User login
VA Touts Telehealth Success Before House Panel
In fiscal year (FY) 2015, VA conducted 2.14 million telehealth visits, reaching more than 677,000 veterans. Telehealth “remains a critical strategy in ensuring veterans can access health care when and where they need it,” Kevin Galpin, MD, acting executive director for telehealth at the VHA told the House Committee on Veterans Affairs earlier this month. “With the support of Congress, we have an opportunity to shape the future and ensure that VA is leveraging cutting-edge technology to provide convenient, accessible, high-quality care to all veterans.”
Related: Madhulika Agarwal on Telehealth at the VHA
Telemental health, in particular, also has seen significant growth. From 2002 through July 2, 2016, Galpin reported, more than 2 million telemental health visits have been provided to more than 389,400 unique veterans. And use of telehealth in the Greater Los Angeles Health Care System alone increased by 61,500, including more than 20,000 telehealth visits, which reached more than 6,000 veterans in southern California.
“For the past 10 years, I have studied many telehealth models and have been most impressed by the VA model as both exemplary and successful,” Herb Rogove, DO, FCCM, FACP, president and chief executive officer, C30 Telemedicine and former board member of the American Telemedicine Association, reported in a statement to the committee.
Related: Telejustice: Reaching Incarcerated Veterans via Telehealth
The VA is testing a new system that will allow veterans to access telehealth from their personal mobile device, smartphone, tablet, or computer. The VA Video Connect (VVC) is currently undergoing field testing for real-time access to VA care and will be fully encrypted to protect patient information. It will complement the VA’s current offerings of home telehealth, using VA-provided devices and store-and-forward telehealth, which allows users to asynchronously acquire and store clinical information (such as data, images, sound, and video) that then can be examined by a provider at another location for clinical evaluation.
Related: Patients Benefit From ICU Telemedicine
Other important telehealth developments include:
- In FY 2015, more than 57,000 rehabilitation encounters for more than 33,000 unique veterans occurred using home telehealth.
- Store-and-forward telehealth has been particularly successful for dermatologic and retinal diagnosis and triage.
- The National Telemental Health Centers have provided access and consults to more than 4,600 veterans at more than 120 sites.
- The Tele-Intensive Care program links VA intensive care units to a central monitoring hub.
- Telesurgical consultation is being used to “enhance the diagnosis, the coordination of care, and the triage of surgical patients.”
In fiscal year (FY) 2015, VA conducted 2.14 million telehealth visits, reaching more than 677,000 veterans. Telehealth “remains a critical strategy in ensuring veterans can access health care when and where they need it,” Kevin Galpin, MD, acting executive director for telehealth at the VHA told the House Committee on Veterans Affairs earlier this month. “With the support of Congress, we have an opportunity to shape the future and ensure that VA is leveraging cutting-edge technology to provide convenient, accessible, high-quality care to all veterans.”
Related: Madhulika Agarwal on Telehealth at the VHA
Telemental health, in particular, also has seen significant growth. From 2002 through July 2, 2016, Galpin reported, more than 2 million telemental health visits have been provided to more than 389,400 unique veterans. And use of telehealth in the Greater Los Angeles Health Care System alone increased by 61,500, including more than 20,000 telehealth visits, which reached more than 6,000 veterans in southern California.
“For the past 10 years, I have studied many telehealth models and have been most impressed by the VA model as both exemplary and successful,” Herb Rogove, DO, FCCM, FACP, president and chief executive officer, C30 Telemedicine and former board member of the American Telemedicine Association, reported in a statement to the committee.
Related: Telejustice: Reaching Incarcerated Veterans via Telehealth
The VA is testing a new system that will allow veterans to access telehealth from their personal mobile device, smartphone, tablet, or computer. The VA Video Connect (VVC) is currently undergoing field testing for real-time access to VA care and will be fully encrypted to protect patient information. It will complement the VA’s current offerings of home telehealth, using VA-provided devices and store-and-forward telehealth, which allows users to asynchronously acquire and store clinical information (such as data, images, sound, and video) that then can be examined by a provider at another location for clinical evaluation.
Related: Patients Benefit From ICU Telemedicine
Other important telehealth developments include:
- In FY 2015, more than 57,000 rehabilitation encounters for more than 33,000 unique veterans occurred using home telehealth.
- Store-and-forward telehealth has been particularly successful for dermatologic and retinal diagnosis and triage.
- The National Telemental Health Centers have provided access and consults to more than 4,600 veterans at more than 120 sites.
- The Tele-Intensive Care program links VA intensive care units to a central monitoring hub.
- Telesurgical consultation is being used to “enhance the diagnosis, the coordination of care, and the triage of surgical patients.”
In fiscal year (FY) 2015, VA conducted 2.14 million telehealth visits, reaching more than 677,000 veterans. Telehealth “remains a critical strategy in ensuring veterans can access health care when and where they need it,” Kevin Galpin, MD, acting executive director for telehealth at the VHA told the House Committee on Veterans Affairs earlier this month. “With the support of Congress, we have an opportunity to shape the future and ensure that VA is leveraging cutting-edge technology to provide convenient, accessible, high-quality care to all veterans.”
Related: Madhulika Agarwal on Telehealth at the VHA
Telemental health, in particular, also has seen significant growth. From 2002 through July 2, 2016, Galpin reported, more than 2 million telemental health visits have been provided to more than 389,400 unique veterans. And use of telehealth in the Greater Los Angeles Health Care System alone increased by 61,500, including more than 20,000 telehealth visits, which reached more than 6,000 veterans in southern California.
“For the past 10 years, I have studied many telehealth models and have been most impressed by the VA model as both exemplary and successful,” Herb Rogove, DO, FCCM, FACP, president and chief executive officer, C30 Telemedicine and former board member of the American Telemedicine Association, reported in a statement to the committee.
Related: Telejustice: Reaching Incarcerated Veterans via Telehealth
The VA is testing a new system that will allow veterans to access telehealth from their personal mobile device, smartphone, tablet, or computer. The VA Video Connect (VVC) is currently undergoing field testing for real-time access to VA care and will be fully encrypted to protect patient information. It will complement the VA’s current offerings of home telehealth, using VA-provided devices and store-and-forward telehealth, which allows users to asynchronously acquire and store clinical information (such as data, images, sound, and video) that then can be examined by a provider at another location for clinical evaluation.
Related: Patients Benefit From ICU Telemedicine
Other important telehealth developments include:
- In FY 2015, more than 57,000 rehabilitation encounters for more than 33,000 unique veterans occurred using home telehealth.
- Store-and-forward telehealth has been particularly successful for dermatologic and retinal diagnosis and triage.
- The National Telemental Health Centers have provided access and consults to more than 4,600 veterans at more than 120 sites.
- The Tele-Intensive Care program links VA intensive care units to a central monitoring hub.
- Telesurgical consultation is being used to “enhance the diagnosis, the coordination of care, and the triage of surgical patients.”
Tips for using EMRs effectively
All young physicians are adept at using electronic medical records. Do you agree? If so, you’d be wrong. It’s true that young, so-called “digital-native” physicians have more training and experience using EMRs, compared with those who trained in the days of paper charts. But young physicians are also inexperienced at caring for patients, and using a keyboard adds complexity to an already difficult task. Some struggle with the sheer volume of work that EMRs create, while others wrestle with the intrusive computer in the exam room. The former is a complex problem, and solving it involves improving both system and individual work flows. The latter is one I’ve had great success with when coaching inexperienced doctors.
One of my roles at Kaiser Permanente, San Diego, is to coach new physicians to help them perform at their best. In particular, we provide one-on-one help for physicians to optimize the quality of service they provide. More often than not, young physicians benefit from optimizing their work flow as much as from modifying their bedside manner.
Here are five common tips I share with them to improve their service while using EMRs:
• Preview coming attractions. High-quality interactions require that prep work be done before the visit begins. Before seeing your patient, review his or her record to learn about the medical history, particularly any recent important health issues. This is true even if the problem is not related to your specialty. This sends a strong signal to your patient that you know and care about him or her as a person.
• Connect with your patient first, then turn to HealthConnect (our version of the EPIC electronic record). For every patient, every visit, spend the first few minutes giving your undivided attention to them while in the room. Conversely, entering the room and logging on the computer immediately diminishes the quality of the experience for patients.
• Ask permission, not forgiveness. When you must use the EMR to review or to chart, ask permission first. Try something like, “This is important. Do you mind if I start typing some of this to be sure it is captured in your record?” I’ve never seen a patient object if you start typing. If they did, then the time isn’t right for you to go to the EMR, and it would best for you to address their concern first.
• Share the screen. Many patients love to see their chart. It’s like giving them a backstage pass. It’s also a great way to keep them engaged while you talk about their issues. Point things out to them and use it to engage in discussion. The better informed your patients are, the more likely they will evaluate you favorably, and the more likely they are to adhere to your advice.
• Complete diagnoses and write any prescriptions while in the room. This is a wonderful opportunity to engage with your patients on the risks and benefits of what you recommend, to review your specific instructions, and to allow them to see their diagnoses written out. Close with a printed copy of what just transpired. The act of giving something tangible makes the encounter feel complete, while also increasing patients’ retention of key information and their likelihood of following up as directed.
As more young physicians join us in the workforce, we know that it doesn’t matter much if you grew up with Facebook and Snapchat; using EMRs effectively is a learned skill that all of us can improve upon.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
All young physicians are adept at using electronic medical records. Do you agree? If so, you’d be wrong. It’s true that young, so-called “digital-native” physicians have more training and experience using EMRs, compared with those who trained in the days of paper charts. But young physicians are also inexperienced at caring for patients, and using a keyboard adds complexity to an already difficult task. Some struggle with the sheer volume of work that EMRs create, while others wrestle with the intrusive computer in the exam room. The former is a complex problem, and solving it involves improving both system and individual work flows. The latter is one I’ve had great success with when coaching inexperienced doctors.
One of my roles at Kaiser Permanente, San Diego, is to coach new physicians to help them perform at their best. In particular, we provide one-on-one help for physicians to optimize the quality of service they provide. More often than not, young physicians benefit from optimizing their work flow as much as from modifying their bedside manner.
Here are five common tips I share with them to improve their service while using EMRs:
• Preview coming attractions. High-quality interactions require that prep work be done before the visit begins. Before seeing your patient, review his or her record to learn about the medical history, particularly any recent important health issues. This is true even if the problem is not related to your specialty. This sends a strong signal to your patient that you know and care about him or her as a person.
• Connect with your patient first, then turn to HealthConnect (our version of the EPIC electronic record). For every patient, every visit, spend the first few minutes giving your undivided attention to them while in the room. Conversely, entering the room and logging on the computer immediately diminishes the quality of the experience for patients.
• Ask permission, not forgiveness. When you must use the EMR to review or to chart, ask permission first. Try something like, “This is important. Do you mind if I start typing some of this to be sure it is captured in your record?” I’ve never seen a patient object if you start typing. If they did, then the time isn’t right for you to go to the EMR, and it would best for you to address their concern first.
• Share the screen. Many patients love to see their chart. It’s like giving them a backstage pass. It’s also a great way to keep them engaged while you talk about their issues. Point things out to them and use it to engage in discussion. The better informed your patients are, the more likely they will evaluate you favorably, and the more likely they are to adhere to your advice.
• Complete diagnoses and write any prescriptions while in the room. This is a wonderful opportunity to engage with your patients on the risks and benefits of what you recommend, to review your specific instructions, and to allow them to see their diagnoses written out. Close with a printed copy of what just transpired. The act of giving something tangible makes the encounter feel complete, while also increasing patients’ retention of key information and their likelihood of following up as directed.
As more young physicians join us in the workforce, we know that it doesn’t matter much if you grew up with Facebook and Snapchat; using EMRs effectively is a learned skill that all of us can improve upon.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
All young physicians are adept at using electronic medical records. Do you agree? If so, you’d be wrong. It’s true that young, so-called “digital-native” physicians have more training and experience using EMRs, compared with those who trained in the days of paper charts. But young physicians are also inexperienced at caring for patients, and using a keyboard adds complexity to an already difficult task. Some struggle with the sheer volume of work that EMRs create, while others wrestle with the intrusive computer in the exam room. The former is a complex problem, and solving it involves improving both system and individual work flows. The latter is one I’ve had great success with when coaching inexperienced doctors.
One of my roles at Kaiser Permanente, San Diego, is to coach new physicians to help them perform at their best. In particular, we provide one-on-one help for physicians to optimize the quality of service they provide. More often than not, young physicians benefit from optimizing their work flow as much as from modifying their bedside manner.
Here are five common tips I share with them to improve their service while using EMRs:
• Preview coming attractions. High-quality interactions require that prep work be done before the visit begins. Before seeing your patient, review his or her record to learn about the medical history, particularly any recent important health issues. This is true even if the problem is not related to your specialty. This sends a strong signal to your patient that you know and care about him or her as a person.
• Connect with your patient first, then turn to HealthConnect (our version of the EPIC electronic record). For every patient, every visit, spend the first few minutes giving your undivided attention to them while in the room. Conversely, entering the room and logging on the computer immediately diminishes the quality of the experience for patients.
• Ask permission, not forgiveness. When you must use the EMR to review or to chart, ask permission first. Try something like, “This is important. Do you mind if I start typing some of this to be sure it is captured in your record?” I’ve never seen a patient object if you start typing. If they did, then the time isn’t right for you to go to the EMR, and it would best for you to address their concern first.
• Share the screen. Many patients love to see their chart. It’s like giving them a backstage pass. It’s also a great way to keep them engaged while you talk about their issues. Point things out to them and use it to engage in discussion. The better informed your patients are, the more likely they will evaluate you favorably, and the more likely they are to adhere to your advice.
• Complete diagnoses and write any prescriptions while in the room. This is a wonderful opportunity to engage with your patients on the risks and benefits of what you recommend, to review your specific instructions, and to allow them to see their diagnoses written out. Close with a printed copy of what just transpired. The act of giving something tangible makes the encounter feel complete, while also increasing patients’ retention of key information and their likelihood of following up as directed.
As more young physicians join us in the workforce, we know that it doesn’t matter much if you grew up with Facebook and Snapchat; using EMRs effectively is a learned skill that all of us can improve upon.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
TEP hernia repair patients have significant QOL improvements
The majority of patients who have undergone laparoscopic totally extraperitoneal groin hernia repair report mild or no symptoms 2 years after the operation, results of a large prospective study indicate.
Researchers assessed 293 patients – 93% of whom were male – who underwent laparoscopic totally extraperitoneal (TEP) groin hernia repair, both before and 3 weeks, 6 months, 1 year, and 2 years after their operation, using the 36-Item Short Form Survey (v2), Surgical Outcomes Measurement System, and Carolinas Comfort Scale.
The study, published in the July issue of the Journal of the American College of Surgeons, found that 98% of individuals reported no or nonbothersome symptoms of sensation of mesh, 95% reported the same for pain, and 97% reported the same for movement limitations when assessed using the Carolinas Comfort Scale 2 years after surgery.
Pain scores, as measured by the Surgical Outcomes Measurement System, also improved significantly from baseline to 2 years after surgery (10 vs. 7.5; P = .025), and at all postoperative points, patients said they were highly satisfied with their quality of life.
“This study found that laparoscopic TEP groin hernia repair improves patient quality of life significantly, as evidenced by two generic and one procedure-specific quality of life instruments,” wrote Matthew E. Gitelis and his colleagues at the department of surgery at NorthShore University HealthSystem, Evanston, Ill. “Additionally, the procedure can be performed safely with minimal morbidity and low recurrence rates.”
According to the 36-Item Short Form Survey, patients showed significant improvements in physical functioning at 2 years after surgery, but not at 3 weeks, 6 months, or 1 year postoperatively. Pain scores initially increased at 3 weeks after surgery, compared with baseline, decreased to baseline levels at 6 months, then improved significantly at 1 and 2 years after surgery.
While surgery did not appear to affect energy/fatigue scores or emotional well-being, patients did report significant improvements in social functioning and role limitations (J Am Coll Surg. 2016 Jul;223:153-161). On average, patients used narcotic pain medication for 2.5 days after surgery, and returned to work and daily activities after 5.4 days.
The study also examined the technical outcomes of the operations, which were all performed by four surgeons specializing in minimally invasive and bariatric surgery at three sites across an academic-affiliated hospital system.
The authors said the decision was made to study the outcomes from more experienced surgeons because of the steep learning curves and specialized skill set required for laparoscopic techniques.
“Looking at the technical outcomes of our cohort as they relate to recurrence rates and complications, we continue to show the importance of reporting the experience of high-volume centers,” they wrote. “Our goal is to better understand the details and duration of quality of life outcomes so that we can better address patient expectations and provide important information used in the decision-making process for patients undergoing an elective procedure.”
There were 66 complications overall, most of which were from seroma (25 patients), hematoma (13 patients), and urinary retention (21 patients), with 7 cases of wound infection reported. Eight patients (2.2%) experienced a hernia recurrence.
“It is worth noting that, in the middle of our study, in an effort to decrease long-term postoperative pain, we switched to lighter-weight mesh (Physiomesh) from the polyester mesh (Parietex anatomical) used previously,” the authors reported. “Carolinas Comfort Scale scores at 1 year did confirm decreased pain scores; however, we also saw significantly higher rates of recurrence during that period.”
No conflicts of interest were declared.
The majority of patients who have undergone laparoscopic totally extraperitoneal groin hernia repair report mild or no symptoms 2 years after the operation, results of a large prospective study indicate.
Researchers assessed 293 patients – 93% of whom were male – who underwent laparoscopic totally extraperitoneal (TEP) groin hernia repair, both before and 3 weeks, 6 months, 1 year, and 2 years after their operation, using the 36-Item Short Form Survey (v2), Surgical Outcomes Measurement System, and Carolinas Comfort Scale.
The study, published in the July issue of the Journal of the American College of Surgeons, found that 98% of individuals reported no or nonbothersome symptoms of sensation of mesh, 95% reported the same for pain, and 97% reported the same for movement limitations when assessed using the Carolinas Comfort Scale 2 years after surgery.
Pain scores, as measured by the Surgical Outcomes Measurement System, also improved significantly from baseline to 2 years after surgery (10 vs. 7.5; P = .025), and at all postoperative points, patients said they were highly satisfied with their quality of life.
“This study found that laparoscopic TEP groin hernia repair improves patient quality of life significantly, as evidenced by two generic and one procedure-specific quality of life instruments,” wrote Matthew E. Gitelis and his colleagues at the department of surgery at NorthShore University HealthSystem, Evanston, Ill. “Additionally, the procedure can be performed safely with minimal morbidity and low recurrence rates.”
According to the 36-Item Short Form Survey, patients showed significant improvements in physical functioning at 2 years after surgery, but not at 3 weeks, 6 months, or 1 year postoperatively. Pain scores initially increased at 3 weeks after surgery, compared with baseline, decreased to baseline levels at 6 months, then improved significantly at 1 and 2 years after surgery.
While surgery did not appear to affect energy/fatigue scores or emotional well-being, patients did report significant improvements in social functioning and role limitations (J Am Coll Surg. 2016 Jul;223:153-161). On average, patients used narcotic pain medication for 2.5 days after surgery, and returned to work and daily activities after 5.4 days.
The study also examined the technical outcomes of the operations, which were all performed by four surgeons specializing in minimally invasive and bariatric surgery at three sites across an academic-affiliated hospital system.
The authors said the decision was made to study the outcomes from more experienced surgeons because of the steep learning curves and specialized skill set required for laparoscopic techniques.
“Looking at the technical outcomes of our cohort as they relate to recurrence rates and complications, we continue to show the importance of reporting the experience of high-volume centers,” they wrote. “Our goal is to better understand the details and duration of quality of life outcomes so that we can better address patient expectations and provide important information used in the decision-making process for patients undergoing an elective procedure.”
There were 66 complications overall, most of which were from seroma (25 patients), hematoma (13 patients), and urinary retention (21 patients), with 7 cases of wound infection reported. Eight patients (2.2%) experienced a hernia recurrence.
“It is worth noting that, in the middle of our study, in an effort to decrease long-term postoperative pain, we switched to lighter-weight mesh (Physiomesh) from the polyester mesh (Parietex anatomical) used previously,” the authors reported. “Carolinas Comfort Scale scores at 1 year did confirm decreased pain scores; however, we also saw significantly higher rates of recurrence during that period.”
No conflicts of interest were declared.
The majority of patients who have undergone laparoscopic totally extraperitoneal groin hernia repair report mild or no symptoms 2 years after the operation, results of a large prospective study indicate.
Researchers assessed 293 patients – 93% of whom were male – who underwent laparoscopic totally extraperitoneal (TEP) groin hernia repair, both before and 3 weeks, 6 months, 1 year, and 2 years after their operation, using the 36-Item Short Form Survey (v2), Surgical Outcomes Measurement System, and Carolinas Comfort Scale.
The study, published in the July issue of the Journal of the American College of Surgeons, found that 98% of individuals reported no or nonbothersome symptoms of sensation of mesh, 95% reported the same for pain, and 97% reported the same for movement limitations when assessed using the Carolinas Comfort Scale 2 years after surgery.
Pain scores, as measured by the Surgical Outcomes Measurement System, also improved significantly from baseline to 2 years after surgery (10 vs. 7.5; P = .025), and at all postoperative points, patients said they were highly satisfied with their quality of life.
“This study found that laparoscopic TEP groin hernia repair improves patient quality of life significantly, as evidenced by two generic and one procedure-specific quality of life instruments,” wrote Matthew E. Gitelis and his colleagues at the department of surgery at NorthShore University HealthSystem, Evanston, Ill. “Additionally, the procedure can be performed safely with minimal morbidity and low recurrence rates.”
According to the 36-Item Short Form Survey, patients showed significant improvements in physical functioning at 2 years after surgery, but not at 3 weeks, 6 months, or 1 year postoperatively. Pain scores initially increased at 3 weeks after surgery, compared with baseline, decreased to baseline levels at 6 months, then improved significantly at 1 and 2 years after surgery.
While surgery did not appear to affect energy/fatigue scores or emotional well-being, patients did report significant improvements in social functioning and role limitations (J Am Coll Surg. 2016 Jul;223:153-161). On average, patients used narcotic pain medication for 2.5 days after surgery, and returned to work and daily activities after 5.4 days.
The study also examined the technical outcomes of the operations, which were all performed by four surgeons specializing in minimally invasive and bariatric surgery at three sites across an academic-affiliated hospital system.
The authors said the decision was made to study the outcomes from more experienced surgeons because of the steep learning curves and specialized skill set required for laparoscopic techniques.
“Looking at the technical outcomes of our cohort as they relate to recurrence rates and complications, we continue to show the importance of reporting the experience of high-volume centers,” they wrote. “Our goal is to better understand the details and duration of quality of life outcomes so that we can better address patient expectations and provide important information used in the decision-making process for patients undergoing an elective procedure.”
There were 66 complications overall, most of which were from seroma (25 patients), hematoma (13 patients), and urinary retention (21 patients), with 7 cases of wound infection reported. Eight patients (2.2%) experienced a hernia recurrence.
“It is worth noting that, in the middle of our study, in an effort to decrease long-term postoperative pain, we switched to lighter-weight mesh (Physiomesh) from the polyester mesh (Parietex anatomical) used previously,” the authors reported. “Carolinas Comfort Scale scores at 1 year did confirm decreased pain scores; however, we also saw significantly higher rates of recurrence during that period.”
No conflicts of interest were declared.
FROM JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Key clinical point: The majority of patients who have undergone laparoscopic totally extraperitoneal groin hernia repair report mild or no symptoms 2 years after the operation.
Major finding: More 90% of patients experience no or nonbothersome symptoms of sensation of mesh, pain or movement limitations at 2 years after laparoscopic totally extraperitoneal groin hernia repair.
Data source: Prospective study in 293 patients undergoing laparoscopic totally extraperitoneal groin hernia repair.
Disclosures: No conflicts of interest were declared.
Treg-boosting strategy prevents GVHD in mice

Photo by Aaron Logan
A treatment strategy that increases the production of regulatory T cells (Tregs) can prevent graft-versus-host disease (GVHD) in mice, according to research published in The Journal of Experimental Medicine.
One way to prevent GVHD after allogeneic hematopoietic stem cell transplant (allo-HSCT) is to co-transplant large numbers of Tregs, which can suppress the donor cells’ effects on healthy tissue without affecting their ability to kill tumor cells.
This approach is challenging, however, because the Tregs must first be isolated from the donor’s peripheral blood or bone marrow and then cultivated in the lab to produce sufficient numbers for transplant.
Andreas Beilhack, MD, of University Hospital Würzburg in Germany, and his colleagues have found a way to overcome this obstacle, at least in mice.
The team developed a protein agonist called STAR2, which selectively activates TNFR2. The researchers noted that TNF and its receptors, TNFR1 and TNFR2, have been shown to play a crucial role in both GVHD and the graft-versus-leukemia effect.
With their experiments, Dr Beilhack and his colleagues showed that STAR2 binds to TNFR2, activating a signaling pathway that increases the number of natural Tregs in vitro and in vivo.
The team also tested STAR2 in mice with lymphoma. Pretreating the mice with STAR2 protected them from developing GVHD after allo-HSCT. And the donor-derived cells retained their ability to kill lymphoma cells.
In addition, the researchers found that a slightly modified version of STAR2 has a similar effect on human Tregs, which suggests this approach could also prevent GVHD in humans undergoing allo-HSCT.
“Furthermore, this strategy may be beneficial for other pathological settings in which elevated numbers of regulatory T cells are desirable, such as autoimmune diseases and solid organ transplantation,” Dr Beilhack said. ![]()

Photo by Aaron Logan
A treatment strategy that increases the production of regulatory T cells (Tregs) can prevent graft-versus-host disease (GVHD) in mice, according to research published in The Journal of Experimental Medicine.
One way to prevent GVHD after allogeneic hematopoietic stem cell transplant (allo-HSCT) is to co-transplant large numbers of Tregs, which can suppress the donor cells’ effects on healthy tissue without affecting their ability to kill tumor cells.
This approach is challenging, however, because the Tregs must first be isolated from the donor’s peripheral blood or bone marrow and then cultivated in the lab to produce sufficient numbers for transplant.
Andreas Beilhack, MD, of University Hospital Würzburg in Germany, and his colleagues have found a way to overcome this obstacle, at least in mice.
The team developed a protein agonist called STAR2, which selectively activates TNFR2. The researchers noted that TNF and its receptors, TNFR1 and TNFR2, have been shown to play a crucial role in both GVHD and the graft-versus-leukemia effect.
With their experiments, Dr Beilhack and his colleagues showed that STAR2 binds to TNFR2, activating a signaling pathway that increases the number of natural Tregs in vitro and in vivo.
The team also tested STAR2 in mice with lymphoma. Pretreating the mice with STAR2 protected them from developing GVHD after allo-HSCT. And the donor-derived cells retained their ability to kill lymphoma cells.
In addition, the researchers found that a slightly modified version of STAR2 has a similar effect on human Tregs, which suggests this approach could also prevent GVHD in humans undergoing allo-HSCT.
“Furthermore, this strategy may be beneficial for other pathological settings in which elevated numbers of regulatory T cells are desirable, such as autoimmune diseases and solid organ transplantation,” Dr Beilhack said. ![]()

Photo by Aaron Logan
A treatment strategy that increases the production of regulatory T cells (Tregs) can prevent graft-versus-host disease (GVHD) in mice, according to research published in The Journal of Experimental Medicine.
One way to prevent GVHD after allogeneic hematopoietic stem cell transplant (allo-HSCT) is to co-transplant large numbers of Tregs, which can suppress the donor cells’ effects on healthy tissue without affecting their ability to kill tumor cells.
This approach is challenging, however, because the Tregs must first be isolated from the donor’s peripheral blood or bone marrow and then cultivated in the lab to produce sufficient numbers for transplant.
Andreas Beilhack, MD, of University Hospital Würzburg in Germany, and his colleagues have found a way to overcome this obstacle, at least in mice.
The team developed a protein agonist called STAR2, which selectively activates TNFR2. The researchers noted that TNF and its receptors, TNFR1 and TNFR2, have been shown to play a crucial role in both GVHD and the graft-versus-leukemia effect.
With their experiments, Dr Beilhack and his colleagues showed that STAR2 binds to TNFR2, activating a signaling pathway that increases the number of natural Tregs in vitro and in vivo.
The team also tested STAR2 in mice with lymphoma. Pretreating the mice with STAR2 protected them from developing GVHD after allo-HSCT. And the donor-derived cells retained their ability to kill lymphoma cells.
In addition, the researchers found that a slightly modified version of STAR2 has a similar effect on human Tregs, which suggests this approach could also prevent GVHD in humans undergoing allo-HSCT.
“Furthermore, this strategy may be beneficial for other pathological settings in which elevated numbers of regulatory T cells are desirable, such as autoimmune diseases and solid organ transplantation,” Dr Beilhack said. ![]()
Genome-editing approach could treat SCD

and a sickled one
Image by Betty Pace
CRISPR-Cas9-mediated genome editing might be a feasible approach for treating sickle cell disease (SCD), according to a group of researchers.
The team used CRISPR to edit hematopoietic stem and progenitor cells (HSPCs) from patients with SCD, which resulted in the production of red blood cells (RBCs) that had enough fetal hemoglobin to be healthy.
The researchers believe this approach might prove effective in treating beta-thalassemia as well.
“Our approach to gene editing is informed by the known benefits of hereditary persistence of fetal hemoglobin,” said study author Mitchell J. Weiss, MD, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“It has been known for some time that individuals with genetic mutations that persistently elevate fetal hemoglobin are resistant to the symptoms of sickle cell disease and beta-thalassemia . . . . We have found a way to use CRISPR gene editing to produce similar benefits.”
Dr Weiss and his colleagues described this method in Nature Medicine.
The researchers noted that SCD and beta-thalassemia become symptomatic when fetal gamma-globin expression from 2 genes, HBG1 and HBG2, decreases and the expression of adult beta-globin increases, which shifts RBC hemoglobin from the fetal form to the adult form.
Reversing this shift can raise levels of fetal hemoglobin and ameliorate the symptoms of beta-thalassemia or SCD.
The team also pointed out that, in people with a benign genetic condition known as hereditary persistence of fetal hemoglobin (HPFH), mutations attenuate gamma-globin-to-beta-globin switching, which causes high levels of fetal hemoglobin expression throughout the patients’ lives.
So the researchers set out to mimic this phenomenon in HSPCs from patients with SCD.
The team performed CRISPR–Cas9-mediated genome editing of the HSPCs to mutate a 13-nt sequence present in the promoters of the HBG1 and HBG2 genes.
In this way, they were able to recapitulate a naturally occurring HPFH-associated mutation, so the HSPCs produced RBCs with increased fetal hemoglobin levels.
“Our work has identified a potential DNA target for genome-editing-mediated therapy and offers proof-of-principle for a possible approach to treat sickle cell and beta-thalassemia,” Dr Weiss said.
“We have been able to snip that DNA target using CRISPR, remove a short segment in a ‘control section’ of DNA that stimulates gamma-to-beta switching, and join the ends back up to produce sustained elevation of fetal hemoglobin levels in adult red blood cells.”
Recently, scientists have used several genome-editing approaches to manipulate HSPCs for the possible treatment of SCD and beta-thalassemia, including repair of specific disease-causing mutations and other strategies to inhibit gamma-to-beta switching.
“Our results represent an additional approach to these existing innovative strategies and compare favorably in terms of the levels of fetal hemoglobin that are produced by our experimental system,” Dr Weiss said.
He and his colleagues noted that, at this stage, it is still too early to begin clinical trials of their approach. The researchers want to refine the genome-editing process and perform other experiments to minimize potentially harmful off-target mutations before clinical trials are considered.
In addition, they said it will be important to compare the different genome-editing approaches head-to-head to determine which is safest and most effective. ![]()

and a sickled one
Image by Betty Pace
CRISPR-Cas9-mediated genome editing might be a feasible approach for treating sickle cell disease (SCD), according to a group of researchers.
The team used CRISPR to edit hematopoietic stem and progenitor cells (HSPCs) from patients with SCD, which resulted in the production of red blood cells (RBCs) that had enough fetal hemoglobin to be healthy.
The researchers believe this approach might prove effective in treating beta-thalassemia as well.
“Our approach to gene editing is informed by the known benefits of hereditary persistence of fetal hemoglobin,” said study author Mitchell J. Weiss, MD, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“It has been known for some time that individuals with genetic mutations that persistently elevate fetal hemoglobin are resistant to the symptoms of sickle cell disease and beta-thalassemia . . . . We have found a way to use CRISPR gene editing to produce similar benefits.”
Dr Weiss and his colleagues described this method in Nature Medicine.
The researchers noted that SCD and beta-thalassemia become symptomatic when fetal gamma-globin expression from 2 genes, HBG1 and HBG2, decreases and the expression of adult beta-globin increases, which shifts RBC hemoglobin from the fetal form to the adult form.
Reversing this shift can raise levels of fetal hemoglobin and ameliorate the symptoms of beta-thalassemia or SCD.
The team also pointed out that, in people with a benign genetic condition known as hereditary persistence of fetal hemoglobin (HPFH), mutations attenuate gamma-globin-to-beta-globin switching, which causes high levels of fetal hemoglobin expression throughout the patients’ lives.
So the researchers set out to mimic this phenomenon in HSPCs from patients with SCD.
The team performed CRISPR–Cas9-mediated genome editing of the HSPCs to mutate a 13-nt sequence present in the promoters of the HBG1 and HBG2 genes.
In this way, they were able to recapitulate a naturally occurring HPFH-associated mutation, so the HSPCs produced RBCs with increased fetal hemoglobin levels.
“Our work has identified a potential DNA target for genome-editing-mediated therapy and offers proof-of-principle for a possible approach to treat sickle cell and beta-thalassemia,” Dr Weiss said.
“We have been able to snip that DNA target using CRISPR, remove a short segment in a ‘control section’ of DNA that stimulates gamma-to-beta switching, and join the ends back up to produce sustained elevation of fetal hemoglobin levels in adult red blood cells.”
Recently, scientists have used several genome-editing approaches to manipulate HSPCs for the possible treatment of SCD and beta-thalassemia, including repair of specific disease-causing mutations and other strategies to inhibit gamma-to-beta switching.
“Our results represent an additional approach to these existing innovative strategies and compare favorably in terms of the levels of fetal hemoglobin that are produced by our experimental system,” Dr Weiss said.
He and his colleagues noted that, at this stage, it is still too early to begin clinical trials of their approach. The researchers want to refine the genome-editing process and perform other experiments to minimize potentially harmful off-target mutations before clinical trials are considered.
In addition, they said it will be important to compare the different genome-editing approaches head-to-head to determine which is safest and most effective. ![]()

and a sickled one
Image by Betty Pace
CRISPR-Cas9-mediated genome editing might be a feasible approach for treating sickle cell disease (SCD), according to a group of researchers.
The team used CRISPR to edit hematopoietic stem and progenitor cells (HSPCs) from patients with SCD, which resulted in the production of red blood cells (RBCs) that had enough fetal hemoglobin to be healthy.
The researchers believe this approach might prove effective in treating beta-thalassemia as well.
“Our approach to gene editing is informed by the known benefits of hereditary persistence of fetal hemoglobin,” said study author Mitchell J. Weiss, MD, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“It has been known for some time that individuals with genetic mutations that persistently elevate fetal hemoglobin are resistant to the symptoms of sickle cell disease and beta-thalassemia . . . . We have found a way to use CRISPR gene editing to produce similar benefits.”
Dr Weiss and his colleagues described this method in Nature Medicine.
The researchers noted that SCD and beta-thalassemia become symptomatic when fetal gamma-globin expression from 2 genes, HBG1 and HBG2, decreases and the expression of adult beta-globin increases, which shifts RBC hemoglobin from the fetal form to the adult form.
Reversing this shift can raise levels of fetal hemoglobin and ameliorate the symptoms of beta-thalassemia or SCD.
The team also pointed out that, in people with a benign genetic condition known as hereditary persistence of fetal hemoglobin (HPFH), mutations attenuate gamma-globin-to-beta-globin switching, which causes high levels of fetal hemoglobin expression throughout the patients’ lives.
So the researchers set out to mimic this phenomenon in HSPCs from patients with SCD.
The team performed CRISPR–Cas9-mediated genome editing of the HSPCs to mutate a 13-nt sequence present in the promoters of the HBG1 and HBG2 genes.
In this way, they were able to recapitulate a naturally occurring HPFH-associated mutation, so the HSPCs produced RBCs with increased fetal hemoglobin levels.
“Our work has identified a potential DNA target for genome-editing-mediated therapy and offers proof-of-principle for a possible approach to treat sickle cell and beta-thalassemia,” Dr Weiss said.
“We have been able to snip that DNA target using CRISPR, remove a short segment in a ‘control section’ of DNA that stimulates gamma-to-beta switching, and join the ends back up to produce sustained elevation of fetal hemoglobin levels in adult red blood cells.”
Recently, scientists have used several genome-editing approaches to manipulate HSPCs for the possible treatment of SCD and beta-thalassemia, including repair of specific disease-causing mutations and other strategies to inhibit gamma-to-beta switching.
“Our results represent an additional approach to these existing innovative strategies and compare favorably in terms of the levels of fetal hemoglobin that are produced by our experimental system,” Dr Weiss said.
He and his colleagues noted that, at this stage, it is still too early to begin clinical trials of their approach. The researchers want to refine the genome-editing process and perform other experiments to minimize potentially harmful off-target mutations before clinical trials are considered.
In addition, they said it will be important to compare the different genome-editing approaches head-to-head to determine which is safest and most effective. ![]()
Drug no longer in development for DLBCL, other cancers

