User login
2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines
Recommendations
Each recommendation has been mapped from the NHLBI grading format to the American College of Cardiology/American Heart Association Class of Recommendation/Level of Evidence (ACC/AHA COR/LOE) construct and is expressed in both formats. Because of the inherent differences in grading systems and the clinical questions driving the recommendations, alignment between the NHLBI and ACC/AHA formats is in some cases imperfect. Definitions for the NHLBI strength of recommendation (A-E, N) and quality of evidence (High, Moderate, Low) and the ACC/AHA levels of the evidence (LOE: A-C) and classes of recommendations (COR: I-III) are provided at the end of the "Major Recommendations" field.
Summary of Recommendations for Lifestyle Management
Diet
Low-density lipoprotein cholesterol (LDL-C): Advise adults who would benefit from LDL-C lowering* to:
- Consume a dietary pattern that emphasizes intake of vegetables, fruits, and whole grains; includes low-fat dairy products, poultry, fish, legumes, nontropical vegetable oils, and nuts; and limits intake of sweets, sugar-sweetened beverages, and red meats. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
- Adapt this dietary pattern to appropriate calorie requirements, personal and cultural food preferences, and nutrition therapy for other medical conditions (including diabetes).
- Achieve this pattern by following plans such as the Dietary Approaches to Stop Hypertension (DASH) dietary pattern, the U.S. Department of Agriculture (USDA) Food Pattern, or the AHA Diet.
- Aim for a dietary pattern that achieves 5% to 6% of calories from saturated fat. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
- Reduce percent of calories from saturated fat. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
- Reduce percent of calories from trans fat. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
Blood pressure (BP): Advise adults who would benefit from BP lowering to:
- Consume a dietary pattern that emphasizes intake of vegetables, fruits, and whole grains; includes low-fat dairy products, poultry, fish, legumes, nontropical vegetable oils, and nuts; and limits intake of sweets, sugar-sweetened beverages, and red meats. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
- Adapt this dietary pattern to appropriate calorie requirements, personal and cultural food preferences, and nutrition therapy for other medical conditions (including diabetes).
- Achieve this pattern by following plans such as the DASH dietary pattern, the USDA Food Pattern, or the AHA Diet.
- Lower sodium intake. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
- a. Consume no more than 2,400 mg of sodium/d; b. Further reduction of sodium intake to 1,500 mg/d can result in even greater reduction in BP; and c. Even without achieving these goals, reducing sodium intake by at least 1,000 mg/d lowers BP. NHLBI Grade: B (Moderate); ACC/AHA COR: IIa; ACC/AHA LOE: B
- Combine the DASH dietary pattern with lower sodium intake. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
Physical Activity
Lipids
- In general, advise adults to engage in aerobic physical activity to reduce LDL-C and non-high-density lipoprotein cholesterol (non–HDL-C): 3–4 sessions per week, lasting on average 40 minutes per session, and involving moderate- to vigorous-intensity physical activity. NHLBI Grade: B (Moderate); ACC/AHA COR: IIa; ACC/AHA LOE: A
BP
- In general, advise adults to engage in aerobic physical activity to lower BP: 3 to 4 sessions per week, lasting on average 40 minutes per session, and involving moderate- to vigorous-intensity physical activity. NHLBI Grade: B (Moderate); ACC/AHA COR: IIa; ACC/AHA LOE: A
*Refer to the NGC summary 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines.
See Tables 7-10, 13, 15, and 16 in the original guideline document for additional diet and physical activity guidelines and resources.
Definitions:
NHLBI Grading of the Strength of Recommendations
| Grade | Strength of Recommendation* |
|---|---|
| A | Strong recommendation There is high certainty based on evidence that the net benefit† is substantial. |
| B | Moderate recommendation There is moderate certainty based on evidence that the net benefit is moderate to substantial, or there is high certainty that the net benefit is moderate. |
| C | Weak recommendation There is at least moderate certainty based on evidence that there is a small net benefit. |
| D | Recommendation against There is at least moderate certainty based on evidence that there is no net benefit or that risks/harms outweigh benefits. |
| E | Expert opinion ("There is insufficient evidence or evidence is unclear or conflicting, but this is what the Work Group recommends.") Net benefit is unclear. Balance of benefits and harms cannot be determined because of no evidence, insufficient evidence, unclear evidence, or conflicting evidence, but the Work Group thought it was important to provide clinical guidance and make a recommendation. Further research is recommended in this area. |
| N | No recommendation for or against ("There is insufficient evidence or evidence is unclear or conflicting.") Net benefit is unclear. Balance of benefits and harms cannot be determined because of no evidence, insufficient evidence, unclear evidence, or conflicting evidence, and the Work Group thought no recommendation should be made. Further research is recommended in this area. |
*In most cases, the strength of the recommendation should be closely aligned with the quality of the evidence; however, under some circumstances, there may be valid reasons for making recommendations that are not closely aligned with the quality of the evidence (e.g., strong recommendation when the evidence quality is moderate, such as smoking cessation to reduce cardiovascular disease [CVD] risk or ordering an electrocardiogram [ECG] as part of the initial diagnostic work-up for a patient presenting with possible myocardial infarction [MI]). Those situations should be limited and the rationale explained clearly by the Work Group.
†Net benefit is defined as benefits minus risks/harms of the service/intervention.
NHLBI Quality Rating of the Strength of Evidence
| Type of Evidence | Quality Rating* |
|---|---|
| High |
| Moderate |
| Low |
*In some cases, other evidence, such as large all-or-none case series (e.g., jumping from airplanes or tall structures), can represent high- or moderate-quality evidence. In such cases, the rationale for the evidence rating exception should be explained by the Work Group and clearly justified.
†"Well-designed, well-executed" refers to studies that directly address the question; use adequate randomization, blinding, and allocation concealment; are adequately powered; use intention-to-treat analyses; and have high follow-up rates.
‡Limitations include concerns with the design and execution of a study that result in decreased confidence in the true estimate of the effect. Examples of such limitations include but are not limited to: inadequate randomization, lack of blinding of study participants or outcome assessors, inadequate power, outcomes of interest that are not prespecified for the primary outcomes, low follow-up rates, and findings based on subgroup analyses. Whether the limitations are considered minor or major is based on the number and severity of flaws in design or execution. Rules for determining whether the limitations are considered minor or major and how they will affect rating of the individual studies will be developed collaboratively with the methodology team.
§Nonrandomized controlled studies refer to intervention studies where assignment to intervention and comparison groups is not random (e.g., quasi-experimental study design).
¶Observational studies include prospective and retrospective cohort, case-control, and cross-sectional studies.
Applying Classification of Recommendations and Level of Evidence
| Size of Treatment Effect | |||||||
|---|---|---|---|---|---|---|---|
| CLASS I Benefit >>> Risk Procedure/Treatment SHOULD be performed/ administered | CLASS IIa Benefit >> Risk Additional studies with focused objectives needed IT IS REASONABLE to perform procedure/administer treatment | CLASS IIb Benefit ≥ Risk Additional studies with broad objectives needed; additional registry data would be helpful Procedure/Treatment MAY BE CONSIDERED | CLASS III No Benefit or Class III Harm | ||||
| Procedure/Test | Treatment | ||||||
| COR III: No Benefit | Not helpful | No proven benefit | |||||
| COR III: Harm | Excess cost without benefit or harmful | Harmful to patients | |||||
| Estimate of Certainty (Precision) of Treatment Effect | LEVEL A Multiple populations evaluated* Data derived from multiple randomized clinical trials or meta-analyses |
|
|
|
| ||
| LEVEL B Limited populations evaluated* Data derived from a single randomized trial or nonrandomized studies |
|
|
|
| |||
| LEVEL C Very limited populations evaluated* Only consensus opinion of experts, case studies, or standard of care |
|
|
|
| |||
A recommendation with Level of Evidence B or C does not imply the recommendation is weak. Many important clinical questions addressed in the guidelines do not lend themselves to clinical trials. Even when randomized trials are unavailable, there may be a very clear clinical consensus that a particular test or therapy is useful or effective.
*Data available from clinical trials or registries about the usefulness/efficacy in different subpopulations, such as sex, age, history of diabetes, history of prior myocardial infarction, history of heart failure, and prior aspirin use.
†For comparative-effectiveness recommendations (Class I and IIa; Level of Evidence A and B only), studies that support the use of comparator verbs should involve direct comparisons of the treatments or strategies being evaluated.
Recommendations
Each recommendation has been mapped from the NHLBI grading format to the American College of Cardiology/American Heart Association Class of Recommendation/Level of Evidence (ACC/AHA COR/LOE) construct and is expressed in both formats. Because of the inherent differences in grading systems and the clinical questions driving the recommendations, alignment between the NHLBI and ACC/AHA formats is in some cases imperfect. Definitions for the NHLBI strength of recommendation (A-E, N) and quality of evidence (High, Moderate, Low) and the ACC/AHA levels of the evidence (LOE: A-C) and classes of recommendations (COR: I-III) are provided at the end of the "Major Recommendations" field.
Summary of Recommendations for Lifestyle Management
Diet
Low-density lipoprotein cholesterol (LDL-C): Advise adults who would benefit from LDL-C lowering* to:
- Consume a dietary pattern that emphasizes intake of vegetables, fruits, and whole grains; includes low-fat dairy products, poultry, fish, legumes, nontropical vegetable oils, and nuts; and limits intake of sweets, sugar-sweetened beverages, and red meats. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
- Adapt this dietary pattern to appropriate calorie requirements, personal and cultural food preferences, and nutrition therapy for other medical conditions (including diabetes).
- Achieve this pattern by following plans such as the Dietary Approaches to Stop Hypertension (DASH) dietary pattern, the U.S. Department of Agriculture (USDA) Food Pattern, or the AHA Diet.
- Aim for a dietary pattern that achieves 5% to 6% of calories from saturated fat. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
- Reduce percent of calories from saturated fat. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
- Reduce percent of calories from trans fat. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
Blood pressure (BP): Advise adults who would benefit from BP lowering to:
- Consume a dietary pattern that emphasizes intake of vegetables, fruits, and whole grains; includes low-fat dairy products, poultry, fish, legumes, nontropical vegetable oils, and nuts; and limits intake of sweets, sugar-sweetened beverages, and red meats. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
- Adapt this dietary pattern to appropriate calorie requirements, personal and cultural food preferences, and nutrition therapy for other medical conditions (including diabetes).
- Achieve this pattern by following plans such as the DASH dietary pattern, the USDA Food Pattern, or the AHA Diet.
- Lower sodium intake. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
- a. Consume no more than 2,400 mg of sodium/d; b. Further reduction of sodium intake to 1,500 mg/d can result in even greater reduction in BP; and c. Even without achieving these goals, reducing sodium intake by at least 1,000 mg/d lowers BP. NHLBI Grade: B (Moderate); ACC/AHA COR: IIa; ACC/AHA LOE: B
- Combine the DASH dietary pattern with lower sodium intake. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
Physical Activity
Lipids
- In general, advise adults to engage in aerobic physical activity to reduce LDL-C and non-high-density lipoprotein cholesterol (non–HDL-C): 3–4 sessions per week, lasting on average 40 minutes per session, and involving moderate- to vigorous-intensity physical activity. NHLBI Grade: B (Moderate); ACC/AHA COR: IIa; ACC/AHA LOE: A
BP
- In general, advise adults to engage in aerobic physical activity to lower BP: 3 to 4 sessions per week, lasting on average 40 minutes per session, and involving moderate- to vigorous-intensity physical activity. NHLBI Grade: B (Moderate); ACC/AHA COR: IIa; ACC/AHA LOE: A
*Refer to the NGC summary 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines.
See Tables 7-10, 13, 15, and 16 in the original guideline document for additional diet and physical activity guidelines and resources.
Definitions:
NHLBI Grading of the Strength of Recommendations
| Grade | Strength of Recommendation* |
|---|---|
| A | Strong recommendation There is high certainty based on evidence that the net benefit† is substantial. |
| B | Moderate recommendation There is moderate certainty based on evidence that the net benefit is moderate to substantial, or there is high certainty that the net benefit is moderate. |
| C | Weak recommendation There is at least moderate certainty based on evidence that there is a small net benefit. |
| D | Recommendation against There is at least moderate certainty based on evidence that there is no net benefit or that risks/harms outweigh benefits. |
| E | Expert opinion ("There is insufficient evidence or evidence is unclear or conflicting, but this is what the Work Group recommends.") Net benefit is unclear. Balance of benefits and harms cannot be determined because of no evidence, insufficient evidence, unclear evidence, or conflicting evidence, but the Work Group thought it was important to provide clinical guidance and make a recommendation. Further research is recommended in this area. |
| N | No recommendation for or against ("There is insufficient evidence or evidence is unclear or conflicting.") Net benefit is unclear. Balance of benefits and harms cannot be determined because of no evidence, insufficient evidence, unclear evidence, or conflicting evidence, and the Work Group thought no recommendation should be made. Further research is recommended in this area. |
*In most cases, the strength of the recommendation should be closely aligned with the quality of the evidence; however, under some circumstances, there may be valid reasons for making recommendations that are not closely aligned with the quality of the evidence (e.g., strong recommendation when the evidence quality is moderate, such as smoking cessation to reduce cardiovascular disease [CVD] risk or ordering an electrocardiogram [ECG] as part of the initial diagnostic work-up for a patient presenting with possible myocardial infarction [MI]). Those situations should be limited and the rationale explained clearly by the Work Group.
†Net benefit is defined as benefits minus risks/harms of the service/intervention.
NHLBI Quality Rating of the Strength of Evidence
| Type of Evidence | Quality Rating* |
|---|---|
| High |
| Moderate |
| Low |
*In some cases, other evidence, such as large all-or-none case series (e.g., jumping from airplanes or tall structures), can represent high- or moderate-quality evidence. In such cases, the rationale for the evidence rating exception should be explained by the Work Group and clearly justified.
†"Well-designed, well-executed" refers to studies that directly address the question; use adequate randomization, blinding, and allocation concealment; are adequately powered; use intention-to-treat analyses; and have high follow-up rates.
‡Limitations include concerns with the design and execution of a study that result in decreased confidence in the true estimate of the effect. Examples of such limitations include but are not limited to: inadequate randomization, lack of blinding of study participants or outcome assessors, inadequate power, outcomes of interest that are not prespecified for the primary outcomes, low follow-up rates, and findings based on subgroup analyses. Whether the limitations are considered minor or major is based on the number and severity of flaws in design or execution. Rules for determining whether the limitations are considered minor or major and how they will affect rating of the individual studies will be developed collaboratively with the methodology team.
§Nonrandomized controlled studies refer to intervention studies where assignment to intervention and comparison groups is not random (e.g., quasi-experimental study design).
¶Observational studies include prospective and retrospective cohort, case-control, and cross-sectional studies.
Applying Classification of Recommendations and Level of Evidence
| Size of Treatment Effect | |||||||
|---|---|---|---|---|---|---|---|
| CLASS I Benefit >>> Risk Procedure/Treatment SHOULD be performed/ administered | CLASS IIa Benefit >> Risk Additional studies with focused objectives needed IT IS REASONABLE to perform procedure/administer treatment | CLASS IIb Benefit ≥ Risk Additional studies with broad objectives needed; additional registry data would be helpful Procedure/Treatment MAY BE CONSIDERED | CLASS III No Benefit or Class III Harm | ||||
| Procedure/Test | Treatment | ||||||
| COR III: No Benefit | Not helpful | No proven benefit | |||||
| COR III: Harm | Excess cost without benefit or harmful | Harmful to patients | |||||
| Estimate of Certainty (Precision) of Treatment Effect | LEVEL A Multiple populations evaluated* Data derived from multiple randomized clinical trials or meta-analyses |
|
|
|
| ||
| LEVEL B Limited populations evaluated* Data derived from a single randomized trial or nonrandomized studies |
|
|
|
| |||
| LEVEL C Very limited populations evaluated* Only consensus opinion of experts, case studies, or standard of care |
|
|
|
| |||
A recommendation with Level of Evidence B or C does not imply the recommendation is weak. Many important clinical questions addressed in the guidelines do not lend themselves to clinical trials. Even when randomized trials are unavailable, there may be a very clear clinical consensus that a particular test or therapy is useful or effective.
*Data available from clinical trials or registries about the usefulness/efficacy in different subpopulations, such as sex, age, history of diabetes, history of prior myocardial infarction, history of heart failure, and prior aspirin use.
†For comparative-effectiveness recommendations (Class I and IIa; Level of Evidence A and B only), studies that support the use of comparator verbs should involve direct comparisons of the treatments or strategies being evaluated.
Recommendations
Each recommendation has been mapped from the NHLBI grading format to the American College of Cardiology/American Heart Association Class of Recommendation/Level of Evidence (ACC/AHA COR/LOE) construct and is expressed in both formats. Because of the inherent differences in grading systems and the clinical questions driving the recommendations, alignment between the NHLBI and ACC/AHA formats is in some cases imperfect. Definitions for the NHLBI strength of recommendation (A-E, N) and quality of evidence (High, Moderate, Low) and the ACC/AHA levels of the evidence (LOE: A-C) and classes of recommendations (COR: I-III) are provided at the end of the "Major Recommendations" field.
Summary of Recommendations for Lifestyle Management
Diet
Low-density lipoprotein cholesterol (LDL-C): Advise adults who would benefit from LDL-C lowering* to:
- Consume a dietary pattern that emphasizes intake of vegetables, fruits, and whole grains; includes low-fat dairy products, poultry, fish, legumes, nontropical vegetable oils, and nuts; and limits intake of sweets, sugar-sweetened beverages, and red meats. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
- Adapt this dietary pattern to appropriate calorie requirements, personal and cultural food preferences, and nutrition therapy for other medical conditions (including diabetes).
- Achieve this pattern by following plans such as the Dietary Approaches to Stop Hypertension (DASH) dietary pattern, the U.S. Department of Agriculture (USDA) Food Pattern, or the AHA Diet.
- Aim for a dietary pattern that achieves 5% to 6% of calories from saturated fat. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
- Reduce percent of calories from saturated fat. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
- Reduce percent of calories from trans fat. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
Blood pressure (BP): Advise adults who would benefit from BP lowering to:
- Consume a dietary pattern that emphasizes intake of vegetables, fruits, and whole grains; includes low-fat dairy products, poultry, fish, legumes, nontropical vegetable oils, and nuts; and limits intake of sweets, sugar-sweetened beverages, and red meats. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
- Adapt this dietary pattern to appropriate calorie requirements, personal and cultural food preferences, and nutrition therapy for other medical conditions (including diabetes).
- Achieve this pattern by following plans such as the DASH dietary pattern, the USDA Food Pattern, or the AHA Diet.
- Lower sodium intake. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
- a. Consume no more than 2,400 mg of sodium/d; b. Further reduction of sodium intake to 1,500 mg/d can result in even greater reduction in BP; and c. Even without achieving these goals, reducing sodium intake by at least 1,000 mg/d lowers BP. NHLBI Grade: B (Moderate); ACC/AHA COR: IIa; ACC/AHA LOE: B
- Combine the DASH dietary pattern with lower sodium intake. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
Physical Activity
Lipids
- In general, advise adults to engage in aerobic physical activity to reduce LDL-C and non-high-density lipoprotein cholesterol (non–HDL-C): 3–4 sessions per week, lasting on average 40 minutes per session, and involving moderate- to vigorous-intensity physical activity. NHLBI Grade: B (Moderate); ACC/AHA COR: IIa; ACC/AHA LOE: A
BP
- In general, advise adults to engage in aerobic physical activity to lower BP: 3 to 4 sessions per week, lasting on average 40 minutes per session, and involving moderate- to vigorous-intensity physical activity. NHLBI Grade: B (Moderate); ACC/AHA COR: IIa; ACC/AHA LOE: A
*Refer to the NGC summary 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines.
See Tables 7-10, 13, 15, and 16 in the original guideline document for additional diet and physical activity guidelines and resources.
Definitions:
NHLBI Grading of the Strength of Recommendations
| Grade | Strength of Recommendation* |
|---|---|
| A | Strong recommendation There is high certainty based on evidence that the net benefit† is substantial. |
| B | Moderate recommendation There is moderate certainty based on evidence that the net benefit is moderate to substantial, or there is high certainty that the net benefit is moderate. |
| C | Weak recommendation There is at least moderate certainty based on evidence that there is a small net benefit. |
| D | Recommendation against There is at least moderate certainty based on evidence that there is no net benefit or that risks/harms outweigh benefits. |
| E | Expert opinion ("There is insufficient evidence or evidence is unclear or conflicting, but this is what the Work Group recommends.") Net benefit is unclear. Balance of benefits and harms cannot be determined because of no evidence, insufficient evidence, unclear evidence, or conflicting evidence, but the Work Group thought it was important to provide clinical guidance and make a recommendation. Further research is recommended in this area. |
| N | No recommendation for or against ("There is insufficient evidence or evidence is unclear or conflicting.") Net benefit is unclear. Balance of benefits and harms cannot be determined because of no evidence, insufficient evidence, unclear evidence, or conflicting evidence, and the Work Group thought no recommendation should be made. Further research is recommended in this area. |
*In most cases, the strength of the recommendation should be closely aligned with the quality of the evidence; however, under some circumstances, there may be valid reasons for making recommendations that are not closely aligned with the quality of the evidence (e.g., strong recommendation when the evidence quality is moderate, such as smoking cessation to reduce cardiovascular disease [CVD] risk or ordering an electrocardiogram [ECG] as part of the initial diagnostic work-up for a patient presenting with possible myocardial infarction [MI]). Those situations should be limited and the rationale explained clearly by the Work Group.
†Net benefit is defined as benefits minus risks/harms of the service/intervention.
NHLBI Quality Rating of the Strength of Evidence
| Type of Evidence | Quality Rating* |
|---|---|
| High |
| Moderate |
| Low |
*In some cases, other evidence, such as large all-or-none case series (e.g., jumping from airplanes or tall structures), can represent high- or moderate-quality evidence. In such cases, the rationale for the evidence rating exception should be explained by the Work Group and clearly justified.
†"Well-designed, well-executed" refers to studies that directly address the question; use adequate randomization, blinding, and allocation concealment; are adequately powered; use intention-to-treat analyses; and have high follow-up rates.
‡Limitations include concerns with the design and execution of a study that result in decreased confidence in the true estimate of the effect. Examples of such limitations include but are not limited to: inadequate randomization, lack of blinding of study participants or outcome assessors, inadequate power, outcomes of interest that are not prespecified for the primary outcomes, low follow-up rates, and findings based on subgroup analyses. Whether the limitations are considered minor or major is based on the number and severity of flaws in design or execution. Rules for determining whether the limitations are considered minor or major and how they will affect rating of the individual studies will be developed collaboratively with the methodology team.
§Nonrandomized controlled studies refer to intervention studies where assignment to intervention and comparison groups is not random (e.g., quasi-experimental study design).
¶Observational studies include prospective and retrospective cohort, case-control, and cross-sectional studies.
Applying Classification of Recommendations and Level of Evidence
| Size of Treatment Effect | |||||||
|---|---|---|---|---|---|---|---|
| CLASS I Benefit >>> Risk Procedure/Treatment SHOULD be performed/ administered | CLASS IIa Benefit >> Risk Additional studies with focused objectives needed IT IS REASONABLE to perform procedure/administer treatment | CLASS IIb Benefit ≥ Risk Additional studies with broad objectives needed; additional registry data would be helpful Procedure/Treatment MAY BE CONSIDERED | CLASS III No Benefit or Class III Harm | ||||
| Procedure/Test | Treatment | ||||||
| COR III: No Benefit | Not helpful | No proven benefit | |||||
| COR III: Harm | Excess cost without benefit or harmful | Harmful to patients | |||||
| Estimate of Certainty (Precision) of Treatment Effect | LEVEL A Multiple populations evaluated* Data derived from multiple randomized clinical trials or meta-analyses |
|
|
|
| ||
| LEVEL B Limited populations evaluated* Data derived from a single randomized trial or nonrandomized studies |
|
|
|
| |||
| LEVEL C Very limited populations evaluated* Only consensus opinion of experts, case studies, or standard of care |
|
|
|
| |||
A recommendation with Level of Evidence B or C does not imply the recommendation is weak. Many important clinical questions addressed in the guidelines do not lend themselves to clinical trials. Even when randomized trials are unavailable, there may be a very clear clinical consensus that a particular test or therapy is useful or effective.
*Data available from clinical trials or registries about the usefulness/efficacy in different subpopulations, such as sex, age, history of diabetes, history of prior myocardial infarction, history of heart failure, and prior aspirin use.
†For comparative-effectiveness recommendations (Class I and IIa; Level of Evidence A and B only), studies that support the use of comparator verbs should involve direct comparisons of the treatments or strategies being evaluated.
OBJECTIVE: To evaluate evidence that particular dietary patterns, nutrient intake, and levels and types of physical activity can play a major role in cardiovascular disease (CVD) prevention and treatment through effects on modifiable CVD risk factors (i.e., blood pressure [BP] and lipids).
Guidelines are copyright © 2014 American College of Cardiology/American Heart Association. All rights reserved. The summary is provided by the Agency for Healthcare Research and Quality.
2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines.
Recommendations
Each recommendation has been mapped from the NHLBI grading format to the American College of Cardiology/American Heart Association Class of Recommendation/Level of Evidence (ACC/AHA COR/LOE) construct and is expressed in both formats. Because of the inherent differences in grading systems and the clinical questions driving the recommendations, alignment between the NHLBI and ACC/AHA formats is in some cases imperfect. Definitions for the NHLBI strength of recommendation (A-E, N) and quality of evidence (High, Moderate, Low) and the ACC/AHA levels of the evidence (LOE: A-C) and classes of recommendations (COR: I-III) are provided at the end of the "Major Recommendations" field.
What's New in the Guideline?
Focus on Atherosclerotic Cardiovascular Disease (ASCVD Risk) Reduction: 4 Statin Benefit Groups
1. This guideline is based on a comprehensive set of data from randomized control trials (RCTs) from which 4 statin benefit groups were identified that focus efforts to reduce ASCVD events in secondary and primary prevention.
2. This guideline identifies high-intensity and moderate-intensity statin therapy for use in secondary and primary prevention.
A New Perspective on Low-density Lipoprotein Cholesterol (LDL-C) and/or Non–High-density Lipoprotein Cholesterol (HDL-C) Treatment Goals
1. The Expert Panel was unable to find RCT evidence to support continued use of specific LDL-C or non–HDL-C treatment targets.
2. The appropriate intensity of statin therapy should be used to reduce ASCVD risk in those most likely to benefit.
3. Nonstatin therapies, as compared with statin therapy, do not provide acceptable ASCVD risk-reduction benefits relative to their potential for adverse effects in the routine prevention of ASCVD.
Global Risk Assessment for Primary Prevention
1. This guideline recommends use of the new Pooled Cohort Equations to estimate 10-year ASCVD risk in both white and black men and women.
2. By more accurately identifying higher-risk individuals for statin therapy, the guideline focuses statin therapy on those most likely to benefit.
3. It also indicates, on the basis of RCT data, those high-risk groups that might not benefit.
4. This guideline recommends a discussion between clinicians and patients before initiation of statin therapy.
Safety Recommendations
1. This guideline used RCTs to identify important safety considerations in individuals receiving treatment of blood cholesterol to reduce ASCVD risk.
2. Using RCTs to determine statin adverse effects facilitates understanding of the net benefit from statin therapy.
3. This guideline provides expert guidance on management of statin-associated adverse effects, including muscle symptoms.
Role of Biomarkers and Noninvasive Tests
1. Treatment decisions in selected individuals who are not included in the 4 statin benefit groups may be informed by other factors as recommended by the Risk Assessment Work Group and Blood Cholesterol Expert Panel.
Future Updates to the Blood Cholesterol Guideline
1. This is a comprehensive guideline for the evidence-based treatment of blood cholesterol to reduce ASCVD risk.
2. Future updates will build on this foundation to provide expert guidance on the management of complex lipid disorders and incorporate refinements in risk stratification based on critical review of emerging data.
3. RCTs comparing alternative treatment strategies are needed in order to inform future evidence-based guidelines for the optimum ASCVD risk-reduction approach.
Note: See Appendix 5 in the original guideline document for an expanded discussion of what's new in the guideline.
Recommendations for Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults—Statin Treatment
Treatment Targets
1. The Expert Panel makes no recommendations for or against specific LDL-C or non–HDL-C targets for the primary or secondary prevention of ASCVD. NHLBI Grade: N (No recommendation); ACC/AHA COR: n/a; ACC/AHA LOE: n/a
Secondary Prevention
1. High-intensity statin therapy should be initiated or continued as first-line therapy in women and men ≤75 years of age who have clinical ASCVD*, unless contraindicated. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
2. In individuals with clinical ASCVD* in whom high-intensity statin therapy would otherwise be used, when high-intensity statin therapy is contraindicated† or when characteristics predisposing to statin-associated adverse effects are present, moderate-intensity statin should be used as the second option if tolerated (see "Safety of Statins," below). NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
3. In individuals with clinical ASCVD >75 years of age, it is reasonable to evaluate the potential for ASCVD risk-reduction benefits and for adverse effects and drug–drug interactions and to consider patient preferences when initiating a moderate- or high-intensity statin. It is reasonable to continue statin therapy in those who are tolerating it. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: B (Heart Protection Study Collaborative Group, 2002; Cholesterol Treatment Trialists' [CTT] Collaboration et al., 2010; Tikkanen et al., 2009; Holmes et al., 2006; Akushevich et al., 2012; Wolff, Starfield &, Anderson, 2002; Fried et al., "Effects," 2011; Robinson et al., 2007; Porock et al., 2005; Stineman et al., 2012; Schonberg et al., 2011; Fried et al., "Health outcome," 2011; Barry & Edgman-Levitan, 2012; Man-Son-Hing, Gage, & Montgomery, 2005; Fried et al., 2002; Ditto et al., 1996; Rosenfeld, Wenger, & Kagawa-Singer, 2000; Nease et al., 1995; Glynn et al., 2010; Shepherd et al., 2002; Trompet et al., 2010; Gray et al., 2011; LaCroix et al., 2008; Hippisley-Cox et al., 2005; Forman et al., 2011)
Primary Prevention in Individuals ≥21 Years of Age with LDL-C ≥190 mg/dL
1. Individuals with LDL-C ≥190 mg/dL or triglycerides ≥500 mg/dL should be evaluated for secondary causes of hyperlipidemia (see Table 6 in the original guideline document). NHLBI Grade: B (Moderate); ACC/AHA COR: I‡; ACC/AHA LOE: B (Berglund et al., 2012; Miller et al., 2011)
2. Adults ≥21 years of age with primary LDL-C ≥190 mg/dL should be treated with statin therapy (10-year ASCVD risk estimation is not required) NHLBI Grade: B (Moderate); ACC/AHA COR: I§; ACC/AHA LOE: B:
- Use high-intensity statin therapy unless contraindicated.
- For individuals unable to tolerate high-intensity statin therapy, use the maximum tolerated statin intensity.
3. For individuals ≥21 years of age with an untreated primary LDL-C ≥190 mg/dL, it is reasonable to intensify statin therapy to achieve at least a 50% LDL-C reduction. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: B (CTT Collaboration et al., 2010; LaRosa et al., 2005; Pedersen et al., 2005; Cannon et al., 2004; Ridker et al, 2008; Baigent et al., 2005)
4. For individuals ≥21 years of age with an untreated primary LDL-C ≥190 mg/dL, after the maximum intensity of statin therapy has been achieved, addition of a nonstatin drug may be considered to further lower LDL-C. Evaluate the potential for ASCVD risk-reduction benefits, adverse effects, and drug–drug interactions, and consider patient preferences. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIb; ACC/AHA LOE: C (Thompson, Packard, & Stone, 2004)
Primary Prevention in Individuals with Diabetes and LDL-C 70–189 mg/dL
1. Moderate-intensity statin therapy should be initiated or continued for adults 40 to 75 years of age with diabetes. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
2. High-intensity statin therapy is reasonable for adults 40 to 75 years of age with diabetes with a ≥7.5% estimated 10-year ASCVD risk‖ unless contraindicated. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: B (Ridker et al., 2008; Ridker et al., 2012)
3. In adults with diabetes, who are <40 years of age or >75 years of age, or with LDL <70 mg/dL, it is reasonable to evaluate the potential for ASCVD benefits and for adverse effects and drug–drug interactions and to consider patient preferences when deciding to initiate, continue, or intensify statin therapy. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: C (Roffi, Angiolillo, & Kappetein, 2011; Nathan et al., 2005; Rhodes et al., 2012; Paynter et al., 2011; Elley et al., 2010; Stevens et al., 2004; Bibbins-Domingo et al., 2007; Daniels et al., 2009; Jacob & Cho, 2010; Bainey & Jugdutt, 2009)
Primary Prevention in Individuals without Diabetes and with LDL-C 70–189 mg/dL
1. The Pooled Cohort Equations should be used to estimate 10-year ASCVD‖ risk for individuals with LDL-C 70–189 mg/dL without clinical ASCVD* to guide initiation of statin therapy for the primary prevention of ASCVD. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: I; ACC/AHA LOE: B (Goff et al., 2014)
2. Adults 40 to 75 years of age with LDL-C 70–189 mg/dL, without clinical ASCVD* or diabetes, and with an estimated 10-year ASCVD‖ risk ≥7.5% should be treated with moderate- to high-intensity statin therapy. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
3. It is reasonable to offer treatment with a moderate-intensity statin to adults 40 to 75 years of age, with LDL-C 70–189 mg/dL, without clinical ASCVD* or diabetes, and with an estimated 10-year ASCVD‖ risk of 5% to <7.5%. NHLBI Grade: C (Weak); ACC/AHA COR: IIa; ACC/AHA LOE: B
4. Before initiation of statin therapy for the primary prevention of ASCVD in adults with LDL-C 70–189 mg/dL without clinical ASCVD* or diabetes, it is reasonable for clinicians and patients to engage in a discussion that considers the potential for ASCVD risk-reduction benefits and for adverse effects and drug–drug interactions, as well as patient preferences for treatment. NHBLI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: C (Yu et al., 2013)
5. In adults with LDL-C <190 mg/dL who are not otherwise identified in a statin benefit group, or for whom after quantitative risk assessment a risk-based treatment decision is uncertain, additional factors¶ may be considered to inform treatment decision making. In these individuals, statin therapy for primary prevention may be considered after evaluation of the potential for ASCVD risk-reduction benefits, adverse effects, and drug–drug interactions and consider patient preferences. NHBLI Grade: E (Expert Opinion); ACC/AHA COR: IIb; ACC/AHA LOE: C (Goff et al., 2014; CTT Collaborators et al., 2012)
Heart Failure and Hemodialysis
1. The Expert Panel makes no recommendations regarding the initiation or discontinuation of statins in patients with NYHA class II–IV ischemic systolic heart failure or in patients on maintenance hemodialysis. NHBLI Grade: N (No Recommendation); ACC/AHA COR: n/a; ACC/AHA LOE: n/a
*Clinical ASCVD includes acute coronary syndromes, history of myocardial infarction (MI), stable or unstable angina, coronary or other arterial revascularization, stroke, transient ischaemic attack (TIA), or peripheral arterial disease presumed to be of atherosclerotic origin.
†Contraindications, warnings, and precautions are defined for each statin according to the manufacturer's prescribing information ("Lescol," 2012; "Pravachol," 2012; "Livalo," 2012; "Zocor," 2012; "Mevacor," 2012; "Lipitor," 2012; "Crestor," 2013).
‡Individuals with secondary causes of hyperlipidemia were excluded from RCTs reviewed. A triglyceride level ≥500 mg/dL was an exclusion criterion for almost all RCTs. Therefore, ruling out secondary causes is necessary to avoid inappropriate statin therapy.
§No RCTs included only individuals with LDL-C ≥190 mg/dL. However, many trials did include individuals with LDL-C ≥190 mg/dL, and all of these trials consistently demonstrated a reduction in ASCVD events. In addition, the Cholesterol Treatment Trialists meta-analyses have shown that each 39-mg/dL reduction in LDL-C with statin therapy reduced ASCVD events by 22%, and the relative reductions in ASCVD events were consistent across the range of LDL-C levels. Therefore, individuals with primary LDL-C ≥190 mg/dL should be treated with statin therapy.
ǁEstimated 10-year or "hard" ASCVD risk includes first occurrence of nonfatal MI, coronary heart disease death, and nonfatal and fatal stroke as used by the Risk Assessment Work Group in developing the Pooled Cohort Equations.
¶These factors may include primary LDL-C ≥160 mg/dL or other evidence of genetic hyperlipidemias; family history of premature ASCVD with onset <55 years of age in a first-degree male relative or <65 years of age in a first-degree female relative; high-sensitivity C-reactive protein ≥2 mg/L; coronary artery calcium (CAC) score ≥300 Agatston units or ≥75th percentile for age, sex, and ethnicity (for additional information, see http://www.mesa-nhlbi.org/CACReference.aspx ![]()
See Table 5 in the original guideline document for high-, moderate-, and low-intensity statin therapies used in the RCTs reviewed by the Expert Panel.
Statin Safety Recommendations
Safety
1. To maximize the safety of statins, selection of the appropriate statin and dose in men and nonpregnant/nonnursing women should be based on patient characteristics, level of ASCVD* risk, and potential for adverse effects. Moderate-intensity statin therapy should be used in individuals in whom high-intensity statin therapy would otherwise be recommended when characteristics predisposing them to statin-associated adverse effects are present. Characteristics predisposing individuals to statin adverse effects include but are not limited to: NHBLI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: B
- Multiple or serious comorbidities, including impaired renal or hepatic function
- History of previous statin intolerance or muscle disorders
- Unexplained alanine aminotransferase (ALT) elevations ≥3 times the upper limit of normal (ULN)
- Patient characteristics or concomitant use of drugs affecting statin metabolism
- Age >75 years
Additional characteristics that could modify the decision to use higher statin intensities might include but are not limited to:
- History of hemorrhagic stroke
- Asian ancestry
2a. Creatine kinase (CK) should not be routinely measured in individuals receiving statin therapy. NHBLI Grade: A (Strong); ACC/AHA COR: III: No Benefit; ACC/AHA LOE: A
2b. Baseline measurement of CK is reasonable for individuals believed to be at increased risk for adverse muscle events because of a personal or family history of statin intolerance or muscle disease, clinical presentation, or concomitant drug therapy that might increase the risk of myopathy. NHBLI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: C (Eckel, 2010)
2c. During statin therapy, it is reasonable to measure CK in individuals with muscle symptoms, including pain, tenderness, stiffness, cramping, weakness, or generalized fatigue. NHBLI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: C (Eckel, 2010)
3a. Baseline measurement of hepatic transaminase levels (ALT) should be performed before initiation of statin therapy. NHBLI Grade: B (Moderate); ACC/AHA COR: I†; ACC/AHA LOE: B
3b. During statin therapy, it is reasonable to measure hepatic function if symptoms suggesting hepatotoxicity arise (e.g., unusual fatigue or weakness, loss of appetite, abdominal pain, dark-colored urine, or yellowing of the skin or sclera). NHBLI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: C (U.S. Food and Drug Administration, 2012)
4. Decreasing the statin dose may be considered when 2 consecutive values of LDL-C levels are <40 mg/dL. NHBLI Grade: C (Weak); ACC/AHA COR: IIb; ACC/AHA LOE: C
5. It may be harmful to initiate simvastatin at 80 mg daily or increase the dose of simvastatin to 80 mg daily. NHBLI Grade: B (Moderate); ACC/AHA COR: III: Harm; ACC/AHA LOE: A ("Zocor," 2012; U.S. Food and Drug Administration, 2010)
6. Individuals receiving statin therapy should be evaluated for new-onset diabetes according to the current diabetes screening guidelines (American Diabetes Association, 2013). Those who develop diabetes during statin therapy should be encouraged to adhere to a heart-healthy dietary pattern, engage in physical activity, achieve and maintain a healthy body weight, cease tobacco use, and continue statin therapy to reduce their risk of ASCVD events. NHBLI Grade: B (Moderate); ACC/AHA COR: I‡; ACC/AHA LOE: B
7. For individuals taking any dose of statins, it is reasonable to use caution in individuals >75 years of age, as well as in individuals who are taking concomitant medications that alter drug metabolism, taking multiple drugs, or taking drugs for conditions that require complex medication regimens (e.g., those who have undergone solid organ transplantation or are receiving treatment for human immunodeficiency virus [HIV]). A review of the manufacturer's prescribing information may be useful before initiation of any cholesterol-lowering drug. NHBLI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: C (Heart Protection Study Collaborative Group, 2002; "Lescol," 2012; "Pravachol," 2012; "Livalo," 2012; "Zocor," 2012; "Mevacor," 2012; "Lipitor," 2012; "Crestor," 2013; U.S. Food and Drug Administration, 2012; Rawlins, 2008; Schwartz et al., 2001; Shepherd et al., 2006)
8. It is reasonable to evaluate and treat muscle symptoms, including pain, tenderness, stiffness, cramping, weakness, or fatigue, in statin-treated patients according to the following management algorithm: NHBLI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: B (Taylor et al., 2011; Eckel, 2010; Baigent et al., 2010; Mills et al., 2008; Dale et al., 2007)
- To avoid unnecessary discontinuation of statins, obtain a history of prior or current muscle symptoms to establish a baseline before initiation of statin therapy.
- If unexplained severe muscle symptoms or fatigue develop during statin therapy, promptly discontinue the statin and address the possibility of rhabdomyolysis by evaluating CK and creatinine and performing urinalysis for myoglobinuria.
- If mild to moderate muscle symptoms develop during statin therapy:
- Discontinue the statin until the symptoms can be evaluated.
- Evaluate the patient for other conditions that might increase the risk for muscle symptoms (e.g., hypothyroidism, reduced renal or hepatic function, rheumatologic disorders such as polymyalgia rheumatica, steroid myopathy, vitamin D deficiency, or primary muscle diseases).
- If muscle symptoms resolve, and if no contraindication exists, give the patient the original or a lower dose of the same statin to establish a causal relationship between the muscle symptoms and statin therapy.
- If a causal relationship exists, discontinue the original statin. Once muscle symptoms resolve, use a low dose of a different statin.
- Once a low dose of a statin is tolerated, gradually increase the dose as tolerated.
- If, after 2 months without statin treatment, muscle symptoms or elevated CK levels do not resolve completely, consider other causes of muscle symptoms listed above.
- If persistent muscle symptoms are determined to arise from a condition unrelated to statin therapy, or if the predisposing condition has been treated, resume statin therapy at the original dose.
9. For individuals presenting with a confusional state or memory impairment while on statin therapy, it may be reasonable to evaluate the patient for nonstatin causes, such as exposure to other drugs, as well as for systemic and neuropsychiatric causes, in addition to the possibility of adverse effects associated with statin drug therapy. NHBLI Grade: E (Expert Opinion); ACC/AHA COR: IIb; ACC/AHA LOE: C (Shepherd et al., 2002; U.S. Food and Drug Administration, 2012; Collins et al., 2004; Roberts, 2009)
*Based on the presence of clinical ASCVD, diabetes, LDL-C ≥190 mg/dL, or level of estimated 10-year ASCVD risk.
†Individuals with elevated ALT levels (usually >1.5 or 2 times ULN) were excluded from RCT participation. Unexplained ALT ≥3 times ULN is a contraindication to statin therapy as listed in manufacturer's prescribing information.
‡Statin use is associated with a very modest excess risk of new-onset diabetes in RCTs and meta-analyses of RCTs (i.e., ∼0.1 excess cases per 100 individuals treated for 1 year with moderate-intensity statin therapy and ∼0.3 excess cases per 100 individuals treated for 1 year with high-intensity statin therapy. The increased risk of new-onset diabetes appears to be confined to those with risk factors for diabetes. These individuals are also at higher risk of ASCVD because of these risk factors. Therefore, if a statin-treated individual develops diabetes as detected by current diabetes screening guidelines, he or she should be counseled to adhere to a heart-healthy dietary pattern, engage in physical activity, achieve and maintain a healthy body weight, cease tobacco use, and continue statin therapy to reduce the risk of ASCVD events.
Nonstatin Safety Recommendations
Safety of Niacin
1. Baseline hepatic transaminases, fasting blood glucose or hemoglobin A1c, and uric acid should be obtained before initiation of niacin, and again during up-titration to a maintenance dose and every 6 months thereafter. NHLBI Grade: B (Moderate); ACC/AHA COR: I; ACC/AHA LOE: B
2. Niacin should not be used if:
- Hepatic transaminase elevations are higher than 2 to 3 times ULN. NHLBI Grade: A (Strong); ACC/AHA COR: III: Harm; ACC/AHA LOE: B
- Persistent severe cutaneous symptoms, persistent hyperglycemia, acute gout, or unexplained abdominal pain or gastrointestinal symptoms occur. NHLBI Grade: B (Moderate); ACC/AHA COR: III: Harm; ACC/AHA LOE: B
- New-onset atrial fibrillation or weight loss occurs. NHLBI Grade: C (Weak); ACC/AHA COR: III: Harm; ACC/AHA LOE: B
3. In individuals with adverse effects from niacin, the potential for ASCVD benefits and the potential for adverse effects should be reconsidered before reinitiation of niacin therapy. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: I; ACC/AHA LOE: B (AIM-HIGH Investigators et al., 2011; "Clofibrate and niacin in coronary heart disease," 1975; Guyton & Bays, 2007; Brown & Zhao, 2008; Grundy et al., 2002)
4. To reduce the frequency and severity of adverse cutaneous symptoms, it is reasonable to: NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: C (AIM-HIGH Investigators et al., 2011; "Clofibrate and niacin in coronary heart disease," 1975; Guyton & Bays, 2007; Brown & Zhao, 2008; Grundy et al., 2002)
- Start niacin at a low dose and titrate to a higher dose over a period of weeks as tolerated.
- Take niacin with food or premedicate with aspirin 325 mg 30 minutes before niacin dosing to alleviate flushing symptoms.
- If an extended-release preparation is used, increase the dose of extended-release niacin from 500 mg to a maximum of 2,000 mg/day over 4 to 8 weeks, with the dose of extended-release niacin increasing not more than weekly.
- If immediate-release niacin is chosen, start at a dose of 100 mg 3 times daily and up-titrate to 3 g/day, divided into 2 or 3 doses.
Safety of Bile Acid Sequestrants (BAS)
1. BAS should not be used in individuals with baseline fasting triglyceride levels ≥300 mg/dL or type III hyperlipoproteinemia, because severe triglyceride elevations might occur. (A fasting lipid panel should be obtained before BAS is initiated, 3 months after initiation, and every 6 to 12 months thereafter.) NHLBI Grade: C (Weak); ACC/AHA COR: III: Harm; ACC/AHA LOE: B
2. It is reasonable to use BAS with caution if baseline triglyceride levels are 250 to 299 mg/dL, and evaluate a fasting lipid panel in 4 to 6 weeks after initiation. Discontinue the BAS if triglycerides exceed 400 mg/dL. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: C (Crouse, 1987)
Safety of Cholesterol-Absorption Inhibitors
1. It is reasonable to obtain baseline hepatic transaminases before initiation of ezetimibe. When ezetimibe is coadministered with a statin, monitor transaminase levels as clinically indicated, and discontinue ezetimibe if persistent ALT elevations ≥3 times ULN occur. NHLBI Grade: C (Weak); ACC/AHA COR: IIa; ACC/AHA LOE: B
Safety of Fibrates
1. Gemfibrozil should not be initiated in patients on statin therapy because of an increased risk for muscle symptoms and rhabdomyolysis. NHLBI Grade: B (Moderate); ACC/AHA COR: III: Harm; ACC/AHA LOE: B
2. Fenofibrate may be considered concomitantly with a low- or moderate-intensity statin only if the benefits from ASCVD risk reduction or triglyceride lowering when triglycerides are ≥500 mg/dL are judged to outweigh the potential risk for adverse effects. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIb; ACC/AHA LOE: C (ACCORD Study Group et al., 2010)
3. Renal status should be evaluated before fenofibrate initiation, within 3 months after initiation, and every 6 months thereafter. Assess renal safety with both a serum creatinine level and an estimated glomerular filtration rate (eGFR) based on creatinine. NHLBI Grade: B (Moderate); ACC/AHA COR: I; ACC/AHA LOE: B
- Fenofibrate should not be used if moderate or severe renal impairment, defined as eGFR <30 mL/min per 1.73 m2, is present. ACC/AHA COR: III: Harm; ACC/AHA LOE: B
- If eGFR is between 30 and 59 mL/min per 1.73 m2, the dose of fenofibrate should not exceed 54 mg/day.*
- If, during follow-up, the eGFR decreases persistently to ≤30 mL/min per 1.73 m2, fenofibrate should be discontinued.
*Consult the manufacturer's prescribing information as there are several forms of fenofibrate available.
Safety of Omega-3 Fatty Acids
1. If eicosapentaenoic acid (EPA) and/or docosahexanoic acid (DHA) are used for the management of severe hypertriglyceridemia, defined as triglycerides ≥500 mg/dL, it is reasonable to evaluate the patient for gastrointestinal disturbances, skin changes, and bleeding. NHLBI Grade: C (Weak); ACC/AHA COR: IIa; ACC/AHA LOE: B
Recommendations for Monitoring, Optimizing, and Addressing Insufficient Response to Statin Therapy
Monitoring Statin Therapy
1. Adherence to medication and lifestyle, therapeutic response to statin therapy, and safety should be regularly assessed. This should also include a fasting lipid panel performed within 4–12 weeks after initiation or dose adjustment, and every 3–12 months thereafter. Other safety measurements should be measured as clinically indicated. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
Optimizing Statin Therapy
1. The maximum tolerated intensity of statin should be used in individuals for whom a high- or moderate-intensity statin is recommended but not tolerated. NHLBI Grade: B (Moderate); ACC/AHA COR: I*; ACC/AHA LOE: B
Insufficient Response to Statin Therapy
1. In individuals who have a less-than-anticipated therapeutic response or are intolerant of the recommended intensity of statin therapy, the following should be performed: NHLBI Grade A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
- Reinforce medication adherence.
- Reinforce adherence to intensive lifestyle changes.
- Exclude secondary causes of hyperlipidemia.
2. It is reasonable to use the following as indicators of anticipated therapeutic response to the recommended intensity of statin therapy. Focus is on the intensity of the statin therapy. As an aid to monitoring: NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: B (LaRosa et al., 2005; Pedersen et al., 2005; Cannon et al., 2004; Amarenco et al., 2006; Thompson & HEART-UK LDL Apheresis Working Group, 2008; Schwertz & Badellino, 2008)
- High-intensity statin therapy† generally results in an average LDL-C reduction of ≥50% from the untreated baseline.
- Moderate-intensity statin therapy generally results in an average LDL-C reduction of 30% to <50% from the untreated baseline.
- LDL-C levels and percents reduction are to be used only to assess response to therapy and adherence. They are not to be used as performance standards.
3. In individuals at higher ASCVD risk receiving the maximum tolerated intensity of statin therapy who continue to have a less-than-anticipated therapeutic response, addition of nonstatin cholesterol-lowering drug(s) may be considered if the ASCVD risk-reduction benefits outweigh the potential for adverse effects. Higher-risk individuals include: NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIb: ACC/AHA LOE: C (AIM-HIGH Investigators et al., 2011; ACCORD Study Group et al., 2010; Rossebo et al., 2007; Sharp Collaborative Group, 2010; Yokoyama, Origasa, & JELIS Investigators, 2003)
- Individuals with clinical ASCVD‡ <75 years of age.
- Individuals with baseline LDL-C ≥190 mg/dL.
- Individuals 40 to 75 years of age with diabetes.
Preference should be given to nonstatin cholesterol-lowering drugs shown to reduce ASCVD events in RCTs.
4. In individuals who are candidates for statin treatment but are completely statin intolerant, it is reasonable to use nonstatin cholesterol-lowering drugs that have been shown to reduce ASCVD events in RCTs if the ASCVD risk-reduction benefits outweigh the potential for adverse effects. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: B (Eckel, 2010; "Clofibrate and niacin in coronary heart disease," 1975; Frick et al., 1987; Lipid Research Clinics Program, 1984; "The Lipid Research Clinics Coronary Primary Prevention Trial results. II.," 1984; Rubins et al., 1999; Keech et al., 2005; HPS2-THRIVE Collaborative Group, 2013)
*Several RCTs found that low-intensity and low-moderate–intensity statin therapy reduced ASCVD events. In addition, the Cholesterol Treatment Trialists meta-analyses found that each 39-mg/dL reduction in LDL-C reduces ASCVD risk by 22%. Therefore, the Panel considered that submaximal statin therapy should be used to reduce ASCVD risk in those unable to tolerate moderate- or high-intensity statin therapy.
†In those already on a statin, in whom baseline LDL-C is unknown, an LDL-C level <100 mg/dL was observed in most individuals receiving high-intensity statin therapy.
‡Clinical ASCVD includes acute coronary syndromes, or a history of myocardial infarction, stable or unstable angina, coronary or other arterial revascularization, stroke, transient ischemic attack, or peripheral arterial disease presumed to be of atherosclerotic origin.
Definitions:
NHLBI Grading of the Strength of Recommendations
| Grade | Strength of Recommendation* |
|---|---|
| A | Strong recommendation There is high certainty based on evidence that the net benefit† is substantial. |
| B | Moderate recommendation There is moderate certainty based on evidence that the net benefit is moderate to substantial, or there is high certainty that the net benefit is moderate. |
| C | Weak recommendation There is at least moderate certainty based on evidence that there is a small net benefit. |
| D | Recommendation against There is at least moderate certainty based on evidence that there is no net benefit or that risks/harms outweigh benefits. |
| E | Expert opinion ("There is insufficient evidence or evidence is unclear or conflicting, but this is what the Work Group recommends.") Net benefit is unclear. Balance of benefits and harms cannot be determined because of no evidence, insufficient evidence, unclear evidence, or conflicting evidence, but the Work Group thought it was important to provide clinical guidance and make a recommendation. Further research is recommended in this area. |
| N | No recommendation for or against ("There is insufficient evidence or evidence is unclear or conflicting.") Net benefit is unclear. Balance of benefits and harms cannot be determined because of no evidence, insufficient evidence, unclear evidence, or conflicting evidence, and the Work Group thought no recommendation should be made. Further research is recommended in this area. |
*In most cases, the strength of the recommendation should be closely aligned with the quality of the evidence; however, under some circumstances, there may be valid reasons for making recommendations that are not closely aligned with the quality of the evidence (e.g., strong recommendation when the evidence quality is moderate, such as smoking cessation to reduce cardiovascular disease [CVD] risk or ordering an electrocardiogram [ECG] as part of the initial diagnostic work-up for a patient presenting with possible myocardial infarction [MI]). Those situations should be limited and the rationale explained clearly by the Work Group.
†Net benefit is defined as benefits minus risks/harms of the service/intervention.
NHLBI Quality Rating of the Strength of Evidence
| Type of Evidence | Quality Rating* |
|---|---|
| High |
| Moderate |
| Low |
*In some cases, other evidence, such as large all-or-none case series (e.g., jumping from airplanes or tall structures), can represent high- or moderate-quality evidence. In such cases, the rationale for the evidence rating exception should be explained by the Work Group and clearly justified.
†"Well-designed, well-executed" refers to studies that directly address the question; use adequate randomization, blinding, and allocation concealment; are adequately powered; use intention-to-treat analyses; and have high follow-up rates.
‡Limitations include concerns with the design and execution of a study that result in decreased confidence in the true estimate of the effect. Examples of such limitations include but are not limited to: inadequate randomization, lack of blinding of study participants or outcome assessors, inadequate power, outcomes of interest that are not prespecified for the primary outcomes, low follow-up rates, and findings based on subgroup analyses. Whether the limitations are considered minor or major is based on the number and severity of flaws in design or execution. Rules for determining whether the limitations are considered minor or major and how they will affect rating of the individual studies will be developed collaboratively with the methodology team.
§Nonrandomized controlled studies refer to intervention studies where assignment to intervention and comparison groups is not random (e.g., quasi-experimental study design).
¶Observational studies include prospective and retrospective cohort, case-control, and cross-sectional studies.
Applying Classification of Recommendations and Level of Evidence
| Size of Treatment Effect | |||||||
|---|---|---|---|---|---|---|---|
| CLASS I Benefit >>> Risk Procedure/Treatment SHOULD be performed/ administered | CLASS IIa Benefit >> Risk Additional studies with focused objectives needed IT IS REASONABLE to perform procedure/administer treatment | CLASS IIb Benefit ≥ Risk Additional studies with broad objectives needed; additional registry data would be helpful Procedure/Treatment MAY BE CONSIDERED | CLASS III No Benefit or Class III Harm | ||||
| Procedure/Test | Treatment | ||||||
| COR III: No Benefit | Not helpful | No proven benefit | |||||
| COR III: Harm | Excess cost without benefit or harmful | Harmful to patients | |||||
| Estimate of Certainty (Precision) of Treatment Effect | LEVEL A Multiple populations evaluated* Data derived from multiple randomized clinical trials or meta-analyses |
|
|
|
| ||
| LEVEL B Limited populations evaluated* Data derived from a single randomized trial or nonrandomized studies |
|
|
|
| |||
| LEVEL C Very limited populations evaluated* Only consensus opinion of experts, case studies, or standard of care |
|
|
|
| |||
A recommendation with Level of Evidence B or C does not imply that the recommendation is weak. Many important clinical questions addressed in the guidelines do not lend themselves to clinical trials. Although randomized trials are unavailable, there may be a very clear clinical consensus that a particular test or therapy is useful or effective.
*Data available from clinical trials or registries about the usefulness/efficacy in different subpopulations, such as sex, age, history of diabetes, history of prior myocardial infarction, history of heart failure, and prior aspirin use.
†For comparative-effectiveness recommendations (Class I and IIa; Level of Evidence A and B only), studies that support the use of comparator verbs should involve direct comparisons of the treatments or strategies being evaluated.
- Summary of Statin Initiation Recommendations for the Treatment of Blood Cholesterol to Reduce ASCVD Risk in Adults
- Initiating Statin Therapy in Individuals with Clinical ASCVD
- Initiating Statin Therapy in Individuals without Clinical ASCVD
- Statin Therapy: Monitoring Therapeutic Response and Adherence
Recommendations
Each recommendation has been mapped from the NHLBI grading format to the American College of Cardiology/American Heart Association Class of Recommendation/Level of Evidence (ACC/AHA COR/LOE) construct and is expressed in both formats. Because of the inherent differences in grading systems and the clinical questions driving the recommendations, alignment between the NHLBI and ACC/AHA formats is in some cases imperfect. Definitions for the NHLBI strength of recommendation (A-E, N) and quality of evidence (High, Moderate, Low) and the ACC/AHA levels of the evidence (LOE: A-C) and classes of recommendations (COR: I-III) are provided at the end of the "Major Recommendations" field.
What's New in the Guideline?
Focus on Atherosclerotic Cardiovascular Disease (ASCVD Risk) Reduction: 4 Statin Benefit Groups
1. This guideline is based on a comprehensive set of data from randomized control trials (RCTs) from which 4 statin benefit groups were identified that focus efforts to reduce ASCVD events in secondary and primary prevention.
2. This guideline identifies high-intensity and moderate-intensity statin therapy for use in secondary and primary prevention.
A New Perspective on Low-density Lipoprotein Cholesterol (LDL-C) and/or Non–High-density Lipoprotein Cholesterol (HDL-C) Treatment Goals
1. The Expert Panel was unable to find RCT evidence to support continued use of specific LDL-C or non–HDL-C treatment targets.
2. The appropriate intensity of statin therapy should be used to reduce ASCVD risk in those most likely to benefit.
3. Nonstatin therapies, as compared with statin therapy, do not provide acceptable ASCVD risk-reduction benefits relative to their potential for adverse effects in the routine prevention of ASCVD.
Global Risk Assessment for Primary Prevention
1. This guideline recommends use of the new Pooled Cohort Equations to estimate 10-year ASCVD risk in both white and black men and women.
2. By more accurately identifying higher-risk individuals for statin therapy, the guideline focuses statin therapy on those most likely to benefit.
3. It also indicates, on the basis of RCT data, those high-risk groups that might not benefit.
4. This guideline recommends a discussion between clinicians and patients before initiation of statin therapy.
Safety Recommendations
1. This guideline used RCTs to identify important safety considerations in individuals receiving treatment of blood cholesterol to reduce ASCVD risk.
2. Using RCTs to determine statin adverse effects facilitates understanding of the net benefit from statin therapy.
3. This guideline provides expert guidance on management of statin-associated adverse effects, including muscle symptoms.
Role of Biomarkers and Noninvasive Tests
1. Treatment decisions in selected individuals who are not included in the 4 statin benefit groups may be informed by other factors as recommended by the Risk Assessment Work Group and Blood Cholesterol Expert Panel.
Future Updates to the Blood Cholesterol Guideline
1. This is a comprehensive guideline for the evidence-based treatment of blood cholesterol to reduce ASCVD risk.
2. Future updates will build on this foundation to provide expert guidance on the management of complex lipid disorders and incorporate refinements in risk stratification based on critical review of emerging data.
3. RCTs comparing alternative treatment strategies are needed in order to inform future evidence-based guidelines for the optimum ASCVD risk-reduction approach.
Note: See Appendix 5 in the original guideline document for an expanded discussion of what's new in the guideline.
Recommendations for Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults—Statin Treatment
Treatment Targets
1. The Expert Panel makes no recommendations for or against specific LDL-C or non–HDL-C targets for the primary or secondary prevention of ASCVD. NHLBI Grade: N (No recommendation); ACC/AHA COR: n/a; ACC/AHA LOE: n/a
Secondary Prevention
1. High-intensity statin therapy should be initiated or continued as first-line therapy in women and men ≤75 years of age who have clinical ASCVD*, unless contraindicated. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
2. In individuals with clinical ASCVD* in whom high-intensity statin therapy would otherwise be used, when high-intensity statin therapy is contraindicated† or when characteristics predisposing to statin-associated adverse effects are present, moderate-intensity statin should be used as the second option if tolerated (see "Safety of Statins," below). NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
3. In individuals with clinical ASCVD >75 years of age, it is reasonable to evaluate the potential for ASCVD risk-reduction benefits and for adverse effects and drug–drug interactions and to consider patient preferences when initiating a moderate- or high-intensity statin. It is reasonable to continue statin therapy in those who are tolerating it. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: B (Heart Protection Study Collaborative Group, 2002; Cholesterol Treatment Trialists' [CTT] Collaboration et al., 2010; Tikkanen et al., 2009; Holmes et al., 2006; Akushevich et al., 2012; Wolff, Starfield &, Anderson, 2002; Fried et al., "Effects," 2011; Robinson et al., 2007; Porock et al., 2005; Stineman et al., 2012; Schonberg et al., 2011; Fried et al., "Health outcome," 2011; Barry & Edgman-Levitan, 2012; Man-Son-Hing, Gage, & Montgomery, 2005; Fried et al., 2002; Ditto et al., 1996; Rosenfeld, Wenger, & Kagawa-Singer, 2000; Nease et al., 1995; Glynn et al., 2010; Shepherd et al., 2002; Trompet et al., 2010; Gray et al., 2011; LaCroix et al., 2008; Hippisley-Cox et al., 2005; Forman et al., 2011)
Primary Prevention in Individuals ≥21 Years of Age with LDL-C ≥190 mg/dL
1. Individuals with LDL-C ≥190 mg/dL or triglycerides ≥500 mg/dL should be evaluated for secondary causes of hyperlipidemia (see Table 6 in the original guideline document). NHLBI Grade: B (Moderate); ACC/AHA COR: I‡; ACC/AHA LOE: B (Berglund et al., 2012; Miller et al., 2011)
2. Adults ≥21 years of age with primary LDL-C ≥190 mg/dL should be treated with statin therapy (10-year ASCVD risk estimation is not required) NHLBI Grade: B (Moderate); ACC/AHA COR: I§; ACC/AHA LOE: B:
- Use high-intensity statin therapy unless contraindicated.
- For individuals unable to tolerate high-intensity statin therapy, use the maximum tolerated statin intensity.
3. For individuals ≥21 years of age with an untreated primary LDL-C ≥190 mg/dL, it is reasonable to intensify statin therapy to achieve at least a 50% LDL-C reduction. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: B (CTT Collaboration et al., 2010; LaRosa et al., 2005; Pedersen et al., 2005; Cannon et al., 2004; Ridker et al, 2008; Baigent et al., 2005)
4. For individuals ≥21 years of age with an untreated primary LDL-C ≥190 mg/dL, after the maximum intensity of statin therapy has been achieved, addition of a nonstatin drug may be considered to further lower LDL-C. Evaluate the potential for ASCVD risk-reduction benefits, adverse effects, and drug–drug interactions, and consider patient preferences. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIb; ACC/AHA LOE: C (Thompson, Packard, & Stone, 2004)
Primary Prevention in Individuals with Diabetes and LDL-C 70–189 mg/dL
1. Moderate-intensity statin therapy should be initiated or continued for adults 40 to 75 years of age with diabetes. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
2. High-intensity statin therapy is reasonable for adults 40 to 75 years of age with diabetes with a ≥7.5% estimated 10-year ASCVD risk‖ unless contraindicated. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: B (Ridker et al., 2008; Ridker et al., 2012)
3. In adults with diabetes, who are <40 years of age or >75 years of age, or with LDL <70 mg/dL, it is reasonable to evaluate the potential for ASCVD benefits and for adverse effects and drug–drug interactions and to consider patient preferences when deciding to initiate, continue, or intensify statin therapy. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: C (Roffi, Angiolillo, & Kappetein, 2011; Nathan et al., 2005; Rhodes et al., 2012; Paynter et al., 2011; Elley et al., 2010; Stevens et al., 2004; Bibbins-Domingo et al., 2007; Daniels et al., 2009; Jacob & Cho, 2010; Bainey & Jugdutt, 2009)
Primary Prevention in Individuals without Diabetes and with LDL-C 70–189 mg/dL
1. The Pooled Cohort Equations should be used to estimate 10-year ASCVD‖ risk for individuals with LDL-C 70–189 mg/dL without clinical ASCVD* to guide initiation of statin therapy for the primary prevention of ASCVD. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: I; ACC/AHA LOE: B (Goff et al., 2014)
2. Adults 40 to 75 years of age with LDL-C 70–189 mg/dL, without clinical ASCVD* or diabetes, and with an estimated 10-year ASCVD‖ risk ≥7.5% should be treated with moderate- to high-intensity statin therapy. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
3. It is reasonable to offer treatment with a moderate-intensity statin to adults 40 to 75 years of age, with LDL-C 70–189 mg/dL, without clinical ASCVD* or diabetes, and with an estimated 10-year ASCVD‖ risk of 5% to <7.5%. NHLBI Grade: C (Weak); ACC/AHA COR: IIa; ACC/AHA LOE: B
4. Before initiation of statin therapy for the primary prevention of ASCVD in adults with LDL-C 70–189 mg/dL without clinical ASCVD* or diabetes, it is reasonable for clinicians and patients to engage in a discussion that considers the potential for ASCVD risk-reduction benefits and for adverse effects and drug–drug interactions, as well as patient preferences for treatment. NHBLI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: C (Yu et al., 2013)
5. In adults with LDL-C <190 mg/dL who are not otherwise identified in a statin benefit group, or for whom after quantitative risk assessment a risk-based treatment decision is uncertain, additional factors¶ may be considered to inform treatment decision making. In these individuals, statin therapy for primary prevention may be considered after evaluation of the potential for ASCVD risk-reduction benefits, adverse effects, and drug–drug interactions and consider patient preferences. NHBLI Grade: E (Expert Opinion); ACC/AHA COR: IIb; ACC/AHA LOE: C (Goff et al., 2014; CTT Collaborators et al., 2012)
Heart Failure and Hemodialysis
1. The Expert Panel makes no recommendations regarding the initiation or discontinuation of statins in patients with NYHA class II–IV ischemic systolic heart failure or in patients on maintenance hemodialysis. NHBLI Grade: N (No Recommendation); ACC/AHA COR: n/a; ACC/AHA LOE: n/a
*Clinical ASCVD includes acute coronary syndromes, history of myocardial infarction (MI), stable or unstable angina, coronary or other arterial revascularization, stroke, transient ischaemic attack (TIA), or peripheral arterial disease presumed to be of atherosclerotic origin.
†Contraindications, warnings, and precautions are defined for each statin according to the manufacturer's prescribing information ("Lescol," 2012; "Pravachol," 2012; "Livalo," 2012; "Zocor," 2012; "Mevacor," 2012; "Lipitor," 2012; "Crestor," 2013).
‡Individuals with secondary causes of hyperlipidemia were excluded from RCTs reviewed. A triglyceride level ≥500 mg/dL was an exclusion criterion for almost all RCTs. Therefore, ruling out secondary causes is necessary to avoid inappropriate statin therapy.
§No RCTs included only individuals with LDL-C ≥190 mg/dL. However, many trials did include individuals with LDL-C ≥190 mg/dL, and all of these trials consistently demonstrated a reduction in ASCVD events. In addition, the Cholesterol Treatment Trialists meta-analyses have shown that each 39-mg/dL reduction in LDL-C with statin therapy reduced ASCVD events by 22%, and the relative reductions in ASCVD events were consistent across the range of LDL-C levels. Therefore, individuals with primary LDL-C ≥190 mg/dL should be treated with statin therapy.
ǁEstimated 10-year or "hard" ASCVD risk includes first occurrence of nonfatal MI, coronary heart disease death, and nonfatal and fatal stroke as used by the Risk Assessment Work Group in developing the Pooled Cohort Equations.
¶These factors may include primary LDL-C ≥160 mg/dL or other evidence of genetic hyperlipidemias; family history of premature ASCVD with onset <55 years of age in a first-degree male relative or <65 years of age in a first-degree female relative; high-sensitivity C-reactive protein ≥2 mg/L; coronary artery calcium (CAC) score ≥300 Agatston units or ≥75th percentile for age, sex, and ethnicity (for additional information, see http://www.mesa-nhlbi.org/CACReference.aspx ![]()
See Table 5 in the original guideline document for high-, moderate-, and low-intensity statin therapies used in the RCTs reviewed by the Expert Panel.
Statin Safety Recommendations
Safety
1. To maximize the safety of statins, selection of the appropriate statin and dose in men and nonpregnant/nonnursing women should be based on patient characteristics, level of ASCVD* risk, and potential for adverse effects. Moderate-intensity statin therapy should be used in individuals in whom high-intensity statin therapy would otherwise be recommended when characteristics predisposing them to statin-associated adverse effects are present. Characteristics predisposing individuals to statin adverse effects include but are not limited to: NHBLI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: B
- Multiple or serious comorbidities, including impaired renal or hepatic function
- History of previous statin intolerance or muscle disorders
- Unexplained alanine aminotransferase (ALT) elevations ≥3 times the upper limit of normal (ULN)
- Patient characteristics or concomitant use of drugs affecting statin metabolism
- Age >75 years
Additional characteristics that could modify the decision to use higher statin intensities might include but are not limited to:
- History of hemorrhagic stroke
- Asian ancestry
2a. Creatine kinase (CK) should not be routinely measured in individuals receiving statin therapy. NHBLI Grade: A (Strong); ACC/AHA COR: III: No Benefit; ACC/AHA LOE: A
2b. Baseline measurement of CK is reasonable for individuals believed to be at increased risk for adverse muscle events because of a personal or family history of statin intolerance or muscle disease, clinical presentation, or concomitant drug therapy that might increase the risk of myopathy. NHBLI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: C (Eckel, 2010)
2c. During statin therapy, it is reasonable to measure CK in individuals with muscle symptoms, including pain, tenderness, stiffness, cramping, weakness, or generalized fatigue. NHBLI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: C (Eckel, 2010)
3a. Baseline measurement of hepatic transaminase levels (ALT) should be performed before initiation of statin therapy. NHBLI Grade: B (Moderate); ACC/AHA COR: I†; ACC/AHA LOE: B
3b. During statin therapy, it is reasonable to measure hepatic function if symptoms suggesting hepatotoxicity arise (e.g., unusual fatigue or weakness, loss of appetite, abdominal pain, dark-colored urine, or yellowing of the skin or sclera). NHBLI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: C (U.S. Food and Drug Administration, 2012)
4. Decreasing the statin dose may be considered when 2 consecutive values of LDL-C levels are <40 mg/dL. NHBLI Grade: C (Weak); ACC/AHA COR: IIb; ACC/AHA LOE: C
5. It may be harmful to initiate simvastatin at 80 mg daily or increase the dose of simvastatin to 80 mg daily. NHBLI Grade: B (Moderate); ACC/AHA COR: III: Harm; ACC/AHA LOE: A ("Zocor," 2012; U.S. Food and Drug Administration, 2010)
6. Individuals receiving statin therapy should be evaluated for new-onset diabetes according to the current diabetes screening guidelines (American Diabetes Association, 2013). Those who develop diabetes during statin therapy should be encouraged to adhere to a heart-healthy dietary pattern, engage in physical activity, achieve and maintain a healthy body weight, cease tobacco use, and continue statin therapy to reduce their risk of ASCVD events. NHBLI Grade: B (Moderate); ACC/AHA COR: I‡; ACC/AHA LOE: B
7. For individuals taking any dose of statins, it is reasonable to use caution in individuals >75 years of age, as well as in individuals who are taking concomitant medications that alter drug metabolism, taking multiple drugs, or taking drugs for conditions that require complex medication regimens (e.g., those who have undergone solid organ transplantation or are receiving treatment for human immunodeficiency virus [HIV]). A review of the manufacturer's prescribing information may be useful before initiation of any cholesterol-lowering drug. NHBLI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: C (Heart Protection Study Collaborative Group, 2002; "Lescol," 2012; "Pravachol," 2012; "Livalo," 2012; "Zocor," 2012; "Mevacor," 2012; "Lipitor," 2012; "Crestor," 2013; U.S. Food and Drug Administration, 2012; Rawlins, 2008; Schwartz et al., 2001; Shepherd et al., 2006)
8. It is reasonable to evaluate and treat muscle symptoms, including pain, tenderness, stiffness, cramping, weakness, or fatigue, in statin-treated patients according to the following management algorithm: NHBLI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: B (Taylor et al., 2011; Eckel, 2010; Baigent et al., 2010; Mills et al., 2008; Dale et al., 2007)
- To avoid unnecessary discontinuation of statins, obtain a history of prior or current muscle symptoms to establish a baseline before initiation of statin therapy.
- If unexplained severe muscle symptoms or fatigue develop during statin therapy, promptly discontinue the statin and address the possibility of rhabdomyolysis by evaluating CK and creatinine and performing urinalysis for myoglobinuria.
- If mild to moderate muscle symptoms develop during statin therapy:
- Discontinue the statin until the symptoms can be evaluated.
- Evaluate the patient for other conditions that might increase the risk for muscle symptoms (e.g., hypothyroidism, reduced renal or hepatic function, rheumatologic disorders such as polymyalgia rheumatica, steroid myopathy, vitamin D deficiency, or primary muscle diseases).
- If muscle symptoms resolve, and if no contraindication exists, give the patient the original or a lower dose of the same statin to establish a causal relationship between the muscle symptoms and statin therapy.
- If a causal relationship exists, discontinue the original statin. Once muscle symptoms resolve, use a low dose of a different statin.
- Once a low dose of a statin is tolerated, gradually increase the dose as tolerated.
- If, after 2 months without statin treatment, muscle symptoms or elevated CK levels do not resolve completely, consider other causes of muscle symptoms listed above.
- If persistent muscle symptoms are determined to arise from a condition unrelated to statin therapy, or if the predisposing condition has been treated, resume statin therapy at the original dose.
9. For individuals presenting with a confusional state or memory impairment while on statin therapy, it may be reasonable to evaluate the patient for nonstatin causes, such as exposure to other drugs, as well as for systemic and neuropsychiatric causes, in addition to the possibility of adverse effects associated with statin drug therapy. NHBLI Grade: E (Expert Opinion); ACC/AHA COR: IIb; ACC/AHA LOE: C (Shepherd et al., 2002; U.S. Food and Drug Administration, 2012; Collins et al., 2004; Roberts, 2009)
*Based on the presence of clinical ASCVD, diabetes, LDL-C ≥190 mg/dL, or level of estimated 10-year ASCVD risk.
†Individuals with elevated ALT levels (usually >1.5 or 2 times ULN) were excluded from RCT participation. Unexplained ALT ≥3 times ULN is a contraindication to statin therapy as listed in manufacturer's prescribing information.
‡Statin use is associated with a very modest excess risk of new-onset diabetes in RCTs and meta-analyses of RCTs (i.e., ∼0.1 excess cases per 100 individuals treated for 1 year with moderate-intensity statin therapy and ∼0.3 excess cases per 100 individuals treated for 1 year with high-intensity statin therapy. The increased risk of new-onset diabetes appears to be confined to those with risk factors for diabetes. These individuals are also at higher risk of ASCVD because of these risk factors. Therefore, if a statin-treated individual develops diabetes as detected by current diabetes screening guidelines, he or she should be counseled to adhere to a heart-healthy dietary pattern, engage in physical activity, achieve and maintain a healthy body weight, cease tobacco use, and continue statin therapy to reduce the risk of ASCVD events.
Nonstatin Safety Recommendations
Safety of Niacin
1. Baseline hepatic transaminases, fasting blood glucose or hemoglobin A1c, and uric acid should be obtained before initiation of niacin, and again during up-titration to a maintenance dose and every 6 months thereafter. NHLBI Grade: B (Moderate); ACC/AHA COR: I; ACC/AHA LOE: B
2. Niacin should not be used if:
- Hepatic transaminase elevations are higher than 2 to 3 times ULN. NHLBI Grade: A (Strong); ACC/AHA COR: III: Harm; ACC/AHA LOE: B
- Persistent severe cutaneous symptoms, persistent hyperglycemia, acute gout, or unexplained abdominal pain or gastrointestinal symptoms occur. NHLBI Grade: B (Moderate); ACC/AHA COR: III: Harm; ACC/AHA LOE: B
- New-onset atrial fibrillation or weight loss occurs. NHLBI Grade: C (Weak); ACC/AHA COR: III: Harm; ACC/AHA LOE: B
3. In individuals with adverse effects from niacin, the potential for ASCVD benefits and the potential for adverse effects should be reconsidered before reinitiation of niacin therapy. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: I; ACC/AHA LOE: B (AIM-HIGH Investigators et al., 2011; "Clofibrate and niacin in coronary heart disease," 1975; Guyton & Bays, 2007; Brown & Zhao, 2008; Grundy et al., 2002)
4. To reduce the frequency and severity of adverse cutaneous symptoms, it is reasonable to: NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: C (AIM-HIGH Investigators et al., 2011; "Clofibrate and niacin in coronary heart disease," 1975; Guyton & Bays, 2007; Brown & Zhao, 2008; Grundy et al., 2002)
- Start niacin at a low dose and titrate to a higher dose over a period of weeks as tolerated.
- Take niacin with food or premedicate with aspirin 325 mg 30 minutes before niacin dosing to alleviate flushing symptoms.
- If an extended-release preparation is used, increase the dose of extended-release niacin from 500 mg to a maximum of 2,000 mg/day over 4 to 8 weeks, with the dose of extended-release niacin increasing not more than weekly.
- If immediate-release niacin is chosen, start at a dose of 100 mg 3 times daily and up-titrate to 3 g/day, divided into 2 or 3 doses.
Safety of Bile Acid Sequestrants (BAS)
1. BAS should not be used in individuals with baseline fasting triglyceride levels ≥300 mg/dL or type III hyperlipoproteinemia, because severe triglyceride elevations might occur. (A fasting lipid panel should be obtained before BAS is initiated, 3 months after initiation, and every 6 to 12 months thereafter.) NHLBI Grade: C (Weak); ACC/AHA COR: III: Harm; ACC/AHA LOE: B
2. It is reasonable to use BAS with caution if baseline triglyceride levels are 250 to 299 mg/dL, and evaluate a fasting lipid panel in 4 to 6 weeks after initiation. Discontinue the BAS if triglycerides exceed 400 mg/dL. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: C (Crouse, 1987)
Safety of Cholesterol-Absorption Inhibitors
1. It is reasonable to obtain baseline hepatic transaminases before initiation of ezetimibe. When ezetimibe is coadministered with a statin, monitor transaminase levels as clinically indicated, and discontinue ezetimibe if persistent ALT elevations ≥3 times ULN occur. NHLBI Grade: C (Weak); ACC/AHA COR: IIa; ACC/AHA LOE: B
Safety of Fibrates
1. Gemfibrozil should not be initiated in patients on statin therapy because of an increased risk for muscle symptoms and rhabdomyolysis. NHLBI Grade: B (Moderate); ACC/AHA COR: III: Harm; ACC/AHA LOE: B
2. Fenofibrate may be considered concomitantly with a low- or moderate-intensity statin only if the benefits from ASCVD risk reduction or triglyceride lowering when triglycerides are ≥500 mg/dL are judged to outweigh the potential risk for adverse effects. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIb; ACC/AHA LOE: C (ACCORD Study Group et al., 2010)
3. Renal status should be evaluated before fenofibrate initiation, within 3 months after initiation, and every 6 months thereafter. Assess renal safety with both a serum creatinine level and an estimated glomerular filtration rate (eGFR) based on creatinine. NHLBI Grade: B (Moderate); ACC/AHA COR: I; ACC/AHA LOE: B
- Fenofibrate should not be used if moderate or severe renal impairment, defined as eGFR <30 mL/min per 1.73 m2, is present. ACC/AHA COR: III: Harm; ACC/AHA LOE: B
- If eGFR is between 30 and 59 mL/min per 1.73 m2, the dose of fenofibrate should not exceed 54 mg/day.*
- If, during follow-up, the eGFR decreases persistently to ≤30 mL/min per 1.73 m2, fenofibrate should be discontinued.
*Consult the manufacturer's prescribing information as there are several forms of fenofibrate available.
Safety of Omega-3 Fatty Acids
1. If eicosapentaenoic acid (EPA) and/or docosahexanoic acid (DHA) are used for the management of severe hypertriglyceridemia, defined as triglycerides ≥500 mg/dL, it is reasonable to evaluate the patient for gastrointestinal disturbances, skin changes, and bleeding. NHLBI Grade: C (Weak); ACC/AHA COR: IIa; ACC/AHA LOE: B
Recommendations for Monitoring, Optimizing, and Addressing Insufficient Response to Statin Therapy
Monitoring Statin Therapy
1. Adherence to medication and lifestyle, therapeutic response to statin therapy, and safety should be regularly assessed. This should also include a fasting lipid panel performed within 4–12 weeks after initiation or dose adjustment, and every 3–12 months thereafter. Other safety measurements should be measured as clinically indicated. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
Optimizing Statin Therapy
1. The maximum tolerated intensity of statin should be used in individuals for whom a high- or moderate-intensity statin is recommended but not tolerated. NHLBI Grade: B (Moderate); ACC/AHA COR: I*; ACC/AHA LOE: B
Insufficient Response to Statin Therapy
1. In individuals who have a less-than-anticipated therapeutic response or are intolerant of the recommended intensity of statin therapy, the following should be performed: NHLBI Grade A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
- Reinforce medication adherence.
- Reinforce adherence to intensive lifestyle changes.
- Exclude secondary causes of hyperlipidemia.
2. It is reasonable to use the following as indicators of anticipated therapeutic response to the recommended intensity of statin therapy. Focus is on the intensity of the statin therapy. As an aid to monitoring: NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: B (LaRosa et al., 2005; Pedersen et al., 2005; Cannon et al., 2004; Amarenco et al., 2006; Thompson & HEART-UK LDL Apheresis Working Group, 2008; Schwertz & Badellino, 2008)
- High-intensity statin therapy† generally results in an average LDL-C reduction of ≥50% from the untreated baseline.
- Moderate-intensity statin therapy generally results in an average LDL-C reduction of 30% to <50% from the untreated baseline.
- LDL-C levels and percents reduction are to be used only to assess response to therapy and adherence. They are not to be used as performance standards.
3. In individuals at higher ASCVD risk receiving the maximum tolerated intensity of statin therapy who continue to have a less-than-anticipated therapeutic response, addition of nonstatin cholesterol-lowering drug(s) may be considered if the ASCVD risk-reduction benefits outweigh the potential for adverse effects. Higher-risk individuals include: NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIb: ACC/AHA LOE: C (AIM-HIGH Investigators et al., 2011; ACCORD Study Group et al., 2010; Rossebo et al., 2007; Sharp Collaborative Group, 2010; Yokoyama, Origasa, & JELIS Investigators, 2003)
- Individuals with clinical ASCVD‡ <75 years of age.
- Individuals with baseline LDL-C ≥190 mg/dL.
- Individuals 40 to 75 years of age with diabetes.
Preference should be given to nonstatin cholesterol-lowering drugs shown to reduce ASCVD events in RCTs.
4. In individuals who are candidates for statin treatment but are completely statin intolerant, it is reasonable to use nonstatin cholesterol-lowering drugs that have been shown to reduce ASCVD events in RCTs if the ASCVD risk-reduction benefits outweigh the potential for adverse effects. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: B (Eckel, 2010; "Clofibrate and niacin in coronary heart disease," 1975; Frick et al., 1987; Lipid Research Clinics Program, 1984; "The Lipid Research Clinics Coronary Primary Prevention Trial results. II.," 1984; Rubins et al., 1999; Keech et al., 2005; HPS2-THRIVE Collaborative Group, 2013)
*Several RCTs found that low-intensity and low-moderate–intensity statin therapy reduced ASCVD events. In addition, the Cholesterol Treatment Trialists meta-analyses found that each 39-mg/dL reduction in LDL-C reduces ASCVD risk by 22%. Therefore, the Panel considered that submaximal statin therapy should be used to reduce ASCVD risk in those unable to tolerate moderate- or high-intensity statin therapy.
†In those already on a statin, in whom baseline LDL-C is unknown, an LDL-C level <100 mg/dL was observed in most individuals receiving high-intensity statin therapy.
‡Clinical ASCVD includes acute coronary syndromes, or a history of myocardial infarction, stable or unstable angina, coronary or other arterial revascularization, stroke, transient ischemic attack, or peripheral arterial disease presumed to be of atherosclerotic origin.
Definitions:
NHLBI Grading of the Strength of Recommendations
| Grade | Strength of Recommendation* |
|---|---|
| A | Strong recommendation There is high certainty based on evidence that the net benefit† is substantial. |
| B | Moderate recommendation There is moderate certainty based on evidence that the net benefit is moderate to substantial, or there is high certainty that the net benefit is moderate. |
| C | Weak recommendation There is at least moderate certainty based on evidence that there is a small net benefit. |
| D | Recommendation against There is at least moderate certainty based on evidence that there is no net benefit or that risks/harms outweigh benefits. |
| E | Expert opinion ("There is insufficient evidence or evidence is unclear or conflicting, but this is what the Work Group recommends.") Net benefit is unclear. Balance of benefits and harms cannot be determined because of no evidence, insufficient evidence, unclear evidence, or conflicting evidence, but the Work Group thought it was important to provide clinical guidance and make a recommendation. Further research is recommended in this area. |
| N | No recommendation for or against ("There is insufficient evidence or evidence is unclear or conflicting.") Net benefit is unclear. Balance of benefits and harms cannot be determined because of no evidence, insufficient evidence, unclear evidence, or conflicting evidence, and the Work Group thought no recommendation should be made. Further research is recommended in this area. |
*In most cases, the strength of the recommendation should be closely aligned with the quality of the evidence; however, under some circumstances, there may be valid reasons for making recommendations that are not closely aligned with the quality of the evidence (e.g., strong recommendation when the evidence quality is moderate, such as smoking cessation to reduce cardiovascular disease [CVD] risk or ordering an electrocardiogram [ECG] as part of the initial diagnostic work-up for a patient presenting with possible myocardial infarction [MI]). Those situations should be limited and the rationale explained clearly by the Work Group.
†Net benefit is defined as benefits minus risks/harms of the service/intervention.
NHLBI Quality Rating of the Strength of Evidence
| Type of Evidence | Quality Rating* |
|---|---|
| High |
| Moderate |
| Low |
*In some cases, other evidence, such as large all-or-none case series (e.g., jumping from airplanes or tall structures), can represent high- or moderate-quality evidence. In such cases, the rationale for the evidence rating exception should be explained by the Work Group and clearly justified.
†"Well-designed, well-executed" refers to studies that directly address the question; use adequate randomization, blinding, and allocation concealment; are adequately powered; use intention-to-treat analyses; and have high follow-up rates.
‡Limitations include concerns with the design and execution of a study that result in decreased confidence in the true estimate of the effect. Examples of such limitations include but are not limited to: inadequate randomization, lack of blinding of study participants or outcome assessors, inadequate power, outcomes of interest that are not prespecified for the primary outcomes, low follow-up rates, and findings based on subgroup analyses. Whether the limitations are considered minor or major is based on the number and severity of flaws in design or execution. Rules for determining whether the limitations are considered minor or major and how they will affect rating of the individual studies will be developed collaboratively with the methodology team.
§Nonrandomized controlled studies refer to intervention studies where assignment to intervention and comparison groups is not random (e.g., quasi-experimental study design).
¶Observational studies include prospective and retrospective cohort, case-control, and cross-sectional studies.
Applying Classification of Recommendations and Level of Evidence
| Size of Treatment Effect | |||||||
|---|---|---|---|---|---|---|---|
| CLASS I Benefit >>> Risk Procedure/Treatment SHOULD be performed/ administered | CLASS IIa Benefit >> Risk Additional studies with focused objectives needed IT IS REASONABLE to perform procedure/administer treatment | CLASS IIb Benefit ≥ Risk Additional studies with broad objectives needed; additional registry data would be helpful Procedure/Treatment MAY BE CONSIDERED | CLASS III No Benefit or Class III Harm | ||||
| Procedure/Test | Treatment | ||||||
| COR III: No Benefit | Not helpful | No proven benefit | |||||
| COR III: Harm | Excess cost without benefit or harmful | Harmful to patients | |||||
| Estimate of Certainty (Precision) of Treatment Effect | LEVEL A Multiple populations evaluated* Data derived from multiple randomized clinical trials or meta-analyses |
|
|
|
| ||
| LEVEL B Limited populations evaluated* Data derived from a single randomized trial or nonrandomized studies |
|
|
|
| |||
| LEVEL C Very limited populations evaluated* Only consensus opinion of experts, case studies, or standard of care |
|
|
|
| |||
A recommendation with Level of Evidence B or C does not imply that the recommendation is weak. Many important clinical questions addressed in the guidelines do not lend themselves to clinical trials. Although randomized trials are unavailable, there may be a very clear clinical consensus that a particular test or therapy is useful or effective.
*Data available from clinical trials or registries about the usefulness/efficacy in different subpopulations, such as sex, age, history of diabetes, history of prior myocardial infarction, history of heart failure, and prior aspirin use.
†For comparative-effectiveness recommendations (Class I and IIa; Level of Evidence A and B only), studies that support the use of comparator verbs should involve direct comparisons of the treatments or strategies being evaluated.
- Summary of Statin Initiation Recommendations for the Treatment of Blood Cholesterol to Reduce ASCVD Risk in Adults
- Initiating Statin Therapy in Individuals with Clinical ASCVD
- Initiating Statin Therapy in Individuals without Clinical ASCVD
- Statin Therapy: Monitoring Therapeutic Response and Adherence
Recommendations
Each recommendation has been mapped from the NHLBI grading format to the American College of Cardiology/American Heart Association Class of Recommendation/Level of Evidence (ACC/AHA COR/LOE) construct and is expressed in both formats. Because of the inherent differences in grading systems and the clinical questions driving the recommendations, alignment between the NHLBI and ACC/AHA formats is in some cases imperfect. Definitions for the NHLBI strength of recommendation (A-E, N) and quality of evidence (High, Moderate, Low) and the ACC/AHA levels of the evidence (LOE: A-C) and classes of recommendations (COR: I-III) are provided at the end of the "Major Recommendations" field.
What's New in the Guideline?
Focus on Atherosclerotic Cardiovascular Disease (ASCVD Risk) Reduction: 4 Statin Benefit Groups
1. This guideline is based on a comprehensive set of data from randomized control trials (RCTs) from which 4 statin benefit groups were identified that focus efforts to reduce ASCVD events in secondary and primary prevention.
2. This guideline identifies high-intensity and moderate-intensity statin therapy for use in secondary and primary prevention.
A New Perspective on Low-density Lipoprotein Cholesterol (LDL-C) and/or Non–High-density Lipoprotein Cholesterol (HDL-C) Treatment Goals
1. The Expert Panel was unable to find RCT evidence to support continued use of specific LDL-C or non–HDL-C treatment targets.
2. The appropriate intensity of statin therapy should be used to reduce ASCVD risk in those most likely to benefit.
3. Nonstatin therapies, as compared with statin therapy, do not provide acceptable ASCVD risk-reduction benefits relative to their potential for adverse effects in the routine prevention of ASCVD.
Global Risk Assessment for Primary Prevention
1. This guideline recommends use of the new Pooled Cohort Equations to estimate 10-year ASCVD risk in both white and black men and women.
2. By more accurately identifying higher-risk individuals for statin therapy, the guideline focuses statin therapy on those most likely to benefit.
3. It also indicates, on the basis of RCT data, those high-risk groups that might not benefit.
4. This guideline recommends a discussion between clinicians and patients before initiation of statin therapy.
Safety Recommendations
1. This guideline used RCTs to identify important safety considerations in individuals receiving treatment of blood cholesterol to reduce ASCVD risk.
2. Using RCTs to determine statin adverse effects facilitates understanding of the net benefit from statin therapy.
3. This guideline provides expert guidance on management of statin-associated adverse effects, including muscle symptoms.
Role of Biomarkers and Noninvasive Tests
1. Treatment decisions in selected individuals who are not included in the 4 statin benefit groups may be informed by other factors as recommended by the Risk Assessment Work Group and Blood Cholesterol Expert Panel.
Future Updates to the Blood Cholesterol Guideline
1. This is a comprehensive guideline for the evidence-based treatment of blood cholesterol to reduce ASCVD risk.
2. Future updates will build on this foundation to provide expert guidance on the management of complex lipid disorders and incorporate refinements in risk stratification based on critical review of emerging data.
3. RCTs comparing alternative treatment strategies are needed in order to inform future evidence-based guidelines for the optimum ASCVD risk-reduction approach.
Note: See Appendix 5 in the original guideline document for an expanded discussion of what's new in the guideline.
Recommendations for Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults—Statin Treatment
Treatment Targets
1. The Expert Panel makes no recommendations for or against specific LDL-C or non–HDL-C targets for the primary or secondary prevention of ASCVD. NHLBI Grade: N (No recommendation); ACC/AHA COR: n/a; ACC/AHA LOE: n/a
Secondary Prevention
1. High-intensity statin therapy should be initiated or continued as first-line therapy in women and men ≤75 years of age who have clinical ASCVD*, unless contraindicated. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
2. In individuals with clinical ASCVD* in whom high-intensity statin therapy would otherwise be used, when high-intensity statin therapy is contraindicated† or when characteristics predisposing to statin-associated adverse effects are present, moderate-intensity statin should be used as the second option if tolerated (see "Safety of Statins," below). NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
3. In individuals with clinical ASCVD >75 years of age, it is reasonable to evaluate the potential for ASCVD risk-reduction benefits and for adverse effects and drug–drug interactions and to consider patient preferences when initiating a moderate- or high-intensity statin. It is reasonable to continue statin therapy in those who are tolerating it. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: B (Heart Protection Study Collaborative Group, 2002; Cholesterol Treatment Trialists' [CTT] Collaboration et al., 2010; Tikkanen et al., 2009; Holmes et al., 2006; Akushevich et al., 2012; Wolff, Starfield &, Anderson, 2002; Fried et al., "Effects," 2011; Robinson et al., 2007; Porock et al., 2005; Stineman et al., 2012; Schonberg et al., 2011; Fried et al., "Health outcome," 2011; Barry & Edgman-Levitan, 2012; Man-Son-Hing, Gage, & Montgomery, 2005; Fried et al., 2002; Ditto et al., 1996; Rosenfeld, Wenger, & Kagawa-Singer, 2000; Nease et al., 1995; Glynn et al., 2010; Shepherd et al., 2002; Trompet et al., 2010; Gray et al., 2011; LaCroix et al., 2008; Hippisley-Cox et al., 2005; Forman et al., 2011)
Primary Prevention in Individuals ≥21 Years of Age with LDL-C ≥190 mg/dL
1. Individuals with LDL-C ≥190 mg/dL or triglycerides ≥500 mg/dL should be evaluated for secondary causes of hyperlipidemia (see Table 6 in the original guideline document). NHLBI Grade: B (Moderate); ACC/AHA COR: I‡; ACC/AHA LOE: B (Berglund et al., 2012; Miller et al., 2011)
2. Adults ≥21 years of age with primary LDL-C ≥190 mg/dL should be treated with statin therapy (10-year ASCVD risk estimation is not required) NHLBI Grade: B (Moderate); ACC/AHA COR: I§; ACC/AHA LOE: B:
- Use high-intensity statin therapy unless contraindicated.
- For individuals unable to tolerate high-intensity statin therapy, use the maximum tolerated statin intensity.
3. For individuals ≥21 years of age with an untreated primary LDL-C ≥190 mg/dL, it is reasonable to intensify statin therapy to achieve at least a 50% LDL-C reduction. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: B (CTT Collaboration et al., 2010; LaRosa et al., 2005; Pedersen et al., 2005; Cannon et al., 2004; Ridker et al, 2008; Baigent et al., 2005)
4. For individuals ≥21 years of age with an untreated primary LDL-C ≥190 mg/dL, after the maximum intensity of statin therapy has been achieved, addition of a nonstatin drug may be considered to further lower LDL-C. Evaluate the potential for ASCVD risk-reduction benefits, adverse effects, and drug–drug interactions, and consider patient preferences. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIb; ACC/AHA LOE: C (Thompson, Packard, & Stone, 2004)
Primary Prevention in Individuals with Diabetes and LDL-C 70–189 mg/dL
1. Moderate-intensity statin therapy should be initiated or continued for adults 40 to 75 years of age with diabetes. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
2. High-intensity statin therapy is reasonable for adults 40 to 75 years of age with diabetes with a ≥7.5% estimated 10-year ASCVD risk‖ unless contraindicated. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: B (Ridker et al., 2008; Ridker et al., 2012)
3. In adults with diabetes, who are <40 years of age or >75 years of age, or with LDL <70 mg/dL, it is reasonable to evaluate the potential for ASCVD benefits and for adverse effects and drug–drug interactions and to consider patient preferences when deciding to initiate, continue, or intensify statin therapy. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: C (Roffi, Angiolillo, & Kappetein, 2011; Nathan et al., 2005; Rhodes et al., 2012; Paynter et al., 2011; Elley et al., 2010; Stevens et al., 2004; Bibbins-Domingo et al., 2007; Daniels et al., 2009; Jacob & Cho, 2010; Bainey & Jugdutt, 2009)
Primary Prevention in Individuals without Diabetes and with LDL-C 70–189 mg/dL
1. The Pooled Cohort Equations should be used to estimate 10-year ASCVD‖ risk for individuals with LDL-C 70–189 mg/dL without clinical ASCVD* to guide initiation of statin therapy for the primary prevention of ASCVD. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: I; ACC/AHA LOE: B (Goff et al., 2014)
2. Adults 40 to 75 years of age with LDL-C 70–189 mg/dL, without clinical ASCVD* or diabetes, and with an estimated 10-year ASCVD‖ risk ≥7.5% should be treated with moderate- to high-intensity statin therapy. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
3. It is reasonable to offer treatment with a moderate-intensity statin to adults 40 to 75 years of age, with LDL-C 70–189 mg/dL, without clinical ASCVD* or diabetes, and with an estimated 10-year ASCVD‖ risk of 5% to <7.5%. NHLBI Grade: C (Weak); ACC/AHA COR: IIa; ACC/AHA LOE: B
4. Before initiation of statin therapy for the primary prevention of ASCVD in adults with LDL-C 70–189 mg/dL without clinical ASCVD* or diabetes, it is reasonable for clinicians and patients to engage in a discussion that considers the potential for ASCVD risk-reduction benefits and for adverse effects and drug–drug interactions, as well as patient preferences for treatment. NHBLI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: C (Yu et al., 2013)
5. In adults with LDL-C <190 mg/dL who are not otherwise identified in a statin benefit group, or for whom after quantitative risk assessment a risk-based treatment decision is uncertain, additional factors¶ may be considered to inform treatment decision making. In these individuals, statin therapy for primary prevention may be considered after evaluation of the potential for ASCVD risk-reduction benefits, adverse effects, and drug–drug interactions and consider patient preferences. NHBLI Grade: E (Expert Opinion); ACC/AHA COR: IIb; ACC/AHA LOE: C (Goff et al., 2014; CTT Collaborators et al., 2012)
Heart Failure and Hemodialysis
1. The Expert Panel makes no recommendations regarding the initiation or discontinuation of statins in patients with NYHA class II–IV ischemic systolic heart failure or in patients on maintenance hemodialysis. NHBLI Grade: N (No Recommendation); ACC/AHA COR: n/a; ACC/AHA LOE: n/a
*Clinical ASCVD includes acute coronary syndromes, history of myocardial infarction (MI), stable or unstable angina, coronary or other arterial revascularization, stroke, transient ischaemic attack (TIA), or peripheral arterial disease presumed to be of atherosclerotic origin.
†Contraindications, warnings, and precautions are defined for each statin according to the manufacturer's prescribing information ("Lescol," 2012; "Pravachol," 2012; "Livalo," 2012; "Zocor," 2012; "Mevacor," 2012; "Lipitor," 2012; "Crestor," 2013).
‡Individuals with secondary causes of hyperlipidemia were excluded from RCTs reviewed. A triglyceride level ≥500 mg/dL was an exclusion criterion for almost all RCTs. Therefore, ruling out secondary causes is necessary to avoid inappropriate statin therapy.
§No RCTs included only individuals with LDL-C ≥190 mg/dL. However, many trials did include individuals with LDL-C ≥190 mg/dL, and all of these trials consistently demonstrated a reduction in ASCVD events. In addition, the Cholesterol Treatment Trialists meta-analyses have shown that each 39-mg/dL reduction in LDL-C with statin therapy reduced ASCVD events by 22%, and the relative reductions in ASCVD events were consistent across the range of LDL-C levels. Therefore, individuals with primary LDL-C ≥190 mg/dL should be treated with statin therapy.
ǁEstimated 10-year or "hard" ASCVD risk includes first occurrence of nonfatal MI, coronary heart disease death, and nonfatal and fatal stroke as used by the Risk Assessment Work Group in developing the Pooled Cohort Equations.
¶These factors may include primary LDL-C ≥160 mg/dL or other evidence of genetic hyperlipidemias; family history of premature ASCVD with onset <55 years of age in a first-degree male relative or <65 years of age in a first-degree female relative; high-sensitivity C-reactive protein ≥2 mg/L; coronary artery calcium (CAC) score ≥300 Agatston units or ≥75th percentile for age, sex, and ethnicity (for additional information, see http://www.mesa-nhlbi.org/CACReference.aspx ![]()
See Table 5 in the original guideline document for high-, moderate-, and low-intensity statin therapies used in the RCTs reviewed by the Expert Panel.
Statin Safety Recommendations
Safety
1. To maximize the safety of statins, selection of the appropriate statin and dose in men and nonpregnant/nonnursing women should be based on patient characteristics, level of ASCVD* risk, and potential for adverse effects. Moderate-intensity statin therapy should be used in individuals in whom high-intensity statin therapy would otherwise be recommended when characteristics predisposing them to statin-associated adverse effects are present. Characteristics predisposing individuals to statin adverse effects include but are not limited to: NHBLI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: B
- Multiple or serious comorbidities, including impaired renal or hepatic function
- History of previous statin intolerance or muscle disorders
- Unexplained alanine aminotransferase (ALT) elevations ≥3 times the upper limit of normal (ULN)
- Patient characteristics or concomitant use of drugs affecting statin metabolism
- Age >75 years
Additional characteristics that could modify the decision to use higher statin intensities might include but are not limited to:
- History of hemorrhagic stroke
- Asian ancestry
2a. Creatine kinase (CK) should not be routinely measured in individuals receiving statin therapy. NHBLI Grade: A (Strong); ACC/AHA COR: III: No Benefit; ACC/AHA LOE: A
2b. Baseline measurement of CK is reasonable for individuals believed to be at increased risk for adverse muscle events because of a personal or family history of statin intolerance or muscle disease, clinical presentation, or concomitant drug therapy that might increase the risk of myopathy. NHBLI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: C (Eckel, 2010)
2c. During statin therapy, it is reasonable to measure CK in individuals with muscle symptoms, including pain, tenderness, stiffness, cramping, weakness, or generalized fatigue. NHBLI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: C (Eckel, 2010)
3a. Baseline measurement of hepatic transaminase levels (ALT) should be performed before initiation of statin therapy. NHBLI Grade: B (Moderate); ACC/AHA COR: I†; ACC/AHA LOE: B
3b. During statin therapy, it is reasonable to measure hepatic function if symptoms suggesting hepatotoxicity arise (e.g., unusual fatigue or weakness, loss of appetite, abdominal pain, dark-colored urine, or yellowing of the skin or sclera). NHBLI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: C (U.S. Food and Drug Administration, 2012)
4. Decreasing the statin dose may be considered when 2 consecutive values of LDL-C levels are <40 mg/dL. NHBLI Grade: C (Weak); ACC/AHA COR: IIb; ACC/AHA LOE: C
5. It may be harmful to initiate simvastatin at 80 mg daily or increase the dose of simvastatin to 80 mg daily. NHBLI Grade: B (Moderate); ACC/AHA COR: III: Harm; ACC/AHA LOE: A ("Zocor," 2012; U.S. Food and Drug Administration, 2010)
6. Individuals receiving statin therapy should be evaluated for new-onset diabetes according to the current diabetes screening guidelines (American Diabetes Association, 2013). Those who develop diabetes during statin therapy should be encouraged to adhere to a heart-healthy dietary pattern, engage in physical activity, achieve and maintain a healthy body weight, cease tobacco use, and continue statin therapy to reduce their risk of ASCVD events. NHBLI Grade: B (Moderate); ACC/AHA COR: I‡; ACC/AHA LOE: B
7. For individuals taking any dose of statins, it is reasonable to use caution in individuals >75 years of age, as well as in individuals who are taking concomitant medications that alter drug metabolism, taking multiple drugs, or taking drugs for conditions that require complex medication regimens (e.g., those who have undergone solid organ transplantation or are receiving treatment for human immunodeficiency virus [HIV]). A review of the manufacturer's prescribing information may be useful before initiation of any cholesterol-lowering drug. NHBLI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: C (Heart Protection Study Collaborative Group, 2002; "Lescol," 2012; "Pravachol," 2012; "Livalo," 2012; "Zocor," 2012; "Mevacor," 2012; "Lipitor," 2012; "Crestor," 2013; U.S. Food and Drug Administration, 2012; Rawlins, 2008; Schwartz et al., 2001; Shepherd et al., 2006)
8. It is reasonable to evaluate and treat muscle symptoms, including pain, tenderness, stiffness, cramping, weakness, or fatigue, in statin-treated patients according to the following management algorithm: NHBLI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: B (Taylor et al., 2011; Eckel, 2010; Baigent et al., 2010; Mills et al., 2008; Dale et al., 2007)
- To avoid unnecessary discontinuation of statins, obtain a history of prior or current muscle symptoms to establish a baseline before initiation of statin therapy.
- If unexplained severe muscle symptoms or fatigue develop during statin therapy, promptly discontinue the statin and address the possibility of rhabdomyolysis by evaluating CK and creatinine and performing urinalysis for myoglobinuria.
- If mild to moderate muscle symptoms develop during statin therapy:
- Discontinue the statin until the symptoms can be evaluated.
- Evaluate the patient for other conditions that might increase the risk for muscle symptoms (e.g., hypothyroidism, reduced renal or hepatic function, rheumatologic disorders such as polymyalgia rheumatica, steroid myopathy, vitamin D deficiency, or primary muscle diseases).
- If muscle symptoms resolve, and if no contraindication exists, give the patient the original or a lower dose of the same statin to establish a causal relationship between the muscle symptoms and statin therapy.
- If a causal relationship exists, discontinue the original statin. Once muscle symptoms resolve, use a low dose of a different statin.
- Once a low dose of a statin is tolerated, gradually increase the dose as tolerated.
- If, after 2 months without statin treatment, muscle symptoms or elevated CK levels do not resolve completely, consider other causes of muscle symptoms listed above.
- If persistent muscle symptoms are determined to arise from a condition unrelated to statin therapy, or if the predisposing condition has been treated, resume statin therapy at the original dose.
9. For individuals presenting with a confusional state or memory impairment while on statin therapy, it may be reasonable to evaluate the patient for nonstatin causes, such as exposure to other drugs, as well as for systemic and neuropsychiatric causes, in addition to the possibility of adverse effects associated with statin drug therapy. NHBLI Grade: E (Expert Opinion); ACC/AHA COR: IIb; ACC/AHA LOE: C (Shepherd et al., 2002; U.S. Food and Drug Administration, 2012; Collins et al., 2004; Roberts, 2009)
*Based on the presence of clinical ASCVD, diabetes, LDL-C ≥190 mg/dL, or level of estimated 10-year ASCVD risk.
†Individuals with elevated ALT levels (usually >1.5 or 2 times ULN) were excluded from RCT participation. Unexplained ALT ≥3 times ULN is a contraindication to statin therapy as listed in manufacturer's prescribing information.
‡Statin use is associated with a very modest excess risk of new-onset diabetes in RCTs and meta-analyses of RCTs (i.e., ∼0.1 excess cases per 100 individuals treated for 1 year with moderate-intensity statin therapy and ∼0.3 excess cases per 100 individuals treated for 1 year with high-intensity statin therapy. The increased risk of new-onset diabetes appears to be confined to those with risk factors for diabetes. These individuals are also at higher risk of ASCVD because of these risk factors. Therefore, if a statin-treated individual develops diabetes as detected by current diabetes screening guidelines, he or she should be counseled to adhere to a heart-healthy dietary pattern, engage in physical activity, achieve and maintain a healthy body weight, cease tobacco use, and continue statin therapy to reduce the risk of ASCVD events.
Nonstatin Safety Recommendations
Safety of Niacin
1. Baseline hepatic transaminases, fasting blood glucose or hemoglobin A1c, and uric acid should be obtained before initiation of niacin, and again during up-titration to a maintenance dose and every 6 months thereafter. NHLBI Grade: B (Moderate); ACC/AHA COR: I; ACC/AHA LOE: B
2. Niacin should not be used if:
- Hepatic transaminase elevations are higher than 2 to 3 times ULN. NHLBI Grade: A (Strong); ACC/AHA COR: III: Harm; ACC/AHA LOE: B
- Persistent severe cutaneous symptoms, persistent hyperglycemia, acute gout, or unexplained abdominal pain or gastrointestinal symptoms occur. NHLBI Grade: B (Moderate); ACC/AHA COR: III: Harm; ACC/AHA LOE: B
- New-onset atrial fibrillation or weight loss occurs. NHLBI Grade: C (Weak); ACC/AHA COR: III: Harm; ACC/AHA LOE: B
3. In individuals with adverse effects from niacin, the potential for ASCVD benefits and the potential for adverse effects should be reconsidered before reinitiation of niacin therapy. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: I; ACC/AHA LOE: B (AIM-HIGH Investigators et al., 2011; "Clofibrate and niacin in coronary heart disease," 1975; Guyton & Bays, 2007; Brown & Zhao, 2008; Grundy et al., 2002)
4. To reduce the frequency and severity of adverse cutaneous symptoms, it is reasonable to: NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: C (AIM-HIGH Investigators et al., 2011; "Clofibrate and niacin in coronary heart disease," 1975; Guyton & Bays, 2007; Brown & Zhao, 2008; Grundy et al., 2002)
- Start niacin at a low dose and titrate to a higher dose over a period of weeks as tolerated.
- Take niacin with food or premedicate with aspirin 325 mg 30 minutes before niacin dosing to alleviate flushing symptoms.
- If an extended-release preparation is used, increase the dose of extended-release niacin from 500 mg to a maximum of 2,000 mg/day over 4 to 8 weeks, with the dose of extended-release niacin increasing not more than weekly.
- If immediate-release niacin is chosen, start at a dose of 100 mg 3 times daily and up-titrate to 3 g/day, divided into 2 or 3 doses.
Safety of Bile Acid Sequestrants (BAS)
1. BAS should not be used in individuals with baseline fasting triglyceride levels ≥300 mg/dL or type III hyperlipoproteinemia, because severe triglyceride elevations might occur. (A fasting lipid panel should be obtained before BAS is initiated, 3 months after initiation, and every 6 to 12 months thereafter.) NHLBI Grade: C (Weak); ACC/AHA COR: III: Harm; ACC/AHA LOE: B
2. It is reasonable to use BAS with caution if baseline triglyceride levels are 250 to 299 mg/dL, and evaluate a fasting lipid panel in 4 to 6 weeks after initiation. Discontinue the BAS if triglycerides exceed 400 mg/dL. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: C (Crouse, 1987)
Safety of Cholesterol-Absorption Inhibitors
1. It is reasonable to obtain baseline hepatic transaminases before initiation of ezetimibe. When ezetimibe is coadministered with a statin, monitor transaminase levels as clinically indicated, and discontinue ezetimibe if persistent ALT elevations ≥3 times ULN occur. NHLBI Grade: C (Weak); ACC/AHA COR: IIa; ACC/AHA LOE: B
Safety of Fibrates
1. Gemfibrozil should not be initiated in patients on statin therapy because of an increased risk for muscle symptoms and rhabdomyolysis. NHLBI Grade: B (Moderate); ACC/AHA COR: III: Harm; ACC/AHA LOE: B
2. Fenofibrate may be considered concomitantly with a low- or moderate-intensity statin only if the benefits from ASCVD risk reduction or triglyceride lowering when triglycerides are ≥500 mg/dL are judged to outweigh the potential risk for adverse effects. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIb; ACC/AHA LOE: C (ACCORD Study Group et al., 2010)
3. Renal status should be evaluated before fenofibrate initiation, within 3 months after initiation, and every 6 months thereafter. Assess renal safety with both a serum creatinine level and an estimated glomerular filtration rate (eGFR) based on creatinine. NHLBI Grade: B (Moderate); ACC/AHA COR: I; ACC/AHA LOE: B
- Fenofibrate should not be used if moderate or severe renal impairment, defined as eGFR <30 mL/min per 1.73 m2, is present. ACC/AHA COR: III: Harm; ACC/AHA LOE: B
- If eGFR is between 30 and 59 mL/min per 1.73 m2, the dose of fenofibrate should not exceed 54 mg/day.*
- If, during follow-up, the eGFR decreases persistently to ≤30 mL/min per 1.73 m2, fenofibrate should be discontinued.
*Consult the manufacturer's prescribing information as there are several forms of fenofibrate available.
Safety of Omega-3 Fatty Acids
1. If eicosapentaenoic acid (EPA) and/or docosahexanoic acid (DHA) are used for the management of severe hypertriglyceridemia, defined as triglycerides ≥500 mg/dL, it is reasonable to evaluate the patient for gastrointestinal disturbances, skin changes, and bleeding. NHLBI Grade: C (Weak); ACC/AHA COR: IIa; ACC/AHA LOE: B
Recommendations for Monitoring, Optimizing, and Addressing Insufficient Response to Statin Therapy
Monitoring Statin Therapy
1. Adherence to medication and lifestyle, therapeutic response to statin therapy, and safety should be regularly assessed. This should also include a fasting lipid panel performed within 4–12 weeks after initiation or dose adjustment, and every 3–12 months thereafter. Other safety measurements should be measured as clinically indicated. NHLBI Grade: A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
Optimizing Statin Therapy
1. The maximum tolerated intensity of statin should be used in individuals for whom a high- or moderate-intensity statin is recommended but not tolerated. NHLBI Grade: B (Moderate); ACC/AHA COR: I*; ACC/AHA LOE: B
Insufficient Response to Statin Therapy
1. In individuals who have a less-than-anticipated therapeutic response or are intolerant of the recommended intensity of statin therapy, the following should be performed: NHLBI Grade A (Strong); ACC/AHA COR: I; ACC/AHA LOE: A
- Reinforce medication adherence.
- Reinforce adherence to intensive lifestyle changes.
- Exclude secondary causes of hyperlipidemia.
2. It is reasonable to use the following as indicators of anticipated therapeutic response to the recommended intensity of statin therapy. Focus is on the intensity of the statin therapy. As an aid to monitoring: NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: B (LaRosa et al., 2005; Pedersen et al., 2005; Cannon et al., 2004; Amarenco et al., 2006; Thompson & HEART-UK LDL Apheresis Working Group, 2008; Schwertz & Badellino, 2008)
- High-intensity statin therapy† generally results in an average LDL-C reduction of ≥50% from the untreated baseline.
- Moderate-intensity statin therapy generally results in an average LDL-C reduction of 30% to <50% from the untreated baseline.
- LDL-C levels and percents reduction are to be used only to assess response to therapy and adherence. They are not to be used as performance standards.
3. In individuals at higher ASCVD risk receiving the maximum tolerated intensity of statin therapy who continue to have a less-than-anticipated therapeutic response, addition of nonstatin cholesterol-lowering drug(s) may be considered if the ASCVD risk-reduction benefits outweigh the potential for adverse effects. Higher-risk individuals include: NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIb: ACC/AHA LOE: C (AIM-HIGH Investigators et al., 2011; ACCORD Study Group et al., 2010; Rossebo et al., 2007; Sharp Collaborative Group, 2010; Yokoyama, Origasa, & JELIS Investigators, 2003)
- Individuals with clinical ASCVD‡ <75 years of age.
- Individuals with baseline LDL-C ≥190 mg/dL.
- Individuals 40 to 75 years of age with diabetes.
Preference should be given to nonstatin cholesterol-lowering drugs shown to reduce ASCVD events in RCTs.
4. In individuals who are candidates for statin treatment but are completely statin intolerant, it is reasonable to use nonstatin cholesterol-lowering drugs that have been shown to reduce ASCVD events in RCTs if the ASCVD risk-reduction benefits outweigh the potential for adverse effects. NHLBI Grade: E (Expert Opinion); ACC/AHA COR: IIa; ACC/AHA LOE: B (Eckel, 2010; "Clofibrate and niacin in coronary heart disease," 1975; Frick et al., 1987; Lipid Research Clinics Program, 1984; "The Lipid Research Clinics Coronary Primary Prevention Trial results. II.," 1984; Rubins et al., 1999; Keech et al., 2005; HPS2-THRIVE Collaborative Group, 2013)
*Several RCTs found that low-intensity and low-moderate–intensity statin therapy reduced ASCVD events. In addition, the Cholesterol Treatment Trialists meta-analyses found that each 39-mg/dL reduction in LDL-C reduces ASCVD risk by 22%. Therefore, the Panel considered that submaximal statin therapy should be used to reduce ASCVD risk in those unable to tolerate moderate- or high-intensity statin therapy.
†In those already on a statin, in whom baseline LDL-C is unknown, an LDL-C level <100 mg/dL was observed in most individuals receiving high-intensity statin therapy.
‡Clinical ASCVD includes acute coronary syndromes, or a history of myocardial infarction, stable or unstable angina, coronary or other arterial revascularization, stroke, transient ischemic attack, or peripheral arterial disease presumed to be of atherosclerotic origin.
Definitions:
NHLBI Grading of the Strength of Recommendations
| Grade | Strength of Recommendation* |
|---|---|
| A | Strong recommendation There is high certainty based on evidence that the net benefit† is substantial. |
| B | Moderate recommendation There is moderate certainty based on evidence that the net benefit is moderate to substantial, or there is high certainty that the net benefit is moderate. |
| C | Weak recommendation There is at least moderate certainty based on evidence that there is a small net benefit. |
| D | Recommendation against There is at least moderate certainty based on evidence that there is no net benefit or that risks/harms outweigh benefits. |
| E | Expert opinion ("There is insufficient evidence or evidence is unclear or conflicting, but this is what the Work Group recommends.") Net benefit is unclear. Balance of benefits and harms cannot be determined because of no evidence, insufficient evidence, unclear evidence, or conflicting evidence, but the Work Group thought it was important to provide clinical guidance and make a recommendation. Further research is recommended in this area. |
| N | No recommendation for or against ("There is insufficient evidence or evidence is unclear or conflicting.") Net benefit is unclear. Balance of benefits and harms cannot be determined because of no evidence, insufficient evidence, unclear evidence, or conflicting evidence, and the Work Group thought no recommendation should be made. Further research is recommended in this area. |
*In most cases, the strength of the recommendation should be closely aligned with the quality of the evidence; however, under some circumstances, there may be valid reasons for making recommendations that are not closely aligned with the quality of the evidence (e.g., strong recommendation when the evidence quality is moderate, such as smoking cessation to reduce cardiovascular disease [CVD] risk or ordering an electrocardiogram [ECG] as part of the initial diagnostic work-up for a patient presenting with possible myocardial infarction [MI]). Those situations should be limited and the rationale explained clearly by the Work Group.
†Net benefit is defined as benefits minus risks/harms of the service/intervention.
NHLBI Quality Rating of the Strength of Evidence
| Type of Evidence | Quality Rating* |
|---|---|
| High |
| Moderate |
| Low |
*In some cases, other evidence, such as large all-or-none case series (e.g., jumping from airplanes or tall structures), can represent high- or moderate-quality evidence. In such cases, the rationale for the evidence rating exception should be explained by the Work Group and clearly justified.
†"Well-designed, well-executed" refers to studies that directly address the question; use adequate randomization, blinding, and allocation concealment; are adequately powered; use intention-to-treat analyses; and have high follow-up rates.
‡Limitations include concerns with the design and execution of a study that result in decreased confidence in the true estimate of the effect. Examples of such limitations include but are not limited to: inadequate randomization, lack of blinding of study participants or outcome assessors, inadequate power, outcomes of interest that are not prespecified for the primary outcomes, low follow-up rates, and findings based on subgroup analyses. Whether the limitations are considered minor or major is based on the number and severity of flaws in design or execution. Rules for determining whether the limitations are considered minor or major and how they will affect rating of the individual studies will be developed collaboratively with the methodology team.
§Nonrandomized controlled studies refer to intervention studies where assignment to intervention and comparison groups is not random (e.g., quasi-experimental study design).
¶Observational studies include prospective and retrospective cohort, case-control, and cross-sectional studies.
Applying Classification of Recommendations and Level of Evidence
| Size of Treatment Effect | |||||||
|---|---|---|---|---|---|---|---|
| CLASS I Benefit >>> Risk Procedure/Treatment SHOULD be performed/ administered | CLASS IIa Benefit >> Risk Additional studies with focused objectives needed IT IS REASONABLE to perform procedure/administer treatment | CLASS IIb Benefit ≥ Risk Additional studies with broad objectives needed; additional registry data would be helpful Procedure/Treatment MAY BE CONSIDERED | CLASS III No Benefit or Class III Harm | ||||
| Procedure/Test | Treatment | ||||||
| COR III: No Benefit | Not helpful | No proven benefit | |||||
| COR III: Harm | Excess cost without benefit or harmful | Harmful to patients | |||||
| Estimate of Certainty (Precision) of Treatment Effect | LEVEL A Multiple populations evaluated* Data derived from multiple randomized clinical trials or meta-analyses |
|
|
|
| ||
| LEVEL B Limited populations evaluated* Data derived from a single randomized trial or nonrandomized studies |
|
|
|
| |||
| LEVEL C Very limited populations evaluated* Only consensus opinion of experts, case studies, or standard of care |
|
|
|
| |||
A recommendation with Level of Evidence B or C does not imply that the recommendation is weak. Many important clinical questions addressed in the guidelines do not lend themselves to clinical trials. Although randomized trials are unavailable, there may be a very clear clinical consensus that a particular test or therapy is useful or effective.
*Data available from clinical trials or registries about the usefulness/efficacy in different subpopulations, such as sex, age, history of diabetes, history of prior myocardial infarction, history of heart failure, and prior aspirin use.
†For comparative-effectiveness recommendations (Class I and IIa; Level of Evidence A and B only), studies that support the use of comparator verbs should involve direct comparisons of the treatments or strategies being evaluated.
- Summary of Statin Initiation Recommendations for the Treatment of Blood Cholesterol to Reduce ASCVD Risk in Adults
- Initiating Statin Therapy in Individuals with Clinical ASCVD
- Initiating Statin Therapy in Individuals without Clinical ASCVD
- Statin Therapy: Monitoring Therapeutic Response and Adherence
OBJECTIVE: To update the clinical practice recommendations for the treatment of blood cholesterol levels to reduce atherosclerotic cardiovascular disease (ASCVD) risk using data from randomized controlled trials (RCTs) and systematic reviews and meta-analyses of RCTs. To provide a strong, evidence-based foundation for the treatment of cholesterol for the primary and secondary prevention of ASCVD in women and men
Guidelines are copyright © 2014 American College of Cardiology/American Heart Association. All rights reserved. The summary is provided by the Agency for Healthcare Research and Quality.
LMWH should replace warfarin, doc says
SAN FRANCISCO—Low-molecular-weight heparin (LMWH) should replace warfarin as thromboprophylaxis in cancer patients, according to a speaker at the 2014 ASH Annual Meeting.
Results of the phase 3 CATCH trial showed that long-term treatment with the LMWH tinzaparin was associated with a 35% lower risk of recurrent venous thromboembolism (VTE) when compared to warfarin, although the difference between the treatment arms was not statistically significant.
Patients who received tinzaparin did have a significantly lower risk of symptomatic deep vein thrombosis (DVT) and clinically relevant, non-major bleeding.
However, there was no difference between the treatment arms with regard to major bleeding or overall mortality.
Agnes Y.Y. Lee, MD, of the University of British Columbia and Vancouver Coastal Health in British Columbia, Canada, presented these results at ASH as LBA-2.*
“CATCH is the largest randomized trial studying treatment of cancer-associated thrombosis,” she said. “It provides confirmatory data for improved efficacy of low-molecular-weight heparin over warfarin.”
The trial included 900 cancer patients from 164 centers around the world. The mean patient age was 59 (range, 18-89), and 59% were female. The most common cancers were gynecologic, colorectal, upper gastrointestinal, and lung.
Patients were stratified by geographic region, tumor characteristics, and history of VTE. They were randomized to receive tinzaparin at 175 IU/kg once daily for 6 months (n=449) or initial tinzaparin at 175 IU/kg once daily for 5 to 10 days overlapped and followed by dose-adjusted warfarin for 6 months (n=451).
In all, 416 patients completed treatment with tinzaparin, and 401 completed warfarin treatment. The patients were followed up to 6 months or death, whichever came first.
Efficacy data
The primary efficacy outcome was recurrent VTE, which included symptomatic DVT and/or pulmonary embolism (PE), incidental proximal DVT and/or PE, and fatal PE.
The rate of recurrent VTE was 7.2% in the tinzaparin arm and 10.5% in the warfarin arm (hazard ratio [HR]=0.65, P=0.07). This represents a 35% reduction in recurrent VTE with the LMWH.
In the per-protocol analysis, the rates of recurrent VTE were 8.3% and 12.7%, respectively (HR=0.62), which translates to a 38% reduction in recurrent VTE with tinzaparin.
“Pre-specified efficacy analyses further showed that tinzaparin significantly reduced symptomatic, recurrent DVT by 52%,” Dr Lee noted. “There were very few symptomatic PEs, equal numbers of fatal PEs occurred in each arm, and there were only 2 incidental thrombotic events, both in the warfarin arm.”
Symptomatic, non-fatal DVT occurred in 12 patients (2.7%) in the tinzaparin arm and 24 (5.3%) in the warfarin arm (HR=0.48, P=0.04). Symptomatic, non-fatal PE occurred in 3 patients (0.7%) and 2 patients (0.4%), respectively. And fatal PE occurred in 17 patients (3.8%) in each arm (HR=0.96).
“We were clearly disappointed that our primary efficacy outcome did not achieve statistical significance,” Dr Lee said. “But our sample size was based on an estimated recurrent [VTE] rate of 12.6% in the warfarin group, and we only saw a 10% [sic] recurrence. So, basically, our study was slightly underpowered to achieve statistical significance.”
“I think that, given the symptomatic DVT results, as well as the per-protocol analysis, in additon to all the previous data on low-molecular-weight heparin, this is still very strong confirmatory data that low-molecular-weight heparin is more effective than warfarin therapy in treating cancer patients with thrombosis.”
Safety and mortality
The primary safety endpoint was major bleeding, which occurred in 2.9% of patients in the tinzaparin arm and 2.6% in the warfarin arm (HR=0.89).
The rate of clinically relevant, non-major bleeding was 11.1% and 16.2%, respectively (HR=0.69, P=0.03).
“Tinzaparin reduced the rate of clinically relevant, non-major bleeding by 31%,” Dr Lee noted.
On the other hand, there was no significant difference between the arms with regard to 180-day overall mortality, which was 34.2% in the tinzaparin arm and 32.3% in the warfarin arm (HR=1.08).
This research was sponsored by LEO Pharma, the company developing tinzaparin (Innohep). ![]()
*Information in the abstract differs from that presented at the meeting.
SAN FRANCISCO—Low-molecular-weight heparin (LMWH) should replace warfarin as thromboprophylaxis in cancer patients, according to a speaker at the 2014 ASH Annual Meeting.
Results of the phase 3 CATCH trial showed that long-term treatment with the LMWH tinzaparin was associated with a 35% lower risk of recurrent venous thromboembolism (VTE) when compared to warfarin, although the difference between the treatment arms was not statistically significant.
Patients who received tinzaparin did have a significantly lower risk of symptomatic deep vein thrombosis (DVT) and clinically relevant, non-major bleeding.
However, there was no difference between the treatment arms with regard to major bleeding or overall mortality.
Agnes Y.Y. Lee, MD, of the University of British Columbia and Vancouver Coastal Health in British Columbia, Canada, presented these results at ASH as LBA-2.*
“CATCH is the largest randomized trial studying treatment of cancer-associated thrombosis,” she said. “It provides confirmatory data for improved efficacy of low-molecular-weight heparin over warfarin.”
The trial included 900 cancer patients from 164 centers around the world. The mean patient age was 59 (range, 18-89), and 59% were female. The most common cancers were gynecologic, colorectal, upper gastrointestinal, and lung.
Patients were stratified by geographic region, tumor characteristics, and history of VTE. They were randomized to receive tinzaparin at 175 IU/kg once daily for 6 months (n=449) or initial tinzaparin at 175 IU/kg once daily for 5 to 10 days overlapped and followed by dose-adjusted warfarin for 6 months (n=451).
In all, 416 patients completed treatment with tinzaparin, and 401 completed warfarin treatment. The patients were followed up to 6 months or death, whichever came first.
Efficacy data
The primary efficacy outcome was recurrent VTE, which included symptomatic DVT and/or pulmonary embolism (PE), incidental proximal DVT and/or PE, and fatal PE.
The rate of recurrent VTE was 7.2% in the tinzaparin arm and 10.5% in the warfarin arm (hazard ratio [HR]=0.65, P=0.07). This represents a 35% reduction in recurrent VTE with the LMWH.
In the per-protocol analysis, the rates of recurrent VTE were 8.3% and 12.7%, respectively (HR=0.62), which translates to a 38% reduction in recurrent VTE with tinzaparin.
“Pre-specified efficacy analyses further showed that tinzaparin significantly reduced symptomatic, recurrent DVT by 52%,” Dr Lee noted. “There were very few symptomatic PEs, equal numbers of fatal PEs occurred in each arm, and there were only 2 incidental thrombotic events, both in the warfarin arm.”
Symptomatic, non-fatal DVT occurred in 12 patients (2.7%) in the tinzaparin arm and 24 (5.3%) in the warfarin arm (HR=0.48, P=0.04). Symptomatic, non-fatal PE occurred in 3 patients (0.7%) and 2 patients (0.4%), respectively. And fatal PE occurred in 17 patients (3.8%) in each arm (HR=0.96).
“We were clearly disappointed that our primary efficacy outcome did not achieve statistical significance,” Dr Lee said. “But our sample size was based on an estimated recurrent [VTE] rate of 12.6% in the warfarin group, and we only saw a 10% [sic] recurrence. So, basically, our study was slightly underpowered to achieve statistical significance.”
“I think that, given the symptomatic DVT results, as well as the per-protocol analysis, in additon to all the previous data on low-molecular-weight heparin, this is still very strong confirmatory data that low-molecular-weight heparin is more effective than warfarin therapy in treating cancer patients with thrombosis.”
Safety and mortality
The primary safety endpoint was major bleeding, which occurred in 2.9% of patients in the tinzaparin arm and 2.6% in the warfarin arm (HR=0.89).
The rate of clinically relevant, non-major bleeding was 11.1% and 16.2%, respectively (HR=0.69, P=0.03).
“Tinzaparin reduced the rate of clinically relevant, non-major bleeding by 31%,” Dr Lee noted.
On the other hand, there was no significant difference between the arms with regard to 180-day overall mortality, which was 34.2% in the tinzaparin arm and 32.3% in the warfarin arm (HR=1.08).
This research was sponsored by LEO Pharma, the company developing tinzaparin (Innohep). ![]()
*Information in the abstract differs from that presented at the meeting.
SAN FRANCISCO—Low-molecular-weight heparin (LMWH) should replace warfarin as thromboprophylaxis in cancer patients, according to a speaker at the 2014 ASH Annual Meeting.
Results of the phase 3 CATCH trial showed that long-term treatment with the LMWH tinzaparin was associated with a 35% lower risk of recurrent venous thromboembolism (VTE) when compared to warfarin, although the difference between the treatment arms was not statistically significant.
Patients who received tinzaparin did have a significantly lower risk of symptomatic deep vein thrombosis (DVT) and clinically relevant, non-major bleeding.
However, there was no difference between the treatment arms with regard to major bleeding or overall mortality.
Agnes Y.Y. Lee, MD, of the University of British Columbia and Vancouver Coastal Health in British Columbia, Canada, presented these results at ASH as LBA-2.*
“CATCH is the largest randomized trial studying treatment of cancer-associated thrombosis,” she said. “It provides confirmatory data for improved efficacy of low-molecular-weight heparin over warfarin.”
The trial included 900 cancer patients from 164 centers around the world. The mean patient age was 59 (range, 18-89), and 59% were female. The most common cancers were gynecologic, colorectal, upper gastrointestinal, and lung.
Patients were stratified by geographic region, tumor characteristics, and history of VTE. They were randomized to receive tinzaparin at 175 IU/kg once daily for 6 months (n=449) or initial tinzaparin at 175 IU/kg once daily for 5 to 10 days overlapped and followed by dose-adjusted warfarin for 6 months (n=451).
In all, 416 patients completed treatment with tinzaparin, and 401 completed warfarin treatment. The patients were followed up to 6 months or death, whichever came first.
Efficacy data
The primary efficacy outcome was recurrent VTE, which included symptomatic DVT and/or pulmonary embolism (PE), incidental proximal DVT and/or PE, and fatal PE.
The rate of recurrent VTE was 7.2% in the tinzaparin arm and 10.5% in the warfarin arm (hazard ratio [HR]=0.65, P=0.07). This represents a 35% reduction in recurrent VTE with the LMWH.
In the per-protocol analysis, the rates of recurrent VTE were 8.3% and 12.7%, respectively (HR=0.62), which translates to a 38% reduction in recurrent VTE with tinzaparin.
“Pre-specified efficacy analyses further showed that tinzaparin significantly reduced symptomatic, recurrent DVT by 52%,” Dr Lee noted. “There were very few symptomatic PEs, equal numbers of fatal PEs occurred in each arm, and there were only 2 incidental thrombotic events, both in the warfarin arm.”
Symptomatic, non-fatal DVT occurred in 12 patients (2.7%) in the tinzaparin arm and 24 (5.3%) in the warfarin arm (HR=0.48, P=0.04). Symptomatic, non-fatal PE occurred in 3 patients (0.7%) and 2 patients (0.4%), respectively. And fatal PE occurred in 17 patients (3.8%) in each arm (HR=0.96).
“We were clearly disappointed that our primary efficacy outcome did not achieve statistical significance,” Dr Lee said. “But our sample size was based on an estimated recurrent [VTE] rate of 12.6% in the warfarin group, and we only saw a 10% [sic] recurrence. So, basically, our study was slightly underpowered to achieve statistical significance.”
“I think that, given the symptomatic DVT results, as well as the per-protocol analysis, in additon to all the previous data on low-molecular-weight heparin, this is still very strong confirmatory data that low-molecular-weight heparin is more effective than warfarin therapy in treating cancer patients with thrombosis.”
Safety and mortality
The primary safety endpoint was major bleeding, which occurred in 2.9% of patients in the tinzaparin arm and 2.6% in the warfarin arm (HR=0.89).
The rate of clinically relevant, non-major bleeding was 11.1% and 16.2%, respectively (HR=0.69, P=0.03).
“Tinzaparin reduced the rate of clinically relevant, non-major bleeding by 31%,” Dr Lee noted.
On the other hand, there was no significant difference between the arms with regard to 180-day overall mortality, which was 34.2% in the tinzaparin arm and 32.3% in the warfarin arm (HR=1.08).
This research was sponsored by LEO Pharma, the company developing tinzaparin (Innohep). ![]()
*Information in the abstract differs from that presented at the meeting.
Study confirms IDH2 as therapeutic target in AML, MDS

