User login
Disease-Modifying Treatment Changes in Clinical Practice
ORLANDO—Patients with multiple sclerosis (MS) and their physicians still consider self-injected immunomodulating medications as first-line agents, according to the results of a study presented at the ACTRIMS 2017 Forum. The results, based on data from a community health–based suburban neurology practice, also indicated that a smaller percentage than expected of patients on injectable medications switched to an oral medication, and a majority of untreated patients at the initial visit chose to star
There are currently 14 FDA-approved immunomodulating medications available for MS and one currently awaiting approval. “This has resulted in patients, in consultation with physicians, having the opportunity to switch from medications that are self injected to medications taken orally or by IV infusion,” said Susan M. Rubin, MD, and colleagues from the Department of Neurology at NorthShore University HealthSystem in Evanston, Illinois. “We speculated that this would result in a high level of treatment changes away from self-injected treatments to the newer options,” Dr. Rubin and colleagues said.
They optimized their electronic medical record by building structured clinical documentation support (SCDS) tools specific to MS practice that standardize initial and annual follow-up visits, write progress notes, and capture data. The toolkit they built documents immunomodulating medications taken, tracks efficacy and adverse events, and notes reasons for discontinuation.
Patients with MS who were referred to the Department of Neurology at NorthShore University HealthSystem were evaluated at initial and annual follow-up visits using SCDS tools by one of three subspecialty neurologists. The researchers created descriptive reports of their cohort, including gender, age at disease onset, disease duration, use of immunomodulating medications, and Expanded Disability Status Scale scores. Patient-reported treatments at their initial visit were compared with treatments at their first annual follow-up visit.
Of the 105 patients in the study, 78% were female. Disease duration was zero to 43 years, with a mean duration of six years. Nearly three-quarters (74%) were not on an immunomodulating medication at first visit. Of those on medication at first visit, 77% were taking an injectable medication. At the annual follow-up visit, 51% started or changed medication, and 49% remained on the same medication. Of the patients who started treatment, 65% started a self-injection medication, 26% started an oral medication, and 9% started an infusion agent.
“Despite the availability of new treatments,” the researchers said, “patients and their physicians were generally content with the current treatment.” They hypothesized that safety concerns reduced the likelihood of change. “It appears that both patients and physicians prioritized safety over possibly greater efficacy when switching medication.”
—Glenn S. Williams
ORLANDO—Patients with multiple sclerosis (MS) and their physicians still consider self-injected immunomodulating medications as first-line agents, according to the results of a study presented at the ACTRIMS 2017 Forum. The results, based on data from a community health–based suburban neurology practice, also indicated that a smaller percentage than expected of patients on injectable medications switched to an oral medication, and a majority of untreated patients at the initial visit chose to star
There are currently 14 FDA-approved immunomodulating medications available for MS and one currently awaiting approval. “This has resulted in patients, in consultation with physicians, having the opportunity to switch from medications that are self injected to medications taken orally or by IV infusion,” said Susan M. Rubin, MD, and colleagues from the Department of Neurology at NorthShore University HealthSystem in Evanston, Illinois. “We speculated that this would result in a high level of treatment changes away from self-injected treatments to the newer options,” Dr. Rubin and colleagues said.
They optimized their electronic medical record by building structured clinical documentation support (SCDS) tools specific to MS practice that standardize initial and annual follow-up visits, write progress notes, and capture data. The toolkit they built documents immunomodulating medications taken, tracks efficacy and adverse events, and notes reasons for discontinuation.
Patients with MS who were referred to the Department of Neurology at NorthShore University HealthSystem were evaluated at initial and annual follow-up visits using SCDS tools by one of three subspecialty neurologists. The researchers created descriptive reports of their cohort, including gender, age at disease onset, disease duration, use of immunomodulating medications, and Expanded Disability Status Scale scores. Patient-reported treatments at their initial visit were compared with treatments at their first annual follow-up visit.
Of the 105 patients in the study, 78% were female. Disease duration was zero to 43 years, with a mean duration of six years. Nearly three-quarters (74%) were not on an immunomodulating medication at first visit. Of those on medication at first visit, 77% were taking an injectable medication. At the annual follow-up visit, 51% started or changed medication, and 49% remained on the same medication. Of the patients who started treatment, 65% started a self-injection medication, 26% started an oral medication, and 9% started an infusion agent.
“Despite the availability of new treatments,” the researchers said, “patients and their physicians were generally content with the current treatment.” They hypothesized that safety concerns reduced the likelihood of change. “It appears that both patients and physicians prioritized safety over possibly greater efficacy when switching medication.”
—Glenn S. Williams
ORLANDO—Patients with multiple sclerosis (MS) and their physicians still consider self-injected immunomodulating medications as first-line agents, according to the results of a study presented at the ACTRIMS 2017 Forum. The results, based on data from a community health–based suburban neurology practice, also indicated that a smaller percentage than expected of patients on injectable medications switched to an oral medication, and a majority of untreated patients at the initial visit chose to star
There are currently 14 FDA-approved immunomodulating medications available for MS and one currently awaiting approval. “This has resulted in patients, in consultation with physicians, having the opportunity to switch from medications that are self injected to medications taken orally or by IV infusion,” said Susan M. Rubin, MD, and colleagues from the Department of Neurology at NorthShore University HealthSystem in Evanston, Illinois. “We speculated that this would result in a high level of treatment changes away from self-injected treatments to the newer options,” Dr. Rubin and colleagues said.
They optimized their electronic medical record by building structured clinical documentation support (SCDS) tools specific to MS practice that standardize initial and annual follow-up visits, write progress notes, and capture data. The toolkit they built documents immunomodulating medications taken, tracks efficacy and adverse events, and notes reasons for discontinuation.
Patients with MS who were referred to the Department of Neurology at NorthShore University HealthSystem were evaluated at initial and annual follow-up visits using SCDS tools by one of three subspecialty neurologists. The researchers created descriptive reports of their cohort, including gender, age at disease onset, disease duration, use of immunomodulating medications, and Expanded Disability Status Scale scores. Patient-reported treatments at their initial visit were compared with treatments at their first annual follow-up visit.
Of the 105 patients in the study, 78% were female. Disease duration was zero to 43 years, with a mean duration of six years. Nearly three-quarters (74%) were not on an immunomodulating medication at first visit. Of those on medication at first visit, 77% were taking an injectable medication. At the annual follow-up visit, 51% started or changed medication, and 49% remained on the same medication. Of the patients who started treatment, 65% started a self-injection medication, 26% started an oral medication, and 9% started an infusion agent.
“Despite the availability of new treatments,” the researchers said, “patients and their physicians were generally content with the current treatment.” They hypothesized that safety concerns reduced the likelihood of change. “It appears that both patients and physicians prioritized safety over possibly greater efficacy when switching medication.”
—Glenn S. Williams
Can Vitamin D Benefit Patients With MS?
Vitamin D as a Risk Factor
Epidemiologic literature first suggested that vitamin D status might be related to the risk of MS. Researchers demonstrated that MS prevalence increases with distance from the equator. A series of retrospective and case–control studies subsequently suggested that patients with MS had lower levels of vitamin D than healthy individuals. These data, however, left open the possibility that having MS and its associated intolerance of heat led to reduced sun exposure, and thus lower levels of vitamin D.
In 2006, Munger and colleagues prospectively examined serum samples obtained from more than seven million US military personnel. They found that, among whites, the risk of MS significantly decreased with increasing levels of 25-hydroxyvitamin D. The effect was most significant in people with vitamin D levels higher than 40 ng/mL. The same association was observed in a later Swedish study that used 30 ng/mL as its threshold for vitamin D sufficiency. In 2016, Munger et al found that insufficient maternal vitamin D during pregnancy may increase the risk of MS in offspring.
Although research by Lucas and colleagues indicated an inverse association between serum vitamin D level and risk of MS, they found a stronger inverse association between ultraviolet (UV) light exposure and risk of MS. The strength of the latter association did not change, whether exposure was measured by skin damage or self-report. In 2017, however, Nielsen and colleagues compared serum vitamin D levels in newborns who subsequently developed MS with those of newborns who did not develop MS. They found a strong association between higher neonatal levels of vitamin D and lower risk of subsequent MS. “One could argue [that] this [result] makes the vitamin D hypothesis stronger than the UV [hypothesis], since the babies, in all likelihood, had not been exposed to much UV [light] at the time they were born,” said Dr. Mowry.
Vitamin D as a Prognostic Factor
Other research has suggested that serum vitamin D level may predict disease activity in MS. Dr. Mowry and colleagues evaluated blood samples taken from children who presented for longitudinal follow-up at pediatric MS centers. The total follow-up period was approximately 18 months. After adjusting for covariates, they found a strong association between higher levels of vitamin D and lower risk of subsequent relapse. “Each 10-ng/mL higher level of vitamin D … was associated with about a one-third reduction in the risk of subsequent relapse,” said Dr. Mowry. A prospective study conducted in Australia found similar results.
In 2012, Dr. Mowry and colleagues measured vitamin D levels in blood samples from 469 patients with relapsing-remitting MS or clinically isolated syndrome (CIS). They found that each additional 10-ng/mL increment of vitamin D level was associated with an approximately 15% lower risk of subsequent new T2 lesions and with an approximately 32% reduced risk of subsequent gadolinium-enhancing lesions. Higher levels of vitamin D also were associated with lower risk of subsequent relapse, but this finding was not statistically significant.
To discover whether vitamin D influences markers known to predict long-term disability, Dr. Mowry and colleagues examined data from a study of atorvastatin in 65 patients with CIS. They measured vitamin D levels at baseline and at month six, and the follow-up period was as long as 18 months. They found that each additional 10-ng/mL increment in vitamin D level was associated with an additional 7.8 mL of preserved gray matter volume. They also observed a trend toward an inverse association between vitamin D levels and the composite end point of three or more new T2 lesions or one or more relapses within a year.
Is Vitamin D Supplementation Appropriate?
“Just because [vitamin D] is available over the counter does not make it safe or effective,” and the supplement should be studied further in clinical trials, said Dr. Mowry. In 2010, Burton et al found that a dose of as much as 40,000 IU/day of vitamin D was safe in the short term and might have immunomodulatory effects in patients with MS. Furthermore, a small Finnish study suggested that a dose of 20,000 IU/week of vitamin D was safe in patients with MS, and also might slow the accumulation of disability.
Hupperts et al studied patients with relapsing-remitting MS who were receiving interferon beta-1a. They randomized 229 participants to vitamin D or placebo and followed them for 48 weeks. In preliminary analyses, the investigators found no difference between treatment groups with respect to the outcome of no evidence of disease activity. Patients who received vitamin D had a lower annualized relapse rate than controls, but the difference was not statistically significant. The active group did have significantly fewer gadolinium-enhancing lesions and new T2 hyperintense lesions, compared with controls, however.
In addition, Dr. Mowry and colleagues are comparing the effects of 5,000-IU and 600-IU doses of vitamin D in patients with MS who are receiving glatiramer acetate. The ongoing study is sponsored by the National MS Society. European studies of the clinical benefit of vitamin D also are under way.
Although the benefits of vitamin D are not completely understood, many neurologists recommend supplementation to their patients with MS. Pharmacokinetic studies have not shown a difference between daily, weekly, or monthly dosing regimens. “As long as you give the same dose of vitamin D, you will get the levels … to the same general area,” said Dr. Mowry. Nevertheless, some studies in other patient populations suggest that very high doses of vitamin D given monthly are probably toxic.
Many studies have suggested that vitamin D3 may be more potent than vitamin D2. “I tend to use [vitamin] D3 when I am supplementing,” said Dr. Mowry. “I aim for levels between 40 and 60 ng/mL, based on our observational data.... For my patients, that largely means they need somewhere between 2,000 and 4,000 IU/day, although sometimes more. I usually recheck the level in three months, based on what we know about the kinetics of vitamin D supplementation. I am cautious in individuals who may be at risk for hypercalcemia or hypercalciuria.”
—Erik Greb
Suggested Reading
Burton JM, Kimball S, Vieth R, et al. A phase I/II dose-escalation trial of vitamin D3 and calcium in multiple sclerosis. Neurology. 2010;74(23):1852-1859.
Mowry EM. Vitamin D: evidence for its role as a prognostic factor in multiple sclerosis. J Neurol Sci. 2011; 311(1-2):19-22.
Mowry EM, Pelletier D, Gao Z, et al. Vitamin D in clinically isolated syndrome: evidence for possible neuroprotection. Eur J Neurol. 2016;23(2):327-332.
Mowry EM, Waubant E, McCulloch CE, et al. Vitamin D status predicts new brain magnetic resonance imaging activity in multiple sclerosis. Ann Neurol. 2012;72(2):234-240.
Munger KL, Åivo J, Hongell K, et al. Vitamin D status during pregnancy and risk of multiple sclerosis in offspring of women in the Finnish Maternity Cohort. JAMA Neurol. 2016;73(5):515-519.
Munger KL, Levin LI, Hollis BW, et al. Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis. JAMA. 2006;296(23):2832-2838.
Nielsen NM, Munger KL, Koch-Henriksen N, et al. Neonatal vitamin D status and risk of multiple sclerosis: a population-based case-control study. Neurology. 2017;88(1):44-51.
Tremlett H, van der Mei IA, Pittas F, et al. Monthly ambient sunlight, infections and relapse rates in multiple sclerosis. Neuroepidemiology. 2008;31(4):271-279.
Vitamin D as a Risk Factor
Epidemiologic literature first suggested that vitamin D status might be related to the risk of MS. Researchers demonstrated that MS prevalence increases with distance from the equator. A series of retrospective and case–control studies subsequently suggested that patients with MS had lower levels of vitamin D than healthy individuals. These data, however, left open the possibility that having MS and its associated intolerance of heat led to reduced sun exposure, and thus lower levels of vitamin D.
In 2006, Munger and colleagues prospectively examined serum samples obtained from more than seven million US military personnel. They found that, among whites, the risk of MS significantly decreased with increasing levels of 25-hydroxyvitamin D. The effect was most significant in people with vitamin D levels higher than 40 ng/mL. The same association was observed in a later Swedish study that used 30 ng/mL as its threshold for vitamin D sufficiency. In 2016, Munger et al found that insufficient maternal vitamin D during pregnancy may increase the risk of MS in offspring.
Although research by Lucas and colleagues indicated an inverse association between serum vitamin D level and risk of MS, they found a stronger inverse association between ultraviolet (UV) light exposure and risk of MS. The strength of the latter association did not change, whether exposure was measured by skin damage or self-report. In 2017, however, Nielsen and colleagues compared serum vitamin D levels in newborns who subsequently developed MS with those of newborns who did not develop MS. They found a strong association between higher neonatal levels of vitamin D and lower risk of subsequent MS. “One could argue [that] this [result] makes the vitamin D hypothesis stronger than the UV [hypothesis], since the babies, in all likelihood, had not been exposed to much UV [light] at the time they were born,” said Dr. Mowry.
Vitamin D as a Prognostic Factor
Other research has suggested that serum vitamin D level may predict disease activity in MS. Dr. Mowry and colleagues evaluated blood samples taken from children who presented for longitudinal follow-up at pediatric MS centers. The total follow-up period was approximately 18 months. After adjusting for covariates, they found a strong association between higher levels of vitamin D and lower risk of subsequent relapse. “Each 10-ng/mL higher level of vitamin D … was associated with about a one-third reduction in the risk of subsequent relapse,” said Dr. Mowry. A prospective study conducted in Australia found similar results.
In 2012, Dr. Mowry and colleagues measured vitamin D levels in blood samples from 469 patients with relapsing-remitting MS or clinically isolated syndrome (CIS). They found that each additional 10-ng/mL increment of vitamin D level was associated with an approximately 15% lower risk of subsequent new T2 lesions and with an approximately 32% reduced risk of subsequent gadolinium-enhancing lesions. Higher levels of vitamin D also were associated with lower risk of subsequent relapse, but this finding was not statistically significant.
To discover whether vitamin D influences markers known to predict long-term disability, Dr. Mowry and colleagues examined data from a study of atorvastatin in 65 patients with CIS. They measured vitamin D levels at baseline and at month six, and the follow-up period was as long as 18 months. They found that each additional 10-ng/mL increment in vitamin D level was associated with an additional 7.8 mL of preserved gray matter volume. They also observed a trend toward an inverse association between vitamin D levels and the composite end point of three or more new T2 lesions or one or more relapses within a year.
Is Vitamin D Supplementation Appropriate?
“Just because [vitamin D] is available over the counter does not make it safe or effective,” and the supplement should be studied further in clinical trials, said Dr. Mowry. In 2010, Burton et al found that a dose of as much as 40,000 IU/day of vitamin D was safe in the short term and might have immunomodulatory effects in patients with MS. Furthermore, a small Finnish study suggested that a dose of 20,000 IU/week of vitamin D was safe in patients with MS, and also might slow the accumulation of disability.
Hupperts et al studied patients with relapsing-remitting MS who were receiving interferon beta-1a. They randomized 229 participants to vitamin D or placebo and followed them for 48 weeks. In preliminary analyses, the investigators found no difference between treatment groups with respect to the outcome of no evidence of disease activity. Patients who received vitamin D had a lower annualized relapse rate than controls, but the difference was not statistically significant. The active group did have significantly fewer gadolinium-enhancing lesions and new T2 hyperintense lesions, compared with controls, however.
In addition, Dr. Mowry and colleagues are comparing the effects of 5,000-IU and 600-IU doses of vitamin D in patients with MS who are receiving glatiramer acetate. The ongoing study is sponsored by the National MS Society. European studies of the clinical benefit of vitamin D also are under way.
Although the benefits of vitamin D are not completely understood, many neurologists recommend supplementation to their patients with MS. Pharmacokinetic studies have not shown a difference between daily, weekly, or monthly dosing regimens. “As long as you give the same dose of vitamin D, you will get the levels … to the same general area,” said Dr. Mowry. Nevertheless, some studies in other patient populations suggest that very high doses of vitamin D given monthly are probably toxic.
Many studies have suggested that vitamin D3 may be more potent than vitamin D2. “I tend to use [vitamin] D3 when I am supplementing,” said Dr. Mowry. “I aim for levels between 40 and 60 ng/mL, based on our observational data.... For my patients, that largely means they need somewhere between 2,000 and 4,000 IU/day, although sometimes more. I usually recheck the level in three months, based on what we know about the kinetics of vitamin D supplementation. I am cautious in individuals who may be at risk for hypercalcemia or hypercalciuria.”
