User login
Screening for intimate partner violence and abuse of elderly and vulnerable adults
The U.S. Preventive Services Task Force has released updated recommendations regarding screening for intimate partner violence and abuse of elderly and vulnerable adults. While their previous recommendations in 2004 gave intimate partner violence screening an "I" recommendation, meaning that the evidence was inconclusive regarding the balance of benefits and intimate partner violence harms, the current recommendation has been upgraded to a "B" recommendation, meaning there is moderate certainty that there is a net benefit from screening. This puts the USPSTF recommendation in alignment with those of most other groups, including the American Medical Association and the *American College of Obstetricians and Gynecologists.
Forms of abuse
The recommendations regarding intimate partner violence in these guidelines refer to physical, sexual, or psychological abuse of women of reproductive age by a current or former partner or spouse. The issue of intimate partner violence is important because research shows that approximately 31% of women and 26% of men have experienced intimate partner violence within their lifetime, and that intimate partner violence is usually undetected. It is also estimated that these numbers are likely to be low because of underreporting. In one large study, the 1-year incidence of abuse was 8% within the last year and 15% within the last 5 years. Approximately 1.5%-5% of pregnant women report being abused. Among older and vulnerable adults, the rate of physical, psychological, or sexual abuse; neglect; or financial exploitation is estimated to be between 2% and 10%.
Intimate partner violence has important and long-lasting effects on victims. Harmful effects include immediate injuries resulting from direct trauma as well as long-term physical and mental health consequences. Long-term physical consequences include sexually transmitted diseases, unintended pregnancy, and worse pregnancy outcomes, as well as higher rates of chronic pain, gastrointestinal disorders, migraine headaches, and disability. Long-term mental health consequences include depression, post-traumatic stress disorder, anxiety disorders, substance abuse, and a higher rate of suicide.
Screening of women
Intimate partner violence in women can be detected with a high level of certainty. There are specific factors that can influence the chances that an individual is at risk for intimate partner violence and can alert clinicians to have increased vigilance for abuse. These risk factors have four categories. The first category is individual, focusing on an individual’s self-esteem. The second is relationship, which focuses on marriage conflict and stability within relationships. Third is community, which is looking at socioeconomic background. Fourth are the societal factors of traditional gender roles.
Many screening instruments exist that have been carefully studied. For instance, the HITS instrument, available in English and Spanish, is a four-item questionnaire that asks about being hurt, insulted, screamed at, or threatened. In one study, it had a sensitivity of 86% and a specificity of 99% for detecting intimate partner violence. The interval for screening is not clear.
Treatment
Once intimate partner violence among women is detected, many approaches are available to help these women. For example, one trial was set up to test the effectiveness of a mentoring support group vs. usual care. All women who entered this trial had discussed intimate partner violence with their primary care physician. After the intervention program, the women who were in the intervention group had significantly reduced scores of abuse as opposed to the comparison group. Another example is a study of pregnant women who reported abuse, who were then randomized to a counseling intervention vs. usual care. Women in the counseling group had decreased pregnancy coercion and were more likely to discontinue an unhealthy or unsafe relationship.
Approaches vary from counseling to social work interventions brought to peoples’ homes, information cards, referral to community services, and mentoring support services. It appears that varied interventions decrease recurrent abuse. There is no reported harm in screening for intimate partner violence. It is necessary for the primary care doctor to be aware of the laws specific to intimate partner violence reporting and privacy within the doctor’s specific region.
Elderly and vulnerable adults
In contrast to screening for intimate partner violence in women, there is a lack of evidence for abuse screening in elderly and vulnerable adult populations. There is a lack of evidence on the benefits of detection and, surprisingly, a lack of evidence on the benefits of early intervention. It is also possible that the harms of detecting abuse in this group may be different, although the risk appears to be small. Some potential harm includes shame, guilt, fear of retaliation, and abandonment by caretakers who have been accused of abuse.
While the evidence to support screening elderly and vulnerable adults is limited, state and local laws vary about the obligation and logistics of reporting elderly abuse. A main conclusion of the USPSTF is that more evidence-based research needs to be done for the population of elderly and vulnerable adults.
Bottom line
Intimate partner violence is common, affecting a quarter of all adults at some point in their life. The mental and physical effects of intimate partner violence can be severe and long-lasting. Screening for intimate partner violence is effective, and effective interventions can be carried out to help women who are victims of intimate partner violence. The USPSTF recommends routine screening of women of reproductive age for intimate partner violence. The data on screening for abuse in the elderly and vulnerable adults is insufficient for the USPSTF to make a recommendation for or against screening.
Reference
• Screening for Intimate Partner Violence and Abuse of Elderly and Vulnerable Adults: U.S. Preventive Services Task Force Recommendation Statement. (Ann. Intern. Med. 2013:158;478-86).
Ms. Skolnik attends Drexel University, Philadelphia, and is a research assistant at the Children’s Hospital of Pennsylvania. Dr. Clouse is an associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital.
*Correction 1/23/14: A previous version of this article misstated the name of the American College of Obstetricians and Gynecologists. This version has been updated.
The U.S. Preventive Services Task Force has released updated recommendations regarding screening for intimate partner violence and abuse of elderly and vulnerable adults. While their previous recommendations in 2004 gave intimate partner violence screening an "I" recommendation, meaning that the evidence was inconclusive regarding the balance of benefits and intimate partner violence harms, the current recommendation has been upgraded to a "B" recommendation, meaning there is moderate certainty that there is a net benefit from screening. This puts the USPSTF recommendation in alignment with those of most other groups, including the American Medical Association and the *American College of Obstetricians and Gynecologists.
Forms of abuse
The recommendations regarding intimate partner violence in these guidelines refer to physical, sexual, or psychological abuse of women of reproductive age by a current or former partner or spouse. The issue of intimate partner violence is important because research shows that approximately 31% of women and 26% of men have experienced intimate partner violence within their lifetime, and that intimate partner violence is usually undetected. It is also estimated that these numbers are likely to be low because of underreporting. In one large study, the 1-year incidence of abuse was 8% within the last year and 15% within the last 5 years. Approximately 1.5%-5% of pregnant women report being abused. Among older and vulnerable adults, the rate of physical, psychological, or sexual abuse; neglect; or financial exploitation is estimated to be between 2% and 10%.
Intimate partner violence has important and long-lasting effects on victims. Harmful effects include immediate injuries resulting from direct trauma as well as long-term physical and mental health consequences. Long-term physical consequences include sexually transmitted diseases, unintended pregnancy, and worse pregnancy outcomes, as well as higher rates of chronic pain, gastrointestinal disorders, migraine headaches, and disability. Long-term mental health consequences include depression, post-traumatic stress disorder, anxiety disorders, substance abuse, and a higher rate of suicide.
Screening of women
Intimate partner violence in women can be detected with a high level of certainty. There are specific factors that can influence the chances that an individual is at risk for intimate partner violence and can alert clinicians to have increased vigilance for abuse. These risk factors have four categories. The first category is individual, focusing on an individual’s self-esteem. The second is relationship, which focuses on marriage conflict and stability within relationships. Third is community, which is looking at socioeconomic background. Fourth are the societal factors of traditional gender roles.
Many screening instruments exist that have been carefully studied. For instance, the HITS instrument, available in English and Spanish, is a four-item questionnaire that asks about being hurt, insulted, screamed at, or threatened. In one study, it had a sensitivity of 86% and a specificity of 99% for detecting intimate partner violence. The interval for screening is not clear.
Treatment
Once intimate partner violence among women is detected, many approaches are available to help these women. For example, one trial was set up to test the effectiveness of a mentoring support group vs. usual care. All women who entered this trial had discussed intimate partner violence with their primary care physician. After the intervention program, the women who were in the intervention group had significantly reduced scores of abuse as opposed to the comparison group. Another example is a study of pregnant women who reported abuse, who were then randomized to a counseling intervention vs. usual care. Women in the counseling group had decreased pregnancy coercion and were more likely to discontinue an unhealthy or unsafe relationship.
Approaches vary from counseling to social work interventions brought to peoples’ homes, information cards, referral to community services, and mentoring support services. It appears that varied interventions decrease recurrent abuse. There is no reported harm in screening for intimate partner violence. It is necessary for the primary care doctor to be aware of the laws specific to intimate partner violence reporting and privacy within the doctor’s specific region.
Elderly and vulnerable adults
In contrast to screening for intimate partner violence in women, there is a lack of evidence for abuse screening in elderly and vulnerable adult populations. There is a lack of evidence on the benefits of detection and, surprisingly, a lack of evidence on the benefits of early intervention. It is also possible that the harms of detecting abuse in this group may be different, although the risk appears to be small. Some potential harm includes shame, guilt, fear of retaliation, and abandonment by caretakers who have been accused of abuse.
While the evidence to support screening elderly and vulnerable adults is limited, state and local laws vary about the obligation and logistics of reporting elderly abuse. A main conclusion of the USPSTF is that more evidence-based research needs to be done for the population of elderly and vulnerable adults.
Bottom line
Intimate partner violence is common, affecting a quarter of all adults at some point in their life. The mental and physical effects of intimate partner violence can be severe and long-lasting. Screening for intimate partner violence is effective, and effective interventions can be carried out to help women who are victims of intimate partner violence. The USPSTF recommends routine screening of women of reproductive age for intimate partner violence. The data on screening for abuse in the elderly and vulnerable adults is insufficient for the USPSTF to make a recommendation for or against screening.
Reference
• Screening for Intimate Partner Violence and Abuse of Elderly and Vulnerable Adults: U.S. Preventive Services Task Force Recommendation Statement. (Ann. Intern. Med. 2013:158;478-86).
Ms. Skolnik attends Drexel University, Philadelphia, and is a research assistant at the Children’s Hospital of Pennsylvania. Dr. Clouse is an associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital.
*Correction 1/23/14: A previous version of this article misstated the name of the American College of Obstetricians and Gynecologists. This version has been updated.
The U.S. Preventive Services Task Force has released updated recommendations regarding screening for intimate partner violence and abuse of elderly and vulnerable adults. While their previous recommendations in 2004 gave intimate partner violence screening an "I" recommendation, meaning that the evidence was inconclusive regarding the balance of benefits and intimate partner violence harms, the current recommendation has been upgraded to a "B" recommendation, meaning there is moderate certainty that there is a net benefit from screening. This puts the USPSTF recommendation in alignment with those of most other groups, including the American Medical Association and the *American College of Obstetricians and Gynecologists.
Forms of abuse
The recommendations regarding intimate partner violence in these guidelines refer to physical, sexual, or psychological abuse of women of reproductive age by a current or former partner or spouse. The issue of intimate partner violence is important because research shows that approximately 31% of women and 26% of men have experienced intimate partner violence within their lifetime, and that intimate partner violence is usually undetected. It is also estimated that these numbers are likely to be low because of underreporting. In one large study, the 1-year incidence of abuse was 8% within the last year and 15% within the last 5 years. Approximately 1.5%-5% of pregnant women report being abused. Among older and vulnerable adults, the rate of physical, psychological, or sexual abuse; neglect; or financial exploitation is estimated to be between 2% and 10%.
Intimate partner violence has important and long-lasting effects on victims. Harmful effects include immediate injuries resulting from direct trauma as well as long-term physical and mental health consequences. Long-term physical consequences include sexually transmitted diseases, unintended pregnancy, and worse pregnancy outcomes, as well as higher rates of chronic pain, gastrointestinal disorders, migraine headaches, and disability. Long-term mental health consequences include depression, post-traumatic stress disorder, anxiety disorders, substance abuse, and a higher rate of suicide.
Screening of women
Intimate partner violence in women can be detected with a high level of certainty. There are specific factors that can influence the chances that an individual is at risk for intimate partner violence and can alert clinicians to have increased vigilance for abuse. These risk factors have four categories. The first category is individual, focusing on an individual’s self-esteem. The second is relationship, which focuses on marriage conflict and stability within relationships. Third is community, which is looking at socioeconomic background. Fourth are the societal factors of traditional gender roles.
Many screening instruments exist that have been carefully studied. For instance, the HITS instrument, available in English and Spanish, is a four-item questionnaire that asks about being hurt, insulted, screamed at, or threatened. In one study, it had a sensitivity of 86% and a specificity of 99% for detecting intimate partner violence. The interval for screening is not clear.
Treatment
Once intimate partner violence among women is detected, many approaches are available to help these women. For example, one trial was set up to test the effectiveness of a mentoring support group vs. usual care. All women who entered this trial had discussed intimate partner violence with their primary care physician. After the intervention program, the women who were in the intervention group had significantly reduced scores of abuse as opposed to the comparison group. Another example is a study of pregnant women who reported abuse, who were then randomized to a counseling intervention vs. usual care. Women in the counseling group had decreased pregnancy coercion and were more likely to discontinue an unhealthy or unsafe relationship.
Approaches vary from counseling to social work interventions brought to peoples’ homes, information cards, referral to community services, and mentoring support services. It appears that varied interventions decrease recurrent abuse. There is no reported harm in screening for intimate partner violence. It is necessary for the primary care doctor to be aware of the laws specific to intimate partner violence reporting and privacy within the doctor’s specific region.
Elderly and vulnerable adults
In contrast to screening for intimate partner violence in women, there is a lack of evidence for abuse screening in elderly and vulnerable adult populations. There is a lack of evidence on the benefits of detection and, surprisingly, a lack of evidence on the benefits of early intervention. It is also possible that the harms of detecting abuse in this group may be different, although the risk appears to be small. Some potential harm includes shame, guilt, fear of retaliation, and abandonment by caretakers who have been accused of abuse.
While the evidence to support screening elderly and vulnerable adults is limited, state and local laws vary about the obligation and logistics of reporting elderly abuse. A main conclusion of the USPSTF is that more evidence-based research needs to be done for the population of elderly and vulnerable adults.
Bottom line
Intimate partner violence is common, affecting a quarter of all adults at some point in their life. The mental and physical effects of intimate partner violence can be severe and long-lasting. Screening for intimate partner violence is effective, and effective interventions can be carried out to help women who are victims of intimate partner violence. The USPSTF recommends routine screening of women of reproductive age for intimate partner violence. The data on screening for abuse in the elderly and vulnerable adults is insufficient for the USPSTF to make a recommendation for or against screening.
Reference
• Screening for Intimate Partner Violence and Abuse of Elderly and Vulnerable Adults: U.S. Preventive Services Task Force Recommendation Statement. (Ann. Intern. Med. 2013:158;478-86).
Ms. Skolnik attends Drexel University, Philadelphia, and is a research assistant at the Children’s Hospital of Pennsylvania. Dr. Clouse is an associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital.
*Correction 1/23/14: A previous version of this article misstated the name of the American College of Obstetricians and Gynecologists. This version has been updated.
Five steps to becoming a primary care leader
With ever more data demonstrating that patient-centered medical homes are the core of successful ACOs, it’s becoming clear that primary care physicians can have a meaningful role in the accountable care movement. In fact, primary care physicians have the opportunity to lead ACO development.
Some primary care physicians have stepped up to leadership and have been very successful. Others want to but don’t know where to start, because there is no precedent for this.
So, what’s required to make a primary care physician a successful ACO leader? It begins with these five fundamental steps:
1. Be the most prepared person in the room. Before you lead, you must understand. And understanding ACOs isn’t a lengthy process. You truly can become one of the most knowledgeable people about ACOs in a matter of hours, not weeks. As you start developing an ACO or collaborative care initiative, your knowledge and positive informed contributions will earn you the respect and confidence of others – foundations upon which leadership rests.
2. Get out of your silo. Accountable care is a team game. Be part of that team by networking intentionally with other primary care physicians, specialists, and hospital administrators. Seek out ways to interact. There is a window of opportunity for the physician willing to bridge gaps.
3. Exercise quiet leadership. There is no need to seize the podium and tell others what to do. That will backfire, of course. Facilitate discussions, and ask others leading questions to find out what they think. Convene breakfasts with members of the medical staff in your community. Engage hospital leadership. An informed primary care physician ACO champion soon will be a much-desired commodity. Lead from behind, as it were. Your goal is to increase awareness and buy-in to a vision, and ideally, it should be the group consensus. You do not need or want to be getting the credit.
4. Do the due diligence. Find out what is going on. What’s out there in your market? Are there medical home networks forming ACOs in your state? What is Medicaid considering? What are the private payers considering?
5. Be wise about who will welcome your leadership. Start with public and private payers. They want higher quality at lower cost, and they’re coming to understand the advantages of the medical home–centric ACO in achieving these goals. Thus, they’re more open to primary care medical home leadership. Enlightened specialists and hospitals are embracing primary care leadership for the same reason. They want to ride the winning horse, and the medical home–centric ACO is often that choice. Others who aren’t as enlightened won’t welcome the loss of control and will resist.
Will leadership be worth it? In our experience, primary care physician leadership has clearly been worth it to those physicians who pursue it, for four reasons. First, their ACO or collaborative care organization is more likely to be successful. Second, their ACO’s savings pool is bigger, and its outcomes are better. Third, they’ve enjoyed restoring the multispecialty collegiality from their days of medical training. And finally, their contributions have been more valuable – and the ACO payments to them based on contributions have been correspondingly more substantial.
Mr. Bobbitt is a senior partner and head of the health law group at the Smith Anderson law firm in Raleigh, N.C. He has many years of experience assisting physicians form integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at [email protected] or 919-821-6612.
With ever more data demonstrating that patient-centered medical homes are the core of successful ACOs, it’s becoming clear that primary care physicians can have a meaningful role in the accountable care movement. In fact, primary care physicians have the opportunity to lead ACO development.
Some primary care physicians have stepped up to leadership and have been very successful. Others want to but don’t know where to start, because there is no precedent for this.
So, what’s required to make a primary care physician a successful ACO leader? It begins with these five fundamental steps:
1. Be the most prepared person in the room. Before you lead, you must understand. And understanding ACOs isn’t a lengthy process. You truly can become one of the most knowledgeable people about ACOs in a matter of hours, not weeks. As you start developing an ACO or collaborative care initiative, your knowledge and positive informed contributions will earn you the respect and confidence of others – foundations upon which leadership rests.
2. Get out of your silo. Accountable care is a team game. Be part of that team by networking intentionally with other primary care physicians, specialists, and hospital administrators. Seek out ways to interact. There is a window of opportunity for the physician willing to bridge gaps.
3. Exercise quiet leadership. There is no need to seize the podium and tell others what to do. That will backfire, of course. Facilitate discussions, and ask others leading questions to find out what they think. Convene breakfasts with members of the medical staff in your community. Engage hospital leadership. An informed primary care physician ACO champion soon will be a much-desired commodity. Lead from behind, as it were. Your goal is to increase awareness and buy-in to a vision, and ideally, it should be the group consensus. You do not need or want to be getting the credit.
4. Do the due diligence. Find out what is going on. What’s out there in your market? Are there medical home networks forming ACOs in your state? What is Medicaid considering? What are the private payers considering?
5. Be wise about who will welcome your leadership. Start with public and private payers. They want higher quality at lower cost, and they’re coming to understand the advantages of the medical home–centric ACO in achieving these goals. Thus, they’re more open to primary care medical home leadership. Enlightened specialists and hospitals are embracing primary care leadership for the same reason. They want to ride the winning horse, and the medical home–centric ACO is often that choice. Others who aren’t as enlightened won’t welcome the loss of control and will resist.
Will leadership be worth it? In our experience, primary care physician leadership has clearly been worth it to those physicians who pursue it, for four reasons. First, their ACO or collaborative care organization is more likely to be successful. Second, their ACO’s savings pool is bigger, and its outcomes are better. Third, they’ve enjoyed restoring the multispecialty collegiality from their days of medical training. And finally, their contributions have been more valuable – and the ACO payments to them based on contributions have been correspondingly more substantial.
Mr. Bobbitt is a senior partner and head of the health law group at the Smith Anderson law firm in Raleigh, N.C. He has many years of experience assisting physicians form integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at [email protected] or 919-821-6612.
With ever more data demonstrating that patient-centered medical homes are the core of successful ACOs, it’s becoming clear that primary care physicians can have a meaningful role in the accountable care movement. In fact, primary care physicians have the opportunity to lead ACO development.
Some primary care physicians have stepped up to leadership and have been very successful. Others want to but don’t know where to start, because there is no precedent for this.
So, what’s required to make a primary care physician a successful ACO leader? It begins with these five fundamental steps:
1. Be the most prepared person in the room. Before you lead, you must understand. And understanding ACOs isn’t a lengthy process. You truly can become one of the most knowledgeable people about ACOs in a matter of hours, not weeks. As you start developing an ACO or collaborative care initiative, your knowledge and positive informed contributions will earn you the respect and confidence of others – foundations upon which leadership rests.
2. Get out of your silo. Accountable care is a team game. Be part of that team by networking intentionally with other primary care physicians, specialists, and hospital administrators. Seek out ways to interact. There is a window of opportunity for the physician willing to bridge gaps.
3. Exercise quiet leadership. There is no need to seize the podium and tell others what to do. That will backfire, of course. Facilitate discussions, and ask others leading questions to find out what they think. Convene breakfasts with members of the medical staff in your community. Engage hospital leadership. An informed primary care physician ACO champion soon will be a much-desired commodity. Lead from behind, as it were. Your goal is to increase awareness and buy-in to a vision, and ideally, it should be the group consensus. You do not need or want to be getting the credit.
4. Do the due diligence. Find out what is going on. What’s out there in your market? Are there medical home networks forming ACOs in your state? What is Medicaid considering? What are the private payers considering?
5. Be wise about who will welcome your leadership. Start with public and private payers. They want higher quality at lower cost, and they’re coming to understand the advantages of the medical home–centric ACO in achieving these goals. Thus, they’re more open to primary care medical home leadership. Enlightened specialists and hospitals are embracing primary care leadership for the same reason. They want to ride the winning horse, and the medical home–centric ACO is often that choice. Others who aren’t as enlightened won’t welcome the loss of control and will resist.
Will leadership be worth it? In our experience, primary care physician leadership has clearly been worth it to those physicians who pursue it, for four reasons. First, their ACO or collaborative care organization is more likely to be successful. Second, their ACO’s savings pool is bigger, and its outcomes are better. Third, they’ve enjoyed restoring the multispecialty collegiality from their days of medical training. And finally, their contributions have been more valuable – and the ACO payments to them based on contributions have been correspondingly more substantial.
Mr. Bobbitt is a senior partner and head of the health law group at the Smith Anderson law firm in Raleigh, N.C. He has many years of experience assisting physicians form integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author at [email protected] or 919-821-6612.
Perspectives on the New Curriculum
The Training Program Experience
By Mara B. Antonoff, M.D., Resident Medical Editor
The new thoracic surgery curriculum has arrived. Debuting this past summer, the curriculum resulted as a joint endeavor of several key organizations heavily vested in thoracic surgical education, with the aim of providing a web-based, multimedia repository of educational materials, accompanied by a formal structure and schedule of weekly topic coverage. Conceptually, the new curriculum has much to offer, with immense theoretical benefits to both the teacher and the student. But what about in practice? Now several months after its launch, the materials provided via the Moodle site and WebBrain have been accessed by the majority of training programs in this country.
How are these tools being utilized by the various programs, and what feedback do they have based on their experiences? The goal of this article will be to explore the various usage patterns of several institutions and their strategies for implementing the materials and integrating them with on-the-ground educational activities. Both the strengths and drawbacks from a programmatic standpoint will be addressed. As you read this article, perhaps you will be motivated to take another look at the curriculum, with new ideas as to how it might best suit your program’s needs.
At Oregon Health and Science University (OHSU), the new curriculum was officially introduced to the trainees and faculty members in a very formal and organized manner, heavily employing the provided instructional videos to become quickly oriented to the new system ("How-To: Utilizing the Thoracic Surgery Brain WebBrain," by Dr. Craig Baker; "How-To: Navigating Moodle," by Dr. Ara Vaporciyan; and "Overview of Teaching Cardiothoracic Surgery" – all available from the Moodle site, http:// jctse.mrooms.net, under Resources on the right hand column). OHSU Program Coordinator Jill Rose reports that she also received helpful information about accessing the curriculum when she attended the "Educate the Educators" course in June, sponsored by the Joint Council on Thoracic Surgery Education (JCTSE). Ms. Rose states, "Faculty and learners enthusiastically adopted this new curriculum and immediately put it to use at least twice a week." When the weekly emails come out, the relevant articles and videos are sent to the trainees and faculty members in the form of a reminder email, including links to the online videos and all related PDF’s as attachments. The residents and fellows then engage in formal curriculum review sessions with faculty, students, and mid-level practitioners – covering the cardiac topics on Monday mornings and thoracic topics on Friday mornings.
At Loma Linda University Health, the residents meet with a faculty moderator on a weekly basis to cover the materials related to the weekly Thoracic Surgery Curriculum topics. The style of presentation is left to the discretion of the attending surgeon, with the majority of the didactic sessions following an oral-board, case-based scenario format. Rather than directly accessing the Moodle pages and WebBrain site, the majority of the faculty and trainees have found that they prefer to have the materials provided to them as hard copies. Consequently, these materials are downloaded and distributed by the program coordinator on a weekly basis.
As with any new educational program, there may be a need for adjustments in initial plans and utilization based on early experiences. For the first few months following release of the curriculum, the Loma Linda group aimed to cover two topics per week – cardiac on Monday mornings and thoracic on Thursday mornings. However, with a tremendous amount of material available for each topic, they ultimately decided to transition to a single weekly session.
While the Loma Linda program has attempted to adhere to the schedule according to the weekly curriculum emails, other programs have chosen to utilize the available materials within the framework of alternative curricular schedules. Rose Haselden, the program coordinator at the Medical University of South Carolina (MUSC), explains that they created their own timeline for covering the materials, based on their specific needs and objectives.
Dr. John Ikonomidis, program director at MUSC, recalls being quick to adopt the new thoracic surgery curriculum. He states, "We were very impressed with its scope and current referencing. When it became available, we went through its entire corpus and divided it into sections which could be covered in 30 minutes. Then we developed a schedule where two topics (one adult or pediatric cardiac and one thoracic) would be covered in our weekly one-hour didactic sessions." Dr. Ikonomidis continues, "The residents are expected to read the material beforehand and faculty are assigned to quiz the residents during the session." In this way, the MUSC program has found a way to use the full breadth of materials, but tailoring the exact learning objectives for their trainees.
While some programs have taken to re-organizing the materials and producing hard copies of the resources for the residents, others have chosen to use the curriculum in its native structure, as a freestanding means of educational supplementation. At Washington University in St. Louis, the trainees are taught how to access the materials and encouraged to both follow the weekly thoracic surgery curriculum emails for independent reading and to utilize the immense resources available for investigating topics relevant to specific cases, conferences, and research interests. Dr. Marc Moon, program director at Washington University, explains that "we have not utilized the materials in any formal, assigned manner; rather, we choose to use the curriculum as a resource for independent study, encouraging our residents to access the multimedia materials both for at-home study and point-of-care reference." Dr. Moon expresses gratitude for the new curriculum, reporting that the faculty members "are grateful that our trainees are able to access these curricular materials through the WebBrain and Moodle, as they serve as an outstanding educational supplement to a high volume operative experience." Dr. Moon further emphasizes, "We find that the new curriculum functions as an excellent adjunct to our clinical teaching."
There are a number of proposed strengths to the new curriculum – its breadth, its ease of access, its correlation with the educational objectives of the American Board of Thoracic Surgery. But what are the benefits being identified from the level of the training program? Dr. Paul Schipper, program director at OHSU, expresses appreciation for the greater volume of material accessible by the trainees, as compared with the older curriculum previously sponsored by the Thoracic Surgery Directors Association (TSDA). States Dr. Schipper, "We’ve been using the TSDA emailed curriculum for several years. With the release of WebBrain, we’ve switched over and been very pleased. Residents are accessing the material and digging deeper into it than previously. In our teaching sessions, we are spending more time on applying the material and less time on explaining it, and I think this is good." Appreciation for the breadth and depth of the material was also noted by Dr. Moon, who identifies the program’s strengths as its ease of access, its large volume, and its applicability to a wide range of educational needs.
Despite the generally laudatory praise, there have been a few issues identified by the training programs that could benefit from some improvement.
Certainly, this is not surprising, as with any educational program, practice and feedback are necessary to optimize the execution for the users. Further, with a resource collection of such enormity, minor tweaks will likely continue in the background at all times in order to ensure ongoing quality-control.
In considering further revision, Dr. Wallen raises some concerns regarding format. He states that "all the moving around on the links makes people crazy," and, for this reason, at Loma Linda, all of the materials are distributed from the WebBrain to the faculty and trainees by the program coordinator. "Otherwise, we would have a revolt," Dr. Jason Wallen explains, This distaste for accessing the materials via the WebBrain is not shared by all users, but it provides feedback, suggesting that changes could be made to optimize formatting to increase ease of use.
Certainly, the leaders in the TSDA, JCTSE, and Thoracic Surgery Residents Association (TSRA) who contributed to the development of the new curriculum are eager for this kind of feedback, welcoming all users to provide constructive criticism. Dr. Ara Vaporciyan, program director at the University of Texas MD Anderson Cancer Center, co-chair of the TSDA/JCTSE Curriculum Committee, and one of the 4 section editors for the curriculum itself, has been a key player in the development of the new curriculum.
States Dr. Vaporciyan, "I never expected this to be perfect on the first try and this is exactly the feedback we need. If we can start an honest conversation about the flaws in the system we can better allocate resources to fixing the most pervasive issues."
Despite the challenges that have been identified, Dr. Wallen remains positive about the curriculum, stating, "We are excited to have an electronic curriculum that our residents can access from anywhere that includes readings and multimedia content. We anticipate that following the curriculum will enhance our residents’ performance on future inservice exams and pave the path to certification."
