User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Home-grown apps for ObGyn clerkship students
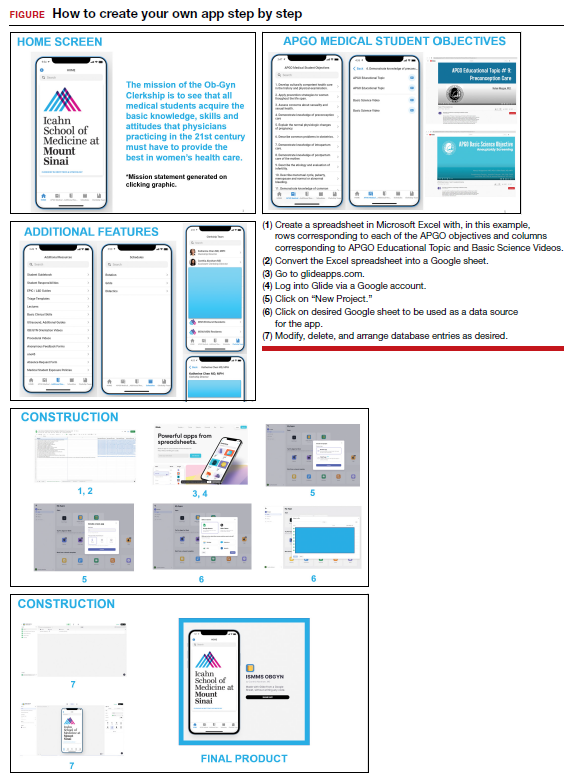
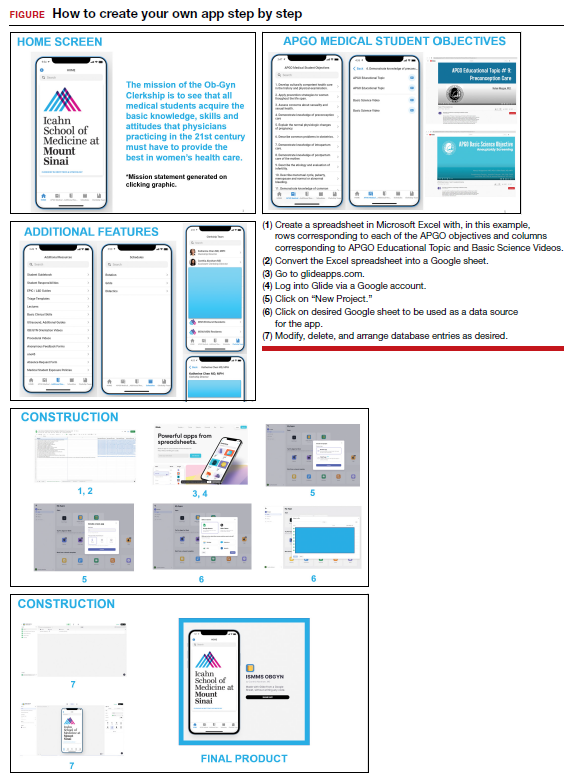
Technology has revolutionized how we access information. One example is the increased use of mobile applications (apps). On the surface, building a new app may seem a daunting and intimidating task. However, new software—such as Glide (glideapps.com)—make it easy for anyone to design, build, and launch a custom web app within hours. This software is free for basic apps but does offer an upgrade for those wanting more professional services (glide-apps.com/pro). Here, by way of example, we identify an area of need and walk the reader
through the process of making an app.
Although there are many apps aimed at educating users on different aspects of obstetrics and gynecology, few are focused on undergraduate medical education (UME). With the assistance of Glide app building software, we created an app focused on providing rapid access to resources aimed at fulfilling medical student objectives from the Association of Professors of Gynecology and Obstetrics (APGO).1 We included 16 of the APGO objectives. On clicking an objective, the user is taken to a screen with links to associated APGO Educational Topic Video and Basic Science Videos. Basic Science Video links were included in order to provide longitudinal learning between the pre-clinical and clinical years of UME. We also created a tab for additional educational resources (including excerpts from the APGO Basic Clinical Skills Curriculum).2 We eventually added two other tabs: one for clerkship schedules that allows students to organize their daily schedule and another that facilitates quick contact with members of the clerkship team. As expected, the app was well-received by our students.
The steps needed for you to make your own app are listed in the FIGURE along with accompanying images for easy navigation. ●
- Association of Professors of Gynecology and Obstetrics (APGO) Medical Student Educational Objectives, 11th ed;2019.
- Association of Professors of Gynecology and Obstetrics (APGO) Basic Clinical Skills Curriculum. Updated 2017.
Technology has revolutionized how we access information. One example is the increased use of mobile applications (apps). On the surface, building a new app may seem a daunting and intimidating task. However, new software—such as Glide (glideapps.com)—make it easy for anyone to design, build, and launch a custom web app within hours. This software is free for basic apps but does offer an upgrade for those wanting more professional services (glide-apps.com/pro). Here, by way of example, we identify an area of need and walk the reader
through the process of making an app.
Although there are many apps aimed at educating users on different aspects of obstetrics and gynecology, few are focused on undergraduate medical education (UME). With the assistance of Glide app building software, we created an app focused on providing rapid access to resources aimed at fulfilling medical student objectives from the Association of Professors of Gynecology and Obstetrics (APGO).1 We included 16 of the APGO objectives. On clicking an objective, the user is taken to a screen with links to associated APGO Educational Topic Video and Basic Science Videos. Basic Science Video links were included in order to provide longitudinal learning between the pre-clinical and clinical years of UME. We also created a tab for additional educational resources (including excerpts from the APGO Basic Clinical Skills Curriculum).2 We eventually added two other tabs: one for clerkship schedules that allows students to organize their daily schedule and another that facilitates quick contact with members of the clerkship team. As expected, the app was well-received by our students.
The steps needed for you to make your own app are listed in the FIGURE along with accompanying images for easy navigation. ●
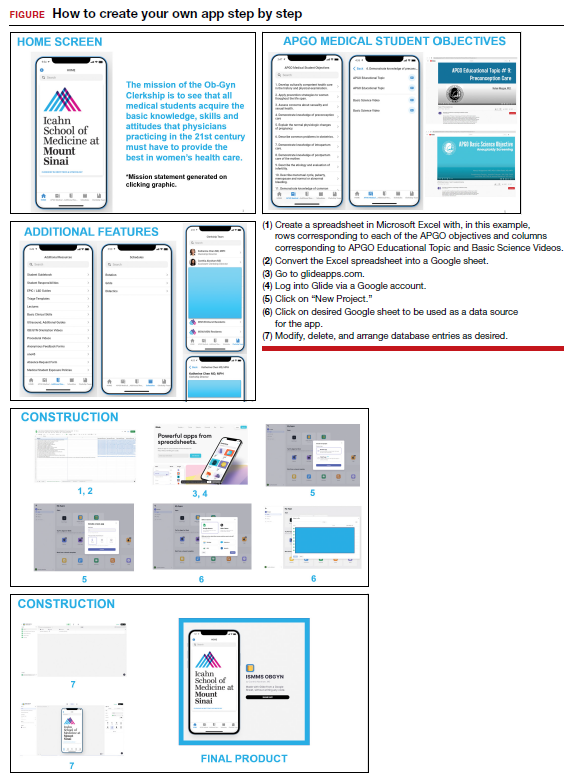
Technology has revolutionized how we access information. One example is the increased use of mobile applications (apps). On the surface, building a new app may seem a daunting and intimidating task. However, new software—such as Glide (glideapps.com)—make it easy for anyone to design, build, and launch a custom web app within hours. This software is free for basic apps but does offer an upgrade for those wanting more professional services (glide-apps.com/pro). Here, by way of example, we identify an area of need and walk the reader
through the process of making an app.
Although there are many apps aimed at educating users on different aspects of obstetrics and gynecology, few are focused on undergraduate medical education (UME). With the assistance of Glide app building software, we created an app focused on providing rapid access to resources aimed at fulfilling medical student objectives from the Association of Professors of Gynecology and Obstetrics (APGO).1 We included 16 of the APGO objectives. On clicking an objective, the user is taken to a screen with links to associated APGO Educational Topic Video and Basic Science Videos. Basic Science Video links were included in order to provide longitudinal learning between the pre-clinical and clinical years of UME. We also created a tab for additional educational resources (including excerpts from the APGO Basic Clinical Skills Curriculum).2 We eventually added two other tabs: one for clerkship schedules that allows students to organize their daily schedule and another that facilitates quick contact with members of the clerkship team. As expected, the app was well-received by our students.
The steps needed for you to make your own app are listed in the FIGURE along with accompanying images for easy navigation. ●
- Association of Professors of Gynecology and Obstetrics (APGO) Medical Student Educational Objectives, 11th ed;2019.
- Association of Professors of Gynecology and Obstetrics (APGO) Basic Clinical Skills Curriculum. Updated 2017.
- Association of Professors of Gynecology and Obstetrics (APGO) Medical Student Educational Objectives, 11th ed;2019.
- Association of Professors of Gynecology and Obstetrics (APGO) Basic Clinical Skills Curriculum. Updated 2017.
Going Beyond Hydroquinone: Alternative Skin Lightening Agents
Disorders of hyperpigmentation—melasma, postinflammatory hyperpigmentation, lichen planus pigmentosus, erythema dyschromicum perstans, and pigmented contact dermatitis, among others—are common and challenging to treat. Although they can affect individuals of all skin types, they most commonly are seen in skin of color; in fact, dyspigmentation is one of the most common chief concerns for which individuals of color see a dermatologist.1,2
For many years, hydroquinone (HQ) was one of the main options available for use as a lightening agent. Although effective, it has the risk of causing irritant dermatitis, potentially leading to further dyspigmentation, in addition to the risk of ochronosis with long-term use. It remains an important and useful treatment for pigmentary disorders, but there are numerous other lightening agents that also can be considered in the treatment of disorders of hyperpigmentation.
Herein, we provide recommendations for traditional and newer non-HQ lightening agents that can be considered when treating disorders of hyperpigmentation.
Traditional Non-HQ Lightening Agents
Retinoids—Retinoids are topical vitamin A derivatives that have been used safely and effectively for decades in the treatment of pigmentary disorders. Retinoids have multiple mechanisms of action in improving pigmentation. In addition to impeding tyrosinase induction, they inhibit pigment transfer to keratinocytes and lead to accelerated pigment loss due to epidermal shedding.3 Over-the-counter formulations include retinol, retinaldehyde, and adapalene. Prescription formulations include tretinoin and tazarotene in different strengths and vehicle formulations.4
Glycolic Acid—Glycolic acid is derived from sugarcane and is considered an α-hydroxy acid that leads to rapid desquamation of pigmented keratinocytes.5 Glycolic acid can not only be used in chemical peels but also in topical creams. It is the most common α-hydroxy acid peel and is sometimes paired with HQ and other topical lightening agents for increased penetration. Glycolic acid peels are available in concentrations of 20% to 70% and can be used at various depths. When used incorrectly, it can cause redness, burning, and even skin discoloration; however, when used at the proper concentrations and depth according to Fitzpatrick skin type, there typically are no notable adverse effects, and clinical results are favorable.
Kojic Acid—Kojic acid is a natural metabolite derived from fungi and is widely used in Asian countries. It works by inhibiting the catecholase activity of tyrosinase6 and typically is available in concentrations of 1% to 4%. A study suggested that a concentration of 1% or less typically is safe to use for prolonged periods without adverse effects. Although not more effective than HQ as a monotherapy, kojic acid has been shown to haveimproved efficacy when used in combination with other lightening agents.7
Azelaic Acid—Azelaic acid works by inhibiting tyrosinase, mitochondrial oxidoreductase activation, and DNA synthesis. It preferentially targets heavily pigmented melanocytes and possesses anti-inflammatory and antibacterial properties.8 A 20% concentration of azelaic acid was compared to HQ 4% for the treatment of melasma, and results revealed that the liposomal form of azelaic acid was considerably more tolerable than HQ 4% and also more effective.9
Licorice Extracts—Licorice extracts have been safely used in several cosmeceutical skin lightening products.10 The main active compounds in licorice root are glabridin and liquiritin, which work to disperse melanin. These compounds often are used topically at concentrations of 10% to 40%. A study by Amer and Metwalli11 found that topical liquiritin produced a reduction of pigmentary intensity, with 80% of patients showing an excellent response, which was described as no difference between the previously pigmented area and the normal skin surrounding it.
Aloesin—Aloesin is a low-molecular-weight glycoprotein found in aloe vera plants. Its mechanism of action includes competitive inhibition of the dihydroxyphenylalanine oxidation site, resulting in the inhibition of tyrosinase.12 It often is combined with arbutin for an enhanced lightening effect.
Niacinamide—Niacinamide is a form of vitamin B3 that works by suppressing the transfer of melanosomes to keratinocytes.13 In addition to its skin lightening effects, it also is photoprotective and antimicrobial, and its tolerability and safety have led to its inclusion in many cosmeceutical and prescription products.14
Ascorbic Acid—Ascorbic acid affects the monopherase activity of tyrosinase, thus reducing the synthesis of melanin. It also serves as an antioxidant in the skin by preventing the production of free radicals that can induce melanogenesis.15 Although it tends to be well tolerated with a low adverse effect profile, its relative instability and varying permeability can present a challenge. It is less effective as a monotherapy, so it often is combined with other lightening ingredients for greater efficacy.
Corticosteroids—Topical corticosteroids are anti-inflammatory and impact melanogenesis, though the mechanism of action of the latter has not been fully elucidated.16,17 Low- to mid-potency topical steroids often are used in conjunction with skin lightening products to diminish irritation and decrease inflammation.18 However, prolonged use of corticosteroids can lead to cutaneous adverse effects such as striae, hypopigmentation, and acne, as well as systemic side effects if there is sufficient absorption over time.
Soybean Extracts—Soybean extracts contain serine protease inhibitors that reduce the transfer of melanosomes into keratinocytes by inhibiting the PAR-2 (protease-activated receptor 2) pathway.19,20
Ellagic Acid—Ellagic acid is found in common plants such as eucalyptus and strawberry as well as green tea.21 It works as an antioxidant and decreases melanogenesis through inhibition of tyrosinase activity.
Paper Mulberry—Paper mulberry extract comes from the roots of the Broussonetia papyrifera tree and functions by inhibiting tyrosinase activity. It is widely used in South Africa and Europe.22
Resveratrol—Resveratrol is an ingredient extracted from Morus alba L and functions as an antimelanogentic agent by directly inhibiting tyrosinase as well as transcriptional and posttranscriptional processing of tyrosinase.23 It also holds antiproliferative, anti-inflammatory, and antioxidant properties and has widely been used for antiaging and skin lightening purposes.24
Newer Non-HQ Lightening Agents
Silymarin—Silymarin (also known as milk thistle [Silybum marianum]), is a polyphenolic flavonoid that possesses anticarcinogenic, antioxidant, and anti-inflammatory properties. It prevents melanin production in a dose-dependent manner by inhibiting levodopa (L-dopa) oxidation activity of tyrosinase and also reduces the expression of tyrosinase protein.25 In combination with vitamins C and E and hexylresorcinol, silymarin has been found to reduce the effects of photodamage, brighten skin, improve evenness and lines, as well as improve global facial appearance.26
Malassezin—Malassezin is an indole produced by Malessezia furfur yeast and has recently been investigated for melanogenesis suppression. Grimes et al27 assessed the efficacy of topical malassezin in 7 patients with facial hyperpigmentation applied twice daily for 14 weeks. Punch biopsies were taken at weeks 0, 8, 14, and 22. Biopsies from weeks 8 and 14 demonstrated reduced epidermal melanin compared to baseline in all participants; however, at 22 weeks, biopsies showed no difference in melanin content compared to baseline, indicating a temporary process induced by the malassezin.27 More clinical studies are needed to investigate this further.
N-acetyl-glucosamine—N-acetyl-glucosamine is an aminosaccharide that inhibits the glycosylation of tyrosinase as well as its function in melanogenesis.28 It is synthesized and included in topical products for wound healing, rhytides, moisturization, and pigmentation disorders.
Topical Tranexamic Acid—Tranexamic acid traditionally has been used orally for the treatment of menorrhagia but also has been found to be beneficial as a therapy for hyperpigmentation and erythema. Tranexamic acid interferes with plasmin activity, thus indirectly inhibiting melanogenesis while also inhibiting angiogenesis by targeting vascular endothelial growth factor (VEGF) receptors.29 It also leads to an increase in the levels of β-endorphin and μ-opioid receptors as well as the expression of estrogen receptor β on the surface of mast cells.30 Its oral benefit led to the development of topical formulations, typically in 2% to 5% concentrations. It has proven particularly beneficial in the treatment of melasma due to its effects on improving pigmentation, erythema, and skin barrier function.31 Topical tranexamic acid has a relatively high safety profile, with minor side effects such as transient skin irritation and erythema being reported.32
Cysteamine—Cysteamine inhibits tyrosinase, peroxidase, and chelating copper ions necessary for melanogenesis. It has proven to be effective in treating melasma and chronic severe postinflammatory hyperpigmentation when used in a 5% cream formulation.33,34 Lima et al35 were the first to compare the effects of topical cysteamine to HQ in the treatment of facial melasma. They found that the mean reduction in modified Melasma Area and Severity Index score was 24% for cysteamine and 41% for HQ after 60 days. There were no severe adverse effects with either treatment group.35
Final Thoughts
Hydroquinone remains the gold standard for treatment of hyperpigmentation; however, its side-effect profile and risk of ochronosis with long-term use has ushered in various other safe and effective skin lightening agents that can be used as monotherapies or in combination with other lightening agents. Many of these products also can be used effectively with procedural treatments such as chemical peels, lasers, and microneedling for enhanced absorption and efficacy. As newer agents are developed, additional well-designed studies will be needed to determine their safety and efficacy in different skin types as well as their role in the treatment of pigmentary disorders.
