User login
Less competition equals higher healthcare costs

Credit: Petr Kratochvil
Medical practices in less competitive markets charge more for their services, according to a study published in JAMA.
The study, based on US healthcare data from 2010, provides new information about the effects of competition on prices for office visits paid by preferred provider organizations (PPOs).
“The research comes out of trying to understand some dramatic changes that have occurred in the healthcare system over a couple of decades,” said Laurence Baker, PhD, of the Stanford University School of Medicine in California.
One such change is the shift from practices with one or two doctors toward larger, more complex organizations with many physicians. An impact of this can be reduced competition among physician practices.
Dr Baker and his colleagues sought to understand how variation in the amount of competition within a region affects the amounts doctors are paid.
The researchers assessed the relationship between competition and prices paid by PPOs for the most commonly billed services within 10 prominent physician specialties—internal medicine, family practice, cardiology, dermatology, gastroenterology, neurology, general surgery, orthopedics, urology, and otolaryngology.
To establish what prices various medical practices were paid for services, the team used Truven Analytics MarketScan Commercial Claims and Encounters database, which contains the prices paid to physicians for more than 49 million privately insured people from all over the US. They obtained the number of claims and the mean price paid for each service in 1058 counties representing all 50 states.
To measure competitiveness, the researchers drew inspiration from the business world. Using Medicare data, they adapted a standard economic competition measure to track physician practice competition for different US regions.
The Hirschman-Herfindahl Index (HHI) uses the relative sizes of practices to measure market concentration. A higher HHI indicates a less competitive market, and a lower HHI indicates higher competition.
Less competition, higher prices
The researchers found that less competition among physician practices was associated with higher prices paid by private PPOs for office visits.
Across 10 types of office visits, the difference in the HHI was associated with average prices for office visits 8.3% to 16.1% higher. In a more conservative model, the difference in the HHI was associated with 3.5% to 5.4% higher average prices.
The researchers pointed out that, in 2011, privately insured individuals in the US spent nearly $250 billion on physician services. In that context, these small percentage increases could translate to tens of billions of dollars in extra spending.
The team also found that, between 2003 and 2010, prices increased more rapidly in areas that were less competitive. Even when there is no change in HHI, practices in less competitive areas could continue to drive up prices.
“These larger organizations might have better processes in place to optimize care,” said Kate Bundorf, PhD, also of the Stanford University School of Medicine.
“But our research also points out [that we] have to think about the effect on prices and try to balance those two things when we think about how to form policy about these organizations.”
Dr Baker echoed that sentiment.
“Sometimes, it can be tempting to say our goals for the healthcare system should be only about taking care of patients and doing it as well as possible,” he said. “We don’t want to worry about the economics. But the truth is, we do have to worry about the prices because the bill does come, even if you wish it wouldn’t.” ![]()

Credit: Petr Kratochvil
Medical practices in less competitive markets charge more for their services, according to a study published in JAMA.
The study, based on US healthcare data from 2010, provides new information about the effects of competition on prices for office visits paid by preferred provider organizations (PPOs).
“The research comes out of trying to understand some dramatic changes that have occurred in the healthcare system over a couple of decades,” said Laurence Baker, PhD, of the Stanford University School of Medicine in California.
One such change is the shift from practices with one or two doctors toward larger, more complex organizations with many physicians. An impact of this can be reduced competition among physician practices.
Dr Baker and his colleagues sought to understand how variation in the amount of competition within a region affects the amounts doctors are paid.
The researchers assessed the relationship between competition and prices paid by PPOs for the most commonly billed services within 10 prominent physician specialties—internal medicine, family practice, cardiology, dermatology, gastroenterology, neurology, general surgery, orthopedics, urology, and otolaryngology.
To establish what prices various medical practices were paid for services, the team used Truven Analytics MarketScan Commercial Claims and Encounters database, which contains the prices paid to physicians for more than 49 million privately insured people from all over the US. They obtained the number of claims and the mean price paid for each service in 1058 counties representing all 50 states.
To measure competitiveness, the researchers drew inspiration from the business world. Using Medicare data, they adapted a standard economic competition measure to track physician practice competition for different US regions.
The Hirschman-Herfindahl Index (HHI) uses the relative sizes of practices to measure market concentration. A higher HHI indicates a less competitive market, and a lower HHI indicates higher competition.
Less competition, higher prices
The researchers found that less competition among physician practices was associated with higher prices paid by private PPOs for office visits.
Across 10 types of office visits, the difference in the HHI was associated with average prices for office visits 8.3% to 16.1% higher. In a more conservative model, the difference in the HHI was associated with 3.5% to 5.4% higher average prices.
The researchers pointed out that, in 2011, privately insured individuals in the US spent nearly $250 billion on physician services. In that context, these small percentage increases could translate to tens of billions of dollars in extra spending.
The team also found that, between 2003 and 2010, prices increased more rapidly in areas that were less competitive. Even when there is no change in HHI, practices in less competitive areas could continue to drive up prices.
“These larger organizations might have better processes in place to optimize care,” said Kate Bundorf, PhD, also of the Stanford University School of Medicine.
“But our research also points out [that we] have to think about the effect on prices and try to balance those two things when we think about how to form policy about these organizations.”
Dr Baker echoed that sentiment.
“Sometimes, it can be tempting to say our goals for the healthcare system should be only about taking care of patients and doing it as well as possible,” he said. “We don’t want to worry about the economics. But the truth is, we do have to worry about the prices because the bill does come, even if you wish it wouldn’t.” ![]()

Credit: Petr Kratochvil
Medical practices in less competitive markets charge more for their services, according to a study published in JAMA.
The study, based on US healthcare data from 2010, provides new information about the effects of competition on prices for office visits paid by preferred provider organizations (PPOs).
“The research comes out of trying to understand some dramatic changes that have occurred in the healthcare system over a couple of decades,” said Laurence Baker, PhD, of the Stanford University School of Medicine in California.
One such change is the shift from practices with one or two doctors toward larger, more complex organizations with many physicians. An impact of this can be reduced competition among physician practices.
Dr Baker and his colleagues sought to understand how variation in the amount of competition within a region affects the amounts doctors are paid.
The researchers assessed the relationship between competition and prices paid by PPOs for the most commonly billed services within 10 prominent physician specialties—internal medicine, family practice, cardiology, dermatology, gastroenterology, neurology, general surgery, orthopedics, urology, and otolaryngology.
To establish what prices various medical practices were paid for services, the team used Truven Analytics MarketScan Commercial Claims and Encounters database, which contains the prices paid to physicians for more than 49 million privately insured people from all over the US. They obtained the number of claims and the mean price paid for each service in 1058 counties representing all 50 states.
To measure competitiveness, the researchers drew inspiration from the business world. Using Medicare data, they adapted a standard economic competition measure to track physician practice competition for different US regions.
The Hirschman-Herfindahl Index (HHI) uses the relative sizes of practices to measure market concentration. A higher HHI indicates a less competitive market, and a lower HHI indicates higher competition.
Less competition, higher prices
The researchers found that less competition among physician practices was associated with higher prices paid by private PPOs for office visits.
Across 10 types of office visits, the difference in the HHI was associated with average prices for office visits 8.3% to 16.1% higher. In a more conservative model, the difference in the HHI was associated with 3.5% to 5.4% higher average prices.
The researchers pointed out that, in 2011, privately insured individuals in the US spent nearly $250 billion on physician services. In that context, these small percentage increases could translate to tens of billions of dollars in extra spending.
The team also found that, between 2003 and 2010, prices increased more rapidly in areas that were less competitive. Even when there is no change in HHI, practices in less competitive areas could continue to drive up prices.
“These larger organizations might have better processes in place to optimize care,” said Kate Bundorf, PhD, also of the Stanford University School of Medicine.
“But our research also points out [that we] have to think about the effect on prices and try to balance those two things when we think about how to form policy about these organizations.”
Dr Baker echoed that sentiment.
“Sometimes, it can be tempting to say our goals for the healthcare system should be only about taking care of patients and doing it as well as possible,” he said. “We don’t want to worry about the economics. But the truth is, we do have to worry about the prices because the bill does come, even if you wish it wouldn’t.” ![]()
Docs often don’t know about patients’ CVCs

A multicenter study showed that roughly 1 in 5 physicians did not know when a hospitalized patient had a central venous catheter (CVC) in place.
Hospitalists were the least likely to know of a CVC’s presence, followed by general medicine teaching attendings, interns, and residents.
These findings raise questions about patient safety, as CVCs pose a risk of bloodstream infection and thrombosis, both of which can be prevented by removing catheters that are no longer necessary.
“We know that central venous catheters are invaluable for the safe and comprehensive care of some hospitalized patients, but just as they are helpful, they can be harmful,” said study author Vineet Chopra, MD, of the University of Michigan Health System in Ann Arbor.
“The key to preventing complications is to remove devices when they are no longer necessary, but that requires knowing they are there in the first place. Our findings suggest that patient safety may be jeopardized if medical providers don’t improve their practices regarding device awareness.”
Dr Chopra and his colleagues reported their findings in the Annals of Internal Medicine.
The study included 990 patients and 1881 clinical assessments at 3 academic medical centers in the US. Responses from interns (n=454), residents and physician extenders (n=513), general medicine teaching attendings (n=245), subspecialty attendings (n=176), intensivists (n=95), and hospitalists (n=398) were included.
The overall prevalence of CVCs was 21.1%, 60.3% of which were peripherally inserted central catheters (PICCs). The remaining CVCs were triple-lumen catheters inserted in the neck (19.6%), chest (11.5%), or groin (8.6%).
In all, 21.2% of clinicians interviewed did not know when a patient had a CVC in place. And 5.6% of clinicians said a patient had a CVC when there was no device in place.
Hospitalists were most likely to be unaware of a CVC (30.5%), followed by general medicine teaching attendings (25.8%), interns (19.1%), and residents (13.8%).
When assessed by service, critical care physicians were the least likely to be unaware of a CVC (12.6%), compared to general medicine teaching attendings/hospitalists (26.2%) and clinicians in other subspecialties (22.5%). Awareness was best among specialties that used CVCs often, such as cardiology and oncology.
Lack of awareness was greatest for PICCs; 25.1% of clinicians were unaware of a PICC’s presence, and 15.6% were unaware of a triple lumen catheter’s presence.
“These findings have important patient safety and policy implications for health systems nationwide,” Dr Chopra said, “because they suggest that removal of clinically unnecessary catheters may be limited by lack of awareness by providers, especially in non-intensive care settings.” ![]()

A multicenter study showed that roughly 1 in 5 physicians did not know when a hospitalized patient had a central venous catheter (CVC) in place.
Hospitalists were the least likely to know of a CVC’s presence, followed by general medicine teaching attendings, interns, and residents.
These findings raise questions about patient safety, as CVCs pose a risk of bloodstream infection and thrombosis, both of which can be prevented by removing catheters that are no longer necessary.
“We know that central venous catheters are invaluable for the safe and comprehensive care of some hospitalized patients, but just as they are helpful, they can be harmful,” said study author Vineet Chopra, MD, of the University of Michigan Health System in Ann Arbor.
“The key to preventing complications is to remove devices when they are no longer necessary, but that requires knowing they are there in the first place. Our findings suggest that patient safety may be jeopardized if medical providers don’t improve their practices regarding device awareness.”
Dr Chopra and his colleagues reported their findings in the Annals of Internal Medicine.
The study included 990 patients and 1881 clinical assessments at 3 academic medical centers in the US. Responses from interns (n=454), residents and physician extenders (n=513), general medicine teaching attendings (n=245), subspecialty attendings (n=176), intensivists (n=95), and hospitalists (n=398) were included.
The overall prevalence of CVCs was 21.1%, 60.3% of which were peripherally inserted central catheters (PICCs). The remaining CVCs were triple-lumen catheters inserted in the neck (19.6%), chest (11.5%), or groin (8.6%).
In all, 21.2% of clinicians interviewed did not know when a patient had a CVC in place. And 5.6% of clinicians said a patient had a CVC when there was no device in place.
Hospitalists were most likely to be unaware of a CVC (30.5%), followed by general medicine teaching attendings (25.8%), interns (19.1%), and residents (13.8%).
When assessed by service, critical care physicians were the least likely to be unaware of a CVC (12.6%), compared to general medicine teaching attendings/hospitalists (26.2%) and clinicians in other subspecialties (22.5%). Awareness was best among specialties that used CVCs often, such as cardiology and oncology.
Lack of awareness was greatest for PICCs; 25.1% of clinicians were unaware of a PICC’s presence, and 15.6% were unaware of a triple lumen catheter’s presence.
“These findings have important patient safety and policy implications for health systems nationwide,” Dr Chopra said, “because they suggest that removal of clinically unnecessary catheters may be limited by lack of awareness by providers, especially in non-intensive care settings.” ![]()

A multicenter study showed that roughly 1 in 5 physicians did not know when a hospitalized patient had a central venous catheter (CVC) in place.
Hospitalists were the least likely to know of a CVC’s presence, followed by general medicine teaching attendings, interns, and residents.
These findings raise questions about patient safety, as CVCs pose a risk of bloodstream infection and thrombosis, both of which can be prevented by removing catheters that are no longer necessary.
“We know that central venous catheters are invaluable for the safe and comprehensive care of some hospitalized patients, but just as they are helpful, they can be harmful,” said study author Vineet Chopra, MD, of the University of Michigan Health System in Ann Arbor.
“The key to preventing complications is to remove devices when they are no longer necessary, but that requires knowing they are there in the first place. Our findings suggest that patient safety may be jeopardized if medical providers don’t improve their practices regarding device awareness.”
Dr Chopra and his colleagues reported their findings in the Annals of Internal Medicine.
The study included 990 patients and 1881 clinical assessments at 3 academic medical centers in the US. Responses from interns (n=454), residents and physician extenders (n=513), general medicine teaching attendings (n=245), subspecialty attendings (n=176), intensivists (n=95), and hospitalists (n=398) were included.
The overall prevalence of CVCs was 21.1%, 60.3% of which were peripherally inserted central catheters (PICCs). The remaining CVCs were triple-lumen catheters inserted in the neck (19.6%), chest (11.5%), or groin (8.6%).
In all, 21.2% of clinicians interviewed did not know when a patient had a CVC in place. And 5.6% of clinicians said a patient had a CVC when there was no device in place.
Hospitalists were most likely to be unaware of a CVC (30.5%), followed by general medicine teaching attendings (25.8%), interns (19.1%), and residents (13.8%).
When assessed by service, critical care physicians were the least likely to be unaware of a CVC (12.6%), compared to general medicine teaching attendings/hospitalists (26.2%) and clinicians in other subspecialties (22.5%). Awareness was best among specialties that used CVCs often, such as cardiology and oncology.
Lack of awareness was greatest for PICCs; 25.1% of clinicians were unaware of a PICC’s presence, and 15.6% were unaware of a triple lumen catheter’s presence.
“These findings have important patient safety and policy implications for health systems nationwide,” Dr Chopra said, “because they suggest that removal of clinically unnecessary catheters may be limited by lack of awareness by providers, especially in non-intensive care settings.” ![]()
ID CONSULT: Influenza virus and pneumococci dance together
Most practitioners know that the flu vaccine has been proven to reduce the frequency of middle ear infections, sinusitis, and pneumonia. However, how that happens is not as clear. My group has been studying the details of the interaction between flu virus and pneumococci to unravel the steps in the dance between the flu virus and the pneumococcus in the nasopharynx that results in significant respiratory diseases. Pneumococci live in the posterior part of the nose and upper pharynx as commensal bacteria in all of us, harmlessly present in relatively low numbers. The bacteria are so common that studies to detect pneumococci in the nasopharynx discover their presence in up to 80% of infants and young children, and about 20% of adults at any one time. The bacteria are harmless in patients that have a competent immune system unless an intercurrent viral upper respiratory infection (URI) occurs.
