User login
New Framework for Quality Improvement
Improving healthcare means taking an efficacious intervention from one setting and effectively implementing it somewhere else.
“It is this key element of adapting what works to new settings that sets improvement in contrast to clinical research. The study of these complex systems will therefore require different methods of inquiry,” according to a recently published paper in the International Journal for Quality in Health Care titled “How Do We Learn about Improving Health Care: A Call for a New Epistemological Paradigm.”
“In biomedical sciences, we’re used to a golden standard that is the randomized controlled trial,” says lead author M. Rashad Massoud, MD, MPH, senior vice president, Quality & Performance Institute, University Research Co., LLC. “Of course, the nature of what we’re trying to do does not lend itself to that type of evaluation. It means that we can’t have an either/or situation where we either continue as we are or we go to flip side—which then inhibits the very nature of improvement from taking place, which is very contextual, very much adaptive in nature. There has to be a happy medium in between, where we can continue to do the improvements without inhibiting them and, at the same time, improve the rigor of the work.”
A new framework for how we learn about improvement could help in the design, implementation, and evaluation of QI by strengthening attribution and better understanding variations in effectiveness in different contexts, the authors assert.
“This will in turn allow us to understand which activities, under which conditions, are most effective at achieving sustained results in health outcomes,” the authors write.
In seeking a new framework for learning about QI, the authors suggest that the following questions must be considered:
- Did the improvements work?
- Why did they work?
- How do we know that the results can be attributed to the changes made?
- How can we replicate them?
“I think hospitalists would probably welcome the idea that not only can they measure improvements in the work that they’re doing but can actually do that in a more rigorous way and actually attribute the results they’re getting to the work that they’re doing,” Dr. Massoud says.
Reference
- Massoud MR, Barry D, Murphy A, Albrecht Y, Sax S, Parchman M. How do we learn about improving health care: a call for a new epistemological paradigm. Intl J Quality Health Care. doi:10.1093/intqhc/mzw039.
Improving healthcare means taking an efficacious intervention from one setting and effectively implementing it somewhere else.
“It is this key element of adapting what works to new settings that sets improvement in contrast to clinical research. The study of these complex systems will therefore require different methods of inquiry,” according to a recently published paper in the International Journal for Quality in Health Care titled “How Do We Learn about Improving Health Care: A Call for a New Epistemological Paradigm.”
“In biomedical sciences, we’re used to a golden standard that is the randomized controlled trial,” says lead author M. Rashad Massoud, MD, MPH, senior vice president, Quality & Performance Institute, University Research Co., LLC. “Of course, the nature of what we’re trying to do does not lend itself to that type of evaluation. It means that we can’t have an either/or situation where we either continue as we are or we go to flip side—which then inhibits the very nature of improvement from taking place, which is very contextual, very much adaptive in nature. There has to be a happy medium in between, where we can continue to do the improvements without inhibiting them and, at the same time, improve the rigor of the work.”
A new framework for how we learn about improvement could help in the design, implementation, and evaluation of QI by strengthening attribution and better understanding variations in effectiveness in different contexts, the authors assert.
“This will in turn allow us to understand which activities, under which conditions, are most effective at achieving sustained results in health outcomes,” the authors write.
In seeking a new framework for learning about QI, the authors suggest that the following questions must be considered:
- Did the improvements work?
- Why did they work?
- How do we know that the results can be attributed to the changes made?
- How can we replicate them?
“I think hospitalists would probably welcome the idea that not only can they measure improvements in the work that they’re doing but can actually do that in a more rigorous way and actually attribute the results they’re getting to the work that they’re doing,” Dr. Massoud says.
Reference
- Massoud MR, Barry D, Murphy A, Albrecht Y, Sax S, Parchman M. How do we learn about improving health care: a call for a new epistemological paradigm. Intl J Quality Health Care. doi:10.1093/intqhc/mzw039.
Improving healthcare means taking an efficacious intervention from one setting and effectively implementing it somewhere else.
“It is this key element of adapting what works to new settings that sets improvement in contrast to clinical research. The study of these complex systems will therefore require different methods of inquiry,” according to a recently published paper in the International Journal for Quality in Health Care titled “How Do We Learn about Improving Health Care: A Call for a New Epistemological Paradigm.”
“In biomedical sciences, we’re used to a golden standard that is the randomized controlled trial,” says lead author M. Rashad Massoud, MD, MPH, senior vice president, Quality & Performance Institute, University Research Co., LLC. “Of course, the nature of what we’re trying to do does not lend itself to that type of evaluation. It means that we can’t have an either/or situation where we either continue as we are or we go to flip side—which then inhibits the very nature of improvement from taking place, which is very contextual, very much adaptive in nature. There has to be a happy medium in between, where we can continue to do the improvements without inhibiting them and, at the same time, improve the rigor of the work.”
A new framework for how we learn about improvement could help in the design, implementation, and evaluation of QI by strengthening attribution and better understanding variations in effectiveness in different contexts, the authors assert.
“This will in turn allow us to understand which activities, under which conditions, are most effective at achieving sustained results in health outcomes,” the authors write.
In seeking a new framework for learning about QI, the authors suggest that the following questions must be considered:
- Did the improvements work?
- Why did they work?
- How do we know that the results can be attributed to the changes made?
- How can we replicate them?
“I think hospitalists would probably welcome the idea that not only can they measure improvements in the work that they’re doing but can actually do that in a more rigorous way and actually attribute the results they’re getting to the work that they’re doing,” Dr. Massoud says.
Reference
- Massoud MR, Barry D, Murphy A, Albrecht Y, Sax S, Parchman M. How do we learn about improving health care: a call for a new epistemological paradigm. Intl J Quality Health Care. doi:10.1093/intqhc/mzw039.
Applying Military Principles to HM Leadership
Hospitalists are more than doctors—they are also leaders in their organizations, which is why a new book by retired Army Lieutenant General Mark Hertling is relevant to what they do every day. Hertling, whose numerous military awards include the Legion of Merit, the Bronze Star, and the Purple Heart, is the author of Growing Physician Leaders: Empowering Doctors to Improve Our Healthcare, which applies his four decades of military leadership to the world of healthcare.
He wrote the book not long after designing the first physician leader course at Florida Hospital in Orlando.
“Many of the administrators and other doctors saw the changes in the doctors, nurses, and administrators who graduated from the course, and they asked me to write down what we had done,” he says. “The book is partially a description of the course, but it’s also a primer on the basics of leadership.”
The book tells readers how to understand what kind of leader they can be as well as how to better understand the motivations of others; it also outlines a variety of influence techniques they can employ to get things done.
“One of the things we drive home is that all physicians are leaders, whether they are in a leadership role or not,” Hertling says.
One of the concepts he outlines is “leading up”—how to influence your bosses to do the things you want them to do. “What we do during this lesson is show readers how they are other people’s bosses, too,” he says, “and that they need to listen to their own people, too, and allow their folks to contribute to the organizational goals.”
Hospitalists are more than doctors—they are also leaders in their organizations, which is why a new book by retired Army Lieutenant General Mark Hertling is relevant to what they do every day. Hertling, whose numerous military awards include the Legion of Merit, the Bronze Star, and the Purple Heart, is the author of Growing Physician Leaders: Empowering Doctors to Improve Our Healthcare, which applies his four decades of military leadership to the world of healthcare.
He wrote the book not long after designing the first physician leader course at Florida Hospital in Orlando.
“Many of the administrators and other doctors saw the changes in the doctors, nurses, and administrators who graduated from the course, and they asked me to write down what we had done,” he says. “The book is partially a description of the course, but it’s also a primer on the basics of leadership.”
The book tells readers how to understand what kind of leader they can be as well as how to better understand the motivations of others; it also outlines a variety of influence techniques they can employ to get things done.
“One of the things we drive home is that all physicians are leaders, whether they are in a leadership role or not,” Hertling says.
One of the concepts he outlines is “leading up”—how to influence your bosses to do the things you want them to do. “What we do during this lesson is show readers how they are other people’s bosses, too,” he says, “and that they need to listen to their own people, too, and allow their folks to contribute to the organizational goals.”
Hospitalists are more than doctors—they are also leaders in their organizations, which is why a new book by retired Army Lieutenant General Mark Hertling is relevant to what they do every day. Hertling, whose numerous military awards include the Legion of Merit, the Bronze Star, and the Purple Heart, is the author of Growing Physician Leaders: Empowering Doctors to Improve Our Healthcare, which applies his four decades of military leadership to the world of healthcare.
He wrote the book not long after designing the first physician leader course at Florida Hospital in Orlando.
“Many of the administrators and other doctors saw the changes in the doctors, nurses, and administrators who graduated from the course, and they asked me to write down what we had done,” he says. “The book is partially a description of the course, but it’s also a primer on the basics of leadership.”
The book tells readers how to understand what kind of leader they can be as well as how to better understand the motivations of others; it also outlines a variety of influence techniques they can employ to get things done.
“One of the things we drive home is that all physicians are leaders, whether they are in a leadership role or not,” Hertling says.
One of the concepts he outlines is “leading up”—how to influence your bosses to do the things you want them to do. “What we do during this lesson is show readers how they are other people’s bosses, too,” he says, “and that they need to listen to their own people, too, and allow their folks to contribute to the organizational goals.”
Obinutuzumab approved to treat FL

The European Commission (EC) has approved the use of obinutuzumab (Gazyvaro), an anti-CD20 monoclonal antibody, in patients with follicular lymphoma (FL).
The approval means obinutuzumab can be given, first in combination with bendamustine and then alone as maintenance therapy, to FL patients who did not respond to, progressed during, or progressed up to 6 months after treatment with rituximab or a rituximab-containing regimen.
Obinutuzumab was previously granted approval by the EC for use in combination with chlorambucil to treat patients with previously untreated chronic lymphocytic leukemia and comorbidities that make them unsuitable for full-dose fludarabine-based therapy.
Obinutuzumab is being developed by Roche. The drug is marketed as Gazyvaro in the European Union and Switzerland but as Gazyva in the rest of the world.
GADOLIN trial
The EC’s approval of obinutuzumab in FL is based on results from the phase 3 GADOLIN trial. The study included 413 patients with rituximab-refractory non-Hodgkin lymphoma, including 321 patients with FL, 46 with marginal zone lymphoma, and 28 with small lymphocytic lymphoma.
The patients were randomized to receive bendamustine alone (control arm) or a combination of bendamustine and obinutuzumab followed by obinutuzumab maintenance (every 2 months for 2 years or until progression).
The primary endpoint of the study was progression-free survival (PFS), as assessed by an independent review committee (IRC). The secondary endpoints were PFS assessed by investigator review, best overall response, complete response (CR), partial response (PR), duration of response, overall survival, and safety profile.
Among patients with FL, the obinutuzumab regimen improved PFS compared to bendamustine alone, as assessed by the IRC (hazard ratio [HR]=0.48, P<0.0001). The median PFS was not reached in patients receiving the obinutuzumab regimen but was 13.8 months in those receiving bendamustine alone.
Investigator-assessed PFS was consistent with IRC-assessed PFS. Investigators said the median PFS with the obinutuzumab regimen was more than double that with bendamustine alone—29.2 months vs 13.7 months (HR=0.48, P<0.0001).
The best overall response for patients receiving the obinutuzumab regimen was 78.7% (15.5% CR, 63.2% PR), compared to 74.7% (18.7% CR, 56% PR) for those receiving bendamustine alone, as assessed by the IRC.
The median duration of response was not reached for patients receiving the obinutuzumab regimen and was 11.6 months for those receiving bendamustine alone.
The median overall survival has not yet been reached in either study arm.
The most common grade 3/4 adverse events observed in patients receiving the obinutuzumab regimen were neutropenia (33%), infusion reactions (11%), and thrombocytopenia (10%).
