User login
IgG4-related disease can strike any organ system
SNOWMASS, COLO. – Progress in the understanding and treatment of immunoglobulin G4–related disease is occurring “at lightning speed,” John H. Stone, MD, said at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
Eight or nine years ago no one had heard of immunoglobulin G4–related disease (IgG4-RD). Today, because of the broad swath the disease cuts, it’s a hot research topic in every subspecialty of medicine as well as surgery, pathology, and radiology.
This new understanding of IgG4-RD, he added, is opening the door to novel treatments.
“This is not a new disease. It was there when we were all in medical school, and for hundreds of years before that. But it’s really only in the last decade that we have come to understand that the disease can affect literally every organ system in the body with syndromes that we once thought were isolated organ-specific syndromes but we now recognize are part of a multiorgan disease currently called IgG4-related disease,” the rheumatologist said.
IgG4-RD is an immune-mediated fibroinflammatory condition characterized histopathologically by three hallmark features in involved tissue: obliterative phlebitis, storiform fibrosis, and a dense lymphoplasmacytic infiltrate.
Clinically, IgG4-RD often presents as a mass lesion that can affect any organ.
“I have many patients who’ve undergone modified Whipple procedures because they were thought to have adenocarcinoma of the pancreas,” according to Dr. Stone.
Other common presentations include Riedel’s thyroiditis, autoimmune pancreatitis, sclerosing cholangitis, sialadenitis, dacryoadenitis, periaortitis, an eosinophilic rash, and pseudotumor of the lung, lymph nodes, or orbits.
“Retroperitoneal fibrosis is a common and underappreciated manifestation. It may be the most common subsyndrome associated with IgG4-related disease,” he observed.
Another common presentation involves atopic disease – asthma, allergic rhinitis, eczema, eosinophilia, nasal polyps – developing out of the blue in middle age or later life. This observation led some other investigators to posit that IgG4-RD is a T-helper type 2–driven disease, an assertion debunked by Dr. Stone and coworkers (Allergy. 2014 Feb;69[2]:269-72).
Dr. Stone and his coinvestigators have published the largest series of patients with biopsy-proven IgG4-RD reported to date (Arthritis Rheumatol. 2015 Sep; 67[9]:2466-75). The average age at disease onset was 50 years. Of note, multiorgan involvement was the norm: 24% of patients had two organs involved, and 38% had three or more.
Analysis of this large patient series has led Dr. Stone to a surprising conclusion about the nature of IgG4-RD: “We have greatly overemphasized the importance of IgG4 in this condition,” he asserted.
Indeed, a mere 51% of the patients with clinically active untreated IgG4-RD in his series had an elevated serum IgG level. Dr. Stone characterized IgG4 as “kind of a wimpy antibody” incapable of driving the disease process because it is a noninflammatory immunoglobulin. This has led to speculation that IgG4 functions as what he termed an “antigen sink,” attempting to bind antigen at sites of inflammation.
But while an elevated serum IgG4 is of limited utility for diagnostic purposes, Dr. Stone and coworkers have demonstrated that it is of value as a predictor of relapse. Among patients with a treatment-induced remission, those in the top quartile in terms of baseline pretreatment serum IgG4 were 6.2-fold more likely to relapse (Rheumatology [Oxford]. 2016 Jun;55[6]:1000-8).
“This is a very useful marker for patients who are going to need chronic ongoing therapy. The notion of putting such patients on steroids for months and years is not appealing,” he said.
Levels of circulating plasmablasts as measured by peripheral blood flow cytometry, especially IgG4-positive plasmablasts, have proven much more helpful than serum IgG4 levels as a diagnostic tool, a reliable biomarker of disease activity, and a therapeutic target. Levels of these short-lived CD19+CD38+CD27+ plasmablasts are enormously elevated independent of serum IgG4 in patients with active IgG4-RD.
“One of the questions I’m most often asked is whether IgG4-related disease is a premalignant condition. My answer is no. The plasmablast expansion is oligoclonal, not polyclonal,” Dr. Stone continued.
He described IgG4-RD as “a continuous dance between T cells and B cells.” The latest thinking regarding pathogenesis is that type 2 T follicular helper cells activate B cells, which become memory B cells or plasmablasts. These activated B cells and plasmablasts present antigen to CD4+ cytotoxic T cells at sites of disease. Dr. Stone and his coinvestigators recently identified these CD4+ cytotoxic T cells as a novel population of clonally expanded T cells with SLAMF7 as a surface marker. The cells secrete interferon-gamma, interleukin-1, and transforming growth factor-beta, all of which are capable of driving the intense fibrosis characteristic of IgG4-RD. In addition, these CD4+ cytotoxic T cells secrete granzyme B and perforin, previously thought to be released mainly by natural killer T cells.
Joint American College of Rheumatology/European League Against Rheumatism classification criteria for the disease are expected to be finalized this winter at the Third International Symposium on IgG4-Related Diseases.
Treatment with rituxumab
Glucocorticoids remain the first-line therapy in IgG4-related disease, but it’s essential to bear in mind that their long-term efficacy in this immune-mediated fibroinflammatory disease is the exception rather than the rule, Dr. Stone said at the symposium.
Dr. Stone was a coauthor of an international expert consensus statement on the treatment of IgG4-related disease (IgG4-RD), which emphasized that point (Arthritis Rheumatol. 2015 Jul;67[7]:1688-99).
“I typically start with prednisone at 40 mg/day, and there’s a dramatic response in these patients. Then I taper them off after 2-3 months. If 2-3 months doesn’t put them into a long-term sustained remission, it’s time to go to something else,” said Dr. Stone.
So what’s the next move, then, after steroids fail? Dr. Stone was a pioneer in the strikingly successful use of B cell depletion via rituximab (Rituxan) in patients with IgG4-RD. First he and his coinvestigators demonstrated that this off-label use of rituximab led to rapid clinical and histologic improvement (Ann Rheum Dis. 2015 Jun; 74[6]:1171-7), then they showed it also causes levels of circulating plasmablasts, serum IgG4, and biomarkers of fibrosis to plunge, suggesting B cell depletion may halt the destructive process of collagen deposition that characterizes this immune-related disease (Ann Rheum Dis. 2015 Dec;74[12]:2236-43). They have also reported that patients with very elevated baseline serum IgG4 levels are at more than sixfold increased risk of relapse at a median of 244 days from their first rituximab infusion (Rheumatology [Oxford]. 2016 Jun;55[6]:1000-8).
The success with rituximab is just one example of how improved understanding of the pathophysiology of IgG4-RD has opened the door to novel treatments. Dr. Stone is the lead investigator in an ongoing phase II, open-label study in which 15 patients with active IgG4-RD will receive intravenous XmAb5871 every 2 weeks for 6 months to evaluate the effect on the IgG4-RD Responder Index. XmAb5871 is a monoclonal antibody that binds to CD19 and FCgammaRIIb in order to downregulate activated B cells and plasmablasts. It is also being developed for treatment of systemic lupus erythematosus.
Dr. Stone and his coinvestigators are working on a therapeutic approach to IgG4-RD that targets antigen presentation by activated B cells to CD4+ cytotoxic T cells at sites of disease. These CD4+ cytotoxic T cells contain signaling lymphocyte activation molecule F7 (SLAMF7) as a surface marker. Elotuzumab (Empliciti), an immunostimulatory humanized monoclonal antibody targeting SLAMF7, is already on the market for treatment of multiple myeloma, he noted.
Dr. Stone reported receiving IgG4-RD-related research funding from and serving as a consultant to Genentech and Xencor, which is developing XmAb5871.
SNOWMASS, COLO. – Progress in the understanding and treatment of immunoglobulin G4–related disease is occurring “at lightning speed,” John H. Stone, MD, said at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
Eight or nine years ago no one had heard of immunoglobulin G4–related disease (IgG4-RD). Today, because of the broad swath the disease cuts, it’s a hot research topic in every subspecialty of medicine as well as surgery, pathology, and radiology.
This new understanding of IgG4-RD, he added, is opening the door to novel treatments.
“This is not a new disease. It was there when we were all in medical school, and for hundreds of years before that. But it’s really only in the last decade that we have come to understand that the disease can affect literally every organ system in the body with syndromes that we once thought were isolated organ-specific syndromes but we now recognize are part of a multiorgan disease currently called IgG4-related disease,” the rheumatologist said.
IgG4-RD is an immune-mediated fibroinflammatory condition characterized histopathologically by three hallmark features in involved tissue: obliterative phlebitis, storiform fibrosis, and a dense lymphoplasmacytic infiltrate.
Clinically, IgG4-RD often presents as a mass lesion that can affect any organ.
“I have many patients who’ve undergone modified Whipple procedures because they were thought to have adenocarcinoma of the pancreas,” according to Dr. Stone.
Other common presentations include Riedel’s thyroiditis, autoimmune pancreatitis, sclerosing cholangitis, sialadenitis, dacryoadenitis, periaortitis, an eosinophilic rash, and pseudotumor of the lung, lymph nodes, or orbits.
“Retroperitoneal fibrosis is a common and underappreciated manifestation. It may be the most common subsyndrome associated with IgG4-related disease,” he observed.
Another common presentation involves atopic disease – asthma, allergic rhinitis, eczema, eosinophilia, nasal polyps – developing out of the blue in middle age or later life. This observation led some other investigators to posit that IgG4-RD is a T-helper type 2–driven disease, an assertion debunked by Dr. Stone and coworkers (Allergy. 2014 Feb;69[2]:269-72).
Dr. Stone and his coinvestigators have published the largest series of patients with biopsy-proven IgG4-RD reported to date (Arthritis Rheumatol. 2015 Sep; 67[9]:2466-75). The average age at disease onset was 50 years. Of note, multiorgan involvement was the norm: 24% of patients had two organs involved, and 38% had three or more.
Analysis of this large patient series has led Dr. Stone to a surprising conclusion about the nature of IgG4-RD: “We have greatly overemphasized the importance of IgG4 in this condition,” he asserted.
Indeed, a mere 51% of the patients with clinically active untreated IgG4-RD in his series had an elevated serum IgG level. Dr. Stone characterized IgG4 as “kind of a wimpy antibody” incapable of driving the disease process because it is a noninflammatory immunoglobulin. This has led to speculation that IgG4 functions as what he termed an “antigen sink,” attempting to bind antigen at sites of inflammation.
But while an elevated serum IgG4 is of limited utility for diagnostic purposes, Dr. Stone and coworkers have demonstrated that it is of value as a predictor of relapse. Among patients with a treatment-induced remission, those in the top quartile in terms of baseline pretreatment serum IgG4 were 6.2-fold more likely to relapse (Rheumatology [Oxford]. 2016 Jun;55[6]:1000-8).
“This is a very useful marker for patients who are going to need chronic ongoing therapy. The notion of putting such patients on steroids for months and years is not appealing,” he said.
Levels of circulating plasmablasts as measured by peripheral blood flow cytometry, especially IgG4-positive plasmablasts, have proven much more helpful than serum IgG4 levels as a diagnostic tool, a reliable biomarker of disease activity, and a therapeutic target. Levels of these short-lived CD19+CD38+CD27+ plasmablasts are enormously elevated independent of serum IgG4 in patients with active IgG4-RD.
“One of the questions I’m most often asked is whether IgG4-related disease is a premalignant condition. My answer is no. The plasmablast expansion is oligoclonal, not polyclonal,” Dr. Stone continued.
He described IgG4-RD as “a continuous dance between T cells and B cells.” The latest thinking regarding pathogenesis is that type 2 T follicular helper cells activate B cells, which become memory B cells or plasmablasts. These activated B cells and plasmablasts present antigen to CD4+ cytotoxic T cells at sites of disease. Dr. Stone and his coinvestigators recently identified these CD4+ cytotoxic T cells as a novel population of clonally expanded T cells with SLAMF7 as a surface marker. The cells secrete interferon-gamma, interleukin-1, and transforming growth factor-beta, all of which are capable of driving the intense fibrosis characteristic of IgG4-RD. In addition, these CD4+ cytotoxic T cells secrete granzyme B and perforin, previously thought to be released mainly by natural killer T cells.
Joint American College of Rheumatology/European League Against Rheumatism classification criteria for the disease are expected to be finalized this winter at the Third International Symposium on IgG4-Related Diseases.
Treatment with rituxumab
Glucocorticoids remain the first-line therapy in IgG4-related disease, but it’s essential to bear in mind that their long-term efficacy in this immune-mediated fibroinflammatory disease is the exception rather than the rule, Dr. Stone said at the symposium.
Dr. Stone was a coauthor of an international expert consensus statement on the treatment of IgG4-related disease (IgG4-RD), which emphasized that point (Arthritis Rheumatol. 2015 Jul;67[7]:1688-99).
“I typically start with prednisone at 40 mg/day, and there’s a dramatic response in these patients. Then I taper them off after 2-3 months. If 2-3 months doesn’t put them into a long-term sustained remission, it’s time to go to something else,” said Dr. Stone.
So what’s the next move, then, after steroids fail? Dr. Stone was a pioneer in the strikingly successful use of B cell depletion via rituximab (Rituxan) in patients with IgG4-RD. First he and his coinvestigators demonstrated that this off-label use of rituximab led to rapid clinical and histologic improvement (Ann Rheum Dis. 2015 Jun; 74[6]:1171-7), then they showed it also causes levels of circulating plasmablasts, serum IgG4, and biomarkers of fibrosis to plunge, suggesting B cell depletion may halt the destructive process of collagen deposition that characterizes this immune-related disease (Ann Rheum Dis. 2015 Dec;74[12]:2236-43). They have also reported that patients with very elevated baseline serum IgG4 levels are at more than sixfold increased risk of relapse at a median of 244 days from their first rituximab infusion (Rheumatology [Oxford]. 2016 Jun;55[6]:1000-8).
The success with rituximab is just one example of how improved understanding of the pathophysiology of IgG4-RD has opened the door to novel treatments. Dr. Stone is the lead investigator in an ongoing phase II, open-label study in which 15 patients with active IgG4-RD will receive intravenous XmAb5871 every 2 weeks for 6 months to evaluate the effect on the IgG4-RD Responder Index. XmAb5871 is a monoclonal antibody that binds to CD19 and FCgammaRIIb in order to downregulate activated B cells and plasmablasts. It is also being developed for treatment of systemic lupus erythematosus.
Dr. Stone and his coinvestigators are working on a therapeutic approach to IgG4-RD that targets antigen presentation by activated B cells to CD4+ cytotoxic T cells at sites of disease. These CD4+ cytotoxic T cells contain signaling lymphocyte activation molecule F7 (SLAMF7) as a surface marker. Elotuzumab (Empliciti), an immunostimulatory humanized monoclonal antibody targeting SLAMF7, is already on the market for treatment of multiple myeloma, he noted.
Dr. Stone reported receiving IgG4-RD-related research funding from and serving as a consultant to Genentech and Xencor, which is developing XmAb5871.
SNOWMASS, COLO. – Progress in the understanding and treatment of immunoglobulin G4–related disease is occurring “at lightning speed,” John H. Stone, MD, said at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
Eight or nine years ago no one had heard of immunoglobulin G4–related disease (IgG4-RD). Today, because of the broad swath the disease cuts, it’s a hot research topic in every subspecialty of medicine as well as surgery, pathology, and radiology.
This new understanding of IgG4-RD, he added, is opening the door to novel treatments.
“This is not a new disease. It was there when we were all in medical school, and for hundreds of years before that. But it’s really only in the last decade that we have come to understand that the disease can affect literally every organ system in the body with syndromes that we once thought were isolated organ-specific syndromes but we now recognize are part of a multiorgan disease currently called IgG4-related disease,” the rheumatologist said.
IgG4-RD is an immune-mediated fibroinflammatory condition characterized histopathologically by three hallmark features in involved tissue: obliterative phlebitis, storiform fibrosis, and a dense lymphoplasmacytic infiltrate.
Clinically, IgG4-RD often presents as a mass lesion that can affect any organ.
“I have many patients who’ve undergone modified Whipple procedures because they were thought to have adenocarcinoma of the pancreas,” according to Dr. Stone.
Other common presentations include Riedel’s thyroiditis, autoimmune pancreatitis, sclerosing cholangitis, sialadenitis, dacryoadenitis, periaortitis, an eosinophilic rash, and pseudotumor of the lung, lymph nodes, or orbits.
“Retroperitoneal fibrosis is a common and underappreciated manifestation. It may be the most common subsyndrome associated with IgG4-related disease,” he observed.
Another common presentation involves atopic disease – asthma, allergic rhinitis, eczema, eosinophilia, nasal polyps – developing out of the blue in middle age or later life. This observation led some other investigators to posit that IgG4-RD is a T-helper type 2–driven disease, an assertion debunked by Dr. Stone and coworkers (Allergy. 2014 Feb;69[2]:269-72).
Dr. Stone and his coinvestigators have published the largest series of patients with biopsy-proven IgG4-RD reported to date (Arthritis Rheumatol. 2015 Sep; 67[9]:2466-75). The average age at disease onset was 50 years. Of note, multiorgan involvement was the norm: 24% of patients had two organs involved, and 38% had three or more.
Analysis of this large patient series has led Dr. Stone to a surprising conclusion about the nature of IgG4-RD: “We have greatly overemphasized the importance of IgG4 in this condition,” he asserted.
Indeed, a mere 51% of the patients with clinically active untreated IgG4-RD in his series had an elevated serum IgG level. Dr. Stone characterized IgG4 as “kind of a wimpy antibody” incapable of driving the disease process because it is a noninflammatory immunoglobulin. This has led to speculation that IgG4 functions as what he termed an “antigen sink,” attempting to bind antigen at sites of inflammation.
But while an elevated serum IgG4 is of limited utility for diagnostic purposes, Dr. Stone and coworkers have demonstrated that it is of value as a predictor of relapse. Among patients with a treatment-induced remission, those in the top quartile in terms of baseline pretreatment serum IgG4 were 6.2-fold more likely to relapse (Rheumatology [Oxford]. 2016 Jun;55[6]:1000-8).
“This is a very useful marker for patients who are going to need chronic ongoing therapy. The notion of putting such patients on steroids for months and years is not appealing,” he said.
Levels of circulating plasmablasts as measured by peripheral blood flow cytometry, especially IgG4-positive plasmablasts, have proven much more helpful than serum IgG4 levels as a diagnostic tool, a reliable biomarker of disease activity, and a therapeutic target. Levels of these short-lived CD19+CD38+CD27+ plasmablasts are enormously elevated independent of serum IgG4 in patients with active IgG4-RD.
“One of the questions I’m most often asked is whether IgG4-related disease is a premalignant condition. My answer is no. The plasmablast expansion is oligoclonal, not polyclonal,” Dr. Stone continued.
He described IgG4-RD as “a continuous dance between T cells and B cells.” The latest thinking regarding pathogenesis is that type 2 T follicular helper cells activate B cells, which become memory B cells or plasmablasts. These activated B cells and plasmablasts present antigen to CD4+ cytotoxic T cells at sites of disease. Dr. Stone and his coinvestigators recently identified these CD4+ cytotoxic T cells as a novel population of clonally expanded T cells with SLAMF7 as a surface marker. The cells secrete interferon-gamma, interleukin-1, and transforming growth factor-beta, all of which are capable of driving the intense fibrosis characteristic of IgG4-RD. In addition, these CD4+ cytotoxic T cells secrete granzyme B and perforin, previously thought to be released mainly by natural killer T cells.
Joint American College of Rheumatology/European League Against Rheumatism classification criteria for the disease are expected to be finalized this winter at the Third International Symposium on IgG4-Related Diseases.
Treatment with rituxumab
Glucocorticoids remain the first-line therapy in IgG4-related disease, but it’s essential to bear in mind that their long-term efficacy in this immune-mediated fibroinflammatory disease is the exception rather than the rule, Dr. Stone said at the symposium.
Dr. Stone was a coauthor of an international expert consensus statement on the treatment of IgG4-related disease (IgG4-RD), which emphasized that point (Arthritis Rheumatol. 2015 Jul;67[7]:1688-99).
“I typically start with prednisone at 40 mg/day, and there’s a dramatic response in these patients. Then I taper them off after 2-3 months. If 2-3 months doesn’t put them into a long-term sustained remission, it’s time to go to something else,” said Dr. Stone.
So what’s the next move, then, after steroids fail? Dr. Stone was a pioneer in the strikingly successful use of B cell depletion via rituximab (Rituxan) in patients with IgG4-RD. First he and his coinvestigators demonstrated that this off-label use of rituximab led to rapid clinical and histologic improvement (Ann Rheum Dis. 2015 Jun; 74[6]:1171-7), then they showed it also causes levels of circulating plasmablasts, serum IgG4, and biomarkers of fibrosis to plunge, suggesting B cell depletion may halt the destructive process of collagen deposition that characterizes this immune-related disease (Ann Rheum Dis. 2015 Dec;74[12]:2236-43). They have also reported that patients with very elevated baseline serum IgG4 levels are at more than sixfold increased risk of relapse at a median of 244 days from their first rituximab infusion (Rheumatology [Oxford]. 2016 Jun;55[6]:1000-8).
The success with rituximab is just one example of how improved understanding of the pathophysiology of IgG4-RD has opened the door to novel treatments. Dr. Stone is the lead investigator in an ongoing phase II, open-label study in which 15 patients with active IgG4-RD will receive intravenous XmAb5871 every 2 weeks for 6 months to evaluate the effect on the IgG4-RD Responder Index. XmAb5871 is a monoclonal antibody that binds to CD19 and FCgammaRIIb in order to downregulate activated B cells and plasmablasts. It is also being developed for treatment of systemic lupus erythematosus.
Dr. Stone and his coinvestigators are working on a therapeutic approach to IgG4-RD that targets antigen presentation by activated B cells to CD4+ cytotoxic T cells at sites of disease. These CD4+ cytotoxic T cells contain signaling lymphocyte activation molecule F7 (SLAMF7) as a surface marker. Elotuzumab (Empliciti), an immunostimulatory humanized monoclonal antibody targeting SLAMF7, is already on the market for treatment of multiple myeloma, he noted.