The trigger in pathogenesis of pneumococcal infections is a viral URI, and particularly influenza infection. The combination of pneumococci and flu in the nose can cause compromise in all four aspects of host defense: 1) structural change, 2) physiologic change, 3) innate immunity change, and 4) adaptive immunity change. Structural change is swelling of the nasal passageways, Eustachian tube, osteomeatal sinus pathway, and tracheobronchial tree. Physiologic change is increased mucus production and reduced cilia beat, resulting in stasis of thickened mucus in the respiratory tree. Thus the stage is set for compromise in the immune response.
Innate immunity basically translates to the response of neutrophils, macrophages, and lymphocytes that are resident in the respiratory pathways or migrate there in response to signals from the site of infection that a problem is brewing. To start the process of innate immunity, chemicals are released from resident epithelial cells, lymphocytes, and neutrophils/macrophages. The chemicals are called cytokines and chemokines. The viruses enter the epithelial cells of the nasopharynx and tracheobronchial tree, and leave a change on the surface of the epithelial cells that alerts lymphocytes to kill and destroy those cells harboring virus. Neutrophils and macrophages ingest the bacteria by recognizing surface proteins on the bacteria that are foreign. Sometimes that is all that is needed, and the host clears the infection. But sometimes the innate response is not enough.
The innate response is good and bad. The bad part is that the release of the cytokines and chemokines and the migration of immune cells to the site of infection results in the release of even more cytokines and chemokines that cause increased inflammation. Microbes love inflammation. The inflammation caused by the virus, such as flu virus, creates a very favorable environment for the pneumococci. So the pneumococci start to reproduce in abundance. Then when the secretions of the nose are swept into the Eustachian tube and middle ear or the sinus drainage pathways and then to the sinuses or into the trachea and bronchi and then the lungs, we see the clinical manifestations of acute otitis media, sinusitis, or pneumonia. The innate response failed.
The adaptive response – as the word implies – is when the immune cells recognize and adapt to the presence of foreign microbes by recognizing their presence, migrating to lymph nodes and spleen, communicating with each other, and consequently multiplying into great numbers. The interaction between the immune cells – T cells and B cells – in the lymph node and migration back to the site of infection takes a few days to occur (3-5 days) if the host has prior immunity from prior infections or vaccination. If there is no prior immunity and no vaccination, then it takes 10-14 days for the adaptive immunity response to kick in and clear the infection. During that extra time, the pneumococci are gaining in numbers, causing more inflammation, and we see those clinical signs of fever, redness, and swelling at the site of infection, and pain.
So influenza can cause all of the events above by itself, but when the virus dances with the pneumococci, and the pneumococci benefit from the partnership, that is the most frequent cause of acute otitis media, sinusitis, and pneumonia. And all of that could have been prevented in most of our patients if they only got their annual flu vaccine.
Dr. Pichichero, a specialist in pediatric infectious diseases, is director of the Research Institute, Rochester (N.Y.) General Hospital. He is also a pediatrician at Legacy Pediatrics in Rochester. The study was supported by a National Institutes of Health grant. Dr. Pichichero said he had no relevant financial disclosures. Email him at [email protected].
Most practitioners know that the flu vaccine has been proven to reduce the frequency of middle ear infections, sinusitis, and pneumonia. However, how that happens is not as clear. My group has been studying the details of the interaction between flu virus and pneumococci to unravel the steps in the dance between the flu virus and the pneumococcus in the nasopharynx that results in significant respiratory diseases. Pneumococci live in the posterior part of the nose and upper pharynx as commensal bacteria in all of us, harmlessly present in relatively low numbers. The bacteria are so common that studies to detect pneumococci in the nasopharynx discover their presence in up to 80% of infants and young children, and about 20% of adults at any one time. The bacteria are harmless in patients that have a competent immune system unless an intercurrent viral upper respiratory infection (URI) occurs.
The trigger in pathogenesis of pneumococcal infections is a viral URI, and particularly influenza infection. The combination of pneumococci and flu in the nose can cause compromise in all four aspects of host defense: 1) structural change, 2) physiologic change, 3) innate immunity change, and 4) adaptive immunity change. Structural change is swelling of the nasal passageways, Eustachian tube, osteomeatal sinus pathway, and tracheobronchial tree. Physiologic change is increased mucus production and reduced cilia beat, resulting in stasis of thickened mucus in the respiratory tree. Thus the stage is set for compromise in the immune response.
Innate immunity basically translates to the response of neutrophils, macrophages, and lymphocytes that are resident in the respiratory pathways or migrate there in response to signals from the site of infection that a problem is brewing. To start the process of innate immunity, chemicals are released from resident epithelial cells, lymphocytes, and neutrophils/macrophages. The chemicals are called cytokines and chemokines. The viruses enter the epithelial cells of the nasopharynx and tracheobronchial tree, and leave a change on the surface of the epithelial cells that alerts lymphocytes to kill and destroy those cells harboring virus. Neutrophils and macrophages ingest the bacteria by recognizing surface proteins on the bacteria that are foreign. Sometimes that is all that is needed, and the host clears the infection. But sometimes the innate response is not enough.
The innate response is good and bad. The bad part is that the release of the cytokines and chemokines and the migration of immune cells to the site of infection results in the release of even more cytokines and chemokines that cause increased inflammation. Microbes love inflammation. The inflammation caused by the virus, such as flu virus, creates a very favorable environment for the pneumococci. So the pneumococci start to reproduce in abundance. Then when the secretions of the nose are swept into the Eustachian tube and middle ear or the sinus drainage pathways and then to the sinuses or into the trachea and bronchi and then the lungs, we see the clinical manifestations of acute otitis media, sinusitis, or pneumonia. The innate response failed.
The adaptive response – as the word implies – is when the immune cells recognize and adapt to the presence of foreign microbes by recognizing their presence, migrating to lymph nodes and spleen, communicating with each other, and consequently multiplying into great numbers. The interaction between the immune cells – T cells and B cells – in the lymph node and migration back to the site of infection takes a few days to occur (3-5 days) if the host has prior immunity from prior infections or vaccination. If there is no prior immunity and no vaccination, then it takes 10-14 days for the adaptive immunity response to kick in and clear the infection. During that extra time, the pneumococci are gaining in numbers, causing more inflammation, and we see those clinical signs of fever, redness, and swelling at the site of infection, and pain.
So influenza can cause all of the events above by itself, but when the virus dances with the pneumococci, and the pneumococci benefit from the partnership, that is the most frequent cause of acute otitis media, sinusitis, and pneumonia. And all of that could have been prevented in most of our patients if they only got their annual flu vaccine.
Dr. Pichichero, a specialist in pediatric infectious diseases, is director of the Research Institute, Rochester (N.Y.) General Hospital. He is also a pediatrician at Legacy Pediatrics in Rochester. The study was supported by a National Institutes of Health grant. Dr. Pichichero said he had no relevant financial disclosures. Email him at [email protected].
Most practitioners know that the flu vaccine has been proven to reduce the frequency of middle ear infections, sinusitis, and pneumonia. However, how that happens is not as clear. My group has been studying the details of the interaction between flu virus and pneumococci to unravel the steps in the dance between the flu virus and the pneumococcus in the nasopharynx that results in significant respiratory diseases. Pneumococci live in the posterior part of the nose and upper pharynx as commensal bacteria in all of us, harmlessly present in relatively low numbers. The bacteria are so common that studies to detect pneumococci in the nasopharynx discover their presence in up to 80% of infants and young children, and about 20% of adults at any one time. The bacteria are harmless in patients that have a competent immune system unless an intercurrent viral upper respiratory infection (URI) occurs.
The trigger in pathogenesis of pneumococcal infections is a viral URI, and particularly influenza infection. The combination of pneumococci and flu in the nose can cause compromise in all four aspects of host defense: 1) structural change, 2) physiologic change, 3) innate immunity change, and 4) adaptive immunity change. Structural change is swelling of the nasal passageways, Eustachian tube, osteomeatal sinus pathway, and tracheobronchial tree. Physiologic change is increased mucus production and reduced cilia beat, resulting in stasis of thickened mucus in the respiratory tree. Thus the stage is set for compromise in the immune response.
Innate immunity basically translates to the response of neutrophils, macrophages, and lymphocytes that are resident in the respiratory pathways or migrate there in response to signals from the site of infection that a problem is brewing. To start the process of innate immunity, chemicals are released from resident epithelial cells, lymphocytes, and neutrophils/macrophages. The chemicals are called cytokines and chemokines. The viruses enter the epithelial cells of the nasopharynx and tracheobronchial tree, and leave a change on the surface of the epithelial cells that alerts lymphocytes to kill and destroy those cells harboring virus. Neutrophils and macrophages ingest the bacteria by recognizing surface proteins on the bacteria that are foreign. Sometimes that is all that is needed, and the host clears the infection. But sometimes the innate response is not enough.
The innate response is good and bad. The bad part is that the release of the cytokines and chemokines and the migration of immune cells to the site of infection results in the release of even more cytokines and chemokines that cause increased inflammation. Microbes love inflammation. The inflammation caused by the virus, such as flu virus, creates a very favorable environment for the pneumococci. So the pneumococci start to reproduce in abundance. Then when the secretions of the nose are swept into the Eustachian tube and middle ear or the sinus drainage pathways and then to the sinuses or into the trachea and bronchi and then the lungs, we see the clinical manifestations of acute otitis media, sinusitis, or pneumonia. The innate response failed.
The adaptive response – as the word implies – is when the immune cells recognize and adapt to the presence of foreign microbes by recognizing their presence, migrating to lymph nodes and spleen, communicating with each other, and consequently multiplying into great numbers. The interaction between the immune cells – T cells and B cells – in the lymph node and migration back to the site of infection takes a few days to occur (3-5 days) if the host has prior immunity from prior infections or vaccination. If there is no prior immunity and no vaccination, then it takes 10-14 days for the adaptive immunity response to kick in and clear the infection. During that extra time, the pneumococci are gaining in numbers, causing more inflammation, and we see those clinical signs of fever, redness, and swelling at the site of infection, and pain.
So influenza can cause all of the events above by itself, but when the virus dances with the pneumococci, and the pneumococci benefit from the partnership, that is the most frequent cause of acute otitis media, sinusitis, and pneumonia. And all of that could have been prevented in most of our patients if they only got their annual flu vaccine.
Dr. Pichichero, a specialist in pediatric infectious diseases, is director of the Research Institute, Rochester (N.Y.) General Hospital. He is also a pediatrician at Legacy Pediatrics in Rochester. The study was supported by a National Institutes of Health grant. Dr. Pichichero said he had no relevant financial disclosures. Email him at [email protected].
Gun ownership in patients with dementia
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Acting strange after trying to ‘get numb’
CASE Numb and confused
Mr. L, age 17, is admitted to the hospital after ingesting 24 diphenhydramine 25-mg tablets in 3 hours as a possible suicide attempt. His parents witnessed him behaving strangely and brought him to the hospital. They state that their son was visibly agitated and acting inappropriately. He was seen talking to birds, trees, and the walls of the house.
Mr. L says he is upset because he broke up with his girlfriend a week earlier after she asked if they could “take a break.” He says that he took the diphenhydramine because he wanted to “get numb” to deal with the emotional stress caused by the break-up.
After the break-up, Mr. L experienced middle-to-late insomnia and was unable to get more than 3 or 4 hours of sleep a night. He reports significant fatigue, depressed mood, anhedonia, impaired concentration, and psychomotor retardation. He denies homicidal ideation or auditory and visual hallucinations.
As an aside, Mr. L reports that, for the past year, he had difficulties with gender identity, sometimes thinking that he might be better off if he had been born a girl and that he felt uncomfortable in a male body.
Which treatment option would you choose for Mr. L’s substance abuse?
a) refer him to a 12-step program
b) begin supportive measures
c) administer activated charcoal
d) prescribe a benzodiazepine to control agitation
The authors’ observations
As youths gain increasing access to medical and pharmaceutical knowledge through the Internet and other sources, it appears that adolescent drug abuse has, in part, shifted toward more easily attainable over-the-counter (OTC) medications. Diphenhydramine, a first-generation antihistamine, can be abused for its effects on the CNS, such as disturbed coordination, irritability, paresthesia, blurred vision, and depression. Effects of diphenhydramine are increased by the presence of alcohol, monoamine oxidase inhibitors, diazepam, hypnotics, sedatives, tranquilizers, and other CNS depressants. In 2011, diphenhydramine abuse was involved in 19,012 emergency room visits, of which 9,301 were for drug-related suicide attempts.1
Diphenhydramine is an inverse agonist of the histamine H1 receptor.2 It is a member of the ethanolamine subclass of antihistaminergic agents.3 By reversing the effects of histamine on capillaries, diphenhydramine can reduce the intensity of allergic symptoms. Diphenhydramine also crosses the blood–brain barrier and antagonizes H1 receptors centrally.
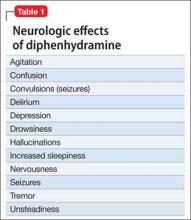
Used as a common sleep aid and allergy medication, the drug works primarily as an H1 receptor partial agonist, but also is a strong competitive antagonist at muscarinic acetylcholine receptors.4 It is abused for its sedative effects and its capacity to cause delirium and hallucinations.5 Diphenhydramine can have a stimulatory effect in children and young adults, instead of the sedating properties seen in adults.6 Such misuse is concerning because diphenhydramine overdose can lead to delirium, confusion, and hallucinations, tachycardia, seizures, mydriasis, xerostomia, urinary retention, ileus, anhidrosis, and hyperthermia. In severe cases it has been associated with cardiac arrhythmias, rhabdomyolysis, status epilepticus, and death.4,6 Neurologic symptoms of diphenhydramine overdose are listed in Table 1.
HISTORY Polysubstance abuse
Mr. L has a 2-year history of major depressive disorder and a history of Cannabis abuse with physiological dependence; Robitussin (base active ingredient, guaifenesin) and hydrocodone abuse with physiological dependence; 3,4-methylenedioxymethamphetamine (MDMA) abuse; and diphenhydramine abuse. He also has a history of gender dysphoria, although he reports that these feelings have become less severe over the past year.
Mr. L attends bi-weekly appointments with an outpatient psychiatrist and reportedly adheres to his medication regimen: fluoxetine, 40 mg/d, and risperidone, 1 mg at bedtime. He denies previous suicidal ideation, suicide attempts, homicidal ideation, or homicidal attempts. He reports no history of physical, sexual, or emotional abuse. He gets good grades in school and has no outstanding academic problems.
Mr. L began using Cannabis at age 14; his last use was 3 weeks before admission. He is guarded about his use of Robitussin, hydrocodone, and MDMA. However, Mr. L reports that he has researched diphenhydramine on the internet and believes that he can safely take up to 1,200 mg without overdosing. He reports normally taking 450 mg of diphenhydramine daily. Mr. L reports difficulty urinating after using diphenhydramine but no other physical complaints.
Mr. L lives with his father and stepmother and has a history of one psychiatric hospitalization at a different facility 2 months ago, followed by outpatient therapy. He obtained his Graduate Equivalency Diploma (GED) and plans to attend college.
At age 5, Mr. L emigrated from Turkey to the United States with his parents. His mother returned to Turkey when he was age 6 and has had no contact with her son since. Whenever Mr. L visits Turkey with his father, the patient refuses to see her, as per collaterals. He gets along well with his stepmother, who is his maternal aunt. Mr. L has been bullied at school and reportedly has few friends.
On mental status examination, Mr. L has an appropriate appearance and appears to be his stated age. He shows good eye contact and is cooperative. Muscle tone and gait are within normal limits. He has no abnormal movements. Speech, thought processes, and associations are normal. He denies auditory hallucinations, visual hallucinations, suicidal ideation (although he presented with a probable suicide attempt), or homicidal ideation. No delusions are elicited.