The most common adverse events of any grade were infusion reactions (69%), neutropenia (35%), nausea (54%), fatigue (39%), cough (26%), diarrhea (27%), constipation (19%), fever (18%), thrombocytopenia (15%), vomiting (22%), upper respiratory tract infection (13%), decreased appetite (18%), joint or muscle pain (12%), sinusitis (12%), anemia (12%), general weakness (11%), and urinary tract infection (10%). ![]()

The European Commission (EC) has approved the use of obinutuzumab (Gazyvaro), an anti-CD20 monoclonal antibody, in patients with follicular lymphoma (FL).
The approval means obinutuzumab can be given, first in combination with bendamustine and then alone as maintenance therapy, to FL patients who did not respond to, progressed during, or progressed up to 6 months after treatment with rituximab or a rituximab-containing regimen.
Obinutuzumab was previously granted approval by the EC for use in combination with chlorambucil to treat patients with previously untreated chronic lymphocytic leukemia and comorbidities that make them unsuitable for full-dose fludarabine-based therapy.
Obinutuzumab is being developed by Roche. The drug is marketed as Gazyvaro in the European Union and Switzerland but as Gazyva in the rest of the world.
GADOLIN trial
The EC’s approval of obinutuzumab in FL is based on results from the phase 3 GADOLIN trial. The study included 413 patients with rituximab-refractory non-Hodgkin lymphoma, including 321 patients with FL, 46 with marginal zone lymphoma, and 28 with small lymphocytic lymphoma.
The patients were randomized to receive bendamustine alone (control arm) or a combination of bendamustine and obinutuzumab followed by obinutuzumab maintenance (every 2 months for 2 years or until progression).
The primary endpoint of the study was progression-free survival (PFS), as assessed by an independent review committee (IRC). The secondary endpoints were PFS assessed by investigator review, best overall response, complete response (CR), partial response (PR), duration of response, overall survival, and safety profile.
Among patients with FL, the obinutuzumab regimen improved PFS compared to bendamustine alone, as assessed by the IRC (hazard ratio [HR]=0.48, P<0.0001). The median PFS was not reached in patients receiving the obinutuzumab regimen but was 13.8 months in those receiving bendamustine alone.
Investigator-assessed PFS was consistent with IRC-assessed PFS. Investigators said the median PFS with the obinutuzumab regimen was more than double that with bendamustine alone—29.2 months vs 13.7 months (HR=0.48, P<0.0001).
The best overall response for patients receiving the obinutuzumab regimen was 78.7% (15.5% CR, 63.2% PR), compared to 74.7% (18.7% CR, 56% PR) for those receiving bendamustine alone, as assessed by the IRC.
The median duration of response was not reached for patients receiving the obinutuzumab regimen and was 11.6 months for those receiving bendamustine alone.
The median overall survival has not yet been reached in either study arm.
The most common grade 3/4 adverse events observed in patients receiving the obinutuzumab regimen were neutropenia (33%), infusion reactions (11%), and thrombocytopenia (10%).
The most common adverse events of any grade were infusion reactions (69%), neutropenia (35%), nausea (54%), fatigue (39%), cough (26%), diarrhea (27%), constipation (19%), fever (18%), thrombocytopenia (15%), vomiting (22%), upper respiratory tract infection (13%), decreased appetite (18%), joint or muscle pain (12%), sinusitis (12%), anemia (12%), general weakness (11%), and urinary tract infection (10%). ![]()

The European Commission (EC) has approved the use of obinutuzumab (Gazyvaro), an anti-CD20 monoclonal antibody, in patients with follicular lymphoma (FL).
The approval means obinutuzumab can be given, first in combination with bendamustine and then alone as maintenance therapy, to FL patients who did not respond to, progressed during, or progressed up to 6 months after treatment with rituximab or a rituximab-containing regimen.
Obinutuzumab was previously granted approval by the EC for use in combination with chlorambucil to treat patients with previously untreated chronic lymphocytic leukemia and comorbidities that make them unsuitable for full-dose fludarabine-based therapy.
Obinutuzumab is being developed by Roche. The drug is marketed as Gazyvaro in the European Union and Switzerland but as Gazyva in the rest of the world.
GADOLIN trial
The EC’s approval of obinutuzumab in FL is based on results from the phase 3 GADOLIN trial. The study included 413 patients with rituximab-refractory non-Hodgkin lymphoma, including 321 patients with FL, 46 with marginal zone lymphoma, and 28 with small lymphocytic lymphoma.
The patients were randomized to receive bendamustine alone (control arm) or a combination of bendamustine and obinutuzumab followed by obinutuzumab maintenance (every 2 months for 2 years or until progression).
The primary endpoint of the study was progression-free survival (PFS), as assessed by an independent review committee (IRC). The secondary endpoints were PFS assessed by investigator review, best overall response, complete response (CR), partial response (PR), duration of response, overall survival, and safety profile.
Among patients with FL, the obinutuzumab regimen improved PFS compared to bendamustine alone, as assessed by the IRC (hazard ratio [HR]=0.48, P<0.0001). The median PFS was not reached in patients receiving the obinutuzumab regimen but was 13.8 months in those receiving bendamustine alone.
Investigator-assessed PFS was consistent with IRC-assessed PFS. Investigators said the median PFS with the obinutuzumab regimen was more than double that with bendamustine alone—29.2 months vs 13.7 months (HR=0.48, P<0.0001).
The best overall response for patients receiving the obinutuzumab regimen was 78.7% (15.5% CR, 63.2% PR), compared to 74.7% (18.7% CR, 56% PR) for those receiving bendamustine alone, as assessed by the IRC.
The median duration of response was not reached for patients receiving the obinutuzumab regimen and was 11.6 months for those receiving bendamustine alone.
The median overall survival has not yet been reached in either study arm.
The most common grade 3/4 adverse events observed in patients receiving the obinutuzumab regimen were neutropenia (33%), infusion reactions (11%), and thrombocytopenia (10%).
The most common adverse events of any grade were infusion reactions (69%), neutropenia (35%), nausea (54%), fatigue (39%), cough (26%), diarrhea (27%), constipation (19%), fever (18%), thrombocytopenia (15%), vomiting (22%), upper respiratory tract infection (13%), decreased appetite (18%), joint or muscle pain (12%), sinusitis (12%), anemia (12%), general weakness (11%), and urinary tract infection (10%). ![]()
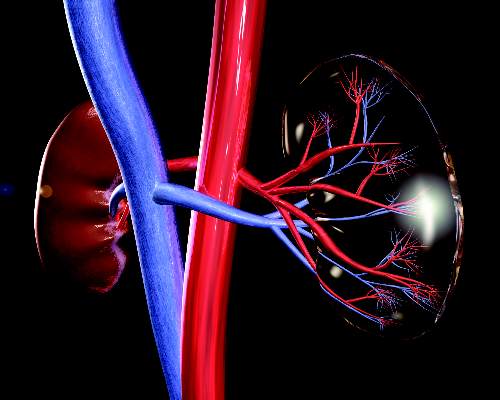
Empagliflozin slows renal disease progression in type 2 diabetes
Empagliflozin was associated with a significant 39% decrease in risk of new or worsening nephropathy, compared with placebo among adults with type 2 diabetes at high risk for cardiovascular events, based on a secondary analysis of the phase III, randomized, double-blind EMPA-REG OUTCOME trial.
“Patients in the empagliflozin group also had a significantly lower risk of progression to macroalbuminuria or clinically relevant renal outcomes, such as a doubling of the serum creatinine level and initiation of renal-replacement therapy, than did those in the placebo group,” Dr. Christoph Wanner of Würzburg (Germany) University Clinic, and his associates reported in the June 14 New England Journal of Medicine.
Empagliflozin(Jardiance) is a selective sodium–glucose cotransporter-2 inhibitor that was approved in the United States in 2014 to improve glycemic control among patients with type 2 diabetes mellitus. In the initial analysis of the EMPA-REG OUTCOME trial, empagliflozin was associated with a significantly lower rate of cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke, as compared with placebo among patients with type 2 diabetes at high cardiovascular risk (N Engl J Med. 2015 Nov 26 doi: 10.1056/NEJMoa1504720).
For the current secondary analysis, Dr. Wanner and his associates focused on renal microvascular outcomes, including new or worsening nephropathy (macroalbuminuria, defined as greater than 300 mg of urinary albumin/gram of creatinine), a doubling of the serum creatinine level accompanied by an epidermal growth factor receptor (eGFR) of less than or equal to 45 mL/minute per 1.73 m2of body surface area, a new need for renal-replacement therapy, and death from renal disease. A total of 7,020 patients with type 2 diabetes and an eGFR of at least 30 mL/minute per 1.73 m2 of body-surface area received either 10 mg or 25 mg of empagliflozin or placebo once daily, plus standard diabetes care (N Engl J Med. 2016 Jun 14. doi: 10.1056/NEJMoa1515920).
New or worsening nephropathy occurred among 525 (12.7%) patients who received empagliflozin, compared with 388 (18.8%) patients who received placebo, for a statistically significant 39% decrease in relative risk of this outcome (hazard ratio, 0.61; P less than .001). This benefit persisted at both doses of empagliflozin, among patients with and without baseline chronic kidney disease (eGFR greater than or equal to 60 mL/min/1.73m2), and across other subgroups stratified by sex, race, body mass index, number of cardiovascular risk factors, and diabetes history and treatment.
A total of 70 patients (1.5%) in the empagliflozin group had a doubling of serum creatinine, vs. 60 patients (2.6%) in the placebo group, for a significant relative risk reduction of 44% (hazard ratio, 0.56; P less than .001). In addition, the proportion of patients starting renal-replacement therapy was twice as high in the placebo group than in the empagliflozin group (0.6% and 0.3%, respectively; HR, 0.45; P less .01).
The groups did not significantly differ in the rate of incident albuminuria, the researchers said. “There were three deaths from renal disease in the empagliflozin group (0.1%) and none in the placebo group,” they added.
The study uncovered no safety signals related to hypoglycemia, diabetic ketoacidosis, thromboembolic events, bone fractures, or volume depletion, the investigators said. Rates of overall adverse events, serious adverse events, and adverse events leading to treatment discontinuation were similar across groups. Rates of complicated urinary tract infections did not significantly vary according to treatment or based on the presence or absence of chronic kidney disease (CKD).Although empagliflozin was associated with a doubling in the rate of urosepsis, these events were rare, affecting only 0.3% and 0.7% of patients with baseline CKD and 0.1% and 0.2% of patients without baseline CKD.
The study was funded by the Boehringer Ingelheim and Eli Lilly and the Diabetes Alliance. Dr. Wanner disclosed grant support from the European Foundation for the Study of Diabetes and personal fees from Boehringer Ingelheim, Janssen, and Novo Nordisk.
[In the EMPA-REG OUTCOME trial,] empagliflozin was associated with a slower progression of kidney disease and lower rates of clinically relevant renal events than was placebo when added to standard of care in patients at high cardiovascular risk. [In the LEADER trial,] the rate of the first occurrence of death from cardiovascular causes, nonfatal myocardial infarction, or nonfatal stroke among patients with type 2 diabetes mellitus was lower with liraglutide than placebo.
Why do the EMPA-REG OUTCOME and LEADER trials show cardiovascular and microvascular benefit, whereas other trials have come close yet have not shown similar results? Although there may have been differences among the participants that account for the positive results, such differences alone do not fully explain the [findings]. We are left with differences that appear encouraging, yet are not a “home run” with regard to the management of diabetes. In the coming years, controlled and comparative effectiveness trials that uniformly combine newer agents with older agents may help to delineate an event more effective treatment plan for the millions of people whose lives are affected by type 2 diabetes.
Dr. Julie R. Ingelfinger is employed by the New England Journal of Medicine as deputy editor. Dr. Clifford J. Rosen is at the Center for Clinical and Translational Research, Maine Medical Center Research Institute, Scarborough, and is an associate editor for the New England Journal of Medicine. These comments are from their accompanying editorial (N Engl J Med. 2016 Jun 14. doi: 10.1056/NEJMe1607413).
