User login
Overcoming death anxiety: Understanding our lives and legacies
Disappointment – “I failed this exam, my life is ruined” or regret – “I am getting a divorce, I wasted so much of my life.” Patients present with a wide variety of complaints that can be understood as a form of death anxiety.
Fundamentally, patients come to see us to understand and explain their lives. One can reinterpret this as a patient asking, “If I died today, would my life have been good enough?” or “When I die, how will I look back at this moment in time and judge the choices I made?”
Other patients come to us attempting to use the same maladaptive defenses that did not serve them well in the past in the hopes of achieving a new outcome that will validate their lives. While it may be understandable that a child dissociates when facing abuse, hoping that this defense mechanism – as an adult – will work, it is unlikely to be fruitful and will certainly not validate or repair the past. This hope to repair one’s past can be interpreted as a fear of death – “I cannot die without correcting this.” This psychic conflict can intensify if one does not adopt a more adaptive understanding of his or her life.
Death anxiety is the feeling associated with the finality of life. Not only is life final, but a constant reminder of that fact is the idea that any one moment is final. Other than in science fiction, one cannot return to a prior moment and repair the past in the hope of a better future. Time goes only in one direction and death is the natural outcome of all life.
Death may have some evolutionary purpose that encourages the promotion of newer and more fitter genes, but one doesn’t have to consider its origin and reason to admit death’s constancy throughout humanity. People die and that is an anxiety-provoking fact of life. Death anxiety can feel especially tangible in our connected world. In a world of constant news, it can feel – for many people – that if your house wasn’t displaced because of global warming or that you are not a war refugee, you don’t deserve to be seen and heard.
This can be a particularly strong feeling for and among physicians, who don’t think that the mental health challenges generated by their own tough circumstances deserve to be labeled a mental disorder, so they designate themselves as having “burnout”1 – as they don’t deserve the sympathy of having the clinically significant impairments of “depression.” Our traumas don’t seem important enough to deserve notice, and thus we may feel like we could die without ever having truly mattered.
This can also be applied in the reverse fashion. Certain individuals, like celebrities, live such extravagant lives that our simpler achievements can feel futile in comparison. While the neighbor’s grass has always felt greener, we are now constantly exposed to perfectly manicured lawns on social media. When compounded, the idea that our successes and our pains are both simultaneously irrelevant can lead one to have very palpable death anxiety – my life will never matter if none of the things I do matter, or my life will never matter because I will never achieve the requisite number of “likes” or “views” on social media required to believe that one’s life was worth living.
A way of alleviating death anxiety can be through the concept of legacy, or what we leave behind. How will people remember me? Will people remember me, or will I disappear like a shadow into the distant memory of my near and dear ones? The idea of being forgotten or lost to memory is intolerable to some and can be a strong driving force to “make a name” for oneself. For those who crave fame, whether a celebrity or a generous alumnus, part of this is likely related to remaining well known after death. After all, one can argue that you are not truly dead as long as you continue to live in the memory and/or genes of others.
Legacy thus serves as a form of posthumous transitional object; a way of calming our fears about how we will be remembered. For many, reconciling their feelings towards their legacy is an avenue to tame death anxiety.
A case study
The case of Mr. B illustrates this. As a 72-year-old male with a long history of generalized anxiety, he once had a nightmare as a child, similar to the plot of Sleeping Beauty. In his dream, he walks up a spiral staircase in a castle and touches the spindle on a spinning wheel, thus ending his life. The dream was vivid and marked him.
His fear of death has subsequently reared its head throughout his life. In more recent years, he has suffered from cardiovascular disease. Although he is now quite stable on his current cardiac medications, he is constantly fearful that he will experience a cardiac event while asleep and suddenly die. He is so anxious about not waking up in the morning that falling asleep is nearly impossible.
Mr. B is single, with no close family besides a sister who lives in another state. He has a dog and few friends. He worries about what will happen to his dog if he doesn’t wake up in the morning, but perhaps most distressing to him is “there’s so much left for me to do, I have so much to write!” As an accomplished author, he continues to write, and hopes to publish many more novels in his lifetime. It is unsurprising that someone without a strong social network may fear death and feel pressured to somehow make a mark on the world before the curtain falls. It is scary to think that even without us, life goes on.
By bringing to Mr. B’s attention that his ever-present anxiety is rooted in fear of death, he was able to gain more insight into his own defensive behaviors. By confronting his death anxiety and processing his definition of a life well lived together in therapy, he’s acknowledged his lack of social connection as demoralizing, and has made significant strides to remedy this. He’s been able to focus on a more fulfilling life day to day, with less emphasis on his to-do list and aspirations. Instead, he’s connected more with his faith and members of his church. He’s gotten close to several neighbors and enjoys long dinners with them on his back patio.
At a recent meeting, he confessed that he feels “lighter” and not as fearful about sudden cardiac death, and thus has noticed that his overall anxiety has diminished greatly. He concluded that experiencing meaningful relationships in the present moment would give him greater joy than spending his remaining time engaged in preserving a future identity for himself. It seems elementary, but if we look within, we may find that we all suffer similarly: How much of our daily actions, thoughts, and fears are tied to the looming threat of death?
Conclusion
While modern psychiatry continues to advance with better understandings of our neurobiology, improved knowledge of pathophysiological processes of mental illness, and expanding discovery of novel pharmacotherapeutics, the modern psychiatrist should not forget fundamental truths of behavior and humanity that were once the staple of psychiatry.
Death anxiety is one of those truths; it is the ultimate stressor that we will all face and should be regular study and practice for psychiatrists. In this article, we explored some of those facets most meaningful to us but recommend you expand your study to the many more available.
Patients often come to physicians seeking validation of their lives or trying to use the same maladaptive defense mechanisms that did not serve them well in the past to achieve a better outcome.
In today’s world, death anxiety can feel palpable due to the constant exposure to global news and social media that can make us feel irrelevant. However, legacy, or what we leave behind, can serve as a way to alleviate death anxiety. For many, reconciling their feelings toward their legacy is an avenue to tame death anxiety. Therapy can help individuals gain insight into their defensive behaviors and process their definition of a life well lived. By focusing on a life worth living, individuals can alleviate their death anxiety and gain a sense of fulfillment.
Dr. Akkoor is a psychiatry resident at the University of California, San Diego. She is interested in immigrant mental health, ethics, consultation-liaison psychiatry, and medical education. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. Dr. Badre and Dr. Akkoor have no conflicts of interest.
Reference
1. Badre N. Burnout: A concept that rebrands mental illness for professionals. Clinical Psychiatry News. 2020 Mar 5.
Disappointment – “I failed this exam, my life is ruined” or regret – “I am getting a divorce, I wasted so much of my life.” Patients present with a wide variety of complaints that can be understood as a form of death anxiety.
Fundamentally, patients come to see us to understand and explain their lives. One can reinterpret this as a patient asking, “If I died today, would my life have been good enough?” or “When I die, how will I look back at this moment in time and judge the choices I made?”
Other patients come to us attempting to use the same maladaptive defenses that did not serve them well in the past in the hopes of achieving a new outcome that will validate their lives. While it may be understandable that a child dissociates when facing abuse, hoping that this defense mechanism – as an adult – will work, it is unlikely to be fruitful and will certainly not validate or repair the past. This hope to repair one’s past can be interpreted as a fear of death – “I cannot die without correcting this.” This psychic conflict can intensify if one does not adopt a more adaptive understanding of his or her life.
Death anxiety is the feeling associated with the finality of life. Not only is life final, but a constant reminder of that fact is the idea that any one moment is final. Other than in science fiction, one cannot return to a prior moment and repair the past in the hope of a better future. Time goes only in one direction and death is the natural outcome of all life.
Death may have some evolutionary purpose that encourages the promotion of newer and more fitter genes, but one doesn’t have to consider its origin and reason to admit death’s constancy throughout humanity. People die and that is an anxiety-provoking fact of life. Death anxiety can feel especially tangible in our connected world. In a world of constant news, it can feel – for many people – that if your house wasn’t displaced because of global warming or that you are not a war refugee, you don’t deserve to be seen and heard.
This can be a particularly strong feeling for and among physicians, who don’t think that the mental health challenges generated by their own tough circumstances deserve to be labeled a mental disorder, so they designate themselves as having “burnout”1 – as they don’t deserve the sympathy of having the clinically significant impairments of “depression.” Our traumas don’t seem important enough to deserve notice, and thus we may feel like we could die without ever having truly mattered.
This can also be applied in the reverse fashion. Certain individuals, like celebrities, live such extravagant lives that our simpler achievements can feel futile in comparison. While the neighbor’s grass has always felt greener, we are now constantly exposed to perfectly manicured lawns on social media. When compounded, the idea that our successes and our pains are both simultaneously irrelevant can lead one to have very palpable death anxiety – my life will never matter if none of the things I do matter, or my life will never matter because I will never achieve the requisite number of “likes” or “views” on social media required to believe that one’s life was worth living.
A way of alleviating death anxiety can be through the concept of legacy, or what we leave behind. How will people remember me? Will people remember me, or will I disappear like a shadow into the distant memory of my near and dear ones? The idea of being forgotten or lost to memory is intolerable to some and can be a strong driving force to “make a name” for oneself. For those who crave fame, whether a celebrity or a generous alumnus, part of this is likely related to remaining well known after death. After all, one can argue that you are not truly dead as long as you continue to live in the memory and/or genes of others.
Legacy thus serves as a form of posthumous transitional object; a way of calming our fears about how we will be remembered. For many, reconciling their feelings towards their legacy is an avenue to tame death anxiety.
A case study
The case of Mr. B illustrates this. As a 72-year-old male with a long history of generalized anxiety, he once had a nightmare as a child, similar to the plot of Sleeping Beauty. In his dream, he walks up a spiral staircase in a castle and touches the spindle on a spinning wheel, thus ending his life. The dream was vivid and marked him.
His fear of death has subsequently reared its head throughout his life. In more recent years, he has suffered from cardiovascular disease. Although he is now quite stable on his current cardiac medications, he is constantly fearful that he will experience a cardiac event while asleep and suddenly die. He is so anxious about not waking up in the morning that falling asleep is nearly impossible.
Mr. B is single, with no close family besides a sister who lives in another state. He has a dog and few friends. He worries about what will happen to his dog if he doesn’t wake up in the morning, but perhaps most distressing to him is “there’s so much left for me to do, I have so much to write!” As an accomplished author, he continues to write, and hopes to publish many more novels in his lifetime. It is unsurprising that someone without a strong social network may fear death and feel pressured to somehow make a mark on the world before the curtain falls. It is scary to think that even without us, life goes on.
By bringing to Mr. B’s attention that his ever-present anxiety is rooted in fear of death, he was able to gain more insight into his own defensive behaviors. By confronting his death anxiety and processing his definition of a life well lived together in therapy, he’s acknowledged his lack of social connection as demoralizing, and has made significant strides to remedy this. He’s been able to focus on a more fulfilling life day to day, with less emphasis on his to-do list and aspirations. Instead, he’s connected more with his faith and members of his church. He’s gotten close to several neighbors and enjoys long dinners with them on his back patio.
At a recent meeting, he confessed that he feels “lighter” and not as fearful about sudden cardiac death, and thus has noticed that his overall anxiety has diminished greatly. He concluded that experiencing meaningful relationships in the present moment would give him greater joy than spending his remaining time engaged in preserving a future identity for himself. It seems elementary, but if we look within, we may find that we all suffer similarly: How much of our daily actions, thoughts, and fears are tied to the looming threat of death?
Conclusion
While modern psychiatry continues to advance with better understandings of our neurobiology, improved knowledge of pathophysiological processes of mental illness, and expanding discovery of novel pharmacotherapeutics, the modern psychiatrist should not forget fundamental truths of behavior and humanity that were once the staple of psychiatry.
Death anxiety is one of those truths; it is the ultimate stressor that we will all face and should be regular study and practice for psychiatrists. In this article, we explored some of those facets most meaningful to us but recommend you expand your study to the many more available.
Patients often come to physicians seeking validation of their lives or trying to use the same maladaptive defense mechanisms that did not serve them well in the past to achieve a better outcome.
In today’s world, death anxiety can feel palpable due to the constant exposure to global news and social media that can make us feel irrelevant. However, legacy, or what we leave behind, can serve as a way to alleviate death anxiety. For many, reconciling their feelings toward their legacy is an avenue to tame death anxiety. Therapy can help individuals gain insight into their defensive behaviors and process their definition of a life well lived. By focusing on a life worth living, individuals can alleviate their death anxiety and gain a sense of fulfillment.
Dr. Akkoor is a psychiatry resident at the University of California, San Diego. She is interested in immigrant mental health, ethics, consultation-liaison psychiatry, and medical education. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. Dr. Badre and Dr. Akkoor have no conflicts of interest.
Reference
1. Badre N. Burnout: A concept that rebrands mental illness for professionals. Clinical Psychiatry News. 2020 Mar 5.
Disappointment – “I failed this exam, my life is ruined” or regret – “I am getting a divorce, I wasted so much of my life.” Patients present with a wide variety of complaints that can be understood as a form of death anxiety.
Fundamentally, patients come to see us to understand and explain their lives. One can reinterpret this as a patient asking, “If I died today, would my life have been good enough?” or “When I die, how will I look back at this moment in time and judge the choices I made?”
Other patients come to us attempting to use the same maladaptive defenses that did not serve them well in the past in the hopes of achieving a new outcome that will validate their lives. While it may be understandable that a child dissociates when facing abuse, hoping that this defense mechanism – as an adult – will work, it is unlikely to be fruitful and will certainly not validate or repair the past. This hope to repair one’s past can be interpreted as a fear of death – “I cannot die without correcting this.” This psychic conflict can intensify if one does not adopt a more adaptive understanding of his or her life.
Death anxiety is the feeling associated with the finality of life. Not only is life final, but a constant reminder of that fact is the idea that any one moment is final. Other than in science fiction, one cannot return to a prior moment and repair the past in the hope of a better future. Time goes only in one direction and death is the natural outcome of all life.
Death may have some evolutionary purpose that encourages the promotion of newer and more fitter genes, but one doesn’t have to consider its origin and reason to admit death’s constancy throughout humanity. People die and that is an anxiety-provoking fact of life. Death anxiety can feel especially tangible in our connected world. In a world of constant news, it can feel – for many people – that if your house wasn’t displaced because of global warming or that you are not a war refugee, you don’t deserve to be seen and heard.
This can be a particularly strong feeling for and among physicians, who don’t think that the mental health challenges generated by their own tough circumstances deserve to be labeled a mental disorder, so they designate themselves as having “burnout”1 – as they don’t deserve the sympathy of having the clinically significant impairments of “depression.” Our traumas don’t seem important enough to deserve notice, and thus we may feel like we could die without ever having truly mattered.
This can also be applied in the reverse fashion. Certain individuals, like celebrities, live such extravagant lives that our simpler achievements can feel futile in comparison. While the neighbor’s grass has always felt greener, we are now constantly exposed to perfectly manicured lawns on social media. When compounded, the idea that our successes and our pains are both simultaneously irrelevant can lead one to have very palpable death anxiety – my life will never matter if none of the things I do matter, or my life will never matter because I will never achieve the requisite number of “likes” or “views” on social media required to believe that one’s life was worth living.
A way of alleviating death anxiety can be through the concept of legacy, or what we leave behind. How will people remember me? Will people remember me, or will I disappear like a shadow into the distant memory of my near and dear ones? The idea of being forgotten or lost to memory is intolerable to some and can be a strong driving force to “make a name” for oneself. For those who crave fame, whether a celebrity or a generous alumnus, part of this is likely related to remaining well known after death. After all, one can argue that you are not truly dead as long as you continue to live in the memory and/or genes of others.
Legacy thus serves as a form of posthumous transitional object; a way of calming our fears about how we will be remembered. For many, reconciling their feelings towards their legacy is an avenue to tame death anxiety.
A case study
The case of Mr. B illustrates this. As a 72-year-old male with a long history of generalized anxiety, he once had a nightmare as a child, similar to the plot of Sleeping Beauty. In his dream, he walks up a spiral staircase in a castle and touches the spindle on a spinning wheel, thus ending his life. The dream was vivid and marked him.
His fear of death has subsequently reared its head throughout his life. In more recent years, he has suffered from cardiovascular disease. Although he is now quite stable on his current cardiac medications, he is constantly fearful that he will experience a cardiac event while asleep and suddenly die. He is so anxious about not waking up in the morning that falling asleep is nearly impossible.
Mr. B is single, with no close family besides a sister who lives in another state. He has a dog and few friends. He worries about what will happen to his dog if he doesn’t wake up in the morning, but perhaps most distressing to him is “there’s so much left for me to do, I have so much to write!” As an accomplished author, he continues to write, and hopes to publish many more novels in his lifetime. It is unsurprising that someone without a strong social network may fear death and feel pressured to somehow make a mark on the world before the curtain falls. It is scary to think that even without us, life goes on.
By bringing to Mr. B’s attention that his ever-present anxiety is rooted in fear of death, he was able to gain more insight into his own defensive behaviors. By confronting his death anxiety and processing his definition of a life well lived together in therapy, he’s acknowledged his lack of social connection as demoralizing, and has made significant strides to remedy this. He’s been able to focus on a more fulfilling life day to day, with less emphasis on his to-do list and aspirations. Instead, he’s connected more with his faith and members of his church. He’s gotten close to several neighbors and enjoys long dinners with them on his back patio.
At a recent meeting, he confessed that he feels “lighter” and not as fearful about sudden cardiac death, and thus has noticed that his overall anxiety has diminished greatly. He concluded that experiencing meaningful relationships in the present moment would give him greater joy than spending his remaining time engaged in preserving a future identity for himself. It seems elementary, but if we look within, we may find that we all suffer similarly: How much of our daily actions, thoughts, and fears are tied to the looming threat of death?
Conclusion
While modern psychiatry continues to advance with better understandings of our neurobiology, improved knowledge of pathophysiological processes of mental illness, and expanding discovery of novel pharmacotherapeutics, the modern psychiatrist should not forget fundamental truths of behavior and humanity that were once the staple of psychiatry.
Death anxiety is one of those truths; it is the ultimate stressor that we will all face and should be regular study and practice for psychiatrists. In this article, we explored some of those facets most meaningful to us but recommend you expand your study to the many more available.
Patients often come to physicians seeking validation of their lives or trying to use the same maladaptive defense mechanisms that did not serve them well in the past to achieve a better outcome.
In today’s world, death anxiety can feel palpable due to the constant exposure to global news and social media that can make us feel irrelevant. However, legacy, or what we leave behind, can serve as a way to alleviate death anxiety. For many, reconciling their feelings toward their legacy is an avenue to tame death anxiety. Therapy can help individuals gain insight into their defensive behaviors and process their definition of a life well lived. By focusing on a life worth living, individuals can alleviate their death anxiety and gain a sense of fulfillment.
Dr. Akkoor is a psychiatry resident at the University of California, San Diego. She is interested in immigrant mental health, ethics, consultation-liaison psychiatry, and medical education. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. Dr. Badre and Dr. Akkoor have no conflicts of interest.
Reference
1. Badre N. Burnout: A concept that rebrands mental illness for professionals. Clinical Psychiatry News. 2020 Mar 5.
Preventing breaks and falls in older adults
LONG BEACH, CALIF. – Ms. S had recently arrived home after a stay at a skilled nursing facility to recover from a hip fracture resulting from osteoporosis. For many patients, follow-up care would have included a DEXA scan or a prescription for a bisphosphonate from a primary care clinician not trained in geriatrics.
But the 85-year-old received care that went further and that is considered best practice for the management of geriatric fractures: A physical therapist visited her after discharge and provided education on the importance of maintaining mobility. Ms. S also underwent assessment for fall risk and gait balance, and a team of multidisciplinary clinicians managed other factors, from postural hypotension to footwear and foot problems.
Sonja Rosen, MD, professor of medicine and chief of geriatric medicine at Cedars-Sinai Medical Center, Los Angeles, talked about Ms. S as part of a panel discussion on applying the “Geriatric 5Ms” for patients with osteoporosis at the annual meeting of the American Geriatrics Society.
“You have to figure out why they are falling and help them not fall again,” Dr. Rosen said.
Approximately 10 million Americans have osteoporosis, and another 44 million have low bone density. One in two women and up to one in four men will experience a bone fracture as a result of osteoporosis, according to the Bone Health and Osteoporosis Foundation.
, which involves considering the care preferences and goals for health care outcomes of individuals.
Ms. S eventually visited a geriatrician through the Cedars-Sinai Geriatric Fracture Program, which has been shown to lower costs and shorten hospital stays. In the program, she was advised to use a walker. Initially, she saw the aid as a hindrance – she felt she should be able to walk without it, like before. But with education, she learned that it is impossible to predict falls and that the walking aid could reduce her risk of a stumble.
Dr. Rosen said clinicians should address any vision problems, prescriptions for psychotropic drugs,which can affect balance, and heart rate and rhythm abnormalities, and they should suggest modifications to the home environment, such as installing grab bars in showers and removing rugs that can easily be tripped over.
The program at Cedars-Sinai, like similar initiatives, offers a team with resources that some clinicians may not have access to, such as a care coordinator and bone-health coach. But health care providers can utilize aspects, such as making referrals to community exercise classes.
Dr. Rosen and her colleagues studied the effects of such exercise programs and found that the programs lessen loneliness and social isolation. Fear of falling decreased in 75% of participants, “which is so key to these postfracture patients in getting back out into the world and engaging in their prior level of functional status,” Dr. Rosen said.
The second ‘M’: Medication management
The second “M,” medications, can help clinicians sequence osteoporosis drugs, depending on patient characteristics and scenarios.
Cathleen Colon-Emeric, MD, MHS, chief of geriatrics at Duke University, in Durham, N.C., dived into the case history of Ms. S, who had hypertension and insomnia in addition to osteoporosis.
First-line treatment for Ms. S – and for most patients – was an oral bisphosphonate, Dr. Colon-Emeric said. Compared with placebo, the drugs decrease the risk of overall osteoporotic fractures by nearly 40% (odds ratio, 0.62). But the medications are linked to injury of the esophageal mucosa. This risk is decreased when a patient stays upright for 30 minutes after taking oral bisphosphonates. Dr. Colon-Emeric displayed a slide of a woman receiving a pedicure at a nail salon.
“The picture of the pedicure is to share the wonderful idea I got from one skilled nursing facility I was working with, who makes sure they do safe administration to prevent esophagitis in their patients by having them all go to a spa day, where they all sit up and get their nails done while they wait their 30 minutes [after taking the pill] sitting up safely,” Dr. Colon-Emeric said.
This strategy drew applause from the audience.
Dr. Colon-Emeric advised that clinicians use judgment in the interpretation of results from the Fracture Risk Assessment Tool (FRAX). Incorporating race into estimates of fracture risk has pros and cons. While there are racial and ethnic differences in average bone density, the data for race calibrations to estimate risk are dated, she said. Clinicians should compare FRAX estimates with and without race input to help patients understand a range of risks.
Some patients may be reluctant to begin taking osteoporosis drugs because of misinformation originating from inaccurate news reports or anecdotes from friends. Dr. Colon-Emeric advised clinicians to remind patients that one in five who experience a fracture will have another injury in the following 2 years.
“A major osteoporotic fracture is akin to a heart attack; it has a very similar 1-year mortality rate and a very similar rate of a subsequent secondary event,” Dr. Colon-Emeric said. “We have a class of medications that decrease both those risks by nearly a third.”
Shared decision-making can help patients understand the risks and benefits of treatment, she said.
“People are really scared about the side effects,” Michelle Keller, PhD, MPH, a research scientist at Cedars-Sinai who attended the session, said. “The idea that a “bone attack” is like a heart attack gets the message across.”
Mind and multicomplexity
Medical complexity of a patient must be considered when making decisions on treatment, according to Joshua Niznik, PharmD, PhD, assistant professor of medicine in the Center for Aging and Health at the University of North Carolina at Chapel Hill.
“Medical complexity is an acknowledgment of the entire person, the burden of their multiple chronic conditions, advanced illnesses, and also their biopsychosocial needs and how those together might augment treatment selection and decision-making,” Dr. Niznik said.
Studies by Dr. Niznik and others have shown that swallowing difficulties, severe dementia, and being older than 90 are linked with a lower likelihood of receiving treatment for osteoporosis.
But therapies for fracture prevention, especially bisphosphonates, appear to be at least as effective for adults with medical complexity as they are for people without such conditions, Dr. Niznik said. Physicians must consider the potential treatment burden and the likelihood of benefit, he said.
Dr. Niznik’s research has shown a lack of strong evidence on how clinicians can manage patients in nursing homes. In some cases, deprescribing is reasonable, such as for patients who have undergone treatment for several years and whose life expectancy is less than 2 years.
“In the absence of any of those, if they are not already treated for osteoporosis, it makes sense to initiate treatment at that time,” Dr. Niznik said.
Matters most: Patient input
Clinicians need to educate patients on how long they must undergo a treatment before they experience benefits, according to Sarah D. Berry, MD, MPH, associate professor of medicine at Harvard Medical School, in Boston.
A meta-analysis of studies that included more than 20,000 women who were randomly assigned to receive bisphosphonate or placebo found that one nonvertebral fracture was avoided during a 12-month period for every 100 persons treated. One hip fracture was avoided during a 20-month period for every 200 patients treated.
“In general, in persons with a 2-year life expectancy, time to benefit favors bisphosphonate use,” Dr. Berry said. “Anabolics may have an even quicker time to benefit.”
Dr. Berry said a shared a decision-making model can help clinicians facilitate discussions that help patients prioritize goals and compare options while considering results, benefits, and harms. And she offered a final tip: Use tools with absolute risk reduction to convey risks and benefits, as the relative risk calculations overestimate how effective treatment will be.
Dr. Rosen has disclosed no relevant financial relationships. Dr. Colon-Emeric has received grants from the National Institutes of Health and VA Health Services Research and Development Funding; has served as endpoint adjudication chair for UCB Pharma; and has received royalties from Wolters Kluwer. Dr. Niznik has received funding from the National Institute of Aging and the Centers for Disease Control and Prevention. Dr. Berry has received funding from the NIH and royalties from Wolters Kluwer.
A version of this article originally appeared on Medscape.com.
LONG BEACH, CALIF. – Ms. S had recently arrived home after a stay at a skilled nursing facility to recover from a hip fracture resulting from osteoporosis. For many patients, follow-up care would have included a DEXA scan or a prescription for a bisphosphonate from a primary care clinician not trained in geriatrics.
But the 85-year-old received care that went further and that is considered best practice for the management of geriatric fractures: A physical therapist visited her after discharge and provided education on the importance of maintaining mobility. Ms. S also underwent assessment for fall risk and gait balance, and a team of multidisciplinary clinicians managed other factors, from postural hypotension to footwear and foot problems.
Sonja Rosen, MD, professor of medicine and chief of geriatric medicine at Cedars-Sinai Medical Center, Los Angeles, talked about Ms. S as part of a panel discussion on applying the “Geriatric 5Ms” for patients with osteoporosis at the annual meeting of the American Geriatrics Society.
“You have to figure out why they are falling and help them not fall again,” Dr. Rosen said.
Approximately 10 million Americans have osteoporosis, and another 44 million have low bone density. One in two women and up to one in four men will experience a bone fracture as a result of osteoporosis, according to the Bone Health and Osteoporosis Foundation.
, which involves considering the care preferences and goals for health care outcomes of individuals.
Ms. S eventually visited a geriatrician through the Cedars-Sinai Geriatric Fracture Program, which has been shown to lower costs and shorten hospital stays. In the program, she was advised to use a walker. Initially, she saw the aid as a hindrance – she felt she should be able to walk without it, like before. But with education, she learned that it is impossible to predict falls and that the walking aid could reduce her risk of a stumble.
Dr. Rosen said clinicians should address any vision problems, prescriptions for psychotropic drugs,which can affect balance, and heart rate and rhythm abnormalities, and they should suggest modifications to the home environment, such as installing grab bars in showers and removing rugs that can easily be tripped over.
The program at Cedars-Sinai, like similar initiatives, offers a team with resources that some clinicians may not have access to, such as a care coordinator and bone-health coach. But health care providers can utilize aspects, such as making referrals to community exercise classes.
Dr. Rosen and her colleagues studied the effects of such exercise programs and found that the programs lessen loneliness and social isolation. Fear of falling decreased in 75% of participants, “which is so key to these postfracture patients in getting back out into the world and engaging in their prior level of functional status,” Dr. Rosen said.
The second ‘M’: Medication management
The second “M,” medications, can help clinicians sequence osteoporosis drugs, depending on patient characteristics and scenarios.
Cathleen Colon-Emeric, MD, MHS, chief of geriatrics at Duke University, in Durham, N.C., dived into the case history of Ms. S, who had hypertension and insomnia in addition to osteoporosis.
First-line treatment for Ms. S – and for most patients – was an oral bisphosphonate, Dr. Colon-Emeric said. Compared with placebo, the drugs decrease the risk of overall osteoporotic fractures by nearly 40% (odds ratio, 0.62). But the medications are linked to injury of the esophageal mucosa. This risk is decreased when a patient stays upright for 30 minutes after taking oral bisphosphonates. Dr. Colon-Emeric displayed a slide of a woman receiving a pedicure at a nail salon.
“The picture of the pedicure is to share the wonderful idea I got from one skilled nursing facility I was working with, who makes sure they do safe administration to prevent esophagitis in their patients by having them all go to a spa day, where they all sit up and get their nails done while they wait their 30 minutes [after taking the pill] sitting up safely,” Dr. Colon-Emeric said.
This strategy drew applause from the audience.
Dr. Colon-Emeric advised that clinicians use judgment in the interpretation of results from the Fracture Risk Assessment Tool (FRAX). Incorporating race into estimates of fracture risk has pros and cons. While there are racial and ethnic differences in average bone density, the data for race calibrations to estimate risk are dated, she said. Clinicians should compare FRAX estimates with and without race input to help patients understand a range of risks.
Some patients may be reluctant to begin taking osteoporosis drugs because of misinformation originating from inaccurate news reports or anecdotes from friends. Dr. Colon-Emeric advised clinicians to remind patients that one in five who experience a fracture will have another injury in the following 2 years.
