User login
Psychosis and catatonia after dancing with a dangerous partner
CASE Rigid, frightened, and mute
Mr. D, age 23, presents for evaluation immediately after discharge from another hospital, where he had been treated for altered mental status.
Ten days earlier, Mr. D’s friends obtained 2C-B (2,5-dimethoxy-4-bromophenethylamine), from the “Darknet,” an underground niche of the Internet. He ingested 20 mg of 2C-B in powder form. Although his friends recovered from a “safe trip,” Mr. D decompensated rapidly over the next few days with persistent psychosis, experiencing both auditory and visual hallucinations. He is “acting strange“ at work, and trying to find “hidden codes” in data. Mr. D also has persistent thought disorganization. He speaks of “connections” between people and things, and says that he is an alien in a spaceship. His friends and family report that he is talking rapidly and is sleeping only 2 or 3 hours each night. Mr. D abruptly quit his job as an analyst a few days after taking the drug.
Mr. D is a single, Ivy League-educated man and is described as hardworking and analytical. His family denies any recent mood changes or life stressors. They report that 1 month ago, Mr. D began smoking marijuana daily. He has no significant medical or psychiatric history, and no family history of psychiatric disorders.
What is your most likely diagnosis for Mr. D?
a) delirium due to a general medical condition
b) substance-induced psychotic disorder
c) catatonia due to a general medical condition
d) schizophrenia
e) bipolar I disorder, currently manic, with psychosis
The authors’ observations
Ring-substituted phenethylamines, commonly known as 2Cs, are designer drugs that are emerging as new substances of abuse.1 2C-B belongs to the phenethylamine subclass of monoamine alkaloids that includes more familiar drugs such as amphetamines, methamphetamines, and 3,4-methylenedioxy-methamphetamine (MDMA).2 It was first synthesized in 1974 by Alexander Shulgin, later described in his book Phenethylamines I Have Known and Loved: A Chemical Love Story, and its hallucinogenic activity is reported to be similar to LSD, mescaline, and psilocybin.3 The literature is scant on the acute effects of 2C intoxication or long-term sequelae of 2C ingestion.1 Most available information regarding the pharmacology of 2C-B comes from users who have reported their drug experiences on blogs, Web sites and forums, and in the media.4
2C-B usually is taken orally in powder or tablet form, in a dose of 10 to 50 mg.4 After an onset period of 20 to 90 minutes, the drug’s effect reaches maximum effect in 15 to 30 minutes, then plateaus for 2 to 7 hours, and comes down within 1 to 2 hours.4 2C-B is known to be orally active, and its hallucinogenic effects are mediated by its actions as a partial serotonin 5HT-2A and 5HT-2C receptor agonist.5 Entactogenic-stimulating effects have been reported at low doses (4 to 10 mg), whereas visual hallucinations with intense colors and object distortion have been reported at moderate doses (10 to 20 mg).4
2C-B, which users often take at parties or raves, appeared on the drug market in the mid 1980s and early 1990s under the names Nexus, Erox, Performax, Toonies, Bromo, Spectrum, and Venus and marketed as a replacement for MDMA after it became a Schedule I drug in the United States.4,6 Some users consume 2C-B in combination with other illicit drugs, including MDMA (called a “party pack”) or LSD (referred to as a “banana split”).6
According to the U.S. Drug Enforcement Agency, law enforcement authorities first seized 2C-B laboratories in California in 1986 and Arizona in 1992.6 Distribution of the drug has been sporadic since it became Schedule I in 1995, and it has been seized from several states, including Virginia, Nevada, Maine, Illinois, Missouri, South Dakota, and Kansas.6
EXAMINATION Passive and mute
On examination, Mr. D is lying in bed with eyes closed and extremities extended in an odd, rigid posture. He is resistant to attempts at passive movement, is nonresponsive to verbal commands, and is mute. A review of vital signs shows tachycardia, 110 beats per minute, but the physical exam is otherwise unremarkable. His Bush-Francis Catatonia Rating Scale (BFCRS) score is 17, indicating a diagnosis of catatonia. Mini-Mental Status Examination cannot be completed because Mr. D is unable to participate.
Laboratory studies reveal an elevated creatinine kinase (CK) level of 356 U/L. Results of a complete blood count, comprehensive metabolic panel, urinalysis, and thyroid-stimulating hormone are normal. Blood alcohol level is <10 mg/dL. Acetaminophen and salicylate levels are normal (<5 mg/dL). Records from his recent hospitalization reveal normal head CT, chest radiography, EEG, and urinalysis, and a negative urine drug screen.
What is the next step in managing Mr. D’s catatonic symptoms?
a) IV normal saline
b) IV lorazepam
c) emergent electroconvulsive therapy (ECT)
d) IM haloperidol
e) IM olanzapine
TREATMENT Saline and psychotropics
While in the emergency room, Mr. D receives 2 L of IV saline. His CK level falls to 137 U/L. A challenge with IV lorazepam, 2 mg, also is performed. Mr. D becomes talkative and follows commands with fluid movements, but his disorganized, delusional thoughts persist. BFCRS score has improved to 9 (Table 1). He is admitted to the psychiatric unit and started on oral lorazepam, 2 mg, 3 times daily, for catatonia, and olanzapine, 10 mg/d, for psychosis.
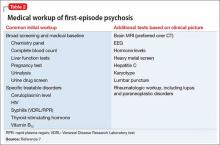
The differential diagnosis for Mr. D’s psychosis includes substance-induced psychotic disorder, schizophrenia, bipolar disorder, and psychosis with another organic cause (Table 2).7 Further medical workup is completed, including a urine drug screen, testing for HIV, hepatitis B, syphilis, lead and heavy metals, ceruloplasmin, vitamin B12, folate, antinuclear antibody, sedimentation rate, and brain MRI. Cannabinoids are detected in his urine drug screen. Another urine sample is sent to an outside lab to test for several synthetic drugs, including MDMA, 3,4-methylenedioxy- N-ethyl-amphetamine, 2C-B, 2C-C, 2C-I, and 2C-P, results of which also are negative.
By the second day of hospitalization, Mr. D appears less disorganized but continues to complain of “scrambled thoughts” and appears guarded. Despite initial response to IV lorazepam and its continuation in oral form, over the next day Mr. D appears more psychomotor-slowed, with motor stiffness. His score on the BFCRS increases, with significant posturing; vital signs remain stable, however.
What is your next step in managing his catatonic symptoms?
a) increase olanzapine
b) decrease olanzapine
c) decrease lorazepam
d) emergent ECT
e) switch to haloperidol
The authors’ observations
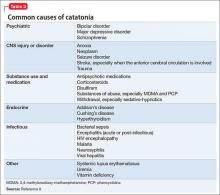
Although catatonia can be associated with a mood or psychotic disorder, it also can be induced by a medication or general medical condition (Table 3).8 It is thought that catatonia is associated with decreased γ-aminobutyric acid (GABA) and dopamine D2 receptor activity, and increased N-methyl-d-aspartate (NMDA) receptor activity.9 Antipsychotics could worsen catatonia through D2 blockade. Benzodiazepines, however, improve catatonia by increasing GABA and decreasing NMDA receptor activity. In this case, Mr. D was naïve to antipsychotics and seemed to be sensitive to them, as evidenced by his worsening symptoms.
Which condition should be considered in the differential diagnosis?
a) parkinsonian-hyperpyrexia syndrome
b) neuroleptic malignant syndrome (NMS)
c) stiff person syndrome
d) serotonin syndrome
e) CNS infection
The authors’ observations
NMS, catatonia, and parkinsonian-hyperpyrexia syndrome are all related to diminished action of dopamine at the D2 receptor. Although the mechanism of catatonia is not completely understood, NMS is thought to be caused by blockade at the D2 receptors by antipsychotics, whereas parkinsonian-hyperpyrexia syndrome is related to withdrawal of dopamine agonists. Because of the similarity in symptoms and proposed mechanisms, some experts hypothesize that NMS is a drug-induced malignant catatonia.10,11 Interestingly, NMS and catatonia respond to withdrawal of antipsychotics, and addition of benzodiazepines and ECT.
Mr. D showed posturing and other behavioral abnormalities, which are less common in NMS. Furthermore, although he had episodes of mild tachycardia, autonomic dysregulation—a hallmark of NMS—was not found. Given the common shared deficiency of activity at the D2 receptor in both NMS and catatonia, antipsychotics could cause or worsen either condition.
TREATMENT ECT
Mr. D’s olanzapine dosage is decreased to 2.5 mg/d. His catatonic symptoms improve with each dosage of oral lorazepam; however, effects seem to lessen and last for shorter periods over the following day. Additionally, Mr. D again becomes more disorganized, stiff, and unable to feed or bathe himself, and develops episodes of mild tachycardia.
Given Mr. D’s partial and poorly sustained response to lorazepam, a trial of ECT is pursued. On the third day of hospitalization, he receives ECT with bi-frontal lead placement at 25% energy. Concurrently, olanzapine is discontinued because of worsening muscle stiffness and concern about neuroleptic sensitivity. His BFCRS score after ECT is 2, and he is noted to be more interactive on the inpatient unit. He continues to receive ECT 3 times a week, with notable improvement, but ongoing psychotic symptoms and catatonic symptoms partially reemerge between ECT treatments. Lead placement is changed to bi-temporal by the third treatment, and the energy setting is increased from 25% to 50%, and to 75% by the sixth treatment. An additional nighttime dose of oral lorazepam, 2 mg, is added after the sixth treatment, in an attempt to reduce “wearing off” by morning.
After the seventh treatment, Mr. D is able to maintain logical conversation without re-emergence of catatonic symptoms over 2 days, signifying a turning point in the treatment course. The ECT energy setting is decreased to 50% to minimize potential memory deficits. His insight into his illness and treatment dramatically improve over the next few days. ECT is discontinued after the tenth treatment and Mr. D is discharged home to the care of his family.
The authors’ observations
Randomized clinical trials studying the effectiveness of ECT for catatonia are limited. Much of what we know about ECT comes from case reports that describe excellent outcomes for a variety of treatment-resistant illnesses, including catatonia in mood disorders, schizophrenia, autism, and other organic brain disease.12
Although benzodiazepines often are the first-line treatment for catatonia caused by any underlying illness, one study showed only 1 of 41 patients achieved remission with benzodiazepines, compared with 100% of those treated with ECT13; another study supported these results with 8 of 9 lorazepam non-responders responding to ECT.14 There are few case reports of substance-induced catatonia in the absence of other chronic mental illness, although none report use of ECT. However, a study showed no significant difference in the effectiveness of ECT for catatonia caused by an affective disorder or schizophrenia.15
Mr. D’s case exemplifies complete remission of catatonia induced by a psychoactive substance.
OUTCOME Steady improvement
Mr. D is followed in the outpatient clinic for 1 month after discharge; lorazepam is tapered successfully. During this time frame, psychotic and catatonic symptoms do not re-emerge. He reports some initial working memory deficits that improve steadily. There is no evidence of any significant psychiatric signs or symptoms, including neurovegetative symptoms of depression, mania or hypomania, perceptual disturbances, or disorganized thoughts or behaviors. He remains abstinent from alcohol, tobacco, and all psychoactive substances.
Bottom Line
Persistent psychosis and catatonia after the use of newer designer drugs such as 2C-B are rare, but these drugs carry serious potential complications that clinicians should be aware of. Benzodiazepines and electroconvulsive therapy have been proved effective for catatonia that is related to a number of psychiatric illnesses, often resulting in good outcomes. However, current evidence on their use is limited, particularly regarding treatment of substance-induced psychosis and catatonia.
Related Resources
• Meyer MR, Maurer HH. Metabolism of designer drugs of abuse: an updated review. Curr Drug Metab. 2010;11(5):468-482.
• Rickli A, Luethi D, Reinisch J, et al. Receptor interaction profiles of novel N-2-methoxybenzyl (NBOMe) derivatives of 2,5-dimethoxy-substituted phenethylamines (2C drugs). Neuropharmacology. 2015;99:546-553.
Drug Brand Names
Haloperidol • Haldol
Lorazepam • Ativan
Olanzapine • Zyprexa
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Dean BV, Stellpflug SJ, Burnett AM, et al. 2C or not 2C: phenethylamine designer drug review. J Med Toxicol. 2013;9(2):172-178.
2. Hill SL, Thomas SH. Clinical toxicology of newer recreational drugs. Clin Toxicol (Phila). 2011;49(8):705-719.
3. Shulgin A, Shulgin A. PiHKAL: a chemical love story. Berkley, CA: Transform Press; 1991.
4. Papoutsis I, Nikolaou P, Stefanidou M, et al. 25B-NBOMe and its precursor 2C-B: modern trends and hidden dangers. Forensic Toxicology. 2015;3(1):1-11.
5. Caudevilla-Gálligo F, Riba J, Ventura M, et al. 4-Bromo-2, 5-dimethoxyphenethylamine (2C-B): presence in the recreational drug market in Spain, pattern of use and subjective effects. J Psychopharmacol. 2012;26(7):1026-1035.
6. National Drug Intelligence Center. Information bulletin: 2C-B (Nexus) reappears on the club drug scene. http:// www.Justice.gov/archive/ndic/pubs0/665. Published May 2001. Accessed June 12, 2015.
7. Freudenreich O, Schulz SC, Goff DC. Initial medical work-up of first episode psychosis: a conceptual review. Early Interv Psychiatry. 2009;3(1):10-18.
8. Masand PS, Levenson JL, et al. Mania, catatonia, and psychosis. In: Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. Washington, DC: American Psychiatric Publishing; 2005: 239-241.
9. Carroll BT. The universal field of hypothesis of catatonia and neuroleptic malignant syndrome. CNS Spectr. 2000;5(7):26-33.
10. Lee JW. Neuroleptic-induced catatonia: clinical presentation, response to benzodiazepines, and relationship to neuroleptic malignant syndrome. J Clin Psychopharmacol. 2010;30(1):3-10.
11. Vancaester E, Santens P. Catatonia and neuroleptic malignant syndrome: two sides of a coin? Acta Neurol Belg. 2007;107(2):47-50.
12. Sienaert P, Dhossche DM, Vancampfort D, et al. A clinical review of the treatment of catatonia. Front Psychiatry. 2014;5:181.
13. Hatta K, Miyakawa K, Ota T, et al. Maximal response to electroconvulsive therapy for the treatment of catatonic symptoms. J ECT. 2007;23(4):233-235.
14. Payee H, Chandrasekaran R, Raju GV. Catatonic syndrome: treatment response to Lorazepam. Indian J Psychiatry. 1999;41(1):49-53.
15. Rohland BM, Carroll BT, Jacoby RG. ECT in the treatment of the catatonic syndrome. J Affect Disord. 1993;29(4):255-261.
3,4-methylenedioxy-methamphetamine, MDMA, Phenethylamines I Have Known and Loved: A Chemical Love Story, LSD, substance abuse, substance use
CASE Rigid, frightened, and mute
Mr. D, age 23, presents for evaluation immediately after discharge from another hospital, where he had been treated for altered mental status.
Ten days earlier, Mr. D’s friends obtained 2C-B (2,5-dimethoxy-4-bromophenethylamine), from the “Darknet,” an underground niche of the Internet. He ingested 20 mg of 2C-B in powder form. Although his friends recovered from a “safe trip,” Mr. D decompensated rapidly over the next few days with persistent psychosis, experiencing both auditory and visual hallucinations. He is “acting strange“ at work, and trying to find “hidden codes” in data. Mr. D also has persistent thought disorganization. He speaks of “connections” between people and things, and says that he is an alien in a spaceship. His friends and family report that he is talking rapidly and is sleeping only 2 or 3 hours each night. Mr. D abruptly quit his job as an analyst a few days after taking the drug.
Mr. D is a single, Ivy League-educated man and is described as hardworking and analytical. His family denies any recent mood changes or life stressors. They report that 1 month ago, Mr. D began smoking marijuana daily. He has no significant medical or psychiatric history, and no family history of psychiatric disorders.
What is your most likely diagnosis for Mr. D?
a) delirium due to a general medical condition
b) substance-induced psychotic disorder
c) catatonia due to a general medical condition
d) schizophrenia
e) bipolar I disorder, currently manic, with psychosis
The authors’ observations
Ring-substituted phenethylamines, commonly known as 2Cs, are designer drugs that are emerging as new substances of abuse.1 2C-B belongs to the phenethylamine subclass of monoamine alkaloids that includes more familiar drugs such as amphetamines, methamphetamines, and 3,4-methylenedioxy-methamphetamine (MDMA).2 It was first synthesized in 1974 by Alexander Shulgin, later described in his book Phenethylamines I Have Known and Loved: A Chemical Love Story, and its hallucinogenic activity is reported to be similar to LSD, mescaline, and psilocybin.3 The literature is scant on the acute effects of 2C intoxication or long-term sequelae of 2C ingestion.1 Most available information regarding the pharmacology of 2C-B comes from users who have reported their drug experiences on blogs, Web sites and forums, and in the media.4
2C-B usually is taken orally in powder or tablet form, in a dose of 10 to 50 mg.4 After an onset period of 20 to 90 minutes, the drug’s effect reaches maximum effect in 15 to 30 minutes, then plateaus for 2 to 7 hours, and comes down within 1 to 2 hours.4 2C-B is known to be orally active, and its hallucinogenic effects are mediated by its actions as a partial serotonin 5HT-2A and 5HT-2C receptor agonist.5 Entactogenic-stimulating effects have been reported at low doses (4 to 10 mg), whereas visual hallucinations with intense colors and object distortion have been reported at moderate doses (10 to 20 mg).4
2C-B, which users often take at parties or raves, appeared on the drug market in the mid 1980s and early 1990s under the names Nexus, Erox, Performax, Toonies, Bromo, Spectrum, and Venus and marketed as a replacement for MDMA after it became a Schedule I drug in the United States.4,6 Some users consume 2C-B in combination with other illicit drugs, including MDMA (called a “party pack”) or LSD (referred to as a “banana split”).6
According to the U.S. Drug Enforcement Agency, law enforcement authorities first seized 2C-B laboratories in California in 1986 and Arizona in 1992.6 Distribution of the drug has been sporadic since it became Schedule I in 1995, and it has been seized from several states, including Virginia, Nevada, Maine, Illinois, Missouri, South Dakota, and Kansas.6
EXAMINATION Passive and mute
On examination, Mr. D is lying in bed with eyes closed and extremities extended in an odd, rigid posture. He is resistant to attempts at passive movement, is nonresponsive to verbal commands, and is mute. A review of vital signs shows tachycardia, 110 beats per minute, but the physical exam is otherwise unremarkable. His Bush-Francis Catatonia Rating Scale (BFCRS) score is 17, indicating a diagnosis of catatonia. Mini-Mental Status Examination cannot be completed because Mr. D is unable to participate.
Laboratory studies reveal an elevated creatinine kinase (CK) level of 356 U/L. Results of a complete blood count, comprehensive metabolic panel, urinalysis, and thyroid-stimulating hormone are normal. Blood alcohol level is <10 mg/dL. Acetaminophen and salicylate levels are normal (<5 mg/dL). Records from his recent hospitalization reveal normal head CT, chest radiography, EEG, and urinalysis, and a negative urine drug screen.
What is the next step in managing Mr. D’s catatonic symptoms?
a) IV normal saline
b) IV lorazepam
c) emergent electroconvulsive therapy (ECT)
d) IM haloperidol
e) IM olanzapine
TREATMENT Saline and psychotropics
While in the emergency room, Mr. D receives 2 L of IV saline. His CK level falls to 137 U/L. A challenge with IV lorazepam, 2 mg, also is performed. Mr. D becomes talkative and follows commands with fluid movements, but his disorganized, delusional thoughts persist. BFCRS score has improved to 9 (Table 1). He is admitted to the psychiatric unit and started on oral lorazepam, 2 mg, 3 times daily, for catatonia, and olanzapine, 10 mg/d, for psychosis.
The differential diagnosis for Mr. D’s psychosis includes substance-induced psychotic disorder, schizophrenia, bipolar disorder, and psychosis with another organic cause (Table 2).7 Further medical workup is completed, including a urine drug screen, testing for HIV, hepatitis B, syphilis, lead and heavy metals, ceruloplasmin, vitamin B12, folate, antinuclear antibody, sedimentation rate, and brain MRI. Cannabinoids are detected in his urine drug screen. Another urine sample is sent to an outside lab to test for several synthetic drugs, including MDMA, 3,4-methylenedioxy- N-ethyl-amphetamine, 2C-B, 2C-C, 2C-I, and 2C-P, results of which also are negative.
By the second day of hospitalization, Mr. D appears less disorganized but continues to complain of “scrambled thoughts” and appears guarded. Despite initial response to IV lorazepam and its continuation in oral form, over the next day Mr. D appears more psychomotor-slowed, with motor stiffness. His score on the BFCRS increases, with significant posturing; vital signs remain stable, however.
What is your next step in managing his catatonic symptoms?
a) increase olanzapine
b) decrease olanzapine
c) decrease lorazepam
d) emergent ECT
e) switch to haloperidol
The authors’ observations
Although catatonia can be associated with a mood or psychotic disorder, it also can be induced by a medication or general medical condition (Table 3).8 It is thought that catatonia is associated with decreased γ-aminobutyric acid (GABA) and dopamine D2 receptor activity, and increased N-methyl-d-aspartate (NMDA) receptor activity.9 Antipsychotics could worsen catatonia through D2 blockade. Benzodiazepines, however, improve catatonia by increasing GABA and decreasing NMDA receptor activity. In this case, Mr. D was naïve to antipsychotics and seemed to be sensitive to them, as evidenced by his worsening symptoms.
Which condition should be considered in the differential diagnosis?
a) parkinsonian-hyperpyrexia syndrome
b) neuroleptic malignant syndrome (NMS)
c) stiff person syndrome
d) serotonin syndrome
e) CNS infection
The authors’ observations
NMS, catatonia, and parkinsonian-hyperpyrexia syndrome are all related to diminished action of dopamine at the D2 receptor. Although the mechanism of catatonia is not completely understood, NMS is thought to be caused by blockade at the D2 receptors by antipsychotics, whereas parkinsonian-hyperpyrexia syndrome is related to withdrawal of dopamine agonists. Because of the similarity in symptoms and proposed mechanisms, some experts hypothesize that NMS is a drug-induced malignant catatonia.10,11 Interestingly, NMS and catatonia respond to withdrawal of antipsychotics, and addition of benzodiazepines and ECT.
Mr. D showed posturing and other behavioral abnormalities, which are less common in NMS. Furthermore, although he had episodes of mild tachycardia, autonomic dysregulation—a hallmark of NMS—was not found. Given the common shared deficiency of activity at the D2 receptor in both NMS and catatonia, antipsychotics could cause or worsen either condition.
TREATMENT ECT
Mr. D’s olanzapine dosage is decreased to 2.5 mg/d. His catatonic symptoms improve with each dosage of oral lorazepam; however, effects seem to lessen and last for shorter periods over the following day. Additionally, Mr. D again becomes more disorganized, stiff, and unable to feed or bathe himself, and develops episodes of mild tachycardia.
Given Mr. D’s partial and poorly sustained response to lorazepam, a trial of ECT is pursued. On the third day of hospitalization, he receives ECT with bi-frontal lead placement at 25% energy. Concurrently, olanzapine is discontinued because of worsening muscle stiffness and concern about neuroleptic sensitivity. His BFCRS score after ECT is 2, and he is noted to be more interactive on the inpatient unit. He continues to receive ECT 3 times a week, with notable improvement, but ongoing psychotic symptoms and catatonic symptoms partially reemerge between ECT treatments. Lead placement is changed to bi-temporal by the third treatment, and the energy setting is increased from 25% to 50%, and to 75% by the sixth treatment. An additional nighttime dose of oral lorazepam, 2 mg, is added after the sixth treatment, in an attempt to reduce “wearing off” by morning.
After the seventh treatment, Mr. D is able to maintain logical conversation without re-emergence of catatonic symptoms over 2 days, signifying a turning point in the treatment course. The ECT energy setting is decreased to 50% to minimize potential memory deficits. His insight into his illness and treatment dramatically improve over the next few days. ECT is discontinued after the tenth treatment and Mr. D is discharged home to the care of his family.
The authors’ observations
Randomized clinical trials studying the effectiveness of ECT for catatonia are limited. Much of what we know about ECT comes from case reports that describe excellent outcomes for a variety of treatment-resistant illnesses, including catatonia in mood disorders, schizophrenia, autism, and other organic brain disease.12
Although benzodiazepines often are the first-line treatment for catatonia caused by any underlying illness, one study showed only 1 of 41 patients achieved remission with benzodiazepines, compared with 100% of those treated with ECT13; another study supported these results with 8 of 9 lorazepam non-responders responding to ECT.14 There are few case reports of substance-induced catatonia in the absence of other chronic mental illness, although none report use of ECT. However, a study showed no significant difference in the effectiveness of ECT for catatonia caused by an affective disorder or schizophrenia.15
Mr. D’s case exemplifies complete remission of catatonia induced by a psychoactive substance.
OUTCOME Steady improvement
Mr. D is followed in the outpatient clinic for 1 month after discharge; lorazepam is tapered successfully. During this time frame, psychotic and catatonic symptoms do not re-emerge. He reports some initial working memory deficits that improve steadily. There is no evidence of any significant psychiatric signs or symptoms, including neurovegetative symptoms of depression, mania or hypomania, perceptual disturbances, or disorganized thoughts or behaviors. He remains abstinent from alcohol, tobacco, and all psychoactive substances.
Bottom Line
Persistent psychosis and catatonia after the use of newer designer drugs such as 2C-B are rare, but these drugs carry serious potential complications that clinicians should be aware of. Benzodiazepines and electroconvulsive therapy have been proved effective for catatonia that is related to a number of psychiatric illnesses, often resulting in good outcomes. However, current evidence on their use is limited, particularly regarding treatment of substance-induced psychosis and catatonia.
Related Resources
• Meyer MR, Maurer HH. Metabolism of designer drugs of abuse: an updated review. Curr Drug Metab. 2010;11(5):468-482.
• Rickli A, Luethi D, Reinisch J, et al. Receptor interaction profiles of novel N-2-methoxybenzyl (NBOMe) derivatives of 2,5-dimethoxy-substituted phenethylamines (2C drugs). Neuropharmacology. 2015;99:546-553.
Drug Brand Names
Haloperidol • Haldol
Lorazepam • Ativan
Olanzapine • Zyprexa
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE Rigid, frightened, and mute
Mr. D, age 23, presents for evaluation immediately after discharge from another hospital, where he had been treated for altered mental status.
Ten days earlier, Mr. D’s friends obtained 2C-B (2,5-dimethoxy-4-bromophenethylamine), from the “Darknet,” an underground niche of the Internet. He ingested 20 mg of 2C-B in powder form. Although his friends recovered from a “safe trip,” Mr. D decompensated rapidly over the next few days with persistent psychosis, experiencing both auditory and visual hallucinations. He is “acting strange“ at work, and trying to find “hidden codes” in data. Mr. D also has persistent thought disorganization. He speaks of “connections” between people and things, and says that he is an alien in a spaceship. His friends and family report that he is talking rapidly and is sleeping only 2 or 3 hours each night. Mr. D abruptly quit his job as an analyst a few days after taking the drug.
Mr. D is a single, Ivy League-educated man and is described as hardworking and analytical. His family denies any recent mood changes or life stressors. They report that 1 month ago, Mr. D began smoking marijuana daily. He has no significant medical or psychiatric history, and no family history of psychiatric disorders.
What is your most likely diagnosis for Mr. D?
a) delirium due to a general medical condition
b) substance-induced psychotic disorder
c) catatonia due to a general medical condition
d) schizophrenia
e) bipolar I disorder, currently manic, with psychosis
The authors’ observations
Ring-substituted phenethylamines, commonly known as 2Cs, are designer drugs that are emerging as new substances of abuse.1 2C-B belongs to the phenethylamine subclass of monoamine alkaloids that includes more familiar drugs such as amphetamines, methamphetamines, and 3,4-methylenedioxy-methamphetamine (MDMA).2 It was first synthesized in 1974 by Alexander Shulgin, later described in his book Phenethylamines I Have Known and Loved: A Chemical Love Story, and its hallucinogenic activity is reported to be similar to LSD, mescaline, and psilocybin.3 The literature is scant on the acute effects of 2C intoxication or long-term sequelae of 2C ingestion.1 Most available information regarding the pharmacology of 2C-B comes from users who have reported their drug experiences on blogs, Web sites and forums, and in the media.4
2C-B usually is taken orally in powder or tablet form, in a dose of 10 to 50 mg.4 After an onset period of 20 to 90 minutes, the drug’s effect reaches maximum effect in 15 to 30 minutes, then plateaus for 2 to 7 hours, and comes down within 1 to 2 hours.4 2C-B is known to be orally active, and its hallucinogenic effects are mediated by its actions as a partial serotonin 5HT-2A and 5HT-2C receptor agonist.5 Entactogenic-stimulating effects have been reported at low doses (4 to 10 mg), whereas visual hallucinations with intense colors and object distortion have been reported at moderate doses (10 to 20 mg).4
2C-B, which users often take at parties or raves, appeared on the drug market in the mid 1980s and early 1990s under the names Nexus, Erox, Performax, Toonies, Bromo, Spectrum, and Venus and marketed as a replacement for MDMA after it became a Schedule I drug in the United States.4,6 Some users consume 2C-B in combination with other illicit drugs, including MDMA (called a “party pack”) or LSD (referred to as a “banana split”).6
According to the U.S. Drug Enforcement Agency, law enforcement authorities first seized 2C-B laboratories in California in 1986 and Arizona in 1992.6 Distribution of the drug has been sporadic since it became Schedule I in 1995, and it has been seized from several states, including Virginia, Nevada, Maine, Illinois, Missouri, South Dakota, and Kansas.6
EXAMINATION Passive and mute
On examination, Mr. D is lying in bed with eyes closed and extremities extended in an odd, rigid posture. He is resistant to attempts at passive movement, is nonresponsive to verbal commands, and is mute. A review of vital signs shows tachycardia, 110 beats per minute, but the physical exam is otherwise unremarkable. His Bush-Francis Catatonia Rating Scale (BFCRS) score is 17, indicating a diagnosis of catatonia. Mini-Mental Status Examination cannot be completed because Mr. D is unable to participate.
Laboratory studies reveal an elevated creatinine kinase (CK) level of 356 U/L. Results of a complete blood count, comprehensive metabolic panel, urinalysis, and thyroid-stimulating hormone are normal. Blood alcohol level is <10 mg/dL. Acetaminophen and salicylate levels are normal (<5 mg/dL). Records from his recent hospitalization reveal normal head CT, chest radiography, EEG, and urinalysis, and a negative urine drug screen.
What is the next step in managing Mr. D’s catatonic symptoms?
a) IV normal saline
b) IV lorazepam
c) emergent electroconvulsive therapy (ECT)
d) IM haloperidol
e) IM olanzapine
TREATMENT Saline and psychotropics
While in the emergency room, Mr. D receives 2 L of IV saline. His CK level falls to 137 U/L. A challenge with IV lorazepam, 2 mg, also is performed. Mr. D becomes talkative and follows commands with fluid movements, but his disorganized, delusional thoughts persist. BFCRS score has improved to 9 (Table 1). He is admitted to the psychiatric unit and started on oral lorazepam, 2 mg, 3 times daily, for catatonia, and olanzapine, 10 mg/d, for psychosis.
The differential diagnosis for Mr. D’s psychosis includes substance-induced psychotic disorder, schizophrenia, bipolar disorder, and psychosis with another organic cause (Table 2).7 Further medical workup is completed, including a urine drug screen, testing for HIV, hepatitis B, syphilis, lead and heavy metals, ceruloplasmin, vitamin B12, folate, antinuclear antibody, sedimentation rate, and brain MRI. Cannabinoids are detected in his urine drug screen. Another urine sample is sent to an outside lab to test for several synthetic drugs, including MDMA, 3,4-methylenedioxy- N-ethyl-amphetamine, 2C-B, 2C-C, 2C-I, and 2C-P, results of which also are negative.
By the second day of hospitalization, Mr. D appears less disorganized but continues to complain of “scrambled thoughts” and appears guarded. Despite initial response to IV lorazepam and its continuation in oral form, over the next day Mr. D appears more psychomotor-slowed, with motor stiffness. His score on the BFCRS increases, with significant posturing; vital signs remain stable, however.
What is your next step in managing his catatonic symptoms?
a) increase olanzapine
b) decrease olanzapine
c) decrease lorazepam
d) emergent ECT
e) switch to haloperidol
The authors’ observations
Although catatonia can be associated with a mood or psychotic disorder, it also can be induced by a medication or general medical condition (Table 3).8 It is thought that catatonia is associated with decreased γ-aminobutyric acid (GABA) and dopamine D2 receptor activity, and increased N-methyl-d-aspartate (NMDA) receptor activity.9 Antipsychotics could worsen catatonia through D2 blockade. Benzodiazepines, however, improve catatonia by increasing GABA and decreasing NMDA receptor activity. In this case, Mr. D was naïve to antipsychotics and seemed to be sensitive to them, as evidenced by his worsening symptoms.
Which condition should be considered in the differential diagnosis?
a) parkinsonian-hyperpyrexia syndrome
b) neuroleptic malignant syndrome (NMS)
c) stiff person syndrome
d) serotonin syndrome
e) CNS infection
The authors’ observations
NMS, catatonia, and parkinsonian-hyperpyrexia syndrome are all related to diminished action of dopamine at the D2 receptor. Although the mechanism of catatonia is not completely understood, NMS is thought to be caused by blockade at the D2 receptors by antipsychotics, whereas parkinsonian-hyperpyrexia syndrome is related to withdrawal of dopamine agonists. Because of the similarity in symptoms and proposed mechanisms, some experts hypothesize that NMS is a drug-induced malignant catatonia.10,11 Interestingly, NMS and catatonia respond to withdrawal of antipsychotics, and addition of benzodiazepines and ECT.
Mr. D showed posturing and other behavioral abnormalities, which are less common in NMS. Furthermore, although he had episodes of mild tachycardia, autonomic dysregulation—a hallmark of NMS—was not found. Given the common shared deficiency of activity at the D2 receptor in both NMS and catatonia, antipsychotics could cause or worsen either condition.
TREATMENT ECT
Mr. D’s olanzapine dosage is decreased to 2.5 mg/d. His catatonic symptoms improve with each dosage of oral lorazepam; however, effects seem to lessen and last for shorter periods over the following day. Additionally, Mr. D again becomes more disorganized, stiff, and unable to feed or bathe himself, and develops episodes of mild tachycardia.
Given Mr. D’s partial and poorly sustained response to lorazepam, a trial of ECT is pursued. On the third day of hospitalization, he receives ECT with bi-frontal lead placement at 25% energy. Concurrently, olanzapine is discontinued because of worsening muscle stiffness and concern about neuroleptic sensitivity. His BFCRS score after ECT is 2, and he is noted to be more interactive on the inpatient unit. He continues to receive ECT 3 times a week, with notable improvement, but ongoing psychotic symptoms and catatonic symptoms partially reemerge between ECT treatments. Lead placement is changed to bi-temporal by the third treatment, and the energy setting is increased from 25% to 50%, and to 75% by the sixth treatment. An additional nighttime dose of oral lorazepam, 2 mg, is added after the sixth treatment, in an attempt to reduce “wearing off” by morning.
After the seventh treatment, Mr. D is able to maintain logical conversation without re-emergence of catatonic symptoms over 2 days, signifying a turning point in the treatment course. The ECT energy setting is decreased to 50% to minimize potential memory deficits. His insight into his illness and treatment dramatically improve over the next few days. ECT is discontinued after the tenth treatment and Mr. D is discharged home to the care of his family.
