User login
Many patients’ severe asthma remains uncontrolled
ATLANTA – More than half of patients severe asthma have disease that remains uncontrolled at their index date of treatment, and 39% remained uncontrolled at 12 months of follow-up, results from a large single specialty practice study showed.
“Severe asthma accounts for only 5%-10% of all asthma [in] patients but at least half of the health care costs, and it’s a significant burden to those who suffer from it,” study author Brian D. Stone, MD, said in an interview at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
The mean age of patients was 44.4 years, 67% were female, 78% were white, 77% had concomitant rhinitis, 21% had sinusitis, and 44% had allergic sensitivities. The mean baseline prebronchodilation FEV1 and FEV1% predicted were 2.45 L and 79.7%, respectively. The mean baseline ACT score was 17, with 61% of patients having ACT scores of 19 or lower, indicating poor symptom control.
Using National Asthma Education and Prevention Program criteria, the researchers found that 52% of patients had uncontrolled asthma at the index date and 39% remained uncontrolled at 12 months of follow-up. In an effort to better manage their severe asthma, more than one-third of patients on Step 4 therapy and 60% of patients on Step 5 therapy changed their asthma controller medications during follow-up.
“As an asthma specialist, I hoped that more [of these patients] would have come under control. These are the most difficult patients to treat,” said Dr. Stone, who practices at Allergy Partners of San Diego. “It’s a population that deserves special attention, and interventions are probably going to be on multiple levels, depending on what type of severe persistent asthma they have. More therapies are needed.”
He acknowledged certain limitations of the study, including the fact that patients were treated by specialists in allergy, asthma, and immunology and, therefore, may not represent the general population with asthma.
The study was supported by AstraZeneca. Dr. Stone reported having no relevant financial disclosures.
ATLANTA – More than half of patients severe asthma have disease that remains uncontrolled at their index date of treatment, and 39% remained uncontrolled at 12 months of follow-up, results from a large single specialty practice study showed.
“Severe asthma accounts for only 5%-10% of all asthma [in] patients but at least half of the health care costs, and it’s a significant burden to those who suffer from it,” study author Brian D. Stone, MD, said in an interview at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
The mean age of patients was 44.4 years, 67% were female, 78% were white, 77% had concomitant rhinitis, 21% had sinusitis, and 44% had allergic sensitivities. The mean baseline prebronchodilation FEV1 and FEV1% predicted were 2.45 L and 79.7%, respectively. The mean baseline ACT score was 17, with 61% of patients having ACT scores of 19 or lower, indicating poor symptom control.
Using National Asthma Education and Prevention Program criteria, the researchers found that 52% of patients had uncontrolled asthma at the index date and 39% remained uncontrolled at 12 months of follow-up. In an effort to better manage their severe asthma, more than one-third of patients on Step 4 therapy and 60% of patients on Step 5 therapy changed their asthma controller medications during follow-up.
“As an asthma specialist, I hoped that more [of these patients] would have come under control. These are the most difficult patients to treat,” said Dr. Stone, who practices at Allergy Partners of San Diego. “It’s a population that deserves special attention, and interventions are probably going to be on multiple levels, depending on what type of severe persistent asthma they have. More therapies are needed.”
He acknowledged certain limitations of the study, including the fact that patients were treated by specialists in allergy, asthma, and immunology and, therefore, may not represent the general population with asthma.
The study was supported by AstraZeneca. Dr. Stone reported having no relevant financial disclosures.
ATLANTA – More than half of patients severe asthma have disease that remains uncontrolled at their index date of treatment, and 39% remained uncontrolled at 12 months of follow-up, results from a large single specialty practice study showed.
“Severe asthma accounts for only 5%-10% of all asthma [in] patients but at least half of the health care costs, and it’s a significant burden to those who suffer from it,” study author Brian D. Stone, MD, said in an interview at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
The mean age of patients was 44.4 years, 67% were female, 78% were white, 77% had concomitant rhinitis, 21% had sinusitis, and 44% had allergic sensitivities. The mean baseline prebronchodilation FEV1 and FEV1% predicted were 2.45 L and 79.7%, respectively. The mean baseline ACT score was 17, with 61% of patients having ACT scores of 19 or lower, indicating poor symptom control.
Using National Asthma Education and Prevention Program criteria, the researchers found that 52% of patients had uncontrolled asthma at the index date and 39% remained uncontrolled at 12 months of follow-up. In an effort to better manage their severe asthma, more than one-third of patients on Step 4 therapy and 60% of patients on Step 5 therapy changed their asthma controller medications during follow-up.
“As an asthma specialist, I hoped that more [of these patients] would have come under control. These are the most difficult patients to treat,” said Dr. Stone, who practices at Allergy Partners of San Diego. “It’s a population that deserves special attention, and interventions are probably going to be on multiple levels, depending on what type of severe persistent asthma they have. More therapies are needed.”
He acknowledged certain limitations of the study, including the fact that patients were treated by specialists in allergy, asthma, and immunology and, therefore, may not represent the general population with asthma.
The study was supported by AstraZeneca. Dr. Stone reported having no relevant financial disclosures.
AT THE 2017 AAAAI ANNUAL MEETING
Key clinical point:
Major finding: More than half of patients with severe asthma (52%) had uncontrolled disease at the index date of treatment, and 39% remained uncontrolled at 12 months of follow-up.
Data source: A retrospective review of 12,922 patients aged 12 years and older with severe asthma who were treated between Jan. 1, 2010, and April 30, 2016.
Disclosures: The study was supported by AstraZeneca. Dr. Stone reported no relevant financial disclosures.
Robot-assisted surgery: Twice the price
HOUSTON – Robot-assisted operations for inguinal hernia repair (IHR) and cholecystectomy have grown steadily in recent years, but these procedures can be done equally well by traditional operations at a fraction of the cost, according to a study from Geisinger Medical Center in Pennsylvania.
Ellen Vogels, DO, of Geisinger, reported results of a study of 1,248 cholecystectomies and 723 initial IHRs from 2007 to 2016. The cholecystectomies were done via robot-assisted surgery or laparoscopy in the hospital or via laparoscopy in an ambulatory surgery center (ASC). The IHRs were done robotically, open, or laparoscopically in the hospital, or open or laparoscopically in an ASC.
Dr. Vogels quoted statistics from the ECRI Institute that showed robotic surgery procedures have increased 178% between 2009 and 2014, and the two procedures the group studied are the most frequently performed robotic procedures.
Within the Geisinger system, the study found a 3:1 cost disparity for IHR: $6,292 total cost for hospital-based robotic surgery vs. $3,421 for ASC-based laparoscopy IHR and $1,853 for ASC-based open repair. For cholecystectomy, the disparity isn’t as wide – it’s 2:1 – but is still significant: Total costs for hospital-based robotic surgery are $6,057 vs. $3,443 for ASC-based cholecystectomy and $3,270 for hospital-based laparoscopic cholecystectomy (the study did not include any open cholecystectomies).
Total costs not only include costs for the procedure but also all related pre- and postoperative care. The cost analysis did not account for the cost of the robot, including maintenance contracts, or costs for laparoscopic instruments. Variable costs also ranged from about $3,000 for robotic IHR to $942 for ASC open repair – which means the lowest per-procedure cost for the latter was around $900.
“Translating this into the fact that cholecystectomies and inguinal hernia repairs are the most often performed general surgery procedures, ambulatory surgery centers can save over $60 billion over the next 10 years in just overhead costs as well as increased efficiency,” Dr. Vogels said.
The study also found access issues depending on where patients had their operations. “As far as service and access in our institution alone, we found that patients going to the main hospital spent as much as two times longer getting these procedures done as compared to the ambulatory surgery centers,” Dr. Vogels said.
Robotic procedures also required longer operative times, the study found – an average of 109 minutes for IHR vs. about an hour for ASC procedures and hospital-based open surgery (but averaging 78 minutes for in-hospital laparoscopy); and 73 minutes for robotic cholecystectomy, 60 minutes for hospital laparoscopy, and 45 minutes for ASC laparoscopy.
Robotic session moderator Dmitry Oleynikov, MD, FACS, of the University of Nebraska Medical Center, Omaha, asked Dr. Vogels if putting a robotic platform in an ambulatory surgery setting would make it more cost effective.
That’s not practical from a cost or efficiency perspective, she said.