Mr. L shows poor judgment about his drug use and situation. He demonstrates limited insight, because he says his only goal is to get out of the hospital. He is alert, awake, and oriented to person, place, and time. He shows no memory or knowledge impairment. He appears euthymic with an inappropriate and constricted affect. On neurologic exam, he had mild tremors in his hands. The authors’ observationsTreatment for diphenhydramine overdose should begin quickly to prevent life-threatening effects and reduce the risk for mortality. The toxin can be removed from the patient’s GI tract with activated charcoal or gastric lavage if the patient presents within 1 hour of ingesting the substance. Administering IV fluids will prevent dehydration. Cardiac functioning is monitored and benzodiazepines could be administered to manage seizures.
Key elements of a toxicologic physical examination include:
• eyes: pupillary size, symmetry, and response to light (vertical or horizontal nystagmus)
• oropharynx: moist or dry mucous membranes, presence or absence of the gag reflex, distinctive odors
• abdomen: presence or absence and quality of bowel sounds
• skin: warm and dry, warm and sweaty, or cool
• neurologic: level of consciousness and mental status, presence of tremors, seizures, or other movement disorders, presence or absence and quality of deep tendon reflexes.7
If a child or adolescent patient cannot communicate how much of a drug he (she) has ingested, questions to ask parents or other informants include:
• Was the medication purchased recently, and if so was the bottle or box full before the patient took the pills?
• If the medication was not new, how many pills were in the bottle before the patient got to it?
• If the medication was prescribed, how many pills were originally prescribed, when was the medication prescribed, and how many pills were already taken prior to the patient getting to the bottle?
• How many pills were left in the bottle?
• How many pills were seen around the area where the patient was found?
• How many pills were found in the patient’s mouth?7
Recommendations
It is well known that OTC medication abuse is a growing medical problem (Table 2). Antihistamines, including diphenhydramine, are readily available to minors and adults. Because of the powerful sedating effects of antihistamines, many adolescent health practitioners give them to patients who have insomnia as a sleep aid.8 As in our case, antihistamines are used recreationally for their hallucinogenic effects, at dosages of 300 to 700 mg.9 Severe symptoms of toxicity, such as delirium and psychosis, seizures, and coma, occur at dosages ≥1,000 mg.9
With growing abuse of these medications, we aim to encourage detailed history taking about abuse of OTC drugs, especially diphenhydramine in adolescent patients.
Outcome Improvement, discharge
Mr. L is given a dual diagnosis of diphenhydramine-induced psychotic disorder with
hallucinations and diphenhydramine-induced depressive disorder, both with onset during intoxication. He also is given a provisional diagnosis of psychotic disorder not otherwise specified and major depressive disorder. Last, he is given a diagnosis of Cannabis dependence with physiological dependence, MDMA abuse, hydrocodone abuse, and Robitussin abuse.
Mr. L is maintained on fluoxetine, 40 mg/d, and risperidone, 1 mg at bedtime and 0.5 mg in the morning. He receives milieu, individual, group, recreational, and medical therapy while in the hospital. Symptoms abate and he is discharged with a plan to follow up with outpatient providers.
Bottom Line
Abuse of over-the-counter (OTC) drugs, such as diphenhydramine, among youths is a growing problem. Remember to question adolescents who appear intoxicated or to have overdosed not only about abuse of alcohol and illicit substances but also of common—and easily and legally accessible—OTC drugs.
Related Resources
• Carr BC. Efficacy, abuse, and toxicity of over-the-counter cough and cold medicines in the pediatric population. Curr Opin Pediatr. 2006;18(2):184-188.
• Thomas A, Nallur DG, Jones N, et al. Diphenhydramine abuse and detoxification: a brief review and case report. J Psychopharmacol. 2009;23(1):101-105.
Drug Brand Names
Diazepam • Valium Hydrocodone • Vicodin
Diphenhydramine • Benadryl Risperidone • Risperdal
Fluoxetine • Prozac
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. U.S. Department of Health and Human Services. Drug Abuse Warning Network, 2011: National estimates of drug-related emergency department visits. http://www.samhsa. gov/data/2k13/DAWN2k11ED/DAWN2k11ED.htm. Published May 2013. Accessed on September 29, 2014.
2. Yamashiro K, Kiryu J, Tsujikawa A, et al. Suppressive effects of histamine H1 receptor antagonist diphenhydramine on the leukocyte infiltration during endotoxin-induced uveitis. Exp Eye Res. 2001;73(1):69-80.
3. Skidgel RA, Kaplan AP, Erdos EG. Histamine, bradykinin, and their antagonists. In: Brunton L, Chabner B, Knollman B, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 12th ed. New York, NY: McGraw Hill; 2011: 911-935.
4. Vearrier D, Curtis JA. Case files of the medical toxicology fellowship at Drexel University. Rhabdomyolysis and compartment syndrome following acute diphenhydramine overdose. J Med Toxicol. 2011;7(3):213-219.
5. Ho M, Tsai K, Liu C. Diphenhydramine overdose related delirium: a case report. Journal of Emergency and Critical Care Medicine. 2006;17(2):77-79.
6. Krenzelok EP, Anderson GM, Mirick M. Massive diphenhydramine overdose resulting in death. Ann Emerg Med. 1982;11(4):212-213.
7. Inaba AS. Toxicologic teasers: Testing your knowledge of clinical toxicology. Hawaii Med J. 1998;57(4):471-473.
8. Kaplan SL. Busner J. The use of prn and stat medication in three child psychiatric inpatient settings. Psychopharmacol Bull. 1997;33(1):161-164.
9. Radovanovic D, Meier PJ, Guirguis M, et al. Dose-dependent toxicity of diphenhydramine overdose. Hum Exp Toxicol. 2000;19(9):489-495.
CASE Numb and confused
Mr. L, age 17, is admitted to the hospital after ingesting 24 diphenhydramine 25-mg tablets in 3 hours as a possible suicide attempt. His parents witnessed him behaving strangely and brought him to the hospital. They state that their son was visibly agitated and acting inappropriately. He was seen talking to birds, trees, and the walls of the house.
Mr. L says he is upset because he broke up with his girlfriend a week earlier after she asked if they could “take a break.” He says that he took the diphenhydramine because he wanted to “get numb” to deal with the emotional stress caused by the break-up.
After the break-up, Mr. L experienced middle-to-late insomnia and was unable to get more than 3 or 4 hours of sleep a night. He reports significant fatigue, depressed mood, anhedonia, impaired concentration, and psychomotor retardation. He denies homicidal ideation or auditory and visual hallucinations.
As an aside, Mr. L reports that, for the past year, he had difficulties with gender identity, sometimes thinking that he might be better off if he had been born a girl and that he felt uncomfortable in a male body.
Which treatment option would you choose for Mr. L’s substance abuse?
a) refer him to a 12-step program
b) begin supportive measures
c) administer activated charcoal
d) prescribe a benzodiazepine to control agitation
The authors’ observations
As youths gain increasing access to medical and pharmaceutical knowledge through the Internet and other sources, it appears that adolescent drug abuse has, in part, shifted toward more easily attainable over-the-counter (OTC) medications. Diphenhydramine, a first-generation antihistamine, can be abused for its effects on the CNS, such as disturbed coordination, irritability, paresthesia, blurred vision, and depression. Effects of diphenhydramine are increased by the presence of alcohol, monoamine oxidase inhibitors, diazepam, hypnotics, sedatives, tranquilizers, and other CNS depressants. In 2011, diphenhydramine abuse was involved in 19,012 emergency room visits, of which 9,301 were for drug-related suicide attempts.1
Diphenhydramine is an inverse agonist of the histamine H1 receptor.2 It is a member of the ethanolamine subclass of antihistaminergic agents.3 By reversing the effects of histamine on capillaries, diphenhydramine can reduce the intensity of allergic symptoms. Diphenhydramine also crosses the blood–brain barrier and antagonizes H1 receptors centrally.
Used as a common sleep aid and allergy medication, the drug works primarily as an H1 receptor partial agonist, but also is a strong competitive antagonist at muscarinic acetylcholine receptors.4 It is abused for its sedative effects and its capacity to cause delirium and hallucinations.5 Diphenhydramine can have a stimulatory effect in children and young adults, instead of the sedating properties seen in adults.6 Such misuse is concerning because diphenhydramine overdose can lead to delirium, confusion, and hallucinations, tachycardia, seizures, mydriasis, xerostomia, urinary retention, ileus, anhidrosis, and hyperthermia. In severe cases it has been associated with cardiac arrhythmias, rhabdomyolysis, status epilepticus, and death.4,6 Neurologic symptoms of diphenhydramine overdose are listed in Table 1.
HISTORY Polysubstance abuse
Mr. L has a 2-year history of major depressive disorder and a history of Cannabis abuse with physiological dependence; Robitussin (base active ingredient, guaifenesin) and hydrocodone abuse with physiological dependence; 3,4-methylenedioxymethamphetamine (MDMA) abuse; and diphenhydramine abuse. He also has a history of gender dysphoria, although he reports that these feelings have become less severe over the past year.
Mr. L attends bi-weekly appointments with an outpatient psychiatrist and reportedly adheres to his medication regimen: fluoxetine, 40 mg/d, and risperidone, 1 mg at bedtime. He denies previous suicidal ideation, suicide attempts, homicidal ideation, or homicidal attempts. He reports no history of physical, sexual, or emotional abuse. He gets good grades in school and has no outstanding academic problems.
Mr. L began using Cannabis at age 14; his last use was 3 weeks before admission. He is guarded about his use of Robitussin, hydrocodone, and MDMA. However, Mr. L reports that he has researched diphenhydramine on the internet and believes that he can safely take up to 1,200 mg without overdosing. He reports normally taking 450 mg of diphenhydramine daily. Mr. L reports difficulty urinating after using diphenhydramine but no other physical complaints.
Mr. L lives with his father and stepmother and has a history of one psychiatric hospitalization at a different facility 2 months ago, followed by outpatient therapy. He obtained his Graduate Equivalency Diploma (GED) and plans to attend college.
At age 5, Mr. L emigrated from Turkey to the United States with his parents. His mother returned to Turkey when he was age 6 and has had no contact with her son since. Whenever Mr. L visits Turkey with his father, the patient refuses to see her, as per collaterals. He gets along well with his stepmother, who is his maternal aunt. Mr. L has been bullied at school and reportedly has few friends.
On mental status examination, Mr. L has an appropriate appearance and appears to be his stated age. He shows good eye contact and is cooperative. Muscle tone and gait are within normal limits. He has no abnormal movements. Speech, thought processes, and associations are normal. He denies auditory hallucinations, visual hallucinations, suicidal ideation (although he presented with a probable suicide attempt), or homicidal ideation. No delusions are elicited.
Mr. L shows poor judgment about his drug use and situation. He demonstrates limited insight, because he says his only goal is to get out of the hospital. He is alert, awake, and oriented to person, place, and time. He shows no memory or knowledge impairment. He appears euthymic with an inappropriate and constricted affect. On neurologic exam, he had mild tremors in his hands. The authors’ observationsTreatment for diphenhydramine overdose should begin quickly to prevent life-threatening effects and reduce the risk for mortality. The toxin can be removed from the patient’s GI tract with activated charcoal or gastric lavage if the patient presents within 1 hour of ingesting the substance. Administering IV fluids will prevent dehydration. Cardiac functioning is monitored and benzodiazepines could be administered to manage seizures.
Key elements of a toxicologic physical examination include:
• eyes: pupillary size, symmetry, and response to light (vertical or horizontal nystagmus)
• oropharynx: moist or dry mucous membranes, presence or absence of the gag reflex, distinctive odors
• abdomen: presence or absence and quality of bowel sounds
• skin: warm and dry, warm and sweaty, or cool
• neurologic: level of consciousness and mental status, presence of tremors, seizures, or other movement disorders, presence or absence and quality of deep tendon reflexes.7
If a child or adolescent patient cannot communicate how much of a drug he (she) has ingested, questions to ask parents or other informants include:
• Was the medication purchased recently, and if so was the bottle or box full before the patient took the pills?
• If the medication was not new, how many pills were in the bottle before the patient got to it?
• If the medication was prescribed, how many pills were originally prescribed, when was the medication prescribed, and how many pills were already taken prior to the patient getting to the bottle?
• How many pills were left in the bottle?
• How many pills were seen around the area where the patient was found?
• How many pills were found in the patient’s mouth?7
Recommendations
It is well known that OTC medication abuse is a growing medical problem (Table 2). Antihistamines, including diphenhydramine, are readily available to minors and adults. Because of the powerful sedating effects of antihistamines, many adolescent health practitioners give them to patients who have insomnia as a sleep aid.8 As in our case, antihistamines are used recreationally for their hallucinogenic effects, at dosages of 300 to 700 mg.9 Severe symptoms of toxicity, such as delirium and psychosis, seizures, and coma, occur at dosages ≥1,000 mg.9
With growing abuse of these medications, we aim to encourage detailed history taking about abuse of OTC drugs, especially diphenhydramine in adolescent patients.
Outcome Improvement, discharge
Mr. L is given a dual diagnosis of diphenhydramine-induced psychotic disorder with
hallucinations and diphenhydramine-induced depressive disorder, both with onset during intoxication. He also is given a provisional diagnosis of psychotic disorder not otherwise specified and major depressive disorder. Last, he is given a diagnosis of Cannabis dependence with physiological dependence, MDMA abuse, hydrocodone abuse, and Robitussin abuse.
Mr. L is maintained on fluoxetine, 40 mg/d, and risperidone, 1 mg at bedtime and 0.5 mg in the morning. He receives milieu, individual, group, recreational, and medical therapy while in the hospital. Symptoms abate and he is discharged with a plan to follow up with outpatient providers.
Bottom Line
Abuse of over-the-counter (OTC) drugs, such as diphenhydramine, among youths is a growing problem. Remember to question adolescents who appear intoxicated or to have overdosed not only about abuse of alcohol and illicit substances but also of common—and easily and legally accessible—OTC drugs.
Related Resources
• Carr BC. Efficacy, abuse, and toxicity of over-the-counter cough and cold medicines in the pediatric population. Curr Opin Pediatr. 2006;18(2):184-188.
• Thomas A, Nallur DG, Jones N, et al. Diphenhydramine abuse and detoxification: a brief review and case report. J Psychopharmacol. 2009;23(1):101-105.
Drug Brand Names
Diazepam • Valium Hydrocodone • Vicodin
Diphenhydramine • Benadryl Risperidone • Risperdal
Fluoxetine • Prozac
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE Numb and confused
Mr. L, age 17, is admitted to the hospital after ingesting 24 diphenhydramine 25-mg tablets in 3 hours as a possible suicide attempt. His parents witnessed him behaving strangely and brought him to the hospital. They state that their son was visibly agitated and acting inappropriately. He was seen talking to birds, trees, and the walls of the house.
Mr. L says he is upset because he broke up with his girlfriend a week earlier after she asked if they could “take a break.” He says that he took the diphenhydramine because he wanted to “get numb” to deal with the emotional stress caused by the break-up.
After the break-up, Mr. L experienced middle-to-late insomnia and was unable to get more than 3 or 4 hours of sleep a night. He reports significant fatigue, depressed mood, anhedonia, impaired concentration, and psychomotor retardation. He denies homicidal ideation or auditory and visual hallucinations.
As an aside, Mr. L reports that, for the past year, he had difficulties with gender identity, sometimes thinking that he might be better off if he had been born a girl and that he felt uncomfortable in a male body.
