User login
Health Policy Scholars for 2016 selected
A total of 17 surgeons have been selected to serve as Health Policy Scholars and participate in the Leadership Program for Health Policy and Management, June 12-18 at the Heller School for Social Policy and Management, Brandeis University, Waltham, MA.
Each scholarship includes attendance at the weeklong intensive course, followed by a year’s service in a health policy–related capacity to the American College of Surgeons (ACS) and the surgical specialty society cosponsoring the awardee.
This year’s scholars are as follows:
• ACS Health Policy Scholar for General Surgery: Subhasis Misra, MB, BS, MS, FACS, Texas Tech University Health Sciences Center School of Medicine, Amarillo
• ACS Health Policy Scholar for General Surgery: SreyRam Kuy, MD, MHS, Louisiana State University, Shreveport
• ACS/American Association of Neurological Surgeons Health Policy Scholar: Kimon Bekelis, MD, Dartmouth-Hitchcock Medical Center, Lebanon, NH
• ACS/American Academy of Otolaryngology–Head & Neck Surgery Health Policy Scholar: Alex J. McKinlay, MD, FACS, Darnall Army Medical Center, Fort Hood, TX
• ACS/American Association for the Surgery of Trauma Health Policy Scholar: Saman Arbabi, MD, FACS, Harborview Medical Center, Seattle, WA
• ACS/American Pediatric Surgery Association Health Policy Scholar: David P. Bliss Jr., MD, FACS, Children’s Medical Center, Dallas, TX
• ACS/American Surgical Association Health Policy Scholar: Eileen M. Bulger, MD, FACS, University of Washington, Seattle
• ACS/American Society of Breast Surgeons Health Policy Scholar: Alyssa D. Throckmorton, MD, FACS, Baptist Medical Group, Nashville, TN
• ACS/American Society of Colon and Rectal Surgeons Health Policy Scholar: Jose G. Guillem, MD, FACS, Memorial Sloan Kettering Cancer Center, New York, NY
• ACS/American Society of Plastic Surgeons Health Policy Scholar: Malcolm Z. Roth, MD, FACS, Albany Medical Center, NY
• ACS/American Urogynecologic Society Health Policy Scholar: Mallika Anand, MD, Spectrum Health Medical Group, Grand Rapids, MI
• ACS/American Urological Association Health Policy Scholar: Thomas Rechtschaffen, MD, FACS, Advanced Urology Centers of New York, Yonkers
• ACS/Eastern Association for the Surgery of Trauma Health Policy Scholar: Alexander L. Eastman, MD, MPH, FACS, University of Texas Southwestern Medical Center, Dallas
• ACS/New England Society of Surgery Health Policy Scholar: Christopher S. Muratore, MD, FACS, Hasbro Children’s Hospital/Rhode Island Hospital, Providence
• ACS/Society for Surgery of the Alimentary Tract Health Policy Scholar: Guilherme Mussi Rocha Campos, MD, FACS, Virginia Commonwealth University, Richmond
• ACS/The Society of Thoracic Surgeons Health Policy Scholar: Daniel T. Engelman, MD, FACS, Baystate Medical Center, Springfield, MA
• ACS/Society for Vascular Surgery Health Policy Scholar: Matthew Jay Sideman, MD, FACS, University of Texas Health Sciences Center, San Antonio
A total of 17 surgeons have been selected to serve as Health Policy Scholars and participate in the Leadership Program for Health Policy and Management, June 12-18 at the Heller School for Social Policy and Management, Brandeis University, Waltham, MA.
Each scholarship includes attendance at the weeklong intensive course, followed by a year’s service in a health policy–related capacity to the American College of Surgeons (ACS) and the surgical specialty society cosponsoring the awardee.
This year’s scholars are as follows:
• ACS Health Policy Scholar for General Surgery: Subhasis Misra, MB, BS, MS, FACS, Texas Tech University Health Sciences Center School of Medicine, Amarillo
• ACS Health Policy Scholar for General Surgery: SreyRam Kuy, MD, MHS, Louisiana State University, Shreveport
• ACS/American Association of Neurological Surgeons Health Policy Scholar: Kimon Bekelis, MD, Dartmouth-Hitchcock Medical Center, Lebanon, NH
• ACS/American Academy of Otolaryngology–Head & Neck Surgery Health Policy Scholar: Alex J. McKinlay, MD, FACS, Darnall Army Medical Center, Fort Hood, TX
• ACS/American Association for the Surgery of Trauma Health Policy Scholar: Saman Arbabi, MD, FACS, Harborview Medical Center, Seattle, WA
• ACS/American Pediatric Surgery Association Health Policy Scholar: David P. Bliss Jr., MD, FACS, Children’s Medical Center, Dallas, TX
• ACS/American Surgical Association Health Policy Scholar: Eileen M. Bulger, MD, FACS, University of Washington, Seattle
• ACS/American Society of Breast Surgeons Health Policy Scholar: Alyssa D. Throckmorton, MD, FACS, Baptist Medical Group, Nashville, TN
• ACS/American Society of Colon and Rectal Surgeons Health Policy Scholar: Jose G. Guillem, MD, FACS, Memorial Sloan Kettering Cancer Center, New York, NY
• ACS/American Society of Plastic Surgeons Health Policy Scholar: Malcolm Z. Roth, MD, FACS, Albany Medical Center, NY
• ACS/American Urogynecologic Society Health Policy Scholar: Mallika Anand, MD, Spectrum Health Medical Group, Grand Rapids, MI
• ACS/American Urological Association Health Policy Scholar: Thomas Rechtschaffen, MD, FACS, Advanced Urology Centers of New York, Yonkers
• ACS/Eastern Association for the Surgery of Trauma Health Policy Scholar: Alexander L. Eastman, MD, MPH, FACS, University of Texas Southwestern Medical Center, Dallas
• ACS/New England Society of Surgery Health Policy Scholar: Christopher S. Muratore, MD, FACS, Hasbro Children’s Hospital/Rhode Island Hospital, Providence
• ACS/Society for Surgery of the Alimentary Tract Health Policy Scholar: Guilherme Mussi Rocha Campos, MD, FACS, Virginia Commonwealth University, Richmond
• ACS/The Society of Thoracic Surgeons Health Policy Scholar: Daniel T. Engelman, MD, FACS, Baystate Medical Center, Springfield, MA
• ACS/Society for Vascular Surgery Health Policy Scholar: Matthew Jay Sideman, MD, FACS, University of Texas Health Sciences Center, San Antonio
A total of 17 surgeons have been selected to serve as Health Policy Scholars and participate in the Leadership Program for Health Policy and Management, June 12-18 at the Heller School for Social Policy and Management, Brandeis University, Waltham, MA.
Each scholarship includes attendance at the weeklong intensive course, followed by a year’s service in a health policy–related capacity to the American College of Surgeons (ACS) and the surgical specialty society cosponsoring the awardee.
This year’s scholars are as follows:
• ACS Health Policy Scholar for General Surgery: Subhasis Misra, MB, BS, MS, FACS, Texas Tech University Health Sciences Center School of Medicine, Amarillo
• ACS Health Policy Scholar for General Surgery: SreyRam Kuy, MD, MHS, Louisiana State University, Shreveport
• ACS/American Association of Neurological Surgeons Health Policy Scholar: Kimon Bekelis, MD, Dartmouth-Hitchcock Medical Center, Lebanon, NH
• ACS/American Academy of Otolaryngology–Head & Neck Surgery Health Policy Scholar: Alex J. McKinlay, MD, FACS, Darnall Army Medical Center, Fort Hood, TX
• ACS/American Association for the Surgery of Trauma Health Policy Scholar: Saman Arbabi, MD, FACS, Harborview Medical Center, Seattle, WA
• ACS/American Pediatric Surgery Association Health Policy Scholar: David P. Bliss Jr., MD, FACS, Children’s Medical Center, Dallas, TX
• ACS/American Surgical Association Health Policy Scholar: Eileen M. Bulger, MD, FACS, University of Washington, Seattle
• ACS/American Society of Breast Surgeons Health Policy Scholar: Alyssa D. Throckmorton, MD, FACS, Baptist Medical Group, Nashville, TN
• ACS/American Society of Colon and Rectal Surgeons Health Policy Scholar: Jose G. Guillem, MD, FACS, Memorial Sloan Kettering Cancer Center, New York, NY
• ACS/American Society of Plastic Surgeons Health Policy Scholar: Malcolm Z. Roth, MD, FACS, Albany Medical Center, NY
• ACS/American Urogynecologic Society Health Policy Scholar: Mallika Anand, MD, Spectrum Health Medical Group, Grand Rapids, MI
• ACS/American Urological Association Health Policy Scholar: Thomas Rechtschaffen, MD, FACS, Advanced Urology Centers of New York, Yonkers
• ACS/Eastern Association for the Surgery of Trauma Health Policy Scholar: Alexander L. Eastman, MD, MPH, FACS, University of Texas Southwestern Medical Center, Dallas
• ACS/New England Society of Surgery Health Policy Scholar: Christopher S. Muratore, MD, FACS, Hasbro Children’s Hospital/Rhode Island Hospital, Providence
• ACS/Society for Surgery of the Alimentary Tract Health Policy Scholar: Guilherme Mussi Rocha Campos, MD, FACS, Virginia Commonwealth University, Richmond
• ACS/The Society of Thoracic Surgeons Health Policy Scholar: Daniel T. Engelman, MD, FACS, Baystate Medical Center, Springfield, MA
• ACS/Society for Vascular Surgery Health Policy Scholar: Matthew Jay Sideman, MD, FACS, University of Texas Health Sciences Center, San Antonio
Award named in honor of Dr. Clowes available for 2017
The American College of Surgeons (ACS) is pleased to offer the George H. A. Clowes, Jr., MD, FACS, Memorial Research Career Development Award for 2017—made possible through the generosity of The Clowes Fund, Inc., of Indianapolis, IN. This award, consisting of a stipend of $45,000 for each of five years that is non-renewable thereafter, supports the research of a promising young surgical investigator. The closing date for receipt of completed 2017 applications and all related documents is August 1, 2016.
The criteria for selection of the recipient of this award are as follows:
• The award is restricted to a Fellow or an Associate Fellow of the ACS who has completed an accredited residency in general surgery within the last seven years (exclusive of time off for maternity leave, military deployment, or medical leave) and has received a full-time faculty appointment at a medical school accredited by the Liaison Committee on Medical Education in the U.S. or by the Committee for Accreditation of Canadian Medical Schools in Canada. The applicant’s academic appointment may not be above the level of assistant professor. Applicants should provide evidence (by publication or otherwise) of productive initial efforts in laboratory research.
• The award may be used for salary support or other purposes at the discretion of the recipient and the institution. Indirect costs are not paid to the recipient or to the recipient’s institution.
• The ACS Scholarships Committee will not consider applicants who have already received research career development awards from professional societies. The committee will give preference to applicants who have received or are working toward a K08 or K23 National Institutes of Health (NIH) grant. The recipient is responsible for notifying the College’s Scholarships Administrator and requesting approval of funding from another source.
• The administrator (dean or fiscal officer) and the head of the applicant’s department or administrative unit must approve the application. This approval must include a commitment to continuation of the academic position and facilities for research throughout the period of the award. In addition, the approval should specify that at least 50 percent of the applicant’s time will be spent conducting the research proposed in the application. This percentage may run concurrently with the time requirements of NIH or other accepted funding.
