User login
Kangaroo mother care may cut death risk for premature babies by a third
, according to new research published online in BMJ Global Health.
Starting the contact, which involves mothers carrying the newborn in a sling, within 24 hours of birth and continuing it for at least 8 hours a day both appear to amplify the effect on reducing mortality and infection, the paper states.
Sindhu Sivanandan, MD, with the department of neonatology at Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India, and Mari Jeeva Sankar, MD, in the pediatrics department of the All India Institute of Medical Sciences, New Delhi, looked at existing studies to compare KMC with conventional care and to compare starting the intervention within 24 hours of birth versus a later start.
Their review looked at 31 trials that included 15,559 low-birthweight and preterm infants collectively. Of the 31 trials, 27 studies compared KMC with conventional care and four compared early with late initiation of KMC.
Mortality risk reduction
Analysis showed that, compared with conventional care, KMC appeared to cut mortality risk by 32% (relative risk, 0.68; 95% confidence interval, 0.53-0.86) during birth hospitalization or by 28 days after birth, while it seemed to reduce the risk of severe infection, such as sepsis, by 15% (RR, 0.85; 95% CI, 0.76-0.96; low-certainty evidence.)
That mortality-risk reduction was found regardless of gestational age or weight of the child at enrolment, time of starting KMC, and whether the intervention was started in a hospital or community.
The studies that had compared early with late-initiated KMC showed a reduction in neonatal mortality of 33%.
Low- and middle-income countries have the highest rates of premature births (gestational age of less than 37 weeks) and low birthweight (less than 2,500 grams). Premature births and low birthweight both are key causes of death and disability.
The World Health Organization recommends KMC as the standard of care among low birthweight infants after clinical stabilization. The American Academy of Pediatrics also promotes immediate KMC.
Relevance in the U.S.
Grace Chan, MD, MPH, PhD, an epidemiologist and pediatrician with the Harvard School of Public Health, Boston, said though the practice is promoted by the WHO and AAP, recommendations to families vary widely by providers.
She said the health benefits for KMC are numerous. One of the biggest is that skin-to-skin contact can help transfer heat to newborns who may have trouble regulating their own temperature. That is especially important in cold climates in places where there may be insufficient indoor heat.
She said it’s well-known that preterm babies are at higher risk for apnea, and listening to a mother’s heartbeat may stimulate the child to breathe regularly.
Additionally with KMC, there’s an inherent benefit of a mother or caregiver being able to see any change in a newborn’s color immediately when the baby is held so closely, as opposed to a nurse watching several babies at a time in a neonatal intensive care unit.
This is evidence that starting KMC right away is important, because the risk of death for premature and low-weight newborns is highest in the first 24 hours of life, Dr. Chan noted.
Barriers of time
There are some barriers, she noted, in that mothers or other caregivers caring for several young children may not have the time to carry a child in a sling for 8 or more hours at a time.
The authors conclude that their findings have policy implications, particularly for low- and middle-income countries: “KMC should be provided to all low birth weight and preterm infants irrespective of the settings – both health facilities and at home,” they wrote.
The authors caution that, “very low birth weight, extremely preterm neonates, and severely unstable neonates were often excluded from studies. More evidence is needed before extrapolating the study results in these high-risk groups.”
The study authors and Dr. Chan report no relevant financial relationships.
, according to new research published online in BMJ Global Health.
Starting the contact, which involves mothers carrying the newborn in a sling, within 24 hours of birth and continuing it for at least 8 hours a day both appear to amplify the effect on reducing mortality and infection, the paper states.
Sindhu Sivanandan, MD, with the department of neonatology at Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India, and Mari Jeeva Sankar, MD, in the pediatrics department of the All India Institute of Medical Sciences, New Delhi, looked at existing studies to compare KMC with conventional care and to compare starting the intervention within 24 hours of birth versus a later start.
Their review looked at 31 trials that included 15,559 low-birthweight and preterm infants collectively. Of the 31 trials, 27 studies compared KMC with conventional care and four compared early with late initiation of KMC.
Mortality risk reduction
Analysis showed that, compared with conventional care, KMC appeared to cut mortality risk by 32% (relative risk, 0.68; 95% confidence interval, 0.53-0.86) during birth hospitalization or by 28 days after birth, while it seemed to reduce the risk of severe infection, such as sepsis, by 15% (RR, 0.85; 95% CI, 0.76-0.96; low-certainty evidence.)
That mortality-risk reduction was found regardless of gestational age or weight of the child at enrolment, time of starting KMC, and whether the intervention was started in a hospital or community.
The studies that had compared early with late-initiated KMC showed a reduction in neonatal mortality of 33%.
Low- and middle-income countries have the highest rates of premature births (gestational age of less than 37 weeks) and low birthweight (less than 2,500 grams). Premature births and low birthweight both are key causes of death and disability.
The World Health Organization recommends KMC as the standard of care among low birthweight infants after clinical stabilization. The American Academy of Pediatrics also promotes immediate KMC.
Relevance in the U.S.
Grace Chan, MD, MPH, PhD, an epidemiologist and pediatrician with the Harvard School of Public Health, Boston, said though the practice is promoted by the WHO and AAP, recommendations to families vary widely by providers.
She said the health benefits for KMC are numerous. One of the biggest is that skin-to-skin contact can help transfer heat to newborns who may have trouble regulating their own temperature. That is especially important in cold climates in places where there may be insufficient indoor heat.
She said it’s well-known that preterm babies are at higher risk for apnea, and listening to a mother’s heartbeat may stimulate the child to breathe regularly.
Additionally with KMC, there’s an inherent benefit of a mother or caregiver being able to see any change in a newborn’s color immediately when the baby is held so closely, as opposed to a nurse watching several babies at a time in a neonatal intensive care unit.
This is evidence that starting KMC right away is important, because the risk of death for premature and low-weight newborns is highest in the first 24 hours of life, Dr. Chan noted.
Barriers of time
There are some barriers, she noted, in that mothers or other caregivers caring for several young children may not have the time to carry a child in a sling for 8 or more hours at a time.
The authors conclude that their findings have policy implications, particularly for low- and middle-income countries: “KMC should be provided to all low birth weight and preterm infants irrespective of the settings – both health facilities and at home,” they wrote.
The authors caution that, “very low birth weight, extremely preterm neonates, and severely unstable neonates were often excluded from studies. More evidence is needed before extrapolating the study results in these high-risk groups.”
The study authors and Dr. Chan report no relevant financial relationships.
, according to new research published online in BMJ Global Health.
Starting the contact, which involves mothers carrying the newborn in a sling, within 24 hours of birth and continuing it for at least 8 hours a day both appear to amplify the effect on reducing mortality and infection, the paper states.
Sindhu Sivanandan, MD, with the department of neonatology at Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India, and Mari Jeeva Sankar, MD, in the pediatrics department of the All India Institute of Medical Sciences, New Delhi, looked at existing studies to compare KMC with conventional care and to compare starting the intervention within 24 hours of birth versus a later start.
Their review looked at 31 trials that included 15,559 low-birthweight and preterm infants collectively. Of the 31 trials, 27 studies compared KMC with conventional care and four compared early with late initiation of KMC.
Mortality risk reduction
Analysis showed that, compared with conventional care, KMC appeared to cut mortality risk by 32% (relative risk, 0.68; 95% confidence interval, 0.53-0.86) during birth hospitalization or by 28 days after birth, while it seemed to reduce the risk of severe infection, such as sepsis, by 15% (RR, 0.85; 95% CI, 0.76-0.96; low-certainty evidence.)
That mortality-risk reduction was found regardless of gestational age or weight of the child at enrolment, time of starting KMC, and whether the intervention was started in a hospital or community.
The studies that had compared early with late-initiated KMC showed a reduction in neonatal mortality of 33%.
Low- and middle-income countries have the highest rates of premature births (gestational age of less than 37 weeks) and low birthweight (less than 2,500 grams). Premature births and low birthweight both are key causes of death and disability.
The World Health Organization recommends KMC as the standard of care among low birthweight infants after clinical stabilization. The American Academy of Pediatrics also promotes immediate KMC.
Relevance in the U.S.
Grace Chan, MD, MPH, PhD, an epidemiologist and pediatrician with the Harvard School of Public Health, Boston, said though the practice is promoted by the WHO and AAP, recommendations to families vary widely by providers.
She said the health benefits for KMC are numerous. One of the biggest is that skin-to-skin contact can help transfer heat to newborns who may have trouble regulating their own temperature. That is especially important in cold climates in places where there may be insufficient indoor heat.
She said it’s well-known that preterm babies are at higher risk for apnea, and listening to a mother’s heartbeat may stimulate the child to breathe regularly.
Additionally with KMC, there’s an inherent benefit of a mother or caregiver being able to see any change in a newborn’s color immediately when the baby is held so closely, as opposed to a nurse watching several babies at a time in a neonatal intensive care unit.
This is evidence that starting KMC right away is important, because the risk of death for premature and low-weight newborns is highest in the first 24 hours of life, Dr. Chan noted.
Barriers of time
There are some barriers, she noted, in that mothers or other caregivers caring for several young children may not have the time to carry a child in a sling for 8 or more hours at a time.
The authors conclude that their findings have policy implications, particularly for low- and middle-income countries: “KMC should be provided to all low birth weight and preterm infants irrespective of the settings – both health facilities and at home,” they wrote.
The authors caution that, “very low birth weight, extremely preterm neonates, and severely unstable neonates were often excluded from studies. More evidence is needed before extrapolating the study results in these high-risk groups.”
The study authors and Dr. Chan report no relevant financial relationships.
FROM BMJ GLOBAL HEALTH
What’s best for patients who are dying of anorexia?
SAN FRANCISCO – The patient at a Florida eating disorder clinic said she was eating plenty even though she acknowledged purging once a week. But her vitals told a different story: Her body mass index (BMI) was 12.2, down from 14.8 a couple of years before – a dangerously low value.
While the woman agreed that she needed to gain weight, she refused advice to pursue residential or inpatient treatment. This left her team with a big dilemma: Should they force her into care because she wouldn’t eat? Was that even possible under the law? Did she have the capacity to make decisions about her future? What other alternatives were there?
Determining the best course of action in cases like this is anything but simple, Dr. Cacodcar said. To make matters more complicated, .
“At least in my state of Florida, we know that it can be very, very hard to get patients expert care,” said Dr. Cacodcar. And, she said, it can be even tougher for certain types of patients, such as those that are LGBTQ and those who have severe illness but don’t meet the criteria.
As Dr. Cacodcar noted, the APA released new practice guidelines regarding eating disorders earlier this year, marking their first update since 2006. The guidelines highlight research that suggests nearly 1% – 0.8% – of the U.S. population will develop AN over their lifetimes. Recent studies also suggest that eating disorder numbers rose during the pandemic, with one analysis finding that patients under inpatient care doubled in 2020.
“Mortality rates are high for anorexia nervosa, up to 10 times higher than matched controls,” Dr. Cacodcar said. “It has the highest mortality rate of the psychiatric diseases with the exception of opioid use disorder.”
As for outcomes, she pointed to a 2019 study that surveyed 387 parents who had children with eating disorders, mostly AN. Only 20% made a full recovery. “The farther you get out from the onset of anorexia, the less likely you are to achieve recovery,” Dr. Cacodcar said. “A lot of the control behaviors become very automatic.”
Determining capacity
In some cases of AN, psychiatrists must determine whether they have the capacity to make decisions about treatment, said Gabriel Jerkins, MD, a chief resident of psychiatry at the University of Florida. At issue is “the ability of the individual to comprehend the information being disclosed in regard to their condition, as well as the nature and potential risks and benefits of the proposed treatment alternatives. They include of course, no treatment at all.”
“We know psychiatric conditions can limit one’s ability to appreciate consequence,” he said.
One option is to seek to institutionalize patients with severe AN because they are a danger to themselves. Clinicians opted to not do this in the case of the patient profiled by Dr. Cacodcar, the one with the BMI of 12.2 who didn’t want inpatient or residential care. (A 5-foot-8 person with a BMI of 12.2 would weigh 80 pounds.)
“The main reason we did not hospitalize her is because an appropriate level of care was not going to be readily available,” Dr. Cacodcar said, and her treatment would have been substandard.
Fortunately, the woman did return after a couple of months and accept residential care. No facility in Florida was willing to accept her because of her low BMI, but she did find one in North Carolina, where she stayed for 2 months. She’s doing well, and her BMI is now 21, Dr. Cacodcar said.
The patient’s story shows that involuntary hospitalization “is not necessarily the best course of action,” Dr. Cacodcar said. “It wasn’t necessarily going to be in the patient’s best interest.”
In another case, a 22-year-old woman had severe AN. She had been a gymnast and dancer, Dr. Jerkins said, “and I include that here only because of how commonly we see that kind of demographic information in patients with anorexia nervosa.”
Her BMI was 17.5, and clinicians discussed feeding her through a feeding tube. She still had “no insight that her symptoms were related to an underlying eating disorder,” Dr. Jerkins said, raising questions about her capacity. “Is it sufficient that the patient understand that she’s underweight?”
Ultimately, he said, she received a feeding tube at a time when her BMI had dropped to 16.3. She suffered from an infection but ultimately she improved and has stabilized at a BMI of around 19, he said.
“I do wonder if allowing her to have some control of how to pursue treatment in this case was therapeutic in a way,” he said, especially since matters of control are deeply ingrained in AN.
A former physical trainer, the patient had a BMI of 17.6. The University of Florida’s eating disorder clinic sent her to an out-of-state residential program, but she was discharged when her blood glucose dipped dangerously low as she compulsively exercised. Her BMI dipped to 16.2.
Dr. Schmidt had the patient involuntarily committed upon her return, but she went home after 12 days with no change in her weight. Ultimately, the patient was referred to an eating disorder center in Colorado for medical stabilization where she was given a feeding tube. But her medical situation was so dire that she was discharged to her home, where she went on hospice and died.
“I’m not arguing for or against the term ‘terminal anorexia.’ But this case does make me think about it,” said Dr. Schmidt. She was referring to a controversial term used by some clinicians to refer to patients who face inevitable death from AN. “Unfortunately,” wrote the authors of a recent report proposing a clinical definition, “these patients and their carers often receive minimal support from eating disorders health professionals who are conflicted about terminal care, and who are hampered and limited by the paucity of literature on end-of-life care for those with anorexia nervosa.”
SAN FRANCISCO – The patient at a Florida eating disorder clinic said she was eating plenty even though she acknowledged purging once a week. But her vitals told a different story: Her body mass index (BMI) was 12.2, down from 14.8 a couple of years before – a dangerously low value.
While the woman agreed that she needed to gain weight, she refused advice to pursue residential or inpatient treatment. This left her team with a big dilemma: Should they force her into care because she wouldn’t eat? Was that even possible under the law? Did she have the capacity to make decisions about her future? What other alternatives were there?
Determining the best course of action in cases like this is anything but simple, Dr. Cacodcar said. To make matters more complicated, .
“At least in my state of Florida, we know that it can be very, very hard to get patients expert care,” said Dr. Cacodcar. And, she said, it can be even tougher for certain types of patients, such as those that are LGBTQ and those who have severe illness but don’t meet the criteria.
As Dr. Cacodcar noted, the APA released new practice guidelines regarding eating disorders earlier this year, marking their first update since 2006. The guidelines highlight research that suggests nearly 1% – 0.8% – of the U.S. population will develop AN over their lifetimes. Recent studies also suggest that eating disorder numbers rose during the pandemic, with one analysis finding that patients under inpatient care doubled in 2020.
