User login
Blending classic clinical skills with new technology
Now that we can order MRI studies on a break from rounds walking to Starbucks, utilize portable ultrasounds to direct IV line placement, and use dual-energy CT to detect a gout attack that has not yet occurred, it seems like a romantic anachronism to extol the ongoing virtues of the seemingly lost art of the physical examination. Back “in the day,” the giants of medicine roamed the halls with their natural instruments of palpation and percussion and their skills in observation and auscultation. They were giants because they stood out then, just as skilled diagnosticians stand out today using an upgraded set of tools. Some physicians a few decades ago were able to recognize, describe, and diagnose late-stage endocarditis with a stethoscope, a magnifying glass, and an ophthalmoscope. The giants of today recognize the patient with endocarditis and document its presence using transesophageal echocardiography before the peripheral eponymous stigmata of Janeway and Osler appear or the blood cultures turn positive. The physical examination, history, diagnostic reasoning, and clinical technology are all essential for a blend that provides efficient and effective medical care. The blending is the challenge.
Clinicians are not created equal. We learn and prioritize our skills in different ways. But if we are not taught to value and trust the physical examination, if we don’t have the opportunity to see it influence patient management in positive ways, we may eschew it and instead indiscriminately use easily available laboratory and imaging tests—a more expensive and often misleading strategic approach. Today while in clinic, I saw a 54-year-old woman for evaluation of possible lupus who had arthritis of the hands and a high positive antinuclear antibody titer, but negative or normal results on other, previously ordered tests, including anti-DNA, rheumatoid factor, anti-cyclic citrullinated peptide, hepatitis C studies, complement levels, and another half-dozen immune serologic tests. On examination, she had typical nodular osteoarthritis of the proximal and distal interphalangeal joints of her hand with squaring of her thumbs. The antinuclear antibody was most likely associated with her previously diagnosed autoimmune thyroid disease.
In an editorial in this issue of the Journal, Dr. Salvatore Mangione, the author of a book on physical diagnosis,1 cites a recent study indicating that the most common recognized diagnostic error related to the physical examination is that the appropriate examination isn’t done.2 I would add to that my concerns over the new common custom of cutting and pasting the findings from earlier physical examinations into later progress notes in the electronic record. So much for the value of being able to recognize “changing murmurs” when diagnosing infectious endocarditis.
The apparent efficiency (reflected in length of stay) and availability of technology, as well as a lack of physician skill and time, are often cited as reasons for the demise of the physical examination. Yet this does not need to be the case. If I had trained with portable ultrasonography readily available to confirm or refute my impressions, my skills at detecting low-grade synovitis would surely be better than they are. With a gold standard at hand, which may be technology or at times a skilled mentor, our examinations can be refined if we want them to be.
But the issue of limited physician time must be addressed. Efficiency is a critical concept in preserving how we practice and perform the physical examination. When we know what we are looking for, we are more likely to find it if it is present, or to have confidence that it is not present. I am far more likely to recognize a loud pulmonic second heart sound if I suspect that the dyspneic patient I am examining has pulmonary hypertension associated with her scleroderma than if I am doing a perfunctory cardiac auscultation in a patient admitted with cellulitis. Appropriate focus provides power to the directed physical examination. If I am looking for the cause of unexplained fevers, I will do a purposeful axillary and epitrochlear lymph node examination. I am not mindlessly probing the flesh.
Nishigori and colleagues have written of the “hypothesis-driven” physical examination.3 Busy clinicians, they say, don’t have time to perform a head-to-toe, by-the-book physical examination. Instead, we should, by a dynamic process, formulate a differential diagnosis from the history and other initial information, and then perform the directed physical examination in earnest, looking for evidence to support or refute our diagnostic hypothesis—and thus redirect it. Plus, in a nice break from electronic charting, we can actually explain our thought processes to the patient as we perform the examination.
This approach makes sense to me as both intellectually satisfying and clinically efficient. And then we can consider which lab tests and technologic gadgetry we should order, while walking to get the café latte we ordered with our cell phone app.
New technology can support and not necessarily replace old habits.
- Mangione S. Physical Diagnosis Secrets, 2nd ed. Philadelphia: Mosby/Elsevier, 2008.
- Verghese A, Charlton B, Kassirer JP, Ramsey M, Ioannidis JP. Inadequacies of physical examination as a cause of medical errors and adverse events: a collection of vignettes. Am J Med 2015; 128:1322–1324.
- Nishigori H, Masuda K, Kikukawa M, et al. A model teaching session for the hypothesis-driven physical examination. Medical Teacher 2011; 33:410–417.
Now that we can order MRI studies on a break from rounds walking to Starbucks, utilize portable ultrasounds to direct IV line placement, and use dual-energy CT to detect a gout attack that has not yet occurred, it seems like a romantic anachronism to extol the ongoing virtues of the seemingly lost art of the physical examination. Back “in the day,” the giants of medicine roamed the halls with their natural instruments of palpation and percussion and their skills in observation and auscultation. They were giants because they stood out then, just as skilled diagnosticians stand out today using an upgraded set of tools. Some physicians a few decades ago were able to recognize, describe, and diagnose late-stage endocarditis with a stethoscope, a magnifying glass, and an ophthalmoscope. The giants of today recognize the patient with endocarditis and document its presence using transesophageal echocardiography before the peripheral eponymous stigmata of Janeway and Osler appear or the blood cultures turn positive. The physical examination, history, diagnostic reasoning, and clinical technology are all essential for a blend that provides efficient and effective medical care. The blending is the challenge.
Clinicians are not created equal. We learn and prioritize our skills in different ways. But if we are not taught to value and trust the physical examination, if we don’t have the opportunity to see it influence patient management in positive ways, we may eschew it and instead indiscriminately use easily available laboratory and imaging tests—a more expensive and often misleading strategic approach. Today while in clinic, I saw a 54-year-old woman for evaluation of possible lupus who had arthritis of the hands and a high positive antinuclear antibody titer, but negative or normal results on other, previously ordered tests, including anti-DNA, rheumatoid factor, anti-cyclic citrullinated peptide, hepatitis C studies, complement levels, and another half-dozen immune serologic tests. On examination, she had typical nodular osteoarthritis of the proximal and distal interphalangeal joints of her hand with squaring of her thumbs. The antinuclear antibody was most likely associated with her previously diagnosed autoimmune thyroid disease.
In an editorial in this issue of the Journal, Dr. Salvatore Mangione, the author of a book on physical diagnosis,1 cites a recent study indicating that the most common recognized diagnostic error related to the physical examination is that the appropriate examination isn’t done.2 I would add to that my concerns over the new common custom of cutting and pasting the findings from earlier physical examinations into later progress notes in the electronic record. So much for the value of being able to recognize “changing murmurs” when diagnosing infectious endocarditis.
The apparent efficiency (reflected in length of stay) and availability of technology, as well as a lack of physician skill and time, are often cited as reasons for the demise of the physical examination. Yet this does not need to be the case. If I had trained with portable ultrasonography readily available to confirm or refute my impressions, my skills at detecting low-grade synovitis would surely be better than they are. With a gold standard at hand, which may be technology or at times a skilled mentor, our examinations can be refined if we want them to be.
But the issue of limited physician time must be addressed. Efficiency is a critical concept in preserving how we practice and perform the physical examination. When we know what we are looking for, we are more likely to find it if it is present, or to have confidence that it is not present. I am far more likely to recognize a loud pulmonic second heart sound if I suspect that the dyspneic patient I am examining has pulmonary hypertension associated with her scleroderma than if I am doing a perfunctory cardiac auscultation in a patient admitted with cellulitis. Appropriate focus provides power to the directed physical examination. If I am looking for the cause of unexplained fevers, I will do a purposeful axillary and epitrochlear lymph node examination. I am not mindlessly probing the flesh.
Nishigori and colleagues have written of the “hypothesis-driven” physical examination.3 Busy clinicians, they say, don’t have time to perform a head-to-toe, by-the-book physical examination. Instead, we should, by a dynamic process, formulate a differential diagnosis from the history and other initial information, and then perform the directed physical examination in earnest, looking for evidence to support or refute our diagnostic hypothesis—and thus redirect it. Plus, in a nice break from electronic charting, we can actually explain our thought processes to the patient as we perform the examination.
This approach makes sense to me as both intellectually satisfying and clinically efficient. And then we can consider which lab tests and technologic gadgetry we should order, while walking to get the café latte we ordered with our cell phone app.
New technology can support and not necessarily replace old habits.
Now that we can order MRI studies on a break from rounds walking to Starbucks, utilize portable ultrasounds to direct IV line placement, and use dual-energy CT to detect a gout attack that has not yet occurred, it seems like a romantic anachronism to extol the ongoing virtues of the seemingly lost art of the physical examination. Back “in the day,” the giants of medicine roamed the halls with their natural instruments of palpation and percussion and their skills in observation and auscultation. They were giants because they stood out then, just as skilled diagnosticians stand out today using an upgraded set of tools. Some physicians a few decades ago were able to recognize, describe, and diagnose late-stage endocarditis with a stethoscope, a magnifying glass, and an ophthalmoscope. The giants of today recognize the patient with endocarditis and document its presence using transesophageal echocardiography before the peripheral eponymous stigmata of Janeway and Osler appear or the blood cultures turn positive. The physical examination, history, diagnostic reasoning, and clinical technology are all essential for a blend that provides efficient and effective medical care. The blending is the challenge.
Clinicians are not created equal. We learn and prioritize our skills in different ways. But if we are not taught to value and trust the physical examination, if we don’t have the opportunity to see it influence patient management in positive ways, we may eschew it and instead indiscriminately use easily available laboratory and imaging tests—a more expensive and often misleading strategic approach. Today while in clinic, I saw a 54-year-old woman for evaluation of possible lupus who had arthritis of the hands and a high positive antinuclear antibody titer, but negative or normal results on other, previously ordered tests, including anti-DNA, rheumatoid factor, anti-cyclic citrullinated peptide, hepatitis C studies, complement levels, and another half-dozen immune serologic tests. On examination, she had typical nodular osteoarthritis of the proximal and distal interphalangeal joints of her hand with squaring of her thumbs. The antinuclear antibody was most likely associated with her previously diagnosed autoimmune thyroid disease.
In an editorial in this issue of the Journal, Dr. Salvatore Mangione, the author of a book on physical diagnosis,1 cites a recent study indicating that the most common recognized diagnostic error related to the physical examination is that the appropriate examination isn’t done.2 I would add to that my concerns over the new common custom of cutting and pasting the findings from earlier physical examinations into later progress notes in the electronic record. So much for the value of being able to recognize “changing murmurs” when diagnosing infectious endocarditis.
The apparent efficiency (reflected in length of stay) and availability of technology, as well as a lack of physician skill and time, are often cited as reasons for the demise of the physical examination. Yet this does not need to be the case. If I had trained with portable ultrasonography readily available to confirm or refute my impressions, my skills at detecting low-grade synovitis would surely be better than they are. With a gold standard at hand, which may be technology or at times a skilled mentor, our examinations can be refined if we want them to be.
But the issue of limited physician time must be addressed. Efficiency is a critical concept in preserving how we practice and perform the physical examination. When we know what we are looking for, we are more likely to find it if it is present, or to have confidence that it is not present. I am far more likely to recognize a loud pulmonic second heart sound if I suspect that the dyspneic patient I am examining has pulmonary hypertension associated with her scleroderma than if I am doing a perfunctory cardiac auscultation in a patient admitted with cellulitis. Appropriate focus provides power to the directed physical examination. If I am looking for the cause of unexplained fevers, I will do a purposeful axillary and epitrochlear lymph node examination. I am not mindlessly probing the flesh.
Nishigori and colleagues have written of the “hypothesis-driven” physical examination.3 Busy clinicians, they say, don’t have time to perform a head-to-toe, by-the-book physical examination. Instead, we should, by a dynamic process, formulate a differential diagnosis from the history and other initial information, and then perform the directed physical examination in earnest, looking for evidence to support or refute our diagnostic hypothesis—and thus redirect it. Plus, in a nice break from electronic charting, we can actually explain our thought processes to the patient as we perform the examination.
This approach makes sense to me as both intellectually satisfying and clinically efficient. And then we can consider which lab tests and technologic gadgetry we should order, while walking to get the café latte we ordered with our cell phone app.
New technology can support and not necessarily replace old habits.
- Mangione S. Physical Diagnosis Secrets, 2nd ed. Philadelphia: Mosby/Elsevier, 2008.
- Verghese A, Charlton B, Kassirer JP, Ramsey M, Ioannidis JP. Inadequacies of physical examination as a cause of medical errors and adverse events: a collection of vignettes. Am J Med 2015; 128:1322–1324.
- Nishigori H, Masuda K, Kikukawa M, et al. A model teaching session for the hypothesis-driven physical examination. Medical Teacher 2011; 33:410–417.
- Mangione S. Physical Diagnosis Secrets, 2nd ed. Philadelphia: Mosby/Elsevier, 2008.
- Verghese A, Charlton B, Kassirer JP, Ramsey M, Ioannidis JP. Inadequacies of physical examination as a cause of medical errors and adverse events: a collection of vignettes. Am J Med 2015; 128:1322–1324.
- Nishigori H, Masuda K, Kikukawa M, et al. A model teaching session for the hypothesis-driven physical examination. Medical Teacher 2011; 33:410–417.
Life after breast, prostate, and colon cancer: Primary care’s role
In 2015, about 1.6 million Americans received a diagnosis of cancer.1 In 2012, when 13.7 million people were living with cancer in the United States, the estimated 5-year survival rate of all cancers was 66.5%.1 Today, breast, prostate, and colon cancers have 5-year survival rates of 89.4%, 98.9%, and 64.9%, respectively.
With this rising trend in survival, primary care physicians have been steadily assuming the long-term care of these patients. The phrase “cancer survivorship” was coined by the National Comprehensive Cancer Network to describe the experience of living with, through, and beyond a cancer diagnosis.2
As cancer becomes a chronic medical condition, the primary care physician assumes a vital role in the treatment of the unique and evolving needs of this patient population.
This article discusses the specific needs of patients surviving breast, prostate, and colon cancer with special focus on surveillance guidelines for recurrence, development of concomitant malignancies, assessment of psychosocial and physical effects, and disease conditions related to the treatment of cancer itself.
FOLLOW-UP CARE AND SURVEILLANCE
Follow-up care in patients being treated for cancer is vital to survivorship. It includes promoting healthy living, managing treatment side effects, and monitoring for long-term side effects and possible recurrence.
Patients previously treated for malignancy are more susceptible to second primary cancers, for an array of reasons including the effects of prior treatment, shared environmental exposures such as smoking, and genetic susceptibility.2 Therefore, it is important for the primary care physician to recognize signs and symptoms and to screen cancer survivors appropriately. The American Society of Clinical Oncology (ASCO) has developed evidence-based recommendations for follow-up care,3 which we review here.
Breast cancer
For breast cancer patients, history and physical examinations are recommended every 3 to 6 months for the first 3 years, every 6 to 12 months in years 4 and 5, and annually thereafter.3
A repeat mammogram should be performed 1 year after the initial mammogram that led to the diagnosis. If the patient underwent radiation therapy, a repeat mammogram of the affected breast should be done 6 months after completion of radiation. Finally, a mammogram should be done every 6 to 12 months thereafter.3 It is also recommended that patients perform a monthly breast self-examination, but this does not replace the annual mammogram.3
Women who are treated with tamoxifen should have an annual gynecologic assessment if they have a uterus and should be encouraged to discuss any abnormal vaginal bleeding with their physician, given the increased risk of uterine cancer.2
ASCO does not recommend routine use of complete blood cell counts, complete metabolic panels, bone scans, chest radiography, computed tomography, ultrasonography, positron-emission tomography, or tumor markers in patients who are asymptomatic.3
Prostate cancer
ASCO’s recommendations for patients recovering from prostate cancer include regular histories and physical examinations and general health promotion. Prostate-specific antigen (PSA) testing is recommended every 6 to 12 months for the first 5 years after treatment and annually thereafter. More frequent PSA testing may be required in men at higher risk of recurrence or in patients who may undergo additional treatment, including radiation and surgery.4 Higher risk of disease recurrence is thought to depend on disease-specific factors at the time of original diagnosis including pretreatment PSA, Gleason score, and tumor stage.4 This should be discussed between the oncologist and primary care physician.
In regard to digital rectal examinations, the oncologist and primary care physician should jointly determine the frequency of examination. The frequency of digital rectal examinations remains an area of controversy due to their low sensitivity for detecting recurrences. Digital rectal examinations may be omitted in patients with undetectable levels of PSA.4
In regard to second primary malignancies, prostate cancer survivors who have undergone pelvic radiation therapy have a slightly higher risk of bladder and colorectal cancer. The lifetime incidence of bladder cancer after pelvic radiation is 5% to 6%, compared with 2.4% in the general population.1,5 A prostate cancer survivor presenting with hematuria should be referred to a urologist for cystoscopy and evaluation of the upper urinary tract to rule out cancer.4
Similarly, patients presenting with rectal bleeding should be referred to a gastroenterologist and the treating radiation oncologist for complete evaluation. The risk of rectal cancer after pelvic radiation therapy increases to about the same level as in someone who has a first-degree relative with colorectal cancer.5 Therefore, it is recommended that patients undergo screening for colorectal cancer in conjunction with existing evidence-based guidelines. There is no evidence to suggest that increased intensity of screening improves overall or disease-specific survival.4
Colon cancer
In patients with resected colorectal cancer, continued surveillance is important to evaluate for recurrent cancer as well as for metachronous neoplasms. Consensus statements indicate that surveillance colonoscopy should be continued for those who have undergone surgical resection for stage I, II, or III colon or rectal cancers, and for those patients with stage IV who have undergone surgical resection with curative intent.6
Patients who undergo curative resection of rectal or colon cancer should have a colonoscopy 1 year after resection or 1 year after the colonoscopy was performed, to clear the colon of synchronous disease. Subsequently, if the colonoscopy done at 1 year is normal, the interval before the next colonoscopy is 3 years. If that colonoscopy is normal, the next colonoscopy is in 5 years. Time intervals may be shorter if there is evidence of hereditary nonpolyposis colorectal cancer or adenoma.
Patients who underwent low anterior resection of rectal cancer should undergo periodic examination of the rectum to evaluate for local recurrence. Although effectiveness is not proven, endoscopic ultrasonography or flexible sigmoidoscopy is suggested at 3- to 6-month intervals for the first 2 to 3 years after resection. This is independent of colonoscopy.6,7
Additionally, ASCO recommends a history and physical examination and carcinoembryonic antigen testing every 3 to 6 months for the first 5 years. Computed tomography of the chest, abdomen, and pelvis should be done annually for the first 3 years after the end of treatment.7
HEALTH PROMOTION
Maintaining a healthy body weight and a nutritionally balanced diet should be encouraged in all cancer survivors. Poor diet, lack of exercise, excessive alcohol consumption, and smoking reduce quality of life and increase the risk of cancer.2
Diet
Numerous studies have looked at dietary modifications and risk reduction, and although there is no consensus on specific dietary guidelines, there is consensus that diet modification to maintain normal body weight will improve overall quality of life.8 Patients should be encouraged to consume a well-balanced diet consisting mostly of fruits, vegetables, whole grains, and beans, and to limit consumption of animal protein.8
There is little evidence to support taking vitamins or other dietary supplements to prevent or control cancer or to prevent its recurrence. The primary care physician should assess supplement use on a regular basis during office visits.2
Exercise
Rest is an important component of the initial recovery process. Too much inactivity, however, leads to loss of physical conditioning and muscle strength. This in turn may negatively affect a patient’s ability to perform activities of daily living and may worsen fatigue associated with treatment.