- Woolery-Lloyd H, Kammer JN. Treatment of hyperpigmentation. Semin Cutan Med Surg. 2011;30:171-175. doi:10.1016/j.sder.2011.06.004
- Desai SR. Hyperpigmentation therapy: a review. J Clin Aesthet Dermatol. 2014;7:13-17.
- Kligman AM, Willis I. A new formula for depigmenting human skin. Arch Dermatol. 1975;111:40-48.
- Kligman AM, Grove GL, Hirose R, et al. Topical tretinoin for photoaged skin. J Am Acad Dermatol. 1986;15(4 pt 2):836-859. doi:10.1016/s0190-9622(86)70242-9
- Sharad J. Glycolic acid peel therapy—a current review. Clin Cosmet Investig Dermatol. 2013;6:281-288. doi:10.2147/CCID.S34029
- Nautiyal A, Wairkar S. Management of hyperpigmentation: current treatments and emerging therapies. Pigment Cell Melanoma Res. 2021;34:1000-1014. doi:10.1111/pcmr.12986
- Saeedi M, Eslamifar M, Khezri K. Kojic acid applications in cosmetic and pharmaceutical preparations. Biomed Pharmacother. 2019;110:582-593. doi:10.1016/j.biopha.2018.12.006
- Schulte BC, Wu W, Rosen T. Azelaic acid: evidence-based update on mechanism of action and clinical application. J Drugs Dermatol. 2015;14:964-968.
- Akl EM. Liposomal azelaic acid 20% cream vs hydroquinone 4% cream as adjuvant to oral tranexamic acid in melasma: a comparative study [published online April 7, 2021]. J Dermatol Treat. doi:10.1080/09546634.2021.1905765
- Holloway VL. Ethnic cosmetic products. Dermatol Clin. 2003;21:743-749. doi:10.1016/s0733-8635(03)00089-5
- Amer M, Metwalli M. Topical liquiritin improves melasma. Int J Dermatol. 2000;39:299-301. doi:10.1046/j.1365-4362.2000.00943.x
- Jones K, Hughes J, Hong M, et al. Modulation of melanogenesis by aloesin: a competitive inhibitor of tyrosinase. Pigment Cell Res. 2002;15:335-340. doi:10.1034/j.1600-0749.2002.02014.x
- Hakozaki T, Minwalla L, Zhuang J, et al. The effect of niacinamide on reducing cutaneous pigmentation and suppression of melanosome transfer. Br J Dermatol. 2002;147:20-31. doi:10.1046/j.1365-2133.2002.04834.x
- Wohlrab J, Kreft D. Niacinamide—mechanisms of action and its topical use in dermatology. Skin Pharmacol Physiol. 2014;27:311-315. doi:10.1159/000359974
- Fitzpatrick RE, Rostan EF. Double-blind, half-face study comparing topical vitamin C and vehicle for rejuvenation of photodamage. Dermatol Surg. 2002;28:231-236. doi:10.1046/j.1524-4725.2002.01129.x
- Mehta AB, Nadkarni NJ, Patil SP, et al. Topical corticosteroids in dermatology. Indian J Dermatol Venereol Leprol. 2016;82:371-378. doi:10.4103/0378-6323.178903
- Petit L, Piérard GE. Skin-lightening products revisited. Int J Cosmet Sci. 2003;25:169-181. doi:10.1046/j.1467-2494.2003.00182.x
- Kanwar AJ, Dhar S, Kaur S. Treatment of melasma with potent topical corticosteroids. Dermatol Basel Switz. 1994;188:170. doi:10.1159/000247129
- Paine C, Sharlow E, Liebel F, et al. An alternative approach to depigmentation by soybean extracts via inhibition of the PAR-2 pathway. J Invest Dermatol. 2001;116:587-595. doi:10.1046/j.1523-1747.2001.01291.x
- Seiberg M, Paine C, Sharlow E, et al. Inhibition of melanosome transfer results in skin lightening. J Invest Dermatol. 2000;115:162-167. doi:10.1046/j.1523-1747.2000.00035.x
- Shimogaki H, Tanaka Y, Tamai H, et al. In vitro and in vivo evaluation of ellagic acid on melanogenesis inhibition. Int J Cosmet Sci. 2000;22:291-303. doi:10.1046/j.1467-2494.2000.00023.x
- Rendon MI, Gaviria JI. Review of skin-lightening agents. Dermatol Surg. 2005;31(7 pt 2):886-889; discussion 889. doi:10.1111/j.1524-4725.2005.31736
- Na JI, Shin JW, Choi HR, et al. Resveratrol as a multifunctional topical hypopigmenting agent [published online February 22, 2019]. Int J Mol Sci. 2019;20:956. doi:10.3390/ijms20040956
- Ratz-Łyko A, Arct J. Resveratrol as an active ingredient for cosmetic and dermatological applications: a review. J Cosmet Laser Ther. 2019;21:84-90. doi:10.1080/14764172.2018.1469767
- Choo SJ, Ryoo IJ, Kim YH, et al. Silymarin inhibits melanin synthesis in melanocyte cells. J Pharm Pharmacol. 2009;61:663-667. doi:10.1211/jpp/61.05.0016
- Draelos ZD, Diaz I, Cohen A, et al. A novel skin brightening topical technology. J Cosmet Dermatol. 2020;19:3280-3285. doi:10.1111/jocd.13741
- Grimes P, Bhawan J, Howell M, et al. Histopathological changes induced by malassezin: a novel natural microbiome indole for treatment of facial hyperpigmentation. J Drugs Dermatol. 2022;21:141-145. doi:10.36849/jdd.6596
- Bissett DL. Glucosamine: an ingredient with skin and other benefits. J Cosmet Dermatol. 2006;5:309-315. doi:10.1111/j.1473-2165.2006.00277.x
- Zhu JW, Ni YJ, Tong XY, et al. Tranexamic acid inhibits angiogenesis and melanogenesis in vitro by targeting VEGF receptors. Int J Med Sci. 2020;17:903-911. doi:10.7150/ijms.44188
- Hiramoto K, Yamate Y, Sugiyama D, et al. Tranexamic acid inhibits the plasma and non-irradiated skin markers of photoaging induced by long-term UVA eye irradiation in female mice. Biomed Pharmacother. 2018;107:54-58. doi:10.1016/j.biopha.2018.07.146
- da Silva Souza ID, Lampe L, Winn D. New topical tranexamic acid derivative for the improvement of hyperpigmentation and inflammation in the sun-damaged skin. J Cosmet Dermatol. 2021;20:561-565. doi:10.1111/jocd.13545
- Kim HJ, Moon SH, Cho SH, et al. Efficacy and safety of tranexamic acid in melasma: a meta-analysis and systematic review. Acta Derm Venereol. 2017;97:776-781. doi:10.2340/00015555-2668
- Mathe N, Balogun M, Yoo J. A case report on the use of topical cysteamine 5% cream in the management of refractory postinflammatory hyperpigmentation (PIH) resistant to triple combination cream (hydroquinone, topical corticosteroids, and retinoids). J Cosmet Dermatol. 2021;20:204-206. doi:10.1111/jocd.13755
- Mansouri P, Farshi S, Hashemi Z, et al. Evaluation of the efficacy of cysteamine 5% cream in the treatment of epidermal melasma: a randomized double-blind placebo-controlled trial. Br J Dermatol. 2015;173:209-217. doi:10.1111/bjd.13424
- Lima PB, Dias JAF, Cassiano D, et al. A comparative study of topical 5% cysteamine versus 4% hydroquinone in the treatment of facial melasma in women. Int J Dermatol. 2020;59:1531-1536. doi:10.1111/ijd.15146
Disorders of hyperpigmentation—melasma, postinflammatory hyperpigmentation, lichen planus pigmentosus, erythema dyschromicum perstans, and pigmented contact dermatitis, among others—are common and challenging to treat. Although they can affect individuals of all skin types, they most commonly are seen in skin of color; in fact, dyspigmentation is one of the most common chief concerns for which individuals of color see a dermatologist.1,2
For many years, hydroquinone (HQ) was one of the main options available for use as a lightening agent. Although effective, it has the risk of causing irritant dermatitis, potentially leading to further dyspigmentation, in addition to the risk of ochronosis with long-term use. It remains an important and useful treatment for pigmentary disorders, but there are numerous other lightening agents that also can be considered in the treatment of disorders of hyperpigmentation.
Herein, we provide recommendations for traditional and newer non-HQ lightening agents that can be considered when treating disorders of hyperpigmentation.
Traditional Non-HQ Lightening Agents
Retinoids—Retinoids are topical vitamin A derivatives that have been used safely and effectively for decades in the treatment of pigmentary disorders. Retinoids have multiple mechanisms of action in improving pigmentation. In addition to impeding tyrosinase induction, they inhibit pigment transfer to keratinocytes and lead to accelerated pigment loss due to epidermal shedding.3 Over-the-counter formulations include retinol, retinaldehyde, and adapalene. Prescription formulations include tretinoin and tazarotene in different strengths and vehicle formulations.4
Glycolic Acid—Glycolic acid is derived from sugarcane and is considered an α-hydroxy acid that leads to rapid desquamation of pigmented keratinocytes.5 Glycolic acid can not only be used in chemical peels but also in topical creams. It is the most common α-hydroxy acid peel and is sometimes paired with HQ and other topical lightening agents for increased penetration. Glycolic acid peels are available in concentrations of 20% to 70% and can be used at various depths. When used incorrectly, it can cause redness, burning, and even skin discoloration; however, when used at the proper concentrations and depth according to Fitzpatrick skin type, there typically are no notable adverse effects, and clinical results are favorable.
Kojic Acid—Kojic acid is a natural metabolite derived from fungi and is widely used in Asian countries. It works by inhibiting the catecholase activity of tyrosinase6 and typically is available in concentrations of 1% to 4%. A study suggested that a concentration of 1% or less typically is safe to use for prolonged periods without adverse effects. Although not more effective than HQ as a monotherapy, kojic acid has been shown to haveimproved efficacy when used in combination with other lightening agents.7
Azelaic Acid—Azelaic acid works by inhibiting tyrosinase, mitochondrial oxidoreductase activation, and DNA synthesis. It preferentially targets heavily pigmented melanocytes and possesses anti-inflammatory and antibacterial properties.8 A 20% concentration of azelaic acid was compared to HQ 4% for the treatment of melasma, and results revealed that the liposomal form of azelaic acid was considerably more tolerable than HQ 4% and also more effective.9
Licorice Extracts—Licorice extracts have been safely used in several cosmeceutical skin lightening products.10 The main active compounds in licorice root are glabridin and liquiritin, which work to disperse melanin. These compounds often are used topically at concentrations of 10% to 40%. A study by Amer and Metwalli11 found that topical liquiritin produced a reduction of pigmentary intensity, with 80% of patients showing an excellent response, which was described as no difference between the previously pigmented area and the normal skin surrounding it.
Aloesin—Aloesin is a low-molecular-weight glycoprotein found in aloe vera plants. Its mechanism of action includes competitive inhibition of the dihydroxyphenylalanine oxidation site, resulting in the inhibition of tyrosinase.12 It often is combined with arbutin for an enhanced lightening effect.
Niacinamide—Niacinamide is a form of vitamin B3 that works by suppressing the transfer of melanosomes to keratinocytes.13 In addition to its skin lightening effects, it also is photoprotective and antimicrobial, and its tolerability and safety have led to its inclusion in many cosmeceutical and prescription products.14
Ascorbic Acid—Ascorbic acid affects the monopherase activity of tyrosinase, thus reducing the synthesis of melanin. It also serves as an antioxidant in the skin by preventing the production of free radicals that can induce melanogenesis.15 Although it tends to be well tolerated with a low adverse effect profile, its relative instability and varying permeability can present a challenge. It is less effective as a monotherapy, so it often is combined with other lightening ingredients for greater efficacy.
Corticosteroids—Topical corticosteroids are anti-inflammatory and impact melanogenesis, though the mechanism of action of the latter has not been fully elucidated.16,17 Low- to mid-potency topical steroids often are used in conjunction with skin lightening products to diminish irritation and decrease inflammation.18 However, prolonged use of corticosteroids can lead to cutaneous adverse effects such as striae, hypopigmentation, and acne, as well as systemic side effects if there is sufficient absorption over time.
Soybean Extracts—Soybean extracts contain serine protease inhibitors that reduce the transfer of melanosomes into keratinocytes by inhibiting the PAR-2 (protease-activated receptor 2) pathway.19,20
Ellagic Acid—Ellagic acid is found in common plants such as eucalyptus and strawberry as well as green tea.21 It works as an antioxidant and decreases melanogenesis through inhibition of tyrosinase activity.
Paper Mulberry—Paper mulberry extract comes from the roots of the Broussonetia papyrifera tree and functions by inhibiting tyrosinase activity. It is widely used in South Africa and Europe.22
Resveratrol—Resveratrol is an ingredient extracted from Morus alba L and functions as an antimelanogentic agent by directly inhibiting tyrosinase as well as transcriptional and posttranscriptional processing of tyrosinase.23 It also holds antiproliferative, anti-inflammatory, and antioxidant properties and has widely been used for antiaging and skin lightening purposes.24
Newer Non-HQ Lightening Agents
Silymarin—Silymarin (also known as milk thistle [Silybum marianum]), is a polyphenolic flavonoid that possesses anticarcinogenic, antioxidant, and anti-inflammatory properties. It prevents melanin production in a dose-dependent manner by inhibiting levodopa (L-dopa) oxidation activity of tyrosinase and also reduces the expression of tyrosinase protein.25 In combination with vitamins C and E and hexylresorcinol, silymarin has been found to reduce the effects of photodamage, brighten skin, improve evenness and lines, as well as improve global facial appearance.26
Malassezin—Malassezin is an indole produced by Malessezia furfur yeast and has recently been investigated for melanogenesis suppression. Grimes et al27 assessed the efficacy of topical malassezin in 7 patients with facial hyperpigmentation applied twice daily for 14 weeks. Punch biopsies were taken at weeks 0, 8, 14, and 22. Biopsies from weeks 8 and 14 demonstrated reduced epidermal melanin compared to baseline in all participants; however, at 22 weeks, biopsies showed no difference in melanin content compared to baseline, indicating a temporary process induced by the malassezin.27 More clinical studies are needed to investigate this further.
N-acetyl-glucosamine—N-acetyl-glucosamine is an aminosaccharide that inhibits the glycosylation of tyrosinase as well as its function in melanogenesis.28 It is synthesized and included in topical products for wound healing, rhytides, moisturization, and pigmentation disorders.
Topical Tranexamic Acid—Tranexamic acid traditionally has been used orally for the treatment of menorrhagia but also has been found to be beneficial as a therapy for hyperpigmentation and erythema. Tranexamic acid interferes with plasmin activity, thus indirectly inhibiting melanogenesis while also inhibiting angiogenesis by targeting vascular endothelial growth factor (VEGF) receptors.29 It also leads to an increase in the levels of β-endorphin and μ-opioid receptors as well as the expression of estrogen receptor β on the surface of mast cells.30 Its oral benefit led to the development of topical formulations, typically in 2% to 5% concentrations. It has proven particularly beneficial in the treatment of melasma due to its effects on improving pigmentation, erythema, and skin barrier function.31 Topical tranexamic acid has a relatively high safety profile, with minor side effects such as transient skin irritation and erythema being reported.32
Cysteamine—Cysteamine inhibits tyrosinase, peroxidase, and chelating copper ions necessary for melanogenesis. It has proven to be effective in treating melasma and chronic severe postinflammatory hyperpigmentation when used in a 5% cream formulation.33,34 Lima et al35 were the first to compare the effects of topical cysteamine to HQ in the treatment of facial melasma. They found that the mean reduction in modified Melasma Area and Severity Index score was 24% for cysteamine and 41% for HQ after 60 days. There were no severe adverse effects with either treatment group.35
Final Thoughts
Hydroquinone remains the gold standard for treatment of hyperpigmentation; however, its side-effect profile and risk of ochronosis with long-term use has ushered in various other safe and effective skin lightening agents that can be used as monotherapies or in combination with other lightening agents. Many of these products also can be used effectively with procedural treatments such as chemical peels, lasers, and microneedling for enhanced absorption and efficacy. As newer agents are developed, additional well-designed studies will be needed to determine their safety and efficacy in different skin types as well as their role in the treatment of pigmentary disorders.
Disorders of hyperpigmentation—melasma, postinflammatory hyperpigmentation, lichen planus pigmentosus, erythema dyschromicum perstans, and pigmented contact dermatitis, among others—are common and challenging to treat. Although they can affect individuals of all skin types, they most commonly are seen in skin of color; in fact, dyspigmentation is one of the most common chief concerns for which individuals of color see a dermatologist.1,2
For many years, hydroquinone (HQ) was one of the main options available for use as a lightening agent. Although effective, it has the risk of causing irritant dermatitis, potentially leading to further dyspigmentation, in addition to the risk of ochronosis with long-term use. It remains an important and useful treatment for pigmentary disorders, but there are numerous other lightening agents that also can be considered in the treatment of disorders of hyperpigmentation.
Herein, we provide recommendations for traditional and newer non-HQ lightening agents that can be considered when treating disorders of hyperpigmentation.
