User login
What’s in the pipeline for female sexual problems?
LAS VEGAS – Female desire and sexual function involve a complicated and interconnected cascade of hormones and neurotransmitters, each providing a potential target for modulation in cases of low desire or sexual dysfunction.
There are some pharmacologic options available now and more drugs in the pipeline, Dr. Roya Rezaee said at the NAMS 2015 annual meeting.
Dr. Rezaee, codirector of the Program for Sexual Health and Vulvovaginal Disorders at University Hospitals Case Medical Center, Cleveland, explained how each treatment acts in the chemical cascade of desire and sexual response.* Though much remains unknown, researchers have identified neurochemical pathways of desire and arousal that act on the brain stem, the hypothalamus, and the amygdala.
Among the neurotransmitters and neurohormones thought to promote female sexual function, dopamine and melanocortin are associated with attention and desire, while norepinephrine and oxytocin are more directly related to arousal. Estrogen and testosterone function as excitatory neurohormones. Serotonin, because it is associated with satiety, may be inhibitory, as are prolactin and the endogenous opioids and endocannabinoids.
In the peripheral tissues, the presence of sex hormones maintains general genital function. For example, estradiol not only promotes vaginal lubrication, but also helps maintain adequate blood flow to the vagina and clitoris. Exogenous testosterone can directly influence the amount of unbound estrogen as well as testosterone, said Dr. Rezaee. Higher testosterone levels downregulate sex hormone–binding globulin, increasing circulating levels of free estrogen and testosterone.
“For women, low testosterone does not always correlate with low desire, but testosterone administration has been shown to be efficacious for low desire,” Dr. Rezaee said. “People are still writing prescriptions for testosterone off label, because a lot of us believe in the data,” she said, adding that a 2009 Cochrane review showed a good safety profile for testosterone.
Targeting dopaminergic pathways to increase desire, an extended-release daily oral combination of trazodone and bupropion, to be marketed as Lorexys, is about to begin phase III clinical trials. Bupropion, a norepinephrine and dopamine reuptake inhibitor, has been known to have prosexual side effects, Dr. Rezaee said. Both ingredients in Lorexys are currently approved as antidepressants.
Increasing available norepinephrine may help with focus and attention, and increase subjective sexual excitement. However, the ADHD and antidepressant medications that increase norepinephrine carry significant side effects and should not be what physicians use to help their patients with low desire, Dr. Rezaee said.
“Serotonin may have a role in low desire by acting as a sexual satiety signal, and SSRIs are serotonergic agents that inhibit desire, arousal, and orgasm in the brain and in the tissue,” she said.
However, there are seven known families of serotonin receptors, and selective modulation specifically of the 5-hydroxytryptamine receptor 1A and 5-HT2A receptors may have prosexual effects. The newly approved medication flibanserin (Addyi) is a selective agonist for 5-HT1A and an antagonist for 5-HT2A receptors. Flibanserin is also thought to produce upregulation in dopamine and norepinephrine in the prefrontal cortex, combating the satiety signals from serotonin and leading to increased desire.
Other medications that are 5-HT1A agonists with potential prosexual effects include buspirone (Buspar) and trazodone (Desyrel, Oleptro).
Blockade of phosphodiesterase type 5 (PDE5) permits relaxation of smooth muscles in arterial walls and increases blood flow to erectile tissues. PDE5 inhibitors such as sildenafil (Viagra) may be of benefit to some women as well, said Dr. Rezaee, though they do not address low desire.
“Newer data support the use of PDE5 inhibitors with women who suffer from SSRI-induced orgasmic complaints of increased latency or decreased intensity, or anorgasmia,” she said. A dose of 25-50 mg of sildenafil 1 hour before sexual activity may help these patients, she advised.
Phase II trials have been completed for two other combination drugs to treat female sexual problems. Lybrido is a combination of testosterone and sildenafil, while Lybridos combines testosterone with buspirone. Both products are oral tablets, taken on demand.
Bremelanotide is a first-in-class drug in development as a melanocortin agonist. This drug, meant to be used on demand to activate an endogenous pathway that increases attention and desire, is in phase III clinical trials.
Dr. Rezaee reported having no relevant financial disclosures.
[email protected]
On Twitter @karioakes
*Correction, 10/20/2015: An earlier version of this story misstated Dr. Rezaee's title.
LAS VEGAS – Female desire and sexual function involve a complicated and interconnected cascade of hormones and neurotransmitters, each providing a potential target for modulation in cases of low desire or sexual dysfunction.
There are some pharmacologic options available now and more drugs in the pipeline, Dr. Roya Rezaee said at the NAMS 2015 annual meeting.
Dr. Rezaee, codirector of the Program for Sexual Health and Vulvovaginal Disorders at University Hospitals Case Medical Center, Cleveland, explained how each treatment acts in the chemical cascade of desire and sexual response.* Though much remains unknown, researchers have identified neurochemical pathways of desire and arousal that act on the brain stem, the hypothalamus, and the amygdala.
Among the neurotransmitters and neurohormones thought to promote female sexual function, dopamine and melanocortin are associated with attention and desire, while norepinephrine and oxytocin are more directly related to arousal. Estrogen and testosterone function as excitatory neurohormones. Serotonin, because it is associated with satiety, may be inhibitory, as are prolactin and the endogenous opioids and endocannabinoids.
In the peripheral tissues, the presence of sex hormones maintains general genital function. For example, estradiol not only promotes vaginal lubrication, but also helps maintain adequate blood flow to the vagina and clitoris. Exogenous testosterone can directly influence the amount of unbound estrogen as well as testosterone, said Dr. Rezaee. Higher testosterone levels downregulate sex hormone–binding globulin, increasing circulating levels of free estrogen and testosterone.
“For women, low testosterone does not always correlate with low desire, but testosterone administration has been shown to be efficacious for low desire,” Dr. Rezaee said. “People are still writing prescriptions for testosterone off label, because a lot of us believe in the data,” she said, adding that a 2009 Cochrane review showed a good safety profile for testosterone.
Targeting dopaminergic pathways to increase desire, an extended-release daily oral combination of trazodone and bupropion, to be marketed as Lorexys, is about to begin phase III clinical trials. Bupropion, a norepinephrine and dopamine reuptake inhibitor, has been known to have prosexual side effects, Dr. Rezaee said. Both ingredients in Lorexys are currently approved as antidepressants.
Increasing available norepinephrine may help with focus and attention, and increase subjective sexual excitement. However, the ADHD and antidepressant medications that increase norepinephrine carry significant side effects and should not be what physicians use to help their patients with low desire, Dr. Rezaee said.
“Serotonin may have a role in low desire by acting as a sexual satiety signal, and SSRIs are serotonergic agents that inhibit desire, arousal, and orgasm in the brain and in the tissue,” she said.
However, there are seven known families of serotonin receptors, and selective modulation specifically of the 5-hydroxytryptamine receptor 1A and 5-HT2A receptors may have prosexual effects. The newly approved medication flibanserin (Addyi) is a selective agonist for 5-HT1A and an antagonist for 5-HT2A receptors. Flibanserin is also thought to produce upregulation in dopamine and norepinephrine in the prefrontal cortex, combating the satiety signals from serotonin and leading to increased desire.
Other medications that are 5-HT1A agonists with potential prosexual effects include buspirone (Buspar) and trazodone (Desyrel, Oleptro).
Blockade of phosphodiesterase type 5 (PDE5) permits relaxation of smooth muscles in arterial walls and increases blood flow to erectile tissues. PDE5 inhibitors such as sildenafil (Viagra) may be of benefit to some women as well, said Dr. Rezaee, though they do not address low desire.
“Newer data support the use of PDE5 inhibitors with women who suffer from SSRI-induced orgasmic complaints of increased latency or decreased intensity, or anorgasmia,” she said. A dose of 25-50 mg of sildenafil 1 hour before sexual activity may help these patients, she advised.
Phase II trials have been completed for two other combination drugs to treat female sexual problems. Lybrido is a combination of testosterone and sildenafil, while Lybridos combines testosterone with buspirone. Both products are oral tablets, taken on demand.
Bremelanotide is a first-in-class drug in development as a melanocortin agonist. This drug, meant to be used on demand to activate an endogenous pathway that increases attention and desire, is in phase III clinical trials.
Dr. Rezaee reported having no relevant financial disclosures.
[email protected]
On Twitter @karioakes
*Correction, 10/20/2015: An earlier version of this story misstated Dr. Rezaee's title.
LAS VEGAS – Female desire and sexual function involve a complicated and interconnected cascade of hormones and neurotransmitters, each providing a potential target for modulation in cases of low desire or sexual dysfunction.
There are some pharmacologic options available now and more drugs in the pipeline, Dr. Roya Rezaee said at the NAMS 2015 annual meeting.
Dr. Rezaee, codirector of the Program for Sexual Health and Vulvovaginal Disorders at University Hospitals Case Medical Center, Cleveland, explained how each treatment acts in the chemical cascade of desire and sexual response.* Though much remains unknown, researchers have identified neurochemical pathways of desire and arousal that act on the brain stem, the hypothalamus, and the amygdala.
Among the neurotransmitters and neurohormones thought to promote female sexual function, dopamine and melanocortin are associated with attention and desire, while norepinephrine and oxytocin are more directly related to arousal. Estrogen and testosterone function as excitatory neurohormones. Serotonin, because it is associated with satiety, may be inhibitory, as are prolactin and the endogenous opioids and endocannabinoids.
In the peripheral tissues, the presence of sex hormones maintains general genital function. For example, estradiol not only promotes vaginal lubrication, but also helps maintain adequate blood flow to the vagina and clitoris. Exogenous testosterone can directly influence the amount of unbound estrogen as well as testosterone, said Dr. Rezaee. Higher testosterone levels downregulate sex hormone–binding globulin, increasing circulating levels of free estrogen and testosterone.
“For women, low testosterone does not always correlate with low desire, but testosterone administration has been shown to be efficacious for low desire,” Dr. Rezaee said. “People are still writing prescriptions for testosterone off label, because a lot of us believe in the data,” she said, adding that a 2009 Cochrane review showed a good safety profile for testosterone.
