User login
Revision technique treats graft dysfunction after esophageal reconstruction
Ingestion of caustic substances like alkali, acid, and bleaches that call for esophageal surgery is relatively rare, and the study of dealing with postsurgery complications even rarer, but a team of surgeons from a large public referral hospital in Paris has collected enough cases over the first years of this century to report that a form of revision surgery in these cases can yield good outcomes with acceptable morbidity, according to a study in the Journal of Thoracic and Cardiovascular Surgery (2016;152:1378-85).
Thibault Voron, MD, and coauthors at Hôpitaux Saint-Louis and the University of Paris performed revision cervicosternolaparotomy (CSLap) on 55 patients from 1999 to 2015. Two patients (4%) died and the severe morbidity rate was 27%, but the long-term functional success rate was 85%. “Of note, these figures compare favorably with results of primary esophageal reconstruction for caustic injuries in the literature,” Dr. Voron and colleagues said. Overall the study authors performed revision surgery on 100 patients, with the remaining 45 undergoing repair through a limited approach. There were no significant differences in characteristics between the two groups.
Primary esophageal reconstruction for caustic injuries can usually be done at referral centers with good results, but up to half of these patients can have late complications, consisting mostly of strictures and redundancy that can cause loss of function, Dr. Voron and coauthors said. Published series have reported revision surgery in 15%-38% of patients (Dis Esophagus. 2008;21:E1-5; Dis Esophagus. 1999;12:7-9), but revision surgery itself is difficult to accomplish.
CSLap involves a large operative field from the jaw to the pubis. It starts with a comprehensive neck exploration through the previous cervical incision or with a median laparotomy to rule out a limited-approach repair. CSLap was undertaken when the graft was too short for a tension-free anastomosis. After the upper part of the graft was dissected from the thoracic inlet, the abdomen was opened for dissection of the abdominal part of the transplant. All scar tissues and strictures were excised after the transplant release, and a new anastomosis was constructed in healthy tissues. In cases involving life-threatening complications, patient survival prevailed over graft preservation and reconstruction of digestive continuity. The operations took up to 10 hours, with 8 hours, 20 minutes the median.
Dr. Voron and coauthors identified two distinct indications for CSLap: graft strictures in 43 (78%) of patients to rescue the primary conduit and reconstruct the cervical anastomosis and a need to access the retrosternal space to treat graft-related complications. “Graft lengthening was definitely not the issue in this situation,” Dr. Voron and colleagues said of the latter indication.
Four patients had emergency revision CSLap for spontaneous graft perforation and complications related to caustic reingestion. None died and one patient had preservation of the primary conduit. “Retrosternal grafts can be quickly removed by blunt dissection in life-threatening circumstances; however, if reasonable chances to recover the transplant exist, CSLap exploration can be justified,” Dr. Voron and coauthors said.
CSLap offers a few advantages in these situations: Transplant release provides significant lengthening of the graft that enables preservation of the primary conduit and redo of the cervical anastomosis in most patients, and it allows direct access to the retrosternal space if needed, Dr. Voron and coauthors said.
Dr. Voron and coauthors had no financial relationships to disclose.
This series by Dr. Voron and coauthors was “truly remarkable,” given the rarity of esophageal caustic injuries and even rarer occasion of revision surgery, Victor A. Ferraris, MD, PhD, of the University of Kentucky, Lexington, said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152:1386-7). He attributed the series size to the authors’ clinical setting in a trauma entry point for Europe’s largest hospital system – the same hospital that received victims of the terrorist attack at the Bataclan concert hall in Paris in November 2015.
“Voron and coauthors clearly have the benefit of a large referral population and vast medical infrastructure in the Assistance Publique-Hôpitaux de Paris,” Dr. Ferraris said. That volume certainly factors into their ability to achieve “very good outcomes,” he said.
“This seems to be an argument in favor of localization of resources to a single center,” Dr. Ferraris said. “Dr. Voron and coauthors have translated their experience into knowledge that can help other surgeons deal with this difficult problem.”
Dr. Ferraris had no financial relationships to disclose.
This series by Dr. Voron and coauthors was “truly remarkable,” given the rarity of esophageal caustic injuries and even rarer occasion of revision surgery, Victor A. Ferraris, MD, PhD, of the University of Kentucky, Lexington, said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152:1386-7). He attributed the series size to the authors’ clinical setting in a trauma entry point for Europe’s largest hospital system – the same hospital that received victims of the terrorist attack at the Bataclan concert hall in Paris in November 2015.
“Voron and coauthors clearly have the benefit of a large referral population and vast medical infrastructure in the Assistance Publique-Hôpitaux de Paris,” Dr. Ferraris said. That volume certainly factors into their ability to achieve “very good outcomes,” he said.
“This seems to be an argument in favor of localization of resources to a single center,” Dr. Ferraris said. “Dr. Voron and coauthors have translated their experience into knowledge that can help other surgeons deal with this difficult problem.”
Dr. Ferraris had no financial relationships to disclose.
This series by Dr. Voron and coauthors was “truly remarkable,” given the rarity of esophageal caustic injuries and even rarer occasion of revision surgery, Victor A. Ferraris, MD, PhD, of the University of Kentucky, Lexington, said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152:1386-7). He attributed the series size to the authors’ clinical setting in a trauma entry point for Europe’s largest hospital system – the same hospital that received victims of the terrorist attack at the Bataclan concert hall in Paris in November 2015.
“Voron and coauthors clearly have the benefit of a large referral population and vast medical infrastructure in the Assistance Publique-Hôpitaux de Paris,” Dr. Ferraris said. That volume certainly factors into their ability to achieve “very good outcomes,” he said.
“This seems to be an argument in favor of localization of resources to a single center,” Dr. Ferraris said. “Dr. Voron and coauthors have translated their experience into knowledge that can help other surgeons deal with this difficult problem.”
Dr. Ferraris had no financial relationships to disclose.
Ingestion of caustic substances like alkali, acid, and bleaches that call for esophageal surgery is relatively rare, and the study of dealing with postsurgery complications even rarer, but a team of surgeons from a large public referral hospital in Paris has collected enough cases over the first years of this century to report that a form of revision surgery in these cases can yield good outcomes with acceptable morbidity, according to a study in the Journal of Thoracic and Cardiovascular Surgery (2016;152:1378-85).
Thibault Voron, MD, and coauthors at Hôpitaux Saint-Louis and the University of Paris performed revision cervicosternolaparotomy (CSLap) on 55 patients from 1999 to 2015. Two patients (4%) died and the severe morbidity rate was 27%, but the long-term functional success rate was 85%. “Of note, these figures compare favorably with results of primary esophageal reconstruction for caustic injuries in the literature,” Dr. Voron and colleagues said. Overall the study authors performed revision surgery on 100 patients, with the remaining 45 undergoing repair through a limited approach. There were no significant differences in characteristics between the two groups.
Primary esophageal reconstruction for caustic injuries can usually be done at referral centers with good results, but up to half of these patients can have late complications, consisting mostly of strictures and redundancy that can cause loss of function, Dr. Voron and coauthors said. Published series have reported revision surgery in 15%-38% of patients (Dis Esophagus. 2008;21:E1-5; Dis Esophagus. 1999;12:7-9), but revision surgery itself is difficult to accomplish.
CSLap involves a large operative field from the jaw to the pubis. It starts with a comprehensive neck exploration through the previous cervical incision or with a median laparotomy to rule out a limited-approach repair. CSLap was undertaken when the graft was too short for a tension-free anastomosis. After the upper part of the graft was dissected from the thoracic inlet, the abdomen was opened for dissection of the abdominal part of the transplant. All scar tissues and strictures were excised after the transplant release, and a new anastomosis was constructed in healthy tissues. In cases involving life-threatening complications, patient survival prevailed over graft preservation and reconstruction of digestive continuity. The operations took up to 10 hours, with 8 hours, 20 minutes the median.
Dr. Voron and coauthors identified two distinct indications for CSLap: graft strictures in 43 (78%) of patients to rescue the primary conduit and reconstruct the cervical anastomosis and a need to access the retrosternal space to treat graft-related complications. “Graft lengthening was definitely not the issue in this situation,” Dr. Voron and colleagues said of the latter indication.
Four patients had emergency revision CSLap for spontaneous graft perforation and complications related to caustic reingestion. None died and one patient had preservation of the primary conduit. “Retrosternal grafts can be quickly removed by blunt dissection in life-threatening circumstances; however, if reasonable chances to recover the transplant exist, CSLap exploration can be justified,” Dr. Voron and coauthors said.
CSLap offers a few advantages in these situations: Transplant release provides significant lengthening of the graft that enables preservation of the primary conduit and redo of the cervical anastomosis in most patients, and it allows direct access to the retrosternal space if needed, Dr. Voron and coauthors said.
Dr. Voron and coauthors had no financial relationships to disclose.
Ingestion of caustic substances like alkali, acid, and bleaches that call for esophageal surgery is relatively rare, and the study of dealing with postsurgery complications even rarer, but a team of surgeons from a large public referral hospital in Paris has collected enough cases over the first years of this century to report that a form of revision surgery in these cases can yield good outcomes with acceptable morbidity, according to a study in the Journal of Thoracic and Cardiovascular Surgery (2016;152:1378-85).
Thibault Voron, MD, and coauthors at Hôpitaux Saint-Louis and the University of Paris performed revision cervicosternolaparotomy (CSLap) on 55 patients from 1999 to 2015. Two patients (4%) died and the severe morbidity rate was 27%, but the long-term functional success rate was 85%. “Of note, these figures compare favorably with results of primary esophageal reconstruction for caustic injuries in the literature,” Dr. Voron and colleagues said. Overall the study authors performed revision surgery on 100 patients, with the remaining 45 undergoing repair through a limited approach. There were no significant differences in characteristics between the two groups.
Primary esophageal reconstruction for caustic injuries can usually be done at referral centers with good results, but up to half of these patients can have late complications, consisting mostly of strictures and redundancy that can cause loss of function, Dr. Voron and coauthors said. Published series have reported revision surgery in 15%-38% of patients (Dis Esophagus. 2008;21:E1-5; Dis Esophagus. 1999;12:7-9), but revision surgery itself is difficult to accomplish.
CSLap involves a large operative field from the jaw to the pubis. It starts with a comprehensive neck exploration through the previous cervical incision or with a median laparotomy to rule out a limited-approach repair. CSLap was undertaken when the graft was too short for a tension-free anastomosis. After the upper part of the graft was dissected from the thoracic inlet, the abdomen was opened for dissection of the abdominal part of the transplant. All scar tissues and strictures were excised after the transplant release, and a new anastomosis was constructed in healthy tissues. In cases involving life-threatening complications, patient survival prevailed over graft preservation and reconstruction of digestive continuity. The operations took up to 10 hours, with 8 hours, 20 minutes the median.
Dr. Voron and coauthors identified two distinct indications for CSLap: graft strictures in 43 (78%) of patients to rescue the primary conduit and reconstruct the cervical anastomosis and a need to access the retrosternal space to treat graft-related complications. “Graft lengthening was definitely not the issue in this situation,” Dr. Voron and colleagues said of the latter indication.
Four patients had emergency revision CSLap for spontaneous graft perforation and complications related to caustic reingestion. None died and one patient had preservation of the primary conduit. “Retrosternal grafts can be quickly removed by blunt dissection in life-threatening circumstances; however, if reasonable chances to recover the transplant exist, CSLap exploration can be justified,” Dr. Voron and coauthors said.
CSLap offers a few advantages in these situations: Transplant release provides significant lengthening of the graft that enables preservation of the primary conduit and redo of the cervical anastomosis in most patients, and it allows direct access to the retrosternal space if needed, Dr. Voron and coauthors said.
Dr. Voron and coauthors had no financial relationships to disclose.
Key clinical point: Cervicosternolaparotomy revision surgery for graft dysfunction after esophageal reconstruction for caustic injuries can achieve good results with acceptable morbidity.
Major finding: Functional success rate after revision CSLap was 85% after a mean follow-up of 4.4 years.
Data source: 55 patients who underwent CSLap revision surgery between 1999 and 2015 at a single center.
Disclosures: Dr. Voron and coauthors had no financial relationships to disclose.