Traditional Non-HQ Lightening Agents
Retinoids—Retinoids are topical vitamin A derivatives that have been used safely and effectively for decades in the treatment of pigmentary disorders. Retinoids have multiple mechanisms of action in improving pigmentation. In addition to impeding tyrosinase induction, they inhibit pigment transfer to keratinocytes and lead to accelerated pigment loss due to epidermal shedding.3 Over-the-counter formulations include retinol, retinaldehyde, and adapalene. Prescription formulations include tretinoin and tazarotene in different strengths and vehicle formulations.4
Glycolic Acid—Glycolic acid is derived from sugarcane and is considered an α-hydroxy acid that leads to rapid desquamation of pigmented keratinocytes.5 Glycolic acid can not only be used in chemical peels but also in topical creams. It is the most common α-hydroxy acid peel and is sometimes paired with HQ and other topical lightening agents for increased penetration. Glycolic acid peels are available in concentrations of 20% to 70% and can be used at various depths. When used incorrectly, it can cause redness, burning, and even skin discoloration; however, when used at the proper concentrations and depth according to Fitzpatrick skin type, there typically are no notable adverse effects, and clinical results are favorable.
Kojic Acid—Kojic acid is a natural metabolite derived from fungi and is widely used in Asian countries. It works by inhibiting the catecholase activity of tyrosinase6 and typically is available in concentrations of 1% to 4%. A study suggested that a concentration of 1% or less typically is safe to use for prolonged periods without adverse effects. Although not more effective than HQ as a monotherapy, kojic acid has been shown to haveimproved efficacy when used in combination with other lightening agents.7
Azelaic Acid—Azelaic acid works by inhibiting tyrosinase, mitochondrial oxidoreductase activation, and DNA synthesis. It preferentially targets heavily pigmented melanocytes and possesses anti-inflammatory and antibacterial properties.8 A 20% concentration of azelaic acid was compared to HQ 4% for the treatment of melasma, and results revealed that the liposomal form of azelaic acid was considerably more tolerable than HQ 4% and also more effective.9
Licorice Extracts—Licorice extracts have been safely used in several cosmeceutical skin lightening products.10 The main active compounds in licorice root are glabridin and liquiritin, which work to disperse melanin. These compounds often are used topically at concentrations of 10% to 40%. A study by Amer and Metwalli11 found that topical liquiritin produced a reduction of pigmentary intensity, with 80% of patients showing an excellent response, which was described as no difference between the previously pigmented area and the normal skin surrounding it.
Aloesin—Aloesin is a low-molecular-weight glycoprotein found in aloe vera plants. Its mechanism of action includes competitive inhibition of the dihydroxyphenylalanine oxidation site, resulting in the inhibition of tyrosinase.12 It often is combined with arbutin for an enhanced lightening effect.
Niacinamide—Niacinamide is a form of vitamin B3 that works by suppressing the transfer of melanosomes to keratinocytes.13 In addition to its skin lightening effects, it also is photoprotective and antimicrobial, and its tolerability and safety have led to its inclusion in many cosmeceutical and prescription products.14
Ascorbic Acid—Ascorbic acid affects the monopherase activity of tyrosinase, thus reducing the synthesis of melanin. It also serves as an antioxidant in the skin by preventing the production of free radicals that can induce melanogenesis.15 Although it tends to be well tolerated with a low adverse effect profile, its relative instability and varying permeability can present a challenge. It is less effective as a monotherapy, so it often is combined with other lightening ingredients for greater efficacy.
Corticosteroids—Topical corticosteroids are anti-inflammatory and impact melanogenesis, though the mechanism of action of the latter has not been fully elucidated.16,17 Low- to mid-potency topical steroids often are used in conjunction with skin lightening products to diminish irritation and decrease inflammation.18 However, prolonged use of corticosteroids can lead to cutaneous adverse effects such as striae, hypopigmentation, and acne, as well as systemic side effects if there is sufficient absorption over time.
Soybean Extracts—Soybean extracts contain serine protease inhibitors that reduce the transfer of melanosomes into keratinocytes by inhibiting the PAR-2 (protease-activated receptor 2) pathway.19,20
Ellagic Acid—Ellagic acid is found in common plants such as eucalyptus and strawberry as well as green tea.21 It works as an antioxidant and decreases melanogenesis through inhibition of tyrosinase activity.
Paper Mulberry—Paper mulberry extract comes from the roots of the Broussonetia papyrifera tree and functions by inhibiting tyrosinase activity. It is widely used in South Africa and Europe.22
Resveratrol—Resveratrol is an ingredient extracted from Morus alba L and functions as an antimelanogentic agent by directly inhibiting tyrosinase as well as transcriptional and posttranscriptional processing of tyrosinase.23 It also holds antiproliferative, anti-inflammatory, and antioxidant properties and has widely been used for antiaging and skin lightening purposes.24
Newer Non-HQ Lightening Agents
Silymarin—Silymarin (also known as milk thistle [Silybum marianum]), is a polyphenolic flavonoid that possesses anticarcinogenic, antioxidant, and anti-inflammatory properties. It prevents melanin production in a dose-dependent manner by inhibiting levodopa (L-dopa) oxidation activity of tyrosinase and also reduces the expression of tyrosinase protein.25 In combination with vitamins C and E and hexylresorcinol, silymarin has been found to reduce the effects of photodamage, brighten skin, improve evenness and lines, as well as improve global facial appearance.26
Malassezin—Malassezin is an indole produced by Malessezia furfur yeast and has recently been investigated for melanogenesis suppression. Grimes et al27 assessed the efficacy of topical malassezin in 7 patients with facial hyperpigmentation applied twice daily for 14 weeks. Punch biopsies were taken at weeks 0, 8, 14, and 22. Biopsies from weeks 8 and 14 demonstrated reduced epidermal melanin compared to baseline in all participants; however, at 22 weeks, biopsies showed no difference in melanin content compared to baseline, indicating a temporary process induced by the malassezin.27 More clinical studies are needed to investigate this further.
N-acetyl-glucosamine—N-acetyl-glucosamine is an aminosaccharide that inhibits the glycosylation of tyrosinase as well as its function in melanogenesis.28 It is synthesized and included in topical products for wound healing, rhytides, moisturization, and pigmentation disorders.
Topical Tranexamic Acid—Tranexamic acid traditionally has been used orally for the treatment of menorrhagia but also has been found to be beneficial as a therapy for hyperpigmentation and erythema. Tranexamic acid interferes with plasmin activity, thus indirectly inhibiting melanogenesis while also inhibiting angiogenesis by targeting vascular endothelial growth factor (VEGF) receptors.29 It also leads to an increase in the levels of β-endorphin and μ-opioid receptors as well as the expression of estrogen receptor β on the surface of mast cells.30 Its oral benefit led to the development of topical formulations, typically in 2% to 5% concentrations. It has proven particularly beneficial in the treatment of melasma due to its effects on improving pigmentation, erythema, and skin barrier function.31 Topical tranexamic acid has a relatively high safety profile, with minor side effects such as transient skin irritation and erythema being reported.32
Cysteamine—Cysteamine inhibits tyrosinase, peroxidase, and chelating copper ions necessary for melanogenesis. It has proven to be effective in treating melasma and chronic severe postinflammatory hyperpigmentation when used in a 5% cream formulation.33,34 Lima et al35 were the first to compare the effects of topical cysteamine to HQ in the treatment of facial melasma. They found that the mean reduction in modified Melasma Area and Severity Index score was 24% for cysteamine and 41% for HQ after 60 days. There were no severe adverse effects with either treatment group.35
Final Thoughts
Hydroquinone remains the gold standard for treatment of hyperpigmentation; however, its side-effect profile and risk of ochronosis with long-term use has ushered in various other safe and effective skin lightening agents that can be used as monotherapies or in combination with other lightening agents. Many of these products also can be used effectively with procedural treatments such as chemical peels, lasers, and microneedling for enhanced absorption and efficacy. As newer agents are developed, additional well-designed studies will be needed to determine their safety and efficacy in different skin types as well as their role in the treatment of pigmentary disorders.
- Woolery-Lloyd H, Kammer JN. Treatment of hyperpigmentation. Semin Cutan Med Surg. 2011;30:171-175. doi:10.1016/j.sder.2011.06.004
- Desai SR. Hyperpigmentation therapy: a review. J Clin Aesthet Dermatol. 2014;7:13-17.
- Kligman AM, Willis I. A new formula for depigmenting human skin. Arch Dermatol. 1975;111:40-48.
- Kligman AM, Grove GL, Hirose R, et al. Topical tretinoin for photoaged skin. J Am Acad Dermatol. 1986;15(4 pt 2):836-859. doi:10.1016/s0190-9622(86)70242-9
- Sharad J. Glycolic acid peel therapy—a current review. Clin Cosmet Investig Dermatol. 2013;6:281-288. doi:10.2147/CCID.S34029
- Nautiyal A, Wairkar S. Management of hyperpigmentation: current treatments and emerging therapies. Pigment Cell Melanoma Res. 2021;34:1000-1014. doi:10.1111/pcmr.12986
- Saeedi M, Eslamifar M, Khezri K. Kojic acid applications in cosmetic and pharmaceutical preparations. Biomed Pharmacother. 2019;110:582-593. doi:10.1016/j.biopha.2018.12.006
- Schulte BC, Wu W, Rosen T. Azelaic acid: evidence-based update on mechanism of action and clinical application. J Drugs Dermatol. 2015;14:964-968.
- Akl EM. Liposomal azelaic acid 20% cream vs hydroquinone 4% cream as adjuvant to oral tranexamic acid in melasma: a comparative study [published online April 7, 2021]. J Dermatol Treat. doi:10.1080/09546634.2021.1905765
- Holloway VL. Ethnic cosmetic products. Dermatol Clin. 2003;21:743-749. doi:10.1016/s0733-8635(03)00089-5
- Amer M, Metwalli M. Topical liquiritin improves melasma. Int J Dermatol. 2000;39:299-301. doi:10.1046/j.1365-4362.2000.00943.x
- Jones K, Hughes J, Hong M, et al. Modulation of melanogenesis by aloesin: a competitive inhibitor of tyrosinase. Pigment Cell Res. 2002;15:335-340. doi:10.1034/j.1600-0749.2002.02014.x
- Hakozaki T, Minwalla L, Zhuang J, et al. The effect of niacinamide on reducing cutaneous pigmentation and suppression of melanosome transfer. Br J Dermatol. 2002;147:20-31. doi:10.1046/j.1365-2133.2002.04834.x
- Wohlrab J, Kreft D. Niacinamide—mechanisms of action and its topical use in dermatology. Skin Pharmacol Physiol. 2014;27:311-315. doi:10.1159/000359974
- Fitzpatrick RE, Rostan EF. Double-blind, half-face study comparing topical vitamin C and vehicle for rejuvenation of photodamage. Dermatol Surg. 2002;28:231-236. doi:10.1046/j.1524-4725.2002.01129.x
- Mehta AB, Nadkarni NJ, Patil SP, et al. Topical corticosteroids in dermatology. Indian J Dermatol Venereol Leprol. 2016;82:371-378. doi:10.4103/0378-6323.178903
- Petit L, Piérard GE. Skin-lightening products revisited. Int J Cosmet Sci. 2003;25:169-181. doi:10.1046/j.1467-2494.2003.00182.x
- Kanwar AJ, Dhar S, Kaur S. Treatment of melasma with potent topical corticosteroids. Dermatol Basel Switz. 1994;188:170. doi:10.1159/000247129
- Paine C, Sharlow E, Liebel F, et al. An alternative approach to depigmentation by soybean extracts via inhibition of the PAR-2 pathway. J Invest Dermatol. 2001;116:587-595. doi:10.1046/j.1523-1747.2001.01291.x
- Seiberg M, Paine C, Sharlow E, et al. Inhibition of melanosome transfer results in skin lightening. J Invest Dermatol. 2000;115:162-167. doi:10.1046/j.1523-1747.2000.00035.x
- Shimogaki H, Tanaka Y, Tamai H, et al. In vitro and in vivo evaluation of ellagic acid on melanogenesis inhibition. Int J Cosmet Sci. 2000;22:291-303. doi:10.1046/j.1467-2494.2000.00023.x
- Rendon MI, Gaviria JI. Review of skin-lightening agents. Dermatol Surg. 2005;31(7 pt 2):886-889; discussion 889. doi:10.1111/j.1524-4725.2005.31736
- Na JI, Shin JW, Choi HR, et al. Resveratrol as a multifunctional topical hypopigmenting agent [published online February 22, 2019]. Int J Mol Sci. 2019;20:956. doi:10.3390/ijms20040956
- Ratz-Łyko A, Arct J. Resveratrol as an active ingredient for cosmetic and dermatological applications: a review. J Cosmet Laser Ther. 2019;21:84-90. doi:10.1080/14764172.2018.1469767
- Choo SJ, Ryoo IJ, Kim YH, et al. Silymarin inhibits melanin synthesis in melanocyte cells. J Pharm Pharmacol. 2009;61:663-667. doi:10.1211/jpp/61.05.0016
- Draelos ZD, Diaz I, Cohen A, et al. A novel skin brightening topical technology. J Cosmet Dermatol. 2020;19:3280-3285. doi:10.1111/jocd.13741
- Grimes P, Bhawan J, Howell M, et al. Histopathological changes induced by malassezin: a novel natural microbiome indole for treatment of facial hyperpigmentation. J Drugs Dermatol. 2022;21:141-145. doi:10.36849/jdd.6596
- Bissett DL. Glucosamine: an ingredient with skin and other benefits. J Cosmet Dermatol. 2006;5:309-315. doi:10.1111/j.1473-2165.2006.00277.x
- Zhu JW, Ni YJ, Tong XY, et al. Tranexamic acid inhibits angiogenesis and melanogenesis in vitro by targeting VEGF receptors. Int J Med Sci. 2020;17:903-911. doi:10.7150/ijms.44188
- Hiramoto K, Yamate Y, Sugiyama D, et al. Tranexamic acid inhibits the plasma and non-irradiated skin markers of photoaging induced by long-term UVA eye irradiation in female mice. Biomed Pharmacother. 2018;107:54-58. doi:10.1016/j.biopha.2018.07.146
- da Silva Souza ID, Lampe L, Winn D. New topical tranexamic acid derivative for the improvement of hyperpigmentation and inflammation in the sun-damaged skin. J Cosmet Dermatol. 2021;20:561-565. doi:10.1111/jocd.13545
- Kim HJ, Moon SH, Cho SH, et al. Efficacy and safety of tranexamic acid in melasma: a meta-analysis and systematic review. Acta Derm Venereol. 2017;97:776-781. doi:10.2340/00015555-2668
- Mathe N, Balogun M, Yoo J. A case report on the use of topical cysteamine 5% cream in the management of refractory postinflammatory hyperpigmentation (PIH) resistant to triple combination cream (hydroquinone, topical corticosteroids, and retinoids). J Cosmet Dermatol. 2021;20:204-206. doi:10.1111/jocd.13755
- Mansouri P, Farshi S, Hashemi Z, et al. Evaluation of the efficacy of cysteamine 5% cream in the treatment of epidermal melasma: a randomized double-blind placebo-controlled trial. Br J Dermatol. 2015;173:209-217. doi:10.1111/bjd.13424
- Lima PB, Dias JAF, Cassiano D, et al. A comparative study of topical 5% cysteamine versus 4% hydroquinone in the treatment of facial melasma in women. Int J Dermatol. 2020;59:1531-1536. doi:10.1111/ijd.15146
- Woolery-Lloyd H, Kammer JN. Treatment of hyperpigmentation. Semin Cutan Med Surg. 2011;30:171-175. doi:10.1016/j.sder.2011.06.004
- Desai SR. Hyperpigmentation therapy: a review. J Clin Aesthet Dermatol. 2014;7:13-17.
- Kligman AM, Willis I. A new formula for depigmenting human skin. Arch Dermatol. 1975;111:40-48.
- Kligman AM, Grove GL, Hirose R, et al. Topical tretinoin for photoaged skin. J Am Acad Dermatol. 1986;15(4 pt 2):836-859. doi:10.1016/s0190-9622(86)70242-9
- Sharad J. Glycolic acid peel therapy—a current review. Clin Cosmet Investig Dermatol. 2013;6:281-288. doi:10.2147/CCID.S34029
- Nautiyal A, Wairkar S. Management of hyperpigmentation: current treatments and emerging therapies. Pigment Cell Melanoma Res. 2021;34:1000-1014. doi:10.1111/pcmr.12986
- Saeedi M, Eslamifar M, Khezri K. Kojic acid applications in cosmetic and pharmaceutical preparations. Biomed Pharmacother. 2019;110:582-593. doi:10.1016/j.biopha.2018.12.006
- Schulte BC, Wu W, Rosen T. Azelaic acid: evidence-based update on mechanism of action and clinical application. J Drugs Dermatol. 2015;14:964-968.