The authors’ observations
Randomized clinical trials studying the effectiveness of ECT for catatonia are limited. Much of what we know about ECT comes from case reports that describe excellent outcomes for a variety of treatment-resistant illnesses, including catatonia in mood disorders, schizophrenia, autism, and other organic brain disease.12
Although benzodiazepines often are the first-line treatment for catatonia caused by any underlying illness, one study showed only 1 of 41 patients achieved remission with benzodiazepines, compared with 100% of those treated with ECT13; another study supported these results with 8 of 9 lorazepam non-responders responding to ECT.14 There are few case reports of substance-induced catatonia in the absence of other chronic mental illness, although none report use of ECT. However, a study showed no significant difference in the effectiveness of ECT for catatonia caused by an affective disorder or schizophrenia.15
Mr. D’s case exemplifies complete remission of catatonia induced by a psychoactive substance.
OUTCOME Steady improvement
Mr. D is followed in the outpatient clinic for 1 month after discharge; lorazepam is tapered successfully. During this time frame, psychotic and catatonic symptoms do not re-emerge. He reports some initial working memory deficits that improve steadily. There is no evidence of any significant psychiatric signs or symptoms, including neurovegetative symptoms of depression, mania or hypomania, perceptual disturbances, or disorganized thoughts or behaviors. He remains abstinent from alcohol, tobacco, and all psychoactive substances.
Bottom Line
Persistent psychosis and catatonia after the use of newer designer drugs such as 2C-B are rare, but these drugs carry serious potential complications that clinicians should be aware of. Benzodiazepines and electroconvulsive therapy have been proved effective for catatonia that is related to a number of psychiatric illnesses, often resulting in good outcomes. However, current evidence on their use is limited, particularly regarding treatment of substance-induced psychosis and catatonia.
Related Resources
• Meyer MR, Maurer HH. Metabolism of designer drugs of abuse: an updated review. Curr Drug Metab. 2010;11(5):468-482.
• Rickli A, Luethi D, Reinisch J, et al. Receptor interaction profiles of novel N-2-methoxybenzyl (NBOMe) derivatives of 2,5-dimethoxy-substituted phenethylamines (2C drugs). Neuropharmacology. 2015;99:546-553.
Drug Brand Names
Haloperidol • Haldol
Lorazepam • Ativan
Olanzapine • Zyprexa
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Dean BV, Stellpflug SJ, Burnett AM, et al. 2C or not 2C: phenethylamine designer drug review. J Med Toxicol. 2013;9(2):172-178.
2. Hill SL, Thomas SH. Clinical toxicology of newer recreational drugs. Clin Toxicol (Phila). 2011;49(8):705-719.
3. Shulgin A, Shulgin A. PiHKAL: a chemical love story. Berkley, CA: Transform Press; 1991.
4. Papoutsis I, Nikolaou P, Stefanidou M, et al. 25B-NBOMe and its precursor 2C-B: modern trends and hidden dangers. Forensic Toxicology. 2015;3(1):1-11.
5. Caudevilla-Gálligo F, Riba J, Ventura M, et al. 4-Bromo-2, 5-dimethoxyphenethylamine (2C-B): presence in the recreational drug market in Spain, pattern of use and subjective effects. J Psychopharmacol. 2012;26(7):1026-1035.
6. National Drug Intelligence Center. Information bulletin: 2C-B (Nexus) reappears on the club drug scene. http:// www.Justice.gov/archive/ndic/pubs0/665. Published May 2001. Accessed June 12, 2015.
7. Freudenreich O, Schulz SC, Goff DC. Initial medical work-up of first episode psychosis: a conceptual review. Early Interv Psychiatry. 2009;3(1):10-18.
8. Masand PS, Levenson JL, et al. Mania, catatonia, and psychosis. In: Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. Washington, DC: American Psychiatric Publishing; 2005: 239-241.
9. Carroll BT. The universal field of hypothesis of catatonia and neuroleptic malignant syndrome. CNS Spectr. 2000;5(7):26-33.
10. Lee JW. Neuroleptic-induced catatonia: clinical presentation, response to benzodiazepines, and relationship to neuroleptic malignant syndrome. J Clin Psychopharmacol. 2010;30(1):3-10.
11. Vancaester E, Santens P. Catatonia and neuroleptic malignant syndrome: two sides of a coin? Acta Neurol Belg. 2007;107(2):47-50.
12. Sienaert P, Dhossche DM, Vancampfort D, et al. A clinical review of the treatment of catatonia. Front Psychiatry. 2014;5:181.
13. Hatta K, Miyakawa K, Ota T, et al. Maximal response to electroconvulsive therapy for the treatment of catatonic symptoms. J ECT. 2007;23(4):233-235.
14. Payee H, Chandrasekaran R, Raju GV. Catatonic syndrome: treatment response to Lorazepam. Indian J Psychiatry. 1999;41(1):49-53.
15. Rohland BM, Carroll BT, Jacoby RG. ECT in the treatment of the catatonic syndrome. J Affect Disord. 1993;29(4):255-261.
1. Dean BV, Stellpflug SJ, Burnett AM, et al. 2C or not 2C: phenethylamine designer drug review. J Med Toxicol. 2013;9(2):172-178.
2. Hill SL, Thomas SH. Clinical toxicology of newer recreational drugs. Clin Toxicol (Phila). 2011;49(8):705-719.
3. Shulgin A, Shulgin A. PiHKAL: a chemical love story. Berkley, CA: Transform Press; 1991.
4. Papoutsis I, Nikolaou P, Stefanidou M, et al. 25B-NBOMe and its precursor 2C-B: modern trends and hidden dangers. Forensic Toxicology. 2015;3(1):1-11.
5. Caudevilla-Gálligo F, Riba J, Ventura M, et al. 4-Bromo-2, 5-dimethoxyphenethylamine (2C-B): presence in the recreational drug market in Spain, pattern of use and subjective effects. J Psychopharmacol. 2012;26(7):1026-1035.
6. National Drug Intelligence Center. Information bulletin: 2C-B (Nexus) reappears on the club drug scene. http:// www.Justice.gov/archive/ndic/pubs0/665. Published May 2001. Accessed June 12, 2015.
7. Freudenreich O, Schulz SC, Goff DC. Initial medical work-up of first episode psychosis: a conceptual review. Early Interv Psychiatry. 2009;3(1):10-18.
8. Masand PS, Levenson JL, et al. Mania, catatonia, and psychosis. In: Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. Washington, DC: American Psychiatric Publishing; 2005: 239-241.
9. Carroll BT. The universal field of hypothesis of catatonia and neuroleptic malignant syndrome. CNS Spectr. 2000;5(7):26-33.
10. Lee JW. Neuroleptic-induced catatonia: clinical presentation, response to benzodiazepines, and relationship to neuroleptic malignant syndrome. J Clin Psychopharmacol. 2010;30(1):3-10.
11. Vancaester E, Santens P. Catatonia and neuroleptic malignant syndrome: two sides of a coin? Acta Neurol Belg. 2007;107(2):47-50.
12. Sienaert P, Dhossche DM, Vancampfort D, et al. A clinical review of the treatment of catatonia. Front Psychiatry. 2014;5:181.
13. Hatta K, Miyakawa K, Ota T, et al. Maximal response to electroconvulsive therapy for the treatment of catatonic symptoms. J ECT. 2007;23(4):233-235.
14. Payee H, Chandrasekaran R, Raju GV. Catatonic syndrome: treatment response to Lorazepam. Indian J Psychiatry. 1999;41(1):49-53.
15. Rohland BM, Carroll BT, Jacoby RG. ECT in the treatment of the catatonic syndrome. J Affect Disord. 1993;29(4):255-261.
3,4-methylenedioxy-methamphetamine, MDMA, Phenethylamines I Have Known and Loved: A Chemical Love Story, LSD, substance abuse, substance use
3,4-methylenedioxy-methamphetamine, MDMA, Phenethylamines I Have Known and Loved: A Chemical Love Story, LSD, substance abuse, substance use
A Streak of Trouble in Fingernail?
A 14-year-old girl is brought to dermatology by her mother, following referral from her pediatrician for evaluation of fingernail changes. Initially, a faint brown streak was observed in the nail of her left fourth finger. Over time, the spot darkened and widened, and the adjacent nail plate flattened.
A few weeks before presentation to dermatology, the adjacent cuticle darkened. The patient denies any sensitivity in the area. Her mother denies any significant or relevant medical history.
EXAMINATION
The dark brown streak measures 4.5 mm in width and runs longitudinally the entire length of the nail plate. The discolored area coincides exactly with flattening of the nail plate, which, when viewed on edge, also exhibits darkening. Significantly, the adjacent cuticle is similarly affected.
No changes are observed on other digits. The child is of Native American ancestry, with type IV skin.
What is the diagnosis?
DISCUSSION
Generically, this problem is termed melanonychia; this case represents the most common type, longitudinal melanonychia (LM). Typically, it originates in the nail matrix with increased melanin production; this causes darkening of the onchocytes, which migrate distally as the nail plate grows.
This benign version is an extremely common problem, especially in darker-skinned patients. Almost 100% of African-Americans older than 50 have it, often in several nails, as do 77% of African Americans older than 20 and 10% to 20% of Japanese persons. Comparatively, only 1% to 2% of white individuals are affected.
The main significance of LM, of course, is the fact that it can represent melanoma, which, for a variety of reasons, is often belatedly identified in subungual areas and is therefore associated with relatively poor survival. Five-year survival rates for subungual melanoma are around 30%, while 10-year survival is only 13%—much lower than for melanomas elsewhere on the body. For example, patients with melanomas removed from other areas of the hand demonstrate 100% five-year survival rates.
Subungual melanoma presenting in this manner is considered one of the so-called acrolentiginous melanomas, which present in peripheral “acral” locations (eg, scalp, soles, mucosal surfaces). While these are not inherently more dangerous in terms of biologic behavior, they tend to escape detection because of their location and (often) atypical appearance, thus having more time in which to become invasive.
Perhaps the most useful and puzzling conundrum associated with acrolentiginous melanomas is this: Darker-skinned patients are, in general, at low risk for melanoma compared to fair-skinned redheads and blondes. However, when dark-skinned patients do develop melanoma, it tends to manifest in an acral area (one reason why melanoma in these patients has a relatively poor prognosis).
Darkening under or in the nails can have other causes; it has been associated with Cushing disease, Addison disease, and alkaptonuria, to name just a few. It can also be associated with skin diseases, including psoriasis, Darier disease, lichen planus, and lichen striatus. A number of drugs, among them minocycline, can produce focal discoloration in or under the nails.
This subungual lesion was biopsied at its proximal origin, under digital block and using a tourniquet. The 3-mm punch specimen was sent for pathologic examination, which showed benign nevoid tissue—effectively ruling out melanoma. Even if the nail is permanently deformed, this was considered a small price to pay for the patient’s peace of mind.
TAKE-HOME LEARNING POINTS
• Dark streaks under fingernails are common in those with darker skin, in whom they often appear in multiple fingers. In the absence of change, these are usually safe.
• The related conundrum is that when those with darker skin develop melanoma, the subungual areas, or other light-skinned areas (sole, mouth, palms), are often where it manifests.
• New and/or changing areas of subungual pigmentation need to be referred to dermatology for evaluation and possible biopsy.
• When this discoloration also involves the adjacent cuticle or other perionychial skin, even more urgency is added to the referral.
A 14-year-old girl is brought to dermatology by her mother, following referral from her pediatrician for evaluation of fingernail changes. Initially, a faint brown streak was observed in the nail of her left fourth finger. Over time, the spot darkened and widened, and the adjacent nail plate flattened.
A few weeks before presentation to dermatology, the adjacent cuticle darkened. The patient denies any sensitivity in the area. Her mother denies any significant or relevant medical history.
EXAMINATION
The dark brown streak measures 4.5 mm in width and runs longitudinally the entire length of the nail plate. The discolored area coincides exactly with flattening of the nail plate, which, when viewed on edge, also exhibits darkening. Significantly, the adjacent cuticle is similarly affected.
No changes are observed on other digits. The child is of Native American ancestry, with type IV skin.
What is the diagnosis?
DISCUSSION
Generically, this problem is termed melanonychia; this case represents the most common type, longitudinal melanonychia (LM). Typically, it originates in the nail matrix with increased melanin production; this causes darkening of the onchocytes, which migrate distally as the nail plate grows.
This benign version is an extremely common problem, especially in darker-skinned patients. Almost 100% of African-Americans older than 50 have it, often in several nails, as do 77% of African Americans older than 20 and 10% to 20% of Japanese persons. Comparatively, only 1% to 2% of white individuals are affected.
The main significance of LM, of course, is the fact that it can represent melanoma, which, for a variety of reasons, is often belatedly identified in subungual areas and is therefore associated with relatively poor survival. Five-year survival rates for subungual melanoma are around 30%, while 10-year survival is only 13%—much lower than for melanomas elsewhere on the body. For example, patients with melanomas removed from other areas of the hand demonstrate 100% five-year survival rates.
Subungual melanoma presenting in this manner is considered one of the so-called acrolentiginous melanomas, which present in peripheral “acral” locations (eg, scalp, soles, mucosal surfaces). While these are not inherently more dangerous in terms of biologic behavior, they tend to escape detection because of their location and (often) atypical appearance, thus having more time in which to become invasive.
Perhaps the most useful and puzzling conundrum associated with acrolentiginous melanomas is this: Darker-skinned patients are, in general, at low risk for melanoma compared to fair-skinned redheads and blondes. However, when dark-skinned patients do develop melanoma, it tends to manifest in an acral area (one reason why melanoma in these patients has a relatively poor prognosis).
Darkening under or in the nails can have other causes; it has been associated with Cushing disease, Addison disease, and alkaptonuria, to name just a few. It can also be associated with skin diseases, including psoriasis, Darier disease, lichen planus, and lichen striatus. A number of drugs, among them minocycline, can produce focal discoloration in or under the nails.
This subungual lesion was biopsied at its proximal origin, under digital block and using a tourniquet. The 3-mm punch specimen was sent for pathologic examination, which showed benign nevoid tissue—effectively ruling out melanoma. Even if the nail is permanently deformed, this was considered a small price to pay for the patient’s peace of mind.
TAKE-HOME LEARNING POINTS
• Dark streaks under fingernails are common in those with darker skin, in whom they often appear in multiple fingers. In the absence of change, these are usually safe.
• The related conundrum is that when those with darker skin develop melanoma, the subungual areas, or other light-skinned areas (sole, mouth, palms), are often where it manifests.
• New and/or changing areas of subungual pigmentation need to be referred to dermatology for evaluation and possible biopsy.
• When this discoloration also involves the adjacent cuticle or other perionychial skin, even more urgency is added to the referral.
A 14-year-old girl is brought to dermatology by her mother, following referral from her pediatrician for evaluation of fingernail changes. Initially, a faint brown streak was observed in the nail of her left fourth finger. Over time, the spot darkened and widened, and the adjacent nail plate flattened.
A few weeks before presentation to dermatology, the adjacent cuticle darkened. The patient denies any sensitivity in the area. Her mother denies any significant or relevant medical history.
EXAMINATION
The dark brown streak measures 4.5 mm in width and runs longitudinally the entire length of the nail plate. The discolored area coincides exactly with flattening of the nail plate, which, when viewed on edge, also exhibits darkening. Significantly, the adjacent cuticle is similarly affected.
No changes are observed on other digits. The child is of Native American ancestry, with type IV skin.
What is the diagnosis?
DISCUSSION
Generically, this problem is termed melanonychia; this case represents the most common type, longitudinal melanonychia (LM). Typically, it originates in the nail matrix with increased melanin production; this causes darkening of the onchocytes, which migrate distally as the nail plate grows.
This benign version is an extremely common problem, especially in darker-skinned patients. Almost 100% of African-Americans older than 50 have it, often in several nails, as do 77% of African Americans older than 20 and 10% to 20% of Japanese persons. Comparatively, only 1% to 2% of white individuals are affected.
The main significance of LM, of course, is the fact that it can represent melanoma, which, for a variety of reasons, is often belatedly identified in subungual areas and is therefore associated with relatively poor survival. Five-year survival rates for subungual melanoma are around 30%, while 10-year survival is only 13%—much lower than for melanomas elsewhere on the body. For example, patients with melanomas removed from other areas of the hand demonstrate 100% five-year survival rates.
Subungual melanoma presenting in this manner is considered one of the so-called acrolentiginous melanomas, which present in peripheral “acral” locations (eg, scalp, soles, mucosal surfaces). While these are not inherently more dangerous in terms of biologic behavior, they tend to escape detection because of their location and (often) atypical appearance, thus having more time in which to become invasive.
Perhaps the most useful and puzzling conundrum associated with acrolentiginous melanomas is this: Darker-skinned patients are, in general, at low risk for melanoma compared to fair-skinned redheads and blondes. However, when dark-skinned patients do develop melanoma, it tends to manifest in an acral area (one reason why melanoma in these patients has a relatively poor prognosis).
Darkening under or in the nails can have other causes; it has been associated with Cushing disease, Addison disease, and alkaptonuria, to name just a few. It can also be associated with skin diseases, including psoriasis, Darier disease, lichen planus, and lichen striatus. A number of drugs, among them minocycline, can produce focal discoloration in or under the nails.
This subungual lesion was biopsied at its proximal origin, under digital block and using a tourniquet. The 3-mm punch specimen was sent for pathologic examination, which showed benign nevoid tissue—effectively ruling out melanoma. Even if the nail is permanently deformed, this was considered a small price to pay for the patient’s peace of mind.
TAKE-HOME LEARNING POINTS
• Dark streaks under fingernails are common in those with darker skin, in whom they often appear in multiple fingers. In the absence of change, these are usually safe.
• The related conundrum is that when those with darker skin develop melanoma, the subungual areas, or other light-skinned areas (sole, mouth, palms), are often where it manifests.
• New and/or changing areas of subungual pigmentation need to be referred to dermatology for evaluation and possible biopsy.
• When this discoloration also involves the adjacent cuticle or other perionychial skin, even more urgency is added to the referral.
Botulinum toxin for depression? An idea that’s raising some eyebrows
Psychiatry is experiencing a major paradigm shift.1 No longer is depression a disease of norepinephrine and serotonin deficiency. Today, we are exploring inflammation, methylation, epigenetics, and neuroplasticity as major players; we are using innovative treatment interventions such as ketamine, magnets, psilocin, anti-inflammatories, and even botulinum toxin.
In 2006, dermatologist Eric Finzi, MD, PhD, reported a case series of 10 depressed patients who were given a single course of botulinum toxin A (BTA, onabotulinum-toxinA) injections in the forehead.2 After 2 months, 9 out of the 10 patients were no longer depressed. The 10th patient, who reported improvement in symptoms but not remission, was the only patient with bipolar depression.
As a psychiatrist (M.M.) and a dermatologist (J.R.), we conducted a randomized controlled trial3 to challenge the difficult-to-swallow notion that a cosmetic intervention could help severely depressed patients. After reporting our positive findings and hearing numerous encouraging patient testimonials, we present a favorable review on the treatment of depression using BTA. We also present the top 10 questions we are asked at lectures about this novel treatment.
A deadly toxin used to treat medical conditions
Botulinum toxin is one of the deadliest substance known to man.4 It was named after the gram-positive bacterium Clostridium botulinum, which causes so-called floppy baby syndrome in infants who eat contaminated honey. Botulinum toxin prevents nerves from releasing acetylcholine, which causes muscle paralysis.
In the wrong hands, botulinum toxin can be exploited for chemical warfare.4 However, doctors are using it to treat >50 medical conditions, including migraine, cervical dystonia, strabismus, overactive bladder, urinary incontinence, excessive sweating, muscle spasm, and now depression.5,6 In 2014, BTA was the top cosmetic treatment in the United States, with >3 million procedures performed, generating more than 1 billion dollars in revenue.7
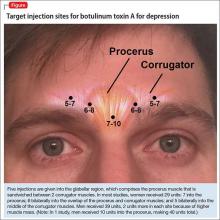
The most common site injected with BTA for cosmetic treatments is the glabellar region, which is the area directly above and in between the eyebrows (ie, the lower forehead). The glabella comprises 2 main muscles: the central procerus flanked by a pair of corrugators (Figure). When expressing fear, anger, sadness, or anguish, these muscles contract, causing the appearance of 2 vertical wrinkles, referred to as the “11s.” The wrinkles also can form the shape of an upside-down “U,” known as the omega sign.8 BTA prevents contraction of these muscles and therefore prevents the appearance of a furrowed brow. During cosmetic procedures, approximately 20 to 50 units of BTA are spread out over 5 glabellar injection sites.9 A similar technique is being used in studies of BTA for depression2,3,10,11 (Figure).
BTA for depression is new to the mental health world but, before psychiatrists caught on, dermatologists were aware that BTA could improve quality of life,12 reduce negative emotions,13 and increase feelings of well-being.14
The evidence
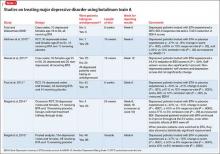
To date, there have been 2 case series,2,15 3 randomized control trials (RCTs),3,10,11 1 pooled analysis,16,17 and 1 meta-analysis18 looking at botulinum for depression (Table 1).2,10,11,15-17 In each trial, a single treatment of BTA (ie, 1 doctor’s visit; 29 to 40 units of BTA distributed into 5 glabellar injections sites), was the intervention studied.2
The first case series, by Finzi and Wasserman2 is described above. A second case series, published in 2013, describes 50 female patients, one-half depressed and one-half non-depressed, all of whom received 20 units of BTA into the glabella.15 At 12 weeks, depression scores in the depressed group had decreased by 54% (14.9 point drop on Beck Depression Inventory [BDI], P < .001) and self-esteem scores had increased significantly. In non-depressed participants, depression scores and self-esteem scores remained constant throughout the 12 weeks.
A pooled analysis reported results of 3 RCTs16,17 consisting of a total of 134 depressed patients, males and females age 18 to 65 who received BTA (n = 59) or placebo (n = 74) into the glabellar region. At the end of 6 weeks, BDI scores in the depressed group had decreased by 47.4% (14.3 points) compared with a 16.2% decrease (5.1 points) in the placebo group. This corresponds to a 52.5% vs 8.0% response rate and a 42.4% vs 8.0% remission rate, respectively (Table 1,1,2,10,11,15-17). There was no difference between the 2 groups in sex, age, depression severity, and number of antidepressants being taken. Females received 29 units and males received 10 to 11 units more to account for higher muscle mass (Figure).
Depression as measured by the physician-administered Hamilton Depression Rating Scale (HAM-D) and the Montgomery-Åsberg Depression Rating Scale showed similar reduction in overall scores (−45.7% vs −14.6%), response rates (54.2% vs 10.7%) and remission rates (30.5% vs 6.7%) with BTA.
Although these improvements in depression scores do not reach those seen with electroconvulsive therapy,19,20 they are comparable to placebo-controlled studies of antidepressants.21,22
Doesn’t this technique work because people who look better, feel better?
Aesthetic improvement alone is unlikely to explain the entire story. A recent study showed that improvement in wrinkle score did not correlate with improvement in mood.23 Furthermore, some patients in RCTs did not like the cosmetic effects of BTA but still reported feeling less depressed after treatment.10
How might it work?
Several theories about the mechanism of action have been proposed:
• The facial feedback hypothesis dates to Charles Darwin in 1872: Facial movements influence emotional states. Numerous studies have confirmed this. Strack et al24 found that patients asked to smile while reading comics found them to be funnier. Ekman et al25 found that imitating angry facial expressions made body temperature and heart rate rise. Dialectical behavioral therapy expert Marsha Linehan recognized the importance of modifying facial expressions (from grimacing to smiling) and posture (from clenched fists to open hands) when feeling distressed, because it is hard to feel “willful” when your “mind is going one way and your body is going another.”26 Accordingly, for a person who continuously “looks” depressed or distressed, reducing the anguished facial expression using botulinum toxin might diminish the entwined negative emotions.
• A more pleasant facial expression improves social interactions, which leads to improvement in self-esteem and mood. Social biologists argue that (1) we are attracted to those who have more pleasant facial expressions and (2) we steer clear of those who appear angry or depressed (a negative facial expression, such as a growling dog, is perceived as a threat). Therefore, anyone who looks depressed might have less rewarding interpersonal interactions, which can contribute to a poor mood.
On a similar note, mirror neurons are regions in the brain that are activated by witnessing another person’s emotional cues. When our mirror neurons light up, we can feel an observed experience, which is why we often feel nervous around anxious people, or cringe when we see others get hurt, or why we might prefer engaging with people who appear happier. It is possible that, after BTA injection, a person’s social connectivity is improved because of a more positive reciprocal firing of mirror neurons.
• BTA leads to direct and indirect neurochemical changes in the brain that can reduce depression. Functional MRI studies have shown that after glabellar BTA injections, the amygdala was less responsive to negative stimuli.27,28 For example, patients who were treated with BTA and then shown pictures of angry people had an attenuated amygdala response to the photos.
This is an important finding, especially for patients who have been traumatized. After a traumatic event, the amygdala “remembers” what happened, which is good, in some ways (it prevents us from getting into a similar dangerous situation), but bad in others (the traumatized amygdala may falsely perceive a non-threatening stimuli as threatening). A hypervigilant amygdala can lead to an out-of-proportion fear response, depression, and anxiety. Therefore, quelling an overactive amygdala with BTA could improve emotional dysregulation and posttraumatic disorders.
Many of our patients reported that, after BTA injection, “traumatic events didn’t feel as traumatizing,” as one said. The emotional pain and rumination that often follow a life stressor “does not overstay its welcome” and patients are able to “move on” more quickly.
It is unknown why the amygdala is quieted after BTA; researchers hypothesize that BTA suppresses facial feedback signals from the forehead branch of the trigeminal nerve to the brain. Another hypothesis is that BTA is directly transported by the trigeminal nerve into the brain and exerts central pharmacological effects on the amygdala.29 This theory has only been studied in rat models.30
When does it start working? How long does it last?
From what we know, BTA for depression could start working as early as 2 weeks and could last as long as 6 months. In one RCT, the earliest follow-up was 2 weeks,10 at which time the depressed patients had responded to botulinum toxin (P ≤ .05). In the other 2 controlled trials, the earliest follow-up was 3 weeks, at which time a more robust response was seen (P < .001). Aesthetically, BTA usually lasts 3 months. It is unclear how long the antidepressant effects last but, in the longest trial,3 depression symptoms continued to improve at 6 months, after cosmetic effects had worn off.
These findings raise a series of questions:
• Do mood effects outlast cosmetic effects? If so, why?
• Does botulinum toxin start to work sooner than 2 weeks?
• Will adherence improve if a patient has to be treated only every 6 months?
In our clinical experience, depressed patients who responded to BTA injection report a slow resurfacing of depressive symptoms 4 to 6 months after treatment, at which point they usually return for “maintenance treatment” (same dosing, same injection configuration).
Will psychiatrists administer the treatment?
Any physician or physician extender can, when properly trained, inject BTA. The question is: Do psychiatrists want to? Administrating botulinum toxin requires more labor and preparation than prescribing a drug (Table 2,31) and requires placing hands on patients. Depending on the type of psychiatric practice, this may be a “deal-breaker” for some providers, such as those in a psychoanalytic practice who might worry about boundaries.
As a basis for comparison, despite several indications for BTA for headache and neurologic conditions, few neurologists have added botulinum toxin to their practice. Dermatologists who are comfortable seeing psychiatric patients or family practitioners, who are already set up for injection procedures, could become custodians of this intervention.
Which patients are candidates for the treatment?
Patients with anxious or agitated depression might be ideal candidates for BTA injection. A recent study looked at predictors of response: Patients with a high agitation score (as measured on item 9 of the HAM-D) were more likely to respond, with a sensitivity of 100%, a specificity of 56%, and an overall precision of 78%.32 So far, no other predictors of response have been clearly identified. Higher baseline wrinkle scores do not predict better response.23 Sex and age do not have any predictive value. The treatment appears to be equally effective in males and females; because only a handful of males have been treated (n = 14), however, these patients need to be studied further.
Is botulinum toxin better as monotherapy or augmentation strategy?
So far, it appears to be equally effective as monotherapy or augmentation strategy,16 but more studies are needed.
How expensive is it?
Estimates of patient cost include the cost of the product and the professional fee for injection. As a point of reference, for cosmetic purposes, depending on practice location, dermatologists charge $11 to $20 per unit of BTA. Therefore, 1 treatment of BTA for depression (29 to 40 units) can cost a patient $319 to $800.
When treating a patient with BTA for medical indications, such as tension headache, insurance often reimburses the physician for the BTA at cost (paid with a J code: J0585) and pay an injection fee (a procedure code) of $150 to $200. A recent analysis of cost-effectiveness estimated that BTA for depression would cost a patient $1,200 to $1,600 annually.33 Compared with the price of branded medications (eg, $500 to $2,000 annually)33 plus weekly psychotherapy (eg, $2,000 to $5,000 annually), BTA may be a cost-effective option for patients who do not respond to conventional treatments. Of course, for patients who tolerate and respond to generic medications or have a therapist who charges on a sliding scale, BTA is not the most cost-effective option.
What about injecting other areas of the face?
We’ve thought about it but haven’t tried it. There are several muscles around the mouth that allow us to smile and frown. BTA injections in the depressor anguli oris, a muscle around the mouth that is largely responsible for frowning, could treat depression. However, if the mechanism of action is via amygdala desensitization through the trigeminal nerve, treating mouth frown muscles might not work.
Is it safe?
BTA in the glabella has an exceptionally good safety profile.9,31,34 Adverse reactions, which include eyelid droop, pain, bruising, and redness at the injection site, are minor and temporary.9 In addition, BTA has few drug–drug interactions. The biggest complaint for most patients is discomfort upon injection, which often is described as feeling like “an ant bite.”
In the pooled analysis of RCTs, apart from local irritation immediately after injection, temporary headache was the only relevant, and possibly treatment-related, adverse event. Headache occurred in 13.6% (n = 8) of the BTA group and 9.3% (n = 7) of the placebo group (P = .44). Compared with antidepressants such as citalopram, where approximately 38.6% of patients report a moderate or severe side-effect burden,21 BTA is well tolerated.
Are other studies underway?
Larger studies are being conducted,35 mainly to confirm what pilot studies have shown. It would be interesting to discover other predictors of response and if different dosing and injection configurations could strengthen the response rate and extend the duration of effect.
Because of the cosmetic effects of BTA, further studies are needed to address the problem of blinding. In earlier studies, raters were blinded during appointments because patients wore surgical caps that covered their glabellar region.3,10 Patients did not know their treatment intervention, but 52% to 90% of patients guessed correctly.3,10,11 Although unblinding is a common problem in “blinded” trials in which some researchers have reported >75% of participants and raters guessed the intervention correctly,36 it is a particularly sensitive area in studies that involve a change in appearance because it is almost impossible to prevent someone from looking in a mirror.
Summing up
Botulinum toxin for depression is not ready for prime time. The FDA has not approved its use for psychiatric indications, and Medicare and commercial insurance do not reimburse for this procedure as a treatment for depression. Patients who request BTA for depression must be informed that this use is off-label.
For now, we recommend psychotherapy or medication management, or both, for most patients with major depression. In addition, until larger studies are done, we recommend that patients who are interested in BTA for depression use it as an add-on to conventional treatment. However, if larger studies replicate the findings of the smaller studies we have described, botulinum toxin could become a novel therapeutic agent in the fight against depression.
Bottom Line
In pilot studies, botulinum toxin A (BTA) has shown efficacy in improving symptoms of depression. Although considered safe, BTA is not FDA-approved for psychiatric indications, and Medicare and commercial insurance do not reimburse for this procedure for depression. Larger studies are underway to determine if this novel treatment can be introduced into practice.
Related Resources
• Wollmer MA, Magid M, Kruger THC. Botulinum toxin treatment in depression. In: Bewley A, Taylor RE, Reichenberg JS, et al, eds. Practical psychodermatology. Hoboken, NJ: John Wiley & Sons; 2014:216-219.
• Botox for depression. www.botoxfordepression.com.
• Botox and depression. www.botoxanddepression.com.
Drug Brand Names
Botulinum toxin A • Botox
Citalopram • Celexa
Acknowledgments
We thank the Brain and Behavior Research Foundation for granting Dr. Magid a young investigator award and for continuing to invest in innovative research ideas. We thank Dr. Eric Finzi, MD, PhD, Axel Wollmer, MD, and Tillmann Krüger, MD, for their continued collaboration in this area of research.
Disclosures
In July 2011, Dr. Magid received a young investigator award from the Brain and Behavior Research Foundation for her study on treating depression using botulinum toxin (Grant number 17648). In November 2012, after completion and as a result of the study on treating depression using botulinum toxin, Dr. Magid became a consultant with Allergan to discuss study findings. In September 2015, Dr. Magid became a speaker for IPSEN Innovation. Dr. Reichenberg is married to Dr. Magid. Dr. Reichenberg has no other conflicts of interest to disclose.
1. Nasrallah HA. 10 Recent paradigm shifts in the neurobiology and treatment of depression. Current Psychiatry. 2015;14(2):10-13.
2. Finzi E, Wasserman E. Treatment of depression with botulinum toxin A: a case series. Dermatol Surg. 2006;32(5):645-649; discussion 649-650.
3. Magid M, Reichenberg JS, Poth PE, et al. Treatment of major depressive disorder using botulinum toxin A: a 24-week randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2014;75(8):837-844.
4. Koussoulakos S. Botulinum neurotoxin: the ugly duckling. Eur Neurol. 2008;61(6):331-342.
5. Chen S. Clinical uses of botulinum neurotoxins: current indications, limitations and future developments. Toxins (Basel). 2012;4(10):913-939.
6. Bhidayasiri R, Truong DD. Expanding use of botulinum toxin. J Neurol Sci. 2005;235(1-1):1-9.
7. Cosmetic surgery national data bank statistics. American Society for Asethetic Plastic Surgery. http://www.surgery. org/sites/default/files/2014-Stats.pdf. Published 2014. Accessed May 30, 2015.
8. Shorter E. Darwin’s contribution to psychiatry. Br J Psychiatry. 2009;195(6):473-474.
9. Winter L, Spiegel J. Botulinum toxin type-A in the treatment of glabellar lines. Clin Cosmet Investig Dermatol. 2009;3:1-4.
10. Wollmer MA, de Boer C, Kalak N, et al. Facing depression with botulinum toxin: a randomized controlled trial. J Psychiatr Res. 2012;46(5):574-581.
11. Finzi E, Rosenthal NE. Treatment of depression with onabotulinumtoxinA: a randomized, double-blind, placebo controlled trial. J Psychiatr Res. 2014;52:1-6.
12. Hexsel D, Brum C, Porto MD, et al. Quality of life and satisfaction of patients after full-face injections of abobotulinum toxin type A: a randomized, phase IV clinical trial. J Drugs Dermatol. 2013;12(12):1363-1367.
13. Lewis MB, Bowler PJ. Botulinum toxin cosmetic therapy correlates with a more positive mood. J Cosmet Dermatol. 2009;8(1):24-26.
14. Sommer B, Zschocke I, Bergfeld D, et al. Satisfaction of patients after treatment with botulinum toxin for dynamic facial lines. Dermatol Surg. 2003;29(5):456-460.
15. Hexsel D, Brum C, Siega C, et al. Evaluation of self‐esteem and depression symptoms in depressed and nondepressed subjects treated with onabotulinumtoxina for glabellar lines. Dermatol Surg. 2013;39(7):1088-1096.
16. Magid M, Reichenberg JS, Finzi E, et al. Treating depression with botulinum toxin: update and meta-analysis from clinic trials. Paper presented at: XVI World Congress of Psychiatry; September 14-18, 2014; Madrid, Spain.
17. Magid M, Finzi E, Kruger TH, et al. Treating depression with botulinum toxin: a pooled analysis of randomized controlled trials. Pharmacopsychiatry. 2015;48(6):205-210.
18. Parsaik A, Mascarenhas S, Hashmi A, et al. Role of botulinum toxin in depression: a systematic review and meta-analysis. J Psychiatr Pract. In press.