Which treatment option would you choose for Mr. L’s substance abuse?
a) refer him to a 12-step program
b) begin supportive measures
c) administer activated charcoal
d) prescribe a benzodiazepine to control agitation
The authors’ observations
As youths gain increasing access to medical and pharmaceutical knowledge through the Internet and other sources, it appears that adolescent drug abuse has, in part, shifted toward more easily attainable over-the-counter (OTC) medications. Diphenhydramine, a first-generation antihistamine, can be abused for its effects on the CNS, such as disturbed coordination, irritability, paresthesia, blurred vision, and depression. Effects of diphenhydramine are increased by the presence of alcohol, monoamine oxidase inhibitors, diazepam, hypnotics, sedatives, tranquilizers, and other CNS depressants. In 2011, diphenhydramine abuse was involved in 19,012 emergency room visits, of which 9,301 were for drug-related suicide attempts.1
Diphenhydramine is an inverse agonist of the histamine H1 receptor.2 It is a member of the ethanolamine subclass of antihistaminergic agents.3 By reversing the effects of histamine on capillaries, diphenhydramine can reduce the intensity of allergic symptoms. Diphenhydramine also crosses the blood–brain barrier and antagonizes H1 receptors centrally.
Used as a common sleep aid and allergy medication, the drug works primarily as an H1 receptor partial agonist, but also is a strong competitive antagonist at muscarinic acetylcholine receptors.4 It is abused for its sedative effects and its capacity to cause delirium and hallucinations.5 Diphenhydramine can have a stimulatory effect in children and young adults, instead of the sedating properties seen in adults.6 Such misuse is concerning because diphenhydramine overdose can lead to delirium, confusion, and hallucinations, tachycardia, seizures, mydriasis, xerostomia, urinary retention, ileus, anhidrosis, and hyperthermia. In severe cases it has been associated with cardiac arrhythmias, rhabdomyolysis, status epilepticus, and death.4,6 Neurologic symptoms of diphenhydramine overdose are listed in Table 1.
HISTORY Polysubstance abuse
Mr. L has a 2-year history of major depressive disorder and a history of Cannabis abuse with physiological dependence; Robitussin (base active ingredient, guaifenesin) and hydrocodone abuse with physiological dependence; 3,4-methylenedioxymethamphetamine (MDMA) abuse; and diphenhydramine abuse. He also has a history of gender dysphoria, although he reports that these feelings have become less severe over the past year.
Mr. L attends bi-weekly appointments with an outpatient psychiatrist and reportedly adheres to his medication regimen: fluoxetine, 40 mg/d, and risperidone, 1 mg at bedtime. He denies previous suicidal ideation, suicide attempts, homicidal ideation, or homicidal attempts. He reports no history of physical, sexual, or emotional abuse. He gets good grades in school and has no outstanding academic problems.
Mr. L began using Cannabis at age 14; his last use was 3 weeks before admission. He is guarded about his use of Robitussin, hydrocodone, and MDMA. However, Mr. L reports that he has researched diphenhydramine on the internet and believes that he can safely take up to 1,200 mg without overdosing. He reports normally taking 450 mg of diphenhydramine daily. Mr. L reports difficulty urinating after using diphenhydramine but no other physical complaints.
Mr. L lives with his father and stepmother and has a history of one psychiatric hospitalization at a different facility 2 months ago, followed by outpatient therapy. He obtained his Graduate Equivalency Diploma (GED) and plans to attend college.
At age 5, Mr. L emigrated from Turkey to the United States with his parents. His mother returned to Turkey when he was age 6 and has had no contact with her son since. Whenever Mr. L visits Turkey with his father, the patient refuses to see her, as per collaterals. He gets along well with his stepmother, who is his maternal aunt. Mr. L has been bullied at school and reportedly has few friends.
On mental status examination, Mr. L has an appropriate appearance and appears to be his stated age. He shows good eye contact and is cooperative. Muscle tone and gait are within normal limits. He has no abnormal movements. Speech, thought processes, and associations are normal. He denies auditory hallucinations, visual hallucinations, suicidal ideation (although he presented with a probable suicide attempt), or homicidal ideation. No delusions are elicited.
Mr. L shows poor judgment about his drug use and situation. He demonstrates limited insight, because he says his only goal is to get out of the hospital. He is alert, awake, and oriented to person, place, and time. He shows no memory or knowledge impairment. He appears euthymic with an inappropriate and constricted affect. On neurologic exam, he had mild tremors in his hands. The authors’ observationsTreatment for diphenhydramine overdose should begin quickly to prevent life-threatening effects and reduce the risk for mortality. The toxin can be removed from the patient’s GI tract with activated charcoal or gastric lavage if the patient presents within 1 hour of ingesting the substance. Administering IV fluids will prevent dehydration. Cardiac functioning is monitored and benzodiazepines could be administered to manage seizures.
Key elements of a toxicologic physical examination include:
• eyes: pupillary size, symmetry, and response to light (vertical or horizontal nystagmus)
• oropharynx: moist or dry mucous membranes, presence or absence of the gag reflex, distinctive odors
• abdomen: presence or absence and quality of bowel sounds
• skin: warm and dry, warm and sweaty, or cool
• neurologic: level of consciousness and mental status, presence of tremors, seizures, or other movement disorders, presence or absence and quality of deep tendon reflexes.7
If a child or adolescent patient cannot communicate how much of a drug he (she) has ingested, questions to ask parents or other informants include:
• Was the medication purchased recently, and if so was the bottle or box full before the patient took the pills?
• If the medication was not new, how many pills were in the bottle before the patient got to it?
• If the medication was prescribed, how many pills were originally prescribed, when was the medication prescribed, and how many pills were already taken prior to the patient getting to the bottle?
• How many pills were left in the bottle?
• How many pills were seen around the area where the patient was found?
• How many pills were found in the patient’s mouth?7
Recommendations
It is well known that OTC medication abuse is a growing medical problem (Table 2). Antihistamines, including diphenhydramine, are readily available to minors and adults. Because of the powerful sedating effects of antihistamines, many adolescent health practitioners give them to patients who have insomnia as a sleep aid.8 As in our case, antihistamines are used recreationally for their hallucinogenic effects, at dosages of 300 to 700 mg.9 Severe symptoms of toxicity, such as delirium and psychosis, seizures, and coma, occur at dosages ≥1,000 mg.9
With growing abuse of these medications, we aim to encourage detailed history taking about abuse of OTC drugs, especially diphenhydramine in adolescent patients.
Outcome Improvement, discharge
Mr. L is given a dual diagnosis of diphenhydramine-induced psychotic disorder with
hallucinations and diphenhydramine-induced depressive disorder, both with onset during intoxication. He also is given a provisional diagnosis of psychotic disorder not otherwise specified and major depressive disorder. Last, he is given a diagnosis of Cannabis dependence with physiological dependence, MDMA abuse, hydrocodone abuse, and Robitussin abuse.
Mr. L is maintained on fluoxetine, 40 mg/d, and risperidone, 1 mg at bedtime and 0.5 mg in the morning. He receives milieu, individual, group, recreational, and medical therapy while in the hospital. Symptoms abate and he is discharged with a plan to follow up with outpatient providers.
Bottom Line
Abuse of over-the-counter (OTC) drugs, such as diphenhydramine, among youths is a growing problem. Remember to question adolescents who appear intoxicated or to have overdosed not only about abuse of alcohol and illicit substances but also of common—and easily and legally accessible—OTC drugs.
Related Resources
• Carr BC. Efficacy, abuse, and toxicity of over-the-counter cough and cold medicines in the pediatric population. Curr Opin Pediatr. 2006;18(2):184-188.
• Thomas A, Nallur DG, Jones N, et al. Diphenhydramine abuse and detoxification: a brief review and case report. J Psychopharmacol. 2009;23(1):101-105.
Drug Brand Names
Diazepam • Valium Hydrocodone • Vicodin
Diphenhydramine • Benadryl Risperidone • Risperdal
Fluoxetine • Prozac
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. U.S. Department of Health and Human Services. Drug Abuse Warning Network, 2011: National estimates of drug-related emergency department visits. http://www.samhsa. gov/data/2k13/DAWN2k11ED/DAWN2k11ED.htm. Published May 2013. Accessed on September 29, 2014.
2. Yamashiro K, Kiryu J, Tsujikawa A, et al. Suppressive effects of histamine H1 receptor antagonist diphenhydramine on the leukocyte infiltration during endotoxin-induced uveitis. Exp Eye Res. 2001;73(1):69-80.
3. Skidgel RA, Kaplan AP, Erdos EG. Histamine, bradykinin, and their antagonists. In: Brunton L, Chabner B, Knollman B, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 12th ed. New York, NY: McGraw Hill; 2011: 911-935.
4. Vearrier D, Curtis JA. Case files of the medical toxicology fellowship at Drexel University. Rhabdomyolysis and compartment syndrome following acute diphenhydramine overdose. J Med Toxicol. 2011;7(3):213-219.
5. Ho M, Tsai K, Liu C. Diphenhydramine overdose related delirium: a case report. Journal of Emergency and Critical Care Medicine. 2006;17(2):77-79.
6. Krenzelok EP, Anderson GM, Mirick M. Massive diphenhydramine overdose resulting in death. Ann Emerg Med. 1982;11(4):212-213.
7. Inaba AS. Toxicologic teasers: Testing your knowledge of clinical toxicology. Hawaii Med J. 1998;57(4):471-473.
8. Kaplan SL. Busner J. The use of prn and stat medication in three child psychiatric inpatient settings. Psychopharmacol Bull. 1997;33(1):161-164.
9. Radovanovic D, Meier PJ, Guirguis M, et al. Dose-dependent toxicity of diphenhydramine overdose. Hum Exp Toxicol. 2000;19(9):489-495.
1. U.S. Department of Health and Human Services. Drug Abuse Warning Network, 2011: National estimates of drug-related emergency department visits. http://www.samhsa. gov/data/2k13/DAWN2k11ED/DAWN2k11ED.htm. Published May 2013. Accessed on September 29, 2014.
2. Yamashiro K, Kiryu J, Tsujikawa A, et al. Suppressive effects of histamine H1 receptor antagonist diphenhydramine on the leukocyte infiltration during endotoxin-induced uveitis. Exp Eye Res. 2001;73(1):69-80.
3. Skidgel RA, Kaplan AP, Erdos EG. Histamine, bradykinin, and their antagonists. In: Brunton L, Chabner B, Knollman B, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 12th ed. New York, NY: McGraw Hill; 2011: 911-935.
4. Vearrier D, Curtis JA. Case files of the medical toxicology fellowship at Drexel University. Rhabdomyolysis and compartment syndrome following acute diphenhydramine overdose. J Med Toxicol. 2011;7(3):213-219.
5. Ho M, Tsai K, Liu C. Diphenhydramine overdose related delirium: a case report. Journal of Emergency and Critical Care Medicine. 2006;17(2):77-79.
6. Krenzelok EP, Anderson GM, Mirick M. Massive diphenhydramine overdose resulting in death. Ann Emerg Med. 1982;11(4):212-213.
7. Inaba AS. Toxicologic teasers: Testing your knowledge of clinical toxicology. Hawaii Med J. 1998;57(4):471-473.
8. Kaplan SL. Busner J. The use of prn and stat medication in three child psychiatric inpatient settings. Psychopharmacol Bull. 1997;33(1):161-164.
9. Radovanovic D, Meier PJ, Guirguis M, et al. Dose-dependent toxicity of diphenhydramine overdose. Hum Exp Toxicol. 2000;19(9):489-495.
How to assess the merits of psychological and neuropsychological test evaluations
Psychological and neuropsychological test evaluations, like all consultative diagnostic services, can vary in quality and clinical utility. Many of these examinations provide valuable insights and helpful recommendations; regrettably, some assessments are only marginally beneficial and can contribute to diagnostic confusion and uncertainty.
When weighing the pros and cons of evaluations, consider these best practices.
Gold-standard tests ought to be in-cluded in the assessment. These include (but are not limited to) the Wechsler Adult Intelligence Scale-Fourth Edition (WAIS-IV); Wechsler Memory Scale-Fourth Edition (WMS-IV); Delis-Kaplan Executive Function System (D-KEFS); Wechsler Individual Achievement Test-Third Edition (WIAT-III); and the Minnesota Multiphasic Personality Inventory-2 (MMPI-2). These tests have a strong evidence base that:
• demonstrates good reliability (ie, produce consistent and accurate scores across examiners and time intervals and are relatively free of measurement error)
• demonstrates good validity (ie, have been shown to measure aspects of psychological and neuropsychological functioning that they claim to measure).
Many gold-standard tests are normed on national samples and are stratified by age, sex, ethnicity or race, educational level, and geographic region. They also include normative data based on the performance of patients who have neuropsychiatric syndromes often seen by psychiatrists in practice.1
The test battery ought to comprise cognitive and neuropsychological measures as well as affective and behavioral measures. When feasible, these tests should be supplemented by informant-based measures of neuropsychiatric functioning to obtain a comprehensive assessment of the patient’s capacities and skills.
An estimated premorbid baseline should be established. This is done by taking a relevant history and administering tests, such as the National Adult Reading Test (NART), that can be used to compare against current test performance. This testing-in-context approach helps differentiate long-term limitations in information processing, which might be attributed to a DSM-5 intellectual disability, specific learning disorder, or other neurodevelopmental disorder, from a known or suspected recent neurobehavioral change.
Tests in the assessment should tap a broad set of neurobehavioral functions. Doing so ensures that, when a patient is referred with a change in cognition or other aspects of mental status, it will be easier to determine whether clinically significant score discrepancies exist across different ability and skill domains. Such dissociations in performance can have important implications for the differential diagnosis and everyday functioning.
Tests that are sensitive to a patient’s over-reporting of symptoms should be used as part of the evaluation in cases of suspected malingering—especially subtle simulation that might elude identification with brief screening-level measures.2 These tests can include the Test of Memory Malingering (TOMM) and the Structured Interview of Reported Symptoms, 2nd edition (SIRS-2).
Test recommendations ought to be grounded in findings; practical; and relatively easy to implement. They also should be consistent with the treatment setting and the patient’s lifestyle, values, and treatment preferences.3
Disclosure
Dr. Pollak reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Geisinger KF, Bracken BA, Carlson JF, et al, eds. APA handbook of testing and assessment in psychology. Washington, DC: American Psychological Association Press; 2013.
2. Brady MC, Scher LM, Newman W. “I just saw Big Bird. He was 100 feet tall!” Malingering in the emergency department. Current Psychiatry. 2013;12(10):33-38,40.
3. McHugh RK, Whitton SW, Peckham AD, et al. Patient p for psychological vs pharmacologic treatment of psychiatric disorders: a meta-analytic review. J Clin Psychiatry. 2013;74(6):595-602.
Psychological and neuropsychological test evaluations, like all consultative diagnostic services, can vary in quality and clinical utility. Many of these examinations provide valuable insights and helpful recommendations; regrettably, some assessments are only marginally beneficial and can contribute to diagnostic confusion and uncertainty.
When weighing the pros and cons of evaluations, consider these best practices.
Gold-standard tests ought to be in-cluded in the assessment. These include (but are not limited to) the Wechsler Adult Intelligence Scale-Fourth Edition (WAIS-IV); Wechsler Memory Scale-Fourth Edition (WMS-IV); Delis-Kaplan Executive Function System (D-KEFS); Wechsler Individual Achievement Test-Third Edition (WIAT-III); and the Minnesota Multiphasic Personality Inventory-2 (MMPI-2). These tests have a strong evidence base that:
• demonstrates good reliability (ie, produce consistent and accurate scores across examiners and time intervals and are relatively free of measurement error)
• demonstrates good validity (ie, have been shown to measure aspects of psychological and neuropsychological functioning that they claim to measure).