in the Moscone Center
SAN FRANCISCO—The first-in-human study of AG-221 has confirmed IDH2 as a therapeutic target in acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS), according to investigators.
From the first dose of therapy, the high plasma level observed in patients “translates into a drastic decrease in 2-HG,” said Eytan M. Stein, MD, of Memorial Sloan Kettering Cancer Center in New York.
Mutations in IDH1 and IDH2 result in the accumulation of the oncometabolite 2-HG. And high levels of 2-HG prompt epigenetic changes to the cell, resulting in impaired cellular differentiation.
“By cycle 1, day 15, at all dose levels, there was fantastic inhibition of 2-HG,” Dr Stein said. “Indeed, this drastic inhibition of 2-HG led to profound clinical benefit.”
He presented interim results of the phase 1 study of AG-221 at the 2014 ASH Annual Meeting (abstract 115).*
The investigators have treated 73 patients with advanced IDH2-mutation-positive hematologic malignancies since the study began in September 2013.
Patients were a median age of 67 years (range, 33-90), and 74% had IDH2 R140 mutations. Most had relapsed/refractory AML (n=55), and the rest had MDS (n=6), untreated AML (n=5), chronic myelomonocytic leukemia (n=5), and myeloid sarcoma (n=1).
Patients received AG-221 as a single agent orally, once or twice a day, continuously, in 28-day cycles. Four dose-expansion cohorts at 100 mg each day were added last October.
To date, the maximum tolerated dose has not been reached, with the highest cumulative daily dose being 300 mg. Investigators observed a single dose-limiting toxicity in 1 patient: grade 5 hypoxia with fungal pneumonia and septic shock.
As of the data cutoff on October 1, 2014, 38 patients were still on therapy, and 35 had discontinued. Five patients withdrew after achieving complete remission (CR) in order to pursue allogeneic transplant.
Dr Stein pointed out that although the median number of prior chemotherapy regimens for the entire cohort was 2, “all of the patients who went on study were predicted to have dismal outcomes with conventional therapy.”
Safety
The therapy was well tolerated, with the most common adverse events (AEs) overall being typical for patients with advanced AML: nausea (23%), pyrexia (19%), and diarrhea (17%).
The majority of serious AEs were disease-related and unrelated to the study drug, Dr Stein said. Thirteen patients experienced 21 serious AEs that were possibly or probably related to treatment.
Investigators observed treatment-related leukocytosis in 3 patients, “but we think that is a differentiating effect of the study drug,” Dr Stein said.
He also pointed out that there was no increase in AEs with increased dose of the drug.
Of the 11 deaths reported, 9 were unrelated to the drug, and 2—sepsis/hypoxia and atrial flutter—were possibly related. The 30-day and 60-day all-cause mortality rates were 4.1% and 13.7%, respectively.
Efficacy
Of the 45 patients who were treated for at least 1 cycle and were evaluable for efficacy, 15 achieved a CR (n=6) or a CR with incomplete blood count recovery. The overall response rate is 56% (25/45).
“Responses appear durable,” Dr Stein commented, “and 90% of responders have had a response duration of at least 3 months, with the earliest patients on study having had durable responses for over 6 months.”
Many of the durable responses are partial remissions, he noted.
Seventeen patients have stable disease, and many of these patients remain on study. Two patients had progressive disease.
“Patients with stable disease have remained on study for a similar amount of time as the responders,” Dr Stein said, “suggesting that, despite the lack of a formal partial remission, many patients are deriving clinical benefit from study treatment.”
This study was sponsored by Agios Pharmaceuticals Inc., the company developing AG-221 in collaboration with Celgene.
Previous results from this study were presented at the 2014 EHA Annual Congress. Based on those results, AG-221 received fast track designation from the US Food and Drug Administration. ![]()
*Data in the presentation were updated from the abstract.