“Mortality rates are high for anorexia nervosa, up to 10 times higher than matched controls,” Dr. Cacodcar said. “It has the highest mortality rate of the psychiatric diseases with the exception of opioid use disorder.”
As for outcomes, she pointed to a 2019 study that surveyed 387 parents who had children with eating disorders, mostly AN. Only 20% made a full recovery. “The farther you get out from the onset of anorexia, the less likely you are to achieve recovery,” Dr. Cacodcar said. “A lot of the control behaviors become very automatic.”
Determining capacity
In some cases of AN, psychiatrists must determine whether they have the capacity to make decisions about treatment, said Gabriel Jerkins, MD, a chief resident of psychiatry at the University of Florida. At issue is “the ability of the individual to comprehend the information being disclosed in regard to their condition, as well as the nature and potential risks and benefits of the proposed treatment alternatives. They include of course, no treatment at all.”
“We know psychiatric conditions can limit one’s ability to appreciate consequence,” he said.
One option is to seek to institutionalize patients with severe AN because they are a danger to themselves. Clinicians opted to not do this in the case of the patient profiled by Dr. Cacodcar, the one with the BMI of 12.2 who didn’t want inpatient or residential care. (A 5-foot-8 person with a BMI of 12.2 would weigh 80 pounds.)
“The main reason we did not hospitalize her is because an appropriate level of care was not going to be readily available,” Dr. Cacodcar said, and her treatment would have been substandard.
Fortunately, the woman did return after a couple of months and accept residential care. No facility in Florida was willing to accept her because of her low BMI, but she did find one in North Carolina, where she stayed for 2 months. She’s doing well, and her BMI is now 21, Dr. Cacodcar said.
The patient’s story shows that involuntary hospitalization “is not necessarily the best course of action,” Dr. Cacodcar said. “It wasn’t necessarily going to be in the patient’s best interest.”
In another case, a 22-year-old woman had severe AN. She had been a gymnast and dancer, Dr. Jerkins said, “and I include that here only because of how commonly we see that kind of demographic information in patients with anorexia nervosa.”
Her BMI was 17.5, and clinicians discussed feeding her through a feeding tube. She still had “no insight that her symptoms were related to an underlying eating disorder,” Dr. Jerkins said, raising questions about her capacity. “Is it sufficient that the patient understand that she’s underweight?”
Ultimately, he said, she received a feeding tube at a time when her BMI had dropped to 16.3. She suffered from an infection but ultimately she improved and has stabilized at a BMI of around 19, he said.
“I do wonder if allowing her to have some control of how to pursue treatment in this case was therapeutic in a way,” he said, especially since matters of control are deeply ingrained in AN.
A former physical trainer, the patient had a BMI of 17.6. The University of Florida’s eating disorder clinic sent her to an out-of-state residential program, but she was discharged when her blood glucose dipped dangerously low as she compulsively exercised. Her BMI dipped to 16.2.
Dr. Schmidt had the patient involuntarily committed upon her return, but she went home after 12 days with no change in her weight. Ultimately, the patient was referred to an eating disorder center in Colorado for medical stabilization where she was given a feeding tube. But her medical situation was so dire that she was discharged to her home, where she went on hospice and died.
“I’m not arguing for or against the term ‘terminal anorexia.’ But this case does make me think about it,” said Dr. Schmidt. She was referring to a controversial term used by some clinicians to refer to patients who face inevitable death from AN. “Unfortunately,” wrote the authors of a recent report proposing a clinical definition, “these patients and their carers often receive minimal support from eating disorders health professionals who are conflicted about terminal care, and who are hampered and limited by the paucity of literature on end-of-life care for those with anorexia nervosa.”
SAN FRANCISCO – The patient at a Florida eating disorder clinic said she was eating plenty even though she acknowledged purging once a week. But her vitals told a different story: Her body mass index (BMI) was 12.2, down from 14.8 a couple of years before – a dangerously low value.
While the woman agreed that she needed to gain weight, she refused advice to pursue residential or inpatient treatment. This left her team with a big dilemma: Should they force her into care because she wouldn’t eat? Was that even possible under the law? Did she have the capacity to make decisions about her future? What other alternatives were there?
Determining the best course of action in cases like this is anything but simple, Dr. Cacodcar said. To make matters more complicated, .
“At least in my state of Florida, we know that it can be very, very hard to get patients expert care,” said Dr. Cacodcar. And, she said, it can be even tougher for certain types of patients, such as those that are LGBTQ and those who have severe illness but don’t meet the criteria.
As Dr. Cacodcar noted, the APA released new practice guidelines regarding eating disorders earlier this year, marking their first update since 2006. The guidelines highlight research that suggests nearly 1% – 0.8% – of the U.S. population will develop AN over their lifetimes. Recent studies also suggest that eating disorder numbers rose during the pandemic, with one analysis finding that patients under inpatient care doubled in 2020.
“Mortality rates are high for anorexia nervosa, up to 10 times higher than matched controls,” Dr. Cacodcar said. “It has the highest mortality rate of the psychiatric diseases with the exception of opioid use disorder.”
As for outcomes, she pointed to a 2019 study that surveyed 387 parents who had children with eating disorders, mostly AN. Only 20% made a full recovery. “The farther you get out from the onset of anorexia, the less likely you are to achieve recovery,” Dr. Cacodcar said. “A lot of the control behaviors become very automatic.”
Determining capacity
In some cases of AN, psychiatrists must determine whether they have the capacity to make decisions about treatment, said Gabriel Jerkins, MD, a chief resident of psychiatry at the University of Florida. At issue is “the ability of the individual to comprehend the information being disclosed in regard to their condition, as well as the nature and potential risks and benefits of the proposed treatment alternatives. They include of course, no treatment at all.”
“We know psychiatric conditions can limit one’s ability to appreciate consequence,” he said.
One option is to seek to institutionalize patients with severe AN because they are a danger to themselves. Clinicians opted to not do this in the case of the patient profiled by Dr. Cacodcar, the one with the BMI of 12.2 who didn’t want inpatient or residential care. (A 5-foot-8 person with a BMI of 12.2 would weigh 80 pounds.)
“The main reason we did not hospitalize her is because an appropriate level of care was not going to be readily available,” Dr. Cacodcar said, and her treatment would have been substandard.
Fortunately, the woman did return after a couple of months and accept residential care. No facility in Florida was willing to accept her because of her low BMI, but she did find one in North Carolina, where she stayed for 2 months. She’s doing well, and her BMI is now 21, Dr. Cacodcar said.
The patient’s story shows that involuntary hospitalization “is not necessarily the best course of action,” Dr. Cacodcar said. “It wasn’t necessarily going to be in the patient’s best interest.”
In another case, a 22-year-old woman had severe AN. She had been a gymnast and dancer, Dr. Jerkins said, “and I include that here only because of how commonly we see that kind of demographic information in patients with anorexia nervosa.”
Her BMI was 17.5, and clinicians discussed feeding her through a feeding tube. She still had “no insight that her symptoms were related to an underlying eating disorder,” Dr. Jerkins said, raising questions about her capacity. “Is it sufficient that the patient understand that she’s underweight?”
Ultimately, he said, she received a feeding tube at a time when her BMI had dropped to 16.3. She suffered from an infection but ultimately she improved and has stabilized at a BMI of around 19, he said.
“I do wonder if allowing her to have some control of how to pursue treatment in this case was therapeutic in a way,” he said, especially since matters of control are deeply ingrained in AN.
A former physical trainer, the patient had a BMI of 17.6. The University of Florida’s eating disorder clinic sent her to an out-of-state residential program, but she was discharged when her blood glucose dipped dangerously low as she compulsively exercised. Her BMI dipped to 16.2.
Dr. Schmidt had the patient involuntarily committed upon her return, but she went home after 12 days with no change in her weight. Ultimately, the patient was referred to an eating disorder center in Colorado for medical stabilization where she was given a feeding tube. But her medical situation was so dire that she was discharged to her home, where she went on hospice and died.
“I’m not arguing for or against the term ‘terminal anorexia.’ But this case does make me think about it,” said Dr. Schmidt. She was referring to a controversial term used by some clinicians to refer to patients who face inevitable death from AN. “Unfortunately,” wrote the authors of a recent report proposing a clinical definition, “these patients and their carers often receive minimal support from eating disorders health professionals who are conflicted about terminal care, and who are hampered and limited by the paucity of literature on end-of-life care for those with anorexia nervosa.”
AT APA 2023
Alcohol dependence in teens tied to subsequent depression
TOPLINE
Alcohol dependence, but not consumption, at age 18 years increases the risk for depression at age 24 years.
METHODOLOGY
- The study included 3,902 mostly White adolescents, about 58% female, born in England from April 1991 to December 1992, who were part of the Avon Longitudinal Study of Parents and Children (ALSPAC) that examined genetic and environmental determinants of health and development.
- Participants completed the self-report Alcohol Use Disorders Identification Test (AUDIT) between the ages of 16 and 23 years, a period when average alcohol use increases rapidly.
- The primary outcome was probability for depression at age 24 years, using the Clinical Interview Schedule Revised (CIS-R), a self-administered computerized clinical assessment of common mental disorder symptoms during the past week.
- Researchers assessed frequency and quantity of alcohol consumption as well as alcohol dependence.
- Confounders included sex, housing type, maternal education and depressive symptoms, parents’ alcohol use, conduct problems at age 4 years, being bullied, and smoking status.
TAKEAWAYS
- After adjustments, alcohol dependence at age 18 years was associated with depression at age 24 years (unstandardized probit coefficient 0.13; 95% confidence interval, 0.02-0.25; P = .019)
- The relationship appeared to persist for alcohol dependence at each age of the growth curve (17-22 years).
- There was no evidence that frequency or quantity of alcohol consumption at age 18 was significantly associated with depression at age 24, suggesting these factors may not increase the risk for later depression unless there are also features of dependency.
IN PRACTICE
“Our findings suggest that preventing alcohol dependence during adolescence, or treating it early, could reduce the risk of depression,” which could have important public health implications, the researchers write.
STUDY DETAILS
The study was carried out by researchers at the University of Bristol; University College London; Critical Thinking Unit, Public Health Directorate, NHS; University of Nottingham, all in the United Kingdom. It was published online in Lancet Psychiatry
LIMITATIONS
There was substantial attrition in the ALSPAC cohort from birth to age 24 years. The sample was recruited from one U.K. region and most participants were White. Measures of alcohol consumption and dependence excluded some features of abuse. And as this is an observational study, the possibility of residual confounding can’t be excluded.
DISCLOSURES
The investigators report no relevant disclosures. The study received support from the UK Medical Research Council and Alcohol Research UK.
A version of this article first appeared on Medscape.com.
TOPLINE
Alcohol dependence, but not consumption, at age 18 years increases the risk for depression at age 24 years.
METHODOLOGY
- The study included 3,902 mostly White adolescents, about 58% female, born in England from April 1991 to December 1992, who were part of the Avon Longitudinal Study of Parents and Children (ALSPAC) that examined genetic and environmental determinants of health and development.
- Participants completed the self-report Alcohol Use Disorders Identification Test (AUDIT) between the ages of 16 and 23 years, a period when average alcohol use increases rapidly.
- The primary outcome was probability for depression at age 24 years, using the Clinical Interview Schedule Revised (CIS-R), a self-administered computerized clinical assessment of common mental disorder symptoms during the past week.
- Researchers assessed frequency and quantity of alcohol consumption as well as alcohol dependence.
- Confounders included sex, housing type, maternal education and depressive symptoms, parents’ alcohol use, conduct problems at age 4 years, being bullied, and smoking status.
TAKEAWAYS
- After adjustments, alcohol dependence at age 18 years was associated with depression at age 24 years (unstandardized probit coefficient 0.13; 95% confidence interval, 0.02-0.25; P = .019)
- The relationship appeared to persist for alcohol dependence at each age of the growth curve (17-22 years).
- There was no evidence that frequency or quantity of alcohol consumption at age 18 was significantly associated with depression at age 24, suggesting these factors may not increase the risk for later depression unless there are also features of dependency.
IN PRACTICE
“Our findings suggest that preventing alcohol dependence during adolescence, or treating it early, could reduce the risk of depression,” which could have important public health implications, the researchers write.
STUDY DETAILS
The study was carried out by researchers at the University of Bristol; University College London; Critical Thinking Unit, Public Health Directorate, NHS; University of Nottingham, all in the United Kingdom. It was published online in Lancet Psychiatry
LIMITATIONS
There was substantial attrition in the ALSPAC cohort from birth to age 24 years. The sample was recruited from one U.K. region and most participants were White. Measures of alcohol consumption and dependence excluded some features of abuse. And as this is an observational study, the possibility of residual confounding can’t be excluded.
DISCLOSURES
The investigators report no relevant disclosures. The study received support from the UK Medical Research Council and Alcohol Research UK.
A version of this article first appeared on Medscape.com.
TOPLINE
Alcohol dependence, but not consumption, at age 18 years increases the risk for depression at age 24 years.
METHODOLOGY
- The study included 3,902 mostly White adolescents, about 58% female, born in England from April 1991 to December 1992, who were part of the Avon Longitudinal Study of Parents and Children (ALSPAC) that examined genetic and environmental determinants of health and development.
- Participants completed the self-report Alcohol Use Disorders Identification Test (AUDIT) between the ages of 16 and 23 years, a period when average alcohol use increases rapidly.
- The primary outcome was probability for depression at age 24 years, using the Clinical Interview Schedule Revised (CIS-R), a self-administered computerized clinical assessment of common mental disorder symptoms during the past week.
- Researchers assessed frequency and quantity of alcohol consumption as well as alcohol dependence.
- Confounders included sex, housing type, maternal education and depressive symptoms, parents’ alcohol use, conduct problems at age 4 years, being bullied, and smoking status.
TAKEAWAYS
- After adjustments, alcohol dependence at age 18 years was associated with depression at age 24 years (unstandardized probit coefficient 0.13; 95% confidence interval, 0.02-0.25; P = .019)
- The relationship appeared to persist for alcohol dependence at each age of the growth curve (17-22 years).
- There was no evidence that frequency or quantity of alcohol consumption at age 18 was significantly associated with depression at age 24, suggesting these factors may not increase the risk for later depression unless there are also features of dependency.
IN PRACTICE
“Our findings suggest that preventing alcohol dependence during adolescence, or treating it early, could reduce the risk of depression,” which could have important public health implications, the researchers write.
STUDY DETAILS
The study was carried out by researchers at the University of Bristol; University College London; Critical Thinking Unit, Public Health Directorate, NHS; University of Nottingham, all in the United Kingdom. It was published online in Lancet Psychiatry
LIMITATIONS
There was substantial attrition in the ALSPAC cohort from birth to age 24 years. The sample was recruited from one U.K. region and most participants were White. Measures of alcohol consumption and dependence excluded some features of abuse. And as this is an observational study, the possibility of residual confounding can’t be excluded.
DISCLOSURES
The investigators report no relevant disclosures. The study received support from the UK Medical Research Council and Alcohol Research UK.
A version of this article first appeared on Medscape.com.
Widespread carboplatin, cisplatin shortages: NCCN survey
The survey, which included responses from 27 NCCN member institutions, revealed that 93% are experiencing a shortage of carboplatin and that 70% have reported a shortage of cisplatin.
“This is an unacceptable situation,” Robert W. Carlson, MD, NCCN’s chief executive offer, said in the statement released by the network.
“We are hearing from oncologists and pharmacists across the country who have to scramble to find appropriate alternatives for treating their patients with cancer right now,” Dr. Carlson said. And while the survey results show patients are still able to get lifesaving care, “it comes at a burden to our overtaxed medical facilities.”