Dr. Ikonomidis shares Dr. Wallen’s enthusiasm, summarizing that his "residents are constantly engaged and we believe that their learning efficiency has increased." Notes Dr. Schipper, "I am hopeful that this system will stay current and realize and appreciate the effort this has and will take to do so."
Certainly, the new curriculum has already been heavily utilized and appreciated by a number of training programs. While there will always be minor adjustments to be made, the innovators behind the Thoracic Surgery WebBrain and Moodle site are receptive to feedback and clearly dedicated to its ongoing growth.
Perhaps this article has encouraged those of you that aren’t using the curriculum regularly to incorporate it into your institution’s educational structure. For those of you already heavily engaged, perhaps you’ve been inspired to try some new strategies of implementation. Moreover, for all users of the system – trainees, educators, and coordinators – regardless of your program’s current level of use, the take-home message from the creators of the curriculum is that you are encouraged to provide feedback to allow evolution and improvement of the program.
The Trainee Experience
By Sanford M. Zeigler, M.D., Resident Medical Editor
Dr. Antonoff has detailed how different programs have chosen to implement the new curriculum. Of course, in order for the curriculum to work in any setting, people have to actually sit down, access the material, and learn from it. The modules need to be easily accessible, logically organized, and appropriate for the audience for which they are intended. To that end, the folks behind the new curriculum worked diligently to organize all the material into the WebBrain format, which attempts to organize the content by the logic of the human brain, using mind maps, and Moodle, which compartmentalizes the readings into individual curricular assignments that are served up on each resident’s personal Moodle page.
The overall architecture of the WebBrain is very organic; the "Brain" is split into four main branches, comprised of Foundations of Surgery, Cardiovascular, Thoracic, and Congenital headings. From these, the subject matter continues to divide and subdivide again until you reach a terminal branch, where the reader can open a number of different sources, both primary and secondary, on a given subject. The brains’ power lies in the connections that can be made across these fluid boundaries. An example can be seen with one reference that discusses MRI imaging of pericardial disease and cardiac masses. When this is selected, the thought leads the reader back to both the pericardial disease heading and the cardiac tumors heading. The subject selection feature allows the reader to wander throughout the entire WebBrain in a free-flowing but logical manner. Connections across different subjects are, at this point, still rarely utilized. The cross-referencing feature could be a boon for more junior integrated residents and general surgery residents if more of the basic concepts section were connected to cardiac and thoracic subjects, and could allow more self-directed reading to residents that find the time to do so. The WebBrain has some basic search functionality embedded in it that could be used to help understand specific clinical scenarios as they are encountered. Layered upon all of the subject matter are tags, which correspond to the weekly curricular readings. If trainees search for the tag "CV08," for example, they will be directed to each source with that tag, bringing the weekly source matter right to the front. Thus, the WebBrain can be used as a guide for casual reading, as a reference for a particular question or clinical scenario encountered in practice, and also as the source for material covered in didactic session.
The Moodle interface is the gateway to the WebBrain. While it may sound easier to deliver the contents of the WebBrain to each resident rather than go through Moodle, this interface serves two functions. In order to license the content for the curriculum, publishers of many of the textbooks require tight security to prevent unauthorized duplication of the materials. Moodle, by requiring a unique login to access the single WebBrain, provides that security and also allows the WebBrain to be modified in the Cloud, rather than at the level of the end-user. Moodle also provides other testing and tracking tools that have not been completely rolled out. Over the coming months, its full architecture will be used to incorporate quizzes, collaborative message boards, and personal tracking to help residents and their program directors ensure that the material is being covered adequately.
Nearly every resident and faculty member I asked about the new curriculum agreed that the update in content and delivery was badly needed. As an intern in an integrated cardiothoracic surgery program, I remember feeling very jealous of my general surgery colleagues’ access to the SCORE portal, which gave them an easily navigable curriculum accessible from anywhere, with instruction in everything from basic science and physiology to advanced surgical diagnosis and technique. The rollout of the Moodle interface and Web Brain content is the first step to a similar, comprehensive compendium of the necessary knowledge to master cardiac and thoracic surgery.
Response to the rollout has been generally positive from the residents. Most residents agree that the content provides a great sample of landmark papers, lecture videos, book chapters, and consensus statements. A fellow Stanford resident, George Dimeling, wrote: "I like the weekly focus and the topic organization. The content is good, but tough to access." The articles and chapters are often more up to date than printed textbooks, and, once the reader accesses the Brain, are instantly viewable with no further log ins or downloads.
Of course, for a busy resident, it may not always be possible to cover a long book chapter quickly, and the primary literature sometimes fails to cover an entire topic. Justin Schaffer, another Stanford resident, offered this thought: "There’s either a short paper or a 40-page book chapter – there is no solid review of the subject matter. They need something like the Doty lecture series and the TSRA publications to get you warmed up if you don’t have all that time." In fact, the WebBrain incorporates many chapters of the TSRA Cardiothoracic Review book, and the TSRA Clinical Scenarios were added to Moodle on Dec. 12.
One of the more common complaints had little to do with the content but more to do with delivery. At my own institution, most of our hospital computers run an outdated copy of Internet Explorer and have restricted access to update or install a new browser. The out-of-date or restricted software packages that are pervasive in institutional machines nullify many of the advantages of the WebBrain/Moodle format, as the majority of computers at Stanford Hospital cannot access the WebBrain. Furthermore, the WebBrain interface can be laggy and slow even with compatible software.
Others have complained that it is not always easy to find the readings, especially if a program does not follow one of the standardized curricula included with the rollout. First, one must find which content they are responsible for via departmental website or reference to the curricula. Next, the resident logs into the Moodle room, and the proper WebBrain course is launched, then each article for the week is selected and downloaded. Only after that can the content be read, saved, or printed. Using the tag function is helpful, but each time a tagged article is selected, the resident is taken away from the search and to the specific content area, away from the other material assigned for the week. Though it isn’t very difficult to navigate back to the search, all of the steps above make it a bit more of a process to access the material than is convenient for a resident trying to fit in readings between cases or while waiting to round. The new software is a definite improvement, yet still has not reached its full potential.
As Dr. Antonoff pointed out, one residency program has easily overcome this obstacle by consolidating and emailing the appropriate material every week. While the Moodle portion of the curriculum still sees limited functionality, this is probably the best solution to all of the problems. If the articles are in your mailbox, they are accessible anywhere, without the bother of logging in and navigating the Brain.
I discussed this with Dr. Jim Fann, who has been very involved in developing the curriculum, and he explained that direct delivery of the content to each resident had been part of the original goal. As mentioned before, however, publishers require that the delivery of the material is secure from unauthorized duplication. Within the context of an individual institution, those issues are less confining. While individual programs work to integrate the material into their own traditions, it may be worthwhile to designate a resident or office staff member to be in charge of distributing the week’s reading. One little-recognized feature of Moodle is the ability to upload calendars. Perhaps this area could be used by each program to keep the curricular and departmental calendars adjacent to the WebBrain link for easier access.
The recent changes in cardiothoracic surgical education have been myriad, and the rollout of the new curriculum is one of the most pervasive and visible signs of that change. The new curriculum has been designed and updated to reflect not only updates in medical knowledge and consensus, but also changes in the demographic of the cardiothoracic surgery resident and new paradigms in surgical education. The content and delivery systems, while not perfect, remain an ever improving work in progress, which aims to bring cardiothoracic surgical education into the collaborative, cloud based learning era while broadening its reach to both green cardiothoracic surgery interns and traditional fellows with a full general surgery residency behind them. All things considered, the rollout has been very successful, and as more functionality is added and bugs are worked out, things can only improve.
The Training Program Experience
By Mara B. Antonoff, M.D., Resident Medical Editor
The new thoracic surgery curriculum has arrived. Debuting this past summer, the curriculum resulted as a joint endeavor of several key organizations heavily vested in thoracic surgical education, with the aim of providing a web-based, multimedia repository of educational materials, accompanied by a formal structure and schedule of weekly topic coverage. Conceptually, the new curriculum has much to offer, with immense theoretical benefits to both the teacher and the student. But what about in practice? Now several months after its launch, the materials provided via the Moodle site and WebBrain have been accessed by the majority of training programs in this country.
How are these tools being utilized by the various programs, and what feedback do they have based on their experiences? The goal of this article will be to explore the various usage patterns of several institutions and their strategies for implementing the materials and integrating them with on-the-ground educational activities. Both the strengths and drawbacks from a programmatic standpoint will be addressed. As you read this article, perhaps you will be motivated to take another look at the curriculum, with new ideas as to how it might best suit your program’s needs.
At Oregon Health and Science University (OHSU), the new curriculum was officially introduced to the trainees and faculty members in a very formal and organized manner, heavily employing the provided instructional videos to become quickly oriented to the new system ("How-To: Utilizing the Thoracic Surgery Brain WebBrain," by Dr. Craig Baker; "How-To: Navigating Moodle," by Dr. Ara Vaporciyan; and "Overview of Teaching Cardiothoracic Surgery" – all available from the Moodle site, http:// jctse.mrooms.net, under Resources on the right hand column). OHSU Program Coordinator Jill Rose reports that she also received helpful information about accessing the curriculum when she attended the "Educate the Educators" course in June, sponsored by the Joint Council on Thoracic Surgery Education (JCTSE). Ms. Rose states, "Faculty and learners enthusiastically adopted this new curriculum and immediately put it to use at least twice a week." When the weekly emails come out, the relevant articles and videos are sent to the trainees and faculty members in the form of a reminder email, including links to the online videos and all related PDF’s as attachments. The residents and fellows then engage in formal curriculum review sessions with faculty, students, and mid-level practitioners – covering the cardiac topics on Monday mornings and thoracic topics on Friday mornings.
At Loma Linda University Health, the residents meet with a faculty moderator on a weekly basis to cover the materials related to the weekly Thoracic Surgery Curriculum topics. The style of presentation is left to the discretion of the attending surgeon, with the majority of the didactic sessions following an oral-board, case-based scenario format. Rather than directly accessing the Moodle pages and WebBrain site, the majority of the faculty and trainees have found that they prefer to have the materials provided to them as hard copies. Consequently, these materials are downloaded and distributed by the program coordinator on a weekly basis.
As with any new educational program, there may be a need for adjustments in initial plans and utilization based on early experiences. For the first few months following release of the curriculum, the Loma Linda group aimed to cover two topics per week – cardiac on Monday mornings and thoracic on Thursday mornings. However, with a tremendous amount of material available for each topic, they ultimately decided to transition to a single weekly session.
While the Loma Linda program has attempted to adhere to the schedule according to the weekly curriculum emails, other programs have chosen to utilize the available materials within the framework of alternative curricular schedules. Rose Haselden, the program coordinator at the Medical University of South Carolina (MUSC), explains that they created their own timeline for covering the materials, based on their specific needs and objectives.
Dr. John Ikonomidis, program director at MUSC, recalls being quick to adopt the new thoracic surgery curriculum. He states, "We were very impressed with its scope and current referencing. When it became available, we went through its entire corpus and divided it into sections which could be covered in 30 minutes. Then we developed a schedule where two topics (one adult or pediatric cardiac and one thoracic) would be covered in our weekly one-hour didactic sessions." Dr. Ikonomidis continues, "The residents are expected to read the material beforehand and faculty are assigned to quiz the residents during the session." In this way, the MUSC program has found a way to use the full breadth of materials, but tailoring the exact learning objectives for their trainees.
While some programs have taken to re-organizing the materials and producing hard copies of the resources for the residents, others have chosen to use the curriculum in its native structure, as a freestanding means of educational supplementation. At Washington University in St. Louis, the trainees are taught how to access the materials and encouraged to both follow the weekly thoracic surgery curriculum emails for independent reading and to utilize the immense resources available for investigating topics relevant to specific cases, conferences, and research interests. Dr. Marc Moon, program director at Washington University, explains that "we have not utilized the materials in any formal, assigned manner; rather, we choose to use the curriculum as a resource for independent study, encouraging our residents to access the multimedia materials both for at-home study and point-of-care reference." Dr. Moon expresses gratitude for the new curriculum, reporting that the faculty members "are grateful that our trainees are able to access these curricular materials through the WebBrain and Moodle, as they serve as an outstanding educational supplement to a high volume operative experience." Dr. Moon further emphasizes, "We find that the new curriculum functions as an excellent adjunct to our clinical teaching."
There are a number of proposed strengths to the new curriculum – its breadth, its ease of access, its correlation with the educational objectives of the American Board of Thoracic Surgery. But what are the benefits being identified from the level of the training program? Dr. Paul Schipper, program director at OHSU, expresses appreciation for the greater volume of material accessible by the trainees, as compared with the older curriculum previously sponsored by the Thoracic Surgery Directors Association (TSDA). States Dr. Schipper, "We’ve been using the TSDA emailed curriculum for several years. With the release of WebBrain, we’ve switched over and been very pleased. Residents are accessing the material and digging deeper into it than previously. In our teaching sessions, we are spending more time on applying the material and less time on explaining it, and I think this is good." Appreciation for the breadth and depth of the material was also noted by Dr. Moon, who identifies the program’s strengths as its ease of access, its large volume, and its applicability to a wide range of educational needs.
Despite the generally laudatory praise, there have been a few issues identified by the training programs that could benefit from some improvement.
Certainly, this is not surprising, as with any educational program, practice and feedback are necessary to optimize the execution for the users. Further, with a resource collection of such enormity, minor tweaks will likely continue in the background at all times in order to ensure ongoing quality-control.
In considering further revision, Dr. Wallen raises some concerns regarding format. He states that "all the moving around on the links makes people crazy," and, for this reason, at Loma Linda, all of the materials are distributed from the WebBrain to the faculty and trainees by the program coordinator. "Otherwise, we would have a revolt," Dr. Jason Wallen explains, This distaste for accessing the materials via the WebBrain is not shared by all users, but it provides feedback, suggesting that changes could be made to optimize formatting to increase ease of use.
Certainly, the leaders in the TSDA, JCTSE, and Thoracic Surgery Residents Association (TSRA) who contributed to the development of the new curriculum are eager for this kind of feedback, welcoming all users to provide constructive criticism. Dr. Ara Vaporciyan, program director at the University of Texas MD Anderson Cancer Center, co-chair of the TSDA/JCTSE Curriculum Committee, and one of the 4 section editors for the curriculum itself, has been a key player in the development of the new curriculum.
States Dr. Vaporciyan, "I never expected this to be perfect on the first try and this is exactly the feedback we need. If we can start an honest conversation about the flaws in the system we can better allocate resources to fixing the most pervasive issues."
Despite the challenges that have been identified, Dr. Wallen remains positive about the curriculum, stating, "We are excited to have an electronic curriculum that our residents can access from anywhere that includes readings and multimedia content. We anticipate that following the curriculum will enhance our residents’ performance on future inservice exams and pave the path to certification."
Dr. Ikonomidis shares Dr. Wallen’s enthusiasm, summarizing that his "residents are constantly engaged and we believe that their learning efficiency has increased." Notes Dr. Schipper, "I am hopeful that this system will stay current and realize and appreciate the effort this has and will take to do so."
Certainly, the new curriculum has already been heavily utilized and appreciated by a number of training programs. While there will always be minor adjustments to be made, the innovators behind the Thoracic Surgery WebBrain and Moodle site are receptive to feedback and clearly dedicated to its ongoing growth.
Perhaps this article has encouraged those of you that aren’t using the curriculum regularly to incorporate it into your institution’s educational structure. For those of you already heavily engaged, perhaps you’ve been inspired to try some new strategies of implementation. Moreover, for all users of the system – trainees, educators, and coordinators – regardless of your program’s current level of use, the take-home message from the creators of the curriculum is that you are encouraged to provide feedback to allow evolution and improvement of the program.
The Trainee Experience
By Sanford M. Zeigler, M.D., Resident Medical Editor
Dr. Antonoff has detailed how different programs have chosen to implement the new curriculum. Of course, in order for the curriculum to work in any setting, people have to actually sit down, access the material, and learn from it. The modules need to be easily accessible, logically organized, and appropriate for the audience for which they are intended. To that end, the folks behind the new curriculum worked diligently to organize all the material into the WebBrain format, which attempts to organize the content by the logic of the human brain, using mind maps, and Moodle, which compartmentalizes the readings into individual curricular assignments that are served up on each resident’s personal Moodle page.
The overall architecture of the WebBrain is very organic; the "Brain" is split into four main branches, comprised of Foundations of Surgery, Cardiovascular, Thoracic, and Congenital headings. From these, the subject matter continues to divide and subdivide again until you reach a terminal branch, where the reader can open a number of different sources, both primary and secondary, on a given subject. The brains’ power lies in the connections that can be made across these fluid boundaries. An example can be seen with one reference that discusses MRI imaging of pericardial disease and cardiac masses. When this is selected, the thought leads the reader back to both the pericardial disease heading and the cardiac tumors heading. The subject selection feature allows the reader to wander throughout the entire WebBrain in a free-flowing but logical manner. Connections across different subjects are, at this point, still rarely utilized. The cross-referencing feature could be a boon for more junior integrated residents and general surgery residents if more of the basic concepts section were connected to cardiac and thoracic subjects, and could allow more self-directed reading to residents that find the time to do so. The WebBrain has some basic search functionality embedded in it that could be used to help understand specific clinical scenarios as they are encountered. Layered upon all of the subject matter are tags, which correspond to the weekly curricular readings. If trainees search for the tag "CV08," for example, they will be directed to each source with that tag, bringing the weekly source matter right to the front. Thus, the WebBrain can be used as a guide for casual reading, as a reference for a particular question or clinical scenario encountered in practice, and also as the source for material covered in didactic session.
The Moodle interface is the gateway to the WebBrain. While it may sound easier to deliver the contents of the WebBrain to each resident rather than go through Moodle, this interface serves two functions. In order to license the content for the curriculum, publishers of many of the textbooks require tight security to prevent unauthorized duplication of the materials. Moodle, by requiring a unique login to access the single WebBrain, provides that security and also allows the WebBrain to be modified in the Cloud, rather than at the level of the end-user. Moodle also provides other testing and tracking tools that have not been completely rolled out. Over the coming months, its full architecture will be used to incorporate quizzes, collaborative message boards, and personal tracking to help residents and their program directors ensure that the material is being covered adequately.
Nearly every resident and faculty member I asked about the new curriculum agreed that the update in content and delivery was badly needed. As an intern in an integrated cardiothoracic surgery program, I remember feeling very jealous of my general surgery colleagues’ access to the SCORE portal, which gave them an easily navigable curriculum accessible from anywhere, with instruction in everything from basic science and physiology to advanced surgical diagnosis and technique. The rollout of the Moodle interface and Web Brain content is the first step to a similar, comprehensive compendium of the necessary knowledge to master cardiac and thoracic surgery.
Response to the rollout has been generally positive from the residents. Most residents agree that the content provides a great sample of landmark papers, lecture videos, book chapters, and consensus statements. A fellow Stanford resident, George Dimeling, wrote: "I like the weekly focus and the topic organization. The content is good, but tough to access." The articles and chapters are often more up to date than printed textbooks, and, once the reader accesses the Brain, are instantly viewable with no further log ins or downloads.
Of course, for a busy resident, it may not always be possible to cover a long book chapter quickly, and the primary literature sometimes fails to cover an entire topic. Justin Schaffer, another Stanford resident, offered this thought: "There’s either a short paper or a 40-page book chapter – there is no solid review of the subject matter. They need something like the Doty lecture series and the TSRA publications to get you warmed up if you don’t have all that time." In fact, the WebBrain incorporates many chapters of the TSRA Cardiothoracic Review book, and the TSRA Clinical Scenarios were added to Moodle on Dec. 12.
One of the more common complaints had little to do with the content but more to do with delivery. At my own institution, most of our hospital computers run an outdated copy of Internet Explorer and have restricted access to update or install a new browser. The out-of-date or restricted software packages that are pervasive in institutional machines nullify many of the advantages of the WebBrain/Moodle format, as the majority of computers at Stanford Hospital cannot access the WebBrain. Furthermore, the WebBrain interface can be laggy and slow even with compatible software.
Others have complained that it is not always easy to find the readings, especially if a program does not follow one of the standardized curricula included with the rollout. First, one must find which content they are responsible for via departmental website or reference to the curricula. Next, the resident logs into the Moodle room, and the proper WebBrain course is launched, then each article for the week is selected and downloaded. Only after that can the content be read, saved, or printed. Using the tag function is helpful, but each time a tagged article is selected, the resident is taken away from the search and to the specific content area, away from the other material assigned for the week. Though it isn’t very difficult to navigate back to the search, all of the steps above make it a bit more of a process to access the material than is convenient for a resident trying to fit in readings between cases or while waiting to round. The new software is a definite improvement, yet still has not reached its full potential.
As Dr. Antonoff pointed out, one residency program has easily overcome this obstacle by consolidating and emailing the appropriate material every week. While the Moodle portion of the curriculum still sees limited functionality, this is probably the best solution to all of the problems. If the articles are in your mailbox, they are accessible anywhere, without the bother of logging in and navigating the Brain.
I discussed this with Dr. Jim Fann, who has been very involved in developing the curriculum, and he explained that direct delivery of the content to each resident had been part of the original goal. As mentioned before, however, publishers require that the delivery of the material is secure from unauthorized duplication. Within the context of an individual institution, those issues are less confining. While individual programs work to integrate the material into their own traditions, it may be worthwhile to designate a resident or office staff member to be in charge of distributing the week’s reading. One little-recognized feature of Moodle is the ability to upload calendars. Perhaps this area could be used by each program to keep the curricular and departmental calendars adjacent to the WebBrain link for easier access.
The recent changes in cardiothoracic surgical education have been myriad, and the rollout of the new curriculum is one of the most pervasive and visible signs of that change. The new curriculum has been designed and updated to reflect not only updates in medical knowledge and consensus, but also changes in the demographic of the cardiothoracic surgery resident and new paradigms in surgical education. The content and delivery systems, while not perfect, remain an ever improving work in progress, which aims to bring cardiothoracic surgical education into the collaborative, cloud based learning era while broadening its reach to both green cardiothoracic surgery interns and traditional fellows with a full general surgery residency behind them. All things considered, the rollout has been very successful, and as more functionality is added and bugs are worked out, things can only improve.
The Training Program Experience
By Mara B. Antonoff, M.D., Resident Medical Editor
The new thoracic surgery curriculum has arrived. Debuting this past summer, the curriculum resulted as a joint endeavor of several key organizations heavily vested in thoracic surgical education, with the aim of providing a web-based, multimedia repository of educational materials, accompanied by a formal structure and schedule of weekly topic coverage. Conceptually, the new curriculum has much to offer, with immense theoretical benefits to both the teacher and the student. But what about in practice? Now several months after its launch, the materials provided via the Moodle site and WebBrain have been accessed by the majority of training programs in this country.
How are these tools being utilized by the various programs, and what feedback do they have based on their experiences? The goal of this article will be to explore the various usage patterns of several institutions and their strategies for implementing the materials and integrating them with on-the-ground educational activities. Both the strengths and drawbacks from a programmatic standpoint will be addressed. As you read this article, perhaps you will be motivated to take another look at the curriculum, with new ideas as to how it might best suit your program’s needs.
At Oregon Health and Science University (OHSU), the new curriculum was officially introduced to the trainees and faculty members in a very formal and organized manner, heavily employing the provided instructional videos to become quickly oriented to the new system ("How-To: Utilizing the Thoracic Surgery Brain WebBrain," by Dr. Craig Baker; "How-To: Navigating Moodle," by Dr. Ara Vaporciyan; and "Overview of Teaching Cardiothoracic Surgery" – all available from the Moodle site, http:// jctse.mrooms.net, under Resources on the right hand column). OHSU Program Coordinator Jill Rose reports that she also received helpful information about accessing the curriculum when she attended the "Educate the Educators" course in June, sponsored by the Joint Council on Thoracic Surgery Education (JCTSE). Ms. Rose states, "Faculty and learners enthusiastically adopted this new curriculum and immediately put it to use at least twice a week." When the weekly emails come out, the relevant articles and videos are sent to the trainees and faculty members in the form of a reminder email, including links to the online videos and all related PDF’s as attachments. The residents and fellows then engage in formal curriculum review sessions with faculty, students, and mid-level practitioners – covering the cardiac topics on Monday mornings and thoracic topics on Friday mornings.
At Loma Linda University Health, the residents meet with a faculty moderator on a weekly basis to cover the materials related to the weekly Thoracic Surgery Curriculum topics. The style of presentation is left to the discretion of the attending surgeon, with the majority of the didactic sessions following an oral-board, case-based scenario format. Rather than directly accessing the Moodle pages and WebBrain site, the majority of the faculty and trainees have found that they prefer to have the materials provided to them as hard copies. Consequently, these materials are downloaded and distributed by the program coordinator on a weekly basis.
As with any new educational program, there may be a need for adjustments in initial plans and utilization based on early experiences. For the first few months following release of the curriculum, the Loma Linda group aimed to cover two topics per week – cardiac on Monday mornings and thoracic on Thursday mornings. However, with a tremendous amount of material available for each topic, they ultimately decided to transition to a single weekly session.
While the Loma Linda program has attempted to adhere to the schedule according to the weekly curriculum emails, other programs have chosen to utilize the available materials within the framework of alternative curricular schedules. Rose Haselden, the program coordinator at the Medical University of South Carolina (MUSC), explains that they created their own timeline for covering the materials, based on their specific needs and objectives.
Dr. John Ikonomidis, program director at MUSC, recalls being quick to adopt the new thoracic surgery curriculum. He states, "We were very impressed with its scope and current referencing. When it became available, we went through its entire corpus and divided it into sections which could be covered in 30 minutes. Then we developed a schedule where two topics (one adult or pediatric cardiac and one thoracic) would be covered in our weekly one-hour didactic sessions." Dr. Ikonomidis continues, "The residents are expected to read the material beforehand and faculty are assigned to quiz the residents during the session." In this way, the MUSC program has found a way to use the full breadth of materials, but tailoring the exact learning objectives for their trainees.
While some programs have taken to re-organizing the materials and producing hard copies of the resources for the residents, others have chosen to use the curriculum in its native structure, as a freestanding means of educational supplementation. At Washington University in St. Louis, the trainees are taught how to access the materials and encouraged to both follow the weekly thoracic surgery curriculum emails for independent reading and to utilize the immense resources available for investigating topics relevant to specific cases, conferences, and research interests. Dr. Marc Moon, program director at Washington University, explains that "we have not utilized the materials in any formal, assigned manner; rather, we choose to use the curriculum as a resource for independent study, encouraging our residents to access the multimedia materials both for at-home study and point-of-care reference." Dr. Moon expresses gratitude for the new curriculum, reporting that the faculty members "are grateful that our trainees are able to access these curricular materials through the WebBrain and Moodle, as they serve as an outstanding educational supplement to a high volume operative experience." Dr. Moon further emphasizes, "We find that the new curriculum functions as an excellent adjunct to our clinical teaching."
There are a number of proposed strengths to the new curriculum – its breadth, its ease of access, its correlation with the educational objectives of the American Board of Thoracic Surgery. But what are the benefits being identified from the level of the training program? Dr. Paul Schipper, program director at OHSU, expresses appreciation for the greater volume of material accessible by the trainees, as compared with the older curriculum previously sponsored by the Thoracic Surgery Directors Association (TSDA). States Dr. Schipper, "We’ve been using the TSDA emailed curriculum for several years. With the release of WebBrain, we’ve switched over and been very pleased. Residents are accessing the material and digging deeper into it than previously. In our teaching sessions, we are spending more time on applying the material and less time on explaining it, and I think this is good." Appreciation for the breadth and depth of the material was also noted by Dr. Moon, who identifies the program’s strengths as its ease of access, its large volume, and its applicability to a wide range of educational needs.
Despite the generally laudatory praise, there have been a few issues identified by the training programs that could benefit from some improvement.
Certainly, this is not surprising, as with any educational program, practice and feedback are necessary to optimize the execution for the users. Further, with a resource collection of such enormity, minor tweaks will likely continue in the background at all times in order to ensure ongoing quality-control.
In considering further revision, Dr. Wallen raises some concerns regarding format. He states that "all the moving around on the links makes people crazy," and, for this reason, at Loma Linda, all of the materials are distributed from the WebBrain to the faculty and trainees by the program coordinator. "Otherwise, we would have a revolt," Dr. Jason Wallen explains, This distaste for accessing the materials via the WebBrain is not shared by all users, but it provides feedback, suggesting that changes could be made to optimize formatting to increase ease of use.
Certainly, the leaders in the TSDA, JCTSE, and Thoracic Surgery Residents Association (TSRA) who contributed to the development of the new curriculum are eager for this kind of feedback, welcoming all users to provide constructive criticism. Dr. Ara Vaporciyan, program director at the University of Texas MD Anderson Cancer Center, co-chair of the TSDA/JCTSE Curriculum Committee, and one of the 4 section editors for the curriculum itself, has been a key player in the development of the new curriculum.
States Dr. Vaporciyan, "I never expected this to be perfect on the first try and this is exactly the feedback we need. If we can start an honest conversation about the flaws in the system we can better allocate resources to fixing the most pervasive issues."
Despite the challenges that have been identified, Dr. Wallen remains positive about the curriculum, stating, "We are excited to have an electronic curriculum that our residents can access from anywhere that includes readings and multimedia content. We anticipate that following the curriculum will enhance our residents’ performance on future inservice exams and pave the path to certification."
Dr. Ikonomidis shares Dr. Wallen’s enthusiasm, summarizing that his "residents are constantly engaged and we believe that their learning efficiency has increased." Notes Dr. Schipper, "I am hopeful that this system will stay current and realize and appreciate the effort this has and will take to do so."
