User login
Shelving of AHCA a win for patients, experts say
SAN DIEGO – The decision by House Republicans to withdraw the American Health Care Act on March 24, 2017 was a victory for the health care of all Americans, especially older, sicker, and poorer patients, according to Nitin S. Damle, MD.
“It was a terrible bill,” Dr. Damle, president of the American College of Physicians, said during a press briefing at the annual meeting of the ACP. “Fortunately it will not become law at this point, but the story doesn’t really end here. The Trump Administration needs to decide whether it’s going to help faithfully implement the Affordable Care Act or sabotage it, either by action or inaction. It’s also important that we turn the page and begin the hard work of engaging with the administration and Congress on a bipartisan agenda to improve American health care.”
The ACHA would have eliminated the federal requirement that insurers cover 10 categories of essential benefits including emergency care, maternity services, and hospitalization, leaving it to states to decide. It also eliminated the requirement that Medicaid cover the same essential benefits. According to Dr. Damle, the AHCA’s age-based tax credits “were too low and the deductibles were going to be too high for older people and poorer patients, because insurers would have been allowed to charge older patients up to five times more than younger patients for their coverage.” For example, the CBO found that under the bill a 64-year-old male who makes $26,500 a year would have to pay $14,600 out of pocket for insurance in the non-group market, compared to $1,700 under the existing ACA, a 750% increase.
“In my practice, I have many older and sicker patients who would have been left behind had this become law, patients with diseases like congestive heart failure, diabetes, chronic obstructive pulmonary disease from smoking who require frequent and ongoing monitoring of their medications, development of any complications from their disease, and sometimes even need home-based support,” Dr. Damle said.
Robert B. Doherty, senior vice president of governmental affairs and public policy for the ACP, described efforts to roll back the ACA as “unchartered” territory. “I have never in the past seen an administration trying to roll back coverage on millions of people,” he said. “This history of the US has been incremental expansion of coverage since the creation of Medicare and Medicaid in 1965.” He acknowledged certain shortcomings of the ACA, including uneven participation by insurers from state to state, and “deductibles may be too high, and premiums too high for some people. On the other hand, the ACA has achieved an historic reduction in the uninsured rate in the United States. More than 20 million people have gained coverage, and according to the CDC, only 8.2% of Americans are without health insurance, an historic low. It’s still too high, but we’re basically 92% of the way to universal coverage in the U.S.”
Mr. Doherty expressed concern that legislative efforts to roll back the ACA could re-emerge. “The Republicans are still talking about bringing it back,” he said. “You can’t take it for granted because Republicans have been promising repeal and replace [legislation] for seven years now, and I think they want to move forward. I think we have to remain vigilant. We have to put pressure on the [Trump] administration to make sure they faithfully execute the law, which they swore to do when they took office. Then we have to reach out and say there are problems that need to be addressed, bipartisan solutions to stabilize the [health insurance] markets and to address other issues like the crushing administrative burden on physicians. You have to start by accepting that the ACA is the law of the land. We need to build upon it and improve it, not repeal it.”
SAN DIEGO – The decision by House Republicans to withdraw the American Health Care Act on March 24, 2017 was a victory for the health care of all Americans, especially older, sicker, and poorer patients, according to Nitin S. Damle, MD.
“It was a terrible bill,” Dr. Damle, president of the American College of Physicians, said during a press briefing at the annual meeting of the ACP. “Fortunately it will not become law at this point, but the story doesn’t really end here. The Trump Administration needs to decide whether it’s going to help faithfully implement the Affordable Care Act or sabotage it, either by action or inaction. It’s also important that we turn the page and begin the hard work of engaging with the administration and Congress on a bipartisan agenda to improve American health care.”
The ACHA would have eliminated the federal requirement that insurers cover 10 categories of essential benefits including emergency care, maternity services, and hospitalization, leaving it to states to decide. It also eliminated the requirement that Medicaid cover the same essential benefits. According to Dr. Damle, the AHCA’s age-based tax credits “were too low and the deductibles were going to be too high for older people and poorer patients, because insurers would have been allowed to charge older patients up to five times more than younger patients for their coverage.” For example, the CBO found that under the bill a 64-year-old male who makes $26,500 a year would have to pay $14,600 out of pocket for insurance in the non-group market, compared to $1,700 under the existing ACA, a 750% increase.
“In my practice, I have many older and sicker patients who would have been left behind had this become law, patients with diseases like congestive heart failure, diabetes, chronic obstructive pulmonary disease from smoking who require frequent and ongoing monitoring of their medications, development of any complications from their disease, and sometimes even need home-based support,” Dr. Damle said.
Robert B. Doherty, senior vice president of governmental affairs and public policy for the ACP, described efforts to roll back the ACA as “unchartered” territory. “I have never in the past seen an administration trying to roll back coverage on millions of people,” he said. “This history of the US has been incremental expansion of coverage since the creation of Medicare and Medicaid in 1965.” He acknowledged certain shortcomings of the ACA, including uneven participation by insurers from state to state, and “deductibles may be too high, and premiums too high for some people. On the other hand, the ACA has achieved an historic reduction in the uninsured rate in the United States. More than 20 million people have gained coverage, and according to the CDC, only 8.2% of Americans are without health insurance, an historic low. It’s still too high, but we’re basically 92% of the way to universal coverage in the U.S.”
Mr. Doherty expressed concern that legislative efforts to roll back the ACA could re-emerge. “The Republicans are still talking about bringing it back,” he said. “You can’t take it for granted because Republicans have been promising repeal and replace [legislation] for seven years now, and I think they want to move forward. I think we have to remain vigilant. We have to put pressure on the [Trump] administration to make sure they faithfully execute the law, which they swore to do when they took office. Then we have to reach out and say there are problems that need to be addressed, bipartisan solutions to stabilize the [health insurance] markets and to address other issues like the crushing administrative burden on physicians. You have to start by accepting that the ACA is the law of the land. We need to build upon it and improve it, not repeal it.”
SAN DIEGO – The decision by House Republicans to withdraw the American Health Care Act on March 24, 2017 was a victory for the health care of all Americans, especially older, sicker, and poorer patients, according to Nitin S. Damle, MD.
“It was a terrible bill,” Dr. Damle, president of the American College of Physicians, said during a press briefing at the annual meeting of the ACP. “Fortunately it will not become law at this point, but the story doesn’t really end here. The Trump Administration needs to decide whether it’s going to help faithfully implement the Affordable Care Act or sabotage it, either by action or inaction. It’s also important that we turn the page and begin the hard work of engaging with the administration and Congress on a bipartisan agenda to improve American health care.”
The ACHA would have eliminated the federal requirement that insurers cover 10 categories of essential benefits including emergency care, maternity services, and hospitalization, leaving it to states to decide. It also eliminated the requirement that Medicaid cover the same essential benefits. According to Dr. Damle, the AHCA’s age-based tax credits “were too low and the deductibles were going to be too high for older people and poorer patients, because insurers would have been allowed to charge older patients up to five times more than younger patients for their coverage.” For example, the CBO found that under the bill a 64-year-old male who makes $26,500 a year would have to pay $14,600 out of pocket for insurance in the non-group market, compared to $1,700 under the existing ACA, a 750% increase.
“In my practice, I have many older and sicker patients who would have been left behind had this become law, patients with diseases like congestive heart failure, diabetes, chronic obstructive pulmonary disease from smoking who require frequent and ongoing monitoring of their medications, development of any complications from their disease, and sometimes even need home-based support,” Dr. Damle said.
Robert B. Doherty, senior vice president of governmental affairs and public policy for the ACP, described efforts to roll back the ACA as “unchartered” territory. “I have never in the past seen an administration trying to roll back coverage on millions of people,” he said. “This history of the US has been incremental expansion of coverage since the creation of Medicare and Medicaid in 1965.” He acknowledged certain shortcomings of the ACA, including uneven participation by insurers from state to state, and “deductibles may be too high, and premiums too high for some people. On the other hand, the ACA has achieved an historic reduction in the uninsured rate in the United States. More than 20 million people have gained coverage, and according to the CDC, only 8.2% of Americans are without health insurance, an historic low. It’s still too high, but we’re basically 92% of the way to universal coverage in the U.S.”
Mr. Doherty expressed concern that legislative efforts to roll back the ACA could re-emerge. “The Republicans are still talking about bringing it back,” he said. “You can’t take it for granted because Republicans have been promising repeal and replace [legislation] for seven years now, and I think they want to move forward. I think we have to remain vigilant. We have to put pressure on the [Trump] administration to make sure they faithfully execute the law, which they swore to do when they took office. Then we have to reach out and say there are problems that need to be addressed, bipartisan solutions to stabilize the [health insurance] markets and to address other issues like the crushing administrative burden on physicians. You have to start by accepting that the ACA is the law of the land. We need to build upon it and improve it, not repeal it.”
AT ACP INTERNAL MEDICINE
Clinical Challenges - April 2017 What's Your Diagnosis?
What's Your Diagnosis?
Answer to “What’s your diagnosis?” on page X: Pseudoachalasia in paraneoplastic syndrome, with radiographic documentation of onset and evolution
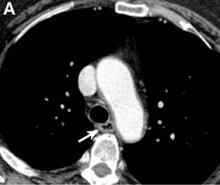
A barium esophagogram revealed an esophagus with characteristic features of achalasia: dilatation, retention of air and fluid, and a “bird’s beak” configuration distally (Figure E). Botulinum injection into the distal esophagus provided the patient with partial relief of her swallowing symptoms.
Evidence supporting the diagnosis of pseudoachalasia associated with paraneoplastic syndrome in this patient is 1) the development of characteristic features of achalasia in association with SCLC, the cancer that is most often associated with paraneoplastic achalasia;1 2) a serum antibody characteristic of SCLC-associated paraneoplastic syndrome; 3) peripheral neuropathy attributed to paraneoplastic syndrome; and 4) absence of an obstructive neoplasm at the gastroesophageal junction.
Pseudoachalasia associated with malignancy may occur by one of three mechanisms1-3: 1) Primary or secondary carcinoma located at or near the gastroesophageal junction, 2) neural invasion of the esophagus, or 3) as a component of the paraneoplastic syndrome. Pseudoachalasia associated with a paraneoplastic syndrome is rare (an estimated 1 in 750,000), although it may be becoming more common.1 The relatively rapid onset of dysphagia is a reported feature of pseudoachalasia, in contrast with the more gradual onset in primary achalasia. Our report documents radiographically the progression within a few months from a normal-diameter esophagus to a very dilated, poorly functioning esophagus. We know of no similar report. Botulinum toxin injection has been reported effective in a few cases.1
References
1. Katzka, D.A., Farrugia, G., Arora, A.S., et al. Achalasia secondary to neoplasia: a disease with a changing differential diagnosis. Dis Esophagus. 2012;25:331-6.
2. Liu, W., Fackler, W., Rice, T.W., et al. The pathogenesis of pseudoachalasia (A clinicopathological study of 13 cases of a rare entity). Am J Surg Pathol. 2002;26:784-8.
3. Gockel, J., Eckardt, V.F., Scmitt, T., et al. Pseudoachalasia: a case series and analysis of the literature. Scand J Gastroenterol. 2005;40:378-85.
Answer to “What’s your diagnosis?” on page X: Pseudoachalasia in paraneoplastic syndrome, with radiographic documentation of onset and evolution
A barium esophagogram revealed an esophagus with characteristic features of achalasia: dilatation, retention of air and fluid, and a “bird’s beak” configuration distally (Figure E). Botulinum injection into the distal esophagus provided the patient with partial relief of her swallowing symptoms.
Evidence supporting the diagnosis of pseudoachalasia associated with paraneoplastic syndrome in this patient is 1) the development of characteristic features of achalasia in association with SCLC, the cancer that is most often associated with paraneoplastic achalasia;1 2) a serum antibody characteristic of SCLC-associated paraneoplastic syndrome; 3) peripheral neuropathy attributed to paraneoplastic syndrome; and 4) absence of an obstructive neoplasm at the gastroesophageal junction.
Pseudoachalasia associated with malignancy may occur by one of three mechanisms1-3: 1) Primary or secondary carcinoma located at or near the gastroesophageal junction, 2) neural invasion of the esophagus, or 3) as a component of the paraneoplastic syndrome. Pseudoachalasia associated with a paraneoplastic syndrome is rare (an estimated 1 in 750,000), although it may be becoming more common.1 The relatively rapid onset of dysphagia is a reported feature of pseudoachalasia, in contrast with the more gradual onset in primary achalasia. Our report documents radiographically the progression within a few months from a normal-diameter esophagus to a very dilated, poorly functioning esophagus. We know of no similar report. Botulinum toxin injection has been reported effective in a few cases.1
References
1. Katzka, D.A., Farrugia, G., Arora, A.S., et al. Achalasia secondary to neoplasia: a disease with a changing differential diagnosis. Dis Esophagus. 2012;25:331-6.
2. Liu, W., Fackler, W., Rice, T.W., et al. The pathogenesis of pseudoachalasia (A clinicopathological study of 13 cases of a rare entity). Am J Surg Pathol. 2002;26:784-8.
3. Gockel, J., Eckardt, V.F., Scmitt, T., et al. Pseudoachalasia: a case series and analysis of the literature. Scand J Gastroenterol. 2005;40:378-85.
Answer to “What’s your diagnosis?” on page X: Pseudoachalasia in paraneoplastic syndrome, with radiographic documentation of onset and evolution
A barium esophagogram revealed an esophagus with characteristic features of achalasia: dilatation, retention of air and fluid, and a “bird’s beak” configuration distally (Figure E). Botulinum injection into the distal esophagus provided the patient with partial relief of her swallowing symptoms.
