User login
Perceptions of Readmitted Patients
Over 14% of all patients hospitalized in the United States are readmitted within 30 days of discharge.1 Numerous studies have used administrative data in order to identify clinical and operational predictors of readmission. However, few studies have explored patients' perspectives on readmission.27 As a result, we know little about potentially modifiable challenges which patients face during the transition from hospital to home. Lack of understanding of the patient perspective has hampered the ability of hospitals to create interventions which address these underlying causes of readmissions.
Patients with low socioeconomic status (SES) are up to 43% more likely to require readmission than their higher‐SES counterparts,8, 9 and qualitative data has described unique challenges faced by low‐SES patients during transition.2 Our objectives were to understand the transition experiences of readmitted patients and to compare these experiences across SES and diagnostic categories.
METHODS
Development of a Survey Instrument
A collaborative team of physicians, nurses, and social workers used a previously defined conceptual framework,10 literature search, and expert interviews to construct a 36‐item survey that addressed the following domains: preparedness for prior discharge; delays in care‐seeking; medication adherence; follow‐up with a primary care provider (PCP); and overarching challenges faced during transition which contributed to readmission. Each question had multiple answer choices including Other which allowed patients to provide open‐ended answers; patients could select all answer choices that applied. Prior to administration, the survey was pretested with 15 random patients and revised to improve reliability and comprehensibility. (See Supporting Information, Survey Script Versions 1.0 and 2.0, in the online version of this article.)
Sampling Strategy and Patient Enrollment
Patients were eligible to participate if they: 1) had capacity to complete an interview; and 2) were readmitted within 30 days of a prior discharge from the Hospital of the University of Pennsylvania (HUP), a 695‐bed academic medical center, or Penn Presbyterian Medical Center (PPMC), a 317‐bed affiliated community hospital. Both hospitals are located in Philadelphia and serve a population which is 45.4% privately insured, 33.5% insured by Medicare, and 21.2% uninsured or insured by Medicaid. We excluded readmissions that were planned or from another facility because these were less sensitive to patient domains such as adherence, access, and social support.
Eligible participants were identified by survey administrators (bedside nurses, social workers, or clinical resource managers) on the day of hospital readmission. Because data were being used immediately for quality improvement, the Institutional Review Board (IRB) waived the need for consent. Administrators typically took 10 minutes to conduct the survey in‐person and record responses directly into patients' electronic medical record (EMR). Inpatient care teams could view responses in real time and work to resolve identified challenges prior to patients' discharge.
Between November 10, 2010 and July 5, 2011, 3881 patients were readmitted to study hospitals. Five hundred eighty‐four readmissions were ineligible for the study because they lacked capacity, were planned readmissions, or were readmitted from another facility. This left 3297 eligible individuals. We surveyed 1084 individuals yielding a response rate of 32.9%11; the remainder either refused the survey, or were not approached for the survey due to time restraints of administrators. Characteristics of responders and nonresponders are displayed in Table 1, and were similar in all measured categories with the exception of age (58.0 vs 55.7, P 0.01) and the number of 60‐day readmissions (2.0 vs 1.3, P 0.01).
| Characteristics of Patients | Survey Sample (n = 1084) | Not in Survey Sample (n = 2797) | P Value* |
|---|---|---|---|
| |||
| Age mean (SD) | 55.7 (16.6) | 58.0 (18.2) | 0.01 |
| Gender, n (%) | 0.88 | ||
| Male | 546 (50.4%) | 1428 (51.1%) | |
| Race, n (%) | 0.96 | ||
| Black | 502 (46.4%) | 1146 (41.3%) | |
| White | 504 (46.6%) | 1362 (49.1%) | |
| Principal discharge diagnosis, n (%) | 0.98 | ||
| Medical | |||
| Acute on chronic systolic heart failure | 44 (4.6%) | 23 (1.3%) | |
| Acute renal failure | 24 (2.5%) | 29 (1.7%) | |
| Surgical | |||
| Postoperative infection | 48 (14.8%) | 53 (5.2%) | |
| Digestive system problems | 17 (5.2%) | 23 (2.2%) | |
| APR‐DRG score, n (%) | 0.13 | ||
| 0 (Not assigned) | 9 (0.7%) | 28 (1.0%) | |
| 1 (Minor) | 113 (10.1%) | 628 (22.7%) | |
| 2 (Moderate) | 338 (31.4%) | 881 (31.8%) | |
| 3 (Major) | 470 (43.7%) | 883 (31.9%) | |
| 4 (Extreme) | 154 (14.3%) | 369 (13.3%) | |
| Length of stay mean (SD) | 6.2 (6.9) | 6.5 (10.1) | 0.33 |
| Insurance payer, n (%) | 0.77 | ||
| Uninsured/Medicaid | 234 (21.6%) | 489 (17.5%) | |
| Medicaid + Medicare | 85 (7.84%) | 172 (6.2%) | |
| Medicare | 345 (31.8%) | 878 (31.5%) | |
| Private | 420 (38.8%) | 1253 (44.9%) | |
| No. of 60‐d readmissions mean (SD) | 1.3 (0.02) | 2.0 (0.02) | 0.01 |
Statistical Analysis
Survey responses were extracted from the EMR and linked with patient clinical and demographic data. Variables pertaining to hospitalization, such as admitting service and principal diagnosis, were associated with patients' index hospitalization rather than the readmission. A trained research assistant extracted open‐ended free‐text answers to any survey questions marked, Other and coded them using a grounded theory approach.12
In our primary analysis, we described challenges reported by readmitted patients. In a secondary analysis, we tested for differences in transition challenges by SES using lack of insurance or Medicaid as a proxy for low SES. Using insurance status as a marker for material aspects of SES is well‐described in health services research.1316 In addition, income data from our institution demonstrated that 86.5% of uninsured and Medicaid patients have a median household income below $15,000. We tested for differences by diagnostic category using the index admitting service (medical vs surgical) as a proxy for diagnostic category (Table 2).
| Low vs High SES (ref) OR (95% CI) | Medical vs Surgical (ref) OR (95% CI) | |
|---|---|---|
| ||
| Unprepared for DC | 1.3 (0.9, 1.9) | 1.0 (0.7, 1.6) |
| Understanding DC instructions | 2.7 (1.1, 6.6) | 1.7 (0.5, 5.8) |
| Executing DC instructions | 2.2 (1.1, 4.4) | 1.6 (0.6, 3.7) |
| Activities of daily living | 1.0 (0.6, 1.5) | 1.1 (0.7, 1.7) |
| Medication access | 1.6 (0.9, 2.8) | 2.3 (1.0, 4.9) |
| Medication adherence | 1.8 (1.2, 3.0) | 2.6 (1.2, 5.4) |
| Lack of social support | 2.0 (1.2, 3.6) | 2.3 (1.0, 5.2) |
| Lack of food, transportation, telephone | 2.6 (1.1, 6.1) | 7.1 (0.9, 53.2) |
| Substance abuse | 6.7 (2.3, 19.2) | 1.5 (0.4, 5.2) |
We compared continuous variables using the two‐sample t test and categorical variables using Pearson's chi‐square test. The Cuzick nonparametric test was used to test for trends across ordered groups. We used multivariable logistic regression models to estimate the association between each binary transition challenge outcome and predictors: SES and diagnostic group. These models were adjusted for potential confounders: age, gender, length of stay, and severity of illness, as determined by All Patient Refined‐Diagnosis Related Groups (APR‐DRGs). We did not adjust for race because it was strongly correlated with SES in our dataset (P 0.0001). Confounders were included in final models if their association with outcomes had a P value less than 0.10. Analyses were performed using the STATA software package, version 11.0 (StataCorp LP, College Station, TX). The survey was approved by the University of Pennsylvania IRB.
RESULTS
Patient Characteristics
We surveyed 1084 unique individuals; 50.4% of participants were male, 46.4% were black. The most common index principal diagnosis in the medical group was systolic heart failure (4.6%), while the most common index principal diagnosis in the surgical group was postoperative infection (14.8%) (Table 1).
Discharge Preparedness, Medication Adherence, and PCP Follow‐up
At the time of prior discharge, 86.4% of respondents felt that they had been prepared for self‐care. 80.3% reported being able to take all discharge medications as prescribed. The most common reasons for not being able to take medications included: 1) side effects or worry about side effects (13.1%); 2) trouble paying for medications (10.7%); and 3) lack of transportation to the pharmacy (8.4%). Since their prior discharge, 52.9% of participants reported that they had visited a PCP; 28.7% of participants report being referred by their PCP to the emergency room for readmission.
Transition Challenges in Overall Survey Sample
During the transition from hospital to home, 45.5% of readmitted patients reported experiencing challenges which contributed to readmission. The most commonly reported issues contributing to readmission were: 1) feeling unprepared for discharge (11.8%); 2) difficulty performing activities of daily living (ADLs) (10.6%); 3) trouble adhering to discharge medications (5.7%); 4) difficulty accessing discharge medications (5.0%); and 5) lack of social support (4.7%).
Transition Challenges by Subgroup
Low‐SES patients were more likely than high‐SES patients to report difficulty understanding (odds ratio [OR] 2.7; 95% confidence interval [CI] 1.1, 6.6) and executing (OR 2.2; 95% CI 1.1, 4.4) discharge instructions, difficulty adhering to medications (OR 1.8; 95% CI 1.2, 3.0), lack of social support (OR 2.0; 95% CI 1.2, 3.6), lack of basic resources (OR 2.6; 95% CI 1.1, 6.1), and substance abuse (OR 6.7; 95% CI 2.3, 19.2) as perceived reasons for readmission. Of the patients who described Other issues contributing to readmission, low‐SES patients most commonly described stress or depression (49.0%), while high‐SES patients most commonly reported a recurrence of symptoms (74.8%). Medical and surgical patients had similar odds of facing each transition challenge with one exception: medical patients were more likely to report difficulty adhering to medications (OR 2.6; 95% CI 1.2, 5.4).
DISCUSSION
Several findings from this study are of interest to practicing hospitalists or hospital administrators. First, of the issues to which patients most commonly attributed readmission, lack of discharge preparedness is the only one which occurs during index hospitalization; in order to address most transition challenges, hospitals must think beyond their walls. By penalizing hospitals for excess rates of readmission, The Hospital Readmission Reduction Program (HRRP) will effectively hold hospitals accountable for addressing issues which occur in patients' homes and communities.17 Hospitals that have robust partnerships with community pharmacies, social service agencies, and PCPs may have the most influence on these issues and the most success in reducing readmissions. Second, consistent with other literature describing increased rates of readmission with enhanced PCP follow‐up,18 our findings demonstrate that PCPs often refer their patients to the emergency room for readmission. This suggests that PCP follow‐up, while perhaps essential for patient care, may not necessarily reduce readmissions and may actually facilitate readmission. Third, this study describes underlying reasons for patient nonadherence with discharge medications: side effects, cost, and transportation. Targeted interventions to improve adherence may include floor‐based pharmacists who counsel on side effects, determine co‐pays prior to discharge, and encourage patients to fill prescriptions from the hospital pharmacy to avoid transportation barriers.
Finally, and perhaps most importantly, these data suggest that one transition experience does not fit all. Patients with low SES appear to have a distinct and challenging transition experience. Currently, there is an emphasis on tailoring transition interventions to specific disease populations, such as patients with congestive heart failure. Our study suggests that it may be more effective to tailor interventions for low‐SES patients across diagnostic category, helping these patients gain access to outpatient medical resources and address competing issues, such as food insecurity or substance abuse.
Our study has several limitations. First, the low survey response rate makes it susceptible to nonresponse bias. Second, survey administration by a member of the care team may have increased social desirability bias. Third, because it was important to the study team to incorporate our survey into hospital workflow, survey responses were recorded directly into the EMR which limited administrators to recording a yes response for each answer choice which the participant endorsed. Therefore, in our dataset, we are unable to distinguish a definite no from a missing response; however, the survey was short, making it unlikely that questions were skipped. Fourth, closed‐ended questions may have failed to capture the range of participant responses, although the inclusion of an open‐ended answer choice ameliorates this issue. Finally, we are unable to draw conclusions regarding association of survey responses with the risk of readmission, because this study was administered only to readmitted patients.
CONCLUSIONS
This report of patients' perspectives challenges many commonly held assumptions regarding readmission. Readmission reflects not only the quality of hospital care, but a variety of factors in patients' homes and communities. PCP follow‐up, while perhaps critical for patient care, may not be a panacea for reducing hospital readmissions. Targeted medication counseling focused on side effects, co‐pay, and medication delivery may address patients' underlying reasons for nonadherence. And most importantly, one transition experience does not fit all. Hospitalists and administrators must tailor interventions to address challenges reported by their patients, particularly those of low SES.
Acknowledgements
The authors are grateful to the Society of General Internal Medicine (SGIM) for selecting our abstract Perceptions of Readmitted Patients on the Transition From Hospital to Home as a Lipkin Award Finalist during the 2012 SGIM National Meeting.
Disclosures: Support for this study was provided by a grant from the Leonard Davis Institute of Health Economics. Dr Grande has received honoraria from the Johns Hopkins University CME Program; has a consultancy with the National Nursing Centers Consortium; and has received grant support from, or has grants pending with, the HealthWell Foundation, the National Human Genome Research Institute, and the Agency for Healthcare Research and Quality. Dr Shannon is the founder of a biotech company, Ventrigen, LLC; is a senior fellow at IHI; is on the scientific advisory boards for Glasgow Smith Klein, Pfizer, Merck, and Value Capture; and is a member of the Board of Directors of the ABIM.
- ,,,.All‐Cause Readmissions by Payer and Age, 2008: Statistical Brief #115. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs.Rockville, MD:Agency for Health Care Policy and Research; February 2006–June2011.
- ,,.Understanding rehospitalization risk: can hospital discharge be modified to reduce recurrent hospitalization?J Hosp Med.2007;2(5):297–304.
- ,,.Patients' and caregivers' transition from hospital to home: needs and recommendations.Home Health Care Serv Q.1999;17(3):27–48.
- ,,.Reasons for readmission in heart failure: perspectives of patients, caregivers, cardiologists, and heart failure nurses.Heart Lung.2009;38(5):427–434.
- ,.Psychiatric rehospitalization of the severely mentally ill: patient and staff perspectives.Nurs Res.1992;41(5):301–305.
- ,,,,,.Continuity of care and monitoring pain after discharge: patient perspective.J Adv Nurs.2010;66(1):40–48.
- ,,,.Going home from hospital: the carer/patient dyad.J Adv Nurs.2001;35(2):206–217.
- ,,.The impact of patient socioeconomic status and other social factors on readmission. A prospective study in 4 Massachusetts hospitals.Inquiry.1994;31(2):163–172.
- ,,,.Redefining readmission risk factors for general medicine patients.J Hosp Med.2011;6(2):54–60.
- ,.Hospital readmissions—not just a measure of quality.JAMA.2011;306(16):1796–1797.
- American Association for Public Opinion Research (AAPOR).Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys.7th ed.Deerfield, IL:AAPOR;2011.
- ,.The Discovery of Grounded Theory: Strategies for Qualitative Research.New York:Aldine;1967.
- ,,,.The relation between health insurance coverage and clinical outcomes among women with breast cancer.N Engl J Med.1993;329(5):326–331.
- ,,,,,.Neighborhood socioeconomic status, Medicaid coverage and medical management of myocardial infarction: atherosclerosis risk in communities (ARIC) community surveillance.BMC Public Health.2010;10:632.
- ,,,,.Effects of practice setting on quality of lipid‐lowering management in patients with coronary artery disease.Am J Cardiol.1998;81(12):1416–1420.
- .Income Data by Insurance Category.2012.
- ,.Hospital readmissions and the Affordable Care Act: paying for coordinated quality care.JAMA.2011;306(16):1794–1795.
- ,,.Does increased access to primary care reduce hospital readmissions?N Engl J Med.1996;334(22):1441–1447.
Over 14% of all patients hospitalized in the United States are readmitted within 30 days of discharge.1 Numerous studies have used administrative data in order to identify clinical and operational predictors of readmission. However, few studies have explored patients' perspectives on readmission.27 As a result, we know little about potentially modifiable challenges which patients face during the transition from hospital to home. Lack of understanding of the patient perspective has hampered the ability of hospitals to create interventions which address these underlying causes of readmissions.
Patients with low socioeconomic status (SES) are up to 43% more likely to require readmission than their higher‐SES counterparts,8, 9 and qualitative data has described unique challenges faced by low‐SES patients during transition.2 Our objectives were to understand the transition experiences of readmitted patients and to compare these experiences across SES and diagnostic categories.
METHODS
Development of a Survey Instrument
A collaborative team of physicians, nurses, and social workers used a previously defined conceptual framework,10 literature search, and expert interviews to construct a 36‐item survey that addressed the following domains: preparedness for prior discharge; delays in care‐seeking; medication adherence; follow‐up with a primary care provider (PCP); and overarching challenges faced during transition which contributed to readmission. Each question had multiple answer choices including Other which allowed patients to provide open‐ended answers; patients could select all answer choices that applied. Prior to administration, the survey was pretested with 15 random patients and revised to improve reliability and comprehensibility. (See Supporting Information, Survey Script Versions 1.0 and 2.0, in the online version of this article.)
Sampling Strategy and Patient Enrollment
Patients were eligible to participate if they: 1) had capacity to complete an interview; and 2) were readmitted within 30 days of a prior discharge from the Hospital of the University of Pennsylvania (HUP), a 695‐bed academic medical center, or Penn Presbyterian Medical Center (PPMC), a 317‐bed affiliated community hospital. Both hospitals are located in Philadelphia and serve a population which is 45.4% privately insured, 33.5% insured by Medicare, and 21.2% uninsured or insured by Medicaid. We excluded readmissions that were planned or from another facility because these were less sensitive to patient domains such as adherence, access, and social support.
Eligible participants were identified by survey administrators (bedside nurses, social workers, or clinical resource managers) on the day of hospital readmission. Because data were being used immediately for quality improvement, the Institutional Review Board (IRB) waived the need for consent. Administrators typically took 10 minutes to conduct the survey in‐person and record responses directly into patients' electronic medical record (EMR). Inpatient care teams could view responses in real time and work to resolve identified challenges prior to patients' discharge.
Between November 10, 2010 and July 5, 2011, 3881 patients were readmitted to study hospitals. Five hundred eighty‐four readmissions were ineligible for the study because they lacked capacity, were planned readmissions, or were readmitted from another facility. This left 3297 eligible individuals. We surveyed 1084 individuals yielding a response rate of 32.9%11; the remainder either refused the survey, or were not approached for the survey due to time restraints of administrators. Characteristics of responders and nonresponders are displayed in Table 1, and were similar in all measured categories with the exception of age (58.0 vs 55.7, P 0.01) and the number of 60‐day readmissions (2.0 vs 1.3, P 0.01).
| Characteristics of Patients | Survey Sample (n = 1084) | Not in Survey Sample (n = 2797) | P Value* |
|---|---|---|---|
| |||
| Age mean (SD) | 55.7 (16.6) | 58.0 (18.2) | 0.01 |
| Gender, n (%) | 0.88 | ||
| Male | 546 (50.4%) | 1428 (51.1%) | |
| Race, n (%) | 0.96 | ||
| Black | 502 (46.4%) | 1146 (41.3%) | |
| White | 504 (46.6%) | 1362 (49.1%) | |
| Principal discharge diagnosis, n (%) | 0.98 | ||
| Medical | |||
| Acute on chronic systolic heart failure | 44 (4.6%) | 23 (1.3%) | |
| Acute renal failure | 24 (2.5%) | 29 (1.7%) | |
| Surgical | |||
| Postoperative infection | 48 (14.8%) | 53 (5.2%) | |
| Digestive system problems | 17 (5.2%) | 23 (2.2%) | |
| APR‐DRG score, n (%) | 0.13 | ||
| 0 (Not assigned) | 9 (0.7%) | 28 (1.0%) | |
| 1 (Minor) | 113 (10.1%) | 628 (22.7%) | |
| 2 (Moderate) | 338 (31.4%) | 881 (31.8%) | |
| 3 (Major) | 470 (43.7%) | 883 (31.9%) | |
| 4 (Extreme) | 154 (14.3%) | 369 (13.3%) | |
| Length of stay mean (SD) | 6.2 (6.9) | 6.5 (10.1) | 0.33 |
| Insurance payer, n (%) | 0.77 | ||
| Uninsured/Medicaid | 234 (21.6%) | 489 (17.5%) | |
| Medicaid + Medicare | 85 (7.84%) | 172 (6.2%) | |
| Medicare | 345 (31.8%) | 878 (31.5%) | |
| Private | 420 (38.8%) | 1253 (44.9%) | |
| No. of 60‐d readmissions mean (SD) | 1.3 (0.02) | 2.0 (0.02) | 0.01 |
Statistical Analysis
Survey responses were extracted from the EMR and linked with patient clinical and demographic data. Variables pertaining to hospitalization, such as admitting service and principal diagnosis, were associated with patients' index hospitalization rather than the readmission. A trained research assistant extracted open‐ended free‐text answers to any survey questions marked, Other and coded them using a grounded theory approach.12
In our primary analysis, we described challenges reported by readmitted patients. In a secondary analysis, we tested for differences in transition challenges by SES using lack of insurance or Medicaid as a proxy for low SES. Using insurance status as a marker for material aspects of SES is well‐described in health services research.1316 In addition, income data from our institution demonstrated that 86.5% of uninsured and Medicaid patients have a median household income below $15,000. We tested for differences by diagnostic category using the index admitting service (medical vs surgical) as a proxy for diagnostic category (Table 2).
| Low vs High SES (ref) OR (95% CI) | Medical vs Surgical (ref) OR (95% CI) | |
|---|---|---|
| ||
| Unprepared for DC | 1.3 (0.9, 1.9) | 1.0 (0.7, 1.6) |
| Understanding DC instructions | 2.7 (1.1, 6.6) | 1.7 (0.5, 5.8) |
| Executing DC instructions | 2.2 (1.1, 4.4) | 1.6 (0.6, 3.7) |
| Activities of daily living | 1.0 (0.6, 1.5) | 1.1 (0.7, 1.7) |
| Medication access | 1.6 (0.9, 2.8) | 2.3 (1.0, 4.9) |
| Medication adherence | 1.8 (1.2, 3.0) | 2.6 (1.2, 5.4) |
| Lack of social support | 2.0 (1.2, 3.6) | 2.3 (1.0, 5.2) |
| Lack of food, transportation, telephone | 2.6 (1.1, 6.1) | 7.1 (0.9, 53.2) |
| Substance abuse | 6.7 (2.3, 19.2) | 1.5 (0.4, 5.2) |
We compared continuous variables using the two‐sample t test and categorical variables using Pearson's chi‐square test. The Cuzick nonparametric test was used to test for trends across ordered groups. We used multivariable logistic regression models to estimate the association between each binary transition challenge outcome and predictors: SES and diagnostic group. These models were adjusted for potential confounders: age, gender, length of stay, and severity of illness, as determined by All Patient Refined‐Diagnosis Related Groups (APR‐DRGs). We did not adjust for race because it was strongly correlated with SES in our dataset (P 0.0001). Confounders were included in final models if their association with outcomes had a P value less than 0.10. Analyses were performed using the STATA software package, version 11.0 (StataCorp LP, College Station, TX). The survey was approved by the University of Pennsylvania IRB.
RESULTS
Patient Characteristics
We surveyed 1084 unique individuals; 50.4% of participants were male, 46.4% were black. The most common index principal diagnosis in the medical group was systolic heart failure (4.6%), while the most common index principal diagnosis in the surgical group was postoperative infection (14.8%) (Table 1).
Discharge Preparedness, Medication Adherence, and PCP Follow‐up
At the time of prior discharge, 86.4% of respondents felt that they had been prepared for self‐care. 80.3% reported being able to take all discharge medications as prescribed. The most common reasons for not being able to take medications included: 1) side effects or worry about side effects (13.1%); 2) trouble paying for medications (10.7%); and 3) lack of transportation to the pharmacy (8.4%). Since their prior discharge, 52.9% of participants reported that they had visited a PCP; 28.7% of participants report being referred by their PCP to the emergency room for readmission.
Transition Challenges in Overall Survey Sample
During the transition from hospital to home, 45.5% of readmitted patients reported experiencing challenges which contributed to readmission. The most commonly reported issues contributing to readmission were: 1) feeling unprepared for discharge (11.8%); 2) difficulty performing activities of daily living (ADLs) (10.6%); 3) trouble adhering to discharge medications (5.7%); 4) difficulty accessing discharge medications (5.0%); and 5) lack of social support (4.7%).
Transition Challenges by Subgroup
Low‐SES patients were more likely than high‐SES patients to report difficulty understanding (odds ratio [OR] 2.7; 95% confidence interval [CI] 1.1, 6.6) and executing (OR 2.2; 95% CI 1.1, 4.4) discharge instructions, difficulty adhering to medications (OR 1.8; 95% CI 1.2, 3.0), lack of social support (OR 2.0; 95% CI 1.2, 3.6), lack of basic resources (OR 2.6; 95% CI 1.1, 6.1), and substance abuse (OR 6.7; 95% CI 2.3, 19.2) as perceived reasons for readmission. Of the patients who described Other issues contributing to readmission, low‐SES patients most commonly described stress or depression (49.0%), while high‐SES patients most commonly reported a recurrence of symptoms (74.8%). Medical and surgical patients had similar odds of facing each transition challenge with one exception: medical patients were more likely to report difficulty adhering to medications (OR 2.6; 95% CI 1.2, 5.4).
DISCUSSION
Several findings from this study are of interest to practicing hospitalists or hospital administrators. First, of the issues to which patients most commonly attributed readmission, lack of discharge preparedness is the only one which occurs during index hospitalization; in order to address most transition challenges, hospitals must think beyond their walls. By penalizing hospitals for excess rates of readmission, The Hospital Readmission Reduction Program (HRRP) will effectively hold hospitals accountable for addressing issues which occur in patients' homes and communities.17 Hospitals that have robust partnerships with community pharmacies, social service agencies, and PCPs may have the most influence on these issues and the most success in reducing readmissions. Second, consistent with other literature describing increased rates of readmission with enhanced PCP follow‐up,18 our findings demonstrate that PCPs often refer their patients to the emergency room for readmission. This suggests that PCP follow‐up, while perhaps essential for patient care, may not necessarily reduce readmissions and may actually facilitate readmission. Third, this study describes underlying reasons for patient nonadherence with discharge medications: side effects, cost, and transportation. Targeted interventions to improve adherence may include floor‐based pharmacists who counsel on side effects, determine co‐pays prior to discharge, and encourage patients to fill prescriptions from the hospital pharmacy to avoid transportation barriers.
Finally, and perhaps most importantly, these data suggest that one transition experience does not fit all. Patients with low SES appear to have a distinct and challenging transition experience. Currently, there is an emphasis on tailoring transition interventions to specific disease populations, such as patients with congestive heart failure. Our study suggests that it may be more effective to tailor interventions for low‐SES patients across diagnostic category, helping these patients gain access to outpatient medical resources and address competing issues, such as food insecurity or substance abuse.
Our study has several limitations. First, the low survey response rate makes it susceptible to nonresponse bias. Second, survey administration by a member of the care team may have increased social desirability bias. Third, because it was important to the study team to incorporate our survey into hospital workflow, survey responses were recorded directly into the EMR which limited administrators to recording a yes response for each answer choice which the participant endorsed. Therefore, in our dataset, we are unable to distinguish a definite no from a missing response; however, the survey was short, making it unlikely that questions were skipped. Fourth, closed‐ended questions may have failed to capture the range of participant responses, although the inclusion of an open‐ended answer choice ameliorates this issue. Finally, we are unable to draw conclusions regarding association of survey responses with the risk of readmission, because this study was administered only to readmitted patients.
CONCLUSIONS
This report of patients' perspectives challenges many commonly held assumptions regarding readmission. Readmission reflects not only the quality of hospital care, but a variety of factors in patients' homes and communities. PCP follow‐up, while perhaps critical for patient care, may not be a panacea for reducing hospital readmissions. Targeted medication counseling focused on side effects, co‐pay, and medication delivery may address patients' underlying reasons for nonadherence. And most importantly, one transition experience does not fit all. Hospitalists and administrators must tailor interventions to address challenges reported by their patients, particularly those of low SES.
Acknowledgements
The authors are grateful to the Society of General Internal Medicine (SGIM) for selecting our abstract Perceptions of Readmitted Patients on the Transition From Hospital to Home as a Lipkin Award Finalist during the 2012 SGIM National Meeting.
Disclosures: Support for this study was provided by a grant from the Leonard Davis Institute of Health Economics. Dr Grande has received honoraria from the Johns Hopkins University CME Program; has a consultancy with the National Nursing Centers Consortium; and has received grant support from, or has grants pending with, the HealthWell Foundation, the National Human Genome Research Institute, and the Agency for Healthcare Research and Quality. Dr Shannon is the founder of a biotech company, Ventrigen, LLC; is a senior fellow at IHI; is on the scientific advisory boards for Glasgow Smith Klein, Pfizer, Merck, and Value Capture; and is a member of the Board of Directors of the ABIM.
Over 14% of all patients hospitalized in the United States are readmitted within 30 days of discharge.1 Numerous studies have used administrative data in order to identify clinical and operational predictors of readmission. However, few studies have explored patients' perspectives on readmission.27 As a result, we know little about potentially modifiable challenges which patients face during the transition from hospital to home. Lack of understanding of the patient perspective has hampered the ability of hospitals to create interventions which address these underlying causes of readmissions.
Patients with low socioeconomic status (SES) are up to 43% more likely to require readmission than their higher‐SES counterparts,8, 9 and qualitative data has described unique challenges faced by low‐SES patients during transition.2 Our objectives were to understand the transition experiences of readmitted patients and to compare these experiences across SES and diagnostic categories.
METHODS
Development of a Survey Instrument
A collaborative team of physicians, nurses, and social workers used a previously defined conceptual framework,10 literature search, and expert interviews to construct a 36‐item survey that addressed the following domains: preparedness for prior discharge; delays in care‐seeking; medication adherence; follow‐up with a primary care provider (PCP); and overarching challenges faced during transition which contributed to readmission. Each question had multiple answer choices including Other which allowed patients to provide open‐ended answers; patients could select all answer choices that applied. Prior to administration, the survey was pretested with 15 random patients and revised to improve reliability and comprehensibility. (See Supporting Information, Survey Script Versions 1.0 and 2.0, in the online version of this article.)
Sampling Strategy and Patient Enrollment
Patients were eligible to participate if they: 1) had capacity to complete an interview; and 2) were readmitted within 30 days of a prior discharge from the Hospital of the University of Pennsylvania (HUP), a 695‐bed academic medical center, or Penn Presbyterian Medical Center (PPMC), a 317‐bed affiliated community hospital. Both hospitals are located in Philadelphia and serve a population which is 45.4% privately insured, 33.5% insured by Medicare, and 21.2% uninsured or insured by Medicaid. We excluded readmissions that were planned or from another facility because these were less sensitive to patient domains such as adherence, access, and social support.
Eligible participants were identified by survey administrators (bedside nurses, social workers, or clinical resource managers) on the day of hospital readmission. Because data were being used immediately for quality improvement, the Institutional Review Board (IRB) waived the need for consent. Administrators typically took 10 minutes to conduct the survey in‐person and record responses directly into patients' electronic medical record (EMR). Inpatient care teams could view responses in real time and work to resolve identified challenges prior to patients' discharge.
Between November 10, 2010 and July 5, 2011, 3881 patients were readmitted to study hospitals. Five hundred eighty‐four readmissions were ineligible for the study because they lacked capacity, were planned readmissions, or were readmitted from another facility. This left 3297 eligible individuals. We surveyed 1084 individuals yielding a response rate of 32.9%11; the remainder either refused the survey, or were not approached for the survey due to time restraints of administrators. Characteristics of responders and nonresponders are displayed in Table 1, and were similar in all measured categories with the exception of age (58.0 vs 55.7, P 0.01) and the number of 60‐day readmissions (2.0 vs 1.3, P 0.01).
| Characteristics of Patients | Survey Sample (n = 1084) | Not in Survey Sample (n = 2797) | P Value* |
|---|---|---|---|
| |||
| Age mean (SD) | 55.7 (16.6) | 58.0 (18.2) | 0.01 |
| Gender, n (%) | 0.88 | ||
| Male | 546 (50.4%) | 1428 (51.1%) | |
| Race, n (%) | 0.96 | ||
| Black | 502 (46.4%) | 1146 (41.3%) | |
| White | 504 (46.6%) | 1362 (49.1%) | |
| Principal discharge diagnosis, n (%) | 0.98 | ||
| Medical | |||
| Acute on chronic systolic heart failure | 44 (4.6%) | 23 (1.3%) | |
| Acute renal failure | 24 (2.5%) | 29 (1.7%) | |
| Surgical | |||
| Postoperative infection | 48 (14.8%) | 53 (5.2%) | |
| Digestive system problems | 17 (5.2%) | 23 (2.2%) | |
| APR‐DRG score, n (%) | 0.13 | ||
| 0 (Not assigned) | 9 (0.7%) | 28 (1.0%) | |
| 1 (Minor) | 113 (10.1%) | 628 (22.7%) | |
| 2 (Moderate) | 338 (31.4%) | 881 (31.8%) | |
| 3 (Major) | 470 (43.7%) | 883 (31.9%) | |
| 4 (Extreme) | 154 (14.3%) | 369 (13.3%) | |
| Length of stay mean (SD) | 6.2 (6.9) | 6.5 (10.1) | 0.33 |
| Insurance payer, n (%) | 0.77 | ||
| Uninsured/Medicaid | 234 (21.6%) | 489 (17.5%) | |
| Medicaid + Medicare | 85 (7.84%) | 172 (6.2%) | |
| Medicare | 345 (31.8%) | 878 (31.5%) | |
| Private | 420 (38.8%) | 1253 (44.9%) | |
| No. of 60‐d readmissions mean (SD) | 1.3 (0.02) | 2.0 (0.02) | 0.01 |
Statistical Analysis
Survey responses were extracted from the EMR and linked with patient clinical and demographic data. Variables pertaining to hospitalization, such as admitting service and principal diagnosis, were associated with patients' index hospitalization rather than the readmission. A trained research assistant extracted open‐ended free‐text answers to any survey questions marked, Other and coded them using a grounded theory approach.12
In our primary analysis, we described challenges reported by readmitted patients. In a secondary analysis, we tested for differences in transition challenges by SES using lack of insurance or Medicaid as a proxy for low SES. Using insurance status as a marker for material aspects of SES is well‐described in health services research.1316 In addition, income data from our institution demonstrated that 86.5% of uninsured and Medicaid patients have a median household income below $15,000. We tested for differences by diagnostic category using the index admitting service (medical vs surgical) as a proxy for diagnostic category (Table 2).
| Low vs High SES (ref) OR (95% CI) | Medical vs Surgical (ref) OR (95% CI) | |
|---|---|---|
| ||
| Unprepared for DC | 1.3 (0.9, 1.9) | 1.0 (0.7, 1.6) |
| Understanding DC instructions | 2.7 (1.1, 6.6) | 1.7 (0.5, 5.8) |
| Executing DC instructions | 2.2 (1.1, 4.4) | 1.6 (0.6, 3.7) |
| Activities of daily living | 1.0 (0.6, 1.5) | 1.1 (0.7, 1.7) |
| Medication access | 1.6 (0.9, 2.8) | 2.3 (1.0, 4.9) |
| Medication adherence | 1.8 (1.2, 3.0) | 2.6 (1.2, 5.4) |
| Lack of social support | 2.0 (1.2, 3.6) | 2.3 (1.0, 5.2) |
| Lack of food, transportation, telephone | 2.6 (1.1, 6.1) | 7.1 (0.9, 53.2) |
| Substance abuse | 6.7 (2.3, 19.2) | 1.5 (0.4, 5.2) |
We compared continuous variables using the two‐sample t test and categorical variables using Pearson's chi‐square test. The Cuzick nonparametric test was used to test for trends across ordered groups. We used multivariable logistic regression models to estimate the association between each binary transition challenge outcome and predictors: SES and diagnostic group. These models were adjusted for potential confounders: age, gender, length of stay, and severity of illness, as determined by All Patient Refined‐Diagnosis Related Groups (APR‐DRGs). We did not adjust for race because it was strongly correlated with SES in our dataset (P 0.0001). Confounders were included in final models if their association with outcomes had a P value less than 0.10. Analyses were performed using the STATA software package, version 11.0 (StataCorp LP, College Station, TX). The survey was approved by the University of Pennsylvania IRB.
RESULTS
Patient Characteristics
We surveyed 1084 unique individuals; 50.4% of participants were male, 46.4% were black. The most common index principal diagnosis in the medical group was systolic heart failure (4.6%), while the most common index principal diagnosis in the surgical group was postoperative infection (14.8%) (Table 1).
Discharge Preparedness, Medication Adherence, and PCP Follow‐up
At the time of prior discharge, 86.4% of respondents felt that they had been prepared for self‐care. 80.3% reported being able to take all discharge medications as prescribed. The most common reasons for not being able to take medications included: 1) side effects or worry about side effects (13.1%); 2) trouble paying for medications (10.7%); and 3) lack of transportation to the pharmacy (8.4%). Since their prior discharge, 52.9% of participants reported that they had visited a PCP; 28.7% of participants report being referred by their PCP to the emergency room for readmission.
Transition Challenges in Overall Survey Sample
During the transition from hospital to home, 45.5% of readmitted patients reported experiencing challenges which contributed to readmission. The most commonly reported issues contributing to readmission were: 1) feeling unprepared for discharge (11.8%); 2) difficulty performing activities of daily living (ADLs) (10.6%); 3) trouble adhering to discharge medications (5.7%); 4) difficulty accessing discharge medications (5.0%); and 5) lack of social support (4.7%).
Transition Challenges by Subgroup
Low‐SES patients were more likely than high‐SES patients to report difficulty understanding (odds ratio [OR] 2.7; 95% confidence interval [CI] 1.1, 6.6) and executing (OR 2.2; 95% CI 1.1, 4.4) discharge instructions, difficulty adhering to medications (OR 1.8; 95% CI 1.2, 3.0), lack of social support (OR 2.0; 95% CI 1.2, 3.6), lack of basic resources (OR 2.6; 95% CI 1.1, 6.1), and substance abuse (OR 6.7; 95% CI 2.3, 19.2) as perceived reasons for readmission. Of the patients who described Other issues contributing to readmission, low‐SES patients most commonly described stress or depression (49.0%), while high‐SES patients most commonly reported a recurrence of symptoms (74.8%). Medical and surgical patients had similar odds of facing each transition challenge with one exception: medical patients were more likely to report difficulty adhering to medications (OR 2.6; 95% CI 1.2, 5.4).
DISCUSSION
Several findings from this study are of interest to practicing hospitalists or hospital administrators. First, of the issues to which patients most commonly attributed readmission, lack of discharge preparedness is the only one which occurs during index hospitalization; in order to address most transition challenges, hospitals must think beyond their walls. By penalizing hospitals for excess rates of readmission, The Hospital Readmission Reduction Program (HRRP) will effectively hold hospitals accountable for addressing issues which occur in patients' homes and communities.17 Hospitals that have robust partnerships with community pharmacies, social service agencies, and PCPs may have the most influence on these issues and the most success in reducing readmissions. Second, consistent with other literature describing increased rates of readmission with enhanced PCP follow‐up,18 our findings demonstrate that PCPs often refer their patients to the emergency room for readmission. This suggests that PCP follow‐up, while perhaps essential for patient care, may not necessarily reduce readmissions and may actually facilitate readmission. Third, this study describes underlying reasons for patient nonadherence with discharge medications: side effects, cost, and transportation. Targeted interventions to improve adherence may include floor‐based pharmacists who counsel on side effects, determine co‐pays prior to discharge, and encourage patients to fill prescriptions from the hospital pharmacy to avoid transportation barriers.
Finally, and perhaps most importantly, these data suggest that one transition experience does not fit all. Patients with low SES appear to have a distinct and challenging transition experience. Currently, there is an emphasis on tailoring transition interventions to specific disease populations, such as patients with congestive heart failure. Our study suggests that it may be more effective to tailor interventions for low‐SES patients across diagnostic category, helping these patients gain access to outpatient medical resources and address competing issues, such as food insecurity or substance abuse.
Our study has several limitations. First, the low survey response rate makes it susceptible to nonresponse bias. Second, survey administration by a member of the care team may have increased social desirability bias. Third, because it was important to the study team to incorporate our survey into hospital workflow, survey responses were recorded directly into the EMR which limited administrators to recording a yes response for each answer choice which the participant endorsed. Therefore, in our dataset, we are unable to distinguish a definite no from a missing response; however, the survey was short, making it unlikely that questions were skipped. Fourth, closed‐ended questions may have failed to capture the range of participant responses, although the inclusion of an open‐ended answer choice ameliorates this issue. Finally, we are unable to draw conclusions regarding association of survey responses with the risk of readmission, because this study was administered only to readmitted patients.
CONCLUSIONS
This report of patients' perspectives challenges many commonly held assumptions regarding readmission. Readmission reflects not only the quality of hospital care, but a variety of factors in patients' homes and communities. PCP follow‐up, while perhaps critical for patient care, may not be a panacea for reducing hospital readmissions. Targeted medication counseling focused on side effects, co‐pay, and medication delivery may address patients' underlying reasons for nonadherence. And most importantly, one transition experience does not fit all. Hospitalists and administrators must tailor interventions to address challenges reported by their patients, particularly those of low SES.
Acknowledgements
The authors are grateful to the Society of General Internal Medicine (SGIM) for selecting our abstract Perceptions of Readmitted Patients on the Transition From Hospital to Home as a Lipkin Award Finalist during the 2012 SGIM National Meeting.
Disclosures: Support for this study was provided by a grant from the Leonard Davis Institute of Health Economics. Dr Grande has received honoraria from the Johns Hopkins University CME Program; has a consultancy with the National Nursing Centers Consortium; and has received grant support from, or has grants pending with, the HealthWell Foundation, the National Human Genome Research Institute, and the Agency for Healthcare Research and Quality. Dr Shannon is the founder of a biotech company, Ventrigen, LLC; is a senior fellow at IHI; is on the scientific advisory boards for Glasgow Smith Klein, Pfizer, Merck, and Value Capture; and is a member of the Board of Directors of the ABIM.
- ,,,.All‐Cause Readmissions by Payer and Age, 2008: Statistical Brief #115. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs.Rockville, MD:Agency for Health Care Policy and Research; February 2006–June2011.
- ,,.Understanding rehospitalization risk: can hospital discharge be modified to reduce recurrent hospitalization?J Hosp Med.2007;2(5):297–304.
- ,,.Patients' and caregivers' transition from hospital to home: needs and recommendations.Home Health Care Serv Q.1999;17(3):27–48.
- ,,.Reasons for readmission in heart failure: perspectives of patients, caregivers, cardiologists, and heart failure nurses.Heart Lung.2009;38(5):427–434.
- ,.Psychiatric rehospitalization of the severely mentally ill: patient and staff perspectives.Nurs Res.1992;41(5):301–305.
- ,,,,,.Continuity of care and monitoring pain after discharge: patient perspective.J Adv Nurs.2010;66(1):40–48.
- ,,,.Going home from hospital: the carer/patient dyad.J Adv Nurs.2001;35(2):206–217.
- ,,.The impact of patient socioeconomic status and other social factors on readmission. A prospective study in 4 Massachusetts hospitals.Inquiry.1994;31(2):163–172.
- ,,,.Redefining readmission risk factors for general medicine patients.J Hosp Med.2011;6(2):54–60.
- ,.Hospital readmissions—not just a measure of quality.JAMA.2011;306(16):1796–1797.
- American Association for Public Opinion Research (AAPOR).Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys.7th ed.Deerfield, IL:AAPOR;2011.
- ,.The Discovery of Grounded Theory: Strategies for Qualitative Research.New York:Aldine;1967.
- ,,,.The relation between health insurance coverage and clinical outcomes among women with breast cancer.N Engl J Med.1993;329(5):326–331.
- ,,,,,.Neighborhood socioeconomic status, Medicaid coverage and medical management of myocardial infarction: atherosclerosis risk in communities (ARIC) community surveillance.BMC Public Health.2010;10:632.
- ,,,,.Effects of practice setting on quality of lipid‐lowering management in patients with coronary artery disease.Am J Cardiol.1998;81(12):1416–1420.
- .Income Data by Insurance Category.2012.
- ,.Hospital readmissions and the Affordable Care Act: paying for coordinated quality care.JAMA.2011;306(16):1794–1795.
- ,,.Does increased access to primary care reduce hospital readmissions?N Engl J Med.1996;334(22):1441–1447.
- ,,,.All‐Cause Readmissions by Payer and Age, 2008: Statistical Brief #115. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs.Rockville, MD:Agency for Health Care Policy and Research; February 2006–June2011.
- ,,.Understanding rehospitalization risk: can hospital discharge be modified to reduce recurrent hospitalization?J Hosp Med.2007;2(5):297–304.
- ,,.Patients' and caregivers' transition from hospital to home: needs and recommendations.Home Health Care Serv Q.1999;17(3):27–48.
- ,,.Reasons for readmission in heart failure: perspectives of patients, caregivers, cardiologists, and heart failure nurses.Heart Lung.2009;38(5):427–434.
- ,.Psychiatric rehospitalization of the severely mentally ill: patient and staff perspectives.Nurs Res.1992;41(5):301–305.
- ,,,,,.Continuity of care and monitoring pain after discharge: patient perspective.J Adv Nurs.2010;66(1):40–48.
- ,,,.Going home from hospital: the carer/patient dyad.J Adv Nurs.2001;35(2):206–217.
- ,,.The impact of patient socioeconomic status and other social factors on readmission. A prospective study in 4 Massachusetts hospitals.Inquiry.1994;31(2):163–172.
- ,,,.Redefining readmission risk factors for general medicine patients.J Hosp Med.2011;6(2):54–60.
- ,.Hospital readmissions—not just a measure of quality.JAMA.2011;306(16):1796–1797.
- American Association for Public Opinion Research (AAPOR).Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys.7th ed.Deerfield, IL:AAPOR;2011.
- ,.The Discovery of Grounded Theory: Strategies for Qualitative Research.New York:Aldine;1967.
- ,,,.The relation between health insurance coverage and clinical outcomes among women with breast cancer.N Engl J Med.1993;329(5):326–331.
- ,,,,,.Neighborhood socioeconomic status, Medicaid coverage and medical management of myocardial infarction: atherosclerosis risk in communities (ARIC) community surveillance.BMC Public Health.2010;10:632.
- ,,,,.Effects of practice setting on quality of lipid‐lowering management in patients with coronary artery disease.Am J Cardiol.1998;81(12):1416–1420.
- .Income Data by Insurance Category.2012.
- ,.Hospital readmissions and the Affordable Care Act: paying for coordinated quality care.JAMA.2011;306(16):1794–1795.
- ,,.Does increased access to primary care reduce hospital readmissions?N Engl J Med.1996;334(22):1441–1447.
Let Lip Defect Size Drive Treatment
SAN DIEGO – Principles for lip repair are based on size and location of the defect, etiology of the lesions, and patient age and gender, said Dr. Michael A. Keefe.
Surgical goals of lip reconstruction are to cover the skin and oral lining, leave a semblance of a vermilion and an adequate stomal diameter, make sure sensation is intact, and ensure that the patient has a competent oral sphincter. "The vermilion is the most visible component of the lips, and it’s also the sensory unit of the lip," Dr. Keefe said at a meeting on superficial anatomy and cutaneous surgery. The meeting was sponsored by the University of California, San Diego, School of Medicine and the Scripps Clinic.
"Scars are very well hidden at the vermilion-cutaneous border. If you have to cross the vermilion-cutaneous junction, cross at 90 degrees."
Lower Lip
The lower vermilion is the most affected target of solar radiation injury. In cases of premalignant lesions such as actinic cheilitis or leukoplakia, Dr. Keefe, a plastic surgeon with the division of head and neck surgery at Sharp Rees-Stealy Medical Group in San Diego, said he often performs a total vermilionectomy (lip shave). This involves resection from the white roll to the contact area with opposite lip. "Primary closure is possible," he said. "You can get tension and dehiscence and flattening of the lip, but generally it heals up pretty well. An option for vermilion reconstruction of larger defects is the buccal mucosal advancement flap, which involves elevating the mucosa deep to salivary glands and superficial to the orbicularis oris muscle."
An advantage of treating the lower lip is that there is increased soft tissue laxity and there is no Cupid’s bow, philtrum, or nose, "so it’s nice that there are no dominant central structures," he said. "The downside is that you have to be mindful of the effect of gravity on the repair, so there is a greater need for tone to prevent drooling and incompetence."
He recommends a staged approach based on the extent of the defect and the age of the patient. For small defects (those less than one-third of the lip size) he uses primary closure. Options for medium defects (those that involve one-third to two-thirds of the lip size) include the Estlander flap, the Abbe flap, Bernard Burow’s procedure, the Karapandzic flap, and the stairstep repair, while the options for large defects (those that involve more than two-thirds of the lip size) include Bernard Burow’s procedure, the Karapandzic flap, and the free flap. "You have a lot of tools, depending on what you feel comfortable with," Dr. Keefe said.
Upper Lip
Cancerous tumors of the upper lip are less common, "but there are some unique structures to pay attention to, including the nose, columella, Cupid’s bow, and the philtrum," he said. "In men there’s a hair-bearing skin issue, but scars can be disguised in a mustache."
The aesthetic subunits to keep in mind, he continued, are the medial subunit, which is one-half of the philtrum, and the lateral subunit, which consists of the philtral column, the nostril sill, the alar base, and the nasolabial crease. Primary closure is used for upper lip defects that involve less than one-third of the lip size. "You can make some perialar crescentic skin excisions, which can help advance things," Dr. Keefe said.