Dr. Stone reported receiving IgG4-RD-related research funding from and serving as a consultant to Genentech and Xencor, which is developing XmAb5871.
EXPERT ANALYSIS FROM THE WINTER RHEUMATOLOGY SYMPOSIUM
Twenty-five states at highest flu activity level
Flu activity in the United States continued to increase as half of the states reached the highest level of influenza-like illness (ILI) activity in the week ending Feb. 11, according to the Centers for Disease Control and Prevention.
For the week, the 25 states at level 10 on the CDC’s 1-10 scale of ILI activity were joined in the high range by Illinois and Kentucky at level 9 and Iowa at level 8, the CDC reported. The previous week, there were 23 states in the high range.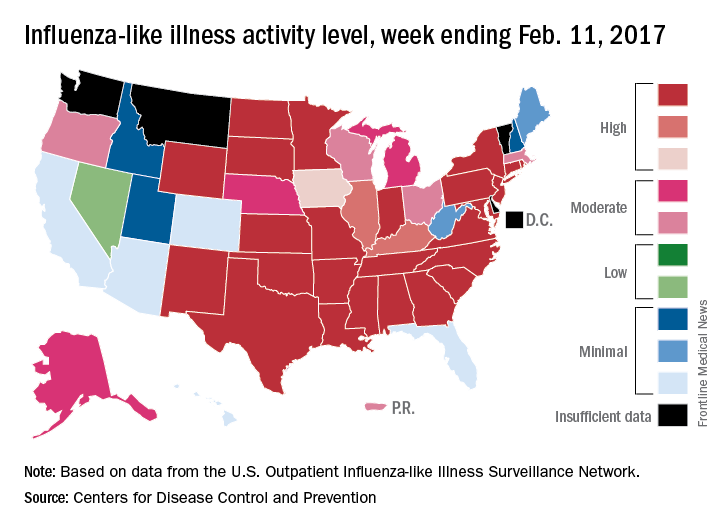
Of the nine flu-related pediatric deaths reported to the CDC during the latest week, eight occurred in earlier weeks. For the 2016-2017 season so far, 29 flu-related pediatric deaths have been reported, the CDC said.
Flu activity in the United States continued to increase as half of the states reached the highest level of influenza-like illness (ILI) activity in the week ending Feb. 11, according to the Centers for Disease Control and Prevention.
For the week, the 25 states at level 10 on the CDC’s 1-10 scale of ILI activity were joined in the high range by Illinois and Kentucky at level 9 and Iowa at level 8, the CDC reported. The previous week, there were 23 states in the high range.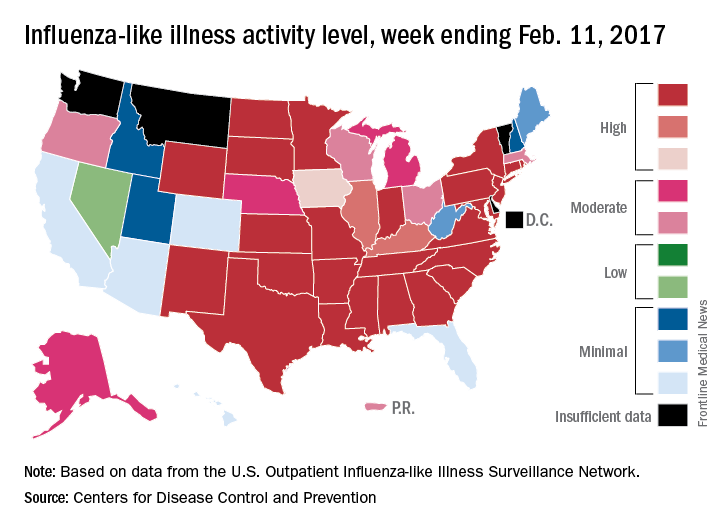
Of the nine flu-related pediatric deaths reported to the CDC during the latest week, eight occurred in earlier weeks. For the 2016-2017 season so far, 29 flu-related pediatric deaths have been reported, the CDC said.
Flu activity in the United States continued to increase as half of the states reached the highest level of influenza-like illness (ILI) activity in the week ending Feb. 11, according to the Centers for Disease Control and Prevention.
For the week, the 25 states at level 10 on the CDC’s 1-10 scale of ILI activity were joined in the high range by Illinois and Kentucky at level 9 and Iowa at level 8, the CDC reported. The previous week, there were 23 states in the high range.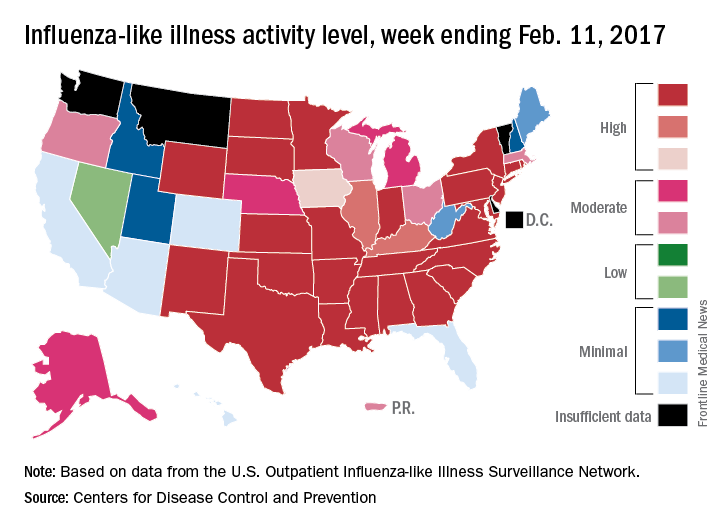
Of the nine flu-related pediatric deaths reported to the CDC during the latest week, eight occurred in earlier weeks. For the 2016-2017 season so far, 29 flu-related pediatric deaths have been reported, the CDC said.
Treating psychopathology in developmentally disabled tricky
LAS VEGAS – Individuals with intellectual disability experience behavioral and psychiatric illness at higher rates than the general population, according to Bryan H. King, MD.
“Increasingly, these individuals are showing up in all of our clinical practices,” Dr. King said at an annual psychopharmacology update held by the Nevada Psychiatric Association. “In this area, it’s not so much that the population doesn’t experience psychiatric illness, but the diagnosis can be challenging because the presentation of symptoms may be different. For someone who can’t articulate whether they’re feeling anxious, fearful, or nervous, it’s more challenging to make a diagnosis.”
More than 10 years ago, researchers from the University of North Carolina at Chapel Hill compared health disparities between adults with developmental disabilities in North Carolina and adults in the state with other disabilities and adults without disabilities (Public Health Rep. 2004;114[4]:418-26). They found those in the developmental disability group had a similar or greater risk of having high blood pressure, cardiovascular disease, diabetes, and chronic pain, compared with nondisabled adults. In addition, 24% of adults in the developmental disability group reported having either no one to talk to about personal things or often felt lonely.
A more recent, large national study found that, compared with adults with no autism diagnoses, those diagnosed with autism had significantly increased rates for all psychiatric disorders, including depression, anxiety, bipolar disorder, obsessive-compulsive disorder, schizophrenia (a more than 20-fold increased rate), and suicide attempts (Autism. 2015;19[7]:814-23). In addition, nearly all medical conditions such as obesity and dyslipidemia were significantly more common in adults with autism.
Results from a separate study of 371 adults with intellectual disabilities found that 40% had at least one mental health disorder and 45% had at least one moderate or severe behavior problem (Soc Psychiatry Psychiatr Epidemiol. 2016;51:767-76). In addition, the highest ratios of unmet to met need were found with respect to sexuality issues and with respect to mental health problems.
Once a diagnosis is made, Dr. King said patients who have developmental disabilities should be treated in the same way as patients who do not. “There is a tremendous amount of heterogeneity in this population,” he said. “If you are confident that you have someone before you who has depression, the treatment for depression is going to proceed in the same ways it does for someone without the condition. Let that guide the way for medications you are going to use.”
In a recent edition of Current Opinion in Psychiatry, authors Na Young Ji, MD, and Robert L. Findling, MD, reviewed current evidence-based pharmacotherapy options for mental health problems in people with intellectual disability (Curr Opin Psychiatry. 2016;29:103-25). Their five key points were:
1. “Antipsychotics, particularly risperidone, appear to be effective in reducing problem behaviors associated with intellectual disability.
2. “For attention-deficit/hyperactivity disorder symptoms, methylphenidate has been shown to be effective, and atomoxetine and alpha-agonists might be beneficial.
3. “Lithium might be effective in reducing aggression. Evidence for the use of antiepileptic drugs, anxiolytics, and naltrexone for management of problem behaviors is insufficient to draw conclusions.
4. “Antidepressants are often poorly tolerated and do not appear to be effective in decreasing repetitive or stereotypic behaviors associated with intellectual disability.
5. “Melatonin appears to improve sleep in people with intellectual disability.”
Dr. King noted that the data for using lithium in people with intellectual disability “are very old. There’s been nothing recent to help us fine-tune the indications.” He said naltrexone is among the best studied in this population, “especially for self-injurious behavior. The two large placebo-controlled trials were negative. In my own clinical experience, I have not seen it helpful.”
Dr. King disclosed that he has received research funding from the National Institutes of Health, Janssen, and Roche. He also is a consultant for Care Management Technologies and Neurotrope.
LAS VEGAS – Individuals with intellectual disability experience behavioral and psychiatric illness at higher rates than the general population, according to Bryan H. King, MD.
“Increasingly, these individuals are showing up in all of our clinical practices,” Dr. King said at an annual psychopharmacology update held by the Nevada Psychiatric Association. “In this area, it’s not so much that the population doesn’t experience psychiatric illness, but the diagnosis can be challenging because the presentation of symptoms may be different. For someone who can’t articulate whether they’re feeling anxious, fearful, or nervous, it’s more challenging to make a diagnosis.”
More than 10 years ago, researchers from the University of North Carolina at Chapel Hill compared health disparities between adults with developmental disabilities in North Carolina and adults in the state with other disabilities and adults without disabilities (Public Health Rep. 2004;114[4]:418-26). They found those in the developmental disability group had a similar or greater risk of having high blood pressure, cardiovascular disease, diabetes, and chronic pain, compared with nondisabled adults. In addition, 24% of adults in the developmental disability group reported having either no one to talk to about personal things or often felt lonely.
A more recent, large national study found that, compared with adults with no autism diagnoses, those diagnosed with autism had significantly increased rates for all psychiatric disorders, including depression, anxiety, bipolar disorder, obsessive-compulsive disorder, schizophrenia (a more than 20-fold increased rate), and suicide attempts (Autism. 2015;19[7]:814-23). In addition, nearly all medical conditions such as obesity and dyslipidemia were significantly more common in adults with autism.
Results from a separate study of 371 adults with intellectual disabilities found that 40% had at least one mental health disorder and 45% had at least one moderate or severe behavior problem (Soc Psychiatry Psychiatr Epidemiol. 2016;51:767-76). In addition, the highest ratios of unmet to met need were found with respect to sexuality issues and with respect to mental health problems.
Once a diagnosis is made, Dr. King said patients who have developmental disabilities should be treated in the same way as patients who do not. “There is a tremendous amount of heterogeneity in this population,” he said. “If you are confident that you have someone before you who has depression, the treatment for depression is going to proceed in the same ways it does for someone without the condition. Let that guide the way for medications you are going to use.”
In a recent edition of Current Opinion in Psychiatry, authors Na Young Ji, MD, and Robert L. Findling, MD, reviewed current evidence-based pharmacotherapy options for mental health problems in people with intellectual disability (Curr Opin Psychiatry. 2016;29:103-25). Their five key points were:
1. “Antipsychotics, particularly risperidone, appear to be effective in reducing problem behaviors associated with intellectual disability.
2. “For attention-deficit/hyperactivity disorder symptoms, methylphenidate has been shown to be effective, and atomoxetine and alpha-agonists might be beneficial.
3. “Lithium might be effective in reducing aggression. Evidence for the use of antiepileptic drugs, anxiolytics, and naltrexone for management of problem behaviors is insufficient to draw conclusions.
4. “Antidepressants are often poorly tolerated and do not appear to be effective in decreasing repetitive or stereotypic behaviors associated with intellectual disability.
5. “Melatonin appears to improve sleep in people with intellectual disability.”
Dr. King noted that the data for using lithium in people with intellectual disability “are very old. There’s been nothing recent to help us fine-tune the indications.” He said naltrexone is among the best studied in this population, “especially for self-injurious behavior. The two large placebo-controlled trials were negative. In my own clinical experience, I have not seen it helpful.”
Dr. King disclosed that he has received research funding from the National Institutes of Health, Janssen, and Roche. He also is a consultant for Care Management Technologies and Neurotrope.
LAS VEGAS – Individuals with intellectual disability experience behavioral and psychiatric illness at higher rates than the general population, according to Bryan H. King, MD.
“Increasingly, these individuals are showing up in all of our clinical practices,” Dr. King said at an annual psychopharmacology update held by the Nevada Psychiatric Association. “In this area, it’s not so much that the population doesn’t experience psychiatric illness, but the diagnosis can be challenging because the presentation of symptoms may be different. For someone who can’t articulate whether they’re feeling anxious, fearful, or nervous, it’s more challenging to make a diagnosis.”
More than 10 years ago, researchers from the University of North Carolina at Chapel Hill compared health disparities between adults with developmental disabilities in North Carolina and adults in the state with other disabilities and adults without disabilities (Public Health Rep. 2004;114[4]:418-26). They found those in the developmental disability group had a similar or greater risk of having high blood pressure, cardiovascular disease, diabetes, and chronic pain, compared with nondisabled adults. In addition, 24% of adults in the developmental disability group reported having either no one to talk to about personal things or often felt lonely.
A more recent, large national study found that, compared with adults with no autism diagnoses, those diagnosed with autism had significantly increased rates for all psychiatric disorders, including depression, anxiety, bipolar disorder, obsessive-compulsive disorder, schizophrenia (a more than 20-fold increased rate), and suicide attempts (Autism. 2015;19[7]:814-23). In addition, nearly all medical conditions such as obesity and dyslipidemia were significantly more common in adults with autism.
Results from a separate study of 371 adults with intellectual disabilities found that 40% had at least one mental health disorder and 45% had at least one moderate or severe behavior problem (Soc Psychiatry Psychiatr Epidemiol. 2016;51:767-76). In addition, the highest ratios of unmet to met need were found with respect to sexuality issues and with respect to mental health problems.
Once a diagnosis is made, Dr. King said patients who have developmental disabilities should be treated in the same way as patients who do not. “There is a tremendous amount of heterogeneity in this population,” he said. “If you are confident that you have someone before you who has depression, the treatment for depression is going to proceed in the same ways it does for someone without the condition. Let that guide the way for medications you are going to use.”
In a recent edition of Current Opinion in Psychiatry, authors Na Young Ji, MD, and Robert L. Findling, MD, reviewed current evidence-based pharmacotherapy options for mental health problems in people with intellectual disability (Curr Opin Psychiatry. 2016;29:103-25). Their five key points were:
1. “Antipsychotics, particularly risperidone, appear to be effective in reducing problem behaviors associated with intellectual disability.
2. “For attention-deficit/hyperactivity disorder symptoms, methylphenidate has been shown to be effective, and atomoxetine and alpha-agonists might be beneficial.
3. “Lithium might be effective in reducing aggression. Evidence for the use of antiepileptic drugs, anxiolytics, and naltrexone for management of problem behaviors is insufficient to draw conclusions.
4. “Antidepressants are often poorly tolerated and do not appear to be effective in decreasing repetitive or stereotypic behaviors associated with intellectual disability.
5. “Melatonin appears to improve sleep in people with intellectual disability.”
Dr. King noted that the data for using lithium in people with intellectual disability “are very old. There’s been nothing recent to help us fine-tune the indications.” He said naltrexone is among the best studied in this population, “especially for self-injurious behavior. The two large placebo-controlled trials were negative. In my own clinical experience, I have not seen it helpful.”
Dr. King disclosed that he has received research funding from the National Institutes of Health, Janssen, and Roche. He also is a consultant for Care Management Technologies and Neurotrope.
EXPERT ANALYSIS AT THE NPA PSYCHOPHARMACOLOGY UPDATE
Lupus Erythematosus Tumidus of the Scalp Masquerading as Alopecia Areata
Lupus erythematosus tumidus (LET) is a relatively rare condition but may simply be underdiagnosed in the literature. It presents as urticarialike papules and plaques in sun-exposed areas, characterized by induration and erythema. Lesions occur on the face, neck, upper extremities, and trunk and heal without scarring.1,2 Rarely, lesions can show fine scaling and associated pruritus, but most often the lesions are asymptomatic.3
Case Report
A 45-year-old woman presented with 2 asymptomatic self-described bald spots on the top of the head of 2 months’ duration. The patient denied prior treatment of the lesions and noted one patch was resolving. She reported no involvement of the eyebrows, eyelashes, and axillary and pubic hair. A review of systems was negative. The patient denied personal or family history of lupus, thyroid disease, or vitiligo.
Clinical examination revealed a 1.1-cm round patch of nonscarring alopecia on the right vertex scalp and a 0.9-cm round patch of nonscarring alopecia with moderate hair regrowth on the left vertex scalp. There was no erythema, scaling, or induration. The rest of the scalp was normal in appearance and the eyebrows and eyelashes were uninvolved. The patient was diagnosed with alopecia areata and was treated with 10 mg/mL of intralesional triamcinolone once monthly for 4 months.