19. Scott AI, ed. The ECT handbook, 2nd ed. The third report of the Royal College of Psychiatrists’ Special Committee of ECT. London, United Kingdom: The Royal College of Psychiatrists; 2005.
20. Ren J, Li H, Palaniyappan L, et al. Repetitive transcranial magnetic stimulation versus electroconvulsive therapy for major depression: a systematic review and meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2014;51:181-189.
21. Trivedi MH, Rush AJ, Wisniewski SR, et al; STAR*D Study Team. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR* D: implications for clinical practice. Am J Psychiatry. 2006;163(1):28-40.
22. Gibbons RD, Hur K, Brown CH, et al. Benefits from antidepressants: synthesis of 6-week patient-level outcomes from double-blind placebo-controlled randomized trials of fluoxetine and venlafaxine. Arch Gen Psychiatry. 2012;69(6):572-579.
23. Reichenberg JS, Magid M, Keeling B. Botulinum toxin for depression: does the presence of rhytids predict response? Presented at: Texas Dermatology Society; May 2015; Bastrop, Texas.
24. Strack F, Martin LL, Stepper S. Inhibiting and facilitating conditions of the human smile: a nonobtrusive test of the facial feedback hypothesis. J Pers Soc Psychol. 1988;54(5):768-777.
25. Ekman P, Levenson RW, Friesen WV. Autonomic nervous system activity distinguishes among emotions. Science. 1983;221(4616):1208-1210.
26. Linehan MM. DBT skills training manual, 2nd ed. New York, NY: Guilford Publications; 2014.
27. Hennenlotter A, Dresel C, Castrop F, et al. The link between facial feedback and neural activity within central circuitries of emotion—new insights from botulinum toxin-induced denervation of frown muscles. Cereb Cortex. 2009;19(3):537-542.
28. Kim MJ, Neta M, Davis FC, et al. Botulinum toxin-induced facial muscle paralysis affects amygdala responses to the perception of emotional expressions: preliminary findings from an A-B-A design. Biol Mood Anxiety Disord. 2014;4:11.
29. Mazzocchio R, Caleo M. More than at the neuromuscular synapse: actions of botulinum neurotoxin A in the central nervous system. Neuroscientist. 2015;21(1):44-61.
30. Antonucci F, Rossi C, Gianfranceschi L, et al. Long-distance retrograde effects of botulinum neurotoxin A. J Neurosci. 2008;28(14):3689-3696.
31. U.S. Food and Drug Administration. Medication guide: botox. http://www.fda.gov/downloads/drugs/drugsafety/ucm176360.pdf. Updated September 2013. Accessed June 7, 2015.
32. Wollmer MA, Kalak N, Jung S, et al. Agitation predicts response of depression to botulinum toxin treatment in a randomized controlled trial. Front Psychiatry. 2014;5:36.
33. Beer K. Cost effectiveness of botulinum toxins for the treatment of depression: preliminary observations. J Drugs Dermatol. 2010;9(1):27-30.
34. Brin MF, Boodhoo TI, Pogoda JM, et al. Safety and tolerability of onabotulinumtoxinA in the treatment of facial lines: a meta-analysis of individual patient data from global clinical registration studies in 1678 participants. J Am Acad Dermatol. 2009;61(6):961-970.e1-11.
35. Botulinum toxin and depression. ClinicalTrials.gov. https:// clinicaltrials.gov/ct2/results?term=botulinum+toxin+and+ depression&Search=Search. Accessed June 1, 2015.
36. Rabkin JG, Markowitz JS, Stewart J, et al. How blind is blind? Assessment of patient and doctor medication guesses in a placebo-controlled trial of imipramine and phenelzine. Psychiatry Res. 1986;19(1):75-86.
Psychiatry is experiencing a major paradigm shift.1 No longer is depression a disease of norepinephrine and serotonin deficiency. Today, we are exploring inflammation, methylation, epigenetics, and neuroplasticity as major players; we are using innovative treatment interventions such as ketamine, magnets, psilocin, anti-inflammatories, and even botulinum toxin.
In 2006, dermatologist Eric Finzi, MD, PhD, reported a case series of 10 depressed patients who were given a single course of botulinum toxin A (BTA, onabotulinum-toxinA) injections in the forehead.2 After 2 months, 9 out of the 10 patients were no longer depressed. The 10th patient, who reported improvement in symptoms but not remission, was the only patient with bipolar depression.
As a psychiatrist (M.M.) and a dermatologist (J.R.), we conducted a randomized controlled trial3 to challenge the difficult-to-swallow notion that a cosmetic intervention could help severely depressed patients. After reporting our positive findings and hearing numerous encouraging patient testimonials, we present a favorable review on the treatment of depression using BTA. We also present the top 10 questions we are asked at lectures about this novel treatment.
A deadly toxin used to treat medical conditions
Botulinum toxin is one of the deadliest substance known to man.4 It was named after the gram-positive bacterium Clostridium botulinum, which causes so-called floppy baby syndrome in infants who eat contaminated honey. Botulinum toxin prevents nerves from releasing acetylcholine, which causes muscle paralysis.
In the wrong hands, botulinum toxin can be exploited for chemical warfare.4 However, doctors are using it to treat >50 medical conditions, including migraine, cervical dystonia, strabismus, overactive bladder, urinary incontinence, excessive sweating, muscle spasm, and now depression.5,6 In 2014, BTA was the top cosmetic treatment in the United States, with >3 million procedures performed, generating more than 1 billion dollars in revenue.7
The most common site injected with BTA for cosmetic treatments is the glabellar region, which is the area directly above and in between the eyebrows (ie, the lower forehead). The glabella comprises 2 main muscles: the central procerus flanked by a pair of corrugators (Figure). When expressing fear, anger, sadness, or anguish, these muscles contract, causing the appearance of 2 vertical wrinkles, referred to as the “11s.” The wrinkles also can form the shape of an upside-down “U,” known as the omega sign.8 BTA prevents contraction of these muscles and therefore prevents the appearance of a furrowed brow. During cosmetic procedures, approximately 20 to 50 units of BTA are spread out over 5 glabellar injection sites.9 A similar technique is being used in studies of BTA for depression2,3,10,11 (Figure).
BTA for depression is new to the mental health world but, before psychiatrists caught on, dermatologists were aware that BTA could improve quality of life,12 reduce negative emotions,13 and increase feelings of well-being.14
The evidence
To date, there have been 2 case series,2,15 3 randomized control trials (RCTs),3,10,11 1 pooled analysis,16,17 and 1 meta-analysis18 looking at botulinum for depression (Table 1).2,10,11,15-17 In each trial, a single treatment of BTA (ie, 1 doctor’s visit; 29 to 40 units of BTA distributed into 5 glabellar injections sites), was the intervention studied.2
The first case series, by Finzi and Wasserman2 is described above. A second case series, published in 2013, describes 50 female patients, one-half depressed and one-half non-depressed, all of whom received 20 units of BTA into the glabella.15 At 12 weeks, depression scores in the depressed group had decreased by 54% (14.9 point drop on Beck Depression Inventory [BDI], P < .001) and self-esteem scores had increased significantly. In non-depressed participants, depression scores and self-esteem scores remained constant throughout the 12 weeks.
A pooled analysis reported results of 3 RCTs16,17 consisting of a total of 134 depressed patients, males and females age 18 to 65 who received BTA (n = 59) or placebo (n = 74) into the glabellar region. At the end of 6 weeks, BDI scores in the depressed group had decreased by 47.4% (14.3 points) compared with a 16.2% decrease (5.1 points) in the placebo group. This corresponds to a 52.5% vs 8.0% response rate and a 42.4% vs 8.0% remission rate, respectively (Table 1,1,2,10,11,15-17). There was no difference between the 2 groups in sex, age, depression severity, and number of antidepressants being taken. Females received 29 units and males received 10 to 11 units more to account for higher muscle mass (Figure).
Depression as measured by the physician-administered Hamilton Depression Rating Scale (HAM-D) and the Montgomery-Åsberg Depression Rating Scale showed similar reduction in overall scores (−45.7% vs −14.6%), response rates (54.2% vs 10.7%) and remission rates (30.5% vs 6.7%) with BTA.
Although these improvements in depression scores do not reach those seen with electroconvulsive therapy,19,20 they are comparable to placebo-controlled studies of antidepressants.21,22
Doesn’t this technique work because people who look better, feel better?
Aesthetic improvement alone is unlikely to explain the entire story. A recent study showed that improvement in wrinkle score did not correlate with improvement in mood.23 Furthermore, some patients in RCTs did not like the cosmetic effects of BTA but still reported feeling less depressed after treatment.10
How might it work?
Several theories about the mechanism of action have been proposed:
• The facial feedback hypothesis dates to Charles Darwin in 1872: Facial movements influence emotional states. Numerous studies have confirmed this. Strack et al24 found that patients asked to smile while reading comics found them to be funnier. Ekman et al25 found that imitating angry facial expressions made body temperature and heart rate rise. Dialectical behavioral therapy expert Marsha Linehan recognized the importance of modifying facial expressions (from grimacing to smiling) and posture (from clenched fists to open hands) when feeling distressed, because it is hard to feel “willful” when your “mind is going one way and your body is going another.”26 Accordingly, for a person who continuously “looks” depressed or distressed, reducing the anguished facial expression using botulinum toxin might diminish the entwined negative emotions.
• A more pleasant facial expression improves social interactions, which leads to improvement in self-esteem and mood. Social biologists argue that (1) we are attracted to those who have more pleasant facial expressions and (2) we steer clear of those who appear angry or depressed (a negative facial expression, such as a growling dog, is perceived as a threat). Therefore, anyone who looks depressed might have less rewarding interpersonal interactions, which can contribute to a poor mood.
On a similar note, mirror neurons are regions in the brain that are activated by witnessing another person’s emotional cues. When our mirror neurons light up, we can feel an observed experience, which is why we often feel nervous around anxious people, or cringe when we see others get hurt, or why we might prefer engaging with people who appear happier. It is possible that, after BTA injection, a person’s social connectivity is improved because of a more positive reciprocal firing of mirror neurons.
• BTA leads to direct and indirect neurochemical changes in the brain that can reduce depression. Functional MRI studies have shown that after glabellar BTA injections, the amygdala was less responsive to negative stimuli.27,28 For example, patients who were treated with BTA and then shown pictures of angry people had an attenuated amygdala response to the photos.
This is an important finding, especially for patients who have been traumatized. After a traumatic event, the amygdala “remembers” what happened, which is good, in some ways (it prevents us from getting into a similar dangerous situation), but bad in others (the traumatized amygdala may falsely perceive a non-threatening stimuli as threatening). A hypervigilant amygdala can lead to an out-of-proportion fear response, depression, and anxiety. Therefore, quelling an overactive amygdala with BTA could improve emotional dysregulation and posttraumatic disorders.
Many of our patients reported that, after BTA injection, “traumatic events didn’t feel as traumatizing,” as one said. The emotional pain and rumination that often follow a life stressor “does not overstay its welcome” and patients are able to “move on” more quickly.
It is unknown why the amygdala is quieted after BTA; researchers hypothesize that BTA suppresses facial feedback signals from the forehead branch of the trigeminal nerve to the brain. Another hypothesis is that BTA is directly transported by the trigeminal nerve into the brain and exerts central pharmacological effects on the amygdala.29 This theory has only been studied in rat models.30
When does it start working? How long does it last?
From what we know, BTA for depression could start working as early as 2 weeks and could last as long as 6 months. In one RCT, the earliest follow-up was 2 weeks,10 at which time the depressed patients had responded to botulinum toxin (P ≤ .05). In the other 2 controlled trials, the earliest follow-up was 3 weeks, at which time a more robust response was seen (P < .001). Aesthetically, BTA usually lasts 3 months. It is unclear how long the antidepressant effects last but, in the longest trial,3 depression symptoms continued to improve at 6 months, after cosmetic effects had worn off.
These findings raise a series of questions:
• Do mood effects outlast cosmetic effects? If so, why?
• Does botulinum toxin start to work sooner than 2 weeks?
• Will adherence improve if a patient has to be treated only every 6 months?
In our clinical experience, depressed patients who responded to BTA injection report a slow resurfacing of depressive symptoms 4 to 6 months after treatment, at which point they usually return for “maintenance treatment” (same dosing, same injection configuration).
Will psychiatrists administer the treatment?
Any physician or physician extender can, when properly trained, inject BTA. The question is: Do psychiatrists want to? Administrating botulinum toxin requires more labor and preparation than prescribing a drug (Table 2,31) and requires placing hands on patients. Depending on the type of psychiatric practice, this may be a “deal-breaker” for some providers, such as those in a psychoanalytic practice who might worry about boundaries.
As a basis for comparison, despite several indications for BTA for headache and neurologic conditions, few neurologists have added botulinum toxin to their practice. Dermatologists who are comfortable seeing psychiatric patients or family practitioners, who are already set up for injection procedures, could become custodians of this intervention.
Which patients are candidates for the treatment?
Patients with anxious or agitated depression might be ideal candidates for BTA injection. A recent study looked at predictors of response: Patients with a high agitation score (as measured on item 9 of the HAM-D) were more likely to respond, with a sensitivity of 100%, a specificity of 56%, and an overall precision of 78%.32 So far, no other predictors of response have been clearly identified. Higher baseline wrinkle scores do not predict better response.23 Sex and age do not have any predictive value. The treatment appears to be equally effective in males and females; because only a handful of males have been treated (n = 14), however, these patients need to be studied further.
Is botulinum toxin better as monotherapy or augmentation strategy?
So far, it appears to be equally effective as monotherapy or augmentation strategy,16 but more studies are needed.
How expensive is it?
Estimates of patient cost include the cost of the product and the professional fee for injection. As a point of reference, for cosmetic purposes, depending on practice location, dermatologists charge $11 to $20 per unit of BTA. Therefore, 1 treatment of BTA for depression (29 to 40 units) can cost a patient $319 to $800.
When treating a patient with BTA for medical indications, such as tension headache, insurance often reimburses the physician for the BTA at cost (paid with a J code: J0585) and pay an injection fee (a procedure code) of $150 to $200. A recent analysis of cost-effectiveness estimated that BTA for depression would cost a patient $1,200 to $1,600 annually.33 Compared with the price of branded medications (eg, $500 to $2,000 annually)33 plus weekly psychotherapy (eg, $2,000 to $5,000 annually), BTA may be a cost-effective option for patients who do not respond to conventional treatments. Of course, for patients who tolerate and respond to generic medications or have a therapist who charges on a sliding scale, BTA is not the most cost-effective option.
What about injecting other areas of the face?
We’ve thought about it but haven’t tried it. There are several muscles around the mouth that allow us to smile and frown. BTA injections in the depressor anguli oris, a muscle around the mouth that is largely responsible for frowning, could treat depression. However, if the mechanism of action is via amygdala desensitization through the trigeminal nerve, treating mouth frown muscles might not work.
Is it safe?
BTA in the glabella has an exceptionally good safety profile.9,31,34 Adverse reactions, which include eyelid droop, pain, bruising, and redness at the injection site, are minor and temporary.9 In addition, BTA has few drug–drug interactions. The biggest complaint for most patients is discomfort upon injection, which often is described as feeling like “an ant bite.”
In the pooled analysis of RCTs, apart from local irritation immediately after injection, temporary headache was the only relevant, and possibly treatment-related, adverse event. Headache occurred in 13.6% (n = 8) of the BTA group and 9.3% (n = 7) of the placebo group (P = .44). Compared with antidepressants such as citalopram, where approximately 38.6% of patients report a moderate or severe side-effect burden,21 BTA is well tolerated.
Are other studies underway?
Larger studies are being conducted,35 mainly to confirm what pilot studies have shown. It would be interesting to discover other predictors of response and if different dosing and injection configurations could strengthen the response rate and extend the duration of effect.
Because of the cosmetic effects of BTA, further studies are needed to address the problem of blinding. In earlier studies, raters were blinded during appointments because patients wore surgical caps that covered their glabellar region.3,10 Patients did not know their treatment intervention, but 52% to 90% of patients guessed correctly.3,10,11 Although unblinding is a common problem in “blinded” trials in which some researchers have reported >75% of participants and raters guessed the intervention correctly,36 it is a particularly sensitive area in studies that involve a change in appearance because it is almost impossible to prevent someone from looking in a mirror.
Summing up
Botulinum toxin for depression is not ready for prime time. The FDA has not approved its use for psychiatric indications, and Medicare and commercial insurance do not reimburse for this procedure as a treatment for depression. Patients who request BTA for depression must be informed that this use is off-label.
For now, we recommend psychotherapy or medication management, or both, for most patients with major depression. In addition, until larger studies are done, we recommend that patients who are interested in BTA for depression use it as an add-on to conventional treatment. However, if larger studies replicate the findings of the smaller studies we have described, botulinum toxin could become a novel therapeutic agent in the fight against depression.
Bottom Line
In pilot studies, botulinum toxin A (BTA) has shown efficacy in improving symptoms of depression. Although considered safe, BTA is not FDA-approved for psychiatric indications, and Medicare and commercial insurance do not reimburse for this procedure for depression. Larger studies are underway to determine if this novel treatment can be introduced into practice.
Related Resources
• Wollmer MA, Magid M, Kruger THC. Botulinum toxin treatment in depression. In: Bewley A, Taylor RE, Reichenberg JS, et al, eds. Practical psychodermatology. Hoboken, NJ: John Wiley & Sons; 2014:216-219.
• Botox for depression. www.botoxfordepression.com.
• Botox and depression. www.botoxanddepression.com.
Drug Brand Names
Botulinum toxin A • Botox
Citalopram • Celexa
Acknowledgments
We thank the Brain and Behavior Research Foundation for granting Dr. Magid a young investigator award and for continuing to invest in innovative research ideas. We thank Dr. Eric Finzi, MD, PhD, Axel Wollmer, MD, and Tillmann Krüger, MD, for their continued collaboration in this area of research.
Disclosures
In July 2011, Dr. Magid received a young investigator award from the Brain and Behavior Research Foundation for her study on treating depression using botulinum toxin (Grant number 17648). In November 2012, after completion and as a result of the study on treating depression using botulinum toxin, Dr. Magid became a consultant with Allergan to discuss study findings. In September 2015, Dr. Magid became a speaker for IPSEN Innovation. Dr. Reichenberg is married to Dr. Magid. Dr. Reichenberg has no other conflicts of interest to disclose.
Psychiatry is experiencing a major paradigm shift.1 No longer is depression a disease of norepinephrine and serotonin deficiency. Today, we are exploring inflammation, methylation, epigenetics, and neuroplasticity as major players; we are using innovative treatment interventions such as ketamine, magnets, psilocin, anti-inflammatories, and even botulinum toxin.
In 2006, dermatologist Eric Finzi, MD, PhD, reported a case series of 10 depressed patients who were given a single course of botulinum toxin A (BTA, onabotulinum-toxinA) injections in the forehead.2 After 2 months, 9 out of the 10 patients were no longer depressed. The 10th patient, who reported improvement in symptoms but not remission, was the only patient with bipolar depression.
As a psychiatrist (M.M.) and a dermatologist (J.R.), we conducted a randomized controlled trial3 to challenge the difficult-to-swallow notion that a cosmetic intervention could help severely depressed patients. After reporting our positive findings and hearing numerous encouraging patient testimonials, we present a favorable review on the treatment of depression using BTA. We also present the top 10 questions we are asked at lectures about this novel treatment.
A deadly toxin used to treat medical conditions
Botulinum toxin is one of the deadliest substance known to man.4 It was named after the gram-positive bacterium Clostridium botulinum, which causes so-called floppy baby syndrome in infants who eat contaminated honey. Botulinum toxin prevents nerves from releasing acetylcholine, which causes muscle paralysis.
In the wrong hands, botulinum toxin can be exploited for chemical warfare.4 However, doctors are using it to treat >50 medical conditions, including migraine, cervical dystonia, strabismus, overactive bladder, urinary incontinence, excessive sweating, muscle spasm, and now depression.5,6 In 2014, BTA was the top cosmetic treatment in the United States, with >3 million procedures performed, generating more than 1 billion dollars in revenue.7
The most common site injected with BTA for cosmetic treatments is the glabellar region, which is the area directly above and in between the eyebrows (ie, the lower forehead). The glabella comprises 2 main muscles: the central procerus flanked by a pair of corrugators (Figure). When expressing fear, anger, sadness, or anguish, these muscles contract, causing the appearance of 2 vertical wrinkles, referred to as the “11s.” The wrinkles also can form the shape of an upside-down “U,” known as the omega sign.8 BTA prevents contraction of these muscles and therefore prevents the appearance of a furrowed brow. During cosmetic procedures, approximately 20 to 50 units of BTA are spread out over 5 glabellar injection sites.9 A similar technique is being used in studies of BTA for depression2,3,10,11 (Figure).
BTA for depression is new to the mental health world but, before psychiatrists caught on, dermatologists were aware that BTA could improve quality of life,12 reduce negative emotions,13 and increase feelings of well-being.14
The evidence
To date, there have been 2 case series,2,15 3 randomized control trials (RCTs),3,10,11 1 pooled analysis,16,17 and 1 meta-analysis18 looking at botulinum for depression (Table 1).2,10,11,15-17 In each trial, a single treatment of BTA (ie, 1 doctor’s visit; 29 to 40 units of BTA distributed into 5 glabellar injections sites), was the intervention studied.2
The first case series, by Finzi and Wasserman2 is described above. A second case series, published in 2013, describes 50 female patients, one-half depressed and one-half non-depressed, all of whom received 20 units of BTA into the glabella.15 At 12 weeks, depression scores in the depressed group had decreased by 54% (14.9 point drop on Beck Depression Inventory [BDI], P < .001) and self-esteem scores had increased significantly. In non-depressed participants, depression scores and self-esteem scores remained constant throughout the 12 weeks.
A pooled analysis reported results of 3 RCTs16,17 consisting of a total of 134 depressed patients, males and females age 18 to 65 who received BTA (n = 59) or placebo (n = 74) into the glabellar region. At the end of 6 weeks, BDI scores in the depressed group had decreased by 47.4% (14.3 points) compared with a 16.2% decrease (5.1 points) in the placebo group. This corresponds to a 52.5% vs 8.0% response rate and a 42.4% vs 8.0% remission rate, respectively (Table 1,1,2,10,11,15-17). There was no difference between the 2 groups in sex, age, depression severity, and number of antidepressants being taken. Females received 29 units and males received 10 to 11 units more to account for higher muscle mass (Figure).
Depression as measured by the physician-administered Hamilton Depression Rating Scale (HAM-D) and the Montgomery-Åsberg Depression Rating Scale showed similar reduction in overall scores (−45.7% vs −14.6%), response rates (54.2% vs 10.7%) and remission rates (30.5% vs 6.7%) with BTA.
Although these improvements in depression scores do not reach those seen with electroconvulsive therapy,19,20 they are comparable to placebo-controlled studies of antidepressants.21,22
Doesn’t this technique work because people who look better, feel better?
Aesthetic improvement alone is unlikely to explain the entire story. A recent study showed that improvement in wrinkle score did not correlate with improvement in mood.23 Furthermore, some patients in RCTs did not like the cosmetic effects of BTA but still reported feeling less depressed after treatment.10
How might it work?
Several theories about the mechanism of action have been proposed:
• The facial feedback hypothesis dates to Charles Darwin in 1872: Facial movements influence emotional states. Numerous studies have confirmed this. Strack et al24 found that patients asked to smile while reading comics found them to be funnier. Ekman et al25 found that imitating angry facial expressions made body temperature and heart rate rise. Dialectical behavioral therapy expert Marsha Linehan recognized the importance of modifying facial expressions (from grimacing to smiling) and posture (from clenched fists to open hands) when feeling distressed, because it is hard to feel “willful” when your “mind is going one way and your body is going another.”26 Accordingly, for a person who continuously “looks” depressed or distressed, reducing the anguished facial expression using botulinum toxin might diminish the entwined negative emotions.
• A more pleasant facial expression improves social interactions, which leads to improvement in self-esteem and mood. Social biologists argue that (1) we are attracted to those who have more pleasant facial expressions and (2) we steer clear of those who appear angry or depressed (a negative facial expression, such as a growling dog, is perceived as a threat). Therefore, anyone who looks depressed might have less rewarding interpersonal interactions, which can contribute to a poor mood.
On a similar note, mirror neurons are regions in the brain that are activated by witnessing another person’s emotional cues. When our mirror neurons light up, we can feel an observed experience, which is why we often feel nervous around anxious people, or cringe when we see others get hurt, or why we might prefer engaging with people who appear happier. It is possible that, after BTA injection, a person’s social connectivity is improved because of a more positive reciprocal firing of mirror neurons.
• BTA leads to direct and indirect neurochemical changes in the brain that can reduce depression. Functional MRI studies have shown that after glabellar BTA injections, the amygdala was less responsive to negative stimuli.27,28 For example, patients who were treated with BTA and then shown pictures of angry people had an attenuated amygdala response to the photos.
This is an important finding, especially for patients who have been traumatized. After a traumatic event, the amygdala “remembers” what happened, which is good, in some ways (it prevents us from getting into a similar dangerous situation), but bad in others (the traumatized amygdala may falsely perceive a non-threatening stimuli as threatening). A hypervigilant amygdala can lead to an out-of-proportion fear response, depression, and anxiety. Therefore, quelling an overactive amygdala with BTA could improve emotional dysregulation and posttraumatic disorders.
Many of our patients reported that, after BTA injection, “traumatic events didn’t feel as traumatizing,” as one said. The emotional pain and rumination that often follow a life stressor “does not overstay its welcome” and patients are able to “move on” more quickly.
It is unknown why the amygdala is quieted after BTA; researchers hypothesize that BTA suppresses facial feedback signals from the forehead branch of the trigeminal nerve to the brain. Another hypothesis is that BTA is directly transported by the trigeminal nerve into the brain and exerts central pharmacological effects on the amygdala.29 This theory has only been studied in rat models.30
When does it start working? How long does it last?
From what we know, BTA for depression could start working as early as 2 weeks and could last as long as 6 months. In one RCT, the earliest follow-up was 2 weeks,10 at which time the depressed patients had responded to botulinum toxin (P ≤ .05). In the other 2 controlled trials, the earliest follow-up was 3 weeks, at which time a more robust response was seen (P < .001). Aesthetically, BTA usually lasts 3 months. It is unclear how long the antidepressant effects last but, in the longest trial,3 depression symptoms continued to improve at 6 months, after cosmetic effects had worn off.
These findings raise a series of questions:
• Do mood effects outlast cosmetic effects? If so, why?
• Does botulinum toxin start to work sooner than 2 weeks?
• Will adherence improve if a patient has to be treated only every 6 months?
In our clinical experience, depressed patients who responded to BTA injection report a slow resurfacing of depressive symptoms 4 to 6 months after treatment, at which point they usually return for “maintenance treatment” (same dosing, same injection configuration).
Will psychiatrists administer the treatment?
Any physician or physician extender can, when properly trained, inject BTA. The question is: Do psychiatrists want to? Administrating botulinum toxin requires more labor and preparation than prescribing a drug (Table 2,31) and requires placing hands on patients. Depending on the type of psychiatric practice, this may be a “deal-breaker” for some providers, such as those in a psychoanalytic practice who might worry about boundaries.
As a basis for comparison, despite several indications for BTA for headache and neurologic conditions, few neurologists have added botulinum toxin to their practice. Dermatologists who are comfortable seeing psychiatric patients or family practitioners, who are already set up for injection procedures, could become custodians of this intervention.
Which patients are candidates for the treatment?
Patients with anxious or agitated depression might be ideal candidates for BTA injection. A recent study looked at predictors of response: Patients with a high agitation score (as measured on item 9 of the HAM-D) were more likely to respond, with a sensitivity of 100%, a specificity of 56%, and an overall precision of 78%.32 So far, no other predictors of response have been clearly identified. Higher baseline wrinkle scores do not predict better response.23 Sex and age do not have any predictive value. The treatment appears to be equally effective in males and females; because only a handful of males have been treated (n = 14), however, these patients need to be studied further.
Is botulinum toxin better as monotherapy or augmentation strategy?
So far, it appears to be equally effective as monotherapy or augmentation strategy,16 but more studies are needed.
How expensive is it?
Estimates of patient cost include the cost of the product and the professional fee for injection. As a point of reference, for cosmetic purposes, depending on practice location, dermatologists charge $11 to $20 per unit of BTA. Therefore, 1 treatment of BTA for depression (29 to 40 units) can cost a patient $319 to $800.
When treating a patient with BTA for medical indications, such as tension headache, insurance often reimburses the physician for the BTA at cost (paid with a J code: J0585) and pay an injection fee (a procedure code) of $150 to $200. A recent analysis of cost-effectiveness estimated that BTA for depression would cost a patient $1,200 to $1,600 annually.33 Compared with the price of branded medications (eg, $500 to $2,000 annually)33 plus weekly psychotherapy (eg, $2,000 to $5,000 annually), BTA may be a cost-effective option for patients who do not respond to conventional treatments. Of course, for patients who tolerate and respond to generic medications or have a therapist who charges on a sliding scale, BTA is not the most cost-effective option.
What about injecting other areas of the face?
We’ve thought about it but haven’t tried it. There are several muscles around the mouth that allow us to smile and frown. BTA injections in the depressor anguli oris, a muscle around the mouth that is largely responsible for frowning, could treat depression. However, if the mechanism of action is via amygdala desensitization through the trigeminal nerve, treating mouth frown muscles might not work.
Is it safe?
BTA in the glabella has an exceptionally good safety profile.9,31,34 Adverse reactions, which include eyelid droop, pain, bruising, and redness at the injection site, are minor and temporary.9 In addition, BTA has few drug–drug interactions. The biggest complaint for most patients is discomfort upon injection, which often is described as feeling like “an ant bite.”
In the pooled analysis of RCTs, apart from local irritation immediately after injection, temporary headache was the only relevant, and possibly treatment-related, adverse event. Headache occurred in 13.6% (n = 8) of the BTA group and 9.3% (n = 7) of the placebo group (P = .44). Compared with antidepressants such as citalopram, where approximately 38.6% of patients report a moderate or severe side-effect burden,21 BTA is well tolerated.
Are other studies underway?
Larger studies are being conducted,35 mainly to confirm what pilot studies have shown. It would be interesting to discover other predictors of response and if different dosing and injection configurations could strengthen the response rate and extend the duration of effect.
Because of the cosmetic effects of BTA, further studies are needed to address the problem of blinding. In earlier studies, raters were blinded during appointments because patients wore surgical caps that covered their glabellar region.3,10 Patients did not know their treatment intervention, but 52% to 90% of patients guessed correctly.3,10,11 Although unblinding is a common problem in “blinded” trials in which some researchers have reported >75% of participants and raters guessed the intervention correctly,36 it is a particularly sensitive area in studies that involve a change in appearance because it is almost impossible to prevent someone from looking in a mirror.
Summing up
Botulinum toxin for depression is not ready for prime time. The FDA has not approved its use for psychiatric indications, and Medicare and commercial insurance do not reimburse for this procedure as a treatment for depression. Patients who request BTA for depression must be informed that this use is off-label.
For now, we recommend psychotherapy or medication management, or both, for most patients with major depression. In addition, until larger studies are done, we recommend that patients who are interested in BTA for depression use it as an add-on to conventional treatment. However, if larger studies replicate the findings of the smaller studies we have described, botulinum toxin could become a novel therapeutic agent in the fight against depression.
Bottom Line
In pilot studies, botulinum toxin A (BTA) has shown efficacy in improving symptoms of depression. Although considered safe, BTA is not FDA-approved for psychiatric indications, and Medicare and commercial insurance do not reimburse for this procedure for depression. Larger studies are underway to determine if this novel treatment can be introduced into practice.
Related Resources
• Wollmer MA, Magid M, Kruger THC. Botulinum toxin treatment in depression. In: Bewley A, Taylor RE, Reichenberg JS, et al, eds. Practical psychodermatology. Hoboken, NJ: John Wiley & Sons; 2014:216-219.
• Botox for depression. www.botoxfordepression.com.
• Botox and depression. www.botoxanddepression.com.
Drug Brand Names
Botulinum toxin A • Botox
Citalopram • Celexa
Acknowledgments
We thank the Brain and Behavior Research Foundation for granting Dr. Magid a young investigator award and for continuing to invest in innovative research ideas. We thank Dr. Eric Finzi, MD, PhD, Axel Wollmer, MD, and Tillmann Krüger, MD, for their continued collaboration in this area of research.
Disclosures
In July 2011, Dr. Magid received a young investigator award from the Brain and Behavior Research Foundation for her study on treating depression using botulinum toxin (Grant number 17648). In November 2012, after completion and as a result of the study on treating depression using botulinum toxin, Dr. Magid became a consultant with Allergan to discuss study findings. In September 2015, Dr. Magid became a speaker for IPSEN Innovation. Dr. Reichenberg is married to Dr. Magid. Dr. Reichenberg has no other conflicts of interest to disclose.
1. Nasrallah HA. 10 Recent paradigm shifts in the neurobiology and treatment of depression. Current Psychiatry. 2015;14(2):10-13.
2. Finzi E, Wasserman E. Treatment of depression with botulinum toxin A: a case series. Dermatol Surg. 2006;32(5):645-649; discussion 649-650.
3. Magid M, Reichenberg JS, Poth PE, et al. Treatment of major depressive disorder using botulinum toxin A: a 24-week randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2014;75(8):837-844.
4. Koussoulakos S. Botulinum neurotoxin: the ugly duckling. Eur Neurol. 2008;61(6):331-342.
5. Chen S. Clinical uses of botulinum neurotoxins: current indications, limitations and future developments. Toxins (Basel). 2012;4(10):913-939.
6. Bhidayasiri R, Truong DD. Expanding use of botulinum toxin. J Neurol Sci. 2005;235(1-1):1-9.
7. Cosmetic surgery national data bank statistics. American Society for Asethetic Plastic Surgery. http://www.surgery. org/sites/default/files/2014-Stats.pdf. Published 2014. Accessed May 30, 2015.
8. Shorter E. Darwin’s contribution to psychiatry. Br J Psychiatry. 2009;195(6):473-474.
9. Winter L, Spiegel J. Botulinum toxin type-A in the treatment of glabellar lines. Clin Cosmet Investig Dermatol. 2009;3:1-4.
10. Wollmer MA, de Boer C, Kalak N, et al. Facing depression with botulinum toxin: a randomized controlled trial. J Psychiatr Res. 2012;46(5):574-581.
11. Finzi E, Rosenthal NE. Treatment of depression with onabotulinumtoxinA: a randomized, double-blind, placebo controlled trial. J Psychiatr Res. 2014;52:1-6.
12. Hexsel D, Brum C, Porto MD, et al. Quality of life and satisfaction of patients after full-face injections of abobotulinum toxin type A: a randomized, phase IV clinical trial. J Drugs Dermatol. 2013;12(12):1363-1367.
13. Lewis MB, Bowler PJ. Botulinum toxin cosmetic therapy correlates with a more positive mood. J Cosmet Dermatol. 2009;8(1):24-26.
14. Sommer B, Zschocke I, Bergfeld D, et al. Satisfaction of patients after treatment with botulinum toxin for dynamic facial lines. Dermatol Surg. 2003;29(5):456-460.
15. Hexsel D, Brum C, Siega C, et al. Evaluation of self‐esteem and depression symptoms in depressed and nondepressed subjects treated with onabotulinumtoxina for glabellar lines. Dermatol Surg. 2013;39(7):1088-1096.
16. Magid M, Reichenberg JS, Finzi E, et al. Treating depression with botulinum toxin: update and meta-analysis from clinic trials. Paper presented at: XVI World Congress of Psychiatry; September 14-18, 2014; Madrid, Spain.
17. Magid M, Finzi E, Kruger TH, et al. Treating depression with botulinum toxin: a pooled analysis of randomized controlled trials. Pharmacopsychiatry. 2015;48(6):205-210.