[In the EMPA-REG OUTCOME trial,] empagliflozin was associated with a slower progression of kidney disease and lower rates of clinically relevant renal events than was placebo when added to standard of care in patients at high cardiovascular risk. [In the LEADER trial,] the rate of the first occurrence of death from cardiovascular causes, nonfatal myocardial infarction, or nonfatal stroke among patients with type 2 diabetes mellitus was lower with liraglutide than placebo.
Why do the EMPA-REG OUTCOME and LEADER trials show cardiovascular and microvascular benefit, whereas other trials have come close yet have not shown similar results? Although there may have been differences among the participants that account for the positive results, such differences alone do not fully explain the [findings]. We are left with differences that appear encouraging, yet are not a “home run” with regard to the management of diabetes. In the coming years, controlled and comparative effectiveness trials that uniformly combine newer agents with older agents may help to delineate an event more effective treatment plan for the millions of people whose lives are affected by type 2 diabetes.
Dr. Julie R. Ingelfinger is employed by the New England Journal of Medicine as deputy editor. Dr. Clifford J. Rosen is at the Center for Clinical and Translational Research, Maine Medical Center Research Institute, Scarborough, and is an associate editor for the New England Journal of Medicine. These comments are from their accompanying editorial (N Engl J Med. 2016 Jun 14. doi: 10.1056/NEJMe1607413).
[In the EMPA-REG OUTCOME trial,] empagliflozin was associated with a slower progression of kidney disease and lower rates of clinically relevant renal events than was placebo when added to standard of care in patients at high cardiovascular risk. [In the LEADER trial,] the rate of the first occurrence of death from cardiovascular causes, nonfatal myocardial infarction, or nonfatal stroke among patients with type 2 diabetes mellitus was lower with liraglutide than placebo.
Why do the EMPA-REG OUTCOME and LEADER trials show cardiovascular and microvascular benefit, whereas other trials have come close yet have not shown similar results? Although there may have been differences among the participants that account for the positive results, such differences alone do not fully explain the [findings]. We are left with differences that appear encouraging, yet are not a “home run” with regard to the management of diabetes. In the coming years, controlled and comparative effectiveness trials that uniformly combine newer agents with older agents may help to delineate an event more effective treatment plan for the millions of people whose lives are affected by type 2 diabetes.
Dr. Julie R. Ingelfinger is employed by the New England Journal of Medicine as deputy editor. Dr. Clifford J. Rosen is at the Center for Clinical and Translational Research, Maine Medical Center Research Institute, Scarborough, and is an associate editor for the New England Journal of Medicine. These comments are from their accompanying editorial (N Engl J Med. 2016 Jun 14. doi: 10.1056/NEJMe1607413).
Empagliflozin was associated with a significant 39% decrease in risk of new or worsening nephropathy, compared with placebo among adults with type 2 diabetes at high risk for cardiovascular events, based on a secondary analysis of the phase III, randomized, double-blind EMPA-REG OUTCOME trial.
“Patients in the empagliflozin group also had a significantly lower risk of progression to macroalbuminuria or clinically relevant renal outcomes, such as a doubling of the serum creatinine level and initiation of renal-replacement therapy, than did those in the placebo group,” Dr. Christoph Wanner of Würzburg (Germany) University Clinic, and his associates reported in the June 14 New England Journal of Medicine.
Empagliflozin(Jardiance) is a selective sodium–glucose cotransporter-2 inhibitor that was approved in the United States in 2014 to improve glycemic control among patients with type 2 diabetes mellitus. In the initial analysis of the EMPA-REG OUTCOME trial, empagliflozin was associated with a significantly lower rate of cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke, as compared with placebo among patients with type 2 diabetes at high cardiovascular risk (N Engl J Med. 2015 Nov 26 doi: 10.1056/NEJMoa1504720).
For the current secondary analysis, Dr. Wanner and his associates focused on renal microvascular outcomes, including new or worsening nephropathy (macroalbuminuria, defined as greater than 300 mg of urinary albumin/gram of creatinine), a doubling of the serum creatinine level accompanied by an epidermal growth factor receptor (eGFR) of less than or equal to 45 mL/minute per 1.73 m2of body surface area, a new need for renal-replacement therapy, and death from renal disease. A total of 7,020 patients with type 2 diabetes and an eGFR of at least 30 mL/minute per 1.73 m2 of body-surface area received either 10 mg or 25 mg of empagliflozin or placebo once daily, plus standard diabetes care (N Engl J Med. 2016 Jun 14. doi: 10.1056/NEJMoa1515920).
New or worsening nephropathy occurred among 525 (12.7%) patients who received empagliflozin, compared with 388 (18.8%) patients who received placebo, for a statistically significant 39% decrease in relative risk of this outcome (hazard ratio, 0.61; P less than .001). This benefit persisted at both doses of empagliflozin, among patients with and without baseline chronic kidney disease (eGFR greater than or equal to 60 mL/min/1.73m2), and across other subgroups stratified by sex, race, body mass index, number of cardiovascular risk factors, and diabetes history and treatment.
A total of 70 patients (1.5%) in the empagliflozin group had a doubling of serum creatinine, vs. 60 patients (2.6%) in the placebo group, for a significant relative risk reduction of 44% (hazard ratio, 0.56; P less than .001). In addition, the proportion of patients starting renal-replacement therapy was twice as high in the placebo group than in the empagliflozin group (0.6% and 0.3%, respectively; HR, 0.45; P less .01).
The groups did not significantly differ in the rate of incident albuminuria, the researchers said. “There were three deaths from renal disease in the empagliflozin group (0.1%) and none in the placebo group,” they added.
The study uncovered no safety signals related to hypoglycemia, diabetic ketoacidosis, thromboembolic events, bone fractures, or volume depletion, the investigators said. Rates of overall adverse events, serious adverse events, and adverse events leading to treatment discontinuation were similar across groups. Rates of complicated urinary tract infections did not significantly vary according to treatment or based on the presence or absence of chronic kidney disease (CKD).Although empagliflozin was associated with a doubling in the rate of urosepsis, these events were rare, affecting only 0.3% and 0.7% of patients with baseline CKD and 0.1% and 0.2% of patients without baseline CKD.
The study was funded by the Boehringer Ingelheim and Eli Lilly and the Diabetes Alliance. Dr. Wanner disclosed grant support from the European Foundation for the Study of Diabetes and personal fees from Boehringer Ingelheim, Janssen, and Novo Nordisk.
Empagliflozin was associated with a significant 39% decrease in risk of new or worsening nephropathy, compared with placebo among adults with type 2 diabetes at high risk for cardiovascular events, based on a secondary analysis of the phase III, randomized, double-blind EMPA-REG OUTCOME trial.
“Patients in the empagliflozin group also had a significantly lower risk of progression to macroalbuminuria or clinically relevant renal outcomes, such as a doubling of the serum creatinine level and initiation of renal-replacement therapy, than did those in the placebo group,” Dr. Christoph Wanner of Würzburg (Germany) University Clinic, and his associates reported in the June 14 New England Journal of Medicine.
Empagliflozin(Jardiance) is a selective sodium–glucose cotransporter-2 inhibitor that was approved in the United States in 2014 to improve glycemic control among patients with type 2 diabetes mellitus. In the initial analysis of the EMPA-REG OUTCOME trial, empagliflozin was associated with a significantly lower rate of cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke, as compared with placebo among patients with type 2 diabetes at high cardiovascular risk (N Engl J Med. 2015 Nov 26 doi: 10.1056/NEJMoa1504720).
For the current secondary analysis, Dr. Wanner and his associates focused on renal microvascular outcomes, including new or worsening nephropathy (macroalbuminuria, defined as greater than 300 mg of urinary albumin/gram of creatinine), a doubling of the serum creatinine level accompanied by an epidermal growth factor receptor (eGFR) of less than or equal to 45 mL/minute per 1.73 m2of body surface area, a new need for renal-replacement therapy, and death from renal disease. A total of 7,020 patients with type 2 diabetes and an eGFR of at least 30 mL/minute per 1.73 m2 of body-surface area received either 10 mg or 25 mg of empagliflozin or placebo once daily, plus standard diabetes care (N Engl J Med. 2016 Jun 14. doi: 10.1056/NEJMoa1515920).
New or worsening nephropathy occurred among 525 (12.7%) patients who received empagliflozin, compared with 388 (18.8%) patients who received placebo, for a statistically significant 39% decrease in relative risk of this outcome (hazard ratio, 0.61; P less than .001). This benefit persisted at both doses of empagliflozin, among patients with and without baseline chronic kidney disease (eGFR greater than or equal to 60 mL/min/1.73m2), and across other subgroups stratified by sex, race, body mass index, number of cardiovascular risk factors, and diabetes history and treatment.
A total of 70 patients (1.5%) in the empagliflozin group had a doubling of serum creatinine, vs. 60 patients (2.6%) in the placebo group, for a significant relative risk reduction of 44% (hazard ratio, 0.56; P less than .001). In addition, the proportion of patients starting renal-replacement therapy was twice as high in the placebo group than in the empagliflozin group (0.6% and 0.3%, respectively; HR, 0.45; P less .01).
The groups did not significantly differ in the rate of incident albuminuria, the researchers said. “There were three deaths from renal disease in the empagliflozin group (0.1%) and none in the placebo group,” they added.
The study uncovered no safety signals related to hypoglycemia, diabetic ketoacidosis, thromboembolic events, bone fractures, or volume depletion, the investigators said. Rates of overall adverse events, serious adverse events, and adverse events leading to treatment discontinuation were similar across groups. Rates of complicated urinary tract infections did not significantly vary according to treatment or based on the presence or absence of chronic kidney disease (CKD).Although empagliflozin was associated with a doubling in the rate of urosepsis, these events were rare, affecting only 0.3% and 0.7% of patients with baseline CKD and 0.1% and 0.2% of patients without baseline CKD.
The study was funded by the Boehringer Ingelheim and Eli Lilly and the Diabetes Alliance. Dr. Wanner disclosed grant support from the European Foundation for the Study of Diabetes and personal fees from Boehringer Ingelheim, Janssen, and Novo Nordisk.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Compared with placebo, empagliflozin was associated with better renal outcomes among patients with type 2 diabetes and high cardiovascular risk.
Major finding: New or worsening nephropathy affected 525 (12.7%) empagliflozin patients, vs. 388 (18.8%) placebo patients (HR, 0.61; P less than .001).
Data source: A secondary analysis of data for 4,124 patients from the international, phase III, double-blind EMPA-REG OUTCOMES trial.
Disclosures: The study was funded by the Boehringer Ingelheim and Eli Lilly and the Diabetes Alliance. Dr. Wanner disclosed grant support from the European Foundation for the Study of Diabetes and personal fees from Boehringer Ingelheim, Janssen, and Novo Nordisk.
Skin patch testing pinpoints dietary triggers of IBS
SAN DIEGO – About 90% of patients reported improvement in symptoms of irritable bowel syndrome after avoiding type 4 food allergens identified by skin patch testing, according to an uncontrolled study.
Furthermore, 69% of patients reported at least moderate improvement after eliminating foods to which they reacted, said Dr. Michael Stierstorfer, a dermatologist at East Penn Dermatology in North Wales, Pa., who partnered with gastroenterologists at Temple University to conduct the study. “This raises questions about a possible overlap between IBS and allergic contact enteritis,” the researchers stated in a poster presented at the annual Digestive Disease Week.
Irritable bowel syndrome is often treatment refractory and tends to elude conventional diagnostics. That was the case for Dr. Stierstorfer, who several years ago developed symptoms of IBS with constipation (IBS-C) that eventually affected him about half the time, he said in an interview. A hydrogen breath test, upper endoscopy, colonoscopy, abdominal/pelvic CT, and tests for gluten-sensitive enteropathy and parasites revealed no abnormalities except decreased small intestinal motility, he said.
But after “flaring badly” twice when he ate Indian food, he began to suspect a cause. “I stopped eating garlic and within a day, I was absolutely fine,” Dr. Stierstorfer said. “The symptoms recurred only if I accidentally ate garlic again.”