“A major osteoporotic fracture is akin to a heart attack; it has a very similar 1-year mortality rate and a very similar rate of a subsequent secondary event,” Dr. Colon-Emeric said. “We have a class of medications that decrease both those risks by nearly a third.”
Shared decision-making can help patients understand the risks and benefits of treatment, she said.
“People are really scared about the side effects,” Michelle Keller, PhD, MPH, a research scientist at Cedars-Sinai who attended the session, said. “The idea that a “bone attack” is like a heart attack gets the message across.”
Mind and multicomplexity
Medical complexity of a patient must be considered when making decisions on treatment, according to Joshua Niznik, PharmD, PhD, assistant professor of medicine in the Center for Aging and Health at the University of North Carolina at Chapel Hill.
“Medical complexity is an acknowledgment of the entire person, the burden of their multiple chronic conditions, advanced illnesses, and also their biopsychosocial needs and how those together might augment treatment selection and decision-making,” Dr. Niznik said.
Studies by Dr. Niznik and others have shown that swallowing difficulties, severe dementia, and being older than 90 are linked with a lower likelihood of receiving treatment for osteoporosis.
But therapies for fracture prevention, especially bisphosphonates, appear to be at least as effective for adults with medical complexity as they are for people without such conditions, Dr. Niznik said. Physicians must consider the potential treatment burden and the likelihood of benefit, he said.
Dr. Niznik’s research has shown a lack of strong evidence on how clinicians can manage patients in nursing homes. In some cases, deprescribing is reasonable, such as for patients who have undergone treatment for several years and whose life expectancy is less than 2 years.
“In the absence of any of those, if they are not already treated for osteoporosis, it makes sense to initiate treatment at that time,” Dr. Niznik said.
Matters most: Patient input
Clinicians need to educate patients on how long they must undergo a treatment before they experience benefits, according to Sarah D. Berry, MD, MPH, associate professor of medicine at Harvard Medical School, in Boston.
A meta-analysis of studies that included more than 20,000 women who were randomly assigned to receive bisphosphonate or placebo found that one nonvertebral fracture was avoided during a 12-month period for every 100 persons treated. One hip fracture was avoided during a 20-month period for every 200 patients treated.
“In general, in persons with a 2-year life expectancy, time to benefit favors bisphosphonate use,” Dr. Berry said. “Anabolics may have an even quicker time to benefit.”
Dr. Berry said a shared a decision-making model can help clinicians facilitate discussions that help patients prioritize goals and compare options while considering results, benefits, and harms. And she offered a final tip: Use tools with absolute risk reduction to convey risks and benefits, as the relative risk calculations overestimate how effective treatment will be.
Dr. Rosen has disclosed no relevant financial relationships. Dr. Colon-Emeric has received grants from the National Institutes of Health and VA Health Services Research and Development Funding; has served as endpoint adjudication chair for UCB Pharma; and has received royalties from Wolters Kluwer. Dr. Niznik has received funding from the National Institute of Aging and the Centers for Disease Control and Prevention. Dr. Berry has received funding from the NIH and royalties from Wolters Kluwer.
A version of this article originally appeared on Medscape.com.
LONG BEACH, CALIF. – Ms. S had recently arrived home after a stay at a skilled nursing facility to recover from a hip fracture resulting from osteoporosis. For many patients, follow-up care would have included a DEXA scan or a prescription for a bisphosphonate from a primary care clinician not trained in geriatrics.
But the 85-year-old received care that went further and that is considered best practice for the management of geriatric fractures: A physical therapist visited her after discharge and provided education on the importance of maintaining mobility. Ms. S also underwent assessment for fall risk and gait balance, and a team of multidisciplinary clinicians managed other factors, from postural hypotension to footwear and foot problems.
Sonja Rosen, MD, professor of medicine and chief of geriatric medicine at Cedars-Sinai Medical Center, Los Angeles, talked about Ms. S as part of a panel discussion on applying the “Geriatric 5Ms” for patients with osteoporosis at the annual meeting of the American Geriatrics Society.
“You have to figure out why they are falling and help them not fall again,” Dr. Rosen said.
Approximately 10 million Americans have osteoporosis, and another 44 million have low bone density. One in two women and up to one in four men will experience a bone fracture as a result of osteoporosis, according to the Bone Health and Osteoporosis Foundation.
, which involves considering the care preferences and goals for health care outcomes of individuals.
Ms. S eventually visited a geriatrician through the Cedars-Sinai Geriatric Fracture Program, which has been shown to lower costs and shorten hospital stays. In the program, she was advised to use a walker. Initially, she saw the aid as a hindrance – she felt she should be able to walk without it, like before. But with education, she learned that it is impossible to predict falls and that the walking aid could reduce her risk of a stumble.
Dr. Rosen said clinicians should address any vision problems, prescriptions for psychotropic drugs,which can affect balance, and heart rate and rhythm abnormalities, and they should suggest modifications to the home environment, such as installing grab bars in showers and removing rugs that can easily be tripped over.
The program at Cedars-Sinai, like similar initiatives, offers a team with resources that some clinicians may not have access to, such as a care coordinator and bone-health coach. But health care providers can utilize aspects, such as making referrals to community exercise classes.
Dr. Rosen and her colleagues studied the effects of such exercise programs and found that the programs lessen loneliness and social isolation. Fear of falling decreased in 75% of participants, “which is so key to these postfracture patients in getting back out into the world and engaging in their prior level of functional status,” Dr. Rosen said.
The second ‘M’: Medication management
The second “M,” medications, can help clinicians sequence osteoporosis drugs, depending on patient characteristics and scenarios.
Cathleen Colon-Emeric, MD, MHS, chief of geriatrics at Duke University, in Durham, N.C., dived into the case history of Ms. S, who had hypertension and insomnia in addition to osteoporosis.
First-line treatment for Ms. S – and for most patients – was an oral bisphosphonate, Dr. Colon-Emeric said. Compared with placebo, the drugs decrease the risk of overall osteoporotic fractures by nearly 40% (odds ratio, 0.62). But the medications are linked to injury of the esophageal mucosa. This risk is decreased when a patient stays upright for 30 minutes after taking oral bisphosphonates. Dr. Colon-Emeric displayed a slide of a woman receiving a pedicure at a nail salon.
“The picture of the pedicure is to share the wonderful idea I got from one skilled nursing facility I was working with, who makes sure they do safe administration to prevent esophagitis in their patients by having them all go to a spa day, where they all sit up and get their nails done while they wait their 30 minutes [after taking the pill] sitting up safely,” Dr. Colon-Emeric said.
This strategy drew applause from the audience.
Dr. Colon-Emeric advised that clinicians use judgment in the interpretation of results from the Fracture Risk Assessment Tool (FRAX). Incorporating race into estimates of fracture risk has pros and cons. While there are racial and ethnic differences in average bone density, the data for race calibrations to estimate risk are dated, she said. Clinicians should compare FRAX estimates with and without race input to help patients understand a range of risks.
Some patients may be reluctant to begin taking osteoporosis drugs because of misinformation originating from inaccurate news reports or anecdotes from friends. Dr. Colon-Emeric advised clinicians to remind patients that one in five who experience a fracture will have another injury in the following 2 years.
“A major osteoporotic fracture is akin to a heart attack; it has a very similar 1-year mortality rate and a very similar rate of a subsequent secondary event,” Dr. Colon-Emeric said. “We have a class of medications that decrease both those risks by nearly a third.”
Shared decision-making can help patients understand the risks and benefits of treatment, she said.
“People are really scared about the side effects,” Michelle Keller, PhD, MPH, a research scientist at Cedars-Sinai who attended the session, said. “The idea that a “bone attack” is like a heart attack gets the message across.”
Mind and multicomplexity
Medical complexity of a patient must be considered when making decisions on treatment, according to Joshua Niznik, PharmD, PhD, assistant professor of medicine in the Center for Aging and Health at the University of North Carolina at Chapel Hill.
“Medical complexity is an acknowledgment of the entire person, the burden of their multiple chronic conditions, advanced illnesses, and also their biopsychosocial needs and how those together might augment treatment selection and decision-making,” Dr. Niznik said.
Studies by Dr. Niznik and others have shown that swallowing difficulties, severe dementia, and being older than 90 are linked with a lower likelihood of receiving treatment for osteoporosis.
But therapies for fracture prevention, especially bisphosphonates, appear to be at least as effective for adults with medical complexity as they are for people without such conditions, Dr. Niznik said. Physicians must consider the potential treatment burden and the likelihood of benefit, he said.
Dr. Niznik’s research has shown a lack of strong evidence on how clinicians can manage patients in nursing homes. In some cases, deprescribing is reasonable, such as for patients who have undergone treatment for several years and whose life expectancy is less than 2 years.
“In the absence of any of those, if they are not already treated for osteoporosis, it makes sense to initiate treatment at that time,” Dr. Niznik said.
Matters most: Patient input
Clinicians need to educate patients on how long they must undergo a treatment before they experience benefits, according to Sarah D. Berry, MD, MPH, associate professor of medicine at Harvard Medical School, in Boston.
A meta-analysis of studies that included more than 20,000 women who were randomly assigned to receive bisphosphonate or placebo found that one nonvertebral fracture was avoided during a 12-month period for every 100 persons treated. One hip fracture was avoided during a 20-month period for every 200 patients treated.
“In general, in persons with a 2-year life expectancy, time to benefit favors bisphosphonate use,” Dr. Berry said. “Anabolics may have an even quicker time to benefit.”
Dr. Berry said a shared a decision-making model can help clinicians facilitate discussions that help patients prioritize goals and compare options while considering results, benefits, and harms. And she offered a final tip: Use tools with absolute risk reduction to convey risks and benefits, as the relative risk calculations overestimate how effective treatment will be.
Dr. Rosen has disclosed no relevant financial relationships. Dr. Colon-Emeric has received grants from the National Institutes of Health and VA Health Services Research and Development Funding; has served as endpoint adjudication chair for UCB Pharma; and has received royalties from Wolters Kluwer. Dr. Niznik has received funding from the National Institute of Aging and the Centers for Disease Control and Prevention. Dr. Berry has received funding from the NIH and royalties from Wolters Kluwer.
A version of this article originally appeared on Medscape.com.
AT AGS 2023
Revisiting our approach to behavioral health referrals
Approximately 1 in 4 people ages 18 years and older and 1 in 3 people ages 18 to 25 years had a mental illness in the past year, according to the 2021 National Survey of Drug Use and Health.1 The survey also found that adults ages 18 to 25 years had the highest rate of serious mental illness but the lowest treatment rate compared to other adult age groups.1 Unfortunately, more than 60% of patients receiving mental health treatment fail to benefit to a clinically meaningful degree.2
However, there is growing evidence that referring patients to behavioral health practitioners (BHPs) with outcome-measured skills that meet the patient’s specific needs can have a dramatic and positive impact. There are 2 main steps to pairing patients with an appropriate BHP: (1) use of measurement-based care data that can be analyzed at the patient and therapist level, and (2) data-driven referrals that pair patients with BHPs based on such routine outcome monitoring data (paired-on outcome data).
Psychotherapy’s slow road toward measurement-based care
Routine outcome monitoring is the systematic measurement of symptoms and functioning during treatment. It serves multiple functions, including program evaluation and benchmarking of patient improvement rates. Moreover, routine outcome monitoring–derived feedback (based on repeated patient outcome measurements) can inform personalized and responsive care decisions throughout treatment.
For all intents and purposes,
- routinely administered symptom/functioning measure, ideally before each clinical encounter,
- practitioner review of these patient-level data,
- patient review of these data with their practitioner, and
- collaborative reevaluation of the person-specific treatment plan informed by these data.
CASE SCENARIO
Violeta W is a 33-year-old woman who presented to her family physician for her annual wellness exam. Prior to the exam, the medical assistant administered a Patient Health Questionnaire-9 (PHQ-9) to screen for depressive symptoms. Ms. W’s score was 20 out of 27, suggestive of depression. To further assess the severity of depressive symptoms and their effect on daily function, the physician reviewed responses to the questionnaire with her and discussed treatment options. Ms. W was most interested in trying a low-dose selective serotonin reuptake inhibitor (SSRI).
At her follow-up visit 4 weeks later, the medical assistant re-administered the PHQ-9. The physician then reviewed Ms. W’s responses with her and, based on Ms. W’s subjective report and objective symptoms (still a score of 20 out of 27 on the PHQ-9), increased her SSRI dose. At each subsequent visit, Ms. W completed a PHQ-9 and reviewed responses and depressive symptoms with her physician.
The value of measurement-based care in mental health care
A narrative review by Lewis et al3 of 21 randomized controlled clinical trials (RCTs) across a range of age groups (eg, adolescents, young adults, adults), disorders (eg, anxiety, mood), and settings (eg, outpatient, inpatient) found that in at least 9 review articles, measurement-based care was associated with significantly improved outcomes vs usual care (ie, treatment without routine outcome monitoring plus feedback). The average increase in treatment effect size was about 30% when treatment was accompanied by measurement-based care.3
Continue to: Moreover, a recent within-patient meta-analysis...
Moreover, a recent within-patient meta-analysis by de Jong et al4 shows that measurement-based care yields a small but significant increase in therapeutic outcomes (d = .15). Use of measurement-based care also is associated with improved communication between the patient and therapist.5 In pharmacotherapy practice, measurement-based care has been shown to predict rapid dose increases and changes in medication, when necessary; faster recovery rates; higher response rates to treatment3; and fewer dropouts.4
Perhaps one of the best-studied benefits of measurement-based mental health care is the ability to predict deterioration in care (ie, patients who are off-track in a way that practitioners often miss without the help of routine outcome monitoring data).6,7 Studies show that without a data-informed approach to care, some forms of psychotherapy or therapy with BHPs who are not sufficiently skilled in treating a given diagnosis increase symptoms or create significant harmful and iatrogenic effects.8-10 Conversely, the meta-analysis by de Jong et al4 found a lower percentage of deterioration in patients receiving measurement-based care. The difference in deterioration was significant: An average of 5.4% of patients in control conditions deteriorated compared to an average of 4.6% in feedback (measurement-based care) groups. There were even larger effect sizes when therapists received training in the feedback system.4
Routine outcome monitoring without a dialogue between patient and practitioner about the assessments (eg, ignoring complete measurement-based care requirements) may be inadequate. A recent review by Muir et al6 found no differences in patient outcomes when data were used solely for aggregate quality improvement activities, suggesting the need for practitioners to review results of routine outcome monitoring assessments with patients and use data to alter care when necessary.
Measurement-based care is believed to deliver benefits and reduce harm by enhancing and encouraging active patient involvement, improving patient understanding of symptoms, promoting better communication, and facilitating better care coordination.3 The benefits of measurement-based care can be enhanced with a comprehensive core routine outcome monitoring tool and the level of monitoring-generated information delivered for multiple stakeholders (eg, patient, therapist, clinic).11
A look at multidimensional assessment
The features of routine outcome monitoring tools vary significantly.12 Some measures assess single-symptom or problem domains (eg, PHQ-9 for depression or Generalized Anxiety Disorder-7 [GAD-7] scale for anxiety) or multiple dimensions (multidimensional routine outcome monitoring). Multidimensional routine outcome monitoring may have benefits over single-domain measures. Single-domain measures and the subscales or factors of more comprehensive multidimensional routine outcome monitoring assessments should possess adequate specificity and sensitivity.
Continue to: Some recent research findings...
Some recent research findings question the construct validity of brief single-domain measures of common presenting problems, such as depression and anxiety. For example, results from a factor analysis of the PHQ-9 and GAD-7 scale in patients with traumatic brain injury suggest these tools measure 1 psychological construct that includes depression and the cognitive components of anxiety (eg, worry)13—a finding consistent with those of other tools.14 Similarly, a larger study of 7763 BH patients found that a single factor accounted for most of the variance of the 2 combined measures, with no set of factors meeting the exacting standards used to develop multidimensional routine outcome monitoring.15 These findings suggest that the PHQ-9 and GAD-7 largely overlap and are not measuring different aspects of health as most practitioners believe (eg, depression and anxiety).
In commonly used assessments, multiple-factor analytic studies with high standards have supported the construct validity of domain-specific subscales, indicating that the various questions tap into different constructs of psychological health.14,16,17
Beyond multiple domain–specific indicators, multidimensional routine outcome measurements provide a global total score that minimizes Type I (false-positive conclusion) and Type II (false-negative conclusion) errors in tracking patient improvement or deterioration.18 As one would expect, multidimensional routine outcome monitoring generally includes more items than single-domain measures; however, this comes with a trade-off. If there are specificity and sensitivity concerns with an ultra-brief single-domain measure, an alternative to a core multidimensional routine outcome measurement is to aggregate a series of single-domain measures into a battery of patient self-reports. However, this approach may take longer for patients to complete since they would have to shift among the varying response sets and wording across the unique single-domain measures.
In addition, the standardization/normalization of multidimensional routine outcome monitoring likely makes interpretation easier than referring to norms and clinical severity cutoffs for many distinct measures. Furthermore, increased specificity enhances predictive power and allows BHPs to screen and track other conditions besides depression and anxiety. (It is worth noting that there are no known studies that have looked at the difference in time to administer or ease of interpretation of multidimensional routine outcome monitoring tools vs multiple single-domain measures.)
Two multidimensional routine outcome monitoring tools that cover a comprehensive series of discrete symptom and functional domains are the Treatment Outcome Package12 and Counseling Center Assessment of Psychological Symptoms.16 These tools, which include subscales beyond general depression and anxiety (eg, sleep, substance misuse, social conflict), take 7 to 10 minutes to complete and provide outcome results across 12 symptom and 8 functional dimensions. As an example, the Treatment Outcome Package has good psychometric qualities (eg, reliability, construct and concurrent validity) for adults,12 children,14,19 and adolescents,19 and can be administered through a secure online data collection portal. The Counseling Center Assessment of Psychological Symptoms has demonstrated high construct validity and good convergent validity.16 These assessments can be administered in paper or digital (eg, electronic medical record portal, smartphone) format.20
Continue to: CASE SCENARIO
CASE SCENARIO
Ms. W’s physician asked her to go online using her phone and answer the questions in the Treatment Outcome Package. Her results, which she viewed with her physician, were displayed in graph form (FIGURE). Her scores were represented in Z scores normalized to the general population, with “0” representing the general, nontreatment-seeking population average and positive scores representing the number of standard deviations (SDs) more severe than the general population average.
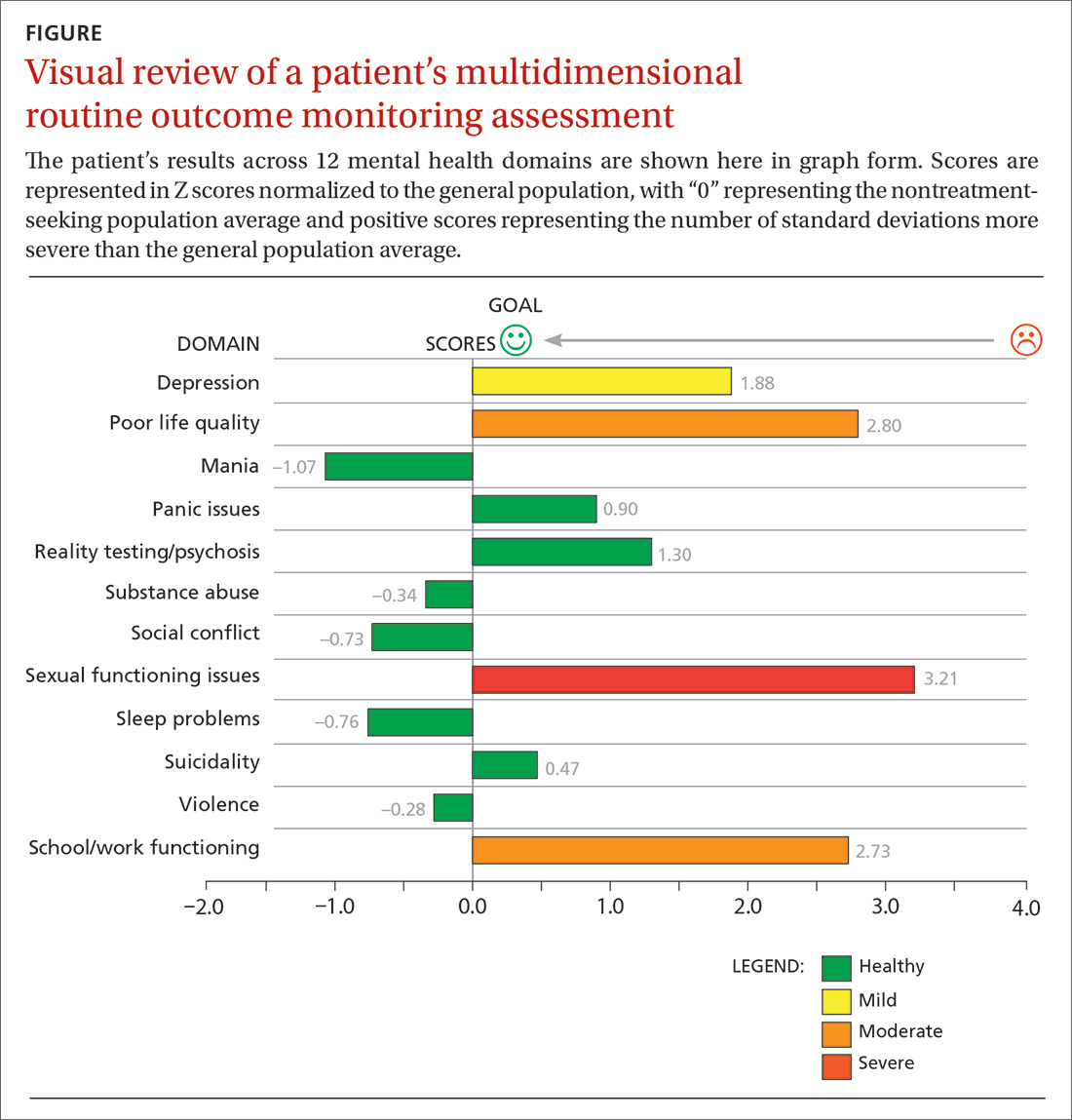
Although this assessment scored Ms. W’s clinically elevated depression as mild, it revealed abnormalities in 3 other domains. Sexual functioning issues represented the most abnormal domain at greater than 3 SDs (more severe than the general population), followed by poor life quality and school/work functioning.
After reviewing Ms. W’s report, her physician decided that pharmacologic management alone (for depression) was not the most appropriate treatment course. Therefore, her physician recommended psychotherapy in addition to the SSRI she was taking. Ms. W agreed to a customized referral for psychotherapy.
Data-driven referrals
When psychotherapy is chosen as a treatment, the individual BHP is an active component of that treatment. Consequently, it is essential to customize referrals to match a patient’s most elevated mental health concerns with a therapist who will most effectively treat those domains. It is rare for a BHP to be skilled in treating every mental health domain.9 Multiple studies have shown that BHPs have identifiable treatment skills in specific domains, which physicians should consider when making referrals.9,21,22 These studies demonstrate the utility of aggregating patient-level routine outcome monitoring data to better understand therapist-level (and ultimately clinic- and system-level) outcomes.
Additionally, recent research has tested this idea prospectively. An RCT funded by the Patient-Centered Outcome Research Institute and published in JAMA Psychiatry showed a significant and positive effect on patient outcomes (ie, reductions in general impairment, impairment involving a patient’s most elevated domain, and global distress) using paired-on outcome data matching vs as-usual matching protocols (eg, therapist self-defined areas of specialty).22 In the RCT, the most effective matching protocol was a combination of eliminating harm and matching the patient on their 3 most problematic domains (the highest match level). These patients ended care as healthy as the general population after 16 weeks of treatment. A random 1-year follow-up assessment from the original RCT showed that most patients who had been matched had maintained their improvement.23
Continue to: Therefore, a multidimensional routine outcome...
Therefore, a multidimensional routine outcome monitoring tool can be used to identify a BHP’s relative strengths and weaknesses across multiple outcome domains. Within a system of care, a sample of BHPs will possess varying outcome-domain profiles. When a new patient is seeking a referral to a BHP, these profiles (or domain-specific outcome track records) can be used to support paired-on outcome data matching. Specifically, a new patient completes the multidimensional routine outcome monitoring tool at pretreatment, and the results reveal the outcome domains on which the patient is most clinically severe. This pattern of domain-specific severity then can be used to pair the new patient with a BHP who has demonstrated success in addressing the same outcome domain(s). This approach matches a new patient to a BHP with established expertise based on routine outcome monitoring.
Retrospective and prospective studies have found that most BHPs have stable performance in their strengths and weaknesses.11,21 One study found that assessing BHP performance with their most recent 30 patients can reliably predict future performance with their next 30 patients.24 This predictability in a practitioner’s outcomes suggests report cards that are updated frequently can be utilized to make case assignments within BH or referrals to a specific BHP from primary care.
Making a paired-on outcome data–matched referral
Making customized BH referrals requires access to information about a practitioner’s previous routine outcome monitoring data per clinical domain (eg, suicidality, violence, quality of life) from their most recent patients. Previous research suggests that follow-up data from a minimum of 15 patients is necessary to make a reliable evaluation of a practitioner’s strengths and weaknesses (ie, effectiveness “report card”) per clinical domain.24
Few, if any, physicians have access to this level of updated outcome data from their referral network. To facilitate widespread use of paired-on outcome data matching, a new Web system (MatchedTherapists.com) will allow the general public and PCPs to access these grades. As a public service option, this site currently allows for a self-assessment using the Treatment Outcome Package. Pending versions will generate paired-on outcome data grades, and users will receive a list of local therapists available for in-person appointments as well as therapists available for virtual appointments. The paired-on outcome data grades are delivered in school-based letter grades. An “A+,” for example, represents the best matching grade. Users also will be able to sort and filter results for other criteria such as telemedicine, insurance, age, gender, and appointment availability. Currently, there are more than 77,000 therapists listed on the site nationwide. A basic listing is free.
CASE SCENARIO
After Ms. W took the multidimensional routine outcome assessment online, she received a list of therapists rank-ordered by paired-on outcome data grade, with the “A+” matches listed first. Three of the best-matched referrals accepted her insurance and were willing to see her through telemedicine. Therapists with available in-person appointments had a “B” grade. After discussing the options with her physician, Ms. W opted for telehealth counseling with the therapist whose profile she liked best. The therapist and PCP tracked her progress through routine outcome monitoring reporting until all her symptoms became subclinical.
Continue to: The future of a "referral bridge"
The future of a “referral bridge”
In this article, we present a solution to a common issue faced by mental health care patients: failure to benefit meaningfully from mental health treatment. Matching patients to specific BHPs based on effectiveness data regarding the therapist’s strengths and skills can improve patient outcomes and reduce harm. In addition, patients appear to value this approach. A Robert Wood Johnson Foundation–funded study demonstrated that patients value seeing practitioners who have a track record of successfully treating previous patients with similar issues.25,26 In many cases, patients indicated they would prioritize this matching process over other factors such as practitioners with a higher number of years of experience or the same demographic characteristics as the patient.25,26
These findings may represent a new area in the science of health care. Over the past century, major advances in diagnosis and treatment—the 2 primary pillars of health care—have turned the art of medicine into a science. However, the art of making referrals has not advanced commensurately, as there has been little attention focused on the “referral bridge” between these 2 pillars. As the studies reviewed in this paper demonstrate, a referral bridge deserves exploration in all fields of medicine.
CORRESPONDENCE
David R. Kraus, PhD, 1 Speen Street, Framingham, MA 01701; [email protected]
1. HHS. 2021 National Survey of Drug Use and Health (NSDUH) Releases. Accessed March 29, 2023. www.samhsa.gov/data/release/2021-national-survey-drug-use-and-health-nsduh-releases
2. Barkham M, Lambert, MJ. The efficacy and effectiveness of psychological therapies. In: Barkham M, Lutz W, Castonguay LG, eds. Bergin and Garfield’s Handbook of Psychotherapy and Behavior Change: 50th Anniversary Edition. 7th ed. John Wiley & Sons, Inc; 2021:135-189.
