User login
Fetal Spina Bifida Surgery: Balancing Access and Outcomes
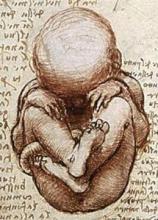
Most medical decisions come down to weighing risks and benefits, and trying to ensure that the balance falls to the good.
About 18 months ago, the diminutive medical and surgical niche that’s fetal surgery (fewer than 1,000 U.S. fetal surgical procedures are done annually) came out with the blockbuster finding that fetal surgery to repair myelomeningoceles and blunt the complications of spina bifida was relatively safe and produced substantial benefits, compared with more conventional treatments that affected infants and children undergo when treatment starts after birth.
To help ensure an adequate number of cases in MOMS (Management of Myelomeningocele Study) to produce a meaningful result in a reasonable amount of time, the couple of dozen or so U.S. medical centers that offer fetal surgery agreed to limit fetal-myelomeningocele repair to three U.S. locations: the Children’s Hospital of Philadelphia (CHOP); Monroe Carell Jr. Children’s Hospital at Vanderbilt University in Nashville, Tenn.; and the University of California, San Francisco (UCSF). Even when all U.S. cases were funneled into these three sites during 8 years, the study enrolled all of 183 cases. The landmark 2011 report on outcomes in MOMS 1 year following birth had data on the first 158 cases (78 fetuses that underwent in utero myelomeningocele repair and 80 control pregnancies for which interventions occurred after birth).
The fetal-myelomeningocele repair world quickly began to change once the New England Journal paper came out in March 2011. The surgery was no longer investigational, and other U.S. centers could get into the act, if they wanted, and if they dared.
During the nearly 18 months since then, about five new programs jumped into the myelomeningocele-repair pool. That number is a little uncertain because no one keeps "official" tabs on who does the surgery, nor is there any official tally of how many fetal repairs are done, or their results. What is clear is that in the 18 months since the MOMS report, roughly 100 fetal myelomeningocele repairs were done in the United States, more than during 8 years of MOMS from February 2003 through the end of 2010.
And, at least as of now, no information is on record for how those 100 or so most recent cases have fared, including the outcomes from the new programs. That’s largely because it takes at least a year following delivery of a repaired fetus to have outcome results with follow-up similar to MOMS, and if you do the math, that means the outcomes from even the first post-MOMS cases are just now trickling in.
The risk-benefit balance at work here is this: Can new centers offer fetal myelomeningocele repairs – an understandably challenging technical undertaking – to boost access to mothers and their affected fetuses, while at the same time ensuring that their outcomes are at least as good as what happened in MOMS? It’s a question that’s not yet been answered.
It’s also a question that so troubled officials at the Eunice Kennedy Shriver National Institute of Child Health and Human Development – the U.S. agency that funded MOMS – that soon after the MOMS result came out, the institute took the unusual step of organizing a panel of experts to come up with guidelines on what a program should have in place if it wanted to venture into the fetal-myelomeningocele repair business. Those recommendations are still in process and are expected out before the end of this year. A preview was offered in June by some UCSF clinicians, but I’ve been told that their summary of the pending guidelines is not completely up to date.
The wider-access issue is very real. I spoke about it with Dr. Foong-Yen Lim, surgical director of the fetal care center at Cincinnati Children’s Hospital, one of the newbie programs that began offering this fetal surgery post MOMS, and that as of mid-August had done 10 cases. Having fetal-myelomeningocele repair available at more U.S. sites is important because during MOMS, when only three sites were available, he knew of cases in which the parents of affected fetuses opted not to go out of town for fetal repair because they could not afford it or could not deal with the relocation. Of course, some patients also might have not wanted to commit to being part a study knowing that once in, they had a 50-50 chance of randomization to standard care.
Dr. Lim told me how deeply he felt the responsibility he and his associates took on when they decided to start offering fetal-myelomeningocele repair and thereby boost access for affected families in the Cincinnati area. "People who take on this procedure need to ask themselves ‘Are we doing as good a job as the other places?’ " he said. He also told me that Cincinnati Children’s counselors make it clear to prospective families that if they prefer, they could travel to CHOP, Vanderbilt, or UCSF, the U.S. sites with the most experience and best-documented track records.
It’s all a balance of risk and benefit.
–Mitchel L. Zoler (on Twitter @mitchelzoler)
Most medical decisions come down to weighing risks and benefits, and trying to ensure that the balance falls to the good.
About 18 months ago, the diminutive medical and surgical niche that’s fetal surgery (fewer than 1,000 U.S. fetal surgical procedures are done annually) came out with the blockbuster finding that fetal surgery to repair myelomeningoceles and blunt the complications of spina bifida was relatively safe and produced substantial benefits, compared with more conventional treatments that affected infants and children undergo when treatment starts after birth.
To help ensure an adequate number of cases in MOMS (Management of Myelomeningocele Study) to produce a meaningful result in a reasonable amount of time, the couple of dozen or so U.S. medical centers that offer fetal surgery agreed to limit fetal-myelomeningocele repair to three U.S. locations: the Children’s Hospital of Philadelphia (CHOP); Monroe Carell Jr. Children’s Hospital at Vanderbilt University in Nashville, Tenn.; and the University of California, San Francisco (UCSF). Even when all U.S. cases were funneled into these three sites during 8 years, the study enrolled all of 183 cases. The landmark 2011 report on outcomes in MOMS 1 year following birth had data on the first 158 cases (78 fetuses that underwent in utero myelomeningocele repair and 80 control pregnancies for which interventions occurred after birth).
The fetal-myelomeningocele repair world quickly began to change once the New England Journal paper came out in March 2011. The surgery was no longer investigational, and other U.S. centers could get into the act, if they wanted, and if they dared.
During the nearly 18 months since then, about five new programs jumped into the myelomeningocele-repair pool. That number is a little uncertain because no one keeps "official" tabs on who does the surgery, nor is there any official tally of how many fetal repairs are done, or their results. What is clear is that in the 18 months since the MOMS report, roughly 100 fetal myelomeningocele repairs were done in the United States, more than during 8 years of MOMS from February 2003 through the end of 2010.
And, at least as of now, no information is on record for how those 100 or so most recent cases have fared, including the outcomes from the new programs. That’s largely because it takes at least a year following delivery of a repaired fetus to have outcome results with follow-up similar to MOMS, and if you do the math, that means the outcomes from even the first post-MOMS cases are just now trickling in.
The risk-benefit balance at work here is this: Can new centers offer fetal myelomeningocele repairs – an understandably challenging technical undertaking – to boost access to mothers and their affected fetuses, while at the same time ensuring that their outcomes are at least as good as what happened in MOMS? It’s a question that’s not yet been answered.
It’s also a question that so troubled officials at the Eunice Kennedy Shriver National Institute of Child Health and Human Development – the U.S. agency that funded MOMS – that soon after the MOMS result came out, the institute took the unusual step of organizing a panel of experts to come up with guidelines on what a program should have in place if it wanted to venture into the fetal-myelomeningocele repair business. Those recommendations are still in process and are expected out before the end of this year. A preview was offered in June by some UCSF clinicians, but I’ve been told that their summary of the pending guidelines is not completely up to date.
The wider-access issue is very real. I spoke about it with Dr. Foong-Yen Lim, surgical director of the fetal care center at Cincinnati Children’s Hospital, one of the newbie programs that began offering this fetal surgery post MOMS, and that as of mid-August had done 10 cases. Having fetal-myelomeningocele repair available at more U.S. sites is important because during MOMS, when only three sites were available, he knew of cases in which the parents of affected fetuses opted not to go out of town for fetal repair because they could not afford it or could not deal with the relocation. Of course, some patients also might have not wanted to commit to being part a study knowing that once in, they had a 50-50 chance of randomization to standard care.
Dr. Lim told me how deeply he felt the responsibility he and his associates took on when they decided to start offering fetal-myelomeningocele repair and thereby boost access for affected families in the Cincinnati area. "People who take on this procedure need to ask themselves ‘Are we doing as good a job as the other places?’ " he said. He also told me that Cincinnati Children’s counselors make it clear to prospective families that if they prefer, they could travel to CHOP, Vanderbilt, or UCSF, the U.S. sites with the most experience and best-documented track records.
It’s all a balance of risk and benefit.
–Mitchel L. Zoler (on Twitter @mitchelzoler)
Most medical decisions come down to weighing risks and benefits, and trying to ensure that the balance falls to the good.
About 18 months ago, the diminutive medical and surgical niche that’s fetal surgery (fewer than 1,000 U.S. fetal surgical procedures are done annually) came out with the blockbuster finding that fetal surgery to repair myelomeningoceles and blunt the complications of spina bifida was relatively safe and produced substantial benefits, compared with more conventional treatments that affected infants and children undergo when treatment starts after birth.
To help ensure an adequate number of cases in MOMS (Management of Myelomeningocele Study) to produce a meaningful result in a reasonable amount of time, the couple of dozen or so U.S. medical centers that offer fetal surgery agreed to limit fetal-myelomeningocele repair to three U.S. locations: the Children’s Hospital of Philadelphia (CHOP); Monroe Carell Jr. Children’s Hospital at Vanderbilt University in Nashville, Tenn.; and the University of California, San Francisco (UCSF). Even when all U.S. cases were funneled into these three sites during 8 years, the study enrolled all of 183 cases. The landmark 2011 report on outcomes in MOMS 1 year following birth had data on the first 158 cases (78 fetuses that underwent in utero myelomeningocele repair and 80 control pregnancies for which interventions occurred after birth).
The fetal-myelomeningocele repair world quickly began to change once the New England Journal paper came out in March 2011. The surgery was no longer investigational, and other U.S. centers could get into the act, if they wanted, and if they dared.
During the nearly 18 months since then, about five new programs jumped into the myelomeningocele-repair pool. That number is a little uncertain because no one keeps "official" tabs on who does the surgery, nor is there any official tally of how many fetal repairs are done, or their results. What is clear is that in the 18 months since the MOMS report, roughly 100 fetal myelomeningocele repairs were done in the United States, more than during 8 years of MOMS from February 2003 through the end of 2010.
And, at least as of now, no information is on record for how those 100 or so most recent cases have fared, including the outcomes from the new programs. That’s largely because it takes at least a year following delivery of a repaired fetus to have outcome results with follow-up similar to MOMS, and if you do the math, that means the outcomes from even the first post-MOMS cases are just now trickling in.
The risk-benefit balance at work here is this: Can new centers offer fetal myelomeningocele repairs – an understandably challenging technical undertaking – to boost access to mothers and their affected fetuses, while at the same time ensuring that their outcomes are at least as good as what happened in MOMS? It’s a question that’s not yet been answered.
It’s also a question that so troubled officials at the Eunice Kennedy Shriver National Institute of Child Health and Human Development – the U.S. agency that funded MOMS – that soon after the MOMS result came out, the institute took the unusual step of organizing a panel of experts to come up with guidelines on what a program should have in place if it wanted to venture into the fetal-myelomeningocele repair business. Those recommendations are still in process and are expected out before the end of this year. A preview was offered in June by some UCSF clinicians, but I’ve been told that their summary of the pending guidelines is not completely up to date.
The wider-access issue is very real. I spoke about it with Dr. Foong-Yen Lim, surgical director of the fetal care center at Cincinnati Children’s Hospital, one of the newbie programs that began offering this fetal surgery post MOMS, and that as of mid-August had done 10 cases. Having fetal-myelomeningocele repair available at more U.S. sites is important because during MOMS, when only three sites were available, he knew of cases in which the parents of affected fetuses opted not to go out of town for fetal repair because they could not afford it or could not deal with the relocation. Of course, some patients also might have not wanted to commit to being part a study knowing that once in, they had a 50-50 chance of randomization to standard care.
Dr. Lim told me how deeply he felt the responsibility he and his associates took on when they decided to start offering fetal-myelomeningocele repair and thereby boost access for affected families in the Cincinnati area. "People who take on this procedure need to ask themselves ‘Are we doing as good a job as the other places?’ " he said. He also told me that Cincinnati Children’s counselors make it clear to prospective families that if they prefer, they could travel to CHOP, Vanderbilt, or UCSF, the U.S. sites with the most experience and best-documented track records.
It’s all a balance of risk and benefit.
–Mitchel L. Zoler (on Twitter @mitchelzoler)
Putting ECGs to the Test
Electrocardiography to test a child’s heart prior to sports participation can help identify some – but not all – causes of sudden cardiac death.
Offering this test is not without debate, however, whether your patient is a young athlete about to start a sports program or a student about to start stimulant medication for attention-deficit/hyperactivity disorder.
Your clinical judgment remains paramount, as ECG screening before sports is not mandated in the United States, but placing your patient in one of the following three categories can help guide diagnosis and management:
• Asymptomatic child, normal physical exam. Most of the patients you see for a sports evaluation will be asymptomatic. Perform the physical examination and take a thorough history, with a specific look for any signs of sudden cardiac death such as family history or previous symptoms. In general, this evaluation will suffice and you will not need to order blood assays or other tests. If you want to augment your evaluation by ordering an ECG, you will be ahead of the curve. Most pediatricians manage these kids whether they order an ECG or not. If you’re uncertain or uncomfortable for any reason at this point, consider referral.
• Symptomatic child. Children in this group may describe palpitations, chest pain, and/or an instance when they felt they were about to pass out (syncope or presyncope). The symptomatic child should be evaluated further if you have any clinical concerns, and ECG is a good starting point. Unless you feel very comfortable, consider specialist consultation and comanagement of these patients. Watch especially for exercise-related syncope. For me, passing out with exercise is a red flag because it’s one of the few specific signs of structural heart disease. At a minimum, evaluations of rhythm (ECG) and structure (echocardiography) are indicated, and sometimes an electrophysiology work-up can be helpful.
• Asymptomatic child, some examination findings. Some asymptomatic children have a potentially relevant clinical finding, such as a murmur. Most innocent murmurs are monitored appropriately in the primary care setting, but referral is more strongly suggested for murmurs of concern, which include holosystolic murmurs, grade 3-6 murmurs, and diastolic murmurs. An ECG is still an excellent starting point, but you have a choice. Some pediatric cardiologists also would recommend an echocardiogram or just a referral to them for further work-up. You don’t always have to rush to echocardiography. (Some would argue there are too many echoes ordered right off the bat, and I think there are too few initial ECGs ordered.)
Much of your management strategy depends on your comfort level. Most pediatricians can read an ECG and immediately know that something is not right if they see a significantly prolonged QT interval or WPW (Wolff-Parkinson-White syndrome) changes. I’ve learned, however, that most of the pediatricians at our institution would be uncomfortable making the call regarding some of the more subtle ECG findings. Many pediatricians’ offices do not have ECG equipment, so the patient will be sent elsewhere anyway.
Screening Before an ADHD Regimen
Consideration of ECG screening also comes up prior to prescription of an ADHD stimulant medication.
Unfortunately, a small number of deaths have been associated with use of these medications. Some of those patients had underlying congenital and structural heart disease that some believe could have been identified with a simple ECG. Most people would agree to some sort of cardiovascular monitoring, such as blood pressure or heart rate measurements. Complicating matters is the increased risk of ADHD in children with congenital heart anomalies.
Proceeding with an ECG screen doesn’t rule out prescribing the ADHD medicine, according to the recommendation, but it might be worthwhile to have a pediatric cardiologist manage any particular clinical concerns.
False-Positive Results
ECGs are safe and very inexpensive if you already have the equipment. The biggest debate about ECGs in the world of sports medicine centers on high false-positive rates. Depending on how the ECG is read and which criteria you use, the false positive rate can be as low as 2% or as high as 15%. Using the right criteria removes some of the unnecessary false positives and can reduce the rate to a more acceptable 2%-5%. In my opinion, that rate is low enough to justify offering low-cost ECGs for those who would like to be screened.