Hepatitis Outlook: October 2016
If you work on the front lines of medical care treating patients with hepatitis, you may not have time to review all the hepatitis research that enters the medical literature every month. Here’s a quick look at some notable news items and journal articles published over the past month, covering a variety of the major hepatitis viruses.
The overall incidence of occult hepatitis B infection (OBI) and window period (WP) infections was found to be low – at 1 in 6,503 and 1 in 24,214 donations respectively – during a study of transfusion associated HBV infection in India.
A Korean study found tenofovir disoproxil fumarate (TDF) mono–rescue therapy to be a reasonable option in chronic hepatitis B virus patients with lamivudine resistance and entecavir resistance. However, the authors said combination therapy should be considered in patients with high baseline HBV DNA levels.
The Hepavax-Gene TF vaccine was equally effective and non-inferior to the Engerix-B vaccine in terms of prevention of mother-to-child hepatitis B virus transmission in neonates born to mothers positive for HBsAg, according to a study in the Pediatric Infectious Disease Journal.
Interferon alfa (IFN-alfa)–based antiviral therapy of hepatitis delta virus infection was independently associated with a lower likelihood for clinical disease progression, according to a German study.
A study of hepatitis C–infected patients in Australian prisons found that bonding and linking social capital can be valuable resources in promoting HCV treatment awareness, uptake, and adherence, and that peer-based programs are likely to be influential in promoting HCV outcomes in the prison setting.
An analysis in Hepatology found that hepatitis C virus testing interventions resulted in an increase in birth cohort testing, compared with standard of care, but also increased costs, although the results support more widespread adoption of BC testing, compared with the other interventions.
A health education program at substance dependence treatment centers in Portugal improved significantly patient knowledge about hepatitis C, even among patients with high baseline knowledge, and increased the rate of referral to liver specialists.
A single-center trial of direct-acting antivirals in treatment-naive patients with chronic hepatitis C virus genotype (GT)1 or 3 infection supported the use of 8-week DAA treatment regimens that maintain high efficacy, even for patients infected with HCV GT3 infection.
Results from the OSIRIS study revealed that simeprevir plus sofosbuvir for 12 weeks achieved a 100% sustained virologic response rate in hepatitis C virus genotype 4-infected patients with or without compensated cirrhosis.
A literature review found that the polymorphism interferon-lambda 4 (IFNL4) ss469415590 was significantly associated with sustained virologic response in hepatitis C virus genotype 1-infected patients, irrespective of race, and has a tendency to be associated with HCV GT2/3 patients.
The overall incidence of occult hepatitis B infection and window period infections was found to be low at 1 in 6,503 and 1 in 24,214 donations, respectively, in a study of South Indian blood donors.
The introduction of universal mass vaccination against hepatitis A in countries with intermediate endemicity for HAV infection led to a considerable decrease in the incidence of hepatitis A in vaccinated and in non-vaccinated age groups alike.
A systematic review in the Journal of Viral Hepatitis found a higher incidence of hepatitis C virus in women, compared with men who inject drugs.
A recent study found that treatment for 6 weeks with ledipasvir plus sofosbuvir was well tolerated and highly effective in patients with acute hepatitis C virus genotype 1 monoinfection.
A Spanish study found that response-guided therapy with boceprevir in combination with pegylated interferon-alfa 2a/ribavirin for HCV-HIV coinfected patients led to overall sustained virologic response rates of 67% but only 51% in patients with cirrhosis.
[email protected]
On Twitter @richpizzi
If you work on the front lines of medical care treating patients with hepatitis, you may not have time to review all the hepatitis research that enters the medical literature every month. Here’s a quick look at some notable news items and journal articles published over the past month, covering a variety of the major hepatitis viruses.
The overall incidence of occult hepatitis B infection (OBI) and window period (WP) infections was found to be low – at 1 in 6,503 and 1 in 24,214 donations respectively – during a study of transfusion associated HBV infection in India.
A Korean study found tenofovir disoproxil fumarate (TDF) mono–rescue therapy to be a reasonable option in chronic hepatitis B virus patients with lamivudine resistance and entecavir resistance. However, the authors said combination therapy should be considered in patients with high baseline HBV DNA levels.
The Hepavax-Gene TF vaccine was equally effective and non-inferior to the Engerix-B vaccine in terms of prevention of mother-to-child hepatitis B virus transmission in neonates born to mothers positive for HBsAg, according to a study in the Pediatric Infectious Disease Journal.
Interferon alfa (IFN-alfa)–based antiviral therapy of hepatitis delta virus infection was independently associated with a lower likelihood for clinical disease progression, according to a German study.
A study of hepatitis C–infected patients in Australian prisons found that bonding and linking social capital can be valuable resources in promoting HCV treatment awareness, uptake, and adherence, and that peer-based programs are likely to be influential in promoting HCV outcomes in the prison setting.
An analysis in Hepatology found that hepatitis C virus testing interventions resulted in an increase in birth cohort testing, compared with standard of care, but also increased costs, although the results support more widespread adoption of BC testing, compared with the other interventions.
A health education program at substance dependence treatment centers in Portugal improved significantly patient knowledge about hepatitis C, even among patients with high baseline knowledge, and increased the rate of referral to liver specialists.
A single-center trial of direct-acting antivirals in treatment-naive patients with chronic hepatitis C virus genotype (GT)1 or 3 infection supported the use of 8-week DAA treatment regimens that maintain high efficacy, even for patients infected with HCV GT3 infection.
Results from the OSIRIS study revealed that simeprevir plus sofosbuvir for 12 weeks achieved a 100% sustained virologic response rate in hepatitis C virus genotype 4-infected patients with or without compensated cirrhosis.
A literature review found that the polymorphism interferon-lambda 4 (IFNL4) ss469415590 was significantly associated with sustained virologic response in hepatitis C virus genotype 1-infected patients, irrespective of race, and has a tendency to be associated with HCV GT2/3 patients.
The overall incidence of occult hepatitis B infection and window period infections was found to be low at 1 in 6,503 and 1 in 24,214 donations, respectively, in a study of South Indian blood donors.
The introduction of universal mass vaccination against hepatitis A in countries with intermediate endemicity for HAV infection led to a considerable decrease in the incidence of hepatitis A in vaccinated and in non-vaccinated age groups alike.
A systematic review in the Journal of Viral Hepatitis found a higher incidence of hepatitis C virus in women, compared with men who inject drugs.
A recent study found that treatment for 6 weeks with ledipasvir plus sofosbuvir was well tolerated and highly effective in patients with acute hepatitis C virus genotype 1 monoinfection.
A Spanish study found that response-guided therapy with boceprevir in combination with pegylated interferon-alfa 2a/ribavirin for HCV-HIV coinfected patients led to overall sustained virologic response rates of 67% but only 51% in patients with cirrhosis.
[email protected]
On Twitter @richpizzi
If you work on the front lines of medical care treating patients with hepatitis, you may not have time to review all the hepatitis research that enters the medical literature every month. Here’s a quick look at some notable news items and journal articles published over the past month, covering a variety of the major hepatitis viruses.
The overall incidence of occult hepatitis B infection (OBI) and window period (WP) infections was found to be low – at 1 in 6,503 and 1 in 24,214 donations respectively – during a study of transfusion associated HBV infection in India.
A Korean study found tenofovir disoproxil fumarate (TDF) mono–rescue therapy to be a reasonable option in chronic hepatitis B virus patients with lamivudine resistance and entecavir resistance. However, the authors said combination therapy should be considered in patients with high baseline HBV DNA levels.
The Hepavax-Gene TF vaccine was equally effective and non-inferior to the Engerix-B vaccine in terms of prevention of mother-to-child hepatitis B virus transmission in neonates born to mothers positive for HBsAg, according to a study in the Pediatric Infectious Disease Journal.
Interferon alfa (IFN-alfa)–based antiviral therapy of hepatitis delta virus infection was independently associated with a lower likelihood for clinical disease progression, according to a German study.
A study of hepatitis C–infected patients in Australian prisons found that bonding and linking social capital can be valuable resources in promoting HCV treatment awareness, uptake, and adherence, and that peer-based programs are likely to be influential in promoting HCV outcomes in the prison setting.
An analysis in Hepatology found that hepatitis C virus testing interventions resulted in an increase in birth cohort testing, compared with standard of care, but also increased costs, although the results support more widespread adoption of BC testing, compared with the other interventions.
A health education program at substance dependence treatment centers in Portugal improved significantly patient knowledge about hepatitis C, even among patients with high baseline knowledge, and increased the rate of referral to liver specialists.
A single-center trial of direct-acting antivirals in treatment-naive patients with chronic hepatitis C virus genotype (GT)1 or 3 infection supported the use of 8-week DAA treatment regimens that maintain high efficacy, even for patients infected with HCV GT3 infection.
Results from the OSIRIS study revealed that simeprevir plus sofosbuvir for 12 weeks achieved a 100% sustained virologic response rate in hepatitis C virus genotype 4-infected patients with or without compensated cirrhosis.
A literature review found that the polymorphism interferon-lambda 4 (IFNL4) ss469415590 was significantly associated with sustained virologic response in hepatitis C virus genotype 1-infected patients, irrespective of race, and has a tendency to be associated with HCV GT2/3 patients.
The overall incidence of occult hepatitis B infection and window period infections was found to be low at 1 in 6,503 and 1 in 24,214 donations, respectively, in a study of South Indian blood donors.
The introduction of universal mass vaccination against hepatitis A in countries with intermediate endemicity for HAV infection led to a considerable decrease in the incidence of hepatitis A in vaccinated and in non-vaccinated age groups alike.
A systematic review in the Journal of Viral Hepatitis found a higher incidence of hepatitis C virus in women, compared with men who inject drugs.
A recent study found that treatment for 6 weeks with ledipasvir plus sofosbuvir was well tolerated and highly effective in patients with acute hepatitis C virus genotype 1 monoinfection.
A Spanish study found that response-guided therapy with boceprevir in combination with pegylated interferon-alfa 2a/ribavirin for HCV-HIV coinfected patients led to overall sustained virologic response rates of 67% but only 51% in patients with cirrhosis.
[email protected]
On Twitter @richpizzi
Adjunctive brexpiprazole improves cognitive function in major depression
VIENNA – Adjunctive brexpiprazole in patients with an inadequate response to antidepressant monotherapy for major depressive disorder resulted in clinically meaningful improvement in multiple aspects of functional impairment, including cognitive dysfunction, in three open-label exploratory studies, Ross A. Baker, PhD, reported at the annual congress of the European College of Neuropsychopharmacology.
Clinician-rated depressive symptoms also showed significant improvement once brexpiprazole (Rexulti) was on board, added Dr. Baker of Otsuka Pharmaceutical in Princeton, N.J.
But fatigue and cognitive impairment are another matter. They are now recognized as core aspects of major depression. Even after patients’ depressive symptoms have gone into remission, lingering cognitive dysfunction often impairs performance at work or school, social life, and family/home life. Antidepressants don’t improve this depression-related cognitive impairment. This was the impetus for the three open-label exploratory studies, which addressed these common problems of functional disability and cognitive impairment in different populations with major depressive disorder. The target dose of brexpiprazole in all three studies was 2 mg per day in addition to whatever antidepressant medication patients were already on.
One 12-week study included 47 young patients working at a job or in school. Their mean baseline score on the Sheehan Disability Scale (SDS) was 6.5; a score of 5 or more on the 0-10 scale indicates significant functional impairment in the three domains covered by the SDS: home responsibilities, social life, and work or school performance.
After 12 weeks of adjunctive brexpiprazole, the patients’ mean SDS score had improved by 3.7 points. The improvement was significant across all three domains in this study, as well as in the other two open-label studies.
Patients also demonstrated significant improvement on the Cognitive and Physical Functioning Questionnaire (CPFQ), a self-rated scale that addresses cognitive impairment and executive function. The CPFQ consists of seven items, each scored 1-6, with a higher score indicating worse function in that domain. After 12 weeks on adjunctive brexpiprazole, the young patients experienced a mean 8.1-point improvement from a baseline CPFQ score of 26.1.
Another study included 37 patients with prominent anxiety as a feature of their major depressive disorder. Over the course of 6 weeks of treatment, their mean SDS score improved by 3.6 points from a baseline of 6.5. Also, their CPFQ score fell by 9.9 points from a baseline of 29.3.