Many gold-standard tests are normed on national samples and are stratified by age, sex, ethnicity or race, educational level, and geographic region. They also include normative data based on the performance of patients who have neuropsychiatric syndromes often seen by psychiatrists in practice.1
The test battery ought to comprise cognitive and neuropsychological measures as well as affective and behavioral measures. When feasible, these tests should be supplemented by informant-based measures of neuropsychiatric functioning to obtain a comprehensive assessment of the patient’s capacities and skills.
An estimated premorbid baseline should be established. This is done by taking a relevant history and administering tests, such as the National Adult Reading Test (NART), that can be used to compare against current test performance. This testing-in-context approach helps differentiate long-term limitations in information processing, which might be attributed to a DSM-5 intellectual disability, specific learning disorder, or other neurodevelopmental disorder, from a known or suspected recent neurobehavioral change.
Tests in the assessment should tap a broad set of neurobehavioral functions. Doing so ensures that, when a patient is referred with a change in cognition or other aspects of mental status, it will be easier to determine whether clinically significant score discrepancies exist across different ability and skill domains. Such dissociations in performance can have important implications for the differential diagnosis and everyday functioning.
Tests that are sensitive to a patient’s over-reporting of symptoms should be used as part of the evaluation in cases of suspected malingering—especially subtle simulation that might elude identification with brief screening-level measures.2 These tests can include the Test of Memory Malingering (TOMM) and the Structured Interview of Reported Symptoms, 2nd edition (SIRS-2).
Test recommendations ought to be grounded in findings; practical; and relatively easy to implement. They also should be consistent with the treatment setting and the patient’s lifestyle, values, and treatment preferences.3
Disclosure
Dr. Pollak reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Psychological and neuropsychological test evaluations, like all consultative diagnostic services, can vary in quality and clinical utility. Many of these examinations provide valuable insights and helpful recommendations; regrettably, some assessments are only marginally beneficial and can contribute to diagnostic confusion and uncertainty.
When weighing the pros and cons of evaluations, consider these best practices.
Gold-standard tests ought to be in-cluded in the assessment. These include (but are not limited to) the Wechsler Adult Intelligence Scale-Fourth Edition (WAIS-IV); Wechsler Memory Scale-Fourth Edition (WMS-IV); Delis-Kaplan Executive Function System (D-KEFS); Wechsler Individual Achievement Test-Third Edition (WIAT-III); and the Minnesota Multiphasic Personality Inventory-2 (MMPI-2). These tests have a strong evidence base that:
• demonstrates good reliability (ie, produce consistent and accurate scores across examiners and time intervals and are relatively free of measurement error)
• demonstrates good validity (ie, have been shown to measure aspects of psychological and neuropsychological functioning that they claim to measure).
Many gold-standard tests are normed on national samples and are stratified by age, sex, ethnicity or race, educational level, and geographic region. They also include normative data based on the performance of patients who have neuropsychiatric syndromes often seen by psychiatrists in practice.1
The test battery ought to comprise cognitive and neuropsychological measures as well as affective and behavioral measures. When feasible, these tests should be supplemented by informant-based measures of neuropsychiatric functioning to obtain a comprehensive assessment of the patient’s capacities and skills.
An estimated premorbid baseline should be established. This is done by taking a relevant history and administering tests, such as the National Adult Reading Test (NART), that can be used to compare against current test performance. This testing-in-context approach helps differentiate long-term limitations in information processing, which might be attributed to a DSM-5 intellectual disability, specific learning disorder, or other neurodevelopmental disorder, from a known or suspected recent neurobehavioral change.
Tests in the assessment should tap a broad set of neurobehavioral functions. Doing so ensures that, when a patient is referred with a change in cognition or other aspects of mental status, it will be easier to determine whether clinically significant score discrepancies exist across different ability and skill domains. Such dissociations in performance can have important implications for the differential diagnosis and everyday functioning.
Tests that are sensitive to a patient’s over-reporting of symptoms should be used as part of the evaluation in cases of suspected malingering—especially subtle simulation that might elude identification with brief screening-level measures.2 These tests can include the Test of Memory Malingering (TOMM) and the Structured Interview of Reported Symptoms, 2nd edition (SIRS-2).
Test recommendations ought to be grounded in findings; practical; and relatively easy to implement. They also should be consistent with the treatment setting and the patient’s lifestyle, values, and treatment preferences.3
Disclosure
Dr. Pollak reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Geisinger KF, Bracken BA, Carlson JF, et al, eds. APA handbook of testing and assessment in psychology. Washington, DC: American Psychological Association Press; 2013.
2. Brady MC, Scher LM, Newman W. “I just saw Big Bird. He was 100 feet tall!” Malingering in the emergency department. Current Psychiatry. 2013;12(10):33-38,40.
3. McHugh RK, Whitton SW, Peckham AD, et al. Patient p for psychological vs pharmacologic treatment of psychiatric disorders: a meta-analytic review. J Clin Psychiatry. 2013;74(6):595-602.
1. Geisinger KF, Bracken BA, Carlson JF, et al, eds. APA handbook of testing and assessment in psychology. Washington, DC: American Psychological Association Press; 2013.
2. Brady MC, Scher LM, Newman W. “I just saw Big Bird. He was 100 feet tall!” Malingering in the emergency department. Current Psychiatry. 2013;12(10):33-38,40.
3. McHugh RK, Whitton SW, Peckham AD, et al. Patient p for psychological vs pharmacologic treatment of psychiatric disorders: a meta-analytic review. J Clin Psychiatry. 2013;74(6):595-602.
Physician groups: Fix interoperability before advancing with meaningful use
Physician groups are growing increasingly frustrated with the focus on meaningful use of electronic health records at the expense of creating an interoperable health information technology infrastructure and are calling on the Department of Health & Human Services to step up on interoperability.
In an Oct. 15 letter to HHS Secretary Sylvia Burwell, a number of groups cited the HHS Office of the National Coordinator for Health Information Technology’s finding that less than 14% of physicians are able to electronically transmit health information outside of their organization because of a lack of EHR interoperability and other issues.
“These barriers to data exchange proliferated as a result of a variety of factors [including] strict MU [meaningful use] requirements and deadlines that do not provide sufficient time to focus on achieving interoperability. This dynamic is also in part due to the strict EHR certification requirements that have forced all stakeholders involved to focus on meeting MU measures as opposed to developing more innovative technological solutions that will enhance patient care and safety while growing the marketplace.”
Groups signing the letter include the American Academy of Family Physicians, American Medical Association, Medical Group Management Association, National Rural Health Association and a number of health care systems.
The letter also notes that in addition to interoperability, usability remains an issue that causes disruption in provider workflow and diverts resources away from patient care, noting that “vendors are limited from addressing these concerns as they focus on meeting increasingly complex certification requirements.”
Among its recommendations, the groups asked for HHS to recognize that the vendor community needs time to develop, test, and implement updates to meet new criteria and should be afforded that time “before continuing on with subsequent stages of the MU program. Testing and achievement of specific performance benchmarks should occur before providers are held accountable for any MU requirements.”
The letter comes as an advisory committee to the Office of the National Coordinator (ONC) is making a same-day recommendation that it delays or staggers meaningful use stage 3 to shift focus on achieving meaningful interoperability and addressing other infrastructure issues.
In its October 2014 report to Congress, the ONC acknowledged issues related to interoperability and other issues that are presenting a barrier for health IT to achieve potential.
“Despite progress in establishing standards and services to support health information exchange and interoperability, practice patterns have not changed to the point that health care providers share patient health information electronically across organizational, vendor, and geographic boundaries,” the report states. “Patient electronic health information needs to be available for appropriate use in solving major challenges, such as providing more effective care and informing and accelerating scientific research.”
To that end, ONC released during an Oct. 15 advisory committee meeting some top-level aspects of its 10-year framework on how it will improve interoperability, which is scheduled to be formalized in March 2015.
According to draft materials, the roadmap calls for health care providers to be able to send, receive, find, and use a basic set of essential health information. By 2020, more granular information should be accessible across systems, which would lead to improved quality and reduced costs. By 2024, the interoperability vision, with systems communicating in full, will lead to a learning health system and facilitate ubiquitous precision medicine.
Separately, AMA in an Oct. 14 letter to CMS and ONC criticized the meaningful use program and offered a series of recommendations to fix it before movement to stage 3 of the program. The group wants to see more flexibility in requirements physicians need to meet requirements, expanding hardship exemptions for all stages, improving quality reporting, and addressing physician EHR usability challenges.
“Many of the MU requirements were designed to increase patient choice and quality of care,” the AMA writes. “Unfortunately, many of these requirements, especially those in the latter phases of the MU program, are having the opposite effect. Oftentimes the requirements decrease the efficiency of patient visits.”
AMA also called on CMS and ONC to “study the total cost of compliance with MU to understand the impact this program is having on practice.”
Physician groups are growing increasingly frustrated with the focus on meaningful use of electronic health records at the expense of creating an interoperable health information technology infrastructure and are calling on the Department of Health & Human Services to step up on interoperability.
In an Oct. 15 letter to HHS Secretary Sylvia Burwell, a number of groups cited the HHS Office of the National Coordinator for Health Information Technology’s finding that less than 14% of physicians are able to electronically transmit health information outside of their organization because of a lack of EHR interoperability and other issues.
“These barriers to data exchange proliferated as a result of a variety of factors [including] strict MU [meaningful use] requirements and deadlines that do not provide sufficient time to focus on achieving interoperability. This dynamic is also in part due to the strict EHR certification requirements that have forced all stakeholders involved to focus on meeting MU measures as opposed to developing more innovative technological solutions that will enhance patient care and safety while growing the marketplace.”
Groups signing the letter include the American Academy of Family Physicians, American Medical Association, Medical Group Management Association, National Rural Health Association and a number of health care systems.
The letter also notes that in addition to interoperability, usability remains an issue that causes disruption in provider workflow and diverts resources away from patient care, noting that “vendors are limited from addressing these concerns as they focus on meeting increasingly complex certification requirements.”
Among its recommendations, the groups asked for HHS to recognize that the vendor community needs time to develop, test, and implement updates to meet new criteria and should be afforded that time “before continuing on with subsequent stages of the MU program. Testing and achievement of specific performance benchmarks should occur before providers are held accountable for any MU requirements.”
The letter comes as an advisory committee to the Office of the National Coordinator (ONC) is making a same-day recommendation that it delays or staggers meaningful use stage 3 to shift focus on achieving meaningful interoperability and addressing other infrastructure issues.
In its October 2014 report to Congress, the ONC acknowledged issues related to interoperability and other issues that are presenting a barrier for health IT to achieve potential.
“Despite progress in establishing standards and services to support health information exchange and interoperability, practice patterns have not changed to the point that health care providers share patient health information electronically across organizational, vendor, and geographic boundaries,” the report states. “Patient electronic health information needs to be available for appropriate use in solving major challenges, such as providing more effective care and informing and accelerating scientific research.”
To that end, ONC released during an Oct. 15 advisory committee meeting some top-level aspects of its 10-year framework on how it will improve interoperability, which is scheduled to be formalized in March 2015.
According to draft materials, the roadmap calls for health care providers to be able to send, receive, find, and use a basic set of essential health information. By 2020, more granular information should be accessible across systems, which would lead to improved quality and reduced costs. By 2024, the interoperability vision, with systems communicating in full, will lead to a learning health system and facilitate ubiquitous precision medicine.
Separately, AMA in an Oct. 14 letter to CMS and ONC criticized the meaningful use program and offered a series of recommendations to fix it before movement to stage 3 of the program. The group wants to see more flexibility in requirements physicians need to meet requirements, expanding hardship exemptions for all stages, improving quality reporting, and addressing physician EHR usability challenges.
“Many of the MU requirements were designed to increase patient choice and quality of care,” the AMA writes. “Unfortunately, many of these requirements, especially those in the latter phases of the MU program, are having the opposite effect. Oftentimes the requirements decrease the efficiency of patient visits.”
AMA also called on CMS and ONC to “study the total cost of compliance with MU to understand the impact this program is having on practice.”
Physician groups are growing increasingly frustrated with the focus on meaningful use of electronic health records at the expense of creating an interoperable health information technology infrastructure and are calling on the Department of Health & Human Services to step up on interoperability.
In an Oct. 15 letter to HHS Secretary Sylvia Burwell, a number of groups cited the HHS Office of the National Coordinator for Health Information Technology’s finding that less than 14% of physicians are able to electronically transmit health information outside of their organization because of a lack of EHR interoperability and other issues.
“These barriers to data exchange proliferated as a result of a variety of factors [including] strict MU [meaningful use] requirements and deadlines that do not provide sufficient time to focus on achieving interoperability. This dynamic is also in part due to the strict EHR certification requirements that have forced all stakeholders involved to focus on meeting MU measures as opposed to developing more innovative technological solutions that will enhance patient care and safety while growing the marketplace.”
Groups signing the letter include the American Academy of Family Physicians, American Medical Association, Medical Group Management Association, National Rural Health Association and a number of health care systems.
The letter also notes that in addition to interoperability, usability remains an issue that causes disruption in provider workflow and diverts resources away from patient care, noting that “vendors are limited from addressing these concerns as they focus on meeting increasingly complex certification requirements.”
Among its recommendations, the groups asked for HHS to recognize that the vendor community needs time to develop, test, and implement updates to meet new criteria and should be afforded that time “before continuing on with subsequent stages of the MU program. Testing and achievement of specific performance benchmarks should occur before providers are held accountable for any MU requirements.”
The letter comes as an advisory committee to the Office of the National Coordinator (ONC) is making a same-day recommendation that it delays or staggers meaningful use stage 3 to shift focus on achieving meaningful interoperability and addressing other infrastructure issues.
In its October 2014 report to Congress, the ONC acknowledged issues related to interoperability and other issues that are presenting a barrier for health IT to achieve potential.
“Despite progress in establishing standards and services to support health information exchange and interoperability, practice patterns have not changed to the point that health care providers share patient health information electronically across organizational, vendor, and geographic boundaries,” the report states. “Patient electronic health information needs to be available for appropriate use in solving major challenges, such as providing more effective care and informing and accelerating scientific research.”
To that end, ONC released during an Oct. 15 advisory committee meeting some top-level aspects of its 10-year framework on how it will improve interoperability, which is scheduled to be formalized in March 2015.
According to draft materials, the roadmap calls for health care providers to be able to send, receive, find, and use a basic set of essential health information. By 2020, more granular information should be accessible across systems, which would lead to improved quality and reduced costs. By 2024, the interoperability vision, with systems communicating in full, will lead to a learning health system and facilitate ubiquitous precision medicine.
Separately, AMA in an Oct. 14 letter to CMS and ONC criticized the meaningful use program and offered a series of recommendations to fix it before movement to stage 3 of the program. The group wants to see more flexibility in requirements physicians need to meet requirements, expanding hardship exemptions for all stages, improving quality reporting, and addressing physician EHR usability challenges.
“Many of the MU requirements were designed to increase patient choice and quality of care,” the AMA writes. “Unfortunately, many of these requirements, especially those in the latter phases of the MU program, are having the opposite effect. Oftentimes the requirements decrease the efficiency of patient visits.”
AMA also called on CMS and ONC to “study the total cost of compliance with MU to understand the impact this program is having on practice.”
Point/Counterpoint: Endo first for the treatment of infrainguinal PAD?
The BASIL study originally published in the Lancet in 2005 (366:1925-34) and subsequently reiterated in multiple publications proposes that an endovascular approach should be utilized as the first invasive treatment modality in patients with infrainguinal peripheral arterial disease whose life expectancy is less than 2 years. By contrast, those patients expected to live beyond 2 years usually should be offered bypass surgery first, especially where a vein is available as a conduit. However, as can be seen from this month’s Point/Counterpoint by Dr. George Meier III and Dr. Michael S. Conte, the debate still rages as to the benefit of open vs. endovascular procedures for these patients. We encourage readers to voice their opinions in our “Letters to the Editor” section, as well as by participating in our web-based Quick Poll to the right of this story. - Dr. Russell Samson, Medical Editor, Vascular Specialist
POINT/COUNTERPOINT
Yes, endo is generally the way to go.