Interestingly, some of the false-positive findings are not as concerning among young athletes. Examples are an incomplete right bundle branch block, early repolarization, isolated QRS voltage criteria for left ventricular hypertrophy, and first-degree atrioventricular block. Some experts argue that if we remove these specific findings, we will be left primarily with the most concerning ones and thus can improve the false-positive rate.
This greater reliability may be reflected by emerging ECG-screening programs across this country. We at Loyola University Health System are in the process of trying to develop one of the first ECG-screening programs at a medical center. Precedents from ECG guidelines for older athletes may be adaptable to protect pediatric patients; about half of large university athletic programs perform ECG screening. In addition, the majority of professional athletes undergo cardiac evaluations.
Dr. Jayanthi is with the department of family medicine and the department of orthopaedic surgery and rehabilitation and also the medical director of primary care sports medicine at Loyola University Chicago in Maywood, Ill. Dr. Jayanthi said that he had no relevant financial disclosures.
Electrocardiography to test a child’s heart prior to sports participation can help identify some – but not all – causes of sudden cardiac death.
Offering this test is not without debate, however, whether your patient is a young athlete about to start a sports program or a student about to start stimulant medication for attention-deficit/hyperactivity disorder.
Your clinical judgment remains paramount, as ECG screening before sports is not mandated in the United States, but placing your patient in one of the following three categories can help guide diagnosis and management:
• Asymptomatic child, normal physical exam. Most of the patients you see for a sports evaluation will be asymptomatic. Perform the physical examination and take a thorough history, with a specific look for any signs of sudden cardiac death such as family history or previous symptoms. In general, this evaluation will suffice and you will not need to order blood assays or other tests. If you want to augment your evaluation by ordering an ECG, you will be ahead of the curve. Most pediatricians manage these kids whether they order an ECG or not. If you’re uncertain or uncomfortable for any reason at this point, consider referral.
• Symptomatic child. Children in this group may describe palpitations, chest pain, and/or an instance when they felt they were about to pass out (syncope or presyncope). The symptomatic child should be evaluated further if you have any clinical concerns, and ECG is a good starting point. Unless you feel very comfortable, consider specialist consultation and comanagement of these patients. Watch especially for exercise-related syncope. For me, passing out with exercise is a red flag because it’s one of the few specific signs of structural heart disease. At a minimum, evaluations of rhythm (ECG) and structure (echocardiography) are indicated, and sometimes an electrophysiology work-up can be helpful.
• Asymptomatic child, some examination findings. Some asymptomatic children have a potentially relevant clinical finding, such as a murmur. Most innocent murmurs are monitored appropriately in the primary care setting, but referral is more strongly suggested for murmurs of concern, which include holosystolic murmurs, grade 3-6 murmurs, and diastolic murmurs. An ECG is still an excellent starting point, but you have a choice. Some pediatric cardiologists also would recommend an echocardiogram or just a referral to them for further work-up. You don’t always have to rush to echocardiography. (Some would argue there are too many echoes ordered right off the bat, and I think there are too few initial ECGs ordered.)
Much of your management strategy depends on your comfort level. Most pediatricians can read an ECG and immediately know that something is not right if they see a significantly prolonged QT interval or WPW (Wolff-Parkinson-White syndrome) changes. I’ve learned, however, that most of the pediatricians at our institution would be uncomfortable making the call regarding some of the more subtle ECG findings. Many pediatricians’ offices do not have ECG equipment, so the patient will be sent elsewhere anyway.
Screening Before an ADHD Regimen
Consideration of ECG screening also comes up prior to prescription of an ADHD stimulant medication.
Unfortunately, a small number of deaths have been associated with use of these medications. Some of those patients had underlying congenital and structural heart disease that some believe could have been identified with a simple ECG. Most people would agree to some sort of cardiovascular monitoring, such as blood pressure or heart rate measurements. Complicating matters is the increased risk of ADHD in children with congenital heart anomalies.
Proceeding with an ECG screen doesn’t rule out prescribing the ADHD medicine, according to the recommendation, but it might be worthwhile to have a pediatric cardiologist manage any particular clinical concerns.
False-Positive Results
ECGs are safe and very inexpensive if you already have the equipment. The biggest debate about ECGs in the world of sports medicine centers on high false-positive rates. Depending on how the ECG is read and which criteria you use, the false positive rate can be as low as 2% or as high as 15%. Using the right criteria removes some of the unnecessary false positives and can reduce the rate to a more acceptable 2%-5%. In my opinion, that rate is low enough to justify offering low-cost ECGs for those who would like to be screened.
Interestingly, some of the false-positive findings are not as concerning among young athletes. Examples are an incomplete right bundle branch block, early repolarization, isolated QRS voltage criteria for left ventricular hypertrophy, and first-degree atrioventricular block. Some experts argue that if we remove these specific findings, we will be left primarily with the most concerning ones and thus can improve the false-positive rate.
This greater reliability may be reflected by emerging ECG-screening programs across this country. We at Loyola University Health System are in the process of trying to develop one of the first ECG-screening programs at a medical center. Precedents from ECG guidelines for older athletes may be adaptable to protect pediatric patients; about half of large university athletic programs perform ECG screening. In addition, the majority of professional athletes undergo cardiac evaluations.
Dr. Jayanthi is with the department of family medicine and the department of orthopaedic surgery and rehabilitation and also the medical director of primary care sports medicine at Loyola University Chicago in Maywood, Ill. Dr. Jayanthi said that he had no relevant financial disclosures.
Electrocardiography to test a child’s heart prior to sports participation can help identify some – but not all – causes of sudden cardiac death.
Offering this test is not without debate, however, whether your patient is a young athlete about to start a sports program or a student about to start stimulant medication for attention-deficit/hyperactivity disorder.
Your clinical judgment remains paramount, as ECG screening before sports is not mandated in the United States, but placing your patient in one of the following three categories can help guide diagnosis and management:
• Asymptomatic child, normal physical exam. Most of the patients you see for a sports evaluation will be asymptomatic. Perform the physical examination and take a thorough history, with a specific look for any signs of sudden cardiac death such as family history or previous symptoms. In general, this evaluation will suffice and you will not need to order blood assays or other tests. If you want to augment your evaluation by ordering an ECG, you will be ahead of the curve. Most pediatricians manage these kids whether they order an ECG or not. If you’re uncertain or uncomfortable for any reason at this point, consider referral.
• Symptomatic child. Children in this group may describe palpitations, chest pain, and/or an instance when they felt they were about to pass out (syncope or presyncope). The symptomatic child should be evaluated further if you have any clinical concerns, and ECG is a good starting point. Unless you feel very comfortable, consider specialist consultation and comanagement of these patients. Watch especially for exercise-related syncope. For me, passing out with exercise is a red flag because it’s one of the few specific signs of structural heart disease. At a minimum, evaluations of rhythm (ECG) and structure (echocardiography) are indicated, and sometimes an electrophysiology work-up can be helpful.
• Asymptomatic child, some examination findings. Some asymptomatic children have a potentially relevant clinical finding, such as a murmur. Most innocent murmurs are monitored appropriately in the primary care setting, but referral is more strongly suggested for murmurs of concern, which include holosystolic murmurs, grade 3-6 murmurs, and diastolic murmurs. An ECG is still an excellent starting point, but you have a choice. Some pediatric cardiologists also would recommend an echocardiogram or just a referral to them for further work-up. You don’t always have to rush to echocardiography. (Some would argue there are too many echoes ordered right off the bat, and I think there are too few initial ECGs ordered.)
Much of your management strategy depends on your comfort level. Most pediatricians can read an ECG and immediately know that something is not right if they see a significantly prolonged QT interval or WPW (Wolff-Parkinson-White syndrome) changes. I’ve learned, however, that most of the pediatricians at our institution would be uncomfortable making the call regarding some of the more subtle ECG findings. Many pediatricians’ offices do not have ECG equipment, so the patient will be sent elsewhere anyway.
Screening Before an ADHD Regimen
Consideration of ECG screening also comes up prior to prescription of an ADHD stimulant medication.
Unfortunately, a small number of deaths have been associated with use of these medications. Some of those patients had underlying congenital and structural heart disease that some believe could have been identified with a simple ECG. Most people would agree to some sort of cardiovascular monitoring, such as blood pressure or heart rate measurements. Complicating matters is the increased risk of ADHD in children with congenital heart anomalies.
Proceeding with an ECG screen doesn’t rule out prescribing the ADHD medicine, according to the recommendation, but it might be worthwhile to have a pediatric cardiologist manage any particular clinical concerns.
False-Positive Results
ECGs are safe and very inexpensive if you already have the equipment. The biggest debate about ECGs in the world of sports medicine centers on high false-positive rates. Depending on how the ECG is read and which criteria you use, the false positive rate can be as low as 2% or as high as 15%. Using the right criteria removes some of the unnecessary false positives and can reduce the rate to a more acceptable 2%-5%. In my opinion, that rate is low enough to justify offering low-cost ECGs for those who would like to be screened.
Interestingly, some of the false-positive findings are not as concerning among young athletes. Examples are an incomplete right bundle branch block, early repolarization, isolated QRS voltage criteria for left ventricular hypertrophy, and first-degree atrioventricular block. Some experts argue that if we remove these specific findings, we will be left primarily with the most concerning ones and thus can improve the false-positive rate.
This greater reliability may be reflected by emerging ECG-screening programs across this country. We at Loyola University Health System are in the process of trying to develop one of the first ECG-screening programs at a medical center. Precedents from ECG guidelines for older athletes may be adaptable to protect pediatric patients; about half of large university athletic programs perform ECG screening. In addition, the majority of professional athletes undergo cardiac evaluations.
Dr. Jayanthi is with the department of family medicine and the department of orthopaedic surgery and rehabilitation and also the medical director of primary care sports medicine at Loyola University Chicago in Maywood, Ill. Dr. Jayanthi said that he had no relevant financial disclosures.
The Images Are Great, But Do They Help?
The advances in cardiac imaging that have taken place in the last few years have provided amazing visualization of cardiac function in health and disease. Imaging has also enabled us to target areas of the heart for medical and surgical intervention.
The images are so slick that we have been known to e-mail them to our patients to show them how clever we are. I am told that they have been used to liven up cocktail parties. In a larger sense, however, few new concepts have emerged as a result of these imaging advances that physiologists and anatomists have not already elegantly described in the past.
We have been obsessed with the possibility that imaging of the heart and the coronary vessels would unlock the mysteries of acute coronary events and provide predictive information of subsequent myocardial infarction. The advances in computed tomography – first with the exercise electrocardiogram (with and without radiographic imaging), followed by coronary angiography, and most recently with CT coronary angiography – are only the most recent attempts to identify the culprit in this long-running quest for the triggers of acute coronary events.
And yet, the answer eludes us. Even when we were able to image the atherosclerotic plaque itself, we found that new events occurred in seemingly normal vessels. So it is not surprising that the ROMICAT II (Rule Out Myocardial Infarction II) study – the most recent study evaluating emergency department patients with acute chest pain using CT angiography – failed to provide any new insight into the diagnosis and prediction of the acute coronary syndrome. Compared with standard evaluation, CT angiography failed to show any clinical benefit other than shortening the average stay in the ED by 7.6 hours (which is unquestionably a quality benefit if your emergency department is anything like mine).
ROMICAT II did show that coronary events were rare in this highly selected patient population who were aged 40-74 years, had no history of coronary artery disease or ischemic electrocardiographic abnormalities, and had normal troponin assays. In the succeeding 28 days following emergency evaluation, there were no acute coronary events detected, and there were only eight adverse cardiac events observed.
Because of the unlikely occurrence of coronary events, these patients can best be dealt with in a nonemergency setting. Both CT angiography and standard testing led to further tests during the 28-day follow-up, including exercise echocardiograms (with or without nuclear imaging) and coronary angiography in roughly three-fourths of the patients. Revascularization was performed in 10% of the population.
So why are we even testing these patients and exposing them to all of the exigencies of ED and hospital admission? We are clearly not providing any service to them. At the same time, we are exposing them to increased radiation and the hazard of the testing procedures themselves. Some would say that the testing was driven by the risks of malpractice litigation. This study should provide some "cover" for that concern, which is undoubtedly real.
The continuing dependence on imaging technology to solve clinical problems has led to the numbing of our ability to perform cognitive processing of clinical data. Heart failure is no longer a clinical entity; it is an echocardiography image. The acute coronary syndrome is not a clinical syndrome, but rather an acquired image or blood test. Daily ward rounds have evolved into a hierarchical listing of the next imaging test to be performed on the patient in order to solve the clinical problem at hand. Consequently, the approach to the patient is no longer a quest to understand what is probable, but a search for the improbable.
A continuous barrage of publications in the medical and lay press has addressed the dollars wasted on imaging procedures, with seemingly little letup in the use of these technologies. Clearly, in the "zero-sum game" world of modern medicine, these costs will ultimately come out of physician’s income. Beyond that, we should realize that they add very little to the care of our patients and may actually add to their risks.
Dr. Goldstein, medical editor of Cardiology News, is a professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
The advances in cardiac imaging that have taken place in the last few years have provided amazing visualization of cardiac function in health and disease. Imaging has also enabled us to target areas of the heart for medical and surgical intervention.
The images are so slick that we have been known to e-mail them to our patients to show them how clever we are. I am told that they have been used to liven up cocktail parties. In a larger sense, however, few new concepts have emerged as a result of these imaging advances that physiologists and anatomists have not already elegantly described in the past.
We have been obsessed with the possibility that imaging of the heart and the coronary vessels would unlock the mysteries of acute coronary events and provide predictive information of subsequent myocardial infarction. The advances in computed tomography – first with the exercise electrocardiogram (with and without radiographic imaging), followed by coronary angiography, and most recently with CT coronary angiography – are only the most recent attempts to identify the culprit in this long-running quest for the triggers of acute coronary events.
And yet, the answer eludes us. Even when we were able to image the atherosclerotic plaque itself, we found that new events occurred in seemingly normal vessels. So it is not surprising that the ROMICAT II (Rule Out Myocardial Infarction II) study – the most recent study evaluating emergency department patients with acute chest pain using CT angiography – failed to provide any new insight into the diagnosis and prediction of the acute coronary syndrome. Compared with standard evaluation, CT angiography failed to show any clinical benefit other than shortening the average stay in the ED by 7.6 hours (which is unquestionably a quality benefit if your emergency department is anything like mine).
ROMICAT II did show that coronary events were rare in this highly selected patient population who were aged 40-74 years, had no history of coronary artery disease or ischemic electrocardiographic abnormalities, and had normal troponin assays. In the succeeding 28 days following emergency evaluation, there were no acute coronary events detected, and there were only eight adverse cardiac events observed.
Because of the unlikely occurrence of coronary events, these patients can best be dealt with in a nonemergency setting. Both CT angiography and standard testing led to further tests during the 28-day follow-up, including exercise echocardiograms (with or without nuclear imaging) and coronary angiography in roughly three-fourths of the patients. Revascularization was performed in 10% of the population.
So why are we even testing these patients and exposing them to all of the exigencies of ED and hospital admission? We are clearly not providing any service to them. At the same time, we are exposing them to increased radiation and the hazard of the testing procedures themselves. Some would say that the testing was driven by the risks of malpractice litigation. This study should provide some "cover" for that concern, which is undoubtedly real.
The continuing dependence on imaging technology to solve clinical problems has led to the numbing of our ability to perform cognitive processing of clinical data. Heart failure is no longer a clinical entity; it is an echocardiography image. The acute coronary syndrome is not a clinical syndrome, but rather an acquired image or blood test. Daily ward rounds have evolved into a hierarchical listing of the next imaging test to be performed on the patient in order to solve the clinical problem at hand. Consequently, the approach to the patient is no longer a quest to understand what is probable, but a search for the improbable.