“When you look at the cost of the ASCs, specifically in the hernia group, the lowest-cost hernia repair is about $800; with the robot it’s going to be significantly higher than that, up to three times higher than that,” Dr. Vogels replied. “Then you’re also changing all those simple ambulatory surgery procedures to more involved robotic procedures, so it’s hard to justify doing that in the ASC.”
Dr. Vogels and her coauthors had no relevant financial disclosures.
HOUSTON – Robot-assisted operations for inguinal hernia repair (IHR) and cholecystectomy have grown steadily in recent years, but these procedures can be done equally well by traditional operations at a fraction of the cost, according to a study from Geisinger Medical Center in Pennsylvania.
Ellen Vogels, DO, of Geisinger, reported results of a study of 1,248 cholecystectomies and 723 initial IHRs from 2007 to 2016. The cholecystectomies were done via robot-assisted surgery or laparoscopy in the hospital or via laparoscopy in an ambulatory surgery center (ASC). The IHRs were done robotically, open, or laparoscopically in the hospital, or open or laparoscopically in an ASC.
Dr. Vogels quoted statistics from the ECRI Institute that showed robotic surgery procedures have increased 178% between 2009 and 2014, and the two procedures the group studied are the most frequently performed robotic procedures.
Within the Geisinger system, the study found a 3:1 cost disparity for IHR: $6,292 total cost for hospital-based robotic surgery vs. $3,421 for ASC-based laparoscopy IHR and $1,853 for ASC-based open repair. For cholecystectomy, the disparity isn’t as wide – it’s 2:1 – but is still significant: Total costs for hospital-based robotic surgery are $6,057 vs. $3,443 for ASC-based cholecystectomy and $3,270 for hospital-based laparoscopic cholecystectomy (the study did not include any open cholecystectomies).
Total costs not only include costs for the procedure but also all related pre- and postoperative care. The cost analysis did not account for the cost of the robot, including maintenance contracts, or costs for laparoscopic instruments. Variable costs also ranged from about $3,000 for robotic IHR to $942 for ASC open repair – which means the lowest per-procedure cost for the latter was around $900.
“Translating this into the fact that cholecystectomies and inguinal hernia repairs are the most often performed general surgery procedures, ambulatory surgery centers can save over $60 billion over the next 10 years in just overhead costs as well as increased efficiency,” Dr. Vogels said.
The study also found access issues depending on where patients had their operations. “As far as service and access in our institution alone, we found that patients going to the main hospital spent as much as two times longer getting these procedures done as compared to the ambulatory surgery centers,” Dr. Vogels said.
Robotic procedures also required longer operative times, the study found – an average of 109 minutes for IHR vs. about an hour for ASC procedures and hospital-based open surgery (but averaging 78 minutes for in-hospital laparoscopy); and 73 minutes for robotic cholecystectomy, 60 minutes for hospital laparoscopy, and 45 minutes for ASC laparoscopy.
Robotic session moderator Dmitry Oleynikov, MD, FACS, of the University of Nebraska Medical Center, Omaha, asked Dr. Vogels if putting a robotic platform in an ambulatory surgery setting would make it more cost effective.
That’s not practical from a cost or efficiency perspective, she said.
“When you look at the cost of the ASCs, specifically in the hernia group, the lowest-cost hernia repair is about $800; with the robot it’s going to be significantly higher than that, up to three times higher than that,” Dr. Vogels replied. “Then you’re also changing all those simple ambulatory surgery procedures to more involved robotic procedures, so it’s hard to justify doing that in the ASC.”
Dr. Vogels and her coauthors had no relevant financial disclosures.
HOUSTON – Robot-assisted operations for inguinal hernia repair (IHR) and cholecystectomy have grown steadily in recent years, but these procedures can be done equally well by traditional operations at a fraction of the cost, according to a study from Geisinger Medical Center in Pennsylvania.
Ellen Vogels, DO, of Geisinger, reported results of a study of 1,248 cholecystectomies and 723 initial IHRs from 2007 to 2016. The cholecystectomies were done via robot-assisted surgery or laparoscopy in the hospital or via laparoscopy in an ambulatory surgery center (ASC). The IHRs were done robotically, open, or laparoscopically in the hospital, or open or laparoscopically in an ASC.
Dr. Vogels quoted statistics from the ECRI Institute that showed robotic surgery procedures have increased 178% between 2009 and 2014, and the two procedures the group studied are the most frequently performed robotic procedures.
Within the Geisinger system, the study found a 3:1 cost disparity for IHR: $6,292 total cost for hospital-based robotic surgery vs. $3,421 for ASC-based laparoscopy IHR and $1,853 for ASC-based open repair. For cholecystectomy, the disparity isn’t as wide – it’s 2:1 – but is still significant: Total costs for hospital-based robotic surgery are $6,057 vs. $3,443 for ASC-based cholecystectomy and $3,270 for hospital-based laparoscopic cholecystectomy (the study did not include any open cholecystectomies).
Total costs not only include costs for the procedure but also all related pre- and postoperative care. The cost analysis did not account for the cost of the robot, including maintenance contracts, or costs for laparoscopic instruments. Variable costs also ranged from about $3,000 for robotic IHR to $942 for ASC open repair – which means the lowest per-procedure cost for the latter was around $900.
“Translating this into the fact that cholecystectomies and inguinal hernia repairs are the most often performed general surgery procedures, ambulatory surgery centers can save over $60 billion over the next 10 years in just overhead costs as well as increased efficiency,” Dr. Vogels said.
The study also found access issues depending on where patients had their operations. “As far as service and access in our institution alone, we found that patients going to the main hospital spent as much as two times longer getting these procedures done as compared to the ambulatory surgery centers,” Dr. Vogels said.
Robotic procedures also required longer operative times, the study found – an average of 109 minutes for IHR vs. about an hour for ASC procedures and hospital-based open surgery (but averaging 78 minutes for in-hospital laparoscopy); and 73 minutes for robotic cholecystectomy, 60 minutes for hospital laparoscopy, and 45 minutes for ASC laparoscopy.
Robotic session moderator Dmitry Oleynikov, MD, FACS, of the University of Nebraska Medical Center, Omaha, asked Dr. Vogels if putting a robotic platform in an ambulatory surgery setting would make it more cost effective.
That’s not practical from a cost or efficiency perspective, she said.
“When you look at the cost of the ASCs, specifically in the hernia group, the lowest-cost hernia repair is about $800; with the robot it’s going to be significantly higher than that, up to three times higher than that,” Dr. Vogels replied. “Then you’re also changing all those simple ambulatory surgery procedures to more involved robotic procedures, so it’s hard to justify doing that in the ASC.”
Dr. Vogels and her coauthors had no relevant financial disclosures.
AT SAGES 2017
Key clinical point: Outcomes for robot-assisted inguinal hernia repair and cholecystectomy are similar to those for outpatient open and laparoscopic procedures.
Major finding: Robotic IHR costs up to three times more than open outpatient surgery, and robotic cholecystectomy costs twice as much as outpatient surgery.
Data source: Study of 1,971 in-hospital robotic, laparoscopic, and open procedures, and outpatient laparoscopic and open operations done from 2007 to 2016 at Geisinger Medical Center.
Disclosures: Dr. Vogels and coauthors reported having no financial disclosures.
Video: Try ‘PLISSIT’ to address postcancer sexual health
NATIONAL HARBOR, MD. – Comprehensive care of patients with gynecologic malignancies should include a sensitive and thorough assessment of sexual health.
In a video interview at the annual meeting of the Society of Gynecologic Oncology, Don Dizon, MD, of Massachusetts General Hospital, Boston, gives a series of practical tips to help physicians take a thorough sexual health history and provide information and guidance for patients and their partners.
Dr. Dizon, professor of gynecologic oncology and director of the oncology sexual health clinic at Brigham and Women’s Hospital, also in Boston, said that he likes to begin with the PLISSIT model, where patients are given permission (P) to talk about sexual problems. Then, the clinician gives the patient limited (LI) scientific or clinical information about the situation, followed by specific suggestions (SS) that might help. Finally, patients may be referred to mental health providers or sex counselors for intensive therapy (IT) if needed.