Targeting dopaminergic pathways to increase desire, an extended-release daily oral combination of trazodone and bupropion, to be marketed as Lorexys, is about to begin phase III clinical trials. Bupropion, a norepinephrine and dopamine reuptake inhibitor, has been known to have prosexual side effects, Dr. Rezaee said. Both ingredients in Lorexys are currently approved as antidepressants.
Increasing available norepinephrine may help with focus and attention, and increase subjective sexual excitement. However, the ADHD and antidepressant medications that increase norepinephrine carry significant side effects and should not be what physicians use to help their patients with low desire, Dr. Rezaee said.
“Serotonin may have a role in low desire by acting as a sexual satiety signal, and SSRIs are serotonergic agents that inhibit desire, arousal, and orgasm in the brain and in the tissue,” she said.
However, there are seven known families of serotonin receptors, and selective modulation specifically of the 5-hydroxytryptamine receptor 1A and 5-HT2A receptors may have prosexual effects. The newly approved medication flibanserin (Addyi) is a selective agonist for 5-HT1A and an antagonist for 5-HT2A receptors. Flibanserin is also thought to produce upregulation in dopamine and norepinephrine in the prefrontal cortex, combating the satiety signals from serotonin and leading to increased desire.
Other medications that are 5-HT1A agonists with potential prosexual effects include buspirone (Buspar) and trazodone (Desyrel, Oleptro).
Blockade of phosphodiesterase type 5 (PDE5) permits relaxation of smooth muscles in arterial walls and increases blood flow to erectile tissues. PDE5 inhibitors such as sildenafil (Viagra) may be of benefit to some women as well, said Dr. Rezaee, though they do not address low desire.
“Newer data support the use of PDE5 inhibitors with women who suffer from SSRI-induced orgasmic complaints of increased latency or decreased intensity, or anorgasmia,” she said. A dose of 25-50 mg of sildenafil 1 hour before sexual activity may help these patients, she advised.
Phase II trials have been completed for two other combination drugs to treat female sexual problems. Lybrido is a combination of testosterone and sildenafil, while Lybridos combines testosterone with buspirone. Both products are oral tablets, taken on demand.
Bremelanotide is a first-in-class drug in development as a melanocortin agonist. This drug, meant to be used on demand to activate an endogenous pathway that increases attention and desire, is in phase III clinical trials.
Dr. Rezaee reported having no relevant financial disclosures.
[email protected]
On Twitter @karioakes
*Correction, 10/20/2015: An earlier version of this story misstated Dr. Rezaee's title.
EXPERT ANALYSIS FROM THE NAMS 2015 ANNUAL MEETING
Anticoagulant Reversal Agent Praxbind Gets Approved
The U.S. Food and Drug Administration on Friday gave accelerated approval to Boehringer Ingelheim's Praxbind (idarucizumab) for use in patients who are taking the anticoagulant Pradaxa (dabigatran) during emergency situations when there is a need to reverse Pradaxa's blood-thinning effects.
"The anticoagulant effects of Pradaxa are important and life-saving for some patients, but there are situations where reversal of the drug's effects is medically necessary," Dr. Richard Pazdur, director of the Office of Hematology and Oncology Products in the FDA's Center for Drug Evaluation and Research, said in a statement.
"Today's approval offers the medical community an important tool for managing patients taking Pradaxa in emergency or life-threatening situations when bleeding can't be controlled," he added.
The FDA approved Pradaxa in 2010 to prevent stroke and systemic blood clots in patients with atrial fibrillation, as well as for the treatment and prevention of deep venous thrombosis and pulmonary embolism.
Praxbind is the first reversal agent approved specifically for Pradaxa and works by binding to the drug compound to neutralize its effect, the FDA said.
The U.S. Food and Drug Administration on Friday gave accelerated approval to Boehringer Ingelheim's Praxbind (idarucizumab) for use in patients who are taking the anticoagulant Pradaxa (dabigatran) during emergency situations when there is a need to reverse Pradaxa's blood-thinning effects.
"The anticoagulant effects of Pradaxa are important and life-saving for some patients, but there are situations where reversal of the drug's effects is medically necessary," Dr. Richard Pazdur, director of the Office of Hematology and Oncology Products in the FDA's Center for Drug Evaluation and Research, said in a statement.
"Today's approval offers the medical community an important tool for managing patients taking Pradaxa in emergency or life-threatening situations when bleeding can't be controlled," he added.
The FDA approved Pradaxa in 2010 to prevent stroke and systemic blood clots in patients with atrial fibrillation, as well as for the treatment and prevention of deep venous thrombosis and pulmonary embolism.
Praxbind is the first reversal agent approved specifically for Pradaxa and works by binding to the drug compound to neutralize its effect, the FDA said.
The U.S. Food and Drug Administration on Friday gave accelerated approval to Boehringer Ingelheim's Praxbind (idarucizumab) for use in patients who are taking the anticoagulant Pradaxa (dabigatran) during emergency situations when there is a need to reverse Pradaxa's blood-thinning effects.
"The anticoagulant effects of Pradaxa are important and life-saving for some patients, but there are situations where reversal of the drug's effects is medically necessary," Dr. Richard Pazdur, director of the Office of Hematology and Oncology Products in the FDA's Center for Drug Evaluation and Research, said in a statement.
"Today's approval offers the medical community an important tool for managing patients taking Pradaxa in emergency or life-threatening situations when bleeding can't be controlled," he added.
The FDA approved Pradaxa in 2010 to prevent stroke and systemic blood clots in patients with atrial fibrillation, as well as for the treatment and prevention of deep venous thrombosis and pulmonary embolism.
Praxbind is the first reversal agent approved specifically for Pradaxa and works by binding to the drug compound to neutralize its effect, the FDA said.
ACS: Less pneumonia, fewer deaths with ketamine for rib fracture pain
CHICAGO – Ketamine is a safe and simple alternative to epidural anesthesia for pain control in the setting of multiple rib fractures, investigators from the Jacobi Medical Center in the Bronx (N.Y.) concluded after reviewing their experience with the drug.
Epidural analgesia has been the standard for controlling pain after multiple rib fractures, but epidurals are sometimes contraindicated in trauma, especially with back and neck injuries. There’s also a bleeding risk, and the need for an on-call anesthesia team to place them, something not all hospitals have.
Those problems – and the success Jacobi surgeons reported with ketamine pain control after thoracotomy – led the hospital to switch to a ketamine-based rib fracture protocol in 2007.
“As far as we know, we are the only people doing this routinely for multiple rib fractures,” Dr. Joelle Getrajdman, a second-year surgery resident at the medical center, said at the annual clinical congress of the American College of Surgeons.
Patients there with two or more rib fractures get a low-dose peripheral intravenous infusion of ketamine 0.05 mg/kg per hour while in the ICU and step-down unit, along with other pain medications as indicated. The hospital discontinues ketamine once patients leave the step-down unit to prevent diversion for illicit use.
To see how well the protocol has worked, the investigators reviewed all 128 adult trauma patients who received ketamine for multiple rib fractures from 2007 to 2014.
These patients were 60 years old on average, with a median of six rib fractures, many of them bilateral. Almost half had injury severity scores above 15, and most had chest Abbreviated Injury Scores of at least 3. Pneumo- and hemothoraces were common. Patients spent a mean of 6 days in the surgical ICU and 13 days in the hospital.
Along with ketamine, almost all had a morphine or hydromorphone (Dilaudid) patient-controlled analgesia (PCA) pumps, more than half received IV ketorolac (Toradol), and about 40% IV Tylenol. Only 14% had paravertebral or intercostal blocks.
Fourteen patients (10.9%) developed pneumonia, and four (3.1%) died, which compares favorably with outcomes in patients receiving epidurals. Historically, epidural analgesia for multiple traumatic rib fractures has been associated with about an 18% pneumonia rate, and about 9% mortality.
Ketamine side effects were minimal; none of the patients had hallucinations or tachycardia, and three (2.3%) were hypotensive on the drug.
Jacobi’s database did not record how many times patients used their PCA pumps, so the study did not have a direct measure of pain control. The investigators plan to look into this question prospectively.
Even so, when patients hurt from rib fractures, they breathe shallowly, which puts them at risk for pneumonia and death. “We have lower rates” of both than with epidurals, “so you could extrapolate that we must be controlling pain better,” Dr. Getrajdman said.
Ketamine at high doses is an anesthetic, but at lower doses it’s an antagonist of N-methyl-D-aspartate (NMDA), and a mild opioid receptor agonist, “so we can give patients the same amount of morphine but achieve a higher analgesic effect,” she said.
Ketamine had been the subject of intense interest in recent years for pain control in a wide variety of settings, as well as for psychiatric and other problems. Clinicaltrials.gov currently lists 138 open investigations of the drug.
Among them is a randomized trial from the Medical College of Wisconsin pitting ketamine against placebo for rib fracture pain following blunt trauma.
Dr. Getrajdman has no disclosures, and there was no outside funding for the work.
CHICAGO – Ketamine is a safe and simple alternative to epidural anesthesia for pain control in the setting of multiple rib fractures, investigators from the Jacobi Medical Center in the Bronx (N.Y.) concluded after reviewing their experience with the drug.
Epidural analgesia has been the standard for controlling pain after multiple rib fractures, but epidurals are sometimes contraindicated in trauma, especially with back and neck injuries. There’s also a bleeding risk, and the need for an on-call anesthesia team to place them, something not all hospitals have.
Those problems – and the success Jacobi surgeons reported with ketamine pain control after thoracotomy – led the hospital to switch to a ketamine-based rib fracture protocol in 2007.
“As far as we know, we are the only people doing this routinely for multiple rib fractures,” Dr. Joelle Getrajdman, a second-year surgery resident at the medical center, said at the annual clinical congress of the American College of Surgeons.