in the Moscone Center
SAN FRANCISCO—The first-in-human study of AG-221 has confirmed IDH2 as a therapeutic target in acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS), according to investigators.
From the first dose of therapy, the high plasma level observed in patients “translates into a drastic decrease in 2-HG,” said Eytan M. Stein, MD, of Memorial Sloan Kettering Cancer Center in New York.
Mutations in IDH1 and IDH2 result in the accumulation of the oncometabolite 2-HG. And high levels of 2-HG prompt epigenetic changes to the cell, resulting in impaired cellular differentiation.
“By cycle 1, day 15, at all dose levels, there was fantastic inhibition of 2-HG,” Dr Stein said. “Indeed, this drastic inhibition of 2-HG led to profound clinical benefit.”
He presented interim results of the phase 1 study of AG-221 at the 2014 ASH Annual Meeting (abstract 115).*
The investigators have treated 73 patients with advanced IDH2-mutation-positive hematologic malignancies since the study began in September 2013.
Patients were a median age of 67 years (range, 33-90), and 74% had IDH2 R140 mutations. Most had relapsed/refractory AML (n=55), and the rest had MDS (n=6), untreated AML (n=5), chronic myelomonocytic leukemia (n=5), and myeloid sarcoma (n=1).
Patients received AG-221 as a single agent orally, once or twice a day, continuously, in 28-day cycles. Four dose-expansion cohorts at 100 mg each day were added last October.
To date, the maximum tolerated dose has not been reached, with the highest cumulative daily dose being 300 mg. Investigators observed a single dose-limiting toxicity in 1 patient: grade 5 hypoxia with fungal pneumonia and septic shock.
As of the data cutoff on October 1, 2014, 38 patients were still on therapy, and 35 had discontinued. Five patients withdrew after achieving complete remission (CR) in order to pursue allogeneic transplant.
Dr Stein pointed out that although the median number of prior chemotherapy regimens for the entire cohort was 2, “all of the patients who went on study were predicted to have dismal outcomes with conventional therapy.”
Safety
The therapy was well tolerated, with the most common adverse events (AEs) overall being typical for patients with advanced AML: nausea (23%), pyrexia (19%), and diarrhea (17%).
The majority of serious AEs were disease-related and unrelated to the study drug, Dr Stein said. Thirteen patients experienced 21 serious AEs that were possibly or probably related to treatment.
Investigators observed treatment-related leukocytosis in 3 patients, “but we think that is a differentiating effect of the study drug,” Dr Stein said.
He also pointed out that there was no increase in AEs with increased dose of the drug.
Of the 11 deaths reported, 9 were unrelated to the drug, and 2—sepsis/hypoxia and atrial flutter—were possibly related. The 30-day and 60-day all-cause mortality rates were 4.1% and 13.7%, respectively.
Efficacy
Of the 45 patients who were treated for at least 1 cycle and were evaluable for efficacy, 15 achieved a CR (n=6) or a CR with incomplete blood count recovery. The overall response rate is 56% (25/45).
“Responses appear durable,” Dr Stein commented, “and 90% of responders have had a response duration of at least 3 months, with the earliest patients on study having had durable responses for over 6 months.”
Many of the durable responses are partial remissions, he noted.
Seventeen patients have stable disease, and many of these patients remain on study. Two patients had progressive disease.
“Patients with stable disease have remained on study for a similar amount of time as the responders,” Dr Stein said, “suggesting that, despite the lack of a formal partial remission, many patients are deriving clinical benefit from study treatment.”
This study was sponsored by Agios Pharmaceuticals Inc., the company developing AG-221 in collaboration with Celgene.
Previous results from this study were presented at the 2014 EHA Annual Congress. Based on those results, AG-221 received fast track designation from the US Food and Drug Administration. ![]()
*Data in the presentation were updated from the abstract.