For centrally located medium-sized defects of the upper lip, he often uses primary closure with perialar crescentic skin excisions. "If it’s greater than one-half of the lip size, you can add an Abbe flap," he said. "That’s nice because that recreates the philtrum area."
For medially located medium-sized defects of the upper lip, "you can use the Abbe flap if the commissure is not involved and the Estlander flap if the commissure is involved."
Options for cases with large defects and adequate cheek tissue, he said, include the reverse Karapandzic flap, the reverse fan flap, inverted Bernard Burow’s procedure, superiorly based cheek flaps, and the bilateral levator anguli oris flap combined with the Abbe flap. Options for cases with inadequate cheek tissue include the distal pedicle flap and the free flap.
Repair Risks
A lot of these patients have medical problems," he said. "When you do your first injection to resect the tumor or put the lip back together, make sure you don’t cause a myocardial infarction. Generally you should be comfortable with patients who have an INR [International Normalized Ratio] of 2.5 and below."
For patients with large cancerous tumors of the lip, be mindful of lymphatic drainage, because larger tumors have an increased risk of metastases, said Dr. Keefe. For tumors larger than 2 cm in length or 6 mm in spread, or if there is perineural spread, the patient should be referred for radiation therapy.
Dr. Keefe said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Principles for lip repair are based on size and location of the defect, etiology of the lesions, and patient age and gender, said Dr. Michael A. Keefe.
Surgical goals of lip reconstruction are to cover the skin and oral lining, leave a semblance of a vermilion and an adequate stomal diameter, make sure sensation is intact, and ensure that the patient has a competent oral sphincter. "The vermilion is the most visible component of the lips, and it’s also the sensory unit of the lip," Dr. Keefe said at a meeting on superficial anatomy and cutaneous surgery. The meeting was sponsored by the University of California, San Diego, School of Medicine and the Scripps Clinic.
"Scars are very well hidden at the vermilion-cutaneous border. If you have to cross the vermilion-cutaneous junction, cross at 90 degrees."
Lower Lip
The lower vermilion is the most affected target of solar radiation injury. In cases of premalignant lesions such as actinic cheilitis or leukoplakia, Dr. Keefe, a plastic surgeon with the division of head and neck surgery at Sharp Rees-Stealy Medical Group in San Diego, said he often performs a total vermilionectomy (lip shave). This involves resection from the white roll to the contact area with opposite lip. "Primary closure is possible," he said. "You can get tension and dehiscence and flattening of the lip, but generally it heals up pretty well. An option for vermilion reconstruction of larger defects is the buccal mucosal advancement flap, which involves elevating the mucosa deep to salivary glands and superficial to the orbicularis oris muscle."
An advantage of treating the lower lip is that there is increased soft tissue laxity and there is no Cupid’s bow, philtrum, or nose, "so it’s nice that there are no dominant central structures," he said. "The downside is that you have to be mindful of the effect of gravity on the repair, so there is a greater need for tone to prevent drooling and incompetence."
He recommends a staged approach based on the extent of the defect and the age of the patient. For small defects (those less than one-third of the lip size) he uses primary closure. Options for medium defects (those that involve one-third to two-thirds of the lip size) include the Estlander flap, the Abbe flap, Bernard Burow’s procedure, the Karapandzic flap, and the stairstep repair, while the options for large defects (those that involve more than two-thirds of the lip size) include Bernard Burow’s procedure, the Karapandzic flap, and the free flap. "You have a lot of tools, depending on what you feel comfortable with," Dr. Keefe said.
Upper Lip
Cancerous tumors of the upper lip are less common, "but there are some unique structures to pay attention to, including the nose, columella, Cupid’s bow, and the philtrum," he said. "In men there’s a hair-bearing skin issue, but scars can be disguised in a mustache."
The aesthetic subunits to keep in mind, he continued, are the medial subunit, which is one-half of the philtrum, and the lateral subunit, which consists of the philtral column, the nostril sill, the alar base, and the nasolabial crease. Primary closure is used for upper lip defects that involve less than one-third of the lip size. "You can make some perialar crescentic skin excisions, which can help advance things," Dr. Keefe said.
For centrally located medium-sized defects of the upper lip, he often uses primary closure with perialar crescentic skin excisions. "If it’s greater than one-half of the lip size, you can add an Abbe flap," he said. "That’s nice because that recreates the philtrum area."
For medially located medium-sized defects of the upper lip, "you can use the Abbe flap if the commissure is not involved and the Estlander flap if the commissure is involved."
Options for cases with large defects and adequate cheek tissue, he said, include the reverse Karapandzic flap, the reverse fan flap, inverted Bernard Burow’s procedure, superiorly based cheek flaps, and the bilateral levator anguli oris flap combined with the Abbe flap. Options for cases with inadequate cheek tissue include the distal pedicle flap and the free flap.
Repair Risks
A lot of these patients have medical problems," he said. "When you do your first injection to resect the tumor or put the lip back together, make sure you don’t cause a myocardial infarction. Generally you should be comfortable with patients who have an INR [International Normalized Ratio] of 2.5 and below."
For patients with large cancerous tumors of the lip, be mindful of lymphatic drainage, because larger tumors have an increased risk of metastases, said Dr. Keefe. For tumors larger than 2 cm in length or 6 mm in spread, or if there is perineural spread, the patient should be referred for radiation therapy.
Dr. Keefe said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Principles for lip repair are based on size and location of the defect, etiology of the lesions, and patient age and gender, said Dr. Michael A. Keefe.
Surgical goals of lip reconstruction are to cover the skin and oral lining, leave a semblance of a vermilion and an adequate stomal diameter, make sure sensation is intact, and ensure that the patient has a competent oral sphincter. "The vermilion is the most visible component of the lips, and it’s also the sensory unit of the lip," Dr. Keefe said at a meeting on superficial anatomy and cutaneous surgery. The meeting was sponsored by the University of California, San Diego, School of Medicine and the Scripps Clinic.
"Scars are very well hidden at the vermilion-cutaneous border. If you have to cross the vermilion-cutaneous junction, cross at 90 degrees."
Lower Lip
The lower vermilion is the most affected target of solar radiation injury. In cases of premalignant lesions such as actinic cheilitis or leukoplakia, Dr. Keefe, a plastic surgeon with the division of head and neck surgery at Sharp Rees-Stealy Medical Group in San Diego, said he often performs a total vermilionectomy (lip shave). This involves resection from the white roll to the contact area with opposite lip. "Primary closure is possible," he said. "You can get tension and dehiscence and flattening of the lip, but generally it heals up pretty well. An option for vermilion reconstruction of larger defects is the buccal mucosal advancement flap, which involves elevating the mucosa deep to salivary glands and superficial to the orbicularis oris muscle."
An advantage of treating the lower lip is that there is increased soft tissue laxity and there is no Cupid’s bow, philtrum, or nose, "so it’s nice that there are no dominant central structures," he said. "The downside is that you have to be mindful of the effect of gravity on the repair, so there is a greater need for tone to prevent drooling and incompetence."
He recommends a staged approach based on the extent of the defect and the age of the patient. For small defects (those less than one-third of the lip size) he uses primary closure. Options for medium defects (those that involve one-third to two-thirds of the lip size) include the Estlander flap, the Abbe flap, Bernard Burow’s procedure, the Karapandzic flap, and the stairstep repair, while the options for large defects (those that involve more than two-thirds of the lip size) include Bernard Burow’s procedure, the Karapandzic flap, and the free flap. "You have a lot of tools, depending on what you feel comfortable with," Dr. Keefe said.
Upper Lip
Cancerous tumors of the upper lip are less common, "but there are some unique structures to pay attention to, including the nose, columella, Cupid’s bow, and the philtrum," he said. "In men there’s a hair-bearing skin issue, but scars can be disguised in a mustache."
The aesthetic subunits to keep in mind, he continued, are the medial subunit, which is one-half of the philtrum, and the lateral subunit, which consists of the philtral column, the nostril sill, the alar base, and the nasolabial crease. Primary closure is used for upper lip defects that involve less than one-third of the lip size. "You can make some perialar crescentic skin excisions, which can help advance things," Dr. Keefe said.
For centrally located medium-sized defects of the upper lip, he often uses primary closure with perialar crescentic skin excisions. "If it’s greater than one-half of the lip size, you can add an Abbe flap," he said. "That’s nice because that recreates the philtrum area."
For medially located medium-sized defects of the upper lip, "you can use the Abbe flap if the commissure is not involved and the Estlander flap if the commissure is involved."
Options for cases with large defects and adequate cheek tissue, he said, include the reverse Karapandzic flap, the reverse fan flap, inverted Bernard Burow’s procedure, superiorly based cheek flaps, and the bilateral levator anguli oris flap combined with the Abbe flap. Options for cases with inadequate cheek tissue include the distal pedicle flap and the free flap.
Repair Risks
A lot of these patients have medical problems," he said. "When you do your first injection to resect the tumor or put the lip back together, make sure you don’t cause a myocardial infarction. Generally you should be comfortable with patients who have an INR [International Normalized Ratio] of 2.5 and below."
For patients with large cancerous tumors of the lip, be mindful of lymphatic drainage, because larger tumors have an increased risk of metastases, said Dr. Keefe. For tumors larger than 2 cm in length or 6 mm in spread, or if there is perineural spread, the patient should be referred for radiation therapy.
Dr. Keefe said that he had no relevant financial conflicts to disclose.
AT A MEETING ON SUPERFICIAL ANATOMY AND CUTANEOUS SURGERY
Appropriate Use of Automobile Child Restraints Found Inadequate
A low proportion of Americans use appropriate automobile restraints for their children, according to a study published online Aug. 7 in American Journal of Preventive Medicine.
Child passenger restraints fall short in three specific areas: Few children ride in rear-facing seats after the age of 1 year, fewer than 2% of those aged 7 and older use a booster seat, and too many in all age groups sit in the front seat. In every age group, children of racial minorities showed much lower use of appropriate child passenger restraints than white children.
"The most important finding from this study is that, while age and racial disparities exist, overall few children are using the restraints recommended for their age group, and many children ... are sitting in the front seat," Dr. Michelle L. Macy of the department of emergency medicine, child health evaluation and research unit, University of Michigan, Ann Arbor, said in a press statement accompanying the report.
According to American Academy of Pediatrics guidelines for child passenger safety, children should remain rear facing in safety seats until at least 2 years of age, should transition to a forward-facing car seat with a five-point harness and continue to use it for as long as possible up to the highest weight or height allowed by the manufacturer, should then transition to a booster seat until they fit properly into an adult seat belt (usually age 11 or older), and should always ride in the back seat until age 13.
Dr. Macy and Dr. Gary L. Freed, also of the university, performed a secondary analysis of data collected by the National Highway Traffic Safety Administration in its annual nationwide surveys of the use of child passenger restraints in 2007, 2008, and 2009. This included direct observation of 21,476 children under age 13 as they were driven to community sites such as gas stations, fast food restaurants, recreation centers, and child care facilities, supplemented by brief interviews with the drivers.
The children were recorded as belonging to one of three mutually exclusive categories: those using age-appropriate child passenger restraints, children making a premature transition to restraints appropriate only to older children, and those using no restraints.
A total of 59% of the children were white, 11% were black, 21% were Hispanic, and 9% were of other races.
Overall, the use of appropriate automobile restraints was low. Even in the age group (infants and toddlers) and racial group (whites) most likely to use appropriate child passenger restraints, only 17% of children were found to be restrained according to AAP guidelines that were current at the time of the study.
Nearly all children in every racial group transitioned to a front-facing car seat well before age 2 years.
At ages 4 and 5 years, 16% of whites, 35% of blacks, 26% of Hispanics, and 27% of other racial groups were prematurely transitioned to adult seat belts, the investigators said (Am. J. Prev. Med. 2012 Aug. 7 [doi:10.1016/j.amepre.2012.05.023]).
Many children younger than age 6 were front-seat passengers, and the proportion rose with increasing age, the investigators said. One in seven 6- to 7-year-olds, one-fourth of 8- to 10-year olds, and more than a third of 11- to 12-year-olds rode in the front seat.
Minority race was the most predominant factor associated with inappropriate use of child passenger restraints, demonstrating "that not all children have been reached equally by community-based public education campaigns and the passage of child safety seat laws in 48 states," Dr. Macy and Dr. Freed said.
In this study, racial differences in seat belt use may have been a marker for disparities in socioeconomic status, education, or English proficiency. These factors may have interfered with a family’s ability to own safety seats or to access information on child passenger safety. Culturally specific programs are needed to address these issues, the investigators noted.
Several other factors also correlated with inappropriate use of child passenger restraints. Drivers who failed to use seat belts themselves were much more likely to forgo appropriate restraints for their child passengers. Drivers of cars, as opposed to drivers of vans or sport-utility vehicles, were less likely to use appropriate restraints for their child passengers. And drivers in the Midwest, as opposed to those in the Northeastern U.S., also were less likely to do so.
Child passengers of very young drivers (aged 16-24 years) also were less likely to be using appropriate restraints and more likely to be riding in the front seat. Vehicles with four or more child passengers were more likely to carry unrestrained child passengers and children in the front seat. This last factor might be attributable to the limited number of seat belt positions available in the back seat.
In contrast, two factors that showed no association with appropriate child restraints were the sex of the child and the sex of the driver.
These study findings show that there are substantial opportunities for clinicians to improve child passenger safety by counseling patients and parents at routine office visits, Dr. Macy and Dr. Freed added.
The investigators reported no relevant financial conflicts.
A low proportion of Americans use appropriate automobile restraints for their children, according to a study published online Aug. 7 in American Journal of Preventive Medicine.
Child passenger restraints fall short in three specific areas: Few children ride in rear-facing seats after the age of 1 year, fewer than 2% of those aged 7 and older use a booster seat, and too many in all age groups sit in the front seat. In every age group, children of racial minorities showed much lower use of appropriate child passenger restraints than white children.
"The most important finding from this study is that, while age and racial disparities exist, overall few children are using the restraints recommended for their age group, and many children ... are sitting in the front seat," Dr. Michelle L. Macy of the department of emergency medicine, child health evaluation and research unit, University of Michigan, Ann Arbor, said in a press statement accompanying the report.
According to American Academy of Pediatrics guidelines for child passenger safety, children should remain rear facing in safety seats until at least 2 years of age, should transition to a forward-facing car seat with a five-point harness and continue to use it for as long as possible up to the highest weight or height allowed by the manufacturer, should then transition to a booster seat until they fit properly into an adult seat belt (usually age 11 or older), and should always ride in the back seat until age 13.
Dr. Macy and Dr. Gary L. Freed, also of the university, performed a secondary analysis of data collected by the National Highway Traffic Safety Administration in its annual nationwide surveys of the use of child passenger restraints in 2007, 2008, and 2009. This included direct observation of 21,476 children under age 13 as they were driven to community sites such as gas stations, fast food restaurants, recreation centers, and child care facilities, supplemented by brief interviews with the drivers.
The children were recorded as belonging to one of three mutually exclusive categories: those using age-appropriate child passenger restraints, children making a premature transition to restraints appropriate only to older children, and those using no restraints.
A total of 59% of the children were white, 11% were black, 21% were Hispanic, and 9% were of other races.
Overall, the use of appropriate automobile restraints was low. Even in the age group (infants and toddlers) and racial group (whites) most likely to use appropriate child passenger restraints, only 17% of children were found to be restrained according to AAP guidelines that were current at the time of the study.
Nearly all children in every racial group transitioned to a front-facing car seat well before age 2 years.
At ages 4 and 5 years, 16% of whites, 35% of blacks, 26% of Hispanics, and 27% of other racial groups were prematurely transitioned to adult seat belts, the investigators said (Am. J. Prev. Med. 2012 Aug. 7 [doi:10.1016/j.amepre.2012.05.023]).
Many children younger than age 6 were front-seat passengers, and the proportion rose with increasing age, the investigators said. One in seven 6- to 7-year-olds, one-fourth of 8- to 10-year olds, and more than a third of 11- to 12-year-olds rode in the front seat.
Minority race was the most predominant factor associated with inappropriate use of child passenger restraints, demonstrating "that not all children have been reached equally by community-based public education campaigns and the passage of child safety seat laws in 48 states," Dr. Macy and Dr. Freed said.
In this study, racial differences in seat belt use may have been a marker for disparities in socioeconomic status, education, or English proficiency. These factors may have interfered with a family’s ability to own safety seats or to access information on child passenger safety. Culturally specific programs are needed to address these issues, the investigators noted.
Several other factors also correlated with inappropriate use of child passenger restraints. Drivers who failed to use seat belts themselves were much more likely to forgo appropriate restraints for their child passengers. Drivers of cars, as opposed to drivers of vans or sport-utility vehicles, were less likely to use appropriate restraints for their child passengers. And drivers in the Midwest, as opposed to those in the Northeastern U.S., also were less likely to do so.
Child passengers of very young drivers (aged 16-24 years) also were less likely to be using appropriate restraints and more likely to be riding in the front seat. Vehicles with four or more child passengers were more likely to carry unrestrained child passengers and children in the front seat. This last factor might be attributable to the limited number of seat belt positions available in the back seat.
In contrast, two factors that showed no association with appropriate child restraints were the sex of the child and the sex of the driver.
These study findings show that there are substantial opportunities for clinicians to improve child passenger safety by counseling patients and parents at routine office visits, Dr. Macy and Dr. Freed added.
The investigators reported no relevant financial conflicts.
A low proportion of Americans use appropriate automobile restraints for their children, according to a study published online Aug. 7 in American Journal of Preventive Medicine.
Child passenger restraints fall short in three specific areas: Few children ride in rear-facing seats after the age of 1 year, fewer than 2% of those aged 7 and older use a booster seat, and too many in all age groups sit in the front seat. In every age group, children of racial minorities showed much lower use of appropriate child passenger restraints than white children.
"The most important finding from this study is that, while age and racial disparities exist, overall few children are using the restraints recommended for their age group, and many children ... are sitting in the front seat," Dr. Michelle L. Macy of the department of emergency medicine, child health evaluation and research unit, University of Michigan, Ann Arbor, said in a press statement accompanying the report.
According to American Academy of Pediatrics guidelines for child passenger safety, children should remain rear facing in safety seats until at least 2 years of age, should transition to a forward-facing car seat with a five-point harness and continue to use it for as long as possible up to the highest weight or height allowed by the manufacturer, should then transition to a booster seat until they fit properly into an adult seat belt (usually age 11 or older), and should always ride in the back seat until age 13.
Dr. Macy and Dr. Gary L. Freed, also of the university, performed a secondary analysis of data collected by the National Highway Traffic Safety Administration in its annual nationwide surveys of the use of child passenger restraints in 2007, 2008, and 2009. This included direct observation of 21,476 children under age 13 as they were driven to community sites such as gas stations, fast food restaurants, recreation centers, and child care facilities, supplemented by brief interviews with the drivers.
The children were recorded as belonging to one of three mutually exclusive categories: those using age-appropriate child passenger restraints, children making a premature transition to restraints appropriate only to older children, and those using no restraints.
A total of 59% of the children were white, 11% were black, 21% were Hispanic, and 9% were of other races.
Overall, the use of appropriate automobile restraints was low. Even in the age group (infants and toddlers) and racial group (whites) most likely to use appropriate child passenger restraints, only 17% of children were found to be restrained according to AAP guidelines that were current at the time of the study.
Nearly all children in every racial group transitioned to a front-facing car seat well before age 2 years.
At ages 4 and 5 years, 16% of whites, 35% of blacks, 26% of Hispanics, and 27% of other racial groups were prematurely transitioned to adult seat belts, the investigators said (Am. J. Prev. Med. 2012 Aug. 7 [doi:10.1016/j.amepre.2012.05.023]).
Many children younger than age 6 were front-seat passengers, and the proportion rose with increasing age, the investigators said. One in seven 6- to 7-year-olds, one-fourth of 8- to 10-year olds, and more than a third of 11- to 12-year-olds rode in the front seat.
Minority race was the most predominant factor associated with inappropriate use of child passenger restraints, demonstrating "that not all children have been reached equally by community-based public education campaigns and the passage of child safety seat laws in 48 states," Dr. Macy and Dr. Freed said.
In this study, racial differences in seat belt use may have been a marker for disparities in socioeconomic status, education, or English proficiency. These factors may have interfered with a family’s ability to own safety seats or to access information on child passenger safety. Culturally specific programs are needed to address these issues, the investigators noted.
Several other factors also correlated with inappropriate use of child passenger restraints. Drivers who failed to use seat belts themselves were much more likely to forgo appropriate restraints for their child passengers. Drivers of cars, as opposed to drivers of vans or sport-utility vehicles, were less likely to use appropriate restraints for their child passengers. And drivers in the Midwest, as opposed to those in the Northeastern U.S., also were less likely to do so.
Child passengers of very young drivers (aged 16-24 years) also were less likely to be using appropriate restraints and more likely to be riding in the front seat. Vehicles with four or more child passengers were more likely to carry unrestrained child passengers and children in the front seat. This last factor might be attributable to the limited number of seat belt positions available in the back seat.
In contrast, two factors that showed no association with appropriate child restraints were the sex of the child and the sex of the driver.
These study findings show that there are substantial opportunities for clinicians to improve child passenger safety by counseling patients and parents at routine office visits, Dr. Macy and Dr. Freed added.
The investigators reported no relevant financial conflicts.
FROM AMERICAN JOURNAL OF PREVENTIVE MEDICINE
Major Finding: Contrary to safety recommendations, few children use rear-facing car seats after age 1 year, fewer than 2% of those aged 7 and older use booster seats, and too many in all age groups ride in the front seat.
Data Source: This was a secondary analysis of data collected in NHTSA 2007-2009 national surveys of booster seat use among 21,476 children.
Disclosures: Dr. Macy and Dr. Freed reported no relevant financial conflicts.
Price Break Ahead for Fidaxomicin for C. Diff. Diarrhea
Hospitals will soon get a break on the price of fidaxomicin tablets for treatment of Clostridium difficile–associated diarrhea, thanks to a new add-on payment from Medicare.
Officials at the Centers for Medicare and Medicaid Services granted a new technology add-on payment for fidaxomicin tablets (Dificid) administered in the hospital. The new payment, which can be as high as $868 for a full course of the macrolide antibacterial drug, will begin on Oct. 1. The add-on payment is in addition to the standard Medicare payment for the treatment of C. difficile–associated diarrhea (CDAD).
The CMS included details about the add-on payment in the final regulation for the Inpatient Prospective Payment System.
Medicare typically only provides the add-on payment for new technologies associated with procedures, such grafts or stents. But after hearing about the clinical performance of the drug, Medicare officials agreed to grant the extra payment to hospitals. In the final rule, CMS officials wrote that the oral antibiotic has the potential "to decrease hospitalizations and physician office visits, and reduce the recurrence of CDAD, as well as to improve the quality of life for patients who have been diagnosed with CDAD."
The CMS provides add-on payments to hospitals to help subsidize the cost of treatments that are new and costly but that potentially offer a significant clinical benefit for Medicare beneficiaries. The payments are offered in addition to the standard DRG (diagnosis-related group) payment and can be up to 50% of the cost of the treatment for 2-3 years.
The CMS will issue guidance in the future on how hospitals can code to receive the add-on payment for Dificid.
Hospitals will soon get a break on the price of fidaxomicin tablets for treatment of Clostridium difficile–associated diarrhea, thanks to a new add-on payment from Medicare.
Officials at the Centers for Medicare and Medicaid Services granted a new technology add-on payment for fidaxomicin tablets (Dificid) administered in the hospital. The new payment, which can be as high as $868 for a full course of the macrolide antibacterial drug, will begin on Oct. 1. The add-on payment is in addition to the standard Medicare payment for the treatment of C. difficile–associated diarrhea (CDAD).
The CMS included details about the add-on payment in the final regulation for the Inpatient Prospective Payment System.
Medicare typically only provides the add-on payment for new technologies associated with procedures, such grafts or stents. But after hearing about the clinical performance of the drug, Medicare officials agreed to grant the extra payment to hospitals. In the final rule, CMS officials wrote that the oral antibiotic has the potential "to decrease hospitalizations and physician office visits, and reduce the recurrence of CDAD, as well as to improve the quality of life for patients who have been diagnosed with CDAD."
The CMS provides add-on payments to hospitals to help subsidize the cost of treatments that are new and costly but that potentially offer a significant clinical benefit for Medicare beneficiaries. The payments are offered in addition to the standard DRG (diagnosis-related group) payment and can be up to 50% of the cost of the treatment for 2-3 years.
The CMS will issue guidance in the future on how hospitals can code to receive the add-on payment for Dificid.
Hospitals will soon get a break on the price of fidaxomicin tablets for treatment of Clostridium difficile–associated diarrhea, thanks to a new add-on payment from Medicare.
Officials at the Centers for Medicare and Medicaid Services granted a new technology add-on payment for fidaxomicin tablets (Dificid) administered in the hospital. The new payment, which can be as high as $868 for a full course of the macrolide antibacterial drug, will begin on Oct. 1. The add-on payment is in addition to the standard Medicare payment for the treatment of C. difficile–associated diarrhea (CDAD).
The CMS included details about the add-on payment in the final regulation for the Inpatient Prospective Payment System.
Medicare typically only provides the add-on payment for new technologies associated with procedures, such grafts or stents. But after hearing about the clinical performance of the drug, Medicare officials agreed to grant the extra payment to hospitals. In the final rule, CMS officials wrote that the oral antibiotic has the potential "to decrease hospitalizations and physician office visits, and reduce the recurrence of CDAD, as well as to improve the quality of life for patients who have been diagnosed with CDAD."
The CMS provides add-on payments to hospitals to help subsidize the cost of treatments that are new and costly but that potentially offer a significant clinical benefit for Medicare beneficiaries. The payments are offered in addition to the standard DRG (diagnosis-related group) payment and can be up to 50% of the cost of the treatment for 2-3 years.
The CMS will issue guidance in the future on how hospitals can code to receive the add-on payment for Dificid.
Duty-Hour Surveys Separate Interns, Program Directors
Interns beginning their surgical training under the new resident duty-hour standards appear to be less pessimistic than program directors, but they still show significant concern that these new regulations will have a detrimental effect on the quality of their training, according to the results of separate surveys of surgical interns in general surgery residency programs and national surgical program directors.
The Accreditation Council for Graduate Medical Education (ACGME) implemented the new standards in July 2011 to include increased supervision and a 16-hour shift maximum for postgraduate year 1 residents, according to a report published in the June issue of Archives of Surgery.
In the summer of 2011, the researchers surveyed all 215 surgical interns in 11 general surgical residency programs distributed across the country to assess their perceptions of how the new duty-hour requirements would affect continuity of care, resident fatigue, and development in the six core ACGME competencies, according to Dr. Ryan M. Antiel of the Mayo Clinic, Rochester, Minn., and his colleagues. Perceptions were measured using a 3-point scale (increase, decrease, no change) for each item. A total of 179 (83.3%) completed the survey. Most respondents (68.7%) were men and were younger than 29 years of age (73%), with 102 categorical interns (57%) and 76 preliminary interns (42.5%), and 1 nonrespondent to this question (Arch. Surg. 2012;147:536-41).
Results of the resident survey were compared with those of an earlier survey of 134 program directors conducted by Dr. Antiel and his colleagues (Mayo Clin. Proc. 2011;86:185-91).
The great majority of the interns (80.3%) indicated that the new restrictions would decrease their ability to achieve continuity with hospitalized patients, and more than half (57.6%) stated that there would be a decrease in the coordination of patient care. Slightly fewer than half (48%) believed it would interfere with their acquisition of new medical knowledge.
"Most of the surgical interns (67.4%) believed that the duty-hour restrictions will decrease their time spent in the operating room," the researchers added. They also indicated that the new standards would decrease their development of surgical skills (52.8%); their time spent with patients on the floor (51.1%); and their overall educational experience (51.1%). Categorical interns were significantly more likely to believe that the changes would decrease both quality and safety of patient care (odds ratio, 2.6).
However, some optimism was also expressed: In all, 61.5% of interns believed that the new standards would decrease resident fatigue; 66.5% indicated that the new hours would increase or not change quality and safety of patient care; 72.1% indicated the same for the ability to effectively communicate with patients, families, and other health professionals; 74.7% indicated the same for the resident’s investigation and self-evaluation of their own patient care; and 70.2% felt that the impact would be neutral or favorable in the area of responsiveness to patient needs that supersede self-interest.
Compared with the program directors surveyed, a significantly higher proportion of interns believed that the new changes would improve or not change residents’ performance. And a significantly larger percentage of program directors agreed that the new changes would decrease coordination of patient care and residents’ acquisition of medical knowledge (76.9% vs. 48.0%). Perhaps most notably in terms of cross-perceptions, most interns (61.5%) believed that the new changes would decrease fatigue, whereas 85.1% of program directors believed that the new hours would increase fatigue, presumably by increasing the intensity of effort and accomplishments required in that shorter amount of time, according to the authors.
The researchers pointed out several limitations to their study beyond those intrinsic to surveys. Attitudes of residents may change over time, although the survey was most concerned with the perception of incoming interns. Also, program directors were not chosen randomly, and some regions may have been underrepresented. In addition, attitudes cannot be taken as evidence of the actual results of duty-hour restrictions on training, only the perceptions of that effect. But in the absence of defined metrics for assessing the effect of duty-hour restrictions on training, the attitudes of those most involved in training may be the best metric available, they noted.
"As residency programs attempt to adapt to the new regulations, surgical interns have significant concerns about the implications of these regulations on their training. The opinions of these interns, although markedly more optimistic than those of surgical program directors, reflect a persistent concern within the surgical community regarding the effects of work-hour restrictions on surgical training," they concluded.
The authors had no disclosures.
Eliminating two important limitations of this study might have put the interns more "in sync" with the program directors. First, large university programs constituted 10 of the 11 surveyed, and I suspect that those residents would be less concerned about duty-hour restrictions (because more of them subsequently choose fellowships and are less likely to go straight into general surgery practice) than would those from nonuniversity or community programs. Second, for 42.5% of the interns surveyed, there was no distinction made between those hoping to go into general surgery vs. those on track for surgical subspecialties, who are less likely to be concerned for the same reason of expecting additional training.
Even when we ignore the limitations of this study, I believe it shows that the "line in the sand" for the entire surgical community – residents and attendings – is no further resident duty-hour restrictions.
Mark L. Friedell, M.D., is from the department of surgery at the University of Missouri–Kansas City. His remarks are abstracted from an invited critique that accompanied the article (Arch. Surg. 2012;147:541). He reported having no disclosures.
Eliminating two important limitations of this study might have put the interns more "in sync" with the program directors. First, large university programs constituted 10 of the 11 surveyed, and I suspect that those residents would be less concerned about duty-hour restrictions (because more of them subsequently choose fellowships and are less likely to go straight into general surgery practice) than would those from nonuniversity or community programs. Second, for 42.5% of the interns surveyed, there was no distinction made between those hoping to go into general surgery vs. those on track for surgical subspecialties, who are less likely to be concerned for the same reason of expecting additional training.
Even when we ignore the limitations of this study, I believe it shows that the "line in the sand" for the entire surgical community – residents and attendings – is no further resident duty-hour restrictions.
Mark L. Friedell, M.D., is from the department of surgery at the University of Missouri–Kansas City. His remarks are abstracted from an invited critique that accompanied the article (Arch. Surg. 2012;147:541). He reported having no disclosures.
Eliminating two important limitations of this study might have put the interns more "in sync" with the program directors. First, large university programs constituted 10 of the 11 surveyed, and I suspect that those residents would be less concerned about duty-hour restrictions (because more of them subsequently choose fellowships and are less likely to go straight into general surgery practice) than would those from nonuniversity or community programs. Second, for 42.5% of the interns surveyed, there was no distinction made between those hoping to go into general surgery vs. those on track for surgical subspecialties, who are less likely to be concerned for the same reason of expecting additional training.
Even when we ignore the limitations of this study, I believe it shows that the "line in the sand" for the entire surgical community – residents and attendings – is no further resident duty-hour restrictions.
Mark L. Friedell, M.D., is from the department of surgery at the University of Missouri–Kansas City. His remarks are abstracted from an invited critique that accompanied the article (Arch. Surg. 2012;147:541). He reported having no disclosures.
Interns beginning their surgical training under the new resident duty-hour standards appear to be less pessimistic than program directors, but they still show significant concern that these new regulations will have a detrimental effect on the quality of their training, according to the results of separate surveys of surgical interns in general surgery residency programs and national surgical program directors.
The Accreditation Council for Graduate Medical Education (ACGME) implemented the new standards in July 2011 to include increased supervision and a 16-hour shift maximum for postgraduate year 1 residents, according to a report published in the June issue of Archives of Surgery.
In the summer of 2011, the researchers surveyed all 215 surgical interns in 11 general surgical residency programs distributed across the country to assess their perceptions of how the new duty-hour requirements would affect continuity of care, resident fatigue, and development in the six core ACGME competencies, according to Dr. Ryan M. Antiel of the Mayo Clinic, Rochester, Minn., and his colleagues. Perceptions were measured using a 3-point scale (increase, decrease, no change) for each item. A total of 179 (83.3%) completed the survey. Most respondents (68.7%) were men and were younger than 29 years of age (73%), with 102 categorical interns (57%) and 76 preliminary interns (42.5%), and 1 nonrespondent to this question (Arch. Surg. 2012;147:536-41).
Results of the resident survey were compared with those of an earlier survey of 134 program directors conducted by Dr. Antiel and his colleagues (Mayo Clin. Proc. 2011;86:185-91).
The great majority of the interns (80.3%) indicated that the new restrictions would decrease their ability to achieve continuity with hospitalized patients, and more than half (57.6%) stated that there would be a decrease in the coordination of patient care. Slightly fewer than half (48%) believed it would interfere with their acquisition of new medical knowledge.
"Most of the surgical interns (67.4%) believed that the duty-hour restrictions will decrease their time spent in the operating room," the researchers added. They also indicated that the new standards would decrease their development of surgical skills (52.8%); their time spent with patients on the floor (51.1%); and their overall educational experience (51.1%). Categorical interns were significantly more likely to believe that the changes would decrease both quality and safety of patient care (odds ratio, 2.6).
However, some optimism was also expressed: In all, 61.5% of interns believed that the new standards would decrease resident fatigue; 66.5% indicated that the new hours would increase or not change quality and safety of patient care; 72.1% indicated the same for the ability to effectively communicate with patients, families, and other health professionals; 74.7% indicated the same for the resident’s investigation and self-evaluation of their own patient care; and 70.2% felt that the impact would be neutral or favorable in the area of responsiveness to patient needs that supersede self-interest.
Compared with the program directors surveyed, a significantly higher proportion of interns believed that the new changes would improve or not change residents’ performance. And a significantly larger percentage of program directors agreed that the new changes would decrease coordination of patient care and residents’ acquisition of medical knowledge (76.9% vs. 48.0%). Perhaps most notably in terms of cross-perceptions, most interns (61.5%) believed that the new changes would decrease fatigue, whereas 85.1% of program directors believed that the new hours would increase fatigue, presumably by increasing the intensity of effort and accomplishments required in that shorter amount of time, according to the authors.
The researchers pointed out several limitations to their study beyond those intrinsic to surveys. Attitudes of residents may change over time, although the survey was most concerned with the perception of incoming interns. Also, program directors were not chosen randomly, and some regions may have been underrepresented. In addition, attitudes cannot be taken as evidence of the actual results of duty-hour restrictions on training, only the perceptions of that effect. But in the absence of defined metrics for assessing the effect of duty-hour restrictions on training, the attitudes of those most involved in training may be the best metric available, they noted.
"As residency programs attempt to adapt to the new regulations, surgical interns have significant concerns about the implications of these regulations on their training. The opinions of these interns, although markedly more optimistic than those of surgical program directors, reflect a persistent concern within the surgical community regarding the effects of work-hour restrictions on surgical training," they concluded.
The authors had no disclosures.
Interns beginning their surgical training under the new resident duty-hour standards appear to be less pessimistic than program directors, but they still show significant concern that these new regulations will have a detrimental effect on the quality of their training, according to the results of separate surveys of surgical interns in general surgery residency programs and national surgical program directors.
The Accreditation Council for Graduate Medical Education (ACGME) implemented the new standards in July 2011 to include increased supervision and a 16-hour shift maximum for postgraduate year 1 residents, according to a report published in the June issue of Archives of Surgery.
In the summer of 2011, the researchers surveyed all 215 surgical interns in 11 general surgical residency programs distributed across the country to assess their perceptions of how the new duty-hour requirements would affect continuity of care, resident fatigue, and development in the six core ACGME competencies, according to Dr. Ryan M. Antiel of the Mayo Clinic, Rochester, Minn., and his colleagues. Perceptions were measured using a 3-point scale (increase, decrease, no change) for each item. A total of 179 (83.3%) completed the survey. Most respondents (68.7%) were men and were younger than 29 years of age (73%), with 102 categorical interns (57%) and 76 preliminary interns (42.5%), and 1 nonrespondent to this question (Arch. Surg. 2012;147:536-41).
Results of the resident survey were compared with those of an earlier survey of 134 program directors conducted by Dr. Antiel and his colleagues (Mayo Clin. Proc. 2011;86:185-91).
The great majority of the interns (80.3%) indicated that the new restrictions would decrease their ability to achieve continuity with hospitalized patients, and more than half (57.6%) stated that there would be a decrease in the coordination of patient care. Slightly fewer than half (48%) believed it would interfere with their acquisition of new medical knowledge.
"Most of the surgical interns (67.4%) believed that the duty-hour restrictions will decrease their time spent in the operating room," the researchers added. They also indicated that the new standards would decrease their development of surgical skills (52.8%); their time spent with patients on the floor (51.1%); and their overall educational experience (51.1%). Categorical interns were significantly more likely to believe that the changes would decrease both quality and safety of patient care (odds ratio, 2.6).
However, some optimism was also expressed: In all, 61.5% of interns believed that the new standards would decrease resident fatigue; 66.5% indicated that the new hours would increase or not change quality and safety of patient care; 72.1% indicated the same for the ability to effectively communicate with patients, families, and other health professionals; 74.7% indicated the same for the resident’s investigation and self-evaluation of their own patient care; and 70.2% felt that the impact would be neutral or favorable in the area of responsiveness to patient needs that supersede self-interest.
Compared with the program directors surveyed, a significantly higher proportion of interns believed that the new changes would improve or not change residents’ performance. And a significantly larger percentage of program directors agreed that the new changes would decrease coordination of patient care and residents’ acquisition of medical knowledge (76.9% vs. 48.0%). Perhaps most notably in terms of cross-perceptions, most interns (61.5%) believed that the new changes would decrease fatigue, whereas 85.1% of program directors believed that the new hours would increase fatigue, presumably by increasing the intensity of effort and accomplishments required in that shorter amount of time, according to the authors.
The researchers pointed out several limitations to their study beyond those intrinsic to surveys. Attitudes of residents may change over time, although the survey was most concerned with the perception of incoming interns. Also, program directors were not chosen randomly, and some regions may have been underrepresented. In addition, attitudes cannot be taken as evidence of the actual results of duty-hour restrictions on training, only the perceptions of that effect. But in the absence of defined metrics for assessing the effect of duty-hour restrictions on training, the attitudes of those most involved in training may be the best metric available, they noted.
"As residency programs attempt to adapt to the new regulations, surgical interns have significant concerns about the implications of these regulations on their training. The opinions of these interns, although markedly more optimistic than those of surgical program directors, reflect a persistent concern within the surgical community regarding the effects of work-hour restrictions on surgical training," they concluded.
The authors had no disclosures.
Major Finding: The majority of interns (80.3%) thought the new restrictions would decrease their ability to achieved continuity with hospitalized patients and that there would be a decrease in the coordination of patient care (57.6%). Fewer than half (48%) believed it would interfere with their acquisition of new medical knowledge.
Data Source: Researchers analyzed the results of a survey of 215 surgical interns in general surgery residency programs and compared them with those of an earlier survey of 134 national surgical program directors.
Disclosures: The authors reported they had no financial disclosures.
Hospitalist‐Led Medicine ED Team
Emergency department (ED) crowding leads to ambulance diversion,1 which can delay care and worsen outcomes, including mortality.2 A national survey showed that 90% of EDs were overcrowded, and 70% reported time on diversion.3 One of the causes of ED crowding is boarding of admitted patients.4 Boarding admitted patients decreases quality of care and satisfaction.57
Improved ED triage, bedside registration, physical expansion of hospitals, and regional ambulance programs have been implemented to decrease ED diversion.812 Despite these attempts, ED diversion continues to be prevalent.
Interventions involving hospitalists have been tested to improve throughput and quality of care for admitted medicine patients boarded in the ED. Howell and colleagues decreased ED diversion through active bed management by hospitalists.13 Briones and colleagues dedicated a hospitalist team to patients boarded in the ED and improved their quality of care.14
Denver Health Medical Center (DHMC) is an urban, academic safety net hospital. In 2009, the ED saw an average of 133 patients daily and an average of 25 were admitted to the medical service. DHMC's ED diversion rate was a mean of 12.4% in 2009. Boarded medicine patients occupied 16% of ED medicine bed capacity. Teaching and nonteaching medical floor teams cared for patients in the ED awaiting inpatient beds, who were the last to be seen. Nursing supervisors transferred boarded patients from the ED to hospital units. Patients with the greatest duration of time in the ED had priority for open beds.
ED diversion is costly.15, 16 DHMC implemented codified diversion criteria, calling the administrator on‐call prior to diversion, and increasing frequency of rounding in the ED, with no sustained effect seen in the rate of ED diversion.
In 2009, the DHMC Hospital Medicine Service addressed the issue of ED crowding, ED diversion, and care of boarded ED patients by creating a hospital medicine ED (HMED) team with 2 functions: (1) to provide ongoing care for medicine patients in the ED awaiting inpatient beds; and (2) to work with nursing supervisors to improve patient flow by adding physician clinical expertise to bed management.
METHODS
Setting and Design
This study took place at DHMC, a 477licensed‐bed academic safety net hospital in Denver, Colorado. We used a prepost design to assess measures of patient flow and timeliness of care. We surveyed ED attendings and nursing supervisors after the intervention to determine perceptions of the HMED team. This study was approved by the local institutional review board (IRB protocol number 09‐0892).
Intervention
In 2009, DHMC, which uses Toyota Lean for quality improvement, performed a Rapid Improvement Event (RIE) to address ED diversion and care of admitted patients boarded in the ED. The RIE team consisted of hospital medicine physicians, ED physicians, social workers, and nurses. Over a 4‐day period, the team examined the present state, created an ideal future state, devised a solution, and tested this solution.
Based upon the results of the RIE, DHMC implemented an HMED team to care for admitted patients boarded in the ED and assist in active bed management. The HMED team is a 24/7 service. During the day shift, the HMED team is composed of 1 dedicated attending and 1 allied health provider (AHP). Since the medicine services were already staffing existing patients in the ED, the 2.0 full‐time equivalent (FTE) needed to staff the HMED team attending and the AHP was reallocated from existing FTE within the hospitalist division. During the evening and night shifts, the HMED team's responsibilities were rolled into existing hospitalist duties.
The HMED team provides clinical care for 2 groups of patients in the ED. The first group represents admitted patients who are still awaiting a medicine ward bed as of 7:00 AM. The HMED team provides ongoing care until discharge from the ED or transfer to a medicine floor. The second group of patients includes new admissions that need to stay in the ED due to a lack of available medicine floor beds. For these patients, the HMED team initiates and continues care until discharge from the ED or transfer to a medical floor (Figure 1).
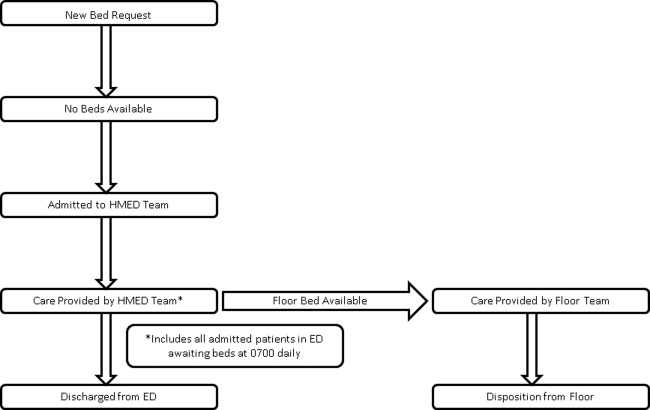
The physician on the HMED team assists nursing supervisors with bed management by providing detailed clinical knowledge, including proximity to discharge as well as updated information on telemetry and intensive care unit (ICU) appropriateness. The HMED team's physician maintains constant knowledge of hospital census via an electronic bed board, and communicates regularly with medical floors about anticipated discharges and transfers to understand the hospital's patient flow status (Figure 2).
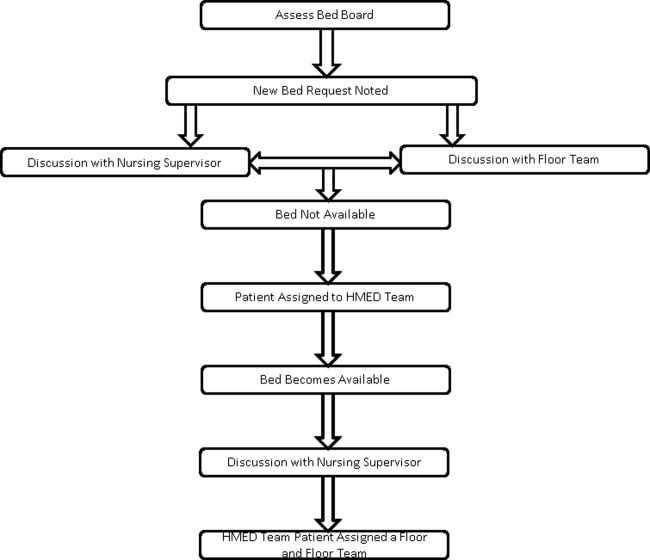
The RIE that resulted in the HMED team was part of the Inpatient Medicine Value Stream, which had the overall goal of saving DHMC $300,000 for 2009. Ten RIEs were planned for this value stream in 2009, with an average of $30,000 of savings expected from each RIE.
Determination of ED Diversion Time
DHMC places responsibility for putting the hospital on an ED Diversion status in the hands of the Emergency Medicine Attending Physician. Diversion is categorized as either due to: (1) excessive ED volume for available ED bedsfull or nearly full department, or full resuscitation rooms without the ability to release a room; or (2) excessive boardingmore than 12 admitted patients awaiting beds in the ED. Other reasons for diversion, such as acute, excessive resource utilization (multiple patients from a single event) and temporary limitation of resources (critical equipment becoming inoperative), are also infrequent causes of diversion that are recorded. The elapsed time during which the ED is on diversion status is recorded and reported as a percentage of the total time on a monthly basis.
Determination of ED Diversion Costs
The cost of diversion at DHMC is calculated by multiplying the average number of ambulance drop‐offs per hour times the number of diversion hours to determine the number of missed patients. The historical mean charges for each ambulance patient are used to determine total missed charge opportunity, which is then applied to the hospital realization rate to calculate missed revenue. In addition, the marginal costs related to Denver Health Medical Plan patients that were unable to be repatriated to DHMC from outlying hospitals, as a result of diversion, is added to the net missed revenue figure. This figure is then divided by the number of diversion hours for the year to determine the cost of each diversion hour. For 2009, the cost of each hour of diversion at DHMC was $5000.
Statistical Analysis
All analyses were performed using SAS Enterprise Guide 4.1 (SAS Institute, Inc, Cary, NC). A Student t test or Wilcoxon rank sum test was used to compare continuous variables, and a chi‐square test was used to compare categorical variables.
Our primary outcome was ED diversion due to hospital bed capacity. These data are recorded, maintained, and analyzed by a DHMC internally developed emergency medical services information system (EMeSIS) that interfaces with computerized laboratory reporting systems, and stores, in part, demographic data as well as real‐time data related to the timing of patient encounters for all patients evaluated in the ED. To assess the effect of the intervention on ED diversion, the proportion of total hours on diversion due to medicine bed capacity was compared preimplementation and postimplementation with a chi‐squared test.
Secondary outcomes for patient flow included: (1) the proportion of patients discharged within 8 hours of transfer to a medical floor; and (2) the proportion of admitted medicine patients discharged from the ED. These data were gathered from the Denver Health Data Warehouse which pools data from both administrative and clinical applications used in patient care. Chi‐squared tests were also used to compare secondary outcomes preintervention and postintervention.
To measure the quality and safety of the HMED team, pre‐ED and post‐ED length of stay (LOS), 48‐hour patient return rate, intensive care unit (ICU) transfer rate, and the total LOS for patients admitted to the HMED team and handed off to a medicine floor team were assessed with the Student t test. To assess timeliness of clinical care provided to boarded medicine patients, self‐reported rounding times were compared preintervention and postintervention with the Student t test.
To assess satisfaction with the HMED team, an anonymous paper survey was administered to ED attendings and nursing supervisors 1 year after the intervention was introduced. The survey consisted of 5 questions, and used a 5‐point Likert scale ranging from strongly disagree (1) to strongly agree (5). Those answering agree or strongly agree were compared to those who were neutral, disagreed, or strongly disagreed.