Evidence supporting the diagnosis of pseudoachalasia associated with paraneoplastic syndrome in this patient is 1) the development of characteristic features of achalasia in association with SCLC, the cancer that is most often associated with paraneoplastic achalasia;1 2) a serum antibody characteristic of SCLC-associated paraneoplastic syndrome; 3) peripheral neuropathy attributed to paraneoplastic syndrome; and 4) absence of an obstructive neoplasm at the gastroesophageal junction.
Pseudoachalasia associated with malignancy may occur by one of three mechanisms1-3: 1) Primary or secondary carcinoma located at or near the gastroesophageal junction, 2) neural invasion of the esophagus, or 3) as a component of the paraneoplastic syndrome. Pseudoachalasia associated with a paraneoplastic syndrome is rare (an estimated 1 in 750,000), although it may be becoming more common.1 The relatively rapid onset of dysphagia is a reported feature of pseudoachalasia, in contrast with the more gradual onset in primary achalasia. Our report documents radiographically the progression within a few months from a normal-diameter esophagus to a very dilated, poorly functioning esophagus. We know of no similar report. Botulinum toxin injection has been reported effective in a few cases.1
References
1. Katzka, D.A., Farrugia, G., Arora, A.S., et al. Achalasia secondary to neoplasia: a disease with a changing differential diagnosis. Dis Esophagus. 2012;25:331-6.
2. Liu, W., Fackler, W., Rice, T.W., et al. The pathogenesis of pseudoachalasia (A clinicopathological study of 13 cases of a rare entity). Am J Surg Pathol. 2002;26:784-8.
3. Gockel, J., Eckardt, V.F., Scmitt, T., et al. Pseudoachalasia: a case series and analysis of the literature. Scand J Gastroenterol. 2005;40:378-85.
What's Your Diagnosis?
What's Your Diagnosis?
By William R. Brown, MD, and Elizabeth K. Dee, MD.
Published previously in Gastroenterology (2013;144:34, 252).
A 67-year-old woman with neuroendocrine small-cell lung cancer (SCLC), recurrent after chemotherapy and radiation therapy, complained of recent-onset dysphagia. She noticed regurgitation of liquids and some solid-food dysphagia. She had lost 20 pounds in the past 2 months. She had no past history of gastroesophageal reflux symptoms or esophagitis. Physical examination reveals no significant abnormalities, but she had had a peripheral sensory neuropathy that improved with treatment of her SCLC. Laboratory tests are unremarkable except for a positive Hu immunoglobulin (Ig)G serum anti-neuronal nuclear antibody test – an antibody that is associated with SCLC.
April 2017 Quiz 2
Q2. Answer: C
Rationale: MALT lymphomas are associated with H. pylori infection in 80%-90% of cases. H. pylori triggers a B-cell clonal expansion leading to lymphoma. Detection of chronic H. pylori using histology is directly dependent on the number of mucosal biopsies. Negative H. pylori testing should prompt an alternative test for H. pylori (either breath or stool antigen test). Treatment of H. pylori is successful in achieving complete remission in up to 80% of cases. Surveillance after treatment of MALT lymphoma is indicated, though the exact protocol has not been established.
References
1. ASGE Standards of Practice Committee. The role of endoscopy in management of premalignant and malignant conditions of the stomach. Gastrointest Endosc. 2015 82(1):1-8.
2. Gisbert J.P., Calvet X. Review article: common misconceptions in the management of Helicobacter pylori-associated gastric MALT-lymphoma. Aliment Pharmacol Ther. 2011 Nov;34(9):1047-62.
Q2. Answer: C
Rationale: MALT lymphomas are associated with H. pylori infection in 80%-90% of cases. H. pylori triggers a B-cell clonal expansion leading to lymphoma. Detection of chronic H. pylori using histology is directly dependent on the number of mucosal biopsies. Negative H. pylori testing should prompt an alternative test for H. pylori (either breath or stool antigen test). Treatment of H. pylori is successful in achieving complete remission in up to 80% of cases. Surveillance after treatment of MALT lymphoma is indicated, though the exact protocol has not been established.
References
1. ASGE Standards of Practice Committee. The role of endoscopy in management of premalignant and malignant conditions of the stomach. Gastrointest Endosc. 2015 82(1):1-8.
2. Gisbert J.P., Calvet X. Review article: common misconceptions in the management of Helicobacter pylori-associated gastric MALT-lymphoma. Aliment Pharmacol Ther. 2011 Nov;34(9):1047-62.
Q2. Answer: C
Rationale: MALT lymphomas are associated with H. pylori infection in 80%-90% of cases. H. pylori triggers a B-cell clonal expansion leading to lymphoma. Detection of chronic H. pylori using histology is directly dependent on the number of mucosal biopsies. Negative H. pylori testing should prompt an alternative test for H. pylori (either breath or stool antigen test). Treatment of H. pylori is successful in achieving complete remission in up to 80% of cases. Surveillance after treatment of MALT lymphoma is indicated, though the exact protocol has not been established.
References
1. ASGE Standards of Practice Committee. The role of endoscopy in management of premalignant and malignant conditions of the stomach. Gastrointest Endosc. 2015 82(1):1-8.
2. Gisbert J.P., Calvet X. Review article: common misconceptions in the management of Helicobacter pylori-associated gastric MALT-lymphoma. Aliment Pharmacol Ther. 2011 Nov;34(9):1047-62.
Q2. A 56-year-old woman presents with epigastric pain and is found to have a 3-cm submucosal mass with thickened rugal folds in the gastric body. Biopsies of the mass show mucosa-associated lymphoid tissue (MALT lymphoma). There is no evidence of Helicobacter pylori infection in the biopsies.
April 2017 Quiz 1
Q1. Answer: A
While heartburn responds well to acid suppression with a proton pump inhibitor, regurgitation does not necessarily improve. It is well known that reflux persists despite acid suppression; in some patients, this manifests as troublesome postprandial regurgitation. Transient LES relaxations (TLESRs) are the prime mechanism for persisting reflex, in patients both with and without hiatal hernias.
Baclofen, a gamma amino butyric acid B (GABA-B) agonist, inhibits TLESRs and has potential to improve persisting regurgitation. Metoclopramide has been demonstrated to have no adjunctive value in treating reflux disease. Hyoscyamine and sucralfate are similarly not of particular benefit in this setting. Cholesytramine is a bile salt binding resin that has value in the management of postcholecystectomy diarrhea.
References
1. Kahrilas P.J., Jonsson A., Denison H., et al. Regurgitation is less responsive to acid suppression than heartburn in patients with gastroesophageal reflux disease. Clin Gastroenterol Hepatol. 2012;10(6):612-9.
2. Vela M.F., Camacho-Lobato L., Srinivasan R., et al. Simultaneous intraesophageal impedance and pH measurement of acid and nonacid gastroesophageal reflux: effect of omeprazole. Gastroenterology. 2001 Jun;120(7):1599-606.
3. Vela M.F., Tutuian R, Katz PO, et al. Baclofen decreases acid and non-acid post-prandial gastro-oesophageal reflux measured by combined multichannel intraluminal impedance and pH. Aliment Pharmacol Ther. 2003 Jan;17(2):243-51.
Q1. Answer: A
While heartburn responds well to acid suppression with a proton pump inhibitor, regurgitation does not necessarily improve. It is well known that reflux persists despite acid suppression; in some patients, this manifests as troublesome postprandial regurgitation. Transient LES relaxations (TLESRs) are the prime mechanism for persisting reflex, in patients both with and without hiatal hernias.
Baclofen, a gamma amino butyric acid B (GABA-B) agonist, inhibits TLESRs and has potential to improve persisting regurgitation. Metoclopramide has been demonstrated to have no adjunctive value in treating reflux disease. Hyoscyamine and sucralfate are similarly not of particular benefit in this setting. Cholesytramine is a bile salt binding resin that has value in the management of postcholecystectomy diarrhea.
References
1. Kahrilas P.J., Jonsson A., Denison H., et al. Regurgitation is less responsive to acid suppression than heartburn in patients with gastroesophageal reflux disease. Clin Gastroenterol Hepatol. 2012;10(6):612-9.
2. Vela M.F., Camacho-Lobato L., Srinivasan R., et al. Simultaneous intraesophageal impedance and pH measurement of acid and nonacid gastroesophageal reflux: effect of omeprazole. Gastroenterology. 2001 Jun;120(7):1599-606.
3. Vela M.F., Tutuian R, Katz PO, et al. Baclofen decreases acid and non-acid post-prandial gastro-oesophageal reflux measured by combined multichannel intraluminal impedance and pH. Aliment Pharmacol Ther. 2003 Jan;17(2):243-51.
Q1. Answer: A
While heartburn responds well to acid suppression with a proton pump inhibitor, regurgitation does not necessarily improve. It is well known that reflux persists despite acid suppression; in some patients, this manifests as troublesome postprandial regurgitation. Transient LES relaxations (TLESRs) are the prime mechanism for persisting reflex, in patients both with and without hiatal hernias.
Baclofen, a gamma amino butyric acid B (GABA-B) agonist, inhibits TLESRs and has potential to improve persisting regurgitation. Metoclopramide has been demonstrated to have no adjunctive value in treating reflux disease. Hyoscyamine and sucralfate are similarly not of particular benefit in this setting. Cholesytramine is a bile salt binding resin that has value in the management of postcholecystectomy diarrhea.
References
1. Kahrilas P.J., Jonsson A., Denison H., et al. Regurgitation is less responsive to acid suppression than heartburn in patients with gastroesophageal reflux disease. Clin Gastroenterol Hepatol. 2012;10(6):612-9.
2. Vela M.F., Camacho-Lobato L., Srinivasan R., et al. Simultaneous intraesophageal impedance and pH measurement of acid and nonacid gastroesophageal reflux: effect of omeprazole. Gastroenterology. 2001 Jun;120(7):1599-606.
3. Vela M.F., Tutuian R, Katz PO, et al. Baclofen decreases acid and non-acid post-prandial gastro-oesophageal reflux measured by combined multichannel intraluminal impedance and pH. Aliment Pharmacol Ther. 2003 Jan;17(2):243-51.
Q1. A 25-year-old woman presents with postprandial regurgitation, typically after dinner. She initially had both heartburn and regurgitation. After she started esomeprazole 40 mg once a day 8 weeks ago, her heartburn completely resolved. An upper endoscopy, performed due to ongoing regurgitation symptoms, reveals a normal esophagus, and a 2-cm sliding hiatal hernia.
Don’t shy away from vaginal salpingectomy
SAN ANTONIO – Surgeons at Houston Methodist Hospital reported a 75% success rate in removing both fallopian tubes during vaginal hysterectomy in a study presented at the annual scientific meeting of the Society of Gynecologic Surgeons.
Serous ovarian carcinoma is now thought to arise from the distal fallopian tube, and it’s estimated that salpingectomy prevents diagnosis of ovarian cancer in 1 in 225 women and death from ovarian cancer in 1 in 450 women. The American Congress of Obstetricians and Gynecologists recommends that surgeons and patients “discuss the potential benefits of the removal of the fallopian tubes” during hysterectomy in women not having an oophorectomy.
The findings from the Houston team show that “it’s feasible in most cases, with very little risk,” said Danielle Antosh, MD, lead investigator and director of the Center for Restorative Pelvic Medicine at Houston Methodist Urogynecology Associates.
“People are doing laparoscopic hysterectomies or robotic hysterectomies” to get at the fallopian tubes, “but they shouldn’t be deterred from trying to remove the fallopian tubes vaginally,” Dr. Antosh said at the SGS 2017 meeting. When women are having a vaginal hysterectomy, “why not try to remove the fallopian tubes? It’s something I would definitely consider counseling your patients about.”
Dr. Antosh said that residents should be taught how to perform salpingectomy during vaginal hysterectomy. “I think it is definitely feasible for residents to do.” Technically, “it’s a lot easier than removing the ovaries” vaginally, she said.
The 70 women in the study were undergoing vaginal hysterectomies by attending physicians for benign reasons, mostly uterine prolapse, followed by heavy menstrual flow and fibroids. In total, 52 (75%) had successful concomitant bilateral vaginal salpingectomies, and 7 additional women had one tube removed. Success was more likely with increasing parity and a history of prolapse. Most of the failures were because the tubes were too high in the pelvis or there were adhesions from prior adnexal surgery. Even with prior adnexal surgery, however, the success rate was 50%.
Vaginal salpingectomy added a mean of 11 minutes to surgery and a mean of 5 mL blood loss. There were no complications reported from including salpingectomy with vaginal hysterectomy. The study wasn’t powered to detect an impact on menopause symptoms, but there was a decrease in menopause symptoms at 16 week follow-up in the salpingectomy group, perhaps related to less sexual dysfunction and urinary incontinence.
The mean age in the study was 51 years, and mean body mass index was 27 kg/m2. There were no malignancies found on tubal pathology.
Five women were transferred to an abdominal approach because of a large uterus or discovery of ovarian pathology. None were transferred for the purpose of salpingectomy.
There was no external funding for the study, and the investigators reported no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – Surgeons at Houston Methodist Hospital reported a 75% success rate in removing both fallopian tubes during vaginal hysterectomy in a study presented at the annual scientific meeting of the Society of Gynecologic Surgeons.