18. Parsaik A, Mascarenhas S, Hashmi A, et al. Role of botulinum toxin in depression: a systematic review and meta-analysis. J Psychiatr Pract. In press.
19. Scott AI, ed. The ECT handbook, 2nd ed. The third report of the Royal College of Psychiatrists’ Special Committee of ECT. London, United Kingdom: The Royal College of Psychiatrists; 2005.
20. Ren J, Li H, Palaniyappan L, et al. Repetitive transcranial magnetic stimulation versus electroconvulsive therapy for major depression: a systematic review and meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2014;51:181-189.
21. Trivedi MH, Rush AJ, Wisniewski SR, et al; STAR*D Study Team. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR* D: implications for clinical practice. Am J Psychiatry. 2006;163(1):28-40.
22. Gibbons RD, Hur K, Brown CH, et al. Benefits from antidepressants: synthesis of 6-week patient-level outcomes from double-blind placebo-controlled randomized trials of fluoxetine and venlafaxine. Arch Gen Psychiatry. 2012;69(6):572-579.
23. Reichenberg JS, Magid M, Keeling B. Botulinum toxin for depression: does the presence of rhytids predict response? Presented at: Texas Dermatology Society; May 2015; Bastrop, Texas.
24. Strack F, Martin LL, Stepper S. Inhibiting and facilitating conditions of the human smile: a nonobtrusive test of the facial feedback hypothesis. J Pers Soc Psychol. 1988;54(5):768-777.
25. Ekman P, Levenson RW, Friesen WV. Autonomic nervous system activity distinguishes among emotions. Science. 1983;221(4616):1208-1210.
26. Linehan MM. DBT skills training manual, 2nd ed. New York, NY: Guilford Publications; 2014.
27. Hennenlotter A, Dresel C, Castrop F, et al. The link between facial feedback and neural activity within central circuitries of emotion—new insights from botulinum toxin-induced denervation of frown muscles. Cereb Cortex. 2009;19(3):537-542.
28. Kim MJ, Neta M, Davis FC, et al. Botulinum toxin-induced facial muscle paralysis affects amygdala responses to the perception of emotional expressions: preliminary findings from an A-B-A design. Biol Mood Anxiety Disord. 2014;4:11.
29. Mazzocchio R, Caleo M. More than at the neuromuscular synapse: actions of botulinum neurotoxin A in the central nervous system. Neuroscientist. 2015;21(1):44-61.
30. Antonucci F, Rossi C, Gianfranceschi L, et al. Long-distance retrograde effects of botulinum neurotoxin A. J Neurosci. 2008;28(14):3689-3696.
31. U.S. Food and Drug Administration. Medication guide: botox. http://www.fda.gov/downloads/drugs/drugsafety/ucm176360.pdf. Updated September 2013. Accessed June 7, 2015.
32. Wollmer MA, Kalak N, Jung S, et al. Agitation predicts response of depression to botulinum toxin treatment in a randomized controlled trial. Front Psychiatry. 2014;5:36.
33. Beer K. Cost effectiveness of botulinum toxins for the treatment of depression: preliminary observations. J Drugs Dermatol. 2010;9(1):27-30.
34. Brin MF, Boodhoo TI, Pogoda JM, et al. Safety and tolerability of onabotulinumtoxinA in the treatment of facial lines: a meta-analysis of individual patient data from global clinical registration studies in 1678 participants. J Am Acad Dermatol. 2009;61(6):961-970.e1-11.
35. Botulinum toxin and depression. ClinicalTrials.gov. https:// clinicaltrials.gov/ct2/results?term=botulinum+toxin+and+ depression&Search=Search. Accessed June 1, 2015.
36. Rabkin JG, Markowitz JS, Stewart J, et al. How blind is blind? Assessment of patient and doctor medication guesses in a placebo-controlled trial of imipramine and phenelzine. Psychiatry Res. 1986;19(1):75-86.
1. Nasrallah HA. 10 Recent paradigm shifts in the neurobiology and treatment of depression. Current Psychiatry. 2015;14(2):10-13.
2. Finzi E, Wasserman E. Treatment of depression with botulinum toxin A: a case series. Dermatol Surg. 2006;32(5):645-649; discussion 649-650.
3. Magid M, Reichenberg JS, Poth PE, et al. Treatment of major depressive disorder using botulinum toxin A: a 24-week randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2014;75(8):837-844.
4. Koussoulakos S. Botulinum neurotoxin: the ugly duckling. Eur Neurol. 2008;61(6):331-342.
5. Chen S. Clinical uses of botulinum neurotoxins: current indications, limitations and future developments. Toxins (Basel). 2012;4(10):913-939.
6. Bhidayasiri R, Truong DD. Expanding use of botulinum toxin. J Neurol Sci. 2005;235(1-1):1-9.
7. Cosmetic surgery national data bank statistics. American Society for Asethetic Plastic Surgery. http://www.surgery. org/sites/default/files/2014-Stats.pdf. Published 2014. Accessed May 30, 2015.
8. Shorter E. Darwin’s contribution to psychiatry. Br J Psychiatry. 2009;195(6):473-474.
9. Winter L, Spiegel J. Botulinum toxin type-A in the treatment of glabellar lines. Clin Cosmet Investig Dermatol. 2009;3:1-4.
10. Wollmer MA, de Boer C, Kalak N, et al. Facing depression with botulinum toxin: a randomized controlled trial. J Psychiatr Res. 2012;46(5):574-581.
11. Finzi E, Rosenthal NE. Treatment of depression with onabotulinumtoxinA: a randomized, double-blind, placebo controlled trial. J Psychiatr Res. 2014;52:1-6.
12. Hexsel D, Brum C, Porto MD, et al. Quality of life and satisfaction of patients after full-face injections of abobotulinum toxin type A: a randomized, phase IV clinical trial. J Drugs Dermatol. 2013;12(12):1363-1367.
13. Lewis MB, Bowler PJ. Botulinum toxin cosmetic therapy correlates with a more positive mood. J Cosmet Dermatol. 2009;8(1):24-26.
14. Sommer B, Zschocke I, Bergfeld D, et al. Satisfaction of patients after treatment with botulinum toxin for dynamic facial lines. Dermatol Surg. 2003;29(5):456-460.
15. Hexsel D, Brum C, Siega C, et al. Evaluation of self‐esteem and depression symptoms in depressed and nondepressed subjects treated with onabotulinumtoxina for glabellar lines. Dermatol Surg. 2013;39(7):1088-1096.
16. Magid M, Reichenberg JS, Finzi E, et al. Treating depression with botulinum toxin: update and meta-analysis from clinic trials. Paper presented at: XVI World Congress of Psychiatry; September 14-18, 2014; Madrid, Spain.
17. Magid M, Finzi E, Kruger TH, et al. Treating depression with botulinum toxin: a pooled analysis of randomized controlled trials. Pharmacopsychiatry. 2015;48(6):205-210.
18. Parsaik A, Mascarenhas S, Hashmi A, et al. Role of botulinum toxin in depression: a systematic review and meta-analysis. J Psychiatr Pract. In press.
19. Scott AI, ed. The ECT handbook, 2nd ed. The third report of the Royal College of Psychiatrists’ Special Committee of ECT. London, United Kingdom: The Royal College of Psychiatrists; 2005.
20. Ren J, Li H, Palaniyappan L, et al. Repetitive transcranial magnetic stimulation versus electroconvulsive therapy for major depression: a systematic review and meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2014;51:181-189.
21. Trivedi MH, Rush AJ, Wisniewski SR, et al; STAR*D Study Team. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR* D: implications for clinical practice. Am J Psychiatry. 2006;163(1):28-40.
22. Gibbons RD, Hur K, Brown CH, et al. Benefits from antidepressants: synthesis of 6-week patient-level outcomes from double-blind placebo-controlled randomized trials of fluoxetine and venlafaxine. Arch Gen Psychiatry. 2012;69(6):572-579.
23. Reichenberg JS, Magid M, Keeling B. Botulinum toxin for depression: does the presence of rhytids predict response? Presented at: Texas Dermatology Society; May 2015; Bastrop, Texas.
24. Strack F, Martin LL, Stepper S. Inhibiting and facilitating conditions of the human smile: a nonobtrusive test of the facial feedback hypothesis. J Pers Soc Psychol. 1988;54(5):768-777.
25. Ekman P, Levenson RW, Friesen WV. Autonomic nervous system activity distinguishes among emotions. Science. 1983;221(4616):1208-1210.
26. Linehan MM. DBT skills training manual, 2nd ed. New York, NY: Guilford Publications; 2014.
27. Hennenlotter A, Dresel C, Castrop F, et al. The link between facial feedback and neural activity within central circuitries of emotion—new insights from botulinum toxin-induced denervation of frown muscles. Cereb Cortex. 2009;19(3):537-542.
28. Kim MJ, Neta M, Davis FC, et al. Botulinum toxin-induced facial muscle paralysis affects amygdala responses to the perception of emotional expressions: preliminary findings from an A-B-A design. Biol Mood Anxiety Disord. 2014;4:11.
29. Mazzocchio R, Caleo M. More than at the neuromuscular synapse: actions of botulinum neurotoxin A in the central nervous system. Neuroscientist. 2015;21(1):44-61.
30. Antonucci F, Rossi C, Gianfranceschi L, et al. Long-distance retrograde effects of botulinum neurotoxin A. J Neurosci. 2008;28(14):3689-3696.
31. U.S. Food and Drug Administration. Medication guide: botox. http://www.fda.gov/downloads/drugs/drugsafety/ucm176360.pdf. Updated September 2013. Accessed June 7, 2015.
32. Wollmer MA, Kalak N, Jung S, et al. Agitation predicts response of depression to botulinum toxin treatment in a randomized controlled trial. Front Psychiatry. 2014;5:36.
33. Beer K. Cost effectiveness of botulinum toxins for the treatment of depression: preliminary observations. J Drugs Dermatol. 2010;9(1):27-30.
34. Brin MF, Boodhoo TI, Pogoda JM, et al. Safety and tolerability of onabotulinumtoxinA in the treatment of facial lines: a meta-analysis of individual patient data from global clinical registration studies in 1678 participants. J Am Acad Dermatol. 2009;61(6):961-970.e1-11.
35. Botulinum toxin and depression. ClinicalTrials.gov. https:// clinicaltrials.gov/ct2/results?term=botulinum+toxin+and+ depression&Search=Search. Accessed June 1, 2015.
36. Rabkin JG, Markowitz JS, Stewart J, et al. How blind is blind? Assessment of patient and doctor medication guesses in a placebo-controlled trial of imipramine and phenelzine. Psychiatry Res. 1986;19(1):75-86.
EADV: Hidradenitis suppurativa carries high cardiovascular risk
COPENHAGEN – Hidradenitis suppurativa, a common, chronic, inflammatory scarring skin disease of the hair follicles, is a red flag signaling elevated levels of multiple cardiovascular risk factors, according to a systematic review and meta-analysis.
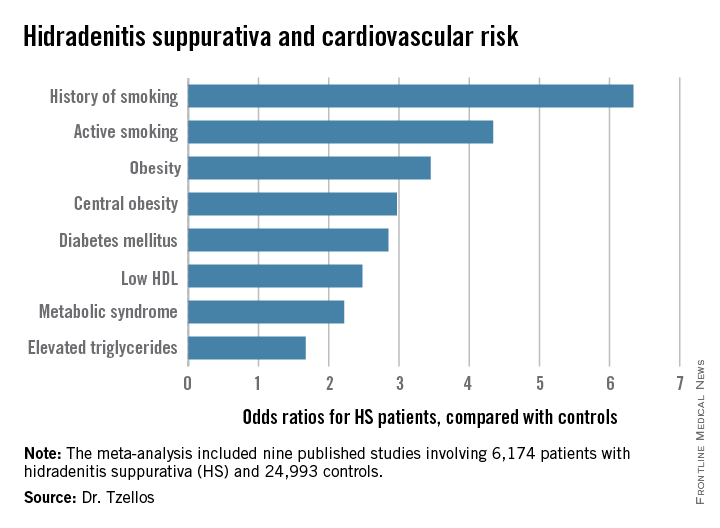
“The need for screening of hidradenitis suppurativa patients for modifiable cardiovascular risk is emphasized,” Dr. Thrasyvoulos Tzellos said in presenting the findings at the annual congress of the European Academy of Dermatology and Venereology.
For such a common and dramatically destructive disease, hidradenitis suppurativa (HS) was underresearched until recently. Investigative interest grew as the tumor necrosis factor inhibitor adalimumab (Humira) underwent development as a novel therapy for what has been traditionally a notoriously difficult to treat disease. The biologic agent received Food and Drug Administration marketing approval in October as the first and only approved treatment for HS.
Dr. Tzellos’s meta-analysis included nine published studies totaling 6,174 HS patients and 24,993 controls. Five studies were case control, and the other four were cross sectional. An indicator of the recent explosive research interest in HS can be seen in the fact that 80% of all the HS patients included in the meta-analysis come from two studies published within just the last year, one from Massachusetts General Hospital (J Am Acad Dermatol. 2014 Dec;71[6]:1144-50) and the other from Israel (Br J Dermatol. 2015 Aug;173[2]:464-70).
Not all the studies examined the same cardiovascular risk factors. For example, only six of nine studies looked at diabetes mellitus as an endpoint. Of those studies that did, diabetes occurred in 856 of 5,685 HS patients, a rate 2.85-fold higher than in controls, according to Dr. Tzellos of University Hospital of North Norway in Troms.
The only cardiovascular risk factor examined that was not significantly more common among patients with HS than controls was hypertension. The 1.57-fold increased likelihood of hypertension among HS patients didn’t achieve statistical significance.
Although patients whose HS was treated exclusively in outpatient settings had significantly higher levels of cardiovascular risk factors than did controls, risk levels were consistently higher still in patients who had been hospitalized for HS.
A meta-analysis such as this cannot address causality, leaving open the question of whether increased cardiovascular risk factors are intrinsic to HS, or the debilitating recurrent skin disease causes affected patients to take a defeatest attitude toward maintenance of a healthy lifestyle.
Dr. Tzellos reported having no financial conflicts regarding this meta-analysis, carried out with academic funding.
COPENHAGEN – Hidradenitis suppurativa, a common, chronic, inflammatory scarring skin disease of the hair follicles, is a red flag signaling elevated levels of multiple cardiovascular risk factors, according to a systematic review and meta-analysis.
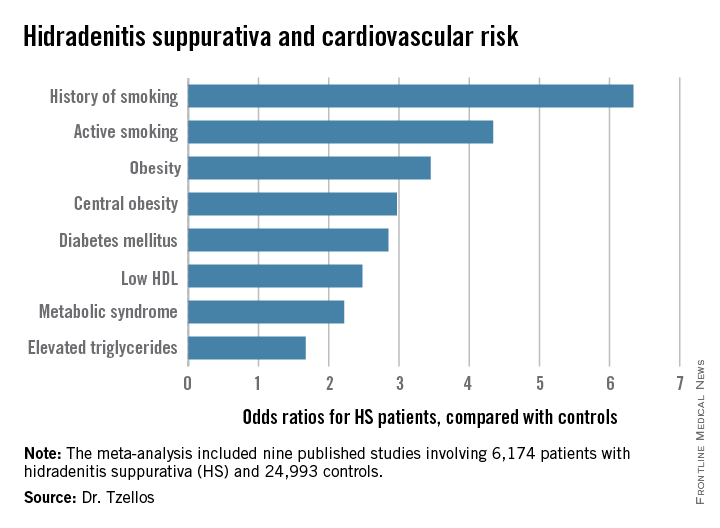
“The need for screening of hidradenitis suppurativa patients for modifiable cardiovascular risk is emphasized,” Dr. Thrasyvoulos Tzellos said in presenting the findings at the annual congress of the European Academy of Dermatology and Venereology.
For such a common and dramatically destructive disease, hidradenitis suppurativa (HS) was underresearched until recently. Investigative interest grew as the tumor necrosis factor inhibitor adalimumab (Humira) underwent development as a novel therapy for what has been traditionally a notoriously difficult to treat disease. The biologic agent received Food and Drug Administration marketing approval in October as the first and only approved treatment for HS.
Dr. Tzellos’s meta-analysis included nine published studies totaling 6,174 HS patients and 24,993 controls. Five studies were case control, and the other four were cross sectional. An indicator of the recent explosive research interest in HS can be seen in the fact that 80% of all the HS patients included in the meta-analysis come from two studies published within just the last year, one from Massachusetts General Hospital (J Am Acad Dermatol. 2014 Dec;71[6]:1144-50) and the other from Israel (Br J Dermatol. 2015 Aug;173[2]:464-70).
Not all the studies examined the same cardiovascular risk factors. For example, only six of nine studies looked at diabetes mellitus as an endpoint. Of those studies that did, diabetes occurred in 856 of 5,685 HS patients, a rate 2.85-fold higher than in controls, according to Dr. Tzellos of University Hospital of North Norway in Troms.
The only cardiovascular risk factor examined that was not significantly more common among patients with HS than controls was hypertension. The 1.57-fold increased likelihood of hypertension among HS patients didn’t achieve statistical significance.
Although patients whose HS was treated exclusively in outpatient settings had significantly higher levels of cardiovascular risk factors than did controls, risk levels were consistently higher still in patients who had been hospitalized for HS.
A meta-analysis such as this cannot address causality, leaving open the question of whether increased cardiovascular risk factors are intrinsic to HS, or the debilitating recurrent skin disease causes affected patients to take a defeatest attitude toward maintenance of a healthy lifestyle.
Dr. Tzellos reported having no financial conflicts regarding this meta-analysis, carried out with academic funding.
COPENHAGEN – Hidradenitis suppurativa, a common, chronic, inflammatory scarring skin disease of the hair follicles, is a red flag signaling elevated levels of multiple cardiovascular risk factors, according to a systematic review and meta-analysis.
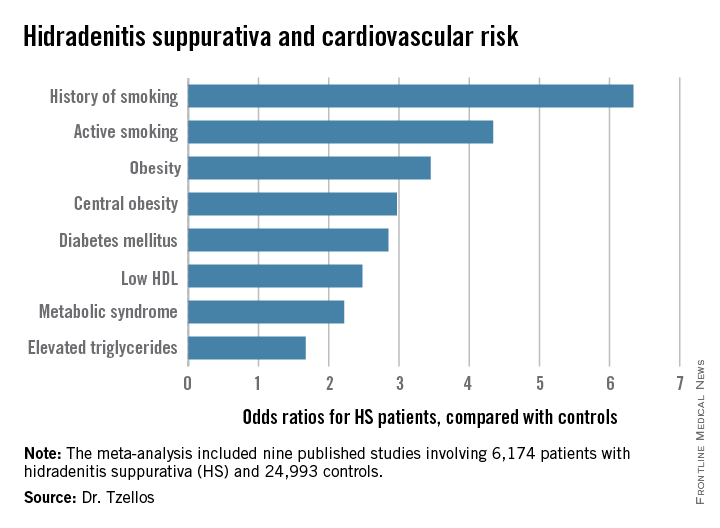
“The need for screening of hidradenitis suppurativa patients for modifiable cardiovascular risk is emphasized,” Dr. Thrasyvoulos Tzellos said in presenting the findings at the annual congress of the European Academy of Dermatology and Venereology.
For such a common and dramatically destructive disease, hidradenitis suppurativa (HS) was underresearched until recently. Investigative interest grew as the tumor necrosis factor inhibitor adalimumab (Humira) underwent development as a novel therapy for what has been traditionally a notoriously difficult to treat disease. The biologic agent received Food and Drug Administration marketing approval in October as the first and only approved treatment for HS.
Dr. Tzellos’s meta-analysis included nine published studies totaling 6,174 HS patients and 24,993 controls. Five studies were case control, and the other four were cross sectional. An indicator of the recent explosive research interest in HS can be seen in the fact that 80% of all the HS patients included in the meta-analysis come from two studies published within just the last year, one from Massachusetts General Hospital (J Am Acad Dermatol. 2014 Dec;71[6]:1144-50) and the other from Israel (Br J Dermatol. 2015 Aug;173[2]:464-70).
Not all the studies examined the same cardiovascular risk factors. For example, only six of nine studies looked at diabetes mellitus as an endpoint. Of those studies that did, diabetes occurred in 856 of 5,685 HS patients, a rate 2.85-fold higher than in controls, according to Dr. Tzellos of University Hospital of North Norway in Troms.
The only cardiovascular risk factor examined that was not significantly more common among patients with HS than controls was hypertension. The 1.57-fold increased likelihood of hypertension among HS patients didn’t achieve statistical significance.
Although patients whose HS was treated exclusively in outpatient settings had significantly higher levels of cardiovascular risk factors than did controls, risk levels were consistently higher still in patients who had been hospitalized for HS.
A meta-analysis such as this cannot address causality, leaving open the question of whether increased cardiovascular risk factors are intrinsic to HS, or the debilitating recurrent skin disease causes affected patients to take a defeatest attitude toward maintenance of a healthy lifestyle.
Dr. Tzellos reported having no financial conflicts regarding this meta-analysis, carried out with academic funding.
AT THE EADV CONGRESS
Key clinical point: Be vigilant in screening for modifiable cardiovascular risk factors in patients with hidradenitis suppurativa.
Major finding: Hidradenitis suppurativa patients were 2.85-fold more likely than controls to have diabetes, 2.22-fold more likely to have metabolic syndrome, and 4.34-fold more likely to be active smokers.
Data source: A meta-analysis of nine published studies totaling 6,174 hidradenitis suppurativa patients and 24,993 controls.
Disclosures: The presenter reported having no financial conflicts regarding this meta-analysis, carried out with academic funding.
AAP backs zero tolerance for headfirst hits in football
WASHINGTON – Teaching young athletes to tackle with their heads up and enforcing rules against illegal headfirst hits can reduce the risks of concussions in youth football, according to a new policy statement by the American Academy of Pediatrics.
An emphasis on proper tackling technique and implementing strategies to reduce head hits maintains the integrity of the game while reducing the most serious injuries as well as subconcussive hits, Dr. Gregory L. Landry, Fellow of the American Academy of Pediatrics (FAAP), and professor of pediatrics and orthopedics at the University of Wisconsin–Madison, said in his plenary talk at the annual meeting of the American Academy of Pediatrics.
Dr. Landry, along with Dr. William P. Meehan III, FAAP, led the Council on Sports Medicine and Fitness in writing the AAP’s policy statement on tackling in youth football (Pediatrics 2015 Oct 25. doi: 10.1542/peds.2015-3282).
In response to growing calls to ban tackling entirely in youth football, and calls to eliminate football from high school sports, the council reviewed the evidence on youth tackling, concussions, and other injuries in football to reach the seven conclusions outlined in the policy statement, Dr. Landry said.
“Most injuries sustained during participation in youth football are minor, including injuries to the head and neck,” according to the policy statement. “The incidences of severe injuries, catastrophic injuries, and concussion, however, are higher in football than most other team sports and appear to increase with age.”
During his talk, Dr. Landry noted that catastrophic injuries occur more frequently in gymnastics and wrestling than in football. Among all youth football injuries, 3.4% are neurologic and 2.5% are fractures. Half are contusions, 16.7% are sprains, and 9.3% are strains.
Within football, young players tend to have far lower rates of concussions, compared to older players. In one 2-year observational study, the overall concussion rates of 7.4 per 1,000 athletic exposures broke down to 4.3 per 1,000 exposures for fourth- and fifth-graders and 14.4 per 1,000 exposures for eighth-graders. On the low end, another study found a concussion rate of 1.8 per 1,000 exposures, with a rate of 0.24 for practices and 6.2 for games.
“One of the common themes is that game rate is always higher than practice rates,” Dr. Landry said. “Running backs seem to be at the highest risk for injuries.”
In addition, tackling is the most common player activity at the time of the injury and at the time of severe injury. “The act of tackling is, in fact, risky business,” Dr. Landry said.
One reason for this relates to improvement in football safety equipment, he explained.
“As football helmets began to improve, football players began leading with their heads instead of their shoulders,” he said. “Leading with the head increases the risk of both concussion and spinal injury. The priority must be that the head must be up when a player tackles someone. The proper way to tackle is leading with the chest.”
A key study showing the effect that heads-up tackling instruction can have on concussion rates involved comparisons with teams taught Heads Up Football, “a comprehensive program developed by USA Football to advance player safety,” according to the program’s website. During the 2014 football season in Indiana, researchers compared teams that participated in the Heads Up program with teams that did not and with a third group of Pop Warner–affiliated teams that had reduced the number of full body contact practices.
Among 71,262 athletic exposures, the rate was lowest for the teams that were both Pop Warner affiliated and Heads Up affiliated, with a rate of 0.97 concussions per 1,000 athletic exposures. The teams involved in neither program had a rate of 7.32 concussions per 1,000 exposures, but even the Heads Up–only teams had a rate more than twice as low, with 2.73 per 1,000 exposures, revealing the importance of not tackling head first, Dr. Landry said.
“That’s the problem with American football – the whole game has changed,” he said, regarding the shift in tackling technique. “And you’re seeing this at the college level and at the professional level.”
In light of the way the game has changed and the risks it presented, the council offered seven conclusions and recommendations in its policy statement:
1. Officials and coaches must enforce the rules of the game, moving toward “zero tolerance of illegal, headfirst hits.” The statement notes a current “culture of tolerance” regarding headfirst tackling. “This culture has to change to one that protects the head for both the tackler and those players being tackled,” the committee stated. “Stronger sanctions for contact to the head, especially of a defenseless player, should be considered, up to and including expulsion from the game.”
2. Although eliminating tackling from football would likely cause a decrease in overall and severe or catastrophic injuries, it would also change essential aspects of the game. “Participants in football must decide whether the potential health risks of sustaining these injuries are outweighed by the recreational benefits associated with proper tackling,” the committee stated. Dr. Landry compared the game to hockey. “In ice hockey, if you don’t check, it’s still ice hockey,” he said. “But with football, removing tackling fundamentally changes the game.”
3. Football leagues should consider expanding their options to include football teams without tackling, such as flag football, for those who want to play without the additional risks from tackling. But youth flag football has not been studied, Dr. Landry pointed out, and some adult studies have shown higher rates of injuries, so youth flag football requires more study.
4. Officials and coaches should look for and implement ways to reduce the number of hits to the head that players experience. “If subconcussive blows to the head result in negative long-term effects on health, then limiting impacts to the head should reduce the risk of these long-term health problems,” the committee stated while acknowledging the need for more research in this area.
5. A theoretical risk exists that delaying the age when athletes learn tackling could lead it to become more dangerous. “Once tackling is introduced, athletes who have no previous experience with tackling would be exposed to collisions for the first time at an age at which speeds are faster, collision forces are greater, and injury risk is higher,” the committee stated. “Lack of experience with tackling and being tackled may lead to an increase in the number and severity of injuries once tackling is introduced.” Dr. Landry acknowledged that the risk is theoretical and hasn’t been studied but perhaps needs to be.
6. Neck strengthening might lessen the risk of concussions with head hits, though little scientific evidence exists to support this hypothesis. “Physical therapists, athletic trainers, or strength and conditioning specialists with expertise in the strengthening and conditioning of pediatric athletes are best qualified to help young football players achieve the neck strength that will help prevent injuries,” the committee stated.
7. Football teams should have athletic trainers present at organized football games and practices since research supports a link between trainers’ presence and a lower incidence of sports-related injuries.
Dr. Landry’s overall message focused on ways to reduce risks without ending football. “Let’s not ban the game,” he said. “Let’s just make it safer.”
Dr. Landry has no financial disclosures but had his college tuition paid by playing football, served as team physician for the University of Wisconsin football team for many seasons, and grew up as the son of a high school football coach. Dr. Meehan is involved in researched partly funded by the National Football League Players Association, and he receives compensation from ABC-Clio Publishing, Wolters Kluwer, and Springer International Publishing for works he has authored.
WASHINGTON – Teaching young athletes to tackle with their heads up and enforcing rules against illegal headfirst hits can reduce the risks of concussions in youth football, according to a new policy statement by the American Academy of Pediatrics.
An emphasis on proper tackling technique and implementing strategies to reduce head hits maintains the integrity of the game while reducing the most serious injuries as well as subconcussive hits, Dr. Gregory L. Landry, Fellow of the American Academy of Pediatrics (FAAP), and professor of pediatrics and orthopedics at the University of Wisconsin–Madison, said in his plenary talk at the annual meeting of the American Academy of Pediatrics.
Dr. Landry, along with Dr. William P. Meehan III, FAAP, led the Council on Sports Medicine and Fitness in writing the AAP’s policy statement on tackling in youth football (Pediatrics 2015 Oct 25. doi: 10.1542/peds.2015-3282).
In response to growing calls to ban tackling entirely in youth football, and calls to eliminate football from high school sports, the council reviewed the evidence on youth tackling, concussions, and other injuries in football to reach the seven conclusions outlined in the policy statement, Dr. Landry said.
“Most injuries sustained during participation in youth football are minor, including injuries to the head and neck,” according to the policy statement. “The incidences of severe injuries, catastrophic injuries, and concussion, however, are higher in football than most other team sports and appear to increase with age.”
During his talk, Dr. Landry noted that catastrophic injuries occur more frequently in gymnastics and wrestling than in football. Among all youth football injuries, 3.4% are neurologic and 2.5% are fractures. Half are contusions, 16.7% are sprains, and 9.3% are strains.
Within football, young players tend to have far lower rates of concussions, compared to older players. In one 2-year observational study, the overall concussion rates of 7.4 per 1,000 athletic exposures broke down to 4.3 per 1,000 exposures for fourth- and fifth-graders and 14.4 per 1,000 exposures for eighth-graders. On the low end, another study found a concussion rate of 1.8 per 1,000 exposures, with a rate of 0.24 for practices and 6.2 for games.
“One of the common themes is that game rate is always higher than practice rates,” Dr. Landry said. “Running backs seem to be at the highest risk for injuries.”
In addition, tackling is the most common player activity at the time of the injury and at the time of severe injury. “The act of tackling is, in fact, risky business,” Dr. Landry said.
One reason for this relates to improvement in football safety equipment, he explained.
“As football helmets began to improve, football players began leading with their heads instead of their shoulders,” he said. “Leading with the head increases the risk of both concussion and spinal injury. The priority must be that the head must be up when a player tackles someone. The proper way to tackle is leading with the chest.”
A key study showing the effect that heads-up tackling instruction can have on concussion rates involved comparisons with teams taught Heads Up Football, “a comprehensive program developed by USA Football to advance player safety,” according to the program’s website. During the 2014 football season in Indiana, researchers compared teams that participated in the Heads Up program with teams that did not and with a third group of Pop Warner–affiliated teams that had reduced the number of full body contact practices.
Among 71,262 athletic exposures, the rate was lowest for the teams that were both Pop Warner affiliated and Heads Up affiliated, with a rate of 0.97 concussions per 1,000 athletic exposures. The teams involved in neither program had a rate of 7.32 concussions per 1,000 exposures, but even the Heads Up–only teams had a rate more than twice as low, with 2.73 per 1,000 exposures, revealing the importance of not tackling head first, Dr. Landry said.
“That’s the problem with American football – the whole game has changed,” he said, regarding the shift in tackling technique. “And you’re seeing this at the college level and at the professional level.”
In light of the way the game has changed and the risks it presented, the council offered seven conclusions and recommendations in its policy statement:
1. Officials and coaches must enforce the rules of the game, moving toward “zero tolerance of illegal, headfirst hits.” The statement notes a current “culture of tolerance” regarding headfirst tackling. “This culture has to change to one that protects the head for both the tackler and those players being tackled,” the committee stated. “Stronger sanctions for contact to the head, especially of a defenseless player, should be considered, up to and including expulsion from the game.”
2. Although eliminating tackling from football would likely cause a decrease in overall and severe or catastrophic injuries, it would also change essential aspects of the game. “Participants in football must decide whether the potential health risks of sustaining these injuries are outweighed by the recreational benefits associated with proper tackling,” the committee stated. Dr. Landry compared the game to hockey. “In ice hockey, if you don’t check, it’s still ice hockey,” he said. “But with football, removing tackling fundamentally changes the game.”
3. Football leagues should consider expanding their options to include football teams without tackling, such as flag football, for those who want to play without the additional risks from tackling. But youth flag football has not been studied, Dr. Landry pointed out, and some adult studies have shown higher rates of injuries, so youth flag football requires more study.
4. Officials and coaches should look for and implement ways to reduce the number of hits to the head that players experience. “If subconcussive blows to the head result in negative long-term effects on health, then limiting impacts to the head should reduce the risk of these long-term health problems,” the committee stated while acknowledging the need for more research in this area.
5. A theoretical risk exists that delaying the age when athletes learn tackling could lead it to become more dangerous. “Once tackling is introduced, athletes who have no previous experience with tackling would be exposed to collisions for the first time at an age at which speeds are faster, collision forces are greater, and injury risk is higher,” the committee stated. “Lack of experience with tackling and being tackled may lead to an increase in the number and severity of injuries once tackling is introduced.” Dr. Landry acknowledged that the risk is theoretical and hasn’t been studied but perhaps needs to be.
6. Neck strengthening might lessen the risk of concussions with head hits, though little scientific evidence exists to support this hypothesis. “Physical therapists, athletic trainers, or strength and conditioning specialists with expertise in the strengthening and conditioning of pediatric athletes are best qualified to help young football players achieve the neck strength that will help prevent injuries,” the committee stated.
7. Football teams should have athletic trainers present at organized football games and practices since research supports a link between trainers’ presence and a lower incidence of sports-related injuries.
Dr. Landry’s overall message focused on ways to reduce risks without ending football. “Let’s not ban the game,” he said. “Let’s just make it safer.”
Dr. Landry has no financial disclosures but had his college tuition paid by playing football, served as team physician for the University of Wisconsin football team for many seasons, and grew up as the son of a high school football coach. Dr. Meehan is involved in researched partly funded by the National Football League Players Association, and he receives compensation from ABC-Clio Publishing, Wolters Kluwer, and Springer International Publishing for works he has authored.
WASHINGTON – Teaching young athletes to tackle with their heads up and enforcing rules against illegal headfirst hits can reduce the risks of concussions in youth football, according to a new policy statement by the American Academy of Pediatrics.
An emphasis on proper tackling technique and implementing strategies to reduce head hits maintains the integrity of the game while reducing the most serious injuries as well as subconcussive hits, Dr. Gregory L. Landry, Fellow of the American Academy of Pediatrics (FAAP), and professor of pediatrics and orthopedics at the University of Wisconsin–Madison, said in his plenary talk at the annual meeting of the American Academy of Pediatrics.
Dr. Landry, along with Dr. William P. Meehan III, FAAP, led the Council on Sports Medicine and Fitness in writing the AAP’s policy statement on tackling in youth football (Pediatrics 2015 Oct 25. doi: 10.1542/peds.2015-3282).
In response to growing calls to ban tackling entirely in youth football, and calls to eliminate football from high school sports, the council reviewed the evidence on youth tackling, concussions, and other injuries in football to reach the seven conclusions outlined in the policy statement, Dr. Landry said.
“Most injuries sustained during participation in youth football are minor, including injuries to the head and neck,” according to the policy statement. “The incidences of severe injuries, catastrophic injuries, and concussion, however, are higher in football than most other team sports and appear to increase with age.”
During his talk, Dr. Landry noted that catastrophic injuries occur more frequently in gymnastics and wrestling than in football. Among all youth football injuries, 3.4% are neurologic and 2.5% are fractures. Half are contusions, 16.7% are sprains, and 9.3% are strains.
Within football, young players tend to have far lower rates of concussions, compared to older players. In one 2-year observational study, the overall concussion rates of 7.4 per 1,000 athletic exposures broke down to 4.3 per 1,000 exposures for fourth- and fifth-graders and 14.4 per 1,000 exposures for eighth-graders. On the low end, another study found a concussion rate of 1.8 per 1,000 exposures, with a rate of 0.24 for practices and 6.2 for games.
“One of the common themes is that game rate is always higher than practice rates,” Dr. Landry said. “Running backs seem to be at the highest risk for injuries.”