3. Lewis CC, Boyd M, Puspitasari A, et al. Implementing measurement-based care in behavioral health: a review. JAMA Psychiatry. 2019;76:324-335. doi: 10.1001/jamapsychiatry.2018.3329
4. de Jong K, Conijn JM, Gallagher RAV, et al. Using progress feedback to improve outcomes and reduce drop-out, treatment duration, and deterioration: a multilevel meta-analysis. Clin Psychol Rev. 2021;85:102002. doi: 10.1016/j.cpr.2021.102002
5. Carlier IVE, Meuldijk D, Van Vliet IM, et al. Routine outcome monitoring and feedback on physical or mental health status: evidence and theory. J Eval Clin Pract. 2012;18:104-110. doi: 10.1111/j.1365-2753.2010.01543.x
6. Muir HJ, Coyne AE, Morrison NR, et al. Ethical implications of routine outcomes monitoring for patients, psychotherapists, and mental health care systems. Psychotherapy (Chic). 2019;56:459-469. doi: 10.1037/pst0000246
7. Hannan C, Lambert MJ, Harmon C, et al. A lab test and algorithms for identifying clients at risk for treatment failure. J Clin Psychol. 2005;61:155-163. doi: 10.1002/jclp.20108
8. Castonguay LG, Boswell JF, Constantino MJ, et al. Training implications of harmful effects of psychological treatments. Am Psychol. 2010;65:34-49. doi: 10.1037/a0017330
9. Kraus DR, Castonguay LG, Boswell JF, et al. Therapist effectiveness: implications for accountability and patient care. Psychother Res. 2011;21:267-276. doi: 10.1080/10503307.2011.563249
10. Lilienfeld SO. Psychological treatments that cause harm. Perspect Psychol Sci. 2007;2:53-70. doi: 10.1111/j.1745-6916.2007.00029.x
11. Boswell JF, Constantino MJ, Kraus DR, et al. The expanding relevance of routinely collected outcome data for mental health care decision making. Adm Policy Ment Health. 2016;43:482-491. doi: 10.1007/s10488-015-0649-6
12. Lyon AR, Lewis CC, Boyd MR, et al. Capabilities and characteristics of digital measurement feedback systems: results from a comprehensive review. Adm Policy Ment Health. 2016;43:441-466. doi: 10.1007/s10488-016-0719-4
13. Teymoori A, Gorbunova A, Haghish FE, et al. Factorial structure and validity of depression (PHQ-9) and anxiety (GAD-7) scales after traumatic brain injury. J Clin Med. 2020;9:873. doi: 10.3390/jcm9030873
14. Kraus DR, Seligman DA, Jordan JR. Validation of a behavioral health treatment outcome and assessment tool designed for naturalistic settings: the Treatment Outcome Package. J Clin Psychol. 2005;61:285‐314. doi: 10.1002/jclp.20084
15. Boothroyd L, Dagnan D, Muncer S. Psychometric analysis of the Generalized Anxiety Disorder Scale and the Patient Health Questionnaire using Mokken scaling and confirmatory factor analysis. Health Prim Care. 2018;2:1-4. doi: 10.15761/HPC.1000145
16. Locke BD, Buzolitz JS, Lei PW, et al. Development of the Counseling Center Assessment of Psychological Symptoms-62 (CCAPS-62). J Couns Psychol. 2011;58:97-109. doi: 10.1037/a0021282
17. Kraus DR, Boswell JF, Wright AGC, et al. Factor structure of the treatment outcome package for children. J Clin Psychol. 2010;66:627-640. doi: 10.1002/jclp.20675
18. McAleavey AA, Nordberg SS, Kraus D, et al. Errors in treatment outcome monitoring: implications for real-world psychotherapy. Can Psychol. 2010;53:105-114. doi: 10.1037/a0027833
19. Baxter EE, Alexander PC, Kraus DR, et al. Concurrent validation of the Treatment Outcome Package (TOP) for children and adolescents. J Child Fam Stud. 2016;25:2415-2422. doi: 10.1007/s10826-016-0419-4
20. Gual-Montolio P, Martínez-Borba V, Bretón-López JM, et al. How are information and communication technologies supporting routine outcome monitoring and measurement-based care in psychotherapy? A systematic review. Int J Environ Res Public Health. 2020;17:3170. doi: 10.3390/ijerph17093170
21. Kraus DR, Bentley JH, Alexander PC, et al. Predicting therapist effectiveness from their own practice-based evidence. J Consult Clin Psychol. 2016;84:473‐483. doi: 10.1037/ccp0000083
22. Constantino MJ, Boswell JF, Coyne AE, et al. Effect of matching therapists to patients vs assignment as usual on adult psychotherapy outcomes. A randomized clinical trial. JAMA Psychiatry. 2021;78:960-969. doi: 10.1001/jamapsychiatry.2021.1221
23. Constantino MJ, Boswell JF, Kraus DR, et al. Matching patients with therapists to improve mental health care. Patient-Centered Outcomes Research Institute (PCORI). 2021. Accessed March 1, 2023. www.pcori.org/research-results/2015/matching-patients-therapists-improve-mental-health-care
24. Institute of Medicine. Committee on Crossing the Quality Chasm: Adaptation to Mental Health and Addictive Disorders. Improving the Quality of Health Care for Mental and Substance-Use Conditions. National Academies Press; 2006. Accessed February 21, 2023. https://nap.nationalacademies.org/read/11470/chapter/1
25. Boswell JF, Constantino MJ, Oswald JM, et al. A multimethod study of mental health care patients’ attitudes toward clinician-level performance information. Psychiatr Serv. 2021;72:452-456. doi: 10.1176/appi.ps.202000366
26. Boswell JF, Constantino MJ, Oswald JM, et al. Mental health care consumers’ relative valuing of clinician performance information. J Consult Clin Psychol. 2018;86:301‐308. doi: 10.1037/ccp0000264
Approximately 1 in 4 people ages 18 years and older and 1 in 3 people ages 18 to 25 years had a mental illness in the past year, according to the 2021 National Survey of Drug Use and Health.1 The survey also found that adults ages 18 to 25 years had the highest rate of serious mental illness but the lowest treatment rate compared to other adult age groups.1 Unfortunately, more than 60% of patients receiving mental health treatment fail to benefit to a clinically meaningful degree.2
However, there is growing evidence that referring patients to behavioral health practitioners (BHPs) with outcome-measured skills that meet the patient’s specific needs can have a dramatic and positive impact. There are 2 main steps to pairing patients with an appropriate BHP: (1) use of measurement-based care data that can be analyzed at the patient and therapist level, and (2) data-driven referrals that pair patients with BHPs based on such routine outcome monitoring data (paired-on outcome data).
Psychotherapy’s slow road toward measurement-based care
Routine outcome monitoring is the systematic measurement of symptoms and functioning during treatment. It serves multiple functions, including program evaluation and benchmarking of patient improvement rates. Moreover, routine outcome monitoring–derived feedback (based on repeated patient outcome measurements) can inform personalized and responsive care decisions throughout treatment.
For all intents and purposes,
- routinely administered symptom/functioning measure, ideally before each clinical encounter,
- practitioner review of these patient-level data,
- patient review of these data with their practitioner, and
- collaborative reevaluation of the person-specific treatment plan informed by these data.
CASE SCENARIO
Violeta W is a 33-year-old woman who presented to her family physician for her annual wellness exam. Prior to the exam, the medical assistant administered a Patient Health Questionnaire-9 (PHQ-9) to screen for depressive symptoms. Ms. W’s score was 20 out of 27, suggestive of depression. To further assess the severity of depressive symptoms and their effect on daily function, the physician reviewed responses to the questionnaire with her and discussed treatment options. Ms. W was most interested in trying a low-dose selective serotonin reuptake inhibitor (SSRI).
At her follow-up visit 4 weeks later, the medical assistant re-administered the PHQ-9. The physician then reviewed Ms. W’s responses with her and, based on Ms. W’s subjective report and objective symptoms (still a score of 20 out of 27 on the PHQ-9), increased her SSRI dose. At each subsequent visit, Ms. W completed a PHQ-9 and reviewed responses and depressive symptoms with her physician.
The value of measurement-based care in mental health care
A narrative review by Lewis et al3 of 21 randomized controlled clinical trials (RCTs) across a range of age groups (eg, adolescents, young adults, adults), disorders (eg, anxiety, mood), and settings (eg, outpatient, inpatient) found that in at least 9 review articles, measurement-based care was associated with significantly improved outcomes vs usual care (ie, treatment without routine outcome monitoring plus feedback). The average increase in treatment effect size was about 30% when treatment was accompanied by measurement-based care.3
Continue to: Moreover, a recent within-patient meta-analysis...
Moreover, a recent within-patient meta-analysis by de Jong et al4 shows that measurement-based care yields a small but significant increase in therapeutic outcomes (d = .15). Use of measurement-based care also is associated with improved communication between the patient and therapist.5 In pharmacotherapy practice, measurement-based care has been shown to predict rapid dose increases and changes in medication, when necessary; faster recovery rates; higher response rates to treatment3; and fewer dropouts.4
Perhaps one of the best-studied benefits of measurement-based mental health care is the ability to predict deterioration in care (ie, patients who are off-track in a way that practitioners often miss without the help of routine outcome monitoring data).6,7 Studies show that without a data-informed approach to care, some forms of psychotherapy or therapy with BHPs who are not sufficiently skilled in treating a given diagnosis increase symptoms or create significant harmful and iatrogenic effects.8-10 Conversely, the meta-analysis by de Jong et al4 found a lower percentage of deterioration in patients receiving measurement-based care. The difference in deterioration was significant: An average of 5.4% of patients in control conditions deteriorated compared to an average of 4.6% in feedback (measurement-based care) groups. There were even larger effect sizes when therapists received training in the feedback system.4
Routine outcome monitoring without a dialogue between patient and practitioner about the assessments (eg, ignoring complete measurement-based care requirements) may be inadequate. A recent review by Muir et al6 found no differences in patient outcomes when data were used solely for aggregate quality improvement activities, suggesting the need for practitioners to review results of routine outcome monitoring assessments with patients and use data to alter care when necessary.
Measurement-based care is believed to deliver benefits and reduce harm by enhancing and encouraging active patient involvement, improving patient understanding of symptoms, promoting better communication, and facilitating better care coordination.3 The benefits of measurement-based care can be enhanced with a comprehensive core routine outcome monitoring tool and the level of monitoring-generated information delivered for multiple stakeholders (eg, patient, therapist, clinic).11
A look at multidimensional assessment
The features of routine outcome monitoring tools vary significantly.12 Some measures assess single-symptom or problem domains (eg, PHQ-9 for depression or Generalized Anxiety Disorder-7 [GAD-7] scale for anxiety) or multiple dimensions (multidimensional routine outcome monitoring). Multidimensional routine outcome monitoring may have benefits over single-domain measures. Single-domain measures and the subscales or factors of more comprehensive multidimensional routine outcome monitoring assessments should possess adequate specificity and sensitivity.
Continue to: Some recent research findings...
Some recent research findings question the construct validity of brief single-domain measures of common presenting problems, such as depression and anxiety. For example, results from a factor analysis of the PHQ-9 and GAD-7 scale in patients with traumatic brain injury suggest these tools measure 1 psychological construct that includes depression and the cognitive components of anxiety (eg, worry)13—a finding consistent with those of other tools.14 Similarly, a larger study of 7763 BH patients found that a single factor accounted for most of the variance of the 2 combined measures, with no set of factors meeting the exacting standards used to develop multidimensional routine outcome monitoring.15 These findings suggest that the PHQ-9 and GAD-7 largely overlap and are not measuring different aspects of health as most practitioners believe (eg, depression and anxiety).
In commonly used assessments, multiple-factor analytic studies with high standards have supported the construct validity of domain-specific subscales, indicating that the various questions tap into different constructs of psychological health.14,16,17
Beyond multiple domain–specific indicators, multidimensional routine outcome measurements provide a global total score that minimizes Type I (false-positive conclusion) and Type II (false-negative conclusion) errors in tracking patient improvement or deterioration.18 As one would expect, multidimensional routine outcome monitoring generally includes more items than single-domain measures; however, this comes with a trade-off. If there are specificity and sensitivity concerns with an ultra-brief single-domain measure, an alternative to a core multidimensional routine outcome measurement is to aggregate a series of single-domain measures into a battery of patient self-reports. However, this approach may take longer for patients to complete since they would have to shift among the varying response sets and wording across the unique single-domain measures.
In addition, the standardization/normalization of multidimensional routine outcome monitoring likely makes interpretation easier than referring to norms and clinical severity cutoffs for many distinct measures. Furthermore, increased specificity enhances predictive power and allows BHPs to screen and track other conditions besides depression and anxiety. (It is worth noting that there are no known studies that have looked at the difference in time to administer or ease of interpretation of multidimensional routine outcome monitoring tools vs multiple single-domain measures.)
Two multidimensional routine outcome monitoring tools that cover a comprehensive series of discrete symptom and functional domains are the Treatment Outcome Package12 and Counseling Center Assessment of Psychological Symptoms.16 These tools, which include subscales beyond general depression and anxiety (eg, sleep, substance misuse, social conflict), take 7 to 10 minutes to complete and provide outcome results across 12 symptom and 8 functional dimensions. As an example, the Treatment Outcome Package has good psychometric qualities (eg, reliability, construct and concurrent validity) for adults,12 children,14,19 and adolescents,19 and can be administered through a secure online data collection portal. The Counseling Center Assessment of Psychological Symptoms has demonstrated high construct validity and good convergent validity.16 These assessments can be administered in paper or digital (eg, electronic medical record portal, smartphone) format.20
Continue to: CASE SCENARIO
CASE SCENARIO
Ms. W’s physician asked her to go online using her phone and answer the questions in the Treatment Outcome Package. Her results, which she viewed with her physician, were displayed in graph form (FIGURE). Her scores were represented in Z scores normalized to the general population, with “0” representing the general, nontreatment-seeking population average and positive scores representing the number of standard deviations (SDs) more severe than the general population average.
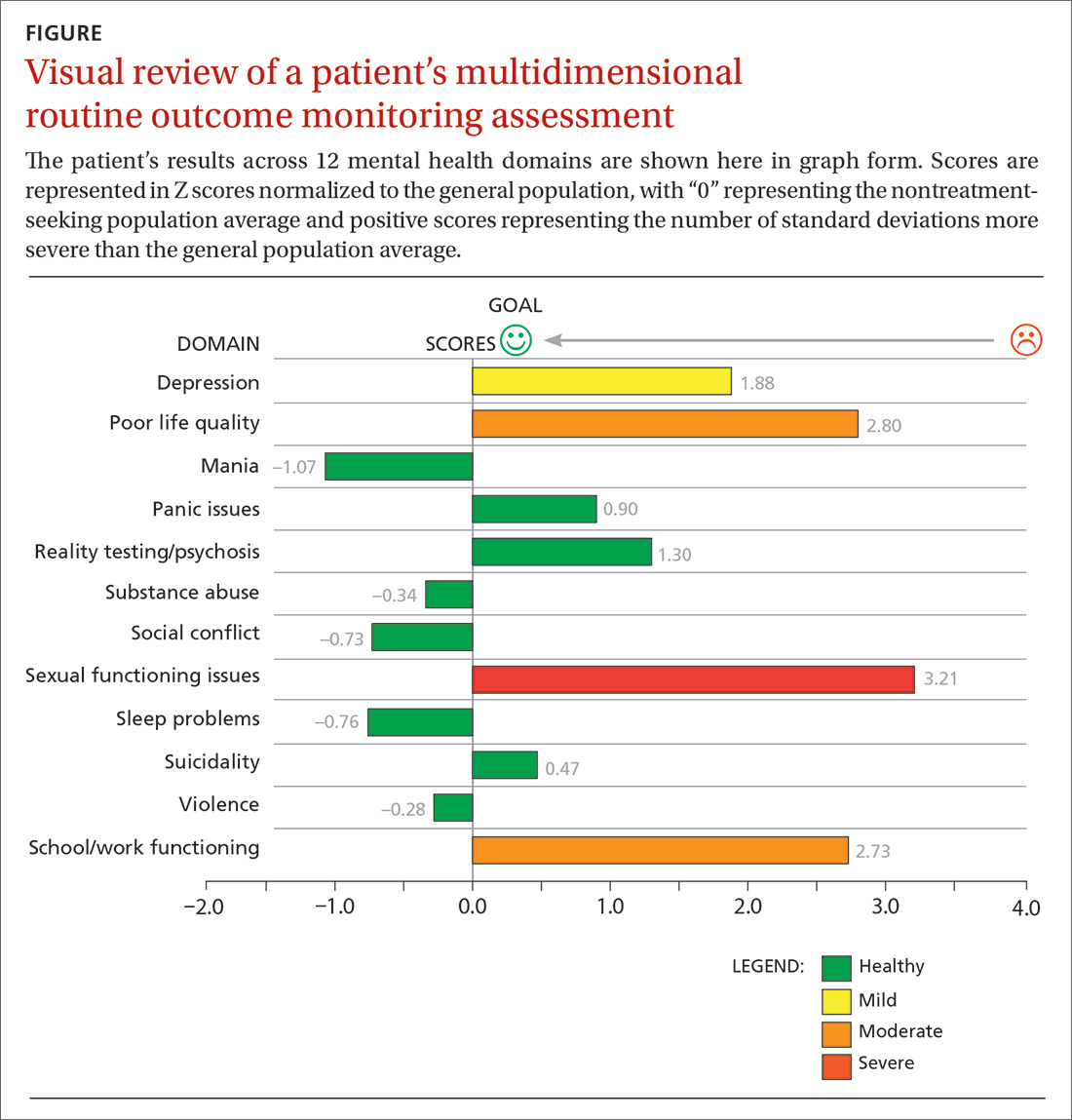
Although this assessment scored Ms. W’s clinically elevated depression as mild, it revealed abnormalities in 3 other domains. Sexual functioning issues represented the most abnormal domain at greater than 3 SDs (more severe than the general population), followed by poor life quality and school/work functioning.
After reviewing Ms. W’s report, her physician decided that pharmacologic management alone (for depression) was not the most appropriate treatment course. Therefore, her physician recommended psychotherapy in addition to the SSRI she was taking. Ms. W agreed to a customized referral for psychotherapy.
Data-driven referrals
When psychotherapy is chosen as a treatment, the individual BHP is an active component of that treatment. Consequently, it is essential to customize referrals to match a patient’s most elevated mental health concerns with a therapist who will most effectively treat those domains. It is rare for a BHP to be skilled in treating every mental health domain.9 Multiple studies have shown that BHPs have identifiable treatment skills in specific domains, which physicians should consider when making referrals.9,21,22 These studies demonstrate the utility of aggregating patient-level routine outcome monitoring data to better understand therapist-level (and ultimately clinic- and system-level) outcomes.
Additionally, recent research has tested this idea prospectively. An RCT funded by the Patient-Centered Outcome Research Institute and published in JAMA Psychiatry showed a significant and positive effect on patient outcomes (ie, reductions in general impairment, impairment involving a patient’s most elevated domain, and global distress) using paired-on outcome data matching vs as-usual matching protocols (eg, therapist self-defined areas of specialty).22 In the RCT, the most effective matching protocol was a combination of eliminating harm and matching the patient on their 3 most problematic domains (the highest match level). These patients ended care as healthy as the general population after 16 weeks of treatment. A random 1-year follow-up assessment from the original RCT showed that most patients who had been matched had maintained their improvement.23
Continue to: Therefore, a multidimensional routine outcome...
Therefore, a multidimensional routine outcome monitoring tool can be used to identify a BHP’s relative strengths and weaknesses across multiple outcome domains. Within a system of care, a sample of BHPs will possess varying outcome-domain profiles. When a new patient is seeking a referral to a BHP, these profiles (or domain-specific outcome track records) can be used to support paired-on outcome data matching. Specifically, a new patient completes the multidimensional routine outcome monitoring tool at pretreatment, and the results reveal the outcome domains on which the patient is most clinically severe. This pattern of domain-specific severity then can be used to pair the new patient with a BHP who has demonstrated success in addressing the same outcome domain(s). This approach matches a new patient to a BHP with established expertise based on routine outcome monitoring.
Retrospective and prospective studies have found that most BHPs have stable performance in their strengths and weaknesses.11,21 One study found that assessing BHP performance with their most recent 30 patients can reliably predict future performance with their next 30 patients.24 This predictability in a practitioner’s outcomes suggests report cards that are updated frequently can be utilized to make case assignments within BH or referrals to a specific BHP from primary care.
Making a paired-on outcome data–matched referral
Making customized BH referrals requires access to information about a practitioner’s previous routine outcome monitoring data per clinical domain (eg, suicidality, violence, quality of life) from their most recent patients. Previous research suggests that follow-up data from a minimum of 15 patients is necessary to make a reliable evaluation of a practitioner’s strengths and weaknesses (ie, effectiveness “report card”) per clinical domain.24
Few, if any, physicians have access to this level of updated outcome data from their referral network. To facilitate widespread use of paired-on outcome data matching, a new Web system (MatchedTherapists.com) will allow the general public and PCPs to access these grades. As a public service option, this site currently allows for a self-assessment using the Treatment Outcome Package. Pending versions will generate paired-on outcome data grades, and users will receive a list of local therapists available for in-person appointments as well as therapists available for virtual appointments. The paired-on outcome data grades are delivered in school-based letter grades. An “A+,” for example, represents the best matching grade. Users also will be able to sort and filter results for other criteria such as telemedicine, insurance, age, gender, and appointment availability. Currently, there are more than 77,000 therapists listed on the site nationwide. A basic listing is free.
CASE SCENARIO
After Ms. W took the multidimensional routine outcome assessment online, she received a list of therapists rank-ordered by paired-on outcome data grade, with the “A+” matches listed first. Three of the best-matched referrals accepted her insurance and were willing to see her through telemedicine. Therapists with available in-person appointments had a “B” grade. After discussing the options with her physician, Ms. W opted for telehealth counseling with the therapist whose profile she liked best. The therapist and PCP tracked her progress through routine outcome monitoring reporting until all her symptoms became subclinical.
Continue to: The future of a "referral bridge"
The future of a “referral bridge”
In this article, we present a solution to a common issue faced by mental health care patients: failure to benefit meaningfully from mental health treatment. Matching patients to specific BHPs based on effectiveness data regarding the therapist’s strengths and skills can improve patient outcomes and reduce harm. In addition, patients appear to value this approach. A Robert Wood Johnson Foundation–funded study demonstrated that patients value seeing practitioners who have a track record of successfully treating previous patients with similar issues.25,26 In many cases, patients indicated they would prioritize this matching process over other factors such as practitioners with a higher number of years of experience or the same demographic characteristics as the patient.25,26
These findings may represent a new area in the science of health care. Over the past century, major advances in diagnosis and treatment—the 2 primary pillars of health care—have turned the art of medicine into a science. However, the art of making referrals has not advanced commensurately, as there has been little attention focused on the “referral bridge” between these 2 pillars. As the studies reviewed in this paper demonstrate, a referral bridge deserves exploration in all fields of medicine.
CORRESPONDENCE
David R. Kraus, PhD, 1 Speen Street, Framingham, MA 01701; [email protected]
Approximately 1 in 4 people ages 18 years and older and 1 in 3 people ages 18 to 25 years had a mental illness in the past year, according to the 2021 National Survey of Drug Use and Health.1 The survey also found that adults ages 18 to 25 years had the highest rate of serious mental illness but the lowest treatment rate compared to other adult age groups.1 Unfortunately, more than 60% of patients receiving mental health treatment fail to benefit to a clinically meaningful degree.2
However, there is growing evidence that referring patients to behavioral health practitioners (BHPs) with outcome-measured skills that meet the patient’s specific needs can have a dramatic and positive impact. There are 2 main steps to pairing patients with an appropriate BHP: (1) use of measurement-based care data that can be analyzed at the patient and therapist level, and (2) data-driven referrals that pair patients with BHPs based on such routine outcome monitoring data (paired-on outcome data).
Psychotherapy’s slow road toward measurement-based care
Routine outcome monitoring is the systematic measurement of symptoms and functioning during treatment. It serves multiple functions, including program evaluation and benchmarking of patient improvement rates. Moreover, routine outcome monitoring–derived feedback (based on repeated patient outcome measurements) can inform personalized and responsive care decisions throughout treatment.
For all intents and purposes,
- routinely administered symptom/functioning measure, ideally before each clinical encounter,
- practitioner review of these patient-level data,
- patient review of these data with their practitioner, and
- collaborative reevaluation of the person-specific treatment plan informed by these data.
CASE SCENARIO
Violeta W is a 33-year-old woman who presented to her family physician for her annual wellness exam. Prior to the exam, the medical assistant administered a Patient Health Questionnaire-9 (PHQ-9) to screen for depressive symptoms. Ms. W’s score was 20 out of 27, suggestive of depression. To further assess the severity of depressive symptoms and their effect on daily function, the physician reviewed responses to the questionnaire with her and discussed treatment options. Ms. W was most interested in trying a low-dose selective serotonin reuptake inhibitor (SSRI).
At her follow-up visit 4 weeks later, the medical assistant re-administered the PHQ-9. The physician then reviewed Ms. W’s responses with her and, based on Ms. W’s subjective report and objective symptoms (still a score of 20 out of 27 on the PHQ-9), increased her SSRI dose. At each subsequent visit, Ms. W completed a PHQ-9 and reviewed responses and depressive symptoms with her physician.
The value of measurement-based care in mental health care
A narrative review by Lewis et al3 of 21 randomized controlled clinical trials (RCTs) across a range of age groups (eg, adolescents, young adults, adults), disorders (eg, anxiety, mood), and settings (eg, outpatient, inpatient) found that in at least 9 review articles, measurement-based care was associated with significantly improved outcomes vs usual care (ie, treatment without routine outcome monitoring plus feedback). The average increase in treatment effect size was about 30% when treatment was accompanied by measurement-based care.3
Continue to: Moreover, a recent within-patient meta-analysis...
Moreover, a recent within-patient meta-analysis by de Jong et al4 shows that measurement-based care yields a small but significant increase in therapeutic outcomes (d = .15). Use of measurement-based care also is associated with improved communication between the patient and therapist.5 In pharmacotherapy practice, measurement-based care has been shown to predict rapid dose increases and changes in medication, when necessary; faster recovery rates; higher response rates to treatment3; and fewer dropouts.4
Perhaps one of the best-studied benefits of measurement-based mental health care is the ability to predict deterioration in care (ie, patients who are off-track in a way that practitioners often miss without the help of routine outcome monitoring data).6,7 Studies show that without a data-informed approach to care, some forms of psychotherapy or therapy with BHPs who are not sufficiently skilled in treating a given diagnosis increase symptoms or create significant harmful and iatrogenic effects.8-10 Conversely, the meta-analysis by de Jong et al4 found a lower percentage of deterioration in patients receiving measurement-based care. The difference in deterioration was significant: An average of 5.4% of patients in control conditions deteriorated compared to an average of 4.6% in feedback (measurement-based care) groups. There were even larger effect sizes when therapists received training in the feedback system.4
Routine outcome monitoring without a dialogue between patient and practitioner about the assessments (eg, ignoring complete measurement-based care requirements) may be inadequate. A recent review by Muir et al6 found no differences in patient outcomes when data were used solely for aggregate quality improvement activities, suggesting the need for practitioners to review results of routine outcome monitoring assessments with patients and use data to alter care when necessary.
Measurement-based care is believed to deliver benefits and reduce harm by enhancing and encouraging active patient involvement, improving patient understanding of symptoms, promoting better communication, and facilitating better care coordination.3 The benefits of measurement-based care can be enhanced with a comprehensive core routine outcome monitoring tool and the level of monitoring-generated information delivered for multiple stakeholders (eg, patient, therapist, clinic).11
A look at multidimensional assessment
The features of routine outcome monitoring tools vary significantly.12 Some measures assess single-symptom or problem domains (eg, PHQ-9 for depression or Generalized Anxiety Disorder-7 [GAD-7] scale for anxiety) or multiple dimensions (multidimensional routine outcome monitoring). Multidimensional routine outcome monitoring may have benefits over single-domain measures. Single-domain measures and the subscales or factors of more comprehensive multidimensional routine outcome monitoring assessments should possess adequate specificity and sensitivity.
Continue to: Some recent research findings...
Some recent research findings question the construct validity of brief single-domain measures of common presenting problems, such as depression and anxiety. For example, results from a factor analysis of the PHQ-9 and GAD-7 scale in patients with traumatic brain injury suggest these tools measure 1 psychological construct that includes depression and the cognitive components of anxiety (eg, worry)13—a finding consistent with those of other tools.14 Similarly, a larger study of 7763 BH patients found that a single factor accounted for most of the variance of the 2 combined measures, with no set of factors meeting the exacting standards used to develop multidimensional routine outcome monitoring.15 These findings suggest that the PHQ-9 and GAD-7 largely overlap and are not measuring different aspects of health as most practitioners believe (eg, depression and anxiety).
In commonly used assessments, multiple-factor analytic studies with high standards have supported the construct validity of domain-specific subscales, indicating that the various questions tap into different constructs of psychological health.14,16,17
Beyond multiple domain–specific indicators, multidimensional routine outcome measurements provide a global total score that minimizes Type I (false-positive conclusion) and Type II (false-negative conclusion) errors in tracking patient improvement or deterioration.18 As one would expect, multidimensional routine outcome monitoring generally includes more items than single-domain measures; however, this comes with a trade-off. If there are specificity and sensitivity concerns with an ultra-brief single-domain measure, an alternative to a core multidimensional routine outcome measurement is to aggregate a series of single-domain measures into a battery of patient self-reports. However, this approach may take longer for patients to complete since they would have to shift among the varying response sets and wording across the unique single-domain measures.
In addition, the standardization/normalization of multidimensional routine outcome monitoring likely makes interpretation easier than referring to norms and clinical severity cutoffs for many distinct measures. Furthermore, increased specificity enhances predictive power and allows BHPs to screen and track other conditions besides depression and anxiety. (It is worth noting that there are no known studies that have looked at the difference in time to administer or ease of interpretation of multidimensional routine outcome monitoring tools vs multiple single-domain measures.)
Two multidimensional routine outcome monitoring tools that cover a comprehensive series of discrete symptom and functional domains are the Treatment Outcome Package12 and Counseling Center Assessment of Psychological Symptoms.16 These tools, which include subscales beyond general depression and anxiety (eg, sleep, substance misuse, social conflict), take 7 to 10 minutes to complete and provide outcome results across 12 symptom and 8 functional dimensions. As an example, the Treatment Outcome Package has good psychometric qualities (eg, reliability, construct and concurrent validity) for adults,12 children,14,19 and adolescents,19 and can be administered through a secure online data collection portal. The Counseling Center Assessment of Psychological Symptoms has demonstrated high construct validity and good convergent validity.16 These assessments can be administered in paper or digital (eg, electronic medical record portal, smartphone) format.20
Continue to: CASE SCENARIO
CASE SCENARIO
Ms. W’s physician asked her to go online using her phone and answer the questions in the Treatment Outcome Package. Her results, which she viewed with her physician, were displayed in graph form (FIGURE). Her scores were represented in Z scores normalized to the general population, with “0” representing the general, nontreatment-seeking population average and positive scores representing the number of standard deviations (SDs) more severe than the general population average.