Serous ovarian carcinoma is now thought to arise from the distal fallopian tube, and it’s estimated that salpingectomy prevents diagnosis of ovarian cancer in 1 in 225 women and death from ovarian cancer in 1 in 450 women. The American Congress of Obstetricians and Gynecologists recommends that surgeons and patients “discuss the potential benefits of the removal of the fallopian tubes” during hysterectomy in women not having an oophorectomy.
The findings from the Houston team show that “it’s feasible in most cases, with very little risk,” said Danielle Antosh, MD, lead investigator and director of the Center for Restorative Pelvic Medicine at Houston Methodist Urogynecology Associates.
“People are doing laparoscopic hysterectomies or robotic hysterectomies” to get at the fallopian tubes, “but they shouldn’t be deterred from trying to remove the fallopian tubes vaginally,” Dr. Antosh said at the SGS 2017 meeting. When women are having a vaginal hysterectomy, “why not try to remove the fallopian tubes? It’s something I would definitely consider counseling your patients about.”
Dr. Antosh said that residents should be taught how to perform salpingectomy during vaginal hysterectomy. “I think it is definitely feasible for residents to do.” Technically, “it’s a lot easier than removing the ovaries” vaginally, she said.
The 70 women in the study were undergoing vaginal hysterectomies by attending physicians for benign reasons, mostly uterine prolapse, followed by heavy menstrual flow and fibroids. In total, 52 (75%) had successful concomitant bilateral vaginal salpingectomies, and 7 additional women had one tube removed. Success was more likely with increasing parity and a history of prolapse. Most of the failures were because the tubes were too high in the pelvis or there were adhesions from prior adnexal surgery. Even with prior adnexal surgery, however, the success rate was 50%.
Vaginal salpingectomy added a mean of 11 minutes to surgery and a mean of 5 mL blood loss. There were no complications reported from including salpingectomy with vaginal hysterectomy. The study wasn’t powered to detect an impact on menopause symptoms, but there was a decrease in menopause symptoms at 16 week follow-up in the salpingectomy group, perhaps related to less sexual dysfunction and urinary incontinence.
The mean age in the study was 51 years, and mean body mass index was 27 kg/m2. There were no malignancies found on tubal pathology.
Five women were transferred to an abdominal approach because of a large uterus or discovery of ovarian pathology. None were transferred for the purpose of salpingectomy.
There was no external funding for the study, and the investigators reported no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – Surgeons at Houston Methodist Hospital reported a 75% success rate in removing both fallopian tubes during vaginal hysterectomy in a study presented at the annual scientific meeting of the Society of Gynecologic Surgeons.
Serous ovarian carcinoma is now thought to arise from the distal fallopian tube, and it’s estimated that salpingectomy prevents diagnosis of ovarian cancer in 1 in 225 women and death from ovarian cancer in 1 in 450 women. The American Congress of Obstetricians and Gynecologists recommends that surgeons and patients “discuss the potential benefits of the removal of the fallopian tubes” during hysterectomy in women not having an oophorectomy.
The findings from the Houston team show that “it’s feasible in most cases, with very little risk,” said Danielle Antosh, MD, lead investigator and director of the Center for Restorative Pelvic Medicine at Houston Methodist Urogynecology Associates.
“People are doing laparoscopic hysterectomies or robotic hysterectomies” to get at the fallopian tubes, “but they shouldn’t be deterred from trying to remove the fallopian tubes vaginally,” Dr. Antosh said at the SGS 2017 meeting. When women are having a vaginal hysterectomy, “why not try to remove the fallopian tubes? It’s something I would definitely consider counseling your patients about.”
Dr. Antosh said that residents should be taught how to perform salpingectomy during vaginal hysterectomy. “I think it is definitely feasible for residents to do.” Technically, “it’s a lot easier than removing the ovaries” vaginally, she said.
The 70 women in the study were undergoing vaginal hysterectomies by attending physicians for benign reasons, mostly uterine prolapse, followed by heavy menstrual flow and fibroids. In total, 52 (75%) had successful concomitant bilateral vaginal salpingectomies, and 7 additional women had one tube removed. Success was more likely with increasing parity and a history of prolapse. Most of the failures were because the tubes were too high in the pelvis or there were adhesions from prior adnexal surgery. Even with prior adnexal surgery, however, the success rate was 50%.
Vaginal salpingectomy added a mean of 11 minutes to surgery and a mean of 5 mL blood loss. There were no complications reported from including salpingectomy with vaginal hysterectomy. The study wasn’t powered to detect an impact on menopause symptoms, but there was a decrease in menopause symptoms at 16 week follow-up in the salpingectomy group, perhaps related to less sexual dysfunction and urinary incontinence.
The mean age in the study was 51 years, and mean body mass index was 27 kg/m2. There were no malignancies found on tubal pathology.
Five women were transferred to an abdominal approach because of a large uterus or discovery of ovarian pathology. None were transferred for the purpose of salpingectomy.
There was no external funding for the study, and the investigators reported no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
AT SGS 2017
Key clinical point:
Major finding: Three-quarters of women undergoing vaginal hysterectomy for benign reasons had successful concomitant bilateral vaginal salpingectomy.
Data source: A single-center, observational study among 70 women undergoing vaginal hysterectomy for benign reasons.
Disclosures: There was no external funding and the investigators reported no relevant financial disclosures.
FDA: Recall of select EpiPen products
Meridian Medical Technologies has issued a voluntary recall for 13 lots of EpiPen products, according to a press release from the U.S. Food and Drug Administration.
The voluntary recall includes EpiPen and EpiPen Jr. Auto-Injector distributed between Dec. 17, 2015, and July 1, 2016 by Mylan Specialty. Products included in the recall may contain a defective part which would prevent the device from activating.
Consumers who need their EpiPens should keep them until a they obtain a replacement, the FDA recommended.
Find the full press release on the FDA website.
Meridian Medical Technologies has issued a voluntary recall for 13 lots of EpiPen products, according to a press release from the U.S. Food and Drug Administration.
The voluntary recall includes EpiPen and EpiPen Jr. Auto-Injector distributed between Dec. 17, 2015, and July 1, 2016 by Mylan Specialty. Products included in the recall may contain a defective part which would prevent the device from activating.
Consumers who need their EpiPens should keep them until a they obtain a replacement, the FDA recommended.
Find the full press release on the FDA website.
Meridian Medical Technologies has issued a voluntary recall for 13 lots of EpiPen products, according to a press release from the U.S. Food and Drug Administration.
The voluntary recall includes EpiPen and EpiPen Jr. Auto-Injector distributed between Dec. 17, 2015, and July 1, 2016 by Mylan Specialty. Products included in the recall may contain a defective part which would prevent the device from activating.
Consumers who need their EpiPens should keep them until a they obtain a replacement, the FDA recommended.
Find the full press release on the FDA website.
Make assessment of immunization status of older adults routine
ATLANTA – In the opinion of John M. Kelso, MD, assessment of immunization status in older adults should be a routine part of all visits.
“Don’t assume that your patients are getting their vaccines someplace else,” he said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. “We should be taking advantage of the fact that these patients are in our offices.”
Inactivated influenza vaccine (IIV3)
For adults aged 65 and older, the high-dose, trivalent version of the flu vaccine (60 micrograms of hemagglutinin per strain, or IIV3-HD) may be preferable to the standard dose of 15 micrograms of hemagglutinin per strain (IIV3-SD). A study of nearly 32,000 patients found that IIV3-HD induced significantly higher antibody responses and provided better protection against laboratory-confirmed influenza, compared with IIV3-SD (N Engl J Med. 2014;371:635-45). The relative efficacy of high dose vs. standard dose was 24.2%. “That means that one-quarter of all breakthrough influenza illnesses could be prevented if IIV3HD were used instead of IIV3-SD,” Dr. Kelso said.
Another approach is to use an adjuvanted influenza vaccine, which contains the standard 15 micrograms of influenza antigen but the adjuvant is MF59, a squalene-based oil-in-water emulsion. One small study of 282 patients aged 65 and older showed the adjuvanted vaccine to be more effective than the unadjuvanted vaccine (Vaccine. 2013;51:1622-8).
The Centers for Disease Control and Prevention does not express a preference for the high-dose or adjuvanted vaccine, but rather stresses the importance of influenza vaccination with whatever age-appropriate IIV formulation is available at the time of the patient’s visit.
The 13-valent pneumococcal conjugate vaccine (PCV13) and the 23-valent pneumococcal polysaccharide vaccine (PPSV23)
All adults who turn 65 years of age should receive the PCV13, followed 1 year later by the PPSV23. For those who already received the PPSV23 after age 65 years of age, they should receive the PCV13 at least 1 year later. “The real bulk of hospitalizations and fatalities from invasive pneumococcal disease are happening to people over 65 year of age,” said Dr. Kelso, who is also a clinical professor of pediatrics and internal medicine at the University of California, San Diego “So there’s a real need here for vaccination.”
Tdap
This should be administered to all adolescents and adults regardless of interval since their last tetanus-diphtheria vaccine. “This includes those age 65 years of age and older in whom the vaccine has been found to be equally safe and immunogenic,” Dr. Kelso said. “This is important not only to prevent pertussis in older adults, but also to prevent them from spreading the disease to infants where it can be fatal.”
Zoster vaccine
One in three adults will develop zoster during their lifetime, he said, and one million episodes occur in the United States each year. Common complications include postherpetic neuralgia and eye involvement that can result in loss of vision. The CDC recommends routine vaccination of all immunocompetent persons over age 60 with one dose of zoster vaccine. “Persons who report a previous episode of zoster can be vaccinated but it is not indicated to treat acute zoster, to prevent persons with acute zoster from developing postherpetic neuralgia, or to treat ongoing postherpetic neuralgia,” Dr. Kelso said.
He reported having no relevant financial disclosures.
ATLANTA – In the opinion of John M. Kelso, MD, assessment of immunization status in older adults should be a routine part of all visits.
“Don’t assume that your patients are getting their vaccines someplace else,” he said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. “We should be taking advantage of the fact that these patients are in our offices.”
Inactivated influenza vaccine (IIV3)
For adults aged 65 and older, the high-dose, trivalent version of the flu vaccine (60 micrograms of hemagglutinin per strain, or IIV3-HD) may be preferable to the standard dose of 15 micrograms of hemagglutinin per strain (IIV3-SD). A study of nearly 32,000 patients found that IIV3-HD induced significantly higher antibody responses and provided better protection against laboratory-confirmed influenza, compared with IIV3-SD (N Engl J Med. 2014;371:635-45). The relative efficacy of high dose vs. standard dose was 24.2%. “That means that one-quarter of all breakthrough influenza illnesses could be prevented if IIV3HD were used instead of IIV3-SD,” Dr. Kelso said.
Another approach is to use an adjuvanted influenza vaccine, which contains the standard 15 micrograms of influenza antigen but the adjuvant is MF59, a squalene-based oil-in-water emulsion. One small study of 282 patients aged 65 and older showed the adjuvanted vaccine to be more effective than the unadjuvanted vaccine (Vaccine. 2013;51:1622-8).
The Centers for Disease Control and Prevention does not express a preference for the high-dose or adjuvanted vaccine, but rather stresses the importance of influenza vaccination with whatever age-appropriate IIV formulation is available at the time of the patient’s visit.
The 13-valent pneumococcal conjugate vaccine (PCV13) and the 23-valent pneumococcal polysaccharide vaccine (PPSV23)
All adults who turn 65 years of age should receive the PCV13, followed 1 year later by the PPSV23. For those who already received the PPSV23 after age 65 years of age, they should receive the PCV13 at least 1 year later. “The real bulk of hospitalizations and fatalities from invasive pneumococcal disease are happening to people over 65 year of age,” said Dr. Kelso, who is also a clinical professor of pediatrics and internal medicine at the University of California, San Diego “So there’s a real need here for vaccination.”
Tdap
This should be administered to all adolescents and adults regardless of interval since their last tetanus-diphtheria vaccine. “This includes those age 65 years of age and older in whom the vaccine has been found to be equally safe and immunogenic,” Dr. Kelso said. “This is important not only to prevent pertussis in older adults, but also to prevent them from spreading the disease to infants where it can be fatal.”
Zoster vaccine
One in three adults will develop zoster during their lifetime, he said, and one million episodes occur in the United States each year. Common complications include postherpetic neuralgia and eye involvement that can result in loss of vision. The CDC recommends routine vaccination of all immunocompetent persons over age 60 with one dose of zoster vaccine. “Persons who report a previous episode of zoster can be vaccinated but it is not indicated to treat acute zoster, to prevent persons with acute zoster from developing postherpetic neuralgia, or to treat ongoing postherpetic neuralgia,” Dr. Kelso said.
He reported having no relevant financial disclosures.
ATLANTA – In the opinion of John M. Kelso, MD, assessment of immunization status in older adults should be a routine part of all visits.
“Don’t assume that your patients are getting their vaccines someplace else,” he said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. “We should be taking advantage of the fact that these patients are in our offices.”
Inactivated influenza vaccine (IIV3)
For adults aged 65 and older, the high-dose, trivalent version of the flu vaccine (60 micrograms of hemagglutinin per strain, or IIV3-HD) may be preferable to the standard dose of 15 micrograms of hemagglutinin per strain (IIV3-SD). A study of nearly 32,000 patients found that IIV3-HD induced significantly higher antibody responses and provided better protection against laboratory-confirmed influenza, compared with IIV3-SD (N Engl J Med. 2014;371:635-45). The relative efficacy of high dose vs. standard dose was 24.2%. “That means that one-quarter of all breakthrough influenza illnesses could be prevented if IIV3HD were used instead of IIV3-SD,” Dr. Kelso said.