ProNAi Therapeutics recently announced its decision to stop development of PNT2258, a drug designed to treat cancers characterized by overexpression of BCL2.
In June, the company suspended development of PNT2258, closing enrollment in a phase 2 trial of patients with relapsed/refractory diffuse large B-cell lymphoma (DLBCL) and a phase 2 trial of patients with Richter’s transformation.
Now, ProNAi has said it does not plan to resume development of the drug.
“[N]o further investment in PNT2258 or the underlying DNAi platform by ProNAi is contemplated, and the company subsequently has closed its research facility based in Plymouth, Michigan, which supported these programs,” the company said in a statement.
About PNT2258
PNT2258 consists of a single-stranded, 24-base DNAi oligonucleotide known as PNT100 that is encapsulated in lipid nanoparticles.
The DNAi technology platform is based on a discovery that single-stranded DNA oligonucleotides can interact with genomic DNA to interfere with oncogenes. PNT100 DNAi is designed to target a genetic regulatory region associated with BCL2.
Last March, PNT2258 was granted orphan drug designation from the US Food and Drug Administration for the treatment of DLBCL.
ProNAi initially suspended the development of PNT2258 in June, following a review of interim data from the phase 2 Wolverine trial. The company said the drug produced “modest efficacy” in this trial, but it seemed the data were not “robust enough” to justify continued development of PNT2258.
“We have decided to suspend development of PNT2258 pending further review of these data in order to determine next steps for both this asset and the DNAi platform,” Nick Glover, president and CEO of ProNAi, said at the time.
The Wolverine trial was designed to evaluate the safety and efficacy of PNT2258 monotherapy in 61 patients with relapsed/refractory DLBCL.
ProNAi reported interim safety and efficacy data as of April 25, 2016, for the first 37 subjects enrolled. The response rate was 8.1% overall (n=37) and 15.8% in the response-evaluable subgroup (n=19).
Subjects were considered response-evaluable if they met the amended eligibility criteria—a performance status of 0 to 1, 1 to 3 prior systemic treatment regimens, and receipt of at least 8 doses of PNT2258 within 35 days of starting therapy.
PNT2258 was also being evaluated in patients with Richter’s transformation in the phase 2 Brighton study. In June, ProNAi said it had enrolled 5 subjects in this study, and 4 had discontinued. No responses were observed.
“On the basis of these interim assessments, we have decided to close the Wolverine and Brighton studies to further enrollment of new subjects,” Barbara Klencke, chief development officer of ProNAi, said at the time.
PNT2258 was evaluated in 2 prior studies as well. In a phase 1 study (NCT01191775), PNT2258 was given to 22 subjects with advanced solid tumors. The drug was considered well tolerated at doses ranging from 1 mg/m2 through 150 mg/m2.
A pilot study of PNT2258 (NCT01733238) enrolled 13 subjects with relapsed/refractory B-cell non-Hodgkin lymphoma. Responses were observed in subjects with DLBCL and those with follicular lymphoma.
Six subjects were progression-free at 12 months, and progression-free survival extended to 2 years and beyond in 4 subjects. The majority of the adverse events were grade 1 or 2. ![]()

ProNAi Therapeutics recently announced its decision to stop development of PNT2258, a drug designed to treat cancers characterized by overexpression of BCL2.
In June, the company suspended development of PNT2258, closing enrollment in a phase 2 trial of patients with relapsed/refractory diffuse large B-cell lymphoma (DLBCL) and a phase 2 trial of patients with Richter’s transformation.
Now, ProNAi has said it does not plan to resume development of the drug.
“[N]o further investment in PNT2258 or the underlying DNAi platform by ProNAi is contemplated, and the company subsequently has closed its research facility based in Plymouth, Michigan, which supported these programs,” the company said in a statement.
About PNT2258
PNT2258 consists of a single-stranded, 24-base DNAi oligonucleotide known as PNT100 that is encapsulated in lipid nanoparticles.
The DNAi technology platform is based on a discovery that single-stranded DNA oligonucleotides can interact with genomic DNA to interfere with oncogenes. PNT100 DNAi is designed to target a genetic regulatory region associated with BCL2.
Last March, PNT2258 was granted orphan drug designation from the US Food and Drug Administration for the treatment of DLBCL.
ProNAi initially suspended the development of PNT2258 in June, following a review of interim data from the phase 2 Wolverine trial. The company said the drug produced “modest efficacy” in this trial, but it seemed the data were not “robust enough” to justify continued development of PNT2258.
“We have decided to suspend development of PNT2258 pending further review of these data in order to determine next steps for both this asset and the DNAi platform,” Nick Glover, president and CEO of ProNAi, said at the time.
The Wolverine trial was designed to evaluate the safety and efficacy of PNT2258 monotherapy in 61 patients with relapsed/refractory DLBCL.
ProNAi reported interim safety and efficacy data as of April 25, 2016, for the first 37 subjects enrolled. The response rate was 8.1% overall (n=37) and 15.8% in the response-evaluable subgroup (n=19).
Subjects were considered response-evaluable if they met the amended eligibility criteria—a performance status of 0 to 1, 1 to 3 prior systemic treatment regimens, and receipt of at least 8 doses of PNT2258 within 35 days of starting therapy.
PNT2258 was also being evaluated in patients with Richter’s transformation in the phase 2 Brighton study. In June, ProNAi said it had enrolled 5 subjects in this study, and 4 had discontinued. No responses were observed.
“On the basis of these interim assessments, we have decided to close the Wolverine and Brighton studies to further enrollment of new subjects,” Barbara Klencke, chief development officer of ProNAi, said at the time.
PNT2258 was evaluated in 2 prior studies as well. In a phase 1 study (NCT01191775), PNT2258 was given to 22 subjects with advanced solid tumors. The drug was considered well tolerated at doses ranging from 1 mg/m2 through 150 mg/m2.
A pilot study of PNT2258 (NCT01733238) enrolled 13 subjects with relapsed/refractory B-cell non-Hodgkin lymphoma. Responses were observed in subjects with DLBCL and those with follicular lymphoma.
Six subjects were progression-free at 12 months, and progression-free survival extended to 2 years and beyond in 4 subjects. The majority of the adverse events were grade 1 or 2. ![]()

ProNAi Therapeutics recently announced its decision to stop development of PNT2258, a drug designed to treat cancers characterized by overexpression of BCL2.
In June, the company suspended development of PNT2258, closing enrollment in a phase 2 trial of patients with relapsed/refractory diffuse large B-cell lymphoma (DLBCL) and a phase 2 trial of patients with Richter’s transformation.
Now, ProNAi has said it does not plan to resume development of the drug.
“[N]o further investment in PNT2258 or the underlying DNAi platform by ProNAi is contemplated, and the company subsequently has closed its research facility based in Plymouth, Michigan, which supported these programs,” the company said in a statement.
About PNT2258
PNT2258 consists of a single-stranded, 24-base DNAi oligonucleotide known as PNT100 that is encapsulated in lipid nanoparticles.
The DNAi technology platform is based on a discovery that single-stranded DNA oligonucleotides can interact with genomic DNA to interfere with oncogenes. PNT100 DNAi is designed to target a genetic regulatory region associated with BCL2.
Last March, PNT2258 was granted orphan drug designation from the US Food and Drug Administration for the treatment of DLBCL.
ProNAi initially suspended the development of PNT2258 in June, following a review of interim data from the phase 2 Wolverine trial. The company said the drug produced “modest efficacy” in this trial, but it seemed the data were not “robust enough” to justify continued development of PNT2258.
“We have decided to suspend development of PNT2258 pending further review of these data in order to determine next steps for both this asset and the DNAi platform,” Nick Glover, president and CEO of ProNAi, said at the time.
The Wolverine trial was designed to evaluate the safety and efficacy of PNT2258 monotherapy in 61 patients with relapsed/refractory DLBCL.
ProNAi reported interim safety and efficacy data as of April 25, 2016, for the first 37 subjects enrolled. The response rate was 8.1% overall (n=37) and 15.8% in the response-evaluable subgroup (n=19).
Subjects were considered response-evaluable if they met the amended eligibility criteria—a performance status of 0 to 1, 1 to 3 prior systemic treatment regimens, and receipt of at least 8 doses of PNT2258 within 35 days of starting therapy.
PNT2258 was also being evaluated in patients with Richter’s transformation in the phase 2 Brighton study. In June, ProNAi said it had enrolled 5 subjects in this study, and 4 had discontinued. No responses were observed.
“On the basis of these interim assessments, we have decided to close the Wolverine and Brighton studies to further enrollment of new subjects,” Barbara Klencke, chief development officer of ProNAi, said at the time.
PNT2258 was evaluated in 2 prior studies as well. In a phase 1 study (NCT01191775), PNT2258 was given to 22 subjects with advanced solid tumors. The drug was considered well tolerated at doses ranging from 1 mg/m2 through 150 mg/m2.
A pilot study of PNT2258 (NCT01733238) enrolled 13 subjects with relapsed/refractory B-cell non-Hodgkin lymphoma. Responses were observed in subjects with DLBCL and those with follicular lymphoma.
Six subjects were progression-free at 12 months, and progression-free survival extended to 2 years and beyond in 4 subjects. The majority of the adverse events were grade 1 or 2. ![]()
Pulmonary complications affect cancer survivors long-term

Photo by Bill Branson
A new study suggests that survivors of childhood cancer may be plagued by pulmonary complications related to treatment well into their adult lives.
The research indicated that the cumulative incidence of pulmonary complications continues to increase up to 25 years from a patient’s initial cancer diagnosis.
In addition, platinum-based chemotherapy and higher doses of radiation were linked to an increased risk of death from pulmonary causes.
Andrew C. Dietz, MD, of Children’s Hospital Los Angeles in California, and his colleagues reported these findings in Cancer.
The researchers analyzed data from 20,690 five-year cancer survivors who participated in the Childhood Cancer Survivor Study to determine the incidence of death from pulmonary causes.
The team also assessed the incidence of various pulmonary complications in 14,316 of those cancer survivors (who completed a baseline survey and/or 1 of 2 follow-up surveys years later), comparing the results to those seen in a control group of 4027 cancer survivor siblings.
About 34% of the 14,316 cancer survivors had been diagnosed with acute leukemia, and about 21% were diagnosed with Hodgkin or non-Hodgkin lymphoma.
The cancer survivors’ median age at diagnosis was 7 (range, 0-21), and their median age at evaluation was 32 (range, 6-59). The median time from diagnosis was 25 years (range, 5-39).
Compared with controls, cancer survivors were more likely to be male, black, and Hispanic. Cancer survivors were slightly younger and more likely to report a history of congestive heart failure, but they were less likely to be overweight/obese or have ever smoked at the time of the baseline survey.
Results
By age 45, the cumulative incidence of any pulmonary condition was 29.6% among cancer survivors and 26.5% among controls (P=0.001).
The cancer survivors were more likely than controls to report chronic cough (rate ratio [RR]=1.6), the need for extra oxygen (RR=1.8), lung fibrosis (RR=3.5), and recurrent pneumonia (RR=2.0).
Among cancer survivors, the risk of asthma was significantly associated with exposure to asparaginase. Chronic cough was significantly associated with chest wall or lung surgery, anthracyclines, hydroxyurea, and lung radiation doses ≥15 Gy.
Emphysema was significantly associated with lomustine. The need for extra oxygen was significantly associated with hematopoietic stem cell transplant, chest wall or lung surgery, and lung radiation doses ≥10 Gy.
Lung fibrosis was significantly associated with chest wall or lung surgery, asparaginase, platinum-based chemotherapy, and lung radiation doses ≥10 Gy. Recurrent pneumonia was significantly associated with lung radiation doses ≥15 Gy.
The standardized mortality ratio for death from pulmonary causes among all eligible cancer survivors (n=20,690) was 5.9. Pulmonary death was significantly associated with exposure to platinum-based agents and lung radiation doses ≥10 Gy.
“This study adds to our understanding of specific, long-term risks to pulmonary health for survivors of childhood cancer and will help refine guidelines for appropriate screening, health surveillance, and counseling,” said study author Daniel A. Mulrooney, MD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
He added that this knowledge could potentially contribute to the design and testing of better, targeted interventions to decrease adverse pulmonary events in this population. ![]()

Photo by Bill Branson
A new study suggests that survivors of childhood cancer may be plagued by pulmonary complications related to treatment well into their adult lives.
The research indicated that the cumulative incidence of pulmonary complications continues to increase up to 25 years from a patient’s initial cancer diagnosis.
In addition, platinum-based chemotherapy and higher doses of radiation were linked to an increased risk of death from pulmonary causes.
Andrew C. Dietz, MD, of Children’s Hospital Los Angeles in California, and his colleagues reported these findings in Cancer.
The researchers analyzed data from 20,690 five-year cancer survivors who participated in the Childhood Cancer Survivor Study to determine the incidence of death from pulmonary causes.
The team also assessed the incidence of various pulmonary complications in 14,316 of those cancer survivors (who completed a baseline survey and/or 1 of 2 follow-up surveys years later), comparing the results to those seen in a control group of 4027 cancer survivor siblings.
About 34% of the 14,316 cancer survivors had been diagnosed with acute leukemia, and about 21% were diagnosed with Hodgkin or non-Hodgkin lymphoma.
The cancer survivors’ median age at diagnosis was 7 (range, 0-21), and their median age at evaluation was 32 (range, 6-59). The median time from diagnosis was 25 years (range, 5-39).
Compared with controls, cancer survivors were more likely to be male, black, and Hispanic. Cancer survivors were slightly younger and more likely to report a history of congestive heart failure, but they were less likely to be overweight/obese or have ever smoked at the time of the baseline survey.
Results
By age 45, the cumulative incidence of any pulmonary condition was 29.6% among cancer survivors and 26.5% among controls (P=0.001).
The cancer survivors were more likely than controls to report chronic cough (rate ratio [RR]=1.6), the need for extra oxygen (RR=1.8), lung fibrosis (RR=3.5), and recurrent pneumonia (RR=2.0).
Among cancer survivors, the risk of asthma was significantly associated with exposure to asparaginase. Chronic cough was significantly associated with chest wall or lung surgery, anthracyclines, hydroxyurea, and lung radiation doses ≥15 Gy.
Emphysema was significantly associated with lomustine. The need for extra oxygen was significantly associated with hematopoietic stem cell transplant, chest wall or lung surgery, and lung radiation doses ≥10 Gy.
Lung fibrosis was significantly associated with chest wall or lung surgery, asparaginase, platinum-based chemotherapy, and lung radiation doses ≥10 Gy. Recurrent pneumonia was significantly associated with lung radiation doses ≥15 Gy.
The standardized mortality ratio for death from pulmonary causes among all eligible cancer survivors (n=20,690) was 5.9. Pulmonary death was significantly associated with exposure to platinum-based agents and lung radiation doses ≥10 Gy.
“This study adds to our understanding of specific, long-term risks to pulmonary health for survivors of childhood cancer and will help refine guidelines for appropriate screening, health surveillance, and counseling,” said study author Daniel A. Mulrooney, MD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
He added that this knowledge could potentially contribute to the design and testing of better, targeted interventions to decrease adverse pulmonary events in this population. ![]()

Photo by Bill Branson
A new study suggests that survivors of childhood cancer may be plagued by pulmonary complications related to treatment well into their adult lives.
The research indicated that the cumulative incidence of pulmonary complications continues to increase up to 25 years from a patient’s initial cancer diagnosis.
In addition, platinum-based chemotherapy and higher doses of radiation were linked to an increased risk of death from pulmonary causes.
Andrew C. Dietz, MD, of Children’s Hospital Los Angeles in California, and his colleagues reported these findings in Cancer.
The researchers analyzed data from 20,690 five-year cancer survivors who participated in the Childhood Cancer Survivor Study to determine the incidence of death from pulmonary causes.
The team also assessed the incidence of various pulmonary complications in 14,316 of those cancer survivors (who completed a baseline survey and/or 1 of 2 follow-up surveys years later), comparing the results to those seen in a control group of 4027 cancer survivor siblings.
About 34% of the 14,316 cancer survivors had been diagnosed with acute leukemia, and about 21% were diagnosed with Hodgkin or non-Hodgkin lymphoma.
The cancer survivors’ median age at diagnosis was 7 (range, 0-21), and their median age at evaluation was 32 (range, 6-59). The median time from diagnosis was 25 years (range, 5-39).
Compared with controls, cancer survivors were more likely to be male, black, and Hispanic. Cancer survivors were slightly younger and more likely to report a history of congestive heart failure, but they were less likely to be overweight/obese or have ever smoked at the time of the baseline survey.
Results
By age 45, the cumulative incidence of any pulmonary condition was 29.6% among cancer survivors and 26.5% among controls (P=0.001).
The cancer survivors were more likely than controls to report chronic cough (rate ratio [RR]=1.6), the need for extra oxygen (RR=1.8), lung fibrosis (RR=3.5), and recurrent pneumonia (RR=2.0).
Among cancer survivors, the risk of asthma was significantly associated with exposure to asparaginase. Chronic cough was significantly associated with chest wall or lung surgery, anthracyclines, hydroxyurea, and lung radiation doses ≥15 Gy.
Emphysema was significantly associated with lomustine. The need for extra oxygen was significantly associated with hematopoietic stem cell transplant, chest wall or lung surgery, and lung radiation doses ≥10 Gy.
Lung fibrosis was significantly associated with chest wall or lung surgery, asparaginase, platinum-based chemotherapy, and lung radiation doses ≥10 Gy. Recurrent pneumonia was significantly associated with lung radiation doses ≥15 Gy.
The standardized mortality ratio for death from pulmonary causes among all eligible cancer survivors (n=20,690) was 5.9. Pulmonary death was significantly associated with exposure to platinum-based agents and lung radiation doses ≥10 Gy.
“This study adds to our understanding of specific, long-term risks to pulmonary health for survivors of childhood cancer and will help refine guidelines for appropriate screening, health surveillance, and counseling,” said study author Daniel A. Mulrooney, MD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
He added that this knowledge could potentially contribute to the design and testing of better, targeted interventions to decrease adverse pulmonary events in this population. ![]()
Postpartum Depression Screening
Maternal postpartum depression occurs in 5% to 25% of all mothers, and up to 40% to 60% in high‐risk populations such as low‐income women.[1, 2, 3, 4] Children of affected mothers suffer negative health consequences such as decreased physical growth, poor maternalchild bond, problem behavior, and child abuse.[5, 6, 7] Timely recognition of symptoms and treatment may improve child outcomes.[8] Published guidelines recommend pediatricians screen for postpartum depression at infant 1‐, 2‐, 4‐, and 6‐month outpatient visits.[9] There are no current guidelines for or studies of screening in general inpatient settings, although emergency rooms[10] and neonatal intensive care units (NICUs)[11] have been examined. Pediatric hospitalization may offer an additional opportunity for expanding screening and intervention.
Augmenting outpatient screening practices with additional inpatient screening would have several benefits. Infant health problems have been associated with postpartum depression, and therefore mothers in the hospital may be at higher risk.[12] Inpatient screening would also improve access to mothers not screened as outpatients. Missed screening could occur due to physician discomfort with screening, time constraints during busy office visits, or noncompliance with recommended visit schedules.[13, 14, 15, 16] Finally, inpatient providers would benefit from understanding the psychosocial milieu of children now under their care. Recent studies note hospital discharges may be improved and readmissions reduced by assessing socioeconomic risk factors during hospitalization.[17] The evidence‐based Peds Effective Discharge: Better Handoff to Home through Safer Transitions Better Outcomes by Optimizing Safe Transitions (Pedi‐BOOST) toolkit specifically recommends an assessment of parental psychiatric issues.[18] Postpartum depression strongly correlates with impaired maternalchild bonding,[19] which in turn negatively affects mothers' engagement with healthcare providers.[20] This could impact patient education and recommendations provided during hospitalization.
Therefore, we sought to perform postpartum depression screening during infant hospitalizations. Our primary goal was to determine rate of postpartum depression in our population and proportion of women previously unscreened who could be captured by inpatient screening. We additionally aimed to determine the proportion of women with poor maternalinfant bond. Our next goal was to identify maternal or infant factors associated with positive postpartum depression screening. Finally, we performed follow‐up calls to determine if in‐hospital interventions resulted in formal postpartum depression diagnosis, use of recommended referrals, improved maternalchild bond, and decreased symptoms of depression over time.
METHODS
Patient Selection
We conducted a prospective observational study on a convenience sample of mothers at Children's Hospital Los Angeles (CHLA), a large, urban, tertiary care hospital. Biological mothers of infants 1 year of age admitted to medicalsurgical floors and assigned to pediatric hospitalist teams between April 1, 2013 and July 30, 2014 were eligible for inclusion. Mothers were required to be age 18 years or older and able to speak and read English or Spanish. Mothers of infants aged 2 weeks were excluded to avoid confusing postpartum depression with maternal baby blues, a distinct entity causing milder symptoms of depression that should resolve by 2 weeks.[21] In an effort to reduce the impact of stress associated with prolonged hospitalization on Edinburgh Postpartum Depression Scale (EPDS) scores, we excluded mothers of children already hospitalized >72 hours. Visits from participants who were readmitted or previously enrolled in the study were excluded. All study procedures were approved by the CHLA Institutional Review Board.
Measures
After giving informed consent, mothers completed demographic forms about themselves and their infants. A 4‐item Likert scale assessed self‐perceived support from family and friends. Past mental health problems were assessed via 10‐item checklist. Self‐reported infant comorbidities and reason for hospitalization were confirmed by chart review for International Classification of Diseases, Ninth Revision diagnoses present on admission and reason for discharge. Next, mothers filled out a maternalinfant bonding scale (MIB)[22] and the EPDS,[23, 24] which has been validated in both English and Spanish.[25] There are no formal cutoffs for the MIB; higher scores indicate worse bonding. Out of a possible 30, a score of 10 or higher on the EPDS was considered a positive screen, indicating risk for postpartum depression. Scores less than 10 were negative screens, and those mothers were determined not at risk.[24] The last EPDS question asks, The thought of harming myself has occurred to me. Any mothers answering yes, quite often, sometimes, or hardly ever were further interviewed and treated per a suicidality operating protocol.
Counseling and Referral
All EPDS mothers were informed of results and did not receive further intervention during hospitalization. For EPDS+ mothers, individual social workers responded to referrals placed by the study team into infant charts and delivered 1‐on‐1 counseling. Social workers received study education prior to initiation and midway through patient recruitment and provided mothers with an educational handout, referral sheet listing online resources of local mental health clinics accepting postpartum depression patients, and help‐line numbers. Mothers who identified a primary doctor were encouraged to follow up with them.
Follow‐up
In order to assess intervention effect over time, all mothers (both EPDS+ and EPDS) were called 3 and 6 months ( 1 week) postenrollment and rescreened with the EPDS and MIB. They also answered a short survey assessing whether they spoke further to a doctor about postpartum depression; used a referral resource; received a formal postpartum depression diagnosis; and if their children visited the ER, urgent care, or hospital again since discharge. Mothers who again screened EPDS+ or newly converted to EPDS+ were provided counseling and referral via phone.
Sample Size Calculation
A priori power analysis determined a sample size of 310 mothers was required to estimate the rate of postpartum depression at CHLA with 5% precision and a 95% confidence level, assuming an estimated prevalence of 27.9% based on prior studies.[26] At this prevalence rate, screening 310 mothers was also predicted to yield at least 77 positive screens on the EPDS, yielding an appropriate sample to detect EPDS score improvements over time. This number was based on previous studies showing reduction in EPDS of 35% following appropriate referral,[26, 27] assuming 15% attrition at both the 3‐month and 6‐month follow‐up sampling points.
Statistical Analysis
After data collection was complete, characteristics between EPDS+ and EPDS groups were compared using 2 tests for dichotomous outcomes and t tests for continuous variables. Multiple logistic regression was then used to compare specific factors associated with positive EPDS screens (P 0.05). Linear regression assessed the relationship between EPDS and MIB scores. Change in average EPDS and MIB scores at the time of first successful follow‐up call between women who did and did not seek further postpartum depression evaluation were compared via 2‐way repeated measures analysis of variance. Statistical analyses were performed using R software.[28]
RESULTS
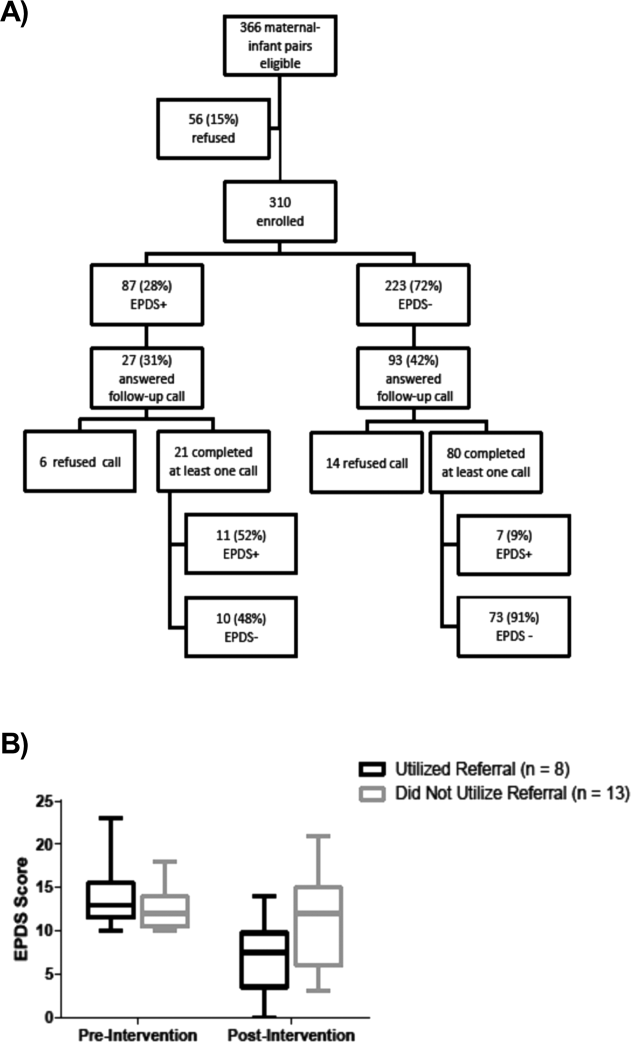
Out of 366 motherinfant pairs, 56 (15%) refused, and 310 (85%) mothers were fully enrolled (Figure 1A). Mothers had an average age of 28.17 years, were 68.3% Hispanic/Latina by self‐report, and 45.2% were married. Infants were an average of 4.24 months old, 81.9% were born term (>37 weeks), and 64.8% were previously healthy (Table 1).
| Characteristic | All Participants, n = 310 |
|---|---|
| |
| Maternal characteristics | |
| Age, y* | 28.17 6.18 |
| Race/ethnicity | |
| White | 48 (15.5%) |
| Black | 25 (8.1%) |
| Hispanic | 211(68.3%) |
| Other | 25 (8.1%) |
| EPDS language | |
| English | 231 (74.5%) |
| Spanish | 79 (25.5%) |
| People in home | 5 (4, 6) |
| No. of children | 2 (1, 3) |
| Relationship | |
| Married | 140 (45.2%) |
| In a relationship | 105 (33.9%) |
| Single | 62 (20%) |
| Any breastfeeding | 142 (45.8%) |
| Unsupportive social network | 54 (17.4%) |
| Some psychiatric disorder | 47 (15.2%) |
| MIB score | 6 (3, 10) |
| Infant characteristics | |
| Age, mo* | 4.24 3.19 |
| Gestational age, wk | 39 (37, 40) |
| Prior admission | 113 (36.5%) |
| Any comorbidity | 109 (35.2%) |
| Congenital heart disease | 27 (8.7%) |
| Neurodevelopmental | 22 (7.1%) |
| Any medical device needed | 38 (12.3%) |