In addition, tackling is the most common player activity at the time of the injury and at the time of severe injury. “The act of tackling is, in fact, risky business,” Dr. Landry said.
One reason for this relates to improvement in football safety equipment, he explained.
“As football helmets began to improve, football players began leading with their heads instead of their shoulders,” he said. “Leading with the head increases the risk of both concussion and spinal injury. The priority must be that the head must be up when a player tackles someone. The proper way to tackle is leading with the chest.”
A key study showing the effect that heads-up tackling instruction can have on concussion rates involved comparisons with teams taught Heads Up Football, “a comprehensive program developed by USA Football to advance player safety,” according to the program’s website. During the 2014 football season in Indiana, researchers compared teams that participated in the Heads Up program with teams that did not and with a third group of Pop Warner–affiliated teams that had reduced the number of full body contact practices.
Among 71,262 athletic exposures, the rate was lowest for the teams that were both Pop Warner affiliated and Heads Up affiliated, with a rate of 0.97 concussions per 1,000 athletic exposures. The teams involved in neither program had a rate of 7.32 concussions per 1,000 exposures, but even the Heads Up–only teams had a rate more than twice as low, with 2.73 per 1,000 exposures, revealing the importance of not tackling head first, Dr. Landry said.
“That’s the problem with American football – the whole game has changed,” he said, regarding the shift in tackling technique. “And you’re seeing this at the college level and at the professional level.”
In light of the way the game has changed and the risks it presented, the council offered seven conclusions and recommendations in its policy statement:
1. Officials and coaches must enforce the rules of the game, moving toward “zero tolerance of illegal, headfirst hits.” The statement notes a current “culture of tolerance” regarding headfirst tackling. “This culture has to change to one that protects the head for both the tackler and those players being tackled,” the committee stated. “Stronger sanctions for contact to the head, especially of a defenseless player, should be considered, up to and including expulsion from the game.”
2. Although eliminating tackling from football would likely cause a decrease in overall and severe or catastrophic injuries, it would also change essential aspects of the game. “Participants in football must decide whether the potential health risks of sustaining these injuries are outweighed by the recreational benefits associated with proper tackling,” the committee stated. Dr. Landry compared the game to hockey. “In ice hockey, if you don’t check, it’s still ice hockey,” he said. “But with football, removing tackling fundamentally changes the game.”
3. Football leagues should consider expanding their options to include football teams without tackling, such as flag football, for those who want to play without the additional risks from tackling. But youth flag football has not been studied, Dr. Landry pointed out, and some adult studies have shown higher rates of injuries, so youth flag football requires more study.
4. Officials and coaches should look for and implement ways to reduce the number of hits to the head that players experience. “If subconcussive blows to the head result in negative long-term effects on health, then limiting impacts to the head should reduce the risk of these long-term health problems,” the committee stated while acknowledging the need for more research in this area.
5. A theoretical risk exists that delaying the age when athletes learn tackling could lead it to become more dangerous. “Once tackling is introduced, athletes who have no previous experience with tackling would be exposed to collisions for the first time at an age at which speeds are faster, collision forces are greater, and injury risk is higher,” the committee stated. “Lack of experience with tackling and being tackled may lead to an increase in the number and severity of injuries once tackling is introduced.” Dr. Landry acknowledged that the risk is theoretical and hasn’t been studied but perhaps needs to be.
6. Neck strengthening might lessen the risk of concussions with head hits, though little scientific evidence exists to support this hypothesis. “Physical therapists, athletic trainers, or strength and conditioning specialists with expertise in the strengthening and conditioning of pediatric athletes are best qualified to help young football players achieve the neck strength that will help prevent injuries,” the committee stated.
7. Football teams should have athletic trainers present at organized football games and practices since research supports a link between trainers’ presence and a lower incidence of sports-related injuries.
Dr. Landry’s overall message focused on ways to reduce risks without ending football. “Let’s not ban the game,” he said. “Let’s just make it safer.”
Dr. Landry has no financial disclosures but had his college tuition paid by playing football, served as team physician for the University of Wisconsin football team for many seasons, and grew up as the son of a high school football coach. Dr. Meehan is involved in researched partly funded by the National Football League Players Association, and he receives compensation from ABC-Clio Publishing, Wolters Kluwer, and Springer International Publishing for works he has authored.
AT THE AAP NATIONAL CONFERENCE
New Warfarin Measure Aids in Anticoagulation Ranking
NEW YORK - A novel warfarin composite measure (WCM) that combines percent time in therapeutic range (TTR) and international normalized ratio (INR) variability might be useful in comparing anticoagulation clinic performance rankings, researchers report.
TTR reflects the intensity of anticoagulation, whereas INR variability reflects its stability. Both are important measures of anticoagulation quality, and previous studies have suggested their combination provides added value.
Dr. Zayd Razouki from Durham VA Medical Center in North Carolina and colleagues developed the WCM, which combines standardized TTR and standardized log INR variability, and examined its feasibility for profiling anticoagulation clinics in the Veterans Health Administration.
WCM's hazard ratios for fatal bleeding and ischemic stroke were greater with very poor control or poor control, compared with those with TTR or INR variability, the researchers report in Circulation Cardiovascular Quality and Outcomes, online September 29.
In contrast, WCM's hazard ratios for major bleeding were larger than those with INR variability but not significantly different from those with TTR.
As for patient level outcomes, WCM was no better than TTR or INR variability.
At the anticoagulation clinic level, WCM reconciled moderately well the discordance in rankings that occurred when using TTR or INR variability separately.
"We would recommend the use of WCM as a performance measure for clinic profiling, as it seems to identify different clinics as outliers," the researchers conclude. "Both on an empirical and a theoretical basis, WCM captures more completely relevant dimensions of anticoagulation control than its component measures."
Dr. Gabriel Vanerio from CASMU Arrhythmia Service in Montevideo, Uruguay, recently demonstrated the usefulness of INR variability for assessing anticoagulation quality. While admitting that the WCM is "very well constructed," he said by email, "I do not believe that this new measurement will be clinically useful."
Instead, Dr. Vanerio suggested that physicians should take home "the importance of anticoagulation quality control" as the main message of this report.
Dr. Razouki did not respond to a request for comments.
NEW YORK - A novel warfarin composite measure (WCM) that combines percent time in therapeutic range (TTR) and international normalized ratio (INR) variability might be useful in comparing anticoagulation clinic performance rankings, researchers report.
TTR reflects the intensity of anticoagulation, whereas INR variability reflects its stability. Both are important measures of anticoagulation quality, and previous studies have suggested their combination provides added value.
Dr. Zayd Razouki from Durham VA Medical Center in North Carolina and colleagues developed the WCM, which combines standardized TTR and standardized log INR variability, and examined its feasibility for profiling anticoagulation clinics in the Veterans Health Administration.
WCM's hazard ratios for fatal bleeding and ischemic stroke were greater with very poor control or poor control, compared with those with TTR or INR variability, the researchers report in Circulation Cardiovascular Quality and Outcomes, online September 29.
In contrast, WCM's hazard ratios for major bleeding were larger than those with INR variability but not significantly different from those with TTR.
As for patient level outcomes, WCM was no better than TTR or INR variability.
At the anticoagulation clinic level, WCM reconciled moderately well the discordance in rankings that occurred when using TTR or INR variability separately.
"We would recommend the use of WCM as a performance measure for clinic profiling, as it seems to identify different clinics as outliers," the researchers conclude. "Both on an empirical and a theoretical basis, WCM captures more completely relevant dimensions of anticoagulation control than its component measures."
Dr. Gabriel Vanerio from CASMU Arrhythmia Service in Montevideo, Uruguay, recently demonstrated the usefulness of INR variability for assessing anticoagulation quality. While admitting that the WCM is "very well constructed," he said by email, "I do not believe that this new measurement will be clinically useful."
Instead, Dr. Vanerio suggested that physicians should take home "the importance of anticoagulation quality control" as the main message of this report.
Dr. Razouki did not respond to a request for comments.
NEW YORK - A novel warfarin composite measure (WCM) that combines percent time in therapeutic range (TTR) and international normalized ratio (INR) variability might be useful in comparing anticoagulation clinic performance rankings, researchers report.
TTR reflects the intensity of anticoagulation, whereas INR variability reflects its stability. Both are important measures of anticoagulation quality, and previous studies have suggested their combination provides added value.
Dr. Zayd Razouki from Durham VA Medical Center in North Carolina and colleagues developed the WCM, which combines standardized TTR and standardized log INR variability, and examined its feasibility for profiling anticoagulation clinics in the Veterans Health Administration.
WCM's hazard ratios for fatal bleeding and ischemic stroke were greater with very poor control or poor control, compared with those with TTR or INR variability, the researchers report in Circulation Cardiovascular Quality and Outcomes, online September 29.
In contrast, WCM's hazard ratios for major bleeding were larger than those with INR variability but not significantly different from those with TTR.
As for patient level outcomes, WCM was no better than TTR or INR variability.
At the anticoagulation clinic level, WCM reconciled moderately well the discordance in rankings that occurred when using TTR or INR variability separately.
"We would recommend the use of WCM as a performance measure for clinic profiling, as it seems to identify different clinics as outliers," the researchers conclude. "Both on an empirical and a theoretical basis, WCM captures more completely relevant dimensions of anticoagulation control than its component measures."
Dr. Gabriel Vanerio from CASMU Arrhythmia Service in Montevideo, Uruguay, recently demonstrated the usefulness of INR variability for assessing anticoagulation quality. While admitting that the WCM is "very well constructed," he said by email, "I do not believe that this new measurement will be clinically useful."
Instead, Dr. Vanerio suggested that physicians should take home "the importance of anticoagulation quality control" as the main message of this report.
Dr. Razouki did not respond to a request for comments.
The fellowship of motherhood
I expected that having a baby as a pediatric subspecialty fellow was going to be a challenge. But I could never have anticipated how scary it would feel to step into the world on the other side of the clinic door. My friends invited me to join a breastfeeding support group on social media “so that I knew I wasn’t the only one up with my baby at 3 a.m.” I learned a lot more than that.
I learned that some mothers trust anecdotes from strangers more than advice from their pediatricians. They recount unsatisfying visits with their pediatricians and then ask other mothers to comment on the advice. As I sifted through a lot of nonscientific and sometimes medically dangerous advice, I also was offered a new perspective. Many mothers will lie to their pediatricians about sleeping and feeding habits because they don’t want to be judged or don’t want another canned answer. Instead of engaging in discussion, they nod, smile, and return to their online support groups.
Very little literature exists on how to partner with mothers to guide them through the breastfeeding journey. These are intimate and individual journeys for each mother and often for each new child. For most mothers who choose to breastfeed, their infant is asking them to learn a new endurance sport, and the body and mind have to start running a marathon on day 1. Breastfeeding consumes nearly every waking moment of at least the first 6 weeks of the infant’s life. It is the most important, stressful, and wonderful part of their young child’s life to date. Pediatricians need to understand and offer advice that reflects this struggle.
So how do we expect pediatricians to help new mothers when our pediatrics residencies lack a basic breastfeeding curriculum? We need to fix it soon because breastfeeding mothers expect evidence-based breastfeeding advice, and as I learned online, they may even fire you if they don’t like what they hear. Although many pediatricians may feel uncomfortable with counseling an adult woman about her body or even treating her, the American Academy of Pediatrics recommends that we do so (Pediatrics 2012 Mar;129[3]:e827-41). There are even resources available to guide billing of extended breastfeeding visits.
The basic science of breastfeeding and how to counsel on common concerns need to be represented in our residency curriculums, as a lack of training early on can perpetuate itself in practice, leading to pediatricians who give outdated advice, reassure when they should counsel further, or give the mother the impression her concerns are irrelevant. Mothers expect more of us when it comes to breastfeeding, and we should expect it of ourselves.
In the meantime, some resources I found helpful were:
• “The Nursing Mother’s Companion,” by Kathleen Huggins (Boston: Harvard Common Press, 2010). This is a great book to help those in training really understand the stresses and common concerns of breastfeeding moms.
• newborns.stanford.edu/Breastfeeding. This is a good online source for those who want a quick tutorial about the early days of breastfeeding.
• AAP Breastfeeding Residency Curriculum (www2.aap.org/breastfeeding/curriculum/medical_knowledge.html). These are learning modules to build knowledge of lactation pathophysiology and how to address mothers’ common concerns.
• www.drmilk.org. This is a support group for breastfeeding moms who are doctors.
Dr. Fricchione is a pediatric infectious diseases fellow at McGaw Medical Center of Northwestern University and the Ann and Robert H. Lurie Children’s Hospital of Chicago.
I expected that having a baby as a pediatric subspecialty fellow was going to be a challenge. But I could never have anticipated how scary it would feel to step into the world on the other side of the clinic door. My friends invited me to join a breastfeeding support group on social media “so that I knew I wasn’t the only one up with my baby at 3 a.m.” I learned a lot more than that.
I learned that some mothers trust anecdotes from strangers more than advice from their pediatricians. They recount unsatisfying visits with their pediatricians and then ask other mothers to comment on the advice. As I sifted through a lot of nonscientific and sometimes medically dangerous advice, I also was offered a new perspective. Many mothers will lie to their pediatricians about sleeping and feeding habits because they don’t want to be judged or don’t want another canned answer. Instead of engaging in discussion, they nod, smile, and return to their online support groups.
Very little literature exists on how to partner with mothers to guide them through the breastfeeding journey. These are intimate and individual journeys for each mother and often for each new child. For most mothers who choose to breastfeed, their infant is asking them to learn a new endurance sport, and the body and mind have to start running a marathon on day 1. Breastfeeding consumes nearly every waking moment of at least the first 6 weeks of the infant’s life. It is the most important, stressful, and wonderful part of their young child’s life to date. Pediatricians need to understand and offer advice that reflects this struggle.
So how do we expect pediatricians to help new mothers when our pediatrics residencies lack a basic breastfeeding curriculum? We need to fix it soon because breastfeeding mothers expect evidence-based breastfeeding advice, and as I learned online, they may even fire you if they don’t like what they hear. Although many pediatricians may feel uncomfortable with counseling an adult woman about her body or even treating her, the American Academy of Pediatrics recommends that we do so (Pediatrics 2012 Mar;129[3]:e827-41). There are even resources available to guide billing of extended breastfeeding visits.
The basic science of breastfeeding and how to counsel on common concerns need to be represented in our residency curriculums, as a lack of training early on can perpetuate itself in practice, leading to pediatricians who give outdated advice, reassure when they should counsel further, or give the mother the impression her concerns are irrelevant. Mothers expect more of us when it comes to breastfeeding, and we should expect it of ourselves.
In the meantime, some resources I found helpful were:
• “The Nursing Mother’s Companion,” by Kathleen Huggins (Boston: Harvard Common Press, 2010). This is a great book to help those in training really understand the stresses and common concerns of breastfeeding moms.
• newborns.stanford.edu/Breastfeeding. This is a good online source for those who want a quick tutorial about the early days of breastfeeding.
• AAP Breastfeeding Residency Curriculum (www2.aap.org/breastfeeding/curriculum/medical_knowledge.html). These are learning modules to build knowledge of lactation pathophysiology and how to address mothers’ common concerns.
• www.drmilk.org. This is a support group for breastfeeding moms who are doctors.
Dr. Fricchione is a pediatric infectious diseases fellow at McGaw Medical Center of Northwestern University and the Ann and Robert H. Lurie Children’s Hospital of Chicago.
I expected that having a baby as a pediatric subspecialty fellow was going to be a challenge. But I could never have anticipated how scary it would feel to step into the world on the other side of the clinic door. My friends invited me to join a breastfeeding support group on social media “so that I knew I wasn’t the only one up with my baby at 3 a.m.” I learned a lot more than that.
I learned that some mothers trust anecdotes from strangers more than advice from their pediatricians. They recount unsatisfying visits with their pediatricians and then ask other mothers to comment on the advice. As I sifted through a lot of nonscientific and sometimes medically dangerous advice, I also was offered a new perspective. Many mothers will lie to their pediatricians about sleeping and feeding habits because they don’t want to be judged or don’t want another canned answer. Instead of engaging in discussion, they nod, smile, and return to their online support groups.
Very little literature exists on how to partner with mothers to guide them through the breastfeeding journey. These are intimate and individual journeys for each mother and often for each new child. For most mothers who choose to breastfeed, their infant is asking them to learn a new endurance sport, and the body and mind have to start running a marathon on day 1. Breastfeeding consumes nearly every waking moment of at least the first 6 weeks of the infant’s life. It is the most important, stressful, and wonderful part of their young child’s life to date. Pediatricians need to understand and offer advice that reflects this struggle.
So how do we expect pediatricians to help new mothers when our pediatrics residencies lack a basic breastfeeding curriculum? We need to fix it soon because breastfeeding mothers expect evidence-based breastfeeding advice, and as I learned online, they may even fire you if they don’t like what they hear. Although many pediatricians may feel uncomfortable with counseling an adult woman about her body or even treating her, the American Academy of Pediatrics recommends that we do so (Pediatrics 2012 Mar;129[3]:e827-41). There are even resources available to guide billing of extended breastfeeding visits.
The basic science of breastfeeding and how to counsel on common concerns need to be represented in our residency curriculums, as a lack of training early on can perpetuate itself in practice, leading to pediatricians who give outdated advice, reassure when they should counsel further, or give the mother the impression her concerns are irrelevant. Mothers expect more of us when it comes to breastfeeding, and we should expect it of ourselves.
In the meantime, some resources I found helpful were:
• “The Nursing Mother’s Companion,” by Kathleen Huggins (Boston: Harvard Common Press, 2010). This is a great book to help those in training really understand the stresses and common concerns of breastfeeding moms.
• newborns.stanford.edu/Breastfeeding. This is a good online source for those who want a quick tutorial about the early days of breastfeeding.
• AAP Breastfeeding Residency Curriculum (www2.aap.org/breastfeeding/curriculum/medical_knowledge.html). These are learning modules to build knowledge of lactation pathophysiology and how to address mothers’ common concerns.
• www.drmilk.org. This is a support group for breastfeeding moms who are doctors.
Dr. Fricchione is a pediatric infectious diseases fellow at McGaw Medical Center of Northwestern University and the Ann and Robert H. Lurie Children’s Hospital of Chicago.
An under-recognized epidemic of elder abuse needs your awareness and action
In its simplest form, elder abuse refers to the intentional infliction of injury or neglect of an older adult by a caregiver. The 5 primary types of elder abuse include neglect, physical, financial, psychological/emotional, and sexual, with a subtype of social abuse that falls under psychological/emotional abuse.
Differentiating abuse from the normal sequelae of physiologic aging can be difficult; therefore, early identification and awareness of risk factors is key, as well as detailed documentation of the patient encounter. As soon as abuse is suspected, clinicians should report it to Adult Protective Services (APS) for further investigation. In terms of prevention, regular screening for elder abuse is still up for debate, but as the incidence of elder abuse continues to rise so should research and preventive efforts to combat this growing public health concern.
What is ‘elder abuse’?According to the Elder Abuse Prevention, Identification, and Treatment Act of 1985, elder abuse is:
…willful infliction of injury, unreasonable confinement, intimidation or cruel punishment with resulting physical harm or pain or mental anguish or the willful deprivation by a caretaker of goods or services which are necessary to avoid physical harm, mental anguish or mental illness.1
There are 2 main components to this definition:
• an older adult has suffered injury or deprivation
• another person is responsible for causing or failing to prevent it.2
Although definitions vary, it generally is accepted that, for elder abuse to occur, it must take place within a relationship of trust.3
An ‘older adult’ is a person age ≥65, representing 14% of the U.S. population.4
According to U.S. Census Bureau data, there were 40 million older adults in 20105;
recent data project that this number will rise to 90 million by 2060 as Baby Boomers age.6 Studies suggest that as many as 10% of older adults in the United States experience elder abuse each year2; one study estimated that 6% of older adults in the community experienced significant abuse in the past month.7
Although elder abuse can occur in any setting, it takes place most often in the community. A survey of state APSs in 2000 showed that 60.7% of abuse was domestic; only 8.3% of incidents occurred in institutional settings.8 The annual direct medical costs associated with elder abuse injury in the United States are estimated at $5.3 billion, which is likely to increase with anticipated growth of the geriatric population.9
Although the number of older adults and the incidence of elder abuse are on the rise, as few as 1 in 14 cases is reported to authorities10; health care providers are some of the least likely of involved parties to report suspected abuse. One study found that 63% of physicians never asked about elder abuse, and only 31% reported encountering it in the previous 12 months.11 A busy clinician—ie, one who sees 20 to 40 geriatric patients a day—has a high likelihood of encountering at least 1 victim of elder abuse,2 yet many cases go unrecognized.
Types of abuseElder abuse comprises 5 categories12:
• neglect (58.5% of cases)
• physical (15.7%)
• financial (12.3%)
• psychological and emotional (7.3%)
• sexual (0.04%).
Social abuse is considered a subtype of psychological and emotional abuse. All “other” types of abuse constitute 5.1% cases; 0.06% are of unknown type.12
Neglect is (1) failure of the caregiver to provide life necessities or (2) the responsible person’s refusal to permit others to provide appropriate care.3 This is one of the most common types of elder abuse in residential facilities. Signs of neglect include dehydration, depression, fecal impaction, and malnutrition (Table).4 The prevalence of dehydration in nursing home patients is reported to be as high as 35%, which may be the result of passive or active withholding of liquids (ie, decreasing hydration to reduce the need to change the resident’s clothing or bedding).4 Other forms of neglect include medication misuse (overdosing or underdosing) and self-neglect, which occurs among people living alone and often is listed as a subtype of neglect, but is controversial because it does not involve another person.
Financial exploitation is the illegal or improper use, or mismanagement, of a person’s money, property, or financial resources3—often, to his (her) detriment. Estimates are that 1 of every 20 older adults has been subject to financial abuse at some point in their life.15 There should be a high index of suspicion for financial exploitation when one notices unexplained changes in power of attorney, wills, or other legal documents; missing checks, money, or belongings.16 In the past, adult children were most likely to be financial abusers; in recent years, however, the abuser is more often a spouse—especially a second spouse.17 Bankers, accountants, and other financial advisors are among those trained to identify risk factors for financial abuse; they are encouraged to caution clients about this possibility.18
Psychological and emotional abuse occurs when a caregiver inflicts mental stress on an older adult by actions and threats that cause fear, violence, isolation, deprivation, or feelings of shame and powerlessness.3 Examples are threatening to put the older adult in a nursing home or verbally abusing him (her). Suspect this type of abuse when a caregiver refuses to leave the older adult or speaks for him, or if the older adult expresses fear in the presence of the caregiver.4 This type of abuse also is prevalent in nursing homes and other long-term care facilities.19
Sexual abuse involves nonconsensual touching or sexual activities (rape, language, exploitive behavior) that are threatened or forced on an older adult.16 Sexual abuse is more common in frail or dependent persons.3 Physical exam findings—particularly dysuria, tender genitalia, and evidence of sexually transmitted infections4—are required to identify sexual abuse, along with signs of depression and display of fear.
Social abuse can be considered a subtype of psychological and emotional abuse, in which a caregiver denies an older adult contact with family and friends or deprives him from access to transportation. Other examples include not allowing the older adult to use the telephone, monitoring phone calls, and claiming that his friends or family are “interfering.”20 Intentionally embarrassing an older adult in front of others also can be considered social abuse.
Technology, particularly smart phones and social media, can complicate and exacerbate elder abuse:
• In July 2013, employees of a Wisconsin nursing home were found with videos and photographs of residents bathing and of a nude resident who had a bowel obstruction being mocked.21
• In May 2014, employees of a nursing home in Massachusetts recorded themselves physically and verbally abusing several older adults with Alzheimer’s disease, including one episode of the employees “hitting the woman on her arms, flicking her ears and then pinching the woman’s nose closed.” The employees also possessed a photograph of her naked.22
• In June 2015, an employee of a nursing home in Indiana was accused of taking
photos of a resident naked and sharing them on the messaging application Snapchat,23 in which images disappear 10 seconds after they are viewed.
As technology evolves, caregivers are finding more cunning ways to abuse older adults. Considering current events and trends in this area, technology as a gateway to elder abuse should be of growing concern.
Risk factorsA 2013 literature review on elder abuse reported that the most important risk factors are related to relationship (family disharmony, poor or conflicting relationships) and environment (a low level of social support),3 although other variables can play a role. Regardless of these findings, it is important to recognize that (1) elder abuse is not a necessary consequence in a family with many risk factors and (2) elder abuse can occur in the absence of any risk factors.
As a whole, women are at a higher risk of abuse, particularly when combined with loneliness, poor social support, cohabitation (especially family members), substance abuse, cognitive impairment, and dementia and other mental health problems.4 Other risk factors include functional deficiency, poor physical health or frailty, low income or wealth, and trauma or past abuse.3
Lower income, poor health, low social support, and belonging to a non-white racial group put an older adult at risk for neglect; female sex is a specific risk factor for sexual assault.15 One study found that, among older adults who suffered physical, mental, or cognitive impairment, 1 of every 4 was at risk of abuse.7
Mental illness. Dementia puts an older adult at higher risk because of increased
caregiver stress resulting from disruptive and aggressive behaviors2; the same is true when the older adult suffers another mental illness, such as anxiety, depression, schizophrenia or bipolar disorder. Presumably, older adults with any of these disorders are at risk of financial and psychological and emotional abuse because of their decreased social support, lack of independence, and inability to hold a job—leaving their caregiver to shoulder more responsibilities and with more opportunities to inflict abuse. In addition, an older adult suffering from depression can feel helpless and unworthy, possibly making him more susceptible to psychological and emotional abuse, and less likely to seek help.
More research is needed to establish racial and ethnic differences in the risk of abuse. Some research states that older adults who are a member of a minority are at greater risk of abuse; however, the difference dissipates after adjusting for variables such as income and social support.24 Cultural confounders, such as varying interpretations of the same set of interactions between older adults, need to be examined further.
Sexual orientation. Identifying one’s self as a lesbian, gay, bisexual, or transgender (LGBT) person is an additional risk factor for elder abuse. In 1997, a report described a nursing home employee who refused to bathe a resident because he didn’t want to “touch the lesbian.”25 Despite evolving attitudes in society toward support and acceptance of sexual orientation, fear of homophobia still prevents some LGBT older adults from seeking help when they have been abused because of their orientation—especially ones who have internalized that
homophobia and feel that they are unworthy of seeking help.25
In addition, health care providers and nursing home staff members might neglect the particular care needs of LGBT older adults, intentionally or unintentionally. APS staff and providers must be cognizant of underlying biases and exhibit respect when assisting LGBT clients.
Approximately 75% of caregivers of older adults are family members; 70% are female26; and most are adult children, spouses, and partners of those receiving care.27 Male caregivers age ≥40 are more likely to be the abuser, however, especially when they possess any of these risk factors: fatigue, burnout, medical illness, mental illness, lack of financial and support services, family history of abusive behavior, and substance abuse.4 People who commit elder abuse also tend to be significantly dependent on the person they are abusing.2 In some cases, and especially when the abuser is financially needy, caregivers turn to elder abuse to obtain resources from the victim.2
From your standpoint as a practitioner, it is important to determine the root cause of elder abuse. According to one review,28 family members with mental illness or a history of substance abuse, or who are stressed by the burden of caregiving, abuse older adults at a higher rate than family members who are not affected in those ways. Depression in particular is a common characteristic of abusers,2 often secondary to the stress of caring for an older adult.
Abuse caused by stress can be addressed by referral to a support group and counseling for the caregiver; psychiatric conditions, such as depression, might be better treated with pharmacotherapy. Evaluate for depression and posttraumatic stress disorder (PTSD) in both the abuser and the abused,29 and for other mental health issues that might compound the situation. It is possible for you to have 2 patients: the older adult and his caregiver. Regardless of the challenge,keep in mind that the older adult’s safety is your priority.
Consequences for the abusedThe abused adult is at risk of a number of serious physical and psychological consequences.30 They tend to have a shorter lifespan, after adjusting for other variables associated with increased mortality.
The reason for shortened lifespan is multifactorial30:
• Bruises, abrasions, and fractures may take longer to heal because of diminished skin and bone regeneration.
• Diseases that affect the heart, lungs, and kidneys might prevent the person from bouncing back from major stressors caused by abuse, such as blood loss, severe injury, and pain.
• Injury from abuse can exacerbate an underlying illness.
• Elder abuse also is associated with increased emergency department use, hospitalization (including readmission within 30 days), and nursing home placement.31
Elder abuse can lead to depression, shame, and guilt; increased isolation; and
increased risk of alcohol abuse and substance use.31 A study found that victims of
elder abuse are significantly more depressed than non-victims.32
In the same study, being a victim of abuse was found to be the second-strongest
predictor of depression, after the state of one’s health.32 Other potential psychiatric
consequences of abuse that need further study include increased risk of developing
fear and anxiety disorders; learned helplessness; and PTSD.33 According to LoFaso,
“depression and anxiety can consume their days and leave them emotionally and
physically frail.”29 Such feelings make these older adults less likely to resolve abuse or break off relations with the abuser.32
Because mental illness can be a risk factor for, and a consequence of, elder abuse,
be aware of such complications and address them appropriately. Keep in mind that older adults are more likely to visit a primary care practitioner than a psychiatrist for a routine health check-up or evaluation of initial cognition-related problems; however, they are more likely to see a psychiatrist for advanced neuropsychiatric problems such as dementia, paranoia, delusions, hallucinations, and insomnia. Adequate education on elder abuse should not be limited to a single medical specialty because it can present in several clinical settings.
Identifying abuseIdentification of elder abuse in the home poses a greater challenge to clinicians than abuse in an institutional setting because it is not directly observable. Compounding this is the lack of unified standards for identifying and dealing with elder abuse. It is first necessary for you to determine the likelihood that abuse or neglect occurred, which can be difficult because the signs of elder abuse and manifestations of normal aging often are similar. You also must establish whether (1) the abused person will accept intervention and (2) the abused person who refuses intervention has the capacity to make that decision. Both of these conditions will guide your approach to management.2
Obtain the history from several sources; review the records; and carefully examine patterns of injury, in particular assessing functional status and level of dependency on the caregiver. Explanations that do not match injuries signal the need for further investigation and examination.
To help differentiate elder abuse from normal physiologic aging, look at the skin for bruises, rashes that do not heal, and ulcers—all of which could be signs of abuse or neglect. Keep in mind that bruising generally is more common in older adults because of the slower turnover rate of epidermal cells; physiologic bruising tends to occur on dorsal aspects of the hands and arms.4 In contrast, bruising secondary to neglect or physical abuse can manifest as a subgaleal hematoma (caused by traumatic hair pulling), tracking in the peritoneum after genital trauma, Battle’s sign, and raccoon eyes, among other findings.4
In addition, larger bruises (>5 cm in diameter) are more likely the result of elder abuse.34 To complicate matters, many older persons are taking anticoagulant therapy, making bruising more likely. In addition, be on the lookout for burns during the physical exam. Evidence suggests that at least 10% of burns caused by battery and assault occur in the context of elder abuse; most burn facilities do not have formal guidelines for screening for abuse and neglect, however.35 According to one retrospective study, the most common causes of burns in older adults are hot water scalds and radiator contact, and the mortality rate of older burn patients in general is higher than among the overall population.36
Falls and fractures are common among older adults, regardless of whether they are
abused, because of polypharmacy, underlying medical conditions, and functional
limitations. Many abusers, however, use these factors to cover up intentional injury
that might have resulted in the older person falling, including overmedication (a form of physical abuse) and withholding a necessary walking aid (a form of neglect). Maintain a high index of suspicion of elder abuse when (1) the caregiver’s and the older adult’s stories of an injury don’t add up and (2) physical findings that might have been caused by abuse are present.
A number of psychiatric and cognitive symptoms suggest other types of elder abuse. Take note of emotional upset, agitation, and unusual behaviors37—especially if you can follow the patient over time to observe marked changes in the presentation. Likewise, be aware of proposed alterations in guardianship, which should be evaluated by a forensic psychiatrist with analysis of medical history, social attachments, home environment, self-care, and finances.38 Such evaluation should provide clues to the motivation behind a change of guardianship and will help to determine if elder abuse should be suspected.
Brandi et al37 provided an informative table that identifies pertinent signs, symptoms, and other findings that clinicians should be aware of to support a suspicion of elder abuse (Table).
Documentation is of utmost importance in evaluating potential elder abuse; keep in mind that the medical record might be used in an investigation of abuse by social workers, law enforcement, and prosecutors. Your records should be legible, clearly indicate who the main caregiver is and what his (her) responsibilities are, and specify who is present at your encounter with the patient.4 Document your observations of patient behavior, reactions to questions, and family dynamics and conflicts16; make note of warning signs such as fear, silence, and inability to interview the patient alone.
In addition to written documentation, take photographs of injuries, with a ruler in the image to record their size. Serial photographs are helpful; so are photographs from a variety of distances (close-up, regional, wholebody) to capture detail and place the wound in the context of a specific area of the body.4
Safety is paramount. Given the findings of the history and physical exam, it is necessary to determine whether it is safe for the patient to return home with the caregiver, or if alternate accommodations or resources, such as a social worker or a support group, are required. Include details of planned follow-up in your evaluation, and offer consideration of possible psychiatric disorders that can develop as a result of such abuse.
ReportingElder abuse is a criminal offense in all states.39 A clinician who has reasonable suspicion that elder abuse occurred must report it, regardless of whether the proof of abuse is concrete.40 At a point of reasonable suspicion, immediately contact APS, law enforcement, and a social worker. Adult Protective Services, modeled after Child Protective Services, is typically administered by local and state health
departments.41
After a report is filed with APS, an assigned social worker makes an in-person home visit to investigate the allegation and determine whether elder abuse is substantiated, partially substantiated, or unsubstantiated.16 In most states, elder abuse reporting is not anonymous because follow-up may be needed to provide additional evidence, especially if the report was made by a health care provider.16
No federal standard exists for states to follow when defining and addressing elder abuse, which can complicate identification and reporting of abuse. Laws governing elder abuse do not allow states to determine the fate of the older adult, who can decide for himself (herself) whether to use or waive protective services.42 Older adults might choose not to report abuse because of shame, intimidation, or fear,43 or to protect a caregiver, who often is a family member.
Elder abuse reports can come from a variety of sources; convincing evidence is, as noted, unnecessary to report it. Health care providers are mandated reporters, but
it is believed that the number of clinicians who report elder abuse based on suspicion is far below what it should be. One study found that 94% of physicians said that they either were unable to prove that the abuse had occurred or decided not to report it.11 Another study found that only 1.4% of elder abuse cases reported to APS come from physicians.44
There are several possible reasons for underreporting elder abuse, including (1) the difficulty of distinguishing elder abuse and neglect from sequelae of normal aging and (2) the fact that cognitive and functional impairment of the abused person makes it difficult, even impossible, to establish the narrative of how the abuse happened. Nursing homes in particular provide a high level of oversight because residents have an average of ≥3 functional deficits.4 Other reasons for underreporting—some of which are difficult to understand, and excuse, in a clinician—are:
• subtlety of signs
• victim denial
• ignorance of reporting procedures
• inadequate training
• lack of information about resources
• concern about losing physician–patient rapport
• concern about involvement in the legal system
• time limitations
• doubt about the effectiveness of APS.16
Assessing capacityThe older adult’s wishes must be respected unless a health care provider or the legal system determines that he lacks functional capacity to make decisions.16
How is capacity evaluated? A capacity evaluation has 3 components:
• Comprehension is a person’s factual understanding of the situation, including
consequences and alternatives
• Free choice is a person’s voluntary decision to accept or reject a proposed treatment, free of coercion (in this setting, free choice is the older adult’s decision whether to report the abuse)
• Reliability is a person’s ability to provide a consistent choice over time.45
Most capacity evaluations are conducted by clinical interview. No single, brief test is used universally, and there is the possibility of inter-rater variability.45 Examples of tests used to assess capacity are the Folstein Mini-Mental Status Examination and the MacArthur Competence Assessment Tool-Treatment45; the latter is a structured interview that incorporates information specific to the individual patient’s decision-making situation.46 Regardless of the approach, the psychiatrist-evaluator ensures that the older adult has been given the appropriate information
to provide informed consent about the situation.47
If the evaluator determines that a person lacks capacity to make decisions, efforts should be made to determine if the cause of that impairment is reversible.47 Older adults who have dementia or other underlying psychiatric condition that impairs cognition might benefit from more education on their situation; ones who appear fearful of consequences should be introduced to a trusted advisor to assist in making competent judgments.47
If the older adult is found to lack capacity, a substitute decision-maker must be sought.47 Many states have statutes specifying the order in which family members are contacted.48 The need to appoint an advisor can become knotty because the suspected abuser often is a family member; clinicians and others involved in identifying a decision-maker to speak on behalf of an older adult should choose carefully.