Accordingly, the National Comprehensive Cancer Network recommends at least 150 minutes of moderate activity and up to 75 minutes of more rigorous activity divided throughout the week.2,8 The regimen should include endurance and muscle strength training, which aid in balance, bone, health, and functional status. The intensity of exercise should be increased in a stepwise fashion, taking into account individual capabilities and limitations.2
Cancer survivors may need specific exercise recommendations and supervised programs to ensure safety and limit long-term side effects of their treatment. For example:
Patients with neuropathy should have their stability, balance, and gait assessed before starting a new program. These patients may benefit from an aerobic exercise program that includes riding a stationary bike rather than running.
Patients with poor bone health should have their fracture risk assessed.
Those with an ostomy bag should empty the bag before physical activity. They should avoid contact sports and activities that increase intra-abdominal pressure.
Patients suffering from lymphedema should wear compression garments when engaging in physical activity. They should undergo baseline and periodic reevaluation of the lymphedema and initiate strength training in the affected body part only if the lymphedema is stable (ie, no need for therapy for 3 months, no recent infections requiring antibiotics, and no change in circumference > 10%).2
Mental health
Health promotion should focus not only on the physical health of the patient, but also on his or her emotional and psychological well-being. As they make the transition from cancer patient to survivor, many individuals may develop or have worsening depression and anxiety due to fear of recurrence. These feelings of powerlessness can linger for years after the initial treatment.
Patients should be screened regularly for signs and symptoms of depression by asking about their family and social support. Referral to support groups, psychologists, and psychiatrists may be warranted.9
MITIGATING CANCER-RELATED FATIGUE
Cancer-related fatigue involves a patient’s subjective sense of physical, emotional, and cognitive exhaustion related to cancer or treatment that is disproportionate to that expected from recent daily activity.2 Fatigue is a common complaint among survivors and can occur months to years after treatment ends.10
Patients should be screened for fatigue at regular intervals. The primary care physician should focus the history to include information regarding the onset, pattern, duration, associated factors, assessment of other treatable comorbidities, medications, psychological well-being, nutritional status, and pain level of each patient who complains of fatigue.
Laboratory tests for treatable causes of fatigue include:
- A complete blood cell count to evaluate for anemia
- A comprehensive metabolic panel to evaluate electrolytes, renal function, and hepatic function
- The thyroid-stimulating hormone level to evaluate thyroid function, particularly in breast cancer patients who have received radiation therapy.2
If no organic cause is uncovered, the focus should shift to lifestyle interventions as the treatment of choice. The treatment of fatigue in this situation is increased physical activity with the goals discussed above. Psychological intervention may be required with cognitive behavioral therapy, psychological and supportive therapies, education on sleep hygiene, and possible sleep restriction.
If alternative causes of fatigue are ruled out and physical and psychological support fails to reduce symptoms, the practitioner can consider a psychostimulant such as methylphenidate, but this should be used cautiously.2
SEXUAL DYSFUNCTION
Intimate relationships and sexuality are an important part of life and are affected by a variety of factors including physical health, psychological well-being, body image perception, and overall status of relationships. As a side effect of chemotherapy, cancer survivors may complain of erectile dysfunction, penile shortening, dyspareunia, vaginal dryness, decreased libido, anorgasmy, and changes in body image. These issues are frequently unaddressed, whether due to the physician’s discomfort in discussing the topic or to the patient’s embarrassment and reluctance to discuss the matter.11
Breast cancer patients may experience sexual dysfunction both during and after treatment due to a combination of systemic effects of treatment, changes in physical appearance leading to impaired body image, strains on partner relationships, and psychological sequelae of diagnosis and treatment of cancer.12 Manipulation and radiation to the breast affect sexual functioning by altering body contour and image. Additionally, chemotherapy can lead to early menopause and hormonal alterations due to endocrine therapies, which can negatively affect sexual organs.11
Studies have shown that treatment with tamoxifen causes less sexual dysfunction than do aromatase inhibitors. In the Arimidex, Tamoxifen, Alone or in Combination trial, therapy with anastrozole was associated with more vaginal dryness, dyspareunia, and decreased libido compared with tamoxifen.12
Treatment requires a comprehensive history, a physical examination, and a discussion of relationship satisfaction with the patient.
Vaginal dryness and dyspareunia can be treated with vaginal lubricants and moisturizers. Moisturizers are effective if used multiple times per week, whereas lubricants can be used on demand. Low-dose vaginal estrogen preparations can be used in select patients with severe vaginal dryness; the goal should be discussed. Hormone replacement therapy is contraindicated in breast cancer survivors due to the risk of recurrence.11
Prostate cancer survivors. Up to 70% of men felt their quality of life and sexual function were adversely affected after the diagnosis and treatment.13,14 Erectile dysfunction following radical prostatectomy and radiation therapy remains one of the leading causes of sexual dysfunction.14–15 Erectile dysfunction is multifactorial, with both psychogenic and organic causes. Comorbidities must be considered including hypertension, diabetes, hyperlipidemia, and smoking. Early penile rehabilitation is a proposed treatment strategy.14
First-line therapy for penile rehabilitation includes introduction of daily low-dose phosphodiesterase type 5 inhibitors as early as the time of catheter removal to within the first month after surgery. The need for daily dosing vs on-demand dosing has been controversial.15 Two large multicenter, double-blind studies had conflicting outcomes. The first reported that in men receiving nightly sildenafil (50 or 100 mg) after radical prostatectomy, 27% had increased return of spontaneous erectile function vs 4% with placebo16; the second study showed no difference between nightly and on-demand dosing.17 The consensus is that a phosphodiesterase type 5 inhibitor should be initiated early.
Second-line therapy includes intracavernosal injections and vacuum erection devices. Finally, a penile prosthesis implant can be offered to patients who have responded poorly to medical therapy.13
Colorectal cancer survivors suffer from sexually related problems similar to those stated above, including erectile dysfunction, ejaculation problems, dyspareunia, vaginal dryness, and decreased enjoyment.18 These patients should be provided treatments similar to those described above. In addition, they may suffer from body image issues, particularly those with a permanent ostomy.9
Sexual dysfunction is a multifaceted problem for patients. Encouraging couples to discuss sexual intimacy frequently helps to reveal and cope with the problems, whether physical or psychological. It is the primary care physician’s role to recognize any sexual concerns and refer to the appropriate specialist.
OSTEOPOROSIS
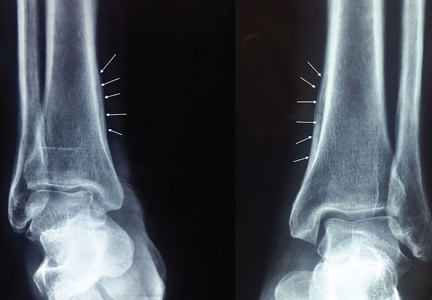
Osteoporosis is a metabolic bone disease characterized by low bone mineral density. As a result, bones become weak and fracture more easily from minor injuries.
Risk factors for osteoporosis include female sex, family history, advanced age, low body weight, low calcium and vitamin D levels, sedentary lifestyle, smoking, and low estrogen levels.19 Cancer treatment places patients at a greater risk for osteoporosis, particularly for those patients with chemotherapy-induced ovarian failure, those treated with aromatase inhibitors, men receiving androgen-deprivation therapy, and patients on glucocorticoid therapy. The morbidity and mortality associated with bone loss can be prevented with appropriate screening, lifestyle changes, and therapy.2
According to the National Osteoporosis Foundation Guideline for Preventing and Treating Osteoporosis, all men and postmenopausal women age 50 and older should be evaluated clinically for osteoporosis risk to determine the need for bone mineral density testing.2,19 The US Preventive Services Task Force recommends bone mineral density testing in all women age 65 and older, and for women 60 to 64 who are at high risk for bone loss. ASCO agrees, and further suggests bone mineral density screening for women with breast cancer who have risk factors such as positive family history, body weight less than 70 kg, and prior nontraumatic fracture, as well as for postmenopausal women of any age receiving aromatase inhibitors and for premenopausal women with therapy-induced ovarian failure.11
Androgen deprivation therapy is a mainstay of treatment in recurrent and metastatic prostate cancer. The effect is severe hypogonadism with reductions in serum testosterone levels. Androgen deprivation therapy accelerates bone turnover, decreases bone mineral density, and contributes to fracture risk. The National Comprehensive Cancer Network additionally suggests measuring bone mineral density at baseline for all men receiving androgen deprivation therapy or other medications associated with bone loss, repeating it 1 year after androgen deprivation therapy and then every 2 years, or as clinically indicated.20
The gold standard for measuring bone mineral density is dual-energy x-ray absorptiometry. The World Health Organization FRAX tool uses bone mineral density and several clinical factors to estimate the risk of fracture in the next 10 years, which can help guide therapy. Cancer patients with elevated fracture risk should be evaluated every 2 years. Counseling should be provided to address modifiable risk factors such as smoking, alcohol consumption, physical inactivity, and low calcium and vitamin D intake. Therapy should be strongly considered in patients with a bone mineral density below a T-score of –2.0. 2,19
Treatment begins with lifestyle modifications such as weight-bearing exercises to improve balance and muscle strength and to prevent falls, and adequate intake of calcium (≥ 1,200 mg daily) and vitamin D (800–1,000 IU daily) for adults age 50 and older. Treatment with bisphosphonates may be required.2,11,20
NEUROPATHY
Many chemotherapeutic agents can lead to neuropathy and can result in long-term disability in patients. Patients treated with taxane- and platinum-based chemotherapy are at particular risk.
Paclitaxel, used in the treatment of breast, ovarian, and lung cancer, can lead to distal neuropathy. This neuropathy commonly has a stocking-and-glove distribution and is primarily sensory; however, it may have motor and autonomic components. The neuropathy typically lessens when the medication is stopped, although in some patients it can persist and lead to long-term disability.
Treatment can include massage. Medications such as gabapentin and pregabalin can also be used, but randomized controlled trials do not support them, as they predominantly treat the tingling rather than the numbness.11
BLADDER AND BOWEL DYSFUNCTION
Urinary incontinence and dysfunction are frequent complications in prostate cancer survivors. Urinary function should be discussed regularly with patients, addressing quality of the urinary stream, difficulty emptying the bladder, timing, and incontinence.4 Urinary incontinence is frequently seen in postprostatectomy patients.
The cornerstone of treating urinary incontinence is determining the cause of the incontinence, whether it is stress or urge incontinence, or both.21 For those patients with urge incontinence alone, practitioners can address the problem with a combination of behavior modification, pelvic floor exercises, and anticholinergic medications such as oxybutynin. If the problem stems from difficulty initiating or a slow stream, physicians may consider alpha-blockers.4,21 If the incontinence is persistent, bothersome, and has components of stress incontinence, the patient should be referred to a urologist for urodynamic testing, cystoscopy, and surgical evaluation for possible placement of a male urethral sling or artificial urinary sphincter.21
Colorectal cancer survivors, particularly those who received radiation therapy, are at high risk of bowel dysfunction such as chronic diarrhea and stool incontinence. Patients should be educated about this possible side effect. Symptoms of bowel dysfunction can affect body image and interfere with social functioning and overall quality of life. Patients should be provided with coping tools such as antidiarrheal medication, stool bulking agents, changes in diet, and protective underwear.
CARDIOVASCULAR DISEASE
Evidence suggests that certain types of chemotherapy and radiation therapy increase the risk of cardiovascular disease. Prostate cancer survivors treated with androgen deprivation therapy, particularly those more than 75 years old, are at increased risk of cardiovascular disease and diabetes.22
It is recommended that men be screened with fasting plasma glucose at baseline and yearly thereafter while receiving androgen deprivation therapy. Lipid panel testing should be done 1 year from initiation of androgen deprivation therapy and then, if results are normal, every 5 years or as clinically warranted. The focus should be on primary prevention with emphasis on smoking cessation, treating hypertension per guidelines, lifestyle modifications, and treatment with aspirin and statins when clinically appropriate.20
Radiation therapy, chemotherapy, and endocrine therapy have all been suggested to lead to cardiotoxicity in breast cancer patients. Anthracycline-based chemotherapies have a well-recognized association with cardiomyopathy. Factors associated with increased risk of anthracycline-induced cardiomyopathy include older age, hypertension, pre-existing coronary artery disease, and previous mediastinal radiation.
Early detection of cardiomyopathy may lead to avoidance of irreversible cardiotoxicity, but there are currently no clear guidelines for cardiac screening in breast cancer survivors. If cardiomyopathy is detected, treatment should include beta-blockers and angiotensin-converting enzyme inhibitors as well as modification of other cardiovascular risk factors.11
A SURVIVORSHIP CARE PLAN
There is life beyond the diagnosis of cancer. As patients are living longer, with an estimated 5-year survival rate of 66.5% of all cancers in the United States, there must be a transition of care from the oncologist to the primary care physician.1 While the oncologist will remain involved in the initial years of follow-up care, these visits will go from twice a year to once a year, and eventually the patient will make a full transition to care by the primary care physician. The timing of this changeover varies from physician to physician, but the primary care physician is ultimately responsible for the follow-up.
A tool to ease this transition is a survivorship care plan. The goal of a survivorship care plan is to individualize a follow-up plan while keeping in mind the necessary surveillance as outlined. These care plans are created with the patient and oncologist and then brought to the primary care physician. While there is an abundance of literature regarding the creation and initiation of survivorship care plans, the success of these plans is uncertain. Ultimately, the goal of a survivorship care plan is to create open dialogue among the oncologist, the primary care physician, and the patient. This unique patient population requires close follow-up by a multidisciplinary team with the primary care physician serving as the steward.
- National Cancer Institute (NIH). Surveillance, Epidemiology, and End Results Program. SEER cancer stat fact sheets. http://seer.cancer.gov/statfacts. Accessed March 6, 2017.
- National Comprehensive Cancer Network (NCCN). NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines Survivorship: 2015. www.nccn.org/professionals/physician_gls/pdf/survivorship.pdf. Accessed March 6, 2017.
- Khatcheressian JL, Hurley P, Bantug E, et al. Breast cancer follow-up and management after primary treatment: American Society of Clinical Oncology Clinical Practice Guideline update. J Clin Oncol 2013; 31:961–965.
- Resnick MJ, Lacchetti C, Bergman J, et al. Prostate cancer survivorship care guideline: American Society of Clinical Oncology Clinical Practice Guideline endorsement. J Clin Oncol 2015; 33:1078–1085.
- Sountoulides P, Koletsas N, Kikidakis D, Paschalidis K, Sofikitis N. Secondary malignancies following radiotherapy for prostate cancer. Ther Adv Urol 2010; 2:119–125.
- Rex DK, Kahi CJ, Levin B, et al. Guidelines for colonoscopy surveillance after cancer resection: a consensus update by the American Cancer Society and US Multi-Society Task Force on Colorectal Cancer. CA Cancer J Clin 2006; 56:160–168.
- Meyerhardt JA, Mangu PB, Flynn PJ, et al; American Society of Clinical Oncology. Follow-up care, surveillance protocol, and secondary prevention measures for survivors of colorectal cancer: American Society of Clinical Oncology clinical practice guideline endorsement. J Clin Oncol 2013; 31:4465–4470.
- Davies NJ, Batehup L, Thomas R. The role of diet and physical activity in breast, colorectal, and prostate cancer survivorship: a review of the literature. Br J Cancer 2011; 105(suppl 1):S52–S73.
- Miller K, editor. Excellent Care for Cancer Survivors: A Guide to Fully Meet Their Needs in Medical Offices and in the Community (Praeger Series on Contemporary Health & Living). 1st ed. Santa Barbara, CA: Praeger; 2012.
- Stanton AL, Rowland JH, Ganz PA. Life after diagnosis and treatment of cancer in adulthood: contributions from psychosocial oncology research. Am Psychol 2015; 70:159–174.
- Stan D, Loprinzi CL, Ruddy KJ. Breast cancer survivorship issues. Hematol Oncol Clin North Am 2013; 27:805–827.
- Fallowfield L, Cella D, Cuzick J, Francis S, Locker G, Howell A. Quality of life of postmenopausal women in the Arimidex, Tamoxifen, Alone or in Combination (ATAC) Adjuvant Breast Cancer Trial. J Clin Oncol 2004; 22:426–471.
- Chung E, Gillman M. Prostate cancer survivorship: a review of erectile dysfunction and penile rehabilitation after prostate cancer therapy. Med J Aust 2014; 200:582–585.
- Sherer BA, Levine LA. Current management of erectile dysfunction in prostate cancer survivors. Curr Opin Urol 2014; 24:401–416.
- Chung E, Brock G. Sexual rehabilitation and cancer survivorship: a state of art review of current literature and management strategies in male sexual dysfunction among prostate cancer survivors. J Sex Med 2013; 10(suppl 1):102–111.
- Padma-Nathan H, McCullough AR, Levine LA, et al; Study Group. Randomized, double-blind, placebo-controlled study of postoperative nightly sildenafil citrate for the prevention of erectile dysfunction after bilateral nerve-sparing radical prostatectomy. Int J Impot Res 2008; 20:479–486.
- Montorsi F, Brock G, Lee J, et al. Effect of nightly versus on-demand vardenafil on recovery of erectile function in men following bilateral nerve-sparing radical prostatectomy. Eur Urol 2008; 54:924–931.
- Den Oudsten BL, Traa MJ, Thong MS, et al. Higher prevalence of sexual dysfunction in colon and rectal cancer survivors compared with the normative population: a population-based study. Eur J Cancer 2012; 48:3161–3170.
- National Osteoporosis Foundation (NOF). http://nof.org. Accessed March 3, 2017.
- Saylor PJ, Keating NL, Smith MR. Prostate cancer survivorship: prevention and treatment of the adverse effects of androgen deprivation therapy. J Gen Intern Med 2009; 24(suppl 2):S389–S394.
- Gupta S, Peterson AC. Stress urinary incontinence in the prostate cancer survivor. Curr Opin Urol 2014; 24:395–400.
- Morgans AK, Fan KH, Koyama T, et al. Influence of age on incident diabetes and cardiovascular disease in prostate cancer survivors receiving androgen deprivation therapy. J Urol 2015; 193:1226–1231.
In 2015, about 1.6 million Americans received a diagnosis of cancer.1 In 2012, when 13.7 million people were living with cancer in the United States, the estimated 5-year survival rate of all cancers was 66.5%.1 Today, breast, prostate, and colon cancers have 5-year survival rates of 89.4%, 98.9%, and 64.9%, respectively.
With this rising trend in survival, primary care physicians have been steadily assuming the long-term care of these patients. The phrase “cancer survivorship” was coined by the National Comprehensive Cancer Network to describe the experience of living with, through, and beyond a cancer diagnosis.2
As cancer becomes a chronic medical condition, the primary care physician assumes a vital role in the treatment of the unique and evolving needs of this patient population.
This article discusses the specific needs of patients surviving breast, prostate, and colon cancer with special focus on surveillance guidelines for recurrence, development of concomitant malignancies, assessment of psychosocial and physical effects, and disease conditions related to the treatment of cancer itself.
FOLLOW-UP CARE AND SURVEILLANCE
Follow-up care in patients being treated for cancer is vital to survivorship. It includes promoting healthy living, managing treatment side effects, and monitoring for long-term side effects and possible recurrence.
Patients previously treated for malignancy are more susceptible to second primary cancers, for an array of reasons including the effects of prior treatment, shared environmental exposures such as smoking, and genetic susceptibility.2 Therefore, it is important for the primary care physician to recognize signs and symptoms and to screen cancer survivors appropriately. The American Society of Clinical Oncology (ASCO) has developed evidence-based recommendations for follow-up care,3 which we review here.