A continuous barrage of publications in the medical and lay press has addressed the dollars wasted on imaging procedures, with seemingly little letup in the use of these technologies. Clearly, in the "zero-sum game" world of modern medicine, these costs will ultimately come out of physician’s income. Beyond that, we should realize that they add very little to the care of our patients and may actually add to their risks.
Dr. Goldstein, medical editor of Cardiology News, is a professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
The advances in cardiac imaging that have taken place in the last few years have provided amazing visualization of cardiac function in health and disease. Imaging has also enabled us to target areas of the heart for medical and surgical intervention.
The images are so slick that we have been known to e-mail them to our patients to show them how clever we are. I am told that they have been used to liven up cocktail parties. In a larger sense, however, few new concepts have emerged as a result of these imaging advances that physiologists and anatomists have not already elegantly described in the past.
We have been obsessed with the possibility that imaging of the heart and the coronary vessels would unlock the mysteries of acute coronary events and provide predictive information of subsequent myocardial infarction. The advances in computed tomography – first with the exercise electrocardiogram (with and without radiographic imaging), followed by coronary angiography, and most recently with CT coronary angiography – are only the most recent attempts to identify the culprit in this long-running quest for the triggers of acute coronary events.
And yet, the answer eludes us. Even when we were able to image the atherosclerotic plaque itself, we found that new events occurred in seemingly normal vessels. So it is not surprising that the ROMICAT II (Rule Out Myocardial Infarction II) study – the most recent study evaluating emergency department patients with acute chest pain using CT angiography – failed to provide any new insight into the diagnosis and prediction of the acute coronary syndrome. Compared with standard evaluation, CT angiography failed to show any clinical benefit other than shortening the average stay in the ED by 7.6 hours (which is unquestionably a quality benefit if your emergency department is anything like mine).
ROMICAT II did show that coronary events were rare in this highly selected patient population who were aged 40-74 years, had no history of coronary artery disease or ischemic electrocardiographic abnormalities, and had normal troponin assays. In the succeeding 28 days following emergency evaluation, there were no acute coronary events detected, and there were only eight adverse cardiac events observed.
Because of the unlikely occurrence of coronary events, these patients can best be dealt with in a nonemergency setting. Both CT angiography and standard testing led to further tests during the 28-day follow-up, including exercise echocardiograms (with or without nuclear imaging) and coronary angiography in roughly three-fourths of the patients. Revascularization was performed in 10% of the population.
So why are we even testing these patients and exposing them to all of the exigencies of ED and hospital admission? We are clearly not providing any service to them. At the same time, we are exposing them to increased radiation and the hazard of the testing procedures themselves. Some would say that the testing was driven by the risks of malpractice litigation. This study should provide some "cover" for that concern, which is undoubtedly real.
The continuing dependence on imaging technology to solve clinical problems has led to the numbing of our ability to perform cognitive processing of clinical data. Heart failure is no longer a clinical entity; it is an echocardiography image. The acute coronary syndrome is not a clinical syndrome, but rather an acquired image or blood test. Daily ward rounds have evolved into a hierarchical listing of the next imaging test to be performed on the patient in order to solve the clinical problem at hand. Consequently, the approach to the patient is no longer a quest to understand what is probable, but a search for the improbable.
A continuous barrage of publications in the medical and lay press has addressed the dollars wasted on imaging procedures, with seemingly little letup in the use of these technologies. Clearly, in the "zero-sum game" world of modern medicine, these costs will ultimately come out of physician’s income. Beyond that, we should realize that they add very little to the care of our patients and may actually add to their risks.
Dr. Goldstein, medical editor of Cardiology News, is a professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
Acetyl-l-Carnitine Yields Mixed Results for Chemo-Induced Neuropathy
CHICAGO – The impact of acetyl-l-carnitine on chemotherapy-induced peripheral neuropathy may depend largely on the clinical context and patient population, a pair of phase III trials suggests.
Acetyl-l-carnitine (ALC), a natural substance marketed over the counter as a dietary supplement, is popular among cancer patients as a result of preclinical and early-phase data in chemotherapy-related neuropathy and also a study in patients with diabetes-related peripheral neuropathy.
But in a trial among 409 U.S. women receiving adjuvant chemotherapy for breast cancer, those who took ALC not only had no decrease in the development of peripheral neuropathy symptoms relative to peers who were given a placebo, but actually had an increase. And they had a higher rate of serious neuropathy, too.
In contrast, in a trial among more than 200 Chinese patients with various cancers who had peripheral neuropathy from previous chemotherapy, those who took ALC were more likely than those who took a placebo to have an improvement of at least one grade in their neuropathy. They also were more likely to have improvements in fatigue and strength.
Taken together, the two trials, which were reported in a poster discussion session at the annual meeting of the American Society of Clinical Oncology, provide yet another cautionary lesson on the complexity of combining conventional and complementary therapies.
"The use of ALC for prevention is not recommended, and I would say, based on [these results], should be cautioned against. It will be interesting to see the carnitine data and to understand, as much as possible, why the trial was negative," commented Debra L. Barton, Ph.D., of the Mayo Clinic in Rochester, Minn., who was invited to discuss the research. "Further studies are needed to really understand if ALC should be used to treat peripheral neuropathy."
ALC for Prevention of Peripheral Neuropathy
In the first trial, Southwest Oncology Group (SWOG) protocol S0715, investigators led by Dr. Dawn L. Hershman randomized women receiving adjuvant taxane chemotherapy for early breast cancer evenly to either oral ALC 1,000 mg three times daily or matching placebo, for 24 weeks.
Compared with their counterparts in the placebo group, women in the ALC group were more likely to have a greater than 5-point adjusted decrease on the neurotoxicity subscale of the Functional Assessment of Cancer Therapy–Taxane (FACT-NTX) instrument at 12 weeks (odds ratio, 1.48; P = .08) and also at 24 weeks (38% vs. 28%; OR, 1.57; P = .05).
This magnitude of worsening is clinically meaningful, maintained Dr. Hershman of Columbia University in New York, "so this is not like a lot of studies where you find a statistically significant difference that’s not clinically meaningful."
In addition, the incidence of grade 3/4 neurotoxicity was 3.8% with ALC, much higher than the 0.5% seen with placebo.
Patients in the ALC group also had scores on the FACT trial outcome index subscale (FACT-TOI), an overall measure of function, that were on average 3.5 points lower (worse) than those among their placebo counterparts (P = .03). There were no significant differences between groups in terms of fatigue and other toxicities.
The investigators have collected biosamples and will be assessing potential biological correlates with peripheral neuropathy outcomes, according to Dr. Hershman.
"We are looking at DNA, oxidative stress, and carnitine levels to better understand the mechanisms of chemotherapy-induced peripheral neuropathy to begin with, because there is not a whole lot known in terms of mechanism," she said. "If we can figure out what makes people worse, then we will maybe be able to figure out how to make people better from a more mechanistic standpoint, because there are very few drugs to treat chemotherapy-induced peripheral neuropathy."
An obvious concern from the trial’s findings is that ALC may somehow potentiate the neurotoxic effects of taxanes. "Based on these data, physicians should be telling patients not to take ALC during adjuvant chemotherapy," Dr. Hershman concluded. "You need to talk to patients. We know from the literature that overwhelmingly large number of patients take supplements during chemotherapy and afterward, many of which have not been tested. It’s important to get that history from patients."
Dr. Barton, the discussant, praised the trial’s rigorous methodology and proposed that there may have been several reasons for the lack of ALC benefit in preventing neuropathy, despite compelling earlier data.
Previous prevention research was done in animals and thus may not translate to humans, she said. And a positive trial for treatment in humans used intravenous administration, which may result in different bioavailability. Finally, "ALC capsules needed to be taken three times a day, and they are rather large, and these patients were, after all, on chemotherapy. They were likely nauseated [and] dyspeptic, and taking what some might call a horse pill three times a day could not have been an easy task. The study did use pill diaries, but we know those aren’t a perfect tool for adherence."
"The great thing is that the study collected blood and they are able to look at carnitine levels," Dr. Barton said. "So if carnitine is up in the group that got acetyl-carnitine and not in the group that got placebo, well, I think that pretty much confirms that this just didn’t work."
ALC for Treatment of Peripheral Neuropathy
In the second trial, protocol ZHAOKE-2007L03540, investigators led by Dr. Yuanjue Sun of the Sixth Affiliated Hospital of Shanghai (China) Jiao Tong University, enrolled 239 patients who had cancer of various types and stages, had completed chemotherapy, and had had at least grade 2 peripheral neuropathy for up to 6 months.
They were randomly assigned to receive either oral ALC at a dose of 3 g/day or matching placebo, for 8 weeks, with outcomes assessed at clinic visits or by telephone.
Analyses showed that compared with their counterparts in the placebo group, patients in the ALC group were more likely to have had an improvement of at least one grade in their neuropathy, both at 8 weeks (51% vs. 24%; P less than .001) and at 12 weeks (58% vs. 40%; P less than .001).
In terms of secondary outcomes, the ALC group was also more likely to have had an improvement in cancer-related fatigue (31% vs. 20%; P = .048), physical strength (29% vs. 13%; P = .02), and electrophysiology in peripheral nerves (75% vs. 58%; P = .02).
The two groups had statistically indistinguishable rates of adverse events (20% vs. 15%) and adverse reactions (6% vs. 5%). The most common events were gastrointestinal ones and skin allergies.
"This is the first time to confirm that ALC has a positive effect to cure chemotherapy-induced peripheral neuropathy in the Chinese population," Dr. Sun commented through a translator.
"I think the very important thing for this trial is, it is a different kind of patient population. Before this, most clinical trials were performed in [whites] or maybe Americans. This is an only-Asian [population]," he noted, and it is possible that there are genetic differences in how ALC is metabolized.
Dr. Barton, the discussant, took a cautionary view, saying that "there are some things to consider before going out and telling patients to consider acetyl-carnitine for their peripheral neuropathy."
It was unclear from the results reported whether the two treatment groups were well balanced and what criteria were used to define improvement for the secondary outcomes, she noted. Additionally, "outcome measures were all provider graded, [and there were] no self-report measures, so it is difficult to understand the impact of treatment on symptoms, particularly from the patient perspective," she noted.
Dr. Hershman, Dr. Sun, and Dr. Barton disclosed no relevant conflicts of interest; the ZHAOKE-2007L03540 trial was sponsored by Lee’s Pharmaceutical Limited.
CHICAGO – The impact of acetyl-l-carnitine on chemotherapy-induced peripheral neuropathy may depend largely on the clinical context and patient population, a pair of phase III trials suggests.
Acetyl-l-carnitine (ALC), a natural substance marketed over the counter as a dietary supplement, is popular among cancer patients as a result of preclinical and early-phase data in chemotherapy-related neuropathy and also a study in patients with diabetes-related peripheral neuropathy.
But in a trial among 409 U.S. women receiving adjuvant chemotherapy for breast cancer, those who took ALC not only had no decrease in the development of peripheral neuropathy symptoms relative to peers who were given a placebo, but actually had an increase. And they had a higher rate of serious neuropathy, too.
In contrast, in a trial among more than 200 Chinese patients with various cancers who had peripheral neuropathy from previous chemotherapy, those who took ALC were more likely than those who took a placebo to have an improvement of at least one grade in their neuropathy. They also were more likely to have improvements in fatigue and strength.
Taken together, the two trials, which were reported in a poster discussion session at the annual meeting of the American Society of Clinical Oncology, provide yet another cautionary lesson on the complexity of combining conventional and complementary therapies.
"The use of ALC for prevention is not recommended, and I would say, based on [these results], should be cautioned against. It will be interesting to see the carnitine data and to understand, as much as possible, why the trial was negative," commented Debra L. Barton, Ph.D., of the Mayo Clinic in Rochester, Minn., who was invited to discuss the research. "Further studies are needed to really understand if ALC should be used to treat peripheral neuropathy."
ALC for Prevention of Peripheral Neuropathy
In the first trial, Southwest Oncology Group (SWOG) protocol S0715, investigators led by Dr. Dawn L. Hershman randomized women receiving adjuvant taxane chemotherapy for early breast cancer evenly to either oral ALC 1,000 mg three times daily or matching placebo, for 24 weeks.
Compared with their counterparts in the placebo group, women in the ALC group were more likely to have a greater than 5-point adjusted decrease on the neurotoxicity subscale of the Functional Assessment of Cancer Therapy–Taxane (FACT-NTX) instrument at 12 weeks (odds ratio, 1.48; P = .08) and also at 24 weeks (38% vs. 28%; OR, 1.57; P = .05).
This magnitude of worsening is clinically meaningful, maintained Dr. Hershman of Columbia University in New York, "so this is not like a lot of studies where you find a statistically significant difference that’s not clinically meaningful."
In addition, the incidence of grade 3/4 neurotoxicity was 3.8% with ALC, much higher than the 0.5% seen with placebo.
Patients in the ALC group also had scores on the FACT trial outcome index subscale (FACT-TOI), an overall measure of function, that were on average 3.5 points lower (worse) than those among their placebo counterparts (P = .03). There were no significant differences between groups in terms of fatigue and other toxicities.
The investigators have collected biosamples and will be assessing potential biological correlates with peripheral neuropathy outcomes, according to Dr. Hershman.
"We are looking at DNA, oxidative stress, and carnitine levels to better understand the mechanisms of chemotherapy-induced peripheral neuropathy to begin with, because there is not a whole lot known in terms of mechanism," she said. "If we can figure out what makes people worse, then we will maybe be able to figure out how to make people better from a more mechanistic standpoint, because there are very few drugs to treat chemotherapy-induced peripheral neuropathy."
An obvious concern from the trial’s findings is that ALC may somehow potentiate the neurotoxic effects of taxanes. "Based on these data, physicians should be telling patients not to take ALC during adjuvant chemotherapy," Dr. Hershman concluded. "You need to talk to patients. We know from the literature that overwhelmingly large number of patients take supplements during chemotherapy and afterward, many of which have not been tested. It’s important to get that history from patients."
Dr. Barton, the discussant, praised the trial’s rigorous methodology and proposed that there may have been several reasons for the lack of ALC benefit in preventing neuropathy, despite compelling earlier data.
Previous prevention research was done in animals and thus may not translate to humans, she said. And a positive trial for treatment in humans used intravenous administration, which may result in different bioavailability. Finally, "ALC capsules needed to be taken three times a day, and they are rather large, and these patients were, after all, on chemotherapy. They were likely nauseated [and] dyspeptic, and taking what some might call a horse pill three times a day could not have been an easy task. The study did use pill diaries, but we know those aren’t a perfect tool for adherence."
"The great thing is that the study collected blood and they are able to look at carnitine levels," Dr. Barton said. "So if carnitine is up in the group that got acetyl-carnitine and not in the group that got placebo, well, I think that pretty much confirms that this just didn’t work."
ALC for Treatment of Peripheral Neuropathy
In the second trial, protocol ZHAOKE-2007L03540, investigators led by Dr. Yuanjue Sun of the Sixth Affiliated Hospital of Shanghai (China) Jiao Tong University, enrolled 239 patients who had cancer of various types and stages, had completed chemotherapy, and had had at least grade 2 peripheral neuropathy for up to 6 months.
They were randomly assigned to receive either oral ALC at a dose of 3 g/day or matching placebo, for 8 weeks, with outcomes assessed at clinic visits or by telephone.
Analyses showed that compared with their counterparts in the placebo group, patients in the ALC group were more likely to have had an improvement of at least one grade in their neuropathy, both at 8 weeks (51% vs. 24%; P less than .001) and at 12 weeks (58% vs. 40%; P less than .001).
In terms of secondary outcomes, the ALC group was also more likely to have had an improvement in cancer-related fatigue (31% vs. 20%; P = .048), physical strength (29% vs. 13%; P = .02), and electrophysiology in peripheral nerves (75% vs. 58%; P = .02).