(B) Postenrollment change in mean Edinburgh Postpartum Depression Scale (EPDS) score of all initially EPDS mothers who completed at least 1 follow‐up phone call, separated by if they did or did not seek referral. Mothers using referral (either spoke with physician or used resource sheet) had significantly larger reduction in score. Statistical analysis by analysis of variance, P < 0.05.
Eighty‐seven (28%) mothers were EPDS+; 223 (72%) were EPDS. Only 42 mothers reported previous postpartum depression screening since the birth of their most recent child. However, 30 infants were 1 month in age, thus outside recommended screening range. Eliminating these infants revealed a 14.6% rate of appropriate prior screening. Higher EPDS scores were associated with higher (worse) MIB scores by linear regression ( = 0.11, P 0.001). The vast majority (77%) of mothers scored a 0 or 1 on the MIB scale, indicating good bonding; further statistical comparison using the MIB scale as a secondary outcome was therefore inappropriate.
On bivariate logistic regression, Hispanic/Latina women were less likely to be EPDS+ (odds ratio [OR]: 0.43; 95% CI: 0.23‐0.84) compared to white/Caucasian women. Mothers who identified Spanish as their primary language and took the Spanish EPDS had lower odds of a positive screen (OR: 0.47; 95% CI: 0.25‐0.88). The racial differences did not persist on multivariate analysis (OR: 0.64; 95% CI: 0.30‐1.38) (Table 2). Maternal characteristics identified as potential risk factors for positive screens were poor social support (OR: 3.58; 95% CI: 1.95‐6.59) and history of a prior psychiatric diagnosis (OR: 5.07; 95% CI: 2.65‐9.72). There were no differences in age, number of children or people living in the home, relationship status, or breastfeeding rates by EPDS score.
| OR | 95% CI | P Value | |
|---|---|---|---|
| |||
| Maternal characteristics | |||
| Maternal age | 0.99 | 0.95‐1.03 | 0.660 |
| Race | |||
| White | Reference | ||
| Black | 0.93 | 0.35‐2.50 | 0.891 |
| Hispanic | 0.43 | 0.23‐0.84 | 0.013 |
| Other | 0.54 | 0.19‐1.55 | 0.254 |
| EPDS language | 0.47 | 0.25‐0.88 | 0.020 |
| People in home | 1.02 | 0.89‐1.16 | 0.799 |
| No. of children | 1.02 | 0.85‐1.23 | 0.819 |
| Relationship | |||
| Married | Reference | ||
| In a relationship | 0.93 | 0.52‐1.65 | 0.802 |
| Single | 1.37 | 0.72‐2.62 | 0.333 |
| Unsupportive social network | 3.58 | 1.95‐6.59 | 0.0001 |
| Some psychiatric disorder | 5.07 | 2.65‐9.72 | 0.0001 |
| Infant characteristics | |||
| Gestational age | 0.96 | 0.87‐1.04 | 0.316 |
| Prior admission | 0.83 | 0.49‐1.39 | 0.476 |
| Any comorbidity | 1.03 | 0.92‐1.18 | 0.551 |
| Congenital heart disease | 1.87 | 0.83‐4.22 | 0.130 |
| Neurodevelopmental | 3.41 | 1.41‐8.21 | 0.006 |
| Any medical device needed | 1.59 | 0.78‐3.24 | 0.201 |
| Multivariate logistic regression | |||
| Race | |||
| White | Reference | ||
| Black | 0.87 | 0.28‐2.70 | 0.812 |
| Hispanic | 0.64 | 0.30‐1.38 | 0.258 |
| Other | 0.88 | 0.29‐2.74 | 0.831 |
| Unsupportive social network | 4.40 | 2.27‐8.53 | 0.0001 |
| Psychiatric disorder | 5.02 | 2.49‐10.15 | 0.0001 |
| Neurodevelopmental comorbidity | 2.78 | 1.03‐7.52 | 0.004 |
Infant characteristics were next examined. Children of EPDS+ and EPDS mothers were similar in age, number of prior hospital admissions, gestational age at birth, and overall use of medical equipment (Table 2). To examine the effect of illness leading to hospitalization on EPDS+ risk, discharge diagnoses were collected and grouped into categories. Infants of EPDS+ mothers were more likely hospitalized for neurologic illness (P = 0.008) (see Supporting Table 1 in the online version of this article), but otherwise similar.
We next compared differences in long‐term infant comorbidities. The rate of having any comorbidity was similar between children of EPDS+ and EPDS mothers (39.1% vs 33.6%; P = 0.551). However, children of EPDS+ mothers were more likely to have mental retardation, hydrocephalus, or require ventriculoperitoneal shunt (VPS); however, the overall number of infants with each comorbidity was low. A neurodevelopmental comorbidity variable was created combining mental retardation, cerebral palsy, epilepsy, hydrocephalus, craniosynostosis, and VPS, resulting in 22 (7.1%) unique infants with 1 or more of these conditions. Having an infant with a neurodevelopmental comorbidity was a risk factor for positive postpartum depression screen (OR: 3.41; 95% CI: 1.41‐8.21). This continued to be significant (OR: 2.78; 95% CI: 1.03‐7.52) (Table 2) when controlling for maternal race/ethnicity, psychiatric history, and social support in multivariate logistic regression.
To determine if women screened followed through with recommendations, participants were called 3 and 6 months postenrollment. We attempted to call all women and successfully reached 120; 19 (16%) refused the call. One hundred one of the original 310 enrolled (33%) completed at least 1 follow‐up call; 47 at 3 months, 40 at 6 months, and only 14 (14%) responded at both time points. Due to this response rate, the first call at either 3 or 6 months was used as a single follow‐up time point for statistical analysis. A slightly higher proportion of EPDS‐ mothers (80/223, 36%) completed calls compared to EPDS+ mothers (21/87, 24%; P = 0.047).
Of 21 mothers initially EPDS+ who completed a follow‐up call, 10 (48%) later screened negative. Seven of these 10 (70%) reported discussing postpartum depression with their physician or using provided referral resources in the interim; 1 woman both spoke to a doctor and used a referral resource. One additional woman used resources, but repeat EPDS was still positive (Table 3). Reasons cited for not seeking evaluation included too busy (n = 4) and lost paperwork (n = 1), or no reason was given (n = 2). Mothers utilizing appropriate follow‐up had reduction in scores compared to those not (F(1,19) = 5.743, P = 0.027), although all scores decreased over time (F(1,19) = 11.54, P = 0.0030) (Figure 1B).
| Changes in Characteristics Following Enrollment | Positive EPDS, N = 21 | Negative EPDS, N = 80 | P Value |
|---|---|---|---|
| |||
| Repeat EPDS negative | 10 (47.6%) | 73 (91.3%) | 0.001 |
| Spoke to a doctor about PD | 6 (28.6%) | 27 (33.7%) | 0.360 |
| Used a study referral resource | 3 (14.3%) | NA | |
| Received a formal diagnosis of PD | 1 (4.7%) | 1 (1.3%) | 0.325 |
| Healthcare utilization* | |||
| No. of ER visits | 0 (00.5) | 0 (02) | 0.074 |
| No. of urgent care visits | 0 (00.5) | 0 (00) | 0.136 |
| No. of hospitalizations | 0 (00) | 0 (01) | 0.021 |
| Repeat MIB score | 1.09 0.38 | 0.69 0.17 | 0.357 |
Of 80 women initially EPDS, most stayed negative (73/80, 91%), but 7 (9%) became EPDS+. These mothers received education and referral information over the phone, but none completed a subsequent call. Infants of mothers initially EPDS had a higher frequency of hospitalization postenrollment compared to EPDS+ mothers (P = 0.021) (Table 3). Two (33%) mothers who converted from EPDS to EPDS+ had infants readmitted in the follow‐up period.
DISCUSSION
This study demonstrated almost a third of mothers of hospitalized infants are at risk for postpartum depression and most had not been previously screened. Stress due to hospitalization did not seem to falsely elevate EPDS scores; the proportion of EPDS+ mothers matched our prestudy prediction (28% vs 27.9%). Follow‐up calls indicated that EPDS+ mothers not pursuing further evaluation tended to remain EPDS+. Higher (worse) MIB score was strongly correlated to increased EPDS score as expected, supporting screening accuracy. Our results suggest that postpartum depression screening in hospital settings can be used to complement outpatient practice and capture mothers who would otherwise be missed.
Although we were able to screen, it is difficult to know whether this correctly identified mothers with postpartum depression. Only 2 mothers reported subsequent official diagnosis of postpartum depression, and 1 of these was EPDS originally. This reflects weakness of our survey‐based design; we only know if the mother self‐reported a formal diagnosis of postpartum depression, because we do not have access to their medical charts. We also had higher than expected loss to follow up (67%), leaving 66 initially EPDS+ mothers with unknown eventual diagnoses. The EPDS has been validated in multiple populations and has a positive predictive value ranging from 23% to 93%.[23] Therefore, somewhere between 20 and 80 women in our study should meet diagnostic criteria for postpartum depression. A limitation of children's hospital‐based screening with the EPDS is lack of adult‐trained psychiatrists who could immediately follow screening with diagnosis. Such integration may already be possible at community or hospital‐within‐a‐hospital models, and could be trialed at children's hospitals. Regardless, participation in the study seemed to increase mothers' awareness of postpartum depression. Prior to enrollment, only 14.6% of subjects reported discussing postpartum depression with a physician, although recall bias likely contributed to some mothers not remembering a screen. Promisingly, on follow‐up, 37% of called participants reported they discussed postpartum depression with a doctor following their child's hospital discharge.
Our study identified low social support and history of past psychiatric diagnosis as maternal risk factors for EPDS+ screens, which is consistent with previous reports.[29] There was a slight increase in subsequent infant hospitalizations in the EPDS group, which is contrary to reports stating that increased healthcare utilization is associated with postpartum depression.[30] However, most studies have shown an increase in only acute or emergency room care visits[30, 31] and no association between maternal depression and infant hospitalization.[30, 32] In our study, the median number of hospitalizations for both groups was 0, indicating overall low utilization. Because 2 of the mothers who converted from EPDS to EPDS+ had children readmitted, this underscores the benefit of reassessment at each medical encounter. A large proportion of mothers (36.5%) reported that the infant had been previously hospitalized, adding another potential missed screening opportunity. Our study supports others advocating repeated screenings and suggests mothers should be screened at any medical encounter that occurs in the first postpartum year.
We identified neurodevelopmental illness as the major infant characteristic associated with postpartum depression risk. Conversely, Garfield et al. did not find correlation between poorer Neurobiologic Risk Score and increased maternal depression risk in a NICU setting.[11] Perhaps our population of older and mainly full‐term infants makes consequences of neurologic insult more obvious and affects mothers more significantly. Cheng et al. reported that 26.9% of mothers of children with cognitive delay reported high depressive symptoms, compared with 17.4% of mothers of typically developing children at 4 years of age.[33] Another body of evidence suggests maternal emotional state during pregnancy influences neurodevelopmental outcome in the child. Maternal anxiety or depression has been associated with altered placental function, reduced infant gray matter density, and worse cognitive function.[34, 35] Therefore, future research may focus on mothers of infants with neurodevelopmental disease to better understand this relationship.
There were several limitations to this study. Some data collected by a survey are subject to information bias. Women may report a more supportive social network than actually exists or omit history of mental health diagnoses. We attempted to control for this by using validated measures where possible and performing chart review to verify reported infant characteristics. Our population was overwhelmingly Hispanic/Latina, and a third of infants were not previously healthy, which limits applicability to other settings. We used a convenience method that could introduce sampling bias. Our hospital's overall patient demographic is 65% Hispanic, which is similar to the 68% sampled in our study. In addition, the proportions of infant diagnoses approximate the overall rates at CHLA, so we feel our sample was fairly representative. There is a general consensus that depression studies have recruitment difficulties.[36] In the unlikely event that all 56 of women who declined to participate were EPDS+, overall proportion of at‐risk mothers would rise to 39%. If our study does show slight underestimation of risk, that would only mean more potential for intervention if screening were mandatory. Another weakness was high loss to follow‐up, which led us to combine the 3‐ and 6‐month follow‐up calls into 1 outcome. Sixty percent of calls used in analysis occurred at 3 months, so long‐term maintenance of improved EPDS scores remains unclear. Although conducting repeat EPDS via phone may affect honest answering of sensitive questions, other studies have used this technique successfully.[4]
CONCLUSION
This is the first study evaluating a screening program for maternal postpartum depression during infant hospitalizations. In our population, risk factors for positive postpartum depression screening were low social support, history of maternal psychiatric diagnosis, and having an infant with neurodevelopmental disease. We believe mothers should receive postpartum depression screening at all medical encounters during the child's first year.
Acknowledgements
The authors thank the CHLA Department of Social Work and the USC Required Scholarly Projects program, and specifically Joseph DeSena and Humberto Avila, for project assistance.
Disclosures: Dr. Trost is an Institutional Career Development Program Scholar through the Southern California Clinical and Translational Science Institute (SC‐CTSI) at the University of Southern California Keck School of Medicine. The content is solely the responsibility of the author(s) and does not represent the official view of the SC‐CTSI. Dr. Trost conceptualized and designed the study, drafted the initial manuscript, and approved the final manuscript as submitted. Dr. Molas‐Torreblanca co‐designed the study, reviewed and revised the manuscript, and approved the final manuscript as submitted. Ms. Man coordinated and supervised hospital data collection, critically reviewed the manuscript, and approved the final manuscript as submitted. Mr. Casillas coordinated and supervised the phone call data collection, critically reviewed the manuscript, and approved the final manuscript as submitted. Ms. Sapir coordinated the referral process for enrolled patients, supervised the design of patient handouts, and critically reviewed and approved the final manuscript as submitted. Dr. Schrager guided study design, supervised the statistical analysis of the final data, critically reviewed and revised the manuscript, and approved the final manuscript as submitted. The authors report no conflicts of interest.
- , , , , . Maternal depressive symptoms and infant health practices among low‐income women. Pediatrics. 2004;113(6):e523–e529.
- , , , et al.; Duke University Evidence‐based Practice Center. Effective Health Care Program. Efficacy and safety of screening for postpartum depression. Comparative effectiveness review number 106. Rockville, MD: Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services; 2013: Available at: https://www.effectivehealthcare.ahrq.gov/ehc/products/379/1437/postpartum‐screening‐report‐130409.pdf. Date accessed Jan 10 2016.
- , , , , . Prevalence rates and demographic characteristics associated with depression in pregnancy and the postpartum. J Consult Clin Psychol. 1989;57(2):269–274.
- , , , , . Screening for depression in the postpartum period: a comparison of three instruments. J Womens Health (Larchmt). 2008;17(4):585–596.
- , , , . Are maternal depression or symptom severity associated with breastfeeding intention or outcomes? J Clin Psychiatry. 2010;71(8):1069–1078.
- , , , , . Impact of maternal depressive symptoms on growth of preschool‐ and school‐aged children. Pediatrics. 2012;130(4):e847–e855.
- , , , , . The timing of maternal depressive symptoms and mothers' parenting practices with young children: implications for pediatric practice. Pediatrics. 2006;118(1):e174–e182.
- , , , , . Improvements in maternal depression as a mediator of intervention effects on early childhood problem behavior. Dev Psychopathol. 2009;21(2):417–439.
- ; Committee on Psychosocial Aspects of Child and Family Health American Academy of Pediatrics. Incorporating recognition and management of perinatal and postpartum depression into pediatric practice. Pediatrics. 2010;126(5):1032–1039.
- , , . Screening for postpartum depression in a pediatric emergency department. Pediatr Emerg Care. 2011;27(9):795–800.
- , , , et al. Risk factors for postpartum depressive symptoms in low‐income women with very low‐birth‐weight infants. Adv Neonatal Care. 2015;15(1):E3–E8.
- , , . Impact of infant health problems on postnatal depression: pilot study to evaluate a health visiting system. Psychiatry Clin Neurosci. 2006;60(2):182–189.
- , , , , , . Primary care pediatricians' roles and perceived responsibilities in the identification and management of maternal depression. Pediatrics. 2002;110(6):1169–1176.
- , , , et al. Does education influence pediatricians' perceptions of physician‐specific barriers for maternal depression? Clin Pediatr (Phila). 2008;47(7):670–678.
- , , , . Pediatricians' views of postpartum depression: a self‐administered survey. Arch Womens Ment Health. 2004;7(4):231–236.
- . Compliance with well‐child visit recommendations: evidence from the Medical Expenditure Panel Survey, 2000–2002. Pediatrics. 2006;118(6):e1766–e1778.
- , , , et al. A framework of pediatric hospital discharge care informed by legislation, research, and practice. JAMA Pediatr. 2014;168(10):955–962; quiz 965–966.
- , , . Pedi‐BOOST. Peds Effective Discharge: Better Handoff to Home through Safer Transitions. 2013. https://www.hospitalmedicine.org/Web/Quality___Innovation/Implementation_Toolkit/pediBoost/Best_Practices/Best_Practices.aspx Accessed Jan 10 2016.
- , , , et al. Effects of maternal depressive symptomatology during pregnancy and the postpartum period on infant‐mother attachment. Psychiatry Clin Neurosci. 2014;68(8):631–639.
- , , , , . Examining maternal depression and attachment insecurity as moderators of the impacts of home visiting for at‐risk mothers and infants. J Consult Clin Psychol. 2009;77(4):788–799.
- , . Postpartum mood disorders: diagnosis and treatment guidelines. J Clin Psychiatry. 1998;59(suppl 2):34–40.
- , , , , . A new Mother‐to‐Infant Bonding Scale: links with early maternal mood. Arch Womens Ment Health. 2005;8(1):45–51.
- , , , , . A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatr Scand. 2009;119(5):350–364.
- , , . Detection of postnatal depression. Development of the 10‐item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–786.
- , , , . Validation of the Edinburgh Postnatal Depression Scale (EPDS) in Spanish mothers. J Affect Disord. 2003;75(1):71–76.
- , , , et al. TRIPPD: a practice‐based network effectiveness study of postpartum depression screening and management. Ann Fam Med. 2012;10(4):320–329.
- , , , , . Detection of postpartum depressive symptoms by screening at well‐child visits. Pediatrics. 2004;113(3 pt 1):551–558.
- R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing: 2013. Available at: http://www.R‐project.org. Accessed Jan 10 2016.
- , , , , . Biological and psychosocial predictors of postpartum depression: systematic review and call for integration. Annu Rev Clin Psychol. 2015;11:99–137.
- , , , et al. Maternal depressive symptoms and children's receipt of health care in the first 3 years of life. Pediatrics. 2005;115(2):306–314.
- , . Maternal factors and child's health care use. Soc Sci Med. 1995;40(5):623–628.
- , , , , . Women's health after pregnancy and child outcomes at age 3 years: a prospective cohort study. Am J Public Health. 2002;92(8):1312–1318.
- , , , . The influence of children's cognitive delay and behavior problems on maternal depression. J Pediatr. 2015;167(3):679–686.
- , , , , . Maternal prenatal symptoms of depression and down regulation of placental monoamine oxidase A expression. J Psychosom Res. 2013;75(4):341–345.
- , , , , . High pregnancy anxiety during mid‐gestation is associated with decreased gray matter density in 6–9‐year‐old children. Psychoneuroendocrinology. 2010;35(1):141–153.
- , , , , . Factors affecting recruitment into depression trials: Systematic review, meta‐synthesis and conceptual framework. J Affect Disord. 2015;172:274–290.
Maternal postpartum depression occurs in 5% to 25% of all mothers, and up to 40% to 60% in high‐risk populations such as low‐income women.[1, 2, 3, 4] Children of affected mothers suffer negative health consequences such as decreased physical growth, poor maternalchild bond, problem behavior, and child abuse.[5, 6, 7] Timely recognition of symptoms and treatment may improve child outcomes.[8] Published guidelines recommend pediatricians screen for postpartum depression at infant 1‐, 2‐, 4‐, and 6‐month outpatient visits.[9] There are no current guidelines for or studies of screening in general inpatient settings, although emergency rooms[10] and neonatal intensive care units (NICUs)[11] have been examined. Pediatric hospitalization may offer an additional opportunity for expanding screening and intervention.
Augmenting outpatient screening practices with additional inpatient screening would have several benefits. Infant health problems have been associated with postpartum depression, and therefore mothers in the hospital may be at higher risk.[12] Inpatient screening would also improve access to mothers not screened as outpatients. Missed screening could occur due to physician discomfort with screening, time constraints during busy office visits, or noncompliance with recommended visit schedules.[13, 14, 15, 16] Finally, inpatient providers would benefit from understanding the psychosocial milieu of children now under their care. Recent studies note hospital discharges may be improved and readmissions reduced by assessing socioeconomic risk factors during hospitalization.[17] The evidence‐based Peds Effective Discharge: Better Handoff to Home through Safer Transitions Better Outcomes by Optimizing Safe Transitions (Pedi‐BOOST) toolkit specifically recommends an assessment of parental psychiatric issues.[18] Postpartum depression strongly correlates with impaired maternalchild bonding,[19] which in turn negatively affects mothers' engagement with healthcare providers.[20] This could impact patient education and recommendations provided during hospitalization.
Therefore, we sought to perform postpartum depression screening during infant hospitalizations. Our primary goal was to determine rate of postpartum depression in our population and proportion of women previously unscreened who could be captured by inpatient screening. We additionally aimed to determine the proportion of women with poor maternalinfant bond. Our next goal was to identify maternal or infant factors associated with positive postpartum depression screening. Finally, we performed follow‐up calls to determine if in‐hospital interventions resulted in formal postpartum depression diagnosis, use of recommended referrals, improved maternalchild bond, and decreased symptoms of depression over time.
METHODS
Patient Selection
We conducted a prospective observational study on a convenience sample of mothers at Children's Hospital Los Angeles (CHLA), a large, urban, tertiary care hospital. Biological mothers of infants 1 year of age admitted to medicalsurgical floors and assigned to pediatric hospitalist teams between April 1, 2013 and July 30, 2014 were eligible for inclusion. Mothers were required to be age 18 years or older and able to speak and read English or Spanish. Mothers of infants aged 2 weeks were excluded to avoid confusing postpartum depression with maternal baby blues, a distinct entity causing milder symptoms of depression that should resolve by 2 weeks.[21] In an effort to reduce the impact of stress associated with prolonged hospitalization on Edinburgh Postpartum Depression Scale (EPDS) scores, we excluded mothers of children already hospitalized >72 hours. Visits from participants who were readmitted or previously enrolled in the study were excluded. All study procedures were approved by the CHLA Institutional Review Board.
Measures
After giving informed consent, mothers completed demographic forms about themselves and their infants. A 4‐item Likert scale assessed self‐perceived support from family and friends. Past mental health problems were assessed via 10‐item checklist. Self‐reported infant comorbidities and reason for hospitalization were confirmed by chart review for International Classification of Diseases, Ninth Revision diagnoses present on admission and reason for discharge. Next, mothers filled out a maternalinfant bonding scale (MIB)[22] and the EPDS,[23, 24] which has been validated in both English and Spanish.[25] There are no formal cutoffs for the MIB; higher scores indicate worse bonding. Out of a possible 30, a score of 10 or higher on the EPDS was considered a positive screen, indicating risk for postpartum depression. Scores less than 10 were negative screens, and those mothers were determined not at risk.[24] The last EPDS question asks, The thought of harming myself has occurred to me. Any mothers answering yes, quite often, sometimes, or hardly ever were further interviewed and treated per a suicidality operating protocol.
Counseling and Referral
All EPDS mothers were informed of results and did not receive further intervention during hospitalization. For EPDS+ mothers, individual social workers responded to referrals placed by the study team into infant charts and delivered 1‐on‐1 counseling. Social workers received study education prior to initiation and midway through patient recruitment and provided mothers with an educational handout, referral sheet listing online resources of local mental health clinics accepting postpartum depression patients, and help‐line numbers. Mothers who identified a primary doctor were encouraged to follow up with them.
Follow‐up
In order to assess intervention effect over time, all mothers (both EPDS+ and EPDS) were called 3 and 6 months ( 1 week) postenrollment and rescreened with the EPDS and MIB. They also answered a short survey assessing whether they spoke further to a doctor about postpartum depression; used a referral resource; received a formal postpartum depression diagnosis; and if their children visited the ER, urgent care, or hospital again since discharge. Mothers who again screened EPDS+ or newly converted to EPDS+ were provided counseling and referral via phone.
Sample Size Calculation
A priori power analysis determined a sample size of 310 mothers was required to estimate the rate of postpartum depression at CHLA with 5% precision and a 95% confidence level, assuming an estimated prevalence of 27.9% based on prior studies.[26] At this prevalence rate, screening 310 mothers was also predicted to yield at least 77 positive screens on the EPDS, yielding an appropriate sample to detect EPDS score improvements over time. This number was based on previous studies showing reduction in EPDS of 35% following appropriate referral,[26, 27] assuming 15% attrition at both the 3‐month and 6‐month follow‐up sampling points.
Statistical Analysis
After data collection was complete, characteristics between EPDS+ and EPDS groups were compared using 2 tests for dichotomous outcomes and t tests for continuous variables. Multiple logistic regression was then used to compare specific factors associated with positive EPDS screens (P 0.05). Linear regression assessed the relationship between EPDS and MIB scores. Change in average EPDS and MIB scores at the time of first successful follow‐up call between women who did and did not seek further postpartum depression evaluation were compared via 2‐way repeated measures analysis of variance. Statistical analyses were performed using R software.[28]
RESULTS
Out of 366 motherinfant pairs, 56 (15%) refused, and 310 (85%) mothers were fully enrolled (Figure 1A). Mothers had an average age of 28.17 years, were 68.3% Hispanic/Latina by self‐report, and 45.2% were married. Infants were an average of 4.24 months old, 81.9% were born term (>37 weeks), and 64.8% were previously healthy (Table 1).
| Characteristic | All Participants, n = 310 |
|---|---|
| |
| Maternal characteristics | |
| Age, y* | 28.17 6.18 |
| Race/ethnicity | |
| White | 48 (15.5%) |
| Black | 25 (8.1%) |
| Hispanic | 211(68.3%) |
| Other | 25 (8.1%) |
| EPDS language | |
| English | 231 (74.5%) |
| Spanish | 79 (25.5%) |
| People in home | 5 (4, 6) |
| No. of children | 2 (1, 3) |
| Relationship | |
| Married | 140 (45.2%) |
| In a relationship | 105 (33.9%) |
| Single | 62 (20%) |
| Any breastfeeding | 142 (45.8%) |
| Unsupportive social network | 54 (17.4%) |
| Some psychiatric disorder | 47 (15.2%) |
| MIB score | 6 (3, 10) |
| Infant characteristics | |
| Age, mo* | 4.24 3.19 |
| Gestational age, wk | 39 (37, 40) |
| Prior admission | 113 (36.5%) |
| Any comorbidity | 109 (35.2%) |
| Congenital heart disease | 27 (8.7%) |
| Neurodevelopmental | 22 (7.1%) |
| Any medical device needed | 38 (12.3%) |