Another approach is to use an adjuvanted influenza vaccine, which contains the standard 15 micrograms of influenza antigen but the adjuvant is MF59, a squalene-based oil-in-water emulsion. One small study of 282 patients aged 65 and older showed the adjuvanted vaccine to be more effective than the unadjuvanted vaccine (Vaccine. 2013;51:1622-8).
The Centers for Disease Control and Prevention does not express a preference for the high-dose or adjuvanted vaccine, but rather stresses the importance of influenza vaccination with whatever age-appropriate IIV formulation is available at the time of the patient’s visit.
The 13-valent pneumococcal conjugate vaccine (PCV13) and the 23-valent pneumococcal polysaccharide vaccine (PPSV23)
All adults who turn 65 years of age should receive the PCV13, followed 1 year later by the PPSV23. For those who already received the PPSV23 after age 65 years of age, they should receive the PCV13 at least 1 year later. “The real bulk of hospitalizations and fatalities from invasive pneumococcal disease are happening to people over 65 year of age,” said Dr. Kelso, who is also a clinical professor of pediatrics and internal medicine at the University of California, San Diego “So there’s a real need here for vaccination.”
Tdap
This should be administered to all adolescents and adults regardless of interval since their last tetanus-diphtheria vaccine. “This includes those age 65 years of age and older in whom the vaccine has been found to be equally safe and immunogenic,” Dr. Kelso said. “This is important not only to prevent pertussis in older adults, but also to prevent them from spreading the disease to infants where it can be fatal.”
Zoster vaccine
One in three adults will develop zoster during their lifetime, he said, and one million episodes occur in the United States each year. Common complications include postherpetic neuralgia and eye involvement that can result in loss of vision. The CDC recommends routine vaccination of all immunocompetent persons over age 60 with one dose of zoster vaccine. “Persons who report a previous episode of zoster can be vaccinated but it is not indicated to treat acute zoster, to prevent persons with acute zoster from developing postherpetic neuralgia, or to treat ongoing postherpetic neuralgia,” Dr. Kelso said.
He reported having no relevant financial disclosures.
EXPERT ANALYSIS AT THE 2017 AAAAI ANNUAL MEETING
Post-exposure doxycycline halves STIs among MSM
SEATTLE – When men who have sex with men were given doxycycline and told to take it after unprotected sex, the incidence of sexually transmitted infections dropped 47% over about 9 months in France.
“We were quite surprised to see” such a strong effect, especially since it was achieved with “a very low use of doxycycline, less than two pills per week” among the 232 men in the study, said lead investigator Jean-Michel Molina, MD, of St. Louis Hospital, Paris.
Sexually transmitted infections (STIs) are especially high among men who have sex with men (MSM), and several of the physicians in Dr. Molina’s audience were glad to hear of an intervention that puts a dent in a difficult problem. Even so, he stressed repeatedly that prophylactic antibiotics for STIs aren’t ready for general practice; the concern is inducing resistance by a too-liberal use. He and his team are analyzing samples they collected for emerging resistance.
“We need to be careful,” Dr. Molina said “these are results from a limited number of people” with short follow-up. “We need more research,” he added.
However, with such low antibiotic pressure, less than two pills a week, resistance might be unlikely. Syphilis and chlamydia might also be less likely to build resistance than gonorrhea, he noted.
All the subjects were in a post-exposure HIV prophylaxis trial. Given the risk of STIs in that setting, it “was a great opportunity to” study the intervention, Dr. Molina said.
His team randomized 116 men to take two 100 mg pills of doxycycline within 72 hours of condomless sexual intercourse, without exceeding six pills per week. They were given enough pills to cover their exposures from unprotected sex, so they didn’t have to make frequent visits to the study clinic. The other 116 men were randomized to observation.
Men in both groups came in every 8 weeks for HIV and syphilis serology tests, and PCR tests of urine and anal and oral swabs for chlamydia and gonorrhea. The median follow-up was 8.7 months.
Twenty-eight patients in the doxycycline group caught a new STI (24%, 37.7 events per 100 patient years) versus 45 in the observation arm (38.8%, 69.7 events per 100 patient years). Doxycycline prophylaxis almost halved the risk (HR 0.53, 95% CI 0.33-0.85, P = .008). More than two-thirds of the infections in both groups were asymptomatic.
The doxycycline group took a median of seven pills/month; eight patients (7%) stopped using the drug due to gastrointestinal side effects.
There was no significant change in sexual behavior in the study arms. Both groups reported a median of about 5-10 sexual partners at each 2 month follow-up visit, and most reported anal sex without a condom. The men were an average of about 40 years old.
Dr. Molina is a consultant for Merck and Viiv, and a speaker and researcher for Gilead, which was one of several funders of the work.
[email protected]
On Twitter @IDPractitioner
SEATTLE – When men who have sex with men were given doxycycline and told to take it after unprotected sex, the incidence of sexually transmitted infections dropped 47% over about 9 months in France.
“We were quite surprised to see” such a strong effect, especially since it was achieved with “a very low use of doxycycline, less than two pills per week” among the 232 men in the study, said lead investigator Jean-Michel Molina, MD, of St. Louis Hospital, Paris.
Sexually transmitted infections (STIs) are especially high among men who have sex with men (MSM), and several of the physicians in Dr. Molina’s audience were glad to hear of an intervention that puts a dent in a difficult problem. Even so, he stressed repeatedly that prophylactic antibiotics for STIs aren’t ready for general practice; the concern is inducing resistance by a too-liberal use. He and his team are analyzing samples they collected for emerging resistance.
“We need to be careful,” Dr. Molina said “these are results from a limited number of people” with short follow-up. “We need more research,” he added.
However, with such low antibiotic pressure, less than two pills a week, resistance might be unlikely. Syphilis and chlamydia might also be less likely to build resistance than gonorrhea, he noted.
All the subjects were in a post-exposure HIV prophylaxis trial. Given the risk of STIs in that setting, it “was a great opportunity to” study the intervention, Dr. Molina said.
His team randomized 116 men to take two 100 mg pills of doxycycline within 72 hours of condomless sexual intercourse, without exceeding six pills per week. They were given enough pills to cover their exposures from unprotected sex, so they didn’t have to make frequent visits to the study clinic. The other 116 men were randomized to observation.
Men in both groups came in every 8 weeks for HIV and syphilis serology tests, and PCR tests of urine and anal and oral swabs for chlamydia and gonorrhea. The median follow-up was 8.7 months.
Twenty-eight patients in the doxycycline group caught a new STI (24%, 37.7 events per 100 patient years) versus 45 in the observation arm (38.8%, 69.7 events per 100 patient years). Doxycycline prophylaxis almost halved the risk (HR 0.53, 95% CI 0.33-0.85, P = .008). More than two-thirds of the infections in both groups were asymptomatic.
The doxycycline group took a median of seven pills/month; eight patients (7%) stopped using the drug due to gastrointestinal side effects.
There was no significant change in sexual behavior in the study arms. Both groups reported a median of about 5-10 sexual partners at each 2 month follow-up visit, and most reported anal sex without a condom. The men were an average of about 40 years old.
Dr. Molina is a consultant for Merck and Viiv, and a speaker and researcher for Gilead, which was one of several funders of the work.
[email protected]
On Twitter @IDPractitioner
SEATTLE – When men who have sex with men were given doxycycline and told to take it after unprotected sex, the incidence of sexually transmitted infections dropped 47% over about 9 months in France.
“We were quite surprised to see” such a strong effect, especially since it was achieved with “a very low use of doxycycline, less than two pills per week” among the 232 men in the study, said lead investigator Jean-Michel Molina, MD, of St. Louis Hospital, Paris.
Sexually transmitted infections (STIs) are especially high among men who have sex with men (MSM), and several of the physicians in Dr. Molina’s audience were glad to hear of an intervention that puts a dent in a difficult problem. Even so, he stressed repeatedly that prophylactic antibiotics for STIs aren’t ready for general practice; the concern is inducing resistance by a too-liberal use. He and his team are analyzing samples they collected for emerging resistance.
“We need to be careful,” Dr. Molina said “these are results from a limited number of people” with short follow-up. “We need more research,” he added.
However, with such low antibiotic pressure, less than two pills a week, resistance might be unlikely. Syphilis and chlamydia might also be less likely to build resistance than gonorrhea, he noted.
All the subjects were in a post-exposure HIV prophylaxis trial. Given the risk of STIs in that setting, it “was a great opportunity to” study the intervention, Dr. Molina said.
His team randomized 116 men to take two 100 mg pills of doxycycline within 72 hours of condomless sexual intercourse, without exceeding six pills per week. They were given enough pills to cover their exposures from unprotected sex, so they didn’t have to make frequent visits to the study clinic. The other 116 men were randomized to observation.
Men in both groups came in every 8 weeks for HIV and syphilis serology tests, and PCR tests of urine and anal and oral swabs for chlamydia and gonorrhea. The median follow-up was 8.7 months.
Twenty-eight patients in the doxycycline group caught a new STI (24%, 37.7 events per 100 patient years) versus 45 in the observation arm (38.8%, 69.7 events per 100 patient years). Doxycycline prophylaxis almost halved the risk (HR 0.53, 95% CI 0.33-0.85, P = .008). More than two-thirds of the infections in both groups were asymptomatic.
The doxycycline group took a median of seven pills/month; eight patients (7%) stopped using the drug due to gastrointestinal side effects.
There was no significant change in sexual behavior in the study arms. Both groups reported a median of about 5-10 sexual partners at each 2 month follow-up visit, and most reported anal sex without a condom. The men were an average of about 40 years old.
Dr. Molina is a consultant for Merck and Viiv, and a speaker and researcher for Gilead, which was one of several funders of the work.
[email protected]
On Twitter @IDPractitioner
AT CROI 2017
Key clinical point:
Major finding: Twenty-eight patients in the doxycycline group caught a new STI (24%, 37.7 events per 100 patient years) versus 45 in the observation arm (38.8%, 69.7 events per 100 patient years).
Data source: Randomized, open-label trial of 232 MSM.
Disclosures: The lead investigator is a consultant for Merck and Viiv, and a speaker and researcher for Gilead, which was one of several funders of the work.
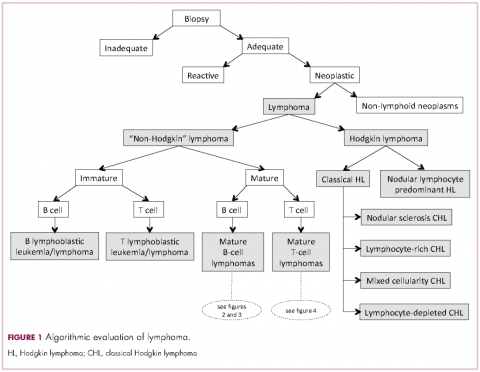
Demystifying the diagnosis and classification of lymphoma: a guide to the hematopathologist’s galaxy
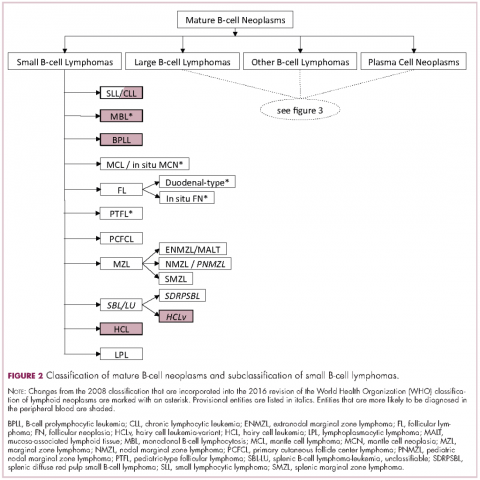
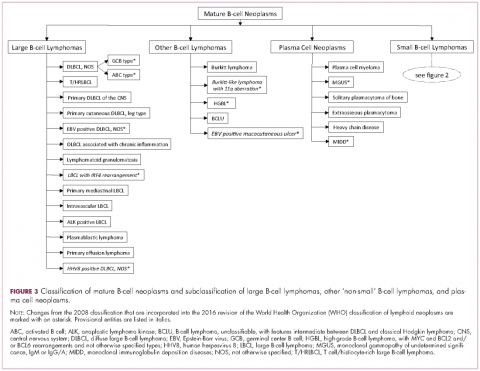
Lymphomas constitute a very heterogeneous group of neoplasms with diverse clinical presentations, prognoses, and responses to therapy. Approximately 80,500 new cases of lymphoma are expected to be diagnosed in the United States in 2017, of which about one quarter will lead to the death of the patient.1 Perhaps more so than any other group of neoplasms, the diagnosis of lymphoma involves the integration of a multiplicity of clinical, histologic and immunophenotypic findings and, on occasion, cytogenetic and molecular results as well. An accurate diagnosis of lymphoma, usually rendered by hematopathologists, allows hematologists/oncologists to treat patients appropriately. Herein we will describe a simplified approach to the diagnosis and classification of lymphomas (Figure 1).
Lymphoma classification
Lymphomas are clonal neoplasms characterized by the expansion of abnormal lymphoid cells that may develop in any organ but commonly involve lymph nodes. The fourth edition of the World Health Organization (WHO) Classification of Tumours of Haematopoietic and Lymphoid tissues, published in 2008, is the official and most current guideline used for diagnosis of lymphoid neoplasms.2 The WHO scheme classifies lymphomas according to the type of cell from which they are derived (mature and immature B cells, T cells, or natural killer (NK) cells, findings determined by their morphology and immunophenotype) and their clinical, cytogenetic, and/or molecular features. This official classification is currently being updated3 and is expected to be published in full in 2017, at which time it is anticipated to include definitions for more than 70 distinct neoplasms.