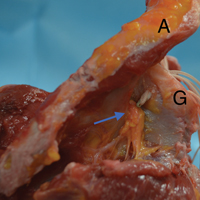
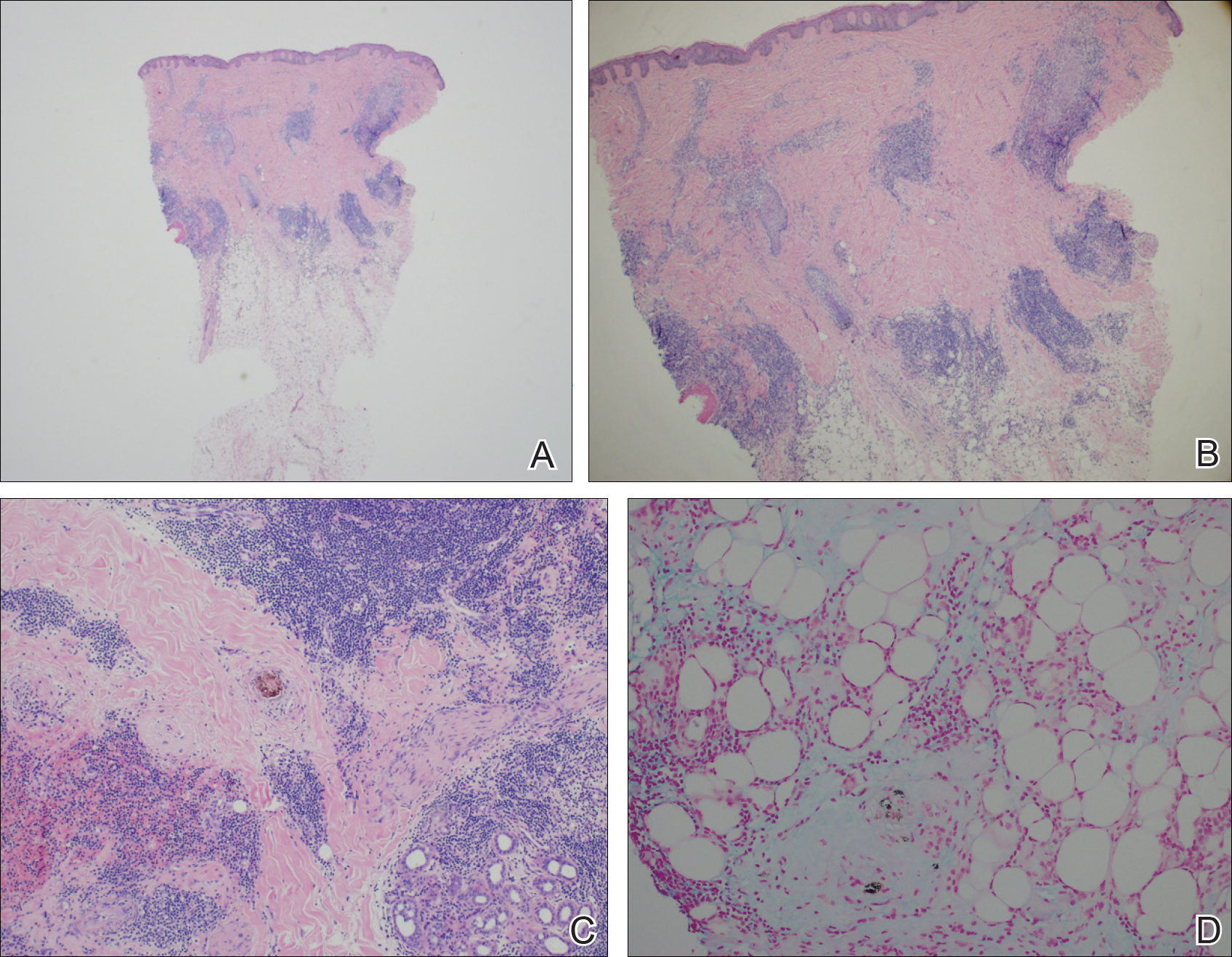
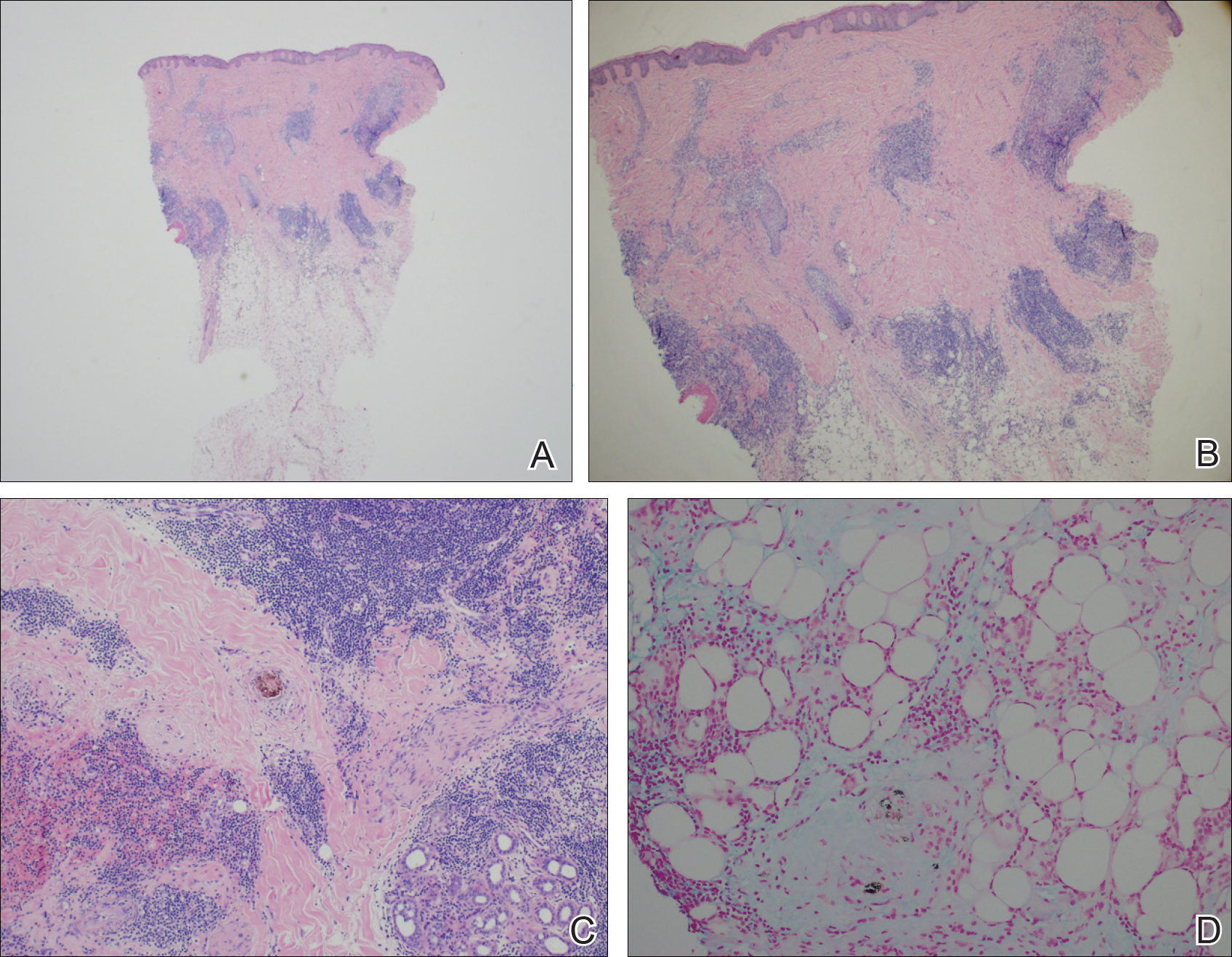
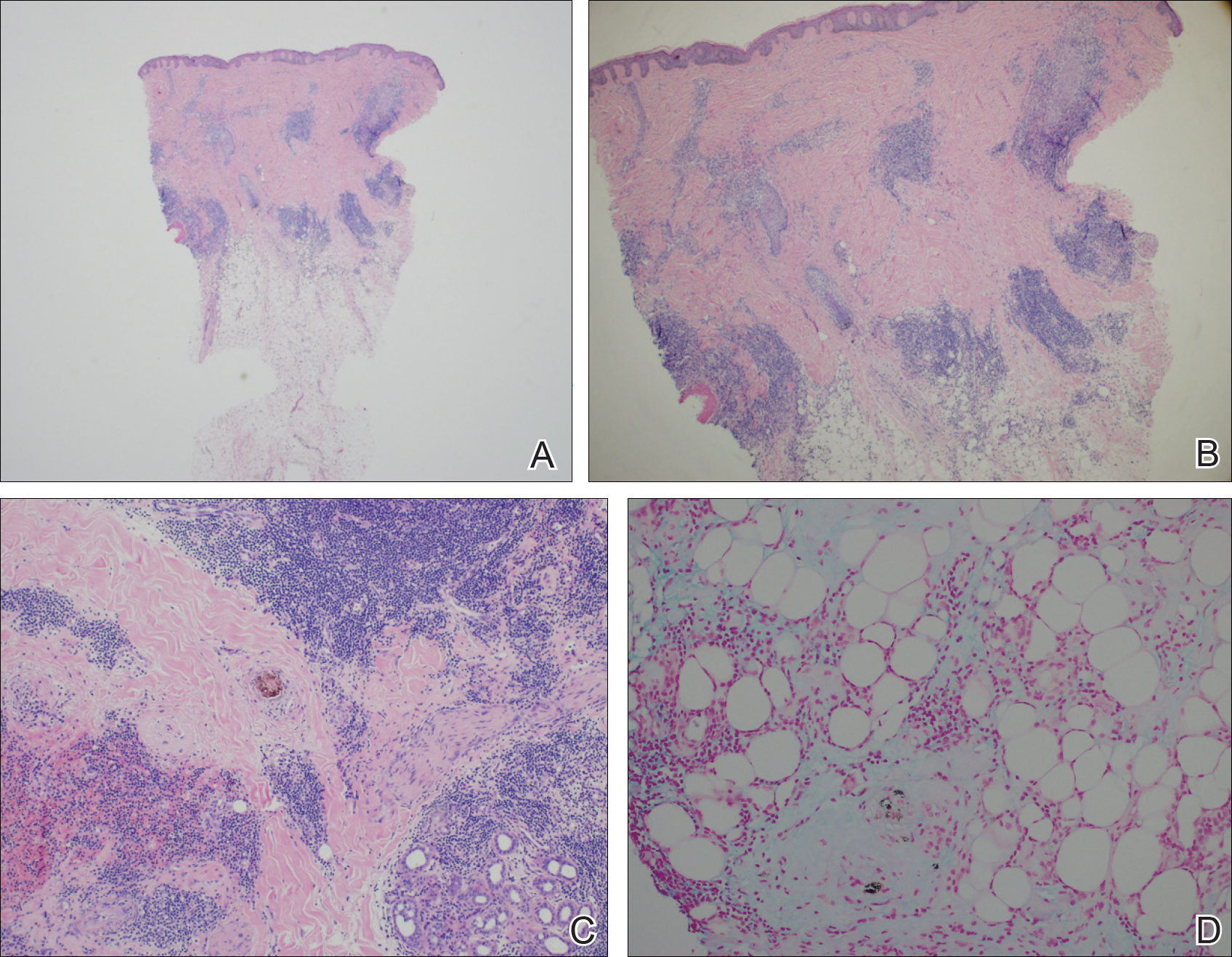
The patient initially showed improvement with moderate hair regrowth. After 4 months of treatment, she developed 3 new 1- to 1.5-cm erythematous alopecic patches on the vertex scalp and had worsening in the initial patches (Figure 1). Given the resistance to standard therapy and the onset of multiple new areas with evidence of inflammatory involvement, a punch biopsy was performed. Histopathologic examination revealed a fairly unremarkable epidermis and a dense dermal inflammatory infiltrate that was present both in the superficial and deep dermis (Figure 2). The inflammatory cells, which appeared to be predominantly comprised of lymphocytes, had a predilection for the vasculature but also were observed within the interstitial dermis. Additionally, mucin appeared to be slightly increased in the deep dermis. The lymphocytic phenotype was confirmed by immunohistochemical studies for CD20 and CD3. The most likely possibilities for this reaction pattern were LET, Jessner lymphocytic infiltrate of the skin (JLIS), gyrate erythema, and lymphoma; however, the immunohistochemical studies effectively ruled out lymphoma. Additionally, there was pronounced dermal mucin noted in the specimen. The patient was diagnosed with LET of the scalp based on the constellation of findings.

Comment
The classification of LET as a single unique entity or disease process sui generis has been in flux in the last decade. Its similarities to JLIS and other forms of chronic cutaneous lupus erythematosus (CCLE) have brought debate.4-6 In 1930, Gougerot and Burnier7 documented the first case of LET in the literature, describing smooth, infiltrated, erythematous lesions with no desquamation or other superficial changes seen in 5 patients.
In 2000, interest in LET and other forms of CCLE was increasing, and reports in the literature paralleled. That year, Kuhn et al4 reported 40 cases of LET, characterizing the clinical and histological features of each case to demonstrate that LET should be separate from other forms of CCLE. Until then, it is likely that many lesions that should have been classified as LET were instead classified as various forms of CCLE. The investigators maintained that LET also should be distinct from JLIS because it is associated with UV exposure.4 Kuhn et al8 reviewed phototesting in 60 patients with LET in 2001 and confirmed this subset was the most photosensitive type of lupus erythematosus.
In general, the histopathologic and immunohistochemical studies in LET and JLIS can be quite similar. Relatively distinguishing histopathologic findings in JLIS include no evidence of epidermal atrophy, basal vacuolar change, or follicular plugging, as well as negative immunofluorescence studies. Both entities show a predominantly T-cell population with a smaller component of B cells and thus a distinction cannot be made based on relative proportions of T and B cells in lesions.2
In 2003, Alexiades-Armenakas et al6 determined immunohistochemical criteria for LET, finding a predominance of T cells and more CD4 lymphocytes than CD8 lymphocytes with a mean ratio of roughly 3 to 1. Their study results maintained LET should be classified as a form of CCLE due to the chronicity of the lesions, the serologic profile with negative anti–double-stranded DNA, anticentromere, anti-Smith, anti-Ro/Sjögren syndrome antigen A, anti-La/Sjögren syndrome antigen B, and anti-nuclear ribonucleoprotein antibodies and the rare association with systemic disease.6 This conclusion was further solidified by a review published that same year citing unique histopathological features when compared to subacute cutaneous LE and discoid lupus erythematosus.5
This case illustrates the importance of histologic evaluation in determining the correct diagnosis in a patient with alopecia areata recalcitrant to treatment. Including LET in the differential of alopecic patches on the scalp could prove beneficial for patients, as LET responds well to antimalarial drugs and photoprotection.9 This patient had a normal antinuclear antibody panel and no signs or symptoms of systemic lupus. It was recommended that she avoid sun exposure and begin treatment with hydroxychloroquine but she declined. At a follow-up visit 6 months later she reported the lesions had improved, but a permanent wig had been sewn over the area, so it could not be examined.
- Lee L, Werth V. Rheumatologic disease. In: Bolognia JL, Jorizzo JL, Rapini RP, eds. Dermatology. Vol 2. 3rd ed. Mosby Elsevier; 2008:615-629.
- Weedon D. The lichenoid reaction pattern. In: Weedon D. Skin Pathology. 2nd ed. Edinburgh, Scotland: Churchill Livingstone; 2002:35-70.
- Dekle CL, Mannes KD, Davis LS, et al. Lupus tumidus. J Am Acad Dermatol. 1999;41:250-253.
- Kuhn A, Richter-Hintz D, Oslislo C, et al. Lupus erythematosus tumidus—a neglected subset of cutaneous lupus erythematosus: report of 40 cases. Arch Dermatol. 2000;136:1033-1041.
- Kuhn A, Sonntag M, Ruzicka T, et al. Histopathologic findings in lupus erythematosus tumidus: review of 80 patients. J Am Acad Dermatol. 2003;48:901-908.
- Alexiades-Armenakas MR, Baldassano M, Bince B, et al. Tumid lupus erythematosus: criteria for classification with immunohistochemical analysis. Arthritis Rheum. 2003;49:494-500.
- Gougerot H, Burnier R. Lupuse rythe mateux “tumidus.” Bull Soc Fr Dermatol Syph. 1930;37:1291-1292.
- Kuhn A, Sonntag M, Richter-Hintz D, et al. Phototesting in lupus erythematosus tumidus—review of 60 patients. Photochem Photobiol. 2001;73:532-536.
- Cozzani E, Christana K, Rongioletti F, et al. Lupus erythematosus tumidus: clinical, histopathological and serological aspects and therapy response of 21 patients. Eur J Dermatol. 2010;20:797-801.
Lupus erythematosus tumidus (LET) is a relatively rare condition but may simply be underdiagnosed in the literature. It presents as urticarialike papules and plaques in sun-exposed areas, characterized by induration and erythema. Lesions occur on the face, neck, upper extremities, and trunk and heal without scarring.1,2 Rarely, lesions can show fine scaling and associated pruritus, but most often the lesions are asymptomatic.3
Case Report
A 45-year-old woman presented with 2 asymptomatic self-described bald spots on the top of the head of 2 months’ duration. The patient denied prior treatment of the lesions and noted one patch was resolving. She reported no involvement of the eyebrows, eyelashes, and axillary and pubic hair. A review of systems was negative. The patient denied personal or family history of lupus, thyroid disease, or vitiligo.
Clinical examination revealed a 1.1-cm round patch of nonscarring alopecia on the right vertex scalp and a 0.9-cm round patch of nonscarring alopecia with moderate hair regrowth on the left vertex scalp. There was no erythema, scaling, or induration. The rest of the scalp was normal in appearance and the eyebrows and eyelashes were uninvolved. The patient was diagnosed with alopecia areata and was treated with 10 mg/mL of intralesional triamcinolone once monthly for 4 months.
The patient initially showed improvement with moderate hair regrowth. After 4 months of treatment, she developed 3 new 1- to 1.5-cm erythematous alopecic patches on the vertex scalp and had worsening in the initial patches (Figure 1). Given the resistance to standard therapy and the onset of multiple new areas with evidence of inflammatory involvement, a punch biopsy was performed. Histopathologic examination revealed a fairly unremarkable epidermis and a dense dermal inflammatory infiltrate that was present both in the superficial and deep dermis (Figure 2). The inflammatory cells, which appeared to be predominantly comprised of lymphocytes, had a predilection for the vasculature but also were observed within the interstitial dermis. Additionally, mucin appeared to be slightly increased in the deep dermis. The lymphocytic phenotype was confirmed by immunohistochemical studies for CD20 and CD3. The most likely possibilities for this reaction pattern were LET, Jessner lymphocytic infiltrate of the skin (JLIS), gyrate erythema, and lymphoma; however, the immunohistochemical studies effectively ruled out lymphoma. Additionally, there was pronounced dermal mucin noted in the specimen. The patient was diagnosed with LET of the scalp based on the constellation of findings.

Comment
The classification of LET as a single unique entity or disease process sui generis has been in flux in the last decade. Its similarities to JLIS and other forms of chronic cutaneous lupus erythematosus (CCLE) have brought debate.4-6 In 1930, Gougerot and Burnier7 documented the first case of LET in the literature, describing smooth, infiltrated, erythematous lesions with no desquamation or other superficial changes seen in 5 patients.
In 2000, interest in LET and other forms of CCLE was increasing, and reports in the literature paralleled. That year, Kuhn et al4 reported 40 cases of LET, characterizing the clinical and histological features of each case to demonstrate that LET should be separate from other forms of CCLE. Until then, it is likely that many lesions that should have been classified as LET were instead classified as various forms of CCLE. The investigators maintained that LET also should be distinct from JLIS because it is associated with UV exposure.4 Kuhn et al8 reviewed phototesting in 60 patients with LET in 2001 and confirmed this subset was the most photosensitive type of lupus erythematosus.
In general, the histopathologic and immunohistochemical studies in LET and JLIS can be quite similar. Relatively distinguishing histopathologic findings in JLIS include no evidence of epidermal atrophy, basal vacuolar change, or follicular plugging, as well as negative immunofluorescence studies. Both entities show a predominantly T-cell population with a smaller component of B cells and thus a distinction cannot be made based on relative proportions of T and B cells in lesions.2
In 2003, Alexiades-Armenakas et al6 determined immunohistochemical criteria for LET, finding a predominance of T cells and more CD4 lymphocytes than CD8 lymphocytes with a mean ratio of roughly 3 to 1. Their study results maintained LET should be classified as a form of CCLE due to the chronicity of the lesions, the serologic profile with negative anti–double-stranded DNA, anticentromere, anti-Smith, anti-Ro/Sjögren syndrome antigen A, anti-La/Sjögren syndrome antigen B, and anti-nuclear ribonucleoprotein antibodies and the rare association with systemic disease.6 This conclusion was further solidified by a review published that same year citing unique histopathological features when compared to subacute cutaneous LE and discoid lupus erythematosus.5
This case illustrates the importance of histologic evaluation in determining the correct diagnosis in a patient with alopecia areata recalcitrant to treatment. Including LET in the differential of alopecic patches on the scalp could prove beneficial for patients, as LET responds well to antimalarial drugs and photoprotection.9 This patient had a normal antinuclear antibody panel and no signs or symptoms of systemic lupus. It was recommended that she avoid sun exposure and begin treatment with hydroxychloroquine but she declined. At a follow-up visit 6 months later she reported the lesions had improved, but a permanent wig had been sewn over the area, so it could not be examined.
Lupus erythematosus tumidus (LET) is a relatively rare condition but may simply be underdiagnosed in the literature. It presents as urticarialike papules and plaques in sun-exposed areas, characterized by induration and erythema. Lesions occur on the face, neck, upper extremities, and trunk and heal without scarring.1,2 Rarely, lesions can show fine scaling and associated pruritus, but most often the lesions are asymptomatic.3
Case Report
A 45-year-old woman presented with 2 asymptomatic self-described bald spots on the top of the head of 2 months’ duration. The patient denied prior treatment of the lesions and noted one patch was resolving. She reported no involvement of the eyebrows, eyelashes, and axillary and pubic hair. A review of systems was negative. The patient denied personal or family history of lupus, thyroid disease, or vitiligo.
Clinical examination revealed a 1.1-cm round patch of nonscarring alopecia on the right vertex scalp and a 0.9-cm round patch of nonscarring alopecia with moderate hair regrowth on the left vertex scalp. There was no erythema, scaling, or induration. The rest of the scalp was normal in appearance and the eyebrows and eyelashes were uninvolved. The patient was diagnosed with alopecia areata and was treated with 10 mg/mL of intralesional triamcinolone once monthly for 4 months.
The patient initially showed improvement with moderate hair regrowth. After 4 months of treatment, she developed 3 new 1- to 1.5-cm erythematous alopecic patches on the vertex scalp and had worsening in the initial patches (Figure 1). Given the resistance to standard therapy and the onset of multiple new areas with evidence of inflammatory involvement, a punch biopsy was performed. Histopathologic examination revealed a fairly unremarkable epidermis and a dense dermal inflammatory infiltrate that was present both in the superficial and deep dermis (Figure 2). The inflammatory cells, which appeared to be predominantly comprised of lymphocytes, had a predilection for the vasculature but also were observed within the interstitial dermis. Additionally, mucin appeared to be slightly increased in the deep dermis. The lymphocytic phenotype was confirmed by immunohistochemical studies for CD20 and CD3. The most likely possibilities for this reaction pattern were LET, Jessner lymphocytic infiltrate of the skin (JLIS), gyrate erythema, and lymphoma; however, the immunohistochemical studies effectively ruled out lymphoma. Additionally, there was pronounced dermal mucin noted in the specimen. The patient was diagnosed with LET of the scalp based on the constellation of findings.

Comment
The classification of LET as a single unique entity or disease process sui generis has been in flux in the last decade. Its similarities to JLIS and other forms of chronic cutaneous lupus erythematosus (CCLE) have brought debate.4-6 In 1930, Gougerot and Burnier7 documented the first case of LET in the literature, describing smooth, infiltrated, erythematous lesions with no desquamation or other superficial changes seen in 5 patients.
In 2000, interest in LET and other forms of CCLE was increasing, and reports in the literature paralleled. That year, Kuhn et al4 reported 40 cases of LET, characterizing the clinical and histological features of each case to demonstrate that LET should be separate from other forms of CCLE. Until then, it is likely that many lesions that should have been classified as LET were instead classified as various forms of CCLE. The investigators maintained that LET also should be distinct from JLIS because it is associated with UV exposure.4 Kuhn et al8 reviewed phototesting in 60 patients with LET in 2001 and confirmed this subset was the most photosensitive type of lupus erythematosus.
In general, the histopathologic and immunohistochemical studies in LET and JLIS can be quite similar. Relatively distinguishing histopathologic findings in JLIS include no evidence of epidermal atrophy, basal vacuolar change, or follicular plugging, as well as negative immunofluorescence studies. Both entities show a predominantly T-cell population with a smaller component of B cells and thus a distinction cannot be made based on relative proportions of T and B cells in lesions.2
In 2003, Alexiades-Armenakas et al6 determined immunohistochemical criteria for LET, finding a predominance of T cells and more CD4 lymphocytes than CD8 lymphocytes with a mean ratio of roughly 3 to 1. Their study results maintained LET should be classified as a form of CCLE due to the chronicity of the lesions, the serologic profile with negative anti–double-stranded DNA, anticentromere, anti-Smith, anti-Ro/Sjögren syndrome antigen A, anti-La/Sjögren syndrome antigen B, and anti-nuclear ribonucleoprotein antibodies and the rare association with systemic disease.6 This conclusion was further solidified by a review published that same year citing unique histopathological features when compared to subacute cutaneous LE and discoid lupus erythematosus.5
This case illustrates the importance of histologic evaluation in determining the correct diagnosis in a patient with alopecia areata recalcitrant to treatment. Including LET in the differential of alopecic patches on the scalp could prove beneficial for patients, as LET responds well to antimalarial drugs and photoprotection.9 This patient had a normal antinuclear antibody panel and no signs or symptoms of systemic lupus. It was recommended that she avoid sun exposure and begin treatment with hydroxychloroquine but she declined. At a follow-up visit 6 months later she reported the lesions had improved, but a permanent wig had been sewn over the area, so it could not be examined.