“It’s also important not to confuse terminology,” said Dr. Dizon. “Intimacy is experienced very differently between men and women. Women experience intimacy through arousal, desire, and, when desire is satisfied, that’s intimacy. Intercourse is not a part of that equation.” For men, he said, intimacy is more often experienced through intercourse. “So the disconnect is greater after cancer is diagnosed,” making it especially important to acknowledge problems sensitively, and to helps patients and partners find a way forward.
“The word I like to use is ‘play,’ ” said Dr. Dizon. When a renegotiation of an intimate relationship is framed in terms of play, the pressure is off, and “men can wrap their hands around that idea,” he said.
Dr. Dizon sits on the board of the Patty Brisben Foundation and the Young Survival Coalition.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @karioakes
NATIONAL HARBOR, MD. – Comprehensive care of patients with gynecologic malignancies should include a sensitive and thorough assessment of sexual health.
In a video interview at the annual meeting of the Society of Gynecologic Oncology, Don Dizon, MD, of Massachusetts General Hospital, Boston, gives a series of practical tips to help physicians take a thorough sexual health history and provide information and guidance for patients and their partners.
Dr. Dizon, professor of gynecologic oncology and director of the oncology sexual health clinic at Brigham and Women’s Hospital, also in Boston, said that he likes to begin with the PLISSIT model, where patients are given permission (P) to talk about sexual problems. Then, the clinician gives the patient limited (LI) scientific or clinical information about the situation, followed by specific suggestions (SS) that might help. Finally, patients may be referred to mental health providers or sex counselors for intensive therapy (IT) if needed.
“It’s also important not to confuse terminology,” said Dr. Dizon. “Intimacy is experienced very differently between men and women. Women experience intimacy through arousal, desire, and, when desire is satisfied, that’s intimacy. Intercourse is not a part of that equation.” For men, he said, intimacy is more often experienced through intercourse. “So the disconnect is greater after cancer is diagnosed,” making it especially important to acknowledge problems sensitively, and to helps patients and partners find a way forward.
“The word I like to use is ‘play,’ ” said Dr. Dizon. When a renegotiation of an intimate relationship is framed in terms of play, the pressure is off, and “men can wrap their hands around that idea,” he said.
Dr. Dizon sits on the board of the Patty Brisben Foundation and the Young Survival Coalition.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @karioakes
NATIONAL HARBOR, MD. – Comprehensive care of patients with gynecologic malignancies should include a sensitive and thorough assessment of sexual health.
In a video interview at the annual meeting of the Society of Gynecologic Oncology, Don Dizon, MD, of Massachusetts General Hospital, Boston, gives a series of practical tips to help physicians take a thorough sexual health history and provide information and guidance for patients and their partners.
Dr. Dizon, professor of gynecologic oncology and director of the oncology sexual health clinic at Brigham and Women’s Hospital, also in Boston, said that he likes to begin with the PLISSIT model, where patients are given permission (P) to talk about sexual problems. Then, the clinician gives the patient limited (LI) scientific or clinical information about the situation, followed by specific suggestions (SS) that might help. Finally, patients may be referred to mental health providers or sex counselors for intensive therapy (IT) if needed.
“It’s also important not to confuse terminology,” said Dr. Dizon. “Intimacy is experienced very differently between men and women. Women experience intimacy through arousal, desire, and, when desire is satisfied, that’s intimacy. Intercourse is not a part of that equation.” For men, he said, intimacy is more often experienced through intercourse. “So the disconnect is greater after cancer is diagnosed,” making it especially important to acknowledge problems sensitively, and to helps patients and partners find a way forward.
“The word I like to use is ‘play,’ ” said Dr. Dizon. When a renegotiation of an intimate relationship is framed in terms of play, the pressure is off, and “men can wrap their hands around that idea,” he said.
Dr. Dizon sits on the board of the Patty Brisben Foundation and the Young Survival Coalition.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @karioakes
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Following the Trajectory of PTSD
Does the course of posttraumatic stress disorder (PTSD) differ depending on whether the person is in the military or has left? Researchers from Naval Health Research Center and the VA wondered whether separation from the military could create a “significant disruption of routine, order, and structure,” which might exacerbate PTSD symptoms, and would the symptoms subside as the veteran adjusted to civilian life?
Using data from the Millennium Cohort Study, researchers examined trajectories of PTSD among 22,080 military personnel across 4 time points, about 3 years apart, from 2001 to 2013. They compared trajectories between people who separated before the second time point or remained in the military across the entire study period. The researchers assessed PTSD screening and symptoms using the PTSD Checklist-Civilian, for which higher scores represent more severe symptoms.
The researchers say 4 distinct classes described symptom trajectories: resilient, delayed onset, improving, and elevated-recovering. Overall, the trajectories were similar for veterans and active-duty personnel. Veterans had a higher likelihood of screening positive for PTSD at baseline before separation and were more likely to newly screen positive for PTSD at waves 2, 3, and 4. Of participants who screened positive for PTSD, veterans had more severe symptoms compared with active-duty personnel at baseline but not at any subsequent assessments.
However, differences between the “elevated-recovering” classes grew over time, showing that veterans did not recover as soon or as “dramatically,” the researchers say. This might be due to symptoms being exacerbated by the change in routine.
The good news is that most veterans and active-duty personnel fell into the resilient class (82% and 87%, respectively). The researchers cite other studies that have found resilience is the most common response to PTSD.
The researchers noted several risk factors for slower recovery, such as lower physical well-being and a history of multiple life stressors. The “delayed onset” group may be a good target for interventions, they suggest. This group reported high use of VA care, but still 26% reported no VA care, indicating that they could benefit from continued efforts to identify and treat them.
Does the course of posttraumatic stress disorder (PTSD) differ depending on whether the person is in the military or has left? Researchers from Naval Health Research Center and the VA wondered whether separation from the military could create a “significant disruption of routine, order, and structure,” which might exacerbate PTSD symptoms, and would the symptoms subside as the veteran adjusted to civilian life?
Using data from the Millennium Cohort Study, researchers examined trajectories of PTSD among 22,080 military personnel across 4 time points, about 3 years apart, from 2001 to 2013. They compared trajectories between people who separated before the second time point or remained in the military across the entire study period. The researchers assessed PTSD screening and symptoms using the PTSD Checklist-Civilian, for which higher scores represent more severe symptoms.
The researchers say 4 distinct classes described symptom trajectories: resilient, delayed onset, improving, and elevated-recovering. Overall, the trajectories were similar for veterans and active-duty personnel. Veterans had a higher likelihood of screening positive for PTSD at baseline before separation and were more likely to newly screen positive for PTSD at waves 2, 3, and 4. Of participants who screened positive for PTSD, veterans had more severe symptoms compared with active-duty personnel at baseline but not at any subsequent assessments.
However, differences between the “elevated-recovering” classes grew over time, showing that veterans did not recover as soon or as “dramatically,” the researchers say. This might be due to symptoms being exacerbated by the change in routine.
The good news is that most veterans and active-duty personnel fell into the resilient class (82% and 87%, respectively). The researchers cite other studies that have found resilience is the most common response to PTSD.
The researchers noted several risk factors for slower recovery, such as lower physical well-being and a history of multiple life stressors. The “delayed onset” group may be a good target for interventions, they suggest. This group reported high use of VA care, but still 26% reported no VA care, indicating that they could benefit from continued efforts to identify and treat them.
Does the course of posttraumatic stress disorder (PTSD) differ depending on whether the person is in the military or has left? Researchers from Naval Health Research Center and the VA wondered whether separation from the military could create a “significant disruption of routine, order, and structure,” which might exacerbate PTSD symptoms, and would the symptoms subside as the veteran adjusted to civilian life?
Using data from the Millennium Cohort Study, researchers examined trajectories of PTSD among 22,080 military personnel across 4 time points, about 3 years apart, from 2001 to 2013. They compared trajectories between people who separated before the second time point or remained in the military across the entire study period. The researchers assessed PTSD screening and symptoms using the PTSD Checklist-Civilian, for which higher scores represent more severe symptoms.
The researchers say 4 distinct classes described symptom trajectories: resilient, delayed onset, improving, and elevated-recovering. Overall, the trajectories were similar for veterans and active-duty personnel. Veterans had a higher likelihood of screening positive for PTSD at baseline before separation and were more likely to newly screen positive for PTSD at waves 2, 3, and 4. Of participants who screened positive for PTSD, veterans had more severe symptoms compared with active-duty personnel at baseline but not at any subsequent assessments.
