User login
Value-based cancer care and the patient perspective
The business of cancer care is in transition. Driven by the Centers for Medicare & Medicaid Services’ (CMS) Oncology Care Model (OCM) program, practices around the country are working to re-engineer the way they provide services, and the way they charge for those services. The implicit goal of all this is to manage (as in reduce) the overall cost of cancer care. A more frequently stated goal is to improve value, typically defined as outcome (numerator) relative to cost (denominator). Alternative payment models are challenged to assess the value of transformational improvement in cancer care.
Click on the PDF icon at the top of this introduction to read the full article.
The business of cancer care is in transition. Driven by the Centers for Medicare & Medicaid Services’ (CMS) Oncology Care Model (OCM) program, practices around the country are working to re-engineer the way they provide services, and the way they charge for those services. The implicit goal of all this is to manage (as in reduce) the overall cost of cancer care. A more frequently stated goal is to improve value, typically defined as outcome (numerator) relative to cost (denominator). Alternative payment models are challenged to assess the value of transformational improvement in cancer care.
Click on the PDF icon at the top of this introduction to read the full article.
The business of cancer care is in transition. Driven by the Centers for Medicare & Medicaid Services’ (CMS) Oncology Care Model (OCM) program, practices around the country are working to re-engineer the way they provide services, and the way they charge for those services. The implicit goal of all this is to manage (as in reduce) the overall cost of cancer care. A more frequently stated goal is to improve value, typically defined as outcome (numerator) relative to cost (denominator). Alternative payment models are challenged to assess the value of transformational improvement in cancer care.
Click on the PDF icon at the top of this introduction to read the full article.
Tibial Tubercle Fracture After Bone–Patellar Tendon–Bone Autograft
A fracture occurring after anterior cruciate ligament (ACL) reconstruction is rare, and rarer still when it involves the harvest site of a bone—patellar tendon—bone (BPTB) autograft. The vast majority of fractures described in the literature are patellar, with the weak point along the patellar bone cut. A number of fractures generally also occur through the bone tunnels in both hamstring and BPTB grafts. However, only 2 cases of tibial tubercle fracture after BPTB graft have been published, and we expound on them in this case report.1,2 The patient provided written informed consent for print and electronic publication of this case report.
Case Report
Eight years after undergoing successful left ACL reconstruction with ipsilateral BPTB graft, a 45-year-old man developed a graft rupture and demonstrated recurrent instability. He requested revision reconstruction, again with a BPTB construct. In the operating room, he was prepared and draped in the usual sterile fashion, and left ACL reconstruction was performed with right-knee central-third BPTB graft.
During surgery, the left knee was arthroscopically examined, and residual ACL graft from the initial reconstruction was removed. Notchplasty was performed, and the residual femoral interference screw was removed from the 12:30 position. A transtibial approach was used, with a 10-mm reamer brought through the proximal tibia, the posterior tibial ACL footprint, and the 2:00 distal femoral position, with 30 mm of femoral condyle drilled, leaving 1 mm of posterior femoral cortex.
After the right leg was exsanguinated, a central-third patellar tendon graft was harvested through a longitudinal incision with a 22-mm × 10-mm patellar plug, a 10-mm patellar graft, and a 22-mm × 11-mm tibial plug. The graft was prepared, the left tibia was overreamed, and the graft was passed. The graft was fixed with a 7-mm × 23-mm biointerference screw in the femur, trialed, and fixed with an 8-mm × 23-mm interference screw in the tibia. Excess bone graft was packed in the patellar defect in the right knee. The rent in the patellar tendon was closed. The rest of the incision was closed, and the patient was placed in an immobilizer and a cold therapy device (Polar Care; Breg, Inc).
At 2-week follow-up, the patient reported having slipped on ice and flexed the right knee, causing a pop, pain, and limitation in range of motion (ROM; 0°-70°).
The patient returned to the operating room 5 days later and underwent open reduction and internal fixation (ORIF) of the tibial tubercle avulsion. After sterile preparation and draping, the previous incision was used. The bony fragment was isolated and the hematoma débrided. Repair was performed with two No. 2 running locked FiberWire sutures (Arthrex) placed through bony drill holes in the fragment (1 medial, 1 lateral). The fragment was reduced and the sutures tied, with further fixation provided with a DePuy Synthes small-fragment 3.5-mm cortical screw with washer. A No. 5 Ethibond suture (Ethicon) was then placed as a secondary cerclage figure-of-8 stitch to protect the repair.
The patient was seen in follow-up 6 weeks after right ACL reconstruction and 4 weeks after left tibial tubercle ORIF. He continued with right knee restrictions, with the weight-bearing brace locked in extension. Left knee ROM was more than 0° to 90° even before any formal physical therapy. At this point, the patient began physical therapy on both knees with ROM limited to 0° to 30° and weight-bearing as tolerated on the right knee (no restrictions on the left knee).
Discussion
Cases of tibial tubercle fracture after BPTB autograft harvest are extremely rare in the published literature. PubMed and Cochrane Review searches revealed only 2—1 in the ipsilateral knee as ACL fixation1 and 1 in the contralateral knee.2 The middle third of the patellar tendon has been used for ACL reconstruction for more than 50 years, which supports the extreme rarity of this complication.3 Tibial tubercle fractures are so rare that they are not even mentioned in reviews of ACL complications.4 These fractures are universally treated with ORIF.1,2
Far more common but still rare, fracture-type complications involve the extensor mechanism and the tibial plateau. Patellar fractures have been documented as occurring in 0.2% to 2.3% of cases.5-7 One paper reported a fracture in 1.3% of cases at a mean of 57 days, with roughly half caused by trauma and the other half having atraumatic causes.8 Lee and colleagues9 found a 0.2% complication rate for all BPTB grafts in 1725 consecutive patients. Although some patients were treated nonoperatively, others underwent operative fixation. Time to clinical and radiographic healing was 7 and 10 weeks, respectively.
Tibial plateau fracture after BPTB harvest is a rare complication, with 11 cases reported in the literature.10 In 4 of those cases, the proposed mechanism of fracture was a stress riser resulting from the synergistic weakness of the tibial harvest site combined with the tibial tunnel reducing proximal tibial bone strength.11-14 The mechanism of injury varied from traumatic to insufficiency fracture, with fixation varying with fracture displacement.
Tibial tubercle fracture after BPTB harvest is extremely rare, with the present case being only the third published in the literature. Like most reported post-ACL reconstruction extensor mechanism disruptions, our case resulted from a traumatic event at an interval after surgery. All other tibial tubercle fracture post-ACL reconstruction disruptions occurred within 2 weeks after surgery.1,2 Sudden tension on the extensor mechanism secondary to hyperflexion caused a fracture through a weakened tibial tubercle with avulsion of the remaining tendon in 2 of the 3 cases, with the third being a lower stress popping noise that occurred during a pivot to stand.1
The residual defect after tibial bone block harvest could represent a weakening of the tubercle by loss of structural bone and by development of stress risers. The previous reports of tibial tubercle fracture after BPTB harvest documented a similar methodology: Use a bone saw and osteotomes to harvest a trapezoidal tibial bone plug 10 mm to 11 mm wide and 22 cm to 35 cm long. As previously documented, we suggest taking care with saw cuts and osteotomes so as not to weaken the proximal tibia or distal patella more than is necessary.1,2 Before surgery, patients should be warned about the possibility of extensor mechanism injuries with use of BPTB grafts.
Conclusion
Tibial tubercle fracture after BPTB harvest for ACL reconstruction is an extremely rare complication. Treatment is ORIF of the tubercle fragment, with a delay in ACL rehabilitation in cases involving the ipsilateral knee.
Am J Orthop. 2016;45(7):E469-E471. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
1. Acton KJ, Dowd GS. Fracture of the tibial tubercle following anterior cruciate ligament reconstruction. Knee. 2002;9(2):157-159.
2. Busfield BT, Safran MR, Cannon WD. Extensor mechanism disruption after contralateral middle third patellar tendon harvest for anterior cruciate ligament revision reconstruction. Arthroscopy. 2005;21(10):1268.e1-e1268.e6.
3. Jones KG. Reconstruction of the anterior cruciate ligament. A technique using the central one-third of the patellar ligament. J Bone Joint Surg Am. 1963;45(5):925-932.
4. Tjoumakaris FP, Herz-Brown AL, Bowers AL, Sennett BJ, Bernstein J. Complications in brief: anterior cruciate ligament reconstruction. Clin Orthop Relat Res. 2012;470(2):630-636.
5. Morgan-Jones RL, Cross TM, Caldwell B, Cross MJ. “Silent” transverse patellar fracture following anterior cruciate ligament reconstruction. Arthroscopy. 2001;17(9):997-999.
6. Viola R, Vianello R. Three cases of patella fracture in 1,320 anterior cruciate ligament reconstructions with bone–patellar tendon–bone autograft. Arthroscopy. 1999;15(1):93-97.
7. Berg EE. Management of patella fractures associated with central third bone–patella tendon–bone autograft ACL reconstructions. Arthroscopy. 1996;12(6):756-759.
8. Stein DA, Hunt SA, Rosen JE, Sherman OH. The incidence and outcome of patella fractures after anterior cruciate ligament reconstruction. Arthroscopy. 2002;18(6):578-583.
9. Lee GH, McCulloch P, Cole BJ, Bush-Joseph CA, Bach BR Jr. The incidence of acute patellar tendon harvest complications for anterior cruciate ligament reconstruction. Arthroscopy. 2008;24(2):162-166.
10. Wong JJ, Muir B. Insufficiency fracture of the tibial plateau after anterior cruciate ligament reconstructive surgery: a case report and review of the literature. J Can Chiropr Assoc. 2013;57(2):123-131.
11. Morgan E, Steensen RN. Traumatic proximal tibial fracture following anterior cruciate ligament reconstruction. Am J Knee Surg. 1998;11(3):193-194.
12. Delcogliano A, Chiossi S, Caporaso A, Franzese S, Menghi A. Tibial plateau fracture after arthroscopic anterior cruciate ligament reconstruction. Arthroscopy. 2001;17(4):E16.
13. Mithöfer K, Gill TJ, Vrahas MS. Tibial plateau fracture following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2004;12(4):325-328.
14. Moen KY, Boynton MD, Raasch WG. Fracture of the proximal tibia after anterior cruciate ligament reconstruction: a case report. Am J Orthop. 1998;27(9):629-630.
A fracture occurring after anterior cruciate ligament (ACL) reconstruction is rare, and rarer still when it involves the harvest site of a bone—patellar tendon—bone (BPTB) autograft. The vast majority of fractures described in the literature are patellar, with the weak point along the patellar bone cut. A number of fractures generally also occur through the bone tunnels in both hamstring and BPTB grafts. However, only 2 cases of tibial tubercle fracture after BPTB graft have been published, and we expound on them in this case report.1,2 The patient provided written informed consent for print and electronic publication of this case report.
Case Report
Eight years after undergoing successful left ACL reconstruction with ipsilateral BPTB graft, a 45-year-old man developed a graft rupture and demonstrated recurrent instability. He requested revision reconstruction, again with a BPTB construct. In the operating room, he was prepared and draped in the usual sterile fashion, and left ACL reconstruction was performed with right-knee central-third BPTB graft.
During surgery, the left knee was arthroscopically examined, and residual ACL graft from the initial reconstruction was removed. Notchplasty was performed, and the residual femoral interference screw was removed from the 12:30 position. A transtibial approach was used, with a 10-mm reamer brought through the proximal tibia, the posterior tibial ACL footprint, and the 2:00 distal femoral position, with 30 mm of femoral condyle drilled, leaving 1 mm of posterior femoral cortex.
After the right leg was exsanguinated, a central-third patellar tendon graft was harvested through a longitudinal incision with a 22-mm × 10-mm patellar plug, a 10-mm patellar graft, and a 22-mm × 11-mm tibial plug. The graft was prepared, the left tibia was overreamed, and the graft was passed. The graft was fixed with a 7-mm × 23-mm biointerference screw in the femur, trialed, and fixed with an 8-mm × 23-mm interference screw in the tibia. Excess bone graft was packed in the patellar defect in the right knee. The rent in the patellar tendon was closed. The rest of the incision was closed, and the patient was placed in an immobilizer and a cold therapy device (Polar Care; Breg, Inc).
At 2-week follow-up, the patient reported having slipped on ice and flexed the right knee, causing a pop, pain, and limitation in range of motion (ROM; 0°-70°).
The patient returned to the operating room 5 days later and underwent open reduction and internal fixation (ORIF) of the tibial tubercle avulsion. After sterile preparation and draping, the previous incision was used. The bony fragment was isolated and the hematoma débrided. Repair was performed with two No. 2 running locked FiberWire sutures (Arthrex) placed through bony drill holes in the fragment (1 medial, 1 lateral). The fragment was reduced and the sutures tied, with further fixation provided with a DePuy Synthes small-fragment 3.5-mm cortical screw with washer. A No. 5 Ethibond suture (Ethicon) was then placed as a secondary cerclage figure-of-8 stitch to protect the repair.
The patient was seen in follow-up 6 weeks after right ACL reconstruction and 4 weeks after left tibial tubercle ORIF. He continued with right knee restrictions, with the weight-bearing brace locked in extension. Left knee ROM was more than 0° to 90° even before any formal physical therapy. At this point, the patient began physical therapy on both knees with ROM limited to 0° to 30° and weight-bearing as tolerated on the right knee (no restrictions on the left knee).
Discussion
Cases of tibial tubercle fracture after BPTB autograft harvest are extremely rare in the published literature. PubMed and Cochrane Review searches revealed only 2—1 in the ipsilateral knee as ACL fixation1 and 1 in the contralateral knee.2 The middle third of the patellar tendon has been used for ACL reconstruction for more than 50 years, which supports the extreme rarity of this complication.3 Tibial tubercle fractures are so rare that they are not even mentioned in reviews of ACL complications.4 These fractures are universally treated with ORIF.1,2
Far more common but still rare, fracture-type complications involve the extensor mechanism and the tibial plateau. Patellar fractures have been documented as occurring in 0.2% to 2.3% of cases.5-7 One paper reported a fracture in 1.3% of cases at a mean of 57 days, with roughly half caused by trauma and the other half having atraumatic causes.8 Lee and colleagues9 found a 0.2% complication rate for all BPTB grafts in 1725 consecutive patients. Although some patients were treated nonoperatively, others underwent operative fixation. Time to clinical and radiographic healing was 7 and 10 weeks, respectively.