The NCCN called on the federal government, the pharmaceutical industry, providers, and payers to take steps to “help mitigate any impacts” from this cancer drug shortage.
“We need to work together to improve the current situation and prevent it from happening again in the future,” Dr. Carlson stressed.
Carboplatin and cisplatin, which are frequently used together for systemic treatment, are highly effective therapies prescribed to treat many cancer types, including lung, breast, and prostate cancers, as well as leukemias and lymphomas. An estimated 500,000 new patients with cancer receive these agents each year.
The current survey, conducted over the last week of May, found that 100% of responding centers are able to continue to treat patients who need cisplatin without delays.
The same cannot be said for carboplatin: only 64% of centers said they are still able to continue treating all current patients receiving the platinum-based therapy. Among 19 responding centers, 20% reported that they were continuing carboplatin regimens for some but not all patients. And 16% reported treatment delays from having to obtain prior authorization for modified treatment plans, though none reported denials.
“Carboplatin has been in short supply for months but in the last 4 weeks has reached a critical stage,” according to one survey comment. “Without additional inventory many of our sites will be out of drug by early next week.”
In response to the survey question, “Is your center experiencing a shortage of carboplatin,” others made similar comments:
- “Current shipments from established manufacturers have been paused.”
- “The supply of carboplatin available is not meeting our demands.”
- “Without additional supply in early June, we will have to implement several shortage mitigation strategies.”
Survey respondents also addressed whether manufacturers or suppliers have provided any indication of when these drugs will become readily available again. For both drugs, about 60% of respondents said no. And for those who do receive updates, many noted that the “information is tentative and variable.”
Respondents indicated that other cancer agents, including methotrexate (67%) and 5FU (26%), are also in short supply at their centers.
The shortage and the uncertainty as to when it will end are forcing some centers to develop conservation and mitigation strategies.
The NCCN has broadly outlined how the federal government, the pharmaceutical industry, providers, and payers can help with prevention and mitigation. The NCCN has called on the federal government and the pharmaceutical industry to work to secure a steady supply of core anticancer drugs and has asked payers to “put patients first and provide flexible and efficient systems of providing coverage for alternative therapies replacing anti-cancer drugs that are unavailable or in shortage.”
Overall, the survey results “demonstrate the widespread impact of the chemotherapy shortage,” said Alyssa Schatz, MSW, senior director of policy and advocacy for NCCN. “We hope that by sharing this survey and calling for united action across the oncology community, we can come together to prevent future drug shortages and ensure quality, effective, equitable, and accessible cancer care for all.”
A version of this article first appeared on Medscape.com.
The survey, which included responses from 27 NCCN member institutions, revealed that 93% are experiencing a shortage of carboplatin and that 70% have reported a shortage of cisplatin.
“This is an unacceptable situation,” Robert W. Carlson, MD, NCCN’s chief executive offer, said in the statement released by the network.
“We are hearing from oncologists and pharmacists across the country who have to scramble to find appropriate alternatives for treating their patients with cancer right now,” Dr. Carlson said. And while the survey results show patients are still able to get lifesaving care, “it comes at a burden to our overtaxed medical facilities.”
The NCCN called on the federal government, the pharmaceutical industry, providers, and payers to take steps to “help mitigate any impacts” from this cancer drug shortage.
“We need to work together to improve the current situation and prevent it from happening again in the future,” Dr. Carlson stressed.
Carboplatin and cisplatin, which are frequently used together for systemic treatment, are highly effective therapies prescribed to treat many cancer types, including lung, breast, and prostate cancers, as well as leukemias and lymphomas. An estimated 500,000 new patients with cancer receive these agents each year.
The current survey, conducted over the last week of May, found that 100% of responding centers are able to continue to treat patients who need cisplatin without delays.
The same cannot be said for carboplatin: only 64% of centers said they are still able to continue treating all current patients receiving the platinum-based therapy. Among 19 responding centers, 20% reported that they were continuing carboplatin regimens for some but not all patients. And 16% reported treatment delays from having to obtain prior authorization for modified treatment plans, though none reported denials.
“Carboplatin has been in short supply for months but in the last 4 weeks has reached a critical stage,” according to one survey comment. “Without additional inventory many of our sites will be out of drug by early next week.”
In response to the survey question, “Is your center experiencing a shortage of carboplatin,” others made similar comments:
- “Current shipments from established manufacturers have been paused.”
- “The supply of carboplatin available is not meeting our demands.”
- “Without additional supply in early June, we will have to implement several shortage mitigation strategies.”
Survey respondents also addressed whether manufacturers or suppliers have provided any indication of when these drugs will become readily available again. For both drugs, about 60% of respondents said no. And for those who do receive updates, many noted that the “information is tentative and variable.”
Respondents indicated that other cancer agents, including methotrexate (67%) and 5FU (26%), are also in short supply at their centers.
The shortage and the uncertainty as to when it will end are forcing some centers to develop conservation and mitigation strategies.
The NCCN has broadly outlined how the federal government, the pharmaceutical industry, providers, and payers can help with prevention and mitigation. The NCCN has called on the federal government and the pharmaceutical industry to work to secure a steady supply of core anticancer drugs and has asked payers to “put patients first and provide flexible and efficient systems of providing coverage for alternative therapies replacing anti-cancer drugs that are unavailable or in shortage.”
Overall, the survey results “demonstrate the widespread impact of the chemotherapy shortage,” said Alyssa Schatz, MSW, senior director of policy and advocacy for NCCN. “We hope that by sharing this survey and calling for united action across the oncology community, we can come together to prevent future drug shortages and ensure quality, effective, equitable, and accessible cancer care for all.”
A version of this article first appeared on Medscape.com.
The survey, which included responses from 27 NCCN member institutions, revealed that 93% are experiencing a shortage of carboplatin and that 70% have reported a shortage of cisplatin.
“This is an unacceptable situation,” Robert W. Carlson, MD, NCCN’s chief executive offer, said in the statement released by the network.
“We are hearing from oncologists and pharmacists across the country who have to scramble to find appropriate alternatives for treating their patients with cancer right now,” Dr. Carlson said. And while the survey results show patients are still able to get lifesaving care, “it comes at a burden to our overtaxed medical facilities.”
The NCCN called on the federal government, the pharmaceutical industry, providers, and payers to take steps to “help mitigate any impacts” from this cancer drug shortage.
“We need to work together to improve the current situation and prevent it from happening again in the future,” Dr. Carlson stressed.
Carboplatin and cisplatin, which are frequently used together for systemic treatment, are highly effective therapies prescribed to treat many cancer types, including lung, breast, and prostate cancers, as well as leukemias and lymphomas. An estimated 500,000 new patients with cancer receive these agents each year.
The current survey, conducted over the last week of May, found that 100% of responding centers are able to continue to treat patients who need cisplatin without delays.
The same cannot be said for carboplatin: only 64% of centers said they are still able to continue treating all current patients receiving the platinum-based therapy. Among 19 responding centers, 20% reported that they were continuing carboplatin regimens for some but not all patients. And 16% reported treatment delays from having to obtain prior authorization for modified treatment plans, though none reported denials.
“Carboplatin has been in short supply for months but in the last 4 weeks has reached a critical stage,” according to one survey comment. “Without additional inventory many of our sites will be out of drug by early next week.”
In response to the survey question, “Is your center experiencing a shortage of carboplatin,” others made similar comments:
- “Current shipments from established manufacturers have been paused.”
- “The supply of carboplatin available is not meeting our demands.”
- “Without additional supply in early June, we will have to implement several shortage mitigation strategies.”
Survey respondents also addressed whether manufacturers or suppliers have provided any indication of when these drugs will become readily available again. For both drugs, about 60% of respondents said no. And for those who do receive updates, many noted that the “information is tentative and variable.”
Respondents indicated that other cancer agents, including methotrexate (67%) and 5FU (26%), are also in short supply at their centers.
The shortage and the uncertainty as to when it will end are forcing some centers to develop conservation and mitigation strategies.
The NCCN has broadly outlined how the federal government, the pharmaceutical industry, providers, and payers can help with prevention and mitigation. The NCCN has called on the federal government and the pharmaceutical industry to work to secure a steady supply of core anticancer drugs and has asked payers to “put patients first and provide flexible and efficient systems of providing coverage for alternative therapies replacing anti-cancer drugs that are unavailable or in shortage.”
Overall, the survey results “demonstrate the widespread impact of the chemotherapy shortage,” said Alyssa Schatz, MSW, senior director of policy and advocacy for NCCN. “We hope that by sharing this survey and calling for united action across the oncology community, we can come together to prevent future drug shortages and ensure quality, effective, equitable, and accessible cancer care for all.”
A version of this article first appeared on Medscape.com.
‘Strikingly positive’ effect of novel MS agent
AURORA, COLO. –
“We should be very excited about these results, which are better than expected and fundamentally tackle autoimmunity,” said study investigator Gavin Giovannoni, MD, PhD, chair of neurology at the Blizard Institute of Barts, London, and the London School of Medicine and Dentistry. “It will be interesting to see if this treatment reestablishes immune tolerance and induces long-term remission,” he said.
The late-breaking study was presented at the annual meeting of the Consortium of Multiple Sclerosis Centers.
Significant lesion reduction
With a variety of disease-modifying therapies available for MS, frexalimab would be unique as a novel second-generation monoclonal antibody designed to block the costimulatory CD40/CD40L cellular pathway. Importantly, the mechanism is believed to potentially modify T- and B-cell activation and innate immune cell function, for an effect of reducing inflammation without depleting B cells.
To investigate the drug’s efficacy and safety, Dr. Giovannoni and his colleagues conducted the phase 2, multicenter trial, in which 129 participants with relapsing MS were randomized to one of four groups – high-dose frexalimab (n = 52); low-dose frexalimab (n = 51); or placebo (n = 12 high-dose, n = 14 low-dose), for the 12-week placebo-controlled period, followed by an open-label extension period that is currently ongoing.
Among 125 participants who completed the study’s 12-week double-blind period, those receiving high-dose frexalimab had an 89% greater reduction in the number of new gadolinium-enhancing T1-lesions, compared with the pooled placebo group (P = .0004), meeting the study’s primary endpoint. After 24 weeks, as many as 96% of those in the high-dose frexalimab arm were free of gadolinium-enhanced T1 lesions.
The frexalimab low-dose group also had a lower, but significant, reduction in the number of new gadolinium-enhanced T1-lesions of 79% versus the pooled placebo group (P = .0021).
Both of the frexalimab groups also had reductions in enlarging T2-lesions and total gadolinium-enhanced T1-lesions.
In the high-dose group, data on 38 participants with open-label data from week 37 showed no new gadolinium-enhanced lesions.
In terms of safety, frexalimab was well tolerated over the 12-week study, with headache and COVID-19 reported among 4% or fewer participants. No serious adverse events were reported.
Looking ahead at safety, Dr. Giovannoni noted that “a known unknown is infections, but this is a problem with all therapies that work via immunosuppressive mechanisms, not only therapies targeting CD40L.” That said, “we didn’t see a big infection signal in the trial, which is reassuring. It also shows the immune system has built-in redundancy and many mechanisms to fight infections,” he added.
In his newsletter, Dr. Giovannoni characterized the study’s results as “strikingly positive,” adding that they “are the most exciting to emerge in MS in the last 12-24 months.”
Overall, “these are the first randomized controlled phase 2 data for a CD40L inhibitor in MS and indicate potential for further development of frexalimab as a high-efficacy therapy,” the investigators noted. “Frexalimab led to a pronounced reduction of new gadolinium-enhancing lesions by 3 months and was well-tolerated,” they added.
An intriguing mechanism
Commenting on the study, Salim Chahin, MD, an assistant professor of neurology in the John L. Trotter MS Center in the department of neurology at Washington University, St. Louis, said that frexalimab represents an intriguing mechanistic approach to MS.
“In the world of MS and neuroimmunology, this is indeed a unique mechanism that has not been explored before,” Dr. Chahin said.
“Therapies targeting CD40 and CD40L are not new but were previously associated with unfavorable side effects, mainly thromboembolic events that halted their development,” he said, noting that the drug appears to avoid these side effects, providing good phase 2 efficacy data.
Dr. Chahin agreed that the phase 3 data will be watched closely for further safety and efficacy issues. “Indeed, it is difficult to interpret the occurrence of COVID-19 infections, given the timing of the phase 2 study, or their severity, but based on the mechanism of action, it is possible that this drug will be associated with a more favorable safety profile than some of the currently approved MS treatments,” Dr. Chahin said.
“But phase 3 trial data are much needed to clarify the immunosuppressive risk.”
The study received funding from Sanofi. Dr. Giovannoni’s disclosures include current or recent relationships with AbbVie, Aslan, Atara Bio, Biogen, BMS-Celgene, GlaxoSmithKline, Janssen/J&J, Japanese Tobacco, Jazz Pharmaceuticals, LifNano, Merck & Co, Merck KGaA/EMD, Moderna, Serono, Moderna, Novartis, Sandoz, Sanofi, and Roche/Genentech. Dr. Chahin reports no relevant financial relationships.
A version of this article first appears on Medscape.com.
AURORA, COLO. –
“We should be very excited about these results, which are better than expected and fundamentally tackle autoimmunity,” said study investigator Gavin Giovannoni, MD, PhD, chair of neurology at the Blizard Institute of Barts, London, and the London School of Medicine and Dentistry. “It will be interesting to see if this treatment reestablishes immune tolerance and induces long-term remission,” he said.
The late-breaking study was presented at the annual meeting of the Consortium of Multiple Sclerosis Centers.
Significant lesion reduction
With a variety of disease-modifying therapies available for MS, frexalimab would be unique as a novel second-generation monoclonal antibody designed to block the costimulatory CD40/CD40L cellular pathway. Importantly, the mechanism is believed to potentially modify T- and B-cell activation and innate immune cell function, for an effect of reducing inflammation without depleting B cells.
To investigate the drug’s efficacy and safety, Dr. Giovannoni and his colleagues conducted the phase 2, multicenter trial, in which 129 participants with relapsing MS were randomized to one of four groups – high-dose frexalimab (n = 52); low-dose frexalimab (n = 51); or placebo (n = 12 high-dose, n = 14 low-dose), for the 12-week placebo-controlled period, followed by an open-label extension period that is currently ongoing.
Among 125 participants who completed the study’s 12-week double-blind period, those receiving high-dose frexalimab had an 89% greater reduction in the number of new gadolinium-enhancing T1-lesions, compared with the pooled placebo group (P = .0004), meeting the study’s primary endpoint. After 24 weeks, as many as 96% of those in the high-dose frexalimab arm were free of gadolinium-enhanced T1 lesions.
The frexalimab low-dose group also had a lower, but significant, reduction in the number of new gadolinium-enhanced T1-lesions of 79% versus the pooled placebo group (P = .0021).
Both of the frexalimab groups also had reductions in enlarging T2-lesions and total gadolinium-enhanced T1-lesions.
In the high-dose group, data on 38 participants with open-label data from week 37 showed no new gadolinium-enhanced lesions.
In terms of safety, frexalimab was well tolerated over the 12-week study, with headache and COVID-19 reported among 4% or fewer participants. No serious adverse events were reported.
Looking ahead at safety, Dr. Giovannoni noted that “a known unknown is infections, but this is a problem with all therapies that work via immunosuppressive mechanisms, not only therapies targeting CD40L.” That said, “we didn’t see a big infection signal in the trial, which is reassuring. It also shows the immune system has built-in redundancy and many mechanisms to fight infections,” he added.