By Dr. George Meier III
Endovascular treatment of lower-extremity arterial disease has rapidly expanded, now approaching the standard for treatment of patients with lower-extremity disease. While open bypass remains a gold standard for the clinical treatment of limb-threatening ischemia, there are many limitations to the use of open surgery.
First and foremost, open surgical intervention represents pain and suffering for the patient as well as a delayed recovery, compared with endovascular treatment. All other factors being equal, most patients would prefer a less-invasive approach to minimize these factors and to maximize the speed of recovery. Open surgical interventions typically require 6 weeks or longer to get back to a functional status even remotely close to the patient’s initial level of function. With more severe tissue loss or with greater pain preoperatively, the difficulty of getting the patient back to full functional status remains problematic. In John Porter’s classic paper published in the Journal of Vascular Surgery in 1998,1 wound complications occurred in 24% of the patients with a 5-year survival rate of only 49% in this relatively young population, average age 66 years. Repeat operations to maintain graft patency, treat wound complications, or treat recurrent or contralateral ischemia were required in 54% of the patients and 23% ultimately required major limb amputation.
Of the 112 patients in this study, only 14.3% achieved the ideal surgical result of an uncomplicated operation: long-term symptom relief, maintenance of functional status, and no recurrence or repeat operations. These are sobering statistics for anyone facing open revascularization for critical limb ischemia.
The BASIL trial is often put forward as an example of the best data available currently to define patient treatments in patients with critical limb ischemia.2 Despite this, BASIL was a flawed trial from the beginning because of the difficulties of truly randomizing patients with vascular disease to open surgical treatment vs. percutaneous treatment. First, all patients had to be appropriate candidates for both open and endovascular treatment. In the real world, we readily recognize that the luxury of this choice is not available to many of our patients. A lack of conduit or increased surgical risk results in endovascular treatment being the only management option for many. Additionally, patient preference increasingly plays a role in treatment selection, obviously increasing the likelihood of less invasive percutaneous treatment. Yes, the mortality of open bypass in BASIL is reported to be in the 1%-3% range, but this population has been carefully selected based on screening and treatment of underlying cardiac disease. The true incidence of cardiovascular disease is impossible to determine since significant cardiac disease negated randomization.
Unfortunately, even with all of the advances in endovascular treatments the results of percutaneous treatment have never reached the results of open bypass. Nonetheless, while the success may not be as great the risks are not as high either. The main challenge to endovascular treatment is the durability of the intervention. While we can usually treat pre-existing disease in the lower-extremity arterial tree, maintaining patency and durability is the challenge. As my esteemed colleague has noted, failure of endovascular treatment in the BASIL trial resulted in significantly worse outcomes for open bypass in those patients. While much was made about this fact when the BASIL trial was published, endovascular treatment after open failure has even a worse outcome than did open treatment after endovascular failure. The truth of the matter is that, for obvious reasons, failure begets failure.
Generally, there are two imaging approaches to defining the extent of vascular disease: first, contrast angiography via percutaneous access; and second, CT angiography using intravenous contrast. If contrast angiography is undertaken to diagnose the extent of disease, then it is a relatively limited extrapolation to treat the patient’s disease percutaneously at the time of the diagnostic angiogram. For this reason, I discuss with all patients coming for diagnostic angiography the issue of endovascular treatment. It is rare that we make patients worse with an attempt at endovascular treatment by an experienced interventionalist. Similarly, it is rare that we alter a bypass level based on an attempt at endovascular treatment. If, in my opinion, the risk of an attempted endovascular treatment is acceptable, then this is done at the time of the diagnostic angiogram. Patients appreciate this discussion prior to proceeding with diagnostic angiography.
What about inadequate autogenous conduit? Even my counterpoint opponent has published a documented 20% risk of absent or inadequate ipsilateral greater saphenous vein.3 While he and his colleagues have documented excellent results using contralateral greater saphenous vein, there is still an inevitable morbidity and, yes, even a mortality risk associated with contralateral leg vein harvest. While in a good cardiac risk patient this may be negligible, we are again facing an ever more complex and medically ill patient population to subject to vascular treatment. It is in this setting that many vascular surgeons move to prosthetic conduits for the treatment of the patient’s vascular disease. While this may provide a short-term fix for the conduit problem, in the long term the risk of sudden, uncompensated failure of limb perfusion by prosthetic graft failure may often result in a higher risk procedure at a time when the patient may be older and more severely limited. Endovascular treatment is clearly a reasonable alternative in patients where autogenous conduit is not readily available.
While this debate will inevitably continue as long as practitioners have bias toward either open or endovascular management of vascular disease, one thing is for certain: We will continue to extend the limits of treatment to ever more ill and complex patients. While we have been very successful at performing fewer and fewer morbid interventions for limb-threatening vascular disease, these patients continue to be increasingly challenging to manage.
As the overall population continues to age, the need for less invasive treatment of limb-threatening vascular disease will continue to grow. And, yes, I agree that vascular surgeons in the role of interventionalist or surgeon are the leadership for the management of CLI in the future.
Dr. Meier is professor and chief of vascular surgery at the University of Cincinnati.
References
1. J. Vasc. Surg. 1998;27:256-63; discussion 264-6
3. J. Vasc. Surg. 2002:35:1085-92
No: A selective approach remains the key.
By Dr. MICHAEL S. CONTE
Recently the term “pandemic” has been applied to the growing global impact of peripheral artery disease (PAD), currently estimated to afflict more than 200 million individuals.1 The term “critical limb ischemia” (CLI), connoting the most advanced stage of PAD with imminent limb threat, is inadequately defined2 but likely encompasses 1%-3% of PAD. Aging of the global population and the increasing prevalence of diabetes are fueling increases in CLI and its impact on public health. While traditionally treated largely by vascular surgeons plying the open bypass trade, the ongoing development and market dispersion of catheter-based technologies for CLI has led to major secular changes.
Recent estimates suggest that upward of 5 billion dollars are spent annually on CLI in the Medicare population.3, 4 Increasing volumes and costs associated with revascularizations for CLI are a major driver, yet recent data suggest that regional spending in the United States is widely disparate and not directly associated with amputation rates.5 Thus defining effectiveness and value in CLI care has become a major challenge to the vascular community.
In current everyday practice, clinicians are faced with making treatment choices for CLI patients based on limited data and lots of anecdote. While the “open vs. endo” debate goes on, in many ways it has become less broadly relevant as the sophisticated clinician recognizes the real challenge lies in defining which approach to apply first in the right patient, at the right time. The only randomized, controlled trial (RCT) done in the field, the BASIL trial,6 is more than a decade old. However its findings remain important. For patients with “severe limb ischemia” likely to survive for at least 2 years, open bypass surgery offered better outcomes over angioplasty as an initial strategy.7 Moreover, the finding in BASIL that patients undergoing bypass after prior failed angioplasty did poorly,8 suggesting “no free lunch” for endovascular failures, has since been confirmed in other large registry studies.9
Simply stated, failure matters in CLI. And although endovascular techniques have continued to improve, the growing epidemic of restenosis shows no signs of abating.10 As in the case of percutaneous coronary intervention (PCI), we will know when endo results are meaningfully improved in PAD when the procedure volume curves actually flatten, not continue to grow geometrically.
So, in selecting the optimal strategy for CLI today, let’s focus on what we seem to know and try to apply an evidence-based mentality. We know that open bypass surgery is an effective and versatile treatment, but one that carries real morbidity (10%-20%) and some mortality (1%-3%). Among many large studies, the PREVENT III multicenter trial provides benchmark data on perioperative and 1-year outcomes.11
We know that the quality of the vein is the critical technical determinant of success, and arterial anatomy is less influential as long as there is outflow to the foot.12 We know that poor quality veins, prosthetics, and other alternatives are much inferior in CLI. And we know that there is a subset of CLI patients who are at high risk for adverse surgical outcomes.13, 14 However one defines them, up to 10% of patients in the large surgical series are in a high-risk group and may not experience meaningful benefit. For endovascular treatments, the data are less clear but certain trends have been consistent. Multilevel disease, long-segment occlusions, heavily calcified lesions, and more advanced tissue loss are negative predictors of clinical success.
Thus at first glance the weaknesses of the two strategies are largely complementary.15 When I encounter an average-risk CLI patient, with an adequate saphenous vein and more than one unfavorable endo factor, I am inclined towards bypass first.
Conversely, endo-favorable anatomy in higher risk patients is a no-brainer. Lots of people fall in the middle, and a significant minority should be considered for primary amputation. Currently my practice is roughly 50% bypass surgery-first in CLI.
Endovascular innovations have made a huge impact on vascular practice, and the leadership of many vascular surgeons (e.g., my esteemed counterpoint author) has been central to advancing the field. Better wires and catheters, retrograde approaches, and drug-eluting technologies continue to be developed at a dizzying pace.
We are all continually learning. Unfortunately, we lack good objective evidence to support most of the expanding armamentarium for CLI. However it is abundantly clear that technical (angiographic) success and clinical success are far apart, which is no surprise. What is surprising is an unsettlingly common lack of honesty about such an obvious fact. Are we all guilty of looking through rose-colored glasses?
Is it really such big news that patency actually matters for most patients with CLI? Technologies will not improve quickly enough if there is no market imperative to make them better. If we continue to buy and use things that are frequently ineffective, or don’t measure it carefully, where is the motivation?
No matter the lens through which one looks at the CLI field, it is desperate for improvement. We need much better technologies that provide longer lasting solutions for patients. We need better diagnostics to predict disease progression and responses to treatment.
We need some new medical or biological therapies that truly alleviate suffering. And we largely lack data on comparative effectiveness, and value, to support thoughtful application of our current treatment arsenal.
Most importantly what we need now is less dogma, and a lot more science. Over more than two decades, multiple RCTs comparing medical, interventional and surgical therapies for coronary artery disease have formed the basis for practice guidelines.
By comparison, our field is nearly incoherent both to vascular specialists and referring physicians. It will not be easy, but this can be done in PAD as well, and the vascular community must embrace it. Moreover it is imperative that vascular surgeons help to lead these multidisciplinary efforts, and develop evidence-based global guidelines to guide best practice in CLI.16 The recent funding of the BEST-CLI trial in the United States and the BASIL-2 trial in the United Kingdom demonstrate the importance to public health and offer great opportunities.
Until better evidence is available, a rational approach to limb salvage requires flexibility, understanding of the factors predicting success/failure for each modality, and the continued use of open bypass surgery as the initial treatment option for a significant number of patients.
And for the sake of our most vulnerable patients, we better keep training vascular surgeons to do all of it well.
Dr. Conte is professor and chief, division of vascular & endovascular surgery and the Edwin J. Wylie, M.D. Chair in Vascular Surgery at the University of California, San Francisco.
References
2. J. Vasc. Surg. 2014;59:220-34
7. J. Vasc. Surg. 2010;51:5S-17S
8. J. Vasc. Surg. 2010;51:18S-31S
9. J. Vasc. Surg. 2011;54:730-6
10. J. Amer. Heart Assoc. 2013;2:e000345
11. J. Vasc. Surg. 2006;43:742-51
12. J. Vasc. Surg. 2007;46:1180-90
13. J. Vasc. Surg. 2009;50:769-75
14. J. Vasc. Surg. 2010;52:1218-25
15. J. Vasc. Surg. 2013;57:8S-13S16. J. Vasc. Surg. 2014;59:510
The BASIL study originally published in the Lancet in 2005 (366:1925-34) and subsequently reiterated in multiple publications proposes that an endovascular approach should be utilized as the first invasive treatment modality in patients with infrainguinal peripheral arterial disease whose life expectancy is less than 2 years. By contrast, those patients expected to live beyond 2 years usually should be offered bypass surgery first, especially where a vein is available as a conduit. However, as can be seen from this month’s Point/Counterpoint by Dr. George Meier III and Dr. Michael S. Conte, the debate still rages as to the benefit of open vs. endovascular procedures for these patients. We encourage readers to voice their opinions in our “Letters to the Editor” section, as well as by participating in our web-based Quick Poll to the right of this story. - Dr. Russell Samson, Medical Editor, Vascular Specialist
POINT/COUNTERPOINT
Yes, endo is generally the way to go.
By Dr. George Meier III
Endovascular treatment of lower-extremity arterial disease has rapidly expanded, now approaching the standard for treatment of patients with lower-extremity disease. While open bypass remains a gold standard for the clinical treatment of limb-threatening ischemia, there are many limitations to the use of open surgery.
First and foremost, open surgical intervention represents pain and suffering for the patient as well as a delayed recovery, compared with endovascular treatment. All other factors being equal, most patients would prefer a less-invasive approach to minimize these factors and to maximize the speed of recovery. Open surgical interventions typically require 6 weeks or longer to get back to a functional status even remotely close to the patient’s initial level of function. With more severe tissue loss or with greater pain preoperatively, the difficulty of getting the patient back to full functional status remains problematic. In John Porter’s classic paper published in the Journal of Vascular Surgery in 1998,1 wound complications occurred in 24% of the patients with a 5-year survival rate of only 49% in this relatively young population, average age 66 years. Repeat operations to maintain graft patency, treat wound complications, or treat recurrent or contralateral ischemia were required in 54% of the patients and 23% ultimately required major limb amputation.
Of the 112 patients in this study, only 14.3% achieved the ideal surgical result of an uncomplicated operation: long-term symptom relief, maintenance of functional status, and no recurrence or repeat operations. These are sobering statistics for anyone facing open revascularization for critical limb ischemia.
The BASIL trial is often put forward as an example of the best data available currently to define patient treatments in patients with critical limb ischemia.2 Despite this, BASIL was a flawed trial from the beginning because of the difficulties of truly randomizing patients with vascular disease to open surgical treatment vs. percutaneous treatment. First, all patients had to be appropriate candidates for both open and endovascular treatment. In the real world, we readily recognize that the luxury of this choice is not available to many of our patients. A lack of conduit or increased surgical risk results in endovascular treatment being the only management option for many. Additionally, patient preference increasingly plays a role in treatment selection, obviously increasing the likelihood of less invasive percutaneous treatment. Yes, the mortality of open bypass in BASIL is reported to be in the 1%-3% range, but this population has been carefully selected based on screening and treatment of underlying cardiac disease. The true incidence of cardiovascular disease is impossible to determine since significant cardiac disease negated randomization.
Unfortunately, even with all of the advances in endovascular treatments the results of percutaneous treatment have never reached the results of open bypass. Nonetheless, while the success may not be as great the risks are not as high either. The main challenge to endovascular treatment is the durability of the intervention. While we can usually treat pre-existing disease in the lower-extremity arterial tree, maintaining patency and durability is the challenge. As my esteemed colleague has noted, failure of endovascular treatment in the BASIL trial resulted in significantly worse outcomes for open bypass in those patients. While much was made about this fact when the BASIL trial was published, endovascular treatment after open failure has even a worse outcome than did open treatment after endovascular failure. The truth of the matter is that, for obvious reasons, failure begets failure.
Generally, there are two imaging approaches to defining the extent of vascular disease: first, contrast angiography via percutaneous access; and second, CT angiography using intravenous contrast. If contrast angiography is undertaken to diagnose the extent of disease, then it is a relatively limited extrapolation to treat the patient’s disease percutaneously at the time of the diagnostic angiogram. For this reason, I discuss with all patients coming for diagnostic angiography the issue of endovascular treatment. It is rare that we make patients worse with an attempt at endovascular treatment by an experienced interventionalist. Similarly, it is rare that we alter a bypass level based on an attempt at endovascular treatment. If, in my opinion, the risk of an attempted endovascular treatment is acceptable, then this is done at the time of the diagnostic angiogram. Patients appreciate this discussion prior to proceeding with diagnostic angiography.