Tibial plateau fracture after BPTB harvest is a rare complication, with 11 cases reported in the literature.10 In 4 of those cases, the proposed mechanism of fracture was a stress riser resulting from the synergistic weakness of the tibial harvest site combined with the tibial tunnel reducing proximal tibial bone strength.11-14 The mechanism of injury varied from traumatic to insufficiency fracture, with fixation varying with fracture displacement.
Tibial tubercle fracture after BPTB harvest is extremely rare, with the present case being only the third published in the literature. Like most reported post-ACL reconstruction extensor mechanism disruptions, our case resulted from a traumatic event at an interval after surgery. All other tibial tubercle fracture post-ACL reconstruction disruptions occurred within 2 weeks after surgery.1,2 Sudden tension on the extensor mechanism secondary to hyperflexion caused a fracture through a weakened tibial tubercle with avulsion of the remaining tendon in 2 of the 3 cases, with the third being a lower stress popping noise that occurred during a pivot to stand.1
The residual defect after tibial bone block harvest could represent a weakening of the tubercle by loss of structural bone and by development of stress risers. The previous reports of tibial tubercle fracture after BPTB harvest documented a similar methodology: Use a bone saw and osteotomes to harvest a trapezoidal tibial bone plug 10 mm to 11 mm wide and 22 cm to 35 cm long. As previously documented, we suggest taking care with saw cuts and osteotomes so as not to weaken the proximal tibia or distal patella more than is necessary.1,2 Before surgery, patients should be warned about the possibility of extensor mechanism injuries with use of BPTB grafts.
Conclusion
Tibial tubercle fracture after BPTB harvest for ACL reconstruction is an extremely rare complication. Treatment is ORIF of the tubercle fragment, with a delay in ACL rehabilitation in cases involving the ipsilateral knee.
Am J Orthop. 2016;45(7):E469-E471. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
A fracture occurring after anterior cruciate ligament (ACL) reconstruction is rare, and rarer still when it involves the harvest site of a bone—patellar tendon—bone (BPTB) autograft. The vast majority of fractures described in the literature are patellar, with the weak point along the patellar bone cut. A number of fractures generally also occur through the bone tunnels in both hamstring and BPTB grafts. However, only 2 cases of tibial tubercle fracture after BPTB graft have been published, and we expound on them in this case report.1,2 The patient provided written informed consent for print and electronic publication of this case report.
Case Report
Eight years after undergoing successful left ACL reconstruction with ipsilateral BPTB graft, a 45-year-old man developed a graft rupture and demonstrated recurrent instability. He requested revision reconstruction, again with a BPTB construct. In the operating room, he was prepared and draped in the usual sterile fashion, and left ACL reconstruction was performed with right-knee central-third BPTB graft.
During surgery, the left knee was arthroscopically examined, and residual ACL graft from the initial reconstruction was removed. Notchplasty was performed, and the residual femoral interference screw was removed from the 12:30 position. A transtibial approach was used, with a 10-mm reamer brought through the proximal tibia, the posterior tibial ACL footprint, and the 2:00 distal femoral position, with 30 mm of femoral condyle drilled, leaving 1 mm of posterior femoral cortex.
After the right leg was exsanguinated, a central-third patellar tendon graft was harvested through a longitudinal incision with a 22-mm × 10-mm patellar plug, a 10-mm patellar graft, and a 22-mm × 11-mm tibial plug. The graft was prepared, the left tibia was overreamed, and the graft was passed. The graft was fixed with a 7-mm × 23-mm biointerference screw in the femur, trialed, and fixed with an 8-mm × 23-mm interference screw in the tibia. Excess bone graft was packed in the patellar defect in the right knee. The rent in the patellar tendon was closed. The rest of the incision was closed, and the patient was placed in an immobilizer and a cold therapy device (Polar Care; Breg, Inc).
At 2-week follow-up, the patient reported having slipped on ice and flexed the right knee, causing a pop, pain, and limitation in range of motion (ROM; 0°-70°).
The patient returned to the operating room 5 days later and underwent open reduction and internal fixation (ORIF) of the tibial tubercle avulsion. After sterile preparation and draping, the previous incision was used. The bony fragment was isolated and the hematoma débrided. Repair was performed with two No. 2 running locked FiberWire sutures (Arthrex) placed through bony drill holes in the fragment (1 medial, 1 lateral). The fragment was reduced and the sutures tied, with further fixation provided with a DePuy Synthes small-fragment 3.5-mm cortical screw with washer. A No. 5 Ethibond suture (Ethicon) was then placed as a secondary cerclage figure-of-8 stitch to protect the repair.
The patient was seen in follow-up 6 weeks after right ACL reconstruction and 4 weeks after left tibial tubercle ORIF. He continued with right knee restrictions, with the weight-bearing brace locked in extension. Left knee ROM was more than 0° to 90° even before any formal physical therapy. At this point, the patient began physical therapy on both knees with ROM limited to 0° to 30° and weight-bearing as tolerated on the right knee (no restrictions on the left knee).
Discussion
Cases of tibial tubercle fracture after BPTB autograft harvest are extremely rare in the published literature. PubMed and Cochrane Review searches revealed only 2—1 in the ipsilateral knee as ACL fixation1 and 1 in the contralateral knee.2 The middle third of the patellar tendon has been used for ACL reconstruction for more than 50 years, which supports the extreme rarity of this complication.3 Tibial tubercle fractures are so rare that they are not even mentioned in reviews of ACL complications.4 These fractures are universally treated with ORIF.1,2
Far more common but still rare, fracture-type complications involve the extensor mechanism and the tibial plateau. Patellar fractures have been documented as occurring in 0.2% to 2.3% of cases.5-7 One paper reported a fracture in 1.3% of cases at a mean of 57 days, with roughly half caused by trauma and the other half having atraumatic causes.8 Lee and colleagues9 found a 0.2% complication rate for all BPTB grafts in 1725 consecutive patients. Although some patients were treated nonoperatively, others underwent operative fixation. Time to clinical and radiographic healing was 7 and 10 weeks, respectively.
Tibial plateau fracture after BPTB harvest is a rare complication, with 11 cases reported in the literature.10 In 4 of those cases, the proposed mechanism of fracture was a stress riser resulting from the synergistic weakness of the tibial harvest site combined with the tibial tunnel reducing proximal tibial bone strength.11-14 The mechanism of injury varied from traumatic to insufficiency fracture, with fixation varying with fracture displacement.
Tibial tubercle fracture after BPTB harvest is extremely rare, with the present case being only the third published in the literature. Like most reported post-ACL reconstruction extensor mechanism disruptions, our case resulted from a traumatic event at an interval after surgery. All other tibial tubercle fracture post-ACL reconstruction disruptions occurred within 2 weeks after surgery.1,2 Sudden tension on the extensor mechanism secondary to hyperflexion caused a fracture through a weakened tibial tubercle with avulsion of the remaining tendon in 2 of the 3 cases, with the third being a lower stress popping noise that occurred during a pivot to stand.1
The residual defect after tibial bone block harvest could represent a weakening of the tubercle by loss of structural bone and by development of stress risers. The previous reports of tibial tubercle fracture after BPTB harvest documented a similar methodology: Use a bone saw and osteotomes to harvest a trapezoidal tibial bone plug 10 mm to 11 mm wide and 22 cm to 35 cm long. As previously documented, we suggest taking care with saw cuts and osteotomes so as not to weaken the proximal tibia or distal patella more than is necessary.1,2 Before surgery, patients should be warned about the possibility of extensor mechanism injuries with use of BPTB grafts.
Conclusion
Tibial tubercle fracture after BPTB harvest for ACL reconstruction is an extremely rare complication. Treatment is ORIF of the tubercle fragment, with a delay in ACL rehabilitation in cases involving the ipsilateral knee.
Am J Orthop. 2016;45(7):E469-E471. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
1. Acton KJ, Dowd GS. Fracture of the tibial tubercle following anterior cruciate ligament reconstruction. Knee. 2002;9(2):157-159.
2. Busfield BT, Safran MR, Cannon WD. Extensor mechanism disruption after contralateral middle third patellar tendon harvest for anterior cruciate ligament revision reconstruction. Arthroscopy. 2005;21(10):1268.e1-e1268.e6.
3. Jones KG. Reconstruction of the anterior cruciate ligament. A technique using the central one-third of the patellar ligament. J Bone Joint Surg Am. 1963;45(5):925-932.
4. Tjoumakaris FP, Herz-Brown AL, Bowers AL, Sennett BJ, Bernstein J. Complications in brief: anterior cruciate ligament reconstruction. Clin Orthop Relat Res. 2012;470(2):630-636.
5. Morgan-Jones RL, Cross TM, Caldwell B, Cross MJ. “Silent” transverse patellar fracture following anterior cruciate ligament reconstruction. Arthroscopy. 2001;17(9):997-999.
6. Viola R, Vianello R. Three cases of patella fracture in 1,320 anterior cruciate ligament reconstructions with bone–patellar tendon–bone autograft. Arthroscopy. 1999;15(1):93-97.
7. Berg EE. Management of patella fractures associated with central third bone–patella tendon–bone autograft ACL reconstructions. Arthroscopy. 1996;12(6):756-759.
8. Stein DA, Hunt SA, Rosen JE, Sherman OH. The incidence and outcome of patella fractures after anterior cruciate ligament reconstruction. Arthroscopy. 2002;18(6):578-583.
9. Lee GH, McCulloch P, Cole BJ, Bush-Joseph CA, Bach BR Jr. The incidence of acute patellar tendon harvest complications for anterior cruciate ligament reconstruction. Arthroscopy. 2008;24(2):162-166.
10. Wong JJ, Muir B. Insufficiency fracture of the tibial plateau after anterior cruciate ligament reconstructive surgery: a case report and review of the literature. J Can Chiropr Assoc. 2013;57(2):123-131.
11. Morgan E, Steensen RN. Traumatic proximal tibial fracture following anterior cruciate ligament reconstruction. Am J Knee Surg. 1998;11(3):193-194.
12. Delcogliano A, Chiossi S, Caporaso A, Franzese S, Menghi A. Tibial plateau fracture after arthroscopic anterior cruciate ligament reconstruction. Arthroscopy. 2001;17(4):E16.
13. Mithöfer K, Gill TJ, Vrahas MS. Tibial plateau fracture following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2004;12(4):325-328.
14. Moen KY, Boynton MD, Raasch WG. Fracture of the proximal tibia after anterior cruciate ligament reconstruction: a case report. Am J Orthop. 1998;27(9):629-630.
1. Acton KJ, Dowd GS. Fracture of the tibial tubercle following anterior cruciate ligament reconstruction. Knee. 2002;9(2):157-159.
2. Busfield BT, Safran MR, Cannon WD. Extensor mechanism disruption after contralateral middle third patellar tendon harvest for anterior cruciate ligament revision reconstruction. Arthroscopy. 2005;21(10):1268.e1-e1268.e6.
3. Jones KG. Reconstruction of the anterior cruciate ligament. A technique using the central one-third of the patellar ligament. J Bone Joint Surg Am. 1963;45(5):925-932.
4. Tjoumakaris FP, Herz-Brown AL, Bowers AL, Sennett BJ, Bernstein J. Complications in brief: anterior cruciate ligament reconstruction. Clin Orthop Relat Res. 2012;470(2):630-636.
5. Morgan-Jones RL, Cross TM, Caldwell B, Cross MJ. “Silent” transverse patellar fracture following anterior cruciate ligament reconstruction. Arthroscopy. 2001;17(9):997-999.
6. Viola R, Vianello R. Three cases of patella fracture in 1,320 anterior cruciate ligament reconstructions with bone–patellar tendon–bone autograft. Arthroscopy. 1999;15(1):93-97.
7. Berg EE. Management of patella fractures associated with central third bone–patella tendon–bone autograft ACL reconstructions. Arthroscopy. 1996;12(6):756-759.
8. Stein DA, Hunt SA, Rosen JE, Sherman OH. The incidence and outcome of patella fractures after anterior cruciate ligament reconstruction. Arthroscopy. 2002;18(6):578-583.
9. Lee GH, McCulloch P, Cole BJ, Bush-Joseph CA, Bach BR Jr. The incidence of acute patellar tendon harvest complications for anterior cruciate ligament reconstruction. Arthroscopy. 2008;24(2):162-166.
10. Wong JJ, Muir B. Insufficiency fracture of the tibial plateau after anterior cruciate ligament reconstructive surgery: a case report and review of the literature. J Can Chiropr Assoc. 2013;57(2):123-131.
11. Morgan E, Steensen RN. Traumatic proximal tibial fracture following anterior cruciate ligament reconstruction. Am J Knee Surg. 1998;11(3):193-194.
12. Delcogliano A, Chiossi S, Caporaso A, Franzese S, Menghi A. Tibial plateau fracture after arthroscopic anterior cruciate ligament reconstruction. Arthroscopy. 2001;17(4):E16.
13. Mithöfer K, Gill TJ, Vrahas MS. Tibial plateau fracture following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2004;12(4):325-328.
14. Moen KY, Boynton MD, Raasch WG. Fracture of the proximal tibia after anterior cruciate ligament reconstruction: a case report. Am J Orthop. 1998;27(9):629-630.
Surgeon general’s addiction report calls for better integrated care
Primary and emergency care providers must step up prevention efforts and the use of state-of-the-art medicine when treating patients with addiction, according to the first-ever U.S. Surgeon General’s report on alcohol, drugs, and health.
In the report, “Facing Addiction in America,” Surgeon General Vivek H. Murthy, MD, called on health care providers to increase access to care and approach addiction and substance use disorders as they would any other chronic health condition.
“We must help everyone see that addiction is not a character flaw – it is a chronic illness that we must approach with the same skill and compassion with which we approach heart disease, diabetes, and cancer,” Dr. Murthy explained.