The two groups had statistically indistinguishable rates of adverse events (20% vs. 15%) and adverse reactions (6% vs. 5%). The most common events were gastrointestinal ones and skin allergies.
"This is the first time to confirm that ALC has a positive effect to cure chemotherapy-induced peripheral neuropathy in the Chinese population," Dr. Sun commented through a translator.
"I think the very important thing for this trial is, it is a different kind of patient population. Before this, most clinical trials were performed in [whites] or maybe Americans. This is an only-Asian [population]," he noted, and it is possible that there are genetic differences in how ALC is metabolized.
Dr. Barton, the discussant, took a cautionary view, saying that "there are some things to consider before going out and telling patients to consider acetyl-carnitine for their peripheral neuropathy."
It was unclear from the results reported whether the two treatment groups were well balanced and what criteria were used to define improvement for the secondary outcomes, she noted. Additionally, "outcome measures were all provider graded, [and there were] no self-report measures, so it is difficult to understand the impact of treatment on symptoms, particularly from the patient perspective," she noted.
Dr. Hershman, Dr. Sun, and Dr. Barton disclosed no relevant conflicts of interest; the ZHAOKE-2007L03540 trial was sponsored by Lee’s Pharmaceutical Limited.
CHICAGO – The impact of acetyl-l-carnitine on chemotherapy-induced peripheral neuropathy may depend largely on the clinical context and patient population, a pair of phase III trials suggests.
Acetyl-l-carnitine (ALC), a natural substance marketed over the counter as a dietary supplement, is popular among cancer patients as a result of preclinical and early-phase data in chemotherapy-related neuropathy and also a study in patients with diabetes-related peripheral neuropathy.
But in a trial among 409 U.S. women receiving adjuvant chemotherapy for breast cancer, those who took ALC not only had no decrease in the development of peripheral neuropathy symptoms relative to peers who were given a placebo, but actually had an increase. And they had a higher rate of serious neuropathy, too.
In contrast, in a trial among more than 200 Chinese patients with various cancers who had peripheral neuropathy from previous chemotherapy, those who took ALC were more likely than those who took a placebo to have an improvement of at least one grade in their neuropathy. They also were more likely to have improvements in fatigue and strength.
Taken together, the two trials, which were reported in a poster discussion session at the annual meeting of the American Society of Clinical Oncology, provide yet another cautionary lesson on the complexity of combining conventional and complementary therapies.
"The use of ALC for prevention is not recommended, and I would say, based on [these results], should be cautioned against. It will be interesting to see the carnitine data and to understand, as much as possible, why the trial was negative," commented Debra L. Barton, Ph.D., of the Mayo Clinic in Rochester, Minn., who was invited to discuss the research. "Further studies are needed to really understand if ALC should be used to treat peripheral neuropathy."
ALC for Prevention of Peripheral Neuropathy
In the first trial, Southwest Oncology Group (SWOG) protocol S0715, investigators led by Dr. Dawn L. Hershman randomized women receiving adjuvant taxane chemotherapy for early breast cancer evenly to either oral ALC 1,000 mg three times daily or matching placebo, for 24 weeks.
Compared with their counterparts in the placebo group, women in the ALC group were more likely to have a greater than 5-point adjusted decrease on the neurotoxicity subscale of the Functional Assessment of Cancer Therapy–Taxane (FACT-NTX) instrument at 12 weeks (odds ratio, 1.48; P = .08) and also at 24 weeks (38% vs. 28%; OR, 1.57; P = .05).
This magnitude of worsening is clinically meaningful, maintained Dr. Hershman of Columbia University in New York, "so this is not like a lot of studies where you find a statistically significant difference that’s not clinically meaningful."
In addition, the incidence of grade 3/4 neurotoxicity was 3.8% with ALC, much higher than the 0.5% seen with placebo.
Patients in the ALC group also had scores on the FACT trial outcome index subscale (FACT-TOI), an overall measure of function, that were on average 3.5 points lower (worse) than those among their placebo counterparts (P = .03). There were no significant differences between groups in terms of fatigue and other toxicities.
The investigators have collected biosamples and will be assessing potential biological correlates with peripheral neuropathy outcomes, according to Dr. Hershman.
"We are looking at DNA, oxidative stress, and carnitine levels to better understand the mechanisms of chemotherapy-induced peripheral neuropathy to begin with, because there is not a whole lot known in terms of mechanism," she said. "If we can figure out what makes people worse, then we will maybe be able to figure out how to make people better from a more mechanistic standpoint, because there are very few drugs to treat chemotherapy-induced peripheral neuropathy."
An obvious concern from the trial’s findings is that ALC may somehow potentiate the neurotoxic effects of taxanes. "Based on these data, physicians should be telling patients not to take ALC during adjuvant chemotherapy," Dr. Hershman concluded. "You need to talk to patients. We know from the literature that overwhelmingly large number of patients take supplements during chemotherapy and afterward, many of which have not been tested. It’s important to get that history from patients."
Dr. Barton, the discussant, praised the trial’s rigorous methodology and proposed that there may have been several reasons for the lack of ALC benefit in preventing neuropathy, despite compelling earlier data.
Previous prevention research was done in animals and thus may not translate to humans, she said. And a positive trial for treatment in humans used intravenous administration, which may result in different bioavailability. Finally, "ALC capsules needed to be taken three times a day, and they are rather large, and these patients were, after all, on chemotherapy. They were likely nauseated [and] dyspeptic, and taking what some might call a horse pill three times a day could not have been an easy task. The study did use pill diaries, but we know those aren’t a perfect tool for adherence."
"The great thing is that the study collected blood and they are able to look at carnitine levels," Dr. Barton said. "So if carnitine is up in the group that got acetyl-carnitine and not in the group that got placebo, well, I think that pretty much confirms that this just didn’t work."
ALC for Treatment of Peripheral Neuropathy
In the second trial, protocol ZHAOKE-2007L03540, investigators led by Dr. Yuanjue Sun of the Sixth Affiliated Hospital of Shanghai (China) Jiao Tong University, enrolled 239 patients who had cancer of various types and stages, had completed chemotherapy, and had had at least grade 2 peripheral neuropathy for up to 6 months.
They were randomly assigned to receive either oral ALC at a dose of 3 g/day or matching placebo, for 8 weeks, with outcomes assessed at clinic visits or by telephone.
Analyses showed that compared with their counterparts in the placebo group, patients in the ALC group were more likely to have had an improvement of at least one grade in their neuropathy, both at 8 weeks (51% vs. 24%; P less than .001) and at 12 weeks (58% vs. 40%; P less than .001).
In terms of secondary outcomes, the ALC group was also more likely to have had an improvement in cancer-related fatigue (31% vs. 20%; P = .048), physical strength (29% vs. 13%; P = .02), and electrophysiology in peripheral nerves (75% vs. 58%; P = .02).
The two groups had statistically indistinguishable rates of adverse events (20% vs. 15%) and adverse reactions (6% vs. 5%). The most common events were gastrointestinal ones and skin allergies.
"This is the first time to confirm that ALC has a positive effect to cure chemotherapy-induced peripheral neuropathy in the Chinese population," Dr. Sun commented through a translator.
"I think the very important thing for this trial is, it is a different kind of patient population. Before this, most clinical trials were performed in [whites] or maybe Americans. This is an only-Asian [population]," he noted, and it is possible that there are genetic differences in how ALC is metabolized.
Dr. Barton, the discussant, took a cautionary view, saying that "there are some things to consider before going out and telling patients to consider acetyl-carnitine for their peripheral neuropathy."
It was unclear from the results reported whether the two treatment groups were well balanced and what criteria were used to define improvement for the secondary outcomes, she noted. Additionally, "outcome measures were all provider graded, [and there were] no self-report measures, so it is difficult to understand the impact of treatment on symptoms, particularly from the patient perspective," she noted.
Dr. Hershman, Dr. Sun, and Dr. Barton disclosed no relevant conflicts of interest; the ZHAOKE-2007L03540 trial was sponsored by Lee’s Pharmaceutical Limited.
AT THE ANNUAL MEETING OF THE AMERICAN SOCIETY OF CLINICAL ONCOLOGY
Major Finding: Patients taking ALC for prevention were more likely to have a greater than 5-point worsening of FACT-NTX score (38% vs. 28%), whereas patients taking ALC for treatment were more likely to have an improvement of at least one grade in neuropathy (51% vs. 24%).
Data Source: Investigators presented separate, randomized, placebo-controlled phase III trials among 410 women receiving adjuvant taxane chemotherapy for breast cancer and 239 patients with cancer and chemotherapy-induced peripheral neuropathy.
Disclosures: Dr. Hershman, Dr. Sun, and Dr. Barton disclosed no relevant conflicts of interest; the ZHAOKE-2007L03540 trial was sponsored by Lee’s Pharmaceutical Limited.
Partner Violence, Reproductive Coercion Are Teen Problems
If your practice sees adolescent patients and you’re not identifying intimate partner violence or coercion on a regular basis, it’s time to ask, "Why not?"
It’s there, it’s more common than you may suspect, and it often produces lifelong health consequences. Not enough teenagers are reporting it – and not enough physicians are asking about it – for a slew of reasons.
Increased attention to these problems in recent years has generated some handy resources for physicians to improve prevention, detection, and responses to intimate partner violence and sexual or reproductive coercion.
More than half (53%) of 1,278 women aged 16-29 years who were seen at family planning clinics reported physical or sexual violence by intimate partners, 19% reported pregnancy coercion, and 15% reported birth control sabotage in one study (Contraception 2010;81:316-22).
Some 40% of 448 females aged 14-20 years who were seen at five urban adolescent clinics said they had experienced intimate partner violence in a separate study (Matern. Child Health J. 2010;14:910-7). A survey of 10th and 11th graders found that more than half of the girls and 13% of boys reported sexual coercion, defined as sexual behaviors involving verbal coercion, threats of force, or use of drugs or alcohol (Violence Vict. 1995;10:299-313).
In a survey of 1,430 seventh graders in three states that was conducted by the Robert Wood Johnson Foundation, 37% said they had witnessed physical dating violence against a peer, 37% reported experiencing psychological dating abuse, and – during the prior 6 month – 15% experienced physical dating abuse and 31% experienced electronic dating aggression.
In a survey of 305 school counselors, the majority (71%) had not received formal training on adolescent dating violence (ADV). Eighty-one percent said their school did not have a protocol to respond to incidents of ADV, and 83% said the school did not conduct periodic student surveys that included questions that mentioned ADV (Pediatrics 2012;130:202-10).
Adolescents overwhelmingly want health care providers to ask about intimate partner violence and coercion, other studies have shown. So, why aren’t they telling you about it, even if you ask?
You may not be asking in the right way, nor asking often enough, Dr. Harise Stein said at Stanford (Calif.) University’s annual pediatric update and preconference.
Teens aged 15-19 years have the highest rates of intimate partner violence and stalking of any age group, yet they report only an estimated 1 in 11 episodes of dating-related violence, said Dr. Stein, an ob.gyn at the university. She is a member of the Santa Clara County (Calif.) Domestic Violence Council.
One in six U.S. women experience rape – "which I think is a national disgrace," she said – and 32% of first rapes occur in female victims aged 12-17-years. In that age group, 36% of rapists are intimate partners, and 33% are acquaintances, according to a 2006 U.S. Department of Justice report.
Abuse during adolescence interferes with emotional development and has been associated with mental and physical illness both during the teen years and carried forward into adulthood, she said. It can exacerbate asthma, headaches, or other chronic illnesses. Consider abuse in the diagnostic differential when you see an adolescent who has developed school problems, increased isolation, personality changes, mental health issues, an eating disorder, substance abuse, cutting and other forms of self-harm, or suicidal ideology, Dr. Stein said.
Vague physical symptoms or symptoms that don’t make sense are red flags for possible abuse, as are chronic pain symptoms (especially headaches), or unexplained worsening of chronic illness. New sexually transmitted infections, an unplanned pregnancy, or a request for emergency contraception open a window to ask about abuse.
Suspicious injuries may result from abuse. Slap marks, scratches, bruises, welts, cuts, or muscle sprains are typical signs in adolescents, but most common are soft tissue injuries of the forearms (held up to defend against blows), face, head, and neck, Dr. Stein said.
The prevalence of being choked to unconsciousness is "very underappreciated by health care workers" because half the time choking leaves no immediate external signs on the neck, she said. The teenager may wake up on the floor and not remember what happened. Only 10 seconds of strangulation can induce unconsciousness, and every second after that causes brain damage. Laryngeal edema over the following 24-48 hours can create airway emergencies. Brain cell death from the choking may cause problems in memory, reasoning, and concentration for several weeks. At least 10% of adult abused women who obtain restraining orders are estimated to have been choked to unconsciousness. Data are lacking for teens.
Teens in abusive relationships are four to six times more likely to get pregnant than are other teens, and 25% of pregnant teens are in abusive relationships, compared with 4%-8% of pregnant adults, Dr. Stein said.
The American Academy of Pediatrics and the American College of Obstetricians and Gynecologists (ACOG) recommend screening for dating abuse (Pediatrics 2009;124:393-402; Obstet. Gynecol. 2012;119:412-7) – perhaps starting as early at age 11, according to AAP’s Bright Futures – and educating preteens and teens about healthy relationships, she said.
Remember a key lesson from Adolescence 101: Teens are more likely to open up if you start with open-ended questions like "How’s school?" instead of pointed questions, or if you approach the topic obliquely by bringing up bullying as something a lot of people are talking about, and use that as a lead-in to talking about relationships. Focus on behaviors, not "abuse," Dr. Stein said.
Adolescents get most of their advice on health topics from peers, so use that to your advantage by giving your patients materials about healthy relationships and resources for abused teens, and telling them it’s "for a friend," if you suspect the patient or a friend is at risk.
To detect intimate partner violence and coercion, watch for it– but also make your office a place where teens will feel comfortable talking about it. Make informational materials available in nonconspicuous places. Explain confidentiality up front in teen visits.
Dr. Eve Espey learned some of these lessons in a vivid way. A patient and her boyfriend came to the emergency department, and an HCG test suggested that she had an ectopic pregnancy. She refused emergency treatment. Once the boyfriend left the room, she admitted that she’d just had an abortion, and didn’t want him to know because she feared he’d be violent. A nurse had screened her and asked specifically about domestic violence, but with the boyfriend in the room, she couldn’t discuss it.
"We made changes after that," said Dr. Espey, professor of ob.gyn. at the University of New Mexico, Albuquerque, and chair of ACOG’s Working Group on Long-Acting Reversible Contraception. "We talk to every woman by herself. We tell them it’s part of our protocol," she said at ACOG’s annual meeting.
A February 2012 opinion published by ACOG’s Committee on Health Care for Underserved Women calls on physicians to screen all women for intimate partner violence at periodic intervals, to offer ongoing support, and to review prevention and referral options with patients. Intimate partner violence is most common during the reproductive years, so it’s important to screen several times during obstetric care, including at the first prenatal visit, at least once per trimester, and at the postpartum checkup, the committee recommended. The opinion paper includes sample questions (Obstet. Gynecol. 2012;119:412-7).
Dr. Espey recommends that ob.gyns. screen patients for intimate partner violence and reproductive coercion at most contraceptive visits, again not by immediate blunt questions like, "Are you safe at home?" but in a more circuitous, conversational way.
"The goal is not disclosure. Just engaging in the conversation is a great first step," she said.
When a patient does reveal intimate partner violence but is not ready to make changes, help the patient avoid unintended pregnancy by separating out the issue of reproductive coercion (in which a partner sabotages birth control or coerces the person to have or terminate a pregnancy), Dr. Espey said.
Talk about contraceptive methods that are less detectable by partners, for example. Long-acting reversible contraceptive methods are less vulnerable to tampering, but hormonal methods that eliminate periods may not work for women whose cycles are being closely monitored by a partner. The string on an IUD can be cut before insertion so that a partner cannot pull it out. If the IUD already is inserted, you’ll need to remove it and cut the string and reinsert it, because cutting the string just at the cervix leaves it potentially detectable, she said. Pills for emergency contraception can be stored in a vitamin bottle to avoid detection.