Certainly, the new curriculum has already been heavily utilized and appreciated by a number of training programs. While there will always be minor adjustments to be made, the innovators behind the Thoracic Surgery WebBrain and Moodle site are receptive to feedback and clearly dedicated to its ongoing growth.
Perhaps this article has encouraged those of you that aren’t using the curriculum regularly to incorporate it into your institution’s educational structure. For those of you already heavily engaged, perhaps you’ve been inspired to try some new strategies of implementation. Moreover, for all users of the system – trainees, educators, and coordinators – regardless of your program’s current level of use, the take-home message from the creators of the curriculum is that you are encouraged to provide feedback to allow evolution and improvement of the program.
The Trainee Experience
By Sanford M. Zeigler, M.D., Resident Medical Editor
Dr. Antonoff has detailed how different programs have chosen to implement the new curriculum. Of course, in order for the curriculum to work in any setting, people have to actually sit down, access the material, and learn from it. The modules need to be easily accessible, logically organized, and appropriate for the audience for which they are intended. To that end, the folks behind the new curriculum worked diligently to organize all the material into the WebBrain format, which attempts to organize the content by the logic of the human brain, using mind maps, and Moodle, which compartmentalizes the readings into individual curricular assignments that are served up on each resident’s personal Moodle page.
The overall architecture of the WebBrain is very organic; the "Brain" is split into four main branches, comprised of Foundations of Surgery, Cardiovascular, Thoracic, and Congenital headings. From these, the subject matter continues to divide and subdivide again until you reach a terminal branch, where the reader can open a number of different sources, both primary and secondary, on a given subject. The brains’ power lies in the connections that can be made across these fluid boundaries. An example can be seen with one reference that discusses MRI imaging of pericardial disease and cardiac masses. When this is selected, the thought leads the reader back to both the pericardial disease heading and the cardiac tumors heading. The subject selection feature allows the reader to wander throughout the entire WebBrain in a free-flowing but logical manner. Connections across different subjects are, at this point, still rarely utilized. The cross-referencing feature could be a boon for more junior integrated residents and general surgery residents if more of the basic concepts section were connected to cardiac and thoracic subjects, and could allow more self-directed reading to residents that find the time to do so. The WebBrain has some basic search functionality embedded in it that could be used to help understand specific clinical scenarios as they are encountered. Layered upon all of the subject matter are tags, which correspond to the weekly curricular readings. If trainees search for the tag "CV08," for example, they will be directed to each source with that tag, bringing the weekly source matter right to the front. Thus, the WebBrain can be used as a guide for casual reading, as a reference for a particular question or clinical scenario encountered in practice, and also as the source for material covered in didactic session.
The Moodle interface is the gateway to the WebBrain. While it may sound easier to deliver the contents of the WebBrain to each resident rather than go through Moodle, this interface serves two functions. In order to license the content for the curriculum, publishers of many of the textbooks require tight security to prevent unauthorized duplication of the materials. Moodle, by requiring a unique login to access the single WebBrain, provides that security and also allows the WebBrain to be modified in the Cloud, rather than at the level of the end-user. Moodle also provides other testing and tracking tools that have not been completely rolled out. Over the coming months, its full architecture will be used to incorporate quizzes, collaborative message boards, and personal tracking to help residents and their program directors ensure that the material is being covered adequately.
Nearly every resident and faculty member I asked about the new curriculum agreed that the update in content and delivery was badly needed. As an intern in an integrated cardiothoracic surgery program, I remember feeling very jealous of my general surgery colleagues’ access to the SCORE portal, which gave them an easily navigable curriculum accessible from anywhere, with instruction in everything from basic science and physiology to advanced surgical diagnosis and technique. The rollout of the Moodle interface and Web Brain content is the first step to a similar, comprehensive compendium of the necessary knowledge to master cardiac and thoracic surgery.
Response to the rollout has been generally positive from the residents. Most residents agree that the content provides a great sample of landmark papers, lecture videos, book chapters, and consensus statements. A fellow Stanford resident, George Dimeling, wrote: "I like the weekly focus and the topic organization. The content is good, but tough to access." The articles and chapters are often more up to date than printed textbooks, and, once the reader accesses the Brain, are instantly viewable with no further log ins or downloads.
Of course, for a busy resident, it may not always be possible to cover a long book chapter quickly, and the primary literature sometimes fails to cover an entire topic. Justin Schaffer, another Stanford resident, offered this thought: "There’s either a short paper or a 40-page book chapter – there is no solid review of the subject matter. They need something like the Doty lecture series and the TSRA publications to get you warmed up if you don’t have all that time." In fact, the WebBrain incorporates many chapters of the TSRA Cardiothoracic Review book, and the TSRA Clinical Scenarios were added to Moodle on Dec. 12.
One of the more common complaints had little to do with the content but more to do with delivery. At my own institution, most of our hospital computers run an outdated copy of Internet Explorer and have restricted access to update or install a new browser. The out-of-date or restricted software packages that are pervasive in institutional machines nullify many of the advantages of the WebBrain/Moodle format, as the majority of computers at Stanford Hospital cannot access the WebBrain. Furthermore, the WebBrain interface can be laggy and slow even with compatible software.
Others have complained that it is not always easy to find the readings, especially if a program does not follow one of the standardized curricula included with the rollout. First, one must find which content they are responsible for via departmental website or reference to the curricula. Next, the resident logs into the Moodle room, and the proper WebBrain course is launched, then each article for the week is selected and downloaded. Only after that can the content be read, saved, or printed. Using the tag function is helpful, but each time a tagged article is selected, the resident is taken away from the search and to the specific content area, away from the other material assigned for the week. Though it isn’t very difficult to navigate back to the search, all of the steps above make it a bit more of a process to access the material than is convenient for a resident trying to fit in readings between cases or while waiting to round. The new software is a definite improvement, yet still has not reached its full potential.
As Dr. Antonoff pointed out, one residency program has easily overcome this obstacle by consolidating and emailing the appropriate material every week. While the Moodle portion of the curriculum still sees limited functionality, this is probably the best solution to all of the problems. If the articles are in your mailbox, they are accessible anywhere, without the bother of logging in and navigating the Brain.
I discussed this with Dr. Jim Fann, who has been very involved in developing the curriculum, and he explained that direct delivery of the content to each resident had been part of the original goal. As mentioned before, however, publishers require that the delivery of the material is secure from unauthorized duplication. Within the context of an individual institution, those issues are less confining. While individual programs work to integrate the material into their own traditions, it may be worthwhile to designate a resident or office staff member to be in charge of distributing the week’s reading. One little-recognized feature of Moodle is the ability to upload calendars. Perhaps this area could be used by each program to keep the curricular and departmental calendars adjacent to the WebBrain link for easier access.
The recent changes in cardiothoracic surgical education have been myriad, and the rollout of the new curriculum is one of the most pervasive and visible signs of that change. The new curriculum has been designed and updated to reflect not only updates in medical knowledge and consensus, but also changes in the demographic of the cardiothoracic surgery resident and new paradigms in surgical education. The content and delivery systems, while not perfect, remain an ever improving work in progress, which aims to bring cardiothoracic surgical education into the collaborative, cloud based learning era while broadening its reach to both green cardiothoracic surgery interns and traditional fellows with a full general surgery residency behind them. All things considered, the rollout has been very successful, and as more functionality is added and bugs are worked out, things can only improve.
When ADHD doesn’t improve, check medication adherence first
NEW YORK – Assessing nonresponsiveness to attention-deficit/hyperactivity disorder treatment requires a bit of detective work, according to Dr. Laurence L. Greenhill.
The reason can be as simple as a little kid not being able to swallow a big pill, or as complex as a dysfunctional family dynamic that interferes with medication adherence. But once the problem is rooted out and addressed, most refractory patients can experience a good response, Dr. Greenhill said at a psychopharmacology update held by the American Academy of Child and Adolescent Psychiatry.
Since primary care physicians usually continue to manage children who respond to ADHD medications, psychiatrists are usually the ones who see nonresponders, said Dr. Greenhill, a child and adolescent psychiatrist at the New York Psychiatric Institute.
Medication nonadherence, the most common cause of a failure to improve, can arise from numerous situations.
On the simple side, it might be a matter of finding the right form of medication; a liquid or sprinkle capsule might be much easier for a child to take than a pill. And not all pills are created equally easy to take.
"For example, [the osmotic controlled release oral delivery system methylphenidate] just went off patent, and generics are now available. But some of these generics are much bigger. In fact, one of the 18-mg pills is twice as large as the patent medicine, and lots of kids can’t swallow it," he said.
The ADHD medication guide published by Long Island Jewish Hospital can be a helpful tool when working with parents on this issue. It lists all the Food and Drug Administration–approved medications for ADHD, with full-size photographs of each capsule, tablet, or pill.
Some generics are not pharmacokinetically or pharmacodynamically identical to the original formulation, Dr. Greenhill noted. Although the drug has to be molecularly identical and dose identical, "the ascending dose curve and duration of action need not be matched." Some generic formulations do fall into this problematic category. "For this reason, I try to encourage parents to get the brand," said Dr. Greenhill, adding that he has no financial interest in any of the drugs.
Medication nonadherence also can be attributable to uncomfortable or even intolerable side effects. These can include gastrointestinal issues, trouble sleeping, lack of appetite, restlessness, irritability, and "feeling fidgety."
Dosage adjustments or a medication change might be in order. For appetite issues, recommend giving the medication after meals, and reassure parents it’s OK to let a child eat later in the evening, when hunger may return.
It’s important to get the child’s growth records from the pediatrician, and plot height and weight curves every 6 months. If there’s a consistent fall-off, consider lowering the dose or changing to another drug.
Contrary to widely held belief, stimulants don’t pose significant cardiac risks to most children. A baseline electrocardiogram is really only necessary for a child who has a family history of sudden cardiac death or a personal history of syncope or cardiac abnormalities. Blood pressure and pulse should be monitored at every visit.
Melatonin is worth a try for youngsters whose ADHD meds interfere with good sleep, Dr. Greenhill said.
"I would start at 1 mg/night and work up," he said. "Starting at a high dose can actually shut off the naturally occurring melatonin. Plasma levels peak about an hour after taking it, so timing is important. I usually start with it about 3 hours before the scheduled sleeping time and then adjust."
Family dynamics also can play a big role in medication nonadherence. "ADHD families are often poor at scheduling activities, sometimes to the extent that parents are the ones who forget to give the medication. They also might not have a clear idea of how to give it, and just leave it on the kitchen table, making it the child’s responsibility to take it every day.
"If this is a child who can’t remember to bring homework back from school, then how is he going to remember to stay on schedule with medication?"
If it’s clear that parents are having difficulty in this area, the simplest thing to do is send the medicine to school and ask the nurse to administer it. Switching to a long-acting form might help, too, since it’s just easier to remember to take one pill than to take two.
The ADHD Parents Medication Guide is a great resource that can be used to get parents actively involved with the child’s drug therapy, Dr. Greenhill said. Developed by the American Psychiatric Association and the American Academy of Child and Adolescent Psychiatry, the online guide is designed to help families and physicians work together to make the best decisions about a child’s care.
Dr. Greenhill is on the advisory board of Quotient, which manufactures an ADHD testing system, and is a consultant for the Health Information Technology Lab.
NEW YORK – Assessing nonresponsiveness to attention-deficit/hyperactivity disorder treatment requires a bit of detective work, according to Dr. Laurence L. Greenhill.
The reason can be as simple as a little kid not being able to swallow a big pill, or as complex as a dysfunctional family dynamic that interferes with medication adherence. But once the problem is rooted out and addressed, most refractory patients can experience a good response, Dr. Greenhill said at a psychopharmacology update held by the American Academy of Child and Adolescent Psychiatry.
Since primary care physicians usually continue to manage children who respond to ADHD medications, psychiatrists are usually the ones who see nonresponders, said Dr. Greenhill, a child and adolescent psychiatrist at the New York Psychiatric Institute.
Medication nonadherence, the most common cause of a failure to improve, can arise from numerous situations.
On the simple side, it might be a matter of finding the right form of medication; a liquid or sprinkle capsule might be much easier for a child to take than a pill. And not all pills are created equally easy to take.
"For example, [the osmotic controlled release oral delivery system methylphenidate] just went off patent, and generics are now available. But some of these generics are much bigger. In fact, one of the 18-mg pills is twice as large as the patent medicine, and lots of kids can’t swallow it," he said.
The ADHD medication guide published by Long Island Jewish Hospital can be a helpful tool when working with parents on this issue. It lists all the Food and Drug Administration–approved medications for ADHD, with full-size photographs of each capsule, tablet, or pill.
Some generics are not pharmacokinetically or pharmacodynamically identical to the original formulation, Dr. Greenhill noted. Although the drug has to be molecularly identical and dose identical, "the ascending dose curve and duration of action need not be matched." Some generic formulations do fall into this problematic category. "For this reason, I try to encourage parents to get the brand," said Dr. Greenhill, adding that he has no financial interest in any of the drugs.
Medication nonadherence also can be attributable to uncomfortable or even intolerable side effects. These can include gastrointestinal issues, trouble sleeping, lack of appetite, restlessness, irritability, and "feeling fidgety."
Dosage adjustments or a medication change might be in order. For appetite issues, recommend giving the medication after meals, and reassure parents it’s OK to let a child eat later in the evening, when hunger may return.
It’s important to get the child’s growth records from the pediatrician, and plot height and weight curves every 6 months. If there’s a consistent fall-off, consider lowering the dose or changing to another drug.
Contrary to widely held belief, stimulants don’t pose significant cardiac risks to most children. A baseline electrocardiogram is really only necessary for a child who has a family history of sudden cardiac death or a personal history of syncope or cardiac abnormalities. Blood pressure and pulse should be monitored at every visit.
Melatonin is worth a try for youngsters whose ADHD meds interfere with good sleep, Dr. Greenhill said.
"I would start at 1 mg/night and work up," he said. "Starting at a high dose can actually shut off the naturally occurring melatonin. Plasma levels peak about an hour after taking it, so timing is important. I usually start with it about 3 hours before the scheduled sleeping time and then adjust."
Family dynamics also can play a big role in medication nonadherence. "ADHD families are often poor at scheduling activities, sometimes to the extent that parents are the ones who forget to give the medication. They also might not have a clear idea of how to give it, and just leave it on the kitchen table, making it the child’s responsibility to take it every day.
"If this is a child who can’t remember to bring homework back from school, then how is he going to remember to stay on schedule with medication?"
If it’s clear that parents are having difficulty in this area, the simplest thing to do is send the medicine to school and ask the nurse to administer it. Switching to a long-acting form might help, too, since it’s just easier to remember to take one pill than to take two.
The ADHD Parents Medication Guide is a great resource that can be used to get parents actively involved with the child’s drug therapy, Dr. Greenhill said. Developed by the American Psychiatric Association and the American Academy of Child and Adolescent Psychiatry, the online guide is designed to help families and physicians work together to make the best decisions about a child’s care.
Dr. Greenhill is on the advisory board of Quotient, which manufactures an ADHD testing system, and is a consultant for the Health Information Technology Lab.
NEW YORK – Assessing nonresponsiveness to attention-deficit/hyperactivity disorder treatment requires a bit of detective work, according to Dr. Laurence L. Greenhill.
The reason can be as simple as a little kid not being able to swallow a big pill, or as complex as a dysfunctional family dynamic that interferes with medication adherence. But once the problem is rooted out and addressed, most refractory patients can experience a good response, Dr. Greenhill said at a psychopharmacology update held by the American Academy of Child and Adolescent Psychiatry.
Since primary care physicians usually continue to manage children who respond to ADHD medications, psychiatrists are usually the ones who see nonresponders, said Dr. Greenhill, a child and adolescent psychiatrist at the New York Psychiatric Institute.
Medication nonadherence, the most common cause of a failure to improve, can arise from numerous situations.
On the simple side, it might be a matter of finding the right form of medication; a liquid or sprinkle capsule might be much easier for a child to take than a pill. And not all pills are created equally easy to take.
"For example, [the osmotic controlled release oral delivery system methylphenidate] just went off patent, and generics are now available. But some of these generics are much bigger. In fact, one of the 18-mg pills is twice as large as the patent medicine, and lots of kids can’t swallow it," he said.
The ADHD medication guide published by Long Island Jewish Hospital can be a helpful tool when working with parents on this issue. It lists all the Food and Drug Administration–approved medications for ADHD, with full-size photographs of each capsule, tablet, or pill.
Some generics are not pharmacokinetically or pharmacodynamically identical to the original formulation, Dr. Greenhill noted. Although the drug has to be molecularly identical and dose identical, "the ascending dose curve and duration of action need not be matched." Some generic formulations do fall into this problematic category. "For this reason, I try to encourage parents to get the brand," said Dr. Greenhill, adding that he has no financial interest in any of the drugs.
Medication nonadherence also can be attributable to uncomfortable or even intolerable side effects. These can include gastrointestinal issues, trouble sleeping, lack of appetite, restlessness, irritability, and "feeling fidgety."
Dosage adjustments or a medication change might be in order. For appetite issues, recommend giving the medication after meals, and reassure parents it’s OK to let a child eat later in the evening, when hunger may return.
It’s important to get the child’s growth records from the pediatrician, and plot height and weight curves every 6 months. If there’s a consistent fall-off, consider lowering the dose or changing to another drug.
Contrary to widely held belief, stimulants don’t pose significant cardiac risks to most children. A baseline electrocardiogram is really only necessary for a child who has a family history of sudden cardiac death or a personal history of syncope or cardiac abnormalities. Blood pressure and pulse should be monitored at every visit.
Melatonin is worth a try for youngsters whose ADHD meds interfere with good sleep, Dr. Greenhill said.
"I would start at 1 mg/night and work up," he said. "Starting at a high dose can actually shut off the naturally occurring melatonin. Plasma levels peak about an hour after taking it, so timing is important. I usually start with it about 3 hours before the scheduled sleeping time and then adjust."
Family dynamics also can play a big role in medication nonadherence. "ADHD families are often poor at scheduling activities, sometimes to the extent that parents are the ones who forget to give the medication. They also might not have a clear idea of how to give it, and just leave it on the kitchen table, making it the child’s responsibility to take it every day.
"If this is a child who can’t remember to bring homework back from school, then how is he going to remember to stay on schedule with medication?"
If it’s clear that parents are having difficulty in this area, the simplest thing to do is send the medicine to school and ask the nurse to administer it. Switching to a long-acting form might help, too, since it’s just easier to remember to take one pill than to take two.
The ADHD Parents Medication Guide is a great resource that can be used to get parents actively involved with the child’s drug therapy, Dr. Greenhill said. Developed by the American Psychiatric Association and the American Academy of Child and Adolescent Psychiatry, the online guide is designed to help families and physicians work together to make the best decisions about a child’s care.
Dr. Greenhill is on the advisory board of Quotient, which manufactures an ADHD testing system, and is a consultant for the Health Information Technology Lab.
EXPERT ANALYSIS FROM THE PSYCHOPHARMACOLOGY UPDATE INSTITUTE
ACA exchanges limiting for patients with blood cancers, report suggests

Credit: CDC
A new report suggests that many health plans in the insurance exchanges mandated by the Affordable Care Act (ACA) will impose high out-of-pocket costs for patients with hematologic malignancies and provide limited access to specialty treatment centers.
Furthermore, although the plans analyzed appear to provide adequate coverage of hematology/oncology drugs, most require prior authorization.
In other words, the insurer must be notified and may not approve the purchase of a drug based on medical evidence or other criteria.
This report, “2014 Individual Exchange Policies in Four States: An Early Look for Patients with Blood Cancers,” was commissioned by the Leukemia & Lymphoma Society and prepared by Milliman, Inc.
It provides a look at the 2014 individual benefit designs, coverage benefits, and premiums for policies sold on 4 state health insurance exchanges—California, New York, Florida, and Texas—with a focus on items of interest for patients with hematologic malignancies.
“[W]hile many new rules under ACA make obtaining insurance easier for people with blood cancers, such as prohibiting companies from turning away patients with pre-existing conditions and eliminating lifetime coverage limitations, the Milliman report identifies several areas of concern that we want cancer patients to be aware of and policymakers to address,” said Mark Velleca, MD, PhD, chief policy and advocacy officer of the Leukemia & Lymphoma Society.
Premium costs
To compare monthly premium rates, the report’s authors captured rates for a 50-year-old non-smoker with an annual income of $90,000 residing in Houston, Los Angeles, Miami, or New York City.
They found considerable variation according to plan type and location, but overall, plans were cheapest in Houston. Monthly premiums for Houston ranged from $234 to $520. The range was $274 to $566 for Los Angeles, $277 to $635 for Miami, and $307 to $896 for New York.
The ranges reflect the costs according to plan type. Each insurer offers 4 different health plans: Platinum (about 10% cost-sharing), Gold (roughly 20%), Silver (roughly 30%), and Bronze (roughly 40%).
Cost-sharing
The authors noted that the lower-tier Bronze and Silver plans require significant cost-sharing for patients. The report revealed high deductibles in the health plans, sometimes nearly as high as the out-of-pocket ceiling.
Deductibles for the Silver and Bronze plans are often at least $2000 and $4000, respectively, for individuals. The maximum out-of-pocket limits set for 2014 are $6350 for an individual policy and $12,799 for a family policy.
Some insurers offer plans in some states with lower out-of-pocket limits. However, the out-of-pocket limit does not apply to non-covered drugs or treatment centers.
Drug coverage
When analyzing drug coverage, the authors decided to look at 3 drugs used to treat chronic myeloid leukemia—imatinib (Gleevec), nilotinib (Tasigna), and dasatinib (Sprycel)—and 5 drugs used to treat multiple myeloma—thalidomide (Thalomid), lenalidomide (Revlimid), pomalidomide (Pomalyst), cyclophosphamide (Cytoxan), and melphalan (Alkeran).
Most of the insurers require prior authorization for these drugs, but most of them cover all 3 chronic myeloid leukemia drugs and a majority of the myeloma drugs. Pomalyst and Cytoxan are often not covered, although most insurers do cover generic cyclophosphamide.
Network adequacy
Most of the insurers studied do not cover all NCI-designated cancer and transplant centers, and a few do not cover any of these centers. The authors said this could discourage patient enrollment in these plans or mean that a patient’s recommended treatment is not covered.
And since it is unlikely that any out-of-network expenses will count toward a patient’s out-of-pocket maximum, cancer patients could accumulate thousands of dollars of medical expenses and never reach their out-of-pocket maximum.
The authors did note, however, that satisfactory cancer care can be provided outside of NCI-designated cancer and transplant centers.
For more details, see the full report. ![]()

Credit: CDC
A new report suggests that many health plans in the insurance exchanges mandated by the Affordable Care Act (ACA) will impose high out-of-pocket costs for patients with hematologic malignancies and provide limited access to specialty treatment centers.
Furthermore, although the plans analyzed appear to provide adequate coverage of hematology/oncology drugs, most require prior authorization.
In other words, the insurer must be notified and may not approve the purchase of a drug based on medical evidence or other criteria.
This report, “2014 Individual Exchange Policies in Four States: An Early Look for Patients with Blood Cancers,” was commissioned by the Leukemia & Lymphoma Society and prepared by Milliman, Inc.
It provides a look at the 2014 individual benefit designs, coverage benefits, and premiums for policies sold on 4 state health insurance exchanges—California, New York, Florida, and Texas—with a focus on items of interest for patients with hematologic malignancies.
“[W]hile many new rules under ACA make obtaining insurance easier for people with blood cancers, such as prohibiting companies from turning away patients with pre-existing conditions and eliminating lifetime coverage limitations, the Milliman report identifies several areas of concern that we want cancer patients to be aware of and policymakers to address,” said Mark Velleca, MD, PhD, chief policy and advocacy officer of the Leukemia & Lymphoma Society.
Premium costs
To compare monthly premium rates, the report’s authors captured rates for a 50-year-old non-smoker with an annual income of $90,000 residing in Houston, Los Angeles, Miami, or New York City.
They found considerable variation according to plan type and location, but overall, plans were cheapest in Houston. Monthly premiums for Houston ranged from $234 to $520. The range was $274 to $566 for Los Angeles, $277 to $635 for Miami, and $307 to $896 for New York.
The ranges reflect the costs according to plan type. Each insurer offers 4 different health plans: Platinum (about 10% cost-sharing), Gold (roughly 20%), Silver (roughly 30%), and Bronze (roughly 40%).
Cost-sharing
The authors noted that the lower-tier Bronze and Silver plans require significant cost-sharing for patients. The report revealed high deductibles in the health plans, sometimes nearly as high as the out-of-pocket ceiling.
Deductibles for the Silver and Bronze plans are often at least $2000 and $4000, respectively, for individuals. The maximum out-of-pocket limits set for 2014 are $6350 for an individual policy and $12,799 for a family policy.
Some insurers offer plans in some states with lower out-of-pocket limits. However, the out-of-pocket limit does not apply to non-covered drugs or treatment centers.
Drug coverage
When analyzing drug coverage, the authors decided to look at 3 drugs used to treat chronic myeloid leukemia—imatinib (Gleevec), nilotinib (Tasigna), and dasatinib (Sprycel)—and 5 drugs used to treat multiple myeloma—thalidomide (Thalomid), lenalidomide (Revlimid), pomalidomide (Pomalyst), cyclophosphamide (Cytoxan), and melphalan (Alkeran).
Most of the insurers require prior authorization for these drugs, but most of them cover all 3 chronic myeloid leukemia drugs and a majority of the myeloma drugs. Pomalyst and Cytoxan are often not covered, although most insurers do cover generic cyclophosphamide.
Network adequacy
Most of the insurers studied do not cover all NCI-designated cancer and transplant centers, and a few do not cover any of these centers. The authors said this could discourage patient enrollment in these plans or mean that a patient’s recommended treatment is not covered.
And since it is unlikely that any out-of-network expenses will count toward a patient’s out-of-pocket maximum, cancer patients could accumulate thousands of dollars of medical expenses and never reach their out-of-pocket maximum.
The authors did note, however, that satisfactory cancer care can be provided outside of NCI-designated cancer and transplant centers.
For more details, see the full report. ![]()

Credit: CDC
A new report suggests that many health plans in the insurance exchanges mandated by the Affordable Care Act (ACA) will impose high out-of-pocket costs for patients with hematologic malignancies and provide limited access to specialty treatment centers.
Furthermore, although the plans analyzed appear to provide adequate coverage of hematology/oncology drugs, most require prior authorization.
In other words, the insurer must be notified and may not approve the purchase of a drug based on medical evidence or other criteria.
This report, “2014 Individual Exchange Policies in Four States: An Early Look for Patients with Blood Cancers,” was commissioned by the Leukemia & Lymphoma Society and prepared by Milliman, Inc.
It provides a look at the 2014 individual benefit designs, coverage benefits, and premiums for policies sold on 4 state health insurance exchanges—California, New York, Florida, and Texas—with a focus on items of interest for patients with hematologic malignancies.
“[W]hile many new rules under ACA make obtaining insurance easier for people with blood cancers, such as prohibiting companies from turning away patients with pre-existing conditions and eliminating lifetime coverage limitations, the Milliman report identifies several areas of concern that we want cancer patients to be aware of and policymakers to address,” said Mark Velleca, MD, PhD, chief policy and advocacy officer of the Leukemia & Lymphoma Society.
Premium costs
To compare monthly premium rates, the report’s authors captured rates for a 50-year-old non-smoker with an annual income of $90,000 residing in Houston, Los Angeles, Miami, or New York City.
They found considerable variation according to plan type and location, but overall, plans were cheapest in Houston. Monthly premiums for Houston ranged from $234 to $520. The range was $274 to $566 for Los Angeles, $277 to $635 for Miami, and $307 to $896 for New York.
The ranges reflect the costs according to plan type. Each insurer offers 4 different health plans: Platinum (about 10% cost-sharing), Gold (roughly 20%), Silver (roughly 30%), and Bronze (roughly 40%).
Cost-sharing
The authors noted that the lower-tier Bronze and Silver plans require significant cost-sharing for patients. The report revealed high deductibles in the health plans, sometimes nearly as high as the out-of-pocket ceiling.
Deductibles for the Silver and Bronze plans are often at least $2000 and $4000, respectively, for individuals. The maximum out-of-pocket limits set for 2014 are $6350 for an individual policy and $12,799 for a family policy.
Some insurers offer plans in some states with lower out-of-pocket limits. However, the out-of-pocket limit does not apply to non-covered drugs or treatment centers.
Drug coverage
When analyzing drug coverage, the authors decided to look at 3 drugs used to treat chronic myeloid leukemia—imatinib (Gleevec), nilotinib (Tasigna), and dasatinib (Sprycel)—and 5 drugs used to treat multiple myeloma—thalidomide (Thalomid), lenalidomide (Revlimid), pomalidomide (Pomalyst), cyclophosphamide (Cytoxan), and melphalan (Alkeran).
Most of the insurers require prior authorization for these drugs, but most of them cover all 3 chronic myeloid leukemia drugs and a majority of the myeloma drugs. Pomalyst and Cytoxan are often not covered, although most insurers do cover generic cyclophosphamide.
Network adequacy
Most of the insurers studied do not cover all NCI-designated cancer and transplant centers, and a few do not cover any of these centers. The authors said this could discourage patient enrollment in these plans or mean that a patient’s recommended treatment is not covered.
And since it is unlikely that any out-of-network expenses will count toward a patient’s out-of-pocket maximum, cancer patients could accumulate thousands of dollars of medical expenses and never reach their out-of-pocket maximum.
The authors did note, however, that satisfactory cancer care can be provided outside of NCI-designated cancer and transplant centers.