In addition to offering an action plan to address substance use of all kinds, the surgeon general’s report updates the public on the state of the art of addiction science, and includes chapters on neurobiology, prevention, treatment, recovery, health systems integration, and recommendations for the future.
Data from 2015 show that more than 27 million people in the United States used illicit drugs or misuse prescription medications, while a quarter of the entire adult and adolescent population reported binge drinking in the past month. However, only 10% of those with a substance use disorder received relevant specialty care.
For the more than 40% of those with substance use disorders who have a comorbid mental health condition, less than half were treated for either, according to the federal Substance Abuse and Mental Health Services Administration.
That treatment gap is the direct result of lack of access to affordable care, shame, discrimination, and the lack of screening for substance misuse and substance use disorders in the primary care setting, Dr. Murthy wrote.
To address the gap, the surgeon general laid out a plan that starts with increasing community-wide substance use prevention efforts, such as enforcement of underage drinking laws and DUI laws, and offering needle exchange programs.
Dr. Murthy also called for a coordinated public health response to addiction, including an overhaul of criminal justice where substance use is concerned, and an emphasis on preventing known risk factors for substance misuse.
The report underscores the need for a better trained and integrated health care workforce equipped to treat addiction as a chronic disease in the general health care setting, enforcement of addiction and mental health parity laws, and the delivery of services based on the latest research into the psychosocial and biological underpinnings of substance use.
Surgeon General Murthy also used the report to urge professional medical associations to advocate for more access to medication-assisted treatment and prescription drug monitoring programs, and to create evidence-based guidelines for integrating substance use disorder treatment.
The American Medical Association responded positively to the report. In a statement, AMA President Andrew W. Gurman, MD, called it a “crucial starting point” and praised its “important guidance for the nation to see that addiction is a chronic disease and must be treated as such.”
While also supporting the report, others in the addiction medicine field pointed out that such starting points had come and gone before.
“As a profession, we saw what was happening 10 years ago, but there was no strong [push] to respond, for a variety of factors,” Ako Jacintho, MD, director of addiction medicine for HealthRIGHT 360, a California community health network, said in an interview.
“The professional medical societies such as the AMA and the American Academy of Family Physicians should have put more pressure on the American Board of Medical Specialties a decade ago to create an addiction medicine subspecialty,” Dr. Jacintho observed.
Access to addiction specialty care would be wider by now had the ABMS not continued to allow psychiatrists to maintain their hold on the specialty, according to Dr. Jacintho, a family physician who treats patients with addictions.
Earlier this year, the ABMS announced it will certify the subspecialty of addiction medicine through the American Board of Preventive Medicine. A date for the first examination is pending.
With the surgeon general’s imprimatur, Dr. Jacintho expects physicians will be more aware that they should at least screen for substance use. He also predicted the report will lead to more patients demanding that addiction treatment services be made available in the primary care setting – and that practitioners will respond, either by subspecializing in addiction, or by otherwise integrating it into their practices.
That should be easier to do with the recently passed Comprehensive Addiction and Recovery Act of 2016, which expands access to medication-assisted treatment for addiction, Dr. Jacintho said.
Dr. Murthy also urged pharmaceutical companies to continue developing abuse-deterrent formulations of opioids, and to prioritize development of nonopioid alternatives for pain relief.
But the surgeon general’s report does not go far enough, given that five times more Americans suffer from chronic pain than have an opioid use disorder, according to William Maixner, DDS, PhD, professor of anesthesiology and director of Duke University’s Center for Translational Pain Medicine, Durham, N.C.
“There is an interrelationship between this very overt substance abuse epidemic and the subtler and larger covert epidemic of chronic pain,” Dr. Maixner said in a statement. “What it has in common with a huge portion of the substance abuse epidemic is opioids.”
Dr. Maixner said he hoped the report would put greater emphasis on developing alternatives to opioids for pain management, “which would eliminate this key pathway to abuse.
“We have a fundamental problem when we are trying to manage pain for the 100 million people who have some form of chronic pain, and opioids are among the few therapies available that work,” he noted.
The surgeon general’s report also urges researchers to become activists to ensure their findings are not “misrepresented” in public policy debates.
“It’s time to change how we view addiction,” said Dr. Murthy. “Not as a moral failing, but as a chronic illness that must be treated with skill, urgency, and compassion. The way we address this crisis is a test for America.”
[email protected]
On Twitter @whitneymcknight
Primary and emergency care providers must step up prevention efforts and the use of state-of-the-art medicine when treating patients with addiction, according to the first-ever U.S. Surgeon General’s report on alcohol, drugs, and health.
In the report, “Facing Addiction in America,” Surgeon General Vivek H. Murthy, MD, called on health care providers to increase access to care and approach addiction and substance use disorders as they would any other chronic health condition.
“We must help everyone see that addiction is not a character flaw – it is a chronic illness that we must approach with the same skill and compassion with which we approach heart disease, diabetes, and cancer,” Dr. Murthy explained.
In addition to offering an action plan to address substance use of all kinds, the surgeon general’s report updates the public on the state of the art of addiction science, and includes chapters on neurobiology, prevention, treatment, recovery, health systems integration, and recommendations for the future.
Data from 2015 show that more than 27 million people in the United States used illicit drugs or misuse prescription medications, while a quarter of the entire adult and adolescent population reported binge drinking in the past month. However, only 10% of those with a substance use disorder received relevant specialty care.
For the more than 40% of those with substance use disorders who have a comorbid mental health condition, less than half were treated for either, according to the federal Substance Abuse and Mental Health Services Administration.
That treatment gap is the direct result of lack of access to affordable care, shame, discrimination, and the lack of screening for substance misuse and substance use disorders in the primary care setting, Dr. Murthy wrote.
To address the gap, the surgeon general laid out a plan that starts with increasing community-wide substance use prevention efforts, such as enforcement of underage drinking laws and DUI laws, and offering needle exchange programs.
Dr. Murthy also called for a coordinated public health response to addiction, including an overhaul of criminal justice where substance use is concerned, and an emphasis on preventing known risk factors for substance misuse.
The report underscores the need for a better trained and integrated health care workforce equipped to treat addiction as a chronic disease in the general health care setting, enforcement of addiction and mental health parity laws, and the delivery of services based on the latest research into the psychosocial and biological underpinnings of substance use.
Surgeon General Murthy also used the report to urge professional medical associations to advocate for more access to medication-assisted treatment and prescription drug monitoring programs, and to create evidence-based guidelines for integrating substance use disorder treatment.
The American Medical Association responded positively to the report. In a statement, AMA President Andrew W. Gurman, MD, called it a “crucial starting point” and praised its “important guidance for the nation to see that addiction is a chronic disease and must be treated as such.”
While also supporting the report, others in the addiction medicine field pointed out that such starting points had come and gone before.
“As a profession, we saw what was happening 10 years ago, but there was no strong [push] to respond, for a variety of factors,” Ako Jacintho, MD, director of addiction medicine for HealthRIGHT 360, a California community health network, said in an interview.
“The professional medical societies such as the AMA and the American Academy of Family Physicians should have put more pressure on the American Board of Medical Specialties a decade ago to create an addiction medicine subspecialty,” Dr. Jacintho observed.
Access to addiction specialty care would be wider by now had the ABMS not continued to allow psychiatrists to maintain their hold on the specialty, according to Dr. Jacintho, a family physician who treats patients with addictions.
Earlier this year, the ABMS announced it will certify the subspecialty of addiction medicine through the American Board of Preventive Medicine. A date for the first examination is pending.
With the surgeon general’s imprimatur, Dr. Jacintho expects physicians will be more aware that they should at least screen for substance use. He also predicted the report will lead to more patients demanding that addiction treatment services be made available in the primary care setting – and that practitioners will respond, either by subspecializing in addiction, or by otherwise integrating it into their practices.
That should be easier to do with the recently passed Comprehensive Addiction and Recovery Act of 2016, which expands access to medication-assisted treatment for addiction, Dr. Jacintho said.
Dr. Murthy also urged pharmaceutical companies to continue developing abuse-deterrent formulations of opioids, and to prioritize development of nonopioid alternatives for pain relief.
But the surgeon general’s report does not go far enough, given that five times more Americans suffer from chronic pain than have an opioid use disorder, according to William Maixner, DDS, PhD, professor of anesthesiology and director of Duke University’s Center for Translational Pain Medicine, Durham, N.C.
“There is an interrelationship between this very overt substance abuse epidemic and the subtler and larger covert epidemic of chronic pain,” Dr. Maixner said in a statement. “What it has in common with a huge portion of the substance abuse epidemic is opioids.”
Dr. Maixner said he hoped the report would put greater emphasis on developing alternatives to opioids for pain management, “which would eliminate this key pathway to abuse.
“We have a fundamental problem when we are trying to manage pain for the 100 million people who have some form of chronic pain, and opioids are among the few therapies available that work,” he noted.
The surgeon general’s report also urges researchers to become activists to ensure their findings are not “misrepresented” in public policy debates.
“It’s time to change how we view addiction,” said Dr. Murthy. “Not as a moral failing, but as a chronic illness that must be treated with skill, urgency, and compassion. The way we address this crisis is a test for America.”
[email protected]
On Twitter @whitneymcknight
Primary and emergency care providers must step up prevention efforts and the use of state-of-the-art medicine when treating patients with addiction, according to the first-ever U.S. Surgeon General’s report on alcohol, drugs, and health.
In the report, “Facing Addiction in America,” Surgeon General Vivek H. Murthy, MD, called on health care providers to increase access to care and approach addiction and substance use disorders as they would any other chronic health condition.
“We must help everyone see that addiction is not a character flaw – it is a chronic illness that we must approach with the same skill and compassion with which we approach heart disease, diabetes, and cancer,” Dr. Murthy explained.
In addition to offering an action plan to address substance use of all kinds, the surgeon general’s report updates the public on the state of the art of addiction science, and includes chapters on neurobiology, prevention, treatment, recovery, health systems integration, and recommendations for the future.
Data from 2015 show that more than 27 million people in the United States used illicit drugs or misuse prescription medications, while a quarter of the entire adult and adolescent population reported binge drinking in the past month. However, only 10% of those with a substance use disorder received relevant specialty care.
For the more than 40% of those with substance use disorders who have a comorbid mental health condition, less than half were treated for either, according to the federal Substance Abuse and Mental Health Services Administration.
That treatment gap is the direct result of lack of access to affordable care, shame, discrimination, and the lack of screening for substance misuse and substance use disorders in the primary care setting, Dr. Murthy wrote.
To address the gap, the surgeon general laid out a plan that starts with increasing community-wide substance use prevention efforts, such as enforcement of underage drinking laws and DUI laws, and offering needle exchange programs.
Dr. Murthy also called for a coordinated public health response to addiction, including an overhaul of criminal justice where substance use is concerned, and an emphasis on preventing known risk factors for substance misuse.
The report underscores the need for a better trained and integrated health care workforce equipped to treat addiction as a chronic disease in the general health care setting, enforcement of addiction and mental health parity laws, and the delivery of services based on the latest research into the psychosocial and biological underpinnings of substance use.
Surgeon General Murthy also used the report to urge professional medical associations to advocate for more access to medication-assisted treatment and prescription drug monitoring programs, and to create evidence-based guidelines for integrating substance use disorder treatment.
The American Medical Association responded positively to the report. In a statement, AMA President Andrew W. Gurman, MD, called it a “crucial starting point” and praised its “important guidance for the nation to see that addiction is a chronic disease and must be treated as such.”
While also supporting the report, others in the addiction medicine field pointed out that such starting points had come and gone before.
“As a profession, we saw what was happening 10 years ago, but there was no strong [push] to respond, for a variety of factors,” Ako Jacintho, MD, director of addiction medicine for HealthRIGHT 360, a California community health network, said in an interview.
“The professional medical societies such as the AMA and the American Academy of Family Physicians should have put more pressure on the American Board of Medical Specialties a decade ago to create an addiction medicine subspecialty,” Dr. Jacintho observed.
Access to addiction specialty care would be wider by now had the ABMS not continued to allow psychiatrists to maintain their hold on the specialty, according to Dr. Jacintho, a family physician who treats patients with addictions.
Earlier this year, the ABMS announced it will certify the subspecialty of addiction medicine through the American Board of Preventive Medicine. A date for the first examination is pending.
With the surgeon general’s imprimatur, Dr. Jacintho expects physicians will be more aware that they should at least screen for substance use. He also predicted the report will lead to more patients demanding that addiction treatment services be made available in the primary care setting – and that practitioners will respond, either by subspecializing in addiction, or by otherwise integrating it into their practices.
That should be easier to do with the recently passed Comprehensive Addiction and Recovery Act of 2016, which expands access to medication-assisted treatment for addiction, Dr. Jacintho said.
Dr. Murthy also urged pharmaceutical companies to continue developing abuse-deterrent formulations of opioids, and to prioritize development of nonopioid alternatives for pain relief.
But the surgeon general’s report does not go far enough, given that five times more Americans suffer from chronic pain than have an opioid use disorder, according to William Maixner, DDS, PhD, professor of anesthesiology and director of Duke University’s Center for Translational Pain Medicine, Durham, N.C.
“There is an interrelationship between this very overt substance abuse epidemic and the subtler and larger covert epidemic of chronic pain,” Dr. Maixner said in a statement. “What it has in common with a huge portion of the substance abuse epidemic is opioids.”
Dr. Maixner said he hoped the report would put greater emphasis on developing alternatives to opioids for pain management, “which would eliminate this key pathway to abuse.
“We have a fundamental problem when we are trying to manage pain for the 100 million people who have some form of chronic pain, and opioids are among the few therapies available that work,” he noted.
The surgeon general’s report also urges researchers to become activists to ensure their findings are not “misrepresented” in public policy debates.
“It’s time to change how we view addiction,” said Dr. Murthy. “Not as a moral failing, but as a chronic illness that must be treated with skill, urgency, and compassion. The way we address this crisis is a test for America.”