(B) Postenrollment change in mean Edinburgh Postpartum Depression Scale (EPDS) score of all initially EPDS mothers who completed at least 1 follow‐up phone call, separated by if they did or did not seek referral. Mothers using referral (either spoke with physician or used resource sheet) had significantly larger reduction in score. Statistical analysis by analysis of variance, P < 0.05.
Eighty‐seven (28%) mothers were EPDS+; 223 (72%) were EPDS. Only 42 mothers reported previous postpartum depression screening since the birth of their most recent child. However, 30 infants were 1 month in age, thus outside recommended screening range. Eliminating these infants revealed a 14.6% rate of appropriate prior screening. Higher EPDS scores were associated with higher (worse) MIB scores by linear regression ( = 0.11, P 0.001). The vast majority (77%) of mothers scored a 0 or 1 on the MIB scale, indicating good bonding; further statistical comparison using the MIB scale as a secondary outcome was therefore inappropriate.
On bivariate logistic regression, Hispanic/Latina women were less likely to be EPDS+ (odds ratio [OR]: 0.43; 95% CI: 0.23‐0.84) compared to white/Caucasian women. Mothers who identified Spanish as their primary language and took the Spanish EPDS had lower odds of a positive screen (OR: 0.47; 95% CI: 0.25‐0.88). The racial differences did not persist on multivariate analysis (OR: 0.64; 95% CI: 0.30‐1.38) (Table 2). Maternal characteristics identified as potential risk factors for positive screens were poor social support (OR: 3.58; 95% CI: 1.95‐6.59) and history of a prior psychiatric diagnosis (OR: 5.07; 95% CI: 2.65‐9.72). There were no differences in age, number of children or people living in the home, relationship status, or breastfeeding rates by EPDS score.
| OR | 95% CI | P Value | |
|---|---|---|---|
| |||
| Maternal characteristics | |||
| Maternal age | 0.99 | 0.95‐1.03 | 0.660 |
| Race | |||
| White | Reference | ||
| Black | 0.93 | 0.35‐2.50 | 0.891 |
| Hispanic | 0.43 | 0.23‐0.84 | 0.013 |
| Other | 0.54 | 0.19‐1.55 | 0.254 |
| EPDS language | 0.47 | 0.25‐0.88 | 0.020 |
| People in home | 1.02 | 0.89‐1.16 | 0.799 |
| No. of children | 1.02 | 0.85‐1.23 | 0.819 |
| Relationship | |||
| Married | Reference | ||
| In a relationship | 0.93 | 0.52‐1.65 | 0.802 |
| Single | 1.37 | 0.72‐2.62 | 0.333 |
| Unsupportive social network | 3.58 | 1.95‐6.59 | 0.0001 |
| Some psychiatric disorder | 5.07 | 2.65‐9.72 | 0.0001 |
| Infant characteristics | |||
| Gestational age | 0.96 | 0.87‐1.04 | 0.316 |
| Prior admission | 0.83 | 0.49‐1.39 | 0.476 |
| Any comorbidity | 1.03 | 0.92‐1.18 | 0.551 |
| Congenital heart disease | 1.87 | 0.83‐4.22 | 0.130 |
| Neurodevelopmental | 3.41 | 1.41‐8.21 | 0.006 |
| Any medical device needed | 1.59 | 0.78‐3.24 | 0.201 |
| Multivariate logistic regression | |||
| Race | |||
| White | Reference | ||
| Black | 0.87 | 0.28‐2.70 | 0.812 |
| Hispanic | 0.64 | 0.30‐1.38 | 0.258 |
| Other | 0.88 | 0.29‐2.74 | 0.831 |
| Unsupportive social network | 4.40 | 2.27‐8.53 | 0.0001 |
| Psychiatric disorder | 5.02 | 2.49‐10.15 | 0.0001 |
| Neurodevelopmental comorbidity | 2.78 | 1.03‐7.52 | 0.004 |
Infant characteristics were next examined. Children of EPDS+ and EPDS mothers were similar in age, number of prior hospital admissions, gestational age at birth, and overall use of medical equipment (Table 2). To examine the effect of illness leading to hospitalization on EPDS+ risk, discharge diagnoses were collected and grouped into categories. Infants of EPDS+ mothers were more likely hospitalized for neurologic illness (P = 0.008) (see Supporting Table 1 in the online version of this article), but otherwise similar.
We next compared differences in long‐term infant comorbidities. The rate of having any comorbidity was similar between children of EPDS+ and EPDS mothers (39.1% vs 33.6%; P = 0.551). However, children of EPDS+ mothers were more likely to have mental retardation, hydrocephalus, or require ventriculoperitoneal shunt (VPS); however, the overall number of infants with each comorbidity was low. A neurodevelopmental comorbidity variable was created combining mental retardation, cerebral palsy, epilepsy, hydrocephalus, craniosynostosis, and VPS, resulting in 22 (7.1%) unique infants with 1 or more of these conditions. Having an infant with a neurodevelopmental comorbidity was a risk factor for positive postpartum depression screen (OR: 3.41; 95% CI: 1.41‐8.21). This continued to be significant (OR: 2.78; 95% CI: 1.03‐7.52) (Table 2) when controlling for maternal race/ethnicity, psychiatric history, and social support in multivariate logistic regression.
To determine if women screened followed through with recommendations, participants were called 3 and 6 months postenrollment. We attempted to call all women and successfully reached 120; 19 (16%) refused the call. One hundred one of the original 310 enrolled (33%) completed at least 1 follow‐up call; 47 at 3 months, 40 at 6 months, and only 14 (14%) responded at both time points. Due to this response rate, the first call at either 3 or 6 months was used as a single follow‐up time point for statistical analysis. A slightly higher proportion of EPDS‐ mothers (80/223, 36%) completed calls compared to EPDS+ mothers (21/87, 24%; P = 0.047).
Of 21 mothers initially EPDS+ who completed a follow‐up call, 10 (48%) later screened negative. Seven of these 10 (70%) reported discussing postpartum depression with their physician or using provided referral resources in the interim; 1 woman both spoke to a doctor and used a referral resource. One additional woman used resources, but repeat EPDS was still positive (Table 3). Reasons cited for not seeking evaluation included too busy (n = 4) and lost paperwork (n = 1), or no reason was given (n = 2). Mothers utilizing appropriate follow‐up had reduction in scores compared to those not (F(1,19) = 5.743, P = 0.027), although all scores decreased over time (F(1,19) = 11.54, P = 0.0030) (Figure 1B).
| Changes in Characteristics Following Enrollment | Positive EPDS, N = 21 | Negative EPDS, N = 80 | P Value |
|---|---|---|---|
| |||
| Repeat EPDS negative | 10 (47.6%) | 73 (91.3%) | 0.001 |
| Spoke to a doctor about PD | 6 (28.6%) | 27 (33.7%) | 0.360 |
| Used a study referral resource | 3 (14.3%) | NA | |
| Received a formal diagnosis of PD | 1 (4.7%) | 1 (1.3%) | 0.325 |
| Healthcare utilization* | |||
| No. of ER visits | 0 (00.5) | 0 (02) | 0.074 |
| No. of urgent care visits | 0 (00.5) | 0 (00) | 0.136 |
| No. of hospitalizations | 0 (00) | 0 (01) | 0.021 |
| Repeat MIB score | 1.09 0.38 | 0.69 0.17 | 0.357 |
Of 80 women initially EPDS, most stayed negative (73/80, 91%), but 7 (9%) became EPDS+. These mothers received education and referral information over the phone, but none completed a subsequent call. Infants of mothers initially EPDS had a higher frequency of hospitalization postenrollment compared to EPDS+ mothers (P = 0.021) (Table 3). Two (33%) mothers who converted from EPDS to EPDS+ had infants readmitted in the follow‐up period.
DISCUSSION
This study demonstrated almost a third of mothers of hospitalized infants are at risk for postpartum depression and most had not been previously screened. Stress due to hospitalization did not seem to falsely elevate EPDS scores; the proportion of EPDS+ mothers matched our prestudy prediction (28% vs 27.9%). Follow‐up calls indicated that EPDS+ mothers not pursuing further evaluation tended to remain EPDS+. Higher (worse) MIB score was strongly correlated to increased EPDS score as expected, supporting screening accuracy. Our results suggest that postpartum depression screening in hospital settings can be used to complement outpatient practice and capture mothers who would otherwise be missed.
Although we were able to screen, it is difficult to know whether this correctly identified mothers with postpartum depression. Only 2 mothers reported subsequent official diagnosis of postpartum depression, and 1 of these was EPDS originally. This reflects weakness of our survey‐based design; we only know if the mother self‐reported a formal diagnosis of postpartum depression, because we do not have access to their medical charts. We also had higher than expected loss to follow up (67%), leaving 66 initially EPDS+ mothers with unknown eventual diagnoses. The EPDS has been validated in multiple populations and has a positive predictive value ranging from 23% to 93%.[23] Therefore, somewhere between 20 and 80 women in our study should meet diagnostic criteria for postpartum depression. A limitation of children's hospital‐based screening with the EPDS is lack of adult‐trained psychiatrists who could immediately follow screening with diagnosis. Such integration may already be possible at community or hospital‐within‐a‐hospital models, and could be trialed at children's hospitals. Regardless, participation in the study seemed to increase mothers' awareness of postpartum depression. Prior to enrollment, only 14.6% of subjects reported discussing postpartum depression with a physician, although recall bias likely contributed to some mothers not remembering a screen. Promisingly, on follow‐up, 37% of called participants reported they discussed postpartum depression with a doctor following their child's hospital discharge.
Our study identified low social support and history of past psychiatric diagnosis as maternal risk factors for EPDS+ screens, which is consistent with previous reports.[29] There was a slight increase in subsequent infant hospitalizations in the EPDS group, which is contrary to reports stating that increased healthcare utilization is associated with postpartum depression.[30] However, most studies have shown an increase in only acute or emergency room care visits[30, 31] and no association between maternal depression and infant hospitalization.[30, 32] In our study, the median number of hospitalizations for both groups was 0, indicating overall low utilization. Because 2 of the mothers who converted from EPDS to EPDS+ had children readmitted, this underscores the benefit of reassessment at each medical encounter. A large proportion of mothers (36.5%) reported that the infant had been previously hospitalized, adding another potential missed screening opportunity. Our study supports others advocating repeated screenings and suggests mothers should be screened at any medical encounter that occurs in the first postpartum year.
We identified neurodevelopmental illness as the major infant characteristic associated with postpartum depression risk. Conversely, Garfield et al. did not find correlation between poorer Neurobiologic Risk Score and increased maternal depression risk in a NICU setting.[11] Perhaps our population of older and mainly full‐term infants makes consequences of neurologic insult more obvious and affects mothers more significantly. Cheng et al. reported that 26.9% of mothers of children with cognitive delay reported high depressive symptoms, compared with 17.4% of mothers of typically developing children at 4 years of age.[33] Another body of evidence suggests maternal emotional state during pregnancy influences neurodevelopmental outcome in the child. Maternal anxiety or depression has been associated with altered placental function, reduced infant gray matter density, and worse cognitive function.[34, 35] Therefore, future research may focus on mothers of infants with neurodevelopmental disease to better understand this relationship.
There were several limitations to this study. Some data collected by a survey are subject to information bias. Women may report a more supportive social network than actually exists or omit history of mental health diagnoses. We attempted to control for this by using validated measures where possible and performing chart review to verify reported infant characteristics. Our population was overwhelmingly Hispanic/Latina, and a third of infants were not previously healthy, which limits applicability to other settings. We used a convenience method that could introduce sampling bias. Our hospital's overall patient demographic is 65% Hispanic, which is similar to the 68% sampled in our study. In addition, the proportions of infant diagnoses approximate the overall rates at CHLA, so we feel our sample was fairly representative. There is a general consensus that depression studies have recruitment difficulties.[36] In the unlikely event that all 56 of women who declined to participate were EPDS+, overall proportion of at‐risk mothers would rise to 39%. If our study does show slight underestimation of risk, that would only mean more potential for intervention if screening were mandatory. Another weakness was high loss to follow‐up, which led us to combine the 3‐ and 6‐month follow‐up calls into 1 outcome. Sixty percent of calls used in analysis occurred at 3 months, so long‐term maintenance of improved EPDS scores remains unclear. Although conducting repeat EPDS via phone may affect honest answering of sensitive questions, other studies have used this technique successfully.[4]
CONCLUSION
This is the first study evaluating a screening program for maternal postpartum depression during infant hospitalizations. In our population, risk factors for positive postpartum depression screening were low social support, history of maternal psychiatric diagnosis, and having an infant with neurodevelopmental disease. We believe mothers should receive postpartum depression screening at all medical encounters during the child's first year.
Acknowledgements
The authors thank the CHLA Department of Social Work and the USC Required Scholarly Projects program, and specifically Joseph DeSena and Humberto Avila, for project assistance.
Disclosures: Dr. Trost is an Institutional Career Development Program Scholar through the Southern California Clinical and Translational Science Institute (SC‐CTSI) at the University of Southern California Keck School of Medicine. The content is solely the responsibility of the author(s) and does not represent the official view of the SC‐CTSI. Dr. Trost conceptualized and designed the study, drafted the initial manuscript, and approved the final manuscript as submitted. Dr. Molas‐Torreblanca co‐designed the study, reviewed and revised the manuscript, and approved the final manuscript as submitted. Ms. Man coordinated and supervised hospital data collection, critically reviewed the manuscript, and approved the final manuscript as submitted. Mr. Casillas coordinated and supervised the phone call data collection, critically reviewed the manuscript, and approved the final manuscript as submitted. Ms. Sapir coordinated the referral process for enrolled patients, supervised the design of patient handouts, and critically reviewed and approved the final manuscript as submitted. Dr. Schrager guided study design, supervised the statistical analysis of the final data, critically reviewed and revised the manuscript, and approved the final manuscript as submitted. The authors report no conflicts of interest.
Maternal postpartum depression occurs in 5% to 25% of all mothers, and up to 40% to 60% in high‐risk populations such as low‐income women.[1, 2, 3, 4] Children of affected mothers suffer negative health consequences such as decreased physical growth, poor maternalchild bond, problem behavior, and child abuse.[5, 6, 7] Timely recognition of symptoms and treatment may improve child outcomes.[8] Published guidelines recommend pediatricians screen for postpartum depression at infant 1‐, 2‐, 4‐, and 6‐month outpatient visits.[9] There are no current guidelines for or studies of screening in general inpatient settings, although emergency rooms[10] and neonatal intensive care units (NICUs)[11] have been examined. Pediatric hospitalization may offer an additional opportunity for expanding screening and intervention.
Augmenting outpatient screening practices with additional inpatient screening would have several benefits. Infant health problems have been associated with postpartum depression, and therefore mothers in the hospital may be at higher risk.[12] Inpatient screening would also improve access to mothers not screened as outpatients. Missed screening could occur due to physician discomfort with screening, time constraints during busy office visits, or noncompliance with recommended visit schedules.[13, 14, 15, 16] Finally, inpatient providers would benefit from understanding the psychosocial milieu of children now under their care. Recent studies note hospital discharges may be improved and readmissions reduced by assessing socioeconomic risk factors during hospitalization.[17] The evidence‐based Peds Effective Discharge: Better Handoff to Home through Safer Transitions Better Outcomes by Optimizing Safe Transitions (Pedi‐BOOST) toolkit specifically recommends an assessment of parental psychiatric issues.[18] Postpartum depression strongly correlates with impaired maternalchild bonding,[19] which in turn negatively affects mothers' engagement with healthcare providers.[20] This could impact patient education and recommendations provided during hospitalization.
Therefore, we sought to perform postpartum depression screening during infant hospitalizations. Our primary goal was to determine rate of postpartum depression in our population and proportion of women previously unscreened who could be captured by inpatient screening. We additionally aimed to determine the proportion of women with poor maternalinfant bond. Our next goal was to identify maternal or infant factors associated with positive postpartum depression screening. Finally, we performed follow‐up calls to determine if in‐hospital interventions resulted in formal postpartum depression diagnosis, use of recommended referrals, improved maternalchild bond, and decreased symptoms of depression over time.
METHODS
Patient Selection
We conducted a prospective observational study on a convenience sample of mothers at Children's Hospital Los Angeles (CHLA), a large, urban, tertiary care hospital. Biological mothers of infants 1 year of age admitted to medicalsurgical floors and assigned to pediatric hospitalist teams between April 1, 2013 and July 30, 2014 were eligible for inclusion. Mothers were required to be age 18 years or older and able to speak and read English or Spanish. Mothers of infants aged 2 weeks were excluded to avoid confusing postpartum depression with maternal baby blues, a distinct entity causing milder symptoms of depression that should resolve by 2 weeks.[21] In an effort to reduce the impact of stress associated with prolonged hospitalization on Edinburgh Postpartum Depression Scale (EPDS) scores, we excluded mothers of children already hospitalized >72 hours. Visits from participants who were readmitted or previously enrolled in the study were excluded. All study procedures were approved by the CHLA Institutional Review Board.
Measures
After giving informed consent, mothers completed demographic forms about themselves and their infants. A 4‐item Likert scale assessed self‐perceived support from family and friends. Past mental health problems were assessed via 10‐item checklist. Self‐reported infant comorbidities and reason for hospitalization were confirmed by chart review for International Classification of Diseases, Ninth Revision diagnoses present on admission and reason for discharge. Next, mothers filled out a maternalinfant bonding scale (MIB)[22] and the EPDS,[23, 24] which has been validated in both English and Spanish.[25] There are no formal cutoffs for the MIB; higher scores indicate worse bonding. Out of a possible 30, a score of 10 or higher on the EPDS was considered a positive screen, indicating risk for postpartum depression. Scores less than 10 were negative screens, and those mothers were determined not at risk.[24] The last EPDS question asks, The thought of harming myself has occurred to me. Any mothers answering yes, quite often, sometimes, or hardly ever were further interviewed and treated per a suicidality operating protocol.
Counseling and Referral
All EPDS mothers were informed of results and did not receive further intervention during hospitalization. For EPDS+ mothers, individual social workers responded to referrals placed by the study team into infant charts and delivered 1‐on‐1 counseling. Social workers received study education prior to initiation and midway through patient recruitment and provided mothers with an educational handout, referral sheet listing online resources of local mental health clinics accepting postpartum depression patients, and help‐line numbers. Mothers who identified a primary doctor were encouraged to follow up with them.
Follow‐up
In order to assess intervention effect over time, all mothers (both EPDS+ and EPDS) were called 3 and 6 months ( 1 week) postenrollment and rescreened with the EPDS and MIB. They also answered a short survey assessing whether they spoke further to a doctor about postpartum depression; used a referral resource; received a formal postpartum depression diagnosis; and if their children visited the ER, urgent care, or hospital again since discharge. Mothers who again screened EPDS+ or newly converted to EPDS+ were provided counseling and referral via phone.
Sample Size Calculation
A priori power analysis determined a sample size of 310 mothers was required to estimate the rate of postpartum depression at CHLA with 5% precision and a 95% confidence level, assuming an estimated prevalence of 27.9% based on prior studies.[26] At this prevalence rate, screening 310 mothers was also predicted to yield at least 77 positive screens on the EPDS, yielding an appropriate sample to detect EPDS score improvements over time. This number was based on previous studies showing reduction in EPDS of 35% following appropriate referral,[26, 27] assuming 15% attrition at both the 3‐month and 6‐month follow‐up sampling points.
Statistical Analysis
After data collection was complete, characteristics between EPDS+ and EPDS groups were compared using 2 tests for dichotomous outcomes and t tests for continuous variables. Multiple logistic regression was then used to compare specific factors associated with positive EPDS screens (P 0.05). Linear regression assessed the relationship between EPDS and MIB scores. Change in average EPDS and MIB scores at the time of first successful follow‐up call between women who did and did not seek further postpartum depression evaluation were compared via 2‐way repeated measures analysis of variance. Statistical analyses were performed using R software.[28]
RESULTS
Out of 366 motherinfant pairs, 56 (15%) refused, and 310 (85%) mothers were fully enrolled (Figure 1A). Mothers had an average age of 28.17 years, were 68.3% Hispanic/Latina by self‐report, and 45.2% were married. Infants were an average of 4.24 months old, 81.9% were born term (>37 weeks), and 64.8% were previously healthy (Table 1).
| Characteristic | All Participants, n = 310 |
|---|---|
| |
| Maternal characteristics | |
| Age, y* | 28.17 6.18 |
| Race/ethnicity | |
| White | 48 (15.5%) |
| Black | 25 (8.1%) |
| Hispanic | 211(68.3%) |
| Other | 25 (8.1%) |
| EPDS language | |
| English | 231 (74.5%) |
| Spanish | 79 (25.5%) |
| People in home | 5 (4, 6) |
| No. of children | 2 (1, 3) |
| Relationship | |
| Married | 140 (45.2%) |
| In a relationship | 105 (33.9%) |
| Single | 62 (20%) |
| Any breastfeeding | 142 (45.8%) |
| Unsupportive social network | 54 (17.4%) |
| Some psychiatric disorder | 47 (15.2%) |
| MIB score | 6 (3, 10) |
| Infant characteristics | |
| Age, mo* | 4.24 3.19 |
| Gestational age, wk | 39 (37, 40) |
| Prior admission | 113 (36.5%) |
| Any comorbidity | 109 (35.2%) |
| Congenital heart disease | 27 (8.7%) |
| Neurodevelopmental | 22 (7.1%) |
| Any medical device needed | 38 (12.3%) |