In his newsletter, Dr. Giovannoni characterized the study’s results as “strikingly positive,” adding that they “are the most exciting to emerge in MS in the last 12-24 months.”
Overall, “these are the first randomized controlled phase 2 data for a CD40L inhibitor in MS and indicate potential for further development of frexalimab as a high-efficacy therapy,” the investigators noted. “Frexalimab led to a pronounced reduction of new gadolinium-enhancing lesions by 3 months and was well-tolerated,” they added.
An intriguing mechanism
Commenting on the study, Salim Chahin, MD, an assistant professor of neurology in the John L. Trotter MS Center in the department of neurology at Washington University, St. Louis, said that frexalimab represents an intriguing mechanistic approach to MS.
“In the world of MS and neuroimmunology, this is indeed a unique mechanism that has not been explored before,” Dr. Chahin said.
“Therapies targeting CD40 and CD40L are not new but were previously associated with unfavorable side effects, mainly thromboembolic events that halted their development,” he said, noting that the drug appears to avoid these side effects, providing good phase 2 efficacy data.
Dr. Chahin agreed that the phase 3 data will be watched closely for further safety and efficacy issues. “Indeed, it is difficult to interpret the occurrence of COVID-19 infections, given the timing of the phase 2 study, or their severity, but based on the mechanism of action, it is possible that this drug will be associated with a more favorable safety profile than some of the currently approved MS treatments,” Dr. Chahin said.
“But phase 3 trial data are much needed to clarify the immunosuppressive risk.”
The study received funding from Sanofi. Dr. Giovannoni’s disclosures include current or recent relationships with AbbVie, Aslan, Atara Bio, Biogen, BMS-Celgene, GlaxoSmithKline, Janssen/J&J, Japanese Tobacco, Jazz Pharmaceuticals, LifNano, Merck & Co, Merck KGaA/EMD, Moderna, Serono, Moderna, Novartis, Sandoz, Sanofi, and Roche/Genentech. Dr. Chahin reports no relevant financial relationships.
A version of this article first appears on Medscape.com.
AURORA, COLO. –
“We should be very excited about these results, which are better than expected and fundamentally tackle autoimmunity,” said study investigator Gavin Giovannoni, MD, PhD, chair of neurology at the Blizard Institute of Barts, London, and the London School of Medicine and Dentistry. “It will be interesting to see if this treatment reestablishes immune tolerance and induces long-term remission,” he said.
The late-breaking study was presented at the annual meeting of the Consortium of Multiple Sclerosis Centers.
Significant lesion reduction
With a variety of disease-modifying therapies available for MS, frexalimab would be unique as a novel second-generation monoclonal antibody designed to block the costimulatory CD40/CD40L cellular pathway. Importantly, the mechanism is believed to potentially modify T- and B-cell activation and innate immune cell function, for an effect of reducing inflammation without depleting B cells.
To investigate the drug’s efficacy and safety, Dr. Giovannoni and his colleagues conducted the phase 2, multicenter trial, in which 129 participants with relapsing MS were randomized to one of four groups – high-dose frexalimab (n = 52); low-dose frexalimab (n = 51); or placebo (n = 12 high-dose, n = 14 low-dose), for the 12-week placebo-controlled period, followed by an open-label extension period that is currently ongoing.
Among 125 participants who completed the study’s 12-week double-blind period, those receiving high-dose frexalimab had an 89% greater reduction in the number of new gadolinium-enhancing T1-lesions, compared with the pooled placebo group (P = .0004), meeting the study’s primary endpoint. After 24 weeks, as many as 96% of those in the high-dose frexalimab arm were free of gadolinium-enhanced T1 lesions.
The frexalimab low-dose group also had a lower, but significant, reduction in the number of new gadolinium-enhanced T1-lesions of 79% versus the pooled placebo group (P = .0021).
Both of the frexalimab groups also had reductions in enlarging T2-lesions and total gadolinium-enhanced T1-lesions.
In the high-dose group, data on 38 participants with open-label data from week 37 showed no new gadolinium-enhanced lesions.
In terms of safety, frexalimab was well tolerated over the 12-week study, with headache and COVID-19 reported among 4% or fewer participants. No serious adverse events were reported.
Looking ahead at safety, Dr. Giovannoni noted that “a known unknown is infections, but this is a problem with all therapies that work via immunosuppressive mechanisms, not only therapies targeting CD40L.” That said, “we didn’t see a big infection signal in the trial, which is reassuring. It also shows the immune system has built-in redundancy and many mechanisms to fight infections,” he added.
In his newsletter, Dr. Giovannoni characterized the study’s results as “strikingly positive,” adding that they “are the most exciting to emerge in MS in the last 12-24 months.”
Overall, “these are the first randomized controlled phase 2 data for a CD40L inhibitor in MS and indicate potential for further development of frexalimab as a high-efficacy therapy,” the investigators noted. “Frexalimab led to a pronounced reduction of new gadolinium-enhancing lesions by 3 months and was well-tolerated,” they added.
An intriguing mechanism
Commenting on the study, Salim Chahin, MD, an assistant professor of neurology in the John L. Trotter MS Center in the department of neurology at Washington University, St. Louis, said that frexalimab represents an intriguing mechanistic approach to MS.
“In the world of MS and neuroimmunology, this is indeed a unique mechanism that has not been explored before,” Dr. Chahin said.
“Therapies targeting CD40 and CD40L are not new but were previously associated with unfavorable side effects, mainly thromboembolic events that halted their development,” he said, noting that the drug appears to avoid these side effects, providing good phase 2 efficacy data.
Dr. Chahin agreed that the phase 3 data will be watched closely for further safety and efficacy issues. “Indeed, it is difficult to interpret the occurrence of COVID-19 infections, given the timing of the phase 2 study, or their severity, but based on the mechanism of action, it is possible that this drug will be associated with a more favorable safety profile than some of the currently approved MS treatments,” Dr. Chahin said.
“But phase 3 trial data are much needed to clarify the immunosuppressive risk.”
The study received funding from Sanofi. Dr. Giovannoni’s disclosures include current or recent relationships with AbbVie, Aslan, Atara Bio, Biogen, BMS-Celgene, GlaxoSmithKline, Janssen/J&J, Japanese Tobacco, Jazz Pharmaceuticals, LifNano, Merck & Co, Merck KGaA/EMD, Moderna, Serono, Moderna, Novartis, Sandoz, Sanofi, and Roche/Genentech. Dr. Chahin reports no relevant financial relationships.
A version of this article first appears on Medscape.com.
At CMSC 2023
After backlash, publisher to retract article that surveyed parents of children with gender dysphoria, says coauthor
The move is “due to concerns about lack of informed consent,” according to tweets by one of the paper’s authors.
The article, “Rapid Onset Gender Dysphoria: Parent Reports on 1655 Possible Cases,” was published in March in the Archives of Sexual Behavior. It has not been cited in the scientific literature, according to Clarivate’s Web of Science, but Altmetric, which tracks the online attention papers receive, ranks the article in the top 1% of all articles of a similar age.
Rapid Onset Gender Dysphoria (ROGD) is, the article stated, a “controversial theory” that “common cultural beliefs, values, and preoccupations cause some adolescents (especially female adolescents) to attribute their social problems, feelings, and mental health issues to gender dysphoria,” and that “youth with ROGD falsely believe that they are transgender,” in part due to social influences.
Michael Bailey, a psychology professor at Northwestern University in Evanston, Ill., and the paper’s corresponding author, tweeted: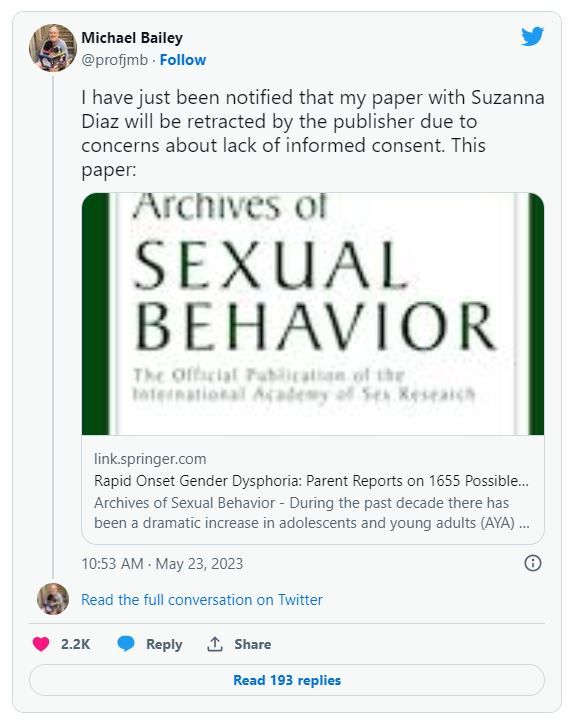
Bailey told Retraction Watch that he would “respond when [he] can” to our request for comment, following “new developments on our end.” Neither Springer Nature nor Kenneth Zucker, editor in chief of Archives of Sexual Behavior, has responded to similar requests.
The paper reported the results of a survey of parents who contacted the website ParentsofROGDKids.com, with which the first author is affiliated. According to the abstract, the authors found:
“Pre-existing mental health issues were common, and youths with these issues were more likely than those without them to have socially and medically transitioned. Parents reported that they had often felt pressured by clinicians to affirm their AYA [adolescent and young adult] child’s new gender and support their transition. According to the parents, AYA children’s mental health deteriorated considerably after social transition.”
Soon after publication, the paper attracted criticism that its method of gathering study participants was biased, and that the authors ignored information that didn’t support the theory of ROGD.
Archives of Sexual Behavior is the official publication of the International Academy of Sex Research, which tweeted on April 19:
The episode prompted a May 5 “Open Letter in Support of Dr. Kenneth Zucker and the Need to Promote Robust Scientific Debate” from the Foundation Against Intolerance and Racism that has now been signed by nearly 2000 people.
On May 10, the following publisher’s note was added to the article:
“readers are alerted that concerns have been raised regarding methodology as described in this article. The publisher is currently investigating this matter and a further response will follow the conclusion of this investigation.
Six days later, the publisher removed the article’s supplementary information “due to a lack of documented consent by study participants.”
The story may feel familiar to readers who recall what happened to another paper in 2018. In that paper, Brown University’s Lisa Littman coined the term ROGD. Following a backlash, Brown took down a press release touting the results, and the paper was eventually republished with corrections.
Bailey has been accused of mistreating transgender research participants, but an investigation by bioethicist Alice Dreger found that of the many accusations, “almost none appear to have been legitimate.”
In a post on UnHerd earlier this month, Bailey responded to the reported concerns about the study lacking approval by an Institutional Review Board (IRB), and that the way the participants were recruited biased the results.
IRB approval was not necessary, Bailey wrote, because Suzanna Diaz, the first author who collected the data, was not affiliated with an institution that required it. “Suzanna Diaz” is a pseudonym for “the mother of a gender dysphoric child she believes has ROGD” who wishes to remain anonymous for the sake of her family, Bailey wrote.
The paper included the following statement about its ethical approval:
“The first author and creator of the survey is not affiliated with any university or hospital. Thus, she did not seek approval from an IRB. After seeing a presentation of preliminary survey results by the first author, the second author suggested the data to be analyzed and submitted as an academic article (he was not involved in collecting the data). The second author consulted with his university’s IRB, who declined to certify the study because data were already collected. However, they advised that publishing the results was likely ethical provided data were deidentified. Editor’s note: After I reviewed the manuscript, I concluded that its publication is ethically appropriate, consistent with Springer policy.”
In his UnHerd post, Bailey quoted from the journal’s submission guidelines:
“If a study has not been granted ethics committee approval prior to commencing, retrospective ethics approval usually cannot be obtained and it may not be possible to consider the manuscript for peer review. The decision on whether to proceed to peer review in such cases is at the Editor’s discretion.”
“Regarding the methodological limitations of the study, these were addressed forthrightly and thoroughly in our article,” Bailey wrote.
Adam Marcus, a cofounder of Retraction Watch, is an editor at this news organization.
A version of this article first appeared on RetractionWatch.com.
The move is “due to concerns about lack of informed consent,” according to tweets by one of the paper’s authors.
The article, “Rapid Onset Gender Dysphoria: Parent Reports on 1655 Possible Cases,” was published in March in the Archives of Sexual Behavior. It has not been cited in the scientific literature, according to Clarivate’s Web of Science, but Altmetric, which tracks the online attention papers receive, ranks the article in the top 1% of all articles of a similar age.
Rapid Onset Gender Dysphoria (ROGD) is, the article stated, a “controversial theory” that “common cultural beliefs, values, and preoccupations cause some adolescents (especially female adolescents) to attribute their social problems, feelings, and mental health issues to gender dysphoria,” and that “youth with ROGD falsely believe that they are transgender,” in part due to social influences.
Michael Bailey, a psychology professor at Northwestern University in Evanston, Ill., and the paper’s corresponding author, tweeted: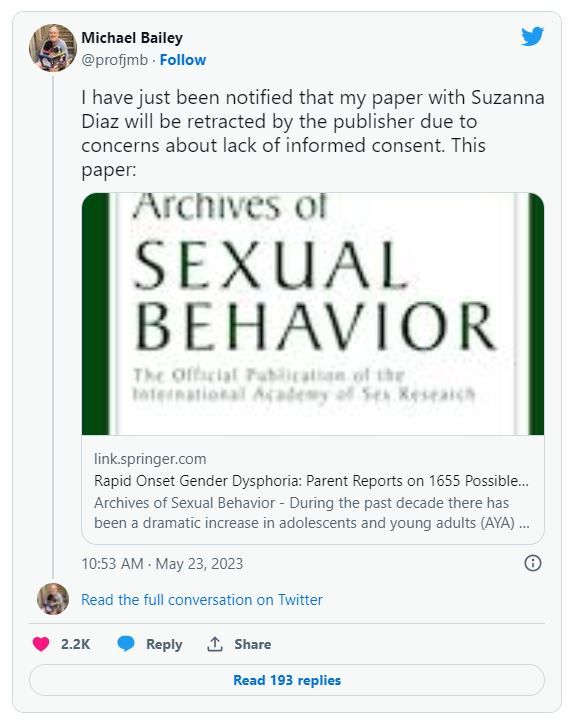
Bailey told Retraction Watch that he would “respond when [he] can” to our request for comment, following “new developments on our end.” Neither Springer Nature nor Kenneth Zucker, editor in chief of Archives of Sexual Behavior, has responded to similar requests.
The paper reported the results of a survey of parents who contacted the website ParentsofROGDKids.com, with which the first author is affiliated. According to the abstract, the authors found:
“Pre-existing mental health issues were common, and youths with these issues were more likely than those without them to have socially and medically transitioned. Parents reported that they had often felt pressured by clinicians to affirm their AYA [adolescent and young adult] child’s new gender and support their transition. According to the parents, AYA children’s mental health deteriorated considerably after social transition.”
Soon after publication, the paper attracted criticism that its method of gathering study participants was biased, and that the authors ignored information that didn’t support the theory of ROGD.
Archives of Sexual Behavior is the official publication of the International Academy of Sex Research, which tweeted on April 19:
The episode prompted a May 5 “Open Letter in Support of Dr. Kenneth Zucker and the Need to Promote Robust Scientific Debate” from the Foundation Against Intolerance and Racism that has now been signed by nearly 2000 people.
On May 10, the following publisher’s note was added to the article:
“readers are alerted that concerns have been raised regarding methodology as described in this article. The publisher is currently investigating this matter and a further response will follow the conclusion of this investigation.
Six days later, the publisher removed the article’s supplementary information “due to a lack of documented consent by study participants.”