Patients there with two or more rib fractures get a low-dose peripheral intravenous infusion of ketamine 0.05 mg/kg per hour while in the ICU and step-down unit, along with other pain medications as indicated. The hospital discontinues ketamine once patients leave the step-down unit to prevent diversion for illicit use.
To see how well the protocol has worked, the investigators reviewed all 128 adult trauma patients who received ketamine for multiple rib fractures from 2007 to 2014.
These patients were 60 years old on average, with a median of six rib fractures, many of them bilateral. Almost half had injury severity scores above 15, and most had chest Abbreviated Injury Scores of at least 3. Pneumo- and hemothoraces were common. Patients spent a mean of 6 days in the surgical ICU and 13 days in the hospital.
Along with ketamine, almost all had a morphine or hydromorphone (Dilaudid) patient-controlled analgesia (PCA) pumps, more than half received IV ketorolac (Toradol), and about 40% IV Tylenol. Only 14% had paravertebral or intercostal blocks.
Fourteen patients (10.9%) developed pneumonia, and four (3.1%) died, which compares favorably with outcomes in patients receiving epidurals. Historically, epidural analgesia for multiple traumatic rib fractures has been associated with about an 18% pneumonia rate, and about 9% mortality.
Ketamine side effects were minimal; none of the patients had hallucinations or tachycardia, and three (2.3%) were hypotensive on the drug.
Jacobi’s database did not record how many times patients used their PCA pumps, so the study did not have a direct measure of pain control. The investigators plan to look into this question prospectively.
Even so, when patients hurt from rib fractures, they breathe shallowly, which puts them at risk for pneumonia and death. “We have lower rates” of both than with epidurals, “so you could extrapolate that we must be controlling pain better,” Dr. Getrajdman said.
Ketamine at high doses is an anesthetic, but at lower doses it’s an antagonist of N-methyl-D-aspartate (NMDA), and a mild opioid receptor agonist, “so we can give patients the same amount of morphine but achieve a higher analgesic effect,” she said.
Ketamine had been the subject of intense interest in recent years for pain control in a wide variety of settings, as well as for psychiatric and other problems. Clinicaltrials.gov currently lists 138 open investigations of the drug.
Among them is a randomized trial from the Medical College of Wisconsin pitting ketamine against placebo for rib fracture pain following blunt trauma.
Dr. Getrajdman has no disclosures, and there was no outside funding for the work.
CHICAGO – Ketamine is a safe and simple alternative to epidural anesthesia for pain control in the setting of multiple rib fractures, investigators from the Jacobi Medical Center in the Bronx (N.Y.) concluded after reviewing their experience with the drug.
Epidural analgesia has been the standard for controlling pain after multiple rib fractures, but epidurals are sometimes contraindicated in trauma, especially with back and neck injuries. There’s also a bleeding risk, and the need for an on-call anesthesia team to place them, something not all hospitals have.
Those problems – and the success Jacobi surgeons reported with ketamine pain control after thoracotomy – led the hospital to switch to a ketamine-based rib fracture protocol in 2007.
“As far as we know, we are the only people doing this routinely for multiple rib fractures,” Dr. Joelle Getrajdman, a second-year surgery resident at the medical center, said at the annual clinical congress of the American College of Surgeons.
Patients there with two or more rib fractures get a low-dose peripheral intravenous infusion of ketamine 0.05 mg/kg per hour while in the ICU and step-down unit, along with other pain medications as indicated. The hospital discontinues ketamine once patients leave the step-down unit to prevent diversion for illicit use.
To see how well the protocol has worked, the investigators reviewed all 128 adult trauma patients who received ketamine for multiple rib fractures from 2007 to 2014.
These patients were 60 years old on average, with a median of six rib fractures, many of them bilateral. Almost half had injury severity scores above 15, and most had chest Abbreviated Injury Scores of at least 3. Pneumo- and hemothoraces were common. Patients spent a mean of 6 days in the surgical ICU and 13 days in the hospital.
Along with ketamine, almost all had a morphine or hydromorphone (Dilaudid) patient-controlled analgesia (PCA) pumps, more than half received IV ketorolac (Toradol), and about 40% IV Tylenol. Only 14% had paravertebral or intercostal blocks.
Fourteen patients (10.9%) developed pneumonia, and four (3.1%) died, which compares favorably with outcomes in patients receiving epidurals. Historically, epidural analgesia for multiple traumatic rib fractures has been associated with about an 18% pneumonia rate, and about 9% mortality.
Ketamine side effects were minimal; none of the patients had hallucinations or tachycardia, and three (2.3%) were hypotensive on the drug.
Jacobi’s database did not record how many times patients used their PCA pumps, so the study did not have a direct measure of pain control. The investigators plan to look into this question prospectively.
Even so, when patients hurt from rib fractures, they breathe shallowly, which puts them at risk for pneumonia and death. “We have lower rates” of both than with epidurals, “so you could extrapolate that we must be controlling pain better,” Dr. Getrajdman said.
Ketamine at high doses is an anesthetic, but at lower doses it’s an antagonist of N-methyl-D-aspartate (NMDA), and a mild opioid receptor agonist, “so we can give patients the same amount of morphine but achieve a higher analgesic effect,” she said.
Ketamine had been the subject of intense interest in recent years for pain control in a wide variety of settings, as well as for psychiatric and other problems. Clinicaltrials.gov currently lists 138 open investigations of the drug.
Among them is a randomized trial from the Medical College of Wisconsin pitting ketamine against placebo for rib fracture pain following blunt trauma.
Dr. Getrajdman has no disclosures, and there was no outside funding for the work.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Patients with multiple rib fractures treated with ketamine for pain control had less risk of pneumonia and death than did patients receiving epidural for pain.
Major finding: Overall, 14 ketamine patients (10.9%) developed pneumonia, and four (3.1%) died.
Data source: Review of 128 rib fracture patients.
Disclosures: The lead investigator has no disclosures, and there was no outside funding for the work.
Study reveals potential drivers of CLL

Photo courtesy of Dana-
Farber Cancer Institute
Researchers say they have identified dozens of genetic abnormalities that may drive chronic lymphocytic leukemia (CLL), including some that were never before linked to human cancer.
The team began to trace how some of these abnormalities affect the course of the disease and its susceptibility to treatment.
And they started tracking the evolutionary path of CLL as its genome spawns new groups and subgroups of tumor cells in a single patient.
“Sequencing the DNA of CLL has taught us a great deal about the genetic basis of the disease,” said Catherine Wu, MD, of Dana-Farber Cancer Institute in Boston, Massachusetts.
“Previous studies, however, were limited by the relatively small number of tumor tissue samples analyzed and by the fact that those samples were taken at different stages of the treatment process from patients treated with different drug agents.”
“In our new study, we wanted to determine if analyzing tissue samples from a large, similarly treated group of patients provides the statistical power necessary to study the disease in all its genetic diversity, to draw connections between certain mutations and the aggressiveness of the disease, and to chart the emergence of new mutations and their role in helping the disease advance. Our results demonstrate the range of insights to be gained by this approach.”
Dr Wu and her colleagues reported these results in Nature.
The researchers collected tumor and normal tissue samples from 538 patients with CLL and performed whole-exome sequencing on each sample.
In this way, the team identified 44 putative CLL driver genes, including 18 CLL mutated drivers that were previously identified and 26 additional putative CLL genes. About 34% of the CLL samples harbored a mutation in at least 1 of these 26 genes.
Nearly 9% of the patients had mutations in CLL genes in the MAPK-ERK pathway. The researchers therefore believe that further exploration of MAPK-ERK pathway inhibitors may be warranted.
The team found that mutations differed between IGHV-mutated and unmutated CLL. IGHV-unmutated CLL tended to have a higher proportion of most driving mutations, while only 3 driver genes were enriched in IGHV-mutated CLL—del(13q), MYD88, and CHD2.
The researchers also discovered that certain mutations were common in patients who had already undergone treatment.
Previous treatment was associated with enrichment in TP53 and BIRC3 mutations del(17p) and del(11q), as well as in mutated DDX3X and MAP2K1. The team therefore believes these mutations may help CLL rebound after initial therapy.
Another key finding was that therapy tended to produce shorter remissions in patients with mutations in TP53 or SF3B1.
“We found that genomic evolution after therapy is the rule rather than the exception,” Dr Wu noted. “Certain mutations were present in a greater number of leukemia cells within a sample after relapse, showing that these mutations, presumably, allow the tumor to persevere.” ![]()

Photo courtesy of Dana-
Farber Cancer Institute
Researchers say they have identified dozens of genetic abnormalities that may drive chronic lymphocytic leukemia (CLL), including some that were never before linked to human cancer.
The team began to trace how some of these abnormalities affect the course of the disease and its susceptibility to treatment.
And they started tracking the evolutionary path of CLL as its genome spawns new groups and subgroups of tumor cells in a single patient.
“Sequencing the DNA of CLL has taught us a great deal about the genetic basis of the disease,” said Catherine Wu, MD, of Dana-Farber Cancer Institute in Boston, Massachusetts.
“Previous studies, however, were limited by the relatively small number of tumor tissue samples analyzed and by the fact that those samples were taken at different stages of the treatment process from patients treated with different drug agents.”
“In our new study, we wanted to determine if analyzing tissue samples from a large, similarly treated group of patients provides the statistical power necessary to study the disease in all its genetic diversity, to draw connections between certain mutations and the aggressiveness of the disease, and to chart the emergence of new mutations and their role in helping the disease advance. Our results demonstrate the range of insights to be gained by this approach.”
Dr Wu and her colleagues reported these results in Nature.
The researchers collected tumor and normal tissue samples from 538 patients with CLL and performed whole-exome sequencing on each sample.
In this way, the team identified 44 putative CLL driver genes, including 18 CLL mutated drivers that were previously identified and 26 additional putative CLL genes. About 34% of the CLL samples harbored a mutation in at least 1 of these 26 genes.
Nearly 9% of the patients had mutations in CLL genes in the MAPK-ERK pathway. The researchers therefore believe that further exploration of MAPK-ERK pathway inhibitors may be warranted.