- Akl EM. Liposomal azelaic acid 20% cream vs hydroquinone 4% cream as adjuvant to oral tranexamic acid in melasma: a comparative study [published online April 7, 2021]. J Dermatol Treat. doi:10.1080/09546634.2021.1905765
- Holloway VL. Ethnic cosmetic products. Dermatol Clin. 2003;21:743-749. doi:10.1016/s0733-8635(03)00089-5
- Amer M, Metwalli M. Topical liquiritin improves melasma. Int J Dermatol. 2000;39:299-301. doi:10.1046/j.1365-4362.2000.00943.x
- Jones K, Hughes J, Hong M, et al. Modulation of melanogenesis by aloesin: a competitive inhibitor of tyrosinase. Pigment Cell Res. 2002;15:335-340. doi:10.1034/j.1600-0749.2002.02014.x
- Hakozaki T, Minwalla L, Zhuang J, et al. The effect of niacinamide on reducing cutaneous pigmentation and suppression of melanosome transfer. Br J Dermatol. 2002;147:20-31. doi:10.1046/j.1365-2133.2002.04834.x
- Wohlrab J, Kreft D. Niacinamide—mechanisms of action and its topical use in dermatology. Skin Pharmacol Physiol. 2014;27:311-315. doi:10.1159/000359974
- Fitzpatrick RE, Rostan EF. Double-blind, half-face study comparing topical vitamin C and vehicle for rejuvenation of photodamage. Dermatol Surg. 2002;28:231-236. doi:10.1046/j.1524-4725.2002.01129.x
- Mehta AB, Nadkarni NJ, Patil SP, et al. Topical corticosteroids in dermatology. Indian J Dermatol Venereol Leprol. 2016;82:371-378. doi:10.4103/0378-6323.178903
- Petit L, Piérard GE. Skin-lightening products revisited. Int J Cosmet Sci. 2003;25:169-181. doi:10.1046/j.1467-2494.2003.00182.x
- Kanwar AJ, Dhar S, Kaur S. Treatment of melasma with potent topical corticosteroids. Dermatol Basel Switz. 1994;188:170. doi:10.1159/000247129
- Paine C, Sharlow E, Liebel F, et al. An alternative approach to depigmentation by soybean extracts via inhibition of the PAR-2 pathway. J Invest Dermatol. 2001;116:587-595. doi:10.1046/j.1523-1747.2001.01291.x
- Seiberg M, Paine C, Sharlow E, et al. Inhibition of melanosome transfer results in skin lightening. J Invest Dermatol. 2000;115:162-167. doi:10.1046/j.1523-1747.2000.00035.x
- Shimogaki H, Tanaka Y, Tamai H, et al. In vitro and in vivo evaluation of ellagic acid on melanogenesis inhibition. Int J Cosmet Sci. 2000;22:291-303. doi:10.1046/j.1467-2494.2000.00023.x
- Rendon MI, Gaviria JI. Review of skin-lightening agents. Dermatol Surg. 2005;31(7 pt 2):886-889; discussion 889. doi:10.1111/j.1524-4725.2005.31736
- Na JI, Shin JW, Choi HR, et al. Resveratrol as a multifunctional topical hypopigmenting agent [published online February 22, 2019]. Int J Mol Sci. 2019;20:956. doi:10.3390/ijms20040956
- Ratz-Łyko A, Arct J. Resveratrol as an active ingredient for cosmetic and dermatological applications: a review. J Cosmet Laser Ther. 2019;21:84-90. doi:10.1080/14764172.2018.1469767
- Choo SJ, Ryoo IJ, Kim YH, et al. Silymarin inhibits melanin synthesis in melanocyte cells. J Pharm Pharmacol. 2009;61:663-667. doi:10.1211/jpp/61.05.0016
- Draelos ZD, Diaz I, Cohen A, et al. A novel skin brightening topical technology. J Cosmet Dermatol. 2020;19:3280-3285. doi:10.1111/jocd.13741
- Grimes P, Bhawan J, Howell M, et al. Histopathological changes induced by malassezin: a novel natural microbiome indole for treatment of facial hyperpigmentation. J Drugs Dermatol. 2022;21:141-145. doi:10.36849/jdd.6596
- Bissett DL. Glucosamine: an ingredient with skin and other benefits. J Cosmet Dermatol. 2006;5:309-315. doi:10.1111/j.1473-2165.2006.00277.x
- Zhu JW, Ni YJ, Tong XY, et al. Tranexamic acid inhibits angiogenesis and melanogenesis in vitro by targeting VEGF receptors. Int J Med Sci. 2020;17:903-911. doi:10.7150/ijms.44188
- Hiramoto K, Yamate Y, Sugiyama D, et al. Tranexamic acid inhibits the plasma and non-irradiated skin markers of photoaging induced by long-term UVA eye irradiation in female mice. Biomed Pharmacother. 2018;107:54-58. doi:10.1016/j.biopha.2018.07.146
- da Silva Souza ID, Lampe L, Winn D. New topical tranexamic acid derivative for the improvement of hyperpigmentation and inflammation in the sun-damaged skin. J Cosmet Dermatol. 2021;20:561-565. doi:10.1111/jocd.13545
- Kim HJ, Moon SH, Cho SH, et al. Efficacy and safety of tranexamic acid in melasma: a meta-analysis and systematic review. Acta Derm Venereol. 2017;97:776-781. doi:10.2340/00015555-2668
- Mathe N, Balogun M, Yoo J. A case report on the use of topical cysteamine 5% cream in the management of refractory postinflammatory hyperpigmentation (PIH) resistant to triple combination cream (hydroquinone, topical corticosteroids, and retinoids). J Cosmet Dermatol. 2021;20:204-206. doi:10.1111/jocd.13755
- Mansouri P, Farshi S, Hashemi Z, et al. Evaluation of the efficacy of cysteamine 5% cream in the treatment of epidermal melasma: a randomized double-blind placebo-controlled trial. Br J Dermatol. 2015;173:209-217. doi:10.1111/bjd.13424
- Lima PB, Dias JAF, Cassiano D, et al. A comparative study of topical 5% cysteamine versus 4% hydroquinone in the treatment of facial melasma in women. Int J Dermatol. 2020;59:1531-1536. doi:10.1111/ijd.15146
Pseudocirrhosis in breast cancer may signal liver metastases
CHICAGO – Pseudocirrhosis appears radiographically similar to cirrhosis, but lacks its classic pathologic features.
The study is the largest cohort of patients with pseudocirrhosis studied to date. “It provides important clinical information about the natural history of this condition to help oncologists better understand which patients develop this condition and what complications are most common. Interestingly, we found that patients who developed ascites had a worse overall survival than patients who did not develop ascites, which was not previously reported,” said Laura Huppert, MD, who presented the findings during a poster session at the annual meeting of the American Society of Clinical Oncology.
Pseudocirrhosis is commonly found in patients with metastatic breast cancer and can lead to ascites and varices, among other complications. “These problems can be quite debilitating and even life-threatening for our patients. In order to better diagnose and treat our patients with pseudocirrhosis, we first wanted to understand the natural history of this condition, including which patients develop it, what treatments they have received, and what complications are most frequent,” said Dr. Huppert, MD, who is a hematology/oncology fellow at the University of California, San Francisco.
The study was retrospective, making it impossible to determine causality. “It is possible that the biology of HR+ disease predisposes patients to the development of pseudocirrhosis through mechanisms that are not yet elucidated. Alternatively, this may be due to the fact that patients with HR+ disease tend to have longer survival and are on systemic therapy for longer periods of time, allowing more time for pseudocirrhosis to develop in response to systemic therapy,” Dr. Huppert said.
In future work, Dr. Huppert plans to examine a control arm of patients with liver disease who do not develop pseudocirrhosis to gain a better understanding of factors that might cause the condition. She also hopes to work with hepatologists to determine if new antifibrosis agents might be applicable to pseudocirrhosis. “There may be interesting things we can learn from other disease states and apply to this condition,” she said.
The researchers analyzed data from 120 patients with pseudocirrhosis. 82.5% of patients were HR+/HER2–, 11.7% were HR+/HER2+, 2.5% were HR–/HER2+, and 3.3% were triple negative. Liver metastases were present in all patients, and 82.5% had more than 15 liver lesions.
A total of 92.5% of patients had previously undergone chemotherapy before pseudocirrhosis was identified, and the median time to diagnosis of pseudocirrhosis after diagnosis of liver metastases was 18.7 months. 50% of patients with pseudocirrhosis had stable or responding disease. After pseudocirrhosis diagnosis, patients underwent a median of 1.0 additional lines of therapy, and the median overall survival following pseudocirrhosis diagnosis was 7.9 months. A total of 80.8% of patients went on to be diagnosed with ascites, 17.5% with esophageal varices, 21.7% with splenomegaly, 10.0% with gastrointestinal bleeding, and 9.2% with hepatic encephalopathy.
Patients with radiographic evidence of ascites survived an average of 42.8 months after metastatic breast cancer diagnosis, while those without ascites survived an average of 76.2 months (P < .001).
Specialty care was rare: Just 7.5% of patients received a GI/hepatology consultation.
Dr. Huppert has no relevant financial disclosures.
CHICAGO – Pseudocirrhosis appears radiographically similar to cirrhosis, but lacks its classic pathologic features.
The study is the largest cohort of patients with pseudocirrhosis studied to date. “It provides important clinical information about the natural history of this condition to help oncologists better understand which patients develop this condition and what complications are most common. Interestingly, we found that patients who developed ascites had a worse overall survival than patients who did not develop ascites, which was not previously reported,” said Laura Huppert, MD, who presented the findings during a poster session at the annual meeting of the American Society of Clinical Oncology.
Pseudocirrhosis is commonly found in patients with metastatic breast cancer and can lead to ascites and varices, among other complications. “These problems can be quite debilitating and even life-threatening for our patients. In order to better diagnose and treat our patients with pseudocirrhosis, we first wanted to understand the natural history of this condition, including which patients develop it, what treatments they have received, and what complications are most frequent,” said Dr. Huppert, MD, who is a hematology/oncology fellow at the University of California, San Francisco.
The study was retrospective, making it impossible to determine causality. “It is possible that the biology of HR+ disease predisposes patients to the development of pseudocirrhosis through mechanisms that are not yet elucidated. Alternatively, this may be due to the fact that patients with HR+ disease tend to have longer survival and are on systemic therapy for longer periods of time, allowing more time for pseudocirrhosis to develop in response to systemic therapy,” Dr. Huppert said.
In future work, Dr. Huppert plans to examine a control arm of patients with liver disease who do not develop pseudocirrhosis to gain a better understanding of factors that might cause the condition. She also hopes to work with hepatologists to determine if new antifibrosis agents might be applicable to pseudocirrhosis. “There may be interesting things we can learn from other disease states and apply to this condition,” she said.
The researchers analyzed data from 120 patients with pseudocirrhosis. 82.5% of patients were HR+/HER2–, 11.7% were HR+/HER2+, 2.5% were HR–/HER2+, and 3.3% were triple negative. Liver metastases were present in all patients, and 82.5% had more than 15 liver lesions.
A total of 92.5% of patients had previously undergone chemotherapy before pseudocirrhosis was identified, and the median time to diagnosis of pseudocirrhosis after diagnosis of liver metastases was 18.7 months. 50% of patients with pseudocirrhosis had stable or responding disease. After pseudocirrhosis diagnosis, patients underwent a median of 1.0 additional lines of therapy, and the median overall survival following pseudocirrhosis diagnosis was 7.9 months. A total of 80.8% of patients went on to be diagnosed with ascites, 17.5% with esophageal varices, 21.7% with splenomegaly, 10.0% with gastrointestinal bleeding, and 9.2% with hepatic encephalopathy.
Patients with radiographic evidence of ascites survived an average of 42.8 months after metastatic breast cancer diagnosis, while those without ascites survived an average of 76.2 months (P < .001).
Specialty care was rare: Just 7.5% of patients received a GI/hepatology consultation.
Dr. Huppert has no relevant financial disclosures.
CHICAGO – Pseudocirrhosis appears radiographically similar to cirrhosis, but lacks its classic pathologic features.
The study is the largest cohort of patients with pseudocirrhosis studied to date. “It provides important clinical information about the natural history of this condition to help oncologists better understand which patients develop this condition and what complications are most common. Interestingly, we found that patients who developed ascites had a worse overall survival than patients who did not develop ascites, which was not previously reported,” said Laura Huppert, MD, who presented the findings during a poster session at the annual meeting of the American Society of Clinical Oncology.
Pseudocirrhosis is commonly found in patients with metastatic breast cancer and can lead to ascites and varices, among other complications. “These problems can be quite debilitating and even life-threatening for our patients. In order to better diagnose and treat our patients with pseudocirrhosis, we first wanted to understand the natural history of this condition, including which patients develop it, what treatments they have received, and what complications are most frequent,” said Dr. Huppert, MD, who is a hematology/oncology fellow at the University of California, San Francisco.
The study was retrospective, making it impossible to determine causality. “It is possible that the biology of HR+ disease predisposes patients to the development of pseudocirrhosis through mechanisms that are not yet elucidated. Alternatively, this may be due to the fact that patients with HR+ disease tend to have longer survival and are on systemic therapy for longer periods of time, allowing more time for pseudocirrhosis to develop in response to systemic therapy,” Dr. Huppert said.
In future work, Dr. Huppert plans to examine a control arm of patients with liver disease who do not develop pseudocirrhosis to gain a better understanding of factors that might cause the condition. She also hopes to work with hepatologists to determine if new antifibrosis agents might be applicable to pseudocirrhosis. “There may be interesting things we can learn from other disease states and apply to this condition,” she said.
The researchers analyzed data from 120 patients with pseudocirrhosis. 82.5% of patients were HR+/HER2–, 11.7% were HR+/HER2+, 2.5% were HR–/HER2+, and 3.3% were triple negative. Liver metastases were present in all patients, and 82.5% had more than 15 liver lesions.
A total of 92.5% of patients had previously undergone chemotherapy before pseudocirrhosis was identified, and the median time to diagnosis of pseudocirrhosis after diagnosis of liver metastases was 18.7 months. 50% of patients with pseudocirrhosis had stable or responding disease. After pseudocirrhosis diagnosis, patients underwent a median of 1.0 additional lines of therapy, and the median overall survival following pseudocirrhosis diagnosis was 7.9 months. A total of 80.8% of patients went on to be diagnosed with ascites, 17.5% with esophageal varices, 21.7% with splenomegaly, 10.0% with gastrointestinal bleeding, and 9.2% with hepatic encephalopathy.
Patients with radiographic evidence of ascites survived an average of 42.8 months after metastatic breast cancer diagnosis, while those without ascites survived an average of 76.2 months (P < .001).
Specialty care was rare: Just 7.5% of patients received a GI/hepatology consultation.
Dr. Huppert has no relevant financial disclosures.
AT ASCO 2022
Excess weight may ward off infection in breast cancer treatment
– a potentially deadly outcome that can occur as a result of chemotherapy treatment.
The study was presented at the annual meeting of the American Society of Clinical Oncology.
It is known that body mass index can affect breast cancer risk and prognosis, but it is not known if BMI can affect how well endocrine therapy works in a given patient. In the PALLAS clinical trial, Georg Pfeiler, MD, Medical University of Vienna, and colleagues, conducted an analysis of 5,698 patients with early hormone receptor–positive breast cancer receiving endocrine therapy with or without palbociclib. Dr. Pfeiler found that women who are overweight or obese had significantly less frequent and less severe cases of neutropenia. With fewer or less severe cases of neutropenia, there were also fewer interruptions in palbociclib treatment.
“One explanation for the lower discontinuation rates may be that the distributional volume of the drug is higher in overweight and obese patients leading to lower serum drug concentrations. It could also be influenced by differences in pharmacokinetics with respect to hyperinsulinemia,” said Dr. Pfeiler, who leads the Oncological Breast Outpatient Clinic and Bone Health Outpatient Clinic at the Medical University of Vienna.
The PALLAS trial compared the combination of palbociclib and adjuvant endocrine therapy with endocrine therapy alone in 5,698 women with early breast cancer. Patients were categorized according to BMI as underweight (BMI < 18.5 kg/m2), normal weight (BMI 18.5-24.9), overweight (BMI, 25-29.9), and obese (> 30). The investigators analyzed differences in adverse events, time to early discontinuation of palbociclib, and in time to invasive disease-free survival.
At baseline, of 5,698 patients, 68 (1.2%) were underweight, 2,082 (36.5%) were of normal weight, 1,818 (31.9%) were overweight, and, 1,730 (30.4%) were obese. In patients treated with palbociclib, neutropenia was the primary toxicity leading to treatment discontinuation with rates of 21.1% in normal-weight patients, 14.0% of overweight patients, and 5.9% of obese patients, respectively.
Significantly different rates of all-grade neutropenia were observed in normal weight, overweight, and obese participants with regard to total (88.5%, 85.7% and 74.7%), as well as grade 3 (64.1%, 62.0% and 43.9%) and grade 4 neutropenia (7.0%, 3.6% and 2.0%), respectively. The lower frequency and severity of neutropenia observed in overweight and obese patients was associated with a significantly lower treatment discontinuation rate over time when compared with normal-weight patients (overweight vs. normal weight: HR, 0.73; 95% CI 0.63-0.84; P < .0001, and obese vs. normal weight: HR, 0.65; 95% CI, 0.56-0.75; P < .0001). There was, however, despite these observations, no statistically significant improvement in invasive disease survival with the addition of palbociclib to endocrine therapy in any weight category (normal weight: HR, 0.84; 95% CI 0.63-1.12; overweight: HR, 1.10; 95% CI 0.82-1.49; and obese: HR, 0.95; 95% CI, 0.69-1.30).
“This is an early analysis, and should be interpreted with caution, especially with regard to disease outcomes. The findings may reduce concerns over hematologic side effects in the overweight and obese. In the future there may be an important impact if it turns out after longer-term follow-up that palbociclib has been underdosed in the overweight and obese. We may need BMI-adapted dose management,” said Dr. Pfeiler, who is currently working on a longer-term follow-up study of the PALLAS group.
The analysis found no significant correlation between weight and occurrence of invasive disease events.
Dr. Pfeiler disclosed honoraria and grants from Pfizer. The study was funded by Alliance Foundation Trials.