RESULTS
The ED saw 48,595 patients during the intervention period (August 1, 2009June 30,2010) which did not differ statistically from the 50,469 patients seen in the control period (August 1, 2008June 30, 2009). The number of admissions to the medicine service during the control period (9727) and intervention period (10,013), and the number of total medical/surgical admissions during the control (20,716) and intervention (20,574) periods did not statistically differ. ED staffing during the intervention did not change. The overall number of licensed beds did not increase during the study period. During the control period, staffed medical/surgical beds increased from 395 to 400 beds, while the number of staffed medical/surgical beds decreased from 400 to 397 beds during the intervention period. Patient characteristics were similar during the 2 time periods, with the exception of race (Table 1).
| Patients Admitted to Medicine and Transferred to a Medicine Floor | Pre | Post | P Value |
|---|---|---|---|
| |||
| No. | 1901 | 1828 | |
| Age* | 53 15 | 54 14 | 0.59 |
| Gender (% male) | 55% | 52% | 0.06 |
| Race (% white) | 40% | 34% | <0.0001 |
| Insurance (% insured) | 67% | 63% | 0.08 |
| Charlson Comorbidity Index | 1.0 [1.0, 1.0] | 1.0 [1.0, 1.0] | 0.52 |
Diversion Hours
After implementation of the HMED team, there was a relative reduction of diversion due to medicine bed capacity of 27% (4.5%3.3%; P < 0.01) (Table 2). During the same time period, the relative proportion of hours on diversion due to ED capacity decreased by 55% (9.9%5.4%).
| Pre | Post | P Value | |
|---|---|---|---|
| |||
| Divert hours due to bed capacity (%, hours)* | 4.5% (3624) | 3.3% (3624) | 0.009 |
| Admitted ED patients transferred to floor | |||
| Discharged within 8 h (%, N) | 1.3% (1901) | 0.5% (1828) | 0.03 |
| Boarded patients rounded on in the ED and transferred to the medical floor | |||
| Total length of stay (days, N) | 2.6 [2.4, 3.2] (154) | 2.5 [2.4, 2.6] (364) | 0.21 |
| All discharges and transfers to the floor | |||
| Discharged from ED [%, (N)] | 4.9% (2009) | 7.5% (1981) | <0.001 |
| ED length of stay [hours, (N)] | 12:09 8:44 (2009) | 12:48 10:00 (1981) | 0.46 |
| Return to hospital <48 h [%, (N)] | 4.6% (2009) | 4.8% (1981) | 0.75 |
| Transfer to the ICU [%, (N)] | 3.3% (2009) | 4.2% (1981) | 0.13 |
Bed Management and Patient Flow
The HMED team rounded on boarded ED patients a mean of 2 hours and 9 minutes earlier (10:59 AM 1:09 vs 8:50 AM 1:20; P < 0.0001). After implementation of the HMED team, patients transferred to a medicine floor and discharged within 8 hours decreased relatively by 67% (1.5%0.5%; P < 0.01), and discharges from the ED of admitted medicine patients increased relatively by 61% (4.9%7.9%; P < 0.001) (Table 2). ED LOS, total LOS, 48‐hour returns to the ED, and ICU transfer rate for patients managed by the HMED team did not change (Table 2).
Perception and Satisfaction
Nine out of 15 (60%) ED attendings and 7 out of 8 (87%) nursing supervisors responded to the survey. The survey demonstrated that ED attendings and nursing supervisors believe the HMED team improves clinical care for boarded patients, communication, collegiality, and patient flow (Table 3).
| Postimplementation of the HMED Team | Total (n = 16) | ED Attendings (n = 9) | Nursing Supervisors (n = 7) |
|---|---|---|---|
| |||
| Quality of care has improved | 94 | 89 | 100 |
| Communication has improved | 94 | 89 | 100 |
| Collegiality and clinical decision‐making has improved | 94 | 100 | 89 |
| Patient flow has improved | 81 | 67 | 100 |
| HMED team is an asset to DHMC | 94 | 89 | 100 |
Financial
The 27% relative reduction in ED diversion due to hospital bed capacity extrapolates to 105.1 hours a year of decreased diversion, accounting for $525,600 of increased annual revenues.
DISCUSSION
This study suggests that an HMED team can decrease ED diversion, due to hospital bed capacity, by improving patient flow and timeliness of care for boarded medicine patients in the ED.
After participating in bed management, ED diversion due to a lack of medicine beds decreased. This is consistent with findings by Howell and colleagues who were able to improve throughput and decrease ED diversion with active bed management.13 Howell and colleagues decreased diversion hours due to temporary ED overload, and diversion hours due to a lack of telemetry or critical care beds. At DHMC, diversion is attributed to either a lack of ED capacity or lack of hospital beds. The primary outcome was the diversion rate due to lack of hospital beds, but it is possible that increased discharges directly from the ED contributed to the decrease in diversion due to ED capacity, underestimating the effect our intervention had on total ED diversion. There were no other initiatives to decrease diversion due to ED capacity during the study periods, and ED capacity and volume did not change during the intervention period.
While there were no statistically significant changes in staffed medical/surgical beds or medicine admissions, staffed medical/surgical beds during the intervention period decreased while there were more admissions to medicine. Both of these variables would increase diversion, resulting in an underestimation of the effect of the intervention.
Howell and colleagues improved throughput in the ED by implementing a service which provided active bed management without clinical responsibilities,13 while Briones and colleagues improved clinical care of patients boarded in the ED without affecting throughput.14 The HMED team improved throughput and decreased ED diversion while improving timeliness of care and perception of care quality for patients boarding in the ED.
By decreasing unnecessary transfers to medicine units and increasing discharges from the ED, patient flow was improved. While there was no difference in ED LOS, there was a trend towards decreased total LOS. A larger sample size or a longer period of observation would be necessary to determine if the trend toward decreased total LOS is statistically significant. ED LOS may not have been decreased because patients who would have been sent to the floor only to be discharged within 8 hours were kept in the ED to expedite testing and discharge, while sicker patients were sent to the medical floor. This decreased the turnover time of inpatient beds and allowed more boarded patients to be moved to floor units.
There was concern that an HMED team would fragment care, which would lead to an increased LOS for those patients who were transferred to a medical floor and cared for by an additional medicine team before discharge.17 As noted, there was a trend towards a decreased LOS for patients initially cared for by the HMED team.
In this intervention, hospital medicine physicians provided information regarding ongoing care of patients boarded in the ED to nursing supervisors. Prior to the intervention, nursing supervisors relied upon information from the ED staff and the boarded patient's time in the ED to assign a medical floor. However, ED staff was not providing care to boarded patients and did not know the most up‐to‐date status of the patient. This queuing process and lack of communication resulted in patients ready for discharge being transferred to floor beds and discharged within a few hours of transfer. The HMED team allowed nursing supervisors to have direct knowledge regarding clinical status, including telemetry and ICU criteria (similar to Howell and colleagues13), and readiness for discharge from the physician taking care of the patient.
By managing boarded patients, an HMED team can improve timeliness and coordination of care. Prior to the intervention, boarded ED patients were the last to be seen on rounds. The HMED team rounds only in the ED, expediting care and discharges. The increased proportion of boarded patients discharged from the ED by the HMED team is consistent with Briones and colleagues' clinically oriented team managing boarding patients in the ED.14
Potential adverse effects of our intervention included increased returns to the ED, increased ICU transfer rate, and decreased housestaff satisfaction. There was no increase in the 48‐hour return rate and no increase in the ICU transfer rate for patients cared for by the HMED team. Housestaff at DHMC are satisfied with the HMED team, since the presence of the HMED team allows them to concentrate on patients on the medical floors.
This intervention provides DHMC with an additional $525,600 in revenue annually. Since existing FTE were reallocated to create the HMED team, no additional FTE were required. In our facility, AHPs take on duties of housestaff. However, only 1 physician may be needed to staff an HMED team. This physician's clinical productivity is about 75% of other physicians; therefore, 25% of time is spent in bed management. At DHMC, other medicine teams picked up for the decreased clinical productivity of the HMED team, so the budget was neutral. However, using 2 FTE to staff 1 physician daily for 365 days a year, one would need to allocate 0.5 physician FTE (0.25 decrease in clinical productivity 2 FTE) for an HMED team.
Our study has several limitations. As a single center study, our findings may not extrapolate to other settings. The study used historical controls, therefore, undetected confounders may exist. We could not control for simultaneous changes in the hospital, however, we did not know of any other concurrent interventions aimed at decreasing ED diversion. Also, the decision to admit or not is partially based on individual ED attendings, which causes variability in practice. Finally, while we were able to measure rounding times as a process measure to reflect timeliness of care and staff perceptions of quality of care, due to our data infrastructure and the way our housestaff and attendings rotate, we were not able to assess more downstream measures of quality of care.
CONCLUSION
ED crowding decreases throughput and worsens clinical care; there are few proven solutions. This study demonstrates an intervention that reduced the percentage of patients transferred to a medicine floor and discharged within 8 hours, increased the number of discharges from the ED of admitted medicine patients, and decreased ED diversion while improving the timeliness of clinical care for patients boarded in the ED.
Acknowledgements
Disclosure: Nothing to report.
- ,,.Access block causes emergency department overcrowding and ambulance diversion in Perth, Western Australia.Emerg Med J.2005;22:351–354.
- ,,,.The relationship between distance to hospital and patient mortality in emergencies: an observational study.Emerg Med J.2007;24:665–668.
- Institute of Medicine.Committee on the Future of Emergency Care in the United States Health System.Hospital‐Based Emergency Care: At the Breaking Point.Washington, DC:National Academies Press;2007.
- ,.Systematic review of emergency department crowding: causes, effects, and solutions.Ann Emerg Med.2008;52:126–136.
- ,.Emergency department crowding is associated with poor care for patients with severe pain.Ann Emerg Med.2008;51:1–5.
- ,,, et al.The impact of emergency department crowding measures on time to antibiotics for patients with community‐acquired pneumonia.Ann Emerg Med.2007;50:510–516.
- ,,, et al;for the DELAYED‐ED Study Group.Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit.Crit Care Med.2007;35:1477–1483.
- ,,, et al.Impact of a triage liaison physician on emergency department overcrowding and throughput: a randomized controlled trial.Acad Emerg Med.2007;14:702–708.
- ,,.Strategies for dealing with emergency department overcrowding: a one‐year study on how bedside registration affects patient throughput times.Emerg Med J.2007;32:337–342.
- ,,, et al.The effect of emergency department expansion on emergency department overcrowding.Acad Emerg Med.2007;14:338–343.
- ,,,,,.Effect of increased ICU capacity on emergency department length of stay and ambulance diversion.Ann Emerg Med.2005;5:471–478.
- ,,,,.Ambulance diversion reduction: the Sacramento solution.Am J Emerg Med.2006;357:608–613.
- ,,,,,.Active bed management by hospitalists and emergency department throughput.Ann Intern Med.2008;149:804–810.
- ,,, et al.A model of hospitalist role in the care of admitted patients in the emergency department.J Hosp Med.2010;5:360–364.
- ,,,,.Ambulance diversion and lost hospital revenues.Ann Emerg Med.2006;48(6):702–710.
- ,,,.The financial impact of ambulance diversion and patient elopements.Acad Emerg Med.2007;14(1):58–62.
- ,,,,.The impact of fragmentation of hospitalist care on length of stay.J. Hosp. Med.2010;5:335–338.
Emergency department (ED) crowding leads to ambulance diversion,1 which can delay care and worsen outcomes, including mortality.2 A national survey showed that 90% of EDs were overcrowded, and 70% reported time on diversion.3 One of the causes of ED crowding is boarding of admitted patients.4 Boarding admitted patients decreases quality of care and satisfaction.57
Improved ED triage, bedside registration, physical expansion of hospitals, and regional ambulance programs have been implemented to decrease ED diversion.812 Despite these attempts, ED diversion continues to be prevalent.
Interventions involving hospitalists have been tested to improve throughput and quality of care for admitted medicine patients boarded in the ED. Howell and colleagues decreased ED diversion through active bed management by hospitalists.13 Briones and colleagues dedicated a hospitalist team to patients boarded in the ED and improved their quality of care.14
Denver Health Medical Center (DHMC) is an urban, academic safety net hospital. In 2009, the ED saw an average of 133 patients daily and an average of 25 were admitted to the medical service. DHMC's ED diversion rate was a mean of 12.4% in 2009. Boarded medicine patients occupied 16% of ED medicine bed capacity. Teaching and nonteaching medical floor teams cared for patients in the ED awaiting inpatient beds, who were the last to be seen. Nursing supervisors transferred boarded patients from the ED to hospital units. Patients with the greatest duration of time in the ED had priority for open beds.
ED diversion is costly.15, 16 DHMC implemented codified diversion criteria, calling the administrator on‐call prior to diversion, and increasing frequency of rounding in the ED, with no sustained effect seen in the rate of ED diversion.
In 2009, the DHMC Hospital Medicine Service addressed the issue of ED crowding, ED diversion, and care of boarded ED patients by creating a hospital medicine ED (HMED) team with 2 functions: (1) to provide ongoing care for medicine patients in the ED awaiting inpatient beds; and (2) to work with nursing supervisors to improve patient flow by adding physician clinical expertise to bed management.
METHODS
Setting and Design
This study took place at DHMC, a 477licensed‐bed academic safety net hospital in Denver, Colorado. We used a prepost design to assess measures of patient flow and timeliness of care. We surveyed ED attendings and nursing supervisors after the intervention to determine perceptions of the HMED team. This study was approved by the local institutional review board (IRB protocol number 09‐0892).
Intervention
In 2009, DHMC, which uses Toyota Lean for quality improvement, performed a Rapid Improvement Event (RIE) to address ED diversion and care of admitted patients boarded in the ED. The RIE team consisted of hospital medicine physicians, ED physicians, social workers, and nurses. Over a 4‐day period, the team examined the present state, created an ideal future state, devised a solution, and tested this solution.
Based upon the results of the RIE, DHMC implemented an HMED team to care for admitted patients boarded in the ED and assist in active bed management. The HMED team is a 24/7 service. During the day shift, the HMED team is composed of 1 dedicated attending and 1 allied health provider (AHP). Since the medicine services were already staffing existing patients in the ED, the 2.0 full‐time equivalent (FTE) needed to staff the HMED team attending and the AHP was reallocated from existing FTE within the hospitalist division. During the evening and night shifts, the HMED team's responsibilities were rolled into existing hospitalist duties.
The HMED team provides clinical care for 2 groups of patients in the ED. The first group represents admitted patients who are still awaiting a medicine ward bed as of 7:00 AM. The HMED team provides ongoing care until discharge from the ED or transfer to a medicine floor. The second group of patients includes new admissions that need to stay in the ED due to a lack of available medicine floor beds. For these patients, the HMED team initiates and continues care until discharge from the ED or transfer to a medical floor (Figure 1).
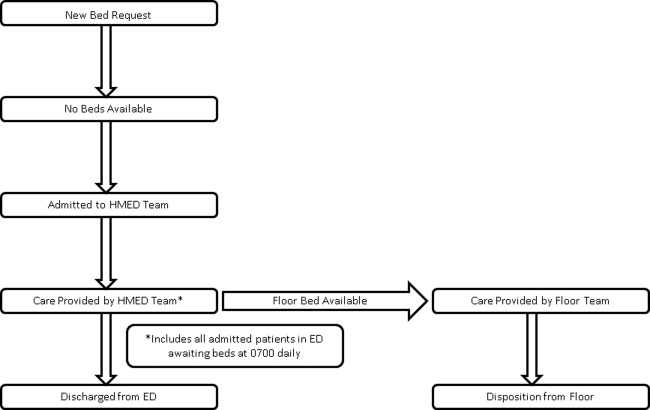
The physician on the HMED team assists nursing supervisors with bed management by providing detailed clinical knowledge, including proximity to discharge as well as updated information on telemetry and intensive care unit (ICU) appropriateness. The HMED team's physician maintains constant knowledge of hospital census via an electronic bed board, and communicates regularly with medical floors about anticipated discharges and transfers to understand the hospital's patient flow status (Figure 2).
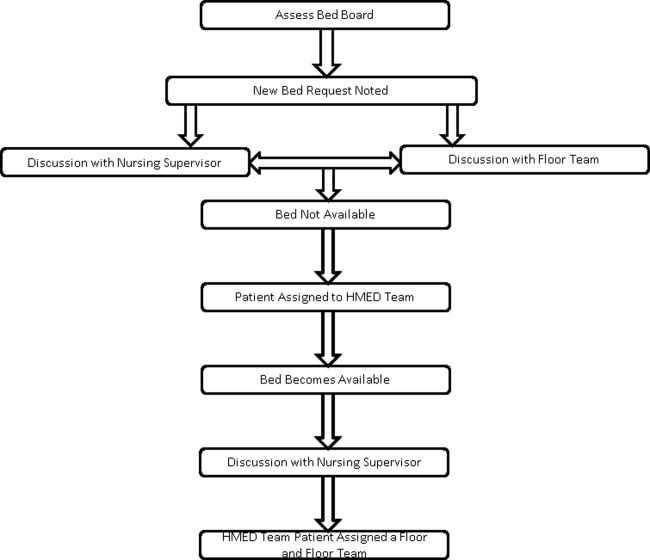
The RIE that resulted in the HMED team was part of the Inpatient Medicine Value Stream, which had the overall goal of saving DHMC $300,000 for 2009. Ten RIEs were planned for this value stream in 2009, with an average of $30,000 of savings expected from each RIE.
Determination of ED Diversion Time
DHMC places responsibility for putting the hospital on an ED Diversion status in the hands of the Emergency Medicine Attending Physician. Diversion is categorized as either due to: (1) excessive ED volume for available ED bedsfull or nearly full department, or full resuscitation rooms without the ability to release a room; or (2) excessive boardingmore than 12 admitted patients awaiting beds in the ED. Other reasons for diversion, such as acute, excessive resource utilization (multiple patients from a single event) and temporary limitation of resources (critical equipment becoming inoperative), are also infrequent causes of diversion that are recorded. The elapsed time during which the ED is on diversion status is recorded and reported as a percentage of the total time on a monthly basis.
Determination of ED Diversion Costs
The cost of diversion at DHMC is calculated by multiplying the average number of ambulance drop‐offs per hour times the number of diversion hours to determine the number of missed patients. The historical mean charges for each ambulance patient are used to determine total missed charge opportunity, which is then applied to the hospital realization rate to calculate missed revenue. In addition, the marginal costs related to Denver Health Medical Plan patients that were unable to be repatriated to DHMC from outlying hospitals, as a result of diversion, is added to the net missed revenue figure. This figure is then divided by the number of diversion hours for the year to determine the cost of each diversion hour. For 2009, the cost of each hour of diversion at DHMC was $5000.
Statistical Analysis
All analyses were performed using SAS Enterprise Guide 4.1 (SAS Institute, Inc, Cary, NC). A Student t test or Wilcoxon rank sum test was used to compare continuous variables, and a chi‐square test was used to compare categorical variables.
Our primary outcome was ED diversion due to hospital bed capacity. These data are recorded, maintained, and analyzed by a DHMC internally developed emergency medical services information system (EMeSIS) that interfaces with computerized laboratory reporting systems, and stores, in part, demographic data as well as real‐time data related to the timing of patient encounters for all patients evaluated in the ED. To assess the effect of the intervention on ED diversion, the proportion of total hours on diversion due to medicine bed capacity was compared preimplementation and postimplementation with a chi‐squared test.
Secondary outcomes for patient flow included: (1) the proportion of patients discharged within 8 hours of transfer to a medical floor; and (2) the proportion of admitted medicine patients discharged from the ED. These data were gathered from the Denver Health Data Warehouse which pools data from both administrative and clinical applications used in patient care. Chi‐squared tests were also used to compare secondary outcomes preintervention and postintervention.
To measure the quality and safety of the HMED team, pre‐ED and post‐ED length of stay (LOS), 48‐hour patient return rate, intensive care unit (ICU) transfer rate, and the total LOS for patients admitted to the HMED team and handed off to a medicine floor team were assessed with the Student t test. To assess timeliness of clinical care provided to boarded medicine patients, self‐reported rounding times were compared preintervention and postintervention with the Student t test.
To assess satisfaction with the HMED team, an anonymous paper survey was administered to ED attendings and nursing supervisors 1 year after the intervention was introduced. The survey consisted of 5 questions, and used a 5‐point Likert scale ranging from strongly disagree (1) to strongly agree (5). Those answering agree or strongly agree were compared to those who were neutral, disagreed, or strongly disagreed.
RESULTS
The ED saw 48,595 patients during the intervention period (August 1, 2009June 30,2010) which did not differ statistically from the 50,469 patients seen in the control period (August 1, 2008June 30, 2009). The number of admissions to the medicine service during the control period (9727) and intervention period (10,013), and the number of total medical/surgical admissions during the control (20,716) and intervention (20,574) periods did not statistically differ. ED staffing during the intervention did not change. The overall number of licensed beds did not increase during the study period. During the control period, staffed medical/surgical beds increased from 395 to 400 beds, while the number of staffed medical/surgical beds decreased from 400 to 397 beds during the intervention period. Patient characteristics were similar during the 2 time periods, with the exception of race (Table 1).
| Patients Admitted to Medicine and Transferred to a Medicine Floor | Pre | Post | P Value |
|---|---|---|---|
| |||
| No. | 1901 | 1828 | |
| Age* | 53 15 | 54 14 | 0.59 |
| Gender (% male) | 55% | 52% | 0.06 |
| Race (% white) | 40% | 34% | <0.0001 |
| Insurance (% insured) | 67% | 63% | 0.08 |
| Charlson Comorbidity Index | 1.0 [1.0, 1.0] | 1.0 [1.0, 1.0] | 0.52 |
Diversion Hours
After implementation of the HMED team, there was a relative reduction of diversion due to medicine bed capacity of 27% (4.5%3.3%; P < 0.01) (Table 2). During the same time period, the relative proportion of hours on diversion due to ED capacity decreased by 55% (9.9%5.4%).
| Pre | Post | P Value | |
|---|---|---|---|
| |||
| Divert hours due to bed capacity (%, hours)* | 4.5% (3624) | 3.3% (3624) | 0.009 |
| Admitted ED patients transferred to floor | |||
| Discharged within 8 h (%, N) | 1.3% (1901) | 0.5% (1828) | 0.03 |
| Boarded patients rounded on in the ED and transferred to the medical floor | |||
| Total length of stay (days, N) | 2.6 [2.4, 3.2] (154) | 2.5 [2.4, 2.6] (364) | 0.21 |
| All discharges and transfers to the floor | |||
| Discharged from ED [%, (N)] | 4.9% (2009) | 7.5% (1981) | <0.001 |
| ED length of stay [hours, (N)] | 12:09 8:44 (2009) | 12:48 10:00 (1981) | 0.46 |
| Return to hospital <48 h [%, (N)] | 4.6% (2009) | 4.8% (1981) | 0.75 |
| Transfer to the ICU [%, (N)] | 3.3% (2009) | 4.2% (1981) | 0.13 |
Bed Management and Patient Flow
The HMED team rounded on boarded ED patients a mean of 2 hours and 9 minutes earlier (10:59 AM 1:09 vs 8:50 AM 1:20; P < 0.0001). After implementation of the HMED team, patients transferred to a medicine floor and discharged within 8 hours decreased relatively by 67% (1.5%0.5%; P < 0.01), and discharges from the ED of admitted medicine patients increased relatively by 61% (4.9%7.9%; P < 0.001) (Table 2). ED LOS, total LOS, 48‐hour returns to the ED, and ICU transfer rate for patients managed by the HMED team did not change (Table 2).
Perception and Satisfaction
Nine out of 15 (60%) ED attendings and 7 out of 8 (87%) nursing supervisors responded to the survey. The survey demonstrated that ED attendings and nursing supervisors believe the HMED team improves clinical care for boarded patients, communication, collegiality, and patient flow (Table 3).
| Postimplementation of the HMED Team | Total (n = 16) | ED Attendings (n = 9) | Nursing Supervisors (n = 7) |
|---|---|---|---|
| |||
| Quality of care has improved | 94 | 89 | 100 |
| Communication has improved | 94 | 89 | 100 |
| Collegiality and clinical decision‐making has improved | 94 | 100 | 89 |
| Patient flow has improved | 81 | 67 | 100 |
| HMED team is an asset to DHMC | 94 | 89 | 100 |
Financial
The 27% relative reduction in ED diversion due to hospital bed capacity extrapolates to 105.1 hours a year of decreased diversion, accounting for $525,600 of increased annual revenues.
DISCUSSION
This study suggests that an HMED team can decrease ED diversion, due to hospital bed capacity, by improving patient flow and timeliness of care for boarded medicine patients in the ED.
After participating in bed management, ED diversion due to a lack of medicine beds decreased. This is consistent with findings by Howell and colleagues who were able to improve throughput and decrease ED diversion with active bed management.13 Howell and colleagues decreased diversion hours due to temporary ED overload, and diversion hours due to a lack of telemetry or critical care beds. At DHMC, diversion is attributed to either a lack of ED capacity or lack of hospital beds. The primary outcome was the diversion rate due to lack of hospital beds, but it is possible that increased discharges directly from the ED contributed to the decrease in diversion due to ED capacity, underestimating the effect our intervention had on total ED diversion. There were no other initiatives to decrease diversion due to ED capacity during the study periods, and ED capacity and volume did not change during the intervention period.
While there were no statistically significant changes in staffed medical/surgical beds or medicine admissions, staffed medical/surgical beds during the intervention period decreased while there were more admissions to medicine. Both of these variables would increase diversion, resulting in an underestimation of the effect of the intervention.
Howell and colleagues improved throughput in the ED by implementing a service which provided active bed management without clinical responsibilities,13 while Briones and colleagues improved clinical care of patients boarded in the ED without affecting throughput.14 The HMED team improved throughput and decreased ED diversion while improving timeliness of care and perception of care quality for patients boarding in the ED.
By decreasing unnecessary transfers to medicine units and increasing discharges from the ED, patient flow was improved. While there was no difference in ED LOS, there was a trend towards decreased total LOS. A larger sample size or a longer period of observation would be necessary to determine if the trend toward decreased total LOS is statistically significant. ED LOS may not have been decreased because patients who would have been sent to the floor only to be discharged within 8 hours were kept in the ED to expedite testing and discharge, while sicker patients were sent to the medical floor. This decreased the turnover time of inpatient beds and allowed more boarded patients to be moved to floor units.
There was concern that an HMED team would fragment care, which would lead to an increased LOS for those patients who were transferred to a medical floor and cared for by an additional medicine team before discharge.17 As noted, there was a trend towards a decreased LOS for patients initially cared for by the HMED team.
In this intervention, hospital medicine physicians provided information regarding ongoing care of patients boarded in the ED to nursing supervisors. Prior to the intervention, nursing supervisors relied upon information from the ED staff and the boarded patient's time in the ED to assign a medical floor. However, ED staff was not providing care to boarded patients and did not know the most up‐to‐date status of the patient. This queuing process and lack of communication resulted in patients ready for discharge being transferred to floor beds and discharged within a few hours of transfer. The HMED team allowed nursing supervisors to have direct knowledge regarding clinical status, including telemetry and ICU criteria (similar to Howell and colleagues13), and readiness for discharge from the physician taking care of the patient.
By managing boarded patients, an HMED team can improve timeliness and coordination of care. Prior to the intervention, boarded ED patients were the last to be seen on rounds. The HMED team rounds only in the ED, expediting care and discharges. The increased proportion of boarded patients discharged from the ED by the HMED team is consistent with Briones and colleagues' clinically oriented team managing boarding patients in the ED.14
Potential adverse effects of our intervention included increased returns to the ED, increased ICU transfer rate, and decreased housestaff satisfaction. There was no increase in the 48‐hour return rate and no increase in the ICU transfer rate for patients cared for by the HMED team. Housestaff at DHMC are satisfied with the HMED team, since the presence of the HMED team allows them to concentrate on patients on the medical floors.
This intervention provides DHMC with an additional $525,600 in revenue annually. Since existing FTE were reallocated to create the HMED team, no additional FTE were required. In our facility, AHPs take on duties of housestaff. However, only 1 physician may be needed to staff an HMED team. This physician's clinical productivity is about 75% of other physicians; therefore, 25% of time is spent in bed management. At DHMC, other medicine teams picked up for the decreased clinical productivity of the HMED team, so the budget was neutral. However, using 2 FTE to staff 1 physician daily for 365 days a year, one would need to allocate 0.5 physician FTE (0.25 decrease in clinical productivity 2 FTE) for an HMED team.
Our study has several limitations. As a single center study, our findings may not extrapolate to other settings. The study used historical controls, therefore, undetected confounders may exist. We could not control for simultaneous changes in the hospital, however, we did not know of any other concurrent interventions aimed at decreasing ED diversion. Also, the decision to admit or not is partially based on individual ED attendings, which causes variability in practice. Finally, while we were able to measure rounding times as a process measure to reflect timeliness of care and staff perceptions of quality of care, due to our data infrastructure and the way our housestaff and attendings rotate, we were not able to assess more downstream measures of quality of care.
CONCLUSION
ED crowding decreases throughput and worsens clinical care; there are few proven solutions. This study demonstrates an intervention that reduced the percentage of patients transferred to a medicine floor and discharged within 8 hours, increased the number of discharges from the ED of admitted medicine patients, and decreased ED diversion while improving the timeliness of clinical care for patients boarded in the ED.
Acknowledgements
Disclosure: Nothing to report.
Emergency department (ED) crowding leads to ambulance diversion,1 which can delay care and worsen outcomes, including mortality.2 A national survey showed that 90% of EDs were overcrowded, and 70% reported time on diversion.3 One of the causes of ED crowding is boarding of admitted patients.4 Boarding admitted patients decreases quality of care and satisfaction.57
Improved ED triage, bedside registration, physical expansion of hospitals, and regional ambulance programs have been implemented to decrease ED diversion.812 Despite these attempts, ED diversion continues to be prevalent.
Interventions involving hospitalists have been tested to improve throughput and quality of care for admitted medicine patients boarded in the ED. Howell and colleagues decreased ED diversion through active bed management by hospitalists.13 Briones and colleagues dedicated a hospitalist team to patients boarded in the ED and improved their quality of care.14
Denver Health Medical Center (DHMC) is an urban, academic safety net hospital. In 2009, the ED saw an average of 133 patients daily and an average of 25 were admitted to the medical service. DHMC's ED diversion rate was a mean of 12.4% in 2009. Boarded medicine patients occupied 16% of ED medicine bed capacity. Teaching and nonteaching medical floor teams cared for patients in the ED awaiting inpatient beds, who were the last to be seen. Nursing supervisors transferred boarded patients from the ED to hospital units. Patients with the greatest duration of time in the ED had priority for open beds.
ED diversion is costly.15, 16 DHMC implemented codified diversion criteria, calling the administrator on‐call prior to diversion, and increasing frequency of rounding in the ED, with no sustained effect seen in the rate of ED diversion.
In 2009, the DHMC Hospital Medicine Service addressed the issue of ED crowding, ED diversion, and care of boarded ED patients by creating a hospital medicine ED (HMED) team with 2 functions: (1) to provide ongoing care for medicine patients in the ED awaiting inpatient beds; and (2) to work with nursing supervisors to improve patient flow by adding physician clinical expertise to bed management.
METHODS
Setting and Design
This study took place at DHMC, a 477licensed‐bed academic safety net hospital in Denver, Colorado. We used a prepost design to assess measures of patient flow and timeliness of care. We surveyed ED attendings and nursing supervisors after the intervention to determine perceptions of the HMED team. This study was approved by the local institutional review board (IRB protocol number 09‐0892).
Intervention
In 2009, DHMC, which uses Toyota Lean for quality improvement, performed a Rapid Improvement Event (RIE) to address ED diversion and care of admitted patients boarded in the ED. The RIE team consisted of hospital medicine physicians, ED physicians, social workers, and nurses. Over a 4‐day period, the team examined the present state, created an ideal future state, devised a solution, and tested this solution.
Based upon the results of the RIE, DHMC implemented an HMED team to care for admitted patients boarded in the ED and assist in active bed management. The HMED team is a 24/7 service. During the day shift, the HMED team is composed of 1 dedicated attending and 1 allied health provider (AHP). Since the medicine services were already staffing existing patients in the ED, the 2.0 full‐time equivalent (FTE) needed to staff the HMED team attending and the AHP was reallocated from existing FTE within the hospitalist division. During the evening and night shifts, the HMED team's responsibilities were rolled into existing hospitalist duties.
The HMED team provides clinical care for 2 groups of patients in the ED. The first group represents admitted patients who are still awaiting a medicine ward bed as of 7:00 AM. The HMED team provides ongoing care until discharge from the ED or transfer to a medicine floor. The second group of patients includes new admissions that need to stay in the ED due to a lack of available medicine floor beds. For these patients, the HMED team initiates and continues care until discharge from the ED or transfer to a medical floor (Figure 1).
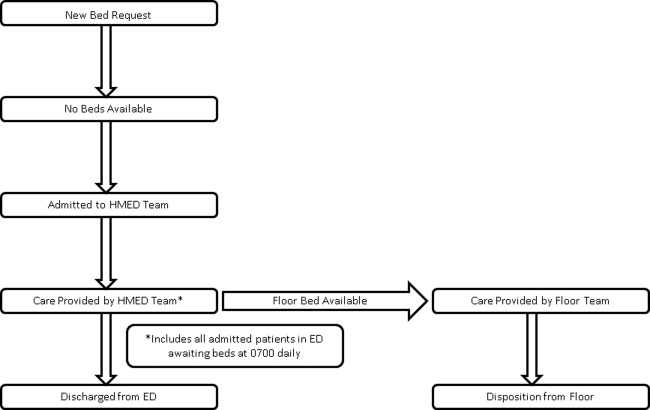
The physician on the HMED team assists nursing supervisors with bed management by providing detailed clinical knowledge, including proximity to discharge as well as updated information on telemetry and intensive care unit (ICU) appropriateness. The HMED team's physician maintains constant knowledge of hospital census via an electronic bed board, and communicates regularly with medical floors about anticipated discharges and transfers to understand the hospital's patient flow status (Figure 2).
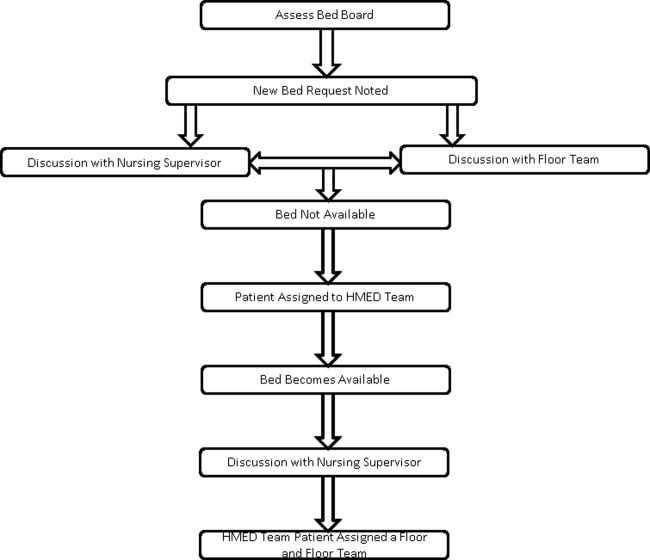
The RIE that resulted in the HMED team was part of the Inpatient Medicine Value Stream, which had the overall goal of saving DHMC $300,000 for 2009. Ten RIEs were planned for this value stream in 2009, with an average of $30,000 of savings expected from each RIE.
Determination of ED Diversion Time
DHMC places responsibility for putting the hospital on an ED Diversion status in the hands of the Emergency Medicine Attending Physician. Diversion is categorized as either due to: (1) excessive ED volume for available ED bedsfull or nearly full department, or full resuscitation rooms without the ability to release a room; or (2) excessive boardingmore than 12 admitted patients awaiting beds in the ED. Other reasons for diversion, such as acute, excessive resource utilization (multiple patients from a single event) and temporary limitation of resources (critical equipment becoming inoperative), are also infrequent causes of diversion that are recorded. The elapsed time during which the ED is on diversion status is recorded and reported as a percentage of the total time on a monthly basis.
Determination of ED Diversion Costs
The cost of diversion at DHMC is calculated by multiplying the average number of ambulance drop‐offs per hour times the number of diversion hours to determine the number of missed patients. The historical mean charges for each ambulance patient are used to determine total missed charge opportunity, which is then applied to the hospital realization rate to calculate missed revenue. In addition, the marginal costs related to Denver Health Medical Plan patients that were unable to be repatriated to DHMC from outlying hospitals, as a result of diversion, is added to the net missed revenue figure. This figure is then divided by the number of diversion hours for the year to determine the cost of each diversion hour. For 2009, the cost of each hour of diversion at DHMC was $5000.
Statistical Analysis
All analyses were performed using SAS Enterprise Guide 4.1 (SAS Institute, Inc, Cary, NC). A Student t test or Wilcoxon rank sum test was used to compare continuous variables, and a chi‐square test was used to compare categorical variables.
Our primary outcome was ED diversion due to hospital bed capacity. These data are recorded, maintained, and analyzed by a DHMC internally developed emergency medical services information system (EMeSIS) that interfaces with computerized laboratory reporting systems, and stores, in part, demographic data as well as real‐time data related to the timing of patient encounters for all patients evaluated in the ED. To assess the effect of the intervention on ED diversion, the proportion of total hours on diversion due to medicine bed capacity was compared preimplementation and postimplementation with a chi‐squared test.
Secondary outcomes for patient flow included: (1) the proportion of patients discharged within 8 hours of transfer to a medical floor; and (2) the proportion of admitted medicine patients discharged from the ED. These data were gathered from the Denver Health Data Warehouse which pools data from both administrative and clinical applications used in patient care. Chi‐squared tests were also used to compare secondary outcomes preintervention and postintervention.
To measure the quality and safety of the HMED team, pre‐ED and post‐ED length of stay (LOS), 48‐hour patient return rate, intensive care unit (ICU) transfer rate, and the total LOS for patients admitted to the HMED team and handed off to a medicine floor team were assessed with the Student t test. To assess timeliness of clinical care provided to boarded medicine patients, self‐reported rounding times were compared preintervention and postintervention with the Student t test.
To assess satisfaction with the HMED team, an anonymous paper survey was administered to ED attendings and nursing supervisors 1 year after the intervention was introduced. The survey consisted of 5 questions, and used a 5‐point Likert scale ranging from strongly disagree (1) to strongly agree (5). Those answering agree or strongly agree were compared to those who were neutral, disagreed, or strongly disagreed.
RESULTS
The ED saw 48,595 patients during the intervention period (August 1, 2009June 30,2010) which did not differ statistically from the 50,469 patients seen in the control period (August 1, 2008June 30, 2009). The number of admissions to the medicine service during the control period (9727) and intervention period (10,013), and the number of total medical/surgical admissions during the control (20,716) and intervention (20,574) periods did not statistically differ. ED staffing during the intervention did not change. The overall number of licensed beds did not increase during the study period. During the control period, staffed medical/surgical beds increased from 395 to 400 beds, while the number of staffed medical/surgical beds decreased from 400 to 397 beds during the intervention period. Patient characteristics were similar during the 2 time periods, with the exception of race (Table 1).
| Patients Admitted to Medicine and Transferred to a Medicine Floor | Pre | Post | P Value |
|---|---|---|---|
| |||
| No. | 1901 | 1828 | |
| Age* | 53 15 | 54 14 | 0.59 |
| Gender (% male) | 55% | 52% | 0.06 |
| Race (% white) | 40% | 34% | <0.0001 |
| Insurance (% insured) | 67% | 63% | 0.08 |
| Charlson Comorbidity Index | 1.0 [1.0, 1.0] | 1.0 [1.0, 1.0] | 0.52 |
Diversion Hours
After implementation of the HMED team, there was a relative reduction of diversion due to medicine bed capacity of 27% (4.5%3.3%; P < 0.01) (Table 2). During the same time period, the relative proportion of hours on diversion due to ED capacity decreased by 55% (9.9%5.4%).
| Pre | Post | P Value | |
|---|---|---|---|
| |||
| Divert hours due to bed capacity (%, hours)* | 4.5% (3624) | 3.3% (3624) | 0.009 |
| Admitted ED patients transferred to floor | |||
| Discharged within 8 h (%, N) | 1.3% (1901) | 0.5% (1828) | 0.03 |
| Boarded patients rounded on in the ED and transferred to the medical floor | |||
| Total length of stay (days, N) | 2.6 [2.4, 3.2] (154) | 2.5 [2.4, 2.6] (364) | 0.21 |
| All discharges and transfers to the floor | |||
| Discharged from ED [%, (N)] | 4.9% (2009) | 7.5% (1981) | <0.001 |
| ED length of stay [hours, (N)] | 12:09 8:44 (2009) | 12:48 10:00 (1981) | 0.46 |
| Return to hospital <48 h [%, (N)] | 4.6% (2009) | 4.8% (1981) | 0.75 |
| Transfer to the ICU [%, (N)] | 3.3% (2009) | 4.2% (1981) | 0.13 |
Bed Management and Patient Flow
The HMED team rounded on boarded ED patients a mean of 2 hours and 9 minutes earlier (10:59 AM 1:09 vs 8:50 AM 1:20; P < 0.0001). After implementation of the HMED team, patients transferred to a medicine floor and discharged within 8 hours decreased relatively by 67% (1.5%0.5%; P < 0.01), and discharges from the ED of admitted medicine patients increased relatively by 61% (4.9%7.9%; P < 0.001) (Table 2). ED LOS, total LOS, 48‐hour returns to the ED, and ICU transfer rate for patients managed by the HMED team did not change (Table 2).
Perception and Satisfaction
Nine out of 15 (60%) ED attendings and 7 out of 8 (87%) nursing supervisors responded to the survey. The survey demonstrated that ED attendings and nursing supervisors believe the HMED team improves clinical care for boarded patients, communication, collegiality, and patient flow (Table 3).
| Postimplementation of the HMED Team | Total (n = 16) | ED Attendings (n = 9) | Nursing Supervisors (n = 7) |
|---|---|---|---|
| |||
| Quality of care has improved | 94 | 89 | 100 |
| Communication has improved | 94 | 89 | 100 |
| Collegiality and clinical decision‐making has improved | 94 | 100 | 89 |
| Patient flow has improved | 81 | 67 | 100 |
| HMED team is an asset to DHMC | 94 | 89 | 100 |
Financial
The 27% relative reduction in ED diversion due to hospital bed capacity extrapolates to 105.1 hours a year of decreased diversion, accounting for $525,600 of increased annual revenues.
DISCUSSION
This study suggests that an HMED team can decrease ED diversion, due to hospital bed capacity, by improving patient flow and timeliness of care for boarded medicine patients in the ED.
After participating in bed management, ED diversion due to a lack of medicine beds decreased. This is consistent with findings by Howell and colleagues who were able to improve throughput and decrease ED diversion with active bed management.13 Howell and colleagues decreased diversion hours due to temporary ED overload, and diversion hours due to a lack of telemetry or critical care beds. At DHMC, diversion is attributed to either a lack of ED capacity or lack of hospital beds. The primary outcome was the diversion rate due to lack of hospital beds, but it is possible that increased discharges directly from the ED contributed to the decrease in diversion due to ED capacity, underestimating the effect our intervention had on total ED diversion. There were no other initiatives to decrease diversion due to ED capacity during the study periods, and ED capacity and volume did not change during the intervention period.
While there were no statistically significant changes in staffed medical/surgical beds or medicine admissions, staffed medical/surgical beds during the intervention period decreased while there were more admissions to medicine. Both of these variables would increase diversion, resulting in an underestimation of the effect of the intervention.
Howell and colleagues improved throughput in the ED by implementing a service which provided active bed management without clinical responsibilities,13 while Briones and colleagues improved clinical care of patients boarded in the ED without affecting throughput.14 The HMED team improved throughput and decreased ED diversion while improving timeliness of care and perception of care quality for patients boarding in the ED.
By decreasing unnecessary transfers to medicine units and increasing discharges from the ED, patient flow was improved. While there was no difference in ED LOS, there was a trend towards decreased total LOS. A larger sample size or a longer period of observation would be necessary to determine if the trend toward decreased total LOS is statistically significant. ED LOS may not have been decreased because patients who would have been sent to the floor only to be discharged within 8 hours were kept in the ED to expedite testing and discharge, while sicker patients were sent to the medical floor. This decreased the turnover time of inpatient beds and allowed more boarded patients to be moved to floor units.
There was concern that an HMED team would fragment care, which would lead to an increased LOS for those patients who were transferred to a medical floor and cared for by an additional medicine team before discharge.17 As noted, there was a trend towards a decreased LOS for patients initially cared for by the HMED team.
In this intervention, hospital medicine physicians provided information regarding ongoing care of patients boarded in the ED to nursing supervisors. Prior to the intervention, nursing supervisors relied upon information from the ED staff and the boarded patient's time in the ED to assign a medical floor. However, ED staff was not providing care to boarded patients and did not know the most up‐to‐date status of the patient. This queuing process and lack of communication resulted in patients ready for discharge being transferred to floor beds and discharged within a few hours of transfer. The HMED team allowed nursing supervisors to have direct knowledge regarding clinical status, including telemetry and ICU criteria (similar to Howell and colleagues13), and readiness for discharge from the physician taking care of the patient.
By managing boarded patients, an HMED team can improve timeliness and coordination of care. Prior to the intervention, boarded ED patients were the last to be seen on rounds. The HMED team rounds only in the ED, expediting care and discharges. The increased proportion of boarded patients discharged from the ED by the HMED team is consistent with Briones and colleagues' clinically oriented team managing boarding patients in the ED.14
Potential adverse effects of our intervention included increased returns to the ED, increased ICU transfer rate, and decreased housestaff satisfaction. There was no increase in the 48‐hour return rate and no increase in the ICU transfer rate for patients cared for by the HMED team. Housestaff at DHMC are satisfied with the HMED team, since the presence of the HMED team allows them to concentrate on patients on the medical floors.
This intervention provides DHMC with an additional $525,600 in revenue annually. Since existing FTE were reallocated to create the HMED team, no additional FTE were required. In our facility, AHPs take on duties of housestaff. However, only 1 physician may be needed to staff an HMED team. This physician's clinical productivity is about 75% of other physicians; therefore, 25% of time is spent in bed management. At DHMC, other medicine teams picked up for the decreased clinical productivity of the HMED team, so the budget was neutral. However, using 2 FTE to staff 1 physician daily for 365 days a year, one would need to allocate 0.5 physician FTE (0.25 decrease in clinical productivity 2 FTE) for an HMED team.
Our study has several limitations. As a single center study, our findings may not extrapolate to other settings. The study used historical controls, therefore, undetected confounders may exist. We could not control for simultaneous changes in the hospital, however, we did not know of any other concurrent interventions aimed at decreasing ED diversion. Also, the decision to admit or not is partially based on individual ED attendings, which causes variability in practice. Finally, while we were able to measure rounding times as a process measure to reflect timeliness of care and staff perceptions of quality of care, due to our data infrastructure and the way our housestaff and attendings rotate, we were not able to assess more downstream measures of quality of care.
CONCLUSION
ED crowding decreases throughput and worsens clinical care; there are few proven solutions. This study demonstrates an intervention that reduced the percentage of patients transferred to a medicine floor and discharged within 8 hours, increased the number of discharges from the ED of admitted medicine patients, and decreased ED diversion while improving the timeliness of clinical care for patients boarded in the ED.
Acknowledgements
Disclosure: Nothing to report.
- ,,.Access block causes emergency department overcrowding and ambulance diversion in Perth, Western Australia.Emerg Med J.2005;22:351–354.
- ,,,.The relationship between distance to hospital and patient mortality in emergencies: an observational study.Emerg Med J.2007;24:665–668.
- Institute of Medicine.Committee on the Future of Emergency Care in the United States Health System.Hospital‐Based Emergency Care: At the Breaking Point.Washington, DC:National Academies Press;2007.
- ,.Systematic review of emergency department crowding: causes, effects, and solutions.Ann Emerg Med.2008;52:126–136.
- ,.Emergency department crowding is associated with poor care for patients with severe pain.Ann Emerg Med.2008;51:1–5.
- ,,, et al.The impact of emergency department crowding measures on time to antibiotics for patients with community‐acquired pneumonia.Ann Emerg Med.2007;50:510–516.
- ,,, et al;for the DELAYED‐ED Study Group.Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit.Crit Care Med.2007;35:1477–1483.
- ,,, et al.Impact of a triage liaison physician on emergency department overcrowding and throughput: a randomized controlled trial.Acad Emerg Med.2007;14:702–708.
- ,,.Strategies for dealing with emergency department overcrowding: a one‐year study on how bedside registration affects patient throughput times.Emerg Med J.2007;32:337–342.
- ,,, et al.The effect of emergency department expansion on emergency department overcrowding.Acad Emerg Med.2007;14:338–343.
- ,,,,,.Effect of increased ICU capacity on emergency department length of stay and ambulance diversion.Ann Emerg Med.2005;5:471–478.
- ,,,,.Ambulance diversion reduction: the Sacramento solution.Am J Emerg Med.2006;357:608–613.
- ,,,,,.Active bed management by hospitalists and emergency department throughput.Ann Intern Med.2008;149:804–810.
- ,,, et al.A model of hospitalist role in the care of admitted patients in the emergency department.J Hosp Med.2010;5:360–364.
- ,,,,.Ambulance diversion and lost hospital revenues.Ann Emerg Med.2006;48(6):702–710.
- ,,,.The financial impact of ambulance diversion and patient elopements.Acad Emerg Med.2007;14(1):58–62.
- ,,,,.The impact of fragmentation of hospitalist care on length of stay.J. Hosp. Med.2010;5:335–338.
- ,,.Access block causes emergency department overcrowding and ambulance diversion in Perth, Western Australia.Emerg Med J.2005;22:351–354.
- ,,,.The relationship between distance to hospital and patient mortality in emergencies: an observational study.Emerg Med J.2007;24:665–668.
- Institute of Medicine.Committee on the Future of Emergency Care in the United States Health System.Hospital‐Based Emergency Care: At the Breaking Point.Washington, DC:National Academies Press;2007.
- ,.Systematic review of emergency department crowding: causes, effects, and solutions.Ann Emerg Med.2008;52:126–136.
- ,.Emergency department crowding is associated with poor care for patients with severe pain.Ann Emerg Med.2008;51:1–5.
- ,,, et al.The impact of emergency department crowding measures on time to antibiotics for patients with community‐acquired pneumonia.Ann Emerg Med.2007;50:510–516.
- ,,, et al;for the DELAYED‐ED Study Group.Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit.Crit Care Med.2007;35:1477–1483.
- ,,, et al.Impact of a triage liaison physician on emergency department overcrowding and throughput: a randomized controlled trial.Acad Emerg Med.2007;14:702–708.