• The applicant must submit, in addition to the application form, an NIH-style biosketch, a detailed research plan of up to eight pages in length, and a proposed budget for the five-year period of the award. The applicant also is required to submit a cover letter of no more than one page describing his or her career objectives, how these career objectives will be achieved, and how the research protocol furthers the applicant’s career development. The ACS Scholarships Committee requires an annual written narrative and financial progress report from the recipient; annual renewal will be based on these reports.
• While holding the award, the recipient is required to attend the Clinical Congress of the ACS; the 2017 recipient will be expected to attend the 2018, 2020, and 2022 Clinical Congresses and present reports to the Scholarships Committee and its guests.
• Upon completion of the five-year funding period, the recipient will be required to submit a final narrative report summarizing research progress and providing information regarding current academic rank, sources of research support, and future plans. The recipient also is required to apply to the Scientific Forum at the conclusion of the award period.
The application form must be completed online and may be posted on the ACS website at facs.org/member-services/scholarships/research/acsclowes. Contact the Scholarships Administrator at [email protected] for additional information.
The American College of Surgeons (ACS) is pleased to offer the George H. A. Clowes, Jr., MD, FACS, Memorial Research Career Development Award for 2017—made possible through the generosity of The Clowes Fund, Inc., of Indianapolis, IN. This award, consisting of a stipend of $45,000 for each of five years that is non-renewable thereafter, supports the research of a promising young surgical investigator. The closing date for receipt of completed 2017 applications and all related documents is August 1, 2016.
The criteria for selection of the recipient of this award are as follows:
• The award is restricted to a Fellow or an Associate Fellow of the ACS who has completed an accredited residency in general surgery within the last seven years (exclusive of time off for maternity leave, military deployment, or medical leave) and has received a full-time faculty appointment at a medical school accredited by the Liaison Committee on Medical Education in the U.S. or by the Committee for Accreditation of Canadian Medical Schools in Canada. The applicant’s academic appointment may not be above the level of assistant professor. Applicants should provide evidence (by publication or otherwise) of productive initial efforts in laboratory research.
• The award may be used for salary support or other purposes at the discretion of the recipient and the institution. Indirect costs are not paid to the recipient or to the recipient’s institution.
• The ACS Scholarships Committee will not consider applicants who have already received research career development awards from professional societies. The committee will give preference to applicants who have received or are working toward a K08 or K23 National Institutes of Health (NIH) grant. The recipient is responsible for notifying the College’s Scholarships Administrator and requesting approval of funding from another source.
• The administrator (dean or fiscal officer) and the head of the applicant’s department or administrative unit must approve the application. This approval must include a commitment to continuation of the academic position and facilities for research throughout the period of the award. In addition, the approval should specify that at least 50 percent of the applicant’s time will be spent conducting the research proposed in the application. This percentage may run concurrently with the time requirements of NIH or other accepted funding.
• The applicant must submit, in addition to the application form, an NIH-style biosketch, a detailed research plan of up to eight pages in length, and a proposed budget for the five-year period of the award. The applicant also is required to submit a cover letter of no more than one page describing his or her career objectives, how these career objectives will be achieved, and how the research protocol furthers the applicant’s career development. The ACS Scholarships Committee requires an annual written narrative and financial progress report from the recipient; annual renewal will be based on these reports.
• While holding the award, the recipient is required to attend the Clinical Congress of the ACS; the 2017 recipient will be expected to attend the 2018, 2020, and 2022 Clinical Congresses and present reports to the Scholarships Committee and its guests.
• Upon completion of the five-year funding period, the recipient will be required to submit a final narrative report summarizing research progress and providing information regarding current academic rank, sources of research support, and future plans. The recipient also is required to apply to the Scientific Forum at the conclusion of the award period.
The application form must be completed online and may be posted on the ACS website at facs.org/member-services/scholarships/research/acsclowes. Contact the Scholarships Administrator at [email protected] for additional information.
The American College of Surgeons (ACS) is pleased to offer the George H. A. Clowes, Jr., MD, FACS, Memorial Research Career Development Award for 2017—made possible through the generosity of The Clowes Fund, Inc., of Indianapolis, IN. This award, consisting of a stipend of $45,000 for each of five years that is non-renewable thereafter, supports the research of a promising young surgical investigator. The closing date for receipt of completed 2017 applications and all related documents is August 1, 2016.
The criteria for selection of the recipient of this award are as follows:
• The award is restricted to a Fellow or an Associate Fellow of the ACS who has completed an accredited residency in general surgery within the last seven years (exclusive of time off for maternity leave, military deployment, or medical leave) and has received a full-time faculty appointment at a medical school accredited by the Liaison Committee on Medical Education in the U.S. or by the Committee for Accreditation of Canadian Medical Schools in Canada. The applicant’s academic appointment may not be above the level of assistant professor. Applicants should provide evidence (by publication or otherwise) of productive initial efforts in laboratory research.
• The award may be used for salary support or other purposes at the discretion of the recipient and the institution. Indirect costs are not paid to the recipient or to the recipient’s institution.
• The ACS Scholarships Committee will not consider applicants who have already received research career development awards from professional societies. The committee will give preference to applicants who have received or are working toward a K08 or K23 National Institutes of Health (NIH) grant. The recipient is responsible for notifying the College’s Scholarships Administrator and requesting approval of funding from another source.
• The administrator (dean or fiscal officer) and the head of the applicant’s department or administrative unit must approve the application. This approval must include a commitment to continuation of the academic position and facilities for research throughout the period of the award. In addition, the approval should specify that at least 50 percent of the applicant’s time will be spent conducting the research proposed in the application. This percentage may run concurrently with the time requirements of NIH or other accepted funding.
• The applicant must submit, in addition to the application form, an NIH-style biosketch, a detailed research plan of up to eight pages in length, and a proposed budget for the five-year period of the award. The applicant also is required to submit a cover letter of no more than one page describing his or her career objectives, how these career objectives will be achieved, and how the research protocol furthers the applicant’s career development. The ACS Scholarships Committee requires an annual written narrative and financial progress report from the recipient; annual renewal will be based on these reports.
• While holding the award, the recipient is required to attend the Clinical Congress of the ACS; the 2017 recipient will be expected to attend the 2018, 2020, and 2022 Clinical Congresses and present reports to the Scholarships Committee and its guests.
• Upon completion of the five-year funding period, the recipient will be required to submit a final narrative report summarizing research progress and providing information regarding current academic rank, sources of research support, and future plans. The recipient also is required to apply to the Scientific Forum at the conclusion of the award period.
The application form must be completed online and may be posted on the ACS website at facs.org/member-services/scholarships/research/acsclowes. Contact the Scholarships Administrator at [email protected] for additional information.
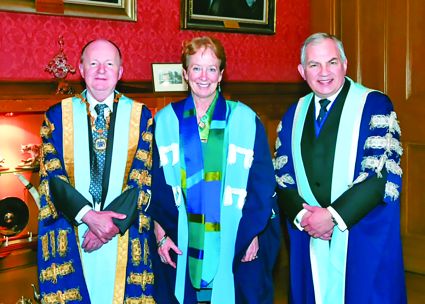
Dr. Julie Ann Freischlag inducted into Royal College of Surgeons of Edinburgh
Julie Ann Freischlag, MD, FACS, vice-chancellor for human health sciences; dean, University of California (UC) Davis School of Medicine; and Past-Chair, American College of Surgeons Board of Regents, and former President of the Society for Vascular Surgery was inducted into the Royal College of Surgeons of Edinburgh (RCSEd) on April 22.
For more than 15 years, Dr. Freischlag has led education and training programs at medical schools in her role as professor and chair of surgery and vascular surgery departments. Dr. Freischlag also has more than 25 years of experience leading patient care services as chief of surgery or vascular surgery.
Dr. Freischlag currently oversees UC Davis Health System’s academic, research, and clinical programs, including the School of Medicine, the Betty Irene Moore School of Nursing, the 1,000-member physician practice group, and UC Davis Medical Center, a 619-bed acute care hospital. Before joining UC Davis, she served as professor and chair, surgery department, and surgeon-in-chief at Johns Hopkins Medical Institutions, Baltimore, MD. At Johns Hopkins, she led initiatives to expand research, add specialty clinical services, improve patient-centered care and patient safety, redesign the surgical training program, and enhance academic career paths for faculty.
Established in 1505, the RCSEd is among the world’s oldest surgical organizations, and admittance into its fellowship is based on professional prominence. With a worldwide membership, the RCSEd pursues excellence and advancement in surgical and dental practice via education, training, and examinations.
Julie Ann Freischlag, MD, FACS, vice-chancellor for human health sciences; dean, University of California (UC) Davis School of Medicine; and Past-Chair, American College of Surgeons Board of Regents, and former President of the Society for Vascular Surgery was inducted into the Royal College of Surgeons of Edinburgh (RCSEd) on April 22.
For more than 15 years, Dr. Freischlag has led education and training programs at medical schools in her role as professor and chair of surgery and vascular surgery departments. Dr. Freischlag also has more than 25 years of experience leading patient care services as chief of surgery or vascular surgery.
Dr. Freischlag currently oversees UC Davis Health System’s academic, research, and clinical programs, including the School of Medicine, the Betty Irene Moore School of Nursing, the 1,000-member physician practice group, and UC Davis Medical Center, a 619-bed acute care hospital. Before joining UC Davis, she served as professor and chair, surgery department, and surgeon-in-chief at Johns Hopkins Medical Institutions, Baltimore, MD. At Johns Hopkins, she led initiatives to expand research, add specialty clinical services, improve patient-centered care and patient safety, redesign the surgical training program, and enhance academic career paths for faculty.
Established in 1505, the RCSEd is among the world’s oldest surgical organizations, and admittance into its fellowship is based on professional prominence. With a worldwide membership, the RCSEd pursues excellence and advancement in surgical and dental practice via education, training, and examinations.
Julie Ann Freischlag, MD, FACS, vice-chancellor for human health sciences; dean, University of California (UC) Davis School of Medicine; and Past-Chair, American College of Surgeons Board of Regents, and former President of the Society for Vascular Surgery was inducted into the Royal College of Surgeons of Edinburgh (RCSEd) on April 22.
For more than 15 years, Dr. Freischlag has led education and training programs at medical schools in her role as professor and chair of surgery and vascular surgery departments. Dr. Freischlag also has more than 25 years of experience leading patient care services as chief of surgery or vascular surgery.
Dr. Freischlag currently oversees UC Davis Health System’s academic, research, and clinical programs, including the School of Medicine, the Betty Irene Moore School of Nursing, the 1,000-member physician practice group, and UC Davis Medical Center, a 619-bed acute care hospital. Before joining UC Davis, she served as professor and chair, surgery department, and surgeon-in-chief at Johns Hopkins Medical Institutions, Baltimore, MD. At Johns Hopkins, she led initiatives to expand research, add specialty clinical services, improve patient-centered care and patient safety, redesign the surgical training program, and enhance academic career paths for faculty.
Established in 1505, the RCSEd is among the world’s oldest surgical organizations, and admittance into its fellowship is based on professional prominence. With a worldwide membership, the RCSEd pursues excellence and advancement in surgical and dental practice via education, training, and examinations.