- Lee L, Werth V. Rheumatologic disease. In: Bolognia JL, Jorizzo JL, Rapini RP, eds. Dermatology. Vol 2. 3rd ed. Mosby Elsevier; 2008:615-629.
- Weedon D. The lichenoid reaction pattern. In: Weedon D. Skin Pathology. 2nd ed. Edinburgh, Scotland: Churchill Livingstone; 2002:35-70.
- Dekle CL, Mannes KD, Davis LS, et al. Lupus tumidus. J Am Acad Dermatol. 1999;41:250-253.
- Kuhn A, Richter-Hintz D, Oslislo C, et al. Lupus erythematosus tumidus—a neglected subset of cutaneous lupus erythematosus: report of 40 cases. Arch Dermatol. 2000;136:1033-1041.
- Kuhn A, Sonntag M, Ruzicka T, et al. Histopathologic findings in lupus erythematosus tumidus: review of 80 patients. J Am Acad Dermatol. 2003;48:901-908.
- Alexiades-Armenakas MR, Baldassano M, Bince B, et al. Tumid lupus erythematosus: criteria for classification with immunohistochemical analysis. Arthritis Rheum. 2003;49:494-500.
- Gougerot H, Burnier R. Lupuse rythe mateux “tumidus.” Bull Soc Fr Dermatol Syph. 1930;37:1291-1292.
- Kuhn A, Sonntag M, Richter-Hintz D, et al. Phototesting in lupus erythematosus tumidus—review of 60 patients. Photochem Photobiol. 2001;73:532-536.
- Cozzani E, Christana K, Rongioletti F, et al. Lupus erythematosus tumidus: clinical, histopathological and serological aspects and therapy response of 21 patients. Eur J Dermatol. 2010;20:797-801.
- Lee L, Werth V. Rheumatologic disease. In: Bolognia JL, Jorizzo JL, Rapini RP, eds. Dermatology. Vol 2. 3rd ed. Mosby Elsevier; 2008:615-629.
- Weedon D. The lichenoid reaction pattern. In: Weedon D. Skin Pathology. 2nd ed. Edinburgh, Scotland: Churchill Livingstone; 2002:35-70.
- Dekle CL, Mannes KD, Davis LS, et al. Lupus tumidus. J Am Acad Dermatol. 1999;41:250-253.
- Kuhn A, Richter-Hintz D, Oslislo C, et al. Lupus erythematosus tumidus—a neglected subset of cutaneous lupus erythematosus: report of 40 cases. Arch Dermatol. 2000;136:1033-1041.
- Kuhn A, Sonntag M, Ruzicka T, et al. Histopathologic findings in lupus erythematosus tumidus: review of 80 patients. J Am Acad Dermatol. 2003;48:901-908.
- Alexiades-Armenakas MR, Baldassano M, Bince B, et al. Tumid lupus erythematosus: criteria for classification with immunohistochemical analysis. Arthritis Rheum. 2003;49:494-500.
- Gougerot H, Burnier R. Lupuse rythe mateux “tumidus.” Bull Soc Fr Dermatol Syph. 1930;37:1291-1292.
- Kuhn A, Sonntag M, Richter-Hintz D, et al. Phototesting in lupus erythematosus tumidus—review of 60 patients. Photochem Photobiol. 2001;73:532-536.
- Cozzani E, Christana K, Rongioletti F, et al. Lupus erythematosus tumidus: clinical, histopathological and serological aspects and therapy response of 21 patients. Eur J Dermatol. 2010;20:797-801.
Practice Points
- Lupus erythematosus tumidus (LET) of the scalp can mimic alopecia areata on clinical presentation.
- A unique variant of chronic cutaneous lupus erythematosus, LET presents in sun-exposed areas without any corresponding systemic signs.
- Lupus erythematosus tumidus may respond well to antimalarial drugs.
Collaborative care aids seniors’ mild depression
A collaborative care model significantly mitigated mild depression in adults aged 65 and older, compared with usual care in the short term, based on data from 705 patients. The findings were published online Feb. 21.
“There is limited research about older people with mild depressive disorders who have insufficient levels of depressive symptoms to meet diagnostic criteria (called subclinical, subthreshold, or subsyndromal depression) but also reduced quality of life and function,” wrote Simon Gilbody, PhD, of the University of York (England) and colleagues. However, subthreshold depression increases the risk of a severe depressive illness, the researchers added.
Overall, patients in the collaborative care group improved from an average score of 7.8 at baseline to 5.4 after 4 months; the usual care group improved from an average of 7.8 at baseline to 6.7 at 4 months. The difference in scores persisted at 12 months in the secondary analysis (JAMA. 2017;317:728-37. doi: 10.1001/jama.2017.0130). “For populations with case-level depression, a successful treatment outcome has been defined as 5 points on the PHQ-9,” the researchers noted. “This magnitude of benefit was not observed in either group of the trial when comparing scores before and after treatment, although this result would be anticipated given the lower baseline PHQ-9 scores in populations with subthreshold depression.’
The study participants came from 32 primary care practices in northern England; the average age was 77 years, and 58% were women.
The results were limited by several factors, including the absence of a standardized interview to diagnose depression, differences in retention and attrition between groups, and the absence of long-term follow-up, “and further research is needed to assess longer-term efficacy,” the researchers said.
Neither Dr. Gilbody nor his colleagues had financial conflicts to disclose.
The CASPER trial “provides the first evidence that collaborative care may benefit patients with subthreshold depression,” Kurt Kroenke, MD, wrote in an accompanying editorial. In addition to the improvements on the Patient Health Questionnaire and the reduction in risk of progression to threshold level depression, the findings further support the use of behavioral activation, which was the core treatment in the study, he said. “Strong evidence for the effectiveness of behavioral activation was provided by the recent COBRA trial. … and behavioral activation was found to be noninferior to cognitive-behavioral therapy for the outcome of depression,” he wrote. However, more research is needed before clinicians routinely expand treatment beyond major depression to include subthreshold depression, Dr. Kroenke noted. Key factors include the variable rate of progression from subthreshold depression to major depression, the duration and context of subthreshold depression, patient preferences, and the possible role of antidepressants, he noted. However, the CASPER findings show “new evidence that collaborative care improves outcomes for at least some patients with subthreshold depression,” Dr. Kroenke said. “Patients with persistent symptoms, functional impairment, and a desire for treatment may particularly benefit,” he added (JAMA. 2017;317:702-4).
Kurt Kroenke, MD, is affiliated with the VA Health Services Research and Development Service Center for Health Communication and Information, Regenstrief Institute and Indiana University, both in Indianapolis. He had no financial conflicts to disclose.
The CASPER trial “provides the first evidence that collaborative care may benefit patients with subthreshold depression,” Kurt Kroenke, MD, wrote in an accompanying editorial. In addition to the improvements on the Patient Health Questionnaire and the reduction in risk of progression to threshold level depression, the findings further support the use of behavioral activation, which was the core treatment in the study, he said. “Strong evidence for the effectiveness of behavioral activation was provided by the recent COBRA trial. … and behavioral activation was found to be noninferior to cognitive-behavioral therapy for the outcome of depression,” he wrote. However, more research is needed before clinicians routinely expand treatment beyond major depression to include subthreshold depression, Dr. Kroenke noted. Key factors include the variable rate of progression from subthreshold depression to major depression, the duration and context of subthreshold depression, patient preferences, and the possible role of antidepressants, he noted. However, the CASPER findings show “new evidence that collaborative care improves outcomes for at least some patients with subthreshold depression,” Dr. Kroenke said. “Patients with persistent symptoms, functional impairment, and a desire for treatment may particularly benefit,” he added (JAMA. 2017;317:702-4).
Kurt Kroenke, MD, is affiliated with the VA Health Services Research and Development Service Center for Health Communication and Information, Regenstrief Institute and Indiana University, both in Indianapolis. He had no financial conflicts to disclose.
The CASPER trial “provides the first evidence that collaborative care may benefit patients with subthreshold depression,” Kurt Kroenke, MD, wrote in an accompanying editorial. In addition to the improvements on the Patient Health Questionnaire and the reduction in risk of progression to threshold level depression, the findings further support the use of behavioral activation, which was the core treatment in the study, he said. “Strong evidence for the effectiveness of behavioral activation was provided by the recent COBRA trial. … and behavioral activation was found to be noninferior to cognitive-behavioral therapy for the outcome of depression,” he wrote. However, more research is needed before clinicians routinely expand treatment beyond major depression to include subthreshold depression, Dr. Kroenke noted. Key factors include the variable rate of progression from subthreshold depression to major depression, the duration and context of subthreshold depression, patient preferences, and the possible role of antidepressants, he noted. However, the CASPER findings show “new evidence that collaborative care improves outcomes for at least some patients with subthreshold depression,” Dr. Kroenke said. “Patients with persistent symptoms, functional impairment, and a desire for treatment may particularly benefit,” he added (JAMA. 2017;317:702-4).
Kurt Kroenke, MD, is affiliated with the VA Health Services Research and Development Service Center for Health Communication and Information, Regenstrief Institute and Indiana University, both in Indianapolis. He had no financial conflicts to disclose.
A collaborative care model significantly mitigated mild depression in adults aged 65 and older, compared with usual care in the short term, based on data from 705 patients. The findings were published online Feb. 21.
“There is limited research about older people with mild depressive disorders who have insufficient levels of depressive symptoms to meet diagnostic criteria (called subclinical, subthreshold, or subsyndromal depression) but also reduced quality of life and function,” wrote Simon Gilbody, PhD, of the University of York (England) and colleagues. However, subthreshold depression increases the risk of a severe depressive illness, the researchers added.
Overall, patients in the collaborative care group improved from an average score of 7.8 at baseline to 5.4 after 4 months; the usual care group improved from an average of 7.8 at baseline to 6.7 at 4 months. The difference in scores persisted at 12 months in the secondary analysis (JAMA. 2017;317:728-37. doi: 10.1001/jama.2017.0130). “For populations with case-level depression, a successful treatment outcome has been defined as 5 points on the PHQ-9,” the researchers noted. “This magnitude of benefit was not observed in either group of the trial when comparing scores before and after treatment, although this result would be anticipated given the lower baseline PHQ-9 scores in populations with subthreshold depression.’
The study participants came from 32 primary care practices in northern England; the average age was 77 years, and 58% were women.
The results were limited by several factors, including the absence of a standardized interview to diagnose depression, differences in retention and attrition between groups, and the absence of long-term follow-up, “and further research is needed to assess longer-term efficacy,” the researchers said.
Neither Dr. Gilbody nor his colleagues had financial conflicts to disclose.
A collaborative care model significantly mitigated mild depression in adults aged 65 and older, compared with usual care in the short term, based on data from 705 patients. The findings were published online Feb. 21.
“There is limited research about older people with mild depressive disorders who have insufficient levels of depressive symptoms to meet diagnostic criteria (called subclinical, subthreshold, or subsyndromal depression) but also reduced quality of life and function,” wrote Simon Gilbody, PhD, of the University of York (England) and colleagues. However, subthreshold depression increases the risk of a severe depressive illness, the researchers added.
Overall, patients in the collaborative care group improved from an average score of 7.8 at baseline to 5.4 after 4 months; the usual care group improved from an average of 7.8 at baseline to 6.7 at 4 months. The difference in scores persisted at 12 months in the secondary analysis (JAMA. 2017;317:728-37. doi: 10.1001/jama.2017.0130). “For populations with case-level depression, a successful treatment outcome has been defined as 5 points on the PHQ-9,” the researchers noted. “This magnitude of benefit was not observed in either group of the trial when comparing scores before and after treatment, although this result would be anticipated given the lower baseline PHQ-9 scores in populations with subthreshold depression.’
The study participants came from 32 primary care practices in northern England; the average age was 77 years, and 58% were women.
The results were limited by several factors, including the absence of a standardized interview to diagnose depression, differences in retention and attrition between groups, and the absence of long-term follow-up, “and further research is needed to assess longer-term efficacy,” the researchers said.
Neither Dr. Gilbody nor his colleagues had financial conflicts to disclose.
FROM JAMA
Key clinical point: Collaborative care reduced subthreshold depression in older adults, compared with usual care after 4 months.
Major finding: Older adults with subthreshold depression who received collaborative care had lower depression scores on the Patient Health Questionnaire than those who received usual care after 4 months (average scores 5.4 and 6.7, respectively).
Data source: A randomized trial of 705 adults aged 65 years and older with subthreshold depression.
Disclosures: The researchers had no financial conflicts to disclose.
Hope on the horizon for novel antidepressants
LAS VEGAS – There remains a great unmet need for more effective and rapidly acting treatments for major depressive disorder, and research is revealing that both new and existing drugs may help, according to one expert.
One argument for additional treatment options is the current rate of suicide in the United States, which ranks as the 10th leading cause of death among persons aged 10 years and older, Gerard Sanacora, MD, PhD, said at an annual psychopharmacology update held by the Nevada Psychiatric Association. Another argument for new antidepressants stems from the results of the STAR*D trial, which found that 37% of patients with major depressive disorder who were treated with citalopram monotherapy had remission with the first treatment.
Dr. Sanacora, who is also director of the Yale Depression Research Program, said that there is a reconceptualization of how clinicians think about the pathophysiology of depression and the path to novel treatment development. A variety of novel pharmacologic and somatic treatments, with new mechanisms of action, are currently undergoing validation for treatment-resistant depression. These include glutamatergic, GABAergic, opioid, and anti‐inflammatory drugs.
Drugs that modulate GABAergic and glutamatergic neurotransmission have anxiolytic and antidepressant activities in rodent models of depression. In addition, the robust, rapid, and relatively sustained antidepressant effects of low-dose ketamine have been observed in double-blind placebo crossover trials in patients with treatment-resistant major depression (Biol Psych. 2000 Feb 15;47[4]:351-4 and Arch Gen Psych. 2006 Aug;63[8]:856-64). Currently, Dr. Sanacora said, more than 80 clinics in the United States provide ketamine therapy, yet clinicians face balancing the potential benefits of the drug with inherent limitations of the ketamine studies to date. These include the fact that the study drug blinding is ineffective; the optimal dose, route, or frequency has not been determined; the duration of effect is unknown; the long-term effectiveness and safety are unclear; and the moderators and mediators of response are unknown.
Results from a National Institutes of Mental Health–funded double-blind, placebo-controlled study examining various doses of ketamine in treatment-resistant depression are anticipated sometime this year. In 2013, a trial sponsored by Janssen Research & Development titled a Study to Evaluate the Safety and Efficacy of Intranasal Esketamine in Treatment-Resistant Depression (SYNAPSE) set out to assess the efficacy and dose response of intranasal esketamine (panel A: 28 mg, 56 mg, and 84 mg; panel B: 14 mg and 56 mg), compared with placebo, in improving depressive symptoms in participants with treatment-resistant depression. The researchers found a positive effect of esketamine vs. saline placebo with some evidence of a dose-response curve, suggesting higher doses to be more effective. Some published studies suggest that chronic ketamine use causes impairments in working memory and other cognitive effects (Addiction. 2009 Jan;104[1]:77-87 and Front Psych. 2014 Dec 4;5:149), while others have found that ketamine does not cause memory deficits when given on up to six occasions (Int J Neuropsychopharmacol. 2014 Jun 25;17[11]:1805-13 and J Psychopharmacol. 2014 Apr 3;28[6]:536-44).
Another drug being studied for major depressive disorder is the investigational agent SAGE-547, an allosteric neurosteroid modulator of both synaptic and extrasynaptic GABA receptors. Preliminary results from a double-blind, placebo-controlled phase II trial in 21 patients with postpartum depression showed that the Hamilton Rating Scale for Depression (HAM-D) total score was reduced by SAGE-547, compared with placebo, at 60 hours (P = .008).
Buprenorphine, a partial mu opioid agonist commonly used in addiction treatment, may also play a future role in helping patients with treatment-resistant depression. One randomized study of 88 patients found that those who took very low doses of buprenorphine for 2 or 4 weeks had significantly lower scores on the Beck Suicide Ideation Scale, compared with their counterparts on placebo (Am J Psychiatry. 2016 May 1;173[5]491-8).
Drugs with anti-inflammatory properties may also have a role. One study of 60 patients found that the tumor necrosis factor–alpha antagonist infliximab may benefit patients with treatment-resistant depression who have high inflammatory biomarkers at baseline (JAMA Psychiatry. 2013 Jan;70[1]:31-41).
“Active participation in clinical research efforts is critical to the advancement of future treatment approaches,” he said.
Dr. Sanacora disclosed having received consulting fees and/or research agreements from numerous industry sources. In addition, free medication was provided to Dr. Sanacora by sanofi‐aventis for a study sponsored by the National Institutes of Health.
LAS VEGAS – There remains a great unmet need for more effective and rapidly acting treatments for major depressive disorder, and research is revealing that both new and existing drugs may help, according to one expert.
One argument for additional treatment options is the current rate of suicide in the United States, which ranks as the 10th leading cause of death among persons aged 10 years and older, Gerard Sanacora, MD, PhD, said at an annual psychopharmacology update held by the Nevada Psychiatric Association. Another argument for new antidepressants stems from the results of the STAR*D trial, which found that 37% of patients with major depressive disorder who were treated with citalopram monotherapy had remission with the first treatment.
Dr. Sanacora, who is also director of the Yale Depression Research Program, said that there is a reconceptualization of how clinicians think about the pathophysiology of depression and the path to novel treatment development. A variety of novel pharmacologic and somatic treatments, with new mechanisms of action, are currently undergoing validation for treatment-resistant depression. These include glutamatergic, GABAergic, opioid, and anti‐inflammatory drugs.
Drugs that modulate GABAergic and glutamatergic neurotransmission have anxiolytic and antidepressant activities in rodent models of depression. In addition, the robust, rapid, and relatively sustained antidepressant effects of low-dose ketamine have been observed in double-blind placebo crossover trials in patients with treatment-resistant major depression (Biol Psych. 2000 Feb 15;47[4]:351-4 and Arch Gen Psych. 2006 Aug;63[8]:856-64). Currently, Dr. Sanacora said, more than 80 clinics in the United States provide ketamine therapy, yet clinicians face balancing the potential benefits of the drug with inherent limitations of the ketamine studies to date. These include the fact that the study drug blinding is ineffective; the optimal dose, route, or frequency has not been determined; the duration of effect is unknown; the long-term effectiveness and safety are unclear; and the moderators and mediators of response are unknown.
Results from a National Institutes of Mental Health–funded double-blind, placebo-controlled study examining various doses of ketamine in treatment-resistant depression are anticipated sometime this year. In 2013, a trial sponsored by Janssen Research & Development titled a Study to Evaluate the Safety and Efficacy of Intranasal Esketamine in Treatment-Resistant Depression (SYNAPSE) set out to assess the efficacy and dose response of intranasal esketamine (panel A: 28 mg, 56 mg, and 84 mg; panel B: 14 mg and 56 mg), compared with placebo, in improving depressive symptoms in participants with treatment-resistant depression. The researchers found a positive effect of esketamine vs. saline placebo with some evidence of a dose-response curve, suggesting higher doses to be more effective. Some published studies suggest that chronic ketamine use causes impairments in working memory and other cognitive effects (Addiction. 2009 Jan;104[1]:77-87 and Front Psych. 2014 Dec 4;5:149), while others have found that ketamine does not cause memory deficits when given on up to six occasions (Int J Neuropsychopharmacol. 2014 Jun 25;17[11]:1805-13 and J Psychopharmacol. 2014 Apr 3;28[6]:536-44).
Another drug being studied for major depressive disorder is the investigational agent SAGE-547, an allosteric neurosteroid modulator of both synaptic and extrasynaptic GABA receptors. Preliminary results from a double-blind, placebo-controlled phase II trial in 21 patients with postpartum depression showed that the Hamilton Rating Scale for Depression (HAM-D) total score was reduced by SAGE-547, compared with placebo, at 60 hours (P = .008).
Buprenorphine, a partial mu opioid agonist commonly used in addiction treatment, may also play a future role in helping patients with treatment-resistant depression. One randomized study of 88 patients found that those who took very low doses of buprenorphine for 2 or 4 weeks had significantly lower scores on the Beck Suicide Ideation Scale, compared with their counterparts on placebo (Am J Psychiatry. 2016 May 1;173[5]491-8).
Drugs with anti-inflammatory properties may also have a role. One study of 60 patients found that the tumor necrosis factor–alpha antagonist infliximab may benefit patients with treatment-resistant depression who have high inflammatory biomarkers at baseline (JAMA Psychiatry. 2013 Jan;70[1]:31-41).
“Active participation in clinical research efforts is critical to the advancement of future treatment approaches,” he said.
Dr. Sanacora disclosed having received consulting fees and/or research agreements from numerous industry sources. In addition, free medication was provided to Dr. Sanacora by sanofi‐aventis for a study sponsored by the National Institutes of Health.
LAS VEGAS – There remains a great unmet need for more effective and rapidly acting treatments for major depressive disorder, and research is revealing that both new and existing drugs may help, according to one expert.
One argument for additional treatment options is the current rate of suicide in the United States, which ranks as the 10th leading cause of death among persons aged 10 years and older, Gerard Sanacora, MD, PhD, said at an annual psychopharmacology update held by the Nevada Psychiatric Association. Another argument for new antidepressants stems from the results of the STAR*D trial, which found that 37% of patients with major depressive disorder who were treated with citalopram monotherapy had remission with the first treatment.