Studies had refuted links between IBS and type 1 hypersensitivity but had not explored the role of type 4 (delayed) hypersensitivity in the disorder, Dr. Stierstorfer discovered. “Dermatologists do patch testing all the time for patients with refractory eczema to search for type 4 allergic contact factors that might be causing their rash,” he said. “I performed a patch test of garlic on myself to look for a type 4 allergy, and it was strongly positive. I thought I probably wasn’t the only person walking around with symptoms that mimicked IBS but were really from a type 4 food allergy.”
He tested that idea by skin patch testing 50 patients with IBS symptoms whom he recruited through his dermatology practice. In all, 30 (60%) patients reacted to at least one food allergen, of whom 14 (46%) reported symptomatic improvement after eliminating the suspected triggers from their diets. The findings appeared in the March 2013 Journal of the American Academy of Dermatology (68:377-84).
Next, Dr. Stierstorfer partnered with Dr. Grace Shin, a 3rd-year gastroenterology fellow at Temple University, Philadelphia, and her colleagues. Together, they tested 57 patients with physician-diagnosed IBS with diarrhea (about 43% of patients), IBS with constipation (16%), mixed IBS (30%), or unsubtyped IBS (11%). Patients averaged 41 years of age (standard deviation, 15 years) and 77% were female. Each patient had between 118 and 122 individual allergen patches placed on his or her back. Two days later, the patches were removed and the skin evaluated for macular erythema consistent with a type 4 hypersensitivity reaction. The patients were checked again a day or 2 later to catch any highly delayed reactions.
In all, 56 patients (98%) showed evidence of at least one hypersensitivity, and most reacted to between two and three allergens, Dr. Stierstorfer said. The most commonly identified triggers were cinnamon bark (35 patients; 61%) and sodium bisulfite (26 patients; 46%). At baseline, patients rated their abdominal pain or discomfort at an average of 6.7 on a 10-point severity scale (SD, 2.3 points). After 2-4 weeks of avoiding allergens to which they developed macular edema, they reported a mean 4.4-point improvement in their abdominal symptoms (SD, 2.7 points; P less than .001).
The patients also reported an average 5.8-point improvement on a 10-point scale of global IBS symptom severity (SD, 3.2 points; P less than .001). Overall, 91% of patients reported at least partial relief of abdominal symptoms, while 89% of patients reported at least partial relief of global symptoms, the investigators reported.
Based on these results, “food-related type 4 hypersensitivity reactions may contribute to the pathogenesis of IBS and IBS-like symptoms,” Dr. Shin said in an interview. “The idea of allergic contact enteritis intrigued me, because it made me think that some patients diagnosed with IBS, especially IBS with diarrhea, might benefit from allergy testing when the standard approaches don’t work.”
Another dietary intervention for IBS, the low-FODMAP diet, can help relieve symptoms, “but it’s a hard diet to follow,” Dr. Shin added. “Being able to focus on eliminating one or two things would be easier than eliminating multiple classes of foods that are so common to an American diet.”
Next, the team is planning a controlled trial of the skin patch test. “There is still more validation work to do,” said Dr. Stierstorfer. “But I think this shows that looking at something from a unique perspective – in this case, a dermatologic perspective for a GI problem – can result in a new approach, and potentially an advance in medicine.”
Dr. Shin had no disclosures. Dr. Stierstorfer disclosed financial ties to IBS Centers for Advanced Food Allergy Testing.
SAN DIEGO – About 90% of patients reported improvement in symptoms of irritable bowel syndrome after avoiding type 4 food allergens identified by skin patch testing, according to an uncontrolled study.
Furthermore, 69% of patients reported at least moderate improvement after eliminating foods to which they reacted, said Dr. Michael Stierstorfer, a dermatologist at East Penn Dermatology in North Wales, Pa., who partnered with gastroenterologists at Temple University to conduct the study. “This raises questions about a possible overlap between IBS and allergic contact enteritis,” the researchers stated in a poster presented at the annual Digestive Disease Week.
Irritable bowel syndrome is often treatment refractory and tends to elude conventional diagnostics. That was the case for Dr. Stierstorfer, who several years ago developed symptoms of IBS with constipation (IBS-C) that eventually affected him about half the time, he said in an interview. A hydrogen breath test, upper endoscopy, colonoscopy, abdominal/pelvic CT, and tests for gluten-sensitive enteropathy and parasites revealed no abnormalities except decreased small intestinal motility, he said.
But after “flaring badly” twice when he ate Indian food, he began to suspect a cause. “I stopped eating garlic and within a day, I was absolutely fine,” Dr. Stierstorfer said. “The symptoms recurred only if I accidentally ate garlic again.”
Studies had refuted links between IBS and type 1 hypersensitivity but had not explored the role of type 4 (delayed) hypersensitivity in the disorder, Dr. Stierstorfer discovered. “Dermatologists do patch testing all the time for patients with refractory eczema to search for type 4 allergic contact factors that might be causing their rash,” he said. “I performed a patch test of garlic on myself to look for a type 4 allergy, and it was strongly positive. I thought I probably wasn’t the only person walking around with symptoms that mimicked IBS but were really from a type 4 food allergy.”
He tested that idea by skin patch testing 50 patients with IBS symptoms whom he recruited through his dermatology practice. In all, 30 (60%) patients reacted to at least one food allergen, of whom 14 (46%) reported symptomatic improvement after eliminating the suspected triggers from their diets. The findings appeared in the March 2013 Journal of the American Academy of Dermatology (68:377-84).
Next, Dr. Stierstorfer partnered with Dr. Grace Shin, a 3rd-year gastroenterology fellow at Temple University, Philadelphia, and her colleagues. Together, they tested 57 patients with physician-diagnosed IBS with diarrhea (about 43% of patients), IBS with constipation (16%), mixed IBS (30%), or unsubtyped IBS (11%). Patients averaged 41 years of age (standard deviation, 15 years) and 77% were female. Each patient had between 118 and 122 individual allergen patches placed on his or her back. Two days later, the patches were removed and the skin evaluated for macular erythema consistent with a type 4 hypersensitivity reaction. The patients were checked again a day or 2 later to catch any highly delayed reactions.
In all, 56 patients (98%) showed evidence of at least one hypersensitivity, and most reacted to between two and three allergens, Dr. Stierstorfer said. The most commonly identified triggers were cinnamon bark (35 patients; 61%) and sodium bisulfite (26 patients; 46%). At baseline, patients rated their abdominal pain or discomfort at an average of 6.7 on a 10-point severity scale (SD, 2.3 points). After 2-4 weeks of avoiding allergens to which they developed macular edema, they reported a mean 4.4-point improvement in their abdominal symptoms (SD, 2.7 points; P less than .001).
The patients also reported an average 5.8-point improvement on a 10-point scale of global IBS symptom severity (SD, 3.2 points; P less than .001). Overall, 91% of patients reported at least partial relief of abdominal symptoms, while 89% of patients reported at least partial relief of global symptoms, the investigators reported.
Based on these results, “food-related type 4 hypersensitivity reactions may contribute to the pathogenesis of IBS and IBS-like symptoms,” Dr. Shin said in an interview. “The idea of allergic contact enteritis intrigued me, because it made me think that some patients diagnosed with IBS, especially IBS with diarrhea, might benefit from allergy testing when the standard approaches don’t work.”
Another dietary intervention for IBS, the low-FODMAP diet, can help relieve symptoms, “but it’s a hard diet to follow,” Dr. Shin added. “Being able to focus on eliminating one or two things would be easier than eliminating multiple classes of foods that are so common to an American diet.”
Next, the team is planning a controlled trial of the skin patch test. “There is still more validation work to do,” said Dr. Stierstorfer. “But I think this shows that looking at something from a unique perspective – in this case, a dermatologic perspective for a GI problem – can result in a new approach, and potentially an advance in medicine.”
Dr. Shin had no disclosures. Dr. Stierstorfer disclosed financial ties to IBS Centers for Advanced Food Allergy Testing.
SAN DIEGO – About 90% of patients reported improvement in symptoms of irritable bowel syndrome after avoiding type 4 food allergens identified by skin patch testing, according to an uncontrolled study.
Furthermore, 69% of patients reported at least moderate improvement after eliminating foods to which they reacted, said Dr. Michael Stierstorfer, a dermatologist at East Penn Dermatology in North Wales, Pa., who partnered with gastroenterologists at Temple University to conduct the study. “This raises questions about a possible overlap between IBS and allergic contact enteritis,” the researchers stated in a poster presented at the annual Digestive Disease Week.
Irritable bowel syndrome is often treatment refractory and tends to elude conventional diagnostics. That was the case for Dr. Stierstorfer, who several years ago developed symptoms of IBS with constipation (IBS-C) that eventually affected him about half the time, he said in an interview. A hydrogen breath test, upper endoscopy, colonoscopy, abdominal/pelvic CT, and tests for gluten-sensitive enteropathy and parasites revealed no abnormalities except decreased small intestinal motility, he said.
But after “flaring badly” twice when he ate Indian food, he began to suspect a cause. “I stopped eating garlic and within a day, I was absolutely fine,” Dr. Stierstorfer said. “The symptoms recurred only if I accidentally ate garlic again.”
Studies had refuted links between IBS and type 1 hypersensitivity but had not explored the role of type 4 (delayed) hypersensitivity in the disorder, Dr. Stierstorfer discovered. “Dermatologists do patch testing all the time for patients with refractory eczema to search for type 4 allergic contact factors that might be causing their rash,” he said. “I performed a patch test of garlic on myself to look for a type 4 allergy, and it was strongly positive. I thought I probably wasn’t the only person walking around with symptoms that mimicked IBS but were really from a type 4 food allergy.”
He tested that idea by skin patch testing 50 patients with IBS symptoms whom he recruited through his dermatology practice. In all, 30 (60%) patients reacted to at least one food allergen, of whom 14 (46%) reported symptomatic improvement after eliminating the suspected triggers from their diets. The findings appeared in the March 2013 Journal of the American Academy of Dermatology (68:377-84).
Next, Dr. Stierstorfer partnered with Dr. Grace Shin, a 3rd-year gastroenterology fellow at Temple University, Philadelphia, and her colleagues. Together, they tested 57 patients with physician-diagnosed IBS with diarrhea (about 43% of patients), IBS with constipation (16%), mixed IBS (30%), or unsubtyped IBS (11%). Patients averaged 41 years of age (standard deviation, 15 years) and 77% were female. Each patient had between 118 and 122 individual allergen patches placed on his or her back. Two days later, the patches were removed and the skin evaluated for macular erythema consistent with a type 4 hypersensitivity reaction. The patients were checked again a day or 2 later to catch any highly delayed reactions.
In all, 56 patients (98%) showed evidence of at least one hypersensitivity, and most reacted to between two and three allergens, Dr. Stierstorfer said. The most commonly identified triggers were cinnamon bark (35 patients; 61%) and sodium bisulfite (26 patients; 46%). At baseline, patients rated their abdominal pain or discomfort at an average of 6.7 on a 10-point severity scale (SD, 2.3 points). After 2-4 weeks of avoiding allergens to which they developed macular edema, they reported a mean 4.4-point improvement in their abdominal symptoms (SD, 2.7 points; P less than .001).
The patients also reported an average 5.8-point improvement on a 10-point scale of global IBS symptom severity (SD, 3.2 points; P less than .001). Overall, 91% of patients reported at least partial relief of abdominal symptoms, while 89% of patients reported at least partial relief of global symptoms, the investigators reported.
Based on these results, “food-related type 4 hypersensitivity reactions may contribute to the pathogenesis of IBS and IBS-like symptoms,” Dr. Shin said in an interview. “The idea of allergic contact enteritis intrigued me, because it made me think that some patients diagnosed with IBS, especially IBS with diarrhea, might benefit from allergy testing when the standard approaches don’t work.”
Another dietary intervention for IBS, the low-FODMAP diet, can help relieve symptoms, “but it’s a hard diet to follow,” Dr. Shin added. “Being able to focus on eliminating one or two things would be easier than eliminating multiple classes of foods that are so common to an American diet.”