- ,,.Strategies for dealing with emergency department overcrowding: a one‐year study on how bedside registration affects patient throughput times.Emerg Med J.2007;32:337–342.
- ,,, et al.The effect of emergency department expansion on emergency department overcrowding.Acad Emerg Med.2007;14:338–343.
- ,,,,,.Effect of increased ICU capacity on emergency department length of stay and ambulance diversion.Ann Emerg Med.2005;5:471–478.
- ,,,,.Ambulance diversion reduction: the Sacramento solution.Am J Emerg Med.2006;357:608–613.
- ,,,,,.Active bed management by hospitalists and emergency department throughput.Ann Intern Med.2008;149:804–810.
- ,,, et al.A model of hospitalist role in the care of admitted patients in the emergency department.J Hosp Med.2010;5:360–364.
- ,,,,.Ambulance diversion and lost hospital revenues.Ann Emerg Med.2006;48(6):702–710.
- ,,,.The financial impact of ambulance diversion and patient elopements.Acad Emerg Med.2007;14(1):58–62.
- ,,,,.The impact of fragmentation of hospitalist care on length of stay.J. Hosp. Med.2010;5:335–338.
Copyright © 2012 Society of Hospital Medicine
Hospital Medicine in the IM Clerkship
Hospital medicine is growing rapidly across the nation with more than 30,000 active hospitalists in more than 90% of all hospitals across the country.1 Although initially focused in the community sector, hospitalists have had an increasing presence within academic centers. The University Healthsystem Consortium 2006 survey found that hospitalists were practicing in 86% of university hospitals, and the average age of the hospital medicine programs was only 4.6 years.2 This changing inpatient work force has had consequences on medical education with an increased hospitalist presence in both resident and student training. The full effects of this have not yet been completely elucidated.
Initially met by educators with apprehension, there is a growing body of literature to suggest that hospitalists are perceived by students to be more effective clinical teachers than non‐hospitalists.3, 4 Multiple studies have demonstrated improved trainee satisfaction, attending teaching efficacy, trainee's perception of attending knowledge, and attending involvement in patient care decisions when working with hospitalists.58 Early concerns regarding diminished trainee autonomy are not supported by the available data.4
However, the extent to which hospitalists are involved in teaching Internal Medicine (IM) to medical students is not known. A study reported in 2000 suggests that hospitalists are prevalent within education.9 Over the past decade though, the hospitalist movement has grown exponentially; the role of hospitalists within teaching activities have likely changed significantly over this same time period. Hospital medicine is the fastest growing medical specialty in this country. In order to determine the role of hospitalists in medical student education within the United States and Canada, we queried clerkship directors in Internal Medicine as part of the 2010 annual Clerkship Directors in Internal Medicine (CDIM) survey.
METHODS
In June 2010, CDIM surveyed its North American institutional members, which represents 107 of 143 Departments of Medicine in the US and Canada. CDIM membership consists of university affiliated academic programs with a medical school. In 2009, 52% were public/state‐funded institutions, 40% were private medical schools, and 3% were military. All CDIM institutional members were sent an electronic mail cover message that explained the purpose of the survey and contained a link to the confidential electronic survey. Nonrespondents were contacted up to 3 additional times by e‐mail and once by telephone. Participants were blinded to any specific hypothesis of the study. The institutional review board (IRB) at Case Western Reserve University reviewed the protocol and determined that the CDIM Survey research protocol did not fit the definition of human subjects' research per 45 CFR 46.102, and declared the study exempt from further IRB review.
Survey Development
A call for questions was issued to CDIM members in the Fall of 2009. In all, 11 topics were submitted for inclusion in the 2010 CDIM Survey. Members of the CDIM Research Committee reviewed submissions and identified 4 different topics of interest: write‐ups (history and physicals [H and Ps]), social networking, ambulatory and inpatient training, and the role of hospitalists. Questions were reviewed, organized, and edited by members of the CDIM Research Committee. Questions were then presented to CDIM Council and further revised. The CDIM Research Committee members then completed an initial draft of the online survey and submitted this for another review by the CDIM Council.
Survey Content
The final version of the survey consisted of a total of 60 items over 4 different topics, with additional questions soliciting background information. Some sections contained items that branched (or involved skip‐logic) so that respondents could bypass sections that were not relevant to them. The section on hospital medicine was comprised of 6 multiple choice and 2 free response questions designed to explore the role of hospitalists in clinical education and educational leadership positions. Questions posed asked clerkship directors to identify if hospitalists serve as teaching attendings, the percentage of students that rotate with hospitalists, whether students rotate with attending hospitalists on services without residents, medical student's interactions with hospitalists during call requirements, the formal educational sessions conducted by academic hospitalists, the educational administrative positions held by hospitalists, and other clinical responsibilities teaching physicians hold while on teaching services. Descriptive statistics were used to analyze the data. A chi‐square test of association was done to evaluate for statistical significance.
RESULTS
Eighty‐two (77%) of 107 departments of medicine responded to the survey. At these academic institutions, the majority of departments indicated that hospitalists serve as teaching attendings at their teaching hospital (91%).
We summarize clerkship directors' responses regarding the percentage of students that rotate with academic hospitalists in Table 1. At 20 medical schools (24%), up to one‐quarter of students rotate with hospitalists. At 23 medical schools (28%), one‐quarter to one‐half of students rotate with hospitalists. Ten departments (12%) indicated that 50% to 75% of students rotate with hospitalists, and 22 departments (27%) reported that 75% to 100% of their students are taught by hospitalists in the clinical setting.
| Percentage of Students | Respondents n = 82 (%) |
|---|---|
| 0 | 7 (9) |
| 125 | 20 (24) |
| 2650 | 23 (28) |
| 5175 | 10 (12) |
| 76100 | 22 (27) |
Most students work with hospitalists on resident teaching services. However, 7 departments (9%) indicated that medical students doing their core clerkship rotate with hospitalists on non‐resident covered services. Few formal educational sessions are conducted by hospitalists (Table 2). In 19 of the IM clerkships (23%), hospitalists conduct no formalized educational sessions. Forty‐two departments (51%) report that up to a quarter of these sessions are conducted by hospitalists. Eight (10%) report more than half of the formal educational sessions are conducted by academic hospitalists.
| Percentage of Didactic Sessions | Respondents n = 82 (%) |
|---|---|
| 0 | 19 (23) |
| 125 | 42 (51) |
| 2650 | 10 (12) |
| 5175 | 3 (4) |
| 76100 | 5 (6) |
| No formal education sessions in clerkship | 3 (4) |
Clerkship directors reported that hospitalists play a role during student call experiences. The majority of respondents reported that students are directly supervised by a combination of residents and/or in‐house hospitalists (Table 3). Thirty‐three departments (42%) answered that in‐house hospitalists are involved in supervising core IM clerkship students during their nighttime call requirements. Students are supervised directly by residents at 59 (72%). Eight departments (10%) reported that students do not interact with hospitalists during call requirements. Three reported that in‐house hospitalists supervise students without residents (4%). Seven departments (9%) reported no call requirement, and 4 (5%) were unable to answer the question.
| Respondents n = 82 (%)* | |
|---|---|
| |
| Students are directly supervised by in‐house hospitalists | 33 (42) |
| Students are directly supervised by residents | 59 (72) |
| Students do not interact with hospitalists during call | 8 (10) |
| There is no call requirement | 7 (7) |
| Don't know/other | 4 (5) |
When asked to identify positions hospitalists hold in educational administration, 16 departments (20%) reported that academic hospitalists hold no educational administrative positions at their institution (Figure 1). Fourteen (17%) responded that academic hospitalists only have roles in patient safety. Eight (10%) reported other unspecified as the only administrative position at their institution. The remaining 44 departments of medicine (53%) responding reported that academic hospitalists hold clerkship and/or residency program leadership roles. In 7 departments (9%), the clerkship director is a hospitalist. At all programs in which this is the case, academic hospitalists hold additional educational administrative roles. The associate clerkship director was reported to be a hospitalist in 18 departments (22%). Site clerkship directors are hospitalists in 8 (10%). In residency education, hospitalists are slightly less prevalent. One participant responded that the residency program director was a hospitalist, while in 18 departments (22%), the hospitalists have roles as associate residency program directors.
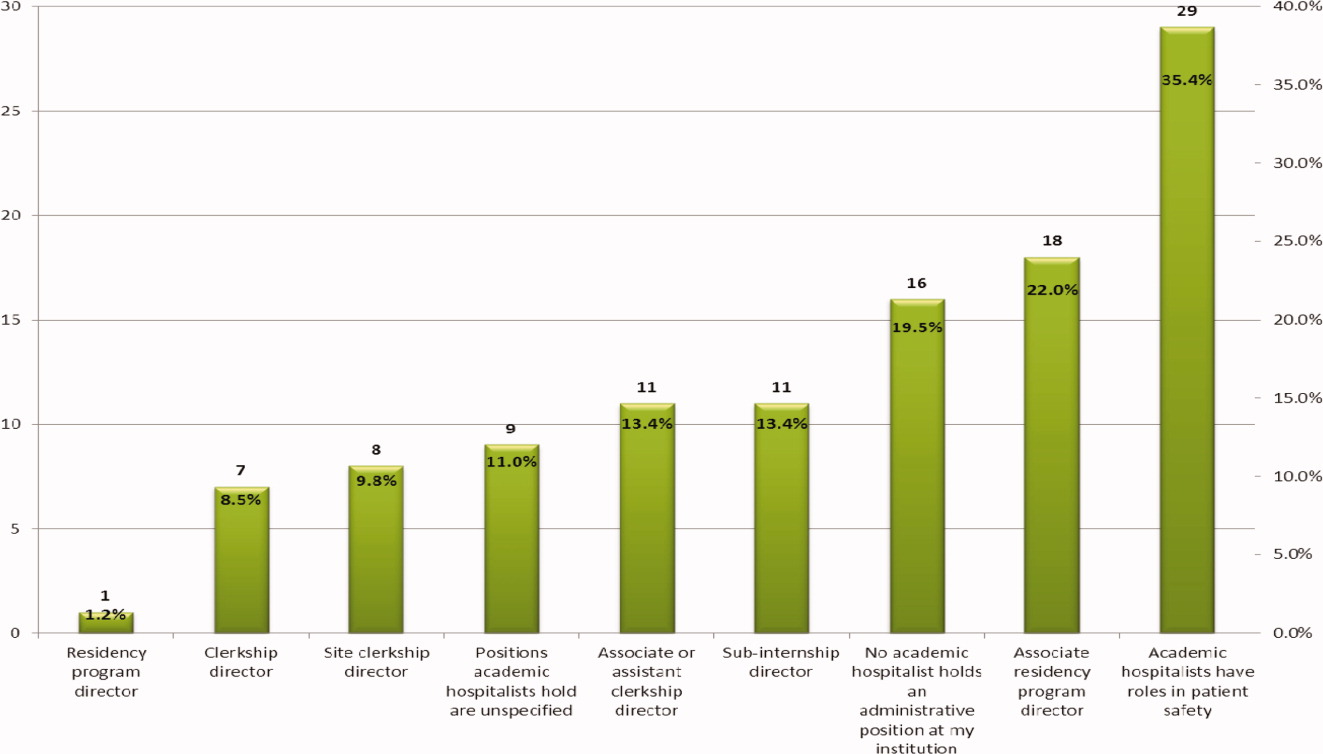
Respondents were asked to comment on other clinical responsibilities for teaching attendings while on‐service. Thirteen (16%) indicated that teaching hospitalists had other clinical responsibilities, whereas 43 (52%) non‐hospitalist teaching attendings were reported to have other clinical responsibilities while on teaching service ( = 33.09, P < 0.0001). The additional responsibilities for teaching hospitalists included general medicine consults (3 programs), quality initiatives (2 programs), clinics (2 programs), additional nonteaching service patients (2 programs), and educational commitments (4 programs). Responsibilities identified for non‐hospitalist teaching attendings were primarily outpatient clinics (29 programs) or were unspecified (14 programs).
DISCUSSION
Over the past decade, hospital medicine has grown exponentially. This clinical growth has been mirrored in medical education. Our study finds that hospitalists teach in core Internal Medicine clerkships in the large majority of Departments of Internal Medicine throughout the US and Canada. Compared to 2000, in which approximately 50% of IM departments employed hospitalists and 80% of these worked with medical students (roughly 40% of all departments),9 we find that 91% of academic IM programs utilize hospitalists for core clerkship education. However, the majority of respondents (72%) reported that less than 25% of formal educational sessions were conducted by academic hospitalists during their core Internal Medicine clerkship. Thus, although hospitalists appear to be involved heavily in supervising medical students during the IM clerkship, the primary teaching modalities utilized appear to be informal. This may be due to the relative youth of the hospitalist movement, with newer faculty being less frequently recruited to conduct didactics. Alternatively, this may result from an historical reliance on subspecialists for Internal Medicine lectures (ie, renal failure lectures are given by a nephrologist, chest pain lectures are given by a cardiologist).
Our study shows that a significant number of hospitalists are involved in student overnight calls. Notably, almost half of the students doing overnight calls were supervised by in‐house hospitalists. This is an expected trend, particularly in the current environment in which intern night hours have been limited and extended shifts are less common.10 Residency programs have frequently shifted to night float systems, the value of which is unknown with regards to education and patient safety.11 Experienced attendings in the hospital afford a unique educational opportunity for third year medical students, and it appears they are being utilized as such.
Although the majority of core IM clerkship students rotate with resident teaching services, we found a small but measureable number of students who are on resident uncovered services. The educational efficacy of this model is not fully defined. In the subinternship setting, resident uncovered teaching hospitalist services were rated equivalently as compared to resident covered teaching services on measures of supervision, faculty assessment, the frequency and value of teaching sessions, and educational value of patient problems. However, students on uncovered services scored these lower on knowledge learned, intellectual discussions, and patient variety.12 Based on this feedback, caution should be taken in assigning more junior students to uncovered hospitalist services. This is especially true in the post‐duty hour setting which has already prompted concern related to student exposure to basic medical conditions.13
Despite the level of hospitalist involvement in core clerkship education, few clerkship directors are hospitalists. However, more than half of the Departments of Internal Medicine report hospitalists in some clerkship or residency educational position. Our survey did not address more senior College of Medicine leadership roles, and may, in fact, underrepresent educational leadership positions. Additionally, a large number of hospitalist have additional roles in patient safety, underscoring hospital medicine's leadership in this important niche post in the Institute of Medicine (IOM) report To Err is Human.14
Our findings indicate that hospitalists are significantly less likely to have additional clinical commitments while on‐service as compared to non‐hospitalist teaching attending. Non‐hospitalist teaching attendings were reported to frequently have outpatient clinic duties while teaching on the inpatient service. Conventional wisdom suggests that educators who are able to focus on teaching activities primarily will likely be better teachers. To date, literature has shown notable learner satisfaction with hospitalist educators.3, 4 However, there are no data on teaching efficacy and learning outcomes. Further studies need to explore the relationship between hospitalist attending status and improved trainee education.
Our study has several limitations. Our report is a survey of institutional members of CDIM. Since not all Departments of Medicine within Schools of Medicine have membership in CDIM, our results may have sampling bias. Additionally, our survey only asked clerkship directors in one discipline to report educational practices. There may be variability at different educational sites that are not captured by the responses. The Society of Hospital Medicine defines a hospitalist as a physician who specializes in the practice of hospital medicine, however, there remains some ambiguity with regards to how much inpatient focus is necessary to employ the term, and this may lead to errors in reporting. Nonetheless, our response rate of 82% is quite high, and suggests that this survey is reflective of national trends.
In summary, hospitalists are involved in medical student education in the majority of Departments of Internal Medicine throughout the US and Canada. They frequently supervise students in‐house at night, and some students rotate on non‐resident covered services. Hospitalists have a notable presence in academic education leadership positions and have significantly less outside clinical responsibilities, allowing them greater focus on teaching. Further studies should to be conducted to determine the effects of hospitalists on learning outcomes. Additional data is needed to determine the influence of hospitalists on students' attitudes and career choices with regards to Internal Medicine.
Acknowledgements
Disclosure: Nothing to report.
- Medical Group Management Association and Society of Hospital Medicine.State of Hospital Medicine: 2011 Report Based on 2010 Data.Franktown, CO:Glacier Publishing Services;2011.
- University HealthSystem Consortium. Role of the Hospitalist 2006 Field Brief.Oak Brook, IL:University HealthSystem Consortium;2006.
- ,.Hospitalist educators: future of inpatient internal medicine training.Mt Sinai J Med.2008;75(5):430–435.
- ,,,.Effect of hospitalist attending physicians on trainee educational experiences: a systematic review.J Hosp Med.2009;4(8):490–498.
- ,.Implications of the hospitalist model for medical students' education.Acad Med.2001;76(4):324–330.
- ,,,,.Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164(17):1866–1871.
- ,.Third‐year medical students' evaluation of hospitalist and nonhospitalist faculty during the inpatient portion of their pediatrics clerkships.J Hosp Med.2007;2(1):17–22.
- ,,,,,.Effect of a pediatric hospitalist system on housestaff education and experience.Arch Pediatr Adolesc Med.2002;156(9):877–883.
- ,,,,.The presence of hospitalists in medical education.Acad Med.2000;75(10 suppl):S34–S36.
- Accreditation Council for Graduate Medical Education (ACGME). Common Program Requirements, Effective July 1,2011. Available at: http://www.acgme‐2010standards.org/pdf/Common_Program_Requirements_07012011.pdf. Accessed on 4 October 2012.
- ,,.Systematic review: association of shift length, protected sleep time, and night float with patient care, residents' health, and education.Ann Intern Med.2010;153(12):829–842.
- ,,,,.Medical subinternship: student experience on a resident uncovered hospitalist service.Teach Learn Med.2008;20(1):18–21.
- ,,,,,.Medical student patient experiences before and after duty hour regulation and hospitalist support.J Gen Intern Med.2010;25(3):207–210.
- ,,.To Err Is Human: Building a Safer Health Care System.Washington, DC:National Academy Press;2000.
Hospital medicine is growing rapidly across the nation with more than 30,000 active hospitalists in more than 90% of all hospitals across the country.1 Although initially focused in the community sector, hospitalists have had an increasing presence within academic centers. The University Healthsystem Consortium 2006 survey found that hospitalists were practicing in 86% of university hospitals, and the average age of the hospital medicine programs was only 4.6 years.2 This changing inpatient work force has had consequences on medical education with an increased hospitalist presence in both resident and student training. The full effects of this have not yet been completely elucidated.
Initially met by educators with apprehension, there is a growing body of literature to suggest that hospitalists are perceived by students to be more effective clinical teachers than non‐hospitalists.3, 4 Multiple studies have demonstrated improved trainee satisfaction, attending teaching efficacy, trainee's perception of attending knowledge, and attending involvement in patient care decisions when working with hospitalists.58 Early concerns regarding diminished trainee autonomy are not supported by the available data.4
However, the extent to which hospitalists are involved in teaching Internal Medicine (IM) to medical students is not known. A study reported in 2000 suggests that hospitalists are prevalent within education.9 Over the past decade though, the hospitalist movement has grown exponentially; the role of hospitalists within teaching activities have likely changed significantly over this same time period. Hospital medicine is the fastest growing medical specialty in this country. In order to determine the role of hospitalists in medical student education within the United States and Canada, we queried clerkship directors in Internal Medicine as part of the 2010 annual Clerkship Directors in Internal Medicine (CDIM) survey.
METHODS
In June 2010, CDIM surveyed its North American institutional members, which represents 107 of 143 Departments of Medicine in the US and Canada. CDIM membership consists of university affiliated academic programs with a medical school. In 2009, 52% were public/state‐funded institutions, 40% were private medical schools, and 3% were military. All CDIM institutional members were sent an electronic mail cover message that explained the purpose of the survey and contained a link to the confidential electronic survey. Nonrespondents were contacted up to 3 additional times by e‐mail and once by telephone. Participants were blinded to any specific hypothesis of the study. The institutional review board (IRB) at Case Western Reserve University reviewed the protocol and determined that the CDIM Survey research protocol did not fit the definition of human subjects' research per 45 CFR 46.102, and declared the study exempt from further IRB review.
Survey Development
A call for questions was issued to CDIM members in the Fall of 2009. In all, 11 topics were submitted for inclusion in the 2010 CDIM Survey. Members of the CDIM Research Committee reviewed submissions and identified 4 different topics of interest: write‐ups (history and physicals [H and Ps]), social networking, ambulatory and inpatient training, and the role of hospitalists. Questions were reviewed, organized, and edited by members of the CDIM Research Committee. Questions were then presented to CDIM Council and further revised. The CDIM Research Committee members then completed an initial draft of the online survey and submitted this for another review by the CDIM Council.
Survey Content
The final version of the survey consisted of a total of 60 items over 4 different topics, with additional questions soliciting background information. Some sections contained items that branched (or involved skip‐logic) so that respondents could bypass sections that were not relevant to them. The section on hospital medicine was comprised of 6 multiple choice and 2 free response questions designed to explore the role of hospitalists in clinical education and educational leadership positions. Questions posed asked clerkship directors to identify if hospitalists serve as teaching attendings, the percentage of students that rotate with hospitalists, whether students rotate with attending hospitalists on services without residents, medical student's interactions with hospitalists during call requirements, the formal educational sessions conducted by academic hospitalists, the educational administrative positions held by hospitalists, and other clinical responsibilities teaching physicians hold while on teaching services. Descriptive statistics were used to analyze the data. A chi‐square test of association was done to evaluate for statistical significance.
RESULTS
Eighty‐two (77%) of 107 departments of medicine responded to the survey. At these academic institutions, the majority of departments indicated that hospitalists serve as teaching attendings at their teaching hospital (91%).
We summarize clerkship directors' responses regarding the percentage of students that rotate with academic hospitalists in Table 1. At 20 medical schools (24%), up to one‐quarter of students rotate with hospitalists. At 23 medical schools (28%), one‐quarter to one‐half of students rotate with hospitalists. Ten departments (12%) indicated that 50% to 75% of students rotate with hospitalists, and 22 departments (27%) reported that 75% to 100% of their students are taught by hospitalists in the clinical setting.
| Percentage of Students | Respondents n = 82 (%) |
|---|---|
| 0 | 7 (9) |
| 125 | 20 (24) |
| 2650 | 23 (28) |
| 5175 | 10 (12) |
| 76100 | 22 (27) |
Most students work with hospitalists on resident teaching services. However, 7 departments (9%) indicated that medical students doing their core clerkship rotate with hospitalists on non‐resident covered services. Few formal educational sessions are conducted by hospitalists (Table 2). In 19 of the IM clerkships (23%), hospitalists conduct no formalized educational sessions. Forty‐two departments (51%) report that up to a quarter of these sessions are conducted by hospitalists. Eight (10%) report more than half of the formal educational sessions are conducted by academic hospitalists.
| Percentage of Didactic Sessions | Respondents n = 82 (%) |
|---|---|
| 0 | 19 (23) |
| 125 | 42 (51) |
| 2650 | 10 (12) |
| 5175 | 3 (4) |
| 76100 | 5 (6) |
| No formal education sessions in clerkship | 3 (4) |
Clerkship directors reported that hospitalists play a role during student call experiences. The majority of respondents reported that students are directly supervised by a combination of residents and/or in‐house hospitalists (Table 3). Thirty‐three departments (42%) answered that in‐house hospitalists are involved in supervising core IM clerkship students during their nighttime call requirements. Students are supervised directly by residents at 59 (72%). Eight departments (10%) reported that students do not interact with hospitalists during call requirements. Three reported that in‐house hospitalists supervise students without residents (4%). Seven departments (9%) reported no call requirement, and 4 (5%) were unable to answer the question.
| Respondents n = 82 (%)* | |
|---|---|
| |
| Students are directly supervised by in‐house hospitalists | 33 (42) |
| Students are directly supervised by residents | 59 (72) |
| Students do not interact with hospitalists during call | 8 (10) |
| There is no call requirement | 7 (7) |
| Don't know/other | 4 (5) |
When asked to identify positions hospitalists hold in educational administration, 16 departments (20%) reported that academic hospitalists hold no educational administrative positions at their institution (Figure 1). Fourteen (17%) responded that academic hospitalists only have roles in patient safety. Eight (10%) reported other unspecified as the only administrative position at their institution. The remaining 44 departments of medicine (53%) responding reported that academic hospitalists hold clerkship and/or residency program leadership roles. In 7 departments (9%), the clerkship director is a hospitalist. At all programs in which this is the case, academic hospitalists hold additional educational administrative roles. The associate clerkship director was reported to be a hospitalist in 18 departments (22%). Site clerkship directors are hospitalists in 8 (10%). In residency education, hospitalists are slightly less prevalent. One participant responded that the residency program director was a hospitalist, while in 18 departments (22%), the hospitalists have roles as associate residency program directors.
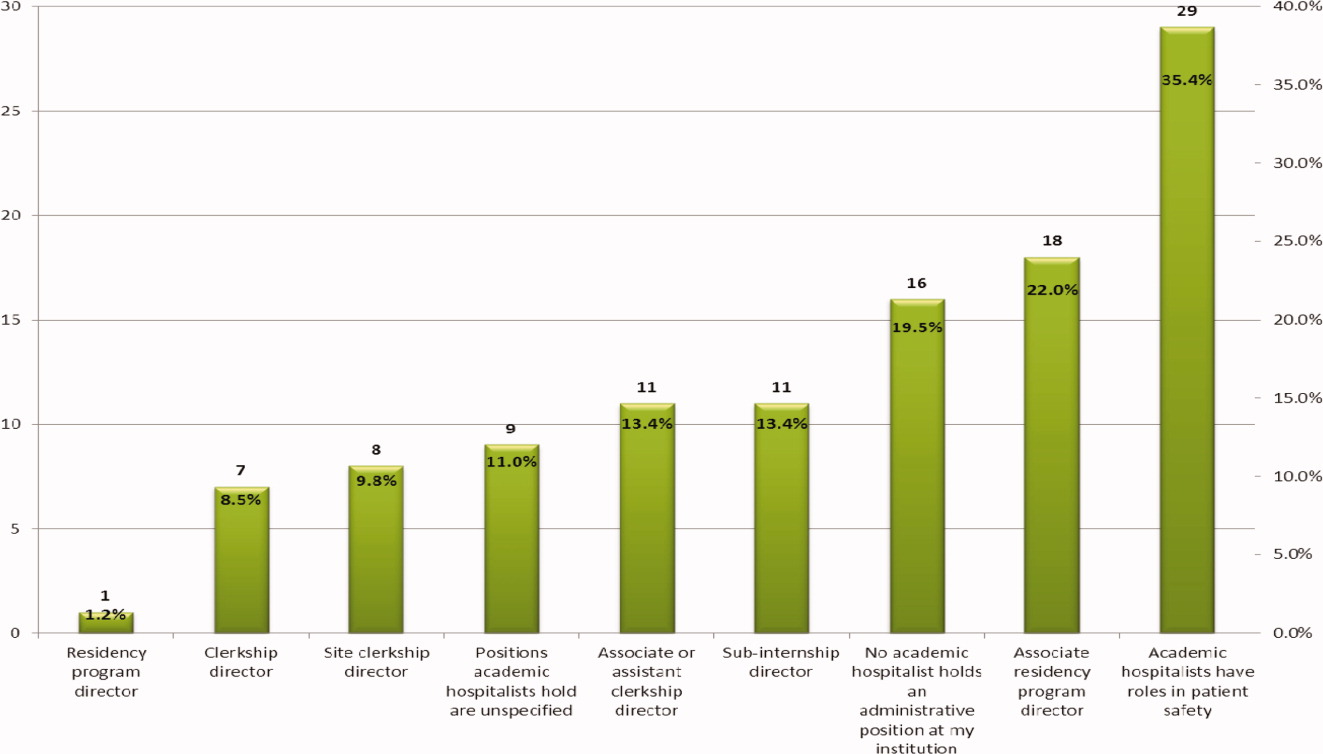
Respondents were asked to comment on other clinical responsibilities for teaching attendings while on‐service. Thirteen (16%) indicated that teaching hospitalists had other clinical responsibilities, whereas 43 (52%) non‐hospitalist teaching attendings were reported to have other clinical responsibilities while on teaching service ( = 33.09, P < 0.0001). The additional responsibilities for teaching hospitalists included general medicine consults (3 programs), quality initiatives (2 programs), clinics (2 programs), additional nonteaching service patients (2 programs), and educational commitments (4 programs). Responsibilities identified for non‐hospitalist teaching attendings were primarily outpatient clinics (29 programs) or were unspecified (14 programs).
DISCUSSION
Over the past decade, hospital medicine has grown exponentially. This clinical growth has been mirrored in medical education. Our study finds that hospitalists teach in core Internal Medicine clerkships in the large majority of Departments of Internal Medicine throughout the US and Canada. Compared to 2000, in which approximately 50% of IM departments employed hospitalists and 80% of these worked with medical students (roughly 40% of all departments),9 we find that 91% of academic IM programs utilize hospitalists for core clerkship education. However, the majority of respondents (72%) reported that less than 25% of formal educational sessions were conducted by academic hospitalists during their core Internal Medicine clerkship. Thus, although hospitalists appear to be involved heavily in supervising medical students during the IM clerkship, the primary teaching modalities utilized appear to be informal. This may be due to the relative youth of the hospitalist movement, with newer faculty being less frequently recruited to conduct didactics. Alternatively, this may result from an historical reliance on subspecialists for Internal Medicine lectures (ie, renal failure lectures are given by a nephrologist, chest pain lectures are given by a cardiologist).
Our study shows that a significant number of hospitalists are involved in student overnight calls. Notably, almost half of the students doing overnight calls were supervised by in‐house hospitalists. This is an expected trend, particularly in the current environment in which intern night hours have been limited and extended shifts are less common.10 Residency programs have frequently shifted to night float systems, the value of which is unknown with regards to education and patient safety.11 Experienced attendings in the hospital afford a unique educational opportunity for third year medical students, and it appears they are being utilized as such.
Although the majority of core IM clerkship students rotate with resident teaching services, we found a small but measureable number of students who are on resident uncovered services. The educational efficacy of this model is not fully defined. In the subinternship setting, resident uncovered teaching hospitalist services were rated equivalently as compared to resident covered teaching services on measures of supervision, faculty assessment, the frequency and value of teaching sessions, and educational value of patient problems. However, students on uncovered services scored these lower on knowledge learned, intellectual discussions, and patient variety.12 Based on this feedback, caution should be taken in assigning more junior students to uncovered hospitalist services. This is especially true in the post‐duty hour setting which has already prompted concern related to student exposure to basic medical conditions.13
Despite the level of hospitalist involvement in core clerkship education, few clerkship directors are hospitalists. However, more than half of the Departments of Internal Medicine report hospitalists in some clerkship or residency educational position. Our survey did not address more senior College of Medicine leadership roles, and may, in fact, underrepresent educational leadership positions. Additionally, a large number of hospitalist have additional roles in patient safety, underscoring hospital medicine's leadership in this important niche post in the Institute of Medicine (IOM) report To Err is Human.14
Our findings indicate that hospitalists are significantly less likely to have additional clinical commitments while on‐service as compared to non‐hospitalist teaching attending. Non‐hospitalist teaching attendings were reported to frequently have outpatient clinic duties while teaching on the inpatient service. Conventional wisdom suggests that educators who are able to focus on teaching activities primarily will likely be better teachers. To date, literature has shown notable learner satisfaction with hospitalist educators.3, 4 However, there are no data on teaching efficacy and learning outcomes. Further studies need to explore the relationship between hospitalist attending status and improved trainee education.
Our study has several limitations. Our report is a survey of institutional members of CDIM. Since not all Departments of Medicine within Schools of Medicine have membership in CDIM, our results may have sampling bias. Additionally, our survey only asked clerkship directors in one discipline to report educational practices. There may be variability at different educational sites that are not captured by the responses. The Society of Hospital Medicine defines a hospitalist as a physician who specializes in the practice of hospital medicine, however, there remains some ambiguity with regards to how much inpatient focus is necessary to employ the term, and this may lead to errors in reporting. Nonetheless, our response rate of 82% is quite high, and suggests that this survey is reflective of national trends.
In summary, hospitalists are involved in medical student education in the majority of Departments of Internal Medicine throughout the US and Canada. They frequently supervise students in‐house at night, and some students rotate on non‐resident covered services. Hospitalists have a notable presence in academic education leadership positions and have significantly less outside clinical responsibilities, allowing them greater focus on teaching. Further studies should to be conducted to determine the effects of hospitalists on learning outcomes. Additional data is needed to determine the influence of hospitalists on students' attitudes and career choices with regards to Internal Medicine.
Acknowledgements
Disclosure: Nothing to report.
Hospital medicine is growing rapidly across the nation with more than 30,000 active hospitalists in more than 90% of all hospitals across the country.1 Although initially focused in the community sector, hospitalists have had an increasing presence within academic centers. The University Healthsystem Consortium 2006 survey found that hospitalists were practicing in 86% of university hospitals, and the average age of the hospital medicine programs was only 4.6 years.2 This changing inpatient work force has had consequences on medical education with an increased hospitalist presence in both resident and student training. The full effects of this have not yet been completely elucidated.
Initially met by educators with apprehension, there is a growing body of literature to suggest that hospitalists are perceived by students to be more effective clinical teachers than non‐hospitalists.3, 4 Multiple studies have demonstrated improved trainee satisfaction, attending teaching efficacy, trainee's perception of attending knowledge, and attending involvement in patient care decisions when working with hospitalists.58 Early concerns regarding diminished trainee autonomy are not supported by the available data.4
However, the extent to which hospitalists are involved in teaching Internal Medicine (IM) to medical students is not known. A study reported in 2000 suggests that hospitalists are prevalent within education.9 Over the past decade though, the hospitalist movement has grown exponentially; the role of hospitalists within teaching activities have likely changed significantly over this same time period. Hospital medicine is the fastest growing medical specialty in this country. In order to determine the role of hospitalists in medical student education within the United States and Canada, we queried clerkship directors in Internal Medicine as part of the 2010 annual Clerkship Directors in Internal Medicine (CDIM) survey.
METHODS
In June 2010, CDIM surveyed its North American institutional members, which represents 107 of 143 Departments of Medicine in the US and Canada. CDIM membership consists of university affiliated academic programs with a medical school. In 2009, 52% were public/state‐funded institutions, 40% were private medical schools, and 3% were military. All CDIM institutional members were sent an electronic mail cover message that explained the purpose of the survey and contained a link to the confidential electronic survey. Nonrespondents were contacted up to 3 additional times by e‐mail and once by telephone. Participants were blinded to any specific hypothesis of the study. The institutional review board (IRB) at Case Western Reserve University reviewed the protocol and determined that the CDIM Survey research protocol did not fit the definition of human subjects' research per 45 CFR 46.102, and declared the study exempt from further IRB review.
Survey Development
A call for questions was issued to CDIM members in the Fall of 2009. In all, 11 topics were submitted for inclusion in the 2010 CDIM Survey. Members of the CDIM Research Committee reviewed submissions and identified 4 different topics of interest: write‐ups (history and physicals [H and Ps]), social networking, ambulatory and inpatient training, and the role of hospitalists. Questions were reviewed, organized, and edited by members of the CDIM Research Committee. Questions were then presented to CDIM Council and further revised. The CDIM Research Committee members then completed an initial draft of the online survey and submitted this for another review by the CDIM Council.
Survey Content
The final version of the survey consisted of a total of 60 items over 4 different topics, with additional questions soliciting background information. Some sections contained items that branched (or involved skip‐logic) so that respondents could bypass sections that were not relevant to them. The section on hospital medicine was comprised of 6 multiple choice and 2 free response questions designed to explore the role of hospitalists in clinical education and educational leadership positions. Questions posed asked clerkship directors to identify if hospitalists serve as teaching attendings, the percentage of students that rotate with hospitalists, whether students rotate with attending hospitalists on services without residents, medical student's interactions with hospitalists during call requirements, the formal educational sessions conducted by academic hospitalists, the educational administrative positions held by hospitalists, and other clinical responsibilities teaching physicians hold while on teaching services. Descriptive statistics were used to analyze the data. A chi‐square test of association was done to evaluate for statistical significance.
RESULTS
Eighty‐two (77%) of 107 departments of medicine responded to the survey. At these academic institutions, the majority of departments indicated that hospitalists serve as teaching attendings at their teaching hospital (91%).
We summarize clerkship directors' responses regarding the percentage of students that rotate with academic hospitalists in Table 1. At 20 medical schools (24%), up to one‐quarter of students rotate with hospitalists. At 23 medical schools (28%), one‐quarter to one‐half of students rotate with hospitalists. Ten departments (12%) indicated that 50% to 75% of students rotate with hospitalists, and 22 departments (27%) reported that 75% to 100% of their students are taught by hospitalists in the clinical setting.
| Percentage of Students | Respondents n = 82 (%) |
|---|---|
| 0 | 7 (9) |
| 125 | 20 (24) |
| 2650 | 23 (28) |
| 5175 | 10 (12) |
| 76100 | 22 (27) |
Most students work with hospitalists on resident teaching services. However, 7 departments (9%) indicated that medical students doing their core clerkship rotate with hospitalists on non‐resident covered services. Few formal educational sessions are conducted by hospitalists (Table 2). In 19 of the IM clerkships (23%), hospitalists conduct no formalized educational sessions. Forty‐two departments (51%) report that up to a quarter of these sessions are conducted by hospitalists. Eight (10%) report more than half of the formal educational sessions are conducted by academic hospitalists.
| Percentage of Didactic Sessions | Respondents n = 82 (%) |
|---|---|
| 0 | 19 (23) |
| 125 | 42 (51) |
| 2650 | 10 (12) |
| 5175 | 3 (4) |
| 76100 | 5 (6) |
| No formal education sessions in clerkship | 3 (4) |
Clerkship directors reported that hospitalists play a role during student call experiences. The majority of respondents reported that students are directly supervised by a combination of residents and/or in‐house hospitalists (Table 3). Thirty‐three departments (42%) answered that in‐house hospitalists are involved in supervising core IM clerkship students during their nighttime call requirements. Students are supervised directly by residents at 59 (72%). Eight departments (10%) reported that students do not interact with hospitalists during call requirements. Three reported that in‐house hospitalists supervise students without residents (4%). Seven departments (9%) reported no call requirement, and 4 (5%) were unable to answer the question.
| Respondents n = 82 (%)* | |
|---|---|
| |
| Students are directly supervised by in‐house hospitalists | 33 (42) |
| Students are directly supervised by residents | 59 (72) |
| Students do not interact with hospitalists during call | 8 (10) |
| There is no call requirement | 7 (7) |
| Don't know/other | 4 (5) |
When asked to identify positions hospitalists hold in educational administration, 16 departments (20%) reported that academic hospitalists hold no educational administrative positions at their institution (Figure 1). Fourteen (17%) responded that academic hospitalists only have roles in patient safety. Eight (10%) reported other unspecified as the only administrative position at their institution. The remaining 44 departments of medicine (53%) responding reported that academic hospitalists hold clerkship and/or residency program leadership roles. In 7 departments (9%), the clerkship director is a hospitalist. At all programs in which this is the case, academic hospitalists hold additional educational administrative roles. The associate clerkship director was reported to be a hospitalist in 18 departments (22%). Site clerkship directors are hospitalists in 8 (10%). In residency education, hospitalists are slightly less prevalent. One participant responded that the residency program director was a hospitalist, while in 18 departments (22%), the hospitalists have roles as associate residency program directors.
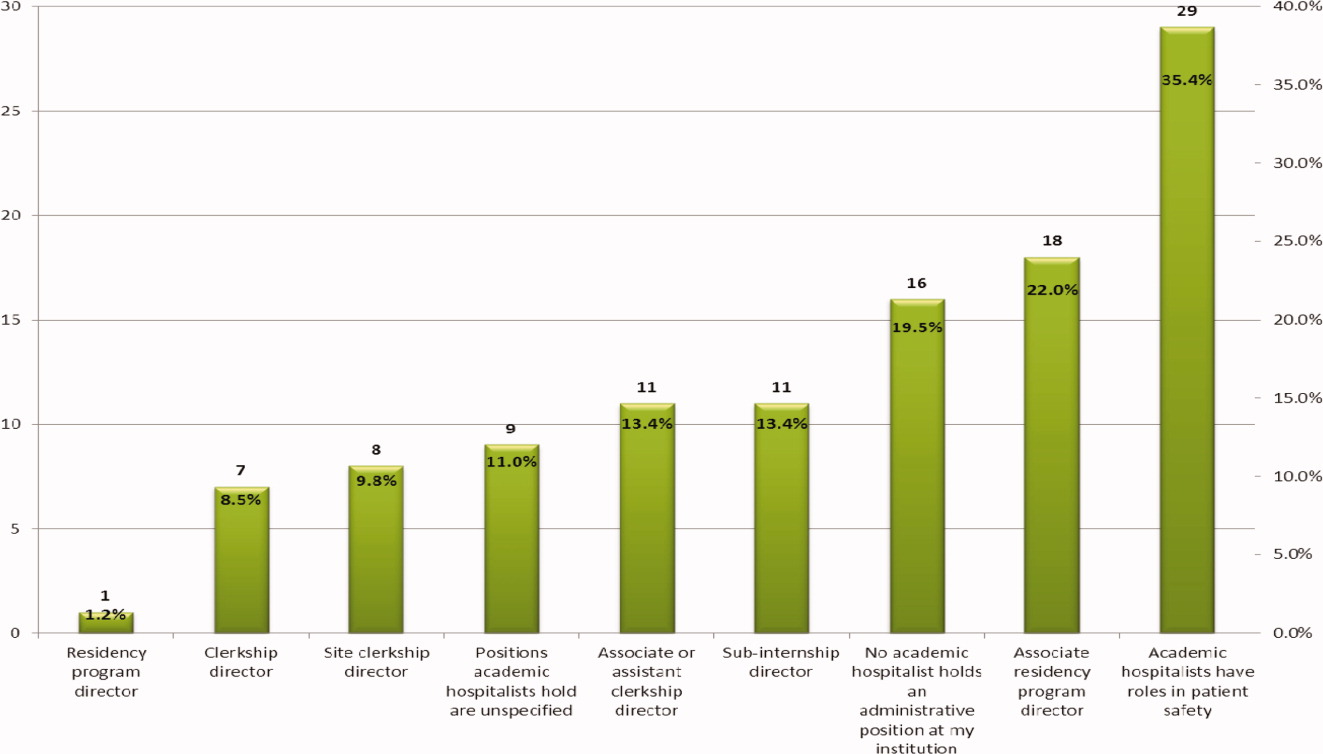
Respondents were asked to comment on other clinical responsibilities for teaching attendings while on‐service. Thirteen (16%) indicated that teaching hospitalists had other clinical responsibilities, whereas 43 (52%) non‐hospitalist teaching attendings were reported to have other clinical responsibilities while on teaching service ( = 33.09, P < 0.0001). The additional responsibilities for teaching hospitalists included general medicine consults (3 programs), quality initiatives (2 programs), clinics (2 programs), additional nonteaching service patients (2 programs), and educational commitments (4 programs). Responsibilities identified for non‐hospitalist teaching attendings were primarily outpatient clinics (29 programs) or were unspecified (14 programs).
DISCUSSION
Over the past decade, hospital medicine has grown exponentially. This clinical growth has been mirrored in medical education. Our study finds that hospitalists teach in core Internal Medicine clerkships in the large majority of Departments of Internal Medicine throughout the US and Canada. Compared to 2000, in which approximately 50% of IM departments employed hospitalists and 80% of these worked with medical students (roughly 40% of all departments),9 we find that 91% of academic IM programs utilize hospitalists for core clerkship education. However, the majority of respondents (72%) reported that less than 25% of formal educational sessions were conducted by academic hospitalists during their core Internal Medicine clerkship. Thus, although hospitalists appear to be involved heavily in supervising medical students during the IM clerkship, the primary teaching modalities utilized appear to be informal. This may be due to the relative youth of the hospitalist movement, with newer faculty being less frequently recruited to conduct didactics. Alternatively, this may result from an historical reliance on subspecialists for Internal Medicine lectures (ie, renal failure lectures are given by a nephrologist, chest pain lectures are given by a cardiologist).
Our study shows that a significant number of hospitalists are involved in student overnight calls. Notably, almost half of the students doing overnight calls were supervised by in‐house hospitalists. This is an expected trend, particularly in the current environment in which intern night hours have been limited and extended shifts are less common.10 Residency programs have frequently shifted to night float systems, the value of which is unknown with regards to education and patient safety.11 Experienced attendings in the hospital afford a unique educational opportunity for third year medical students, and it appears they are being utilized as such.
Although the majority of core IM clerkship students rotate with resident teaching services, we found a small but measureable number of students who are on resident uncovered services. The educational efficacy of this model is not fully defined. In the subinternship setting, resident uncovered teaching hospitalist services were rated equivalently as compared to resident covered teaching services on measures of supervision, faculty assessment, the frequency and value of teaching sessions, and educational value of patient problems. However, students on uncovered services scored these lower on knowledge learned, intellectual discussions, and patient variety.12 Based on this feedback, caution should be taken in assigning more junior students to uncovered hospitalist services. This is especially true in the post‐duty hour setting which has already prompted concern related to student exposure to basic medical conditions.13
Despite the level of hospitalist involvement in core clerkship education, few clerkship directors are hospitalists. However, more than half of the Departments of Internal Medicine report hospitalists in some clerkship or residency educational position. Our survey did not address more senior College of Medicine leadership roles, and may, in fact, underrepresent educational leadership positions. Additionally, a large number of hospitalist have additional roles in patient safety, underscoring hospital medicine's leadership in this important niche post in the Institute of Medicine (IOM) report To Err is Human.14
Our findings indicate that hospitalists are significantly less likely to have additional clinical commitments while on‐service as compared to non‐hospitalist teaching attending. Non‐hospitalist teaching attendings were reported to frequently have outpatient clinic duties while teaching on the inpatient service. Conventional wisdom suggests that educators who are able to focus on teaching activities primarily will likely be better teachers. To date, literature has shown notable learner satisfaction with hospitalist educators.3, 4 However, there are no data on teaching efficacy and learning outcomes. Further studies need to explore the relationship between hospitalist attending status and improved trainee education.
Our study has several limitations. Our report is a survey of institutional members of CDIM. Since not all Departments of Medicine within Schools of Medicine have membership in CDIM, our results may have sampling bias. Additionally, our survey only asked clerkship directors in one discipline to report educational practices. There may be variability at different educational sites that are not captured by the responses. The Society of Hospital Medicine defines a hospitalist as a physician who specializes in the practice of hospital medicine, however, there remains some ambiguity with regards to how much inpatient focus is necessary to employ the term, and this may lead to errors in reporting. Nonetheless, our response rate of 82% is quite high, and suggests that this survey is reflective of national trends.
In summary, hospitalists are involved in medical student education in the majority of Departments of Internal Medicine throughout the US and Canada. They frequently supervise students in‐house at night, and some students rotate on non‐resident covered services. Hospitalists have a notable presence in academic education leadership positions and have significantly less outside clinical responsibilities, allowing them greater focus on teaching. Further studies should to be conducted to determine the effects of hospitalists on learning outcomes. Additional data is needed to determine the influence of hospitalists on students' attitudes and career choices with regards to Internal Medicine.
Acknowledgements
Disclosure: Nothing to report.
- Medical Group Management Association and Society of Hospital Medicine.State of Hospital Medicine: 2011 Report Based on 2010 Data.Franktown, CO:Glacier Publishing Services;2011.
- University HealthSystem Consortium. Role of the Hospitalist 2006 Field Brief.Oak Brook, IL:University HealthSystem Consortium;2006.
- ,.Hospitalist educators: future of inpatient internal medicine training.Mt Sinai J Med.2008;75(5):430–435.
- ,,,.Effect of hospitalist attending physicians on trainee educational experiences: a systematic review.J Hosp Med.2009;4(8):490–498.
- ,.Implications of the hospitalist model for medical students' education.Acad Med.2001;76(4):324–330.
- ,,,,.Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164(17):1866–1871.
- ,.Third‐year medical students' evaluation of hospitalist and nonhospitalist faculty during the inpatient portion of their pediatrics clerkships.J Hosp Med.2007;2(1):17–22.
- ,,,,,.Effect of a pediatric hospitalist system on housestaff education and experience.Arch Pediatr Adolesc Med.2002;156(9):877–883.
- ,,,,.The presence of hospitalists in medical education.Acad Med.2000;75(10 suppl):S34–S36.
- Accreditation Council for Graduate Medical Education (ACGME). Common Program Requirements, Effective July 1,2011. Available at: http://www.acgme‐2010standards.org/pdf/Common_Program_Requirements_07012011.pdf. Accessed on 4 October 2012.
- ,,.Systematic review: association of shift length, protected sleep time, and night float with patient care, residents' health, and education.Ann Intern Med.2010;153(12):829–842.
- ,,,,.Medical subinternship: student experience on a resident uncovered hospitalist service.Teach Learn Med.2008;20(1):18–21.
- ,,,,,.Medical student patient experiences before and after duty hour regulation and hospitalist support.J Gen Intern Med.2010;25(3):207–210.
- ,,.To Err Is Human: Building a Safer Health Care System.Washington, DC:National Academy Press;2000.
- Medical Group Management Association and Society of Hospital Medicine.State of Hospital Medicine: 2011 Report Based on 2010 Data.Franktown, CO:Glacier Publishing Services;2011.
- University HealthSystem Consortium. Role of the Hospitalist 2006 Field Brief.Oak Brook, IL:University HealthSystem Consortium;2006.
- ,.Hospitalist educators: future of inpatient internal medicine training.Mt Sinai J Med.2008;75(5):430–435.
- ,,,.Effect of hospitalist attending physicians on trainee educational experiences: a systematic review.J Hosp Med.2009;4(8):490–498.
- ,.Implications of the hospitalist model for medical students' education.Acad Med.2001;76(4):324–330.