[email protected]
On Twitter @whitneymcknight
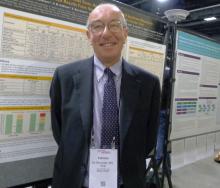
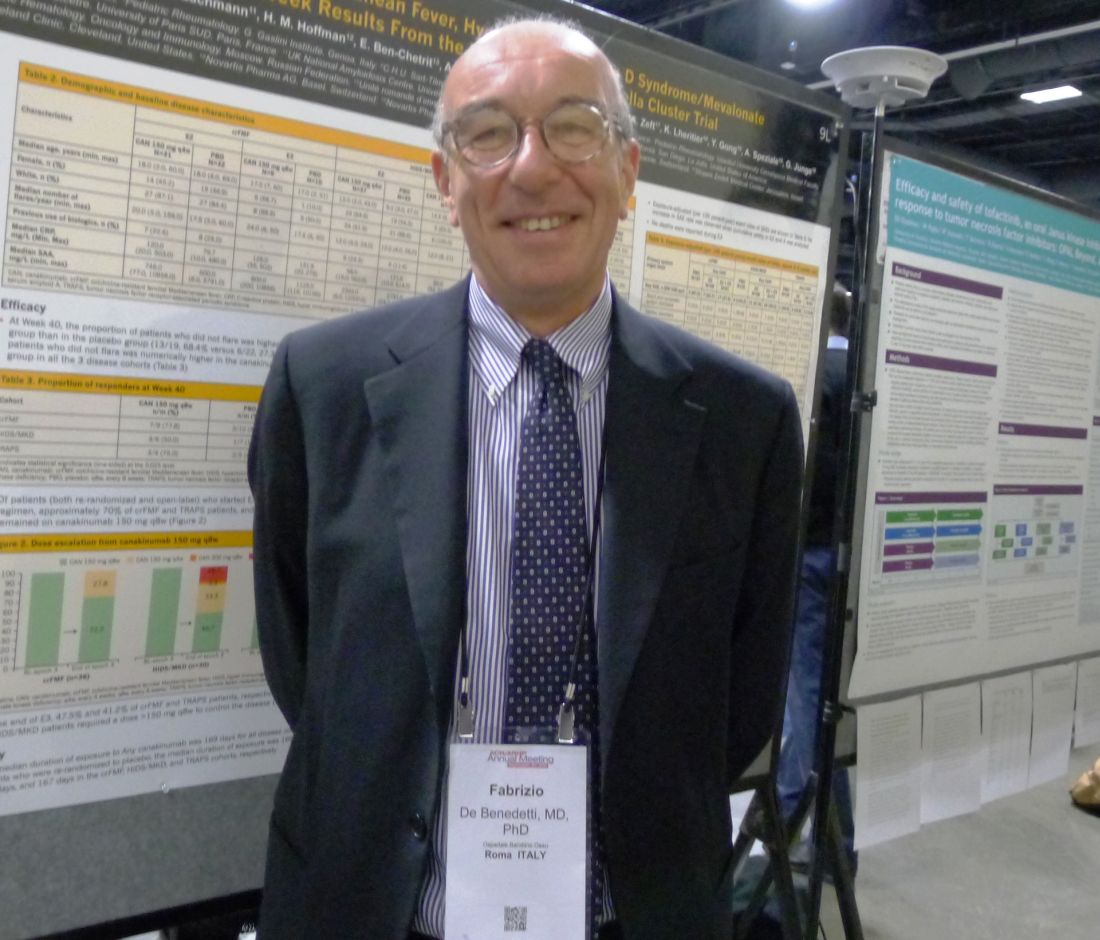
Canakinumab controls periodic fever syndromes in post-flare and maintenance dosing
WASHINGTON – Prolonged dosing with canakinumab, an anti-interleukin-1beta monoclonal antibody, confirmed its efficacy in controlling flares in three rare autoinflammatory diseases grouped as periodic fever syndromes: familial Mediterranean fever, hyperimmunoglobulin D syndrome/mevalonate kinase deficiency, and TNF receptor–associated periodic syndrome.
“Colchicine is effective in the majority of patients with FMF [familial Mediterranean fever]. However, patients with resistance to colchicine and patients with HIDS/MKD [hyperimmunoglobulin D syndrome/mevalonate kinase deficiency] or TRAPS [TNF receptor–associated periodic syndrome] have no available therapy until now. The diseases have different mechanisms and different genetic causes, but overlapping and different clinical features and a common mediator. They are all characterized by recurrent fever, joint pain, and involvement of various organs. In addition to greatly affecting the quality of life, the major complication is amyloidosis. Clinical studies and animal studies suggested that IL-1beta was involved in the pathogenesis of these diseases, and canakinumab [Ilaris] targets IL-1beta,” explained Fabrizio De Benedetti, MD, a pediatric rheumatologist at Bambino Gesu Children’s Hospital in Rome.
Following the 16-week, double-blind, randomized treatment phase of the CLUSTER trial, responders at the standard dose of 150 mg (or 2 mg/kg for patients weighing 40 kg or less) every 4 weeks were rerandomized in a 24-week randomized withdrawal phase, followed by a 72-week open-label phase.
At the annual meeting of the American College of Rheumatology, Dr. De Benedetti presented results of the 24-week randomized withdrawal phase in which 42 patients who showed complete response (defined as resolution of index flare and no new flare in the 16 week duration of the randomized controlled phase of the study) after being initially randomized to canakinumab 150 mg every 4 weeks were then rerandomized 1:1 to canakinumab 150 mg every 8 weeks versus placebo. He also presented results for patients who failed placebo during the initial 16-week randomized treatment period; went to open-label rescue treatment with canakinumab; and then, in the 24-week maintenance period, began taking open-label canakinumab 150 mg every 8 weeks. Overall, 160 patients had evaluable data for the maintenance dosing period.
The end point of this phase on a maintenance dose of canakinumab 150 mg every 8 weeks was the proportion of patients who maintained disease control and had no flare, meaning Physician Global Assessment was less than 2 and C-reactive protein was less than 30 mg/L between week 16 and week 40 after rerandomization. Patients who experienced a flare during this time could be escalated up to canakinumab 300 mg every 4 weeks.
At week 40, the proportion of responders was higher in the canakinumab-treated group, compared with placebo, at 68% versus 27%, respectively, but the difference was not statistically significant, Dr. De Benedetti reported.
The percentage of patients on canakinumab who maintained their response by week 40 was higher in each disease group, compared with placebo, but not to a statistically significant extent. The response rates were 78% vs. 30% for FMF; 50% vs. 14% for HIDS/MKD; and 75% vs. 40% for TRAPS. Only 10% of FMF and 8% of TRAPS patients required titration of canakinumab up to 300 mg every 4 weeks, compared with 29% of HIDS/MKD patients, he said.
No new safety findings were reported and there was no accumulation of toxicity. A total of 139 adverse events was reported among all patients in the placebo arm (including the double-blind and prolonged dosing phases), and 8 of these were deemed serious adverse events. The rate of serious adverse events was 85 per 100 patient-years. Among canakinumab-treated patients, the rates of serious adverse events were 34 per 100 patient-years for FMF, 34 per 100 for HIDS/MKD, and 19 per 100 for TRAPS.
“The results of this trial confirm the long-term efficacy of canakinumab in these rare diseases and provide information on the long-term dose needed to control disease, with about half of the patients with FMF or TRAPS and about one-third of those with HIDS/MKD showing no flare at a prolonged dose of 150 mg every 8 weeks,” Dr. De Benedetti said.
The study was supported by Novartis, which markets canakinumab. Dr. De Benedetti disclosed financial ties with Novartis, Pfizer, AbbVie, Roche, Novimmune, and Bristol-Myers Squibb.
WASHINGTON – Prolonged dosing with canakinumab, an anti-interleukin-1beta monoclonal antibody, confirmed its efficacy in controlling flares in three rare autoinflammatory diseases grouped as periodic fever syndromes: familial Mediterranean fever, hyperimmunoglobulin D syndrome/mevalonate kinase deficiency, and TNF receptor–associated periodic syndrome.
“Colchicine is effective in the majority of patients with FMF [familial Mediterranean fever]. However, patients with resistance to colchicine and patients with HIDS/MKD [hyperimmunoglobulin D syndrome/mevalonate kinase deficiency] or TRAPS [TNF receptor–associated periodic syndrome] have no available therapy until now. The diseases have different mechanisms and different genetic causes, but overlapping and different clinical features and a common mediator. They are all characterized by recurrent fever, joint pain, and involvement of various organs. In addition to greatly affecting the quality of life, the major complication is amyloidosis. Clinical studies and animal studies suggested that IL-1beta was involved in the pathogenesis of these diseases, and canakinumab [Ilaris] targets IL-1beta,” explained Fabrizio De Benedetti, MD, a pediatric rheumatologist at Bambino Gesu Children’s Hospital in Rome.
Following the 16-week, double-blind, randomized treatment phase of the CLUSTER trial, responders at the standard dose of 150 mg (or 2 mg/kg for patients weighing 40 kg or less) every 4 weeks were rerandomized in a 24-week randomized withdrawal phase, followed by a 72-week open-label phase.
At the annual meeting of the American College of Rheumatology, Dr. De Benedetti presented results of the 24-week randomized withdrawal phase in which 42 patients who showed complete response (defined as resolution of index flare and no new flare in the 16 week duration of the randomized controlled phase of the study) after being initially randomized to canakinumab 150 mg every 4 weeks were then rerandomized 1:1 to canakinumab 150 mg every 8 weeks versus placebo. He also presented results for patients who failed placebo during the initial 16-week randomized treatment period; went to open-label rescue treatment with canakinumab; and then, in the 24-week maintenance period, began taking open-label canakinumab 150 mg every 8 weeks. Overall, 160 patients had evaluable data for the maintenance dosing period.
The end point of this phase on a maintenance dose of canakinumab 150 mg every 8 weeks was the proportion of patients who maintained disease control and had no flare, meaning Physician Global Assessment was less than 2 and C-reactive protein was less than 30 mg/L between week 16 and week 40 after rerandomization. Patients who experienced a flare during this time could be escalated up to canakinumab 300 mg every 4 weeks.
At week 40, the proportion of responders was higher in the canakinumab-treated group, compared with placebo, at 68% versus 27%, respectively, but the difference was not statistically significant, Dr. De Benedetti reported.
The percentage of patients on canakinumab who maintained their response by week 40 was higher in each disease group, compared with placebo, but not to a statistically significant extent. The response rates were 78% vs. 30% for FMF; 50% vs. 14% for HIDS/MKD; and 75% vs. 40% for TRAPS. Only 10% of FMF and 8% of TRAPS patients required titration of canakinumab up to 300 mg every 4 weeks, compared with 29% of HIDS/MKD patients, he said.
No new safety findings were reported and there was no accumulation of toxicity. A total of 139 adverse events was reported among all patients in the placebo arm (including the double-blind and prolonged dosing phases), and 8 of these were deemed serious adverse events. The rate of serious adverse events was 85 per 100 patient-years. Among canakinumab-treated patients, the rates of serious adverse events were 34 per 100 patient-years for FMF, 34 per 100 for HIDS/MKD, and 19 per 100 for TRAPS.
“The results of this trial confirm the long-term efficacy of canakinumab in these rare diseases and provide information on the long-term dose needed to control disease, with about half of the patients with FMF or TRAPS and about one-third of those with HIDS/MKD showing no flare at a prolonged dose of 150 mg every 8 weeks,” Dr. De Benedetti said.
The study was supported by Novartis, which markets canakinumab. Dr. De Benedetti disclosed financial ties with Novartis, Pfizer, AbbVie, Roche, Novimmune, and Bristol-Myers Squibb.
WASHINGTON – Prolonged dosing with canakinumab, an anti-interleukin-1beta monoclonal antibody, confirmed its efficacy in controlling flares in three rare autoinflammatory diseases grouped as periodic fever syndromes: familial Mediterranean fever, hyperimmunoglobulin D syndrome/mevalonate kinase deficiency, and TNF receptor–associated periodic syndrome.
“Colchicine is effective in the majority of patients with FMF [familial Mediterranean fever]. However, patients with resistance to colchicine and patients with HIDS/MKD [hyperimmunoglobulin D syndrome/mevalonate kinase deficiency] or TRAPS [TNF receptor–associated periodic syndrome] have no available therapy until now. The diseases have different mechanisms and different genetic causes, but overlapping and different clinical features and a common mediator. They are all characterized by recurrent fever, joint pain, and involvement of various organs. In addition to greatly affecting the quality of life, the major complication is amyloidosis. Clinical studies and animal studies suggested that IL-1beta was involved in the pathogenesis of these diseases, and canakinumab [Ilaris] targets IL-1beta,” explained Fabrizio De Benedetti, MD, a pediatric rheumatologist at Bambino Gesu Children’s Hospital in Rome.
Following the 16-week, double-blind, randomized treatment phase of the CLUSTER trial, responders at the standard dose of 150 mg (or 2 mg/kg for patients weighing 40 kg or less) every 4 weeks were rerandomized in a 24-week randomized withdrawal phase, followed by a 72-week open-label phase.
At the annual meeting of the American College of Rheumatology, Dr. De Benedetti presented results of the 24-week randomized withdrawal phase in which 42 patients who showed complete response (defined as resolution of index flare and no new flare in the 16 week duration of the randomized controlled phase of the study) after being initially randomized to canakinumab 150 mg every 4 weeks were then rerandomized 1:1 to canakinumab 150 mg every 8 weeks versus placebo. He also presented results for patients who failed placebo during the initial 16-week randomized treatment period; went to open-label rescue treatment with canakinumab; and then, in the 24-week maintenance period, began taking open-label canakinumab 150 mg every 8 weeks. Overall, 160 patients had evaluable data for the maintenance dosing period.
The end point of this phase on a maintenance dose of canakinumab 150 mg every 8 weeks was the proportion of patients who maintained disease control and had no flare, meaning Physician Global Assessment was less than 2 and C-reactive protein was less than 30 mg/L between week 16 and week 40 after rerandomization. Patients who experienced a flare during this time could be escalated up to canakinumab 300 mg every 4 weeks.
At week 40, the proportion of responders was higher in the canakinumab-treated group, compared with placebo, at 68% versus 27%, respectively, but the difference was not statistically significant, Dr. De Benedetti reported.