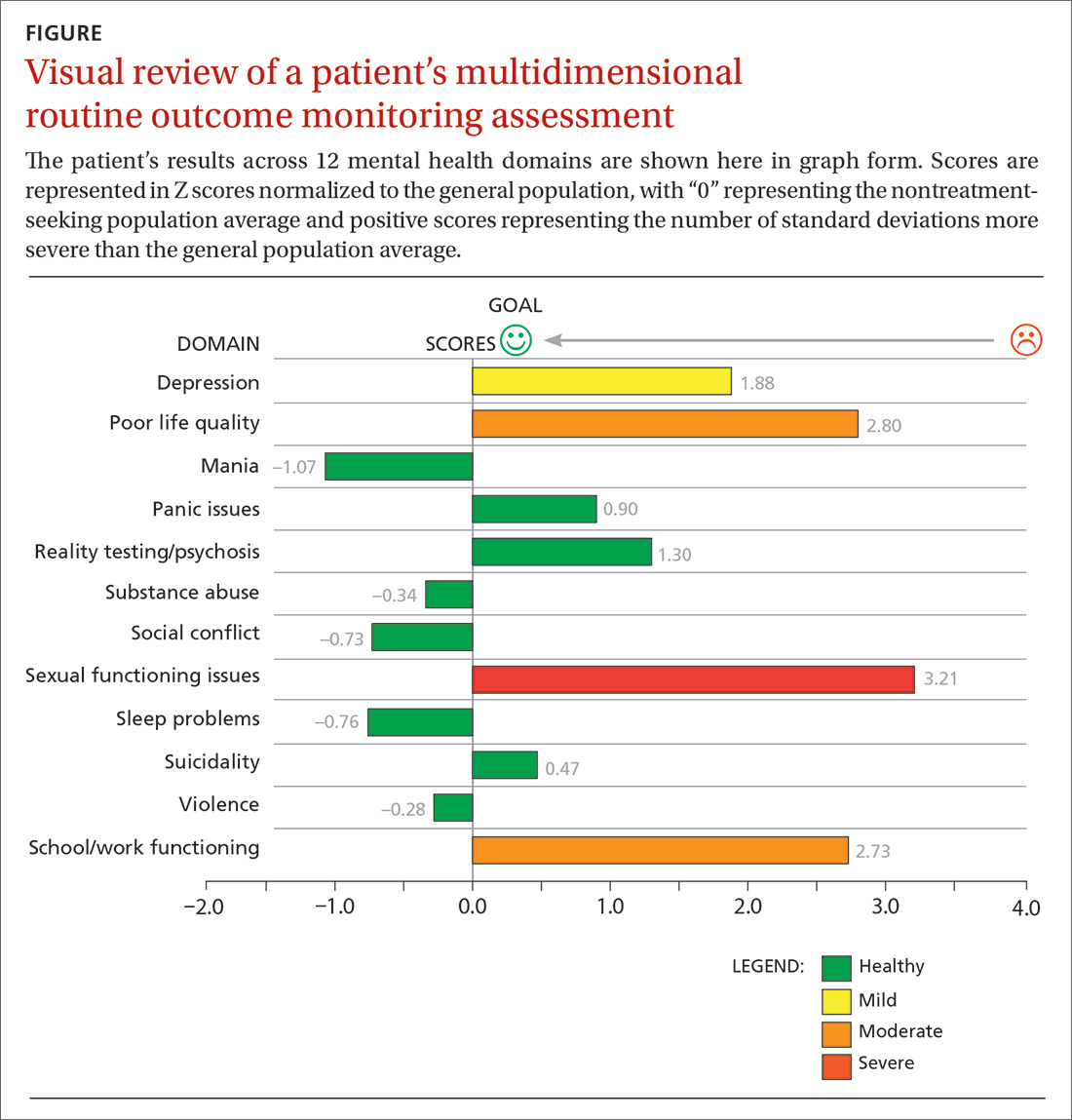
Although this assessment scored Ms. W’s clinically elevated depression as mild, it revealed abnormalities in 3 other domains. Sexual functioning issues represented the most abnormal domain at greater than 3 SDs (more severe than the general population), followed by poor life quality and school/work functioning.
After reviewing Ms. W’s report, her physician decided that pharmacologic management alone (for depression) was not the most appropriate treatment course. Therefore, her physician recommended psychotherapy in addition to the SSRI she was taking. Ms. W agreed to a customized referral for psychotherapy.
Data-driven referrals
When psychotherapy is chosen as a treatment, the individual BHP is an active component of that treatment. Consequently, it is essential to customize referrals to match a patient’s most elevated mental health concerns with a therapist who will most effectively treat those domains. It is rare for a BHP to be skilled in treating every mental health domain.9 Multiple studies have shown that BHPs have identifiable treatment skills in specific domains, which physicians should consider when making referrals.9,21,22 These studies demonstrate the utility of aggregating patient-level routine outcome monitoring data to better understand therapist-level (and ultimately clinic- and system-level) outcomes.
Additionally, recent research has tested this idea prospectively. An RCT funded by the Patient-Centered Outcome Research Institute and published in JAMA Psychiatry showed a significant and positive effect on patient outcomes (ie, reductions in general impairment, impairment involving a patient’s most elevated domain, and global distress) using paired-on outcome data matching vs as-usual matching protocols (eg, therapist self-defined areas of specialty).22 In the RCT, the most effective matching protocol was a combination of eliminating harm and matching the patient on their 3 most problematic domains (the highest match level). These patients ended care as healthy as the general population after 16 weeks of treatment. A random 1-year follow-up assessment from the original RCT showed that most patients who had been matched had maintained their improvement.23
Continue to: Therefore, a multidimensional routine outcome...
Therefore, a multidimensional routine outcome monitoring tool can be used to identify a BHP’s relative strengths and weaknesses across multiple outcome domains. Within a system of care, a sample of BHPs will possess varying outcome-domain profiles. When a new patient is seeking a referral to a BHP, these profiles (or domain-specific outcome track records) can be used to support paired-on outcome data matching. Specifically, a new patient completes the multidimensional routine outcome monitoring tool at pretreatment, and the results reveal the outcome domains on which the patient is most clinically severe. This pattern of domain-specific severity then can be used to pair the new patient with a BHP who has demonstrated success in addressing the same outcome domain(s). This approach matches a new patient to a BHP with established expertise based on routine outcome monitoring.
Retrospective and prospective studies have found that most BHPs have stable performance in their strengths and weaknesses.11,21 One study found that assessing BHP performance with their most recent 30 patients can reliably predict future performance with their next 30 patients.24 This predictability in a practitioner’s outcomes suggests report cards that are updated frequently can be utilized to make case assignments within BH or referrals to a specific BHP from primary care.
Making a paired-on outcome data–matched referral
Making customized BH referrals requires access to information about a practitioner’s previous routine outcome monitoring data per clinical domain (eg, suicidality, violence, quality of life) from their most recent patients. Previous research suggests that follow-up data from a minimum of 15 patients is necessary to make a reliable evaluation of a practitioner’s strengths and weaknesses (ie, effectiveness “report card”) per clinical domain.24
Few, if any, physicians have access to this level of updated outcome data from their referral network. To facilitate widespread use of paired-on outcome data matching, a new Web system (MatchedTherapists.com) will allow the general public and PCPs to access these grades. As a public service option, this site currently allows for a self-assessment using the Treatment Outcome Package. Pending versions will generate paired-on outcome data grades, and users will receive a list of local therapists available for in-person appointments as well as therapists available for virtual appointments. The paired-on outcome data grades are delivered in school-based letter grades. An “A+,” for example, represents the best matching grade. Users also will be able to sort and filter results for other criteria such as telemedicine, insurance, age, gender, and appointment availability. Currently, there are more than 77,000 therapists listed on the site nationwide. A basic listing is free.
CASE SCENARIO
After Ms. W took the multidimensional routine outcome assessment online, she received a list of therapists rank-ordered by paired-on outcome data grade, with the “A+” matches listed first. Three of the best-matched referrals accepted her insurance and were willing to see her through telemedicine. Therapists with available in-person appointments had a “B” grade. After discussing the options with her physician, Ms. W opted for telehealth counseling with the therapist whose profile she liked best. The therapist and PCP tracked her progress through routine outcome monitoring reporting until all her symptoms became subclinical.
Continue to: The future of a "referral bridge"
The future of a “referral bridge”
In this article, we present a solution to a common issue faced by mental health care patients: failure to benefit meaningfully from mental health treatment. Matching patients to specific BHPs based on effectiveness data regarding the therapist’s strengths and skills can improve patient outcomes and reduce harm. In addition, patients appear to value this approach. A Robert Wood Johnson Foundation–funded study demonstrated that patients value seeing practitioners who have a track record of successfully treating previous patients with similar issues.25,26 In many cases, patients indicated they would prioritize this matching process over other factors such as practitioners with a higher number of years of experience or the same demographic characteristics as the patient.25,26
These findings may represent a new area in the science of health care. Over the past century, major advances in diagnosis and treatment—the 2 primary pillars of health care—have turned the art of medicine into a science. However, the art of making referrals has not advanced commensurately, as there has been little attention focused on the “referral bridge” between these 2 pillars. As the studies reviewed in this paper demonstrate, a referral bridge deserves exploration in all fields of medicine.
CORRESPONDENCE
David R. Kraus, PhD, 1 Speen Street, Framingham, MA 01701; [email protected]
1. HHS. 2021 National Survey of Drug Use and Health (NSDUH) Releases. Accessed March 29, 2023. www.samhsa.gov/data/release/2021-national-survey-drug-use-and-health-nsduh-releases
2. Barkham M, Lambert, MJ. The efficacy and effectiveness of psychological therapies. In: Barkham M, Lutz W, Castonguay LG, eds. Bergin and Garfield’s Handbook of Psychotherapy and Behavior Change: 50th Anniversary Edition. 7th ed. John Wiley & Sons, Inc; 2021:135-189.
3. Lewis CC, Boyd M, Puspitasari A, et al. Implementing measurement-based care in behavioral health: a review. JAMA Psychiatry. 2019;76:324-335. doi: 10.1001/jamapsychiatry.2018.3329
4. de Jong K, Conijn JM, Gallagher RAV, et al. Using progress feedback to improve outcomes and reduce drop-out, treatment duration, and deterioration: a multilevel meta-analysis. Clin Psychol Rev. 2021;85:102002. doi: 10.1016/j.cpr.2021.102002
5. Carlier IVE, Meuldijk D, Van Vliet IM, et al. Routine outcome monitoring and feedback on physical or mental health status: evidence and theory. J Eval Clin Pract. 2012;18:104-110. doi: 10.1111/j.1365-2753.2010.01543.x
6. Muir HJ, Coyne AE, Morrison NR, et al. Ethical implications of routine outcomes monitoring for patients, psychotherapists, and mental health care systems. Psychotherapy (Chic). 2019;56:459-469. doi: 10.1037/pst0000246
7. Hannan C, Lambert MJ, Harmon C, et al. A lab test and algorithms for identifying clients at risk for treatment failure. J Clin Psychol. 2005;61:155-163. doi: 10.1002/jclp.20108
8. Castonguay LG, Boswell JF, Constantino MJ, et al. Training implications of harmful effects of psychological treatments. Am Psychol. 2010;65:34-49. doi: 10.1037/a0017330
9. Kraus DR, Castonguay LG, Boswell JF, et al. Therapist effectiveness: implications for accountability and patient care. Psychother Res. 2011;21:267-276. doi: 10.1080/10503307.2011.563249
10. Lilienfeld SO. Psychological treatments that cause harm. Perspect Psychol Sci. 2007;2:53-70. doi: 10.1111/j.1745-6916.2007.00029.x
11. Boswell JF, Constantino MJ, Kraus DR, et al. The expanding relevance of routinely collected outcome data for mental health care decision making. Adm Policy Ment Health. 2016;43:482-491. doi: 10.1007/s10488-015-0649-6
12. Lyon AR, Lewis CC, Boyd MR, et al. Capabilities and characteristics of digital measurement feedback systems: results from a comprehensive review. Adm Policy Ment Health. 2016;43:441-466. doi: 10.1007/s10488-016-0719-4
13. Teymoori A, Gorbunova A, Haghish FE, et al. Factorial structure and validity of depression (PHQ-9) and anxiety (GAD-7) scales after traumatic brain injury. J Clin Med. 2020;9:873. doi: 10.3390/jcm9030873
14. Kraus DR, Seligman DA, Jordan JR. Validation of a behavioral health treatment outcome and assessment tool designed for naturalistic settings: the Treatment Outcome Package. J Clin Psychol. 2005;61:285‐314. doi: 10.1002/jclp.20084
15. Boothroyd L, Dagnan D, Muncer S. Psychometric analysis of the Generalized Anxiety Disorder Scale and the Patient Health Questionnaire using Mokken scaling and confirmatory factor analysis. Health Prim Care. 2018;2:1-4. doi: 10.15761/HPC.1000145
16. Locke BD, Buzolitz JS, Lei PW, et al. Development of the Counseling Center Assessment of Psychological Symptoms-62 (CCAPS-62). J Couns Psychol. 2011;58:97-109. doi: 10.1037/a0021282
17. Kraus DR, Boswell JF, Wright AGC, et al. Factor structure of the treatment outcome package for children. J Clin Psychol. 2010;66:627-640. doi: 10.1002/jclp.20675
18. McAleavey AA, Nordberg SS, Kraus D, et al. Errors in treatment outcome monitoring: implications for real-world psychotherapy. Can Psychol. 2010;53:105-114. doi: 10.1037/a0027833
19. Baxter EE, Alexander PC, Kraus DR, et al. Concurrent validation of the Treatment Outcome Package (TOP) for children and adolescents. J Child Fam Stud. 2016;25:2415-2422. doi: 10.1007/s10826-016-0419-4
20. Gual-Montolio P, Martínez-Borba V, Bretón-López JM, et al. How are information and communication technologies supporting routine outcome monitoring and measurement-based care in psychotherapy? A systematic review. Int J Environ Res Public Health. 2020;17:3170. doi: 10.3390/ijerph17093170
21. Kraus DR, Bentley JH, Alexander PC, et al. Predicting therapist effectiveness from their own practice-based evidence. J Consult Clin Psychol. 2016;84:473‐483. doi: 10.1037/ccp0000083
22. Constantino MJ, Boswell JF, Coyne AE, et al. Effect of matching therapists to patients vs assignment as usual on adult psychotherapy outcomes. A randomized clinical trial. JAMA Psychiatry. 2021;78:960-969. doi: 10.1001/jamapsychiatry.2021.1221
23. Constantino MJ, Boswell JF, Kraus DR, et al. Matching patients with therapists to improve mental health care. Patient-Centered Outcomes Research Institute (PCORI). 2021. Accessed March 1, 2023. www.pcori.org/research-results/2015/matching-patients-therapists-improve-mental-health-care
24. Institute of Medicine. Committee on Crossing the Quality Chasm: Adaptation to Mental Health and Addictive Disorders. Improving the Quality of Health Care for Mental and Substance-Use Conditions. National Academies Press; 2006. Accessed February 21, 2023. https://nap.nationalacademies.org/read/11470/chapter/1
25. Boswell JF, Constantino MJ, Oswald JM, et al. A multimethod study of mental health care patients’ attitudes toward clinician-level performance information. Psychiatr Serv. 2021;72:452-456. doi: 10.1176/appi.ps.202000366
26. Boswell JF, Constantino MJ, Oswald JM, et al. Mental health care consumers’ relative valuing of clinician performance information. J Consult Clin Psychol. 2018;86:301‐308. doi: 10.1037/ccp0000264
1. HHS. 2021 National Survey of Drug Use and Health (NSDUH) Releases. Accessed March 29, 2023. www.samhsa.gov/data/release/2021-national-survey-drug-use-and-health-nsduh-releases
2. Barkham M, Lambert, MJ. The efficacy and effectiveness of psychological therapies. In: Barkham M, Lutz W, Castonguay LG, eds. Bergin and Garfield’s Handbook of Psychotherapy and Behavior Change: 50th Anniversary Edition. 7th ed. John Wiley & Sons, Inc; 2021:135-189.
3. Lewis CC, Boyd M, Puspitasari A, et al. Implementing measurement-based care in behavioral health: a review. JAMA Psychiatry. 2019;76:324-335. doi: 10.1001/jamapsychiatry.2018.3329
4. de Jong K, Conijn JM, Gallagher RAV, et al. Using progress feedback to improve outcomes and reduce drop-out, treatment duration, and deterioration: a multilevel meta-analysis. Clin Psychol Rev. 2021;85:102002. doi: 10.1016/j.cpr.2021.102002
5. Carlier IVE, Meuldijk D, Van Vliet IM, et al. Routine outcome monitoring and feedback on physical or mental health status: evidence and theory. J Eval Clin Pract. 2012;18:104-110. doi: 10.1111/j.1365-2753.2010.01543.x
6. Muir HJ, Coyne AE, Morrison NR, et al. Ethical implications of routine outcomes monitoring for patients, psychotherapists, and mental health care systems. Psychotherapy (Chic). 2019;56:459-469. doi: 10.1037/pst0000246
7. Hannan C, Lambert MJ, Harmon C, et al. A lab test and algorithms for identifying clients at risk for treatment failure. J Clin Psychol. 2005;61:155-163. doi: 10.1002/jclp.20108
8. Castonguay LG, Boswell JF, Constantino MJ, et al. Training implications of harmful effects of psychological treatments. Am Psychol. 2010;65:34-49. doi: 10.1037/a0017330
9. Kraus DR, Castonguay LG, Boswell JF, et al. Therapist effectiveness: implications for accountability and patient care. Psychother Res. 2011;21:267-276. doi: 10.1080/10503307.2011.563249
10. Lilienfeld SO. Psychological treatments that cause harm. Perspect Psychol Sci. 2007;2:53-70. doi: 10.1111/j.1745-6916.2007.00029.x
11. Boswell JF, Constantino MJ, Kraus DR, et al. The expanding relevance of routinely collected outcome data for mental health care decision making. Adm Policy Ment Health. 2016;43:482-491. doi: 10.1007/s10488-015-0649-6
12. Lyon AR, Lewis CC, Boyd MR, et al. Capabilities and characteristics of digital measurement feedback systems: results from a comprehensive review. Adm Policy Ment Health. 2016;43:441-466. doi: 10.1007/s10488-016-0719-4
13. Teymoori A, Gorbunova A, Haghish FE, et al. Factorial structure and validity of depression (PHQ-9) and anxiety (GAD-7) scales after traumatic brain injury. J Clin Med. 2020;9:873. doi: 10.3390/jcm9030873
14. Kraus DR, Seligman DA, Jordan JR. Validation of a behavioral health treatment outcome and assessment tool designed for naturalistic settings: the Treatment Outcome Package. J Clin Psychol. 2005;61:285‐314. doi: 10.1002/jclp.20084
15. Boothroyd L, Dagnan D, Muncer S. Psychometric analysis of the Generalized Anxiety Disorder Scale and the Patient Health Questionnaire using Mokken scaling and confirmatory factor analysis. Health Prim Care. 2018;2:1-4. doi: 10.15761/HPC.1000145
16. Locke BD, Buzolitz JS, Lei PW, et al. Development of the Counseling Center Assessment of Psychological Symptoms-62 (CCAPS-62). J Couns Psychol. 2011;58:97-109. doi: 10.1037/a0021282
17. Kraus DR, Boswell JF, Wright AGC, et al. Factor structure of the treatment outcome package for children. J Clin Psychol. 2010;66:627-640. doi: 10.1002/jclp.20675
18. McAleavey AA, Nordberg SS, Kraus D, et al. Errors in treatment outcome monitoring: implications for real-world psychotherapy. Can Psychol. 2010;53:105-114. doi: 10.1037/a0027833
19. Baxter EE, Alexander PC, Kraus DR, et al. Concurrent validation of the Treatment Outcome Package (TOP) for children and adolescents. J Child Fam Stud. 2016;25:2415-2422. doi: 10.1007/s10826-016-0419-4
20. Gual-Montolio P, Martínez-Borba V, Bretón-López JM, et al. How are information and communication technologies supporting routine outcome monitoring and measurement-based care in psychotherapy? A systematic review. Int J Environ Res Public Health. 2020;17:3170. doi: 10.3390/ijerph17093170
21. Kraus DR, Bentley JH, Alexander PC, et al. Predicting therapist effectiveness from their own practice-based evidence. J Consult Clin Psychol. 2016;84:473‐483. doi: 10.1037/ccp0000083
22. Constantino MJ, Boswell JF, Coyne AE, et al. Effect of matching therapists to patients vs assignment as usual on adult psychotherapy outcomes. A randomized clinical trial. JAMA Psychiatry. 2021;78:960-969. doi: 10.1001/jamapsychiatry.2021.1221
23. Constantino MJ, Boswell JF, Kraus DR, et al. Matching patients with therapists to improve mental health care. Patient-Centered Outcomes Research Institute (PCORI). 2021. Accessed March 1, 2023. www.pcori.org/research-results/2015/matching-patients-therapists-improve-mental-health-care
24. Institute of Medicine. Committee on Crossing the Quality Chasm: Adaptation to Mental Health and Addictive Disorders. Improving the Quality of Health Care for Mental and Substance-Use Conditions. National Academies Press; 2006. Accessed February 21, 2023. https://nap.nationalacademies.org/read/11470/chapter/1
25. Boswell JF, Constantino MJ, Oswald JM, et al. A multimethod study of mental health care patients’ attitudes toward clinician-level performance information. Psychiatr Serv. 2021;72:452-456. doi: 10.1176/appi.ps.202000366
26. Boswell JF, Constantino MJ, Oswald JM, et al. Mental health care consumers’ relative valuing of clinician performance information. J Consult Clin Psychol. 2018;86:301‐308. doi: 10.1037/ccp0000264
Mohs surgery workforce continues to increase
SEATTLE – At least for now, and that has been the case for the past 5 years.
Using CMS billing codes as a surrogate, the researchers found that there was a steady increase in the number of physicians who billed from 2015 to 2020. With the exception of 2020, which was the height of the COVID-19 pandemic, the number of times that a specific code was billed for increased on average by 4.7% annually.
“Thus, if the attrition rate remains stable, even with changes in board certification and potential payer eligibility restrictions, the number of physicians will continue to increase,” study author Ji Won Ahn, MD, who specializes in dermatology and Mohs surgery at University of Pittsburgh Medical Center, said at the annual meeting of the American College of Mohs Surgery, where she presented the results.
The growth in the number of Mohs surgeons has been fueled by several factors, including a rising incidence of skin cancer as well as the superior cure rates and cosmetic outcomes with the procedure. Reimbursement has been favorable and training pathways have expanded. A 2019 retrospective study reported that there were 2,240 dermatologists who performed Mohs surgery in the United States, with nearly all of them (94.6%) residing in metropolitan areas.
Dr. Ahn explained that it was important to define the workforce because of several new factors that will be affecting it in the future. “With the establishment of Micrographic Surgery and Dermatologic Oncology [MSDO] board certification that went into effect 2 years ago, potential future payer eligibility restrictions may be coming,” she said. “The adequacy of the Mohs surgery workforce is an important consideration.”
Another issue is that new board certification will be limited to fellowship-trained physicians after the first 5 years. “We wanted to compare these numbers with the fellowship numbers,” she said. “Although fellowship numbers are something that the college potentially has the power to change.”
Dr. Ahn and colleagues used the Centers for Medicare & Medicaid Services database to evaluate the use of the Current Procedural Terminology (CPT) code 17311, which is one of the most common billing codes for Mohs micrographic technique. Looking at data from 2015-2020, they found that there was an annual increase in the number of unique national provider identifiers (NPIs) billing for 17311, at an average rate of 75.6 per year.
The total number of times that 17311 was billed also increased from 2015 to 2019 at an average rate of 4.7% per year but declined in 2020 by 8.4%. “Overall, there was an average of 135 new NPIs that appeared and an average of 59.4 NPIs that stopped billing for 17311,” thus, an attrition rate of 59 surgeons, Dr. Ahn explained.
She emphasized that notably, the number of approved MSDO fellowship spots has remained stable since 2016 and is about 92 to 93 per year. “There are about 135 new surgeons and about two-thirds are new fellowship graduates,” she said.
The researchers were also interested in seeing how saturated each surgeon was and looked at the approximate number of cases that they were handling.
Of the physicians who billed 17311 through CMS, over 26% billed less than 100 times and more than 45% billed less than 200 times, and over 80% billed less than 500 times.
“One might be able to conclude that there might be some potential flexibility depending on the future need for surgeons,” she said.
The study was limited by several factors, one being that the researchers looked only at CPT code 17311 and not other designated codes for Mohs surgery. Other factors such as staff and space limitations were not accounted for since only billing data were used.
Dr. Ahn and her team are going to continue their work, and the next steps are to look at geographic trends and monitor for insurance network eligibility changes. “We are currently doing a workforce survey so we can better understand our current workforce rather than just historical data,” she concluded.
Asked to comment on the results, Vishal Patel, MD, assistant professor of dermatology and director of the cutaneous oncology program at George Washington University, Washington, who was not involved with the study, noted that the increase in the “billing rates of the first stage of Mohs micrographic surgery highlights not only the growing skin cancer epidemic, but also the number of providers who are providing these services. This underscores the importance of standardized training guidelines and board certifications of Mohs micrographic surgeons to assure high levels of patient care and the appropriate use of Mohs micrographic surgery,” he said.
No external funding of the study was reported. Dr. Ahn reported no relevant financial relationships. Dr. Patel is a consultant for Sanofi, Regeneron, and Almirall.
A version of this article originally appeared on Medscape.com.
SEATTLE – At least for now, and that has been the case for the past 5 years.
Using CMS billing codes as a surrogate, the researchers found that there was a steady increase in the number of physicians who billed from 2015 to 2020. With the exception of 2020, which was the height of the COVID-19 pandemic, the number of times that a specific code was billed for increased on average by 4.7% annually.
“Thus, if the attrition rate remains stable, even with changes in board certification and potential payer eligibility restrictions, the number of physicians will continue to increase,” study author Ji Won Ahn, MD, who specializes in dermatology and Mohs surgery at University of Pittsburgh Medical Center, said at the annual meeting of the American College of Mohs Surgery, where she presented the results.
The growth in the number of Mohs surgeons has been fueled by several factors, including a rising incidence of skin cancer as well as the superior cure rates and cosmetic outcomes with the procedure. Reimbursement has been favorable and training pathways have expanded. A 2019 retrospective study reported that there were 2,240 dermatologists who performed Mohs surgery in the United States, with nearly all of them (94.6%) residing in metropolitan areas.
Dr. Ahn explained that it was important to define the workforce because of several new factors that will be affecting it in the future. “With the establishment of Micrographic Surgery and Dermatologic Oncology [MSDO] board certification that went into effect 2 years ago, potential future payer eligibility restrictions may be coming,” she said. “The adequacy of the Mohs surgery workforce is an important consideration.”
Another issue is that new board certification will be limited to fellowship-trained physicians after the first 5 years. “We wanted to compare these numbers with the fellowship numbers,” she said. “Although fellowship numbers are something that the college potentially has the power to change.”
Dr. Ahn and colleagues used the Centers for Medicare & Medicaid Services database to evaluate the use of the Current Procedural Terminology (CPT) code 17311, which is one of the most common billing codes for Mohs micrographic technique. Looking at data from 2015-2020, they found that there was an annual increase in the number of unique national provider identifiers (NPIs) billing for 17311, at an average rate of 75.6 per year.
The total number of times that 17311 was billed also increased from 2015 to 2019 at an average rate of 4.7% per year but declined in 2020 by 8.4%. “Overall, there was an average of 135 new NPIs that appeared and an average of 59.4 NPIs that stopped billing for 17311,” thus, an attrition rate of 59 surgeons, Dr. Ahn explained.
She emphasized that notably, the number of approved MSDO fellowship spots has remained stable since 2016 and is about 92 to 93 per year. “There are about 135 new surgeons and about two-thirds are new fellowship graduates,” she said.
The researchers were also interested in seeing how saturated each surgeon was and looked at the approximate number of cases that they were handling.
Of the physicians who billed 17311 through CMS, over 26% billed less than 100 times and more than 45% billed less than 200 times, and over 80% billed less than 500 times.
“One might be able to conclude that there might be some potential flexibility depending on the future need for surgeons,” she said.
The study was limited by several factors, one being that the researchers looked only at CPT code 17311 and not other designated codes for Mohs surgery. Other factors such as staff and space limitations were not accounted for since only billing data were used.
Dr. Ahn and her team are going to continue their work, and the next steps are to look at geographic trends and monitor for insurance network eligibility changes. “We are currently doing a workforce survey so we can better understand our current workforce rather than just historical data,” she concluded.
Asked to comment on the results, Vishal Patel, MD, assistant professor of dermatology and director of the cutaneous oncology program at George Washington University, Washington, who was not involved with the study, noted that the increase in the “billing rates of the first stage of Mohs micrographic surgery highlights not only the growing skin cancer epidemic, but also the number of providers who are providing these services. This underscores the importance of standardized training guidelines and board certifications of Mohs micrographic surgeons to assure high levels of patient care and the appropriate use of Mohs micrographic surgery,” he said.
No external funding of the study was reported. Dr. Ahn reported no relevant financial relationships. Dr. Patel is a consultant for Sanofi, Regeneron, and Almirall.
A version of this article originally appeared on Medscape.com.
SEATTLE – At least for now, and that has been the case for the past 5 years.
Using CMS billing codes as a surrogate, the researchers found that there was a steady increase in the number of physicians who billed from 2015 to 2020. With the exception of 2020, which was the height of the COVID-19 pandemic, the number of times that a specific code was billed for increased on average by 4.7% annually.
“Thus, if the attrition rate remains stable, even with changes in board certification and potential payer eligibility restrictions, the number of physicians will continue to increase,” study author Ji Won Ahn, MD, who specializes in dermatology and Mohs surgery at University of Pittsburgh Medical Center, said at the annual meeting of the American College of Mohs Surgery, where she presented the results.
The growth in the number of Mohs surgeons has been fueled by several factors, including a rising incidence of skin cancer as well as the superior cure rates and cosmetic outcomes with the procedure. Reimbursement has been favorable and training pathways have expanded. A 2019 retrospective study reported that there were 2,240 dermatologists who performed Mohs surgery in the United States, with nearly all of them (94.6%) residing in metropolitan areas.
Dr. Ahn explained that it was important to define the workforce because of several new factors that will be affecting it in the future. “With the establishment of Micrographic Surgery and Dermatologic Oncology [MSDO] board certification that went into effect 2 years ago, potential future payer eligibility restrictions may be coming,” she said. “The adequacy of the Mohs surgery workforce is an important consideration.”
Another issue is that new board certification will be limited to fellowship-trained physicians after the first 5 years. “We wanted to compare these numbers with the fellowship numbers,” she said. “Although fellowship numbers are something that the college potentially has the power to change.”
Dr. Ahn and colleagues used the Centers for Medicare & Medicaid Services database to evaluate the use of the Current Procedural Terminology (CPT) code 17311, which is one of the most common billing codes for Mohs micrographic technique. Looking at data from 2015-2020, they found that there was an annual increase in the number of unique national provider identifiers (NPIs) billing for 17311, at an average rate of 75.6 per year.