– a potentially deadly outcome that can occur as a result of chemotherapy treatment.
The study was presented at the annual meeting of the American Society of Clinical Oncology.
It is known that body mass index can affect breast cancer risk and prognosis, but it is not known if BMI can affect how well endocrine therapy works in a given patient. In the PALLAS clinical trial, Georg Pfeiler, MD, Medical University of Vienna, and colleagues, conducted an analysis of 5,698 patients with early hormone receptor–positive breast cancer receiving endocrine therapy with or without palbociclib. Dr. Pfeiler found that women who are overweight or obese had significantly less frequent and less severe cases of neutropenia. With fewer or less severe cases of neutropenia, there were also fewer interruptions in palbociclib treatment.
“One explanation for the lower discontinuation rates may be that the distributional volume of the drug is higher in overweight and obese patients leading to lower serum drug concentrations. It could also be influenced by differences in pharmacokinetics with respect to hyperinsulinemia,” said Dr. Pfeiler, who leads the Oncological Breast Outpatient Clinic and Bone Health Outpatient Clinic at the Medical University of Vienna.
The PALLAS trial compared the combination of palbociclib and adjuvant endocrine therapy with endocrine therapy alone in 5,698 women with early breast cancer. Patients were categorized according to BMI as underweight (BMI < 18.5 kg/m2), normal weight (BMI 18.5-24.9), overweight (BMI, 25-29.9), and obese (> 30). The investigators analyzed differences in adverse events, time to early discontinuation of palbociclib, and in time to invasive disease-free survival.
At baseline, of 5,698 patients, 68 (1.2%) were underweight, 2,082 (36.5%) were of normal weight, 1,818 (31.9%) were overweight, and, 1,730 (30.4%) were obese. In patients treated with palbociclib, neutropenia was the primary toxicity leading to treatment discontinuation with rates of 21.1% in normal-weight patients, 14.0% of overweight patients, and 5.9% of obese patients, respectively.
Significantly different rates of all-grade neutropenia were observed in normal weight, overweight, and obese participants with regard to total (88.5%, 85.7% and 74.7%), as well as grade 3 (64.1%, 62.0% and 43.9%) and grade 4 neutropenia (7.0%, 3.6% and 2.0%), respectively. The lower frequency and severity of neutropenia observed in overweight and obese patients was associated with a significantly lower treatment discontinuation rate over time when compared with normal-weight patients (overweight vs. normal weight: HR, 0.73; 95% CI 0.63-0.84; P < .0001, and obese vs. normal weight: HR, 0.65; 95% CI, 0.56-0.75; P < .0001). There was, however, despite these observations, no statistically significant improvement in invasive disease survival with the addition of palbociclib to endocrine therapy in any weight category (normal weight: HR, 0.84; 95% CI 0.63-1.12; overweight: HR, 1.10; 95% CI 0.82-1.49; and obese: HR, 0.95; 95% CI, 0.69-1.30).
“This is an early analysis, and should be interpreted with caution, especially with regard to disease outcomes. The findings may reduce concerns over hematologic side effects in the overweight and obese. In the future there may be an important impact if it turns out after longer-term follow-up that palbociclib has been underdosed in the overweight and obese. We may need BMI-adapted dose management,” said Dr. Pfeiler, who is currently working on a longer-term follow-up study of the PALLAS group.
The analysis found no significant correlation between weight and occurrence of invasive disease events.
Dr. Pfeiler disclosed honoraria and grants from Pfizer. The study was funded by Alliance Foundation Trials.
– a potentially deadly outcome that can occur as a result of chemotherapy treatment.
The study was presented at the annual meeting of the American Society of Clinical Oncology.
It is known that body mass index can affect breast cancer risk and prognosis, but it is not known if BMI can affect how well endocrine therapy works in a given patient. In the PALLAS clinical trial, Georg Pfeiler, MD, Medical University of Vienna, and colleagues, conducted an analysis of 5,698 patients with early hormone receptor–positive breast cancer receiving endocrine therapy with or without palbociclib. Dr. Pfeiler found that women who are overweight or obese had significantly less frequent and less severe cases of neutropenia. With fewer or less severe cases of neutropenia, there were also fewer interruptions in palbociclib treatment.
“One explanation for the lower discontinuation rates may be that the distributional volume of the drug is higher in overweight and obese patients leading to lower serum drug concentrations. It could also be influenced by differences in pharmacokinetics with respect to hyperinsulinemia,” said Dr. Pfeiler, who leads the Oncological Breast Outpatient Clinic and Bone Health Outpatient Clinic at the Medical University of Vienna.
The PALLAS trial compared the combination of palbociclib and adjuvant endocrine therapy with endocrine therapy alone in 5,698 women with early breast cancer. Patients were categorized according to BMI as underweight (BMI < 18.5 kg/m2), normal weight (BMI 18.5-24.9), overweight (BMI, 25-29.9), and obese (> 30). The investigators analyzed differences in adverse events, time to early discontinuation of palbociclib, and in time to invasive disease-free survival.
At baseline, of 5,698 patients, 68 (1.2%) were underweight, 2,082 (36.5%) were of normal weight, 1,818 (31.9%) were overweight, and, 1,730 (30.4%) were obese. In patients treated with palbociclib, neutropenia was the primary toxicity leading to treatment discontinuation with rates of 21.1% in normal-weight patients, 14.0% of overweight patients, and 5.9% of obese patients, respectively.
Significantly different rates of all-grade neutropenia were observed in normal weight, overweight, and obese participants with regard to total (88.5%, 85.7% and 74.7%), as well as grade 3 (64.1%, 62.0% and 43.9%) and grade 4 neutropenia (7.0%, 3.6% and 2.0%), respectively. The lower frequency and severity of neutropenia observed in overweight and obese patients was associated with a significantly lower treatment discontinuation rate over time when compared with normal-weight patients (overweight vs. normal weight: HR, 0.73; 95% CI 0.63-0.84; P < .0001, and obese vs. normal weight: HR, 0.65; 95% CI, 0.56-0.75; P < .0001). There was, however, despite these observations, no statistically significant improvement in invasive disease survival with the addition of palbociclib to endocrine therapy in any weight category (normal weight: HR, 0.84; 95% CI 0.63-1.12; overweight: HR, 1.10; 95% CI 0.82-1.49; and obese: HR, 0.95; 95% CI, 0.69-1.30).
“This is an early analysis, and should be interpreted with caution, especially with regard to disease outcomes. The findings may reduce concerns over hematologic side effects in the overweight and obese. In the future there may be an important impact if it turns out after longer-term follow-up that palbociclib has been underdosed in the overweight and obese. We may need BMI-adapted dose management,” said Dr. Pfeiler, who is currently working on a longer-term follow-up study of the PALLAS group.
The analysis found no significant correlation between weight and occurrence of invasive disease events.
Dr. Pfeiler disclosed honoraria and grants from Pfizer. The study was funded by Alliance Foundation Trials.
FROM ASCO 2022
Women with HER2+ metastatic breast cancer are living longer
When a patient first presents to a doctor with signs and symptoms of having breast cancer that has metastasized to other parts of the body, the prospects of long-term survival are dim. But now, a new study presented at the annual meeting of the American Society of Clinical Oncology suggests that women with metastatic HER2+ breast cancer are generally living longer, compared with women treated in previous years.
Between 2010 and 2018, the overall survival for 5,576 women (99% women) with HER2+ metastatic breast cancer enrolled in this study improved 5.6% each year of the study. The study also showed a 6.4% improvement in breast cancer–specific death rates year over year.
“These highlights coincide with significant therapeutic advances for HER2+ metastatic breast cancer over the past decade. We need to continue our research efforts to identify better treatments for our patients so we can continue to improve the prognosis of these patients,” said study author Jose Pablo Leone, MD, a medical oncologist with Dana-Farber Cancer Institute, Boston.
The study, which is based on an evaluation of data from the Surveillance, Epidemiology and End Results database, found factors associated with shorter survival included older age, Black race, lower income, and the presence of visceral or brain metastases. Long-term survival of more than 5 years was associated with younger age, White race, and higher income, but also having fewer metastatic sites and estrogen receptor (ER)/progesterone receptor (PR) positivity.
“We also found specific factors that were only associated with shorter overall survival, such as the presence of metastases in the brain, liver, or lung. The lack of metastasis in these sites was not associated with longer overall survival. In contrast, a lower number of metastatic sites, regardless of the location of those sites were associated with longer overall survival but not short-term survival,” Dr. Leone said.
A total of 63.3% of patients in the study survived less than 2 years while 37.8% lived 5 years or more, and 26.8% lived longer than 8 years. Factors associated with less than 2 years in overall survival were older age (odds ratio, 3.76), Black race (OR 1.5), nonductal nonlobular (OR, 4.64), brain metastases (OR, 2.95), liver metastases (OR, 1.98), lung metastases (OR, 1.56), ER/PR negativity (OR, 1.74), and lower income (OR, 1.62). Factors associated with longer survival of 5 years or more included younger age (OR, 2.85), White race (OR, 1.7), fewer metastatic organ sites (OR, 2.6), ER/PR positivity (OR, 1.27), and higher income (OR, 3.31).
Dr. Leone said that, while involvement of specific visceral sites (brain, liver, lung) was associated with shorter overall survival, the odds of living longer than 5 years was not associated with those sites. In contrast, the number of sites was associated with longer overall survival, but not shorter overall survival regardless of location. “While fewer number of metastatic sites were associated with higher odds of overall survival greater than 5 years, the number of metastatic sites was not associated with the odds of overall survival of being less than 2 years,” he said.
A limitation of the study included the retrospective nature of the study. “Treatment data are unavailable, so we cannot quantify the impact of various treatments on the odds of survival,” Dr. Leone said.
This study was not funded.
When a patient first presents to a doctor with signs and symptoms of having breast cancer that has metastasized to other parts of the body, the prospects of long-term survival are dim. But now, a new study presented at the annual meeting of the American Society of Clinical Oncology suggests that women with metastatic HER2+ breast cancer are generally living longer, compared with women treated in previous years.
Between 2010 and 2018, the overall survival for 5,576 women (99% women) with HER2+ metastatic breast cancer enrolled in this study improved 5.6% each year of the study. The study also showed a 6.4% improvement in breast cancer–specific death rates year over year.
“These highlights coincide with significant therapeutic advances for HER2+ metastatic breast cancer over the past decade. We need to continue our research efforts to identify better treatments for our patients so we can continue to improve the prognosis of these patients,” said study author Jose Pablo Leone, MD, a medical oncologist with Dana-Farber Cancer Institute, Boston.
The study, which is based on an evaluation of data from the Surveillance, Epidemiology and End Results database, found factors associated with shorter survival included older age, Black race, lower income, and the presence of visceral or brain metastases. Long-term survival of more than 5 years was associated with younger age, White race, and higher income, but also having fewer metastatic sites and estrogen receptor (ER)/progesterone receptor (PR) positivity.
“We also found specific factors that were only associated with shorter overall survival, such as the presence of metastases in the brain, liver, or lung. The lack of metastasis in these sites was not associated with longer overall survival. In contrast, a lower number of metastatic sites, regardless of the location of those sites were associated with longer overall survival but not short-term survival,” Dr. Leone said.
A total of 63.3% of patients in the study survived less than 2 years while 37.8% lived 5 years or more, and 26.8% lived longer than 8 years. Factors associated with less than 2 years in overall survival were older age (odds ratio, 3.76), Black race (OR 1.5), nonductal nonlobular (OR, 4.64), brain metastases (OR, 2.95), liver metastases (OR, 1.98), lung metastases (OR, 1.56), ER/PR negativity (OR, 1.74), and lower income (OR, 1.62). Factors associated with longer survival of 5 years or more included younger age (OR, 2.85), White race (OR, 1.7), fewer metastatic organ sites (OR, 2.6), ER/PR positivity (OR, 1.27), and higher income (OR, 3.31).
Dr. Leone said that, while involvement of specific visceral sites (brain, liver, lung) was associated with shorter overall survival, the odds of living longer than 5 years was not associated with those sites. In contrast, the number of sites was associated with longer overall survival, but not shorter overall survival regardless of location. “While fewer number of metastatic sites were associated with higher odds of overall survival greater than 5 years, the number of metastatic sites was not associated with the odds of overall survival of being less than 2 years,” he said.
A limitation of the study included the retrospective nature of the study. “Treatment data are unavailable, so we cannot quantify the impact of various treatments on the odds of survival,” Dr. Leone said.
This study was not funded.
When a patient first presents to a doctor with signs and symptoms of having breast cancer that has metastasized to other parts of the body, the prospects of long-term survival are dim. But now, a new study presented at the annual meeting of the American Society of Clinical Oncology suggests that women with metastatic HER2+ breast cancer are generally living longer, compared with women treated in previous years.
Between 2010 and 2018, the overall survival for 5,576 women (99% women) with HER2+ metastatic breast cancer enrolled in this study improved 5.6% each year of the study. The study also showed a 6.4% improvement in breast cancer–specific death rates year over year.
“These highlights coincide with significant therapeutic advances for HER2+ metastatic breast cancer over the past decade. We need to continue our research efforts to identify better treatments for our patients so we can continue to improve the prognosis of these patients,” said study author Jose Pablo Leone, MD, a medical oncologist with Dana-Farber Cancer Institute, Boston.
The study, which is based on an evaluation of data from the Surveillance, Epidemiology and End Results database, found factors associated with shorter survival included older age, Black race, lower income, and the presence of visceral or brain metastases. Long-term survival of more than 5 years was associated with younger age, White race, and higher income, but also having fewer metastatic sites and estrogen receptor (ER)/progesterone receptor (PR) positivity.
“We also found specific factors that were only associated with shorter overall survival, such as the presence of metastases in the brain, liver, or lung. The lack of metastasis in these sites was not associated with longer overall survival. In contrast, a lower number of metastatic sites, regardless of the location of those sites were associated with longer overall survival but not short-term survival,” Dr. Leone said.
A total of 63.3% of patients in the study survived less than 2 years while 37.8% lived 5 years or more, and 26.8% lived longer than 8 years. Factors associated with less than 2 years in overall survival were older age (odds ratio, 3.76), Black race (OR 1.5), nonductal nonlobular (OR, 4.64), brain metastases (OR, 2.95), liver metastases (OR, 1.98), lung metastases (OR, 1.56), ER/PR negativity (OR, 1.74), and lower income (OR, 1.62). Factors associated with longer survival of 5 years or more included younger age (OR, 2.85), White race (OR, 1.7), fewer metastatic organ sites (OR, 2.6), ER/PR positivity (OR, 1.27), and higher income (OR, 3.31).
Dr. Leone said that, while involvement of specific visceral sites (brain, liver, lung) was associated with shorter overall survival, the odds of living longer than 5 years was not associated with those sites. In contrast, the number of sites was associated with longer overall survival, but not shorter overall survival regardless of location. “While fewer number of metastatic sites were associated with higher odds of overall survival greater than 5 years, the number of metastatic sites was not associated with the odds of overall survival of being less than 2 years,” he said.
A limitation of the study included the retrospective nature of the study. “Treatment data are unavailable, so we cannot quantify the impact of various treatments on the odds of survival,” Dr. Leone said.
This study was not funded.
FROM ASCO 2022
Monkeypox largely a mystery for pregnant people
With monkeypox now circulating in the United States, expecting mothers may worry about what might happen if they contract the infection while pregnant.
As of today, 25 cases of monkeypox have been confirmed in the United States since the outbreak began in early May, according to the U.S. Centers for Disease Control and Prevention. Although none of those cases has involved a pregnant person, the World Health Organization says monkeypox can pass from mother to fetus before delivery or to newborns by close contact during and after birth.
The case count could grow as the agency continues to investigate potential infections of the virus. In a conference call Friday, health officials stressed the importance of contact tracing, testing, and vaccine treatment.
As physicians in the United States are scrambling for information on ways to treat patients, a new study, published in Ultrasound in Obstetrics & Gynecology, could help clinicians better care for pregnant people infected with monkeypox. The authors advise consistently monitoring the fetus for infection and conducting regular ultrasounds, among other precautions.
Asma Khalil, MBBCh, MD, a professor of obstetrics and fetal medicine at St. George’s University, London, and lead author of the new study, said the monkeypox outbreak outside Africa caught many clinicians by surprise.
“We quickly realized very few physicians caring for pregnant women knew anything at all about monkeypox and how it affects pregnancy,” Dr. Khalil told this news organization. “Clinicians caring for pregnant women are likely to be faced soon with pregnant women concerned they may have the infection – because they have a rash, for example – or indeed pregnant women who do have the infection.”
According to the CDC, monkeypox can be transmitted through direct contact with the rash, sores, or scabs caused by the virus, as well as contact with clothing, bedding, towels, or other surfaces used by an infected person. Respiratory droplets and oral fluids from a person with monkeypox have also been linked to spread of the virus, as has sexual activity.
Although the condition is rarely fatal, infants and young children are at the greatest risk of developing severe symptoms, health officials said.
The U.S. Food and Drug Administration has approved a monkeypox vaccine, Jynneos (Bavarian Nordic A/S), for general use, but it has not been specifically approved for pregnant people. However, a study of 300 pregnant women who received the vaccine reported no adverse reactions or failed pregnancies linked to the shots.
The new review suggests that women who have a confirmed infection during pregnancy should have a doctor closely monitor the fetus until birth.
If the fetus is over 26 weeks or if the mother is unwell, the fetus should be cared for with heart monitoring, either by a doctor or remotely every 2-3 days. Ultrasounds should be performed regularly to confirm that the fetus is still growing well and that the placenta is functioning properly.