For more details, see the full report. ![]()
State-of-the-Art Wound Healing: Skin Substitutes for Chronic Wounds
Should you communicate with patients online?
A lot of mythology regarding the new Health Insurance Portability and Accountability Act rules (which I discussed in detail a few months ago) continues to circulate. One of the biggest myths is that e-mail communication with patients is now forbidden, so let’s debunk that one right now.
Here is a statement lifted verbatim from the official HIPAA web site (FAQ section):
"Patients may initiate communications with a provider using e-mail. If this situation occurs, the health care provider can assume (unless the patient has explicitly stated otherwise) that e-mail communications are acceptable to the individual.
"If the provider feels the patient may not be aware of the possible risks of using unencrypted e-mail, or has concerns about potential liability, the provider can alert the patient of those risks, and let the patient decide whether to continue e-mail communications."
Okay, so it’s permissible – but is it a good idea? Aside from the obvious privacy issues, many physicians balk at taking on one more unreimbursed demand on their time. While no one denies that these concerns are real, there also are real benefits to be gained from properly managed online communication – among them increased practice efficiency, and increased quality of care and satisfaction for patients.
I started giving one of my e-mail addresses to selected patients several years ago as an experiment, hoping to take some pressure off of our overloaded telephone system. The patients were grateful for simplified and more direct access, and I appreciated the decrease in phone messages and interruptions while I was seeing patients. I also noticed a decrease in those frustrating, unnecessary office visits – you know, "The rash is completely gone, but you told me to come back ..."
In general, I have found that the advantages for everyone involved (not least my nurses and receptionists) far outweigh the problems. And now, newer technologies such as encryption, web-based messaging, and integrated online communication should go a long way toward assuaging privacy concerns.
Encryption software is now inexpensive, readily available, and easily added to most e-mail systems. Packages are available from companies such as EMC, Hilgraeve, Kryptiq, Proofpoint, Axway, and ZixCorp, among many others. (As always, I have no financial interest in any company mentioned in this column.)
Rather than simply encrypting their e-mail, increasing numbers of physicians are opting for the route taken by most online banking and shopping sites: a secure website. Patients sign onto it and send a message to your office. Physicians or staffers are notified in their regular e-mail of messages on the website, and then they post a reply to the patient on the site that can only be accessed by the patient. The patient is notified of the practice’s reply in his or her regular e-mail. Web-based messaging services can be incorporated into existing practice sites or can stand on their own. Medfusion, MyDocOnline, and RelayHealth are among the many vendors that offer secure cloud-based messaging services.
A big advantage of using such a service is that you’re partnering with a vendor who has to stay on top of HIPAA and other privacy requirements. Another is the option of using electronic forms, or templates. Templates ensure that patients’ messages include the information needed to process prescription refill requests, or to adequately describe their problems and provide some clinical assessment data for the physician or nurse. They also can be designed to triage messages to the front- and back-office staff, so that time is not wasted bouncing messages around the office until the proper responder is found.
Many electronic health record systems now allow you to integrate a web-based messaging system. Advantages here include the ability to view the patient’s medical record from home or anywhere else before answering the communication, and the fact that all messages automatically become a part of the patient’s record. Electronic health record vendors that provide this type of system include Allscripts, CompuGroup Medical, Cerner, Epic, GE Medical Systems, NextGen, McKesson, and Siemens.
As with any cloud-based service, insist on multiple layers of security, uninterruptible power sources, instant switchover to backup hardware in the event of a crash, and frequent, reliable backups.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is a clinical associate professor of dermatology at Seton Hall University School of Graduate Medical Education in South Orange, N.J. Dr. Eastern is a two-time past president of the Dermatological Society of New Jersey, and currently serves on its executive board. He holds teaching positions at several hospitals and has delivered more than 500 academic speaking presentations. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Skin & Allergy News.
A lot of mythology regarding the new Health Insurance Portability and Accountability Act rules (which I discussed in detail a few months ago) continues to circulate. One of the biggest myths is that e-mail communication with patients is now forbidden, so let’s debunk that one right now.
Here is a statement lifted verbatim from the official HIPAA web site (FAQ section):
"Patients may initiate communications with a provider using e-mail. If this situation occurs, the health care provider can assume (unless the patient has explicitly stated otherwise) that e-mail communications are acceptable to the individual.
"If the provider feels the patient may not be aware of the possible risks of using unencrypted e-mail, or has concerns about potential liability, the provider can alert the patient of those risks, and let the patient decide whether to continue e-mail communications."
Okay, so it’s permissible – but is it a good idea? Aside from the obvious privacy issues, many physicians balk at taking on one more unreimbursed demand on their time. While no one denies that these concerns are real, there also are real benefits to be gained from properly managed online communication – among them increased practice efficiency, and increased quality of care and satisfaction for patients.
I started giving one of my e-mail addresses to selected patients several years ago as an experiment, hoping to take some pressure off of our overloaded telephone system. The patients were grateful for simplified and more direct access, and I appreciated the decrease in phone messages and interruptions while I was seeing patients. I also noticed a decrease in those frustrating, unnecessary office visits – you know, "The rash is completely gone, but you told me to come back ..."
In general, I have found that the advantages for everyone involved (not least my nurses and receptionists) far outweigh the problems. And now, newer technologies such as encryption, web-based messaging, and integrated online communication should go a long way toward assuaging privacy concerns.
Encryption software is now inexpensive, readily available, and easily added to most e-mail systems. Packages are available from companies such as EMC, Hilgraeve, Kryptiq, Proofpoint, Axway, and ZixCorp, among many others. (As always, I have no financial interest in any company mentioned in this column.)
Rather than simply encrypting their e-mail, increasing numbers of physicians are opting for the route taken by most online banking and shopping sites: a secure website. Patients sign onto it and send a message to your office. Physicians or staffers are notified in their regular e-mail of messages on the website, and then they post a reply to the patient on the site that can only be accessed by the patient. The patient is notified of the practice’s reply in his or her regular e-mail. Web-based messaging services can be incorporated into existing practice sites or can stand on their own. Medfusion, MyDocOnline, and RelayHealth are among the many vendors that offer secure cloud-based messaging services.
A big advantage of using such a service is that you’re partnering with a vendor who has to stay on top of HIPAA and other privacy requirements. Another is the option of using electronic forms, or templates. Templates ensure that patients’ messages include the information needed to process prescription refill requests, or to adequately describe their problems and provide some clinical assessment data for the physician or nurse. They also can be designed to triage messages to the front- and back-office staff, so that time is not wasted bouncing messages around the office until the proper responder is found.
Many electronic health record systems now allow you to integrate a web-based messaging system. Advantages here include the ability to view the patient’s medical record from home or anywhere else before answering the communication, and the fact that all messages automatically become a part of the patient’s record. Electronic health record vendors that provide this type of system include Allscripts, CompuGroup Medical, Cerner, Epic, GE Medical Systems, NextGen, McKesson, and Siemens.
As with any cloud-based service, insist on multiple layers of security, uninterruptible power sources, instant switchover to backup hardware in the event of a crash, and frequent, reliable backups.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is a clinical associate professor of dermatology at Seton Hall University School of Graduate Medical Education in South Orange, N.J. Dr. Eastern is a two-time past president of the Dermatological Society of New Jersey, and currently serves on its executive board. He holds teaching positions at several hospitals and has delivered more than 500 academic speaking presentations. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Skin & Allergy News.
A lot of mythology regarding the new Health Insurance Portability and Accountability Act rules (which I discussed in detail a few months ago) continues to circulate. One of the biggest myths is that e-mail communication with patients is now forbidden, so let’s debunk that one right now.
Here is a statement lifted verbatim from the official HIPAA web site (FAQ section):
"Patients may initiate communications with a provider using e-mail. If this situation occurs, the health care provider can assume (unless the patient has explicitly stated otherwise) that e-mail communications are acceptable to the individual.
"If the provider feels the patient may not be aware of the possible risks of using unencrypted e-mail, or has concerns about potential liability, the provider can alert the patient of those risks, and let the patient decide whether to continue e-mail communications."
Okay, so it’s permissible – but is it a good idea? Aside from the obvious privacy issues, many physicians balk at taking on one more unreimbursed demand on their time. While no one denies that these concerns are real, there also are real benefits to be gained from properly managed online communication – among them increased practice efficiency, and increased quality of care and satisfaction for patients.
I started giving one of my e-mail addresses to selected patients several years ago as an experiment, hoping to take some pressure off of our overloaded telephone system. The patients were grateful for simplified and more direct access, and I appreciated the decrease in phone messages and interruptions while I was seeing patients. I also noticed a decrease in those frustrating, unnecessary office visits – you know, "The rash is completely gone, but you told me to come back ..."
In general, I have found that the advantages for everyone involved (not least my nurses and receptionists) far outweigh the problems. And now, newer technologies such as encryption, web-based messaging, and integrated online communication should go a long way toward assuaging privacy concerns.
Encryption software is now inexpensive, readily available, and easily added to most e-mail systems. Packages are available from companies such as EMC, Hilgraeve, Kryptiq, Proofpoint, Axway, and ZixCorp, among many others. (As always, I have no financial interest in any company mentioned in this column.)
Rather than simply encrypting their e-mail, increasing numbers of physicians are opting for the route taken by most online banking and shopping sites: a secure website. Patients sign onto it and send a message to your office. Physicians or staffers are notified in their regular e-mail of messages on the website, and then they post a reply to the patient on the site that can only be accessed by the patient. The patient is notified of the practice’s reply in his or her regular e-mail. Web-based messaging services can be incorporated into existing practice sites or can stand on their own. Medfusion, MyDocOnline, and RelayHealth are among the many vendors that offer secure cloud-based messaging services.
A big advantage of using such a service is that you’re partnering with a vendor who has to stay on top of HIPAA and other privacy requirements. Another is the option of using electronic forms, or templates. Templates ensure that patients’ messages include the information needed to process prescription refill requests, or to adequately describe their problems and provide some clinical assessment data for the physician or nurse. They also can be designed to triage messages to the front- and back-office staff, so that time is not wasted bouncing messages around the office until the proper responder is found.
Many electronic health record systems now allow you to integrate a web-based messaging system. Advantages here include the ability to view the patient’s medical record from home or anywhere else before answering the communication, and the fact that all messages automatically become a part of the patient’s record. Electronic health record vendors that provide this type of system include Allscripts, CompuGroup Medical, Cerner, Epic, GE Medical Systems, NextGen, McKesson, and Siemens.
As with any cloud-based service, insist on multiple layers of security, uninterruptible power sources, instant switchover to backup hardware in the event of a crash, and frequent, reliable backups.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is a clinical associate professor of dermatology at Seton Hall University School of Graduate Medical Education in South Orange, N.J. Dr. Eastern is a two-time past president of the Dermatological Society of New Jersey, and currently serves on its executive board. He holds teaching positions at several hospitals and has delivered more than 500 academic speaking presentations. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Skin & Allergy News.
CTLs prove effective against EBV lymphomas

Cytotoxic T lymphocytes (CTLs) targeting Epstein-Barr virus (EBV) proteins appear to be a promising treatment option for patients with aggressive lymphomas.
Researchers tested the autologous CTLs in a cohort of 50 patients with Hodgkin or non-Hodgkin lymphoma.
The treatment produced responses in about 62% of patients with relapsed or refractory disease.
And it sustained remissions in roughly 93% of patients who were at a high risk of relapse.
Catherine Bollard, MD, of the Children’s National Medical Center in Washington, DC, and her colleagues reported these results in the Journal of Clinical Oncology.
The investigators noted that about 40% of lymphoma patients have tumor cells expressing the type II latency EBV antigens latent membrane protein 1 (LMP1) and LMP2. But T cells specific for these antigens are present in low numbers and may not “recognize” the tumors they should attack.
So Dr Bollard and her colleagues decided to test the effects of infusing LMP-directed CTLs into 50 patients with EBV-positive lymphomas.
The researchers used adenoviral vector-transduced dendritic cells and EBV-transformed B–lymphoblastoid cell lines as antigen-presenting cells to activate and expand LMP-specific T cells.
For some patients, the team used an adenoviral vector encoding the LMP2 antigen alone (n=17). And for others, they used a vector encoding both LMP1 and LMP2 (n=33).
Twenty-nine of the patients were in remission when they received CTL infusions, but they were at a high risk of relapse. The remaining 21 patients had relapsed or refractory disease at the time of CTL infusion.
Twenty-seven of the 29 patients who received CTLs as an adjuvant treatment remained in remission from their disease at 3.1 years after treatment.
However, the 2-year event-free survival rate was 82% for this group of patients. None of them died of lymphoma, but 9 died from complications associated with the chemotherapy and radiation they had received.
“That’s why this research is important,” Dr Bollard said. “Patients with lymphomas traditionally have a good cure rate with chemotherapy and radiation. What kills them is the side effects of those treatments—second cancers, lung, and heart disease.”
Of the 21 patients with relapsed or refractory disease, 13 responded to CTL infusions. And 11 patients achieved a complete response.
In this group, the 2-year event-free survival rate was about 50%, regardless of whether patients received CTLs directed against LMP1/2 or LMP2 alone.
The investigators found that responses were associated with effector and central memory LMP1-specific CTLs but not with the patient’s type of lymphoma or lymphopenic status.
Even those patients with limited in vivo expansion of LMP-directed CTLs achieved complete responses. And this effect was associated with epitope spreading.
“This is a targeted therapeutic approach that we hope can be used early in the disease to treat relapse,” Dr Bollard said. “We saw good outcomes here. Eventually, it could be a front-line therapy.”
The researchers noted that the difficulty of tailoring CTLs for each patient has been cited as a barrier to this type of treatment. But currently available treatments can be expensive and induce severe side effects that require hospitalization.
“Although we spend some time making the cells, patients go home with few side effects and few associated hospital costs,” said study author Cliona Rooney, PhD, of the Baylor College of Medicine in Houston, Texas. “It can be less costly than chemotherapy.”
In this study, the investigators did not see any toxicities attributable to CTL infusion. One patient did have CNS deterioration 2 weeks after infusion, but this was attributed to disease progression.
And another patient developed respiratory complications about 4 weeks after a second CTL infusion. But this was attributed to an intercurrent infection, and the patient made a complete recovery. ![]()

Cytotoxic T lymphocytes (CTLs) targeting Epstein-Barr virus (EBV) proteins appear to be a promising treatment option for patients with aggressive lymphomas.
Researchers tested the autologous CTLs in a cohort of 50 patients with Hodgkin or non-Hodgkin lymphoma.
The treatment produced responses in about 62% of patients with relapsed or refractory disease.
And it sustained remissions in roughly 93% of patients who were at a high risk of relapse.
Catherine Bollard, MD, of the Children’s National Medical Center in Washington, DC, and her colleagues reported these results in the Journal of Clinical Oncology.
The investigators noted that about 40% of lymphoma patients have tumor cells expressing the type II latency EBV antigens latent membrane protein 1 (LMP1) and LMP2. But T cells specific for these antigens are present in low numbers and may not “recognize” the tumors they should attack.
So Dr Bollard and her colleagues decided to test the effects of infusing LMP-directed CTLs into 50 patients with EBV-positive lymphomas.
The researchers used adenoviral vector-transduced dendritic cells and EBV-transformed B–lymphoblastoid cell lines as antigen-presenting cells to activate and expand LMP-specific T cells.
For some patients, the team used an adenoviral vector encoding the LMP2 antigen alone (n=17). And for others, they used a vector encoding both LMP1 and LMP2 (n=33).
Twenty-nine of the patients were in remission when they received CTL infusions, but they were at a high risk of relapse. The remaining 21 patients had relapsed or refractory disease at the time of CTL infusion.
Twenty-seven of the 29 patients who received CTLs as an adjuvant treatment remained in remission from their disease at 3.1 years after treatment.
However, the 2-year event-free survival rate was 82% for this group of patients. None of them died of lymphoma, but 9 died from complications associated with the chemotherapy and radiation they had received.
“That’s why this research is important,” Dr Bollard said. “Patients with lymphomas traditionally have a good cure rate with chemotherapy and radiation. What kills them is the side effects of those treatments—second cancers, lung, and heart disease.”
Of the 21 patients with relapsed or refractory disease, 13 responded to CTL infusions. And 11 patients achieved a complete response.
In this group, the 2-year event-free survival rate was about 50%, regardless of whether patients received CTLs directed against LMP1/2 or LMP2 alone.
The investigators found that responses were associated with effector and central memory LMP1-specific CTLs but not with the patient’s type of lymphoma or lymphopenic status.
Even those patients with limited in vivo expansion of LMP-directed CTLs achieved complete responses. And this effect was associated with epitope spreading.
“This is a targeted therapeutic approach that we hope can be used early in the disease to treat relapse,” Dr Bollard said. “We saw good outcomes here. Eventually, it could be a front-line therapy.”
The researchers noted that the difficulty of tailoring CTLs for each patient has been cited as a barrier to this type of treatment. But currently available treatments can be expensive and induce severe side effects that require hospitalization.
“Although we spend some time making the cells, patients go home with few side effects and few associated hospital costs,” said study author Cliona Rooney, PhD, of the Baylor College of Medicine in Houston, Texas. “It can be less costly than chemotherapy.”
In this study, the investigators did not see any toxicities attributable to CTL infusion. One patient did have CNS deterioration 2 weeks after infusion, but this was attributed to disease progression.
And another patient developed respiratory complications about 4 weeks after a second CTL infusion. But this was attributed to an intercurrent infection, and the patient made a complete recovery. ![]()

Cytotoxic T lymphocytes (CTLs) targeting Epstein-Barr virus (EBV) proteins appear to be a promising treatment option for patients with aggressive lymphomas.
Researchers tested the autologous CTLs in a cohort of 50 patients with Hodgkin or non-Hodgkin lymphoma.
The treatment produced responses in about 62% of patients with relapsed or refractory disease.
And it sustained remissions in roughly 93% of patients who were at a high risk of relapse.
Catherine Bollard, MD, of the Children’s National Medical Center in Washington, DC, and her colleagues reported these results in the Journal of Clinical Oncology.
The investigators noted that about 40% of lymphoma patients have tumor cells expressing the type II latency EBV antigens latent membrane protein 1 (LMP1) and LMP2. But T cells specific for these antigens are present in low numbers and may not “recognize” the tumors they should attack.
So Dr Bollard and her colleagues decided to test the effects of infusing LMP-directed CTLs into 50 patients with EBV-positive lymphomas.
The researchers used adenoviral vector-transduced dendritic cells and EBV-transformed B–lymphoblastoid cell lines as antigen-presenting cells to activate and expand LMP-specific T cells.
For some patients, the team used an adenoviral vector encoding the LMP2 antigen alone (n=17). And for others, they used a vector encoding both LMP1 and LMP2 (n=33).
Twenty-nine of the patients were in remission when they received CTL infusions, but they were at a high risk of relapse. The remaining 21 patients had relapsed or refractory disease at the time of CTL infusion.
Twenty-seven of the 29 patients who received CTLs as an adjuvant treatment remained in remission from their disease at 3.1 years after treatment.
However, the 2-year event-free survival rate was 82% for this group of patients. None of them died of lymphoma, but 9 died from complications associated with the chemotherapy and radiation they had received.
“That’s why this research is important,” Dr Bollard said. “Patients with lymphomas traditionally have a good cure rate with chemotherapy and radiation. What kills them is the side effects of those treatments—second cancers, lung, and heart disease.”
Of the 21 patients with relapsed or refractory disease, 13 responded to CTL infusions. And 11 patients achieved a complete response.
In this group, the 2-year event-free survival rate was about 50%, regardless of whether patients received CTLs directed against LMP1/2 or LMP2 alone.
The investigators found that responses were associated with effector and central memory LMP1-specific CTLs but not with the patient’s type of lymphoma or lymphopenic status.
Even those patients with limited in vivo expansion of LMP-directed CTLs achieved complete responses. And this effect was associated with epitope spreading.
“This is a targeted therapeutic approach that we hope can be used early in the disease to treat relapse,” Dr Bollard said. “We saw good outcomes here. Eventually, it could be a front-line therapy.”
The researchers noted that the difficulty of tailoring CTLs for each patient has been cited as a barrier to this type of treatment. But currently available treatments can be expensive and induce severe side effects that require hospitalization.
“Although we spend some time making the cells, patients go home with few side effects and few associated hospital costs,” said study author Cliona Rooney, PhD, of the Baylor College of Medicine in Houston, Texas. “It can be less costly than chemotherapy.”
In this study, the investigators did not see any toxicities attributable to CTL infusion. One patient did have CNS deterioration 2 weeks after infusion, but this was attributed to disease progression.
And another patient developed respiratory complications about 4 weeks after a second CTL infusion. But this was attributed to an intercurrent infection, and the patient made a complete recovery. ![]()
Structured Peer Observation of Teaching
Hospitalists are increasingly responsible for educating students and housestaff in internal medicine.[1] Because the quality of teaching is an important factor in learning,[2, 3, 4] leaders in medical education have expressed concern over the rapid shift of teaching responsibilities to this new group of educators.[5, 6, 7, 8] Moreover, recent changes in duty hour restrictions have strained both student and resident education,[9, 10] necessitating the optimization of inpatient teaching.[11, 12] Many hospitalists have recently finished residency and have not had formal training in clinical teaching. Collectively, most hospital medicine groups are early in their careers, have significant clinical obligations,[13] and may not have the bandwidth or expertise to provide faculty development for improving clinical teaching.
Rationally designed and theoretically sound faculty development to improve inpatient clinical teaching is required to meet this challenge. There are a limited number of reports describing faculty development focused on strengthening the teaching of hospitalists, and only 3 utilized direct observation and feedback, 1 of which involved peer observation in the clinical setting.[14, 15, 16] This 2011 report described a narrative method of peer observation and feedback but did not assess for efficacy of the program.[16] To our knowledge, there have been no studies of structured peer observation and feedback to optimize hospitalist attendings' teaching which have evaluated the efficacy of the intervention.
We developed a faculty development program based on peer observation and feedback based on actual teaching practices, using structured feedback anchored in validated and observable measures of effective teaching. We hypothesized that participation in the program would increase confidence in key teaching skills, increase confidence in the ability to give and receive peer feedback, and strengthen attitudes toward peer observation and feedback.
METHODS
Subjects and Setting
The study was conducted at a 570‐bed academic, tertiary care medical center affiliated with an internal medicine residency program of 180 housestaff. Internal medicine ward attendings rotate during 2‐week blocks, and are asked to give formal teaching rounds 3 or 4 times a week (these sessions are distinct from teaching which may happen while rounding on patients). Ward teams are composed of 1 senior resident, 2 interns, and 1 to 2 medical students. The majority of internal medicine ward attendings are hospitalist faculty, hospital medicine fellows, or medicine chief residents. Because outpatient general internists and subspecialists only occasionally attend on the wards, we refer to ward attendings as attending hospitalists in this article. All attending hospitalists were eligible to participate if they attended on the wards at least twice during the academic year. The institutional review board at the University of California, San Francisco approved this study.
Theoretical Framework
We reviewed the literature to optimize our program in 3 conceptual domains: (1) overall structure of the program, (2) definition of effective teaching and (3) effective delivery of feedback.
Over‐reliance on didactics that are disconnected from the work environment is a weakness of traditional faculty development. Individuals may attempt to apply what they have learned, but receiving feedback on their actual workplace practices may be difficult. A recent perspective responds to this fragmentation by conceptualizing faculty development as embedded in both a faculty development community and a workplace community. This model emphasizes translating what faculty have learned in the classroom into practice, and highlights the importance of coaching in the workplace.[17] In accordance with this framework, we designed our program to reach beyond isolated workshops to effectively penetrate the workplace community.
We selected the Stanford Faculty Development Program (SFDP) framework for optimal clinical teaching as our model for recognizing and improving teaching skills. The SFDP was developed as a theory‐based intensive feedback method to improve teaching skills,[18, 19] and has been shown to improve teaching in the ambulatory[20] and inpatient settings.[21, 22] In this widely disseminated framework,[23, 24] excellent clinical teaching is grounded in optimizing observable behaviors organized around 7 domains.[18] A 26‐item instrument to evaluate clinical teaching (SFDP‐26) has been developed based on this framework[25] and has been validated in multiple settings.[26, 27] High‐quality teaching, as defined by the SFDP framework, has been correlated with improved educational outcomes in internal medicine clerkship students.[4]
Feedback is crucial to optimizing teaching,[28, 29, 30] particularly when it incorporates consultation[31] and narrative comments.[32] Peer feedback has several advantages over feedback from learners or from other non‐peer observers (such as supervisors or other evaluators). First, the observers benefit by gaining insight into their own weaknesses and potential areas for growth as teachers.[33, 34] Additionally, collegial observation and feedback may promote supportive teaching relationships between faculty.[35] Furthermore, peer review overcomes the biases that may be present in learner evaluations.[36] We established a 3‐stage feedback technique based on a previously described method.[37] In the first step, the observer elicits self‐appraisal from the speaker. Next, the observer provides specific, behaviorally anchored feedback in the form of 3 reinforcing comments and 2 constructive comments. Finally, the observer elicits a reflection on the feedback and helps develop a plan to improve teaching in future opportunities. We used a dyad model (paired participants repeatedly observe and give feedback to each other) to support mutual benefit and reciprocity between attendings.
Intervention
Using a modified Delphi approach, 5 medical education experts selected the 10 items that are most easily observable and salient to formal attending teaching rounds from the SFDP‐26 teaching assessment tool. A structured observation form was created, which included a checklist of the 10 selected items, space for note taking, and a template for narrative feedback (Figure 1).
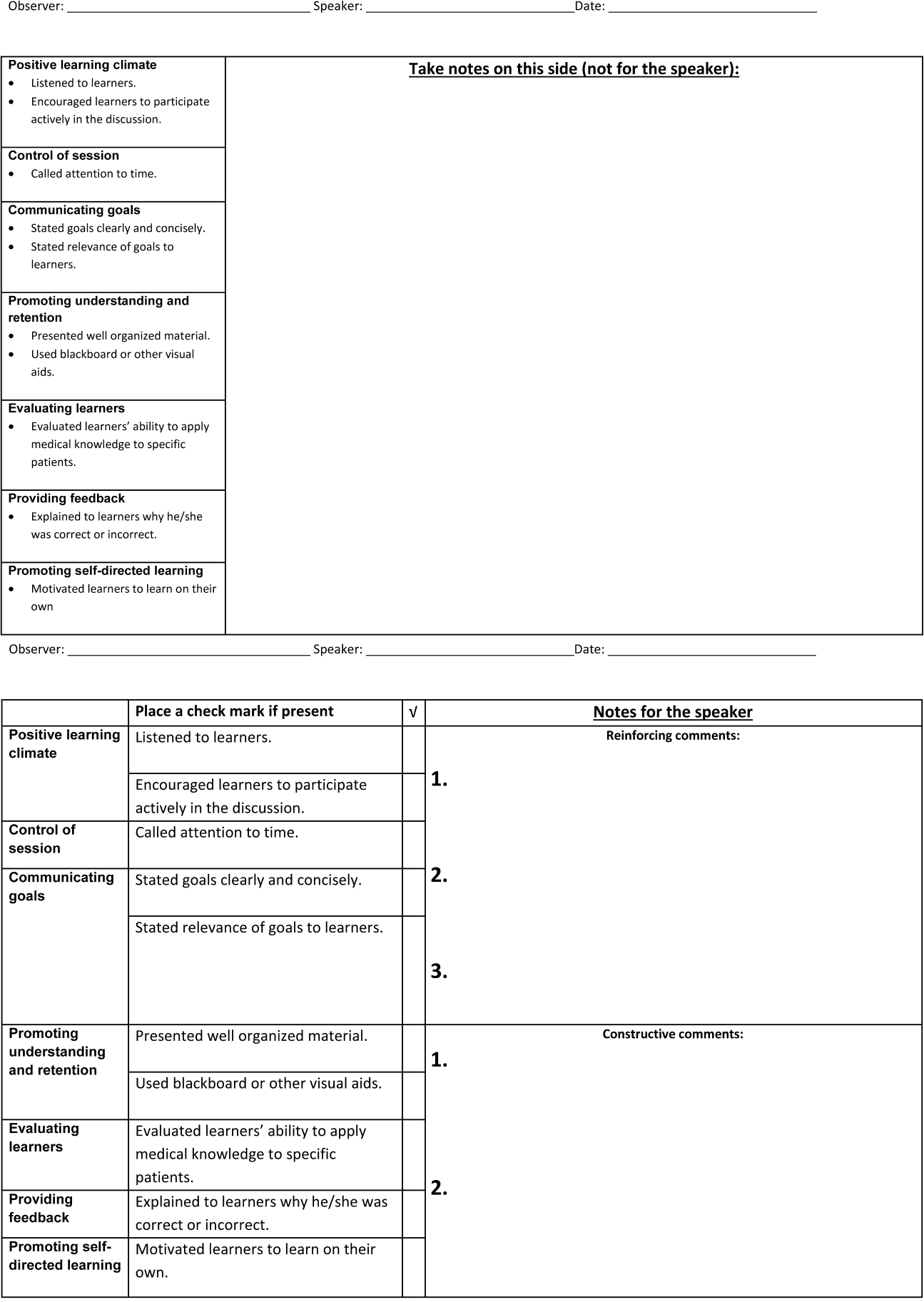
We introduced the SFDP framework during a 2‐hour initial training session. Participants watched videos of teaching, learned to identify the 10 selected teaching behaviors, developed appropriate constructive and reinforcing comments, and practiced giving and receiving peer feedback.