The percentage of patients on canakinumab who maintained their response by week 40 was higher in each disease group, compared with placebo, but not to a statistically significant extent. The response rates were 78% vs. 30% for FMF; 50% vs. 14% for HIDS/MKD; and 75% vs. 40% for TRAPS. Only 10% of FMF and 8% of TRAPS patients required titration of canakinumab up to 300 mg every 4 weeks, compared with 29% of HIDS/MKD patients, he said.
No new safety findings were reported and there was no accumulation of toxicity. A total of 139 adverse events was reported among all patients in the placebo arm (including the double-blind and prolonged dosing phases), and 8 of these were deemed serious adverse events. The rate of serious adverse events was 85 per 100 patient-years. Among canakinumab-treated patients, the rates of serious adverse events were 34 per 100 patient-years for FMF, 34 per 100 for HIDS/MKD, and 19 per 100 for TRAPS.
“The results of this trial confirm the long-term efficacy of canakinumab in these rare diseases and provide information on the long-term dose needed to control disease, with about half of the patients with FMF or TRAPS and about one-third of those with HIDS/MKD showing no flare at a prolonged dose of 150 mg every 8 weeks,” Dr. De Benedetti said.
The study was supported by Novartis, which markets canakinumab. Dr. De Benedetti disclosed financial ties with Novartis, Pfizer, AbbVie, Roche, Novimmune, and Bristol-Myers Squibb.
AT THE ACR ANNUAL MEETING
Key clinical point:
Major finding: At week 40, the proportion of responders was higher in the canakinumab-treated group (68%), compared with placebo (27%), but the difference was not statistically significant.
Data source: A phase III, randomized, double-blind, 16-week, placebo-controlled trial of 181 patients, followed by a 24-week withdrawal phase rerandomizing 42 responders, with all other patients continuing on canakinumab.
Disclosures: The study was supported by Novartis, which markets canakinumab. Dr. De Benedetti disclosed financial ties with Novartis, Pfizer, AbbVie, Roche, Novimmune, and Bristol-Myers Squibb.
Scott Kaatz, DO, uses SHM to Engage Future Hospitalists
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Log on to www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Scott Kaatz, DO, MSc, FACP, SFHM, a hospitalist at Henry Ford Hospital in Detroit. In addition to being an active SHM member, he is immediate past president of SHM’s Michigan Chapter and has been involved in multiple mentored implementation (MI) programs offered by SHM’s Center for Hospital Innovation and Improvement.
Question: What inspired you to begin working in hospital medicine and later join and become so involved with SHM?
Answer: For most of my career, I’ve been at Henry Ford Hospital in Detroit, including during my internal medicine residency. After residency, I was a primary-care physician there, and I rounded three to four months out of the year in the hospital with traditional house staff model. Four years ago, I transitioned to another role as a chief quality officer at Hurley Medical Center in Flint, Mich. While in Flint, I didn’t have a clinic and was strictly a hospitalist, spending about four months a year rounding.
When my career path led me to mostly inpatient work in the hospital, I became more involved not only with hospital medicine but with SHM. As of this past June, I went back home to Henry Ford as a full-time hospitalist. I now focus my attention on hospital medicine for eight months of the year, with some protected time for faculty development and scholarly activities for residents and junior faculty in the division of hospital medicine.
Q: How has your involvement with SHM’s mentored implementation programs impacted your practice and led to improved patient care?
A: After participating in the venous thromboembolism (VTE) mentored implementation program, I became a participant as a mentee site for I-PASS, a program focused on improving communication between providers during patient handoffs. During my time with the I-PASS team, I could sense the commitment and energy to improving handoffs not only at my site but at other participant sites nationwide during our regular check-in calls. Mentored implementation programs are brilliant because they go beyond providing sites with data, a few research papers, and some written recommendations. They really dig down into the true spirit of mentoring with a team.
At Hurley Medical Center, we went “all in” with our pediatric residency. What was most encouraging was that by the end of the year, the I-PASS recommendations and processes were standard practice and fully integrated into the culture and workflow of the care teams.
I applaud these programs tremendously. That’s really how you impact change, and it’s the spark, energy, and momentum from both mentors and mentees that keeps the team on track.
Q: You are the immediate past president of the Michigan Chapter of SHM. What have been some of the biggest benefits of being involved with an SHM chapter?
A: When I first became involved with SHM, there had been a Northern Michigan Chapter, but since SHM seeks to have regional chapters that cater to local audiences, I and some of my colleagues set out to develop a Southern Michigan Chapter. We developed our chapter and designed our meetings with support from SHM’s Chapter Support Committee.
At a typical meeting, we typically host an hour of cocktails with some hors d’oeuvres to provide an opportunity for networking and fellowship. The personal connections are at the heart of these meetings. From the content side, we always have a speaker to talk about issues germane to hospitalists. These are not just run-of-the-mill grand rounds discussions but rather information on clinical updates or the business and policy side of hospital medicine.
In our chapter, we also cycle leadership each year, using a “see one, do one, teach one” approach with our vice president-elect, president, and immediate past president to ensure proper development and continuity.
Moving forward, we are trying to reach out to medical students on a more regular basis. If you’re in your third year of medical school, it’s beneficial to start talking informally to hospitalists from multiple organizations in the state and get a feel for what a career in hospital medicine is like. How amazing would it be to walk in and interview for residency with a person you had dinner with a few months ago?
Q: SHM’s Board of Directors recently approved a Chapter Development Fund to support innovative initiatives that drive engagement on a local level. Explain the potential impact you see this having on chapters and, more broadly, SHM’s membership and hospital medicine.
A: Since our chapter’s inception, we have been able to expand our reach and stream our content to other parts of the state on the Internet. Part of the reason we have been able to do this is due to support from a Chapter Development Fund recently approved by SHM’s Board of Directors. As a result, we have turned our Southern Michigan Chapter into a statewide chapter with virtual sites. At the last meeting, we had over 75 attendees between our physical site and our “satellite site” in Michigan.
Our next project is to apply for funding to provide first- and second-year residents with free membership for a year through our chapter to expose them to the resources SHM has available to them and get their foot in the door with the organization. At a recent co-sponsored statewide meeting with the American College of Physicians, we were able to sign up 20 residents as new members of SHM, and our chapter paid their dues as an investment into our specialty.
Q: Any closing thoughts?
A: If there’s one thing I haven’t yet shared that I feel quite passionately about, it’s that SHM has such a robust library of educational resources that all hospitalists should be aware of, especially SHM’s annual meeting. It’s extraordinarily clinical and features a sizeable amount of content for grassroots clinicians and hospital leaders, including the best speakers in the field. On top of the educational components, the networking possibilities with hospitalists across the country make the annual meeting a prime example of the value SHM offers.
I’ve also been fortunate to have been involved with developing enduring materials on SHM’s Learning Portal, some of which are available without cost due to grant funding. The fact that SHM has pursued this funding and made some of these resources available to hospitalists outside of SHM’s membership embodies the organization’s mission of not only teaching doctors how to take better care of patients but helping patients get better—one of many reasons I am proud to be an active member. TH
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Log on to www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Scott Kaatz, DO, MSc, FACP, SFHM, a hospitalist at Henry Ford Hospital in Detroit. In addition to being an active SHM member, he is immediate past president of SHM’s Michigan Chapter and has been involved in multiple mentored implementation (MI) programs offered by SHM’s Center for Hospital Innovation and Improvement.
Question: What inspired you to begin working in hospital medicine and later join and become so involved with SHM?
Answer: For most of my career, I’ve been at Henry Ford Hospital in Detroit, including during my internal medicine residency. After residency, I was a primary-care physician there, and I rounded three to four months out of the year in the hospital with traditional house staff model. Four years ago, I transitioned to another role as a chief quality officer at Hurley Medical Center in Flint, Mich. While in Flint, I didn’t have a clinic and was strictly a hospitalist, spending about four months a year rounding.
When my career path led me to mostly inpatient work in the hospital, I became more involved not only with hospital medicine but with SHM. As of this past June, I went back home to Henry Ford as a full-time hospitalist. I now focus my attention on hospital medicine for eight months of the year, with some protected time for faculty development and scholarly activities for residents and junior faculty in the division of hospital medicine.
Q: How has your involvement with SHM’s mentored implementation programs impacted your practice and led to improved patient care?
A: After participating in the venous thromboembolism (VTE) mentored implementation program, I became a participant as a mentee site for I-PASS, a program focused on improving communication between providers during patient handoffs. During my time with the I-PASS team, I could sense the commitment and energy to improving handoffs not only at my site but at other participant sites nationwide during our regular check-in calls. Mentored implementation programs are brilliant because they go beyond providing sites with data, a few research papers, and some written recommendations. They really dig down into the true spirit of mentoring with a team.
At Hurley Medical Center, we went “all in” with our pediatric residency. What was most encouraging was that by the end of the year, the I-PASS recommendations and processes were standard practice and fully integrated into the culture and workflow of the care teams.
I applaud these programs tremendously. That’s really how you impact change, and it’s the spark, energy, and momentum from both mentors and mentees that keeps the team on track.
Q: You are the immediate past president of the Michigan Chapter of SHM. What have been some of the biggest benefits of being involved with an SHM chapter?
A: When I first became involved with SHM, there had been a Northern Michigan Chapter, but since SHM seeks to have regional chapters that cater to local audiences, I and some of my colleagues set out to develop a Southern Michigan Chapter. We developed our chapter and designed our meetings with support from SHM’s Chapter Support Committee.
At a typical meeting, we typically host an hour of cocktails with some hors d’oeuvres to provide an opportunity for networking and fellowship. The personal connections are at the heart of these meetings. From the content side, we always have a speaker to talk about issues germane to hospitalists. These are not just run-of-the-mill grand rounds discussions but rather information on clinical updates or the business and policy side of hospital medicine.
In our chapter, we also cycle leadership each year, using a “see one, do one, teach one” approach with our vice president-elect, president, and immediate past president to ensure proper development and continuity.
Moving forward, we are trying to reach out to medical students on a more regular basis. If you’re in your third year of medical school, it’s beneficial to start talking informally to hospitalists from multiple organizations in the state and get a feel for what a career in hospital medicine is like. How amazing would it be to walk in and interview for residency with a person you had dinner with a few months ago?
Q: SHM’s Board of Directors recently approved a Chapter Development Fund to support innovative initiatives that drive engagement on a local level. Explain the potential impact you see this having on chapters and, more broadly, SHM’s membership and hospital medicine.
A: Since our chapter’s inception, we have been able to expand our reach and stream our content to other parts of the state on the Internet. Part of the reason we have been able to do this is due to support from a Chapter Development Fund recently approved by SHM’s Board of Directors. As a result, we have turned our Southern Michigan Chapter into a statewide chapter with virtual sites. At the last meeting, we had over 75 attendees between our physical site and our “satellite site” in Michigan.
Our next project is to apply for funding to provide first- and second-year residents with free membership for a year through our chapter to expose them to the resources SHM has available to them and get their foot in the door with the organization. At a recent co-sponsored statewide meeting with the American College of Physicians, we were able to sign up 20 residents as new members of SHM, and our chapter paid their dues as an investment into our specialty.
Q: Any closing thoughts?
A: If there’s one thing I haven’t yet shared that I feel quite passionately about, it’s that SHM has such a robust library of educational resources that all hospitalists should be aware of, especially SHM’s annual meeting. It’s extraordinarily clinical and features a sizeable amount of content for grassroots clinicians and hospital leaders, including the best speakers in the field. On top of the educational components, the networking possibilities with hospitalists across the country make the annual meeting a prime example of the value SHM offers.
I’ve also been fortunate to have been involved with developing enduring materials on SHM’s Learning Portal, some of which are available without cost due to grant funding. The fact that SHM has pursued this funding and made some of these resources available to hospitalists outside of SHM’s membership embodies the organization’s mission of not only teaching doctors how to take better care of patients but helping patients get better—one of many reasons I am proud to be an active member. TH
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Log on to www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Scott Kaatz, DO, MSc, FACP, SFHM, a hospitalist at Henry Ford Hospital in Detroit. In addition to being an active SHM member, he is immediate past president of SHM’s Michigan Chapter and has been involved in multiple mentored implementation (MI) programs offered by SHM’s Center for Hospital Innovation and Improvement.
Question: What inspired you to begin working in hospital medicine and later join and become so involved with SHM?
Answer: For most of my career, I’ve been at Henry Ford Hospital in Detroit, including during my internal medicine residency. After residency, I was a primary-care physician there, and I rounded three to four months out of the year in the hospital with traditional house staff model. Four years ago, I transitioned to another role as a chief quality officer at Hurley Medical Center in Flint, Mich. While in Flint, I didn’t have a clinic and was strictly a hospitalist, spending about four months a year rounding.
When my career path led me to mostly inpatient work in the hospital, I became more involved not only with hospital medicine but with SHM. As of this past June, I went back home to Henry Ford as a full-time hospitalist. I now focus my attention on hospital medicine for eight months of the year, with some protected time for faculty development and scholarly activities for residents and junior faculty in the division of hospital medicine.
Q: How has your involvement with SHM’s mentored implementation programs impacted your practice and led to improved patient care?
A: After participating in the venous thromboembolism (VTE) mentored implementation program, I became a participant as a mentee site for I-PASS, a program focused on improving communication between providers during patient handoffs. During my time with the I-PASS team, I could sense the commitment and energy to improving handoffs not only at my site but at other participant sites nationwide during our regular check-in calls. Mentored implementation programs are brilliant because they go beyond providing sites with data, a few research papers, and some written recommendations. They really dig down into the true spirit of mentoring with a team.
At Hurley Medical Center, we went “all in” with our pediatric residency. What was most encouraging was that by the end of the year, the I-PASS recommendations and processes were standard practice and fully integrated into the culture and workflow of the care teams.
I applaud these programs tremendously. That’s really how you impact change, and it’s the spark, energy, and momentum from both mentors and mentees that keeps the team on track.
Q: You are the immediate past president of the Michigan Chapter of SHM. What have been some of the biggest benefits of being involved with an SHM chapter?