The total number of times that 17311 was billed also increased from 2015 to 2019 at an average rate of 4.7% per year but declined in 2020 by 8.4%. “Overall, there was an average of 135 new NPIs that appeared and an average of 59.4 NPIs that stopped billing for 17311,” thus, an attrition rate of 59 surgeons, Dr. Ahn explained.
She emphasized that notably, the number of approved MSDO fellowship spots has remained stable since 2016 and is about 92 to 93 per year. “There are about 135 new surgeons and about two-thirds are new fellowship graduates,” she said.
The researchers were also interested in seeing how saturated each surgeon was and looked at the approximate number of cases that they were handling.
Of the physicians who billed 17311 through CMS, over 26% billed less than 100 times and more than 45% billed less than 200 times, and over 80% billed less than 500 times.
“One might be able to conclude that there might be some potential flexibility depending on the future need for surgeons,” she said.
The study was limited by several factors, one being that the researchers looked only at CPT code 17311 and not other designated codes for Mohs surgery. Other factors such as staff and space limitations were not accounted for since only billing data were used.
Dr. Ahn and her team are going to continue their work, and the next steps are to look at geographic trends and monitor for insurance network eligibility changes. “We are currently doing a workforce survey so we can better understand our current workforce rather than just historical data,” she concluded.
Asked to comment on the results, Vishal Patel, MD, assistant professor of dermatology and director of the cutaneous oncology program at George Washington University, Washington, who was not involved with the study, noted that the increase in the “billing rates of the first stage of Mohs micrographic surgery highlights not only the growing skin cancer epidemic, but also the number of providers who are providing these services. This underscores the importance of standardized training guidelines and board certifications of Mohs micrographic surgeons to assure high levels of patient care and the appropriate use of Mohs micrographic surgery,” he said.
No external funding of the study was reported. Dr. Ahn reported no relevant financial relationships. Dr. Patel is a consultant for Sanofi, Regeneron, and Almirall.
A version of this article originally appeared on Medscape.com.
AT ACMS 2023
Clinical Advances in Myasthenia Gravis From AAN 2023
Clinical advances in myasthenia gravis from the 2023 American Academy of Neurology (AAN) Annual Meeting include the association between fatigue and disease severity and promising results from three ongoing trials of novel therapies, as reported by Dr Nicholas Silvestri, from the University at Buffalo, Buffalo, New York.
Dr Silvestri begins by discussing a study of autoantibodies in patients with seronegative disease, which highlighted the potential for impaired B-cell tolerance, and goes on to examine research underscoring the association between fatigue and disease severity, as well as anxiety and depression.
Moving on to novel therapies, Dr Silvestri reviews a combined analysis of three trials of rozanolixizumab, which demonstrated the drug's encouraging efficacy and favorable safety profile.
Next, he turns to the ADAPT+ trial, which showed that efgartigimod continued to have an improved clinical response after patients rolled over from the initial ADAPT trial to ADAPT+, with no new safety signals apparent.
Finally, Dr Silvestri looks at data from the postmarketing registry of eculizumab, which revealed how a significant proportion of patients were able discontinue or reduce their other medications once they started the drug.
--
Nicholas J. Silvestri, MD, Associate Professor, Department of Neurology, Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, Buffalo, New York
Nicholas J. Silvestri, MD, has disclosed the following relevant financial relationships:
Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: argenx; Alexion; Immunovant; UCB
Serve(d) as a speaker or a member of a speakers bureau for: argenx; Alexion
Clinical advances in myasthenia gravis from the 2023 American Academy of Neurology (AAN) Annual Meeting include the association between fatigue and disease severity and promising results from three ongoing trials of novel therapies, as reported by Dr Nicholas Silvestri, from the University at Buffalo, Buffalo, New York.
Dr Silvestri begins by discussing a study of autoantibodies in patients with seronegative disease, which highlighted the potential for impaired B-cell tolerance, and goes on to examine research underscoring the association between fatigue and disease severity, as well as anxiety and depression.
Moving on to novel therapies, Dr Silvestri reviews a combined analysis of three trials of rozanolixizumab, which demonstrated the drug's encouraging efficacy and favorable safety profile.
Next, he turns to the ADAPT+ trial, which showed that efgartigimod continued to have an improved clinical response after patients rolled over from the initial ADAPT trial to ADAPT+, with no new safety signals apparent.
Finally, Dr Silvestri looks at data from the postmarketing registry of eculizumab, which revealed how a significant proportion of patients were able discontinue or reduce their other medications once they started the drug.
--
Nicholas J. Silvestri, MD, Associate Professor, Department of Neurology, Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, Buffalo, New York
Nicholas J. Silvestri, MD, has disclosed the following relevant financial relationships:
Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: argenx; Alexion; Immunovant; UCB
Serve(d) as a speaker or a member of a speakers bureau for: argenx; Alexion
Clinical advances in myasthenia gravis from the 2023 American Academy of Neurology (AAN) Annual Meeting include the association between fatigue and disease severity and promising results from three ongoing trials of novel therapies, as reported by Dr Nicholas Silvestri, from the University at Buffalo, Buffalo, New York.
Dr Silvestri begins by discussing a study of autoantibodies in patients with seronegative disease, which highlighted the potential for impaired B-cell tolerance, and goes on to examine research underscoring the association between fatigue and disease severity, as well as anxiety and depression.
Moving on to novel therapies, Dr Silvestri reviews a combined analysis of three trials of rozanolixizumab, which demonstrated the drug's encouraging efficacy and favorable safety profile.
Next, he turns to the ADAPT+ trial, which showed that efgartigimod continued to have an improved clinical response after patients rolled over from the initial ADAPT trial to ADAPT+, with no new safety signals apparent.
Finally, Dr Silvestri looks at data from the postmarketing registry of eculizumab, which revealed how a significant proportion of patients were able discontinue or reduce their other medications once they started the drug.
--
Nicholas J. Silvestri, MD, Associate Professor, Department of Neurology, Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, Buffalo, New York
Nicholas J. Silvestri, MD, has disclosed the following relevant financial relationships:
Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: argenx; Alexion; Immunovant; UCB
Serve(d) as a speaker or a member of a speakers bureau for: argenx; Alexion

Atezolizumab is associated with enhanced response in triple-negative breast cancer
based on final data from a randomized trial.
The IMpassion031 trial showed significant improvement in pathological complete response (pCR) with the addition of atezolizumab to chemotherapy, as well as an acceptable safety profile, said Carlos H. Barrios, MD, of the Latin American Cooperative Oncology Group, Oncoclinicas, in Porto Allegre, Brazil, at the European Society for Medical Oncology (ESMO) Breast Cancer annual congress. Those findings were published in the Lancet in 2020.
Dr. Barrios reported data from a final analysis of the IMpassion031 trial, with data on event-free survival (EFS), disease-free survival (DFS) and overall survival (OS) in the intent-to-treat (ITT) and PD-L1–positive populations.
In the study, patients with early triple-negative breast cancer (eTNBC) and a primary tumor greater than 2 cm were randomized to 840 mg of atezolizumab once every 2 weeks plus a neoadjuvant chemotherapy regimen of nab-paclitaxel 125 mg/m2 once weekly for 12 weeks, followed by doxorubicin 60 mg/m2 plus cyclophosphamide 600 mg/m2 once every 2 weeks for 8 weeks. A total of 333 patients were randomized (165 atezolizumab and 168 placebo). Patients were stratified by stage II versus stage III, and by status of PD-L1, a protein that can predict treatment response (PD-L1 less than 1% vs. 1% or higher).
The primary endpoints (previously reported) were pathological complete response (pCR) in the ITT and PD-L1 populations. After a median follow-up of 39 months, the pCR was 58% in patients treated with atezolizumab versus 41% in those treated with neoadjuvant chemotherapy alone (P = .0044) in the ITT population, Dr. Barrios said. The added benefit from atezolizumab occurred regardless of the status of PD-L1.
Dr. Barrios reported the secondary outcomes of EFS, DFS, and OS in the intent-to-treat and PD-L1–positive populations. “This is a descriptive analysis, with no statistical comparison,” he emphasized.
The 2-year data on EFS, DFS, and OS consistently favored atezolizumab across key clinical subgroups, Dr. Barrios said. In the ITT population, 2-year EFS, DFS, and OS was 85%, 87%, and 95%, respectively, in the atezolizumab group and 80%, 83%, and 90%, respectively, in the placebo group. The results were similar, irrespective of PD-L1 status.
In the PD-L1–positive population, 2-year EFS, DFS, and OS was 89%, 91%, and 95%, respectively, in atezolizumab patients and 80%, 87%, and 91% in placebo patients.
Among patients without pCR at the time of surgery, 14 of 70 patients (20%) in the atezolizumab group and 33 of 99 patients (33%) in the placebo group received additional adjuvant systemic therapy. The most common adjunctive therapy was capecitabine.
As for safety, no new safety signals or treatment-related deaths were observed in the study. Overall, 70% of atezolizumab patients and 62% of placebo patients experienced grade 3 or 4 adverse events (AEs); 59% and 54% of which were treatment related. A total of 1% of patients in each group experienced grade 5 AEs. A total of 25% of atezolizumab patients and 20% of placebo patients experienced AEs leading to treatment discontinuation.
In a further exploratory analysis, pCR was highly predictive of long-term outcomes. Exploratory analysis of circulating tumor DNA (ctDNA) showed clearance in 89% of atezolizumab patients and 86% of placebo patients by the time of surgery.
Looking at the relationship between ctDNA, DFS, and OS, positive ctDNA was associated with a worse prognosis following surgery. As demonstrated in previous studies, pCR patients with negative ctDNA had the best DFS and OS. “In non-pCR patients with positive ctDNA, a numerical trend suggests improved overall survival with atezolizumab,” although the caveat is the very small numbers, Dr. Barrios said.
More research is needed, but in the final analysis, the significant pCR benefit seen with the addition of atezolizumab to chemotherapy for eTNBC translated into numerically improved EFS, DFS and OS, said Dr. Barrios. Additionally, “we should further analyze ctDNA to help select patients for further therapy.”
In a question-and-answer session, Dr. Barrios was asked how the results compared with other studies.
“We should not overinterpret the results,” he said. However, “what the IMpassion031 study shows is consistency; the results are aligned with previous studies addressing the same question of introducing immunotherapy,” in the patient population. Although the numbers in the IMpassion031 study did not reach statistical significance, it is important to recognize that they reflect previous research.
“In my opinion, looking at the whole field, immunotherapy is something we need to consider as part of the treatment of these patients,” said Dr. Barrios. However, more research is needed to better identify which patients do and do not need chemotherapy.
Phase 2 data show increased response with added atezolizumab for PD-L1–negative patients
In a second study known as ABSCG-52/ATHENE, researchers evaluated neoadjuvant atezolizumab in combination with dual HER2 blockade plus epirubicin for the treatment of patients with early HER2-positive breast cancer.
For most of these patients, the current standard of care is neoadjuvant dual HER2 blockade with trastuzumab (T) and pertuzumab (P) plus poly-chemotherapy, said Gabriel Rinnerthaler, MD, of the Salzburg (Austria) Cancer Research Institute, said in his presentation at the meeting. However, de-escalation of chemotherapy has been a major focus of research in recent years, and more research is needed on a combination of anthracyclines, such as epirubicin and idarubicin, and immune-checkpoint modulators.
In the phase 2 study, the researchers randomized patients with previously untreated, histologically confirmed HER2-positive early breast cancer (defined as a clinical prognostic stage cT1c–4a-d, N0-3, M0) in a 1:1 ratio to two 3-weekly cycles of a chemotherapy-free induction phase (part 1) with TP plus 1,200 mg atezolizumab (TP-A) or TP alone.
“We hypothesized that the additive effect of immune checkpoint inhibitors plus anti-HER2 therapy and chemotherapy would not be linear,” he said.
At the end of this period, all patients underwent four cycles of TP-A in combination with epirubicin (part 2). The primary endpoint was pCR (defined as absence of invasive cancer in the breast and axillary nodes, or ypT0/Tis ypN0) in the overall study population, and a pCR of 40% was considered a positive result.
A total of 29 patients were randomized to TP-A and 29 to TP alone in nine treatment centers in Austria. The study population ranged from 33 to 82 years, with a median age of 57 years. Most patients (72.4%) had hormone receptor (HR)–positive tumors; a total of 45 patients had stage IIA cancer, and 13 had stage IIB.
The primary endpoint of pCR occurred in 35 patients overall (60.3%). In a univariate analysis, the response rates were lower in HR-positive patients, in premenopausal patients, and in histologies other than NST (invasive carcinoma of no special type), Dr. Rinnerthaler said, but none of the differences were statistically significant, likely because of the small numbers in each group.
In an exploratory analysis of the ITT population with available PD-L1 data, the pCR was 69.2% for PD-L1–negative patients and 55.2% for PD-L1–positive patients.
“We observed the highest pCR rates in PD-L1–negative patients treated in the TP-A group and the lowest in PD-L1–positive patients treated with TP alone,” Dr. Rinnerthaler said.
No new safety concerns were observed during the study, Dr. Rinnerthaler noted. AEs of grade 3 or higher occurred in 17 patients (29.3%), including 9 in the TP-A group and 8 in the TP group. The most common AEs in both groups were nausea, diarrhea, and fatigue. No AEs of special interest of grade 3 or higher (defined as immune-related AEs, cardiac disorders, or infusion-related reactions) were observed.
The study findings were limited by the small sample size, but the resulting pCR rate of 60.3% was higher than the predefined threshold of 40% and supports additional research, said Dr. Rinnerthaler.
“For HER2-positive early breast cancer, a neoadjuvant chemotherapy de-escalation immunotherapy regimen with trastuzumab, pertuzumab, atezolizumab, and epirubicin is highly effective and safe and merits further investigation,” he concluded.
During a question-and-answer session, Dr. Rinnerthaler was asked why pCR increased in PD-L1 negative patients.
Previous data have shown that PD-L1 is up-regulated in certain tumors, and may serve as a surrogate for sensitivity, he said. In previous studies the additional effect of atezolizumab was seen in a PD-L1–negative group.
Dr. Rinnerthaler said he hopes to clarify this question when his research team reviews biopsy data from baseline and after the induction phase.
Defining response is key to de-escalation
In the IMpassion031 trial, “what we saw is a tendency to better outcomes for those patients who received atezolizumab,” said Matteo Lambertini, MD, of the University of Genova (Italy), who served as discussant for the two studies. The IMpassion031 study raises the question of where we are in the use of immuno-oncology for eTNBC. The study is now one of five neoadjuvant trials in this population.
Dr. Lambertini cited the KEYNOTE-522 study, which showed significant results in EFS. However, sample sizes and statistical design were different between these studies. “I think we need large studies of data in the adjuvant and postneoadjuvant setting for patients with triple-negative breast cancer.”
Postneoadjuvant considerations from the IMpassion031 trial showed good outcomes with no additional benefit of an immune checkpoint inhibitors.
For those patients with a pCR, it is definitely time to de-escalate treatment,” he said. In patients without pCR, escalation is needed, but an improved definition of pCR is also needed.
With regard to the ATHENE study, “it may be considered a positive study because the threshold of 40% was reached,” he said. The question is what is the optimum chemotherapy backbone. There appears to be no added benefit to adding an immune checkpoint inhibitor.
There are needs for defining the role of immunotherapy in HER2-positive breast cancer and more biomarker research to inform patient selection and study design, he said.
Finally, “I am not sure that the addition of an immune checkpoint inhibitor can be considered a de-escalation,” he noted.
IMpassion031 was supported by F. Hoffmann–La Roche. Dr. Barrio disclosed financial relationships with numerous companies. ABSCG-52/ATHENE was supported by the Austrian Breast and Colorectal Cancer Study Group and Roche Austria. Dr. Rinnerthaler disclosed relationships with multiple companies including Amgen, Daiichi Sankyo, Lilly, Gilead, MSD, Novartis, Pfizer, Roche, Seagen, and Pierre Fabre. Dr. Lambertini disclosed relationships with multiple companies including Roche, Novartis, AstraZeneca, Lilly, Exact Sciences, Pfizer, MSD, Seagen, Gilead, Takeda, Sandoz, Ipsen, Libbs, Knight, and Daiichi Sankyo.
based on final data from a randomized trial.
The IMpassion031 trial showed significant improvement in pathological complete response (pCR) with the addition of atezolizumab to chemotherapy, as well as an acceptable safety profile, said Carlos H. Barrios, MD, of the Latin American Cooperative Oncology Group, Oncoclinicas, in Porto Allegre, Brazil, at the European Society for Medical Oncology (ESMO) Breast Cancer annual congress. Those findings were published in the Lancet in 2020.
Dr. Barrios reported data from a final analysis of the IMpassion031 trial, with data on event-free survival (EFS), disease-free survival (DFS) and overall survival (OS) in the intent-to-treat (ITT) and PD-L1–positive populations.
In the study, patients with early triple-negative breast cancer (eTNBC) and a primary tumor greater than 2 cm were randomized to 840 mg of atezolizumab once every 2 weeks plus a neoadjuvant chemotherapy regimen of nab-paclitaxel 125 mg/m2 once weekly for 12 weeks, followed by doxorubicin 60 mg/m2 plus cyclophosphamide 600 mg/m2 once every 2 weeks for 8 weeks. A total of 333 patients were randomized (165 atezolizumab and 168 placebo). Patients were stratified by stage II versus stage III, and by status of PD-L1, a protein that can predict treatment response (PD-L1 less than 1% vs. 1% or higher).
The primary endpoints (previously reported) were pathological complete response (pCR) in the ITT and PD-L1 populations. After a median follow-up of 39 months, the pCR was 58% in patients treated with atezolizumab versus 41% in those treated with neoadjuvant chemotherapy alone (P = .0044) in the ITT population, Dr. Barrios said. The added benefit from atezolizumab occurred regardless of the status of PD-L1.
Dr. Barrios reported the secondary outcomes of EFS, DFS, and OS in the intent-to-treat and PD-L1–positive populations. “This is a descriptive analysis, with no statistical comparison,” he emphasized.
The 2-year data on EFS, DFS, and OS consistently favored atezolizumab across key clinical subgroups, Dr. Barrios said. In the ITT population, 2-year EFS, DFS, and OS was 85%, 87%, and 95%, respectively, in the atezolizumab group and 80%, 83%, and 90%, respectively, in the placebo group. The results were similar, irrespective of PD-L1 status.
In the PD-L1–positive population, 2-year EFS, DFS, and OS was 89%, 91%, and 95%, respectively, in atezolizumab patients and 80%, 87%, and 91% in placebo patients.
Among patients without pCR at the time of surgery, 14 of 70 patients (20%) in the atezolizumab group and 33 of 99 patients (33%) in the placebo group received additional adjuvant systemic therapy. The most common adjunctive therapy was capecitabine.
As for safety, no new safety signals or treatment-related deaths were observed in the study. Overall, 70% of atezolizumab patients and 62% of placebo patients experienced grade 3 or 4 adverse events (AEs); 59% and 54% of which were treatment related. A total of 1% of patients in each group experienced grade 5 AEs. A total of 25% of atezolizumab patients and 20% of placebo patients experienced AEs leading to treatment discontinuation.
In a further exploratory analysis, pCR was highly predictive of long-term outcomes. Exploratory analysis of circulating tumor DNA (ctDNA) showed clearance in 89% of atezolizumab patients and 86% of placebo patients by the time of surgery.
Looking at the relationship between ctDNA, DFS, and OS, positive ctDNA was associated with a worse prognosis following surgery. As demonstrated in previous studies, pCR patients with negative ctDNA had the best DFS and OS. “In non-pCR patients with positive ctDNA, a numerical trend suggests improved overall survival with atezolizumab,” although the caveat is the very small numbers, Dr. Barrios said.
More research is needed, but in the final analysis, the significant pCR benefit seen with the addition of atezolizumab to chemotherapy for eTNBC translated into numerically improved EFS, DFS and OS, said Dr. Barrios. Additionally, “we should further analyze ctDNA to help select patients for further therapy.”
In a question-and-answer session, Dr. Barrios was asked how the results compared with other studies.
“We should not overinterpret the results,” he said. However, “what the IMpassion031 study shows is consistency; the results are aligned with previous studies addressing the same question of introducing immunotherapy,” in the patient population. Although the numbers in the IMpassion031 study did not reach statistical significance, it is important to recognize that they reflect previous research.
“In my opinion, looking at the whole field, immunotherapy is something we need to consider as part of the treatment of these patients,” said Dr. Barrios. However, more research is needed to better identify which patients do and do not need chemotherapy.
Phase 2 data show increased response with added atezolizumab for PD-L1–negative patients
In a second study known as ABSCG-52/ATHENE, researchers evaluated neoadjuvant atezolizumab in combination with dual HER2 blockade plus epirubicin for the treatment of patients with early HER2-positive breast cancer.
For most of these patients, the current standard of care is neoadjuvant dual HER2 blockade with trastuzumab (T) and pertuzumab (P) plus poly-chemotherapy, said Gabriel Rinnerthaler, MD, of the Salzburg (Austria) Cancer Research Institute, said in his presentation at the meeting. However, de-escalation of chemotherapy has been a major focus of research in recent years, and more research is needed on a combination of anthracyclines, such as epirubicin and idarubicin, and immune-checkpoint modulators.
In the phase 2 study, the researchers randomized patients with previously untreated, histologically confirmed HER2-positive early breast cancer (defined as a clinical prognostic stage cT1c–4a-d, N0-3, M0) in a 1:1 ratio to two 3-weekly cycles of a chemotherapy-free induction phase (part 1) with TP plus 1,200 mg atezolizumab (TP-A) or TP alone.
“We hypothesized that the additive effect of immune checkpoint inhibitors plus anti-HER2 therapy and chemotherapy would not be linear,” he said.
At the end of this period, all patients underwent four cycles of TP-A in combination with epirubicin (part 2). The primary endpoint was pCR (defined as absence of invasive cancer in the breast and axillary nodes, or ypT0/Tis ypN0) in the overall study population, and a pCR of 40% was considered a positive result.
A total of 29 patients were randomized to TP-A and 29 to TP alone in nine treatment centers in Austria. The study population ranged from 33 to 82 years, with a median age of 57 years. Most patients (72.4%) had hormone receptor (HR)–positive tumors; a total of 45 patients had stage IIA cancer, and 13 had stage IIB.
The primary endpoint of pCR occurred in 35 patients overall (60.3%). In a univariate analysis, the response rates were lower in HR-positive patients, in premenopausal patients, and in histologies other than NST (invasive carcinoma of no special type), Dr. Rinnerthaler said, but none of the differences were statistically significant, likely because of the small numbers in each group.
In an exploratory analysis of the ITT population with available PD-L1 data, the pCR was 69.2% for PD-L1–negative patients and 55.2% for PD-L1–positive patients.
“We observed the highest pCR rates in PD-L1–negative patients treated in the TP-A group and the lowest in PD-L1–positive patients treated with TP alone,” Dr. Rinnerthaler said.
No new safety concerns were observed during the study, Dr. Rinnerthaler noted. AEs of grade 3 or higher occurred in 17 patients (29.3%), including 9 in the TP-A group and 8 in the TP group. The most common AEs in both groups were nausea, diarrhea, and fatigue. No AEs of special interest of grade 3 or higher (defined as immune-related AEs, cardiac disorders, or infusion-related reactions) were observed.
The study findings were limited by the small sample size, but the resulting pCR rate of 60.3% was higher than the predefined threshold of 40% and supports additional research, said Dr. Rinnerthaler.
“For HER2-positive early breast cancer, a neoadjuvant chemotherapy de-escalation immunotherapy regimen with trastuzumab, pertuzumab, atezolizumab, and epirubicin is highly effective and safe and merits further investigation,” he concluded.
During a question-and-answer session, Dr. Rinnerthaler was asked why pCR increased in PD-L1 negative patients.
Previous data have shown that PD-L1 is up-regulated in certain tumors, and may serve as a surrogate for sensitivity, he said. In previous studies the additional effect of atezolizumab was seen in a PD-L1–negative group.
Dr. Rinnerthaler said he hopes to clarify this question when his research team reviews biopsy data from baseline and after the induction phase.
Defining response is key to de-escalation
In the IMpassion031 trial, “what we saw is a tendency to better outcomes for those patients who received atezolizumab,” said Matteo Lambertini, MD, of the University of Genova (Italy), who served as discussant for the two studies. The IMpassion031 study raises the question of where we are in the use of immuno-oncology for eTNBC. The study is now one of five neoadjuvant trials in this population.
Dr. Lambertini cited the KEYNOTE-522 study, which showed significant results in EFS. However, sample sizes and statistical design were different between these studies. “I think we need large studies of data in the adjuvant and postneoadjuvant setting for patients with triple-negative breast cancer.”
Postneoadjuvant considerations from the IMpassion031 trial showed good outcomes with no additional benefit of an immune checkpoint inhibitors.
For those patients with a pCR, it is definitely time to de-escalate treatment,” he said. In patients without pCR, escalation is needed, but an improved definition of pCR is also needed.
With regard to the ATHENE study, “it may be considered a positive study because the threshold of 40% was reached,” he said. The question is what is the optimum chemotherapy backbone. There appears to be no added benefit to adding an immune checkpoint inhibitor.
There are needs for defining the role of immunotherapy in HER2-positive breast cancer and more biomarker research to inform patient selection and study design, he said.
Finally, “I am not sure that the addition of an immune checkpoint inhibitor can be considered a de-escalation,” he noted.
IMpassion031 was supported by F. Hoffmann–La Roche. Dr. Barrio disclosed financial relationships with numerous companies. ABSCG-52/ATHENE was supported by the Austrian Breast and Colorectal Cancer Study Group and Roche Austria. Dr. Rinnerthaler disclosed relationships with multiple companies including Amgen, Daiichi Sankyo, Lilly, Gilead, MSD, Novartis, Pfizer, Roche, Seagen, and Pierre Fabre. Dr. Lambertini disclosed relationships with multiple companies including Roche, Novartis, AstraZeneca, Lilly, Exact Sciences, Pfizer, MSD, Seagen, Gilead, Takeda, Sandoz, Ipsen, Libbs, Knight, and Daiichi Sankyo.
based on final data from a randomized trial.
The IMpassion031 trial showed significant improvement in pathological complete response (pCR) with the addition of atezolizumab to chemotherapy, as well as an acceptable safety profile, said Carlos H. Barrios, MD, of the Latin American Cooperative Oncology Group, Oncoclinicas, in Porto Allegre, Brazil, at the European Society for Medical Oncology (ESMO) Breast Cancer annual congress. Those findings were published in the Lancet in 2020.
Dr. Barrios reported data from a final analysis of the IMpassion031 trial, with data on event-free survival (EFS), disease-free survival (DFS) and overall survival (OS) in the intent-to-treat (ITT) and PD-L1–positive populations.
In the study, patients with early triple-negative breast cancer (eTNBC) and a primary tumor greater than 2 cm were randomized to 840 mg of atezolizumab once every 2 weeks plus a neoadjuvant chemotherapy regimen of nab-paclitaxel 125 mg/m2 once weekly for 12 weeks, followed by doxorubicin 60 mg/m2 plus cyclophosphamide 600 mg/m2 once every 2 weeks for 8 weeks. A total of 333 patients were randomized (165 atezolizumab and 168 placebo). Patients were stratified by stage II versus stage III, and by status of PD-L1, a protein that can predict treatment response (PD-L1 less than 1% vs. 1% or higher).
The primary endpoints (previously reported) were pathological complete response (pCR) in the ITT and PD-L1 populations. After a median follow-up of 39 months, the pCR was 58% in patients treated with atezolizumab versus 41% in those treated with neoadjuvant chemotherapy alone (P = .0044) in the ITT population, Dr. Barrios said. The added benefit from atezolizumab occurred regardless of the status of PD-L1.
Dr. Barrios reported the secondary outcomes of EFS, DFS, and OS in the intent-to-treat and PD-L1–positive populations. “This is a descriptive analysis, with no statistical comparison,” he emphasized.
The 2-year data on EFS, DFS, and OS consistently favored atezolizumab across key clinical subgroups, Dr. Barrios said. In the ITT population, 2-year EFS, DFS, and OS was 85%, 87%, and 95%, respectively, in the atezolizumab group and 80%, 83%, and 90%, respectively, in the placebo group. The results were similar, irrespective of PD-L1 status.
In the PD-L1–positive population, 2-year EFS, DFS, and OS was 89%, 91%, and 95%, respectively, in atezolizumab patients and 80%, 87%, and 91% in placebo patients.
Among patients without pCR at the time of surgery, 14 of 70 patients (20%) in the atezolizumab group and 33 of 99 patients (33%) in the placebo group received additional adjuvant systemic therapy. The most common adjunctive therapy was capecitabine.
As for safety, no new safety signals or treatment-related deaths were observed in the study. Overall, 70% of atezolizumab patients and 62% of placebo patients experienced grade 3 or 4 adverse events (AEs); 59% and 54% of which were treatment related. A total of 1% of patients in each group experienced grade 5 AEs. A total of 25% of atezolizumab patients and 20% of placebo patients experienced AEs leading to treatment discontinuation.
In a further exploratory analysis, pCR was highly predictive of long-term outcomes. Exploratory analysis of circulating tumor DNA (ctDNA) showed clearance in 89% of atezolizumab patients and 86% of placebo patients by the time of surgery.
Looking at the relationship between ctDNA, DFS, and OS, positive ctDNA was associated with a worse prognosis following surgery. As demonstrated in previous studies, pCR patients with negative ctDNA had the best DFS and OS. “In non-pCR patients with positive ctDNA, a numerical trend suggests improved overall survival with atezolizumab,” although the caveat is the very small numbers, Dr. Barrios said.
More research is needed, but in the final analysis, the significant pCR benefit seen with the addition of atezolizumab to chemotherapy for eTNBC translated into numerically improved EFS, DFS and OS, said Dr. Barrios. Additionally, “we should further analyze ctDNA to help select patients for further therapy.”
In a question-and-answer session, Dr. Barrios was asked how the results compared with other studies.