in the Moscone Center
SAN FRANCISCO—The first-in-human study of AG-221 has confirmed IDH2 as a therapeutic target in acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS), according to investigators.
From the first dose of therapy, the high plasma level observed in patients “translates into a drastic decrease in 2-HG,” said Eytan M. Stein, MD, of Memorial Sloan Kettering Cancer Center in New York.
Mutations in IDH1 and IDH2 result in the accumulation of the oncometabolite 2-HG. And high levels of 2-HG prompt epigenetic changes to the cell, resulting in impaired cellular differentiation.
“By cycle 1, day 15, at all dose levels, there was fantastic inhibition of 2-HG,” Dr Stein said. “Indeed, this drastic inhibition of 2-HG led to profound clinical benefit.”
He presented interim results of the phase 1 study of AG-221 at the 2014 ASH Annual Meeting (abstract 115).*
The investigators have treated 73 patients with advanced IDH2-mutation-positive hematologic malignancies since the study began in September 2013.
Patients were a median age of 67 years (range, 33-90), and 74% had IDH2 R140 mutations. Most had relapsed/refractory AML (n=55), and the rest had MDS (n=6), untreated AML (n=5), chronic myelomonocytic leukemia (n=5), and myeloid sarcoma (n=1).
Patients received AG-221 as a single agent orally, once or twice a day, continuously, in 28-day cycles. Four dose-expansion cohorts at 100 mg each day were added last October.
To date, the maximum tolerated dose has not been reached, with the highest cumulative daily dose being 300 mg. Investigators observed a single dose-limiting toxicity in 1 patient: grade 5 hypoxia with fungal pneumonia and septic shock.
As of the data cutoff on October 1, 2014, 38 patients were still on therapy, and 35 had discontinued. Five patients withdrew after achieving complete remission (CR) in order to pursue allogeneic transplant.
Dr Stein pointed out that although the median number of prior chemotherapy regimens for the entire cohort was 2, “all of the patients who went on study were predicted to have dismal outcomes with conventional therapy.”
Safety
The therapy was well tolerated, with the most common adverse events (AEs) overall being typical for patients with advanced AML: nausea (23%), pyrexia (19%), and diarrhea (17%).
The majority of serious AEs were disease-related and unrelated to the study drug, Dr Stein said. Thirteen patients experienced 21 serious AEs that were possibly or probably related to treatment.
Investigators observed treatment-related leukocytosis in 3 patients, “but we think that is a differentiating effect of the study drug,” Dr Stein said.
He also pointed out that there was no increase in AEs with increased dose of the drug.
Of the 11 deaths reported, 9 were unrelated to the drug, and 2—sepsis/hypoxia and atrial flutter—were possibly related. The 30-day and 60-day all-cause mortality rates were 4.1% and 13.7%, respectively.
Efficacy
Of the 45 patients who were treated for at least 1 cycle and were evaluable for efficacy, 15 achieved a CR (n=6) or a CR with incomplete blood count recovery. The overall response rate is 56% (25/45).
“Responses appear durable,” Dr Stein commented, “and 90% of responders have had a response duration of at least 3 months, with the earliest patients on study having had durable responses for over 6 months.”
Many of the durable responses are partial remissions, he noted.
Seventeen patients have stable disease, and many of these patients remain on study. Two patients had progressive disease.
“Patients with stable disease have remained on study for a similar amount of time as the responders,” Dr Stein said, “suggesting that, despite the lack of a formal partial remission, many patients are deriving clinical benefit from study treatment.”
This study was sponsored by Agios Pharmaceuticals Inc., the company developing AG-221 in collaboration with Celgene.
Previous results from this study were presented at the 2014 EHA Annual Congress. Based on those results, AG-221 received fast track designation from the US Food and Drug Administration. ![]()
*Data in the presentation were updated from the abstract.
Referring Smokers to Quitlines
Telephone-based programs to encourage and support quitting smoking—known as “quitlines”—have been established as effective both clinically and in the “real world.” However, quitlines rely on smokers calling in for them to work. Researchers from the Tobacco Cessation and Prevention Program and the Massachusetts Department of Public Health, both in Boston, say being referred to quitlines by their health care providers might help even more smokers quit.
The researchers collected data for 2,737 provider-referred and 530 self-referred smokers from the Massachusetts Smokers’ Helpline, which offers evidence-based proactive telephone counseling sessions, nicotine replacement therapy (NRT), and self-help materials. They then examined differences in demographics, service utilization, and quit outcomes. The primary outcome was quit status at the 6- to 8-month follow-up.
Twenty percent of provider-referred clients quit smoking; 26% of self-referred clients quit. Provider-referred smokers who used the quitline services had higher odds of quitting, compared with those who used methods not including a quitline. However, the provider-referral model was limited by lower enrollment, lower use, and poorer outcomes compared with self-referred services. Patients aged 18 to 34 years and those aged > 65 years had the best chances of quitting and staying smoke-free. Patients referred from private practices were more likely to quit than were those referred from a hospital.
Provider-referred smokers who read the self-help materials had 1.2 times the odds of quitting compared with those who didn’t. Using any amount of the 2-week supply of NRT doubled the odds of quitting. Clients who used a combination of counseling and NRT had the greatest success, with more than triple the chances of quitting, compared with clients who did neither.
Self-referred smokers also had good results, although not usually as quickly as provider-referred smokers, who saw significantly improved outcomes after 3 counseling sessions. It took 4 sessions for the self-referred smokers to see the same results.
Readiness to quit was an important predictor of success. Tobacco dependence also predicted quitting success. Clients in both groups who could wait > 30 minutes before smoking their first cigarette had better luck than did those who had to smoke immediately after waking.
The researchers suggest some ways to improve the provider-referred model. One is to offer more support for smokers from lower socioeconomic levels. According to other research, those smokers may need more treatment content and access to more intensive pharmacotherapy, the researchers say.
It might also help all quitline clients, they add, to minimize the wait time between referral and actual provision of service. Longer wait times can “increase the room for ambivalence for any smoker,” they note, “but may be especially detrimental for provider-referred smokers who are less ready to make a quit attempt.”
And what is the provider’s role in assessing patient readiness to quit and preparing patients for the quitline services? In reality, the researchers say, not all patients have received an evidence-based intervention or are ready to quit when they are enrolled. Moreover, many are lost in the callback process. Using 3 callback attempts, the Massachusetts quitline only reaches 40% of their potential quitters. Upping the callback rate to 5 attempts raises the reach slightly, to 50%. That shows the need, the researchers say, for better and more frequent provider training, outreach, feedback reporting, clinical champions on site, and systems support.
Source
Song G, Landau AS, Gorin TJ, Keithly L. Am J Prev Med. 2014;47(4):392-402.
doi: 10.1016/j.amepre.2014.05.043.
Telephone-based programs to encourage and support quitting smoking—known as “quitlines”—have been established as effective both clinically and in the “real world.” However, quitlines rely on smokers calling in for them to work. Researchers from the Tobacco Cessation and Prevention Program and the Massachusetts Department of Public Health, both in Boston, say being referred to quitlines by their health care providers might help even more smokers quit.
The researchers collected data for 2,737 provider-referred and 530 self-referred smokers from the Massachusetts Smokers’ Helpline, which offers evidence-based proactive telephone counseling sessions, nicotine replacement therapy (NRT), and self-help materials. They then examined differences in demographics, service utilization, and quit outcomes. The primary outcome was quit status at the 6- to 8-month follow-up.
Twenty percent of provider-referred clients quit smoking; 26% of self-referred clients quit. Provider-referred smokers who used the quitline services had higher odds of quitting, compared with those who used methods not including a quitline. However, the provider-referral model was limited by lower enrollment, lower use, and poorer outcomes compared with self-referred services. Patients aged 18 to 34 years and those aged > 65 years had the best chances of quitting and staying smoke-free. Patients referred from private practices were more likely to quit than were those referred from a hospital.
Provider-referred smokers who read the self-help materials had 1.2 times the odds of quitting compared with those who didn’t. Using any amount of the 2-week supply of NRT doubled the odds of quitting. Clients who used a combination of counseling and NRT had the greatest success, with more than triple the chances of quitting, compared with clients who did neither.
Self-referred smokers also had good results, although not usually as quickly as provider-referred smokers, who saw significantly improved outcomes after 3 counseling sessions. It took 4 sessions for the self-referred smokers to see the same results.
Readiness to quit was an important predictor of success. Tobacco dependence also predicted quitting success. Clients in both groups who could wait > 30 minutes before smoking their first cigarette had better luck than did those who had to smoke immediately after waking.
The researchers suggest some ways to improve the provider-referred model. One is to offer more support for smokers from lower socioeconomic levels. According to other research, those smokers may need more treatment content and access to more intensive pharmacotherapy, the researchers say.
It might also help all quitline clients, they add, to minimize the wait time between referral and actual provision of service. Longer wait times can “increase the room for ambivalence for any smoker,” they note, “but may be especially detrimental for provider-referred smokers who are less ready to make a quit attempt.”
And what is the provider’s role in assessing patient readiness to quit and preparing patients for the quitline services? In reality, the researchers say, not all patients have received an evidence-based intervention or are ready to quit when they are enrolled. Moreover, many are lost in the callback process. Using 3 callback attempts, the Massachusetts quitline only reaches 40% of their potential quitters. Upping the callback rate to 5 attempts raises the reach slightly, to 50%. That shows the need, the researchers say, for better and more frequent provider training, outreach, feedback reporting, clinical champions on site, and systems support.
Source
Song G, Landau AS, Gorin TJ, Keithly L. Am J Prev Med. 2014;47(4):392-402.
doi: 10.1016/j.amepre.2014.05.043.
Telephone-based programs to encourage and support quitting smoking—known as “quitlines”—have been established as effective both clinically and in the “real world.” However, quitlines rely on smokers calling in for them to work. Researchers from the Tobacco Cessation and Prevention Program and the Massachusetts Department of Public Health, both in Boston, say being referred to quitlines by their health care providers might help even more smokers quit.
The researchers collected data for 2,737 provider-referred and 530 self-referred smokers from the Massachusetts Smokers’ Helpline, which offers evidence-based proactive telephone counseling sessions, nicotine replacement therapy (NRT), and self-help materials. They then examined differences in demographics, service utilization, and quit outcomes. The primary outcome was quit status at the 6- to 8-month follow-up.
Twenty percent of provider-referred clients quit smoking; 26% of self-referred clients quit. Provider-referred smokers who used the quitline services had higher odds of quitting, compared with those who used methods not including a quitline. However, the provider-referral model was limited by lower enrollment, lower use, and poorer outcomes compared with self-referred services. Patients aged 18 to 34 years and those aged > 65 years had the best chances of quitting and staying smoke-free. Patients referred from private practices were more likely to quit than were those referred from a hospital.
Provider-referred smokers who read the self-help materials had 1.2 times the odds of quitting compared with those who didn’t. Using any amount of the 2-week supply of NRT doubled the odds of quitting. Clients who used a combination of counseling and NRT had the greatest success, with more than triple the chances of quitting, compared with clients who did neither.
Self-referred smokers also had good results, although not usually as quickly as provider-referred smokers, who saw significantly improved outcomes after 3 counseling sessions. It took 4 sessions for the self-referred smokers to see the same results.
Readiness to quit was an important predictor of success. Tobacco dependence also predicted quitting success. Clients in both groups who could wait > 30 minutes before smoking their first cigarette had better luck than did those who had to smoke immediately after waking.
The researchers suggest some ways to improve the provider-referred model. One is to offer more support for smokers from lower socioeconomic levels. According to other research, those smokers may need more treatment content and access to more intensive pharmacotherapy, the researchers say.
It might also help all quitline clients, they add, to minimize the wait time between referral and actual provision of service. Longer wait times can “increase the room for ambivalence for any smoker,” they note, “but may be especially detrimental for provider-referred smokers who are less ready to make a quit attempt.”
And what is the provider’s role in assessing patient readiness to quit and preparing patients for the quitline services? In reality, the researchers say, not all patients have received an evidence-based intervention or are ready to quit when they are enrolled. Moreover, many are lost in the callback process. Using 3 callback attempts, the Massachusetts quitline only reaches 40% of their potential quitters. Upping the callback rate to 5 attempts raises the reach slightly, to 50%. That shows the need, the researchers say, for better and more frequent provider training, outreach, feedback reporting, clinical champions on site, and systems support.
Source
Song G, Landau AS, Gorin TJ, Keithly L. Am J Prev Med. 2014;47(4):392-402.
doi: 10.1016/j.amepre.2014.05.043.
Amount of blood transfused doesn’t affect long-term mortality