A: When I first became involved with SHM, there had been a Northern Michigan Chapter, but since SHM seeks to have regional chapters that cater to local audiences, I and some of my colleagues set out to develop a Southern Michigan Chapter. We developed our chapter and designed our meetings with support from SHM’s Chapter Support Committee.
At a typical meeting, we typically host an hour of cocktails with some hors d’oeuvres to provide an opportunity for networking and fellowship. The personal connections are at the heart of these meetings. From the content side, we always have a speaker to talk about issues germane to hospitalists. These are not just run-of-the-mill grand rounds discussions but rather information on clinical updates or the business and policy side of hospital medicine.
In our chapter, we also cycle leadership each year, using a “see one, do one, teach one” approach with our vice president-elect, president, and immediate past president to ensure proper development and continuity.
Moving forward, we are trying to reach out to medical students on a more regular basis. If you’re in your third year of medical school, it’s beneficial to start talking informally to hospitalists from multiple organizations in the state and get a feel for what a career in hospital medicine is like. How amazing would it be to walk in and interview for residency with a person you had dinner with a few months ago?
Q: SHM’s Board of Directors recently approved a Chapter Development Fund to support innovative initiatives that drive engagement on a local level. Explain the potential impact you see this having on chapters and, more broadly, SHM’s membership and hospital medicine.
A: Since our chapter’s inception, we have been able to expand our reach and stream our content to other parts of the state on the Internet. Part of the reason we have been able to do this is due to support from a Chapter Development Fund recently approved by SHM’s Board of Directors. As a result, we have turned our Southern Michigan Chapter into a statewide chapter with virtual sites. At the last meeting, we had over 75 attendees between our physical site and our “satellite site” in Michigan.
Our next project is to apply for funding to provide first- and second-year residents with free membership for a year through our chapter to expose them to the resources SHM has available to them and get their foot in the door with the organization. At a recent co-sponsored statewide meeting with the American College of Physicians, we were able to sign up 20 residents as new members of SHM, and our chapter paid their dues as an investment into our specialty.
Q: Any closing thoughts?
A: If there’s one thing I haven’t yet shared that I feel quite passionately about, it’s that SHM has such a robust library of educational resources that all hospitalists should be aware of, especially SHM’s annual meeting. It’s extraordinarily clinical and features a sizeable amount of content for grassroots clinicians and hospital leaders, including the best speakers in the field. On top of the educational components, the networking possibilities with hospitalists across the country make the annual meeting a prime example of the value SHM offers.
I’ve also been fortunate to have been involved with developing enduring materials on SHM’s Learning Portal, some of which are available without cost due to grant funding. The fact that SHM has pursued this funding and made some of these resources available to hospitalists outside of SHM’s membership embodies the organization’s mission of not only teaching doctors how to take better care of patients but helping patients get better—one of many reasons I am proud to be an active member. TH
FDA approves new uses for drug in MM

Photo courtesy of Janssen
The US Food and Drug Administration (FDA) has approved new indications for the monoclonal antibody daratumumab (Darzalex®).
The drug is now approved for use in combination with lenalidomide and dexamethasone or bortezomib and dexamethasone to treat patients with multiple myeloma (MM) who have received at least 1 prior therapy.
This approval comes 3 months after a supplemental biologics license application was submitted to the FDA.
The application was granted priority review last month, and the FDA granted daratumumab breakthrough therapy designation in July.
Daratumumab is the first CD38-directed cytolytic antibody approved anywhere in the world.
The drug received accelerated approval from the FDA in November of last year for use as monotherapy in MM patients who have received at least 3 prior lines of therapy, including a proteasome inhibitor and an immunomodulatory agent, or MM patients who are double refractory to a proteasome inhibitor and immunomodulatory agent.
Daratumumab is being developed by Janssen Biotech, Inc. under an exclusive worldwide license from Genmab. For the full prescribing information, visit www.DARZALEX.com.
Phase 3 trials
The FDA’s latest approval of daratumumab was based on data from the phase 3 POLLUX and CASTOR trials.
In the POLLUX trial, researchers compared treatment with lenalidomide and dexamethasone to treatment with daratumumab, lenalidomide, and dexamethasone in patients with relapsed or refractory MM.
Patients who received daratumumab in combination had a significantly higher response rate and longer progression-free survival than patients who received the 2-drug combination.
However, treatment with daratumumab was associated with infusion-related reactions and a higher incidence of neutropenia.
Results from this trial were published in NEJM in October.
In the CASTOR trial, researchers compared treatment with bortezomib and dexamethasone to treatment with daratumumab, bortezomib, and dexamethasone in patients with previously treated MM.
Patients who received the 3-drug combination had a higher response rate, longer progression-free survival, and a higher incidence of grade 3/4 adverse events than those who received the 2-drug combination.
Results from this trial were published in NEJM in August. ![]()

Photo courtesy of Janssen
The US Food and Drug Administration (FDA) has approved new indications for the monoclonal antibody daratumumab (Darzalex®).
The drug is now approved for use in combination with lenalidomide and dexamethasone or bortezomib and dexamethasone to treat patients with multiple myeloma (MM) who have received at least 1 prior therapy.
This approval comes 3 months after a supplemental biologics license application was submitted to the FDA.
The application was granted priority review last month, and the FDA granted daratumumab breakthrough therapy designation in July.
Daratumumab is the first CD38-directed cytolytic antibody approved anywhere in the world.
The drug received accelerated approval from the FDA in November of last year for use as monotherapy in MM patients who have received at least 3 prior lines of therapy, including a proteasome inhibitor and an immunomodulatory agent, or MM patients who are double refractory to a proteasome inhibitor and immunomodulatory agent.
Daratumumab is being developed by Janssen Biotech, Inc. under an exclusive worldwide license from Genmab. For the full prescribing information, visit www.DARZALEX.com.
Phase 3 trials
The FDA’s latest approval of daratumumab was based on data from the phase 3 POLLUX and CASTOR trials.
In the POLLUX trial, researchers compared treatment with lenalidomide and dexamethasone to treatment with daratumumab, lenalidomide, and dexamethasone in patients with relapsed or refractory MM.
Patients who received daratumumab in combination had a significantly higher response rate and longer progression-free survival than patients who received the 2-drug combination.
However, treatment with daratumumab was associated with infusion-related reactions and a higher incidence of neutropenia.
Results from this trial were published in NEJM in October.
In the CASTOR trial, researchers compared treatment with bortezomib and dexamethasone to treatment with daratumumab, bortezomib, and dexamethasone in patients with previously treated MM.
Patients who received the 3-drug combination had a higher response rate, longer progression-free survival, and a higher incidence of grade 3/4 adverse events than those who received the 2-drug combination.
Results from this trial were published in NEJM in August. ![]()

Photo courtesy of Janssen
The US Food and Drug Administration (FDA) has approved new indications for the monoclonal antibody daratumumab (Darzalex®).
The drug is now approved for use in combination with lenalidomide and dexamethasone or bortezomib and dexamethasone to treat patients with multiple myeloma (MM) who have received at least 1 prior therapy.
This approval comes 3 months after a supplemental biologics license application was submitted to the FDA.
The application was granted priority review last month, and the FDA granted daratumumab breakthrough therapy designation in July.
Daratumumab is the first CD38-directed cytolytic antibody approved anywhere in the world.
The drug received accelerated approval from the FDA in November of last year for use as monotherapy in MM patients who have received at least 3 prior lines of therapy, including a proteasome inhibitor and an immunomodulatory agent, or MM patients who are double refractory to a proteasome inhibitor and immunomodulatory agent.
Daratumumab is being developed by Janssen Biotech, Inc. under an exclusive worldwide license from Genmab. For the full prescribing information, visit www.DARZALEX.com.
Phase 3 trials
The FDA’s latest approval of daratumumab was based on data from the phase 3 POLLUX and CASTOR trials.
In the POLLUX trial, researchers compared treatment with lenalidomide and dexamethasone to treatment with daratumumab, lenalidomide, and dexamethasone in patients with relapsed or refractory MM.
Patients who received daratumumab in combination had a significantly higher response rate and longer progression-free survival than patients who received the 2-drug combination.
However, treatment with daratumumab was associated with infusion-related reactions and a higher incidence of neutropenia.
Results from this trial were published in NEJM in October.
In the CASTOR trial, researchers compared treatment with bortezomib and dexamethasone to treatment with daratumumab, bortezomib, and dexamethasone in patients with previously treated MM.
Patients who received the 3-drug combination had a higher response rate, longer progression-free survival, and a higher incidence of grade 3/4 adverse events than those who received the 2-drug combination.
Results from this trial were published in NEJM in August. ![]()
ALL subtype ‘highly prevalent’ in adults

Photo courtesy of St. Jude
Children’s Research Hospital
Researchers have found evidence to suggest that a high-risk subtype of acute lymphoblastic leukemia (ALL) is “highly prevalent” in adults with ALL.
In a study of nearly 800 adults with ALL, roughly a quarter of the patients had Philadelphia chromosome-like (Ph-like) ALL.
Patients with Ph-like ALL had inferior overall survival (OS) and event-free survival (EFS), but most of them also had kinase-activating alterations that suggest they might respond well to tyrosine kinase inhibitors.
The researchers reported these findings in the Journal of Clinical Oncology.
“This study establishes that a large percentage of adults with ALL have this high-risk subtype,” said study author Charles Mullighan, MD, MBBS, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“The finding provides a compelling reason to identify those with Ph-like ALL and move forward with clinical trials of these targeted therapies in combination with current chemotherapeutic regimens.”
This study builds on previous research, which suggested that Ph-like ALL becomes more common with age, is associated with poor prognosis, and is characterized by genomic alterations that appear to make patients responsive to treatment with tyrosine kinase inhibitors.
“Our 2014 findings that the prevalence of Ph-like ALL increased with age and was particularly common in young adults generated tremendous interest because adult ALL is difficult to treat,” Dr Mullighan said. “In this study, we determined that the prevalence remains high across the age spectrum of adults with ALL.”
Prevalence and outcomes
The study included 798 adults who were between the ages of 21 and 86 when diagnosed with ALL. A total of 194 patients (24%) had Ph-like ALL.
The incidence of Ph-like ALL was 27.9% among young adults (ages 21 to 39), 20.4% in adults (ages 40 to 59), and 24.0% in older adults (ages 60 to 86).
Patients with Ph-like ALL had significantly inferior 5-year OS compared to patients with non-Ph-like ALL—23.8% and 52.4%, respectively (P<0.001). The same was true for 5-year EFS—22.5% and 49.3%, respectively (P<0.001).
Among Ph-like ALL patients, the 5-year EFS rates were 40.4% for young adults, 29.8% for adults, and 18.9% for older adults. The 5-year OS rates were 45.2%, 35.1%, and 16.2%, respectively.
Genomic analysis
The researchers performed genomic analysis of 180 of the Ph-like ALL cases and found that 88% had kinase-activating alterations.
This included CRLF2 rearrangements in 51% of cases, JAK2 or EPOR rearrangements in 12.4%, ABL class fusions in 9.8%, other JAK-STAT sequence mutations in 7.2%, other kinase alterations in 4.1%, and Ras pathway mutations in 3.6%.
“Our comprehensive sequencing showed that Ph-like ALL in adults is the most genetically diverse subtype of leukemia that has been described,” said study author Kathryn Roberts, PhD, of St. Jude.
“Cumulatively, more than 50 different chromosomal rearrangements involving 15 different kinases and cytokine receptors have been identified. In this study, we identified 11 chromosomal rearrangements that are new to Ph-like ALL.”
These 11 rearrangements are FIP1L1-PDGFRA, SNX29-PDGFRB, SMU1-JAK2, ZNF340-JAK2, THADA-EPOR, SMARCA4-TYK2, ZNF340-TYK2, ZYMM2-FLT3, DNTT-BLNK, TMEM2-PTK2B, and KANK1-CBL1.
The diversity of kinase-activating alterations in Ph-like ALL has important clinical implications, said study author Hagop Kantarjian, MD, of the University of Texas MD Anderson Cancer Center in Houston.
“It is important that we now identify patients with Ph-like ALL at diagnosis to provide optimal treatment with targeted agents,” he said.
The findings also highlight the importance of centralized comprehensive genomic sequencing for patients, said study author Elisabeth Paietta, PhD, of the Montefiore Health System and Albert Einstein College of Medicine in Bronx, New York.
“Lymphoblasts from almost half of the patients with Ph-like ALL harbor a genomic rearrangement of CRLF2, which can be detected by flow cytometry using an antibody to CRLF2,” Dr Paietta said. “This is very important as it allows a quick characterization of this Ph-like ALL subtype prior to any detailed sequencing.” ![]()

Photo courtesy of St. Jude
Children’s Research Hospital
Researchers have found evidence to suggest that a high-risk subtype of acute lymphoblastic leukemia (ALL) is “highly prevalent” in adults with ALL.
In a study of nearly 800 adults with ALL, roughly a quarter of the patients had Philadelphia chromosome-like (Ph-like) ALL.
Patients with Ph-like ALL had inferior overall survival (OS) and event-free survival (EFS), but most of them also had kinase-activating alterations that suggest they might respond well to tyrosine kinase inhibitors.
The researchers reported these findings in the Journal of Clinical Oncology.
“This study establishes that a large percentage of adults with ALL have this high-risk subtype,” said study author Charles Mullighan, MD, MBBS, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“The finding provides a compelling reason to identify those with Ph-like ALL and move forward with clinical trials of these targeted therapies in combination with current chemotherapeutic regimens.”
This study builds on previous research, which suggested that Ph-like ALL becomes more common with age, is associated with poor prognosis, and is characterized by genomic alterations that appear to make patients responsive to treatment with tyrosine kinase inhibitors.
“Our 2014 findings that the prevalence of Ph-like ALL increased with age and was particularly common in young adults generated tremendous interest because adult ALL is difficult to treat,” Dr Mullighan said. “In this study, we determined that the prevalence remains high across the age spectrum of adults with ALL.”
Prevalence and outcomes
The study included 798 adults who were between the ages of 21 and 86 when diagnosed with ALL. A total of 194 patients (24%) had Ph-like ALL.