Dr. Sanacora, who is also director of the Yale Depression Research Program, said that there is a reconceptualization of how clinicians think about the pathophysiology of depression and the path to novel treatment development. A variety of novel pharmacologic and somatic treatments, with new mechanisms of action, are currently undergoing validation for treatment-resistant depression. These include glutamatergic, GABAergic, opioid, and anti‐inflammatory drugs.
Drugs that modulate GABAergic and glutamatergic neurotransmission have anxiolytic and antidepressant activities in rodent models of depression. In addition, the robust, rapid, and relatively sustained antidepressant effects of low-dose ketamine have been observed in double-blind placebo crossover trials in patients with treatment-resistant major depression (Biol Psych. 2000 Feb 15;47[4]:351-4 and Arch Gen Psych. 2006 Aug;63[8]:856-64). Currently, Dr. Sanacora said, more than 80 clinics in the United States provide ketamine therapy, yet clinicians face balancing the potential benefits of the drug with inherent limitations of the ketamine studies to date. These include the fact that the study drug blinding is ineffective; the optimal dose, route, or frequency has not been determined; the duration of effect is unknown; the long-term effectiveness and safety are unclear; and the moderators and mediators of response are unknown.
Results from a National Institutes of Mental Health–funded double-blind, placebo-controlled study examining various doses of ketamine in treatment-resistant depression are anticipated sometime this year. In 2013, a trial sponsored by Janssen Research & Development titled a Study to Evaluate the Safety and Efficacy of Intranasal Esketamine in Treatment-Resistant Depression (SYNAPSE) set out to assess the efficacy and dose response of intranasal esketamine (panel A: 28 mg, 56 mg, and 84 mg; panel B: 14 mg and 56 mg), compared with placebo, in improving depressive symptoms in participants with treatment-resistant depression. The researchers found a positive effect of esketamine vs. saline placebo with some evidence of a dose-response curve, suggesting higher doses to be more effective. Some published studies suggest that chronic ketamine use causes impairments in working memory and other cognitive effects (Addiction. 2009 Jan;104[1]:77-87 and Front Psych. 2014 Dec 4;5:149), while others have found that ketamine does not cause memory deficits when given on up to six occasions (Int J Neuropsychopharmacol. 2014 Jun 25;17[11]:1805-13 and J Psychopharmacol. 2014 Apr 3;28[6]:536-44).
Another drug being studied for major depressive disorder is the investigational agent SAGE-547, an allosteric neurosteroid modulator of both synaptic and extrasynaptic GABA receptors. Preliminary results from a double-blind, placebo-controlled phase II trial in 21 patients with postpartum depression showed that the Hamilton Rating Scale for Depression (HAM-D) total score was reduced by SAGE-547, compared with placebo, at 60 hours (P = .008).
Buprenorphine, a partial mu opioid agonist commonly used in addiction treatment, may also play a future role in helping patients with treatment-resistant depression. One randomized study of 88 patients found that those who took very low doses of buprenorphine for 2 or 4 weeks had significantly lower scores on the Beck Suicide Ideation Scale, compared with their counterparts on placebo (Am J Psychiatry. 2016 May 1;173[5]491-8).
Drugs with anti-inflammatory properties may also have a role. One study of 60 patients found that the tumor necrosis factor–alpha antagonist infliximab may benefit patients with treatment-resistant depression who have high inflammatory biomarkers at baseline (JAMA Psychiatry. 2013 Jan;70[1]:31-41).
“Active participation in clinical research efforts is critical to the advancement of future treatment approaches,” he said.
Dr. Sanacora disclosed having received consulting fees and/or research agreements from numerous industry sources. In addition, free medication was provided to Dr. Sanacora by sanofi‐aventis for a study sponsored by the National Institutes of Health.
EXPERT ANALYSIS FROM THE NPA PSYCHOPHARMACOLOGY UPDATE
Light therapy eases Parkinson’s-related sleep disturbances
Light therapy significantly reduced excessive daytime sleepiness, improved sleep quality, decreased overnight awakenings, shortened sleep latency, enhanced daytime alertness and activity level, and improved motor symptoms in patients with Parkinson’s disease, according to a report published online Feb. 20 in JAMA Neurology.
The noninvasive, nonpharmacologic treatment was well tolerated, and patient adherence was excellent in a small, multicenter, randomized controlled trial. Light therapy is widely available as a treatment for several sleep and psychiatric disorders and is “relatively easy to prescribe and incorporate into a clinical practice,” said Aleksandar Videnovic, MD, of the department of neurology at Massachusetts General Hospital and the division of sleep medicine at Harvard Medical School, both in Boston, and his associates.
To assess the safety and efficacy of light therapy as a novel treatment for PD, they studied 31 adults (age range, 32-77 years) who had a mean disease duration of 6 years. These study participants were randomly assigned to use 1 hour of exposure to 10,000 lux of bright light (16 patients in the intervention group) or 1 hour of exposure to less than 300 lux of dim red light (15 control subjects) every morning and every afternoon for 2 weeks.
The study participants – 13 men and 18 women – also wore actigraphy monitors all day and all night, completed daily sleep diaries, and noted daytime sleepiness in a log every 2 hours, 3 days per week.
Bright light significantly improved excessive daytime sleepiness as measured by the Epworth Sleepiness Scale and self-reported alertness during wake time, as well as several sleep metrics such as overall sleep quality, overnight awakenings, and ease of falling asleep. All the patients in the intervention group reported being more refreshed in the mornings during the study period, as compared with baseline.
Light therapy also improved overall PD severity as measured by the Unified Parkinson’s Disease Rating Scale, particularly in scores related to activities of daily living and motor symptoms. Moreover, this effect persisted during the 2-week washout period after treatment was discontinued, Dr. Videnovic and his associates said (JAMA Neurol. 2017 Feb 20. doi: 10.1001/jamaneurol.2016.5192).
The treatment was well tolerated. In the intervention group, one patient reported headache and another sleepiness, and in the control group one patient reported itchy eyes. The effects resolved spontaneously, and neither lead to treatment withdrawal.
“Based on these results, the next logical step is to optimize various parameters of light therapy (e.g., intensity, duration, and wavelength) not only for impaired sleep and alertness but also for other motor and nonmotor manifestation of PD,” the investigators wrote.
A major limitation of this study was that exposure to ambient light throughout the day was not measured. Some people in the control group received as much or even more light exposure than those assigned to bright-light therapy. “Future studies may be more strict in controlling such exposures,” Dr. Videnovic and his associates said.
This study was supported by the National Parkinson Foundation and the National Institutes of Health. Dr. Videnovic reported having no relevant financial disclosures. One of his associates reported ties to Merck, Phillips, Eisai, and Teva.
The study by Dr. Videnovic and his associates is important because it introduces a new concept into the much-studied phenomenon of sleep disturbances in Parkinson’s disease.
The authors demonstrated that chronobiological interventions can be used therapeutically in PD. Accounting for circadian physiology also sets a new standard for future studies of sleep, nighttime wakefulness, and daytime function not only in PD but, it is hoped, in other diseases as well.
Birgit Högl, MD, is with the department of neurology at the Medical University of Innsbruck (Austria). She reported receiving honoraria as a speaker, advisory board member, or consultant from UCB, Otsuka, Lundbeck, Lilly, Axovant, AbbVie, Mundipharma, Benevolent Bio, and Janssen Cilag, and travel support from Habel Medizintechnik and Vivisol. Dr. Högl made these remarks in an editorial (JAMA Neurol. 2017 Feb 20. doi: 10.1001/jamaneurol.2016.5519) accompanying the report by Dr. Videnovic and his colleagues.
The study by Dr. Videnovic and his associates is important because it introduces a new concept into the much-studied phenomenon of sleep disturbances in Parkinson’s disease.
The authors demonstrated that chronobiological interventions can be used therapeutically in PD. Accounting for circadian physiology also sets a new standard for future studies of sleep, nighttime wakefulness, and daytime function not only in PD but, it is hoped, in other diseases as well.
Birgit Högl, MD, is with the department of neurology at the Medical University of Innsbruck (Austria). She reported receiving honoraria as a speaker, advisory board member, or consultant from UCB, Otsuka, Lundbeck, Lilly, Axovant, AbbVie, Mundipharma, Benevolent Bio, and Janssen Cilag, and travel support from Habel Medizintechnik and Vivisol. Dr. Högl made these remarks in an editorial (JAMA Neurol. 2017 Feb 20. doi: 10.1001/jamaneurol.2016.5519) accompanying the report by Dr. Videnovic and his colleagues.
The study by Dr. Videnovic and his associates is important because it introduces a new concept into the much-studied phenomenon of sleep disturbances in Parkinson’s disease.
The authors demonstrated that chronobiological interventions can be used therapeutically in PD. Accounting for circadian physiology also sets a new standard for future studies of sleep, nighttime wakefulness, and daytime function not only in PD but, it is hoped, in other diseases as well.
Birgit Högl, MD, is with the department of neurology at the Medical University of Innsbruck (Austria). She reported receiving honoraria as a speaker, advisory board member, or consultant from UCB, Otsuka, Lundbeck, Lilly, Axovant, AbbVie, Mundipharma, Benevolent Bio, and Janssen Cilag, and travel support from Habel Medizintechnik and Vivisol. Dr. Högl made these remarks in an editorial (JAMA Neurol. 2017 Feb 20. doi: 10.1001/jamaneurol.2016.5519) accompanying the report by Dr. Videnovic and his colleagues.
Light therapy significantly reduced excessive daytime sleepiness, improved sleep quality, decreased overnight awakenings, shortened sleep latency, enhanced daytime alertness and activity level, and improved motor symptoms in patients with Parkinson’s disease, according to a report published online Feb. 20 in JAMA Neurology.
The noninvasive, nonpharmacologic treatment was well tolerated, and patient adherence was excellent in a small, multicenter, randomized controlled trial. Light therapy is widely available as a treatment for several sleep and psychiatric disorders and is “relatively easy to prescribe and incorporate into a clinical practice,” said Aleksandar Videnovic, MD, of the department of neurology at Massachusetts General Hospital and the division of sleep medicine at Harvard Medical School, both in Boston, and his associates.
To assess the safety and efficacy of light therapy as a novel treatment for PD, they studied 31 adults (age range, 32-77 years) who had a mean disease duration of 6 years. These study participants were randomly assigned to use 1 hour of exposure to 10,000 lux of bright light (16 patients in the intervention group) or 1 hour of exposure to less than 300 lux of dim red light (15 control subjects) every morning and every afternoon for 2 weeks.
The study participants – 13 men and 18 women – also wore actigraphy monitors all day and all night, completed daily sleep diaries, and noted daytime sleepiness in a log every 2 hours, 3 days per week.
Bright light significantly improved excessive daytime sleepiness as measured by the Epworth Sleepiness Scale and self-reported alertness during wake time, as well as several sleep metrics such as overall sleep quality, overnight awakenings, and ease of falling asleep. All the patients in the intervention group reported being more refreshed in the mornings during the study period, as compared with baseline.
Light therapy also improved overall PD severity as measured by the Unified Parkinson’s Disease Rating Scale, particularly in scores related to activities of daily living and motor symptoms. Moreover, this effect persisted during the 2-week washout period after treatment was discontinued, Dr. Videnovic and his associates said (JAMA Neurol. 2017 Feb 20. doi: 10.1001/jamaneurol.2016.5192).
The treatment was well tolerated. In the intervention group, one patient reported headache and another sleepiness, and in the control group one patient reported itchy eyes. The effects resolved spontaneously, and neither lead to treatment withdrawal.
“Based on these results, the next logical step is to optimize various parameters of light therapy (e.g., intensity, duration, and wavelength) not only for impaired sleep and alertness but also for other motor and nonmotor manifestation of PD,” the investigators wrote.
A major limitation of this study was that exposure to ambient light throughout the day was not measured. Some people in the control group received as much or even more light exposure than those assigned to bright-light therapy. “Future studies may be more strict in controlling such exposures,” Dr. Videnovic and his associates said.
This study was supported by the National Parkinson Foundation and the National Institutes of Health. Dr. Videnovic reported having no relevant financial disclosures. One of his associates reported ties to Merck, Phillips, Eisai, and Teva.
Light therapy significantly reduced excessive daytime sleepiness, improved sleep quality, decreased overnight awakenings, shortened sleep latency, enhanced daytime alertness and activity level, and improved motor symptoms in patients with Parkinson’s disease, according to a report published online Feb. 20 in JAMA Neurology.
The noninvasive, nonpharmacologic treatment was well tolerated, and patient adherence was excellent in a small, multicenter, randomized controlled trial. Light therapy is widely available as a treatment for several sleep and psychiatric disorders and is “relatively easy to prescribe and incorporate into a clinical practice,” said Aleksandar Videnovic, MD, of the department of neurology at Massachusetts General Hospital and the division of sleep medicine at Harvard Medical School, both in Boston, and his associates.
To assess the safety and efficacy of light therapy as a novel treatment for PD, they studied 31 adults (age range, 32-77 years) who had a mean disease duration of 6 years. These study participants were randomly assigned to use 1 hour of exposure to 10,000 lux of bright light (16 patients in the intervention group) or 1 hour of exposure to less than 300 lux of dim red light (15 control subjects) every morning and every afternoon for 2 weeks.
The study participants – 13 men and 18 women – also wore actigraphy monitors all day and all night, completed daily sleep diaries, and noted daytime sleepiness in a log every 2 hours, 3 days per week.
Bright light significantly improved excessive daytime sleepiness as measured by the Epworth Sleepiness Scale and self-reported alertness during wake time, as well as several sleep metrics such as overall sleep quality, overnight awakenings, and ease of falling asleep. All the patients in the intervention group reported being more refreshed in the mornings during the study period, as compared with baseline.
Light therapy also improved overall PD severity as measured by the Unified Parkinson’s Disease Rating Scale, particularly in scores related to activities of daily living and motor symptoms. Moreover, this effect persisted during the 2-week washout period after treatment was discontinued, Dr. Videnovic and his associates said (JAMA Neurol. 2017 Feb 20. doi: 10.1001/jamaneurol.2016.5192).
The treatment was well tolerated. In the intervention group, one patient reported headache and another sleepiness, and in the control group one patient reported itchy eyes. The effects resolved spontaneously, and neither lead to treatment withdrawal.
“Based on these results, the next logical step is to optimize various parameters of light therapy (e.g., intensity, duration, and wavelength) not only for impaired sleep and alertness but also for other motor and nonmotor manifestation of PD,” the investigators wrote.
A major limitation of this study was that exposure to ambient light throughout the day was not measured. Some people in the control group received as much or even more light exposure than those assigned to bright-light therapy. “Future studies may be more strict in controlling such exposures,” Dr. Videnovic and his associates said.
This study was supported by the National Parkinson Foundation and the National Institutes of Health. Dr. Videnovic reported having no relevant financial disclosures. One of his associates reported ties to Merck, Phillips, Eisai, and Teva.
FROM JAMA NEUROLOGY
Key clinical point:
Major finding: Compared with a control condition, bright light significantly improved excessive daytime sleepiness as measured by the Epworth Sleepiness Scale and self-reported alertness during wake time.
Data source: A randomized controlled trial involving 31 adults with Parkinson’s disease–related sleep disturbances.
Disclosures: This study was supported by the National Parkinson Foundation and the National Institutes of Health. Dr. Videnovic reported having no relevant financial disclosures. One of his associates reported ties to Merck, Phillips, Eisai, and Teva.
Safety of Superior Labrum Anterior and Posterior (SLAP) Repair Posterior to Biceps Tendon Is Improved With a Percutaneous Approach
Take-Home Points
- Anchors placed posterior to the biceps during SLAP repair are at risk for glenoid vault penetration and/or suprascapular nerve (SSN) injury.
- Vault penetration and SSN injury are avoided by using a Port of Wilmington (PW) portal instead of an anterior portal.
- A percutaneous PW portal is safe and passes through the rotator cuff muscle only.
Since being classified by Snyder and colleagues,1 various arthroscopic techniques have been used to repair superior labrum anterior and posterior (SLAP) tears, particularly type II tears. Despite being commonly performed, repairs of SLAP lesions remain challenging. There is high variability in the rate of good/excellent functional outcomes and athletes’ return to previous level of play after SLAP repairs.2,3 Furthermore, the rate of complications after SLAP repair is as high as 5%.4
One of the most common complications of repair of a type II SLAP tear is nerve injury.4 In particular, suprascapular nerve (SSN) injury has occurred after arthroscopic repair of SLAP tears.5,6 Three cadaveric studies have demonstrated that glenoid vault penetration is common during placement of knotted anchors for SLAP repair and that the SSN is at risk during placement of these anchors.7-9 However, 2 of the 3 studies used only an anterior portal in their evaluation of anchor placement. Safety of anchor placement posterior to the biceps tendon may be improved with a percutaneous approach using a Port of Wilmington (PW) portal.10,11 No studies have evaluated the risk of glenoid vault penetration and SSN injury with shorter knotless anchors.
We conducted a study to compare a standard anterosuperolateral (ASL) portal with a percutaneous PW portal for knotless anchors placed posterior to the biceps tendon during repair of SLAP tears. We hypothesized that anchors placed through the PW portal would be less likely to penetrate the glenoid vault and would be farther from the SSN in the event of bone penetration.
Materials and Methods
Six matched pairs of fresh human cadaveric shoulders were used in this study. Each specimen included the scapula, the clavicle, and the humerus. All 6 specimens were male, and their mean age was 41.2 years (range, 23-59 years). Shoulder arthroscopy was performed for placement of SLAP anchors, and open dissection followed.
Anchor Placement
The scapula was clamped and the shoulder placed in the lateral decubitus position with 30° of abduction, 20° of forward flexion, and neutral rotation.10 A standard posterior glenohumeral viewing portal was established and a 30° arthroscope inserted. Both shoulders of each matched pair were randomly assigned to anchor placement through either an ASL portal or a PW portal. Two anchors were placed in the superior glenoid to simulate repair of a posterior SLAP tear.11 Each was a 2.9-mm short (12.5-mm) knotless anchor (BioComposite PushLock; Arthrex) that included a polyetheretherketone (PEEK) eyelet for threading sutures before anchor placement. A drill guide was inserted according to manufacturer guidelines, and a 2.9-mm drill was used to make a bone socket 18 mm deep. The anchor eyelet was loaded with suture tape (Labral Tape; Arthrex), and the anchor and suture were inserted into the socket. The sutures were left uncut to aid in anchor visualization during open dissection. On a right shoulder, the first anchor was placed just posterior to the biceps tendon, at 11 o’clock, and the second anchor about 1 cm posterior to the first, at 10 o’clock. All anchors were placed by an arthroscopy fellowship–trained shoulder surgeon. Before placement, anchor location was confirmed by another arthroscopy fellowship–trained shoulder surgeon.
The ASL portal was created, with an 18-gauge spinal needle and an outside-in technique, about 1 cm lateral to the anterolateral corner of the acromion.
In the opposite shoulder, the PW portal was created, with a percutaneous technique, about 1 cm anterior and 1 cm lateral to the posterolateral corner of the acromion. An 18-gauge spinal needle was inserted to allow a 45° angle of approach to the posterosuperior glenoid.11
Cadaveric Dissection
After anchor placement, another shoulder surgeon performed the dissection. Skin, subcutaneous tissue, deltoid, and clavicle were removed. In the percutaneous specimens, PW portal location relative to rotator cuff was recorded before cuff removal. After overlying soft tissues were removed from a specimen, the anchors were examined for glenoid vault penetration. In the setting of vault penetration, digital calipers were used to measure the shortest distance from anchor to SSN.
Results
In the ASL portal group, 8 (66.7%) of 12 anchors (4/6 at 11 o’clock, 4/6 at 10 o’clock) penetrated the medial glenoid vault.
In the PW portal group, 2 (16.7%) of 12 anchors (1/6 at 11 o’clock, 1/6 at 10 o’clock, both from a single specimen) penetrated the medial glenoid vault. Actually, in each case the eyelet and not the anchor penetrated the vault. In the penetration cases, distance to SSN was 20 mm for the 11 o’clock anchor and 8 mm for the 10 o’clock anchor (Table). Of the 6 portals, 3 passed through the supraspinatus muscle, 2 through the infraspinatus musculotendinous junction, and 1 through the infraspinatus muscle.
Discussion
Our study findings support the hypothesis that SLAP repair anchors placed posterior to the biceps tendon are more likely to remain in bone with use of a percutaneous approach relative to an ASL approach. Our findings also support the growing body of evidence that such anchors placed with an anterior approach increase the risk for SSN injury.
Three other cadaveric studies have evaluated anchor placement for SLAP repair. Chan and colleagues7 evaluated drill penetration during bone socket preparation for SLAP repair in 21 matched pairs of formalin-embalmed cadavers. A 20-mm drill was used for correspondence to a 14.5-mm anchor, though no anchors were inserted, and sockets were created in an open manner. Through a mimicked ASL portal, 1 socket was made anterior to the biceps tendon, at 1 o’clock; then, through a mimicked PW portal, 2 sockets were made posterior to the tendon, at 11 o’clock and 9 to 10 o’clock. Glenoid vault penetration occurred in 29% of the 42 anterior sockets, but only 1 anchor (2.4%) touched the SSN. Penetration did not occur with the 11 o’clock anchors. The 9 to 10 o’clock anchor was at highest risk for SSN injury (9.5%, 4 cases). The study was limited by lack of anchor placement and open creation of bone sockets in embalmed cadavers.
Koh and colleagues8 evaluated arthroscopic placement of anterior SLAP anchors in 6 matched pairs of fresh-frozen cadavers. Through an ASL portal, each 14.5-mm knotted anchor was placed anterior to the biceps tendon, at 1 o’clock. As in the study by Chan and colleagues,7 drill depth was 20 mm. Notably, anchors were seated 2 mm beyond manufacturer recommendations, and the cadavers were of Asian origin, likely indicating smaller glenoids compared to specimens from North America or Europe. All 12 anchors penetrated the glenoid vault; mean distance to SSN was 3.1 mm.
