User login
Do cosmetic breast implants hinder the detection of malignancy and reduce breast cancer–specific survival?
Most epidemiologic studies have found no elevated risk of breast cancer among women who undergo cosmetic breast augmentation. However, there is concern that implants, which are radio-opaque, may limit our ability to diagnose malignancies at an early stage using screening mammography.
In this study, investigators compared the stage distribution of breast cancers at diagnosis and documented breast cancer–specific survival among women with and without cosmetic breast implants. Twelve cross-sectional studies published after 2000 in the United States had evaluated stage distribution of breast cancer among women with and without cosmetic implants. As stated above, investigators found an elevated risk of nonlocalized breast cancer among women with implants in their meta-analysis of these studies (OR, 1.26), but this elevated risk did not achieve statistical significance. A second analysis of five studies found an elevated risk of breast cancer–specific mortality (OR, 1.38), compared with the general population (no implants), which did achieve significance.
MRI may be helpful—but is the expense justified?
More than 300,000 women underwent cosmetic breast augmentation in 2011 in the United States, an increase of roughly 800% since the early 1990s. The impaired visualization of breast tissue via mammography in these women ranges from 22% to 83%. In addition, the implants limit compression of the breasts during mammography, and capsular contraction further contributes to this problem.
Magnetic resonance imaging (MRI) may be helpful in screening women with cosmetic breast implants, but this technology is expensive, and evidence supporting its routine use in this population is limited.
Some mammographers use special techniques to better visualize the breast tissue of women with implants. These techniques include displacing the implant posteriorly and pulling the breast tissue in front of it. However, even with such strategies, as much as one-third of the breast tissue may be inadequately assessed.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
These findings underscore the importance of sharing the risks of nonlocalized breast malignancy and increased breast cancer mortality with patients who are considering cosmetic breast implants, as well as with women who have already undergone this common procedure. Future studies are needed to address relevant issues, including the role of 3-D (tomosynthesis) technology in screening women with breast implants and optimal screening intervals in this subgroup.
ANDREW M. KAUNITZ, MD
We want to hear from you. Tell us what you think.
Most epidemiologic studies have found no elevated risk of breast cancer among women who undergo cosmetic breast augmentation. However, there is concern that implants, which are radio-opaque, may limit our ability to diagnose malignancies at an early stage using screening mammography.
In this study, investigators compared the stage distribution of breast cancers at diagnosis and documented breast cancer–specific survival among women with and without cosmetic breast implants. Twelve cross-sectional studies published after 2000 in the United States had evaluated stage distribution of breast cancer among women with and without cosmetic implants. As stated above, investigators found an elevated risk of nonlocalized breast cancer among women with implants in their meta-analysis of these studies (OR, 1.26), but this elevated risk did not achieve statistical significance. A second analysis of five studies found an elevated risk of breast cancer–specific mortality (OR, 1.38), compared with the general population (no implants), which did achieve significance.
MRI may be helpful—but is the expense justified?
More than 300,000 women underwent cosmetic breast augmentation in 2011 in the United States, an increase of roughly 800% since the early 1990s. The impaired visualization of breast tissue via mammography in these women ranges from 22% to 83%. In addition, the implants limit compression of the breasts during mammography, and capsular contraction further contributes to this problem.
Magnetic resonance imaging (MRI) may be helpful in screening women with cosmetic breast implants, but this technology is expensive, and evidence supporting its routine use in this population is limited.
Some mammographers use special techniques to better visualize the breast tissue of women with implants. These techniques include displacing the implant posteriorly and pulling the breast tissue in front of it. However, even with such strategies, as much as one-third of the breast tissue may be inadequately assessed.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
These findings underscore the importance of sharing the risks of nonlocalized breast malignancy and increased breast cancer mortality with patients who are considering cosmetic breast implants, as well as with women who have already undergone this common procedure. Future studies are needed to address relevant issues, including the role of 3-D (tomosynthesis) technology in screening women with breast implants and optimal screening intervals in this subgroup.
ANDREW M. KAUNITZ, MD
We want to hear from you. Tell us what you think.
Most epidemiologic studies have found no elevated risk of breast cancer among women who undergo cosmetic breast augmentation. However, there is concern that implants, which are radio-opaque, may limit our ability to diagnose malignancies at an early stage using screening mammography.
In this study, investigators compared the stage distribution of breast cancers at diagnosis and documented breast cancer–specific survival among women with and without cosmetic breast implants. Twelve cross-sectional studies published after 2000 in the United States had evaluated stage distribution of breast cancer among women with and without cosmetic implants. As stated above, investigators found an elevated risk of nonlocalized breast cancer among women with implants in their meta-analysis of these studies (OR, 1.26), but this elevated risk did not achieve statistical significance. A second analysis of five studies found an elevated risk of breast cancer–specific mortality (OR, 1.38), compared with the general population (no implants), which did achieve significance.
MRI may be helpful—but is the expense justified?
More than 300,000 women underwent cosmetic breast augmentation in 2011 in the United States, an increase of roughly 800% since the early 1990s. The impaired visualization of breast tissue via mammography in these women ranges from 22% to 83%. In addition, the implants limit compression of the breasts during mammography, and capsular contraction further contributes to this problem.
Magnetic resonance imaging (MRI) may be helpful in screening women with cosmetic breast implants, but this technology is expensive, and evidence supporting its routine use in this population is limited.
Some mammographers use special techniques to better visualize the breast tissue of women with implants. These techniques include displacing the implant posteriorly and pulling the breast tissue in front of it. However, even with such strategies, as much as one-third of the breast tissue may be inadequately assessed.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
These findings underscore the importance of sharing the risks of nonlocalized breast malignancy and increased breast cancer mortality with patients who are considering cosmetic breast implants, as well as with women who have already undergone this common procedure. Future studies are needed to address relevant issues, including the role of 3-D (tomosynthesis) technology in screening women with breast implants and optimal screening intervals in this subgroup.
ANDREW M. KAUNITZ, MD
We want to hear from you. Tell us what you think.
The “Canoe” Technique to Insert Lumbar Pedicle Screws: Consistent, Safe, and Simple
Successful treatment of chronic vaginitis
Gadzooks! In preparing for the morning office practice session you notice that two patients with chronic vaginitis have been scheduled back to back in 15-minute slots.
Ms. A has chronic bacterial vaginosis. Ms. B has chronic yeast vaginitis. What are you going to do?
Chronic bacterial vaginosis
The normal vaginal microbiome is dominated by Lactobacillus crispatus and Lactobacillus jensenii. These organisms produce hydrogen peroxide and keep the vaginal pH ≤4.5. When Gardnerella vaginalis and associated anaerobic bacteria gain dominance in the vagina, bacterial vaginosis ensues. This infection is characterized by1:
- homogenous, thin, grayish-white discharge that smoothly coats the vaginal epithelium
- pH >4.5
- fishy odor when potassium hydroxide is added to a sample of the discharge
- clue cells on a saline wet mount.
Why is it prone to recur? If bacterial vaginosis was a simple infection, treatment with metronidazole or clindamycin should be very effective. But in many women the relief from symptoms provided by a single course of antibiotics is short-lived, and many patients experience recurrent bacterial vaginosis in the next few months.
The cause of this resistance to antibiotic treatment may be that G vaginalis and other anaerobes, such as Atopobium species, aggregate in vaginal biofilms that prevent the antibiotic from reaching the organism.2 The biofilm provides a safe haven for the bacteria to regrow following a single course of treatment.3 In addition, the nutrient-limited environment inside the encapsulated biofilm helps the bacteria to resist the toxic effects of the antibiotic.4
Another potential mechanism for bacterial vaginosis recurrence is that women destined to develop repeat infection often harbor G vaginalis encapsulated in biofilms in the mouth. These extravaginal bacteria often are found again in the vagina, suggesting that bacterial vaginosis can be acquired from extravaginal bacterial reservoirs.5 Investigators are developing approaches, such as intravaginal treatment with DNase, to destroy the vaginal biofilm in order to enhance the efficacy of antibiotic treatment.6
Treatment
Options for initial infection. There are three treatments for an initial occurrence of bacterial vaginosis7:
- oral metronidazole 500 mg twice daily for 7 days
- 0.75% metronidazole gel one applicator intravaginally once daily for 5 days, or
- 2% clindamycin cream one applicator intravaginally at bedtime for 7 days.
Long-term metronidazole for recurrence. Approximately half of women who respond to initial treatment will have bacterial vaginosis again within 1 year. If vaginitis caused by recurrent bacterial vaginosisis diagnosed, a prolonged course of antibiotic treatment is warranted. Treatment starts with an induction regimen of the standard treatments listed in the paragraph above. This is followed by a long-term maintenance regimen using 0.75% metronidazole vaginal gel one applicator twice weekly for 4 to 6 months.8
Recurrent Candida vulvovaginitis
Four or more occurrences of symptomatic Candida vulvovaginitis in 12 months indicates recurrent infection. Recurrence is usually caused by reinfection with the same organism from a vaginal reservoir. For women with such repeat infection, vaginal cultures should be obtained to confirm Candida and to search for treatment-resistant species, such as Candida glabrata. (Many C glabrata organisms are resistant to standard fluconazole treatment.)
Treatment options
Long courses of oral or vaginal antimycotic agents can be effective treatment for recurrent Candida vulvovaginitis.
Fluconazole. One regimen is fluconazole 150 mg orally every 72 hours for 3 doses, followed by fluconazole 150 mg once weekly for 6 months.9 If patients relapse from this regimen, then the vaginitis should be retreated with fluconazole 150 mg orally every 72 hours for 3 doses, followed by fluconazole 150 mg weekly for 12 months.
Boric acid. If C glabrata is thought to be the cause of the infection, it may be difficult to eradicate with fluconazole. A regimen to treat recurrent vaginitis caused by C glabrata is intravaginal boric acid, a 600 mg capsule once nightly for 14 days.10,11This medication is not FDA-approved for this purpose and must be made by a compounding pharmacy. Boric acid can be fatal if swallowed rather than used intravaginally. Care must be taken to avoid access to these capsules by children.
Boric acid vaginal capsules also can be used to treat chronic bacterial vaginosis in combination with antibiotic therapy.12
Flucytosine. An alternative regimen to treat C glabrata is flucytosine vaginal cream one applicator nightly for 14 days. This vaginal cream must be compounded because it is not available as a commercial medication.
You are armed and ready
In retrospect, you realize that the morning office session schedule is going to be fine. You will treat Ms. A with a long course of metronidazole and Ms. B with a long course of fluconazole. Hopefully, they will both find relief from their symptoms.
Tell us what you think, at [email protected]. Please include your name and city and state.
- Eschenbach DA, Hillier S, Critchlow C, Stevens C, DeRouen T, Holmes KK. Diagnosis and clinical manifestations of bacterial vaginosis. Am J Obstet Gynecol. 1988;158(4):819–828.
- Swidinski A, Mendling W, Loening-Baucke V, et al. Adherent biofilms in bacterial vaginosis.Obstet Gynecol. 2005;106(5 pt 1):1013–1023.
- Swidinski A, Mendling W, Loening-Baucke V, et al. An adherent Gardnerella vaginalis biofilm persists on the vaginal epithelium after standard therapy with oral metronidazole. Am J Obstet Gynecol. 2008;198(1):97e1–e6.
- Monds RD, O’Toole GA. The developmental model of microbial biofilm: ten years of a paradigm up for review. Trends Microbiol. 2009;17(2):73–87.
- Marrazzo JM, Friedler TL, Srinivasan S, et al. Extravaginal reservoirs of vaginal bacteria as risk factors for incident bacterial vaginosis. J Infect Dis. 2012;205(10):1580–1588.
- Hymes SR, Randis TM, Sun TY, Ratner AJ. DNase inhibits Gardnerella vaginalis biofilms in vitro and in vivo. J Infect Dis. 2013;207(10):1491–1497.
- Workowski KA, Berman S; Centers for Disease Control and Prevention (CDC). Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep. 2010; 59(RR-12):1–110.
- Sobel JD, Ferris D, Schwebke J, et al. Suppressive antibacterial therapy with 0.75% metronidazole vaginal gel to prevent recurrent bacterial vaginosis. Am J Obstet Gynecol. 2006;194(5):1283–1289.
- Sobel JD, Wiesenfeld HC, Martens M, et al. Maintenance fluconazole therapy for recurrent vulvovaginal candidiasis. N Engl J Med. 2004;351(9):876–883.
- Savini V, Catavitello C, Bianco A, Balbinot A, D’Antonio F, D’Antonio D. Azole resistant Candida glabrata vulvovaginitis treated with boric acid. Eur J Obstet Gynecol Reprod Biol. 2009;147(1):112.
- Iavazzo C, Gkegkes ID, Zarkada IM, Falagas ME. Boric acid for recurrent vulvovaginal candidiasis: the clinical evidence. J Womens Health(Larchmt). 2011;20(8):1245–1255.
- Reichman O, Akins R, Sobel JD. Boric acid addition to suppressive antimicrobial therapy for recurrent bacterial vaginosis. Sex Transm Dis. 2009;36(11):732–734.
Gadzooks! In preparing for the morning office practice session you notice that two patients with chronic vaginitis have been scheduled back to back in 15-minute slots.
Ms. A has chronic bacterial vaginosis. Ms. B has chronic yeast vaginitis. What are you going to do?
Chronic bacterial vaginosis
The normal vaginal microbiome is dominated by Lactobacillus crispatus and Lactobacillus jensenii. These organisms produce hydrogen peroxide and keep the vaginal pH ≤4.5. When Gardnerella vaginalis and associated anaerobic bacteria gain dominance in the vagina, bacterial vaginosis ensues. This infection is characterized by1:
- homogenous, thin, grayish-white discharge that smoothly coats the vaginal epithelium
- pH >4.5
- fishy odor when potassium hydroxide is added to a sample of the discharge
- clue cells on a saline wet mount.
Why is it prone to recur? If bacterial vaginosis was a simple infection, treatment with metronidazole or clindamycin should be very effective. But in many women the relief from symptoms provided by a single course of antibiotics is short-lived, and many patients experience recurrent bacterial vaginosis in the next few months.
The cause of this resistance to antibiotic treatment may be that G vaginalis and other anaerobes, such as Atopobium species, aggregate in vaginal biofilms that prevent the antibiotic from reaching the organism.2 The biofilm provides a safe haven for the bacteria to regrow following a single course of treatment.3 In addition, the nutrient-limited environment inside the encapsulated biofilm helps the bacteria to resist the toxic effects of the antibiotic.4
Another potential mechanism for bacterial vaginosis recurrence is that women destined to develop repeat infection often harbor G vaginalis encapsulated in biofilms in the mouth. These extravaginal bacteria often are found again in the vagina, suggesting that bacterial vaginosis can be acquired from extravaginal bacterial reservoirs.5 Investigators are developing approaches, such as intravaginal treatment with DNase, to destroy the vaginal biofilm in order to enhance the efficacy of antibiotic treatment.6
Treatment
Options for initial infection. There are three treatments for an initial occurrence of bacterial vaginosis7:
- oral metronidazole 500 mg twice daily for 7 days
- 0.75% metronidazole gel one applicator intravaginally once daily for 5 days, or
- 2% clindamycin cream one applicator intravaginally at bedtime for 7 days.
Long-term metronidazole for recurrence. Approximately half of women who respond to initial treatment will have bacterial vaginosis again within 1 year. If vaginitis caused by recurrent bacterial vaginosisis diagnosed, a prolonged course of antibiotic treatment is warranted. Treatment starts with an induction regimen of the standard treatments listed in the paragraph above. This is followed by a long-term maintenance regimen using 0.75% metronidazole vaginal gel one applicator twice weekly for 4 to 6 months.8
Recurrent Candida vulvovaginitis
Four or more occurrences of symptomatic Candida vulvovaginitis in 12 months indicates recurrent infection. Recurrence is usually caused by reinfection with the same organism from a vaginal reservoir. For women with such repeat infection, vaginal cultures should be obtained to confirm Candida and to search for treatment-resistant species, such as Candida glabrata. (Many C glabrata organisms are resistant to standard fluconazole treatment.)
Treatment options
Long courses of oral or vaginal antimycotic agents can be effective treatment for recurrent Candida vulvovaginitis.
Fluconazole. One regimen is fluconazole 150 mg orally every 72 hours for 3 doses, followed by fluconazole 150 mg once weekly for 6 months.9 If patients relapse from this regimen, then the vaginitis should be retreated with fluconazole 150 mg orally every 72 hours for 3 doses, followed by fluconazole 150 mg weekly for 12 months.
Boric acid. If C glabrata is thought to be the cause of the infection, it may be difficult to eradicate with fluconazole. A regimen to treat recurrent vaginitis caused by C glabrata is intravaginal boric acid, a 600 mg capsule once nightly for 14 days.10,11This medication is not FDA-approved for this purpose and must be made by a compounding pharmacy. Boric acid can be fatal if swallowed rather than used intravaginally. Care must be taken to avoid access to these capsules by children.
Boric acid vaginal capsules also can be used to treat chronic bacterial vaginosis in combination with antibiotic therapy.12
Flucytosine. An alternative regimen to treat C glabrata is flucytosine vaginal cream one applicator nightly for 14 days. This vaginal cream must be compounded because it is not available as a commercial medication.
You are armed and ready
In retrospect, you realize that the morning office session schedule is going to be fine. You will treat Ms. A with a long course of metronidazole and Ms. B with a long course of fluconazole. Hopefully, they will both find relief from their symptoms.
Tell us what you think, at [email protected]. Please include your name and city and state.
Gadzooks! In preparing for the morning office practice session you notice that two patients with chronic vaginitis have been scheduled back to back in 15-minute slots.
Ms. A has chronic bacterial vaginosis. Ms. B has chronic yeast vaginitis. What are you going to do?
Chronic bacterial vaginosis
The normal vaginal microbiome is dominated by Lactobacillus crispatus and Lactobacillus jensenii. These organisms produce hydrogen peroxide and keep the vaginal pH ≤4.5. When Gardnerella vaginalis and associated anaerobic bacteria gain dominance in the vagina, bacterial vaginosis ensues. This infection is characterized by1:
- homogenous, thin, grayish-white discharge that smoothly coats the vaginal epithelium
- pH >4.5
- fishy odor when potassium hydroxide is added to a sample of the discharge
- clue cells on a saline wet mount.
Why is it prone to recur? If bacterial vaginosis was a simple infection, treatment with metronidazole or clindamycin should be very effective. But in many women the relief from symptoms provided by a single course of antibiotics is short-lived, and many patients experience recurrent bacterial vaginosis in the next few months.
The cause of this resistance to antibiotic treatment may be that G vaginalis and other anaerobes, such as Atopobium species, aggregate in vaginal biofilms that prevent the antibiotic from reaching the organism.2 The biofilm provides a safe haven for the bacteria to regrow following a single course of treatment.3 In addition, the nutrient-limited environment inside the encapsulated biofilm helps the bacteria to resist the toxic effects of the antibiotic.4
Another potential mechanism for bacterial vaginosis recurrence is that women destined to develop repeat infection often harbor G vaginalis encapsulated in biofilms in the mouth. These extravaginal bacteria often are found again in the vagina, suggesting that bacterial vaginosis can be acquired from extravaginal bacterial reservoirs.5 Investigators are developing approaches, such as intravaginal treatment with DNase, to destroy the vaginal biofilm in order to enhance the efficacy of antibiotic treatment.6
Treatment
Options for initial infection. There are three treatments for an initial occurrence of bacterial vaginosis7:
- oral metronidazole 500 mg twice daily for 7 days
- 0.75% metronidazole gel one applicator intravaginally once daily for 5 days, or
- 2% clindamycin cream one applicator intravaginally at bedtime for 7 days.
Long-term metronidazole for recurrence. Approximately half of women who respond to initial treatment will have bacterial vaginosis again within 1 year. If vaginitis caused by recurrent bacterial vaginosisis diagnosed, a prolonged course of antibiotic treatment is warranted. Treatment starts with an induction regimen of the standard treatments listed in the paragraph above. This is followed by a long-term maintenance regimen using 0.75% metronidazole vaginal gel one applicator twice weekly for 4 to 6 months.8
Recurrent Candida vulvovaginitis
Four or more occurrences of symptomatic Candida vulvovaginitis in 12 months indicates recurrent infection. Recurrence is usually caused by reinfection with the same organism from a vaginal reservoir. For women with such repeat infection, vaginal cultures should be obtained to confirm Candida and to search for treatment-resistant species, such as Candida glabrata. (Many C glabrata organisms are resistant to standard fluconazole treatment.)
Treatment options
Long courses of oral or vaginal antimycotic agents can be effective treatment for recurrent Candida vulvovaginitis.
Fluconazole. One regimen is fluconazole 150 mg orally every 72 hours for 3 doses, followed by fluconazole 150 mg once weekly for 6 months.9 If patients relapse from this regimen, then the vaginitis should be retreated with fluconazole 150 mg orally every 72 hours for 3 doses, followed by fluconazole 150 mg weekly for 12 months.
Boric acid. If C glabrata is thought to be the cause of the infection, it may be difficult to eradicate with fluconazole. A regimen to treat recurrent vaginitis caused by C glabrata is intravaginal boric acid, a 600 mg capsule once nightly for 14 days.10,11This medication is not FDA-approved for this purpose and must be made by a compounding pharmacy. Boric acid can be fatal if swallowed rather than used intravaginally. Care must be taken to avoid access to these capsules by children.
Boric acid vaginal capsules also can be used to treat chronic bacterial vaginosis in combination with antibiotic therapy.12
Flucytosine. An alternative regimen to treat C glabrata is flucytosine vaginal cream one applicator nightly for 14 days. This vaginal cream must be compounded because it is not available as a commercial medication.
You are armed and ready
In retrospect, you realize that the morning office session schedule is going to be fine. You will treat Ms. A with a long course of metronidazole and Ms. B with a long course of fluconazole. Hopefully, they will both find relief from their symptoms.
Tell us what you think, at [email protected]. Please include your name and city and state.
- Eschenbach DA, Hillier S, Critchlow C, Stevens C, DeRouen T, Holmes KK. Diagnosis and clinical manifestations of bacterial vaginosis. Am J Obstet Gynecol. 1988;158(4):819–828.
- Swidinski A, Mendling W, Loening-Baucke V, et al. Adherent biofilms in bacterial vaginosis.Obstet Gynecol. 2005;106(5 pt 1):1013–1023.
- Swidinski A, Mendling W, Loening-Baucke V, et al. An adherent Gardnerella vaginalis biofilm persists on the vaginal epithelium after standard therapy with oral metronidazole. Am J Obstet Gynecol. 2008;198(1):97e1–e6.
- Monds RD, O’Toole GA. The developmental model of microbial biofilm: ten years of a paradigm up for review. Trends Microbiol. 2009;17(2):73–87.
- Marrazzo JM, Friedler TL, Srinivasan S, et al. Extravaginal reservoirs of vaginal bacteria as risk factors for incident bacterial vaginosis. J Infect Dis. 2012;205(10):1580–1588.
- Hymes SR, Randis TM, Sun TY, Ratner AJ. DNase inhibits Gardnerella vaginalis biofilms in vitro and in vivo. J Infect Dis. 2013;207(10):1491–1497.
- Workowski KA, Berman S; Centers for Disease Control and Prevention (CDC). Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep. 2010; 59(RR-12):1–110.