However, differences between the “elevated-recovering” classes grew over time, showing that veterans did not recover as soon or as “dramatically,” the researchers say. This might be due to symptoms being exacerbated by the change in routine.
The good news is that most veterans and active-duty personnel fell into the resilient class (82% and 87%, respectively). The researchers cite other studies that have found resilience is the most common response to PTSD.
The researchers noted several risk factors for slower recovery, such as lower physical well-being and a history of multiple life stressors. The “delayed onset” group may be a good target for interventions, they suggest. This group reported high use of VA care, but still 26% reported no VA care, indicating that they could benefit from continued efforts to identify and treat them.
Rare Cancer Gets Timely Right Treatment
Be careful not to assume multiple cancerous lesions are advanced stage metastatic cancer, caution clinicians from H Plus Yangji Hospital in Seoul, and Inje University Haeundae Paik Hospital in Busan, both in the Republic of Korea. They came close to making that mistake.
Related: A Mysterious Massive Hemorrhage
The researchers reported on a patient who was on the verge of getting only palliative care for advanced laryngeal cancer with multiple lung metastases, when in fact he was a candidate for curative-aim chemotherapy. Thanks to a “meticulous approach,” the researchers switched their plan in time.
The patient was referred to their hospital because of symptoms such as “foreign body sensation” and voice change. A smoker for 45 years, he stopped 5 years before. A physical examination revealed that lymph nodes in the neck, axillary, and inguinal areas were not enlarged. Blood count and laboratory data were all normal, but a computed tomography (CT) scan and MRI revealed that the patient had an unusual constellation of simultaneous triple primary cancers: laryngeal supraglottic cancer, small cell lung cancer (SCLC), and squamous cell lung cancer.
Head and neck cancer with synchronous or metachronous lung cancers during follow-up isn’t rare, the clinicians say. But their patient’s case is uncommon because the coexistence of SCLC and squamous cell lung cancer has rarely been reported.
Related: Finding Synchronous Cancers
Supraglottic laryngeal cancer is usually diagnosed in the advanced stages with cervical lymph node metastasis because of its nonspecific presenting symptoms and its anatomic characteristics, including a rich lymphatic network, the researchers say. That was why at the initial presentation they presumed the patient had advanced metastatic cancer. If there had not been “high suspicion” or effort to confirm the 2 distinct lung masses by invasive diagnostic procedures, the patient would have received the expected palliative treatment and not the curative-aim treatment.
After the patient received concurrent chemoradiation therapy with weekly cisplatin, the supraglottic laryngeal cancer was “markedly decreased” without newly developed cervical lymph node metastasis. A follow-up chest CT showed partial response for the SCLC in the left upper lobe; the squamous cell lung cancer in the right lower lobe remained stable. The patient was given additional chemotherapy with etoposide and cisplatin. He has survived without recurrence.
Related: Timeliness of Lung Cancer Diagnosis and Treatment
Source:
Kim EK, Kim JY, Kim BM, Lim SN. BMJ Case Rep. 2017;2017.
doi: 10.1136/bcr-2016-216305.
Be careful not to assume multiple cancerous lesions are advanced stage metastatic cancer, caution clinicians from H Plus Yangji Hospital in Seoul, and Inje University Haeundae Paik Hospital in Busan, both in the Republic of Korea. They came close to making that mistake.
Related: A Mysterious Massive Hemorrhage
The researchers reported on a patient who was on the verge of getting only palliative care for advanced laryngeal cancer with multiple lung metastases, when in fact he was a candidate for curative-aim chemotherapy. Thanks to a “meticulous approach,” the researchers switched their plan in time.
The patient was referred to their hospital because of symptoms such as “foreign body sensation” and voice change. A smoker for 45 years, he stopped 5 years before. A physical examination revealed that lymph nodes in the neck, axillary, and inguinal areas were not enlarged. Blood count and laboratory data were all normal, but a computed tomography (CT) scan and MRI revealed that the patient had an unusual constellation of simultaneous triple primary cancers: laryngeal supraglottic cancer, small cell lung cancer (SCLC), and squamous cell lung cancer.
Head and neck cancer with synchronous or metachronous lung cancers during follow-up isn’t rare, the clinicians say. But their patient’s case is uncommon because the coexistence of SCLC and squamous cell lung cancer has rarely been reported.
Related: Finding Synchronous Cancers
Supraglottic laryngeal cancer is usually diagnosed in the advanced stages with cervical lymph node metastasis because of its nonspecific presenting symptoms and its anatomic characteristics, including a rich lymphatic network, the researchers say. That was why at the initial presentation they presumed the patient had advanced metastatic cancer. If there had not been “high suspicion” or effort to confirm the 2 distinct lung masses by invasive diagnostic procedures, the patient would have received the expected palliative treatment and not the curative-aim treatment.
After the patient received concurrent chemoradiation therapy with weekly cisplatin, the supraglottic laryngeal cancer was “markedly decreased” without newly developed cervical lymph node metastasis. A follow-up chest CT showed partial response for the SCLC in the left upper lobe; the squamous cell lung cancer in the right lower lobe remained stable. The patient was given additional chemotherapy with etoposide and cisplatin. He has survived without recurrence.
Related: Timeliness of Lung Cancer Diagnosis and Treatment
Source:
Kim EK, Kim JY, Kim BM, Lim SN. BMJ Case Rep. 2017;2017.
doi: 10.1136/bcr-2016-216305.
Be careful not to assume multiple cancerous lesions are advanced stage metastatic cancer, caution clinicians from H Plus Yangji Hospital in Seoul, and Inje University Haeundae Paik Hospital in Busan, both in the Republic of Korea. They came close to making that mistake.
Related: A Mysterious Massive Hemorrhage
The researchers reported on a patient who was on the verge of getting only palliative care for advanced laryngeal cancer with multiple lung metastases, when in fact he was a candidate for curative-aim chemotherapy. Thanks to a “meticulous approach,” the researchers switched their plan in time.
The patient was referred to their hospital because of symptoms such as “foreign body sensation” and voice change. A smoker for 45 years, he stopped 5 years before. A physical examination revealed that lymph nodes in the neck, axillary, and inguinal areas were not enlarged. Blood count and laboratory data were all normal, but a computed tomography (CT) scan and MRI revealed that the patient had an unusual constellation of simultaneous triple primary cancers: laryngeal supraglottic cancer, small cell lung cancer (SCLC), and squamous cell lung cancer.
Head and neck cancer with synchronous or metachronous lung cancers during follow-up isn’t rare, the clinicians say. But their patient’s case is uncommon because the coexistence of SCLC and squamous cell lung cancer has rarely been reported.
Related: Finding Synchronous Cancers
Supraglottic laryngeal cancer is usually diagnosed in the advanced stages with cervical lymph node metastasis because of its nonspecific presenting symptoms and its anatomic characteristics, including a rich lymphatic network, the researchers say. That was why at the initial presentation they presumed the patient had advanced metastatic cancer. If there had not been “high suspicion” or effort to confirm the 2 distinct lung masses by invasive diagnostic procedures, the patient would have received the expected palliative treatment and not the curative-aim treatment.
After the patient received concurrent chemoradiation therapy with weekly cisplatin, the supraglottic laryngeal cancer was “markedly decreased” without newly developed cervical lymph node metastasis. A follow-up chest CT showed partial response for the SCLC in the left upper lobe; the squamous cell lung cancer in the right lower lobe remained stable. The patient was given additional chemotherapy with etoposide and cisplatin. He has survived without recurrence.
Related: Timeliness of Lung Cancer Diagnosis and Treatment
Source:
Kim EK, Kim JY, Kim BM, Lim SN. BMJ Case Rep. 2017;2017.
doi: 10.1136/bcr-2016-216305.
Warfarin, aspirin linked to higher risk of ICH in AFib
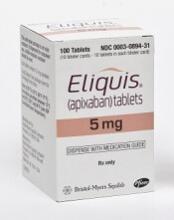
An analysis of data from the ARISTOTLE trial suggests patients with atrial fibrillation (AFib) have a higher risk of intracranial hemorrhage (ICH) when they receive warfarin as opposed to apixaban.
The analysis also indicates that concomitant aspirin use increases the risk of ICH among AFib patients taking either warfarin or apixaban as stroke prophylaxis.