“We should not overinterpret the results,” he said. However, “what the IMpassion031 study shows is consistency; the results are aligned with previous studies addressing the same question of introducing immunotherapy,” in the patient population. Although the numbers in the IMpassion031 study did not reach statistical significance, it is important to recognize that they reflect previous research.
“In my opinion, looking at the whole field, immunotherapy is something we need to consider as part of the treatment of these patients,” said Dr. Barrios. However, more research is needed to better identify which patients do and do not need chemotherapy.
Phase 2 data show increased response with added atezolizumab for PD-L1–negative patients
In a second study known as ABSCG-52/ATHENE, researchers evaluated neoadjuvant atezolizumab in combination with dual HER2 blockade plus epirubicin for the treatment of patients with early HER2-positive breast cancer.
For most of these patients, the current standard of care is neoadjuvant dual HER2 blockade with trastuzumab (T) and pertuzumab (P) plus poly-chemotherapy, said Gabriel Rinnerthaler, MD, of the Salzburg (Austria) Cancer Research Institute, said in his presentation at the meeting. However, de-escalation of chemotherapy has been a major focus of research in recent years, and more research is needed on a combination of anthracyclines, such as epirubicin and idarubicin, and immune-checkpoint modulators.
In the phase 2 study, the researchers randomized patients with previously untreated, histologically confirmed HER2-positive early breast cancer (defined as a clinical prognostic stage cT1c–4a-d, N0-3, M0) in a 1:1 ratio to two 3-weekly cycles of a chemotherapy-free induction phase (part 1) with TP plus 1,200 mg atezolizumab (TP-A) or TP alone.
“We hypothesized that the additive effect of immune checkpoint inhibitors plus anti-HER2 therapy and chemotherapy would not be linear,” he said.
At the end of this period, all patients underwent four cycles of TP-A in combination with epirubicin (part 2). The primary endpoint was pCR (defined as absence of invasive cancer in the breast and axillary nodes, or ypT0/Tis ypN0) in the overall study population, and a pCR of 40% was considered a positive result.
A total of 29 patients were randomized to TP-A and 29 to TP alone in nine treatment centers in Austria. The study population ranged from 33 to 82 years, with a median age of 57 years. Most patients (72.4%) had hormone receptor (HR)–positive tumors; a total of 45 patients had stage IIA cancer, and 13 had stage IIB.
The primary endpoint of pCR occurred in 35 patients overall (60.3%). In a univariate analysis, the response rates were lower in HR-positive patients, in premenopausal patients, and in histologies other than NST (invasive carcinoma of no special type), Dr. Rinnerthaler said, but none of the differences were statistically significant, likely because of the small numbers in each group.
In an exploratory analysis of the ITT population with available PD-L1 data, the pCR was 69.2% for PD-L1–negative patients and 55.2% for PD-L1–positive patients.
“We observed the highest pCR rates in PD-L1–negative patients treated in the TP-A group and the lowest in PD-L1–positive patients treated with TP alone,” Dr. Rinnerthaler said.
No new safety concerns were observed during the study, Dr. Rinnerthaler noted. AEs of grade 3 or higher occurred in 17 patients (29.3%), including 9 in the TP-A group and 8 in the TP group. The most common AEs in both groups were nausea, diarrhea, and fatigue. No AEs of special interest of grade 3 or higher (defined as immune-related AEs, cardiac disorders, or infusion-related reactions) were observed.
The study findings were limited by the small sample size, but the resulting pCR rate of 60.3% was higher than the predefined threshold of 40% and supports additional research, said Dr. Rinnerthaler.
“For HER2-positive early breast cancer, a neoadjuvant chemotherapy de-escalation immunotherapy regimen with trastuzumab, pertuzumab, atezolizumab, and epirubicin is highly effective and safe and merits further investigation,” he concluded.
During a question-and-answer session, Dr. Rinnerthaler was asked why pCR increased in PD-L1 negative patients.
Previous data have shown that PD-L1 is up-regulated in certain tumors, and may serve as a surrogate for sensitivity, he said. In previous studies the additional effect of atezolizumab was seen in a PD-L1–negative group.
Dr. Rinnerthaler said he hopes to clarify this question when his research team reviews biopsy data from baseline and after the induction phase.
Defining response is key to de-escalation
In the IMpassion031 trial, “what we saw is a tendency to better outcomes for those patients who received atezolizumab,” said Matteo Lambertini, MD, of the University of Genova (Italy), who served as discussant for the two studies. The IMpassion031 study raises the question of where we are in the use of immuno-oncology for eTNBC. The study is now one of five neoadjuvant trials in this population.
Dr. Lambertini cited the KEYNOTE-522 study, which showed significant results in EFS. However, sample sizes and statistical design were different between these studies. “I think we need large studies of data in the adjuvant and postneoadjuvant setting for patients with triple-negative breast cancer.”
Postneoadjuvant considerations from the IMpassion031 trial showed good outcomes with no additional benefit of an immune checkpoint inhibitors.
For those patients with a pCR, it is definitely time to de-escalate treatment,” he said. In patients without pCR, escalation is needed, but an improved definition of pCR is also needed.
With regard to the ATHENE study, “it may be considered a positive study because the threshold of 40% was reached,” he said. The question is what is the optimum chemotherapy backbone. There appears to be no added benefit to adding an immune checkpoint inhibitor.
There are needs for defining the role of immunotherapy in HER2-positive breast cancer and more biomarker research to inform patient selection and study design, he said.
Finally, “I am not sure that the addition of an immune checkpoint inhibitor can be considered a de-escalation,” he noted.
IMpassion031 was supported by F. Hoffmann–La Roche. Dr. Barrio disclosed financial relationships with numerous companies. ABSCG-52/ATHENE was supported by the Austrian Breast and Colorectal Cancer Study Group and Roche Austria. Dr. Rinnerthaler disclosed relationships with multiple companies including Amgen, Daiichi Sankyo, Lilly, Gilead, MSD, Novartis, Pfizer, Roche, Seagen, and Pierre Fabre. Dr. Lambertini disclosed relationships with multiple companies including Roche, Novartis, AstraZeneca, Lilly, Exact Sciences, Pfizer, MSD, Seagen, Gilead, Takeda, Sandoz, Ipsen, Libbs, Knight, and Daiichi Sankyo.
FROM ESMO BREAST CANCER 2023
Impact of an Educational and Laboratory Stewardship Intervention on Inpatient COVID-19 Therapeutics at a Veterans Affairs Medical Center
Throughout the COVID-19 pandemic, health care professionals (HCPs), including emergency medicine physicians and hospitalists, have been continuously challenged to maintain an up-to-date clinical practice on COVID-19 therapeutics as new evidence emerged.1,2 In the early part of the pandemic, these included not only appropriate and time-sensitive prescriptions of COVID-19 therapeutics, such as remdesivir and dexamethasone, but also judicious use of empiric antibiotics given the low prevalence for bacterial coinfection in early disease.3-6 Alongside this, curbing the excessive laboratory testing of these patients during the pandemic was important not only to minimize costs but also to reduce potential iatrogenic harm and extended length of stay (LOS).7
At the beginning of the pandemic in March 2020 at the US Department of Veterans Affairs (VA) North Texas Health Care System (VANTHCS) Dallas VA Medical Center (DVAMC), we attempted to provide therapeutic guidance for physicians primarily through direct infectious disease (ID) consultation (in-person or electronic).8 This was secondarily supported by a pharmacist and ID physician–curated “living guidance” document on COVID-19 care accessible to all physicians through the DVAMC electronic health record (EHR) and intranet.
As the alpha variant (lineage B.1.1.7) of COVID-19 began spreading throughout North Texas in the winter of 2020, we implemented a targeted educational intervention toward the hospitalist group taking care of patients with COVID-19 with the primary goal of improving the accuracy of COVID-19 therapeutics while minimizing the consultative burden on ID clinical and pharmacy staff. This initiative consisted of (1) proactive guideline dissemination through email and text messages; (2) virtual didactics; and (3) physician reminders during the consultation process. Our ultimate aims were to improve hospitalist-led appropriate prescriptions of remdesivir and dexamethasone, reducing empiric antibiotic days of therapy in patients with COVID-19 at low risk of bacterial coinfection, and reducing laboratory orders that were not indicated for the management of these patients. Following this intervention and the resolution of the second wave, we retrospectively assessed the temporal trends of COVID-19 practices by hospitalists and associated patterns of ID consultation in the DVAMC from October 1, 2020, to March 31, 2021.
METHODS
The educational intervention was carried out at the DVAMC, a 1A high complex facility with more than 200 inpatient beds and part of the VANTHCS. During the study period, patients admitted with COVID-19 were located either on a closed floor (managed by the hospitalist team) or in a closed intensive care unit (ICU) (managed by the pulmonary/critical care team) contingent on the level of care or oxygen supplementation required. ID and other subspecialties provided consultation services as requested by hospitalists or ICU teams either electronically or in person. During the study period, 66 hospitalists were involved in the care of the patients: 59 (89.5%) permanent staff, 4 (6.0%) fee-basis physicians, and 3 (4.5%) moonlighting fellows.
Educational Initiative
We delivered educational sessions to the hospitalists, using collaboration software with video meeting capability every 1 to 2 months beginning in December 2020. An additional session focused on reducing empiric antibiotic prescriptions was also delivered to the emergency medicine department, based on feedback from the hospitalist group. The content for the educational sessions came from informal surveys of both ID trainees assigned to the consultation service and hospitalists, covering the following topics: understanding the stages of COVID-19 illness (virologic replication vs inflammatory) and rationales for therapy; assessing disease severity; indications and use of remdesivir; indications and use of dexamethasone; assessing for bacterial coinfections; when an ID consultation is required; management algorithm for COVID-19; and locating guidelines on the intranet. About 15 to 20 physicians participated in each session. In addition, slides of these didactics and updated institutional COVID-19 guidelines were disseminated to the hospitalist group via email and text messaging. We also linked the intranet institution guidelines in our communication, including a revised user-friendly flowchart (eAppendix).
Laboratory Stewardship Initiative
Laboratory stewardship initiatives were implemented by modifying suggested orders on the admission of patients with COVID-19 and directly educating hospitalist and emergency medicine physicians on evidence-based laboratory orders. At the beginning of the pandemic, a broad admission order set was established at DVAMC, based on the then limited knowledge of the course of infection with COVID-19. This order set allowed the admitting physicians to efficiently order laboratory tests for patients, especially during the demanding increase in patient volume experienced by DVAMC.
As new evidence emerged during the pandemic, many of the laboratory orders were reviewed for clinical utility during care for the patient with COVID-19 per the latest guidance. In December 2020, the admission orders for patients with COVID-19 were revised to reflect better laboratory stewardship to reduce cost and harm. The ID section revised the laboratory orders and disseminated the new order set to admitting physicians. Specifically, the admission order set removed the following laboratory tests available for selection: routine blood cultures, interleukin 6 (IL-6) level, and Legionella sputum culture. These laboratory orders were removed based on the lack of supporting evidence in persons admitted with COVID-19.9 In addition to modification of the admission order set, educational sessions were held with hospitalists to disseminate knowledge of the new changes and address any concerns.
Observations of Care
This study was approved by the VANTHCS Institutional Review Board (protocol code 20-047). Records were retrospectively reviewed for patients admitted to DVAMC for COVID-19 under hospitalist care (patients admitted directly to the ICU were excluded) from October 1, 2020, to March 31, 2021. Age, sex, race and ethnicity, and comorbidities were collected from the EHR. In addition clinical measures such as maximum oxygen requirement during admission (none, nasal cannula of 2-4 L/min, high flow/bilevel positive airway pressure [BiPAP] or mechanical ventilation), proven presence of coinfection (defined as the isolation of a probable pathogen in pure culture and/or clinically determined by ID specialist evaluation), and the average LOS also were collected. For laboratory stewardship data, a retrospective chart review was conducted to determine the total number of blood cultures obtained within 24 hours of admission per month during the study period. Both IL-6 levels and Legionella sputum culture data were collected as the total number of laboratory orders per month, as it was assumed that most of these orders were obtained for patients admitted with COVID-19.
Individual patient-level data were extracted to calculate monthly percentages of ID consultations for COVID-19 by the hospitalist team, adherence to institutional guidelines for dexamethasone and remdesivir prescriptions, and empiric antibiotic prescriptions for patients with COVID-19, including use of a priori adjudication criteria to determine justified vs unjustified empiric use. These criteria included asymmetric chest X-ray infiltrates concerning for bacterial pneumonia; peripheral white blood cell count > 11 K/μL; critical respiratory failure in the emergency department (ED) and being transferred to the ICU; and ID consultation recommended. Because the total number of antibiotics was not being analyzed but rather just the use of antibiotics for the justified and unjustified groups, antibiotic days were reported as the length of therapy (LOT).10 A subset analysis was performed on antibiotic prescriptions by the hospitalist group focusing on those with mild-to-moderate oxygen requirements (no high flow, noninvasive or invasive ventilatory methods) and excluding infections with a proven microbiologic entity.
Differences in demographic and clinical characteristics of patients with COVID-19 admitted from October 1, 2020, to March 31, 2021, were assessed using ANOVA, χ2, and Kruskal-Wallis test. χ2 was used to compare the difference in total laboratory orders for routine blood cultures, IL-6 levels, and Legionella sputum cultures between pre-intervention (October to December 2020) and postintervention (January to March 2021). These pre- and postintervention periods were determined based on the timing of revised admission orders in the EHR and initiation of focused educational sessions starting in late December 2020 and early January 2021. Linear regressions were used to examine the possible 6-month trend of the percentage of patients receiving ID consultation for appropriate dexamethasone prescriptions, appropriate remdesivir prescriptions, appropriate antibiotic coadministration, and mean number of antibiotic days per patient. Linear and logistic regression were also used to assess the trend in LOS over the 6 months while adjusting for age, race and ethnicity, sex, and coinfections. All analyses were performed using SAS 9.4. Statistical significance was defined as P < .05.
RESULTS
From October 1, 2020, to March 31, 2021, there were 565 admissions for COVID-19, which peaked in January 2021 with 163. Analysis of the patient characteristics showed no statistically significant difference for age, sex, oxygen requirements during admission, or proven presence of coinfection between the months of interest (Table 1).
The number of blood cultures obtained in the first 24 hours of admission significantly decreased from 58.1% of admissions in October 2020 to 34.8% of admissions in March 2021 (P < .01) (Table 2).
We observed trends that coincided with the educational efforts. The rate of dexamethasone and remdesivir prescriptions for eligible patients that followed guidelines without ID consultation grew from 0% to 22.2% (P < .01) and 0% to 16.7% (P = .01), respectively. The remaining correct prescriptions for dexamethasone or remdesivir were instituted only after ID consultation. These improvements were seen in tandem with decreased reliance on ID consultation for admitted patients with COVID-19 overall (86.5% in October 2020 to 56.5% in March 2021; P < .01).
After applying a priori justified antibiotic use criteria, we found that the overall degree of empiric unjustified antibiotic use remained high for patients admitted with COVID-19 (36.5%-60.3%) and was largely driven by prescriptions from the ED. However, further analysis revealed a statistically significant decrease in empiric antibiotic LOT per patient during the study period from 3.0 days in October 2020 to 0.9 days in March 2021 (P < .01). In addition, there was a statistically significant change in the mean (SD) LOS, which decreased from 16.3 (17.8) days in October 2020 to 9.7 (13.0) days in March 2021 (P = .02).
DISCUSSION
As the COVID-19 pandemic has evolved, the ability to enact up-to-date guidance is crucial to streamlining patient care, improving time to COVID-19–specific therapies, and minimizing the burden on subspecialty consultation services. At DVAMC, we initiated a targeted and deliberate educational effort directed toward hospitalist and ED groups combined with a laboratory stewardship effort over 6 months to improve the implementation of COVID-19 therapeutics, reduce empiric antibiotic use without reliance on ID consultation services, and reduce the number of unnecessary laboratory orders for admitted patients with COVID-19. During this time, we observed modest but statistically significant improvements in the accuracy of dexamethasone and remdesivir prescribing. In addition, we observed statistically significant improvement in the average LOT per patient regarding antibiotic use and overall decreased LOS. These improvements were seen in parallel with decreasing requests for ID consultation, suggesting that they were attributable in part to increasing self-confidence and efficacy in COVID-19 practices by the hospitalist group. Modification of the COVID-19 admission order set for our facility resulted in substantial decreases in orders for blood cultures, IL-6 levels, and sputum cultures for Legionella.
ID consultation, either in person or remotely, has been instrumental in assisting physicians in COVID-19 management and has been shown to reduce morbidity, mortality, and patient LOS in other infections.11,12 However, in scenarios where ID consultation is not available or in limited supply, accessibility, familiarity, and confidence of primary practitioners to use therapeutic guidance material are integral. Frequent and accessible guidance for the management of COVID-19 has been provided by the National Institutes of Health and the Infectious Diseases Society of America.13,14 Other mechanisms of assisting physicians in both test ordering and therapeutics include clinical decision support tools built into the EHR and the use of a smartphone digital application.15 Guidance needs to be adapted to the context of the facility, including available resources and specific restrictions and/or prohibitions on therapeutics (eg, mandatory ID consultation or approval). In our facility, while COVID-19 therapeutic living guidance documents were maintained and accessible through the intranet, proactive dissemination and redirection were important steps in enabling the use of these documents.
Limitations
We acknowledge several limitations to this study. Most important, the correlations we observed do not represent causation. Our analysis was not designed to ascertain the direct impact of any single or combined educational and laboratory stewardship intervention from this study, and we acknowledge that the improvements in part could be related to increased experience and confidence with COVID-19 management that occurred over time independent of our programs. Furthermore, we acknowledge that several areas of COVID-19 management did not improve over time (such as overall empiric antibiotic use from the ED) or had very modest improvements (hospitalist-initiated remdesivir use). These results underscore the complex dynamics and contextual barriers to rapidly implementing guideline-based care at VANTHCS. Potential factors include insufficient reach to all physicians, variable learner motivation, and therapeutic momentum of antibiotic use carried forward from the ED.16,17 These factors should be considered as grounds for further study. Another limitation was the inability to track viewership and engagement of our COVID-19 guidance document. Without the use metrics, it is difficult to know the individual impact of the document regarding the changing trends in COVID-19 management we observed during the study period.
Conclusions
We report improvements in COVID-19 therapeutic prescriptions and the use of antibiotics and laboratory testing over 6 months at the DVAMC. This was correlated with a deliberate COVID-19 educational initiative that included antibiotic and laboratory stewardship interventions with simultaneous decreased reliance on ID consultation. These efforts lend support to the proof of the principle of combined educational and laboratory stewardship interventions to improve the care of COVID-19 patients, especially where ID support may not be available or is accessed remotely.
1. Dagens A, Sigfrid L, Cai E, et al. Scope, quality, and inclusivity of clinical guidelines produced early in the covid-19 pandemic: rapid review. BMJ. 2020;369:m1936. Published 2020 May 26. doi:10.1136/bmj.m1936
2. Dhivagaran T, Abbas U, Butt F, Arunasalam L, Chang O. Critical appraisal of clinical practice guidelines for the management of COVID-19: protocol for a systematic review. Syst Rev. 2021;10(1):317. Published 2021 Dec 22. doi:10.1186/s13643-021-01871-7
3. Garcia-Vidal C, Sanjuan G, Moreno-García E, et al. Incidence of co-infections and superinfections in hospitalized patients with COVID-19: a retrospective cohort study. Clin Microbiol Infect. 2021;27(1):83-88. doi:10.1016/j.cmi.2020.07.041
4. Karaba SM, Jones G, Helsel T, et al. Prevalence of co-infection at the time of hospital admission in covid-19 patients, a multicenter study. Open Forum Infect Dis. 2020;8(1):ofaa578. Published 2020 Dec 21. doi:10.1093/ofid/ofaa578
5. RECOVERY Collaborative Group, Horby P, Lim WS, et al. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2021;384(8):693-704. doi:10.1056/NEJMoa2021436
6. Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the treatment of covid-19 - final report. N Engl J Med. 2020;383(19):1813-1826. doi:10.1056/NEJMoa2007764
7. Durant TJS, Peaper DR, Ferguson D, Schulz WL. Impact of COVID-19 pandemic on laboratory utilization. J Appl Lab Med. 2020;5(6):1194-1205. doi:10.1093/jalm/jfaa121
8. Yagnik KJ, Saad HA, King HL, Bedimo RJ, Lehmann CU, Medford RJ. Characteristics and outcomes of infectious diseases electronic COVID-19 consultations at a multisite academic health system. Cureus. 2021;13(11):e19203. Published 2021 Nov 2. doi:10.7759/cureus.19203
9. Rawson TM, Moore LSP, Zhu N, et al. Bacterial and fungal coinfection in individuals with coronavirus: a rapid review to support COVID-19 antimicrobial prescribing. Clin Infect Dis. 2020;71(9):2459-2468. doi:10.1093/cid/ciaa530
10. Yarrington ME, Moehring RW. Basic, advanced, and novel metrics to guide antibiotic use assessments. Curr Treat Options Infect Dis. 2019;11(2):145-160. doi:10.1007/s40506-019-00188-3
11. Bai AD, Showler A, Burry L, et al. Impact of infectious disease consultation on quality of care, mortality, and length of stay in Staphylococcus aureus bacteremia: results from a large multicenter cohort study. Clin Infect Dis. 2015;60(10):1451-1461. doi:10.1093/cid/civ120
12. Mejia-Chew C, O’Halloran JA, Olsen MA, et al. Effect of infectious disease consultation on mortality and treatment of patients with candida bloodstream infections: a retrospective, cohort study. Lancet Infect Dis. 2019;19(12):1336-1344. doi:10.1016/S1473-3099(19)30405-0
13. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health (US); April 21, 2021. Accessed February 14, 2023. https://files.covid19treatmentguidelines.nih.gov/guidelines/covid19treatmentguidelines.pdf
14. Bhimraj A, Morgan RL, Shumaker AH, et al. Infectious Diseases Society of America guidelines on the treatment and management of patients with COVID-19. Clin Infect Dis. 2020;ciaa478. doi:10.1093/cid/ciaa478
15. Suraj V, Del Vecchio Fitz C, Kleiman LB, et al. SMART COVID Navigator, a clinical decision support tool for COVID-19 treatment: design and development study. J Med Internet Res. 2022;24(2):e29279. Published 2022 Feb 18. doi:10.2196/29279
16. Pendharkar SR, Minty E, Shukalek CB, et al. Description of a multi-faceted COVID-19 pandemic physician workforce plan at a multi-site academic health system. J Gen Intern Med. 2021;36(5):1310-1318. doi:10.1007/s11606-020-06543-1
17. Pulia MS, Wolf I, Schulz LT, Pop-Vicas A, Schwei RJ, Lindenauer PK. COVID-19: an emerging threat to antibiotic stewardship in the emergency department. West J Emerg Med. 2020;21(5):1283-1286. Published 2020 Aug 7. doi:10.5811/westjem.2020.7.48848
Throughout the COVID-19 pandemic, health care professionals (HCPs), including emergency medicine physicians and hospitalists, have been continuously challenged to maintain an up-to-date clinical practice on COVID-19 therapeutics as new evidence emerged.1,2 In the early part of the pandemic, these included not only appropriate and time-sensitive prescriptions of COVID-19 therapeutics, such as remdesivir and dexamethasone, but also judicious use of empiric antibiotics given the low prevalence for bacterial coinfection in early disease.3-6 Alongside this, curbing the excessive laboratory testing of these patients during the pandemic was important not only to minimize costs but also to reduce potential iatrogenic harm and extended length of stay (LOS).7
At the beginning of the pandemic in March 2020 at the US Department of Veterans Affairs (VA) North Texas Health Care System (VANTHCS) Dallas VA Medical Center (DVAMC), we attempted to provide therapeutic guidance for physicians primarily through direct infectious disease (ID) consultation (in-person or electronic).8 This was secondarily supported by a pharmacist and ID physician–curated “living guidance” document on COVID-19 care accessible to all physicians through the DVAMC electronic health record (EHR) and intranet.
As the alpha variant (lineage B.1.1.7) of COVID-19 began spreading throughout North Texas in the winter of 2020, we implemented a targeted educational intervention toward the hospitalist group taking care of patients with COVID-19 with the primary goal of improving the accuracy of COVID-19 therapeutics while minimizing the consultative burden on ID clinical and pharmacy staff. This initiative consisted of (1) proactive guideline dissemination through email and text messages; (2) virtual didactics; and (3) physician reminders during the consultation process. Our ultimate aims were to improve hospitalist-led appropriate prescriptions of remdesivir and dexamethasone, reducing empiric antibiotic days of therapy in patients with COVID-19 at low risk of bacterial coinfection, and reducing laboratory orders that were not indicated for the management of these patients. Following this intervention and the resolution of the second wave, we retrospectively assessed the temporal trends of COVID-19 practices by hospitalists and associated patterns of ID consultation in the DVAMC from October 1, 2020, to March 31, 2021.
METHODS
The educational intervention was carried out at the DVAMC, a 1A high complex facility with more than 200 inpatient beds and part of the VANTHCS. During the study period, patients admitted with COVID-19 were located either on a closed floor (managed by the hospitalist team) or in a closed intensive care unit (ICU) (managed by the pulmonary/critical care team) contingent on the level of care or oxygen supplementation required. ID and other subspecialties provided consultation services as requested by hospitalists or ICU teams either electronically or in person. During the study period, 66 hospitalists were involved in the care of the patients: 59 (89.5%) permanent staff, 4 (6.0%) fee-basis physicians, and 3 (4.5%) moonlighting fellows.
Educational Initiative
We delivered educational sessions to the hospitalists, using collaboration software with video meeting capability every 1 to 2 months beginning in December 2020. An additional session focused on reducing empiric antibiotic prescriptions was also delivered to the emergency medicine department, based on feedback from the hospitalist group. The content for the educational sessions came from informal surveys of both ID trainees assigned to the consultation service and hospitalists, covering the following topics: understanding the stages of COVID-19 illness (virologic replication vs inflammatory) and rationales for therapy; assessing disease severity; indications and use of remdesivir; indications and use of dexamethasone; assessing for bacterial coinfections; when an ID consultation is required; management algorithm for COVID-19; and locating guidelines on the intranet. About 15 to 20 physicians participated in each session. In addition, slides of these didactics and updated institutional COVID-19 guidelines were disseminated to the hospitalist group via email and text messaging. We also linked the intranet institution guidelines in our communication, including a revised user-friendly flowchart (eAppendix).
Laboratory Stewardship Initiative
Laboratory stewardship initiatives were implemented by modifying suggested orders on the admission of patients with COVID-19 and directly educating hospitalist and emergency medicine physicians on evidence-based laboratory orders. At the beginning of the pandemic, a broad admission order set was established at DVAMC, based on the then limited knowledge of the course of infection with COVID-19. This order set allowed the admitting physicians to efficiently order laboratory tests for patients, especially during the demanding increase in patient volume experienced by DVAMC.
As new evidence emerged during the pandemic, many of the laboratory orders were reviewed for clinical utility during care for the patient with COVID-19 per the latest guidance. In December 2020, the admission orders for patients with COVID-19 were revised to reflect better laboratory stewardship to reduce cost and harm. The ID section revised the laboratory orders and disseminated the new order set to admitting physicians. Specifically, the admission order set removed the following laboratory tests available for selection: routine blood cultures, interleukin 6 (IL-6) level, and Legionella sputum culture. These laboratory orders were removed based on the lack of supporting evidence in persons admitted with COVID-19.9 In addition to modification of the admission order set, educational sessions were held with hospitalists to disseminate knowledge of the new changes and address any concerns.
Observations of Care
This study was approved by the VANTHCS Institutional Review Board (protocol code 20-047). Records were retrospectively reviewed for patients admitted to DVAMC for COVID-19 under hospitalist care (patients admitted directly to the ICU were excluded) from October 1, 2020, to March 31, 2021. Age, sex, race and ethnicity, and comorbidities were collected from the EHR. In addition clinical measures such as maximum oxygen requirement during admission (none, nasal cannula of 2-4 L/min, high flow/bilevel positive airway pressure [BiPAP] or mechanical ventilation), proven presence of coinfection (defined as the isolation of a probable pathogen in pure culture and/or clinically determined by ID specialist evaluation), and the average LOS also were collected. For laboratory stewardship data, a retrospective chart review was conducted to determine the total number of blood cultures obtained within 24 hours of admission per month during the study period. Both IL-6 levels and Legionella sputum culture data were collected as the total number of laboratory orders per month, as it was assumed that most of these orders were obtained for patients admitted with COVID-19.
Individual patient-level data were extracted to calculate monthly percentages of ID consultations for COVID-19 by the hospitalist team, adherence to institutional guidelines for dexamethasone and remdesivir prescriptions, and empiric antibiotic prescriptions for patients with COVID-19, including use of a priori adjudication criteria to determine justified vs unjustified empiric use. These criteria included asymmetric chest X-ray infiltrates concerning for bacterial pneumonia; peripheral white blood cell count > 11 K/μL; critical respiratory failure in the emergency department (ED) and being transferred to the ICU; and ID consultation recommended. Because the total number of antibiotics was not being analyzed but rather just the use of antibiotics for the justified and unjustified groups, antibiotic days were reported as the length of therapy (LOT).10 A subset analysis was performed on antibiotic prescriptions by the hospitalist group focusing on those with mild-to-moderate oxygen requirements (no high flow, noninvasive or invasive ventilatory methods) and excluding infections with a proven microbiologic entity.
Differences in demographic and clinical characteristics of patients with COVID-19 admitted from October 1, 2020, to March 31, 2021, were assessed using ANOVA, χ2, and Kruskal-Wallis test. χ2 was used to compare the difference in total laboratory orders for routine blood cultures, IL-6 levels, and Legionella sputum cultures between pre-intervention (October to December 2020) and postintervention (January to March 2021). These pre- and postintervention periods were determined based on the timing of revised admission orders in the EHR and initiation of focused educational sessions starting in late December 2020 and early January 2021. Linear regressions were used to examine the possible 6-month trend of the percentage of patients receiving ID consultation for appropriate dexamethasone prescriptions, appropriate remdesivir prescriptions, appropriate antibiotic coadministration, and mean number of antibiotic days per patient. Linear and logistic regression were also used to assess the trend in LOS over the 6 months while adjusting for age, race and ethnicity, sex, and coinfections. All analyses were performed using SAS 9.4. Statistical significance was defined as P < .05.