- Sobel JD, Ferris D, Schwebke J, et al. Suppressive antibacterial therapy with 0.75% metronidazole vaginal gel to prevent recurrent bacterial vaginosis. Am J Obstet Gynecol. 2006;194(5):1283–1289.
- Sobel JD, Wiesenfeld HC, Martens M, et al. Maintenance fluconazole therapy for recurrent vulvovaginal candidiasis. N Engl J Med. 2004;351(9):876–883.
- Savini V, Catavitello C, Bianco A, Balbinot A, D’Antonio F, D’Antonio D. Azole resistant Candida glabrata vulvovaginitis treated with boric acid. Eur J Obstet Gynecol Reprod Biol. 2009;147(1):112.
- Iavazzo C, Gkegkes ID, Zarkada IM, Falagas ME. Boric acid for recurrent vulvovaginal candidiasis: the clinical evidence. J Womens Health(Larchmt). 2011;20(8):1245–1255.
- Reichman O, Akins R, Sobel JD. Boric acid addition to suppressive antimicrobial therapy for recurrent bacterial vaginosis. Sex Transm Dis. 2009;36(11):732–734.
- Eschenbach DA, Hillier S, Critchlow C, Stevens C, DeRouen T, Holmes KK. Diagnosis and clinical manifestations of bacterial vaginosis. Am J Obstet Gynecol. 1988;158(4):819–828.
- Swidinski A, Mendling W, Loening-Baucke V, et al. Adherent biofilms in bacterial vaginosis.Obstet Gynecol. 2005;106(5 pt 1):1013–1023.
- Swidinski A, Mendling W, Loening-Baucke V, et al. An adherent Gardnerella vaginalis biofilm persists on the vaginal epithelium after standard therapy with oral metronidazole. Am J Obstet Gynecol. 2008;198(1):97e1–e6.
- Monds RD, O’Toole GA. The developmental model of microbial biofilm: ten years of a paradigm up for review. Trends Microbiol. 2009;17(2):73–87.
- Marrazzo JM, Friedler TL, Srinivasan S, et al. Extravaginal reservoirs of vaginal bacteria as risk factors for incident bacterial vaginosis. J Infect Dis. 2012;205(10):1580–1588.
- Hymes SR, Randis TM, Sun TY, Ratner AJ. DNase inhibits Gardnerella vaginalis biofilms in vitro and in vivo. J Infect Dis. 2013;207(10):1491–1497.
- Workowski KA, Berman S; Centers for Disease Control and Prevention (CDC). Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep. 2010; 59(RR-12):1–110.
- Sobel JD, Ferris D, Schwebke J, et al. Suppressive antibacterial therapy with 0.75% metronidazole vaginal gel to prevent recurrent bacterial vaginosis. Am J Obstet Gynecol. 2006;194(5):1283–1289.
- Sobel JD, Wiesenfeld HC, Martens M, et al. Maintenance fluconazole therapy for recurrent vulvovaginal candidiasis. N Engl J Med. 2004;351(9):876–883.
- Savini V, Catavitello C, Bianco A, Balbinot A, D’Antonio F, D’Antonio D. Azole resistant Candida glabrata vulvovaginitis treated with boric acid. Eur J Obstet Gynecol Reprod Biol. 2009;147(1):112.
- Iavazzo C, Gkegkes ID, Zarkada IM, Falagas ME. Boric acid for recurrent vulvovaginal candidiasis: the clinical evidence. J Womens Health(Larchmt). 2011;20(8):1245–1255.
- Reichman O, Akins R, Sobel JD. Boric acid addition to suppressive antimicrobial therapy for recurrent bacterial vaginosis. Sex Transm Dis. 2009;36(11):732–734.
Type IIb Bony Mallet Finger: Is Anatomical Reduction of the Fracture Necessary?
Travelers' diarrhea: Prevention, treatment, and post-trip evaluation
1. Recommend antibiotic chemoprophylaxis for travelers at high risk for travelers’ diarrhea (TD) and those at high risk for complications. It is also appropriate for travelers who have an inflexible itinerary. B
2. Recommend bismuth subsalicylate chemoprophylaxis for travelers at high risk for TD who are willing to comply with the regimen and want to avoid antibiotic prophylaxis. B
3. Advise travelers to initiate self-treatment for TD with a fluoroquinolone (or azithromycin, if in South or Southeast Asia) at the onset of diarrhea if it is bloody or accompanied by fever. A
NOTE: This practice recommendation in the print version of this article stated that travelers should also take loperamide; however, both the Centers for Disease Control and Prevention and the Infectious Diseases Society of America advise against the use of loperamide by travelers with fever or bloody diarrhea [corrected August 27, 2013].
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
A 40-year-old female patient, a childhood immigrant from India, is seeking advice regarding her upcoming 2-week trip to Mumbai. She is taking her 2 children, ages 16 years and 16 months, to visit their grandparents for the first time. She has made this trip alone a few times and has invariably experienced short bouts of self-limited diarrheal illness. She wonders what she might do to prevent travelers’ diarrhea. Her only medical problem is rheumatoid arthritis, which has been well controlled with methotrexate. Her children are healthy. What would you recommend?
Recommendations regarding travelers’ diarrhea (TD) address prevention and management. Prevention encompasses advice about personal behaviors and the use of chemoprophylaxis (antimicrobial and non-antimicrobial) and vaccinations. Since international travelers are known to treat themselves for diarrheal illnesses during their trips,1 recommendations regarding management should assume self-treatment and include the use of both antibiotics and non-antibiotic remedies. Pretravel recommendations will of course be most effective if they account for the individual’s risk for TD.
Innate patient susceptibility, destination, and dietary choices determine TD risk
TD is generally defined as the passage of 3 of more loose stools in a 24-hour period, with associated symptoms of enteric infection—eg, fever, nausea, vomiting, or abdominal cramping. Defined in this manner, TD is thought to occur in 60% to 70% of individuals who travel from developed countries to less-developed countries.2,4 Risk of TD is influenced both by intrinsic personal factors and by factors specific to the trip.
Personal risk factorsIndividual variation in susceptibility to TD might result from a genetic predisposition arising from single nucleotide polymorphisms governing various inflammatory marker proteins.5 A history of multiple episodes of TD, especially if fellow travelers were spared, can suggest this kind of individual susceptibility. Other factors that increase vulnerability to TD are immunodeficiency, achlorhydric states such as atrophic gastritis, and chronic use of proton pump inhibitors.6,7 However, the trip itself is much more important in assessing risk for TD.
Trip-related risk factors
The destination. The most salient risk factor for TD is the geographic destination. Regions of the world can be divided into TD risk strata:2
- Very high: South Asia
- High: South America, Sub-Saharan Africa
- Medium: Central America, Mexico, Caribbean, Middle East, North Africa, Southeast Asia, Oceania
- Low: Europe, North America (excluding Mexico), Australasia, Northeast Asia.
Particularly notable countries, in descending order of risk, are Nepal, India, Myanmar, Bolivia, Sri Lanka, Ecuador, Peru, Kenya, and Guatemala.2
Dietary choices. Additionally, since travelers acquire TD by ingesting food or beverages contaminated with pathogenic fecal microbes, dietary behaviors during the trip affect their susceptibility. At least risk are business travelers and tourists who confine their activities to more affluent settings in which food and beverages are prepared and stored hygienically.1,4,8,9 At greater risk are travelers who immerse themselves in local culture, visiting locations that are more impoverished and not as well equipped with sanitation systems, especially if their stay is at least 2 to 3 weeks.1,4,8,9
Also, the older a traveler is, the lower his or her risk of TD.1,9 An exception to this might be infants whose diet consists solely of breast milk or formula prepared under sanitary conditions.
Mandates and options for preventing TD
Emphasize food and beverage precautions
It might be reasonable to expect that travelers who are circumspect about their food and beverage choices on trips will be able to avoid TD. Indeed, this is the basis for the aphorism, “Boil it, peel it, or forget it.” Guidelines routinely recommend that travelers restrict their selection of foods to those that have been well cooked and are served while still very hot, and to fruits and vegetables that they peel themselves. Likewise, they should drink only beverages that have been boiled or are in sealed bottles or under carbonation and served without ice.10-12 Many travelers might find these recommendations too restrictive to follow faithfully. Moreover, studies suggest it may not be possible for even the most assiduous traveler to fully avoid the risk of TD.13,14 The hygienic characteristics of the travel destination may be more determinative, as illustrated by the successful reduction of TD rates in Jamaica by improving sanitation in tourist resorts.15
Antibiotic chemoprophylaxis: A debated practice with limited consensusThe etiologic agents of TD are multiple and vary somewhat in predominance according to geographic region.3,16,17 TABLE 1 depicts variance by region.16 The most common pathogens are strains of the bacterium Escherichia coli, particularly enterotoxigenic (ETEC), enteroaggregative (EAEC), and enteropathogenic (EPEC) strains.16 Other bacteria of importance are Campylobacter, Salmonella, and Shigella. Viruses, particularly norovirus (notably connected with cruise ships), can also cause TD, although it is implicated in no more than 17% of cases.18 Parasitic pathogens are even less common causes of TD (4%-10%) and mainly involve the protozoa, Giardia lamblia, and, to a lesser extent, Entamoeba histolytica and Cryptosporidium.
Although some pathogens often have a characteristic presentation—such as frothy, greasy diarrhea in the case of G lamblia—they generally cannot be reliably distinguished from one another clinically. Notably, up to 50% of stool samples from TD patients do not yield any pathogen,16 raising the suspicion that current diagnostic technology is not sufficiently sensitive to routinely identify certain bacteria.
There is no consensus on recommending antibiotic chemoprophylaxis against TD.
Opponents of this practice10-12,19,20 point out that TD is generally a brief (3-5 days), self-limited illness. Moreover, concerns about antibiotic resistance have come to pass. Previously used agents, trimethoprim-sulfamethoxazole and doxycycline, are no longer effective in preventing or treating TD. In addition, antibiotic use carries the risk of allergic reactions as well as other adverse effects including, ironically, the development of antibiotic-associated diarrhea and Clostridium difficile diarrhea.
Proponents of antibiotic chemoprophylaxis21,22 point to its demonstrated efficacy in reducing the risk of TD by 4% to 40%.11 They also argue that at least 20% to 25% of travelers who get TD must significantly curtail their activities for a day or more.1,23 This change in travel plans is associated not only with significant personal loss but also imposes a financial burden.23 Furthermore, TD is known to have longer-term effects. Up to 10% of sufferers develop postinfectious irritable bowel syndrome (PI-IBS) that can last for 5 or 6 years.21,22,24,25 It is not known, however, whether the use of antibiotic chemoprophylaxis significantly reduces the incidence of PI-IBS.
Finally, the luminal antibiotic, rifaximin, nonabsorbable as it is, is very well-tolerated and holds promise for not inciting antibiotic resistance.22 However, while its efficacy in preventing TD has been demonstrated in various settings,22,26,27 it is not approved by the US Food and Drug Administration for this indication. Also, concerns persist that it might not be effective in preventing TD caused by invasive pathogens.19
Indications on which all agree. Even opponents of antibiotic chemoprophylaxis grant that it is probably warranted for 2 groups of travelers.10-12 The first is those whose trip schedule is of such importance that any deviation would be intolerable. The second is travelers with comorbidities that would render them at high risk for serious inconvenience or illness if they developed TD. Examples of the latter include patients with enterostomies, mobility impairments, immune suppression, inflammatory bowel disease, and renal or metabolic diseases.
Chemoprophylaxis regimens. If you prescribe an antibiotic prophylactically, consider daily doses of a fluoroquinolone (eg, ciprofloxacin 500 mg orally once daily, not twice daily as for treatment) or rifaximin 200 mg orally once or twice a day, for no longer than 2 to 3 weeks.10
Non-antimicrobial chemoprophylaxis
Bismuth subsalicylate has reduced the incidence of TD from 40% to just 14% when taken in doses of 2 chewable tablets or 60 mL of liquid 4 times daily. 11,19,22 However, the dosing frequency can hinder adherence. Moreover, the relatively high doses required raise the risk of adverse drug reactions such as blackening of the tongue and stool, nausea, constipation, Reye syndrome (in children under 12 years), and possibly tinnitus. The salicylate component of the drug poses a threat to patients with aspirin allergy, renal disease, and those taking anticoagulants. Drug interactions with probenecid and methotrexate are also possible. Bismuth is not recommended for use for longer than 3 weeks, or for children younger than 3 years or pregnant women in their third trimester.
Other non-antimicrobial chemoprophylaxis agents include probiotics such as Lactobacillus andSaccharomyces. These preparations of bacteria and fungi are marketed either singly or in blends of varying composition and proportion. The evidence is divided on their efficacy, and even though some meta-analyses have concluded probiotics such as Saccharomyces boulardii are useful in preventing TD, endorsement in clinical guidelines is muted.10-12,28-30
Immunizations have limited value so farNatural immunity to E coli gastrointestinal infection among indigenous people in less developed countries has raised the possibility of a role for vaccines in preventing TD. Some strains of ETEC produce a heat-labile toxin (LT) that bears significant resemblance to the toxin produced by Vibrio cholerae. Therefore, the oral cholera vaccine, Dukoral, has been marketed outside the United States for the prevention of TD.19,22 However, only ≤7% of TD cases worldwide would be prevented by routine use of this vaccine.31 A transdermal LT vaccine, which involves the antigen-presenting Langerhans cells in the superficial skin layers, is promising but not yet available for routine use.19,22
Treating TD and associated symptoms
Antibiotic treatment
Given that most cases of TD are caused by bacterial pathogens, antibiotics are considered the mainstay of treatment. Concerns about the ill effects of antibiotic use in the case of enterohemorrhagic E coli(EHEC O157:H7) can be allayed because this strain is rarely a cause of TD.9Patient factors that increase vulnerability to TD are immunodeficiency, achlorhydric states such as atrophic gastritis, and chronic use of proton pump inhibitors.
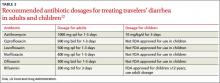
Consider local resistance patterns and risk of invasive infection. Which antibiotic to recommend is governed by the antibiotic resistance patterns prevalent in the travel destinations and by the risk of infection by invasive pathogens. Invasive TD is generally caused by Campylobacter, Shigella, or Salmonella and manifests clinically with bloody diarrhea, fever, or both. Rifaximin at a dose of 200 mg orally 3 times daily is effective for noninvasive TD.31,32 However, travelers who develop invasive TD need an alternative to rifaximin. (Those who advocate reserving antibiotic treatment only for invasive diarrhea will not see a role for rifaximin in the first place.) In most invasive cases, a fluoroquinolone will suffice.10-12,19,32 However, increasing prevalence of fluoroquinolone-resistantCampylobacter species has been reported in South and Southeast Asia. In those locations, azithromycin is an effective alternative, albeit with risk of nausea.33TABLE 212 provides details of recommended antibiotic dosages for adults and children. The duration of treatment is generally 1 day unless symptoms persist, in which case a 3-day course is recommended.10-12,19,32 If the traveler experiences persistent, new, or worsening symptoms beyond this point, immediate evaluation by a physician is required.
Non-antibiotic treatment
The antimotility agent loperamide is a well-established antidiarrheal agent. Its effective and safe use as an adjunct to antibiotics in the treatment of TD has been demonstrated in several studies.10-12,19,32,34 It is generally not used to treat children with TD9
No other non-antibiotic treatment for TD has significant guideline or clinical trial support. Bismuth subsalicylate can be helpful as an antidiarrheal agent,35 but is not often recommended because the regimen makes adherence difficult and because antibiotics and loperamide are effective.
Oral rehydration is usually a mainstay of treating gastrointestinal disease among infants and children. However, it, too, has a limited role in cases of TD because dehydration is not usually a significant part of the clinical presentation, perhaps because vomiting is not often prominent.
CASE Advice regarding safe food and beverage choices is essential for the patient and her children. Despite the increased risk for TD due to her history and her use of the immunosuppressant methotrexate, she decides not to pursue antibiotic prophylaxis. Bismuth is also contraindicated because of the methotrexate. Her teenage daughter declines bismuth prophylaxis, and her toddler is too young for it.
The patient does accept a prescription for azithromycin for her and her daughters in case they experience TD. This choice is appropriate given the destination of India and concern about Campylobacterresistance to fluoroquinolones. You also recommend loperamide for use by the mother and older child, in conjunction with the antibiotic.
Two weeks after their trip abroad, the travelers return for an office visit. On the trip, the mother and toddler suffered diarrhea, which responded well to your recommended management. The older child was well during the trip, but she developed diarrhea, abdominal pain, and anorexia one week after returning to the United States. These symptoms have persisted despite a 3-day course of azithromycin and loperamide.
Post-travel evaluation
TD generally occurs within one to 2 weeks of arrival at the travel destination and usually lasts no longer than 4 to 5 days.19 This scenario is typical of a bacterial infection. When it occurs later or lasts longer, or both, consider several alternative possibilities.19,36 First, the likelihood of a protozoal parasitic infection is increased. Although giardiasis is most likely, other protozoa such as Entamoeba, Cyclospora, Isospora, and Cryptosporidium are also possibilities. Second, if diarrhea persists, it might be due, not to continued infection, but to a self-limited post-infectious enteropathy or to PI-IBS. Third, TD is known to precipitate the clinical manifestation of underlying gastrointestinal disorders such as inflammatory bowel disease (IBD), celiac disease, or even cancer.37
With an atypical disease course, it’s advisable to send 3 stool samples for laboratory evaluation for ova and parasites and for antigen assays for Giardia. If results of these tests are negative, given the difficulty inherent in diagnosing Giardia, consider empiric treatment with metronidazole in lieu of duodenal sampling.36 If the diarrhea persists, investigate serologic markers for celiac disease and IBD. If these are not revealing, referral for colonoscopy is prudent.
CASE The teenager’s 3 stool samples were negative for ova and parasites and for Giardia antigen. Following empirical treatment with oral metronidazole 250 mg, 3 times daily for 7 days, the diarrhea resolved.
CORRESPONDENCE Dilip Nair, MD, Joan C. Edwards School of Medicine at Marshall University, 1600 Medical Center Drive, Suite 1500, Huntington, WV 25701; [email protected]
1. Hill DR. Occurrence and self-treatment of diarrhea in a large cohort of Americans traveling to developing countries. Am J Trop Med Hyg. 2000;62:585–589.
2. Greenwood Z, Black J, Weld L, et al. for the GeoSentinel Surveillance Network. Gastrointestinal infection among international travelers globally. J Travel Med. 2008;15:221–228.
3. DuPont HL. Systematic review: the epidemiology and clinical features of travellers’ diarrhoea. Aliment Pharmacol Ther. 2009;30:187–196.
4. Steffen R, Tornieporth N, Clemens SA, et al. Epidemiology of travelers’ diarrhea: details of a global survey. J Travel Med. 2004;11:231–237.
5. de la Cabada Bauche J, DuPont HL. New developments in traveler’s diarrhea. Gastroenterol Hepatol. 2011;7:88–95.
6. Cabada MM, White AC. Travelers’ diarrhea: an update on susceptibility, prevention, and treatment. Curr Gastroenterol Rep. 2008;10:473–479.
7. Ericsson CD. Travellers with pre-existing medical conditions. Int J Antimicrob Agents. 2003;21:181–188.
8. Cabada MM, Maldonado F, Quispe W, et al. Risk factors associated with diarrhea among international visitors to Cuzco, Peru. Am J Trop Med Hyg. 2006;75:968–972.
9. Mackell S. Traveler’s diarrhea in the pediatric population: etiology and impact. Clin Infect Dis. 2005;41(suppl 8):S547–S552.
10. Hill DR, Ericsson CD, Pearson RD, et al. The practice of travel medicine: guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2006;43:1499–1539.
11. Connor BA. Travelers’ diarrhea. Available at:http://wwwnc.cdc.gov/travel/yellowbook/2012/chapter-2-the-pre-travel-consultation/travelers-diarrhea.htm. Accessed August 20, 2012.
12. Advice for travelers. Treat Guidel Med Lett. 2012;10:45–56.
13. Shlim DR. Looking for evidence that personal hygiene precautions prevent travelers’ diarrhea. Clin Infect Dis. 2005;41(suppl 8):S531–S535.
14. Laverone E, Boccalini S, Bechini A, et al. Travelers’ compliance to prophylactic measures and behavior during stay abroad: results of a retrospective study of subjects returning to a travel medicine center in Italy. J Travel Med. 2006;13:338–344.
15. Ashley DV, Walters C, Dockery-Brown C, et al. Interventions to prevent and control food-borne diseases associated with a reduction in traveler’s diarrhea in tourists to Jamaica. J Travel Med. 2004;11:364–367.
16. Shah N, DuPont HL, Ramsey DJ. Global etiology of travelers’ diarrhea: systematic review from 1973 to the present. Am J Trop Med Hyg. 2009;80:609–614.
17. Riddle MS, Sanders JW, Putnam SD, et al. Incidence, etiology, and impact of diarrhea among long-term travelers (US military and similar populations): a systematic review. Am J Trop Med Hyg. 2006;74:891–900.
18. Koo HL, Ajami NJ, Jiang ZD, et al. Noroviruses as a cause of diarrhea in travelers to Guatemala, India, and Mexico. J Clin Microbiol. 2010;48:1673–1676.
19. Hill DR, Ryan ET. Management of travellers’ diarrhoea. BMJ. 2008;337:863–867.
20. Rendi-Wagner P, Kollaritsch H. Drug prophylaxis for travelers’ diarrhea. Clin Infect Dis. 2002;34:628–633.
21. Pimentel M, Riddle MS. Prevention of traveler’s diarrhea: a call to reconvene. Clin Infect Dis. 2008;46:151–152.
22. DuPont HL. Systematic review: prevention of travellers’ diarrhoea. Aliment Pharmacol Ther. 2008;27:741–751.
23. Wang M, Szucs TD, Steffen R. Economic aspects of travelers’ diarrhea. J Travel Med. 2008;15:110–118.
24. Neal KR, Barker L, Spiller RC. Prognosis in post-infective irritable bowel syndrome: a six year follow up study. Gut. 2002;51:410–413.
25. Tornblom H, Holmvall P, Svenungsson B, et al. Gastrointestinal symptoms after infectious diarrhea: a five-year follow-up in a Swedish cohort of adults. Clin Gastroenterol Hepatol. 2007;5:461–464.
26. DuPont HL, Jiang ZD, Okhuysen PC, et al. A randomized, double-blind, placebo-controlled trial of rifaximin to prevent travelers’ diarrhea. Ann Intern Med. 2005;142:805–812.
27. Taylor DN, McKenzie R, Durbin A, et al. Rifaximin, a nonabsorbed oral antibiotic, prevents shigellosis after experimental challenge. Clin Infect Dis. 2006;42:1283–1288.
28. Sazawal S, Hiremath G, Dhingra U, et al. Efficacy of probiotics in prevention of acute diarrhoea: a meta-analysis of masked, randomised, placebo-controlled trials. Lancet Infect Dis. 2006;6:374–382.
29. Bri V, Buffet P, Genty S, et al. Absence of efficacy of nonviable Lactobacillus acidophilus for the prevention of traveler’s diarrhea: a randomized, double-blind, controlled study. Clin Infect Dis. 2006;43:1170–1175.
30. Hill DR, Ford L, Lalloo DG. Oral cholera vaccines—use in clinical practice. Lancet Infect Dis. 2006;6:361–373.
31. Taylor DN, Bourgeois AL, Ericsson CD, et al. A randomized double-blind, multicenter study of rifaximin compared with placebo and with ciprofloxacin in the treatment of travelers’ diarrhea. Am J Trop Med Hyg. 2006;74:1060–1066.