Prevention and screeningKey to reducing the prevalence of elder abuse in the community is formulating
strategies for prevention and screening. The American Medical Association recommends that clinicians “incorporate routine questions related to elder abuse and neglect into daily practice.”49 Older adults might not admit to abuse or neglect unless they are asked; speak to patients at eye level, keep questions simple, direct, and nonjudgmental, and assure them (1) that discussions are confidential and (2) that their safety is your primary goal.50,51
Comprehensive approaches to questioning patients are available and often recommended for screening for elder abuse.4 However, screening in the office setting often involves short, directly administered questionnaires.49 For example, the Health and Safety Screen developed at the University of Maine comprises 6 questions52:
• Has anyone close to you called you names or insulted you recently?
• Are you afraid of anyone in your life?
• Are you able to use the telephone anytime you want to?
• Has anyone forced you to do things you didn’t want to do?
• Has anyone taken things or money that belong to you without your OK?
• Has anyone close to you tried to hurt you or harm you recently?
Because of time constraints and lack of a universal standard, there is debate whether regular elder abuse screening is time-effective. It often is recommended, therefore, that clinicians in primary care (1) refer older adults with risk factors for abuse to geriatric medical teams trained in these measures and (2) perform periodic follow-up on such patients4 (Figure).
• New York City Elder Abuse Center encourages collaboration among health, mental health, and community justice organizations.28 The program involves a number of resources for addressing elder abuse, such as promoting staff awareness of risk factors for, and signs of, abuse, and screening for mental health problems in the abused.
• The Elder Justice Act, enacted in 2010 to combat elder abuse, provides federal funds and resources to prevent, detect, treat, and intervene to stop abuse and, when appropriate, to prosecute abusers.53
This Web Exclusive Table provides a 7-point summary reference guide for understanding and preventing elder abuse in your practice.
BOTTOM LINEIdentification of elder abuse can be difficult because signs and symptoms of abuse closely resemble physiologic aging. Older adults with identifiable risk factors should be screened for abuse; time constraints make universal screening impossible at this time. In the future, multidisciplinary approaches likely will make elder abuse more easily identifiable through the combined work of health care providers, law enforcement agencies, banks, and other institutions—with the ultimate goal of protecting older adults in the community from abuse.
Related Resources
• Frazão SL, Correia AM, Norton P, et al. Physical abuse against elderly persons in institutional settings. J Forensic Leg Med. 2015;36:54-60.
• Sorrentino R. Performing capacity evaluations: what’s expected from your consult. Current Psychiatry. 2014;13(1):41-44.
Disclosures
Ms. Hubert reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products. Dr. Gupta is a member of the speakers’ bureau of Alkermes, Allergan, Avanir Pharmaceuticals, Takeda Pharmaceutical, Lundbeck, Otsuka Pharmaceutical, and Sunovion Pharmaceuticals.
1. The Elder Abuse Prevention, Identification, and Treatment Act of 1985, HR 1674, 99th Cong (1985).
2. Lachs MS, Pillemer K. Elder abuse. Lancet. 2004;364(9441):1263-1272.
3. Johannesen M, LoGiudice D. Elder abuse: a systematic review of risk factors in community-dwelling elders. Age Ageing. 2013;42(3):292-298.
4. Gibbs LM, Mosqueda L, eds. Medical implications of elder abuse and neglect. Clin Geriatr Med. 2014;30(4):xv-xvi. doi: 10.1016/j.cger.2014.08.015.
5. Werner CA. The Older Population: 2010. U.S. Census Bureau. http://webcache.googleusercontent.com/search?q=cache:hCCb_pcnO6QJ :ht tps://www.census.gov/prod/cen2010/briefs/c2010br-09.pdf+&cd=1&hl=en&ct=clnk&gl=uss. Issued November 2011. Accessed October 10, 2015.
6. Himes CL. Elderly Americans. Population Bulletin. 2002;56(4):1-41.
7. Cooper C, Selwood A, Livingston G. The prevalence of elder abuse and neglect: a systematic review. Age Ageing. 2008;37(2):151-60.
8. Teaster PB. A response to the abuse of vulnerable adults: the 2000 Survey of State Adult Protective Services. The National Center on Elder Abuse. http://www.ncea.aoa.gov/Resources/Publication/docs/apsreport030703.pdf. 2003.
Accessed October 22, 2015.
9. Mouton CP, Rodabough RJ, Rovi SL, et al. Prevalence and 3-year incidence of abuse among postmenopausal women. Am J Public Health. 2004;94(4):605-612.
10. Acierno R, Hernandez MA, Amstadter AB, et al. Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: the National Elder Mistreatment Study. Am J Public Health. 2010;100(2):292-297.
11. Kennedy RD. Elder abuse and neglect: the experience, knowledge, and attitudes of primary care physicians. Fam Med. 2005;37(7):481-485.
12. Statistic Brain Research Institute. Elderly abuse statistics. http://www.statisticbrain.com/elderly-abuse-statistics. Accessed June 22, 2015.
13. Lachs MS, Bachman R, Williams CS, et al. Resident-to-resident elder mistreatment and police contact in nursing homes: findings from a population-based cohort. J Am Geriatr Soc. 2007;55(6):840-845.
14. Lachs M, Bachman R, Williams C, et al. Older adults as crime victims, perpetrators, witnesses, and complainants: a population-based study of police interactions. J Elder Abuse Negl. 2005;16(4):25-40.
15. Acierno R, Hernandez-Tejada M, Muzzy W, et al. National Elder Mistreatment Study. Washington, DC: National Institute of Justice; 2009.
16. Dong XQ. Elder abuse: systematic review and implications for practice. J Am Geriatr Soc. 2015;63(6):1214-1238.
17. Freedman M. The growing epidemic of financial elder abuse. The Tax Advisor. http://www.cpa2biz.com/Content/media/PRODUCER_CONTENT/Newsletters/
Articles_2007/Tax/Financial_Elder_Abuse.jsp. Published November 2007. Accessed June 24, 2015.
18. Consumer Financial Protection Bureau. Protection for older Americans. http://www.consumerfinance.gov/olderamericans. Accessed June 22, 2015.
19. Castle NG. Nursing home deficiency citations for abuse. J Appl Gerontol. 2011;30(6):719-743.
20. Elder Abuse Prevention Unit. Social abuse. http://www.eapu.com.au/elder-abuse/social-abuse. Published 2014. Accessed June 24, 2015.
21. Former nursing home employees allegedly photographed naked resident. United Press International. http://www.upi.com/Top_News/US/2013/07/03/Former-nursinghome-employees-allegedly-photographed-nakedresidents/
65801372893020. Published July 3, 2013. Accessed June 24, 2015.
22. Miller N. Two charged with elder assault at an assisted living facility. MetroWest Daily News. http://www.metrowestdailynews.com/article/20140506/
NEWS/140507587. Updated May 7, 2014. Accessed June 24, 2015.
23. Jorgensen J. New charges filed in nursing home case.WHAS11. http://www.whas11.com/story/news/local/2015/06/24/new-charges-filed-in-nursing-homecase/29243183/. Published June 24, 2015. Accessed June 27, 2015.
24. Hermandez-Tejada MA, Amstadter A, Muzzy W, et al. The National Elder Mistreatment Study: race and ethnicity findings. J Elder Abuse Negl. 2013;25(4):281-293.
25. Cooks-Daniels L. Lesbian, gay male, bisexual and transgendered elders: elder abuse and neglect issues. J Elder Abuse Negl. 1998;9(2):35-49.
26. Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist. 1980;20(6):649-655.
27. Tatara T, Blumerman Kuzmeskus L, Duckhorn E, et al. The National Center on Elder Abuse Incidence Study: final report. http://aoa.gov/AoA_Programs/Elder_Rights/Elder_Abuse/docs/ABuseReport_Full.pdf. Published September 1998. Accessed October 19, 2015.
28. Rosen AL. Where mental health and elder abuse intersect. Generations. 2014;38(3):75-79.
29. LoFaso V. The role of the primary physician in assessing and treating the mental health concerns of elder abuse victims. NYC Elder Abuse Center eNewsletter.nyceac.com/wp-content/uploads/2013/03/Exploring-the-IntersectionofElder-Abuse-and-Mental-Health_eNewsletter.pdf. Published March 12, 2013. Accessed August 20, 2015.
30. Lachs MS, Williams CS, O’Brien S, et al. The mortality of elder mistreatment. JAMA. 1998;280(5):428-432.
31. Dyer CB, Pavlik VN, Murphy KP, et al. The high prevalence of depression and dementia in elder abuse or neglect. J Am Geriatr Soc. 2000;48(2):205-208.
32. Pillemer K, Prescott D. Psychological effects of elder abuse: a research note. J Elder Abuse Negl. 1988;1(1):65-73.
33. Elder abuse: consequences. Centers for Disease Control and Prevention. http://www.cdc.gov/violenceprevention/elderabuse/consequences.html. Updated June 22, 2015.Accessed August 20, 2015.
34. Wiglesworth A, Austin R, Corona M, et al. Bruising as a marker of physical elder abuse. J Am Geriatr Soc. 2009;57(7):1191-1196.
35. Peck MD. Epidemiology of burns throughout the World. Part II: intentional burns in adults. Burns. 2012;38(5):630-637.
36. 2014 National Burn Repository; report of data between 2004-2013. American Burn Association. http://www.ameriburn.org/2014NBRAnnualReport.pdf. Published 2014. Accessed June 26, 2015.
37. Brandi B, Dyer CB, Heisler CJ, et al. Systemic responses to elder abuse. In: Brandi B, Dyer CB, Heisler CJ, eds. Elder abuse detection and intervention: a collaborative approach. New York, NY: Spring Publishing Company; 2007:79-100.
38. Welner M. Guardianship. The Forensic Panel. http://www.forensicpanel.com/expert_services/psychiatry/civil_law/guardianship.html. Accessed August 20, 2015.
39. Watson E. Elder abuse: definition, types and statistics, and elder abuse (mistreatment and neglect) laws. Journal of Legal Nurse Consulting. 2013;24(2):40-42.
40. National Center on Elder Abuse Administration on Aging. Reporting abuse. http://www.ncea.aoa.gov/Stop_Abuse/Get_Help/Report/index.aspx. Accessed August 18, 2015.
41. Mukherjee D. Organizational structures of elder abuse reporting systems. Administration in Social Work. 2011;35(5):517-531.
42. Costin LB, Karger HJ, Stoesz H. The politics of child abuse in America. New York, NY: Oxford University Press; 1996.
43. Thomson MJ, Lietzau LK, Doty MM, et al. An analysis of elder abuse rates in Milwaukee County. WMJ. 2011;110(6):271-276.
44. Teaster PB, Dugar TA, Mendiondo MS, et al; The National Committee for the Prevention of Elder Abuse; The National Adult Protective Services Association. The 2004 Survey of State Adult Protective Services: Abuse of Adults 60 Years and Older. http://www.ncea.aoa.gov/Resources/Publication/docs/APS_2004NCEASurvey.pdf. Published March 2007. Accessed October 19, 2015.
45. Sorrentino R. Performing capacity evaluations: what’s expected from your consult. Current Psychiatry. 2014;13(1):41-44.
46. Grisso T, Appelbaum PS. MacArthur competence assessment tool for treatment (MacCAT-T). Sarasota, FL: Professional Resources Press; 1998.
47. Appelbaum PS. Clinical practice. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;35(18):1834-1840.
48. Wynn S. Decision by surrogates: An overview of surrogate consent laws in the United States. Bifocal: A Journal of the ABA Commission on Bar and Aging. 2014;36(1). http://www.americanbar.org/publications/bifocal/vol_36/
issue_1_october2014/default_surrogate_consent_statutes.html. Accessed October 22, 2015.
49. American Medical Association. Diagnostic and treatment guidelines on elder abuse and neglect. Chicago, IL: American Medical Association; 1992.
50. Harrell R, Toronjo C, McLaughlin J, et al. How geriatricians identify elder abuse and neglect. Am J Med Sci. 2002;323(1):34-38.
51. Ahmad M, Lachs MS. Elder abuse and neglect: what physicians can and should do. Cleve Clin J Med. 2002; 69(10):801-808.
52. Elder abuse screening protocol for physicians: lessons learned from the Maine Partners for Elder Protection Pilot Project. University of Maine Center on Aging. http://umcoa.siteturbine.com/uploaded_files/mainecenteronaging.umaine.edu/files/elderabusescreeningmanual.pdf. Published May 2, 2007. Accessed August 20, 2015.
53. What is the Elder Justice Act? USC Davis School of Gerontology. http://gerontology.usc.edu/resources/articles/what-is-the-elder-justice-act/. Published 2015. Accessed October 20, 2015.
In its simplest form, elder abuse refers to the intentional infliction of injury or neglect of an older adult by a caregiver. The 5 primary types of elder abuse include neglect, physical, financial, psychological/emotional, and sexual, with a subtype of social abuse that falls under psychological/emotional abuse.
Differentiating abuse from the normal sequelae of physiologic aging can be difficult; therefore, early identification and awareness of risk factors is key, as well as detailed documentation of the patient encounter. As soon as abuse is suspected, clinicians should report it to Adult Protective Services (APS) for further investigation. In terms of prevention, regular screening for elder abuse is still up for debate, but as the incidence of elder abuse continues to rise so should research and preventive efforts to combat this growing public health concern.
What is ‘elder abuse’?According to the Elder Abuse Prevention, Identification, and Treatment Act of 1985, elder abuse is:
…willful infliction of injury, unreasonable confinement, intimidation or cruel punishment with resulting physical harm or pain or mental anguish or the willful deprivation by a caretaker of goods or services which are necessary to avoid physical harm, mental anguish or mental illness.1
There are 2 main components to this definition:
• an older adult has suffered injury or deprivation
• another person is responsible for causing or failing to prevent it.2
Although definitions vary, it generally is accepted that, for elder abuse to occur, it must take place within a relationship of trust.3
An ‘older adult’ is a person age ≥65, representing 14% of the U.S. population.4
According to U.S. Census Bureau data, there were 40 million older adults in 20105;
recent data project that this number will rise to 90 million by 2060 as Baby Boomers age.6 Studies suggest that as many as 10% of older adults in the United States experience elder abuse each year2; one study estimated that 6% of older adults in the community experienced significant abuse in the past month.7
Although elder abuse can occur in any setting, it takes place most often in the community. A survey of state APSs in 2000 showed that 60.7% of abuse was domestic; only 8.3% of incidents occurred in institutional settings.8 The annual direct medical costs associated with elder abuse injury in the United States are estimated at $5.3 billion, which is likely to increase with anticipated growth of the geriatric population.9
Although the number of older adults and the incidence of elder abuse are on the rise, as few as 1 in 14 cases is reported to authorities10; health care providers are some of the least likely of involved parties to report suspected abuse. One study found that 63% of physicians never asked about elder abuse, and only 31% reported encountering it in the previous 12 months.11 A busy clinician—ie, one who sees 20 to 40 geriatric patients a day—has a high likelihood of encountering at least 1 victim of elder abuse,2 yet many cases go unrecognized.
Types of abuseElder abuse comprises 5 categories12:
• neglect (58.5% of cases)
• physical (15.7%)
• financial (12.3%)
• psychological and emotional (7.3%)
• sexual (0.04%).
Social abuse is considered a subtype of psychological and emotional abuse. All “other” types of abuse constitute 5.1% cases; 0.06% are of unknown type.12
Neglect is (1) failure of the caregiver to provide life necessities or (2) the responsible person’s refusal to permit others to provide appropriate care.3 This is one of the most common types of elder abuse in residential facilities. Signs of neglect include dehydration, depression, fecal impaction, and malnutrition (Table).4 The prevalence of dehydration in nursing home patients is reported to be as high as 35%, which may be the result of passive or active withholding of liquids (ie, decreasing hydration to reduce the need to change the resident’s clothing or bedding).4 Other forms of neglect include medication misuse (overdosing or underdosing) and self-neglect, which occurs among people living alone and often is listed as a subtype of neglect, but is controversial because it does not involve another person.
Financial exploitation is the illegal or improper use, or mismanagement, of a person’s money, property, or financial resources3—often, to his (her) detriment. Estimates are that 1 of every 20 older adults has been subject to financial abuse at some point in their life.15 There should be a high index of suspicion for financial exploitation when one notices unexplained changes in power of attorney, wills, or other legal documents; missing checks, money, or belongings.16 In the past, adult children were most likely to be financial abusers; in recent years, however, the abuser is more often a spouse—especially a second spouse.17 Bankers, accountants, and other financial advisors are among those trained to identify risk factors for financial abuse; they are encouraged to caution clients about this possibility.18
Psychological and emotional abuse occurs when a caregiver inflicts mental stress on an older adult by actions and threats that cause fear, violence, isolation, deprivation, or feelings of shame and powerlessness.3 Examples are threatening to put the older adult in a nursing home or verbally abusing him (her). Suspect this type of abuse when a caregiver refuses to leave the older adult or speaks for him, or if the older adult expresses fear in the presence of the caregiver.4 This type of abuse also is prevalent in nursing homes and other long-term care facilities.19
Sexual abuse involves nonconsensual touching or sexual activities (rape, language, exploitive behavior) that are threatened or forced on an older adult.16 Sexual abuse is more common in frail or dependent persons.3 Physical exam findings—particularly dysuria, tender genitalia, and evidence of sexually transmitted infections4—are required to identify sexual abuse, along with signs of depression and display of fear.
Social abuse can be considered a subtype of psychological and emotional abuse, in which a caregiver denies an older adult contact with family and friends or deprives him from access to transportation. Other examples include not allowing the older adult to use the telephone, monitoring phone calls, and claiming that his friends or family are “interfering.”20 Intentionally embarrassing an older adult in front of others also can be considered social abuse.
Technology, particularly smart phones and social media, can complicate and exacerbate elder abuse:
• In July 2013, employees of a Wisconsin nursing home were found with videos and photographs of residents bathing and of a nude resident who had a bowel obstruction being mocked.21
• In May 2014, employees of a nursing home in Massachusetts recorded themselves physically and verbally abusing several older adults with Alzheimer’s disease, including one episode of the employees “hitting the woman on her arms, flicking her ears and then pinching the woman’s nose closed.” The employees also possessed a photograph of her naked.22
• In June 2015, an employee of a nursing home in Indiana was accused of taking
photos of a resident naked and sharing them on the messaging application Snapchat,23 in which images disappear 10 seconds after they are viewed.
As technology evolves, caregivers are finding more cunning ways to abuse older adults. Considering current events and trends in this area, technology as a gateway to elder abuse should be of growing concern.
Risk factorsA 2013 literature review on elder abuse reported that the most important risk factors are related to relationship (family disharmony, poor or conflicting relationships) and environment (a low level of social support),3 although other variables can play a role. Regardless of these findings, it is important to recognize that (1) elder abuse is not a necessary consequence in a family with many risk factors and (2) elder abuse can occur in the absence of any risk factors.
As a whole, women are at a higher risk of abuse, particularly when combined with loneliness, poor social support, cohabitation (especially family members), substance abuse, cognitive impairment, and dementia and other mental health problems.4 Other risk factors include functional deficiency, poor physical health or frailty, low income or wealth, and trauma or past abuse.3
Lower income, poor health, low social support, and belonging to a non-white racial group put an older adult at risk for neglect; female sex is a specific risk factor for sexual assault.15 One study found that, among older adults who suffered physical, mental, or cognitive impairment, 1 of every 4 was at risk of abuse.7
Mental illness. Dementia puts an older adult at higher risk because of increased
caregiver stress resulting from disruptive and aggressive behaviors2; the same is true when the older adult suffers another mental illness, such as anxiety, depression, schizophrenia or bipolar disorder. Presumably, older adults with any of these disorders are at risk of financial and psychological and emotional abuse because of their decreased social support, lack of independence, and inability to hold a job—leaving their caregiver to shoulder more responsibilities and with more opportunities to inflict abuse. In addition, an older adult suffering from depression can feel helpless and unworthy, possibly making him more susceptible to psychological and emotional abuse, and less likely to seek help.
More research is needed to establish racial and ethnic differences in the risk of abuse. Some research states that older adults who are a member of a minority are at greater risk of abuse; however, the difference dissipates after adjusting for variables such as income and social support.24 Cultural confounders, such as varying interpretations of the same set of interactions between older adults, need to be examined further.
Sexual orientation. Identifying one’s self as a lesbian, gay, bisexual, or transgender (LGBT) person is an additional risk factor for elder abuse. In 1997, a report described a nursing home employee who refused to bathe a resident because he didn’t want to “touch the lesbian.”25 Despite evolving attitudes in society toward support and acceptance of sexual orientation, fear of homophobia still prevents some LGBT older adults from seeking help when they have been abused because of their orientation—especially ones who have internalized that
homophobia and feel that they are unworthy of seeking help.25
In addition, health care providers and nursing home staff members might neglect the particular care needs of LGBT older adults, intentionally or unintentionally. APS staff and providers must be cognizant of underlying biases and exhibit respect when assisting LGBT clients.
Approximately 75% of caregivers of older adults are family members; 70% are female26; and most are adult children, spouses, and partners of those receiving care.27 Male caregivers age ≥40 are more likely to be the abuser, however, especially when they possess any of these risk factors: fatigue, burnout, medical illness, mental illness, lack of financial and support services, family history of abusive behavior, and substance abuse.4 People who commit elder abuse also tend to be significantly dependent on the person they are abusing.2 In some cases, and especially when the abuser is financially needy, caregivers turn to elder abuse to obtain resources from the victim.2
From your standpoint as a practitioner, it is important to determine the root cause of elder abuse. According to one review,28 family members with mental illness or a history of substance abuse, or who are stressed by the burden of caregiving, abuse older adults at a higher rate than family members who are not affected in those ways. Depression in particular is a common characteristic of abusers,2 often secondary to the stress of caring for an older adult.
Abuse caused by stress can be addressed by referral to a support group and counseling for the caregiver; psychiatric conditions, such as depression, might be better treated with pharmacotherapy. Evaluate for depression and posttraumatic stress disorder (PTSD) in both the abuser and the abused,29 and for other mental health issues that might compound the situation. It is possible for you to have 2 patients: the older adult and his caregiver. Regardless of the challenge,keep in mind that the older adult’s safety is your priority.
Consequences for the abusedThe abused adult is at risk of a number of serious physical and psychological consequences.30 They tend to have a shorter lifespan, after adjusting for other variables associated with increased mortality.
The reason for shortened lifespan is multifactorial30:
• Bruises, abrasions, and fractures may take longer to heal because of diminished skin and bone regeneration.
• Diseases that affect the heart, lungs, and kidneys might prevent the person from bouncing back from major stressors caused by abuse, such as blood loss, severe injury, and pain.
• Injury from abuse can exacerbate an underlying illness.
• Elder abuse also is associated with increased emergency department use, hospitalization (including readmission within 30 days), and nursing home placement.31
Elder abuse can lead to depression, shame, and guilt; increased isolation; and
increased risk of alcohol abuse and substance use.31 A study found that victims of
elder abuse are significantly more depressed than non-victims.32
In the same study, being a victim of abuse was found to be the second-strongest
predictor of depression, after the state of one’s health.32 Other potential psychiatric
consequences of abuse that need further study include increased risk of developing
fear and anxiety disorders; learned helplessness; and PTSD.33 According to LoFaso,
“depression and anxiety can consume their days and leave them emotionally and
physically frail.”29 Such feelings make these older adults less likely to resolve abuse or break off relations with the abuser.32
Because mental illness can be a risk factor for, and a consequence of, elder abuse,
be aware of such complications and address them appropriately. Keep in mind that older adults are more likely to visit a primary care practitioner than a psychiatrist for a routine health check-up or evaluation of initial cognition-related problems; however, they are more likely to see a psychiatrist for advanced neuropsychiatric problems such as dementia, paranoia, delusions, hallucinations, and insomnia. Adequate education on elder abuse should not be limited to a single medical specialty because it can present in several clinical settings.
Identifying abuseIdentification of elder abuse in the home poses a greater challenge to clinicians than abuse in an institutional setting because it is not directly observable. Compounding this is the lack of unified standards for identifying and dealing with elder abuse. It is first necessary for you to determine the likelihood that abuse or neglect occurred, which can be difficult because the signs of elder abuse and manifestations of normal aging often are similar. You also must establish whether (1) the abused person will accept intervention and (2) the abused person who refuses intervention has the capacity to make that decision. Both of these conditions will guide your approach to management.2
Obtain the history from several sources; review the records; and carefully examine patterns of injury, in particular assessing functional status and level of dependency on the caregiver. Explanations that do not match injuries signal the need for further investigation and examination.
To help differentiate elder abuse from normal physiologic aging, look at the skin for bruises, rashes that do not heal, and ulcers—all of which could be signs of abuse or neglect. Keep in mind that bruising generally is more common in older adults because of the slower turnover rate of epidermal cells; physiologic bruising tends to occur on dorsal aspects of the hands and arms.4 In contrast, bruising secondary to neglect or physical abuse can manifest as a subgaleal hematoma (caused by traumatic hair pulling), tracking in the peritoneum after genital trauma, Battle’s sign, and raccoon eyes, among other findings.4
In addition, larger bruises (>5 cm in diameter) are more likely the result of elder abuse.34 To complicate matters, many older persons are taking anticoagulant therapy, making bruising more likely. In addition, be on the lookout for burns during the physical exam. Evidence suggests that at least 10% of burns caused by battery and assault occur in the context of elder abuse; most burn facilities do not have formal guidelines for screening for abuse and neglect, however.35 According to one retrospective study, the most common causes of burns in older adults are hot water scalds and radiator contact, and the mortality rate of older burn patients in general is higher than among the overall population.36
Falls and fractures are common among older adults, regardless of whether they are
abused, because of polypharmacy, underlying medical conditions, and functional
limitations. Many abusers, however, use these factors to cover up intentional injury
that might have resulted in the older person falling, including overmedication (a form of physical abuse) and withholding a necessary walking aid (a form of neglect). Maintain a high index of suspicion of elder abuse when (1) the caregiver’s and the older adult’s stories of an injury don’t add up and (2) physical findings that might have been caused by abuse are present.
A number of psychiatric and cognitive symptoms suggest other types of elder abuse. Take note of emotional upset, agitation, and unusual behaviors37—especially if you can follow the patient over time to observe marked changes in the presentation. Likewise, be aware of proposed alterations in guardianship, which should be evaluated by a forensic psychiatrist with analysis of medical history, social attachments, home environment, self-care, and finances.38 Such evaluation should provide clues to the motivation behind a change of guardianship and will help to determine if elder abuse should be suspected.
Brandi et al37 provided an informative table that identifies pertinent signs, symptoms, and other findings that clinicians should be aware of to support a suspicion of elder abuse (Table).
Documentation is of utmost importance in evaluating potential elder abuse; keep in mind that the medical record might be used in an investigation of abuse by social workers, law enforcement, and prosecutors. Your records should be legible, clearly indicate who the main caregiver is and what his (her) responsibilities are, and specify who is present at your encounter with the patient.4 Document your observations of patient behavior, reactions to questions, and family dynamics and conflicts16; make note of warning signs such as fear, silence, and inability to interview the patient alone.
In addition to written documentation, take photographs of injuries, with a ruler in the image to record their size. Serial photographs are helpful; so are photographs from a variety of distances (close-up, regional, wholebody) to capture detail and place the wound in the context of a specific area of the body.4
Safety is paramount. Given the findings of the history and physical exam, it is necessary to determine whether it is safe for the patient to return home with the caregiver, or if alternate accommodations or resources, such as a social worker or a support group, are required. Include details of planned follow-up in your evaluation, and offer consideration of possible psychiatric disorders that can develop as a result of such abuse.
ReportingElder abuse is a criminal offense in all states.39 A clinician who has reasonable suspicion that elder abuse occurred must report it, regardless of whether the proof of abuse is concrete.40 At a point of reasonable suspicion, immediately contact APS, law enforcement, and a social worker. Adult Protective Services, modeled after Child Protective Services, is typically administered by local and state health
departments.41
After a report is filed with APS, an assigned social worker makes an in-person home visit to investigate the allegation and determine whether elder abuse is substantiated, partially substantiated, or unsubstantiated.16 In most states, elder abuse reporting is not anonymous because follow-up may be needed to provide additional evidence, especially if the report was made by a health care provider.16
No federal standard exists for states to follow when defining and addressing elder abuse, which can complicate identification and reporting of abuse. Laws governing elder abuse do not allow states to determine the fate of the older adult, who can decide for himself (herself) whether to use or waive protective services.42 Older adults might choose not to report abuse because of shame, intimidation, or fear,43 or to protect a caregiver, who often is a family member.
Elder abuse reports can come from a variety of sources; convincing evidence is, as noted, unnecessary to report it. Health care providers are mandated reporters, but
it is believed that the number of clinicians who report elder abuse based on suspicion is far below what it should be. One study found that 94% of physicians said that they either were unable to prove that the abuse had occurred or decided not to report it.11 Another study found that only 1.4% of elder abuse cases reported to APS come from physicians.44
There are several possible reasons for underreporting elder abuse, including (1) the difficulty of distinguishing elder abuse and neglect from sequelae of normal aging and (2) the fact that cognitive and functional impairment of the abused person makes it difficult, even impossible, to establish the narrative of how the abuse happened. Nursing homes in particular provide a high level of oversight because residents have an average of ≥3 functional deficits.4 Other reasons for underreporting—some of which are difficult to understand, and excuse, in a clinician—are:
• subtlety of signs
• victim denial
• ignorance of reporting procedures
• inadequate training
• lack of information about resources
• concern about losing physician–patient rapport
• concern about involvement in the legal system
• time limitations
• doubt about the effectiveness of APS.16
Assessing capacityThe older adult’s wishes must be respected unless a health care provider or the legal system determines that he lacks functional capacity to make decisions.16
How is capacity evaluated? A capacity evaluation has 3 components:
• Comprehension is a person’s factual understanding of the situation, including
consequences and alternatives
• Free choice is a person’s voluntary decision to accept or reject a proposed treatment, free of coercion (in this setting, free choice is the older adult’s decision whether to report the abuse)
• Reliability is a person’s ability to provide a consistent choice over time.45
Most capacity evaluations are conducted by clinical interview. No single, brief test is used universally, and there is the possibility of inter-rater variability.45 Examples of tests used to assess capacity are the Folstein Mini-Mental Status Examination and the MacArthur Competence Assessment Tool-Treatment45; the latter is a structured interview that incorporates information specific to the individual patient’s decision-making situation.46 Regardless of the approach, the psychiatrist-evaluator ensures that the older adult has been given the appropriate information
to provide informed consent about the situation.47
If the evaluator determines that a person lacks capacity to make decisions, efforts should be made to determine if the cause of that impairment is reversible.47 Older adults who have dementia or other underlying psychiatric condition that impairs cognition might benefit from more education on their situation; ones who appear fearful of consequences should be introduced to a trusted advisor to assist in making competent judgments.47
If the older adult is found to lack capacity, a substitute decision-maker must be sought.47 Many states have statutes specifying the order in which family members are contacted.48 The need to appoint an advisor can become knotty because the suspected abuser often is a family member; clinicians and others involved in identifying a decision-maker to speak on behalf of an older adult should choose carefully.
Prevention and screeningKey to reducing the prevalence of elder abuse in the community is formulating
strategies for prevention and screening. The American Medical Association recommends that clinicians “incorporate routine questions related to elder abuse and neglect into daily practice.”49 Older adults might not admit to abuse or neglect unless they are asked; speak to patients at eye level, keep questions simple, direct, and nonjudgmental, and assure them (1) that discussions are confidential and (2) that their safety is your primary goal.50,51
Comprehensive approaches to questioning patients are available and often recommended for screening for elder abuse.4 However, screening in the office setting often involves short, directly administered questionnaires.49 For example, the Health and Safety Screen developed at the University of Maine comprises 6 questions52:
• Has anyone close to you called you names or insulted you recently?
• Are you afraid of anyone in your life?
• Are you able to use the telephone anytime you want to?
• Has anyone forced you to do things you didn’t want to do?
• Has anyone taken things or money that belong to you without your OK?
• Has anyone close to you tried to hurt you or harm you recently?
Because of time constraints and lack of a universal standard, there is debate whether regular elder abuse screening is time-effective. It often is recommended, therefore, that clinicians in primary care (1) refer older adults with risk factors for abuse to geriatric medical teams trained in these measures and (2) perform periodic follow-up on such patients4 (Figure).
• New York City Elder Abuse Center encourages collaboration among health, mental health, and community justice organizations.28 The program involves a number of resources for addressing elder abuse, such as promoting staff awareness of risk factors for, and signs of, abuse, and screening for mental health problems in the abused.
• The Elder Justice Act, enacted in 2010 to combat elder abuse, provides federal funds and resources to prevent, detect, treat, and intervene to stop abuse and, when appropriate, to prosecute abusers.53
This Web Exclusive Table provides a 7-point summary reference guide for understanding and preventing elder abuse in your practice.
BOTTOM LINEIdentification of elder abuse can be difficult because signs and symptoms of abuse closely resemble physiologic aging. Older adults with identifiable risk factors should be screened for abuse; time constraints make universal screening impossible at this time. In the future, multidisciplinary approaches likely will make elder abuse more easily identifiable through the combined work of health care providers, law enforcement agencies, banks, and other institutions—with the ultimate goal of protecting older adults in the community from abuse.
Related Resources
• Frazão SL, Correia AM, Norton P, et al. Physical abuse against elderly persons in institutional settings. J Forensic Leg Med. 2015;36:54-60.
• Sorrentino R. Performing capacity evaluations: what’s expected from your consult. Current Psychiatry. 2014;13(1):41-44.
Disclosures
Ms. Hubert reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products. Dr. Gupta is a member of the speakers’ bureau of Alkermes, Allergan, Avanir Pharmaceuticals, Takeda Pharmaceutical, Lundbeck, Otsuka Pharmaceutical, and Sunovion Pharmaceuticals.
In its simplest form, elder abuse refers to the intentional infliction of injury or neglect of an older adult by a caregiver. The 5 primary types of elder abuse include neglect, physical, financial, psychological/emotional, and sexual, with a subtype of social abuse that falls under psychological/emotional abuse.
Differentiating abuse from the normal sequelae of physiologic aging can be difficult; therefore, early identification and awareness of risk factors is key, as well as detailed documentation of the patient encounter. As soon as abuse is suspected, clinicians should report it to Adult Protective Services (APS) for further investigation. In terms of prevention, regular screening for elder abuse is still up for debate, but as the incidence of elder abuse continues to rise so should research and preventive efforts to combat this growing public health concern.