RESULTS
From October 1, 2020, to March 31, 2021, there were 565 admissions for COVID-19, which peaked in January 2021 with 163. Analysis of the patient characteristics showed no statistically significant difference for age, sex, oxygen requirements during admission, or proven presence of coinfection between the months of interest (Table 1).
The number of blood cultures obtained in the first 24 hours of admission significantly decreased from 58.1% of admissions in October 2020 to 34.8% of admissions in March 2021 (P < .01) (Table 2).
We observed trends that coincided with the educational efforts. The rate of dexamethasone and remdesivir prescriptions for eligible patients that followed guidelines without ID consultation grew from 0% to 22.2% (P < .01) and 0% to 16.7% (P = .01), respectively. The remaining correct prescriptions for dexamethasone or remdesivir were instituted only after ID consultation. These improvements were seen in tandem with decreased reliance on ID consultation for admitted patients with COVID-19 overall (86.5% in October 2020 to 56.5% in March 2021; P < .01).
After applying a priori justified antibiotic use criteria, we found that the overall degree of empiric unjustified antibiotic use remained high for patients admitted with COVID-19 (36.5%-60.3%) and was largely driven by prescriptions from the ED. However, further analysis revealed a statistically significant decrease in empiric antibiotic LOT per patient during the study period from 3.0 days in October 2020 to 0.9 days in March 2021 (P < .01). In addition, there was a statistically significant change in the mean (SD) LOS, which decreased from 16.3 (17.8) days in October 2020 to 9.7 (13.0) days in March 2021 (P = .02).
DISCUSSION
As the COVID-19 pandemic has evolved, the ability to enact up-to-date guidance is crucial to streamlining patient care, improving time to COVID-19–specific therapies, and minimizing the burden on subspecialty consultation services. At DVAMC, we initiated a targeted and deliberate educational effort directed toward hospitalist and ED groups combined with a laboratory stewardship effort over 6 months to improve the implementation of COVID-19 therapeutics, reduce empiric antibiotic use without reliance on ID consultation services, and reduce the number of unnecessary laboratory orders for admitted patients with COVID-19. During this time, we observed modest but statistically significant improvements in the accuracy of dexamethasone and remdesivir prescribing. In addition, we observed statistically significant improvement in the average LOT per patient regarding antibiotic use and overall decreased LOS. These improvements were seen in parallel with decreasing requests for ID consultation, suggesting that they were attributable in part to increasing self-confidence and efficacy in COVID-19 practices by the hospitalist group. Modification of the COVID-19 admission order set for our facility resulted in substantial decreases in orders for blood cultures, IL-6 levels, and sputum cultures for Legionella.
ID consultation, either in person or remotely, has been instrumental in assisting physicians in COVID-19 management and has been shown to reduce morbidity, mortality, and patient LOS in other infections.11,12 However, in scenarios where ID consultation is not available or in limited supply, accessibility, familiarity, and confidence of primary practitioners to use therapeutic guidance material are integral. Frequent and accessible guidance for the management of COVID-19 has been provided by the National Institutes of Health and the Infectious Diseases Society of America.13,14 Other mechanisms of assisting physicians in both test ordering and therapeutics include clinical decision support tools built into the EHR and the use of a smartphone digital application.15 Guidance needs to be adapted to the context of the facility, including available resources and specific restrictions and/or prohibitions on therapeutics (eg, mandatory ID consultation or approval). In our facility, while COVID-19 therapeutic living guidance documents were maintained and accessible through the intranet, proactive dissemination and redirection were important steps in enabling the use of these documents.
Limitations
We acknowledge several limitations to this study. Most important, the correlations we observed do not represent causation. Our analysis was not designed to ascertain the direct impact of any single or combined educational and laboratory stewardship intervention from this study, and we acknowledge that the improvements in part could be related to increased experience and confidence with COVID-19 management that occurred over time independent of our programs. Furthermore, we acknowledge that several areas of COVID-19 management did not improve over time (such as overall empiric antibiotic use from the ED) or had very modest improvements (hospitalist-initiated remdesivir use). These results underscore the complex dynamics and contextual barriers to rapidly implementing guideline-based care at VANTHCS. Potential factors include insufficient reach to all physicians, variable learner motivation, and therapeutic momentum of antibiotic use carried forward from the ED.16,17 These factors should be considered as grounds for further study. Another limitation was the inability to track viewership and engagement of our COVID-19 guidance document. Without the use metrics, it is difficult to know the individual impact of the document regarding the changing trends in COVID-19 management we observed during the study period.
Conclusions
We report improvements in COVID-19 therapeutic prescriptions and the use of antibiotics and laboratory testing over 6 months at the DVAMC. This was correlated with a deliberate COVID-19 educational initiative that included antibiotic and laboratory stewardship interventions with simultaneous decreased reliance on ID consultation. These efforts lend support to the proof of the principle of combined educational and laboratory stewardship interventions to improve the care of COVID-19 patients, especially where ID support may not be available or is accessed remotely.
Throughout the COVID-19 pandemic, health care professionals (HCPs), including emergency medicine physicians and hospitalists, have been continuously challenged to maintain an up-to-date clinical practice on COVID-19 therapeutics as new evidence emerged.1,2 In the early part of the pandemic, these included not only appropriate and time-sensitive prescriptions of COVID-19 therapeutics, such as remdesivir and dexamethasone, but also judicious use of empiric antibiotics given the low prevalence for bacterial coinfection in early disease.3-6 Alongside this, curbing the excessive laboratory testing of these patients during the pandemic was important not only to minimize costs but also to reduce potential iatrogenic harm and extended length of stay (LOS).7
At the beginning of the pandemic in March 2020 at the US Department of Veterans Affairs (VA) North Texas Health Care System (VANTHCS) Dallas VA Medical Center (DVAMC), we attempted to provide therapeutic guidance for physicians primarily through direct infectious disease (ID) consultation (in-person or electronic).8 This was secondarily supported by a pharmacist and ID physician–curated “living guidance” document on COVID-19 care accessible to all physicians through the DVAMC electronic health record (EHR) and intranet.
As the alpha variant (lineage B.1.1.7) of COVID-19 began spreading throughout North Texas in the winter of 2020, we implemented a targeted educational intervention toward the hospitalist group taking care of patients with COVID-19 with the primary goal of improving the accuracy of COVID-19 therapeutics while minimizing the consultative burden on ID clinical and pharmacy staff. This initiative consisted of (1) proactive guideline dissemination through email and text messages; (2) virtual didactics; and (3) physician reminders during the consultation process. Our ultimate aims were to improve hospitalist-led appropriate prescriptions of remdesivir and dexamethasone, reducing empiric antibiotic days of therapy in patients with COVID-19 at low risk of bacterial coinfection, and reducing laboratory orders that were not indicated for the management of these patients. Following this intervention and the resolution of the second wave, we retrospectively assessed the temporal trends of COVID-19 practices by hospitalists and associated patterns of ID consultation in the DVAMC from October 1, 2020, to March 31, 2021.
METHODS
The educational intervention was carried out at the DVAMC, a 1A high complex facility with more than 200 inpatient beds and part of the VANTHCS. During the study period, patients admitted with COVID-19 were located either on a closed floor (managed by the hospitalist team) or in a closed intensive care unit (ICU) (managed by the pulmonary/critical care team) contingent on the level of care or oxygen supplementation required. ID and other subspecialties provided consultation services as requested by hospitalists or ICU teams either electronically or in person. During the study period, 66 hospitalists were involved in the care of the patients: 59 (89.5%) permanent staff, 4 (6.0%) fee-basis physicians, and 3 (4.5%) moonlighting fellows.
Educational Initiative
We delivered educational sessions to the hospitalists, using collaboration software with video meeting capability every 1 to 2 months beginning in December 2020. An additional session focused on reducing empiric antibiotic prescriptions was also delivered to the emergency medicine department, based on feedback from the hospitalist group. The content for the educational sessions came from informal surveys of both ID trainees assigned to the consultation service and hospitalists, covering the following topics: understanding the stages of COVID-19 illness (virologic replication vs inflammatory) and rationales for therapy; assessing disease severity; indications and use of remdesivir; indications and use of dexamethasone; assessing for bacterial coinfections; when an ID consultation is required; management algorithm for COVID-19; and locating guidelines on the intranet. About 15 to 20 physicians participated in each session. In addition, slides of these didactics and updated institutional COVID-19 guidelines were disseminated to the hospitalist group via email and text messaging. We also linked the intranet institution guidelines in our communication, including a revised user-friendly flowchart (eAppendix).
Laboratory Stewardship Initiative
Laboratory stewardship initiatives were implemented by modifying suggested orders on the admission of patients with COVID-19 and directly educating hospitalist and emergency medicine physicians on evidence-based laboratory orders. At the beginning of the pandemic, a broad admission order set was established at DVAMC, based on the then limited knowledge of the course of infection with COVID-19. This order set allowed the admitting physicians to efficiently order laboratory tests for patients, especially during the demanding increase in patient volume experienced by DVAMC.
As new evidence emerged during the pandemic, many of the laboratory orders were reviewed for clinical utility during care for the patient with COVID-19 per the latest guidance. In December 2020, the admission orders for patients with COVID-19 were revised to reflect better laboratory stewardship to reduce cost and harm. The ID section revised the laboratory orders and disseminated the new order set to admitting physicians. Specifically, the admission order set removed the following laboratory tests available for selection: routine blood cultures, interleukin 6 (IL-6) level, and Legionella sputum culture. These laboratory orders were removed based on the lack of supporting evidence in persons admitted with COVID-19.9 In addition to modification of the admission order set, educational sessions were held with hospitalists to disseminate knowledge of the new changes and address any concerns.
Observations of Care
This study was approved by the VANTHCS Institutional Review Board (protocol code 20-047). Records were retrospectively reviewed for patients admitted to DVAMC for COVID-19 under hospitalist care (patients admitted directly to the ICU were excluded) from October 1, 2020, to March 31, 2021. Age, sex, race and ethnicity, and comorbidities were collected from the EHR. In addition clinical measures such as maximum oxygen requirement during admission (none, nasal cannula of 2-4 L/min, high flow/bilevel positive airway pressure [BiPAP] or mechanical ventilation), proven presence of coinfection (defined as the isolation of a probable pathogen in pure culture and/or clinically determined by ID specialist evaluation), and the average LOS also were collected. For laboratory stewardship data, a retrospective chart review was conducted to determine the total number of blood cultures obtained within 24 hours of admission per month during the study period. Both IL-6 levels and Legionella sputum culture data were collected as the total number of laboratory orders per month, as it was assumed that most of these orders were obtained for patients admitted with COVID-19.
Individual patient-level data were extracted to calculate monthly percentages of ID consultations for COVID-19 by the hospitalist team, adherence to institutional guidelines for dexamethasone and remdesivir prescriptions, and empiric antibiotic prescriptions for patients with COVID-19, including use of a priori adjudication criteria to determine justified vs unjustified empiric use. These criteria included asymmetric chest X-ray infiltrates concerning for bacterial pneumonia; peripheral white blood cell count > 11 K/μL; critical respiratory failure in the emergency department (ED) and being transferred to the ICU; and ID consultation recommended. Because the total number of antibiotics was not being analyzed but rather just the use of antibiotics for the justified and unjustified groups, antibiotic days were reported as the length of therapy (LOT).10 A subset analysis was performed on antibiotic prescriptions by the hospitalist group focusing on those with mild-to-moderate oxygen requirements (no high flow, noninvasive or invasive ventilatory methods) and excluding infections with a proven microbiologic entity.
Differences in demographic and clinical characteristics of patients with COVID-19 admitted from October 1, 2020, to March 31, 2021, were assessed using ANOVA, χ2, and Kruskal-Wallis test. χ2 was used to compare the difference in total laboratory orders for routine blood cultures, IL-6 levels, and Legionella sputum cultures between pre-intervention (October to December 2020) and postintervention (January to March 2021). These pre- and postintervention periods were determined based on the timing of revised admission orders in the EHR and initiation of focused educational sessions starting in late December 2020 and early January 2021. Linear regressions were used to examine the possible 6-month trend of the percentage of patients receiving ID consultation for appropriate dexamethasone prescriptions, appropriate remdesivir prescriptions, appropriate antibiotic coadministration, and mean number of antibiotic days per patient. Linear and logistic regression were also used to assess the trend in LOS over the 6 months while adjusting for age, race and ethnicity, sex, and coinfections. All analyses were performed using SAS 9.4. Statistical significance was defined as P < .05.
RESULTS
From October 1, 2020, to March 31, 2021, there were 565 admissions for COVID-19, which peaked in January 2021 with 163. Analysis of the patient characteristics showed no statistically significant difference for age, sex, oxygen requirements during admission, or proven presence of coinfection between the months of interest (Table 1).
The number of blood cultures obtained in the first 24 hours of admission significantly decreased from 58.1% of admissions in October 2020 to 34.8% of admissions in March 2021 (P < .01) (Table 2).
We observed trends that coincided with the educational efforts. The rate of dexamethasone and remdesivir prescriptions for eligible patients that followed guidelines without ID consultation grew from 0% to 22.2% (P < .01) and 0% to 16.7% (P = .01), respectively. The remaining correct prescriptions for dexamethasone or remdesivir were instituted only after ID consultation. These improvements were seen in tandem with decreased reliance on ID consultation for admitted patients with COVID-19 overall (86.5% in October 2020 to 56.5% in March 2021; P < .01).
After applying a priori justified antibiotic use criteria, we found that the overall degree of empiric unjustified antibiotic use remained high for patients admitted with COVID-19 (36.5%-60.3%) and was largely driven by prescriptions from the ED. However, further analysis revealed a statistically significant decrease in empiric antibiotic LOT per patient during the study period from 3.0 days in October 2020 to 0.9 days in March 2021 (P < .01). In addition, there was a statistically significant change in the mean (SD) LOS, which decreased from 16.3 (17.8) days in October 2020 to 9.7 (13.0) days in March 2021 (P = .02).
DISCUSSION
As the COVID-19 pandemic has evolved, the ability to enact up-to-date guidance is crucial to streamlining patient care, improving time to COVID-19–specific therapies, and minimizing the burden on subspecialty consultation services. At DVAMC, we initiated a targeted and deliberate educational effort directed toward hospitalist and ED groups combined with a laboratory stewardship effort over 6 months to improve the implementation of COVID-19 therapeutics, reduce empiric antibiotic use without reliance on ID consultation services, and reduce the number of unnecessary laboratory orders for admitted patients with COVID-19. During this time, we observed modest but statistically significant improvements in the accuracy of dexamethasone and remdesivir prescribing. In addition, we observed statistically significant improvement in the average LOT per patient regarding antibiotic use and overall decreased LOS. These improvements were seen in parallel with decreasing requests for ID consultation, suggesting that they were attributable in part to increasing self-confidence and efficacy in COVID-19 practices by the hospitalist group. Modification of the COVID-19 admission order set for our facility resulted in substantial decreases in orders for blood cultures, IL-6 levels, and sputum cultures for Legionella.
ID consultation, either in person or remotely, has been instrumental in assisting physicians in COVID-19 management and has been shown to reduce morbidity, mortality, and patient LOS in other infections.11,12 However, in scenarios where ID consultation is not available or in limited supply, accessibility, familiarity, and confidence of primary practitioners to use therapeutic guidance material are integral. Frequent and accessible guidance for the management of COVID-19 has been provided by the National Institutes of Health and the Infectious Diseases Society of America.13,14 Other mechanisms of assisting physicians in both test ordering and therapeutics include clinical decision support tools built into the EHR and the use of a smartphone digital application.15 Guidance needs to be adapted to the context of the facility, including available resources and specific restrictions and/or prohibitions on therapeutics (eg, mandatory ID consultation or approval). In our facility, while COVID-19 therapeutic living guidance documents were maintained and accessible through the intranet, proactive dissemination and redirection were important steps in enabling the use of these documents.
Limitations
We acknowledge several limitations to this study. Most important, the correlations we observed do not represent causation. Our analysis was not designed to ascertain the direct impact of any single or combined educational and laboratory stewardship intervention from this study, and we acknowledge that the improvements in part could be related to increased experience and confidence with COVID-19 management that occurred over time independent of our programs. Furthermore, we acknowledge that several areas of COVID-19 management did not improve over time (such as overall empiric antibiotic use from the ED) or had very modest improvements (hospitalist-initiated remdesivir use). These results underscore the complex dynamics and contextual barriers to rapidly implementing guideline-based care at VANTHCS. Potential factors include insufficient reach to all physicians, variable learner motivation, and therapeutic momentum of antibiotic use carried forward from the ED.16,17 These factors should be considered as grounds for further study. Another limitation was the inability to track viewership and engagement of our COVID-19 guidance document. Without the use metrics, it is difficult to know the individual impact of the document regarding the changing trends in COVID-19 management we observed during the study period.
Conclusions
We report improvements in COVID-19 therapeutic prescriptions and the use of antibiotics and laboratory testing over 6 months at the DVAMC. This was correlated with a deliberate COVID-19 educational initiative that included antibiotic and laboratory stewardship interventions with simultaneous decreased reliance on ID consultation. These efforts lend support to the proof of the principle of combined educational and laboratory stewardship interventions to improve the care of COVID-19 patients, especially where ID support may not be available or is accessed remotely.
1. Dagens A, Sigfrid L, Cai E, et al. Scope, quality, and inclusivity of clinical guidelines produced early in the covid-19 pandemic: rapid review. BMJ. 2020;369:m1936. Published 2020 May 26. doi:10.1136/bmj.m1936
2. Dhivagaran T, Abbas U, Butt F, Arunasalam L, Chang O. Critical appraisal of clinical practice guidelines for the management of COVID-19: protocol for a systematic review. Syst Rev. 2021;10(1):317. Published 2021 Dec 22. doi:10.1186/s13643-021-01871-7
3. Garcia-Vidal C, Sanjuan G, Moreno-García E, et al. Incidence of co-infections and superinfections in hospitalized patients with COVID-19: a retrospective cohort study. Clin Microbiol Infect. 2021;27(1):83-88. doi:10.1016/j.cmi.2020.07.041
4. Karaba SM, Jones G, Helsel T, et al. Prevalence of co-infection at the time of hospital admission in covid-19 patients, a multicenter study. Open Forum Infect Dis. 2020;8(1):ofaa578. Published 2020 Dec 21. doi:10.1093/ofid/ofaa578
5. RECOVERY Collaborative Group, Horby P, Lim WS, et al. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2021;384(8):693-704. doi:10.1056/NEJMoa2021436
6. Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the treatment of covid-19 - final report. N Engl J Med. 2020;383(19):1813-1826. doi:10.1056/NEJMoa2007764
7. Durant TJS, Peaper DR, Ferguson D, Schulz WL. Impact of COVID-19 pandemic on laboratory utilization. J Appl Lab Med. 2020;5(6):1194-1205. doi:10.1093/jalm/jfaa121
8. Yagnik KJ, Saad HA, King HL, Bedimo RJ, Lehmann CU, Medford RJ. Characteristics and outcomes of infectious diseases electronic COVID-19 consultations at a multisite academic health system. Cureus. 2021;13(11):e19203. Published 2021 Nov 2. doi:10.7759/cureus.19203
9. Rawson TM, Moore LSP, Zhu N, et al. Bacterial and fungal coinfection in individuals with coronavirus: a rapid review to support COVID-19 antimicrobial prescribing. Clin Infect Dis. 2020;71(9):2459-2468. doi:10.1093/cid/ciaa530
10. Yarrington ME, Moehring RW. Basic, advanced, and novel metrics to guide antibiotic use assessments. Curr Treat Options Infect Dis. 2019;11(2):145-160. doi:10.1007/s40506-019-00188-3
11. Bai AD, Showler A, Burry L, et al. Impact of infectious disease consultation on quality of care, mortality, and length of stay in Staphylococcus aureus bacteremia: results from a large multicenter cohort study. Clin Infect Dis. 2015;60(10):1451-1461. doi:10.1093/cid/civ120
12. Mejia-Chew C, O’Halloran JA, Olsen MA, et al. Effect of infectious disease consultation on mortality and treatment of patients with candida bloodstream infections: a retrospective, cohort study. Lancet Infect Dis. 2019;19(12):1336-1344. doi:10.1016/S1473-3099(19)30405-0
13. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health (US); April 21, 2021. Accessed February 14, 2023. https://files.covid19treatmentguidelines.nih.gov/guidelines/covid19treatmentguidelines.pdf
14. Bhimraj A, Morgan RL, Shumaker AH, et al. Infectious Diseases Society of America guidelines on the treatment and management of patients with COVID-19. Clin Infect Dis. 2020;ciaa478. doi:10.1093/cid/ciaa478
15. Suraj V, Del Vecchio Fitz C, Kleiman LB, et al. SMART COVID Navigator, a clinical decision support tool for COVID-19 treatment: design and development study. J Med Internet Res. 2022;24(2):e29279. Published 2022 Feb 18. doi:10.2196/29279
16. Pendharkar SR, Minty E, Shukalek CB, et al. Description of a multi-faceted COVID-19 pandemic physician workforce plan at a multi-site academic health system. J Gen Intern Med. 2021;36(5):1310-1318. doi:10.1007/s11606-020-06543-1
17. Pulia MS, Wolf I, Schulz LT, Pop-Vicas A, Schwei RJ, Lindenauer PK. COVID-19: an emerging threat to antibiotic stewardship in the emergency department. West J Emerg Med. 2020;21(5):1283-1286. Published 2020 Aug 7. doi:10.5811/westjem.2020.7.48848
1. Dagens A, Sigfrid L, Cai E, et al. Scope, quality, and inclusivity of clinical guidelines produced early in the covid-19 pandemic: rapid review. BMJ. 2020;369:m1936. Published 2020 May 26. doi:10.1136/bmj.m1936
2. Dhivagaran T, Abbas U, Butt F, Arunasalam L, Chang O. Critical appraisal of clinical practice guidelines for the management of COVID-19: protocol for a systematic review. Syst Rev. 2021;10(1):317. Published 2021 Dec 22. doi:10.1186/s13643-021-01871-7
3. Garcia-Vidal C, Sanjuan G, Moreno-García E, et al. Incidence of co-infections and superinfections in hospitalized patients with COVID-19: a retrospective cohort study. Clin Microbiol Infect. 2021;27(1):83-88. doi:10.1016/j.cmi.2020.07.041
4. Karaba SM, Jones G, Helsel T, et al. Prevalence of co-infection at the time of hospital admission in covid-19 patients, a multicenter study. Open Forum Infect Dis. 2020;8(1):ofaa578. Published 2020 Dec 21. doi:10.1093/ofid/ofaa578
5. RECOVERY Collaborative Group, Horby P, Lim WS, et al. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2021;384(8):693-704. doi:10.1056/NEJMoa2021436
6. Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the treatment of covid-19 - final report. N Engl J Med. 2020;383(19):1813-1826. doi:10.1056/NEJMoa2007764
7. Durant TJS, Peaper DR, Ferguson D, Schulz WL. Impact of COVID-19 pandemic on laboratory utilization. J Appl Lab Med. 2020;5(6):1194-1205. doi:10.1093/jalm/jfaa121
8. Yagnik KJ, Saad HA, King HL, Bedimo RJ, Lehmann CU, Medford RJ. Characteristics and outcomes of infectious diseases electronic COVID-19 consultations at a multisite academic health system. Cureus. 2021;13(11):e19203. Published 2021 Nov 2. doi:10.7759/cureus.19203
9. Rawson TM, Moore LSP, Zhu N, et al. Bacterial and fungal coinfection in individuals with coronavirus: a rapid review to support COVID-19 antimicrobial prescribing. Clin Infect Dis. 2020;71(9):2459-2468. doi:10.1093/cid/ciaa530
10. Yarrington ME, Moehring RW. Basic, advanced, and novel metrics to guide antibiotic use assessments. Curr Treat Options Infect Dis. 2019;11(2):145-160. doi:10.1007/s40506-019-00188-3
11. Bai AD, Showler A, Burry L, et al. Impact of infectious disease consultation on quality of care, mortality, and length of stay in Staphylococcus aureus bacteremia: results from a large multicenter cohort study. Clin Infect Dis. 2015;60(10):1451-1461. doi:10.1093/cid/civ120
12. Mejia-Chew C, O’Halloran JA, Olsen MA, et al. Effect of infectious disease consultation on mortality and treatment of patients with candida bloodstream infections: a retrospective, cohort study. Lancet Infect Dis. 2019;19(12):1336-1344. doi:10.1016/S1473-3099(19)30405-0
13. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health (US); April 21, 2021. Accessed February 14, 2023. https://files.covid19treatmentguidelines.nih.gov/guidelines/covid19treatmentguidelines.pdf
14. Bhimraj A, Morgan RL, Shumaker AH, et al. Infectious Diseases Society of America guidelines on the treatment and management of patients with COVID-19. Clin Infect Dis. 2020;ciaa478. doi:10.1093/cid/ciaa478
15. Suraj V, Del Vecchio Fitz C, Kleiman LB, et al. SMART COVID Navigator, a clinical decision support tool for COVID-19 treatment: design and development study. J Med Internet Res. 2022;24(2):e29279. Published 2022 Feb 18. doi:10.2196/29279
16. Pendharkar SR, Minty E, Shukalek CB, et al. Description of a multi-faceted COVID-19 pandemic physician workforce plan at a multi-site academic health system. J Gen Intern Med. 2021;36(5):1310-1318. doi:10.1007/s11606-020-06543-1
17. Pulia MS, Wolf I, Schulz LT, Pop-Vicas A, Schwei RJ, Lindenauer PK. COVID-19: an emerging threat to antibiotic stewardship in the emergency department. West J Emerg Med. 2020;21(5):1283-1286. Published 2020 Aug 7. doi:10.5811/westjem.2020.7.48848
CDC: Drug-resistant ringworm reported in New York
BY ALICIA AULT
The in New York.
Tinea, or ringworm, one of the most common fungal infections, is responsible for almost 5 million outpatient visits and 690 hospitalizations annually, according to the CDC.
Over the past 10 years, severe, antifungal-resistant tinea has spread in South Asia, in part because of the rise of a new dermatophyte species known as Trichophyton indotineae, wrote the authors of a report on the two patients with the drug-resistant strain. This epidemic “has likely been driven by misuse and overuse of topical antifungals and corticosteroids,” added the authors, in Morbidity and Mortality Weekly Report.
The cases were detected by a New York City dermatologist. In the first case, a 28-year-old woman developed a widespread pruritic eruption in the summer of 2021. She did not consult a dermatologist until December, when she was in the third trimester of pregnancy. She had large, annular, scaly, pruritic plaques on her neck, abdomen, pubic region, and buttocks, but had no underlying medical conditions, no known exposures to someone with a similar rash, and no recent international travel history.
After she gave birth in January, she started oral terbinafine therapy but had no improvement after 2 weeks. Clinicians administered a 4-week course of itraconazole, which resolved the infection.
The second patient, a 47-year-old woman with no medical conditions, developed a rash while in Bangladesh in the summer of 2022. Other family members had a similar rash. She was treated with topical antifungal and steroid combination creams but had no resolution. Back in the United States, she was prescribed hydrocortisone 2.5% ointment and diphenhydramine, clotrimazole cream, and terbinafine cream in three successive emergency department visits. In December 2022, dermatologists, observing widespread, discrete, scaly, annular, pruritic plaques on the thighs and buttocks, prescribed a 4-week course of oral terbinafine. When the rash did not resolve, she was given 4 weeks of griseofulvin. The rash persisted, although there was 80% improvement. Clinicians are now considering itraconazole. The woman’s son and husband are also being evaluated, as they have similar rashes.
In both cases, skin culture isolates were initially identified as Trichophyton mentagrophytes. Further analysis at the New York State Department of Health’s lab, using Sanger sequencing of the internal transcribed spacer region of the ribosomal gene, followed by phylogenetic analysis, identified the isolates as T. indotineae.
The authors note that culture-based techniques used by most clinical laboratories typically misidentify T. indotineae as T. mentagrophytes or T. interdigitale. Genomic sequencing must be used to properly identify T. indotineae, they wrote.
Clinicians should consider T. indotineae in patients with widespread ringworm, especially if they do not improve with topical antifungals or oral terbinafine, said the authors. If T. indotineae is suspected, state or local public health departments can direct clinicians to testing.
The authors report no relevant financial relationships.
BY ALICIA AULT
The in New York.
Tinea, or ringworm, one of the most common fungal infections, is responsible for almost 5 million outpatient visits and 690 hospitalizations annually, according to the CDC.
Over the past 10 years, severe, antifungal-resistant tinea has spread in South Asia, in part because of the rise of a new dermatophyte species known as Trichophyton indotineae, wrote the authors of a report on the two patients with the drug-resistant strain. This epidemic “has likely been driven by misuse and overuse of topical antifungals and corticosteroids,” added the authors, in Morbidity and Mortality Weekly Report.
The cases were detected by a New York City dermatologist. In the first case, a 28-year-old woman developed a widespread pruritic eruption in the summer of 2021. She did not consult a dermatologist until December, when she was in the third trimester of pregnancy. She had large, annular, scaly, pruritic plaques on her neck, abdomen, pubic region, and buttocks, but had no underlying medical conditions, no known exposures to someone with a similar rash, and no recent international travel history.
After she gave birth in January, she started oral terbinafine therapy but had no improvement after 2 weeks. Clinicians administered a 4-week course of itraconazole, which resolved the infection.
The second patient, a 47-year-old woman with no medical conditions, developed a rash while in Bangladesh in the summer of 2022. Other family members had a similar rash. She was treated with topical antifungal and steroid combination creams but had no resolution. Back in the United States, she was prescribed hydrocortisone 2.5% ointment and diphenhydramine, clotrimazole cream, and terbinafine cream in three successive emergency department visits. In December 2022, dermatologists, observing widespread, discrete, scaly, annular, pruritic plaques on the thighs and buttocks, prescribed a 4-week course of oral terbinafine. When the rash did not resolve, she was given 4 weeks of griseofulvin. The rash persisted, although there was 80% improvement. Clinicians are now considering itraconazole. The woman’s son and husband are also being evaluated, as they have similar rashes.