Further into the pregnancy, monitoring should include measurements of the fetus and detailed assessment of the fetal organs and the amniotic fluid. Once the infection is resolved, the risk to the fetus is small, according to Dr. Khalil. However, since data are limited, she recommended an ultrasound scan every 2-4 weeks. At birth, for the protection of the infant and the mother, the baby should be isolated until infection is no longer a risk.
The Royal College of Obstetricians & Gynaecologists is preparing guidance on the management of monkeypox in pregnant people, Dr. Khalil said. The American College of Obstetricians and Gynecologists said it is “relying on the CDC for the time being,” according to a spokesperson for ACOG.
“There is a clear need for further research in this area,” Dr. Khalil said. “The current outbreak is an ideal opportunity to make this happen.”
Dr. Khalil has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
With monkeypox now circulating in the United States, expecting mothers may worry about what might happen if they contract the infection while pregnant.
As of today, 25 cases of monkeypox have been confirmed in the United States since the outbreak began in early May, according to the U.S. Centers for Disease Control and Prevention. Although none of those cases has involved a pregnant person, the World Health Organization says monkeypox can pass from mother to fetus before delivery or to newborns by close contact during and after birth.
The case count could grow as the agency continues to investigate potential infections of the virus. In a conference call Friday, health officials stressed the importance of contact tracing, testing, and vaccine treatment.
As physicians in the United States are scrambling for information on ways to treat patients, a new study, published in Ultrasound in Obstetrics & Gynecology, could help clinicians better care for pregnant people infected with monkeypox. The authors advise consistently monitoring the fetus for infection and conducting regular ultrasounds, among other precautions.
Asma Khalil, MBBCh, MD, a professor of obstetrics and fetal medicine at St. George’s University, London, and lead author of the new study, said the monkeypox outbreak outside Africa caught many clinicians by surprise.
“We quickly realized very few physicians caring for pregnant women knew anything at all about monkeypox and how it affects pregnancy,” Dr. Khalil told this news organization. “Clinicians caring for pregnant women are likely to be faced soon with pregnant women concerned they may have the infection – because they have a rash, for example – or indeed pregnant women who do have the infection.”
According to the CDC, monkeypox can be transmitted through direct contact with the rash, sores, or scabs caused by the virus, as well as contact with clothing, bedding, towels, or other surfaces used by an infected person. Respiratory droplets and oral fluids from a person with monkeypox have also been linked to spread of the virus, as has sexual activity.
Although the condition is rarely fatal, infants and young children are at the greatest risk of developing severe symptoms, health officials said.
The U.S. Food and Drug Administration has approved a monkeypox vaccine, Jynneos (Bavarian Nordic A/S), for general use, but it has not been specifically approved for pregnant people. However, a study of 300 pregnant women who received the vaccine reported no adverse reactions or failed pregnancies linked to the shots.
The new review suggests that women who have a confirmed infection during pregnancy should have a doctor closely monitor the fetus until birth.
If the fetus is over 26 weeks or if the mother is unwell, the fetus should be cared for with heart monitoring, either by a doctor or remotely every 2-3 days. Ultrasounds should be performed regularly to confirm that the fetus is still growing well and that the placenta is functioning properly.
Further into the pregnancy, monitoring should include measurements of the fetus and detailed assessment of the fetal organs and the amniotic fluid. Once the infection is resolved, the risk to the fetus is small, according to Dr. Khalil. However, since data are limited, she recommended an ultrasound scan every 2-4 weeks. At birth, for the protection of the infant and the mother, the baby should be isolated until infection is no longer a risk.
The Royal College of Obstetricians & Gynaecologists is preparing guidance on the management of monkeypox in pregnant people, Dr. Khalil said. The American College of Obstetricians and Gynecologists said it is “relying on the CDC for the time being,” according to a spokesperson for ACOG.
“There is a clear need for further research in this area,” Dr. Khalil said. “The current outbreak is an ideal opportunity to make this happen.”
Dr. Khalil has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
With monkeypox now circulating in the United States, expecting mothers may worry about what might happen if they contract the infection while pregnant.
As of today, 25 cases of monkeypox have been confirmed in the United States since the outbreak began in early May, according to the U.S. Centers for Disease Control and Prevention. Although none of those cases has involved a pregnant person, the World Health Organization says monkeypox can pass from mother to fetus before delivery or to newborns by close contact during and after birth.
The case count could grow as the agency continues to investigate potential infections of the virus. In a conference call Friday, health officials stressed the importance of contact tracing, testing, and vaccine treatment.
As physicians in the United States are scrambling for information on ways to treat patients, a new study, published in Ultrasound in Obstetrics & Gynecology, could help clinicians better care for pregnant people infected with monkeypox. The authors advise consistently monitoring the fetus for infection and conducting regular ultrasounds, among other precautions.
Asma Khalil, MBBCh, MD, a professor of obstetrics and fetal medicine at St. George’s University, London, and lead author of the new study, said the monkeypox outbreak outside Africa caught many clinicians by surprise.
“We quickly realized very few physicians caring for pregnant women knew anything at all about monkeypox and how it affects pregnancy,” Dr. Khalil told this news organization. “Clinicians caring for pregnant women are likely to be faced soon with pregnant women concerned they may have the infection – because they have a rash, for example – or indeed pregnant women who do have the infection.”
According to the CDC, monkeypox can be transmitted through direct contact with the rash, sores, or scabs caused by the virus, as well as contact with clothing, bedding, towels, or other surfaces used by an infected person. Respiratory droplets and oral fluids from a person with monkeypox have also been linked to spread of the virus, as has sexual activity.
Although the condition is rarely fatal, infants and young children are at the greatest risk of developing severe symptoms, health officials said.
The U.S. Food and Drug Administration has approved a monkeypox vaccine, Jynneos (Bavarian Nordic A/S), for general use, but it has not been specifically approved for pregnant people. However, a study of 300 pregnant women who received the vaccine reported no adverse reactions or failed pregnancies linked to the shots.
The new review suggests that women who have a confirmed infection during pregnancy should have a doctor closely monitor the fetus until birth.
If the fetus is over 26 weeks or if the mother is unwell, the fetus should be cared for with heart monitoring, either by a doctor or remotely every 2-3 days. Ultrasounds should be performed regularly to confirm that the fetus is still growing well and that the placenta is functioning properly.
Further into the pregnancy, monitoring should include measurements of the fetus and detailed assessment of the fetal organs and the amniotic fluid. Once the infection is resolved, the risk to the fetus is small, according to Dr. Khalil. However, since data are limited, she recommended an ultrasound scan every 2-4 weeks. At birth, for the protection of the infant and the mother, the baby should be isolated until infection is no longer a risk.
The Royal College of Obstetricians & Gynaecologists is preparing guidance on the management of monkeypox in pregnant people, Dr. Khalil said. The American College of Obstetricians and Gynecologists said it is “relying on the CDC for the time being,” according to a spokesperson for ACOG.
“There is a clear need for further research in this area,” Dr. Khalil said. “The current outbreak is an ideal opportunity to make this happen.”
Dr. Khalil has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Women with high-risk pregnancies could die if Roe is overturned
Kendra Joseph of San Antonio, Tex., had given up on the idea of having a second child. At 40 years old, and with a daughter pleading for a sibling, she and her husband were nervous about the risk of trying for another child due to her advanced maternal age. Mrs. Joseph had ended an earlier pregnancy at 15 weeks after finding out her son had Edwards syndrome, a genetic trait that’s fatal in most cases.
Now a new Texas law that bans abortion past 6 weeks would mean that if either she or her baby were at risk of dying, she might still have to carry the baby to term. For Mrs. Joseph, it wasn’t worth the risk at first. Then in February, just as they had decided against another baby, the couple found out they were expecting. She’s thrilled about her pregnancy, but it’s also been a nervewracking few months.
“It’s scary being pregnant anyway,” she says, “but these new restrictions add a layer of stress.”
Twenty-eight states could ban or tightly restrict abortion if the Supreme Court overturns the landmark Roe v. Wade decision. A leaked draft of the court’s opinion has been widely interpreted as signaling that the court will overturn the law. This means that women who are at a higher risk of pregnancy complications or those who have chronic conditions before getting pregnant could be at risk of dying if they can’t get an abortion.
According to the CDC, the maternal mortality rate in the United States in 2020 was 23.8 deaths per 100,000 live births – among the highest in the developed world. The rate is eight times as high as it is in countries like the Netherlands, Norway, and New Zealand.
“Many of the women I take care of have a pregnancy that presents a real and present danger to their health, and this often goes along with the fact that they’re very unlikely to have a healthy baby,” says Chavi Karkowsky, MD, a maternal fetal medicine specialist at Montefiore Medical Center, New York.
Maternal mortality, she says, can be caused by health conditions that some women may not know about before getting pregnant. (For example, finding out she had cervical cancer at a prenatal visit and then having to choose between chemotherapy and her baby.) And there are also life-threatening conditions caused by pregnancy, like preeclampsia, which can cause high blood pressure and kidney damage, as well as gestational diabetes. Research has also shown that the risk of maternal mortality increases with age.
University of Colorado researchers, in a study published in the journal Demography, found that banning abortion nationwide would lead to a 20% increase in maternal death. For Black women, the increase in mortality could be as high as 33%, due to higher rates of poverty and less access to health care, says Amanda Stevenson, PhD, a sociologist at the University of Colorado and one of the study’s authors. Black women in the U.S. are more than three times as likely to die as a result of pregnancy complications due to poor exposure to health care, structural racism, and chronic health conditions, according to the CDC.
If Roe v. Wade is overturned, more women will likely die because remaining pregnant poses a far greater mortality risk for them than the risk associated with an abortion, says Dr. Stevenson.
For women with high-risk pregnancies who need an abortion, traveling out of state puts them at a health risk, says Jamila Perritt, MD, an ob.gyn. in Washington, D.C. and president of Physicians for Reproductive Health. In places where abortion is restricted, it can cause significant delays in accessing medical care. “Abortion is a time-sensitive procedure, and as the pregnancy progresses, it can become increasingly difficult to find a clinic that will provide care,” she says.
She recalls one of her patients who had a heart problem that required a pregnancy to be ended. The patient at first had to travel to find a doctor who could evaluate her unique condition, then go out of state to get an abortion. All the while, the clock was ticking and her health was at risk. In this case, the patient had the money to travel out of state, find child care, and pay for the procedure.
“This was a resourced individual, and while this was difficult for her, it wasn’t impossible,” says Dr. Perritt.
Many of the states with the highest maternal mortality rates, including Louisiana, Texas, Arkansas, Alabama, South Carolina, and Georgia, also plan to strictly limit abortions or ban them completely. Some abortion opponents insist this won’t harm mothers.
“The pro-life movement loves both babies and moms,” says Sarah Zagorski, a spokeswoman for Louisiana Right to Life. “It is a tragedy that Louisiana has high mortality rates among pregnant women. However, legal abortion does not improve these rates.”
But for many women who need an abortion, statewide bans may make it hard to get. This worries Kendra Joseph, who’s now 18 weeks into her pregnancy.
“I try to put the bad things that could happen out of my mind, but it’s really hard when you’re dealing with these totally unnecessary and cruel restrictions. We as women, we’re just losing so much,” she says.
A version of this article first appeared on WebMD.com.
Kendra Joseph of San Antonio, Tex., had given up on the idea of having a second child. At 40 years old, and with a daughter pleading for a sibling, she and her husband were nervous about the risk of trying for another child due to her advanced maternal age. Mrs. Joseph had ended an earlier pregnancy at 15 weeks after finding out her son had Edwards syndrome, a genetic trait that’s fatal in most cases.
Now a new Texas law that bans abortion past 6 weeks would mean that if either she or her baby were at risk of dying, she might still have to carry the baby to term. For Mrs. Joseph, it wasn’t worth the risk at first. Then in February, just as they had decided against another baby, the couple found out they were expecting. She’s thrilled about her pregnancy, but it’s also been a nervewracking few months.
“It’s scary being pregnant anyway,” she says, “but these new restrictions add a layer of stress.”
Twenty-eight states could ban or tightly restrict abortion if the Supreme Court overturns the landmark Roe v. Wade decision. A leaked draft of the court’s opinion has been widely interpreted as signaling that the court will overturn the law. This means that women who are at a higher risk of pregnancy complications or those who have chronic conditions before getting pregnant could be at risk of dying if they can’t get an abortion.
According to the CDC, the maternal mortality rate in the United States in 2020 was 23.8 deaths per 100,000 live births – among the highest in the developed world. The rate is eight times as high as it is in countries like the Netherlands, Norway, and New Zealand.
“Many of the women I take care of have a pregnancy that presents a real and present danger to their health, and this often goes along with the fact that they’re very unlikely to have a healthy baby,” says Chavi Karkowsky, MD, a maternal fetal medicine specialist at Montefiore Medical Center, New York.
Maternal mortality, she says, can be caused by health conditions that some women may not know about before getting pregnant. (For example, finding out she had cervical cancer at a prenatal visit and then having to choose between chemotherapy and her baby.) And there are also life-threatening conditions caused by pregnancy, like preeclampsia, which can cause high blood pressure and kidney damage, as well as gestational diabetes. Research has also shown that the risk of maternal mortality increases with age.
University of Colorado researchers, in a study published in the journal Demography, found that banning abortion nationwide would lead to a 20% increase in maternal death. For Black women, the increase in mortality could be as high as 33%, due to higher rates of poverty and less access to health care, says Amanda Stevenson, PhD, a sociologist at the University of Colorado and one of the study’s authors. Black women in the U.S. are more than three times as likely to die as a result of pregnancy complications due to poor exposure to health care, structural racism, and chronic health conditions, according to the CDC.
If Roe v. Wade is overturned, more women will likely die because remaining pregnant poses a far greater mortality risk for them than the risk associated with an abortion, says Dr. Stevenson.
For women with high-risk pregnancies who need an abortion, traveling out of state puts them at a health risk, says Jamila Perritt, MD, an ob.gyn. in Washington, D.C. and president of Physicians for Reproductive Health. In places where abortion is restricted, it can cause significant delays in accessing medical care. “Abortion is a time-sensitive procedure, and as the pregnancy progresses, it can become increasingly difficult to find a clinic that will provide care,” she says.
She recalls one of her patients who had a heart problem that required a pregnancy to be ended. The patient at first had to travel to find a doctor who could evaluate her unique condition, then go out of state to get an abortion. All the while, the clock was ticking and her health was at risk. In this case, the patient had the money to travel out of state, find child care, and pay for the procedure.
“This was a resourced individual, and while this was difficult for her, it wasn’t impossible,” says Dr. Perritt.
Many of the states with the highest maternal mortality rates, including Louisiana, Texas, Arkansas, Alabama, South Carolina, and Georgia, also plan to strictly limit abortions or ban them completely. Some abortion opponents insist this won’t harm mothers.
“The pro-life movement loves both babies and moms,” says Sarah Zagorski, a spokeswoman for Louisiana Right to Life. “It is a tragedy that Louisiana has high mortality rates among pregnant women. However, legal abortion does not improve these rates.”
But for many women who need an abortion, statewide bans may make it hard to get. This worries Kendra Joseph, who’s now 18 weeks into her pregnancy.
“I try to put the bad things that could happen out of my mind, but it’s really hard when you’re dealing with these totally unnecessary and cruel restrictions. We as women, we’re just losing so much,” she says.
A version of this article first appeared on WebMD.com.
Kendra Joseph of San Antonio, Tex., had given up on the idea of having a second child. At 40 years old, and with a daughter pleading for a sibling, she and her husband were nervous about the risk of trying for another child due to her advanced maternal age. Mrs. Joseph had ended an earlier pregnancy at 15 weeks after finding out her son had Edwards syndrome, a genetic trait that’s fatal in most cases.
Now a new Texas law that bans abortion past 6 weeks would mean that if either she or her baby were at risk of dying, she might still have to carry the baby to term. For Mrs. Joseph, it wasn’t worth the risk at first. Then in February, just as they had decided against another baby, the couple found out they were expecting. She’s thrilled about her pregnancy, but it’s also been a nervewracking few months.
“It’s scary being pregnant anyway,” she says, “but these new restrictions add a layer of stress.”
Twenty-eight states could ban or tightly restrict abortion if the Supreme Court overturns the landmark Roe v. Wade decision. A leaked draft of the court’s opinion has been widely interpreted as signaling that the court will overturn the law. This means that women who are at a higher risk of pregnancy complications or those who have chronic conditions before getting pregnant could be at risk of dying if they can’t get an abortion.
According to the CDC, the maternal mortality rate in the United States in 2020 was 23.8 deaths per 100,000 live births – among the highest in the developed world. The rate is eight times as high as it is in countries like the Netherlands, Norway, and New Zealand.
“Many of the women I take care of have a pregnancy that presents a real and present danger to their health, and this often goes along with the fact that they’re very unlikely to have a healthy baby,” says Chavi Karkowsky, MD, a maternal fetal medicine specialist at Montefiore Medical Center, New York.
Maternal mortality, she says, can be caused by health conditions that some women may not know about before getting pregnant. (For example, finding out she had cervical cancer at a prenatal visit and then having to choose between chemotherapy and her baby.) And there are also life-threatening conditions caused by pregnancy, like preeclampsia, which can cause high blood pressure and kidney damage, as well as gestational diabetes. Research has also shown that the risk of maternal mortality increases with age.