Dyads were created on the basis of predetermined attending schedules. Participants were asked to observe and be observed twice during attending teaching rounds over the course of the academic year. Attending teaching rounds were defined as any preplanned didactic activity for ward teams. The structured observation forms were returned to the study coordinators after the observer had given feedback to the presenter. A copy of the feedback without the observer's notes was also given to each speaker. At the midpoint of the academic year, a refresher session was offered to reinforce those teaching behaviors that were the least frequently performed to date. All participants received a $50.00
Measurements and Data Collection
Participants were given a pre‐ and post‐program survey. The surveys included questions assessing confidence in ability to give feedback, receive feedback without feeling defensive, and teach effectively, as well as attitudes toward peer observation. The postprogram survey was administered at the end of the year and additionally assessed the self‐rated performance of the 10 selected teaching behaviors. A retrospective pre‐ and post‐program assessment was used for this outcome, because this method can be more reliable when participants initially may not have sufficient insight to accurately assess their own competence in specific measures.[21] The post‐program survey also included 4 questions assessing satisfaction with aspects of the program. All questions were structured as statements to which the respondent indicated degree of agreement using a 5‐point Likert scale, where 1=strongly disagree and 5=strongly agree. Structured observation forms used by participants were collected throughout the year to assess frequency of performance of the 10 selected teaching behaviors.
Statistical Analysis
We only analyzed the pre‐ and post‐program surveys that could be matched using anonymous identifiers provided by participants. For both prospective and retrospective measures, mean values and standard deviations were calculated. Wilcoxon signed rank tests for nonparametric data were performed to obtain P values. For all comparisons, a P value of <0.05 was considered significant. All comparisons were performed using Stata version 10 (StataCorp, College Station, TX).
RESULTS
Participant Characteristics and Participation in Program
Of the 37 eligible attending hospitalists, 22 (59%) enrolled. Fourteen were hospital medicine faculty, 6 were hospital medicine fellows, and 2 were internal medicine chief residents. The averagestandard deviation (SD) number of years as a ward attending was 2.2 years2.1. Seventeen (77%) reported previously having been observed and given feedback by a colleague, and 9 (41%) reported previously observing a colleague for the purpose of giving feedback.
All 22 participants attended 1 of 2, 2‐hour training sessions. Ten participants attended an hour‐long midyear refresher session. A total of 19 observation and feedback sessions took place; 15 of them occurred in the first half of the academic year. Fifteen attending hospitalists participated in at least 1 observed teaching session. Of the 11 dyads, 6 completed at least 1 observation of each other. Two dyads performed 2 observations of each other.
Fifteen participants (68% of those enrolled) completed both the pre‐ and post‐program surveys. Among these respondents, the average number of years attending was 2.92.2 years. Eight (53%) reported previously having been observed and given feedback by a colleague, and 7 (47%) reported previously observing a colleague for the purpose of giving feedback. For this subset of participants, the averageSD frequency of being observed during the program was 1.30.7, and observing was 1.10.8.
Confidence in Ability to Give Feedback, Receive Feedback, and Teach Effectively
In comparison of pre‐ and post‐intervention measures, participants indicated increased confidence in their ability to evaluate their colleagues and provide feedback in all domains queried. Participants also indicated increased confidence in the efficacy of their feedback to improve their colleagues' teaching skills. Participating in the program did not significantly change pre‐intervention levels of confidence in ability to receive feedback without being defensive or confidence in ability to use feedback to improve teaching skills (Table 1).
| Statement | Mean Pre | SD | Mean Post | SD | P |
|---|---|---|---|---|---|
| |||||
| I can accurately assess my colleagues' teaching skills. | 3.20 | 0.86 | 4.07 | 0.59 | 0.004 |
| I can give accurate feedback to my colleagues regarding their teaching skills. | 3.40 | 0.63 | 4.20 | 0.56 | 0.002 |
| I can give feedback in a way that that my colleague will not feel defensive about their teaching skills. | 3.60 | 0.63 | 4.20 | 0.56 | 0.046 |
| My feedback will improve my colleagues' teaching skills. | 3.40 | 0.51 | 3.93 | 0.59 | 0.011 |
| I can receive feedback from a colleague without being defensive about my teaching skills. | 3.87 | 0.92 | 4.27 | 0.59 | 0.156 |
| I can use feedback from a colleague to improve my teaching skills. | 4.33 | 0.82 | 4.47 | 0.64 | 0.607 |
| I am confident in my ability to teach students and residents during attending rounds.a | 3.21 | 0.89 | 3.71 | 0.83 | 0.026 |
| I am confident in my knowledge of components of effective teaching.a | 3.21 | 0.89 | 3.71 | 0.99 | 0.035 |
| Learners regard me as an effective teacher.a | 3.14 | 0.66 | 3.64 | 0.74 | 0.033 |
Self‐Rated Performance of 10 Selected Teaching Behaviors
In retrospective assessment, participants felt that their performance had improved in all 10 teaching behaviors after the intervention. This perceived improvement reached statistical significance in 8 of the 10 selected behaviors (Table 2).
| SFDP Framework Category From Skeff et al.[18] | When I Give Attending Rounds, I Generally . | Mean Pre | SD | Mean Post | SD | P |
|---|---|---|---|---|---|---|
| ||||||
| 1. Establishing a positive learning climate | Listen to learners | 4.27 | 0.59 | 4.53 | 0.52 | 0.046 |
| Encourage learners to participate actively in the discussion | 4.07 | 0.70 | 4.60 | 0.51 | 0.009 | |
| 2. Controlling the teaching session | Call attention to time | 3.33 | 0.98 | 4.27 | 0.59 | 0.004 |
| 3. Communicating goals | State goals clearly and concisely | 3.40 | 0.63 | 4.27 | 0.59 | 0.001 |
| State relevance of goals to learners | 3.40 | 0.74 | 4.20 | 0.68 | 0.002 | |
| 4. Promoting understanding and retention | Present well‐organized material | 3.87 | 0.64 | 4.07 | 0.70 | 0.083 |
| Use blackboard or other visual aids | 4.27 | 0.88 | 4.47 | 0.74 | 0.158 | |
| 5. Evaluating the learners | Evaluate learners' ability to apply medical knowledge to specific patients | 3.33 | 0.98 | 4.00 | 0.76 | 0.005 |
| 6. Providing feedback to the learners | Explain to learners why he/she was correct or incorrect | 3.47 | 1.13 | 4.13 | 0.64 | 0.009 |
| 7. Promoting self‐directed learning | Motivate learners to learn on their own | 3.20 | 0.86 | 3.73 | 0.70 | 0.005 |
Attitudes Toward Peer Observation and Feedback
There were no significant changes in attitudes toward observation and feedback on teaching. A strong preprogram belief that observation and feedback can improve teaching skills increased slightly, but not significantly, after the program. Participants remained largely neutral in expectation of discomfort with giving or receiving peer feedback. Prior to the program, there was a slight tendency to believe that observation and feedback is more effective when done by more skilled and experienced colleagues; this belief diminished, but not significantly (Table 3).
| Statement | Mean Pre | SD | Mean Post | SD | P |
|---|---|---|---|---|---|
| |||||
| Being observed and receiving feedback can improve my teaching skills. | 4.47 | 1.06 | 4.60 | 0.51 | 0.941 |
| My teaching skills cannot improve without observation with feedback. | 2.93 | 1.39 | 3.47 | 1.30 | 0.188 |
| Observation with feedback is most effective when done by colleagues who are expert educators. | 3.53 | 0.83 | 3.33 | 0.98 | 0.180 |
| Observation with feedback is most effective when done by colleagues who have been teaching many years. | 3.40 | 0.91 | 3.07 | 1.03 | 0.143 |
| The thought of observing and giving feedback to my colleagues makes me uncomfortable. | 3.13 | 0.92 | 3.00 | 1.13 | 0.565 |
| The thought of being observed by a colleague and receiving feedback makes me uncomfortable. | 3.20 | 0.94 | 3.27 | 1.22 | 0.747 |
Program Evaluation
There were a variable number of responses to the program evaluation questions. The majority of participants found the program to be very beneficial (1=strongly disagree, 5=strongly agree [n, meanSD]): My teaching has improved as a result of this program (n=14, 4.90.3). Both giving (n=11, 4.21.6) and receiving (n=13, 4.61.1) feedback were felt to have improved teaching skills. There was strong agreement from respondents that they would participate in the program in the future: I am likely to participate in this program in the future (n=12, 4.60.9).
DISCUSSION
Previous studies have shown that teaching skills are unlikely to improve without feedback,[28, 29, 30] yet feedback for hospitalists is usually limited to summative, end‐rotation evaluations from learners, disconnected from the teaching encounter. Our theory‐based, rationally designed peer observation and feedback program resulted in increased confidence in the ability to give feedback, receive feedback, and teach effectively. Participation did not result in negative attitudes toward giving and receiving feedback from colleagues. Participants self‐reported increased performance of important teaching behaviors. Most participants rated the program very highly, and endorsed improved teaching skills as a result of the program.
Our experience provides several lessons for other groups considering the implementation of peer feedback to strengthen teaching. First, we suggest that hospitalist groups may expect variable degrees of participation in a voluntary peer feedback program. In our program, 41% of eligible attendings did not participate. We did not specifically investigate why; we speculate that they may not have had the time, believed that their teaching skills were already strong, or they may have been daunted at the idea of peer review. It is also possible that participants were a self‐selected group who were the most motivated to strengthen their teaching. Second, we note the steep decline in the number of observations in the second half of the year. Informal assessment for reasons for the drop‐off suggested that after initial enthusiasm for the program, navigating the logistics of observing the same peer in the second half of the year proved to be prohibitive to many participants. Therefore, future versions of peer feedback programs may benefit from removing the dyad requirement and encouraging all participants to observe one another whenever possible.
With these lessons in mind, we believe that a peer observation program could be implemented by other hospital medicine groups. The program does not require extensive content expertise or senior faculty but does require engaged leadership and interested and motivated faculty. Groups could identify an individual in their group with an interest in clinical teaching who could then be responsible for creating the training session (materials available upon request). We believe that with only a small upfront investment, most hospital medicine groups could use this as a model to build a peer observation program aimed at improving clinical teaching.
Our study has several limitations. As noted above, our participation rate was 59%, and the number of participating attendings declined through the year. We did not examine whether our program resulted in advances in the knowledge, skills, or attitudes of the learners; because each attending teaching session was unique, it was not possible to measure changes in learner knowledge. Our primary outcome measures relied on self‐assessment rather than higher order and more objective measures of teaching efficacy. Furthermore, our results may not be generalizable to other programs, given the heterogeneity in service structures and teaching practices across the country. This was an uncontrolled study; some of the outcomes may have naturally occurred independent of the intervention due to the natural evolution of clinical teaching. As with any educational intervention that integrates multiple strategies, we are not able to discern if the improved outcomes were the result of the initial didactic sessions, the refresher sessions, or the peer feedback itself. Serial assessments of frequency of teaching behaviors were not done due to the low number of observations in the second half of the program. Finally, our 10‐item tool derived from the validated SFDP‐26 tool is not itself a validated assessment of teaching.
We acknowledge that the increased confidence seen in our participants does not necessarily predict improved performance. Although increased confidence in core skills is a necessary step that can lead to changes in behavior, further studies are needed to determine whether the increase in faculty confidence that results from peer observation and feedback translates into improved educational outcomes.
The pressure on hospitalists to be excellent teachers is here to stay. Resources to train these faculty are scarce, yet we must prioritize faculty development in teaching to optimize the training of future physicians. Our data illustrate the benefits of peer observation and feedback. Hospitalist programs should consider this option in addressing the professional development needs of their faculty.
Acknowledgements
The authors thank Zachary Martin for administrative support for the program; Gurpreet Dhaliwal, MD, and Patricia O'Sullivan, PhD, for aid in program development; and John Amory, MD, MPH, for critical review of the manuscript. The authors thank the University of California, San Francisco Office of Medical Education for funding this work with an Educational Research Grant.
Disclosures: Funding: UCSF Office of Medical Education Educational Research Grant. Ethics approval: approved by UCSF Committee on Human Research. Previous presentations: Previous versions of this work were presented as an oral presentation at the University of California at San Francisco Medical Education Day, San Francisco, California, April 27, 2012, and as a poster presentation at the Society for General Internal Medicine 35th Annual Meeting, Orlando, Florida, May 912, 2012. The authors report no conflicts of interest.
- , , . Hospitalist involvement in internal medicine residencies. J Hosp Med. 2009;4(8):471–475.
- , , , , , . Is there a relationship between attending physicians' and residents' teaching skills and students' examination scores? Acad Med. 2000;75(11):1144–1146.
- , , . Six‐year documentation of the association between excellent clinical teaching and improved students' examination performances. Acad Med. 2000;75(10 suppl):S62–S64.
- , . Effect of clinical teaching on student performance during a medicine clerkship. Am J Med. 2001;110(3):205–209.
- , . Implications of the hospitalist model for medical students' education. Acad Med. 2001;76(4):324–330.
- . On educating and being a physician in the hospitalist era. Am J Med. 2001;111(9B):45S–47S.
- , . The role of hospitalists in medical education. Am J Med. 1999;107(4):305–309.
- , , , , , . Challenges and opportunities in academic hospital medicine: report from the academic hospital medicine summit. J Gen Intern Med. 2009;24(5):636–641.
- , , , et al. Impact of duty hour regulations on medical students' education: views of key clinical faculty. J Gen Intern Med. 2008;23(7):1084–1089.
- , , , , , . The impact of resident duty hours reform on the internal medicine core clerkship: results from the clerkship directors in internal medicine survey. Acad Med. 2006;81(12):1038–1044.
- , , , . Effects of resident work hour limitations on faculty professional lives. J Gen Intern Med. 2008;23(7):1077–1083.
- , . Teaching internal medicine residents in the new era. Inpatient attending with duty‐hour regulations. J Gen Intern Med. 2006;21(5):447–452.
- , , , . Survey of US academic hospitalist leaders about mentorship and academic activities in hospitalist groups. J Hosp Med. 2011;6(1):5–9.
- , , , . Using observed structured teaching exercises (OSTE) to enhance hospitalist teaching during family centered rounds. J Hosp Med. 2011;6(7):423–427.
- , , , . Investing in the future: building an academic hospitalist faculty development program. J Hosp Med. 2011;6(3):161–166.
- , , , . How to become a better clinical teacher: a collaborative peer observation process. Med Teach. 2011;33(2):151–155.
- , . Reframing research on faculty development. Acad Med. 2011;86(4):421–428.
- , , , et al. The Stanford faculty development program: a dissemination approach to faculty development for medical teachers. Teach Learn Med. 1992;4(3):180–187.
- . Evaluation of a method for improving the teaching performance of attending physicians. Am J Med. 1983;75(3):465–470.
- , , , . The impact of the Stanford Faculty Development Program on ambulatory teaching behavior. J Gen Intern Med. 2006;21(5):430–434.
- , , . Evaluation of a medical faculty development program: a comparison of traditional pre/post and retrospective pre/post self‐assessment ratings. Eval Health Prof. 1992;15(3):350–366.
- , , , , . Evaluation of the seminar method to improve clinical teaching. J Gen Intern Med. 1986;1(5):315–322.
- , , , , . Regional teaching improvement programs for community‐based teachers. Am J Med. 1999;106(1):76–80.
- , , , . Improving clinical teaching. Evaluation of a national dissemination program. Arch Intern Med. 1992;152(6):1156–1161.
- , , , . Factorial validation of a widely disseminated educational framework for evaluating clinical teachers. Acad Med. 1998;73(6):688–695.
- , , , . Student and resident evaluations of faculty—how reliable are they? Factorial validation of an educational framework using residents' evaluations of clinician‐educators. Acad Med. 1999;74(10):S25–S27.
- , . Students' global assessments of clinical teachers: a reliable and valid measure of teaching effectiveness. Acad Med. 1998;73(10 suppl):S72–S74.
- . The practice of giving feedback to improve teaching: what is effective? J Higher Educ. 1993;64(5):574–593.
- , , , et al. Faculty development. A resource for clinical teachers. J Gen Intern Med. 1997;12(suppl 2):S56–S63.
- , , , et al. A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME guide no. 8. Med Teach. 2006;28(6):497–526.
- , . Strategies for improving teaching practices: a comprehensive approach to faculty development. Acad Med. 1998;73(4):387–396.
- , . Relationship between systematic feedback to faculty and ratings of clinical teaching. Acad Med. 1996;71(10):1100–1102.
- . Lessons learned from a peer review of bedside teaching. Acad Med. 2004;79(4):343–346.
- , , , . Evaluating an instrument for the peer review of inpatient teaching. Med Teach. 2003;25(2):131–135.
- , , . Twelve tips for peer observation of teaching. Med Teach. 2007;29(4):297–300.
- , . Assessing the quality of teaching. Am J Med. 1999;106(4):381–384.
- , , , , , . To the point: medical education reviews—providing feedback. Am J Obstet Gynecol. 2007;196(6):508–513.
Hospitalists are increasingly responsible for educating students and housestaff in internal medicine.[1] Because the quality of teaching is an important factor in learning,[2, 3, 4] leaders in medical education have expressed concern over the rapid shift of teaching responsibilities to this new group of educators.[5, 6, 7, 8] Moreover, recent changes in duty hour restrictions have strained both student and resident education,[9, 10] necessitating the optimization of inpatient teaching.[11, 12] Many hospitalists have recently finished residency and have not had formal training in clinical teaching. Collectively, most hospital medicine groups are early in their careers, have significant clinical obligations,[13] and may not have the bandwidth or expertise to provide faculty development for improving clinical teaching.
Rationally designed and theoretically sound faculty development to improve inpatient clinical teaching is required to meet this challenge. There are a limited number of reports describing faculty development focused on strengthening the teaching of hospitalists, and only 3 utilized direct observation and feedback, 1 of which involved peer observation in the clinical setting.[14, 15, 16] This 2011 report described a narrative method of peer observation and feedback but did not assess for efficacy of the program.[16] To our knowledge, there have been no studies of structured peer observation and feedback to optimize hospitalist attendings' teaching which have evaluated the efficacy of the intervention.
We developed a faculty development program based on peer observation and feedback based on actual teaching practices, using structured feedback anchored in validated and observable measures of effective teaching. We hypothesized that participation in the program would increase confidence in key teaching skills, increase confidence in the ability to give and receive peer feedback, and strengthen attitudes toward peer observation and feedback.
METHODS
Subjects and Setting
The study was conducted at a 570‐bed academic, tertiary care medical center affiliated with an internal medicine residency program of 180 housestaff. Internal medicine ward attendings rotate during 2‐week blocks, and are asked to give formal teaching rounds 3 or 4 times a week (these sessions are distinct from teaching which may happen while rounding on patients). Ward teams are composed of 1 senior resident, 2 interns, and 1 to 2 medical students. The majority of internal medicine ward attendings are hospitalist faculty, hospital medicine fellows, or medicine chief residents. Because outpatient general internists and subspecialists only occasionally attend on the wards, we refer to ward attendings as attending hospitalists in this article. All attending hospitalists were eligible to participate if they attended on the wards at least twice during the academic year. The institutional review board at the University of California, San Francisco approved this study.
Theoretical Framework
We reviewed the literature to optimize our program in 3 conceptual domains: (1) overall structure of the program, (2) definition of effective teaching and (3) effective delivery of feedback.
Over‐reliance on didactics that are disconnected from the work environment is a weakness of traditional faculty development. Individuals may attempt to apply what they have learned, but receiving feedback on their actual workplace practices may be difficult. A recent perspective responds to this fragmentation by conceptualizing faculty development as embedded in both a faculty development community and a workplace community. This model emphasizes translating what faculty have learned in the classroom into practice, and highlights the importance of coaching in the workplace.[17] In accordance with this framework, we designed our program to reach beyond isolated workshops to effectively penetrate the workplace community.
We selected the Stanford Faculty Development Program (SFDP) framework for optimal clinical teaching as our model for recognizing and improving teaching skills. The SFDP was developed as a theory‐based intensive feedback method to improve teaching skills,[18, 19] and has been shown to improve teaching in the ambulatory[20] and inpatient settings.[21, 22] In this widely disseminated framework,[23, 24] excellent clinical teaching is grounded in optimizing observable behaviors organized around 7 domains.[18] A 26‐item instrument to evaluate clinical teaching (SFDP‐26) has been developed based on this framework[25] and has been validated in multiple settings.[26, 27] High‐quality teaching, as defined by the SFDP framework, has been correlated with improved educational outcomes in internal medicine clerkship students.[4]
Feedback is crucial to optimizing teaching,[28, 29, 30] particularly when it incorporates consultation[31] and narrative comments.[32] Peer feedback has several advantages over feedback from learners or from other non‐peer observers (such as supervisors or other evaluators). First, the observers benefit by gaining insight into their own weaknesses and potential areas for growth as teachers.[33, 34] Additionally, collegial observation and feedback may promote supportive teaching relationships between faculty.[35] Furthermore, peer review overcomes the biases that may be present in learner evaluations.[36] We established a 3‐stage feedback technique based on a previously described method.[37] In the first step, the observer elicits self‐appraisal from the speaker. Next, the observer provides specific, behaviorally anchored feedback in the form of 3 reinforcing comments and 2 constructive comments. Finally, the observer elicits a reflection on the feedback and helps develop a plan to improve teaching in future opportunities. We used a dyad model (paired participants repeatedly observe and give feedback to each other) to support mutual benefit and reciprocity between attendings.
Intervention
Using a modified Delphi approach, 5 medical education experts selected the 10 items that are most easily observable and salient to formal attending teaching rounds from the SFDP‐26 teaching assessment tool. A structured observation form was created, which included a checklist of the 10 selected items, space for note taking, and a template for narrative feedback (Figure 1).
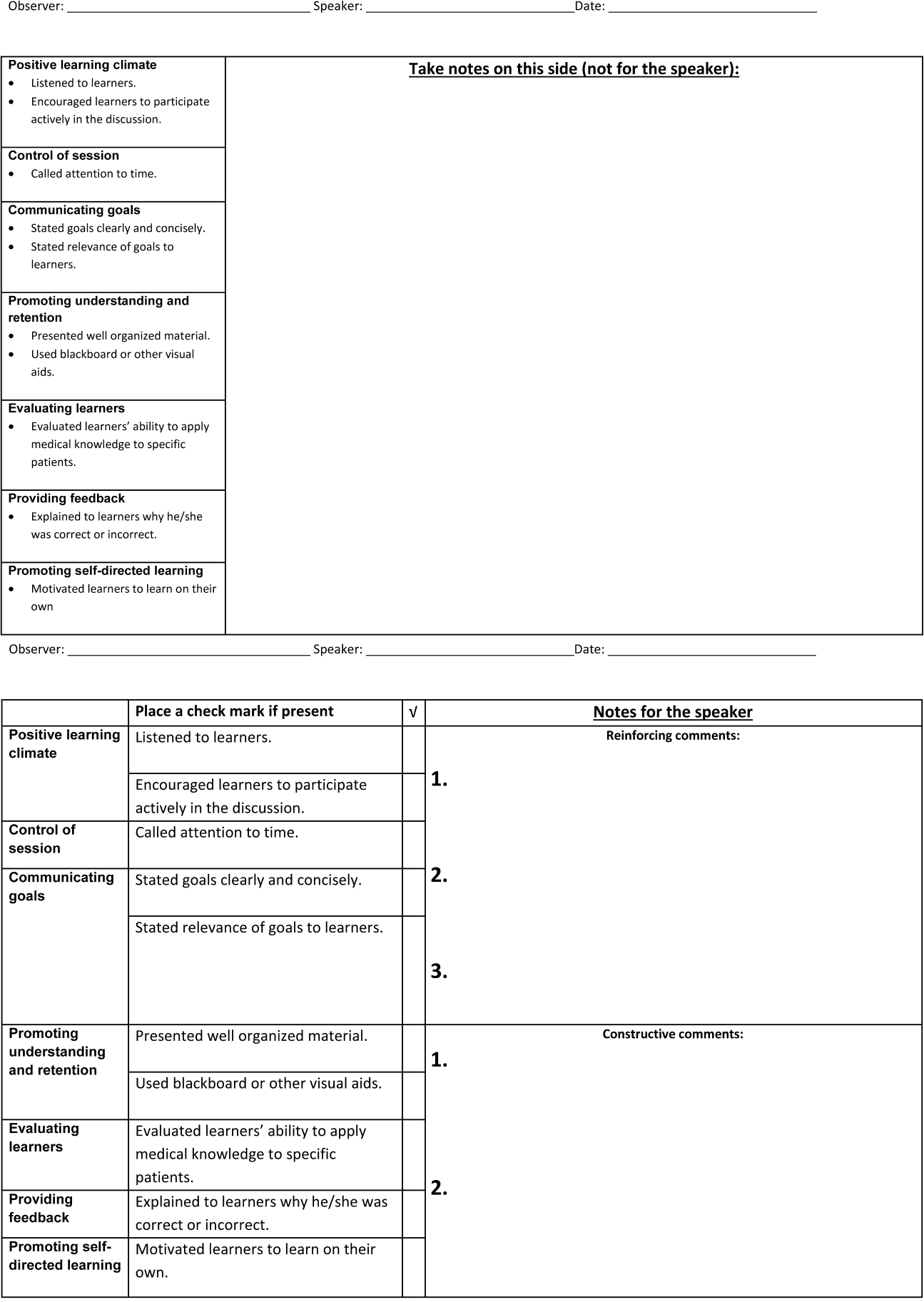
We introduced the SFDP framework during a 2‐hour initial training session. Participants watched videos of teaching, learned to identify the 10 selected teaching behaviors, developed appropriate constructive and reinforcing comments, and practiced giving and receiving peer feedback.
Dyads were created on the basis of predetermined attending schedules. Participants were asked to observe and be observed twice during attending teaching rounds over the course of the academic year. Attending teaching rounds were defined as any preplanned didactic activity for ward teams. The structured observation forms were returned to the study coordinators after the observer had given feedback to the presenter. A copy of the feedback without the observer's notes was also given to each speaker. At the midpoint of the academic year, a refresher session was offered to reinforce those teaching behaviors that were the least frequently performed to date. All participants received a $50.00
Measurements and Data Collection
Participants were given a pre‐ and post‐program survey. The surveys included questions assessing confidence in ability to give feedback, receive feedback without feeling defensive, and teach effectively, as well as attitudes toward peer observation. The postprogram survey was administered at the end of the year and additionally assessed the self‐rated performance of the 10 selected teaching behaviors. A retrospective pre‐ and post‐program assessment was used for this outcome, because this method can be more reliable when participants initially may not have sufficient insight to accurately assess their own competence in specific measures.[21] The post‐program survey also included 4 questions assessing satisfaction with aspects of the program. All questions were structured as statements to which the respondent indicated degree of agreement using a 5‐point Likert scale, where 1=strongly disagree and 5=strongly agree. Structured observation forms used by participants were collected throughout the year to assess frequency of performance of the 10 selected teaching behaviors.
Statistical Analysis
We only analyzed the pre‐ and post‐program surveys that could be matched using anonymous identifiers provided by participants. For both prospective and retrospective measures, mean values and standard deviations were calculated. Wilcoxon signed rank tests for nonparametric data were performed to obtain P values. For all comparisons, a P value of <0.05 was considered significant. All comparisons were performed using Stata version 10 (StataCorp, College Station, TX).
RESULTS
Participant Characteristics and Participation in Program
Of the 37 eligible attending hospitalists, 22 (59%) enrolled. Fourteen were hospital medicine faculty, 6 were hospital medicine fellows, and 2 were internal medicine chief residents. The averagestandard deviation (SD) number of years as a ward attending was 2.2 years2.1. Seventeen (77%) reported previously having been observed and given feedback by a colleague, and 9 (41%) reported previously observing a colleague for the purpose of giving feedback.
All 22 participants attended 1 of 2, 2‐hour training sessions. Ten participants attended an hour‐long midyear refresher session. A total of 19 observation and feedback sessions took place; 15 of them occurred in the first half of the academic year. Fifteen attending hospitalists participated in at least 1 observed teaching session. Of the 11 dyads, 6 completed at least 1 observation of each other. Two dyads performed 2 observations of each other.
Fifteen participants (68% of those enrolled) completed both the pre‐ and post‐program surveys. Among these respondents, the average number of years attending was 2.92.2 years. Eight (53%) reported previously having been observed and given feedback by a colleague, and 7 (47%) reported previously observing a colleague for the purpose of giving feedback. For this subset of participants, the averageSD frequency of being observed during the program was 1.30.7, and observing was 1.10.8.