Breast cancer
For breast cancer patients, history and physical examinations are recommended every 3 to 6 months for the first 3 years, every 6 to 12 months in years 4 and 5, and annually thereafter.3
A repeat mammogram should be performed 1 year after the initial mammogram that led to the diagnosis. If the patient underwent radiation therapy, a repeat mammogram of the affected breast should be done 6 months after completion of radiation. Finally, a mammogram should be done every 6 to 12 months thereafter.3 It is also recommended that patients perform a monthly breast self-examination, but this does not replace the annual mammogram.3
Women who are treated with tamoxifen should have an annual gynecologic assessment if they have a uterus and should be encouraged to discuss any abnormal vaginal bleeding with their physician, given the increased risk of uterine cancer.2
ASCO does not recommend routine use of complete blood cell counts, complete metabolic panels, bone scans, chest radiography, computed tomography, ultrasonography, positron-emission tomography, or tumor markers in patients who are asymptomatic.3
Prostate cancer
ASCO’s recommendations for patients recovering from prostate cancer include regular histories and physical examinations and general health promotion. Prostate-specific antigen (PSA) testing is recommended every 6 to 12 months for the first 5 years after treatment and annually thereafter. More frequent PSA testing may be required in men at higher risk of recurrence or in patients who may undergo additional treatment, including radiation and surgery.4 Higher risk of disease recurrence is thought to depend on disease-specific factors at the time of original diagnosis including pretreatment PSA, Gleason score, and tumor stage.4 This should be discussed between the oncologist and primary care physician.
In regard to digital rectal examinations, the oncologist and primary care physician should jointly determine the frequency of examination. The frequency of digital rectal examinations remains an area of controversy due to their low sensitivity for detecting recurrences. Digital rectal examinations may be omitted in patients with undetectable levels of PSA.4
In regard to second primary malignancies, prostate cancer survivors who have undergone pelvic radiation therapy have a slightly higher risk of bladder and colorectal cancer. The lifetime incidence of bladder cancer after pelvic radiation is 5% to 6%, compared with 2.4% in the general population.1,5 A prostate cancer survivor presenting with hematuria should be referred to a urologist for cystoscopy and evaluation of the upper urinary tract to rule out cancer.4
Similarly, patients presenting with rectal bleeding should be referred to a gastroenterologist and the treating radiation oncologist for complete evaluation. The risk of rectal cancer after pelvic radiation therapy increases to about the same level as in someone who has a first-degree relative with colorectal cancer.5 Therefore, it is recommended that patients undergo screening for colorectal cancer in conjunction with existing evidence-based guidelines. There is no evidence to suggest that increased intensity of screening improves overall or disease-specific survival.4
Colon cancer
In patients with resected colorectal cancer, continued surveillance is important to evaluate for recurrent cancer as well as for metachronous neoplasms. Consensus statements indicate that surveillance colonoscopy should be continued for those who have undergone surgical resection for stage I, II, or III colon or rectal cancers, and for those patients with stage IV who have undergone surgical resection with curative intent.6
Patients who undergo curative resection of rectal or colon cancer should have a colonoscopy 1 year after resection or 1 year after the colonoscopy was performed, to clear the colon of synchronous disease. Subsequently, if the colonoscopy done at 1 year is normal, the interval before the next colonoscopy is 3 years. If that colonoscopy is normal, the next colonoscopy is in 5 years. Time intervals may be shorter if there is evidence of hereditary nonpolyposis colorectal cancer or adenoma.
Patients who underwent low anterior resection of rectal cancer should undergo periodic examination of the rectum to evaluate for local recurrence. Although effectiveness is not proven, endoscopic ultrasonography or flexible sigmoidoscopy is suggested at 3- to 6-month intervals for the first 2 to 3 years after resection. This is independent of colonoscopy.6,7
Additionally, ASCO recommends a history and physical examination and carcinoembryonic antigen testing every 3 to 6 months for the first 5 years. Computed tomography of the chest, abdomen, and pelvis should be done annually for the first 3 years after the end of treatment.7
HEALTH PROMOTION
Maintaining a healthy body weight and a nutritionally balanced diet should be encouraged in all cancer survivors. Poor diet, lack of exercise, excessive alcohol consumption, and smoking reduce quality of life and increase the risk of cancer.2
Diet
Numerous studies have looked at dietary modifications and risk reduction, and although there is no consensus on specific dietary guidelines, there is consensus that diet modification to maintain normal body weight will improve overall quality of life.8 Patients should be encouraged to consume a well-balanced diet consisting mostly of fruits, vegetables, whole grains, and beans, and to limit consumption of animal protein.8
There is little evidence to support taking vitamins or other dietary supplements to prevent or control cancer or to prevent its recurrence. The primary care physician should assess supplement use on a regular basis during office visits.2
Exercise
Rest is an important component of the initial recovery process. Too much inactivity, however, leads to loss of physical conditioning and muscle strength. This in turn may negatively affect a patient’s ability to perform activities of daily living and may worsen fatigue associated with treatment.
Accordingly, the National Comprehensive Cancer Network recommends at least 150 minutes of moderate activity and up to 75 minutes of more rigorous activity divided throughout the week.2,8 The regimen should include endurance and muscle strength training, which aid in balance, bone, health, and functional status. The intensity of exercise should be increased in a stepwise fashion, taking into account individual capabilities and limitations.2
Cancer survivors may need specific exercise recommendations and supervised programs to ensure safety and limit long-term side effects of their treatment. For example:
Patients with neuropathy should have their stability, balance, and gait assessed before starting a new program. These patients may benefit from an aerobic exercise program that includes riding a stationary bike rather than running.
Patients with poor bone health should have their fracture risk assessed.
Those with an ostomy bag should empty the bag before physical activity. They should avoid contact sports and activities that increase intra-abdominal pressure.
Patients suffering from lymphedema should wear compression garments when engaging in physical activity. They should undergo baseline and periodic reevaluation of the lymphedema and initiate strength training in the affected body part only if the lymphedema is stable (ie, no need for therapy for 3 months, no recent infections requiring antibiotics, and no change in circumference > 10%).2
Mental health
Health promotion should focus not only on the physical health of the patient, but also on his or her emotional and psychological well-being. As they make the transition from cancer patient to survivor, many individuals may develop or have worsening depression and anxiety due to fear of recurrence. These feelings of powerlessness can linger for years after the initial treatment.
Patients should be screened regularly for signs and symptoms of depression by asking about their family and social support. Referral to support groups, psychologists, and psychiatrists may be warranted.9
MITIGATING CANCER-RELATED FATIGUE
Cancer-related fatigue involves a patient’s subjective sense of physical, emotional, and cognitive exhaustion related to cancer or treatment that is disproportionate to that expected from recent daily activity.2 Fatigue is a common complaint among survivors and can occur months to years after treatment ends.10
Patients should be screened for fatigue at regular intervals. The primary care physician should focus the history to include information regarding the onset, pattern, duration, associated factors, assessment of other treatable comorbidities, medications, psychological well-being, nutritional status, and pain level of each patient who complains of fatigue.
Laboratory tests for treatable causes of fatigue include:
- A complete blood cell count to evaluate for anemia
- A comprehensive metabolic panel to evaluate electrolytes, renal function, and hepatic function
- The thyroid-stimulating hormone level to evaluate thyroid function, particularly in breast cancer patients who have received radiation therapy.2
If no organic cause is uncovered, the focus should shift to lifestyle interventions as the treatment of choice. The treatment of fatigue in this situation is increased physical activity with the goals discussed above. Psychological intervention may be required with cognitive behavioral therapy, psychological and supportive therapies, education on sleep hygiene, and possible sleep restriction.
If alternative causes of fatigue are ruled out and physical and psychological support fails to reduce symptoms, the practitioner can consider a psychostimulant such as methylphenidate, but this should be used cautiously.2
SEXUAL DYSFUNCTION
Intimate relationships and sexuality are an important part of life and are affected by a variety of factors including physical health, psychological well-being, body image perception, and overall status of relationships. As a side effect of chemotherapy, cancer survivors may complain of erectile dysfunction, penile shortening, dyspareunia, vaginal dryness, decreased libido, anorgasmy, and changes in body image. These issues are frequently unaddressed, whether due to the physician’s discomfort in discussing the topic or to the patient’s embarrassment and reluctance to discuss the matter.11
Breast cancer patients may experience sexual dysfunction both during and after treatment due to a combination of systemic effects of treatment, changes in physical appearance leading to impaired body image, strains on partner relationships, and psychological sequelae of diagnosis and treatment of cancer.12 Manipulation and radiation to the breast affect sexual functioning by altering body contour and image. Additionally, chemotherapy can lead to early menopause and hormonal alterations due to endocrine therapies, which can negatively affect sexual organs.11
Studies have shown that treatment with tamoxifen causes less sexual dysfunction than do aromatase inhibitors. In the Arimidex, Tamoxifen, Alone or in Combination trial, therapy with anastrozole was associated with more vaginal dryness, dyspareunia, and decreased libido compared with tamoxifen.12
Treatment requires a comprehensive history, a physical examination, and a discussion of relationship satisfaction with the patient.
Vaginal dryness and dyspareunia can be treated with vaginal lubricants and moisturizers. Moisturizers are effective if used multiple times per week, whereas lubricants can be used on demand. Low-dose vaginal estrogen preparations can be used in select patients with severe vaginal dryness; the goal should be discussed. Hormone replacement therapy is contraindicated in breast cancer survivors due to the risk of recurrence.11
Prostate cancer survivors. Up to 70% of men felt their quality of life and sexual function were adversely affected after the diagnosis and treatment.13,14 Erectile dysfunction following radical prostatectomy and radiation therapy remains one of the leading causes of sexual dysfunction.14–15 Erectile dysfunction is multifactorial, with both psychogenic and organic causes. Comorbidities must be considered including hypertension, diabetes, hyperlipidemia, and smoking. Early penile rehabilitation is a proposed treatment strategy.14
First-line therapy for penile rehabilitation includes introduction of daily low-dose phosphodiesterase type 5 inhibitors as early as the time of catheter removal to within the first month after surgery. The need for daily dosing vs on-demand dosing has been controversial.15 Two large multicenter, double-blind studies had conflicting outcomes. The first reported that in men receiving nightly sildenafil (50 or 100 mg) after radical prostatectomy, 27% had increased return of spontaneous erectile function vs 4% with placebo16; the second study showed no difference between nightly and on-demand dosing.17 The consensus is that a phosphodiesterase type 5 inhibitor should be initiated early.
Second-line therapy includes intracavernosal injections and vacuum erection devices. Finally, a penile prosthesis implant can be offered to patients who have responded poorly to medical therapy.13
Colorectal cancer survivors suffer from sexually related problems similar to those stated above, including erectile dysfunction, ejaculation problems, dyspareunia, vaginal dryness, and decreased enjoyment.18 These patients should be provided treatments similar to those described above. In addition, they may suffer from body image issues, particularly those with a permanent ostomy.9
Sexual dysfunction is a multifaceted problem for patients. Encouraging couples to discuss sexual intimacy frequently helps to reveal and cope with the problems, whether physical or psychological. It is the primary care physician’s role to recognize any sexual concerns and refer to the appropriate specialist.
OSTEOPOROSIS
Osteoporosis is a metabolic bone disease characterized by low bone mineral density. As a result, bones become weak and fracture more easily from minor injuries.
Risk factors for osteoporosis include female sex, family history, advanced age, low body weight, low calcium and vitamin D levels, sedentary lifestyle, smoking, and low estrogen levels.19 Cancer treatment places patients at a greater risk for osteoporosis, particularly for those patients with chemotherapy-induced ovarian failure, those treated with aromatase inhibitors, men receiving androgen-deprivation therapy, and patients on glucocorticoid therapy. The morbidity and mortality associated with bone loss can be prevented with appropriate screening, lifestyle changes, and therapy.2
According to the National Osteoporosis Foundation Guideline for Preventing and Treating Osteoporosis, all men and postmenopausal women age 50 and older should be evaluated clinically for osteoporosis risk to determine the need for bone mineral density testing.2,19 The US Preventive Services Task Force recommends bone mineral density testing in all women age 65 and older, and for women 60 to 64 who are at high risk for bone loss. ASCO agrees, and further suggests bone mineral density screening for women with breast cancer who have risk factors such as positive family history, body weight less than 70 kg, and prior nontraumatic fracture, as well as for postmenopausal women of any age receiving aromatase inhibitors and for premenopausal women with therapy-induced ovarian failure.11
Androgen deprivation therapy is a mainstay of treatment in recurrent and metastatic prostate cancer. The effect is severe hypogonadism with reductions in serum testosterone levels. Androgen deprivation therapy accelerates bone turnover, decreases bone mineral density, and contributes to fracture risk. The National Comprehensive Cancer Network additionally suggests measuring bone mineral density at baseline for all men receiving androgen deprivation therapy or other medications associated with bone loss, repeating it 1 year after androgen deprivation therapy and then every 2 years, or as clinically indicated.20
The gold standard for measuring bone mineral density is dual-energy x-ray absorptiometry. The World Health Organization FRAX tool uses bone mineral density and several clinical factors to estimate the risk of fracture in the next 10 years, which can help guide therapy. Cancer patients with elevated fracture risk should be evaluated every 2 years. Counseling should be provided to address modifiable risk factors such as smoking, alcohol consumption, physical inactivity, and low calcium and vitamin D intake. Therapy should be strongly considered in patients with a bone mineral density below a T-score of –2.0. 2,19
Treatment begins with lifestyle modifications such as weight-bearing exercises to improve balance and muscle strength and to prevent falls, and adequate intake of calcium (≥ 1,200 mg daily) and vitamin D (800–1,000 IU daily) for adults age 50 and older. Treatment with bisphosphonates may be required.2,11,20
NEUROPATHY
Many chemotherapeutic agents can lead to neuropathy and can result in long-term disability in patients. Patients treated with taxane- and platinum-based chemotherapy are at particular risk.
Paclitaxel, used in the treatment of breast, ovarian, and lung cancer, can lead to distal neuropathy. This neuropathy commonly has a stocking-and-glove distribution and is primarily sensory; however, it may have motor and autonomic components. The neuropathy typically lessens when the medication is stopped, although in some patients it can persist and lead to long-term disability.
Treatment can include massage. Medications such as gabapentin and pregabalin can also be used, but randomized controlled trials do not support them, as they predominantly treat the tingling rather than the numbness.11
BLADDER AND BOWEL DYSFUNCTION
Urinary incontinence and dysfunction are frequent complications in prostate cancer survivors. Urinary function should be discussed regularly with patients, addressing quality of the urinary stream, difficulty emptying the bladder, timing, and incontinence.4 Urinary incontinence is frequently seen in postprostatectomy patients.
The cornerstone of treating urinary incontinence is determining the cause of the incontinence, whether it is stress or urge incontinence, or both.21 For those patients with urge incontinence alone, practitioners can address the problem with a combination of behavior modification, pelvic floor exercises, and anticholinergic medications such as oxybutynin. If the problem stems from difficulty initiating or a slow stream, physicians may consider alpha-blockers.4,21 If the incontinence is persistent, bothersome, and has components of stress incontinence, the patient should be referred to a urologist for urodynamic testing, cystoscopy, and surgical evaluation for possible placement of a male urethral sling or artificial urinary sphincter.21
Colorectal cancer survivors, particularly those who received radiation therapy, are at high risk of bowel dysfunction such as chronic diarrhea and stool incontinence. Patients should be educated about this possible side effect. Symptoms of bowel dysfunction can affect body image and interfere with social functioning and overall quality of life. Patients should be provided with coping tools such as antidiarrheal medication, stool bulking agents, changes in diet, and protective underwear.
CARDIOVASCULAR DISEASE
Evidence suggests that certain types of chemotherapy and radiation therapy increase the risk of cardiovascular disease. Prostate cancer survivors treated with androgen deprivation therapy, particularly those more than 75 years old, are at increased risk of cardiovascular disease and diabetes.22
It is recommended that men be screened with fasting plasma glucose at baseline and yearly thereafter while receiving androgen deprivation therapy. Lipid panel testing should be done 1 year from initiation of androgen deprivation therapy and then, if results are normal, every 5 years or as clinically warranted. The focus should be on primary prevention with emphasis on smoking cessation, treating hypertension per guidelines, lifestyle modifications, and treatment with aspirin and statins when clinically appropriate.20
Radiation therapy, chemotherapy, and endocrine therapy have all been suggested to lead to cardiotoxicity in breast cancer patients. Anthracycline-based chemotherapies have a well-recognized association with cardiomyopathy. Factors associated with increased risk of anthracycline-induced cardiomyopathy include older age, hypertension, pre-existing coronary artery disease, and previous mediastinal radiation.
Early detection of cardiomyopathy may lead to avoidance of irreversible cardiotoxicity, but there are currently no clear guidelines for cardiac screening in breast cancer survivors. If cardiomyopathy is detected, treatment should include beta-blockers and angiotensin-converting enzyme inhibitors as well as modification of other cardiovascular risk factors.11
A SURVIVORSHIP CARE PLAN
There is life beyond the diagnosis of cancer. As patients are living longer, with an estimated 5-year survival rate of 66.5% of all cancers in the United States, there must be a transition of care from the oncologist to the primary care physician.1 While the oncologist will remain involved in the initial years of follow-up care, these visits will go from twice a year to once a year, and eventually the patient will make a full transition to care by the primary care physician. The timing of this changeover varies from physician to physician, but the primary care physician is ultimately responsible for the follow-up.
A tool to ease this transition is a survivorship care plan. The goal of a survivorship care plan is to individualize a follow-up plan while keeping in mind the necessary surveillance as outlined. These care plans are created with the patient and oncologist and then brought to the primary care physician. While there is an abundance of literature regarding the creation and initiation of survivorship care plans, the success of these plans is uncertain. Ultimately, the goal of a survivorship care plan is to create open dialogue among the oncologist, the primary care physician, and the patient. This unique patient population requires close follow-up by a multidisciplinary team with the primary care physician serving as the steward.
In 2015, about 1.6 million Americans received a diagnosis of cancer.1 In 2012, when 13.7 million people were living with cancer in the United States, the estimated 5-year survival rate of all cancers was 66.5%.1 Today, breast, prostate, and colon cancers have 5-year survival rates of 89.4%, 98.9%, and 64.9%, respectively.
With this rising trend in survival, primary care physicians have been steadily assuming the long-term care of these patients. The phrase “cancer survivorship” was coined by the National Comprehensive Cancer Network to describe the experience of living with, through, and beyond a cancer diagnosis.2
As cancer becomes a chronic medical condition, the primary care physician assumes a vital role in the treatment of the unique and evolving needs of this patient population.
This article discusses the specific needs of patients surviving breast, prostate, and colon cancer with special focus on surveillance guidelines for recurrence, development of concomitant malignancies, assessment of psychosocial and physical effects, and disease conditions related to the treatment of cancer itself.
FOLLOW-UP CARE AND SURVEILLANCE
Follow-up care in patients being treated for cancer is vital to survivorship. It includes promoting healthy living, managing treatment side effects, and monitoring for long-term side effects and possible recurrence.
Patients previously treated for malignancy are more susceptible to second primary cancers, for an array of reasons including the effects of prior treatment, shared environmental exposures such as smoking, and genetic susceptibility.2 Therefore, it is important for the primary care physician to recognize signs and symptoms and to screen cancer survivors appropriately. The American Society of Clinical Oncology (ASCO) has developed evidence-based recommendations for follow-up care,3 which we review here.