Morgan and colleagues9 compared anterior and ASL portals created for SLAP repairs in 10 matched-pair cadavers. Anchors were placed at 1 o’clock, 11 o’clock, and 10 o’clock. As in the studies by Chan and colleagues7 and Koh and colleagues,8 14.5-mm knotted anchors were used. One anterior anchor (10%) placed through an ASL portal penetrated the cortex by 1 mm, and 2 anterior anchors (20%) placed through anterior portals penetrated the cortex (1 was completely out of the bone). Overall, 65% of 11 o’clock anchors and 100% of 10 o’clock anchors violated the glenoid vault. With the 11 o’clock anchors, mean distance to SSN was 6 mm for ASL portals and 4.2 mm for anterior portals; with the 10 o’clock anchors, mean distance to SSN was 8 mm for ASL portals and 2.1 mm for anterior portals.
Overall, the results of these 3 studies suggest that, with use of ASL portals, placement of SLAP anchors anterior to the biceps tendon is safe. Using the same portals, however, anchors placed posterior to the tendon are at higher risk for glenoid vault penetration. Supporting these findings are our study’s penetration rates: 66.7% for anchors placed through ASL portals and 16.7% for anchors placed through percutaneous PW portals. The different rates are not surprising given that the coracoid process projects anterior to the glenoid and provides additional bone stock for placement of anchors anteriorly vs posteriorly. Therefore, with percutaneous PW portals, the approach angle directs the anchor toward the bone of the coracoid base. Furthermore, the SSN passes nearest the posterior aspect of the glenoid. In a study by Shishido and Kikuchi,12 the distance from the posterior rim of the glenoid to the SSN was 18 mm, and from the superior rim was 29 mm. Therefore, anchors placed with an anterior approach naturally are directed toward the SSN.
In addition to portal placement and approach angle, anchor length likely affects the risks for glenoid vault penetration and SSN injury.
One limitation of this study was the small number of cadavers, all of which were male. Female cadavers and cadavers of other ethnic origins likely have smaller glenoid vaults, and thus their inclusion would have altered our results. This issue was well described in studies mentioned in this article, and our goal was simply to compare ASL portals with percutaneous PW portals, so we think it does not change the fact that the risks for glenoid vault penetration and SSN injury are reduced with use of PW portals for anchors placed posterior to the biceps tendon.
Conclusion
This study was the first to examine glenoid vault penetration and SSN proximity with short anchors for SLAP repair. The risk for glenoid vault penetration during repair of SLAP tears posterior to the biceps tendon was reduced by anchor placement with a percutaneous posterior approach. The percutaneous posterior approach also directs the anchor away from the SSN.
Am J Orthop. 2017;46(1):E60-E64. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
1. Snyder SJ, Banas MP, Karzel RP. An analysis of 140 injuries to the superior glenoid labrum. J Shoulder Elbow Surg. 1995;4(4):243-248.
2. Denard PJ, Lädermann A, Burkhart SS. Long-term outcome after arthroscopic repair of type II SLAP lesions: results according to age and workers’ compensation status. Arthroscopy. 2012;28(4):451-457.
3. Gorantla K, Gill C, Wright RW. The outcome of type II SLAP repair: a systematic review. Arthroscopy. 2010;26(4):537-545.
4. Weber SC, Martin DF, Seiler JG 3rd, Harrast JJ. Superior labrum anterior and posterior lesions of the shoulder: incidence rates, complications, and outcomes as reported by American Board of Orthopedic Surgery. Part II candidates. Am J Sports Med. 2012;40(7):1538-1543.
5. Kim SH, Koh YG, Sung CH, Moon HK, Park YS. Iatrogenic suprascapular nerve injury after repair of type II SLAP lesion. Arthroscopy. 2010;26(7):1005-1008.
6. Yoo JC, Lee YS, Ahn JH, Park JH, Kang HJ, Koh KH. Isolated suprascapular nerve injury below the spinoglenoid notch after SLAP repair. J Shoulder Elbow Surg. 2009;18(4):e27-e29.
7. Chan H, Beaupre LA, Bouliane MJ. Injury of the suprascapular nerve during arthroscopic repair of superior labral tears: an anatomic study. J Shoulder Elbow Surg. 2010;19(5):709-715.
8. Koh KH, Park WH, Lim TK, Yoo JC. Medial perforation of the glenoid neck following SLAP repair places the suprascapular nerve at risk: a cadaveric study. J Shoulder Elbow Surg. 2011;20(2):245-250.
9. Morgan RT, Henn RF 3rd, Paryavi E, Dreese J. Injury to the suprascapular nerve during superior labrum anterior and posterior repair: is a rotator interval portal safer than an anterosuperior portal? Arthroscopy. 2014;30(11):1418-1423.
10. Lo IK, Lind CC, Burkhart SS. Glenohumeral arthroscopy portals established using an outside-in technique: neurovascular anatomy at risk. Arthroscopy. 2004;20(6):596-602.
11. Morgan CD, Burkhart SS, Palmeri M, Gillespie M. Type II SLAP lesions: three subtypes and their relationships to superior instability and rotator cuff tears. Arthroscopy. 1998;14(6):553-565.
12. Shishido H, Kikuchi S. Injury of the suprascapular nerve in shoulder surgery: an anatomic study. J Shoulder Elbow Surg. 2001;10(4):372-376.
13. Uggen C, Wei A, Glousman RE, et al. Biomechanical comparison of knotless anchor repair versus simple suture repair for type II SLAP lesions. Arthroscopy. 2009;25(10):1085-1092.
14. Kim SH, Crater RB, Hargens AR. Movement-induced knot migration after anterior stabilization in the shoulder. Arthroscopy. 2013;29(3):485-490.
Take-Home Points
- Anchors placed posterior to the biceps during SLAP repair are at risk for glenoid vault penetration and/or suprascapular nerve (SSN) injury.
- Vault penetration and SSN injury are avoided by using a Port of Wilmington (PW) portal instead of an anterior portal.
- A percutaneous PW portal is safe and passes through the rotator cuff muscle only.
Since being classified by Snyder and colleagues,1 various arthroscopic techniques have been used to repair superior labrum anterior and posterior (SLAP) tears, particularly type II tears. Despite being commonly performed, repairs of SLAP lesions remain challenging. There is high variability in the rate of good/excellent functional outcomes and athletes’ return to previous level of play after SLAP repairs.2,3 Furthermore, the rate of complications after SLAP repair is as high as 5%.4
One of the most common complications of repair of a type II SLAP tear is nerve injury.4 In particular, suprascapular nerve (SSN) injury has occurred after arthroscopic repair of SLAP tears.5,6 Three cadaveric studies have demonstrated that glenoid vault penetration is common during placement of knotted anchors for SLAP repair and that the SSN is at risk during placement of these anchors.7-9 However, 2 of the 3 studies used only an anterior portal in their evaluation of anchor placement. Safety of anchor placement posterior to the biceps tendon may be improved with a percutaneous approach using a Port of Wilmington (PW) portal.10,11 No studies have evaluated the risk of glenoid vault penetration and SSN injury with shorter knotless anchors.
We conducted a study to compare a standard anterosuperolateral (ASL) portal with a percutaneous PW portal for knotless anchors placed posterior to the biceps tendon during repair of SLAP tears. We hypothesized that anchors placed through the PW portal would be less likely to penetrate the glenoid vault and would be farther from the SSN in the event of bone penetration.
Materials and Methods
Six matched pairs of fresh human cadaveric shoulders were used in this study. Each specimen included the scapula, the clavicle, and the humerus. All 6 specimens were male, and their mean age was 41.2 years (range, 23-59 years). Shoulder arthroscopy was performed for placement of SLAP anchors, and open dissection followed.
Anchor Placement
The scapula was clamped and the shoulder placed in the lateral decubitus position with 30° of abduction, 20° of forward flexion, and neutral rotation.10 A standard posterior glenohumeral viewing portal was established and a 30° arthroscope inserted. Both shoulders of each matched pair were randomly assigned to anchor placement through either an ASL portal or a PW portal. Two anchors were placed in the superior glenoid to simulate repair of a posterior SLAP tear.11 Each was a 2.9-mm short (12.5-mm) knotless anchor (BioComposite PushLock; Arthrex) that included a polyetheretherketone (PEEK) eyelet for threading sutures before anchor placement. A drill guide was inserted according to manufacturer guidelines, and a 2.9-mm drill was used to make a bone socket 18 mm deep. The anchor eyelet was loaded with suture tape (Labral Tape; Arthrex), and the anchor and suture were inserted into the socket. The sutures were left uncut to aid in anchor visualization during open dissection. On a right shoulder, the first anchor was placed just posterior to the biceps tendon, at 11 o’clock, and the second anchor about 1 cm posterior to the first, at 10 o’clock. All anchors were placed by an arthroscopy fellowship–trained shoulder surgeon. Before placement, anchor location was confirmed by another arthroscopy fellowship–trained shoulder surgeon.
The ASL portal was created, with an 18-gauge spinal needle and an outside-in technique, about 1 cm lateral to the anterolateral corner of the acromion.
In the opposite shoulder, the PW portal was created, with a percutaneous technique, about 1 cm anterior and 1 cm lateral to the posterolateral corner of the acromion. An 18-gauge spinal needle was inserted to allow a 45° angle of approach to the posterosuperior glenoid.11
Cadaveric Dissection
After anchor placement, another shoulder surgeon performed the dissection. Skin, subcutaneous tissue, deltoid, and clavicle were removed. In the percutaneous specimens, PW portal location relative to rotator cuff was recorded before cuff removal. After overlying soft tissues were removed from a specimen, the anchors were examined for glenoid vault penetration. In the setting of vault penetration, digital calipers were used to measure the shortest distance from anchor to SSN.
Results
In the ASL portal group, 8 (66.7%) of 12 anchors (4/6 at 11 o’clock, 4/6 at 10 o’clock) penetrated the medial glenoid vault.
In the PW portal group, 2 (16.7%) of 12 anchors (1/6 at 11 o’clock, 1/6 at 10 o’clock, both from a single specimen) penetrated the medial glenoid vault. Actually, in each case the eyelet and not the anchor penetrated the vault. In the penetration cases, distance to SSN was 20 mm for the 11 o’clock anchor and 8 mm for the 10 o’clock anchor (Table). Of the 6 portals, 3 passed through the supraspinatus muscle, 2 through the infraspinatus musculotendinous junction, and 1 through the infraspinatus muscle.
Discussion
Our study findings support the hypothesis that SLAP repair anchors placed posterior to the biceps tendon are more likely to remain in bone with use of a percutaneous approach relative to an ASL approach. Our findings also support the growing body of evidence that such anchors placed with an anterior approach increase the risk for SSN injury.
Three other cadaveric studies have evaluated anchor placement for SLAP repair. Chan and colleagues7 evaluated drill penetration during bone socket preparation for SLAP repair in 21 matched pairs of formalin-embalmed cadavers. A 20-mm drill was used for correspondence to a 14.5-mm anchor, though no anchors were inserted, and sockets were created in an open manner. Through a mimicked ASL portal, 1 socket was made anterior to the biceps tendon, at 1 o’clock; then, through a mimicked PW portal, 2 sockets were made posterior to the tendon, at 11 o’clock and 9 to 10 o’clock. Glenoid vault penetration occurred in 29% of the 42 anterior sockets, but only 1 anchor (2.4%) touched the SSN. Penetration did not occur with the 11 o’clock anchors. The 9 to 10 o’clock anchor was at highest risk for SSN injury (9.5%, 4 cases). The study was limited by lack of anchor placement and open creation of bone sockets in embalmed cadavers.
Koh and colleagues8 evaluated arthroscopic placement of anterior SLAP anchors in 6 matched pairs of fresh-frozen cadavers. Through an ASL portal, each 14.5-mm knotted anchor was placed anterior to the biceps tendon, at 1 o’clock. As in the study by Chan and colleagues,7 drill depth was 20 mm. Notably, anchors were seated 2 mm beyond manufacturer recommendations, and the cadavers were of Asian origin, likely indicating smaller glenoids compared to specimens from North America or Europe. All 12 anchors penetrated the glenoid vault; mean distance to SSN was 3.1 mm.
Morgan and colleagues9 compared anterior and ASL portals created for SLAP repairs in 10 matched-pair cadavers. Anchors were placed at 1 o’clock, 11 o’clock, and 10 o’clock. As in the studies by Chan and colleagues7 and Koh and colleagues,8 14.5-mm knotted anchors were used. One anterior anchor (10%) placed through an ASL portal penetrated the cortex by 1 mm, and 2 anterior anchors (20%) placed through anterior portals penetrated the cortex (1 was completely out of the bone). Overall, 65% of 11 o’clock anchors and 100% of 10 o’clock anchors violated the glenoid vault. With the 11 o’clock anchors, mean distance to SSN was 6 mm for ASL portals and 4.2 mm for anterior portals; with the 10 o’clock anchors, mean distance to SSN was 8 mm for ASL portals and 2.1 mm for anterior portals.
Overall, the results of these 3 studies suggest that, with use of ASL portals, placement of SLAP anchors anterior to the biceps tendon is safe. Using the same portals, however, anchors placed posterior to the tendon are at higher risk for glenoid vault penetration. Supporting these findings are our study’s penetration rates: 66.7% for anchors placed through ASL portals and 16.7% for anchors placed through percutaneous PW portals. The different rates are not surprising given that the coracoid process projects anterior to the glenoid and provides additional bone stock for placement of anchors anteriorly vs posteriorly. Therefore, with percutaneous PW portals, the approach angle directs the anchor toward the bone of the coracoid base. Furthermore, the SSN passes nearest the posterior aspect of the glenoid. In a study by Shishido and Kikuchi,12 the distance from the posterior rim of the glenoid to the SSN was 18 mm, and from the superior rim was 29 mm. Therefore, anchors placed with an anterior approach naturally are directed toward the SSN.
In addition to portal placement and approach angle, anchor length likely affects the risks for glenoid vault penetration and SSN injury.
One limitation of this study was the small number of cadavers, all of which were male. Female cadavers and cadavers of other ethnic origins likely have smaller glenoid vaults, and thus their inclusion would have altered our results. This issue was well described in studies mentioned in this article, and our goal was simply to compare ASL portals with percutaneous PW portals, so we think it does not change the fact that the risks for glenoid vault penetration and SSN injury are reduced with use of PW portals for anchors placed posterior to the biceps tendon.
Conclusion
This study was the first to examine glenoid vault penetration and SSN proximity with short anchors for SLAP repair. The risk for glenoid vault penetration during repair of SLAP tears posterior to the biceps tendon was reduced by anchor placement with a percutaneous posterior approach. The percutaneous posterior approach also directs the anchor away from the SSN.
Am J Orthop. 2017;46(1):E60-E64. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
Take-Home Points
- Anchors placed posterior to the biceps during SLAP repair are at risk for glenoid vault penetration and/or suprascapular nerve (SSN) injury.
- Vault penetration and SSN injury are avoided by using a Port of Wilmington (PW) portal instead of an anterior portal.
- A percutaneous PW portal is safe and passes through the rotator cuff muscle only.
Since being classified by Snyder and colleagues,1 various arthroscopic techniques have been used to repair superior labrum anterior and posterior (SLAP) tears, particularly type II tears. Despite being commonly performed, repairs of SLAP lesions remain challenging. There is high variability in the rate of good/excellent functional outcomes and athletes’ return to previous level of play after SLAP repairs.2,3 Furthermore, the rate of complications after SLAP repair is as high as 5%.4
One of the most common complications of repair of a type II SLAP tear is nerve injury.4 In particular, suprascapular nerve (SSN) injury has occurred after arthroscopic repair of SLAP tears.5,6 Three cadaveric studies have demonstrated that glenoid vault penetration is common during placement of knotted anchors for SLAP repair and that the SSN is at risk during placement of these anchors.7-9 However, 2 of the 3 studies used only an anterior portal in their evaluation of anchor placement. Safety of anchor placement posterior to the biceps tendon may be improved with a percutaneous approach using a Port of Wilmington (PW) portal.10,11 No studies have evaluated the risk of glenoid vault penetration and SSN injury with shorter knotless anchors.
We conducted a study to compare a standard anterosuperolateral (ASL) portal with a percutaneous PW portal for knotless anchors placed posterior to the biceps tendon during repair of SLAP tears. We hypothesized that anchors placed through the PW portal would be less likely to penetrate the glenoid vault and would be farther from the SSN in the event of bone penetration.
Materials and Methods
Six matched pairs of fresh human cadaveric shoulders were used in this study. Each specimen included the scapula, the clavicle, and the humerus. All 6 specimens were male, and their mean age was 41.2 years (range, 23-59 years). Shoulder arthroscopy was performed for placement of SLAP anchors, and open dissection followed.
Anchor Placement
The scapula was clamped and the shoulder placed in the lateral decubitus position with 30° of abduction, 20° of forward flexion, and neutral rotation.10 A standard posterior glenohumeral viewing portal was established and a 30° arthroscope inserted. Both shoulders of each matched pair were randomly assigned to anchor placement through either an ASL portal or a PW portal. Two anchors were placed in the superior glenoid to simulate repair of a posterior SLAP tear.11 Each was a 2.9-mm short (12.5-mm) knotless anchor (BioComposite PushLock; Arthrex) that included a polyetheretherketone (PEEK) eyelet for threading sutures before anchor placement. A drill guide was inserted according to manufacturer guidelines, and a 2.9-mm drill was used to make a bone socket 18 mm deep. The anchor eyelet was loaded with suture tape (Labral Tape; Arthrex), and the anchor and suture were inserted into the socket. The sutures were left uncut to aid in anchor visualization during open dissection. On a right shoulder, the first anchor was placed just posterior to the biceps tendon, at 11 o’clock, and the second anchor about 1 cm posterior to the first, at 10 o’clock. All anchors were placed by an arthroscopy fellowship–trained shoulder surgeon. Before placement, anchor location was confirmed by another arthroscopy fellowship–trained shoulder surgeon.
The ASL portal was created, with an 18-gauge spinal needle and an outside-in technique, about 1 cm lateral to the anterolateral corner of the acromion.
In the opposite shoulder, the PW portal was created, with a percutaneous technique, about 1 cm anterior and 1 cm lateral to the posterolateral corner of the acromion. An 18-gauge spinal needle was inserted to allow a 45° angle of approach to the posterosuperior glenoid.11
Cadaveric Dissection
After anchor placement, another shoulder surgeon performed the dissection. Skin, subcutaneous tissue, deltoid, and clavicle were removed. In the percutaneous specimens, PW portal location relative to rotator cuff was recorded before cuff removal. After overlying soft tissues were removed from a specimen, the anchors were examined for glenoid vault penetration. In the setting of vault penetration, digital calipers were used to measure the shortest distance from anchor to SSN.
Results
In the ASL portal group, 8 (66.7%) of 12 anchors (4/6 at 11 o’clock, 4/6 at 10 o’clock) penetrated the medial glenoid vault.
In the PW portal group, 2 (16.7%) of 12 anchors (1/6 at 11 o’clock, 1/6 at 10 o’clock, both from a single specimen) penetrated the medial glenoid vault. Actually, in each case the eyelet and not the anchor penetrated the vault. In the penetration cases, distance to SSN was 20 mm for the 11 o’clock anchor and 8 mm for the 10 o’clock anchor (Table). Of the 6 portals, 3 passed through the supraspinatus muscle, 2 through the infraspinatus musculotendinous junction, and 1 through the infraspinatus muscle.
Discussion
Our study findings support the hypothesis that SLAP repair anchors placed posterior to the biceps tendon are more likely to remain in bone with use of a percutaneous approach relative to an ASL approach. Our findings also support the growing body of evidence that such anchors placed with an anterior approach increase the risk for SSN injury.
Three other cadaveric studies have evaluated anchor placement for SLAP repair. Chan and colleagues7 evaluated drill penetration during bone socket preparation for SLAP repair in 21 matched pairs of formalin-embalmed cadavers. A 20-mm drill was used for correspondence to a 14.5-mm anchor, though no anchors were inserted, and sockets were created in an open manner. Through a mimicked ASL portal, 1 socket was made anterior to the biceps tendon, at 1 o’clock; then, through a mimicked PW portal, 2 sockets were made posterior to the tendon, at 11 o’clock and 9 to 10 o’clock. Glenoid vault penetration occurred in 29% of the 42 anterior sockets, but only 1 anchor (2.4%) touched the SSN. Penetration did not occur with the 11 o’clock anchors. The 9 to 10 o’clock anchor was at highest risk for SSN injury (9.5%, 4 cases). The study was limited by lack of anchor placement and open creation of bone sockets in embalmed cadavers.
Koh and colleagues8 evaluated arthroscopic placement of anterior SLAP anchors in 6 matched pairs of fresh-frozen cadavers. Through an ASL portal, each 14.5-mm knotted anchor was placed anterior to the biceps tendon, at 1 o’clock. As in the study by Chan and colleagues,7 drill depth was 20 mm. Notably, anchors were seated 2 mm beyond manufacturer recommendations, and the cadavers were of Asian origin, likely indicating smaller glenoids compared to specimens from North America or Europe. All 12 anchors penetrated the glenoid vault; mean distance to SSN was 3.1 mm.
Morgan and colleagues9 compared anterior and ASL portals created for SLAP repairs in 10 matched-pair cadavers. Anchors were placed at 1 o’clock, 11 o’clock, and 10 o’clock. As in the studies by Chan and colleagues7 and Koh and colleagues,8 14.5-mm knotted anchors were used. One anterior anchor (10%) placed through an ASL portal penetrated the cortex by 1 mm, and 2 anterior anchors (20%) placed through anterior portals penetrated the cortex (1 was completely out of the bone). Overall, 65% of 11 o’clock anchors and 100% of 10 o’clock anchors violated the glenoid vault. With the 11 o’clock anchors, mean distance to SSN was 6 mm for ASL portals and 4.2 mm for anterior portals; with the 10 o’clock anchors, mean distance to SSN was 8 mm for ASL portals and 2.1 mm for anterior portals.