32. DuPont HL, Ericsson CD, Farthing MJG, et al. Expert review of the evidence base for self-therapy of travelers’ diarrhea. J Travel Med. 2009;16:161–171.
33. Tribble DR, Sanders JW, Pang LW, et al. Traveler’s diarrhea in Thailand: randomized, double-blind trial comparing single-dose and 3-day azithromycin-based regimens with a 3-day levofloxacin regimen. Clin Infect Dis. 2007;44:338–346.
34. Riddle MS, Arnold S, Tribble DR. Effect of adjunctive loperamide in combination with antibiotics on treatment outcomes in travelers’ diarrhea: a systematic review and meta-analysis. Clin Infect Dis. 2008;47:1007–1014.
35. Steffen R. Worldwide efficacy of bismuth subsalicylate in the treatment of travelers’ diarrhea. Rev Infect Dis. 1990;12(suppl 1):S80–S86.
36. Connor BA. Persistent travelers’ diarrhea. Available at:http://wwwnc.cdc.gov/travel/yellowbook/2012/chapter-5-post-travel-evaluation/persistent-travelers-diarrhea.htm. Accessed August 20, 2012.
37.Landzberg BR, Connor BA. Persistent diarrhea in the returning traveler: think beyond persistent infection. Scand J Gastroenterol. 2005;40:112–114.
1. Recommend antibiotic chemoprophylaxis for travelers at high risk for travelers’ diarrhea (TD) and those at high risk for complications. It is also appropriate for travelers who have an inflexible itinerary. B
2. Recommend bismuth subsalicylate chemoprophylaxis for travelers at high risk for TD who are willing to comply with the regimen and want to avoid antibiotic prophylaxis. B
3. Advise travelers to initiate self-treatment for TD with a fluoroquinolone (or azithromycin, if in South or Southeast Asia) at the onset of diarrhea if it is bloody or accompanied by fever. A
NOTE: This practice recommendation in the print version of this article stated that travelers should also take loperamide; however, both the Centers for Disease Control and Prevention and the Infectious Diseases Society of America advise against the use of loperamide by travelers with fever or bloody diarrhea [corrected August 27, 2013].
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
A 40-year-old female patient, a childhood immigrant from India, is seeking advice regarding her upcoming 2-week trip to Mumbai. She is taking her 2 children, ages 16 years and 16 months, to visit their grandparents for the first time. She has made this trip alone a few times and has invariably experienced short bouts of self-limited diarrheal illness. She wonders what she might do to prevent travelers’ diarrhea. Her only medical problem is rheumatoid arthritis, which has been well controlled with methotrexate. Her children are healthy. What would you recommend?
Recommendations regarding travelers’ diarrhea (TD) address prevention and management. Prevention encompasses advice about personal behaviors and the use of chemoprophylaxis (antimicrobial and non-antimicrobial) and vaccinations. Since international travelers are known to treat themselves for diarrheal illnesses during their trips,1 recommendations regarding management should assume self-treatment and include the use of both antibiotics and non-antibiotic remedies. Pretravel recommendations will of course be most effective if they account for the individual’s risk for TD.
Innate patient susceptibility, destination, and dietary choices determine TD risk
TD is generally defined as the passage of 3 of more loose stools in a 24-hour period, with associated symptoms of enteric infection—eg, fever, nausea, vomiting, or abdominal cramping. Defined in this manner, TD is thought to occur in 60% to 70% of individuals who travel from developed countries to less-developed countries.2,4 Risk of TD is influenced both by intrinsic personal factors and by factors specific to the trip.
Personal risk factorsIndividual variation in susceptibility to TD might result from a genetic predisposition arising from single nucleotide polymorphisms governing various inflammatory marker proteins.5 A history of multiple episodes of TD, especially if fellow travelers were spared, can suggest this kind of individual susceptibility. Other factors that increase vulnerability to TD are immunodeficiency, achlorhydric states such as atrophic gastritis, and chronic use of proton pump inhibitors.6,7 However, the trip itself is much more important in assessing risk for TD.
Trip-related risk factors
The destination. The most salient risk factor for TD is the geographic destination. Regions of the world can be divided into TD risk strata:2
- Very high: South Asia
- High: South America, Sub-Saharan Africa
- Medium: Central America, Mexico, Caribbean, Middle East, North Africa, Southeast Asia, Oceania
- Low: Europe, North America (excluding Mexico), Australasia, Northeast Asia.
Particularly notable countries, in descending order of risk, are Nepal, India, Myanmar, Bolivia, Sri Lanka, Ecuador, Peru, Kenya, and Guatemala.2
Dietary choices. Additionally, since travelers acquire TD by ingesting food or beverages contaminated with pathogenic fecal microbes, dietary behaviors during the trip affect their susceptibility. At least risk are business travelers and tourists who confine their activities to more affluent settings in which food and beverages are prepared and stored hygienically.1,4,8,9 At greater risk are travelers who immerse themselves in local culture, visiting locations that are more impoverished and not as well equipped with sanitation systems, especially if their stay is at least 2 to 3 weeks.1,4,8,9
Also, the older a traveler is, the lower his or her risk of TD.1,9 An exception to this might be infants whose diet consists solely of breast milk or formula prepared under sanitary conditions.
Mandates and options for preventing TD
Emphasize food and beverage precautions
It might be reasonable to expect that travelers who are circumspect about their food and beverage choices on trips will be able to avoid TD. Indeed, this is the basis for the aphorism, “Boil it, peel it, or forget it.” Guidelines routinely recommend that travelers restrict their selection of foods to those that have been well cooked and are served while still very hot, and to fruits and vegetables that they peel themselves. Likewise, they should drink only beverages that have been boiled or are in sealed bottles or under carbonation and served without ice.10-12 Many travelers might find these recommendations too restrictive to follow faithfully. Moreover, studies suggest it may not be possible for even the most assiduous traveler to fully avoid the risk of TD.13,14 The hygienic characteristics of the travel destination may be more determinative, as illustrated by the successful reduction of TD rates in Jamaica by improving sanitation in tourist resorts.15
Antibiotic chemoprophylaxis: A debated practice with limited consensusThe etiologic agents of TD are multiple and vary somewhat in predominance according to geographic region.3,16,17 TABLE 1 depicts variance by region.16 The most common pathogens are strains of the bacterium Escherichia coli, particularly enterotoxigenic (ETEC), enteroaggregative (EAEC), and enteropathogenic (EPEC) strains.16 Other bacteria of importance are Campylobacter, Salmonella, and Shigella. Viruses, particularly norovirus (notably connected with cruise ships), can also cause TD, although it is implicated in no more than 17% of cases.18 Parasitic pathogens are even less common causes of TD (4%-10%) and mainly involve the protozoa, Giardia lamblia, and, to a lesser extent, Entamoeba histolytica and Cryptosporidium.
Although some pathogens often have a characteristic presentation—such as frothy, greasy diarrhea in the case of G lamblia—they generally cannot be reliably distinguished from one another clinically. Notably, up to 50% of stool samples from TD patients do not yield any pathogen,16 raising the suspicion that current diagnostic technology is not sufficiently sensitive to routinely identify certain bacteria.
There is no consensus on recommending antibiotic chemoprophylaxis against TD.
Opponents of this practice10-12,19,20 point out that TD is generally a brief (3-5 days), self-limited illness. Moreover, concerns about antibiotic resistance have come to pass. Previously used agents, trimethoprim-sulfamethoxazole and doxycycline, are no longer effective in preventing or treating TD. In addition, antibiotic use carries the risk of allergic reactions as well as other adverse effects including, ironically, the development of antibiotic-associated diarrhea and Clostridium difficile diarrhea.
Proponents of antibiotic chemoprophylaxis21,22 point to its demonstrated efficacy in reducing the risk of TD by 4% to 40%.11 They also argue that at least 20% to 25% of travelers who get TD must significantly curtail their activities for a day or more.1,23 This change in travel plans is associated not only with significant personal loss but also imposes a financial burden.23 Furthermore, TD is known to have longer-term effects. Up to 10% of sufferers develop postinfectious irritable bowel syndrome (PI-IBS) that can last for 5 or 6 years.21,22,24,25 It is not known, however, whether the use of antibiotic chemoprophylaxis significantly reduces the incidence of PI-IBS.
Finally, the luminal antibiotic, rifaximin, nonabsorbable as it is, is very well-tolerated and holds promise for not inciting antibiotic resistance.22 However, while its efficacy in preventing TD has been demonstrated in various settings,22,26,27 it is not approved by the US Food and Drug Administration for this indication. Also, concerns persist that it might not be effective in preventing TD caused by invasive pathogens.19
Indications on which all agree. Even opponents of antibiotic chemoprophylaxis grant that it is probably warranted for 2 groups of travelers.10-12 The first is those whose trip schedule is of such importance that any deviation would be intolerable. The second is travelers with comorbidities that would render them at high risk for serious inconvenience or illness if they developed TD. Examples of the latter include patients with enterostomies, mobility impairments, immune suppression, inflammatory bowel disease, and renal or metabolic diseases.
Chemoprophylaxis regimens. If you prescribe an antibiotic prophylactically, consider daily doses of a fluoroquinolone (eg, ciprofloxacin 500 mg orally once daily, not twice daily as for treatment) or rifaximin 200 mg orally once or twice a day, for no longer than 2 to 3 weeks.10
Non-antimicrobial chemoprophylaxis
Bismuth subsalicylate has reduced the incidence of TD from 40% to just 14% when taken in doses of 2 chewable tablets or 60 mL of liquid 4 times daily. 11,19,22 However, the dosing frequency can hinder adherence. Moreover, the relatively high doses required raise the risk of adverse drug reactions such as blackening of the tongue and stool, nausea, constipation, Reye syndrome (in children under 12 years), and possibly tinnitus. The salicylate component of the drug poses a threat to patients with aspirin allergy, renal disease, and those taking anticoagulants. Drug interactions with probenecid and methotrexate are also possible. Bismuth is not recommended for use for longer than 3 weeks, or for children younger than 3 years or pregnant women in their third trimester.
Other non-antimicrobial chemoprophylaxis agents include probiotics such as Lactobacillus andSaccharomyces. These preparations of bacteria and fungi are marketed either singly or in blends of varying composition and proportion. The evidence is divided on their efficacy, and even though some meta-analyses have concluded probiotics such as Saccharomyces boulardii are useful in preventing TD, endorsement in clinical guidelines is muted.10-12,28-30
Immunizations have limited value so farNatural immunity to E coli gastrointestinal infection among indigenous people in less developed countries has raised the possibility of a role for vaccines in preventing TD. Some strains of ETEC produce a heat-labile toxin (LT) that bears significant resemblance to the toxin produced by Vibrio cholerae. Therefore, the oral cholera vaccine, Dukoral, has been marketed outside the United States for the prevention of TD.19,22 However, only ≤7% of TD cases worldwide would be prevented by routine use of this vaccine.31 A transdermal LT vaccine, which involves the antigen-presenting Langerhans cells in the superficial skin layers, is promising but not yet available for routine use.19,22
Treating TD and associated symptoms
Antibiotic treatment
Given that most cases of TD are caused by bacterial pathogens, antibiotics are considered the mainstay of treatment. Concerns about the ill effects of antibiotic use in the case of enterohemorrhagic E coli(EHEC O157:H7) can be allayed because this strain is rarely a cause of TD.9Patient factors that increase vulnerability to TD are immunodeficiency, achlorhydric states such as atrophic gastritis, and chronic use of proton pump inhibitors.
Consider local resistance patterns and risk of invasive infection. Which antibiotic to recommend is governed by the antibiotic resistance patterns prevalent in the travel destinations and by the risk of infection by invasive pathogens. Invasive TD is generally caused by Campylobacter, Shigella, or Salmonella and manifests clinically with bloody diarrhea, fever, or both. Rifaximin at a dose of 200 mg orally 3 times daily is effective for noninvasive TD.31,32 However, travelers who develop invasive TD need an alternative to rifaximin. (Those who advocate reserving antibiotic treatment only for invasive diarrhea will not see a role for rifaximin in the first place.) In most invasive cases, a fluoroquinolone will suffice.10-12,19,32 However, increasing prevalence of fluoroquinolone-resistantCampylobacter species has been reported in South and Southeast Asia. In those locations, azithromycin is an effective alternative, albeit with risk of nausea.33TABLE 212 provides details of recommended antibiotic dosages for adults and children. The duration of treatment is generally 1 day unless symptoms persist, in which case a 3-day course is recommended.10-12,19,32 If the traveler experiences persistent, new, or worsening symptoms beyond this point, immediate evaluation by a physician is required.
Non-antibiotic treatment
The antimotility agent loperamide is a well-established antidiarrheal agent. Its effective and safe use as an adjunct to antibiotics in the treatment of TD has been demonstrated in several studies.10-12,19,32,34 It is generally not used to treat children with TD9
No other non-antibiotic treatment for TD has significant guideline or clinical trial support. Bismuth subsalicylate can be helpful as an antidiarrheal agent,35 but is not often recommended because the regimen makes adherence difficult and because antibiotics and loperamide are effective.
Oral rehydration is usually a mainstay of treating gastrointestinal disease among infants and children. However, it, too, has a limited role in cases of TD because dehydration is not usually a significant part of the clinical presentation, perhaps because vomiting is not often prominent.
CASE Advice regarding safe food and beverage choices is essential for the patient and her children. Despite the increased risk for TD due to her history and her use of the immunosuppressant methotrexate, she decides not to pursue antibiotic prophylaxis. Bismuth is also contraindicated because of the methotrexate. Her teenage daughter declines bismuth prophylaxis, and her toddler is too young for it.
The patient does accept a prescription for azithromycin for her and her daughters in case they experience TD. This choice is appropriate given the destination of India and concern about Campylobacterresistance to fluoroquinolones. You also recommend loperamide for use by the mother and older child, in conjunction with the antibiotic.
Two weeks after their trip abroad, the travelers return for an office visit. On the trip, the mother and toddler suffered diarrhea, which responded well to your recommended management. The older child was well during the trip, but she developed diarrhea, abdominal pain, and anorexia one week after returning to the United States. These symptoms have persisted despite a 3-day course of azithromycin and loperamide.
Post-travel evaluation
TD generally occurs within one to 2 weeks of arrival at the travel destination and usually lasts no longer than 4 to 5 days.19 This scenario is typical of a bacterial infection. When it occurs later or lasts longer, or both, consider several alternative possibilities.19,36 First, the likelihood of a protozoal parasitic infection is increased. Although giardiasis is most likely, other protozoa such as Entamoeba, Cyclospora, Isospora, and Cryptosporidium are also possibilities. Second, if diarrhea persists, it might be due, not to continued infection, but to a self-limited post-infectious enteropathy or to PI-IBS. Third, TD is known to precipitate the clinical manifestation of underlying gastrointestinal disorders such as inflammatory bowel disease (IBD), celiac disease, or even cancer.37
With an atypical disease course, it’s advisable to send 3 stool samples for laboratory evaluation for ova and parasites and for antigen assays for Giardia. If results of these tests are negative, given the difficulty inherent in diagnosing Giardia, consider empiric treatment with metronidazole in lieu of duodenal sampling.36 If the diarrhea persists, investigate serologic markers for celiac disease and IBD. If these are not revealing, referral for colonoscopy is prudent.
CASE The teenager’s 3 stool samples were negative for ova and parasites and for Giardia antigen. Following empirical treatment with oral metronidazole 250 mg, 3 times daily for 7 days, the diarrhea resolved.
CORRESPONDENCE Dilip Nair, MD, Joan C. Edwards School of Medicine at Marshall University, 1600 Medical Center Drive, Suite 1500, Huntington, WV 25701; [email protected]
1. Recommend antibiotic chemoprophylaxis for travelers at high risk for travelers’ diarrhea (TD) and those at high risk for complications. It is also appropriate for travelers who have an inflexible itinerary. B
2. Recommend bismuth subsalicylate chemoprophylaxis for travelers at high risk for TD who are willing to comply with the regimen and want to avoid antibiotic prophylaxis. B
3. Advise travelers to initiate self-treatment for TD with a fluoroquinolone (or azithromycin, if in South or Southeast Asia) at the onset of diarrhea if it is bloody or accompanied by fever. A
NOTE: This practice recommendation in the print version of this article stated that travelers should also take loperamide; however, both the Centers for Disease Control and Prevention and the Infectious Diseases Society of America advise against the use of loperamide by travelers with fever or bloody diarrhea [corrected August 27, 2013].
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
A 40-year-old female patient, a childhood immigrant from India, is seeking advice regarding her upcoming 2-week trip to Mumbai. She is taking her 2 children, ages 16 years and 16 months, to visit their grandparents for the first time. She has made this trip alone a few times and has invariably experienced short bouts of self-limited diarrheal illness. She wonders what she might do to prevent travelers’ diarrhea. Her only medical problem is rheumatoid arthritis, which has been well controlled with methotrexate. Her children are healthy. What would you recommend?
Recommendations regarding travelers’ diarrhea (TD) address prevention and management. Prevention encompasses advice about personal behaviors and the use of chemoprophylaxis (antimicrobial and non-antimicrobial) and vaccinations. Since international travelers are known to treat themselves for diarrheal illnesses during their trips,1 recommendations regarding management should assume self-treatment and include the use of both antibiotics and non-antibiotic remedies. Pretravel recommendations will of course be most effective if they account for the individual’s risk for TD.
Innate patient susceptibility, destination, and dietary choices determine TD risk
TD is generally defined as the passage of 3 of more loose stools in a 24-hour period, with associated symptoms of enteric infection—eg, fever, nausea, vomiting, or abdominal cramping. Defined in this manner, TD is thought to occur in 60% to 70% of individuals who travel from developed countries to less-developed countries.2,4 Risk of TD is influenced both by intrinsic personal factors and by factors specific to the trip.
Personal risk factorsIndividual variation in susceptibility to TD might result from a genetic predisposition arising from single nucleotide polymorphisms governing various inflammatory marker proteins.5 A history of multiple episodes of TD, especially if fellow travelers were spared, can suggest this kind of individual susceptibility. Other factors that increase vulnerability to TD are immunodeficiency, achlorhydric states such as atrophic gastritis, and chronic use of proton pump inhibitors.6,7 However, the trip itself is much more important in assessing risk for TD.
Trip-related risk factors
The destination. The most salient risk factor for TD is the geographic destination. Regions of the world can be divided into TD risk strata:2
- Very high: South Asia
- High: South America, Sub-Saharan Africa
- Medium: Central America, Mexico, Caribbean, Middle East, North Africa, Southeast Asia, Oceania
- Low: Europe, North America (excluding Mexico), Australasia, Northeast Asia.
Particularly notable countries, in descending order of risk, are Nepal, India, Myanmar, Bolivia, Sri Lanka, Ecuador, Peru, Kenya, and Guatemala.2
Dietary choices. Additionally, since travelers acquire TD by ingesting food or beverages contaminated with pathogenic fecal microbes, dietary behaviors during the trip affect their susceptibility. At least risk are business travelers and tourists who confine their activities to more affluent settings in which food and beverages are prepared and stored hygienically.1,4,8,9 At greater risk are travelers who immerse themselves in local culture, visiting locations that are more impoverished and not as well equipped with sanitation systems, especially if their stay is at least 2 to 3 weeks.1,4,8,9
Also, the older a traveler is, the lower his or her risk of TD.1,9 An exception to this might be infants whose diet consists solely of breast milk or formula prepared under sanitary conditions.
Mandates and options for preventing TD
Emphasize food and beverage precautions
It might be reasonable to expect that travelers who are circumspect about their food and beverage choices on trips will be able to avoid TD. Indeed, this is the basis for the aphorism, “Boil it, peel it, or forget it.” Guidelines routinely recommend that travelers restrict their selection of foods to those that have been well cooked and are served while still very hot, and to fruits and vegetables that they peel themselves. Likewise, they should drink only beverages that have been boiled or are in sealed bottles or under carbonation and served without ice.10-12 Many travelers might find these recommendations too restrictive to follow faithfully. Moreover, studies suggest it may not be possible for even the most assiduous traveler to fully avoid the risk of TD.13,14 The hygienic characteristics of the travel destination may be more determinative, as illustrated by the successful reduction of TD rates in Jamaica by improving sanitation in tourist resorts.15
Antibiotic chemoprophylaxis: A debated practice with limited consensusThe etiologic agents of TD are multiple and vary somewhat in predominance according to geographic region.3,16,17 TABLE 1 depicts variance by region.16 The most common pathogens are strains of the bacterium Escherichia coli, particularly enterotoxigenic (ETEC), enteroaggregative (EAEC), and enteropathogenic (EPEC) strains.16 Other bacteria of importance are Campylobacter, Salmonella, and Shigella. Viruses, particularly norovirus (notably connected with cruise ships), can also cause TD, although it is implicated in no more than 17% of cases.18 Parasitic pathogens are even less common causes of TD (4%-10%) and mainly involve the protozoa, Giardia lamblia, and, to a lesser extent, Entamoeba histolytica and Cryptosporidium.
Although some pathogens often have a characteristic presentation—such as frothy, greasy diarrhea in the case of G lamblia—they generally cannot be reliably distinguished from one another clinically. Notably, up to 50% of stool samples from TD patients do not yield any pathogen,16 raising the suspicion that current diagnostic technology is not sufficiently sensitive to routinely identify certain bacteria.
There is no consensus on recommending antibiotic chemoprophylaxis against TD.
Opponents of this practice10-12,19,20 point out that TD is generally a brief (3-5 days), self-limited illness. Moreover, concerns about antibiotic resistance have come to pass. Previously used agents, trimethoprim-sulfamethoxazole and doxycycline, are no longer effective in preventing or treating TD. In addition, antibiotic use carries the risk of allergic reactions as well as other adverse effects including, ironically, the development of antibiotic-associated diarrhea and Clostridium difficile diarrhea.
Proponents of antibiotic chemoprophylaxis21,22 point to its demonstrated efficacy in reducing the risk of TD by 4% to 40%.11 They also argue that at least 20% to 25% of travelers who get TD must significantly curtail their activities for a day or more.1,23 This change in travel plans is associated not only with significant personal loss but also imposes a financial burden.23 Furthermore, TD is known to have longer-term effects. Up to 10% of sufferers develop postinfectious irritable bowel syndrome (PI-IBS) that can last for 5 or 6 years.21,22,24,25 It is not known, however, whether the use of antibiotic chemoprophylaxis significantly reduces the incidence of PI-IBS.
Finally, the luminal antibiotic, rifaximin, nonabsorbable as it is, is very well-tolerated and holds promise for not inciting antibiotic resistance.22 However, while its efficacy in preventing TD has been demonstrated in various settings,22,26,27 it is not approved by the US Food and Drug Administration for this indication. Also, concerns persist that it might not be effective in preventing TD caused by invasive pathogens.19
Indications on which all agree. Even opponents of antibiotic chemoprophylaxis grant that it is probably warranted for 2 groups of travelers.10-12 The first is those whose trip schedule is of such importance that any deviation would be intolerable. The second is travelers with comorbidities that would render them at high risk for serious inconvenience or illness if they developed TD. Examples of the latter include patients with enterostomies, mobility impairments, immune suppression, inflammatory bowel disease, and renal or metabolic diseases.