Her practice keeps laminated copies handy of a color-coded chart from the Centers for Disease Control and Prevention that helps clinicians quickly identify which forms of contraception are medically appropriate for particular patients – and showing that long-active contraceptives usually are an option. The "Summary Chart of U.S. Medical Eligibility Criteria for Contraceptive Use" is free.
She also lets patients who get an abortion know that they can say they’ve had a miscarriage, if they need to. "Women don’t realize that abortion cannot be detected. Tell them," she said.
These discussions plant the seeds for women to grow into readiness to leave abusive relationships, Dr. Espey said. Of course, keep in mind any legal requirements in your state to report abuse.
Adolescents often feel more comfortable being asked initially about abuse and coercion if it’s asked electronically, Virginia A. Duplessis said at ACOG’s annual meeting. In live conversations, "We’re moving from ‘Have you ever been punched, slapped, or kicked?’ to more nuanced conversation," said Ms. Duplessis, a program manager for Futures Without Violence, a nonprofit organization formerly known as the Family Violence Prevention Fund, headquartered in San Francisco.
Teens may not understand that violence and coercion are not acceptable ways to show love, she said.
Dr. Stein also pointed to a segment of the Tyra Banks television talk show that’s posted online, in which adolescents in the audience had trouble identifying types of abuse other than physical abuse.
Other times, the patient may have the knowledge, but feel unable to act on it. Ms. Duplessis described her frustration in a previous job as a community educator when teens who had condoms or birth control pills and knew how to use them kept reporting that they weren’t used. It’s not that they were dumb or apathetic, she finally learned; reproductive coercion often was the problem. The girls feared the consequences of negotiating condom use more than they feared pregnancy, or their partners threw away their pills.
That frustration with patients who do not follow a plan of care is one reason that clinicians don’t screen for intimate partner violence, she said. They also may not be comfortable starting conversations on this topic, or don’t ask because they don’t know what to do if a patient discloses intimate partner violence or coercion.
Futures Without Violence offers free materials to clinicians to simplify screening, such as folding wallet-size "safety cards" to give patients that list screening questions and resources.
Ms. Duplessis manages Project Connect, a national public health initiative to prevent violence against women through efforts focused on adolescent health, reproductive health, and home visiting programs. Funded by the U.S. Office on Women’s Health, Project Connect’s 10 geographically and ethnically diverse sites explore new ways to prevent, identify, and respond to domestic and sexual violence.
In a randomized, controlled pilot trial, a community-based intervention achieved some success (Contraception 2011;83:274-80). Clinicians asked 906 women at four family planning clinics questions about intimate partner violence and sexual and reproductive coercion, and reviewed the "safety cards" they gave to patients. The intervention took less than a minute of time in some cases, or longer if a positive screen led to more discussion.
Among women who had experienced recent partner violence, those in the intervention group were 71% less likely to report pregnancy coercion and 63% more likely to end an unhealthy or unsafe relationship, compared with a control group who got usual care.
Data suggest that reducing adolescent relationship abuse should reduce rates of substance abuse, teen pregnancy, depression, eating disorders, suicide, school dropouts, and adult intimate partner violence, Dr. Stein said.
For the past 4 years, she has reviewed the literature on the effects of abuse and has sent out monthly updates to interested parties. During that time, her monthly summary has grown from three to six pages. Attention to intimate partner violence and coercion is increasing, and every clinician plays a role, she said.
Dr. Stein, Dr. Espey and Ms. Duplessis recommended the following resources:
• ACOG and Futures Without Violence cobranded a guide for clinicians, "Addressing Intimate Partner Violence, Reproductive and Sexual Coercion." The 56-page pamphlet includes sample scripts for talking with patients, advice on managing someone who screens positive, quality assessment tools for clinical practices, and links to resources including a clinician training kit, "safety cards" for patients, and more.
• The "Healthcare Education, Assessment and Response Tool for Teen Relationships (HEART) Primer" is another free comprehensive toolkit to help clinicians recognize and decrease adolescent relationship abuse and sexual and reproductive coercion, offered by the California Adolescent Health Collaborative.
• The National Center for Youth Law created legal guides for Arizona, California, Maine, Michigan, and Ohio for "When Teens Disclose Dating Violence to Health Care Providers: A Guide to Confidentiality and Reporting Laws."
• Dr. Stein sends monthly e-mail updates about the literature on the effects of abuse. To get on her list, e-mail [email protected].
Dr. Stein, Dr. Espey, and Ms. Duplessis reported having no financial disclosures.
If your practice sees adolescent patients and you’re not identifying intimate partner violence or coercion on a regular basis, it’s time to ask, "Why not?"
It’s there, it’s more common than you may suspect, and it often produces lifelong health consequences. Not enough teenagers are reporting it – and not enough physicians are asking about it – for a slew of reasons.
Increased attention to these problems in recent years has generated some handy resources for physicians to improve prevention, detection, and responses to intimate partner violence and sexual or reproductive coercion.
More than half (53%) of 1,278 women aged 16-29 years who were seen at family planning clinics reported physical or sexual violence by intimate partners, 19% reported pregnancy coercion, and 15% reported birth control sabotage in one study (Contraception 2010;81:316-22).
Some 40% of 448 females aged 14-20 years who were seen at five urban adolescent clinics said they had experienced intimate partner violence in a separate study (Matern. Child Health J. 2010;14:910-7). A survey of 10th and 11th graders found that more than half of the girls and 13% of boys reported sexual coercion, defined as sexual behaviors involving verbal coercion, threats of force, or use of drugs or alcohol (Violence Vict. 1995;10:299-313).
In a survey of 1,430 seventh graders in three states that was conducted by the Robert Wood Johnson Foundation, 37% said they had witnessed physical dating violence against a peer, 37% reported experiencing psychological dating abuse, and – during the prior 6 month – 15% experienced physical dating abuse and 31% experienced electronic dating aggression.
In a survey of 305 school counselors, the majority (71%) had not received formal training on adolescent dating violence (ADV). Eighty-one percent said their school did not have a protocol to respond to incidents of ADV, and 83% said the school did not conduct periodic student surveys that included questions that mentioned ADV (Pediatrics 2012;130:202-10).
Adolescents overwhelmingly want health care providers to ask about intimate partner violence and coercion, other studies have shown. So, why aren’t they telling you about it, even if you ask?
You may not be asking in the right way, nor asking often enough, Dr. Harise Stein said at Stanford (Calif.) University’s annual pediatric update and preconference.
Teens aged 15-19 years have the highest rates of intimate partner violence and stalking of any age group, yet they report only an estimated 1 in 11 episodes of dating-related violence, said Dr. Stein, an ob.gyn at the university. She is a member of the Santa Clara County (Calif.) Domestic Violence Council.
One in six U.S. women experience rape – "which I think is a national disgrace," she said – and 32% of first rapes occur in female victims aged 12-17-years. In that age group, 36% of rapists are intimate partners, and 33% are acquaintances, according to a 2006 U.S. Department of Justice report.
Abuse during adolescence interferes with emotional development and has been associated with mental and physical illness both during the teen years and carried forward into adulthood, she said. It can exacerbate asthma, headaches, or other chronic illnesses. Consider abuse in the diagnostic differential when you see an adolescent who has developed school problems, increased isolation, personality changes, mental health issues, an eating disorder, substance abuse, cutting and other forms of self-harm, or suicidal ideology, Dr. Stein said.
Vague physical symptoms or symptoms that don’t make sense are red flags for possible abuse, as are chronic pain symptoms (especially headaches), or unexplained worsening of chronic illness. New sexually transmitted infections, an unplanned pregnancy, or a request for emergency contraception open a window to ask about abuse.
Suspicious injuries may result from abuse. Slap marks, scratches, bruises, welts, cuts, or muscle sprains are typical signs in adolescents, but most common are soft tissue injuries of the forearms (held up to defend against blows), face, head, and neck, Dr. Stein said.
The prevalence of being choked to unconsciousness is "very underappreciated by health care workers" because half the time choking leaves no immediate external signs on the neck, she said. The teenager may wake up on the floor and not remember what happened. Only 10 seconds of strangulation can induce unconsciousness, and every second after that causes brain damage. Laryngeal edema over the following 24-48 hours can create airway emergencies. Brain cell death from the choking may cause problems in memory, reasoning, and concentration for several weeks. At least 10% of adult abused women who obtain restraining orders are estimated to have been choked to unconsciousness. Data are lacking for teens.
Teens in abusive relationships are four to six times more likely to get pregnant than are other teens, and 25% of pregnant teens are in abusive relationships, compared with 4%-8% of pregnant adults, Dr. Stein said.
The American Academy of Pediatrics and the American College of Obstetricians and Gynecologists (ACOG) recommend screening for dating abuse (Pediatrics 2009;124:393-402; Obstet. Gynecol. 2012;119:412-7) – perhaps starting as early at age 11, according to AAP’s Bright Futures – and educating preteens and teens about healthy relationships, she said.
Remember a key lesson from Adolescence 101: Teens are more likely to open up if you start with open-ended questions like "How’s school?" instead of pointed questions, or if you approach the topic obliquely by bringing up bullying as something a lot of people are talking about, and use that as a lead-in to talking about relationships. Focus on behaviors, not "abuse," Dr. Stein said.
Adolescents get most of their advice on health topics from peers, so use that to your advantage by giving your patients materials about healthy relationships and resources for abused teens, and telling them it’s "for a friend," if you suspect the patient or a friend is at risk.
To detect intimate partner violence and coercion, watch for it– but also make your office a place where teens will feel comfortable talking about it. Make informational materials available in nonconspicuous places. Explain confidentiality up front in teen visits.
Dr. Eve Espey learned some of these lessons in a vivid way. A patient and her boyfriend came to the emergency department, and an HCG test suggested that she had an ectopic pregnancy. She refused emergency treatment. Once the boyfriend left the room, she admitted that she’d just had an abortion, and didn’t want him to know because she feared he’d be violent. A nurse had screened her and asked specifically about domestic violence, but with the boyfriend in the room, she couldn’t discuss it.
"We made changes after that," said Dr. Espey, professor of ob.gyn. at the University of New Mexico, Albuquerque, and chair of ACOG’s Working Group on Long-Acting Reversible Contraception. "We talk to every woman by herself. We tell them it’s part of our protocol," she said at ACOG’s annual meeting.
A February 2012 opinion published by ACOG’s Committee on Health Care for Underserved Women calls on physicians to screen all women for intimate partner violence at periodic intervals, to offer ongoing support, and to review prevention and referral options with patients. Intimate partner violence is most common during the reproductive years, so it’s important to screen several times during obstetric care, including at the first prenatal visit, at least once per trimester, and at the postpartum checkup, the committee recommended. The opinion paper includes sample questions (Obstet. Gynecol. 2012;119:412-7).
Dr. Espey recommends that ob.gyns. screen patients for intimate partner violence and reproductive coercion at most contraceptive visits, again not by immediate blunt questions like, "Are you safe at home?" but in a more circuitous, conversational way.
"The goal is not disclosure. Just engaging in the conversation is a great first step," she said.
When a patient does reveal intimate partner violence but is not ready to make changes, help the patient avoid unintended pregnancy by separating out the issue of reproductive coercion (in which a partner sabotages birth control or coerces the person to have or terminate a pregnancy), Dr. Espey said.
Talk about contraceptive methods that are less detectable by partners, for example. Long-acting reversible contraceptive methods are less vulnerable to tampering, but hormonal methods that eliminate periods may not work for women whose cycles are being closely monitored by a partner. The string on an IUD can be cut before insertion so that a partner cannot pull it out. If the IUD already is inserted, you’ll need to remove it and cut the string and reinsert it, because cutting the string just at the cervix leaves it potentially detectable, she said. Pills for emergency contraception can be stored in a vitamin bottle to avoid detection.
Her practice keeps laminated copies handy of a color-coded chart from the Centers for Disease Control and Prevention that helps clinicians quickly identify which forms of contraception are medically appropriate for particular patients – and showing that long-active contraceptives usually are an option. The "Summary Chart of U.S. Medical Eligibility Criteria for Contraceptive Use" is free.
She also lets patients who get an abortion know that they can say they’ve had a miscarriage, if they need to. "Women don’t realize that abortion cannot be detected. Tell them," she said.
These discussions plant the seeds for women to grow into readiness to leave abusive relationships, Dr. Espey said. Of course, keep in mind any legal requirements in your state to report abuse.
Adolescents often feel more comfortable being asked initially about abuse and coercion if it’s asked electronically, Virginia A. Duplessis said at ACOG’s annual meeting. In live conversations, "We’re moving from ‘Have you ever been punched, slapped, or kicked?’ to more nuanced conversation," said Ms. Duplessis, a program manager for Futures Without Violence, a nonprofit organization formerly known as the Family Violence Prevention Fund, headquartered in San Francisco.
Teens may not understand that violence and coercion are not acceptable ways to show love, she said.
Dr. Stein also pointed to a segment of the Tyra Banks television talk show that’s posted online, in which adolescents in the audience had trouble identifying types of abuse other than physical abuse.
Other times, the patient may have the knowledge, but feel unable to act on it. Ms. Duplessis described her frustration in a previous job as a community educator when teens who had condoms or birth control pills and knew how to use them kept reporting that they weren’t used. It’s not that they were dumb or apathetic, she finally learned; reproductive coercion often was the problem. The girls feared the consequences of negotiating condom use more than they feared pregnancy, or their partners threw away their pills.
That frustration with patients who do not follow a plan of care is one reason that clinicians don’t screen for intimate partner violence, she said. They also may not be comfortable starting conversations on this topic, or don’t ask because they don’t know what to do if a patient discloses intimate partner violence or coercion.
Futures Without Violence offers free materials to clinicians to simplify screening, such as folding wallet-size "safety cards" to give patients that list screening questions and resources.
Ms. Duplessis manages Project Connect, a national public health initiative to prevent violence against women through efforts focused on adolescent health, reproductive health, and home visiting programs. Funded by the U.S. Office on Women’s Health, Project Connect’s 10 geographically and ethnically diverse sites explore new ways to prevent, identify, and respond to domestic and sexual violence.
In a randomized, controlled pilot trial, a community-based intervention achieved some success (Contraception 2011;83:274-80). Clinicians asked 906 women at four family planning clinics questions about intimate partner violence and sexual and reproductive coercion, and reviewed the "safety cards" they gave to patients. The intervention took less than a minute of time in some cases, or longer if a positive screen led to more discussion.
Among women who had experienced recent partner violence, those in the intervention group were 71% less likely to report pregnancy coercion and 63% more likely to end an unhealthy or unsafe relationship, compared with a control group who got usual care.
Data suggest that reducing adolescent relationship abuse should reduce rates of substance abuse, teen pregnancy, depression, eating disorders, suicide, school dropouts, and adult intimate partner violence, Dr. Stein said.
For the past 4 years, she has reviewed the literature on the effects of abuse and has sent out monthly updates to interested parties. During that time, her monthly summary has grown from three to six pages. Attention to intimate partner violence and coercion is increasing, and every clinician plays a role, she said.
Dr. Stein, Dr. Espey and Ms. Duplessis recommended the following resources:
• ACOG and Futures Without Violence cobranded a guide for clinicians, "Addressing Intimate Partner Violence, Reproductive and Sexual Coercion." The 56-page pamphlet includes sample scripts for talking with patients, advice on managing someone who screens positive, quality assessment tools for clinical practices, and links to resources including a clinician training kit, "safety cards" for patients, and more.
• The "Healthcare Education, Assessment and Response Tool for Teen Relationships (HEART) Primer" is another free comprehensive toolkit to help clinicians recognize and decrease adolescent relationship abuse and sexual and reproductive coercion, offered by the California Adolescent Health Collaborative.
