User login
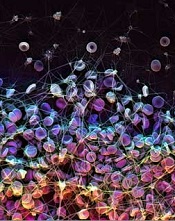
to form a blood clot
Credit: James Weaver
Researchers have developed a coating that can prevent blood and bacteria from adhering to the surface of medical devices.
The coating repelled blood from more than 20 medically relevant substrates, suppressed biofilm formation, and prevented coagulation in an animal model for at least 8 hours.
The researchers believe this technology could reduce the use of anticoagulants and help prevent thrombotic occlusion and biofouling of medical devices.
The idea for the coating evolved from a surface technology known as “slippery liquid-infused porous surfaces (SLIPS),” which was developed by Joanna Aizenberg, PhD, of Harvard University’s Wyss Institute for Biologically Inspired Engineering.
Inspired by the slippery surface of the carnivorous pitcher plant, which enables the plant to capture insects, SLIPS can repel nearly any material. The liquid layer on the surface provides a barrier to everything from ice to crude oil and blood.
“Traditional SLIPS uses porous, textured surface substrates to immobilize the liquid layer, whereas medical surfaces are mostly flat and smooth,” Dr Aizenberg said. “So we further adapted our approach by capitalizing on the natural roughness of chemically modified surfaces of medical devices.”
She and her colleagues described this work in Nature Biotechnology.
The researchers developed a super-repellent coating that can be adhered to existing, approved medical devices. In a 2-step surface-coating process, they chemically attached a monolayer of perfluorocarbon, which is similar to Teflon.
Then, they added a layer of liquid perfluorocarbon, which is widely used in medicine for applications such as liquid ventilation for infants with breathing challenges, blood substitution, and eye surgery. The team calls the tethered perfluorocarbon plus the liquid layer a “tethered-liquid perfluorocarbon surface (TLP)”.
TLP worked seamlessly when coated on more than 20 different medical surfaces, including plastics, glasses, and metals.
The researchers also implanted medical-grade tubing and catheters coated with TLP in large blood vessels in pigs, and the coating prevented blood from clotting for at least 8 hours without the use of anticoagulants.
TLP-treated medical tubing was stored for more than a year under normal temperature and humidity conditions and still prevented clot formation, repelling fibrin and platelets.
The TLP surface remained stable under the full range of clinically relevant physiological shear stresses, or rates of blood flow seen in catheters and central lines, all the way up to dialysis machines.
When the bacteria Pseudomonas aeruginosa were grown in TLP-coated medical tubing for more than 6 weeks, less than 1 in a billion bacteria were able to adhere. Central lines coated with TLP significantly reduced sepsis from central-line associated bloodstream infections.
Out of curiosity, the researchers even tested a TLP-coated surface with a gecko, whose footpads contain hair-like structures with tremendous adhesive strength. And the gecko was unable to hold on.
“We were wonderfully surprised by how well the TLP coating worked, particularly in vivo without heparin,” said Anna Waterhouse, PhD, of the Wyss Institute.
“Usually, the blood will start to clot within an hour in the extracorporeal circuit, so our experiments really demonstrate the clinical relevance of this new coating.” ![]()
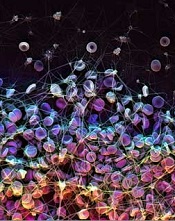
to form a blood clot
Credit: James Weaver
Researchers have developed a coating that can prevent blood and bacteria from adhering to the surface of medical devices.
The coating repelled blood from more than 20 medically relevant substrates, suppressed biofilm formation, and prevented coagulation in an animal model for at least 8 hours.
The researchers believe this technology could reduce the use of anticoagulants and help prevent thrombotic occlusion and biofouling of medical devices.
The idea for the coating evolved from a surface technology known as “slippery liquid-infused porous surfaces (SLIPS),” which was developed by Joanna Aizenberg, PhD, of Harvard University’s Wyss Institute for Biologically Inspired Engineering.
Inspired by the slippery surface of the carnivorous pitcher plant, which enables the plant to capture insects, SLIPS can repel nearly any material. The liquid layer on the surface provides a barrier to everything from ice to crude oil and blood.
“Traditional SLIPS uses porous, textured surface substrates to immobilize the liquid layer, whereas medical surfaces are mostly flat and smooth,” Dr Aizenberg said. “So we further adapted our approach by capitalizing on the natural roughness of chemically modified surfaces of medical devices.”
She and her colleagues described this work in Nature Biotechnology.
The researchers developed a super-repellent coating that can be adhered to existing, approved medical devices. In a 2-step surface-coating process, they chemically attached a monolayer of perfluorocarbon, which is similar to Teflon.