Lymphomas are broadly and informally classified as Hodgkin lymphomas (HLs) and non-Hodgkin lymphomas (NHLs), based on the differences these two groups show in their clinical presentation, treatment, prognosis, and proportion of neoplastic cells, among others. NHLs are by far the most common type of lymphomas, accounting for approximately 90% of all new cases of lymphoma in the United States and 70% worldwide.1,2 NHLs are a very heterogeneous group of B-, T-, or NK-cell neoplasms that, in turn, can also be informally subclassified as low-grade (or indolent) or high-grade (or aggressive) according to their predicted clinical behavior. HLs are comparatively rare, less heterogeneous, uniformly of B-cell origin and, in the case of classical Hodgkin lymphoma, highly curable.1,2 It is beyond the scope of this manuscript to outline the features of each of the >70 specific entities, but the reader is referred elsewhere for more detail and encouraged to become familiarized with the complexity, challenges, and beauty of lymphoma diagnosis.2,3
Biopsy procedure
A correct diagnosis begins with an adequate biopsy procedure. It is essential that biopsy specimens for lymphoma evaluation be submitted fresh and unfixed, because some crucial analyses such as flow cytometry or conventional cytogenetics can only be performed on fresh tissue. Indeed, it is important for the hematologist/oncologist and/or surgeon and/or interventional radiologist to converse with the hematopathologist prior to and even during some procedures to ensure the correct processing of the specimen. Also, it is important to limit the compression of the specimen and the excessive use of cauterization during the biopsy procedure, both of which cause artifacts that may render impossible the interpretation of the histopathologic findings.
Given that the diagnosis of lymphoma is based not only on the cytologic details of the lymphoma cells but also on the architectural pattern with which they infiltrate an organ, the larger the biopsy specimen, the easier it will be for a hematopathologist to identify the pattern. In addition, excisional biopsies frequently contain more diagnostic tissue than needle core biopsies and this provides pathologists with the option to submit tissue fragments for ancillary tests that require unfixed tissue as noted above. Needle core biopsies of lymph nodes are increasingly being used because of their association with fewer complications and lower cost than excisional biopsies. However, needle core biopsies provide only a glimpse of the pattern of infiltration and may not be completely representative of the architecture. Therefore, excisional lymph node biopsies of lymph nodes are preferred over needle core biopsies, recognizing that in the setting of deeply seated lymph nodes, needle core biopsies may be the only or the best surgical option.
Clinical presentation
Accurate diagnosis of lymphoma cannot take place in a vacuum. The hematopathologist’s initial approach to the diagnosis of lymphoid processes in tissue biopsies should begin with a thorough review of the clinical history, although some pathology laboratories may not have immediate access to this information. The hematopathologist should evaluate factors such as age, gender, location of the tumor, symptomatology, medications, serology, and prior history of malignancy, immunosuppression or immunodeficiency in every case. Other important but frequently omitted parts of the clinical history are the patient’s occupation, history of exposure to animals, and the presence of tattoos, which may be associated with certain reactive lymphadenopathies.
Histomorphologic evaluation
Despite the plethora of new and increasingly sophisticated tools, histologic and morphologic analysis still remains the cornerstone of diagnosis in hematopathology. However, for the characterization of an increasing number of reactive and neoplastic lymphoid processes, hematopathologists may also require immunophenotypic, molecular, and cytogenetic tests for an accurate diagnosis. Upon review of the clinical information, a microscopic evaluation of the tissue submitted for processing by the histology laboratory will be performed. The results of concurrent flow cytometric evaluation (performed on fresh unfixed material) should also be available in most if not all cases before the H&E-stained slides are available for review. Upon receipt of H&E-stained slides, the hematopathologist will evaluate the quality of the submitted specimen, since many diagnostic difficulties stem from suboptimal techniques related to the biopsy procedure, fixation, processing, cutting, or staining (Figure 1). If deemed suitable for accurate diagnosis, a search for signs of preservation or disruption of the organ that was biopsied will follow. The identification of certain morphologic patterns aids the hematopathologist in answering the first question: “what organ is this and is this consistent with what is indicated on the requisition?” This is usually immediately followed by “is this sufficient and adequate material for a diagnosis?” and “is there any normal architecture?” If the architecture is not normal, “is this alteration due to a reactive or a neoplastic process?” If neoplastic, “is it lymphoma or a non-hematolymphoid neoplasm?”
Both reactive and neoplastic processes have variably unique morphologic features that if properly recognized, guide the subsequent testing. However, some reactive and neoplastic processes can present with overlapping features, and even after extensive immunophenotypic evaluation and the performance of ancillary studies, it may not be possible to conclusively determine its nature. If the lymph node architecture is altered or effaced, the predominant pattern of infiltration (eg, nodular, diffuse, interfollicular, intrasinusoidal) and the degree of alteration of the normal architecture is evaluated, usually at low magnification. When the presence of an infiltrate is recognized, its components must be characterized. If the infiltrate is composed of a homogeneous expansion of lymphoid cells that disrupts or replaces the normal lymphoid architecture, a lymphoma will be suspected or diagnosed. The pattern of distribution of the cells along with their individual morphologic characteristics (ie, size, nuclear shape, chromatin configuration, nucleoli, amount and hue of cytoplasm) are key factors for the diagnosis and classification of the lymphoma that will guide subsequent testing. The immunophenotypic analysis (by immunohistochemistry, flow cytometry or a combination of both) may confirm the reactive or neoplastic nature of the process, and its subclassification. B-cell lymphomas, in particular have variable and distinctive histologic features: as a diffuse infiltrate of large mature lymphoid cells (eg, diffuse large B-cell lymphoma), an expansion of immature lymphoid cells (lymphoblastic lymphoma), and a nodular infiltrate of small, intermediate and/or mature large B cells (eg, follicular lymphoma).
Mature T-cell lymphomas may display similar histologic, features but they can be quite heterogeneous with an infiltrate composed of one predominant cell type or a mixture of small, medium-sized, and large atypical lymphoid cells (on occasion with abundant clear cytoplasm) and a variable number of eosinophils, plasma cells, macrophages (including granulomas), and B cells. HLs most commonly efface the lymph node architecture with a nodular or diffuse infiltrate variably composed of reactive lymphocytes, granulocytes, macrophages, and plasma cells and usually a minority of large neoplastic cells (Hodgkin/Reed-Sternberg cells and/or lymphocyte predominant cells).
Once the H&E-stained slides are evaluated and a diagnosis of lymphoma is suspected or established, the hematopathologist will attempt to determine whether it has mature or immature features, and whether low- or high-grade morphologic characteristics are present. The maturity of lymphoid cells is generally determined by the nature of the chromatin, which if “fine” and homogeneous (with or without a conspicuous nucleolus) will usually, but not always, be considered immature, whereas clumped, vesicular or hyperchromatic chromatin is generally, but not always, associated with maturity. If the chromatin displays immature features, the differential diagnosis will mainly include B- and T-lymphoblastic lymphomas, but also blastoid variants of mature neoplasm such as mantle cell lymphoma, and follicular lymphoma, as well as high-grade B-cell lymphomas. Features associated with low-grade lymphomas (eg, follicular lymphoma, small lymphocytic lymphoma/chronic lymphocytic leukemia, marginal zone lymphoma, lymphoplasmacytic lymphoma) include small cell morphology, mature chromatin, absence of a significant number of mitoses or apoptotic cells, and a low proliferation index as shown by immunohistochemistry for Ki67. High-grade lymphomas, such as lymphoblastic lymphoma, Burkitt lymphoma, or certain large B-cell lymphomas tend to show opposite features, and some of the mature entities are frequently associated with MYC rearrangements. Of note, immature lymphomas tend to be clinically high grade, but not all clinically high-grade lymphomas are immature. Conversely, the majority of low-grade lymphomas are usually mature.
Immunophenotypic evaluation
Immunophenotypic evaluation is essential because the lineage of lymphoma cells cannot be determined by morphology alone. The immunophenotype is the combination of proteins/markers (eg, CD20, CD3, TdT) expressed by cells. Usually, it is evaluated by immunohistochemistry and/or flow cytometry, which help determine the proportion of lymphoid cells that express a certain marker and its location and intensity within the cells. While immunohistochemistry is normally performed on formalin-fixed and paraffin-embedded tissue, flow cytometry can be evaluated only on fresh unfixed tissue. Flow cytometry has the advantage over immunohistochemistry of being faster and better at simultaneously identifying coexpression of multiple markers on multiple cell populations. However, certain markers can only be evaluated by immunohistochemistry.
The immunophenotypic analysis will in most cases reveal whether the lymphomas is of B-, T- or NK-cell origin, and whether a lymphoma subtype associated immunophenotype is present. Typical pan B-cell antigens include PAX5, CD19, and CD79a (CD20 is less broadly expressed throughout B-cell differentiation, although it is usually evident in most mature B-cell lymphomas), and typical pan T-cell antigens include CD2, CD5, and CD7. The immature or mature nature of a lymphoma can also be confirmed by evaluation of the immunophenotype. Immature lymphomas commonly express one or more of TdT, CD10, or CD34; T-lymphoblastic lymphoma cells may also coexpress CD1a. The majority of NHLs and all HLs are derived from (or reflect) B cells at different stages of maturation. Mature B-cell lymphomas are the most common type of lymphoma and typically, but not always, express pan B-cell markers as well as surface membrane immunoglobulin, with the latter also most useful in assessing clonality via a determination of light chain restriction. Some mature B-cell lymphomas tend to acquire markers that are either never physiologically expressed by normal mature B cells (eg, cyclin D1 in mantle cell lymphoma, or BCL2 in germinal center B cells in follicular lymphoma) or only expressed in a minor fraction (eg, CD5 that is characteristically expressed in small lymphocytic and mantle cell lymphoma). The most common mature B-cell lymphomas include diffuse large B-cell lymphoma, follicular lymphoma, small lymphocytic lymphoma, mantle cell lymphoma, marginal zone lymphoma, Burkitt lymphoma, and lymphoplasmacytic lymphoma (Figures 2 and 3). Classical HLs are also lymphomas of B-cell origin that demonstrate diminished preservation of their B-cell immunophenotype (as evidenced by the dim expression of PAX5 but absence of most other pan B-cell antigens), expression of CD30, variable expression of CD15, and loss of CD45 (Figure 1). In contrast, nodular lymphocyte predominant HL shows a preserved B-cell immunophenotypic program and expression of CD45, typically without CD30 and CD15. Of note, the evaluation of the immunophenotype of the neoplastic cells in HL is routinely assessed by immunohistochemistry because most flow cytometry laboratories cannot reliably detect and characterize the low numbers of these cells.
Mature T-cell lymphomas generally express one or more T-cell markers, and tend to display a T-helper (CD4-positive) or cytotoxic (CD8-positive) immunophenotype and may show loss of markers expressed by most normal T-cells (eg, CD5, CD7; Figure 4). However, a subset of them may express markers not commonly detected in normal T cells, such as ALK. NK-cell lymphomas lack surface CD3 (expressing only cytoplasmic CD3) and CD5 but express some pan T-cell antigens (such as CD2 and CD7) as well as CD16 and/or CD56.
Patients with primary or acquired immune dysfunction are at risk for development of lymphoma and other less clearly defined lymphoproliferative disorders, the majority of which are associated with infection of the lymphoid cells with Epstein-Barr virus (EBV). Therefore, evaluation with chromogenic in situ hybridization for an EBV-encoded early RNA (EBER1) is routinely performed in these cases; it is thus essential that the hematopathologist be informed of the altered immune system of the patient. If lymphoma develops, they may be morphologically similar to those that appear in immunocompetent patients, which specifically in the post-transplant setting are known as monomorphic post-transplant lymphoproliferative disorders (PTLD). If the PTLD does not meet the criteria for any of the recognized types of lymphoma, it may be best characterized as a polymorphic PTLD.
Once the lineage (B-, T-, or NK-cell) of the mature lymphoma has been established, the sum (and on occasion the gestalt) of the clinical, morphologic, immunophenotypic and other findings will be considered for the subclassification of the neoplasm.
Cytogenetic and molecular evaluation
If the morphologic and immunophenotypic analysis is inconclusive or nondiagnostic, then molecular and/or cytogenetic testing may further aid in the characterization of the process. Some of available molecular tests include analyses for the rearrangements of the variable region of the immunoglobulin (IG) or T-cell receptor (TCR) genes and for mutations on specific genes. The identification of specific mutations not only confirms the clonal nature of the process but, on occasion, it may also help subclassify the lymphoma, whereas IG or TCR rearrangement studies are used to establish whether a lymphoid expansion is polyclonal or monoclonal. The molecular findings should not be evaluated in isolation, because not all monoclonal rearrangements are diagnostic of lymphoma, and not all lymphomas will show a monoclonal rearrangement. Other methodologies that can aid in the identification of a clonal process or specific genetic abnormalities include metaphase cytogenetics (karyotyping) and fluorescence in situ hybridization (FISH). If any cytogenetic abnormalities are found in sufficient numbers (and constitutional abnormalities are excluded), their identification indicates the presence of a clonal process. Also, some cytogenetic abnormalities are characteristic of certain lymphomas. However, they may be neither 100% diagnostically sensitive nor diagnostically specific, for example, the hallmark t(14;18)/IGH-BCL2 is not present in all follicular lymphomas and not all lymphomas with this translocation are follicular lymphomas. Whereas FISH is generally performed on a minimum of 200 cells, compared with typically 20 metaphase by “conventional” karyotyping, and is therefore considered to have higher analytical sensitivity, it evaluates only for the presence or absence of the abnormality being investigated with a given set of probes, and therefore other abnormalities, if present, will not be identified. The value of FISH cytogenetic studies is perhaps best illustrated in the need to diagnose double hit lymphomas, amongst other scenarios. The detection of certain mutations can aid in the diagnosis of certain lymphomas, such as MYD88 in lymphoplasmacytic lymphoma, prognosis of others, such as in follicular lymphoma and identify pathways that may be precisely therapeutically targeted.