—Erik Greb
Suggested Reading
Burton JM, Kimball S, Vieth R, et al. A phase I/II dose-escalation trial of vitamin D3 and calcium in multiple sclerosis. Neurology. 2010;74(23):1852-1859.
Mowry EM. Vitamin D: evidence for its role as a prognostic factor in multiple sclerosis. J Neurol Sci. 2011; 311(1-2):19-22.
Mowry EM, Pelletier D, Gao Z, et al. Vitamin D in clinically isolated syndrome: evidence for possible neuroprotection. Eur J Neurol. 2016;23(2):327-332.
Mowry EM, Waubant E, McCulloch CE, et al. Vitamin D status predicts new brain magnetic resonance imaging activity in multiple sclerosis. Ann Neurol. 2012;72(2):234-240.
Munger KL, Åivo J, Hongell K, et al. Vitamin D status during pregnancy and risk of multiple sclerosis in offspring of women in the Finnish Maternity Cohort. JAMA Neurol. 2016;73(5):515-519.
Munger KL, Levin LI, Hollis BW, et al. Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis. JAMA. 2006;296(23):2832-2838.
Nielsen NM, Munger KL, Koch-Henriksen N, et al. Neonatal vitamin D status and risk of multiple sclerosis: a population-based case-control study. Neurology. 2017;88(1):44-51.
Tremlett H, van der Mei IA, Pittas F, et al. Monthly ambient sunlight, infections and relapse rates in multiple sclerosis. Neuroepidemiology. 2008;31(4):271-279.
Vitamin D as a Risk Factor
Epidemiologic literature first suggested that vitamin D status might be related to the risk of MS. Researchers demonstrated that MS prevalence increases with distance from the equator. A series of retrospective and case–control studies subsequently suggested that patients with MS had lower levels of vitamin D than healthy individuals. These data, however, left open the possibility that having MS and its associated intolerance of heat led to reduced sun exposure, and thus lower levels of vitamin D.
In 2006, Munger and colleagues prospectively examined serum samples obtained from more than seven million US military personnel. They found that, among whites, the risk of MS significantly decreased with increasing levels of 25-hydroxyvitamin D. The effect was most significant in people with vitamin D levels higher than 40 ng/mL. The same association was observed in a later Swedish study that used 30 ng/mL as its threshold for vitamin D sufficiency. In 2016, Munger et al found that insufficient maternal vitamin D during pregnancy may increase the risk of MS in offspring.
Although research by Lucas and colleagues indicated an inverse association between serum vitamin D level and risk of MS, they found a stronger inverse association between ultraviolet (UV) light exposure and risk of MS. The strength of the latter association did not change, whether exposure was measured by skin damage or self-report. In 2017, however, Nielsen and colleagues compared serum vitamin D levels in newborns who subsequently developed MS with those of newborns who did not develop MS. They found a strong association between higher neonatal levels of vitamin D and lower risk of subsequent MS. “One could argue [that] this [result] makes the vitamin D hypothesis stronger than the UV [hypothesis], since the babies, in all likelihood, had not been exposed to much UV [light] at the time they were born,” said Dr. Mowry.
Vitamin D as a Prognostic Factor
Other research has suggested that serum vitamin D level may predict disease activity in MS. Dr. Mowry and colleagues evaluated blood samples taken from children who presented for longitudinal follow-up at pediatric MS centers. The total follow-up period was approximately 18 months. After adjusting for covariates, they found a strong association between higher levels of vitamin D and lower risk of subsequent relapse. “Each 10-ng/mL higher level of vitamin D … was associated with about a one-third reduction in the risk of subsequent relapse,” said Dr. Mowry. A prospective study conducted in Australia found similar results.
In 2012, Dr. Mowry and colleagues measured vitamin D levels in blood samples from 469 patients with relapsing-remitting MS or clinically isolated syndrome (CIS). They found that each additional 10-ng/mL increment of vitamin D level was associated with an approximately 15% lower risk of subsequent new T2 lesions and with an approximately 32% reduced risk of subsequent gadolinium-enhancing lesions. Higher levels of vitamin D also were associated with lower risk of subsequent relapse, but this finding was not statistically significant.
To discover whether vitamin D influences markers known to predict long-term disability, Dr. Mowry and colleagues examined data from a study of atorvastatin in 65 patients with CIS. They measured vitamin D levels at baseline and at month six, and the follow-up period was as long as 18 months. They found that each additional 10-ng/mL increment in vitamin D level was associated with an additional 7.8 mL of preserved gray matter volume. They also observed a trend toward an inverse association between vitamin D levels and the composite end point of three or more new T2 lesions or one or more relapses within a year.
Is Vitamin D Supplementation Appropriate?
“Just because [vitamin D] is available over the counter does not make it safe or effective,” and the supplement should be studied further in clinical trials, said Dr. Mowry. In 2010, Burton et al found that a dose of as much as 40,000 IU/day of vitamin D was safe in the short term and might have immunomodulatory effects in patients with MS. Furthermore, a small Finnish study suggested that a dose of 20,000 IU/week of vitamin D was safe in patients with MS, and also might slow the accumulation of disability.
Hupperts et al studied patients with relapsing-remitting MS who were receiving interferon beta-1a. They randomized 229 participants to vitamin D or placebo and followed them for 48 weeks. In preliminary analyses, the investigators found no difference between treatment groups with respect to the outcome of no evidence of disease activity. Patients who received vitamin D had a lower annualized relapse rate than controls, but the difference was not statistically significant. The active group did have significantly fewer gadolinium-enhancing lesions and new T2 hyperintense lesions, compared with controls, however.
In addition, Dr. Mowry and colleagues are comparing the effects of 5,000-IU and 600-IU doses of vitamin D in patients with MS who are receiving glatiramer acetate. The ongoing study is sponsored by the National MS Society. European studies of the clinical benefit of vitamin D also are under way.
Although the benefits of vitamin D are not completely understood, many neurologists recommend supplementation to their patients with MS. Pharmacokinetic studies have not shown a difference between daily, weekly, or monthly dosing regimens. “As long as you give the same dose of vitamin D, you will get the levels … to the same general area,” said Dr. Mowry. Nevertheless, some studies in other patient populations suggest that very high doses of vitamin D given monthly are probably toxic.
Many studies have suggested that vitamin D3 may be more potent than vitamin D2. “I tend to use [vitamin] D3 when I am supplementing,” said Dr. Mowry. “I aim for levels between 40 and 60 ng/mL, based on our observational data.... For my patients, that largely means they need somewhere between 2,000 and 4,000 IU/day, although sometimes more. I usually recheck the level in three months, based on what we know about the kinetics of vitamin D supplementation. I am cautious in individuals who may be at risk for hypercalcemia or hypercalciuria.”
—Erik Greb
Suggested Reading
Burton JM, Kimball S, Vieth R, et al. A phase I/II dose-escalation trial of vitamin D3 and calcium in multiple sclerosis. Neurology. 2010;74(23):1852-1859.
Mowry EM. Vitamin D: evidence for its role as a prognostic factor in multiple sclerosis. J Neurol Sci. 2011; 311(1-2):19-22.
Mowry EM, Pelletier D, Gao Z, et al. Vitamin D in clinically isolated syndrome: evidence for possible neuroprotection. Eur J Neurol. 2016;23(2):327-332.
Mowry EM, Waubant E, McCulloch CE, et al. Vitamin D status predicts new brain magnetic resonance imaging activity in multiple sclerosis. Ann Neurol. 2012;72(2):234-240.
Munger KL, Åivo J, Hongell K, et al. Vitamin D status during pregnancy and risk of multiple sclerosis in offspring of women in the Finnish Maternity Cohort. JAMA Neurol. 2016;73(5):515-519.
Munger KL, Levin LI, Hollis BW, et al. Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis. JAMA. 2006;296(23):2832-2838.
Nielsen NM, Munger KL, Koch-Henriksen N, et al. Neonatal vitamin D status and risk of multiple sclerosis: a population-based case-control study. Neurology. 2017;88(1):44-51.
Tremlett H, van der Mei IA, Pittas F, et al. Monthly ambient sunlight, infections and relapse rates in multiple sclerosis. Neuroepidemiology. 2008;31(4):271-279.
Which treatments for pelvic floor disorders are backed by evidence?
EXPERT COMMENTARY
Care of women with pelvic floor disorders, primarily urinary incontinence and POP, involves:
- assessing the patient’s symptoms and determining how bothersome they are
- educating the patient about her condition and the options for treatment
- initiating treatment with the most conservative and least invasive therapies.
Safe treatments include PFMT and pessaries, and both can be effective. However, since approximately 25% of women experience one or more pelvic floor disorders during their life, surgical repair of these disorders is common. The lifetime risk of surgery for stress urinary incontinence (SUI) or POP is 20%,1 and one-third of patients will undergo reoperation for the same condition. Midurethral mesh slings are the gold standard for surgical management of SUI.2 Use of transvaginal mesh for primary prolapse repairs, however, is associated with challenging adverse effects, and its use should be reserved for carefully selected patients.
Data from 3 recent studies contribute to our evidence base on various treatments for pelvic floor disorders.
Details of the studies
PFMT for secondary prevention of POP. In a study conducted in the United Kingdom and New Zealand, Hagen and colleagues randomly assigned 414 women with POP, with or without symptoms, to an intervention group or a control group. The women had previously participated in a longitudinal study of postpartum pelvic floor function. Participants in the intervention group (n = 207) received 5 formal sessions of PFMT over 16 weeks, followed by Pilates-based classes focused on pelvic floor exercises; those in the control group (n = 207) received an informational leaflet about prolapse and lifestyle. The primary outcome was self-reported prolapse symptoms, assessed with the POP Symptom Score (POP-SS) at 2 years.
At study end, the mean (SD) POP-SS score in the intervention group was 3.2 (3.4), compared with a mean (SD) score of 4.2 (4.4) in the control group (adjusted mean difference, −1.01; 95% confidence interval [CI], −1.70 to −0.33; P = .004).
Investigators’ interpretation. The researchers concluded that the participants in the PFMT group had a small but significant—and clinically important—decrease in prolapse symptoms.
The PROSPECT study: Standard versus augmented surgical repair. In a multicenter trial in the United Kingdom by Glazener and associates, 1,352 women with symptomatic POP were randomly allocated to surgical repair with native tissue alone (standard repair) or to standard surgical repair augmented either with polypropylene mesh or with biological graft. The primary outcomes were participant-reported prolapse symptoms (assessed with POP-SS) and prolapse-related quality of life scores; these were measured at 1 year and at 2 years.
One year after surgery, failure rates (defined as prolapse beyond the hymen) were similar in all groups (range, 14%–18%); serious adverse events were also similar in all surgical groups (range, 6%–10%). Overall, 6% of women underwent reoperation for recurrent symptoms. Among women randomly assigned to repair with mesh, 12% to 14% experienced mesh-related adverse events; three-quarters of these women ultimately required surgical excision of the mesh.
Study takeaway. Thus, in terms of effectiveness, quality of life, and adverse effects, augmentation of a vaginal surgical repair with either mesh or graft material did not improve the outcomes of women with POP.
Adverse events after surgical procedures for pelvic floor disorders. In Scotland, Morling and colleagues performed a retrospective observational cohort study of first-time surgeries for SUI (mesh or colposuspension; 16,660 procedures) and prolapse (mesh or native tissue; 18,986 procedures).
After 5 years of follow-up, women who underwent midurethral mesh sling placement or colposuspension had similar rates of repeat surgery for recurrent SUI (adjusted incidence rate ratio, 0.90; 95% CI, 0.73–1.11). Use of mesh slings was associated with fewer immediate complications (adjusted relative risk, 0.44; 95% CI, 0.36–0.55) compared with nonmesh surgery.
Among women who underwent surgery for prolapse, those who had anterior and posterior repair with mesh experienced higher late complication rates than those who underwent native tissue repair. Risk for subsequent prolapse repair was similar with mesh and native-tissue procedures.
Authors’ commentary. The researchers noted that their data support the use of mesh procedures for incontinence but additional research on longer-term outcomes would be useful. However, for prolapse repair, the study results do not decidedly favor any one vault repair procedure.
--Meadow M. Good, DO
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Wu JM, Matthews CA, Conover MM, Pate V, Funk MJ. Lifetime risk of stress incontinence or pelvic organ prolapse surgery. Obstet Gynecol. 2014;123(6):1201–1206.
- Nager C, Tulikangas P, Miller D, Rovner E, Goldman H. Position statement on mesh midurethral slings for stress urinary incontinence. Female Pelvic Med Reconstr Surg. 2014;20(3):123–125.
EXPERT COMMENTARY
Care of women with pelvic floor disorders, primarily urinary incontinence and POP, involves:
- assessing the patient’s symptoms and determining how bothersome they are
- educating the patient about her condition and the options for treatment
- initiating treatment with the most conservative and least invasive therapies.
Safe treatments include PFMT and pessaries, and both can be effective. However, since approximately 25% of women experience one or more pelvic floor disorders during their life, surgical repair of these disorders is common. The lifetime risk of surgery for stress urinary incontinence (SUI) or POP is 20%,1 and one-third of patients will undergo reoperation for the same condition. Midurethral mesh slings are the gold standard for surgical management of SUI.2 Use of transvaginal mesh for primary prolapse repairs, however, is associated with challenging adverse effects, and its use should be reserved for carefully selected patients.
Data from 3 recent studies contribute to our evidence base on various treatments for pelvic floor disorders.
Details of the studies
PFMT for secondary prevention of POP. In a study conducted in the United Kingdom and New Zealand, Hagen and colleagues randomly assigned 414 women with POP, with or without symptoms, to an intervention group or a control group. The women had previously participated in a longitudinal study of postpartum pelvic floor function. Participants in the intervention group (n = 207) received 5 formal sessions of PFMT over 16 weeks, followed by Pilates-based classes focused on pelvic floor exercises; those in the control group (n = 207) received an informational leaflet about prolapse and lifestyle. The primary outcome was self-reported prolapse symptoms, assessed with the POP Symptom Score (POP-SS) at 2 years.
At study end, the mean (SD) POP-SS score in the intervention group was 3.2 (3.4), compared with a mean (SD) score of 4.2 (4.4) in the control group (adjusted mean difference, −1.01; 95% confidence interval [CI], −1.70 to −0.33; P = .004).
Investigators’ interpretation. The researchers concluded that the participants in the PFMT group had a small but significant—and clinically important—decrease in prolapse symptoms.
The PROSPECT study: Standard versus augmented surgical repair. In a multicenter trial in the United Kingdom by Glazener and associates, 1,352 women with symptomatic POP were randomly allocated to surgical repair with native tissue alone (standard repair) or to standard surgical repair augmented either with polypropylene mesh or with biological graft. The primary outcomes were participant-reported prolapse symptoms (assessed with POP-SS) and prolapse-related quality of life scores; these were measured at 1 year and at 2 years.
One year after surgery, failure rates (defined as prolapse beyond the hymen) were similar in all groups (range, 14%–18%); serious adverse events were also similar in all surgical groups (range, 6%–10%). Overall, 6% of women underwent reoperation for recurrent symptoms. Among women randomly assigned to repair with mesh, 12% to 14% experienced mesh-related adverse events; three-quarters of these women ultimately required surgical excision of the mesh.
Study takeaway. Thus, in terms of effectiveness, quality of life, and adverse effects, augmentation of a vaginal surgical repair with either mesh or graft material did not improve the outcomes of women with POP.
Adverse events after surgical procedures for pelvic floor disorders. In Scotland, Morling and colleagues performed a retrospective observational cohort study of first-time surgeries for SUI (mesh or colposuspension; 16,660 procedures) and prolapse (mesh or native tissue; 18,986 procedures).
After 5 years of follow-up, women who underwent midurethral mesh sling placement or colposuspension had similar rates of repeat surgery for recurrent SUI (adjusted incidence rate ratio, 0.90; 95% CI, 0.73–1.11). Use of mesh slings was associated with fewer immediate complications (adjusted relative risk, 0.44; 95% CI, 0.36–0.55) compared with nonmesh surgery.
Among women who underwent surgery for prolapse, those who had anterior and posterior repair with mesh experienced higher late complication rates than those who underwent native tissue repair. Risk for subsequent prolapse repair was similar with mesh and native-tissue procedures.
Authors’ commentary. The researchers noted that their data support the use of mesh procedures for incontinence but additional research on longer-term outcomes would be useful. However, for prolapse repair, the study results do not decidedly favor any one vault repair procedure.
--Meadow M. Good, DO
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
EXPERT COMMENTARY
Care of women with pelvic floor disorders, primarily urinary incontinence and POP, involves:
- assessing the patient’s symptoms and determining how bothersome they are
- educating the patient about her condition and the options for treatment
- initiating treatment with the most conservative and least invasive therapies.
Safe treatments include PFMT and pessaries, and both can be effective. However, since approximately 25% of women experience one or more pelvic floor disorders during their life, surgical repair of these disorders is common. The lifetime risk of surgery for stress urinary incontinence (SUI) or POP is 20%,1 and one-third of patients will undergo reoperation for the same condition. Midurethral mesh slings are the gold standard for surgical management of SUI.2 Use of transvaginal mesh for primary prolapse repairs, however, is associated with challenging adverse effects, and its use should be reserved for carefully selected patients.
Data from 3 recent studies contribute to our evidence base on various treatments for pelvic floor disorders.
Details of the studies
PFMT for secondary prevention of POP. In a study conducted in the United Kingdom and New Zealand, Hagen and colleagues randomly assigned 414 women with POP, with or without symptoms, to an intervention group or a control group. The women had previously participated in a longitudinal study of postpartum pelvic floor function. Participants in the intervention group (n = 207) received 5 formal sessions of PFMT over 16 weeks, followed by Pilates-based classes focused on pelvic floor exercises; those in the control group (n = 207) received an informational leaflet about prolapse and lifestyle. The primary outcome was self-reported prolapse symptoms, assessed with the POP Symptom Score (POP-SS) at 2 years.
At study end, the mean (SD) POP-SS score in the intervention group was 3.2 (3.4), compared with a mean (SD) score of 4.2 (4.4) in the control group (adjusted mean difference, −1.01; 95% confidence interval [CI], −1.70 to −0.33; P = .004).