• The National Center for Youth Law created legal guides for Arizona, California, Maine, Michigan, and Ohio for "When Teens Disclose Dating Violence to Health Care Providers: A Guide to Confidentiality and Reporting Laws."
• Dr. Stein sends monthly e-mail updates about the literature on the effects of abuse. To get on her list, e-mail [email protected].
Dr. Stein, Dr. Espey, and Ms. Duplessis reported having no financial disclosures.
If your practice sees adolescent patients and you’re not identifying intimate partner violence or coercion on a regular basis, it’s time to ask, "Why not?"
It’s there, it’s more common than you may suspect, and it often produces lifelong health consequences. Not enough teenagers are reporting it – and not enough physicians are asking about it – for a slew of reasons.
Increased attention to these problems in recent years has generated some handy resources for physicians to improve prevention, detection, and responses to intimate partner violence and sexual or reproductive coercion.
More than half (53%) of 1,278 women aged 16-29 years who were seen at family planning clinics reported physical or sexual violence by intimate partners, 19% reported pregnancy coercion, and 15% reported birth control sabotage in one study (Contraception 2010;81:316-22).
Some 40% of 448 females aged 14-20 years who were seen at five urban adolescent clinics said they had experienced intimate partner violence in a separate study (Matern. Child Health J. 2010;14:910-7). A survey of 10th and 11th graders found that more than half of the girls and 13% of boys reported sexual coercion, defined as sexual behaviors involving verbal coercion, threats of force, or use of drugs or alcohol (Violence Vict. 1995;10:299-313).
In a survey of 1,430 seventh graders in three states that was conducted by the Robert Wood Johnson Foundation, 37% said they had witnessed physical dating violence against a peer, 37% reported experiencing psychological dating abuse, and – during the prior 6 month – 15% experienced physical dating abuse and 31% experienced electronic dating aggression.
In a survey of 305 school counselors, the majority (71%) had not received formal training on adolescent dating violence (ADV). Eighty-one percent said their school did not have a protocol to respond to incidents of ADV, and 83% said the school did not conduct periodic student surveys that included questions that mentioned ADV (Pediatrics 2012;130:202-10).
Adolescents overwhelmingly want health care providers to ask about intimate partner violence and coercion, other studies have shown. So, why aren’t they telling you about it, even if you ask?
You may not be asking in the right way, nor asking often enough, Dr. Harise Stein said at Stanford (Calif.) University’s annual pediatric update and preconference.
Teens aged 15-19 years have the highest rates of intimate partner violence and stalking of any age group, yet they report only an estimated 1 in 11 episodes of dating-related violence, said Dr. Stein, an ob.gyn at the university. She is a member of the Santa Clara County (Calif.) Domestic Violence Council.
One in six U.S. women experience rape – "which I think is a national disgrace," she said – and 32% of first rapes occur in female victims aged 12-17-years. In that age group, 36% of rapists are intimate partners, and 33% are acquaintances, according to a 2006 U.S. Department of Justice report.
Abuse during adolescence interferes with emotional development and has been associated with mental and physical illness both during the teen years and carried forward into adulthood, she said. It can exacerbate asthma, headaches, or other chronic illnesses. Consider abuse in the diagnostic differential when you see an adolescent who has developed school problems, increased isolation, personality changes, mental health issues, an eating disorder, substance abuse, cutting and other forms of self-harm, or suicidal ideology, Dr. Stein said.
Vague physical symptoms or symptoms that don’t make sense are red flags for possible abuse, as are chronic pain symptoms (especially headaches), or unexplained worsening of chronic illness. New sexually transmitted infections, an unplanned pregnancy, or a request for emergency contraception open a window to ask about abuse.
Suspicious injuries may result from abuse. Slap marks, scratches, bruises, welts, cuts, or muscle sprains are typical signs in adolescents, but most common are soft tissue injuries of the forearms (held up to defend against blows), face, head, and neck, Dr. Stein said.
The prevalence of being choked to unconsciousness is "very underappreciated by health care workers" because half the time choking leaves no immediate external signs on the neck, she said. The teenager may wake up on the floor and not remember what happened. Only 10 seconds of strangulation can induce unconsciousness, and every second after that causes brain damage. Laryngeal edema over the following 24-48 hours can create airway emergencies. Brain cell death from the choking may cause problems in memory, reasoning, and concentration for several weeks. At least 10% of adult abused women who obtain restraining orders are estimated to have been choked to unconsciousness. Data are lacking for teens.
Teens in abusive relationships are four to six times more likely to get pregnant than are other teens, and 25% of pregnant teens are in abusive relationships, compared with 4%-8% of pregnant adults, Dr. Stein said.
The American Academy of Pediatrics and the American College of Obstetricians and Gynecologists (ACOG) recommend screening for dating abuse (Pediatrics 2009;124:393-402; Obstet. Gynecol. 2012;119:412-7) – perhaps starting as early at age 11, according to AAP’s Bright Futures – and educating preteens and teens about healthy relationships, she said.
Remember a key lesson from Adolescence 101: Teens are more likely to open up if you start with open-ended questions like "How’s school?" instead of pointed questions, or if you approach the topic obliquely by bringing up bullying as something a lot of people are talking about, and use that as a lead-in to talking about relationships. Focus on behaviors, not "abuse," Dr. Stein said.
Adolescents get most of their advice on health topics from peers, so use that to your advantage by giving your patients materials about healthy relationships and resources for abused teens, and telling them it’s "for a friend," if you suspect the patient or a friend is at risk.
To detect intimate partner violence and coercion, watch for it– but also make your office a place where teens will feel comfortable talking about it. Make informational materials available in nonconspicuous places. Explain confidentiality up front in teen visits.
Dr. Eve Espey learned some of these lessons in a vivid way. A patient and her boyfriend came to the emergency department, and an HCG test suggested that she had an ectopic pregnancy. She refused emergency treatment. Once the boyfriend left the room, she admitted that she’d just had an abortion, and didn’t want him to know because she feared he’d be violent. A nurse had screened her and asked specifically about domestic violence, but with the boyfriend in the room, she couldn’t discuss it.
"We made changes after that," said Dr. Espey, professor of ob.gyn. at the University of New Mexico, Albuquerque, and chair of ACOG’s Working Group on Long-Acting Reversible Contraception. "We talk to every woman by herself. We tell them it’s part of our protocol," she said at ACOG’s annual meeting.
A February 2012 opinion published by ACOG’s Committee on Health Care for Underserved Women calls on physicians to screen all women for intimate partner violence at periodic intervals, to offer ongoing support, and to review prevention and referral options with patients. Intimate partner violence is most common during the reproductive years, so it’s important to screen several times during obstetric care, including at the first prenatal visit, at least once per trimester, and at the postpartum checkup, the committee recommended. The opinion paper includes sample questions (Obstet. Gynecol. 2012;119:412-7).
Dr. Espey recommends that ob.gyns. screen patients for intimate partner violence and reproductive coercion at most contraceptive visits, again not by immediate blunt questions like, "Are you safe at home?" but in a more circuitous, conversational way.
"The goal is not disclosure. Just engaging in the conversation is a great first step," she said.
When a patient does reveal intimate partner violence but is not ready to make changes, help the patient avoid unintended pregnancy by separating out the issue of reproductive coercion (in which a partner sabotages birth control or coerces the person to have or terminate a pregnancy), Dr. Espey said.
Talk about contraceptive methods that are less detectable by partners, for example. Long-acting reversible contraceptive methods are less vulnerable to tampering, but hormonal methods that eliminate periods may not work for women whose cycles are being closely monitored by a partner. The string on an IUD can be cut before insertion so that a partner cannot pull it out. If the IUD already is inserted, you’ll need to remove it and cut the string and reinsert it, because cutting the string just at the cervix leaves it potentially detectable, she said. Pills for emergency contraception can be stored in a vitamin bottle to avoid detection.
Her practice keeps laminated copies handy of a color-coded chart from the Centers for Disease Control and Prevention that helps clinicians quickly identify which forms of contraception are medically appropriate for particular patients – and showing that long-active contraceptives usually are an option. The "Summary Chart of U.S. Medical Eligibility Criteria for Contraceptive Use" is free.
She also lets patients who get an abortion know that they can say they’ve had a miscarriage, if they need to. "Women don’t realize that abortion cannot be detected. Tell them," she said.
These discussions plant the seeds for women to grow into readiness to leave abusive relationships, Dr. Espey said. Of course, keep in mind any legal requirements in your state to report abuse.
Adolescents often feel more comfortable being asked initially about abuse and coercion if it’s asked electronically, Virginia A. Duplessis said at ACOG’s annual meeting. In live conversations, "We’re moving from ‘Have you ever been punched, slapped, or kicked?’ to more nuanced conversation," said Ms. Duplessis, a program manager for Futures Without Violence, a nonprofit organization formerly known as the Family Violence Prevention Fund, headquartered in San Francisco.
Teens may not understand that violence and coercion are not acceptable ways to show love, she said.
Dr. Stein also pointed to a segment of the Tyra Banks television talk show that’s posted online, in which adolescents in the audience had trouble identifying types of abuse other than physical abuse.
Other times, the patient may have the knowledge, but feel unable to act on it. Ms. Duplessis described her frustration in a previous job as a community educator when teens who had condoms or birth control pills and knew how to use them kept reporting that they weren’t used. It’s not that they were dumb or apathetic, she finally learned; reproductive coercion often was the problem. The girls feared the consequences of negotiating condom use more than they feared pregnancy, or their partners threw away their pills.
That frustration with patients who do not follow a plan of care is one reason that clinicians don’t screen for intimate partner violence, she said. They also may not be comfortable starting conversations on this topic, or don’t ask because they don’t know what to do if a patient discloses intimate partner violence or coercion.
Futures Without Violence offers free materials to clinicians to simplify screening, such as folding wallet-size "safety cards" to give patients that list screening questions and resources.
Ms. Duplessis manages Project Connect, a national public health initiative to prevent violence against women through efforts focused on adolescent health, reproductive health, and home visiting programs. Funded by the U.S. Office on Women’s Health, Project Connect’s 10 geographically and ethnically diverse sites explore new ways to prevent, identify, and respond to domestic and sexual violence.
In a randomized, controlled pilot trial, a community-based intervention achieved some success (Contraception 2011;83:274-80). Clinicians asked 906 women at four family planning clinics questions about intimate partner violence and sexual and reproductive coercion, and reviewed the "safety cards" they gave to patients. The intervention took less than a minute of time in some cases, or longer if a positive screen led to more discussion.
Among women who had experienced recent partner violence, those in the intervention group were 71% less likely to report pregnancy coercion and 63% more likely to end an unhealthy or unsafe relationship, compared with a control group who got usual care.
Data suggest that reducing adolescent relationship abuse should reduce rates of substance abuse, teen pregnancy, depression, eating disorders, suicide, school dropouts, and adult intimate partner violence, Dr. Stein said.
For the past 4 years, she has reviewed the literature on the effects of abuse and has sent out monthly updates to interested parties. During that time, her monthly summary has grown from three to six pages. Attention to intimate partner violence and coercion is increasing, and every clinician plays a role, she said.
Dr. Stein, Dr. Espey and Ms. Duplessis recommended the following resources:
• ACOG and Futures Without Violence cobranded a guide for clinicians, "Addressing Intimate Partner Violence, Reproductive and Sexual Coercion." The 56-page pamphlet includes sample scripts for talking with patients, advice on managing someone who screens positive, quality assessment tools for clinical practices, and links to resources including a clinician training kit, "safety cards" for patients, and more.
• The "Healthcare Education, Assessment and Response Tool for Teen Relationships (HEART) Primer" is another free comprehensive toolkit to help clinicians recognize and decrease adolescent relationship abuse and sexual and reproductive coercion, offered by the California Adolescent Health Collaborative.
• The National Center for Youth Law created legal guides for Arizona, California, Maine, Michigan, and Ohio for "When Teens Disclose Dating Violence to Health Care Providers: A Guide to Confidentiality and Reporting Laws."
• Dr. Stein sends monthly e-mail updates about the literature on the effects of abuse. To get on her list, e-mail [email protected].
Dr. Stein, Dr. Espey, and Ms. Duplessis reported having no financial disclosures.
Still No Implementation Date Set for ICD-10
A new implementation date for the 10th revision of the International Statistical Classification of Diseases coding system (ICD-10) isn't expected to be known until after the November election, says a coding specialist. But hospitalists and others should not take that as a sign to just sit around and wait for a date.
"We're probably not going to hear anything until after the election is finished," says Brenda Edwards, CPC, CPMA, a coding and compliance specialist with Kansas Medical Mutual Insurance Co. and a trainer with AAPC. "The thing that's worrisome, though, is people think this delay we have encountered is a time to sit back and do nothing, but really we’re almost burning money by not doing anything."
An outcry from many physicians led the U.S. Department of Health and Human Services to delay the planned October 2013 implementation date. No new date has been announced.
Edwards urges physicians, billing specialists, and group leaders to use the delay as an opportunity to better prepare for the implementation. She suggests checking with vendors and preparing training programs to help adjust to the new coding initiative, which will quadruple the number of billing codes to 68,000.
"Everyone at this point should still be moving forward," she says.
At the same time, the Centers for Medicare & Medicaid Services (CMS) is seeking public comment on a new version of its ICD-10 readiness assessment. Those interested in weighing in can learn more here.
A new implementation date for the 10th revision of the International Statistical Classification of Diseases coding system (ICD-10) isn't expected to be known until after the November election, says a coding specialist. But hospitalists and others should not take that as a sign to just sit around and wait for a date.
"We're probably not going to hear anything until after the election is finished," says Brenda Edwards, CPC, CPMA, a coding and compliance specialist with Kansas Medical Mutual Insurance Co. and a trainer with AAPC. "The thing that's worrisome, though, is people think this delay we have encountered is a time to sit back and do nothing, but really we’re almost burning money by not doing anything."
An outcry from many physicians led the U.S. Department of Health and Human Services to delay the planned October 2013 implementation date. No new date has been announced.
Edwards urges physicians, billing specialists, and group leaders to use the delay as an opportunity to better prepare for the implementation. She suggests checking with vendors and preparing training programs to help adjust to the new coding initiative, which will quadruple the number of billing codes to 68,000.
"Everyone at this point should still be moving forward," she says.
At the same time, the Centers for Medicare & Medicaid Services (CMS) is seeking public comment on a new version of its ICD-10 readiness assessment. Those interested in weighing in can learn more here.
A new implementation date for the 10th revision of the International Statistical Classification of Diseases coding system (ICD-10) isn't expected to be known until after the November election, says a coding specialist. But hospitalists and others should not take that as a sign to just sit around and wait for a date.
"We're probably not going to hear anything until after the election is finished," says Brenda Edwards, CPC, CPMA, a coding and compliance specialist with Kansas Medical Mutual Insurance Co. and a trainer with AAPC. "The thing that's worrisome, though, is people think this delay we have encountered is a time to sit back and do nothing, but really we’re almost burning money by not doing anything."
An outcry from many physicians led the U.S. Department of Health and Human Services to delay the planned October 2013 implementation date. No new date has been announced.
Edwards urges physicians, billing specialists, and group leaders to use the delay as an opportunity to better prepare for the implementation. She suggests checking with vendors and preparing training programs to help adjust to the new coding initiative, which will quadruple the number of billing codes to 68,000.
"Everyone at this point should still be moving forward," she says.
At the same time, the Centers for Medicare & Medicaid Services (CMS) is seeking public comment on a new version of its ICD-10 readiness assessment. Those interested in weighing in can learn more here.
TH.org Survey: VTE Prophylaxis a Gray Area for Some Hospitalists
Six out of 7 respondents to an unscientific survey at the-hospitalist.org correctly answered the question "Which patient being discharged DOES NOT require VTE prophylaxis?" while 14% of respondents answered incorrectly, according to veteran hospitalists who reviewed survey results.
