak, and I would talk to guys and that was it. It wasn’t bad at all.”
Dr. Maag told no one that he was a doctor because he didn’t want to be treated differently. The anonymity led to interesting tidbits from other inmates about the best pill mills in the area for example, how to make crack cocaine, and selling items for drugs. On his last day in jail, the other inmates learned from his discharge paperwork that Dr. Maag was a physician.
“One of the corrections officers said: ‘You’re a doctor? We’ve never had a doctor in here before!’” Dr. Maag remembers. “He said: ‘What did a doctor do to get into jail?’ I said: ‘Do you really want to know?’ ”
About the time that Dr. Maag was released from jail, the Florida Board of Medicine learned of his charges and began reviewing his case. Mr. Fayard presented the same facts to the board and argued for Dr. Maag to keep his license, emphasizing the offenses in which he was convicted were significantly less severe than the original felonies charged. The board agreed to dismiss the case.
“The probable cause panel for the board of medicine considered the complaint that has been filed against your client in the above referenced case,” Peter Delia, then-assistant general counsel for the Florida Department of Health, wrote in a letter dated April 27, 2016. “After careful review of all information and evidence obtained in this case, the panel determined that probable cause of a violation does not exist and directed this case to be closed.”
A short-lived celebration
Once home, Dr. Maag was on house arrest, but he was granted permission to travel for work. He continued to practice emergency medicine. After several months, authorities dropped the house arrest, and a judge canceled his probation early. It appeared the road rage incident was finally behind him.
But a year later, in 2018, the doctor received a letter from the Centers for Medicare & Medicaid Services informing him that because of his charges, his Medicare number had been revoked in November 2015.
“It took them 3 years to find me and tell me, even though I never moved,” he said. “Medicare said because I never reported this, they were hitting me up with falsification of documentation because I had signed other Medicare paperwork saying I had never been barred from Medicare, because I didn’t know that I was.”
Dr. Maag hired a different attorney to help him fight the 3-year enrollment ban. He requested reconsideration from CMS, but a hearing officer in October 2017 upheld the revocation. Because his privileges had been revoked in 2015, Dr. Maag’s practice group had to return all money billed by Dr. Maag to Medicare over the 3-year period, which totaled about $190,000.
A CMS spokeswoman declined to comment about Dr. Maag’s case, referring a reporter for this news organization to an administrative law judge’s decision that summarizes the agency’s findings.
According to the summary, in separate reconsidered determinations, the CMS hearing officer concluded that the revocation was proper under section 424.535(a)(3). The regulation, enacted in 2011, allows CMS to revoke billing privileges if a provider was convicted of a federal or state felony within the preceding 10 years that the agency determines is detrimental to the Medicare program and its beneficiaries.
The hearing officer reasoned that Dr. Maag “had been convicted of a felony that is akin to assault and, even if it were not, his actions showed a reckless disregard for the safety of others.” She concluded also that CMS could appropriately revoke Dr. Maag’s Medicare enrollment because he did not report his felony conviction within 30 days as required.
Dr. Maag went through several phases of fighting the revocation, including an appeal to the Department of Health & Human Services Departmental Appeals Board. He argued that his plea was a no-contest plea, which is not considered an admission of guilt. Dr. Maag and his attorney provided CMS a 15-page paper about his background, education, career accomplishments, and patient care history. They emphasized that Dr. Maag had never harmed or threatened a patient, and that his offense had nothing to do with his practice.
In February 2021, Judge Carolyn Cozad Hughes, an administrative law judge with CMS, upheld the 3-year revocation. In her decision, she wrote that for purposes of revocation under CMS law, “convicted” means that a judgment of conviction has been entered by a federal, state, or local court regardless of whether the judgment of conviction has been expunged or otherwise removed. She disagreed with Dr. Maag’s contention that his was a crime against property and, therefore, not akin to any of the felony offenses enumerated under the revocation section, which are crimes against persons.
“Even disregarding the allegations contained in the probable cause affidavit, Petitioner cannot escape the undisputed fact, established by his conviction and his own admissions, that the ‘property’ he so ‘willfully and maliciously’ damaged was a motorcycle traveling at a high rate of speed, and, that two young people were sitting atop that motorcycle,” Judge Hughes wrote. “Moreover, as part of the same conduct, he was charged – and convicted – of misdemeanor reckless driving with ‘willful and wanton disregard for the safety of persons or property.’ Thus, even accepting Petitioner’s description of the events, he unquestionably showed no regard for the safety of the young people on that motorcycle.”