Investigators’ interpretation. The researchers concluded that the participants in the PFMT group had a small but significant—and clinically important—decrease in prolapse symptoms.
The PROSPECT study: Standard versus augmented surgical repair. In a multicenter trial in the United Kingdom by Glazener and associates, 1,352 women with symptomatic POP were randomly allocated to surgical repair with native tissue alone (standard repair) or to standard surgical repair augmented either with polypropylene mesh or with biological graft. The primary outcomes were participant-reported prolapse symptoms (assessed with POP-SS) and prolapse-related quality of life scores; these were measured at 1 year and at 2 years.
One year after surgery, failure rates (defined as prolapse beyond the hymen) were similar in all groups (range, 14%–18%); serious adverse events were also similar in all surgical groups (range, 6%–10%). Overall, 6% of women underwent reoperation for recurrent symptoms. Among women randomly assigned to repair with mesh, 12% to 14% experienced mesh-related adverse events; three-quarters of these women ultimately required surgical excision of the mesh.
Study takeaway. Thus, in terms of effectiveness, quality of life, and adverse effects, augmentation of a vaginal surgical repair with either mesh or graft material did not improve the outcomes of women with POP.
Adverse events after surgical procedures for pelvic floor disorders. In Scotland, Morling and colleagues performed a retrospective observational cohort study of first-time surgeries for SUI (mesh or colposuspension; 16,660 procedures) and prolapse (mesh or native tissue; 18,986 procedures).
After 5 years of follow-up, women who underwent midurethral mesh sling placement or colposuspension had similar rates of repeat surgery for recurrent SUI (adjusted incidence rate ratio, 0.90; 95% CI, 0.73–1.11). Use of mesh slings was associated with fewer immediate complications (adjusted relative risk, 0.44; 95% CI, 0.36–0.55) compared with nonmesh surgery.
Among women who underwent surgery for prolapse, those who had anterior and posterior repair with mesh experienced higher late complication rates than those who underwent native tissue repair. Risk for subsequent prolapse repair was similar with mesh and native-tissue procedures.
Authors’ commentary. The researchers noted that their data support the use of mesh procedures for incontinence but additional research on longer-term outcomes would be useful. However, for prolapse repair, the study results do not decidedly favor any one vault repair procedure.
--Meadow M. Good, DO
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Wu JM, Matthews CA, Conover MM, Pate V, Funk MJ. Lifetime risk of stress incontinence or pelvic organ prolapse surgery. Obstet Gynecol. 2014;123(6):1201–1206.
- Nager C, Tulikangas P, Miller D, Rovner E, Goldman H. Position statement on mesh midurethral slings for stress urinary incontinence. Female Pelvic Med Reconstr Surg. 2014;20(3):123–125.
- Wu JM, Matthews CA, Conover MM, Pate V, Funk MJ. Lifetime risk of stress incontinence or pelvic organ prolapse surgery. Obstet Gynecol. 2014;123(6):1201–1206.
- Nager C, Tulikangas P, Miller D, Rovner E, Goldman H. Position statement on mesh midurethral slings for stress urinary incontinence. Female Pelvic Med Reconstr Surg. 2014;20(3):123–125.
Justice Department joins lawsuit alleging massive Medicare fraud by UnitedHealth
The Justice Department has joined a California whistle-blower’s lawsuit that accuses insurance giant UnitedHealth Group of fraud in its popular Medicare Advantage health plans.
Justice officials filed legal papers to intervene in the suit, first brought by whistle-blower James Swoben in 2009, on Friday in federal court in Los Angeles. On Monday, they sought a court order to combine Mr. Swoben’s case with that of another whistle-blower.
Mr. Swoben has accused the insurer of “gaming” the Medicare Advantage payment system by “making patients look sicker than they are,” said his attorney, William K. Hanagami. Mr. Hanagami said the combined cases could prove to be among the “larger frauds” ever against Medicare, with damages that he speculates could top $1 billion.
UnitedHealth spokesman Matt Burns denied any wrongdoing by the company. “We are honored to serve millions of seniors through Medicare Advantage, proud of the access to quality health care we provided, and confident we complied with program rules,” he wrote in an email.
Mr. Burns also said that “litigating against Medicare Advantage plans to create new rules through the courts will not fix widely acknowledged government policy shortcomings or help Medicare Advantage members and is wrong.”
Medicare Advantage is a popular alternative to traditional Medicare. The privately run health plans have enrolled more than 18 million elderly and people with disabilities – about a third of those eligible for Medicare – at a cost to taxpayers of more than $150 billion a year.
Although the plans generally enjoy strong support in Congress, they have been the target of at least a half-dozen whistle-blower lawsuits alleging patterns of overbilling and fraud. In most of the prior cases, Justice Department officials have decided not to intervene, which often limits the financial recovery by the government and also by whistle-blowers, who can be awarded a portion of recovered funds. A decision to intervene means that the Justice Department is taking over the investigation of the case, greatly raising the stakes.
“This is a very big development and sends a strong signal that the Trump administration is very serious when it comes to fighting fraud in the health care arena,” said Patrick Burns, associate director of Taxpayers Against Fraud in Washington, a nonprofit supported by whistle-blowers and their lawyers. Burns said the “winners here are going to be American taxpayers.”
Patrick Burns also contends that the cases against UnitedHealth could potentially exceed $1 billion in damages, which would place them among the top two or three whistle-blower–prompted cases on record.
“This is not one company engaged in episodic bad behavior, but a lucrative business plan that appears to be national in scope,” he said.
On Monday, the government said it wants to consolidate the Swoben case with another whistle-blower action filed in 2011 by former UnitedHealth executive Benjamin Poehling and unsealed in March by a federal judge. Mr. Poehling also has alleged that the insurer generated hundreds of millions of dollars or more in overpayments.
When Congress created the current Medicare Advantage program in 2003, it expected to pay higher rates for sicker patients than for people in good health using a formula called a risk score.
But, overspending tied to inflated risk scores has repeatedly been cited by government auditors, including the Government Accountability Office. A series of articles published in 2014 by the Center for Public Integrity found that these improper payments have cost taxpayers tens of billions of dollars.
“If the goal of fraud is to artificially increase risk scores and you do that wholesale, that results in some rather significant dollars,” Mr. Hanagami said.
David Lipschutz, senior policy attorney for the Center for Medicare Advocacy, a nonprofit offering legal assistance and other resources for those eligible for Medicare, said his group is “deeply concerned by ongoing improper payments” to Medicare Advantage health plans.
These overpayments “undermine the finances of the overall Medicare program,” he said in an emailed statement. He said his group supports “more rigorous oversight” of payments made to the health plans.
The two whistle-blower complaints allege that UnitedHealth has had a practice of asking the government to reimburse it for underpayments but did not report claims for which it had received too much money, despite knowing some of these claims had inflated risk scores.
The federal Centers for Medicare & Medicaid Services said in draft regulations issued in January 2014 that it would begin requiring that Medicare Advantage plans report any improper payment – either too much or too little.
These reviews “cannot be designed only to identify diagnoses that would trigger additional payments,” the proposal stated.
But CMS backed off the regulation’s reporting requirements in the face of opposition from the insurance industry. The agency didn’t say why it did so.
The Justice Department said in an April 2016 amicus brief in the Swoben case that the CMS decision not to move ahead with the reporting regulation “does not relieve defendants of the broad obligation to exercise due diligence in ensuring the accuracy” of claims submitted for payment.
The Justice Department concluded in the brief that the insurers “chose not to connect the dots,” even though they knew of both overpayments and underpayments. Instead, the insurers “acted in a deliberately ignorant or reckless manner in falsely certifying the accuracy, completeness, and truthfulness of submitted data,” the 2016 brief states.
The Justice Department has said it also is investigating risk-score payments to other Medicare Advantage insurers, but has not said whether it plans to take action against any of them.
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
The Justice Department has joined a California whistle-blower’s lawsuit that accuses insurance giant UnitedHealth Group of fraud in its popular Medicare Advantage health plans.
Justice officials filed legal papers to intervene in the suit, first brought by whistle-blower James Swoben in 2009, on Friday in federal court in Los Angeles. On Monday, they sought a court order to combine Mr. Swoben’s case with that of another whistle-blower.
Mr. Swoben has accused the insurer of “gaming” the Medicare Advantage payment system by “making patients look sicker than they are,” said his attorney, William K. Hanagami. Mr. Hanagami said the combined cases could prove to be among the “larger frauds” ever against Medicare, with damages that he speculates could top $1 billion.
UnitedHealth spokesman Matt Burns denied any wrongdoing by the company. “We are honored to serve millions of seniors through Medicare Advantage, proud of the access to quality health care we provided, and confident we complied with program rules,” he wrote in an email.
Mr. Burns also said that “litigating against Medicare Advantage plans to create new rules through the courts will not fix widely acknowledged government policy shortcomings or help Medicare Advantage members and is wrong.”
Medicare Advantage is a popular alternative to traditional Medicare. The privately run health plans have enrolled more than 18 million elderly and people with disabilities – about a third of those eligible for Medicare – at a cost to taxpayers of more than $150 billion a year.
Although the plans generally enjoy strong support in Congress, they have been the target of at least a half-dozen whistle-blower lawsuits alleging patterns of overbilling and fraud. In most of the prior cases, Justice Department officials have decided not to intervene, which often limits the financial recovery by the government and also by whistle-blowers, who can be awarded a portion of recovered funds. A decision to intervene means that the Justice Department is taking over the investigation of the case, greatly raising the stakes.
“This is a very big development and sends a strong signal that the Trump administration is very serious when it comes to fighting fraud in the health care arena,” said Patrick Burns, associate director of Taxpayers Against Fraud in Washington, a nonprofit supported by whistle-blowers and their lawyers. Burns said the “winners here are going to be American taxpayers.”
Patrick Burns also contends that the cases against UnitedHealth could potentially exceed $1 billion in damages, which would place them among the top two or three whistle-blower–prompted cases on record.
“This is not one company engaged in episodic bad behavior, but a lucrative business plan that appears to be national in scope,” he said.
On Monday, the government said it wants to consolidate the Swoben case with another whistle-blower action filed in 2011 by former UnitedHealth executive Benjamin Poehling and unsealed in March by a federal judge. Mr. Poehling also has alleged that the insurer generated hundreds of millions of dollars or more in overpayments.
When Congress created the current Medicare Advantage program in 2003, it expected to pay higher rates for sicker patients than for people in good health using a formula called a risk score.
But, overspending tied to inflated risk scores has repeatedly been cited by government auditors, including the Government Accountability Office. A series of articles published in 2014 by the Center for Public Integrity found that these improper payments have cost taxpayers tens of billions of dollars.
“If the goal of fraud is to artificially increase risk scores and you do that wholesale, that results in some rather significant dollars,” Mr. Hanagami said.
David Lipschutz, senior policy attorney for the Center for Medicare Advocacy, a nonprofit offering legal assistance and other resources for those eligible for Medicare, said his group is “deeply concerned by ongoing improper payments” to Medicare Advantage health plans.
These overpayments “undermine the finances of the overall Medicare program,” he said in an emailed statement. He said his group supports “more rigorous oversight” of payments made to the health plans.
The two whistle-blower complaints allege that UnitedHealth has had a practice of asking the government to reimburse it for underpayments but did not report claims for which it had received too much money, despite knowing some of these claims had inflated risk scores.
The federal Centers for Medicare & Medicaid Services said in draft regulations issued in January 2014 that it would begin requiring that Medicare Advantage plans report any improper payment – either too much or too little.
These reviews “cannot be designed only to identify diagnoses that would trigger additional payments,” the proposal stated.
But CMS backed off the regulation’s reporting requirements in the face of opposition from the insurance industry. The agency didn’t say why it did so.
The Justice Department said in an April 2016 amicus brief in the Swoben case that the CMS decision not to move ahead with the reporting regulation “does not relieve defendants of the broad obligation to exercise due diligence in ensuring the accuracy” of claims submitted for payment.
The Justice Department concluded in the brief that the insurers “chose not to connect the dots,” even though they knew of both overpayments and underpayments. Instead, the insurers “acted in a deliberately ignorant or reckless manner in falsely certifying the accuracy, completeness, and truthfulness of submitted data,” the 2016 brief states.
The Justice Department has said it also is investigating risk-score payments to other Medicare Advantage insurers, but has not said whether it plans to take action against any of them.
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
The Justice Department has joined a California whistle-blower’s lawsuit that accuses insurance giant UnitedHealth Group of fraud in its popular Medicare Advantage health plans.
Justice officials filed legal papers to intervene in the suit, first brought by whistle-blower James Swoben in 2009, on Friday in federal court in Los Angeles. On Monday, they sought a court order to combine Mr. Swoben’s case with that of another whistle-blower.
Mr. Swoben has accused the insurer of “gaming” the Medicare Advantage payment system by “making patients look sicker than they are,” said his attorney, William K. Hanagami. Mr. Hanagami said the combined cases could prove to be among the “larger frauds” ever against Medicare, with damages that he speculates could top $1 billion.
UnitedHealth spokesman Matt Burns denied any wrongdoing by the company. “We are honored to serve millions of seniors through Medicare Advantage, proud of the access to quality health care we provided, and confident we complied with program rules,” he wrote in an email.
Mr. Burns also said that “litigating against Medicare Advantage plans to create new rules through the courts will not fix widely acknowledged government policy shortcomings or help Medicare Advantage members and is wrong.”
Medicare Advantage is a popular alternative to traditional Medicare. The privately run health plans have enrolled more than 18 million elderly and people with disabilities – about a third of those eligible for Medicare – at a cost to taxpayers of more than $150 billion a year.
Although the plans generally enjoy strong support in Congress, they have been the target of at least a half-dozen whistle-blower lawsuits alleging patterns of overbilling and fraud. In most of the prior cases, Justice Department officials have decided not to intervene, which often limits the financial recovery by the government and also by whistle-blowers, who can be awarded a portion of recovered funds. A decision to intervene means that the Justice Department is taking over the investigation of the case, greatly raising the stakes.
“This is a very big development and sends a strong signal that the Trump administration is very serious when it comes to fighting fraud in the health care arena,” said Patrick Burns, associate director of Taxpayers Against Fraud in Washington, a nonprofit supported by whistle-blowers and their lawyers. Burns said the “winners here are going to be American taxpayers.”
Patrick Burns also contends that the cases against UnitedHealth could potentially exceed $1 billion in damages, which would place them among the top two or three whistle-blower–prompted cases on record.
“This is not one company engaged in episodic bad behavior, but a lucrative business plan that appears to be national in scope,” he said.
On Monday, the government said it wants to consolidate the Swoben case with another whistle-blower action filed in 2011 by former UnitedHealth executive Benjamin Poehling and unsealed in March by a federal judge. Mr. Poehling also has alleged that the insurer generated hundreds of millions of dollars or more in overpayments.
When Congress created the current Medicare Advantage program in 2003, it expected to pay higher rates for sicker patients than for people in good health using a formula called a risk score.
But, overspending tied to inflated risk scores has repeatedly been cited by government auditors, including the Government Accountability Office. A series of articles published in 2014 by the Center for Public Integrity found that these improper payments have cost taxpayers tens of billions of dollars.
“If the goal of fraud is to artificially increase risk scores and you do that wholesale, that results in some rather significant dollars,” Mr. Hanagami said.
David Lipschutz, senior policy attorney for the Center for Medicare Advocacy, a nonprofit offering legal assistance and other resources for those eligible for Medicare, said his group is “deeply concerned by ongoing improper payments” to Medicare Advantage health plans.
These overpayments “undermine the finances of the overall Medicare program,” he said in an emailed statement. He said his group supports “more rigorous oversight” of payments made to the health plans.
The two whistle-blower complaints allege that UnitedHealth has had a practice of asking the government to reimburse it for underpayments but did not report claims for which it had received too much money, despite knowing some of these claims had inflated risk scores.
The federal Centers for Medicare & Medicaid Services said in draft regulations issued in January 2014 that it would begin requiring that Medicare Advantage plans report any improper payment – either too much or too little.
These reviews “cannot be designed only to identify diagnoses that would trigger additional payments,” the proposal stated.
But CMS backed off the regulation’s reporting requirements in the face of opposition from the insurance industry. The agency didn’t say why it did so.
The Justice Department said in an April 2016 amicus brief in the Swoben case that the CMS decision not to move ahead with the reporting regulation “does not relieve defendants of the broad obligation to exercise due diligence in ensuring the accuracy” of claims submitted for payment.
The Justice Department concluded in the brief that the insurers “chose not to connect the dots,” even though they knew of both overpayments and underpayments. Instead, the insurers “acted in a deliberately ignorant or reckless manner in falsely certifying the accuracy, completeness, and truthfulness of submitted data,” the 2016 brief states.
The Justice Department has said it also is investigating risk-score payments to other Medicare Advantage insurers, but has not said whether it plans to take action against any of them.
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Can Gene Expression–Based Technologies Help Diagnose MS?
ORLANDO—RNA expression patterns are highly dynamic, even at the earliest stages of multiple sclerosis (MS) pathogenesis, according to research presented at the ACTRIMS 2017 Forum. Machine learning methods trained and validated with these gene targets are a highly accurate tool that could provide actionable data for health care providers who suspect MS.
RNA sequencing was performed to identify differentially expressed protein-coding and noncoding RNA genes at distinct stages of MS, compared with controls. Expression levels of these genes were validated by real-time polymerase chain reaction (PCR) across all 979 subjects recruited. Ratios of gene expression data were used as inputs to train machine learning classifiers capable of multicategory comparisons. An independent validation testing set consisting of individuals across each control
—Glenn S. Williams
ORLANDO—RNA expression patterns are highly dynamic, even at the earliest stages of multiple sclerosis (MS) pathogenesis, according to research presented at the ACTRIMS 2017 Forum. Machine learning methods trained and validated with these gene targets are a highly accurate tool that could provide actionable data for health care providers who suspect MS.