Nearly 200 people responded to the survey, which provided the following answers:
• Hip/knee replacement patients;
• Hip-fracture surgery patients;
• Patients with advanced solid tumors;
• Patients with congestive heart failure; and
• Immobile or bed-bound patients.
The survey ran from June 29 to July 27 and was not limited to physicians. Sixty-six percent of respondents chose "patients with congestive heart failure" as their answer; 20% of respondents chose "patients with advanced solid tumors." Both types of discharged patients do not require VTE prophylaxis, according to the new American College of Chest Physicians (ACCP) guidelines, says Joseph Ming Wah Li, MD, SFHM, FACP, past president of SHM, associate professor of medicine at Harvard Medical School, and hospitalist at Beth Israel Deaconess Medical Center in Boston.
"Hospitalists are familiar with the fact that patients with advanced solid tumors without additional risk factors do not need extended prophylaxis, as per the guidelines put out by ACCP," Dr. Li says. "And patients with congestive heart failure being discharged from the hospital do not need extended thromboprophylaxis, either."
As for the 14% of respondents who chose incorrectly, Gregory Maynard, MD, MSc, SFHM, health sciences professor of medicine at the University of California at San Diego, says extended prophylaxis "may not be on their radar."
"Hospitalists are still struggling to get a consistent approach to inpatient VTE prophylaxis, especially since the ACCP 9 guidelines changed methodologies and provided weaker support for prophylaxis," says Dr. Maynard, senior vice president of SHM's Center for Hospital Innovation and Improvement.
For more information, check out our "Key Clinical Question" outlining VTE prophylaxis guidelines.
Six out of 7 respondents to an unscientific survey at the-hospitalist.org correctly answered the question "Which patient being discharged DOES NOT require VTE prophylaxis?" while 14% of respondents answered incorrectly, according to veteran hospitalists who reviewed survey results.
Nearly 200 people responded to the survey, which provided the following answers:
• Hip/knee replacement patients;
• Hip-fracture surgery patients;
• Patients with advanced solid tumors;
• Patients with congestive heart failure; and
• Immobile or bed-bound patients.
The survey ran from June 29 to July 27 and was not limited to physicians. Sixty-six percent of respondents chose "patients with congestive heart failure" as their answer; 20% of respondents chose "patients with advanced solid tumors." Both types of discharged patients do not require VTE prophylaxis, according to the new American College of Chest Physicians (ACCP) guidelines, says Joseph Ming Wah Li, MD, SFHM, FACP, past president of SHM, associate professor of medicine at Harvard Medical School, and hospitalist at Beth Israel Deaconess Medical Center in Boston.
"Hospitalists are familiar with the fact that patients with advanced solid tumors without additional risk factors do not need extended prophylaxis, as per the guidelines put out by ACCP," Dr. Li says. "And patients with congestive heart failure being discharged from the hospital do not need extended thromboprophylaxis, either."
As for the 14% of respondents who chose incorrectly, Gregory Maynard, MD, MSc, SFHM, health sciences professor of medicine at the University of California at San Diego, says extended prophylaxis "may not be on their radar."
"Hospitalists are still struggling to get a consistent approach to inpatient VTE prophylaxis, especially since the ACCP 9 guidelines changed methodologies and provided weaker support for prophylaxis," says Dr. Maynard, senior vice president of SHM's Center for Hospital Innovation and Improvement.
For more information, check out our "Key Clinical Question" outlining VTE prophylaxis guidelines.
Six out of 7 respondents to an unscientific survey at the-hospitalist.org correctly answered the question "Which patient being discharged DOES NOT require VTE prophylaxis?" while 14% of respondents answered incorrectly, according to veteran hospitalists who reviewed survey results.
Nearly 200 people responded to the survey, which provided the following answers:
• Hip/knee replacement patients;
• Hip-fracture surgery patients;
• Patients with advanced solid tumors;
• Patients with congestive heart failure; and
• Immobile or bed-bound patients.
The survey ran from June 29 to July 27 and was not limited to physicians. Sixty-six percent of respondents chose "patients with congestive heart failure" as their answer; 20% of respondents chose "patients with advanced solid tumors." Both types of discharged patients do not require VTE prophylaxis, according to the new American College of Chest Physicians (ACCP) guidelines, says Joseph Ming Wah Li, MD, SFHM, FACP, past president of SHM, associate professor of medicine at Harvard Medical School, and hospitalist at Beth Israel Deaconess Medical Center in Boston.
"Hospitalists are familiar with the fact that patients with advanced solid tumors without additional risk factors do not need extended prophylaxis, as per the guidelines put out by ACCP," Dr. Li says. "And patients with congestive heart failure being discharged from the hospital do not need extended thromboprophylaxis, either."
As for the 14% of respondents who chose incorrectly, Gregory Maynard, MD, MSc, SFHM, health sciences professor of medicine at the University of California at San Diego, says extended prophylaxis "may not be on their radar."
"Hospitalists are still struggling to get a consistent approach to inpatient VTE prophylaxis, especially since the ACCP 9 guidelines changed methodologies and provided weaker support for prophylaxis," says Dr. Maynard, senior vice president of SHM's Center for Hospital Innovation and Improvement.
For more information, check out our "Key Clinical Question" outlining VTE prophylaxis guidelines.
Welcome to the August Online Issue: Take the SVS Survey
When the Society for Vascular Surgery (SVS) was approached to become involved in assessing vascular out-patient centers (OEC) the Clinical Practices Committee (CPC) convened to examine this topic that was arousing so much interest and concern among providers and patients.
After reviewing the preliminary CPC assessment, the SVS leadership asked two of the committee to develop an editorial for publication in Vascular Specialist. The intent is to survey the SVS membership on this increasingly relevant issue.
So click on the editorial. Read it. And take the easy online, interactive survey at the bottom.
Your views ARE important. They will help shape how SVS deals with this important issue going forward. Let us know your opinions about OECs. There is room for comment after each survey question, but if you have a lengthier opinion, please take the survey and then e-mail us your in-depth comments at [email protected].
When the Society for Vascular Surgery (SVS) was approached to become involved in assessing vascular out-patient centers (OEC) the Clinical Practices Committee (CPC) convened to examine this topic that was arousing so much interest and concern among providers and patients.
After reviewing the preliminary CPC assessment, the SVS leadership asked two of the committee to develop an editorial for publication in Vascular Specialist. The intent is to survey the SVS membership on this increasingly relevant issue.
So click on the editorial. Read it. And take the easy online, interactive survey at the bottom.
Your views ARE important. They will help shape how SVS deals with this important issue going forward. Let us know your opinions about OECs. There is room for comment after each survey question, but if you have a lengthier opinion, please take the survey and then e-mail us your in-depth comments at [email protected].
When the Society for Vascular Surgery (SVS) was approached to become involved in assessing vascular out-patient centers (OEC) the Clinical Practices Committee (CPC) convened to examine this topic that was arousing so much interest and concern among providers and patients.
After reviewing the preliminary CPC assessment, the SVS leadership asked two of the committee to develop an editorial for publication in Vascular Specialist. The intent is to survey the SVS membership on this increasingly relevant issue.
So click on the editorial. Read it. And take the easy online, interactive survey at the bottom.
Your views ARE important. They will help shape how SVS deals with this important issue going forward. Let us know your opinions about OECs. There is room for comment after each survey question, but if you have a lengthier opinion, please take the survey and then e-mail us your in-depth comments at [email protected].
The Recovery Process: Confidentiality and Families
Recovery includes having a good social support system – family members and friends who believe in the patient’s recovery. The health care system fiercely guards the patient’s personal information. How do we as mental health providers best communicate with the patient’s family?
There are differing attitudes about talking with families. In a study by Phyllis Solomon, Ph.D., most providers interpreted confidentiality policies conservatively, and 54 percent were confused about the types of information that are confidential (Psychiatric Serv. 2003;54:1622-8).
The need to ensure that communication is optimal is further demonstrated by the findings of a recently devised instrument called the Confidentiality Issues Test, or CIT. The CIT, as outlined by Tina Marshall, Ph.D., and Dr. Solomon, contains scenarios, descriptions, and questions about confidentiality issues and family members (Am J. Psychiatric Rehab. 2012;15:97-115). The following two questions come from the CIT, and the answer in bold is the correct one.
First Situation
A woman calls you about a patient on your caseload and identifies herself as your patient’s mother. You have no release, but the patient has mentioned that he visits his mother frequently, and you have no reason to believe that the caller is a danger to the patient. The caller says she wants to make sure that her son’s case manager gets certain very important information about his financial and legal situation –information that he often does not mention to staff.
Which answer is correct?
1a. All you can say is that you cannot give out any information about patients without a release, including whether any particular person receives services at your agency.
1b. You are only allowed to take the caller’s name and contact information and tell her that if any information can be released, someone will get back to her.
1c. While stating that you cannot give out any information, you are allowed to ask the caller about the information she is concerned about conveying and say that if it turns out that her son is a patient there, you will make sure the information gets to the right person.
1d. Since the caller is an immediate family member and has important information, you are allowed to confirm that the son is a patient at your agency, but not to release any other information.
Second Situation
A patient has told you (or someone at your agency) that she plans to take an overdose tonight, and has a large number of pills saved up at her apartment. You know that she has a roommate, and you have the roommate’s contact information, but you have no signed release to talk to the roommate.
Which answer is correct?
5a. Even in this situation, you must get a signed release from the patient to be able to call and talk to the roommate about the patient’s safety.
5b. You do not need to have a release to talk to the roommate if there is a question of imminent death or serious injury to the patient, as long as the information you share is restricted to the issue of the consumer’s safety.
5c. Neither of the above choices is correct.
5d. Not sure
Almost 50% of behavioral health providers who completed this test believed that even without revealing any information about a client, they could not listen to a family member or a significant support person without a release from the patient, or were unsure whether they could, according to Dr. Marshall and Dr. Solomon. Staff also indicated that they would attempt to avoid being in a situation where they had to implement a policy that seemed too fraught with difficulties.
Most patients, and especially those with chronic mental illness, need assistance in monitoring and managing symptoms as an important part of recovery. Families are the first to notice symptoms; families bring the patients to the emergency room; and families are most affected by their relative’s disability. Family conflict can arise when the family member does not understand the illness or the symptoms – and does not understand how best to respond to an ill relative. Families want to offer support but need some information about their relative’s illness and treatment. What can you divulge to families?
First, the patient needs to understand the role of the family in managing the illness. When patients understand that their family/friends can be helpful and agree to give the family members ways to be helpful, they usually are willing to have their family members come for a visit. A family consultation clarifies where the boundaries are between the patient, the mental health providers, and the family members. The family member does not need to know "specifics," but does need to know how to respond when difficulties arise so that the family member does not get overly anxious and then does things that are unhelpful.
A conversation with a patient about sharing information with family members might go something like this:
Doctor: "Suzi, if you have a side effect from your medication, what should your husband do? Is the side effect life-threatening, or can you call in the morning to get advice? We have talked about if you have a side effect you call me, and we can discuss it. If your husband gets too worried because your side effect is frightening, then there is conflict about how to manage the symptom. So, if your husband knows what we discuss about side effects, then things at home will be calm. What do you think?"
Patient: "Okay, I understand. That sounds good. The less worried he is, the more he will let me alone."
D: "Are there other situations where you think that if your husband had more information, he might be less anxious and therefore less on your back about things?"
P: "Maybe if he understood my depression more – that I get forgetful or too tired or feeling hopeless ..."
D: "How would it help if he had more information?"
P: "He would not start to talk to me in that angry voice, then get on the phone and complain to his mother."
D: "Do you think he would agree to come in so that we could talk about ways to manage your symptoms?"
P: "Yes, but you have to promise not to talk about other things."
D: "What other things do you not want me to talk to her about?"
P: "I don’t want you telling him that I feel suicidal."
D: "Do you think he knows?"
P: "Yes, but I don’t want him talking about it with me."
D: "Don’t you think he would be more settled if he knew you could successfully use your safety plan? Your plan is for you to do something to distract your thoughts and to counteract the feelings, then to call me or the emergency number if you are needing further help. Remember the plan you have? You have used it a couple of times."
P: "Maybe, yes, perhaps."
D: "Put yourself in his shoes. Wouldn’t you be more comfortable knowing that there is a good safety plan in place?"
P: "I guess so."
D: "Okay, think about it, talk to him, and let’s schedule a meeting. Also, if you want, you can both go to the family support group we have."
P: "Okay, I’ll talk to him."
Staff also can offer nonconfidential information to family members and friends. We make it clear that we are not authorized to acknowledge whether the person is receiving treatment at the agency but can still answer general questions such as those dealing with diagnosis and treatment. We can provide written educational material and information about community resources. We can say that family involvement is important and that with the patient’s agreement, family members and friends can be involved in treatment; and we can listen to whatever they want to tell us.
Here is a quick summary of points to remember when it comes to confidentiality issues:
1. Discuss goals of family involvement with patients.
2. Educate staff about the benefits of involving family.
3. Provide guidance to staff on what to discuss with families and how to talk to families.
4. Ensure that your staff understands what is and what is not confidential information.
5. Remember that you can always listen to what a family member or friend has to say.
6. Keep in mind that serious risk trumps the need for a release of information to family or friends.
Confidentiality is vital. It safeguards patients’ trust and allows patients to work toward their own recovery. There are consent procedures for releasing confidential information, and some agencies have forms specifically designed for families. These forms specify the types of information to be released to a designated family member or significant person, and have a longer time frame of 1 year. These forms allow information to be communicated verbally rather than in writing.
When staff members understand the rationale and goals of involving family and friends, and if they receive training in how to approach patients and their families, willingness will be greater to implement a family-friendly approach to recovery.
Dr. Heru is with the department of psychiatry at the University of Colorado Medical School. She has been a member of the Association of Family Psychiatrists since 2002 and currently serves as the organization’s treasurer. In addition, she is the coauthor of two books on working with families and is the author of numerous articles on this topic.
Recovery includes having a good social support system – family members and friends who believe in the patient’s recovery. The health care system fiercely guards the patient’s personal information. How do we as mental health providers best communicate with the patient’s family?
There are differing attitudes about talking with families. In a study by Phyllis Solomon, Ph.D., most providers interpreted confidentiality policies conservatively, and 54 percent were confused about the types of information that are confidential (Psychiatric Serv. 2003;54:1622-8).
The need to ensure that communication is optimal is further demonstrated by the findings of a recently devised instrument called the Confidentiality Issues Test, or CIT. The CIT, as outlined by Tina Marshall, Ph.D., and Dr. Solomon, contains scenarios, descriptions, and questions about confidentiality issues and family members (Am J. Psychiatric Rehab. 2012;15:97-115). The following two questions come from the CIT, and the answer in bold is the correct one.
First Situation
A woman calls you about a patient on your caseload and identifies herself as your patient’s mother. You have no release, but the patient has mentioned that he visits his mother frequently, and you have no reason to believe that the caller is a danger to the patient. The caller says she wants to make sure that her son’s case manager gets certain very important information about his financial and legal situation –information that he often does not mention to staff.
Which answer is correct?
1a. All you can say is that you cannot give out any information about patients without a release, including whether any particular person receives services at your agency.
1b. You are only allowed to take the caller’s name and contact information and tell her that if any information can be released, someone will get back to her.
1c. While stating that you cannot give out any information, you are allowed to ask the caller about the information she is concerned about conveying and say that if it turns out that her son is a patient there, you will make sure the information gets to the right person.
1d. Since the caller is an immediate family member and has important information, you are allowed to confirm that the son is a patient at your agency, but not to release any other information.
Second Situation
A patient has told you (or someone at your agency) that she plans to take an overdose tonight, and has a large number of pills saved up at her apartment. You know that she has a roommate, and you have the roommate’s contact information, but you have no signed release to talk to the roommate.