- ,,,,.Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164(17):1866–1871.
- ,.Third‐year medical students' evaluation of hospitalist and nonhospitalist faculty during the inpatient portion of their pediatrics clerkships.J Hosp Med.2007;2(1):17–22.
- ,,,,,.Effect of a pediatric hospitalist system on housestaff education and experience.Arch Pediatr Adolesc Med.2002;156(9):877–883.
- ,,,,.The presence of hospitalists in medical education.Acad Med.2000;75(10 suppl):S34–S36.
- Accreditation Council for Graduate Medical Education (ACGME). Common Program Requirements, Effective July 1,2011. Available at: http://www.acgme‐2010standards.org/pdf/Common_Program_Requirements_07012011.pdf. Accessed on 4 October 2012.
- ,,.Systematic review: association of shift length, protected sleep time, and night float with patient care, residents' health, and education.Ann Intern Med.2010;153(12):829–842.
- ,,,,.Medical subinternship: student experience on a resident uncovered hospitalist service.Teach Learn Med.2008;20(1):18–21.
- ,,,,,.Medical student patient experiences before and after duty hour regulation and hospitalist support.J Gen Intern Med.2010;25(3):207–210.
- ,,.To Err Is Human: Building a Safer Health Care System.Washington, DC:National Academy Press;2000.
Copyright © 2012 Society of Hospital Medicine
Overnight Resident Supervision
Postgraduate medical education has traditionally relied on a training model of progressive independence, where housestaff learn patient care through increasing autonomy and decreasing levels of supervision.1 While this framework has little empirical backing, it is grounded in sound educational theory from similar disciplines and endorsed by medical associations.1, 2 The Accreditation Council for Graduate Medical Education (ACGME) recently implemented regulations requiring that first‐year residents have a qualified supervisor physically present or immediately available at all times.3 Previously, oversight by an offsite supervisor (for example, an attending physician at home) was considered adequate. These new regulations, although motivated by patient safety imperatives,4 have elicited concerns that increased supervision may lead to decreased housestaff autonomy and an increased reliance on supervisors for clinical guidance.5 Such changes could ultimately produce less qualified practitioners by the completion of training.
Critics of the current training model point to a patient safety mechanism where housestaff must take responsibility for requesting attending‐level help when situations arise that surpass their skill level.5 For resident physicians, however, the decision to request support is often complex and dependent not only on the clinical question, but also on unique and variable trainee and supervisor factors.6 Survey data from 1999, prior to the current training regulations, showed that increased faculty presence improved resident reports of educational value, quality of patient care, and autonomy.7 A recent survey, performed after the initiation of overnight attending supervision at an academic medical center, demonstrated perceived improvements in educational value and patient‐level outcomes by both faculty and housestaff.8 Whether increased supervision and resident autonomy can coexist remains undetermined.
Overnight rotations for residents (commonly referred to as night float) are often times of little direct or indirect supervision. A recent systematic review of clinical supervision practices for housestaff in all fields found scarce literature on overnight supervision practices.9 There remains limited and conflicting data regarding the quality of patient care provided by the resident night float,10 as well as evidence revealing a low perceived educational value of night rotations when compared with non‐night float rotations.11 Yet in 2006, more than three‐quarters of all internal medicine programs employed night float rotations.12 In response to ACGME guidelines mandating decreased shift lengths with continued restrictions on overall duty hours, it appears likely even more training programs will implement night float systems.
The presence of overnight hospitalists (also known as nocturnists) is growing within the academic setting, yet their role in relation to trainees is either poorly defined13 or independent of housestaff.14 To better understand the impact of increasing levels of supervision on residency training, we investigated housestaff perceptions of education, autonomy, and clinical decision‐making before and after implementation of an in‐hospital, overnight attending physician (nocturnist).
METHODS
The study was conducted at a 570‐bed academic, tertiary care medical center affiliated with an internal medicine residency program of 170 housestaff. At our institution, all first year residents perform a week of intern night float consisting of overnight cross‐coverage of general medicine patients on the floor, step‐down, and intensive care units (ICUs). Second and third year residents each complete 4 to 6 days of resident night float each year at this hospital. They are responsible for assisting the intern night float with cross‐coverage, in addition to admitting general medicine patients to the floor, step‐down unit, and intensive care units. Every night at our medical center, 1 intern night float and 1 resident night float are on duty in the hospital; this is in addition to a resident from the on‐call medicine team and a resident working in the ICU. Prior to July 2010, no internal medicine attending physicians were physically present in the hospital at night. Oversight for the intern and resident night float was provided by the attending physician for the on‐call resident ward team, who was at home and available by pager. The night float housestaff were instructed to contact the responsible attending physician only when a major change in clinical status occurred for hospitalized or newly admitted patients, though this expectation was neither standardized nor monitored.
We established a nocturnist program at the start of the 2010 academic year. The position was staffed by hospitalists from within the Division of Hospital Medicine without the use of moonlighters. Two‐thirds of shifts were filled by 3 dedicated nocturnists with remaining staffing provided by junior hospitalist faculty. The dedicated nocturnists had recently completed their internal medicine residency at our institution. Shift length was 12 hours and dedicated nocturnists worked, on average, 10 shifts per month. The nocturnist filled a critical overnight safety role through mandatory bedside staffing of newly admitted ICU patients within 2 hours of admission, discussion in person or via telephone of newly admitted step‐down unit patients within 6 hours of admission, and direct or indirect supervision of the care of any patients undergoing a major change in clinical status. The overnight hospitalist was also available for clinical questions and to assist housestaff with triaging of overnight admissions. After nocturnist implementation, overnight housestaff received direct supervision or had immediate access to direct supervision, while prior to the nocturnist, residents had access only to indirect supervision.
In addition, the nocturnist admitted medicine patients after 1 AM in a 1:1 ratio with the admitting night float resident, performed medical consults, and provided coverage of non‐teaching medicine services. While actual volume numbers were not obtained, the estimated average of resident admissions per night was 2 to 3, and the number of nocturnist admissions was 1 to 2. The nocturnist also met nightly with night float housestaff for half‐hour didactics focusing on the management of common overnight clinical scenarios. The role of the new nocturnist was described to all housestaff in orientation materials given prior to their night float rotation and their general medicine ward rotation.
We administered pre‐rolling surveys and post‐rolling surveys of internal medicine intern and resident physicians who underwent the night float rotation at our hospital during the 2010 to 2011 academic year. Surveys examined housestaff perceptions of the night float rotation with regard to supervisory roles, educational and clinical value, and clinical decision‐making prior to and after implementation of the nocturnist. Surveys were designed by the study investigators based on prior literature,1, 510 personal experience, and housestaff suggestion, and were refined during works‐in‐progress meetings. Surveys were composed of Likert‐style questions asking housestaff to rate their level of agreement (15, strongly disagree to strongly agree) with statements regarding the supervisory and educational experience of the night float rotation, and to judge their frequency of contact (15, never to always/nightly) with an attending physician for specific clinical scenarios. The clinical scenarios described situations dealing with attendingresident communication around transfers of care, diagnostic evaluation, therapeutic interventions, and adverse events. Scenarios were taken from previous literature describing supervision preferences of faculty and residents during times of critical clinical decision‐making.15
One week prior to the beginning their night float rotation for the 20102011 academic year, housestaff were sent an e‐mail request to complete an online survey asking about their night float rotation during the prior academic year, when no nocturnist was present. One week after completion of their night float rotation for the 20102011 academic year, housestaff received an e‐mail with a link to a post‐survey asking about their recently completed, nocturnist‐supervised, night float rotation. First year residents received only a post‐survey at the completion of their night float rotation, as they would be unable to reflect on prior experience.
Informed consent was imbedded within the e‐mail survey request. Survey requests were sent by a fellow within the Division of Hospital Medicine with a brief message cosigned by an associate program director of the residency program. We did not collect unique identifiers from respondents in order to offer additional assurances to the participants that the survey was anonymous. There was no incentive offered for completion of the survey. Survey data were anonymous and downloaded to a database by a third party. Data were analyzed using Microsoft Excel, and pre‐responses and post‐responses compared using a Student t test. The study was approved by the medical center's Institutional Review Board.
RESULTS
Rates of response for pre‐surveys and post‐surveys were 57% (43 respondents) and 51% (53 respondents), respectively. Due to response rates and in order to convey accurately the perceptions of the training program as a whole, we collapsed responses of the pre‐surveys and post‐surveys based on level of training. After implementation of the overnight attending, we observed a significant increase in the perceived clinical value of the night float rotation (3.95 vs 4.27, P = 0.01) as well as in the adequacy of overnight supervision (3.65 vs 4.30, P < 0.0001; Table 1). There was no reported change in housestaff decision‐making autonomy (4.35 vs 4.45, P = 0.44). In addition, we noted a nonsignificant trend towards an increased perception of the night float rotation as a valuable educational experience (3.83 vs 4.04, P = 0.24). After implementation of the nocturnist, more resident physicians agreed that overnight supervision by an attending positively impacted patient outcomes (3.79 vs 4.30, P = 0.002).
| Statement | Pre‐Nocturnist (n = 43) Mean (SD) | Post‐Nocturnist (n = 53) Mean (SD) | P Value |
|---|---|---|---|
| |||
| Night float is a valuable educational rotation | 3.83 (0.81) | 4.04 (0.83) | 0.24 |
| Night float is a valuable clinical rotation | 3.95 (0.65) | 4.27 (0.59) | 0.01 |
| I have adequate overnight supervision | 3.65 (0.76) | 4.30 (0.72) | <0.0001 |
| I have sufficient autonomy to make clinical decisions | 4.35 (0.57) | 4.45 (0.60) | 0.44 |
| Overnight supervision by an attending positively impacts patient outcomes | 3.79 (0.88) | 4.30 (0.74) | 0.002 |
After implementation of the nocturnist, night float providers demonstrated increased rates of contacting an attending physician overnight (Table 2). There were significantly greater rates of attending contact for transfers from outside facilities (2.00 vs 3.20, P = 0.006) and during times of adverse events (2.51 vs 3.25, P = 0.04). We observed a reported increase in attending contact prior to ordering invasive diagnostic procedures (1.75 vs 2.76, P = 0.004) and noninvasive diagnostic procedures (1.09 vs 1.31, P = 0.03), as well as prior to initiation of intravenous antibiotics (1.11 vs 1.47, P = 0.007) and vasopressors (1.52 vs 2.40, P = 0.004).
| Scenario | Pre‐Nocturnist (n = 42) Mean (SD) | Post‐Nocturnist (n = 51) Mean (SD) | P Value |
|---|---|---|---|
| |||
| Receive transfer from outside facility | 2.00 (1.27) | 3.20 (1.58) | 0.006 |
| Prior to ordering noninvasive diagnostic procedure | 1.09 (0.29) | 1.31 (0.58) | 0.03 |
| Prior to ordering an invasive procedure | 1.75 (0.84) | 2.76 (1.45) | 0.004 |
| Prior to initiation of intravenous antibiotics | 1.11 (0.32) | 1.47 (0.76) | 0.007 |
| Prior to initiation of vasopressors | 1.52 (0.82) | 2.40 (1.49) | 0.004 |
| Patient experiencing adverse event, regardless of cause | 2.51 (1.31) | 3.25 (1.34) | 0.04 |
After initiating the program, the nocturnist became the most commonly contacted overnight provider by the night float housestaff (Table 3). We observed a decrease in peer to peer contact between the night float housestaff and the on‐call overnight resident after implementation of the nocturnist (2.67 vs 2.04, P = 0.006).
| Provider | Pre‐Nocturnist (n = 43) Mean (SD) | Post‐Nocturnist (n = 53) Mean (SD) | P Value |
|---|---|---|---|
| |||
| ICU Fellow | 1.86 (0.70) | 1.86 (0.83) | 0.96 |
| On‐call resident | 2.67 (0.89) | 2.04 (0.92) | 0.006 |
| ICU resident | 2.14 (0.74) | 2.04 (0.91) | 0.56 |
| On‐call medicine attending | 1.41 (0.79) | 1.26 (0.52) | 0.26 |
| Patient's PMD | 1.27 (0.31) | 1.15 (0.41) | 0.31 |
| Referring MD | 1.32 (0.60) | 1.15 (0.45) | 0.11 |
| Nocturnist | 3.59 (1.22) | ||
Attending presence led to increased agreement that there was a defined overnight attending to contact (2.97 vs 1.96, P < 0.0001) and a decreased fear of waking an attending overnight for assistance (3.26 vs 2.72, P = 0.03). Increased attending availability, however, did not change resident physician's fear of revealing knowledge gaps, their desire to make decisions independently, or their belief that contacting an attending would not change a patient's outcome (Table 4).
| Statement | Pre‐Nocturnist (n = 42) Mean (SD) | Post‐Nocturnist (n = 52) Mean (SD) | P Value |
|---|---|---|---|
| |||
| No defined attending to contact | 2.97 (1.35) | 1.96 (0.92) | <0.0001 |
| Fear of waking an attending | 3.26 (1.25) | 2.72 (1.09) | 0.03 |
| Fear of revealing knowledge gaps | 2.26 (1.14) | 2.25 (0.96) | 0.95 |
| Would rather make decision on own | 3.40 (0.93) | 3.03 (1.06) | 0.08 |
| Will not change patient outcome | 3.26 (1.06) | 3.21 (1.03) | 0.81 |
DISCUSSION
The ACGME's new duty hour regulations require that supervision for first‐year residents be provided by a qualified physician (advanced resident, fellow, or attending physician) who is physically present at the hospital. Our study demonstrates that increased direct overnight supervision provided by an in‐house nocturnist enhanced the clinical value of the night float rotation and the perceived quality of patient care. In our study, increased attending supervision did not reduce perceived decision‐making autonomy, and in fact led to increased rates of attending contact during times of critical clinical decision‐making. Such results may help assuage fears that recent regulations mandating enhanced attending supervision will produce less capable practitioners, and offers reassurance that such changes are positively impacting patient care.
Many academic institutions are implementing nocturnists, although their precise roles and responsibilities are still being defined. Our nocturnist program was explicitly designed with housestaff supervision as a core responsibility, with the goal of improving patient safety and housestaff education overnight. We found that availability barriers to attending contact were logically decreased with in‐house faculty presence. Potentially harmful attitudes, however, around requesting support (such as fear of revealing knowledge gaps or the desire to make decisions independently) remained. Furthermore, despite statistically significant increases in contact between faculty and residents at times of critical decision‐making, overall rates of attending contact for diagnostic and therapeutic interventions remained low. It is unknown from our study or previous research, however, what level of contact is appropriate or ideal for many clinical scenarios.
Additionally, we described a novel role of an academic nocturnist at a tertiary care teaching hospital and offered a potential template for the development of academic nocturnists at similar institutions seeking to increase direct overnight supervision. Such roles have not been previously well defined in the literature. Based on our experience, the nocturnist's role was manageable and well utilized by housestaff, particularly for assistance with critically ill patients and overnight triaging. We believe there are a number of factors associated with the success of this role. First, clear guidelines were presented to housestaff and nocturnists regarding expectations for supervision (for example, staffing ICU admissions within 2 hours). These guidelines likely contributed to the increased attending contact observed during critical clinical decision‐making, as well as the perceived improved patient outcomes by our housestaff. Second, the nocturnists were expected to be an integral part of the overnight care team. In many systems, the nocturnists act completely independently of the housestaff teams, creating an additional barrier to contact and communication. In our system, because of clear guidelines and their integral role in staffing overnight admissions, the nocturnists were an essential partner in care for the housestaff. Third, most of the nocturnists had recently completed their residency training at this institution. Although our survey does not directly address this, we believe their knowledge of the hospital, appreciation of the role of the intern and the resident within our system, and understanding of the need to preserve housestaff autonomy were essential to building a successful nocturnist role. Lastly, the nocturnists were not only expected to supervise and staff new admissions, but were also given a teaching expectation. We believe they were viewed by housestaff as qualified teaching attendings, similar to the daytime hospitalist. These findings may provide guidelines for other institutions seeking to balance overnight hospitalist supervision with preserving resident's ability to make autonomous decisions.
There are several limitations to our study. The findings represent the experience of internal medicine housestaff at a single academic, tertiary care medical center and may not be reflective of other institutions or specialties. We asked housestaff to recall night float experiences from the prior year, which may have introduced recall bias, though responses were obtained before participants underwent the new curriculum. Maturation of housestaff over time could have led to changes in perceived autonomy, value of the night float rotation, and rates of attending contact independent of nocturnist implementation. In addition, there may have been unaccounted changes to other elements of the residency program, hospital, or patient volume between rotations. The implementation of the nocturnist, however, was the only major change to our training program that academic year, and there were no significant changes in patient volume, structure of the teaching or non‐resident services, or other policies around resident supervision.
It is possible that the nocturnist may have contributed to reports of increased clinical value and perceived quality of patient care simply by decreasing overnight workload for housestaff, and enhanced supervision and teaching may have played a lesser role. Even if this were true, optimizing resident workload is in itself an important goal for teaching hospitals and residency programs alike in order to maximize patient safety. Inclusion of intern post‐rotation surveys may have influenced data; though, we had no reason to suspect the surveyed interns would respond in a different manner than prior resident groups. The responses of both junior and senior housestaff were pooled; while this potentially weighted the results in favor of higher responding groups, we felt that it conveyed the residents' accurate sentiments on the program. Finally, while we compared two models of overnight supervision, we reported only housestaff perceptions of education, autonomy, patient outcomes, and supervisory contact, and not direct measures of knowledge or patient care. Further research will be required to define the relationship between supervision practices and patient‐level clinical outcomes.
The new ACGME regulations around resident supervision, as well as the broader movement to improve the safety and quality of care, require residency programs to negotiate a delicate balance between providing high‐quality patient care while preserving graduated independence in clinical training. Our study demonstrates that increased overnight supervision by nocturnists with well‐defined supervisory and teaching roles can preserve housestaff autonomy, improve the clinical experience for trainees, increase access to support during times of critical decision‐making, and potentially lead to improved patient outcomes.
Acknowledgements
Disclosures: No authors received commercial support for the submitted work. Dr Arora reports being an editorial board member for Agency for Healthcare Research and Quality (AHRQ) Web M&M, receiving grants from the ACGME for previous work, and receiving payment for speaking on graduate medical education supervision.
- ,,,.Progressive independence in clinical training: a tradition worth defending?Acad Med.2005;80(10 suppl):S106–S111.
- Joint Committee of the Group on Resident Affairs and Organization of Resident Representatives.Patient Safety and Graduate Medical Education.Washington, DC:Association of American Medical Colleges; February2003:6.
- Accreditation Council on Graduate Medical Education.Common Program Requirements. Available at: http://www.acgme.org/acWebsite/home/Common_Program_Requirements_07012011.pdf. Accessed October 16,2011.
- The IOM medical errors report: 5 years later, the journey continues.Qual Lett Health Lead.2005;17(1):2–10.
- .Supervision in medical education: logical fallacies and clear choices.J Grad Med Educ.2010;2(1):141–143.
- ,,,.Preserving professional credibility: grounded theory study of medical trainees' requests for clinical support.BMJ.2009;338:b128.
- ,,,,.Increased faculty presence on inpatient teaching services.Mayo Clin Proc.2004;79(3):332–336.
- ,,,.The effect of overnight in‐house attending coverage on perceptions of care and education on a general medical service.J Grad Med Educ.2010;2(1):53–56.
- ,,, et al.A systematic review: the effect of clinical supervision on patient and residency education outcomes.Acad Med.2012;87(4):428–442.
- ,,,,.Residents' perceptions of a night float system.BMC Med Educ.2009;9:52.
- ,,,.Resident perceptions of the educational value of night float rotations.Teach Learn Med.2010;22(3):196–201.
- ,,,.How do internal medicine residency programs evaluate their resident float experiences?South Med J.2006;99(9):919–923.
- ,,.Hospitalist involvement in internal medicine residencies.J Hosp Med.2009;4(8):471–475.
- ,,, et al.Complying with ACGME resident duty hour restrictions: restructuring the 80 hour workweek to enhance education and patient safety at Texas A81(12):1026–1031.
- ,,,,.On‐call supervision and resident autonomy: from micromanager to absentee attending.Am J Med.2009;122(8):784–788.
Postgraduate medical education has traditionally relied on a training model of progressive independence, where housestaff learn patient care through increasing autonomy and decreasing levels of supervision.1 While this framework has little empirical backing, it is grounded in sound educational theory from similar disciplines and endorsed by medical associations.1, 2 The Accreditation Council for Graduate Medical Education (ACGME) recently implemented regulations requiring that first‐year residents have a qualified supervisor physically present or immediately available at all times.3 Previously, oversight by an offsite supervisor (for example, an attending physician at home) was considered adequate. These new regulations, although motivated by patient safety imperatives,4 have elicited concerns that increased supervision may lead to decreased housestaff autonomy and an increased reliance on supervisors for clinical guidance.5 Such changes could ultimately produce less qualified practitioners by the completion of training.
Critics of the current training model point to a patient safety mechanism where housestaff must take responsibility for requesting attending‐level help when situations arise that surpass their skill level.5 For resident physicians, however, the decision to request support is often complex and dependent not only on the clinical question, but also on unique and variable trainee and supervisor factors.6 Survey data from 1999, prior to the current training regulations, showed that increased faculty presence improved resident reports of educational value, quality of patient care, and autonomy.7 A recent survey, performed after the initiation of overnight attending supervision at an academic medical center, demonstrated perceived improvements in educational value and patient‐level outcomes by both faculty and housestaff.8 Whether increased supervision and resident autonomy can coexist remains undetermined.
Overnight rotations for residents (commonly referred to as night float) are often times of little direct or indirect supervision. A recent systematic review of clinical supervision practices for housestaff in all fields found scarce literature on overnight supervision practices.9 There remains limited and conflicting data regarding the quality of patient care provided by the resident night float,10 as well as evidence revealing a low perceived educational value of night rotations when compared with non‐night float rotations.11 Yet in 2006, more than three‐quarters of all internal medicine programs employed night float rotations.12 In response to ACGME guidelines mandating decreased shift lengths with continued restrictions on overall duty hours, it appears likely even more training programs will implement night float systems.
The presence of overnight hospitalists (also known as nocturnists) is growing within the academic setting, yet their role in relation to trainees is either poorly defined13 or independent of housestaff.14 To better understand the impact of increasing levels of supervision on residency training, we investigated housestaff perceptions of education, autonomy, and clinical decision‐making before and after implementation of an in‐hospital, overnight attending physician (nocturnist).
METHODS
The study was conducted at a 570‐bed academic, tertiary care medical center affiliated with an internal medicine residency program of 170 housestaff. At our institution, all first year residents perform a week of intern night float consisting of overnight cross‐coverage of general medicine patients on the floor, step‐down, and intensive care units (ICUs). Second and third year residents each complete 4 to 6 days of resident night float each year at this hospital. They are responsible for assisting the intern night float with cross‐coverage, in addition to admitting general medicine patients to the floor, step‐down unit, and intensive care units. Every night at our medical center, 1 intern night float and 1 resident night float are on duty in the hospital; this is in addition to a resident from the on‐call medicine team and a resident working in the ICU. Prior to July 2010, no internal medicine attending physicians were physically present in the hospital at night. Oversight for the intern and resident night float was provided by the attending physician for the on‐call resident ward team, who was at home and available by pager. The night float housestaff were instructed to contact the responsible attending physician only when a major change in clinical status occurred for hospitalized or newly admitted patients, though this expectation was neither standardized nor monitored.
We established a nocturnist program at the start of the 2010 academic year. The position was staffed by hospitalists from within the Division of Hospital Medicine without the use of moonlighters. Two‐thirds of shifts were filled by 3 dedicated nocturnists with remaining staffing provided by junior hospitalist faculty. The dedicated nocturnists had recently completed their internal medicine residency at our institution. Shift length was 12 hours and dedicated nocturnists worked, on average, 10 shifts per month. The nocturnist filled a critical overnight safety role through mandatory bedside staffing of newly admitted ICU patients within 2 hours of admission, discussion in person or via telephone of newly admitted step‐down unit patients within 6 hours of admission, and direct or indirect supervision of the care of any patients undergoing a major change in clinical status. The overnight hospitalist was also available for clinical questions and to assist housestaff with triaging of overnight admissions. After nocturnist implementation, overnight housestaff received direct supervision or had immediate access to direct supervision, while prior to the nocturnist, residents had access only to indirect supervision.
In addition, the nocturnist admitted medicine patients after 1 AM in a 1:1 ratio with the admitting night float resident, performed medical consults, and provided coverage of non‐teaching medicine services. While actual volume numbers were not obtained, the estimated average of resident admissions per night was 2 to 3, and the number of nocturnist admissions was 1 to 2. The nocturnist also met nightly with night float housestaff for half‐hour didactics focusing on the management of common overnight clinical scenarios. The role of the new nocturnist was described to all housestaff in orientation materials given prior to their night float rotation and their general medicine ward rotation.
We administered pre‐rolling surveys and post‐rolling surveys of internal medicine intern and resident physicians who underwent the night float rotation at our hospital during the 2010 to 2011 academic year. Surveys examined housestaff perceptions of the night float rotation with regard to supervisory roles, educational and clinical value, and clinical decision‐making prior to and after implementation of the nocturnist. Surveys were designed by the study investigators based on prior literature,1, 510 personal experience, and housestaff suggestion, and were refined during works‐in‐progress meetings. Surveys were composed of Likert‐style questions asking housestaff to rate their level of agreement (15, strongly disagree to strongly agree) with statements regarding the supervisory and educational experience of the night float rotation, and to judge their frequency of contact (15, never to always/nightly) with an attending physician for specific clinical scenarios. The clinical scenarios described situations dealing with attendingresident communication around transfers of care, diagnostic evaluation, therapeutic interventions, and adverse events. Scenarios were taken from previous literature describing supervision preferences of faculty and residents during times of critical clinical decision‐making.15
One week prior to the beginning their night float rotation for the 20102011 academic year, housestaff were sent an e‐mail request to complete an online survey asking about their night float rotation during the prior academic year, when no nocturnist was present. One week after completion of their night float rotation for the 20102011 academic year, housestaff received an e‐mail with a link to a post‐survey asking about their recently completed, nocturnist‐supervised, night float rotation. First year residents received only a post‐survey at the completion of their night float rotation, as they would be unable to reflect on prior experience.
Informed consent was imbedded within the e‐mail survey request. Survey requests were sent by a fellow within the Division of Hospital Medicine with a brief message cosigned by an associate program director of the residency program. We did not collect unique identifiers from respondents in order to offer additional assurances to the participants that the survey was anonymous. There was no incentive offered for completion of the survey. Survey data were anonymous and downloaded to a database by a third party. Data were analyzed using Microsoft Excel, and pre‐responses and post‐responses compared using a Student t test. The study was approved by the medical center's Institutional Review Board.
RESULTS
Rates of response for pre‐surveys and post‐surveys were 57% (43 respondents) and 51% (53 respondents), respectively. Due to response rates and in order to convey accurately the perceptions of the training program as a whole, we collapsed responses of the pre‐surveys and post‐surveys based on level of training. After implementation of the overnight attending, we observed a significant increase in the perceived clinical value of the night float rotation (3.95 vs 4.27, P = 0.01) as well as in the adequacy of overnight supervision (3.65 vs 4.30, P < 0.0001; Table 1). There was no reported change in housestaff decision‐making autonomy (4.35 vs 4.45, P = 0.44). In addition, we noted a nonsignificant trend towards an increased perception of the night float rotation as a valuable educational experience (3.83 vs 4.04, P = 0.24). After implementation of the nocturnist, more resident physicians agreed that overnight supervision by an attending positively impacted patient outcomes (3.79 vs 4.30, P = 0.002).
| Statement | Pre‐Nocturnist (n = 43) Mean (SD) | Post‐Nocturnist (n = 53) Mean (SD) | P Value |
|---|---|---|---|
| |||
| Night float is a valuable educational rotation | 3.83 (0.81) | 4.04 (0.83) | 0.24 |
| Night float is a valuable clinical rotation | 3.95 (0.65) | 4.27 (0.59) | 0.01 |
| I have adequate overnight supervision | 3.65 (0.76) | 4.30 (0.72) | <0.0001 |
| I have sufficient autonomy to make clinical decisions | 4.35 (0.57) | 4.45 (0.60) | 0.44 |
| Overnight supervision by an attending positively impacts patient outcomes | 3.79 (0.88) | 4.30 (0.74) | 0.002 |
After implementation of the nocturnist, night float providers demonstrated increased rates of contacting an attending physician overnight (Table 2). There were significantly greater rates of attending contact for transfers from outside facilities (2.00 vs 3.20, P = 0.006) and during times of adverse events (2.51 vs 3.25, P = 0.04). We observed a reported increase in attending contact prior to ordering invasive diagnostic procedures (1.75 vs 2.76, P = 0.004) and noninvasive diagnostic procedures (1.09 vs 1.31, P = 0.03), as well as prior to initiation of intravenous antibiotics (1.11 vs 1.47, P = 0.007) and vasopressors (1.52 vs 2.40, P = 0.004).
| Scenario | Pre‐Nocturnist (n = 42) Mean (SD) | Post‐Nocturnist (n = 51) Mean (SD) | P Value |
|---|---|---|---|
| |||
| Receive transfer from outside facility | 2.00 (1.27) | 3.20 (1.58) | 0.006 |
| Prior to ordering noninvasive diagnostic procedure | 1.09 (0.29) | 1.31 (0.58) | 0.03 |
| Prior to ordering an invasive procedure | 1.75 (0.84) | 2.76 (1.45) | 0.004 |
| Prior to initiation of intravenous antibiotics | 1.11 (0.32) | 1.47 (0.76) | 0.007 |
| Prior to initiation of vasopressors | 1.52 (0.82) | 2.40 (1.49) | 0.004 |
| Patient experiencing adverse event, regardless of cause | 2.51 (1.31) | 3.25 (1.34) | 0.04 |
After initiating the program, the nocturnist became the most commonly contacted overnight provider by the night float housestaff (Table 3). We observed a decrease in peer to peer contact between the night float housestaff and the on‐call overnight resident after implementation of the nocturnist (2.67 vs 2.04, P = 0.006).
| Provider | Pre‐Nocturnist (n = 43) Mean (SD) | Post‐Nocturnist (n = 53) Mean (SD) | P Value |
|---|---|---|---|
| |||
| ICU Fellow | 1.86 (0.70) | 1.86 (0.83) | 0.96 |
| On‐call resident | 2.67 (0.89) | 2.04 (0.92) | 0.006 |
| ICU resident | 2.14 (0.74) | 2.04 (0.91) | 0.56 |
| On‐call medicine attending | 1.41 (0.79) | 1.26 (0.52) | 0.26 |
| Patient's PMD | 1.27 (0.31) | 1.15 (0.41) | 0.31 |
| Referring MD | 1.32 (0.60) | 1.15 (0.45) | 0.11 |
| Nocturnist | 3.59 (1.22) | ||
Attending presence led to increased agreement that there was a defined overnight attending to contact (2.97 vs 1.96, P < 0.0001) and a decreased fear of waking an attending overnight for assistance (3.26 vs 2.72, P = 0.03). Increased attending availability, however, did not change resident physician's fear of revealing knowledge gaps, their desire to make decisions independently, or their belief that contacting an attending would not change a patient's outcome (Table 4).
| Statement | Pre‐Nocturnist (n = 42) Mean (SD) | Post‐Nocturnist (n = 52) Mean (SD) | P Value |
|---|---|---|---|
| |||
| No defined attending to contact | 2.97 (1.35) | 1.96 (0.92) | <0.0001 |
| Fear of waking an attending | 3.26 (1.25) | 2.72 (1.09) | 0.03 |
| Fear of revealing knowledge gaps | 2.26 (1.14) | 2.25 (0.96) | 0.95 |
| Would rather make decision on own | 3.40 (0.93) | 3.03 (1.06) | 0.08 |
| Will not change patient outcome | 3.26 (1.06) | 3.21 (1.03) | 0.81 |
DISCUSSION
The ACGME's new duty hour regulations require that supervision for first‐year residents be provided by a qualified physician (advanced resident, fellow, or attending physician) who is physically present at the hospital. Our study demonstrates that increased direct overnight supervision provided by an in‐house nocturnist enhanced the clinical value of the night float rotation and the perceived quality of patient care. In our study, increased attending supervision did not reduce perceived decision‐making autonomy, and in fact led to increased rates of attending contact during times of critical clinical decision‐making. Such results may help assuage fears that recent regulations mandating enhanced attending supervision will produce less capable practitioners, and offers reassurance that such changes are positively impacting patient care.
Many academic institutions are implementing nocturnists, although their precise roles and responsibilities are still being defined. Our nocturnist program was explicitly designed with housestaff supervision as a core responsibility, with the goal of improving patient safety and housestaff education overnight. We found that availability barriers to attending contact were logically decreased with in‐house faculty presence. Potentially harmful attitudes, however, around requesting support (such as fear of revealing knowledge gaps or the desire to make decisions independently) remained. Furthermore, despite statistically significant increases in contact between faculty and residents at times of critical decision‐making, overall rates of attending contact for diagnostic and therapeutic interventions remained low. It is unknown from our study or previous research, however, what level of contact is appropriate or ideal for many clinical scenarios.
Additionally, we described a novel role of an academic nocturnist at a tertiary care teaching hospital and offered a potential template for the development of academic nocturnists at similar institutions seeking to increase direct overnight supervision. Such roles have not been previously well defined in the literature. Based on our experience, the nocturnist's role was manageable and well utilized by housestaff, particularly for assistance with critically ill patients and overnight triaging. We believe there are a number of factors associated with the success of this role. First, clear guidelines were presented to housestaff and nocturnists regarding expectations for supervision (for example, staffing ICU admissions within 2 hours). These guidelines likely contributed to the increased attending contact observed during critical clinical decision‐making, as well as the perceived improved patient outcomes by our housestaff. Second, the nocturnists were expected to be an integral part of the overnight care team. In many systems, the nocturnists act completely independently of the housestaff teams, creating an additional barrier to contact and communication. In our system, because of clear guidelines and their integral role in staffing overnight admissions, the nocturnists were an essential partner in care for the housestaff. Third, most of the nocturnists had recently completed their residency training at this institution. Although our survey does not directly address this, we believe their knowledge of the hospital, appreciation of the role of the intern and the resident within our system, and understanding of the need to preserve housestaff autonomy were essential to building a successful nocturnist role. Lastly, the nocturnists were not only expected to supervise and staff new admissions, but were also given a teaching expectation. We believe they were viewed by housestaff as qualified teaching attendings, similar to the daytime hospitalist. These findings may provide guidelines for other institutions seeking to balance overnight hospitalist supervision with preserving resident's ability to make autonomous decisions.
There are several limitations to our study. The findings represent the experience of internal medicine housestaff at a single academic, tertiary care medical center and may not be reflective of other institutions or specialties. We asked housestaff to recall night float experiences from the prior year, which may have introduced recall bias, though responses were obtained before participants underwent the new curriculum. Maturation of housestaff over time could have led to changes in perceived autonomy, value of the night float rotation, and rates of attending contact independent of nocturnist implementation. In addition, there may have been unaccounted changes to other elements of the residency program, hospital, or patient volume between rotations. The implementation of the nocturnist, however, was the only major change to our training program that academic year, and there were no significant changes in patient volume, structure of the teaching or non‐resident services, or other policies around resident supervision.
It is possible that the nocturnist may have contributed to reports of increased clinical value and perceived quality of patient care simply by decreasing overnight workload for housestaff, and enhanced supervision and teaching may have played a lesser role. Even if this were true, optimizing resident workload is in itself an important goal for teaching hospitals and residency programs alike in order to maximize patient safety. Inclusion of intern post‐rotation surveys may have influenced data; though, we had no reason to suspect the surveyed interns would respond in a different manner than prior resident groups. The responses of both junior and senior housestaff were pooled; while this potentially weighted the results in favor of higher responding groups, we felt that it conveyed the residents' accurate sentiments on the program. Finally, while we compared two models of overnight supervision, we reported only housestaff perceptions of education, autonomy, patient outcomes, and supervisory contact, and not direct measures of knowledge or patient care. Further research will be required to define the relationship between supervision practices and patient‐level clinical outcomes.
The new ACGME regulations around resident supervision, as well as the broader movement to improve the safety and quality of care, require residency programs to negotiate a delicate balance between providing high‐quality patient care while preserving graduated independence in clinical training. Our study demonstrates that increased overnight supervision by nocturnists with well‐defined supervisory and teaching roles can preserve housestaff autonomy, improve the clinical experience for trainees, increase access to support during times of critical decision‐making, and potentially lead to improved patient outcomes.
Acknowledgements
Disclosures: No authors received commercial support for the submitted work. Dr Arora reports being an editorial board member for Agency for Healthcare Research and Quality (AHRQ) Web M&M, receiving grants from the ACGME for previous work, and receiving payment for speaking on graduate medical education supervision.
Postgraduate medical education has traditionally relied on a training model of progressive independence, where housestaff learn patient care through increasing autonomy and decreasing levels of supervision.1 While this framework has little empirical backing, it is grounded in sound educational theory from similar disciplines and endorsed by medical associations.1, 2 The Accreditation Council for Graduate Medical Education (ACGME) recently implemented regulations requiring that first‐year residents have a qualified supervisor physically present or immediately available at all times.3 Previously, oversight by an offsite supervisor (for example, an attending physician at home) was considered adequate. These new regulations, although motivated by patient safety imperatives,4 have elicited concerns that increased supervision may lead to decreased housestaff autonomy and an increased reliance on supervisors for clinical guidance.5 Such changes could ultimately produce less qualified practitioners by the completion of training.
Critics of the current training model point to a patient safety mechanism where housestaff must take responsibility for requesting attending‐level help when situations arise that surpass their skill level.5 For resident physicians, however, the decision to request support is often complex and dependent not only on the clinical question, but also on unique and variable trainee and supervisor factors.6 Survey data from 1999, prior to the current training regulations, showed that increased faculty presence improved resident reports of educational value, quality of patient care, and autonomy.7 A recent survey, performed after the initiation of overnight attending supervision at an academic medical center, demonstrated perceived improvements in educational value and patient‐level outcomes by both faculty and housestaff.8 Whether increased supervision and resident autonomy can coexist remains undetermined.
Overnight rotations for residents (commonly referred to as night float) are often times of little direct or indirect supervision. A recent systematic review of clinical supervision practices for housestaff in all fields found scarce literature on overnight supervision practices.9 There remains limited and conflicting data regarding the quality of patient care provided by the resident night float,10 as well as evidence revealing a low perceived educational value of night rotations when compared with non‐night float rotations.11 Yet in 2006, more than three‐quarters of all internal medicine programs employed night float rotations.12 In response to ACGME guidelines mandating decreased shift lengths with continued restrictions on overall duty hours, it appears likely even more training programs will implement night float systems.
The presence of overnight hospitalists (also known as nocturnists) is growing within the academic setting, yet their role in relation to trainees is either poorly defined13 or independent of housestaff.14 To better understand the impact of increasing levels of supervision on residency training, we investigated housestaff perceptions of education, autonomy, and clinical decision‐making before and after implementation of an in‐hospital, overnight attending physician (nocturnist).
METHODS
The study was conducted at a 570‐bed academic, tertiary care medical center affiliated with an internal medicine residency program of 170 housestaff. At our institution, all first year residents perform a week of intern night float consisting of overnight cross‐coverage of general medicine patients on the floor, step‐down, and intensive care units (ICUs). Second and third year residents each complete 4 to 6 days of resident night float each year at this hospital. They are responsible for assisting the intern night float with cross‐coverage, in addition to admitting general medicine patients to the floor, step‐down unit, and intensive care units. Every night at our medical center, 1 intern night float and 1 resident night float are on duty in the hospital; this is in addition to a resident from the on‐call medicine team and a resident working in the ICU. Prior to July 2010, no internal medicine attending physicians were physically present in the hospital at night. Oversight for the intern and resident night float was provided by the attending physician for the on‐call resident ward team, who was at home and available by pager. The night float housestaff were instructed to contact the responsible attending physician only when a major change in clinical status occurred for hospitalized or newly admitted patients, though this expectation was neither standardized nor monitored.
We established a nocturnist program at the start of the 2010 academic year. The position was staffed by hospitalists from within the Division of Hospital Medicine without the use of moonlighters. Two‐thirds of shifts were filled by 3 dedicated nocturnists with remaining staffing provided by junior hospitalist faculty. The dedicated nocturnists had recently completed their internal medicine residency at our institution. Shift length was 12 hours and dedicated nocturnists worked, on average, 10 shifts per month. The nocturnist filled a critical overnight safety role through mandatory bedside staffing of newly admitted ICU patients within 2 hours of admission, discussion in person or via telephone of newly admitted step‐down unit patients within 6 hours of admission, and direct or indirect supervision of the care of any patients undergoing a major change in clinical status. The overnight hospitalist was also available for clinical questions and to assist housestaff with triaging of overnight admissions. After nocturnist implementation, overnight housestaff received direct supervision or had immediate access to direct supervision, while prior to the nocturnist, residents had access only to indirect supervision.
In addition, the nocturnist admitted medicine patients after 1 AM in a 1:1 ratio with the admitting night float resident, performed medical consults, and provided coverage of non‐teaching medicine services. While actual volume numbers were not obtained, the estimated average of resident admissions per night was 2 to 3, and the number of nocturnist admissions was 1 to 2. The nocturnist also met nightly with night float housestaff for half‐hour didactics focusing on the management of common overnight clinical scenarios. The role of the new nocturnist was described to all housestaff in orientation materials given prior to their night float rotation and their general medicine ward rotation.
We administered pre‐rolling surveys and post‐rolling surveys of internal medicine intern and resident physicians who underwent the night float rotation at our hospital during the 2010 to 2011 academic year. Surveys examined housestaff perceptions of the night float rotation with regard to supervisory roles, educational and clinical value, and clinical decision‐making prior to and after implementation of the nocturnist. Surveys were designed by the study investigators based on prior literature,1, 510 personal experience, and housestaff suggestion, and were refined during works‐in‐progress meetings. Surveys were composed of Likert‐style questions asking housestaff to rate their level of agreement (15, strongly disagree to strongly agree) with statements regarding the supervisory and educational experience of the night float rotation, and to judge their frequency of contact (15, never to always/nightly) with an attending physician for specific clinical scenarios. The clinical scenarios described situations dealing with attendingresident communication around transfers of care, diagnostic evaluation, therapeutic interventions, and adverse events. Scenarios were taken from previous literature describing supervision preferences of faculty and residents during times of critical clinical decision‐making.15
One week prior to the beginning their night float rotation for the 20102011 academic year, housestaff were sent an e‐mail request to complete an online survey asking about their night float rotation during the prior academic year, when no nocturnist was present. One week after completion of their night float rotation for the 20102011 academic year, housestaff received an e‐mail with a link to a post‐survey asking about their recently completed, nocturnist‐supervised, night float rotation. First year residents received only a post‐survey at the completion of their night float rotation, as they would be unable to reflect on prior experience.
Informed consent was imbedded within the e‐mail survey request. Survey requests were sent by a fellow within the Division of Hospital Medicine with a brief message cosigned by an associate program director of the residency program. We did not collect unique identifiers from respondents in order to offer additional assurances to the participants that the survey was anonymous. There was no incentive offered for completion of the survey. Survey data were anonymous and downloaded to a database by a third party. Data were analyzed using Microsoft Excel, and pre‐responses and post‐responses compared using a Student t test. The study was approved by the medical center's Institutional Review Board.
RESULTS
Rates of response for pre‐surveys and post‐surveys were 57% (43 respondents) and 51% (53 respondents), respectively. Due to response rates and in order to convey accurately the perceptions of the training program as a whole, we collapsed responses of the pre‐surveys and post‐surveys based on level of training. After implementation of the overnight attending, we observed a significant increase in the perceived clinical value of the night float rotation (3.95 vs 4.27, P = 0.01) as well as in the adequacy of overnight supervision (3.65 vs 4.30, P < 0.0001; Table 1). There was no reported change in housestaff decision‐making autonomy (4.35 vs 4.45, P = 0.44). In addition, we noted a nonsignificant trend towards an increased perception of the night float rotation as a valuable educational experience (3.83 vs 4.04, P = 0.24). After implementation of the nocturnist, more resident physicians agreed that overnight supervision by an attending positively impacted patient outcomes (3.79 vs 4.30, P = 0.002).
| Statement | Pre‐Nocturnist (n = 43) Mean (SD) | Post‐Nocturnist (n = 53) Mean (SD) | P Value |
|---|---|---|---|
| |||
| Night float is a valuable educational rotation | 3.83 (0.81) | 4.04 (0.83) | 0.24 |
| Night float is a valuable clinical rotation | 3.95 (0.65) | 4.27 (0.59) | 0.01 |
| I have adequate overnight supervision | 3.65 (0.76) | 4.30 (0.72) | <0.0001 |
| I have sufficient autonomy to make clinical decisions | 4.35 (0.57) | 4.45 (0.60) | 0.44 |
| Overnight supervision by an attending positively impacts patient outcomes | 3.79 (0.88) | 4.30 (0.74) | 0.002 |
After implementation of the nocturnist, night float providers demonstrated increased rates of contacting an attending physician overnight (Table 2). There were significantly greater rates of attending contact for transfers from outside facilities (2.00 vs 3.20, P = 0.006) and during times of adverse events (2.51 vs 3.25, P = 0.04). We observed a reported increase in attending contact prior to ordering invasive diagnostic procedures (1.75 vs 2.76, P = 0.004) and noninvasive diagnostic procedures (1.09 vs 1.31, P = 0.03), as well as prior to initiation of intravenous antibiotics (1.11 vs 1.47, P = 0.007) and vasopressors (1.52 vs 2.40, P = 0.004).
| Scenario | Pre‐Nocturnist (n = 42) Mean (SD) | Post‐Nocturnist (n = 51) Mean (SD) | P Value |
|---|---|---|---|
| |||
| Receive transfer from outside facility | 2.00 (1.27) | 3.20 (1.58) | 0.006 |
| Prior to ordering noninvasive diagnostic procedure | 1.09 (0.29) | 1.31 (0.58) | 0.03 |
| Prior to ordering an invasive procedure | 1.75 (0.84) | 2.76 (1.45) | 0.004 |
| Prior to initiation of intravenous antibiotics | 1.11 (0.32) | 1.47 (0.76) | 0.007 |
| Prior to initiation of vasopressors | 1.52 (0.82) | 2.40 (1.49) | 0.004 |
| Patient experiencing adverse event, regardless of cause | 2.51 (1.31) | 3.25 (1.34) | 0.04 |
After initiating the program, the nocturnist became the most commonly contacted overnight provider by the night float housestaff (Table 3). We observed a decrease in peer to peer contact between the night float housestaff and the on‐call overnight resident after implementation of the nocturnist (2.67 vs 2.04, P = 0.006).
| Provider | Pre‐Nocturnist (n = 43) Mean (SD) | Post‐Nocturnist (n = 53) Mean (SD) | P Value |
|---|---|---|---|
| |||
| ICU Fellow | 1.86 (0.70) | 1.86 (0.83) | 0.96 |
| On‐call resident | 2.67 (0.89) | 2.04 (0.92) | 0.006 |
| ICU resident | 2.14 (0.74) | 2.04 (0.91) | 0.56 |
| On‐call medicine attending | 1.41 (0.79) | 1.26 (0.52) | 0.26 |
| Patient's PMD | 1.27 (0.31) | 1.15 (0.41) | 0.31 |
| Referring MD | 1.32 (0.60) | 1.15 (0.45) | 0.11 |
| Nocturnist | 3.59 (1.22) | ||
Attending presence led to increased agreement that there was a defined overnight attending to contact (2.97 vs 1.96, P < 0.0001) and a decreased fear of waking an attending overnight for assistance (3.26 vs 2.72, P = 0.03). Increased attending availability, however, did not change resident physician's fear of revealing knowledge gaps, their desire to make decisions independently, or their belief that contacting an attending would not change a patient's outcome (Table 4).
| Statement | Pre‐Nocturnist (n = 42) Mean (SD) | Post‐Nocturnist (n = 52) Mean (SD) | P Value |
|---|---|---|---|
| |||
| No defined attending to contact | 2.97 (1.35) | 1.96 (0.92) | <0.0001 |
| Fear of waking an attending | 3.26 (1.25) | 2.72 (1.09) | 0.03 |
| Fear of revealing knowledge gaps | 2.26 (1.14) | 2.25 (0.96) | 0.95 |
| Would rather make decision on own | 3.40 (0.93) | 3.03 (1.06) | 0.08 |
| Will not change patient outcome | 3.26 (1.06) | 3.21 (1.03) | 0.81 |
DISCUSSION
The ACGME's new duty hour regulations require that supervision for first‐year residents be provided by a qualified physician (advanced resident, fellow, or attending physician) who is physically present at the hospital. Our study demonstrates that increased direct overnight supervision provided by an in‐house nocturnist enhanced the clinical value of the night float rotation and the perceived quality of patient care. In our study, increased attending supervision did not reduce perceived decision‐making autonomy, and in fact led to increased rates of attending contact during times of critical clinical decision‐making. Such results may help assuage fears that recent regulations mandating enhanced attending supervision will produce less capable practitioners, and offers reassurance that such changes are positively impacting patient care.
Many academic institutions are implementing nocturnists, although their precise roles and responsibilities are still being defined. Our nocturnist program was explicitly designed with housestaff supervision as a core responsibility, with the goal of improving patient safety and housestaff education overnight. We found that availability barriers to attending contact were logically decreased with in‐house faculty presence. Potentially harmful attitudes, however, around requesting support (such as fear of revealing knowledge gaps or the desire to make decisions independently) remained. Furthermore, despite statistically significant increases in contact between faculty and residents at times of critical decision‐making, overall rates of attending contact for diagnostic and therapeutic interventions remained low. It is unknown from our study or previous research, however, what level of contact is appropriate or ideal for many clinical scenarios.