In both cases, skin culture isolates were initially identified as Trichophyton mentagrophytes. Further analysis at the New York State Department of Health’s lab, using Sanger sequencing of the internal transcribed spacer region of the ribosomal gene, followed by phylogenetic analysis, identified the isolates as T. indotineae.
The authors note that culture-based techniques used by most clinical laboratories typically misidentify T. indotineae as T. mentagrophytes or T. interdigitale. Genomic sequencing must be used to properly identify T. indotineae, they wrote.
Clinicians should consider T. indotineae in patients with widespread ringworm, especially if they do not improve with topical antifungals or oral terbinafine, said the authors. If T. indotineae is suspected, state or local public health departments can direct clinicians to testing.
The authors report no relevant financial relationships.
BY ALICIA AULT
The in New York.
Tinea, or ringworm, one of the most common fungal infections, is responsible for almost 5 million outpatient visits and 690 hospitalizations annually, according to the CDC.
Over the past 10 years, severe, antifungal-resistant tinea has spread in South Asia, in part because of the rise of a new dermatophyte species known as Trichophyton indotineae, wrote the authors of a report on the two patients with the drug-resistant strain. This epidemic “has likely been driven by misuse and overuse of topical antifungals and corticosteroids,” added the authors, in Morbidity and Mortality Weekly Report.
The cases were detected by a New York City dermatologist. In the first case, a 28-year-old woman developed a widespread pruritic eruption in the summer of 2021. She did not consult a dermatologist until December, when she was in the third trimester of pregnancy. She had large, annular, scaly, pruritic plaques on her neck, abdomen, pubic region, and buttocks, but had no underlying medical conditions, no known exposures to someone with a similar rash, and no recent international travel history.
After she gave birth in January, she started oral terbinafine therapy but had no improvement after 2 weeks. Clinicians administered a 4-week course of itraconazole, which resolved the infection.
The second patient, a 47-year-old woman with no medical conditions, developed a rash while in Bangladesh in the summer of 2022. Other family members had a similar rash. She was treated with topical antifungal and steroid combination creams but had no resolution. Back in the United States, she was prescribed hydrocortisone 2.5% ointment and diphenhydramine, clotrimazole cream, and terbinafine cream in three successive emergency department visits. In December 2022, dermatologists, observing widespread, discrete, scaly, annular, pruritic plaques on the thighs and buttocks, prescribed a 4-week course of oral terbinafine. When the rash did not resolve, she was given 4 weeks of griseofulvin. The rash persisted, although there was 80% improvement. Clinicians are now considering itraconazole. The woman’s son and husband are also being evaluated, as they have similar rashes.
In both cases, skin culture isolates were initially identified as Trichophyton mentagrophytes. Further analysis at the New York State Department of Health’s lab, using Sanger sequencing of the internal transcribed spacer region of the ribosomal gene, followed by phylogenetic analysis, identified the isolates as T. indotineae.
The authors note that culture-based techniques used by most clinical laboratories typically misidentify T. indotineae as T. mentagrophytes or T. interdigitale. Genomic sequencing must be used to properly identify T. indotineae, they wrote.
Clinicians should consider T. indotineae in patients with widespread ringworm, especially if they do not improve with topical antifungals or oral terbinafine, said the authors. If T. indotineae is suspected, state or local public health departments can direct clinicians to testing.
The authors report no relevant financial relationships.
What’s Causing Cancers at Air Force Bases?
It has been a troubling mystery—and yet, is an unsolved one: Last January, at least 9 service members who had worked at Malmstrom Air Force Base (AFB) in Montana were reported to have been diagnosed with non-Hodgkin lymphoma. Then more cancer cases were reported, not only at Malmstrom, but at Francis E. Warren AFB in Wyoming, Minot AFB in North Dakota, and Vandenberg AFB in California. The bases operate the silos that house nuclear warheads carried by Minuteman III intercontinental ballistic missiles (ICBMs).
In all, 36 cancer cases were reported among missileers: 10 developed non-Hodgkin lymphoma, 2 Hodgkin lymphoma, and 24 another form of cancer. Eight of the missileers, the majority of whom served at Malmstrom between 1997 and 2007, have died.
So far, though, the US Air Force (USAF) reports that it has found no current risk factors that could explain the unusual number of cases.
In February, Gen. Thomas Bussiere, commander of Air Force Global Strike Command, approved a study to conduct a formal assessment related to specific cancer concerns and examine the possibility of cancer clusters at ICBM bases. The Missile Community Cancer Study, conducted by the Air Force School of Aerospace Medicine, will look at all ICBM wings, all missileers, and those who maintain, guard, and support the bases. The review also incorporates active-duty medical data, the US Department of Veterans Affairs cancer registry data, mortality data, and public cancer registries.
Missileers may be exposed to a variety of chemicals and toxins. The potential hazardous materials exposure at the missile silos extends to all 3 missile bases, USAF says. The equipment in the launch control center and equipment buildings were identical. However, each of the ICBM bases has specific environmental and agricultural factors that will be considered as studies continue, according to the USAF. The land surrounding missile alert facilities, launch control centers, and launch facilities is not owned by the government; the study teams noted that locations could contain additional unknown agricultural hazards. Procedures for testing and cleaning the facilities vary across installations, creating inconsistencies, according to the USAF.
The study teams recently presented their initial findings. “[O]verall,” they said, “there were no factors identified that would be considered immediate concerns for acute cancer risks,” according to a report from the USAF 711th Human Performance Wing, obtained by the Associated Press.
This isn’t the first time that concerns have been raised about possible cancer clusters at Malmstrom. In 2001, after cases of various cancers from missileers were reported—including cervical, thyroid, Hodgkin lymphoma, and non-Hodgkin lymphoma—the Air Force Institute for Operational Health conducted a site evaluation and sampling for possible chemical and biologic contaminants at their facilities. Results of all tests, the 2005 report said, did not demonstrate any levels above acceptable standards according to state and federal regulations. The survey concluded that launch control centers provide a safe and healthy working environment.
In 2005, following the release of the report, the USAF said “There is not sufficient evidence to consider the possibility of a cancer clustering to justify further investigation.” The research report noted, “[S]ometimes illnesses tend to occur by chance alone and it is not uncommon to see clustering or what has been referred to as ‘perceived clustering’ of conditions, especially when they occur in a close group of people or certain communities as in the military.”
On its website, though, the Air Force Medical Service now says that the findings from 2 decades ago may have changed.
The findings from the new study are not final. The USAF is continuing its investigation, including conducting an epidemiological study of cancers within the missile community. In the meantime, Air Force Global Strike Command Public Affairs says that, in response to the review panel’s recommendations, Gen. Bussiere has directed that facilities be deep cleaned regularly, signage denoting the presence of polychlorinated biphenyls be updated, and burning no longer allowed as a means of destroying classified materials inside the facilities.
Notably, the changes will also include improving communication and coordination between medical personnel and missile community members. Bussiere directed his staff to explore specifically assigning medical professionals to ICBM units, to have a better understanding of the environment and missions. He also ordered further engagement with personnel who work with known occupational hazards to collect more data and information. While awaiting the eventual replacement of the Minuteman III ICBM with the LGM-35A Sentinel, preventive maintenance and environmental upgrades will be prioritized and any upgrade or new piece of equipment will be “scrutinized for hazards.”
The USAF has also established a website to address the missileer community’s concerns.
It has been a troubling mystery—and yet, is an unsolved one: Last January, at least 9 service members who had worked at Malmstrom Air Force Base (AFB) in Montana were reported to have been diagnosed with non-Hodgkin lymphoma. Then more cancer cases were reported, not only at Malmstrom, but at Francis E. Warren AFB in Wyoming, Minot AFB in North Dakota, and Vandenberg AFB in California. The bases operate the silos that house nuclear warheads carried by Minuteman III intercontinental ballistic missiles (ICBMs).
In all, 36 cancer cases were reported among missileers: 10 developed non-Hodgkin lymphoma, 2 Hodgkin lymphoma, and 24 another form of cancer. Eight of the missileers, the majority of whom served at Malmstrom between 1997 and 2007, have died.
So far, though, the US Air Force (USAF) reports that it has found no current risk factors that could explain the unusual number of cases.
In February, Gen. Thomas Bussiere, commander of Air Force Global Strike Command, approved a study to conduct a formal assessment related to specific cancer concerns and examine the possibility of cancer clusters at ICBM bases. The Missile Community Cancer Study, conducted by the Air Force School of Aerospace Medicine, will look at all ICBM wings, all missileers, and those who maintain, guard, and support the bases. The review also incorporates active-duty medical data, the US Department of Veterans Affairs cancer registry data, mortality data, and public cancer registries.
Missileers may be exposed to a variety of chemicals and toxins. The potential hazardous materials exposure at the missile silos extends to all 3 missile bases, USAF says. The equipment in the launch control center and equipment buildings were identical. However, each of the ICBM bases has specific environmental and agricultural factors that will be considered as studies continue, according to the USAF. The land surrounding missile alert facilities, launch control centers, and launch facilities is not owned by the government; the study teams noted that locations could contain additional unknown agricultural hazards. Procedures for testing and cleaning the facilities vary across installations, creating inconsistencies, according to the USAF.
The study teams recently presented their initial findings. “[O]verall,” they said, “there were no factors identified that would be considered immediate concerns for acute cancer risks,” according to a report from the USAF 711th Human Performance Wing, obtained by the Associated Press.
This isn’t the first time that concerns have been raised about possible cancer clusters at Malmstrom. In 2001, after cases of various cancers from missileers were reported—including cervical, thyroid, Hodgkin lymphoma, and non-Hodgkin lymphoma—the Air Force Institute for Operational Health conducted a site evaluation and sampling for possible chemical and biologic contaminants at their facilities. Results of all tests, the 2005 report said, did not demonstrate any levels above acceptable standards according to state and federal regulations. The survey concluded that launch control centers provide a safe and healthy working environment.
In 2005, following the release of the report, the USAF said “There is not sufficient evidence to consider the possibility of a cancer clustering to justify further investigation.” The research report noted, “[S]ometimes illnesses tend to occur by chance alone and it is not uncommon to see clustering or what has been referred to as ‘perceived clustering’ of conditions, especially when they occur in a close group of people or certain communities as in the military.”
On its website, though, the Air Force Medical Service now says that the findings from 2 decades ago may have changed.
The findings from the new study are not final. The USAF is continuing its investigation, including conducting an epidemiological study of cancers within the missile community. In the meantime, Air Force Global Strike Command Public Affairs says that, in response to the review panel’s recommendations, Gen. Bussiere has directed that facilities be deep cleaned regularly, signage denoting the presence of polychlorinated biphenyls be updated, and burning no longer allowed as a means of destroying classified materials inside the facilities.
Notably, the changes will also include improving communication and coordination between medical personnel and missile community members. Bussiere directed his staff to explore specifically assigning medical professionals to ICBM units, to have a better understanding of the environment and missions. He also ordered further engagement with personnel who work with known occupational hazards to collect more data and information. While awaiting the eventual replacement of the Minuteman III ICBM with the LGM-35A Sentinel, preventive maintenance and environmental upgrades will be prioritized and any upgrade or new piece of equipment will be “scrutinized for hazards.”
The USAF has also established a website to address the missileer community’s concerns.
It has been a troubling mystery—and yet, is an unsolved one: Last January, at least 9 service members who had worked at Malmstrom Air Force Base (AFB) in Montana were reported to have been diagnosed with non-Hodgkin lymphoma. Then more cancer cases were reported, not only at Malmstrom, but at Francis E. Warren AFB in Wyoming, Minot AFB in North Dakota, and Vandenberg AFB in California. The bases operate the silos that house nuclear warheads carried by Minuteman III intercontinental ballistic missiles (ICBMs).
In all, 36 cancer cases were reported among missileers: 10 developed non-Hodgkin lymphoma, 2 Hodgkin lymphoma, and 24 another form of cancer. Eight of the missileers, the majority of whom served at Malmstrom between 1997 and 2007, have died.
So far, though, the US Air Force (USAF) reports that it has found no current risk factors that could explain the unusual number of cases.
In February, Gen. Thomas Bussiere, commander of Air Force Global Strike Command, approved a study to conduct a formal assessment related to specific cancer concerns and examine the possibility of cancer clusters at ICBM bases. The Missile Community Cancer Study, conducted by the Air Force School of Aerospace Medicine, will look at all ICBM wings, all missileers, and those who maintain, guard, and support the bases. The review also incorporates active-duty medical data, the US Department of Veterans Affairs cancer registry data, mortality data, and public cancer registries.
Missileers may be exposed to a variety of chemicals and toxins. The potential hazardous materials exposure at the missile silos extends to all 3 missile bases, USAF says. The equipment in the launch control center and equipment buildings were identical. However, each of the ICBM bases has specific environmental and agricultural factors that will be considered as studies continue, according to the USAF. The land surrounding missile alert facilities, launch control centers, and launch facilities is not owned by the government; the study teams noted that locations could contain additional unknown agricultural hazards. Procedures for testing and cleaning the facilities vary across installations, creating inconsistencies, according to the USAF.
The study teams recently presented their initial findings. “[O]verall,” they said, “there were no factors identified that would be considered immediate concerns for acute cancer risks,” according to a report from the USAF 711th Human Performance Wing, obtained by the Associated Press.
This isn’t the first time that concerns have been raised about possible cancer clusters at Malmstrom. In 2001, after cases of various cancers from missileers were reported—including cervical, thyroid, Hodgkin lymphoma, and non-Hodgkin lymphoma—the Air Force Institute for Operational Health conducted a site evaluation and sampling for possible chemical and biologic contaminants at their facilities. Results of all tests, the 2005 report said, did not demonstrate any levels above acceptable standards according to state and federal regulations. The survey concluded that launch control centers provide a safe and healthy working environment.
In 2005, following the release of the report, the USAF said “There is not sufficient evidence to consider the possibility of a cancer clustering to justify further investigation.” The research report noted, “[S]ometimes illnesses tend to occur by chance alone and it is not uncommon to see clustering or what has been referred to as ‘perceived clustering’ of conditions, especially when they occur in a close group of people or certain communities as in the military.”
On its website, though, the Air Force Medical Service now says that the findings from 2 decades ago may have changed.
The findings from the new study are not final. The USAF is continuing its investigation, including conducting an epidemiological study of cancers within the missile community. In the meantime, Air Force Global Strike Command Public Affairs says that, in response to the review panel’s recommendations, Gen. Bussiere has directed that facilities be deep cleaned regularly, signage denoting the presence of polychlorinated biphenyls be updated, and burning no longer allowed as a means of destroying classified materials inside the facilities.
Notably, the changes will also include improving communication and coordination between medical personnel and missile community members. Bussiere directed his staff to explore specifically assigning medical professionals to ICBM units, to have a better understanding of the environment and missions. He also ordered further engagement with personnel who work with known occupational hazards to collect more data and information. While awaiting the eventual replacement of the Minuteman III ICBM with the LGM-35A Sentinel, preventive maintenance and environmental upgrades will be prioritized and any upgrade or new piece of equipment will be “scrutinized for hazards.”
The USAF has also established a website to address the missileer community’s concerns.
Metabolic abnormalities boost obesity-related cancer risk
, and an even higher risk, two- to threefold higher, for specific cancers, such as endometrial, liver, and renal cell cancers, compared with metabolically healthy normal weight.
Even in people with so-called “metabolically healthy” obesity, the risk for overall obesity-related cancer is increased, compared with normal-weight, metabolically healthy individuals; however, the associations here are weaker than in people with metabolically unhealthy obesity.
“The type of metabolic obesity phenotype is important when assessing obesity-related cancer risk,” lead researcher Ming Sun, PhD, from Lund University, Malmö, Sweden, said in an interview. “In general, metabolic aberrations further increased the obesity-induced cancer risk, suggesting that obesity and metabolic aberrations are useful targets for prevention.”
“This synergy means that when obesity and metabolic unhealth occur together, that’s particularly bad,” added Tanja Stocks, PhD, senior author, also of Lund University.
“But the data also highlight that even obesity and overweight alone comprise an increased risk of cancer,” Dr. Stocks noted.
Dr. Sun said the findings have important public health implications, suggesting that “a significant number of cancer cases could potentially be prevented by targeting the coexistence of metabolic problems and obesity, in particular for obesity-related cancers among men.”
The results will be presented as a poster by Dr. Sun at the European Congress on Obesity 2023, being held in Dublin, and have been published in the Journal of the National Cancer Institute.
Metabolically unhealthy obesity worst for cancer risks
Andrew G. Renehan, PhD, FRCS, professor of cancer studies and surgery, University of Manchester, England, welcomed the new work, saying it addresses the issue with very large study numbers. “[It] nicely demonstrates that there are clear examples where metabolically unhealthy overweight and obese phenotypes have increased cancer risk relative to [metabolically] healthy overweight and obese phenotypes,” he said.
“There is a clear need for clinically based research addressing these hypotheses ... but these studies will additionally need to factor in other dimensions such as the selection of treatment for metabolic aberrations, both medical and surgical, and the consequent metabolic control resulting from these interventions,” Dr. Renehan observed.
Vibhu Chittajallu, MD, a gastroenterologist based at University Hospitals Cleveland Medical Center, said it was beneficial to see another study further validating the association of obesity with the development of obesity-associated cancers.
“This is an interesting study [because it focuses] on the role of metabolic syndrome in obesity and how it affects the risk of development of obesity-associated cancers,” he said in an interview.
“I believe that the results of this study further strengthen the need for improved management of obesity and metabolic syndrome to reduce the risk of obesity-associated cancer formation that plays a role in preventable and premature deaths in adult patients with obesity.”
Synergy between metabolic aberrations and obesity, and cancer risk
Dr. Sun and colleagues note that obesity is an established risk factor for several cancers. It is often accompanied by metabolic aberrations, which have been a commonly proposed mechanism to link obesity with cancer. During the last decade, obesity with or without metabolic aberrations – commonly termed “metabolically unhealthy” or “healthy obesity” – has been extensively investigated in the cardiovascular field; however, studies regarding cancer are limited.
According to Dr. Sun, this new study is the first to look at the synergistic effect of unhealthy metabolism and body mass index – the latter was further categorized as normal weight (BMI < 25 kg/m2), overweight (BMI < 30) and obesity (BMI ≤ 30) – and the association with cancer risk, both overall and in relation to site-specific cancers.
Data were drawn from 797,193 European individuals (in Norway, Sweden, and Austria), of whom 23,630 developed an obesity-related cancer during the follow-up period. A metabolic score comprising mid-blood pressure, plasma glucose, and triglycerides was used to provide a measure of healthy or unhealthy metabolic status. Relative risks (hazard ratios) for overall and site-specific cancers were determined. Comparisons were made with metabolically healthy people of normal weight (effectively controls).
When different metabolic scores and BMIs were combined, participants fell into six categories: metabolically unhealthy obesity (6.8% of participants); metabolically healthy obesity (3.4%), metabolically unhealthy overweight (15.4%), metabolically healthy overweight (19.8%), metabolically unhealthy normal weight (12.5%), and metabolically healthy normal weight (42.0%).
Metabolically unhealthy women with obesity had a hazard ratio of 1.43 for overall obesity-related cancers, compared with metabolically healthy women of normal weight. Of particular note were risks of two cancer types in women with metabolically unhealthy obesity: renal cancer, with an HR of 2.43, and endometrial cancer, with an HR of 3.0, compared with controls.
Even in metabolically healthy women with obesity, compared with metabolically healthy women of normal weight, there was an increased risk of endometrial cancer, with an HR of 2.36.
“If you look at individual cancers, in particular endometrial cancer, this seems to be very much driven by obesity and not so much by the metabolic factor,” remarked Dr. Stocks.
In males, compared with metabolically healthy men of normal weight, metabolically unhealthy men with obesity had an overall obesity-related cancer risk HR of 1.91. Specifically, the risk of renal cell cancer was more than doubled, with an HR of 2.59. The HR for colon cancer was 1.85, and that for rectal cancer and pancreatic cancer was similar, both having HRs of 1.32.
Again, risk was lower in metabolically healthy men with obesity, although still higher than for metabolically healthy normal-weight men.
A version of this article first appeared on Medscape.com.
, and an even higher risk, two- to threefold higher, for specific cancers, such as endometrial, liver, and renal cell cancers, compared with metabolically healthy normal weight.
Even in people with so-called “metabolically healthy” obesity, the risk for overall obesity-related cancer is increased, compared with normal-weight, metabolically healthy individuals; however, the associations here are weaker than in people with metabolically unhealthy obesity.
“The type of metabolic obesity phenotype is important when assessing obesity-related cancer risk,” lead researcher Ming Sun, PhD, from Lund University, Malmö, Sweden, said in an interview. “In general, metabolic aberrations further increased the obesity-induced cancer risk, suggesting that obesity and metabolic aberrations are useful targets for prevention.”
“This synergy means that when obesity and metabolic unhealth occur together, that’s particularly bad,” added Tanja Stocks, PhD, senior author, also of Lund University.
“But the data also highlight that even obesity and overweight alone comprise an increased risk of cancer,” Dr. Stocks noted.
Dr. Sun said the findings have important public health implications, suggesting that “a significant number of cancer cases could potentially be prevented by targeting the coexistence of metabolic problems and obesity, in particular for obesity-related cancers among men.”
The results will be presented as a poster by Dr. Sun at the European Congress on Obesity 2023, being held in Dublin, and have been published in the Journal of the National Cancer Institute.
Metabolically unhealthy obesity worst for cancer risks
Andrew G. Renehan, PhD, FRCS, professor of cancer studies and surgery, University of Manchester, England, welcomed the new work, saying it addresses the issue with very large study numbers. “[It] nicely demonstrates that there are clear examples where metabolically unhealthy overweight and obese phenotypes have increased cancer risk relative to [metabolically] healthy overweight and obese phenotypes,” he said.
“There is a clear need for clinically based research addressing these hypotheses ... but these studies will additionally need to factor in other dimensions such as the selection of treatment for metabolic aberrations, both medical and surgical, and the consequent metabolic control resulting from these interventions,” Dr. Renehan observed.
Vibhu Chittajallu, MD, a gastroenterologist based at University Hospitals Cleveland Medical Center, said it was beneficial to see another study further validating the association of obesity with the development of obesity-associated cancers.
“This is an interesting study [because it focuses] on the role of metabolic syndrome in obesity and how it affects the risk of development of obesity-associated cancers,” he said in an interview.
“I believe that the results of this study further strengthen the need for improved management of obesity and metabolic syndrome to reduce the risk of obesity-associated cancer formation that plays a role in preventable and premature deaths in adult patients with obesity.”
Synergy between metabolic aberrations and obesity, and cancer risk
Dr. Sun and colleagues note that obesity is an established risk factor for several cancers. It is often accompanied by metabolic aberrations, which have been a commonly proposed mechanism to link obesity with cancer. During the last decade, obesity with or without metabolic aberrations – commonly termed “metabolically unhealthy” or “healthy obesity” – has been extensively investigated in the cardiovascular field; however, studies regarding cancer are limited.
According to Dr. Sun, this new study is the first to look at the synergistic effect of unhealthy metabolism and body mass index – the latter was further categorized as normal weight (BMI < 25 kg/m2), overweight (BMI < 30) and obesity (BMI ≤ 30) – and the association with cancer risk, both overall and in relation to site-specific cancers.
Data were drawn from 797,193 European individuals (in Norway, Sweden, and Austria), of whom 23,630 developed an obesity-related cancer during the follow-up period. A metabolic score comprising mid-blood pressure, plasma glucose, and triglycerides was used to provide a measure of healthy or unhealthy metabolic status. Relative risks (hazard ratios) for overall and site-specific cancers were determined. Comparisons were made with metabolically healthy people of normal weight (effectively controls).
When different metabolic scores and BMIs were combined, participants fell into six categories: metabolically unhealthy obesity (6.8% of participants); metabolically healthy obesity (3.4%), metabolically unhealthy overweight (15.4%), metabolically healthy overweight (19.8%), metabolically unhealthy normal weight (12.5%), and metabolically healthy normal weight (42.0%).
Metabolically unhealthy women with obesity had a hazard ratio of 1.43 for overall obesity-related cancers, compared with metabolically healthy women of normal weight. Of particular note were risks of two cancer types in women with metabolically unhealthy obesity: renal cancer, with an HR of 2.43, and endometrial cancer, with an HR of 3.0, compared with controls.
Even in metabolically healthy women with obesity, compared with metabolically healthy women of normal weight, there was an increased risk of endometrial cancer, with an HR of 2.36.
“If you look at individual cancers, in particular endometrial cancer, this seems to be very much driven by obesity and not so much by the metabolic factor,” remarked Dr. Stocks.
In males, compared with metabolically healthy men of normal weight, metabolically unhealthy men with obesity had an overall obesity-related cancer risk HR of 1.91. Specifically, the risk of renal cell cancer was more than doubled, with an HR of 2.59. The HR for colon cancer was 1.85, and that for rectal cancer and pancreatic cancer was similar, both having HRs of 1.32.
Again, risk was lower in metabolically healthy men with obesity, although still higher than for metabolically healthy normal-weight men.
A version of this article first appeared on Medscape.com.
, and an even higher risk, two- to threefold higher, for specific cancers, such as endometrial, liver, and renal cell cancers, compared with metabolically healthy normal weight.
Even in people with so-called “metabolically healthy” obesity, the risk for overall obesity-related cancer is increased, compared with normal-weight, metabolically healthy individuals; however, the associations here are weaker than in people with metabolically unhealthy obesity.
“The type of metabolic obesity phenotype is important when assessing obesity-related cancer risk,” lead researcher Ming Sun, PhD, from Lund University, Malmö, Sweden, said in an interview. “In general, metabolic aberrations further increased the obesity-induced cancer risk, suggesting that obesity and metabolic aberrations are useful targets for prevention.”
“This synergy means that when obesity and metabolic unhealth occur together, that’s particularly bad,” added Tanja Stocks, PhD, senior author, also of Lund University.
“But the data also highlight that even obesity and overweight alone comprise an increased risk of cancer,” Dr. Stocks noted.
Dr. Sun said the findings have important public health implications, suggesting that “a significant number of cancer cases could potentially be prevented by targeting the coexistence of metabolic problems and obesity, in particular for obesity-related cancers among men.”
The results will be presented as a poster by Dr. Sun at the European Congress on Obesity 2023, being held in Dublin, and have been published in the Journal of the National Cancer Institute.
Metabolically unhealthy obesity worst for cancer risks
Andrew G. Renehan, PhD, FRCS, professor of cancer studies and surgery, University of Manchester, England, welcomed the new work, saying it addresses the issue with very large study numbers. “[It] nicely demonstrates that there are clear examples where metabolically unhealthy overweight and obese phenotypes have increased cancer risk relative to [metabolically] healthy overweight and obese phenotypes,” he said.
“There is a clear need for clinically based research addressing these hypotheses ... but these studies will additionally need to factor in other dimensions such as the selection of treatment for metabolic aberrations, both medical and surgical, and the consequent metabolic control resulting from these interventions,” Dr. Renehan observed.
Vibhu Chittajallu, MD, a gastroenterologist based at University Hospitals Cleveland Medical Center, said it was beneficial to see another study further validating the association of obesity with the development of obesity-associated cancers.
“This is an interesting study [because it focuses] on the role of metabolic syndrome in obesity and how it affects the risk of development of obesity-associated cancers,” he said in an interview.
“I believe that the results of this study further strengthen the need for improved management of obesity and metabolic syndrome to reduce the risk of obesity-associated cancer formation that plays a role in preventable and premature deaths in adult patients with obesity.”
Synergy between metabolic aberrations and obesity, and cancer risk
Dr. Sun and colleagues note that obesity is an established risk factor for several cancers. It is often accompanied by metabolic aberrations, which have been a commonly proposed mechanism to link obesity with cancer. During the last decade, obesity with or without metabolic aberrations – commonly termed “metabolically unhealthy” or “healthy obesity” – has been extensively investigated in the cardiovascular field; however, studies regarding cancer are limited.
According to Dr. Sun, this new study is the first to look at the synergistic effect of unhealthy metabolism and body mass index – the latter was further categorized as normal weight (BMI < 25 kg/m2), overweight (BMI < 30) and obesity (BMI ≤ 30) – and the association with cancer risk, both overall and in relation to site-specific cancers.
Data were drawn from 797,193 European individuals (in Norway, Sweden, and Austria), of whom 23,630 developed an obesity-related cancer during the follow-up period. A metabolic score comprising mid-blood pressure, plasma glucose, and triglycerides was used to provide a measure of healthy or unhealthy metabolic status. Relative risks (hazard ratios) for overall and site-specific cancers were determined. Comparisons were made with metabolically healthy people of normal weight (effectively controls).
When different metabolic scores and BMIs were combined, participants fell into six categories: metabolically unhealthy obesity (6.8% of participants); metabolically healthy obesity (3.4%), metabolically unhealthy overweight (15.4%), metabolically healthy overweight (19.8%), metabolically unhealthy normal weight (12.5%), and metabolically healthy normal weight (42.0%).
Metabolically unhealthy women with obesity had a hazard ratio of 1.43 for overall obesity-related cancers, compared with metabolically healthy women of normal weight. Of particular note were risks of two cancer types in women with metabolically unhealthy obesity: renal cancer, with an HR of 2.43, and endometrial cancer, with an HR of 3.0, compared with controls.
Even in metabolically healthy women with obesity, compared with metabolically healthy women of normal weight, there was an increased risk of endometrial cancer, with an HR of 2.36.
“If you look at individual cancers, in particular endometrial cancer, this seems to be very much driven by obesity and not so much by the metabolic factor,” remarked Dr. Stocks.
In males, compared with metabolically healthy men of normal weight, metabolically unhealthy men with obesity had an overall obesity-related cancer risk HR of 1.91. Specifically, the risk of renal cell cancer was more than doubled, with an HR of 2.59. The HR for colon cancer was 1.85, and that for rectal cancer and pancreatic cancer was similar, both having HRs of 1.32.
Again, risk was lower in metabolically healthy men with obesity, although still higher than for metabolically healthy normal-weight men.
A version of this article first appeared on Medscape.com.
FROM ECO 2023