Breast cancer
For breast cancer patients, history and physical examinations are recommended every 3 to 6 months for the first 3 years, every 6 to 12 months in years 4 and 5, and annually thereafter.3
A repeat mammogram should be performed 1 year after the initial mammogram that led to the diagnosis. If the patient underwent radiation therapy, a repeat mammogram of the affected breast should be done 6 months after completion of radiation. Finally, a mammogram should be done every 6 to 12 months thereafter.3 It is also recommended that patients perform a monthly breast self-examination, but this does not replace the annual mammogram.3
Women who are treated with tamoxifen should have an annual gynecologic assessment if they have a uterus and should be encouraged to discuss any abnormal vaginal bleeding with their physician, given the increased risk of uterine cancer.2
ASCO does not recommend routine use of complete blood cell counts, complete metabolic panels, bone scans, chest radiography, computed tomography, ultrasonography, positron-emission tomography, or tumor markers in patients who are asymptomatic.3
Prostate cancer
ASCO’s recommendations for patients recovering from prostate cancer include regular histories and physical examinations and general health promotion. Prostate-specific antigen (PSA) testing is recommended every 6 to 12 months for the first 5 years after treatment and annually thereafter. More frequent PSA testing may be required in men at higher risk of recurrence or in patients who may undergo additional treatment, including radiation and surgery.4 Higher risk of disease recurrence is thought to depend on disease-specific factors at the time of original diagnosis including pretreatment PSA, Gleason score, and tumor stage.4 This should be discussed between the oncologist and primary care physician.
In regard to digital rectal examinations, the oncologist and primary care physician should jointly determine the frequency of examination. The frequency of digital rectal examinations remains an area of controversy due to their low sensitivity for detecting recurrences. Digital rectal examinations may be omitted in patients with undetectable levels of PSA.4
In regard to second primary malignancies, prostate cancer survivors who have undergone pelvic radiation therapy have a slightly higher risk of bladder and colorectal cancer. The lifetime incidence of bladder cancer after pelvic radiation is 5% to 6%, compared with 2.4% in the general population.1,5 A prostate cancer survivor presenting with hematuria should be referred to a urologist for cystoscopy and evaluation of the upper urinary tract to rule out cancer.4
Similarly, patients presenting with rectal bleeding should be referred to a gastroenterologist and the treating radiation oncologist for complete evaluation. The risk of rectal cancer after pelvic radiation therapy increases to about the same level as in someone who has a first-degree relative with colorectal cancer.5 Therefore, it is recommended that patients undergo screening for colorectal cancer in conjunction with existing evidence-based guidelines. There is no evidence to suggest that increased intensity of screening improves overall or disease-specific survival.4
Colon cancer
In patients with resected colorectal cancer, continued surveillance is important to evaluate for recurrent cancer as well as for metachronous neoplasms. Consensus statements indicate that surveillance colonoscopy should be continued for those who have undergone surgical resection for stage I, II, or III colon or rectal cancers, and for those patients with stage IV who have undergone surgical resection with curative intent.6
Patients who undergo curative resection of rectal or colon cancer should have a colonoscopy 1 year after resection or 1 year after the colonoscopy was performed, to clear the colon of synchronous disease. Subsequently, if the colonoscopy done at 1 year is normal, the interval before the next colonoscopy is 3 years. If that colonoscopy is normal, the next colonoscopy is in 5 years. Time intervals may be shorter if there is evidence of hereditary nonpolyposis colorectal cancer or adenoma.
Patients who underwent low anterior resection of rectal cancer should undergo periodic examination of the rectum to evaluate for local recurrence. Although effectiveness is not proven, endoscopic ultrasonography or flexible sigmoidoscopy is suggested at 3- to 6-month intervals for the first 2 to 3 years after resection. This is independent of colonoscopy.6,7
Additionally, ASCO recommends a history and physical examination and carcinoembryonic antigen testing every 3 to 6 months for the first 5 years. Computed tomography of the chest, abdomen, and pelvis should be done annually for the first 3 years after the end of treatment.7
HEALTH PROMOTION
Maintaining a healthy body weight and a nutritionally balanced diet should be encouraged in all cancer survivors. Poor diet, lack of exercise, excessive alcohol consumption, and smoking reduce quality of life and increase the risk of cancer.2
Diet
Numerous studies have looked at dietary modifications and risk reduction, and although there is no consensus on specific dietary guidelines, there is consensus that diet modification to maintain normal body weight will improve overall quality of life.8 Patients should be encouraged to consume a well-balanced diet consisting mostly of fruits, vegetables, whole grains, and beans, and to limit consumption of animal protein.8
There is little evidence to support taking vitamins or other dietary supplements to prevent or control cancer or to prevent its recurrence. The primary care physician should assess supplement use on a regular basis during office visits.2
Exercise
Rest is an important component of the initial recovery process. Too much inactivity, however, leads to loss of physical conditioning and muscle strength. This in turn may negatively affect a patient’s ability to perform activities of daily living and may worsen fatigue associated with treatment.
Accordingly, the National Comprehensive Cancer Network recommends at least 150 minutes of moderate activity and up to 75 minutes of more rigorous activity divided throughout the week.2,8 The regimen should include endurance and muscle strength training, which aid in balance, bone, health, and functional status. The intensity of exercise should be increased in a stepwise fashion, taking into account individual capabilities and limitations.2
Cancer survivors may need specific exercise recommendations and supervised programs to ensure safety and limit long-term side effects of their treatment. For example:
Patients with neuropathy should have their stability, balance, and gait assessed before starting a new program. These patients may benefit from an aerobic exercise program that includes riding a stationary bike rather than running.
Patients with poor bone health should have their fracture risk assessed.
Those with an ostomy bag should empty the bag before physical activity. They should avoid contact sports and activities that increase intra-abdominal pressure.
Patients suffering from lymphedema should wear compression garments when engaging in physical activity. They should undergo baseline and periodic reevaluation of the lymphedema and initiate strength training in the affected body part only if the lymphedema is stable (ie, no need for therapy for 3 months, no recent infections requiring antibiotics, and no change in circumference > 10%).2
Mental health
Health promotion should focus not only on the physical health of the patient, but also on his or her emotional and psychological well-being. As they make the transition from cancer patient to survivor, many individuals may develop or have worsening depression and anxiety due to fear of recurrence. These feelings of powerlessness can linger for years after the initial treatment.
Patients should be screened regularly for signs and symptoms of depression by asking about their family and social support. Referral to support groups, psychologists, and psychiatrists may be warranted.9
MITIGATING CANCER-RELATED FATIGUE
Cancer-related fatigue involves a patient’s subjective sense of physical, emotional, and cognitive exhaustion related to cancer or treatment that is disproportionate to that expected from recent daily activity.2 Fatigue is a common complaint among survivors and can occur months to years after treatment ends.10
Patients should be screened for fatigue at regular intervals. The primary care physician should focus the history to include information regarding the onset, pattern, duration, associated factors, assessment of other treatable comorbidities, medications, psychological well-being, nutritional status, and pain level of each patient who complains of fatigue.
Laboratory tests for treatable causes of fatigue include:
- A complete blood cell count to evaluate for anemia
- A comprehensive metabolic panel to evaluate electrolytes, renal function, and hepatic function
- The thyroid-stimulating hormone level to evaluate thyroid function, particularly in breast cancer patients who have received radiation therapy.2
If no organic cause is uncovered, the focus should shift to lifestyle interventions as the treatment of choice. The treatment of fatigue in this situation is increased physical activity with the goals discussed above. Psychological intervention may be required with cognitive behavioral therapy, psychological and supportive therapies, education on sleep hygiene, and possible sleep restriction.
If alternative causes of fatigue are ruled out and physical and psychological support fails to reduce symptoms, the practitioner can consider a psychostimulant such as methylphenidate, but this should be used cautiously.2
SEXUAL DYSFUNCTION
Intimate relationships and sexuality are an important part of life and are affected by a variety of factors including physical health, psychological well-being, body image perception, and overall status of relationships. As a side effect of chemotherapy, cancer survivors may complain of erectile dysfunction, penile shortening, dyspareunia, vaginal dryness, decreased libido, anorgasmy, and changes in body image. These issues are frequently unaddressed, whether due to the physician’s discomfort in discussing the topic or to the patient’s embarrassment and reluctance to discuss the matter.11
Breast cancer patients may experience sexual dysfunction both during and after treatment due to a combination of systemic effects of treatment, changes in physical appearance leading to impaired body image, strains on partner relationships, and psychological sequelae of diagnosis and treatment of cancer.12 Manipulation and radiation to the breast affect sexual functioning by altering body contour and image. Additionally, chemotherapy can lead to early menopause and hormonal alterations due to endocrine therapies, which can negatively affect sexual organs.11
Studies have shown that treatment with tamoxifen causes less sexual dysfunction than do aromatase inhibitors. In the Arimidex, Tamoxifen, Alone or in Combination trial, therapy with anastrozole was associated with more vaginal dryness, dyspareunia, and decreased libido compared with tamoxifen.12
Treatment requires a comprehensive history, a physical examination, and a discussion of relationship satisfaction with the patient.
Vaginal dryness and dyspareunia can be treated with vaginal lubricants and moisturizers. Moisturizers are effective if used multiple times per week, whereas lubricants can be used on demand. Low-dose vaginal estrogen preparations can be used in select patients with severe vaginal dryness; the goal should be discussed. Hormone replacement therapy is contraindicated in breast cancer survivors due to the risk of recurrence.11
Prostate cancer survivors. Up to 70% of men felt their quality of life and sexual function were adversely affected after the diagnosis and treatment.13,14 Erectile dysfunction following radical prostatectomy and radiation therapy remains one of the leading causes of sexual dysfunction.14–15 Erectile dysfunction is multifactorial, with both psychogenic and organic causes. Comorbidities must be considered including hypertension, diabetes, hyperlipidemia, and smoking. Early penile rehabilitation is a proposed treatment strategy.14
First-line therapy for penile rehabilitation includes introduction of daily low-dose phosphodiesterase type 5 inhibitors as early as the time of catheter removal to within the first month after surgery. The need for daily dosing vs on-demand dosing has been controversial.15 Two large multicenter, double-blind studies had conflicting outcomes. The first reported that in men receiving nightly sildenafil (50 or 100 mg) after radical prostatectomy, 27% had increased return of spontaneous erectile function vs 4% with placebo16; the second study showed no difference between nightly and on-demand dosing.17 The consensus is that a phosphodiesterase type 5 inhibitor should be initiated early.
Second-line therapy includes intracavernosal injections and vacuum erection devices. Finally, a penile prosthesis implant can be offered to patients who have responded poorly to medical therapy.13
Colorectal cancer survivors suffer from sexually related problems similar to those stated above, including erectile dysfunction, ejaculation problems, dyspareunia, vaginal dryness, and decreased enjoyment.18 These patients should be provided treatments similar to those described above. In addition, they may suffer from body image issues, particularly those with a permanent ostomy.9
Sexual dysfunction is a multifaceted problem for patients. Encouraging couples to discuss sexual intimacy frequently helps to reveal and cope with the problems, whether physical or psychological. It is the primary care physician’s role to recognize any sexual concerns and refer to the appropriate specialist.
OSTEOPOROSIS
Osteoporosis is a metabolic bone disease characterized by low bone mineral density. As a result, bones become weak and fracture more easily from minor injuries.
Risk factors for osteoporosis include female sex, family history, advanced age, low body weight, low calcium and vitamin D levels, sedentary lifestyle, smoking, and low estrogen levels.19 Cancer treatment places patients at a greater risk for osteoporosis, particularly for those patients with chemotherapy-induced ovarian failure, those treated with aromatase inhibitors, men receiving androgen-deprivation therapy, and patients on glucocorticoid therapy. The morbidity and mortality associated with bone loss can be prevented with appropriate screening, lifestyle changes, and therapy.2
According to the National Osteoporosis Foundation Guideline for Preventing and Treating Osteoporosis, all men and postmenopausal women age 50 and older should be evaluated clinically for osteoporosis risk to determine the need for bone mineral density testing.2,19 The US Preventive Services Task Force recommends bone mineral density testing in all women age 65 and older, and for women 60 to 64 who are at high risk for bone loss. ASCO agrees, and further suggests bone mineral density screening for women with breast cancer who have risk factors such as positive family history, body weight less than 70 kg, and prior nontraumatic fracture, as well as for postmenopausal women of any age receiving aromatase inhibitors and for premenopausal women with therapy-induced ovarian failure.11
Androgen deprivation therapy is a mainstay of treatment in recurrent and metastatic prostate cancer. The effect is severe hypogonadism with reductions in serum testosterone levels. Androgen deprivation therapy accelerates bone turnover, decreases bone mineral density, and contributes to fracture risk. The National Comprehensive Cancer Network additionally suggests measuring bone mineral density at baseline for all men receiving androgen deprivation therapy or other medications associated with bone loss, repeating it 1 year after androgen deprivation therapy and then every 2 years, or as clinically indicated.20
The gold standard for measuring bone mineral density is dual-energy x-ray absorptiometry. The World Health Organization FRAX tool uses bone mineral density and several clinical factors to estimate the risk of fracture in the next 10 years, which can help guide therapy. Cancer patients with elevated fracture risk should be evaluated every 2 years. Counseling should be provided to address modifiable risk factors such as smoking, alcohol consumption, physical inactivity, and low calcium and vitamin D intake. Therapy should be strongly considered in patients with a bone mineral density below a T-score of –2.0. 2,19
Treatment begins with lifestyle modifications such as weight-bearing exercises to improve balance and muscle strength and to prevent falls, and adequate intake of calcium (≥ 1,200 mg daily) and vitamin D (800–1,000 IU daily) for adults age 50 and older. Treatment with bisphosphonates may be required.2,11,20
NEUROPATHY
Many chemotherapeutic agents can lead to neuropathy and can result in long-term disability in patients. Patients treated with taxane- and platinum-based chemotherapy are at particular risk.
Paclitaxel, used in the treatment of breast, ovarian, and lung cancer, can lead to distal neuropathy. This neuropathy commonly has a stocking-and-glove distribution and is primarily sensory; however, it may have motor and autonomic components. The neuropathy typically lessens when the medication is stopped, although in some patients it can persist and lead to long-term disability.
Treatment can include massage. Medications such as gabapentin and pregabalin can also be used, but randomized controlled trials do not support them, as they predominantly treat the tingling rather than the numbness.11
BLADDER AND BOWEL DYSFUNCTION
Urinary incontinence and dysfunction are frequent complications in prostate cancer survivors. Urinary function should be discussed regularly with patients, addressing quality of the urinary stream, difficulty emptying the bladder, timing, and incontinence.4 Urinary incontinence is frequently seen in postprostatectomy patients.
The cornerstone of treating urinary incontinence is determining the cause of the incontinence, whether it is stress or urge incontinence, or both.21 For those patients with urge incontinence alone, practitioners can address the problem with a combination of behavior modification, pelvic floor exercises, and anticholinergic medications such as oxybutynin. If the problem stems from difficulty initiating or a slow stream, physicians may consider alpha-blockers.4,21 If the incontinence is persistent, bothersome, and has components of stress incontinence, the patient should be referred to a urologist for urodynamic testing, cystoscopy, and surgical evaluation for possible placement of a male urethral sling or artificial urinary sphincter.21
Colorectal cancer survivors, particularly those who received radiation therapy, are at high risk of bowel dysfunction such as chronic diarrhea and stool incontinence. Patients should be educated about this possible side effect. Symptoms of bowel dysfunction can affect body image and interfere with social functioning and overall quality of life. Patients should be provided with coping tools such as antidiarrheal medication, stool bulking agents, changes in diet, and protective underwear.
CARDIOVASCULAR DISEASE
Evidence suggests that certain types of chemotherapy and radiation therapy increase the risk of cardiovascular disease. Prostate cancer survivors treated with androgen deprivation therapy, particularly those more than 75 years old, are at increased risk of cardiovascular disease and diabetes.22
It is recommended that men be screened with fasting plasma glucose at baseline and yearly thereafter while receiving androgen deprivation therapy. Lipid panel testing should be done 1 year from initiation of androgen deprivation therapy and then, if results are normal, every 5 years or as clinically warranted. The focus should be on primary prevention with emphasis on smoking cessation, treating hypertension per guidelines, lifestyle modifications, and treatment with aspirin and statins when clinically appropriate.20
Radiation therapy, chemotherapy, and endocrine therapy have all been suggested to lead to cardiotoxicity in breast cancer patients. Anthracycline-based chemotherapies have a well-recognized association with cardiomyopathy. Factors associated with increased risk of anthracycline-induced cardiomyopathy include older age, hypertension, pre-existing coronary artery disease, and previous mediastinal radiation.
Early detection of cardiomyopathy may lead to avoidance of irreversible cardiotoxicity, but there are currently no clear guidelines for cardiac screening in breast cancer survivors. If cardiomyopathy is detected, treatment should include beta-blockers and angiotensin-converting enzyme inhibitors as well as modification of other cardiovascular risk factors.11
A SURVIVORSHIP CARE PLAN
There is life beyond the diagnosis of cancer. As patients are living longer, with an estimated 5-year survival rate of 66.5% of all cancers in the United States, there must be a transition of care from the oncologist to the primary care physician.1 While the oncologist will remain involved in the initial years of follow-up care, these visits will go from twice a year to once a year, and eventually the patient will make a full transition to care by the primary care physician. The timing of this changeover varies from physician to physician, but the primary care physician is ultimately responsible for the follow-up.
A tool to ease this transition is a survivorship care plan. The goal of a survivorship care plan is to individualize a follow-up plan while keeping in mind the necessary surveillance as outlined. These care plans are created with the patient and oncologist and then brought to the primary care physician. While there is an abundance of literature regarding the creation and initiation of survivorship care plans, the success of these plans is uncertain. Ultimately, the goal of a survivorship care plan is to create open dialogue among the oncologist, the primary care physician, and the patient. This unique patient population requires close follow-up by a multidisciplinary team with the primary care physician serving as the steward.
- National Cancer Institute (NIH). Surveillance, Epidemiology, and End Results Program. SEER cancer stat fact sheets. http://seer.cancer.gov/statfacts. Accessed March 6, 2017.
- National Comprehensive Cancer Network (NCCN). NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines Survivorship: 2015. www.nccn.org/professionals/physician_gls/pdf/survivorship.pdf. Accessed March 6, 2017.
- Khatcheressian JL, Hurley P, Bantug E, et al. Breast cancer follow-up and management after primary treatment: American Society of Clinical Oncology Clinical Practice Guideline update. J Clin Oncol 2013; 31:961–965.
- Resnick MJ, Lacchetti C, Bergman J, et al. Prostate cancer survivorship care guideline: American Society of Clinical Oncology Clinical Practice Guideline endorsement. J Clin Oncol 2015; 33:1078–1085.
- Sountoulides P, Koletsas N, Kikidakis D, Paschalidis K, Sofikitis N. Secondary malignancies following radiotherapy for prostate cancer. Ther Adv Urol 2010; 2:119–125.
- Rex DK, Kahi CJ, Levin B, et al. Guidelines for colonoscopy surveillance after cancer resection: a consensus update by the American Cancer Society and US Multi-Society Task Force on Colorectal Cancer. CA Cancer J Clin 2006; 56:160–168.
- Meyerhardt JA, Mangu PB, Flynn PJ, et al; American Society of Clinical Oncology. Follow-up care, surveillance protocol, and secondary prevention measures for survivors of colorectal cancer: American Society of Clinical Oncology clinical practice guideline endorsement. J Clin Oncol 2013; 31:4465–4470.
- Davies NJ, Batehup L, Thomas R. The role of diet and physical activity in breast, colorectal, and prostate cancer survivorship: a review of the literature. Br J Cancer 2011; 105(suppl 1):S52–S73.
- Miller K, editor. Excellent Care for Cancer Survivors: A Guide to Fully Meet Their Needs in Medical Offices and in the Community (Praeger Series on Contemporary Health & Living). 1st ed. Santa Barbara, CA: Praeger; 2012.
- Stanton AL, Rowland JH, Ganz PA. Life after diagnosis and treatment of cancer in adulthood: contributions from psychosocial oncology research. Am Psychol 2015; 70:159–174.