Judge Hughes noted that, although Dr. Maag’s crimes may not be among those specified in the regulation, CMS has broad authority to determine which felonies are detrimental to the best interests of the program and its beneficiaries.
A new career path
Unable to practice emergency medicine and beset with debt, Dr. Maag spiraled into a dark depression. His family had to start using retirement money that he was saving for the future care of his son, who has autism.
“I was suicidal,” he said. “There were two times that I came very close to going out to the woods by my house and hanging myself. All I wanted was to have everything go away. My wife saved my life.”
Slowly, Dr. Maag climbed out of the despondency and began considering new career options. After working and training briefly in hair restoration, Dr. Maag became a hair transplant specialist and opened his own hair restoration practice. It was a way to practice and help patients without having to accept Medicare. Today, he is the founder of Honest Hair Restoration in Bradenton, Fla.
Hair restoration is not the type of medicine that he “was designed to do,” Dr. Maag said, but he has embraced its advantages, such as learning about the business aspects of medicine and having a slower-paced work life. The business, which opened in 2019, is doing well and growing steadily.
Earlier this month, Dr. Maag learned CMS had reinstated his Medicare billing privileges. If an opportunity arises to go back into emergency medicine or urgent care, he is open to the possibilities, he said, but he plans to continue hair restoration for now. He hopes the lessons learned from his road rage incident may help others in similar circumstances.
“If I could go back to that very moment, I would’ve just kept my window up and I wouldn’t have said anything,” Dr. Maag said. “I would’ve kept my mouth shut and gone on about my day. Would I have loved it to have never happened? Yeah, and I’d probably be starting my retirement now. Am I stronger now? Well, I’m probably a hell of a lot wiser. But when all is said and done, I don’t want anybody feeling sorry for me. It was all my doing and I have to live with the consequences.”
Mr. Fayard, the attorney, says the case is a cautionary tale for doctors.
“No one is really above the law,” he said. “There aren’t two legal systems. You can’t just pay a little money and be done. At every level, serious charges have serious ramifications for everyone involved. Law enforcement and judges are not going to care of you’re a physician and you commit a crime. But physicians have a lot more on the line than many others. They can lose their ability to practice.”
A version of this article first appeared on Medscape.com.
Bifidobacteria supplementation regulates newborn immune system
Supplementing breastfed infants with bifidobacteria promotes development of a well-regulated immune system, theoretically reducing risk of immune-mediated conditions like allergies and asthma, according to investigators.
These findings support the importance of early gut colonization with beneficial microbes, an event that may affect the immune system throughout life, reported lead author Bethany M. Henrick, PhD, director of immunology and diagnostics at Evolve Biosystems, Davis, Calif., and adjunct assistant professor at the University of Nebraska, Lincoln, and colleagues.
“Dysbiosis of the infant gut microbiome is common in modern societies and a likely contributing factor to the increased incidences of immune-mediated disorders,” the investigators wrote in Cell. “Therefore, there is great interest in identifying microbial factors that can support healthier immune system imprinting and hopefully prevent cases of allergy, autoimmunity, and possibly other conditions involving the immune system.”
Prevailing theory suggests that the rising incidence of neonatal intestinal dysbiosis – which is typical in developed countries – may be caused by a variety of factors, including cesarean sections; modern hygiene practices; antibiotics, antiseptics, and other medications; diets high in fat and sugar; and infant formula.
According to Dr. Henrick and colleagues, a healthy gut microbiome plays the greatest role in immunological development during the first 3 months post partum; specifically, a lack of bifidobacteria during this time has been linked with increased risks of autoimmunity and enteric inflammation, although underlying immune mechanisms remain unclear.
Bifidobacteria also exemplify the symbiotic relationship between mothers, babies, and beneficial microbes. The investigators pointed out that breast milk contains human milk oligosaccharides (HMOs), which humans cannot digest, but are an excellent source of energy for bifidobacteria and other beneficial microbes, giving them a “selective nutritional advantage.”
Bifidobacteria should therefore be common residents within the infant gut, but this is often not now the case, leading Dr. Henrick and colleagues to zero in on the microbe, in hopes of determining the exactly how beneficial bacteria shape immune development.