Confidence in Ability to Give Feedback, Receive Feedback, and Teach Effectively
In comparison of pre‐ and post‐intervention measures, participants indicated increased confidence in their ability to evaluate their colleagues and provide feedback in all domains queried. Participants also indicated increased confidence in the efficacy of their feedback to improve their colleagues' teaching skills. Participating in the program did not significantly change pre‐intervention levels of confidence in ability to receive feedback without being defensive or confidence in ability to use feedback to improve teaching skills (Table 1).
| Statement | Mean Pre | SD | Mean Post | SD | P |
|---|---|---|---|---|---|
| |||||
| I can accurately assess my colleagues' teaching skills. | 3.20 | 0.86 | 4.07 | 0.59 | 0.004 |
| I can give accurate feedback to my colleagues regarding their teaching skills. | 3.40 | 0.63 | 4.20 | 0.56 | 0.002 |
| I can give feedback in a way that that my colleague will not feel defensive about their teaching skills. | 3.60 | 0.63 | 4.20 | 0.56 | 0.046 |
| My feedback will improve my colleagues' teaching skills. | 3.40 | 0.51 | 3.93 | 0.59 | 0.011 |
| I can receive feedback from a colleague without being defensive about my teaching skills. | 3.87 | 0.92 | 4.27 | 0.59 | 0.156 |
| I can use feedback from a colleague to improve my teaching skills. | 4.33 | 0.82 | 4.47 | 0.64 | 0.607 |
| I am confident in my ability to teach students and residents during attending rounds.a | 3.21 | 0.89 | 3.71 | 0.83 | 0.026 |
| I am confident in my knowledge of components of effective teaching.a | 3.21 | 0.89 | 3.71 | 0.99 | 0.035 |
| Learners regard me as an effective teacher.a | 3.14 | 0.66 | 3.64 | 0.74 | 0.033 |
Self‐Rated Performance of 10 Selected Teaching Behaviors
In retrospective assessment, participants felt that their performance had improved in all 10 teaching behaviors after the intervention. This perceived improvement reached statistical significance in 8 of the 10 selected behaviors (Table 2).
| SFDP Framework Category From Skeff et al.[18] | When I Give Attending Rounds, I Generally . | Mean Pre | SD | Mean Post | SD | P |
|---|---|---|---|---|---|---|
| ||||||
| 1. Establishing a positive learning climate | Listen to learners | 4.27 | 0.59 | 4.53 | 0.52 | 0.046 |
| Encourage learners to participate actively in the discussion | 4.07 | 0.70 | 4.60 | 0.51 | 0.009 | |
| 2. Controlling the teaching session | Call attention to time | 3.33 | 0.98 | 4.27 | 0.59 | 0.004 |
| 3. Communicating goals | State goals clearly and concisely | 3.40 | 0.63 | 4.27 | 0.59 | 0.001 |
| State relevance of goals to learners | 3.40 | 0.74 | 4.20 | 0.68 | 0.002 | |
| 4. Promoting understanding and retention | Present well‐organized material | 3.87 | 0.64 | 4.07 | 0.70 | 0.083 |
| Use blackboard or other visual aids | 4.27 | 0.88 | 4.47 | 0.74 | 0.158 | |
| 5. Evaluating the learners | Evaluate learners' ability to apply medical knowledge to specific patients | 3.33 | 0.98 | 4.00 | 0.76 | 0.005 |
| 6. Providing feedback to the learners | Explain to learners why he/she was correct or incorrect | 3.47 | 1.13 | 4.13 | 0.64 | 0.009 |
| 7. Promoting self‐directed learning | Motivate learners to learn on their own | 3.20 | 0.86 | 3.73 | 0.70 | 0.005 |
Attitudes Toward Peer Observation and Feedback
There were no significant changes in attitudes toward observation and feedback on teaching. A strong preprogram belief that observation and feedback can improve teaching skills increased slightly, but not significantly, after the program. Participants remained largely neutral in expectation of discomfort with giving or receiving peer feedback. Prior to the program, there was a slight tendency to believe that observation and feedback is more effective when done by more skilled and experienced colleagues; this belief diminished, but not significantly (Table 3).
| Statement | Mean Pre | SD | Mean Post | SD | P |
|---|---|---|---|---|---|
| |||||
| Being observed and receiving feedback can improve my teaching skills. | 4.47 | 1.06 | 4.60 | 0.51 | 0.941 |
| My teaching skills cannot improve without observation with feedback. | 2.93 | 1.39 | 3.47 | 1.30 | 0.188 |
| Observation with feedback is most effective when done by colleagues who are expert educators. | 3.53 | 0.83 | 3.33 | 0.98 | 0.180 |
| Observation with feedback is most effective when done by colleagues who have been teaching many years. | 3.40 | 0.91 | 3.07 | 1.03 | 0.143 |
| The thought of observing and giving feedback to my colleagues makes me uncomfortable. | 3.13 | 0.92 | 3.00 | 1.13 | 0.565 |
| The thought of being observed by a colleague and receiving feedback makes me uncomfortable. | 3.20 | 0.94 | 3.27 | 1.22 | 0.747 |
Program Evaluation
There were a variable number of responses to the program evaluation questions. The majority of participants found the program to be very beneficial (1=strongly disagree, 5=strongly agree [n, meanSD]): My teaching has improved as a result of this program (n=14, 4.90.3). Both giving (n=11, 4.21.6) and receiving (n=13, 4.61.1) feedback were felt to have improved teaching skills. There was strong agreement from respondents that they would participate in the program in the future: I am likely to participate in this program in the future (n=12, 4.60.9).
DISCUSSION
Previous studies have shown that teaching skills are unlikely to improve without feedback,[28, 29, 30] yet feedback for hospitalists is usually limited to summative, end‐rotation evaluations from learners, disconnected from the teaching encounter. Our theory‐based, rationally designed peer observation and feedback program resulted in increased confidence in the ability to give feedback, receive feedback, and teach effectively. Participation did not result in negative attitudes toward giving and receiving feedback from colleagues. Participants self‐reported increased performance of important teaching behaviors. Most participants rated the program very highly, and endorsed improved teaching skills as a result of the program.
Our experience provides several lessons for other groups considering the implementation of peer feedback to strengthen teaching. First, we suggest that hospitalist groups may expect variable degrees of participation in a voluntary peer feedback program. In our program, 41% of eligible attendings did not participate. We did not specifically investigate why; we speculate that they may not have had the time, believed that their teaching skills were already strong, or they may have been daunted at the idea of peer review. It is also possible that participants were a self‐selected group who were the most motivated to strengthen their teaching. Second, we note the steep decline in the number of observations in the second half of the year. Informal assessment for reasons for the drop‐off suggested that after initial enthusiasm for the program, navigating the logistics of observing the same peer in the second half of the year proved to be prohibitive to many participants. Therefore, future versions of peer feedback programs may benefit from removing the dyad requirement and encouraging all participants to observe one another whenever possible.
With these lessons in mind, we believe that a peer observation program could be implemented by other hospital medicine groups. The program does not require extensive content expertise or senior faculty but does require engaged leadership and interested and motivated faculty. Groups could identify an individual in their group with an interest in clinical teaching who could then be responsible for creating the training session (materials available upon request). We believe that with only a small upfront investment, most hospital medicine groups could use this as a model to build a peer observation program aimed at improving clinical teaching.
Our study has several limitations. As noted above, our participation rate was 59%, and the number of participating attendings declined through the year. We did not examine whether our program resulted in advances in the knowledge, skills, or attitudes of the learners; because each attending teaching session was unique, it was not possible to measure changes in learner knowledge. Our primary outcome measures relied on self‐assessment rather than higher order and more objective measures of teaching efficacy. Furthermore, our results may not be generalizable to other programs, given the heterogeneity in service structures and teaching practices across the country. This was an uncontrolled study; some of the outcomes may have naturally occurred independent of the intervention due to the natural evolution of clinical teaching. As with any educational intervention that integrates multiple strategies, we are not able to discern if the improved outcomes were the result of the initial didactic sessions, the refresher sessions, or the peer feedback itself. Serial assessments of frequency of teaching behaviors were not done due to the low number of observations in the second half of the program. Finally, our 10‐item tool derived from the validated SFDP‐26 tool is not itself a validated assessment of teaching.
We acknowledge that the increased confidence seen in our participants does not necessarily predict improved performance. Although increased confidence in core skills is a necessary step that can lead to changes in behavior, further studies are needed to determine whether the increase in faculty confidence that results from peer observation and feedback translates into improved educational outcomes.
The pressure on hospitalists to be excellent teachers is here to stay. Resources to train these faculty are scarce, yet we must prioritize faculty development in teaching to optimize the training of future physicians. Our data illustrate the benefits of peer observation and feedback. Hospitalist programs should consider this option in addressing the professional development needs of their faculty.
Acknowledgements
The authors thank Zachary Martin for administrative support for the program; Gurpreet Dhaliwal, MD, and Patricia O'Sullivan, PhD, for aid in program development; and John Amory, MD, MPH, for critical review of the manuscript. The authors thank the University of California, San Francisco Office of Medical Education for funding this work with an Educational Research Grant.
Disclosures: Funding: UCSF Office of Medical Education Educational Research Grant. Ethics approval: approved by UCSF Committee on Human Research. Previous presentations: Previous versions of this work were presented as an oral presentation at the University of California at San Francisco Medical Education Day, San Francisco, California, April 27, 2012, and as a poster presentation at the Society for General Internal Medicine 35th Annual Meeting, Orlando, Florida, May 912, 2012. The authors report no conflicts of interest.
Hospitalists are increasingly responsible for educating students and housestaff in internal medicine.[1] Because the quality of teaching is an important factor in learning,[2, 3, 4] leaders in medical education have expressed concern over the rapid shift of teaching responsibilities to this new group of educators.[5, 6, 7, 8] Moreover, recent changes in duty hour restrictions have strained both student and resident education,[9, 10] necessitating the optimization of inpatient teaching.[11, 12] Many hospitalists have recently finished residency and have not had formal training in clinical teaching. Collectively, most hospital medicine groups are early in their careers, have significant clinical obligations,[13] and may not have the bandwidth or expertise to provide faculty development for improving clinical teaching.
Rationally designed and theoretically sound faculty development to improve inpatient clinical teaching is required to meet this challenge. There are a limited number of reports describing faculty development focused on strengthening the teaching of hospitalists, and only 3 utilized direct observation and feedback, 1 of which involved peer observation in the clinical setting.[14, 15, 16] This 2011 report described a narrative method of peer observation and feedback but did not assess for efficacy of the program.[16] To our knowledge, there have been no studies of structured peer observation and feedback to optimize hospitalist attendings' teaching which have evaluated the efficacy of the intervention.
We developed a faculty development program based on peer observation and feedback based on actual teaching practices, using structured feedback anchored in validated and observable measures of effective teaching. We hypothesized that participation in the program would increase confidence in key teaching skills, increase confidence in the ability to give and receive peer feedback, and strengthen attitudes toward peer observation and feedback.
METHODS
Subjects and Setting
The study was conducted at a 570‐bed academic, tertiary care medical center affiliated with an internal medicine residency program of 180 housestaff. Internal medicine ward attendings rotate during 2‐week blocks, and are asked to give formal teaching rounds 3 or 4 times a week (these sessions are distinct from teaching which may happen while rounding on patients). Ward teams are composed of 1 senior resident, 2 interns, and 1 to 2 medical students. The majority of internal medicine ward attendings are hospitalist faculty, hospital medicine fellows, or medicine chief residents. Because outpatient general internists and subspecialists only occasionally attend on the wards, we refer to ward attendings as attending hospitalists in this article. All attending hospitalists were eligible to participate if they attended on the wards at least twice during the academic year. The institutional review board at the University of California, San Francisco approved this study.
Theoretical Framework
We reviewed the literature to optimize our program in 3 conceptual domains: (1) overall structure of the program, (2) definition of effective teaching and (3) effective delivery of feedback.
Over‐reliance on didactics that are disconnected from the work environment is a weakness of traditional faculty development. Individuals may attempt to apply what they have learned, but receiving feedback on their actual workplace practices may be difficult. A recent perspective responds to this fragmentation by conceptualizing faculty development as embedded in both a faculty development community and a workplace community. This model emphasizes translating what faculty have learned in the classroom into practice, and highlights the importance of coaching in the workplace.[17] In accordance with this framework, we designed our program to reach beyond isolated workshops to effectively penetrate the workplace community.
We selected the Stanford Faculty Development Program (SFDP) framework for optimal clinical teaching as our model for recognizing and improving teaching skills. The SFDP was developed as a theory‐based intensive feedback method to improve teaching skills,[18, 19] and has been shown to improve teaching in the ambulatory[20] and inpatient settings.[21, 22] In this widely disseminated framework,[23, 24] excellent clinical teaching is grounded in optimizing observable behaviors organized around 7 domains.[18] A 26‐item instrument to evaluate clinical teaching (SFDP‐26) has been developed based on this framework[25] and has been validated in multiple settings.[26, 27] High‐quality teaching, as defined by the SFDP framework, has been correlated with improved educational outcomes in internal medicine clerkship students.[4]
Feedback is crucial to optimizing teaching,[28, 29, 30] particularly when it incorporates consultation[31] and narrative comments.[32] Peer feedback has several advantages over feedback from learners or from other non‐peer observers (such as supervisors or other evaluators). First, the observers benefit by gaining insight into their own weaknesses and potential areas for growth as teachers.[33, 34] Additionally, collegial observation and feedback may promote supportive teaching relationships between faculty.[35] Furthermore, peer review overcomes the biases that may be present in learner evaluations.[36] We established a 3‐stage feedback technique based on a previously described method.[37] In the first step, the observer elicits self‐appraisal from the speaker. Next, the observer provides specific, behaviorally anchored feedback in the form of 3 reinforcing comments and 2 constructive comments. Finally, the observer elicits a reflection on the feedback and helps develop a plan to improve teaching in future opportunities. We used a dyad model (paired participants repeatedly observe and give feedback to each other) to support mutual benefit and reciprocity between attendings.
Intervention
Using a modified Delphi approach, 5 medical education experts selected the 10 items that are most easily observable and salient to formal attending teaching rounds from the SFDP‐26 teaching assessment tool. A structured observation form was created, which included a checklist of the 10 selected items, space for note taking, and a template for narrative feedback (Figure 1).
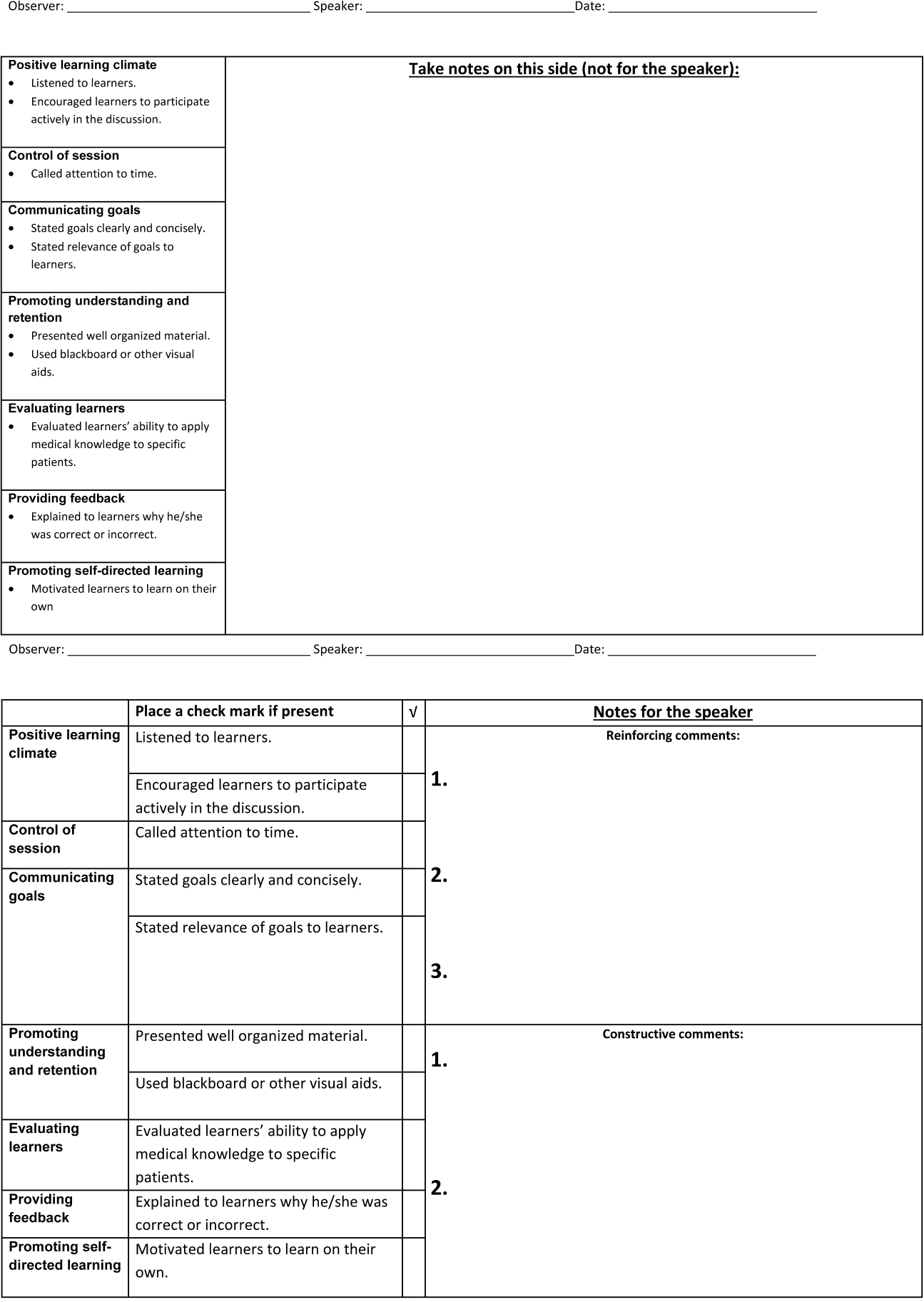
We introduced the SFDP framework during a 2‐hour initial training session. Participants watched videos of teaching, learned to identify the 10 selected teaching behaviors, developed appropriate constructive and reinforcing comments, and practiced giving and receiving peer feedback.
Dyads were created on the basis of predetermined attending schedules. Participants were asked to observe and be observed twice during attending teaching rounds over the course of the academic year. Attending teaching rounds were defined as any preplanned didactic activity for ward teams. The structured observation forms were returned to the study coordinators after the observer had given feedback to the presenter. A copy of the feedback without the observer's notes was also given to each speaker. At the midpoint of the academic year, a refresher session was offered to reinforce those teaching behaviors that were the least frequently performed to date. All participants received a $50.00
Measurements and Data Collection
Participants were given a pre‐ and post‐program survey. The surveys included questions assessing confidence in ability to give feedback, receive feedback without feeling defensive, and teach effectively, as well as attitudes toward peer observation. The postprogram survey was administered at the end of the year and additionally assessed the self‐rated performance of the 10 selected teaching behaviors. A retrospective pre‐ and post‐program assessment was used for this outcome, because this method can be more reliable when participants initially may not have sufficient insight to accurately assess their own competence in specific measures.[21] The post‐program survey also included 4 questions assessing satisfaction with aspects of the program. All questions were structured as statements to which the respondent indicated degree of agreement using a 5‐point Likert scale, where 1=strongly disagree and 5=strongly agree. Structured observation forms used by participants were collected throughout the year to assess frequency of performance of the 10 selected teaching behaviors.
Statistical Analysis
We only analyzed the pre‐ and post‐program surveys that could be matched using anonymous identifiers provided by participants. For both prospective and retrospective measures, mean values and standard deviations were calculated. Wilcoxon signed rank tests for nonparametric data were performed to obtain P values. For all comparisons, a P value of <0.05 was considered significant. All comparisons were performed using Stata version 10 (StataCorp, College Station, TX).
RESULTS
Participant Characteristics and Participation in Program
Of the 37 eligible attending hospitalists, 22 (59%) enrolled. Fourteen were hospital medicine faculty, 6 were hospital medicine fellows, and 2 were internal medicine chief residents. The averagestandard deviation (SD) number of years as a ward attending was 2.2 years2.1. Seventeen (77%) reported previously having been observed and given feedback by a colleague, and 9 (41%) reported previously observing a colleague for the purpose of giving feedback.
All 22 participants attended 1 of 2, 2‐hour training sessions. Ten participants attended an hour‐long midyear refresher session. A total of 19 observation and feedback sessions took place; 15 of them occurred in the first half of the academic year. Fifteen attending hospitalists participated in at least 1 observed teaching session. Of the 11 dyads, 6 completed at least 1 observation of each other. Two dyads performed 2 observations of each other.
Fifteen participants (68% of those enrolled) completed both the pre‐ and post‐program surveys. Among these respondents, the average number of years attending was 2.92.2 years. Eight (53%) reported previously having been observed and given feedback by a colleague, and 7 (47%) reported previously observing a colleague for the purpose of giving feedback. For this subset of participants, the averageSD frequency of being observed during the program was 1.30.7, and observing was 1.10.8.
Confidence in Ability to Give Feedback, Receive Feedback, and Teach Effectively
In comparison of pre‐ and post‐intervention measures, participants indicated increased confidence in their ability to evaluate their colleagues and provide feedback in all domains queried. Participants also indicated increased confidence in the efficacy of their feedback to improve their colleagues' teaching skills. Participating in the program did not significantly change pre‐intervention levels of confidence in ability to receive feedback without being defensive or confidence in ability to use feedback to improve teaching skills (Table 1).
| Statement | Mean Pre | SD | Mean Post | SD | P |
|---|---|---|---|---|---|
| |||||
| I can accurately assess my colleagues' teaching skills. | 3.20 | 0.86 | 4.07 | 0.59 | 0.004 |
| I can give accurate feedback to my colleagues regarding their teaching skills. | 3.40 | 0.63 | 4.20 | 0.56 | 0.002 |
| I can give feedback in a way that that my colleague will not feel defensive about their teaching skills. | 3.60 | 0.63 | 4.20 | 0.56 | 0.046 |
| My feedback will improve my colleagues' teaching skills. | 3.40 | 0.51 | 3.93 | 0.59 | 0.011 |
| I can receive feedback from a colleague without being defensive about my teaching skills. | 3.87 | 0.92 | 4.27 | 0.59 | 0.156 |
| I can use feedback from a colleague to improve my teaching skills. | 4.33 | 0.82 | 4.47 | 0.64 | 0.607 |
| I am confident in my ability to teach students and residents during attending rounds.a | 3.21 | 0.89 | 3.71 | 0.83 | 0.026 |
| I am confident in my knowledge of components of effective teaching.a | 3.21 | 0.89 | 3.71 | 0.99 | 0.035 |
| Learners regard me as an effective teacher.a | 3.14 | 0.66 | 3.64 | 0.74 | 0.033 |
Self‐Rated Performance of 10 Selected Teaching Behaviors
In retrospective assessment, participants felt that their performance had improved in all 10 teaching behaviors after the intervention. This perceived improvement reached statistical significance in 8 of the 10 selected behaviors (Table 2).
| SFDP Framework Category From Skeff et al.[18] | When I Give Attending Rounds, I Generally . | Mean Pre | SD | Mean Post | SD | P |
|---|---|---|---|---|---|---|
| ||||||
| 1. Establishing a positive learning climate | Listen to learners | 4.27 | 0.59 | 4.53 | 0.52 | 0.046 |
| Encourage learners to participate actively in the discussion | 4.07 | 0.70 | 4.60 | 0.51 | 0.009 | |
| 2. Controlling the teaching session | Call attention to time | 3.33 | 0.98 | 4.27 | 0.59 | 0.004 |
| 3. Communicating goals | State goals clearly and concisely | 3.40 | 0.63 | 4.27 | 0.59 | 0.001 |
| State relevance of goals to learners | 3.40 | 0.74 | 4.20 | 0.68 | 0.002 | |
| 4. Promoting understanding and retention | Present well‐organized material | 3.87 | 0.64 | 4.07 | 0.70 | 0.083 |
| Use blackboard or other visual aids | 4.27 | 0.88 | 4.47 | 0.74 | 0.158 | |
| 5. Evaluating the learners | Evaluate learners' ability to apply medical knowledge to specific patients | 3.33 | 0.98 | 4.00 | 0.76 | 0.005 |
| 6. Providing feedback to the learners | Explain to learners why he/she was correct or incorrect | 3.47 | 1.13 | 4.13 | 0.64 | 0.009 |
| 7. Promoting self‐directed learning | Motivate learners to learn on their own | 3.20 | 0.86 | 3.73 | 0.70 | 0.005 |
Attitudes Toward Peer Observation and Feedback
There were no significant changes in attitudes toward observation and feedback on teaching. A strong preprogram belief that observation and feedback can improve teaching skills increased slightly, but not significantly, after the program. Participants remained largely neutral in expectation of discomfort with giving or receiving peer feedback. Prior to the program, there was a slight tendency to believe that observation and feedback is more effective when done by more skilled and experienced colleagues; this belief diminished, but not significantly (Table 3).
| Statement | Mean Pre | SD | Mean Post | SD | P |
|---|---|---|---|---|---|
| |||||
| Being observed and receiving feedback can improve my teaching skills. | 4.47 | 1.06 | 4.60 | 0.51 | 0.941 |
| My teaching skills cannot improve without observation with feedback. | 2.93 | 1.39 | 3.47 | 1.30 | 0.188 |
| Observation with feedback is most effective when done by colleagues who are expert educators. | 3.53 | 0.83 | 3.33 | 0.98 | 0.180 |
| Observation with feedback is most effective when done by colleagues who have been teaching many years. | 3.40 | 0.91 | 3.07 | 1.03 | 0.143 |
| The thought of observing and giving feedback to my colleagues makes me uncomfortable. | 3.13 | 0.92 | 3.00 | 1.13 | 0.565 |
| The thought of being observed by a colleague and receiving feedback makes me uncomfortable. | 3.20 | 0.94 | 3.27 | 1.22 | 0.747 |
Program Evaluation
There were a variable number of responses to the program evaluation questions. The majority of participants found the program to be very beneficial (1=strongly disagree, 5=strongly agree [n, meanSD]): My teaching has improved as a result of this program (n=14, 4.90.3). Both giving (n=11, 4.21.6) and receiving (n=13, 4.61.1) feedback were felt to have improved teaching skills. There was strong agreement from respondents that they would participate in the program in the future: I am likely to participate in this program in the future (n=12, 4.60.9).
DISCUSSION
Previous studies have shown that teaching skills are unlikely to improve without feedback,[28, 29, 30] yet feedback for hospitalists is usually limited to summative, end‐rotation evaluations from learners, disconnected from the teaching encounter. Our theory‐based, rationally designed peer observation and feedback program resulted in increased confidence in the ability to give feedback, receive feedback, and teach effectively. Participation did not result in negative attitudes toward giving and receiving feedback from colleagues. Participants self‐reported increased performance of important teaching behaviors. Most participants rated the program very highly, and endorsed improved teaching skills as a result of the program.
Our experience provides several lessons for other groups considering the implementation of peer feedback to strengthen teaching. First, we suggest that hospitalist groups may expect variable degrees of participation in a voluntary peer feedback program. In our program, 41% of eligible attendings did not participate. We did not specifically investigate why; we speculate that they may not have had the time, believed that their teaching skills were already strong, or they may have been daunted at the idea of peer review. It is also possible that participants were a self‐selected group who were the most motivated to strengthen their teaching. Second, we note the steep decline in the number of observations in the second half of the year. Informal assessment for reasons for the drop‐off suggested that after initial enthusiasm for the program, navigating the logistics of observing the same peer in the second half of the year proved to be prohibitive to many participants. Therefore, future versions of peer feedback programs may benefit from removing the dyad requirement and encouraging all participants to observe one another whenever possible.
With these lessons in mind, we believe that a peer observation program could be implemented by other hospital medicine groups. The program does not require extensive content expertise or senior faculty but does require engaged leadership and interested and motivated faculty. Groups could identify an individual in their group with an interest in clinical teaching who could then be responsible for creating the training session (materials available upon request). We believe that with only a small upfront investment, most hospital medicine groups could use this as a model to build a peer observation program aimed at improving clinical teaching.
Our study has several limitations. As noted above, our participation rate was 59%, and the number of participating attendings declined through the year. We did not examine whether our program resulted in advances in the knowledge, skills, or attitudes of the learners; because each attending teaching session was unique, it was not possible to measure changes in learner knowledge. Our primary outcome measures relied on self‐assessment rather than higher order and more objective measures of teaching efficacy. Furthermore, our results may not be generalizable to other programs, given the heterogeneity in service structures and teaching practices across the country. This was an uncontrolled study; some of the outcomes may have naturally occurred independent of the intervention due to the natural evolution of clinical teaching. As with any educational intervention that integrates multiple strategies, we are not able to discern if the improved outcomes were the result of the initial didactic sessions, the refresher sessions, or the peer feedback itself. Serial assessments of frequency of teaching behaviors were not done due to the low number of observations in the second half of the program. Finally, our 10‐item tool derived from the validated SFDP‐26 tool is not itself a validated assessment of teaching.
We acknowledge that the increased confidence seen in our participants does not necessarily predict improved performance. Although increased confidence in core skills is a necessary step that can lead to changes in behavior, further studies are needed to determine whether the increase in faculty confidence that results from peer observation and feedback translates into improved educational outcomes.
The pressure on hospitalists to be excellent teachers is here to stay. Resources to train these faculty are scarce, yet we must prioritize faculty development in teaching to optimize the training of future physicians. Our data illustrate the benefits of peer observation and feedback. Hospitalist programs should consider this option in addressing the professional development needs of their faculty.
Acknowledgements
The authors thank Zachary Martin for administrative support for the program; Gurpreet Dhaliwal, MD, and Patricia O'Sullivan, PhD, for aid in program development; and John Amory, MD, MPH, for critical review of the manuscript. The authors thank the University of California, San Francisco Office of Medical Education for funding this work with an Educational Research Grant.
Disclosures: Funding: UCSF Office of Medical Education Educational Research Grant. Ethics approval: approved by UCSF Committee on Human Research. Previous presentations: Previous versions of this work were presented as an oral presentation at the University of California at San Francisco Medical Education Day, San Francisco, California, April 27, 2012, and as a poster presentation at the Society for General Internal Medicine 35th Annual Meeting, Orlando, Florida, May 912, 2012. The authors report no conflicts of interest.
- , , . Hospitalist involvement in internal medicine residencies. J Hosp Med. 2009;4(8):471–475.
- , , , , , . Is there a relationship between attending physicians' and residents' teaching skills and students' examination scores? Acad Med. 2000;75(11):1144–1146.
- , , . Six‐year documentation of the association between excellent clinical teaching and improved students' examination performances. Acad Med. 2000;75(10 suppl):S62–S64.