(B) Postenrollment change in mean Edinburgh Postpartum Depression Scale (EPDS) score of all initially EPDS mothers who completed at least 1 follow‐up phone call, separated by if they did or did not seek referral. Mothers using referral (either spoke with physician or used resource sheet) had significantly larger reduction in score. Statistical analysis by analysis of variance, P < 0.05.
Eighty‐seven (28%) mothers were EPDS+; 223 (72%) were EPDS. Only 42 mothers reported previous postpartum depression screening since the birth of their most recent child. However, 30 infants were 1 month in age, thus outside recommended screening range. Eliminating these infants revealed a 14.6% rate of appropriate prior screening. Higher EPDS scores were associated with higher (worse) MIB scores by linear regression ( = 0.11, P 0.001). The vast majority (77%) of mothers scored a 0 or 1 on the MIB scale, indicating good bonding; further statistical comparison using the MIB scale as a secondary outcome was therefore inappropriate.
On bivariate logistic regression, Hispanic/Latina women were less likely to be EPDS+ (odds ratio [OR]: 0.43; 95% CI: 0.23‐0.84) compared to white/Caucasian women. Mothers who identified Spanish as their primary language and took the Spanish EPDS had lower odds of a positive screen (OR: 0.47; 95% CI: 0.25‐0.88). The racial differences did not persist on multivariate analysis (OR: 0.64; 95% CI: 0.30‐1.38) (Table 2). Maternal characteristics identified as potential risk factors for positive screens were poor social support (OR: 3.58; 95% CI: 1.95‐6.59) and history of a prior psychiatric diagnosis (OR: 5.07; 95% CI: 2.65‐9.72). There were no differences in age, number of children or people living in the home, relationship status, or breastfeeding rates by EPDS score.
| OR | 95% CI | P Value | |
|---|---|---|---|
| |||
| Maternal characteristics | |||
| Maternal age | 0.99 | 0.95‐1.03 | 0.660 |
| Race | |||
| White | Reference | ||
| Black | 0.93 | 0.35‐2.50 | 0.891 |
| Hispanic | 0.43 | 0.23‐0.84 | 0.013 |
| Other | 0.54 | 0.19‐1.55 | 0.254 |
| EPDS language | 0.47 | 0.25‐0.88 | 0.020 |
| People in home | 1.02 | 0.89‐1.16 | 0.799 |
| No. of children | 1.02 | 0.85‐1.23 | 0.819 |
| Relationship | |||
| Married | Reference | ||
| In a relationship | 0.93 | 0.52‐1.65 | 0.802 |
| Single | 1.37 | 0.72‐2.62 | 0.333 |
| Unsupportive social network | 3.58 | 1.95‐6.59 | 0.0001 |
| Some psychiatric disorder | 5.07 | 2.65‐9.72 | 0.0001 |
| Infant characteristics | |||
| Gestational age | 0.96 | 0.87‐1.04 | 0.316 |
| Prior admission | 0.83 | 0.49‐1.39 | 0.476 |
| Any comorbidity | 1.03 | 0.92‐1.18 | 0.551 |
| Congenital heart disease | 1.87 | 0.83‐4.22 | 0.130 |
| Neurodevelopmental | 3.41 | 1.41‐8.21 | 0.006 |
| Any medical device needed | 1.59 | 0.78‐3.24 | 0.201 |
| Multivariate logistic regression | |||
| Race | |||
| White | Reference | ||
| Black | 0.87 | 0.28‐2.70 | 0.812 |
| Hispanic | 0.64 | 0.30‐1.38 | 0.258 |
| Other | 0.88 | 0.29‐2.74 | 0.831 |
| Unsupportive social network | 4.40 | 2.27‐8.53 | 0.0001 |
| Psychiatric disorder | 5.02 | 2.49‐10.15 | 0.0001 |
| Neurodevelopmental comorbidity | 2.78 | 1.03‐7.52 | 0.004 |
Infant characteristics were next examined. Children of EPDS+ and EPDS mothers were similar in age, number of prior hospital admissions, gestational age at birth, and overall use of medical equipment (Table 2). To examine the effect of illness leading to hospitalization on EPDS+ risk, discharge diagnoses were collected and grouped into categories. Infants of EPDS+ mothers were more likely hospitalized for neurologic illness (P = 0.008) (see Supporting Table 1 in the online version of this article), but otherwise similar.
We next compared differences in long‐term infant comorbidities. The rate of having any comorbidity was similar between children of EPDS+ and EPDS mothers (39.1% vs 33.6%; P = 0.551). However, children of EPDS+ mothers were more likely to have mental retardation, hydrocephalus, or require ventriculoperitoneal shunt (VPS); however, the overall number of infants with each comorbidity was low. A neurodevelopmental comorbidity variable was created combining mental retardation, cerebral palsy, epilepsy, hydrocephalus, craniosynostosis, and VPS, resulting in 22 (7.1%) unique infants with 1 or more of these conditions. Having an infant with a neurodevelopmental comorbidity was a risk factor for positive postpartum depression screen (OR: 3.41; 95% CI: 1.41‐8.21). This continued to be significant (OR: 2.78; 95% CI: 1.03‐7.52) (Table 2) when controlling for maternal race/ethnicity, psychiatric history, and social support in multivariate logistic regression.
To determine if women screened followed through with recommendations, participants were called 3 and 6 months postenrollment. We attempted to call all women and successfully reached 120; 19 (16%) refused the call. One hundred one of the original 310 enrolled (33%) completed at least 1 follow‐up call; 47 at 3 months, 40 at 6 months, and only 14 (14%) responded at both time points. Due to this response rate, the first call at either 3 or 6 months was used as a single follow‐up time point for statistical analysis. A slightly higher proportion of EPDS‐ mothers (80/223, 36%) completed calls compared to EPDS+ mothers (21/87, 24%; P = 0.047).
Of 21 mothers initially EPDS+ who completed a follow‐up call, 10 (48%) later screened negative. Seven of these 10 (70%) reported discussing postpartum depression with their physician or using provided referral resources in the interim; 1 woman both spoke to a doctor and used a referral resource. One additional woman used resources, but repeat EPDS was still positive (Table 3). Reasons cited for not seeking evaluation included too busy (n = 4) and lost paperwork (n = 1), or no reason was given (n = 2). Mothers utilizing appropriate follow‐up had reduction in scores compared to those not (F(1,19) = 5.743, P = 0.027), although all scores decreased over time (F(1,19) = 11.54, P = 0.0030) (Figure 1B).
| Changes in Characteristics Following Enrollment | Positive EPDS, N = 21 | Negative EPDS, N = 80 | P Value |
|---|---|---|---|
| |||
| Repeat EPDS negative | 10 (47.6%) | 73 (91.3%) | 0.001 |
| Spoke to a doctor about PD | 6 (28.6%) | 27 (33.7%) | 0.360 |
| Used a study referral resource | 3 (14.3%) | NA | |
| Received a formal diagnosis of PD | 1 (4.7%) | 1 (1.3%) | 0.325 |
| Healthcare utilization* | |||
| No. of ER visits | 0 (00.5) | 0 (02) | 0.074 |
| No. of urgent care visits | 0 (00.5) | 0 (00) | 0.136 |
| No. of hospitalizations | 0 (00) | 0 (01) | 0.021 |
| Repeat MIB score | 1.09 0.38 | 0.69 0.17 | 0.357 |
Of 80 women initially EPDS, most stayed negative (73/80, 91%), but 7 (9%) became EPDS+. These mothers received education and referral information over the phone, but none completed a subsequent call. Infants of mothers initially EPDS had a higher frequency of hospitalization postenrollment compared to EPDS+ mothers (P = 0.021) (Table 3). Two (33%) mothers who converted from EPDS to EPDS+ had infants readmitted in the follow‐up period.
DISCUSSION
This study demonstrated almost a third of mothers of hospitalized infants are at risk for postpartum depression and most had not been previously screened. Stress due to hospitalization did not seem to falsely elevate EPDS scores; the proportion of EPDS+ mothers matched our prestudy prediction (28% vs 27.9%). Follow‐up calls indicated that EPDS+ mothers not pursuing further evaluation tended to remain EPDS+. Higher (worse) MIB score was strongly correlated to increased EPDS score as expected, supporting screening accuracy. Our results suggest that postpartum depression screening in hospital settings can be used to complement outpatient practice and capture mothers who would otherwise be missed.
Although we were able to screen, it is difficult to know whether this correctly identified mothers with postpartum depression. Only 2 mothers reported subsequent official diagnosis of postpartum depression, and 1 of these was EPDS originally. This reflects weakness of our survey‐based design; we only know if the mother self‐reported a formal diagnosis of postpartum depression, because we do not have access to their medical charts. We also had higher than expected loss to follow up (67%), leaving 66 initially EPDS+ mothers with unknown eventual diagnoses. The EPDS has been validated in multiple populations and has a positive predictive value ranging from 23% to 93%.[23] Therefore, somewhere between 20 and 80 women in our study should meet diagnostic criteria for postpartum depression. A limitation of children's hospital‐based screening with the EPDS is lack of adult‐trained psychiatrists who could immediately follow screening with diagnosis. Such integration may already be possible at community or hospital‐within‐a‐hospital models, and could be trialed at children's hospitals. Regardless, participation in the study seemed to increase mothers' awareness of postpartum depression. Prior to enrollment, only 14.6% of subjects reported discussing postpartum depression with a physician, although recall bias likely contributed to some mothers not remembering a screen. Promisingly, on follow‐up, 37% of called participants reported they discussed postpartum depression with a doctor following their child's hospital discharge.
Our study identified low social support and history of past psychiatric diagnosis as maternal risk factors for EPDS+ screens, which is consistent with previous reports.[29] There was a slight increase in subsequent infant hospitalizations in the EPDS group, which is contrary to reports stating that increased healthcare utilization is associated with postpartum depression.[30] However, most studies have shown an increase in only acute or emergency room care visits[30, 31] and no association between maternal depression and infant hospitalization.[30, 32] In our study, the median number of hospitalizations for both groups was 0, indicating overall low utilization. Because 2 of the mothers who converted from EPDS to EPDS+ had children readmitted, this underscores the benefit of reassessment at each medical encounter. A large proportion of mothers (36.5%) reported that the infant had been previously hospitalized, adding another potential missed screening opportunity. Our study supports others advocating repeated screenings and suggests mothers should be screened at any medical encounter that occurs in the first postpartum year.
We identified neurodevelopmental illness as the major infant characteristic associated with postpartum depression risk. Conversely, Garfield et al. did not find correlation between poorer Neurobiologic Risk Score and increased maternal depression risk in a NICU setting.[11] Perhaps our population of older and mainly full‐term infants makes consequences of neurologic insult more obvious and affects mothers more significantly. Cheng et al. reported that 26.9% of mothers of children with cognitive delay reported high depressive symptoms, compared with 17.4% of mothers of typically developing children at 4 years of age.[33] Another body of evidence suggests maternal emotional state during pregnancy influences neurodevelopmental outcome in the child. Maternal anxiety or depression has been associated with altered placental function, reduced infant gray matter density, and worse cognitive function.[34, 35] Therefore, future research may focus on mothers of infants with neurodevelopmental disease to better understand this relationship.
There were several limitations to this study. Some data collected by a survey are subject to information bias. Women may report a more supportive social network than actually exists or omit history of mental health diagnoses. We attempted to control for this by using validated measures where possible and performing chart review to verify reported infant characteristics. Our population was overwhelmingly Hispanic/Latina, and a third of infants were not previously healthy, which limits applicability to other settings. We used a convenience method that could introduce sampling bias. Our hospital's overall patient demographic is 65% Hispanic, which is similar to the 68% sampled in our study. In addition, the proportions of infant diagnoses approximate the overall rates at CHLA, so we feel our sample was fairly representative. There is a general consensus that depression studies have recruitment difficulties.[36] In the unlikely event that all 56 of women who declined to participate were EPDS+, overall proportion of at‐risk mothers would rise to 39%. If our study does show slight underestimation of risk, that would only mean more potential for intervention if screening were mandatory. Another weakness was high loss to follow‐up, which led us to combine the 3‐ and 6‐month follow‐up calls into 1 outcome. Sixty percent of calls used in analysis occurred at 3 months, so long‐term maintenance of improved EPDS scores remains unclear. Although conducting repeat EPDS via phone may affect honest answering of sensitive questions, other studies have used this technique successfully.[4]
CONCLUSION
This is the first study evaluating a screening program for maternal postpartum depression during infant hospitalizations. In our population, risk factors for positive postpartum depression screening were low social support, history of maternal psychiatric diagnosis, and having an infant with neurodevelopmental disease. We believe mothers should receive postpartum depression screening at all medical encounters during the child's first year.
Acknowledgements
The authors thank the CHLA Department of Social Work and the USC Required Scholarly Projects program, and specifically Joseph DeSena and Humberto Avila, for project assistance.
Disclosures: Dr. Trost is an Institutional Career Development Program Scholar through the Southern California Clinical and Translational Science Institute (SC‐CTSI) at the University of Southern California Keck School of Medicine. The content is solely the responsibility of the author(s) and does not represent the official view of the SC‐CTSI. Dr. Trost conceptualized and designed the study, drafted the initial manuscript, and approved the final manuscript as submitted. Dr. Molas‐Torreblanca co‐designed the study, reviewed and revised the manuscript, and approved the final manuscript as submitted. Ms. Man coordinated and supervised hospital data collection, critically reviewed the manuscript, and approved the final manuscript as submitted. Mr. Casillas coordinated and supervised the phone call data collection, critically reviewed the manuscript, and approved the final manuscript as submitted. Ms. Sapir coordinated the referral process for enrolled patients, supervised the design of patient handouts, and critically reviewed and approved the final manuscript as submitted. Dr. Schrager guided study design, supervised the statistical analysis of the final data, critically reviewed and revised the manuscript, and approved the final manuscript as submitted. The authors report no conflicts of interest.
- , , , , . Maternal depressive symptoms and infant health practices among low‐income women. Pediatrics. 2004;113(6):e523–e529.
- , , , et al.; Duke University Evidence‐based Practice Center. Effective Health Care Program. Efficacy and safety of screening for postpartum depression. Comparative effectiveness review number 106. Rockville, MD: Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services; 2013: Available at: https://www.effectivehealthcare.ahrq.gov/ehc/products/379/1437/postpartum‐screening‐report‐130409.pdf. Date accessed Jan 10 2016.
- , , , , . Prevalence rates and demographic characteristics associated with depression in pregnancy and the postpartum. J Consult Clin Psychol. 1989;57(2):269–274.
- , , , , . Screening for depression in the postpartum period: a comparison of three instruments. J Womens Health (Larchmt). 2008;17(4):585–596.
- , , , . Are maternal depression or symptom severity associated with breastfeeding intention or outcomes? J Clin Psychiatry. 2010;71(8):1069–1078.
- , , , , . Impact of maternal depressive symptoms on growth of preschool‐ and school‐aged children. Pediatrics. 2012;130(4):e847–e855.
- , , , , . The timing of maternal depressive symptoms and mothers' parenting practices with young children: implications for pediatric practice. Pediatrics. 2006;118(1):e174–e182.
- , , , , . Improvements in maternal depression as a mediator of intervention effects on early childhood problem behavior. Dev Psychopathol. 2009;21(2):417–439.
- ; Committee on Psychosocial Aspects of Child and Family Health American Academy of Pediatrics. Incorporating recognition and management of perinatal and postpartum depression into pediatric practice. Pediatrics. 2010;126(5):1032–1039.
- , , . Screening for postpartum depression in a pediatric emergency department. Pediatr Emerg Care. 2011;27(9):795–800.
- , , , et al. Risk factors for postpartum depressive symptoms in low‐income women with very low‐birth‐weight infants. Adv Neonatal Care. 2015;15(1):E3–E8.
- , , . Impact of infant health problems on postnatal depression: pilot study to evaluate a health visiting system. Psychiatry Clin Neurosci. 2006;60(2):182–189.
- , , , , , . Primary care pediatricians' roles and perceived responsibilities in the identification and management of maternal depression. Pediatrics. 2002;110(6):1169–1176.
- , , , et al. Does education influence pediatricians' perceptions of physician‐specific barriers for maternal depression? Clin Pediatr (Phila). 2008;47(7):670–678.
- , , , . Pediatricians' views of postpartum depression: a self‐administered survey. Arch Womens Ment Health. 2004;7(4):231–236.
- . Compliance with well‐child visit recommendations: evidence from the Medical Expenditure Panel Survey, 2000–2002. Pediatrics. 2006;118(6):e1766–e1778.
- , , , et al. A framework of pediatric hospital discharge care informed by legislation, research, and practice. JAMA Pediatr. 2014;168(10):955–962; quiz 965–966.
- , , . Pedi‐BOOST. Peds Effective Discharge: Better Handoff to Home through Safer Transitions. 2013. https://www.hospitalmedicine.org/Web/Quality___Innovation/Implementation_Toolkit/pediBoost/Best_Practices/Best_Practices.aspx Accessed Jan 10 2016.
- , , , et al. Effects of maternal depressive symptomatology during pregnancy and the postpartum period on infant‐mother attachment. Psychiatry Clin Neurosci. 2014;68(8):631–639.
- , , , , . Examining maternal depression and attachment insecurity as moderators of the impacts of home visiting for at‐risk mothers and infants. J Consult Clin Psychol. 2009;77(4):788–799.
- , . Postpartum mood disorders: diagnosis and treatment guidelines. J Clin Psychiatry. 1998;59(suppl 2):34–40.
- , , , , . A new Mother‐to‐Infant Bonding Scale: links with early maternal mood. Arch Womens Ment Health. 2005;8(1):45–51.
- , , , , . A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatr Scand. 2009;119(5):350–364.
- , , . Detection of postnatal depression. Development of the 10‐item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–786.
- , , , . Validation of the Edinburgh Postnatal Depression Scale (EPDS) in Spanish mothers. J Affect Disord. 2003;75(1):71–76.
- , , , et al. TRIPPD: a practice‐based network effectiveness study of postpartum depression screening and management. Ann Fam Med. 2012;10(4):320–329.
- , , , , . Detection of postpartum depressive symptoms by screening at well‐child visits. Pediatrics. 2004;113(3 pt 1):551–558.
- R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing: 2013. Available at: http://www.R‐project.org. Accessed Jan 10 2016.
- , , , , . Biological and psychosocial predictors of postpartum depression: systematic review and call for integration. Annu Rev Clin Psychol. 2015;11:99–137.
- , , , et al. Maternal depressive symptoms and children's receipt of health care in the first 3 years of life. Pediatrics. 2005;115(2):306–314.
- , . Maternal factors and child's health care use. Soc Sci Med. 1995;40(5):623–628.
- , , , , . Women's health after pregnancy and child outcomes at age 3 years: a prospective cohort study. Am J Public Health. 2002;92(8):1312–1318.
- , , , . The influence of children's cognitive delay and behavior problems on maternal depression. J Pediatr. 2015;167(3):679–686.
- , , , , . Maternal prenatal symptoms of depression and down regulation of placental monoamine oxidase A expression. J Psychosom Res. 2013;75(4):341–345.
- , , , , . High pregnancy anxiety during mid‐gestation is associated with decreased gray matter density in 6–9‐year‐old children. Psychoneuroendocrinology. 2010;35(1):141–153.
- , , , , . Factors affecting recruitment into depression trials: Systematic review, meta‐synthesis and conceptual framework. J Affect Disord. 2015;172:274–290.
- , , , , . Maternal depressive symptoms and infant health practices among low‐income women. Pediatrics. 2004;113(6):e523–e529.
- , , , et al.; Duke University Evidence‐based Practice Center. Effective Health Care Program. Efficacy and safety of screening for postpartum depression. Comparative effectiveness review number 106. Rockville, MD: Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services; 2013: Available at: https://www.effectivehealthcare.ahrq.gov/ehc/products/379/1437/postpartum‐screening‐report‐130409.pdf. Date accessed Jan 10 2016.
- , , , , . Prevalence rates and demographic characteristics associated with depression in pregnancy and the postpartum. J Consult Clin Psychol. 1989;57(2):269–274.
- , , , , . Screening for depression in the postpartum period: a comparison of three instruments. J Womens Health (Larchmt). 2008;17(4):585–596.
- , , , . Are maternal depression or symptom severity associated with breastfeeding intention or outcomes? J Clin Psychiatry. 2010;71(8):1069–1078.
- , , , , . Impact of maternal depressive symptoms on growth of preschool‐ and school‐aged children. Pediatrics. 2012;130(4):e847–e855.
- , , , , . The timing of maternal depressive symptoms and mothers' parenting practices with young children: implications for pediatric practice. Pediatrics. 2006;118(1):e174–e182.
- , , , , . Improvements in maternal depression as a mediator of intervention effects on early childhood problem behavior. Dev Psychopathol. 2009;21(2):417–439.
- ; Committee on Psychosocial Aspects of Child and Family Health American Academy of Pediatrics. Incorporating recognition and management of perinatal and postpartum depression into pediatric practice. Pediatrics. 2010;126(5):1032–1039.
- , , . Screening for postpartum depression in a pediatric emergency department. Pediatr Emerg Care. 2011;27(9):795–800.
- , , , et al. Risk factors for postpartum depressive symptoms in low‐income women with very low‐birth‐weight infants. Adv Neonatal Care. 2015;15(1):E3–E8.
- , , . Impact of infant health problems on postnatal depression: pilot study to evaluate a health visiting system. Psychiatry Clin Neurosci. 2006;60(2):182–189.
- , , , , , . Primary care pediatricians' roles and perceived responsibilities in the identification and management of maternal depression. Pediatrics. 2002;110(6):1169–1176.
- , , , et al. Does education influence pediatricians' perceptions of physician‐specific barriers for maternal depression? Clin Pediatr (Phila). 2008;47(7):670–678.
- , , , . Pediatricians' views of postpartum depression: a self‐administered survey. Arch Womens Ment Health. 2004;7(4):231–236.
- . Compliance with well‐child visit recommendations: evidence from the Medical Expenditure Panel Survey, 2000–2002. Pediatrics. 2006;118(6):e1766–e1778.
- , , , et al. A framework of pediatric hospital discharge care informed by legislation, research, and practice. JAMA Pediatr. 2014;168(10):955–962; quiz 965–966.
- , , . Pedi‐BOOST. Peds Effective Discharge: Better Handoff to Home through Safer Transitions. 2013. https://www.hospitalmedicine.org/Web/Quality___Innovation/Implementation_Toolkit/pediBoost/Best_Practices/Best_Practices.aspx Accessed Jan 10 2016.
- , , , et al. Effects of maternal depressive symptomatology during pregnancy and the postpartum period on infant‐mother attachment. Psychiatry Clin Neurosci. 2014;68(8):631–639.
- , , , , . Examining maternal depression and attachment insecurity as moderators of the impacts of home visiting for at‐risk mothers and infants. J Consult Clin Psychol. 2009;77(4):788–799.
- , . Postpartum mood disorders: diagnosis and treatment guidelines. J Clin Psychiatry. 1998;59(suppl 2):34–40.
- , , , , . A new Mother‐to‐Infant Bonding Scale: links with early maternal mood. Arch Womens Ment Health. 2005;8(1):45–51.
- , , , , . A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatr Scand. 2009;119(5):350–364.
- , , . Detection of postnatal depression. Development of the 10‐item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–786.
- , , , . Validation of the Edinburgh Postnatal Depression Scale (EPDS) in Spanish mothers. J Affect Disord. 2003;75(1):71–76.
- , , , et al. TRIPPD: a practice‐based network effectiveness study of postpartum depression screening and management. Ann Fam Med. 2012;10(4):320–329.
- , , , , . Detection of postpartum depressive symptoms by screening at well‐child visits. Pediatrics. 2004;113(3 pt 1):551–558.
- R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing: 2013. Available at: http://www.R‐project.org. Accessed Jan 10 2016.
- , , , , . Biological and psychosocial predictors of postpartum depression: systematic review and call for integration. Annu Rev Clin Psychol. 2015;11:99–137.
- , , , et al. Maternal depressive symptoms and children's receipt of health care in the first 3 years of life. Pediatrics. 2005;115(2):306–314.
- , . Maternal factors and child's health care use. Soc Sci Med. 1995;40(5):623–628.
- , , , , . Women's health after pregnancy and child outcomes at age 3 years: a prospective cohort study. Am J Public Health. 2002;92(8):1312–1318.
- , , , . The influence of children's cognitive delay and behavior problems on maternal depression. J Pediatr. 2015;167(3):679–686.
- , , , , . Maternal prenatal symptoms of depression and down regulation of placental monoamine oxidase A expression. J Psychosom Res. 2013;75(4):341–345.
- , , , , . High pregnancy anxiety during mid‐gestation is associated with decreased gray matter density in 6–9‐year‐old children. Psychoneuroendocrinology. 2010;35(1):141–153.
- , , , , . Factors affecting recruitment into depression trials: Systematic review, meta‐synthesis and conceptual framework. J Affect Disord. 2015;172:274–290.
Pneumonia Treatment Duration
Pneumonia is the leading inpatient infectious diagnosis for which antimicrobials are prescribed in the United States.[1] Supported by moderate‐ to high‐quality evidence, guidelines produced jointly by the Infectious Diseases Society of America (IDSA) and American Thoracic Society (ATS) recommend treating pneumonia with the shortest appropriate duration of antimicrobial therapy to minimize risk for antimicrobial‐related adverse events.[2, 3, 4]
Evidence supports short duration of therapy for treatment of uncomplicated pneumonia.[3, 4, 5, 6, 7, 8, 9, 10, 11, 12] IDSA/ATS guidelines state, patients with CAP [community‐acquired pneumonia] should be treated for a minimum of 5 days (level 1 evidence), should be afebrile for 4872 hours, and should have no more than 1 CAP‐associated sign of clinical instabilitybefore discontinuation of therapy (level II evidence). (Moderate recommendation.) A longer duration of therapy may be warranted if initial therapy was not active against the identified pathogen or if it was complicated by [abscess, empyema, severe immunosuppression, or] extra‐pulmonary infection such as meningitis or endocarditis. (Weak recommendation; level III evidence).[3] Recommended therapy duration for patients with uncomplicated healthcare‐associated pneumonia (HCAP) who respond to initial therapy is 7 to 8 days unless gram‐negative nonfermenting rods or complications are identified (level I evidence).[4]
Within the Veterans Health Administration (VHA), the Antimicrobial Stewardship Taskforce (ASTF) was created to optimize care by developing, deploying, and monitoring a national‐level strategic plan for antimicrobial therapy management improvements.[13, 14] Although single‐center studies have found antimicrobial therapy for CAP being frequently prescribed for longer than recommended, the reproducibility of this finding across different facilities has not been assessed.[15, 16] The ASTF collaborated with the VHA Center for Medication Safety to assess total duration of antimicrobial therapy prescribed for veterans hospitalized with uncomplicated pneumonia.[17]
METHODS
This retrospective multicenter evaluation was conducted in 30 VHA facilities that volunteered to participate in this project. Inpatients discharged with a primary International Classification of Diseases, Ninth Revision, Clinical Modification (ICD‐9‐CM) diagnosis code for pneumonia (or pneumonia diagnosis secondary to primary sepsis diagnosis) during 2013 were evaluated.[18] Diagnoses, admissions, and patient demographics were identified using Veterans Affairs (VA) integrated databases through the Austin Integrated Technology Center. Up to 200 admissions per facility were randomly selected for review. Clinical pharmacists at each facility performed manual record reviews utilizing a standardized protocol and collection form. Completed cases were uploaded to a central database for analysis. Standardized chart abstraction was facilitated by detailed instructions, a data dictionary, and monthly conference calls.
Inclusion criteria required patient admission to any medical ward including intensive care unit (ICU) wards for 48 hours, receipt of >24 hours inpatient antimicrobial therapy (eg, at least 2 doses of a once‐daily antibiotic), documentation of pneumonia discharge diagnosis, and survival until discharge. Exclusion criteria were: complicated pneumonia (lung abscess, necrotizing pneumonia, thoracentesis performed), significant immunosuppression (cancer chemotherapy or absolute neutrophil count 1500 cell/mm3 within 28 days, organ transplantation, human immunodeficiency virus infection); or extrapulmonary infection (eg, meningitis, endocarditis).[3] Patients were also excluded if directly transferred from another inpatient facility, pneumonia occurred >48 hours after admission, index hospitalization was >14 days, previously hospitalized within 28 days prior to index admission, or discharged without documentation of completing a full course of therapy. In addition, patients who received initial therapy discordant with culture and susceptibility findings, were not clinically stable by discharge, or had gram‐negative nonfermentative bacilli cultured were excluded from analysis because according to the guidelines, either data are lacking to support a short duration of therapy such as initial discordant therapy, or a longer duration of therapy may be warranted such as gram‐negative nonfermentative bacilli and clinical instability at discharge.[4] Our intent for these exclusions was to minimize bias against clinician decision making for cases where a longer duration of therapy may have been appropriate.
Patients meeting all criteria had the following abstracted: demographics; prior healthcare exposures, admitting location (ICU or non‐ICU ward), parameters for calculation of Pneumonia Severity Index (PSI), culture results obtained 48 hours of admission, duration of antimicrobials administered during hospitalization and prescribed upon discharge (or recommendations for outpatient duration in the discharge summary for patients receiving medications from non‐VA sources), daily clinical stability assessment, Clostridium difficile infection (CDI) test results, and readmission or death within 28 days of discharge.[19]
Guideline‐similar CAP therapy duration was defined as a minimum of 5 days of antimicrobials, up to a maximum of 3 additional days beginning the first day the patient was afebrile and exhibited 1 sign of clinical instability (heart rate > 100 beats/minute, respiratory rate >24 breaths/minute, systolic blood pressure 90, oxygen saturation 90% or partial pressure of oxygen 60 mm Hg on room air or baseline O2 requirements, or not returned to baseline mental status).[3] This definition was made by consensus decision of the investigators and was necessary to operationalize the relationship between clinical stability and appropriate duration of therapy. Guideline‐similar HCAP therapy duration was defined as 8 days.[4] CDI was defined in accordance with VA criteria for hospital onset and community‐onset healthcare‐facilityassociated CDI.[20] All‐cause hospital readmission and all‐cause death were defined as inpatient readmission or any death, respectively, within 28 days after discharge for the pneumonia admission.
Demographics, comorbidities, microbiology results, antimicrobial utilization, CDI, readmission, and death rates between guideline‐similar and guideline‐excessive duration of antimicrobial therapy groups were characterized with descriptive statistics, Mann‐Whitney U test, or 2 test as indicated (significance defined as P 0.05). Multivariable logistic regression (SAS version 9.3 [SAS Institute, Cary, NC]) was used to assess association between duration of therapy exceeding recommended guidelines with all‐cause readmission and all‐cause death after adjustment for pertinent covariates. Odds ratios (OR) with 95% confidence intervals ( 95% CI) were reported. This medication utilization evaluation (MUE) was reviewed by the Hines VHA Institutional Review Board for Human Subjects Protection. Based on VHA Policy Handbook 1058.05, which defines operations activities that may constitute research, the board determined that the evaluation constituted quality improvement rather than research, and thus was exempt from VHA Human Subjects Research requirements.
RESULTS
There were 3881 admissions eligible for chart review. After manual chart review of inclusion and exclusion criteria, 1739 (44.8%) patients were available for duration of therapy analysis. (Figure 1). Only 1 admission for each patient was analyzed.
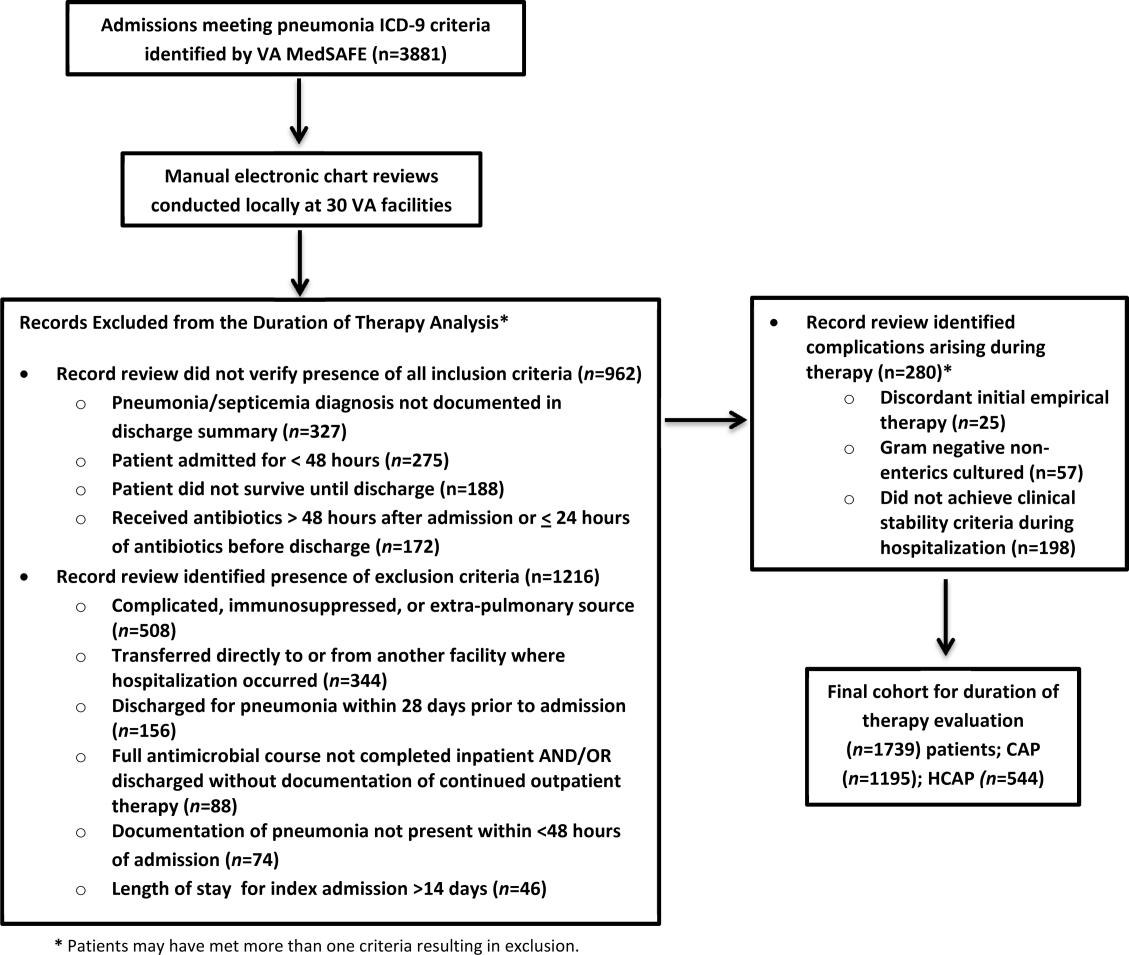
The cohort was comprised primarily of elderly male patients (96.6%) of whom more than two‐thirds were hospitalized for CAP (Table 1). Most patients had significant disease severity as indicated by PSI score; however, only 12% were directly admitted to the ICU. Blood cultures were collected in >95% of cases; lower respiratory cultures were obtained in 39.9% of cases.
| Characteristic | Value |
|---|---|
| |
| Age, y, mean SD | 71.8 (12.7) |
| Gender, male, n (%) | 1,680 (96.6) |
| Living environment at time of index admission, n (%) | |
| Home | 1,416 (81.4) |
| VA community‐based living center | 88 (5.1) |
| Non‐VA long‐term skilled care facility | 95 (5.5) |
| Assisted living facility | 52 (2.9) |
| Not documented | 46 (2.7) |
| Other | 29 (1.7) |
| Prior healthcare exposures, n (%) | |
| Prior hospitalization within last 90 days | 310 (17.8) |
| Residence in a long‐term skilled care facility in last 90 days | 209 (12.0) |
| Chronic dialysis within last 28 days | 52 (3.0) |
| Intravenous antimicrobials within last 28 days | 76 (4.4) |
| Wound, tracheostomy, or ventilator care in last 28 days | 37 (2.1) |
| Community‐acquired pneumonia, n (%) | 1,195 (68.7) |
| Healthcare‐associated pneumonia, n (%) | 544 (31.3) |
| Comorbidities, n (%) | |
| Renal disease | 438 (25.2) |
| Liver disease | 39 (2.2) |
| Congestive heart failure | 436 (25.1) |
| Cerebrovascular disease | 356 (20.4) |
| Neoplastic disease (excluding skin) | 384 (22.1) |
| Severity of illness, n (%) | |
| Pneumonia Severity Index | |
| Class I | 30 (1.8) |
| Class II | 198 (11.4) |
| Class III | 349 (20.1) |
| Class IV | 759 (43.6) |
| Class V | 403 (23.2) |
| Intensive care upon admission | 212 (12.2) |
| Culture collection 48 hours of admission, n (%) | 1,687 (97.0) |
| Blood | 1,631 (96.7) |
| Lower respiratory tract (sputum) | 673 (39.9) |
| Bronchoalveolar lavage | 20 (1.2) |
| Urine | 632 (37.5) |
| Skin/wound | 3 (0.2) |
| Other | 158 (9.4) |
| Facility complexity, n (%) | |
| Level 1a‐c | 1,286 (74.0) |
| Level 2 | 437 (25.1) |
| Level 3 | 16 (0.9) |
Commonly administered antimicrobials during hospitalization and at discharge are summarized in Table 2. Anti‐pseudomonal ‐lactams and antimethicillin‐resistant Staphylococcus aureus antimicrobials were more frequently administered to patients with HCAP, whereas third‐generation cephalosporins and macrolides were more likely to be administered to patients with CAP. Fluoroquinolones were prescribed to 55.3% of patients upon discharge.