It is only recently that the necessary knowledge and techniques to perform studies like this one have become available, the investigators wrote, noting a better understanding of cell-regulatory relationships, advances in immune profiling at the systems level, and new technology that allows for profiling small-volume samples from infants.
The present study involved a series of observational experiments and a small interventional trial.
First, the investigators conducted a wide array of blood- and fecal-based longitudinal analyses from 208 infants in Sweden to characterize immune cell expansion and microbiome colonization of the gut, with a focus on bifidobacteria.
Their results showed that infants lacking bifidobacteria, and HMO-utilization genes (which are expressed by bifidobacteria and other beneficial microbes), had higher levels of systemic inflammation, including increased T helper 2 (Th2) and Th17 responses.
“Infants not colonized by Bifidobacteriaceae or in cases where these microbes fail to expand during the first months of life there is evidence of systemic and intestinal inflammation, increased frequencies of activated immune cells, and reduced levels of regulatory cells indicative of systemic immune dysregulation,” the investigators wrote.
The interventional part of the study involved 60 breastfed infants in California. Twenty-nine of the newborns were given 1.8 x 1010 colony-forming units (CFUs) of B. longum subsp. infantis EVC001 daily from postnatal day 7 to day 28, while the remaining 31 infants were given no supplementation.
Fecal samples were collected on day 6 and day 60. At day 60, supplemented infants had high levels of HMO-utilization genes, plus significantly greater alpha diversity (P = .0001; Wilcoxon), compared with controls. Infants receiving EVC001 also had less inflammatory fecal cytokines, suggesting that microbes expressing HMO-utilization genes cause a shift away from proinflammatory Th2 and Th17 responses, and toward Th1.
“It is not the simple presence of bifidobacteria that is responsible for the immune effects but the metabolic partnership between the bacteria and HMOs,” the investigators noted.
According to principal investigator Petter Brodin, MD, PhD, professor of pediatric immunology at Karolinska Institutet, Solna, Sweden, the findings deserve further investigation.
“Our data indicate that substitution with beneficial microbes efficiently metabolizing HMOs could open a way to prevent cases of immune-mediated diseases, but larger, randomized trials aimed at this will be required to determine this potential,” Dr. Brodin said in an interview.
Carolynn Dude, MD, PhD, assistant professor in the division of maternal-fetal medicine at Emory University, Atlanta, agreed that more work is needed.
“While this study provides some insight into the mechanisms that may set up a newborn for poor health outcomes later in life, the data is still very limited, and more long-term follow-up on these infants is needed before recommending any sort of bacterial supplementation to a newborn,” Dr. Dude said in an interview.
Dr. Brodin and colleagues are planning an array of related studies, including larger clinical trials; further investigations into mechanisms of action; comparisons between the present cohort and infants in Kenya, where immune-mediated diseases are rare; and evaluations of vaccine responses and infectious disease susceptibility.
The study was supported by the European Research Council, the Swedish Research Council, the Marianne & Marcus Wallenberg Foundation, and others. The investigators disclosed relationships with Cytodelics, Scailyte, Kancera, and others. Dr. Dude reported no relevant conflicts of interest.
Supplementing breastfed infants with bifidobacteria promotes development of a well-regulated immune system, theoretically reducing risk of immune-mediated conditions like allergies and asthma, according to investigators.
These findings support the importance of early gut colonization with beneficial microbes, an event that may affect the immune system throughout life, reported lead author Bethany M. Henrick, PhD, director of immunology and diagnostics at Evolve Biosystems, Davis, Calif., and adjunct assistant professor at the University of Nebraska, Lincoln, and colleagues.
“Dysbiosis of the infant gut microbiome is common in modern societies and a likely contributing factor to the increased incidences of immune-mediated disorders,” the investigators wrote in Cell. “Therefore, there is great interest in identifying microbial factors that can support healthier immune system imprinting and hopefully prevent cases of allergy, autoimmunity, and possibly other conditions involving the immune system.”
Prevailing theory suggests that the rising incidence of neonatal intestinal dysbiosis – which is typical in developed countries – may be caused by a variety of factors, including cesarean sections; modern hygiene practices; antibiotics, antiseptics, and other medications; diets high in fat and sugar; and infant formula.
According to Dr. Henrick and colleagues, a healthy gut microbiome plays the greatest role in immunological development during the first 3 months post partum; specifically, a lack of bifidobacteria during this time has been linked with increased risks of autoimmunity and enteric inflammation, although underlying immune mechanisms remain unclear.