RNA sequencing was performed to identify differentially expressed protein-coding and noncoding RNA genes at distinct stages of MS, compared with controls. Expression levels of these genes were validated by real-time polymerase chain reaction (PCR) across all 979 subjects recruited. Ratios of gene expression data were used as inputs to train machine learning classifiers capable of multicategory comparisons. An independent validation testing set consisting of individuals across each control
—Glenn S. Williams
ORLANDO—RNA expression patterns are highly dynamic, even at the earliest stages of multiple sclerosis (MS) pathogenesis, according to research presented at the ACTRIMS 2017 Forum. Machine learning methods trained and validated with these gene targets are a highly accurate tool that could provide actionable data for health care providers who suspect MS.
RNA sequencing was performed to identify differentially expressed protein-coding and noncoding RNA genes at distinct stages of MS, compared with controls. Expression levels of these genes were validated by real-time polymerase chain reaction (PCR) across all 979 subjects recruited. Ratios of gene expression data were used as inputs to train machine learning classifiers capable of multicategory comparisons. An independent validation testing set consisting of individuals across each control
—Glenn S. Williams
Dr. Henri Ford Accorded Honorary Fellowship in RCSEng
Henri R. Ford, MD, MHA, FACS, FAAP, vice-president and surgeon-in-chief, Children’s Hospital Los Angeles; professor of surgery and vice-dean for medical education, Keck School of Medicine, University of Southern California; and member of the American College of Surgeons Board of Regents, was accorded Honorary Fellowship in the Royal College of Surgeons of England (RCSEng) on March 7 in London, U.K.
A world-renowned Haitian-American surgeon, Dr. Ford played a prominent role in organizing and leading medical teams in response to the catastrophic 2010 earthquake in Haiti. Born in Haiti, Dr. Ford regularly returns to his native country to teach, lead operating teams, and assist in developing surgical systems, which the island nation historically has lacked. His accomplishments there are myriad. For example, in May 2015, Dr. Ford led a team of health care professionals that made history by completing the first separation of conjoined twins in Haiti. (Read more about the operation at www.cbsnews.com/news/more-than-just-a-surgery-conjoined-twins-separated-in-haiti/.)
Dr. Ford and his family fled Haiti’s oppressive regime and came to the U.S. when he was 13 years old. He received his medical degree from Harvard Medical School, Boston, MA, and trained in general surgery at Weill Cornell Medical College, New York, NY. He completed his pediatric surgical training at Children’s Hospital of Pittsburgh, PA. Prior to joining Children’s Hospital Los Angeles in 2005, Dr. Ford was professor and chief, division of pediatric surgery, and surgeon-in-chief, Children’s Hospital of Pittsburgh and the University of Pittsburgh School of Medicine.
Su-Anna Boddy, MS, FRCS, council member for the RCSEng, introduced Dr. Ford at the ceremony and spoke of his accomplishments, and Clare Marx, CBE, DL, PRCS, RCSEng president, formally awarded him the honor.
Henri R. Ford, MD, MHA, FACS, FAAP, vice-president and surgeon-in-chief, Children’s Hospital Los Angeles; professor of surgery and vice-dean for medical education, Keck School of Medicine, University of Southern California; and member of the American College of Surgeons Board of Regents, was accorded Honorary Fellowship in the Royal College of Surgeons of England (RCSEng) on March 7 in London, U.K.
A world-renowned Haitian-American surgeon, Dr. Ford played a prominent role in organizing and leading medical teams in response to the catastrophic 2010 earthquake in Haiti. Born in Haiti, Dr. Ford regularly returns to his native country to teach, lead operating teams, and assist in developing surgical systems, which the island nation historically has lacked. His accomplishments there are myriad. For example, in May 2015, Dr. Ford led a team of health care professionals that made history by completing the first separation of conjoined twins in Haiti. (Read more about the operation at www.cbsnews.com/news/more-than-just-a-surgery-conjoined-twins-separated-in-haiti/.)
Dr. Ford and his family fled Haiti’s oppressive regime and came to the U.S. when he was 13 years old. He received his medical degree from Harvard Medical School, Boston, MA, and trained in general surgery at Weill Cornell Medical College, New York, NY. He completed his pediatric surgical training at Children’s Hospital of Pittsburgh, PA. Prior to joining Children’s Hospital Los Angeles in 2005, Dr. Ford was professor and chief, division of pediatric surgery, and surgeon-in-chief, Children’s Hospital of Pittsburgh and the University of Pittsburgh School of Medicine.
Su-Anna Boddy, MS, FRCS, council member for the RCSEng, introduced Dr. Ford at the ceremony and spoke of his accomplishments, and Clare Marx, CBE, DL, PRCS, RCSEng president, formally awarded him the honor.
Henri R. Ford, MD, MHA, FACS, FAAP, vice-president and surgeon-in-chief, Children’s Hospital Los Angeles; professor of surgery and vice-dean for medical education, Keck School of Medicine, University of Southern California; and member of the American College of Surgeons Board of Regents, was accorded Honorary Fellowship in the Royal College of Surgeons of England (RCSEng) on March 7 in London, U.K.
A world-renowned Haitian-American surgeon, Dr. Ford played a prominent role in organizing and leading medical teams in response to the catastrophic 2010 earthquake in Haiti. Born in Haiti, Dr. Ford regularly returns to his native country to teach, lead operating teams, and assist in developing surgical systems, which the island nation historically has lacked. His accomplishments there are myriad. For example, in May 2015, Dr. Ford led a team of health care professionals that made history by completing the first separation of conjoined twins in Haiti. (Read more about the operation at www.cbsnews.com/news/more-than-just-a-surgery-conjoined-twins-separated-in-haiti/.)
Dr. Ford and his family fled Haiti’s oppressive regime and came to the U.S. when he was 13 years old. He received his medical degree from Harvard Medical School, Boston, MA, and trained in general surgery at Weill Cornell Medical College, New York, NY. He completed his pediatric surgical training at Children’s Hospital of Pittsburgh, PA. Prior to joining Children’s Hospital Los Angeles in 2005, Dr. Ford was professor and chief, division of pediatric surgery, and surgeon-in-chief, Children’s Hospital of Pittsburgh and the University of Pittsburgh School of Medicine.
Su-Anna Boddy, MS, FRCS, council member for the RCSEng, introduced Dr. Ford at the ceremony and spoke of his accomplishments, and Clare Marx, CBE, DL, PRCS, RCSEng president, formally awarded him the honor.
Dr. Thomas Starzl, the “Father of Transplantation,” passes away
Thomas E. Starzl, MD, PhD, FACS, known as the “father of transplantation” for his role as the first surgeon to perform a successful human liver transplant and for developing techniques for safe, standardized surgery in the field of transplantation, died March 4 at his home in Pittsburgh, PA. He was 90 years old.
After nearly a decade of laboratory research and surgical practice at institutions such as Northwestern Medical School, Chicago, IL, and Johns Hopkins Hospital, Baltimore, MD, Dr. Starzl performed the world’s first successful liver transplant while practicing at the University of Colorado, Boulder, in 1967. This achievement came at a time when the prevailing medical opinion on the feasibility of liver transplants was pessimistic, but Dr. Starzl’s monumental success led to a newfound clinical interest in the possibilities of allogenic human transplantation. In 1980, he introduced anti-lymphocyte globulin and cyclosporine to his previous development of azathioprine and corticosteroid immunosuppression to prevent organ rejection. It was this advancement that moved organ transplantation from being considered an experimental to a clinically accepted treatment modality.
Dr. Starzl joined the University of Pittsburgh School of Medicine in 1981 as professor of surgery; there, he launched the first liver transplant program in the U.S. Though he retired from clinical and surgical service in 1991 after serving as chief of transplantation services at various Pittsburgh hospitals, he remained at the University of Pittsburgh as distinguished service professor of surgery and director emeritus of the University of Pittsburgh Medical Center’s Thomas E. Starzl Transplantation Institute.
Read about Dr. Starzl’s storied career and a statement from his family at www.news.pitt.edu/news/starzl. For a more thorough account of Dr. Starzl’s accomplishments, visit the University of Pittsburgh’s Dr. Thomas E. Starzl website at www.starzl.pitt.edu/index.html.
Thomas E. Starzl, MD, PhD, FACS, known as the “father of transplantation” for his role as the first surgeon to perform a successful human liver transplant and for developing techniques for safe, standardized surgery in the field of transplantation, died March 4 at his home in Pittsburgh, PA. He was 90 years old.
After nearly a decade of laboratory research and surgical practice at institutions such as Northwestern Medical School, Chicago, IL, and Johns Hopkins Hospital, Baltimore, MD, Dr. Starzl performed the world’s first successful liver transplant while practicing at the University of Colorado, Boulder, in 1967. This achievement came at a time when the prevailing medical opinion on the feasibility of liver transplants was pessimistic, but Dr. Starzl’s monumental success led to a newfound clinical interest in the possibilities of allogenic human transplantation. In 1980, he introduced anti-lymphocyte globulin and cyclosporine to his previous development of azathioprine and corticosteroid immunosuppression to prevent organ rejection. It was this advancement that moved organ transplantation from being considered an experimental to a clinically accepted treatment modality.
Dr. Starzl joined the University of Pittsburgh School of Medicine in 1981 as professor of surgery; there, he launched the first liver transplant program in the U.S. Though he retired from clinical and surgical service in 1991 after serving as chief of transplantation services at various Pittsburgh hospitals, he remained at the University of Pittsburgh as distinguished service professor of surgery and director emeritus of the University of Pittsburgh Medical Center’s Thomas E. Starzl Transplantation Institute.
Read about Dr. Starzl’s storied career and a statement from his family at www.news.pitt.edu/news/starzl. For a more thorough account of Dr. Starzl’s accomplishments, visit the University of Pittsburgh’s Dr. Thomas E. Starzl website at www.starzl.pitt.edu/index.html.
Thomas E. Starzl, MD, PhD, FACS, known as the “father of transplantation” for his role as the first surgeon to perform a successful human liver transplant and for developing techniques for safe, standardized surgery in the field of transplantation, died March 4 at his home in Pittsburgh, PA. He was 90 years old.
After nearly a decade of laboratory research and surgical practice at institutions such as Northwestern Medical School, Chicago, IL, and Johns Hopkins Hospital, Baltimore, MD, Dr. Starzl performed the world’s first successful liver transplant while practicing at the University of Colorado, Boulder, in 1967. This achievement came at a time when the prevailing medical opinion on the feasibility of liver transplants was pessimistic, but Dr. Starzl’s monumental success led to a newfound clinical interest in the possibilities of allogenic human transplantation. In 1980, he introduced anti-lymphocyte globulin and cyclosporine to his previous development of azathioprine and corticosteroid immunosuppression to prevent organ rejection. It was this advancement that moved organ transplantation from being considered an experimental to a clinically accepted treatment modality.
Dr. Starzl joined the University of Pittsburgh School of Medicine in 1981 as professor of surgery; there, he launched the first liver transplant program in the U.S. Though he retired from clinical and surgical service in 1991 after serving as chief of transplantation services at various Pittsburgh hospitals, he remained at the University of Pittsburgh as distinguished service professor of surgery and director emeritus of the University of Pittsburgh Medical Center’s Thomas E. Starzl Transplantation Institute.
Read about Dr. Starzl’s storied career and a statement from his family at www.news.pitt.edu/news/starzl. For a more thorough account of Dr. Starzl’s accomplishments, visit the University of Pittsburgh’s Dr. Thomas E. Starzl website at www.starzl.pitt.edu/index.html.
Pitolisant Reduces Cataplexy Attacks in Narcolepsy
Pitolisant, a histamine H3 receptor inverse agonist, is well tolerated and effectively reduces cataplexy, according to data published in the March issue of Lancet Neurology. If the drug’s effect is confirmed in long-term studies, pitolisant could become a first-line therapy for cataplexy in patients with narcolepsy, who currently have few treatment options, according to the authors.
Two types of drugs are used to treat cataplexy. Antidepressants are used off-label and not well supported by evidence. Sodium oxybate is effective, but may cause serious adverse events.
Zoltán Szakács, MD, a doctor at the State Health Center in Budapest, and colleagues enrolled patients with narcolepsy from 16 sleep centers in nine countries into a randomized, double-blind, placebo-controlled trial. Eligible participants were age 18, had narcolepsy with cataplexy, had at least three cataplexies per week, and had excessive daytime sleepiness. Patients were randomized to pitolisant or placebo once per day. During a three-week flexible dosing period, patients randomized to pitolisant received 5 mg for the first week, 10 mg for the second week, and for the third week, a dose of between 5 mg and 20 mg, on the basis of safety and efficacy. A four-week period of stable dosing followed. Finally, patients underwent a one-week withdrawal period.
In all, 54 patients received pitolisant, and 51 received placebo. During the stable dosing period, the weekly cataplexy rate was decreased by 75% in patients who received pitolisant and by 38% among controls. The effect was significant regardless of the patient’s stable dose of pitolisant. Use of concomitant anticataplectic treatment before study initiation did not affect the results. The drug also improved scores on the Epworth Sleepiness Scale and maintenance of wakefulness test.
The pitolisant group had a significantly higher rate of treatment-related adverse events than did the placebo group (28% vs 12%). The researchers recorded no serious adverse events, but observed one case of severe nausea in the pitolisant group.
The study’s main limitation is that the diagnosis of narcolepsy was based on nonspecific criteria, said Christian R. Baumann, Professor of Neurology at University Hospital Zurich, in an accompanying editorial. “The fact that reported mean sleep latencies in the cohort of Szakács and colleagues (4.2–4.7 min) were higher than those reported in other cohorts, including ours (2.6–2.9 min), leaves some uncertainty about patient inclusion,” he added.
Nevertheless, the study may contribute to the regulatory approval of pitolisant. “This is good news for clinicians, since we need more treatment options to better tailor individualized therapy for patients with narcolepsy,” said Dr. Baumann.
—Erik Greb
Suggested Reading
Szakacs Z, Dauvilliers Y, Mikhaylov V, et al. Safety and efficacy of pitolisant on cataplexy in patients with narcolepsy: a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2017;16(3):200-207.
Baumann CR. Wide implications of a trial on pitolisant for cataplexy. Lancet Neurol. 2017;16(3):173-174.
Pitolisant, a histamine H3 receptor inverse agonist, is well tolerated and effectively reduces cataplexy, according to data published in the March issue of Lancet Neurology. If the drug’s effect is confirmed in long-term studies, pitolisant could become a first-line therapy for cataplexy in patients with narcolepsy, who currently have few treatment options, according to the authors.
Two types of drugs are used to treat cataplexy. Antidepressants are used off-label and not well supported by evidence. Sodium oxybate is effective, but may cause serious adverse events.
Zoltán Szakács, MD, a doctor at the State Health Center in Budapest, and colleagues enrolled patients with narcolepsy from 16 sleep centers in nine countries into a randomized, double-blind, placebo-controlled trial. Eligible participants were age 18, had narcolepsy with cataplexy, had at least three cataplexies per week, and had excessive daytime sleepiness. Patients were randomized to pitolisant or placebo once per day. During a three-week flexible dosing period, patients randomized to pitolisant received 5 mg for the first week, 10 mg for the second week, and for the third week, a dose of between 5 mg and 20 mg, on the basis of safety and efficacy. A four-week period of stable dosing followed. Finally, patients underwent a one-week withdrawal period.
In all, 54 patients received pitolisant, and 51 received placebo. During the stable dosing period, the weekly cataplexy rate was decreased by 75% in patients who received pitolisant and by 38% among controls. The effect was significant regardless of the patient’s stable dose of pitolisant. Use of concomitant anticataplectic treatment before study initiation did not affect the results. The drug also improved scores on the Epworth Sleepiness Scale and maintenance of wakefulness test.
The pitolisant group had a significantly higher rate of treatment-related adverse events than did the placebo group (28% vs 12%). The researchers recorded no serious adverse events, but observed one case of severe nausea in the pitolisant group.
The study’s main limitation is that the diagnosis of narcolepsy was based on nonspecific criteria, said Christian R. Baumann, Professor of Neurology at University Hospital Zurich, in an accompanying editorial. “The fact that reported mean sleep latencies in the cohort of Szakács and colleagues (4.2–4.7 min) were higher than those reported in other cohorts, including ours (2.6–2.9 min), leaves some uncertainty about patient inclusion,” he added.
Nevertheless, the study may contribute to the regulatory approval of pitolisant. “This is good news for clinicians, since we need more treatment options to better tailor individualized therapy for patients with narcolepsy,” said Dr. Baumann.
—Erik Greb
Suggested Reading
Szakacs Z, Dauvilliers Y, Mikhaylov V, et al. Safety and efficacy of pitolisant on cataplexy in patients with narcolepsy: a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2017;16(3):200-207.
Baumann CR. Wide implications of a trial on pitolisant for cataplexy. Lancet Neurol. 2017;16(3):173-174.
Pitolisant, a histamine H3 receptor inverse agonist, is well tolerated and effectively reduces cataplexy, according to data published in the March issue of Lancet Neurology. If the drug’s effect is confirmed in long-term studies, pitolisant could become a first-line therapy for cataplexy in patients with narcolepsy, who currently have few treatment options, according to the authors.
Two types of drugs are used to treat cataplexy. Antidepressants are used off-label and not well supported by evidence. Sodium oxybate is effective, but may cause serious adverse events.
Zoltán Szakács, MD, a doctor at the State Health Center in Budapest, and colleagues enrolled patients with narcolepsy from 16 sleep centers in nine countries into a randomized, double-blind, placebo-controlled trial. Eligible participants were age 18, had narcolepsy with cataplexy, had at least three cataplexies per week, and had excessive daytime sleepiness. Patients were randomized to pitolisant or placebo once per day. During a three-week flexible dosing period, patients randomized to pitolisant received 5 mg for the first week, 10 mg for the second week, and for the third week, a dose of between 5 mg and 20 mg, on the basis of safety and efficacy. A four-week period of stable dosing followed. Finally, patients underwent a one-week withdrawal period.
In all, 54 patients received pitolisant, and 51 received placebo. During the stable dosing period, the weekly cataplexy rate was decreased by 75% in patients who received pitolisant and by 38% among controls. The effect was significant regardless of the patient’s stable dose of pitolisant. Use of concomitant anticataplectic treatment before study initiation did not affect the results. The drug also improved scores on the Epworth Sleepiness Scale and maintenance of wakefulness test.
The pitolisant group had a significantly higher rate of treatment-related adverse events than did the placebo group (28% vs 12%). The researchers recorded no serious adverse events, but observed one case of severe nausea in the pitolisant group.