Credit: UAB Hospital
Long-term mortality is not affected by the amount of blood a patient receives following surgery, according to research published in The Lancet.
Investigators compared a liberal transfusion strategy, in which patients received blood to maintain a hemoglobin level at 100 g/L or higher, and a restrictive strategy, in which patients received blood when hemoglobin levels were lower than 80 g/L or if they had symptoms of anemia.
And, at about 3 years of follow-up, there was no difference in mortality between the two groups.
Jeffrey L. Carson, MD, of Robert Wood Johnson Medical School in New Jersey, and his colleagues conducted this research, analyzing data from the FOCUS trial, which included patients from 47 hospitals in the US and Canada.
The trial enrolled 2016 adults age 50 and older, with a history of or risk factors for cardiovascular disease, who had postoperative hemoglobin concentrations lower than 100 g/L within 3 days of surgery to repair a hip fracture.
Patients were randomized by a central telephone system to the liberal (n=1007) or restrictive (n=1009) transfusion groups. The investigators analyzed the long-term mortality of these patients, which was established by linking participants to national death registries in the US and Canada.
The results revealed no difference in mortality from cardiovascular disease, cancer, or severe infection due to the amount of the blood given after surgery.
This supports the initial results of the FOCUS trial, which Dr Carson and his colleagues published in NEJM in 2011 and which demonstrated the safety of fewer transfusions in the short-term.
For the current analysis, the median duration of follow-up was 3.1 years. Eight hundred and forty-one patients (42%) died during that time—432 in the liberal transfusion group and 409 in the restrictive transfusion group. This difference was not statistically significant, with a hazard ratio of 1.09 and a P value of 0.21.
“There has been a steady decline in the amount of blood in transfusions given to patients in the past 3 to 5 years,” Dr Carson noted. “I think it is very reassuring that we have found that using less blood is okay, not just from a short-term perspective, but also a long-term perspective.”
Medical experts had worried that larger amounts of transfused blood might suppress immune function—which could lead to death from infection or cancer—or that smaller transfusions might worsen a patient’s chronic heart disease by depriving the heart of oxygen and other nutrients that it might have absorbed by pumping more blood.
But in both instances, Dr Carson and his colleagues found no difference in long-term death rates, regardless of the number of transfusions.
Dr Carson noted that there are health conditions, such as heart attacks, where the effects of the two transfusion strategies are less certain. Preliminary evidence suggests heart attack patients need more blood, not less. But additional studies are needed to confirm that. ![]()