The story may feel familiar to readers who recall what happened to another paper in 2018. In that paper, Brown University’s Lisa Littman coined the term ROGD. Following a backlash, Brown took down a press release touting the results, and the paper was eventually republished with corrections.
Bailey has been accused of mistreating transgender research participants, but an investigation by bioethicist Alice Dreger found that of the many accusations, “almost none appear to have been legitimate.”
In a post on UnHerd earlier this month, Bailey responded to the reported concerns about the study lacking approval by an Institutional Review Board (IRB), and that the way the participants were recruited biased the results.
IRB approval was not necessary, Bailey wrote, because Suzanna Diaz, the first author who collected the data, was not affiliated with an institution that required it. “Suzanna Diaz” is a pseudonym for “the mother of a gender dysphoric child she believes has ROGD” who wishes to remain anonymous for the sake of her family, Bailey wrote.
The paper included the following statement about its ethical approval:
“The first author and creator of the survey is not affiliated with any university or hospital. Thus, she did not seek approval from an IRB. After seeing a presentation of preliminary survey results by the first author, the second author suggested the data to be analyzed and submitted as an academic article (he was not involved in collecting the data). The second author consulted with his university’s IRB, who declined to certify the study because data were already collected. However, they advised that publishing the results was likely ethical provided data were deidentified. Editor’s note: After I reviewed the manuscript, I concluded that its publication is ethically appropriate, consistent with Springer policy.”
In his UnHerd post, Bailey quoted from the journal’s submission guidelines:
“If a study has not been granted ethics committee approval prior to commencing, retrospective ethics approval usually cannot be obtained and it may not be possible to consider the manuscript for peer review. The decision on whether to proceed to peer review in such cases is at the Editor’s discretion.”
“Regarding the methodological limitations of the study, these were addressed forthrightly and thoroughly in our article,” Bailey wrote.
Adam Marcus, a cofounder of Retraction Watch, is an editor at this news organization.
A version of this article first appeared on RetractionWatch.com.
The move is “due to concerns about lack of informed consent,” according to tweets by one of the paper’s authors.
The article, “Rapid Onset Gender Dysphoria: Parent Reports on 1655 Possible Cases,” was published in March in the Archives of Sexual Behavior. It has not been cited in the scientific literature, according to Clarivate’s Web of Science, but Altmetric, which tracks the online attention papers receive, ranks the article in the top 1% of all articles of a similar age.
Rapid Onset Gender Dysphoria (ROGD) is, the article stated, a “controversial theory” that “common cultural beliefs, values, and preoccupations cause some adolescents (especially female adolescents) to attribute their social problems, feelings, and mental health issues to gender dysphoria,” and that “youth with ROGD falsely believe that they are transgender,” in part due to social influences.
Michael Bailey, a psychology professor at Northwestern University in Evanston, Ill., and the paper’s corresponding author, tweeted:
Bailey told Retraction Watch that he would “respond when [he] can” to our request for comment, following “new developments on our end.” Neither Springer Nature nor Kenneth Zucker, editor in chief of Archives of Sexual Behavior, has responded to similar requests.
The paper reported the results of a survey of parents who contacted the website ParentsofROGDKids.com, with which the first author is affiliated. According to the abstract, the authors found:
“Pre-existing mental health issues were common, and youths with these issues were more likely than those without them to have socially and medically transitioned. Parents reported that they had often felt pressured by clinicians to affirm their AYA [adolescent and young adult] child’s new gender and support their transition. According to the parents, AYA children’s mental health deteriorated considerably after social transition.”
Soon after publication, the paper attracted criticism that its method of gathering study participants was biased, and that the authors ignored information that didn’t support the theory of ROGD.
Archives of Sexual Behavior is the official publication of the International Academy of Sex Research, which tweeted on April 19:
The episode prompted a May 5 “Open Letter in Support of Dr. Kenneth Zucker and the Need to Promote Robust Scientific Debate” from the Foundation Against Intolerance and Racism that has now been signed by nearly 2000 people.
On May 10, the following publisher’s note was added to the article:
“readers are alerted that concerns have been raised regarding methodology as described in this article. The publisher is currently investigating this matter and a further response will follow the conclusion of this investigation.
Six days later, the publisher removed the article’s supplementary information “due to a lack of documented consent by study participants.”
The story may feel familiar to readers who recall what happened to another paper in 2018. In that paper, Brown University’s Lisa Littman coined the term ROGD. Following a backlash, Brown took down a press release touting the results, and the paper was eventually republished with corrections.
Bailey has been accused of mistreating transgender research participants, but an investigation by bioethicist Alice Dreger found that of the many accusations, “almost none appear to have been legitimate.”
In a post on UnHerd earlier this month, Bailey responded to the reported concerns about the study lacking approval by an Institutional Review Board (IRB), and that the way the participants were recruited biased the results.
IRB approval was not necessary, Bailey wrote, because Suzanna Diaz, the first author who collected the data, was not affiliated with an institution that required it. “Suzanna Diaz” is a pseudonym for “the mother of a gender dysphoric child she believes has ROGD” who wishes to remain anonymous for the sake of her family, Bailey wrote.
The paper included the following statement about its ethical approval:
“The first author and creator of the survey is not affiliated with any university or hospital. Thus, she did not seek approval from an IRB. After seeing a presentation of preliminary survey results by the first author, the second author suggested the data to be analyzed and submitted as an academic article (he was not involved in collecting the data). The second author consulted with his university’s IRB, who declined to certify the study because data were already collected. However, they advised that publishing the results was likely ethical provided data were deidentified. Editor’s note: After I reviewed the manuscript, I concluded that its publication is ethically appropriate, consistent with Springer policy.”
In his UnHerd post, Bailey quoted from the journal’s submission guidelines:
“If a study has not been granted ethics committee approval prior to commencing, retrospective ethics approval usually cannot be obtained and it may not be possible to consider the manuscript for peer review. The decision on whether to proceed to peer review in such cases is at the Editor’s discretion.”
“Regarding the methodological limitations of the study, these were addressed forthrightly and thoroughly in our article,” Bailey wrote.
Adam Marcus, a cofounder of Retraction Watch, is an editor at this news organization.
A version of this article first appeared on RetractionWatch.com.
Management of patients with neuromuscular weakness: The latest CHEST guideline
Patients with neuromuscular diseases (NMD) face an increased risk of respiratory muscle weakness, which can contribute to various health problems. These include chronic respiratory failure, sleep-related breathing disorders, sialorrhea, and reduced cough effectiveness. In collaboration with AASM, AARC, and ATS, CHEST has developed guidelines to help clinicians manage patients with NMD. using the population, intervention, comparator, and outcome (PICO) format using the GRADE (Grading of Recommendations, Assessment, Development, and Evaluations) methodology.
A few of the key recommendations are as follows:
1. Addressing the use and timing of pulmonary function tests (PFT), the panel suggests measuring vital capacity (FVC or SVC), MIP/MEP, SNIP, or PCF in patients with NMD every 6 months.
2. For the detection of respiratory failure and sleep-related breathing disorders in symptomatic patients with NMD who have normal PFT and overnight oximetry (ONO), the panel suggested that clinicians consider polysomnography (PSG) to assess whether noninvasive ventilation (NIV) would be beneficial. Adult patients do not have to have PSG to manage NMD if the PFT or ONO criteria support using NIV.
3. The panel recommends the use of NIV for the treatment of respiratory failure. To guide the initiation of NIV, clinicians can use any fall in FVC to < 80% of predicted with symptoms or FVC to < 50% of predicted without symptoms or SNIP/MIP to < –40 cm H2O or hypercapnia. The panel recommended individualizing treatment.
4. The panel suggested mouth piece ventilation (MPV) for daytime ventilatory support in patients with preserved bulbar function. Its desirable effects include delaying or avoiding tracheostomy and improving speech, cough effectiveness, and coordination of breathing and swallowing.
5. Invasive home mechanical ventilation (MV) by tracheostomy was identified as an acceptable option for patients with progressive respiratory failure, particularly those who were unable to clear secretions. Because of the high costs and caregiver burden, the guideline highlights the need to consider patient preferences, tolerability, the ability to maintain mouthpiece ventilation, and the availability of resources when choosing an appropriate treatment option.
6. The panel suggested practicing clinicians address the management of sialorrhea and airway clearance techniques in patients with NMD, as they face the risk of aspiration and pneumonia. For sialorrhea, the panel suggests starting with a trial of anticholinergic agents, as they are inexpensive and readily available. The panel also provided advice on botulinum toxin therapy and radiation therapy, which have limited data and should be reserved for experienced centers.
7. The panel reviewed data on airway clearance techniques, including glossopharyngeal breathing (GPB), mechanical insufflation-exsufflation (MI-E), also commonly known as cough-assist device, manually assisted cough, lung volume recruitment (LVR) by air stacking, and high-frequency chest wall oscillation (HFCWO). The panel suggested using airway clearance techniques based on local resources, expertise, and shared decision-making with patients.
The panel stressed the importance of respect for patient preferences, treatment goals, and quality of life considerations. The panel emphasized the need to modernize and improve access to ventilatory support for patients with NMD and the role of shared decision-making in improving quality of life and long-term outcomes. The panel also suggests that randomized controlled trials in patients with NMD would help establish a higher grade of evidence.
Dr. Hubel and Dr. Khan are from the Division of Pulmonary Allergy and Critical Care Medicine, Oregon Health and Science University, Portland.
Reference
Khan A et al. Respiratory management of patients with neuromuscular weakness: An American College of Chest Physicians Clinical Practice Guideline and Expert Panel Report [published online ahead of print, 2023 Mar 13]. Chest. 2023;S0012-3692(23)00353-7. doi: 10.1016/j.chest.2023.03.011.
Patients with neuromuscular diseases (NMD) face an increased risk of respiratory muscle weakness, which can contribute to various health problems. These include chronic respiratory failure, sleep-related breathing disorders, sialorrhea, and reduced cough effectiveness. In collaboration with AASM, AARC, and ATS, CHEST has developed guidelines to help clinicians manage patients with NMD. using the population, intervention, comparator, and outcome (PICO) format using the GRADE (Grading of Recommendations, Assessment, Development, and Evaluations) methodology.
A few of the key recommendations are as follows:
1. Addressing the use and timing of pulmonary function tests (PFT), the panel suggests measuring vital capacity (FVC or SVC), MIP/MEP, SNIP, or PCF in patients with NMD every 6 months.
2. For the detection of respiratory failure and sleep-related breathing disorders in symptomatic patients with NMD who have normal PFT and overnight oximetry (ONO), the panel suggested that clinicians consider polysomnography (PSG) to assess whether noninvasive ventilation (NIV) would be beneficial. Adult patients do not have to have PSG to manage NMD if the PFT or ONO criteria support using NIV.
3. The panel recommends the use of NIV for the treatment of respiratory failure. To guide the initiation of NIV, clinicians can use any fall in FVC to < 80% of predicted with symptoms or FVC to < 50% of predicted without symptoms or SNIP/MIP to < –40 cm H2O or hypercapnia. The panel recommended individualizing treatment.
4. The panel suggested mouth piece ventilation (MPV) for daytime ventilatory support in patients with preserved bulbar function. Its desirable effects include delaying or avoiding tracheostomy and improving speech, cough effectiveness, and coordination of breathing and swallowing.
5. Invasive home mechanical ventilation (MV) by tracheostomy was identified as an acceptable option for patients with progressive respiratory failure, particularly those who were unable to clear secretions. Because of the high costs and caregiver burden, the guideline highlights the need to consider patient preferences, tolerability, the ability to maintain mouthpiece ventilation, and the availability of resources when choosing an appropriate treatment option.
6. The panel suggested practicing clinicians address the management of sialorrhea and airway clearance techniques in patients with NMD, as they face the risk of aspiration and pneumonia. For sialorrhea, the panel suggests starting with a trial of anticholinergic agents, as they are inexpensive and readily available. The panel also provided advice on botulinum toxin therapy and radiation therapy, which have limited data and should be reserved for experienced centers.
7. The panel reviewed data on airway clearance techniques, including glossopharyngeal breathing (GPB), mechanical insufflation-exsufflation (MI-E), also commonly known as cough-assist device, manually assisted cough, lung volume recruitment (LVR) by air stacking, and high-frequency chest wall oscillation (HFCWO). The panel suggested using airway clearance techniques based on local resources, expertise, and shared decision-making with patients.
The panel stressed the importance of respect for patient preferences, treatment goals, and quality of life considerations. The panel emphasized the need to modernize and improve access to ventilatory support for patients with NMD and the role of shared decision-making in improving quality of life and long-term outcomes. The panel also suggests that randomized controlled trials in patients with NMD would help establish a higher grade of evidence.
Dr. Hubel and Dr. Khan are from the Division of Pulmonary Allergy and Critical Care Medicine, Oregon Health and Science University, Portland.
Reference
Khan A et al. Respiratory management of patients with neuromuscular weakness: An American College of Chest Physicians Clinical Practice Guideline and Expert Panel Report [published online ahead of print, 2023 Mar 13]. Chest. 2023;S0012-3692(23)00353-7. doi: 10.1016/j.chest.2023.03.011.
Patients with neuromuscular diseases (NMD) face an increased risk of respiratory muscle weakness, which can contribute to various health problems. These include chronic respiratory failure, sleep-related breathing disorders, sialorrhea, and reduced cough effectiveness. In collaboration with AASM, AARC, and ATS, CHEST has developed guidelines to help clinicians manage patients with NMD. using the population, intervention, comparator, and outcome (PICO) format using the GRADE (Grading of Recommendations, Assessment, Development, and Evaluations) methodology.
A few of the key recommendations are as follows:
1. Addressing the use and timing of pulmonary function tests (PFT), the panel suggests measuring vital capacity (FVC or SVC), MIP/MEP, SNIP, or PCF in patients with NMD every 6 months.
2. For the detection of respiratory failure and sleep-related breathing disorders in symptomatic patients with NMD who have normal PFT and overnight oximetry (ONO), the panel suggested that clinicians consider polysomnography (PSG) to assess whether noninvasive ventilation (NIV) would be beneficial. Adult patients do not have to have PSG to manage NMD if the PFT or ONO criteria support using NIV.
3. The panel recommends the use of NIV for the treatment of respiratory failure. To guide the initiation of NIV, clinicians can use any fall in FVC to < 80% of predicted with symptoms or FVC to < 50% of predicted without symptoms or SNIP/MIP to < –40 cm H2O or hypercapnia. The panel recommended individualizing treatment.
4. The panel suggested mouth piece ventilation (MPV) for daytime ventilatory support in patients with preserved bulbar function. Its desirable effects include delaying or avoiding tracheostomy and improving speech, cough effectiveness, and coordination of breathing and swallowing.
5. Invasive home mechanical ventilation (MV) by tracheostomy was identified as an acceptable option for patients with progressive respiratory failure, particularly those who were unable to clear secretions. Because of the high costs and caregiver burden, the guideline highlights the need to consider patient preferences, tolerability, the ability to maintain mouthpiece ventilation, and the availability of resources when choosing an appropriate treatment option.
6. The panel suggested practicing clinicians address the management of sialorrhea and airway clearance techniques in patients with NMD, as they face the risk of aspiration and pneumonia. For sialorrhea, the panel suggests starting with a trial of anticholinergic agents, as they are inexpensive and readily available. The panel also provided advice on botulinum toxin therapy and radiation therapy, which have limited data and should be reserved for experienced centers.