- , . Effect of clinical teaching on student performance during a medicine clerkship. Am J Med. 2001;110(3):205–209.
- , . Implications of the hospitalist model for medical students' education. Acad Med. 2001;76(4):324–330.
- . On educating and being a physician in the hospitalist era. Am J Med. 2001;111(9B):45S–47S.
- , . The role of hospitalists in medical education. Am J Med. 1999;107(4):305–309.
- , , , , , . Challenges and opportunities in academic hospital medicine: report from the academic hospital medicine summit. J Gen Intern Med. 2009;24(5):636–641.
- , , , et al. Impact of duty hour regulations on medical students' education: views of key clinical faculty. J Gen Intern Med. 2008;23(7):1084–1089.
- , , , , , . The impact of resident duty hours reform on the internal medicine core clerkship: results from the clerkship directors in internal medicine survey. Acad Med. 2006;81(12):1038–1044.
- , , , . Effects of resident work hour limitations on faculty professional lives. J Gen Intern Med. 2008;23(7):1077–1083.
- , . Teaching internal medicine residents in the new era. Inpatient attending with duty‐hour regulations. J Gen Intern Med. 2006;21(5):447–452.
- , , , . Survey of US academic hospitalist leaders about mentorship and academic activities in hospitalist groups. J Hosp Med. 2011;6(1):5–9.
- , , , . Using observed structured teaching exercises (OSTE) to enhance hospitalist teaching during family centered rounds. J Hosp Med. 2011;6(7):423–427.
- , , , . Investing in the future: building an academic hospitalist faculty development program. J Hosp Med. 2011;6(3):161–166.
- , , , . How to become a better clinical teacher: a collaborative peer observation process. Med Teach. 2011;33(2):151–155.
- , . Reframing research on faculty development. Acad Med. 2011;86(4):421–428.
- , , , et al. The Stanford faculty development program: a dissemination approach to faculty development for medical teachers. Teach Learn Med. 1992;4(3):180–187.
- . Evaluation of a method for improving the teaching performance of attending physicians. Am J Med. 1983;75(3):465–470.
- , , , . The impact of the Stanford Faculty Development Program on ambulatory teaching behavior. J Gen Intern Med. 2006;21(5):430–434.
- , , . Evaluation of a medical faculty development program: a comparison of traditional pre/post and retrospective pre/post self‐assessment ratings. Eval Health Prof. 1992;15(3):350–366.
- , , , , . Evaluation of the seminar method to improve clinical teaching. J Gen Intern Med. 1986;1(5):315–322.
- , , , , . Regional teaching improvement programs for community‐based teachers. Am J Med. 1999;106(1):76–80.
- , , , . Improving clinical teaching. Evaluation of a national dissemination program. Arch Intern Med. 1992;152(6):1156–1161.
- , , , . Factorial validation of a widely disseminated educational framework for evaluating clinical teachers. Acad Med. 1998;73(6):688–695.
- , , , . Student and resident evaluations of faculty—how reliable are they? Factorial validation of an educational framework using residents' evaluations of clinician‐educators. Acad Med. 1999;74(10):S25–S27.
- , . Students' global assessments of clinical teachers: a reliable and valid measure of teaching effectiveness. Acad Med. 1998;73(10 suppl):S72–S74.
- . The practice of giving feedback to improve teaching: what is effective? J Higher Educ. 1993;64(5):574–593.
- , , , et al. Faculty development. A resource for clinical teachers. J Gen Intern Med. 1997;12(suppl 2):S56–S63.
- , , , et al. A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME guide no. 8. Med Teach. 2006;28(6):497–526.
- , . Strategies for improving teaching practices: a comprehensive approach to faculty development. Acad Med. 1998;73(4):387–396.
- , . Relationship between systematic feedback to faculty and ratings of clinical teaching. Acad Med. 1996;71(10):1100–1102.
- . Lessons learned from a peer review of bedside teaching. Acad Med. 2004;79(4):343–346.
- , , , . Evaluating an instrument for the peer review of inpatient teaching. Med Teach. 2003;25(2):131–135.
- , , . Twelve tips for peer observation of teaching. Med Teach. 2007;29(4):297–300.
- , . Assessing the quality of teaching. Am J Med. 1999;106(4):381–384.
- , , , , , . To the point: medical education reviews—providing feedback. Am J Obstet Gynecol. 2007;196(6):508–513.
- , , . Hospitalist involvement in internal medicine residencies. J Hosp Med. 2009;4(8):471–475.
- , , , , , . Is there a relationship between attending physicians' and residents' teaching skills and students' examination scores? Acad Med. 2000;75(11):1144–1146.
- , , . Six‐year documentation of the association between excellent clinical teaching and improved students' examination performances. Acad Med. 2000;75(10 suppl):S62–S64.
- , . Effect of clinical teaching on student performance during a medicine clerkship. Am J Med. 2001;110(3):205–209.
- , . Implications of the hospitalist model for medical students' education. Acad Med. 2001;76(4):324–330.
- . On educating and being a physician in the hospitalist era. Am J Med. 2001;111(9B):45S–47S.
- , . The role of hospitalists in medical education. Am J Med. 1999;107(4):305–309.
- , , , , , . Challenges and opportunities in academic hospital medicine: report from the academic hospital medicine summit. J Gen Intern Med. 2009;24(5):636–641.
- , , , et al. Impact of duty hour regulations on medical students' education: views of key clinical faculty. J Gen Intern Med. 2008;23(7):1084–1089.
- , , , , , . The impact of resident duty hours reform on the internal medicine core clerkship: results from the clerkship directors in internal medicine survey. Acad Med. 2006;81(12):1038–1044.
- , , , . Effects of resident work hour limitations on faculty professional lives. J Gen Intern Med. 2008;23(7):1077–1083.
- , . Teaching internal medicine residents in the new era. Inpatient attending with duty‐hour regulations. J Gen Intern Med. 2006;21(5):447–452.
- , , , . Survey of US academic hospitalist leaders about mentorship and academic activities in hospitalist groups. J Hosp Med. 2011;6(1):5–9.
- , , , . Using observed structured teaching exercises (OSTE) to enhance hospitalist teaching during family centered rounds. J Hosp Med. 2011;6(7):423–427.
- , , , . Investing in the future: building an academic hospitalist faculty development program. J Hosp Med. 2011;6(3):161–166.
- , , , . How to become a better clinical teacher: a collaborative peer observation process. Med Teach. 2011;33(2):151–155.
- , . Reframing research on faculty development. Acad Med. 2011;86(4):421–428.
- , , , et al. The Stanford faculty development program: a dissemination approach to faculty development for medical teachers. Teach Learn Med. 1992;4(3):180–187.
- . Evaluation of a method for improving the teaching performance of attending physicians. Am J Med. 1983;75(3):465–470.
- , , , . The impact of the Stanford Faculty Development Program on ambulatory teaching behavior. J Gen Intern Med. 2006;21(5):430–434.
- , , . Evaluation of a medical faculty development program: a comparison of traditional pre/post and retrospective pre/post self‐assessment ratings. Eval Health Prof. 1992;15(3):350–366.
- , , , , . Evaluation of the seminar method to improve clinical teaching. J Gen Intern Med. 1986;1(5):315–322.
- , , , , . Regional teaching improvement programs for community‐based teachers. Am J Med. 1999;106(1):76–80.
- , , , . Improving clinical teaching. Evaluation of a national dissemination program. Arch Intern Med. 1992;152(6):1156–1161.
- , , , . Factorial validation of a widely disseminated educational framework for evaluating clinical teachers. Acad Med. 1998;73(6):688–695.
- , , , . Student and resident evaluations of faculty—how reliable are they? Factorial validation of an educational framework using residents' evaluations of clinician‐educators. Acad Med. 1999;74(10):S25–S27.
- , . Students' global assessments of clinical teachers: a reliable and valid measure of teaching effectiveness. Acad Med. 1998;73(10 suppl):S72–S74.
- . The practice of giving feedback to improve teaching: what is effective? J Higher Educ. 1993;64(5):574–593.
- , , , et al. Faculty development. A resource for clinical teachers. J Gen Intern Med. 1997;12(suppl 2):S56–S63.
- , , , et al. A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME guide no. 8. Med Teach. 2006;28(6):497–526.
- , . Strategies for improving teaching practices: a comprehensive approach to faculty development. Acad Med. 1998;73(4):387–396.
- , . Relationship between systematic feedback to faculty and ratings of clinical teaching. Acad Med. 1996;71(10):1100–1102.
- . Lessons learned from a peer review of bedside teaching. Acad Med. 2004;79(4):343–346.
- , , , . Evaluating an instrument for the peer review of inpatient teaching. Med Teach. 2003;25(2):131–135.
- , , . Twelve tips for peer observation of teaching. Med Teach. 2007;29(4):297–300.
- , . Assessing the quality of teaching. Am J Med. 1999;106(4):381–384.
- , , , , , . To the point: medical education reviews—providing feedback. Am J Obstet Gynecol. 2007;196(6):508–513.
© 2014 Society of Hospital Medicine
Discharge Before Noon
Late afternoon hospital discharges are thought to create admission bottlenecks in the emergency department (ED).[1] ED overcrowding increases the length of stay (LOS) of patients[2] and is a major dissatisfier for both patients and staff.[3] In our medical center, ED patients who are admitted after 1:00 pm have a 0.6‐day longer risk‐adjusted LOS than those admitted before 1:00 pm (M. Radford, MD, written communication, March 2012).
Many potential barriers to discharging patients early in the day exist.[4] However, comprehensive discharge planning favorably impacts discharge times.[5] There are limited published data regarding discharging patients early in the day. Studies have focused on improved discharge care coordination,[6, 7] in‐room display of planned discharge time,[8] and a discharge brunch.[9] In January 2012, the calendar month discharge before noon (DBN) percentage for 2 inpatient medicine units in our institution was approximately 7%, well below the organizational goal of 30%. We describe an intervention to sustainably increase the DBN percentage.
METHODS
Setting
The intervention took place on the 17th floor of New York University (NYU) Langone Medical Center's Tisch Hospital, an urban, academic medical center. All patients on the 17th floor received the intervention.
The 17th floor is composed of 2 acute care inpatient medical units17E and 17W. Each unit has 35 medical beds including a 16‐bed medical step down unit (SDU). Medical teams on the floor consist of 4 housestaff teams, a nurse practitioner (NP) team, and an SDU team. Each housestaff and NP team is led by a hospitalist, who is the attending of record for the majority of patients, though some patients on these teams are cared for by private attendings. Medical teams admit patients to any unit based upon bed availability. Nurses are assigned patients by acuity, not by medical team.
Intervention
Kick‐Off Event, Definition of Responsibilities, and Checklist
All stakeholders and front‐line staff were invited to a kickoff event on March 5, 2012. This event included education and discussion about the importance of a safe and early discharge from the patient and staff perspective. Roles in the discharge process were clearly defined and a corresponding checklist was created (Table 1). The checklist was used at least once per day during afternoon interdisciplinary in preparation for next‐day DBNs. Discharge date and time are communicated by the medical team to individual patients and families on the day a patient is identified for DBN. Patients and families did not receive additional orientation to the DBN initiative.
| Discharge Task | Responsible Team Member |
|---|---|
| |
| MD discharge summary and medication reconciliation | Resident or NP |
| Discharge order | Resident or NP |
| Prescription(s) | Resident or NP |
| Communicate discharge date and time to patient/family | Resident/hospitalist/NP |
| Patient education | Nurse |
| RN discharge summary | Nurse |
| Patient belongings/clothing | Nurse |
| Patient education/teaching | Nurse |
| Final labs/tests | Nurse |
| Assess Foley catheter need and remove | Nurse |
| Transportation | Social worker and care manager |
| At‐home services (HHA/HA/private hire) | Social worker and care manager |
| Equipment/supplies (DME, O2, ostomy supplies) | Social worker and care manager |
Interdisciplinary Rounds and DBN Website
In the past, interdisciplinary rounds, attended by each unit's charge nurse (CN), the medical resident or NP, the hospitalist, the team‐based social work (SW), and care management (CM) occurred in the morning between 9:00 am and 10:00 am. With the DBN initiative, additional afternoon interdisciplinary rounds were held at 3:00 pm. These rounds were designed to identify the next day's DBNs. Multidisciplinary team members were asked to complete the checklist responsibilities the same day that DBNs were identified rather than waiting until the day of discharge. A DBN website was created, and CMs were asked to log anticipated DBNs on this site after 3:00 pm rounds. The website generates a daily automated email at 4:30 pm to the DBN listserv with a list of the next day's anticipated DBNs. The listserv includes all hospitalists, residents, NPs, CNs, nurse managers (NM), medical directors, bed management, building services, SWs, and CMs. Additional departments were subsequently added as the DBN initiative became standard of care.
Assistant NMs update the DBN website overnight, adding patients identified by nursing staff as a possible DBN and highlighting changes in the condition of previously identified patients. At 7:00 am, an automated update email is sent by the website to the listserv. The automated emails include the DBN checklist, key phone numbers, and useful links.
Daily Leadership Meeting, Ongoing Process Improvement, and Real‐Time Feedback
Weekdays at 11:00 am, an interdisciplinary leadership meeting occurs with the medical directors, assistant NMs, CNs, and representatives from SW, CM, and hospital administration. At this meeting, all discharges from the previous day are reviewed to identify areas for improvement and trends in barriers to DBN. The current day's expected DBNs are also reviewed to address discharge bottlenecks in real time. Daily feedback was provided via a poster displayed in staff areas with daily DBN statistics.
Reward and Recognition
At the kickoff, a prize system was announced for the conclusion of the first month of the intervention if DBN thresholds were met. Rewards included a pizza party and raffle gift certificates. To hardwire the process, these rewards were repeated at the conclusion of each of the first 3 months of the intervention.
Changes to the Floor
There were notable changes to the floor during the time of this intervention. From October 25, 2012 until January 1, 2013, the hospital was closed after evacuation due to Hurricane Sandy. Units 17E and 17W reopened on January 14, 2013. The NP team was not restarted with the reopening. All other floor processes, including the DBN interventions, were restarted. The time period of floor closure was excluded in this analysis. The initial medical center goal was 30% DBNs. During the intervention period, the goal increased to 40%.
Data Collection and Analysis
Primary Outcome: Calendar Month DBN Percentage
The date and time of discharge are recorded by the discharging nurse or patient unit assistant in our electronic medical record (Epic, Madison WI) at the time the patient leaves the unit. Utilizing NYU's cost accounting system (Enterprise Performance Systems Inc., Chicago, IL), we obtained discharge date and time among inpatients discharged from units 17E and 17W between June 1, 2011 and March 4, 2012 (the baseline period) and March 5, 2012 and June 31, 2013 (the intervention period). Data from October 25, 2012 to the end of January 2013 were excluded due to hospital closure from Hurricane Sandy. The analysis includes 8 months of baseline data and 13 months of intervention data (not counting the excluded months from hospital closure), measuring the extent to which improvement was sustained. To match organizational criteria for DBN, we excluded patients on the units in the patient class observation, deaths, and inpatient hospice.
Patients were identified as DBNs if the discharge time was before 12:01 pm, in accordance with our medical center administration's definition of DBN. Calendar month DBN percentage was calculated by dividing the number of DBN patients during the calendar month by the total number of discharged patients during the calendar month. The proportion of DBNs in the baseline population was compared to the proportion of DBNs in the intervention population. Statistical significance for the change in DBN was evaluated by use of a 2‐tailed z test.
Secondary Outcomes: Observed‐to‐Expected LOS and 30‐Day Readmission Rate
Expected LOS was provided by the University Health Consortium (UHC). UHC calculates a risk‐adjusted LOS for each patient by assigning a severity of illness, selection of a patient population to serve as a basis of the model, and use of statistical regression to assign an expected LOS in days. Observed‐to‐expected (O/E) LOS for each patient is calculated by dividing the expected LOS in days by the observed (actual) LOS in days. The average of the O/E LOS for all patients in the baseline period was compared to the average O/E LOS for all patients in the intervention period. This average was calculated by summing the O/E LOS of all patients in each time period and dividing by the total number of patients. In accordance with our medical center administration's reporting standards, we report the mean of the O/E LOS. For statistical evaluation of this non‐normally distributed continuous variable, we also report the median of the O/E LOS for the baseline and intervention time period and use the Wilcoxon rank sum test to evaluate for statistical significance.
Readmission cases are identified by the clinical quality and effectiveness department at our medical center using the UHC definition of all patients who are readmitted to a hospital within 30 days of discharge from the index admission. The 30‐day readmission rate is calculated by dividing the total number of cases identified as readmissions within 30 days by the total number of admissions over the same time period. This rate was obtained on a calendar‐month basis for patients discharged from the index admission before noon, after noon, and in total. These rates were averaged over the baseline and intervention period. The proportion of 30‐day readmissions in the baseline population was compared to the proportion of 30‐day readmissions in the intervention population. Statistical significance for the change in 30‐day readmissions was evaluated by use of a 2‐tailed z test.
RESULTS
Primary Outcome: Calendar Month DBN Percentage
The calendar month DBN percentage increased in the first month of the intervention, from 16% to 42% (Figure 1). This improvement was sustained throughout the intervention, with an average calendar month DBN percentage of 38% over the 13‐month intervention period. Use of a 2‐tailed z test to compare the pre‐intervention proportion (11%) of patients who were DBN with the post‐intervention proportion (38%) who were DBN showed a statistically significant change (z score 23.6, P = 0.0002). Units 17E and 17W had a combined 2536 total discharges in the baseline period, with 265 patients discharged before noon. In the intervention period, 3277 total discharges occurred, with 1236 patients discharged before noon. The average time of discharge moved 1 hour and 31 minutes, from 3:43 pm in the baseline period to 2:13 pm in the intervention period.
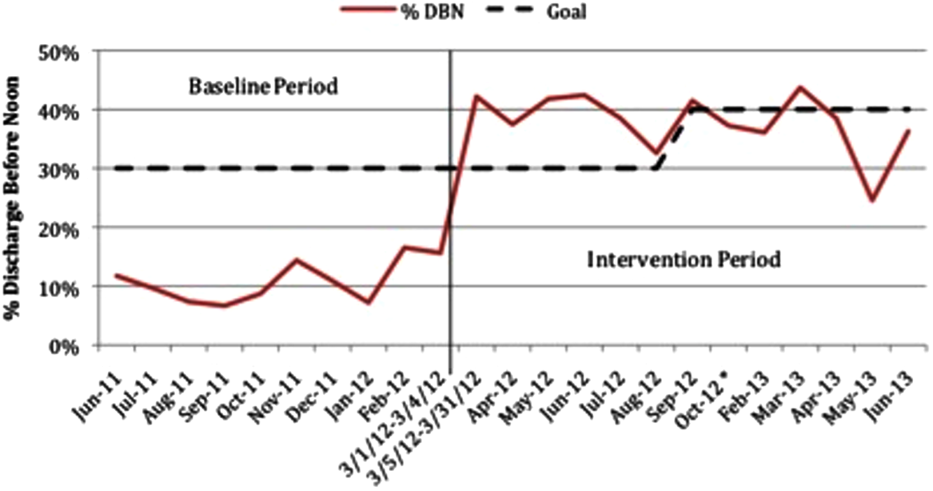
Secondary Outcomes: O/E LOS and 30‐Day Readmission Rate
The average O/E LOS during the baseline period was 1.06, and this declined during the intervention period to 0.96 [Table 2]. Using the Wilcoxon rank sum test, we found a statistically significant difference between the O/E LOS in the baseline (median 0.82) and intervention (median 0.76) periods (P = 0.0001). The average 30‐day readmission rate declined from 14.3% during the baseline to 13.1% during the intervention period. The change in 30‐day readmission rate was not statistically significant (z score=1.3132, P=0.1902). The change in readmission rate was similar and not statistically significant whether the patient was discharged before (13.6% baseline vs 12.6% intervention, P=0.66) or after noon (14.4% baseline vs 13.4% intervention, P=0.35) (Figure 2).
| Units 17E and 17W | Baseline Period | Intervention Period | Change | P Value |
|---|---|---|---|---|
| ||||
| O/E LOS, mean (median) | 1.06 (0.82) | 0.96 (0.76) | 10% | 0.0001a |
| 30‐day readmission rate | 14.3 | 13.1 | 1.2% | 0.1902 |
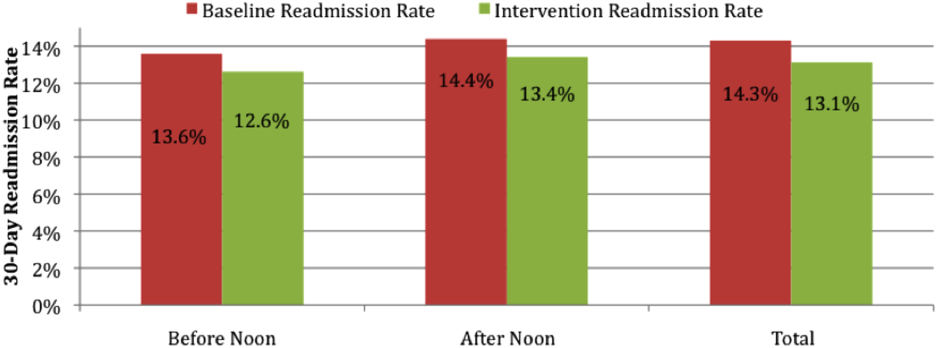
DISCUSSION
Throughput and discharges late in the day are challenges that face all medical centers. We demonstrate that successful and sustainable improvements in DBN are possible. We were able to increase the DBN percentage from 11% in the baseline period to an average of 38% in the 13 months after our intervention. Our success allowed us to surpass our medical center's initial goal of 30% DBN.
The intervention took place on 2 inpatient medical units at an urban, academic medical center. This intervention is likely generalizable to comparable medical centers. The study is limited by the implementation of multiple interventions as part of the DBN initiative at the same time. We are unable to isolate the effect of individual changes. If other medical centers wish to use a similar intervention, we believe the 3 most important parts of our intervention are: (1) kickoff event to engage all staff with a clear definition of roles; (2) daily real‐time feedback, utilizing tools such as unit boards tracking the DBN percentage; and (3) a standardized form of communication for expected DBNs. In our experience, for a DBN to be successful, the team, patient, and family members must be alerted, and discharge plans must be initiated at least 1 day prior to the expected discharge. Attempting to discharge a patient before noon when they have been identified on the day of discharge is a losing proposition, both to achieve a coordinated, safe discharge and for staff and patient satisfaction.
The O/E LOS and 30‐day readmission rate declined over the intervention period, suggesting that there is no negative effect on these metrics. There was concern that staff would choose to keep patients an extra night to allow for an extra DBN the following day. This was actively discouraged during the kickoff event and throughout the intervention period at interdisciplinary rounds and through informal communications. Based upon the decline in O/E LOS, this did not occur. There was also concern that the 30‐day readmission rate may increase if patients are discharged earlier in the day than usual. We observed an actual but not statistically significant decline in 30‐day readmission rate, potentially due to improved communication between team members and earlier identification of expected discharges at the prior day's afternoon DBN rounds. It is unknown if the decline in O/E LOS and 30‐day readmission rate was effected by the DBN initiative. Many other initiatives were ongoing within the medical center that could be effecting these variables. More research is required to better understand the true effect of DBN on LOS and 30‐day readmission rate.
There is limited literature on discharge early in the day. One previous study showed improvement in the DBN percentage on an obstetric floor through the institution of a discharge brunch.[9] Another report showed a modest increase (from 19.6% to 26%) in DBNs with the use of scheduled discharges.[6] This study was of unclear duration and was not specific to medical units. Another study focused on the use of in‐room display boards to document the expected day and time of patient discharge.[8] That report focused on the ability to schedule and achieve the scheduled discharge date and time. The authors describe a trend toward more discharges early in the day but provide no specific data on this effect. The only study looking specifically at discharge early in the day on a medical unit showed improvement in the discharge before 1:00 pm percentage, but was of small size (81 total patients) and short duration (1 month).[7] Our study is of larger size and longer duration, is focused on implementation of a medical service, and provides a comprehensive system that should be reproducible.
There are several next steps to our work. We will continue to monitor the DBN percentage and the ongoing sustainability of the project. We plan to investigate the effect of this rapid and notable increase in DBN percentage on a variety of patient outcomes and hospital metrics, including patient satisfaction, timeliness of ED admissions, intensive care unit transfers to the medical floor, and direct admissions.
Our study demonstrates that increased timely discharge is an achievable and sustainable goal for medical centers. Future work will allow for better understanding of the full effects of such an intervention on patient outcomes and hospital metrics.
- , , , . Impact of admission and discharge peak times on hospital overcrowding. Stud Health Technol Inform. 2011;168:82–88.
- , , , , , . Boarding inpatients in the emergency department increases discharged patient length of stay. J Emerg Med. 2013;44(1):230–235.
- , . Overcrowding in the nation's emergency departments: complex causes and disturbing effects. Ann Emerg Med. 2000;35(1):63–68.
- , , . Caregiver perceptions of the reasons for delayed hospital discharge. Eff Clin Pract. 2001;4(6):250–255.
- , , , et al. Daily multidisciplinary discharge rounds in a trauma center: a little time, well spent. J Trauma. 2009;66(3):880–887.
- , , , . All roads lead to scheduled discharges. Nursing. 2008;38(12):61–63.
- , , , . Discharging patients earlier in the day: a concept worth evaluating. Health Care Manag (Frederick). 2007;26(2):142–146.
- , , , et al. In‐room display of day and time patient is anticipated to leave hospital: a “discharge appointment”. J Hosp Med. 2007;2(1):13–16.
- , . The discharge brunch: reducing chaos and increasing smiles on the OB unit. Nurs Womens Health. 2009;13(5):402–409.
Late afternoon hospital discharges are thought to create admission bottlenecks in the emergency department (ED).[1] ED overcrowding increases the length of stay (LOS) of patients[2] and is a major dissatisfier for both patients and staff.[3] In our medical center, ED patients who are admitted after 1:00 pm have a 0.6‐day longer risk‐adjusted LOS than those admitted before 1:00 pm (M. Radford, MD, written communication, March 2012).
Many potential barriers to discharging patients early in the day exist.[4] However, comprehensive discharge planning favorably impacts discharge times.[5] There are limited published data regarding discharging patients early in the day. Studies have focused on improved discharge care coordination,[6, 7] in‐room display of planned discharge time,[8] and a discharge brunch.[9] In January 2012, the calendar month discharge before noon (DBN) percentage for 2 inpatient medicine units in our institution was approximately 7%, well below the organizational goal of 30%. We describe an intervention to sustainably increase the DBN percentage.
METHODS
Setting
The intervention took place on the 17th floor of New York University (NYU) Langone Medical Center's Tisch Hospital, an urban, academic medical center. All patients on the 17th floor received the intervention.
The 17th floor is composed of 2 acute care inpatient medical units17E and 17W. Each unit has 35 medical beds including a 16‐bed medical step down unit (SDU). Medical teams on the floor consist of 4 housestaff teams, a nurse practitioner (NP) team, and an SDU team. Each housestaff and NP team is led by a hospitalist, who is the attending of record for the majority of patients, though some patients on these teams are cared for by private attendings. Medical teams admit patients to any unit based upon bed availability. Nurses are assigned patients by acuity, not by medical team.
Intervention
Kick‐Off Event, Definition of Responsibilities, and Checklist
All stakeholders and front‐line staff were invited to a kickoff event on March 5, 2012. This event included education and discussion about the importance of a safe and early discharge from the patient and staff perspective. Roles in the discharge process were clearly defined and a corresponding checklist was created (Table 1). The checklist was used at least once per day during afternoon interdisciplinary in preparation for next‐day DBNs. Discharge date and time are communicated by the medical team to individual patients and families on the day a patient is identified for DBN. Patients and families did not receive additional orientation to the DBN initiative.
| Discharge Task | Responsible Team Member |
|---|---|
| |
| MD discharge summary and medication reconciliation | Resident or NP |
| Discharge order | Resident or NP |
| Prescription(s) | Resident or NP |
| Communicate discharge date and time to patient/family | Resident/hospitalist/NP |
| Patient education | Nurse |
| RN discharge summary | Nurse |
| Patient belongings/clothing | Nurse |
| Patient education/teaching | Nurse |
| Final labs/tests | Nurse |
| Assess Foley catheter need and remove | Nurse |
| Transportation | Social worker and care manager |
| At‐home services (HHA/HA/private hire) | Social worker and care manager |
| Equipment/supplies (DME, O2, ostomy supplies) | Social worker and care manager |
Interdisciplinary Rounds and DBN Website
In the past, interdisciplinary rounds, attended by each unit's charge nurse (CN), the medical resident or NP, the hospitalist, the team‐based social work (SW), and care management (CM) occurred in the morning between 9:00 am and 10:00 am. With the DBN initiative, additional afternoon interdisciplinary rounds were held at 3:00 pm. These rounds were designed to identify the next day's DBNs. Multidisciplinary team members were asked to complete the checklist responsibilities the same day that DBNs were identified rather than waiting until the day of discharge. A DBN website was created, and CMs were asked to log anticipated DBNs on this site after 3:00 pm rounds. The website generates a daily automated email at 4:30 pm to the DBN listserv with a list of the next day's anticipated DBNs. The listserv includes all hospitalists, residents, NPs, CNs, nurse managers (NM), medical directors, bed management, building services, SWs, and CMs. Additional departments were subsequently added as the DBN initiative became standard of care.
Assistant NMs update the DBN website overnight, adding patients identified by nursing staff as a possible DBN and highlighting changes in the condition of previously identified patients. At 7:00 am, an automated update email is sent by the website to the listserv. The automated emails include the DBN checklist, key phone numbers, and useful links.