The team found that mutations differed between IGHV-mutated and unmutated CLL. IGHV-unmutated CLL tended to have a higher proportion of most driving mutations, while only 3 driver genes were enriched in IGHV-mutated CLL—del(13q), MYD88, and CHD2.
The researchers also discovered that certain mutations were common in patients who had already undergone treatment.
Previous treatment was associated with enrichment in TP53 and BIRC3 mutations del(17p) and del(11q), as well as in mutated DDX3X and MAP2K1. The team therefore believes these mutations may help CLL rebound after initial therapy.
Another key finding was that therapy tended to produce shorter remissions in patients with mutations in TP53 or SF3B1.
“We found that genomic evolution after therapy is the rule rather than the exception,” Dr Wu noted. “Certain mutations were present in a greater number of leukemia cells within a sample after relapse, showing that these mutations, presumably, allow the tumor to persevere.” ![]()

Photo courtesy of Dana-
Farber Cancer Institute
Researchers say they have identified dozens of genetic abnormalities that may drive chronic lymphocytic leukemia (CLL), including some that were never before linked to human cancer.
The team began to trace how some of these abnormalities affect the course of the disease and its susceptibility to treatment.
And they started tracking the evolutionary path of CLL as its genome spawns new groups and subgroups of tumor cells in a single patient.
“Sequencing the DNA of CLL has taught us a great deal about the genetic basis of the disease,” said Catherine Wu, MD, of Dana-Farber Cancer Institute in Boston, Massachusetts.
“Previous studies, however, were limited by the relatively small number of tumor tissue samples analyzed and by the fact that those samples were taken at different stages of the treatment process from patients treated with different drug agents.”
“In our new study, we wanted to determine if analyzing tissue samples from a large, similarly treated group of patients provides the statistical power necessary to study the disease in all its genetic diversity, to draw connections between certain mutations and the aggressiveness of the disease, and to chart the emergence of new mutations and their role in helping the disease advance. Our results demonstrate the range of insights to be gained by this approach.”
Dr Wu and her colleagues reported these results in Nature.
The researchers collected tumor and normal tissue samples from 538 patients with CLL and performed whole-exome sequencing on each sample.
In this way, the team identified 44 putative CLL driver genes, including 18 CLL mutated drivers that were previously identified and 26 additional putative CLL genes. About 34% of the CLL samples harbored a mutation in at least 1 of these 26 genes.
Nearly 9% of the patients had mutations in CLL genes in the MAPK-ERK pathway. The researchers therefore believe that further exploration of MAPK-ERK pathway inhibitors may be warranted.
The team found that mutations differed between IGHV-mutated and unmutated CLL. IGHV-unmutated CLL tended to have a higher proportion of most driving mutations, while only 3 driver genes were enriched in IGHV-mutated CLL—del(13q), MYD88, and CHD2.
The researchers also discovered that certain mutations were common in patients who had already undergone treatment.
Previous treatment was associated with enrichment in TP53 and BIRC3 mutations del(17p) and del(11q), as well as in mutated DDX3X and MAP2K1. The team therefore believes these mutations may help CLL rebound after initial therapy.
Another key finding was that therapy tended to produce shorter remissions in patients with mutations in TP53 or SF3B1.
“We found that genomic evolution after therapy is the rule rather than the exception,” Dr Wu noted. “Certain mutations were present in a greater number of leukemia cells within a sample after relapse, showing that these mutations, presumably, allow the tumor to persevere.” ![]()
Team identifies problems with preclinical research

Poor study design and the tendency to publish positive—but not negative—results threaten the validity of preclinical research, according to an article published in eLife.
“Only a fraction of drugs that show promise in animals end up proving safe and effective in humans,” said study author Jonathan Kimmelman, PhD, of McGill University in Montreal, Quebec, Canada.
“An important reason is because studies in animals are often not well designed and because positive results have a higher chance of being published. They end up skewing what we think we know about the potential of a drug.”
Dr Kimmelman and his colleagues came to this conclusion after evaluating all published animal studies of sunitinib, a drug used to treat advanced kidney cancer, a rare type of stomach cancer, and rare tumors of the neuroendocrine system.
The investigators found evidence to suggest that studies reporting little or no anticancer effect were simply not published, leading anticancer effects of the drug to be overestimated by as much as 45%.
The team noted, however, that these findings do not raise any concerns about the clinical use of sunitinib.
Dr Kimmelman and his colleagues also found that few studies used practices like blinding or randomization. And it was often unclear how many animals had been tested because the sample size was not reported.
The drug was tested against different cancers, and all types tested showed statistically significant anticancer activity, a result that “strains credibility”, according to Dr Kimmelman.
He added that researchers failed to observe the dose-dependent response to the drug that is known to occur in humans.
Finally, the researchers did not test the drug on a range of animal models, focusing instead on juvenile female mice with a compromised immune system. Malignancies tested in a wider range of animal types, such as mice that have spontaneously developed tumors, showed less extreme effect sizes.
“Preclinical research is plagued by poor design and reporting practices, exposing patients to harmful and inactive agents, wasting time in the lab, and driving up the price of drugs,” Dr Kimmelman said.
“Our findings provide compelling reasons for developing and implementing guidelines for the design and reporting of preclinical studies in cancer, similar to those already in use for stroke, epilepsy, and cardiology.” ![]()

Poor study design and the tendency to publish positive—but not negative—results threaten the validity of preclinical research, according to an article published in eLife.
“Only a fraction of drugs that show promise in animals end up proving safe and effective in humans,” said study author Jonathan Kimmelman, PhD, of McGill University in Montreal, Quebec, Canada.
“An important reason is because studies in animals are often not well designed and because positive results have a higher chance of being published. They end up skewing what we think we know about the potential of a drug.”
Dr Kimmelman and his colleagues came to this conclusion after evaluating all published animal studies of sunitinib, a drug used to treat advanced kidney cancer, a rare type of stomach cancer, and rare tumors of the neuroendocrine system.
The investigators found evidence to suggest that studies reporting little or no anticancer effect were simply not published, leading anticancer effects of the drug to be overestimated by as much as 45%.
The team noted, however, that these findings do not raise any concerns about the clinical use of sunitinib.
Dr Kimmelman and his colleagues also found that few studies used practices like blinding or randomization. And it was often unclear how many animals had been tested because the sample size was not reported.
The drug was tested against different cancers, and all types tested showed statistically significant anticancer activity, a result that “strains credibility”, according to Dr Kimmelman.
He added that researchers failed to observe the dose-dependent response to the drug that is known to occur in humans.
Finally, the researchers did not test the drug on a range of animal models, focusing instead on juvenile female mice with a compromised immune system. Malignancies tested in a wider range of animal types, such as mice that have spontaneously developed tumors, showed less extreme effect sizes.
“Preclinical research is plagued by poor design and reporting practices, exposing patients to harmful and inactive agents, wasting time in the lab, and driving up the price of drugs,” Dr Kimmelman said.
“Our findings provide compelling reasons for developing and implementing guidelines for the design and reporting of preclinical studies in cancer, similar to those already in use for stroke, epilepsy, and cardiology.” ![]()

Poor study design and the tendency to publish positive—but not negative—results threaten the validity of preclinical research, according to an article published in eLife.
“Only a fraction of drugs that show promise in animals end up proving safe and effective in humans,” said study author Jonathan Kimmelman, PhD, of McGill University in Montreal, Quebec, Canada.
“An important reason is because studies in animals are often not well designed and because positive results have a higher chance of being published. They end up skewing what we think we know about the potential of a drug.”
Dr Kimmelman and his colleagues came to this conclusion after evaluating all published animal studies of sunitinib, a drug used to treat advanced kidney cancer, a rare type of stomach cancer, and rare tumors of the neuroendocrine system.
The investigators found evidence to suggest that studies reporting little or no anticancer effect were simply not published, leading anticancer effects of the drug to be overestimated by as much as 45%.
The team noted, however, that these findings do not raise any concerns about the clinical use of sunitinib.
Dr Kimmelman and his colleagues also found that few studies used practices like blinding or randomization. And it was often unclear how many animals had been tested because the sample size was not reported.
The drug was tested against different cancers, and all types tested showed statistically significant anticancer activity, a result that “strains credibility”, according to Dr Kimmelman.
He added that researchers failed to observe the dose-dependent response to the drug that is known to occur in humans.
Finally, the researchers did not test the drug on a range of animal models, focusing instead on juvenile female mice with a compromised immune system. Malignancies tested in a wider range of animal types, such as mice that have spontaneously developed tumors, showed less extreme effect sizes.
“Preclinical research is plagued by poor design and reporting practices, exposing patients to harmful and inactive agents, wasting time in the lab, and driving up the price of drugs,” Dr Kimmelman said.
“Our findings provide compelling reasons for developing and implementing guidelines for the design and reporting of preclinical studies in cancer, similar to those already in use for stroke, epilepsy, and cardiology.” ![]()
IDWeek: Rifapentine had best completion rates for health care workers with latent TB
SAN DIEGO – Health care workers with latent tuberculosis infection (LTBI) were significantly more likely to continue a shorter course of weekly rifapentine plus isoniazid (INH) than daily INH monotherapy, researchers reported at an annual scientific meeting on infectious diseases.
“Consideration should be given to no longer routinely recommending INH for the treatment of LTBI among health care workers,” said Dr. Esther Arguello Perez of Memorial Sloan Kettering Cancer Center, New York.
Health care workers face a greater risk of TB infection than the general population, regardless of the income level in the country where they live; patients with undiagnosed laryngeal or pulmonary TB usually pose the greatest risk, especially during procedures that cause coughing, such as sputum induction and bronchoscopy (Int J Tuberc Lung Dis. 2007;11[6]:593-605).
