User login
The large majority of women who start using a long-acting reversible contraceptive (LARC) find it acceptable and cost effective enough to continue using the method for at least 2 years, findings from a retrospective cohort study suggest.
Investigators performed a chart review to assess continuation rates in a real-world, mixed-payer setting among 8,603 women aged 15-44 years who had a device inserted between 2004 and 2012 at the University of Utah Healthcare System.
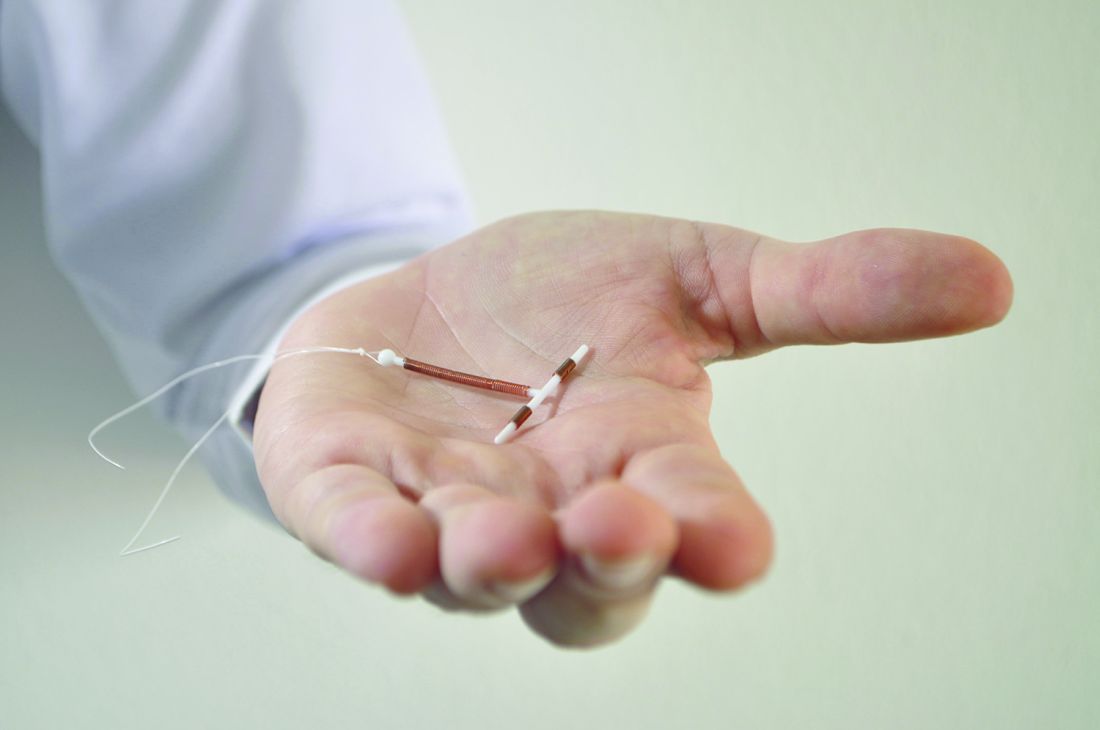
At 2 years, the proportion of women still using the device they had received was 77.8% for the hormonal IUD users, 73.1% for the copper IUD users, and 75.9% for the implant users, according to study findings reported online (Am J Obstet Gynecol. 2017 Feb 8. doi: 10.1016/j.ajog.2017.02.003).
“These data demonstrate a high rate of 2-year continuation of contraceptive devices in a mixed-payer system suggesting user acceptability and confirming that a majority of users reach the point of cost neutrality as demonstrated previously,” Jessica N. Sanders, PhD, of the University of Utah, Salt Lake City, and her colleagues wrote.
In analyses adjusted for potential confounders, compared with copper IUD users, the levonorgestrel IUD users and the implant users had higher adjusted 2-year continuation rates (incidence risk ratio, 1.08 for each).
Additionally, women’s likelihood of continuing use of their contraceptive device for at least 2 years increased with their age at the time of insertion. And women were more likely to still be using their method at that time if they paid for care themselves (incidence risk ratio, 1.13) or were covered by public health insurance (1.04), as compared with those covered by private insurance. Hispanic ethnicity was also associated with 2-year continuation.
“Differences by method type and patient characteristics were small and consistent with previous studies that have demonstrated LARC acceptability across patient demographics,” Dr. Sanders and her coauthors wrote.
Study limitations included possible bias and residual confounding, potentially limited generalizability to other populations of women, and lack of information on pregnancy and obstetric history for the majority of the cohort. But one of the study’s strengths is that it represents actual use, which may differ from prospective studies where participants are reimbursed to continue participation.
Dr. Sanders reported having no relevant conflicts of interest; some of the coauthors are employees of, have affiliations with, and/or own stock in companies that manufacture IUDs and implants. The study was funded in part by Bayer Healthcare.