| Inpatient Antimicrobials Administered* | ||||
|---|---|---|---|---|
| Portion of Cohort Receiving Antimicrobial, n (%), n = 1,739 |
Therapy Duration Similar With Guidelines, n (%), n = 241 |
Therapy Duration Exceeding Guidelines, n (%), n = 1,498 | Significance | |
| Antimicrobials Dispensed or Recommended at Discharge | ||||
| Portion of Cohort Receiving Antimicrobial, n (%), n = 1,471 |
Therapy Duration Similar With Guidelines, n (%), n = 151 |
Therapy Duration Exceeding Guidelines, n (%), n = 1,320 | Significance | |
| ||||
| Third‐generation cephalosporins | 809 (46.5) | 75 (31.1) | 734 (49.0) | 0.001 |
| Fluoroquinolones | 836 (48.1) | 114 (47.3) | 722 (48.2) | 0.80 |
| Macrolides | 788 (45.3) | 90 (37.3) | 698 (46.6) | 0.01 |
| Pseudomonal ‐lactams | 692 (39.8) | 138 (57.3) | 554 (37.0) | 0.01 |
| Anti‐MRSA antimicrobials | 663 (38.1) | 135 (56.0) | 528 (35.3) | 0.01 |
| Other ‐lactams | 139 (8.0) | 10 (4.2) | 129 (8.6) | 0.02 |
| Tetracyclines | 119 (6.8) | 14 (5.8) | 105 (7.0) | 0.49 |
| Other | 97 (5.6) | 15 (6.2) | 82 (5.5) | 0.64 |
| Third‐generation cephalosporins | 285 (19.4) | 27 (17.9) | 258 (19.6) | 0.62 |
| Fluoroquinolones | 813 (55.3) | 95 (62.9) | 718 (54.4) | 0.05 |
| Macrolides | 203 (13.8) | 20 (13.3) | 183 (13.9) | 0.83 |
| Pseudomonal ‐lactams | 31 (2.1) | 4 (2.7) | 27 (2.1) | 0.62 |
| Anti‐MRSA antimicrobials | 45 (3.1) | 6 (4.0) | 39 (3.0) | 0.49 |
| Other ‐lactams | 239 (16.3) | 13 (8.6) | 226 (17.1) | 0.01 |
| Tetracyclines | 95 (6.5) | 10 (6.6) | 85 (6.4) | 0.93 |
| Other | 44 (3.0) | 5 (3.3) | 39 (3.0) | 0.81 |
Overall, 13.9% of patients with uncomplicated pneumonia received guideline‐similar duration of therapy (Table 3). A greater proportion of HCAP patients (29.0%) received guideline‐similar therapy duration as compared to CAP patients (6.9%) (P 0.01 (Table 3). Median duration of therapy was 7 days (interquartile range [IQR] = 78 days) for guideline‐similar therapy compared to 10 days (913 days) for therapy duration in excess of guideline recommendations. Overall, 97.1 % of patients met clinical stability criteria before day 4 of therapy, yet 50% received 4 days of intravenous (IV) therapy (median was 4 days, IQR = 36 days). Antimicrobial therapy was generally completed after discharge, as only 17.3% received their entire treatment course during hospitalization. Median duration of outpatient oral (PO) antimicrobial therapy was twice as long for guideline‐excessive therapy compared to guideline‐similar therapy (6 vs 3 days), whereas duration of inpatient IV and PO antimicrobial therapy was similar. Patients discharged on a fluoroquinolone were more likely to receive guideline‐similar duration of therapy. The VHA classifies facilities into 3 levels of complexity, with lower scores indicating more complex facilities.[21] Guideline‐similar therapy duration occurred in 10.4% of cases in lower complexity facilities (levels 2 and 3),and 15.1% in more complex facilities (level 1) (P = 0.01). The median duration of therapy was similar for more and less complex facilities, respectively (10 days, IQR = 812 days vs 10 days, IQR = 813 days).
| Outcome |
Therapy Duration Similar With IDSA/ATS Guidelines |
Therapy Duration in Excess of IDSA/ATS Guideline Recommendations | Significance |
|---|---|---|---|
| |||
| Antimicrobial duration consistent with guideline recommendations, n (%) | 241 (13.9) | 1,498 (86.1) | NR |
| CAP* | 83 (6.9) | 1,112 (93.1) | NR |
| HCAP* | 158 (29.0) | 386 (71.0) | NR |
| Total days of therapy for pneumonia, median (IQR) | 7 (78) | 10 (913) | NR |
| CAP | 6 (59) | 10 (812) | 0.01 |
| HCAP | 7 (78) | 11 (1014) | 0.01 |
| Days of IV therapy administered for pneumonia, median (IQR) | 4 (37) | 4 (36) | 0.50 |
| Days of PO inpatient therapy administered, median (IQR) | 1 (03) | 1 (03) | 0.78 |
| Days of PO outpatient therapy dispensed at discharge, median (IQR) | 3 (25) | 6 (47) | 0.01 |
| Days of PO outpatient therapy recommended in Discharge Summary for patients without a VA prescription, median (IQR) | 3 (24) | 5 (47) | 0.01 |
| Aggregate 28‐day hospital readmission, n (%) | 42 (17.4) | 183 (12.2) | 0.03 |
| CAP∥# | 7 (8.4) | 112 (10.1) | 0.58 |
| HCAP∥# | 35 (22.2) | 71 (18.4) | 0.28 |
| Aggregate 28‐day CDI rate, n (%) | 6 (2.5) | 9 (0.6) | 0.03 |
| CAP∥** | 1 (1.2) | 6 (0.5) | 0.44 |
| HCAP∥** | 5 (3.2) | 3 (0.8) | 0.04 |
| Aggregate 28‐day death after discharge, n (%) | 6 (2.5) | 52 (3.5) | 0.43 |
| CAP∥** | 1 (1.2) | 33 (3.0) | 0.35 |
| HCAP∥** | 5 (3.2) | 19 (4.9) | 0.37 |
The 28‐day postdischarge all‐cause readmission rate for patients who received guideline‐similar therapy duration was higher (17.4%) than for patients who received therapy duration in excess of guideline recommendations (12.2%) (P = 0.03). After adjustment for covariates associated with readmission (HCAP, age, prior skilled nursing facility residence, PSI score comorbidity elements), we found no evidence that patients who received guideline‐similar therapy duration were more likely to be readmitted than were patients who received guideline‐excessive duration (OR: 1.1 [95% CI: 0.8, 1.7]) (Table 3). Likewise, no difference in 28‐day all‐cause postdischarge mortality was identified between guideline‐similar and guideline‐excessive duration after adjustment for the same covariates (adjusted OR: 0.5 [95% CI: 0.2, 1.2]) (Table 4).
| Model Variables | Odds Ratio | 95% Confidence Interval | P Value |
|---|---|---|---|
| |||
| Readmission model | |||
| Duration of antibiotics | 1.11 | 0.75, 1.64 | 0.62 |
| HCAP | 1.94 | 1.38, 2.72 | 0.01 |
| Age | 1.01 | 1.00, 1.03 | 0.04 |
| Prior skilled nursing facility residence | 0.91 | 0.59, 1.40 | 0.67 |
| PSI score comorbidity elements | |||
| Neoplastic disease | 1.20 | 0.86, 1.67 | 0.29 |
| Liver disease | 1.55 | 0.66, 3.64 | 0.31 |
| CHF | 1.15 | 0.83, 1.59 | 0.41 |
| Cerebrovascular disease | 1.06 | 0.75, 1.50 | 0.75 |
| Renal disease | 1.51 | 1.09, 2.08 | 0.01 |
| Mortality model | |||
| Duration of antibiotics | 0.53 | 0.23, 1.22 | 0.14 |
| HCAP | 2.53 | 1.38, 4.65 | 0.01 |
| Age | 1.06 | 1.03, 1.09 | 0.01 |
| Prior skilled nursing facility residence | 0.79 | 0.38, 1.66 | 0.53 |
| PSI score comorbidity elements | |||
| Neoplastic disease | 1.03 | 0.57, 1.87 | 0.91 |
| Liver disease | 0.001 | 0.001, >999.9 | 0.98 |
| CHF | 0.73 | 0.39, 1.38 | 0.34 |
| Cerebrovascular disease | 0.82 | 0.43, 1.56 | 0.55 |
| Renal disease | 0.72 | 0.39, 1.35 | 0.31 |
CDI cases (n = 15) were too sparse to adequately perform multivariable logistic regression analysis; however, a higher percentage of patients who received guideline‐similar duration of therapy developed CDI compared to patients who received guideline‐excessive duration of therapy (40.0% vs 13.6%, P 0.01). The median duration of therapy for patients who did and did not develop CDI was similar (8 days, IQR = 714 days vs 10 days, IQR = 812 days, P = 0.85, respectively). Patients who developed CDI had a higher rate of HCAP diagnosis (1.5% vs 0.6%; P = 0.06), were more likely to have concomitant non‐pneumonia infection (40.0% vs 9.5%, P 0.01), have chronic comorbidity (86.7% vs 59.1%, P = 0.03), and to have been admitted to the ICU (26.7% vs 12.1%, P = 0.09).
DISCUSSION
IDSA/ATS guidelines for pneumonia duration of therapy generally agree with other professional society guidelines including the British Thoracic Society and National Institute for Health and Care Excellence.[22, 23] In contrast to existing evidence and guideline recommendations, this multi‐centered evaluation identified prolonged durations of antimicrobial therapy prescribed in 93% and 71% of patients with uncomplicated CAP and HCAP (Table 3), respectively.[3, 4, 5, 6, 7, 8, 9, 10, 11, 12] Almost all (97.1%) uncomplicated CAP and HCAP patients met clinical stability criteria before day 4 of hospitalization, yet the median duration of IV therapy was 4 days. Because criteria for IV to PO conversion and the clinical stability definition utilized in this analysis were similar, many patients may have been eligible for PO therapy earlier, favorably impacting length of stay, cost, and adverse effects.[3, 12, 24, 25, 26] Although median days of inpatient PO therapy administered was 1 day (IQR = 03 days), inpatient observation after PO conversion may not be necessary. The duration of PO therapy was based on calendar days, where if a patient received 1 dose of a once daily antibiotic (ie, levofloxacin), they were considered to have received 1 day of inpatient PO antibiotics even if discharged the same day.
Approximately half of all days of therapy occurred after discharge. Although the median therapy duration for inpatients was similar, the median duration of antimicrobials administered upon hospital discharge was twice as long for patients receiving guideline‐excessive compared to guideline‐similar duration of therapy. The median excess in antibiotic duration is almost entirely accounted for by excess outpatient days of therapy. This is an important consideration for antimicrobial stewardship programs that tend to focus on inpatient antimicrobial use.
Noteworthy observations include the low rate of respiratory tract culture collection (41%) and frequent use of fluoroquinolones upon discharge. Collection of respiratory tract cultures is recommended for all patients with HCAP and patients with CAP who have risk factors for resistant pathogens, characteristics that were common in this cohort.[3, 4] Recently, we identified that respiratory culture collection is associated with increased de‐escalation rates in HCAP, and that culture‐negative patients frequently receive fluoroquinolones.[27] IDSA/ATS CAP guidelines discourage empirically switching to PO fluoroquinolone therapy based on bioavailability considerations alone.[3] Further, fluoroquinolones are considered to be associated with high risk of CDI.[28, 29] Prescription of fluoroquinolone upon discharge was associated with guideline‐similar duration of therapy and was not shown to be associated with CDI; however, power to detect differences between exposures to specific antimicrobials and CDI was low.
CDI was more common in patients with CAP (1.2% vs 0.5%) and HCAP (3.2% vs 0.8%) who received duration of therapy similar with guideline recommendations. This observation is confounded, as patients with CDI had significantly greater comorbidity as well as secondary infections and tended to more frequently receive ICU care. There were no differences in adjusted rates of readmission or death between patients receiving guideline‐similar and guideline‐excessive duration of therapy.
Evaluation strengths included exclusion of patients with complicating conditions possibly requiring prolonged antimicrobial treatment courses, which allowed the evaluation to focus on patients most likely to benefit from shorter course therapy. The definition of appropriate therapy duration was based upon daily assessment of clinical stability criteria that paralleled the CAP guidelines. The definition utilized objective parameters while accounting for patient variability in achieving clinical stability criteria. Finally, the analyses of clinical end points suggest that shorter duration of therapy may be as safe and effective as longer duration of therapy in uncomplicated pneumonia.
Limitations include those common to other analyses conducted within the VHA, including a predominantly elderly male cohort.[30] Only ICD‐9‐CM codes consistent with a discharge diagnosis of pneumonia were used to identify the cohort, and clinical impressions not documented in the medical record may have impacted the clinician's treatment duration decisions. The upper limit of appropriate duration of therapy for CAP was arbitrarily set at up to 3 days beyond meeting clinical stability criteria to provide a reasonable duration of appropriate therapy beyond clinical stability to operationalize the duration of therapy recommendations within the context of the IDSA/ATS guidelines. Additionally, CIs for the ORs of readmission and mortality were broad, and thus too imprecise to determine whether guideline‐similar durations increased or decreased readmission or mortality in comparison with therapy that exceeded guideline recommendations. We could not fully assess the potential for association between guideline‐excessive therapy duration and risk for CDI due to sparse cases. Finally, non‐VA prescription data were not available for all patients, and we relied on intended duration of therapy as recommended by the discharging provider in 4.1% of cases.
Most quality assessments of pneumonia treatment have focused on antimicrobial selection and timely administration or conversion from IV to PO therapy.[31, 32] This evaluation identified potential opportunities for expansion of antimicrobial stewardship activities during the transition of care setting. The efficacy of short‐course ‐lactam, macrolide, or fluoroquinolone therapy for CAP appears equivalent to longer treatment regimens with no difference in adverse event rates, suggesting that optimal duration of therapy may be a rational target for quality improvement.[5, 6, 7, 8, 9, 10, 11, 12, 15, 31] Recommendations for HCAP duration of therapy are extrapolated from a prospective multicentered study, which randomized patients with hospital‐acquired pneumonia to receive 8 versus 15 days of therapy, that identified similar outcomes to ours.[4, 12]
Single‐center studies have identified that antimicrobial therapy for pneumonia is frequently prescribed for longer than recommended by guidelines, which found a similar median duration of therapy as our evaluation.[15, 16] Similar to Jenkins et al., we observed a high rate of fluoroquinolone prescriptions upon discharge.[16]
There are few published examples of interventions designed to limit excessive duration of therapy, particularly for antimicrobials prescribed upon hospital discharge.[15, 33, 34] Serial procalcitonin measurements have been used to guide duration of therapy for pneumonia; however, the costbenefit ratio of procalcitonin measurement is unclear.[35, 36] Procalcitonin use was uncommon, and none of the participating facilities in our evaluation utilized a specific algorithm to guide therapy duration. Limited data suggest that patient‐level prospective audit with feedback may be effective. Advic et al. evaluated management of presumed CAP before and after education and prospective feedback to medical teams concerning antimicrobial selection and duration of therapy.[15] The intervention led to a decrease in median duration of therapy from 10 days (IQR = 813 days) to 7 days (IQR = 78 days) without increasing clinical failure or readmission rates. We recently reported a single‐center evaluation in which pharmacists utilizing a decision support tool while performing discharge medication reconciliation were able to reduce excessive mean duration of therapy from 9.5 days ( 2.4 days) to 8.3 days ( 2.9 days) in patients without complicated pneumonia, with a 19.2% reduction in duration of therapy prescribed at discharge.[37] A similar approach utilizing pharmacists performing discharge review has recently been reported in a community hospital.[38]
Future work should recognize that few patients complete their entire course of therapy as inpatients, and the majority of treatment is prescribed upon discharge. Pivotal time points for antimicrobial stewardship intervention include day 2 to 3 of hospitalization when conveying suggestions for antimicrobial de‐escalation and/or IV to PO conversion, and toward the end of hospitalization during discharge planning. Although it may not be feasible for antimicrobial stewards to review all uncomplicated cases of pneumonia during hospitalization, most facilities have a systematic process for reviewing medications during transitions of care. We believe that interventions intended to assess and recommend shortened courses of therapy are appropriate. These interventions should include a mechanism for support by stewardship personnel or other infectious diseases specialists. Based on our evaluation, the ASTF produced and disseminated clinical guidance documents and tools to triage pneumonia case severity and assess response to therapy. Qualified personnel are encouraged to use this information to make recommendations to providers regarding excessive duration of therapy for uncomplicated cases where appropriate. Other work should include an in‐depth assessment of clinical outcomes related to treatment duration, investigation of provider rationale for prolonged treatment, and duration of antimicrobial therapy prescribed upon discharge for other common disease states. Finally, manual chart review to classify uncomplicated cases and related outcomes was laborious, and automated case identification is technologically plausible and should be explored.[39]
In conclusion, this national VHA MUE found that patients with uncomplicated pneumonia were commonly prescribed antimicrobials for the duration of therapy in excess of guideline recommendations. Patients with uncomplicated pneumonia who received therapy duration consistent with guideline recommendations did not have significantly different all‐cause readmission and death rates compared to patients receiving prolonged treatment. Approximately half of all therapy was prescribed upon hospital discharge, and clinicians as well as antimicrobial stewardship programs should consider these findings to address excessive duration of antimicrobial therapy upon hospital discharge.
Acknowledgements
The authors acknowledge Dr. Michael Fine for his assistance with utilization of the Pneumonia Severity Index, Kenneth Bukowski for assisting with development of data collection tools and data management, and members of the Antimicrobial Stewardship Taskforce Implementation Sub‐Committee. Collaborators in the Pneumonia Duration of Therapy Medication Utilization Evaluation Group include: Biloxi VA (VA Gulf Coast): Cheryl Hankins, PharmD, BCPS; Central Alabama VAMC: Lauren Rass, PharmD, BCPS, Kelly Mooney, PharmD, BCPS; Central Arkansas: Nicholas Tinsley, MS, PharmD; Chillicothe VA: Stephen Hanson, PharmD, BCPS, Beth Gallaugher, BSN, RN, Elizabeth Baltenberger, PharmD; Cincinnati VA: Jason Hiett, PharmD, BCPS, Victoria Tate, PharmD, BCPS, Brian Salzman, PharmD; Dorn Medical Center: MaryAnne Maurer, PharmD, BCPS, BCACP, Rebekah Sipes, PharmD, BCACP, Ginger Ervin, PharmD; Dwight D. Eisenhower VAMC: Emily Potter, PharmD; Hudson Valley: Rita Lee Bodine, PharmD, Clement Chen, PharmD, Cristina Fantino, PharmD; James H. Quillen VAMC: Marty Vannoy, PharmD, BCPS, Erin Harshbarger, PharmD, Kristen Nelsen, PharmD; Jesse Brown VAMC: Lisa Young, PharmD, BCPS, AQ‐ID, Andrea Bidlencik, PharmD, BCPS; Kansas City VA: Jamie Guyear, PharmD, AQ‐ID, Ann Ungerman, PharmD, BCPS, Lauri Witt, PharmD, BCACP; Louis Stokes Cleveland VAMC: Amy Hirsch, PharmD, BCPS, Steven Adoryan, PharmD, BCP‐CC, Amanda Miller, PharmD, BCPS; Maine VAMC: Joel Coon, PharmD, Rachel Naida, PharmD, Kelly Grossman, PharmD; Martinsburg VAMC: Kelly Li, PharmD, Sarah Mickanis, PharmD, BCPS; Miami VA Medical Center: Mara Carrasquillo, BS, PharmD, Maribel Toro, PharmD; North Florida/South Georgia Veterans Health System: Nora Morgan, PharmD, Hugh Frank, PharmD, BCPS, BCPP, Sarah Onofrio, PharmD, BCPS; North Texas HCS: Susan Duquaine, PharmD, BCPS, AQ‐ID, Ruben Villaneuva, PharmD, BCPS, Jaela Dahl, PharmD, BCPS; Ozarks: Andrew Siler, PharmD, BCPS, Michele Walker, PharmD, CGP, Jennifer Cole, PharmD, BCPS, BCCCP; Providence VAMC: Kerry LaPlante, PharmD, FCCP, Lindsey Williamson, PharmD; Richmond VA: Daniel Tassone, PharmD, BCPS; Salisbury VAMC: Brett Norem, PharmD, Marrisa Ragonesi, PharmD; San Juan VA: Monica Sanabria‐Seda, PharmD, BCPS, Jaime Velez‐Fores, PharmD, BCPS, AQ‐ID, Norma Ayala‐Burgos, PharmD; Sioux Falls VA: Andrea Aylward, PharmD, BCPS; South Texas HCS: Kelly Echevarria, PharmD, BCPS, AQ‐ID, Manuel Escobar, PharmD; Tennessee Valley HCS: Casey Ryals, PharmD, BCACP, Molly Hurst, PharmD, Jonathan Hale, PharmD; VA Central Iowa Health Care System: Jenny Phabmixay, PharmD, BCPS, Mackenzie Brown, PharmD, BCPS, Cynthia Muthusi, PharmD, BCPS; VA Loma Linda: Tony Chau, PharmD; VA Sierra Nevada: Scott Mambourg, PharmD, BCPS, AAHIVP, Matthew Han, PharmD, Nathan Mihoch, PharmD; VA WNY Healthcare System: Kari Mergenhagen, PharmD, BCPS, AQ‐ID, Christine Ruh, PharmD, BCPS; Veterans Affairs Salt Lake City Health System: Emily Spivak, MD, MHS, Patricia Orlando, PharmD
Disclosures: Karl Madaras‐Kelly is employed full time by Idaho State University and has a without compensation appointment as a clinical pharmacist at the Boise VA Medical Center. He receives grant support unrelated to this work through the Department of Veterans Affairs subcontracted to Idaho State University. Muriel Burk is employed full time through the Department of Veterans Affairs as clinical pharmacy specialist in outcomes and medication safety evaluation. Christina Caplinger was employed by the Department of Veterans Affairs as an infectious diseases fellow at the time this work was completed. She is currently employed by Micromedex. Jefferson Bohan is employed full time by the Department of Veterans Affairs as an infectious diseases fellow. Melinda Neuhauser is employed full time through the Department of Veterans Affairs as a clinical pharmacy specialistinfectious diseases. Matthew Goetz is employed full time through the Department of Veterans Affairs as an infectious diseases physician. Rhongping Zhang is employed full time through the Department of Veterans Affairs as a data analyst. Francesca Cunningham is employed full time through the Department of Veterans Affairs as the director of the VA Center for Medication Safety. This work was supported with resources and use of the Department of Veterans Affairs healthcare system. The views expressed in this article are solely those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs. The authors report no conflicts of interest.
- Centers for Disease Control and Prevention. National hospital discharge survey 2010. Available at: http://www.cdc.gov/nchs/fastats/pneumonia.htm. Accessed December 1, 2014.
- , , , et al. Implementing an antibiotic stewardship program: guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis. 2016;62(10):e51–e77.
- , , , et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community‐acquired pneumonia in adults. Clin Infect Dis. 2007;44(suppl 2):S27–S72.
- American Thoracic Society; Infectious Diseases Society of America. Guidelines for the management of adults with hospital‐acquired, ventilator‐associated, and healthcare‐associated pneumonia. Am J Respir Crit Care Med. 2005;171(4):388–416.
- , , , et al. Short‐ versus long‐course antibacterial therapy for community‐acquired pneumonia: a meta‐analysis. Drugs. 2008;68(13):1841–1854.
- , , , et al. Efficacy of short‐course antibiotic regimens for community‐acquired pneumonia: a meta‐analysis. Am J Med. 2007;120:783–790.
- , , , et al. High‐dose, short‐course levofloxacin for community‐acquired pneumonia: a new treatment paradigm. Clin Infect Dis. 2003;37:752–760.
- , , , et al. Comparison of 7 versus 10 days of antibiotic therapy for hospitalized patients with uncomplicated community‐acquired pneumonia: a prospective. Am J Ther. 1999;6(4):217–222.
- , , , et al. Effectiveness of discontinuing antibiotic treatment after three days versus eight days in mild to moderate‐severe community acquired pneumonia: randomised, double blind trial. BMJ. 2006;332(7554):1355.
- , , , et al. Efficacy of a three day course of azithromycin in moderately severe community‐acquired pneumonia. Eur Respir J. 1995;8(3):398–402.
- , , , et al. Comparison of 8 vs 15 days of antibiotic therapy for ventilator‐associated pneumonia in adults: a randomized trial. JAMA. 2003;290(19):2588–2598.
- , , , et al. Effectiveness of early switch from intravenous to oral antibiotics in severe community acquired pneumonia: multicentre randomized trial. BMJ. 2006;333(7580):1193.
- , , , , . Unnecessary antimicrobial use in the context of Clostridium difficile infection: a call to arms for the Veterans Affairs Antimicrobial Stewardship Task Force. Infect Control Hosp Epidemiol. 2013;34(6):651–653.
- VHA Directive 1031. Antimicrobial stewardship programs. Available at: https://www1.va.gov/vhapublications/ViewPublication.asp?pub_ID=2964. Accessed December 1, 2014.
- , , , et al. Impact of an antimicrobial stewardship intervention on shortening the duration of therapy for community‐acquired pneumonia. Clin Infect Dis. 2012;54:1581–1587.
- , , , et al. Targets for antibiotic and healthcare resource stewardship in inpatient community‐acquired pneumonia: a comparison of management practices with National Guideline Recommendations. Infection. 2013;41(1):135–144.
- , , , , . Pharmacy benefits management in the Veterans Health Administration: 1995 to 2003. Am J Manag Care. 2005;11(2):104–112.
- , , , . Accuracy of administrative data for identifying patients with pneumonia. Am J Med Qual. 2005;20(6):319–328.
- , , , et al. A prediction rule to identify low‐risk patients with community‐acquired pneumonia. N Engl J Med. 1997;336:243–250.
- , , , , . Clostridium difficile infections in Veterans Health Administration acute care facilities. Infect Control Hosp Epidemiol. 2014;35(8):1037–1042.
- , , , , . Organization complexity and primary care providers' perceptions of quality improvement culture within the Veterans Health Administration. Am J Med Qual. 2016;31(2):139–146.
- , , , et al. BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax. 2009;64(suppl 3):iii1–iii55.
- National Institute for Health and Care Excellence. Pneumonia in adults: diagnosis and management. Available at: http://www.nice.org.uk/guidance/cg191. Published December 2014. Accessed May 9, 2016.
- , , , , , . A prospective randomized study of inpatient IV antibiotics for community‐acquired pneumonia: the optimal duration of therapy. Chest. 1996;110(4):965–971.
- , , , et al. Early switch from intravenous to oral antibiotics and early hospital discharge: a prospective observational study of 200 consecutive patients with community‐acquired pneumonia. Arch Intern Med. 1999;159(20):2449–2454.
- , , , . Correlates and economic and clinical outcomes of an adult IV to PO antimicrobial conversion program at an academic medical center in Midwest United States. J Pharm Pract. 2015;28(3):238–248.
- , , , et al. Antimicrobial De‐escalation of treatment for healthcare‐associated pneumonia within the Veterans Healthcare Administration. J Antimicrob Chemother. 2016;71(2):539–546.
- , , , et al. Community‐associated Clostridium difficile infection and antibiotics: a meta‐analysis. J Antimicrob Chemother. 2013;68(9):1951.
- , , , . Meta‐analysis of antibiotics and the risk of community‐associated Clostridium difficle infection. Antimicrob Agents Chemother. 2013;57(5):2326–2332.
- , , , et al. Evaluating diagnosis‐based case‐mix measures: how well do they apply to the VA population? Med Care. 2001;39:692–704.
- , , . What is the role of antimicrobial stewardship in improving outcomes of patients with CAP? Infect Dis Clin North Am. 2013;27(1):211–228.
- , , , et al. Quality of care for elderly patients hospitalized for pneumonia in the United States, 2006 to 2010. JAMA Intern Med. 2014;174(11):1806–1814.
- , , , et al. An evaluation of the impact of antibiotic stewardship on reducing the use of high‐risk antibiotics and its effect on the incidence of Clostridium difficile infection in hospital settings. J Antimicrob Chemother. 2012;67(12):2988–2996.
- , , , et al.; Centers for Disease Control and Prevention. Vital signs: improving antibiotic use among hospitalized patients. MMWR Morb Mortal Wkly Rep. 2014;63(9):194–200.
- , , et al. Effect of procalcitonin‐based guidelines vs standard guidelines on antibiotic use in lower respiratory tract infections: the ProHOSP randomized controlled trial. JAMA. 2009;302(10):1059–1066.
- , , , et al. Cost‐effectiveness of procalcitonin‐guided antibiotic use in community acquired pneumonia. J Gen Intern Med. 2013;28(9):1157–1164.
- , , , , , . Interim evaluation of a Protocol to Optimize the Duration of Pneumonia Therapy at Hospital Discharge. Open Forum Infect Dis. 2015;2(suppl 1):S379.
- , , , et al. Intervention to improve antibiotic selection and shorten treatment durations at the time of hospital discharge. Open Forum Infect Dis. 2015;2(suppl 1):S1.
- , , , et al. Using the electronic medical record to identify community‐acquired pneumonia: toward a replicable automated strategy. PLoS One. 2013;8(8):e70944.
Pneumonia is the leading inpatient infectious diagnosis for which antimicrobials are prescribed in the United States.[1] Supported by moderate‐ to high‐quality evidence, guidelines produced jointly by the Infectious Diseases Society of America (IDSA) and American Thoracic Society (ATS) recommend treating pneumonia with the shortest appropriate duration of antimicrobial therapy to minimize risk for antimicrobial‐related adverse events.[2, 3, 4]
Evidence supports short duration of therapy for treatment of uncomplicated pneumonia.[3, 4, 5, 6, 7, 8, 9, 10, 11, 12] IDSA/ATS guidelines state, patients with CAP [community‐acquired pneumonia] should be treated for a minimum of 5 days (level 1 evidence), should be afebrile for 4872 hours, and should have no more than 1 CAP‐associated sign of clinical instabilitybefore discontinuation of therapy (level II evidence). (Moderate recommendation.) A longer duration of therapy may be warranted if initial therapy was not active against the identified pathogen or if it was complicated by [abscess, empyema, severe immunosuppression, or] extra‐pulmonary infection such as meningitis or endocarditis. (Weak recommendation; level III evidence).[3] Recommended therapy duration for patients with uncomplicated healthcare‐associated pneumonia (HCAP) who respond to initial therapy is 7 to 8 days unless gram‐negative nonfermenting rods or complications are identified (level I evidence).[4]
Within the Veterans Health Administration (VHA), the Antimicrobial Stewardship Taskforce (ASTF) was created to optimize care by developing, deploying, and monitoring a national‐level strategic plan for antimicrobial therapy management improvements.[13, 14] Although single‐center studies have found antimicrobial therapy for CAP being frequently prescribed for longer than recommended, the reproducibility of this finding across different facilities has not been assessed.[15, 16] The ASTF collaborated with the VHA Center for Medication Safety to assess total duration of antimicrobial therapy prescribed for veterans hospitalized with uncomplicated pneumonia.[17]
METHODS
This retrospective multicenter evaluation was conducted in 30 VHA facilities that volunteered to participate in this project. Inpatients discharged with a primary International Classification of Diseases, Ninth Revision, Clinical Modification (ICD‐9‐CM) diagnosis code for pneumonia (or pneumonia diagnosis secondary to primary sepsis diagnosis) during 2013 were evaluated.[18] Diagnoses, admissions, and patient demographics were identified using Veterans Affairs (VA) integrated databases through the Austin Integrated Technology Center. Up to 200 admissions per facility were randomly selected for review. Clinical pharmacists at each facility performed manual record reviews utilizing a standardized protocol and collection form. Completed cases were uploaded to a central database for analysis. Standardized chart abstraction was facilitated by detailed instructions, a data dictionary, and monthly conference calls.
Inclusion criteria required patient admission to any medical ward including intensive care unit (ICU) wards for 48 hours, receipt of >24 hours inpatient antimicrobial therapy (eg, at least 2 doses of a once‐daily antibiotic), documentation of pneumonia discharge diagnosis, and survival until discharge. Exclusion criteria were: complicated pneumonia (lung abscess, necrotizing pneumonia, thoracentesis performed), significant immunosuppression (cancer chemotherapy or absolute neutrophil count 1500 cell/mm3 within 28 days, organ transplantation, human immunodeficiency virus infection); or extrapulmonary infection (eg, meningitis, endocarditis).[3] Patients were also excluded if directly transferred from another inpatient facility, pneumonia occurred >48 hours after admission, index hospitalization was >14 days, previously hospitalized within 28 days prior to index admission, or discharged without documentation of completing a full course of therapy. In addition, patients who received initial therapy discordant with culture and susceptibility findings, were not clinically stable by discharge, or had gram‐negative nonfermentative bacilli cultured were excluded from analysis because according to the guidelines, either data are lacking to support a short duration of therapy such as initial discordant therapy, or a longer duration of therapy may be warranted such as gram‐negative nonfermentative bacilli and clinical instability at discharge.[4] Our intent for these exclusions was to minimize bias against clinician decision making for cases where a longer duration of therapy may have been appropriate.
Patients meeting all criteria had the following abstracted: demographics; prior healthcare exposures, admitting location (ICU or non‐ICU ward), parameters for calculation of Pneumonia Severity Index (PSI), culture results obtained 48 hours of admission, duration of antimicrobials administered during hospitalization and prescribed upon discharge (or recommendations for outpatient duration in the discharge summary for patients receiving medications from non‐VA sources), daily clinical stability assessment, Clostridium difficile infection (CDI) test results, and readmission or death within 28 days of discharge.[19]
Guideline‐similar CAP therapy duration was defined as a minimum of 5 days of antimicrobials, up to a maximum of 3 additional days beginning the first day the patient was afebrile and exhibited 1 sign of clinical instability (heart rate > 100 beats/minute, respiratory rate >24 breaths/minute, systolic blood pressure 90, oxygen saturation 90% or partial pressure of oxygen 60 mm Hg on room air or baseline O2 requirements, or not returned to baseline mental status).[3] This definition was made by consensus decision of the investigators and was necessary to operationalize the relationship between clinical stability and appropriate duration of therapy. Guideline‐similar HCAP therapy duration was defined as 8 days.[4] CDI was defined in accordance with VA criteria for hospital onset and community‐onset healthcare‐facilityassociated CDI.[20] All‐cause hospital readmission and all‐cause death were defined as inpatient readmission or any death, respectively, within 28 days after discharge for the pneumonia admission.
Demographics, comorbidities, microbiology results, antimicrobial utilization, CDI, readmission, and death rates between guideline‐similar and guideline‐excessive duration of antimicrobial therapy groups were characterized with descriptive statistics, Mann‐Whitney U test, or 2 test as indicated (significance defined as P 0.05). Multivariable logistic regression (SAS version 9.3 [SAS Institute, Cary, NC]) was used to assess association between duration of therapy exceeding recommended guidelines with all‐cause readmission and all‐cause death after adjustment for pertinent covariates. Odds ratios (OR) with 95% confidence intervals ( 95% CI) were reported. This medication utilization evaluation (MUE) was reviewed by the Hines VHA Institutional Review Board for Human Subjects Protection. Based on VHA Policy Handbook 1058.05, which defines operations activities that may constitute research, the board determined that the evaluation constituted quality improvement rather than research, and thus was exempt from VHA Human Subjects Research requirements.
RESULTS
There were 3881 admissions eligible for chart review. After manual chart review of inclusion and exclusion criteria, 1739 (44.8%) patients were available for duration of therapy analysis. (Figure 1). Only 1 admission for each patient was analyzed.
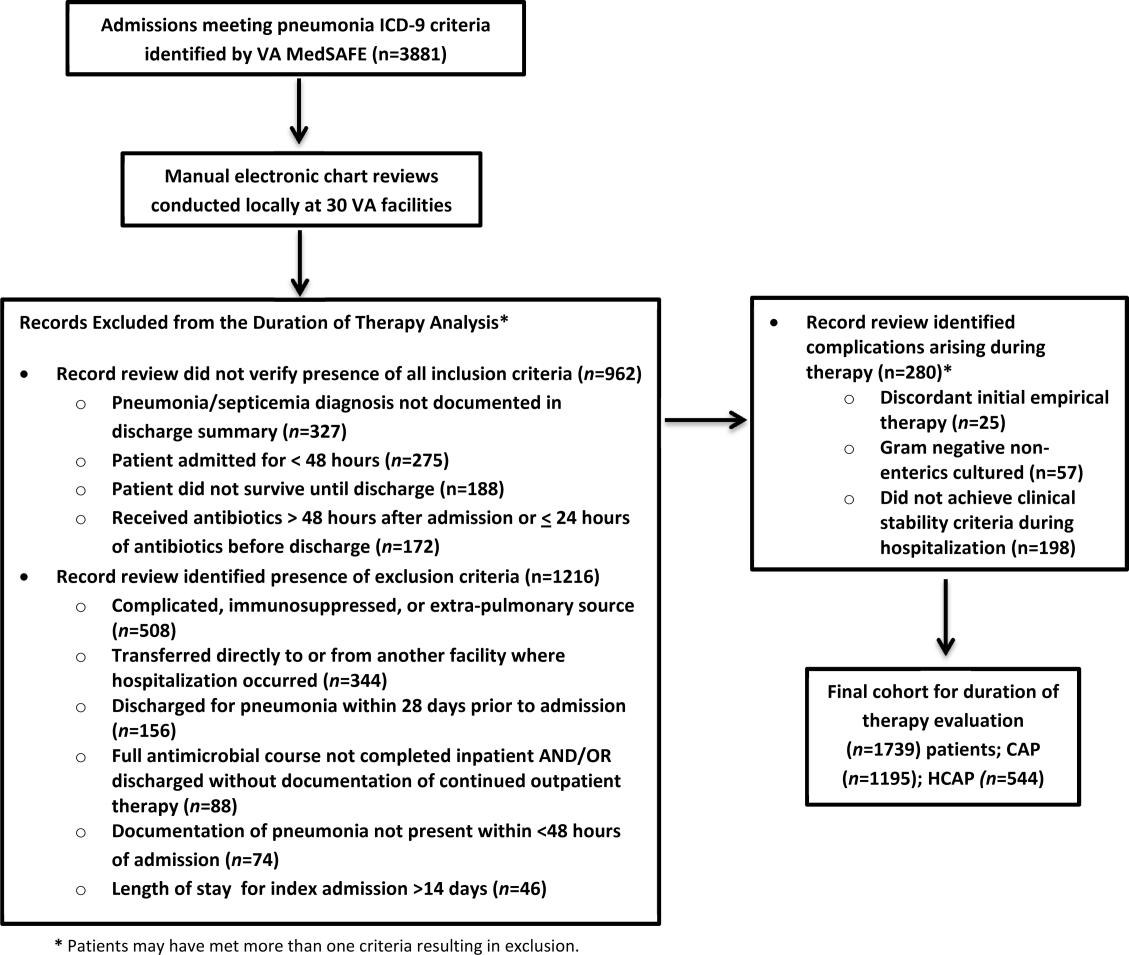
The cohort was comprised primarily of elderly male patients (96.6%) of whom more than two‐thirds were hospitalized for CAP (Table 1). Most patients had significant disease severity as indicated by PSI score; however, only 12% were directly admitted to the ICU. Blood cultures were collected in >95% of cases; lower respiratory cultures were obtained in 39.9% of cases.