Bifidobacteria also exemplify the symbiotic relationship between mothers, babies, and beneficial microbes. The investigators pointed out that breast milk contains human milk oligosaccharides (HMOs), which humans cannot digest, but are an excellent source of energy for bifidobacteria and other beneficial microbes, giving them a “selective nutritional advantage.”
Bifidobacteria should therefore be common residents within the infant gut, but this is often not now the case, leading Dr. Henrick and colleagues to zero in on the microbe, in hopes of determining the exactly how beneficial bacteria shape immune development.
It is only recently that the necessary knowledge and techniques to perform studies like this one have become available, the investigators wrote, noting a better understanding of cell-regulatory relationships, advances in immune profiling at the systems level, and new technology that allows for profiling small-volume samples from infants.
The present study involved a series of observational experiments and a small interventional trial.
First, the investigators conducted a wide array of blood- and fecal-based longitudinal analyses from 208 infants in Sweden to characterize immune cell expansion and microbiome colonization of the gut, with a focus on bifidobacteria.
Their results showed that infants lacking bifidobacteria, and HMO-utilization genes (which are expressed by bifidobacteria and other beneficial microbes), had higher levels of systemic inflammation, including increased T helper 2 (Th2) and Th17 responses.
“Infants not colonized by Bifidobacteriaceae or in cases where these microbes fail to expand during the first months of life there is evidence of systemic and intestinal inflammation, increased frequencies of activated immune cells, and reduced levels of regulatory cells indicative of systemic immune dysregulation,” the investigators wrote.
The interventional part of the study involved 60 breastfed infants in California. Twenty-nine of the newborns were given 1.8 x 1010 colony-forming units (CFUs) of B. longum subsp. infantis EVC001 daily from postnatal day 7 to day 28, while the remaining 31 infants were given no supplementation.
Fecal samples were collected on day 6 and day 60. At day 60, supplemented infants had high levels of HMO-utilization genes, plus significantly greater alpha diversity (P = .0001; Wilcoxon), compared with controls. Infants receiving EVC001 also had less inflammatory fecal cytokines, suggesting that microbes expressing HMO-utilization genes cause a shift away from proinflammatory Th2 and Th17 responses, and toward Th1.
“It is not the simple presence of bifidobacteria that is responsible for the immune effects but the metabolic partnership between the bacteria and HMOs,” the investigators noted.
According to principal investigator Petter Brodin, MD, PhD, professor of pediatric immunology at Karolinska Institutet, Solna, Sweden, the findings deserve further investigation.
“Our data indicate that substitution with beneficial microbes efficiently metabolizing HMOs could open a way to prevent cases of immune-mediated diseases, but larger, randomized trials aimed at this will be required to determine this potential,” Dr. Brodin said in an interview.
Carolynn Dude, MD, PhD, assistant professor in the division of maternal-fetal medicine at Emory University, Atlanta, agreed that more work is needed.
“While this study provides some insight into the mechanisms that may set up a newborn for poor health outcomes later in life, the data is still very limited, and more long-term follow-up on these infants is needed before recommending any sort of bacterial supplementation to a newborn,” Dr. Dude said in an interview.
Dr. Brodin and colleagues are planning an array of related studies, including larger clinical trials; further investigations into mechanisms of action; comparisons between the present cohort and infants in Kenya, where immune-mediated diseases are rare; and evaluations of vaccine responses and infectious disease susceptibility.
The study was supported by the European Research Council, the Swedish Research Council, the Marianne & Marcus Wallenberg Foundation, and others. The investigators disclosed relationships with Cytodelics, Scailyte, Kancera, and others. Dr. Dude reported no relevant conflicts of interest.
Supplementing breastfed infants with bifidobacteria promotes development of a well-regulated immune system, theoretically reducing risk of immune-mediated conditions like allergies and asthma, according to investigators.
These findings support the importance of early gut colonization with beneficial microbes, an event that may affect the immune system throughout life, reported lead author Bethany M. Henrick, PhD, director of immunology and diagnostics at Evolve Biosystems, Davis, Calif., and adjunct assistant professor at the University of Nebraska, Lincoln, and colleagues.
“Dysbiosis of the infant gut microbiome is common in modern societies and a likely contributing factor to the increased incidences of immune-mediated disorders,” the investigators wrote in Cell. “Therefore, there is great interest in identifying microbial factors that can support healthier immune system imprinting and hopefully prevent cases of allergy, autoimmunity, and possibly other conditions involving the immune system.”