Final remarks
The diagnosis of lymphoma can be complex and usually requires the hematopathologist to integrate multiple parameters. The classification of lymphomas is not static, and new entities or variants are continuously described, and the facets of well-known ones refined. While such changes are often to the chagrin of hematologists/oncologists and hematopathologists alike, we should embrace the incorporation of nascent and typically cool data into our practice, as more therapeutically relevant entities are molded.
1. Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2017. CA Cancer J Clin. 2017 ;67(1):7-30.
2. Swerdlow SH, Campo E, Harris NL, et al, eds. WHO classification of tumours of haematopoietic and lymphoid tissues. In: Bosman FT, Jaffe ES, Lakhani SR, Ohgaki H, eds. World Health Organization Classification of Tumours. Lyon, France: IARC; 2008.
3. Swerdlow SH, Campo E, Pileri SA, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016 ;127(20):2375-2390.
Lymphomas constitute a very heterogeneous group of neoplasms with diverse clinical presentations, prognoses, and responses to therapy. Approximately 80,500 new cases of lymphoma are expected to be diagnosed in the United States in 2017, of which about one quarter will lead to the death of the patient.1 Perhaps more so than any other group of neoplasms, the diagnosis of lymphoma involves the integration of a multiplicity of clinical, histologic and immunophenotypic findings and, on occasion, cytogenetic and molecular results as well. An accurate diagnosis of lymphoma, usually rendered by hematopathologists, allows hematologists/oncologists to treat patients appropriately. Herein we will describe a simplified approach to the diagnosis and classification of lymphomas (Figure 1).
Lymphoma classification
Lymphomas are clonal neoplasms characterized by the expansion of abnormal lymphoid cells that may develop in any organ but commonly involve lymph nodes. The fourth edition of the World Health Organization (WHO) Classification of Tumours of Haematopoietic and Lymphoid tissues, published in 2008, is the official and most current guideline used for diagnosis of lymphoid neoplasms.2 The WHO scheme classifies lymphomas according to the type of cell from which they are derived (mature and immature B cells, T cells, or natural killer (NK) cells, findings determined by their morphology and immunophenotype) and their clinical, cytogenetic, and/or molecular features. This official classification is currently being updated3 and is expected to be published in full in 2017, at which time it is anticipated to include definitions for more than 70 distinct neoplasms.
Lymphomas are broadly and informally classified as Hodgkin lymphomas (HLs) and non-Hodgkin lymphomas (NHLs), based on the differences these two groups show in their clinical presentation, treatment, prognosis, and proportion of neoplastic cells, among others. NHLs are by far the most common type of lymphomas, accounting for approximately 90% of all new cases of lymphoma in the United States and 70% worldwide.1,2 NHLs are a very heterogeneous group of B-, T-, or NK-cell neoplasms that, in turn, can also be informally subclassified as low-grade (or indolent) or high-grade (or aggressive) according to their predicted clinical behavior. HLs are comparatively rare, less heterogeneous, uniformly of B-cell origin and, in the case of classical Hodgkin lymphoma, highly curable.1,2 It is beyond the scope of this manuscript to outline the features of each of the >70 specific entities, but the reader is referred elsewhere for more detail and encouraged to become familiarized with the complexity, challenges, and beauty of lymphoma diagnosis.2,3
Biopsy procedure
A correct diagnosis begins with an adequate biopsy procedure. It is essential that biopsy specimens for lymphoma evaluation be submitted fresh and unfixed, because some crucial analyses such as flow cytometry or conventional cytogenetics can only be performed on fresh tissue. Indeed, it is important for the hematologist/oncologist and/or surgeon and/or interventional radiologist to converse with the hematopathologist prior to and even during some procedures to ensure the correct processing of the specimen. Also, it is important to limit the compression of the specimen and the excessive use of cauterization during the biopsy procedure, both of which cause artifacts that may render impossible the interpretation of the histopathologic findings.
Given that the diagnosis of lymphoma is based not only on the cytologic details of the lymphoma cells but also on the architectural pattern with which they infiltrate an organ, the larger the biopsy specimen, the easier it will be for a hematopathologist to identify the pattern. In addition, excisional biopsies frequently contain more diagnostic tissue than needle core biopsies and this provides pathologists with the option to submit tissue fragments for ancillary tests that require unfixed tissue as noted above. Needle core biopsies of lymph nodes are increasingly being used because of their association with fewer complications and lower cost than excisional biopsies. However, needle core biopsies provide only a glimpse of the pattern of infiltration and may not be completely representative of the architecture. Therefore, excisional lymph node biopsies of lymph nodes are preferred over needle core biopsies, recognizing that in the setting of deeply seated lymph nodes, needle core biopsies may be the only or the best surgical option.
Clinical presentation
Accurate diagnosis of lymphoma cannot take place in a vacuum. The hematopathologist’s initial approach to the diagnosis of lymphoid processes in tissue biopsies should begin with a thorough review of the clinical history, although some pathology laboratories may not have immediate access to this information. The hematopathologist should evaluate factors such as age, gender, location of the tumor, symptomatology, medications, serology, and prior history of malignancy, immunosuppression or immunodeficiency in every case. Other important but frequently omitted parts of the clinical history are the patient’s occupation, history of exposure to animals, and the presence of tattoos, which may be associated with certain reactive lymphadenopathies.
Histomorphologic evaluation
Despite the plethora of new and increasingly sophisticated tools, histologic and morphologic analysis still remains the cornerstone of diagnosis in hematopathology. However, for the characterization of an increasing number of reactive and neoplastic lymphoid processes, hematopathologists may also require immunophenotypic, molecular, and cytogenetic tests for an accurate diagnosis. Upon review of the clinical information, a microscopic evaluation of the tissue submitted for processing by the histology laboratory will be performed. The results of concurrent flow cytometric evaluation (performed on fresh unfixed material) should also be available in most if not all cases before the H&E-stained slides are available for review. Upon receipt of H&E-stained slides, the hematopathologist will evaluate the quality of the submitted specimen, since many diagnostic difficulties stem from suboptimal techniques related to the biopsy procedure, fixation, processing, cutting, or staining (Figure 1). If deemed suitable for accurate diagnosis, a search for signs of preservation or disruption of the organ that was biopsied will follow. The identification of certain morphologic patterns aids the hematopathologist in answering the first question: “what organ is this and is this consistent with what is indicated on the requisition?” This is usually immediately followed by “is this sufficient and adequate material for a diagnosis?” and “is there any normal architecture?” If the architecture is not normal, “is this alteration due to a reactive or a neoplastic process?” If neoplastic, “is it lymphoma or a non-hematolymphoid neoplasm?”
Both reactive and neoplastic processes have variably unique morphologic features that if properly recognized, guide the subsequent testing. However, some reactive and neoplastic processes can present with overlapping features, and even after extensive immunophenotypic evaluation and the performance of ancillary studies, it may not be possible to conclusively determine its nature. If the lymph node architecture is altered or effaced, the predominant pattern of infiltration (eg, nodular, diffuse, interfollicular, intrasinusoidal) and the degree of alteration of the normal architecture is evaluated, usually at low magnification. When the presence of an infiltrate is recognized, its components must be characterized. If the infiltrate is composed of a homogeneous expansion of lymphoid cells that disrupts or replaces the normal lymphoid architecture, a lymphoma will be suspected or diagnosed. The pattern of distribution of the cells along with their individual morphologic characteristics (ie, size, nuclear shape, chromatin configuration, nucleoli, amount and hue of cytoplasm) are key factors for the diagnosis and classification of the lymphoma that will guide subsequent testing. The immunophenotypic analysis (by immunohistochemistry, flow cytometry or a combination of both) may confirm the reactive or neoplastic nature of the process, and its subclassification. B-cell lymphomas, in particular have variable and distinctive histologic features: as a diffuse infiltrate of large mature lymphoid cells (eg, diffuse large B-cell lymphoma), an expansion of immature lymphoid cells (lymphoblastic lymphoma), and a nodular infiltrate of small, intermediate and/or mature large B cells (eg, follicular lymphoma).
Mature T-cell lymphomas may display similar histologic, features but they can be quite heterogeneous with an infiltrate composed of one predominant cell type or a mixture of small, medium-sized, and large atypical lymphoid cells (on occasion with abundant clear cytoplasm) and a variable number of eosinophils, plasma cells, macrophages (including granulomas), and B cells. HLs most commonly efface the lymph node architecture with a nodular or diffuse infiltrate variably composed of reactive lymphocytes, granulocytes, macrophages, and plasma cells and usually a minority of large neoplastic cells (Hodgkin/Reed-Sternberg cells and/or lymphocyte predominant cells).
Once the H&E-stained slides are evaluated and a diagnosis of lymphoma is suspected or established, the hematopathologist will attempt to determine whether it has mature or immature features, and whether low- or high-grade morphologic characteristics are present. The maturity of lymphoid cells is generally determined by the nature of the chromatin, which if “fine” and homogeneous (with or without a conspicuous nucleolus) will usually, but not always, be considered immature, whereas clumped, vesicular or hyperchromatic chromatin is generally, but not always, associated with maturity. If the chromatin displays immature features, the differential diagnosis will mainly include B- and T-lymphoblastic lymphomas, but also blastoid variants of mature neoplasm such as mantle cell lymphoma, and follicular lymphoma, as well as high-grade B-cell lymphomas. Features associated with low-grade lymphomas (eg, follicular lymphoma, small lymphocytic lymphoma/chronic lymphocytic leukemia, marginal zone lymphoma, lymphoplasmacytic lymphoma) include small cell morphology, mature chromatin, absence of a significant number of mitoses or apoptotic cells, and a low proliferation index as shown by immunohistochemistry for Ki67. High-grade lymphomas, such as lymphoblastic lymphoma, Burkitt lymphoma, or certain large B-cell lymphomas tend to show opposite features, and some of the mature entities are frequently associated with MYC rearrangements. Of note, immature lymphomas tend to be clinically high grade, but not all clinically high-grade lymphomas are immature. Conversely, the majority of low-grade lymphomas are usually mature.
Immunophenotypic evaluation
Immunophenotypic evaluation is essential because the lineage of lymphoma cells cannot be determined by morphology alone. The immunophenotype is the combination of proteins/markers (eg, CD20, CD3, TdT) expressed by cells. Usually, it is evaluated by immunohistochemistry and/or flow cytometry, which help determine the proportion of lymphoid cells that express a certain marker and its location and intensity within the cells. While immunohistochemistry is normally performed on formalin-fixed and paraffin-embedded tissue, flow cytometry can be evaluated only on fresh unfixed tissue. Flow cytometry has the advantage over immunohistochemistry of being faster and better at simultaneously identifying coexpression of multiple markers on multiple cell populations. However, certain markers can only be evaluated by immunohistochemistry.
The immunophenotypic analysis will in most cases reveal whether the lymphomas is of B-, T- or NK-cell origin, and whether a lymphoma subtype associated immunophenotype is present. Typical pan B-cell antigens include PAX5, CD19, and CD79a (CD20 is less broadly expressed throughout B-cell differentiation, although it is usually evident in most mature B-cell lymphomas), and typical pan T-cell antigens include CD2, CD5, and CD7. The immature or mature nature of a lymphoma can also be confirmed by evaluation of the immunophenotype. Immature lymphomas commonly express one or more of TdT, CD10, or CD34; T-lymphoblastic lymphoma cells may also coexpress CD1a. The majority of NHLs and all HLs are derived from (or reflect) B cells at different stages of maturation. Mature B-cell lymphomas are the most common type of lymphoma and typically, but not always, express pan B-cell markers as well as surface membrane immunoglobulin, with the latter also most useful in assessing clonality via a determination of light chain restriction. Some mature B-cell lymphomas tend to acquire markers that are either never physiologically expressed by normal mature B cells (eg, cyclin D1 in mantle cell lymphoma, or BCL2 in germinal center B cells in follicular lymphoma) or only expressed in a minor fraction (eg, CD5 that is characteristically expressed in small lymphocytic and mantle cell lymphoma). The most common mature B-cell lymphomas include diffuse large B-cell lymphoma, follicular lymphoma, small lymphocytic lymphoma, mantle cell lymphoma, marginal zone lymphoma, Burkitt lymphoma, and lymphoplasmacytic lymphoma (Figures 2 and 3). Classical HLs are also lymphomas of B-cell origin that demonstrate diminished preservation of their B-cell immunophenotype (as evidenced by the dim expression of PAX5 but absence of most other pan B-cell antigens), expression of CD30, variable expression of CD15, and loss of CD45 (Figure 1). In contrast, nodular lymphocyte predominant HL shows a preserved B-cell immunophenotypic program and expression of CD45, typically without CD30 and CD15. Of note, the evaluation of the immunophenotype of the neoplastic cells in HL is routinely assessed by immunohistochemistry because most flow cytometry laboratories cannot reliably detect and characterize the low numbers of these cells.