| Characteristic | Value |
|---|---|
| |
| Age, y, mean SD | 71.8 (12.7) |
| Gender, male, n (%) | 1,680 (96.6) |
| Living environment at time of index admission, n (%) | |
| Home | 1,416 (81.4) |
| VA community‐based living center | 88 (5.1) |
| Non‐VA long‐term skilled care facility | 95 (5.5) |
| Assisted living facility | 52 (2.9) |
| Not documented | 46 (2.7) |
| Other | 29 (1.7) |
| Prior healthcare exposures, n (%) | |
| Prior hospitalization within last 90 days | 310 (17.8) |
| Residence in a long‐term skilled care facility in last 90 days | 209 (12.0) |
| Chronic dialysis within last 28 days | 52 (3.0) |
| Intravenous antimicrobials within last 28 days | 76 (4.4) |
| Wound, tracheostomy, or ventilator care in last 28 days | 37 (2.1) |
| Community‐acquired pneumonia, n (%) | 1,195 (68.7) |
| Healthcare‐associated pneumonia, n (%) | 544 (31.3) |
| Comorbidities, n (%) | |
| Renal disease | 438 (25.2) |
| Liver disease | 39 (2.2) |
| Congestive heart failure | 436 (25.1) |
| Cerebrovascular disease | 356 (20.4) |
| Neoplastic disease (excluding skin) | 384 (22.1) |
| Severity of illness, n (%) | |
| Pneumonia Severity Index | |
| Class I | 30 (1.8) |
| Class II | 198 (11.4) |
| Class III | 349 (20.1) |
| Class IV | 759 (43.6) |
| Class V | 403 (23.2) |
| Intensive care upon admission | 212 (12.2) |
| Culture collection 48 hours of admission, n (%) | 1,687 (97.0) |
| Blood | 1,631 (96.7) |
| Lower respiratory tract (sputum) | 673 (39.9) |
| Bronchoalveolar lavage | 20 (1.2) |
| Urine | 632 (37.5) |
| Skin/wound | 3 (0.2) |
| Other | 158 (9.4) |
| Facility complexity, n (%) | |
| Level 1a‐c | 1,286 (74.0) |
| Level 2 | 437 (25.1) |
| Level 3 | 16 (0.9) |
Commonly administered antimicrobials during hospitalization and at discharge are summarized in Table 2. Anti‐pseudomonal ‐lactams and antimethicillin‐resistant Staphylococcus aureus antimicrobials were more frequently administered to patients with HCAP, whereas third‐generation cephalosporins and macrolides were more likely to be administered to patients with CAP. Fluoroquinolones were prescribed to 55.3% of patients upon discharge.
| Inpatient Antimicrobials Administered* | ||||
|---|---|---|---|---|
| Portion of Cohort Receiving Antimicrobial, n (%), n = 1,739 |
Therapy Duration Similar With Guidelines, n (%), n = 241 |
Therapy Duration Exceeding Guidelines, n (%), n = 1,498 | Significance | |
| Antimicrobials Dispensed or Recommended at Discharge | ||||
| Portion of Cohort Receiving Antimicrobial, n (%), n = 1,471 |
Therapy Duration Similar With Guidelines, n (%), n = 151 |
Therapy Duration Exceeding Guidelines, n (%), n = 1,320 | Significance | |
| ||||
| Third‐generation cephalosporins | 809 (46.5) | 75 (31.1) | 734 (49.0) | 0.001 |
| Fluoroquinolones | 836 (48.1) | 114 (47.3) | 722 (48.2) | 0.80 |
| Macrolides | 788 (45.3) | 90 (37.3) | 698 (46.6) | 0.01 |
| Pseudomonal ‐lactams | 692 (39.8) | 138 (57.3) | 554 (37.0) | 0.01 |
| Anti‐MRSA antimicrobials | 663 (38.1) | 135 (56.0) | 528 (35.3) | 0.01 |
| Other ‐lactams | 139 (8.0) | 10 (4.2) | 129 (8.6) | 0.02 |
| Tetracyclines | 119 (6.8) | 14 (5.8) | 105 (7.0) | 0.49 |
| Other | 97 (5.6) | 15 (6.2) | 82 (5.5) | 0.64 |
| Third‐generation cephalosporins | 285 (19.4) | 27 (17.9) | 258 (19.6) | 0.62 |
| Fluoroquinolones | 813 (55.3) | 95 (62.9) | 718 (54.4) | 0.05 |
| Macrolides | 203 (13.8) | 20 (13.3) | 183 (13.9) | 0.83 |
| Pseudomonal ‐lactams | 31 (2.1) | 4 (2.7) | 27 (2.1) | 0.62 |
| Anti‐MRSA antimicrobials | 45 (3.1) | 6 (4.0) | 39 (3.0) | 0.49 |
| Other ‐lactams | 239 (16.3) | 13 (8.6) | 226 (17.1) | 0.01 |
| Tetracyclines | 95 (6.5) | 10 (6.6) | 85 (6.4) | 0.93 |
| Other | 44 (3.0) | 5 (3.3) | 39 (3.0) | 0.81 |
Overall, 13.9% of patients with uncomplicated pneumonia received guideline‐similar duration of therapy (Table 3). A greater proportion of HCAP patients (29.0%) received guideline‐similar therapy duration as compared to CAP patients (6.9%) (P 0.01 (Table 3). Median duration of therapy was 7 days (interquartile range [IQR] = 78 days) for guideline‐similar therapy compared to 10 days (913 days) for therapy duration in excess of guideline recommendations. Overall, 97.1 % of patients met clinical stability criteria before day 4 of therapy, yet 50% received 4 days of intravenous (IV) therapy (median was 4 days, IQR = 36 days). Antimicrobial therapy was generally completed after discharge, as only 17.3% received their entire treatment course during hospitalization. Median duration of outpatient oral (PO) antimicrobial therapy was twice as long for guideline‐excessive therapy compared to guideline‐similar therapy (6 vs 3 days), whereas duration of inpatient IV and PO antimicrobial therapy was similar. Patients discharged on a fluoroquinolone were more likely to receive guideline‐similar duration of therapy. The VHA classifies facilities into 3 levels of complexity, with lower scores indicating more complex facilities.[21] Guideline‐similar therapy duration occurred in 10.4% of cases in lower complexity facilities (levels 2 and 3),and 15.1% in more complex facilities (level 1) (P = 0.01). The median duration of therapy was similar for more and less complex facilities, respectively (10 days, IQR = 812 days vs 10 days, IQR = 813 days).
| Outcome |
Therapy Duration Similar With IDSA/ATS Guidelines |
Therapy Duration in Excess of IDSA/ATS Guideline Recommendations | Significance |
|---|---|---|---|
| |||
| Antimicrobial duration consistent with guideline recommendations, n (%) | 241 (13.9) | 1,498 (86.1) | NR |
| CAP* | 83 (6.9) | 1,112 (93.1) | NR |
| HCAP* | 158 (29.0) | 386 (71.0) | NR |
| Total days of therapy for pneumonia, median (IQR) | 7 (78) | 10 (913) | NR |
| CAP | 6 (59) | 10 (812) | 0.01 |
| HCAP | 7 (78) | 11 (1014) | 0.01 |
| Days of IV therapy administered for pneumonia, median (IQR) | 4 (37) | 4 (36) | 0.50 |
| Days of PO inpatient therapy administered, median (IQR) | 1 (03) | 1 (03) | 0.78 |
| Days of PO outpatient therapy dispensed at discharge, median (IQR) | 3 (25) | 6 (47) | 0.01 |
| Days of PO outpatient therapy recommended in Discharge Summary for patients without a VA prescription, median (IQR) | 3 (24) | 5 (47) | 0.01 |
| Aggregate 28‐day hospital readmission, n (%) | 42 (17.4) | 183 (12.2) | 0.03 |
| CAP∥# | 7 (8.4) | 112 (10.1) | 0.58 |
| HCAP∥# | 35 (22.2) | 71 (18.4) | 0.28 |
| Aggregate 28‐day CDI rate, n (%) | 6 (2.5) | 9 (0.6) | 0.03 |
| CAP∥** | 1 (1.2) | 6 (0.5) | 0.44 |
| HCAP∥** | 5 (3.2) | 3 (0.8) | 0.04 |
| Aggregate 28‐day death after discharge, n (%) | 6 (2.5) | 52 (3.5) | 0.43 |
| CAP∥** | 1 (1.2) | 33 (3.0) | 0.35 |
| HCAP∥** | 5 (3.2) | 19 (4.9) | 0.37 |
The 28‐day postdischarge all‐cause readmission rate for patients who received guideline‐similar therapy duration was higher (17.4%) than for patients who received therapy duration in excess of guideline recommendations (12.2%) (P = 0.03). After adjustment for covariates associated with readmission (HCAP, age, prior skilled nursing facility residence, PSI score comorbidity elements), we found no evidence that patients who received guideline‐similar therapy duration were more likely to be readmitted than were patients who received guideline‐excessive duration (OR: 1.1 [95% CI: 0.8, 1.7]) (Table 3). Likewise, no difference in 28‐day all‐cause postdischarge mortality was identified between guideline‐similar and guideline‐excessive duration after adjustment for the same covariates (adjusted OR: 0.5 [95% CI: 0.2, 1.2]) (Table 4).
| Model Variables | Odds Ratio | 95% Confidence Interval | P Value |
|---|---|---|---|
| |||
| Readmission model | |||
| Duration of antibiotics | 1.11 | 0.75, 1.64 | 0.62 |
| HCAP | 1.94 | 1.38, 2.72 | 0.01 |
| Age | 1.01 | 1.00, 1.03 | 0.04 |
| Prior skilled nursing facility residence | 0.91 | 0.59, 1.40 | 0.67 |
| PSI score comorbidity elements | |||
| Neoplastic disease | 1.20 | 0.86, 1.67 | 0.29 |
| Liver disease | 1.55 | 0.66, 3.64 | 0.31 |
| CHF | 1.15 | 0.83, 1.59 | 0.41 |
| Cerebrovascular disease | 1.06 | 0.75, 1.50 | 0.75 |
| Renal disease | 1.51 | 1.09, 2.08 | 0.01 |
| Mortality model | |||
| Duration of antibiotics | 0.53 | 0.23, 1.22 | 0.14 |
| HCAP | 2.53 | 1.38, 4.65 | 0.01 |
| Age | 1.06 | 1.03, 1.09 | 0.01 |
| Prior skilled nursing facility residence | 0.79 | 0.38, 1.66 | 0.53 |
| PSI score comorbidity elements | |||
| Neoplastic disease | 1.03 | 0.57, 1.87 | 0.91 |
| Liver disease | 0.001 | 0.001, >999.9 | 0.98 |
| CHF | 0.73 | 0.39, 1.38 | 0.34 |
| Cerebrovascular disease | 0.82 | 0.43, 1.56 | 0.55 |
| Renal disease | 0.72 | 0.39, 1.35 | 0.31 |
CDI cases (n = 15) were too sparse to adequately perform multivariable logistic regression analysis; however, a higher percentage of patients who received guideline‐similar duration of therapy developed CDI compared to patients who received guideline‐excessive duration of therapy (40.0% vs 13.6%, P 0.01). The median duration of therapy for patients who did and did not develop CDI was similar (8 days, IQR = 714 days vs 10 days, IQR = 812 days, P = 0.85, respectively). Patients who developed CDI had a higher rate of HCAP diagnosis (1.5% vs 0.6%; P = 0.06), were more likely to have concomitant non‐pneumonia infection (40.0% vs 9.5%, P 0.01), have chronic comorbidity (86.7% vs 59.1%, P = 0.03), and to have been admitted to the ICU (26.7% vs 12.1%, P = 0.09).
DISCUSSION
IDSA/ATS guidelines for pneumonia duration of therapy generally agree with other professional society guidelines including the British Thoracic Society and National Institute for Health and Care Excellence.[22, 23] In contrast to existing evidence and guideline recommendations, this multi‐centered evaluation identified prolonged durations of antimicrobial therapy prescribed in 93% and 71% of patients with uncomplicated CAP and HCAP (Table 3), respectively.[3, 4, 5, 6, 7, 8, 9, 10, 11, 12] Almost all (97.1%) uncomplicated CAP and HCAP patients met clinical stability criteria before day 4 of hospitalization, yet the median duration of IV therapy was 4 days. Because criteria for IV to PO conversion and the clinical stability definition utilized in this analysis were similar, many patients may have been eligible for PO therapy earlier, favorably impacting length of stay, cost, and adverse effects.[3, 12, 24, 25, 26] Although median days of inpatient PO therapy administered was 1 day (IQR = 03 days), inpatient observation after PO conversion may not be necessary. The duration of PO therapy was based on calendar days, where if a patient received 1 dose of a once daily antibiotic (ie, levofloxacin), they were considered to have received 1 day of inpatient PO antibiotics even if discharged the same day.
Approximately half of all days of therapy occurred after discharge. Although the median therapy duration for inpatients was similar, the median duration of antimicrobials administered upon hospital discharge was twice as long for patients receiving guideline‐excessive compared to guideline‐similar duration of therapy. The median excess in antibiotic duration is almost entirely accounted for by excess outpatient days of therapy. This is an important consideration for antimicrobial stewardship programs that tend to focus on inpatient antimicrobial use.
Noteworthy observations include the low rate of respiratory tract culture collection (41%) and frequent use of fluoroquinolones upon discharge. Collection of respiratory tract cultures is recommended for all patients with HCAP and patients with CAP who have risk factors for resistant pathogens, characteristics that were common in this cohort.[3, 4] Recently, we identified that respiratory culture collection is associated with increased de‐escalation rates in HCAP, and that culture‐negative patients frequently receive fluoroquinolones.[27] IDSA/ATS CAP guidelines discourage empirically switching to PO fluoroquinolone therapy based on bioavailability considerations alone.[3] Further, fluoroquinolones are considered to be associated with high risk of CDI.[28, 29] Prescription of fluoroquinolone upon discharge was associated with guideline‐similar duration of therapy and was not shown to be associated with CDI; however, power to detect differences between exposures to specific antimicrobials and CDI was low.
CDI was more common in patients with CAP (1.2% vs 0.5%) and HCAP (3.2% vs 0.8%) who received duration of therapy similar with guideline recommendations. This observation is confounded, as patients with CDI had significantly greater comorbidity as well as secondary infections and tended to more frequently receive ICU care. There were no differences in adjusted rates of readmission or death between patients receiving guideline‐similar and guideline‐excessive duration of therapy.
Evaluation strengths included exclusion of patients with complicating conditions possibly requiring prolonged antimicrobial treatment courses, which allowed the evaluation to focus on patients most likely to benefit from shorter course therapy. The definition of appropriate therapy duration was based upon daily assessment of clinical stability criteria that paralleled the CAP guidelines. The definition utilized objective parameters while accounting for patient variability in achieving clinical stability criteria. Finally, the analyses of clinical end points suggest that shorter duration of therapy may be as safe and effective as longer duration of therapy in uncomplicated pneumonia.
Limitations include those common to other analyses conducted within the VHA, including a predominantly elderly male cohort.[30] Only ICD‐9‐CM codes consistent with a discharge diagnosis of pneumonia were used to identify the cohort, and clinical impressions not documented in the medical record may have impacted the clinician's treatment duration decisions. The upper limit of appropriate duration of therapy for CAP was arbitrarily set at up to 3 days beyond meeting clinical stability criteria to provide a reasonable duration of appropriate therapy beyond clinical stability to operationalize the duration of therapy recommendations within the context of the IDSA/ATS guidelines. Additionally, CIs for the ORs of readmission and mortality were broad, and thus too imprecise to determine whether guideline‐similar durations increased or decreased readmission or mortality in comparison with therapy that exceeded guideline recommendations. We could not fully assess the potential for association between guideline‐excessive therapy duration and risk for CDI due to sparse cases. Finally, non‐VA prescription data were not available for all patients, and we relied on intended duration of therapy as recommended by the discharging provider in 4.1% of cases.
Most quality assessments of pneumonia treatment have focused on antimicrobial selection and timely administration or conversion from IV to PO therapy.[31, 32] This evaluation identified potential opportunities for expansion of antimicrobial stewardship activities during the transition of care setting. The efficacy of short‐course ‐lactam, macrolide, or fluoroquinolone therapy for CAP appears equivalent to longer treatment regimens with no difference in adverse event rates, suggesting that optimal duration of therapy may be a rational target for quality improvement.[5, 6, 7, 8, 9, 10, 11, 12, 15, 31] Recommendations for HCAP duration of therapy are extrapolated from a prospective multicentered study, which randomized patients with hospital‐acquired pneumonia to receive 8 versus 15 days of therapy, that identified similar outcomes to ours.[4, 12]
Single‐center studies have identified that antimicrobial therapy for pneumonia is frequently prescribed for longer than recommended by guidelines, which found a similar median duration of therapy as our evaluation.[15, 16] Similar to Jenkins et al., we observed a high rate of fluoroquinolone prescriptions upon discharge.[16]
There are few published examples of interventions designed to limit excessive duration of therapy, particularly for antimicrobials prescribed upon hospital discharge.[15, 33, 34] Serial procalcitonin measurements have been used to guide duration of therapy for pneumonia; however, the costbenefit ratio of procalcitonin measurement is unclear.[35, 36] Procalcitonin use was uncommon, and none of the participating facilities in our evaluation utilized a specific algorithm to guide therapy duration. Limited data suggest that patient‐level prospective audit with feedback may be effective. Advic et al. evaluated management of presumed CAP before and after education and prospective feedback to medical teams concerning antimicrobial selection and duration of therapy.[15] The intervention led to a decrease in median duration of therapy from 10 days (IQR = 813 days) to 7 days (IQR = 78 days) without increasing clinical failure or readmission rates. We recently reported a single‐center evaluation in which pharmacists utilizing a decision support tool while performing discharge medication reconciliation were able to reduce excessive mean duration of therapy from 9.5 days ( 2.4 days) to 8.3 days ( 2.9 days) in patients without complicated pneumonia, with a 19.2% reduction in duration of therapy prescribed at discharge.[37] A similar approach utilizing pharmacists performing discharge review has recently been reported in a community hospital.[38]
Future work should recognize that few patients complete their entire course of therapy as inpatients, and the majority of treatment is prescribed upon discharge. Pivotal time points for antimicrobial stewardship intervention include day 2 to 3 of hospitalization when conveying suggestions for antimicrobial de‐escalation and/or IV to PO conversion, and toward the end of hospitalization during discharge planning. Although it may not be feasible for antimicrobial stewards to review all uncomplicated cases of pneumonia during hospitalization, most facilities have a systematic process for reviewing medications during transitions of care. We believe that interventions intended to assess and recommend shortened courses of therapy are appropriate. These interventions should include a mechanism for support by stewardship personnel or other infectious diseases specialists. Based on our evaluation, the ASTF produced and disseminated clinical guidance documents and tools to triage pneumonia case severity and assess response to therapy. Qualified personnel are encouraged to use this information to make recommendations to providers regarding excessive duration of therapy for uncomplicated cases where appropriate. Other work should include an in‐depth assessment of clinical outcomes related to treatment duration, investigation of provider rationale for prolonged treatment, and duration of antimicrobial therapy prescribed upon discharge for other common disease states. Finally, manual chart review to classify uncomplicated cases and related outcomes was laborious, and automated case identification is technologically plausible and should be explored.[39]
In conclusion, this national VHA MUE found that patients with uncomplicated pneumonia were commonly prescribed antimicrobials for the duration of therapy in excess of guideline recommendations. Patients with uncomplicated pneumonia who received therapy duration consistent with guideline recommendations did not have significantly different all‐cause readmission and death rates compared to patients receiving prolonged treatment. Approximately half of all therapy was prescribed upon hospital discharge, and clinicians as well as antimicrobial stewardship programs should consider these findings to address excessive duration of antimicrobial therapy upon hospital discharge.
Acknowledgements
The authors acknowledge Dr. Michael Fine for his assistance with utilization of the Pneumonia Severity Index, Kenneth Bukowski for assisting with development of data collection tools and data management, and members of the Antimicrobial Stewardship Taskforce Implementation Sub‐Committee. Collaborators in the Pneumonia Duration of Therapy Medication Utilization Evaluation Group include: Biloxi VA (VA Gulf Coast): Cheryl Hankins, PharmD, BCPS; Central Alabama VAMC: Lauren Rass, PharmD, BCPS, Kelly Mooney, PharmD, BCPS; Central Arkansas: Nicholas Tinsley, MS, PharmD; Chillicothe VA: Stephen Hanson, PharmD, BCPS, Beth Gallaugher, BSN, RN, Elizabeth Baltenberger, PharmD; Cincinnati VA: Jason Hiett, PharmD, BCPS, Victoria Tate, PharmD, BCPS, Brian Salzman, PharmD; Dorn Medical Center: MaryAnne Maurer, PharmD, BCPS, BCACP, Rebekah Sipes, PharmD, BCACP, Ginger Ervin, PharmD; Dwight D. Eisenhower VAMC: Emily Potter, PharmD; Hudson Valley: Rita Lee Bodine, PharmD, Clement Chen, PharmD, Cristina Fantino, PharmD; James H. Quillen VAMC: Marty Vannoy, PharmD, BCPS, Erin Harshbarger, PharmD, Kristen Nelsen, PharmD; Jesse Brown VAMC: Lisa Young, PharmD, BCPS, AQ‐ID, Andrea Bidlencik, PharmD, BCPS; Kansas City VA: Jamie Guyear, PharmD, AQ‐ID, Ann Ungerman, PharmD, BCPS, Lauri Witt, PharmD, BCACP; Louis Stokes Cleveland VAMC: Amy Hirsch, PharmD, BCPS, Steven Adoryan, PharmD, BCP‐CC, Amanda Miller, PharmD, BCPS; Maine VAMC: Joel Coon, PharmD, Rachel Naida, PharmD, Kelly Grossman, PharmD; Martinsburg VAMC: Kelly Li, PharmD, Sarah Mickanis, PharmD, BCPS; Miami VA Medical Center: Mara Carrasquillo, BS, PharmD, Maribel Toro, PharmD; North Florida/South Georgia Veterans Health System: Nora Morgan, PharmD, Hugh Frank, PharmD, BCPS, BCPP, Sarah Onofrio, PharmD, BCPS; North Texas HCS: Susan Duquaine, PharmD, BCPS, AQ‐ID, Ruben Villaneuva, PharmD, BCPS, Jaela Dahl, PharmD, BCPS; Ozarks: Andrew Siler, PharmD, BCPS, Michele Walker, PharmD, CGP, Jennifer Cole, PharmD, BCPS, BCCCP; Providence VAMC: Kerry LaPlante, PharmD, FCCP, Lindsey Williamson, PharmD; Richmond VA: Daniel Tassone, PharmD, BCPS; Salisbury VAMC: Brett Norem, PharmD, Marrisa Ragonesi, PharmD; San Juan VA: Monica Sanabria‐Seda, PharmD, BCPS, Jaime Velez‐Fores, PharmD, BCPS, AQ‐ID, Norma Ayala‐Burgos, PharmD; Sioux Falls VA: Andrea Aylward, PharmD, BCPS; South Texas HCS: Kelly Echevarria, PharmD, BCPS, AQ‐ID, Manuel Escobar, PharmD; Tennessee Valley HCS: Casey Ryals, PharmD, BCACP, Molly Hurst, PharmD, Jonathan Hale, PharmD; VA Central Iowa Health Care System: Jenny Phabmixay, PharmD, BCPS, Mackenzie Brown, PharmD, BCPS, Cynthia Muthusi, PharmD, BCPS; VA Loma Linda: Tony Chau, PharmD; VA Sierra Nevada: Scott Mambourg, PharmD, BCPS, AAHIVP, Matthew Han, PharmD, Nathan Mihoch, PharmD; VA WNY Healthcare System: Kari Mergenhagen, PharmD, BCPS, AQ‐ID, Christine Ruh, PharmD, BCPS; Veterans Affairs Salt Lake City Health System: Emily Spivak, MD, MHS, Patricia Orlando, PharmD
Disclosures: Karl Madaras‐Kelly is employed full time by Idaho State University and has a without compensation appointment as a clinical pharmacist at the Boise VA Medical Center. He receives grant support unrelated to this work through the Department of Veterans Affairs subcontracted to Idaho State University. Muriel Burk is employed full time through the Department of Veterans Affairs as clinical pharmacy specialist in outcomes and medication safety evaluation. Christina Caplinger was employed by the Department of Veterans Affairs as an infectious diseases fellow at the time this work was completed. She is currently employed by Micromedex. Jefferson Bohan is employed full time by the Department of Veterans Affairs as an infectious diseases fellow. Melinda Neuhauser is employed full time through the Department of Veterans Affairs as a clinical pharmacy specialistinfectious diseases. Matthew Goetz is employed full time through the Department of Veterans Affairs as an infectious diseases physician. Rhongping Zhang is employed full time through the Department of Veterans Affairs as a data analyst. Francesca Cunningham is employed full time through the Department of Veterans Affairs as the director of the VA Center for Medication Safety. This work was supported with resources and use of the Department of Veterans Affairs healthcare system. The views expressed in this article are solely those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs. The authors report no conflicts of interest.
Pneumonia is the leading inpatient infectious diagnosis for which antimicrobials are prescribed in the United States.[1] Supported by moderate‐ to high‐quality evidence, guidelines produced jointly by the Infectious Diseases Society of America (IDSA) and American Thoracic Society (ATS) recommend treating pneumonia with the shortest appropriate duration of antimicrobial therapy to minimize risk for antimicrobial‐related adverse events.[2, 3, 4]
Evidence supports short duration of therapy for treatment of uncomplicated pneumonia.[3, 4, 5, 6, 7, 8, 9, 10, 11, 12] IDSA/ATS guidelines state, patients with CAP [community‐acquired pneumonia] should be treated for a minimum of 5 days (level 1 evidence), should be afebrile for 4872 hours, and should have no more than 1 CAP‐associated sign of clinical instabilitybefore discontinuation of therapy (level II evidence). (Moderate recommendation.) A longer duration of therapy may be warranted if initial therapy was not active against the identified pathogen or if it was complicated by [abscess, empyema, severe immunosuppression, or] extra‐pulmonary infection such as meningitis or endocarditis. (Weak recommendation; level III evidence).[3] Recommended therapy duration for patients with uncomplicated healthcare‐associated pneumonia (HCAP) who respond to initial therapy is 7 to 8 days unless gram‐negative nonfermenting rods or complications are identified (level I evidence).[4]
Within the Veterans Health Administration (VHA), the Antimicrobial Stewardship Taskforce (ASTF) was created to optimize care by developing, deploying, and monitoring a national‐level strategic plan for antimicrobial therapy management improvements.[13, 14] Although single‐center studies have found antimicrobial therapy for CAP being frequently prescribed for longer than recommended, the reproducibility of this finding across different facilities has not been assessed.[15, 16] The ASTF collaborated with the VHA Center for Medication Safety to assess total duration of antimicrobial therapy prescribed for veterans hospitalized with uncomplicated pneumonia.[17]
METHODS
This retrospective multicenter evaluation was conducted in 30 VHA facilities that volunteered to participate in this project. Inpatients discharged with a primary International Classification of Diseases, Ninth Revision, Clinical Modification (ICD‐9‐CM) diagnosis code for pneumonia (or pneumonia diagnosis secondary to primary sepsis diagnosis) during 2013 were evaluated.[18] Diagnoses, admissions, and patient demographics were identified using Veterans Affairs (VA) integrated databases through the Austin Integrated Technology Center. Up to 200 admissions per facility were randomly selected for review. Clinical pharmacists at each facility performed manual record reviews utilizing a standardized protocol and collection form. Completed cases were uploaded to a central database for analysis. Standardized chart abstraction was facilitated by detailed instructions, a data dictionary, and monthly conference calls.
Inclusion criteria required patient admission to any medical ward including intensive care unit (ICU) wards for 48 hours, receipt of >24 hours inpatient antimicrobial therapy (eg, at least 2 doses of a once‐daily antibiotic), documentation of pneumonia discharge diagnosis, and survival until discharge. Exclusion criteria were: complicated pneumonia (lung abscess, necrotizing pneumonia, thoracentesis performed), significant immunosuppression (cancer chemotherapy or absolute neutrophil count 1500 cell/mm3 within 28 days, organ transplantation, human immunodeficiency virus infection); or extrapulmonary infection (eg, meningitis, endocarditis).[3] Patients were also excluded if directly transferred from another inpatient facility, pneumonia occurred >48 hours after admission, index hospitalization was >14 days, previously hospitalized within 28 days prior to index admission, or discharged without documentation of completing a full course of therapy. In addition, patients who received initial therapy discordant with culture and susceptibility findings, were not clinically stable by discharge, or had gram‐negative nonfermentative bacilli cultured were excluded from analysis because according to the guidelines, either data are lacking to support a short duration of therapy such as initial discordant therapy, or a longer duration of therapy may be warranted such as gram‐negative nonfermentative bacilli and clinical instability at discharge.[4] Our intent for these exclusions was to minimize bias against clinician decision making for cases where a longer duration of therapy may have been appropriate.
Patients meeting all criteria had the following abstracted: demographics; prior healthcare exposures, admitting location (ICU or non‐ICU ward), parameters for calculation of Pneumonia Severity Index (PSI), culture results obtained 48 hours of admission, duration of antimicrobials administered during hospitalization and prescribed upon discharge (or recommendations for outpatient duration in the discharge summary for patients receiving medications from non‐VA sources), daily clinical stability assessment, Clostridium difficile infection (CDI) test results, and readmission or death within 28 days of discharge.[19]
Guideline‐similar CAP therapy duration was defined as a minimum of 5 days of antimicrobials, up to a maximum of 3 additional days beginning the first day the patient was afebrile and exhibited 1 sign of clinical instability (heart rate > 100 beats/minute, respiratory rate >24 breaths/minute, systolic blood pressure 90, oxygen saturation 90% or partial pressure of oxygen 60 mm Hg on room air or baseline O2 requirements, or not returned to baseline mental status).[3] This definition was made by consensus decision of the investigators and was necessary to operationalize the relationship between clinical stability and appropriate duration of therapy. Guideline‐similar HCAP therapy duration was defined as 8 days.[4] CDI was defined in accordance with VA criteria for hospital onset and community‐onset healthcare‐facilityassociated CDI.[20] All‐cause hospital readmission and all‐cause death were defined as inpatient readmission or any death, respectively, within 28 days after discharge for the pneumonia admission.
Demographics, comorbidities, microbiology results, antimicrobial utilization, CDI, readmission, and death rates between guideline‐similar and guideline‐excessive duration of antimicrobial therapy groups were characterized with descriptive statistics, Mann‐Whitney U test, or 2 test as indicated (significance defined as P 0.05). Multivariable logistic regression (SAS version 9.3 [SAS Institute, Cary, NC]) was used to assess association between duration of therapy exceeding recommended guidelines with all‐cause readmission and all‐cause death after adjustment for pertinent covariates. Odds ratios (OR) with 95% confidence intervals ( 95% CI) were reported. This medication utilization evaluation (MUE) was reviewed by the Hines VHA Institutional Review Board for Human Subjects Protection. Based on VHA Policy Handbook 1058.05, which defines operations activities that may constitute research, the board determined that the evaluation constituted quality improvement rather than research, and thus was exempt from VHA Human Subjects Research requirements.
RESULTS
There were 3881 admissions eligible for chart review. After manual chart review of inclusion and exclusion criteria, 1739 (44.8%) patients were available for duration of therapy analysis. (Figure 1). Only 1 admission for each patient was analyzed.
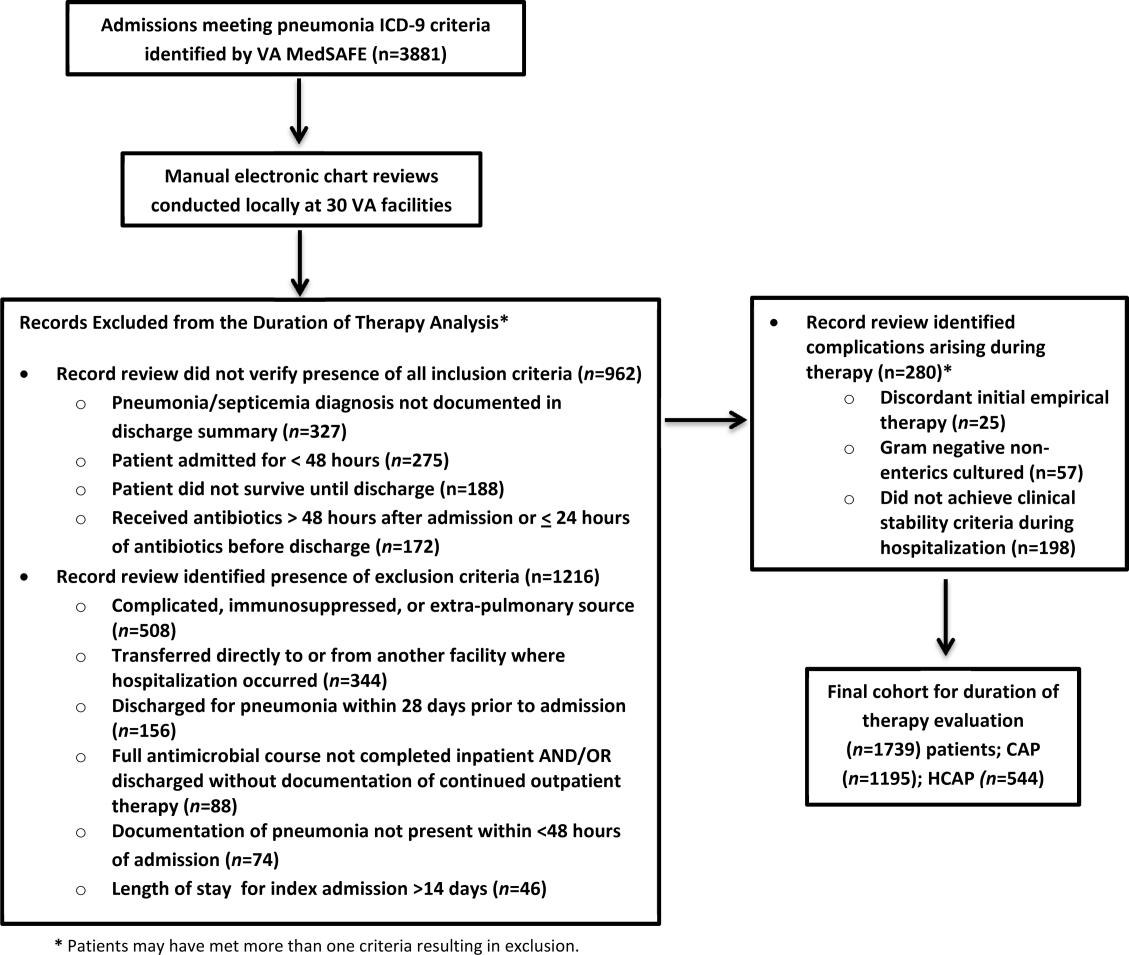
The cohort was comprised primarily of elderly male patients (96.6%) of whom more than two‐thirds were hospitalized for CAP (Table 1). Most patients had significant disease severity as indicated by PSI score; however, only 12% were directly admitted to the ICU. Blood cultures were collected in >95% of cases; lower respiratory cultures were obtained in 39.9% of cases.
| Characteristic | Value |
|---|---|
| |
| Age, y, mean SD | 71.8 (12.7) |
| Gender, male, n (%) | 1,680 (96.6) |
| Living environment at time of index admission, n (%) | |
| Home | 1,416 (81.4) |
| VA community‐based living center | 88 (5.1) |
| Non‐VA long‐term skilled care facility | 95 (5.5) |
| Assisted living facility | 52 (2.9) |
| Not documented | 46 (2.7) |
| Other | 29 (1.7) |
| Prior healthcare exposures, n (%) | |
| Prior hospitalization within last 90 days | 310 (17.8) |
| Residence in a long‐term skilled care facility in last 90 days | 209 (12.0) |
| Chronic dialysis within last 28 days | 52 (3.0) |
| Intravenous antimicrobials within last 28 days | 76 (4.4) |
| Wound, tracheostomy, or ventilator care in last 28 days | 37 (2.1) |
| Community‐acquired pneumonia, n (%) | 1,195 (68.7) |
| Healthcare‐associated pneumonia, n (%) | 544 (31.3) |
| Comorbidities, n (%) | |
| Renal disease | 438 (25.2) |
| Liver disease | 39 (2.2) |
| Congestive heart failure | 436 (25.1) |
| Cerebrovascular disease | 356 (20.4) |
| Neoplastic disease (excluding skin) | 384 (22.1) |
| Severity of illness, n (%) | |
| Pneumonia Severity Index | |
| Class I | 30 (1.8) |
| Class II | 198 (11.4) |
| Class III | 349 (20.1) |
| Class IV | 759 (43.6) |
| Class V | 403 (23.2) |
| Intensive care upon admission | 212 (12.2) |
| Culture collection 48 hours of admission, n (%) | 1,687 (97.0) |
| Blood | 1,631 (96.7) |
| Lower respiratory tract (sputum) | 673 (39.9) |
| Bronchoalveolar lavage | 20 (1.2) |
| Urine | 632 (37.5) |
| Skin/wound | 3 (0.2) |
| Other | 158 (9.4) |
| Facility complexity, n (%) | |
| Level 1a‐c | 1,286 (74.0) |
| Level 2 | 437 (25.1) |
| Level 3 | 16 (0.9) |
Commonly administered antimicrobials during hospitalization and at discharge are summarized in Table 2. Anti‐pseudomonal ‐lactams and antimethicillin‐resistant Staphylococcus aureus antimicrobials were more frequently administered to patients with HCAP, whereas third‐generation cephalosporins and macrolides were more likely to be administered to patients with CAP. Fluoroquinolones were prescribed to 55.3% of patients upon discharge.
| Inpatient Antimicrobials Administered* | ||||
|---|---|---|---|---|
| Portion of Cohort Receiving Antimicrobial, n (%), n = 1,739 |
Therapy Duration Similar With Guidelines, n (%), n = 241 |
Therapy Duration Exceeding Guidelines, n (%), n = 1,498 | Significance | |
| Antimicrobials Dispensed or Recommended at Discharge | ||||
| Portion of Cohort Receiving Antimicrobial, n (%), n = 1,471 |
Therapy Duration Similar With Guidelines, n (%), n = 151 |
Therapy Duration Exceeding Guidelines, n (%), n = 1,320 | Significance | |
| ||||
| Third‐generation cephalosporins | 809 (46.5) | 75 (31.1) | 734 (49.0) | 0.001 |
| Fluoroquinolones | 836 (48.1) | 114 (47.3) | 722 (48.2) | 0.80 |
| Macrolides | 788 (45.3) | 90 (37.3) | 698 (46.6) | 0.01 |
| Pseudomonal ‐lactams | 692 (39.8) | 138 (57.3) | 554 (37.0) | 0.01 |
| Anti‐MRSA antimicrobials | 663 (38.1) | 135 (56.0) | 528 (35.3) | 0.01 |
| Other ‐lactams | 139 (8.0) | 10 (4.2) | 129 (8.6) | 0.02 |
| Tetracyclines | 119 (6.8) | 14 (5.8) | 105 (7.0) | 0.49 |
| Other | 97 (5.6) | 15 (6.2) | 82 (5.5) | 0.64 |
| Third‐generation cephalosporins | 285 (19.4) | 27 (17.9) | 258 (19.6) | 0.62 |
| Fluoroquinolones | 813 (55.3) | 95 (62.9) | 718 (54.4) | 0.05 |
| Macrolides | 203 (13.8) | 20 (13.3) | 183 (13.9) | 0.83 |
| Pseudomonal ‐lactams | 31 (2.1) | 4 (2.7) | 27 (2.1) | 0.62 |
| Anti‐MRSA antimicrobials | 45 (3.1) | 6 (4.0) | 39 (3.0) | 0.49 |
| Other ‐lactams | 239 (16.3) | 13 (8.6) | 226 (17.1) | 0.01 |
| Tetracyclines | 95 (6.5) | 10 (6.6) | 85 (6.4) | 0.93 |
| Other | 44 (3.0) | 5 (3.3) | 39 (3.0) | 0.81 |
Overall, 13.9% of patients with uncomplicated pneumonia received guideline‐similar duration of therapy (Table 3). A greater proportion of HCAP patients (29.0%) received guideline‐similar therapy duration as compared to CAP patients (6.9%) (P 0.01 (Table 3). Median duration of therapy was 7 days (interquartile range [IQR] = 78 days) for guideline‐similar therapy compared to 10 days (913 days) for therapy duration in excess of guideline recommendations. Overall, 97.1 % of patients met clinical stability criteria before day 4 of therapy, yet 50% received 4 days of intravenous (IV) therapy (median was 4 days, IQR = 36 days). Antimicrobial therapy was generally completed after discharge, as only 17.3% received their entire treatment course during hospitalization. Median duration of outpatient oral (PO) antimicrobial therapy was twice as long for guideline‐excessive therapy compared to guideline‐similar therapy (6 vs 3 days), whereas duration of inpatient IV and PO antimicrobial therapy was similar. Patients discharged on a fluoroquinolone were more likely to receive guideline‐similar duration of therapy. The VHA classifies facilities into 3 levels of complexity, with lower scores indicating more complex facilities.[21] Guideline‐similar therapy duration occurred in 10.4% of cases in lower complexity facilities (levels 2 and 3),and 15.1% in more complex facilities (level 1) (P = 0.01). The median duration of therapy was similar for more and less complex facilities, respectively (10 days, IQR = 812 days vs 10 days, IQR = 813 days).