The third study involved 61 patients who had switched antidepressants after an inadequate response. After 6 weeks on adjunctive brexpiprazole, their mean SDS score improved from 6.3 to 3.2, and their CPFQ dropped by 9.9 points from a baseline of 29.3 points.
Increased energy and alertness were commonly reported by participants in all three studies.
MADRS scores improved by a mean of 18.1 points from 28.3 points at baseline in the youth study, by 19.8 points from a baseline of 30.1 in the high-anxiety group, and by 17.3 points from a baseline of 29.6 in the study of patients who’d switched antidepressants.
These exploratory studies were sponsored by Otsuka Pharmaceutical. Dr. Baker is a company employee.
Brexpiprazole also is FDA-approved for treatment of schizophrenia.
VIENNA – Adjunctive brexpiprazole in patients with an inadequate response to antidepressant monotherapy for major depressive disorder resulted in clinically meaningful improvement in multiple aspects of functional impairment, including cognitive dysfunction, in three open-label exploratory studies, Ross A. Baker, PhD, reported at the annual congress of the European College of Neuropsychopharmacology.
Clinician-rated depressive symptoms also showed significant improvement once brexpiprazole (Rexulti) was on board, added Dr. Baker of Otsuka Pharmaceutical in Princeton, N.J.
But fatigue and cognitive impairment are another matter. They are now recognized as core aspects of major depression. Even after patients’ depressive symptoms have gone into remission, lingering cognitive dysfunction often impairs performance at work or school, social life, and family/home life. Antidepressants don’t improve this depression-related cognitive impairment. This was the impetus for the three open-label exploratory studies, which addressed these common problems of functional disability and cognitive impairment in different populations with major depressive disorder. The target dose of brexpiprazole in all three studies was 2 mg per day in addition to whatever antidepressant medication patients were already on.
One 12-week study included 47 young patients working at a job or in school. Their mean baseline score on the Sheehan Disability Scale (SDS) was 6.5; a score of 5 or more on the 0-10 scale indicates significant functional impairment in the three domains covered by the SDS: home responsibilities, social life, and work or school performance.
After 12 weeks of adjunctive brexpiprazole, the patients’ mean SDS score had improved by 3.7 points. The improvement was significant across all three domains in this study, as well as in the other two open-label studies.
Patients also demonstrated significant improvement on the Cognitive and Physical Functioning Questionnaire (CPFQ), a self-rated scale that addresses cognitive impairment and executive function. The CPFQ consists of seven items, each scored 1-6, with a higher score indicating worse function in that domain. After 12 weeks on adjunctive brexpiprazole, the young patients experienced a mean 8.1-point improvement from a baseline CPFQ score of 26.1.
Another study included 37 patients with prominent anxiety as a feature of their major depressive disorder. Over the course of 6 weeks of treatment, their mean SDS score improved by 3.6 points from a baseline of 6.5. Also, their CPFQ score fell by 9.9 points from a baseline of 29.3.
The third study involved 61 patients who had switched antidepressants after an inadequate response. After 6 weeks on adjunctive brexpiprazole, their mean SDS score improved from 6.3 to 3.2, and their CPFQ dropped by 9.9 points from a baseline of 29.3 points.
Increased energy and alertness were commonly reported by participants in all three studies.
MADRS scores improved by a mean of 18.1 points from 28.3 points at baseline in the youth study, by 19.8 points from a baseline of 30.1 in the high-anxiety group, and by 17.3 points from a baseline of 29.6 in the study of patients who’d switched antidepressants.
These exploratory studies were sponsored by Otsuka Pharmaceutical. Dr. Baker is a company employee.
Brexpiprazole also is FDA-approved for treatment of schizophrenia.
VIENNA – Adjunctive brexpiprazole in patients with an inadequate response to antidepressant monotherapy for major depressive disorder resulted in clinically meaningful improvement in multiple aspects of functional impairment, including cognitive dysfunction, in three open-label exploratory studies, Ross A. Baker, PhD, reported at the annual congress of the European College of Neuropsychopharmacology.
Clinician-rated depressive symptoms also showed significant improvement once brexpiprazole (Rexulti) was on board, added Dr. Baker of Otsuka Pharmaceutical in Princeton, N.J.
But fatigue and cognitive impairment are another matter. They are now recognized as core aspects of major depression. Even after patients’ depressive symptoms have gone into remission, lingering cognitive dysfunction often impairs performance at work or school, social life, and family/home life. Antidepressants don’t improve this depression-related cognitive impairment. This was the impetus for the three open-label exploratory studies, which addressed these common problems of functional disability and cognitive impairment in different populations with major depressive disorder. The target dose of brexpiprazole in all three studies was 2 mg per day in addition to whatever antidepressant medication patients were already on.
One 12-week study included 47 young patients working at a job or in school. Their mean baseline score on the Sheehan Disability Scale (SDS) was 6.5; a score of 5 or more on the 0-10 scale indicates significant functional impairment in the three domains covered by the SDS: home responsibilities, social life, and work or school performance.
After 12 weeks of adjunctive brexpiprazole, the patients’ mean SDS score had improved by 3.7 points. The improvement was significant across all three domains in this study, as well as in the other two open-label studies.
Patients also demonstrated significant improvement on the Cognitive and Physical Functioning Questionnaire (CPFQ), a self-rated scale that addresses cognitive impairment and executive function. The CPFQ consists of seven items, each scored 1-6, with a higher score indicating worse function in that domain. After 12 weeks on adjunctive brexpiprazole, the young patients experienced a mean 8.1-point improvement from a baseline CPFQ score of 26.1.
Another study included 37 patients with prominent anxiety as a feature of their major depressive disorder. Over the course of 6 weeks of treatment, their mean SDS score improved by 3.6 points from a baseline of 6.5. Also, their CPFQ score fell by 9.9 points from a baseline of 29.3.
The third study involved 61 patients who had switched antidepressants after an inadequate response. After 6 weeks on adjunctive brexpiprazole, their mean SDS score improved from 6.3 to 3.2, and their CPFQ dropped by 9.9 points from a baseline of 29.3 points.
Increased energy and alertness were commonly reported by participants in all three studies.
MADRS scores improved by a mean of 18.1 points from 28.3 points at baseline in the youth study, by 19.8 points from a baseline of 30.1 in the high-anxiety group, and by 17.3 points from a baseline of 29.6 in the study of patients who’d switched antidepressants.
These exploratory studies were sponsored by Otsuka Pharmaceutical. Dr. Baker is a company employee.
Brexpiprazole also is FDA-approved for treatment of schizophrenia.
AT THE ECNP CONGRESS
Key clinical point:
Major finding: Mean scores on the Sheehan Disability Scale improved by 3.1-3.7 points from a baseline of 6.3-6.5 after 6 or 12 weeks of adjunctive brexpiprazole in three studies.
Data source: The three open-label exploratory studies included a total of 145 patients with major depressive disorder.
Disclosures: The studies were sponsored by Otsuka Pharmaceuticals. The presenter is employed by the company.
Patient with a breast mass: Why did she pursue litigation?
CASE: After routine mammography results, DCIS found
A 49-year-old woman (G2 P2002) with a history of fibrocystic breast disease presented with a left breast mass that she found a month ago on self-examination. The patient faithfully had obtained routine mammograms since age 40. This year, after reporting the mass and with spot films obtained as recommended by the radiologist, a new cluster of microcalcifications was identified on the report: “spot compression” assessment identified a 3-cm mass and noted “s/p breast augmentation.”
The radiologist interpreted the spot films to be benign. His report stated that “15% of breast cancers are not detected by mammogram and breast self-exam is recommended monthly from 40 years of age.”
The gynecologist recommended a 6-month follow up. When the patient complied, the radiologist’s report again noted calcifications believed to be nonmalignant. Six months later, the patient presented with bloody nipple discharge from her left breast with apparent “eczema-like” lesions on the areola. The patient noted that her “left implant felt different.”
The patient’s surgical history included breast augmentation “years ago.” Her family history was negative for breast cancer. Her medications included hormone therapy (conjugated estrogens 0.625 mg with medroxyprogesterone acetate 2.5 mg daily) for vaginal atrophy. Other medical conditions included irritable bowel syndrome (managed with diet), anxiety and mood swings (for which she was taking sertraline), decreased libido, and irregular vaginal bleeding (after the patient refused endometrial sampling, she was switched to oral contraceptives to address the problem). In addition, her hypertension was being treated with hydrochlorothiazide.
At the gynecologist’s suggestion, a dermatology consultation was obtained.
The dermatologist gave a diagnosis of Paget disease with high-grade ductal carcinoma-in-situ (DCIS). The interval from screening mammogram to DCIS diagnosis had been 8 months. The dermatologist referred the patient to a breast surgeon. A discussion ensued between the breast surgeon and the dermatologist concerning the difficulty of making a diagnosis of breast cancer in a woman with breast augmentation.
The patient underwent modified radical mastectomy, and histopathology revealed DCIS with clear margins; lymph nodes were negative.
The patient filed a malpractice suit against the gynecologist related to the delayed breast mass evaluation and management. She remained upset that when she called the gynecologist’s office to convey her concerns regarding the left nipple discharge and implant concerns, “she was blown off.” She felt there was a clear “failure to communicate on critical matters of her health.” She alleged that the gynecologist, not the dermatologist, should have referred her to a breast surgeon.
WHAT 'S THE VERDICT?
In the end, the patient decided not to pursue the lawsuit.
Related article:
Who is liable when a surgical error occurs?
Medical considerations
Breast cancer is the most common female malignancy, with 232,340 cases occurring annually in the United States. It is the second leading cause of cancer-related death in US women.1 For this case discussion, we review the role of breast cancer screening, including breast self-examination and mammography.
Is breast self-examination recommended?