The large majority of women who start using a long-acting reversible contraceptive (LARC) find it acceptable and cost effective enough to continue using the method for at least 2 years, findings from a retrospective cohort study suggest.
Investigators performed a chart review to assess continuation rates in a real-world, mixed-payer setting among 8,603 women aged 15-44 years who had a device inserted between 2004 and 2012 at the University of Utah Healthcare System.
At 2 years, the proportion of women still using the device they had received was 77.8% for the hormonal IUD users, 73.1% for the copper IUD users, and 75.9% for the implant users, according to study findings reported online (Am J Obstet Gynecol. 2017 Feb 8. doi: 10.1016/j.ajog.2017.02.003).
“These data demonstrate a high rate of 2-year continuation of contraceptive devices in a mixed-payer system suggesting user acceptability and confirming that a majority of users reach the point of cost neutrality as demonstrated previously,” Jessica N. Sanders, PhD, of the University of Utah, Salt Lake City, and her colleagues wrote.
In analyses adjusted for potential confounders, compared with copper IUD users, the levonorgestrel IUD users and the implant users had higher adjusted 2-year continuation rates (incidence risk ratio, 1.08 for each).
Additionally, women’s likelihood of continuing use of their contraceptive device for at least 2 years increased with their age at the time of insertion. And women were more likely to still be using their method at that time if they paid for care themselves (incidence risk ratio, 1.13) or were covered by public health insurance (1.04), as compared with those covered by private insurance. Hispanic ethnicity was also associated with 2-year continuation.
“Differences by method type and patient characteristics were small and consistent with previous studies that have demonstrated LARC acceptability across patient demographics,” Dr. Sanders and her coauthors wrote.
Study limitations included possible bias and residual confounding, potentially limited generalizability to other populations of women, and lack of information on pregnancy and obstetric history for the majority of the cohort. But one of the study’s strengths is that it represents actual use, which may differ from prospective studies where participants are reimbursed to continue participation.
Dr. Sanders reported having no relevant conflicts of interest; some of the coauthors are employees of, have affiliations with, and/or own stock in companies that manufacture IUDs and implants. The study was funded in part by Bayer Healthcare.
The large majority of women who start using a long-acting reversible contraceptive (LARC) find it acceptable and cost effective enough to continue using the method for at least 2 years, findings from a retrospective cohort study suggest.
Investigators performed a chart review to assess continuation rates in a real-world, mixed-payer setting among 8,603 women aged 15-44 years who had a device inserted between 2004 and 2012 at the University of Utah Healthcare System.
At 2 years, the proportion of women still using the device they had received was 77.8% for the hormonal IUD users, 73.1% for the copper IUD users, and 75.9% for the implant users, according to study findings reported online (Am J Obstet Gynecol. 2017 Feb 8. doi: 10.1016/j.ajog.2017.02.003).
“These data demonstrate a high rate of 2-year continuation of contraceptive devices in a mixed-payer system suggesting user acceptability and confirming that a majority of users reach the point of cost neutrality as demonstrated previously,” Jessica N. Sanders, PhD, of the University of Utah, Salt Lake City, and her colleagues wrote.
In analyses adjusted for potential confounders, compared with copper IUD users, the levonorgestrel IUD users and the implant users had higher adjusted 2-year continuation rates (incidence risk ratio, 1.08 for each).
Additionally, women’s likelihood of continuing use of their contraceptive device for at least 2 years increased with their age at the time of insertion. And women were more likely to still be using their method at that time if they paid for care themselves (incidence risk ratio, 1.13) or were covered by public health insurance (1.04), as compared with those covered by private insurance. Hispanic ethnicity was also associated with 2-year continuation.
“Differences by method type and patient characteristics were small and consistent with previous studies that have demonstrated LARC acceptability across patient demographics,” Dr. Sanders and her coauthors wrote.
Study limitations included possible bias and residual confounding, potentially limited generalizability to other populations of women, and lack of information on pregnancy and obstetric history for the majority of the cohort. But one of the study’s strengths is that it represents actual use, which may differ from prospective studies where participants are reimbursed to continue participation.
Dr. Sanders reported having no relevant conflicts of interest; some of the coauthors are employees of, have affiliations with, and/or own stock in companies that manufacture IUDs and implants. The study was funded in part by Bayer Healthcare.
FROM THE AMERICAN JOURNAL OF OBSTETRICS & GYNECOLOGY
Key clinical point:
Major finding: The 2-year continuation rate was 77.8% for the levonorgestrel 52 mg IUD, 73.1% for the copper T380A IUD, and 75.9% for the 68 mg etonogestrel implant.
Data source: A single-center retrospective cohort study of 8,603 women who had an IUD or contraceptive implant inserted during a 9-year period.
Disclosures: Dr. Sanders reported having no relevant conflicts of interest; some of the coauthors are employees of, have affiliations with, and/or own stock in companies that manufacture IUDs and implants. The study was funded in part by Bayer Healthcare.