Although occupational TB testing is routine in U.S. health care organizations, more than half of health care workers who start treatment for LTBI historically have failed to finish (Chest. 2010;137[2]:401-9. doi: 10.1378/chest.09-0394). The standard LTBI regimen – 300 mg INH daily for 9 months – has been linked to potentially intolerable adverse effects such as hepatotoxicity, persistent gastrointestinal symptoms, rash, and neuropsychiatric problems (Drug Healthc Patient Saf. 2014;6:145-9. doi: 10.2147/DHPS.S68837).
In a 2011 multicenter trial, investigators reported a significantly higher completion rate for weekly rifapentine plus INH (900 mg each; 82% vs. 69% for daily INH; P < .001). Rates of adverse effects were significantly lower with weekly rifapentine plus INH, although grade 3-4 events and risk of death did not differ between the groups (N Engl J Med. 2011;365:2155-66. doi: 10.1056/NEJMoa1104875). The results of that trial quickly transformed recommendations for LTBI treatment (MMWR. 2011:60(48);1650-53).
Memorial Sloan Kettering implemented weekly rifapentine plus INH for its LTBI personnel in 2011. By 2014, about three-quarters of personnel with LTBI received rifapentine plus INH, while the rest were evenly split between rifampin and INH monotherapy, Dr. Arguello Perez reported at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
To understand how health care workers’ attitudes and treatment acceptance shifted along with practice, the investigators reviewed records from all health care workers at Memorial Sloan Kettering who were diagnosed with LTBI for 2005-2014. Among 930 patients, only 357 (38%) accepted treatment, although 76% of these individuals finished the regimen they started, she noted. Rifapentine plus INH had the highest completion rate (88%), significantly exceeding rates for a 4-month course of daily rifampin (84%) and for 9 months of INH monotherapy (70%; P < .01 for both differences). In contrast, completion rates for rifampin and INH did not significantly differ, Dr. Arguello Perez said.
Notably, LTBI treatment completion rates among health care workers rose by 26% between 2013, when most prescriptions were for rifampin or INH monotherapy, and 2014, when most were for rifapentine plus INH. “Health care workers might be more likely to accept treatment for LTBI if they know about alternatives to INH,” she concluded.
Dr. Arguello Perez and her associates reported no funding sources and had no financial disclosures.
SAN DIEGO – Health care workers with latent tuberculosis infection (LTBI) were significantly more likely to continue a shorter course of weekly rifapentine plus isoniazid (INH) than daily INH monotherapy, researchers reported at an annual scientific meeting on infectious diseases.
“Consideration should be given to no longer routinely recommending INH for the treatment of LTBI among health care workers,” said Dr. Esther Arguello Perez of Memorial Sloan Kettering Cancer Center, New York.
Health care workers face a greater risk of TB infection than the general population, regardless of the income level in the country where they live; patients with undiagnosed laryngeal or pulmonary TB usually pose the greatest risk, especially during procedures that cause coughing, such as sputum induction and bronchoscopy (Int J Tuberc Lung Dis. 2007;11[6]:593-605).
Although occupational TB testing is routine in U.S. health care organizations, more than half of health care workers who start treatment for LTBI historically have failed to finish (Chest. 2010;137[2]:401-9. doi: 10.1378/chest.09-0394). The standard LTBI regimen – 300 mg INH daily for 9 months – has been linked to potentially intolerable adverse effects such as hepatotoxicity, persistent gastrointestinal symptoms, rash, and neuropsychiatric problems (Drug Healthc Patient Saf. 2014;6:145-9. doi: 10.2147/DHPS.S68837).
In a 2011 multicenter trial, investigators reported a significantly higher completion rate for weekly rifapentine plus INH (900 mg each; 82% vs. 69% for daily INH; P < .001). Rates of adverse effects were significantly lower with weekly rifapentine plus INH, although grade 3-4 events and risk of death did not differ between the groups (N Engl J Med. 2011;365:2155-66. doi: 10.1056/NEJMoa1104875). The results of that trial quickly transformed recommendations for LTBI treatment (MMWR. 2011:60(48);1650-53).
Memorial Sloan Kettering implemented weekly rifapentine plus INH for its LTBI personnel in 2011. By 2014, about three-quarters of personnel with LTBI received rifapentine plus INH, while the rest were evenly split between rifampin and INH monotherapy, Dr. Arguello Perez reported at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
To understand how health care workers’ attitudes and treatment acceptance shifted along with practice, the investigators reviewed records from all health care workers at Memorial Sloan Kettering who were diagnosed with LTBI for 2005-2014. Among 930 patients, only 357 (38%) accepted treatment, although 76% of these individuals finished the regimen they started, she noted. Rifapentine plus INH had the highest completion rate (88%), significantly exceeding rates for a 4-month course of daily rifampin (84%) and for 9 months of INH monotherapy (70%; P < .01 for both differences). In contrast, completion rates for rifampin and INH did not significantly differ, Dr. Arguello Perez said.
Notably, LTBI treatment completion rates among health care workers rose by 26% between 2013, when most prescriptions were for rifampin or INH monotherapy, and 2014, when most were for rifapentine plus INH. “Health care workers might be more likely to accept treatment for LTBI if they know about alternatives to INH,” she concluded.
Dr. Arguello Perez and her associates reported no funding sources and had no financial disclosures.
SAN DIEGO – Health care workers with latent tuberculosis infection (LTBI) were significantly more likely to continue a shorter course of weekly rifapentine plus isoniazid (INH) than daily INH monotherapy, researchers reported at an annual scientific meeting on infectious diseases.
“Consideration should be given to no longer routinely recommending INH for the treatment of LTBI among health care workers,” said Dr. Esther Arguello Perez of Memorial Sloan Kettering Cancer Center, New York.
Health care workers face a greater risk of TB infection than the general population, regardless of the income level in the country where they live; patients with undiagnosed laryngeal or pulmonary TB usually pose the greatest risk, especially during procedures that cause coughing, such as sputum induction and bronchoscopy (Int J Tuberc Lung Dis. 2007;11[6]:593-605).
Although occupational TB testing is routine in U.S. health care organizations, more than half of health care workers who start treatment for LTBI historically have failed to finish (Chest. 2010;137[2]:401-9. doi: 10.1378/chest.09-0394). The standard LTBI regimen – 300 mg INH daily for 9 months – has been linked to potentially intolerable adverse effects such as hepatotoxicity, persistent gastrointestinal symptoms, rash, and neuropsychiatric problems (Drug Healthc Patient Saf. 2014;6:145-9. doi: 10.2147/DHPS.S68837).
In a 2011 multicenter trial, investigators reported a significantly higher completion rate for weekly rifapentine plus INH (900 mg each; 82% vs. 69% for daily INH; P < .001). Rates of adverse effects were significantly lower with weekly rifapentine plus INH, although grade 3-4 events and risk of death did not differ between the groups (N Engl J Med. 2011;365:2155-66. doi: 10.1056/NEJMoa1104875). The results of that trial quickly transformed recommendations for LTBI treatment (MMWR. 2011:60(48);1650-53).
Memorial Sloan Kettering implemented weekly rifapentine plus INH for its LTBI personnel in 2011. By 2014, about three-quarters of personnel with LTBI received rifapentine plus INH, while the rest were evenly split between rifampin and INH monotherapy, Dr. Arguello Perez reported at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
To understand how health care workers’ attitudes and treatment acceptance shifted along with practice, the investigators reviewed records from all health care workers at Memorial Sloan Kettering who were diagnosed with LTBI for 2005-2014. Among 930 patients, only 357 (38%) accepted treatment, although 76% of these individuals finished the regimen they started, she noted. Rifapentine plus INH had the highest completion rate (88%), significantly exceeding rates for a 4-month course of daily rifampin (84%) and for 9 months of INH monotherapy (70%; P < .01 for both differences). In contrast, completion rates for rifampin and INH did not significantly differ, Dr. Arguello Perez said.
Notably, LTBI treatment completion rates among health care workers rose by 26% between 2013, when most prescriptions were for rifampin or INH monotherapy, and 2014, when most were for rifapentine plus INH. “Health care workers might be more likely to accept treatment for LTBI if they know about alternatives to INH,” she concluded.
Dr. Arguello Perez and her associates reported no funding sources and had no financial disclosures.
AT IDweek 2015
Key clinical point: Isoniazid monotherapy should not be recommended routinely for health care workers with latent tuberculosis infections.
Major finding: Rates of treatment completion were significantly higher for weekly rifapentine plus isoniazid than for daily isoniazid monotherapy (P < .01).
Data source: Retrospective analysis of all health care workers with LTBI at Memorial Sloan Kettering Cancer Center during 2005-2014.
Disclosures: The researchers reported no funding sources and made no financial disclosures.
Depression, hypertension combo compounds cardiovascular risk
LONDON – The combination of depression and very high systolic blood pressure increased the risk for a major cardiovascular event by 83%, compared with normal blood pressure and no depression, in patients with existing heart disease, diabetes, or stroke.
In a large family practice–based study, the hazard ratio for first hospital admission due to myocardial infarction, stroke or heart failure, or cardiovascular death in patients with high (at least 160 mm Hg) systolic blood pressure who were also depressed was 1.83, a highly significant difference compared with individuals with normal BP and no depression.
The presence of depression also significantly increased the risk for these cardiovascular events by 36% in patients with lower systolic BPs, compared with those with normal BP and no depression.
“Patients with existing heart disease, diabetes, or stroke are more likely to have another heart attack or another stroke or die from heart problems than the general population,” Dr. Bhautesh Jani of the Institute of Health and Wellbeing, University of Glasgow (Scotland), said at the annual congress of the European Society of Cardiology.
“In particular, those who have extremes of blood pressure or those who have depressive symptoms are at higher risk, which has been shown by previous evidence. What is relatively unknown is the combined effect of having extremes of blood pressure and depressive symptoms together, and our study tried to address that problem,” Dr. Jani explained.
The study involved more than 35,500 individuals with existing heart disease, diabetes, or stroke living in Scotland, of whom 3,939 (11%) had at least one major cardiovascular event that needed hospital admission during a 4-year period. Patients had been divided into groups based on their systolic BP, and depressive symptoms were assessed using the Hospital Anxiety and Depression Scale (HADS) during 2008-2009. A HADS score of more than 7 was considered indicative of depression.