University of Colorado researchers, in a study published in the journal Demography, found that banning abortion nationwide would lead to a 20% increase in maternal death. For Black women, the increase in mortality could be as high as 33%, due to higher rates of poverty and less access to health care, says Amanda Stevenson, PhD, a sociologist at the University of Colorado and one of the study’s authors. Black women in the U.S. are more than three times as likely to die as a result of pregnancy complications due to poor exposure to health care, structural racism, and chronic health conditions, according to the CDC.
If Roe v. Wade is overturned, more women will likely die because remaining pregnant poses a far greater mortality risk for them than the risk associated with an abortion, says Dr. Stevenson.
For women with high-risk pregnancies who need an abortion, traveling out of state puts them at a health risk, says Jamila Perritt, MD, an ob.gyn. in Washington, D.C. and president of Physicians for Reproductive Health. In places where abortion is restricted, it can cause significant delays in accessing medical care. “Abortion is a time-sensitive procedure, and as the pregnancy progresses, it can become increasingly difficult to find a clinic that will provide care,” she says.
She recalls one of her patients who had a heart problem that required a pregnancy to be ended. The patient at first had to travel to find a doctor who could evaluate her unique condition, then go out of state to get an abortion. All the while, the clock was ticking and her health was at risk. In this case, the patient had the money to travel out of state, find child care, and pay for the procedure.
“This was a resourced individual, and while this was difficult for her, it wasn’t impossible,” says Dr. Perritt.
Many of the states with the highest maternal mortality rates, including Louisiana, Texas, Arkansas, Alabama, South Carolina, and Georgia, also plan to strictly limit abortions or ban them completely. Some abortion opponents insist this won’t harm mothers.
“The pro-life movement loves both babies and moms,” says Sarah Zagorski, a spokeswoman for Louisiana Right to Life. “It is a tragedy that Louisiana has high mortality rates among pregnant women. However, legal abortion does not improve these rates.”
But for many women who need an abortion, statewide bans may make it hard to get. This worries Kendra Joseph, who’s now 18 weeks into her pregnancy.
“I try to put the bad things that could happen out of my mind, but it’s really hard when you’re dealing with these totally unnecessary and cruel restrictions. We as women, we’re just losing so much,” she says.
A version of this article first appeared on WebMD.com.
Treating bone loss ups survival for breast cancer patients
A final long-term analysis of a study designed to evaluate the safety of a common osteoporosis drug used to treat bone loss in women who were treated for breast cancer, finds the
The final analysis of “Adjuvant Denosumab in Breast Cancer (ABCSG-18)” was presented at the annual meeting of the American Society of Clinical Oncology.
“Adjuvant denosumab should be considered for routine clinical use in postmenopausal patients with HR+ breast cancer on aromatase inhibitors treatment,” said the study’s author Michael Gnant, MD, FACS, director of surgery for the Medical University of Vienna.
Denosumab is currently recommended by ASCO as a treatment option for osteoporosis in patients who were successfully treated for nonmetastatic disease.
ABCSG-18 was a prospective, double-blind, placebo-controlled, phase 3 trial that comprised 3,420 patients (mean age 64.5 years) from 58 treatment centers. It included postmenopausal patients with early HR+ breast cancer who were treated with aromatase inhibitors between 2006 and 2013. Among the patients, 1,711 received denosumab 60 mg and 1,709 received a placebo every 6 months.
The primary endpoint was time to first clinical fracture, and the secondary disease outcome-related endpoints were disease-free survival, bone metastasis–free survival, and overall survival.
The hazard ratio for disease-free survival in the denosumab group was 0.83 (95% confidence interval [CI], 0.71-0.97, P = .02) after a median follow-up of 8 years. Disease-free survival (DFS) was 69.0% in the placebo arm and 74.4% in the denosumab arm, with events occurring in 19.8% of patients overall, including deaths in 8.3%.
Bone metastasis–free survival (BMFS) rates were 81.3% and 85.7% in the placebo and denosumab arms, respectively (HR = 0.81, 95% CI, 0.65-1.00, P = .05). Overall survival was 83.6% and 88.8% in the placebo and denosumab arms, respectively (HR = 0.80; 95% CI, 0.63-1.01, P = .06).
There were no new toxicities, nor was there a single positive case of osteonecrosis of the jaw (ONJ) during the study period, which may be due to the low dosage of denosumab. The bone protection dose of denosumab is much lower than that used for treatment of metastases which can be 12 times higher. In those cases, 4%-6% of patients may develop ONJ. “At these very low doses, even after 30,000 treatment years, we did not observe a single confirmed ONJ case,” he said.
Exploratory observations showed the majority of events to include distant recurrences in bone, liver, and lungs. Analysis revealed a trend toward reduction in contralateral breast cancer in the denosumab arm (24 versus 29 events), with a reduction in second non-breast primary malignancies (101 versus 127 events).
In a much earlier ABCSG-18 study from 2015, the primary endpoint of fracture risk was reduced significantly with denosumab (HR = 0.50, P < .0001), with highly significantly longer time to first clinical fracture, higher percent increase in bone mineral density (P < .0001 for both) and fewer vertebral fractures (P = .009). There is evidence that older generation bisphosphonates have potential beyond bone health, such as reducing metabolism (which benefits bone turnover), and improving breast cancer outcomes. These benefits sparked interest in potential long-term cancer reduction with denosumab, Dr. Gnant said.
“Bone marrow is a putative source of late relapse. Tumor cells can harbor there in a quiescent state for 10-15-20 years, and then for some reason wake up and cause metastases. So, all bone-targeted agents are also evaluated for reductions in cancer which is what we were looking to investigate here in this 15-year data,” he said. Denosumab is more targeted than the bisphosphonates, and directly inhibits the RANK ligand which is an important mediator of osteoclast activation. “This ligand is believed to support metastases in the process of waking up,” Dr. Gnant said.
A limitation of the study is that the outcome endpoints of ABCSG-18 are secondary ones, making the results technically descriptive. The study was sponsored by Amgen.
A final long-term analysis of a study designed to evaluate the safety of a common osteoporosis drug used to treat bone loss in women who were treated for breast cancer, finds the
The final analysis of “Adjuvant Denosumab in Breast Cancer (ABCSG-18)” was presented at the annual meeting of the American Society of Clinical Oncology.
“Adjuvant denosumab should be considered for routine clinical use in postmenopausal patients with HR+ breast cancer on aromatase inhibitors treatment,” said the study’s author Michael Gnant, MD, FACS, director of surgery for the Medical University of Vienna.
Denosumab is currently recommended by ASCO as a treatment option for osteoporosis in patients who were successfully treated for nonmetastatic disease.
ABCSG-18 was a prospective, double-blind, placebo-controlled, phase 3 trial that comprised 3,420 patients (mean age 64.5 years) from 58 treatment centers. It included postmenopausal patients with early HR+ breast cancer who were treated with aromatase inhibitors between 2006 and 2013. Among the patients, 1,711 received denosumab 60 mg and 1,709 received a placebo every 6 months.
The primary endpoint was time to first clinical fracture, and the secondary disease outcome-related endpoints were disease-free survival, bone metastasis–free survival, and overall survival.
The hazard ratio for disease-free survival in the denosumab group was 0.83 (95% confidence interval [CI], 0.71-0.97, P = .02) after a median follow-up of 8 years. Disease-free survival (DFS) was 69.0% in the placebo arm and 74.4% in the denosumab arm, with events occurring in 19.8% of patients overall, including deaths in 8.3%.
Bone metastasis–free survival (BMFS) rates were 81.3% and 85.7% in the placebo and denosumab arms, respectively (HR = 0.81, 95% CI, 0.65-1.00, P = .05). Overall survival was 83.6% and 88.8% in the placebo and denosumab arms, respectively (HR = 0.80; 95% CI, 0.63-1.01, P = .06).
There were no new toxicities, nor was there a single positive case of osteonecrosis of the jaw (ONJ) during the study period, which may be due to the low dosage of denosumab. The bone protection dose of denosumab is much lower than that used for treatment of metastases which can be 12 times higher. In those cases, 4%-6% of patients may develop ONJ. “At these very low doses, even after 30,000 treatment years, we did not observe a single confirmed ONJ case,” he said.
Exploratory observations showed the majority of events to include distant recurrences in bone, liver, and lungs. Analysis revealed a trend toward reduction in contralateral breast cancer in the denosumab arm (24 versus 29 events), with a reduction in second non-breast primary malignancies (101 versus 127 events).
In a much earlier ABCSG-18 study from 2015, the primary endpoint of fracture risk was reduced significantly with denosumab (HR = 0.50, P < .0001), with highly significantly longer time to first clinical fracture, higher percent increase in bone mineral density (P < .0001 for both) and fewer vertebral fractures (P = .009). There is evidence that older generation bisphosphonates have potential beyond bone health, such as reducing metabolism (which benefits bone turnover), and improving breast cancer outcomes. These benefits sparked interest in potential long-term cancer reduction with denosumab, Dr. Gnant said.
“Bone marrow is a putative source of late relapse. Tumor cells can harbor there in a quiescent state for 10-15-20 years, and then for some reason wake up and cause metastases. So, all bone-targeted agents are also evaluated for reductions in cancer which is what we were looking to investigate here in this 15-year data,” he said. Denosumab is more targeted than the bisphosphonates, and directly inhibits the RANK ligand which is an important mediator of osteoclast activation. “This ligand is believed to support metastases in the process of waking up,” Dr. Gnant said.
A limitation of the study is that the outcome endpoints of ABCSG-18 are secondary ones, making the results technically descriptive. The study was sponsored by Amgen.
A final long-term analysis of a study designed to evaluate the safety of a common osteoporosis drug used to treat bone loss in women who were treated for breast cancer, finds the
The final analysis of “Adjuvant Denosumab in Breast Cancer (ABCSG-18)” was presented at the annual meeting of the American Society of Clinical Oncology.
“Adjuvant denosumab should be considered for routine clinical use in postmenopausal patients with HR+ breast cancer on aromatase inhibitors treatment,” said the study’s author Michael Gnant, MD, FACS, director of surgery for the Medical University of Vienna.
Denosumab is currently recommended by ASCO as a treatment option for osteoporosis in patients who were successfully treated for nonmetastatic disease.
ABCSG-18 was a prospective, double-blind, placebo-controlled, phase 3 trial that comprised 3,420 patients (mean age 64.5 years) from 58 treatment centers. It included postmenopausal patients with early HR+ breast cancer who were treated with aromatase inhibitors between 2006 and 2013. Among the patients, 1,711 received denosumab 60 mg and 1,709 received a placebo every 6 months.
The primary endpoint was time to first clinical fracture, and the secondary disease outcome-related endpoints were disease-free survival, bone metastasis–free survival, and overall survival.
The hazard ratio for disease-free survival in the denosumab group was 0.83 (95% confidence interval [CI], 0.71-0.97, P = .02) after a median follow-up of 8 years. Disease-free survival (DFS) was 69.0% in the placebo arm and 74.4% in the denosumab arm, with events occurring in 19.8% of patients overall, including deaths in 8.3%.
Bone metastasis–free survival (BMFS) rates were 81.3% and 85.7% in the placebo and denosumab arms, respectively (HR = 0.81, 95% CI, 0.65-1.00, P = .05). Overall survival was 83.6% and 88.8% in the placebo and denosumab arms, respectively (HR = 0.80; 95% CI, 0.63-1.01, P = .06).
There were no new toxicities, nor was there a single positive case of osteonecrosis of the jaw (ONJ) during the study period, which may be due to the low dosage of denosumab. The bone protection dose of denosumab is much lower than that used for treatment of metastases which can be 12 times higher. In those cases, 4%-6% of patients may develop ONJ. “At these very low doses, even after 30,000 treatment years, we did not observe a single confirmed ONJ case,” he said.
Exploratory observations showed the majority of events to include distant recurrences in bone, liver, and lungs. Analysis revealed a trend toward reduction in contralateral breast cancer in the denosumab arm (24 versus 29 events), with a reduction in second non-breast primary malignancies (101 versus 127 events).
In a much earlier ABCSG-18 study from 2015, the primary endpoint of fracture risk was reduced significantly with denosumab (HR = 0.50, P < .0001), with highly significantly longer time to first clinical fracture, higher percent increase in bone mineral density (P < .0001 for both) and fewer vertebral fractures (P = .009). There is evidence that older generation bisphosphonates have potential beyond bone health, such as reducing metabolism (which benefits bone turnover), and improving breast cancer outcomes. These benefits sparked interest in potential long-term cancer reduction with denosumab, Dr. Gnant said.
“Bone marrow is a putative source of late relapse. Tumor cells can harbor there in a quiescent state for 10-15-20 years, and then for some reason wake up and cause metastases. So, all bone-targeted agents are also evaluated for reductions in cancer which is what we were looking to investigate here in this 15-year data,” he said. Denosumab is more targeted than the bisphosphonates, and directly inhibits the RANK ligand which is an important mediator of osteoclast activation. “This ligand is believed to support metastases in the process of waking up,” Dr. Gnant said.
A limitation of the study is that the outcome endpoints of ABCSG-18 are secondary ones, making the results technically descriptive. The study was sponsored by Amgen.
FROM ASCO 2022
Pembrolizumab before surgery improves survival in early triple negative breast cancer
for improving survival in patients with early triple negative breast cancer (TNBC).
The findings were presented in Chicago June 4 and 5 at the annual meeting of the American Society of Clinical Oncology by study author Lajos Pusztai, MD, D.Phil, director of Breast Cancer Translational Research at Yale University, New Haven, Conn.
KEYNOTE-522 is the first prospective, randomized, placebo-controlled phase 3 trial of pembrolizumab for early-stage TNBC in the neoadjuvant and adjuvant setting.
The study included 1,174 patients (median age 49 years) with previously untreated stage II or III triple-negative breast cancer. Patients were randomly assigned to receive neoadjuvant therapy with four cycles of pembrolizumab (200 mg) or placebo every 3 weeks plus paclitaxel and carboplatin, followed by four cycles of pembrolizumab or placebo plus doxorubicin-cyclophosphamide or epirubicin-cyclophosphamide. After surgery, patients received pembrolizumab or placebeo for 9 cycles or until recurrence or unacceptable toxicity. The primary end points were pathological complete response and event-free survival.
A total of 784 patients were treated with pembrolizumab and chemotherapy, and the second group of 390 patients received a placebo and chemotherapy. After surgery, patients received adjuvant pembrolizumab (pembrolizumab-chemotherapy group) or placebo and chemotherapy for every 3 weeks for up to nine cycles.
The estimated event-free survival at 36 months was 84.5% in the pembrolizumab-chemotherapy group, compared with 76.8% in the placebo-chemotherapy group (hazard ratio for event or death, 0.63; 95% confidence interval, 0.48 to 0.82; P <0.001). Adverse events occurred predominantly during the neoadjuvant phase and were consistent with the established safety profiles of pembrolizumab and chemotherapy.
At the first interim analysis, 64.8% achieved pathological complete response in the pembrolizumab group versus 51.2% in the placebo group. At the fourth interim analysis at 36 months, event-free survival was 76.8% in the placebo arm and 84.5% in the pembrolizumab arm. RCB-0 status was achieved by 63.4% and 56.2% of patients in the pembrolizumab and placebo arms, respectively.
Pembrolizumab did contribute immune-related adverse events, mostly grades 1-2, in about 17% of patients with thyroid function abnormalities most common with most occurring 20 weeks prior to surgical treatment.
Treatment with pembrolizumab added to chemotherapy, compared with chemotherapy alone, shifted residual cancer burden to lower categories across the entire spectrum of patients in the trial.
The hazard ratio for event-free survival with RCB-0, which Dr. Pusztai said is equivalent to a pathologic complete response (pCR), was 0.70 (0.38-1.31). For RCB-1 (minimal residual disease) it was 0.92 (0.39-2.20); for RCB-2 (moderate residual disease) it was 0.52 (0.32-0.82); and for RCB-3 (extensive residual disease) it was 1.24 (0.69-2.23).
“The most important finding is that patients in RCB-2, a group with a moderate amount of residual disease, experienced significant improvement with pembrolizumab. This clearly indicates not only that pembrolizumab leads to higher pCR rates but also that the pembrolizumCR/RCB-0 ... extends to patients who do not achieve pCR,” Dr. Pusztai said.
The benefit, he suggested, could be a result of the adjuvant pembrolizumab maintenance phase.
Patients in the RCB-3 category do poorly regardless of treatment (EFS of 34.6 % and 26.2% in the pembrolizumab and placebo arms, respectively).
“The RCB-3 population represents an unmet medical need, and they will need better drugs, and additional postoperative adjuvant therapy,” Dr. Pusztai said. The current standard of care is capecitabine for 6-8 cycles. Emerging new therapies, such as antibody drug conjugates, will be tested, he said.
In terms of limitations, adjuvant capecitabine was not allowed. “It remains uncertain how much better the RCB-2 and -3 patient outcomes would have been if capecitabine were administered,” he said.
The study was funded by Merck Sharp and Dohme, a subsidiary of Merck. Dr. Pusztai has received consulting fees and honoraria from Merck.
for improving survival in patients with early triple negative breast cancer (TNBC).
The findings were presented in Chicago June 4 and 5 at the annual meeting of the American Society of Clinical Oncology by study author Lajos Pusztai, MD, D.Phil, director of Breast Cancer Translational Research at Yale University, New Haven, Conn.
KEYNOTE-522 is the first prospective, randomized, placebo-controlled phase 3 trial of pembrolizumab for early-stage TNBC in the neoadjuvant and adjuvant setting.