Chemoprophylaxis regimens. If you prescribe an antibiotic prophylactically, consider daily doses of a fluoroquinolone (eg, ciprofloxacin 500 mg orally once daily, not twice daily as for treatment) or rifaximin 200 mg orally once or twice a day, for no longer than 2 to 3 weeks.10
Non-antimicrobial chemoprophylaxis
Bismuth subsalicylate has reduced the incidence of TD from 40% to just 14% when taken in doses of 2 chewable tablets or 60 mL of liquid 4 times daily. 11,19,22 However, the dosing frequency can hinder adherence. Moreover, the relatively high doses required raise the risk of adverse drug reactions such as blackening of the tongue and stool, nausea, constipation, Reye syndrome (in children under 12 years), and possibly tinnitus. The salicylate component of the drug poses a threat to patients with aspirin allergy, renal disease, and those taking anticoagulants. Drug interactions with probenecid and methotrexate are also possible. Bismuth is not recommended for use for longer than 3 weeks, or for children younger than 3 years or pregnant women in their third trimester.
Other non-antimicrobial chemoprophylaxis agents include probiotics such as Lactobacillus andSaccharomyces. These preparations of bacteria and fungi are marketed either singly or in blends of varying composition and proportion. The evidence is divided on their efficacy, and even though some meta-analyses have concluded probiotics such as Saccharomyces boulardii are useful in preventing TD, endorsement in clinical guidelines is muted.10-12,28-30
Immunizations have limited value so farNatural immunity to E coli gastrointestinal infection among indigenous people in less developed countries has raised the possibility of a role for vaccines in preventing TD. Some strains of ETEC produce a heat-labile toxin (LT) that bears significant resemblance to the toxin produced by Vibrio cholerae. Therefore, the oral cholera vaccine, Dukoral, has been marketed outside the United States for the prevention of TD.19,22 However, only ≤7% of TD cases worldwide would be prevented by routine use of this vaccine.31 A transdermal LT vaccine, which involves the antigen-presenting Langerhans cells in the superficial skin layers, is promising but not yet available for routine use.19,22
Treating TD and associated symptoms
Antibiotic treatment
Given that most cases of TD are caused by bacterial pathogens, antibiotics are considered the mainstay of treatment. Concerns about the ill effects of antibiotic use in the case of enterohemorrhagic E coli(EHEC O157:H7) can be allayed because this strain is rarely a cause of TD.9Patient factors that increase vulnerability to TD are immunodeficiency, achlorhydric states such as atrophic gastritis, and chronic use of proton pump inhibitors.
Consider local resistance patterns and risk of invasive infection. Which antibiotic to recommend is governed by the antibiotic resistance patterns prevalent in the travel destinations and by the risk of infection by invasive pathogens. Invasive TD is generally caused by Campylobacter, Shigella, or Salmonella and manifests clinically with bloody diarrhea, fever, or both. Rifaximin at a dose of 200 mg orally 3 times daily is effective for noninvasive TD.31,32 However, travelers who develop invasive TD need an alternative to rifaximin. (Those who advocate reserving antibiotic treatment only for invasive diarrhea will not see a role for rifaximin in the first place.) In most invasive cases, a fluoroquinolone will suffice.10-12,19,32 However, increasing prevalence of fluoroquinolone-resistantCampylobacter species has been reported in South and Southeast Asia. In those locations, azithromycin is an effective alternative, albeit with risk of nausea.33TABLE 212 provides details of recommended antibiotic dosages for adults and children. The duration of treatment is generally 1 day unless symptoms persist, in which case a 3-day course is recommended.10-12,19,32 If the traveler experiences persistent, new, or worsening symptoms beyond this point, immediate evaluation by a physician is required.
Non-antibiotic treatment
The antimotility agent loperamide is a well-established antidiarrheal agent. Its effective and safe use as an adjunct to antibiotics in the treatment of TD has been demonstrated in several studies.10-12,19,32,34 It is generally not used to treat children with TD9
No other non-antibiotic treatment for TD has significant guideline or clinical trial support. Bismuth subsalicylate can be helpful as an antidiarrheal agent,35 but is not often recommended because the regimen makes adherence difficult and because antibiotics and loperamide are effective.
Oral rehydration is usually a mainstay of treating gastrointestinal disease among infants and children. However, it, too, has a limited role in cases of TD because dehydration is not usually a significant part of the clinical presentation, perhaps because vomiting is not often prominent.
CASE Advice regarding safe food and beverage choices is essential for the patient and her children. Despite the increased risk for TD due to her history and her use of the immunosuppressant methotrexate, she decides not to pursue antibiotic prophylaxis. Bismuth is also contraindicated because of the methotrexate. Her teenage daughter declines bismuth prophylaxis, and her toddler is too young for it.
The patient does accept a prescription for azithromycin for her and her daughters in case they experience TD. This choice is appropriate given the destination of India and concern about Campylobacterresistance to fluoroquinolones. You also recommend loperamide for use by the mother and older child, in conjunction with the antibiotic.
Two weeks after their trip abroad, the travelers return for an office visit. On the trip, the mother and toddler suffered diarrhea, which responded well to your recommended management. The older child was well during the trip, but she developed diarrhea, abdominal pain, and anorexia one week after returning to the United States. These symptoms have persisted despite a 3-day course of azithromycin and loperamide.
Post-travel evaluation
TD generally occurs within one to 2 weeks of arrival at the travel destination and usually lasts no longer than 4 to 5 days.19 This scenario is typical of a bacterial infection. When it occurs later or lasts longer, or both, consider several alternative possibilities.19,36 First, the likelihood of a protozoal parasitic infection is increased. Although giardiasis is most likely, other protozoa such as Entamoeba, Cyclospora, Isospora, and Cryptosporidium are also possibilities. Second, if diarrhea persists, it might be due, not to continued infection, but to a self-limited post-infectious enteropathy or to PI-IBS. Third, TD is known to precipitate the clinical manifestation of underlying gastrointestinal disorders such as inflammatory bowel disease (IBD), celiac disease, or even cancer.37
With an atypical disease course, it’s advisable to send 3 stool samples for laboratory evaluation for ova and parasites and for antigen assays for Giardia. If results of these tests are negative, given the difficulty inherent in diagnosing Giardia, consider empiric treatment with metronidazole in lieu of duodenal sampling.36 If the diarrhea persists, investigate serologic markers for celiac disease and IBD. If these are not revealing, referral for colonoscopy is prudent.
CASE The teenager’s 3 stool samples were negative for ova and parasites and for Giardia antigen. Following empirical treatment with oral metronidazole 250 mg, 3 times daily for 7 days, the diarrhea resolved.
CORRESPONDENCE Dilip Nair, MD, Joan C. Edwards School of Medicine at Marshall University, 1600 Medical Center Drive, Suite 1500, Huntington, WV 25701; [email protected]
1. Hill DR. Occurrence and self-treatment of diarrhea in a large cohort of Americans traveling to developing countries. Am J Trop Med Hyg. 2000;62:585–589.
2. Greenwood Z, Black J, Weld L, et al. for the GeoSentinel Surveillance Network. Gastrointestinal infection among international travelers globally. J Travel Med. 2008;15:221–228.
3. DuPont HL. Systematic review: the epidemiology and clinical features of travellers’ diarrhoea. Aliment Pharmacol Ther. 2009;30:187–196.
4. Steffen R, Tornieporth N, Clemens SA, et al. Epidemiology of travelers’ diarrhea: details of a global survey. J Travel Med. 2004;11:231–237.
5. de la Cabada Bauche J, DuPont HL. New developments in traveler’s diarrhea. Gastroenterol Hepatol. 2011;7:88–95.
6. Cabada MM, White AC. Travelers’ diarrhea: an update on susceptibility, prevention, and treatment. Curr Gastroenterol Rep. 2008;10:473–479.
7. Ericsson CD. Travellers with pre-existing medical conditions. Int J Antimicrob Agents. 2003;21:181–188.
8. Cabada MM, Maldonado F, Quispe W, et al. Risk factors associated with diarrhea among international visitors to Cuzco, Peru. Am J Trop Med Hyg. 2006;75:968–972.
9. Mackell S. Traveler’s diarrhea in the pediatric population: etiology and impact. Clin Infect Dis. 2005;41(suppl 8):S547–S552.
10. Hill DR, Ericsson CD, Pearson RD, et al. The practice of travel medicine: guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2006;43:1499–1539.
11. Connor BA. Travelers’ diarrhea. Available at:http://wwwnc.cdc.gov/travel/yellowbook/2012/chapter-2-the-pre-travel-consultation/travelers-diarrhea.htm. Accessed August 20, 2012.
12. Advice for travelers. Treat Guidel Med Lett. 2012;10:45–56.
13. Shlim DR. Looking for evidence that personal hygiene precautions prevent travelers’ diarrhea. Clin Infect Dis. 2005;41(suppl 8):S531–S535.
14. Laverone E, Boccalini S, Bechini A, et al. Travelers’ compliance to prophylactic measures and behavior during stay abroad: results of a retrospective study of subjects returning to a travel medicine center in Italy. J Travel Med. 2006;13:338–344.
15. Ashley DV, Walters C, Dockery-Brown C, et al. Interventions to prevent and control food-borne diseases associated with a reduction in traveler’s diarrhea in tourists to Jamaica. J Travel Med. 2004;11:364–367.
16. Shah N, DuPont HL, Ramsey DJ. Global etiology of travelers’ diarrhea: systematic review from 1973 to the present. Am J Trop Med Hyg. 2009;80:609–614.
17. Riddle MS, Sanders JW, Putnam SD, et al. Incidence, etiology, and impact of diarrhea among long-term travelers (US military and similar populations): a systematic review. Am J Trop Med Hyg. 2006;74:891–900.
18. Koo HL, Ajami NJ, Jiang ZD, et al. Noroviruses as a cause of diarrhea in travelers to Guatemala, India, and Mexico. J Clin Microbiol. 2010;48:1673–1676.
19. Hill DR, Ryan ET. Management of travellers’ diarrhoea. BMJ. 2008;337:863–867.
20. Rendi-Wagner P, Kollaritsch H. Drug prophylaxis for travelers’ diarrhea. Clin Infect Dis. 2002;34:628–633.
21. Pimentel M, Riddle MS. Prevention of traveler’s diarrhea: a call to reconvene. Clin Infect Dis. 2008;46:151–152.
22. DuPont HL. Systematic review: prevention of travellers’ diarrhoea. Aliment Pharmacol Ther. 2008;27:741–751.
23. Wang M, Szucs TD, Steffen R. Economic aspects of travelers’ diarrhea. J Travel Med. 2008;15:110–118.
24. Neal KR, Barker L, Spiller RC. Prognosis in post-infective irritable bowel syndrome: a six year follow up study. Gut. 2002;51:410–413.
25. Tornblom H, Holmvall P, Svenungsson B, et al. Gastrointestinal symptoms after infectious diarrhea: a five-year follow-up in a Swedish cohort of adults. Clin Gastroenterol Hepatol. 2007;5:461–464.
26. DuPont HL, Jiang ZD, Okhuysen PC, et al. A randomized, double-blind, placebo-controlled trial of rifaximin to prevent travelers’ diarrhea. Ann Intern Med. 2005;142:805–812.
27. Taylor DN, McKenzie R, Durbin A, et al. Rifaximin, a nonabsorbed oral antibiotic, prevents shigellosis after experimental challenge. Clin Infect Dis. 2006;42:1283–1288.
28. Sazawal S, Hiremath G, Dhingra U, et al. Efficacy of probiotics in prevention of acute diarrhoea: a meta-analysis of masked, randomised, placebo-controlled trials. Lancet Infect Dis. 2006;6:374–382.
29. Bri V, Buffet P, Genty S, et al. Absence of efficacy of nonviable Lactobacillus acidophilus for the prevention of traveler’s diarrhea: a randomized, double-blind, controlled study. Clin Infect Dis. 2006;43:1170–1175.
30. Hill DR, Ford L, Lalloo DG. Oral cholera vaccines—use in clinical practice. Lancet Infect Dis. 2006;6:361–373.
31. Taylor DN, Bourgeois AL, Ericsson CD, et al. A randomized double-blind, multicenter study of rifaximin compared with placebo and with ciprofloxacin in the treatment of travelers’ diarrhea. Am J Trop Med Hyg. 2006;74:1060–1066.
32. DuPont HL, Ericsson CD, Farthing MJG, et al. Expert review of the evidence base for self-therapy of travelers’ diarrhea. J Travel Med. 2009;16:161–171.
33. Tribble DR, Sanders JW, Pang LW, et al. Traveler’s diarrhea in Thailand: randomized, double-blind trial comparing single-dose and 3-day azithromycin-based regimens with a 3-day levofloxacin regimen. Clin Infect Dis. 2007;44:338–346.
34. Riddle MS, Arnold S, Tribble DR. Effect of adjunctive loperamide in combination with antibiotics on treatment outcomes in travelers’ diarrhea: a systematic review and meta-analysis. Clin Infect Dis. 2008;47:1007–1014.
35. Steffen R. Worldwide efficacy of bismuth subsalicylate in the treatment of travelers’ diarrhea. Rev Infect Dis. 1990;12(suppl 1):S80–S86.
36. Connor BA. Persistent travelers’ diarrhea. Available at:http://wwwnc.cdc.gov/travel/yellowbook/2012/chapter-5-post-travel-evaluation/persistent-travelers-diarrhea.htm. Accessed August 20, 2012.
37.Landzberg BR, Connor BA. Persistent diarrhea in the returning traveler: think beyond persistent infection. Scand J Gastroenterol. 2005;40:112–114.
1. Hill DR. Occurrence and self-treatment of diarrhea in a large cohort of Americans traveling to developing countries. Am J Trop Med Hyg. 2000;62:585–589.
2. Greenwood Z, Black J, Weld L, et al. for the GeoSentinel Surveillance Network. Gastrointestinal infection among international travelers globally. J Travel Med. 2008;15:221–228.
3. DuPont HL. Systematic review: the epidemiology and clinical features of travellers’ diarrhoea. Aliment Pharmacol Ther. 2009;30:187–196.
4. Steffen R, Tornieporth N, Clemens SA, et al. Epidemiology of travelers’ diarrhea: details of a global survey. J Travel Med. 2004;11:231–237.
5. de la Cabada Bauche J, DuPont HL. New developments in traveler’s diarrhea. Gastroenterol Hepatol. 2011;7:88–95.
6. Cabada MM, White AC. Travelers’ diarrhea: an update on susceptibility, prevention, and treatment. Curr Gastroenterol Rep. 2008;10:473–479.
7. Ericsson CD. Travellers with pre-existing medical conditions. Int J Antimicrob Agents. 2003;21:181–188.
8. Cabada MM, Maldonado F, Quispe W, et al. Risk factors associated with diarrhea among international visitors to Cuzco, Peru. Am J Trop Med Hyg. 2006;75:968–972.
9. Mackell S. Traveler’s diarrhea in the pediatric population: etiology and impact. Clin Infect Dis. 2005;41(suppl 8):S547–S552.
10. Hill DR, Ericsson CD, Pearson RD, et al. The practice of travel medicine: guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2006;43:1499–1539.
11. Connor BA. Travelers’ diarrhea. Available at:http://wwwnc.cdc.gov/travel/yellowbook/2012/chapter-2-the-pre-travel-consultation/travelers-diarrhea.htm. Accessed August 20, 2012.
12. Advice for travelers. Treat Guidel Med Lett. 2012;10:45–56.
13. Shlim DR. Looking for evidence that personal hygiene precautions prevent travelers’ diarrhea. Clin Infect Dis. 2005;41(suppl 8):S531–S535.
14. Laverone E, Boccalini S, Bechini A, et al. Travelers’ compliance to prophylactic measures and behavior during stay abroad: results of a retrospective study of subjects returning to a travel medicine center in Italy. J Travel Med. 2006;13:338–344.
15. Ashley DV, Walters C, Dockery-Brown C, et al. Interventions to prevent and control food-borne diseases associated with a reduction in traveler’s diarrhea in tourists to Jamaica. J Travel Med. 2004;11:364–367.
16. Shah N, DuPont HL, Ramsey DJ. Global etiology of travelers’ diarrhea: systematic review from 1973 to the present. Am J Trop Med Hyg. 2009;80:609–614.
17. Riddle MS, Sanders JW, Putnam SD, et al. Incidence, etiology, and impact of diarrhea among long-term travelers (US military and similar populations): a systematic review. Am J Trop Med Hyg. 2006;74:891–900.
18. Koo HL, Ajami NJ, Jiang ZD, et al. Noroviruses as a cause of diarrhea in travelers to Guatemala, India, and Mexico. J Clin Microbiol. 2010;48:1673–1676.
19. Hill DR, Ryan ET. Management of travellers’ diarrhoea. BMJ. 2008;337:863–867.
20. Rendi-Wagner P, Kollaritsch H. Drug prophylaxis for travelers’ diarrhea. Clin Infect Dis. 2002;34:628–633.
21. Pimentel M, Riddle MS. Prevention of traveler’s diarrhea: a call to reconvene. Clin Infect Dis. 2008;46:151–152.
22. DuPont HL. Systematic review: prevention of travellers’ diarrhoea. Aliment Pharmacol Ther. 2008;27:741–751.
23. Wang M, Szucs TD, Steffen R. Economic aspects of travelers’ diarrhea. J Travel Med. 2008;15:110–118.
24. Neal KR, Barker L, Spiller RC. Prognosis in post-infective irritable bowel syndrome: a six year follow up study. Gut. 2002;51:410–413.
25. Tornblom H, Holmvall P, Svenungsson B, et al. Gastrointestinal symptoms after infectious diarrhea: a five-year follow-up in a Swedish cohort of adults. Clin Gastroenterol Hepatol. 2007;5:461–464.
26. DuPont HL, Jiang ZD, Okhuysen PC, et al. A randomized, double-blind, placebo-controlled trial of rifaximin to prevent travelers’ diarrhea. Ann Intern Med. 2005;142:805–812.
27. Taylor DN, McKenzie R, Durbin A, et al. Rifaximin, a nonabsorbed oral antibiotic, prevents shigellosis after experimental challenge. Clin Infect Dis. 2006;42:1283–1288.
28. Sazawal S, Hiremath G, Dhingra U, et al. Efficacy of probiotics in prevention of acute diarrhoea: a meta-analysis of masked, randomised, placebo-controlled trials. Lancet Infect Dis. 2006;6:374–382.
29. Bri V, Buffet P, Genty S, et al. Absence of efficacy of nonviable Lactobacillus acidophilus for the prevention of traveler’s diarrhea: a randomized, double-blind, controlled study. Clin Infect Dis. 2006;43:1170–1175.
30. Hill DR, Ford L, Lalloo DG. Oral cholera vaccines—use in clinical practice. Lancet Infect Dis. 2006;6:361–373.
31. Taylor DN, Bourgeois AL, Ericsson CD, et al. A randomized double-blind, multicenter study of rifaximin compared with placebo and with ciprofloxacin in the treatment of travelers’ diarrhea. Am J Trop Med Hyg. 2006;74:1060–1066.
32. DuPont HL, Ericsson CD, Farthing MJG, et al. Expert review of the evidence base for self-therapy of travelers’ diarrhea. J Travel Med. 2009;16:161–171.
33. Tribble DR, Sanders JW, Pang LW, et al. Traveler’s diarrhea in Thailand: randomized, double-blind trial comparing single-dose and 3-day azithromycin-based regimens with a 3-day levofloxacin regimen. Clin Infect Dis. 2007;44:338–346.
34. Riddle MS, Arnold S, Tribble DR. Effect of adjunctive loperamide in combination with antibiotics on treatment outcomes in travelers’ diarrhea: a systematic review and meta-analysis. Clin Infect Dis. 2008;47:1007–1014.
35. Steffen R. Worldwide efficacy of bismuth subsalicylate in the treatment of travelers’ diarrhea. Rev Infect Dis. 1990;12(suppl 1):S80–S86.
36. Connor BA. Persistent travelers’ diarrhea. Available at:http://wwwnc.cdc.gov/travel/yellowbook/2012/chapter-5-post-travel-evaluation/persistent-travelers-diarrhea.htm. Accessed August 20, 2012.
37.Landzberg BR, Connor BA. Persistent diarrhea in the returning traveler: think beyond persistent infection. Scand J Gastroenterol. 2005;40:112–114.
Long-term increase seen in abdominal sacrocolpopexy failure rates
More than 225,000 operations are performed each year in the United States for pelvic organ prolapse (POP). Abdominal sacrocolpopexy is considered the most durable of these procedures, but long-term outcomes need to be studied, say researchers from University of Utah School of Medicine, Salt Lake City.1 Direct costs for these procedures exceed $1 billion per year, and, as the population ages, the need to treat POP and urinary incontinence will rise.1
The original Colpopexy and Urinary Reduction Efforts (CARE) trial included 322 women without stress urinary incontinence (SUI) who underwent abdominal sacrocolpopexy between 2002 and 2005 for symptomatic POP. Because SUI is a common adverse event following POP surgery, study patients were randomly assigned to receive concomitant Burch urethropexy or no urethropexy.
Details of the study
The extended CARE study enrolled 92% (215/233) of eligible 2-year CARE trial completers. A total of 181 (84%) of the 215 women went on to complete 5 years of follow-up, and 126 (56%) completed 7 years of follow-up. The primary goals of the extended CARE study, as reported in JAMA, were to compare long-term anatomic success rates, stress continence rates, overall pelvic floor symptoms, pelvic-floor–specific quality of life (QOL), and mesh-related adverse events.
RESULTS
Treatment failure probability. Treatment failure was considered symptomatic or anatomic POP, SUI, or overall urinary incontinence score of 3 or greater on the Incontinence Severity Index. The procedure’s failure rates showed a gradual increase over the follow-up, in both the urethropexy group and the no urethropexy group.
Urethropexy vs no urethropexy. By year 7, the estimated probabilities of treatment failure for the urethropexy group versus the no urethropexy group, respectively, were:
- for anatomic POP – 0.27 versus 0.22 (treatment difference of 0.05; 95% confidence interval [CI], 0.161 to 0.271)
- for symptomatic POP – 0.29 versus 0.24 (treatment difference of 0.049; 95% CI, 0.060 to 0.162)
- for composite POP – 0.48 versus 0.34 (treatment difference of 0.134; 95% CI, 0.096 to 0.322)
- for SUI – 0.62 versus 0.77 (treatment difference of 0.153; 95% CI, 0.268 to 0.030)
- for overall urinary incontinence – 0.75 versus 0.81 (treatment difference of 0.064; 95% CI, 0.161 to 0.032).
Mesh erosion probability. By year 2, 3 of the 322 women enrolled in CARE had suture erosion and 17 had mesh erosion. There were 2 additional cases of suture erosion and 6 additional cases of mesh erosion by year 7. All types of mesh eroded. The estimated probability of mesh erosion in the CARE and extended CARE trials at the time of the last known treatment failure (6.18 years) was 10.5% (95% CI, 6.8%-16.1%).
Repeat surgery probability. By year 7, at least 36 of 215 women (16.7%) in the extended CARE trial had additional surgery related to pelvic floor disorders, 11 for recurrent POP, 14 for SUI, and 11 for mesh complications.