Credit: UAB Hospital
Long-term mortality is not affected by the amount of blood a patient receives following surgery, according to research published in The Lancet.
Investigators compared a liberal transfusion strategy, in which patients received blood to maintain a hemoglobin level at 100 g/L or higher, and a restrictive strategy, in which patients received blood when hemoglobin levels were lower than 80 g/L or if they had symptoms of anemia.
And, at about 3 years of follow-up, there was no difference in mortality between the two groups.
Jeffrey L. Carson, MD, of Robert Wood Johnson Medical School in New Jersey, and his colleagues conducted this research, analyzing data from the FOCUS trial, which included patients from 47 hospitals in the US and Canada.
The trial enrolled 2016 adults age 50 and older, with a history of or risk factors for cardiovascular disease, who had postoperative hemoglobin concentrations lower than 100 g/L within 3 days of surgery to repair a hip fracture.
Patients were randomized by a central telephone system to the liberal (n=1007) or restrictive (n=1009) transfusion groups. The investigators analyzed the long-term mortality of these patients, which was established by linking participants to national death registries in the US and Canada.
The results revealed no difference in mortality from cardiovascular disease, cancer, or severe infection due to the amount of the blood given after surgery.
This supports the initial results of the FOCUS trial, which Dr Carson and his colleagues published in NEJM in 2011 and which demonstrated the safety of fewer transfusions in the short-term.
For the current analysis, the median duration of follow-up was 3.1 years. Eight hundred and forty-one patients (42%) died during that time—432 in the liberal transfusion group and 409 in the restrictive transfusion group. This difference was not statistically significant, with a hazard ratio of 1.09 and a P value of 0.21.
“There has been a steady decline in the amount of blood in transfusions given to patients in the past 3 to 5 years,” Dr Carson noted. “I think it is very reassuring that we have found that using less blood is okay, not just from a short-term perspective, but also a long-term perspective.”
Medical experts had worried that larger amounts of transfused blood might suppress immune function—which could lead to death from infection or cancer—or that smaller transfusions might worsen a patient’s chronic heart disease by depriving the heart of oxygen and other nutrients that it might have absorbed by pumping more blood.
But in both instances, Dr Carson and his colleagues found no difference in long-term death rates, regardless of the number of transfusions.
Dr Carson noted that there are health conditions, such as heart attacks, where the effects of the two transfusion strategies are less certain. Preliminary evidence suggests heart attack patients need more blood, not less. But additional studies are needed to confirm that. ![]()

Credit: UAB Hospital
Long-term mortality is not affected by the amount of blood a patient receives following surgery, according to research published in The Lancet.
Investigators compared a liberal transfusion strategy, in which patients received blood to maintain a hemoglobin level at 100 g/L or higher, and a restrictive strategy, in which patients received blood when hemoglobin levels were lower than 80 g/L or if they had symptoms of anemia.
And, at about 3 years of follow-up, there was no difference in mortality between the two groups.
Jeffrey L. Carson, MD, of Robert Wood Johnson Medical School in New Jersey, and his colleagues conducted this research, analyzing data from the FOCUS trial, which included patients from 47 hospitals in the US and Canada.
The trial enrolled 2016 adults age 50 and older, with a history of or risk factors for cardiovascular disease, who had postoperative hemoglobin concentrations lower than 100 g/L within 3 days of surgery to repair a hip fracture.
Patients were randomized by a central telephone system to the liberal (n=1007) or restrictive (n=1009) transfusion groups. The investigators analyzed the long-term mortality of these patients, which was established by linking participants to national death registries in the US and Canada.
The results revealed no difference in mortality from cardiovascular disease, cancer, or severe infection due to the amount of the blood given after surgery.
This supports the initial results of the FOCUS trial, which Dr Carson and his colleagues published in NEJM in 2011 and which demonstrated the safety of fewer transfusions in the short-term.
For the current analysis, the median duration of follow-up was 3.1 years. Eight hundred and forty-one patients (42%) died during that time—432 in the liberal transfusion group and 409 in the restrictive transfusion group. This difference was not statistically significant, with a hazard ratio of 1.09 and a P value of 0.21.
“There has been a steady decline in the amount of blood in transfusions given to patients in the past 3 to 5 years,” Dr Carson noted. “I think it is very reassuring that we have found that using less blood is okay, not just from a short-term perspective, but also a long-term perspective.”
Medical experts had worried that larger amounts of transfused blood might suppress immune function—which could lead to death from infection or cancer—or that smaller transfusions might worsen a patient’s chronic heart disease by depriving the heart of oxygen and other nutrients that it might have absorbed by pumping more blood.
But in both instances, Dr Carson and his colleagues found no difference in long-term death rates, regardless of the number of transfusions.
Dr Carson noted that there are health conditions, such as heart attacks, where the effects of the two transfusion strategies are less certain. Preliminary evidence suggests heart attack patients need more blood, not less. But additional studies are needed to confirm that. ![]()
Team identifies prognostic markers for CN-AML

Researchers say they’ve identified novel prognostic markers for older patients with cytogenetically normal acute myeloid leukemia (CN-AML).
The team examined the expression of long noncoding RNAs (lncRNAs) in patients with CN-AML who were at least 60 years of age.
This revealed a pattern of 48 lncRNAs that predicted both response to standard chemotherapy and overall survival.
The researchers described this discovery in PNAS.
“[Our findings] strongly suggest that lncRNA expression profiles can predict which patients will respond to standard therapy,” said principal investigator Clara D. Bloomfield, MD, of The Ohio State University Comprehensive Cancer Center in Columbus.
“That’s important because it would spare these patients from the toxic side effects of experimental therapies. Patients who are classified in the unfavorable group would receive different therapy: stem cell transplant or a clinical trial using new therapeutic approaches. Thus, this research will help to tailor leukemia therapy to each individual.”
In addition, she said, the study revealed novel targets for the development of new therapies.
Dr Bloomfield and her colleagues began this research by analyzing bone marrow samples from 148 older patients with CN-AML who were treated on Cancer and Leukemia Group B clinical trials. All had received similar chemotherapy regimens.
The researchers first identified the 48 lncRNAs that were most associated with survival. Using these 48 lncRNAs, the team divided patients into two groups: those with a favorable prognostic score and those with an unfavorable score.
The researchers then validated the scores in an independent matched set of 71 similarly treated CN-AML patients and compared patients with an unfavorable score to those with a favorable score.
Results showed that patients with an unfavorable score had a lower complete response (CR) rate—54%, compared to 89% for patients with a favorable score.
Three years after CR, only 7% of patients with an unfavorable score were disease-free, compared with 39% of patients with a favorable score.
Overall survival at 3 years for those with an unfavorable score was 10%, compared to 43% for patients with a favorable score.
Distinct lncRNA profiles were associated with mutations in 6 genes—FLT3, NPM1, CEBPA, IDH2, ASXL1, and RUNX1.
The researchers concluded that lncRNA expression profiles are associated with recurrent mutations, clinical features, and outcome in AML. A fraction of these lncRNAs may have a functional role in leukemogenesis. Furthermore, lncRNAs could be used as biomarkers for outcome in AML. ![]()

Researchers say they’ve identified novel prognostic markers for older patients with cytogenetically normal acute myeloid leukemia (CN-AML).
The team examined the expression of long noncoding RNAs (lncRNAs) in patients with CN-AML who were at least 60 years of age.
This revealed a pattern of 48 lncRNAs that predicted both response to standard chemotherapy and overall survival.
The researchers described this discovery in PNAS.
“[Our findings] strongly suggest that lncRNA expression profiles can predict which patients will respond to standard therapy,” said principal investigator Clara D. Bloomfield, MD, of The Ohio State University Comprehensive Cancer Center in Columbus.
“That’s important because it would spare these patients from the toxic side effects of experimental therapies. Patients who are classified in the unfavorable group would receive different therapy: stem cell transplant or a clinical trial using new therapeutic approaches. Thus, this research will help to tailor leukemia therapy to each individual.”
In addition, she said, the study revealed novel targets for the development of new therapies.
Dr Bloomfield and her colleagues began this research by analyzing bone marrow samples from 148 older patients with CN-AML who were treated on Cancer and Leukemia Group B clinical trials. All had received similar chemotherapy regimens.
The researchers first identified the 48 lncRNAs that were most associated with survival. Using these 48 lncRNAs, the team divided patients into two groups: those with a favorable prognostic score and those with an unfavorable score.
The researchers then validated the scores in an independent matched set of 71 similarly treated CN-AML patients and compared patients with an unfavorable score to those with a favorable score.
Results showed that patients with an unfavorable score had a lower complete response (CR) rate—54%, compared to 89% for patients with a favorable score.
Three years after CR, only 7% of patients with an unfavorable score were disease-free, compared with 39% of patients with a favorable score.
Overall survival at 3 years for those with an unfavorable score was 10%, compared to 43% for patients with a favorable score.
Distinct lncRNA profiles were associated with mutations in 6 genes—FLT3, NPM1, CEBPA, IDH2, ASXL1, and RUNX1.
The researchers concluded that lncRNA expression profiles are associated with recurrent mutations, clinical features, and outcome in AML. A fraction of these lncRNAs may have a functional role in leukemogenesis. Furthermore, lncRNAs could be used as biomarkers for outcome in AML. ![]()

Researchers say they’ve identified novel prognostic markers for older patients with cytogenetically normal acute myeloid leukemia (CN-AML).
The team examined the expression of long noncoding RNAs (lncRNAs) in patients with CN-AML who were at least 60 years of age.
This revealed a pattern of 48 lncRNAs that predicted both response to standard chemotherapy and overall survival.
The researchers described this discovery in PNAS.
“[Our findings] strongly suggest that lncRNA expression profiles can predict which patients will respond to standard therapy,” said principal investigator Clara D. Bloomfield, MD, of The Ohio State University Comprehensive Cancer Center in Columbus.
“That’s important because it would spare these patients from the toxic side effects of experimental therapies. Patients who are classified in the unfavorable group would receive different therapy: stem cell transplant or a clinical trial using new therapeutic approaches. Thus, this research will help to tailor leukemia therapy to each individual.”
In addition, she said, the study revealed novel targets for the development of new therapies.
Dr Bloomfield and her colleagues began this research by analyzing bone marrow samples from 148 older patients with CN-AML who were treated on Cancer and Leukemia Group B clinical trials. All had received similar chemotherapy regimens.
The researchers first identified the 48 lncRNAs that were most associated with survival. Using these 48 lncRNAs, the team divided patients into two groups: those with a favorable prognostic score and those with an unfavorable score.
The researchers then validated the scores in an independent matched set of 71 similarly treated CN-AML patients and compared patients with an unfavorable score to those with a favorable score.
Results showed that patients with an unfavorable score had a lower complete response (CR) rate—54%, compared to 89% for patients with a favorable score.
Three years after CR, only 7% of patients with an unfavorable score were disease-free, compared with 39% of patients with a favorable score.
Overall survival at 3 years for those with an unfavorable score was 10%, compared to 43% for patients with a favorable score.
Distinct lncRNA profiles were associated with mutations in 6 genes—FLT3, NPM1, CEBPA, IDH2, ASXL1, and RUNX1.
The researchers concluded that lncRNA expression profiles are associated with recurrent mutations, clinical features, and outcome in AML. A fraction of these lncRNAs may have a functional role in leukemogenesis. Furthermore, lncRNAs could be used as biomarkers for outcome in AML. ![]()
Barriers to Establishing a PCS
Palliative care (PC) focuses on relieving distressing symptoms such as pain, dyspnea, fatigue, and depression; providing psychological, social, emotional, and spiritual support; and helping patients choose treatments consistent with their values.[1] Palliative care consultation services (PCSs) increase patient and family satisfaction,[2, 3] improve quality of life,[4] reduce resource utilization,[5] and decrease hospital expenditure.[2, 6] Hospitals that fund a PCS typically realize a sizable return on investment and good value, as these services provide better care at lower cost.[7] These benefits provide a strong rationale for all hospitals to establish a PCS. However, only 53% of acute care hospitals in California offer PC services, and only 37% have a hospital‐based PCS.[7] To increase access for patients with serious illness, it is necessary to understand the barriers that hinder the development of PCS. In this study, we asked leaders from hospitals without a PCS to describe these barriers and identify strategies that could overcome them and promote PCSs.
METHODS
In 2011, we surveyed all acute care hospitals in California to assess the prevalence of PCSs in the state. We defined a PCS as an interdisciplinary team that sees patients, identifies needs, makes treatment recommendations, facilitates patient and/or family decision making, and/or directly provides palliative care for patients with life‐threatening illness and their families. Hospitals that did not have a PCS were asked questions regarding plans to establish one (Is there an effort underway to establish a palliative care program in your hospital?), perceived barriers to starting one (What are 3 significant barriers or circumstances that have prevented your hospital from creating a palliative care program?), and ideas for overcoming barriers (What resources, training, policy changes would be most helpful in overcoming those barriers?). Questions that allowed for open‐ended responses were analyzed using a thematic approach.[8] Themes were initially reviewed by 1 researcher (C.J.B.), then refined and confirmed at each stage using an iterative process with other research team members (D.L.O., S.Z.P.) to reduce potential biases. Questions assessing hospital characteristics and status toward establishing a PCS provided a list of possible answers. Frequencies to these responses are reported accordingly.
RESULTS
Surveys were distributed to 376 acute care hospitals in California, of which 360 responded to the survey, resulting in a 96% response rate. Of the 360 hospitals surveyed, 46% (n=166) reported not offering any PCS. Out of the 166 that did not have PCS, 7 stated they had a PCS at some point in the last 5 years, but the program was discontinued. Hospitals without a PCS were largely for profit (75%, n=125), small with 150 beds (72%, n=120), and not affiliated with a system (63%, n=105). Overall, 34% (43/128) of hospitals reported that they had efforts underway to establish one, with 21% (9/43) expecting to start seeing patients within a year. Seventy‐two hospitals (56%, 72/128) reported that providers from local hospices aided them in providing their patients with PC, and that this approach met the needs of their patients. A total of 93 hospitals identified multiple barriers (n=186) to establishing a PCS, of which 162 responses could be categorized into 5 meaningful themes. Regarding strategies to overcome these barriers, 65 hospitals provided 72 responses that could be categorized into 5 meaningful themes (Table 1).
| Barriers and Strategies | Responses, % (n) |
|---|---|
| |
| Main barriers to establishing a PCS | 93 hospitals provided 186 barriers |
| Insufficient funding and/or resources | 31 (58) |
| Insufficient staff to support a PCS | 20 (37) |
| Perceived lack of need for a PCS | 14 (27) |
| Lack of support among nonpalliative care physicians | 13 (25) |
| Competing priorities | 8 (15) |
| Don't know/unsure | 14 (24) |
| Main strategies to overcome barriers to establishing a PCS | 65 hospitals provided 72 strategies |
| Reroute funding to establish a PCS | 28 (20) |
| Explain benefits of PCS to staff and community | 24 (17) |
| Provide a framework for how to establish a PCS | 21 (15) |
| Staff for a PCS | 18 (13) |
| Physician support | 10 (7) |
DISCUSSION
Despite citing obstacles to providing PCSs, one‐third of hospitals surveyed report that they are planning to establish a program. As an alternative, many hospitals without a PCS reported that they provide their patients with PC through partnerships with local hospice services. This approach may provide some hospitals with a practical alternative to having a PCS, especially in smaller institutions where budgets and the need for PC are proportionally small. Future surveys should account for this approach to providing PCS to patients. Sharing the strong evidence of return on investment from PCS[6, 7] with hospital leaders could help overcome the perceived barrier of cost and garner financial support. Training programs and technical assistance provided by the Palliative Care Leadership Center initiative and the Center to Advance Palliative Care have a proven track record in helping hospitals establish a PCS through mentored training,[9] and the End‐of‐Life Nursing Education Consortium has demonstrated effectiveness with nursing education.[10] These programs could provide the resources that many hospitals seek. Educating hospital leaders and clinicians about the evidence for PCSs improving care for patients with serious illness may further help to engender support for PCSs. One barrier that may be more difficult to overcome is the lack of trained PC clinicians. Efforts to educate and train generalist clinicians in primary PC may mitigate this shortfall.[1] Increasing the number of trained primary PC clinicians may also reduce fragmentation in patient care and reduce burden on specialist PC clinicians.[11] Specialty PC clinicians can also lend their expertise to hospitals seeking to start a PCS to achieve the goal of universal access to PCS.
Acknowledgements
The authors thank the Hospital Council of Northern and Central California, the Hospital Council of Southern California, and the Hospital Council of San Diego and Imperial Counties for their support in encouraging their members to participate. The authors also thank all of the respondents for their diligence and care in responding to the survey.
Disclosures
The California HealthCare Foundation provided funding to support the administration of the survey and analysis of findings, as well as limited dissemination of results though the foundation's communication venues. The authors report no conflicts of interest.
- Institute of Medicine. Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life. Washington, DC: The National Academies Press; 2014.
- , , , et al. Impact of an inpatient palliative care team: a randomized control trial. J Palliat Med. 2008;11(2):180–190.
- , , , , . A systematic review of satisfaction with care at the end of life. J Am Geriatr Soc. 2008;56(1):124–129.
- . Health care system factors affecting end‐of‐life care. J Palliat Med. 2005;8(suppl 1):S79–S87.
- , , . Impact of palliative care case management on resource use by patients dying of cancer at a Veterans Affairs medical center. J Palliat Med. 2005;8(1):26–35.
- , , , et al. Cost savings associated with US hospital palliative care consultation programs. Arch Intern Med. 2008;168(16):1783–1790.
- , , . Two steps forward, one step back: changes in palliative care consultation services in California hospitals from 2007 to 2011. J Palliat Med. 2014;17(11):1214–1220.
- , . Using qualitative methods to explore key questions in palliative care. J Palliat Med. 2009;12(8):725–730.
- , , . Center to Advance Palliative Care palliative care consultation service metrics: consensus recommendations. J Palliat Med. 2008;11(10):1294–1298.
- , , , et al. Evaluation of the End‐of‐Life Nursing Education Consortium undergraduate faculty training program. J Palliat Med. 2005;8(1):107–114.
- , . Generalist plus specialist palliative care–creating a more sustainable model. N Engl J Med. 2013;368(13):1173–1175.
Palliative care (PC) focuses on relieving distressing symptoms such as pain, dyspnea, fatigue, and depression; providing psychological, social, emotional, and spiritual support; and helping patients choose treatments consistent with their values.[1] Palliative care consultation services (PCSs) increase patient and family satisfaction,[2, 3] improve quality of life,[4] reduce resource utilization,[5] and decrease hospital expenditure.[2, 6] Hospitals that fund a PCS typically realize a sizable return on investment and good value, as these services provide better care at lower cost.[7] These benefits provide a strong rationale for all hospitals to establish a PCS. However, only 53% of acute care hospitals in California offer PC services, and only 37% have a hospital‐based PCS.[7] To increase access for patients with serious illness, it is necessary to understand the barriers that hinder the development of PCS. In this study, we asked leaders from hospitals without a PCS to describe these barriers and identify strategies that could overcome them and promote PCSs.
METHODS
In 2011, we surveyed all acute care hospitals in California to assess the prevalence of PCSs in the state. We defined a PCS as an interdisciplinary team that sees patients, identifies needs, makes treatment recommendations, facilitates patient and/or family decision making, and/or directly provides palliative care for patients with life‐threatening illness and their families. Hospitals that did not have a PCS were asked questions regarding plans to establish one (Is there an effort underway to establish a palliative care program in your hospital?), perceived barriers to starting one (What are 3 significant barriers or circumstances that have prevented your hospital from creating a palliative care program?), and ideas for overcoming barriers (What resources, training, policy changes would be most helpful in overcoming those barriers?). Questions that allowed for open‐ended responses were analyzed using a thematic approach.[8] Themes were initially reviewed by 1 researcher (C.J.B.), then refined and confirmed at each stage using an iterative process with other research team members (D.L.O., S.Z.P.) to reduce potential biases. Questions assessing hospital characteristics and status toward establishing a PCS provided a list of possible answers. Frequencies to these responses are reported accordingly.
RESULTS
Surveys were distributed to 376 acute care hospitals in California, of which 360 responded to the survey, resulting in a 96% response rate. Of the 360 hospitals surveyed, 46% (n=166) reported not offering any PCS. Out of the 166 that did not have PCS, 7 stated they had a PCS at some point in the last 5 years, but the program was discontinued. Hospitals without a PCS were largely for profit (75%, n=125), small with 150 beds (72%, n=120), and not affiliated with a system (63%, n=105). Overall, 34% (43/128) of hospitals reported that they had efforts underway to establish one, with 21% (9/43) expecting to start seeing patients within a year. Seventy‐two hospitals (56%, 72/128) reported that providers from local hospices aided them in providing their patients with PC, and that this approach met the needs of their patients. A total of 93 hospitals identified multiple barriers (n=186) to establishing a PCS, of which 162 responses could be categorized into 5 meaningful themes. Regarding strategies to overcome these barriers, 65 hospitals provided 72 responses that could be categorized into 5 meaningful themes (Table 1).
| Barriers and Strategies | Responses, % (n) |
|---|---|
| |
| Main barriers to establishing a PCS | 93 hospitals provided 186 barriers |
| Insufficient funding and/or resources | 31 (58) |
| Insufficient staff to support a PCS | 20 (37) |
| Perceived lack of need for a PCS | 14 (27) |
| Lack of support among nonpalliative care physicians | 13 (25) |
| Competing priorities | 8 (15) |
| Don't know/unsure | 14 (24) |
| Main strategies to overcome barriers to establishing a PCS | 65 hospitals provided 72 strategies |
| Reroute funding to establish a PCS | 28 (20) |
| Explain benefits of PCS to staff and community | 24 (17) |
| Provide a framework for how to establish a PCS | 21 (15) |
| Staff for a PCS | 18 (13) |
| Physician support | 10 (7) |
DISCUSSION
Despite citing obstacles to providing PCSs, one‐third of hospitals surveyed report that they are planning to establish a program. As an alternative, many hospitals without a PCS reported that they provide their patients with PC through partnerships with local hospice services. This approach may provide some hospitals with a practical alternative to having a PCS, especially in smaller institutions where budgets and the need for PC are proportionally small. Future surveys should account for this approach to providing PCS to patients. Sharing the strong evidence of return on investment from PCS[6, 7] with hospital leaders could help overcome the perceived barrier of cost and garner financial support. Training programs and technical assistance provided by the Palliative Care Leadership Center initiative and the Center to Advance Palliative Care have a proven track record in helping hospitals establish a PCS through mentored training,[9] and the End‐of‐Life Nursing Education Consortium has demonstrated effectiveness with nursing education.[10] These programs could provide the resources that many hospitals seek. Educating hospital leaders and clinicians about the evidence for PCSs improving care for patients with serious illness may further help to engender support for PCSs. One barrier that may be more difficult to overcome is the lack of trained PC clinicians. Efforts to educate and train generalist clinicians in primary PC may mitigate this shortfall.[1] Increasing the number of trained primary PC clinicians may also reduce fragmentation in patient care and reduce burden on specialist PC clinicians.[11] Specialty PC clinicians can also lend their expertise to hospitals seeking to start a PCS to achieve the goal of universal access to PCS.
Acknowledgements
The authors thank the Hospital Council of Northern and Central California, the Hospital Council of Southern California, and the Hospital Council of San Diego and Imperial Counties for their support in encouraging their members to participate. The authors also thank all of the respondents for their diligence and care in responding to the survey.
Disclosures
The California HealthCare Foundation provided funding to support the administration of the survey and analysis of findings, as well as limited dissemination of results though the foundation's communication venues. The authors report no conflicts of interest.
Palliative care (PC) focuses on relieving distressing symptoms such as pain, dyspnea, fatigue, and depression; providing psychological, social, emotional, and spiritual support; and helping patients choose treatments consistent with their values.[1] Palliative care consultation services (PCSs) increase patient and family satisfaction,[2, 3] improve quality of life,[4] reduce resource utilization,[5] and decrease hospital expenditure.[2, 6] Hospitals that fund a PCS typically realize a sizable return on investment and good value, as these services provide better care at lower cost.[7] These benefits provide a strong rationale for all hospitals to establish a PCS. However, only 53% of acute care hospitals in California offer PC services, and only 37% have a hospital‐based PCS.[7] To increase access for patients with serious illness, it is necessary to understand the barriers that hinder the development of PCS. In this study, we asked leaders from hospitals without a PCS to describe these barriers and identify strategies that could overcome them and promote PCSs.
METHODS
In 2011, we surveyed all acute care hospitals in California to assess the prevalence of PCSs in the state. We defined a PCS as an interdisciplinary team that sees patients, identifies needs, makes treatment recommendations, facilitates patient and/or family decision making, and/or directly provides palliative care for patients with life‐threatening illness and their families. Hospitals that did not have a PCS were asked questions regarding plans to establish one (Is there an effort underway to establish a palliative care program in your hospital?), perceived barriers to starting one (What are 3 significant barriers or circumstances that have prevented your hospital from creating a palliative care program?), and ideas for overcoming barriers (What resources, training, policy changes would be most helpful in overcoming those barriers?). Questions that allowed for open‐ended responses were analyzed using a thematic approach.[8] Themes were initially reviewed by 1 researcher (C.J.B.), then refined and confirmed at each stage using an iterative process with other research team members (D.L.O., S.Z.P.) to reduce potential biases. Questions assessing hospital characteristics and status toward establishing a PCS provided a list of possible answers. Frequencies to these responses are reported accordingly.
RESULTS
Surveys were distributed to 376 acute care hospitals in California, of which 360 responded to the survey, resulting in a 96% response rate. Of the 360 hospitals surveyed, 46% (n=166) reported not offering any PCS. Out of the 166 that did not have PCS, 7 stated they had a PCS at some point in the last 5 years, but the program was discontinued. Hospitals without a PCS were largely for profit (75%, n=125), small with 150 beds (72%, n=120), and not affiliated with a system (63%, n=105). Overall, 34% (43/128) of hospitals reported that they had efforts underway to establish one, with 21% (9/43) expecting to start seeing patients within a year. Seventy‐two hospitals (56%, 72/128) reported that providers from local hospices aided them in providing their patients with PC, and that this approach met the needs of their patients. A total of 93 hospitals identified multiple barriers (n=186) to establishing a PCS, of which 162 responses could be categorized into 5 meaningful themes. Regarding strategies to overcome these barriers, 65 hospitals provided 72 responses that could be categorized into 5 meaningful themes (Table 1).
| Barriers and Strategies | Responses, % (n) |
|---|---|
| |
| Main barriers to establishing a PCS | 93 hospitals provided 186 barriers |
| Insufficient funding and/or resources | 31 (58) |
| Insufficient staff to support a PCS | 20 (37) |
| Perceived lack of need for a PCS | 14 (27) |
| Lack of support among nonpalliative care physicians | 13 (25) |
| Competing priorities | 8 (15) |
| Don't know/unsure | 14 (24) |
| Main strategies to overcome barriers to establishing a PCS | 65 hospitals provided 72 strategies |
| Reroute funding to establish a PCS | 28 (20) |
| Explain benefits of PCS to staff and community | 24 (17) |
| Provide a framework for how to establish a PCS | 21 (15) |
| Staff for a PCS | 18 (13) |
| Physician support | 10 (7) |
DISCUSSION
Despite citing obstacles to providing PCSs, one‐third of hospitals surveyed report that they are planning to establish a program. As an alternative, many hospitals without a PCS reported that they provide their patients with PC through partnerships with local hospice services. This approach may provide some hospitals with a practical alternative to having a PCS, especially in smaller institutions where budgets and the need for PC are proportionally small. Future surveys should account for this approach to providing PCS to patients. Sharing the strong evidence of return on investment from PCS[6, 7] with hospital leaders could help overcome the perceived barrier of cost and garner financial support. Training programs and technical assistance provided by the Palliative Care Leadership Center initiative and the Center to Advance Palliative Care have a proven track record in helping hospitals establish a PCS through mentored training,[9] and the End‐of‐Life Nursing Education Consortium has demonstrated effectiveness with nursing education.[10] These programs could provide the resources that many hospitals seek. Educating hospital leaders and clinicians about the evidence for PCSs improving care for patients with serious illness may further help to engender support for PCSs. One barrier that may be more difficult to overcome is the lack of trained PC clinicians. Efforts to educate and train generalist clinicians in primary PC may mitigate this shortfall.[1] Increasing the number of trained primary PC clinicians may also reduce fragmentation in patient care and reduce burden on specialist PC clinicians.[11] Specialty PC clinicians can also lend their expertise to hospitals seeking to start a PCS to achieve the goal of universal access to PCS.
Acknowledgements
The authors thank the Hospital Council of Northern and Central California, the Hospital Council of Southern California, and the Hospital Council of San Diego and Imperial Counties for their support in encouraging their members to participate. The authors also thank all of the respondents for their diligence and care in responding to the survey.
Disclosures
The California HealthCare Foundation provided funding to support the administration of the survey and analysis of findings, as well as limited dissemination of results though the foundation's communication venues. The authors report no conflicts of interest.
- Institute of Medicine. Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life. Washington, DC: The National Academies Press; 2014.
- , , , et al. Impact of an inpatient palliative care team: a randomized control trial. J Palliat Med. 2008;11(2):180–190.
- , , , , . A systematic review of satisfaction with care at the end of life. J Am Geriatr Soc. 2008;56(1):124–129.
- . Health care system factors affecting end‐of‐life care. J Palliat Med. 2005;8(suppl 1):S79–S87.
- , , . Impact of palliative care case management on resource use by patients dying of cancer at a Veterans Affairs medical center. J Palliat Med. 2005;8(1):26–35.
- , , , et al. Cost savings associated with US hospital palliative care consultation programs. Arch Intern Med. 2008;168(16):1783–1790.
- , , . Two steps forward, one step back: changes in palliative care consultation services in California hospitals from 2007 to 2011. J Palliat Med. 2014;17(11):1214–1220.
- , . Using qualitative methods to explore key questions in palliative care. J Palliat Med. 2009;12(8):725–730.
- , , . Center to Advance Palliative Care palliative care consultation service metrics: consensus recommendations. J Palliat Med. 2008;11(10):1294–1298.
- , , , et al. Evaluation of the End‐of‐Life Nursing Education Consortium undergraduate faculty training program. J Palliat Med. 2005;8(1):107–114.
- , . Generalist plus specialist palliative care–creating a more sustainable model. N Engl J Med. 2013;368(13):1173–1175.
- Institute of Medicine. Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life. Washington, DC: The National Academies Press; 2014.
- , , , et al. Impact of an inpatient palliative care team: a randomized control trial. J Palliat Med. 2008;11(2):180–190.
- , , , , . A systematic review of satisfaction with care at the end of life. J Am Geriatr Soc. 2008;56(1):124–129.
- . Health care system factors affecting end‐of‐life care. J Palliat Med. 2005;8(suppl 1):S79–S87.
- , , . Impact of palliative care case management on resource use by patients dying of cancer at a Veterans Affairs medical center. J Palliat Med. 2005;8(1):26–35.
- , , , et al. Cost savings associated with US hospital palliative care consultation programs. Arch Intern Med. 2008;168(16):1783–1790.
- , , . Two steps forward, one step back: changes in palliative care consultation services in California hospitals from 2007 to 2011. J Palliat Med. 2014;17(11):1214–1220.
- , . Using qualitative methods to explore key questions in palliative care. J Palliat Med. 2009;12(8):725–730.
- , , . Center to Advance Palliative Care palliative care consultation service metrics: consensus recommendations. J Palliat Med. 2008;11(10):1294–1298.
- , , , et al. Evaluation of the End‐of‐Life Nursing Education Consortium undergraduate faculty training program. J Palliat Med. 2005;8(1):107–114.
- , . Generalist plus specialist palliative care–creating a more sustainable model. N Engl J Med. 2013;368(13):1173–1175.
Congenital uterine anomalies: A resource of diagnostic images, Part 2
As detailed in Part 1 of this installment on uterine anomalies, a uterus that has developed abnormally can appear to be normal on 2D sonography and on unenhanced sonohysterography (Figure). Without the application of 3D coronal ultrasonography, accurate identification of the fundal contour, and ultimately the type and classification of the uterine anomaly, is not possible.1-3 Fortunately, the lowered cost (compared with magnetic resonance imaging) and the noninvasive nature of this more detailed imaging modality makes its use convenient to both the physician and the patient.
In part 1 of this 2-part installment of our imaging series, we discussed the frequency with which uterine anomalies occur and their types and classifications, as well as offered an imaging library showing the normal endometrial cavity, arcuate uterus, incomplete (partial) uterine septum, and complete uterine septum. Here, we provide two cases demonstrating 3D sonography of the unicornuate, bicornuate, didelphic, and DES-exposed uterus.
A. | B. 
|
C. 
| D. 
|
E. 
| F. 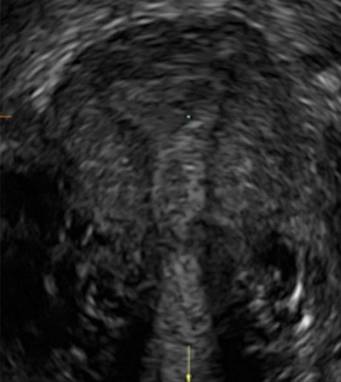
|
G. 
In sagittal view, a uterus with a congenital anomaly can appear normal. Sagittal views of a normal uterus (A) and didelphic uterus (B) and sonohysterogram of a unicornuate uterus (C). Transverse views of a normal (D) and didelphic uterus (E). 3D coronal views of a normal (F) and didelphic uterus (G).
Case 1: Unicornuate uterus
Transverse view of Mirena IUD in right horn and noncommunicating rudimentary left horn.