Prevailing theory suggests that the rising incidence of neonatal intestinal dysbiosis – which is typical in developed countries – may be caused by a variety of factors, including cesarean sections; modern hygiene practices; antibiotics, antiseptics, and other medications; diets high in fat and sugar; and infant formula.
According to Dr. Henrick and colleagues, a healthy gut microbiome plays the greatest role in immunological development during the first 3 months post partum; specifically, a lack of bifidobacteria during this time has been linked with increased risks of autoimmunity and enteric inflammation, although underlying immune mechanisms remain unclear.
Bifidobacteria also exemplify the symbiotic relationship between mothers, babies, and beneficial microbes. The investigators pointed out that breast milk contains human milk oligosaccharides (HMOs), which humans cannot digest, but are an excellent source of energy for bifidobacteria and other beneficial microbes, giving them a “selective nutritional advantage.”
Bifidobacteria should therefore be common residents within the infant gut, but this is often not now the case, leading Dr. Henrick and colleagues to zero in on the microbe, in hopes of determining the exactly how beneficial bacteria shape immune development.
It is only recently that the necessary knowledge and techniques to perform studies like this one have become available, the investigators wrote, noting a better understanding of cell-regulatory relationships, advances in immune profiling at the systems level, and new technology that allows for profiling small-volume samples from infants.
The present study involved a series of observational experiments and a small interventional trial.
First, the investigators conducted a wide array of blood- and fecal-based longitudinal analyses from 208 infants in Sweden to characterize immune cell expansion and microbiome colonization of the gut, with a focus on bifidobacteria.
Their results showed that infants lacking bifidobacteria, and HMO-utilization genes (which are expressed by bifidobacteria and other beneficial microbes), had higher levels of systemic inflammation, including increased T helper 2 (Th2) and Th17 responses.
“Infants not colonized by Bifidobacteriaceae or in cases where these microbes fail to expand during the first months of life there is evidence of systemic and intestinal inflammation, increased frequencies of activated immune cells, and reduced levels of regulatory cells indicative of systemic immune dysregulation,” the investigators wrote.
The interventional part of the study involved 60 breastfed infants in California. Twenty-nine of the newborns were given 1.8 x 1010 colony-forming units (CFUs) of B. longum subsp. infantis EVC001 daily from postnatal day 7 to day 28, while the remaining 31 infants were given no supplementation.
Fecal samples were collected on day 6 and day 60. At day 60, supplemented infants had high levels of HMO-utilization genes, plus significantly greater alpha diversity (P = .0001; Wilcoxon), compared with controls. Infants receiving EVC001 also had less inflammatory fecal cytokines, suggesting that microbes expressing HMO-utilization genes cause a shift away from proinflammatory Th2 and Th17 responses, and toward Th1.
“It is not the simple presence of bifidobacteria that is responsible for the immune effects but the metabolic partnership between the bacteria and HMOs,” the investigators noted.
According to principal investigator Petter Brodin, MD, PhD, professor of pediatric immunology at Karolinska Institutet, Solna, Sweden, the findings deserve further investigation.
“Our data indicate that substitution with beneficial microbes efficiently metabolizing HMOs could open a way to prevent cases of immune-mediated diseases, but larger, randomized trials aimed at this will be required to determine this potential,” Dr. Brodin said in an interview.
Carolynn Dude, MD, PhD, assistant professor in the division of maternal-fetal medicine at Emory University, Atlanta, agreed that more work is needed.
“While this study provides some insight into the mechanisms that may set up a newborn for poor health outcomes later in life, the data is still very limited, and more long-term follow-up on these infants is needed before recommending any sort of bacterial supplementation to a newborn,” Dr. Dude said in an interview.
Dr. Brodin and colleagues are planning an array of related studies, including larger clinical trials; further investigations into mechanisms of action; comparisons between the present cohort and infants in Kenya, where immune-mediated diseases are rare; and evaluations of vaccine responses and infectious disease susceptibility.
The study was supported by the European Research Council, the Swedish Research Council, the Marianne & Marcus Wallenberg Foundation, and others. The investigators disclosed relationships with Cytodelics, Scailyte, Kancera, and others. Dr. Dude reported no relevant conflicts of interest.
FROM CELL