What is ‘elder abuse’?According to the Elder Abuse Prevention, Identification, and Treatment Act of 1985, elder abuse is:
…willful infliction of injury, unreasonable confinement, intimidation or cruel punishment with resulting physical harm or pain or mental anguish or the willful deprivation by a caretaker of goods or services which are necessary to avoid physical harm, mental anguish or mental illness.1
There are 2 main components to this definition:
• an older adult has suffered injury or deprivation
• another person is responsible for causing or failing to prevent it.2
Although definitions vary, it generally is accepted that, for elder abuse to occur, it must take place within a relationship of trust.3
An ‘older adult’ is a person age ≥65, representing 14% of the U.S. population.4
According to U.S. Census Bureau data, there were 40 million older adults in 20105;
recent data project that this number will rise to 90 million by 2060 as Baby Boomers age.6 Studies suggest that as many as 10% of older adults in the United States experience elder abuse each year2; one study estimated that 6% of older adults in the community experienced significant abuse in the past month.7
Although elder abuse can occur in any setting, it takes place most often in the community. A survey of state APSs in 2000 showed that 60.7% of abuse was domestic; only 8.3% of incidents occurred in institutional settings.8 The annual direct medical costs associated with elder abuse injury in the United States are estimated at $5.3 billion, which is likely to increase with anticipated growth of the geriatric population.9
Although the number of older adults and the incidence of elder abuse are on the rise, as few as 1 in 14 cases is reported to authorities10; health care providers are some of the least likely of involved parties to report suspected abuse. One study found that 63% of physicians never asked about elder abuse, and only 31% reported encountering it in the previous 12 months.11 A busy clinician—ie, one who sees 20 to 40 geriatric patients a day—has a high likelihood of encountering at least 1 victim of elder abuse,2 yet many cases go unrecognized.
Types of abuseElder abuse comprises 5 categories12:
• neglect (58.5% of cases)
• physical (15.7%)
• financial (12.3%)
• psychological and emotional (7.3%)
• sexual (0.04%).
Social abuse is considered a subtype of psychological and emotional abuse. All “other” types of abuse constitute 5.1% cases; 0.06% are of unknown type.12
Neglect is (1) failure of the caregiver to provide life necessities or (2) the responsible person’s refusal to permit others to provide appropriate care.3 This is one of the most common types of elder abuse in residential facilities. Signs of neglect include dehydration, depression, fecal impaction, and malnutrition (Table).4 The prevalence of dehydration in nursing home patients is reported to be as high as 35%, which may be the result of passive or active withholding of liquids (ie, decreasing hydration to reduce the need to change the resident’s clothing or bedding).4 Other forms of neglect include medication misuse (overdosing or underdosing) and self-neglect, which occurs among people living alone and often is listed as a subtype of neglect, but is controversial because it does not involve another person.
Financial exploitation is the illegal or improper use, or mismanagement, of a person’s money, property, or financial resources3—often, to his (her) detriment. Estimates are that 1 of every 20 older adults has been subject to financial abuse at some point in their life.15 There should be a high index of suspicion for financial exploitation when one notices unexplained changes in power of attorney, wills, or other legal documents; missing checks, money, or belongings.16 In the past, adult children were most likely to be financial abusers; in recent years, however, the abuser is more often a spouse—especially a second spouse.17 Bankers, accountants, and other financial advisors are among those trained to identify risk factors for financial abuse; they are encouraged to caution clients about this possibility.18
Psychological and emotional abuse occurs when a caregiver inflicts mental stress on an older adult by actions and threats that cause fear, violence, isolation, deprivation, or feelings of shame and powerlessness.3 Examples are threatening to put the older adult in a nursing home or verbally abusing him (her). Suspect this type of abuse when a caregiver refuses to leave the older adult or speaks for him, or if the older adult expresses fear in the presence of the caregiver.4 This type of abuse also is prevalent in nursing homes and other long-term care facilities.19
Sexual abuse involves nonconsensual touching or sexual activities (rape, language, exploitive behavior) that are threatened or forced on an older adult.16 Sexual abuse is more common in frail or dependent persons.3 Physical exam findings—particularly dysuria, tender genitalia, and evidence of sexually transmitted infections4—are required to identify sexual abuse, along with signs of depression and display of fear.
Social abuse can be considered a subtype of psychological and emotional abuse, in which a caregiver denies an older adult contact with family and friends or deprives him from access to transportation. Other examples include not allowing the older adult to use the telephone, monitoring phone calls, and claiming that his friends or family are “interfering.”20 Intentionally embarrassing an older adult in front of others also can be considered social abuse.
Technology, particularly smart phones and social media, can complicate and exacerbate elder abuse:
• In July 2013, employees of a Wisconsin nursing home were found with videos and photographs of residents bathing and of a nude resident who had a bowel obstruction being mocked.21
• In May 2014, employees of a nursing home in Massachusetts recorded themselves physically and verbally abusing several older adults with Alzheimer’s disease, including one episode of the employees “hitting the woman on her arms, flicking her ears and then pinching the woman’s nose closed.” The employees also possessed a photograph of her naked.22
• In June 2015, an employee of a nursing home in Indiana was accused of taking
photos of a resident naked and sharing them on the messaging application Snapchat,23 in which images disappear 10 seconds after they are viewed.
As technology evolves, caregivers are finding more cunning ways to abuse older adults. Considering current events and trends in this area, technology as a gateway to elder abuse should be of growing concern.
Risk factorsA 2013 literature review on elder abuse reported that the most important risk factors are related to relationship (family disharmony, poor or conflicting relationships) and environment (a low level of social support),3 although other variables can play a role. Regardless of these findings, it is important to recognize that (1) elder abuse is not a necessary consequence in a family with many risk factors and (2) elder abuse can occur in the absence of any risk factors.
As a whole, women are at a higher risk of abuse, particularly when combined with loneliness, poor social support, cohabitation (especially family members), substance abuse, cognitive impairment, and dementia and other mental health problems.4 Other risk factors include functional deficiency, poor physical health or frailty, low income or wealth, and trauma or past abuse.3
Lower income, poor health, low social support, and belonging to a non-white racial group put an older adult at risk for neglect; female sex is a specific risk factor for sexual assault.15 One study found that, among older adults who suffered physical, mental, or cognitive impairment, 1 of every 4 was at risk of abuse.7
Mental illness. Dementia puts an older adult at higher risk because of increased
caregiver stress resulting from disruptive and aggressive behaviors2; the same is true when the older adult suffers another mental illness, such as anxiety, depression, schizophrenia or bipolar disorder. Presumably, older adults with any of these disorders are at risk of financial and psychological and emotional abuse because of their decreased social support, lack of independence, and inability to hold a job—leaving their caregiver to shoulder more responsibilities and with more opportunities to inflict abuse. In addition, an older adult suffering from depression can feel helpless and unworthy, possibly making him more susceptible to psychological and emotional abuse, and less likely to seek help.
More research is needed to establish racial and ethnic differences in the risk of abuse. Some research states that older adults who are a member of a minority are at greater risk of abuse; however, the difference dissipates after adjusting for variables such as income and social support.24 Cultural confounders, such as varying interpretations of the same set of interactions between older adults, need to be examined further.
Sexual orientation. Identifying one’s self as a lesbian, gay, bisexual, or transgender (LGBT) person is an additional risk factor for elder abuse. In 1997, a report described a nursing home employee who refused to bathe a resident because he didn’t want to “touch the lesbian.”25 Despite evolving attitudes in society toward support and acceptance of sexual orientation, fear of homophobia still prevents some LGBT older adults from seeking help when they have been abused because of their orientation—especially ones who have internalized that
homophobia and feel that they are unworthy of seeking help.25
In addition, health care providers and nursing home staff members might neglect the particular care needs of LGBT older adults, intentionally or unintentionally. APS staff and providers must be cognizant of underlying biases and exhibit respect when assisting LGBT clients.
Approximately 75% of caregivers of older adults are family members; 70% are female26; and most are adult children, spouses, and partners of those receiving care.27 Male caregivers age ≥40 are more likely to be the abuser, however, especially when they possess any of these risk factors: fatigue, burnout, medical illness, mental illness, lack of financial and support services, family history of abusive behavior, and substance abuse.4 People who commit elder abuse also tend to be significantly dependent on the person they are abusing.2 In some cases, and especially when the abuser is financially needy, caregivers turn to elder abuse to obtain resources from the victim.2
From your standpoint as a practitioner, it is important to determine the root cause of elder abuse. According to one review,28 family members with mental illness or a history of substance abuse, or who are stressed by the burden of caregiving, abuse older adults at a higher rate than family members who are not affected in those ways. Depression in particular is a common characteristic of abusers,2 often secondary to the stress of caring for an older adult.
Abuse caused by stress can be addressed by referral to a support group and counseling for the caregiver; psychiatric conditions, such as depression, might be better treated with pharmacotherapy. Evaluate for depression and posttraumatic stress disorder (PTSD) in both the abuser and the abused,29 and for other mental health issues that might compound the situation. It is possible for you to have 2 patients: the older adult and his caregiver. Regardless of the challenge,keep in mind that the older adult’s safety is your priority.
Consequences for the abusedThe abused adult is at risk of a number of serious physical and psychological consequences.30 They tend to have a shorter lifespan, after adjusting for other variables associated with increased mortality.
The reason for shortened lifespan is multifactorial30:
• Bruises, abrasions, and fractures may take longer to heal because of diminished skin and bone regeneration.
• Diseases that affect the heart, lungs, and kidneys might prevent the person from bouncing back from major stressors caused by abuse, such as blood loss, severe injury, and pain.
• Injury from abuse can exacerbate an underlying illness.
• Elder abuse also is associated with increased emergency department use, hospitalization (including readmission within 30 days), and nursing home placement.31
Elder abuse can lead to depression, shame, and guilt; increased isolation; and
increased risk of alcohol abuse and substance use.31 A study found that victims of
elder abuse are significantly more depressed than non-victims.32
In the same study, being a victim of abuse was found to be the second-strongest
predictor of depression, after the state of one’s health.32 Other potential psychiatric
consequences of abuse that need further study include increased risk of developing
fear and anxiety disorders; learned helplessness; and PTSD.33 According to LoFaso,
“depression and anxiety can consume their days and leave them emotionally and
physically frail.”29 Such feelings make these older adults less likely to resolve abuse or break off relations with the abuser.32
Because mental illness can be a risk factor for, and a consequence of, elder abuse,
be aware of such complications and address them appropriately. Keep in mind that older adults are more likely to visit a primary care practitioner than a psychiatrist for a routine health check-up or evaluation of initial cognition-related problems; however, they are more likely to see a psychiatrist for advanced neuropsychiatric problems such as dementia, paranoia, delusions, hallucinations, and insomnia. Adequate education on elder abuse should not be limited to a single medical specialty because it can present in several clinical settings.
Identifying abuseIdentification of elder abuse in the home poses a greater challenge to clinicians than abuse in an institutional setting because it is not directly observable. Compounding this is the lack of unified standards for identifying and dealing with elder abuse. It is first necessary for you to determine the likelihood that abuse or neglect occurred, which can be difficult because the signs of elder abuse and manifestations of normal aging often are similar. You also must establish whether (1) the abused person will accept intervention and (2) the abused person who refuses intervention has the capacity to make that decision. Both of these conditions will guide your approach to management.2
Obtain the history from several sources; review the records; and carefully examine patterns of injury, in particular assessing functional status and level of dependency on the caregiver. Explanations that do not match injuries signal the need for further investigation and examination.
To help differentiate elder abuse from normal physiologic aging, look at the skin for bruises, rashes that do not heal, and ulcers—all of which could be signs of abuse or neglect. Keep in mind that bruising generally is more common in older adults because of the slower turnover rate of epidermal cells; physiologic bruising tends to occur on dorsal aspects of the hands and arms.4 In contrast, bruising secondary to neglect or physical abuse can manifest as a subgaleal hematoma (caused by traumatic hair pulling), tracking in the peritoneum after genital trauma, Battle’s sign, and raccoon eyes, among other findings.4
In addition, larger bruises (>5 cm in diameter) are more likely the result of elder abuse.34 To complicate matters, many older persons are taking anticoagulant therapy, making bruising more likely. In addition, be on the lookout for burns during the physical exam. Evidence suggests that at least 10% of burns caused by battery and assault occur in the context of elder abuse; most burn facilities do not have formal guidelines for screening for abuse and neglect, however.35 According to one retrospective study, the most common causes of burns in older adults are hot water scalds and radiator contact, and the mortality rate of older burn patients in general is higher than among the overall population.36
Falls and fractures are common among older adults, regardless of whether they are
abused, because of polypharmacy, underlying medical conditions, and functional
limitations. Many abusers, however, use these factors to cover up intentional injury
that might have resulted in the older person falling, including overmedication (a form of physical abuse) and withholding a necessary walking aid (a form of neglect). Maintain a high index of suspicion of elder abuse when (1) the caregiver’s and the older adult’s stories of an injury don’t add up and (2) physical findings that might have been caused by abuse are present.
A number of psychiatric and cognitive symptoms suggest other types of elder abuse. Take note of emotional upset, agitation, and unusual behaviors37—especially if you can follow the patient over time to observe marked changes in the presentation. Likewise, be aware of proposed alterations in guardianship, which should be evaluated by a forensic psychiatrist with analysis of medical history, social attachments, home environment, self-care, and finances.38 Such evaluation should provide clues to the motivation behind a change of guardianship and will help to determine if elder abuse should be suspected.
Brandi et al37 provided an informative table that identifies pertinent signs, symptoms, and other findings that clinicians should be aware of to support a suspicion of elder abuse (Table).
Documentation is of utmost importance in evaluating potential elder abuse; keep in mind that the medical record might be used in an investigation of abuse by social workers, law enforcement, and prosecutors. Your records should be legible, clearly indicate who the main caregiver is and what his (her) responsibilities are, and specify who is present at your encounter with the patient.4 Document your observations of patient behavior, reactions to questions, and family dynamics and conflicts16; make note of warning signs such as fear, silence, and inability to interview the patient alone.
In addition to written documentation, take photographs of injuries, with a ruler in the image to record their size. Serial photographs are helpful; so are photographs from a variety of distances (close-up, regional, wholebody) to capture detail and place the wound in the context of a specific area of the body.4
Safety is paramount. Given the findings of the history and physical exam, it is necessary to determine whether it is safe for the patient to return home with the caregiver, or if alternate accommodations or resources, such as a social worker or a support group, are required. Include details of planned follow-up in your evaluation, and offer consideration of possible psychiatric disorders that can develop as a result of such abuse.
ReportingElder abuse is a criminal offense in all states.39 A clinician who has reasonable suspicion that elder abuse occurred must report it, regardless of whether the proof of abuse is concrete.40 At a point of reasonable suspicion, immediately contact APS, law enforcement, and a social worker. Adult Protective Services, modeled after Child Protective Services, is typically administered by local and state health
departments.41
After a report is filed with APS, an assigned social worker makes an in-person home visit to investigate the allegation and determine whether elder abuse is substantiated, partially substantiated, or unsubstantiated.16 In most states, elder abuse reporting is not anonymous because follow-up may be needed to provide additional evidence, especially if the report was made by a health care provider.16
No federal standard exists for states to follow when defining and addressing elder abuse, which can complicate identification and reporting of abuse. Laws governing elder abuse do not allow states to determine the fate of the older adult, who can decide for himself (herself) whether to use or waive protective services.42 Older adults might choose not to report abuse because of shame, intimidation, or fear,43 or to protect a caregiver, who often is a family member.
Elder abuse reports can come from a variety of sources; convincing evidence is, as noted, unnecessary to report it. Health care providers are mandated reporters, but
it is believed that the number of clinicians who report elder abuse based on suspicion is far below what it should be. One study found that 94% of physicians said that they either were unable to prove that the abuse had occurred or decided not to report it.11 Another study found that only 1.4% of elder abuse cases reported to APS come from physicians.44
There are several possible reasons for underreporting elder abuse, including (1) the difficulty of distinguishing elder abuse and neglect from sequelae of normal aging and (2) the fact that cognitive and functional impairment of the abused person makes it difficult, even impossible, to establish the narrative of how the abuse happened. Nursing homes in particular provide a high level of oversight because residents have an average of ≥3 functional deficits.4 Other reasons for underreporting—some of which are difficult to understand, and excuse, in a clinician—are:
• subtlety of signs
• victim denial
• ignorance of reporting procedures
• inadequate training
• lack of information about resources
• concern about losing physician–patient rapport
• concern about involvement in the legal system
• time limitations
• doubt about the effectiveness of APS.16
Assessing capacityThe older adult’s wishes must be respected unless a health care provider or the legal system determines that he lacks functional capacity to make decisions.16
How is capacity evaluated? A capacity evaluation has 3 components:
• Comprehension is a person’s factual understanding of the situation, including
consequences and alternatives
• Free choice is a person’s voluntary decision to accept or reject a proposed treatment, free of coercion (in this setting, free choice is the older adult’s decision whether to report the abuse)
• Reliability is a person’s ability to provide a consistent choice over time.45
Most capacity evaluations are conducted by clinical interview. No single, brief test is used universally, and there is the possibility of inter-rater variability.45 Examples of tests used to assess capacity are the Folstein Mini-Mental Status Examination and the MacArthur Competence Assessment Tool-Treatment45; the latter is a structured interview that incorporates information specific to the individual patient’s decision-making situation.46 Regardless of the approach, the psychiatrist-evaluator ensures that the older adult has been given the appropriate information
to provide informed consent about the situation.47
If the evaluator determines that a person lacks capacity to make decisions, efforts should be made to determine if the cause of that impairment is reversible.47 Older adults who have dementia or other underlying psychiatric condition that impairs cognition might benefit from more education on their situation; ones who appear fearful of consequences should be introduced to a trusted advisor to assist in making competent judgments.47
If the older adult is found to lack capacity, a substitute decision-maker must be sought.47 Many states have statutes specifying the order in which family members are contacted.48 The need to appoint an advisor can become knotty because the suspected abuser often is a family member; clinicians and others involved in identifying a decision-maker to speak on behalf of an older adult should choose carefully.
Prevention and screeningKey to reducing the prevalence of elder abuse in the community is formulating
strategies for prevention and screening. The American Medical Association recommends that clinicians “incorporate routine questions related to elder abuse and neglect into daily practice.”49 Older adults might not admit to abuse or neglect unless they are asked; speak to patients at eye level, keep questions simple, direct, and nonjudgmental, and assure them (1) that discussions are confidential and (2) that their safety is your primary goal.50,51
Comprehensive approaches to questioning patients are available and often recommended for screening for elder abuse.4 However, screening in the office setting often involves short, directly administered questionnaires.49 For example, the Health and Safety Screen developed at the University of Maine comprises 6 questions52:
• Has anyone close to you called you names or insulted you recently?
• Are you afraid of anyone in your life?
• Are you able to use the telephone anytime you want to?
• Has anyone forced you to do things you didn’t want to do?
• Has anyone taken things or money that belong to you without your OK?
• Has anyone close to you tried to hurt you or harm you recently?
Because of time constraints and lack of a universal standard, there is debate whether regular elder abuse screening is time-effective. It often is recommended, therefore, that clinicians in primary care (1) refer older adults with risk factors for abuse to geriatric medical teams trained in these measures and (2) perform periodic follow-up on such patients4 (Figure).
• New York City Elder Abuse Center encourages collaboration among health, mental health, and community justice organizations.28 The program involves a number of resources for addressing elder abuse, such as promoting staff awareness of risk factors for, and signs of, abuse, and screening for mental health problems in the abused.
• The Elder Justice Act, enacted in 2010 to combat elder abuse, provides federal funds and resources to prevent, detect, treat, and intervene to stop abuse and, when appropriate, to prosecute abusers.53
This Web Exclusive Table provides a 7-point summary reference guide for understanding and preventing elder abuse in your practice.
BOTTOM LINEIdentification of elder abuse can be difficult because signs and symptoms of abuse closely resemble physiologic aging. Older adults with identifiable risk factors should be screened for abuse; time constraints make universal screening impossible at this time. In the future, multidisciplinary approaches likely will make elder abuse more easily identifiable through the combined work of health care providers, law enforcement agencies, banks, and other institutions—with the ultimate goal of protecting older adults in the community from abuse.
Related Resources
• Frazão SL, Correia AM, Norton P, et al. Physical abuse against elderly persons in institutional settings. J Forensic Leg Med. 2015;36:54-60.
• Sorrentino R. Performing capacity evaluations: what’s expected from your consult. Current Psychiatry. 2014;13(1):41-44.
Disclosures
Ms. Hubert reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products. Dr. Gupta is a member of the speakers’ bureau of Alkermes, Allergan, Avanir Pharmaceuticals, Takeda Pharmaceutical, Lundbeck, Otsuka Pharmaceutical, and Sunovion Pharmaceuticals.
1. The Elder Abuse Prevention, Identification, and Treatment Act of 1985, HR 1674, 99th Cong (1985).
2. Lachs MS, Pillemer K. Elder abuse. Lancet. 2004;364(9441):1263-1272.
3. Johannesen M, LoGiudice D. Elder abuse: a systematic review of risk factors in community-dwelling elders. Age Ageing. 2013;42(3):292-298.
4. Gibbs LM, Mosqueda L, eds. Medical implications of elder abuse and neglect. Clin Geriatr Med. 2014;30(4):xv-xvi. doi: 10.1016/j.cger.2014.08.015.
5. Werner CA. The Older Population: 2010. U.S. Census Bureau. http://webcache.googleusercontent.com/search?q=cache:hCCb_pcnO6QJ :ht tps://www.census.gov/prod/cen2010/briefs/c2010br-09.pdf+&cd=1&hl=en&ct=clnk&gl=uss. Issued November 2011. Accessed October 10, 2015.
6. Himes CL. Elderly Americans. Population Bulletin. 2002;56(4):1-41.
7. Cooper C, Selwood A, Livingston G. The prevalence of elder abuse and neglect: a systematic review. Age Ageing. 2008;37(2):151-60.
8. Teaster PB. A response to the abuse of vulnerable adults: the 2000 Survey of State Adult Protective Services. The National Center on Elder Abuse. http://www.ncea.aoa.gov/Resources/Publication/docs/apsreport030703.pdf. 2003.
Accessed October 22, 2015.
9. Mouton CP, Rodabough RJ, Rovi SL, et al. Prevalence and 3-year incidence of abuse among postmenopausal women. Am J Public Health. 2004;94(4):605-612.
10. Acierno R, Hernandez MA, Amstadter AB, et al. Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: the National Elder Mistreatment Study. Am J Public Health. 2010;100(2):292-297.
11. Kennedy RD. Elder abuse and neglect: the experience, knowledge, and attitudes of primary care physicians. Fam Med. 2005;37(7):481-485.
12. Statistic Brain Research Institute. Elderly abuse statistics. http://www.statisticbrain.com/elderly-abuse-statistics. Accessed June 22, 2015.
13. Lachs MS, Bachman R, Williams CS, et al. Resident-to-resident elder mistreatment and police contact in nursing homes: findings from a population-based cohort. J Am Geriatr Soc. 2007;55(6):840-845.
14. Lachs M, Bachman R, Williams C, et al. Older adults as crime victims, perpetrators, witnesses, and complainants: a population-based study of police interactions. J Elder Abuse Negl. 2005;16(4):25-40.
15. Acierno R, Hernandez-Tejada M, Muzzy W, et al. National Elder Mistreatment Study. Washington, DC: National Institute of Justice; 2009.
16. Dong XQ. Elder abuse: systematic review and implications for practice. J Am Geriatr Soc. 2015;63(6):1214-1238.
17. Freedman M. The growing epidemic of financial elder abuse. The Tax Advisor. http://www.cpa2biz.com/Content/media/PRODUCER_CONTENT/Newsletters/
Articles_2007/Tax/Financial_Elder_Abuse.jsp. Published November 2007. Accessed June 24, 2015.
18. Consumer Financial Protection Bureau. Protection for older Americans. http://www.consumerfinance.gov/olderamericans. Accessed June 22, 2015.
19. Castle NG. Nursing home deficiency citations for abuse. J Appl Gerontol. 2011;30(6):719-743.
20. Elder Abuse Prevention Unit. Social abuse. http://www.eapu.com.au/elder-abuse/social-abuse. Published 2014. Accessed June 24, 2015.
21. Former nursing home employees allegedly photographed naked resident. United Press International. http://www.upi.com/Top_News/US/2013/07/03/Former-nursinghome-employees-allegedly-photographed-nakedresidents/
65801372893020. Published July 3, 2013. Accessed June 24, 2015.
22. Miller N. Two charged with elder assault at an assisted living facility. MetroWest Daily News. http://www.metrowestdailynews.com/article/20140506/
NEWS/140507587. Updated May 7, 2014. Accessed June 24, 2015.
23. Jorgensen J. New charges filed in nursing home case.WHAS11. http://www.whas11.com/story/news/local/2015/06/24/new-charges-filed-in-nursing-homecase/29243183/. Published June 24, 2015. Accessed June 27, 2015.
24. Hermandez-Tejada MA, Amstadter A, Muzzy W, et al. The National Elder Mistreatment Study: race and ethnicity findings. J Elder Abuse Negl. 2013;25(4):281-293.
25. Cooks-Daniels L. Lesbian, gay male, bisexual and transgendered elders: elder abuse and neglect issues. J Elder Abuse Negl. 1998;9(2):35-49.
26. Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist. 1980;20(6):649-655.
27. Tatara T, Blumerman Kuzmeskus L, Duckhorn E, et al. The National Center on Elder Abuse Incidence Study: final report. http://aoa.gov/AoA_Programs/Elder_Rights/Elder_Abuse/docs/ABuseReport_Full.pdf. Published September 1998. Accessed October 19, 2015.
28. Rosen AL. Where mental health and elder abuse intersect. Generations. 2014;38(3):75-79.
29. LoFaso V. The role of the primary physician in assessing and treating the mental health concerns of elder abuse victims. NYC Elder Abuse Center eNewsletter.nyceac.com/wp-content/uploads/2013/03/Exploring-the-IntersectionofElder-Abuse-and-Mental-Health_eNewsletter.pdf. Published March 12, 2013. Accessed August 20, 2015.
30. Lachs MS, Williams CS, O’Brien S, et al. The mortality of elder mistreatment. JAMA. 1998;280(5):428-432.
31. Dyer CB, Pavlik VN, Murphy KP, et al. The high prevalence of depression and dementia in elder abuse or neglect. J Am Geriatr Soc. 2000;48(2):205-208.
32. Pillemer K, Prescott D. Psychological effects of elder abuse: a research note. J Elder Abuse Negl. 1988;1(1):65-73.
33. Elder abuse: consequences. Centers for Disease Control and Prevention. http://www.cdc.gov/violenceprevention/elderabuse/consequences.html. Updated June 22, 2015.Accessed August 20, 2015.
34. Wiglesworth A, Austin R, Corona M, et al. Bruising as a marker of physical elder abuse. J Am Geriatr Soc. 2009;57(7):1191-1196.
35. Peck MD. Epidemiology of burns throughout the World. Part II: intentional burns in adults. Burns. 2012;38(5):630-637.
36. 2014 National Burn Repository; report of data between 2004-2013. American Burn Association. http://www.ameriburn.org/2014NBRAnnualReport.pdf. Published 2014. Accessed June 26, 2015.
37. Brandi B, Dyer CB, Heisler CJ, et al. Systemic responses to elder abuse. In: Brandi B, Dyer CB, Heisler CJ, eds. Elder abuse detection and intervention: a collaborative approach. New York, NY: Spring Publishing Company; 2007:79-100.
38. Welner M. Guardianship. The Forensic Panel. http://www.forensicpanel.com/expert_services/psychiatry/civil_law/guardianship.html. Accessed August 20, 2015.
39. Watson E. Elder abuse: definition, types and statistics, and elder abuse (mistreatment and neglect) laws. Journal of Legal Nurse Consulting. 2013;24(2):40-42.
40. National Center on Elder Abuse Administration on Aging. Reporting abuse. http://www.ncea.aoa.gov/Stop_Abuse/Get_Help/Report/index.aspx. Accessed August 18, 2015.
41. Mukherjee D. Organizational structures of elder abuse reporting systems. Administration in Social Work. 2011;35(5):517-531.
42. Costin LB, Karger HJ, Stoesz H. The politics of child abuse in America. New York, NY: Oxford University Press; 1996.
43. Thomson MJ, Lietzau LK, Doty MM, et al. An analysis of elder abuse rates in Milwaukee County. WMJ. 2011;110(6):271-276.
44. Teaster PB, Dugar TA, Mendiondo MS, et al; The National Committee for the Prevention of Elder Abuse; The National Adult Protective Services Association. The 2004 Survey of State Adult Protective Services: Abuse of Adults 60 Years and Older. http://www.ncea.aoa.gov/Resources/Publication/docs/APS_2004NCEASurvey.pdf. Published March 2007. Accessed October 19, 2015.
45. Sorrentino R. Performing capacity evaluations: what’s expected from your consult. Current Psychiatry. 2014;13(1):41-44.
46. Grisso T, Appelbaum PS. MacArthur competence assessment tool for treatment (MacCAT-T). Sarasota, FL: Professional Resources Press; 1998.
47. Appelbaum PS. Clinical practice. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;35(18):1834-1840.
48. Wynn S. Decision by surrogates: An overview of surrogate consent laws in the United States. Bifocal: A Journal of the ABA Commission on Bar and Aging. 2014;36(1). http://www.americanbar.org/publications/bifocal/vol_36/
issue_1_october2014/default_surrogate_consent_statutes.html. Accessed October 22, 2015.
49. American Medical Association. Diagnostic and treatment guidelines on elder abuse and neglect. Chicago, IL: American Medical Association; 1992.
50. Harrell R, Toronjo C, McLaughlin J, et al. How geriatricians identify elder abuse and neglect. Am J Med Sci. 2002;323(1):34-38.
51. Ahmad M, Lachs MS. Elder abuse and neglect: what physicians can and should do. Cleve Clin J Med. 2002; 69(10):801-808.
52. Elder abuse screening protocol for physicians: lessons learned from the Maine Partners for Elder Protection Pilot Project. University of Maine Center on Aging. http://umcoa.siteturbine.com/uploaded_files/mainecenteronaging.umaine.edu/files/elderabusescreeningmanual.pdf. Published May 2, 2007. Accessed August 20, 2015.
53. What is the Elder Justice Act? USC Davis School of Gerontology. http://gerontology.usc.edu/resources/articles/what-is-the-elder-justice-act/. Published 2015. Accessed October 20, 2015.
1. The Elder Abuse Prevention, Identification, and Treatment Act of 1985, HR 1674, 99th Cong (1985).
2. Lachs MS, Pillemer K. Elder abuse. Lancet. 2004;364(9441):1263-1272.
3. Johannesen M, LoGiudice D. Elder abuse: a systematic review of risk factors in community-dwelling elders. Age Ageing. 2013;42(3):292-298.
4. Gibbs LM, Mosqueda L, eds. Medical implications of elder abuse and neglect. Clin Geriatr Med. 2014;30(4):xv-xvi. doi: 10.1016/j.cger.2014.08.015.
5. Werner CA. The Older Population: 2010. U.S. Census Bureau. http://webcache.googleusercontent.com/search?q=cache:hCCb_pcnO6QJ :ht tps://www.census.gov/prod/cen2010/briefs/c2010br-09.pdf+&cd=1&hl=en&ct=clnk&gl=uss. Issued November 2011. Accessed October 10, 2015.
6. Himes CL. Elderly Americans. Population Bulletin. 2002;56(4):1-41.
7. Cooper C, Selwood A, Livingston G. The prevalence of elder abuse and neglect: a systematic review. Age Ageing. 2008;37(2):151-60.
8. Teaster PB. A response to the abuse of vulnerable adults: the 2000 Survey of State Adult Protective Services. The National Center on Elder Abuse. http://www.ncea.aoa.gov/Resources/Publication/docs/apsreport030703.pdf. 2003.
Accessed October 22, 2015.
9. Mouton CP, Rodabough RJ, Rovi SL, et al. Prevalence and 3-year incidence of abuse among postmenopausal women. Am J Public Health. 2004;94(4):605-612.
10. Acierno R, Hernandez MA, Amstadter AB, et al. Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: the National Elder Mistreatment Study. Am J Public Health. 2010;100(2):292-297.
11. Kennedy RD. Elder abuse and neglect: the experience, knowledge, and attitudes of primary care physicians. Fam Med. 2005;37(7):481-485.
12. Statistic Brain Research Institute. Elderly abuse statistics. http://www.statisticbrain.com/elderly-abuse-statistics. Accessed June 22, 2015.
13. Lachs MS, Bachman R, Williams CS, et al. Resident-to-resident elder mistreatment and police contact in nursing homes: findings from a population-based cohort. J Am Geriatr Soc. 2007;55(6):840-845.
14. Lachs M, Bachman R, Williams C, et al. Older adults as crime victims, perpetrators, witnesses, and complainants: a population-based study of police interactions. J Elder Abuse Negl. 2005;16(4):25-40.
15. Acierno R, Hernandez-Tejada M, Muzzy W, et al. National Elder Mistreatment Study. Washington, DC: National Institute of Justice; 2009.
16. Dong XQ. Elder abuse: systematic review and implications for practice. J Am Geriatr Soc. 2015;63(6):1214-1238.
17. Freedman M. The growing epidemic of financial elder abuse. The Tax Advisor. http://www.cpa2biz.com/Content/media/PRODUCER_CONTENT/Newsletters/
Articles_2007/Tax/Financial_Elder_Abuse.jsp. Published November 2007. Accessed June 24, 2015.
18. Consumer Financial Protection Bureau. Protection for older Americans. http://www.consumerfinance.gov/olderamericans. Accessed June 22, 2015.
19. Castle NG. Nursing home deficiency citations for abuse. J Appl Gerontol. 2011;30(6):719-743.
20. Elder Abuse Prevention Unit. Social abuse. http://www.eapu.com.au/elder-abuse/social-abuse. Published 2014. Accessed June 24, 2015.
21. Former nursing home employees allegedly photographed naked resident. United Press International. http://www.upi.com/Top_News/US/2013/07/03/Former-nursinghome-employees-allegedly-photographed-nakedresidents/
65801372893020. Published July 3, 2013. Accessed June 24, 2015.
22. Miller N. Two charged with elder assault at an assisted living facility. MetroWest Daily News. http://www.metrowestdailynews.com/article/20140506/
NEWS/140507587. Updated May 7, 2014. Accessed June 24, 2015.
23. Jorgensen J. New charges filed in nursing home case.WHAS11. http://www.whas11.com/story/news/local/2015/06/24/new-charges-filed-in-nursing-homecase/29243183/. Published June 24, 2015. Accessed June 27, 2015.
24. Hermandez-Tejada MA, Amstadter A, Muzzy W, et al. The National Elder Mistreatment Study: race and ethnicity findings. J Elder Abuse Negl. 2013;25(4):281-293.
25. Cooks-Daniels L. Lesbian, gay male, bisexual and transgendered elders: elder abuse and neglect issues. J Elder Abuse Negl. 1998;9(2):35-49.
26. Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist. 1980;20(6):649-655.
27. Tatara T, Blumerman Kuzmeskus L, Duckhorn E, et al. The National Center on Elder Abuse Incidence Study: final report. http://aoa.gov/AoA_Programs/Elder_Rights/Elder_Abuse/docs/ABuseReport_Full.pdf. Published September 1998. Accessed October 19, 2015.
28. Rosen AL. Where mental health and elder abuse intersect. Generations. 2014;38(3):75-79.
29. LoFaso V. The role of the primary physician in assessing and treating the mental health concerns of elder abuse victims. NYC Elder Abuse Center eNewsletter.nyceac.com/wp-content/uploads/2013/03/Exploring-the-IntersectionofElder-Abuse-and-Mental-Health_eNewsletter.pdf. Published March 12, 2013. Accessed August 20, 2015.
30. Lachs MS, Williams CS, O’Brien S, et al. The mortality of elder mistreatment. JAMA. 1998;280(5):428-432.
31. Dyer CB, Pavlik VN, Murphy KP, et al. The high prevalence of depression and dementia in elder abuse or neglect. J Am Geriatr Soc. 2000;48(2):205-208.