Drs. A. Brent Eastman, Michael Sinclair named UCSF Alumni of the Year
A. Brent Eastman, MD, FACS, a general, vascular, and trauma surgeon from San Diego, CA, and a Past-President of the American College of Surgeons, was one of two Fellows who received the University of California, San Francisco (UCSF) Medical Alumni Association’s 2016 Alumni of the Year awards at the 50th reunion of the UCSF School of Medicine. Michael C. Sinclair, MD, FACS, Allentown, PA, a retired cardiothoracic surgeon, mountain climber, and author of a memoir, No Regrets, No Apologies, also was honored. Alumni Association president Yao Heng, MD, San Francisco, presented the awards to the two 1966 alumni at an April 9 dinner with UCSF Medical School dean Talmadge King, Jr., MD.
Dr. Eastman is a former corporate senior vice-president and chief medical officer of Scripps Health, N. Paul Whittier Endowed Chair of Trauma at Scripps Memorial Hospital, La Jolla, and clinical professor of surgery-trauma at the University of California, San Diego. He is a founder of the San Diego County Trauma System, which is now in its 32nd year and regarded worldwide as a model for trauma care.
Dr. Eastman’s efforts in trauma took him around the world. He was part of a team that cared for thousands of evacuees after Hurricane Katrina in New Orleans, LA, in 2005, and assisted earthquake victims in Haiti in 2010. He has assisted in the development of extensive trauma systems internationally, including throughout India. In addition, he was a visiting surgeon at the U.S. military hospital in Landstuhl, Germany, where he provided care to soldiers injured in the Iraq and Afghanistan wars.
Dr. Sinclair has volunteered for a number of international humanitarian missions in Croatia, Guatemala, Jordan, Pakistan, Libya, and Nigeria and is currently on a two-year tour to provide surgical care and training in Rwanda.
The Alumni of the Year award is regarded as the highest honor bestowed by the UCSF Medical Alumni Association. Each year, alumni from all classes nominate fellow classmates who have demonstrated dedication to the principles of a physician, made significant contributions to medicine, and provided community service.
A. Brent Eastman, MD, FACS, a general, vascular, and trauma surgeon from San Diego, CA, and a Past-President of the American College of Surgeons, was one of two Fellows who received the University of California, San Francisco (UCSF) Medical Alumni Association’s 2016 Alumni of the Year awards at the 50th reunion of the UCSF School of Medicine. Michael C. Sinclair, MD, FACS, Allentown, PA, a retired cardiothoracic surgeon, mountain climber, and author of a memoir, No Regrets, No Apologies, also was honored. Alumni Association president Yao Heng, MD, San Francisco, presented the awards to the two 1966 alumni at an April 9 dinner with UCSF Medical School dean Talmadge King, Jr., MD.
Dr. Eastman is a former corporate senior vice-president and chief medical officer of Scripps Health, N. Paul Whittier Endowed Chair of Trauma at Scripps Memorial Hospital, La Jolla, and clinical professor of surgery-trauma at the University of California, San Diego. He is a founder of the San Diego County Trauma System, which is now in its 32nd year and regarded worldwide as a model for trauma care.
Dr. Eastman’s efforts in trauma took him around the world. He was part of a team that cared for thousands of evacuees after Hurricane Katrina in New Orleans, LA, in 2005, and assisted earthquake victims in Haiti in 2010. He has assisted in the development of extensive trauma systems internationally, including throughout India. In addition, he was a visiting surgeon at the U.S. military hospital in Landstuhl, Germany, where he provided care to soldiers injured in the Iraq and Afghanistan wars.
Dr. Sinclair has volunteered for a number of international humanitarian missions in Croatia, Guatemala, Jordan, Pakistan, Libya, and Nigeria and is currently on a two-year tour to provide surgical care and training in Rwanda.
The Alumni of the Year award is regarded as the highest honor bestowed by the UCSF Medical Alumni Association. Each year, alumni from all classes nominate fellow classmates who have demonstrated dedication to the principles of a physician, made significant contributions to medicine, and provided community service.
A. Brent Eastman, MD, FACS, a general, vascular, and trauma surgeon from San Diego, CA, and a Past-President of the American College of Surgeons, was one of two Fellows who received the University of California, San Francisco (UCSF) Medical Alumni Association’s 2016 Alumni of the Year awards at the 50th reunion of the UCSF School of Medicine. Michael C. Sinclair, MD, FACS, Allentown, PA, a retired cardiothoracic surgeon, mountain climber, and author of a memoir, No Regrets, No Apologies, also was honored. Alumni Association president Yao Heng, MD, San Francisco, presented the awards to the two 1966 alumni at an April 9 dinner with UCSF Medical School dean Talmadge King, Jr., MD.
Dr. Eastman is a former corporate senior vice-president and chief medical officer of Scripps Health, N. Paul Whittier Endowed Chair of Trauma at Scripps Memorial Hospital, La Jolla, and clinical professor of surgery-trauma at the University of California, San Diego. He is a founder of the San Diego County Trauma System, which is now in its 32nd year and regarded worldwide as a model for trauma care.
Dr. Eastman’s efforts in trauma took him around the world. He was part of a team that cared for thousands of evacuees after Hurricane Katrina in New Orleans, LA, in 2005, and assisted earthquake victims in Haiti in 2010. He has assisted in the development of extensive trauma systems internationally, including throughout India. In addition, he was a visiting surgeon at the U.S. military hospital in Landstuhl, Germany, where he provided care to soldiers injured in the Iraq and Afghanistan wars.
Dr. Sinclair has volunteered for a number of international humanitarian missions in Croatia, Guatemala, Jordan, Pakistan, Libya, and Nigeria and is currently on a two-year tour to provide surgical care and training in Rwanda.
The Alumni of the Year award is regarded as the highest honor bestowed by the UCSF Medical Alumni Association. Each year, alumni from all classes nominate fellow classmates who have demonstrated dedication to the principles of a physician, made significant contributions to medicine, and provided community service.
ACS announces 2016 Oweida Scholarship recipient
The Executive Committee of the American College of Surgeons (ACS) Board of Governors has selected the recipient of the 2016 Nizar N. Oweida, MD, FACS, Scholarship of the ACS – Chayanin Musikasinthorn, MD, MPH, FACS, a general and trauma/critical care surgeon, Gallup Indian Medical Center, NM. Dr. Musikasinthorn is a commissioned officer of the U.S. Public Health Service and provides surgical services to members of the local First Nation population, the Navajo people.
The scholarship will enable Dr. Musikasinthorn to attend Clinical Congress 2016, October 16-20 in Washington, DC, to enhance her ability to provide quality surgical care to patients. She will give a presentation at the Scholarships Committee meeting and the Rural Surgery Forum at Clinical Congress.
The Oweida Scholarship was established in 1998 in memory of Dr. Oweida, a general surgeon from a small town in western Pennsylvania. The $5,000 award subsidizes attendance at the annual Clinical Congress, including Postgraduate Course fees.
The Oweida Scholarship provides young surgeons who practice in rural communities with the opportunity to attend the Clinical Congress and benefit from its educational experiences. It is awarded annually.
The requirements for this award are posted to the College website at facs.org/member-services/scholarships/special/oweida. The application deadline for the 2017 Oweida Scholarship is December 15, 2016.
The Executive Committee of the American College of Surgeons (ACS) Board of Governors has selected the recipient of the 2016 Nizar N. Oweida, MD, FACS, Scholarship of the ACS – Chayanin Musikasinthorn, MD, MPH, FACS, a general and trauma/critical care surgeon, Gallup Indian Medical Center, NM. Dr. Musikasinthorn is a commissioned officer of the U.S. Public Health Service and provides surgical services to members of the local First Nation population, the Navajo people.
The scholarship will enable Dr. Musikasinthorn to attend Clinical Congress 2016, October 16-20 in Washington, DC, to enhance her ability to provide quality surgical care to patients. She will give a presentation at the Scholarships Committee meeting and the Rural Surgery Forum at Clinical Congress.
The Oweida Scholarship was established in 1998 in memory of Dr. Oweida, a general surgeon from a small town in western Pennsylvania. The $5,000 award subsidizes attendance at the annual Clinical Congress, including Postgraduate Course fees.
The Oweida Scholarship provides young surgeons who practice in rural communities with the opportunity to attend the Clinical Congress and benefit from its educational experiences. It is awarded annually.
The requirements for this award are posted to the College website at facs.org/member-services/scholarships/special/oweida. The application deadline for the 2017 Oweida Scholarship is December 15, 2016.
The Executive Committee of the American College of Surgeons (ACS) Board of Governors has selected the recipient of the 2016 Nizar N. Oweida, MD, FACS, Scholarship of the ACS – Chayanin Musikasinthorn, MD, MPH, FACS, a general and trauma/critical care surgeon, Gallup Indian Medical Center, NM. Dr. Musikasinthorn is a commissioned officer of the U.S. Public Health Service and provides surgical services to members of the local First Nation population, the Navajo people.
The scholarship will enable Dr. Musikasinthorn to attend Clinical Congress 2016, October 16-20 in Washington, DC, to enhance her ability to provide quality surgical care to patients. She will give a presentation at the Scholarships Committee meeting and the Rural Surgery Forum at Clinical Congress.
The Oweida Scholarship was established in 1998 in memory of Dr. Oweida, a general surgeon from a small town in western Pennsylvania. The $5,000 award subsidizes attendance at the annual Clinical Congress, including Postgraduate Course fees.
The Oweida Scholarship provides young surgeons who practice in rural communities with the opportunity to attend the Clinical Congress and benefit from its educational experiences. It is awarded annually.
The requirements for this award are posted to the College website at facs.org/member-services/scholarships/special/oweida. The application deadline for the 2017 Oweida Scholarship is December 15, 2016.
Register now for ACS NSQIP Conference, July 16−19 in San Diego, CA
Online registration for the 2016 American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP®) Conference, July 16−19 at the Hilton San Diego Bayfront, CA, is open. View the agenda on the conference brochure at facs.org/quality-programs/acs-nsqip/events/annual-conference/agenda. Conference space is limited.
With the theme of Innovate to Make a Difference, interactive workshops, informal meetings, and sessions built around personal perspectives will explore employing innovative approaches and ideas to improve patient safety and improve processes. The conference will include additional pediatric-specific content tailored to fit the needs of ACS NSQIP Pediatric program participants.
Julie A. Freischlag, MD, FACS, vice-chancellor for human health sciences and dean of the school of medicine at the University of California, Davis, will be the keynote speaker. A prominent academic health leader and a national voice for improving health and health care, Dr. Freischlag oversees UC Davis Health System’s academic, research, and clinical programs, including the school of medicine, the Betty Irene Moore School of Nursing, the 1,000-member physician practice group, and UC Davis Medical Center, a 619-bed acute-care hospital. Dr. Freischlag’s speech, Career Satisfaction by Way of Resilience, will highlight ways for health care professionals to find career happiness through flexibility, resiliency, and avoiding burnout.
For details regarding registration, contact Registration Services at 312-202-5244 or [email protected]. For questions about the conference, contact ACS NSQIP staff at 312-202-5261 or [email protected].
Online registration for the 2016 American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP®) Conference, July 16−19 at the Hilton San Diego Bayfront, CA, is open. View the agenda on the conference brochure at facs.org/quality-programs/acs-nsqip/events/annual-conference/agenda. Conference space is limited.