Dr. Jani noted that all the results were adjusted for multiple confounding factors, including age, gender, socioeconomic status, number of comorbid conditions, total cholesterol values, body mass index, and the initiation of antidepressant medication.
“The key implications I would suggest are for secondary prevention and to perhaps focus our resources on monitoring blood pressure and providing treatment in patients with associated depressive symptoms,” Dr. Jani proposed.
Dr. Christi Deaton, professor of clinical nursing research at the University of Cambridge (England), who commented on the study findings, noted that it highlighted the importance of raising awareness among both clinicians and patients of the potential risk associated with a combination of hypertension and depression, particularly among patients with a high level of other risk factors for further cardiovascular events.
“Screening patients for depression is very simple to do and you can start with a couple of questions asking about whether or not the patient felt sad or had low mood, and then go on to use other screening tools,” she observed. “All providers should be screening patients and thinking about the synergy of these two risk factors,” she said.
Other research presented at the ESC Congress by cardiologist Dr. Salim Hayek of Emory University in Atlanta also highlighted the importance of screening for depression, this time in patients with angina. In a study of 5,202 adults enrolled in the university’s biobank between 2004 and 2013 and who underwent left heart catheterization, patients with frequent chest pain were found to have more depressive symptoms than those without angina. Depressive symptoms in this study were assessed using the Patient Health Questionnaire (PHQ-9).
“Chest pain was more frequent in patients with mild depression with and without coronary artery disease, regardless of sex or history of myocardial infarction,” Dr. Hayek said. After multivariate analysis, depression was the most important predictor of frequent chest pain, he added. Other factors independently associated with chest pain frequency were female sex, coronary artery disease severity, history of MI, body mass index, and high blood lipid levels.
“At follow-up, a decrease in depressive symptoms was associated with improvement in chest pain,” Dr. Hayek said, but patients with depression who were revascularized did not show an improvement in chest pain.
The findings suggest that the association between chest pain and depression was independent of the underlying arterial disease and further studies are needed to look at the effect of revascularization and angina relief on depressive symptoms, and conversely if antidepressant medications could help alleviate chest pain.
The study Dr. Jani presented was funded by the Scottish Government. Dr. Jani and Dr. Hayek both reported having no disclosures.
This article was updated February 3, 2016.
LONDON – The combination of depression and very high systolic blood pressure increased the risk for a major cardiovascular event by 83%, compared with normal blood pressure and no depression, in patients with existing heart disease, diabetes, or stroke.
In a large family practice–based study, the hazard ratio for first hospital admission due to myocardial infarction, stroke or heart failure, or cardiovascular death in patients with high (at least 160 mm Hg) systolic blood pressure who were also depressed was 1.83, a highly significant difference compared with individuals with normal BP and no depression.
The presence of depression also significantly increased the risk for these cardiovascular events by 36% in patients with lower systolic BPs, compared with those with normal BP and no depression.
“Patients with existing heart disease, diabetes, or stroke are more likely to have another heart attack or another stroke or die from heart problems than the general population,” Dr. Bhautesh Jani of the Institute of Health and Wellbeing, University of Glasgow (Scotland), said at the annual congress of the European Society of Cardiology.
“In particular, those who have extremes of blood pressure or those who have depressive symptoms are at higher risk, which has been shown by previous evidence. What is relatively unknown is the combined effect of having extremes of blood pressure and depressive symptoms together, and our study tried to address that problem,” Dr. Jani explained.
The study involved more than 35,500 individuals with existing heart disease, diabetes, or stroke living in Scotland, of whom 3,939 (11%) had at least one major cardiovascular event that needed hospital admission during a 4-year period. Patients had been divided into groups based on their systolic BP, and depressive symptoms were assessed using the Hospital Anxiety and Depression Scale (HADS) during 2008-2009. A HADS score of more than 7 was considered indicative of depression.
Dr. Jani noted that all the results were adjusted for multiple confounding factors, including age, gender, socioeconomic status, number of comorbid conditions, total cholesterol values, body mass index, and the initiation of antidepressant medication.
“The key implications I would suggest are for secondary prevention and to perhaps focus our resources on monitoring blood pressure and providing treatment in patients with associated depressive symptoms,” Dr. Jani proposed.
Dr. Christi Deaton, professor of clinical nursing research at the University of Cambridge (England), who commented on the study findings, noted that it highlighted the importance of raising awareness among both clinicians and patients of the potential risk associated with a combination of hypertension and depression, particularly among patients with a high level of other risk factors for further cardiovascular events.
“Screening patients for depression is very simple to do and you can start with a couple of questions asking about whether or not the patient felt sad or had low mood, and then go on to use other screening tools,” she observed. “All providers should be screening patients and thinking about the synergy of these two risk factors,” she said.
Other research presented at the ESC Congress by cardiologist Dr. Salim Hayek of Emory University in Atlanta also highlighted the importance of screening for depression, this time in patients with angina. In a study of 5,202 adults enrolled in the university’s biobank between 2004 and 2013 and who underwent left heart catheterization, patients with frequent chest pain were found to have more depressive symptoms than those without angina. Depressive symptoms in this study were assessed using the Patient Health Questionnaire (PHQ-9).
“Chest pain was more frequent in patients with mild depression with and without coronary artery disease, regardless of sex or history of myocardial infarction,” Dr. Hayek said. After multivariate analysis, depression was the most important predictor of frequent chest pain, he added. Other factors independently associated with chest pain frequency were female sex, coronary artery disease severity, history of MI, body mass index, and high blood lipid levels.
“At follow-up, a decrease in depressive symptoms was associated with improvement in chest pain,” Dr. Hayek said, but patients with depression who were revascularized did not show an improvement in chest pain.
The findings suggest that the association between chest pain and depression was independent of the underlying arterial disease and further studies are needed to look at the effect of revascularization and angina relief on depressive symptoms, and conversely if antidepressant medications could help alleviate chest pain.
The study Dr. Jani presented was funded by the Scottish Government. Dr. Jani and Dr. Hayek both reported having no disclosures.
This article was updated February 3, 2016.
LONDON – The combination of depression and very high systolic blood pressure increased the risk for a major cardiovascular event by 83%, compared with normal blood pressure and no depression, in patients with existing heart disease, diabetes, or stroke.
In a large family practice–based study, the hazard ratio for first hospital admission due to myocardial infarction, stroke or heart failure, or cardiovascular death in patients with high (at least 160 mm Hg) systolic blood pressure who were also depressed was 1.83, a highly significant difference compared with individuals with normal BP and no depression.
The presence of depression also significantly increased the risk for these cardiovascular events by 36% in patients with lower systolic BPs, compared with those with normal BP and no depression.
“Patients with existing heart disease, diabetes, or stroke are more likely to have another heart attack or another stroke or die from heart problems than the general population,” Dr. Bhautesh Jani of the Institute of Health and Wellbeing, University of Glasgow (Scotland), said at the annual congress of the European Society of Cardiology.
“In particular, those who have extremes of blood pressure or those who have depressive symptoms are at higher risk, which has been shown by previous evidence. What is relatively unknown is the combined effect of having extremes of blood pressure and depressive symptoms together, and our study tried to address that problem,” Dr. Jani explained.
The study involved more than 35,500 individuals with existing heart disease, diabetes, or stroke living in Scotland, of whom 3,939 (11%) had at least one major cardiovascular event that needed hospital admission during a 4-year period. Patients had been divided into groups based on their systolic BP, and depressive symptoms were assessed using the Hospital Anxiety and Depression Scale (HADS) during 2008-2009. A HADS score of more than 7 was considered indicative of depression.
Dr. Jani noted that all the results were adjusted for multiple confounding factors, including age, gender, socioeconomic status, number of comorbid conditions, total cholesterol values, body mass index, and the initiation of antidepressant medication.
“The key implications I would suggest are for secondary prevention and to perhaps focus our resources on monitoring blood pressure and providing treatment in patients with associated depressive symptoms,” Dr. Jani proposed.
Dr. Christi Deaton, professor of clinical nursing research at the University of Cambridge (England), who commented on the study findings, noted that it highlighted the importance of raising awareness among both clinicians and patients of the potential risk associated with a combination of hypertension and depression, particularly among patients with a high level of other risk factors for further cardiovascular events.
“Screening patients for depression is very simple to do and you can start with a couple of questions asking about whether or not the patient felt sad or had low mood, and then go on to use other screening tools,” she observed. “All providers should be screening patients and thinking about the synergy of these two risk factors,” she said.
Other research presented at the ESC Congress by cardiologist Dr. Salim Hayek of Emory University in Atlanta also highlighted the importance of screening for depression, this time in patients with angina. In a study of 5,202 adults enrolled in the university’s biobank between 2004 and 2013 and who underwent left heart catheterization, patients with frequent chest pain were found to have more depressive symptoms than those without angina. Depressive symptoms in this study were assessed using the Patient Health Questionnaire (PHQ-9).
“Chest pain was more frequent in patients with mild depression with and without coronary artery disease, regardless of sex or history of myocardial infarction,” Dr. Hayek said. After multivariate analysis, depression was the most important predictor of frequent chest pain, he added. Other factors independently associated with chest pain frequency were female sex, coronary artery disease severity, history of MI, body mass index, and high blood lipid levels.
“At follow-up, a decrease in depressive symptoms was associated with improvement in chest pain,” Dr. Hayek said, but patients with depression who were revascularized did not show an improvement in chest pain.
The findings suggest that the association between chest pain and depression was independent of the underlying arterial disease and further studies are needed to look at the effect of revascularization and angina relief on depressive symptoms, and conversely if antidepressant medications could help alleviate chest pain.
The study Dr. Jani presented was funded by the Scottish Government. Dr. Jani and Dr. Hayek both reported having no disclosures.
This article was updated February 3, 2016.
AT THE ESC CONGRESS 2015
Key clinical point: Better monitoring and management of both hypertension and depression could help reduce further cardiovascular morbidity and mortality.