32. Pillemer K, Prescott D. Psychological effects of elder abuse: a research note. J Elder Abuse Negl. 1988;1(1):65-73.
33. Elder abuse: consequences. Centers for Disease Control and Prevention. http://www.cdc.gov/violenceprevention/elderabuse/consequences.html. Updated June 22, 2015.Accessed August 20, 2015.
34. Wiglesworth A, Austin R, Corona M, et al. Bruising as a marker of physical elder abuse. J Am Geriatr Soc. 2009;57(7):1191-1196.
35. Peck MD. Epidemiology of burns throughout the World. Part II: intentional burns in adults. Burns. 2012;38(5):630-637.
36. 2014 National Burn Repository; report of data between 2004-2013. American Burn Association. http://www.ameriburn.org/2014NBRAnnualReport.pdf. Published 2014. Accessed June 26, 2015.
37. Brandi B, Dyer CB, Heisler CJ, et al. Systemic responses to elder abuse. In: Brandi B, Dyer CB, Heisler CJ, eds. Elder abuse detection and intervention: a collaborative approach. New York, NY: Spring Publishing Company; 2007:79-100.
38. Welner M. Guardianship. The Forensic Panel. http://www.forensicpanel.com/expert_services/psychiatry/civil_law/guardianship.html. Accessed August 20, 2015.
39. Watson E. Elder abuse: definition, types and statistics, and elder abuse (mistreatment and neglect) laws. Journal of Legal Nurse Consulting. 2013;24(2):40-42.
40. National Center on Elder Abuse Administration on Aging. Reporting abuse. http://www.ncea.aoa.gov/Stop_Abuse/Get_Help/Report/index.aspx. Accessed August 18, 2015.
41. Mukherjee D. Organizational structures of elder abuse reporting systems. Administration in Social Work. 2011;35(5):517-531.
42. Costin LB, Karger HJ, Stoesz H. The politics of child abuse in America. New York, NY: Oxford University Press; 1996.
43. Thomson MJ, Lietzau LK, Doty MM, et al. An analysis of elder abuse rates in Milwaukee County. WMJ. 2011;110(6):271-276.
44. Teaster PB, Dugar TA, Mendiondo MS, et al; The National Committee for the Prevention of Elder Abuse; The National Adult Protective Services Association. The 2004 Survey of State Adult Protective Services: Abuse of Adults 60 Years and Older. http://www.ncea.aoa.gov/Resources/Publication/docs/APS_2004NCEASurvey.pdf. Published March 2007. Accessed October 19, 2015.
45. Sorrentino R. Performing capacity evaluations: what’s expected from your consult. Current Psychiatry. 2014;13(1):41-44.
46. Grisso T, Appelbaum PS. MacArthur competence assessment tool for treatment (MacCAT-T). Sarasota, FL: Professional Resources Press; 1998.
47. Appelbaum PS. Clinical practice. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;35(18):1834-1840.
48. Wynn S. Decision by surrogates: An overview of surrogate consent laws in the United States. Bifocal: A Journal of the ABA Commission on Bar and Aging. 2014;36(1). http://www.americanbar.org/publications/bifocal/vol_36/
issue_1_october2014/default_surrogate_consent_statutes.html. Accessed October 22, 2015.
49. American Medical Association. Diagnostic and treatment guidelines on elder abuse and neglect. Chicago, IL: American Medical Association; 1992.
50. Harrell R, Toronjo C, McLaughlin J, et al. How geriatricians identify elder abuse and neglect. Am J Med Sci. 2002;323(1):34-38.
51. Ahmad M, Lachs MS. Elder abuse and neglect: what physicians can and should do. Cleve Clin J Med. 2002; 69(10):801-808.
52. Elder abuse screening protocol for physicians: lessons learned from the Maine Partners for Elder Protection Pilot Project. University of Maine Center on Aging. http://umcoa.siteturbine.com/uploaded_files/mainecenteronaging.umaine.edu/files/elderabusescreeningmanual.pdf. Published May 2, 2007. Accessed August 20, 2015.
53. What is the Elder Justice Act? USC Davis School of Gerontology. http://gerontology.usc.edu/resources/articles/what-is-the-elder-justice-act/. Published 2015. Accessed October 20, 2015.
Painful Lesion Hasn’t Responded to Antibiotics
ANSWER
The correct answer is erythema nodosum (EN; choice “c”), a reactive form of septal panniculitis with many potential triggers.
Erythema induratum (choice “a”) is a manifestation of lobular panniculitis, which affects the fat lobules but not the septae. It too has numerous triggers, but it tends to manifest with more discrete nodules, which eventually open and drain. It is far less common than EN.
Urticaria (choice “b”), also known as hives, presents as itchy, stingy wheals that are typically evanescent (eg, they appear suddenly, within seconds, and disappear within hours). Despite the itching and stinging, urticaria rarely hurts when it presents on the skin.
Erysipelas (choice “d”) is a superficial form of skin infection. More superficial than cellulitis, it usually is caused by a member of the Streptococcus family. It has a bright red appearance and sharply demarcated margins, with a peau d’orange (dimpled, like an orange peel) effect on its surface. It is acute in origin and responds readily to most common antibiotics.
DISCUSSION
Erythema nodosum, a reactive process involving fibrous septae that support and separate subcutaneous adipocytes, is notable for the complete lack of epidermal change (eg, scaling, broken skin, pointing, draining). The incidence is about 2 in 10,000 population, with women outnumbering men at a rate of 4:1 and the 18-to-34 age-group most affected. The anterior leg is involved in the vast majority of cases.
EN often starts with flulike symptoms, followed by the appearance of discrete, bright red nodules, measuring 2 to 4 cm, on the anterior legs; these darken and coalesce over a period of seven to 10 weeks. New lesions can continue to appear for up to six weeks. As they progress, the lesions often become ecchymotic. Idiopathic cases (at least 20%) can last months.
Notable triggers include Crohn disease flares and use of drugs such as sulfa, gold salts, and oral contraceptives. Several infections have been identified as triggers, including strep, mycoplasma, and campylobacter, as well as deep fungal infections (histoplasmosis, blastomycosis, coccidioidomycosis, and sporotrichosis). More unusual causes include pregnancy and diseases such as sarcoidosis, tuberculosis, Behçet disease, and leukemia/lymphoma.
The diagnostic workup for EN includes punch biopsy of deep adipose tissue and throat culture, and when indicated, ASO titer (if strep is suspected) and chest films (to rule out tuberculosis and sarcoid). In most cases, the diagnosis can be made on clinical grounds alone, although the triggering entity may be difficult to identify. The identification and elimination of the underlying trigger is nonetheless crucial for diagnosis and treatment.
That issue aside, most cases of EN resolve with minimal treatment; this can include the use of NSAIDs and elevation of the limbs when possible. In this particular case, the intense pain the patient was experiencing called for stronger therapy (ibuprofen 800 mg tid, plus a two-week taper of prednisone 40 mg). She responded quite well, and the problem was almost totally resolved at a follow-up visit several weeks later.
In the absence of findings to the contrary, it is likely that the trigger for this patient’s EN was strep, given the timing of its manifestation after a sore throat.
ANSWER
The correct answer is erythema nodosum (EN; choice “c”), a reactive form of septal panniculitis with many potential triggers.
Erythema induratum (choice “a”) is a manifestation of lobular panniculitis, which affects the fat lobules but not the septae. It too has numerous triggers, but it tends to manifest with more discrete nodules, which eventually open and drain. It is far less common than EN.
Urticaria (choice “b”), also known as hives, presents as itchy, stingy wheals that are typically evanescent (eg, they appear suddenly, within seconds, and disappear within hours). Despite the itching and stinging, urticaria rarely hurts when it presents on the skin.
Erysipelas (choice “d”) is a superficial form of skin infection. More superficial than cellulitis, it usually is caused by a member of the Streptococcus family. It has a bright red appearance and sharply demarcated margins, with a peau d’orange (dimpled, like an orange peel) effect on its surface. It is acute in origin and responds readily to most common antibiotics.
DISCUSSION
Erythema nodosum, a reactive process involving fibrous septae that support and separate subcutaneous adipocytes, is notable for the complete lack of epidermal change (eg, scaling, broken skin, pointing, draining). The incidence is about 2 in 10,000 population, with women outnumbering men at a rate of 4:1 and the 18-to-34 age-group most affected. The anterior leg is involved in the vast majority of cases.
EN often starts with flulike symptoms, followed by the appearance of discrete, bright red nodules, measuring 2 to 4 cm, on the anterior legs; these darken and coalesce over a period of seven to 10 weeks. New lesions can continue to appear for up to six weeks. As they progress, the lesions often become ecchymotic. Idiopathic cases (at least 20%) can last months.
Notable triggers include Crohn disease flares and use of drugs such as sulfa, gold salts, and oral contraceptives. Several infections have been identified as triggers, including strep, mycoplasma, and campylobacter, as well as deep fungal infections (histoplasmosis, blastomycosis, coccidioidomycosis, and sporotrichosis). More unusual causes include pregnancy and diseases such as sarcoidosis, tuberculosis, Behçet disease, and leukemia/lymphoma.
The diagnostic workup for EN includes punch biopsy of deep adipose tissue and throat culture, and when indicated, ASO titer (if strep is suspected) and chest films (to rule out tuberculosis and sarcoid). In most cases, the diagnosis can be made on clinical grounds alone, although the triggering entity may be difficult to identify. The identification and elimination of the underlying trigger is nonetheless crucial for diagnosis and treatment.
That issue aside, most cases of EN resolve with minimal treatment; this can include the use of NSAIDs and elevation of the limbs when possible. In this particular case, the intense pain the patient was experiencing called for stronger therapy (ibuprofen 800 mg tid, plus a two-week taper of prednisone 40 mg). She responded quite well, and the problem was almost totally resolved at a follow-up visit several weeks later.
In the absence of findings to the contrary, it is likely that the trigger for this patient’s EN was strep, given the timing of its manifestation after a sore throat.
ANSWER
The correct answer is erythema nodosum (EN; choice “c”), a reactive form of septal panniculitis with many potential triggers.
Erythema induratum (choice “a”) is a manifestation of lobular panniculitis, which affects the fat lobules but not the septae. It too has numerous triggers, but it tends to manifest with more discrete nodules, which eventually open and drain. It is far less common than EN.
Urticaria (choice “b”), also known as hives, presents as itchy, stingy wheals that are typically evanescent (eg, they appear suddenly, within seconds, and disappear within hours). Despite the itching and stinging, urticaria rarely hurts when it presents on the skin.
Erysipelas (choice “d”) is a superficial form of skin infection. More superficial than cellulitis, it usually is caused by a member of the Streptococcus family. It has a bright red appearance and sharply demarcated margins, with a peau d’orange (dimpled, like an orange peel) effect on its surface. It is acute in origin and responds readily to most common antibiotics.
DISCUSSION
Erythema nodosum, a reactive process involving fibrous septae that support and separate subcutaneous adipocytes, is notable for the complete lack of epidermal change (eg, scaling, broken skin, pointing, draining). The incidence is about 2 in 10,000 population, with women outnumbering men at a rate of 4:1 and the 18-to-34 age-group most affected. The anterior leg is involved in the vast majority of cases.
EN often starts with flulike symptoms, followed by the appearance of discrete, bright red nodules, measuring 2 to 4 cm, on the anterior legs; these darken and coalesce over a period of seven to 10 weeks. New lesions can continue to appear for up to six weeks. As they progress, the lesions often become ecchymotic. Idiopathic cases (at least 20%) can last months.
Notable triggers include Crohn disease flares and use of drugs such as sulfa, gold salts, and oral contraceptives. Several infections have been identified as triggers, including strep, mycoplasma, and campylobacter, as well as deep fungal infections (histoplasmosis, blastomycosis, coccidioidomycosis, and sporotrichosis). More unusual causes include pregnancy and diseases such as sarcoidosis, tuberculosis, Behçet disease, and leukemia/lymphoma.
The diagnostic workup for EN includes punch biopsy of deep adipose tissue and throat culture, and when indicated, ASO titer (if strep is suspected) and chest films (to rule out tuberculosis and sarcoid). In most cases, the diagnosis can be made on clinical grounds alone, although the triggering entity may be difficult to identify. The identification and elimination of the underlying trigger is nonetheless crucial for diagnosis and treatment.
That issue aside, most cases of EN resolve with minimal treatment; this can include the use of NSAIDs and elevation of the limbs when possible. In this particular case, the intense pain the patient was experiencing called for stronger therapy (ibuprofen 800 mg tid, plus a two-week taper of prednisone 40 mg). She responded quite well, and the problem was almost totally resolved at a follow-up visit several weeks later.
In the absence of findings to the contrary, it is likely that the trigger for this patient’s EN was strep, given the timing of its manifestation after a sore throat.

A 57-year-old woman is referred to dermatology for “cellulitis” that has persisted despite several courses of oral antibiotics (including cephalexin and trimethoprim/sulfamethoxazole). She denies taking any other medications and has no significant medical history. She states that the problem manifested as discrete red nodules, which eventually coalesced into a single large patch. At the time, she had just recovered from a sore throat and still felt a bit ill, although she denies cough, fever, and shortness of breath. Examination reveals a large (12 x 14 cm) red edematous plaque in the skin over her right anterior tibia. The deep intradermal and subdermal edema is exquisitely tender to touch, considerably warmer than the surrounding skin, and highly blanchable. No other changes are noted on the epidermal surface. A deep 5-mm punch biopsy is performed. Results show a dense lymphohistiocytic infiltrate in the pannicular septae.
Is monitoring of plasma antipsychotic levels useful?
Although there has been success in defining the minimum therapeutic response threshold for certain antipsychotics—for example, clozapine (350 to 450 ng/mL), haloperidol (3 to 5 ng/mL), and fluphenazine (0.8 ng/mL)—one aspect of antipsychotic plasma levels not widely discussed is their value as a marker of adherence.
Many schizophrenia patients achieve an optimal response to agents for which there is no depot formulation. For them, maintenance of symptom control depends wholly on oral medication adherence.1 Regrettably, nonadherence with oral antipsychotic treatment is prevalent among patients with schizophrenia; yet, in routine clinical practice, the extent of nonadherence rarely is measured.
Studies have been able to quantify oral medication nonadherence using monitoring devices, such as the Medication Event Monitoring System (MEMS) that electronically records opening of the medication container and strongly correlates with pill count. Although patients knew they were participating in a trial using MEMS technology, only 48% were able to take their medication at least 80% of the time in a 4-week study,2 and only 43% met the 70% adherence threshold in a 6-month trial.3
Clinicians, patients: Unreliable indicators of adherence
Neither clinician rating nor patient self-reporting is a reliable predictor of adherence with an oral medication regimen. In the 6-month adherence trial,3 clinicians estimated that 95% of their patients met the 70% adherence threshold (the actual percentage was 43%); in a 12-week study, clinician ratings correlated weakly with adherence (r = 0.32; P = .001), but patient self-reporting showed no significant correlation (r = 0.18; P = .08) with pill count.4
Clinicians underestimate not only the extent of nonadherence but also the impact that even a brief period of modest nonadherence has on the risk of relapse. In an 18-month prospective study of patients who recently had been given a diagnosis of schizophrenia, and in whom clinician and patient reports were supplemented with a pill count every 1 to 2 weeks and plasma antipsychotic levels every 4 weeks, any period of at least mild nonadherence was significantly predictive of symptom exacerbation or relapse (hazard ratio [HR], 3.4; 95% CI, 1.4–8.4; P < .002).1 Moreover, 50% to 75% adherence for ≥ 2 consecutive weeks increased the HR to 5.8, and moderate nonadherence (<50% for 2.0 to 3.9 weeks) to an HR of 28.5.
There might be a better method already available
Given the poor correlation between a clinician’s judgment and a patient’s actual pill-taking, it is clear that more accurate methods of tracking adherence must be devised. Because MEMS technology is not widely available, and because pill counts require a home visit or a cooperative patient who brings medications to office visits, plasma antipsychotic monitoring potentially is an appealing method of tracking adherence.
Correlation between the plasma antipsychotic level and relapse is not consistently seen in the literature,4 but plasma levels obtained during periods of clinical stability offer the opportunity to define, for the individual patient, a range of drug exposure that is associated with clinical response. The ideal plasma level baseline is obtained at steady state during a presumed period of observed adherence, such as during a hospital stay. Although patients can be nonadherent in the hospital, this setting offers the best proxy for an acute clinical response to a given plasma level. The alternative is to obtain several plasma levels during a period of outpatient clinical stability.
Clinicians must be mindful that changes in the plasma antipsychotic level after hospital discharge might not reflect poor adherence; environmental factors (eg, exposure to cytochrome P450 or P-glycoprotein inducers) can have a significant impact on results. Resumption of smoking is a classic example, and routinely is associated with a 50% reduction in plasma clozapine levels.5
There also is expected variability in plasma antipsychotic levels based on (1) the timing of prior doses with regard to trough levels, and (2) the effects of an occasional missed dose. Nevertheless, in a sample of adherent clozapine-treated patients, investigators found that 98% of patients had a coefficient of variability (CV) of 30% for sequential plasma concentrations (mean CV, 14%).6
Clinicians should inform patients that the plasma antipsychotic level is a tool for helping track treatment engagement before relapse—the same way metabolic monitoring helps track abnormalities that can be associated with future cardiovascular events. (Clinicians also must be charitable with their patients when discussing a significant drop in the plasma antipsychotic level [eg, >30%], acknowledging that many patients often miss doses.)
Using the patient’s input about specific difficulties with a medication regimen, clinicians should strive to find ways to improve oral medication adherence. In many cases, the clinician can assist through medication simplification, consolidation of multiple daily doses, provision of pill boxes, and discussions about long-acting injectable (LAI) antipsychotics.
In short, plasma antipsychotic levels offer an opportunity to have a richer, evidence-based discussion about adherence, beyond the trite, ineffective question “Did you take your medication?” Use of an objective measure can (1) serve as a benchmark for the patient (eg, “You seemed to do better when your clozapine level was above 400 ng/mL”), and (2) remind clinicians of the variable adherence inherent with oral medication regimens.
A note about long-acting injectable antipsychotics
Because nonadherence is seen throughout the course of schizophrenia, discussion of LAI therapy should not be limited to patients with chronic illness. Results of recent naturalistic7 and randomized studies8 show significant reduction in the rate of psychotic relapse and improved symptom control8 among first-episode patients who are taking an LAI. Moreover, compelling data show that most first-episode patients who are taking an oral antipsychotic will accept a recommendation for treatment with an LAI.9
Summing up: 2 Tools for achieving therapeutic success
Monitoring plasma levels of antipsychotics offers a method for quantifying the problem of nonadherence. For many patients, an LAI antipsychotic provides a solution to nonadherence, and the increasing variety of LAI preparations means more options with which to match individual patients.
Clinicians have a limited amount of time to spend with patients in the office, but time spent discussing LAIs is an investment in the patient’s stability and functional outcome. Minutes once spent managing nonadherence can be devoted to understanding the patient’s aspirations and to developing strategies to achieve those goals.
In the end, isn’t that what we’d rather be talking about with our patients?
1. Subotnik KL, Nuechterlein KH, Ventura J, et al. Risperidone nonadherence and return of positive symptoms in the early course of schizophrenia. Am J Psychiatry. 2011;168(3):286-292.
2. Remington G, Teo C, Mann S, et al. Examining levels of antipsychotic adherence to better understand nonadherence. J Clin Psychopharmacol. 2013;33(2):261-263.
3. Byerly MJ, Thompson A, Carmody T, et al. Validity of electronically monitored medication adherence and conventional adherence measures in schizophrenia. Psychiatr Serv. 2007;58(6):844-847.
4. Velligan DI, Wang M, Diamond P, et al. Relationships among subjective and objective measures of adherence to oral antipsychotic medications. Psychiatr Serv. 2007;58(9):1187-1192.
5. Meyer JM. Individual changes in clozapine levels after smoking cessation: results and a predictive model. J Clin Psychopharmacol. 2001;21(6):569-574.
6. Dugan DJ, Ereshefsky L, Toney GB, et al. Dose and interval adherence among stabilized clozapine-treated patients measured by medication event monitoring. Presented at: Meeting of the New Clinical Drug Evaluation Unit; May 30-June 2, 2000; Boca Raton, FL.
7. Tiihonen J, Haukka J, Taylor M, et al. A nationwide cohort study of oral and depot antipsychotics after first hospitalization for schizophrenia. [Erratum in Am J Psychiatry. 2012;169(2):223]. Am J Psychiatry. 2011;168(6):603-609.
8. Subotnik KL, Casaus LR, Ventura J, et al. Long-acting injectable risperidone for relapse prevention and control of breakthrough symptoms after a recent first episode of schizophrenia: a randomized clinical trial. JAMA Psychiatry. 2015;72(8):822-829.
9. Weiden PJ, Schooler NR, Weedon JC, et al. A randomized controlled trial of long-acting injectable risperidone vs continuation on oral atypical antipsychotics for first-episode schizophrenia patients: initial adherence outcome. J Clin Psychiatry. 2009;70(10):1397-1406.
Although there has been success in defining the minimum therapeutic response threshold for certain antipsychotics—for example, clozapine (350 to 450 ng/mL), haloperidol (3 to 5 ng/mL), and fluphenazine (0.8 ng/mL)—one aspect of antipsychotic plasma levels not widely discussed is their value as a marker of adherence.
Many schizophrenia patients achieve an optimal response to agents for which there is no depot formulation. For them, maintenance of symptom control depends wholly on oral medication adherence.1 Regrettably, nonadherence with oral antipsychotic treatment is prevalent among patients with schizophrenia; yet, in routine clinical practice, the extent of nonadherence rarely is measured.
Studies have been able to quantify oral medication nonadherence using monitoring devices, such as the Medication Event Monitoring System (MEMS) that electronically records opening of the medication container and strongly correlates with pill count. Although patients knew they were participating in a trial using MEMS technology, only 48% were able to take their medication at least 80% of the time in a 4-week study,2 and only 43% met the 70% adherence threshold in a 6-month trial.3
Clinicians, patients: Unreliable indicators of adherence
Neither clinician rating nor patient self-reporting is a reliable predictor of adherence with an oral medication regimen. In the 6-month adherence trial,3 clinicians estimated that 95% of their patients met the 70% adherence threshold (the actual percentage was 43%); in a 12-week study, clinician ratings correlated weakly with adherence (r = 0.32; P = .001), but patient self-reporting showed no significant correlation (r = 0.18; P = .08) with pill count.4
Clinicians underestimate not only the extent of nonadherence but also the impact that even a brief period of modest nonadherence has on the risk of relapse. In an 18-month prospective study of patients who recently had been given a diagnosis of schizophrenia, and in whom clinician and patient reports were supplemented with a pill count every 1 to 2 weeks and plasma antipsychotic levels every 4 weeks, any period of at least mild nonadherence was significantly predictive of symptom exacerbation or relapse (hazard ratio [HR], 3.4; 95% CI, 1.4–8.4; P < .002).1 Moreover, 50% to 75% adherence for ≥ 2 consecutive weeks increased the HR to 5.8, and moderate nonadherence (<50% for 2.0 to 3.9 weeks) to an HR of 28.5.
There might be a better method already available
Given the poor correlation between a clinician’s judgment and a patient’s actual pill-taking, it is clear that more accurate methods of tracking adherence must be devised. Because MEMS technology is not widely available, and because pill counts require a home visit or a cooperative patient who brings medications to office visits, plasma antipsychotic monitoring potentially is an appealing method of tracking adherence.
Correlation between the plasma antipsychotic level and relapse is not consistently seen in the literature,4 but plasma levels obtained during periods of clinical stability offer the opportunity to define, for the individual patient, a range of drug exposure that is associated with clinical response. The ideal plasma level baseline is obtained at steady state during a presumed period of observed adherence, such as during a hospital stay. Although patients can be nonadherent in the hospital, this setting offers the best proxy for an acute clinical response to a given plasma level. The alternative is to obtain several plasma levels during a period of outpatient clinical stability.
Clinicians must be mindful that changes in the plasma antipsychotic level after hospital discharge might not reflect poor adherence; environmental factors (eg, exposure to cytochrome P450 or P-glycoprotein inducers) can have a significant impact on results. Resumption of smoking is a classic example, and routinely is associated with a 50% reduction in plasma clozapine levels.5
There also is expected variability in plasma antipsychotic levels based on (1) the timing of prior doses with regard to trough levels, and (2) the effects of an occasional missed dose. Nevertheless, in a sample of adherent clozapine-treated patients, investigators found that 98% of patients had a coefficient of variability (CV) of 30% for sequential plasma concentrations (mean CV, 14%).6
Clinicians should inform patients that the plasma antipsychotic level is a tool for helping track treatment engagement before relapse—the same way metabolic monitoring helps track abnormalities that can be associated with future cardiovascular events. (Clinicians also must be charitable with their patients when discussing a significant drop in the plasma antipsychotic level [eg, >30%], acknowledging that many patients often miss doses.)
Using the patient’s input about specific difficulties with a medication regimen, clinicians should strive to find ways to improve oral medication adherence. In many cases, the clinician can assist through medication simplification, consolidation of multiple daily doses, provision of pill boxes, and discussions about long-acting injectable (LAI) antipsychotics.
In short, plasma antipsychotic levels offer an opportunity to have a richer, evidence-based discussion about adherence, beyond the trite, ineffective question “Did you take your medication?” Use of an objective measure can (1) serve as a benchmark for the patient (eg, “You seemed to do better when your clozapine level was above 400 ng/mL”), and (2) remind clinicians of the variable adherence inherent with oral medication regimens.
A note about long-acting injectable antipsychotics
Because nonadherence is seen throughout the course of schizophrenia, discussion of LAI therapy should not be limited to patients with chronic illness. Results of recent naturalistic7 and randomized studies8 show significant reduction in the rate of psychotic relapse and improved symptom control8 among first-episode patients who are taking an LAI. Moreover, compelling data show that most first-episode patients who are taking an oral antipsychotic will accept a recommendation for treatment with an LAI.9
Summing up: 2 Tools for achieving therapeutic success
Monitoring plasma levels of antipsychotics offers a method for quantifying the problem of nonadherence. For many patients, an LAI antipsychotic provides a solution to nonadherence, and the increasing variety of LAI preparations means more options with which to match individual patients.
Clinicians have a limited amount of time to spend with patients in the office, but time spent discussing LAIs is an investment in the patient’s stability and functional outcome. Minutes once spent managing nonadherence can be devoted to understanding the patient’s aspirations and to developing strategies to achieve those goals.
In the end, isn’t that what we’d rather be talking about with our patients?
Although there has been success in defining the minimum therapeutic response threshold for certain antipsychotics—for example, clozapine (350 to 450 ng/mL), haloperidol (3 to 5 ng/mL), and fluphenazine (0.8 ng/mL)—one aspect of antipsychotic plasma levels not widely discussed is their value as a marker of adherence.
Many schizophrenia patients achieve an optimal response to agents for which there is no depot formulation. For them, maintenance of symptom control depends wholly on oral medication adherence.1 Regrettably, nonadherence with oral antipsychotic treatment is prevalent among patients with schizophrenia; yet, in routine clinical practice, the extent of nonadherence rarely is measured.
Studies have been able to quantify oral medication nonadherence using monitoring devices, such as the Medication Event Monitoring System (MEMS) that electronically records opening of the medication container and strongly correlates with pill count. Although patients knew they were participating in a trial using MEMS technology, only 48% were able to take their medication at least 80% of the time in a 4-week study,2 and only 43% met the 70% adherence threshold in a 6-month trial.3
Clinicians, patients: Unreliable indicators of adherence
Neither clinician rating nor patient self-reporting is a reliable predictor of adherence with an oral medication regimen. In the 6-month adherence trial,3 clinicians estimated that 95% of their patients met the 70% adherence threshold (the actual percentage was 43%); in a 12-week study, clinician ratings correlated weakly with adherence (r = 0.32; P = .001), but patient self-reporting showed no significant correlation (r = 0.18; P = .08) with pill count.4
Clinicians underestimate not only the extent of nonadherence but also the impact that even a brief period of modest nonadherence has on the risk of relapse. In an 18-month prospective study of patients who recently had been given a diagnosis of schizophrenia, and in whom clinician and patient reports were supplemented with a pill count every 1 to 2 weeks and plasma antipsychotic levels every 4 weeks, any period of at least mild nonadherence was significantly predictive of symptom exacerbation or relapse (hazard ratio [HR], 3.4; 95% CI, 1.4–8.4; P < .002).1 Moreover, 50% to 75% adherence for ≥ 2 consecutive weeks increased the HR to 5.8, and moderate nonadherence (<50% for 2.0 to 3.9 weeks) to an HR of 28.5.
There might be a better method already available
Given the poor correlation between a clinician’s judgment and a patient’s actual pill-taking, it is clear that more accurate methods of tracking adherence must be devised. Because MEMS technology is not widely available, and because pill counts require a home visit or a cooperative patient who brings medications to office visits, plasma antipsychotic monitoring potentially is an appealing method of tracking adherence.
Correlation between the plasma antipsychotic level and relapse is not consistently seen in the literature,4 but plasma levels obtained during periods of clinical stability offer the opportunity to define, for the individual patient, a range of drug exposure that is associated with clinical response. The ideal plasma level baseline is obtained at steady state during a presumed period of observed adherence, such as during a hospital stay. Although patients can be nonadherent in the hospital, this setting offers the best proxy for an acute clinical response to a given plasma level. The alternative is to obtain several plasma levels during a period of outpatient clinical stability.
Clinicians must be mindful that changes in the plasma antipsychotic level after hospital discharge might not reflect poor adherence; environmental factors (eg, exposure to cytochrome P450 or P-glycoprotein inducers) can have a significant impact on results. Resumption of smoking is a classic example, and routinely is associated with a 50% reduction in plasma clozapine levels.5
There also is expected variability in plasma antipsychotic levels based on (1) the timing of prior doses with regard to trough levels, and (2) the effects of an occasional missed dose. Nevertheless, in a sample of adherent clozapine-treated patients, investigators found that 98% of patients had a coefficient of variability (CV) of 30% for sequential plasma concentrations (mean CV, 14%).6
Clinicians should inform patients that the plasma antipsychotic level is a tool for helping track treatment engagement before relapse—the same way metabolic monitoring helps track abnormalities that can be associated with future cardiovascular events. (Clinicians also must be charitable with their patients when discussing a significant drop in the plasma antipsychotic level [eg, >30%], acknowledging that many patients often miss doses.)
Using the patient’s input about specific difficulties with a medication regimen, clinicians should strive to find ways to improve oral medication adherence. In many cases, the clinician can assist through medication simplification, consolidation of multiple daily doses, provision of pill boxes, and discussions about long-acting injectable (LAI) antipsychotics.
In short, plasma antipsychotic levels offer an opportunity to have a richer, evidence-based discussion about adherence, beyond the trite, ineffective question “Did you take your medication?” Use of an objective measure can (1) serve as a benchmark for the patient (eg, “You seemed to do better when your clozapine level was above 400 ng/mL”), and (2) remind clinicians of the variable adherence inherent with oral medication regimens.
A note about long-acting injectable antipsychotics
Because nonadherence is seen throughout the course of schizophrenia, discussion of LAI therapy should not be limited to patients with chronic illness. Results of recent naturalistic7 and randomized studies8 show significant reduction in the rate of psychotic relapse and improved symptom control8 among first-episode patients who are taking an LAI. Moreover, compelling data show that most first-episode patients who are taking an oral antipsychotic will accept a recommendation for treatment with an LAI.9
Summing up: 2 Tools for achieving therapeutic success
Monitoring plasma levels of antipsychotics offers a method for quantifying the problem of nonadherence. For many patients, an LAI antipsychotic provides a solution to nonadherence, and the increasing variety of LAI preparations means more options with which to match individual patients.
Clinicians have a limited amount of time to spend with patients in the office, but time spent discussing LAIs is an investment in the patient’s stability and functional outcome. Minutes once spent managing nonadherence can be devoted to understanding the patient’s aspirations and to developing strategies to achieve those goals.
In the end, isn’t that what we’d rather be talking about with our patients?
1. Subotnik KL, Nuechterlein KH, Ventura J, et al. Risperidone nonadherence and return of positive symptoms in the early course of schizophrenia. Am J Psychiatry. 2011;168(3):286-292.
2. Remington G, Teo C, Mann S, et al. Examining levels of antipsychotic adherence to better understand nonadherence. J Clin Psychopharmacol. 2013;33(2):261-263.
3. Byerly MJ, Thompson A, Carmody T, et al. Validity of electronically monitored medication adherence and conventional adherence measures in schizophrenia. Psychiatr Serv. 2007;58(6):844-847.
4. Velligan DI, Wang M, Diamond P, et al. Relationships among subjective and objective measures of adherence to oral antipsychotic medications. Psychiatr Serv. 2007;58(9):1187-1192.
5. Meyer JM. Individual changes in clozapine levels after smoking cessation: results and a predictive model. J Clin Psychopharmacol. 2001;21(6):569-574.
6. Dugan DJ, Ereshefsky L, Toney GB, et al. Dose and interval adherence among stabilized clozapine-treated patients measured by medication event monitoring. Presented at: Meeting of the New Clinical Drug Evaluation Unit; May 30-June 2, 2000; Boca Raton, FL.
7. Tiihonen J, Haukka J, Taylor M, et al. A nationwide cohort study of oral and depot antipsychotics after first hospitalization for schizophrenia. [Erratum in Am J Psychiatry. 2012;169(2):223]. Am J Psychiatry. 2011;168(6):603-609.
8. Subotnik KL, Casaus LR, Ventura J, et al. Long-acting injectable risperidone for relapse prevention and control of breakthrough symptoms after a recent first episode of schizophrenia: a randomized clinical trial. JAMA Psychiatry. 2015;72(8):822-829.
9. Weiden PJ, Schooler NR, Weedon JC, et al. A randomized controlled trial of long-acting injectable risperidone vs continuation on oral atypical antipsychotics for first-episode schizophrenia patients: initial adherence outcome. J Clin Psychiatry. 2009;70(10):1397-1406.
1. Subotnik KL, Nuechterlein KH, Ventura J, et al. Risperidone nonadherence and return of positive symptoms in the early course of schizophrenia. Am J Psychiatry. 2011;168(3):286-292.
2. Remington G, Teo C, Mann S, et al. Examining levels of antipsychotic adherence to better understand nonadherence. J Clin Psychopharmacol. 2013;33(2):261-263.
3. Byerly MJ, Thompson A, Carmody T, et al. Validity of electronically monitored medication adherence and conventional adherence measures in schizophrenia. Psychiatr Serv. 2007;58(6):844-847.
4. Velligan DI, Wang M, Diamond P, et al. Relationships among subjective and objective measures of adherence to oral antipsychotic medications. Psychiatr Serv. 2007;58(9):1187-1192.
5. Meyer JM. Individual changes in clozapine levels after smoking cessation: results and a predictive model. J Clin Psychopharmacol. 2001;21(6):569-574.
6. Dugan DJ, Ereshefsky L, Toney GB, et al. Dose and interval adherence among stabilized clozapine-treated patients measured by medication event monitoring. Presented at: Meeting of the New Clinical Drug Evaluation Unit; May 30-June 2, 2000; Boca Raton, FL.
7. Tiihonen J, Haukka J, Taylor M, et al. A nationwide cohort study of oral and depot antipsychotics after first hospitalization for schizophrenia. [Erratum in Am J Psychiatry. 2012;169(2):223]. Am J Psychiatry. 2011;168(6):603-609.
8. Subotnik KL, Casaus LR, Ventura J, et al. Long-acting injectable risperidone for relapse prevention and control of breakthrough symptoms after a recent first episode of schizophrenia: a randomized clinical trial. JAMA Psychiatry. 2015;72(8):822-829.
9. Weiden PJ, Schooler NR, Weedon JC, et al. A randomized controlled trial of long-acting injectable risperidone vs continuation on oral atypical antipsychotics for first-episode schizophrenia patients: initial adherence outcome. J Clin Psychiatry. 2009;70(10):1397-1406.