With the theme of Innovate to Make a Difference, interactive workshops, informal meetings, and sessions built around personal perspectives will explore employing innovative approaches and ideas to improve patient safety and improve processes. The conference will include additional pediatric-specific content tailored to fit the needs of ACS NSQIP Pediatric program participants.
Julie A. Freischlag, MD, FACS, vice-chancellor for human health sciences and dean of the school of medicine at the University of California, Davis, will be the keynote speaker. A prominent academic health leader and a national voice for improving health and health care, Dr. Freischlag oversees UC Davis Health System’s academic, research, and clinical programs, including the school of medicine, the Betty Irene Moore School of Nursing, the 1,000-member physician practice group, and UC Davis Medical Center, a 619-bed acute-care hospital. Dr. Freischlag’s speech, Career Satisfaction by Way of Resilience, will highlight ways for health care professionals to find career happiness through flexibility, resiliency, and avoiding burnout.
For details regarding registration, contact Registration Services at 312-202-5244 or [email protected]. For questions about the conference, contact ACS NSQIP staff at 312-202-5261 or [email protected].
Online registration for the 2016 American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP®) Conference, July 16−19 at the Hilton San Diego Bayfront, CA, is open. View the agenda on the conference brochure at facs.org/quality-programs/acs-nsqip/events/annual-conference/agenda. Conference space is limited.
With the theme of Innovate to Make a Difference, interactive workshops, informal meetings, and sessions built around personal perspectives will explore employing innovative approaches and ideas to improve patient safety and improve processes. The conference will include additional pediatric-specific content tailored to fit the needs of ACS NSQIP Pediatric program participants.
Julie A. Freischlag, MD, FACS, vice-chancellor for human health sciences and dean of the school of medicine at the University of California, Davis, will be the keynote speaker. A prominent academic health leader and a national voice for improving health and health care, Dr. Freischlag oversees UC Davis Health System’s academic, research, and clinical programs, including the school of medicine, the Betty Irene Moore School of Nursing, the 1,000-member physician practice group, and UC Davis Medical Center, a 619-bed acute-care hospital. Dr. Freischlag’s speech, Career Satisfaction by Way of Resilience, will highlight ways for health care professionals to find career happiness through flexibility, resiliency, and avoiding burnout.
For details regarding registration, contact Registration Services at 312-202-5244 or [email protected]. For questions about the conference, contact ACS NSQIP staff at 312-202-5261 or [email protected].
ACGME announces FIRST trial waiver for 2016−2017
On May 17, the Accreditation Council for Graduate Medical Education (ACGME) announced that it “has issued a multicenter research trial waiver, along with seed funding, to the Flexibility in Duty Hour Requirements for Surgical Trainees (FIRST) Trial for the 2016−2017 academic year, based on the recommendation of the ACGME Review Committee for Surgery.” The ACGME Task Force reviewing Common Program Requirements for residency training in the U.S. determined that, in order to comprehensively evaluate the clinical education and experience environment, “it is premature to issue any proposed modifications to requirements for the upcoming academic year.”
Working together in the best interests of surgical patient safety, the American College of Surgeons and the American Board of Surgery will continue to collect high-quality data during this one-year expansion of the FIRST Trial. In this time, new programs that meet the requirements as of July 1, 2016, will be allowed to enroll in the trial, and those programs already enrolled will be able to add ongoing data to support future reviews of residency program standards. The one-year expansion will conclude in June 2017.
FIRST Trial results were released online February 2 in the New England Journal of Medicine and presented concurrently at the 2016 Academic Surgical Congress in Jacksonville, FL, by the trial’s principal investigator, Karl Y. Bilimoria, MD, MS, FACS. The findings indicated that surgical residents can work more flexible hours than currently allowed by the ACGME without compromising surgical patient safety.
In addition to the patient safety findings, FIRST Trial results indicated that flexibility allowed for greater continuity of patient care, fewer handoffs to other care providers, and increased resident satisfaction. Read the announcement on the ACGME website at www.acgme.org/Portals/0/PDFs/Nasca-Community/NascaLettertotheCommunity-5-17-16.pdf.
On May 17, the Accreditation Council for Graduate Medical Education (ACGME) announced that it “has issued a multicenter research trial waiver, along with seed funding, to the Flexibility in Duty Hour Requirements for Surgical Trainees (FIRST) Trial for the 2016−2017 academic year, based on the recommendation of the ACGME Review Committee for Surgery.” The ACGME Task Force reviewing Common Program Requirements for residency training in the U.S. determined that, in order to comprehensively evaluate the clinical education and experience environment, “it is premature to issue any proposed modifications to requirements for the upcoming academic year.”
Working together in the best interests of surgical patient safety, the American College of Surgeons and the American Board of Surgery will continue to collect high-quality data during this one-year expansion of the FIRST Trial. In this time, new programs that meet the requirements as of July 1, 2016, will be allowed to enroll in the trial, and those programs already enrolled will be able to add ongoing data to support future reviews of residency program standards. The one-year expansion will conclude in June 2017.
FIRST Trial results were released online February 2 in the New England Journal of Medicine and presented concurrently at the 2016 Academic Surgical Congress in Jacksonville, FL, by the trial’s principal investigator, Karl Y. Bilimoria, MD, MS, FACS. The findings indicated that surgical residents can work more flexible hours than currently allowed by the ACGME without compromising surgical patient safety.
In addition to the patient safety findings, FIRST Trial results indicated that flexibility allowed for greater continuity of patient care, fewer handoffs to other care providers, and increased resident satisfaction. Read the announcement on the ACGME website at www.acgme.org/Portals/0/PDFs/Nasca-Community/NascaLettertotheCommunity-5-17-16.pdf.
On May 17, the Accreditation Council for Graduate Medical Education (ACGME) announced that it “has issued a multicenter research trial waiver, along with seed funding, to the Flexibility in Duty Hour Requirements for Surgical Trainees (FIRST) Trial for the 2016−2017 academic year, based on the recommendation of the ACGME Review Committee for Surgery.” The ACGME Task Force reviewing Common Program Requirements for residency training in the U.S. determined that, in order to comprehensively evaluate the clinical education and experience environment, “it is premature to issue any proposed modifications to requirements for the upcoming academic year.”
Working together in the best interests of surgical patient safety, the American College of Surgeons and the American Board of Surgery will continue to collect high-quality data during this one-year expansion of the FIRST Trial. In this time, new programs that meet the requirements as of July 1, 2016, will be allowed to enroll in the trial, and those programs already enrolled will be able to add ongoing data to support future reviews of residency program standards. The one-year expansion will conclude in June 2017.
FIRST Trial results were released online February 2 in the New England Journal of Medicine and presented concurrently at the 2016 Academic Surgical Congress in Jacksonville, FL, by the trial’s principal investigator, Karl Y. Bilimoria, MD, MS, FACS. The findings indicated that surgical residents can work more flexible hours than currently allowed by the ACGME without compromising surgical patient safety.
In addition to the patient safety findings, FIRST Trial results indicated that flexibility allowed for greater continuity of patient care, fewer handoffs to other care providers, and increased resident satisfaction. Read the announcement on the ACGME website at www.acgme.org/Portals/0/PDFs/Nasca-Community/NascaLettertotheCommunity-5-17-16.pdf.
Surgical workforce shortages in rural areas
This month I write about one of the College’s current advocacy efforts directed at ensuring an adequate surgical workforce in underserved and rural areas. Evidence indicates a current and growing shortage of surgeons available to serve the needs of populations in certain parts of the country. A shortage of general surgeons is a clear component to the crisis in health care workforce. Accordingly, the American College of Surgeons (ACS) is urging policy makers to recognize that only surgeons are uniquely qualified to provide certain necessary, lifesaving procedures, which other health professionals are neither trained nor competent to provide.
To determine where these areas of shortage are located and where access to surgical care is thus potentially a challenge, the ACS is strongly supporting the efforts of Representatives Larry Bucshon, MD, FACS (R-Ind.) and Ami Bera, MD (D-Calif.) who recently introduced H.R. 4959, the Ensuring Access to General Surgery Act of 2016. This legislation serves to direct the Secretary of the Department of Health and Human Services (HHS) to conduct a study on the designation of surgical Health Professional Shortage Areas (HPSA).
A variety of federal programs use the HPSA designation to improve access to health care by focusing aid and assistance on specific geographic areas and populations with the greatest unmet needs. The division of HHS known as the Health Resources and Services Administration (HRSA) has developed criteria used to determine whether certain geographic areas, population groups, or facilities may be designated as a HPSA. HPSA designation may be applied to urban or rural geographic areas, specific population groups, medical provider groups, or other public health care facilities. Currently, HRSA limits HPSA designations to shortages in primary care services, dental services, or mental health services.
HRSA has never designated an entity as a HPSA purely based upon a shortage of surgical services. In light of the available evidence relative to the shortage of surgical providers in certain parts of the country, ACS believes that research is necessary to determine exactly what constitutes a surgical shortage area, e.g., establish definitional criteria, with subsequent application of those criteria to determine where areas so defined are located. Such would provide HRSA with a valuable tool to utilize in efforts directed at increasing patient access to surgical care. Ultimately, offering incentives to surgeons to locate or remain in HPSA communities could become critical in guaranteeing all Medicare beneficiaries, regardless of geographic location, have access to quality surgical care. Determining what constitutes a surgical shortage area will serve to help HRSA to appropriately focus its resources.
Accordingly, we need your help and urge you to take action today.
Using the information below, please call your representatives today and urge them to join their colleagues and cosponsor H.R. 4959, the Ensuring Access to General Surgery Act of 2016.
Instructions
Call toll-free: 1-877-996-4464
You will be connected to your representative‘s office. Once you are connected, provide your name and indicate that you are a constituent. You should also be prepared to provide additional contact information for follow-up purposes.
Next, we suggest you use the following message:
• As a surgeon and as your constituent, I urge you to join your colleagues and cosponsor H.R. 4959, the Ensuring Access to General Surgery Act of 2016, which would direct the Secretary of Department of Health and Human Services (HHS) to conduct a study to designate General Surgery Health Professional Shortage Areas (HPSA).
• The division of HHS known as the Health Resources and Services Administration (HRSA) has developed designation criteria in order to determine whether certain geographic areas, population groups, or facilities may be designated as a HPSA.
• HRSA has never designated an entity as a HPSA purely based upon a shortage of surgical services.
• In light of evidence relative to a shortage of surgeons, ACS believes that research is necessary to determine exactly what constitutes a surgical shortage area and subsequently where these areas exist.
Alternatively, for those who were seeking a topic on which to initiate a personal in-district meeting with representatives and their staff as was discussed in last month’s edition of this column, H.R. 4959 presents a prime subject for such in order to have a focused meeting with a specific ask on a “white hat” issue that will surely resonate with members of Congress. Currently, in-district work periods are scheduled for the last week of June, the last two weeks of July, and the entire month of August.
As always, those with questions or concerns, or those who need assistance in setting up an in-district meeting may contact staff of the Division of Advocacy and Health Policy by phone at 202-337-2701 or via e-mail at [email protected].
Thank you for taking the time to engage and take action on this critical issue.
Please encourage your colleagues to do likewise.
Until next month ...
Dr. Patrick V. Bailey is an ACS Fellow, a pediatric surgeon, and Medical Director, Advocacy, for the Division of Advocacy and Health Policy, in the ACS offices in Washington, DC.