7. The panel reviewed data on airway clearance techniques, including glossopharyngeal breathing (GPB), mechanical insufflation-exsufflation (MI-E), also commonly known as cough-assist device, manually assisted cough, lung volume recruitment (LVR) by air stacking, and high-frequency chest wall oscillation (HFCWO). The panel suggested using airway clearance techniques based on local resources, expertise, and shared decision-making with patients.
The panel stressed the importance of respect for patient preferences, treatment goals, and quality of life considerations. The panel emphasized the need to modernize and improve access to ventilatory support for patients with NMD and the role of shared decision-making in improving quality of life and long-term outcomes. The panel also suggests that randomized controlled trials in patients with NMD would help establish a higher grade of evidence.
Dr. Hubel and Dr. Khan are from the Division of Pulmonary Allergy and Critical Care Medicine, Oregon Health and Science University, Portland.
Reference
Khan A et al. Respiratory management of patients with neuromuscular weakness: An American College of Chest Physicians Clinical Practice Guideline and Expert Panel Report [published online ahead of print, 2023 Mar 13]. Chest. 2023;S0012-3692(23)00353-7. doi: 10.1016/j.chest.2023.03.011.
Did an unfair system help ADAURA win on overall survival?
Barry Bonds and Roger Clemens are two world-class baseball players who played well enough to earn enduring respect and admiration. However, their reputations have been permanently tainted by their use of performance-enhancing drugs. Although they are both undeniably gifted, we’ll never know where their natural talent ended and their unfair advantage began.
The medical oncology version of this scenario played out in front of our eyes at the ASCO 2023 Plenary Session featuring the ADAURA trial. In this case, the unfair advantage was clear: Nearly two-thirds of patients in the control arm did not cross over to a standard-of-care treatment at relapse.
The ADAURA trial tested the value of the third-generation oral EGFR inhibitor osimertinib vs. placebo for up to 3 years in patients with a resected stage IB-IIIA non–small cell lung cancer (NSCLC) harboring an activating EGFR mutation. Initially presented in the ASCO 2020 Plenary Session, the preliminary analysis for ADAURA demonstrated a remarkably favorable improvement in disease-free survival (DFS) in the osimertinib arm, which led to its prompt Food and Drug Administration approval in this setting.
At the time, I was among the more vocal critics of the fanfare around this trial. The DFS improvement was impressive but, in this context, represented a low threshold for FDA approval. We already knew that prior trials of other, less effective adjuvant EGFR inhibitors routinely improved DFS but ultimately failed to improve overall survival.
Although in some cases, a DFS benefit can be sufficient to warrant changing practice, I would argue that overall survival is the most critical endpoint in a curative setting by a wide margin. I would also argue that cost should be a consideration for a drug priced at $440,000 over 3 years in the United States. At the very least, we – patients, oncologists, payers – should want to clarify what we get for $440,000 per patient, especially if that money could be better spent on other things.
Of note, we need to know whether the same overall survival may be achieved in this setting by treating only patients whose disease relapses, avoiding both the cost and toxicity of continuous treatment.
The relevance of this question became even more acute when an updated version of the ADAURA trial showed that the DFS benefit from osimertinib began to erode immediately after patients completed active treatment. Although the DFS benefit remained excellent,
The overall survival data – the critical test in my mind – were presented at the ASCO Plenary Session. The results were highly positive, with a hazard ratio for overall survival of 0.49 and a similar benefit observed across all eligible disease stages.
As with the presentation of the DFS data in 2020, these results were accompanied by adulation during the session and fawning in the media. However, a subset of people in the audience, and on Twitter, voiced a major concern: In the control arm, only 38.5% of the patients whose disease had relapsed (79 of 205) ever received osimertinib.
Post-protocol treatment included reassurances that patients in the control arm were offered crossover to osimertinib, but this only occurred starting in April 2020 and only when the treating investigator requested it.
The fact that only a minority of patients in the control arm ever received osimertinib means that ADAURA is not a trial that tests adjuvant osimertinib to osimertinib at relapse, the prevailing standard of care in the United States and the preferred treatment in this setting, based on NCCN guidelines for patients with relapsed/metastatic EGFR mutation–positive NSCLC since the FDA approval in April 2018.
The change in standard of care in the United States and some other countries did not lead to an amendment in the trial, based on the argument that the trial was designed with DFS as the primary endpoint and that patients in the control arm are effectively off trial at relapse. That means patients would receive their country’s standard of care, which may be below, or different from, the standard in the United States or other parts of the world.
While defensible, others considered the low rate of osimertinib delivery in the control arm a serious flaw in the trial design and arguably an ethical problem.
Given this trial design, it’s important to question whether the trial magnified the difference in overall survival between the two arms compared with the standard of care in countries where adjuvant osimertinib will ultimately be marketed. Although I strongly suspect that the overall survival difference would have been significant without the disparity in access to osimertinib in the control arm, we will never know the magnitude of that difference.
With the current design, the trial demonstrates that osimertinib is associated with improved survival in 100% of patients with EGFR mutation–positive NSCLC who receive the agent vs. 38.5% of patients receiving it at some point after relapse.
At the end of the day, ADAURA followed conventional trial rules, which led to a windfall of accolades at the cost of suboptimal care for many of the patients randomly assigned to the control arm.
We need to decide as an oncology community whether we want to accept a system that confers rewards for stakeholders at the expense of patients enrolled in the trial.
We have developed a system that not only permits but depends on global trials enrolling many patients from countries with staging and off-protocol oncology care below standards of care in other parts of the world – effectively condoning and perpetuating disparities in optimal care globally. I am also saddened that some of the most respected leaders in our field have become upset when I question the ethics of accepting this system, one that I believe we have agency to change.
The question here is not whether osimertinib is a good drug; it is remarkably effective for patients with EGFR mutation–positive NSCLC. The question is how to design trials in a fair and balanced way that doesn’t compromise patient care or ethical standards.
If people think my assessment is too harsh, I openly welcome debate.
Bottom line: The ADAURA trial lays bare deeper problems with clinical trial design, and I would challenge readers to reflect on our clinical trial culture in oncology, which offers a system of rules that rewards denying the best identified care for patients on our clinical trials.
At the very least, should we celebrate these wins without fully acknowledging these problems?
Dr. West is clinical associate professor, department of medical oncology, City of Hope Comprehensive Cancer Care, Duarte, Calif. He reported conflicts of interest with Bristol-Myers Squibb, Boehringer Ingelheim, Spectrum, AstraZeneca, Celgene, Genentech/Roche, Pfizer, Merck, and Eli Lilly.
A version of this article first appeared on Medscape.com.
Barry Bonds and Roger Clemens are two world-class baseball players who played well enough to earn enduring respect and admiration. However, their reputations have been permanently tainted by their use of performance-enhancing drugs. Although they are both undeniably gifted, we’ll never know where their natural talent ended and their unfair advantage began.
The medical oncology version of this scenario played out in front of our eyes at the ASCO 2023 Plenary Session featuring the ADAURA trial. In this case, the unfair advantage was clear: Nearly two-thirds of patients in the control arm did not cross over to a standard-of-care treatment at relapse.
The ADAURA trial tested the value of the third-generation oral EGFR inhibitor osimertinib vs. placebo for up to 3 years in patients with a resected stage IB-IIIA non–small cell lung cancer (NSCLC) harboring an activating EGFR mutation. Initially presented in the ASCO 2020 Plenary Session, the preliminary analysis for ADAURA demonstrated a remarkably favorable improvement in disease-free survival (DFS) in the osimertinib arm, which led to its prompt Food and Drug Administration approval in this setting.
At the time, I was among the more vocal critics of the fanfare around this trial. The DFS improvement was impressive but, in this context, represented a low threshold for FDA approval. We already knew that prior trials of other, less effective adjuvant EGFR inhibitors routinely improved DFS but ultimately failed to improve overall survival.
Although in some cases, a DFS benefit can be sufficient to warrant changing practice, I would argue that overall survival is the most critical endpoint in a curative setting by a wide margin. I would also argue that cost should be a consideration for a drug priced at $440,000 over 3 years in the United States. At the very least, we – patients, oncologists, payers – should want to clarify what we get for $440,000 per patient, especially if that money could be better spent on other things.
Of note, we need to know whether the same overall survival may be achieved in this setting by treating only patients whose disease relapses, avoiding both the cost and toxicity of continuous treatment.
The relevance of this question became even more acute when an updated version of the ADAURA trial showed that the DFS benefit from osimertinib began to erode immediately after patients completed active treatment. Although the DFS benefit remained excellent,
The overall survival data – the critical test in my mind – were presented at the ASCO Plenary Session. The results were highly positive, with a hazard ratio for overall survival of 0.49 and a similar benefit observed across all eligible disease stages.
As with the presentation of the DFS data in 2020, these results were accompanied by adulation during the session and fawning in the media. However, a subset of people in the audience, and on Twitter, voiced a major concern: In the control arm, only 38.5% of the patients whose disease had relapsed (79 of 205) ever received osimertinib.
Post-protocol treatment included reassurances that patients in the control arm were offered crossover to osimertinib, but this only occurred starting in April 2020 and only when the treating investigator requested it.
The fact that only a minority of patients in the control arm ever received osimertinib means that ADAURA is not a trial that tests adjuvant osimertinib to osimertinib at relapse, the prevailing standard of care in the United States and the preferred treatment in this setting, based on NCCN guidelines for patients with relapsed/metastatic EGFR mutation–positive NSCLC since the FDA approval in April 2018.
The change in standard of care in the United States and some other countries did not lead to an amendment in the trial, based on the argument that the trial was designed with DFS as the primary endpoint and that patients in the control arm are effectively off trial at relapse. That means patients would receive their country’s standard of care, which may be below, or different from, the standard in the United States or other parts of the world.
While defensible, others considered the low rate of osimertinib delivery in the control arm a serious flaw in the trial design and arguably an ethical problem.
Given this trial design, it’s important to question whether the trial magnified the difference in overall survival between the two arms compared with the standard of care in countries where adjuvant osimertinib will ultimately be marketed. Although I strongly suspect that the overall survival difference would have been significant without the disparity in access to osimertinib in the control arm, we will never know the magnitude of that difference.
With the current design, the trial demonstrates that osimertinib is associated with improved survival in 100% of patients with EGFR mutation–positive NSCLC who receive the agent vs. 38.5% of patients receiving it at some point after relapse.
At the end of the day, ADAURA followed conventional trial rules, which led to a windfall of accolades at the cost of suboptimal care for many of the patients randomly assigned to the control arm.
We need to decide as an oncology community whether we want to accept a system that confers rewards for stakeholders at the expense of patients enrolled in the trial.
We have developed a system that not only permits but depends on global trials enrolling many patients from countries with staging and off-protocol oncology care below standards of care in other parts of the world – effectively condoning and perpetuating disparities in optimal care globally. I am also saddened that some of the most respected leaders in our field have become upset when I question the ethics of accepting this system, one that I believe we have agency to change.
The question here is not whether osimertinib is a good drug; it is remarkably effective for patients with EGFR mutation–positive NSCLC. The question is how to design trials in a fair and balanced way that doesn’t compromise patient care or ethical standards.
If people think my assessment is too harsh, I openly welcome debate.
Bottom line: The ADAURA trial lays bare deeper problems with clinical trial design, and I would challenge readers to reflect on our clinical trial culture in oncology, which offers a system of rules that rewards denying the best identified care for patients on our clinical trials.
At the very least, should we celebrate these wins without fully acknowledging these problems?
Dr. West is clinical associate professor, department of medical oncology, City of Hope Comprehensive Cancer Care, Duarte, Calif. He reported conflicts of interest with Bristol-Myers Squibb, Boehringer Ingelheim, Spectrum, AstraZeneca, Celgene, Genentech/Roche, Pfizer, Merck, and Eli Lilly.
A version of this article first appeared on Medscape.com.
Barry Bonds and Roger Clemens are two world-class baseball players who played well enough to earn enduring respect and admiration. However, their reputations have been permanently tainted by their use of performance-enhancing drugs. Although they are both undeniably gifted, we’ll never know where their natural talent ended and their unfair advantage began.
The medical oncology version of this scenario played out in front of our eyes at the ASCO 2023 Plenary Session featuring the ADAURA trial. In this case, the unfair advantage was clear: Nearly two-thirds of patients in the control arm did not cross over to a standard-of-care treatment at relapse.
The ADAURA trial tested the value of the third-generation oral EGFR inhibitor osimertinib vs. placebo for up to 3 years in patients with a resected stage IB-IIIA non–small cell lung cancer (NSCLC) harboring an activating EGFR mutation. Initially presented in the ASCO 2020 Plenary Session, the preliminary analysis for ADAURA demonstrated a remarkably favorable improvement in disease-free survival (DFS) in the osimertinib arm, which led to its prompt Food and Drug Administration approval in this setting.
At the time, I was among the more vocal critics of the fanfare around this trial. The DFS improvement was impressive but, in this context, represented a low threshold for FDA approval. We already knew that prior trials of other, less effective adjuvant EGFR inhibitors routinely improved DFS but ultimately failed to improve overall survival.
Although in some cases, a DFS benefit can be sufficient to warrant changing practice, I would argue that overall survival is the most critical endpoint in a curative setting by a wide margin. I would also argue that cost should be a consideration for a drug priced at $440,000 over 3 years in the United States. At the very least, we – patients, oncologists, payers – should want to clarify what we get for $440,000 per patient, especially if that money could be better spent on other things.
Of note, we need to know whether the same overall survival may be achieved in this setting by treating only patients whose disease relapses, avoiding both the cost and toxicity of continuous treatment.
The relevance of this question became even more acute when an updated version of the ADAURA trial showed that the DFS benefit from osimertinib began to erode immediately after patients completed active treatment. Although the DFS benefit remained excellent,
The overall survival data – the critical test in my mind – were presented at the ASCO Plenary Session. The results were highly positive, with a hazard ratio for overall survival of 0.49 and a similar benefit observed across all eligible disease stages.
As with the presentation of the DFS data in 2020, these results were accompanied by adulation during the session and fawning in the media. However, a subset of people in the audience, and on Twitter, voiced a major concern: In the control arm, only 38.5% of the patients whose disease had relapsed (79 of 205) ever received osimertinib.
Post-protocol treatment included reassurances that patients in the control arm were offered crossover to osimertinib, but this only occurred starting in April 2020 and only when the treating investigator requested it.
The fact that only a minority of patients in the control arm ever received osimertinib means that ADAURA is not a trial that tests adjuvant osimertinib to osimertinib at relapse, the prevailing standard of care in the United States and the preferred treatment in this setting, based on NCCN guidelines for patients with relapsed/metastatic EGFR mutation–positive NSCLC since the FDA approval in April 2018.
The change in standard of care in the United States and some other countries did not lead to an amendment in the trial, based on the argument that the trial was designed with DFS as the primary endpoint and that patients in the control arm are effectively off trial at relapse. That means patients would receive their country’s standard of care, which may be below, or different from, the standard in the United States or other parts of the world.
While defensible, others considered the low rate of osimertinib delivery in the control arm a serious flaw in the trial design and arguably an ethical problem.
Given this trial design, it’s important to question whether the trial magnified the difference in overall survival between the two arms compared with the standard of care in countries where adjuvant osimertinib will ultimately be marketed. Although I strongly suspect that the overall survival difference would have been significant without the disparity in access to osimertinib in the control arm, we will never know the magnitude of that difference.
With the current design, the trial demonstrates that osimertinib is associated with improved survival in 100% of patients with EGFR mutation–positive NSCLC who receive the agent vs. 38.5% of patients receiving it at some point after relapse.