Recently, medical care has evolved from “breast self-examination” (BSE) to “breast self-awareness.”2 The concept of BSE and concerns about it stem in part from “the Shanghai study.”3 In this prospective randomized trial, 266,064 female textile workers were randomly assigned to “rigorous and repetitive training in BSE” versus no instruction and no BSE performance. The former group had twice as many breast biopsies than the latter group (2,761 biopsies in the BSE group vs 1,505 in the control group). There was no difference in the number of breast cancers diagnosed among the groups—864 in the BSE group and 896 in the control group (relative risk [RR], 0.97; 95% confidence interval [CI], 0.88–1.06; P = .47). Other studies also support lack of efficacy regarding BSE.4
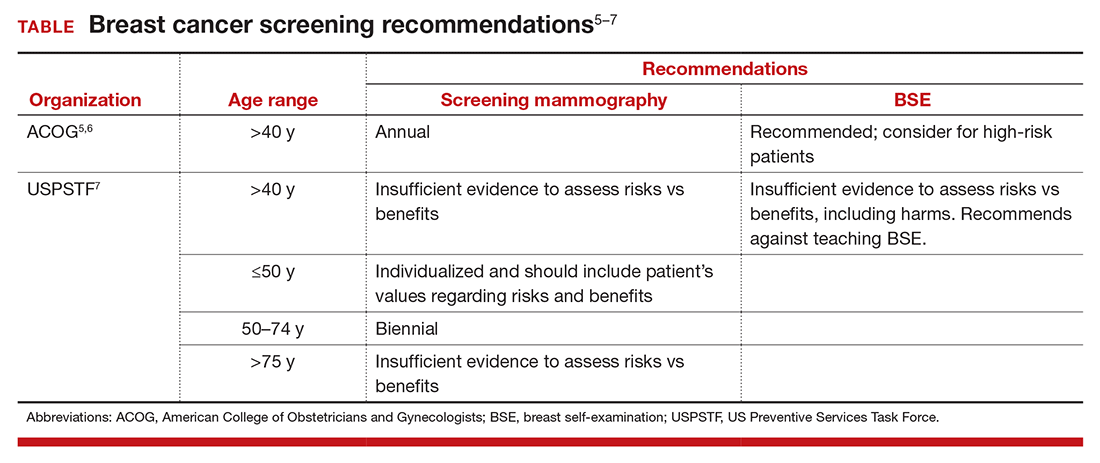
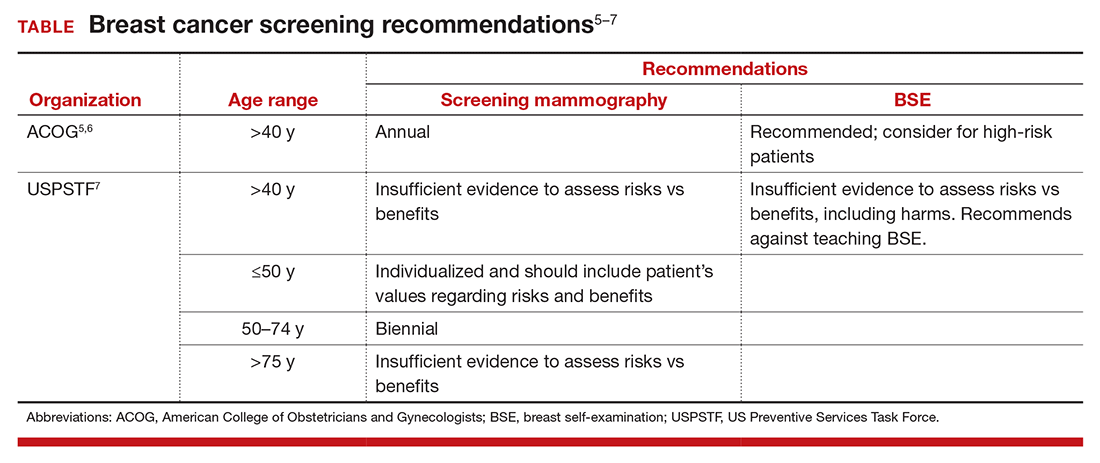
The potential for psychological harm, unnecessary biopsy, and additional imaging in association with false-positive findings is a concern2 (TABLE). The American College of Obstetricians and Gynecologists (ACOG) states, “breast self-examination may be appropriate for certain high-risk populations and for other women who chose to follow this approach.”2,5,6 The US Preventive Services Task Force (USPSTF) guidelines say that there is “insufficient evidence to assess risks vs benefits, including harms,” and recommends against teaching BSE.7 The American Cancer Society puts BSE in the “optional” category.2,8
Is there a middle of the road strategy? Perhaps. The concept of breast-awareness was developed so that women understand how their breasts look and feel.2,5 The concept does not advocate monthly BSE. The Mayo Clinic reported that, of 592 breast cancers, 57% were detected following abnormal screening mammography, 30% by BSE and 14% by clinical examination by a clinician. Furthermore, 38% of women with a palpable abnormality had a normal mammogram within the preceding 13 months.9 McBride and colleagues aptly addressed this: “Healthcare providers can educate their patients that breast awareness, in essence, is a two-step process. First, it requires that women be familiar with their breasts and aware of new changes and, second, have an understanding of the implications of these changes which includes informing their health care provider promptly.”10 The concept of “know what is normal for you” as conveyed by The Susan G. Komen Foundation succinctly encourages communication with patients.2,11
Mammography
The latest technique in mammography is digital or 3D mammography, also known as tomosynthesis. The technique is similar to 2D mammography with the addition of digital cameras. A study published in the radiology literature noted that the 2 methods were equivalent.12 One possible advantage of 3D mammography is that the 3D images are stored in computer files and are more easily incorporated into the electronic medical record.
What about mammography after breast augmentation?
While breast augmentation is not associated with an increase in breast cancer,13 mammography following breast augmentation can be more difficult to interpret and may result in a delay in diagnosis. In a prospective study of asymptomatic women who were diagnosed with breast cancer, 137 had augmentation and 685 did not. Miglioretti and colleagues noted that the sensitivity of screening mammography was lower in the augmentation cohort.14 To enhance accuracy, breast implant displacement views (in which the breast tissue is pulled forward and the implant is displaced posteriorly to improve visualization) have been recommended.15 A retrospective review provides data reporting no effect on interpretation of mammograms following augmentation.16 The American Cancer Society recommends the same screening for women with implants as without implants, starting at age 40 years.17
Paget disease of the breast
Paget disease of the breast was first described by Sir James Paget in 1874. He also defined Paget disease of extramammary tissue, bone, vulva, and penis. Paget disease of the breast is a rare type of cancer in which the skin and nipple are involved frequently in association with DCIS or invasive breast cancer. The skin has an eczema-like appearance. Characteristic Paget (malignant) cells are large with clear cytoplasm (clear halo) and eccentric, hyperchromatic nuclei throughout the dermis. Assessment includes mammography and biopsy with immunohistochemical staining. Treatment varies by case and can include lumpectomy or mastectomy and chemotherapy and/or radiation therapy. Medications, including tamoxifen and anastrazole, have been recommended. Prognosis depends on nodal involvement. The disease is more common in women older than age 50.18
Related article:
The medicolegal considerations of interacting with your patients online
Legal issues: What was the gynecologist’s obligation?
The question remains, did the gynecologist have an obligation to obtain diagnostic mammography and ultrasound of the breast? Would it have been prudent for immediate referral to a breast surgeon? These are critical questions.
Negligence and the standard of care
The malpractice lawsuit against this gynecologist is based on negligence. In essence, it is a claim that the management provided fell below a standard of care that would be given by a reasonably careful and prudent gynecologist under the circumstances. This generally means that the care was less than the profession itself would find acceptable. Here the claim is essentially a diagnostic error claim, a common basis of malpractice.19 The delay in diagnosing breast cancer is a leading cause of malpractice claims against gynecologists.20,21
It is axiomatic that not all bad outcomes are the result of error, and not all errors are a result of an unacceptable standard of care. It is only bad outcomes resulting from careless or negligent errors that give rise to malpractice. But malpractice claims are often filed without knowing whether or not there was negligence—and, as we will see, many of those claims are without merit.
Was there negligence?
Ordinarily the plaintiff/patient must demonstrate that the care by the physician fell below the standard of care and, as a result, the patient suffered an injury. Stated another way, the plaintiff must show that the physician’s actions were unreasonable given all of the circumstances. In this case, the plaintiff must demonstrate that the gynecologist’s care was not appropriate. Failure to refer to another physician or provide additional testing is likely to be the major claim for negligence or inappropriate care.
Did that negligence cause injury?
Even if the plaintiff can demonstrate that the care was negligent, to prevail the plaintiff must also demonstrate that that negligence caused the injury—and that might be difficult.
What injury was caused by the delay in discovering the cancer? It did not apparently lead to the patient’s death. Can it be proven that the delay clearly shortened the patient’s life expectancy or required additional expensive and painful treatment? That may be difficult to demonstrate.
Causation. The causation factor could appear in many cancer or similar medical cases. On one hand, causation is a critical matter, but on the other hand, delay in treating cancer might have a very adverse effect on patients.
In recent years, about half the states have solved this dilemma by recognizing the concept of “loss of chance.”22 Essentially, this means that the health care provider, by delaying treatment, diminished the possibility that the patient would survive or recover fully.
There are significant variations among states in the loss-of-chance concept, many being quite technical.22 Thus, it is possible that a delay that reduced the chance of recovery or survival could be the injury and causal connection between the injury and the negligence. Even in states that recognize the loss-of-chance concept, the patient still must prove loss of chance.
Lessons learned from this case study
- Breast self-awareness has replaced (substituted) breast self-examination
- ACOG recommends breast mammography beginning at age 40 years
- Breast augmentation affects mammographic interpretation
- Prehaps if better communication had been provided initially, the patient would not have sought legal counsel or filed a weak suit
Related article:
Is the smartphone recording while the patient is under anesthesia?
Is this a strong malpractice case?
In the case presented here, it is not clear that the patient could show a meaningful loss of chance. If there is a delay in the breast cancer diagnosis, tumor doubling time would be an issue. While it is impossible to assess growth rate when a breast cancer is in its preclinical microscopic stage, doubling time can be 100 to 200 days. Therefore, it would take 20 years for the tumor to reach a 1- to 2-cm diameter. A log-normal distribution has been suggested for determining tumor growth.23
Although the facts in this case are sketchy, this does not look like a strong malpractice case. Given the expense, difficulty, and length of time it takes to pursue a malpractice case (especially for someone battling cancer), an obvious question is: Why would a patient file a lawsuit in these circumstances? There is no single answer to that, but the hope of getting rich is unlikely a primary motivation. Ironically, many malpractice cases are filed in which there was no error (or at least no negligent error).24
The search for what really happened, or why the bad event happened, is key. In other circumstances, it may be a desire for revenge or to protect other patients from similar bad results. Studies repeatedly have shown a somewhat limited correlation between negligent error and the decision to file a malpractice claim.24–26 In this case, the patient’s sense of being “blown off” during a particularly difficult time may represent the reason why she filed a malpractice lawsuit. Communication gaffes and poor physician-patient relationships undoubtedly contribute to medical malpractice claims.27,28 Improving communication with patients probably improves care, but it also almost certainly reduces the risk of a malpractice claim.29
Why a lawyer would accept this case is also unclear, but that is an issue for another day. Also for another day is the issue of product liability concerning breast implants. Those legal issues and related liability, primarily directed to the manufacturers of the implants, are interesting topics. They are also complex and will be the subject of a future article.
Finally, the patient’s decision to not pursue her lawsuit does not come as a surprise. A relatively small percentage of malpractice claims result in any meaningful financial recovery for the plaintiff. Few cases go to trial, and of those that do result in a verdict, about 75% of the verdicts are in favor of the physician.25,30 Many cases just fade away, either because the plaintiff never pursues them or because they are dismissed by a court at an early stage. Nonetheless, for the physician, even winning a malpractice case is disruptive and difficult. So in addition to ensuring careful, quality, and up-to-date care, a physician should seek to maintain good relationships and communication with patients to reduce the probability of even weak lawsuits being filed.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63(1):11–30.
- Mark K, Temkin S, Terplan M. Breast self-awareness: the evidence behind the euphemism. Obstet Gynecol. 2014;123(4):734–745.
- Thomas D, Gao D, Self S, et al. Randomized trial of breast self-examination in Shanghai: methodology and preliminary results. J Natl Cancer Inst. 1997;89(5):355–365.
- Jones S. Regular self-examination or clinical examination for early detection of breast cancer. Int J Epidemiol. 2008;37(6):1219.
- ACOG Committee on Practice Bulletins–Gynecology. ACOG Practice Bulletin No. 122. American College of Obstetricians and Gynecologists website. http://www.acog.org/Resources-And-Publications/Practice-Bulletins/Committee-on-Practice-Bulletins-Gynecology/Breast-Cancer-Screening. Published August 2011; reaffirmed 2014. Accessed November 10, 2016.
- ACOG Statement on breast cancer screening guidelines. American College of Obstetricians and Gynecologists website. http://www.acog.org/About-ACOG/News-Room/Statements/2016/ACOG-Statement-on-Breast-Cancer-Screening-Guidelines. Published January 11, 2016. Accessed November 10, 2016.
- Final Recommendation Statement: Breast Cancer: Screening. U.S. Preventive Services Task Force web site. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/breast-cancer-screening1. Published September 2016. Accessed November 10, 2016.
- American Cancer Society recommendations for early breast cancer detection in women without breast symptoms. American Cancer Society website. http://www.cancer.org/cancer/breastcancer/moreinformation/breastcancerearlydetection/breast-cancer-early-detection-acs-recs. Updated October 20, 2015. Accessed November 10, 2016.
- Mathis K, Hoskin T, Boughey J, et al. Palpable presentation of breast cancer persists in the era of screening mammography. J Am Coll Surg. 2010;210(3):314–318.
- MacBride M, Pruthi S, Bevers T. The evolution of breast self-examination to breast awareness. Breast J. 2012;18(6):641–643.
- Susan G. Komen Foundation. Breast self-awareness messages. http://ww5.komen.org/Breastcancer/Breastselfawareness.html. Accessed November 10, 2016.
- DelTurco MR, Mantellini P, Ciatto S, et al. Full-field digital versus screen-film mammography: comparative accuracy in concurrent screening cohorts. AJR. 2007;189(4):860–866.
- Susan G. Koman Foundation. Factors that do not increase breast cancer risk: Breast implants. https://ww5.komen.org/BreastCancer/FactorsThatDoNotIncreaseRisk.html. Updated October 28, 2016. Accessed November 10, 2016.
- Miglioretti D, Rutter, C, Geller B, et al. Effect of breast augmentation on the accuracy of mammography and cancer characteristics. JAMA. 2004;291(4):442–450.
- Eklund GW, Busby RC, Miller SH, Job JS. Improved imaging of the augmented breast. Am J Roentgenol. 1988;151(3):469–473.