ABDOMINAL SACROCOLPOPEXY FOR POP IS LESS EFFECTIVE THAN DESIRED
During 7 years of follow-up, abdominal sacrocolpopexy failure rates increased in both the urethropexy group and the no urethropexy group, although urethropexy prevented SUI longer than no urethropexy. “By 5 years, nearly one-third of women met our composite failure definition,” said the authors.1
“Based on our results,” they write, “women considering abdominal sacrocolpopexy should be counseled that this procedure effectively provides relief from POP symptoms; however, the anatomic support deteriorates over time. Adding an anti-incontinence procedure for women continent preoperatively decreases, but does not eliminate, the risk of de novo SUI. Surgical counseling about the ongoing risk of mesh-related events even for abdominal sacrocolpopexy is critical. Women should be aware that symptoms such as vaginal bleeding, discharge, and pain may be due to mesh erosion and should seek help accordingly.”1
We want to hear from you! Tell us what you think.
Reference
1. Nygaard I, Brubaker L, Zyczynski HM, et al. Long-term outcomes following abdominal sacrocolpopexy for pelvic organ prolapse. JAMA. 2013;309(19):2016–2024.
More than 225,000 operations are performed each year in the United States for pelvic organ prolapse (POP). Abdominal sacrocolpopexy is considered the most durable of these procedures, but long-term outcomes need to be studied, say researchers from University of Utah School of Medicine, Salt Lake City.1 Direct costs for these procedures exceed $1 billion per year, and, as the population ages, the need to treat POP and urinary incontinence will rise.1
The original Colpopexy and Urinary Reduction Efforts (CARE) trial included 322 women without stress urinary incontinence (SUI) who underwent abdominal sacrocolpopexy between 2002 and 2005 for symptomatic POP. Because SUI is a common adverse event following POP surgery, study patients were randomly assigned to receive concomitant Burch urethropexy or no urethropexy.
Details of the study
The extended CARE study enrolled 92% (215/233) of eligible 2-year CARE trial completers. A total of 181 (84%) of the 215 women went on to complete 5 years of follow-up, and 126 (56%) completed 7 years of follow-up. The primary goals of the extended CARE study, as reported in JAMA, were to compare long-term anatomic success rates, stress continence rates, overall pelvic floor symptoms, pelvic-floor–specific quality of life (QOL), and mesh-related adverse events.
RESULTS
Treatment failure probability. Treatment failure was considered symptomatic or anatomic POP, SUI, or overall urinary incontinence score of 3 or greater on the Incontinence Severity Index. The procedure’s failure rates showed a gradual increase over the follow-up, in both the urethropexy group and the no urethropexy group.
Urethropexy vs no urethropexy. By year 7, the estimated probabilities of treatment failure for the urethropexy group versus the no urethropexy group, respectively, were:
- for anatomic POP – 0.27 versus 0.22 (treatment difference of 0.05; 95% confidence interval [CI], 0.161 to 0.271)
- for symptomatic POP – 0.29 versus 0.24 (treatment difference of 0.049; 95% CI, 0.060 to 0.162)
- for composite POP – 0.48 versus 0.34 (treatment difference of 0.134; 95% CI, 0.096 to 0.322)
- for SUI – 0.62 versus 0.77 (treatment difference of 0.153; 95% CI, 0.268 to 0.030)
- for overall urinary incontinence – 0.75 versus 0.81 (treatment difference of 0.064; 95% CI, 0.161 to 0.032).
Mesh erosion probability. By year 2, 3 of the 322 women enrolled in CARE had suture erosion and 17 had mesh erosion. There were 2 additional cases of suture erosion and 6 additional cases of mesh erosion by year 7. All types of mesh eroded. The estimated probability of mesh erosion in the CARE and extended CARE trials at the time of the last known treatment failure (6.18 years) was 10.5% (95% CI, 6.8%-16.1%).
Repeat surgery probability. By year 7, at least 36 of 215 women (16.7%) in the extended CARE trial had additional surgery related to pelvic floor disorders, 11 for recurrent POP, 14 for SUI, and 11 for mesh complications.
ABDOMINAL SACROCOLPOPEXY FOR POP IS LESS EFFECTIVE THAN DESIRED
During 7 years of follow-up, abdominal sacrocolpopexy failure rates increased in both the urethropexy group and the no urethropexy group, although urethropexy prevented SUI longer than no urethropexy. “By 5 years, nearly one-third of women met our composite failure definition,” said the authors.1
“Based on our results,” they write, “women considering abdominal sacrocolpopexy should be counseled that this procedure effectively provides relief from POP symptoms; however, the anatomic support deteriorates over time. Adding an anti-incontinence procedure for women continent preoperatively decreases, but does not eliminate, the risk of de novo SUI. Surgical counseling about the ongoing risk of mesh-related events even for abdominal sacrocolpopexy is critical. Women should be aware that symptoms such as vaginal bleeding, discharge, and pain may be due to mesh erosion and should seek help accordingly.”1
We want to hear from you! Tell us what you think.
More than 225,000 operations are performed each year in the United States for pelvic organ prolapse (POP). Abdominal sacrocolpopexy is considered the most durable of these procedures, but long-term outcomes need to be studied, say researchers from University of Utah School of Medicine, Salt Lake City.1 Direct costs for these procedures exceed $1 billion per year, and, as the population ages, the need to treat POP and urinary incontinence will rise.1
The original Colpopexy and Urinary Reduction Efforts (CARE) trial included 322 women without stress urinary incontinence (SUI) who underwent abdominal sacrocolpopexy between 2002 and 2005 for symptomatic POP. Because SUI is a common adverse event following POP surgery, study patients were randomly assigned to receive concomitant Burch urethropexy or no urethropexy.
Details of the study
The extended CARE study enrolled 92% (215/233) of eligible 2-year CARE trial completers. A total of 181 (84%) of the 215 women went on to complete 5 years of follow-up, and 126 (56%) completed 7 years of follow-up. The primary goals of the extended CARE study, as reported in JAMA, were to compare long-term anatomic success rates, stress continence rates, overall pelvic floor symptoms, pelvic-floor–specific quality of life (QOL), and mesh-related adverse events.
RESULTS
Treatment failure probability. Treatment failure was considered symptomatic or anatomic POP, SUI, or overall urinary incontinence score of 3 or greater on the Incontinence Severity Index. The procedure’s failure rates showed a gradual increase over the follow-up, in both the urethropexy group and the no urethropexy group.
Urethropexy vs no urethropexy. By year 7, the estimated probabilities of treatment failure for the urethropexy group versus the no urethropexy group, respectively, were:
- for anatomic POP – 0.27 versus 0.22 (treatment difference of 0.05; 95% confidence interval [CI], 0.161 to 0.271)
- for symptomatic POP – 0.29 versus 0.24 (treatment difference of 0.049; 95% CI, 0.060 to 0.162)
- for composite POP – 0.48 versus 0.34 (treatment difference of 0.134; 95% CI, 0.096 to 0.322)
- for SUI – 0.62 versus 0.77 (treatment difference of 0.153; 95% CI, 0.268 to 0.030)
- for overall urinary incontinence – 0.75 versus 0.81 (treatment difference of 0.064; 95% CI, 0.161 to 0.032).
Mesh erosion probability. By year 2, 3 of the 322 women enrolled in CARE had suture erosion and 17 had mesh erosion. There were 2 additional cases of suture erosion and 6 additional cases of mesh erosion by year 7. All types of mesh eroded. The estimated probability of mesh erosion in the CARE and extended CARE trials at the time of the last known treatment failure (6.18 years) was 10.5% (95% CI, 6.8%-16.1%).
Repeat surgery probability. By year 7, at least 36 of 215 women (16.7%) in the extended CARE trial had additional surgery related to pelvic floor disorders, 11 for recurrent POP, 14 for SUI, and 11 for mesh complications.
ABDOMINAL SACROCOLPOPEXY FOR POP IS LESS EFFECTIVE THAN DESIRED
During 7 years of follow-up, abdominal sacrocolpopexy failure rates increased in both the urethropexy group and the no urethropexy group, although urethropexy prevented SUI longer than no urethropexy. “By 5 years, nearly one-third of women met our composite failure definition,” said the authors.1
“Based on our results,” they write, “women considering abdominal sacrocolpopexy should be counseled that this procedure effectively provides relief from POP symptoms; however, the anatomic support deteriorates over time. Adding an anti-incontinence procedure for women continent preoperatively decreases, but does not eliminate, the risk of de novo SUI. Surgical counseling about the ongoing risk of mesh-related events even for abdominal sacrocolpopexy is critical. Women should be aware that symptoms such as vaginal bleeding, discharge, and pain may be due to mesh erosion and should seek help accordingly.”1
We want to hear from you! Tell us what you think.
Reference
1. Nygaard I, Brubaker L, Zyczynski HM, et al. Long-term outcomes following abdominal sacrocolpopexy for pelvic organ prolapse. JAMA. 2013;309(19):2016–2024.
Reference
1. Nygaard I, Brubaker L, Zyczynski HM, et al. Long-term outcomes following abdominal sacrocolpopexy for pelvic organ prolapse. JAMA. 2013;309(19):2016–2024.
Girl, 13, With a Bump on Her Leg
A girl, age 13 years, 4 months, presented to her primary care provider’s office for a well visit. Among her concerns, she mentioned a “bump” she had had on her right leg “for the past six months, maybe longer.” The area felt irritated when touched or when the patient “ran too much.” She had seen no change in the bump since she first noticed it. The patient knew of no trauma or other preceding factors. She denied any fever or warmth, redness, or ecchymosis to the area.
Medical history was unremarkable except for familial short stature and myopia. The patient was the fifth of eight children born to nonconsanguinous parents. She denied any surgical history or hospitalizations and was premenarcheal. She was up to date on all age-appropriate vaccines, with her meningococcal vaccine administered at that visit.
The patient’s blood pressure was 99/58 mm Hg with an apical pulse rate of 82 beats/min. Her growth parameters were following her curve. Her height was 55” (0.3 percentile); weight, 81 lb (7.5 percentile); and BMI, 18.8 (48.6 percentile).
The physical exam was normal with the exception of the musculoskeletal exam. Examination of the lower extremities revealed a palpable, 4 cm x 5 cm lesion at the right distal medial thigh just proximal to the knee. The lesion could not be visualized but on palpation was tender and firm. There was some question as to whether the lesion itself or inflamed soft tissue overlying the lesion was mobile. No overlying warmth, induration, erythema, or ecchymosis was noted.
Passive and active range of motion was intact at the hip and knee. No lesions to the upper extremities were evident, and no scoliosis was seen.
Blood work was done to rule out certain diagnoses. Results from a complete blood count with differential, lactate dehydrogenase (LDH), parathyroid hormone, lipid profiles, thyroid function, and a comprehensive metabolic profile were unremarkable. A low level of vitamin D 25-OH was detected: 21.7 ng/mL (normal range, 32 to 100 ng/mL).
Distal femur x-rays with posteroanterior, lateral, and oblique views were ordered. The imaging revealed a 3 cm x 3 cm lesion projecting from the “distal, somewhat medial” femur, which was diagnosed as a benign femoral osteochondroma. Significant inflammation to the surrounding soft-tissue structures was observed. A questionable old fracture of the osteochondroma was noted. The remaining bony structures and joints appeared normal.
An ultrasound of the lesion was also ordered to investigate soft-tissue swelling. This revealed a hypoechoic collar around the distal end of the osteochondroma, which could represent a fluid collection, hematoma from trauma, or bursitis. The soft tissues were deemed normal.
Because of the extent of inflammation, the radiologist recommended MRI without contrast to rule out bursitis or trauma to the osteochondroma.
DISCUSSION
Osteochondromas, which may be present in up to 3% of the general population, are the most common benign bone tumors.1-3 An osteochondroma is a cartilage-capped bony projection that arises on the external surface of the bone; it contains a marrow cavity that is continuous with the underlying bone.2,4 The majority of osteochondromas are solitary, accounting for perhaps 85% to 90% of all such lesions, and they are typically nonhereditary; the remaining 10% to 15% of osteochondromas are hereditary multiple osteochondromas or exostoses1,2 (see “Definition of Multiple Exostoses Syndrome”2,5,6,7).
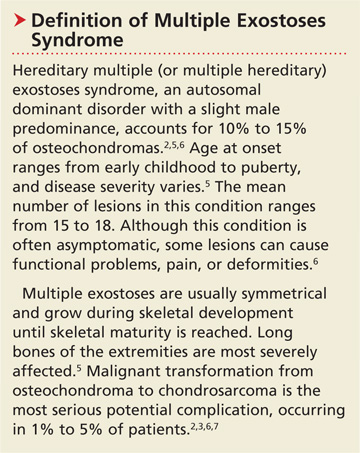
Most lesions are painless and slow growing, and they usually occur in children and adolescents.2 They typically stop growing at skeletal maturity with the closure of the growth plates.3,8,9 There is no predilection for males or females in single lesions.2
Solitary osteochondromas typically appear in the lower extremities and at long tubular bone metaphyses,1-3,10 especially on the femur, humerus, tibia, spine, and hip. Any part of the skeleton can be affected, but 30% of lesions occur on the femur and 40% at either the proximal metaphysis of the tibia or the distal metaphysis of the femur.2,11
Most osteochondromas are asymptomatic and are found incidentally.1,3 However, some patients present with local pain as a result of irritation to adjacent structures, limitation of joint motion, growth disturbance, or fracture of the pedicle.3,4,9,11,12 A very small proportion of patients (no more than 1%) with solitary osteochondromas experience malignant transformation.2,3,6,7 No particular blood work is recommended for patients with solitary osteochondromas.2
Differential Diagnosis
In addition to osteochondromas, several other lesions should be considered in the patient with musculoskeletal lesions (see Table 15,6,13-19).
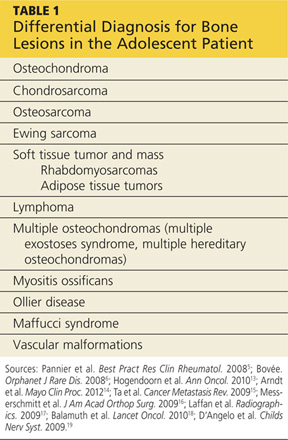
Cartilaginous tumors. Chondrosarcomas are malignant cartilaginous tumors.20-22 They commonly affect long bones, including the humerus and femur, and some flat bones, such as the pelvic bones.13,22 They are most commonly seen in adults, and have no predisposition by gender.13
Chondrosarcomas can be primary (ie, arising de novo) or secondary (developing on preexisting benign cartilaginous neoplasms, including osteochondromas). The majority of chondrosarcomas are slow growing, and they rarely metastasize. It is difficult to differentiate between a benign lesion (such as an osteochondroma) and a chondrosarcoma by either histology or radiology. However, reliable predictors for malignancy include size exceeding 5 cm and location in the axial skeleton.20
Bone tumors.Osteosarcomas are the most common malignant bone tumors in children and adolescents, with 400 to 560 US patients in this age-group diagnosed each year.14-16 Osteosarcomas are uncommon in children younger than 10; their incidence peaks during the early teenage years (median peak age, 16), then declines rapidly among older patients. They are more common in males than females.15
Osteosarcomas commonly develop during periods of rapid bone turnover, such as the adolescent growth spurt. Common sites include the distal femur, proximal humerus, and proximal tibia,15,16 particularly near the knee.13 Usually, osteosarcomas present with nonspecific symptoms, including strain-related pain of several months’ duration, which may disrupt sleep.16 Laboratory findings in affected patients may include elevations in LDH, alkaline phosphatase, and/or ESR.15,23
Physical exam reveals a visible or palpable mass in the affected area, along with decreased joint motion; localized warmth or erythema may also be present. Late signs of osteosarcoma include weight loss, general malaise, and fever. First-line imaging for the patient with a suspected osteosarcoma is x-ray, which will show ill-defined borders, osteoblastic and/or osteolytic features, and an associated soft tissue mass. Advanced imaging, such as MRI, is warranted.16
Ewing sarcoma, the second most common bone tumor in children and adolescents, is an aggressive form of childhood cancer.14,18 Approximately 25% of all Ewing sarcomas arise in soft tissues rather than bones.18 They are more common in whites than in other ethnic groups and have a slight male predominance.13,18 The median age at diagnosis is 15.13 The most common presenting symptoms are tumor related, such as pain or a noticeable mass. While x-rays are usually ordered first, MRI is preferred.18
Soft tissue tumors and masses.Rhabdomyosarcomas are malignancies that account for more than half of the soft tissue sarcomas in children and adolescents. Less than one-fifth of cases occur in the extremities, and most occur in children younger than 10. These lesions have a slight male predominance and are more common in whites than in other patients.14,17,24
Approximately 6% of childhood soft tissue tumors are adipose tissue tumors, which may be benign (eg, lipomas) or malignant (eg, liposarcomas). Lipomas in children account for nearly 4% of all soft tissue tumors and can be classified as superficial (which are often diagnosed clinically) or deep (frequently requiring imaging).25
Lymphomaaccounts for 7% of cancers in US children and adolescents and more than 25% of newly diagnosed cancers in patients between 15 and 19, making it the most common malignancy in adolescents and the third most common in children.26,27 Non-Hodgkin lymphoma is the fourth leading type of malignancy in US adolescents.27 Rarely, lymphomas present with primary event soft tissue involvement.28
Myositis ossificans (MO) is a rare benign disorder involving formation of heterotrophic bone in skeletal muscles and soft tissues.29 Though possible in patients of any age, MO is most commonly seen in adolescents and young adults. Often the result of soft tissue injury (in which case it is referred to as myositis ossificans circumscripta or traumatic), MO develops in areas that are exposed to trauma, such as the anterior thighs or arms. Lesions can be diagnosed via plain x-ray or CT, although MRI and ultrasound can also be useful evaluation tools.17,29,30
Because MO circumscripta typically presents as a painful soft tissue mass, it can be mistaken for a soft tissue sarcoma or an osteosarcoma; radiologic evaluation is required to make the proper diagnosis. Less common forms of MO are myositis ossificans progressiva and myositis ossificans without a history of trauma.29
Ollier diseaseis a rare, nonfamilial disorder characterized by multiple enchondromas (or enchondromatoses), which are distributed asymmetrically with areas of dysplastic cartilage. Enchondromas are benign cartilage tumors that frequently affect long tubular bones along the metaphyses in proximity to the growth plate. The enchondromas result in significant growth abnormalities. About one in 1 million people are diagnosed yearly.5,19 (Similarly, Maffucci syndrome is represented by multiple enchondromas in association with hemangiomas.5)
Ollier disease typically manifests during childhood5 with bone swelling, local pain, and palpable bony masses, which are often associated with bone deformities.19 Patients generally present with an asymmetric shortening of one extremity and the appearance of palpable bony masses on their fingers or toes, which may or may not be associated with pathologic fractures.5,19 In 20% to 50% of patients with Ollier disease, enchondromas are at risk for malignant transformation into chondrosarcomas.5
Vascular malformations. Certain abnormalities of vascular development cause birthmarks and abnormalities of varying degree in underlying tissues.31 They are usually present at birth and grow proportionally to the child’s growth.25,31 However, they can also be seen in later childhood and adolescence.
Radiologic Investigation
Plain radiography of the affected area is the first-line radiologic study to be performed.13 While most osteochondromas can be diagnosed by plain x-ray, cross-sectional imaging via CT or MRI is recommended in lesions with certain characteristics, such as a broad stalk or location in the axial skeleton. Because MRI involves no radiation exposure, it is a particularly good diagnostic tool for children.32
Ultrasound is a good imaging method for evaluating for complications of osteochondromas, including bursa formation or vascular compromise.32
Treatment and Management
Although usually asymptomatic, osteochondroma can trigger some significant symptoms. Osteochondromas are at risk for fracture and can cause body deformities, mechanical joint problems, weakness of the affected limb, numbness, vascular compression, aneurysm, arterial thrombosis, venous thrombosis, pain, acute ischemia, and nerve compression. Clinical signs of malignant transformation include pain, swelling, and increased lesion size.2
Surgical excision is recommended but should be delayed until after the patient has reached skeletal maturity in order to decrease the risk for recurrence.33
Patient Education and Follow-up
In addition to explaining appropriate pain management (eg, NSAIDs), it is especially important for the pediatric NP or PA to encourage the patient with a solitary osteochondroma to follow up with the pediatric orthopedic surgeon. Reasons include the need to monitor growth of the lesion (which is likely to continue in a patient who has not yet reached skeletal maturity) and assess for associated functional or joint problems. Patients should also be advised to seek the specialist’s attention if such problems develop or if pain increases.
Generally, the pediatric clinician should be sufficiently informed to answer questions about this condition from the patient or family. Any follow-up laboratory work recommended by the specialist can also be performed by the pediatric NP or PA.
OUTCOME FOR THE CASE PATIENT
MRI without contrast, as recommended by the radiologist to rule out a bursa or trauma to the osteochondroma, was considered an important part of the follow-up plan. As the patient had not yet reached skeletal maturity, she was referred to a pediatric orthopedic surgeon for possible excision of the lesion, due to its size and the pain associated with running or other exertion.
CONCLUSION
Solitary osteochondromas are the most common benign bone tumors. Although they are generally asymptomatic, pain and other symptoms can arise as a result of irritation to the adjacent structures. In this case, the patient’s chief complaint was an irritating “bump” that she had had on her right leg for at least six months.
Generally, follow-up monitoring of the osteochondroma and orthopedic follow-up care are warranted, at least until the patient reaches skeletal maturity. At that point, surgical excision of the lesion is recommended.
REFERENCES
1. Florez B, Mönckeberg J, Castillo G, Beguiristain J. Solitary osteochondroma long-term follow-up. J Pediatr Orthop B. 2008;17:91-94.
2. Kitsoulis P, Galani V, Stefanaki K, et al. Osteochondromas: review of the clinical, radiological and pathological features. In Vivo. 2008;22:633-646.
3. Ramos-Pascua LR, Sánchez-Herráez S, Alonso-Barrio JA, Alonso-León A. Solitary proximal end of femur osteochondroma: an indication and result of the en bloc resection without hip luxation [in Spanish]. Rev Esp Cir Ortop Traumatol. 2012;56:24-31.
4. Payne WT, Merrell G. Benign bony and soft tissue tumors of the hand. J Hand Surg. 2010;35:1901-1910.
5. Pannier S, Legeai-Mallet L. Hereditary multiple exostoses and enchondromatosis. Best Pract Res Clin Rheumatol. 2008;22:45-54.
6. Bovée JV. Multiple osteochondromas. Orphanet J Rare Dis. 2008;3(3).
7. Staals EL, Bacchini P, Mercuri M, Bertoni F. Dedifferentiated chondrosarcomas arising in preexisting osteochondromas. J Bone Joint Surg Am. 2007;89:987-993.
8. Singh R, Jain M, Siwach R, et al. Large para-articular osteochondroma of the knee joint: a case report. Acta Orthop Traumatol Turc. 2012;46:139-143.
9. Lee JY, Lee S, Joo KB, et al. Intraarticular osteochondroma of shoulder: a case report. Clin Imaging. 2013;37:379-381.
10. Kim Y-C, Ahn JH, Lee JW. Osteochondroma of the distal tibia complicated by a tibialis posterior tendon tear. J Foot Ankle Surg. 2012;51: 660-663.
11. Allagui M, Amara K, Aloui I, et al. Historical giant near-circumferential osteochondroma of the proximal humerus. J Shoulder Elbow Surg. 2010;19:e12-e15.
12. Li M, Luettringhaus T, Walker KR, Cole PA. Operative treatment of femoral neck osteochondroma through a digastric approach in a pediatric patient: a case report and review of the literature. J Pediatr Orthop B. 2012;21:230-234.