| Outcome |
Therapy Duration Similar With IDSA/ATS Guidelines |
Therapy Duration in Excess of IDSA/ATS Guideline Recommendations | Significance |
|---|---|---|---|
| |||
| Antimicrobial duration consistent with guideline recommendations, n (%) | 241 (13.9) | 1,498 (86.1) | NR |
| CAP* | 83 (6.9) | 1,112 (93.1) | NR |
| HCAP* | 158 (29.0) | 386 (71.0) | NR |
| Total days of therapy for pneumonia, median (IQR) | 7 (78) | 10 (913) | NR |
| CAP | 6 (59) | 10 (812) | 0.01 |
| HCAP | 7 (78) | 11 (1014) | 0.01 |
| Days of IV therapy administered for pneumonia, median (IQR) | 4 (37) | 4 (36) | 0.50 |
| Days of PO inpatient therapy administered, median (IQR) | 1 (03) | 1 (03) | 0.78 |
| Days of PO outpatient therapy dispensed at discharge, median (IQR) | 3 (25) | 6 (47) | 0.01 |
| Days of PO outpatient therapy recommended in Discharge Summary for patients without a VA prescription, median (IQR) | 3 (24) | 5 (47) | 0.01 |
| Aggregate 28‐day hospital readmission, n (%) | 42 (17.4) | 183 (12.2) | 0.03 |
| CAP∥# | 7 (8.4) | 112 (10.1) | 0.58 |
| HCAP∥# | 35 (22.2) | 71 (18.4) | 0.28 |
| Aggregate 28‐day CDI rate, n (%) | 6 (2.5) | 9 (0.6) | 0.03 |
| CAP∥** | 1 (1.2) | 6 (0.5) | 0.44 |
| HCAP∥** | 5 (3.2) | 3 (0.8) | 0.04 |
| Aggregate 28‐day death after discharge, n (%) | 6 (2.5) | 52 (3.5) | 0.43 |
| CAP∥** | 1 (1.2) | 33 (3.0) | 0.35 |
| HCAP∥** | 5 (3.2) | 19 (4.9) | 0.37 |
The 28‐day postdischarge all‐cause readmission rate for patients who received guideline‐similar therapy duration was higher (17.4%) than for patients who received therapy duration in excess of guideline recommendations (12.2%) (P = 0.03). After adjustment for covariates associated with readmission (HCAP, age, prior skilled nursing facility residence, PSI score comorbidity elements), we found no evidence that patients who received guideline‐similar therapy duration were more likely to be readmitted than were patients who received guideline‐excessive duration (OR: 1.1 [95% CI: 0.8, 1.7]) (Table 3). Likewise, no difference in 28‐day all‐cause postdischarge mortality was identified between guideline‐similar and guideline‐excessive duration after adjustment for the same covariates (adjusted OR: 0.5 [95% CI: 0.2, 1.2]) (Table 4).
| Model Variables | Odds Ratio | 95% Confidence Interval | P Value |
|---|---|---|---|
| |||
| Readmission model | |||
| Duration of antibiotics | 1.11 | 0.75, 1.64 | 0.62 |
| HCAP | 1.94 | 1.38, 2.72 | 0.01 |
| Age | 1.01 | 1.00, 1.03 | 0.04 |
| Prior skilled nursing facility residence | 0.91 | 0.59, 1.40 | 0.67 |
| PSI score comorbidity elements | |||
| Neoplastic disease | 1.20 | 0.86, 1.67 | 0.29 |
| Liver disease | 1.55 | 0.66, 3.64 | 0.31 |
| CHF | 1.15 | 0.83, 1.59 | 0.41 |
| Cerebrovascular disease | 1.06 | 0.75, 1.50 | 0.75 |
| Renal disease | 1.51 | 1.09, 2.08 | 0.01 |
| Mortality model | |||
| Duration of antibiotics | 0.53 | 0.23, 1.22 | 0.14 |
| HCAP | 2.53 | 1.38, 4.65 | 0.01 |
| Age | 1.06 | 1.03, 1.09 | 0.01 |
| Prior skilled nursing facility residence | 0.79 | 0.38, 1.66 | 0.53 |
| PSI score comorbidity elements | |||
| Neoplastic disease | 1.03 | 0.57, 1.87 | 0.91 |
| Liver disease | 0.001 | 0.001, >999.9 | 0.98 |
| CHF | 0.73 | 0.39, 1.38 | 0.34 |
| Cerebrovascular disease | 0.82 | 0.43, 1.56 | 0.55 |
| Renal disease | 0.72 | 0.39, 1.35 | 0.31 |
CDI cases (n = 15) were too sparse to adequately perform multivariable logistic regression analysis; however, a higher percentage of patients who received guideline‐similar duration of therapy developed CDI compared to patients who received guideline‐excessive duration of therapy (40.0% vs 13.6%, P 0.01). The median duration of therapy for patients who did and did not develop CDI was similar (8 days, IQR = 714 days vs 10 days, IQR = 812 days, P = 0.85, respectively). Patients who developed CDI had a higher rate of HCAP diagnosis (1.5% vs 0.6%; P = 0.06), were more likely to have concomitant non‐pneumonia infection (40.0% vs 9.5%, P 0.01), have chronic comorbidity (86.7% vs 59.1%, P = 0.03), and to have been admitted to the ICU (26.7% vs 12.1%, P = 0.09).
DISCUSSION
IDSA/ATS guidelines for pneumonia duration of therapy generally agree with other professional society guidelines including the British Thoracic Society and National Institute for Health and Care Excellence.[22, 23] In contrast to existing evidence and guideline recommendations, this multi‐centered evaluation identified prolonged durations of antimicrobial therapy prescribed in 93% and 71% of patients with uncomplicated CAP and HCAP (Table 3), respectively.[3, 4, 5, 6, 7, 8, 9, 10, 11, 12] Almost all (97.1%) uncomplicated CAP and HCAP patients met clinical stability criteria before day 4 of hospitalization, yet the median duration of IV therapy was 4 days. Because criteria for IV to PO conversion and the clinical stability definition utilized in this analysis were similar, many patients may have been eligible for PO therapy earlier, favorably impacting length of stay, cost, and adverse effects.[3, 12, 24, 25, 26] Although median days of inpatient PO therapy administered was 1 day (IQR = 03 days), inpatient observation after PO conversion may not be necessary. The duration of PO therapy was based on calendar days, where if a patient received 1 dose of a once daily antibiotic (ie, levofloxacin), they were considered to have received 1 day of inpatient PO antibiotics even if discharged the same day.
Approximately half of all days of therapy occurred after discharge. Although the median therapy duration for inpatients was similar, the median duration of antimicrobials administered upon hospital discharge was twice as long for patients receiving guideline‐excessive compared to guideline‐similar duration of therapy. The median excess in antibiotic duration is almost entirely accounted for by excess outpatient days of therapy. This is an important consideration for antimicrobial stewardship programs that tend to focus on inpatient antimicrobial use.
Noteworthy observations include the low rate of respiratory tract culture collection (41%) and frequent use of fluoroquinolones upon discharge. Collection of respiratory tract cultures is recommended for all patients with HCAP and patients with CAP who have risk factors for resistant pathogens, characteristics that were common in this cohort.[3, 4] Recently, we identified that respiratory culture collection is associated with increased de‐escalation rates in HCAP, and that culture‐negative patients frequently receive fluoroquinolones.[27] IDSA/ATS CAP guidelines discourage empirically switching to PO fluoroquinolone therapy based on bioavailability considerations alone.[3] Further, fluoroquinolones are considered to be associated with high risk of CDI.[28, 29] Prescription of fluoroquinolone upon discharge was associated with guideline‐similar duration of therapy and was not shown to be associated with CDI; however, power to detect differences between exposures to specific antimicrobials and CDI was low.
CDI was more common in patients with CAP (1.2% vs 0.5%) and HCAP (3.2% vs 0.8%) who received duration of therapy similar with guideline recommendations. This observation is confounded, as patients with CDI had significantly greater comorbidity as well as secondary infections and tended to more frequently receive ICU care. There were no differences in adjusted rates of readmission or death between patients receiving guideline‐similar and guideline‐excessive duration of therapy.
Evaluation strengths included exclusion of patients with complicating conditions possibly requiring prolonged antimicrobial treatment courses, which allowed the evaluation to focus on patients most likely to benefit from shorter course therapy. The definition of appropriate therapy duration was based upon daily assessment of clinical stability criteria that paralleled the CAP guidelines. The definition utilized objective parameters while accounting for patient variability in achieving clinical stability criteria. Finally, the analyses of clinical end points suggest that shorter duration of therapy may be as safe and effective as longer duration of therapy in uncomplicated pneumonia.
Limitations include those common to other analyses conducted within the VHA, including a predominantly elderly male cohort.[30] Only ICD‐9‐CM codes consistent with a discharge diagnosis of pneumonia were used to identify the cohort, and clinical impressions not documented in the medical record may have impacted the clinician's treatment duration decisions. The upper limit of appropriate duration of therapy for CAP was arbitrarily set at up to 3 days beyond meeting clinical stability criteria to provide a reasonable duration of appropriate therapy beyond clinical stability to operationalize the duration of therapy recommendations within the context of the IDSA/ATS guidelines. Additionally, CIs for the ORs of readmission and mortality were broad, and thus too imprecise to determine whether guideline‐similar durations increased or decreased readmission or mortality in comparison with therapy that exceeded guideline recommendations. We could not fully assess the potential for association between guideline‐excessive therapy duration and risk for CDI due to sparse cases. Finally, non‐VA prescription data were not available for all patients, and we relied on intended duration of therapy as recommended by the discharging provider in 4.1% of cases.
Most quality assessments of pneumonia treatment have focused on antimicrobial selection and timely administration or conversion from IV to PO therapy.[31, 32] This evaluation identified potential opportunities for expansion of antimicrobial stewardship activities during the transition of care setting. The efficacy of short‐course ‐lactam, macrolide, or fluoroquinolone therapy for CAP appears equivalent to longer treatment regimens with no difference in adverse event rates, suggesting that optimal duration of therapy may be a rational target for quality improvement.[5, 6, 7, 8, 9, 10, 11, 12, 15, 31] Recommendations for HCAP duration of therapy are extrapolated from a prospective multicentered study, which randomized patients with hospital‐acquired pneumonia to receive 8 versus 15 days of therapy, that identified similar outcomes to ours.[4, 12]
Single‐center studies have identified that antimicrobial therapy for pneumonia is frequently prescribed for longer than recommended by guidelines, which found a similar median duration of therapy as our evaluation.[15, 16] Similar to Jenkins et al., we observed a high rate of fluoroquinolone prescriptions upon discharge.[16]
There are few published examples of interventions designed to limit excessive duration of therapy, particularly for antimicrobials prescribed upon hospital discharge.[15, 33, 34] Serial procalcitonin measurements have been used to guide duration of therapy for pneumonia; however, the costbenefit ratio of procalcitonin measurement is unclear.[35, 36] Procalcitonin use was uncommon, and none of the participating facilities in our evaluation utilized a specific algorithm to guide therapy duration. Limited data suggest that patient‐level prospective audit with feedback may be effective. Advic et al. evaluated management of presumed CAP before and after education and prospective feedback to medical teams concerning antimicrobial selection and duration of therapy.[15] The intervention led to a decrease in median duration of therapy from 10 days (IQR = 813 days) to 7 days (IQR = 78 days) without increasing clinical failure or readmission rates. We recently reported a single‐center evaluation in which pharmacists utilizing a decision support tool while performing discharge medication reconciliation were able to reduce excessive mean duration of therapy from 9.5 days ( 2.4 days) to 8.3 days ( 2.9 days) in patients without complicated pneumonia, with a 19.2% reduction in duration of therapy prescribed at discharge.[37] A similar approach utilizing pharmacists performing discharge review has recently been reported in a community hospital.[38]
Future work should recognize that few patients complete their entire course of therapy as inpatients, and the majority of treatment is prescribed upon discharge. Pivotal time points for antimicrobial stewardship intervention include day 2 to 3 of hospitalization when conveying suggestions for antimicrobial de‐escalation and/or IV to PO conversion, and toward the end of hospitalization during discharge planning. Although it may not be feasible for antimicrobial stewards to review all uncomplicated cases of pneumonia during hospitalization, most facilities have a systematic process for reviewing medications during transitions of care. We believe that interventions intended to assess and recommend shortened courses of therapy are appropriate. These interventions should include a mechanism for support by stewardship personnel or other infectious diseases specialists. Based on our evaluation, the ASTF produced and disseminated clinical guidance documents and tools to triage pneumonia case severity and assess response to therapy. Qualified personnel are encouraged to use this information to make recommendations to providers regarding excessive duration of therapy for uncomplicated cases where appropriate. Other work should include an in‐depth assessment of clinical outcomes related to treatment duration, investigation of provider rationale for prolonged treatment, and duration of antimicrobial therapy prescribed upon discharge for other common disease states. Finally, manual chart review to classify uncomplicated cases and related outcomes was laborious, and automated case identification is technologically plausible and should be explored.[39]
In conclusion, this national VHA MUE found that patients with uncomplicated pneumonia were commonly prescribed antimicrobials for the duration of therapy in excess of guideline recommendations. Patients with uncomplicated pneumonia who received therapy duration consistent with guideline recommendations did not have significantly different all‐cause readmission and death rates compared to patients receiving prolonged treatment. Approximately half of all therapy was prescribed upon hospital discharge, and clinicians as well as antimicrobial stewardship programs should consider these findings to address excessive duration of antimicrobial therapy upon hospital discharge.
Acknowledgements
The authors acknowledge Dr. Michael Fine for his assistance with utilization of the Pneumonia Severity Index, Kenneth Bukowski for assisting with development of data collection tools and data management, and members of the Antimicrobial Stewardship Taskforce Implementation Sub‐Committee. Collaborators in the Pneumonia Duration of Therapy Medication Utilization Evaluation Group include: Biloxi VA (VA Gulf Coast): Cheryl Hankins, PharmD, BCPS; Central Alabama VAMC: Lauren Rass, PharmD, BCPS, Kelly Mooney, PharmD, BCPS; Central Arkansas: Nicholas Tinsley, MS, PharmD; Chillicothe VA: Stephen Hanson, PharmD, BCPS, Beth Gallaugher, BSN, RN, Elizabeth Baltenberger, PharmD; Cincinnati VA: Jason Hiett, PharmD, BCPS, Victoria Tate, PharmD, BCPS, Brian Salzman, PharmD; Dorn Medical Center: MaryAnne Maurer, PharmD, BCPS, BCACP, Rebekah Sipes, PharmD, BCACP, Ginger Ervin, PharmD; Dwight D. Eisenhower VAMC: Emily Potter, PharmD; Hudson Valley: Rita Lee Bodine, PharmD, Clement Chen, PharmD, Cristina Fantino, PharmD; James H. Quillen VAMC: Marty Vannoy, PharmD, BCPS, Erin Harshbarger, PharmD, Kristen Nelsen, PharmD; Jesse Brown VAMC: Lisa Young, PharmD, BCPS, AQ‐ID, Andrea Bidlencik, PharmD, BCPS; Kansas City VA: Jamie Guyear, PharmD, AQ‐ID, Ann Ungerman, PharmD, BCPS, Lauri Witt, PharmD, BCACP; Louis Stokes Cleveland VAMC: Amy Hirsch, PharmD, BCPS, Steven Adoryan, PharmD, BCP‐CC, Amanda Miller, PharmD, BCPS; Maine VAMC: Joel Coon, PharmD, Rachel Naida, PharmD, Kelly Grossman, PharmD; Martinsburg VAMC: Kelly Li, PharmD, Sarah Mickanis, PharmD, BCPS; Miami VA Medical Center: Mara Carrasquillo, BS, PharmD, Maribel Toro, PharmD; North Florida/South Georgia Veterans Health System: Nora Morgan, PharmD, Hugh Frank, PharmD, BCPS, BCPP, Sarah Onofrio, PharmD, BCPS; North Texas HCS: Susan Duquaine, PharmD, BCPS, AQ‐ID, Ruben Villaneuva, PharmD, BCPS, Jaela Dahl, PharmD, BCPS; Ozarks: Andrew Siler, PharmD, BCPS, Michele Walker, PharmD, CGP, Jennifer Cole, PharmD, BCPS, BCCCP; Providence VAMC: Kerry LaPlante, PharmD, FCCP, Lindsey Williamson, PharmD; Richmond VA: Daniel Tassone, PharmD, BCPS; Salisbury VAMC: Brett Norem, PharmD, Marrisa Ragonesi, PharmD; San Juan VA: Monica Sanabria‐Seda, PharmD, BCPS, Jaime Velez‐Fores, PharmD, BCPS, AQ‐ID, Norma Ayala‐Burgos, PharmD; Sioux Falls VA: Andrea Aylward, PharmD, BCPS; South Texas HCS: Kelly Echevarria, PharmD, BCPS, AQ‐ID, Manuel Escobar, PharmD; Tennessee Valley HCS: Casey Ryals, PharmD, BCACP, Molly Hurst, PharmD, Jonathan Hale, PharmD; VA Central Iowa Health Care System: Jenny Phabmixay, PharmD, BCPS, Mackenzie Brown, PharmD, BCPS, Cynthia Muthusi, PharmD, BCPS; VA Loma Linda: Tony Chau, PharmD; VA Sierra Nevada: Scott Mambourg, PharmD, BCPS, AAHIVP, Matthew Han, PharmD, Nathan Mihoch, PharmD; VA WNY Healthcare System: Kari Mergenhagen, PharmD, BCPS, AQ‐ID, Christine Ruh, PharmD, BCPS; Veterans Affairs Salt Lake City Health System: Emily Spivak, MD, MHS, Patricia Orlando, PharmD
Disclosures: Karl Madaras‐Kelly is employed full time by Idaho State University and has a without compensation appointment as a clinical pharmacist at the Boise VA Medical Center. He receives grant support unrelated to this work through the Department of Veterans Affairs subcontracted to Idaho State University. Muriel Burk is employed full time through the Department of Veterans Affairs as clinical pharmacy specialist in outcomes and medication safety evaluation. Christina Caplinger was employed by the Department of Veterans Affairs as an infectious diseases fellow at the time this work was completed. She is currently employed by Micromedex. Jefferson Bohan is employed full time by the Department of Veterans Affairs as an infectious diseases fellow. Melinda Neuhauser is employed full time through the Department of Veterans Affairs as a clinical pharmacy specialistinfectious diseases. Matthew Goetz is employed full time through the Department of Veterans Affairs as an infectious diseases physician. Rhongping Zhang is employed full time through the Department of Veterans Affairs as a data analyst. Francesca Cunningham is employed full time through the Department of Veterans Affairs as the director of the VA Center for Medication Safety. This work was supported with resources and use of the Department of Veterans Affairs healthcare system. The views expressed in this article are solely those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs. The authors report no conflicts of interest.
- Centers for Disease Control and Prevention. National hospital discharge survey 2010. Available at: http://www.cdc.gov/nchs/fastats/pneumonia.htm. Accessed December 1, 2014.
- , , , et al. Implementing an antibiotic stewardship program: guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis. 2016;62(10):e51–e77.
- , , , et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community‐acquired pneumonia in adults. Clin Infect Dis. 2007;44(suppl 2):S27–S72.
- American Thoracic Society; Infectious Diseases Society of America. Guidelines for the management of adults with hospital‐acquired, ventilator‐associated, and healthcare‐associated pneumonia. Am J Respir Crit Care Med. 2005;171(4):388–416.
- , , , et al. Short‐ versus long‐course antibacterial therapy for community‐acquired pneumonia: a meta‐analysis. Drugs. 2008;68(13):1841–1854.
- , , , et al. Efficacy of short‐course antibiotic regimens for community‐acquired pneumonia: a meta‐analysis. Am J Med. 2007;120:783–790.
- , , , et al. High‐dose, short‐course levofloxacin for community‐acquired pneumonia: a new treatment paradigm. Clin Infect Dis. 2003;37:752–760.
- , , , et al. Comparison of 7 versus 10 days of antibiotic therapy for hospitalized patients with uncomplicated community‐acquired pneumonia: a prospective. Am J Ther. 1999;6(4):217–222.
- , , , et al. Effectiveness of discontinuing antibiotic treatment after three days versus eight days in mild to moderate‐severe community acquired pneumonia: randomised, double blind trial. BMJ. 2006;332(7554):1355.
- , , , et al. Efficacy of a three day course of azithromycin in moderately severe community‐acquired pneumonia. Eur Respir J. 1995;8(3):398–402.
- , , , et al. Comparison of 8 vs 15 days of antibiotic therapy for ventilator‐associated pneumonia in adults: a randomized trial. JAMA. 2003;290(19):2588–2598.
- , , , et al. Effectiveness of early switch from intravenous to oral antibiotics in severe community acquired pneumonia: multicentre randomized trial. BMJ. 2006;333(7580):1193.
- , , , , . Unnecessary antimicrobial use in the context of Clostridium difficile infection: a call to arms for the Veterans Affairs Antimicrobial Stewardship Task Force. Infect Control Hosp Epidemiol. 2013;34(6):651–653.
- VHA Directive 1031. Antimicrobial stewardship programs. Available at: https://www1.va.gov/vhapublications/ViewPublication.asp?pub_ID=2964. Accessed December 1, 2014.
- , , , et al. Impact of an antimicrobial stewardship intervention on shortening the duration of therapy for community‐acquired pneumonia. Clin Infect Dis. 2012;54:1581–1587.
- , , , et al. Targets for antibiotic and healthcare resource stewardship in inpatient community‐acquired pneumonia: a comparison of management practices with National Guideline Recommendations. Infection. 2013;41(1):135–144.
- , , , , . Pharmacy benefits management in the Veterans Health Administration: 1995 to 2003. Am J Manag Care. 2005;11(2):104–112.
- , , , . Accuracy of administrative data for identifying patients with pneumonia. Am J Med Qual. 2005;20(6):319–328.
- , , , et al. A prediction rule to identify low‐risk patients with community‐acquired pneumonia. N Engl J Med. 1997;336:243–250.
- , , , , . Clostridium difficile infections in Veterans Health Administration acute care facilities. Infect Control Hosp Epidemiol. 2014;35(8):1037–1042.
- , , , , . Organization complexity and primary care providers' perceptions of quality improvement culture within the Veterans Health Administration. Am J Med Qual. 2016;31(2):139–146.
- , , , et al. BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax. 2009;64(suppl 3):iii1–iii55.
- National Institute for Health and Care Excellence. Pneumonia in adults: diagnosis and management. Available at: http://www.nice.org.uk/guidance/cg191. Published December 2014. Accessed May 9, 2016.
- , , , , , . A prospective randomized study of inpatient IV antibiotics for community‐acquired pneumonia: the optimal duration of therapy. Chest. 1996;110(4):965–971.
- , , , et al. Early switch from intravenous to oral antibiotics and early hospital discharge: a prospective observational study of 200 consecutive patients with community‐acquired pneumonia. Arch Intern Med. 1999;159(20):2449–2454.
- , , , . Correlates and economic and clinical outcomes of an adult IV to PO antimicrobial conversion program at an academic medical center in Midwest United States. J Pharm Pract. 2015;28(3):238–248.
- , , , et al. Antimicrobial De‐escalation of treatment for healthcare‐associated pneumonia within the Veterans Healthcare Administration. J Antimicrob Chemother. 2016;71(2):539–546.
- , , , et al. Community‐associated Clostridium difficile infection and antibiotics: a meta‐analysis. J Antimicrob Chemother. 2013;68(9):1951.
- , , , . Meta‐analysis of antibiotics and the risk of community‐associated Clostridium difficle infection. Antimicrob Agents Chemother. 2013;57(5):2326–2332.
- , , , et al. Evaluating diagnosis‐based case‐mix measures: how well do they apply to the VA population? Med Care. 2001;39:692–704.
- , , . What is the role of antimicrobial stewardship in improving outcomes of patients with CAP? Infect Dis Clin North Am. 2013;27(1):211–228.
- , , , et al. Quality of care for elderly patients hospitalized for pneumonia in the United States, 2006 to 2010. JAMA Intern Med. 2014;174(11):1806–1814.
- , , , et al. An evaluation of the impact of antibiotic stewardship on reducing the use of high‐risk antibiotics and its effect on the incidence of Clostridium difficile infection in hospital settings. J Antimicrob Chemother. 2012;67(12):2988–2996.
- , , , et al.; Centers for Disease Control and Prevention. Vital signs: improving antibiotic use among hospitalized patients. MMWR Morb Mortal Wkly Rep. 2014;63(9):194–200.
- , , et al. Effect of procalcitonin‐based guidelines vs standard guidelines on antibiotic use in lower respiratory tract infections: the ProHOSP randomized controlled trial. JAMA. 2009;302(10):1059–1066.
- , , , et al. Cost‐effectiveness of procalcitonin‐guided antibiotic use in community acquired pneumonia. J Gen Intern Med. 2013;28(9):1157–1164.
- , , , , , . Interim evaluation of a Protocol to Optimize the Duration of Pneumonia Therapy at Hospital Discharge. Open Forum Infect Dis. 2015;2(suppl 1):S379.
- , , , et al. Intervention to improve antibiotic selection and shorten treatment durations at the time of hospital discharge. Open Forum Infect Dis. 2015;2(suppl 1):S1.
- , , , et al. Using the electronic medical record to identify community‐acquired pneumonia: toward a replicable automated strategy. PLoS One. 2013;8(8):e70944.
- Centers for Disease Control and Prevention. National hospital discharge survey 2010. Available at: http://www.cdc.gov/nchs/fastats/pneumonia.htm. Accessed December 1, 2014.
- , , , et al. Implementing an antibiotic stewardship program: guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis. 2016;62(10):e51–e77.
- , , , et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community‐acquired pneumonia in adults. Clin Infect Dis. 2007;44(suppl 2):S27–S72.
- American Thoracic Society; Infectious Diseases Society of America. Guidelines for the management of adults with hospital‐acquired, ventilator‐associated, and healthcare‐associated pneumonia. Am J Respir Crit Care Med. 2005;171(4):388–416.
- , , , et al. Short‐ versus long‐course antibacterial therapy for community‐acquired pneumonia: a meta‐analysis. Drugs. 2008;68(13):1841–1854.
- , , , et al. Efficacy of short‐course antibiotic regimens for community‐acquired pneumonia: a meta‐analysis. Am J Med. 2007;120:783–790.
- , , , et al. High‐dose, short‐course levofloxacin for community‐acquired pneumonia: a new treatment paradigm. Clin Infect Dis. 2003;37:752–760.
- , , , et al. Comparison of 7 versus 10 days of antibiotic therapy for hospitalized patients with uncomplicated community‐acquired pneumonia: a prospective. Am J Ther. 1999;6(4):217–222.
- , , , et al. Effectiveness of discontinuing antibiotic treatment after three days versus eight days in mild to moderate‐severe community acquired pneumonia: randomised, double blind trial. BMJ. 2006;332(7554):1355.
- , , , et al. Efficacy of a three day course of azithromycin in moderately severe community‐acquired pneumonia. Eur Respir J. 1995;8(3):398–402.
- , , , et al. Comparison of 8 vs 15 days of antibiotic therapy for ventilator‐associated pneumonia in adults: a randomized trial. JAMA. 2003;290(19):2588–2598.
- , , , et al. Effectiveness of early switch from intravenous to oral antibiotics in severe community acquired pneumonia: multicentre randomized trial. BMJ. 2006;333(7580):1193.
- , , , , . Unnecessary antimicrobial use in the context of Clostridium difficile infection: a call to arms for the Veterans Affairs Antimicrobial Stewardship Task Force. Infect Control Hosp Epidemiol. 2013;34(6):651–653.
- VHA Directive 1031. Antimicrobial stewardship programs. Available at: https://www1.va.gov/vhapublications/ViewPublication.asp?pub_ID=2964. Accessed December 1, 2014.
- , , , et al. Impact of an antimicrobial stewardship intervention on shortening the duration of therapy for community‐acquired pneumonia. Clin Infect Dis. 2012;54:1581–1587.
- , , , et al. Targets for antibiotic and healthcare resource stewardship in inpatient community‐acquired pneumonia: a comparison of management practices with National Guideline Recommendations. Infection. 2013;41(1):135–144.
- , , , , . Pharmacy benefits management in the Veterans Health Administration: 1995 to 2003. Am J Manag Care. 2005;11(2):104–112.
- , , , . Accuracy of administrative data for identifying patients with pneumonia. Am J Med Qual. 2005;20(6):319–328.
- , , , et al. A prediction rule to identify low‐risk patients with community‐acquired pneumonia. N Engl J Med. 1997;336:243–250.
- , , , , . Clostridium difficile infections in Veterans Health Administration acute care facilities. Infect Control Hosp Epidemiol. 2014;35(8):1037–1042.
- , , , , . Organization complexity and primary care providers' perceptions of quality improvement culture within the Veterans Health Administration. Am J Med Qual. 2016;31(2):139–146.
- , , , et al. BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax. 2009;64(suppl 3):iii1–iii55.
- National Institute for Health and Care Excellence. Pneumonia in adults: diagnosis and management. Available at: http://www.nice.org.uk/guidance/cg191. Published December 2014. Accessed May 9, 2016.
- , , , , , . A prospective randomized study of inpatient IV antibiotics for community‐acquired pneumonia: the optimal duration of therapy. Chest. 1996;110(4):965–971.
- , , , et al. Early switch from intravenous to oral antibiotics and early hospital discharge: a prospective observational study of 200 consecutive patients with community‐acquired pneumonia. Arch Intern Med. 1999;159(20):2449–2454.
- , , , . Correlates and economic and clinical outcomes of an adult IV to PO antimicrobial conversion program at an academic medical center in Midwest United States. J Pharm Pract. 2015;28(3):238–248.
- , , , et al. Antimicrobial De‐escalation of treatment for healthcare‐associated pneumonia within the Veterans Healthcare Administration. J Antimicrob Chemother. 2016;71(2):539–546.
- , , , et al. Community‐associated Clostridium difficile infection and antibiotics: a meta‐analysis. J Antimicrob Chemother. 2013;68(9):1951.
- , , , . Meta‐analysis of antibiotics and the risk of community‐associated Clostridium difficle infection. Antimicrob Agents Chemother. 2013;57(5):2326–2332.
- , , , et al. Evaluating diagnosis‐based case‐mix measures: how well do they apply to the VA population? Med Care. 2001;39:692–704.
- , , . What is the role of antimicrobial stewardship in improving outcomes of patients with CAP? Infect Dis Clin North Am. 2013;27(1):211–228.
- , , , et al. Quality of care for elderly patients hospitalized for pneumonia in the United States, 2006 to 2010. JAMA Intern Med. 2014;174(11):1806–1814.
- , , , et al. An evaluation of the impact of antibiotic stewardship on reducing the use of high‐risk antibiotics and its effect on the incidence of Clostridium difficile infection in hospital settings. J Antimicrob Chemother. 2012;67(12):2988–2996.
- , , , et al.; Centers for Disease Control and Prevention. Vital signs: improving antibiotic use among hospitalized patients. MMWR Morb Mortal Wkly Rep. 2014;63(9):194–200.
- , , et al. Effect of procalcitonin‐based guidelines vs standard guidelines on antibiotic use in lower respiratory tract infections: the ProHOSP randomized controlled trial. JAMA. 2009;302(10):1059–1066.
- , , , et al. Cost‐effectiveness of procalcitonin‐guided antibiotic use in community acquired pneumonia. J Gen Intern Med. 2013;28(9):1157–1164.
- , , , , , . Interim evaluation of a Protocol to Optimize the Duration of Pneumonia Therapy at Hospital Discharge. Open Forum Infect Dis. 2015;2(suppl 1):S379.
- , , , et al. Intervention to improve antibiotic selection and shorten treatment durations at the time of hospital discharge. Open Forum Infect Dis. 2015;2(suppl 1):S1.
- , , , et al. Using the electronic medical record to identify community‐acquired pneumonia: toward a replicable automated strategy. PLoS One. 2013;8(8):e70944.
Funding Announced for Alport Syndrome Research
The Alport Syndrome Foundation (ASF), Pedersen Family, and The Kidney Foundation of Canada (KFOC) Research Funding Program have announced that joint funding has been awarded for two new research projects on Alport syndrome, a rare genetic kidney disease.
Dr. Hirofumi Kai of Kumamoto University in Japan has been awarded $100,000 for a two-year study, “Search for Therapeutic Reagents by Modeling Alport Syndrome in Mice and Humans.” Dr. Jeffrey Miner of Washington University in St. Louis has been awarded $100,000 for a one-year study, “5-Ht2b Antagonism as a Strategy to Prevent Renal Function Loss in Alport Syndrome.”
The Alport Syndrome Foundation and its partners have provided more than $2 million for Alport syndrome research and have funded researchers at several universities in the US and in Australia, Japan, Germany and Canada.
Alport syndrome is a rare hereditary kidney disease that causes kidney failure, hearing loss, and vision abnormalities. It leads to kidney failure in 50% of the boys with the predominant, X-linked form of the disease by age 25 and in 90% by age 40. These patients require dialysis or a kidney transplant. Some girls with the syndrome are affected similarly to boys but most see later disease progression and many have milder symptoms.
The Alport Syndrome Foundation (ASF), Pedersen Family, and The Kidney Foundation of Canada (KFOC) Research Funding Program have announced that joint funding has been awarded for two new research projects on Alport syndrome, a rare genetic kidney disease.
Dr. Hirofumi Kai of Kumamoto University in Japan has been awarded $100,000 for a two-year study, “Search for Therapeutic Reagents by Modeling Alport Syndrome in Mice and Humans.” Dr. Jeffrey Miner of Washington University in St. Louis has been awarded $100,000 for a one-year study, “5-Ht2b Antagonism as a Strategy to Prevent Renal Function Loss in Alport Syndrome.”
The Alport Syndrome Foundation and its partners have provided more than $2 million for Alport syndrome research and have funded researchers at several universities in the US and in Australia, Japan, Germany and Canada.
Alport syndrome is a rare hereditary kidney disease that causes kidney failure, hearing loss, and vision abnormalities. It leads to kidney failure in 50% of the boys with the predominant, X-linked form of the disease by age 25 and in 90% by age 40. These patients require dialysis or a kidney transplant. Some girls with the syndrome are affected similarly to boys but most see later disease progression and many have milder symptoms.
The Alport Syndrome Foundation (ASF), Pedersen Family, and The Kidney Foundation of Canada (KFOC) Research Funding Program have announced that joint funding has been awarded for two new research projects on Alport syndrome, a rare genetic kidney disease.
Dr. Hirofumi Kai of Kumamoto University in Japan has been awarded $100,000 for a two-year study, “Search for Therapeutic Reagents by Modeling Alport Syndrome in Mice and Humans.” Dr. Jeffrey Miner of Washington University in St. Louis has been awarded $100,000 for a one-year study, “5-Ht2b Antagonism as a Strategy to Prevent Renal Function Loss in Alport Syndrome.”
The Alport Syndrome Foundation and its partners have provided more than $2 million for Alport syndrome research and have funded researchers at several universities in the US and in Australia, Japan, Germany and Canada.
Alport syndrome is a rare hereditary kidney disease that causes kidney failure, hearing loss, and vision abnormalities. It leads to kidney failure in 50% of the boys with the predominant, X-linked form of the disease by age 25 and in 90% by age 40. These patients require dialysis or a kidney transplant. Some girls with the syndrome are affected similarly to boys but most see later disease progression and many have milder symptoms.