- Kam K, Lee E, Pairwan S, et al. The effect of breast implants on mammogram outcomes. Am Surg. 2015;81(10):1053–1056.
- American Cancer Society. Mammograms and other imaging tests. http://www.cancer.org/acs/groups/cid/documents/webcontent/003178-pdf.pdf. Revised April 25, 2016. Accessed November 10, 2016.
- Dalberg K, Hellborg H, Warnberg F. Paget’s disease of the nipple in a population based cohort. Breast Cancer Res Treat. 2008;111(2):313–319.
- Saber Tehrani A, Lee H, Mathews S, et al. 25-year summary of US malpractice claims for diagnostic errors 1986–2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672–680.
- White AA, Pichert JW, Bledsoe SH, Irwin C, Entman SS. Cause and effect analysis of closed claims in obstetrics and gynecology. Obstet Gynecol. 2005;105(5 pt 1):1031–1038.
- Ward CJ, Green VL. Risk management and medico-legal issues in breast cancer. Clin Obstet Gynecol. 2016;59(2):439–446.
- Guest L, Schap D, Tran T. The “Loss of Chance” rule as a special category of damages in medical malpractice: a state-by-state analysis. J Legal Econ. 2015;21(2):53–107.
- Kuroishi T, Tominaga S, Morimoto T, et al. Tumor growth rate and prognosis of breast cancer mainly detected by mass screening. Jpn J Cancer Res. 1990;81(5):454–462.
- Localio AR, Lawthers AG, Brennan TA, et al. Relation between malpractice claims and adverse events due to negligence: results of the Harvard Medical Practice Study III. N Engl J Medicine. 1991;325(4):245–251.
- Gandhi TK, Kachalia A, Thomas EJ, et al. Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims. Ann Intern Med. 2006;145(7):488–496.
- Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354(19):2024–2033.
- Huntington B, Kuhn N. Communication gaffes: a root cause of malpractice claims. Proc (Bayl Univ Med Cent). 2003;16(2):157–161.
- Moore PJ, Adler NE, Robertson PA. Medical malpractice: the effect of doctor-patient relations on medical patient perceptions and malpractice intentions. West J Med. 2000;173(4):244–250.
- Hickson GB, Jenkins AD. Identifying and addressing communication failures as a means of reducing unnecessary malpractice claims. NC Med J. 2007;68(5):362–364.
- Jena AB, Chandra A, Lakdawalla D, Seabury S. Outcomes of medical malpractice litigation against US physicians. Arch Intern Med. 2012;172(11):892–894.
CASE: After routine mammography results, DCIS found
A 49-year-old woman (G2 P2002) with a history of fibrocystic breast disease presented with a left breast mass that she found a month ago on self-examination. The patient faithfully had obtained routine mammograms since age 40. This year, after reporting the mass and with spot films obtained as recommended by the radiologist, a new cluster of microcalcifications was identified on the report: “spot compression” assessment identified a 3-cm mass and noted “s/p breast augmentation.”
The radiologist interpreted the spot films to be benign. His report stated that “15% of breast cancers are not detected by mammogram and breast self-exam is recommended monthly from 40 years of age.”
The gynecologist recommended a 6-month follow up. When the patient complied, the radiologist’s report again noted calcifications believed to be nonmalignant. Six months later, the patient presented with bloody nipple discharge from her left breast with apparent “eczema-like” lesions on the areola. The patient noted that her “left implant felt different.”
The patient’s surgical history included breast augmentation “years ago.” Her family history was negative for breast cancer. Her medications included hormone therapy (conjugated estrogens 0.625 mg with medroxyprogesterone acetate 2.5 mg daily) for vaginal atrophy. Other medical conditions included irritable bowel syndrome (managed with diet), anxiety and mood swings (for which she was taking sertraline), decreased libido, and irregular vaginal bleeding (after the patient refused endometrial sampling, she was switched to oral contraceptives to address the problem). In addition, her hypertension was being treated with hydrochlorothiazide.
At the gynecologist’s suggestion, a dermatology consultation was obtained.
The dermatologist gave a diagnosis of Paget disease with high-grade ductal carcinoma-in-situ (DCIS). The interval from screening mammogram to DCIS diagnosis had been 8 months. The dermatologist referred the patient to a breast surgeon. A discussion ensued between the breast surgeon and the dermatologist concerning the difficulty of making a diagnosis of breast cancer in a woman with breast augmentation.
The patient underwent modified radical mastectomy, and histopathology revealed DCIS with clear margins; lymph nodes were negative.
The patient filed a malpractice suit against the gynecologist related to the delayed breast mass evaluation and management. She remained upset that when she called the gynecologist’s office to convey her concerns regarding the left nipple discharge and implant concerns, “she was blown off.” She felt there was a clear “failure to communicate on critical matters of her health.” She alleged that the gynecologist, not the dermatologist, should have referred her to a breast surgeon.
WHAT 'S THE VERDICT?
In the end, the patient decided not to pursue the lawsuit.
Related article:
Who is liable when a surgical error occurs?
Medical considerations
Breast cancer is the most common female malignancy, with 232,340 cases occurring annually in the United States. It is the second leading cause of cancer-related death in US women.1 For this case discussion, we review the role of breast cancer screening, including breast self-examination and mammography.
Is breast self-examination recommended?
Recently, medical care has evolved from “breast self-examination” (BSE) to “breast self-awareness.”2 The concept of BSE and concerns about it stem in part from “the Shanghai study.”3 In this prospective randomized trial, 266,064 female textile workers were randomly assigned to “rigorous and repetitive training in BSE” versus no instruction and no BSE performance. The former group had twice as many breast biopsies than the latter group (2,761 biopsies in the BSE group vs 1,505 in the control group). There was no difference in the number of breast cancers diagnosed among the groups—864 in the BSE group and 896 in the control group (relative risk [RR], 0.97; 95% confidence interval [CI], 0.88–1.06; P = .47). Other studies also support lack of efficacy regarding BSE.4
The potential for psychological harm, unnecessary biopsy, and additional imaging in association with false-positive findings is a concern2 (TABLE). The American College of Obstetricians and Gynecologists (ACOG) states, “breast self-examination may be appropriate for certain high-risk populations and for other women who chose to follow this approach.”2,5,6 The US Preventive Services Task Force (USPSTF) guidelines say that there is “insufficient evidence to assess risks vs benefits, including harms,” and recommends against teaching BSE.7 The American Cancer Society puts BSE in the “optional” category.2,8
Is there a middle of the road strategy? Perhaps. The concept of breast-awareness was developed so that women understand how their breasts look and feel.2,5 The concept does not advocate monthly BSE. The Mayo Clinic reported that, of 592 breast cancers, 57% were detected following abnormal screening mammography, 30% by BSE and 14% by clinical examination by a clinician. Furthermore, 38% of women with a palpable abnormality had a normal mammogram within the preceding 13 months.9 McBride and colleagues aptly addressed this: “Healthcare providers can educate their patients that breast awareness, in essence, is a two-step process. First, it requires that women be familiar with their breasts and aware of new changes and, second, have an understanding of the implications of these changes which includes informing their health care provider promptly.”10 The concept of “know what is normal for you” as conveyed by The Susan G. Komen Foundation succinctly encourages communication with patients.2,11
Mammography
The latest technique in mammography is digital or 3D mammography, also known as tomosynthesis. The technique is similar to 2D mammography with the addition of digital cameras. A study published in the radiology literature noted that the 2 methods were equivalent.12 One possible advantage of 3D mammography is that the 3D images are stored in computer files and are more easily incorporated into the electronic medical record.
What about mammography after breast augmentation?
While breast augmentation is not associated with an increase in breast cancer,13 mammography following breast augmentation can be more difficult to interpret and may result in a delay in diagnosis. In a prospective study of asymptomatic women who were diagnosed with breast cancer, 137 had augmentation and 685 did not. Miglioretti and colleagues noted that the sensitivity of screening mammography was lower in the augmentation cohort.14 To enhance accuracy, breast implant displacement views (in which the breast tissue is pulled forward and the implant is displaced posteriorly to improve visualization) have been recommended.15 A retrospective review provides data reporting no effect on interpretation of mammograms following augmentation.16 The American Cancer Society recommends the same screening for women with implants as without implants, starting at age 40 years.17
Paget disease of the breast
Paget disease of the breast was first described by Sir James Paget in 1874. He also defined Paget disease of extramammary tissue, bone, vulva, and penis. Paget disease of the breast is a rare type of cancer in which the skin and nipple are involved frequently in association with DCIS or invasive breast cancer. The skin has an eczema-like appearance. Characteristic Paget (malignant) cells are large with clear cytoplasm (clear halo) and eccentric, hyperchromatic nuclei throughout the dermis. Assessment includes mammography and biopsy with immunohistochemical staining. Treatment varies by case and can include lumpectomy or mastectomy and chemotherapy and/or radiation therapy. Medications, including tamoxifen and anastrazole, have been recommended. Prognosis depends on nodal involvement. The disease is more common in women older than age 50.18
Related article:
The medicolegal considerations of interacting with your patients online
Legal issues: What was the gynecologist’s obligation?
The question remains, did the gynecologist have an obligation to obtain diagnostic mammography and ultrasound of the breast? Would it have been prudent for immediate referral to a breast surgeon? These are critical questions.
Negligence and the standard of care
The malpractice lawsuit against this gynecologist is based on negligence. In essence, it is a claim that the management provided fell below a standard of care that would be given by a reasonably careful and prudent gynecologist under the circumstances. This generally means that the care was less than the profession itself would find acceptable. Here the claim is essentially a diagnostic error claim, a common basis of malpractice.19 The delay in diagnosing breast cancer is a leading cause of malpractice claims against gynecologists.20,21
It is axiomatic that not all bad outcomes are the result of error, and not all errors are a result of an unacceptable standard of care. It is only bad outcomes resulting from careless or negligent errors that give rise to malpractice. But malpractice claims are often filed without knowing whether or not there was negligence—and, as we will see, many of those claims are without merit.
Was there negligence?
Ordinarily the plaintiff/patient must demonstrate that the care by the physician fell below the standard of care and, as a result, the patient suffered an injury. Stated another way, the plaintiff must show that the physician’s actions were unreasonable given all of the circumstances. In this case, the plaintiff must demonstrate that the gynecologist’s care was not appropriate. Failure to refer to another physician or provide additional testing is likely to be the major claim for negligence or inappropriate care.
Did that negligence cause injury?
Even if the plaintiff can demonstrate that the care was negligent, to prevail the plaintiff must also demonstrate that that negligence caused the injury—and that might be difficult.
What injury was caused by the delay in discovering the cancer? It did not apparently lead to the patient’s death. Can it be proven that the delay clearly shortened the patient’s life expectancy or required additional expensive and painful treatment? That may be difficult to demonstrate.
Causation. The causation factor could appear in many cancer or similar medical cases. On one hand, causation is a critical matter, but on the other hand, delay in treating cancer might have a very adverse effect on patients.
In recent years, about half the states have solved this dilemma by recognizing the concept of “loss of chance.”22 Essentially, this means that the health care provider, by delaying treatment, diminished the possibility that the patient would survive or recover fully.
There are significant variations among states in the loss-of-chance concept, many being quite technical.22 Thus, it is possible that a delay that reduced the chance of recovery or survival could be the injury and causal connection between the injury and the negligence. Even in states that recognize the loss-of-chance concept, the patient still must prove loss of chance.
Lessons learned from this case study
- Breast self-awareness has replaced (substituted) breast self-examination
- ACOG recommends breast mammography beginning at age 40 years
- Breast augmentation affects mammographic interpretation
- Prehaps if better communication had been provided initially, the patient would not have sought legal counsel or filed a weak suit
Related article:
Is the smartphone recording while the patient is under anesthesia?
Is this a strong malpractice case?