- Stan D, Loprinzi CL, Ruddy KJ. Breast cancer survivorship issues. Hematol Oncol Clin North Am 2013; 27:805–827.
- Fallowfield L, Cella D, Cuzick J, Francis S, Locker G, Howell A. Quality of life of postmenopausal women in the Arimidex, Tamoxifen, Alone or in Combination (ATAC) Adjuvant Breast Cancer Trial. J Clin Oncol 2004; 22:426–471.
- Chung E, Gillman M. Prostate cancer survivorship: a review of erectile dysfunction and penile rehabilitation after prostate cancer therapy. Med J Aust 2014; 200:582–585.
- Sherer BA, Levine LA. Current management of erectile dysfunction in prostate cancer survivors. Curr Opin Urol 2014; 24:401–416.
- Chung E, Brock G. Sexual rehabilitation and cancer survivorship: a state of art review of current literature and management strategies in male sexual dysfunction among prostate cancer survivors. J Sex Med 2013; 10(suppl 1):102–111.
- Padma-Nathan H, McCullough AR, Levine LA, et al; Study Group. Randomized, double-blind, placebo-controlled study of postoperative nightly sildenafil citrate for the prevention of erectile dysfunction after bilateral nerve-sparing radical prostatectomy. Int J Impot Res 2008; 20:479–486.
- Montorsi F, Brock G, Lee J, et al. Effect of nightly versus on-demand vardenafil on recovery of erectile function in men following bilateral nerve-sparing radical prostatectomy. Eur Urol 2008; 54:924–931.
- Den Oudsten BL, Traa MJ, Thong MS, et al. Higher prevalence of sexual dysfunction in colon and rectal cancer survivors compared with the normative population: a population-based study. Eur J Cancer 2012; 48:3161–3170.
- National Osteoporosis Foundation (NOF). http://nof.org. Accessed March 3, 2017.
- Saylor PJ, Keating NL, Smith MR. Prostate cancer survivorship: prevention and treatment of the adverse effects of androgen deprivation therapy. J Gen Intern Med 2009; 24(suppl 2):S389–S394.
- Gupta S, Peterson AC. Stress urinary incontinence in the prostate cancer survivor. Curr Opin Urol 2014; 24:395–400.
- Morgans AK, Fan KH, Koyama T, et al. Influence of age on incident diabetes and cardiovascular disease in prostate cancer survivors receiving androgen deprivation therapy. J Urol 2015; 193:1226–1231.
- National Cancer Institute (NIH). Surveillance, Epidemiology, and End Results Program. SEER cancer stat fact sheets. http://seer.cancer.gov/statfacts. Accessed March 6, 2017.
- National Comprehensive Cancer Network (NCCN). NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines Survivorship: 2015. www.nccn.org/professionals/physician_gls/pdf/survivorship.pdf. Accessed March 6, 2017.
- Khatcheressian JL, Hurley P, Bantug E, et al. Breast cancer follow-up and management after primary treatment: American Society of Clinical Oncology Clinical Practice Guideline update. J Clin Oncol 2013; 31:961–965.
- Resnick MJ, Lacchetti C, Bergman J, et al. Prostate cancer survivorship care guideline: American Society of Clinical Oncology Clinical Practice Guideline endorsement. J Clin Oncol 2015; 33:1078–1085.
- Sountoulides P, Koletsas N, Kikidakis D, Paschalidis K, Sofikitis N. Secondary malignancies following radiotherapy for prostate cancer. Ther Adv Urol 2010; 2:119–125.
- Rex DK, Kahi CJ, Levin B, et al. Guidelines for colonoscopy surveillance after cancer resection: a consensus update by the American Cancer Society and US Multi-Society Task Force on Colorectal Cancer. CA Cancer J Clin 2006; 56:160–168.
- Meyerhardt JA, Mangu PB, Flynn PJ, et al; American Society of Clinical Oncology. Follow-up care, surveillance protocol, and secondary prevention measures for survivors of colorectal cancer: American Society of Clinical Oncology clinical practice guideline endorsement. J Clin Oncol 2013; 31:4465–4470.
- Davies NJ, Batehup L, Thomas R. The role of diet and physical activity in breast, colorectal, and prostate cancer survivorship: a review of the literature. Br J Cancer 2011; 105(suppl 1):S52–S73.
- Miller K, editor. Excellent Care for Cancer Survivors: A Guide to Fully Meet Their Needs in Medical Offices and in the Community (Praeger Series on Contemporary Health & Living). 1st ed. Santa Barbara, CA: Praeger; 2012.
- Stanton AL, Rowland JH, Ganz PA. Life after diagnosis and treatment of cancer in adulthood: contributions from psychosocial oncology research. Am Psychol 2015; 70:159–174.
- Stan D, Loprinzi CL, Ruddy KJ. Breast cancer survivorship issues. Hematol Oncol Clin North Am 2013; 27:805–827.
- Fallowfield L, Cella D, Cuzick J, Francis S, Locker G, Howell A. Quality of life of postmenopausal women in the Arimidex, Tamoxifen, Alone or in Combination (ATAC) Adjuvant Breast Cancer Trial. J Clin Oncol 2004; 22:426–471.
- Chung E, Gillman M. Prostate cancer survivorship: a review of erectile dysfunction and penile rehabilitation after prostate cancer therapy. Med J Aust 2014; 200:582–585.
- Sherer BA, Levine LA. Current management of erectile dysfunction in prostate cancer survivors. Curr Opin Urol 2014; 24:401–416.
- Chung E, Brock G. Sexual rehabilitation and cancer survivorship: a state of art review of current literature and management strategies in male sexual dysfunction among prostate cancer survivors. J Sex Med 2013; 10(suppl 1):102–111.
- Padma-Nathan H, McCullough AR, Levine LA, et al; Study Group. Randomized, double-blind, placebo-controlled study of postoperative nightly sildenafil citrate for the prevention of erectile dysfunction after bilateral nerve-sparing radical prostatectomy. Int J Impot Res 2008; 20:479–486.
- Montorsi F, Brock G, Lee J, et al. Effect of nightly versus on-demand vardenafil on recovery of erectile function in men following bilateral nerve-sparing radical prostatectomy. Eur Urol 2008; 54:924–931.
- Den Oudsten BL, Traa MJ, Thong MS, et al. Higher prevalence of sexual dysfunction in colon and rectal cancer survivors compared with the normative population: a population-based study. Eur J Cancer 2012; 48:3161–3170.
- National Osteoporosis Foundation (NOF). http://nof.org. Accessed March 3, 2017.
- Saylor PJ, Keating NL, Smith MR. Prostate cancer survivorship: prevention and treatment of the adverse effects of androgen deprivation therapy. J Gen Intern Med 2009; 24(suppl 2):S389–S394.
- Gupta S, Peterson AC. Stress urinary incontinence in the prostate cancer survivor. Curr Opin Urol 2014; 24:395–400.
- Morgans AK, Fan KH, Koyama T, et al. Influence of age on incident diabetes and cardiovascular disease in prostate cancer survivors receiving androgen deprivation therapy. J Urol 2015; 193:1226–1231.
KEY POINTS
- The American Society of Clinical Oncology has developed evidence-based recommendations for follow-up care and surveillance for new and recurrent cancer in cancer survivors. In general, this surveillance should be more frequent in the first months and years after cancer treatment but can become less so as time goes on.
- Health promotion in cancer survivors involves the same advice regarding smoking cessation, diet, exercise, and mental health that all patients require.
- Depending on the type of cancer and treatment, long-term adverse effects include fatigue, sexual dysfunction, osteoporosis, neuropathy, bladder and bowel dysfunction, and cardiovascular disease.
- A survivorship care plan can be drawn up with input from the patient, oncologist, primary care physician, and other caregivers so that everyone can be clear as to what is going on.
Which patients with nonalcoholic fatty liver disease should undergo liver biopsy?
Patients should undergo biopsy to guide management and prognosis if suspected of having steatohepatitis or fibrosis.
WHAT IS NAFLD?
Nonalcoholic fatty liver disease (NAFLD) is the most common form of chronic liver disease in the United States and is the second most common reason for liver transplant.1 It is thought to be the hepatic consequence of systemic insulin resistance and the metabolic syndrome characterized by obesity, dyslipidemia, and type 2 diabetes mellitus.
WHAT IS THE RELATIONSHIP BETWEEN NAFLD AND NASH?
NAFLD is defined by the accumulation of hepatic fat as evidenced by imaging or histologic study and without a coexisting cause of chronic liver disease or a secondary cause of hepatic steatosis, including significant alcohol use, medications, or an inherited or acquired metabolic state.
NAFLD has two subtypes: nonalcoholic fatty liver (NAFL) and nonalcoholic steatohepatitis (NASH). NAFL is characterized by steatosis, including inflammation, in at least 5% of hepatocytes. NASH is defined by a constellation of features that include steatosis, lobular and portal inflammation, and liver cell injury in the form of hepatocyte ballooning.2
Clinically, it is especially important to distinguish patients with the NASH subtype, as most NAFLD patients have steatosis without necroinflammation or fibrosis and do not require medical therapy.
CLINICAL SIGNIFICANCE OF NAFLD: NASH IS WORSE THAN NAFL
NAFL carries an excellent prognosis in terms of histologic progression of liver disease, whereas NASH can histologically progress to fibrosis and, in up to 15% of patients, to cirrhosis.3
Progression of fibrosis poses secondary risks, including complications associated with portal hypertension (ascites, variceal hemorrhage, hepatic encephalopathy), end-stage liver disease, and hepatocellular carcinoma. In Western countries, 4% to 22% of cases of hepatocellular carcinoma are attributed to NAFLD.4
In a 2015 meta-analysis, patients with NAFL and stage 0 fibrosis at baseline progressed 1 stage of fibrosis over 14.3 years, whereas patients with NASH and stage 0 fibrosis experienced an accelerated rate of progression, advancing 1 stage of fibrosis over 7.1 years.5 A systematic review of patients with NASH identified age and inflammation on initial liver biopsy as independent predictors of progression to advanced fibrosis.6
Patients with NAFLD have a higher all-cause mortality rate than patients of the same age and sex without NAFLD.7
HOW SHOULD PATIENTS WITH NAFLD BE EVALUATED?
Initial evaluation of a patient with suspected NAFLD should include a thorough serologic evaluation to exclude coexisting causes of chronic liver disease. Tests include:
- A viral hepatitis panel
- Antinuclear antibody (ANA)
- Antismooth muscle antibody (ASMA)
- Antimitochondrial antibody (AMA)
- Iron studies
- Alpha-1 antitrypsin level
- Ceruloplasmin level.
Aminotransferase levels and imaging studies (ultrasonography, computed tomography, and magnetic resonance imaging) do not reliably convey the degree of NASH and fibrosis.
Biopsy. Whereas sensitive serologic tests have been introduced to detect and diagnose many causes of liver disease, liver biopsy (transjugular or percutaneous) with histologic examination remains the only way to accurately assess the degree of steatosis and, thus, to distinguish NAFL from NASH.2
The Pathology Committee of the NASH Clinical Research Network designed and validated a NAFLD scoring system,8,9 with points allocated for degrees of:
- Steatosis (0–3)
- Lobular inflammation (0–2)
- Hepatocellular ballooning (0–2)
- Fibrosis (0–4).
A NAFLD Activity Score of less than 3 is consistent with “not NASH,” a score of 3 or 4 with borderline NASH, and a score of 5 or more with NASH.8 However, the diagnosis of NASH is not based on the NAFLD scoring system, but rather on the pathologist’s overall evaluation of the liver biopsy.9
The metabolic syndrome is an established risk factor for steatohepatitis in patients with NAFLD, and its presence in patients with persistently elevated liver biochemical tests may help identify those who would benefit from further diagnostic and prognostic evaluation, including liver biopsy.2,10 In addition, a 2008 study that used a decision-tree modeling system demonstrated that early liver biopsy could provide a survival benefit.11
NONINVASIVE TESTING
Since liver biopsy is associated with procedure-related morbidity, mortality, and cost, researchers have been developing noninvasive markers of steatohepatitis and fibrosis.12
The NAFLD fibrosis score—based on patient age, body mass index, hyperglycemia, platelet count, albumin, and ratio of aspartate aminotransferase to alanine aminotransferase—has been shown to have an area under the receiver operating curve of 0.85 for predicting advanced fibrosis, with a negative predictive value of 88% to 93% and a positive predictive value of 82% to 90%.13 The NAFLD fibrosis score can be used to identify patients who may have fibrosis or cirrhosis and can help direct the use of liver biopsy in patients who would benefit from prognostication and potential treatment.
Of note, the NAFLD fibrosis score is only slightly less accurate than the imaging techniques of magnetic resonance elastography and transient elastography, particularly when the relative costs are considered.14
INDICATIONS FOR LIVER BIOPSY
There are two clear indications for liver biopsy in NAFLD.
Before starting any pharmacologic therapy for NAFLD. Most NAFLD patients have steatosis without NASH or fibrosis and do not require medical therapy. Importantly, the available treatments have significant adverse effects—prostate cancer with vitamin E, bladder cancer and weight gain with pioglitazone, and nausea with pentoxifylline.
Diagnosis. Up to 30% of patients have elevated serum ferritin and autoantibodies, including ANA, ASMA, and AMA. Liver biopsy is often needed to exclude hemochromatosis or autoimmune hepatitis.15 Occasionally, a possible confounding drug-induced liver injury may necessitate a liver biopsy.
LIFESTYLE MODIFICATION
The first step in managing patients who have NAFLD is to treat components of the metabolic syndrome, including obesity, dyslipidemia, and type 2 diabetes.
In a randomized controlled trial in 31 obese patients with biopsy-proven NASH,16 intensive lifestyle modification (consisting of diet, behavior modification, and 200 minutes of exercise weekly for 48 weeks) was shown to improve histologic NAFLD Activity Scores, including degrees of steatosis, necrosis, and inflammation. As a result, weight loss of 7% to 9% is generally recommended for patients with NAFLD.
DRUG THERAPIES
Much research has been directed toward identifying risk factors for progression of fibrosis and toward developing new therapies for patients with NAFLD. A 2015 meta-analysis concluded that pentoxifylline and obeticholic acid improve fibrosis, while vitamin E, thiazolidinediones, and obeticholic acid improve necroinflammation associated with NASH.17
Long-term studies are needed to determine the impact of these drugs on NASH-related morbidity, mortality, and need for liver transplant.
TAKE-AWAY POINTS
- NAFLD is the leading cause of chronic liver disease in the United States and is increasing as a reason for liver transplant.
- NASH is associated with the metabolic syndrome and can progress to fibrosis, cirrhosis, and end-stage liver disease. Noninvasive markers such as the NAFLD Activity Score can be useful in identifying patients who may have advanced fibrosis and can select patients who should be directed to liver biopsy for definitive diagnosis.8,9
- Liver biopsy is the gold standard for diagnosing steatohepatitis and fibrosis and is the only diagnostic tool used in clinical trials to direct pharmacotherapy for NASH.
- Liver biopsy should be reserved for patients suspected of having NASH or fibrosis and who might benefit from therapy.
- Liver biopsy is also indicated for those NAFLD patients who have confounding laboratory findings such as an elevated ferritin level and autoantibodies including ANA, ASMA, and AMA.
- Wong RJ, Aquilar M, Cheung R, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology 2015; 148:547–555.
- Chalasani N, Younossi Z, Lavine JE, et al; American Gastroenterological Association; American Association for the Study of Liver Diseases; American College of Gastroenterology. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology 2012; 142:1592–1609.
- Ekstedt M, Franzén LE, Mathiesen UL, et al. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology 2006; 44:865–873.
- Michelotti GA, Machado MV, Diehl AM. NAFLD, NASH and liver cancer. Nat Rev Gastroenterol Hepatol 2013; 10:656–665.
- Singh S, Allen AM, Wang Z, Prokop LJ, Murad MH, Loomba R. Fibrosis progression in nonalcoholic fatty liver vs nonalcoholic steatohepatitis: a systematic review and meta-analysis of paired-biopsy studies. Clin Gastroenterol Hepatol 2015; 13:643–654.
- Argo CK, Northup PG, Al-Osaimi AM, Caldwell SH. Systematic review of risk factors for fibrosis progression in non-alcoholic steatohepatitis. J Hepatol 2009; 51:371–379.
- Adams LA, Lymp JF, St. Sauver J, et al. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology 2005; 129:113–121.
- Kleiner DE, Brunt EM, Van Natta M, et al; Nonalcoholic Steatohepatitis Clinical Research Network. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 2005; 41:1313–1321.
- Brunt EM, Kleiner DE, Wilson LA, Belt P, Neuschwander-Tetri BA; NASH Clinical Research Network (CRN). Nonalcoholic fatty liver disease (NAFLD) activity score and the histopathologic diagnosis in NAFLD: distinct clinicopathologic meanings. Hepatology 2011; 53:810–820.
- Marchesini G, Bugianesi E, Forlani G, et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology 2003; 37:917–923.
- Gaidos JK, Hillner BE, Sanyal AJ. A decision analysis study of the value of a liver biopsy in nonalcoholic steatohepatitis. Liver Int 2008; 28:650–658.
- Musso G, Gambino R, Cassader M, Pagano G. Meta-analysis: natural history of non-alcoholic fatty liver disease (NAFLD) and diagnostic accuracy of non-invasive tests for liver disease severity. Ann Med 2011; 43:617–649.
- Angulo P, Hui JM, Marchesini G, et al. The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology 2007; 45:846–854.
- Imajo K, Kessoku T, Honda Y, et al. Magnetic resonance imaging more accurately classifies steatosis and fibrosis in patients with nonalcoholic fatty liver disease than transient elastography. Gastroenterology 2016; 150:626–637.e7.
- Neuschwander-Tetri BA, Clark JM, Bass NM, et al; NASH Clinical Research Network. Clinical, laboratory and histological associations in adults with nonalcoholic fatty liver disease. Hepatology 2010; 52:913–924.
- Promrat K, Kleiner DE, Niemeier HM, et al. Randomized controlled trial testing the effects of weight loss on nonalcoholic steatohepatitis. Hepatology 2010; 51:121–129.
- Singh S, Khera R, Allen AM, Murad H, Loomba R. Comparative effectiveness of pharmacological interventions for nonalcoholic steatohepatitis: a systematic review and network meta-analysis. Hepatology 2015; 62:1417–1432.
Patients should undergo biopsy to guide management and prognosis if suspected of having steatohepatitis or fibrosis.
WHAT IS NAFLD?
Nonalcoholic fatty liver disease (NAFLD) is the most common form of chronic liver disease in the United States and is the second most common reason for liver transplant.1 It is thought to be the hepatic consequence of systemic insulin resistance and the metabolic syndrome characterized by obesity, dyslipidemia, and type 2 diabetes mellitus.
WHAT IS THE RELATIONSHIP BETWEEN NAFLD AND NASH?
NAFLD is defined by the accumulation of hepatic fat as evidenced by imaging or histologic study and without a coexisting cause of chronic liver disease or a secondary cause of hepatic steatosis, including significant alcohol use, medications, or an inherited or acquired metabolic state.
NAFLD has two subtypes: nonalcoholic fatty liver (NAFL) and nonalcoholic steatohepatitis (NASH). NAFL is characterized by steatosis, including inflammation, in at least 5% of hepatocytes. NASH is defined by a constellation of features that include steatosis, lobular and portal inflammation, and liver cell injury in the form of hepatocyte ballooning.2
Clinically, it is especially important to distinguish patients with the NASH subtype, as most NAFLD patients have steatosis without necroinflammation or fibrosis and do not require medical therapy.