Case 2: Bicornuate uterus, with concave contour
A patient reporting pelvic pain is examined by 2D sonography, which reveals a bicornuate uterus (A). Note the concave fundal contour (arrow), indicating bicornuate uterus, both horns communicating. 3D imaging (B) revealing fundal “dimple” (concave contour, >1 cm), which is indicative of bicornuate uterus. Complete separation of cavities (C).
A. 
B. 
C. 
Case 3: Didelphic uterus
A patient presenting with primary infertility is found to have a didelphic uterus on 2D and 3D imaging. Note complete separation of uterine cavities on transverse, 2D views (A and B). The left horn sagittal, 2D view shows a normal appearing uterus (C). 3D imaging (D).
A. 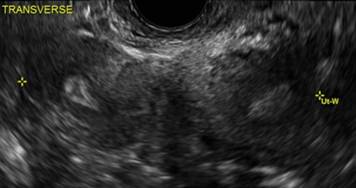
B. 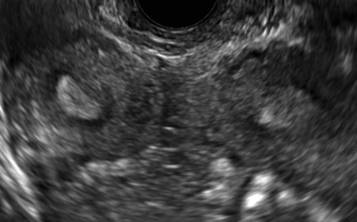
C. 
D. 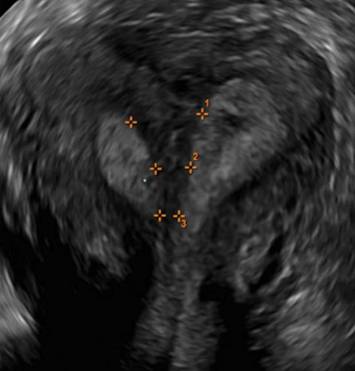
Additional images
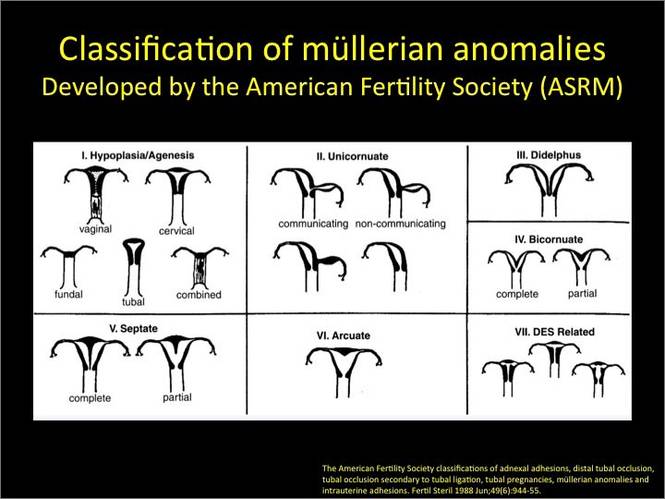
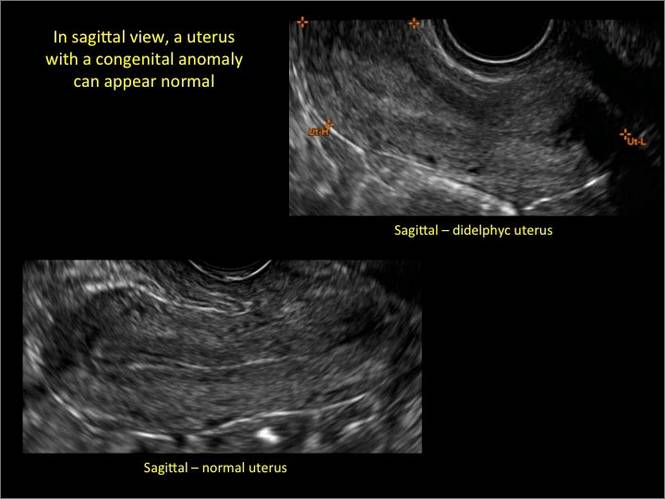
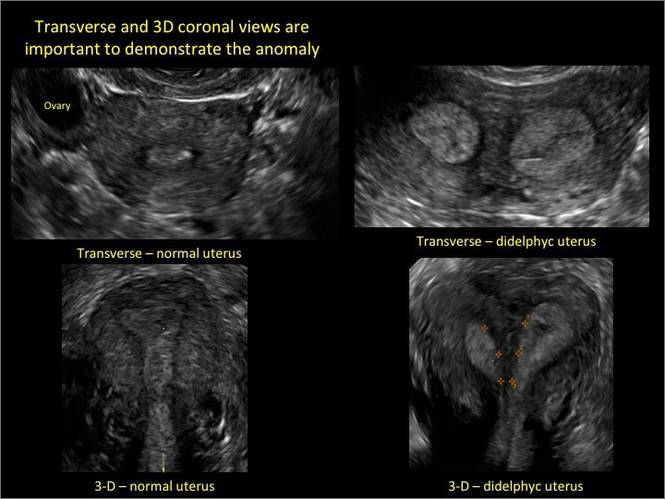
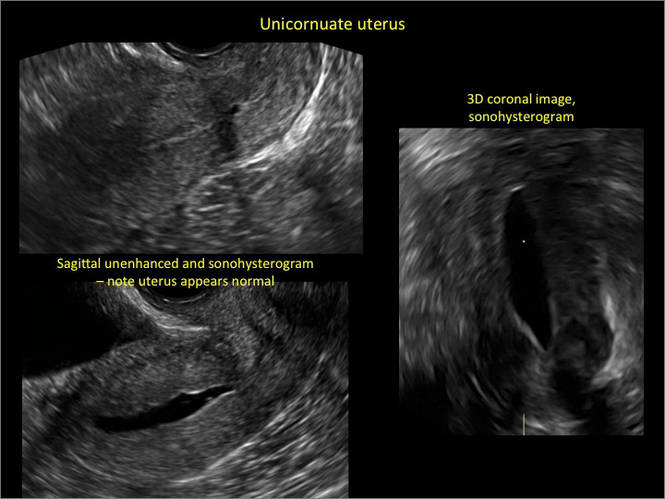
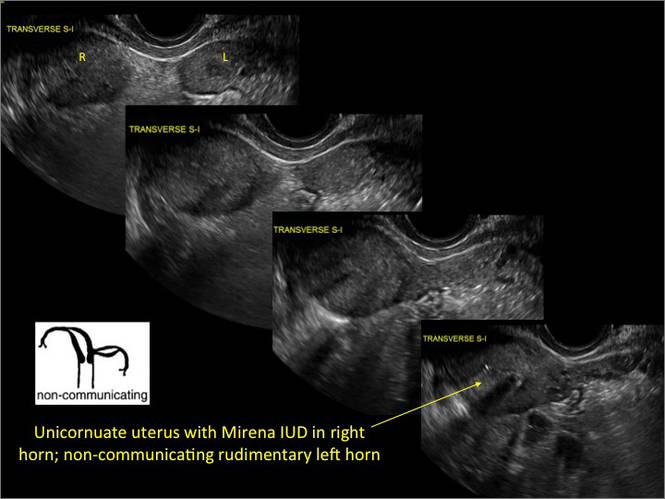
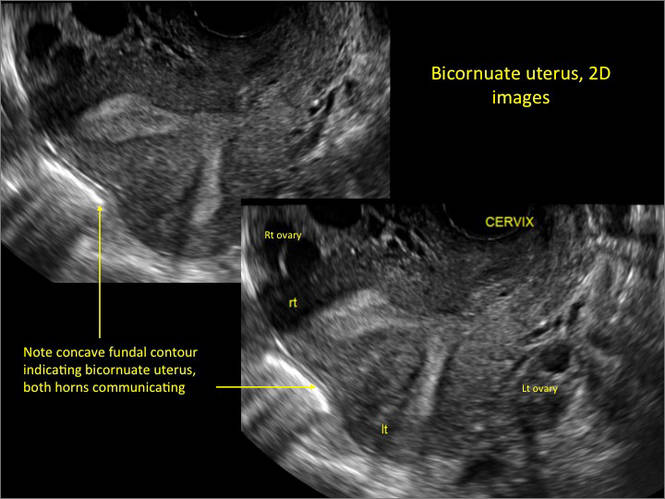
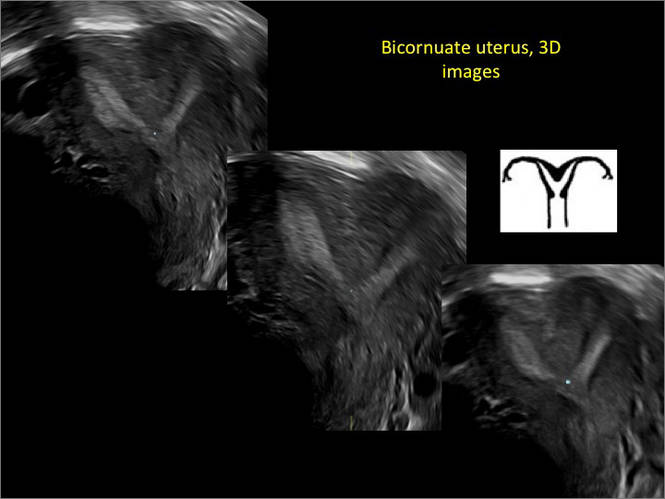
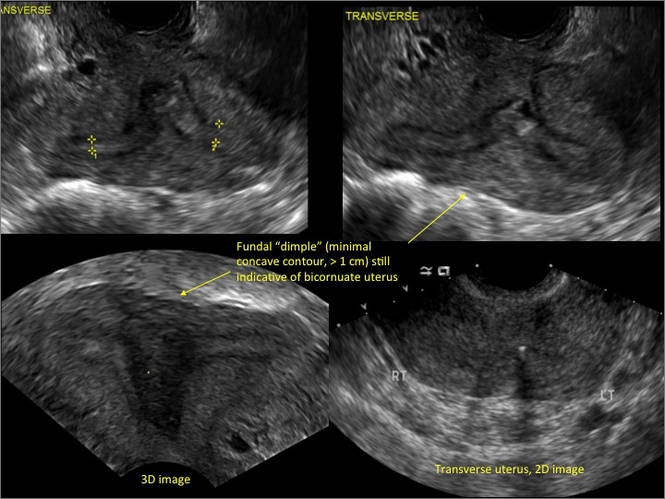
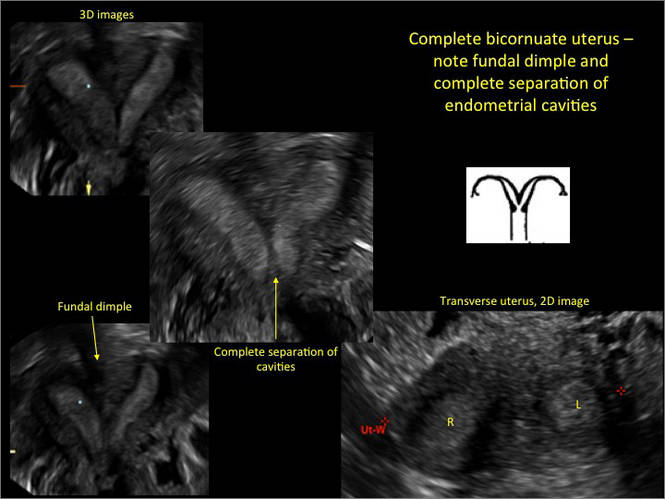
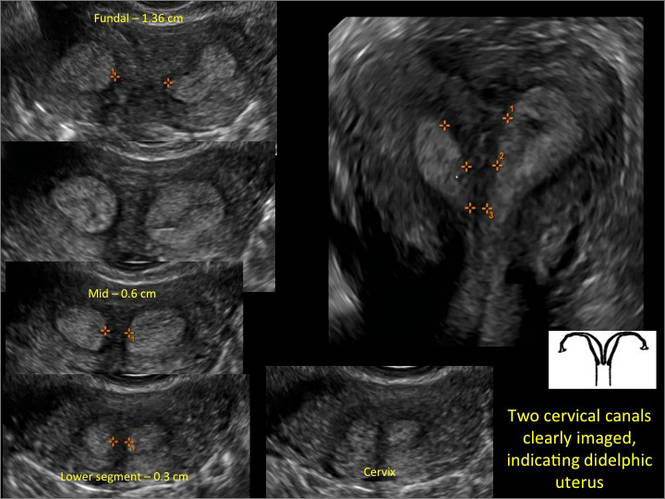

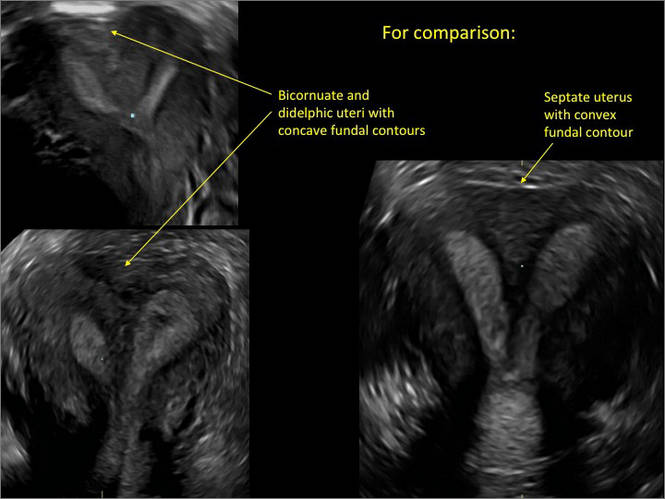
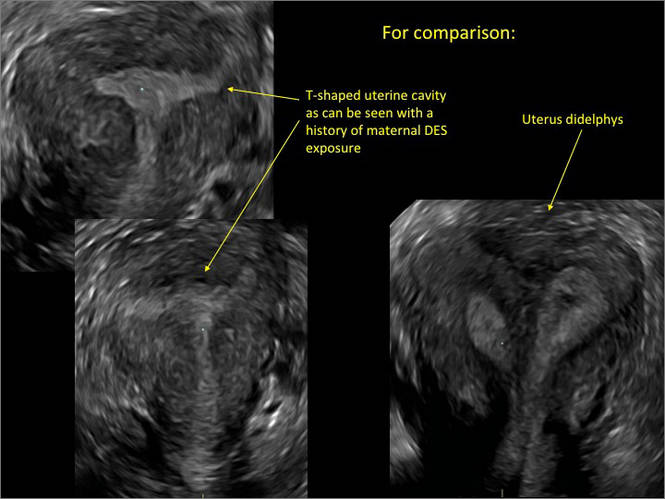
- Deutch T, Bocca S, Oehninger S, et al. Magnetic resonance imaging versus three-dimensional transvaginal ultrasound for the diagnosis of müllerian anomalies [abstract]. Fertil Steril 2006; 86(suppl):S308.15.
- Wu MH, Hsu CC, Huang KE. Detection of congenital müllerian duct anomalies using three-dimensional ultrasound. J Clin Ultrasound 1997; 25:487–492.
- Deutch TD, Abuhamad AZ. The role of 3-dimensional ultrasonography and magnetic resonance imaging in the diagnosis of müllerian duct anomalies: a review of the literature. J Ultrasound Med 2008; 27:413–423.
As detailed in Part 1 of this installment on uterine anomalies, a uterus that has developed abnormally can appear to be normal on 2D sonography and on unenhanced sonohysterography (Figure). Without the application of 3D coronal ultrasonography, accurate identification of the fundal contour, and ultimately the type and classification of the uterine anomaly, is not possible.1-3 Fortunately, the lowered cost (compared with magnetic resonance imaging) and the noninvasive nature of this more detailed imaging modality makes its use convenient to both the physician and the patient.
In part 1 of this 2-part installment of our imaging series, we discussed the frequency with which uterine anomalies occur and their types and classifications, as well as offered an imaging library showing the normal endometrial cavity, arcuate uterus, incomplete (partial) uterine septum, and complete uterine septum. Here, we provide two cases demonstrating 3D sonography of the unicornuate, bicornuate, didelphic, and DES-exposed uterus.
A. | B. 
|
C. 
| D. 
|
E. 
| F. 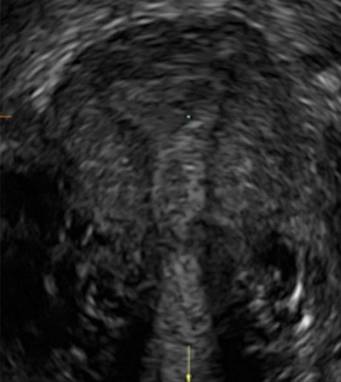
|
G. 
In sagittal view, a uterus with a congenital anomaly can appear normal. Sagittal views of a normal uterus (A) and didelphic uterus (B) and sonohysterogram of a unicornuate uterus (C). Transverse views of a normal (D) and didelphic uterus (E). 3D coronal views of a normal (F) and didelphic uterus (G).
Case 1: Unicornuate uterus
Transverse view of Mirena IUD in right horn and noncommunicating rudimentary left horn.

Case 2: Bicornuate uterus, with concave contour
A patient reporting pelvic pain is examined by 2D sonography, which reveals a bicornuate uterus (A). Note the concave fundal contour (arrow), indicating bicornuate uterus, both horns communicating. 3D imaging (B) revealing fundal “dimple” (concave contour, >1 cm), which is indicative of bicornuate uterus. Complete separation of cavities (C).
A. 
B. 
C. 
Case 3: Didelphic uterus
A patient presenting with primary infertility is found to have a didelphic uterus on 2D and 3D imaging. Note complete separation of uterine cavities on transverse, 2D views (A and B). The left horn sagittal, 2D view shows a normal appearing uterus (C). 3D imaging (D).
A. 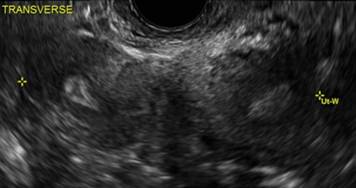
B. 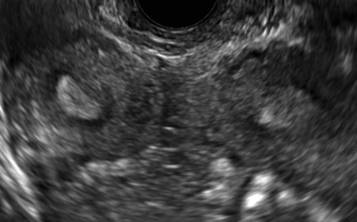
C. 
D. 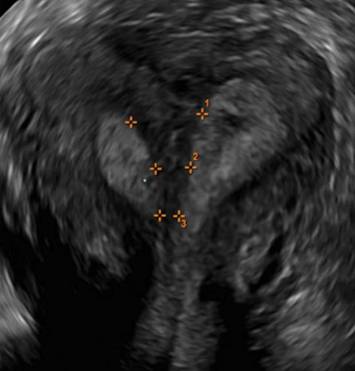
Additional images
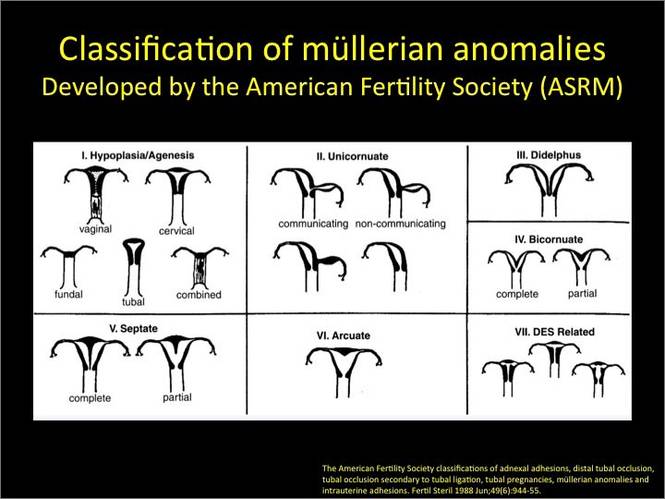
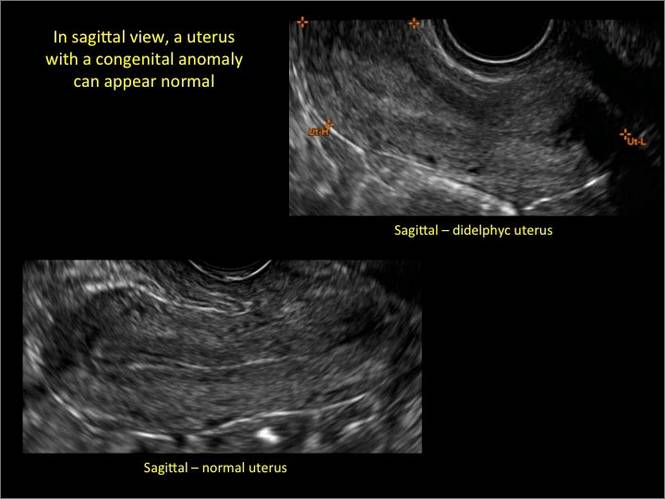
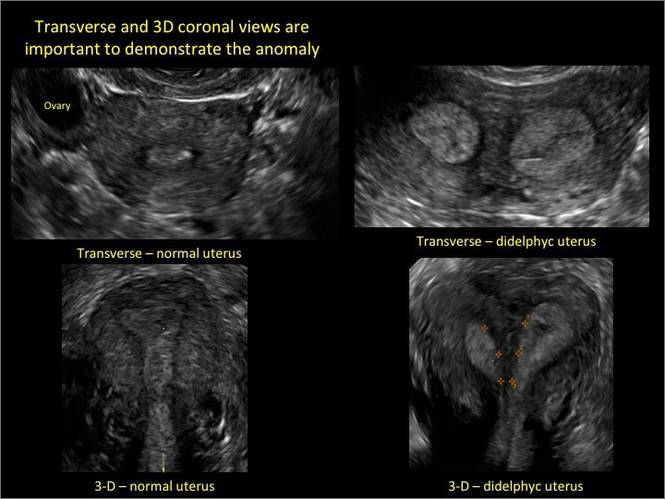
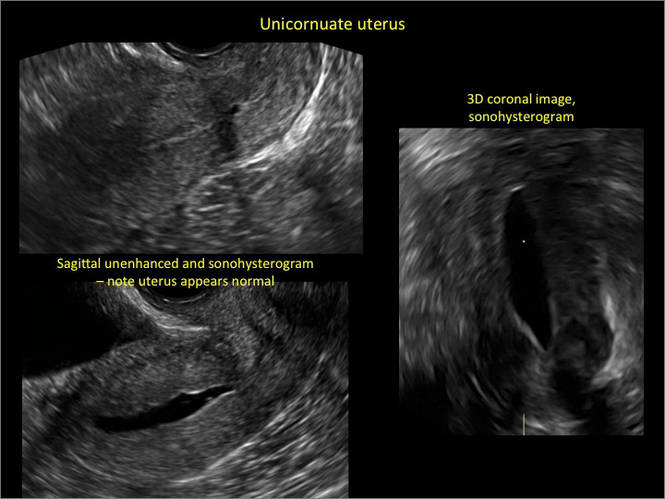
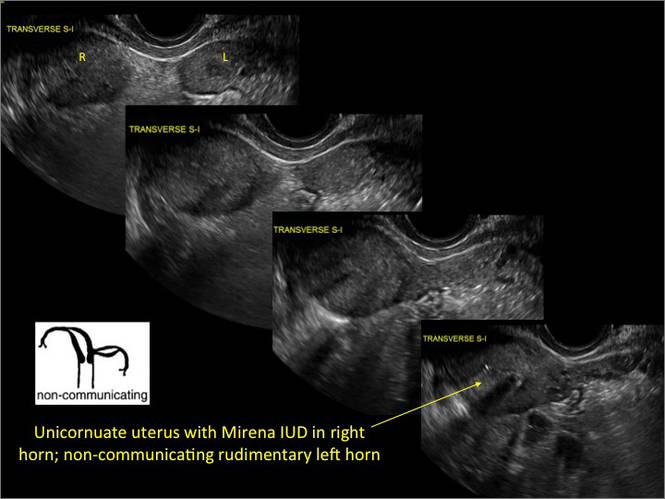
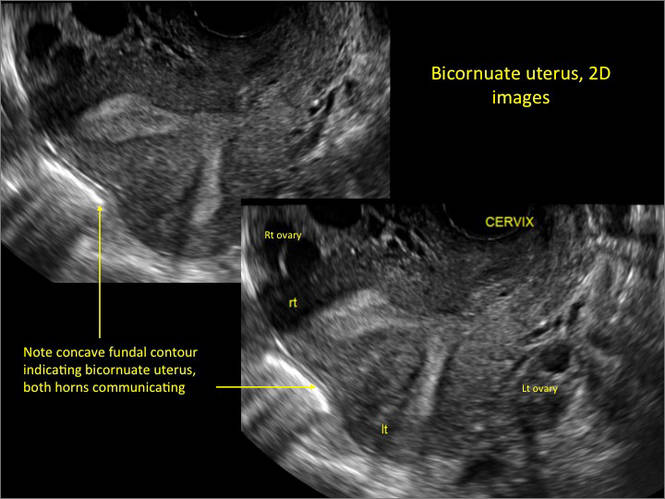
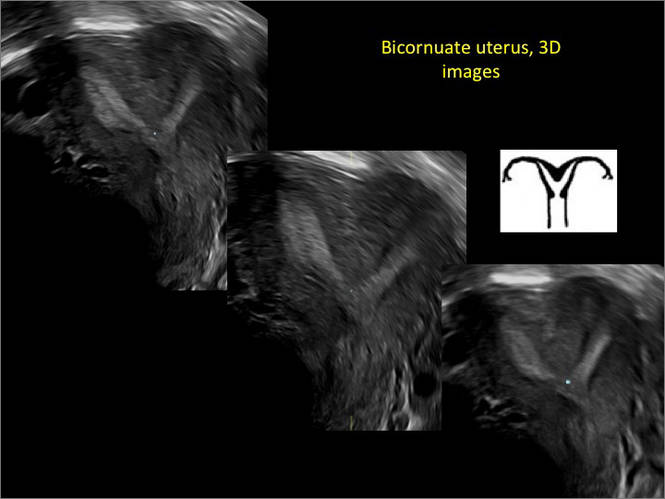
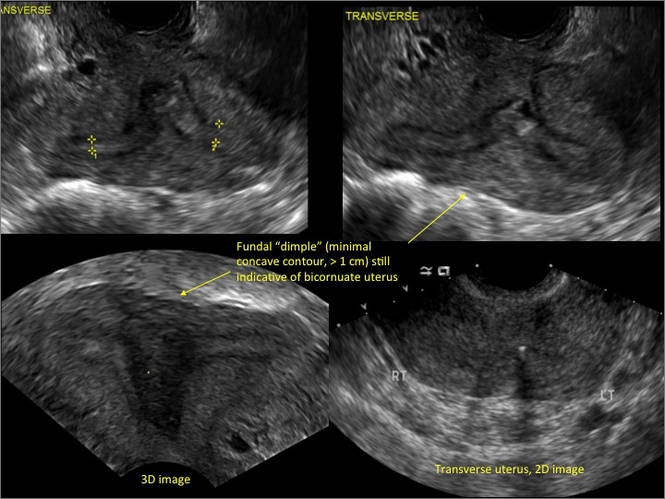
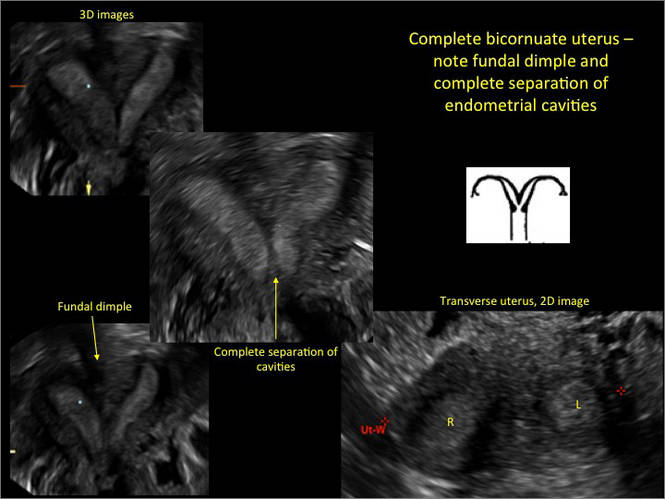
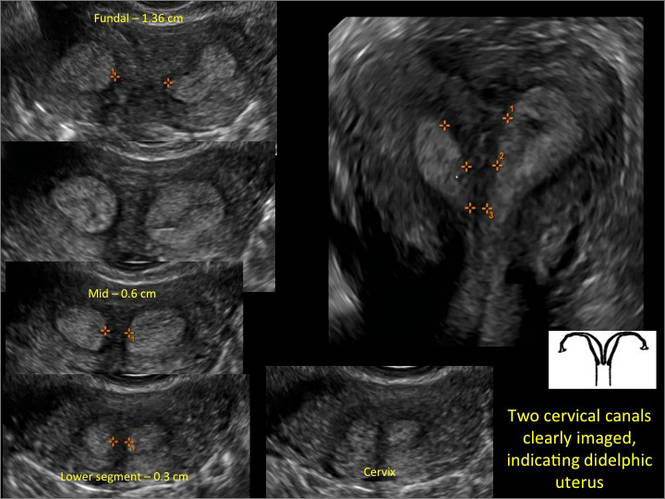