This month I write about one of the College’s current advocacy efforts directed at ensuring an adequate surgical workforce in underserved and rural areas. Evidence indicates a current and growing shortage of surgeons available to serve the needs of populations in certain parts of the country. A shortage of general surgeons is a clear component to the crisis in health care workforce. Accordingly, the American College of Surgeons (ACS) is urging policy makers to recognize that only surgeons are uniquely qualified to provide certain necessary, lifesaving procedures, which other health professionals are neither trained nor competent to provide.
To determine where these areas of shortage are located and where access to surgical care is thus potentially a challenge, the ACS is strongly supporting the efforts of Representatives Larry Bucshon, MD, FACS (R-Ind.) and Ami Bera, MD (D-Calif.) who recently introduced H.R. 4959, the Ensuring Access to General Surgery Act of 2016. This legislation serves to direct the Secretary of the Department of Health and Human Services (HHS) to conduct a study on the designation of surgical Health Professional Shortage Areas (HPSA).
A variety of federal programs use the HPSA designation to improve access to health care by focusing aid and assistance on specific geographic areas and populations with the greatest unmet needs. The division of HHS known as the Health Resources and Services Administration (HRSA) has developed criteria used to determine whether certain geographic areas, population groups, or facilities may be designated as a HPSA. HPSA designation may be applied to urban or rural geographic areas, specific population groups, medical provider groups, or other public health care facilities. Currently, HRSA limits HPSA designations to shortages in primary care services, dental services, or mental health services.
HRSA has never designated an entity as a HPSA purely based upon a shortage of surgical services. In light of the available evidence relative to the shortage of surgical providers in certain parts of the country, ACS believes that research is necessary to determine exactly what constitutes a surgical shortage area, e.g., establish definitional criteria, with subsequent application of those criteria to determine where areas so defined are located. Such would provide HRSA with a valuable tool to utilize in efforts directed at increasing patient access to surgical care. Ultimately, offering incentives to surgeons to locate or remain in HPSA communities could become critical in guaranteeing all Medicare beneficiaries, regardless of geographic location, have access to quality surgical care. Determining what constitutes a surgical shortage area will serve to help HRSA to appropriately focus its resources.
Accordingly, we need your help and urge you to take action today.
Using the information below, please call your representatives today and urge them to join their colleagues and cosponsor H.R. 4959, the Ensuring Access to General Surgery Act of 2016.
Instructions
Call toll-free: 1-877-996-4464
You will be connected to your representative‘s office. Once you are connected, provide your name and indicate that you are a constituent. You should also be prepared to provide additional contact information for follow-up purposes.
Next, we suggest you use the following message:
• As a surgeon and as your constituent, I urge you to join your colleagues and cosponsor H.R. 4959, the Ensuring Access to General Surgery Act of 2016, which would direct the Secretary of Department of Health and Human Services (HHS) to conduct a study to designate General Surgery Health Professional Shortage Areas (HPSA).
• The division of HHS known as the Health Resources and Services Administration (HRSA) has developed designation criteria in order to determine whether certain geographic areas, population groups, or facilities may be designated as a HPSA.
• HRSA has never designated an entity as a HPSA purely based upon a shortage of surgical services.
• In light of evidence relative to a shortage of surgeons, ACS believes that research is necessary to determine exactly what constitutes a surgical shortage area and subsequently where these areas exist.
Alternatively, for those who were seeking a topic on which to initiate a personal in-district meeting with representatives and their staff as was discussed in last month’s edition of this column, H.R. 4959 presents a prime subject for such in order to have a focused meeting with a specific ask on a “white hat” issue that will surely resonate with members of Congress. Currently, in-district work periods are scheduled for the last week of June, the last two weeks of July, and the entire month of August.
As always, those with questions or concerns, or those who need assistance in setting up an in-district meeting may contact staff of the Division of Advocacy and Health Policy by phone at 202-337-2701 or via e-mail at [email protected].
Thank you for taking the time to engage and take action on this critical issue.
Please encourage your colleagues to do likewise.
Until next month ...
Dr. Patrick V. Bailey is an ACS Fellow, a pediatric surgeon, and Medical Director, Advocacy, for the Division of Advocacy and Health Policy, in the ACS offices in Washington, DC.
This month I write about one of the College’s current advocacy efforts directed at ensuring an adequate surgical workforce in underserved and rural areas. Evidence indicates a current and growing shortage of surgeons available to serve the needs of populations in certain parts of the country. A shortage of general surgeons is a clear component to the crisis in health care workforce. Accordingly, the American College of Surgeons (ACS) is urging policy makers to recognize that only surgeons are uniquely qualified to provide certain necessary, lifesaving procedures, which other health professionals are neither trained nor competent to provide.
To determine where these areas of shortage are located and where access to surgical care is thus potentially a challenge, the ACS is strongly supporting the efforts of Representatives Larry Bucshon, MD, FACS (R-Ind.) and Ami Bera, MD (D-Calif.) who recently introduced H.R. 4959, the Ensuring Access to General Surgery Act of 2016. This legislation serves to direct the Secretary of the Department of Health and Human Services (HHS) to conduct a study on the designation of surgical Health Professional Shortage Areas (HPSA).
A variety of federal programs use the HPSA designation to improve access to health care by focusing aid and assistance on specific geographic areas and populations with the greatest unmet needs. The division of HHS known as the Health Resources and Services Administration (HRSA) has developed criteria used to determine whether certain geographic areas, population groups, or facilities may be designated as a HPSA. HPSA designation may be applied to urban or rural geographic areas, specific population groups, medical provider groups, or other public health care facilities. Currently, HRSA limits HPSA designations to shortages in primary care services, dental services, or mental health services.
HRSA has never designated an entity as a HPSA purely based upon a shortage of surgical services. In light of the available evidence relative to the shortage of surgical providers in certain parts of the country, ACS believes that research is necessary to determine exactly what constitutes a surgical shortage area, e.g., establish definitional criteria, with subsequent application of those criteria to determine where areas so defined are located. Such would provide HRSA with a valuable tool to utilize in efforts directed at increasing patient access to surgical care. Ultimately, offering incentives to surgeons to locate or remain in HPSA communities could become critical in guaranteeing all Medicare beneficiaries, regardless of geographic location, have access to quality surgical care. Determining what constitutes a surgical shortage area will serve to help HRSA to appropriately focus its resources.
Accordingly, we need your help and urge you to take action today.
Using the information below, please call your representatives today and urge them to join their colleagues and cosponsor H.R. 4959, the Ensuring Access to General Surgery Act of 2016.
Instructions
Call toll-free: 1-877-996-4464
You will be connected to your representative‘s office. Once you are connected, provide your name and indicate that you are a constituent. You should also be prepared to provide additional contact information for follow-up purposes.
Next, we suggest you use the following message:
• As a surgeon and as your constituent, I urge you to join your colleagues and cosponsor H.R. 4959, the Ensuring Access to General Surgery Act of 2016, which would direct the Secretary of Department of Health and Human Services (HHS) to conduct a study to designate General Surgery Health Professional Shortage Areas (HPSA).
• The division of HHS known as the Health Resources and Services Administration (HRSA) has developed designation criteria in order to determine whether certain geographic areas, population groups, or facilities may be designated as a HPSA.
• HRSA has never designated an entity as a HPSA purely based upon a shortage of surgical services.
• In light of evidence relative to a shortage of surgeons, ACS believes that research is necessary to determine exactly what constitutes a surgical shortage area and subsequently where these areas exist.
Alternatively, for those who were seeking a topic on which to initiate a personal in-district meeting with representatives and their staff as was discussed in last month’s edition of this column, H.R. 4959 presents a prime subject for such in order to have a focused meeting with a specific ask on a “white hat” issue that will surely resonate with members of Congress. Currently, in-district work periods are scheduled for the last week of June, the last two weeks of July, and the entire month of August.
As always, those with questions or concerns, or those who need assistance in setting up an in-district meeting may contact staff of the Division of Advocacy and Health Policy by phone at 202-337-2701 or via e-mail at [email protected].
Thank you for taking the time to engage and take action on this critical issue.
Please encourage your colleagues to do likewise.
Until next month ...
Dr. Patrick V. Bailey is an ACS Fellow, a pediatric surgeon, and Medical Director, Advocacy, for the Division of Advocacy and Health Policy, in the ACS offices in Washington, DC.
Catheter Use Among Teaching Hospitals
Urinary catheter use can be associated with urinary tract infections, delirium, trauma, and immobility.[1] Evidence‐based strategies to reduce inappropriate use are available[2]; however, their application across centers is variable.[3] We aimed to characterize the prevalence and indication for catheters among Canadian teaching hospitals with and without catheter reduction programs.
METHODS
Twelve of 17 postgraduate internal medicine training program directors agreed to participate, and 9 Canadian teaching hospitals enrolled in this prevalence study of urinary catheter use among medical inpatients. Data collection used a standardized form and took place over 5 consecutive weekdays during August 2015. Each site anonymously collected the total number of catheters, total number of inpatient‐days, and indications for use from either the bedside nurse or physician. Appropriate clinical indications were based on the 2009 guidelines from the Healthcare Infection Control Practice Advisory Committee.[4] Potentially inappropriate indications included urine output measurement in noncritically ill patients, and other or unknown indications.[4, 5] A catheter reduction program was defined as the presence of a structured system to monitor and reduce use via: nurse‐directed catheter removal, audit‐feedback of use to providers, physician reminders, and/or automatic stop orders.
The primary outcome was the number of catheter days per 100 inpatient‐days. We used generalized estimating equations to adjust the 95% confidence interval (CI) and P value to account for hospital‐level clustering of the responses. The P values are from a 2‐tailed Wald test against the true log scale parameter being equal to zero. The analysis was performed using R version 3.0.2 using the geepack package (Free Software Foundation, Boston, MA).
The McGill University Health Centre Research Ethics Board approved this study with concomitant authorization at participating sites.