Then, they added a layer of liquid perfluorocarbon, which is widely used in medicine for applications such as liquid ventilation for infants with breathing challenges, blood substitution, and eye surgery. The team calls the tethered perfluorocarbon plus the liquid layer a “tethered-liquid perfluorocarbon surface (TLP)”.
TLP worked seamlessly when coated on more than 20 different medical surfaces, including plastics, glasses, and metals.
The researchers also implanted medical-grade tubing and catheters coated with TLP in large blood vessels in pigs, and the coating prevented blood from clotting for at least 8 hours without the use of anticoagulants.
TLP-treated medical tubing was stored for more than a year under normal temperature and humidity conditions and still prevented clot formation, repelling fibrin and platelets.
The TLP surface remained stable under the full range of clinically relevant physiological shear stresses, or rates of blood flow seen in catheters and central lines, all the way up to dialysis machines.
When the bacteria Pseudomonas aeruginosa were grown in TLP-coated medical tubing for more than 6 weeks, less than 1 in a billion bacteria were able to adhere. Central lines coated with TLP significantly reduced sepsis from central-line associated bloodstream infections.
Out of curiosity, the researchers even tested a TLP-coated surface with a gecko, whose footpads contain hair-like structures with tremendous adhesive strength. And the gecko was unable to hold on.
“We were wonderfully surprised by how well the TLP coating worked, particularly in vivo without heparin,” said Anna Waterhouse, PhD, of the Wyss Institute.
“Usually, the blood will start to clot within an hour in the extracorporeal circuit, so our experiments really demonstrate the clinical relevance of this new coating.” ![]()
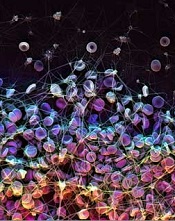
to form a blood clot
Credit: James Weaver
Researchers have developed a coating that can prevent blood and bacteria from adhering to the surface of medical devices.
The coating repelled blood from more than 20 medically relevant substrates, suppressed biofilm formation, and prevented coagulation in an animal model for at least 8 hours.
The researchers believe this technology could reduce the use of anticoagulants and help prevent thrombotic occlusion and biofouling of medical devices.
The idea for the coating evolved from a surface technology known as “slippery liquid-infused porous surfaces (SLIPS),” which was developed by Joanna Aizenberg, PhD, of Harvard University’s Wyss Institute for Biologically Inspired Engineering.
Inspired by the slippery surface of the carnivorous pitcher plant, which enables the plant to capture insects, SLIPS can repel nearly any material. The liquid layer on the surface provides a barrier to everything from ice to crude oil and blood.
“Traditional SLIPS uses porous, textured surface substrates to immobilize the liquid layer, whereas medical surfaces are mostly flat and smooth,” Dr Aizenberg said. “So we further adapted our approach by capitalizing on the natural roughness of chemically modified surfaces of medical devices.”
She and her colleagues described this work in Nature Biotechnology.
The researchers developed a super-repellent coating that can be adhered to existing, approved medical devices. In a 2-step surface-coating process, they chemically attached a monolayer of perfluorocarbon, which is similar to Teflon.
Then, they added a layer of liquid perfluorocarbon, which is widely used in medicine for applications such as liquid ventilation for infants with breathing challenges, blood substitution, and eye surgery. The team calls the tethered perfluorocarbon plus the liquid layer a “tethered-liquid perfluorocarbon surface (TLP)”.
TLP worked seamlessly when coated on more than 20 different medical surfaces, including plastics, glasses, and metals.
The researchers also implanted medical-grade tubing and catheters coated with TLP in large blood vessels in pigs, and the coating prevented blood from clotting for at least 8 hours without the use of anticoagulants.
TLP-treated medical tubing was stored for more than a year under normal temperature and humidity conditions and still prevented clot formation, repelling fibrin and platelets.
The TLP surface remained stable under the full range of clinically relevant physiological shear stresses, or rates of blood flow seen in catheters and central lines, all the way up to dialysis machines.
When the bacteria Pseudomonas aeruginosa were grown in TLP-coated medical tubing for more than 6 weeks, less than 1 in a billion bacteria were able to adhere. Central lines coated with TLP significantly reduced sepsis from central-line associated bloodstream infections.
Out of curiosity, the researchers even tested a TLP-coated surface with a gecko, whose footpads contain hair-like structures with tremendous adhesive strength. And the gecko was unable to hold on.
“We were wonderfully surprised by how well the TLP coating worked, particularly in vivo without heparin,” said Anna Waterhouse, PhD, of the Wyss Institute.
“Usually, the blood will start to clot within an hour in the extracorporeal circuit, so our experiments really demonstrate the clinical relevance of this new coating.” ![]()