“We know that aspirin has only a modest effect in preventing stroke in atrial fibrillation patients, yet it was one of the top predictors of intracranial hemorrhage,” said study author Renato D. Lopes, MD, PhD, of Duke Clinical Research Institute in Durham, North Carolina.
“Our finding demonstrates that aspirin is not as safe as one might think.”
Dr Lopes and his colleagues reported this finding in Blood.
Previous results from the ARISTOTLE trial, published in 2011, suggested that apixaban was superior to warfarin in terms of preventing stroke and systemic embolism, reducing bleeding, and reducing mortality in AFib patients.
However, a report published in 2013 suggested the results of this trial may have been affected by patients at 1 or more clinical trial sites receiving the wrong medication or dose, adverse events going unreported, and records being changed.
Bristol-Myers Squibb and Pfizer (funders of ARISTOTLE) said these issues likely had a negligible effect on the trial results. And the US Food and Drug Administration agreed when it approved apixaban for use in AFib patients in 2013.
Current analysis
For the current analysis, researchers used ARISTOTLE data to investigate the frequency and characteristics of ICH. They analyzed data from 18,140 AFib patients treated with warfarin or apixaban at sites in North America, Latin America, Europe, and Asia.
In all, 174 patients developed ICH. Most of these bleeds were spontaneous (71.2%) rather than traumatic (28.8%).
Apixaban vs warfarin
Patients randomized to receive apixaban had a lower incidence of ICH than those randomized to warfarin—0.33% per year and 0.80% per year, respectively.
The risk of ICH was significantly lower in the apixaban arm than the warfarin arm (hazard ratio [HR]=0.42, 95% CI 0.30–0.58; P<0.0001). The same was true for spontaneous ICH (HR=0.52, 95% CI 190 0.35–0.75; P=0.0006) and traumatic ICH (HR=0.26, 95% CI 0.13–0.53; P=0.0002).
In the warfarin arm, the median time from the most recent international normalized ratio (INR) test to ICH was 13 days (range, 6-21).
Most patients (78.5%) in the warfarin arm who developed ICH had a pre-ICH INR below 3.0. The median INR was 2.6 (range, 2.1-3.0).
Other risk factors
The researchers found that several factors other than study treatment were associated with an increased risk of ICH.
Patients treated at trial sites in Asia (HR=3.19) or Latin America (HR=1.57) had an increased risk of ICH compared to patients treated in Europe.
Each 5-year increase in patient age was associated with an increased risk of ICH (HR=1.25.)
Patients with a prior stroke or transient ischemic attack (HR=1.83) had an increased risk of ICH, as did patients receiving aspirin at baseline (HR=1.37).
The researchers said the increased risk of ICH associated with aspirin use was particularly pronounced in older patients. ![]()
An analysis of data from the ARISTOTLE trial suggests patients with atrial fibrillation (AFib) have a higher risk of intracranial hemorrhage (ICH) when they receive warfarin as opposed to apixaban.
The analysis also indicates that concomitant aspirin use increases the risk of ICH among AFib patients taking either warfarin or apixaban as stroke prophylaxis.
“We know that aspirin has only a modest effect in preventing stroke in atrial fibrillation patients, yet it was one of the top predictors of intracranial hemorrhage,” said study author Renato D. Lopes, MD, PhD, of Duke Clinical Research Institute in Durham, North Carolina.
“Our finding demonstrates that aspirin is not as safe as one might think.”
Dr Lopes and his colleagues reported this finding in Blood.
Previous results from the ARISTOTLE trial, published in 2011, suggested that apixaban was superior to warfarin in terms of preventing stroke and systemic embolism, reducing bleeding, and reducing mortality in AFib patients.
However, a report published in 2013 suggested the results of this trial may have been affected by patients at 1 or more clinical trial sites receiving the wrong medication or dose, adverse events going unreported, and records being changed.
Bristol-Myers Squibb and Pfizer (funders of ARISTOTLE) said these issues likely had a negligible effect on the trial results. And the US Food and Drug Administration agreed when it approved apixaban for use in AFib patients in 2013.
Current analysis
For the current analysis, researchers used ARISTOTLE data to investigate the frequency and characteristics of ICH. They analyzed data from 18,140 AFib patients treated with warfarin or apixaban at sites in North America, Latin America, Europe, and Asia.
In all, 174 patients developed ICH. Most of these bleeds were spontaneous (71.2%) rather than traumatic (28.8%).
Apixaban vs warfarin
Patients randomized to receive apixaban had a lower incidence of ICH than those randomized to warfarin—0.33% per year and 0.80% per year, respectively.
The risk of ICH was significantly lower in the apixaban arm than the warfarin arm (hazard ratio [HR]=0.42, 95% CI 0.30–0.58; P<0.0001). The same was true for spontaneous ICH (HR=0.52, 95% CI 190 0.35–0.75; P=0.0006) and traumatic ICH (HR=0.26, 95% CI 0.13–0.53; P=0.0002).
In the warfarin arm, the median time from the most recent international normalized ratio (INR) test to ICH was 13 days (range, 6-21).
Most patients (78.5%) in the warfarin arm who developed ICH had a pre-ICH INR below 3.0. The median INR was 2.6 (range, 2.1-3.0).
Other risk factors
The researchers found that several factors other than study treatment were associated with an increased risk of ICH.
Patients treated at trial sites in Asia (HR=3.19) or Latin America (HR=1.57) had an increased risk of ICH compared to patients treated in Europe.
Each 5-year increase in patient age was associated with an increased risk of ICH (HR=1.25.)
Patients with a prior stroke or transient ischemic attack (HR=1.83) had an increased risk of ICH, as did patients receiving aspirin at baseline (HR=1.37).
The researchers said the increased risk of ICH associated with aspirin use was particularly pronounced in older patients. ![]()
An analysis of data from the ARISTOTLE trial suggests patients with atrial fibrillation (AFib) have a higher risk of intracranial hemorrhage (ICH) when they receive warfarin as opposed to apixaban.
The analysis also indicates that concomitant aspirin use increases the risk of ICH among AFib patients taking either warfarin or apixaban as stroke prophylaxis.
“We know that aspirin has only a modest effect in preventing stroke in atrial fibrillation patients, yet it was one of the top predictors of intracranial hemorrhage,” said study author Renato D. Lopes, MD, PhD, of Duke Clinical Research Institute in Durham, North Carolina.
“Our finding demonstrates that aspirin is not as safe as one might think.”
Dr Lopes and his colleagues reported this finding in Blood.
Previous results from the ARISTOTLE trial, published in 2011, suggested that apixaban was superior to warfarin in terms of preventing stroke and systemic embolism, reducing bleeding, and reducing mortality in AFib patients.
However, a report published in 2013 suggested the results of this trial may have been affected by patients at 1 or more clinical trial sites receiving the wrong medication or dose, adverse events going unreported, and records being changed.
Bristol-Myers Squibb and Pfizer (funders of ARISTOTLE) said these issues likely had a negligible effect on the trial results. And the US Food and Drug Administration agreed when it approved apixaban for use in AFib patients in 2013.
Current analysis
For the current analysis, researchers used ARISTOTLE data to investigate the frequency and characteristics of ICH. They analyzed data from 18,140 AFib patients treated with warfarin or apixaban at sites in North America, Latin America, Europe, and Asia.
In all, 174 patients developed ICH. Most of these bleeds were spontaneous (71.2%) rather than traumatic (28.8%).
Apixaban vs warfarin
Patients randomized to receive apixaban had a lower incidence of ICH than those randomized to warfarin—0.33% per year and 0.80% per year, respectively.
The risk of ICH was significantly lower in the apixaban arm than the warfarin arm (hazard ratio [HR]=0.42, 95% CI 0.30–0.58; P<0.0001). The same was true for spontaneous ICH (HR=0.52, 95% CI 190 0.35–0.75; P=0.0006) and traumatic ICH (HR=0.26, 95% CI 0.13–0.53; P=0.0002).
In the warfarin arm, the median time from the most recent international normalized ratio (INR) test to ICH was 13 days (range, 6-21).
Most patients (78.5%) in the warfarin arm who developed ICH had a pre-ICH INR below 3.0. The median INR was 2.6 (range, 2.1-3.0).
Other risk factors
The researchers found that several factors other than study treatment were associated with an increased risk of ICH.