RESULTS
The characteristics of participating hospitals are displayed in Table 1. Those with active catheter reduction programs reported established systems for monitoring catheter placement, duration, and catheter‐associated urinary tract infections. More than half of the hospitals lacked a catheter reduction program. Overall, catheters were present on 13.6% of patient‐days (range, 2.3%32.4%). Centers without reduction programs reported higher rates of catheter use both overall and for potentially inappropriate indications. After adjustment for clustering, those with a formal intervention had 8.8 fewer catheter days per 100 patient‐days as compared to those without (9.8 [95% CI: 6.0‐15.6] vs 18.6 [95% CI: 13.0‐26.1], P = 0.03). This meant that the odds of a urinary catheter being present were 2 times (95% CI: 1.0‐3.4) greater in hospitals without reduction programs. Differences in appropriate catheter use did not reach statistical significance.
| Characteristic | Hospital | Overall, n (%)* | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | I | ||
| ||||||||||
| Total beds, n | 442 | 533 | 824 | 505 | 272 | 925 | 650 | 777 | 446 | 5,374 |
| Has system in place to monitor urinary catheter placement | Yes | Yes | Yes | Yes | No | No | No | No | No | N/A |
| Has system in place to monitor duration and/or discontinuation of urinary catheters | Yes | Yes | Yes | No | No | No | No | No | No | N/A |
| Has a system in place for monitoring catheter associated urinary tract infection rates | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | N/A |
| Presence of a UC reduction program | Active | Active | Active | Active | No | No | No | No | No | N/A |
| Duration of UC reduction program, y | 1 | 2 | 1 | 1 | N/A | N/A | N/A | N/A | N/A | N/A |
| Total patient‐days | 425 | 455 | 527 | 405 | 87 | 311 | 285 | 394 | 253 | 3142 |
| Total UC days | 27 | 32 | 42 | 77 | 2 | 36 | 48 | 80 | 82 | 426 |
| UC rate per 100 patient‐days | 6.4 | 7.0 | 8.0 | 19.0 | 2.3 | 11.6 | 16.8 | 20.3 | 32.4 | 13.6 |
| Reported historical UC rate per 100 patient‐days∥ | 12.0 | 16.5 | 18.8 | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Potentially appropriate indications, n (%) | 19 (70) | 25 (78) | 30 (71) | 36 (47) | 0 | 33 (92) | 27 (56) | 32 (40) | 59 (72) | 261 (61) |
| Obstruction | 5 (19) | 11 (34) | 19 (45) | 7 (9) | 0 | 1 (3) | 10 (21) | 20 (25) | 2 (2) | 75 (17.6) |
| Retention | 10 (37) | 9 (28) | 7 (17) | 21 (27) | 0 | 22 (61) | 9 (19) | 11 (14) | 23 (28) | 112 (26.3) |
| Palliative | 4 (15) | 0 | 4 (10) | 8 (10) | 0 | 10 (28) | 5 (10) | 1 (1) | 16 (20) | 93 (21.8) |
| Sacral ulcer | 0 | 5 (16) | 0 | 0 | 0 | 0 | 3 (6) | 0 | 18 (22) | 26 (6.1) |
| Potentially inappropriate indications, n (%) | 8 (30) | 8 (25) | 12 (28) | 50 (65) | 2 (100) | 3 (8) | 21 (44) | 70 (88) | 16 (20) | 190 (45) |
| Urine output | 2 (7) | 0 | 1 (2) | 22 (14) | 2 (100) | 3 (8) | 11 (23) | 50 (35) | 8 (10) | 96 (22.5) |
| Other | 6 (22) | 8 (25) | 10 (24) | 26 (32) | 0 | 0 | 5 (10) | 13 (16) | 0 | 68 (16.0) |
| Unknown | 0 | 0 | 1 (2) | 2 (3) | 0 | 0 | 5 (10) | 7 (9) | 8 (10) | 23 (5.3) |
DISCUSSION
Despite the availability of consensus guidelines for appropriate use and the efforts of movements like Choosing Wisely, many Canadian teaching hospitals have not yet established a urinary catheter reduction program for medical inpatients. Our findings are similar to 2 non‐Canadian studies, which demonstrated that fewer than half of hospitals had implemented control measures.[4, 6] In contrast to those other studies, our study demonstrated that hospitals that employed control measures had reduced rates of catheter use suggesting that systematic, structured efforts are necessary to improve practice.[7, 8]
Ours is the first nation‐wide study in Canada to report urinary catheter rates and the effect of associated reduction programs. Data from the National Healthcare Safety Network suggest our Canadian estimates of urinary catheter rates in medical inpatients are similar to those of the United States (13.6 vs 14.8 catheter days per 100 inpatient‐days, respectively, for general medical inpatients).[9, 10]
Several limitations of this study warrant discussion. First, we sampled only academic institutions at 1 time point, which may not represent annualized rates or rates in community hospitals. However, our findings are similar to those reported in previous studies.[10] Second, our method of consecutive daily audits may have caused individuals to change their behavior knowing that they were being observed, resulting in lower catheter utilization than would have been otherwise present and biasing our estimates of catheter overuse downward. Third, we collected point prevalence data, limiting our ability to make inferences on causality. The key factor(s) contributing to observed differences between hospitals remains unknown. However, pre‐post intervention data available for 3 hospitals suggest that improvements followed active catheter reduction efforts.[7, 8] Fourth, we were unable to obtain outcome data such as catheter‐associated urinary tract infection, delirium, or fall rates. However, catheter reduction is widely recognized as an important first step to reducing preventable harm for hospital patients.
We suggest that the broader uptake of structured models of care that promote early discontinuation of urinary catheters on medical wards is needed to improve their appropriateness. Fortunately, it appears as though a variety of models are effective. Therefore, when it comes to adopting Choosing Wisely's less is more philosophy toward urinary catheter utilization, we suggest that less time be allowed to pass before more proven and structured interventions are universally implemented.
Acknowledgements
The authors are indebted to John Matelski, MSc, for statistical analyses.
Disclosures: The Canadian Society of Internal Medicine and its Choosing Wisely Canada Subcommittee supported this work. The authors report no conflicts of interest.
- , , , et al. Diagnosis, prevention, and treatment of catheter‐associated urinary tract infection in adults: 2009 international clinical practice guidelines from the Infectious Diseases Society of America. Clin Infect Dis. 2010;50(5):625–663.
- , , , et al. Strategies to prevent catheter‐associated urinary tract infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35(5):464–479.
- , , , et al. Preventing catheter‐associated urinary tract infection in the United States: a national comparative study. JAMA Intern Med. 2013;173(10):874–879.
- , , , et al, Healthcare Infection Control Practices Advisory Committee. Guideline for prevention of catheter‐associated urinary tract infections 2009. Infect Control Hosp Epidemiol. 2010;31(4):319–326.
- , , , et al. Are physicians aware of which of their patients have indwelling urinary catheters? Am J Med. 2000;109(6):476–480.
- , , , et al. Adoption of policies to prevent catheter‐associated urinary tract infections in United States intensive care units. Am J Infect Control. 2012;40(8):705–710.
- , , , et al. Medical directive for urinary catheter removal by nurses on general medical wards. JAMA Intern Med. 2016;176(1):113–115.
- , , , et al. Novel low‐resource intervention reduces urinary catheter use and associated urinary tract infections: role of outcome measure bias? Am J Infect Control. 2015;43(4):348–353.
- , , , et al. National Healthcare Safety Network report, data summary for 2013, Device-associated Module. Am J Infect Control. 2015;43(3):206–221.
- , , , et al. Regional variation in urinary catheter use and catheter‐associated urinary tract infection: results from a national collaborative. Infect Control Hosp Epidemiol. 2014;35(suppl 3):S99–S106.
Urinary catheter use can be associated with urinary tract infections, delirium, trauma, and immobility.[1] Evidence‐based strategies to reduce inappropriate use are available[2]; however, their application across centers is variable.[3] We aimed to characterize the prevalence and indication for catheters among Canadian teaching hospitals with and without catheter reduction programs.
METHODS
Twelve of 17 postgraduate internal medicine training program directors agreed to participate, and 9 Canadian teaching hospitals enrolled in this prevalence study of urinary catheter use among medical inpatients. Data collection used a standardized form and took place over 5 consecutive weekdays during August 2015. Each site anonymously collected the total number of catheters, total number of inpatient‐days, and indications for use from either the bedside nurse or physician. Appropriate clinical indications were based on the 2009 guidelines from the Healthcare Infection Control Practice Advisory Committee.[4] Potentially inappropriate indications included urine output measurement in noncritically ill patients, and other or unknown indications.[4, 5] A catheter reduction program was defined as the presence of a structured system to monitor and reduce use via: nurse‐directed catheter removal, audit‐feedback of use to providers, physician reminders, and/or automatic stop orders.
The primary outcome was the number of catheter days per 100 inpatient‐days. We used generalized estimating equations to adjust the 95% confidence interval (CI) and P value to account for hospital‐level clustering of the responses. The P values are from a 2‐tailed Wald test against the true log scale parameter being equal to zero. The analysis was performed using R version 3.0.2 using the geepack package (Free Software Foundation, Boston, MA).
The McGill University Health Centre Research Ethics Board approved this study with concomitant authorization at participating sites.
RESULTS
The characteristics of participating hospitals are displayed in Table 1. Those with active catheter reduction programs reported established systems for monitoring catheter placement, duration, and catheter‐associated urinary tract infections. More than half of the hospitals lacked a catheter reduction program. Overall, catheters were present on 13.6% of patient‐days (range, 2.3%32.4%). Centers without reduction programs reported higher rates of catheter use both overall and for potentially inappropriate indications. After adjustment for clustering, those with a formal intervention had 8.8 fewer catheter days per 100 patient‐days as compared to those without (9.8 [95% CI: 6.0‐15.6] vs 18.6 [95% CI: 13.0‐26.1], P = 0.03). This meant that the odds of a urinary catheter being present were 2 times (95% CI: 1.0‐3.4) greater in hospitals without reduction programs. Differences in appropriate catheter use did not reach statistical significance.
| Characteristic | Hospital | Overall, n (%)* | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | I | ||
| ||||||||||
| Total beds, n | 442 | 533 | 824 | 505 | 272 | 925 | 650 | 777 | 446 | 5,374 |
| Has system in place to monitor urinary catheter placement | Yes | Yes | Yes | Yes | No | No | No | No | No | N/A |
| Has system in place to monitor duration and/or discontinuation of urinary catheters | Yes | Yes | Yes | No | No | No | No | No | No | N/A |
| Has a system in place for monitoring catheter associated urinary tract infection rates | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | N/A |
| Presence of a UC reduction program | Active | Active | Active | Active | No | No | No | No | No | N/A |
| Duration of UC reduction program, y | 1 | 2 | 1 | 1 | N/A | N/A | N/A | N/A | N/A | N/A |
| Total patient‐days | 425 | 455 | 527 | 405 | 87 | 311 | 285 | 394 | 253 | 3142 |
| Total UC days | 27 | 32 | 42 | 77 | 2 | 36 | 48 | 80 | 82 | 426 |
| UC rate per 100 patient‐days | 6.4 | 7.0 | 8.0 | 19.0 | 2.3 | 11.6 | 16.8 | 20.3 | 32.4 | 13.6 |
| Reported historical UC rate per 100 patient‐days∥ | 12.0 | 16.5 | 18.8 | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Potentially appropriate indications, n (%) | 19 (70) | 25 (78) | 30 (71) | 36 (47) | 0 | 33 (92) | 27 (56) | 32 (40) | 59 (72) | 261 (61) |
| Obstruction | 5 (19) | 11 (34) | 19 (45) | 7 (9) | 0 | 1 (3) | 10 (21) | 20 (25) | 2 (2) | 75 (17.6) |
| Retention | 10 (37) | 9 (28) | 7 (17) | 21 (27) | 0 | 22 (61) | 9 (19) | 11 (14) | 23 (28) | 112 (26.3) |
| Palliative | 4 (15) | 0 | 4 (10) | 8 (10) | 0 | 10 (28) | 5 (10) | 1 (1) | 16 (20) | 93 (21.8) |
| Sacral ulcer | 0 | 5 (16) | 0 | 0 | 0 | 0 | 3 (6) | 0 | 18 (22) | 26 (6.1) |
| Potentially inappropriate indications, n (%) | 8 (30) | 8 (25) | 12 (28) | 50 (65) | 2 (100) | 3 (8) | 21 (44) | 70 (88) | 16 (20) | 190 (45) |
| Urine output | 2 (7) | 0 | 1 (2) | 22 (14) | 2 (100) | 3 (8) | 11 (23) | 50 (35) | 8 (10) | 96 (22.5) |
| Other | 6 (22) | 8 (25) | 10 (24) | 26 (32) | 0 | 0 | 5 (10) | 13 (16) | 0 | 68 (16.0) |
| Unknown | 0 | 0 | 1 (2) | 2 (3) | 0 | 0 | 5 (10) | 7 (9) | 8 (10) | 23 (5.3) |
DISCUSSION
Despite the availability of consensus guidelines for appropriate use and the efforts of movements like Choosing Wisely, many Canadian teaching hospitals have not yet established a urinary catheter reduction program for medical inpatients. Our findings are similar to 2 non‐Canadian studies, which demonstrated that fewer than half of hospitals had implemented control measures.[4, 6] In contrast to those other studies, our study demonstrated that hospitals that employed control measures had reduced rates of catheter use suggesting that systematic, structured efforts are necessary to improve practice.[7, 8]
Ours is the first nation‐wide study in Canada to report urinary catheter rates and the effect of associated reduction programs. Data from the National Healthcare Safety Network suggest our Canadian estimates of urinary catheter rates in medical inpatients are similar to those of the United States (13.6 vs 14.8 catheter days per 100 inpatient‐days, respectively, for general medical inpatients).[9, 10]
Several limitations of this study warrant discussion. First, we sampled only academic institutions at 1 time point, which may not represent annualized rates or rates in community hospitals. However, our findings are similar to those reported in previous studies.[10] Second, our method of consecutive daily audits may have caused individuals to change their behavior knowing that they were being observed, resulting in lower catheter utilization than would have been otherwise present and biasing our estimates of catheter overuse downward. Third, we collected point prevalence data, limiting our ability to make inferences on causality. The key factor(s) contributing to observed differences between hospitals remains unknown. However, pre‐post intervention data available for 3 hospitals suggest that improvements followed active catheter reduction efforts.[7, 8] Fourth, we were unable to obtain outcome data such as catheter‐associated urinary tract infection, delirium, or fall rates. However, catheter reduction is widely recognized as an important first step to reducing preventable harm for hospital patients.