The incidence of Ph-like ALL was 27.9% among young adults (ages 21 to 39), 20.4% in adults (ages 40 to 59), and 24.0% in older adults (ages 60 to 86).
Patients with Ph-like ALL had significantly inferior 5-year OS compared to patients with non-Ph-like ALL—23.8% and 52.4%, respectively (P<0.001). The same was true for 5-year EFS—22.5% and 49.3%, respectively (P<0.001).
Among Ph-like ALL patients, the 5-year EFS rates were 40.4% for young adults, 29.8% for adults, and 18.9% for older adults. The 5-year OS rates were 45.2%, 35.1%, and 16.2%, respectively.
Genomic analysis
The researchers performed genomic analysis of 180 of the Ph-like ALL cases and found that 88% had kinase-activating alterations.
This included CRLF2 rearrangements in 51% of cases, JAK2 or EPOR rearrangements in 12.4%, ABL class fusions in 9.8%, other JAK-STAT sequence mutations in 7.2%, other kinase alterations in 4.1%, and Ras pathway mutations in 3.6%.
“Our comprehensive sequencing showed that Ph-like ALL in adults is the most genetically diverse subtype of leukemia that has been described,” said study author Kathryn Roberts, PhD, of St. Jude.
“Cumulatively, more than 50 different chromosomal rearrangements involving 15 different kinases and cytokine receptors have been identified. In this study, we identified 11 chromosomal rearrangements that are new to Ph-like ALL.”
These 11 rearrangements are FIP1L1-PDGFRA, SNX29-PDGFRB, SMU1-JAK2, ZNF340-JAK2, THADA-EPOR, SMARCA4-TYK2, ZNF340-TYK2, ZYMM2-FLT3, DNTT-BLNK, TMEM2-PTK2B, and KANK1-CBL1.
The diversity of kinase-activating alterations in Ph-like ALL has important clinical implications, said study author Hagop Kantarjian, MD, of the University of Texas MD Anderson Cancer Center in Houston.
“It is important that we now identify patients with Ph-like ALL at diagnosis to provide optimal treatment with targeted agents,” he said.
The findings also highlight the importance of centralized comprehensive genomic sequencing for patients, said study author Elisabeth Paietta, PhD, of the Montefiore Health System and Albert Einstein College of Medicine in Bronx, New York.
“Lymphoblasts from almost half of the patients with Ph-like ALL harbor a genomic rearrangement of CRLF2, which can be detected by flow cytometry using an antibody to CRLF2,” Dr Paietta said. “This is very important as it allows a quick characterization of this Ph-like ALL subtype prior to any detailed sequencing.” ![]()

Photo courtesy of St. Jude
Children’s Research Hospital
Researchers have found evidence to suggest that a high-risk subtype of acute lymphoblastic leukemia (ALL) is “highly prevalent” in adults with ALL.
In a study of nearly 800 adults with ALL, roughly a quarter of the patients had Philadelphia chromosome-like (Ph-like) ALL.
Patients with Ph-like ALL had inferior overall survival (OS) and event-free survival (EFS), but most of them also had kinase-activating alterations that suggest they might respond well to tyrosine kinase inhibitors.
The researchers reported these findings in the Journal of Clinical Oncology.
“This study establishes that a large percentage of adults with ALL have this high-risk subtype,” said study author Charles Mullighan, MD, MBBS, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“The finding provides a compelling reason to identify those with Ph-like ALL and move forward with clinical trials of these targeted therapies in combination with current chemotherapeutic regimens.”
This study builds on previous research, which suggested that Ph-like ALL becomes more common with age, is associated with poor prognosis, and is characterized by genomic alterations that appear to make patients responsive to treatment with tyrosine kinase inhibitors.
“Our 2014 findings that the prevalence of Ph-like ALL increased with age and was particularly common in young adults generated tremendous interest because adult ALL is difficult to treat,” Dr Mullighan said. “In this study, we determined that the prevalence remains high across the age spectrum of adults with ALL.”
Prevalence and outcomes
The study included 798 adults who were between the ages of 21 and 86 when diagnosed with ALL. A total of 194 patients (24%) had Ph-like ALL.
The incidence of Ph-like ALL was 27.9% among young adults (ages 21 to 39), 20.4% in adults (ages 40 to 59), and 24.0% in older adults (ages 60 to 86).
Patients with Ph-like ALL had significantly inferior 5-year OS compared to patients with non-Ph-like ALL—23.8% and 52.4%, respectively (P<0.001). The same was true for 5-year EFS—22.5% and 49.3%, respectively (P<0.001).
Among Ph-like ALL patients, the 5-year EFS rates were 40.4% for young adults, 29.8% for adults, and 18.9% for older adults. The 5-year OS rates were 45.2%, 35.1%, and 16.2%, respectively.
Genomic analysis
The researchers performed genomic analysis of 180 of the Ph-like ALL cases and found that 88% had kinase-activating alterations.
This included CRLF2 rearrangements in 51% of cases, JAK2 or EPOR rearrangements in 12.4%, ABL class fusions in 9.8%, other JAK-STAT sequence mutations in 7.2%, other kinase alterations in 4.1%, and Ras pathway mutations in 3.6%.
“Our comprehensive sequencing showed that Ph-like ALL in adults is the most genetically diverse subtype of leukemia that has been described,” said study author Kathryn Roberts, PhD, of St. Jude.
“Cumulatively, more than 50 different chromosomal rearrangements involving 15 different kinases and cytokine receptors have been identified. In this study, we identified 11 chromosomal rearrangements that are new to Ph-like ALL.”
These 11 rearrangements are FIP1L1-PDGFRA, SNX29-PDGFRB, SMU1-JAK2, ZNF340-JAK2, THADA-EPOR, SMARCA4-TYK2, ZNF340-TYK2, ZYMM2-FLT3, DNTT-BLNK, TMEM2-PTK2B, and KANK1-CBL1.
The diversity of kinase-activating alterations in Ph-like ALL has important clinical implications, said study author Hagop Kantarjian, MD, of the University of Texas MD Anderson Cancer Center in Houston.
“It is important that we now identify patients with Ph-like ALL at diagnosis to provide optimal treatment with targeted agents,” he said.
The findings also highlight the importance of centralized comprehensive genomic sequencing for patients, said study author Elisabeth Paietta, PhD, of the Montefiore Health System and Albert Einstein College of Medicine in Bronx, New York.
“Lymphoblasts from almost half of the patients with Ph-like ALL harbor a genomic rearrangement of CRLF2, which can be detected by flow cytometry using an antibody to CRLF2,” Dr Paietta said. “This is very important as it allows a quick characterization of this Ph-like ALL subtype prior to any detailed sequencing.” ![]()
Drug approved to treat hemophilia A in Kuwait
(Elocta) packaging
Photo courtesy of Sobi
The Ministry of Health in Kuwait has approved efmoroctocog alfa (Elocta®), a recombinant human factor VIII Fc-fusion protein, for the treatment of hemophilia A.
It is indicated for both on-demand and prophylactic treatment in hemophilia A patients of all ages.
Efmoroctocog alfa is the first recombinant factor VIII Fc fusion protein therapy approved for the treatment of hemophilia A in the Middle East region.
Efmoroctocog alfa is also approved in the European Union, Switzerland, Iceland, Liechtenstein, Norway, the US, Canada, Australia, New Zealand, Brazil, Taiwan, and Japan.
Efmoroctocog alfa was developed by fusing B-domain deleted factor VIII to the Fc portion of immunoglobulin G subclass 1. It is believed that this enables efmoroctocog alfa to utilize a naturally occurring pathway to prolong the time the therapy remains in the body.
Sobi and Biogen are collaborators in the development and commercialization of efmoroctocog alfa for hemophilia A.
The approval of efmoroctocog alfa in Kuwait was based on data from a pair of phase 3 studies: A-LONG and Kids A-LONG.
A-LONG
The A-LONG study included 165 previously treated males 12 years of age and older with severe hemophilia A. Researchers evaluated individualized and weekly prophylaxis to reduce or prevent bleeding episodes and on-demand dosing to treat bleeding episodes.
Prophylaxis with efmoroctocog alfa resulted in low annualized bleeding rates, and a majority of bleeding episodes were controlled with a single injection of efmoroctocog alfa.
None of the patients developed neutralizing antibodies, efmoroctocog alfa was considered well-tolerated, and the product had a prolonged half-life when compared with recombinant factor VIII.
Kids A-LONG
The Kids A-LONG study included 71 boys (younger than 12) with severe hemophilia A who had at least 50 prior exposure days to factor VIII therapies.
The children saw their median annualized bleeding rate decrease with efmoroctocog alfa, and close to half of the children did not have any bleeding episodes while they were receiving efmoroctocog alfa.
None of the patients developed inhibitors, and researchers said adverse events were typical of a pediatric hemophilia population. ![]()
(Elocta) packaging
Photo courtesy of Sobi
The Ministry of Health in Kuwait has approved efmoroctocog alfa (Elocta®), a recombinant human factor VIII Fc-fusion protein, for the treatment of hemophilia A.
It is indicated for both on-demand and prophylactic treatment in hemophilia A patients of all ages.
Efmoroctocog alfa is the first recombinant factor VIII Fc fusion protein therapy approved for the treatment of hemophilia A in the Middle East region.
Efmoroctocog alfa is also approved in the European Union, Switzerland, Iceland, Liechtenstein, Norway, the US, Canada, Australia, New Zealand, Brazil, Taiwan, and Japan.
Efmoroctocog alfa was developed by fusing B-domain deleted factor VIII to the Fc portion of immunoglobulin G subclass 1. It is believed that this enables efmoroctocog alfa to utilize a naturally occurring pathway to prolong the time the therapy remains in the body.
Sobi and Biogen are collaborators in the development and commercialization of efmoroctocog alfa for hemophilia A.
The approval of efmoroctocog alfa in Kuwait was based on data from a pair of phase 3 studies: A-LONG and Kids A-LONG.
A-LONG
The A-LONG study included 165 previously treated males 12 years of age and older with severe hemophilia A. Researchers evaluated individualized and weekly prophylaxis to reduce or prevent bleeding episodes and on-demand dosing to treat bleeding episodes.
Prophylaxis with efmoroctocog alfa resulted in low annualized bleeding rates, and a majority of bleeding episodes were controlled with a single injection of efmoroctocog alfa.
None of the patients developed neutralizing antibodies, efmoroctocog alfa was considered well-tolerated, and the product had a prolonged half-life when compared with recombinant factor VIII.
Kids A-LONG
The Kids A-LONG study included 71 boys (younger than 12) with severe hemophilia A who had at least 50 prior exposure days to factor VIII therapies.
The children saw their median annualized bleeding rate decrease with efmoroctocog alfa, and close to half of the children did not have any bleeding episodes while they were receiving efmoroctocog alfa.
None of the patients developed inhibitors, and researchers said adverse events were typical of a pediatric hemophilia population. ![]()
(Elocta) packaging
Photo courtesy of Sobi
The Ministry of Health in Kuwait has approved efmoroctocog alfa (Elocta®), a recombinant human factor VIII Fc-fusion protein, for the treatment of hemophilia A.
It is indicated for both on-demand and prophylactic treatment in hemophilia A patients of all ages.
Efmoroctocog alfa is the first recombinant factor VIII Fc fusion protein therapy approved for the treatment of hemophilia A in the Middle East region.
Efmoroctocog alfa is also approved in the European Union, Switzerland, Iceland, Liechtenstein, Norway, the US, Canada, Australia, New Zealand, Brazil, Taiwan, and Japan.
Efmoroctocog alfa was developed by fusing B-domain deleted factor VIII to the Fc portion of immunoglobulin G subclass 1. It is believed that this enables efmoroctocog alfa to utilize a naturally occurring pathway to prolong the time the therapy remains in the body.
Sobi and Biogen are collaborators in the development and commercialization of efmoroctocog alfa for hemophilia A.
The approval of efmoroctocog alfa in Kuwait was based on data from a pair of phase 3 studies: A-LONG and Kids A-LONG.
A-LONG
The A-LONG study included 165 previously treated males 12 years of age and older with severe hemophilia A. Researchers evaluated individualized and weekly prophylaxis to reduce or prevent bleeding episodes and on-demand dosing to treat bleeding episodes.
Prophylaxis with efmoroctocog alfa resulted in low annualized bleeding rates, and a majority of bleeding episodes were controlled with a single injection of efmoroctocog alfa.
None of the patients developed neutralizing antibodies, efmoroctocog alfa was considered well-tolerated, and the product had a prolonged half-life when compared with recombinant factor VIII.
Kids A-LONG
The Kids A-LONG study included 71 boys (younger than 12) with severe hemophilia A who had at least 50 prior exposure days to factor VIII therapies.
The children saw their median annualized bleeding rate decrease with efmoroctocog alfa, and close to half of the children did not have any bleeding episodes while they were receiving efmoroctocog alfa.
None of the patients developed inhibitors, and researchers said adverse events were typical of a pediatric hemophilia population. ![]()
Novel CLL drugs could greatly increase costs

New research suggests the increasing use of oral targeted therapies for chronic lymphocytic leukemia (CLL) could raise US treatment costs for the disease by almost 600%.
Investigators modeled the evolving management of CLL from 2011 to 2025 and found that increasing use of the oral targeted therapies ibrutinib and idelalisib could greatly increase costs for both patients and payers.
The team detailed these findings in the Journal of Clinical Oncology.
“The rising cost of cancer care is a serious concern,” said study author Jagpreet Chhatwal, PhD, of Massachusetts General Hospital in Boston.
“The average cost of annual cancer treatment, which was below $10,000 per patient before 2000, has now increased to more than $100,000. Such increasing trends can limit access to new therapies, potentially undermining their clinical effectiveness. These new drugs are highly effective, but their high costs motivated us to project their changing economic burden and affordability.”
Dr Chhatwal and his colleagues noted that ibrutinib and idelalisib each cost around $130,000 per year, and treatment with these drugs may be continued indefinitely.
So the team set out to determine the potential financial impact of the drugs on payers’ budgets, as well as on Medicare-enrolled patients, who represent the majority of CLL patients in the US.