Major finding: The rate of major cardiovascular events was 83% higher in depressed patients with very high (at least 160 mm Hg) systolic BP, compared with individuals with normal pressure and no depression.
Data source: Large family practice study of 35,537 patients with existing coronary heart disease, diabetes, or stroke followed up for 4 years.
Disclosures: The study Dr. Jani presented was funded by the Scottish Government. Dr. Jani had no disclosures.
EADV: Prophylactic photodynamic therapy benefits transplant recipients
COPENHAGEN – Twice-yearly prophylactic photodynamic therapy for primary prevention of actinic keratoses and squamous cell carcinomas is a novel and effective strategy that addresses the problem of accelerated photocarcinogenesis in organ transplant recipients, according to an interim analysis of a multinational, randomized, controlled trial.
“The overall aim is to prevent squamous cell carcinoma development. Photodynamic therapy is well established for secondary prevention of further AKs, and these very early data show that it can also be used for primary prevention in very high-risk patients,” Dr. Katrine Togsverd-Bo said at the annual congress of the European Academy of Dermatology and Venereology.
Accelerated carcinogenesis on sun-exposed skin is a major concern in organ transplant recipients (OTRs). They experience early onset of multiple AKs, with field cancerization and up to a 100-fold increased risk of squamous cell carcinomas (SCCs). Moreover, their SCCs are at substantially greater risk of metastasis than SCCs occurring in the general population, noted Dr. Togsverd-Bo of Bispebjerg Hospital and the University of Copenhagen.
She presented an interim analysis of an ongoing 5-year prospective randomized trial in 50 renal transplant recipients at academic dermatology centers in Copenhagen, Oslo, and Gothenburg, Sweden. All participants had clinically normal-appearing skin at baseline, with no history of AKs or SCCs. They are undergoing twice-yearly, split-side photodynamic therapy (PDT) on the face, forearm, and hand, with the opposite side serving as the untreated control.
To date, 25 patients have completed 3 years of the study. At 3 years of prospective follow-up by blinded evaluators, 50% of patients had AKs on their untreated side, compared with 26% on the prophylactic PDT side. The collective number of AKs on untreated skin was 43, compared with just 8 AKs on PDT-treated skin. Seven patients had AKs only on their untreated side, six had AKs on both sides, and none had any AKs only on their PDT-treated side.
The twice-yearly prophylactic PDT regimen consists of a 3-hour application of 20% methyl aminolevulinate as a photosensitizer followed by applications of a conventional LED light at 37 J/cm2.
Dr. Togsverd-Bo reported having no financial conflicts regarding her study.
COPENHAGEN – Twice-yearly prophylactic photodynamic therapy for primary prevention of actinic keratoses and squamous cell carcinomas is a novel and effective strategy that addresses the problem of accelerated photocarcinogenesis in organ transplant recipients, according to an interim analysis of a multinational, randomized, controlled trial.
“The overall aim is to prevent squamous cell carcinoma development. Photodynamic therapy is well established for secondary prevention of further AKs, and these very early data show that it can also be used for primary prevention in very high-risk patients,” Dr. Katrine Togsverd-Bo said at the annual congress of the European Academy of Dermatology and Venereology.
Accelerated carcinogenesis on sun-exposed skin is a major concern in organ transplant recipients (OTRs). They experience early onset of multiple AKs, with field cancerization and up to a 100-fold increased risk of squamous cell carcinomas (SCCs). Moreover, their SCCs are at substantially greater risk of metastasis than SCCs occurring in the general population, noted Dr. Togsverd-Bo of Bispebjerg Hospital and the University of Copenhagen.
She presented an interim analysis of an ongoing 5-year prospective randomized trial in 50 renal transplant recipients at academic dermatology centers in Copenhagen, Oslo, and Gothenburg, Sweden. All participants had clinically normal-appearing skin at baseline, with no history of AKs or SCCs. They are undergoing twice-yearly, split-side photodynamic therapy (PDT) on the face, forearm, and hand, with the opposite side serving as the untreated control.
To date, 25 patients have completed 3 years of the study. At 3 years of prospective follow-up by blinded evaluators, 50% of patients had AKs on their untreated side, compared with 26% on the prophylactic PDT side. The collective number of AKs on untreated skin was 43, compared with just 8 AKs on PDT-treated skin. Seven patients had AKs only on their untreated side, six had AKs on both sides, and none had any AKs only on their PDT-treated side.
The twice-yearly prophylactic PDT regimen consists of a 3-hour application of 20% methyl aminolevulinate as a photosensitizer followed by applications of a conventional LED light at 37 J/cm2.
Dr. Togsverd-Bo reported having no financial conflicts regarding her study.
COPENHAGEN – Twice-yearly prophylactic photodynamic therapy for primary prevention of actinic keratoses and squamous cell carcinomas is a novel and effective strategy that addresses the problem of accelerated photocarcinogenesis in organ transplant recipients, according to an interim analysis of a multinational, randomized, controlled trial.
“The overall aim is to prevent squamous cell carcinoma development. Photodynamic therapy is well established for secondary prevention of further AKs, and these very early data show that it can also be used for primary prevention in very high-risk patients,” Dr. Katrine Togsverd-Bo said at the annual congress of the European Academy of Dermatology and Venereology.
Accelerated carcinogenesis on sun-exposed skin is a major concern in organ transplant recipients (OTRs). They experience early onset of multiple AKs, with field cancerization and up to a 100-fold increased risk of squamous cell carcinomas (SCCs). Moreover, their SCCs are at substantially greater risk of metastasis than SCCs occurring in the general population, noted Dr. Togsverd-Bo of Bispebjerg Hospital and the University of Copenhagen.
She presented an interim analysis of an ongoing 5-year prospective randomized trial in 50 renal transplant recipients at academic dermatology centers in Copenhagen, Oslo, and Gothenburg, Sweden. All participants had clinically normal-appearing skin at baseline, with no history of AKs or SCCs. They are undergoing twice-yearly, split-side photodynamic therapy (PDT) on the face, forearm, and hand, with the opposite side serving as the untreated control.
To date, 25 patients have completed 3 years of the study. At 3 years of prospective follow-up by blinded evaluators, 50% of patients had AKs on their untreated side, compared with 26% on the prophylactic PDT side. The collective number of AKs on untreated skin was 43, compared with just 8 AKs on PDT-treated skin. Seven patients had AKs only on their untreated side, six had AKs on both sides, and none had any AKs only on their PDT-treated side.
The twice-yearly prophylactic PDT regimen consists of a 3-hour application of 20% methyl aminolevulinate as a photosensitizer followed by applications of a conventional LED light at 37 J/cm2.
Dr. Togsverd-Bo reported having no financial conflicts regarding her study.
AT THE EADV CONGRESS
Key clinical point: Prophylactic photodynamic therapy is a new and effective strategy for primary prevention of actinic keratoses and squamous cell carcinomas in organ transplant recipients.
Major finding: At 3 years of follow-up, 25 renal transplant recipients collectively had 8 actinic keratoses on the side of their face, forearms, and hands treated with twice-yearly prophylactic photodynamic therapy, compared with 43 AKs on the untreated control side.
Data source: This is an interim 3-year analysis from an ongoing 5-year prospective multinational, randomized, controlled trial involving 50 renal transplant recipients.
Disclosures: The presenter reported having no financial conflicts regarding this ongoing study.
NCCN creates tool to aid treatment decisions

patient and her father
Photo by Rhoda Baer
The National Comprehensive Cancer Network (NCCN) has developed a new tool to accompany its clinical practice guidelines.
The tool—known as NCCN Evidence Blocks™—is designed to provide additional information about guideline recommendations and help inform treatment decisions.
NCCN has already added Evidence Blocks to its guidelines for chronic myelogenous leukemia and multiple myeloma.
The organization hopes to have Evidence Blocks for all of its guidelines by early 2017.
The Evidence Blocks provide a visual representation of 5 key value measures pertaining to guideline recommendations:
- Efficacy of treatment regimens
- Safety of regimens
- Quality and quantity of evidence supporting regimens
- Consistency of evidence supporting regimens
- Affordability of regimens. (This represents an estimate of overall total cost of a therapy, including but not limited to acquisition, administration, inpatient vs outpatient care, supportive care, infusions, toxicity monitoring, antiemetics and growth factors, and hospitalization.)
The Evidence Blocks are graphics of actual blocks that consist of 25 small squares. So each block has 5 rows and 5 columns.
Each of the 5 value measures—efficacy, safety, etc.—has a dedicated column within an Evidence Block, and each row of the Evidence Block represents a rating on a scale of 1 to 5. A score of 1 is unfavorable and a score of 5 is most favorable.
The rating of each value measure is shown by filling in the squares of the dedicated column—such as efficacy—up to the row that represents its assigned score—such as 4.
For example:
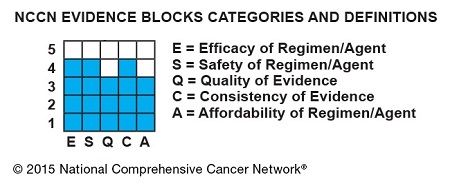
NCCN hopes this visual rating system will help patients and their physicians identify the optimal treatment based on clinical and economic considerations that are of the most value to the patient.
“Some patients will want an emerging therapy even with limited data,” said Robert W. Carlson, MD, chief executive officer of NCCN.
“Others will be most concerned about the expected side effects of the treatment indicated in the safety column. Still others may be very sensitive to cost. By considering the attributes of the range of possible therapies, the healthcare provider and the patient can discuss the benefits and drawbacks of each option and come to a decision most acceptable to the individual.”
By the end of 2015, NCCN expects to publish NCCN Evidence Blocks for systemic therapies (not surgery or radiation therapy) in the NCCN guidelines for breast, colon, non-small cell lung, and rectal cancers.
NCCN Evidence Blocks for systemic therapies are expected to be contained within the complete library of NCCN guidelines by the end of 2016.