Daily Leadership Meeting, Ongoing Process Improvement, and Real‐Time Feedback
Weekdays at 11:00 am, an interdisciplinary leadership meeting occurs with the medical directors, assistant NMs, CNs, and representatives from SW, CM, and hospital administration. At this meeting, all discharges from the previous day are reviewed to identify areas for improvement and trends in barriers to DBN. The current day's expected DBNs are also reviewed to address discharge bottlenecks in real time. Daily feedback was provided via a poster displayed in staff areas with daily DBN statistics.
Reward and Recognition
At the kickoff, a prize system was announced for the conclusion of the first month of the intervention if DBN thresholds were met. Rewards included a pizza party and raffle gift certificates. To hardwire the process, these rewards were repeated at the conclusion of each of the first 3 months of the intervention.
Changes to the Floor
There were notable changes to the floor during the time of this intervention. From October 25, 2012 until January 1, 2013, the hospital was closed after evacuation due to Hurricane Sandy. Units 17E and 17W reopened on January 14, 2013. The NP team was not restarted with the reopening. All other floor processes, including the DBN interventions, were restarted. The time period of floor closure was excluded in this analysis. The initial medical center goal was 30% DBNs. During the intervention period, the goal increased to 40%.
Data Collection and Analysis
Primary Outcome: Calendar Month DBN Percentage
The date and time of discharge are recorded by the discharging nurse or patient unit assistant in our electronic medical record (Epic, Madison WI) at the time the patient leaves the unit. Utilizing NYU's cost accounting system (Enterprise Performance Systems Inc., Chicago, IL), we obtained discharge date and time among inpatients discharged from units 17E and 17W between June 1, 2011 and March 4, 2012 (the baseline period) and March 5, 2012 and June 31, 2013 (the intervention period). Data from October 25, 2012 to the end of January 2013 were excluded due to hospital closure from Hurricane Sandy. The analysis includes 8 months of baseline data and 13 months of intervention data (not counting the excluded months from hospital closure), measuring the extent to which improvement was sustained. To match organizational criteria for DBN, we excluded patients on the units in the patient class observation, deaths, and inpatient hospice.
Patients were identified as DBNs if the discharge time was before 12:01 pm, in accordance with our medical center administration's definition of DBN. Calendar month DBN percentage was calculated by dividing the number of DBN patients during the calendar month by the total number of discharged patients during the calendar month. The proportion of DBNs in the baseline population was compared to the proportion of DBNs in the intervention population. Statistical significance for the change in DBN was evaluated by use of a 2‐tailed z test.
Secondary Outcomes: Observed‐to‐Expected LOS and 30‐Day Readmission Rate
Expected LOS was provided by the University Health Consortium (UHC). UHC calculates a risk‐adjusted LOS for each patient by assigning a severity of illness, selection of a patient population to serve as a basis of the model, and use of statistical regression to assign an expected LOS in days. Observed‐to‐expected (O/E) LOS for each patient is calculated by dividing the expected LOS in days by the observed (actual) LOS in days. The average of the O/E LOS for all patients in the baseline period was compared to the average O/E LOS for all patients in the intervention period. This average was calculated by summing the O/E LOS of all patients in each time period and dividing by the total number of patients. In accordance with our medical center administration's reporting standards, we report the mean of the O/E LOS. For statistical evaluation of this non‐normally distributed continuous variable, we also report the median of the O/E LOS for the baseline and intervention time period and use the Wilcoxon rank sum test to evaluate for statistical significance.
Readmission cases are identified by the clinical quality and effectiveness department at our medical center using the UHC definition of all patients who are readmitted to a hospital within 30 days of discharge from the index admission. The 30‐day readmission rate is calculated by dividing the total number of cases identified as readmissions within 30 days by the total number of admissions over the same time period. This rate was obtained on a calendar‐month basis for patients discharged from the index admission before noon, after noon, and in total. These rates were averaged over the baseline and intervention period. The proportion of 30‐day readmissions in the baseline population was compared to the proportion of 30‐day readmissions in the intervention population. Statistical significance for the change in 30‐day readmissions was evaluated by use of a 2‐tailed z test.
RESULTS
Primary Outcome: Calendar Month DBN Percentage
The calendar month DBN percentage increased in the first month of the intervention, from 16% to 42% (Figure 1). This improvement was sustained throughout the intervention, with an average calendar month DBN percentage of 38% over the 13‐month intervention period. Use of a 2‐tailed z test to compare the pre‐intervention proportion (11%) of patients who were DBN with the post‐intervention proportion (38%) who were DBN showed a statistically significant change (z score 23.6, P = 0.0002). Units 17E and 17W had a combined 2536 total discharges in the baseline period, with 265 patients discharged before noon. In the intervention period, 3277 total discharges occurred, with 1236 patients discharged before noon. The average time of discharge moved 1 hour and 31 minutes, from 3:43 pm in the baseline period to 2:13 pm in the intervention period.
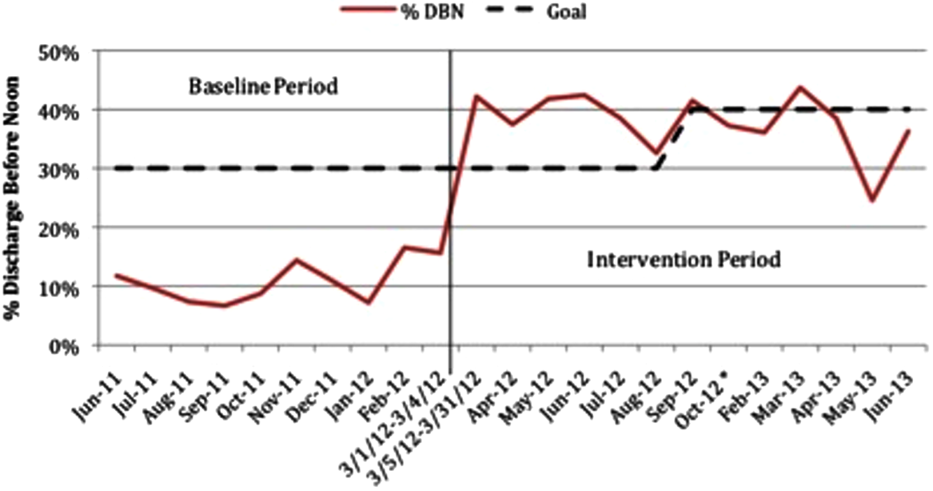
Secondary Outcomes: O/E LOS and 30‐Day Readmission Rate
The average O/E LOS during the baseline period was 1.06, and this declined during the intervention period to 0.96 [Table 2]. Using the Wilcoxon rank sum test, we found a statistically significant difference between the O/E LOS in the baseline (median 0.82) and intervention (median 0.76) periods (P = 0.0001). The average 30‐day readmission rate declined from 14.3% during the baseline to 13.1% during the intervention period. The change in 30‐day readmission rate was not statistically significant (z score=1.3132, P=0.1902). The change in readmission rate was similar and not statistically significant whether the patient was discharged before (13.6% baseline vs 12.6% intervention, P=0.66) or after noon (14.4% baseline vs 13.4% intervention, P=0.35) (Figure 2).
| Units 17E and 17W | Baseline Period | Intervention Period | Change | P Value |
|---|---|---|---|---|
| ||||
| O/E LOS, mean (median) | 1.06 (0.82) | 0.96 (0.76) | 10% | 0.0001a |
| 30‐day readmission rate | 14.3 | 13.1 | 1.2% | 0.1902 |
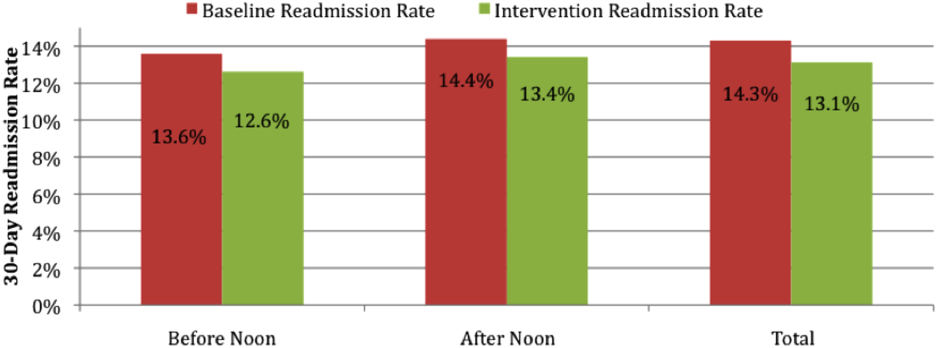
DISCUSSION
Throughput and discharges late in the day are challenges that face all medical centers. We demonstrate that successful and sustainable improvements in DBN are possible. We were able to increase the DBN percentage from 11% in the baseline period to an average of 38% in the 13 months after our intervention. Our success allowed us to surpass our medical center's initial goal of 30% DBN.
The intervention took place on 2 inpatient medical units at an urban, academic medical center. This intervention is likely generalizable to comparable medical centers. The study is limited by the implementation of multiple interventions as part of the DBN initiative at the same time. We are unable to isolate the effect of individual changes. If other medical centers wish to use a similar intervention, we believe the 3 most important parts of our intervention are: (1) kickoff event to engage all staff with a clear definition of roles; (2) daily real‐time feedback, utilizing tools such as unit boards tracking the DBN percentage; and (3) a standardized form of communication for expected DBNs. In our experience, for a DBN to be successful, the team, patient, and family members must be alerted, and discharge plans must be initiated at least 1 day prior to the expected discharge. Attempting to discharge a patient before noon when they have been identified on the day of discharge is a losing proposition, both to achieve a coordinated, safe discharge and for staff and patient satisfaction.
The O/E LOS and 30‐day readmission rate declined over the intervention period, suggesting that there is no negative effect on these metrics. There was concern that staff would choose to keep patients an extra night to allow for an extra DBN the following day. This was actively discouraged during the kickoff event and throughout the intervention period at interdisciplinary rounds and through informal communications. Based upon the decline in O/E LOS, this did not occur. There was also concern that the 30‐day readmission rate may increase if patients are discharged earlier in the day than usual. We observed an actual but not statistically significant decline in 30‐day readmission rate, potentially due to improved communication between team members and earlier identification of expected discharges at the prior day's afternoon DBN rounds. It is unknown if the decline in O/E LOS and 30‐day readmission rate was effected by the DBN initiative. Many other initiatives were ongoing within the medical center that could be effecting these variables. More research is required to better understand the true effect of DBN on LOS and 30‐day readmission rate.
There is limited literature on discharge early in the day. One previous study showed improvement in the DBN percentage on an obstetric floor through the institution of a discharge brunch.[9] Another report showed a modest increase (from 19.6% to 26%) in DBNs with the use of scheduled discharges.[6] This study was of unclear duration and was not specific to medical units. Another study focused on the use of in‐room display boards to document the expected day and time of patient discharge.[8] That report focused on the ability to schedule and achieve the scheduled discharge date and time. The authors describe a trend toward more discharges early in the day but provide no specific data on this effect. The only study looking specifically at discharge early in the day on a medical unit showed improvement in the discharge before 1:00 pm percentage, but was of small size (81 total patients) and short duration (1 month).[7] Our study is of larger size and longer duration, is focused on implementation of a medical service, and provides a comprehensive system that should be reproducible.
There are several next steps to our work. We will continue to monitor the DBN percentage and the ongoing sustainability of the project. We plan to investigate the effect of this rapid and notable increase in DBN percentage on a variety of patient outcomes and hospital metrics, including patient satisfaction, timeliness of ED admissions, intensive care unit transfers to the medical floor, and direct admissions.
Our study demonstrates that increased timely discharge is an achievable and sustainable goal for medical centers. Future work will allow for better understanding of the full effects of such an intervention on patient outcomes and hospital metrics.
Late afternoon hospital discharges are thought to create admission bottlenecks in the emergency department (ED).[1] ED overcrowding increases the length of stay (LOS) of patients[2] and is a major dissatisfier for both patients and staff.[3] In our medical center, ED patients who are admitted after 1:00 pm have a 0.6‐day longer risk‐adjusted LOS than those admitted before 1:00 pm (M. Radford, MD, written communication, March 2012).
Many potential barriers to discharging patients early in the day exist.[4] However, comprehensive discharge planning favorably impacts discharge times.[5] There are limited published data regarding discharging patients early in the day. Studies have focused on improved discharge care coordination,[6, 7] in‐room display of planned discharge time,[8] and a discharge brunch.[9] In January 2012, the calendar month discharge before noon (DBN) percentage for 2 inpatient medicine units in our institution was approximately 7%, well below the organizational goal of 30%. We describe an intervention to sustainably increase the DBN percentage.
METHODS
Setting
The intervention took place on the 17th floor of New York University (NYU) Langone Medical Center's Tisch Hospital, an urban, academic medical center. All patients on the 17th floor received the intervention.
The 17th floor is composed of 2 acute care inpatient medical units17E and 17W. Each unit has 35 medical beds including a 16‐bed medical step down unit (SDU). Medical teams on the floor consist of 4 housestaff teams, a nurse practitioner (NP) team, and an SDU team. Each housestaff and NP team is led by a hospitalist, who is the attending of record for the majority of patients, though some patients on these teams are cared for by private attendings. Medical teams admit patients to any unit based upon bed availability. Nurses are assigned patients by acuity, not by medical team.
Intervention
Kick‐Off Event, Definition of Responsibilities, and Checklist
All stakeholders and front‐line staff were invited to a kickoff event on March 5, 2012. This event included education and discussion about the importance of a safe and early discharge from the patient and staff perspective. Roles in the discharge process were clearly defined and a corresponding checklist was created (Table 1). The checklist was used at least once per day during afternoon interdisciplinary in preparation for next‐day DBNs. Discharge date and time are communicated by the medical team to individual patients and families on the day a patient is identified for DBN. Patients and families did not receive additional orientation to the DBN initiative.
| Discharge Task | Responsible Team Member |
|---|---|
| |
| MD discharge summary and medication reconciliation | Resident or NP |
| Discharge order | Resident or NP |
| Prescription(s) | Resident or NP |
| Communicate discharge date and time to patient/family | Resident/hospitalist/NP |
| Patient education | Nurse |
| RN discharge summary | Nurse |
| Patient belongings/clothing | Nurse |
| Patient education/teaching | Nurse |
| Final labs/tests | Nurse |
| Assess Foley catheter need and remove | Nurse |
| Transportation | Social worker and care manager |
| At‐home services (HHA/HA/private hire) | Social worker and care manager |
| Equipment/supplies (DME, O2, ostomy supplies) | Social worker and care manager |
Interdisciplinary Rounds and DBN Website
In the past, interdisciplinary rounds, attended by each unit's charge nurse (CN), the medical resident or NP, the hospitalist, the team‐based social work (SW), and care management (CM) occurred in the morning between 9:00 am and 10:00 am. With the DBN initiative, additional afternoon interdisciplinary rounds were held at 3:00 pm. These rounds were designed to identify the next day's DBNs. Multidisciplinary team members were asked to complete the checklist responsibilities the same day that DBNs were identified rather than waiting until the day of discharge. A DBN website was created, and CMs were asked to log anticipated DBNs on this site after 3:00 pm rounds. The website generates a daily automated email at 4:30 pm to the DBN listserv with a list of the next day's anticipated DBNs. The listserv includes all hospitalists, residents, NPs, CNs, nurse managers (NM), medical directors, bed management, building services, SWs, and CMs. Additional departments were subsequently added as the DBN initiative became standard of care.
Assistant NMs update the DBN website overnight, adding patients identified by nursing staff as a possible DBN and highlighting changes in the condition of previously identified patients. At 7:00 am, an automated update email is sent by the website to the listserv. The automated emails include the DBN checklist, key phone numbers, and useful links.
Daily Leadership Meeting, Ongoing Process Improvement, and Real‐Time Feedback
Weekdays at 11:00 am, an interdisciplinary leadership meeting occurs with the medical directors, assistant NMs, CNs, and representatives from SW, CM, and hospital administration. At this meeting, all discharges from the previous day are reviewed to identify areas for improvement and trends in barriers to DBN. The current day's expected DBNs are also reviewed to address discharge bottlenecks in real time. Daily feedback was provided via a poster displayed in staff areas with daily DBN statistics.
Reward and Recognition
At the kickoff, a prize system was announced for the conclusion of the first month of the intervention if DBN thresholds were met. Rewards included a pizza party and raffle gift certificates. To hardwire the process, these rewards were repeated at the conclusion of each of the first 3 months of the intervention.
Changes to the Floor
There were notable changes to the floor during the time of this intervention. From October 25, 2012 until January 1, 2013, the hospital was closed after evacuation due to Hurricane Sandy. Units 17E and 17W reopened on January 14, 2013. The NP team was not restarted with the reopening. All other floor processes, including the DBN interventions, were restarted. The time period of floor closure was excluded in this analysis. The initial medical center goal was 30% DBNs. During the intervention period, the goal increased to 40%.
Data Collection and Analysis
Primary Outcome: Calendar Month DBN Percentage
The date and time of discharge are recorded by the discharging nurse or patient unit assistant in our electronic medical record (Epic, Madison WI) at the time the patient leaves the unit. Utilizing NYU's cost accounting system (Enterprise Performance Systems Inc., Chicago, IL), we obtained discharge date and time among inpatients discharged from units 17E and 17W between June 1, 2011 and March 4, 2012 (the baseline period) and March 5, 2012 and June 31, 2013 (the intervention period). Data from October 25, 2012 to the end of January 2013 were excluded due to hospital closure from Hurricane Sandy. The analysis includes 8 months of baseline data and 13 months of intervention data (not counting the excluded months from hospital closure), measuring the extent to which improvement was sustained. To match organizational criteria for DBN, we excluded patients on the units in the patient class observation, deaths, and inpatient hospice.
Patients were identified as DBNs if the discharge time was before 12:01 pm, in accordance with our medical center administration's definition of DBN. Calendar month DBN percentage was calculated by dividing the number of DBN patients during the calendar month by the total number of discharged patients during the calendar month. The proportion of DBNs in the baseline population was compared to the proportion of DBNs in the intervention population. Statistical significance for the change in DBN was evaluated by use of a 2‐tailed z test.
Secondary Outcomes: Observed‐to‐Expected LOS and 30‐Day Readmission Rate
Expected LOS was provided by the University Health Consortium (UHC). UHC calculates a risk‐adjusted LOS for each patient by assigning a severity of illness, selection of a patient population to serve as a basis of the model, and use of statistical regression to assign an expected LOS in days. Observed‐to‐expected (O/E) LOS for each patient is calculated by dividing the expected LOS in days by the observed (actual) LOS in days. The average of the O/E LOS for all patients in the baseline period was compared to the average O/E LOS for all patients in the intervention period. This average was calculated by summing the O/E LOS of all patients in each time period and dividing by the total number of patients. In accordance with our medical center administration's reporting standards, we report the mean of the O/E LOS. For statistical evaluation of this non‐normally distributed continuous variable, we also report the median of the O/E LOS for the baseline and intervention time period and use the Wilcoxon rank sum test to evaluate for statistical significance.
Readmission cases are identified by the clinical quality and effectiveness department at our medical center using the UHC definition of all patients who are readmitted to a hospital within 30 days of discharge from the index admission. The 30‐day readmission rate is calculated by dividing the total number of cases identified as readmissions within 30 days by the total number of admissions over the same time period. This rate was obtained on a calendar‐month basis for patients discharged from the index admission before noon, after noon, and in total. These rates were averaged over the baseline and intervention period. The proportion of 30‐day readmissions in the baseline population was compared to the proportion of 30‐day readmissions in the intervention population. Statistical significance for the change in 30‐day readmissions was evaluated by use of a 2‐tailed z test.
RESULTS
Primary Outcome: Calendar Month DBN Percentage
The calendar month DBN percentage increased in the first month of the intervention, from 16% to 42% (Figure 1). This improvement was sustained throughout the intervention, with an average calendar month DBN percentage of 38% over the 13‐month intervention period. Use of a 2‐tailed z test to compare the pre‐intervention proportion (11%) of patients who were DBN with the post‐intervention proportion (38%) who were DBN showed a statistically significant change (z score 23.6, P = 0.0002). Units 17E and 17W had a combined 2536 total discharges in the baseline period, with 265 patients discharged before noon. In the intervention period, 3277 total discharges occurred, with 1236 patients discharged before noon. The average time of discharge moved 1 hour and 31 minutes, from 3:43 pm in the baseline period to 2:13 pm in the intervention period.
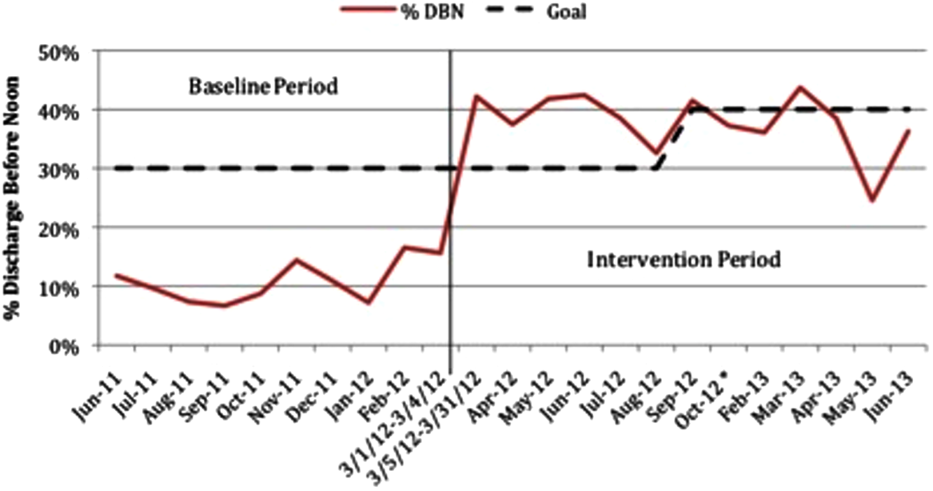
Secondary Outcomes: O/E LOS and 30‐Day Readmission Rate
The average O/E LOS during the baseline period was 1.06, and this declined during the intervention period to 0.96 [Table 2]. Using the Wilcoxon rank sum test, we found a statistically significant difference between the O/E LOS in the baseline (median 0.82) and intervention (median 0.76) periods (P = 0.0001). The average 30‐day readmission rate declined from 14.3% during the baseline to 13.1% during the intervention period. The change in 30‐day readmission rate was not statistically significant (z score=1.3132, P=0.1902). The change in readmission rate was similar and not statistically significant whether the patient was discharged before (13.6% baseline vs 12.6% intervention, P=0.66) or after noon (14.4% baseline vs 13.4% intervention, P=0.35) (Figure 2).
| Units 17E and 17W | Baseline Period | Intervention Period | Change | P Value |
|---|---|---|---|---|
| ||||
| O/E LOS, mean (median) | 1.06 (0.82) | 0.96 (0.76) | 10% | 0.0001a |
| 30‐day readmission rate | 14.3 | 13.1 | 1.2% | 0.1902 |
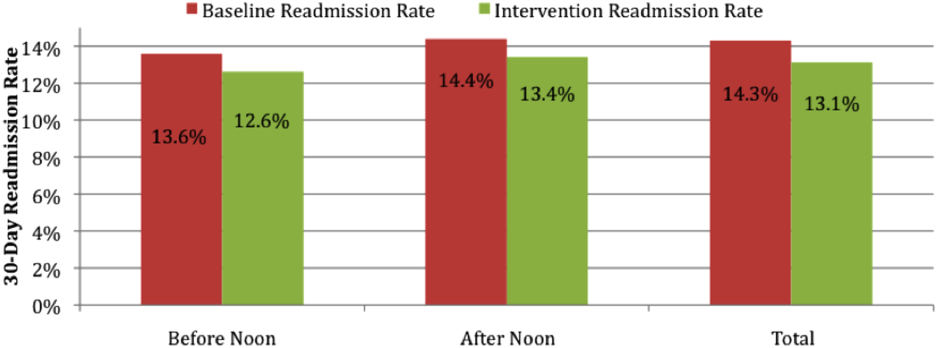
DISCUSSION
Throughput and discharges late in the day are challenges that face all medical centers. We demonstrate that successful and sustainable improvements in DBN are possible. We were able to increase the DBN percentage from 11% in the baseline period to an average of 38% in the 13 months after our intervention. Our success allowed us to surpass our medical center's initial goal of 30% DBN.
The intervention took place on 2 inpatient medical units at an urban, academic medical center. This intervention is likely generalizable to comparable medical centers. The study is limited by the implementation of multiple interventions as part of the DBN initiative at the same time. We are unable to isolate the effect of individual changes. If other medical centers wish to use a similar intervention, we believe the 3 most important parts of our intervention are: (1) kickoff event to engage all staff with a clear definition of roles; (2) daily real‐time feedback, utilizing tools such as unit boards tracking the DBN percentage; and (3) a standardized form of communication for expected DBNs. In our experience, for a DBN to be successful, the team, patient, and family members must be alerted, and discharge plans must be initiated at least 1 day prior to the expected discharge. Attempting to discharge a patient before noon when they have been identified on the day of discharge is a losing proposition, both to achieve a coordinated, safe discharge and for staff and patient satisfaction.
The O/E LOS and 30‐day readmission rate declined over the intervention period, suggesting that there is no negative effect on these metrics. There was concern that staff would choose to keep patients an extra night to allow for an extra DBN the following day. This was actively discouraged during the kickoff event and throughout the intervention period at interdisciplinary rounds and through informal communications. Based upon the decline in O/E LOS, this did not occur. There was also concern that the 30‐day readmission rate may increase if patients are discharged earlier in the day than usual. We observed an actual but not statistically significant decline in 30‐day readmission rate, potentially due to improved communication between team members and earlier identification of expected discharges at the prior day's afternoon DBN rounds. It is unknown if the decline in O/E LOS and 30‐day readmission rate was effected by the DBN initiative. Many other initiatives were ongoing within the medical center that could be effecting these variables. More research is required to better understand the true effect of DBN on LOS and 30‐day readmission rate.
There is limited literature on discharge early in the day. One previous study showed improvement in the DBN percentage on an obstetric floor through the institution of a discharge brunch.[9] Another report showed a modest increase (from 19.6% to 26%) in DBNs with the use of scheduled discharges.[6] This study was of unclear duration and was not specific to medical units. Another study focused on the use of in‐room display boards to document the expected day and time of patient discharge.[8] That report focused on the ability to schedule and achieve the scheduled discharge date and time. The authors describe a trend toward more discharges early in the day but provide no specific data on this effect. The only study looking specifically at discharge early in the day on a medical unit showed improvement in the discharge before 1:00 pm percentage, but was of small size (81 total patients) and short duration (1 month).[7] Our study is of larger size and longer duration, is focused on implementation of a medical service, and provides a comprehensive system that should be reproducible.
There are several next steps to our work. We will continue to monitor the DBN percentage and the ongoing sustainability of the project. We plan to investigate the effect of this rapid and notable increase in DBN percentage on a variety of patient outcomes and hospital metrics, including patient satisfaction, timeliness of ED admissions, intensive care unit transfers to the medical floor, and direct admissions.
Our study demonstrates that increased timely discharge is an achievable and sustainable goal for medical centers. Future work will allow for better understanding of the full effects of such an intervention on patient outcomes and hospital metrics.
- , , , . Impact of admission and discharge peak times on hospital overcrowding. Stud Health Technol Inform. 2011;168:82–88.
- , , , , , . Boarding inpatients in the emergency department increases discharged patient length of stay. J Emerg Med. 2013;44(1):230–235.
- , . Overcrowding in the nation's emergency departments: complex causes and disturbing effects. Ann Emerg Med. 2000;35(1):63–68.
- , , . Caregiver perceptions of the reasons for delayed hospital discharge. Eff Clin Pract. 2001;4(6):250–255.
- , , , et al. Daily multidisciplinary discharge rounds in a trauma center: a little time, well spent. J Trauma. 2009;66(3):880–887.
- , , , . All roads lead to scheduled discharges. Nursing. 2008;38(12):61–63.
- , , , . Discharging patients earlier in the day: a concept worth evaluating. Health Care Manag (Frederick). 2007;26(2):142–146.
- , , , et al. In‐room display of day and time patient is anticipated to leave hospital: a “discharge appointment”. J Hosp Med. 2007;2(1):13–16.
- , . The discharge brunch: reducing chaos and increasing smiles on the OB unit. Nurs Womens Health. 2009;13(5):402–409.
- , , , . Impact of admission and discharge peak times on hospital overcrowding. Stud Health Technol Inform. 2011;168:82–88.
- , , , , , . Boarding inpatients in the emergency department increases discharged patient length of stay. J Emerg Med. 2013;44(1):230–235.
- , . Overcrowding in the nation's emergency departments: complex causes and disturbing effects. Ann Emerg Med. 2000;35(1):63–68.
- , , . Caregiver perceptions of the reasons for delayed hospital discharge. Eff Clin Pract. 2001;4(6):250–255.
- , , , et al. Daily multidisciplinary discharge rounds in a trauma center: a little time, well spent. J Trauma. 2009;66(3):880–887.
- , , , . All roads lead to scheduled discharges. Nursing. 2008;38(12):61–63.
- , , , . Discharging patients earlier in the day: a concept worth evaluating. Health Care Manag (Frederick). 2007;26(2):142–146.
- , , , et al. In‐room display of day and time patient is anticipated to leave hospital: a “discharge appointment”. J Hosp Med. 2007;2(1):13–16.
- , . The discharge brunch: reducing chaos and increasing smiles on the OB unit. Nurs Womens Health. 2009;13(5):402–409.
© 2014 Society of Hospital Medicine