In the case presented here, it is not clear that the patient could show a meaningful loss of chance. If there is a delay in the breast cancer diagnosis, tumor doubling time would be an issue. While it is impossible to assess growth rate when a breast cancer is in its preclinical microscopic stage, doubling time can be 100 to 200 days. Therefore, it would take 20 years for the tumor to reach a 1- to 2-cm diameter. A log-normal distribution has been suggested for determining tumor growth.23
Although the facts in this case are sketchy, this does not look like a strong malpractice case. Given the expense, difficulty, and length of time it takes to pursue a malpractice case (especially for someone battling cancer), an obvious question is: Why would a patient file a lawsuit in these circumstances? There is no single answer to that, but the hope of getting rich is unlikely a primary motivation. Ironically, many malpractice cases are filed in which there was no error (or at least no negligent error).24
The search for what really happened, or why the bad event happened, is key. In other circumstances, it may be a desire for revenge or to protect other patients from similar bad results. Studies repeatedly have shown a somewhat limited correlation between negligent error and the decision to file a malpractice claim.24–26 In this case, the patient’s sense of being “blown off” during a particularly difficult time may represent the reason why she filed a malpractice lawsuit. Communication gaffes and poor physician-patient relationships undoubtedly contribute to medical malpractice claims.27,28 Improving communication with patients probably improves care, but it also almost certainly reduces the risk of a malpractice claim.29
Why a lawyer would accept this case is also unclear, but that is an issue for another day. Also for another day is the issue of product liability concerning breast implants. Those legal issues and related liability, primarily directed to the manufacturers of the implants, are interesting topics. They are also complex and will be the subject of a future article.
Finally, the patient’s decision to not pursue her lawsuit does not come as a surprise. A relatively small percentage of malpractice claims result in any meaningful financial recovery for the plaintiff. Few cases go to trial, and of those that do result in a verdict, about 75% of the verdicts are in favor of the physician.25,30 Many cases just fade away, either because the plaintiff never pursues them or because they are dismissed by a court at an early stage. Nonetheless, for the physician, even winning a malpractice case is disruptive and difficult. So in addition to ensuring careful, quality, and up-to-date care, a physician should seek to maintain good relationships and communication with patients to reduce the probability of even weak lawsuits being filed.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
CASE: After routine mammography results, DCIS found
A 49-year-old woman (G2 P2002) with a history of fibrocystic breast disease presented with a left breast mass that she found a month ago on self-examination. The patient faithfully had obtained routine mammograms since age 40. This year, after reporting the mass and with spot films obtained as recommended by the radiologist, a new cluster of microcalcifications was identified on the report: “spot compression” assessment identified a 3-cm mass and noted “s/p breast augmentation.”
The radiologist interpreted the spot films to be benign. His report stated that “15% of breast cancers are not detected by mammogram and breast self-exam is recommended monthly from 40 years of age.”
The gynecologist recommended a 6-month follow up. When the patient complied, the radiologist’s report again noted calcifications believed to be nonmalignant. Six months later, the patient presented with bloody nipple discharge from her left breast with apparent “eczema-like” lesions on the areola. The patient noted that her “left implant felt different.”
The patient’s surgical history included breast augmentation “years ago.” Her family history was negative for breast cancer. Her medications included hormone therapy (conjugated estrogens 0.625 mg with medroxyprogesterone acetate 2.5 mg daily) for vaginal atrophy. Other medical conditions included irritable bowel syndrome (managed with diet), anxiety and mood swings (for which she was taking sertraline), decreased libido, and irregular vaginal bleeding (after the patient refused endometrial sampling, she was switched to oral contraceptives to address the problem). In addition, her hypertension was being treated with hydrochlorothiazide.
At the gynecologist’s suggestion, a dermatology consultation was obtained.
The dermatologist gave a diagnosis of Paget disease with high-grade ductal carcinoma-in-situ (DCIS). The interval from screening mammogram to DCIS diagnosis had been 8 months. The dermatologist referred the patient to a breast surgeon. A discussion ensued between the breast surgeon and the dermatologist concerning the difficulty of making a diagnosis of breast cancer in a woman with breast augmentation.
The patient underwent modified radical mastectomy, and histopathology revealed DCIS with clear margins; lymph nodes were negative.
The patient filed a malpractice suit against the gynecologist related to the delayed breast mass evaluation and management. She remained upset that when she called the gynecologist’s office to convey her concerns regarding the left nipple discharge and implant concerns, “she was blown off.” She felt there was a clear “failure to communicate on critical matters of her health.” She alleged that the gynecologist, not the dermatologist, should have referred her to a breast surgeon.
WHAT 'S THE VERDICT?
In the end, the patient decided not to pursue the lawsuit.
Related article:
Who is liable when a surgical error occurs?
Medical considerations
Breast cancer is the most common female malignancy, with 232,340 cases occurring annually in the United States. It is the second leading cause of cancer-related death in US women.1 For this case discussion, we review the role of breast cancer screening, including breast self-examination and mammography.
Is breast self-examination recommended?
Recently, medical care has evolved from “breast self-examination” (BSE) to “breast self-awareness.”2 The concept of BSE and concerns about it stem in part from “the Shanghai study.”3 In this prospective randomized trial, 266,064 female textile workers were randomly assigned to “rigorous and repetitive training in BSE” versus no instruction and no BSE performance. The former group had twice as many breast biopsies than the latter group (2,761 biopsies in the BSE group vs 1,505 in the control group). There was no difference in the number of breast cancers diagnosed among the groups—864 in the BSE group and 896 in the control group (relative risk [RR], 0.97; 95% confidence interval [CI], 0.88–1.06; P = .47). Other studies also support lack of efficacy regarding BSE.4
The potential for psychological harm, unnecessary biopsy, and additional imaging in association with false-positive findings is a concern2 (TABLE). The American College of Obstetricians and Gynecologists (ACOG) states, “breast self-examination may be appropriate for certain high-risk populations and for other women who chose to follow this approach.”2,5,6 The US Preventive Services Task Force (USPSTF) guidelines say that there is “insufficient evidence to assess risks vs benefits, including harms,” and recommends against teaching BSE.7 The American Cancer Society puts BSE in the “optional” category.2,8
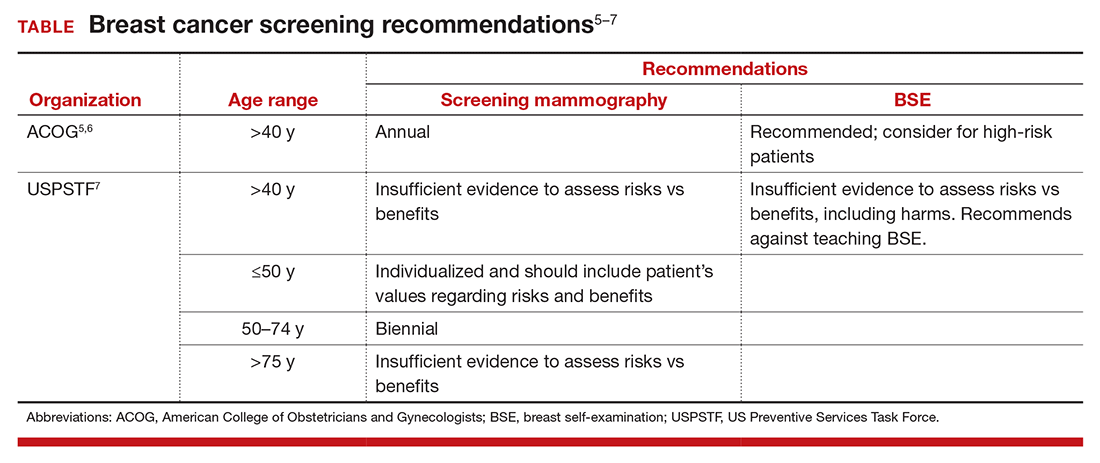
Is there a middle of the road strategy? Perhaps. The concept of breast-awareness was developed so that women understand how their breasts look and feel.2,5 The concept does not advocate monthly BSE. The Mayo Clinic reported that, of 592 breast cancers, 57% were detected following abnormal screening mammography, 30% by BSE and 14% by clinical examination by a clinician. Furthermore, 38% of women with a palpable abnormality had a normal mammogram within the preceding 13 months.9 McBride and colleagues aptly addressed this: “Healthcare providers can educate their patients that breast awareness, in essence, is a two-step process. First, it requires that women be familiar with their breasts and aware of new changes and, second, have an understanding of the implications of these changes which includes informing their health care provider promptly.”10 The concept of “know what is normal for you” as conveyed by The Susan G. Komen Foundation succinctly encourages communication with patients.2,11
Mammography
The latest technique in mammography is digital or 3D mammography, also known as tomosynthesis. The technique is similar to 2D mammography with the addition of digital cameras. A study published in the radiology literature noted that the 2 methods were equivalent.12 One possible advantage of 3D mammography is that the 3D images are stored in computer files and are more easily incorporated into the electronic medical record.
What about mammography after breast augmentation?
While breast augmentation is not associated with an increase in breast cancer,13 mammography following breast augmentation can be more difficult to interpret and may result in a delay in diagnosis. In a prospective study of asymptomatic women who were diagnosed with breast cancer, 137 had augmentation and 685 did not. Miglioretti and colleagues noted that the sensitivity of screening mammography was lower in the augmentation cohort.14 To enhance accuracy, breast implant displacement views (in which the breast tissue is pulled forward and the implant is displaced posteriorly to improve visualization) have been recommended.15 A retrospective review provides data reporting no effect on interpretation of mammograms following augmentation.16 The American Cancer Society recommends the same screening for women with implants as without implants, starting at age 40 years.17
Paget disease of the breast
Paget disease of the breast was first described by Sir James Paget in 1874. He also defined Paget disease of extramammary tissue, bone, vulva, and penis. Paget disease of the breast is a rare type of cancer in which the skin and nipple are involved frequently in association with DCIS or invasive breast cancer. The skin has an eczema-like appearance. Characteristic Paget (malignant) cells are large with clear cytoplasm (clear halo) and eccentric, hyperchromatic nuclei throughout the dermis. Assessment includes mammography and biopsy with immunohistochemical staining. Treatment varies by case and can include lumpectomy or mastectomy and chemotherapy and/or radiation therapy. Medications, including tamoxifen and anastrazole, have been recommended. Prognosis depends on nodal involvement. The disease is more common in women older than age 50.18
Related article:
The medicolegal considerations of interacting with your patients online
Legal issues: What was the gynecologist’s obligation?
The question remains, did the gynecologist have an obligation to obtain diagnostic mammography and ultrasound of the breast? Would it have been prudent for immediate referral to a breast surgeon? These are critical questions.
Negligence and the standard of care
The malpractice lawsuit against this gynecologist is based on negligence. In essence, it is a claim that the management provided fell below a standard of care that would be given by a reasonably careful and prudent gynecologist under the circumstances. This generally means that the care was less than the profession itself would find acceptable. Here the claim is essentially a diagnostic error claim, a common basis of malpractice.19 The delay in diagnosing breast cancer is a leading cause of malpractice claims against gynecologists.20,21
It is axiomatic that not all bad outcomes are the result of error, and not all errors are a result of an unacceptable standard of care. It is only bad outcomes resulting from careless or negligent errors that give rise to malpractice. But malpractice claims are often filed without knowing whether or not there was negligence—and, as we will see, many of those claims are without merit.
Was there negligence?
Ordinarily the plaintiff/patient must demonstrate that the care by the physician fell below the standard of care and, as a result, the patient suffered an injury. Stated another way, the plaintiff must show that the physician’s actions were unreasonable given all of the circumstances. In this case, the plaintiff must demonstrate that the gynecologist’s care was not appropriate. Failure to refer to another physician or provide additional testing is likely to be the major claim for negligence or inappropriate care.
Did that negligence cause injury?
Even if the plaintiff can demonstrate that the care was negligent, to prevail the plaintiff must also demonstrate that that negligence caused the injury—and that might be difficult.
What injury was caused by the delay in discovering the cancer? It did not apparently lead to the patient’s death. Can it be proven that the delay clearly shortened the patient’s life expectancy or required additional expensive and painful treatment? That may be difficult to demonstrate.
Causation. The causation factor could appear in many cancer or similar medical cases. On one hand, causation is a critical matter, but on the other hand, delay in treating cancer might have a very adverse effect on patients.
In recent years, about half the states have solved this dilemma by recognizing the concept of “loss of chance.”22 Essentially, this means that the health care provider, by delaying treatment, diminished the possibility that the patient would survive or recover fully.
There are significant variations among states in the loss-of-chance concept, many being quite technical.22 Thus, it is possible that a delay that reduced the chance of recovery or survival could be the injury and causal connection between the injury and the negligence. Even in states that recognize the loss-of-chance concept, the patient still must prove loss of chance.