In the near term, NCCN will continue to publish 2 sets of guidelines: those including NCCN Evidence Blocks and those without. The Evidence Blocks are not currently published in the NCCN Guidelines for Patients® and are intended for use in the US only.
For more information about NCCN Evidence Blocks, visit NCCN.org/EvidenceBlocks. ![]()

patient and her father
Photo by Rhoda Baer
The National Comprehensive Cancer Network (NCCN) has developed a new tool to accompany its clinical practice guidelines.
The tool—known as NCCN Evidence Blocks™—is designed to provide additional information about guideline recommendations and help inform treatment decisions.
NCCN has already added Evidence Blocks to its guidelines for chronic myelogenous leukemia and multiple myeloma.
The organization hopes to have Evidence Blocks for all of its guidelines by early 2017.
The Evidence Blocks provide a visual representation of 5 key value measures pertaining to guideline recommendations:
- Efficacy of treatment regimens
- Safety of regimens
- Quality and quantity of evidence supporting regimens
- Consistency of evidence supporting regimens
- Affordability of regimens. (This represents an estimate of overall total cost of a therapy, including but not limited to acquisition, administration, inpatient vs outpatient care, supportive care, infusions, toxicity monitoring, antiemetics and growth factors, and hospitalization.)
The Evidence Blocks are graphics of actual blocks that consist of 25 small squares. So each block has 5 rows and 5 columns.
Each of the 5 value measures—efficacy, safety, etc.—has a dedicated column within an Evidence Block, and each row of the Evidence Block represents a rating on a scale of 1 to 5. A score of 1 is unfavorable and a score of 5 is most favorable.
The rating of each value measure is shown by filling in the squares of the dedicated column—such as efficacy—up to the row that represents its assigned score—such as 4.
For example:
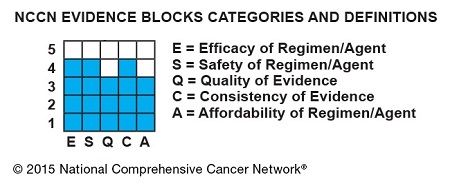
NCCN hopes this visual rating system will help patients and their physicians identify the optimal treatment based on clinical and economic considerations that are of the most value to the patient.
“Some patients will want an emerging therapy even with limited data,” said Robert W. Carlson, MD, chief executive officer of NCCN.
“Others will be most concerned about the expected side effects of the treatment indicated in the safety column. Still others may be very sensitive to cost. By considering the attributes of the range of possible therapies, the healthcare provider and the patient can discuss the benefits and drawbacks of each option and come to a decision most acceptable to the individual.”
By the end of 2015, NCCN expects to publish NCCN Evidence Blocks for systemic therapies (not surgery or radiation therapy) in the NCCN guidelines for breast, colon, non-small cell lung, and rectal cancers.
NCCN Evidence Blocks for systemic therapies are expected to be contained within the complete library of NCCN guidelines by the end of 2016.
In the near term, NCCN will continue to publish 2 sets of guidelines: those including NCCN Evidence Blocks and those without. The Evidence Blocks are not currently published in the NCCN Guidelines for Patients® and are intended for use in the US only.
For more information about NCCN Evidence Blocks, visit NCCN.org/EvidenceBlocks. ![]()

patient and her father
Photo by Rhoda Baer
The National Comprehensive Cancer Network (NCCN) has developed a new tool to accompany its clinical practice guidelines.
The tool—known as NCCN Evidence Blocks™—is designed to provide additional information about guideline recommendations and help inform treatment decisions.
NCCN has already added Evidence Blocks to its guidelines for chronic myelogenous leukemia and multiple myeloma.
The organization hopes to have Evidence Blocks for all of its guidelines by early 2017.
The Evidence Blocks provide a visual representation of 5 key value measures pertaining to guideline recommendations:
- Efficacy of treatment regimens
- Safety of regimens
- Quality and quantity of evidence supporting regimens
- Consistency of evidence supporting regimens
- Affordability of regimens. (This represents an estimate of overall total cost of a therapy, including but not limited to acquisition, administration, inpatient vs outpatient care, supportive care, infusions, toxicity monitoring, antiemetics and growth factors, and hospitalization.)
The Evidence Blocks are graphics of actual blocks that consist of 25 small squares. So each block has 5 rows and 5 columns.
Each of the 5 value measures—efficacy, safety, etc.—has a dedicated column within an Evidence Block, and each row of the Evidence Block represents a rating on a scale of 1 to 5. A score of 1 is unfavorable and a score of 5 is most favorable.
The rating of each value measure is shown by filling in the squares of the dedicated column—such as efficacy—up to the row that represents its assigned score—such as 4.
For example:
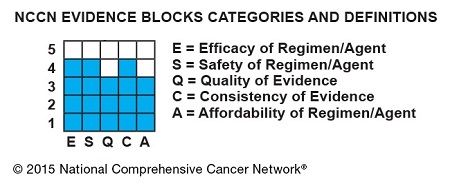
NCCN hopes this visual rating system will help patients and their physicians identify the optimal treatment based on clinical and economic considerations that are of the most value to the patient.
“Some patients will want an emerging therapy even with limited data,” said Robert W. Carlson, MD, chief executive officer of NCCN.
“Others will be most concerned about the expected side effects of the treatment indicated in the safety column. Still others may be very sensitive to cost. By considering the attributes of the range of possible therapies, the healthcare provider and the patient can discuss the benefits and drawbacks of each option and come to a decision most acceptable to the individual.”
By the end of 2015, NCCN expects to publish NCCN Evidence Blocks for systemic therapies (not surgery or radiation therapy) in the NCCN guidelines for breast, colon, non-small cell lung, and rectal cancers.
NCCN Evidence Blocks for systemic therapies are expected to be contained within the complete library of NCCN guidelines by the end of 2016.
In the near term, NCCN will continue to publish 2 sets of guidelines: those including NCCN Evidence Blocks and those without. The Evidence Blocks are not currently published in the NCCN Guidelines for Patients® and are intended for use in the US only.
For more information about NCCN Evidence Blocks, visit NCCN.org/EvidenceBlocks. ![]()
Lithium safe, effective for kids with bipolar type I
Lithium appears to be both safe and effective for the management of bipolar I disorder symptoms in pediatric populations, a recently published study from Pediatrics confirms.
Lead author Dr. Robert L. Findling of Johns Hopkins University and his associates conducted a multicenter, randomized, placebo-controlled outpatient trial, gathering data from 153 participants between the ages of 7 and 17 with bipolar I disorder/manic or mixed episodes. Among the participants, 81 were randomized to receive lithium (n = 53) or placebo (n = 28), for up to 8 weeks. Symptoms of bipolar disorder were assessed using the Young Mania Rating Scale (YMRS) score.
Ultimately, the study found that lithium was effective in reducing manic symptoms in nearly one-half (47%) of these participants, with Overall Clinical Global Impression–Improvement scores favoring lithium (n = 25; 47% very much/much improved), compared with placebo (n = 6; 21% very much/much improved) after 8 weeks. The researchers also noted that lithium use was not associated with weight gain, although they observed a statistically significant increase in thyrotropin concentration among the lithium group. Nausea, headache, and vomiting were the most common side effects.
“This study provides evidence to support the efficacy of lithium in the acute treatment of youths with [bipolar I disorder] who are currently in a manic or mixed state. Lithium had an adverse effect profile that was acceptable for most patients,” the authors wrote.
Read the full article in Pediatrics.
Lithium appears to be both safe and effective for the management of bipolar I disorder symptoms in pediatric populations, a recently published study from Pediatrics confirms.
Lead author Dr. Robert L. Findling of Johns Hopkins University and his associates conducted a multicenter, randomized, placebo-controlled outpatient trial, gathering data from 153 participants between the ages of 7 and 17 with bipolar I disorder/manic or mixed episodes. Among the participants, 81 were randomized to receive lithium (n = 53) or placebo (n = 28), for up to 8 weeks. Symptoms of bipolar disorder were assessed using the Young Mania Rating Scale (YMRS) score.
Ultimately, the study found that lithium was effective in reducing manic symptoms in nearly one-half (47%) of these participants, with Overall Clinical Global Impression–Improvement scores favoring lithium (n = 25; 47% very much/much improved), compared with placebo (n = 6; 21% very much/much improved) after 8 weeks. The researchers also noted that lithium use was not associated with weight gain, although they observed a statistically significant increase in thyrotropin concentration among the lithium group. Nausea, headache, and vomiting were the most common side effects.
“This study provides evidence to support the efficacy of lithium in the acute treatment of youths with [bipolar I disorder] who are currently in a manic or mixed state. Lithium had an adverse effect profile that was acceptable for most patients,” the authors wrote.
Read the full article in Pediatrics.
Lithium appears to be both safe and effective for the management of bipolar I disorder symptoms in pediatric populations, a recently published study from Pediatrics confirms.
Lead author Dr. Robert L. Findling of Johns Hopkins University and his associates conducted a multicenter, randomized, placebo-controlled outpatient trial, gathering data from 153 participants between the ages of 7 and 17 with bipolar I disorder/manic or mixed episodes. Among the participants, 81 were randomized to receive lithium (n = 53) or placebo (n = 28), for up to 8 weeks. Symptoms of bipolar disorder were assessed using the Young Mania Rating Scale (YMRS) score.
Ultimately, the study found that lithium was effective in reducing manic symptoms in nearly one-half (47%) of these participants, with Overall Clinical Global Impression–Improvement scores favoring lithium (n = 25; 47% very much/much improved), compared with placebo (n = 6; 21% very much/much improved) after 8 weeks. The researchers also noted that lithium use was not associated with weight gain, although they observed a statistically significant increase in thyrotropin concentration among the lithium group. Nausea, headache, and vomiting were the most common side effects.
“This study provides evidence to support the efficacy of lithium in the acute treatment of youths with [bipolar I disorder] who are currently in a manic or mixed state. Lithium had an adverse effect profile that was acceptable for most patients,” the authors wrote.
Read the full article in Pediatrics.
FROM PEDIATRICS