Overall, the results of these 3 studies suggest that, with use of ASL portals, placement of SLAP anchors anterior to the biceps tendon is safe. Using the same portals, however, anchors placed posterior to the tendon are at higher risk for glenoid vault penetration. Supporting these findings are our study’s penetration rates: 66.7% for anchors placed through ASL portals and 16.7% for anchors placed through percutaneous PW portals. The different rates are not surprising given that the coracoid process projects anterior to the glenoid and provides additional bone stock for placement of anchors anteriorly vs posteriorly. Therefore, with percutaneous PW portals, the approach angle directs the anchor toward the bone of the coracoid base. Furthermore, the SSN passes nearest the posterior aspect of the glenoid. In a study by Shishido and Kikuchi,12 the distance from the posterior rim of the glenoid to the SSN was 18 mm, and from the superior rim was 29 mm. Therefore, anchors placed with an anterior approach naturally are directed toward the SSN.
In addition to portal placement and approach angle, anchor length likely affects the risks for glenoid vault penetration and SSN injury.
One limitation of this study was the small number of cadavers, all of which were male. Female cadavers and cadavers of other ethnic origins likely have smaller glenoid vaults, and thus their inclusion would have altered our results. This issue was well described in studies mentioned in this article, and our goal was simply to compare ASL portals with percutaneous PW portals, so we think it does not change the fact that the risks for glenoid vault penetration and SSN injury are reduced with use of PW portals for anchors placed posterior to the biceps tendon.
Conclusion
This study was the first to examine glenoid vault penetration and SSN proximity with short anchors for SLAP repair. The risk for glenoid vault penetration during repair of SLAP tears posterior to the biceps tendon was reduced by anchor placement with a percutaneous posterior approach. The percutaneous posterior approach also directs the anchor away from the SSN.
Am J Orthop. 2017;46(1):E60-E64. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
1. Snyder SJ, Banas MP, Karzel RP. An analysis of 140 injuries to the superior glenoid labrum. J Shoulder Elbow Surg. 1995;4(4):243-248.
2. Denard PJ, Lädermann A, Burkhart SS. Long-term outcome after arthroscopic repair of type II SLAP lesions: results according to age and workers’ compensation status. Arthroscopy. 2012;28(4):451-457.
3. Gorantla K, Gill C, Wright RW. The outcome of type II SLAP repair: a systematic review. Arthroscopy. 2010;26(4):537-545.
4. Weber SC, Martin DF, Seiler JG 3rd, Harrast JJ. Superior labrum anterior and posterior lesions of the shoulder: incidence rates, complications, and outcomes as reported by American Board of Orthopedic Surgery. Part II candidates. Am J Sports Med. 2012;40(7):1538-1543.
5. Kim SH, Koh YG, Sung CH, Moon HK, Park YS. Iatrogenic suprascapular nerve injury after repair of type II SLAP lesion. Arthroscopy. 2010;26(7):1005-1008.
6. Yoo JC, Lee YS, Ahn JH, Park JH, Kang HJ, Koh KH. Isolated suprascapular nerve injury below the spinoglenoid notch after SLAP repair. J Shoulder Elbow Surg. 2009;18(4):e27-e29.
7. Chan H, Beaupre LA, Bouliane MJ. Injury of the suprascapular nerve during arthroscopic repair of superior labral tears: an anatomic study. J Shoulder Elbow Surg. 2010;19(5):709-715.
8. Koh KH, Park WH, Lim TK, Yoo JC. Medial perforation of the glenoid neck following SLAP repair places the suprascapular nerve at risk: a cadaveric study. J Shoulder Elbow Surg. 2011;20(2):245-250.
9. Morgan RT, Henn RF 3rd, Paryavi E, Dreese J. Injury to the suprascapular nerve during superior labrum anterior and posterior repair: is a rotator interval portal safer than an anterosuperior portal? Arthroscopy. 2014;30(11):1418-1423.
10. Lo IK, Lind CC, Burkhart SS. Glenohumeral arthroscopy portals established using an outside-in technique: neurovascular anatomy at risk. Arthroscopy. 2004;20(6):596-602.
11. Morgan CD, Burkhart SS, Palmeri M, Gillespie M. Type II SLAP lesions: three subtypes and their relationships to superior instability and rotator cuff tears. Arthroscopy. 1998;14(6):553-565.
12. Shishido H, Kikuchi S. Injury of the suprascapular nerve in shoulder surgery: an anatomic study. J Shoulder Elbow Surg. 2001;10(4):372-376.
13. Uggen C, Wei A, Glousman RE, et al. Biomechanical comparison of knotless anchor repair versus simple suture repair for type II SLAP lesions. Arthroscopy. 2009;25(10):1085-1092.
14. Kim SH, Crater RB, Hargens AR. Movement-induced knot migration after anterior stabilization in the shoulder. Arthroscopy. 2013;29(3):485-490.
1. Snyder SJ, Banas MP, Karzel RP. An analysis of 140 injuries to the superior glenoid labrum. J Shoulder Elbow Surg. 1995;4(4):243-248.
2. Denard PJ, Lädermann A, Burkhart SS. Long-term outcome after arthroscopic repair of type II SLAP lesions: results according to age and workers’ compensation status. Arthroscopy. 2012;28(4):451-457.
3. Gorantla K, Gill C, Wright RW. The outcome of type II SLAP repair: a systematic review. Arthroscopy. 2010;26(4):537-545.
4. Weber SC, Martin DF, Seiler JG 3rd, Harrast JJ. Superior labrum anterior and posterior lesions of the shoulder: incidence rates, complications, and outcomes as reported by American Board of Orthopedic Surgery. Part II candidates. Am J Sports Med. 2012;40(7):1538-1543.
5. Kim SH, Koh YG, Sung CH, Moon HK, Park YS. Iatrogenic suprascapular nerve injury after repair of type II SLAP lesion. Arthroscopy. 2010;26(7):1005-1008.
6. Yoo JC, Lee YS, Ahn JH, Park JH, Kang HJ, Koh KH. Isolated suprascapular nerve injury below the spinoglenoid notch after SLAP repair. J Shoulder Elbow Surg. 2009;18(4):e27-e29.
7. Chan H, Beaupre LA, Bouliane MJ. Injury of the suprascapular nerve during arthroscopic repair of superior labral tears: an anatomic study. J Shoulder Elbow Surg. 2010;19(5):709-715.
8. Koh KH, Park WH, Lim TK, Yoo JC. Medial perforation of the glenoid neck following SLAP repair places the suprascapular nerve at risk: a cadaveric study. J Shoulder Elbow Surg. 2011;20(2):245-250.
9. Morgan RT, Henn RF 3rd, Paryavi E, Dreese J. Injury to the suprascapular nerve during superior labrum anterior and posterior repair: is a rotator interval portal safer than an anterosuperior portal? Arthroscopy. 2014;30(11):1418-1423.
10. Lo IK, Lind CC, Burkhart SS. Glenohumeral arthroscopy portals established using an outside-in technique: neurovascular anatomy at risk. Arthroscopy. 2004;20(6):596-602.
11. Morgan CD, Burkhart SS, Palmeri M, Gillespie M. Type II SLAP lesions: three subtypes and their relationships to superior instability and rotator cuff tears. Arthroscopy. 1998;14(6):553-565.
12. Shishido H, Kikuchi S. Injury of the suprascapular nerve in shoulder surgery: an anatomic study. J Shoulder Elbow Surg. 2001;10(4):372-376.
13. Uggen C, Wei A, Glousman RE, et al. Biomechanical comparison of knotless anchor repair versus simple suture repair for type II SLAP lesions. Arthroscopy. 2009;25(10):1085-1092.
14. Kim SH, Crater RB, Hargens AR. Movement-induced knot migration after anterior stabilization in the shoulder. Arthroscopy. 2013;29(3):485-490.
Medication for life
Some areas of psychiatry would benefit from more controversy. One of them is the prescription of antidepressants to young people dealing with romantic disappointments.
I have seen many young men and women given an antidepressant for the very painful, but ordinary, romantic break-ups characteristic of this phase of life, who then become habituated to the drug. They take the medication indefinitely, their brains accommodate neurophysiologically to the presence of the chemical, and they become unable to discontinue it without intolerable withdrawal symptoms that look like an underlying illness. A parallel phenomenon occurs not infrequently with the use of amphetamines (and other stimulants) for attention-deficit hyperactivity disorder that is at times mistakenly diagnosed in this age group.
Antidepressants for early romantic disappointments
Mr. A, now in his 30s, became sullen and withdrawn at age 16 after a girl refused his romantic approaches. His well-intentioned parents took him to a psychiatrist, who, after a brief evaluation, prescribed fluoxetine. Mr. A is now well adjusted and happily married but unable to get off fluoxetine. Even when it is carefully tapered, 2 or 3 months after it is discontinued, he becomes anxious and depressed. This is an iatrogenic problem. It is not related to goings-on in his mind or his life; rather it is the result of his brain’s accommodation to a medication, producing a serious withdrawal syndrome.
His original psychiatrist made only a descriptive diagnosis. He did not inquire about what was going on in Mr. A’s mind and thus could not make a dynamic diagnosis (that is, a diagnosis of a patient’s central emotional conflicts, ability to function in relation to other people, strengths, and weaknesses). Mr. A, like many adolescents, had a lot of anxiety and guilt about sexual and romantic involvement, and potential success. He defended against his anxiety and guilt by assuring himself life would never work out for him. When the girl he admired rebuffed him, he immediately concluded this would perpetually be his fate, so the girl’s refusal was particularly painful. Mr. A feels that had this dynamic been discussed with him at the time, he may well not have needed medication at all.
Ms. B, like Mr. A, was prescribed antidepressants for depressive reactions to early romantic disappointments. Likewise, she self-punitively convinced herself, despite easily attracting men’s attentions, that these disappointments meant a lifetime alone. Ms. B has a family history of depression (although neither of her brothers struggles with it), and she felt that she needed the medications to help negotiate difficult periods. But should she have been on them for extended periods of time? Therapeutic attention to her emotional conflicts helped her to form lasting relationships, marry, and have children. Unable to get off the medications, she had to deal with the risks of their use during pregnancy, which she then subjected to the same sort of guilty self-accusations as she previously had used to limit her romantic prospects.
Ms. C came to me on three medications – one for each of her significant romantic break-ups. She, too, was depressively self-diminishing, beginning therapy by letting me know all the things she could think of that might make me think less of her. Understanding some of the reasons for her self-deprecation helped her toward better romantic relationships but did not give her the courage to get off her medications. Pregnancy, however, led her to promptly and successfully discontinue an antidepressant and a mood stabilizer (she has never had any symptoms suggestive of manic depression). She remained on a low dose of a selective serotonin reuptake inhibitor, had an uneventful pregnancy, and then fell in love with a charming baby.
Principles for consideration
• Psychiatrists (and other mental health professionals and primary care physicians treating mental illness) should always make a dynamic, and not merely a descriptive, diagnosis. Even with a more clearly biologically driven problem, such as bipolar disorder, the patient’s personality and conflicts matter.
• Psychiatrists should be very judicious about prescribing medications in adolescence and young adulthood, especially for difficulties adapting to the typical events of those phases of life. Expert psychotherapy should be the first choice in these instances.
• Medication, when necessary, should be prescribed for as limited a time as possible. It is important for young people to advance their own development, not feel needlessly beholden to medications, not get iatrogenically dependent on them, and not feel that they have “diseases” they don’t have.
Amphetamines for misdiagnosed ADHD
When Ms. D’s family moved to a new house, she, her brother, and her sister, each attended a new school. Unlike her siblings, Ms. D, who was in high school, had a difficult adjustment. Her grades fell. She was taken to a psychiatrist who diagnosed ADHD and prescribed amphetamines. The psychiatrist paid little attention to her prior lack of difficulty in school or her struggles making new friends. Nor did the psychiatrist learn that Ms. D had to ward off the seductive advances of an older teacher (although Ms. D would likely not have been immediately forthcoming about this at the time).
When Ms. D came to me as a college student, for troubles with anger, anxiety, and some depression, she was religiously taking 70 mg of amphetamines daily. After I learned a bit about her and raised the question of whether she actually had ADHD, and whether it might make sense to consider tapering the amphetamines, she was appalled and looked like a toddler who was afraid I was about to steal her candy. Helping her to get off the unneeded medication was a multiyear process.
First, she had to recognize that it was prescribed to treat a problem she probably didn’t have, and second, that it was failing to help her with the problems she did have. As we attended to some of her actual emotional conflicts, she became willing to experiment with lower doses. She was able to see that her work was little changed as the dose was lowered, and that her difficulties with school had more to do with feelings toward classmates and teachers than with the presence or absence of amphetamines. After a protracted struggle, finally off the medication, she felt in charge of her life and no longer believed there was something inherently wrong with her mind or her brain.
Mr. E was the only son in a high-powered academic family. His older sisters were all intellectual standouts. Early in high school, he received his first B as a grade in a course. He was taken to a pediatrician, diagnosed with ADHD, and put on stimulants. Like Ms. D, he came to believe that he needed them. In college, he began to develop some magical aspects to his thinking, a potential side effect of the stimulants. It was very difficult to help him see either that he had a problem with his thinking or that it might be attributable to the medication.
Principles to consider
• If the ADHD wasn’t there in elementary school or before, it is unlikely that an adolescent or young adult has new-onset ADHD. A new or newly amplified conflict is occurring in the person’s mind and life A dynamic diagnosis, as always, is essential.
• When medication is prescribed for actual ADHD, as with anything else, the question of how long it will be taken must be asked. For life? Until other means of adaptation are accomplished? Until adequate outcome studies of long-term use of the medication are performed?
Helping patients to get off unneeded, or no longer needed, medications can be a difficult task. Their emotional attachments to the medications can be intense and varied. For some, the prescription is a sign of being loved and cared for. For others, it represents a certification of a deficit, appeases guilt about success, and/or attests to the need for special consideration. Insofar as the medication has been helpful, it may have come to be regarded as a dearly loved friend, or even a part of the self.
When medication has been helpful, there is also, of course, concern about the potential return of the difficulties for which it was prescribed. Few patients are told at the time of first prescription that there is potential risk of habituation and return of, or potential exaggeration of, symptoms with discontinuation. This type of discussion is more difficult to have in situations in which a prescription is urgently needed and the patient is reluctant, but is still not often done in those instances in which a prescription is more optional than essential. The picture is seldom simple.
These few comments only scratch the surface of the difficulties doctors and patients face in helping patients to discontinue their medications. Residency programs pay a lot of attention to helping trainees learn to prescribe medications; rarely do they sufficiently educate residents how to help patients discontinue them. The fact that so many residencies currently pay limited attention to interventions apart from medication contributes further to the difficulty.
Medications have saved the life of many a psychiatric patient. Some patients need medication for life. But some end up on medication for life, even in some instances when the medication may not have been needed in the first place. Although it is often a difficult task, we need to do a better job of distinguishing which patients are which.
Dr. Blum is a psychiatrist and psychoanalyst in private practice in Philadelphia. He teaches in the departments of anthropology and psychiatry at the University of Pennsylvania and at the Psychoanalytic Center of Philadelphia.
Some areas of psychiatry would benefit from more controversy. One of them is the prescription of antidepressants to young people dealing with romantic disappointments.
I have seen many young men and women given an antidepressant for the very painful, but ordinary, romantic break-ups characteristic of this phase of life, who then become habituated to the drug. They take the medication indefinitely, their brains accommodate neurophysiologically to the presence of the chemical, and they become unable to discontinue it without intolerable withdrawal symptoms that look like an underlying illness. A parallel phenomenon occurs not infrequently with the use of amphetamines (and other stimulants) for attention-deficit hyperactivity disorder that is at times mistakenly diagnosed in this age group.
Antidepressants for early romantic disappointments
Mr. A, now in his 30s, became sullen and withdrawn at age 16 after a girl refused his romantic approaches. His well-intentioned parents took him to a psychiatrist, who, after a brief evaluation, prescribed fluoxetine. Mr. A is now well adjusted and happily married but unable to get off fluoxetine. Even when it is carefully tapered, 2 or 3 months after it is discontinued, he becomes anxious and depressed. This is an iatrogenic problem. It is not related to goings-on in his mind or his life; rather it is the result of his brain’s accommodation to a medication, producing a serious withdrawal syndrome.
His original psychiatrist made only a descriptive diagnosis. He did not inquire about what was going on in Mr. A’s mind and thus could not make a dynamic diagnosis (that is, a diagnosis of a patient’s central emotional conflicts, ability to function in relation to other people, strengths, and weaknesses). Mr. A, like many adolescents, had a lot of anxiety and guilt about sexual and romantic involvement, and potential success. He defended against his anxiety and guilt by assuring himself life would never work out for him. When the girl he admired rebuffed him, he immediately concluded this would perpetually be his fate, so the girl’s refusal was particularly painful. Mr. A feels that had this dynamic been discussed with him at the time, he may well not have needed medication at all.
Ms. B, like Mr. A, was prescribed antidepressants for depressive reactions to early romantic disappointments. Likewise, she self-punitively convinced herself, despite easily attracting men’s attentions, that these disappointments meant a lifetime alone. Ms. B has a family history of depression (although neither of her brothers struggles with it), and she felt that she needed the medications to help negotiate difficult periods. But should she have been on them for extended periods of time? Therapeutic attention to her emotional conflicts helped her to form lasting relationships, marry, and have children. Unable to get off the medications, she had to deal with the risks of their use during pregnancy, which she then subjected to the same sort of guilty self-accusations as she previously had used to limit her romantic prospects.
Ms. C came to me on three medications – one for each of her significant romantic break-ups. She, too, was depressively self-diminishing, beginning therapy by letting me know all the things she could think of that might make me think less of her. Understanding some of the reasons for her self-deprecation helped her toward better romantic relationships but did not give her the courage to get off her medications. Pregnancy, however, led her to promptly and successfully discontinue an antidepressant and a mood stabilizer (she has never had any symptoms suggestive of manic depression). She remained on a low dose of a selective serotonin reuptake inhibitor, had an uneventful pregnancy, and then fell in love with a charming baby.
Principles for consideration
• Psychiatrists (and other mental health professionals and primary care physicians treating mental illness) should always make a dynamic, and not merely a descriptive, diagnosis. Even with a more clearly biologically driven problem, such as bipolar disorder, the patient’s personality and conflicts matter.
• Psychiatrists should be very judicious about prescribing medications in adolescence and young adulthood, especially for difficulties adapting to the typical events of those phases of life. Expert psychotherapy should be the first choice in these instances.
• Medication, when necessary, should be prescribed for as limited a time as possible. It is important for young people to advance their own development, not feel needlessly beholden to medications, not get iatrogenically dependent on them, and not feel that they have “diseases” they don’t have.
Amphetamines for misdiagnosed ADHD
When Ms. D’s family moved to a new house, she, her brother, and her sister, each attended a new school. Unlike her siblings, Ms. D, who was in high school, had a difficult adjustment. Her grades fell. She was taken to a psychiatrist who diagnosed ADHD and prescribed amphetamines. The psychiatrist paid little attention to her prior lack of difficulty in school or her struggles making new friends. Nor did the psychiatrist learn that Ms. D had to ward off the seductive advances of an older teacher (although Ms. D would likely not have been immediately forthcoming about this at the time).
When Ms. D came to me as a college student, for troubles with anger, anxiety, and some depression, she was religiously taking 70 mg of amphetamines daily. After I learned a bit about her and raised the question of whether she actually had ADHD, and whether it might make sense to consider tapering the amphetamines, she was appalled and looked like a toddler who was afraid I was about to steal her candy. Helping her to get off the unneeded medication was a multiyear process.
First, she had to recognize that it was prescribed to treat a problem she probably didn’t have, and second, that it was failing to help her with the problems she did have. As we attended to some of her actual emotional conflicts, she became willing to experiment with lower doses. She was able to see that her work was little changed as the dose was lowered, and that her difficulties with school had more to do with feelings toward classmates and teachers than with the presence or absence of amphetamines. After a protracted struggle, finally off the medication, she felt in charge of her life and no longer believed there was something inherently wrong with her mind or her brain.
Mr. E was the only son in a high-powered academic family. His older sisters were all intellectual standouts. Early in high school, he received his first B as a grade in a course. He was taken to a pediatrician, diagnosed with ADHD, and put on stimulants. Like Ms. D, he came to believe that he needed them. In college, he began to develop some magical aspects to his thinking, a potential side effect of the stimulants. It was very difficult to help him see either that he had a problem with his thinking or that it might be attributable to the medication.
Principles to consider
• If the ADHD wasn’t there in elementary school or before, it is unlikely that an adolescent or young adult has new-onset ADHD. A new or newly amplified conflict is occurring in the person’s mind and life A dynamic diagnosis, as always, is essential.
• When medication is prescribed for actual ADHD, as with anything else, the question of how long it will be taken must be asked. For life? Until other means of adaptation are accomplished? Until adequate outcome studies of long-term use of the medication are performed?
Helping patients to get off unneeded, or no longer needed, medications can be a difficult task. Their emotional attachments to the medications can be intense and varied. For some, the prescription is a sign of being loved and cared for. For others, it represents a certification of a deficit, appeases guilt about success, and/or attests to the need for special consideration. Insofar as the medication has been helpful, it may have come to be regarded as a dearly loved friend, or even a part of the self.
When medication has been helpful, there is also, of course, concern about the potential return of the difficulties for which it was prescribed. Few patients are told at the time of first prescription that there is potential risk of habituation and return of, or potential exaggeration of, symptoms with discontinuation. This type of discussion is more difficult to have in situations in which a prescription is urgently needed and the patient is reluctant, but is still not often done in those instances in which a prescription is more optional than essential. The picture is seldom simple.