The study’s main limitation is that the diagnosis of narcolepsy was based on nonspecific criteria, said Christian R. Baumann, Professor of Neurology at University Hospital Zurich, in an accompanying editorial. “The fact that reported mean sleep latencies in the cohort of Szakács and colleagues (4.2–4.7 min) were higher than those reported in other cohorts, including ours (2.6–2.9 min), leaves some uncertainty about patient inclusion,” he added.
Nevertheless, the study may contribute to the regulatory approval of pitolisant. “This is good news for clinicians, since we need more treatment options to better tailor individualized therapy for patients with narcolepsy,” said Dr. Baumann.
—Erik Greb
Suggested Reading
Szakacs Z, Dauvilliers Y, Mikhaylov V, et al. Safety and efficacy of pitolisant on cataplexy in patients with narcolepsy: a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2017;16(3):200-207.
Baumann CR. Wide implications of a trial on pitolisant for cataplexy. Lancet Neurol. 2017;16(3):173-174.
Abdominal myomectomy: Patient and surgical technique considerations
CASE Woman with fibroids seeks alternative to hysterectomy
A 42-year-old woman (G2P2) presents to the office for evaluation of heavy menstrual bleeding and known uterine fibroids. Physical examination reveals a 16-week-sized uterus, and ultrasonography shows at least 6 fibroids, 2 of which impinge on the uterine cavity. She does not want to have any more children, but she wishes to avoid a hysterectomy.
Abdominal myomectomy: A good option for many women
Abdominal myomectomy is an underutilized procedure. With fibroids as the indication for surgery, 197,000 hysterectomies were performed in the United States in 2010, compared with approximately 40,000 myomectomies.1,2 Moreover, the rates of both laparoscopic and abdominal myomectomy have decreased following the controversial morcellation advisory issued by the US Food and Drug Administration.3
The differences in the hysterectomy and myomectomy rates might be explained by the many myths ascribed to myomectomy. Such myths include the beliefs that myomectomy, when compared with hysterectomy, is associated with greater risk of visceral injury, more blood loss, poor uterine healing, and high risk of fibroid recurrence, and that myomectomy is unlikely to improve patient symptoms.
Studies show, however, that these beliefs are wrong. The risk of needing treatment for new fibroid growth following myomectomy is low.4 Hysterectomy, compared with myomectomy for similar size uteri, is actually associated with a greater risk of injury to the bowel, bladder, and ureters and with a greater risk of operative hemorrhage. Furthermore, hysterectomy (without oophorectomy) can be associated with early menopause in approximately 10% of women, while myomectomy does not alter ovarian hormones. (See “7 Myomectomy myths debunked,” which appeared in the February 2017 issue of OBG
For women who have serious medical problems (severe anemia, ureteral obstruction) due to uterine fibroids, surgery usually is necessary. In addition, women may request surgery for fibroid-associated quality-of-life concerns, such as heavy menstrual bleeding, infertility, pelvic pressure, urinary frequency, or incontinence. In one prospective study, the authors found that when women were assessed 6 months after undergoing myomectomy, 75% reported experiencing a significant decrease in bothersome symptoms.7
Myomectomy may be considered even for women with large uterine fibroids who desire uterine conservation. In a systematic review of the perioperative morbidity associated with abdominal myomectomy compared with abdominal hysterectomy for fibroids, which included 1,520 women with uterine size up to 16 to 18 weeks, no difference was found in major morbidity rates.8 Investigators who studied 91 women with uterine size ranging from 16 to 36 weeks who underwent abdominal myomectomy reported 1 bowel injury, 1 bladder injury, and 1 reoperation for bowel obstruction; no women had conversion to hysterectomy.9
Since ObGyn residency training emphasizes hysterectomy techniques, many residents receive only limited exposure to myomectomy procedures. Increased exposure to and comfort with myomectomy surgical technique would encourage more gynecologists to offer this option to their patients who desire uterine conservation, including those who do not desire future childbearing.
Imaging techniques are essential in the preoperative evaluation
For women with fibroid-related symptoms who desire surgery with uterine preservation, determining the myomectomy approach (abdominal, laparoscopic/robotic, hysteroscopic) depends on accurate assessment of the size, number, and position of the fibroids. If abdominal myomectomy is planned because of uterine size, the presence of numerous fibroids, or patient choice, transvaginal/transabdominal ultrasonography usually is adequate for anticipating what will be found during surgery. Sonography is readily available and is the least costly imaging technique that can help differentiate fibroids from other pelvic pathology. Although small fibroids may not be seen on sonography, they can be palpated and removed at the time of open surgery.
If submucous fibroids need to be better defined, saline-infusion sonography can be performed. However, if laparoscopic/robotic myomectomy (which precludes accurate palpation during surgery) is being considered, magnetic resonance imaging (MRI) allows the best assessment of the size, number, and position of the fibroids.10 When adenomyosis is considered in the differential diagnosis, MRI is an accurate way to determine its presence and helps in planning the best surgical procedure and approach.
Correct anemia before surgery
Women with fibroids may have anemia requiring correction before surgery to reduce the need for intraoperative or postoperative blood transfusion. Mild iron deficiency anemia can be treated prior to surgery with oral elemental iron 150 to 200 mg per day. Vitamin C 1,000 mg per day helps to increase intestinal iron absorption. Three weeks of treatment with oral iron can increase hemoglobin concentration by 2 g/dL.
For more severe anemia or rapid correction of anemia, intravenous (IV) iron sucrose infusions, 200 mg infused over 2 hours and given 3 times per week for 3 weeks, can increase hemoglobin by 3 g/dL.11 In our ObGyn practice, hematologists manage iron infusions.
Read about abdominal incision technique
Abdominal incision technique
Even a large uterus with multiple fibroids usually can be managed through use of a transverse lower abdominal incision. Prior to reaching the lateral borders of the rectus abdominis, curve the fascial incision cephalad to avoid injury to the ileoinguinal nerves (FIGURE 1). Detaching the midline rectus fascia (linea alba) from the anterior abdominal wall, starting at the pubic symphysis and continuing up to the umbilicus, frees the rectus muscles and allows them to be easily separated (see VIDEO 1). Since fascia is not elastic, these 2 steps are important to allow more room to deliver the uterus through the incision.
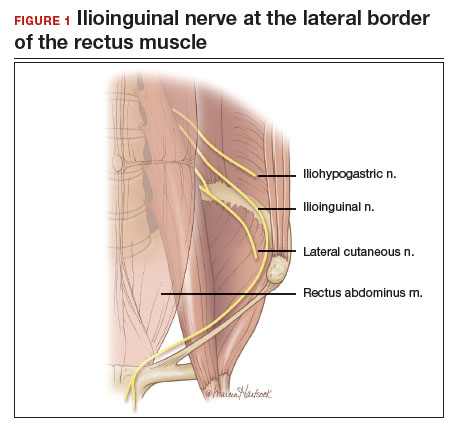
Delivery of the uterus through the incision isolates the surgical field from the bowel, bladder, ureters, and pelvic nerves. Once the uterus is delivered, inspect and palpate it for fibroids. Identify the fundus and the position of the uterine cavity by locating both uterine cornua and imagining a straight line between them. It may be necessary to explore the endometrial cavity to look for and remove submucous fibroids. Then plan the necessary uterine incisions for removing all fibroids (see VIDEO 2).
Read about managing blood loss
4 approaches to managing intraoperative blood loss
In my practice, we employ misoprostol, tranexamic acid, vasopressin, and a uterine and ovarian vessel tourniquet to manage intraoperative blood loss.12 Although no data exist to show that using these methods together is advantageous, they have different mechanisms of action and no negative interactions.
Misoprostol 400 μg inserted vaginally 2 hours before surgery induces myometrial contraction and compression of the uterine vessels. This agent can reduce blood loss by 98 mL per case.12
Tranexamic acid, an antifibrinolytic, is given IV piggyback at the start of surgery at a dose of 10 mg/kg; it can reduce blood loss by 243 mL per case.12
Vasopressin 20 U in 100 mL normal saline, injected below the vascular pseudocapsule, causes vasoconstriction of capillaries and small arterioles and venules and can reduce blood loss by 246 mL per case.12 Intravascular injection should be avoided because rare cases of bradycardia and cardiovascular collapse have been reported.13 Using vasopressin to decrease blood loss during myomectomy is an off-label use of this drug.
Place a tourniquet around the lower uterine segment, including the infundibular pelvic ligaments. Tourniquet use is the most effective way to decrease blood loss during myomectomy, since it can reduce blood loss by 1,870 mL.12 For women who wish to preserve fertility, take care to ensure that the tourniquet does not compromise the tubes. For women who are certain they do not want to preserve fertility, discuss the possibility of performing bilateral salpingectomy to decrease the risk of subsequent tubal (“ovarian”) cancer.
Some surgeons incise the broad ligaments bilaterally and pass the tourniquet through the broad ligaments to avoid compromising blood flow to the ovaries. Occluding the utero- ovarian ligaments with bulldog clamps to control collateral blood flow from the ovarian artery has been described, but the clamps can tear these often enlarged and fragile uterine veins during manipulation of the uterus. Release the tourniquet every 15 to 30 minutes to allow reperfusion of the ovaries. In women with ovarian torsion lasting hours to days, the ovary has been found to resist hypoxia and recover function.14 Antral follicle counts of detorsed and contralateral normal ovaries following a mean of 13 hours of hypoxia are similar 3 months following detorsion.15
Consider blood salvage. For women with multiple or very large fibroids, consider using a salvage-type autologous blood transfusion device, which has been shown to reduce the need for heterologous blood transfusion.16 This device suctions blood from the operative field, mixes it with heparinized saline, and stores the blood in a canister (FIGURE 2). If the patient requires blood reinfusion, the stored blood is washed with saline, filtered, centrifuged, and given back to the patient intravenously. Blood salvage, or cell salvage, avoids the risks of infection and transfusion reaction, and the oxygen transport capacity of salvaged red blood cells is equal to or better than that of stored allogeneic red cells.

Additional surgical considerations
Previous teaching suggested that proper placement of the uterine incisions was an important factor in limiting blood loss. Some authors suggested that vertical uterine incisions would avoid injury to the ascending uterine vessels should inadvertent extension of the incision occur. Other authors proposed horizontal uterine incisions to avoid severing the arcuate vessels that branch off from the ascending uterine arteries and run transversely across the uterus. However, since fibroids distort the normal vascular architecture, it is not possible to entirely avoid severing vessels in the myometrium (FIGURE 3).17 Uterine incisions can therefore be made as needed based on the position of the fibroids and the need to avoid inadvertent extension to the ascending uterine vessels or cornua.17
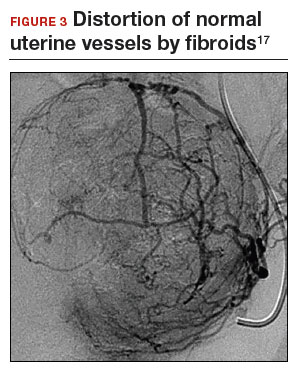
Fibroid anatomy and vascularity. Fibroids are entirely encased within the dense blood supply of a pseudocapsule (FIGURE 4),18 and no distinct “vascular pedicle” exists at the base of the fibroid.19 It is therefore important to extend the uterine incisions down through the entire pseudocapsule until the fibroid is clearly visible. This will identify a less vascular surgical plane, which is deeper than commonly recognized. Once the fibroid is reached, the pseudocapsule can be “wiped away” using a dry laparotomy sponge (see VIDEO 3). Staying under the pseudocapsule reduces bleeding and may preserve the tissue growth factors and neurotransmitters that are thought to promote wound healing.20
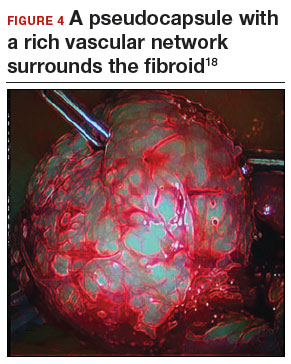
Adhesion prevention. Limiting the number of uterine incisions has been suggested as a way to reduce the risk of postoperative pelvic adhesions. To extract fibroids that are distant from an incision, however, tunnels must be created within the myometrium, and this makes hemostasis within these defects difficult. In that blood increases the risk of adhesion formation, tunneling may be counterproductive. If tunneling incisions are avoided and hemostasis is secured immediately, the risk of adhesion formation should be lessened.
Therefore, make incisions directly over the fibroids. Remove only easily accessed fibroids and promptly close the defects to secure hemostasis. Multiple uterine incisions may be needed; adhesion barriers may help limit adhesion formation.21
On final removal of the tourniquet, carefully inspect for bleeding and perform any necessary re-suturing. We place a pain pump (ON-Q* Pain Relief System, Halyard Health, Inc) for pain management and close the abdominal incision in the standard manner.
Postoperative care: Manage pain, restore function
The pain pump infuser, attached to one soaker catheter above and one below the fascia, provides continuous infusion of bupivacaine to the incision at 4 mL per hour for 4 days. The pain pump greatly reduces the need for postoperative opioids.22 Use of a patient-controlled analgesia pump, with its associated adverse effects (sedation, need for oxygen saturation monitoring, slowing of bowel function) can thus be avoided. The patient’s residual pain is controlled with oral oxycodone or hydrocodone and scheduled nonsteroidal anti-inflammatory drugs.
In my practice, we use an enhanced recovery after surgery (ERAS) protocol designed to reduce postoperative surgical stress and expedite a return to baseline physiologic body functions.23 Excellent well-researched, evidence-based studies support the effectiveness of ERAS in gynecologic and general surgery procedures.24
Pre-emptive, preoperative analgesia (gabapentin and celecoxib) and end-of-case IV acetaminophen are given to reduce the inflammatory response and the need for postoperative opioids. Once it is confirmed that the patient is hemodynamically stable, add ketorolac 30 mg IV every 6 hours on postoperative day 1. Nausea and vomiting prophylaxis includes ondansetron and dexamethasone at the end of surgery, avoidance of bowel edema with restriction of intraoperative and postoperative fluids (euvolemia), early oral feeding, and gum chewing. On the evening of surgery, the urinary catheter is removed to reduce the risk of bladder infection and facilitate ambulation. Encourage sitting at the bedside and early ambulation starting the evening of surgery to reduce risk of thromboembolism and to avoid skeletal muscle weakness and postoperative fatigue.
Most women are able to be discharged on postoperative day 2. They return to the office on postoperative day 5 for removal of the pain pump.
CASE Continued: Fibroids removed via abdominal myomectomy
We performed an abdominal myomectomy through a Pfannenstiel incision. Nine fibroids—3 of which were not seen on MRI—ranging in size from 1 to 7 cm were removed. Intravaginal misoprostol, IV tranexamic acid, subserosal vasopressin, and a uterine vessel tourniquet limited the intraoperative blood loss to 225 mL. After surgery, a pain pump and ERAS protocol allowed the patient to be discharged on postoperative day 2, and she returned to the office on day 5 for removal of the pain pump. Oral pain medication was continued on an as-needed basis.
Acknowledgement
The author would like to thank Stanley West, MD, for generously teaching him the surgical techniques for performing abdominal myomectomy.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Wright JD, Herzog TJ, Tsui J, et al. Nationwide trends in the performance of inpatient hysterectomy in the United States. Obstet Gynecol. 2013;122(2 pt 1):233–241.
- Barrett ML, Weiss AJ, Stocks C, Steiner CA, Myers ER. Statistical brief 200. Procedures to treat benign uterine fibroids in hospital inpatient and hospital-based ambulatory surgery settings, 2013. Healthcare Cost and Utilization Project website. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb200-Procedures-Treat-Uterine-Fibroids.jsp. Published January 2016. Accessed February 9, 2017.
- Stentz NC, Cooney L, Sammel MD, Shah DK. Impact of the Food and Drug Administration (FDA) safety communication on morcellation on surgical practice and perioperative morbidity following myomectomy [abstract p300]. Fertil Steril. 2016;106(3 suppl):e219.
- Hillis SD, Marchbanks PA, Peterson HB. Obstet Gynecol. 1996;87(4):539–543.
- Pritts E, Vanness D, Berek JS, et al. The prevalence of occult leiomyosarcoma at surgery for presumed uterine fibroids: a meta-analysis. Gynecol Surg. 2015;12(3):165–177.
- Bogani G, Cliby WA, Aletti GD. Impact of morcellation on survival outcomes of patients with unexpected uterine leiomyosarcoma: a systematic review and meta-analysis. Gynecol Oncol. 2015;137(1):167–172.
- Dilek S, Ertunc D, Tok EC, Cimen R, Doruk A. The effect of myomectomy on health-related quality of life of women with myoma uteri. J Obstet Gynaecol Res. 2010;36(2):364–369.
- Pundir J, Walawalkar R, Seshadri S, Khalaf Y, El-Toukhy T. Perioperative morbidity associated with abdominal myomectomy compared with total abdominal hysterectomy for uterine fibroids. J Obstet Gynaecol. 2013;33(7):655–662.
- West S, Ruiz R, Parker WH. Abdominal myomectomy in women with very large uterine size. Fertil Steril. 2006;85(1):36–39.
- Dueholm M, Lundorf E, Hansen ES, Ledertoug S, Olesen F. Evaluation of the uterine cavity with magnetic resonance imaging, transvaginal sonography, hysterosonographic examination, and diagnostic hysteroscopy. Fertil Steril. 2001;76(2):350–357.
- Kim YH, Chung HH, Kang SB, Kim SC, Kim YT. Safety and usefulness of intravenous iron sucrose in the management of preoperative anemia in patients with menorrhagia: a phase IV, open-label, prospective, randomized study. Acta Haematol. 2009;121(1):37–41.
- Kongnyuy EJ, Wiysonge CS. Interventions to reduce haemorrhage during myomectomy for fibroids. Cochrane Database Syst Rev. 2014 Aug 15;(8):CD005355.
- Hobo R, Netsu S, Koyasu Y, Tsutsumi O. Bradycardia and cardiac arrest caused by intramyometrial injection of vasopressin during a laparoscopically assisted myomectomy. Obstet Gynecol. 2009;113(2 pt 2):484–486.
- Oelsner G, Cohen SB, Soriano D, Admon D, Mashiach S, Carp H. Minimal surgery for the twisted ischaemic adnexa can preserve ovarian function. Hum Reprod. 2003;18(12):2599–2602.