Patients treated at trial sites in Asia (HR=3.19) or Latin America (HR=1.57) had an increased risk of ICH compared to patients treated in Europe.
Each 5-year increase in patient age was associated with an increased risk of ICH (HR=1.25.)
Patients with a prior stroke or transient ischemic attack (HR=1.83) had an increased risk of ICH, as did patients receiving aspirin at baseline (HR=1.37).
The researchers said the increased risk of ICH associated with aspirin use was particularly pronounced in older patients. ![]()
Studies support Zika screening in entire US blood supply
Results from a pair of studies suggest it is necessary to test for Zika virus in all blood donated in the US, even blood collected outside areas of active Zika transmission.
Last year, the US Food and Drug Administration recommended that all states and US territories screen donated whole blood and blood components for the Zika virus.
Two studies published in Transfusion support that recommendation by revealing the presence of blood donors who tested positive for Zika and may have acquired the infection via travel or sexual contact.
In the first study, researchers screened donor plasma samples using the cobas Zika test. Some of the researchers are employees/contractors of Roche Molecular Systems, Inc., which developed the test.
The study included 358,786 blood donations made in US states. Plasma samples from 23 of the donors were reactive on the first test.
For these cases, the testing lab performed repeat tests with cobas Zika. The lab also simulated minipool testing by diluting a donor sample 1:6 with Zika-negative human plasma. In addition, the reactive samples were sent out for alternate nucleic acid testing and serology testing.
The additional tests suggested 14 of the samples were positive for the Zika virus.
Ten of the 14 donors said they had traveled to an area of active Zika transmission within 90 days of their donation, and 3 of the 10 donors also had a sexual exposure risk. The median time from the end of the donors’ travel to their donation was 25 days (range, 6-71).
Three donors had not traveled to an area of active Zika transmission outside the US, but they lived in Miami-Dade County and were thought to have contracted the virus there.
For the remaining donor, there was no information on travel or sexual exposure risk.
The researchers said minipool testing likely would have identified half of the Zika-positive donations, as only 7 of the 14 donations with probable Zika virus infection were detectable via the simulated minipool testing.
The team also said the estimated specificity of the cobas Zika test was 99.997%.
In the second study, researchers screened donor plasma samples using the Procleix Zika virus assay. Some of the researchers are employees/contractors of Hologic, Inc., and Grifols Diagnostic Solutions, Inc., the companies that co-developed the assay.
The study included 466,834 blood donations in the US (outside of Puerto Rico and Florida). Twenty donor samples were reactive on the initial test.
These 20 samples (and additional samples from these donors) underwent subsequent testing with the Procleix Zika virus assay, real-time polymerase chain reaction, and Zika virus IgG and IgM capture ELISAs.
According to subsequent tests, 5 donors were reactive for Zika virus RNA. All of these donations were collected outside areas of active Zika transmission, but all 5 donors had traveled to areas of active transmission.
The researchers said the estimated specificity of the Procleix Zika virus assay was 99.997%.
The team also reported transfusion of an apheresis platelet donation from 1 of the 5 Zika-positive donors. The recipient of this product did not develop Zika infection, which suggests these units may not be infectious.
However, other researchers previously reported what they believed to be transmission of the Zika virus via platelet transfusion. ![]()
Results from a pair of studies suggest it is necessary to test for Zika virus in all blood donated in the US, even blood collected outside areas of active Zika transmission.
Last year, the US Food and Drug Administration recommended that all states and US territories screen donated whole blood and blood components for the Zika virus.
Two studies published in Transfusion support that recommendation by revealing the presence of blood donors who tested positive for Zika and may have acquired the infection via travel or sexual contact.
In the first study, researchers screened donor plasma samples using the cobas Zika test. Some of the researchers are employees/contractors of Roche Molecular Systems, Inc., which developed the test.
The study included 358,786 blood donations made in US states. Plasma samples from 23 of the donors were reactive on the first test.
For these cases, the testing lab performed repeat tests with cobas Zika. The lab also simulated minipool testing by diluting a donor sample 1:6 with Zika-negative human plasma. In addition, the reactive samples were sent out for alternate nucleic acid testing and serology testing.
The additional tests suggested 14 of the samples were positive for the Zika virus.
Ten of the 14 donors said they had traveled to an area of active Zika transmission within 90 days of their donation, and 3 of the 10 donors also had a sexual exposure risk. The median time from the end of the donors’ travel to their donation was 25 days (range, 6-71).
Three donors had not traveled to an area of active Zika transmission outside the US, but they lived in Miami-Dade County and were thought to have contracted the virus there.
For the remaining donor, there was no information on travel or sexual exposure risk.
The researchers said minipool testing likely would have identified half of the Zika-positive donations, as only 7 of the 14 donations with probable Zika virus infection were detectable via the simulated minipool testing.
The team also said the estimated specificity of the cobas Zika test was 99.997%.
In the second study, researchers screened donor plasma samples using the Procleix Zika virus assay. Some of the researchers are employees/contractors of Hologic, Inc., and Grifols Diagnostic Solutions, Inc., the companies that co-developed the assay.
The study included 466,834 blood donations in the US (outside of Puerto Rico and Florida). Twenty donor samples were reactive on the initial test.
These 20 samples (and additional samples from these donors) underwent subsequent testing with the Procleix Zika virus assay, real-time polymerase chain reaction, and Zika virus IgG and IgM capture ELISAs.
According to subsequent tests, 5 donors were reactive for Zika virus RNA. All of these donations were collected outside areas of active Zika transmission, but all 5 donors had traveled to areas of active transmission.
The researchers said the estimated specificity of the Procleix Zika virus assay was 99.997%.
The team also reported transfusion of an apheresis platelet donation from 1 of the 5 Zika-positive donors. The recipient of this product did not develop Zika infection, which suggests these units may not be infectious.
However, other researchers previously reported what they believed to be transmission of the Zika virus via platelet transfusion. ![]()
Results from a pair of studies suggest it is necessary to test for Zika virus in all blood donated in the US, even blood collected outside areas of active Zika transmission.
Last year, the US Food and Drug Administration recommended that all states and US territories screen donated whole blood and blood components for the Zika virus.
Two studies published in Transfusion support that recommendation by revealing the presence of blood donors who tested positive for Zika and may have acquired the infection via travel or sexual contact.
In the first study, researchers screened donor plasma samples using the cobas Zika test. Some of the researchers are employees/contractors of Roche Molecular Systems, Inc., which developed the test.
The study included 358,786 blood donations made in US states. Plasma samples from 23 of the donors were reactive on the first test.
For these cases, the testing lab performed repeat tests with cobas Zika. The lab also simulated minipool testing by diluting a donor sample 1:6 with Zika-negative human plasma. In addition, the reactive samples were sent out for alternate nucleic acid testing and serology testing.
The additional tests suggested 14 of the samples were positive for the Zika virus.
Ten of the 14 donors said they had traveled to an area of active Zika transmission within 90 days of their donation, and 3 of the 10 donors also had a sexual exposure risk. The median time from the end of the donors’ travel to their donation was 25 days (range, 6-71).
Three donors had not traveled to an area of active Zika transmission outside the US, but they lived in Miami-Dade County and were thought to have contracted the virus there.
For the remaining donor, there was no information on travel or sexual exposure risk.
The researchers said minipool testing likely would have identified half of the Zika-positive donations, as only 7 of the 14 donations with probable Zika virus infection were detectable via the simulated minipool testing.
The team also said the estimated specificity of the cobas Zika test was 99.997%.
In the second study, researchers screened donor plasma samples using the Procleix Zika virus assay. Some of the researchers are employees/contractors of Hologic, Inc., and Grifols Diagnostic Solutions, Inc., the companies that co-developed the assay.
The study included 466,834 blood donations in the US (outside of Puerto Rico and Florida). Twenty donor samples were reactive on the initial test.
These 20 samples (and additional samples from these donors) underwent subsequent testing with the Procleix Zika virus assay, real-time polymerase chain reaction, and Zika virus IgG and IgM capture ELISAs.
According to subsequent tests, 5 donors were reactive for Zika virus RNA. All of these donations were collected outside areas of active Zika transmission, but all 5 donors had traveled to areas of active transmission.
The researchers said the estimated specificity of the Procleix Zika virus assay was 99.997%.