We suggest that the broader uptake of structured models of care that promote early discontinuation of urinary catheters on medical wards is needed to improve their appropriateness. Fortunately, it appears as though a variety of models are effective. Therefore, when it comes to adopting Choosing Wisely's less is more philosophy toward urinary catheter utilization, we suggest that less time be allowed to pass before more proven and structured interventions are universally implemented.
Acknowledgements
The authors are indebted to John Matelski, MSc, for statistical analyses.
Disclosures: The Canadian Society of Internal Medicine and its Choosing Wisely Canada Subcommittee supported this work. The authors report no conflicts of interest.
Urinary catheter use can be associated with urinary tract infections, delirium, trauma, and immobility.[1] Evidence‐based strategies to reduce inappropriate use are available[2]; however, their application across centers is variable.[3] We aimed to characterize the prevalence and indication for catheters among Canadian teaching hospitals with and without catheter reduction programs.
METHODS
Twelve of 17 postgraduate internal medicine training program directors agreed to participate, and 9 Canadian teaching hospitals enrolled in this prevalence study of urinary catheter use among medical inpatients. Data collection used a standardized form and took place over 5 consecutive weekdays during August 2015. Each site anonymously collected the total number of catheters, total number of inpatient‐days, and indications for use from either the bedside nurse or physician. Appropriate clinical indications were based on the 2009 guidelines from the Healthcare Infection Control Practice Advisory Committee.[4] Potentially inappropriate indications included urine output measurement in noncritically ill patients, and other or unknown indications.[4, 5] A catheter reduction program was defined as the presence of a structured system to monitor and reduce use via: nurse‐directed catheter removal, audit‐feedback of use to providers, physician reminders, and/or automatic stop orders.
The primary outcome was the number of catheter days per 100 inpatient‐days. We used generalized estimating equations to adjust the 95% confidence interval (CI) and P value to account for hospital‐level clustering of the responses. The P values are from a 2‐tailed Wald test against the true log scale parameter being equal to zero. The analysis was performed using R version 3.0.2 using the geepack package (Free Software Foundation, Boston, MA).
The McGill University Health Centre Research Ethics Board approved this study with concomitant authorization at participating sites.
RESULTS
The characteristics of participating hospitals are displayed in Table 1. Those with active catheter reduction programs reported established systems for monitoring catheter placement, duration, and catheter‐associated urinary tract infections. More than half of the hospitals lacked a catheter reduction program. Overall, catheters were present on 13.6% of patient‐days (range, 2.3%32.4%). Centers without reduction programs reported higher rates of catheter use both overall and for potentially inappropriate indications. After adjustment for clustering, those with a formal intervention had 8.8 fewer catheter days per 100 patient‐days as compared to those without (9.8 [95% CI: 6.0‐15.6] vs 18.6 [95% CI: 13.0‐26.1], P = 0.03). This meant that the odds of a urinary catheter being present were 2 times (95% CI: 1.0‐3.4) greater in hospitals without reduction programs. Differences in appropriate catheter use did not reach statistical significance.
| Characteristic | Hospital | Overall, n (%)* | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | I | ||
| ||||||||||
| Total beds, n | 442 | 533 | 824 | 505 | 272 | 925 | 650 | 777 | 446 | 5,374 |
| Has system in place to monitor urinary catheter placement | Yes | Yes | Yes | Yes | No | No | No | No | No | N/A |
| Has system in place to monitor duration and/or discontinuation of urinary catheters | Yes | Yes | Yes | No | No | No | No | No | No | N/A |
| Has a system in place for monitoring catheter associated urinary tract infection rates | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | N/A |
| Presence of a UC reduction program | Active | Active | Active | Active | No | No | No | No | No | N/A |
| Duration of UC reduction program, y | 1 | 2 | 1 | 1 | N/A | N/A | N/A | N/A | N/A | N/A |
| Total patient‐days | 425 | 455 | 527 | 405 | 87 | 311 | 285 | 394 | 253 | 3142 |
| Total UC days | 27 | 32 | 42 | 77 | 2 | 36 | 48 | 80 | 82 | 426 |
| UC rate per 100 patient‐days | 6.4 | 7.0 | 8.0 | 19.0 | 2.3 | 11.6 | 16.8 | 20.3 | 32.4 | 13.6 |
| Reported historical UC rate per 100 patient‐days∥ | 12.0 | 16.5 | 18.8 | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Potentially appropriate indications, n (%) | 19 (70) | 25 (78) | 30 (71) | 36 (47) | 0 | 33 (92) | 27 (56) | 32 (40) | 59 (72) | 261 (61) |
| Obstruction | 5 (19) | 11 (34) | 19 (45) | 7 (9) | 0 | 1 (3) | 10 (21) | 20 (25) | 2 (2) | 75 (17.6) |
| Retention | 10 (37) | 9 (28) | 7 (17) | 21 (27) | 0 | 22 (61) | 9 (19) | 11 (14) | 23 (28) | 112 (26.3) |
| Palliative | 4 (15) | 0 | 4 (10) | 8 (10) | 0 | 10 (28) | 5 (10) | 1 (1) | 16 (20) | 93 (21.8) |
| Sacral ulcer | 0 | 5 (16) | 0 | 0 | 0 | 0 | 3 (6) | 0 | 18 (22) | 26 (6.1) |
| Potentially inappropriate indications, n (%) | 8 (30) | 8 (25) | 12 (28) | 50 (65) | 2 (100) | 3 (8) | 21 (44) | 70 (88) | 16 (20) | 190 (45) |
| Urine output | 2 (7) | 0 | 1 (2) | 22 (14) | 2 (100) | 3 (8) | 11 (23) | 50 (35) | 8 (10) | 96 (22.5) |
| Other | 6 (22) | 8 (25) | 10 (24) | 26 (32) | 0 | 0 | 5 (10) | 13 (16) | 0 | 68 (16.0) |
| Unknown | 0 | 0 | 1 (2) | 2 (3) | 0 | 0 | 5 (10) | 7 (9) | 8 (10) | 23 (5.3) |
DISCUSSION
Despite the availability of consensus guidelines for appropriate use and the efforts of movements like Choosing Wisely, many Canadian teaching hospitals have not yet established a urinary catheter reduction program for medical inpatients. Our findings are similar to 2 non‐Canadian studies, which demonstrated that fewer than half of hospitals had implemented control measures.[4, 6] In contrast to those other studies, our study demonstrated that hospitals that employed control measures had reduced rates of catheter use suggesting that systematic, structured efforts are necessary to improve practice.[7, 8]
Ours is the first nation‐wide study in Canada to report urinary catheter rates and the effect of associated reduction programs. Data from the National Healthcare Safety Network suggest our Canadian estimates of urinary catheter rates in medical inpatients are similar to those of the United States (13.6 vs 14.8 catheter days per 100 inpatient‐days, respectively, for general medical inpatients).[9, 10]
Several limitations of this study warrant discussion. First, we sampled only academic institutions at 1 time point, which may not represent annualized rates or rates in community hospitals. However, our findings are similar to those reported in previous studies.[10] Second, our method of consecutive daily audits may have caused individuals to change their behavior knowing that they were being observed, resulting in lower catheter utilization than would have been otherwise present and biasing our estimates of catheter overuse downward. Third, we collected point prevalence data, limiting our ability to make inferences on causality. The key factor(s) contributing to observed differences between hospitals remains unknown. However, pre‐post intervention data available for 3 hospitals suggest that improvements followed active catheter reduction efforts.[7, 8] Fourth, we were unable to obtain outcome data such as catheter‐associated urinary tract infection, delirium, or fall rates. However, catheter reduction is widely recognized as an important first step to reducing preventable harm for hospital patients.
We suggest that the broader uptake of structured models of care that promote early discontinuation of urinary catheters on medical wards is needed to improve their appropriateness. Fortunately, it appears as though a variety of models are effective. Therefore, when it comes to adopting Choosing Wisely's less is more philosophy toward urinary catheter utilization, we suggest that less time be allowed to pass before more proven and structured interventions are universally implemented.
Acknowledgements
The authors are indebted to John Matelski, MSc, for statistical analyses.
Disclosures: The Canadian Society of Internal Medicine and its Choosing Wisely Canada Subcommittee supported this work. The authors report no conflicts of interest.
- , , , et al. Diagnosis, prevention, and treatment of catheter‐associated urinary tract infection in adults: 2009 international clinical practice guidelines from the Infectious Diseases Society of America. Clin Infect Dis. 2010;50(5):625–663.
- , , , et al. Strategies to prevent catheter‐associated urinary tract infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35(5):464–479.
- , , , et al. Preventing catheter‐associated urinary tract infection in the United States: a national comparative study. JAMA Intern Med. 2013;173(10):874–879.
- , , , et al, Healthcare Infection Control Practices Advisory Committee. Guideline for prevention of catheter‐associated urinary tract infections 2009. Infect Control Hosp Epidemiol. 2010;31(4):319–326.
- , , , et al. Are physicians aware of which of their patients have indwelling urinary catheters? Am J Med. 2000;109(6):476–480.
- , , , et al. Adoption of policies to prevent catheter‐associated urinary tract infections in United States intensive care units. Am J Infect Control. 2012;40(8):705–710.
- , , , et al. Medical directive for urinary catheter removal by nurses on general medical wards. JAMA Intern Med. 2016;176(1):113–115.
- , , , et al. Novel low‐resource intervention reduces urinary catheter use and associated urinary tract infections: role of outcome measure bias? Am J Infect Control. 2015;43(4):348–353.