At the end of the day, ADAURA followed conventional trial rules, which led to a windfall of accolades at the cost of suboptimal care for many of the patients randomly assigned to the control arm.
We need to decide as an oncology community whether we want to accept a system that confers rewards for stakeholders at the expense of patients enrolled in the trial.
We have developed a system that not only permits but depends on global trials enrolling many patients from countries with staging and off-protocol oncology care below standards of care in other parts of the world – effectively condoning and perpetuating disparities in optimal care globally. I am also saddened that some of the most respected leaders in our field have become upset when I question the ethics of accepting this system, one that I believe we have agency to change.
The question here is not whether osimertinib is a good drug; it is remarkably effective for patients with EGFR mutation–positive NSCLC. The question is how to design trials in a fair and balanced way that doesn’t compromise patient care or ethical standards.
If people think my assessment is too harsh, I openly welcome debate.
Bottom line: The ADAURA trial lays bare deeper problems with clinical trial design, and I would challenge readers to reflect on our clinical trial culture in oncology, which offers a system of rules that rewards denying the best identified care for patients on our clinical trials.
At the very least, should we celebrate these wins without fully acknowledging these problems?
Dr. West is clinical associate professor, department of medical oncology, City of Hope Comprehensive Cancer Care, Duarte, Calif. He reported conflicts of interest with Bristol-Myers Squibb, Boehringer Ingelheim, Spectrum, AstraZeneca, Celgene, Genentech/Roche, Pfizer, Merck, and Eli Lilly.
A version of this article first appeared on Medscape.com.
Wildfire smoke and air quality: How long could health effects last?
People with moderate to severe asthma, chronic obstructive pulmonary disease, and other risk factors are used to checking air quality warnings before heading outside. But this situation is anything but typical.
Even people not normally at risk can have burning eyes, a runny nose, and a hard time breathing. These are among the symptoms to watch for as health effects of wildfire smoke. Special considerations should be made for people with heart disease, lung disease, and other conditions that put them at increased risk. Those affected can also have trouble sleeping, anxiety, and ongoing mental health issues.
The smoke will stick around the next few days, possibly clearing out early next week when the winds change direction, Weather Channel meteorologist Ari Sarsalari predicted June 8. But that doesn’t mean any physical or mental health effects will clear up as quickly.
“We are seeing dramatic increases in air pollution, and we are seeing increases in patients coming to the ED and the hospital. We expect that this will increase in the days ahead,” said Meredith McCormack, MD, MHS, a volunteer medical spokesperson for the American Lung Association.
“The air quality in our area – Baltimore – and other surrounding areas is not healthy for anyone,” said Dr. McCormack, who specializes in pulmonary and critical care medicine at Johns Hopkins University, Baltimore.
How serious are the health warnings?
Residents of California might be more familiar with the hazards of wildfire smoke, but this is a novel experience for many people along the East Coast. Air quality advisories are popping up on cellphones for people living in Boston, New York, and as far south as Northern Virginia. What should the estimated 75 million to 128 million affected Americans do?
We asked experts to weigh in on when it’s safe or not safe to spend time outside, when to seek medical help, and the best ways for people to protect themselves.
“It’s important to stay indoors and close all windows to reduce exposure to smoke from wildfires. It’s also essential to stay away from any windows that may not have a good seal, in order to minimize any potential exposure to smoke,” said Robert Glatter, MD, editor at large for Medscape Emergency Medicine and an emergency medicine doctor at Lenox Hill Hospital/Northwell Health in New York.
Dr. Glatter noted that placing moist towels under doors and sealing leaking windows can help.
Monitor your symptoms, and contact your doctor or go to urgent care, Dr. McCormack advised, if you see any increase in concerning symptoms. These include shortness of breath, coughing, chest tightness, or wheezing. Also make sure you take recommended medications and have enough on hand, she said.
Fine particles, big concerns
The weather is warming in many parts of the country, and that can mean air conditioning. Adding a MERV 13 filter to a central air conditioning system could reduce exposure to wildfire smoke. Using a portable indoor air purifier with a HEPA filter also can help people without central air conditioning. The filter can help remove small particles in the air but must be replaced regularly.
Smoke from wildfires contains multiple toxins, including heavy metals, carcinogens, and fine particulate matter (PM) under 2.5 microns. Dr. Glatter explained that these particles are about 100 times thinner than a human hair. Because of their size, they can embed deeper into the airways in the lungs and trigger chronic inflammation.
“This has also been linked to increased rates of lung cancer and brain tumors,” he said, based on a 2022 study in Canada.
The effects of smoke from wildfires can continue for many years. After the 2014 Hazelwood coal mine fire, emergency department visits for respiratory conditions and cardiovascular complaints remained higher for up to 2-5 years later, Dr. Glatter said. Again, large quantities of fine particulate matter in the smoke, less than 2.5 microns (PM 2.5), was to blame.
Exposure to smoke from wildfires during pregnancy has also been linked to abnormal fetal growth, preterm birth, as well as low birth weight, a January 2023 preprint on MedRxiv suggested.
Time to wear a mask again?
A properly fitted N95 mask will be the best approach to lessen exposure to smoke from wildfires, “but by itself cannot eliminate all of the risk,” Dr. Glatter said. Surgical masks can add minimal protection, and cloth masks will not provide any significant protection against the damaging effects of smoke from wildfires.
KN95 masks tend to be more comfortable to wear than N95s. But leakage often occurs that can make this type of protection less effective, Dr. Glatter said.
“Masks are important if you need to go outdoors,” Dr. McCormack said. Also, if you’re traveling by car, set the air conditioning system to recirculate to filter the air inside the vehicle, she recommended.
What does that number mean?
The federal government monitors air quality nationwide. In case you’re unfamiliar, the U.S. Air Quality Index includes a color-coded scale for ozone levels and particle pollution, the main concern from wildfire smoke. The lowest risk is the Green or satisfactory air quality category, where air pollution poses little or no risk, with an Index number from 0 to 50.
The index gets progressively more serious, from Yellow for moderate risk (51-100) up to a Maroon category, a hazardous range of 300 or higher on the index. When a Maroon advisory is issued, it means an emergency health warning where “everyone is more likely to be affected.”
How do you know if your outside air is polluted? Your local Air Quality Index (AQI) from the EPA can help. It’s a scale of 0 to 500, and the greater the number, the more harmful pollution in the air. It has six levels: good, moderate, unhealthy for sensitive groups, unhealthy, very unhealthy, and hazardous. You can find it at AirNow.gov.
New York is under an air quality alert until midnight Friday with a current “unhealthy” Index report of 200. The city recorded its worst-ever air quality on Wednesday. The New York State Department of Environmental Conservation warns that fine particulate levels – small particles that can enter a person’s lungs – are the biggest concern.
AirNow.gov warns that western New England down to Washington has air quality in the three worst categories – ranging from unhealthy to very unhealthy and hazardous. The ten worst locations on the U.S. Air Quality Index as of 10 a.m. ET on June 8 include the Wilmington, Del., area with an Index of 241, or “very unhealthy.”
Other “very unhealthy” locations have the following Index readings:
- 244: Suburban Washington/Maryland.
- 252: Southern coastal New Jersey.
- 252: Kent County, Del.
- 270: Philadelphia.
- 291: Greater New Castle County, Del.
- 293: Northern Virginia.
- 293: Metropolitan Washington.
These two locations are in the “hazardous” or health emergency warning category:
- 309: Lehigh Valley, Pa.
- 399: Susquehanna Valley, Pa.
To check an air quality advisory in your area, enter your ZIP code at AirNow.gov.
A version of this article first appeared on WebMD.com.
People with moderate to severe asthma, chronic obstructive pulmonary disease, and other risk factors are used to checking air quality warnings before heading outside. But this situation is anything but typical.
Even people not normally at risk can have burning eyes, a runny nose, and a hard time breathing. These are among the symptoms to watch for as health effects of wildfire smoke. Special considerations should be made for people with heart disease, lung disease, and other conditions that put them at increased risk. Those affected can also have trouble sleeping, anxiety, and ongoing mental health issues.
The smoke will stick around the next few days, possibly clearing out early next week when the winds change direction, Weather Channel meteorologist Ari Sarsalari predicted June 8. But that doesn’t mean any physical or mental health effects will clear up as quickly.
“We are seeing dramatic increases in air pollution, and we are seeing increases in patients coming to the ED and the hospital. We expect that this will increase in the days ahead,” said Meredith McCormack, MD, MHS, a volunteer medical spokesperson for the American Lung Association.
“The air quality in our area – Baltimore – and other surrounding areas is not healthy for anyone,” said Dr. McCormack, who specializes in pulmonary and critical care medicine at Johns Hopkins University, Baltimore.
How serious are the health warnings?
Residents of California might be more familiar with the hazards of wildfire smoke, but this is a novel experience for many people along the East Coast. Air quality advisories are popping up on cellphones for people living in Boston, New York, and as far south as Northern Virginia. What should the estimated 75 million to 128 million affected Americans do?
We asked experts to weigh in on when it’s safe or not safe to spend time outside, when to seek medical help, and the best ways for people to protect themselves.
“It’s important to stay indoors and close all windows to reduce exposure to smoke from wildfires. It’s also essential to stay away from any windows that may not have a good seal, in order to minimize any potential exposure to smoke,” said Robert Glatter, MD, editor at large for Medscape Emergency Medicine and an emergency medicine doctor at Lenox Hill Hospital/Northwell Health in New York.
Dr. Glatter noted that placing moist towels under doors and sealing leaking windows can help.
Monitor your symptoms, and contact your doctor or go to urgent care, Dr. McCormack advised, if you see any increase in concerning symptoms. These include shortness of breath, coughing, chest tightness, or wheezing. Also make sure you take recommended medications and have enough on hand, she said.
Fine particles, big concerns
The weather is warming in many parts of the country, and that can mean air conditioning. Adding a MERV 13 filter to a central air conditioning system could reduce exposure to wildfire smoke. Using a portable indoor air purifier with a HEPA filter also can help people without central air conditioning. The filter can help remove small particles in the air but must be replaced regularly.
Smoke from wildfires contains multiple toxins, including heavy metals, carcinogens, and fine particulate matter (PM) under 2.5 microns. Dr. Glatter explained that these particles are about 100 times thinner than a human hair. Because of their size, they can embed deeper into the airways in the lungs and trigger chronic inflammation.
“This has also been linked to increased rates of lung cancer and brain tumors,” he said, based on a 2022 study in Canada.
The effects of smoke from wildfires can continue for many years. After the 2014 Hazelwood coal mine fire, emergency department visits for respiratory conditions and cardiovascular complaints remained higher for up to 2-5 years later, Dr. Glatter said. Again, large quantities of fine particulate matter in the smoke, less than 2.5 microns (PM 2.5), was to blame.
Exposure to smoke from wildfires during pregnancy has also been linked to abnormal fetal growth, preterm birth, as well as low birth weight, a January 2023 preprint on MedRxiv suggested.
Time to wear a mask again?
A properly fitted N95 mask will be the best approach to lessen exposure to smoke from wildfires, “but by itself cannot eliminate all of the risk,” Dr. Glatter said. Surgical masks can add minimal protection, and cloth masks will not provide any significant protection against the damaging effects of smoke from wildfires.
KN95 masks tend to be more comfortable to wear than N95s. But leakage often occurs that can make this type of protection less effective, Dr. Glatter said.
“Masks are important if you need to go outdoors,” Dr. McCormack said. Also, if you’re traveling by car, set the air conditioning system to recirculate to filter the air inside the vehicle, she recommended.
What does that number mean?
The federal government monitors air quality nationwide. In case you’re unfamiliar, the U.S. Air Quality Index includes a color-coded scale for ozone levels and particle pollution, the main concern from wildfire smoke. The lowest risk is the Green or satisfactory air quality category, where air pollution poses little or no risk, with an Index number from 0 to 50.
The index gets progressively more serious, from Yellow for moderate risk (51-100) up to a Maroon category, a hazardous range of 300 or higher on the index. When a Maroon advisory is issued, it means an emergency health warning where “everyone is more likely to be affected.”
How do you know if your outside air is polluted? Your local Air Quality Index (AQI) from the EPA can help. It’s a scale of 0 to 500, and the greater the number, the more harmful pollution in the air. It has six levels: good, moderate, unhealthy for sensitive groups, unhealthy, very unhealthy, and hazardous. You can find it at AirNow.gov.
New York is under an air quality alert until midnight Friday with a current “unhealthy” Index report of 200. The city recorded its worst-ever air quality on Wednesday. The New York State Department of Environmental Conservation warns that fine particulate levels – small particles that can enter a person’s lungs – are the biggest concern.
AirNow.gov warns that western New England down to Washington has air quality in the three worst categories – ranging from unhealthy to very unhealthy and hazardous. The ten worst locations on the U.S. Air Quality Index as of 10 a.m. ET on June 8 include the Wilmington, Del., area with an Index of 241, or “very unhealthy.”
Other “very unhealthy” locations have the following Index readings:
- 244: Suburban Washington/Maryland.
- 252: Southern coastal New Jersey.
- 252: Kent County, Del.
- 270: Philadelphia.
- 291: Greater New Castle County, Del.
- 293: Northern Virginia.
- 293: Metropolitan Washington.
These two locations are in the “hazardous” or health emergency warning category:
- 309: Lehigh Valley, Pa.
- 399: Susquehanna Valley, Pa.
To check an air quality advisory in your area, enter your ZIP code at AirNow.gov.
A version of this article first appeared on WebMD.com.
People with moderate to severe asthma, chronic obstructive pulmonary disease, and other risk factors are used to checking air quality warnings before heading outside. But this situation is anything but typical.
Even people not normally at risk can have burning eyes, a runny nose, and a hard time breathing. These are among the symptoms to watch for as health effects of wildfire smoke. Special considerations should be made for people with heart disease, lung disease, and other conditions that put them at increased risk. Those affected can also have trouble sleeping, anxiety, and ongoing mental health issues.
The smoke will stick around the next few days, possibly clearing out early next week when the winds change direction, Weather Channel meteorologist Ari Sarsalari predicted June 8. But that doesn’t mean any physical or mental health effects will clear up as quickly.
“We are seeing dramatic increases in air pollution, and we are seeing increases in patients coming to the ED and the hospital. We expect that this will increase in the days ahead,” said Meredith McCormack, MD, MHS, a volunteer medical spokesperson for the American Lung Association.
“The air quality in our area – Baltimore – and other surrounding areas is not healthy for anyone,” said Dr. McCormack, who specializes in pulmonary and critical care medicine at Johns Hopkins University, Baltimore.
How serious are the health warnings?
Residents of California might be more familiar with the hazards of wildfire smoke, but this is a novel experience for many people along the East Coast. Air quality advisories are popping up on cellphones for people living in Boston, New York, and as far south as Northern Virginia. What should the estimated 75 million to 128 million affected Americans do?
We asked experts to weigh in on when it’s safe or not safe to spend time outside, when to seek medical help, and the best ways for people to protect themselves.
“It’s important to stay indoors and close all windows to reduce exposure to smoke from wildfires. It’s also essential to stay away from any windows that may not have a good seal, in order to minimize any potential exposure to smoke,” said Robert Glatter, MD, editor at large for Medscape Emergency Medicine and an emergency medicine doctor at Lenox Hill Hospital/Northwell Health in New York.
Dr. Glatter noted that placing moist towels under doors and sealing leaking windows can help.
Monitor your symptoms, and contact your doctor or go to urgent care, Dr. McCormack advised, if you see any increase in concerning symptoms. These include shortness of breath, coughing, chest tightness, or wheezing. Also make sure you take recommended medications and have enough on hand, she said.