Next, the team is planning a controlled trial of the skin patch test. “There is still more validation work to do,” said Dr. Stierstorfer. “But I think this shows that looking at something from a unique perspective – in this case, a dermatologic perspective for a GI problem – can result in a new approach, and potentially an advance in medicine.”
Dr. Shin had no disclosures. Dr. Stierstorfer disclosed financial ties to IBS Centers for Advanced Food Allergy Testing.
AT DDW® 2016
Key clinical point: Avoiding food allergens identified by skin patch testing significantly improved self-reported symptoms of irritable bowel syndrome.
Major finding: In all, 69% of patients reported at least moderate improvement after eliminating foods to which they reacted.
Data source: A single-arm proof-of-concept study of 57 patients with physician-diagnosed IBS.
Disclosures: Dr. Shin had no disclosures. Dr. Stierstorfer disclosed financial ties to IBS Centers for Advanced Food Allergy Testing.
IASLC lung cancer staging project proposes changes for new TNM classification
The International Association for the Study of Lung Cancer (IASLC) Staging and Prognostic Factors Committee has developed proposals for revision of the T, N, and M categories of the 8th edition of the TNM Classification for lung cancer due to be published in late 2016. The new classification will be enacted in January 2017.
The changes proposed were based on the results of an analysis of a new database of 94,708 cases donated from 35 sources in 16 countries around the world.
The methods used and the proposals made were published in the Journal of Thoracic Oncology (2016;11:39-51).
Candidate proposals for the TNM stage groups were developed in conjunction with proposed changes to the T and M categories, which were previously published (J Thorac Oncol 2015;10:990-1003, and 2015;10:1515-22). There were no proposed changes to the N.
Changes to some T and M descriptors will result in these cases being assigned to a different stage than that to which they would have been assigned in the 7th edition. In addition, some TNM subsets have been moved to a new stage grouping, according to Dr. Peter Goldstraw of Imperial College, London, and his colleagues on behalf of the IASLC Staging and Prognostic Factors Committee.
Major new proposals
T1 changes: Size cut points have further proliferated in the proposals for the 8th edition, and outgrowth of the emphasis on tumor size in the 7th edition, such that size will now be a descriptor in all T categories, according to the authors. New stage groupings proposed divide stage T1 into T1a, T1b, and T1c, based on the new size cut points of 1 cm and 2 cm. This results in these cases (when associated with the categories N0 and M0) being assigned to stages 1A1, 1A2, and 1A3, respectively, which reflects the statistically different prognosis of these cases.
T3, T4 changes: A new group has been created for the most advanced local disease categories, T3 and T4 associated with N3 disease, but category M0. Such cases will now be classified as stage IIIC, reflecting their worse outcomes than seen in cases involving tumors that remain in stage IIIB. The prognosis for stage IIIC cases is similar to that of stage IVA cases, however the researchers justified the separation, based upon the different treatment approaches used for such cases.
M changes: Although cases with intrathoracic metastatic disease to the contralateral lung or with pleural/pericardial dissemination remain classified as M1a disease, the category M1b will now be assigned to cases with a single metastatic deposit (in one organ) and M1a and M1b cases will be moored to a new stage grouping called IVA. The more common situation of multiple metastatic deposits, usually in more than one organ, will be classified as M1c and staged as IVB. Separation of the M1a and M1b categories was maintained both for further data analysis and because some patients with oligometastatic disease are now receiving more aggressive local therapy in addition to systemic treatment, according to the authors.
Other proposals
A variety of more minor changes to stage groupings has also been proposed, some of which will result in a T descriptor being allocated to a higher stage. In some cases, tumors may be allocated to a different T category entirely, leading to a reclassification of stage. Among the examples given were tumors associated with diaphragmatic invasion to TV, which, when associated with N0 disease, will move from stage IIB to IIA.
Impact on treatment
The relationship of the proposed classification changes to treatment decisions is not direct, the authors stated in their discussion. “Although such changes might raise the issue of whether consequent changes to treatment algorithms are needed, it is important to remind ourselves that stage does not dictate treatment. Stage is one, and perhaps the most important, of several prognostic factors that guide the appropriate treatment option[s] to offer the patient. Any change to established treatment algorithms should be based on clinical judgment informed by prospective trials,” they emphasized.
New stage groupings should be used in any trials of novel therapies, they added.
“We hope that the thoracic oncology community finds the proposals of value and that, when accepted, will have a positive impact on the effectiveness of treatment for lung cancer, which will benefit patients around the globe,” the researchers concluded.
The research to develop the new proposals was funded by the IASLC, including funds obtained through unrestricted grants obtained from the pharmaceutical industry. The authors reported no other disclosures.
The 8th edition of the TNM staging is upon us. It is the summary of analysis of 90,000 cases and data collected over 11 years. It behooves every thoracic surgeon taking care of patients with lung cancer to familiarize themselves with the new version. The staging proposal is available as an open access article on the Journal of Thoracic Oncology website.
From a statistical viewpoint, this edition fits the data better than previous editions did. However, from a practical application, it is more cumbersome to use routinely in a busy clinic. One hopes that we can soon say, “There’s an app for that!” Such interfacing will enhance the application of this edition significantly.

|
Dr. Sai Yendamuri |
The new edition of the staging system is particularly important for surgeons for two reasons. The first is the formal recognition that patients with oligometastatic disease have a better prognosis than other stage IV disease and may be amenable to multimodality therapies with curative intent, as is currently performed by select clinical teams. The second is the further refinement of stage I disease with respect to tumor size. Combined with the new histologic classification of adenocarcinoma and its proposed integration with the TNM classification, the debate of sublobar vs. lobar resection for stage I NSCLC will become more nuanced. These implications for the practicing thoracic surgeon make the manuscript mandatory reading.
Dr. Sai Yendamuri is chair, department of thoracic surgery, and director, thoracic surgery research laboratory, and a professor of oncology at Roswell Park Cancer Institute, Buffalo, N.Y. He is also the general thoracic editor for Thoracic Surgery News.
The 8th edition of the TNM staging is upon us. It is the summary of analysis of 90,000 cases and data collected over 11 years. It behooves every thoracic surgeon taking care of patients with lung cancer to familiarize themselves with the new version. The staging proposal is available as an open access article on the Journal of Thoracic Oncology website.
From a statistical viewpoint, this edition fits the data better than previous editions did. However, from a practical application, it is more cumbersome to use routinely in a busy clinic. One hopes that we can soon say, “There’s an app for that!” Such interfacing will enhance the application of this edition significantly.

|
Dr. Sai Yendamuri |
The new edition of the staging system is particularly important for surgeons for two reasons. The first is the formal recognition that patients with oligometastatic disease have a better prognosis than other stage IV disease and may be amenable to multimodality therapies with curative intent, as is currently performed by select clinical teams. The second is the further refinement of stage I disease with respect to tumor size. Combined with the new histologic classification of adenocarcinoma and its proposed integration with the TNM classification, the debate of sublobar vs. lobar resection for stage I NSCLC will become more nuanced. These implications for the practicing thoracic surgeon make the manuscript mandatory reading.
Dr. Sai Yendamuri is chair, department of thoracic surgery, and director, thoracic surgery research laboratory, and a professor of oncology at Roswell Park Cancer Institute, Buffalo, N.Y. He is also the general thoracic editor for Thoracic Surgery News.
The 8th edition of the TNM staging is upon us. It is the summary of analysis of 90,000 cases and data collected over 11 years. It behooves every thoracic surgeon taking care of patients with lung cancer to familiarize themselves with the new version. The staging proposal is available as an open access article on the Journal of Thoracic Oncology website.
From a statistical viewpoint, this edition fits the data better than previous editions did. However, from a practical application, it is more cumbersome to use routinely in a busy clinic. One hopes that we can soon say, “There’s an app for that!” Such interfacing will enhance the application of this edition significantly.

|
Dr. Sai Yendamuri |
The new edition of the staging system is particularly important for surgeons for two reasons. The first is the formal recognition that patients with oligometastatic disease have a better prognosis than other stage IV disease and may be amenable to multimodality therapies with curative intent, as is currently performed by select clinical teams. The second is the further refinement of stage I disease with respect to tumor size. Combined with the new histologic classification of adenocarcinoma and its proposed integration with the TNM classification, the debate of sublobar vs. lobar resection for stage I NSCLC will become more nuanced. These implications for the practicing thoracic surgeon make the manuscript mandatory reading.
Dr. Sai Yendamuri is chair, department of thoracic surgery, and director, thoracic surgery research laboratory, and a professor of oncology at Roswell Park Cancer Institute, Buffalo, N.Y. He is also the general thoracic editor for Thoracic Surgery News.
The International Association for the Study of Lung Cancer (IASLC) Staging and Prognostic Factors Committee has developed proposals for revision of the T, N, and M categories of the 8th edition of the TNM Classification for lung cancer due to be published in late 2016. The new classification will be enacted in January 2017.
The changes proposed were based on the results of an analysis of a new database of 94,708 cases donated from 35 sources in 16 countries around the world.
The methods used and the proposals made were published in the Journal of Thoracic Oncology (2016;11:39-51).
Candidate proposals for the TNM stage groups were developed in conjunction with proposed changes to the T and M categories, which were previously published (J Thorac Oncol 2015;10:990-1003, and 2015;10:1515-22). There were no proposed changes to the N.
Changes to some T and M descriptors will result in these cases being assigned to a different stage than that to which they would have been assigned in the 7th edition. In addition, some TNM subsets have been moved to a new stage grouping, according to Dr. Peter Goldstraw of Imperial College, London, and his colleagues on behalf of the IASLC Staging and Prognostic Factors Committee.
Major new proposals
T1 changes: Size cut points have further proliferated in the proposals for the 8th edition, and outgrowth of the emphasis on tumor size in the 7th edition, such that size will now be a descriptor in all T categories, according to the authors. New stage groupings proposed divide stage T1 into T1a, T1b, and T1c, based on the new size cut points of 1 cm and 2 cm. This results in these cases (when associated with the categories N0 and M0) being assigned to stages 1A1, 1A2, and 1A3, respectively, which reflects the statistically different prognosis of these cases.
T3, T4 changes: A new group has been created for the most advanced local disease categories, T3 and T4 associated with N3 disease, but category M0. Such cases will now be classified as stage IIIC, reflecting their worse outcomes than seen in cases involving tumors that remain in stage IIIB. The prognosis for stage IIIC cases is similar to that of stage IVA cases, however the researchers justified the separation, based upon the different treatment approaches used for such cases.
M changes: Although cases with intrathoracic metastatic disease to the contralateral lung or with pleural/pericardial dissemination remain classified as M1a disease, the category M1b will now be assigned to cases with a single metastatic deposit (in one organ) and M1a and M1b cases will be moored to a new stage grouping called IVA. The more common situation of multiple metastatic deposits, usually in more than one organ, will be classified as M1c and staged as IVB. Separation of the M1a and M1b categories was maintained both for further data analysis and because some patients with oligometastatic disease are now receiving more aggressive local therapy in addition to systemic treatment, according to the authors.
Other proposals
A variety of more minor changes to stage groupings has also been proposed, some of which will result in a T descriptor being allocated to a higher stage. In some cases, tumors may be allocated to a different T category entirely, leading to a reclassification of stage. Among the examples given were tumors associated with diaphragmatic invasion to TV, which, when associated with N0 disease, will move from stage IIB to IIA.
Impact on treatment
The relationship of the proposed classification changes to treatment decisions is not direct, the authors stated in their discussion. “Although such changes might raise the issue of whether consequent changes to treatment algorithms are needed, it is important to remind ourselves that stage does not dictate treatment. Stage is one, and perhaps the most important, of several prognostic factors that guide the appropriate treatment option[s] to offer the patient. Any change to established treatment algorithms should be based on clinical judgment informed by prospective trials,” they emphasized.
New stage groupings should be used in any trials of novel therapies, they added.
“We hope that the thoracic oncology community finds the proposals of value and that, when accepted, will have a positive impact on the effectiveness of treatment for lung cancer, which will benefit patients around the globe,” the researchers concluded.