The investigators developed a model to simulate the evolving management of CLL from 2011 to 2025.
In one scenario, chemoimmunotherapy was the standard of care before 2014, while oral targeted therapies were used for patients with del(17p) and relapsed CLL from 2014 onward and for first-line treatment of CLL from 2016 onward.
The team also modeled a scenario in which chemoimmunotherapy was the standard of care throughout the entire time period and compared the costs between these scenarios.
The model projects that:
- Per-patient lifetime costs for CLL treatment will increase from $147,000 to $604,000 from 2016 onward
- The total out-of-pocket costs for Medicare patients will increase from $9200 to $57,000 for patients initiating treatment from 2016 onward
- The total annual cost of CLL management in the US will rise from $0.74 billion in 2011 to $5.13 billion in 2025, an increase of 590%.
“Such substantial increases in the cost are mainly driven by high drug prices, prolonged treatment duration, and the increase in the number of patients living with CLL,” said study author Qiushi Chen, PhD, of Massachusetts General Hospital.
The investigators also noted that the standard measure used to determine the cost-effectiveness of a medical intervention is whether it costs less than $100,000 for each additional year of life gained. The projected cost-effectiveness ratio of oral targeted therapy in CLL is $189,000 for each year gained.
“At the current average wholesale prices, oral targeted therapies for CLL are not cost-effective, and prices would need to drop by 50% to 70% to become cost-effective,” Dr Chhatwal said.
“We are not recommending that clinicians choose less effective CLL management strategies that do not include oral targeted therapies,” said study author Nitin Jain, MD, of the University of Texas MD Anderson Cancer Center in Houston.
“Instead, we propose that the prices of these drugs need to be reduced to make the treatment cost-effective and more affordable, something we hope may happen with all cancer drugs. We also believe more research is needed to explore whether we can discontinue targeted treatment of patients who have responded well without risking worsening of their health.” ![]()

New research suggests the increasing use of oral targeted therapies for chronic lymphocytic leukemia (CLL) could raise US treatment costs for the disease by almost 600%.
Investigators modeled the evolving management of CLL from 2011 to 2025 and found that increasing use of the oral targeted therapies ibrutinib and idelalisib could greatly increase costs for both patients and payers.
The team detailed these findings in the Journal of Clinical Oncology.
“The rising cost of cancer care is a serious concern,” said study author Jagpreet Chhatwal, PhD, of Massachusetts General Hospital in Boston.
“The average cost of annual cancer treatment, which was below $10,000 per patient before 2000, has now increased to more than $100,000. Such increasing trends can limit access to new therapies, potentially undermining their clinical effectiveness. These new drugs are highly effective, but their high costs motivated us to project their changing economic burden and affordability.”
Dr Chhatwal and his colleagues noted that ibrutinib and idelalisib each cost around $130,000 per year, and treatment with these drugs may be continued indefinitely.
So the team set out to determine the potential financial impact of the drugs on payers’ budgets, as well as on Medicare-enrolled patients, who represent the majority of CLL patients in the US.
The investigators developed a model to simulate the evolving management of CLL from 2011 to 2025.
In one scenario, chemoimmunotherapy was the standard of care before 2014, while oral targeted therapies were used for patients with del(17p) and relapsed CLL from 2014 onward and for first-line treatment of CLL from 2016 onward.
The team also modeled a scenario in which chemoimmunotherapy was the standard of care throughout the entire time period and compared the costs between these scenarios.
The model projects that:
- Per-patient lifetime costs for CLL treatment will increase from $147,000 to $604,000 from 2016 onward
- The total out-of-pocket costs for Medicare patients will increase from $9200 to $57,000 for patients initiating treatment from 2016 onward
- The total annual cost of CLL management in the US will rise from $0.74 billion in 2011 to $5.13 billion in 2025, an increase of 590%.
“Such substantial increases in the cost are mainly driven by high drug prices, prolonged treatment duration, and the increase in the number of patients living with CLL,” said study author Qiushi Chen, PhD, of Massachusetts General Hospital.
The investigators also noted that the standard measure used to determine the cost-effectiveness of a medical intervention is whether it costs less than $100,000 for each additional year of life gained. The projected cost-effectiveness ratio of oral targeted therapy in CLL is $189,000 for each year gained.
“At the current average wholesale prices, oral targeted therapies for CLL are not cost-effective, and prices would need to drop by 50% to 70% to become cost-effective,” Dr Chhatwal said.
“We are not recommending that clinicians choose less effective CLL management strategies that do not include oral targeted therapies,” said study author Nitin Jain, MD, of the University of Texas MD Anderson Cancer Center in Houston.
“Instead, we propose that the prices of these drugs need to be reduced to make the treatment cost-effective and more affordable, something we hope may happen with all cancer drugs. We also believe more research is needed to explore whether we can discontinue targeted treatment of patients who have responded well without risking worsening of their health.” ![]()

New research suggests the increasing use of oral targeted therapies for chronic lymphocytic leukemia (CLL) could raise US treatment costs for the disease by almost 600%.
Investigators modeled the evolving management of CLL from 2011 to 2025 and found that increasing use of the oral targeted therapies ibrutinib and idelalisib could greatly increase costs for both patients and payers.
The team detailed these findings in the Journal of Clinical Oncology.
“The rising cost of cancer care is a serious concern,” said study author Jagpreet Chhatwal, PhD, of Massachusetts General Hospital in Boston.
“The average cost of annual cancer treatment, which was below $10,000 per patient before 2000, has now increased to more than $100,000. Such increasing trends can limit access to new therapies, potentially undermining their clinical effectiveness. These new drugs are highly effective, but their high costs motivated us to project their changing economic burden and affordability.”
Dr Chhatwal and his colleagues noted that ibrutinib and idelalisib each cost around $130,000 per year, and treatment with these drugs may be continued indefinitely.
So the team set out to determine the potential financial impact of the drugs on payers’ budgets, as well as on Medicare-enrolled patients, who represent the majority of CLL patients in the US.
The investigators developed a model to simulate the evolving management of CLL from 2011 to 2025.
In one scenario, chemoimmunotherapy was the standard of care before 2014, while oral targeted therapies were used for patients with del(17p) and relapsed CLL from 2014 onward and for first-line treatment of CLL from 2016 onward.
The team also modeled a scenario in which chemoimmunotherapy was the standard of care throughout the entire time period and compared the costs between these scenarios.
The model projects that:
- Per-patient lifetime costs for CLL treatment will increase from $147,000 to $604,000 from 2016 onward
- The total out-of-pocket costs for Medicare patients will increase from $9200 to $57,000 for patients initiating treatment from 2016 onward
- The total annual cost of CLL management in the US will rise from $0.74 billion in 2011 to $5.13 billion in 2025, an increase of 590%.
“Such substantial increases in the cost are mainly driven by high drug prices, prolonged treatment duration, and the increase in the number of patients living with CLL,” said study author Qiushi Chen, PhD, of Massachusetts General Hospital.
The investigators also noted that the standard measure used to determine the cost-effectiveness of a medical intervention is whether it costs less than $100,000 for each additional year of life gained. The projected cost-effectiveness ratio of oral targeted therapy in CLL is $189,000 for each year gained.
“At the current average wholesale prices, oral targeted therapies for CLL are not cost-effective, and prices would need to drop by 50% to 70% to become cost-effective,” Dr Chhatwal said.
“We are not recommending that clinicians choose less effective CLL management strategies that do not include oral targeted therapies,” said study author Nitin Jain, MD, of the University of Texas MD Anderson Cancer Center in Houston.
“Instead, we propose that the prices of these drugs need to be reduced to make the treatment cost-effective and more affordable, something we hope may happen with all cancer drugs. We also believe more research is needed to explore whether we can discontinue targeted treatment of patients who have responded well without risking worsening of their health.” ![]()
Which Health Care Providers Are Most Likely to Get Vaccinated?
Making it easier for employees to get free flu vaccinations on site—and requiring vaccinations—has helped bump up coverage, according to an online survey conducted for the CDC.
Of 2,316 health care personnel who responded, 79% reported having gotten a flu shot for the 2015-2016 season, up 15.5 percentage points from the 2010-2011 estimate but similar to the 77.3% coverage for 2014-2015.
Physicians are most likely to get vaccinated (95.6%), whereas assistants and aides have the lowest coverage, although it was well above half (64.1%). Nurse practitioners and physician assistants also had a high rate of vaccination (90.3%), followed by nurses (90.1%) and pharmacists (86.5%), and Allied health professionals/technicians/technologists (84.7%).
Related: The Ads Say ‘Get Your Flu Shot Today,’ But It May Be Wiser To Wait
Coverage among staff in long-term care settings was up—from 63.9% in 2014-2015 to 69.2% for 2015-2016—but still consistently lower than the coverage in hospitals and ambulatory care. Coverage in those settings was similar in both seasons. Employer requirements “likely contributed” to the gradual increase in vaccination among health care staff in settings with lowest coverage, the researchers say.
In facilities where vaccination was required, coverage was nearly total (96.5%). But only 61% of health care personnel work in hospitals with vaccination requirements—and that’s at least 27 percentage points higher than the proportion in any other work setting, the researchers say. Aides and assistants reported the lowest prevalence of vaccination requirements (22.5%).
Related: New Vaccination Data & Trends
Next to requirements, cost influenced vaccination response. The majority of vaccinated health care staff got the shots at their workplace. Coverage was highest when free vaccination was available on-site for a day or more.
To boost vaccination among long-term care staff, the CDC and the National Vaccine Program Office offer a web-based tool kit that includes access to resources, strategies, and educational material (www.cdc/gov/flu/toolkit/long-term-care/index.htm). Employers and health care administrators can also check out the Guide to Community Preventive Services, which presents evidence to support on-site vaccination at no or low cost.
Related: Health Care Providers Impact on HPV Vaccination Rates
Source:
Black CL, Yue X, Ball SW, et al. MMWR. 2016;65(38):1026-1031.
Making it easier for employees to get free flu vaccinations on site—and requiring vaccinations—has helped bump up coverage, according to an online survey conducted for the CDC.
Of 2,316 health care personnel who responded, 79% reported having gotten a flu shot for the 2015-2016 season, up 15.5 percentage points from the 2010-2011 estimate but similar to the 77.3% coverage for 2014-2015.
Physicians are most likely to get vaccinated (95.6%), whereas assistants and aides have the lowest coverage, although it was well above half (64.1%). Nurse practitioners and physician assistants also had a high rate of vaccination (90.3%), followed by nurses (90.1%) and pharmacists (86.5%), and Allied health professionals/technicians/technologists (84.7%).
Related: The Ads Say ‘Get Your Flu Shot Today,’ But It May Be Wiser To Wait
Coverage among staff in long-term care settings was up—from 63.9% in 2014-2015 to 69.2% for 2015-2016—but still consistently lower than the coverage in hospitals and ambulatory care. Coverage in those settings was similar in both seasons. Employer requirements “likely contributed” to the gradual increase in vaccination among health care staff in settings with lowest coverage, the researchers say.
In facilities where vaccination was required, coverage was nearly total (96.5%). But only 61% of health care personnel work in hospitals with vaccination requirements—and that’s at least 27 percentage points higher than the proportion in any other work setting, the researchers say. Aides and assistants reported the lowest prevalence of vaccination requirements (22.5%).
Related: New Vaccination Data & Trends
Next to requirements, cost influenced vaccination response. The majority of vaccinated health care staff got the shots at their workplace. Coverage was highest when free vaccination was available on-site for a day or more.
To boost vaccination among long-term care staff, the CDC and the National Vaccine Program Office offer a web-based tool kit that includes access to resources, strategies, and educational material (www.cdc/gov/flu/toolkit/long-term-care/index.htm). Employers and health care administrators can also check out the Guide to Community Preventive Services, which presents evidence to support on-site vaccination at no or low cost.
Related: Health Care Providers Impact on HPV Vaccination Rates
Source:
Black CL, Yue X, Ball SW, et al. MMWR. 2016;65(38):1026-1031.
Making it easier for employees to get free flu vaccinations on site—and requiring vaccinations—has helped bump up coverage, according to an online survey conducted for the CDC.
Of 2,316 health care personnel who responded, 79% reported having gotten a flu shot for the 2015-2016 season, up 15.5 percentage points from the 2010-2011 estimate but similar to the 77.3% coverage for 2014-2015.
Physicians are most likely to get vaccinated (95.6%), whereas assistants and aides have the lowest coverage, although it was well above half (64.1%). Nurse practitioners and physician assistants also had a high rate of vaccination (90.3%), followed by nurses (90.1%) and pharmacists (86.5%), and Allied health professionals/technicians/technologists (84.7%).
Related: The Ads Say ‘Get Your Flu Shot Today,’ But It May Be Wiser To Wait
Coverage among staff in long-term care settings was up—from 63.9% in 2014-2015 to 69.2% for 2015-2016—but still consistently lower than the coverage in hospitals and ambulatory care. Coverage in those settings was similar in both seasons. Employer requirements “likely contributed” to the gradual increase in vaccination among health care staff in settings with lowest coverage, the researchers say.
In facilities where vaccination was required, coverage was nearly total (96.5%). But only 61% of health care personnel work in hospitals with vaccination requirements—and that’s at least 27 percentage points higher than the proportion in any other work setting, the researchers say. Aides and assistants reported the lowest prevalence of vaccination requirements (22.5%).
Related: New Vaccination Data & Trends
Next to requirements, cost influenced vaccination response. The majority of vaccinated health care staff got the shots at their workplace. Coverage was highest when free vaccination was available on-site for a day or more.
To boost vaccination among long-term care staff, the CDC and the National Vaccine Program Office offer a web-based tool kit that includes access to resources, strategies, and educational material (www.cdc/gov/flu/toolkit/long-term-care/index.htm). Employers and health care administrators can also check out the Guide to Community Preventive Services, which presents evidence to support on-site vaccination at no or low cost.
Related: Health Care Providers Impact on HPV Vaccination Rates
Source:
Black CL, Yue X, Ball SW, et al. MMWR. 2016;65(38):1026-1031.