What about inadequate autogenous conduit? Even my counterpoint opponent has published a documented 20% risk of absent or inadequate ipsilateral greater saphenous vein.3 While he and his colleagues have documented excellent results using contralateral greater saphenous vein, there is still an inevitable morbidity and, yes, even a mortality risk associated with contralateral leg vein harvest. While in a good cardiac risk patient this may be negligible, we are again facing an ever more complex and medically ill patient population to subject to vascular treatment. It is in this setting that many vascular surgeons move to prosthetic conduits for the treatment of the patient’s vascular disease. While this may provide a short-term fix for the conduit problem, in the long term the risk of sudden, uncompensated failure of limb perfusion by prosthetic graft failure may often result in a higher risk procedure at a time when the patient may be older and more severely limited. Endovascular treatment is clearly a reasonable alternative in patients where autogenous conduit is not readily available.
While this debate will inevitably continue as long as practitioners have bias toward either open or endovascular management of vascular disease, one thing is for certain: We will continue to extend the limits of treatment to ever more ill and complex patients. While we have been very successful at performing fewer and fewer morbid interventions for limb-threatening vascular disease, these patients continue to be increasingly challenging to manage.
As the overall population continues to age, the need for less invasive treatment of limb-threatening vascular disease will continue to grow. And, yes, I agree that vascular surgeons in the role of interventionalist or surgeon are the leadership for the management of CLI in the future.
Dr. Meier is professor and chief of vascular surgery at the University of Cincinnati.
References
1. J. Vasc. Surg. 1998;27:256-63; discussion 264-6
3. J. Vasc. Surg. 2002:35:1085-92
No: A selective approach remains the key.
By Dr. MICHAEL S. CONTE
Recently the term “pandemic” has been applied to the growing global impact of peripheral artery disease (PAD), currently estimated to afflict more than 200 million individuals.1 The term “critical limb ischemia” (CLI), connoting the most advanced stage of PAD with imminent limb threat, is inadequately defined2 but likely encompasses 1%-3% of PAD. Aging of the global population and the increasing prevalence of diabetes are fueling increases in CLI and its impact on public health. While traditionally treated largely by vascular surgeons plying the open bypass trade, the ongoing development and market dispersion of catheter-based technologies for CLI has led to major secular changes.
Recent estimates suggest that upward of 5 billion dollars are spent annually on CLI in the Medicare population.3, 4 Increasing volumes and costs associated with revascularizations for CLI are a major driver, yet recent data suggest that regional spending in the United States is widely disparate and not directly associated with amputation rates.5 Thus defining effectiveness and value in CLI care has become a major challenge to the vascular community.
In current everyday practice, clinicians are faced with making treatment choices for CLI patients based on limited data and lots of anecdote. While the “open vs. endo” debate goes on, in many ways it has become less broadly relevant as the sophisticated clinician recognizes the real challenge lies in defining which approach to apply first in the right patient, at the right time. The only randomized, controlled trial (RCT) done in the field, the BASIL trial,6 is more than a decade old. However its findings remain important. For patients with “severe limb ischemia” likely to survive for at least 2 years, open bypass surgery offered better outcomes over angioplasty as an initial strategy.7 Moreover, the finding in BASIL that patients undergoing bypass after prior failed angioplasty did poorly,8 suggesting “no free lunch” for endovascular failures, has since been confirmed in other large registry studies.9
Simply stated, failure matters in CLI. And although endovascular techniques have continued to improve, the growing epidemic of restenosis shows no signs of abating.10 As in the case of percutaneous coronary intervention (PCI), we will know when endo results are meaningfully improved in PAD when the procedure volume curves actually flatten, not continue to grow geometrically.
So, in selecting the optimal strategy for CLI today, let’s focus on what we seem to know and try to apply an evidence-based mentality. We know that open bypass surgery is an effective and versatile treatment, but one that carries real morbidity (10%-20%) and some mortality (1%-3%). Among many large studies, the PREVENT III multicenter trial provides benchmark data on perioperative and 1-year outcomes.11
We know that the quality of the vein is the critical technical determinant of success, and arterial anatomy is less influential as long as there is outflow to the foot.12 We know that poor quality veins, prosthetics, and other alternatives are much inferior in CLI. And we know that there is a subset of CLI patients who are at high risk for adverse surgical outcomes.13, 14 However one defines them, up to 10% of patients in the large surgical series are in a high-risk group and may not experience meaningful benefit. For endovascular treatments, the data are less clear but certain trends have been consistent. Multilevel disease, long-segment occlusions, heavily calcified lesions, and more advanced tissue loss are negative predictors of clinical success.
Thus at first glance the weaknesses of the two strategies are largely complementary.15 When I encounter an average-risk CLI patient, with an adequate saphenous vein and more than one unfavorable endo factor, I am inclined towards bypass first.
Conversely, endo-favorable anatomy in higher risk patients is a no-brainer. Lots of people fall in the middle, and a significant minority should be considered for primary amputation. Currently my practice is roughly 50% bypass surgery-first in CLI.
Endovascular innovations have made a huge impact on vascular practice, and the leadership of many vascular surgeons (e.g., my esteemed counterpoint author) has been central to advancing the field. Better wires and catheters, retrograde approaches, and drug-eluting technologies continue to be developed at a dizzying pace.
We are all continually learning. Unfortunately, we lack good objective evidence to support most of the expanding armamentarium for CLI. However it is abundantly clear that technical (angiographic) success and clinical success are far apart, which is no surprise. What is surprising is an unsettlingly common lack of honesty about such an obvious fact. Are we all guilty of looking through rose-colored glasses?
Is it really such big news that patency actually matters for most patients with CLI? Technologies will not improve quickly enough if there is no market imperative to make them better. If we continue to buy and use things that are frequently ineffective, or don’t measure it carefully, where is the motivation?
No matter the lens through which one looks at the CLI field, it is desperate for improvement. We need much better technologies that provide longer lasting solutions for patients. We need better diagnostics to predict disease progression and responses to treatment.
We need some new medical or biological therapies that truly alleviate suffering. And we largely lack data on comparative effectiveness, and value, to support thoughtful application of our current treatment arsenal.
Most importantly what we need now is less dogma, and a lot more science. Over more than two decades, multiple RCTs comparing medical, interventional and surgical therapies for coronary artery disease have formed the basis for practice guidelines.
By comparison, our field is nearly incoherent both to vascular specialists and referring physicians. It will not be easy, but this can be done in PAD as well, and the vascular community must embrace it. Moreover it is imperative that vascular surgeons help to lead these multidisciplinary efforts, and develop evidence-based global guidelines to guide best practice in CLI.16 The recent funding of the BEST-CLI trial in the United States and the BASIL-2 trial in the United Kingdom demonstrate the importance to public health and offer great opportunities.
Until better evidence is available, a rational approach to limb salvage requires flexibility, understanding of the factors predicting success/failure for each modality, and the continued use of open bypass surgery as the initial treatment option for a significant number of patients.
And for the sake of our most vulnerable patients, we better keep training vascular surgeons to do all of it well.
Dr. Conte is professor and chief, division of vascular & endovascular surgery and the Edwin J. Wylie, M.D. Chair in Vascular Surgery at the University of California, San Francisco.
References
2. J. Vasc. Surg. 2014;59:220-34
7. J. Vasc. Surg. 2010;51:5S-17S
8. J. Vasc. Surg. 2010;51:18S-31S
9. J. Vasc. Surg. 2011;54:730-6
10. J. Amer. Heart Assoc. 2013;2:e000345
11. J. Vasc. Surg. 2006;43:742-51
12. J. Vasc. Surg. 2007;46:1180-90
13. J. Vasc. Surg. 2009;50:769-75
14. J. Vasc. Surg. 2010;52:1218-25
15. J. Vasc. Surg. 2013;57:8S-13S16. J. Vasc. Surg. 2014;59:510
The BASIL study originally published in the Lancet in 2005 (366:1925-34) and subsequently reiterated in multiple publications proposes that an endovascular approach should be utilized as the first invasive treatment modality in patients with infrainguinal peripheral arterial disease whose life expectancy is less than 2 years. By contrast, those patients expected to live beyond 2 years usually should be offered bypass surgery first, especially where a vein is available as a conduit. However, as can be seen from this month’s Point/Counterpoint by Dr. George Meier III and Dr. Michael S. Conte, the debate still rages as to the benefit of open vs. endovascular procedures for these patients. We encourage readers to voice their opinions in our “Letters to the Editor” section, as well as by participating in our web-based Quick Poll to the right of this story. - Dr. Russell Samson, Medical Editor, Vascular Specialist
POINT/COUNTERPOINT
Yes, endo is generally the way to go.
By Dr. George Meier III
Endovascular treatment of lower-extremity arterial disease has rapidly expanded, now approaching the standard for treatment of patients with lower-extremity disease. While open bypass remains a gold standard for the clinical treatment of limb-threatening ischemia, there are many limitations to the use of open surgery.
First and foremost, open surgical intervention represents pain and suffering for the patient as well as a delayed recovery, compared with endovascular treatment. All other factors being equal, most patients would prefer a less-invasive approach to minimize these factors and to maximize the speed of recovery. Open surgical interventions typically require 6 weeks or longer to get back to a functional status even remotely close to the patient’s initial level of function. With more severe tissue loss or with greater pain preoperatively, the difficulty of getting the patient back to full functional status remains problematic. In John Porter’s classic paper published in the Journal of Vascular Surgery in 1998,1 wound complications occurred in 24% of the patients with a 5-year survival rate of only 49% in this relatively young population, average age 66 years. Repeat operations to maintain graft patency, treat wound complications, or treat recurrent or contralateral ischemia were required in 54% of the patients and 23% ultimately required major limb amputation.
Of the 112 patients in this study, only 14.3% achieved the ideal surgical result of an uncomplicated operation: long-term symptom relief, maintenance of functional status, and no recurrence or repeat operations. These are sobering statistics for anyone facing open revascularization for critical limb ischemia.
The BASIL trial is often put forward as an example of the best data available currently to define patient treatments in patients with critical limb ischemia.2 Despite this, BASIL was a flawed trial from the beginning because of the difficulties of truly randomizing patients with vascular disease to open surgical treatment vs. percutaneous treatment. First, all patients had to be appropriate candidates for both open and endovascular treatment. In the real world, we readily recognize that the luxury of this choice is not available to many of our patients. A lack of conduit or increased surgical risk results in endovascular treatment being the only management option for many. Additionally, patient preference increasingly plays a role in treatment selection, obviously increasing the likelihood of less invasive percutaneous treatment. Yes, the mortality of open bypass in BASIL is reported to be in the 1%-3% range, but this population has been carefully selected based on screening and treatment of underlying cardiac disease. The true incidence of cardiovascular disease is impossible to determine since significant cardiac disease negated randomization.
Unfortunately, even with all of the advances in endovascular treatments the results of percutaneous treatment have never reached the results of open bypass. Nonetheless, while the success may not be as great the risks are not as high either. The main challenge to endovascular treatment is the durability of the intervention. While we can usually treat pre-existing disease in the lower-extremity arterial tree, maintaining patency and durability is the challenge. As my esteemed colleague has noted, failure of endovascular treatment in the BASIL trial resulted in significantly worse outcomes for open bypass in those patients. While much was made about this fact when the BASIL trial was published, endovascular treatment after open failure has even a worse outcome than did open treatment after endovascular failure. The truth of the matter is that, for obvious reasons, failure begets failure.
Generally, there are two imaging approaches to defining the extent of vascular disease: first, contrast angiography via percutaneous access; and second, CT angiography using intravenous contrast. If contrast angiography is undertaken to diagnose the extent of disease, then it is a relatively limited extrapolation to treat the patient’s disease percutaneously at the time of the diagnostic angiogram. For this reason, I discuss with all patients coming for diagnostic angiography the issue of endovascular treatment. It is rare that we make patients worse with an attempt at endovascular treatment by an experienced interventionalist. Similarly, it is rare that we alter a bypass level based on an attempt at endovascular treatment. If, in my opinion, the risk of an attempted endovascular treatment is acceptable, then this is done at the time of the diagnostic angiogram. Patients appreciate this discussion prior to proceeding with diagnostic angiography.
What about inadequate autogenous conduit? Even my counterpoint opponent has published a documented 20% risk of absent or inadequate ipsilateral greater saphenous vein.3 While he and his colleagues have documented excellent results using contralateral greater saphenous vein, there is still an inevitable morbidity and, yes, even a mortality risk associated with contralateral leg vein harvest. While in a good cardiac risk patient this may be negligible, we are again facing an ever more complex and medically ill patient population to subject to vascular treatment. It is in this setting that many vascular surgeons move to prosthetic conduits for the treatment of the patient’s vascular disease. While this may provide a short-term fix for the conduit problem, in the long term the risk of sudden, uncompensated failure of limb perfusion by prosthetic graft failure may often result in a higher risk procedure at a time when the patient may be older and more severely limited. Endovascular treatment is clearly a reasonable alternative in patients where autogenous conduit is not readily available.
While this debate will inevitably continue as long as practitioners have bias toward either open or endovascular management of vascular disease, one thing is for certain: We will continue to extend the limits of treatment to ever more ill and complex patients. While we have been very successful at performing fewer and fewer morbid interventions for limb-threatening vascular disease, these patients continue to be increasingly challenging to manage.
As the overall population continues to age, the need for less invasive treatment of limb-threatening vascular disease will continue to grow. And, yes, I agree that vascular surgeons in the role of interventionalist or surgeon are the leadership for the management of CLI in the future.
Dr. Meier is professor and chief of vascular surgery at the University of Cincinnati.
References
1. J. Vasc. Surg. 1998;27:256-63; discussion 264-6
3. J. Vasc. Surg. 2002:35:1085-92
No: A selective approach remains the key.
By Dr. MICHAEL S. CONTE
Recently the term “pandemic” has been applied to the growing global impact of peripheral artery disease (PAD), currently estimated to afflict more than 200 million individuals.1 The term “critical limb ischemia” (CLI), connoting the most advanced stage of PAD with imminent limb threat, is inadequately defined2 but likely encompasses 1%-3% of PAD. Aging of the global population and the increasing prevalence of diabetes are fueling increases in CLI and its impact on public health. While traditionally treated largely by vascular surgeons plying the open bypass trade, the ongoing development and market dispersion of catheter-based technologies for CLI has led to major secular changes.
Recent estimates suggest that upward of 5 billion dollars are spent annually on CLI in the Medicare population.3, 4 Increasing volumes and costs associated with revascularizations for CLI are a major driver, yet recent data suggest that regional spending in the United States is widely disparate and not directly associated with amputation rates.5 Thus defining effectiveness and value in CLI care has become a major challenge to the vascular community.
In current everyday practice, clinicians are faced with making treatment choices for CLI patients based on limited data and lots of anecdote. While the “open vs. endo” debate goes on, in many ways it has become less broadly relevant as the sophisticated clinician recognizes the real challenge lies in defining which approach to apply first in the right patient, at the right time. The only randomized, controlled trial (RCT) done in the field, the BASIL trial,6 is more than a decade old. However its findings remain important. For patients with “severe limb ischemia” likely to survive for at least 2 years, open bypass surgery offered better outcomes over angioplasty as an initial strategy.7 Moreover, the finding in BASIL that patients undergoing bypass after prior failed angioplasty did poorly,8 suggesting “no free lunch” for endovascular failures, has since been confirmed in other large registry studies.9
Simply stated, failure matters in CLI. And although endovascular techniques have continued to improve, the growing epidemic of restenosis shows no signs of abating.10 As in the case of percutaneous coronary intervention (PCI), we will know when endo results are meaningfully improved in PAD when the procedure volume curves actually flatten, not continue to grow geometrically.