Fine particles, big concerns
The weather is warming in many parts of the country, and that can mean air conditioning. Adding a MERV 13 filter to a central air conditioning system could reduce exposure to wildfire smoke. Using a portable indoor air purifier with a HEPA filter also can help people without central air conditioning. The filter can help remove small particles in the air but must be replaced regularly.
Smoke from wildfires contains multiple toxins, including heavy metals, carcinogens, and fine particulate matter (PM) under 2.5 microns. Dr. Glatter explained that these particles are about 100 times thinner than a human hair. Because of their size, they can embed deeper into the airways in the lungs and trigger chronic inflammation.
“This has also been linked to increased rates of lung cancer and brain tumors,” he said, based on a 2022 study in Canada.
The effects of smoke from wildfires can continue for many years. After the 2014 Hazelwood coal mine fire, emergency department visits for respiratory conditions and cardiovascular complaints remained higher for up to 2-5 years later, Dr. Glatter said. Again, large quantities of fine particulate matter in the smoke, less than 2.5 microns (PM 2.5), was to blame.
Exposure to smoke from wildfires during pregnancy has also been linked to abnormal fetal growth, preterm birth, as well as low birth weight, a January 2023 preprint on MedRxiv suggested.
Time to wear a mask again?
A properly fitted N95 mask will be the best approach to lessen exposure to smoke from wildfires, “but by itself cannot eliminate all of the risk,” Dr. Glatter said. Surgical masks can add minimal protection, and cloth masks will not provide any significant protection against the damaging effects of smoke from wildfires.
KN95 masks tend to be more comfortable to wear than N95s. But leakage often occurs that can make this type of protection less effective, Dr. Glatter said.
“Masks are important if you need to go outdoors,” Dr. McCormack said. Also, if you’re traveling by car, set the air conditioning system to recirculate to filter the air inside the vehicle, she recommended.
What does that number mean?
The federal government monitors air quality nationwide. In case you’re unfamiliar, the U.S. Air Quality Index includes a color-coded scale for ozone levels and particle pollution, the main concern from wildfire smoke. The lowest risk is the Green or satisfactory air quality category, where air pollution poses little or no risk, with an Index number from 0 to 50.
The index gets progressively more serious, from Yellow for moderate risk (51-100) up to a Maroon category, a hazardous range of 300 or higher on the index. When a Maroon advisory is issued, it means an emergency health warning where “everyone is more likely to be affected.”
How do you know if your outside air is polluted? Your local Air Quality Index (AQI) from the EPA can help. It’s a scale of 0 to 500, and the greater the number, the more harmful pollution in the air. It has six levels: good, moderate, unhealthy for sensitive groups, unhealthy, very unhealthy, and hazardous. You can find it at AirNow.gov.
New York is under an air quality alert until midnight Friday with a current “unhealthy” Index report of 200. The city recorded its worst-ever air quality on Wednesday. The New York State Department of Environmental Conservation warns that fine particulate levels – small particles that can enter a person’s lungs – are the biggest concern.
AirNow.gov warns that western New England down to Washington has air quality in the three worst categories – ranging from unhealthy to very unhealthy and hazardous. The ten worst locations on the U.S. Air Quality Index as of 10 a.m. ET on June 8 include the Wilmington, Del., area with an Index of 241, or “very unhealthy.”
Other “very unhealthy” locations have the following Index readings:
- 244: Suburban Washington/Maryland.
- 252: Southern coastal New Jersey.
- 252: Kent County, Del.
- 270: Philadelphia.
- 291: Greater New Castle County, Del.
- 293: Northern Virginia.
- 293: Metropolitan Washington.
These two locations are in the “hazardous” or health emergency warning category:
- 309: Lehigh Valley, Pa.
- 399: Susquehanna Valley, Pa.
To check an air quality advisory in your area, enter your ZIP code at AirNow.gov.
A version of this article first appeared on WebMD.com.
Halting active inflammation key in treating PIH
CHICAGO –
Dr. Desai, clinical assistant professor in the department of dermatology at the University of Texas Southwestern Medical Center, Dallas, spoke at the Pigmentary Disorders Exchange Symposium, provided by MedscapeLive!
Like all dermatologists, he said at the meeting, he sees lots of acne cases. However, PIH is often the presenting reason for the visit in his practice, which focuses predominantly on skin of color.
“Most of my patients come in not even worried about the acne,” he said. “They come in wanting me to fix the dark spots.”
Inflammation persists
Dermatologists, Dr. Desai said, should educate patients with active PIH resulting from acne or other diseases that even though the condition has been labeled post- inflammatory hyperpigmentation, the inflammation continues to be a problem.
He said, while patients may think PIH is “just scars,” the inflammation is still active and the condition needs to be treated from a skin-lightening perspective but, more importantly, with a focus on halting the inflammation. “If you were to biopsy the areas of hyperpigmentation, you would find a high density of active inflammatory behaviors still present in the skin,” he said.
When treating patients, it’s critical to first treat the underlying skin condition aggressively, he said. “Things like topical retinoids and azelaic acid mechanistically actually make a lot more sense for PIH than even hydroquinone, in some cases, because these therapies are actually anti-inflammatory for many of the diseases we treat.”
Dr. Desai noted that, in patients with darker skin tones, even diseases like seborrheic dermatitis and plaque psoriasis can result in PIH, while in patients with lighter skin tones, the same diseases may leave some residual postinflammatory erythema.
“I think it’s very important, particularly when you’re treating a darker skin–toned patient, to arrest the erythema early on to prevent that further worsening of hyperpigmentation,” he said.
Biopsies important
In cases of PIH, determining the best treatment requires finding out where the pigment is and how deep it is, Dr. Desai said.
He noted dermatologists are often worried about doing biopsies, particularly in patients with darker skin, because of the risk of scarring and keloid formation for those more prone to keloids. The preference is also for a therapeutic effect without using invasive procedures.
“But particularly with PIH, in patients who have been therapeutically challenging, I don’t hesitate to do very small biopsies – 2- and 3-mm punch biopsies – particularly if they are from the head and neck area.”
He suggests doing biopsies on part of the ear, lower jaw line, or the neck area, as these areas tend to heal nicely. “You don’t have to be so concerned about the scarring if you counsel appropriately,” he said.
The biopsy can be valuable in determining whether a very expensive treatment will reach the intended target.
Topical retinoids play an important role as anti-inflammatories for PIH, Dr. Desai said.
He gave an example of a patient with Fitzpatrick skin type IV or V with chronic acne and extensive PIH. “Are you going to effectively tell that patient to apply 4% hydroquinone triple-combination compound across 30 different areas of PIH on their face? The answer is that’s really not very efficient or effective.”
That’s why therapies, such as retinoids, that target the pathogenesis of PIH, particularly the inflammatory component, are important, he added.
Psychological burden
PIH comes with significant stigma and loss of quality of life loss that can last many years.
During another presentation at the meeting, Susan C. Taylor, MD, professor and vice chair of diversity, equity and inclusion in the department of dermatology, at the University of Pennsylvania, Philadelphia, pointed out that in a 2016 study of 324 patients in seven Asian countries, acne-related PIH lasted longer than 1 year in 65.2% of patients and 5 years or longer in 22.3%, significantly affecting their quality of life.
Dr. Desai added that, in a paper recently published in the British Journal of Dermatology, on the impact of postacne hyperpigmentation in patients, the authors pointed out that the reported prevalence of PIH in patients with acne ranges between 45.5% and 87.2%, depending on skin phototype, and that in most cases, PIH takes more than a year to fade.
“Studies have demonstrated that patients with acne and resulting scarring often face stigmatization, leading to quality of life impairment, social withdrawal and body image disorders, which can further contribute to higher risk for depression and social anxiety,” the paper’s authors wrote.
Dr. Desai reported no financial disclosures relevant to his talk.
CHICAGO –
Dr. Desai, clinical assistant professor in the department of dermatology at the University of Texas Southwestern Medical Center, Dallas, spoke at the Pigmentary Disorders Exchange Symposium, provided by MedscapeLive!
Like all dermatologists, he said at the meeting, he sees lots of acne cases. However, PIH is often the presenting reason for the visit in his practice, which focuses predominantly on skin of color.
“Most of my patients come in not even worried about the acne,” he said. “They come in wanting me to fix the dark spots.”
Inflammation persists
Dermatologists, Dr. Desai said, should educate patients with active PIH resulting from acne or other diseases that even though the condition has been labeled post- inflammatory hyperpigmentation, the inflammation continues to be a problem.
He said, while patients may think PIH is “just scars,” the inflammation is still active and the condition needs to be treated from a skin-lightening perspective but, more importantly, with a focus on halting the inflammation. “If you were to biopsy the areas of hyperpigmentation, you would find a high density of active inflammatory behaviors still present in the skin,” he said.
When treating patients, it’s critical to first treat the underlying skin condition aggressively, he said. “Things like topical retinoids and azelaic acid mechanistically actually make a lot more sense for PIH than even hydroquinone, in some cases, because these therapies are actually anti-inflammatory for many of the diseases we treat.”
Dr. Desai noted that, in patients with darker skin tones, even diseases like seborrheic dermatitis and plaque psoriasis can result in PIH, while in patients with lighter skin tones, the same diseases may leave some residual postinflammatory erythema.
“I think it’s very important, particularly when you’re treating a darker skin–toned patient, to arrest the erythema early on to prevent that further worsening of hyperpigmentation,” he said.
Biopsies important
In cases of PIH, determining the best treatment requires finding out where the pigment is and how deep it is, Dr. Desai said.
He noted dermatologists are often worried about doing biopsies, particularly in patients with darker skin, because of the risk of scarring and keloid formation for those more prone to keloids. The preference is also for a therapeutic effect without using invasive procedures.
“But particularly with PIH, in patients who have been therapeutically challenging, I don’t hesitate to do very small biopsies – 2- and 3-mm punch biopsies – particularly if they are from the head and neck area.”
He suggests doing biopsies on part of the ear, lower jaw line, or the neck area, as these areas tend to heal nicely. “You don’t have to be so concerned about the scarring if you counsel appropriately,” he said.
The biopsy can be valuable in determining whether a very expensive treatment will reach the intended target.
Topical retinoids play an important role as anti-inflammatories for PIH, Dr. Desai said.
He gave an example of a patient with Fitzpatrick skin type IV or V with chronic acne and extensive PIH. “Are you going to effectively tell that patient to apply 4% hydroquinone triple-combination compound across 30 different areas of PIH on their face? The answer is that’s really not very efficient or effective.”
That’s why therapies, such as retinoids, that target the pathogenesis of PIH, particularly the inflammatory component, are important, he added.
Psychological burden
PIH comes with significant stigma and loss of quality of life loss that can last many years.
During another presentation at the meeting, Susan C. Taylor, MD, professor and vice chair of diversity, equity and inclusion in the department of dermatology, at the University of Pennsylvania, Philadelphia, pointed out that in a 2016 study of 324 patients in seven Asian countries, acne-related PIH lasted longer than 1 year in 65.2% of patients and 5 years or longer in 22.3%, significantly affecting their quality of life.
Dr. Desai added that, in a paper recently published in the British Journal of Dermatology, on the impact of postacne hyperpigmentation in patients, the authors pointed out that the reported prevalence of PIH in patients with acne ranges between 45.5% and 87.2%, depending on skin phototype, and that in most cases, PIH takes more than a year to fade.
“Studies have demonstrated that patients with acne and resulting scarring often face stigmatization, leading to quality of life impairment, social withdrawal and body image disorders, which can further contribute to higher risk for depression and social anxiety,” the paper’s authors wrote.
Dr. Desai reported no financial disclosures relevant to his talk.
CHICAGO –
Dr. Desai, clinical assistant professor in the department of dermatology at the University of Texas Southwestern Medical Center, Dallas, spoke at the Pigmentary Disorders Exchange Symposium, provided by MedscapeLive!
Like all dermatologists, he said at the meeting, he sees lots of acne cases. However, PIH is often the presenting reason for the visit in his practice, which focuses predominantly on skin of color.
“Most of my patients come in not even worried about the acne,” he said. “They come in wanting me to fix the dark spots.”
Inflammation persists
Dermatologists, Dr. Desai said, should educate patients with active PIH resulting from acne or other diseases that even though the condition has been labeled post- inflammatory hyperpigmentation, the inflammation continues to be a problem.
He said, while patients may think PIH is “just scars,” the inflammation is still active and the condition needs to be treated from a skin-lightening perspective but, more importantly, with a focus on halting the inflammation. “If you were to biopsy the areas of hyperpigmentation, you would find a high density of active inflammatory behaviors still present in the skin,” he said.
When treating patients, it’s critical to first treat the underlying skin condition aggressively, he said. “Things like topical retinoids and azelaic acid mechanistically actually make a lot more sense for PIH than even hydroquinone, in some cases, because these therapies are actually anti-inflammatory for many of the diseases we treat.”
Dr. Desai noted that, in patients with darker skin tones, even diseases like seborrheic dermatitis and plaque psoriasis can result in PIH, while in patients with lighter skin tones, the same diseases may leave some residual postinflammatory erythema.
“I think it’s very important, particularly when you’re treating a darker skin–toned patient, to arrest the erythema early on to prevent that further worsening of hyperpigmentation,” he said.
Biopsies important
In cases of PIH, determining the best treatment requires finding out where the pigment is and how deep it is, Dr. Desai said.
He noted dermatologists are often worried about doing biopsies, particularly in patients with darker skin, because of the risk of scarring and keloid formation for those more prone to keloids. The preference is also for a therapeutic effect without using invasive procedures.
“But particularly with PIH, in patients who have been therapeutically challenging, I don’t hesitate to do very small biopsies – 2- and 3-mm punch biopsies – particularly if they are from the head and neck area.”
He suggests doing biopsies on part of the ear, lower jaw line, or the neck area, as these areas tend to heal nicely. “You don’t have to be so concerned about the scarring if you counsel appropriately,” he said.
The biopsy can be valuable in determining whether a very expensive treatment will reach the intended target.
Topical retinoids play an important role as anti-inflammatories for PIH, Dr. Desai said.
He gave an example of a patient with Fitzpatrick skin type IV or V with chronic acne and extensive PIH. “Are you going to effectively tell that patient to apply 4% hydroquinone triple-combination compound across 30 different areas of PIH on their face? The answer is that’s really not very efficient or effective.”
That’s why therapies, such as retinoids, that target the pathogenesis of PIH, particularly the inflammatory component, are important, he added.
Psychological burden
PIH comes with significant stigma and loss of quality of life loss that can last many years.
During another presentation at the meeting, Susan C. Taylor, MD, professor and vice chair of diversity, equity and inclusion in the department of dermatology, at the University of Pennsylvania, Philadelphia, pointed out that in a 2016 study of 324 patients in seven Asian countries, acne-related PIH lasted longer than 1 year in 65.2% of patients and 5 years or longer in 22.3%, significantly affecting their quality of life.
Dr. Desai added that, in a paper recently published in the British Journal of Dermatology, on the impact of postacne hyperpigmentation in patients, the authors pointed out that the reported prevalence of PIH in patients with acne ranges between 45.5% and 87.2%, depending on skin phototype, and that in most cases, PIH takes more than a year to fade.
“Studies have demonstrated that patients with acne and resulting scarring often face stigmatization, leading to quality of life impairment, social withdrawal and body image disorders, which can further contribute to higher risk for depression and social anxiety,” the paper’s authors wrote.
Dr. Desai reported no financial disclosures relevant to his talk.
AT THE MEDSCAPELIVE! PIGMENTARY DISORDERS SYMPOSIUM