Mature T-cell lymphomas generally express one or more T-cell markers, and tend to display a T-helper (CD4-positive) or cytotoxic (CD8-positive) immunophenotype and may show loss of markers expressed by most normal T-cells (eg, CD5, CD7; Figure 4). However, a subset of them may express markers not commonly detected in normal T cells, such as ALK. NK-cell lymphomas lack surface CD3 (expressing only cytoplasmic CD3) and CD5 but express some pan T-cell antigens (such as CD2 and CD7) as well as CD16 and/or CD56.
Patients with primary or acquired immune dysfunction are at risk for development of lymphoma and other less clearly defined lymphoproliferative disorders, the majority of which are associated with infection of the lymphoid cells with Epstein-Barr virus (EBV). Therefore, evaluation with chromogenic in situ hybridization for an EBV-encoded early RNA (EBER1) is routinely performed in these cases; it is thus essential that the hematopathologist be informed of the altered immune system of the patient. If lymphoma develops, they may be morphologically similar to those that appear in immunocompetent patients, which specifically in the post-transplant setting are known as monomorphic post-transplant lymphoproliferative disorders (PTLD). If the PTLD does not meet the criteria for any of the recognized types of lymphoma, it may be best characterized as a polymorphic PTLD.
Once the lineage (B-, T-, or NK-cell) of the mature lymphoma has been established, the sum (and on occasion the gestalt) of the clinical, morphologic, immunophenotypic and other findings will be considered for the subclassification of the neoplasm.
Cytogenetic and molecular evaluation
If the morphologic and immunophenotypic analysis is inconclusive or nondiagnostic, then molecular and/or cytogenetic testing may further aid in the characterization of the process. Some of available molecular tests include analyses for the rearrangements of the variable region of the immunoglobulin (IG) or T-cell receptor (TCR) genes and for mutations on specific genes. The identification of specific mutations not only confirms the clonal nature of the process but, on occasion, it may also help subclassify the lymphoma, whereas IG or TCR rearrangement studies are used to establish whether a lymphoid expansion is polyclonal or monoclonal. The molecular findings should not be evaluated in isolation, because not all monoclonal rearrangements are diagnostic of lymphoma, and not all lymphomas will show a monoclonal rearrangement. Other methodologies that can aid in the identification of a clonal process or specific genetic abnormalities include metaphase cytogenetics (karyotyping) and fluorescence in situ hybridization (FISH). If any cytogenetic abnormalities are found in sufficient numbers (and constitutional abnormalities are excluded), their identification indicates the presence of a clonal process. Also, some cytogenetic abnormalities are characteristic of certain lymphomas. However, they may be neither 100% diagnostically sensitive nor diagnostically specific, for example, the hallmark t(14;18)/IGH-BCL2 is not present in all follicular lymphomas and not all lymphomas with this translocation are follicular lymphomas. Whereas FISH is generally performed on a minimum of 200 cells, compared with typically 20 metaphase by “conventional” karyotyping, and is therefore considered to have higher analytical sensitivity, it evaluates only for the presence or absence of the abnormality being investigated with a given set of probes, and therefore other abnormalities, if present, will not be identified. The value of FISH cytogenetic studies is perhaps best illustrated in the need to diagnose double hit lymphomas, amongst other scenarios. The detection of certain mutations can aid in the diagnosis of certain lymphomas, such as MYD88 in lymphoplasmacytic lymphoma, prognosis of others, such as in follicular lymphoma and identify pathways that may be precisely therapeutically targeted.
Final remarks
The diagnosis of lymphoma can be complex and usually requires the hematopathologist to integrate multiple parameters. The classification of lymphomas is not static, and new entities or variants are continuously described, and the facets of well-known ones refined. While such changes are often to the chagrin of hematologists/oncologists and hematopathologists alike, we should embrace the incorporation of nascent and typically cool data into our practice, as more therapeutically relevant entities are molded.
Lymphomas constitute a very heterogeneous group of neoplasms with diverse clinical presentations, prognoses, and responses to therapy. Approximately 80,500 new cases of lymphoma are expected to be diagnosed in the United States in 2017, of which about one quarter will lead to the death of the patient.1 Perhaps more so than any other group of neoplasms, the diagnosis of lymphoma involves the integration of a multiplicity of clinical, histologic and immunophenotypic findings and, on occasion, cytogenetic and molecular results as well. An accurate diagnosis of lymphoma, usually rendered by hematopathologists, allows hematologists/oncologists to treat patients appropriately. Herein we will describe a simplified approach to the diagnosis and classification of lymphomas (Figure 1).
Lymphoma classification
Lymphomas are clonal neoplasms characterized by the expansion of abnormal lymphoid cells that may develop in any organ but commonly involve lymph nodes. The fourth edition of the World Health Organization (WHO) Classification of Tumours of Haematopoietic and Lymphoid tissues, published in 2008, is the official and most current guideline used for diagnosis of lymphoid neoplasms.2 The WHO scheme classifies lymphomas according to the type of cell from which they are derived (mature and immature B cells, T cells, or natural killer (NK) cells, findings determined by their morphology and immunophenotype) and their clinical, cytogenetic, and/or molecular features. This official classification is currently being updated3 and is expected to be published in full in 2017, at which time it is anticipated to include definitions for more than 70 distinct neoplasms.
Lymphomas are broadly and informally classified as Hodgkin lymphomas (HLs) and non-Hodgkin lymphomas (NHLs), based on the differences these two groups show in their clinical presentation, treatment, prognosis, and proportion of neoplastic cells, among others. NHLs are by far the most common type of lymphomas, accounting for approximately 90% of all new cases of lymphoma in the United States and 70% worldwide.1,2 NHLs are a very heterogeneous group of B-, T-, or NK-cell neoplasms that, in turn, can also be informally subclassified as low-grade (or indolent) or high-grade (or aggressive) according to their predicted clinical behavior. HLs are comparatively rare, less heterogeneous, uniformly of B-cell origin and, in the case of classical Hodgkin lymphoma, highly curable.1,2 It is beyond the scope of this manuscript to outline the features of each of the >70 specific entities, but the reader is referred elsewhere for more detail and encouraged to become familiarized with the complexity, challenges, and beauty of lymphoma diagnosis.2,3
Biopsy procedure
A correct diagnosis begins with an adequate biopsy procedure. It is essential that biopsy specimens for lymphoma evaluation be submitted fresh and unfixed, because some crucial analyses such as flow cytometry or conventional cytogenetics can only be performed on fresh tissue. Indeed, it is important for the hematologist/oncologist and/or surgeon and/or interventional radiologist to converse with the hematopathologist prior to and even during some procedures to ensure the correct processing of the specimen. Also, it is important to limit the compression of the specimen and the excessive use of cauterization during the biopsy procedure, both of which cause artifacts that may render impossible the interpretation of the histopathologic findings.
Given that the diagnosis of lymphoma is based not only on the cytologic details of the lymphoma cells but also on the architectural pattern with which they infiltrate an organ, the larger the biopsy specimen, the easier it will be for a hematopathologist to identify the pattern. In addition, excisional biopsies frequently contain more diagnostic tissue than needle core biopsies and this provides pathologists with the option to submit tissue fragments for ancillary tests that require unfixed tissue as noted above. Needle core biopsies of lymph nodes are increasingly being used because of their association with fewer complications and lower cost than excisional biopsies. However, needle core biopsies provide only a glimpse of the pattern of infiltration and may not be completely representative of the architecture. Therefore, excisional lymph node biopsies of lymph nodes are preferred over needle core biopsies, recognizing that in the setting of deeply seated lymph nodes, needle core biopsies may be the only or the best surgical option.
Clinical presentation
Accurate diagnosis of lymphoma cannot take place in a vacuum. The hematopathologist’s initial approach to the diagnosis of lymphoid processes in tissue biopsies should begin with a thorough review of the clinical history, although some pathology laboratories may not have immediate access to this information. The hematopathologist should evaluate factors such as age, gender, location of the tumor, symptomatology, medications, serology, and prior history of malignancy, immunosuppression or immunodeficiency in every case. Other important but frequently omitted parts of the clinical history are the patient’s occupation, history of exposure to animals, and the presence of tattoos, which may be associated with certain reactive lymphadenopathies.
Histomorphologic evaluation
Despite the plethora of new and increasingly sophisticated tools, histologic and morphologic analysis still remains the cornerstone of diagnosis in hematopathology. However, for the characterization of an increasing number of reactive and neoplastic lymphoid processes, hematopathologists may also require immunophenotypic, molecular, and cytogenetic tests for an accurate diagnosis. Upon review of the clinical information, a microscopic evaluation of the tissue submitted for processing by the histology laboratory will be performed. The results of concurrent flow cytometric evaluation (performed on fresh unfixed material) should also be available in most if not all cases before the H&E-stained slides are available for review. Upon receipt of H&E-stained slides, the hematopathologist will evaluate the quality of the submitted specimen, since many diagnostic difficulties stem from suboptimal techniques related to the biopsy procedure, fixation, processing, cutting, or staining (Figure 1). If deemed suitable for accurate diagnosis, a search for signs of preservation or disruption of the organ that was biopsied will follow. The identification of certain morphologic patterns aids the hematopathologist in answering the first question: “what organ is this and is this consistent with what is indicated on the requisition?” This is usually immediately followed by “is this sufficient and adequate material for a diagnosis?” and “is there any normal architecture?” If the architecture is not normal, “is this alteration due to a reactive or a neoplastic process?” If neoplastic, “is it lymphoma or a non-hematolymphoid neoplasm?”
Both reactive and neoplastic processes have variably unique morphologic features that if properly recognized, guide the subsequent testing. However, some reactive and neoplastic processes can present with overlapping features, and even after extensive immunophenotypic evaluation and the performance of ancillary studies, it may not be possible to conclusively determine its nature. If the lymph node architecture is altered or effaced, the predominant pattern of infiltration (eg, nodular, diffuse, interfollicular, intrasinusoidal) and the degree of alteration of the normal architecture is evaluated, usually at low magnification. When the presence of an infiltrate is recognized, its components must be characterized. If the infiltrate is composed of a homogeneous expansion of lymphoid cells that disrupts or replaces the normal lymphoid architecture, a lymphoma will be suspected or diagnosed. The pattern of distribution of the cells along with their individual morphologic characteristics (ie, size, nuclear shape, chromatin configuration, nucleoli, amount and hue of cytoplasm) are key factors for the diagnosis and classification of the lymphoma that will guide subsequent testing. The immunophenotypic analysis (by immunohistochemistry, flow cytometry or a combination of both) may confirm the reactive or neoplastic nature of the process, and its subclassification. B-cell lymphomas, in particular have variable and distinctive histologic features: as a diffuse infiltrate of large mature lymphoid cells (eg, diffuse large B-cell lymphoma), an expansion of immature lymphoid cells (lymphoblastic lymphoma), and a nodular infiltrate of small, intermediate and/or mature large B cells (eg, follicular lymphoma).
Mature T-cell lymphomas may display similar histologic, features but they can be quite heterogeneous with an infiltrate composed of one predominant cell type or a mixture of small, medium-sized, and large atypical lymphoid cells (on occasion with abundant clear cytoplasm) and a variable number of eosinophils, plasma cells, macrophages (including granulomas), and B cells. HLs most commonly efface the lymph node architecture with a nodular or diffuse infiltrate variably composed of reactive lymphocytes, granulocytes, macrophages, and plasma cells and usually a minority of large neoplastic cells (Hodgkin/Reed-Sternberg cells and/or lymphocyte predominant cells).
Once the H&E-stained slides are evaluated and a diagnosis of lymphoma is suspected or established, the hematopathologist will attempt to determine whether it has mature or immature features, and whether low- or high-grade morphologic characteristics are present. The maturity of lymphoid cells is generally determined by the nature of the chromatin, which if “fine” and homogeneous (with or without a conspicuous nucleolus) will usually, but not always, be considered immature, whereas clumped, vesicular or hyperchromatic chromatin is generally, but not always, associated with maturity. If the chromatin displays immature features, the differential diagnosis will mainly include B- and T-lymphoblastic lymphomas, but also blastoid variants of mature neoplasm such as mantle cell lymphoma, and follicular lymphoma, as well as high-grade B-cell lymphomas. Features associated with low-grade lymphomas (eg, follicular lymphoma, small lymphocytic lymphoma/chronic lymphocytic leukemia, marginal zone lymphoma, lymphoplasmacytic lymphoma) include small cell morphology, mature chromatin, absence of a significant number of mitoses or apoptotic cells, and a low proliferation index as shown by immunohistochemistry for Ki67. High-grade lymphomas, such as lymphoblastic lymphoma, Burkitt lymphoma, or certain large B-cell lymphomas tend to show opposite features, and some of the mature entities are frequently associated with MYC rearrangements. Of note, immature lymphomas tend to be clinically high grade, but not all clinically high-grade lymphomas are immature. Conversely, the majority of low-grade lymphomas are usually mature.
Immunophenotypic evaluation
Immunophenotypic evaluation is essential because the lineage of lymphoma cells cannot be determined by morphology alone. The immunophenotype is the combination of proteins/markers (eg, CD20, CD3, TdT) expressed by cells. Usually, it is evaluated by immunohistochemistry and/or flow cytometry, which help determine the proportion of lymphoid cells that express a certain marker and its location and intensity within the cells. While immunohistochemistry is normally performed on formalin-fixed and paraffin-embedded tissue, flow cytometry can be evaluated only on fresh unfixed tissue. Flow cytometry has the advantage over immunohistochemistry of being faster and better at simultaneously identifying coexpression of multiple markers on multiple cell populations. However, certain markers can only be evaluated by immunohistochemistry.