Additionally, we described a novel role of an academic nocturnist at a tertiary care teaching hospital and offered a potential template for the development of academic nocturnists at similar institutions seeking to increase direct overnight supervision. Such roles have not been previously well defined in the literature. Based on our experience, the nocturnist's role was manageable and well utilized by housestaff, particularly for assistance with critically ill patients and overnight triaging. We believe there are a number of factors associated with the success of this role. First, clear guidelines were presented to housestaff and nocturnists regarding expectations for supervision (for example, staffing ICU admissions within 2 hours). These guidelines likely contributed to the increased attending contact observed during critical clinical decision‐making, as well as the perceived improved patient outcomes by our housestaff. Second, the nocturnists were expected to be an integral part of the overnight care team. In many systems, the nocturnists act completely independently of the housestaff teams, creating an additional barrier to contact and communication. In our system, because of clear guidelines and their integral role in staffing overnight admissions, the nocturnists were an essential partner in care for the housestaff. Third, most of the nocturnists had recently completed their residency training at this institution. Although our survey does not directly address this, we believe their knowledge of the hospital, appreciation of the role of the intern and the resident within our system, and understanding of the need to preserve housestaff autonomy were essential to building a successful nocturnist role. Lastly, the nocturnists were not only expected to supervise and staff new admissions, but were also given a teaching expectation. We believe they were viewed by housestaff as qualified teaching attendings, similar to the daytime hospitalist. These findings may provide guidelines for other institutions seeking to balance overnight hospitalist supervision with preserving resident's ability to make autonomous decisions.
There are several limitations to our study. The findings represent the experience of internal medicine housestaff at a single academic, tertiary care medical center and may not be reflective of other institutions or specialties. We asked housestaff to recall night float experiences from the prior year, which may have introduced recall bias, though responses were obtained before participants underwent the new curriculum. Maturation of housestaff over time could have led to changes in perceived autonomy, value of the night float rotation, and rates of attending contact independent of nocturnist implementation. In addition, there may have been unaccounted changes to other elements of the residency program, hospital, or patient volume between rotations. The implementation of the nocturnist, however, was the only major change to our training program that academic year, and there were no significant changes in patient volume, structure of the teaching or non‐resident services, or other policies around resident supervision.
It is possible that the nocturnist may have contributed to reports of increased clinical value and perceived quality of patient care simply by decreasing overnight workload for housestaff, and enhanced supervision and teaching may have played a lesser role. Even if this were true, optimizing resident workload is in itself an important goal for teaching hospitals and residency programs alike in order to maximize patient safety. Inclusion of intern post‐rotation surveys may have influenced data; though, we had no reason to suspect the surveyed interns would respond in a different manner than prior resident groups. The responses of both junior and senior housestaff were pooled; while this potentially weighted the results in favor of higher responding groups, we felt that it conveyed the residents' accurate sentiments on the program. Finally, while we compared two models of overnight supervision, we reported only housestaff perceptions of education, autonomy, patient outcomes, and supervisory contact, and not direct measures of knowledge or patient care. Further research will be required to define the relationship between supervision practices and patient‐level clinical outcomes.
The new ACGME regulations around resident supervision, as well as the broader movement to improve the safety and quality of care, require residency programs to negotiate a delicate balance between providing high‐quality patient care while preserving graduated independence in clinical training. Our study demonstrates that increased overnight supervision by nocturnists with well‐defined supervisory and teaching roles can preserve housestaff autonomy, improve the clinical experience for trainees, increase access to support during times of critical decision‐making, and potentially lead to improved patient outcomes.
Acknowledgements
Disclosures: No authors received commercial support for the submitted work. Dr Arora reports being an editorial board member for Agency for Healthcare Research and Quality (AHRQ) Web M&M, receiving grants from the ACGME for previous work, and receiving payment for speaking on graduate medical education supervision.
- ,,,.Progressive independence in clinical training: a tradition worth defending?Acad Med.2005;80(10 suppl):S106–S111.
- Joint Committee of the Group on Resident Affairs and Organization of Resident Representatives.Patient Safety and Graduate Medical Education.Washington, DC:Association of American Medical Colleges; February2003:6.
- Accreditation Council on Graduate Medical Education.Common Program Requirements. Available at: http://www.acgme.org/acWebsite/home/Common_Program_Requirements_07012011.pdf. Accessed October 16,2011.
- The IOM medical errors report: 5 years later, the journey continues.Qual Lett Health Lead.2005;17(1):2–10.
- .Supervision in medical education: logical fallacies and clear choices.J Grad Med Educ.2010;2(1):141–143.
- ,,,.Preserving professional credibility: grounded theory study of medical trainees' requests for clinical support.BMJ.2009;338:b128.
- ,,,,.Increased faculty presence on inpatient teaching services.Mayo Clin Proc.2004;79(3):332–336.
- ,,,.The effect of overnight in‐house attending coverage on perceptions of care and education on a general medical service.J Grad Med Educ.2010;2(1):53–56.
- ,,, et al.A systematic review: the effect of clinical supervision on patient and residency education outcomes.Acad Med.2012;87(4):428–442.
- ,,,,.Residents' perceptions of a night float system.BMC Med Educ.2009;9:52.
- ,,,.Resident perceptions of the educational value of night float rotations.Teach Learn Med.2010;22(3):196–201.
- ,,,.How do internal medicine residency programs evaluate their resident float experiences?South Med J.2006;99(9):919–923.
- ,,.Hospitalist involvement in internal medicine residencies.J Hosp Med.2009;4(8):471–475.
- ,,, et al.Complying with ACGME resident duty hour restrictions: restructuring the 80 hour workweek to enhance education and patient safety at Texas A81(12):1026–1031.
- ,,,,.On‐call supervision and resident autonomy: from micromanager to absentee attending.Am J Med.2009;122(8):784–788.
- ,,,.Progressive independence in clinical training: a tradition worth defending?Acad Med.2005;80(10 suppl):S106–S111.
- Joint Committee of the Group on Resident Affairs and Organization of Resident Representatives.Patient Safety and Graduate Medical Education.Washington, DC:Association of American Medical Colleges; February2003:6.
- Accreditation Council on Graduate Medical Education.Common Program Requirements. Available at: http://www.acgme.org/acWebsite/home/Common_Program_Requirements_07012011.pdf. Accessed October 16,2011.
- The IOM medical errors report: 5 years later, the journey continues.Qual Lett Health Lead.2005;17(1):2–10.
- .Supervision in medical education: logical fallacies and clear choices.J Grad Med Educ.2010;2(1):141–143.
- ,,,.Preserving professional credibility: grounded theory study of medical trainees' requests for clinical support.BMJ.2009;338:b128.
- ,,,,.Increased faculty presence on inpatient teaching services.Mayo Clin Proc.2004;79(3):332–336.
- ,,,.The effect of overnight in‐house attending coverage on perceptions of care and education on a general medical service.J Grad Med Educ.2010;2(1):53–56.
- ,,, et al.A systematic review: the effect of clinical supervision on patient and residency education outcomes.Acad Med.2012;87(4):428–442.
- ,,,,.Residents' perceptions of a night float system.BMC Med Educ.2009;9:52.
- ,,,.Resident perceptions of the educational value of night float rotations.Teach Learn Med.2010;22(3):196–201.
- ,,,.How do internal medicine residency programs evaluate their resident float experiences?South Med J.2006;99(9):919–923.
- ,,.Hospitalist involvement in internal medicine residencies.J Hosp Med.2009;4(8):471–475.
- ,,, et al.Complying with ACGME resident duty hour restrictions: restructuring the 80 hour workweek to enhance education and patient safety at Texas A81(12):1026–1031.
- ,,,,.On‐call supervision and resident autonomy: from micromanager to absentee attending.Am J Med.2009;122(8):784–788.
Copyright © 2012 Society of Hospital Medicine
Innovative Monitoring Technology
Treatment of hospitalized patients is becoming more and more complex as a result of rising patient age, multiple comorbidities, and more complex procedures, yet most are hospitalized in a non‐intensive care unit (non‐ICU) setting. With this rising complexity, a large proportion of hospital patients experience serious adverse events during their hospital stay, including cardiac arrest, respiratory failure, and shock, leading to unplanned admissions to the ICU, and death.1 For patients with unexpected clinical deterioration, delayed or suboptimal intervention is associated with increased morbidity and mortality.2, 3 This has prompted many hospitals to implement some form of a rapid response system (RRS) for early detection of clinical deterioration, and adequate response through rapid response teams (RRT).2, 4, 5 Still, evidence suggests that many of these systems are deficient in the detection and/or the response phase, and do not lead to the expected outcomes in terms of preventing critical events.6, 7
Researchers have established that patients frequently demonstrate clinical signs of deterioration hours before cardiac arrests or urgent transfers to ICUs.8, 9 The importance of timely interventions in many acute clinical conditions like sepsis, acute myocardial infarction, and stroke is also well established.1012 Taking these facts together with the observed shortcomings of most current rapid response systems has led experts to call for a shift of focus from the efferent limb of the RRS (the response team) to the afferent limb (the means of detecting patients at risk and obtaining help).13 A consensus conference held in 2008 emphasized the importance of accurate monitoring of vital signs for all hospitalized patients, and at the same time recommended, if practical and affordable, that all patients be monitored continuously by monitoring technology, which improves patient comfort, is easy to use, and reduces the number of false alerts.13
Technology applications that allow for continuous vital sign monitoring designed for non‐ICU settings may help hospitals achieve meaningful results by providing earlier detection of clinical deterioration, either when implemented as part of an RRS or as a stand‐alone system. To fit this description, monitors would have to be easy to use by the staff, impose little limitation on the patient, and be capable of trend analyses so that they minimize the incidence of false alerts and alert fatigue. We set out to investigate the capability of such a system to predict patient deterioration in a medical floor setting.
METHODS
Patients and Settings
We conducted a feasibility noninterventional study in two 36‐bed medicine units of two tertiary academic medical centers: Sheba Medical Center, Tel Hashomer, and Sapir Medical Center, Kfar Sababoth in Israel. The aim of the study was to define optimal cutoff values for vital signs alerts and define the accuracy of these alerts in predicting clinical deterioration. The study was approved beforehand by the independent Institutional Review Boards of both institutions.
The Earlysense system is a contactless continuous‐measurement monitor for heart rate (HR), respiration rate (RR), and bed motion. It is based on a piezoelectric sensor, sensitive to applied mechanical strain, which is placed under the patient's mattress and functions without the need for contact between patient and device. The Earlysense system was previously shown to measure accurately both HR and RR in sleep laboratory and general ICU settings.14
We chose to evaluate patients who were at increased risk for respiratory failure, which would enable us to capture more events in this study. We thus included, in the study population, patients hospitalized with an admitting diagnosis due to an acute respiratory condition including pneumonia, chronic obstructive pulmonary disease or asthma exacerbation, congestive heart failure with pulmonary edema or congestion, and patients who needed supplemental oxygen on admission. Patients were enrolled only if within the initial 24 hours of hospitalization in the study units. Dementia and inability to sign informed consent were exclusion criteria for enrollment in this study. Patients with a do not resuscitate order were not excluded from enrollment. Patient enrollment took place during the period of January to December of 2008 in Sheba Medical Center and July to November of 2008 in Sapir Medical Center. Since the study was noninterventional, and the Earlysense monitor did not produce alerts for the duration of this study, patients were still monitored by other monitoring devices, such as telemetry and pulse oximeter, as per clinical decision.
Following enrollment and informed consent, the Earlysense sensor was placed under the mattress and connected to the Earlysense bedside monitor that recorded the signals and the interpreted vital signs. The Earlysense system automatically started measuring respiratory rate, heart rate, and motion rate with no need for patient, nurse, or technician involvement, as long as the patient remained in bed. Since this was a noninterventional study, no alerts were produced from the Earlysense monitor, and floor staff was not trained to make clinical decisions based on vital sign data from the device. Patients were monitored for the full extent of their stay in the 2 medical departments. Since we had only 2 monitors at each site, in an attempt to enroll more patients, in cases where patients stayed for more than 2 weeks, a decision was made by the principal investigator whether to continue monitoring or disconnect the sensor and enroll another patient. This was based on an assessment of clinical stability and on how much longer patients were expected to stay in the unit, in an attempt to avoid a situation where a patient was utilizing 1 monitor for a very long period of time. Following patient discharge or discontinuation of the monitor, all data were downloaded to a central server for analysis. A full description of the contactless sensor and monitor was published previously.14, 15 The signal analysis determining the HR and RR from the motion waves is proprietary.
Clinical and Alert Definitions
Patients were followed for major clinical events during their hospitalization. A major clinical event was defined as any one of the following: 1) patient was transferred to an ICU (medical or cardiac); 2) patient was intubated and mechanically ventilated on the floor; or 3) patient had a cardiac arrest while in the unit.
Respiratory rate or heart rate alerts were based on vital sign readings recorded and analyzed retrospectively for this study. The Earlysense system performs signal processing in order to isolate the respiratory and the heart pulse patterns from the signal obtained by the piezoelectric sensor. Each 0.5 seconds, an updated HR reading is established based on analysis of the heart pulse pattern for the last 8 seconds, and an updated RR reading based on analysis of the last 1 minute of the respiration pattern. These specific time periods were intended to provide up‐to‐date HR and RR values, and still reduce possible false HR and RR readings caused by signal artifacts. For defining optimal cutoffs for alerts in an internal validation process, alerts were considered true‐positive if they were followed by a major clinical event within 24 hours. An alert was considered false‐positive (false alert) if no major clinical event occurred in the following 24 hours.
As a secondary outcome, we also analyzed 24‐hour trends to look for correlations with major clinical events. For trend analysis, we grouped together HR and RR readings for 6‐hour periods throughout the day in a running window fashion (data for the last 6 hours was clustered every 3 minutes). We then compared the median of the readings for each period with the corresponding period of the previous day. Post‐hoc alerts were generated when the difference (delta) between medians passed the threshold set. Only 6‐hour time windows with at least 420 valid RR or HR results were included in the analysis.
Data Analysis
In the data analysis, we excluded patients with less than 30 hours of monitoring, allowing us to evaluate the trend analysis for at least one comparable time window. We examined increasing possible cutoff values for the differences in median values that would best predict the clinical events. To find the best possible models, we performed a receiver operating characteristic (ROC) curve analysis. We looked for the optimal cutoff to yield the maximal sum of sensitivity plus specificity, and computed associated statistics (area under the curve [AUC]) and associated confidence interval; if the lower bound of interval was found to be above 0.5, the AUC was significantly different from chance. We determined a P value that tests the null hypothesis that the AUC really equals 0.5. A value below 0.05 was considered significant.
RESULTS
Of 149 patients monitored by the Earlysense system for this study, 113 had at least 30 hours of monitoring. The characteristics of these patients are presented in Table 1. Of these 113 patients, 9 had a major clinical event (8.0%), including 2 patients who were transferred to an ICU, 1 patient who was intubated and ventilated in the study unit and later had a cardiac arrest and died, and 6 more patients who developed cardiac arrest and died in the study units (overall, 10 major clinical events). Comparing patients with a major clinical event to patients without, we found no significant difference in age, gender, body mass index, or comorbidity (Charlson score), however, patients who had a clinical event stayed significantly longer than those without a clinical event (Table 1). On average, time from admission to the major clinical event was 11.6 days (range 228).
| All Patients | Patients Without a Major Clinical Event | Patients With a Major Clinical Event | P (t Test) | |
|---|---|---|---|---|
| ||||
| Patients | 113 | 104 | 9 | |
| Gender (% female) | 45.1 | 46.2 | 33.3 | 0.46 |
| Age, average SD | 69 18 | 69 18.5 | 69 16.4 | 0.99 |
| Body mass index, average (range) | 27 (1752.7) | 27.1 (1752.7) | 25.2 (17.932) | 0.41 |
| Charlson comorbidity score | 1.58 | 1.55 | 1.99 | 0.64 |
| Length of stay (days), average SD | 7.3 5.9 | 6.9 6.0 | 11.9 7.8 | 0.02 |
| Primary diagnosis | ||||
| Pneumonia | 36 | 32 | 4 | |
| CHF | 33 | 31 | 2 | |
| COPD | 17 | 16 | 1 | |
| Other respiratory* | 27 | 25 | 2 | |
Overall, this study included a total of 8628 recording hours for the 113 patients we analyzed. Using the vital signs thresholds found to provide the highest sensitivity and specificity, we recorded 898 RR alerts (average frequency of 2.4 alerts per patient‐day) and 107 HR alerts (average frequency of 0.3 alerts per patient‐day). For the entire study, we have found 63 trend alerts (46 RR and 17 HR) when using thresholds for maximal sensitivity and specificity, at a frequency of 0.2 alerts per patient‐day.
In Table 2, we summarize the sensitivity, specificity, positive predictive value, and negative predictive value of alerts in predicting a major clinical deterioration per patient for both the threshold alerts and the trend alerts. The cutoff values are those of optimal performance (maximal sensitivity plus specificity) along the ROC curves presented in Figure 1. The optimal cutoffs for the threshold alerts were HRs below 40 or above 115 beats/min, and RRs below 8 or above 40 breaths/min. For the trend alerts, when comparing between time periods, we found that a cutoff of a rise of 20 or more beats/min and 5 or more breaths/min corresponded with a maximal sensitivity and specificity, and we used these as the thresholds for the trending alerts.
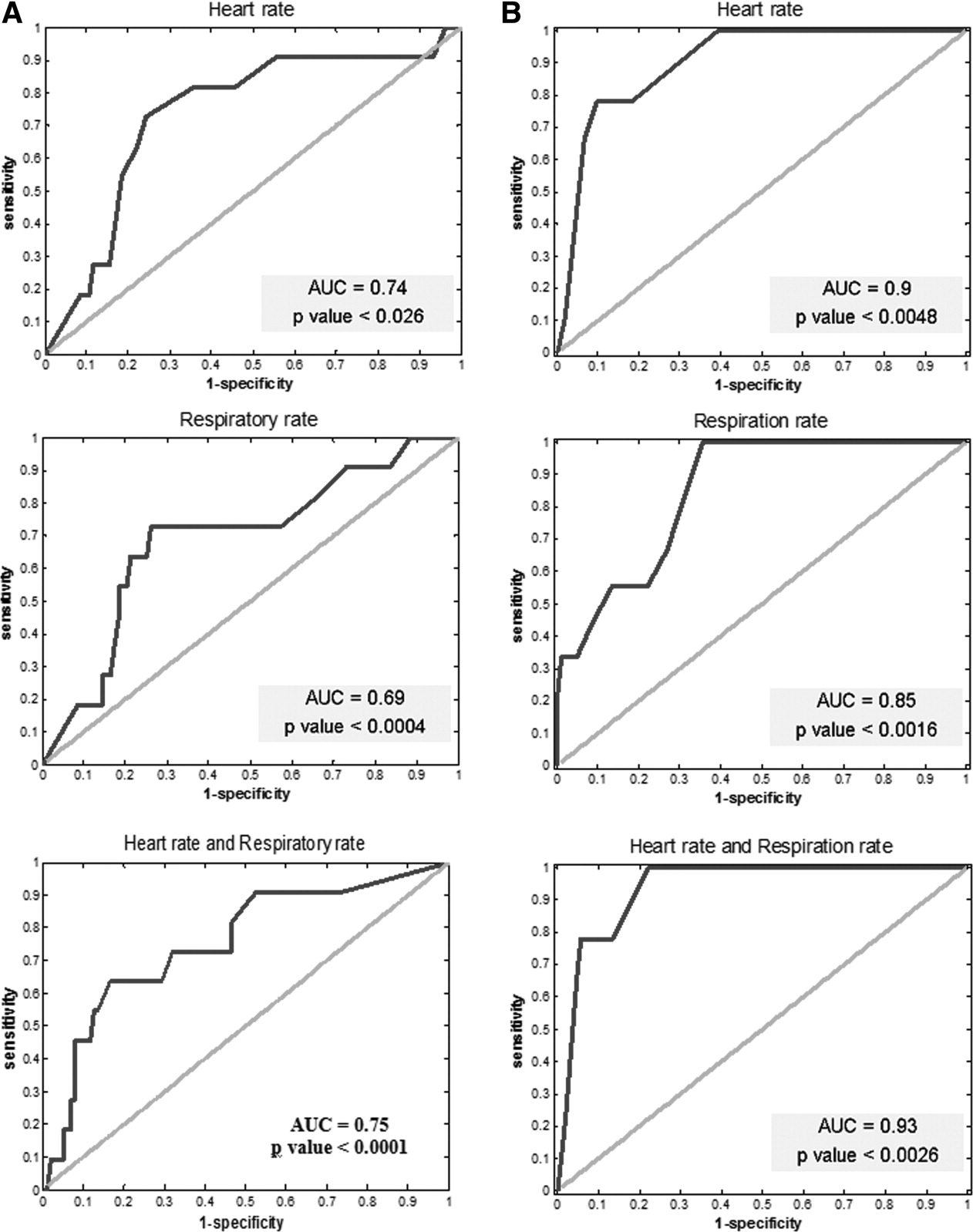
Optimal cutoffs were used when comparing time periods (20/min for HR and 5/min for RR) for maximal sum of sensitivity and specificity. Abbreviations: AUC, area under the curve.
| Sensitivity (%) | Specificity (%) | Positive Predictive Value (%) | Negative Predictive Value (%) | |
|---|---|---|---|---|
| ||||
| Threshold alerts | ||||
| HR* | 82 | 67 | 21 | 97 |
| RR | 64 | 81 | 26 | 95 |
| HR and RR | 55 | 94 | 50 | 95 |
| Trend alerts | ||||
| HR 20 | 78 | 90 | 41 | 97 |
| RR 5 | 100 | 64 | 20 | 100 |
| HR and RR | 78 | 94 | 54 | 98 |
For the determined alerts, out of the 10 clinical events, in 7 cases the alerts would have indicated the deterioration within more than 1 hour from the actual event and within 24 hours prior to the clinical event. In one case, the alert would have indicated the risk within less than 1 hour; in another case, within the 2448 hours window; and in the last case, the alerts would have done so more than 48 hours prior to the event (these last 2 cases were considered false‐negative for our post hoc analysis).
The ROC analysis for both the threshold alerts and the trend alerts for both HR and RR correlated well with the clinical events (P < 0.05 for all models) (Figure 1). When comparing the threshold alerts with the trend alerts, trend alerts had a higher AUC, suggesting that these would be more accurate in alerting for major clinical events. Specifically, the model for HR 6‐hour trend alerts demonstrated a larger AUC (0.9 and 0.85, respectively), while the combination of HR and RR had the largest AUC (0.93).
DISCUSSION
The development of monitoring systems designed for hospitalized patients on non‐ICU floors derives from the need to minimize preventable in‐hospital mortality. This study has explored one such possible solution. Through retrospective definition of optimal alert settings and internal validation within a derivation cohort, we have found the Earlysense monitor to be accurate in predicting major clinical deterioration by using both simple thresholds and a vital signs trend algorithm. We found that the post hoc determined alerts were relatively infrequent. We also found that trend alerts showed greater ability to accurately capture these deteriorations compared with simple alert thresholds, and that using a combination alert based on both HR and RR trends provided the highest accuracy and confidence for predicting clinical deterioration. These results suggest the advantages that smart alerts can bringincreasing sensitivity while lowering the alert burden and reducing the number of false alerts.
An effective and efficient patient monitoring system must be able to quickly detect acute life‐threatening events or subacute patient deterioration that will lead to a life‐threatening event; in addition, this system should have a low false‐positive rate (few false alerts). While a high sensitivity is desirable,16 this usually comes at the cost of lower specificity and higher false‐positive rates. Studies have found alerts from monitoring systems in an ICU and emergency department environment to be tremendously frequent and with an extremely high false‐positive rate.1721 Unsurprisingly, it has been reported that only about 10% of alerts are responded to by the clinical staff.22 In an attempt to improve alert relevancy and accuracy, newly designed integrated monitoring systems for ICUs use alert algorithms and trend analysis performed on data received from multiple vital signs monitors.2327 With the evident need to continuously monitor patients on hospital floors,13, 28 there is a clear gap to‐date in such experience and a need to study the implications for patients and staff as we try to optimize the monitoring tools for this environment.
As more emphasis is placed on the afferent limb of rapid response systems, we can expect to see a greater need for systems able to detect changes in clinical status that might lead to patient deterioration. The intermittent vital sign measurement performed by nurses and support staff on the floors is now regarded as inadequate by itself, because it may not be performed predictably, accurately, or completely.28 Continuous monitoring systems should complement manual intermittent vital signs monitoring and play an important role in bringing the nurse to the patient's side at the right time so that a complete assessment can be done.29, 30 There remains no substitution for a nurse evaluating the patient and making critical decisions based on his or her knowledge of the patient's condition.
While today, both electrocardiographic monitoring (telemetry) and continuous pulse oximetry provide some solution for the need for continuous monitoring on the floors, these carry disadvantages that prevent them from becoming the optimal solution. While telemetry is invaluable for higher risk cardiac patients, significant overuse of this application does occur,31 and most monitored patients gain little cardiac arrest survival benefits.32 Pulse oximetry, although regarded as one of the most important technological advancements in monitoring patients, carries important limitations that might prevent early detection of respiratory failure.33, 34 Furthermore, these 2 modalities require continuous contact of leads/sensors to the patient, a disadvantage when regarding monitoring for low/average risk patients on non‐ICU hospital floors. Related to these disadvantages, the results presented here might position the implementation of the Earlysense monitor as a preferred alternative.
This study has several important limitations. This was a retrospective noninterventional study limited to internal medicine patients. Our patients served as a derivation cohort, alert thresholds were set post hoc, and sensitivity and specificity were internally validated. It remains to be shown that the results shown here can be reproduced in a real‐time interventional study. We only included patients who were considered above average risk within medical wards, as we were hoping to capture more clinical deteriorations with a relatively small cohort. We cannot rule out that our results might be biased and may not similarly apply to all non‐ICU medical patients. Finally, the retrospective nature of this study did not allow us to assess other outcomes of appropriateness, such as staff objective assessment of alert appropriateness or change in clinical management as a result of an alert. When using these devices in the alert mode, alert thresholds may be changed by the clinical staff based on clinical judgment to further lower false alerts and alert frequency. We also did not collect information that could have allowed us to assess clinical usefulness of the alerts compared to routine clinical assessment. Documenting whether the clinical events were suspected beforehand by the clinical teams could have allowed us to assess clinical usefulness. Future interventional studies are needed to validate the Earlysense system prospectively in both medical and surgical floor settings, first using a common alert threshold alerting system and secondly using the smart trend alerts described here.
In conclusion, we found that the Earlysense monitor is able to continuously measure RR and HR, providing low alert frequency. The current study demonstrates the potential of this system to provide timely prediction of patient deterioration. Utilizing a smart trend algorithm has been shown to improve the device's accuracy and reduce associated alert burden and false‐positive alerts.
Acknowledgements
Disclosures: The study was funded by an industry grant provided by Earlysense LTD. Eyal Zimlichman, MD, MSc Ronen Rozenblum, PhD, MPH, and Jeffrey M. Rothschild, MD, MPH, have each received a research grant supported by Earlysense LTD. Martine Szyper‐Kravitz, MD, Avraham Unterman, MD, Howard Amital, MD, MHA, and Yehuda Shoenfeld, MD, report no conflicts of interest. Zvika Shinar, PhD, Tal Klap, and Shiraz Levkovich are employed by Earlysense LTD and are holding equity with the company.
- ,,,,,.Temporal trends in rates of patient harm resulting from medical care.N Engl J Med.2010;363(22):2124–2134.
- ,,, et al.Findings of the first consensus conference on medical emergency teams.Crit Care Med.2006;34(9):2463–2478.
- ,,,,.Inpatient transfers to the intensive care unit: delays are associated with increased mortality and morbidity.J Gen Intern Med.2003;18(2):77–83.
- ,,,,.Redefining in‐hospital resuscitation: the concept of the medical emergency team.Resuscitation.2001;48(2):105–110.
- Institute for Healthcare Improvement (IHI). Protecting 5 million lives from harm. Available at: www.ihi.org/ihi/programs/campaign. Accessed September 8,2011.
- ,,, et al.Introduction of the medical emergency team (MET) system: a cluster‐randomised controlled trial.Lancet.2005;365(9477):2091–2097.
- ,,,,.Rapid response teams: a systematic review and meta‐analysis.Arch Intern Med.2010;170(1):18–26.
- ,,,,,.Recognising clinical instability in hospital patients before cardiac arrest or unplanned admission to intensive care. A pilot study in a tertiary‐care hospital.Med J Aust.1999;171(1):22–25.
- ,,,,,.A comparison of antecedents to cardiac arrests, deaths and emergency intensive care admissions in Australia and New Zealand, and the United Kingdom—the ACADEMIA study.Resuscitation.2004;62(3):275–282.
- ,,, et al.Early goal‐directed therapy in the treatment of severe sepsis and septic shock.N Engl J Med.2001;345(19):1368–1377.
- .Top ten list in myocardial infarction.Chest.2000;118(5):1477–1479.
- ,,, et al.Improvement in stroke mortality in Canada and the United States, 1990 to 2002.Circulation.2006;113(10):1335–1343.
- ,,, et al.“Identifying the hospitalised patient in crisis”—a consensus conference on the afferent limb of rapid response systems.Resuscitation.2010;81(4):375–382.
- ,,,.Contactless respiratory and heart rate monitoring: validation of an innovative tool.J Med Eng Technol.2010;35(7–8):393–398.
- ,,,,,.How is my patient doing? Evaluating hospitalized patients using continuous vital signs monitoring.Isr Med Assoc J.2009;11(6):382–394.
- ,,,,,.Medical device alarms.Biomed Tech (Berl).2011;56(2):73–83.
- ,.Poor prognosis for existing monitors in the intensive care unit.Crit Care Med.1997;25(4):614–619.
- .Crying wolf: false alarms in a pediatric intensive care unit.Crit Care Med.1994;22(6):981–985.
- ,,,,,.Intensive care unit alarms—how many do we need?Crit Care Med.2010;38(2):451–456.
- ,,,,.Alarmed: adverse events in low‐risk patients with chest pain receiving continuous electrocardiographic monitoring in the emergency department. A pilot study.Am J Emerg Med.2006;24(1):62–67.
- ,,,,,.Multicentric study of monitoring alarms in the adult intensive care unit (ICU): a descriptive analysis.Intensive Care Med.1999;25(12):1360–1366.
- .Alarms in the intensive care unit: how can the number of false alarms be reduced?Crit Care.2001;5(4):184–188.
- ,,,,,.Cardiorespiratory instability before and after implementing an integrated monitoring system.Crit Care Med.2011;39(1):65–72.
- ,,.Adaptive change detection in heart rate trend monitoring in anesthetized children.IEEE Trans Biomed Eng.2006;53(11):2211–2219.
- ,,,,,.Defining the incidence of cardiorespiratory instability in patients in step‐down units using an electronic integrated monitoring system.Arch Intern Med.2008;168(12):1300–1308.
- ,,, et al.Implementation of a real‐time computerized sepsis alert in nonintensive care unit patients.Crit Care Med.2011;39(3):469–473.
- ,,,,,.Early prediction of septic shock in hospitalized patients.J Hosp Med.2010;5(1):19–25.
- ,,.Rapid‐response teams.N Engl J Med.2011;365(2):139–146.
- ,,,.An analysis of the causes of adverse events from the Quality in Australian Health Care Study.Med J Aust.1999;170(9):411–415.
- ,.Taking your rapid response team to the next level. Society of Critical Care Medicine;2010. Available at: http://www.sccm.org/Publications/Critical_Connections/Archives/December‐2010/Pages/RapidResponseTeam.aspx. Accessed August 11,year="2011"2011.
- ,.Electrocardiographic monitoring in the hospitalized patient: a diagnostic intervention of uncertain clinical impact.Am J Emerg Med.2008;26(9):1047–1055.
- ,.Continuous electrocardiographic monitoring and cardiac arrest outcomes in 8,932 telemetry ward patients.Acad Emerg Med.2000;7(6):647–652.
- ,.The benefits and pitfalls of pulse oximetry.BMJ.1993;307(6902):457–458.
- ,.Patterns of unexpected in‐hospital deaths: a root cause analysis.Patient Saf Surg.2011;5(1):3.
Treatment of hospitalized patients is becoming more and more complex as a result of rising patient age, multiple comorbidities, and more complex procedures, yet most are hospitalized in a non‐intensive care unit (non‐ICU) setting. With this rising complexity, a large proportion of hospital patients experience serious adverse events during their hospital stay, including cardiac arrest, respiratory failure, and shock, leading to unplanned admissions to the ICU, and death.1 For patients with unexpected clinical deterioration, delayed or suboptimal intervention is associated with increased morbidity and mortality.2, 3 This has prompted many hospitals to implement some form of a rapid response system (RRS) for early detection of clinical deterioration, and adequate response through rapid response teams (RRT).2, 4, 5 Still, evidence suggests that many of these systems are deficient in the detection and/or the response phase, and do not lead to the expected outcomes in terms of preventing critical events.6, 7
Researchers have established that patients frequently demonstrate clinical signs of deterioration hours before cardiac arrests or urgent transfers to ICUs.8, 9 The importance of timely interventions in many acute clinical conditions like sepsis, acute myocardial infarction, and stroke is also well established.1012 Taking these facts together with the observed shortcomings of most current rapid response systems has led experts to call for a shift of focus from the efferent limb of the RRS (the response team) to the afferent limb (the means of detecting patients at risk and obtaining help).13 A consensus conference held in 2008 emphasized the importance of accurate monitoring of vital signs for all hospitalized patients, and at the same time recommended, if practical and affordable, that all patients be monitored continuously by monitoring technology, which improves patient comfort, is easy to use, and reduces the number of false alerts.13
Technology applications that allow for continuous vital sign monitoring designed for non‐ICU settings may help hospitals achieve meaningful results by providing earlier detection of clinical deterioration, either when implemented as part of an RRS or as a stand‐alone system. To fit this description, monitors would have to be easy to use by the staff, impose little limitation on the patient, and be capable of trend analyses so that they minimize the incidence of false alerts and alert fatigue. We set out to investigate the capability of such a system to predict patient deterioration in a medical floor setting.
METHODS
Patients and Settings
We conducted a feasibility noninterventional study in two 36‐bed medicine units of two tertiary academic medical centers: Sheba Medical Center, Tel Hashomer, and Sapir Medical Center, Kfar Sababoth in Israel. The aim of the study was to define optimal cutoff values for vital signs alerts and define the accuracy of these alerts in predicting clinical deterioration. The study was approved beforehand by the independent Institutional Review Boards of both institutions.
The Earlysense system is a contactless continuous‐measurement monitor for heart rate (HR), respiration rate (RR), and bed motion. It is based on a piezoelectric sensor, sensitive to applied mechanical strain, which is placed under the patient's mattress and functions without the need for contact between patient and device. The Earlysense system was previously shown to measure accurately both HR and RR in sleep laboratory and general ICU settings.14
We chose to evaluate patients who were at increased risk for respiratory failure, which would enable us to capture more events in this study. We thus included, in the study population, patients hospitalized with an admitting diagnosis due to an acute respiratory condition including pneumonia, chronic obstructive pulmonary disease or asthma exacerbation, congestive heart failure with pulmonary edema or congestion, and patients who needed supplemental oxygen on admission. Patients were enrolled only if within the initial 24 hours of hospitalization in the study units. Dementia and inability to sign informed consent were exclusion criteria for enrollment in this study. Patients with a do not resuscitate order were not excluded from enrollment. Patient enrollment took place during the period of January to December of 2008 in Sheba Medical Center and July to November of 2008 in Sapir Medical Center. Since the study was noninterventional, and the Earlysense monitor did not produce alerts for the duration of this study, patients were still monitored by other monitoring devices, such as telemetry and pulse oximeter, as per clinical decision.
Following enrollment and informed consent, the Earlysense sensor was placed under the mattress and connected to the Earlysense bedside monitor that recorded the signals and the interpreted vital signs. The Earlysense system automatically started measuring respiratory rate, heart rate, and motion rate with no need for patient, nurse, or technician involvement, as long as the patient remained in bed. Since this was a noninterventional study, no alerts were produced from the Earlysense monitor, and floor staff was not trained to make clinical decisions based on vital sign data from the device. Patients were monitored for the full extent of their stay in the 2 medical departments. Since we had only 2 monitors at each site, in an attempt to enroll more patients, in cases where patients stayed for more than 2 weeks, a decision was made by the principal investigator whether to continue monitoring or disconnect the sensor and enroll another patient. This was based on an assessment of clinical stability and on how much longer patients were expected to stay in the unit, in an attempt to avoid a situation where a patient was utilizing 1 monitor for a very long period of time. Following patient discharge or discontinuation of the monitor, all data were downloaded to a central server for analysis. A full description of the contactless sensor and monitor was published previously.14, 15 The signal analysis determining the HR and RR from the motion waves is proprietary.
Clinical and Alert Definitions
Patients were followed for major clinical events during their hospitalization. A major clinical event was defined as any one of the following: 1) patient was transferred to an ICU (medical or cardiac); 2) patient was intubated and mechanically ventilated on the floor; or 3) patient had a cardiac arrest while in the unit.
Respiratory rate or heart rate alerts were based on vital sign readings recorded and analyzed retrospectively for this study. The Earlysense system performs signal processing in order to isolate the respiratory and the heart pulse patterns from the signal obtained by the piezoelectric sensor. Each 0.5 seconds, an updated HR reading is established based on analysis of the heart pulse pattern for the last 8 seconds, and an updated RR reading based on analysis of the last 1 minute of the respiration pattern. These specific time periods were intended to provide up‐to‐date HR and RR values, and still reduce possible false HR and RR readings caused by signal artifacts. For defining optimal cutoffs for alerts in an internal validation process, alerts were considered true‐positive if they were followed by a major clinical event within 24 hours. An alert was considered false‐positive (false alert) if no major clinical event occurred in the following 24 hours.
As a secondary outcome, we also analyzed 24‐hour trends to look for correlations with major clinical events. For trend analysis, we grouped together HR and RR readings for 6‐hour periods throughout the day in a running window fashion (data for the last 6 hours was clustered every 3 minutes). We then compared the median of the readings for each period with the corresponding period of the previous day. Post‐hoc alerts were generated when the difference (delta) between medians passed the threshold set. Only 6‐hour time windows with at least 420 valid RR or HR results were included in the analysis.
Data Analysis
In the data analysis, we excluded patients with less than 30 hours of monitoring, allowing us to evaluate the trend analysis for at least one comparable time window. We examined increasing possible cutoff values for the differences in median values that would best predict the clinical events. To find the best possible models, we performed a receiver operating characteristic (ROC) curve analysis. We looked for the optimal cutoff to yield the maximal sum of sensitivity plus specificity, and computed associated statistics (area under the curve [AUC]) and associated confidence interval; if the lower bound of interval was found to be above 0.5, the AUC was significantly different from chance. We determined a P value that tests the null hypothesis that the AUC really equals 0.5. A value below 0.05 was considered significant.
RESULTS
Of 149 patients monitored by the Earlysense system for this study, 113 had at least 30 hours of monitoring. The characteristics of these patients are presented in Table 1. Of these 113 patients, 9 had a major clinical event (8.0%), including 2 patients who were transferred to an ICU, 1 patient who was intubated and ventilated in the study unit and later had a cardiac arrest and died, and 6 more patients who developed cardiac arrest and died in the study units (overall, 10 major clinical events). Comparing patients with a major clinical event to patients without, we found no significant difference in age, gender, body mass index, or comorbidity (Charlson score), however, patients who had a clinical event stayed significantly longer than those without a clinical event (Table 1). On average, time from admission to the major clinical event was 11.6 days (range 228).
| All Patients | Patients Without a Major Clinical Event | Patients With a Major Clinical Event | P (t Test) | |
|---|---|---|---|---|
| ||||
| Patients | 113 | 104 | 9 | |
| Gender (% female) | 45.1 | 46.2 | 33.3 | 0.46 |
| Age, average SD | 69 18 | 69 18.5 | 69 16.4 | 0.99 |
| Body mass index, average (range) | 27 (1752.7) | 27.1 (1752.7) | 25.2 (17.932) | 0.41 |
| Charlson comorbidity score | 1.58 | 1.55 | 1.99 | 0.64 |
| Length of stay (days), average SD | 7.3 5.9 | 6.9 6.0 | 11.9 7.8 | 0.02 |
| Primary diagnosis | ||||
| Pneumonia | 36 | 32 | 4 | |
| CHF | 33 | 31 | 2 | |
| COPD | 17 | 16 | 1 | |
| Other respiratory* | 27 | 25 | 2 | |
Overall, this study included a total of 8628 recording hours for the 113 patients we analyzed. Using the vital signs thresholds found to provide the highest sensitivity and specificity, we recorded 898 RR alerts (average frequency of 2.4 alerts per patient‐day) and 107 HR alerts (average frequency of 0.3 alerts per patient‐day). For the entire study, we have found 63 trend alerts (46 RR and 17 HR) when using thresholds for maximal sensitivity and specificity, at a frequency of 0.2 alerts per patient‐day.
In Table 2, we summarize the sensitivity, specificity, positive predictive value, and negative predictive value of alerts in predicting a major clinical deterioration per patient for both the threshold alerts and the trend alerts. The cutoff values are those of optimal performance (maximal sensitivity plus specificity) along the ROC curves presented in Figure 1. The optimal cutoffs for the threshold alerts were HRs below 40 or above 115 beats/min, and RRs below 8 or above 40 breaths/min. For the trend alerts, when comparing between time periods, we found that a cutoff of a rise of 20 or more beats/min and 5 or more breaths/min corresponded with a maximal sensitivity and specificity, and we used these as the thresholds for the trending alerts.
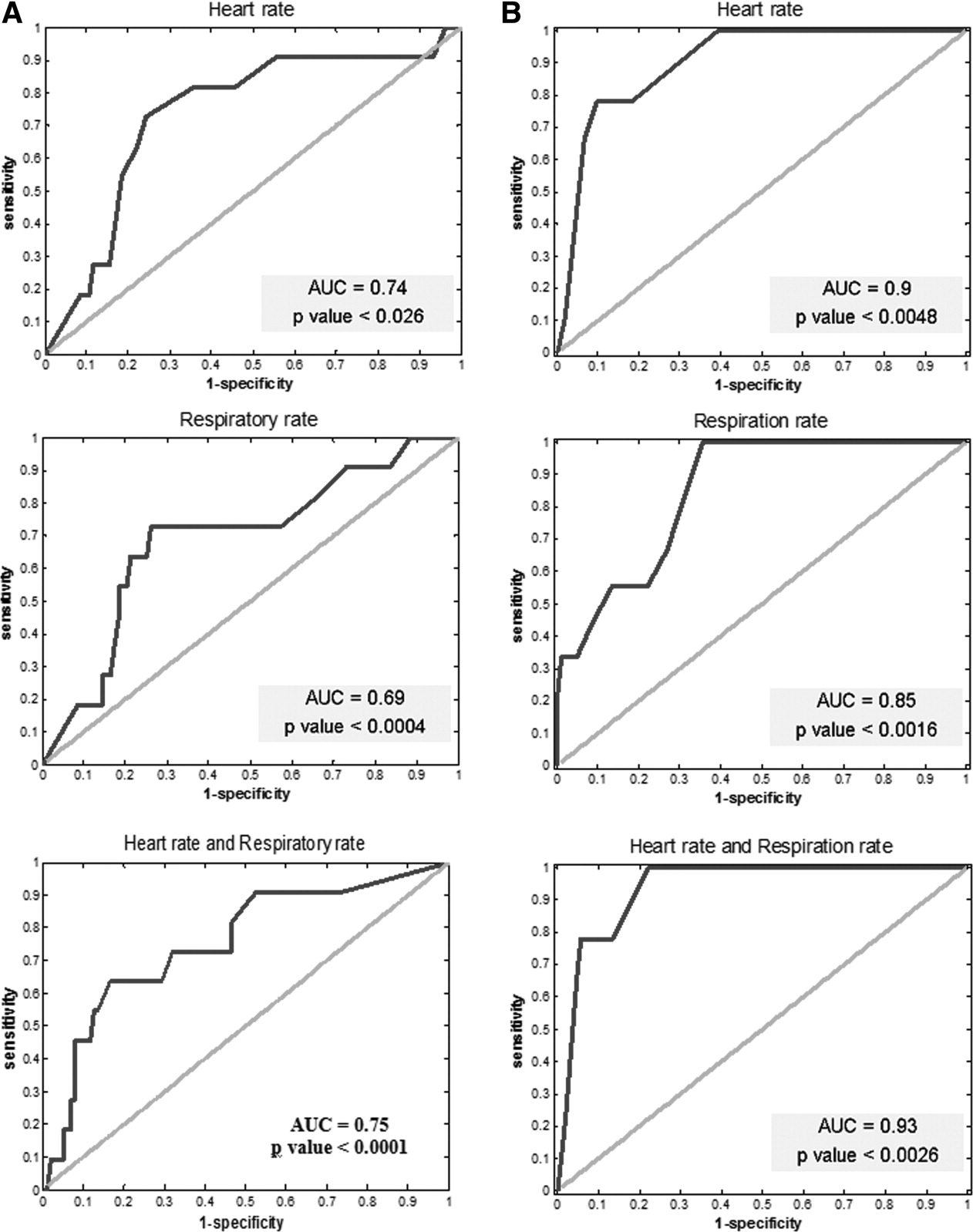
Optimal cutoffs were used when comparing time periods (20/min for HR and 5/min for RR) for maximal sum of sensitivity and specificity. Abbreviations: AUC, area under the curve.
| Sensitivity (%) | Specificity (%) | Positive Predictive Value (%) | Negative Predictive Value (%) | |
|---|---|---|---|---|
| ||||
| Threshold alerts | ||||
| HR* | 82 | 67 | 21 | 97 |
| RR | 64 | 81 | 26 | 95 |
| HR and RR | 55 | 94 | 50 | 95 |
| Trend alerts | ||||
| HR 20 | 78 | 90 | 41 | 97 |
| RR 5 | 100 | 64 | 20 | 100 |
| HR and RR | 78 | 94 | 54 | 98 |
For the determined alerts, out of the 10 clinical events, in 7 cases the alerts would have indicated the deterioration within more than 1 hour from the actual event and within 24 hours prior to the clinical event. In one case, the alert would have indicated the risk within less than 1 hour; in another case, within the 2448 hours window; and in the last case, the alerts would have done so more than 48 hours prior to the event (these last 2 cases were considered false‐negative for our post hoc analysis).
The ROC analysis for both the threshold alerts and the trend alerts for both HR and RR correlated well with the clinical events (P < 0.05 for all models) (Figure 1). When comparing the threshold alerts with the trend alerts, trend alerts had a higher AUC, suggesting that these would be more accurate in alerting for major clinical events. Specifically, the model for HR 6‐hour trend alerts demonstrated a larger AUC (0.9 and 0.85, respectively), while the combination of HR and RR had the largest AUC (0.93).
DISCUSSION
The development of monitoring systems designed for hospitalized patients on non‐ICU floors derives from the need to minimize preventable in‐hospital mortality. This study has explored one such possible solution. Through retrospective definition of optimal alert settings and internal validation within a derivation cohort, we have found the Earlysense monitor to be accurate in predicting major clinical deterioration by using both simple thresholds and a vital signs trend algorithm. We found that the post hoc determined alerts were relatively infrequent. We also found that trend alerts showed greater ability to accurately capture these deteriorations compared with simple alert thresholds, and that using a combination alert based on both HR and RR trends provided the highest accuracy and confidence for predicting clinical deterioration. These results suggest the advantages that smart alerts can bringincreasing sensitivity while lowering the alert burden and reducing the number of false alerts.
An effective and efficient patient monitoring system must be able to quickly detect acute life‐threatening events or subacute patient deterioration that will lead to a life‐threatening event; in addition, this system should have a low false‐positive rate (few false alerts). While a high sensitivity is desirable,16 this usually comes at the cost of lower specificity and higher false‐positive rates. Studies have found alerts from monitoring systems in an ICU and emergency department environment to be tremendously frequent and with an extremely high false‐positive rate.1721 Unsurprisingly, it has been reported that only about 10% of alerts are responded to by the clinical staff.22 In an attempt to improve alert relevancy and accuracy, newly designed integrated monitoring systems for ICUs use alert algorithms and trend analysis performed on data received from multiple vital signs monitors.2327 With the evident need to continuously monitor patients on hospital floors,13, 28 there is a clear gap to‐date in such experience and a need to study the implications for patients and staff as we try to optimize the monitoring tools for this environment.
As more emphasis is placed on the afferent limb of rapid response systems, we can expect to see a greater need for systems able to detect changes in clinical status that might lead to patient deterioration. The intermittent vital sign measurement performed by nurses and support staff on the floors is now regarded as inadequate by itself, because it may not be performed predictably, accurately, or completely.28 Continuous monitoring systems should complement manual intermittent vital signs monitoring and play an important role in bringing the nurse to the patient's side at the right time so that a complete assessment can be done.29, 30 There remains no substitution for a nurse evaluating the patient and making critical decisions based on his or her knowledge of the patient's condition.
While today, both electrocardiographic monitoring (telemetry) and continuous pulse oximetry provide some solution for the need for continuous monitoring on the floors, these carry disadvantages that prevent them from becoming the optimal solution. While telemetry is invaluable for higher risk cardiac patients, significant overuse of this application does occur,31 and most monitored patients gain little cardiac arrest survival benefits.32 Pulse oximetry, although regarded as one of the most important technological advancements in monitoring patients, carries important limitations that might prevent early detection of respiratory failure.33, 34 Furthermore, these 2 modalities require continuous contact of leads/sensors to the patient, a disadvantage when regarding monitoring for low/average risk patients on non‐ICU hospital floors. Related to these disadvantages, the results presented here might position the implementation of the Earlysense monitor as a preferred alternative.