- Yasa C, Dural O, Bastu E, Zorlu M, Demir O, Ugurlucan FG. Impact of laparoscopic ovarian detorsion on ovarian reserve. J Obstet Gynaecol Res. 2017;43(2):298–302.
- Yamada T, Ikeda A, Okamoto Y, Okamoto Y, Kanda T, Ueki M. Intraoperative blood salvage in abdominal simple total hysterectomy for uterine myoma. Int J Gynaecol Obstet. 1997;59(3):233–236.
- Discepola F, Valenti DA, Reinhold C, Tulandi T. Analysis of arterial blood vessels surrounding the myoma: relevance to myomectomy. Obstet Gynecol. 2007;110(6):1301–1303.
- Malavasi A, Cavalotti C, Nicolardi G, et al. The opioid neuropeptides in uterine fibroid pseudocapsules: a putative association with cervical integrity in human reproduction. Gynecol Endocrinol. 2013;29(11):982–988.
- Walocha JA, Litwin JA, Miodonski AJ. Vascular system of intramural leiomyomata revealed by corrosion casting and scanning electron microscopy. Hum Reprod. 2003;18(5):1088–1093.
- Tinelli A, Mynbaev OA, Sparic R, et al. Angiogenesis and vascularization of uterine leiomyoma: clinical value of pseudocapsule containing peptides and neurotransmitters [published online ahead of print March 22, 2016]. Curr Protein Pept Sci. doi:10.2174/1389203717666160322150338.
- Diamond MP. Reduction of adhesions after uterine myomectomy by Seprafilm membrane (HAL-F): a blinded, prospective, randomized, multicenter clinical study. Seprafilm Adhesion Study Group. Fertil Steril. 1996;66(6):904–910.
- Liu SS, Richman JM, Thirlby RC, Wu CL. Efficacy of continuous wound catheters delivering local anesthetic for postoperative analgesia: a quantitative and qualitative systematic review of randomized controlled trials. J Am Coll Surg. 2006;203(6):914–932.
- Lassen K, Soop M, Nygren J, et al; Enhanced Recovery After Surgery (ERAS) Group. Consensus review of optimal perioperative care in colorectal surgery: Enhanced Recovery After Surgery (ERAS) Group recommendations. Arch Surg. 2009;144(10):961–969.
- Kalogera E, Bakkum-Gamez JN, Jankowski CJ, et al. Enhanced recovery in gynecologic surgery. Obstet Gynecol. 2013;122(2 pt 1):319–328.
CASE Woman with fibroids seeks alternative to hysterectomy
A 42-year-old woman (G2P2) presents to the office for evaluation of heavy menstrual bleeding and known uterine fibroids. Physical examination reveals a 16-week-sized uterus, and ultrasonography shows at least 6 fibroids, 2 of which impinge on the uterine cavity. She does not want to have any more children, but she wishes to avoid a hysterectomy.
Abdominal myomectomy: A good option for many women
Abdominal myomectomy is an underutilized procedure. With fibroids as the indication for surgery, 197,000 hysterectomies were performed in the United States in 2010, compared with approximately 40,000 myomectomies.1,2 Moreover, the rates of both laparoscopic and abdominal myomectomy have decreased following the controversial morcellation advisory issued by the US Food and Drug Administration.3
The differences in the hysterectomy and myomectomy rates might be explained by the many myths ascribed to myomectomy. Such myths include the beliefs that myomectomy, when compared with hysterectomy, is associated with greater risk of visceral injury, more blood loss, poor uterine healing, and high risk of fibroid recurrence, and that myomectomy is unlikely to improve patient symptoms.
Studies show, however, that these beliefs are wrong. The risk of needing treatment for new fibroid growth following myomectomy is low.4 Hysterectomy, compared with myomectomy for similar size uteri, is actually associated with a greater risk of injury to the bowel, bladder, and ureters and with a greater risk of operative hemorrhage. Furthermore, hysterectomy (without oophorectomy) can be associated with early menopause in approximately 10% of women, while myomectomy does not alter ovarian hormones. (See “7 Myomectomy myths debunked,” which appeared in the February 2017 issue of OBG
For women who have serious medical problems (severe anemia, ureteral obstruction) due to uterine fibroids, surgery usually is necessary. In addition, women may request surgery for fibroid-associated quality-of-life concerns, such as heavy menstrual bleeding, infertility, pelvic pressure, urinary frequency, or incontinence. In one prospective study, the authors found that when women were assessed 6 months after undergoing myomectomy, 75% reported experiencing a significant decrease in bothersome symptoms.7
Myomectomy may be considered even for women with large uterine fibroids who desire uterine conservation. In a systematic review of the perioperative morbidity associated with abdominal myomectomy compared with abdominal hysterectomy for fibroids, which included 1,520 women with uterine size up to 16 to 18 weeks, no difference was found in major morbidity rates.8 Investigators who studied 91 women with uterine size ranging from 16 to 36 weeks who underwent abdominal myomectomy reported 1 bowel injury, 1 bladder injury, and 1 reoperation for bowel obstruction; no women had conversion to hysterectomy.9
Since ObGyn residency training emphasizes hysterectomy techniques, many residents receive only limited exposure to myomectomy procedures. Increased exposure to and comfort with myomectomy surgical technique would encourage more gynecologists to offer this option to their patients who desire uterine conservation, including those who do not desire future childbearing.
Imaging techniques are essential in the preoperative evaluation
For women with fibroid-related symptoms who desire surgery with uterine preservation, determining the myomectomy approach (abdominal, laparoscopic/robotic, hysteroscopic) depends on accurate assessment of the size, number, and position of the fibroids. If abdominal myomectomy is planned because of uterine size, the presence of numerous fibroids, or patient choice, transvaginal/transabdominal ultrasonography usually is adequate for anticipating what will be found during surgery. Sonography is readily available and is the least costly imaging technique that can help differentiate fibroids from other pelvic pathology. Although small fibroids may not be seen on sonography, they can be palpated and removed at the time of open surgery.
If submucous fibroids need to be better defined, saline-infusion sonography can be performed. However, if laparoscopic/robotic myomectomy (which precludes accurate palpation during surgery) is being considered, magnetic resonance imaging (MRI) allows the best assessment of the size, number, and position of the fibroids.10 When adenomyosis is considered in the differential diagnosis, MRI is an accurate way to determine its presence and helps in planning the best surgical procedure and approach.
Correct anemia before surgery
Women with fibroids may have anemia requiring correction before surgery to reduce the need for intraoperative or postoperative blood transfusion. Mild iron deficiency anemia can be treated prior to surgery with oral elemental iron 150 to 200 mg per day. Vitamin C 1,000 mg per day helps to increase intestinal iron absorption. Three weeks of treatment with oral iron can increase hemoglobin concentration by 2 g/dL.
For more severe anemia or rapid correction of anemia, intravenous (IV) iron sucrose infusions, 200 mg infused over 2 hours and given 3 times per week for 3 weeks, can increase hemoglobin by 3 g/dL.11 In our ObGyn practice, hematologists manage iron infusions.
Read about abdominal incision technique
Abdominal incision technique
Even a large uterus with multiple fibroids usually can be managed through use of a transverse lower abdominal incision. Prior to reaching the lateral borders of the rectus abdominis, curve the fascial incision cephalad to avoid injury to the ileoinguinal nerves (FIGURE 1). Detaching the midline rectus fascia (linea alba) from the anterior abdominal wall, starting at the pubic symphysis and continuing up to the umbilicus, frees the rectus muscles and allows them to be easily separated (see VIDEO 1). Since fascia is not elastic, these 2 steps are important to allow more room to deliver the uterus through the incision.
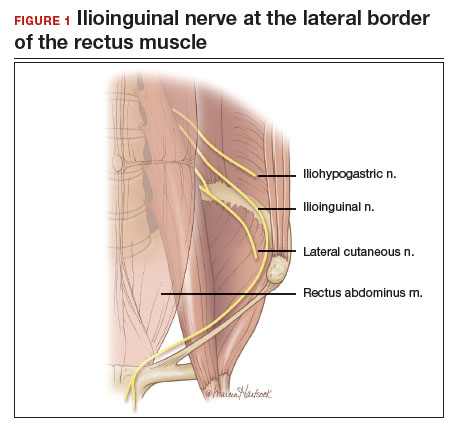
Delivery of the uterus through the incision isolates the surgical field from the bowel, bladder, ureters, and pelvic nerves. Once the uterus is delivered, inspect and palpate it for fibroids. Identify the fundus and the position of the uterine cavity by locating both uterine cornua and imagining a straight line between them. It may be necessary to explore the endometrial cavity to look for and remove submucous fibroids. Then plan the necessary uterine incisions for removing all fibroids (see VIDEO 2).
Read about managing blood loss
4 approaches to managing intraoperative blood loss
In my practice, we employ misoprostol, tranexamic acid, vasopressin, and a uterine and ovarian vessel tourniquet to manage intraoperative blood loss.12 Although no data exist to show that using these methods together is advantageous, they have different mechanisms of action and no negative interactions.
Misoprostol 400 μg inserted vaginally 2 hours before surgery induces myometrial contraction and compression of the uterine vessels. This agent can reduce blood loss by 98 mL per case.12
Tranexamic acid, an antifibrinolytic, is given IV piggyback at the start of surgery at a dose of 10 mg/kg; it can reduce blood loss by 243 mL per case.12
Vasopressin 20 U in 100 mL normal saline, injected below the vascular pseudocapsule, causes vasoconstriction of capillaries and small arterioles and venules and can reduce blood loss by 246 mL per case.12 Intravascular injection should be avoided because rare cases of bradycardia and cardiovascular collapse have been reported.13 Using vasopressin to decrease blood loss during myomectomy is an off-label use of this drug.
Place a tourniquet around the lower uterine segment, including the infundibular pelvic ligaments. Tourniquet use is the most effective way to decrease blood loss during myomectomy, since it can reduce blood loss by 1,870 mL.12 For women who wish to preserve fertility, take care to ensure that the tourniquet does not compromise the tubes. For women who are certain they do not want to preserve fertility, discuss the possibility of performing bilateral salpingectomy to decrease the risk of subsequent tubal (“ovarian”) cancer.
Some surgeons incise the broad ligaments bilaterally and pass the tourniquet through the broad ligaments to avoid compromising blood flow to the ovaries. Occluding the utero- ovarian ligaments with bulldog clamps to control collateral blood flow from the ovarian artery has been described, but the clamps can tear these often enlarged and fragile uterine veins during manipulation of the uterus. Release the tourniquet every 15 to 30 minutes to allow reperfusion of the ovaries. In women with ovarian torsion lasting hours to days, the ovary has been found to resist hypoxia and recover function.14 Antral follicle counts of detorsed and contralateral normal ovaries following a mean of 13 hours of hypoxia are similar 3 months following detorsion.15
Consider blood salvage. For women with multiple or very large fibroids, consider using a salvage-type autologous blood transfusion device, which has been shown to reduce the need for heterologous blood transfusion.16 This device suctions blood from the operative field, mixes it with heparinized saline, and stores the blood in a canister (FIGURE 2). If the patient requires blood reinfusion, the stored blood is washed with saline, filtered, centrifuged, and given back to the patient intravenously. Blood salvage, or cell salvage, avoids the risks of infection and transfusion reaction, and the oxygen transport capacity of salvaged red blood cells is equal to or better than that of stored allogeneic red cells.

Additional surgical considerations
Previous teaching suggested that proper placement of the uterine incisions was an important factor in limiting blood loss. Some authors suggested that vertical uterine incisions would avoid injury to the ascending uterine vessels should inadvertent extension of the incision occur. Other authors proposed horizontal uterine incisions to avoid severing the arcuate vessels that branch off from the ascending uterine arteries and run transversely across the uterus. However, since fibroids distort the normal vascular architecture, it is not possible to entirely avoid severing vessels in the myometrium (FIGURE 3).17 Uterine incisions can therefore be made as needed based on the position of the fibroids and the need to avoid inadvertent extension to the ascending uterine vessels or cornua.17
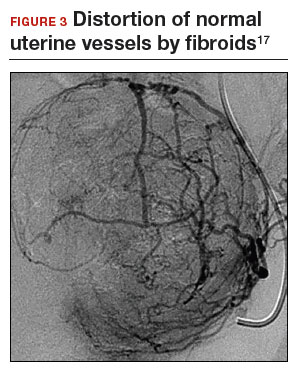
Fibroid anatomy and vascularity. Fibroids are entirely encased within the dense blood supply of a pseudocapsule (FIGURE 4),18 and no distinct “vascular pedicle” exists at the base of the fibroid.19 It is therefore important to extend the uterine incisions down through the entire pseudocapsule until the fibroid is clearly visible. This will identify a less vascular surgical plane, which is deeper than commonly recognized. Once the fibroid is reached, the pseudocapsule can be “wiped away” using a dry laparotomy sponge (see VIDEO 3). Staying under the pseudocapsule reduces bleeding and may preserve the tissue growth factors and neurotransmitters that are thought to promote wound healing.20
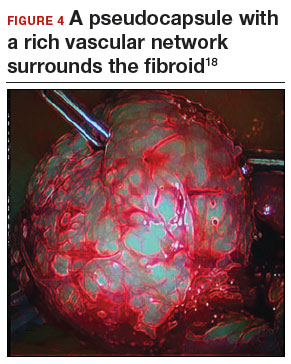
Adhesion prevention. Limiting the number of uterine incisions has been suggested as a way to reduce the risk of postoperative pelvic adhesions. To extract fibroids that are distant from an incision, however, tunnels must be created within the myometrium, and this makes hemostasis within these defects difficult. In that blood increases the risk of adhesion formation, tunneling may be counterproductive. If tunneling incisions are avoided and hemostasis is secured immediately, the risk of adhesion formation should be lessened.
Therefore, make incisions directly over the fibroids. Remove only easily accessed fibroids and promptly close the defects to secure hemostasis. Multiple uterine incisions may be needed; adhesion barriers may help limit adhesion formation.21
On final removal of the tourniquet, carefully inspect for bleeding and perform any necessary re-suturing. We place a pain pump (ON-Q* Pain Relief System, Halyard Health, Inc) for pain management and close the abdominal incision in the standard manner.
Postoperative care: Manage pain, restore function
The pain pump infuser, attached to one soaker catheter above and one below the fascia, provides continuous infusion of bupivacaine to the incision at 4 mL per hour for 4 days. The pain pump greatly reduces the need for postoperative opioids.22 Use of a patient-controlled analgesia pump, with its associated adverse effects (sedation, need for oxygen saturation monitoring, slowing of bowel function) can thus be avoided. The patient’s residual pain is controlled with oral oxycodone or hydrocodone and scheduled nonsteroidal anti-inflammatory drugs.
In my practice, we use an enhanced recovery after surgery (ERAS) protocol designed to reduce postoperative surgical stress and expedite a return to baseline physiologic body functions.23 Excellent well-researched, evidence-based studies support the effectiveness of ERAS in gynecologic and general surgery procedures.24
Pre-emptive, preoperative analgesia (gabapentin and celecoxib) and end-of-case IV acetaminophen are given to reduce the inflammatory response and the need for postoperative opioids. Once it is confirmed that the patient is hemodynamically stable, add ketorolac 30 mg IV every 6 hours on postoperative day 1. Nausea and vomiting prophylaxis includes ondansetron and dexamethasone at the end of surgery, avoidance of bowel edema with restriction of intraoperative and postoperative fluids (euvolemia), early oral feeding, and gum chewing. On the evening of surgery, the urinary catheter is removed to reduce the risk of bladder infection and facilitate ambulation. Encourage sitting at the bedside and early ambulation starting the evening of surgery to reduce risk of thromboembolism and to avoid skeletal muscle weakness and postoperative fatigue.
Most women are able to be discharged on postoperative day 2. They return to the office on postoperative day 5 for removal of the pain pump.
CASE Continued: Fibroids removed via abdominal myomectomy
We performed an abdominal myomectomy through a Pfannenstiel incision. Nine fibroids—3 of which were not seen on MRI—ranging in size from 1 to 7 cm were removed. Intravaginal misoprostol, IV tranexamic acid, subserosal vasopressin, and a uterine vessel tourniquet limited the intraoperative blood loss to 225 mL. After surgery, a pain pump and ERAS protocol allowed the patient to be discharged on postoperative day 2, and she returned to the office on day 5 for removal of the pain pump. Oral pain medication was continued on an as-needed basis.
Acknowledgement
The author would like to thank Stanley West, MD, for generously teaching him the surgical techniques for performing abdominal myomectomy.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
CASE Woman with fibroids seeks alternative to hysterectomy
A 42-year-old woman (G2P2) presents to the office for evaluation of heavy menstrual bleeding and known uterine fibroids. Physical examination reveals a 16-week-sized uterus, and ultrasonography shows at least 6 fibroids, 2 of which impinge on the uterine cavity. She does not want to have any more children, but she wishes to avoid a hysterectomy.
Abdominal myomectomy: A good option for many women
Abdominal myomectomy is an underutilized procedure. With fibroids as the indication for surgery, 197,000 hysterectomies were performed in the United States in 2010, compared with approximately 40,000 myomectomies.1,2 Moreover, the rates of both laparoscopic and abdominal myomectomy have decreased following the controversial morcellation advisory issued by the US Food and Drug Administration.3
The differences in the hysterectomy and myomectomy rates might be explained by the many myths ascribed to myomectomy. Such myths include the beliefs that myomectomy, when compared with hysterectomy, is associated with greater risk of visceral injury, more blood loss, poor uterine healing, and high risk of fibroid recurrence, and that myomectomy is unlikely to improve patient symptoms.