The team also reported transfusion of an apheresis platelet donation from 1 of the 5 Zika-positive donors. The recipient of this product did not develop Zika infection, which suggests these units may not be infectious.
However, other researchers previously reported what they believed to be transmission of the Zika virus via platelet transfusion. ![]()
FDA grants priority review for BLA of CAR T-cell therapy
The US Food and Drug Administration (FDA) has granted priority review for a biologics license application (BLA) for CTL019 (tisagenlecleucel-T), an investigational chimeric antigen receptor (CAR) T-cell therapy.
The BLA is for CTL019 as a treatment for pediatric patients and young adults with relapsed or refractory B-cell acute lymphoblastic leukemia (ALL).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA accepted the BLA for CTL019 yesterday, according to Novartis.
About CTL019
CTL019 consists of autologous T cells expressing a CD19-specific CAR. The therapy was first developed by the University of Pennsylvania.
In 2012, the university and Novartis entered into a global collaboration to further research, develop, and commercialize CAR-T cell therapies, including CTL019. Novartis holds the worldwide rights to CARs developed through the collaboration.
CTL019 already has breakthrough therapy designation for the treatment of adults and children with relapsed/refractory ALL.
Novartis said it is planning additional filings for CTL019 in the US and European Union later this year, including a BLA with the FDA for the treatment of adults with relapsed/refractory diffuse large B-cell lymphoma (DLBCL) and applications for marketing authorization with the European Medicines Agency in relapsed/refractory B-cell ALL and relapsed/refractory DLBCL.
Trials of CTL019 in ALL
The priority review designation for CTL019 is based on results from the Novartis-sponsored ELIANA study (NCT02435849). Results from this international, phase 2 trial were presented at ASH 2016.
The trial enrolled patients who had CD19-positive B-ALL with morphologic marrow tumor involvement at registration (>5% blasts) and were primary refractory, were chemo-refractory after first relapse, had relapsed after second-line therapy, or were ineligible for allogeneic hematopoietic stem cell transplant.
Most patients received fludarabine/cyclophosphamide lymphodepleting chemotherapy followed by a single dose of CTL019.
Three months post-infusion, 82% of patients (41/50) had achieved a complete response or complete response with incomplete blood count recovery.
Nearly half of the patients in the trial (48%) experienced grade 3/4 cytokine release syndrome (CRS), though there were no deaths due to CRS. Fifteen percent of patients experienced grade 3 neurological and psychiatric events, including confusion, delirium, encephalopathy, agitation, and seizure.
The BLA for CTL019 is also supported by results from the phase 2 ENSIGN trial, which were presented at ASH 2016, and results of a pilot study in patients with relapsed/refractory ALL, which were presented at ASH 2015. ![]()
The US Food and Drug Administration (FDA) has granted priority review for a biologics license application (BLA) for CTL019 (tisagenlecleucel-T), an investigational chimeric antigen receptor (CAR) T-cell therapy.
The BLA is for CTL019 as a treatment for pediatric patients and young adults with relapsed or refractory B-cell acute lymphoblastic leukemia (ALL).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA accepted the BLA for CTL019 yesterday, according to Novartis.
About CTL019
CTL019 consists of autologous T cells expressing a CD19-specific CAR. The therapy was first developed by the University of Pennsylvania.
In 2012, the university and Novartis entered into a global collaboration to further research, develop, and commercialize CAR-T cell therapies, including CTL019. Novartis holds the worldwide rights to CARs developed through the collaboration.
CTL019 already has breakthrough therapy designation for the treatment of adults and children with relapsed/refractory ALL.
Novartis said it is planning additional filings for CTL019 in the US and European Union later this year, including a BLA with the FDA for the treatment of adults with relapsed/refractory diffuse large B-cell lymphoma (DLBCL) and applications for marketing authorization with the European Medicines Agency in relapsed/refractory B-cell ALL and relapsed/refractory DLBCL.
Trials of CTL019 in ALL
The priority review designation for CTL019 is based on results from the Novartis-sponsored ELIANA study (NCT02435849). Results from this international, phase 2 trial were presented at ASH 2016.
The trial enrolled patients who had CD19-positive B-ALL with morphologic marrow tumor involvement at registration (>5% blasts) and were primary refractory, were chemo-refractory after first relapse, had relapsed after second-line therapy, or were ineligible for allogeneic hematopoietic stem cell transplant.
Most patients received fludarabine/cyclophosphamide lymphodepleting chemotherapy followed by a single dose of CTL019.
Three months post-infusion, 82% of patients (41/50) had achieved a complete response or complete response with incomplete blood count recovery.
Nearly half of the patients in the trial (48%) experienced grade 3/4 cytokine release syndrome (CRS), though there were no deaths due to CRS. Fifteen percent of patients experienced grade 3 neurological and psychiatric events, including confusion, delirium, encephalopathy, agitation, and seizure.
The BLA for CTL019 is also supported by results from the phase 2 ENSIGN trial, which were presented at ASH 2016, and results of a pilot study in patients with relapsed/refractory ALL, which were presented at ASH 2015. ![]()
The US Food and Drug Administration (FDA) has granted priority review for a biologics license application (BLA) for CTL019 (tisagenlecleucel-T), an investigational chimeric antigen receptor (CAR) T-cell therapy.
The BLA is for CTL019 as a treatment for pediatric patients and young adults with relapsed or refractory B-cell acute lymphoblastic leukemia (ALL).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA accepted the BLA for CTL019 yesterday, according to Novartis.
About CTL019
CTL019 consists of autologous T cells expressing a CD19-specific CAR. The therapy was first developed by the University of Pennsylvania.
In 2012, the university and Novartis entered into a global collaboration to further research, develop, and commercialize CAR-T cell therapies, including CTL019. Novartis holds the worldwide rights to CARs developed through the collaboration.
CTL019 already has breakthrough therapy designation for the treatment of adults and children with relapsed/refractory ALL.
Novartis said it is planning additional filings for CTL019 in the US and European Union later this year, including a BLA with the FDA for the treatment of adults with relapsed/refractory diffuse large B-cell lymphoma (DLBCL) and applications for marketing authorization with the European Medicines Agency in relapsed/refractory B-cell ALL and relapsed/refractory DLBCL.
Trials of CTL019 in ALL
The priority review designation for CTL019 is based on results from the Novartis-sponsored ELIANA study (NCT02435849). Results from this international, phase 2 trial were presented at ASH 2016.
The trial enrolled patients who had CD19-positive B-ALL with morphologic marrow tumor involvement at registration (>5% blasts) and were primary refractory, were chemo-refractory after first relapse, had relapsed after second-line therapy, or were ineligible for allogeneic hematopoietic stem cell transplant.
Most patients received fludarabine/cyclophosphamide lymphodepleting chemotherapy followed by a single dose of CTL019.
Three months post-infusion, 82% of patients (41/50) had achieved a complete response or complete response with incomplete blood count recovery.
Nearly half of the patients in the trial (48%) experienced grade 3/4 cytokine release syndrome (CRS), though there were no deaths due to CRS. Fifteen percent of patients experienced grade 3 neurological and psychiatric events, including confusion, delirium, encephalopathy, agitation, and seizure.
The BLA for CTL019 is also supported by results from the phase 2 ENSIGN trial, which were presented at ASH 2016, and results of a pilot study in patients with relapsed/refractory ALL, which were presented at ASH 2015. ![]()
Team identifies proteins that give malaria parasites ‘superpower’
Researchers say they have identified proteins that enable the malaria parasite Plasmodium falciparum to “walk through cell walls.”
The team believes the proteins—SPECT and PLP1—could be targeted to develop antimalarial drugs or vaccines.
Justin Boddey, PhD, of the Walter and Eliza Hall Institute of Medical Research in Parkville, Victoria, Australia, and his colleagues described this research in Cell Reports.
“The malaria infection cycle begins with a mosquito bite, when parasites are injected into the skin, and then rapidly move to the liver,” Dr Boddey explained. “We have shown that P falciparum employs a technique called cell traversal to quickly move through host cells in their path as they seek out liver cells to infect.”
“Our study identified that P falciparum parasites traverse human cells—effectively walking through cell walls—using 2 proteins called SPECT and PLP1 to achieve this superpower. This allows parasites to get from the skin to the liver very quickly following a mosquito bite.”