CLINICAL SIGNIFICANCE OF NAFLD: NASH IS WORSE THAN NAFL
NAFL carries an excellent prognosis in terms of histologic progression of liver disease, whereas NASH can histologically progress to fibrosis and, in up to 15% of patients, to cirrhosis.3
Progression of fibrosis poses secondary risks, including complications associated with portal hypertension (ascites, variceal hemorrhage, hepatic encephalopathy), end-stage liver disease, and hepatocellular carcinoma. In Western countries, 4% to 22% of cases of hepatocellular carcinoma are attributed to NAFLD.4
In a 2015 meta-analysis, patients with NAFL and stage 0 fibrosis at baseline progressed 1 stage of fibrosis over 14.3 years, whereas patients with NASH and stage 0 fibrosis experienced an accelerated rate of progression, advancing 1 stage of fibrosis over 7.1 years.5 A systematic review of patients with NASH identified age and inflammation on initial liver biopsy as independent predictors of progression to advanced fibrosis.6
Patients with NAFLD have a higher all-cause mortality rate than patients of the same age and sex without NAFLD.7
HOW SHOULD PATIENTS WITH NAFLD BE EVALUATED?
Initial evaluation of a patient with suspected NAFLD should include a thorough serologic evaluation to exclude coexisting causes of chronic liver disease. Tests include:
- A viral hepatitis panel
- Antinuclear antibody (ANA)
- Antismooth muscle antibody (ASMA)
- Antimitochondrial antibody (AMA)
- Iron studies
- Alpha-1 antitrypsin level
- Ceruloplasmin level.
Aminotransferase levels and imaging studies (ultrasonography, computed tomography, and magnetic resonance imaging) do not reliably convey the degree of NASH and fibrosis.
Biopsy. Whereas sensitive serologic tests have been introduced to detect and diagnose many causes of liver disease, liver biopsy (transjugular or percutaneous) with histologic examination remains the only way to accurately assess the degree of steatosis and, thus, to distinguish NAFL from NASH.2
The Pathology Committee of the NASH Clinical Research Network designed and validated a NAFLD scoring system,8,9 with points allocated for degrees of:
- Steatosis (0–3)
- Lobular inflammation (0–2)
- Hepatocellular ballooning (0–2)
- Fibrosis (0–4).
A NAFLD Activity Score of less than 3 is consistent with “not NASH,” a score of 3 or 4 with borderline NASH, and a score of 5 or more with NASH.8 However, the diagnosis of NASH is not based on the NAFLD scoring system, but rather on the pathologist’s overall evaluation of the liver biopsy.9
The metabolic syndrome is an established risk factor for steatohepatitis in patients with NAFLD, and its presence in patients with persistently elevated liver biochemical tests may help identify those who would benefit from further diagnostic and prognostic evaluation, including liver biopsy.2,10 In addition, a 2008 study that used a decision-tree modeling system demonstrated that early liver biopsy could provide a survival benefit.11
NONINVASIVE TESTING
Since liver biopsy is associated with procedure-related morbidity, mortality, and cost, researchers have been developing noninvasive markers of steatohepatitis and fibrosis.12
The NAFLD fibrosis score—based on patient age, body mass index, hyperglycemia, platelet count, albumin, and ratio of aspartate aminotransferase to alanine aminotransferase—has been shown to have an area under the receiver operating curve of 0.85 for predicting advanced fibrosis, with a negative predictive value of 88% to 93% and a positive predictive value of 82% to 90%.13 The NAFLD fibrosis score can be used to identify patients who may have fibrosis or cirrhosis and can help direct the use of liver biopsy in patients who would benefit from prognostication and potential treatment.
Of note, the NAFLD fibrosis score is only slightly less accurate than the imaging techniques of magnetic resonance elastography and transient elastography, particularly when the relative costs are considered.14
INDICATIONS FOR LIVER BIOPSY
There are two clear indications for liver biopsy in NAFLD.
Before starting any pharmacologic therapy for NAFLD. Most NAFLD patients have steatosis without NASH or fibrosis and do not require medical therapy. Importantly, the available treatments have significant adverse effects—prostate cancer with vitamin E, bladder cancer and weight gain with pioglitazone, and nausea with pentoxifylline.
Diagnosis. Up to 30% of patients have elevated serum ferritin and autoantibodies, including ANA, ASMA, and AMA. Liver biopsy is often needed to exclude hemochromatosis or autoimmune hepatitis.15 Occasionally, a possible confounding drug-induced liver injury may necessitate a liver biopsy.
LIFESTYLE MODIFICATION
The first step in managing patients who have NAFLD is to treat components of the metabolic syndrome, including obesity, dyslipidemia, and type 2 diabetes.
In a randomized controlled trial in 31 obese patients with biopsy-proven NASH,16 intensive lifestyle modification (consisting of diet, behavior modification, and 200 minutes of exercise weekly for 48 weeks) was shown to improve histologic NAFLD Activity Scores, including degrees of steatosis, necrosis, and inflammation. As a result, weight loss of 7% to 9% is generally recommended for patients with NAFLD.
DRUG THERAPIES
Much research has been directed toward identifying risk factors for progression of fibrosis and toward developing new therapies for patients with NAFLD. A 2015 meta-analysis concluded that pentoxifylline and obeticholic acid improve fibrosis, while vitamin E, thiazolidinediones, and obeticholic acid improve necroinflammation associated with NASH.17
Long-term studies are needed to determine the impact of these drugs on NASH-related morbidity, mortality, and need for liver transplant.
TAKE-AWAY POINTS
- NAFLD is the leading cause of chronic liver disease in the United States and is increasing as a reason for liver transplant.
- NASH is associated with the metabolic syndrome and can progress to fibrosis, cirrhosis, and end-stage liver disease. Noninvasive markers such as the NAFLD Activity Score can be useful in identifying patients who may have advanced fibrosis and can select patients who should be directed to liver biopsy for definitive diagnosis.8,9
- Liver biopsy is the gold standard for diagnosing steatohepatitis and fibrosis and is the only diagnostic tool used in clinical trials to direct pharmacotherapy for NASH.
- Liver biopsy should be reserved for patients suspected of having NASH or fibrosis and who might benefit from therapy.
- Liver biopsy is also indicated for those NAFLD patients who have confounding laboratory findings such as an elevated ferritin level and autoantibodies including ANA, ASMA, and AMA.
Patients should undergo biopsy to guide management and prognosis if suspected of having steatohepatitis or fibrosis.
WHAT IS NAFLD?
Nonalcoholic fatty liver disease (NAFLD) is the most common form of chronic liver disease in the United States and is the second most common reason for liver transplant.1 It is thought to be the hepatic consequence of systemic insulin resistance and the metabolic syndrome characterized by obesity, dyslipidemia, and type 2 diabetes mellitus.
WHAT IS THE RELATIONSHIP BETWEEN NAFLD AND NASH?
NAFLD is defined by the accumulation of hepatic fat as evidenced by imaging or histologic study and without a coexisting cause of chronic liver disease or a secondary cause of hepatic steatosis, including significant alcohol use, medications, or an inherited or acquired metabolic state.
NAFLD has two subtypes: nonalcoholic fatty liver (NAFL) and nonalcoholic steatohepatitis (NASH). NAFL is characterized by steatosis, including inflammation, in at least 5% of hepatocytes. NASH is defined by a constellation of features that include steatosis, lobular and portal inflammation, and liver cell injury in the form of hepatocyte ballooning.2
Clinically, it is especially important to distinguish patients with the NASH subtype, as most NAFLD patients have steatosis without necroinflammation or fibrosis and do not require medical therapy.
CLINICAL SIGNIFICANCE OF NAFLD: NASH IS WORSE THAN NAFL
NAFL carries an excellent prognosis in terms of histologic progression of liver disease, whereas NASH can histologically progress to fibrosis and, in up to 15% of patients, to cirrhosis.3
Progression of fibrosis poses secondary risks, including complications associated with portal hypertension (ascites, variceal hemorrhage, hepatic encephalopathy), end-stage liver disease, and hepatocellular carcinoma. In Western countries, 4% to 22% of cases of hepatocellular carcinoma are attributed to NAFLD.4
In a 2015 meta-analysis, patients with NAFL and stage 0 fibrosis at baseline progressed 1 stage of fibrosis over 14.3 years, whereas patients with NASH and stage 0 fibrosis experienced an accelerated rate of progression, advancing 1 stage of fibrosis over 7.1 years.5 A systematic review of patients with NASH identified age and inflammation on initial liver biopsy as independent predictors of progression to advanced fibrosis.6
Patients with NAFLD have a higher all-cause mortality rate than patients of the same age and sex without NAFLD.7
HOW SHOULD PATIENTS WITH NAFLD BE EVALUATED?
Initial evaluation of a patient with suspected NAFLD should include a thorough serologic evaluation to exclude coexisting causes of chronic liver disease. Tests include:
- A viral hepatitis panel
- Antinuclear antibody (ANA)
- Antismooth muscle antibody (ASMA)
- Antimitochondrial antibody (AMA)
- Iron studies
- Alpha-1 antitrypsin level
- Ceruloplasmin level.
Aminotransferase levels and imaging studies (ultrasonography, computed tomography, and magnetic resonance imaging) do not reliably convey the degree of NASH and fibrosis.
Biopsy. Whereas sensitive serologic tests have been introduced to detect and diagnose many causes of liver disease, liver biopsy (transjugular or percutaneous) with histologic examination remains the only way to accurately assess the degree of steatosis and, thus, to distinguish NAFL from NASH.2
The Pathology Committee of the NASH Clinical Research Network designed and validated a NAFLD scoring system,8,9 with points allocated for degrees of:
- Steatosis (0–3)
- Lobular inflammation (0–2)
- Hepatocellular ballooning (0–2)
- Fibrosis (0–4).
A NAFLD Activity Score of less than 3 is consistent with “not NASH,” a score of 3 or 4 with borderline NASH, and a score of 5 or more with NASH.8 However, the diagnosis of NASH is not based on the NAFLD scoring system, but rather on the pathologist’s overall evaluation of the liver biopsy.9
The metabolic syndrome is an established risk factor for steatohepatitis in patients with NAFLD, and its presence in patients with persistently elevated liver biochemical tests may help identify those who would benefit from further diagnostic and prognostic evaluation, including liver biopsy.2,10 In addition, a 2008 study that used a decision-tree modeling system demonstrated that early liver biopsy could provide a survival benefit.11
NONINVASIVE TESTING
Since liver biopsy is associated with procedure-related morbidity, mortality, and cost, researchers have been developing noninvasive markers of steatohepatitis and fibrosis.12
The NAFLD fibrosis score—based on patient age, body mass index, hyperglycemia, platelet count, albumin, and ratio of aspartate aminotransferase to alanine aminotransferase—has been shown to have an area under the receiver operating curve of 0.85 for predicting advanced fibrosis, with a negative predictive value of 88% to 93% and a positive predictive value of 82% to 90%.13 The NAFLD fibrosis score can be used to identify patients who may have fibrosis or cirrhosis and can help direct the use of liver biopsy in patients who would benefit from prognostication and potential treatment.
Of note, the NAFLD fibrosis score is only slightly less accurate than the imaging techniques of magnetic resonance elastography and transient elastography, particularly when the relative costs are considered.14
INDICATIONS FOR LIVER BIOPSY
There are two clear indications for liver biopsy in NAFLD.
Before starting any pharmacologic therapy for NAFLD. Most NAFLD patients have steatosis without NASH or fibrosis and do not require medical therapy. Importantly, the available treatments have significant adverse effects—prostate cancer with vitamin E, bladder cancer and weight gain with pioglitazone, and nausea with pentoxifylline.
Diagnosis. Up to 30% of patients have elevated serum ferritin and autoantibodies, including ANA, ASMA, and AMA. Liver biopsy is often needed to exclude hemochromatosis or autoimmune hepatitis.15 Occasionally, a possible confounding drug-induced liver injury may necessitate a liver biopsy.
LIFESTYLE MODIFICATION
The first step in managing patients who have NAFLD is to treat components of the metabolic syndrome, including obesity, dyslipidemia, and type 2 diabetes.
In a randomized controlled trial in 31 obese patients with biopsy-proven NASH,16 intensive lifestyle modification (consisting of diet, behavior modification, and 200 minutes of exercise weekly for 48 weeks) was shown to improve histologic NAFLD Activity Scores, including degrees of steatosis, necrosis, and inflammation. As a result, weight loss of 7% to 9% is generally recommended for patients with NAFLD.
DRUG THERAPIES
Much research has been directed toward identifying risk factors for progression of fibrosis and toward developing new therapies for patients with NAFLD. A 2015 meta-analysis concluded that pentoxifylline and obeticholic acid improve fibrosis, while vitamin E, thiazolidinediones, and obeticholic acid improve necroinflammation associated with NASH.17
Long-term studies are needed to determine the impact of these drugs on NASH-related morbidity, mortality, and need for liver transplant.
TAKE-AWAY POINTS
- NAFLD is the leading cause of chronic liver disease in the United States and is increasing as a reason for liver transplant.
- NASH is associated with the metabolic syndrome and can progress to fibrosis, cirrhosis, and end-stage liver disease. Noninvasive markers such as the NAFLD Activity Score can be useful in identifying patients who may have advanced fibrosis and can select patients who should be directed to liver biopsy for definitive diagnosis.8,9
- Liver biopsy is the gold standard for diagnosing steatohepatitis and fibrosis and is the only diagnostic tool used in clinical trials to direct pharmacotherapy for NASH.
- Liver biopsy should be reserved for patients suspected of having NASH or fibrosis and who might benefit from therapy.
- Liver biopsy is also indicated for those NAFLD patients who have confounding laboratory findings such as an elevated ferritin level and autoantibodies including ANA, ASMA, and AMA.
- Wong RJ, Aquilar M, Cheung R, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology 2015; 148:547–555.
- Chalasani N, Younossi Z, Lavine JE, et al; American Gastroenterological Association; American Association for the Study of Liver Diseases; American College of Gastroenterology. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology 2012; 142:1592–1609.
- Ekstedt M, Franzén LE, Mathiesen UL, et al. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology 2006; 44:865–873.
- Michelotti GA, Machado MV, Diehl AM. NAFLD, NASH and liver cancer. Nat Rev Gastroenterol Hepatol 2013; 10:656–665.
- Singh S, Allen AM, Wang Z, Prokop LJ, Murad MH, Loomba R. Fibrosis progression in nonalcoholic fatty liver vs nonalcoholic steatohepatitis: a systematic review and meta-analysis of paired-biopsy studies. Clin Gastroenterol Hepatol 2015; 13:643–654.
- Argo CK, Northup PG, Al-Osaimi AM, Caldwell SH. Systematic review of risk factors for fibrosis progression in non-alcoholic steatohepatitis. J Hepatol 2009; 51:371–379.
- Adams LA, Lymp JF, St. Sauver J, et al. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology 2005; 129:113–121.
- Kleiner DE, Brunt EM, Van Natta M, et al; Nonalcoholic Steatohepatitis Clinical Research Network. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 2005; 41:1313–1321.
- Brunt EM, Kleiner DE, Wilson LA, Belt P, Neuschwander-Tetri BA; NASH Clinical Research Network (CRN). Nonalcoholic fatty liver disease (NAFLD) activity score and the histopathologic diagnosis in NAFLD: distinct clinicopathologic meanings. Hepatology 2011; 53:810–820.
- Marchesini G, Bugianesi E, Forlani G, et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology 2003; 37:917–923.
- Gaidos JK, Hillner BE, Sanyal AJ. A decision analysis study of the value of a liver biopsy in nonalcoholic steatohepatitis. Liver Int 2008; 28:650–658.
- Musso G, Gambino R, Cassader M, Pagano G. Meta-analysis: natural history of non-alcoholic fatty liver disease (NAFLD) and diagnostic accuracy of non-invasive tests for liver disease severity. Ann Med 2011; 43:617–649.
- Angulo P, Hui JM, Marchesini G, et al. The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology 2007; 45:846–854.
- Imajo K, Kessoku T, Honda Y, et al. Magnetic resonance imaging more accurately classifies steatosis and fibrosis in patients with nonalcoholic fatty liver disease than transient elastography. Gastroenterology 2016; 150:626–637.e7.
- Neuschwander-Tetri BA, Clark JM, Bass NM, et al; NASH Clinical Research Network. Clinical, laboratory and histological associations in adults with nonalcoholic fatty liver disease. Hepatology 2010; 52:913–924.
- Promrat K, Kleiner DE, Niemeier HM, et al. Randomized controlled trial testing the effects of weight loss on nonalcoholic steatohepatitis. Hepatology 2010; 51:121–129.
- Singh S, Khera R, Allen AM, Murad H, Loomba R. Comparative effectiveness of pharmacological interventions for nonalcoholic steatohepatitis: a systematic review and network meta-analysis. Hepatology 2015; 62:1417–1432.
- Wong RJ, Aquilar M, Cheung R, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology 2015; 148:547–555.
- Chalasani N, Younossi Z, Lavine JE, et al; American Gastroenterological Association; American Association for the Study of Liver Diseases; American College of Gastroenterology. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology 2012; 142:1592–1609.
- Ekstedt M, Franzén LE, Mathiesen UL, et al. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology 2006; 44:865–873.
- Michelotti GA, Machado MV, Diehl AM. NAFLD, NASH and liver cancer. Nat Rev Gastroenterol Hepatol 2013; 10:656–665.
- Singh S, Allen AM, Wang Z, Prokop LJ, Murad MH, Loomba R. Fibrosis progression in nonalcoholic fatty liver vs nonalcoholic steatohepatitis: a systematic review and meta-analysis of paired-biopsy studies. Clin Gastroenterol Hepatol 2015; 13:643–654.
- Argo CK, Northup PG, Al-Osaimi AM, Caldwell SH. Systematic review of risk factors for fibrosis progression in non-alcoholic steatohepatitis. J Hepatol 2009; 51:371–379.
- Adams LA, Lymp JF, St. Sauver J, et al. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology 2005; 129:113–121.
- Kleiner DE, Brunt EM, Van Natta M, et al; Nonalcoholic Steatohepatitis Clinical Research Network. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 2005; 41:1313–1321.
- Brunt EM, Kleiner DE, Wilson LA, Belt P, Neuschwander-Tetri BA; NASH Clinical Research Network (CRN). Nonalcoholic fatty liver disease (NAFLD) activity score and the histopathologic diagnosis in NAFLD: distinct clinicopathologic meanings. Hepatology 2011; 53:810–820.
- Marchesini G, Bugianesi E, Forlani G, et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology 2003; 37:917–923.
- Gaidos JK, Hillner BE, Sanyal AJ. A decision analysis study of the value of a liver biopsy in nonalcoholic steatohepatitis. Liver Int 2008; 28:650–658.
- Musso G, Gambino R, Cassader M, Pagano G. Meta-analysis: natural history of non-alcoholic fatty liver disease (NAFLD) and diagnostic accuracy of non-invasive tests for liver disease severity. Ann Med 2011; 43:617–649.
- Angulo P, Hui JM, Marchesini G, et al. The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology 2007; 45:846–854.
- Imajo K, Kessoku T, Honda Y, et al. Magnetic resonance imaging more accurately classifies steatosis and fibrosis in patients with nonalcoholic fatty liver disease than transient elastography. Gastroenterology 2016; 150:626–637.e7.
- Neuschwander-Tetri BA, Clark JM, Bass NM, et al; NASH Clinical Research Network. Clinical, laboratory and histological associations in adults with nonalcoholic fatty liver disease. Hepatology 2010; 52:913–924.
- Promrat K, Kleiner DE, Niemeier HM, et al. Randomized controlled trial testing the effects of weight loss on nonalcoholic steatohepatitis. Hepatology 2010; 51:121–129.