So, in selecting the optimal strategy for CLI today, let’s focus on what we seem to know and try to apply an evidence-based mentality. We know that open bypass surgery is an effective and versatile treatment, but one that carries real morbidity (10%-20%) and some mortality (1%-3%). Among many large studies, the PREVENT III multicenter trial provides benchmark data on perioperative and 1-year outcomes.11
We know that the quality of the vein is the critical technical determinant of success, and arterial anatomy is less influential as long as there is outflow to the foot.12 We know that poor quality veins, prosthetics, and other alternatives are much inferior in CLI. And we know that there is a subset of CLI patients who are at high risk for adverse surgical outcomes.13, 14 However one defines them, up to 10% of patients in the large surgical series are in a high-risk group and may not experience meaningful benefit. For endovascular treatments, the data are less clear but certain trends have been consistent. Multilevel disease, long-segment occlusions, heavily calcified lesions, and more advanced tissue loss are negative predictors of clinical success.
Thus at first glance the weaknesses of the two strategies are largely complementary.15 When I encounter an average-risk CLI patient, with an adequate saphenous vein and more than one unfavorable endo factor, I am inclined towards bypass first.
Conversely, endo-favorable anatomy in higher risk patients is a no-brainer. Lots of people fall in the middle, and a significant minority should be considered for primary amputation. Currently my practice is roughly 50% bypass surgery-first in CLI.
Endovascular innovations have made a huge impact on vascular practice, and the leadership of many vascular surgeons (e.g., my esteemed counterpoint author) has been central to advancing the field. Better wires and catheters, retrograde approaches, and drug-eluting technologies continue to be developed at a dizzying pace.
We are all continually learning. Unfortunately, we lack good objective evidence to support most of the expanding armamentarium for CLI. However it is abundantly clear that technical (angiographic) success and clinical success are far apart, which is no surprise. What is surprising is an unsettlingly common lack of honesty about such an obvious fact. Are we all guilty of looking through rose-colored glasses?
Is it really such big news that patency actually matters for most patients with CLI? Technologies will not improve quickly enough if there is no market imperative to make them better. If we continue to buy and use things that are frequently ineffective, or don’t measure it carefully, where is the motivation?
No matter the lens through which one looks at the CLI field, it is desperate for improvement. We need much better technologies that provide longer lasting solutions for patients. We need better diagnostics to predict disease progression and responses to treatment.
We need some new medical or biological therapies that truly alleviate suffering. And we largely lack data on comparative effectiveness, and value, to support thoughtful application of our current treatment arsenal.
Most importantly what we need now is less dogma, and a lot more science. Over more than two decades, multiple RCTs comparing medical, interventional and surgical therapies for coronary artery disease have formed the basis for practice guidelines.
By comparison, our field is nearly incoherent both to vascular specialists and referring physicians. It will not be easy, but this can be done in PAD as well, and the vascular community must embrace it. Moreover it is imperative that vascular surgeons help to lead these multidisciplinary efforts, and develop evidence-based global guidelines to guide best practice in CLI.16 The recent funding of the BEST-CLI trial in the United States and the BASIL-2 trial in the United Kingdom demonstrate the importance to public health and offer great opportunities.
Until better evidence is available, a rational approach to limb salvage requires flexibility, understanding of the factors predicting success/failure for each modality, and the continued use of open bypass surgery as the initial treatment option for a significant number of patients.
And for the sake of our most vulnerable patients, we better keep training vascular surgeons to do all of it well.
Dr. Conte is professor and chief, division of vascular & endovascular surgery and the Edwin J. Wylie, M.D. Chair in Vascular Surgery at the University of California, San Francisco.
References
2. J. Vasc. Surg. 2014;59:220-34
7. J. Vasc. Surg. 2010;51:5S-17S
8. J. Vasc. Surg. 2010;51:18S-31S
9. J. Vasc. Surg. 2011;54:730-6
10. J. Amer. Heart Assoc. 2013;2:e000345
11. J. Vasc. Surg. 2006;43:742-51
12. J. Vasc. Surg. 2007;46:1180-90
13. J. Vasc. Surg. 2009;50:769-75
14. J. Vasc. Surg. 2010;52:1218-25
15. J. Vasc. Surg. 2013;57:8S-13S16. J. Vasc. Surg. 2014;59:510
Link found between sleep disorders and osteoporosis risk
Patients with sleep disorders are much more likely to develop osteoporosis than are those without sleep disorders, according to Dr. Chia-Ming Yen and her associates.
Patients diagnosed with sleep apnea between 1998 and 2001 had an osteoporosis incidence of nearly 10% at the end of 2010, while those without sleep disorders had incidence of 6.7%. Patients with insomnia developed osteoporosis at a rate of 13.1%, and patients with other sleep disturbances had an incidence of 12.7%, Dr. Yen of the National Formosa University in Taiwan, and her associates reported (Sleep Med. 2014 Aug. 1 [doi:10.1016/j.sleep.2014.07.005]).
Women and the elderly were particularly likely to develop osteoporosis if a sleep disorder was present. Of patients aged 64 years and older who were diagnosed with osteoporosis, 36.2% also had sleep apnea, and 31.9% had another sleep disorder. Incidences of osteoporosis in women in all cases were three to five times higher than those in men, and patients with multiple comorbidities also had an increased risk of osteoporosis, the investigators reported.
The study used data collected from 1996-2010 by the National Health Research Institute of Taiwan.
Patients with sleep disorders are much more likely to develop osteoporosis than are those without sleep disorders, according to Dr. Chia-Ming Yen and her associates.
Patients diagnosed with sleep apnea between 1998 and 2001 had an osteoporosis incidence of nearly 10% at the end of 2010, while those without sleep disorders had incidence of 6.7%. Patients with insomnia developed osteoporosis at a rate of 13.1%, and patients with other sleep disturbances had an incidence of 12.7%, Dr. Yen of the National Formosa University in Taiwan, and her associates reported (Sleep Med. 2014 Aug. 1 [doi:10.1016/j.sleep.2014.07.005]).
Women and the elderly were particularly likely to develop osteoporosis if a sleep disorder was present. Of patients aged 64 years and older who were diagnosed with osteoporosis, 36.2% also had sleep apnea, and 31.9% had another sleep disorder. Incidences of osteoporosis in women in all cases were three to five times higher than those in men, and patients with multiple comorbidities also had an increased risk of osteoporosis, the investigators reported.
The study used data collected from 1996-2010 by the National Health Research Institute of Taiwan.
Patients with sleep disorders are much more likely to develop osteoporosis than are those without sleep disorders, according to Dr. Chia-Ming Yen and her associates.
Patients diagnosed with sleep apnea between 1998 and 2001 had an osteoporosis incidence of nearly 10% at the end of 2010, while those without sleep disorders had incidence of 6.7%. Patients with insomnia developed osteoporosis at a rate of 13.1%, and patients with other sleep disturbances had an incidence of 12.7%, Dr. Yen of the National Formosa University in Taiwan, and her associates reported (Sleep Med. 2014 Aug. 1 [doi:10.1016/j.sleep.2014.07.005]).
Women and the elderly were particularly likely to develop osteoporosis if a sleep disorder was present. Of patients aged 64 years and older who were diagnosed with osteoporosis, 36.2% also had sleep apnea, and 31.9% had another sleep disorder. Incidences of osteoporosis in women in all cases were three to five times higher than those in men, and patients with multiple comorbidities also had an increased risk of osteoporosis, the investigators reported.
The study used data collected from 1996-2010 by the National Health Research Institute of Taiwan.
Enzyme ‘switch’ is key to new treatment strategy for T-ALL
Credit: Thomas Semkow
Blocking the action of an enzyme “switch” needed to activate tumor growth may be a practical strategy for treating T-cell acute lymphoblastic leukemia (T-ALL), new research suggests.
The study showed that this enzyme, JMJD3, acts as a cancer “on” switch by splitting off a chemical methyl group of another protein that is usually methylated by the tumor-suppressing enzyme PRC2.
PRC2 acts, in turn, as an “off” switch for cancer cell proliferation.
The researchers previously showed that this destabilizing and cutting loose of PRC2 leads to activation of the NOTCH1 pathway, a process common to many cancers but especially active in at least half of all people with T-ALL.
The team said the drug manufacturer GlaxoSmithKline is already developing an investigational compound called GSKJ4, whose treatment path follows the biological road map revealed in this research.
“Our investigations are showing incredible promise in fighting this disease at the transcriptional level,” said Iannis Aifantis, PhD, of NYU Langone Medical Center in New York.
“We are blocking the action of enzymes controlling the transcription of proteins involved in leukemia, rather than attempting to directly suppress cancer genes.”
Dr Aifantis and his colleagues described this approach in a letter to Nature.
The group’s findings are the culmination of several years of research to unravel precisely how PRC2 suppresses tumor growth since the team first reported the phenomenon in leukemia.
For the current study, the researchers investigated precisely how demethylation triggers the chain of events that evicts PRC2 from cells, thereby removing PRC2 suppression of NOTCH1, which directly binds to and activates cancer-causing genes.
Specifically, they focused on a protein controlled and methylated by PRC2 called H3K27, as well as two other enzymes closely tied to H3K27—JMJD3 and UTX.
The study showed that JMJD3 was highly active in both mice and human leukemia cells at all stages of tumor growth and development. By contrast, UTX was not overexpressed in leukemia, but it was highly active in noncancerous mouse and human cells.
When mice and human leukemia cells were treated with the experimental drug GSKJ4, JMJD3 activity stopped, and all cancer cells eventually died.
Subsequent experiments showed that, in leukemic JMJD3 knockout mice, NOTCH1 activity declined, while UTX activity remained the same.
The disease also progressed much faster in mice bred without UTX, while mice lived longer if they produced UTX. These findings suggest that UTX production controls several tumor-suppressing genes.
To further confirm their findings, the researchers screened more than 200 blood samples from children and adults with T-ALL, revealing several common mutations in UTX.
Dr Aifantis said plans are underway to test GSKJ4 against human leukemia cells transplanted in mice. Other experiments will use the drug in combination with standard chemotherapy in animals with leukemia.
“Our report serves as a valuable reminder of just how complex cancers like T-cell acute lymphoblastic leukemia can be,” Dr Aifantis said, “and that enzymes can play many, even opposing, roles in both tumor growth and suppression.” ![]()
Credit: Thomas Semkow
Blocking the action of an enzyme “switch” needed to activate tumor growth may be a practical strategy for treating T-cell acute lymphoblastic leukemia (T-ALL), new research suggests.
The study showed that this enzyme, JMJD3, acts as a cancer “on” switch by splitting off a chemical methyl group of another protein that is usually methylated by the tumor-suppressing enzyme PRC2.
PRC2 acts, in turn, as an “off” switch for cancer cell proliferation.
The researchers previously showed that this destabilizing and cutting loose of PRC2 leads to activation of the NOTCH1 pathway, a process common to many cancers but especially active in at least half of all people with T-ALL.
The team said the drug manufacturer GlaxoSmithKline is already developing an investigational compound called GSKJ4, whose treatment path follows the biological road map revealed in this research.
“Our investigations are showing incredible promise in fighting this disease at the transcriptional level,” said Iannis Aifantis, PhD, of NYU Langone Medical Center in New York.
“We are blocking the action of enzymes controlling the transcription of proteins involved in leukemia, rather than attempting to directly suppress cancer genes.”
Dr Aifantis and his colleagues described this approach in a letter to Nature.
The group’s findings are the culmination of several years of research to unravel precisely how PRC2 suppresses tumor growth since the team first reported the phenomenon in leukemia.
For the current study, the researchers investigated precisely how demethylation triggers the chain of events that evicts PRC2 from cells, thereby removing PRC2 suppression of NOTCH1, which directly binds to and activates cancer-causing genes.
Specifically, they focused on a protein controlled and methylated by PRC2 called H3K27, as well as two other enzymes closely tied to H3K27—JMJD3 and UTX.
The study showed that JMJD3 was highly active in both mice and human leukemia cells at all stages of tumor growth and development. By contrast, UTX was not overexpressed in leukemia, but it was highly active in noncancerous mouse and human cells.
When mice and human leukemia cells were treated with the experimental drug GSKJ4, JMJD3 activity stopped, and all cancer cells eventually died.
Subsequent experiments showed that, in leukemic JMJD3 knockout mice, NOTCH1 activity declined, while UTX activity remained the same.
The disease also progressed much faster in mice bred without UTX, while mice lived longer if they produced UTX. These findings suggest that UTX production controls several tumor-suppressing genes.
To further confirm their findings, the researchers screened more than 200 blood samples from children and adults with T-ALL, revealing several common mutations in UTX.
Dr Aifantis said plans are underway to test GSKJ4 against human leukemia cells transplanted in mice. Other experiments will use the drug in combination with standard chemotherapy in animals with leukemia.
“Our report serves as a valuable reminder of just how complex cancers like T-cell acute lymphoblastic leukemia can be,” Dr Aifantis said, “and that enzymes can play many, even opposing, roles in both tumor growth and suppression.” ![]()
Credit: Thomas Semkow
Blocking the action of an enzyme “switch” needed to activate tumor growth may be a practical strategy for treating T-cell acute lymphoblastic leukemia (T-ALL), new research suggests.
The study showed that this enzyme, JMJD3, acts as a cancer “on” switch by splitting off a chemical methyl group of another protein that is usually methylated by the tumor-suppressing enzyme PRC2.
PRC2 acts, in turn, as an “off” switch for cancer cell proliferation.
The researchers previously showed that this destabilizing and cutting loose of PRC2 leads to activation of the NOTCH1 pathway, a process common to many cancers but especially active in at least half of all people with T-ALL.
The team said the drug manufacturer GlaxoSmithKline is already developing an investigational compound called GSKJ4, whose treatment path follows the biological road map revealed in this research.
“Our investigations are showing incredible promise in fighting this disease at the transcriptional level,” said Iannis Aifantis, PhD, of NYU Langone Medical Center in New York.
“We are blocking the action of enzymes controlling the transcription of proteins involved in leukemia, rather than attempting to directly suppress cancer genes.”
Dr Aifantis and his colleagues described this approach in a letter to Nature.
The group’s findings are the culmination of several years of research to unravel precisely how PRC2 suppresses tumor growth since the team first reported the phenomenon in leukemia.
For the current study, the researchers investigated precisely how demethylation triggers the chain of events that evicts PRC2 from cells, thereby removing PRC2 suppression of NOTCH1, which directly binds to and activates cancer-causing genes.
Specifically, they focused on a protein controlled and methylated by PRC2 called H3K27, as well as two other enzymes closely tied to H3K27—JMJD3 and UTX.
The study showed that JMJD3 was highly active in both mice and human leukemia cells at all stages of tumor growth and development. By contrast, UTX was not overexpressed in leukemia, but it was highly active in noncancerous mouse and human cells.
When mice and human leukemia cells were treated with the experimental drug GSKJ4, JMJD3 activity stopped, and all cancer cells eventually died.
Subsequent experiments showed that, in leukemic JMJD3 knockout mice, NOTCH1 activity declined, while UTX activity remained the same.
The disease also progressed much faster in mice bred without UTX, while mice lived longer if they produced UTX. These findings suggest that UTX production controls several tumor-suppressing genes.
To further confirm their findings, the researchers screened more than 200 blood samples from children and adults with T-ALL, revealing several common mutations in UTX.
Dr Aifantis said plans are underway to test GSKJ4 against human leukemia cells transplanted in mice. Other experiments will use the drug in combination with standard chemotherapy in animals with leukemia.
“Our report serves as a valuable reminder of just how complex cancers like T-cell acute lymphoblastic leukemia can be,” Dr Aifantis said, “and that enzymes can play many, even opposing, roles in both tumor growth and suppression.” ![]()