This study has several important limitations. This was a retrospective noninterventional study limited to internal medicine patients. Our patients served as a derivation cohort, alert thresholds were set post hoc, and sensitivity and specificity were internally validated. It remains to be shown that the results shown here can be reproduced in a real‐time interventional study. We only included patients who were considered above average risk within medical wards, as we were hoping to capture more clinical deteriorations with a relatively small cohort. We cannot rule out that our results might be biased and may not similarly apply to all non‐ICU medical patients. Finally, the retrospective nature of this study did not allow us to assess other outcomes of appropriateness, such as staff objective assessment of alert appropriateness or change in clinical management as a result of an alert. When using these devices in the alert mode, alert thresholds may be changed by the clinical staff based on clinical judgment to further lower false alerts and alert frequency. We also did not collect information that could have allowed us to assess clinical usefulness of the alerts compared to routine clinical assessment. Documenting whether the clinical events were suspected beforehand by the clinical teams could have allowed us to assess clinical usefulness. Future interventional studies are needed to validate the Earlysense system prospectively in both medical and surgical floor settings, first using a common alert threshold alerting system and secondly using the smart trend alerts described here.
In conclusion, we found that the Earlysense monitor is able to continuously measure RR and HR, providing low alert frequency. The current study demonstrates the potential of this system to provide timely prediction of patient deterioration. Utilizing a smart trend algorithm has been shown to improve the device's accuracy and reduce associated alert burden and false‐positive alerts.
Acknowledgements
Disclosures: The study was funded by an industry grant provided by Earlysense LTD. Eyal Zimlichman, MD, MSc Ronen Rozenblum, PhD, MPH, and Jeffrey M. Rothschild, MD, MPH, have each received a research grant supported by Earlysense LTD. Martine Szyper‐Kravitz, MD, Avraham Unterman, MD, Howard Amital, MD, MHA, and Yehuda Shoenfeld, MD, report no conflicts of interest. Zvika Shinar, PhD, Tal Klap, and Shiraz Levkovich are employed by Earlysense LTD and are holding equity with the company.
Treatment of hospitalized patients is becoming more and more complex as a result of rising patient age, multiple comorbidities, and more complex procedures, yet most are hospitalized in a non‐intensive care unit (non‐ICU) setting. With this rising complexity, a large proportion of hospital patients experience serious adverse events during their hospital stay, including cardiac arrest, respiratory failure, and shock, leading to unplanned admissions to the ICU, and death.1 For patients with unexpected clinical deterioration, delayed or suboptimal intervention is associated with increased morbidity and mortality.2, 3 This has prompted many hospitals to implement some form of a rapid response system (RRS) for early detection of clinical deterioration, and adequate response through rapid response teams (RRT).2, 4, 5 Still, evidence suggests that many of these systems are deficient in the detection and/or the response phase, and do not lead to the expected outcomes in terms of preventing critical events.6, 7
Researchers have established that patients frequently demonstrate clinical signs of deterioration hours before cardiac arrests or urgent transfers to ICUs.8, 9 The importance of timely interventions in many acute clinical conditions like sepsis, acute myocardial infarction, and stroke is also well established.1012 Taking these facts together with the observed shortcomings of most current rapid response systems has led experts to call for a shift of focus from the efferent limb of the RRS (the response team) to the afferent limb (the means of detecting patients at risk and obtaining help).13 A consensus conference held in 2008 emphasized the importance of accurate monitoring of vital signs for all hospitalized patients, and at the same time recommended, if practical and affordable, that all patients be monitored continuously by monitoring technology, which improves patient comfort, is easy to use, and reduces the number of false alerts.13
Technology applications that allow for continuous vital sign monitoring designed for non‐ICU settings may help hospitals achieve meaningful results by providing earlier detection of clinical deterioration, either when implemented as part of an RRS or as a stand‐alone system. To fit this description, monitors would have to be easy to use by the staff, impose little limitation on the patient, and be capable of trend analyses so that they minimize the incidence of false alerts and alert fatigue. We set out to investigate the capability of such a system to predict patient deterioration in a medical floor setting.
METHODS
Patients and Settings
We conducted a feasibility noninterventional study in two 36‐bed medicine units of two tertiary academic medical centers: Sheba Medical Center, Tel Hashomer, and Sapir Medical Center, Kfar Sababoth in Israel. The aim of the study was to define optimal cutoff values for vital signs alerts and define the accuracy of these alerts in predicting clinical deterioration. The study was approved beforehand by the independent Institutional Review Boards of both institutions.
The Earlysense system is a contactless continuous‐measurement monitor for heart rate (HR), respiration rate (RR), and bed motion. It is based on a piezoelectric sensor, sensitive to applied mechanical strain, which is placed under the patient's mattress and functions without the need for contact between patient and device. The Earlysense system was previously shown to measure accurately both HR and RR in sleep laboratory and general ICU settings.14
We chose to evaluate patients who were at increased risk for respiratory failure, which would enable us to capture more events in this study. We thus included, in the study population, patients hospitalized with an admitting diagnosis due to an acute respiratory condition including pneumonia, chronic obstructive pulmonary disease or asthma exacerbation, congestive heart failure with pulmonary edema or congestion, and patients who needed supplemental oxygen on admission. Patients were enrolled only if within the initial 24 hours of hospitalization in the study units. Dementia and inability to sign informed consent were exclusion criteria for enrollment in this study. Patients with a do not resuscitate order were not excluded from enrollment. Patient enrollment took place during the period of January to December of 2008 in Sheba Medical Center and July to November of 2008 in Sapir Medical Center. Since the study was noninterventional, and the Earlysense monitor did not produce alerts for the duration of this study, patients were still monitored by other monitoring devices, such as telemetry and pulse oximeter, as per clinical decision.
Following enrollment and informed consent, the Earlysense sensor was placed under the mattress and connected to the Earlysense bedside monitor that recorded the signals and the interpreted vital signs. The Earlysense system automatically started measuring respiratory rate, heart rate, and motion rate with no need for patient, nurse, or technician involvement, as long as the patient remained in bed. Since this was a noninterventional study, no alerts were produced from the Earlysense monitor, and floor staff was not trained to make clinical decisions based on vital sign data from the device. Patients were monitored for the full extent of their stay in the 2 medical departments. Since we had only 2 monitors at each site, in an attempt to enroll more patients, in cases where patients stayed for more than 2 weeks, a decision was made by the principal investigator whether to continue monitoring or disconnect the sensor and enroll another patient. This was based on an assessment of clinical stability and on how much longer patients were expected to stay in the unit, in an attempt to avoid a situation where a patient was utilizing 1 monitor for a very long period of time. Following patient discharge or discontinuation of the monitor, all data were downloaded to a central server for analysis. A full description of the contactless sensor and monitor was published previously.14, 15 The signal analysis determining the HR and RR from the motion waves is proprietary.
Clinical and Alert Definitions
Patients were followed for major clinical events during their hospitalization. A major clinical event was defined as any one of the following: 1) patient was transferred to an ICU (medical or cardiac); 2) patient was intubated and mechanically ventilated on the floor; or 3) patient had a cardiac arrest while in the unit.
Respiratory rate or heart rate alerts were based on vital sign readings recorded and analyzed retrospectively for this study. The Earlysense system performs signal processing in order to isolate the respiratory and the heart pulse patterns from the signal obtained by the piezoelectric sensor. Each 0.5 seconds, an updated HR reading is established based on analysis of the heart pulse pattern for the last 8 seconds, and an updated RR reading based on analysis of the last 1 minute of the respiration pattern. These specific time periods were intended to provide up‐to‐date HR and RR values, and still reduce possible false HR and RR readings caused by signal artifacts. For defining optimal cutoffs for alerts in an internal validation process, alerts were considered true‐positive if they were followed by a major clinical event within 24 hours. An alert was considered false‐positive (false alert) if no major clinical event occurred in the following 24 hours.
As a secondary outcome, we also analyzed 24‐hour trends to look for correlations with major clinical events. For trend analysis, we grouped together HR and RR readings for 6‐hour periods throughout the day in a running window fashion (data for the last 6 hours was clustered every 3 minutes). We then compared the median of the readings for each period with the corresponding period of the previous day. Post‐hoc alerts were generated when the difference (delta) between medians passed the threshold set. Only 6‐hour time windows with at least 420 valid RR or HR results were included in the analysis.
Data Analysis
In the data analysis, we excluded patients with less than 30 hours of monitoring, allowing us to evaluate the trend analysis for at least one comparable time window. We examined increasing possible cutoff values for the differences in median values that would best predict the clinical events. To find the best possible models, we performed a receiver operating characteristic (ROC) curve analysis. We looked for the optimal cutoff to yield the maximal sum of sensitivity plus specificity, and computed associated statistics (area under the curve [AUC]) and associated confidence interval; if the lower bound of interval was found to be above 0.5, the AUC was significantly different from chance. We determined a P value that tests the null hypothesis that the AUC really equals 0.5. A value below 0.05 was considered significant.
RESULTS
Of 149 patients monitored by the Earlysense system for this study, 113 had at least 30 hours of monitoring. The characteristics of these patients are presented in Table 1. Of these 113 patients, 9 had a major clinical event (8.0%), including 2 patients who were transferred to an ICU, 1 patient who was intubated and ventilated in the study unit and later had a cardiac arrest and died, and 6 more patients who developed cardiac arrest and died in the study units (overall, 10 major clinical events). Comparing patients with a major clinical event to patients without, we found no significant difference in age, gender, body mass index, or comorbidity (Charlson score), however, patients who had a clinical event stayed significantly longer than those without a clinical event (Table 1). On average, time from admission to the major clinical event was 11.6 days (range 228).
| All Patients | Patients Without a Major Clinical Event | Patients With a Major Clinical Event | P (t Test) | |
|---|---|---|---|---|
| ||||
| Patients | 113 | 104 | 9 | |
| Gender (% female) | 45.1 | 46.2 | 33.3 | 0.46 |
| Age, average SD | 69 18 | 69 18.5 | 69 16.4 | 0.99 |
| Body mass index, average (range) | 27 (1752.7) | 27.1 (1752.7) | 25.2 (17.932) | 0.41 |
| Charlson comorbidity score | 1.58 | 1.55 | 1.99 | 0.64 |
| Length of stay (days), average SD | 7.3 5.9 | 6.9 6.0 | 11.9 7.8 | 0.02 |
| Primary diagnosis | ||||
| Pneumonia | 36 | 32 | 4 | |
| CHF | 33 | 31 | 2 | |
| COPD | 17 | 16 | 1 | |
| Other respiratory* | 27 | 25 | 2 | |
Overall, this study included a total of 8628 recording hours for the 113 patients we analyzed. Using the vital signs thresholds found to provide the highest sensitivity and specificity, we recorded 898 RR alerts (average frequency of 2.4 alerts per patient‐day) and 107 HR alerts (average frequency of 0.3 alerts per patient‐day). For the entire study, we have found 63 trend alerts (46 RR and 17 HR) when using thresholds for maximal sensitivity and specificity, at a frequency of 0.2 alerts per patient‐day.
In Table 2, we summarize the sensitivity, specificity, positive predictive value, and negative predictive value of alerts in predicting a major clinical deterioration per patient for both the threshold alerts and the trend alerts. The cutoff values are those of optimal performance (maximal sensitivity plus specificity) along the ROC curves presented in Figure 1. The optimal cutoffs for the threshold alerts were HRs below 40 or above 115 beats/min, and RRs below 8 or above 40 breaths/min. For the trend alerts, when comparing between time periods, we found that a cutoff of a rise of 20 or more beats/min and 5 or more breaths/min corresponded with a maximal sensitivity and specificity, and we used these as the thresholds for the trending alerts.
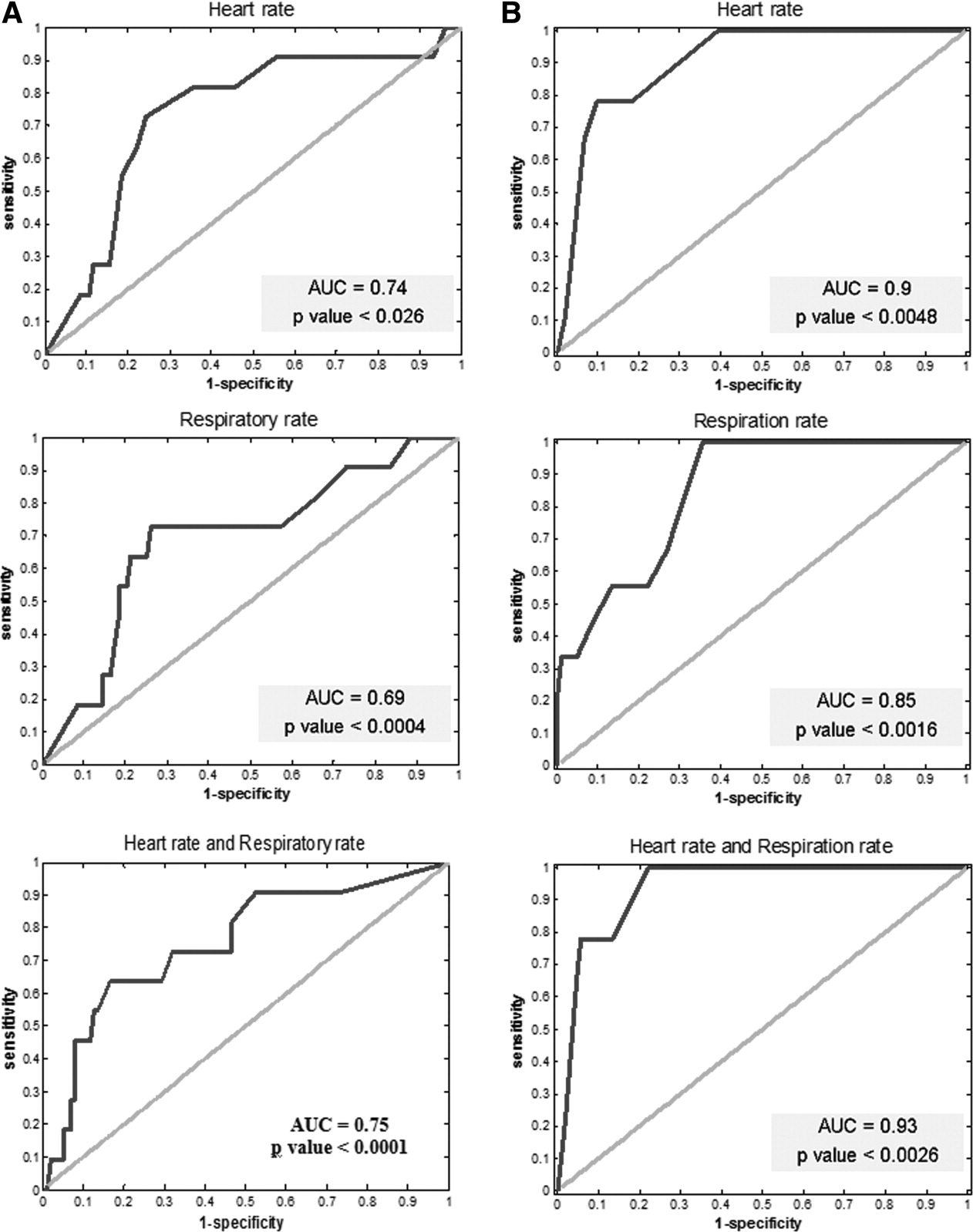
Optimal cutoffs were used when comparing time periods (20/min for HR and 5/min for RR) for maximal sum of sensitivity and specificity. Abbreviations: AUC, area under the curve.
| Sensitivity (%) | Specificity (%) | Positive Predictive Value (%) | Negative Predictive Value (%) | |
|---|---|---|---|---|
| ||||
| Threshold alerts | ||||
| HR* | 82 | 67 | 21 | 97 |
| RR | 64 | 81 | 26 | 95 |
| HR and RR | 55 | 94 | 50 | 95 |
| Trend alerts | ||||
| HR 20 | 78 | 90 | 41 | 97 |
| RR 5 | 100 | 64 | 20 | 100 |
| HR and RR | 78 | 94 | 54 | 98 |
For the determined alerts, out of the 10 clinical events, in 7 cases the alerts would have indicated the deterioration within more than 1 hour from the actual event and within 24 hours prior to the clinical event. In one case, the alert would have indicated the risk within less than 1 hour; in another case, within the 2448 hours window; and in the last case, the alerts would have done so more than 48 hours prior to the event (these last 2 cases were considered false‐negative for our post hoc analysis).
The ROC analysis for both the threshold alerts and the trend alerts for both HR and RR correlated well with the clinical events (P < 0.05 for all models) (Figure 1). When comparing the threshold alerts with the trend alerts, trend alerts had a higher AUC, suggesting that these would be more accurate in alerting for major clinical events. Specifically, the model for HR 6‐hour trend alerts demonstrated a larger AUC (0.9 and 0.85, respectively), while the combination of HR and RR had the largest AUC (0.93).
DISCUSSION
The development of monitoring systems designed for hospitalized patients on non‐ICU floors derives from the need to minimize preventable in‐hospital mortality. This study has explored one such possible solution. Through retrospective definition of optimal alert settings and internal validation within a derivation cohort, we have found the Earlysense monitor to be accurate in predicting major clinical deterioration by using both simple thresholds and a vital signs trend algorithm. We found that the post hoc determined alerts were relatively infrequent. We also found that trend alerts showed greater ability to accurately capture these deteriorations compared with simple alert thresholds, and that using a combination alert based on both HR and RR trends provided the highest accuracy and confidence for predicting clinical deterioration. These results suggest the advantages that smart alerts can bringincreasing sensitivity while lowering the alert burden and reducing the number of false alerts.
An effective and efficient patient monitoring system must be able to quickly detect acute life‐threatening events or subacute patient deterioration that will lead to a life‐threatening event; in addition, this system should have a low false‐positive rate (few false alerts). While a high sensitivity is desirable,16 this usually comes at the cost of lower specificity and higher false‐positive rates. Studies have found alerts from monitoring systems in an ICU and emergency department environment to be tremendously frequent and with an extremely high false‐positive rate.1721 Unsurprisingly, it has been reported that only about 10% of alerts are responded to by the clinical staff.22 In an attempt to improve alert relevancy and accuracy, newly designed integrated monitoring systems for ICUs use alert algorithms and trend analysis performed on data received from multiple vital signs monitors.2327 With the evident need to continuously monitor patients on hospital floors,13, 28 there is a clear gap to‐date in such experience and a need to study the implications for patients and staff as we try to optimize the monitoring tools for this environment.
As more emphasis is placed on the afferent limb of rapid response systems, we can expect to see a greater need for systems able to detect changes in clinical status that might lead to patient deterioration. The intermittent vital sign measurement performed by nurses and support staff on the floors is now regarded as inadequate by itself, because it may not be performed predictably, accurately, or completely.28 Continuous monitoring systems should complement manual intermittent vital signs monitoring and play an important role in bringing the nurse to the patient's side at the right time so that a complete assessment can be done.29, 30 There remains no substitution for a nurse evaluating the patient and making critical decisions based on his or her knowledge of the patient's condition.
While today, both electrocardiographic monitoring (telemetry) and continuous pulse oximetry provide some solution for the need for continuous monitoring on the floors, these carry disadvantages that prevent them from becoming the optimal solution. While telemetry is invaluable for higher risk cardiac patients, significant overuse of this application does occur,31 and most monitored patients gain little cardiac arrest survival benefits.32 Pulse oximetry, although regarded as one of the most important technological advancements in monitoring patients, carries important limitations that might prevent early detection of respiratory failure.33, 34 Furthermore, these 2 modalities require continuous contact of leads/sensors to the patient, a disadvantage when regarding monitoring for low/average risk patients on non‐ICU hospital floors. Related to these disadvantages, the results presented here might position the implementation of the Earlysense monitor as a preferred alternative.
This study has several important limitations. This was a retrospective noninterventional study limited to internal medicine patients. Our patients served as a derivation cohort, alert thresholds were set post hoc, and sensitivity and specificity were internally validated. It remains to be shown that the results shown here can be reproduced in a real‐time interventional study. We only included patients who were considered above average risk within medical wards, as we were hoping to capture more clinical deteriorations with a relatively small cohort. We cannot rule out that our results might be biased and may not similarly apply to all non‐ICU medical patients. Finally, the retrospective nature of this study did not allow us to assess other outcomes of appropriateness, such as staff objective assessment of alert appropriateness or change in clinical management as a result of an alert. When using these devices in the alert mode, alert thresholds may be changed by the clinical staff based on clinical judgment to further lower false alerts and alert frequency. We also did not collect information that could have allowed us to assess clinical usefulness of the alerts compared to routine clinical assessment. Documenting whether the clinical events were suspected beforehand by the clinical teams could have allowed us to assess clinical usefulness. Future interventional studies are needed to validate the Earlysense system prospectively in both medical and surgical floor settings, first using a common alert threshold alerting system and secondly using the smart trend alerts described here.
In conclusion, we found that the Earlysense monitor is able to continuously measure RR and HR, providing low alert frequency. The current study demonstrates the potential of this system to provide timely prediction of patient deterioration. Utilizing a smart trend algorithm has been shown to improve the device's accuracy and reduce associated alert burden and false‐positive alerts.
Acknowledgements
Disclosures: The study was funded by an industry grant provided by Earlysense LTD. Eyal Zimlichman, MD, MSc Ronen Rozenblum, PhD, MPH, and Jeffrey M. Rothschild, MD, MPH, have each received a research grant supported by Earlysense LTD. Martine Szyper‐Kravitz, MD, Avraham Unterman, MD, Howard Amital, MD, MHA, and Yehuda Shoenfeld, MD, report no conflicts of interest. Zvika Shinar, PhD, Tal Klap, and Shiraz Levkovich are employed by Earlysense LTD and are holding equity with the company.
- ,,,,,.Temporal trends in rates of patient harm resulting from medical care.N Engl J Med.2010;363(22):2124–2134.
- ,,, et al.Findings of the first consensus conference on medical emergency teams.Crit Care Med.2006;34(9):2463–2478.
- ,,,,.Inpatient transfers to the intensive care unit: delays are associated with increased mortality and morbidity.J Gen Intern Med.2003;18(2):77–83.
- ,,,,.Redefining in‐hospital resuscitation: the concept of the medical emergency team.Resuscitation.2001;48(2):105–110.
- Institute for Healthcare Improvement (IHI). Protecting 5 million lives from harm. Available at: www.ihi.org/ihi/programs/campaign. Accessed September 8,2011.
- ,,, et al.Introduction of the medical emergency team (MET) system: a cluster‐randomised controlled trial.Lancet.2005;365(9477):2091–2097.
- ,,,,.Rapid response teams: a systematic review and meta‐analysis.Arch Intern Med.2010;170(1):18–26.
- ,,,,,.Recognising clinical instability in hospital patients before cardiac arrest or unplanned admission to intensive care. A pilot study in a tertiary‐care hospital.Med J Aust.1999;171(1):22–25.
- ,,,,,.A comparison of antecedents to cardiac arrests, deaths and emergency intensive care admissions in Australia and New Zealand, and the United Kingdom—the ACADEMIA study.Resuscitation.2004;62(3):275–282.
- ,,, et al.Early goal‐directed therapy in the treatment of severe sepsis and septic shock.N Engl J Med.2001;345(19):1368–1377.
- .Top ten list in myocardial infarction.Chest.2000;118(5):1477–1479.
- ,,, et al.Improvement in stroke mortality in Canada and the United States, 1990 to 2002.Circulation.2006;113(10):1335–1343.
- ,,, et al.“Identifying the hospitalised patient in crisis”—a consensus conference on the afferent limb of rapid response systems.Resuscitation.2010;81(4):375–382.
- ,,,.Contactless respiratory and heart rate monitoring: validation of an innovative tool.J Med Eng Technol.2010;35(7–8):393–398.
- ,,,,,.How is my patient doing? Evaluating hospitalized patients using continuous vital signs monitoring.Isr Med Assoc J.2009;11(6):382–394.
- ,,,,,.Medical device alarms.Biomed Tech (Berl).2011;56(2):73–83.
- ,.Poor prognosis for existing monitors in the intensive care unit.Crit Care Med.1997;25(4):614–619.
- .Crying wolf: false alarms in a pediatric intensive care unit.Crit Care Med.1994;22(6):981–985.
- ,,,,,.Intensive care unit alarms—how many do we need?Crit Care Med.2010;38(2):451–456.
- ,,,,.Alarmed: adverse events in low‐risk patients with chest pain receiving continuous electrocardiographic monitoring in the emergency department. A pilot study.Am J Emerg Med.2006;24(1):62–67.
- ,,,,,.Multicentric study of monitoring alarms in the adult intensive care unit (ICU): a descriptive analysis.Intensive Care Med.1999;25(12):1360–1366.
- .Alarms in the intensive care unit: how can the number of false alarms be reduced?Crit Care.2001;5(4):184–188.
- ,,,,,.Cardiorespiratory instability before and after implementing an integrated monitoring system.Crit Care Med.2011;39(1):65–72.
- ,,.Adaptive change detection in heart rate trend monitoring in anesthetized children.IEEE Trans Biomed Eng.2006;53(11):2211–2219.
- ,,,,,.Defining the incidence of cardiorespiratory instability in patients in step‐down units using an electronic integrated monitoring system.Arch Intern Med.2008;168(12):1300–1308.
- ,,, et al.Implementation of a real‐time computerized sepsis alert in nonintensive care unit patients.Crit Care Med.2011;39(3):469–473.
- ,,,,,.Early prediction of septic shock in hospitalized patients.J Hosp Med.2010;5(1):19–25.
- ,,.Rapid‐response teams.N Engl J Med.2011;365(2):139–146.
- ,,,.An analysis of the causes of adverse events from the Quality in Australian Health Care Study.Med J Aust.1999;170(9):411–415.
- ,.Taking your rapid response team to the next level. Society of Critical Care Medicine;2010. Available at: http://www.sccm.org/Publications/Critical_Connections/Archives/December‐2010/Pages/RapidResponseTeam.aspx. Accessed August 11,year="2011"2011.
- ,.Electrocardiographic monitoring in the hospitalized patient: a diagnostic intervention of uncertain clinical impact.Am J Emerg Med.2008;26(9):1047–1055.
- ,.Continuous electrocardiographic monitoring and cardiac arrest outcomes in 8,932 telemetry ward patients.Acad Emerg Med.2000;7(6):647–652.
- ,.The benefits and pitfalls of pulse oximetry.BMJ.1993;307(6902):457–458.
- ,.Patterns of unexpected in‐hospital deaths: a root cause analysis.Patient Saf Surg.2011;5(1):3.
- ,,,,,.Temporal trends in rates of patient harm resulting from medical care.N Engl J Med.2010;363(22):2124–2134.
- ,,, et al.Findings of the first consensus conference on medical emergency teams.Crit Care Med.2006;34(9):2463–2478.
- ,,,,.Inpatient transfers to the intensive care unit: delays are associated with increased mortality and morbidity.J Gen Intern Med.2003;18(2):77–83.
- ,,,,.Redefining in‐hospital resuscitation: the concept of the medical emergency team.Resuscitation.2001;48(2):105–110.
- Institute for Healthcare Improvement (IHI). Protecting 5 million lives from harm. Available at: www.ihi.org/ihi/programs/campaign. Accessed September 8,2011.
- ,,, et al.Introduction of the medical emergency team (MET) system: a cluster‐randomised controlled trial.Lancet.2005;365(9477):2091–2097.
- ,,,,.Rapid response teams: a systematic review and meta‐analysis.Arch Intern Med.2010;170(1):18–26.
- ,,,,,.Recognising clinical instability in hospital patients before cardiac arrest or unplanned admission to intensive care. A pilot study in a tertiary‐care hospital.Med J Aust.1999;171(1):22–25.
- ,,,,,.A comparison of antecedents to cardiac arrests, deaths and emergency intensive care admissions in Australia and New Zealand, and the United Kingdom—the ACADEMIA study.Resuscitation.2004;62(3):275–282.
- ,,, et al.Early goal‐directed therapy in the treatment of severe sepsis and septic shock.N Engl J Med.2001;345(19):1368–1377.
- .Top ten list in myocardial infarction.Chest.2000;118(5):1477–1479.
- ,,, et al.Improvement in stroke mortality in Canada and the United States, 1990 to 2002.Circulation.2006;113(10):1335–1343.
- ,,, et al.“Identifying the hospitalised patient in crisis”—a consensus conference on the afferent limb of rapid response systems.Resuscitation.2010;81(4):375–382.
- ,,,.Contactless respiratory and heart rate monitoring: validation of an innovative tool.J Med Eng Technol.2010;35(7–8):393–398.
- ,,,,,.How is my patient doing? Evaluating hospitalized patients using continuous vital signs monitoring.Isr Med Assoc J.2009;11(6):382–394.
- ,,,,,.Medical device alarms.Biomed Tech (Berl).2011;56(2):73–83.
- ,.Poor prognosis for existing monitors in the intensive care unit.Crit Care Med.1997;25(4):614–619.
- .Crying wolf: false alarms in a pediatric intensive care unit.Crit Care Med.1994;22(6):981–985.
- ,,,,,.Intensive care unit alarms—how many do we need?Crit Care Med.2010;38(2):451–456.
- ,,,,.Alarmed: adverse events in low‐risk patients with chest pain receiving continuous electrocardiographic monitoring in the emergency department. A pilot study.Am J Emerg Med.2006;24(1):62–67.
- ,,,,,.Multicentric study of monitoring alarms in the adult intensive care unit (ICU): a descriptive analysis.Intensive Care Med.1999;25(12):1360–1366.
- .Alarms in the intensive care unit: how can the number of false alarms be reduced?Crit Care.2001;5(4):184–188.
- ,,,,,.Cardiorespiratory instability before and after implementing an integrated monitoring system.Crit Care Med.2011;39(1):65–72.
- ,,.Adaptive change detection in heart rate trend monitoring in anesthetized children.IEEE Trans Biomed Eng.2006;53(11):2211–2219.
- ,,,,,.Defining the incidence of cardiorespiratory instability in patients in step‐down units using an electronic integrated monitoring system.Arch Intern Med.2008;168(12):1300–1308.
- ,,, et al.Implementation of a real‐time computerized sepsis alert in nonintensive care unit patients.Crit Care Med.2011;39(3):469–473.
- ,,,,,.Early prediction of septic shock in hospitalized patients.J Hosp Med.2010;5(1):19–25.
- ,,.Rapid‐response teams.N Engl J Med.2011;365(2):139–146.
- ,,,.An analysis of the causes of adverse events from the Quality in Australian Health Care Study.Med J Aust.1999;170(9):411–415.
- ,.Taking your rapid response team to the next level. Society of Critical Care Medicine;2010. Available at: http://www.sccm.org/Publications/Critical_Connections/Archives/December‐2010/Pages/RapidResponseTeam.aspx. Accessed August 11,year="2011"2011.
- ,.Electrocardiographic monitoring in the hospitalized patient: a diagnostic intervention of uncertain clinical impact.Am J Emerg Med.2008;26(9):1047–1055.
- ,.Continuous electrocardiographic monitoring and cardiac arrest outcomes in 8,932 telemetry ward patients.Acad Emerg Med.2000;7(6):647–652.
- ,.The benefits and pitfalls of pulse oximetry.BMJ.1993;307(6902):457–458.
- ,.Patterns of unexpected in‐hospital deaths: a root cause analysis.Patient Saf Surg.2011;5(1):3.
Copyright © 2012 Society of Hospital Medicine
Sepsis Outcomes Across Settings
Sepsis is a major cause of death in hospitalized patients.13 It is recommended that patients with sepsis be treated with early appropriate antibiotics, as well as early goal‐directed therapy including fluid and vasopressor support according to evidence‐based guidelines.46 Following such evidence‐based protocols and process‐of‐care interventions has been shown to be associated with better patient outcomes, including decreased mortality.7, 8
Most patients with severe sepsis are cared for in intensive care units (ICUs). At times, there are no beds available in the primary ICU and patients presenting to the hospital with sepsis are cared for in other units. Patients admitted to a non‐preferred clinical inpatient setting are sometimes referred to as overflow.9 ICUs can differ significantly in staffing patterns, equipment, and training.10 It is not known if overflow sepsis patients receive similar care when admitted to non‐primary ICUs.
At our hospital, we have an active bed management system led by the hospitalist division.11 This system includes protocols to place sepsis patients in the overflow ICU if the primary ICU is full. We hypothesized that process‐of‐care interventions would be more strictly adhered to when sepsis patients were in the primary ICU rather than in the overflow unit at our institution.
METHODS
Design
This was a retrospective cohort study of all patients with sepsis admitted to either the primary medical intensive care unit (MICU) or the overflow cardiac intensive care unit (CICU) at our hospital between July 2009 and February 2010. We reviewed the admission database starting with the month of February 2010 and proceeded backwards, month by month, until we reached the target number of patients.
Setting
The study was conducted at our 320‐bed, university‐affiliated academic medical center in Baltimore, MD. The MICU and the CICU are closed units that are located adjacent to each other and have 12 beds each. They are staffed by separate pools of attending physicians trained in pulmonary/critical care medicine and cardiovascular diseases, respectively, and no attending physician attends in both units. During the study period, there were 10 unique MICU and 14 unique CICU attending physicians; while most attending physicians covered the unit for 14 days, none of the physicians were on service more than 2 of the 2‐week blocks (28 days). Each unit is additionally staffed by fellows of the respective specialties, and internal medicine residents and interns belonging to the same residency program (who rotate through both ICUs). Residents and fellows are generally assigned to these ICUs for 4 continuous weeks. The assignment of specific attendings, fellows, and residents to either ICU is performed by individual division administrators on a rotational basis based on residency, fellowship, and faculty service requirements. The teams in each ICU function independently of each other. Clinical care of patients requiring the assistance of the other specialty (pulmonary medicine or cardiology) have guidance conferred via an official consultation. Orders on patients in both ICUs are written by the residents using the same computerized order entry system (CPOE) under the supervision of their attending physicians. The nursing staff is exclusive to each ICU. The respiratory therapists spend time in both units. The nursing and respiratory therapy staff in both ICUs are similarly trained and certified, and have the same patient‐to‐nursing ratios.
Subjects
All patients admitted with a possible diagnosis of sepsis to either the MICU or CICU were identified by querying the hospital electronic triage database called etriage. This Web‐based application is used to admit patients to all the Medicine services at our hospital. We employed a wide case‐finding net using keywords that included pneumonia, sepsis, hypotension, high lactate, hypoxia, UTI (urinary tract infection)/urosepsis, SIRS (systemic inflammatory response syndrome), hypothermia, and respiratory failure. A total of 197 adult patients were identified. The charts and the electronic medical record (EMR) of these patients were then reviewed to determine the presence of a sepsis diagnosis using standard consensus criteria.12 Severe sepsis was defined by sepsis associated with organ dysfunction, hypoperfusion, or hypotension using criteria described by Bone et al.12
Fifty‐six did not meet the criteria for sepsis and were excluded from the analysis. A total of 141 patients were included in the study. This being a pilot study, we did not have any preliminary data regarding adherence to sepsis guidelines in overflow ICUs to calculate appropriate sample size. However, in 2 recent studies of dedicated ICUs (Ferrer et al13 and Castellanos‐Ortega et al14), the averaged adherence to a single measure like checking of lactate level was 27% pre‐intervention and 62% post‐intervention. With alpha level 0.05 and 80% power, one would need 31 patients in each unit to detect such differences with respect to this intervention. Although this data does not necessarily apply to overflow ICUs or for combination of processes, we used a goal of having at least 31 patients in each ICU.
The study was approved by the Johns Hopkins Institutional Review Board. The need for informed consent was waived given the retrospective nature of the study.
Data Extraction Process and Procedures
The clinical data was extracted from the EMR and patient charts using a standardized data extraction instrument, modified from a case report form (CRF) used and validated in previous studies.15, 16 The following procedures were used for the data extraction:
The data extractors included 4 physicians and 1 research assistant and were trained and tested by a single expert in data review and extraction.
Lab data was transcribed directly from the EMR. Calculation of acute physiology and chronic health evaluation (APACHE II) scores were done using the website
http://www.sfar.org/subores2/apache22.html (Socit Franaise d'Anesthsie et de Ranimation). Sepsis‐related organ failure assessment (SOFA) scores were calculated using usual criteria.17Delivery of specific treatments and interventions, including their timing, was extracted from the EMR.
The attending physicians' notes were used as the final source to assign diagnoses such as presence of acute lung injury, site of infection, and record interventions.
Data Analysis
Analyses focused primarily on assessing whether patients were treated differently between the MICU and CICU. The primary exposure variables were the process‐of‐care measures. We specifically used measurement of central venous saturation, checking of lactate level, and administration of antibiotics within 60 minutes in patients with severe sepsis as our primary process‐of‐care measures.13 Continuous variables were reported as mean standard deviation, and Student's t tests were used to compare the 2 groups. Categorical data were expressed as frequency distributions, and chi‐square tests were used to identify differences between the 2 groups. All tests were 2‐tailed with statistical significance set at 0.05. Statistical analysis was performed using SPSS version 19.0. (IBM, Armonk, NY).
To overcome data constraints, we created a dichotomous variable for each of the 3 primary processes‐of‐care (indicating receipt of process or not) and then combined them into 1 dichotomous variable indicating whether or not the patients with severe sepsis received all 3 primary processes‐of‐care. The combined variable was the key independent variable in the model.
We performed logistic regression analysis on patients with severe sepsis. The equation Logit [P(ICU Type = CICU)] = + 1Combined + 2Age describes the framework of the model, with ICU type being the dependent variable, and the combined variable of patients receiving all primary measures being the independent variable and controlled for age. Logistic regression was performed using JMP (SAS Institute, Inc, Cary, NC).
We additionally performed a secondary analysis to explore possible predictors of mortality using a logistic regression model, with the event of death as the dependent variable, and age, APACHE II scores, combined processes‐of‐care, and ICU type included as independent variables.
RESULTS
There were 100 patients admitted to the MICU and 41 patients admitted to the CICU during the study period (Table 1). The majority of the patients were admitted to the ICUs directly from the emergency department (ED) (n = 129), with a small number of patients who were transferred from the Medicine floors (n = 12).
| MICU (N =100) | CICU (N =41) | P Value | |
|---|---|---|---|
| |||
| Age in years, mean SD | 67 14.8 | 72 15.1 | 0.11 |
| Female, n (%) | 57 (57) | 27 (66) | 0.33 |
| Patients with chronic organ insufficiency, n (%) | 59 (59) | 22 (54) | 0.56 |
| Patients with severe sepsis, n (%) | 88 (88) | 21 (51) | <0.001 |
| Patients needing mechanical ventilation, n (%) | 43 (43) | 14 (34) | 0.33 |
| APACHE II score, mean SD | 25.53 9.11 | 24.37 9.53 | 0.50 |
| SOFA score on day 1, mean SD | 7.09 3.55 | 6.71 4.57 | 0.60 |
| Patients with acute lung injury on presentation, n (%) | 8 (8) | 2 (5) | 0.50 |
There were no significant differences between the 2 study groups in terms of age, sex, primary site of infection, mean APACHE II score, SOFA scores on day 1, chronic organ insufficiency, immune suppression, or need for mechanical ventilation (Table 1). The most common site of infection was lung. There were significantly more patients with severe sepsis in the MICU (88% vs 51%, P <0.001).
Sepsis Process‐of‐Care Measures
There were no significant differences in the proportion of severe sepsis patients who had central venous saturation checked (MICU: 46% vs CICU: 41%, P = 0.67), lactate level checked (95% vs 100%, P = 0.37), or received antibiotics within 60 minutes of presentation (75% vs 69%, P = 0.59) (Table 2). Multiple other processes and treatments were delivered similarly, as shown in Table 2.
| Primary Process‐of‐Care Measures (Severe Sepsis Patients) | MICU (N = 88) | CICU (N = 21) | P Value |
|---|---|---|---|
| |||
| Patients with central venous oxygen saturation checked, n (%)* | 31 (46) | 7 (41) | 0.67 |
| Patients with lactate level checked, n (%)* | 58 (95) | 16 (100) | 0.37 |
| Received antibiotics within 60 min, n (%)* | 46 (75) | 11 (69) | 0.59 |
| Patients who had all 3 above processes and treatments, n (%) | 19 (22) | 4 (19) | 0.79 |
| Received vasopressor, n (%) | 25 (28) | 8 (38) | 0.55 |
| ICU Treatments and Processes (All Sepsis Patients) | (N =100) | (N = 41) | |
| Fluid balance 24 h after admission in liters, mean SD | 1.96 2.42 | 1.42 2.63 | 0.24 |
| Patients who received stress dose steroids, n (%) | 11 (11) | 4 (10) | 0.83 |
| Patients who received Drotrecogin alfa, n (%) | 0 (0) | 0 (0) | |
| Morning glucose 24 h after admission in mg/dL, mean SD | 161 111 | 144 80 | 0.38 |
| Received DVT prophylaxis within 24 h of admission, n (%) | 74 (74) | 20 (49) | 0.004 |
| Received GI prophylaxis within 24 h of admission, n (%) | 68 (68) | 18 (44) | 0.012 |
| Received RBC transfusion within 24 h of admission, n (%) | 8 (8) | 7 (17) | 0.11 |
| Received renal replacement therapy, n (%) | 13 (13) | 3 (7) | 0.33 |
| Received a spontaneous breathing trial within 24 h of admission, n (%)* | 4 (11) | 4 (33) | 0.07 |
Logistic regression analysis examining the receipt of all 3 primary processes‐of‐care while controlling for age revealed that the odds of the being in one of the ICUs was not significantly different (P = 0.85). The secondary analysis regression models revealed that only the APACHE II score (odds ratio [OR] = 1.21; confidence interval [CI], 1.121.31) was significantly associated with higher odds of mortality. ICU‐type [MICU vs CICU] (OR = 1.85; CI, 0.428.20), age (OR = 1.01; CI, 0.971.06), and combined processes of care (OR = 0.26; CI, 0.071.01) did not have significant associations with odds of mortality.
A review of microbiologic sensitivities revealed a trend towards significance that the cultured microorganism(s) was likely to be resistant to the initial antibiotics administered in MICU vs CICU (15% vs 5%, respectively, P = 0.09).
Mechanical Ventilation Parameters
The majority of the ventilated patients were admitted to each ICU in assist control (AC) mode. There were no significant differences in categories of mean tidal volume (TV) (P = 0.3), mean plateau pressures (P = 0.12), mean fraction of inspired oxygen (FiO2) (P = 0.95), and mean positive end‐expiratory pressures (PEEP) (P = 0.98) noted across the 2 units at the time of ICU admission, and also 24 hours after ICU admission. Further comparison of measurements of tidal volumes and plateau pressures over 7 days of ICU stay revealed no significant differences in the 2 ICUs (P = 0.40 and 0.57, respectively, on day 7 of ICU admission). There was a trend towards significance in fewer patients in the MICU receiving spontaneous breathing trial within 24 hours of ICU admission (11% vs 33%, P = 0.07) (Table 2).
Patient Outcomes
There were no significant differences in ICU mortality (MICU 19% vs CICU 10%, P = 0.18), or hospital mortality (21% vs 15%, P = 0.38) across the units (Table 3). Mean ICU and hospital length of stay (LOS) and proportion of patients discharged home with unassisted breathing were similar (Table 3).
| Patient Outcomes | MICU (N = 100) | CICU (N = 41) | P Value |
|---|---|---|---|
| |||
| ICU mortality, n (%) | 19 (19) | 4 (10) | 0.18 |
| Hospital mortality, n (%) | 21 (21) | 6 (15) | 0.38 |
| Discharged home with unassisted breathing, n (%) | 33 (33) | 19 (46) | 0.14 |
| ICU length of stay in days, mean SD | 4.78 6.24 | 4.92 6.32 | 0.97 |
| Hospital length of stay in days, mean SD | 9.68 9.22 | 9.73 9.33 | 0.98 |
DISCUSSION
Since sepsis is more commonly treated in the medical ICU and some data suggests that specialty ICUs may be better at providing desired care,18, 19 we believed that patients treated in the MICU would be more likely to receive guideline‐concordant care. The study refutes our a priori hypothesis and reveals that evidence‐based processes‐of‐care associated with improved outcomes for sepsis are similarly implemented at our institution in the primary and overflow ICU. These findings are important, as ICU bed availability is a frequent problem and many hospitals overflow patients to non‐primary ICUs.9, 20
The observed equivalence in the care delivered may be a function of the relatively high number of patients with sepsis treated in the overflow unit, thereby giving the delivery teams enough experience to provide the desired care. An alternative explanation could be that the residents in CICU brought with them the experience from having previously trained in the MICU. Although, some of the care processes for sepsis patients are influenced by the CPOE (with embedded order sets and protocols), it is unlikely that CPOE can fully account for similarity in care because many processes and therapies (like use of steroids, amount of fluid delivered in first 24 hours, packed red blood cells [PRBC] transfusion, and spontaneous breathing trials) are not embedded within order sets.
The significant difference noted in the areas of deep vein thrombosis (DVT) and gastrointestinal (GI) prophylaxis within 24 hours of ICU admission was unexpected. These preventive therapies are included in initial order sets in the CPOE, which prompt physicians to order them as standard‐of‐care. With respect to DVT prophylaxis, we suspect that some of the difference might be attributable to specific contraindications to its use, which could have been more common in one of the units. There were more patients in MICU on mechanical ventilation (although not statistically significant) and with severe sepsis (statistically significant) at time of admission, which might have contributed to the difference noted in use of GI prophylaxis. It is also plausible that these differences might have disappeared if they were reassessed beyond 24 hours into the ICU admission. We cannot rule out the presence of unit‐ and physician‐level differences that contributed to this. Likewise, there was an unexpected trend towards significance, wherein more patients in CICU had spontaneous breathing trials within 24 hours of admission. This might also be explained by the higher number of patients with severe sepsis in the MICU (preempting any weaning attempts). These caveats aside, it is reassuring that, at our institution, admitting septic patients to the first available ICU bed does not adversely affect important processes‐of‐care.
One might ask whether this study's data should reassure other sites who are boarding septic patients in non‐primary ICUs. Irrespective of the number of patients studied or the degree of statistical significance of the associations, an observational study design cannot prove that boarding septic patients in non‐primary ICUs is either safe or unsafe. However, we hope that readers reflect on, and take inventory of, systems issues that may be different between unitswith an eye towards eliminating variation such that all units managing septic patients are primed to deliver guideline‐concordant care. Other hospitals that use CPOE with sepsis order sets, have protocols for sepsis care, and who train nursing and respiratory therapists to meet high standards might be pleased to see that the patients in our study received comparable, high‐quality care across the 2 units. While our data suggests that boarding patients in overflow units may be safe, these findings would need to be replicated at other sites using prospective designs to prove safety.
Length of emergency room stay prior to admission is associated with higher mortality rates.2123 At many hospitals, critical care beds are a scarce resource such that most hospitals have a policy for the triage of patients to critical care beds.24, 25 Lundberg and colleagues' study demonstrated that patients who developed septic shock on the medical wards experienced delays in receipt of intravenous fluids, inotropic agents and transfer to a critical care setting.26 Thus, rather than waiting in the ED or on the medical service for an MICU bed to become available, it may be most wise to admit a critically sick septic patient to the first available ICU bed, even to an overflow ICU. In a recent study by Sidlow and Aggarwal, 1104 patients discharged from the coronary care unit (CCU) with a non‐cardiac primary diagnosis were compared to patients admitted to the MICU in the same hospital.27 The study found no differences in patient mortality, 30‐day readmission rate, hospital LOS, ICU LOS, and safety outcomes of ventilator‐associated pneumonia and catheter‐associated bloodstream infections between ICUs. However, their study did not examine processes‐of‐care delivered between the primary ICU and the overflow unit, and did not validate the primary diagnoses of patients admitted to the ICU.
Several limitations of this study should be considered. First, this study was conducted at a single center. Second, we used a retrospective study design; however, a prospective study randomizing patients to 1 of the 2 units would likely never be possible. Third, the relatively small number of patients limited the power of the study to detect mortality differences between the units. However, this was a pilot study focused on processes of care as opposed to clinical outcomes. Fourth, it is possible that we did not capture every single patient with sepsis with our keyword search. Our use of a previously validated screening process should have limited the number of missed cases.15, 16 Fifth, although the 2 ICUs have exclusive nursing staff and attending physicians, the housestaff and respiratory therapists do rotate between the 2 ICUs and place orders in the common CPOE. The rotating housestaff may certainly represent a source for confounding, but the large numbers (>30) of evenly spread housestaff over the study period minimizes the potential for any trainee to be responsible for a large proportion of observed practice. Sixth, ICU attendings are the physicians of record and could influence the results. Because no attending physician was on service for more than 4 weeks during the study period, and patients were equally spread over this same time, concerns about clustering and biases this may have created should be minimal but cannot be ruled out. Seventh, some interventions and processes, such as antibiotic administration and measurement of lactate, may have been initiated in the ED, thereby decreasing the potential for differences between the groups. Additionally, we cannot rule out the possibility that factors other than bed availability drove the admission process (we found that the relative proportion of patients admitted to overflow ICU during hours of ambulance diversion was similar to the overflow ICU admissions during non‐ambulance diversion hours). It is possible that some selection bias by the hospitalist assigning patients to specific ICUs influenced their triage decisionsalthough all triaging doctors go through the same process of training in active bed management.11 While more patients admitted to the MICU had severe sepsis, there were no differences between groups in APACHE II or SOFA scores. However, we cannot rule out that there were other residual confounders. Finally, in a small number of cases (4/41, 10%), the CICU team consulted the MICU attending for assistance. This input had the potential to reduce disparities in care between the units.
Overflowing patients to non‐primary ICUs occurs in many hospitals. Our study demonstrates that sepsis treatment for overflow patients may be similar to that received in the primary ICU. While a large multicentered and randomized trial could determine whether significant management and outcome differences exist between primary and overflow ICUs, feasibility concerns make it unlikely that such a study will ever be conducted.