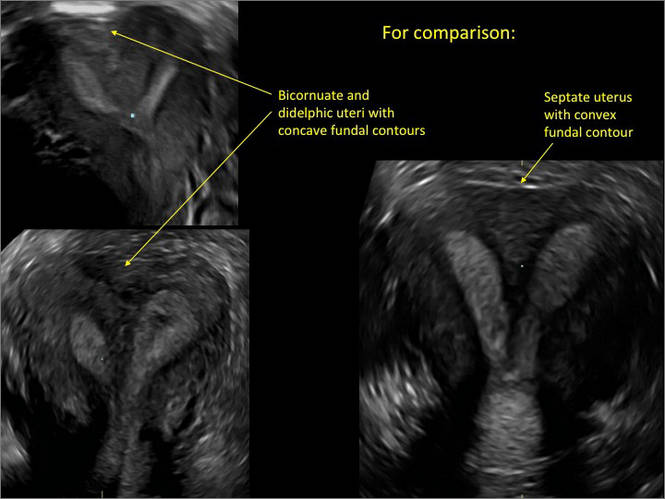
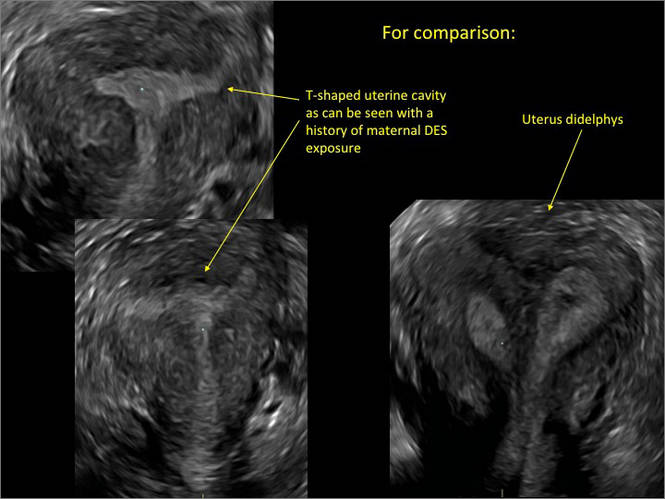
As detailed in Part 1 of this installment on uterine anomalies, a uterus that has developed abnormally can appear to be normal on 2D sonography and on unenhanced sonohysterography (Figure). Without the application of 3D coronal ultrasonography, accurate identification of the fundal contour, and ultimately the type and classification of the uterine anomaly, is not possible.1-3 Fortunately, the lowered cost (compared with magnetic resonance imaging) and the noninvasive nature of this more detailed imaging modality makes its use convenient to both the physician and the patient.
In part 1 of this 2-part installment of our imaging series, we discussed the frequency with which uterine anomalies occur and their types and classifications, as well as offered an imaging library showing the normal endometrial cavity, arcuate uterus, incomplete (partial) uterine septum, and complete uterine septum. Here, we provide two cases demonstrating 3D sonography of the unicornuate, bicornuate, didelphic, and DES-exposed uterus.
A. | B. 
|
C. 
| D. 
|
E. 
| F. 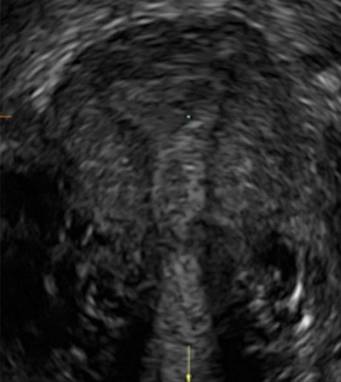
|
G. 
In sagittal view, a uterus with a congenital anomaly can appear normal. Sagittal views of a normal uterus (A) and didelphic uterus (B) and sonohysterogram of a unicornuate uterus (C). Transverse views of a normal (D) and didelphic uterus (E). 3D coronal views of a normal (F) and didelphic uterus (G).
Case 1: Unicornuate uterus
Transverse view of Mirena IUD in right horn and noncommunicating rudimentary left horn.

Case 2: Bicornuate uterus, with concave contour
A patient reporting pelvic pain is examined by 2D sonography, which reveals a bicornuate uterus (A). Note the concave fundal contour (arrow), indicating bicornuate uterus, both horns communicating. 3D imaging (B) revealing fundal “dimple” (concave contour, >1 cm), which is indicative of bicornuate uterus. Complete separation of cavities (C).
A. 
B. 
C. 
Case 3: Didelphic uterus
A patient presenting with primary infertility is found to have a didelphic uterus on 2D and 3D imaging. Note complete separation of uterine cavities on transverse, 2D views (A and B). The left horn sagittal, 2D view shows a normal appearing uterus (C). 3D imaging (D).
A. 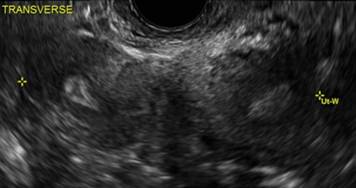
B. 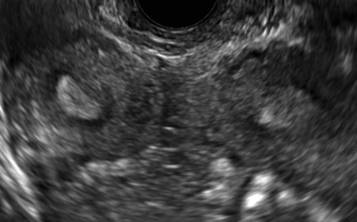
C. 
D. 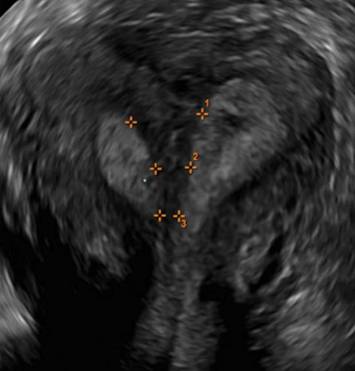
Additional images
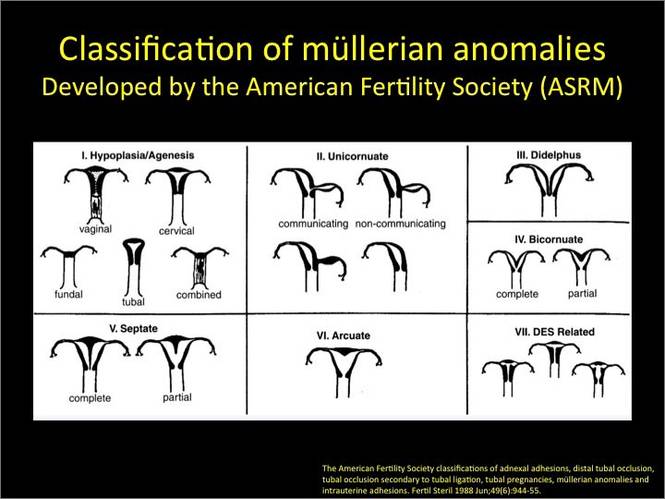
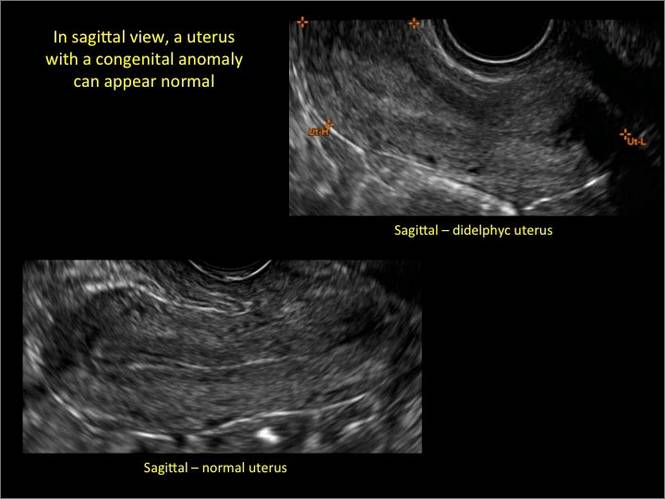
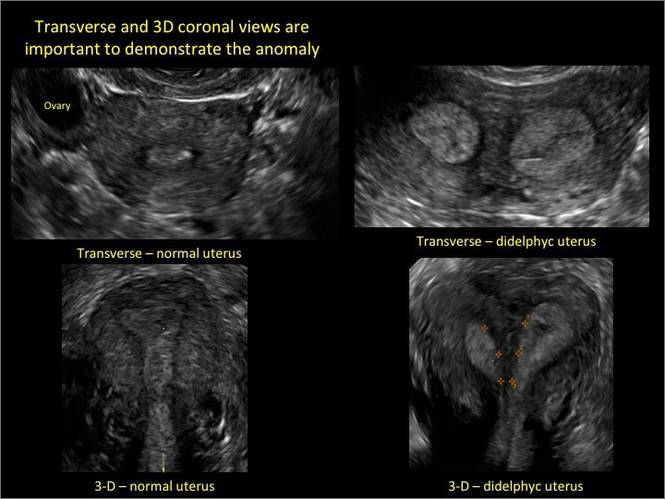
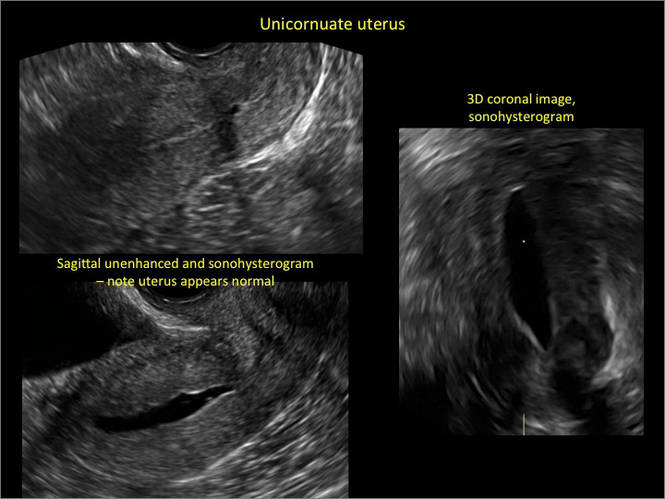
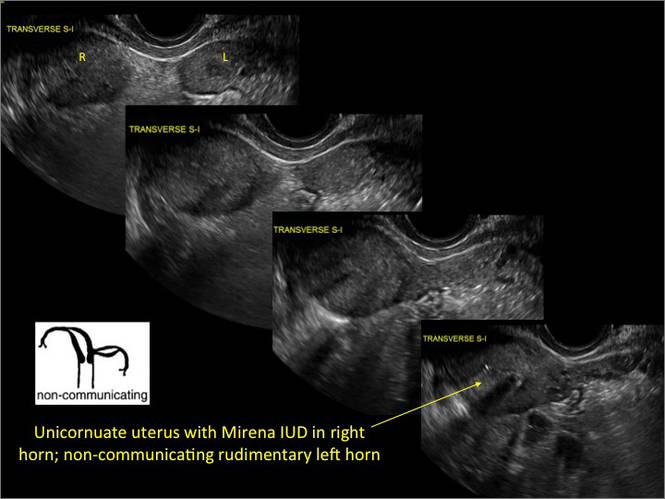
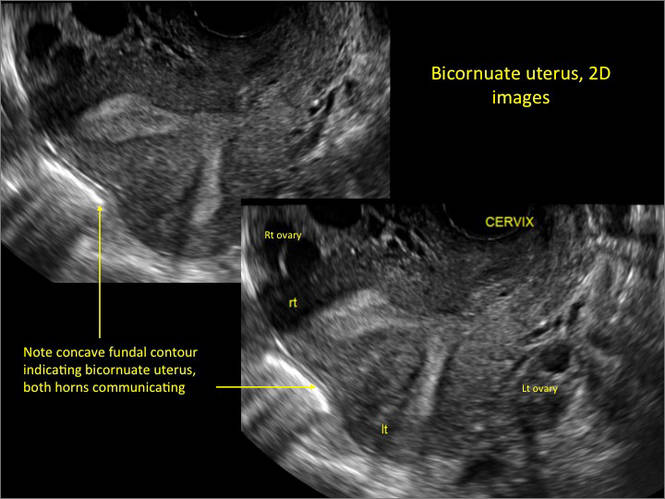
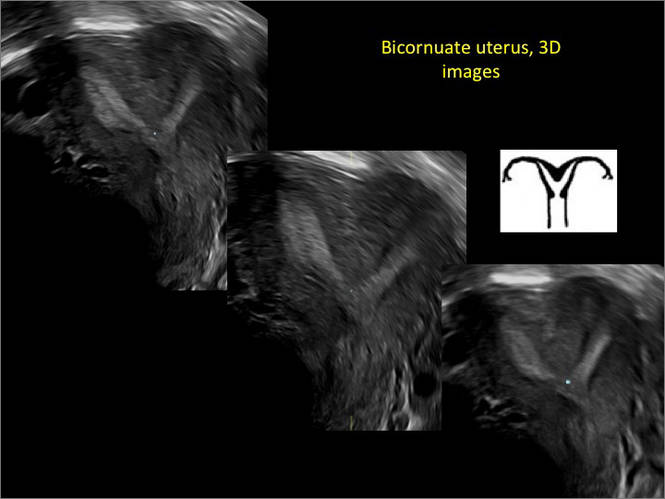
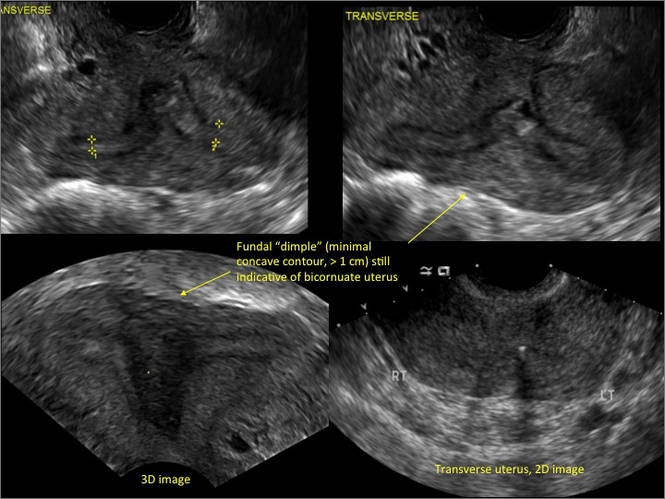
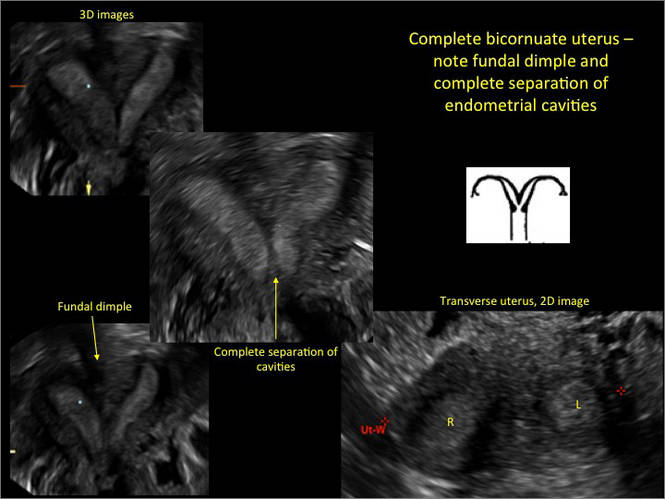
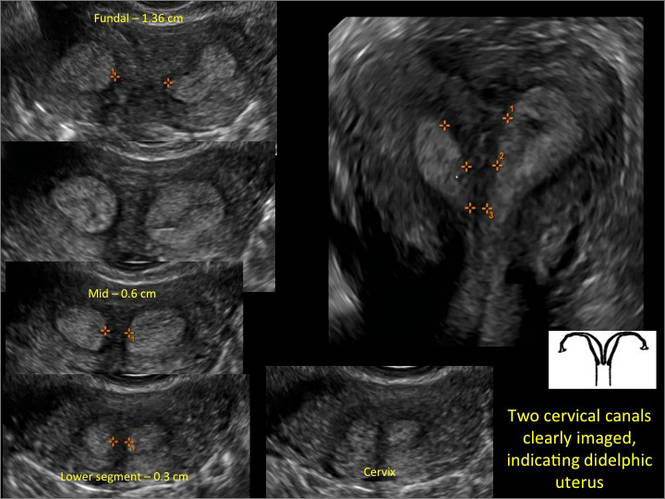

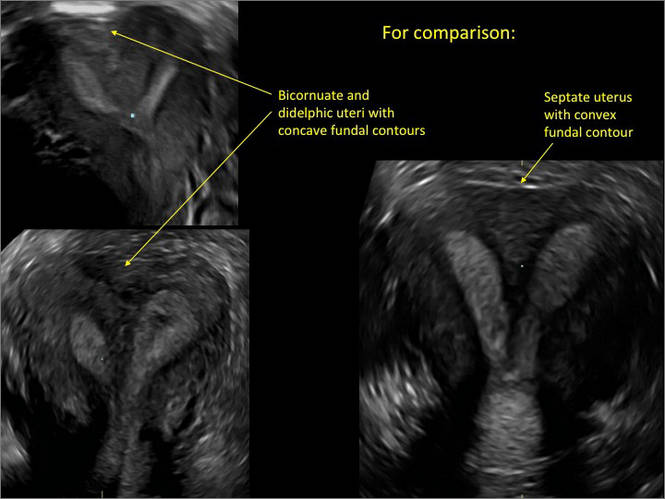
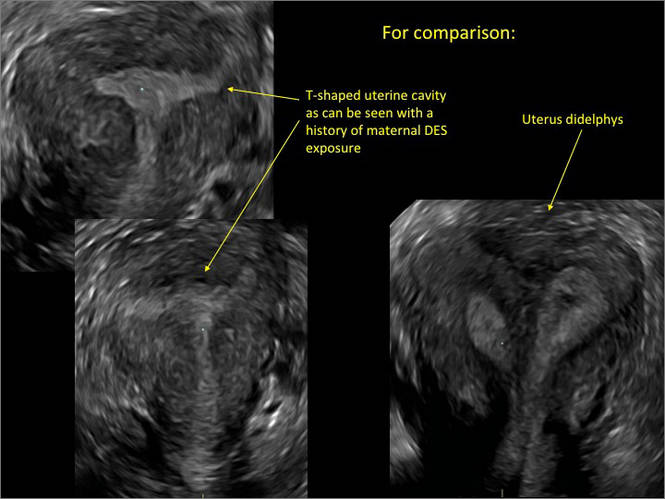
- Deutch T, Bocca S, Oehninger S, et al. Magnetic resonance imaging versus three-dimensional transvaginal ultrasound for the diagnosis of müllerian anomalies [abstract]. Fertil Steril 2006; 86(suppl):S308.15.
- Wu MH, Hsu CC, Huang KE. Detection of congenital müllerian duct anomalies using three-dimensional ultrasound. J Clin Ultrasound 1997; 25:487–492.
- Deutch TD, Abuhamad AZ. The role of 3-dimensional ultrasonography and magnetic resonance imaging in the diagnosis of müllerian duct anomalies: a review of the literature. J Ultrasound Med 2008; 27:413–423.
- Deutch T, Bocca S, Oehninger S, et al. Magnetic resonance imaging versus three-dimensional transvaginal ultrasound for the diagnosis of müllerian anomalies [abstract]. Fertil Steril 2006; 86(suppl):S308.15.
- Wu MH, Hsu CC, Huang KE. Detection of congenital müllerian duct anomalies using three-dimensional ultrasound. J Clin Ultrasound 1997; 25:487–492.
- Deutch TD, Abuhamad AZ. The role of 3-dimensional ultrasonography and magnetic resonance imaging in the diagnosis of müllerian duct anomalies: a review of the literature. J Ultrasound Med 2008; 27:413–423.
CAR-T cell therapy rolls on in pediatric ALL
SAN FRANCISCO – CAR-T cell therapy drove relapsed, refractory acute lymphoblastic leukemia into complete remission in 92% or all but three of 39 children in a phase I/IIa study.
Complete responses were seen within 28 days of receiving a chimeric antigen receptor (CAR)-T cell infusion and have persisted in 15 patients for a year or more, Dr. Stephan A. Grupp reported at the annual meeting of the American Society of Hematology.
Ten relapses have occurred during follow-up of up to 31 months (median 6 months). Half were due to disappearance of the T cells, resulting in CD19-positive relapse, and half were related to antigen escape, resulting in CD19-negative relapse.
Five of the relapsed patients died. No events have been seen in patients who remain in remission after 12 months.
Importantly, CAR-T cell therapy was not used as a bridge to transplant, with only three patients subsequently going on to stem cell transplantation, Dr. Grupp, a pediatric oncologist at the Children’s Hospital of Philadelphia (CHOP) and professor of pediatrics at the University of Pennsylvania, said during a press briefing.
When asked whether CAR-T therapy could be a replacement for transplantation in the future, Dr. Grupp responded, “That would be my fondest hope. We’re not quite there yet, but we’re a lot closer than we used to be.”
The novel immunotherapy first hit the front pages in 2011 after researchers at CHOP and the University of Pennsylvania reported breakthrough results in a handful of children treated with CTL019 cells. T cells are collected from the patient and then genetically reengineered with a CAR directed against tumor B cells expressing the CD19 surface antigen.
More than 130 patients have now been treated by the Pennsylvania team with the CTL019 approach, which received breakthrough therapy status from the Food and Drug Administration in July 2014.
The updated results presented by Dr. Grupp build on those reported earlier this year (N. Engl. J. Med. 2014;371:1507-17) and involve 39 children and young adults. This includes the first 30 pediatric patients with relapsed, refractory ALL treated in the pilot trial. Their median age was 10 years and most were refractory to multiple prior therapies.
At 6 months, the duration of response was 76% and event-free survival was 70%.
The ability of patients to retain their T cells for 6 months or longer was observed in about two-thirds of patients and “is a key point in maintaining remission in these patients,” Dr. Grupp said.
Response rates were independent of disease burden at the time of infusion: 82% response in patients with more than 50% leukemia blast cells, 88% in those with more than 5% blasts, and 100% in those with 0.01%-5% blasts or less than 0.01% blasts.
Patients with higher baseline disease burden (more than 50% blasts), however, were significantly more likely to experience severe cytokine release syndrome (CRS), compared with those with lower disease burden (P < .002).
CRS has been seen across CAR-T cell studies, but there are insufficient data to determine whether this toxicity differs between adult and pediatric patients.
“The key to the cytokine release syndrome, and I believe this carries across platforms and actually may also apply to blinatumomab, is the amplification of the macrophage system through interleukin-6,” Dr. Grupp explained. “This is a classical feedback loop that is actually druggable” using the IL-6 receptor blocker tocilizumab (Actemra).
This strategy produced “remarkable control” of the CRS toxicity, with many of the severe CRS cases experiencing resolution within hours and all cases resolving within 2-3 days, he said.
B-cell aplasia was observed in all responding patients to date and was managed with intravenous immunoglobulin replacement therapy.
The two key questions for the future of CTL019 therapy are toxicity and the logistics of collecting a cell sample and sending it to a centralized manufacturing facility, Dr. Grupp said. This process has already been done on a small scale at CHOP because their cells are made at the University of Pennsylvania. Novartis, which licensed the technology, has built a cell-manufacturing facility and an ongoing phase II study is evaluating whether the technology can be safely rolled out to eight or nine pediatric centers across the country. An adult study will follow, he said.
SAN FRANCISCO – CAR-T cell therapy drove relapsed, refractory acute lymphoblastic leukemia into complete remission in 92% or all but three of 39 children in a phase I/IIa study.
Complete responses were seen within 28 days of receiving a chimeric antigen receptor (CAR)-T cell infusion and have persisted in 15 patients for a year or more, Dr. Stephan A. Grupp reported at the annual meeting of the American Society of Hematology.
Ten relapses have occurred during follow-up of up to 31 months (median 6 months). Half were due to disappearance of the T cells, resulting in CD19-positive relapse, and half were related to antigen escape, resulting in CD19-negative relapse.
Five of the relapsed patients died. No events have been seen in patients who remain in remission after 12 months.
Importantly, CAR-T cell therapy was not used as a bridge to transplant, with only three patients subsequently going on to stem cell transplantation, Dr. Grupp, a pediatric oncologist at the Children’s Hospital of Philadelphia (CHOP) and professor of pediatrics at the University of Pennsylvania, said during a press briefing.
When asked whether CAR-T therapy could be a replacement for transplantation in the future, Dr. Grupp responded, “That would be my fondest hope. We’re not quite there yet, but we’re a lot closer than we used to be.”
The novel immunotherapy first hit the front pages in 2011 after researchers at CHOP and the University of Pennsylvania reported breakthrough results in a handful of children treated with CTL019 cells. T cells are collected from the patient and then genetically reengineered with a CAR directed against tumor B cells expressing the CD19 surface antigen.
More than 130 patients have now been treated by the Pennsylvania team with the CTL019 approach, which received breakthrough therapy status from the Food and Drug Administration in July 2014.
The updated results presented by Dr. Grupp build on those reported earlier this year (N. Engl. J. Med. 2014;371:1507-17) and involve 39 children and young adults. This includes the first 30 pediatric patients with relapsed, refractory ALL treated in the pilot trial. Their median age was 10 years and most were refractory to multiple prior therapies.
At 6 months, the duration of response was 76% and event-free survival was 70%.
The ability of patients to retain their T cells for 6 months or longer was observed in about two-thirds of patients and “is a key point in maintaining remission in these patients,” Dr. Grupp said.
Response rates were independent of disease burden at the time of infusion: 82% response in patients with more than 50% leukemia blast cells, 88% in those with more than 5% blasts, and 100% in those with 0.01%-5% blasts or less than 0.01% blasts.
Patients with higher baseline disease burden (more than 50% blasts), however, were significantly more likely to experience severe cytokine release syndrome (CRS), compared with those with lower disease burden (P < .002).
CRS has been seen across CAR-T cell studies, but there are insufficient data to determine whether this toxicity differs between adult and pediatric patients.
“The key to the cytokine release syndrome, and I believe this carries across platforms and actually may also apply to blinatumomab, is the amplification of the macrophage system through interleukin-6,” Dr. Grupp explained. “This is a classical feedback loop that is actually druggable” using the IL-6 receptor blocker tocilizumab (Actemra).
This strategy produced “remarkable control” of the CRS toxicity, with many of the severe CRS cases experiencing resolution within hours and all cases resolving within 2-3 days, he said.
B-cell aplasia was observed in all responding patients to date and was managed with intravenous immunoglobulin replacement therapy.
The two key questions for the future of CTL019 therapy are toxicity and the logistics of collecting a cell sample and sending it to a centralized manufacturing facility, Dr. Grupp said. This process has already been done on a small scale at CHOP because their cells are made at the University of Pennsylvania. Novartis, which licensed the technology, has built a cell-manufacturing facility and an ongoing phase II study is evaluating whether the technology can be safely rolled out to eight or nine pediatric centers across the country. An adult study will follow, he said.
SAN FRANCISCO – CAR-T cell therapy drove relapsed, refractory acute lymphoblastic leukemia into complete remission in 92% or all but three of 39 children in a phase I/IIa study.
Complete responses were seen within 28 days of receiving a chimeric antigen receptor (CAR)-T cell infusion and have persisted in 15 patients for a year or more, Dr. Stephan A. Grupp reported at the annual meeting of the American Society of Hematology.
Ten relapses have occurred during follow-up of up to 31 months (median 6 months). Half were due to disappearance of the T cells, resulting in CD19-positive relapse, and half were related to antigen escape, resulting in CD19-negative relapse.
Five of the relapsed patients died. No events have been seen in patients who remain in remission after 12 months.
Importantly, CAR-T cell therapy was not used as a bridge to transplant, with only three patients subsequently going on to stem cell transplantation, Dr. Grupp, a pediatric oncologist at the Children’s Hospital of Philadelphia (CHOP) and professor of pediatrics at the University of Pennsylvania, said during a press briefing.
When asked whether CAR-T therapy could be a replacement for transplantation in the future, Dr. Grupp responded, “That would be my fondest hope. We’re not quite there yet, but we’re a lot closer than we used to be.”
The novel immunotherapy first hit the front pages in 2011 after researchers at CHOP and the University of Pennsylvania reported breakthrough results in a handful of children treated with CTL019 cells. T cells are collected from the patient and then genetically reengineered with a CAR directed against tumor B cells expressing the CD19 surface antigen.
More than 130 patients have now been treated by the Pennsylvania team with the CTL019 approach, which received breakthrough therapy status from the Food and Drug Administration in July 2014.
The updated results presented by Dr. Grupp build on those reported earlier this year (N. Engl. J. Med. 2014;371:1507-17) and involve 39 children and young adults. This includes the first 30 pediatric patients with relapsed, refractory ALL treated in the pilot trial. Their median age was 10 years and most were refractory to multiple prior therapies.
At 6 months, the duration of response was 76% and event-free survival was 70%.
The ability of patients to retain their T cells for 6 months or longer was observed in about two-thirds of patients and “is a key point in maintaining remission in these patients,” Dr. Grupp said.
Response rates were independent of disease burden at the time of infusion: 82% response in patients with more than 50% leukemia blast cells, 88% in those with more than 5% blasts, and 100% in those with 0.01%-5% blasts or less than 0.01% blasts.
Patients with higher baseline disease burden (more than 50% blasts), however, were significantly more likely to experience severe cytokine release syndrome (CRS), compared with those with lower disease burden (P < .002).
CRS has been seen across CAR-T cell studies, but there are insufficient data to determine whether this toxicity differs between adult and pediatric patients.
“The key to the cytokine release syndrome, and I believe this carries across platforms and actually may also apply to blinatumomab, is the amplification of the macrophage system through interleukin-6,” Dr. Grupp explained. “This is a classical feedback loop that is actually druggable” using the IL-6 receptor blocker tocilizumab (Actemra).
This strategy produced “remarkable control” of the CRS toxicity, with many of the severe CRS cases experiencing resolution within hours and all cases resolving within 2-3 days, he said.
B-cell aplasia was observed in all responding patients to date and was managed with intravenous immunoglobulin replacement therapy.
The two key questions for the future of CTL019 therapy are toxicity and the logistics of collecting a cell sample and sending it to a centralized manufacturing facility, Dr. Grupp said. This process has already been done on a small scale at CHOP because their cells are made at the University of Pennsylvania. Novartis, which licensed the technology, has built a cell-manufacturing facility and an ongoing phase II study is evaluating whether the technology can be safely rolled out to eight or nine pediatric centers across the country. An adult study will follow, he said.
AT ASH 2014
Key clinical point: CAR-T cell therapy continues to provide durable responses in early studies of children with refractory ALL.
Major finding: Complete remission occurred in 36 of 39 patients (92%) treated with CAR-T cell therapy.
Data source: Phase I/IIa a study in 39 children and young adults with relapsed, refractory acute lymphoblastic leukemia.
Disclosures: The authors reported financial ties with Novartis, the study sponsor.