The study included 1,174 patients (median age 49 years) with previously untreated stage II or III triple-negative breast cancer. Patients were randomly assigned to receive neoadjuvant therapy with four cycles of pembrolizumab (200 mg) or placebo every 3 weeks plus paclitaxel and carboplatin, followed by four cycles of pembrolizumab or placebo plus doxorubicin-cyclophosphamide or epirubicin-cyclophosphamide. After surgery, patients received pembrolizumab or placebeo for 9 cycles or until recurrence or unacceptable toxicity. The primary end points were pathological complete response and event-free survival.
A total of 784 patients were treated with pembrolizumab and chemotherapy, and the second group of 390 patients received a placebo and chemotherapy. After surgery, patients received adjuvant pembrolizumab (pembrolizumab-chemotherapy group) or placebo and chemotherapy for every 3 weeks for up to nine cycles.
The estimated event-free survival at 36 months was 84.5% in the pembrolizumab-chemotherapy group, compared with 76.8% in the placebo-chemotherapy group (hazard ratio for event or death, 0.63; 95% confidence interval, 0.48 to 0.82; P <0.001). Adverse events occurred predominantly during the neoadjuvant phase and were consistent with the established safety profiles of pembrolizumab and chemotherapy.
At the first interim analysis, 64.8% achieved pathological complete response in the pembrolizumab group versus 51.2% in the placebo group. At the fourth interim analysis at 36 months, event-free survival was 76.8% in the placebo arm and 84.5% in the pembrolizumab arm. RCB-0 status was achieved by 63.4% and 56.2% of patients in the pembrolizumab and placebo arms, respectively.
Pembrolizumab did contribute immune-related adverse events, mostly grades 1-2, in about 17% of patients with thyroid function abnormalities most common with most occurring 20 weeks prior to surgical treatment.
Treatment with pembrolizumab added to chemotherapy, compared with chemotherapy alone, shifted residual cancer burden to lower categories across the entire spectrum of patients in the trial.
The hazard ratio for event-free survival with RCB-0, which Dr. Pusztai said is equivalent to a pathologic complete response (pCR), was 0.70 (0.38-1.31). For RCB-1 (minimal residual disease) it was 0.92 (0.39-2.20); for RCB-2 (moderate residual disease) it was 0.52 (0.32-0.82); and for RCB-3 (extensive residual disease) it was 1.24 (0.69-2.23).
“The most important finding is that patients in RCB-2, a group with a moderate amount of residual disease, experienced significant improvement with pembrolizumab. This clearly indicates not only that pembrolizumab leads to higher pCR rates but also that the pembrolizumCR/RCB-0 ... extends to patients who do not achieve pCR,” Dr. Pusztai said.
The benefit, he suggested, could be a result of the adjuvant pembrolizumab maintenance phase.
Patients in the RCB-3 category do poorly regardless of treatment (EFS of 34.6 % and 26.2% in the pembrolizumab and placebo arms, respectively).
“The RCB-3 population represents an unmet medical need, and they will need better drugs, and additional postoperative adjuvant therapy,” Dr. Pusztai said. The current standard of care is capecitabine for 6-8 cycles. Emerging new therapies, such as antibody drug conjugates, will be tested, he said.
In terms of limitations, adjuvant capecitabine was not allowed. “It remains uncertain how much better the RCB-2 and -3 patient outcomes would have been if capecitabine were administered,” he said.
The study was funded by Merck Sharp and Dohme, a subsidiary of Merck. Dr. Pusztai has received consulting fees and honoraria from Merck.
for improving survival in patients with early triple negative breast cancer (TNBC).
The findings were presented in Chicago June 4 and 5 at the annual meeting of the American Society of Clinical Oncology by study author Lajos Pusztai, MD, D.Phil, director of Breast Cancer Translational Research at Yale University, New Haven, Conn.
KEYNOTE-522 is the first prospective, randomized, placebo-controlled phase 3 trial of pembrolizumab for early-stage TNBC in the neoadjuvant and adjuvant setting.
The study included 1,174 patients (median age 49 years) with previously untreated stage II or III triple-negative breast cancer. Patients were randomly assigned to receive neoadjuvant therapy with four cycles of pembrolizumab (200 mg) or placebo every 3 weeks plus paclitaxel and carboplatin, followed by four cycles of pembrolizumab or placebo plus doxorubicin-cyclophosphamide or epirubicin-cyclophosphamide. After surgery, patients received pembrolizumab or placebeo for 9 cycles or until recurrence or unacceptable toxicity. The primary end points were pathological complete response and event-free survival.
A total of 784 patients were treated with pembrolizumab and chemotherapy, and the second group of 390 patients received a placebo and chemotherapy. After surgery, patients received adjuvant pembrolizumab (pembrolizumab-chemotherapy group) or placebo and chemotherapy for every 3 weeks for up to nine cycles.
The estimated event-free survival at 36 months was 84.5% in the pembrolizumab-chemotherapy group, compared with 76.8% in the placebo-chemotherapy group (hazard ratio for event or death, 0.63; 95% confidence interval, 0.48 to 0.82; P <0.001). Adverse events occurred predominantly during the neoadjuvant phase and were consistent with the established safety profiles of pembrolizumab and chemotherapy.
At the first interim analysis, 64.8% achieved pathological complete response in the pembrolizumab group versus 51.2% in the placebo group. At the fourth interim analysis at 36 months, event-free survival was 76.8% in the placebo arm and 84.5% in the pembrolizumab arm. RCB-0 status was achieved by 63.4% and 56.2% of patients in the pembrolizumab and placebo arms, respectively.
Pembrolizumab did contribute immune-related adverse events, mostly grades 1-2, in about 17% of patients with thyroid function abnormalities most common with most occurring 20 weeks prior to surgical treatment.
Treatment with pembrolizumab added to chemotherapy, compared with chemotherapy alone, shifted residual cancer burden to lower categories across the entire spectrum of patients in the trial.
The hazard ratio for event-free survival with RCB-0, which Dr. Pusztai said is equivalent to a pathologic complete response (pCR), was 0.70 (0.38-1.31). For RCB-1 (minimal residual disease) it was 0.92 (0.39-2.20); for RCB-2 (moderate residual disease) it was 0.52 (0.32-0.82); and for RCB-3 (extensive residual disease) it was 1.24 (0.69-2.23).
“The most important finding is that patients in RCB-2, a group with a moderate amount of residual disease, experienced significant improvement with pembrolizumab. This clearly indicates not only that pembrolizumab leads to higher pCR rates but also that the pembrolizumCR/RCB-0 ... extends to patients who do not achieve pCR,” Dr. Pusztai said.
The benefit, he suggested, could be a result of the adjuvant pembrolizumab maintenance phase.
Patients in the RCB-3 category do poorly regardless of treatment (EFS of 34.6 % and 26.2% in the pembrolizumab and placebo arms, respectively).
“The RCB-3 population represents an unmet medical need, and they will need better drugs, and additional postoperative adjuvant therapy,” Dr. Pusztai said. The current standard of care is capecitabine for 6-8 cycles. Emerging new therapies, such as antibody drug conjugates, will be tested, he said.
In terms of limitations, adjuvant capecitabine was not allowed. “It remains uncertain how much better the RCB-2 and -3 patient outcomes would have been if capecitabine were administered,” he said.
The study was funded by Merck Sharp and Dohme, a subsidiary of Merck. Dr. Pusztai has received consulting fees and honoraria from Merck.
FROM ASCO 2022
New treatment outperforms chemo in HER2-low breast cancer
CHICAGO -- Breast cancer patients with low levels of HER2 expression, previously considered untreatable with HER2-targeted therapies, benefited from the anti-HER2 antibody drug conjugate trastuzumab deruxtecan.
“Overall, these results establish HER2 low metastatic breast cancer as a targetable population of breast cancer with trastuzumab deruxtecan as a new standard of care in this setting,” said Shanu Modi, MD, during a press conference held in Chicago at the annual meeting of the American Society of Clinical Oncology, where she presented the results.
“I think the results of this trial clearly will be practice changing,” said ASCO spokesperson and breast cancer expert Jane Lowe Meisel, MD, during the press conference. “I think what this trial does is really extend the benefits of this agent to a whole new group of patients that traditionally is really quite difficult to treat. I think this will offer a wonderful new option for patients and also will really fundamentally change the way we think about HER2 status and how we classify this in our metastatic patients,” Dr. Meisel added.
The conjugate includes the anti-HER2 antibody trastuzumab and the topoisomerase I inhibitor deruxtecan, which interferes with DNA replication. Trastuzumab has demonstrated efficacy in patients with high levels of HER2 expression, and trastuzumab-deruxtecan received FDA approval in May 2022 for the treatment of HER2-positive breast cancer in patients who had previously received an anti-HER2 regimen.
However, anti-HER2 agents had not been shown to benefit HER2-low patients, defined as immunohistochemistry (IHC) 1+ or 2+. About 60% of breast cancer patients traditionally thought of HER2 negative could be classified as HER2 low, according to Dr. Modi, who is a medical oncologist at Memorial Sloan Kettering Cancer Center, New York.
Asked why she thought trastuzumab deruxtecan succeeded where other anti-HER2 therapies failed in this population, Dr. Modi highlighted the nature of the drug conjugate, including a high drug payload and the use of a topoisomerase inhibitor, which is rarely employed against breast cancer. Once released from the antibody, the drug retains its ability to cross cell membranes and enter the tumor microenvironment. That ‘knock on’ effect might allow it to reach neighboring cells that don’t express HER2. “We know HER2 expression is very heterogeneous. I think that’s why, for the first time, we’re seeing activity for a targeted agent,” Dr. Modi said.
The DESTINY-Breast04 study included 557 patients in Asia, Europe, and North America with HR-negative or HR-positive, HER2-low, unresectable, and/or metastatic breast cancer. Patients were randomized to trastuzumab deruxtecan or physician’s choice of several standard chemotherapy drugs. After a median follow-up of 18.4 months, compared with the chemotherapy group, patients in the trastuzumab deruxtecan arm had a 49% reduction in risk of progression and a 36% reduction in mortality. The group also had longer progression-free survival (10.1 months vs. 5.4 months) and overall survival (23.9 months vs. 17.5 months).
Although adverse events were similar between the two groups (52.6% in trastuzumab deruxtecan, 67.4% in chemotherapy), lung toxicity occurred in 12% of the group, and there were 3 fatalities as a result (0.8%). Interstitial lung disease/pneumonitis has been linked to trastuzumab treatment in the past, with one meta-analysis finding a frequency of 2.4% and fatality rate of 0.2%.
Additional studies are in progress to determine the minimum threshold of HER2 expression needed to gain a benefit from trastuzumab deruxtecan treatment.
The study was funded by Daiichi Sankyo, and AstraZeneca. Dr. Modi has advised, consulted for, or received honoraria from Daiichi Sankyo, and AstraZeneca. Dr. Meisel has advised or consulted for Medscape and AstraZeneca.
CHICAGO -- Breast cancer patients with low levels of HER2 expression, previously considered untreatable with HER2-targeted therapies, benefited from the anti-HER2 antibody drug conjugate trastuzumab deruxtecan.
“Overall, these results establish HER2 low metastatic breast cancer as a targetable population of breast cancer with trastuzumab deruxtecan as a new standard of care in this setting,” said Shanu Modi, MD, during a press conference held in Chicago at the annual meeting of the American Society of Clinical Oncology, where she presented the results.
“I think the results of this trial clearly will be practice changing,” said ASCO spokesperson and breast cancer expert Jane Lowe Meisel, MD, during the press conference. “I think what this trial does is really extend the benefits of this agent to a whole new group of patients that traditionally is really quite difficult to treat. I think this will offer a wonderful new option for patients and also will really fundamentally change the way we think about HER2 status and how we classify this in our metastatic patients,” Dr. Meisel added.
The conjugate includes the anti-HER2 antibody trastuzumab and the topoisomerase I inhibitor deruxtecan, which interferes with DNA replication. Trastuzumab has demonstrated efficacy in patients with high levels of HER2 expression, and trastuzumab-deruxtecan received FDA approval in May 2022 for the treatment of HER2-positive breast cancer in patients who had previously received an anti-HER2 regimen.
However, anti-HER2 agents had not been shown to benefit HER2-low patients, defined as immunohistochemistry (IHC) 1+ or 2+. About 60% of breast cancer patients traditionally thought of HER2 negative could be classified as HER2 low, according to Dr. Modi, who is a medical oncologist at Memorial Sloan Kettering Cancer Center, New York.
Asked why she thought trastuzumab deruxtecan succeeded where other anti-HER2 therapies failed in this population, Dr. Modi highlighted the nature of the drug conjugate, including a high drug payload and the use of a topoisomerase inhibitor, which is rarely employed against breast cancer. Once released from the antibody, the drug retains its ability to cross cell membranes and enter the tumor microenvironment. That ‘knock on’ effect might allow it to reach neighboring cells that don’t express HER2. “We know HER2 expression is very heterogeneous. I think that’s why, for the first time, we’re seeing activity for a targeted agent,” Dr. Modi said.
The DESTINY-Breast04 study included 557 patients in Asia, Europe, and North America with HR-negative or HR-positive, HER2-low, unresectable, and/or metastatic breast cancer. Patients were randomized to trastuzumab deruxtecan or physician’s choice of several standard chemotherapy drugs. After a median follow-up of 18.4 months, compared with the chemotherapy group, patients in the trastuzumab deruxtecan arm had a 49% reduction in risk of progression and a 36% reduction in mortality. The group also had longer progression-free survival (10.1 months vs. 5.4 months) and overall survival (23.9 months vs. 17.5 months).
Although adverse events were similar between the two groups (52.6% in trastuzumab deruxtecan, 67.4% in chemotherapy), lung toxicity occurred in 12% of the group, and there were 3 fatalities as a result (0.8%). Interstitial lung disease/pneumonitis has been linked to trastuzumab treatment in the past, with one meta-analysis finding a frequency of 2.4% and fatality rate of 0.2%.
Additional studies are in progress to determine the minimum threshold of HER2 expression needed to gain a benefit from trastuzumab deruxtecan treatment.
The study was funded by Daiichi Sankyo, and AstraZeneca. Dr. Modi has advised, consulted for, or received honoraria from Daiichi Sankyo, and AstraZeneca. Dr. Meisel has advised or consulted for Medscape and AstraZeneca.
CHICAGO -- Breast cancer patients with low levels of HER2 expression, previously considered untreatable with HER2-targeted therapies, benefited from the anti-HER2 antibody drug conjugate trastuzumab deruxtecan.
“Overall, these results establish HER2 low metastatic breast cancer as a targetable population of breast cancer with trastuzumab deruxtecan as a new standard of care in this setting,” said Shanu Modi, MD, during a press conference held in Chicago at the annual meeting of the American Society of Clinical Oncology, where she presented the results.
“I think the results of this trial clearly will be practice changing,” said ASCO spokesperson and breast cancer expert Jane Lowe Meisel, MD, during the press conference. “I think what this trial does is really extend the benefits of this agent to a whole new group of patients that traditionally is really quite difficult to treat. I think this will offer a wonderful new option for patients and also will really fundamentally change the way we think about HER2 status and how we classify this in our metastatic patients,” Dr. Meisel added.
The conjugate includes the anti-HER2 antibody trastuzumab and the topoisomerase I inhibitor deruxtecan, which interferes with DNA replication. Trastuzumab has demonstrated efficacy in patients with high levels of HER2 expression, and trastuzumab-deruxtecan received FDA approval in May 2022 for the treatment of HER2-positive breast cancer in patients who had previously received an anti-HER2 regimen.
However, anti-HER2 agents had not been shown to benefit HER2-low patients, defined as immunohistochemistry (IHC) 1+ or 2+. About 60% of breast cancer patients traditionally thought of HER2 negative could be classified as HER2 low, according to Dr. Modi, who is a medical oncologist at Memorial Sloan Kettering Cancer Center, New York.
Asked why she thought trastuzumab deruxtecan succeeded where other anti-HER2 therapies failed in this population, Dr. Modi highlighted the nature of the drug conjugate, including a high drug payload and the use of a topoisomerase inhibitor, which is rarely employed against breast cancer. Once released from the antibody, the drug retains its ability to cross cell membranes and enter the tumor microenvironment. That ‘knock on’ effect might allow it to reach neighboring cells that don’t express HER2. “We know HER2 expression is very heterogeneous. I think that’s why, for the first time, we’re seeing activity for a targeted agent,” Dr. Modi said.
The DESTINY-Breast04 study included 557 patients in Asia, Europe, and North America with HR-negative or HR-positive, HER2-low, unresectable, and/or metastatic breast cancer. Patients were randomized to trastuzumab deruxtecan or physician’s choice of several standard chemotherapy drugs. After a median follow-up of 18.4 months, compared with the chemotherapy group, patients in the trastuzumab deruxtecan arm had a 49% reduction in risk of progression and a 36% reduction in mortality. The group also had longer progression-free survival (10.1 months vs. 5.4 months) and overall survival (23.9 months vs. 17.5 months).
Although adverse events were similar between the two groups (52.6% in trastuzumab deruxtecan, 67.4% in chemotherapy), lung toxicity occurred in 12% of the group, and there were 3 fatalities as a result (0.8%). Interstitial lung disease/pneumonitis has been linked to trastuzumab treatment in the past, with one meta-analysis finding a frequency of 2.4% and fatality rate of 0.2%.
Additional studies are in progress to determine the minimum threshold of HER2 expression needed to gain a benefit from trastuzumab deruxtecan treatment.
The study was funded by Daiichi Sankyo, and AstraZeneca. Dr. Modi has advised, consulted for, or received honoraria from Daiichi Sankyo, and AstraZeneca. Dr. Meisel has advised or consulted for Medscape and AstraZeneca.
AT ASCO 2022