The immunophenotypic analysis will in most cases reveal whether the lymphomas is of B-, T- or NK-cell origin, and whether a lymphoma subtype associated immunophenotype is present. Typical pan B-cell antigens include PAX5, CD19, and CD79a (CD20 is less broadly expressed throughout B-cell differentiation, although it is usually evident in most mature B-cell lymphomas), and typical pan T-cell antigens include CD2, CD5, and CD7. The immature or mature nature of a lymphoma can also be confirmed by evaluation of the immunophenotype. Immature lymphomas commonly express one or more of TdT, CD10, or CD34; T-lymphoblastic lymphoma cells may also coexpress CD1a. The majority of NHLs and all HLs are derived from (or reflect) B cells at different stages of maturation. Mature B-cell lymphomas are the most common type of lymphoma and typically, but not always, express pan B-cell markers as well as surface membrane immunoglobulin, with the latter also most useful in assessing clonality via a determination of light chain restriction. Some mature B-cell lymphomas tend to acquire markers that are either never physiologically expressed by normal mature B cells (eg, cyclin D1 in mantle cell lymphoma, or BCL2 in germinal center B cells in follicular lymphoma) or only expressed in a minor fraction (eg, CD5 that is characteristically expressed in small lymphocytic and mantle cell lymphoma). The most common mature B-cell lymphomas include diffuse large B-cell lymphoma, follicular lymphoma, small lymphocytic lymphoma, mantle cell lymphoma, marginal zone lymphoma, Burkitt lymphoma, and lymphoplasmacytic lymphoma (Figures 2 and 3). Classical HLs are also lymphomas of B-cell origin that demonstrate diminished preservation of their B-cell immunophenotype (as evidenced by the dim expression of PAX5 but absence of most other pan B-cell antigens), expression of CD30, variable expression of CD15, and loss of CD45 (Figure 1). In contrast, nodular lymphocyte predominant HL shows a preserved B-cell immunophenotypic program and expression of CD45, typically without CD30 and CD15. Of note, the evaluation of the immunophenotype of the neoplastic cells in HL is routinely assessed by immunohistochemistry because most flow cytometry laboratories cannot reliably detect and characterize the low numbers of these cells.
Mature T-cell lymphomas generally express one or more T-cell markers, and tend to display a T-helper (CD4-positive) or cytotoxic (CD8-positive) immunophenotype and may show loss of markers expressed by most normal T-cells (eg, CD5, CD7; Figure 4). However, a subset of them may express markers not commonly detected in normal T cells, such as ALK. NK-cell lymphomas lack surface CD3 (expressing only cytoplasmic CD3) and CD5 but express some pan T-cell antigens (such as CD2 and CD7) as well as CD16 and/or CD56.
Patients with primary or acquired immune dysfunction are at risk for development of lymphoma and other less clearly defined lymphoproliferative disorders, the majority of which are associated with infection of the lymphoid cells with Epstein-Barr virus (EBV). Therefore, evaluation with chromogenic in situ hybridization for an EBV-encoded early RNA (EBER1) is routinely performed in these cases; it is thus essential that the hematopathologist be informed of the altered immune system of the patient. If lymphoma develops, they may be morphologically similar to those that appear in immunocompetent patients, which specifically in the post-transplant setting are known as monomorphic post-transplant lymphoproliferative disorders (PTLD). If the PTLD does not meet the criteria for any of the recognized types of lymphoma, it may be best characterized as a polymorphic PTLD.
Once the lineage (B-, T-, or NK-cell) of the mature lymphoma has been established, the sum (and on occasion the gestalt) of the clinical, morphologic, immunophenotypic and other findings will be considered for the subclassification of the neoplasm.
Cytogenetic and molecular evaluation
If the morphologic and immunophenotypic analysis is inconclusive or nondiagnostic, then molecular and/or cytogenetic testing may further aid in the characterization of the process. Some of available molecular tests include analyses for the rearrangements of the variable region of the immunoglobulin (IG) or T-cell receptor (TCR) genes and for mutations on specific genes. The identification of specific mutations not only confirms the clonal nature of the process but, on occasion, it may also help subclassify the lymphoma, whereas IG or TCR rearrangement studies are used to establish whether a lymphoid expansion is polyclonal or monoclonal. The molecular findings should not be evaluated in isolation, because not all monoclonal rearrangements are diagnostic of lymphoma, and not all lymphomas will show a monoclonal rearrangement. Other methodologies that can aid in the identification of a clonal process or specific genetic abnormalities include metaphase cytogenetics (karyotyping) and fluorescence in situ hybridization (FISH). If any cytogenetic abnormalities are found in sufficient numbers (and constitutional abnormalities are excluded), their identification indicates the presence of a clonal process. Also, some cytogenetic abnormalities are characteristic of certain lymphomas. However, they may be neither 100% diagnostically sensitive nor diagnostically specific, for example, the hallmark t(14;18)/IGH-BCL2 is not present in all follicular lymphomas and not all lymphomas with this translocation are follicular lymphomas. Whereas FISH is generally performed on a minimum of 200 cells, compared with typically 20 metaphase by “conventional” karyotyping, and is therefore considered to have higher analytical sensitivity, it evaluates only for the presence or absence of the abnormality being investigated with a given set of probes, and therefore other abnormalities, if present, will not be identified. The value of FISH cytogenetic studies is perhaps best illustrated in the need to diagnose double hit lymphomas, amongst other scenarios. The detection of certain mutations can aid in the diagnosis of certain lymphomas, such as MYD88 in lymphoplasmacytic lymphoma, prognosis of others, such as in follicular lymphoma and identify pathways that may be precisely therapeutically targeted.
Final remarks
The diagnosis of lymphoma can be complex and usually requires the hematopathologist to integrate multiple parameters. The classification of lymphomas is not static, and new entities or variants are continuously described, and the facets of well-known ones refined. While such changes are often to the chagrin of hematologists/oncologists and hematopathologists alike, we should embrace the incorporation of nascent and typically cool data into our practice, as more therapeutically relevant entities are molded.
1. Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2017. CA Cancer J Clin. 2017 ;67(1):7-30.
2. Swerdlow SH, Campo E, Harris NL, et al, eds. WHO classification of tumours of haematopoietic and lymphoid tissues. In: Bosman FT, Jaffe ES, Lakhani SR, Ohgaki H, eds. World Health Organization Classification of Tumours. Lyon, France: IARC; 2008.
3. Swerdlow SH, Campo E, Pileri SA, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016 ;127(20):2375-2390.
1. Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2017. CA Cancer J Clin. 2017 ;67(1):7-30.
2. Swerdlow SH, Campo E, Harris NL, et al, eds. WHO classification of tumours of haematopoietic and lymphoid tissues. In: Bosman FT, Jaffe ES, Lakhani SR, Ohgaki H, eds. World Health Organization Classification of Tumours. Lyon, France: IARC; 2008.
3. Swerdlow SH, Campo E, Pileri SA, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016 ;127(20):2375-2390.
Quality of life in hypothyroidism is key, but no treatment guide exists
ORLANDO – The quality of life of someone with treated hypothyroidism is worse than that of the general population and requires endocrinologists to think “outside the pill box,” said Anna M. Sawka, MD, PhD, of the University of Toronto, at a spring symposium presented by the American Thyroid Association.
While issues such as whether monotherapy with T4 is the treatment of choice or whether there is a subset of patients who might benefit from treatment with either T4/T3 in combination or even with extract of dessicated thyroid, many patients with treated hypothyroidism continue to feel bad, judging from discussion during the symposium.
As defined by the CDC, health-related quality of life can be energy level, mood, health risks and condition, functional and socioeconomic status. Here, at this meeting, the focus is on treatment. But QoL is so much more than that. It is recorded by the patient; it’s their perceptions. Of the available disease-specific–measures of QoL, many have not been validated.
One group of researchers assessed four QoL assessment questionnaires and gave top rating to the ThyPRO (thyroid-specific patient reported outcome) questionnaire for use in patients with hypothyroidism due to Hashimoto’s disease or thyroidectomy (J Clin Epidemiol. 2016 Oct;78:63-72).
The ThyPRO looks at two factors that are key to QoL in hypothyroidism: satisfaction with thyroid hormone and symptom control.
Looking at hypothyroidism from the perspective of the patient is catching on in endocrinology. Dr. Sawka reviewed data from 6 studies of QoL in people with treated hypothyroidism. The years of the studies ranged from 2002 to 2017 and the number of patients ranged from 58 to 591. While only one study used the ThyPRO, all found that QoL was worse in patients with treated hypothyroidism than in the general population.
Findings from one study based on in-depth interviews with 16 patients, of whom 5 had hypothyroidism and 11 had hyperthyroidism, showed that a key trait of either condition was that of losing control over their physical and mental states, with the hypothyroid group reporting feeling drained while the others said they felt sped up. The signs of hypothyroidism can be attributed to other things, such as aging or stress, and that ambiguity frustrated the patients in the study. Also key was the experience of having to negotiate their disease, with a keen awareness that their endocrinologist did not validate their experience, that they had to look to lab tests to tell them the state of their disease, and they had to deal with functional limitations (Qual Health Research. 2015 Jul;25[7]:945-53).
Dr. Sawka reported that she has no financial disclosures.
ORLANDO – The quality of life of someone with treated hypothyroidism is worse than that of the general population and requires endocrinologists to think “outside the pill box,” said Anna M. Sawka, MD, PhD, of the University of Toronto, at a spring symposium presented by the American Thyroid Association.
While issues such as whether monotherapy with T4 is the treatment of choice or whether there is a subset of patients who might benefit from treatment with either T4/T3 in combination or even with extract of dessicated thyroid, many patients with treated hypothyroidism continue to feel bad, judging from discussion during the symposium.
As defined by the CDC, health-related quality of life can be energy level, mood, health risks and condition, functional and socioeconomic status. Here, at this meeting, the focus is on treatment. But QoL is so much more than that. It is recorded by the patient; it’s their perceptions. Of the available disease-specific–measures of QoL, many have not been validated.
One group of researchers assessed four QoL assessment questionnaires and gave top rating to the ThyPRO (thyroid-specific patient reported outcome) questionnaire for use in patients with hypothyroidism due to Hashimoto’s disease or thyroidectomy (J Clin Epidemiol. 2016 Oct;78:63-72).
The ThyPRO looks at two factors that are key to QoL in hypothyroidism: satisfaction with thyroid hormone and symptom control.
Looking at hypothyroidism from the perspective of the patient is catching on in endocrinology. Dr. Sawka reviewed data from 6 studies of QoL in people with treated hypothyroidism. The years of the studies ranged from 2002 to 2017 and the number of patients ranged from 58 to 591. While only one study used the ThyPRO, all found that QoL was worse in patients with treated hypothyroidism than in the general population.
Findings from one study based on in-depth interviews with 16 patients, of whom 5 had hypothyroidism and 11 had hyperthyroidism, showed that a key trait of either condition was that of losing control over their physical and mental states, with the hypothyroid group reporting feeling drained while the others said they felt sped up. The signs of hypothyroidism can be attributed to other things, such as aging or stress, and that ambiguity frustrated the patients in the study. Also key was the experience of having to negotiate their disease, with a keen awareness that their endocrinologist did not validate their experience, that they had to look to lab tests to tell them the state of their disease, and they had to deal with functional limitations (Qual Health Research. 2015 Jul;25[7]:945-53).
Dr. Sawka reported that she has no financial disclosures.
ORLANDO – The quality of life of someone with treated hypothyroidism is worse than that of the general population and requires endocrinologists to think “outside the pill box,” said Anna M. Sawka, MD, PhD, of the University of Toronto, at a spring symposium presented by the American Thyroid Association.
While issues such as whether monotherapy with T4 is the treatment of choice or whether there is a subset of patients who might benefit from treatment with either T4/T3 in combination or even with extract of dessicated thyroid, many patients with treated hypothyroidism continue to feel bad, judging from discussion during the symposium.
As defined by the CDC, health-related quality of life can be energy level, mood, health risks and condition, functional and socioeconomic status. Here, at this meeting, the focus is on treatment. But QoL is so much more than that. It is recorded by the patient; it’s their perceptions. Of the available disease-specific–measures of QoL, many have not been validated.
One group of researchers assessed four QoL assessment questionnaires and gave top rating to the ThyPRO (thyroid-specific patient reported outcome) questionnaire for use in patients with hypothyroidism due to Hashimoto’s disease or thyroidectomy (J Clin Epidemiol. 2016 Oct;78:63-72).
The ThyPRO looks at two factors that are key to QoL in hypothyroidism: satisfaction with thyroid hormone and symptom control.
Looking at hypothyroidism from the perspective of the patient is catching on in endocrinology. Dr. Sawka reviewed data from 6 studies of QoL in people with treated hypothyroidism. The years of the studies ranged from 2002 to 2017 and the number of patients ranged from 58 to 591. While only one study used the ThyPRO, all found that QoL was worse in patients with treated hypothyroidism than in the general population.
Findings from one study based on in-depth interviews with 16 patients, of whom 5 had hypothyroidism and 11 had hyperthyroidism, showed that a key trait of either condition was that of losing control over their physical and mental states, with the hypothyroid group reporting feeling drained while the others said they felt sped up. The signs of hypothyroidism can be attributed to other things, such as aging or stress, and that ambiguity frustrated the patients in the study. Also key was the experience of having to negotiate their disease, with a keen awareness that their endocrinologist did not validate their experience, that they had to look to lab tests to tell them the state of their disease, and they had to deal with functional limitations (Qual Health Research. 2015 Jul;25[7]:945-53).
Dr. Sawka reported that she has no financial disclosures.
AT AN ATA SYMPOSIUM