Acknowledgements
Disclosure: Dr Wright is a Miller‐Coulson Family Scholar and this work is supported by the Miller‐Coulson family through the Johns Hopkins Center for Innovative Medicine. Dr Sevransky was supported with a grant from National Institute of General Medical Sciences, NIGMS K‐23‐1399. All other authors disclose no relevant or financial conflicts of interest.
- ,,,,,.Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care.Crit Care Med.2001;29(7):1303–1310.
- ,,, et al;for the Milwaukee Initiative in Critical Care Outcomes Research (MICCOR) Group of Investigators.Nationwide trends of severe sepsis in the twenty first century (2000–2007).Chest.2011;140(5):1223–1231.
- ,,,.Rapid increase in hospitalization and mortality rates for severe sepsis in the United States: a trend analysis from 1993 to 2003.Crit Care Med.2007;35(5):1244–1250.
- ,,, et al.Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2008.Crit Care Med.2008;36(1):296–327.
- ,,, et al.Lactate clearance vs central venous oxygen saturation as goals of early sepsis therapy: a randomized clinical trial.JAMA.2010;303(8):739–746.
- ,,, et al.Early goal‐directed therapy in the treatment of severe sepsis and septic shock.N Engl J Med.2001;345(19):1368–1377.
- ,,, et al.Implementation of a bundle of quality indicators for the early management of severe sepsis and septic shock is associated with decreased mortality.Crit Care Med.2007;35(4):1105–1112.
- ,,, et al.Early combination antibiotic therapy yields improved survival compared with monotherapy in septic shock: a propensity‐matched analysis.Crit Care Med.2010;38(9):1773–1785.
- .A new dimension of the PACU: the dilemma of the ICU overflow patient.J Post Anesth Nurs.1994;9(5):297–300.
- ,,, et al.Descriptive analysis of critical care units in the United States.Crit Care Med.1992;20(6):846–863.
- ,,,,,.Active bed management by hospitalists and emergency department throughput.Ann Intern Med.2008;149(11):804–811.
- ,,, et al.Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee, American College of Chest Physicians/Society of Critical Care Medicine.Chest.1992;101(6):1644–1655.
- ,,, et al.Improvement in process of care and outcome after a multicenter severe sepsis educational program in Spain.JAMA.2008;299(19):2294–2303.
- ,,, et al.Impact of the surviving sepsis campaign protocols on hospital length of stay and mortality in septic shock patients: results of a three‐year follow‐up quasi‐experimental study.Crit Care Med.2010;38(4):1036–1043.
- ,,, et al.Study protocol: the improving care of acute lung injury patients (ICAP) study.Crit Care.2006;10(1):R9.
- ,,,,,.Critical illness outcome study: an observational study of protocols and mortality in intensive care units.Open Access J Clin Trials.2011;3(September):55–65.
- ,,, et al.The SOFA (sepsis‐related organ failure assessment) score to describe organ dysfunction/failure: on behalf of the Working Group on Sepsis‐Related Problems of the European Society of Intensive Care Medicine.Intensive Care Med.1996;22(7):707–710.
- ,,,,,.Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review.JAMA.2002;288(17):2151–2162.
- ,,.Do intensivists in ICU improve outcome?Best Pract Res Clin Anaesthesiol.2005;19(1):125–135.
- .Is the postanesthesia care unit becoming an intensive care unit?J Perianesth Nurs.1999;14(2):73–77.
- ,,,,;for the DELAY‐ED Study Group.Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit.Crit Care Med.2007;35(6):1477–1483.
- ,,, et al.Association between timing of intensive care unit admission and outcomes for emergency department patients with community‐acquired pneumonia.Crit Care Med.2009;37(11):2867–2874.
- ,.Association between ambulance diversion and survival among patients with acute myocardial infarction.JAMA.2011;305(23):2440–2447.
- .Civilian triage in the intensive care unit: the ritual of the last bed.Crit Care Med.1993;21(4):598–606.
- ,,,,;for the Values Ethics and Rationing in Critical Care Task Force.Rationing critical care beds: a systematic review.Crit Care Med.2004;32(7):1588–1597.
- ,,, et al.Septic shock: an analysis of outcomes for patients with onset on hospital wards versus intensive care units.Crit Care Med.1998;26(6):1020–1024.
- ,.“The MICU is full”: one hospital's experience with an overflow triage policy.Jt Comm J Qual Patient Saf.2011;37(10):456–460.
Sepsis is a major cause of death in hospitalized patients.13 It is recommended that patients with sepsis be treated with early appropriate antibiotics, as well as early goal‐directed therapy including fluid and vasopressor support according to evidence‐based guidelines.46 Following such evidence‐based protocols and process‐of‐care interventions has been shown to be associated with better patient outcomes, including decreased mortality.7, 8
Most patients with severe sepsis are cared for in intensive care units (ICUs). At times, there are no beds available in the primary ICU and patients presenting to the hospital with sepsis are cared for in other units. Patients admitted to a non‐preferred clinical inpatient setting are sometimes referred to as overflow.9 ICUs can differ significantly in staffing patterns, equipment, and training.10 It is not known if overflow sepsis patients receive similar care when admitted to non‐primary ICUs.
At our hospital, we have an active bed management system led by the hospitalist division.11 This system includes protocols to place sepsis patients in the overflow ICU if the primary ICU is full. We hypothesized that process‐of‐care interventions would be more strictly adhered to when sepsis patients were in the primary ICU rather than in the overflow unit at our institution.
METHODS
Design
This was a retrospective cohort study of all patients with sepsis admitted to either the primary medical intensive care unit (MICU) or the overflow cardiac intensive care unit (CICU) at our hospital between July 2009 and February 2010. We reviewed the admission database starting with the month of February 2010 and proceeded backwards, month by month, until we reached the target number of patients.
Setting
The study was conducted at our 320‐bed, university‐affiliated academic medical center in Baltimore, MD. The MICU and the CICU are closed units that are located adjacent to each other and have 12 beds each. They are staffed by separate pools of attending physicians trained in pulmonary/critical care medicine and cardiovascular diseases, respectively, and no attending physician attends in both units. During the study period, there were 10 unique MICU and 14 unique CICU attending physicians; while most attending physicians covered the unit for 14 days, none of the physicians were on service more than 2 of the 2‐week blocks (28 days). Each unit is additionally staffed by fellows of the respective specialties, and internal medicine residents and interns belonging to the same residency program (who rotate through both ICUs). Residents and fellows are generally assigned to these ICUs for 4 continuous weeks. The assignment of specific attendings, fellows, and residents to either ICU is performed by individual division administrators on a rotational basis based on residency, fellowship, and faculty service requirements. The teams in each ICU function independently of each other. Clinical care of patients requiring the assistance of the other specialty (pulmonary medicine or cardiology) have guidance conferred via an official consultation. Orders on patients in both ICUs are written by the residents using the same computerized order entry system (CPOE) under the supervision of their attending physicians. The nursing staff is exclusive to each ICU. The respiratory therapists spend time in both units. The nursing and respiratory therapy staff in both ICUs are similarly trained and certified, and have the same patient‐to‐nursing ratios.
Subjects
All patients admitted with a possible diagnosis of sepsis to either the MICU or CICU were identified by querying the hospital electronic triage database called etriage. This Web‐based application is used to admit patients to all the Medicine services at our hospital. We employed a wide case‐finding net using keywords that included pneumonia, sepsis, hypotension, high lactate, hypoxia, UTI (urinary tract infection)/urosepsis, SIRS (systemic inflammatory response syndrome), hypothermia, and respiratory failure. A total of 197 adult patients were identified. The charts and the electronic medical record (EMR) of these patients were then reviewed to determine the presence of a sepsis diagnosis using standard consensus criteria.12 Severe sepsis was defined by sepsis associated with organ dysfunction, hypoperfusion, or hypotension using criteria described by Bone et al.12
Fifty‐six did not meet the criteria for sepsis and were excluded from the analysis. A total of 141 patients were included in the study. This being a pilot study, we did not have any preliminary data regarding adherence to sepsis guidelines in overflow ICUs to calculate appropriate sample size. However, in 2 recent studies of dedicated ICUs (Ferrer et al13 and Castellanos‐Ortega et al14), the averaged adherence to a single measure like checking of lactate level was 27% pre‐intervention and 62% post‐intervention. With alpha level 0.05 and 80% power, one would need 31 patients in each unit to detect such differences with respect to this intervention. Although this data does not necessarily apply to overflow ICUs or for combination of processes, we used a goal of having at least 31 patients in each ICU.
The study was approved by the Johns Hopkins Institutional Review Board. The need for informed consent was waived given the retrospective nature of the study.
Data Extraction Process and Procedures
The clinical data was extracted from the EMR and patient charts using a standardized data extraction instrument, modified from a case report form (CRF) used and validated in previous studies.15, 16 The following procedures were used for the data extraction:
The data extractors included 4 physicians and 1 research assistant and were trained and tested by a single expert in data review and extraction.
Lab data was transcribed directly from the EMR. Calculation of acute physiology and chronic health evaluation (APACHE II) scores were done using the website
http://www.sfar.org/subores2/apache22.html (Socit Franaise d'Anesthsie et de Ranimation). Sepsis‐related organ failure assessment (SOFA) scores were calculated using usual criteria.17Delivery of specific treatments and interventions, including their timing, was extracted from the EMR.
The attending physicians' notes were used as the final source to assign diagnoses such as presence of acute lung injury, site of infection, and record interventions.
Data Analysis
Analyses focused primarily on assessing whether patients were treated differently between the MICU and CICU. The primary exposure variables were the process‐of‐care measures. We specifically used measurement of central venous saturation, checking of lactate level, and administration of antibiotics within 60 minutes in patients with severe sepsis as our primary process‐of‐care measures.13 Continuous variables were reported as mean standard deviation, and Student's t tests were used to compare the 2 groups. Categorical data were expressed as frequency distributions, and chi‐square tests were used to identify differences between the 2 groups. All tests were 2‐tailed with statistical significance set at 0.05. Statistical analysis was performed using SPSS version 19.0. (IBM, Armonk, NY).
To overcome data constraints, we created a dichotomous variable for each of the 3 primary processes‐of‐care (indicating receipt of process or not) and then combined them into 1 dichotomous variable indicating whether or not the patients with severe sepsis received all 3 primary processes‐of‐care. The combined variable was the key independent variable in the model.
We performed logistic regression analysis on patients with severe sepsis. The equation Logit [P(ICU Type = CICU)] = + 1Combined + 2Age describes the framework of the model, with ICU type being the dependent variable, and the combined variable of patients receiving all primary measures being the independent variable and controlled for age. Logistic regression was performed using JMP (SAS Institute, Inc, Cary, NC).
We additionally performed a secondary analysis to explore possible predictors of mortality using a logistic regression model, with the event of death as the dependent variable, and age, APACHE II scores, combined processes‐of‐care, and ICU type included as independent variables.
RESULTS
There were 100 patients admitted to the MICU and 41 patients admitted to the CICU during the study period (Table 1). The majority of the patients were admitted to the ICUs directly from the emergency department (ED) (n = 129), with a small number of patients who were transferred from the Medicine floors (n = 12).
| MICU (N =100) | CICU (N =41) | P Value | |
|---|---|---|---|
| |||
| Age in years, mean SD | 67 14.8 | 72 15.1 | 0.11 |
| Female, n (%) | 57 (57) | 27 (66) | 0.33 |
| Patients with chronic organ insufficiency, n (%) | 59 (59) | 22 (54) | 0.56 |
| Patients with severe sepsis, n (%) | 88 (88) | 21 (51) | <0.001 |
| Patients needing mechanical ventilation, n (%) | 43 (43) | 14 (34) | 0.33 |
| APACHE II score, mean SD | 25.53 9.11 | 24.37 9.53 | 0.50 |
| SOFA score on day 1, mean SD | 7.09 3.55 | 6.71 4.57 | 0.60 |
| Patients with acute lung injury on presentation, n (%) | 8 (8) | 2 (5) | 0.50 |
There were no significant differences between the 2 study groups in terms of age, sex, primary site of infection, mean APACHE II score, SOFA scores on day 1, chronic organ insufficiency, immune suppression, or need for mechanical ventilation (Table 1). The most common site of infection was lung. There were significantly more patients with severe sepsis in the MICU (88% vs 51%, P <0.001).
Sepsis Process‐of‐Care Measures
There were no significant differences in the proportion of severe sepsis patients who had central venous saturation checked (MICU: 46% vs CICU: 41%, P = 0.67), lactate level checked (95% vs 100%, P = 0.37), or received antibiotics within 60 minutes of presentation (75% vs 69%, P = 0.59) (Table 2). Multiple other processes and treatments were delivered similarly, as shown in Table 2.
| Primary Process‐of‐Care Measures (Severe Sepsis Patients) | MICU (N = 88) | CICU (N = 21) | P Value |
|---|---|---|---|
| |||
| Patients with central venous oxygen saturation checked, n (%)* | 31 (46) | 7 (41) | 0.67 |
| Patients with lactate level checked, n (%)* | 58 (95) | 16 (100) | 0.37 |
| Received antibiotics within 60 min, n (%)* | 46 (75) | 11 (69) | 0.59 |
| Patients who had all 3 above processes and treatments, n (%) | 19 (22) | 4 (19) | 0.79 |
| Received vasopressor, n (%) | 25 (28) | 8 (38) | 0.55 |
| ICU Treatments and Processes (All Sepsis Patients) | (N =100) | (N = 41) | |
| Fluid balance 24 h after admission in liters, mean SD | 1.96 2.42 | 1.42 2.63 | 0.24 |
| Patients who received stress dose steroids, n (%) | 11 (11) | 4 (10) | 0.83 |
| Patients who received Drotrecogin alfa, n (%) | 0 (0) | 0 (0) | |
| Morning glucose 24 h after admission in mg/dL, mean SD | 161 111 | 144 80 | 0.38 |
| Received DVT prophylaxis within 24 h of admission, n (%) | 74 (74) | 20 (49) | 0.004 |
| Received GI prophylaxis within 24 h of admission, n (%) | 68 (68) | 18 (44) | 0.012 |
| Received RBC transfusion within 24 h of admission, n (%) | 8 (8) | 7 (17) | 0.11 |
| Received renal replacement therapy, n (%) | 13 (13) | 3 (7) | 0.33 |
| Received a spontaneous breathing trial within 24 h of admission, n (%)* | 4 (11) | 4 (33) | 0.07 |
Logistic regression analysis examining the receipt of all 3 primary processes‐of‐care while controlling for age revealed that the odds of the being in one of the ICUs was not significantly different (P = 0.85). The secondary analysis regression models revealed that only the APACHE II score (odds ratio [OR] = 1.21; confidence interval [CI], 1.121.31) was significantly associated with higher odds of mortality. ICU‐type [MICU vs CICU] (OR = 1.85; CI, 0.428.20), age (OR = 1.01; CI, 0.971.06), and combined processes of care (OR = 0.26; CI, 0.071.01) did not have significant associations with odds of mortality.
A review of microbiologic sensitivities revealed a trend towards significance that the cultured microorganism(s) was likely to be resistant to the initial antibiotics administered in MICU vs CICU (15% vs 5%, respectively, P = 0.09).
Mechanical Ventilation Parameters
The majority of the ventilated patients were admitted to each ICU in assist control (AC) mode. There were no significant differences in categories of mean tidal volume (TV) (P = 0.3), mean plateau pressures (P = 0.12), mean fraction of inspired oxygen (FiO2) (P = 0.95), and mean positive end‐expiratory pressures (PEEP) (P = 0.98) noted across the 2 units at the time of ICU admission, and also 24 hours after ICU admission. Further comparison of measurements of tidal volumes and plateau pressures over 7 days of ICU stay revealed no significant differences in the 2 ICUs (P = 0.40 and 0.57, respectively, on day 7 of ICU admission). There was a trend towards significance in fewer patients in the MICU receiving spontaneous breathing trial within 24 hours of ICU admission (11% vs 33%, P = 0.07) (Table 2).
Patient Outcomes
There were no significant differences in ICU mortality (MICU 19% vs CICU 10%, P = 0.18), or hospital mortality (21% vs 15%, P = 0.38) across the units (Table 3). Mean ICU and hospital length of stay (LOS) and proportion of patients discharged home with unassisted breathing were similar (Table 3).
| Patient Outcomes | MICU (N = 100) | CICU (N = 41) | P Value |
|---|---|---|---|
| |||
| ICU mortality, n (%) | 19 (19) | 4 (10) | 0.18 |
| Hospital mortality, n (%) | 21 (21) | 6 (15) | 0.38 |
| Discharged home with unassisted breathing, n (%) | 33 (33) | 19 (46) | 0.14 |
| ICU length of stay in days, mean SD | 4.78 6.24 | 4.92 6.32 | 0.97 |
| Hospital length of stay in days, mean SD | 9.68 9.22 | 9.73 9.33 | 0.98 |
DISCUSSION
Since sepsis is more commonly treated in the medical ICU and some data suggests that specialty ICUs may be better at providing desired care,18, 19 we believed that patients treated in the MICU would be more likely to receive guideline‐concordant care. The study refutes our a priori hypothesis and reveals that evidence‐based processes‐of‐care associated with improved outcomes for sepsis are similarly implemented at our institution in the primary and overflow ICU. These findings are important, as ICU bed availability is a frequent problem and many hospitals overflow patients to non‐primary ICUs.9, 20
The observed equivalence in the care delivered may be a function of the relatively high number of patients with sepsis treated in the overflow unit, thereby giving the delivery teams enough experience to provide the desired care. An alternative explanation could be that the residents in CICU brought with them the experience from having previously trained in the MICU. Although, some of the care processes for sepsis patients are influenced by the CPOE (with embedded order sets and protocols), it is unlikely that CPOE can fully account for similarity in care because many processes and therapies (like use of steroids, amount of fluid delivered in first 24 hours, packed red blood cells [PRBC] transfusion, and spontaneous breathing trials) are not embedded within order sets.
The significant difference noted in the areas of deep vein thrombosis (DVT) and gastrointestinal (GI) prophylaxis within 24 hours of ICU admission was unexpected. These preventive therapies are included in initial order sets in the CPOE, which prompt physicians to order them as standard‐of‐care. With respect to DVT prophylaxis, we suspect that some of the difference might be attributable to specific contraindications to its use, which could have been more common in one of the units. There were more patients in MICU on mechanical ventilation (although not statistically significant) and with severe sepsis (statistically significant) at time of admission, which might have contributed to the difference noted in use of GI prophylaxis. It is also plausible that these differences might have disappeared if they were reassessed beyond 24 hours into the ICU admission. We cannot rule out the presence of unit‐ and physician‐level differences that contributed to this. Likewise, there was an unexpected trend towards significance, wherein more patients in CICU had spontaneous breathing trials within 24 hours of admission. This might also be explained by the higher number of patients with severe sepsis in the MICU (preempting any weaning attempts). These caveats aside, it is reassuring that, at our institution, admitting septic patients to the first available ICU bed does not adversely affect important processes‐of‐care.
One might ask whether this study's data should reassure other sites who are boarding septic patients in non‐primary ICUs. Irrespective of the number of patients studied or the degree of statistical significance of the associations, an observational study design cannot prove that boarding septic patients in non‐primary ICUs is either safe or unsafe. However, we hope that readers reflect on, and take inventory of, systems issues that may be different between unitswith an eye towards eliminating variation such that all units managing septic patients are primed to deliver guideline‐concordant care. Other hospitals that use CPOE with sepsis order sets, have protocols for sepsis care, and who train nursing and respiratory therapists to meet high standards might be pleased to see that the patients in our study received comparable, high‐quality care across the 2 units. While our data suggests that boarding patients in overflow units may be safe, these findings would need to be replicated at other sites using prospective designs to prove safety.
Length of emergency room stay prior to admission is associated with higher mortality rates.2123 At many hospitals, critical care beds are a scarce resource such that most hospitals have a policy for the triage of patients to critical care beds.24, 25 Lundberg and colleagues' study demonstrated that patients who developed septic shock on the medical wards experienced delays in receipt of intravenous fluids, inotropic agents and transfer to a critical care setting.26 Thus, rather than waiting in the ED or on the medical service for an MICU bed to become available, it may be most wise to admit a critically sick septic patient to the first available ICU bed, even to an overflow ICU. In a recent study by Sidlow and Aggarwal, 1104 patients discharged from the coronary care unit (CCU) with a non‐cardiac primary diagnosis were compared to patients admitted to the MICU in the same hospital.27 The study found no differences in patient mortality, 30‐day readmission rate, hospital LOS, ICU LOS, and safety outcomes of ventilator‐associated pneumonia and catheter‐associated bloodstream infections between ICUs. However, their study did not examine processes‐of‐care delivered between the primary ICU and the overflow unit, and did not validate the primary diagnoses of patients admitted to the ICU.
Several limitations of this study should be considered. First, this study was conducted at a single center. Second, we used a retrospective study design; however, a prospective study randomizing patients to 1 of the 2 units would likely never be possible. Third, the relatively small number of patients limited the power of the study to detect mortality differences between the units. However, this was a pilot study focused on processes of care as opposed to clinical outcomes. Fourth, it is possible that we did not capture every single patient with sepsis with our keyword search. Our use of a previously validated screening process should have limited the number of missed cases.15, 16 Fifth, although the 2 ICUs have exclusive nursing staff and attending physicians, the housestaff and respiratory therapists do rotate between the 2 ICUs and place orders in the common CPOE. The rotating housestaff may certainly represent a source for confounding, but the large numbers (>30) of evenly spread housestaff over the study period minimizes the potential for any trainee to be responsible for a large proportion of observed practice. Sixth, ICU attendings are the physicians of record and could influence the results. Because no attending physician was on service for more than 4 weeks during the study period, and patients were equally spread over this same time, concerns about clustering and biases this may have created should be minimal but cannot be ruled out. Seventh, some interventions and processes, such as antibiotic administration and measurement of lactate, may have been initiated in the ED, thereby decreasing the potential for differences between the groups. Additionally, we cannot rule out the possibility that factors other than bed availability drove the admission process (we found that the relative proportion of patients admitted to overflow ICU during hours of ambulance diversion was similar to the overflow ICU admissions during non‐ambulance diversion hours). It is possible that some selection bias by the hospitalist assigning patients to specific ICUs influenced their triage decisionsalthough all triaging doctors go through the same process of training in active bed management.11 While more patients admitted to the MICU had severe sepsis, there were no differences between groups in APACHE II or SOFA scores. However, we cannot rule out that there were other residual confounders. Finally, in a small number of cases (4/41, 10%), the CICU team consulted the MICU attending for assistance. This input had the potential to reduce disparities in care between the units.
Overflowing patients to non‐primary ICUs occurs in many hospitals. Our study demonstrates that sepsis treatment for overflow patients may be similar to that received in the primary ICU. While a large multicentered and randomized trial could determine whether significant management and outcome differences exist between primary and overflow ICUs, feasibility concerns make it unlikely that such a study will ever be conducted.
Acknowledgements
Disclosure: Dr Wright is a Miller‐Coulson Family Scholar and this work is supported by the Miller‐Coulson family through the Johns Hopkins Center for Innovative Medicine. Dr Sevransky was supported with a grant from National Institute of General Medical Sciences, NIGMS K‐23‐1399. All other authors disclose no relevant or financial conflicts of interest.
Sepsis is a major cause of death in hospitalized patients.13 It is recommended that patients with sepsis be treated with early appropriate antibiotics, as well as early goal‐directed therapy including fluid and vasopressor support according to evidence‐based guidelines.46 Following such evidence‐based protocols and process‐of‐care interventions has been shown to be associated with better patient outcomes, including decreased mortality.7, 8
Most patients with severe sepsis are cared for in intensive care units (ICUs). At times, there are no beds available in the primary ICU and patients presenting to the hospital with sepsis are cared for in other units. Patients admitted to a non‐preferred clinical inpatient setting are sometimes referred to as overflow.9 ICUs can differ significantly in staffing patterns, equipment, and training.10 It is not known if overflow sepsis patients receive similar care when admitted to non‐primary ICUs.
At our hospital, we have an active bed management system led by the hospitalist division.11 This system includes protocols to place sepsis patients in the overflow ICU if the primary ICU is full. We hypothesized that process‐of‐care interventions would be more strictly adhered to when sepsis patients were in the primary ICU rather than in the overflow unit at our institution.
METHODS
Design
This was a retrospective cohort study of all patients with sepsis admitted to either the primary medical intensive care unit (MICU) or the overflow cardiac intensive care unit (CICU) at our hospital between July 2009 and February 2010. We reviewed the admission database starting with the month of February 2010 and proceeded backwards, month by month, until we reached the target number of patients.
Setting
The study was conducted at our 320‐bed, university‐affiliated academic medical center in Baltimore, MD. The MICU and the CICU are closed units that are located adjacent to each other and have 12 beds each. They are staffed by separate pools of attending physicians trained in pulmonary/critical care medicine and cardiovascular diseases, respectively, and no attending physician attends in both units. During the study period, there were 10 unique MICU and 14 unique CICU attending physicians; while most attending physicians covered the unit for 14 days, none of the physicians were on service more than 2 of the 2‐week blocks (28 days). Each unit is additionally staffed by fellows of the respective specialties, and internal medicine residents and interns belonging to the same residency program (who rotate through both ICUs). Residents and fellows are generally assigned to these ICUs for 4 continuous weeks. The assignment of specific attendings, fellows, and residents to either ICU is performed by individual division administrators on a rotational basis based on residency, fellowship, and faculty service requirements. The teams in each ICU function independently of each other. Clinical care of patients requiring the assistance of the other specialty (pulmonary medicine or cardiology) have guidance conferred via an official consultation. Orders on patients in both ICUs are written by the residents using the same computerized order entry system (CPOE) under the supervision of their attending physicians. The nursing staff is exclusive to each ICU. The respiratory therapists spend time in both units. The nursing and respiratory therapy staff in both ICUs are similarly trained and certified, and have the same patient‐to‐nursing ratios.
Subjects
All patients admitted with a possible diagnosis of sepsis to either the MICU or CICU were identified by querying the hospital electronic triage database called etriage. This Web‐based application is used to admit patients to all the Medicine services at our hospital. We employed a wide case‐finding net using keywords that included pneumonia, sepsis, hypotension, high lactate, hypoxia, UTI (urinary tract infection)/urosepsis, SIRS (systemic inflammatory response syndrome), hypothermia, and respiratory failure. A total of 197 adult patients were identified. The charts and the electronic medical record (EMR) of these patients were then reviewed to determine the presence of a sepsis diagnosis using standard consensus criteria.12 Severe sepsis was defined by sepsis associated with organ dysfunction, hypoperfusion, or hypotension using criteria described by Bone et al.12
Fifty‐six did not meet the criteria for sepsis and were excluded from the analysis. A total of 141 patients were included in the study. This being a pilot study, we did not have any preliminary data regarding adherence to sepsis guidelines in overflow ICUs to calculate appropriate sample size. However, in 2 recent studies of dedicated ICUs (Ferrer et al13 and Castellanos‐Ortega et al14), the averaged adherence to a single measure like checking of lactate level was 27% pre‐intervention and 62% post‐intervention. With alpha level 0.05 and 80% power, one would need 31 patients in each unit to detect such differences with respect to this intervention. Although this data does not necessarily apply to overflow ICUs or for combination of processes, we used a goal of having at least 31 patients in each ICU.
The study was approved by the Johns Hopkins Institutional Review Board. The need for informed consent was waived given the retrospective nature of the study.
Data Extraction Process and Procedures
The clinical data was extracted from the EMR and patient charts using a standardized data extraction instrument, modified from a case report form (CRF) used and validated in previous studies.15, 16 The following procedures were used for the data extraction:
The data extractors included 4 physicians and 1 research assistant and were trained and tested by a single expert in data review and extraction.
Lab data was transcribed directly from the EMR. Calculation of acute physiology and chronic health evaluation (APACHE II) scores were done using the website
http://www.sfar.org/subores2/apache22.html (Socit Franaise d'Anesthsie et de Ranimation). Sepsis‐related organ failure assessment (SOFA) scores were calculated using usual criteria.17Delivery of specific treatments and interventions, including their timing, was extracted from the EMR.
The attending physicians' notes were used as the final source to assign diagnoses such as presence of acute lung injury, site of infection, and record interventions.
Data Analysis
Analyses focused primarily on assessing whether patients were treated differently between the MICU and CICU. The primary exposure variables were the process‐of‐care measures. We specifically used measurement of central venous saturation, checking of lactate level, and administration of antibiotics within 60 minutes in patients with severe sepsis as our primary process‐of‐care measures.13 Continuous variables were reported as mean standard deviation, and Student's t tests were used to compare the 2 groups. Categorical data were expressed as frequency distributions, and chi‐square tests were used to identify differences between the 2 groups. All tests were 2‐tailed with statistical significance set at 0.05. Statistical analysis was performed using SPSS version 19.0. (IBM, Armonk, NY).
To overcome data constraints, we created a dichotomous variable for each of the 3 primary processes‐of‐care (indicating receipt of process or not) and then combined them into 1 dichotomous variable indicating whether or not the patients with severe sepsis received all 3 primary processes‐of‐care. The combined variable was the key independent variable in the model.
We performed logistic regression analysis on patients with severe sepsis. The equation Logit [P(ICU Type = CICU)] = + 1Combined + 2Age describes the framework of the model, with ICU type being the dependent variable, and the combined variable of patients receiving all primary measures being the independent variable and controlled for age. Logistic regression was performed using JMP (SAS Institute, Inc, Cary, NC).
We additionally performed a secondary analysis to explore possible predictors of mortality using a logistic regression model, with the event of death as the dependent variable, and age, APACHE II scores, combined processes‐of‐care, and ICU type included as independent variables.
RESULTS
There were 100 patients admitted to the MICU and 41 patients admitted to the CICU during the study period (Table 1). The majority of the patients were admitted to the ICUs directly from the emergency department (ED) (n = 129), with a small number of patients who were transferred from the Medicine floors (n = 12).
| MICU (N =100) | CICU (N =41) | P Value | |
|---|---|---|---|
| |||
| Age in years, mean SD | 67 14.8 | 72 15.1 | 0.11 |
| Female, n (%) | 57 (57) | 27 (66) | 0.33 |
| Patients with chronic organ insufficiency, n (%) | 59 (59) | 22 (54) | 0.56 |
| Patients with severe sepsis, n (%) | 88 (88) | 21 (51) | <0.001 |
| Patients needing mechanical ventilation, n (%) | 43 (43) | 14 (34) | 0.33 |
| APACHE II score, mean SD | 25.53 9.11 | 24.37 9.53 | 0.50 |
| SOFA score on day 1, mean SD | 7.09 3.55 | 6.71 4.57 | 0.60 |
| Patients with acute lung injury on presentation, n (%) | 8 (8) | 2 (5) | 0.50 |
There were no significant differences between the 2 study groups in terms of age, sex, primary site of infection, mean APACHE II score, SOFA scores on day 1, chronic organ insufficiency, immune suppression, or need for mechanical ventilation (Table 1). The most common site of infection was lung. There were significantly more patients with severe sepsis in the MICU (88% vs 51%, P <0.001).
Sepsis Process‐of‐Care Measures
There were no significant differences in the proportion of severe sepsis patients who had central venous saturation checked (MICU: 46% vs CICU: 41%, P = 0.67), lactate level checked (95% vs 100%, P = 0.37), or received antibiotics within 60 minutes of presentation (75% vs 69%, P = 0.59) (Table 2). Multiple other processes and treatments were delivered similarly, as shown in Table 2.
| Primary Process‐of‐Care Measures (Severe Sepsis Patients) | MICU (N = 88) | CICU (N = 21) | P Value |
|---|---|---|---|
| |||
| Patients with central venous oxygen saturation checked, n (%)* | 31 (46) | 7 (41) | 0.67 |
| Patients with lactate level checked, n (%)* | 58 (95) | 16 (100) | 0.37 |
| Received antibiotics within 60 min, n (%)* | 46 (75) | 11 (69) | 0.59 |
| Patients who had all 3 above processes and treatments, n (%) | 19 (22) | 4 (19) | 0.79 |
| Received vasopressor, n (%) | 25 (28) | 8 (38) | 0.55 |
| ICU Treatments and Processes (All Sepsis Patients) | (N =100) | (N = 41) | |
| Fluid balance 24 h after admission in liters, mean SD | 1.96 2.42 | 1.42 2.63 | 0.24 |
| Patients who received stress dose steroids, n (%) | 11 (11) | 4 (10) | 0.83 |
| Patients who received Drotrecogin alfa, n (%) | 0 (0) | 0 (0) | |
| Morning glucose 24 h after admission in mg/dL, mean SD | 161 111 | 144 80 | 0.38 |
| Received DVT prophylaxis within 24 h of admission, n (%) | 74 (74) | 20 (49) | 0.004 |
| Received GI prophylaxis within 24 h of admission, n (%) | 68 (68) | 18 (44) | 0.012 |
| Received RBC transfusion within 24 h of admission, n (%) | 8 (8) | 7 (17) | 0.11 |
| Received renal replacement therapy, n (%) | 13 (13) | 3 (7) | 0.33 |
| Received a spontaneous breathing trial within 24 h of admission, n (%)* | 4 (11) | 4 (33) | 0.07 |
Logistic regression analysis examining the receipt of all 3 primary processes‐of‐care while controlling for age revealed that the odds of the being in one of the ICUs was not significantly different (P = 0.85). The secondary analysis regression models revealed that only the APACHE II score (odds ratio [OR] = 1.21; confidence interval [CI], 1.121.31) was significantly associated with higher odds of mortality. ICU‐type [MICU vs CICU] (OR = 1.85; CI, 0.428.20), age (OR = 1.01; CI, 0.971.06), and combined processes of care (OR = 0.26; CI, 0.071.01) did not have significant associations with odds of mortality.
A review of microbiologic sensitivities revealed a trend towards significance that the cultured microorganism(s) was likely to be resistant to the initial antibiotics administered in MICU vs CICU (15% vs 5%, respectively, P = 0.09).
Mechanical Ventilation Parameters
The majority of the ventilated patients were admitted to each ICU in assist control (AC) mode. There were no significant differences in categories of mean tidal volume (TV) (P = 0.3), mean plateau pressures (P = 0.12), mean fraction of inspired oxygen (FiO2) (P = 0.95), and mean positive end‐expiratory pressures (PEEP) (P = 0.98) noted across the 2 units at the time of ICU admission, and also 24 hours after ICU admission. Further comparison of measurements of tidal volumes and plateau pressures over 7 days of ICU stay revealed no significant differences in the 2 ICUs (P = 0.40 and 0.57, respectively, on day 7 of ICU admission). There was a trend towards significance in fewer patients in the MICU receiving spontaneous breathing trial within 24 hours of ICU admission (11% vs 33%, P = 0.07) (Table 2).
Patient Outcomes
There were no significant differences in ICU mortality (MICU 19% vs CICU 10%, P = 0.18), or hospital mortality (21% vs 15%, P = 0.38) across the units (Table 3). Mean ICU and hospital length of stay (LOS) and proportion of patients discharged home with unassisted breathing were similar (Table 3).
| Patient Outcomes | MICU (N = 100) | CICU (N = 41) | P Value |
|---|---|---|---|
| |||
| ICU mortality, n (%) | 19 (19) | 4 (10) | 0.18 |
| Hospital mortality, n (%) | 21 (21) | 6 (15) | 0.38 |
| Discharged home with unassisted breathing, n (%) | 33 (33) | 19 (46) | 0.14 |
| ICU length of stay in days, mean SD | 4.78 6.24 | 4.92 6.32 | 0.97 |
| Hospital length of stay in days, mean SD | 9.68 9.22 | 9.73 9.33 | 0.98 |
DISCUSSION
Since sepsis is more commonly treated in the medical ICU and some data suggests that specialty ICUs may be better at providing desired care,18, 19 we believed that patients treated in the MICU would be more likely to receive guideline‐concordant care. The study refutes our a priori hypothesis and reveals that evidence‐based processes‐of‐care associated with improved outcomes for sepsis are similarly implemented at our institution in the primary and overflow ICU. These findings are important, as ICU bed availability is a frequent problem and many hospitals overflow patients to non‐primary ICUs.9, 20
The observed equivalence in the care delivered may be a function of the relatively high number of patients with sepsis treated in the overflow unit, thereby giving the delivery teams enough experience to provide the desired care. An alternative explanation could be that the residents in CICU brought with them the experience from having previously trained in the MICU. Although, some of the care processes for sepsis patients are influenced by the CPOE (with embedded order sets and protocols), it is unlikely that CPOE can fully account for similarity in care because many processes and therapies (like use of steroids, amount of fluid delivered in first 24 hours, packed red blood cells [PRBC] transfusion, and spontaneous breathing trials) are not embedded within order sets.
The significant difference noted in the areas of deep vein thrombosis (DVT) and gastrointestinal (GI) prophylaxis within 24 hours of ICU admission was unexpected. These preventive therapies are included in initial order sets in the CPOE, which prompt physicians to order them as standard‐of‐care. With respect to DVT prophylaxis, we suspect that some of the difference might be attributable to specific contraindications to its use, which could have been more common in one of the units. There were more patients in MICU on mechanical ventilation (although not statistically significant) and with severe sepsis (statistically significant) at time of admission, which might have contributed to the difference noted in use of GI prophylaxis. It is also plausible that these differences might have disappeared if they were reassessed beyond 24 hours into the ICU admission. We cannot rule out the presence of unit‐ and physician‐level differences that contributed to this. Likewise, there was an unexpected trend towards significance, wherein more patients in CICU had spontaneous breathing trials within 24 hours of admission. This might also be explained by the higher number of patients with severe sepsis in the MICU (preempting any weaning attempts). These caveats aside, it is reassuring that, at our institution, admitting septic patients to the first available ICU bed does not adversely affect important processes‐of‐care.
One might ask whether this study's data should reassure other sites who are boarding septic patients in non‐primary ICUs. Irrespective of the number of patients studied or the degree of statistical significance of the associations, an observational study design cannot prove that boarding septic patients in non‐primary ICUs is either safe or unsafe. However, we hope that readers reflect on, and take inventory of, systems issues that may be different between unitswith an eye towards eliminating variation such that all units managing septic patients are primed to deliver guideline‐concordant care. Other hospitals that use CPOE with sepsis order sets, have protocols for sepsis care, and who train nursing and respiratory therapists to meet high standards might be pleased to see that the patients in our study received comparable, high‐quality care across the 2 units. While our data suggests that boarding patients in overflow units may be safe, these findings would need to be replicated at other sites using prospective designs to prove safety.
Length of emergency room stay prior to admission is associated with higher mortality rates.2123 At many hospitals, critical care beds are a scarce resource such that most hospitals have a policy for the triage of patients to critical care beds.24, 25 Lundberg and colleagues' study demonstrated that patients who developed septic shock on the medical wards experienced delays in receipt of intravenous fluids, inotropic agents and transfer to a critical care setting.26 Thus, rather than waiting in the ED or on the medical service for an MICU bed to become available, it may be most wise to admit a critically sick septic patient to the first available ICU bed, even to an overflow ICU. In a recent study by Sidlow and Aggarwal, 1104 patients discharged from the coronary care unit (CCU) with a non‐cardiac primary diagnosis were compared to patients admitted to the MICU in the same hospital.27 The study found no differences in patient mortality, 30‐day readmission rate, hospital LOS, ICU LOS, and safety outcomes of ventilator‐associated pneumonia and catheter‐associated bloodstream infections between ICUs. However, their study did not examine processes‐of‐care delivered between the primary ICU and the overflow unit, and did not validate the primary diagnoses of patients admitted to the ICU.
Several limitations of this study should be considered. First, this study was conducted at a single center. Second, we used a retrospective study design; however, a prospective study randomizing patients to 1 of the 2 units would likely never be possible. Third, the relatively small number of patients limited the power of the study to detect mortality differences between the units. However, this was a pilot study focused on processes of care as opposed to clinical outcomes. Fourth, it is possible that we did not capture every single patient with sepsis with our keyword search. Our use of a previously validated screening process should have limited the number of missed cases.15, 16 Fifth, although the 2 ICUs have exclusive nursing staff and attending physicians, the housestaff and respiratory therapists do rotate between the 2 ICUs and place orders in the common CPOE. The rotating housestaff may certainly represent a source for confounding, but the large numbers (>30) of evenly spread housestaff over the study period minimizes the potential for any trainee to be responsible for a large proportion of observed practice. Sixth, ICU attendings are the physicians of record and could influence the results. Because no attending physician was on service for more than 4 weeks during the study period, and patients were equally spread over this same time, concerns about clustering and biases this may have created should be minimal but cannot be ruled out. Seventh, some interventions and processes, such as antibiotic administration and measurement of lactate, may have been initiated in the ED, thereby decreasing the potential for differences between the groups. Additionally, we cannot rule out the possibility that factors other than bed availability drove the admission process (we found that the relative proportion of patients admitted to overflow ICU during hours of ambulance diversion was similar to the overflow ICU admissions during non‐ambulance diversion hours). It is possible that some selection bias by the hospitalist assigning patients to specific ICUs influenced their triage decisionsalthough all triaging doctors go through the same process of training in active bed management.11 While more patients admitted to the MICU had severe sepsis, there were no differences between groups in APACHE II or SOFA scores. However, we cannot rule out that there were other residual confounders. Finally, in a small number of cases (4/41, 10%), the CICU team consulted the MICU attending for assistance. This input had the potential to reduce disparities in care between the units.
Overflowing patients to non‐primary ICUs occurs in many hospitals. Our study demonstrates that sepsis treatment for overflow patients may be similar to that received in the primary ICU. While a large multicentered and randomized trial could determine whether significant management and outcome differences exist between primary and overflow ICUs, feasibility concerns make it unlikely that such a study will ever be conducted.
Acknowledgements
Disclosure: Dr Wright is a Miller‐Coulson Family Scholar and this work is supported by the Miller‐Coulson family through the Johns Hopkins Center for Innovative Medicine. Dr Sevransky was supported with a grant from National Institute of General Medical Sciences, NIGMS K‐23‐1399. All other authors disclose no relevant or financial conflicts of interest.
- ,,,,,.Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care.Crit Care Med.2001;29(7):1303–1310.
- ,,, et al;for the Milwaukee Initiative in Critical Care Outcomes Research (MICCOR) Group of Investigators.Nationwide trends of severe sepsis in the twenty first century (2000–2007).Chest.2011;140(5):1223–1231.
- ,,,.Rapid increase in hospitalization and mortality rates for severe sepsis in the United States: a trend analysis from 1993 to 2003.Crit Care Med.2007;35(5):1244–1250.
- ,,, et al.Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2008.Crit Care Med.2008;36(1):296–327.
- ,,, et al.Lactate clearance vs central venous oxygen saturation as goals of early sepsis therapy: a randomized clinical trial.JAMA.2010;303(8):739–746.
- ,,, et al.Early goal‐directed therapy in the treatment of severe sepsis and septic shock.N Engl J Med.2001;345(19):1368–1377.
- ,,, et al.Implementation of a bundle of quality indicators for the early management of severe sepsis and septic shock is associated with decreased mortality.Crit Care Med.2007;35(4):1105–1112.
- ,,, et al.Early combination antibiotic therapy yields improved survival compared with monotherapy in septic shock: a propensity‐matched analysis.Crit Care Med.2010;38(9):1773–1785.
- .A new dimension of the PACU: the dilemma of the ICU overflow patient.J Post Anesth Nurs.1994;9(5):297–300.
- ,,, et al.Descriptive analysis of critical care units in the United States.Crit Care Med.1992;20(6):846–863.
- ,,,,,.Active bed management by hospitalists and emergency department throughput.Ann Intern Med.2008;149(11):804–811.
- ,,, et al.Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee, American College of Chest Physicians/Society of Critical Care Medicine.Chest.1992;101(6):1644–1655.
- ,,, et al.Improvement in process of care and outcome after a multicenter severe sepsis educational program in Spain.JAMA.2008;299(19):2294–2303.
- ,,, et al.Impact of the surviving sepsis campaign protocols on hospital length of stay and mortality in septic shock patients: results of a three‐year follow‐up quasi‐experimental study.Crit Care Med.2010;38(4):1036–1043.
- ,,, et al.Study protocol: the improving care of acute lung injury patients (ICAP) study.Crit Care.2006;10(1):R9.
- ,,,,,.Critical illness outcome study: an observational study of protocols and mortality in intensive care units.Open Access J Clin Trials.2011;3(September):55–65.
- ,,, et al.The SOFA (sepsis‐related organ failure assessment) score to describe organ dysfunction/failure: on behalf of the Working Group on Sepsis‐Related Problems of the European Society of Intensive Care Medicine.Intensive Care Med.1996;22(7):707–710.
- ,,,,,.Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review.JAMA.2002;288(17):2151–2162.
- ,,.Do intensivists in ICU improve outcome?Best Pract Res Clin Anaesthesiol.2005;19(1):125–135.
- .Is the postanesthesia care unit becoming an intensive care unit?J Perianesth Nurs.1999;14(2):73–77.
- ,,,,;for the DELAY‐ED Study Group.Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit.Crit Care Med.2007;35(6):1477–1483.
- ,,, et al.Association between timing of intensive care unit admission and outcomes for emergency department patients with community‐acquired pneumonia.Crit Care Med.2009;37(11):2867–2874.
- ,.Association between ambulance diversion and survival among patients with acute myocardial infarction.JAMA.2011;305(23):2440–2447.
- .Civilian triage in the intensive care unit: the ritual of the last bed.Crit Care Med.1993;21(4):598–606.
- ,,,,;for the Values Ethics and Rationing in Critical Care Task Force.Rationing critical care beds: a systematic review.Crit Care Med.2004;32(7):1588–1597.
- ,,, et al.Septic shock: an analysis of outcomes for patients with onset on hospital wards versus intensive care units.Crit Care Med.1998;26(6):1020–1024.
- ,.“The MICU is full”: one hospital's experience with an overflow triage policy.Jt Comm J Qual Patient Saf.2011;37(10):456–460.
- ,,,,,.Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care.Crit Care Med.2001;29(7):1303–1310.
- ,,, et al;for the Milwaukee Initiative in Critical Care Outcomes Research (MICCOR) Group of Investigators.Nationwide trends of severe sepsis in the twenty first century (2000–2007).Chest.2011;140(5):1223–1231.
- ,,,.Rapid increase in hospitalization and mortality rates for severe sepsis in the United States: a trend analysis from 1993 to 2003.Crit Care Med.2007;35(5):1244–1250.
- ,,, et al.Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2008.Crit Care Med.2008;36(1):296–327.
- ,,, et al.Lactate clearance vs central venous oxygen saturation as goals of early sepsis therapy: a randomized clinical trial.JAMA.2010;303(8):739–746.
- ,,, et al.Early goal‐directed therapy in the treatment of severe sepsis and septic shock.N Engl J Med.2001;345(19):1368–1377.
- ,,, et al.Implementation of a bundle of quality indicators for the early management of severe sepsis and septic shock is associated with decreased mortality.Crit Care Med.2007;35(4):1105–1112.
- ,,, et al.Early combination antibiotic therapy yields improved survival compared with monotherapy in septic shock: a propensity‐matched analysis.Crit Care Med.2010;38(9):1773–1785.
- .A new dimension of the PACU: the dilemma of the ICU overflow patient.J Post Anesth Nurs.1994;9(5):297–300.
- ,,, et al.Descriptive analysis of critical care units in the United States.Crit Care Med.1992;20(6):846–863.
- ,,,,,.Active bed management by hospitalists and emergency department throughput.Ann Intern Med.2008;149(11):804–811.
- ,,, et al.Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee, American College of Chest Physicians/Society of Critical Care Medicine.Chest.1992;101(6):1644–1655.
- ,,, et al.Improvement in process of care and outcome after a multicenter severe sepsis educational program in Spain.JAMA.2008;299(19):2294–2303.
- ,,, et al.Impact of the surviving sepsis campaign protocols on hospital length of stay and mortality in septic shock patients: results of a three‐year follow‐up quasi‐experimental study.Crit Care Med.2010;38(4):1036–1043.
- ,,, et al.Study protocol: the improving care of acute lung injury patients (ICAP) study.Crit Care.2006;10(1):R9.
- ,,,,,.Critical illness outcome study: an observational study of protocols and mortality in intensive care units.Open Access J Clin Trials.2011;3(September):55–65.
- ,,, et al.The SOFA (sepsis‐related organ failure assessment) score to describe organ dysfunction/failure: on behalf of the Working Group on Sepsis‐Related Problems of the European Society of Intensive Care Medicine.Intensive Care Med.1996;22(7):707–710.
- ,,,,,.Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review.JAMA.2002;288(17):2151–2162.
- ,,.Do intensivists in ICU improve outcome?Best Pract Res Clin Anaesthesiol.2005;19(1):125–135.
- .Is the postanesthesia care unit becoming an intensive care unit?J Perianesth Nurs.1999;14(2):73–77.
- ,,,,;for the DELAY‐ED Study Group.Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit.Crit Care Med.2007;35(6):1477–1483.
- ,,, et al.Association between timing of intensive care unit admission and outcomes for emergency department patients with community‐acquired pneumonia.Crit Care Med.2009;37(11):2867–2874.
- ,.Association between ambulance diversion and survival among patients with acute myocardial infarction.JAMA.2011;305(23):2440–2447.
- .Civilian triage in the intensive care unit: the ritual of the last bed.Crit Care Med.1993;21(4):598–606.
- ,,,,;for the Values Ethics and Rationing in Critical Care Task Force.Rationing critical care beds: a systematic review.Crit Care Med.2004;32(7):1588–1597.
- ,,, et al.Septic shock: an analysis of outcomes for patients with onset on hospital wards versus intensive care units.Crit Care Med.1998;26(6):1020–1024.
- ,.“The MICU is full”: one hospital's experience with an overflow triage policy.Jt Comm J Qual Patient Saf.2011;37(10):456–460.
Copyright © 2012 Society of Hospital Medicine