The research to develop the new proposals was funded by the IASLC, including funds obtained through unrestricted grants obtained from the pharmaceutical industry. The authors reported no other disclosures.
The International Association for the Study of Lung Cancer (IASLC) Staging and Prognostic Factors Committee has developed proposals for revision of the T, N, and M categories of the 8th edition of the TNM Classification for lung cancer due to be published in late 2016. The new classification will be enacted in January 2017.
The changes proposed were based on the results of an analysis of a new database of 94,708 cases donated from 35 sources in 16 countries around the world.
The methods used and the proposals made were published in the Journal of Thoracic Oncology (2016;11:39-51).
Candidate proposals for the TNM stage groups were developed in conjunction with proposed changes to the T and M categories, which were previously published (J Thorac Oncol 2015;10:990-1003, and 2015;10:1515-22). There were no proposed changes to the N.
Changes to some T and M descriptors will result in these cases being assigned to a different stage than that to which they would have been assigned in the 7th edition. In addition, some TNM subsets have been moved to a new stage grouping, according to Dr. Peter Goldstraw of Imperial College, London, and his colleagues on behalf of the IASLC Staging and Prognostic Factors Committee.
Major new proposals
T1 changes: Size cut points have further proliferated in the proposals for the 8th edition, and outgrowth of the emphasis on tumor size in the 7th edition, such that size will now be a descriptor in all T categories, according to the authors. New stage groupings proposed divide stage T1 into T1a, T1b, and T1c, based on the new size cut points of 1 cm and 2 cm. This results in these cases (when associated with the categories N0 and M0) being assigned to stages 1A1, 1A2, and 1A3, respectively, which reflects the statistically different prognosis of these cases.
T3, T4 changes: A new group has been created for the most advanced local disease categories, T3 and T4 associated with N3 disease, but category M0. Such cases will now be classified as stage IIIC, reflecting their worse outcomes than seen in cases involving tumors that remain in stage IIIB. The prognosis for stage IIIC cases is similar to that of stage IVA cases, however the researchers justified the separation, based upon the different treatment approaches used for such cases.
M changes: Although cases with intrathoracic metastatic disease to the contralateral lung or with pleural/pericardial dissemination remain classified as M1a disease, the category M1b will now be assigned to cases with a single metastatic deposit (in one organ) and M1a and M1b cases will be moored to a new stage grouping called IVA. The more common situation of multiple metastatic deposits, usually in more than one organ, will be classified as M1c and staged as IVB. Separation of the M1a and M1b categories was maintained both for further data analysis and because some patients with oligometastatic disease are now receiving more aggressive local therapy in addition to systemic treatment, according to the authors.
Other proposals
A variety of more minor changes to stage groupings has also been proposed, some of which will result in a T descriptor being allocated to a higher stage. In some cases, tumors may be allocated to a different T category entirely, leading to a reclassification of stage. Among the examples given were tumors associated with diaphragmatic invasion to TV, which, when associated with N0 disease, will move from stage IIB to IIA.
Impact on treatment
The relationship of the proposed classification changes to treatment decisions is not direct, the authors stated in their discussion. “Although such changes might raise the issue of whether consequent changes to treatment algorithms are needed, it is important to remind ourselves that stage does not dictate treatment. Stage is one, and perhaps the most important, of several prognostic factors that guide the appropriate treatment option[s] to offer the patient. Any change to established treatment algorithms should be based on clinical judgment informed by prospective trials,” they emphasized.
New stage groupings should be used in any trials of novel therapies, they added.
“We hope that the thoracic oncology community finds the proposals of value and that, when accepted, will have a positive impact on the effectiveness of treatment for lung cancer, which will benefit patients around the globe,” the researchers concluded.
The research to develop the new proposals was funded by the IASLC, including funds obtained through unrestricted grants obtained from the pharmaceutical industry. The authors reported no other disclosures.
FROM THE JOURNAL OF THORACIC ONCOLOGY
Key clinical point: New lung cancer classification to become effective January 2017.
Major finding: Size will now be a descriptor in all T categories, according to the authors. New stage groupings proposed dividing stage T1 into T1a, T1b, and T1c, based on the new size cut points of 1 cm and 2 cm.
Data source: The International Association for the Study of Lung Cancer (IASLC) Staging and Prognostic Factors Committee has developed proposals for revision of the T, N, and M categories of the 8th edition of the TNM Classification for lung cancer.
Disclosures: The research to develop the new proposals was funded by the IASLC, including funds obtained through unrestricted grants obtained from the pharmaceutical industry. The authors reported no other disclosures.
Recognizing Contributions Physician Personalities Make to the Greater Good
My family and I recently took a spring break trip out west to see a few national parks. During the trip, we stayed on a family ranch in Utah. It had a wide variety of livestock, including a large number of mules and horses.
During our stay at this family-owned ranch, two things really stood out and made me think:
- The guesthouse we stayed in had an inordinate volume of collections dedicated to the science and art of raising horses and mules. Everywhere one looked you could find a wall-mounted picture, poem, or coffee table book about these species. My favorite, written by the owner of the ranch, John Hauer, was The Natural Superiority of Mules.1
- The second thing I noticed was that every member of the ranch-owning family had fairly strong opinions about which was better—horse or mule. Just to recap the biology, a horse is the product of two horses, whereas a mule is the progeny of a male donkey and a female horse. It turns out that their physical structure and demeanors are very different.
One of the oldest members of the ranch family (who I believe was a “distant uncle”) had a very strong opinion about the superiority of the mule. His opinion was based on selected facts, including that mules are “steadier on their feet” in unstable ground, require less volume and less frequent food and water, and very rarely became ill or need costly veterinary care.
Another mule-favoring family member told us how mules get a “bad rap” for being stubborn when they actually are much smarter and better decision makers than horses. She recalled a famous folklore of a farmer who took his mule out to gather materials from across a field. When the farmer and the mule approached a wooden bridge, the mule absolutely refused to cross the bridge. After much back and forth between the farmer and the mule (involving both coaxing and cussing), the farmer gave up and returned to the farm with the mule. He then took his horse on the same errand. When they came to the same bridge, the horse also hesitated but required little bargaining from the farmer to coax it to cross the bridge. When barely halfway across, a rotten board in the bridge gave way, almost sending both the horse and the farmer to their deaths in the ravine below.
The moral of the folklore is that mules cannot be coaxed (or cussed) into performing behaviors that will put themselves or those around them at risk of injury or death. Mules will stop when exhausted or profoundly dehydrated, for example, whereas a horse will continue on if ordered by their farmer, even to the point of running themselves to their eventual demise.
One of the younger members of the family-owned ranch, however, had very strong opinions on the superiority of the horse. Horses are loyal and unwavering in their dedication to please those that they serve. They will put the needs of others before themselves in most situations and therefore almost always “outperform” a mule in all respects. They are willing and (usually) able to perform in uncertain conditions, even despite some reservations. They are loyal and loving, and they have unique and inquisitive personalities, which makes them fun to raise and to ride any day.
Test Drives
Our family of four went on a ride with some of these animals and randomly got two horses and two mules. Interestingly, during our ride, we all did indeed notice the differences between the horses and the mules.
The horses were seemingly easygoing and quick to please, easily following cues to change direction or course. The mules were more hesitant and seemed to need to understand why they were being asked to do something before they acquiesced to the demand.
And when we approached a narrow rocky downslope, the mules were slow, steady, and confident, whereas the horses were seemingly uncomfortable and less agile. And, indeed in researching mules, they seem to have gotten a very bad rap over time (as evidenced by the term “stubborn as a mule”).
Charles Darwin actually categorized mules as an example of “hybrid vigor,” which is a rare example of when an offspring is actually better in most ways than either of its parents. Compared to its parental species, mules have more intelligence, endurance, longevity, health, speed, height, and agility. Also to their advantage, they have harder skin and hooves, allowing them to weather and endure more treacherous conditions.
With all of this newfound knowledge of the mule, it struck me what remarkable similarity some physicians have with mules and the role that these mules are likely serving within our organizations. These physicians are probably labeled as stubborn, obstinate, resistant, or impatient. But maybe they are actually intelligent, agile, and appropriately cautious. Maybe the resistance they express in the organization is serving to warn others about the rotten wooden bridges.
HM Takeaway
Similar to a ranch, most hospitals probably function best with a healthy combination of horses and mules. So if you get an opportunity, next time you encounter physicians at your hospital acting like mules, you should congratulate them and appreciate their mule-like characteristics. Recognize the contribution these types of physicians are making, in their own way, to the greater good of the organization.
After all, we can’t—and shouldn’t—all be horses. TH
Reference
1. Hauer J. The Natural Superiority of Mules: A Celebration of One of the Most Intelligent, Sure-footed, and Misunderstood Animals in the World. New York, NY: Skyhorse Publishing; 2006.

My family and I recently took a spring break trip out west to see a few national parks. During the trip, we stayed on a family ranch in Utah. It had a wide variety of livestock, including a large number of mules and horses.
During our stay at this family-owned ranch, two things really stood out and made me think:
- The guesthouse we stayed in had an inordinate volume of collections dedicated to the science and art of raising horses and mules. Everywhere one looked you could find a wall-mounted picture, poem, or coffee table book about these species. My favorite, written by the owner of the ranch, John Hauer, was The Natural Superiority of Mules.1
- The second thing I noticed was that every member of the ranch-owning family had fairly strong opinions about which was better—horse or mule. Just to recap the biology, a horse is the product of two horses, whereas a mule is the progeny of a male donkey and a female horse. It turns out that their physical structure and demeanors are very different.
One of the oldest members of the ranch family (who I believe was a “distant uncle”) had a very strong opinion about the superiority of the mule. His opinion was based on selected facts, including that mules are “steadier on their feet” in unstable ground, require less volume and less frequent food and water, and very rarely became ill or need costly veterinary care.
Another mule-favoring family member told us how mules get a “bad rap” for being stubborn when they actually are much smarter and better decision makers than horses. She recalled a famous folklore of a farmer who took his mule out to gather materials from across a field. When the farmer and the mule approached a wooden bridge, the mule absolutely refused to cross the bridge. After much back and forth between the farmer and the mule (involving both coaxing and cussing), the farmer gave up and returned to the farm with the mule. He then took his horse on the same errand. When they came to the same bridge, the horse also hesitated but required little bargaining from the farmer to coax it to cross the bridge. When barely halfway across, a rotten board in the bridge gave way, almost sending both the horse and the farmer to their deaths in the ravine below.
The moral of the folklore is that mules cannot be coaxed (or cussed) into performing behaviors that will put themselves or those around them at risk of injury or death. Mules will stop when exhausted or profoundly dehydrated, for example, whereas a horse will continue on if ordered by their farmer, even to the point of running themselves to their eventual demise.
One of the younger members of the family-owned ranch, however, had very strong opinions on the superiority of the horse. Horses are loyal and unwavering in their dedication to please those that they serve. They will put the needs of others before themselves in most situations and therefore almost always “outperform” a mule in all respects. They are willing and (usually) able to perform in uncertain conditions, even despite some reservations. They are loyal and loving, and they have unique and inquisitive personalities, which makes them fun to raise and to ride any day.
Test Drives
Our family of four went on a ride with some of these animals and randomly got two horses and two mules. Interestingly, during our ride, we all did indeed notice the differences between the horses and the mules.
The horses were seemingly easygoing and quick to please, easily following cues to change direction or course. The mules were more hesitant and seemed to need to understand why they were being asked to do something before they acquiesced to the demand.
And when we approached a narrow rocky downslope, the mules were slow, steady, and confident, whereas the horses were seemingly uncomfortable and less agile. And, indeed in researching mules, they seem to have gotten a very bad rap over time (as evidenced by the term “stubborn as a mule”).
Charles Darwin actually categorized mules as an example of “hybrid vigor,” which is a rare example of when an offspring is actually better in most ways than either of its parents. Compared to its parental species, mules have more intelligence, endurance, longevity, health, speed, height, and agility. Also to their advantage, they have harder skin and hooves, allowing them to weather and endure more treacherous conditions.