Studies show, however, that these beliefs are wrong. The risk of needing treatment for new fibroid growth following myomectomy is low.4 Hysterectomy, compared with myomectomy for similar size uteri, is actually associated with a greater risk of injury to the bowel, bladder, and ureters and with a greater risk of operative hemorrhage. Furthermore, hysterectomy (without oophorectomy) can be associated with early menopause in approximately 10% of women, while myomectomy does not alter ovarian hormones. (See “7 Myomectomy myths debunked,” which appeared in the February 2017 issue of OBG
For women who have serious medical problems (severe anemia, ureteral obstruction) due to uterine fibroids, surgery usually is necessary. In addition, women may request surgery for fibroid-associated quality-of-life concerns, such as heavy menstrual bleeding, infertility, pelvic pressure, urinary frequency, or incontinence. In one prospective study, the authors found that when women were assessed 6 months after undergoing myomectomy, 75% reported experiencing a significant decrease in bothersome symptoms.7
Myomectomy may be considered even for women with large uterine fibroids who desire uterine conservation. In a systematic review of the perioperative morbidity associated with abdominal myomectomy compared with abdominal hysterectomy for fibroids, which included 1,520 women with uterine size up to 16 to 18 weeks, no difference was found in major morbidity rates.8 Investigators who studied 91 women with uterine size ranging from 16 to 36 weeks who underwent abdominal myomectomy reported 1 bowel injury, 1 bladder injury, and 1 reoperation for bowel obstruction; no women had conversion to hysterectomy.9
Since ObGyn residency training emphasizes hysterectomy techniques, many residents receive only limited exposure to myomectomy procedures. Increased exposure to and comfort with myomectomy surgical technique would encourage more gynecologists to offer this option to their patients who desire uterine conservation, including those who do not desire future childbearing.
Imaging techniques are essential in the preoperative evaluation
For women with fibroid-related symptoms who desire surgery with uterine preservation, determining the myomectomy approach (abdominal, laparoscopic/robotic, hysteroscopic) depends on accurate assessment of the size, number, and position of the fibroids. If abdominal myomectomy is planned because of uterine size, the presence of numerous fibroids, or patient choice, transvaginal/transabdominal ultrasonography usually is adequate for anticipating what will be found during surgery. Sonography is readily available and is the least costly imaging technique that can help differentiate fibroids from other pelvic pathology. Although small fibroids may not be seen on sonography, they can be palpated and removed at the time of open surgery.
If submucous fibroids need to be better defined, saline-infusion sonography can be performed. However, if laparoscopic/robotic myomectomy (which precludes accurate palpation during surgery) is being considered, magnetic resonance imaging (MRI) allows the best assessment of the size, number, and position of the fibroids.10 When adenomyosis is considered in the differential diagnosis, MRI is an accurate way to determine its presence and helps in planning the best surgical procedure and approach.
Correct anemia before surgery
Women with fibroids may have anemia requiring correction before surgery to reduce the need for intraoperative or postoperative blood transfusion. Mild iron deficiency anemia can be treated prior to surgery with oral elemental iron 150 to 200 mg per day. Vitamin C 1,000 mg per day helps to increase intestinal iron absorption. Three weeks of treatment with oral iron can increase hemoglobin concentration by 2 g/dL.
For more severe anemia or rapid correction of anemia, intravenous (IV) iron sucrose infusions, 200 mg infused over 2 hours and given 3 times per week for 3 weeks, can increase hemoglobin by 3 g/dL.11 In our ObGyn practice, hematologists manage iron infusions.
Read about abdominal incision technique
Abdominal incision technique
Even a large uterus with multiple fibroids usually can be managed through use of a transverse lower abdominal incision. Prior to reaching the lateral borders of the rectus abdominis, curve the fascial incision cephalad to avoid injury to the ileoinguinal nerves (FIGURE 1). Detaching the midline rectus fascia (linea alba) from the anterior abdominal wall, starting at the pubic symphysis and continuing up to the umbilicus, frees the rectus muscles and allows them to be easily separated (see VIDEO 1). Since fascia is not elastic, these 2 steps are important to allow more room to deliver the uterus through the incision.
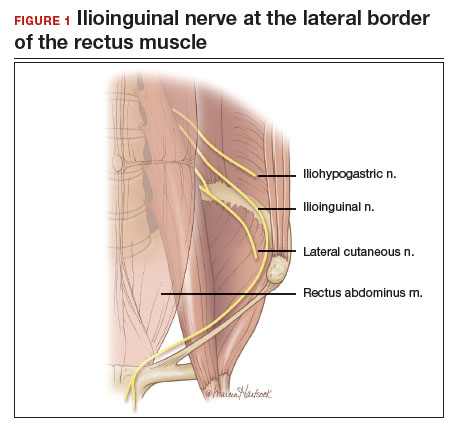
Delivery of the uterus through the incision isolates the surgical field from the bowel, bladder, ureters, and pelvic nerves. Once the uterus is delivered, inspect and palpate it for fibroids. Identify the fundus and the position of the uterine cavity by locating both uterine cornua and imagining a straight line between them. It may be necessary to explore the endometrial cavity to look for and remove submucous fibroids. Then plan the necessary uterine incisions for removing all fibroids (see VIDEO 2).
Read about managing blood loss
4 approaches to managing intraoperative blood loss
In my practice, we employ misoprostol, tranexamic acid, vasopressin, and a uterine and ovarian vessel tourniquet to manage intraoperative blood loss.12 Although no data exist to show that using these methods together is advantageous, they have different mechanisms of action and no negative interactions.
Misoprostol 400 μg inserted vaginally 2 hours before surgery induces myometrial contraction and compression of the uterine vessels. This agent can reduce blood loss by 98 mL per case.12
Tranexamic acid, an antifibrinolytic, is given IV piggyback at the start of surgery at a dose of 10 mg/kg; it can reduce blood loss by 243 mL per case.12
Vasopressin 20 U in 100 mL normal saline, injected below the vascular pseudocapsule, causes vasoconstriction of capillaries and small arterioles and venules and can reduce blood loss by 246 mL per case.12 Intravascular injection should be avoided because rare cases of bradycardia and cardiovascular collapse have been reported.13 Using vasopressin to decrease blood loss during myomectomy is an off-label use of this drug.
Place a tourniquet around the lower uterine segment, including the infundibular pelvic ligaments. Tourniquet use is the most effective way to decrease blood loss during myomectomy, since it can reduce blood loss by 1,870 mL.12 For women who wish to preserve fertility, take care to ensure that the tourniquet does not compromise the tubes. For women who are certain they do not want to preserve fertility, discuss the possibility of performing bilateral salpingectomy to decrease the risk of subsequent tubal (“ovarian”) cancer.
Some surgeons incise the broad ligaments bilaterally and pass the tourniquet through the broad ligaments to avoid compromising blood flow to the ovaries. Occluding the utero- ovarian ligaments with bulldog clamps to control collateral blood flow from the ovarian artery has been described, but the clamps can tear these often enlarged and fragile uterine veins during manipulation of the uterus. Release the tourniquet every 15 to 30 minutes to allow reperfusion of the ovaries. In women with ovarian torsion lasting hours to days, the ovary has been found to resist hypoxia and recover function.14 Antral follicle counts of detorsed and contralateral normal ovaries following a mean of 13 hours of hypoxia are similar 3 months following detorsion.15
Consider blood salvage. For women with multiple or very large fibroids, consider using a salvage-type autologous blood transfusion device, which has been shown to reduce the need for heterologous blood transfusion.16 This device suctions blood from the operative field, mixes it with heparinized saline, and stores the blood in a canister (FIGURE 2). If the patient requires blood reinfusion, the stored blood is washed with saline, filtered, centrifuged, and given back to the patient intravenously. Blood salvage, or cell salvage, avoids the risks of infection and transfusion reaction, and the oxygen transport capacity of salvaged red blood cells is equal to or better than that of stored allogeneic red cells.

Additional surgical considerations
Previous teaching suggested that proper placement of the uterine incisions was an important factor in limiting blood loss. Some authors suggested that vertical uterine incisions would avoid injury to the ascending uterine vessels should inadvertent extension of the incision occur. Other authors proposed horizontal uterine incisions to avoid severing the arcuate vessels that branch off from the ascending uterine arteries and run transversely across the uterus. However, since fibroids distort the normal vascular architecture, it is not possible to entirely avoid severing vessels in the myometrium (FIGURE 3).17 Uterine incisions can therefore be made as needed based on the position of the fibroids and the need to avoid inadvertent extension to the ascending uterine vessels or cornua.17
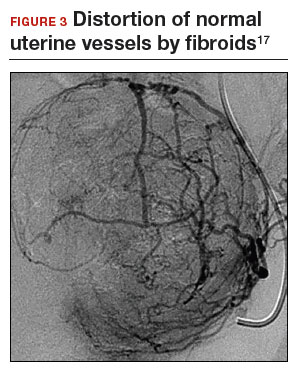
Fibroid anatomy and vascularity. Fibroids are entirely encased within the dense blood supply of a pseudocapsule (FIGURE 4),18 and no distinct “vascular pedicle” exists at the base of the fibroid.19 It is therefore important to extend the uterine incisions down through the entire pseudocapsule until the fibroid is clearly visible. This will identify a less vascular surgical plane, which is deeper than commonly recognized. Once the fibroid is reached, the pseudocapsule can be “wiped away” using a dry laparotomy sponge (see VIDEO 3). Staying under the pseudocapsule reduces bleeding and may preserve the tissue growth factors and neurotransmitters that are thought to promote wound healing.20
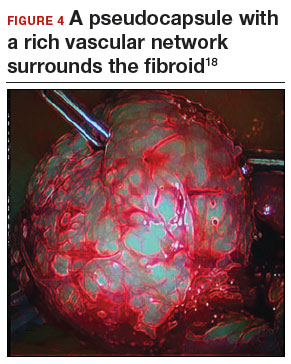
Adhesion prevention. Limiting the number of uterine incisions has been suggested as a way to reduce the risk of postoperative pelvic adhesions. To extract fibroids that are distant from an incision, however, tunnels must be created within the myometrium, and this makes hemostasis within these defects difficult. In that blood increases the risk of adhesion formation, tunneling may be counterproductive. If tunneling incisions are avoided and hemostasis is secured immediately, the risk of adhesion formation should be lessened.
Therefore, make incisions directly over the fibroids. Remove only easily accessed fibroids and promptly close the defects to secure hemostasis. Multiple uterine incisions may be needed; adhesion barriers may help limit adhesion formation.21
On final removal of the tourniquet, carefully inspect for bleeding and perform any necessary re-suturing. We place a pain pump (ON-Q* Pain Relief System, Halyard Health, Inc) for pain management and close the abdominal incision in the standard manner.
Postoperative care: Manage pain, restore function
The pain pump infuser, attached to one soaker catheter above and one below the fascia, provides continuous infusion of bupivacaine to the incision at 4 mL per hour for 4 days. The pain pump greatly reduces the need for postoperative opioids.22 Use of a patient-controlled analgesia pump, with its associated adverse effects (sedation, need for oxygen saturation monitoring, slowing of bowel function) can thus be avoided. The patient’s residual pain is controlled with oral oxycodone or hydrocodone and scheduled nonsteroidal anti-inflammatory drugs.
In my practice, we use an enhanced recovery after surgery (ERAS) protocol designed to reduce postoperative surgical stress and expedite a return to baseline physiologic body functions.23 Excellent well-researched, evidence-based studies support the effectiveness of ERAS in gynecologic and general surgery procedures.24
Pre-emptive, preoperative analgesia (gabapentin and celecoxib) and end-of-case IV acetaminophen are given to reduce the inflammatory response and the need for postoperative opioids. Once it is confirmed that the patient is hemodynamically stable, add ketorolac 30 mg IV every 6 hours on postoperative day 1. Nausea and vomiting prophylaxis includes ondansetron and dexamethasone at the end of surgery, avoidance of bowel edema with restriction of intraoperative and postoperative fluids (euvolemia), early oral feeding, and gum chewing. On the evening of surgery, the urinary catheter is removed to reduce the risk of bladder infection and facilitate ambulation. Encourage sitting at the bedside and early ambulation starting the evening of surgery to reduce risk of thromboembolism and to avoid skeletal muscle weakness and postoperative fatigue.
Most women are able to be discharged on postoperative day 2. They return to the office on postoperative day 5 for removal of the pain pump.
CASE Continued: Fibroids removed via abdominal myomectomy
We performed an abdominal myomectomy through a Pfannenstiel incision. Nine fibroids—3 of which were not seen on MRI—ranging in size from 1 to 7 cm were removed. Intravaginal misoprostol, IV tranexamic acid, subserosal vasopressin, and a uterine vessel tourniquet limited the intraoperative blood loss to 225 mL. After surgery, a pain pump and ERAS protocol allowed the patient to be discharged on postoperative day 2, and she returned to the office on day 5 for removal of the pain pump. Oral pain medication was continued on an as-needed basis.
Acknowledgement
The author would like to thank Stanley West, MD, for generously teaching him the surgical techniques for performing abdominal myomectomy.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Wright JD, Herzog TJ, Tsui J, et al. Nationwide trends in the performance of inpatient hysterectomy in the United States. Obstet Gynecol. 2013;122(2 pt 1):233–241.
- Barrett ML, Weiss AJ, Stocks C, Steiner CA, Myers ER. Statistical brief 200. Procedures to treat benign uterine fibroids in hospital inpatient and hospital-based ambulatory surgery settings, 2013. Healthcare Cost and Utilization Project website. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb200-Procedures-Treat-Uterine-Fibroids.jsp. Published January 2016. Accessed February 9, 2017.
- Stentz NC, Cooney L, Sammel MD, Shah DK. Impact of the Food and Drug Administration (FDA) safety communication on morcellation on surgical practice and perioperative morbidity following myomectomy [abstract p300]. Fertil Steril. 2016;106(3 suppl):e219.
- Hillis SD, Marchbanks PA, Peterson HB. Obstet Gynecol. 1996;87(4):539–543.
- Pritts E, Vanness D, Berek JS, et al. The prevalence of occult leiomyosarcoma at surgery for presumed uterine fibroids: a meta-analysis. Gynecol Surg. 2015;12(3):165–177.
- Bogani G, Cliby WA, Aletti GD. Impact of morcellation on survival outcomes of patients with unexpected uterine leiomyosarcoma: a systematic review and meta-analysis. Gynecol Oncol. 2015;137(1):167–172.
- Dilek S, Ertunc D, Tok EC, Cimen R, Doruk A. The effect of myomectomy on health-related quality of life of women with myoma uteri. J Obstet Gynaecol Res. 2010;36(2):364–369.
- Pundir J, Walawalkar R, Seshadri S, Khalaf Y, El-Toukhy T. Perioperative morbidity associated with abdominal myomectomy compared with total abdominal hysterectomy for uterine fibroids. J Obstet Gynaecol. 2013;33(7):655–662.
- West S, Ruiz R, Parker WH. Abdominal myomectomy in women with very large uterine size. Fertil Steril. 2006;85(1):36–39.
- Dueholm M, Lundorf E, Hansen ES, Ledertoug S, Olesen F. Evaluation of the uterine cavity with magnetic resonance imaging, transvaginal sonography, hysterosonographic examination, and diagnostic hysteroscopy. Fertil Steril. 2001;76(2):350–357.
- Kim YH, Chung HH, Kang SB, Kim SC, Kim YT. Safety and usefulness of intravenous iron sucrose in the management of preoperative anemia in patients with menorrhagia: a phase IV, open-label, prospective, randomized study. Acta Haematol. 2009;121(1):37–41.
- Kongnyuy EJ, Wiysonge CS. Interventions to reduce haemorrhage during myomectomy for fibroids. Cochrane Database Syst Rev. 2014 Aug 15;(8):CD005355.
- Hobo R, Netsu S, Koyasu Y, Tsutsumi O. Bradycardia and cardiac arrest caused by intramyometrial injection of vasopressin during a laparoscopically assisted myomectomy. Obstet Gynecol. 2009;113(2 pt 2):484–486.
- Oelsner G, Cohen SB, Soriano D, Admon D, Mashiach S, Carp H. Minimal surgery for the twisted ischaemic adnexa can preserve ovarian function. Hum Reprod. 2003;18(12):2599–2602.
- Yasa C, Dural O, Bastu E, Zorlu M, Demir O, Ugurlucan FG. Impact of laparoscopic ovarian detorsion on ovarian reserve. J Obstet Gynaecol Res. 2017;43(2):298–302.
- Yamada T, Ikeda A, Okamoto Y, Okamoto Y, Kanda T, Ueki M. Intraoperative blood salvage in abdominal simple total hysterectomy for uterine myoma. Int J Gynaecol Obstet. 1997;59(3):233–236.
- Discepola F, Valenti DA, Reinhold C, Tulandi T. Analysis of arterial blood vessels surrounding the myoma: relevance to myomectomy. Obstet Gynecol. 2007;110(6):1301–1303.
- Malavasi A, Cavalotti C, Nicolardi G, et al. The opioid neuropeptides in uterine fibroid pseudocapsules: a putative association with cervical integrity in human reproduction. Gynecol Endocrinol. 2013;29(11):982–988.
- Walocha JA, Litwin JA, Miodonski AJ. Vascular system of intramural leiomyomata revealed by corrosion casting and scanning electron microscopy. Hum Reprod. 2003;18(5):1088–1093.
- Tinelli A, Mynbaev OA, Sparic R, et al. Angiogenesis and vascularization of uterine leiomyoma: clinical value of pseudocapsule containing peptides and neurotransmitters [published online ahead of print March 22, 2016]. Curr Protein Pept Sci. doi:10.2174/1389203717666160322150338.
- Diamond MP. Reduction of adhesions after uterine myomectomy by Seprafilm membrane (HAL-F): a blinded, prospective, randomized, multicenter clinical study. Seprafilm Adhesion Study Group. Fertil Steril. 1996;66(6):904–910.
- Liu SS, Richman JM, Thirlby RC, Wu CL. Efficacy of continuous wound catheters delivering local anesthetic for postoperative analgesia: a quantitative and qualitative systematic review of randomized controlled trials. J Am Coll Surg. 2006;203(6):914–932.
- Lassen K, Soop M, Nygren J, et al; Enhanced Recovery After Surgery (ERAS) Group. Consensus review of optimal perioperative care in colorectal surgery: Enhanced Recovery After Surgery (ERAS) Group recommendations. Arch Surg. 2009;144(10):961–969.
- Kalogera E, Bakkum-Gamez JN, Jankowski CJ, et al. Enhanced recovery in gynecologic surgery. Obstet Gynecol. 2013;122(2 pt 1):319–328.
- Wright JD, Herzog TJ, Tsui J, et al. Nationwide trends in the performance of inpatient hysterectomy in the United States. Obstet Gynecol. 2013;122(2 pt 1):233–241.