- Singh S, Khera R, Allen AM, Murad H, Loomba R. Comparative effectiveness of pharmacological interventions for nonalcoholic steatohepatitis: a systematic review and network meta-analysis. Hepatology 2015; 62:1417–1432.
Maternal asthma: Management strategies
The incidence of maternal asthma is rising. Based on US national health surveys, the prevalence of asthma during pregnancy is between 3.7% and 8.4%.1 It is the most common respiratory illness of pregnancy.2 Hence, clinicians need to know how asthma affects the mother and the fetus. Appropriate care of asthma during pregnancy is based on several management principles, as reviewed here, and is key to ensuring good outcomes for the mother and the baby.
EFFECT OF PREGNANCY ON ASTHMA CONTROL
Asthma control can vary in pregnancy. About a third of asthmatic women experience a worsening of asthma control with pregnancy, a third remain unchanged, and another third have improvement in asthma symptoms.3 The peak worsening of asthma tends to occur in the sixth month.4 Asthma control also tends to be better in the last month of pregnancy.3
The peak expiratory flow rate was noted to increase with each trimester in a small study of 43 women.5 The authors speculated that a rising progesterone level stimulates cyclic adenosine monophosphate to cause bronchodilation, thereby improving the expiratory flow rate and asthma control. Asthma control tends to follow the pattern experienced in the previous pregnancy: ie, if asthma worsened during the previous pregnancy, the same will be likely in the subsequent pregnancy.3
Two maternal factors that adversely affect asthma severity during pregnancy are the use of asthma medications contrary to guidelines such as those of the Global Initiative for Asthma (http://ginasthma.org/2017-gina-report-global-strategy-for-asthma-management-and-prevention) and inadquate control of asthma before becoming pregnant.6 Pregnancy can bring on stress, and stress is known to worsen asthma. In addition, when patients themselves were interviewed to elucidate the reasons for poor adherence to asthma medications during pregnancy, concerns about medication use, especially corticosteroids, stood out.7 A study based on prescription claims data showed that in the first trimester, there was a significant decline in asthma prescription medications (a 23% decline in inhaled corticosteroids, a 13% decline in short-acting bronchodilator agents, and a 54% decline in rescue corticosteroids).8 Lack of physician education about management of asthma in pregnancy and discomfort with prescribing to pregnant women also affect asthma control.
EFFECT OF ASTHMA ON MATERNAL AND FETAL OUTCOMES
Studies of the effects of asthma on fetal and maternal outcomes have yielded mixed and conflicting results.9 Adverse outcomes that have been shown to be associated with maternal asthma are listed in Table 1. Other studies have not demonstrated an association between asthma in pregnancy and maternal or fetal adverse events.9 Such discrepant findings are due to differences in study population characteristics that make comparisons difficult. A meta-analysis involving more than 1.6 million asthmatic women showed maternal asthma was associated with a 40% greater risk of low birth weight and preterm delivery, a 50% greater risk of preeclampsia, and a 20% greater risk of the baby being small for its gestational age.10
The association of maternal asthma and preterm birth may pose short-term and long-term health risks to the child associated with prematurity.9 Short-term risks with prematurity include infection, respiratory distress syndrome, brain injury, and necrotizing enterocolitis. Long-term risks include neurodevelopmental and behavioral sequelae. Furthermore, asthma exacerbations during pregnancy are associated with a twofold higher risk of low birth weight.11 The benefits of good adherence to asthma regimens during pregnancy outweigh the risks associated with frequent symptoms and exacerbations caused by untreated asthma.12
OUTPATIENT MANAGEMENT OF MATERNAL ASTHMA
Goals
In the 2004 update of the National Asthma Education and Prevention Program (NAEPP) Working Group Report on Managing Asthma During Pregnancy, goals focused mainly on adequate asthma control for maternal health and quality of life, as well as normal fetal maturation (Table 2),12 goals similar to those in nonpregnant asthmatic women.
Assessment and monitoring
Monthly physician visits during pregnancy are recommended for assessment of symptoms and pulmonary function. If symptoms are uncontrolled, therapy must be stepped up, and any trigger for exacerbation, such as gastroesophageal reflux disease (GERD), exposure, or rhinitis, must be treated and eliminated. NAEPP guidelines recommend baseline spirometry at the time of initial assessment.12 At follow-up visits, spirometry is preferred, but measurement of the peak expiratory flow rate usually suffices. Such objective data can help differentiate dyspnea from asthma and from dyspnea that usually accompanies the physiologic changes of pregnancy. In addition, patients should be advised to monitor for adequate fetal activity. If asthma is uncontrolled or poorly controlled, serial fetal ultrasonography should be considered from 32 weeks of gestation, as well as after recovery from an asthma exacerbation. Regular monitoring of the pregnant asthmatic patient by a multidisciplinary team can improve outcomes.13
Avoiding triggers
Patients should be advised to avoid asthma triggers such as pet dander, dust mites, pollen, smoke, mold, and perfumes, as this can decrease symptoms and allow for use of lower doses of medications.12 Additionally, smoking cessation must be strongly encouraged, not only to control maternal asthma, but also to prevent harm to the fetus.
MANAGEMENT OF SPECIFIC TRIGGERS
GERD
Reflux disease often worsens during pregnancy, and it can coexist with asthma and can also exacerbate it.14 Optimal control of GERD helps maintain adequate asthma control. For mild reflux symptoms, lifestyle modifications such as elevating the head of bed, avoiding eating too close to bedtime, and avoiding foods that cause heartburn may be adequate.15,16 If medications are needed, antacids (but not sodium bicarbonate, for fear of metabolic alkalosis) and sucralfate should be considered before using a histamine 2 receptor antagonist such as ranitidine. Proton pump inhibitors should be considered only if reflux symptoms are refractory to other therapies.
Allergic rhinitis
Intranasal corticosteroids are effective against allergic rhinitis in pregnancy (Table 3).12 Montelukast, a leukotriene receptor antagonist, can be used, but data to support its use for allergic rhinitis in pregnancy are limited.
Among antihistamines, second-generation drugs such as cetirizine or loratadine can be considered.12 Oral decongestants such as pseudoephedrine in early pregnancy are associated with a rare congenital fetal abnormality called gastroschisis, caused by vascular disruption.17 Hence, if a nasal decongestant is required in early pregnancy, a local therapy such as an intranasal corticosteroid, short-term oxymetazoline, or an external nasal dilator may be considered.12 These therapies must be combined with avoidance of allergens whenever possible.
Allergies
Diagnostic allergy and skin tests during pregnancy pose a risk of anaphylaxis and thus should be avoided. Instead, the focus should be on obtaining a thorough medical history about exposures and eliminating specific asthma triggers. It is also inadvisable to start allergen immunotherapy during pregnancy because of the risk of anaphylaxis and the effect of treatment on the mother and fetus.18 However, maintenance doses of allergen immunotherapy can be continued during pregnancy.18
Patient education
Because of concern about the risks of taking medications during pregnancy, many women with asthma stop using their inhalers during pregnancy, thus compromising asthma control.8,13 The physician and multidisciplinary team must use every opportunity to emphasize the importance of good asthma control during pregnancy. Inhaler technique should also be reviewed and, if defective, corrected. Again, trigger avoidance and tobacco cessation should be addressed.
Drugs
The NAEPP recommendations state that asthma therapy should be continued during pregnancy, as it is safer both for mother and fetus to avoid exacerbations and uncontrolled asthma.12 Despite this, 25% of primary care physicians instruct their patients to decrease or discontinue their inhaled corticosteroid during pregnancy.19 As with asthma in general, treatment should involve using the lowest dose of drugs that achieves adequate control of symptoms.
In 2015, the US Food and Drug Administration (FDA) amended the labeling rule for medications used in pregnancy and lactation. The previous risk categories A (safest), B, C, D, and X (highest risk) are in the process of being removed from labels for all human prescription drugs and biologic products, to be replaced with a summary of the risks of taking the drug during pregnancy and lactation, a discussion of the data supporting the use, and relevant information to help healthcare providers make prescribing decisions and counsel women about the use of drugs during pregnancy and lactation (www.fda.gov/Drugs/DevelopmentApprovalProcess/DevelopmentResources/Labeling/ucm093307.htm).
ROLES OF CONTROLLER THERAPY AND RESCUE THERAPY
Inhaled corticosteroids
Inhaled corticosteroids are the mainstay of asthma controller therapy during pregnancy. A meta-analysis of 16 studies showed no increased risk of congenital malformations, cesarean delivery, or stillbirth among mothers who used these agents during pregnancy.20 Because there are more safety data for budesonide, it is currently the preferred inhaled corticosteroid during pregnancy.9 However, if a patient’s asthma is controlled with a different corticosteroid before pregnancy, that agent may be continued during pregnancy, especially if it is thought that switching formulations could adversely affect asthma control.12 This is mainly because current data do not prove that other inhaled corticosteroids are unsafe.
Inhaled beta-agonists
Inhaled beta-agonists, both short-acting and long-acting, are used for rescue therapy. Albuterol is the preferred short-acting agent for rescue therapy in pregnant women with asthma.12 Meta-analysis has shown no increased risk of major or minor congenital malformations in pregnant patients who use bronchodilators.20 Long-acting beta-agonists typically are used as add-on therapy when asthma cannot be controlled by an inhaled corticosteroid. They should not be used without a controller medication (ie, an inhaled corticosteroid).
Guidelines for rescue therapy are similar to those for nonpregnant asthmatic patients. Although data are limited as to the gestational effects of long-acting beta-agonists (ie, formoterol, salmeterol), it can be assumed that the toxicologic and pharmacologic profiles are similar to those of the short-acting bronchodilators. Thus, the safety of albuterol can be extended potentially to the long-acting beta-agonists.12
Combining controller and rescue therapy
When asthma is not adequately controlled on inhaled corticosteroids, a long-acting beta-agonist can be added or the dose of corticosteroid can be increased. The 2004 NAEPP guidelines stated that based on available literature, there was no clear advantage of one option over the other.12 A study that compared the 2 approaches found no difference in rates of congenital malformations.21
Leukotriene receptor antagonists
There is little in the literature regarding the use of leukotriene receptor antagonists during pregnancy. However, animal safety data are reassuring,12 and human studies have not found a higher risk of major congenital malformations.22,23 Thus, they are an alternative for patients whose asthma has been well controlled on these agents before pregnancy. Montelukast and zafirlukast are in former FDA pregnancy risk factor category B (probably safe) (Table 3). However, 5-lipoxygenase inhibitors such as zileuton are contraindicated based on animal studies showing teratogenicity.24
Omalizumab
Omalizumab, a recombinant anti-immunoglobulin E antibody, can be used for allergic asthma not controlled with inhaled corticosteroids (Table 3). An analysis of the omalizumab pregnancy registry25 found no significant increase in the rate of major congenital malformations, prematurity, or babies small for gestational age in asthmatic women taking omalizumab 8 weeks before conception or during pregnancy vs pregnant asthmatic women not taking omalizumab. However, this drug carries a risk of anaphylaxis and so should not be started during pregnancy.25
Theophylline
Because of potential toxicity, use of theophylline during pregnancy requires careful monitoring to ensure the serum concentration remains between 5 and 12 µg/mL.12 Drug interactions are also common: for example, alcohol may increase the serum concentration of theophylline, and theophylline may increase the toxic effect of formoterol.
Systemic corticosteroids
Pregnant women with asthma that is not well controlled despite the therapies described above may require a daily oral corticosteroid such as prednisone to achieve adequate control. Oral steroids are also a mainstay of treatment of asthma exacerbation.
Although use of corticosteroids in the first trimester was associated with orofacial cleft in infants,12 these studies did not include many women with asthma. In 2011, a nationwide cohort study from Denmark showed no increase in the risk of orofacial cleft with the use of corticosteroids during pregnancy.26
Preeclampsia, low birth weight, and preterm delivery have been described with corticosteroid use in pregnancy. It is not known whether these problems were a result of corticosteroid use or were due to the uncontrolled nature of the underlying condition that led to the steroid use. Since the risk of uncontrolled asthma to mother and fetus outweighs the risk of systemic corticosteroids, these drugs are recommended when indicated for management of maternal asthma.12
ACUTE EXACERBATIONS REQUIRE AGGRESSIVE MANAGEMENT
Based on a systematic review, 20% of pregnant women with asthma require some intervention for an asthma exacerbation during pregnancy, and 5.8% are admitted to the hospital for an exacerbation.11 Exacerbations were associated with a higher risk of low birth weight compared with rates in women without asthma.
Exacerbations are more common late in the second trimester and are unlikely to occur during labor and delivery.2 The incidence of exacerbations increases with the severity of asthma, from 8% in mild asthma, to 47% in moderate asthma, to 65% in severe asthma.27 Risk factors for exacerbations include poor prenatal care, obesity, and lack of appropriate treatment with inhaled corticosteroids.2 The main triggers are viral respiratory infections and noncompliance with inhaled corticosteroid therapy.11
Asthma exacerbations during pregnancy should be managed aggressively (Table 4),12 as the risk to the fetus of hypoxia far outweighs any risk from asthma medications. Close collaboration between the primary care physician and the obstetrician allows closer monitoring of mother and fetus.
The goal oxygen saturation must be above 95%.12 Signs of acute respiratory failure in a pregnant patient include a partial pressure of arterial oxygen less than 70 mm Hg or a partial pressure of carbon dioxide greater than 35 mm Hg.
In a multicenter study comparing nonpregnant and pregnant women visiting the emergency room for asthma exacerbations,28 pregnant women were less likely to be prescribed systemic corticosteroids either in the emergency room or at the time of hospital discharge, and they were also more likely to describe an ongoing exacerbation at 2-week follow-up. However, a recent study showed a significant increase in systemic corticosteroid treatment in the emergency room (51% to 78% across the time periods, odds ratio 3.11, 95% confidence interval 1.27–7.60, P = .01). There was also an increase in steroid treatment at discharge (42% to 63%, odds ratio 2.49, 95% confidence interval 0.97–6.37, P = .054), though the increase was not statistically significant.29 Although emergency room care for pregnant asthmatic women has improved, this group concluded that further improvement is still warranted, as 1 in 3 women is discharged without corticosteroid treatment.
- Kwon HL, Belanger K, Bracken MB. Asthma prevalence among pregnant and childbearing-aged women in the United States: estimates from national health surveys. Ann Epidemiol 2003; 13:317–324.
- Powell H, Murphy VE, Taylor DR, et al. Management of asthma in pregnancy guided by measurement of fraction of exhaled nitric oxide: a double-blind, randomised controlled trial. Lancet 2011; 378:983–990.
- Schatz M, Harden K, Forsythe A, et al. The course of asthma during pregnancy, post partum, and with successive pregnancies: a prospective analysis. J Allergy Clin Immunol 1988; 81:509–517.
- Gluck JC, Gluck PA. The effect of pregnancy on the course of asthma. Immunol Allergy Clin North Am 2006; 26:63–80.
- Beckmann CA. Peak flow values by gestation in women with asthma. Clin Nurs Res 2008; 17:174–181.
- Belanger K, Hellenbrand ME, Holford TR, Bracken M. Effect of pregnancy on maternal asthma symptoms and medication use. Obstet Gynecol 2010; 115:559–567.
- Lim AS, Stewart K, Abramson MJ, Ryan K, George J. Asthma during pregnancy: the experiences, concerns and views of pregnant women with asthma. J Asthma 2012; 49:474–479.
- Enriquez R, Wu P, Griffin MR, et al. Cessation of asthma medication in early pregnancy. Am J Obstet Gynecol 2006; 195:149–153.
- Bain E, Pierides KL, Clifton VL, et al. Interventions for managing asthma in pregnancy. Cochrane Database Syst Rev 2014; 10:CD010660.
- Murphy VE, Namazy JA, Powell H, et al. A meta-analysis of adverse perinatal outcomes in women with asthma. BJOG 2011; 118:1314–1323.
- Murphy VE, Clifton VL, Gibson PG. Asthma exacerbations during pregnancy: incidence and association with adverse pregnancy outcomes. Thorax 2006; 61:169–176.
- National Heart, Lung, and Blood Institute; National Asthma Education and Prevention Program Asthma and Pregnancy Working Group. NAEPP expert panel report. Managing asthma during pregnancy: recommendations for pharmacologic treatment—2004 update. J Allergy Clin Immunol 2005; 115:34–46.
- Lim AS, Stewart K, Abramson MJ, Walker SP, Smith CL, George J. Multidisciplinary Approach to Management of Maternal Asthma (MAMMA): a randomized controlled trial. Chest 2014; 145:1046–1054.
- Harding SM. Gastroesophageal reflux: a potential asthma trigger. Immunol Allergy Clin North Am 2005; 25:131–148.
- Ahmad S, Mokaddas E. Recent advances in the diagnosis and treatment of multidrug-resistant tuberculosis. Respir Med 2009; 103:1777–1790.
- van der Woude CJ, Metselaar HJ, Danese S. Management of gastrointestinal and liver diseases during pregnancy. Gut 2014; 63:1014–1023.
- Werler MM. Teratogen update: pseudoephedrine. Birth Defects Res A Clin Mol Teratol 2006; 76:445–452.
- Cox L, Nelson H, Lockey R, et al. Allergen immunotherapy: a practice parameter third update. J Allergy Clin Immunol 2011; 127(suppl 1):S1–S55.
- Lim AS, Stewart K, Abramson MJ, George J. Management of asthma in pregnant women by general practitioners: a cross sectional survey. BMC Fam Pract 2011; 12:121.
- Murphy VE, Wang G, Namazy JA, et al. The risk of congenital malformations, perinatal mortality and neonatal hospitalisation among pregnant women with asthma: a systematic review and meta-analysis. BJOG 2013; 120:812–822.
- Eltonsy S, Forget A, Beauchesne MF, Blais L. Risk of congenital malformations for asthmatic pregnant women using a long-acting beta2-agonist and inhaled corticosteroid combination versus higher-dose inhaled corticosteroid monotherapy. J Allergy Clin Immunol 2015; 135:123–130.
- Nelsen LM, Shields KE, Cunningham ML, et al. Congenital malformations among infants born to women receiving montelukast, inhaled corticosteroids, and other asthma medications. J Allergy Clin Immunol 2012; 129:251–254.e1–e6.
- Sarkar M, Koren G, Kalra S, et al. Montelukast use during pregnancy: a multicentre, prospective, comparative study of infant outcomes. Eur J Clin Pharmacol 2009; 65:1259–1264.
- Namazy JA, Schatz M. The safety of asthma medications during pregnancy: an update for clinicians. Ther Adv Respir Dis 2014; 8:103–110.
- Namazy J, Cabana MD, Scheuerle AE, et al. The Xolair Pregnancy Registry (EXPECT): the safety of omalizumab use during pregnancy. J Allergy Clin Immunol 2015; 135:407–412.
- Hviid A, Molgaard-Nielsen D. Corticosteroid use during pregnancy and risk of orofacial clefts. CMAJ 2011; 183:796–804.
- Murphy VE, Gibson P, Talbot PI, Clifton VL. Severe asthma exacerbations during pregnancy. Obstet Gynecol 2005; 106:1046–1054.
- Cydulka RK, Emerman CL, Schreiber D, Molander KH, Woodruff PG, Camargo CA Jr. Acute asthma among pregnant women presenting to the emergency department. Am J Respir Crit Care Med 1999; 160:887–892.
- Hasegawa K, Cydulka RK, Sullivan AF, et al. Improved management of acute asthma among pregnant women presenting to the ED. Chest 2015; 147:406–414.
The incidence of maternal asthma is rising. Based on US national health surveys, the prevalence of asthma during pregnancy is between 3.7% and 8.4%.1 It is the most common respiratory illness of pregnancy.2 Hence, clinicians need to know how asthma affects the mother and the fetus. Appropriate care of asthma during pregnancy is based on several management principles, as reviewed here, and is key to ensuring good outcomes for the mother and the baby.