With all of this newfound knowledge of the mule, it struck me what remarkable similarity some physicians have with mules and the role that these mules are likely serving within our organizations. These physicians are probably labeled as stubborn, obstinate, resistant, or impatient. But maybe they are actually intelligent, agile, and appropriately cautious. Maybe the resistance they express in the organization is serving to warn others about the rotten wooden bridges.
HM Takeaway
Similar to a ranch, most hospitals probably function best with a healthy combination of horses and mules. So if you get an opportunity, next time you encounter physicians at your hospital acting like mules, you should congratulate them and appreciate their mule-like characteristics. Recognize the contribution these types of physicians are making, in their own way, to the greater good of the organization.
After all, we can’t—and shouldn’t—all be horses. TH
Reference
1. Hauer J. The Natural Superiority of Mules: A Celebration of One of the Most Intelligent, Sure-footed, and Misunderstood Animals in the World. New York, NY: Skyhorse Publishing; 2006.

My family and I recently took a spring break trip out west to see a few national parks. During the trip, we stayed on a family ranch in Utah. It had a wide variety of livestock, including a large number of mules and horses.
During our stay at this family-owned ranch, two things really stood out and made me think:
- The guesthouse we stayed in had an inordinate volume of collections dedicated to the science and art of raising horses and mules. Everywhere one looked you could find a wall-mounted picture, poem, or coffee table book about these species. My favorite, written by the owner of the ranch, John Hauer, was The Natural Superiority of Mules.1
- The second thing I noticed was that every member of the ranch-owning family had fairly strong opinions about which was better—horse or mule. Just to recap the biology, a horse is the product of two horses, whereas a mule is the progeny of a male donkey and a female horse. It turns out that their physical structure and demeanors are very different.
One of the oldest members of the ranch family (who I believe was a “distant uncle”) had a very strong opinion about the superiority of the mule. His opinion was based on selected facts, including that mules are “steadier on their feet” in unstable ground, require less volume and less frequent food and water, and very rarely became ill or need costly veterinary care.
Another mule-favoring family member told us how mules get a “bad rap” for being stubborn when they actually are much smarter and better decision makers than horses. She recalled a famous folklore of a farmer who took his mule out to gather materials from across a field. When the farmer and the mule approached a wooden bridge, the mule absolutely refused to cross the bridge. After much back and forth between the farmer and the mule (involving both coaxing and cussing), the farmer gave up and returned to the farm with the mule. He then took his horse on the same errand. When they came to the same bridge, the horse also hesitated but required little bargaining from the farmer to coax it to cross the bridge. When barely halfway across, a rotten board in the bridge gave way, almost sending both the horse and the farmer to their deaths in the ravine below.
The moral of the folklore is that mules cannot be coaxed (or cussed) into performing behaviors that will put themselves or those around them at risk of injury or death. Mules will stop when exhausted or profoundly dehydrated, for example, whereas a horse will continue on if ordered by their farmer, even to the point of running themselves to their eventual demise.
One of the younger members of the family-owned ranch, however, had very strong opinions on the superiority of the horse. Horses are loyal and unwavering in their dedication to please those that they serve. They will put the needs of others before themselves in most situations and therefore almost always “outperform” a mule in all respects. They are willing and (usually) able to perform in uncertain conditions, even despite some reservations. They are loyal and loving, and they have unique and inquisitive personalities, which makes them fun to raise and to ride any day.
Test Drives
Our family of four went on a ride with some of these animals and randomly got two horses and two mules. Interestingly, during our ride, we all did indeed notice the differences between the horses and the mules.
The horses were seemingly easygoing and quick to please, easily following cues to change direction or course. The mules were more hesitant and seemed to need to understand why they were being asked to do something before they acquiesced to the demand.
And when we approached a narrow rocky downslope, the mules were slow, steady, and confident, whereas the horses were seemingly uncomfortable and less agile. And, indeed in researching mules, they seem to have gotten a very bad rap over time (as evidenced by the term “stubborn as a mule”).
Charles Darwin actually categorized mules as an example of “hybrid vigor,” which is a rare example of when an offspring is actually better in most ways than either of its parents. Compared to its parental species, mules have more intelligence, endurance, longevity, health, speed, height, and agility. Also to their advantage, they have harder skin and hooves, allowing them to weather and endure more treacherous conditions.
With all of this newfound knowledge of the mule, it struck me what remarkable similarity some physicians have with mules and the role that these mules are likely serving within our organizations. These physicians are probably labeled as stubborn, obstinate, resistant, or impatient. But maybe they are actually intelligent, agile, and appropriately cautious. Maybe the resistance they express in the organization is serving to warn others about the rotten wooden bridges.
HM Takeaway
Similar to a ranch, most hospitals probably function best with a healthy combination of horses and mules. So if you get an opportunity, next time you encounter physicians at your hospital acting like mules, you should congratulate them and appreciate their mule-like characteristics. Recognize the contribution these types of physicians are making, in their own way, to the greater good of the organization.
After all, we can’t—and shouldn’t—all be horses. TH
Reference
1. Hauer J. The Natural Superiority of Mules: A Celebration of One of the Most Intelligent, Sure-footed, and Misunderstood Animals in the World. New York, NY: Skyhorse Publishing; 2006.

Drug can address unmet need in cHL, doc says

COPENHAGEN—The PD-1 checkpoint inhibitor nivolumab can address an unmet need in patients with classical Hodgkin lymphoma (cHL) who have progressive or relapsed disease, according to a speaker at the 21st Congress of the European Hematology Association.
In the phase 2 Checkmate-205 trial, nivolumab produced an objective response rate of 66% in cHL patients who had relapsed or progressed after autologous hematopoietic stem cell transplant (HSCT) and subsequent brentuximab vedotin.
The median duration of response was 7.8 months, and most patients had a response that was ongoing at the time of analysis.
Although the safety profile of nivolumab was considered “acceptable” by researchers, the drug has been linked to serious complications, including death, among patients who proceeded to allogeneic HSCT after receiving nivolumab.
Still, nivolumab is “an important new therapy to meet the unmet need” in cHL, according to Anas Younes, MD, of Memorial Sloan Kettering Cancer Center in New York, New York.
Dr Younes presented results with nivolumab from cohort B of the Checkmate-205 trial as abstract S793. Checkmate-205 was sponsored by Bristol-Myers Squibb.
Cohort B included 80 cHL patients who had relapsed or progressed after autologous HSCT and post-transplant brentuximab vedotin. (Cohort A included patients who had not previously received brentuximab vedotin.)
The patients’ median age was 37 (range, 18-72), and 64% were male. The median number of prior lines of therapy was 4 (range, 3-15), and 49% of patients had received at least 5 previous lines of therapy.
Seventy-four percent of patients had previously received radiation, 93% had received 1 prior autologous HSCT, and 8% had received 2. All patients had received brentuximab vedotin after transplant, and 54% had not responded to that treatment.
Study treatment
Patients received nivolumab at 3 mg/kg intravenously every 2 weeks until disease progression or unacceptable toxicity.
At a median follow-up of 8.9 months (range, 1.9-11.7), 36% of patients had come off treatment—16% due to disease progression, 5% due to toxicity, 8% because they had gone on to allogeneic HSCT, and 8% for other reasons (the patient’s request, the investigator’s decision, the patient was lost to follow-up, or the reason was not reported).
Dr Younes noted that all patients who stopped nivolumab to undergo HSCT were still alive at the data cut-off.
Efficacy
The objective response rate, per an independent radiologic review committee, was 66%. Nine percent of patients achieved a complete response, 58% had a partial response, 23% had stable disease, and 8% had progressive disease. The committee was unable to determine the status of 4% of patients.
The median time to response was 2.1 months, and the estimated median duration of response was 7.8 months.
“Keep in mind that the majority of patients are still on therapy, so this is expected to improve with time,” Dr Younes said.
The majority of responses (62%) were ongoing at the time of analysis. In an exploratory analysis, the researchers observed that 72% of patients who did not respond to their most recent prior brentuximab vedotin treatment did respond to nivolumab.
At 6 months, the progression-free survival rate was 77%, and the overall survival rate was 99%. The median progression-free survival was 10 months, and the median overall survival has not been reached.
Dr Younes said that, although the follow-up is short, the survival data are “still impressive.”
Safety
Adverse events (AEs) occurred in 99% of patients, grade 3/4 AEs occurred in 40% of patients, and there was 1 grade 5 AE (multi-organ failure due to Epstein-Barr-virus-positive T-cell lymphoma).
Treatment-related AEs occurred in 90% of patients. The most common of these were fatigue (25%), infusion-related reactions (20%), rash (16%), arthralgia (14%), pyrexia (14%), nausea (13%), diarrhea (10%), and pruritus (10%).
Treatment-related serious AEs occurred in 6% of patients and included pyrexia, tumor progression, arrhythmia, infusion reactions, septic meningitis, and pneumonia.
Extended safety follow-up of cHL patients treated in the nivolumab clinical trial program who were subsequently treated with allogeneic HSCT (n=17) revealed complications, including fatal events.
A warning about such complications has been added to the US prescribing information for nivolumab, which was recently granted accelerated approval from the US Food and Drug Administration (FDA) to treat patients with relapsed or refractory cHL who have received an autologous HSCT and post-transplant brentuximab vedotin.
Because of these transplant-related deaths, the FDA has advised that healthcare professionals follow patients closely for early evidence of transplant-related complications, such as hyperacute graft-versus-host disease, severe acute graft-versus-host disease, steroid-requiring febrile syndrome, hepatic veno-occlusive disease, and other immune-mediated adverse reactions.
The FDA has also required that Bristol-Myers Squibb further study the safety of allogeneic HSCT after nivolumab. ![]()

COPENHAGEN—The PD-1 checkpoint inhibitor nivolumab can address an unmet need in patients with classical Hodgkin lymphoma (cHL) who have progressive or relapsed disease, according to a speaker at the 21st Congress of the European Hematology Association.
In the phase 2 Checkmate-205 trial, nivolumab produced an objective response rate of 66% in cHL patients who had relapsed or progressed after autologous hematopoietic stem cell transplant (HSCT) and subsequent brentuximab vedotin.
The median duration of response was 7.8 months, and most patients had a response that was ongoing at the time of analysis.
Although the safety profile of nivolumab was considered “acceptable” by researchers, the drug has been linked to serious complications, including death, among patients who proceeded to allogeneic HSCT after receiving nivolumab.
Still, nivolumab is “an important new therapy to meet the unmet need” in cHL, according to Anas Younes, MD, of Memorial Sloan Kettering Cancer Center in New York, New York.
Dr Younes presented results with nivolumab from cohort B of the Checkmate-205 trial as abstract S793. Checkmate-205 was sponsored by Bristol-Myers Squibb.
Cohort B included 80 cHL patients who had relapsed or progressed after autologous HSCT and post-transplant brentuximab vedotin. (Cohort A included patients who had not previously received brentuximab vedotin.)
The patients’ median age was 37 (range, 18-72), and 64% were male. The median number of prior lines of therapy was 4 (range, 3-15), and 49% of patients had received at least 5 previous lines of therapy.
Seventy-four percent of patients had previously received radiation, 93% had received 1 prior autologous HSCT, and 8% had received 2. All patients had received brentuximab vedotin after transplant, and 54% had not responded to that treatment.
Study treatment
Patients received nivolumab at 3 mg/kg intravenously every 2 weeks until disease progression or unacceptable toxicity.
At a median follow-up of 8.9 months (range, 1.9-11.7), 36% of patients had come off treatment—16% due to disease progression, 5% due to toxicity, 8% because they had gone on to allogeneic HSCT, and 8% for other reasons (the patient’s request, the investigator’s decision, the patient was lost to follow-up, or the reason was not reported).
Dr Younes noted that all patients who stopped nivolumab to undergo HSCT were still alive at the data cut-off.