- , , , et al. National Healthcare Safety Network report, data summary for 2013, Device-associated Module. Am J Infect Control. 2015;43(3):206–221.
- , , , et al. Regional variation in urinary catheter use and catheter‐associated urinary tract infection: results from a national collaborative. Infect Control Hosp Epidemiol. 2014;35(suppl 3):S99–S106.
- , , , et al. Diagnosis, prevention, and treatment of catheter‐associated urinary tract infection in adults: 2009 international clinical practice guidelines from the Infectious Diseases Society of America. Clin Infect Dis. 2010;50(5):625–663.
- , , , et al. Strategies to prevent catheter‐associated urinary tract infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35(5):464–479.
- , , , et al. Preventing catheter‐associated urinary tract infection in the United States: a national comparative study. JAMA Intern Med. 2013;173(10):874–879.
- , , , et al, Healthcare Infection Control Practices Advisory Committee. Guideline for prevention of catheter‐associated urinary tract infections 2009. Infect Control Hosp Epidemiol. 2010;31(4):319–326.
- , , , et al. Are physicians aware of which of their patients have indwelling urinary catheters? Am J Med. 2000;109(6):476–480.
- , , , et al. Adoption of policies to prevent catheter‐associated urinary tract infections in United States intensive care units. Am J Infect Control. 2012;40(8):705–710.
- , , , et al. Medical directive for urinary catheter removal by nurses on general medical wards. JAMA Intern Med. 2016;176(1):113–115.
- , , , et al. Novel low‐resource intervention reduces urinary catheter use and associated urinary tract infections: role of outcome measure bias? Am J Infect Control. 2015;43(4):348–353.
- , , , et al. National Healthcare Safety Network report, data summary for 2013, Device-associated Module. Am J Infect Control. 2015;43(3):206–221.
- , , , et al. Regional variation in urinary catheter use and catheter‐associated urinary tract infection: results from a national collaborative. Infect Control Hosp Epidemiol. 2014;35(suppl 3):S99–S106.
© 2016 Society of Hospital Medicine
Setting up your own RSS feed
Last month, I discussed RSS news feeds as a useful tool for keeping abreast of frequently updated information, such as blog entries, news headlines, audio, and video, without having to visit a multitude of different Web pages each day.
This month, I’ll explain how to set up your own feed, which is useful if you want to increase the readership on your website, or publicize a podcast, or keep your patients abreast of your practice’s latest treatments and procedures. It will also alert you immediately if your name pops up in news or gossip sites.
There are several options, depending on your budget, and how involved you personally want to be in the process: Many Web hosting services will automatically create and update your feed for a monthly fee; so if you already have a professionally hosted website, check to see if your host offers that service. If not, Web services such as Feedity and Rapidfeeds allow you to manage multiple feeds, with automatic updates, so that you will not need to manually update your feed each time you update your website content. Feedity’s software can even generate an RSS file without your having to input each item. Other popular hosting options include Web Hosting Hub, Arvixe, and MyHosting, among many others. (As always, I have no financial interest in any service I mention here.)
Another option, used by many organizations that publish their own articles and news stories, is a content management system (CMS), an application designed to organize, store, and publish content, including tools for adding RSS feeds. Examples include Drupal and Plone – both free, open-source programs.
Alternatively, you can download a stand-alone RSS creation program, then create and update your feed manually. Again, there are many options to choose from. One popular example is RSS Builder, a free, open source RSS creation program that allows you to create RSS files, upload them to your website, and automatically manage them to some extent. Disadvantages of free systems include advertisements (sometimes removable for a monthly fee), scarce or nonexistent technical support, and in many cases, no option to create more than one feed. You may also have to manually add new headlines, links, and descriptive text yourself. Your “free” feed can become quite expensive if you or staffers are forced to spend an inordinate amount of time maintaining it. Paid programs such as FeedForAll allow easier creation and maintenance, and less time commitment.
Once you have chosen your service, create your first feed. The process will differ from program to program, but the general idea is the same for almost all of them. All feeds will need some basic data: A title (which should be the same as your website or podcast); the URL for your website, to help viewers link back to your home page; and a description – a sentence or two describing the general content on the feed.
Once you’ve entered this information, you can start populating the feed with content. Enter in the title of each article, blog post, podcast episode, etc., the URL that links directly to that content, and the publishing date. Each entry should have its own short but sweet description; this is what your readers will see before they choose to click your entry in their RSS readers. You can add author information and further comments if needed. Add a new entry for each piece of content that you want to broadcast.
Most RSS apps suggest that you assign each item in your feed a global unique identifier (GUID), which RSS readers use to determine if an item has been changed or updated. Each feed item should have its own GUID, particularly if multiple items are located at the same URL.
Once you’re done entering in all of your content to your feed, you need to export it to an XML file, which will allow visitors to subscribe to your feed. Then upload the XML file to your website, place it on your homepage, and click the Publish Feed button.
Once your feed is live, consider submitting it to some of the many RSS feed directories (also called aggregate sites) that collect articles from similar interests and can significantly increase your viewership. Search for medically oriented directories, and others that match the interests that your feed addresses, and submit each directory’s URL to your feed’s XML file.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Dermatology News. Write to him at [email protected].
Last month, I discussed RSS news feeds as a useful tool for keeping abreast of frequently updated information, such as blog entries, news headlines, audio, and video, without having to visit a multitude of different Web pages each day.
This month, I’ll explain how to set up your own feed, which is useful if you want to increase the readership on your website, or publicize a podcast, or keep your patients abreast of your practice’s latest treatments and procedures. It will also alert you immediately if your name pops up in news or gossip sites.
There are several options, depending on your budget, and how involved you personally want to be in the process: Many Web hosting services will automatically create and update your feed for a monthly fee; so if you already have a professionally hosted website, check to see if your host offers that service. If not, Web services such as Feedity and Rapidfeeds allow you to manage multiple feeds, with automatic updates, so that you will not need to manually update your feed each time you update your website content. Feedity’s software can even generate an RSS file without your having to input each item. Other popular hosting options include Web Hosting Hub, Arvixe, and MyHosting, among many others. (As always, I have no financial interest in any service I mention here.)
Another option, used by many organizations that publish their own articles and news stories, is a content management system (CMS), an application designed to organize, store, and publish content, including tools for adding RSS feeds. Examples include Drupal and Plone – both free, open-source programs.
Alternatively, you can download a stand-alone RSS creation program, then create and update your feed manually. Again, there are many options to choose from. One popular example is RSS Builder, a free, open source RSS creation program that allows you to create RSS files, upload them to your website, and automatically manage them to some extent. Disadvantages of free systems include advertisements (sometimes removable for a monthly fee), scarce or nonexistent technical support, and in many cases, no option to create more than one feed. You may also have to manually add new headlines, links, and descriptive text yourself. Your “free” feed can become quite expensive if you or staffers are forced to spend an inordinate amount of time maintaining it. Paid programs such as FeedForAll allow easier creation and maintenance, and less time commitment.
Once you have chosen your service, create your first feed. The process will differ from program to program, but the general idea is the same for almost all of them. All feeds will need some basic data: A title (which should be the same as your website or podcast); the URL for your website, to help viewers link back to your home page; and a description – a sentence or two describing the general content on the feed.
Once you’ve entered this information, you can start populating the feed with content. Enter in the title of each article, blog post, podcast episode, etc., the URL that links directly to that content, and the publishing date. Each entry should have its own short but sweet description; this is what your readers will see before they choose to click your entry in their RSS readers. You can add author information and further comments if needed. Add a new entry for each piece of content that you want to broadcast.
Most RSS apps suggest that you assign each item in your feed a global unique identifier (GUID), which RSS readers use to determine if an item has been changed or updated. Each feed item should have its own GUID, particularly if multiple items are located at the same URL.
Once you’re done entering in all of your content to your feed, you need to export it to an XML file, which will allow visitors to subscribe to your feed. Then upload the XML file to your website, place it on your homepage, and click the Publish Feed button.
Once your feed is live, consider submitting it to some of the many RSS feed directories (also called aggregate sites) that collect articles from similar interests and can significantly increase your viewership. Search for medically oriented directories, and others that match the interests that your feed addresses, and submit each directory’s URL to your feed’s XML file.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Dermatology News. Write to him at [email protected].
Last month, I discussed RSS news feeds as a useful tool for keeping abreast of frequently updated information, such as blog entries, news headlines, audio, and video, without having to visit a multitude of different Web pages each day.
This month, I’ll explain how to set up your own feed, which is useful if you want to increase the readership on your website, or publicize a podcast, or keep your patients abreast of your practice’s latest treatments and procedures. It will also alert you immediately if your name pops up in news or gossip sites.
There are several options, depending on your budget, and how involved you personally want to be in the process: Many Web hosting services will automatically create and update your feed for a monthly fee; so if you already have a professionally hosted website, check to see if your host offers that service. If not, Web services such as Feedity and Rapidfeeds allow you to manage multiple feeds, with automatic updates, so that you will not need to manually update your feed each time you update your website content. Feedity’s software can even generate an RSS file without your having to input each item. Other popular hosting options include Web Hosting Hub, Arvixe, and MyHosting, among many others. (As always, I have no financial interest in any service I mention here.)
Another option, used by many organizations that publish their own articles and news stories, is a content management system (CMS), an application designed to organize, store, and publish content, including tools for adding RSS feeds. Examples include Drupal and Plone – both free, open-source programs.
Alternatively, you can download a stand-alone RSS creation program, then create and update your feed manually. Again, there are many options to choose from. One popular example is RSS Builder, a free, open source RSS creation program that allows you to create RSS files, upload them to your website, and automatically manage them to some extent. Disadvantages of free systems include advertisements (sometimes removable for a monthly fee), scarce or nonexistent technical support, and in many cases, no option to create more than one feed. You may also have to manually add new headlines, links, and descriptive text yourself. Your “free” feed can become quite expensive if you or staffers are forced to spend an inordinate amount of time maintaining it. Paid programs such as FeedForAll allow easier creation and maintenance, and less time commitment.
Once you have chosen your service, create your first feed. The process will differ from program to program, but the general idea is the same for almost all of them. All feeds will need some basic data: A title (which should be the same as your website or podcast); the URL for your website, to help viewers link back to your home page; and a description – a sentence or two describing the general content on the feed.
Once you’ve entered this information, you can start populating the feed with content. Enter in the title of each article, blog post, podcast episode, etc., the URL that links directly to that content, and the publishing date. Each entry should have its own short but sweet description; this is what your readers will see before they choose to click your entry in their RSS readers. You can add author information and further comments if needed. Add a new entry for each piece of content that you want to broadcast.
Most RSS apps suggest that you assign each item in your feed a global unique identifier (GUID), which RSS readers use to determine if an item has been changed or updated. Each feed item should have its own GUID, particularly if multiple items are located at the same URL.
Once you’re done entering in all of your content to your feed, you need to export it to an XML file, which will allow visitors to subscribe to your feed. Then upload the XML file to your website, place it on your homepage, and click the Publish Feed button.
Once your feed is live, consider submitting it to some of the many RSS feed directories (also called aggregate sites) that collect articles from similar interests and can significantly increase your viewership. Search for medically oriented directories, and others that match the interests that your feed addresses, and submit each directory’s URL to your feed’s XML file.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Dermatology News. Write to him at [email protected].