These few comments only scratch the surface of the difficulties doctors and patients face in helping patients to discontinue their medications. Residency programs pay a lot of attention to helping trainees learn to prescribe medications; rarely do they sufficiently educate residents how to help patients discontinue them. The fact that so many residencies currently pay limited attention to interventions apart from medication contributes further to the difficulty.
Medications have saved the life of many a psychiatric patient. Some patients need medication for life. But some end up on medication for life, even in some instances when the medication may not have been needed in the first place. Although it is often a difficult task, we need to do a better job of distinguishing which patients are which.
Dr. Blum is a psychiatrist and psychoanalyst in private practice in Philadelphia. He teaches in the departments of anthropology and psychiatry at the University of Pennsylvania and at the Psychoanalytic Center of Philadelphia.
Some areas of psychiatry would benefit from more controversy. One of them is the prescription of antidepressants to young people dealing with romantic disappointments.
I have seen many young men and women given an antidepressant for the very painful, but ordinary, romantic break-ups characteristic of this phase of life, who then become habituated to the drug. They take the medication indefinitely, their brains accommodate neurophysiologically to the presence of the chemical, and they become unable to discontinue it without intolerable withdrawal symptoms that look like an underlying illness. A parallel phenomenon occurs not infrequently with the use of amphetamines (and other stimulants) for attention-deficit hyperactivity disorder that is at times mistakenly diagnosed in this age group.
Antidepressants for early romantic disappointments
Mr. A, now in his 30s, became sullen and withdrawn at age 16 after a girl refused his romantic approaches. His well-intentioned parents took him to a psychiatrist, who, after a brief evaluation, prescribed fluoxetine. Mr. A is now well adjusted and happily married but unable to get off fluoxetine. Even when it is carefully tapered, 2 or 3 months after it is discontinued, he becomes anxious and depressed. This is an iatrogenic problem. It is not related to goings-on in his mind or his life; rather it is the result of his brain’s accommodation to a medication, producing a serious withdrawal syndrome.
His original psychiatrist made only a descriptive diagnosis. He did not inquire about what was going on in Mr. A’s mind and thus could not make a dynamic diagnosis (that is, a diagnosis of a patient’s central emotional conflicts, ability to function in relation to other people, strengths, and weaknesses). Mr. A, like many adolescents, had a lot of anxiety and guilt about sexual and romantic involvement, and potential success. He defended against his anxiety and guilt by assuring himself life would never work out for him. When the girl he admired rebuffed him, he immediately concluded this would perpetually be his fate, so the girl’s refusal was particularly painful. Mr. A feels that had this dynamic been discussed with him at the time, he may well not have needed medication at all.
Ms. B, like Mr. A, was prescribed antidepressants for depressive reactions to early romantic disappointments. Likewise, she self-punitively convinced herself, despite easily attracting men’s attentions, that these disappointments meant a lifetime alone. Ms. B has a family history of depression (although neither of her brothers struggles with it), and she felt that she needed the medications to help negotiate difficult periods. But should she have been on them for extended periods of time? Therapeutic attention to her emotional conflicts helped her to form lasting relationships, marry, and have children. Unable to get off the medications, she had to deal with the risks of their use during pregnancy, which she then subjected to the same sort of guilty self-accusations as she previously had used to limit her romantic prospects.
Ms. C came to me on three medications – one for each of her significant romantic break-ups. She, too, was depressively self-diminishing, beginning therapy by letting me know all the things she could think of that might make me think less of her. Understanding some of the reasons for her self-deprecation helped her toward better romantic relationships but did not give her the courage to get off her medications. Pregnancy, however, led her to promptly and successfully discontinue an antidepressant and a mood stabilizer (she has never had any symptoms suggestive of manic depression). She remained on a low dose of a selective serotonin reuptake inhibitor, had an uneventful pregnancy, and then fell in love with a charming baby.
Principles for consideration
• Psychiatrists (and other mental health professionals and primary care physicians treating mental illness) should always make a dynamic, and not merely a descriptive, diagnosis. Even with a more clearly biologically driven problem, such as bipolar disorder, the patient’s personality and conflicts matter.
• Psychiatrists should be very judicious about prescribing medications in adolescence and young adulthood, especially for difficulties adapting to the typical events of those phases of life. Expert psychotherapy should be the first choice in these instances.
• Medication, when necessary, should be prescribed for as limited a time as possible. It is important for young people to advance their own development, not feel needlessly beholden to medications, not get iatrogenically dependent on them, and not feel that they have “diseases” they don’t have.
Amphetamines for misdiagnosed ADHD
When Ms. D’s family moved to a new house, she, her brother, and her sister, each attended a new school. Unlike her siblings, Ms. D, who was in high school, had a difficult adjustment. Her grades fell. She was taken to a psychiatrist who diagnosed ADHD and prescribed amphetamines. The psychiatrist paid little attention to her prior lack of difficulty in school or her struggles making new friends. Nor did the psychiatrist learn that Ms. D had to ward off the seductive advances of an older teacher (although Ms. D would likely not have been immediately forthcoming about this at the time).
When Ms. D came to me as a college student, for troubles with anger, anxiety, and some depression, she was religiously taking 70 mg of amphetamines daily. After I learned a bit about her and raised the question of whether she actually had ADHD, and whether it might make sense to consider tapering the amphetamines, she was appalled and looked like a toddler who was afraid I was about to steal her candy. Helping her to get off the unneeded medication was a multiyear process.
First, she had to recognize that it was prescribed to treat a problem she probably didn’t have, and second, that it was failing to help her with the problems she did have. As we attended to some of her actual emotional conflicts, she became willing to experiment with lower doses. She was able to see that her work was little changed as the dose was lowered, and that her difficulties with school had more to do with feelings toward classmates and teachers than with the presence or absence of amphetamines. After a protracted struggle, finally off the medication, she felt in charge of her life and no longer believed there was something inherently wrong with her mind or her brain.
Mr. E was the only son in a high-powered academic family. His older sisters were all intellectual standouts. Early in high school, he received his first B as a grade in a course. He was taken to a pediatrician, diagnosed with ADHD, and put on stimulants. Like Ms. D, he came to believe that he needed them. In college, he began to develop some magical aspects to his thinking, a potential side effect of the stimulants. It was very difficult to help him see either that he had a problem with his thinking or that it might be attributable to the medication.
Principles to consider
• If the ADHD wasn’t there in elementary school or before, it is unlikely that an adolescent or young adult has new-onset ADHD. A new or newly amplified conflict is occurring in the person’s mind and life A dynamic diagnosis, as always, is essential.
• When medication is prescribed for actual ADHD, as with anything else, the question of how long it will be taken must be asked. For life? Until other means of adaptation are accomplished? Until adequate outcome studies of long-term use of the medication are performed?
Helping patients to get off unneeded, or no longer needed, medications can be a difficult task. Their emotional attachments to the medications can be intense and varied. For some, the prescription is a sign of being loved and cared for. For others, it represents a certification of a deficit, appeases guilt about success, and/or attests to the need for special consideration. Insofar as the medication has been helpful, it may have come to be regarded as a dearly loved friend, or even a part of the self.
When medication has been helpful, there is also, of course, concern about the potential return of the difficulties for which it was prescribed. Few patients are told at the time of first prescription that there is potential risk of habituation and return of, or potential exaggeration of, symptoms with discontinuation. This type of discussion is more difficult to have in situations in which a prescription is urgently needed and the patient is reluctant, but is still not often done in those instances in which a prescription is more optional than essential. The picture is seldom simple.
These few comments only scratch the surface of the difficulties doctors and patients face in helping patients to discontinue their medications. Residency programs pay a lot of attention to helping trainees learn to prescribe medications; rarely do they sufficiently educate residents how to help patients discontinue them. The fact that so many residencies currently pay limited attention to interventions apart from medication contributes further to the difficulty.
Medications have saved the life of many a psychiatric patient. Some patients need medication for life. But some end up on medication for life, even in some instances when the medication may not have been needed in the first place. Although it is often a difficult task, we need to do a better job of distinguishing which patients are which.
Dr. Blum is a psychiatrist and psychoanalyst in private practice in Philadelphia. He teaches in the departments of anthropology and psychiatry at the University of Pennsylvania and at the Psychoanalytic Center of Philadelphia.
Aortic repair in Loeys-Dietz syndrome requires close follow-up
The knowledge about Loeys-Dietz syndrome has evolved quickly since Hal Dietz, MD, and Bart Loeys, MD, at Johns Hopkins University, Baltimore, first reported on it in 2005. Now, another team of Johns Hopkins investigators have reported that an aggressive approach with aortic root replacement coupled with valve-sparing whenever possible produces favorable results, but that clinicians must follow these patients closely with cardiovascular imaging.
“Growing experience with Loeys-Dietz syndrome has confirmed early impressions of its aggressive nature and proclivity toward aortic catastrophe,” Nishant D. Patel, MD, and his coauthors said in the February issue of the Journal of Thoracic and Cardiovascular Surgery (2017;153:406-12). They reported on results of all 79 patients with Loeys-Dietz syndrome (LDS) who had cardiovascular surgery at Johns Hopkins. There were two (3%) deaths during surgery and eight (10%) late deaths.
Patients with LDS are at risk for dissection early when the aortic root reaches 4 cm. Despite what they termed “favorable” outcomes of surgery, Dr. Patel and his coauthors acknowledged that reintervention rates for this population are high – 19 patients (24%) had subsequent operations. That suggests cardiac surgeons must closely monitor these patients. “Meticulous follow-up with cardiovascular surveillance imaging remains important for management, particularly as clinical LDS subtypes are characterized and more tailored treatment is developed,” Dr. Patel and his coauthors reported.
They advise echocardiography every 3 to 6 months for the first year after surgery and then every 6 to 12 months afterward. Full-body imaging should occur at least every 2 years.
“In particular, patients with type B dissections should be monitored aggressively for aneurysm growth,” Dr. Patel and his coauthors said. They recommend imaging at seven to 14 days after dissection, then repeat imaging at 1, 3, 6, and 12 months, and then yearly thereafter.
They noted that four LDS subtypes have been identified. Although those with LDS1 and 2 subtypes are prone to aortic rupture at an earlier age and at smaller aortic diameters than other connective tissue disorders, the medical and surgical management for all subtypes are similar, Dr. Patel and his coauthors indicated.
“Certain congenital heart defects are more common among patients with LDS, compared with the normal population, including patent ductus arteriosus and mitral valve prolapse/insufficiency,” they said. Genotype is one factor that determines the need for surgery in LDS patients, Dr. Patel and his coauthors said. Others are growth rate, aortic valve function, family history, and severity of noncardiac phenotype.
The 79 patients in the study were divided almost evenly between gender, and the average age at first operation was 24.9 years; 38 were children younger than 18 years and 20 had a previous sternotomy.
Aortic root replacement represented the predominant operation in the group, accounting for 65 operations (82.3%), of which 52 (80%) were valve-sparing procedures and the remainder were composite valve-graft procedures. The other procedures the researchers performed were nine aortic arch replacements (11.4%), three open thoracoabdominal repairs (3.8%) and two ascending aorta replacements (2.5%).
“Valve-sparing root replacement has become a safe and reliable option for appropriately selected younger patients with LDS,” Dr. Patel and his coauthors wrote. Five patients needed a second operation on the aortic valve or root; three of them had a Florida sleeve procedure. “Based on these initial outcomes with the Florida sleeve at our institution, we have abandoned this procedure in favor of conventional valve-sparing root replacement,” Dr. Patel and his coauthors stated.
Dr. Patel and his coauthors had no financial relationships to disclose.
This report by Dr. Patel and his coauthors confirms the need for close surveillance of individuals with Loeys-Dietz syndrome who have had aortic operations, John S. Ikonomidis, MD, PhD, of the Medical University of South Carolina, Charleston, said in his invited commentary (J Thorac Cardiovasc Surg. 2017;153:413-4).
Dr. Ikonomidis noted this study is important because of its population size. “This is probably the largest single-center surgical report of this kind in the world,” he said.
The study highlighted a number of issues germane to LDS patients who have cardiovascular surgery, among them a critical need for genetic testing to help cardiac surgeons determine the disease genotype and what operation to perform, Dr. Ikonomidis said.
But Dr. Ikonomidis also pointed out the variation in aortic root size in the study patients. The smallest root in the series was 2 cm and 21 of 65 patients with a maximum root diameter smaller than 4 cm had root surgery. “This is a testament to the fact that surgical decision making in this population is dependent not just on the known genotype and aortic dimensions, but also on the rate of growth, aortic valve function, severity of noncardiac phenotype, and family history,” Dr. Ikonomidis said.
Dr. Ikonomidis had no financial relationships to disclose.
This report by Dr. Patel and his coauthors confirms the need for close surveillance of individuals with Loeys-Dietz syndrome who have had aortic operations, John S. Ikonomidis, MD, PhD, of the Medical University of South Carolina, Charleston, said in his invited commentary (J Thorac Cardiovasc Surg. 2017;153:413-4).
Dr. Ikonomidis noted this study is important because of its population size. “This is probably the largest single-center surgical report of this kind in the world,” he said.
The study highlighted a number of issues germane to LDS patients who have cardiovascular surgery, among them a critical need for genetic testing to help cardiac surgeons determine the disease genotype and what operation to perform, Dr. Ikonomidis said.
But Dr. Ikonomidis also pointed out the variation in aortic root size in the study patients. The smallest root in the series was 2 cm and 21 of 65 patients with a maximum root diameter smaller than 4 cm had root surgery. “This is a testament to the fact that surgical decision making in this population is dependent not just on the known genotype and aortic dimensions, but also on the rate of growth, aortic valve function, severity of noncardiac phenotype, and family history,” Dr. Ikonomidis said.
Dr. Ikonomidis had no financial relationships to disclose.
This report by Dr. Patel and his coauthors confirms the need for close surveillance of individuals with Loeys-Dietz syndrome who have had aortic operations, John S. Ikonomidis, MD, PhD, of the Medical University of South Carolina, Charleston, said in his invited commentary (J Thorac Cardiovasc Surg. 2017;153:413-4).
Dr. Ikonomidis noted this study is important because of its population size. “This is probably the largest single-center surgical report of this kind in the world,” he said.
The study highlighted a number of issues germane to LDS patients who have cardiovascular surgery, among them a critical need for genetic testing to help cardiac surgeons determine the disease genotype and what operation to perform, Dr. Ikonomidis said.
But Dr. Ikonomidis also pointed out the variation in aortic root size in the study patients. The smallest root in the series was 2 cm and 21 of 65 patients with a maximum root diameter smaller than 4 cm had root surgery. “This is a testament to the fact that surgical decision making in this population is dependent not just on the known genotype and aortic dimensions, but also on the rate of growth, aortic valve function, severity of noncardiac phenotype, and family history,” Dr. Ikonomidis said.
Dr. Ikonomidis had no financial relationships to disclose.
The knowledge about Loeys-Dietz syndrome has evolved quickly since Hal Dietz, MD, and Bart Loeys, MD, at Johns Hopkins University, Baltimore, first reported on it in 2005. Now, another team of Johns Hopkins investigators have reported that an aggressive approach with aortic root replacement coupled with valve-sparing whenever possible produces favorable results, but that clinicians must follow these patients closely with cardiovascular imaging.
“Growing experience with Loeys-Dietz syndrome has confirmed early impressions of its aggressive nature and proclivity toward aortic catastrophe,” Nishant D. Patel, MD, and his coauthors said in the February issue of the Journal of Thoracic and Cardiovascular Surgery (2017;153:406-12). They reported on results of all 79 patients with Loeys-Dietz syndrome (LDS) who had cardiovascular surgery at Johns Hopkins. There were two (3%) deaths during surgery and eight (10%) late deaths.
Patients with LDS are at risk for dissection early when the aortic root reaches 4 cm. Despite what they termed “favorable” outcomes of surgery, Dr. Patel and his coauthors acknowledged that reintervention rates for this population are high – 19 patients (24%) had subsequent operations. That suggests cardiac surgeons must closely monitor these patients. “Meticulous follow-up with cardiovascular surveillance imaging remains important for management, particularly as clinical LDS subtypes are characterized and more tailored treatment is developed,” Dr. Patel and his coauthors reported.
They advise echocardiography every 3 to 6 months for the first year after surgery and then every 6 to 12 months afterward. Full-body imaging should occur at least every 2 years.
“In particular, patients with type B dissections should be monitored aggressively for aneurysm growth,” Dr. Patel and his coauthors said. They recommend imaging at seven to 14 days after dissection, then repeat imaging at 1, 3, 6, and 12 months, and then yearly thereafter.
They noted that four LDS subtypes have been identified. Although those with LDS1 and 2 subtypes are prone to aortic rupture at an earlier age and at smaller aortic diameters than other connective tissue disorders, the medical and surgical management for all subtypes are similar, Dr. Patel and his coauthors indicated.
“Certain congenital heart defects are more common among patients with LDS, compared with the normal population, including patent ductus arteriosus and mitral valve prolapse/insufficiency,” they said. Genotype is one factor that determines the need for surgery in LDS patients, Dr. Patel and his coauthors said. Others are growth rate, aortic valve function, family history, and severity of noncardiac phenotype.
The 79 patients in the study were divided almost evenly between gender, and the average age at first operation was 24.9 years; 38 were children younger than 18 years and 20 had a previous sternotomy.
Aortic root replacement represented the predominant operation in the group, accounting for 65 operations (82.3%), of which 52 (80%) were valve-sparing procedures and the remainder were composite valve-graft procedures. The other procedures the researchers performed were nine aortic arch replacements (11.4%), three open thoracoabdominal repairs (3.8%) and two ascending aorta replacements (2.5%).
“Valve-sparing root replacement has become a safe and reliable option for appropriately selected younger patients with LDS,” Dr. Patel and his coauthors wrote. Five patients needed a second operation on the aortic valve or root; three of them had a Florida sleeve procedure. “Based on these initial outcomes with the Florida sleeve at our institution, we have abandoned this procedure in favor of conventional valve-sparing root replacement,” Dr. Patel and his coauthors stated.
Dr. Patel and his coauthors had no financial relationships to disclose.
The knowledge about Loeys-Dietz syndrome has evolved quickly since Hal Dietz, MD, and Bart Loeys, MD, at Johns Hopkins University, Baltimore, first reported on it in 2005. Now, another team of Johns Hopkins investigators have reported that an aggressive approach with aortic root replacement coupled with valve-sparing whenever possible produces favorable results, but that clinicians must follow these patients closely with cardiovascular imaging.
“Growing experience with Loeys-Dietz syndrome has confirmed early impressions of its aggressive nature and proclivity toward aortic catastrophe,” Nishant D. Patel, MD, and his coauthors said in the February issue of the Journal of Thoracic and Cardiovascular Surgery (2017;153:406-12). They reported on results of all 79 patients with Loeys-Dietz syndrome (LDS) who had cardiovascular surgery at Johns Hopkins. There were two (3%) deaths during surgery and eight (10%) late deaths.
Patients with LDS are at risk for dissection early when the aortic root reaches 4 cm. Despite what they termed “favorable” outcomes of surgery, Dr. Patel and his coauthors acknowledged that reintervention rates for this population are high – 19 patients (24%) had subsequent operations. That suggests cardiac surgeons must closely monitor these patients. “Meticulous follow-up with cardiovascular surveillance imaging remains important for management, particularly as clinical LDS subtypes are characterized and more tailored treatment is developed,” Dr. Patel and his coauthors reported.
They advise echocardiography every 3 to 6 months for the first year after surgery and then every 6 to 12 months afterward. Full-body imaging should occur at least every 2 years.
“In particular, patients with type B dissections should be monitored aggressively for aneurysm growth,” Dr. Patel and his coauthors said. They recommend imaging at seven to 14 days after dissection, then repeat imaging at 1, 3, 6, and 12 months, and then yearly thereafter.
They noted that four LDS subtypes have been identified. Although those with LDS1 and 2 subtypes are prone to aortic rupture at an earlier age and at smaller aortic diameters than other connective tissue disorders, the medical and surgical management for all subtypes are similar, Dr. Patel and his coauthors indicated.
“Certain congenital heart defects are more common among patients with LDS, compared with the normal population, including patent ductus arteriosus and mitral valve prolapse/insufficiency,” they said. Genotype is one factor that determines the need for surgery in LDS patients, Dr. Patel and his coauthors said. Others are growth rate, aortic valve function, family history, and severity of noncardiac phenotype.
The 79 patients in the study were divided almost evenly between gender, and the average age at first operation was 24.9 years; 38 were children younger than 18 years and 20 had a previous sternotomy.
Aortic root replacement represented the predominant operation in the group, accounting for 65 operations (82.3%), of which 52 (80%) were valve-sparing procedures and the remainder were composite valve-graft procedures. The other procedures the researchers performed were nine aortic arch replacements (11.4%), three open thoracoabdominal repairs (3.8%) and two ascending aorta replacements (2.5%).
“Valve-sparing root replacement has become a safe and reliable option for appropriately selected younger patients with LDS,” Dr. Patel and his coauthors wrote. Five patients needed a second operation on the aortic valve or root; three of them had a Florida sleeve procedure. “Based on these initial outcomes with the Florida sleeve at our institution, we have abandoned this procedure in favor of conventional valve-sparing root replacement,” Dr. Patel and his coauthors stated.
Dr. Patel and his coauthors had no financial relationships to disclose.
Key clinical point: Outcomes for aortic surgery in Loeys-Dietz syndrome are favorable, but reintervention rates are high.
Major finding: Patients require close postoperative follow-up with cardiovascular imaging.
Data source: Retrospective review of 79 patients who had cardiovascular surgery for LDS over 26 years at Johns Hopkins University.
Disclosure: Dr. Patel and his coauthors reported having no relevant financial disclosures.