Efficacy
The objective response rate, per an independent radiologic review committee, was 66%. Nine percent of patients achieved a complete response, 58% had a partial response, 23% had stable disease, and 8% had progressive disease. The committee was unable to determine the status of 4% of patients.
The median time to response was 2.1 months, and the estimated median duration of response was 7.8 months.
“Keep in mind that the majority of patients are still on therapy, so this is expected to improve with time,” Dr Younes said.
The majority of responses (62%) were ongoing at the time of analysis. In an exploratory analysis, the researchers observed that 72% of patients who did not respond to their most recent prior brentuximab vedotin treatment did respond to nivolumab.
At 6 months, the progression-free survival rate was 77%, and the overall survival rate was 99%. The median progression-free survival was 10 months, and the median overall survival has not been reached.
Dr Younes said that, although the follow-up is short, the survival data are “still impressive.”
Safety
Adverse events (AEs) occurred in 99% of patients, grade 3/4 AEs occurred in 40% of patients, and there was 1 grade 5 AE (multi-organ failure due to Epstein-Barr-virus-positive T-cell lymphoma).
Treatment-related AEs occurred in 90% of patients. The most common of these were fatigue (25%), infusion-related reactions (20%), rash (16%), arthralgia (14%), pyrexia (14%), nausea (13%), diarrhea (10%), and pruritus (10%).
Treatment-related serious AEs occurred in 6% of patients and included pyrexia, tumor progression, arrhythmia, infusion reactions, septic meningitis, and pneumonia.
Extended safety follow-up of cHL patients treated in the nivolumab clinical trial program who were subsequently treated with allogeneic HSCT (n=17) revealed complications, including fatal events.
A warning about such complications has been added to the US prescribing information for nivolumab, which was recently granted accelerated approval from the US Food and Drug Administration (FDA) to treat patients with relapsed or refractory cHL who have received an autologous HSCT and post-transplant brentuximab vedotin.
Because of these transplant-related deaths, the FDA has advised that healthcare professionals follow patients closely for early evidence of transplant-related complications, such as hyperacute graft-versus-host disease, severe acute graft-versus-host disease, steroid-requiring febrile syndrome, hepatic veno-occlusive disease, and other immune-mediated adverse reactions.
The FDA has also required that Bristol-Myers Squibb further study the safety of allogeneic HSCT after nivolumab. ![]()

COPENHAGEN—The PD-1 checkpoint inhibitor nivolumab can address an unmet need in patients with classical Hodgkin lymphoma (cHL) who have progressive or relapsed disease, according to a speaker at the 21st Congress of the European Hematology Association.
In the phase 2 Checkmate-205 trial, nivolumab produced an objective response rate of 66% in cHL patients who had relapsed or progressed after autologous hematopoietic stem cell transplant (HSCT) and subsequent brentuximab vedotin.
The median duration of response was 7.8 months, and most patients had a response that was ongoing at the time of analysis.
Although the safety profile of nivolumab was considered “acceptable” by researchers, the drug has been linked to serious complications, including death, among patients who proceeded to allogeneic HSCT after receiving nivolumab.
Still, nivolumab is “an important new therapy to meet the unmet need” in cHL, according to Anas Younes, MD, of Memorial Sloan Kettering Cancer Center in New York, New York.
Dr Younes presented results with nivolumab from cohort B of the Checkmate-205 trial as abstract S793. Checkmate-205 was sponsored by Bristol-Myers Squibb.
Cohort B included 80 cHL patients who had relapsed or progressed after autologous HSCT and post-transplant brentuximab vedotin. (Cohort A included patients who had not previously received brentuximab vedotin.)
The patients’ median age was 37 (range, 18-72), and 64% were male. The median number of prior lines of therapy was 4 (range, 3-15), and 49% of patients had received at least 5 previous lines of therapy.
Seventy-four percent of patients had previously received radiation, 93% had received 1 prior autologous HSCT, and 8% had received 2. All patients had received brentuximab vedotin after transplant, and 54% had not responded to that treatment.
Study treatment
Patients received nivolumab at 3 mg/kg intravenously every 2 weeks until disease progression or unacceptable toxicity.
At a median follow-up of 8.9 months (range, 1.9-11.7), 36% of patients had come off treatment—16% due to disease progression, 5% due to toxicity, 8% because they had gone on to allogeneic HSCT, and 8% for other reasons (the patient’s request, the investigator’s decision, the patient was lost to follow-up, or the reason was not reported).
Dr Younes noted that all patients who stopped nivolumab to undergo HSCT were still alive at the data cut-off.
Efficacy
The objective response rate, per an independent radiologic review committee, was 66%. Nine percent of patients achieved a complete response, 58% had a partial response, 23% had stable disease, and 8% had progressive disease. The committee was unable to determine the status of 4% of patients.
The median time to response was 2.1 months, and the estimated median duration of response was 7.8 months.
“Keep in mind that the majority of patients are still on therapy, so this is expected to improve with time,” Dr Younes said.
The majority of responses (62%) were ongoing at the time of analysis. In an exploratory analysis, the researchers observed that 72% of patients who did not respond to their most recent prior brentuximab vedotin treatment did respond to nivolumab.
At 6 months, the progression-free survival rate was 77%, and the overall survival rate was 99%. The median progression-free survival was 10 months, and the median overall survival has not been reached.
Dr Younes said that, although the follow-up is short, the survival data are “still impressive.”
Safety
Adverse events (AEs) occurred in 99% of patients, grade 3/4 AEs occurred in 40% of patients, and there was 1 grade 5 AE (multi-organ failure due to Epstein-Barr-virus-positive T-cell lymphoma).
Treatment-related AEs occurred in 90% of patients. The most common of these were fatigue (25%), infusion-related reactions (20%), rash (16%), arthralgia (14%), pyrexia (14%), nausea (13%), diarrhea (10%), and pruritus (10%).
Treatment-related serious AEs occurred in 6% of patients and included pyrexia, tumor progression, arrhythmia, infusion reactions, septic meningitis, and pneumonia.
Extended safety follow-up of cHL patients treated in the nivolumab clinical trial program who were subsequently treated with allogeneic HSCT (n=17) revealed complications, including fatal events.
A warning about such complications has been added to the US prescribing information for nivolumab, which was recently granted accelerated approval from the US Food and Drug Administration (FDA) to treat patients with relapsed or refractory cHL who have received an autologous HSCT and post-transplant brentuximab vedotin.
Because of these transplant-related deaths, the FDA has advised that healthcare professionals follow patients closely for early evidence of transplant-related complications, such as hyperacute graft-versus-host disease, severe acute graft-versus-host disease, steroid-requiring febrile syndrome, hepatic veno-occlusive disease, and other immune-mediated adverse reactions.
The FDA has also required that Bristol-Myers Squibb further study the safety of allogeneic HSCT after nivolumab. ![]()
AGA Research Foundation announces 2016 class of Research Award winners
At Digestive Disease Week® 2016, the AGA Research Foundation honored its 2016 class of Research Award winners. The AGA Research Awards Program serves to support talented investigators who are pursuing careers in digestive disease research. A research grant from the AGA Research Foundation ensures that a major proportion of the recipient’s time is protected for research.
“The AGA Research Foundation received a record number of applications in 2016 from young investigators working to advance our understanding of digestive and liver diseases,” said Robert S. Sandler, MD, MPH, AGAF, incoming chair of the AGA Research Foundation. “AGA is proud to invest in these 66 talented scientists and looks forward to seeing how each of their research projects will ultimately lead to better care for patients suffering from digestive disorders.”
The AGA Research Awards Program is made possible thanks to the foundation’s generous donors. To show your support for GI research, visit www.gastro.org/donateonline.
The 2016 AGA Research Foundation award recipients can be found here. To learn about upcoming research funding opportunities, visit www.gastro.org/awards.
At Digestive Disease Week® 2016, the AGA Research Foundation honored its 2016 class of Research Award winners. The AGA Research Awards Program serves to support talented investigators who are pursuing careers in digestive disease research. A research grant from the AGA Research Foundation ensures that a major proportion of the recipient’s time is protected for research.
“The AGA Research Foundation received a record number of applications in 2016 from young investigators working to advance our understanding of digestive and liver diseases,” said Robert S. Sandler, MD, MPH, AGAF, incoming chair of the AGA Research Foundation. “AGA is proud to invest in these 66 talented scientists and looks forward to seeing how each of their research projects will ultimately lead to better care for patients suffering from digestive disorders.”
The AGA Research Awards Program is made possible thanks to the foundation’s generous donors. To show your support for GI research, visit www.gastro.org/donateonline.
The 2016 AGA Research Foundation award recipients can be found here. To learn about upcoming research funding opportunities, visit www.gastro.org/awards.
At Digestive Disease Week® 2016, the AGA Research Foundation honored its 2016 class of Research Award winners. The AGA Research Awards Program serves to support talented investigators who are pursuing careers in digestive disease research. A research grant from the AGA Research Foundation ensures that a major proportion of the recipient’s time is protected for research.
“The AGA Research Foundation received a record number of applications in 2016 from young investigators working to advance our understanding of digestive and liver diseases,” said Robert S. Sandler, MD, MPH, AGAF, incoming chair of the AGA Research Foundation. “AGA is proud to invest in these 66 talented scientists and looks forward to seeing how each of their research projects will ultimately lead to better care for patients suffering from digestive disorders.”
The AGA Research Awards Program is made possible thanks to the foundation’s generous donors. To show your support for GI research, visit www.gastro.org/donateonline.
The 2016 AGA Research Foundation award recipients can be found here. To learn about upcoming research funding opportunities, visit www.gastro.org/awards.
Finding Alternatives to Open Surgical Resection for Patients With Epilepsy
Although open surgical resection is considered the gold standard for patients with epilepsy who do not respond to medical therapy, there are several viable alternatives, according to Englot and associates writing in Neurosurgical Review. Among the minimally invasive procedures to consider: stereotactic laser ablation and stereotactic radiosurgery, which the researchers say can offer relatively favorable seizure outcomes, especially in patients with mesial temporary lobe epilepsy. Other options include multiple subpial transections and corpus callosotomy in select patients. Among the palliative procedures to consider are vagus nerve stimulation, deep brain stimulation, and responsive neurostimulation, which the authors say may significantly decrease seizure frequency and improve quality of life.
Englot DJ, Birk H, Chang EF. Seizure outcomes in nonresective epilepsy surgery: an update. Neurosurg Rev. 2016; May 21 [Epub ahead of print]
Although open surgical resection is considered the gold standard for patients with epilepsy who do not respond to medical therapy, there are several viable alternatives, according to Englot and associates writing in Neurosurgical Review. Among the minimally invasive procedures to consider: stereotactic laser ablation and stereotactic radiosurgery, which the researchers say can offer relatively favorable seizure outcomes, especially in patients with mesial temporary lobe epilepsy. Other options include multiple subpial transections and corpus callosotomy in select patients. Among the palliative procedures to consider are vagus nerve stimulation, deep brain stimulation, and responsive neurostimulation, which the authors say may significantly decrease seizure frequency and improve quality of life.
Englot DJ, Birk H, Chang EF. Seizure outcomes in nonresective epilepsy surgery: an update. Neurosurg Rev. 2016; May 21 [Epub ahead of print]
Although open surgical resection is considered the gold standard for patients with epilepsy who do not respond to medical therapy, there are several viable alternatives, according to Englot and associates writing in Neurosurgical Review. Among the minimally invasive procedures to consider: stereotactic laser ablation and stereotactic radiosurgery, which the researchers say can offer relatively favorable seizure outcomes, especially in patients with mesial temporary lobe epilepsy. Other options include multiple subpial transections and corpus callosotomy in select patients. Among the palliative procedures to consider are vagus nerve stimulation, deep brain stimulation, and responsive neurostimulation, which the authors say may significantly decrease seizure frequency and improve quality of life.
Englot DJ, Birk H, Chang EF. Seizure outcomes in nonresective epilepsy surgery: an update. Neurosurg Rev. 2016; May 21 [Epub ahead of print]