Lessons learned from this case study
- Breast self-awareness has replaced (substituted) breast self-examination
- ACOG recommends breast mammography beginning at age 40 years
- Breast augmentation affects mammographic interpretation
- Prehaps if better communication had been provided initially, the patient would not have sought legal counsel or filed a weak suit
Related article:
Is the smartphone recording while the patient is under anesthesia?
Is this a strong malpractice case?
In the case presented here, it is not clear that the patient could show a meaningful loss of chance. If there is a delay in the breast cancer diagnosis, tumor doubling time would be an issue. While it is impossible to assess growth rate when a breast cancer is in its preclinical microscopic stage, doubling time can be 100 to 200 days. Therefore, it would take 20 years for the tumor to reach a 1- to 2-cm diameter. A log-normal distribution has been suggested for determining tumor growth.23
Although the facts in this case are sketchy, this does not look like a strong malpractice case. Given the expense, difficulty, and length of time it takes to pursue a malpractice case (especially for someone battling cancer), an obvious question is: Why would a patient file a lawsuit in these circumstances? There is no single answer to that, but the hope of getting rich is unlikely a primary motivation. Ironically, many malpractice cases are filed in which there was no error (or at least no negligent error).24
The search for what really happened, or why the bad event happened, is key. In other circumstances, it may be a desire for revenge or to protect other patients from similar bad results. Studies repeatedly have shown a somewhat limited correlation between negligent error and the decision to file a malpractice claim.24–26 In this case, the patient’s sense of being “blown off” during a particularly difficult time may represent the reason why she filed a malpractice lawsuit. Communication gaffes and poor physician-patient relationships undoubtedly contribute to medical malpractice claims.27,28 Improving communication with patients probably improves care, but it also almost certainly reduces the risk of a malpractice claim.29
Why a lawyer would accept this case is also unclear, but that is an issue for another day. Also for another day is the issue of product liability concerning breast implants. Those legal issues and related liability, primarily directed to the manufacturers of the implants, are interesting topics. They are also complex and will be the subject of a future article.
Finally, the patient’s decision to not pursue her lawsuit does not come as a surprise. A relatively small percentage of malpractice claims result in any meaningful financial recovery for the plaintiff. Few cases go to trial, and of those that do result in a verdict, about 75% of the verdicts are in favor of the physician.25,30 Many cases just fade away, either because the plaintiff never pursues them or because they are dismissed by a court at an early stage. Nonetheless, for the physician, even winning a malpractice case is disruptive and difficult. So in addition to ensuring careful, quality, and up-to-date care, a physician should seek to maintain good relationships and communication with patients to reduce the probability of even weak lawsuits being filed.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63(1):11–30.
- Mark K, Temkin S, Terplan M. Breast self-awareness: the evidence behind the euphemism. Obstet Gynecol. 2014;123(4):734–745.
- Thomas D, Gao D, Self S, et al. Randomized trial of breast self-examination in Shanghai: methodology and preliminary results. J Natl Cancer Inst. 1997;89(5):355–365.
- Jones S. Regular self-examination or clinical examination for early detection of breast cancer. Int J Epidemiol. 2008;37(6):1219.
- ACOG Committee on Practice Bulletins–Gynecology. ACOG Practice Bulletin No. 122. American College of Obstetricians and Gynecologists website. http://www.acog.org/Resources-And-Publications/Practice-Bulletins/Committee-on-Practice-Bulletins-Gynecology/Breast-Cancer-Screening. Published August 2011; reaffirmed 2014. Accessed November 10, 2016.
- ACOG Statement on breast cancer screening guidelines. American College of Obstetricians and Gynecologists website. http://www.acog.org/About-ACOG/News-Room/Statements/2016/ACOG-Statement-on-Breast-Cancer-Screening-Guidelines. Published January 11, 2016. Accessed November 10, 2016.
- Final Recommendation Statement: Breast Cancer: Screening. U.S. Preventive Services Task Force web site. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/breast-cancer-screening1. Published September 2016. Accessed November 10, 2016.
- American Cancer Society recommendations for early breast cancer detection in women without breast symptoms. American Cancer Society website. http://www.cancer.org/cancer/breastcancer/moreinformation/breastcancerearlydetection/breast-cancer-early-detection-acs-recs. Updated October 20, 2015. Accessed November 10, 2016.
- Mathis K, Hoskin T, Boughey J, et al. Palpable presentation of breast cancer persists in the era of screening mammography. J Am Coll Surg. 2010;210(3):314–318.
- MacBride M, Pruthi S, Bevers T. The evolution of breast self-examination to breast awareness. Breast J. 2012;18(6):641–643.
- Susan G. Komen Foundation. Breast self-awareness messages. http://ww5.komen.org/Breastcancer/Breastselfawareness.html. Accessed November 10, 2016.
- DelTurco MR, Mantellini P, Ciatto S, et al. Full-field digital versus screen-film mammography: comparative accuracy in concurrent screening cohorts. AJR. 2007;189(4):860–866.
- Susan G. Koman Foundation. Factors that do not increase breast cancer risk: Breast implants. https://ww5.komen.org/BreastCancer/FactorsThatDoNotIncreaseRisk.html. Updated October 28, 2016. Accessed November 10, 2016.
- Miglioretti D, Rutter, C, Geller B, et al. Effect of breast augmentation on the accuracy of mammography and cancer characteristics. JAMA. 2004;291(4):442–450.
- Eklund GW, Busby RC, Miller SH, Job JS. Improved imaging of the augmented breast. Am J Roentgenol. 1988;151(3):469–473.
- Kam K, Lee E, Pairwan S, et al. The effect of breast implants on mammogram outcomes. Am Surg. 2015;81(10):1053–1056.
- American Cancer Society. Mammograms and other imaging tests. http://www.cancer.org/acs/groups/cid/documents/webcontent/003178-pdf.pdf. Revised April 25, 2016. Accessed November 10, 2016.
- Dalberg K, Hellborg H, Warnberg F. Paget’s disease of the nipple in a population based cohort. Breast Cancer Res Treat. 2008;111(2):313–319.
- Saber Tehrani A, Lee H, Mathews S, et al. 25-year summary of US malpractice claims for diagnostic errors 1986–2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672–680.
- White AA, Pichert JW, Bledsoe SH, Irwin C, Entman SS. Cause and effect analysis of closed claims in obstetrics and gynecology. Obstet Gynecol. 2005;105(5 pt 1):1031–1038.
- Ward CJ, Green VL. Risk management and medico-legal issues in breast cancer. Clin Obstet Gynecol. 2016;59(2):439–446.
- Guest L, Schap D, Tran T. The “Loss of Chance” rule as a special category of damages in medical malpractice: a state-by-state analysis. J Legal Econ. 2015;21(2):53–107.
- Kuroishi T, Tominaga S, Morimoto T, et al. Tumor growth rate and prognosis of breast cancer mainly detected by mass screening. Jpn J Cancer Res. 1990;81(5):454–462.
- Localio AR, Lawthers AG, Brennan TA, et al. Relation between malpractice claims and adverse events due to negligence: results of the Harvard Medical Practice Study III. N Engl J Medicine. 1991;325(4):245–251.
- Gandhi TK, Kachalia A, Thomas EJ, et al. Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims. Ann Intern Med. 2006;145(7):488–496.
- Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354(19):2024–2033.
- Huntington B, Kuhn N. Communication gaffes: a root cause of malpractice claims. Proc (Bayl Univ Med Cent). 2003;16(2):157–161.
- Moore PJ, Adler NE, Robertson PA. Medical malpractice: the effect of doctor-patient relations on medical patient perceptions and malpractice intentions. West J Med. 2000;173(4):244–250.
- Hickson GB, Jenkins AD. Identifying and addressing communication failures as a means of reducing unnecessary malpractice claims. NC Med J. 2007;68(5):362–364.
- Jena AB, Chandra A, Lakdawalla D, Seabury S. Outcomes of medical malpractice litigation against US physicians. Arch Intern Med. 2012;172(11):892–894.
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63(1):11–30.
- Mark K, Temkin S, Terplan M. Breast self-awareness: the evidence behind the euphemism. Obstet Gynecol. 2014;123(4):734–745.
- Thomas D, Gao D, Self S, et al. Randomized trial of breast self-examination in Shanghai: methodology and preliminary results. J Natl Cancer Inst. 1997;89(5):355–365.
- Jones S. Regular self-examination or clinical examination for early detection of breast cancer. Int J Epidemiol. 2008;37(6):1219.
- ACOG Committee on Practice Bulletins–Gynecology. ACOG Practice Bulletin No. 122. American College of Obstetricians and Gynecologists website. http://www.acog.org/Resources-And-Publications/Practice-Bulletins/Committee-on-Practice-Bulletins-Gynecology/Breast-Cancer-Screening. Published August 2011; reaffirmed 2014. Accessed November 10, 2016.
- ACOG Statement on breast cancer screening guidelines. American College of Obstetricians and Gynecologists website. http://www.acog.org/About-ACOG/News-Room/Statements/2016/ACOG-Statement-on-Breast-Cancer-Screening-Guidelines. Published January 11, 2016. Accessed November 10, 2016.
- Final Recommendation Statement: Breast Cancer: Screening. U.S. Preventive Services Task Force web site. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/breast-cancer-screening1. Published September 2016. Accessed November 10, 2016.
- American Cancer Society recommendations for early breast cancer detection in women without breast symptoms. American Cancer Society website. http://www.cancer.org/cancer/breastcancer/moreinformation/breastcancerearlydetection/breast-cancer-early-detection-acs-recs. Updated October 20, 2015. Accessed November 10, 2016.
- Mathis K, Hoskin T, Boughey J, et al. Palpable presentation of breast cancer persists in the era of screening mammography. J Am Coll Surg. 2010;210(3):314–318.
- MacBride M, Pruthi S, Bevers T. The evolution of breast self-examination to breast awareness. Breast J. 2012;18(6):641–643.
- Susan G. Komen Foundation. Breast self-awareness messages. http://ww5.komen.org/Breastcancer/Breastselfawareness.html. Accessed November 10, 2016.
- DelTurco MR, Mantellini P, Ciatto S, et al. Full-field digital versus screen-film mammography: comparative accuracy in concurrent screening cohorts. AJR. 2007;189(4):860–866.
- Susan G. Koman Foundation. Factors that do not increase breast cancer risk: Breast implants. https://ww5.komen.org/BreastCancer/FactorsThatDoNotIncreaseRisk.html. Updated October 28, 2016. Accessed November 10, 2016.
- Miglioretti D, Rutter, C, Geller B, et al. Effect of breast augmentation on the accuracy of mammography and cancer characteristics. JAMA. 2004;291(4):442–450.
- Eklund GW, Busby RC, Miller SH, Job JS. Improved imaging of the augmented breast. Am J Roentgenol. 1988;151(3):469–473.
- Kam K, Lee E, Pairwan S, et al. The effect of breast implants on mammogram outcomes. Am Surg. 2015;81(10):1053–1056.
- American Cancer Society. Mammograms and other imaging tests. http://www.cancer.org/acs/groups/cid/documents/webcontent/003178-pdf.pdf. Revised April 25, 2016. Accessed November 10, 2016.
- Dalberg K, Hellborg H, Warnberg F. Paget’s disease of the nipple in a population based cohort. Breast Cancer Res Treat. 2008;111(2):313–319.
- Saber Tehrani A, Lee H, Mathews S, et al. 25-year summary of US malpractice claims for diagnostic errors 1986–2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672–680.
- White AA, Pichert JW, Bledsoe SH, Irwin C, Entman SS. Cause and effect analysis of closed claims in obstetrics and gynecology. Obstet Gynecol. 2005;105(5 pt 1):1031–1038.
- Ward CJ, Green VL. Risk management and medico-legal issues in breast cancer. Clin Obstet Gynecol. 2016;59(2):439–446.
- Guest L, Schap D, Tran T. The “Loss of Chance” rule as a special category of damages in medical malpractice: a state-by-state analysis. J Legal Econ. 2015;21(2):53–107.
- Kuroishi T, Tominaga S, Morimoto T, et al. Tumor growth rate and prognosis of breast cancer mainly detected by mass screening. Jpn J Cancer Res. 1990;81(5):454–462.