13. Hogendoorn PC, Athanasou N, Bielack S, et al; ESMO/EUROBONET Working Group. Bone sarcomas: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2010;21 suppl 5:v204-v213.
14. Arndt CAS, Rose PS, Folpe AL, Laack NN. Common musculoskeletal tumors of childhood and adolescence. Mayo Clin Proc. 2012;87:475-487.
15. Ta HT, Dass CR, Choong PF, Dunstan DE. Osteosarcoma treatment: state of the art. Cancer Metastasis Rev. 2009;28:247-263.
16. Messerschmitt PJ, Garcia RM, Abdul-Karim FW, et al. Osteosarcoma. J Am Acad Orthop Surg. 2009;17:515-527.
17. Laffan EE, Ngan B-Y, Navarro OM. Pediatric soft-tissue tumors and pseudotumors: MR imaging features with pathologic correlation: Part 2. Tumors of fibroblastic/myofibroblastic, so-called fibrohistiocytic, muscular, lymphomatous, neurogenic, hair matrix, and uncertain origin. Radiographics. 2009;29:e36.
18. Balamuth NJ, Womer RB. Ewing’s sarcoma. Lancet Oncol. 2010;11(2):184.
19. D’Angelo L, Massimi L, Narducci A, Di Rocco C. Ollier disease. Childs Nerv Syst. 2009;25:647-653.
20. Gelderblom H, Hogendoorn PC, Dijkstra SD, et al. The clinical approach towards chondrosarcoma. Oncologist. 2008;13:320-329.
21. Nosratzehi T, Pakfetrat A. Chondrosarcoma. Zahedan J Res Med Sci. 2013;15:64-64.
22. Prado FO, Nishimoto IN, Perez DE, et al. Head and neck chondrosarcoma: analysis of 16 cases. Br J Oral Maxillofacial Surg. 2009;47:555-557.
23. Kim HJ, Chalmers PN, Morris CD. Pediatric osteogenic sarcoma. Curr Opin Pediatr. 2010;22:61-66.
24. Sultan I, Qaddoumi I, Yaser S, et al. Comparing adult and pediatric rhabdomyosarcoma in the surveillance, epidemiology and end results program, 1973 to 2005: an analysis of 2,600 patients. J Clin Oncol. 2009;27:3391-3397.
25. Navarro OM, Laffan EE, Ngan B-Y. Pediatric soft-tissue tumors and pseudo-tumors: MR imaging features with pathologic correlation: Part 1. Imaging approach, pseudotumors, vascular lesions, and adipocytic tumors. Radiographics. 2009;29:887-906.
26. Gross TG, Termuhlen AM. Pediatric non-Hodgkin lymphoma. Curr Hematol Malig Rep. 2008;3:167-173.
27. Hochberg J, Waxman IM, Kelly KM, et al. Adolescent non-Hodgkin lymphoma and Hodgkin lymphoma: state of the science. Br J Haematol. 2009;144:24-40.
28. Derenzini E, Casadei B, Pellegrini C, et al. Non-Hodgkin lymphomas presenting as soft tissue masses: A single center experience and meta-analysis of the published series. Clin Lymphoma Myeloma Leuk. 2012 Dec 12. [Epub ahead of print]
29. Micheli A, Trapani S, Brizzi I, et al. Myositis ossificans circumscripta: a paediatric case and review of the literature. Eur J Pediatr. 2009;168:523-529.
30. McKenzie G, Raby N, Ritchie D. Non-neoplastic soft-tissue masses. Br J Radiol. 2009;82:775-785.
31. Buckmiller LM, Richter GT, Suen JY. Diagnosis and management of hemangiomas and vascular malformations of the head and neck. Oral Dis. 2010;16:405-418.
32. Khanna G, Bennett DL. Pediatric bone lesions: beyond the plain radiographic evaluation. Semin Roentgenol. 2012;47:90-99.
33. Rijal L, Nepal P, Baral S, et al. Solitary diaphyseal exostosis of femur, how common is it? Eur J Orthop Surg Traumatol. 2011;21:363-365.
A girl, age 13 years, 4 months, presented to her primary care provider’s office for a well visit. Among her concerns, she mentioned a “bump” she had had on her right leg “for the past six months, maybe longer.” The area felt irritated when touched or when the patient “ran too much.” She had seen no change in the bump since she first noticed it. The patient knew of no trauma or other preceding factors. She denied any fever or warmth, redness, or ecchymosis to the area.
Medical history was unremarkable except for familial short stature and myopia. The patient was the fifth of eight children born to nonconsanguinous parents. She denied any surgical history or hospitalizations and was premenarcheal. She was up to date on all age-appropriate vaccines, with her meningococcal vaccine administered at that visit.
The patient’s blood pressure was 99/58 mm Hg with an apical pulse rate of 82 beats/min. Her growth parameters were following her curve. Her height was 55” (0.3 percentile); weight, 81 lb (7.5 percentile); and BMI, 18.8 (48.6 percentile).
The physical exam was normal with the exception of the musculoskeletal exam. Examination of the lower extremities revealed a palpable, 4 cm x 5 cm lesion at the right distal medial thigh just proximal to the knee. The lesion could not be visualized but on palpation was tender and firm. There was some question as to whether the lesion itself or inflamed soft tissue overlying the lesion was mobile. No overlying warmth, induration, erythema, or ecchymosis was noted.
Passive and active range of motion was intact at the hip and knee. No lesions to the upper extremities were evident, and no scoliosis was seen.
Blood work was done to rule out certain diagnoses. Results from a complete blood count with differential, lactate dehydrogenase (LDH), parathyroid hormone, lipid profiles, thyroid function, and a comprehensive metabolic profile were unremarkable. A low level of vitamin D 25-OH was detected: 21.7 ng/mL (normal range, 32 to 100 ng/mL).
Distal femur x-rays with posteroanterior, lateral, and oblique views were ordered. The imaging revealed a 3 cm x 3 cm lesion projecting from the “distal, somewhat medial” femur, which was diagnosed as a benign femoral osteochondroma. Significant inflammation to the surrounding soft-tissue structures was observed. A questionable old fracture of the osteochondroma was noted. The remaining bony structures and joints appeared normal.
An ultrasound of the lesion was also ordered to investigate soft-tissue swelling. This revealed a hypoechoic collar around the distal end of the osteochondroma, which could represent a fluid collection, hematoma from trauma, or bursitis. The soft tissues were deemed normal.
Because of the extent of inflammation, the radiologist recommended MRI without contrast to rule out bursitis or trauma to the osteochondroma.
DISCUSSION
Osteochondromas, which may be present in up to 3% of the general population, are the most common benign bone tumors.1-3 An osteochondroma is a cartilage-capped bony projection that arises on the external surface of the bone; it contains a marrow cavity that is continuous with the underlying bone.2,4 The majority of osteochondromas are solitary, accounting for perhaps 85% to 90% of all such lesions, and they are typically nonhereditary; the remaining 10% to 15% of osteochondromas are hereditary multiple osteochondromas or exostoses1,2 (see “Definition of Multiple Exostoses Syndrome”2,5,6,7).
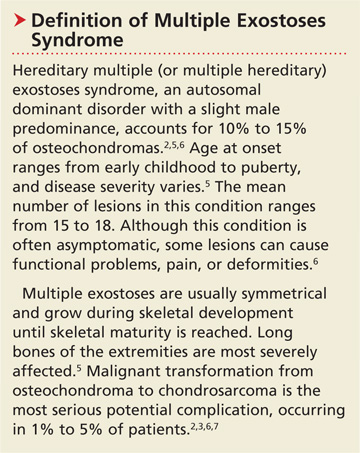
Most lesions are painless and slow growing, and they usually occur in children and adolescents.2 They typically stop growing at skeletal maturity with the closure of the growth plates.3,8,9 There is no predilection for males or females in single lesions.2
Solitary osteochondromas typically appear in the lower extremities and at long tubular bone metaphyses,1-3,10 especially on the femur, humerus, tibia, spine, and hip. Any part of the skeleton can be affected, but 30% of lesions occur on the femur and 40% at either the proximal metaphysis of the tibia or the distal metaphysis of the femur.2,11
Most osteochondromas are asymptomatic and are found incidentally.1,3 However, some patients present with local pain as a result of irritation to adjacent structures, limitation of joint motion, growth disturbance, or fracture of the pedicle.3,4,9,11,12 A very small proportion of patients (no more than 1%) with solitary osteochondromas experience malignant transformation.2,3,6,7 No particular blood work is recommended for patients with solitary osteochondromas.2
Differential Diagnosis
In addition to osteochondromas, several other lesions should be considered in the patient with musculoskeletal lesions (see Table 15,6,13-19).
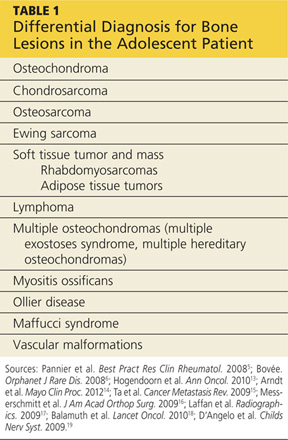
Cartilaginous tumors. Chondrosarcomas are malignant cartilaginous tumors.20-22 They commonly affect long bones, including the humerus and femur, and some flat bones, such as the pelvic bones.13,22 They are most commonly seen in adults, and have no predisposition by gender.13
Chondrosarcomas can be primary (ie, arising de novo) or secondary (developing on preexisting benign cartilaginous neoplasms, including osteochondromas). The majority of chondrosarcomas are slow growing, and they rarely metastasize. It is difficult to differentiate between a benign lesion (such as an osteochondroma) and a chondrosarcoma by either histology or radiology. However, reliable predictors for malignancy include size exceeding 5 cm and location in the axial skeleton.20
Bone tumors.Osteosarcomas are the most common malignant bone tumors in children and adolescents, with 400 to 560 US patients in this age-group diagnosed each year.14-16 Osteosarcomas are uncommon in children younger than 10; their incidence peaks during the early teenage years (median peak age, 16), then declines rapidly among older patients. They are more common in males than females.15
Osteosarcomas commonly develop during periods of rapid bone turnover, such as the adolescent growth spurt. Common sites include the distal femur, proximal humerus, and proximal tibia,15,16 particularly near the knee.13 Usually, osteosarcomas present with nonspecific symptoms, including strain-related pain of several months’ duration, which may disrupt sleep.16 Laboratory findings in affected patients may include elevations in LDH, alkaline phosphatase, and/or ESR.15,23
Physical exam reveals a visible or palpable mass in the affected area, along with decreased joint motion; localized warmth or erythema may also be present. Late signs of osteosarcoma include weight loss, general malaise, and fever. First-line imaging for the patient with a suspected osteosarcoma is x-ray, which will show ill-defined borders, osteoblastic and/or osteolytic features, and an associated soft tissue mass. Advanced imaging, such as MRI, is warranted.16
Ewing sarcoma, the second most common bone tumor in children and adolescents, is an aggressive form of childhood cancer.14,18 Approximately 25% of all Ewing sarcomas arise in soft tissues rather than bones.18 They are more common in whites than in other ethnic groups and have a slight male predominance.13,18 The median age at diagnosis is 15.13 The most common presenting symptoms are tumor related, such as pain or a noticeable mass. While x-rays are usually ordered first, MRI is preferred.18
Soft tissue tumors and masses.Rhabdomyosarcomas are malignancies that account for more than half of the soft tissue sarcomas in children and adolescents. Less than one-fifth of cases occur in the extremities, and most occur in children younger than 10. These lesions have a slight male predominance and are more common in whites than in other patients.14,17,24
Approximately 6% of childhood soft tissue tumors are adipose tissue tumors, which may be benign (eg, lipomas) or malignant (eg, liposarcomas). Lipomas in children account for nearly 4% of all soft tissue tumors and can be classified as superficial (which are often diagnosed clinically) or deep (frequently requiring imaging).25
Lymphomaaccounts for 7% of cancers in US children and adolescents and more than 25% of newly diagnosed cancers in patients between 15 and 19, making it the most common malignancy in adolescents and the third most common in children.26,27 Non-Hodgkin lymphoma is the fourth leading type of malignancy in US adolescents.27 Rarely, lymphomas present with primary event soft tissue involvement.28
Myositis ossificans (MO) is a rare benign disorder involving formation of heterotrophic bone in skeletal muscles and soft tissues.29 Though possible in patients of any age, MO is most commonly seen in adolescents and young adults. Often the result of soft tissue injury (in which case it is referred to as myositis ossificans circumscripta or traumatic), MO develops in areas that are exposed to trauma, such as the anterior thighs or arms. Lesions can be diagnosed via plain x-ray or CT, although MRI and ultrasound can also be useful evaluation tools.17,29,30
Because MO circumscripta typically presents as a painful soft tissue mass, it can be mistaken for a soft tissue sarcoma or an osteosarcoma; radiologic evaluation is required to make the proper diagnosis. Less common forms of MO are myositis ossificans progressiva and myositis ossificans without a history of trauma.29
Ollier diseaseis a rare, nonfamilial disorder characterized by multiple enchondromas (or enchondromatoses), which are distributed asymmetrically with areas of dysplastic cartilage. Enchondromas are benign cartilage tumors that frequently affect long tubular bones along the metaphyses in proximity to the growth plate. The enchondromas result in significant growth abnormalities. About one in 1 million people are diagnosed yearly.5,19 (Similarly, Maffucci syndrome is represented by multiple enchondromas in association with hemangiomas.5)
Ollier disease typically manifests during childhood5 with bone swelling, local pain, and palpable bony masses, which are often associated with bone deformities.19 Patients generally present with an asymmetric shortening of one extremity and the appearance of palpable bony masses on their fingers or toes, which may or may not be associated with pathologic fractures.5,19 In 20% to 50% of patients with Ollier disease, enchondromas are at risk for malignant transformation into chondrosarcomas.5
Vascular malformations. Certain abnormalities of vascular development cause birthmarks and abnormalities of varying degree in underlying tissues.31 They are usually present at birth and grow proportionally to the child’s growth.25,31 However, they can also be seen in later childhood and adolescence.
Radiologic Investigation
Plain radiography of the affected area is the first-line radiologic study to be performed.13 While most osteochondromas can be diagnosed by plain x-ray, cross-sectional imaging via CT or MRI is recommended in lesions with certain characteristics, such as a broad stalk or location in the axial skeleton. Because MRI involves no radiation exposure, it is a particularly good diagnostic tool for children.32
Ultrasound is a good imaging method for evaluating for complications of osteochondromas, including bursa formation or vascular compromise.32
Treatment and Management
Although usually asymptomatic, osteochondroma can trigger some significant symptoms. Osteochondromas are at risk for fracture and can cause body deformities, mechanical joint problems, weakness of the affected limb, numbness, vascular compression, aneurysm, arterial thrombosis, venous thrombosis, pain, acute ischemia, and nerve compression. Clinical signs of malignant transformation include pain, swelling, and increased lesion size.2
Surgical excision is recommended but should be delayed until after the patient has reached skeletal maturity in order to decrease the risk for recurrence.33
Patient Education and Follow-up
In addition to explaining appropriate pain management (eg, NSAIDs), it is especially important for the pediatric NP or PA to encourage the patient with a solitary osteochondroma to follow up with the pediatric orthopedic surgeon. Reasons include the need to monitor growth of the lesion (which is likely to continue in a patient who has not yet reached skeletal maturity) and assess for associated functional or joint problems. Patients should also be advised to seek the specialist’s attention if such problems develop or if pain increases.
Generally, the pediatric clinician should be sufficiently informed to answer questions about this condition from the patient or family. Any follow-up laboratory work recommended by the specialist can also be performed by the pediatric NP or PA.
OUTCOME FOR THE CASE PATIENT
MRI without contrast, as recommended by the radiologist to rule out a bursa or trauma to the osteochondroma, was considered an important part of the follow-up plan. As the patient had not yet reached skeletal maturity, she was referred to a pediatric orthopedic surgeon for possible excision of the lesion, due to its size and the pain associated with running or other exertion.
CONCLUSION
Solitary osteochondromas are the most common benign bone tumors. Although they are generally asymptomatic, pain and other symptoms can arise as a result of irritation to the adjacent structures. In this case, the patient’s chief complaint was an irritating “bump” that she had had on her right leg for at least six months.
Generally, follow-up monitoring of the osteochondroma and orthopedic follow-up care are warranted, at least until the patient reaches skeletal maturity. At that point, surgical excision of the lesion is recommended.
REFERENCES
1. Florez B, Mönckeberg J, Castillo G, Beguiristain J. Solitary osteochondroma long-term follow-up. J Pediatr Orthop B. 2008;17:91-94.
2. Kitsoulis P, Galani V, Stefanaki K, et al. Osteochondromas: review of the clinical, radiological and pathological features. In Vivo. 2008;22:633-646.
3. Ramos-Pascua LR, Sánchez-Herráez S, Alonso-Barrio JA, Alonso-León A. Solitary proximal end of femur osteochondroma: an indication and result of the en bloc resection without hip luxation [in Spanish]. Rev Esp Cir Ortop Traumatol. 2012;56:24-31.
4. Payne WT, Merrell G. Benign bony and soft tissue tumors of the hand. J Hand Surg. 2010;35:1901-1910.
5. Pannier S, Legeai-Mallet L. Hereditary multiple exostoses and enchondromatosis. Best Pract Res Clin Rheumatol. 2008;22:45-54.
6. Bovée JV. Multiple osteochondromas. Orphanet J Rare Dis. 2008;3(3).
7. Staals EL, Bacchini P, Mercuri M, Bertoni F. Dedifferentiated chondrosarcomas arising in preexisting osteochondromas. J Bone Joint Surg Am. 2007;89:987-993.
8. Singh R, Jain M, Siwach R, et al. Large para-articular osteochondroma of the knee joint: a case report. Acta Orthop Traumatol Turc. 2012;46:139-143.
9. Lee JY, Lee S, Joo KB, et al. Intraarticular osteochondroma of shoulder: a case report. Clin Imaging. 2013;37:379-381.
10. Kim Y-C, Ahn JH, Lee JW. Osteochondroma of the distal tibia complicated by a tibialis posterior tendon tear. J Foot Ankle Surg. 2012;51: 660-663.
11. Allagui M, Amara K, Aloui I, et al. Historical giant near-circumferential osteochondroma of the proximal humerus. J Shoulder Elbow Surg. 2010;19:e12-e15.
12. Li M, Luettringhaus T, Walker KR, Cole PA. Operative treatment of femoral neck osteochondroma through a digastric approach in a pediatric patient: a case report and review of the literature. J Pediatr Orthop B. 2012;21:230-234.
13. Hogendoorn PC, Athanasou N, Bielack S, et al; ESMO/EUROBONET Working Group. Bone sarcomas: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2010;21 suppl 5:v204-v213.
14. Arndt CAS, Rose PS, Folpe AL, Laack NN. Common musculoskeletal tumors of childhood and adolescence. Mayo Clin Proc. 2012;87:475-487.
15. Ta HT, Dass CR, Choong PF, Dunstan DE. Osteosarcoma treatment: state of the art. Cancer Metastasis Rev. 2009;28:247-263.
16. Messerschmitt PJ, Garcia RM, Abdul-Karim FW, et al. Osteosarcoma. J Am Acad Orthop Surg. 2009;17:515-527.
17. Laffan EE, Ngan B-Y, Navarro OM. Pediatric soft-tissue tumors and pseudotumors: MR imaging features with pathologic correlation: Part 2. Tumors of fibroblastic/myofibroblastic, so-called fibrohistiocytic, muscular, lymphomatous, neurogenic, hair matrix, and uncertain origin. Radiographics. 2009;29:e36.
18. Balamuth NJ, Womer RB. Ewing’s sarcoma. Lancet Oncol. 2010;11(2):184.
19. D’Angelo L, Massimi L, Narducci A, Di Rocco C. Ollier disease. Childs Nerv Syst. 2009;25:647-653.
20. Gelderblom H, Hogendoorn PC, Dijkstra SD, et al. The clinical approach towards chondrosarcoma. Oncologist. 2008;13:320-329.
21. Nosratzehi T, Pakfetrat A. Chondrosarcoma. Zahedan J Res Med Sci. 2013;15:64-64.
22. Prado FO, Nishimoto IN, Perez DE, et al. Head and neck chondrosarcoma: analysis of 16 cases. Br J Oral Maxillofacial Surg. 2009;47:555-557.
23. Kim HJ, Chalmers PN, Morris CD. Pediatric osteogenic sarcoma. Curr Opin Pediatr. 2010;22:61-66.
24. Sultan I, Qaddoumi I, Yaser S, et al. Comparing adult and pediatric rhabdomyosarcoma in the surveillance, epidemiology and end results program, 1973 to 2005: an analysis of 2,600 patients. J Clin Oncol. 2009;27:3391-3397.
25. Navarro OM, Laffan EE, Ngan B-Y. Pediatric soft-tissue tumors and pseudo-tumors: MR imaging features with pathologic correlation: Part 1. Imaging approach, pseudotumors, vascular lesions, and adipocytic tumors. Radiographics. 2009;29:887-906.
26. Gross TG, Termuhlen AM. Pediatric non-Hodgkin lymphoma. Curr Hematol Malig Rep. 2008;3:167-173.
27. Hochberg J, Waxman IM, Kelly KM, et al. Adolescent non-Hodgkin lymphoma and Hodgkin lymphoma: state of the science. Br J Haematol. 2009;144:24-40.
28. Derenzini E, Casadei B, Pellegrini C, et al. Non-Hodgkin lymphomas presenting as soft tissue masses: A single center experience and meta-analysis of the published series. Clin Lymphoma Myeloma Leuk. 2012 Dec 12. [Epub ahead of print]
29. Micheli A, Trapani S, Brizzi I, et al. Myositis ossificans circumscripta: a paediatric case and review of the literature. Eur J Pediatr. 2009;168:523-529.
30. McKenzie G, Raby N, Ritchie D. Non-neoplastic soft-tissue masses. Br J Radiol. 2009;82:775-785.
31. Buckmiller LM, Richter GT, Suen JY. Diagnosis and management of hemangiomas and vascular malformations of the head and neck. Oral Dis. 2010;16:405-418.
32. Khanna G, Bennett DL. Pediatric bone lesions: beyond the plain radiographic evaluation. Semin Roentgenol. 2012;47:90-99.
33. Rijal L, Nepal P, Baral S, et al. Solitary diaphyseal exostosis of femur, how common is it? Eur J Orthop Surg Traumatol. 2011;21:363-365.
A girl, age 13 years, 4 months, presented to her primary care provider’s office for a well visit. Among her concerns, she mentioned a “bump” she had had on her right leg “for the past six months, maybe longer.” The area felt irritated when touched or when the patient “ran too much.” She had seen no change in the bump since she first noticed it. The patient knew of no trauma or other preceding factors. She denied any fever or warmth, redness, or ecchymosis to the area.
Medical history was unremarkable except for familial short stature and myopia. The patient was the fifth of eight children born to nonconsanguinous parents. She denied any surgical history or hospitalizations and was premenarcheal. She was up to date on all age-appropriate vaccines, with her meningococcal vaccine administered at that visit.
The patient’s blood pressure was 99/58 mm Hg with an apical pulse rate of 82 beats/min. Her growth parameters were following her curve. Her height was 55” (0.3 percentile); weight, 81 lb (7.5 percentile); and BMI, 18.8 (48.6 percentile).