Dr Boddey said pinpointing these proteins was a good avenue for new therapies.
“Our long-term goal is to eradicate malaria, so we have to look at ways of breaking the cycle of infection,” he said. “A vaccine or treatment that halts the liver-stage infection offers the best chance of eradication because it stops parasites before they take hold.” ![]()
Researchers say they have identified proteins that enable the malaria parasite Plasmodium falciparum to “walk through cell walls.”
The team believes the proteins—SPECT and PLP1—could be targeted to develop antimalarial drugs or vaccines.
Justin Boddey, PhD, of the Walter and Eliza Hall Institute of Medical Research in Parkville, Victoria, Australia, and his colleagues described this research in Cell Reports.
“The malaria infection cycle begins with a mosquito bite, when parasites are injected into the skin, and then rapidly move to the liver,” Dr Boddey explained. “We have shown that P falciparum employs a technique called cell traversal to quickly move through host cells in their path as they seek out liver cells to infect.”
“Our study identified that P falciparum parasites traverse human cells—effectively walking through cell walls—using 2 proteins called SPECT and PLP1 to achieve this superpower. This allows parasites to get from the skin to the liver very quickly following a mosquito bite.”
Dr Boddey said pinpointing these proteins was a good avenue for new therapies.
“Our long-term goal is to eradicate malaria, so we have to look at ways of breaking the cycle of infection,” he said. “A vaccine or treatment that halts the liver-stage infection offers the best chance of eradication because it stops parasites before they take hold.” ![]()
Researchers say they have identified proteins that enable the malaria parasite Plasmodium falciparum to “walk through cell walls.”
The team believes the proteins—SPECT and PLP1—could be targeted to develop antimalarial drugs or vaccines.
Justin Boddey, PhD, of the Walter and Eliza Hall Institute of Medical Research in Parkville, Victoria, Australia, and his colleagues described this research in Cell Reports.
“The malaria infection cycle begins with a mosquito bite, when parasites are injected into the skin, and then rapidly move to the liver,” Dr Boddey explained. “We have shown that P falciparum employs a technique called cell traversal to quickly move through host cells in their path as they seek out liver cells to infect.”
“Our study identified that P falciparum parasites traverse human cells—effectively walking through cell walls—using 2 proteins called SPECT and PLP1 to achieve this superpower. This allows parasites to get from the skin to the liver very quickly following a mosquito bite.”
Dr Boddey said pinpointing these proteins was a good avenue for new therapies.
“Our long-term goal is to eradicate malaria, so we have to look at ways of breaking the cycle of infection,” he said. “A vaccine or treatment that halts the liver-stage infection offers the best chance of eradication because it stops parasites before they take hold.” ![]()
Intensely pruritic rash

The linear pattern of the vesicles and their distribution on the patient’s arms prompted the family physician (FP) to suspect that this was a case of allergic contact dermatitis (ACD) caused by exposure to a plant. While drug eruptions can cause all kinds of rashes—including vesicular eruptions—it would be rare for them to cause a perfect linear pattern. Upon further questioning, the FP learned that the patient had been gardening in her backyard a few days before the eruption started. This additional information supported a diagnosis of Rhus dermatitis from poison ivy. (Depending on the plants growing in the region, it could also have been poison oak.)
Toxicodendron (Rhus) dermatitis (poison ivy, poison oak, and poison sumac) is caused by urushiol, which is found in the sap of this plant family. Clinically, a line of vesicles can occur from brushing against one of the plants. The linear pattern can also occur from scratching and dragging the urushiol across pruritic skin with the fingernails. If ACD involves extensive skin areas (>20%), systemic steroid therapy is often required and offers relief within 12 to 24 hours. Severe poison ivy/oak is treated with oral prednisone for 2 to 3 weeks. Methylprednisolone should be avoided because the dose and duration are insufficient and can lead to a rebound contact dermatitis at the end of the short course.
In this case, the patient didn’t need an oral steroid. The patient was happy knowing the diagnosis and that the eruption would go away spontaneously. The FP suggested over-the-counter calamine lotion to sooth the itching and also asked the patient if she wanted a prescription for a topical steroid. The patient said that she would like one as a backup in case the over-the-counter lotion didn’t work, so the FP gave her a prescription for 0.1% triamcinolone cream to be applied once to twice daily.
While the evidence for topical steroids in Rhus dermatitis isn’t strong, the risk of adverse effects from topical steroids is much less than the risks associated with weeks of an oral steroid. During a future visit for her hypertension, the patient indicated that the poison ivy had gone away uneventfully.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Usatine R. Contact dermatitis. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:591-596.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com

The linear pattern of the vesicles and their distribution on the patient’s arms prompted the family physician (FP) to suspect that this was a case of allergic contact dermatitis (ACD) caused by exposure to a plant. While drug eruptions can cause all kinds of rashes—including vesicular eruptions—it would be rare for them to cause a perfect linear pattern. Upon further questioning, the FP learned that the patient had been gardening in her backyard a few days before the eruption started. This additional information supported a diagnosis of Rhus dermatitis from poison ivy. (Depending on the plants growing in the region, it could also have been poison oak.)
Toxicodendron (Rhus) dermatitis (poison ivy, poison oak, and poison sumac) is caused by urushiol, which is found in the sap of this plant family. Clinically, a line of vesicles can occur from brushing against one of the plants. The linear pattern can also occur from scratching and dragging the urushiol across pruritic skin with the fingernails. If ACD involves extensive skin areas (>20%), systemic steroid therapy is often required and offers relief within 12 to 24 hours. Severe poison ivy/oak is treated with oral prednisone for 2 to 3 weeks. Methylprednisolone should be avoided because the dose and duration are insufficient and can lead to a rebound contact dermatitis at the end of the short course.
In this case, the patient didn’t need an oral steroid. The patient was happy knowing the diagnosis and that the eruption would go away spontaneously. The FP suggested over-the-counter calamine lotion to sooth the itching and also asked the patient if she wanted a prescription for a topical steroid. The patient said that she would like one as a backup in case the over-the-counter lotion didn’t work, so the FP gave her a prescription for 0.1% triamcinolone cream to be applied once to twice daily.
While the evidence for topical steroids in Rhus dermatitis isn’t strong, the risk of adverse effects from topical steroids is much less than the risks associated with weeks of an oral steroid. During a future visit for her hypertension, the patient indicated that the poison ivy had gone away uneventfully.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Usatine R. Contact dermatitis. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:591-596.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com

The linear pattern of the vesicles and their distribution on the patient’s arms prompted the family physician (FP) to suspect that this was a case of allergic contact dermatitis (ACD) caused by exposure to a plant. While drug eruptions can cause all kinds of rashes—including vesicular eruptions—it would be rare for them to cause a perfect linear pattern. Upon further questioning, the FP learned that the patient had been gardening in her backyard a few days before the eruption started. This additional information supported a diagnosis of Rhus dermatitis from poison ivy. (Depending on the plants growing in the region, it could also have been poison oak.)
Toxicodendron (Rhus) dermatitis (poison ivy, poison oak, and poison sumac) is caused by urushiol, which is found in the sap of this plant family. Clinically, a line of vesicles can occur from brushing against one of the plants. The linear pattern can also occur from scratching and dragging the urushiol across pruritic skin with the fingernails. If ACD involves extensive skin areas (>20%), systemic steroid therapy is often required and offers relief within 12 to 24 hours. Severe poison ivy/oak is treated with oral prednisone for 2 to 3 weeks. Methylprednisolone should be avoided because the dose and duration are insufficient and can lead to a rebound contact dermatitis at the end of the short course.
In this case, the patient didn’t need an oral steroid. The patient was happy knowing the diagnosis and that the eruption would go away spontaneously. The FP suggested over-the-counter calamine lotion to sooth the itching and also asked the patient if she wanted a prescription for a topical steroid. The patient said that she would like one as a backup in case the over-the-counter lotion didn’t work, so the FP gave her a prescription for 0.1% triamcinolone cream to be applied once to twice daily.
While the evidence for topical steroids in Rhus dermatitis isn’t strong, the risk of adverse effects from topical steroids is much less than the risks associated with weeks of an oral steroid. During a future visit for her hypertension, the patient indicated that the poison ivy had gone away uneventfully.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Usatine R. Contact dermatitis. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:591-596.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com