Which answer is correct?
5a. Even in this situation, you must get a signed release from the patient to be able to call and talk to the roommate about the patient’s safety.
5b. You do not need to have a release to talk to the roommate if there is a question of imminent death or serious injury to the patient, as long as the information you share is restricted to the issue of the consumer’s safety.
5c. Neither of the above choices is correct.
5d. Not sure
Almost 50% of behavioral health providers who completed this test believed that even without revealing any information about a client, they could not listen to a family member or a significant support person without a release from the patient, or were unsure whether they could, according to Dr. Marshall and Dr. Solomon. Staff also indicated that they would attempt to avoid being in a situation where they had to implement a policy that seemed too fraught with difficulties.
Most patients, and especially those with chronic mental illness, need assistance in monitoring and managing symptoms as an important part of recovery. Families are the first to notice symptoms; families bring the patients to the emergency room; and families are most affected by their relative’s disability. Family conflict can arise when the family member does not understand the illness or the symptoms – and does not understand how best to respond to an ill relative. Families want to offer support but need some information about their relative’s illness and treatment. What can you divulge to families?
First, the patient needs to understand the role of the family in managing the illness. When patients understand that their family/friends can be helpful and agree to give the family members ways to be helpful, they usually are willing to have their family members come for a visit. A family consultation clarifies where the boundaries are between the patient, the mental health providers, and the family members. The family member does not need to know "specifics," but does need to know how to respond when difficulties arise so that the family member does not get overly anxious and then does things that are unhelpful.
A conversation with a patient about sharing information with family members might go something like this:
Doctor: "Suzi, if you have a side effect from your medication, what should your husband do? Is the side effect life-threatening, or can you call in the morning to get advice? We have talked about if you have a side effect you call me, and we can discuss it. If your husband gets too worried because your side effect is frightening, then there is conflict about how to manage the symptom. So, if your husband knows what we discuss about side effects, then things at home will be calm. What do you think?"
Patient: "Okay, I understand. That sounds good. The less worried he is, the more he will let me alone."
D: "Are there other situations where you think that if your husband had more information, he might be less anxious and therefore less on your back about things?"
P: "Maybe if he understood my depression more – that I get forgetful or too tired or feeling hopeless ..."
D: "How would it help if he had more information?"
P: "He would not start to talk to me in that angry voice, then get on the phone and complain to his mother."
D: "Do you think he would agree to come in so that we could talk about ways to manage your symptoms?"
P: "Yes, but you have to promise not to talk about other things."
D: "What other things do you not want me to talk to her about?"
P: "I don’t want you telling him that I feel suicidal."
D: "Do you think he knows?"
P: "Yes, but I don’t want him talking about it with me."
D: "Don’t you think he would be more settled if he knew you could successfully use your safety plan? Your plan is for you to do something to distract your thoughts and to counteract the feelings, then to call me or the emergency number if you are needing further help. Remember the plan you have? You have used it a couple of times."
P: "Maybe, yes, perhaps."
D: "Put yourself in his shoes. Wouldn’t you be more comfortable knowing that there is a good safety plan in place?"
P: "I guess so."
D: "Okay, think about it, talk to him, and let’s schedule a meeting. Also, if you want, you can both go to the family support group we have."
P: "Okay, I’ll talk to him."
Staff also can offer nonconfidential information to family members and friends. We make it clear that we are not authorized to acknowledge whether the person is receiving treatment at the agency but can still answer general questions such as those dealing with diagnosis and treatment. We can provide written educational material and information about community resources. We can say that family involvement is important and that with the patient’s agreement, family members and friends can be involved in treatment; and we can listen to whatever they want to tell us.
Here is a quick summary of points to remember when it comes to confidentiality issues:
1. Discuss goals of family involvement with patients.
2. Educate staff about the benefits of involving family.
3. Provide guidance to staff on what to discuss with families and how to talk to families.
4. Ensure that your staff understands what is and what is not confidential information.
5. Remember that you can always listen to what a family member or friend has to say.
6. Keep in mind that serious risk trumps the need for a release of information to family or friends.
Confidentiality is vital. It safeguards patients’ trust and allows patients to work toward their own recovery. There are consent procedures for releasing confidential information, and some agencies have forms specifically designed for families. These forms specify the types of information to be released to a designated family member or significant person, and have a longer time frame of 1 year. These forms allow information to be communicated verbally rather than in writing.
When staff members understand the rationale and goals of involving family and friends, and if they receive training in how to approach patients and their families, willingness will be greater to implement a family-friendly approach to recovery.
Dr. Heru is with the department of psychiatry at the University of Colorado Medical School. She has been a member of the Association of Family Psychiatrists since 2002 and currently serves as the organization’s treasurer. In addition, she is the coauthor of two books on working with families and is the author of numerous articles on this topic.
Recovery includes having a good social support system – family members and friends who believe in the patient’s recovery. The health care system fiercely guards the patient’s personal information. How do we as mental health providers best communicate with the patient’s family?
There are differing attitudes about talking with families. In a study by Phyllis Solomon, Ph.D., most providers interpreted confidentiality policies conservatively, and 54 percent were confused about the types of information that are confidential (Psychiatric Serv. 2003;54:1622-8).
The need to ensure that communication is optimal is further demonstrated by the findings of a recently devised instrument called the Confidentiality Issues Test, or CIT. The CIT, as outlined by Tina Marshall, Ph.D., and Dr. Solomon, contains scenarios, descriptions, and questions about confidentiality issues and family members (Am J. Psychiatric Rehab. 2012;15:97-115). The following two questions come from the CIT, and the answer in bold is the correct one.
First Situation
A woman calls you about a patient on your caseload and identifies herself as your patient’s mother. You have no release, but the patient has mentioned that he visits his mother frequently, and you have no reason to believe that the caller is a danger to the patient. The caller says she wants to make sure that her son’s case manager gets certain very important information about his financial and legal situation –information that he often does not mention to staff.
Which answer is correct?
1a. All you can say is that you cannot give out any information about patients without a release, including whether any particular person receives services at your agency.
1b. You are only allowed to take the caller’s name and contact information and tell her that if any information can be released, someone will get back to her.
1c. While stating that you cannot give out any information, you are allowed to ask the caller about the information she is concerned about conveying and say that if it turns out that her son is a patient there, you will make sure the information gets to the right person.
1d. Since the caller is an immediate family member and has important information, you are allowed to confirm that the son is a patient at your agency, but not to release any other information.
Second Situation
A patient has told you (or someone at your agency) that she plans to take an overdose tonight, and has a large number of pills saved up at her apartment. You know that she has a roommate, and you have the roommate’s contact information, but you have no signed release to talk to the roommate.
Which answer is correct?
5a. Even in this situation, you must get a signed release from the patient to be able to call and talk to the roommate about the patient’s safety.
5b. You do not need to have a release to talk to the roommate if there is a question of imminent death or serious injury to the patient, as long as the information you share is restricted to the issue of the consumer’s safety.
5c. Neither of the above choices is correct.
5d. Not sure
Almost 50% of behavioral health providers who completed this test believed that even without revealing any information about a client, they could not listen to a family member or a significant support person without a release from the patient, or were unsure whether they could, according to Dr. Marshall and Dr. Solomon. Staff also indicated that they would attempt to avoid being in a situation where they had to implement a policy that seemed too fraught with difficulties.
Most patients, and especially those with chronic mental illness, need assistance in monitoring and managing symptoms as an important part of recovery. Families are the first to notice symptoms; families bring the patients to the emergency room; and families are most affected by their relative’s disability. Family conflict can arise when the family member does not understand the illness or the symptoms – and does not understand how best to respond to an ill relative. Families want to offer support but need some information about their relative’s illness and treatment. What can you divulge to families?
First, the patient needs to understand the role of the family in managing the illness. When patients understand that their family/friends can be helpful and agree to give the family members ways to be helpful, they usually are willing to have their family members come for a visit. A family consultation clarifies where the boundaries are between the patient, the mental health providers, and the family members. The family member does not need to know "specifics," but does need to know how to respond when difficulties arise so that the family member does not get overly anxious and then does things that are unhelpful.
A conversation with a patient about sharing information with family members might go something like this:
Doctor: "Suzi, if you have a side effect from your medication, what should your husband do? Is the side effect life-threatening, or can you call in the morning to get advice? We have talked about if you have a side effect you call me, and we can discuss it. If your husband gets too worried because your side effect is frightening, then there is conflict about how to manage the symptom. So, if your husband knows what we discuss about side effects, then things at home will be calm. What do you think?"
Patient: "Okay, I understand. That sounds good. The less worried he is, the more he will let me alone."
D: "Are there other situations where you think that if your husband had more information, he might be less anxious and therefore less on your back about things?"
P: "Maybe if he understood my depression more – that I get forgetful or too tired or feeling hopeless ..."
D: "How would it help if he had more information?"
P: "He would not start to talk to me in that angry voice, then get on the phone and complain to his mother."
D: "Do you think he would agree to come in so that we could talk about ways to manage your symptoms?"
P: "Yes, but you have to promise not to talk about other things."
D: "What other things do you not want me to talk to her about?"
P: "I don’t want you telling him that I feel suicidal."
D: "Do you think he knows?"
P: "Yes, but I don’t want him talking about it with me."
D: "Don’t you think he would be more settled if he knew you could successfully use your safety plan? Your plan is for you to do something to distract your thoughts and to counteract the feelings, then to call me or the emergency number if you are needing further help. Remember the plan you have? You have used it a couple of times."
P: "Maybe, yes, perhaps."
D: "Put yourself in his shoes. Wouldn’t you be more comfortable knowing that there is a good safety plan in place?"
P: "I guess so."
D: "Okay, think about it, talk to him, and let’s schedule a meeting. Also, if you want, you can both go to the family support group we have."
P: "Okay, I’ll talk to him."
Staff also can offer nonconfidential information to family members and friends. We make it clear that we are not authorized to acknowledge whether the person is receiving treatment at the agency but can still answer general questions such as those dealing with diagnosis and treatment. We can provide written educational material and information about community resources. We can say that family involvement is important and that with the patient’s agreement, family members and friends can be involved in treatment; and we can listen to whatever they want to tell us.
Here is a quick summary of points to remember when it comes to confidentiality issues:
1. Discuss goals of family involvement with patients.
2. Educate staff about the benefits of involving family.
3. Provide guidance to staff on what to discuss with families and how to talk to families.
4. Ensure that your staff understands what is and what is not confidential information.
5. Remember that you can always listen to what a family member or friend has to say.
6. Keep in mind that serious risk trumps the need for a release of information to family or friends.
Confidentiality is vital. It safeguards patients’ trust and allows patients to work toward their own recovery. There are consent procedures for releasing confidential information, and some agencies have forms specifically designed for families. These forms specify the types of information to be released to a designated family member or significant person, and have a longer time frame of 1 year. These forms allow information to be communicated verbally rather than in writing.
When staff members understand the rationale and goals of involving family and friends, and if they receive training in how to approach patients and their families, willingness will be greater to implement a family-friendly approach to recovery.
Dr. Heru is with the department of psychiatry at the University of Colorado Medical School. She has been a member of the Association of Family Psychiatrists since 2002 and currently serves as the organization’s treasurer. In addition, she is the coauthor of two books on working with families and is the author of numerous articles on this topic.
CDC Urges Hep C Test for Baby Boomers
The Centers for Disease Control and Prevention recommends that all Americans aged 47-67 years should be tested once for hepatitis C infection, according to a CDC statement published Aug. 16 online. The CDC proposed the recommendation in May 2012.
Data from previous studies suggest that the baby boomers, defined by the CDC as individuals born between 1945 and 1965, are at increased risk for hepatitis C for many reasons, including blood transfusions, hospital exposures, and a possible history of risky behaviors in their younger years. However, many people in this age group are amenable to hepatitis C testing if it is available to them.
According to the CDC statement, "1 in 30 baby boomers has been infected with hepatitis C, and most don’t know it." This life-threatening infection has few symptoms and affects approximately 3.2 million U.S. adults, most of whom are baby boomers, according to the CDC. Hepatitis C is the leading cause of liver transplantation in the United States, and the virus causes serious liver diseases including cirrhosis and liver cancer.
The CDC said in the statement that a one-time hepatitis C test for all baby boomers could potentially identify more than 800,000 additional cases. If treated early, up to 75% of these individuals could be cured, avoiding the costs and serious complications associated with untreated hepatitis C infections. New therapies have recently improved the cure rate significantly.
The CDC encourages clinicians to promote hepatitis C testing to their baby boomer patients.
"Identifying these hidden infections early will allow more baby boomers to receive care and treatment, before they develop life-threatening liver disease," Dr. Kevin Fenton, director of CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD and TB Prevention, said in the CDC statement. One-time hepatitis C testing for baby boomers "could potentially save tens of thousands of lives," he said.
The Centers for Disease Control and Prevention recommends that all Americans aged 47-67 years should be tested once for hepatitis C infection, according to a CDC statement published Aug. 16 online. The CDC proposed the recommendation in May 2012.
Data from previous studies suggest that the baby boomers, defined by the CDC as individuals born between 1945 and 1965, are at increased risk for hepatitis C for many reasons, including blood transfusions, hospital exposures, and a possible history of risky behaviors in their younger years. However, many people in this age group are amenable to hepatitis C testing if it is available to them.
According to the CDC statement, "1 in 30 baby boomers has been infected with hepatitis C, and most don’t know it." This life-threatening infection has few symptoms and affects approximately 3.2 million U.S. adults, most of whom are baby boomers, according to the CDC. Hepatitis C is the leading cause of liver transplantation in the United States, and the virus causes serious liver diseases including cirrhosis and liver cancer.
The CDC said in the statement that a one-time hepatitis C test for all baby boomers could potentially identify more than 800,000 additional cases. If treated early, up to 75% of these individuals could be cured, avoiding the costs and serious complications associated with untreated hepatitis C infections. New therapies have recently improved the cure rate significantly.
The CDC encourages clinicians to promote hepatitis C testing to their baby boomer patients.
"Identifying these hidden infections early will allow more baby boomers to receive care and treatment, before they develop life-threatening liver disease," Dr. Kevin Fenton, director of CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD and TB Prevention, said in the CDC statement. One-time hepatitis C testing for baby boomers "could potentially save tens of thousands of lives," he said.
The Centers for Disease Control and Prevention recommends that all Americans aged 47-67 years should be tested once for hepatitis C infection, according to a CDC statement published Aug. 16 online. The CDC proposed the recommendation in May 2012.
Data from previous studies suggest that the baby boomers, defined by the CDC as individuals born between 1945 and 1965, are at increased risk for hepatitis C for many reasons, including blood transfusions, hospital exposures, and a possible history of risky behaviors in their younger years. However, many people in this age group are amenable to hepatitis C testing if it is available to them.
According to the CDC statement, "1 in 30 baby boomers has been infected with hepatitis C, and most don’t know it." This life-threatening infection has few symptoms and affects approximately 3.2 million U.S. adults, most of whom are baby boomers, according to the CDC. Hepatitis C is the leading cause of liver transplantation in the United States, and the virus causes serious liver diseases including cirrhosis and liver cancer.
The CDC said in the statement that a one-time hepatitis C test for all baby boomers could potentially identify more than 800,000 additional cases. If treated early, up to 75% of these individuals could be cured, avoiding the costs and serious complications associated with untreated hepatitis C infections. New therapies have recently improved the cure rate significantly.
The CDC encourages clinicians to promote hepatitis C testing to their baby boomer patients.
"Identifying these hidden infections early will allow more baby boomers to receive care and treatment, before they develop life-threatening liver disease," Dr. Kevin Fenton, director of CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD and TB Prevention, said in the CDC statement. One-time hepatitis C testing for baby boomers "could potentially save tens of thousands of lives," he said.