- Localio AR, Lawthers AG, Brennan TA, et al. Relation between malpractice claims and adverse events due to negligence: results of the Harvard Medical Practice Study III. N Engl J Medicine. 1991;325(4):245–251.
- Gandhi TK, Kachalia A, Thomas EJ, et al. Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims. Ann Intern Med. 2006;145(7):488–496.
- Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354(19):2024–2033.
- Huntington B, Kuhn N. Communication gaffes: a root cause of malpractice claims. Proc (Bayl Univ Med Cent). 2003;16(2):157–161.
- Moore PJ, Adler NE, Robertson PA. Medical malpractice: the effect of doctor-patient relations on medical patient perceptions and malpractice intentions. West J Med. 2000;173(4):244–250.
- Hickson GB, Jenkins AD. Identifying and addressing communication failures as a means of reducing unnecessary malpractice claims. NC Med J. 2007;68(5):362–364.
- Jena AB, Chandra A, Lakdawalla D, Seabury S. Outcomes of medical malpractice litigation against US physicians. Arch Intern Med. 2012;172(11):892–894.
Management of Daily Glycemic Fluctuations in Patients With Type 2 Diabetes
While type 2 diabetes is commonly seen in primary care, it is difficult to manage successfully over time. This series offers brief eNewsletters written by clinical experts that are designed to assist in the clinical management of patients with type 2 diabetes.
While type 2 diabetes is commonly seen in primary care, it is difficult to manage successfully over time. This series offers brief eNewsletters written by clinical experts that are designed to assist in the clinical management of patients with type 2 diabetes.
While type 2 diabetes is commonly seen in primary care, it is difficult to manage successfully over time. This series offers brief eNewsletters written by clinical experts that are designed to assist in the clinical management of patients with type 2 diabetes.
Mortality Risk for Status Epilepticus Varies With Epilepsy Status
Status epilepticus (SE) significantly increases the all-cause mortality according to a review of more than 82,000 hospitalizations and emergency-department visits. Within this large group were 1,296 patients who presented with only SE, 2,136 patients who had post-epilepsy SE, and nearly 79,000 cases of epilepsy only, which served as controls. Angela M. Malek and associates found a mortality rate of 24.9% among SE only cases, compared with 20% in controls (hazard ratio 1.61) after adjustment for demographic and clinical confounding variables. Patients who presented with post-epilepsy SE had a mortality rate of 29.2% but a hazard ratio of only 1.16.
Malek AM, Wilson DA, Martz GU, et al. Mortality following status epilepticus in persons with and without epilepsy. Seizure. 2016;42:7-13.
Status epilepticus (SE) significantly increases the all-cause mortality according to a review of more than 82,000 hospitalizations and emergency-department visits. Within this large group were 1,296 patients who presented with only SE, 2,136 patients who had post-epilepsy SE, and nearly 79,000 cases of epilepsy only, which served as controls. Angela M. Malek and associates found a mortality rate of 24.9% among SE only cases, compared with 20% in controls (hazard ratio 1.61) after adjustment for demographic and clinical confounding variables. Patients who presented with post-epilepsy SE had a mortality rate of 29.2% but a hazard ratio of only 1.16.
Malek AM, Wilson DA, Martz GU, et al. Mortality following status epilepticus in persons with and without epilepsy. Seizure. 2016;42:7-13.
Status epilepticus (SE) significantly increases the all-cause mortality according to a review of more than 82,000 hospitalizations and emergency-department visits. Within this large group were 1,296 patients who presented with only SE, 2,136 patients who had post-epilepsy SE, and nearly 79,000 cases of epilepsy only, which served as controls. Angela M. Malek and associates found a mortality rate of 24.9% among SE only cases, compared with 20% in controls (hazard ratio 1.61) after adjustment for demographic and clinical confounding variables. Patients who presented with post-epilepsy SE had a mortality rate of 29.2% but a hazard ratio of only 1.16.
Malek AM, Wilson DA, Martz GU, et al. Mortality following status epilepticus in persons with and without epilepsy. Seizure. 2016;42:7-13.
Post-surgical Seizure Linked to Psychogenic Nonepileptic Seizures
Patients who continue to have seizures after epilepsy surgery should be evaluated for psychogenic nonepileptic seizures (PNES), based on a recent retrospective analysis of 1,105 patients. Among this cohort, 697 patients experienced postoperative seizures, and 27 of the 697 had documented PNES, according to Ali A. Asadi-Pooya and associates. Risk factors associated with post–epilepsy surgery PNES included an intelligence quotient (IQ) below 80 and a history of a psychiatric diagnosis.
Asadi-Pooya AA, Asadollahi M, Tinker J, et al. Post–epilepsy surgery psychogenic nonepileptic seizures. Epilepsia. 2016;57(10):1691-1696.
Patients who continue to have seizures after epilepsy surgery should be evaluated for psychogenic nonepileptic seizures (PNES), based on a recent retrospective analysis of 1,105 patients. Among this cohort, 697 patients experienced postoperative seizures, and 27 of the 697 had documented PNES, according to Ali A. Asadi-Pooya and associates. Risk factors associated with post–epilepsy surgery PNES included an intelligence quotient (IQ) below 80 and a history of a psychiatric diagnosis.
Asadi-Pooya AA, Asadollahi M, Tinker J, et al. Post–epilepsy surgery psychogenic nonepileptic seizures. Epilepsia. 2016;57(10):1691-1696.
Patients who continue to have seizures after epilepsy surgery should be evaluated for psychogenic nonepileptic seizures (PNES), based on a recent retrospective analysis of 1,105 patients. Among this cohort, 697 patients experienced postoperative seizures, and 27 of the 697 had documented PNES, according to Ali A. Asadi-Pooya and associates. Risk factors associated with post–epilepsy surgery PNES included an intelligence quotient (IQ) below 80 and a history of a psychiatric diagnosis.
Asadi-Pooya AA, Asadollahi M, Tinker J, et al. Post–epilepsy surgery psychogenic nonepileptic seizures. Epilepsia. 2016;57(10):1691-1696.
Do Epilepsy-related Mutations Make Patients Depressed?
Among relatives of patients with epilepsy, the prevalence of depression is greater among those who believe they have an increased risk of epilepsy because they may have inherited an epilepsy-related mutation. Shawn T. Sorge and his colleagues reached that conclusion after surveying 417 individuals in 104 families in which 4 persons per family had the disease on average. On the other hand, individuals with epilepsy seemed less troubled by the diagnosis: The likelihood of having depression was not related to any potential epilepsy-related mutation among persons who already have epilepsy.
Sorge ST, Hesdorffer DC, Phelan JC, et al. Depression and genetic causal attribution of epilepsy in multiplex epilepsy families. Epilepsia. 2016;57(10):1643-1650.
Among relatives of patients with epilepsy, the prevalence of depression is greater among those who believe they have an increased risk of epilepsy because they may have inherited an epilepsy-related mutation. Shawn T. Sorge and his colleagues reached that conclusion after surveying 417 individuals in 104 families in which 4 persons per family had the disease on average. On the other hand, individuals with epilepsy seemed less troubled by the diagnosis: The likelihood of having depression was not related to any potential epilepsy-related mutation among persons who already have epilepsy.
Sorge ST, Hesdorffer DC, Phelan JC, et al. Depression and genetic causal attribution of epilepsy in multiplex epilepsy families. Epilepsia. 2016;57(10):1643-1650.
Among relatives of patients with epilepsy, the prevalence of depression is greater among those who believe they have an increased risk of epilepsy because they may have inherited an epilepsy-related mutation. Shawn T. Sorge and his colleagues reached that conclusion after surveying 417 individuals in 104 families in which 4 persons per family had the disease on average. On the other hand, individuals with epilepsy seemed less troubled by the diagnosis: The likelihood of having depression was not related to any potential epilepsy-related mutation among persons who already have epilepsy.
Sorge ST, Hesdorffer DC, Phelan JC, et al. Depression and genetic causal attribution of epilepsy in multiplex epilepsy families. Epilepsia. 2016;57(10):1643-1650.
Epilepsy Experts Release Recommendations on Managing Unprovoked Seizures
The American Academy of Neurology and the American Epilepsy Society have released their guidelines on how to manage an adult patient who has had their first unprovoked seizure. Based on their review of the evidence, they recommend that clinicians base their decision about immediately initiating an antiepileptic drug after a first seizure on an individualized assessment. That evaluation should weigh the risk of a second seizure occurring against the adverse effects of the medication, as well as patient preferences. The risk of a second seizure increases if the patient has already suffered a symptomatic brain insult such as a stroke or head trauma, among other risk factors. The guidelines also point out that immediate treatment with an antiepileptic agent reduces the likelihood of additional seizures for 2 years but does not have an impact on long-term prognosis for seizure remission.
Tao JX, Davis AM. Management of an Unprovoked First Seizure in Adults. JAMA. 2016;316(15):1590-1591.
The American Academy of Neurology and the American Epilepsy Society have released their guidelines on how to manage an adult patient who has had their first unprovoked seizure. Based on their review of the evidence, they recommend that clinicians base their decision about immediately initiating an antiepileptic drug after a first seizure on an individualized assessment. That evaluation should weigh the risk of a second seizure occurring against the adverse effects of the medication, as well as patient preferences. The risk of a second seizure increases if the patient has already suffered a symptomatic brain insult such as a stroke or head trauma, among other risk factors. The guidelines also point out that immediate treatment with an antiepileptic agent reduces the likelihood of additional seizures for 2 years but does not have an impact on long-term prognosis for seizure remission.
Tao JX, Davis AM. Management of an Unprovoked First Seizure in Adults. JAMA. 2016;316(15):1590-1591.
The American Academy of Neurology and the American Epilepsy Society have released their guidelines on how to manage an adult patient who has had their first unprovoked seizure. Based on their review of the evidence, they recommend that clinicians base their decision about immediately initiating an antiepileptic drug after a first seizure on an individualized assessment. That evaluation should weigh the risk of a second seizure occurring against the adverse effects of the medication, as well as patient preferences. The risk of a second seizure increases if the patient has already suffered a symptomatic brain insult such as a stroke or head trauma, among other risk factors. The guidelines also point out that immediate treatment with an antiepileptic agent reduces the likelihood of additional seizures for 2 years but does not have an impact on long-term prognosis for seizure remission.
Tao JX, Davis AM. Management of an Unprovoked First Seizure in Adults. JAMA. 2016;316(15):1590-1591.
Temporal Instability Detected in Network Connectivity in Epilepsy
Temporal lobe epilepsy (TLE) is believed to disrupt resting state functional connectivity in the brain. To explore this association in more depth, investigators used group independent component analysis (ICA) to identify the brain’s default mode network (DMN). The DMN has been linked to episodic memory, which does not function normally in patients with TLE. The researchers found functional connectivity instability over time among patients with left and right sided TLE, when compared with healthy controls. The instability within the DMN was most consistently detected within the precuneus region of the brain.
Robinson LF, He X, Barnett P et al. The temporal instability of resting state network connectivity in intractable epilepsy. Hum Brain Mapp. 2016; Sept 15 [Epub ahead of print]
Temporal lobe epilepsy (TLE) is believed to disrupt resting state functional connectivity in the brain. To explore this association in more depth, investigators used group independent component analysis (ICA) to identify the brain’s default mode network (DMN). The DMN has been linked to episodic memory, which does not function normally in patients with TLE. The researchers found functional connectivity instability over time among patients with left and right sided TLE, when compared with healthy controls. The instability within the DMN was most consistently detected within the precuneus region of the brain.
Robinson LF, He X, Barnett P et al. The temporal instability of resting state network connectivity in intractable epilepsy. Hum Brain Mapp. 2016; Sept 15 [Epub ahead of print]
Temporal lobe epilepsy (TLE) is believed to disrupt resting state functional connectivity in the brain. To explore this association in more depth, investigators used group independent component analysis (ICA) to identify the brain’s default mode network (DMN). The DMN has been linked to episodic memory, which does not function normally in patients with TLE. The researchers found functional connectivity instability over time among patients with left and right sided TLE, when compared with healthy controls. The instability within the DMN was most consistently detected within the precuneus region of the brain.
Robinson LF, He X, Barnett P et al. The temporal instability of resting state network connectivity in intractable epilepsy. Hum Brain Mapp. 2016; Sept 15 [Epub ahead of print]