The physical exam was normal with the exception of the musculoskeletal exam. Examination of the lower extremities revealed a palpable, 4 cm x 5 cm lesion at the right distal medial thigh just proximal to the knee. The lesion could not be visualized but on palpation was tender and firm. There was some question as to whether the lesion itself or inflamed soft tissue overlying the lesion was mobile. No overlying warmth, induration, erythema, or ecchymosis was noted.
Passive and active range of motion was intact at the hip and knee. No lesions to the upper extremities were evident, and no scoliosis was seen.
Blood work was done to rule out certain diagnoses. Results from a complete blood count with differential, lactate dehydrogenase (LDH), parathyroid hormone, lipid profiles, thyroid function, and a comprehensive metabolic profile were unremarkable. A low level of vitamin D 25-OH was detected: 21.7 ng/mL (normal range, 32 to 100 ng/mL).
Distal femur x-rays with posteroanterior, lateral, and oblique views were ordered. The imaging revealed a 3 cm x 3 cm lesion projecting from the “distal, somewhat medial” femur, which was diagnosed as a benign femoral osteochondroma. Significant inflammation to the surrounding soft-tissue structures was observed. A questionable old fracture of the osteochondroma was noted. The remaining bony structures and joints appeared normal.
An ultrasound of the lesion was also ordered to investigate soft-tissue swelling. This revealed a hypoechoic collar around the distal end of the osteochondroma, which could represent a fluid collection, hematoma from trauma, or bursitis. The soft tissues were deemed normal.
Because of the extent of inflammation, the radiologist recommended MRI without contrast to rule out bursitis or trauma to the osteochondroma.
DISCUSSION
Osteochondromas, which may be present in up to 3% of the general population, are the most common benign bone tumors.1-3 An osteochondroma is a cartilage-capped bony projection that arises on the external surface of the bone; it contains a marrow cavity that is continuous with the underlying bone.2,4 The majority of osteochondromas are solitary, accounting for perhaps 85% to 90% of all such lesions, and they are typically nonhereditary; the remaining 10% to 15% of osteochondromas are hereditary multiple osteochondromas or exostoses1,2 (see “Definition of Multiple Exostoses Syndrome”2,5,6,7).
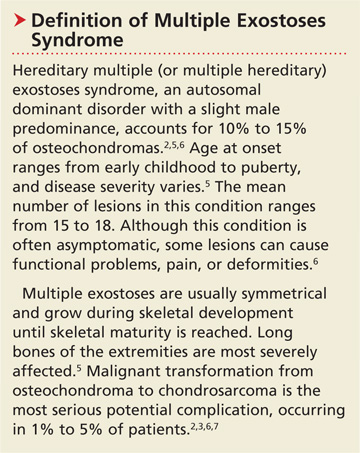
Most lesions are painless and slow growing, and they usually occur in children and adolescents.2 They typically stop growing at skeletal maturity with the closure of the growth plates.3,8,9 There is no predilection for males or females in single lesions.2
Solitary osteochondromas typically appear in the lower extremities and at long tubular bone metaphyses,1-3,10 especially on the femur, humerus, tibia, spine, and hip. Any part of the skeleton can be affected, but 30% of lesions occur on the femur and 40% at either the proximal metaphysis of the tibia or the distal metaphysis of the femur.2,11
Most osteochondromas are asymptomatic and are found incidentally.1,3 However, some patients present with local pain as a result of irritation to adjacent structures, limitation of joint motion, growth disturbance, or fracture of the pedicle.3,4,9,11,12 A very small proportion of patients (no more than 1%) with solitary osteochondromas experience malignant transformation.2,3,6,7 No particular blood work is recommended for patients with solitary osteochondromas.2
Differential Diagnosis
In addition to osteochondromas, several other lesions should be considered in the patient with musculoskeletal lesions (see Table 15,6,13-19).
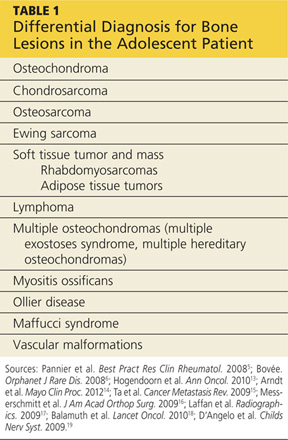
Cartilaginous tumors. Chondrosarcomas are malignant cartilaginous tumors.20-22 They commonly affect long bones, including the humerus and femur, and some flat bones, such as the pelvic bones.13,22 They are most commonly seen in adults, and have no predisposition by gender.13
Chondrosarcomas can be primary (ie, arising de novo) or secondary (developing on preexisting benign cartilaginous neoplasms, including osteochondromas). The majority of chondrosarcomas are slow growing, and they rarely metastasize. It is difficult to differentiate between a benign lesion (such as an osteochondroma) and a chondrosarcoma by either histology or radiology. However, reliable predictors for malignancy include size exceeding 5 cm and location in the axial skeleton.20
Bone tumors.Osteosarcomas are the most common malignant bone tumors in children and adolescents, with 400 to 560 US patients in this age-group diagnosed each year.14-16 Osteosarcomas are uncommon in children younger than 10; their incidence peaks during the early teenage years (median peak age, 16), then declines rapidly among older patients. They are more common in males than females.15
Osteosarcomas commonly develop during periods of rapid bone turnover, such as the adolescent growth spurt. Common sites include the distal femur, proximal humerus, and proximal tibia,15,16 particularly near the knee.13 Usually, osteosarcomas present with nonspecific symptoms, including strain-related pain of several months’ duration, which may disrupt sleep.16 Laboratory findings in affected patients may include elevations in LDH, alkaline phosphatase, and/or ESR.15,23
Physical exam reveals a visible or palpable mass in the affected area, along with decreased joint motion; localized warmth or erythema may also be present. Late signs of osteosarcoma include weight loss, general malaise, and fever. First-line imaging for the patient with a suspected osteosarcoma is x-ray, which will show ill-defined borders, osteoblastic and/or osteolytic features, and an associated soft tissue mass. Advanced imaging, such as MRI, is warranted.16
Ewing sarcoma, the second most common bone tumor in children and adolescents, is an aggressive form of childhood cancer.14,18 Approximately 25% of all Ewing sarcomas arise in soft tissues rather than bones.18 They are more common in whites than in other ethnic groups and have a slight male predominance.13,18 The median age at diagnosis is 15.13 The most common presenting symptoms are tumor related, such as pain or a noticeable mass. While x-rays are usually ordered first, MRI is preferred.18
Soft tissue tumors and masses.Rhabdomyosarcomas are malignancies that account for more than half of the soft tissue sarcomas in children and adolescents. Less than one-fifth of cases occur in the extremities, and most occur in children younger than 10. These lesions have a slight male predominance and are more common in whites than in other patients.14,17,24
Approximately 6% of childhood soft tissue tumors are adipose tissue tumors, which may be benign (eg, lipomas) or malignant (eg, liposarcomas). Lipomas in children account for nearly 4% of all soft tissue tumors and can be classified as superficial (which are often diagnosed clinically) or deep (frequently requiring imaging).25
Lymphomaaccounts for 7% of cancers in US children and adolescents and more than 25% of newly diagnosed cancers in patients between 15 and 19, making it the most common malignancy in adolescents and the third most common in children.26,27 Non-Hodgkin lymphoma is the fourth leading type of malignancy in US adolescents.27 Rarely, lymphomas present with primary event soft tissue involvement.28
Myositis ossificans (MO) is a rare benign disorder involving formation of heterotrophic bone in skeletal muscles and soft tissues.29 Though possible in patients of any age, MO is most commonly seen in adolescents and young adults. Often the result of soft tissue injury (in which case it is referred to as myositis ossificans circumscripta or traumatic), MO develops in areas that are exposed to trauma, such as the anterior thighs or arms. Lesions can be diagnosed via plain x-ray or CT, although MRI and ultrasound can also be useful evaluation tools.17,29,30
Because MO circumscripta typically presents as a painful soft tissue mass, it can be mistaken for a soft tissue sarcoma or an osteosarcoma; radiologic evaluation is required to make the proper diagnosis. Less common forms of MO are myositis ossificans progressiva and myositis ossificans without a history of trauma.29
Ollier diseaseis a rare, nonfamilial disorder characterized by multiple enchondromas (or enchondromatoses), which are distributed asymmetrically with areas of dysplastic cartilage. Enchondromas are benign cartilage tumors that frequently affect long tubular bones along the metaphyses in proximity to the growth plate. The enchondromas result in significant growth abnormalities. About one in 1 million people are diagnosed yearly.5,19 (Similarly, Maffucci syndrome is represented by multiple enchondromas in association with hemangiomas.5)
Ollier disease typically manifests during childhood5 with bone swelling, local pain, and palpable bony masses, which are often associated with bone deformities.19 Patients generally present with an asymmetric shortening of one extremity and the appearance of palpable bony masses on their fingers or toes, which may or may not be associated with pathologic fractures.5,19 In 20% to 50% of patients with Ollier disease, enchondromas are at risk for malignant transformation into chondrosarcomas.5
Vascular malformations. Certain abnormalities of vascular development cause birthmarks and abnormalities of varying degree in underlying tissues.31 They are usually present at birth and grow proportionally to the child’s growth.25,31 However, they can also be seen in later childhood and adolescence.
Radiologic Investigation
Plain radiography of the affected area is the first-line radiologic study to be performed.13 While most osteochondromas can be diagnosed by plain x-ray, cross-sectional imaging via CT or MRI is recommended in lesions with certain characteristics, such as a broad stalk or location in the axial skeleton. Because MRI involves no radiation exposure, it is a particularly good diagnostic tool for children.32
Ultrasound is a good imaging method for evaluating for complications of osteochondromas, including bursa formation or vascular compromise.32
Treatment and Management
Although usually asymptomatic, osteochondroma can trigger some significant symptoms. Osteochondromas are at risk for fracture and can cause body deformities, mechanical joint problems, weakness of the affected limb, numbness, vascular compression, aneurysm, arterial thrombosis, venous thrombosis, pain, acute ischemia, and nerve compression. Clinical signs of malignant transformation include pain, swelling, and increased lesion size.2
Surgical excision is recommended but should be delayed until after the patient has reached skeletal maturity in order to decrease the risk for recurrence.33
Patient Education and Follow-up
In addition to explaining appropriate pain management (eg, NSAIDs), it is especially important for the pediatric NP or PA to encourage the patient with a solitary osteochondroma to follow up with the pediatric orthopedic surgeon. Reasons include the need to monitor growth of the lesion (which is likely to continue in a patient who has not yet reached skeletal maturity) and assess for associated functional or joint problems. Patients should also be advised to seek the specialist’s attention if such problems develop or if pain increases.
Generally, the pediatric clinician should be sufficiently informed to answer questions about this condition from the patient or family. Any follow-up laboratory work recommended by the specialist can also be performed by the pediatric NP or PA.
OUTCOME FOR THE CASE PATIENT
MRI without contrast, as recommended by the radiologist to rule out a bursa or trauma to the osteochondroma, was considered an important part of the follow-up plan. As the patient had not yet reached skeletal maturity, she was referred to a pediatric orthopedic surgeon for possible excision of the lesion, due to its size and the pain associated with running or other exertion.
CONCLUSION
Solitary osteochondromas are the most common benign bone tumors. Although they are generally asymptomatic, pain and other symptoms can arise as a result of irritation to the adjacent structures. In this case, the patient’s chief complaint was an irritating “bump” that she had had on her right leg for at least six months.
Generally, follow-up monitoring of the osteochondroma and orthopedic follow-up care are warranted, at least until the patient reaches skeletal maturity. At that point, surgical excision of the lesion is recommended.
REFERENCES
1. Florez B, Mönckeberg J, Castillo G, Beguiristain J. Solitary osteochondroma long-term follow-up. J Pediatr Orthop B. 2008;17:91-94.
2. Kitsoulis P, Galani V, Stefanaki K, et al. Osteochondromas: review of the clinical, radiological and pathological features. In Vivo. 2008;22:633-646.
3. Ramos-Pascua LR, Sánchez-Herráez S, Alonso-Barrio JA, Alonso-León A. Solitary proximal end of femur osteochondroma: an indication and result of the en bloc resection without hip luxation [in Spanish]. Rev Esp Cir Ortop Traumatol. 2012;56:24-31.
4. Payne WT, Merrell G. Benign bony and soft tissue tumors of the hand. J Hand Surg. 2010;35:1901-1910.
5. Pannier S, Legeai-Mallet L. Hereditary multiple exostoses and enchondromatosis. Best Pract Res Clin Rheumatol. 2008;22:45-54.
6. Bovée JV. Multiple osteochondromas. Orphanet J Rare Dis. 2008;3(3).
7. Staals EL, Bacchini P, Mercuri M, Bertoni F. Dedifferentiated chondrosarcomas arising in preexisting osteochondromas. J Bone Joint Surg Am. 2007;89:987-993.
8. Singh R, Jain M, Siwach R, et al. Large para-articular osteochondroma of the knee joint: a case report. Acta Orthop Traumatol Turc. 2012;46:139-143.
9. Lee JY, Lee S, Joo KB, et al. Intraarticular osteochondroma of shoulder: a case report. Clin Imaging. 2013;37:379-381.
10. Kim Y-C, Ahn JH, Lee JW. Osteochondroma of the distal tibia complicated by a tibialis posterior tendon tear. J Foot Ankle Surg. 2012;51: 660-663.
11. Allagui M, Amara K, Aloui I, et al. Historical giant near-circumferential osteochondroma of the proximal humerus. J Shoulder Elbow Surg. 2010;19:e12-e15.
12. Li M, Luettringhaus T, Walker KR, Cole PA. Operative treatment of femoral neck osteochondroma through a digastric approach in a pediatric patient: a case report and review of the literature. J Pediatr Orthop B. 2012;21:230-234.
13. Hogendoorn PC, Athanasou N, Bielack S, et al; ESMO/EUROBONET Working Group. Bone sarcomas: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2010;21 suppl 5:v204-v213.
14. Arndt CAS, Rose PS, Folpe AL, Laack NN. Common musculoskeletal tumors of childhood and adolescence. Mayo Clin Proc. 2012;87:475-487.
15. Ta HT, Dass CR, Choong PF, Dunstan DE. Osteosarcoma treatment: state of the art. Cancer Metastasis Rev. 2009;28:247-263.
16. Messerschmitt PJ, Garcia RM, Abdul-Karim FW, et al. Osteosarcoma. J Am Acad Orthop Surg. 2009;17:515-527.
17. Laffan EE, Ngan B-Y, Navarro OM. Pediatric soft-tissue tumors and pseudotumors: MR imaging features with pathologic correlation: Part 2. Tumors of fibroblastic/myofibroblastic, so-called fibrohistiocytic, muscular, lymphomatous, neurogenic, hair matrix, and uncertain origin. Radiographics. 2009;29:e36.
18. Balamuth NJ, Womer RB. Ewing’s sarcoma. Lancet Oncol. 2010;11(2):184.
19. D’Angelo L, Massimi L, Narducci A, Di Rocco C. Ollier disease. Childs Nerv Syst. 2009;25:647-653.
20. Gelderblom H, Hogendoorn PC, Dijkstra SD, et al. The clinical approach towards chondrosarcoma. Oncologist. 2008;13:320-329.
21. Nosratzehi T, Pakfetrat A. Chondrosarcoma. Zahedan J Res Med Sci. 2013;15:64-64.
22. Prado FO, Nishimoto IN, Perez DE, et al. Head and neck chondrosarcoma: analysis of 16 cases. Br J Oral Maxillofacial Surg. 2009;47:555-557.
23. Kim HJ, Chalmers PN, Morris CD. Pediatric osteogenic sarcoma. Curr Opin Pediatr. 2010;22:61-66.
24. Sultan I, Qaddoumi I, Yaser S, et al. Comparing adult and pediatric rhabdomyosarcoma in the surveillance, epidemiology and end results program, 1973 to 2005: an analysis of 2,600 patients. J Clin Oncol. 2009;27:3391-3397.
25. Navarro OM, Laffan EE, Ngan B-Y. Pediatric soft-tissue tumors and pseudo-tumors: MR imaging features with pathologic correlation: Part 1. Imaging approach, pseudotumors, vascular lesions, and adipocytic tumors. Radiographics. 2009;29:887-906.
26. Gross TG, Termuhlen AM. Pediatric non-Hodgkin lymphoma. Curr Hematol Malig Rep. 2008;3:167-173.
27. Hochberg J, Waxman IM, Kelly KM, et al. Adolescent non-Hodgkin lymphoma and Hodgkin lymphoma: state of the science. Br J Haematol. 2009;144:24-40.
28. Derenzini E, Casadei B, Pellegrini C, et al. Non-Hodgkin lymphomas presenting as soft tissue masses: A single center experience and meta-analysis of the published series. Clin Lymphoma Myeloma Leuk. 2012 Dec 12. [Epub ahead of print]
29. Micheli A, Trapani S, Brizzi I, et al. Myositis ossificans circumscripta: a paediatric case and review of the literature. Eur J Pediatr. 2009;168:523-529.
30. McKenzie G, Raby N, Ritchie D. Non-neoplastic soft-tissue masses. Br J Radiol. 2009;82:775-785.
31. Buckmiller LM, Richter GT, Suen JY. Diagnosis and management of hemangiomas and vascular malformations of the head and neck. Oral Dis. 2010;16:405-418.
32. Khanna G, Bennett DL. Pediatric bone lesions: beyond the plain radiographic evaluation. Semin Roentgenol. 2012;47:90-99.
33. Rijal L, Nepal P, Baral S, et al. Solitary diaphyseal exostosis of femur, how common is it? Eur J Orthop Surg Traumatol. 2011;21:363-365.
Erratum (Cosmet Dermatol. May 2013:18-26)
Our success with a single-visit smoking cessation intervention
Tobacco use is the leading preventable cause of death and disease in the United States,1 but how best to help patients quit? US Public Health Service guidelines recommend a 2-tiered approach consisting of counseling and pharmaceutical treatment.2 Because primary care physicians are busy caring for other patients, however, and pharmacists in our state can prescribe medication under collaborative practice agreements with physicians, we piloted a single-visit smoking cessation group intervention conducted by a pharmacist (NP) and health coach (HW).
Patients were recruited from 2 primary care practices to participate in a 2-hour group visit that included both behavioral and pharmacologic interventions. Follow-up phone calls and in-person visits with the health coach were made available, but were not part of the structured curriculum.
We used motivational interviewing to assist patients in developing individualized quit plans and offered small rewards for stopping, such as a note pad and 6-month certificate. Patients did not pay for the group visit, but were required to pay for pharmacotherapy (health insurance or out of pocket).
Between September 2011 and May 2012, a total of 35 patients attended one of 7 smoking cessation group visits. Twenty-seven (77%) participants opted for medication or nicotine replacement therapy and 23 (65.7%) used the health coach services.
As of June 2012—with participants ranging from one month to 9 months’ follow-up—23% remained tobacco free. This compares with documented one-year quit rates of 3% to 5% (unassisted), 7% to 16% (with behavioral intervention), and up to 24% with pharmacologic treatment and ongoing behavioral support.3 Similar smoking cessation rates have been described with multiple-session pharmacist-led group visits.4 This pilot program demonstrated that a single group intervention can be performed in a primary care setting with a pharmacist and health coach, freeing physicians to care for other patients.
Challenges include variable reimbursement from insurers for pharmacist-led tobacco cessation group visits and disparate pharmacy policies—pharmacists are not allowed to prescribe medication in every state. Nonetheless, this pilot, funded by Fairview Physician Associates and the University of Minnesota Academic Health Center, represents a promising means of delivering effective preventive services by leveraging team members in a busy primary care clinic.
Nicole Paterson, PharmD, BCPS
Holly Wiest, MA
Lynne Fiscus, MD, MPH
Minneapolis, Minn
1. Centers for Disease Control and Prevention. Annual Smoking-Attributable Mortality, Years of Potential Life Lost, and Productivity Losses—United States, 2000–2004. MMWR. 2008;57:1226–1228.
2. Fiore MC, Jaen CR, Baker TB, et al. Treating tobacco use and dependence: 2008 update—clinical practice guideline. Available at:http://bphc.hrsa.gov/buckets/treatingtobacco.pdf. Accessed July 21, 2012.
3. Laniado-Laborin R. Smoking cessation intervention: an evidence-based approach. Postgrad Med. 2009;122:74–82.
4. Dent LA, Harris KJ, Noonan CW. Randomized trial assessing the effectiveness of a pharmacist-delivered program for smoking cessation. Ann Pharmacother. 2009;43:194–201.
Tobacco use is the leading preventable cause of death and disease in the United States,1 but how best to help patients quit? US Public Health Service guidelines recommend a 2-tiered approach consisting of counseling and pharmaceutical treatment.2 Because primary care physicians are busy caring for other patients, however, and pharmacists in our state can prescribe medication under collaborative practice agreements with physicians, we piloted a single-visit smoking cessation group intervention conducted by a pharmacist (NP) and health coach (HW).
Patients were recruited from 2 primary care practices to participate in a 2-hour group visit that included both behavioral and pharmacologic interventions. Follow-up phone calls and in-person visits with the health coach were made available, but were not part of the structured curriculum.
We used motivational interviewing to assist patients in developing individualized quit plans and offered small rewards for stopping, such as a note pad and 6-month certificate. Patients did not pay for the group visit, but were required to pay for pharmacotherapy (health insurance or out of pocket).
Between September 2011 and May 2012, a total of 35 patients attended one of 7 smoking cessation group visits. Twenty-seven (77%) participants opted for medication or nicotine replacement therapy and 23 (65.7%) used the health coach services.
As of June 2012—with participants ranging from one month to 9 months’ follow-up—23% remained tobacco free. This compares with documented one-year quit rates of 3% to 5% (unassisted), 7% to 16% (with behavioral intervention), and up to 24% with pharmacologic treatment and ongoing behavioral support.3 Similar smoking cessation rates have been described with multiple-session pharmacist-led group visits.4 This pilot program demonstrated that a single group intervention can be performed in a primary care setting with a pharmacist and health coach, freeing physicians to care for other patients.
Challenges include variable reimbursement from insurers for pharmacist-led tobacco cessation group visits and disparate pharmacy policies—pharmacists are not allowed to prescribe medication in every state. Nonetheless, this pilot, funded by Fairview Physician Associates and the University of Minnesota Academic Health Center, represents a promising means of delivering effective preventive services by leveraging team members in a busy primary care clinic.
Nicole Paterson, PharmD, BCPS
Holly Wiest, MA
Lynne Fiscus, MD, MPH
Minneapolis, Minn
Tobacco use is the leading preventable cause of death and disease in the United States,1 but how best to help patients quit? US Public Health Service guidelines recommend a 2-tiered approach consisting of counseling and pharmaceutical treatment.2 Because primary care physicians are busy caring for other patients, however, and pharmacists in our state can prescribe medication under collaborative practice agreements with physicians, we piloted a single-visit smoking cessation group intervention conducted by a pharmacist (NP) and health coach (HW).
Patients were recruited from 2 primary care practices to participate in a 2-hour group visit that included both behavioral and pharmacologic interventions. Follow-up phone calls and in-person visits with the health coach were made available, but were not part of the structured curriculum.
We used motivational interviewing to assist patients in developing individualized quit plans and offered small rewards for stopping, such as a note pad and 6-month certificate. Patients did not pay for the group visit, but were required to pay for pharmacotherapy (health insurance or out of pocket).