- Barrett ML, Weiss AJ, Stocks C, Steiner CA, Myers ER. Statistical brief 200. Procedures to treat benign uterine fibroids in hospital inpatient and hospital-based ambulatory surgery settings, 2013. Healthcare Cost and Utilization Project website. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb200-Procedures-Treat-Uterine-Fibroids.jsp. Published January 2016. Accessed February 9, 2017.
- Stentz NC, Cooney L, Sammel MD, Shah DK. Impact of the Food and Drug Administration (FDA) safety communication on morcellation on surgical practice and perioperative morbidity following myomectomy [abstract p300]. Fertil Steril. 2016;106(3 suppl):e219.
- Hillis SD, Marchbanks PA, Peterson HB. Obstet Gynecol. 1996;87(4):539–543.
- Pritts E, Vanness D, Berek JS, et al. The prevalence of occult leiomyosarcoma at surgery for presumed uterine fibroids: a meta-analysis. Gynecol Surg. 2015;12(3):165–177.
- Bogani G, Cliby WA, Aletti GD. Impact of morcellation on survival outcomes of patients with unexpected uterine leiomyosarcoma: a systematic review and meta-analysis. Gynecol Oncol. 2015;137(1):167–172.
- Dilek S, Ertunc D, Tok EC, Cimen R, Doruk A. The effect of myomectomy on health-related quality of life of women with myoma uteri. J Obstet Gynaecol Res. 2010;36(2):364–369.
- Pundir J, Walawalkar R, Seshadri S, Khalaf Y, El-Toukhy T. Perioperative morbidity associated with abdominal myomectomy compared with total abdominal hysterectomy for uterine fibroids. J Obstet Gynaecol. 2013;33(7):655–662.
- West S, Ruiz R, Parker WH. Abdominal myomectomy in women with very large uterine size. Fertil Steril. 2006;85(1):36–39.
- Dueholm M, Lundorf E, Hansen ES, Ledertoug S, Olesen F. Evaluation of the uterine cavity with magnetic resonance imaging, transvaginal sonography, hysterosonographic examination, and diagnostic hysteroscopy. Fertil Steril. 2001;76(2):350–357.
- Kim YH, Chung HH, Kang SB, Kim SC, Kim YT. Safety and usefulness of intravenous iron sucrose in the management of preoperative anemia in patients with menorrhagia: a phase IV, open-label, prospective, randomized study. Acta Haematol. 2009;121(1):37–41.
- Kongnyuy EJ, Wiysonge CS. Interventions to reduce haemorrhage during myomectomy for fibroids. Cochrane Database Syst Rev. 2014 Aug 15;(8):CD005355.
- Hobo R, Netsu S, Koyasu Y, Tsutsumi O. Bradycardia and cardiac arrest caused by intramyometrial injection of vasopressin during a laparoscopically assisted myomectomy. Obstet Gynecol. 2009;113(2 pt 2):484–486.
- Oelsner G, Cohen SB, Soriano D, Admon D, Mashiach S, Carp H. Minimal surgery for the twisted ischaemic adnexa can preserve ovarian function. Hum Reprod. 2003;18(12):2599–2602.
- Yasa C, Dural O, Bastu E, Zorlu M, Demir O, Ugurlucan FG. Impact of laparoscopic ovarian detorsion on ovarian reserve. J Obstet Gynaecol Res. 2017;43(2):298–302.
- Yamada T, Ikeda A, Okamoto Y, Okamoto Y, Kanda T, Ueki M. Intraoperative blood salvage in abdominal simple total hysterectomy for uterine myoma. Int J Gynaecol Obstet. 1997;59(3):233–236.
- Discepola F, Valenti DA, Reinhold C, Tulandi T. Analysis of arterial blood vessels surrounding the myoma: relevance to myomectomy. Obstet Gynecol. 2007;110(6):1301–1303.
- Malavasi A, Cavalotti C, Nicolardi G, et al. The opioid neuropeptides in uterine fibroid pseudocapsules: a putative association with cervical integrity in human reproduction. Gynecol Endocrinol. 2013;29(11):982–988.
- Walocha JA, Litwin JA, Miodonski AJ. Vascular system of intramural leiomyomata revealed by corrosion casting and scanning electron microscopy. Hum Reprod. 2003;18(5):1088–1093.
- Tinelli A, Mynbaev OA, Sparic R, et al. Angiogenesis and vascularization of uterine leiomyoma: clinical value of pseudocapsule containing peptides and neurotransmitters [published online ahead of print March 22, 2016]. Curr Protein Pept Sci. doi:10.2174/1389203717666160322150338.
- Diamond MP. Reduction of adhesions after uterine myomectomy by Seprafilm membrane (HAL-F): a blinded, prospective, randomized, multicenter clinical study. Seprafilm Adhesion Study Group. Fertil Steril. 1996;66(6):904–910.
- Liu SS, Richman JM, Thirlby RC, Wu CL. Efficacy of continuous wound catheters delivering local anesthetic for postoperative analgesia: a quantitative and qualitative systematic review of randomized controlled trials. J Am Coll Surg. 2006;203(6):914–932.
- Lassen K, Soop M, Nygren J, et al; Enhanced Recovery After Surgery (ERAS) Group. Consensus review of optimal perioperative care in colorectal surgery: Enhanced Recovery After Surgery (ERAS) Group recommendations. Arch Surg. 2009;144(10):961–969.
- Kalogera E, Bakkum-Gamez JN, Jankowski CJ, et al. Enhanced recovery in gynecologic surgery. Obstet Gynecol. 2013;122(2 pt 1):319–328.
Robotics: General surgery goes its own way
HOUSTON – Subspecialties such as urology and gynecology have seen a steady increase in robot-assisted surgery and an offsetting decline in open procedures, but in general surgery, robot-assisted procedures seem to be making gains at the expense of laparoscopy, according to researchers from the University of Nebraska.
In two specific operations, ventral and inguinal hernia repairs (VHR and IHR), the percentage of open procedures has increased or held steady over the 7-year study period while the share of laparoscopic operations declined and robot-assisted surgeries (RAS) increased, Priscila Rodrigues Armijo, MD, reported at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
This shift to RAS rather than laparoscopy could have significant implications because RAS is significantly more costly than laparoscopy, Dr. Armijo said. “In our study, the open procedures were the most expensive, followed by the robot-assisted surgeries and then laparoscopy,” she said. Median direct costs were $14,364 for open procedures, $11,376 for RAS and $7,945 for laparoscopy.
The Nebraska study retrospectively analyzed five different general surgery procedures: colectomy, cholecystectomy, and bariatric procedures in addition to VHR and IHR. The researchers analyzed 857,468 operations entered into the University HealthSystem Consortium Clinical Database Resource Manager from October 2008 to September 2015.
Dr. Armijo explained that the goal was to study trends in general surgery because while several studies have examined trends in urologic and gynecologic surgery, few studies have done so in general surgery.
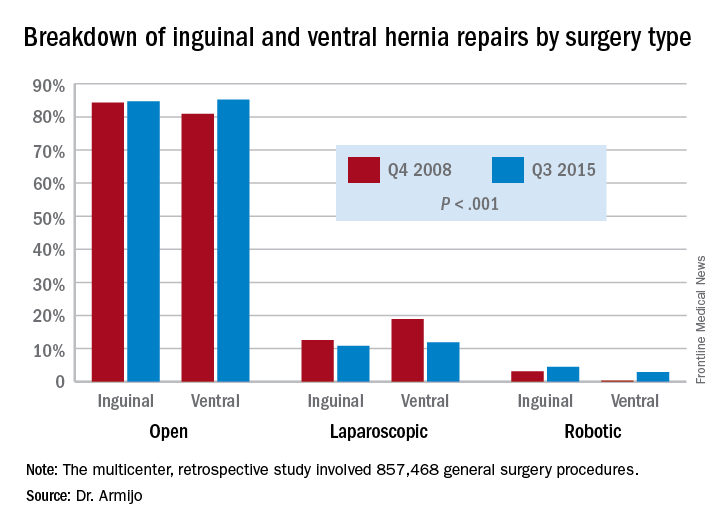
“There was a significant increase in minimally invasive utilizations over time, and robotic surgery increased disproportionately compared to the laparoscope counterpart,” Dr. Armijo said. “And although we cannot prove where those patients are coming from, we believe that, especially for inguinal and ventral hernia repairs, they are coming from laparoscopic surgeons who now are adopting robotic techniques and not from open surgeons switching to the robotic approach.”
In 7 years, the study showed a significant decrease in the share of open procedures in colectomy (from 71.8% to 61.9%), cholecystectomy (35.7% to 27.1%), and bariatric surgery (20.1% to 10.1%), but an increase in both laparoscopic and RAS approaches in these surgeries.
However, in IHR, open procedures held steady at around 84% through the study period, while laparoscopic procedures declined from 12.6% to 10.8% and RAS jumped 3.1% to 4.5%. For VHR, the share of open procedures actually jumped from 80.9% to 85.2%, while the proportion of laparoscopic procedures fell from 18.9% to 11.9% and RAS operations jumped more than tenfold, from 0.2% to 2.9%.
“For ventral hernia repair there was a significant decrease in the laparoscopic approach with a significant increase in both open and robotic procedures, which may be due to new open techniques, including component separation, that have been shown to be more durable as a repair,” Dr. Armijo said. “In addition, those repair techniques are more easily performed with the robotic approach. Laparoscopic surgeons are finding that robotic technology is enabling them to execute surgical tasks, such as suturing mesh.”
Coauthor Dmitry Oleynikov, MD, FACS, disclosed he is a stockholder in Virtual Incision Corp. Dr. Armijo and other coauthors had no financial relationships to disclose.
HOUSTON – Subspecialties such as urology and gynecology have seen a steady increase in robot-assisted surgery and an offsetting decline in open procedures, but in general surgery, robot-assisted procedures seem to be making gains at the expense of laparoscopy, according to researchers from the University of Nebraska.
In two specific operations, ventral and inguinal hernia repairs (VHR and IHR), the percentage of open procedures has increased or held steady over the 7-year study period while the share of laparoscopic operations declined and robot-assisted surgeries (RAS) increased, Priscila Rodrigues Armijo, MD, reported at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
This shift to RAS rather than laparoscopy could have significant implications because RAS is significantly more costly than laparoscopy, Dr. Armijo said. “In our study, the open procedures were the most expensive, followed by the robot-assisted surgeries and then laparoscopy,” she said. Median direct costs were $14,364 for open procedures, $11,376 for RAS and $7,945 for laparoscopy.
The Nebraska study retrospectively analyzed five different general surgery procedures: colectomy, cholecystectomy, and bariatric procedures in addition to VHR and IHR. The researchers analyzed 857,468 operations entered into the University HealthSystem Consortium Clinical Database Resource Manager from October 2008 to September 2015.
Dr. Armijo explained that the goal was to study trends in general surgery because while several studies have examined trends in urologic and gynecologic surgery, few studies have done so in general surgery.
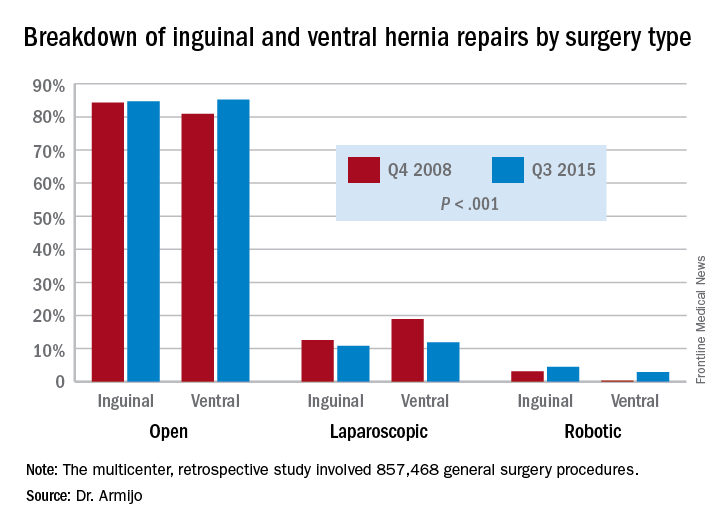
“There was a significant increase in minimally invasive utilizations over time, and robotic surgery increased disproportionately compared to the laparoscope counterpart,” Dr. Armijo said. “And although we cannot prove where those patients are coming from, we believe that, especially for inguinal and ventral hernia repairs, they are coming from laparoscopic surgeons who now are adopting robotic techniques and not from open surgeons switching to the robotic approach.”
In 7 years, the study showed a significant decrease in the share of open procedures in colectomy (from 71.8% to 61.9%), cholecystectomy (35.7% to 27.1%), and bariatric surgery (20.1% to 10.1%), but an increase in both laparoscopic and RAS approaches in these surgeries.
However, in IHR, open procedures held steady at around 84% through the study period, while laparoscopic procedures declined from 12.6% to 10.8% and RAS jumped 3.1% to 4.5%. For VHR, the share of open procedures actually jumped from 80.9% to 85.2%, while the proportion of laparoscopic procedures fell from 18.9% to 11.9% and RAS operations jumped more than tenfold, from 0.2% to 2.9%.
“For ventral hernia repair there was a significant decrease in the laparoscopic approach with a significant increase in both open and robotic procedures, which may be due to new open techniques, including component separation, that have been shown to be more durable as a repair,” Dr. Armijo said. “In addition, those repair techniques are more easily performed with the robotic approach. Laparoscopic surgeons are finding that robotic technology is enabling them to execute surgical tasks, such as suturing mesh.”
Coauthor Dmitry Oleynikov, MD, FACS, disclosed he is a stockholder in Virtual Incision Corp. Dr. Armijo and other coauthors had no financial relationships to disclose.
HOUSTON – Subspecialties such as urology and gynecology have seen a steady increase in robot-assisted surgery and an offsetting decline in open procedures, but in general surgery, robot-assisted procedures seem to be making gains at the expense of laparoscopy, according to researchers from the University of Nebraska.
In two specific operations, ventral and inguinal hernia repairs (VHR and IHR), the percentage of open procedures has increased or held steady over the 7-year study period while the share of laparoscopic operations declined and robot-assisted surgeries (RAS) increased, Priscila Rodrigues Armijo, MD, reported at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
This shift to RAS rather than laparoscopy could have significant implications because RAS is significantly more costly than laparoscopy, Dr. Armijo said. “In our study, the open procedures were the most expensive, followed by the robot-assisted surgeries and then laparoscopy,” she said. Median direct costs were $14,364 for open procedures, $11,376 for RAS and $7,945 for laparoscopy.
The Nebraska study retrospectively analyzed five different general surgery procedures: colectomy, cholecystectomy, and bariatric procedures in addition to VHR and IHR. The researchers analyzed 857,468 operations entered into the University HealthSystem Consortium Clinical Database Resource Manager from October 2008 to September 2015.
Dr. Armijo explained that the goal was to study trends in general surgery because while several studies have examined trends in urologic and gynecologic surgery, few studies have done so in general surgery.
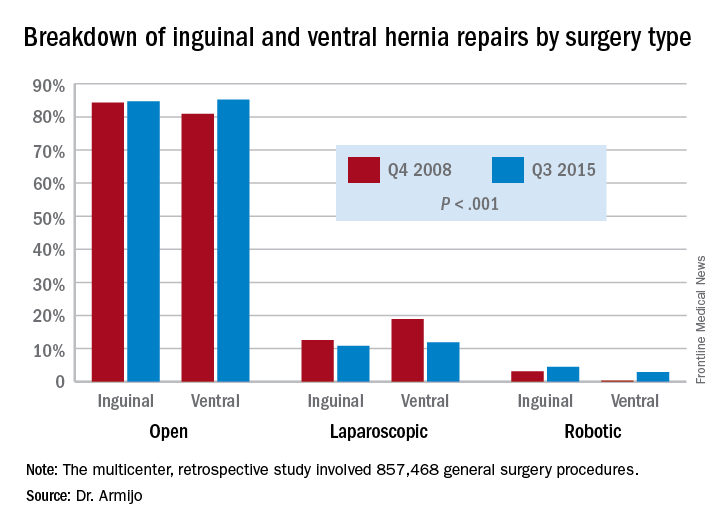
“There was a significant increase in minimally invasive utilizations over time, and robotic surgery increased disproportionately compared to the laparoscope counterpart,” Dr. Armijo said. “And although we cannot prove where those patients are coming from, we believe that, especially for inguinal and ventral hernia repairs, they are coming from laparoscopic surgeons who now are adopting robotic techniques and not from open surgeons switching to the robotic approach.”
In 7 years, the study showed a significant decrease in the share of open procedures in colectomy (from 71.8% to 61.9%), cholecystectomy (35.7% to 27.1%), and bariatric surgery (20.1% to 10.1%), but an increase in both laparoscopic and RAS approaches in these surgeries.
However, in IHR, open procedures held steady at around 84% through the study period, while laparoscopic procedures declined from 12.6% to 10.8% and RAS jumped 3.1% to 4.5%. For VHR, the share of open procedures actually jumped from 80.9% to 85.2%, while the proportion of laparoscopic procedures fell from 18.9% to 11.9% and RAS operations jumped more than tenfold, from 0.2% to 2.9%.
“For ventral hernia repair there was a significant decrease in the laparoscopic approach with a significant increase in both open and robotic procedures, which may be due to new open techniques, including component separation, that have been shown to be more durable as a repair,” Dr. Armijo said. “In addition, those repair techniques are more easily performed with the robotic approach. Laparoscopic surgeons are finding that robotic technology is enabling them to execute surgical tasks, such as suturing mesh.”
Coauthor Dmitry Oleynikov, MD, FACS, disclosed he is a stockholder in Virtual Incision Corp. Dr. Armijo and other coauthors had no financial relationships to disclose.
AT SAGES 2017
Key clinical point: In inguinal and ventral hernia repair, laparoscopic surgeons are more likely than are open surgery counterparts to move to surgical robot.
Major finding: Over the 7-year study period, the share of open ventral hernia repair procedures increased from 80.9% to 85.2%, while the proportion of laparoscopic procedures fell from 18.9% to 11.9% and RAS operations increased from 0.2% to 2.9%.
Data source: Multicenter, retrospective study of 857,468 general surgery procedures from 2008 to 2015 in the University HealthSystem Consortium Clinical Database Resource Manager.
Disclosures: Dr. Armijo reported having no financial disclosures. Coauthor Dmitry Oleynikov, MD, disclosed stock holding in Virtual Incision Corp.