Between September 2011 and May 2012, a total of 35 patients attended one of 7 smoking cessation group visits. Twenty-seven (77%) participants opted for medication or nicotine replacement therapy and 23 (65.7%) used the health coach services.
As of June 2012—with participants ranging from one month to 9 months’ follow-up—23% remained tobacco free. This compares with documented one-year quit rates of 3% to 5% (unassisted), 7% to 16% (with behavioral intervention), and up to 24% with pharmacologic treatment and ongoing behavioral support.3 Similar smoking cessation rates have been described with multiple-session pharmacist-led group visits.4 This pilot program demonstrated that a single group intervention can be performed in a primary care setting with a pharmacist and health coach, freeing physicians to care for other patients.
Challenges include variable reimbursement from insurers for pharmacist-led tobacco cessation group visits and disparate pharmacy policies—pharmacists are not allowed to prescribe medication in every state. Nonetheless, this pilot, funded by Fairview Physician Associates and the University of Minnesota Academic Health Center, represents a promising means of delivering effective preventive services by leveraging team members in a busy primary care clinic.
Nicole Paterson, PharmD, BCPS
Holly Wiest, MA
Lynne Fiscus, MD, MPH
Minneapolis, Minn
1. Centers for Disease Control and Prevention. Annual Smoking-Attributable Mortality, Years of Potential Life Lost, and Productivity Losses—United States, 2000–2004. MMWR. 2008;57:1226–1228.
2. Fiore MC, Jaen CR, Baker TB, et al. Treating tobacco use and dependence: 2008 update—clinical practice guideline. Available at:http://bphc.hrsa.gov/buckets/treatingtobacco.pdf. Accessed July 21, 2012.
3. Laniado-Laborin R. Smoking cessation intervention: an evidence-based approach. Postgrad Med. 2009;122:74–82.
4. Dent LA, Harris KJ, Noonan CW. Randomized trial assessing the effectiveness of a pharmacist-delivered program for smoking cessation. Ann Pharmacother. 2009;43:194–201.
1. Centers for Disease Control and Prevention. Annual Smoking-Attributable Mortality, Years of Potential Life Lost, and Productivity Losses—United States, 2000–2004. MMWR. 2008;57:1226–1228.
2. Fiore MC, Jaen CR, Baker TB, et al. Treating tobacco use and dependence: 2008 update—clinical practice guideline. Available at:http://bphc.hrsa.gov/buckets/treatingtobacco.pdf. Accessed July 21, 2012.
3. Laniado-Laborin R. Smoking cessation intervention: an evidence-based approach. Postgrad Med. 2009;122:74–82.
4. Dent LA, Harris KJ, Noonan CW. Randomized trial assessing the effectiveness of a pharmacist-delivered program for smoking cessation. Ann Pharmacother. 2009;43:194–201.
Should have used other dystocia maneuvers first
gb
AN OBGYN ENCOUNTERED SHOULDER DYSTOCIA. He used fundal pressure and downward lateral traction to free the baby’s shoulder. The child has a brachial plexus injury of the right shoulder, including nerve avulsion, a fractured clavicle, and permanent disfigurement. She underwent surgery; physical and occupational therapy will continue.
PARENTS' CLAIM The standard sequence of maneuvers should have been attempted before fundal pressure and lateral traction were used—the baby was sufficiently oxygenated to allow time for these maneuvers. Excessive lateral traction caused the injury.
DEFENDANTS' DEFENSE The injuries occurred in utero before or while the fetus progressed down the birth canal, and were due to the maternal forces of labor.
VERDICT A $3,070,000 Michigan verdict was returned against the hospital, ObGyn, and ObGyn group.
WHAT IS THE STANDARD SEQUENCE OF MANEUVERS FOR SHOULDER DYSTOCIA?
Read Dr. Robert L. Barbieri’s May Editorial, You are the second responder to a shoulder dystocia emergency. What do you do first? and Dr. Ronald T. Burkman’s March Stop/Start article, Stop all activities that may lead to further shoulder impaction when you suspect possible shoulder dystocia Meconium aspiration leads to brain injury
LATE IN HER PREGNANCY, a woman went to the emergency department (ED) with hypertension; she was discharged the same day. She saw her ObGyns, Dr. A and Dr. B, three times in the next 2 weeks. A day after her last visit, she returned to the ED in active labor. Dr. B assumed her care. Fetal monitoring indicated a nonreassuring heart rate with decelerations. Dr. B administered oxytocin and labor continued.
The baby was born by cesarean delivery after 25 minutes of fetal bradycardia. She was covered in meconium, with a low heart rate and irregular, labored respirations. The baby was transferred to another hospital, where she was treated for pulmonary hypertension, meconium aspiration, and seizures. The child is totally disabled, and will require constant care for life.
PARENTS' CLAIM The mother’s hypertension was not properly treated. Dr. B and the nurse waited too long to perform a cesarean delivery.
DEFENDANTS' DEFENSE Proper prenatal care was provided. There was no reason for additional testing; fetal heart tones at the mother’s last office visit were reactive. There were no clinical signs of a hematoma or cord varix during office visits. An unpredictable, unpreventable umbilical cord hematoma caused ischemia and hypoxia, and the subsequent brain injury. Meconium had been in the amniotic fluid for at least 10 hours due to the ischemic/hypoxic episode. The hematoma formed between her last office visit and when the mother came to the hospital the next day.
VERDICT Settlements were reached with Dr. A and the hospital. An Arkansas defense verdict was returned for Dr. B and the nurse.
14 months' recovery after mass removed
A GYNECOLOGIC ONCOLOGIST operated on a woman in her 50s to remove a large, noncancerous pelvic mass. The patient, discharged on postoperative day 2, was readmitted the next day with a fever (temperature, 103ºF), nausea, vomiting, and abdominal pain. Four days later, the oncologist repaired a perforated bowel and created an ileostomy. Other procedures were needed to drain abscesses and repair fistulas, and resect a large portion of colon due to continuing infection. Treatment lasted 14 months.
PATIENT'S CLAIM The gynecologic oncologist was negligent in failing to timely diagnose and treat the bowel perforation. Earlier repair would have curtailed development of the abscesses and fistulae.
PHYSICIAN'S DEFENSE Any complications the patient experienced were unrelated to any delay in treatment.
VERDICT A $612,237 Michigan verdict was returned.
Colon perforated during abdominal access
WHEN A MORBIDLY OBESE 37-YEAR-OLD WOMAN reported chronic pelvic pain, her gynecologist suspected endometriosis. Conservative treatment failed and the gynecologist offered laparoscopic hysterectomy.
After abdominal insufflation was unsuccessfully attempted twice using a Veress needle, the gynecologist entered the abdomen with a Visiport optical trocar, and continued the procedure. The gynecologist inspected the abdomen before closing but found no injuries.
The patient did not do well after surgery. CT scan detected a bowel perforation on postoperative day 6. During exploratory laparotomy, a through-and-through “bayonet” colon perforation was repaired. Because of the extensive infection, the patient’s surgical wound was left open and several “washouts” were performed; the wound was closed several weeks later. The patient also underwent two adhesiolysis procedures.
PATIENT'S CLAIM Access to the abdomen was not properly performed and caused colon perforation. The injury should have been found and treated earlier.
PHYSICIAN'S DEFENSE The case was settled before trial.
VERDICT A $750,000 Virginia settlement was reached.
READ How to avoid intestinal and urinary tract injuries during gynecologic laparoscopy, by Michael Baggish, MD (Surgical Techniques, October 2012) What caused this C. diff infection after hysterectomy?
AFTER A HYSTERECTOMY, a 42-year-old woman developed a persistent fever and increased white blood cell count. The gynecologist prescribed ciprofloxacin for a urinary tract infection, and discharged the patient from the hospital on postoperative day 4. She returned to the gynecologist’s office with severe abdominal pain and vomiting 4 days after discharge. The gynecologist prescribed an antacid and told her to continue taking ciprofloxacin.
The patient was taken to the ED by ambulance 3 days later. Testing revealed a Clostridium dificule (C. diff) infection. During emergency surgery, a large portion of her colon was resected, and a colostomy was performed. The colostomy was reversed 6 months later. The patient developed an incisional hernia and has abdominal scarring.
PATIENT'S CLAIM Prophylactic antibiotics should have been prescribed before surgery.
Two possible scenarios were presented: 1) A bowel injury occurred during surgery, and ciprofloxacin likely worsened the infection caused by the bowel injury; or 2) ciprofloxacin triggered the C. diff infection that caused leaking colon perforations and subsequent peritonitis.
The colon perforations could have been avoided if the gynecologist had diagnosed and treated the C. diff infection in a timely manner.
PHYSICIAN'S DEFENSE The patient’s symptoms did not suggest a C. diff infection; testing was not necessary. Ciprofloxacin might have allowed the proliferation of the C. diff infection, but the use of the drug was not negligent. The infection was not preventable and could not have been diagnosed earlier.
VERDICT A $776,000 New York verdict was returned.
Brain injury and cerebral palsy: When did this occur?
DURING LABOR AND DELIVERY, there were periods when the fetal heart-rate tracings were nonreassuring with variable decelerations and fetal tachycardia; some variables were severe. The child suffered anoxic encephalopathy that caused neurologic injury and cerebral palsy.
PARENTS' CLAIM The infant suffered numerous hypoxic incidents before cesarean delivery was performed. An earlier cesarean delivery could have prevented the injury.
PHYSICIAN'S DEFENSE The newborn had a normal blood cord gas level of 7.2 pH and Apgar scores of 9 and 10, at 1 and 5 minutes, respectively. Fetal heart-rate tracings did not show evidence of fetal hypoxia. The brain injury likely occurred prior to the onset of labor and was possibly related to a viral encephalopathy.
VERDICT A Virginia defense verdict was returned. These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
gb
AN OBGYN ENCOUNTERED SHOULDER DYSTOCIA. He used fundal pressure and downward lateral traction to free the baby’s shoulder. The child has a brachial plexus injury of the right shoulder, including nerve avulsion, a fractured clavicle, and permanent disfigurement. She underwent surgery; physical and occupational therapy will continue.
PARENTS' CLAIM The standard sequence of maneuvers should have been attempted before fundal pressure and lateral traction were used—the baby was sufficiently oxygenated to allow time for these maneuvers. Excessive lateral traction caused the injury.
DEFENDANTS' DEFENSE The injuries occurred in utero before or while the fetus progressed down the birth canal, and were due to the maternal forces of labor.
VERDICT A $3,070,000 Michigan verdict was returned against the hospital, ObGyn, and ObGyn group.
WHAT IS THE STANDARD SEQUENCE OF MANEUVERS FOR SHOULDER DYSTOCIA?
Read Dr. Robert L. Barbieri’s May Editorial, You are the second responder to a shoulder dystocia emergency. What do you do first? and Dr. Ronald T. Burkman’s March Stop/Start article, Stop all activities that may lead to further shoulder impaction when you suspect possible shoulder dystocia Meconium aspiration leads to brain injury
LATE IN HER PREGNANCY, a woman went to the emergency department (ED) with hypertension; she was discharged the same day. She saw her ObGyns, Dr. A and Dr. B, three times in the next 2 weeks. A day after her last visit, she returned to the ED in active labor. Dr. B assumed her care. Fetal monitoring indicated a nonreassuring heart rate with decelerations. Dr. B administered oxytocin and labor continued.
The baby was born by cesarean delivery after 25 minutes of fetal bradycardia. She was covered in meconium, with a low heart rate and irregular, labored respirations. The baby was transferred to another hospital, where she was treated for pulmonary hypertension, meconium aspiration, and seizures. The child is totally disabled, and will require constant care for life.
PARENTS' CLAIM The mother’s hypertension was not properly treated. Dr. B and the nurse waited too long to perform a cesarean delivery.
DEFENDANTS' DEFENSE Proper prenatal care was provided. There was no reason for additional testing; fetal heart tones at the mother’s last office visit were reactive. There were no clinical signs of a hematoma or cord varix during office visits. An unpredictable, unpreventable umbilical cord hematoma caused ischemia and hypoxia, and the subsequent brain injury. Meconium had been in the amniotic fluid for at least 10 hours due to the ischemic/hypoxic episode. The hematoma formed between her last office visit and when the mother came to the hospital the next day.
VERDICT Settlements were reached with Dr. A and the hospital. An Arkansas defense verdict was returned for Dr. B and the nurse.
14 months' recovery after mass removed
A GYNECOLOGIC ONCOLOGIST operated on a woman in her 50s to remove a large, noncancerous pelvic mass. The patient, discharged on postoperative day 2, was readmitted the next day with a fever (temperature, 103ºF), nausea, vomiting, and abdominal pain. Four days later, the oncologist repaired a perforated bowel and created an ileostomy. Other procedures were needed to drain abscesses and repair fistulas, and resect a large portion of colon due to continuing infection. Treatment lasted 14 months.
PATIENT'S CLAIM The gynecologic oncologist was negligent in failing to timely diagnose and treat the bowel perforation. Earlier repair would have curtailed development of the abscesses and fistulae.
PHYSICIAN'S DEFENSE Any complications the patient experienced were unrelated to any delay in treatment.
VERDICT A $612,237 Michigan verdict was returned.
Colon perforated during abdominal access
WHEN A MORBIDLY OBESE 37-YEAR-OLD WOMAN reported chronic pelvic pain, her gynecologist suspected endometriosis. Conservative treatment failed and the gynecologist offered laparoscopic hysterectomy.
After abdominal insufflation was unsuccessfully attempted twice using a Veress needle, the gynecologist entered the abdomen with a Visiport optical trocar, and continued the procedure. The gynecologist inspected the abdomen before closing but found no injuries.
The patient did not do well after surgery. CT scan detected a bowel perforation on postoperative day 6. During exploratory laparotomy, a through-and-through “bayonet” colon perforation was repaired. Because of the extensive infection, the patient’s surgical wound was left open and several “washouts” were performed; the wound was closed several weeks later. The patient also underwent two adhesiolysis procedures.
PATIENT'S CLAIM Access to the abdomen was not properly performed and caused colon perforation. The injury should have been found and treated earlier.
PHYSICIAN'S DEFENSE The case was settled before trial.
VERDICT A $750,000 Virginia settlement was reached.
READ How to avoid intestinal and urinary tract injuries during gynecologic laparoscopy, by Michael Baggish, MD (Surgical Techniques, October 2012) What caused this C. diff infection after hysterectomy?
AFTER A HYSTERECTOMY, a 42-year-old woman developed a persistent fever and increased white blood cell count. The gynecologist prescribed ciprofloxacin for a urinary tract infection, and discharged the patient from the hospital on postoperative day 4. She returned to the gynecologist’s office with severe abdominal pain and vomiting 4 days after discharge. The gynecologist prescribed an antacid and told her to continue taking ciprofloxacin.
The patient was taken to the ED by ambulance 3 days later. Testing revealed a Clostridium dificule (C. diff) infection. During emergency surgery, a large portion of her colon was resected, and a colostomy was performed. The colostomy was reversed 6 months later. The patient developed an incisional hernia and has abdominal scarring.
PATIENT'S CLAIM Prophylactic antibiotics should have been prescribed before surgery.
Two possible scenarios were presented: 1) A bowel injury occurred during surgery, and ciprofloxacin likely worsened the infection caused by the bowel injury; or 2) ciprofloxacin triggered the C. diff infection that caused leaking colon perforations and subsequent peritonitis.
The colon perforations could have been avoided if the gynecologist had diagnosed and treated the C. diff infection in a timely manner.
PHYSICIAN'S DEFENSE The patient’s symptoms did not suggest a C. diff infection; testing was not necessary. Ciprofloxacin might have allowed the proliferation of the C. diff infection, but the use of the drug was not negligent. The infection was not preventable and could not have been diagnosed earlier.
VERDICT A $776,000 New York verdict was returned.
Brain injury and cerebral palsy: When did this occur?
DURING LABOR AND DELIVERY, there were periods when the fetal heart-rate tracings were nonreassuring with variable decelerations and fetal tachycardia; some variables were severe. The child suffered anoxic encephalopathy that caused neurologic injury and cerebral palsy.
PARENTS' CLAIM The infant suffered numerous hypoxic incidents before cesarean delivery was performed. An earlier cesarean delivery could have prevented the injury.
PHYSICIAN'S DEFENSE The newborn had a normal blood cord gas level of 7.2 pH and Apgar scores of 9 and 10, at 1 and 5 minutes, respectively. Fetal heart-rate tracings did not show evidence of fetal hypoxia. The brain injury likely occurred prior to the onset of labor and was possibly related to a viral encephalopathy.
VERDICT A Virginia defense verdict was returned. These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
gb
AN OBGYN ENCOUNTERED SHOULDER DYSTOCIA. He used fundal pressure and downward lateral traction to free the baby’s shoulder. The child has a brachial plexus injury of the right shoulder, including nerve avulsion, a fractured clavicle, and permanent disfigurement. She underwent surgery; physical and occupational therapy will continue.
PARENTS' CLAIM The standard sequence of maneuvers should have been attempted before fundal pressure and lateral traction were used—the baby was sufficiently oxygenated to allow time for these maneuvers. Excessive lateral traction caused the injury.
DEFENDANTS' DEFENSE The injuries occurred in utero before or while the fetus progressed down the birth canal, and were due to the maternal forces of labor.
VERDICT A $3,070,000 Michigan verdict was returned against the hospital, ObGyn, and ObGyn group.
WHAT IS THE STANDARD SEQUENCE OF MANEUVERS FOR SHOULDER DYSTOCIA?
Read Dr. Robert L. Barbieri’s May Editorial, You are the second responder to a shoulder dystocia emergency. What do you do first? and Dr. Ronald T. Burkman’s March Stop/Start article, Stop all activities that may lead to further shoulder impaction when you suspect possible shoulder dystocia Meconium aspiration leads to brain injury
LATE IN HER PREGNANCY, a woman went to the emergency department (ED) with hypertension; she was discharged the same day. She saw her ObGyns, Dr. A and Dr. B, three times in the next 2 weeks. A day after her last visit, she returned to the ED in active labor. Dr. B assumed her care. Fetal monitoring indicated a nonreassuring heart rate with decelerations. Dr. B administered oxytocin and labor continued.
The baby was born by cesarean delivery after 25 minutes of fetal bradycardia. She was covered in meconium, with a low heart rate and irregular, labored respirations. The baby was transferred to another hospital, where she was treated for pulmonary hypertension, meconium aspiration, and seizures. The child is totally disabled, and will require constant care for life.
PARENTS' CLAIM The mother’s hypertension was not properly treated. Dr. B and the nurse waited too long to perform a cesarean delivery.
DEFENDANTS' DEFENSE Proper prenatal care was provided. There was no reason for additional testing; fetal heart tones at the mother’s last office visit were reactive. There were no clinical signs of a hematoma or cord varix during office visits. An unpredictable, unpreventable umbilical cord hematoma caused ischemia and hypoxia, and the subsequent brain injury. Meconium had been in the amniotic fluid for at least 10 hours due to the ischemic/hypoxic episode. The hematoma formed between her last office visit and when the mother came to the hospital the next day.
VERDICT Settlements were reached with Dr. A and the hospital. An Arkansas defense verdict was returned for Dr. B and the nurse.
14 months' recovery after mass removed
A GYNECOLOGIC ONCOLOGIST operated on a woman in her 50s to remove a large, noncancerous pelvic mass. The patient, discharged on postoperative day 2, was readmitted the next day with a fever (temperature, 103ºF), nausea, vomiting, and abdominal pain. Four days later, the oncologist repaired a perforated bowel and created an ileostomy. Other procedures were needed to drain abscesses and repair fistulas, and resect a large portion of colon due to continuing infection. Treatment lasted 14 months.
PATIENT'S CLAIM The gynecologic oncologist was negligent in failing to timely diagnose and treat the bowel perforation. Earlier repair would have curtailed development of the abscesses and fistulae.
PHYSICIAN'S DEFENSE Any complications the patient experienced were unrelated to any delay in treatment.
VERDICT A $612,237 Michigan verdict was returned.
Colon perforated during abdominal access
WHEN A MORBIDLY OBESE 37-YEAR-OLD WOMAN reported chronic pelvic pain, her gynecologist suspected endometriosis. Conservative treatment failed and the gynecologist offered laparoscopic hysterectomy.
After abdominal insufflation was unsuccessfully attempted twice using a Veress needle, the gynecologist entered the abdomen with a Visiport optical trocar, and continued the procedure. The gynecologist inspected the abdomen before closing but found no injuries.
The patient did not do well after surgery. CT scan detected a bowel perforation on postoperative day 6. During exploratory laparotomy, a through-and-through “bayonet” colon perforation was repaired. Because of the extensive infection, the patient’s surgical wound was left open and several “washouts” were performed; the wound was closed several weeks later. The patient also underwent two adhesiolysis procedures.
PATIENT'S CLAIM Access to the abdomen was not properly performed and caused colon perforation. The injury should have been found and treated earlier.
PHYSICIAN'S DEFENSE The case was settled before trial.
VERDICT A $750,000 Virginia settlement was reached.
READ How to avoid intestinal and urinary tract injuries during gynecologic laparoscopy, by Michael Baggish, MD (Surgical Techniques, October 2012) What caused this C. diff infection after hysterectomy?
AFTER A HYSTERECTOMY, a 42-year-old woman developed a persistent fever and increased white blood cell count. The gynecologist prescribed ciprofloxacin for a urinary tract infection, and discharged the patient from the hospital on postoperative day 4. She returned to the gynecologist’s office with severe abdominal pain and vomiting 4 days after discharge. The gynecologist prescribed an antacid and told her to continue taking ciprofloxacin.
The patient was taken to the ED by ambulance 3 days later. Testing revealed a Clostridium dificule (C. diff) infection. During emergency surgery, a large portion of her colon was resected, and a colostomy was performed. The colostomy was reversed 6 months later. The patient developed an incisional hernia and has abdominal scarring.
PATIENT'S CLAIM Prophylactic antibiotics should have been prescribed before surgery.
Two possible scenarios were presented: 1) A bowel injury occurred during surgery, and ciprofloxacin likely worsened the infection caused by the bowel injury; or 2) ciprofloxacin triggered the C. diff infection that caused leaking colon perforations and subsequent peritonitis.
The colon perforations could have been avoided if the gynecologist had diagnosed and treated the C. diff infection in a timely manner.
PHYSICIAN'S DEFENSE The patient’s symptoms did not suggest a C. diff infection; testing was not necessary. Ciprofloxacin might have allowed the proliferation of the C. diff infection, but the use of the drug was not negligent. The infection was not preventable and could not have been diagnosed earlier.
VERDICT A $776,000 New York verdict was returned.
Brain injury and cerebral palsy: When did this occur?
DURING LABOR AND DELIVERY, there were periods when the fetal heart-rate tracings were nonreassuring with variable decelerations and fetal tachycardia; some variables were severe. The child suffered anoxic encephalopathy that caused neurologic injury and cerebral palsy.
PARENTS' CLAIM The infant suffered numerous hypoxic incidents before cesarean delivery was performed. An earlier cesarean delivery could have prevented the injury.
PHYSICIAN'S DEFENSE The newborn had a normal blood cord gas level of 7.2 pH and Apgar scores of 9 and 10, at 1 and 5 minutes, respectively. Fetal heart-rate tracings did not show evidence of fetal hypoxia. The brain injury likely occurred prior to the onset of labor and was possibly related to a viral encephalopathy.
VERDICT A Virginia defense verdict was returned. These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.