EFFECT OF PREGNANCY ON ASTHMA CONTROL
Asthma control can vary in pregnancy. About a third of asthmatic women experience a worsening of asthma control with pregnancy, a third remain unchanged, and another third have improvement in asthma symptoms.3 The peak worsening of asthma tends to occur in the sixth month.4 Asthma control also tends to be better in the last month of pregnancy.3
The peak expiratory flow rate was noted to increase with each trimester in a small study of 43 women.5 The authors speculated that a rising progesterone level stimulates cyclic adenosine monophosphate to cause bronchodilation, thereby improving the expiratory flow rate and asthma control. Asthma control tends to follow the pattern experienced in the previous pregnancy: ie, if asthma worsened during the previous pregnancy, the same will be likely in the subsequent pregnancy.3
Two maternal factors that adversely affect asthma severity during pregnancy are the use of asthma medications contrary to guidelines such as those of the Global Initiative for Asthma (http://ginasthma.org/2017-gina-report-global-strategy-for-asthma-management-and-prevention) and inadquate control of asthma before becoming pregnant.6 Pregnancy can bring on stress, and stress is known to worsen asthma. In addition, when patients themselves were interviewed to elucidate the reasons for poor adherence to asthma medications during pregnancy, concerns about medication use, especially corticosteroids, stood out.7 A study based on prescription claims data showed that in the first trimester, there was a significant decline in asthma prescription medications (a 23% decline in inhaled corticosteroids, a 13% decline in short-acting bronchodilator agents, and a 54% decline in rescue corticosteroids).8 Lack of physician education about management of asthma in pregnancy and discomfort with prescribing to pregnant women also affect asthma control.
EFFECT OF ASTHMA ON MATERNAL AND FETAL OUTCOMES
Studies of the effects of asthma on fetal and maternal outcomes have yielded mixed and conflicting results.9 Adverse outcomes that have been shown to be associated with maternal asthma are listed in Table 1. Other studies have not demonstrated an association between asthma in pregnancy and maternal or fetal adverse events.9 Such discrepant findings are due to differences in study population characteristics that make comparisons difficult. A meta-analysis involving more than 1.6 million asthmatic women showed maternal asthma was associated with a 40% greater risk of low birth weight and preterm delivery, a 50% greater risk of preeclampsia, and a 20% greater risk of the baby being small for its gestational age.10
The association of maternal asthma and preterm birth may pose short-term and long-term health risks to the child associated with prematurity.9 Short-term risks with prematurity include infection, respiratory distress syndrome, brain injury, and necrotizing enterocolitis. Long-term risks include neurodevelopmental and behavioral sequelae. Furthermore, asthma exacerbations during pregnancy are associated with a twofold higher risk of low birth weight.11 The benefits of good adherence to asthma regimens during pregnancy outweigh the risks associated with frequent symptoms and exacerbations caused by untreated asthma.12
OUTPATIENT MANAGEMENT OF MATERNAL ASTHMA
Goals
In the 2004 update of the National Asthma Education and Prevention Program (NAEPP) Working Group Report on Managing Asthma During Pregnancy, goals focused mainly on adequate asthma control for maternal health and quality of life, as well as normal fetal maturation (Table 2),12 goals similar to those in nonpregnant asthmatic women.
Assessment and monitoring
Monthly physician visits during pregnancy are recommended for assessment of symptoms and pulmonary function. If symptoms are uncontrolled, therapy must be stepped up, and any trigger for exacerbation, such as gastroesophageal reflux disease (GERD), exposure, or rhinitis, must be treated and eliminated. NAEPP guidelines recommend baseline spirometry at the time of initial assessment.12 At follow-up visits, spirometry is preferred, but measurement of the peak expiratory flow rate usually suffices. Such objective data can help differentiate dyspnea from asthma and from dyspnea that usually accompanies the physiologic changes of pregnancy. In addition, patients should be advised to monitor for adequate fetal activity. If asthma is uncontrolled or poorly controlled, serial fetal ultrasonography should be considered from 32 weeks of gestation, as well as after recovery from an asthma exacerbation. Regular monitoring of the pregnant asthmatic patient by a multidisciplinary team can improve outcomes.13
Avoiding triggers
Patients should be advised to avoid asthma triggers such as pet dander, dust mites, pollen, smoke, mold, and perfumes, as this can decrease symptoms and allow for use of lower doses of medications.12 Additionally, smoking cessation must be strongly encouraged, not only to control maternal asthma, but also to prevent harm to the fetus.
MANAGEMENT OF SPECIFIC TRIGGERS
GERD
Reflux disease often worsens during pregnancy, and it can coexist with asthma and can also exacerbate it.14 Optimal control of GERD helps maintain adequate asthma control. For mild reflux symptoms, lifestyle modifications such as elevating the head of bed, avoiding eating too close to bedtime, and avoiding foods that cause heartburn may be adequate.15,16 If medications are needed, antacids (but not sodium bicarbonate, for fear of metabolic alkalosis) and sucralfate should be considered before using a histamine 2 receptor antagonist such as ranitidine. Proton pump inhibitors should be considered only if reflux symptoms are refractory to other therapies.
Allergic rhinitis
Intranasal corticosteroids are effective against allergic rhinitis in pregnancy (Table 3).12 Montelukast, a leukotriene receptor antagonist, can be used, but data to support its use for allergic rhinitis in pregnancy are limited.
Among antihistamines, second-generation drugs such as cetirizine or loratadine can be considered.12 Oral decongestants such as pseudoephedrine in early pregnancy are associated with a rare congenital fetal abnormality called gastroschisis, caused by vascular disruption.17 Hence, if a nasal decongestant is required in early pregnancy, a local therapy such as an intranasal corticosteroid, short-term oxymetazoline, or an external nasal dilator may be considered.12 These therapies must be combined with avoidance of allergens whenever possible.
Allergies
Diagnostic allergy and skin tests during pregnancy pose a risk of anaphylaxis and thus should be avoided. Instead, the focus should be on obtaining a thorough medical history about exposures and eliminating specific asthma triggers. It is also inadvisable to start allergen immunotherapy during pregnancy because of the risk of anaphylaxis and the effect of treatment on the mother and fetus.18 However, maintenance doses of allergen immunotherapy can be continued during pregnancy.18
Patient education
Because of concern about the risks of taking medications during pregnancy, many women with asthma stop using their inhalers during pregnancy, thus compromising asthma control.8,13 The physician and multidisciplinary team must use every opportunity to emphasize the importance of good asthma control during pregnancy. Inhaler technique should also be reviewed and, if defective, corrected. Again, trigger avoidance and tobacco cessation should be addressed.
Drugs
The NAEPP recommendations state that asthma therapy should be continued during pregnancy, as it is safer both for mother and fetus to avoid exacerbations and uncontrolled asthma.12 Despite this, 25% of primary care physicians instruct their patients to decrease or discontinue their inhaled corticosteroid during pregnancy.19 As with asthma in general, treatment should involve using the lowest dose of drugs that achieves adequate control of symptoms.
In 2015, the US Food and Drug Administration (FDA) amended the labeling rule for medications used in pregnancy and lactation. The previous risk categories A (safest), B, C, D, and X (highest risk) are in the process of being removed from labels for all human prescription drugs and biologic products, to be replaced with a summary of the risks of taking the drug during pregnancy and lactation, a discussion of the data supporting the use, and relevant information to help healthcare providers make prescribing decisions and counsel women about the use of drugs during pregnancy and lactation (www.fda.gov/Drugs/DevelopmentApprovalProcess/DevelopmentResources/Labeling/ucm093307.htm).
ROLES OF CONTROLLER THERAPY AND RESCUE THERAPY
Inhaled corticosteroids
Inhaled corticosteroids are the mainstay of asthma controller therapy during pregnancy. A meta-analysis of 16 studies showed no increased risk of congenital malformations, cesarean delivery, or stillbirth among mothers who used these agents during pregnancy.20 Because there are more safety data for budesonide, it is currently the preferred inhaled corticosteroid during pregnancy.9 However, if a patient’s asthma is controlled with a different corticosteroid before pregnancy, that agent may be continued during pregnancy, especially if it is thought that switching formulations could adversely affect asthma control.12 This is mainly because current data do not prove that other inhaled corticosteroids are unsafe.
Inhaled beta-agonists
Inhaled beta-agonists, both short-acting and long-acting, are used for rescue therapy. Albuterol is the preferred short-acting agent for rescue therapy in pregnant women with asthma.12 Meta-analysis has shown no increased risk of major or minor congenital malformations in pregnant patients who use bronchodilators.20 Long-acting beta-agonists typically are used as add-on therapy when asthma cannot be controlled by an inhaled corticosteroid. They should not be used without a controller medication (ie, an inhaled corticosteroid).
Guidelines for rescue therapy are similar to those for nonpregnant asthmatic patients. Although data are limited as to the gestational effects of long-acting beta-agonists (ie, formoterol, salmeterol), it can be assumed that the toxicologic and pharmacologic profiles are similar to those of the short-acting bronchodilators. Thus, the safety of albuterol can be extended potentially to the long-acting beta-agonists.12
Combining controller and rescue therapy
When asthma is not adequately controlled on inhaled corticosteroids, a long-acting beta-agonist can be added or the dose of corticosteroid can be increased. The 2004 NAEPP guidelines stated that based on available literature, there was no clear advantage of one option over the other.12 A study that compared the 2 approaches found no difference in rates of congenital malformations.21
Leukotriene receptor antagonists
There is little in the literature regarding the use of leukotriene receptor antagonists during pregnancy. However, animal safety data are reassuring,12 and human studies have not found a higher risk of major congenital malformations.22,23 Thus, they are an alternative for patients whose asthma has been well controlled on these agents before pregnancy. Montelukast and zafirlukast are in former FDA pregnancy risk factor category B (probably safe) (Table 3). However, 5-lipoxygenase inhibitors such as zileuton are contraindicated based on animal studies showing teratogenicity.24
Omalizumab
Omalizumab, a recombinant anti-immunoglobulin E antibody, can be used for allergic asthma not controlled with inhaled corticosteroids (Table 3). An analysis of the omalizumab pregnancy registry25 found no significant increase in the rate of major congenital malformations, prematurity, or babies small for gestational age in asthmatic women taking omalizumab 8 weeks before conception or during pregnancy vs pregnant asthmatic women not taking omalizumab. However, this drug carries a risk of anaphylaxis and so should not be started during pregnancy.25
Theophylline
Because of potential toxicity, use of theophylline during pregnancy requires careful monitoring to ensure the serum concentration remains between 5 and 12 µg/mL.12 Drug interactions are also common: for example, alcohol may increase the serum concentration of theophylline, and theophylline may increase the toxic effect of formoterol.
Systemic corticosteroids
Pregnant women with asthma that is not well controlled despite the therapies described above may require a daily oral corticosteroid such as prednisone to achieve adequate control. Oral steroids are also a mainstay of treatment of asthma exacerbation.
Although use of corticosteroids in the first trimester was associated with orofacial cleft in infants,12 these studies did not include many women with asthma. In 2011, a nationwide cohort study from Denmark showed no increase in the risk of orofacial cleft with the use of corticosteroids during pregnancy.26
Preeclampsia, low birth weight, and preterm delivery have been described with corticosteroid use in pregnancy. It is not known whether these problems were a result of corticosteroid use or were due to the uncontrolled nature of the underlying condition that led to the steroid use. Since the risk of uncontrolled asthma to mother and fetus outweighs the risk of systemic corticosteroids, these drugs are recommended when indicated for management of maternal asthma.12
ACUTE EXACERBATIONS REQUIRE AGGRESSIVE MANAGEMENT
Based on a systematic review, 20% of pregnant women with asthma require some intervention for an asthma exacerbation during pregnancy, and 5.8% are admitted to the hospital for an exacerbation.11 Exacerbations were associated with a higher risk of low birth weight compared with rates in women without asthma.
Exacerbations are more common late in the second trimester and are unlikely to occur during labor and delivery.2 The incidence of exacerbations increases with the severity of asthma, from 8% in mild asthma, to 47% in moderate asthma, to 65% in severe asthma.27 Risk factors for exacerbations include poor prenatal care, obesity, and lack of appropriate treatment with inhaled corticosteroids.2 The main triggers are viral respiratory infections and noncompliance with inhaled corticosteroid therapy.11
Asthma exacerbations during pregnancy should be managed aggressively (Table 4),12 as the risk to the fetus of hypoxia far outweighs any risk from asthma medications. Close collaboration between the primary care physician and the obstetrician allows closer monitoring of mother and fetus.
The goal oxygen saturation must be above 95%.12 Signs of acute respiratory failure in a pregnant patient include a partial pressure of arterial oxygen less than 70 mm Hg or a partial pressure of carbon dioxide greater than 35 mm Hg.
In a multicenter study comparing nonpregnant and pregnant women visiting the emergency room for asthma exacerbations,28 pregnant women were less likely to be prescribed systemic corticosteroids either in the emergency room or at the time of hospital discharge, and they were also more likely to describe an ongoing exacerbation at 2-week follow-up. However, a recent study showed a significant increase in systemic corticosteroid treatment in the emergency room (51% to 78% across the time periods, odds ratio 3.11, 95% confidence interval 1.27–7.60, P = .01). There was also an increase in steroid treatment at discharge (42% to 63%, odds ratio 2.49, 95% confidence interval 0.97–6.37, P = .054), though the increase was not statistically significant.29 Although emergency room care for pregnant asthmatic women has improved, this group concluded that further improvement is still warranted, as 1 in 3 women is discharged without corticosteroid treatment.
The incidence of maternal asthma is rising. Based on US national health surveys, the prevalence of asthma during pregnancy is between 3.7% and 8.4%.1 It is the most common respiratory illness of pregnancy.2 Hence, clinicians need to know how asthma affects the mother and the fetus. Appropriate care of asthma during pregnancy is based on several management principles, as reviewed here, and is key to ensuring good outcomes for the mother and the baby.
EFFECT OF PREGNANCY ON ASTHMA CONTROL
Asthma control can vary in pregnancy. About a third of asthmatic women experience a worsening of asthma control with pregnancy, a third remain unchanged, and another third have improvement in asthma symptoms.3 The peak worsening of asthma tends to occur in the sixth month.4 Asthma control also tends to be better in the last month of pregnancy.3
The peak expiratory flow rate was noted to increase with each trimester in a small study of 43 women.5 The authors speculated that a rising progesterone level stimulates cyclic adenosine monophosphate to cause bronchodilation, thereby improving the expiratory flow rate and asthma control. Asthma control tends to follow the pattern experienced in the previous pregnancy: ie, if asthma worsened during the previous pregnancy, the same will be likely in the subsequent pregnancy.3
Two maternal factors that adversely affect asthma severity during pregnancy are the use of asthma medications contrary to guidelines such as those of the Global Initiative for Asthma (http://ginasthma.org/2017-gina-report-global-strategy-for-asthma-management-and-prevention) and inadquate control of asthma before becoming pregnant.6 Pregnancy can bring on stress, and stress is known to worsen asthma. In addition, when patients themselves were interviewed to elucidate the reasons for poor adherence to asthma medications during pregnancy, concerns about medication use, especially corticosteroids, stood out.7 A study based on prescription claims data showed that in the first trimester, there was a significant decline in asthma prescription medications (a 23% decline in inhaled corticosteroids, a 13% decline in short-acting bronchodilator agents, and a 54% decline in rescue corticosteroids).8 Lack of physician education about management of asthma in pregnancy and discomfort with prescribing to pregnant women also affect asthma control.
EFFECT OF ASTHMA ON MATERNAL AND FETAL OUTCOMES
Studies of the effects of asthma on fetal and maternal outcomes have yielded mixed and conflicting results.9 Adverse outcomes that have been shown to be associated with maternal asthma are listed in Table 1. Other studies have not demonstrated an association between asthma in pregnancy and maternal or fetal adverse events.9 Such discrepant findings are due to differences in study population characteristics that make comparisons difficult. A meta-analysis involving more than 1.6 million asthmatic women showed maternal asthma was associated with a 40% greater risk of low birth weight and preterm delivery, a 50% greater risk of preeclampsia, and a 20% greater risk of the baby being small for its gestational age.10
The association of maternal asthma and preterm birth may pose short-term and long-term health risks to the child associated with prematurity.9 Short-term risks with prematurity include infection, respiratory distress syndrome, brain injury, and necrotizing enterocolitis. Long-term risks include neurodevelopmental and behavioral sequelae. Furthermore, asthma exacerbations during pregnancy are associated with a twofold higher risk of low birth weight.11 The benefits of good adherence to asthma regimens during pregnancy outweigh the risks associated with frequent symptoms and exacerbations caused by untreated asthma.12
OUTPATIENT MANAGEMENT OF MATERNAL ASTHMA
Goals
In the 2004 update of the National Asthma Education and Prevention Program (NAEPP) Working Group Report on Managing Asthma During Pregnancy, goals focused mainly on adequate asthma control for maternal health and quality of life, as well as normal fetal maturation (Table 2),12 goals similar to those in nonpregnant asthmatic women.
Assessment and monitoring
Monthly physician visits during pregnancy are recommended for assessment of symptoms and pulmonary function. If symptoms are uncontrolled, therapy must be stepped up, and any trigger for exacerbation, such as gastroesophageal reflux disease (GERD), exposure, or rhinitis, must be treated and eliminated. NAEPP guidelines recommend baseline spirometry at the time of initial assessment.12 At follow-up visits, spirometry is preferred, but measurement of the peak expiratory flow rate usually suffices. Such objective data can help differentiate dyspnea from asthma and from dyspnea that usually accompanies the physiologic changes of pregnancy. In addition, patients should be advised to monitor for adequate fetal activity. If asthma is uncontrolled or poorly controlled, serial fetal ultrasonography should be considered from 32 weeks of gestation, as well as after recovery from an asthma exacerbation. Regular monitoring of the pregnant asthmatic patient by a multidisciplinary team can improve outcomes.13
Avoiding triggers
Patients should be advised to avoid asthma triggers such as pet dander, dust mites, pollen, smoke, mold, and perfumes, as this can decrease symptoms and allow for use of lower doses of medications.12 Additionally, smoking cessation must be strongly encouraged, not only to control maternal asthma, but also to prevent harm to the fetus.
MANAGEMENT OF SPECIFIC TRIGGERS
GERD
Reflux disease often worsens during pregnancy, and it can coexist with asthma and can also exacerbate it.14 Optimal control of GERD helps maintain adequate asthma control. For mild reflux symptoms, lifestyle modifications such as elevating the head of bed, avoiding eating too close to bedtime, and avoiding foods that cause heartburn may be adequate.15,16 If medications are needed, antacids (but not sodium bicarbonate, for fear of metabolic alkalosis) and sucralfate should be considered before using a histamine 2 receptor antagonist such as ranitidine. Proton pump inhibitors should be considered only if reflux symptoms are refractory to other therapies.
Allergic rhinitis
Intranasal corticosteroids are effective against allergic rhinitis in pregnancy (Table 3).12 Montelukast, a leukotriene receptor antagonist, can be used, but data to support its use for allergic rhinitis in pregnancy are limited.
Among antihistamines, second-generation drugs such as cetirizine or loratadine can be considered.12 Oral decongestants such as pseudoephedrine in early pregnancy are associated with a rare congenital fetal abnormality called gastroschisis, caused by vascular disruption.17 Hence, if a nasal decongestant is required in early pregnancy, a local therapy such as an intranasal corticosteroid, short-term oxymetazoline, or an external nasal dilator may be considered.12 These therapies must be combined with avoidance of allergens whenever possible.
Allergies
Diagnostic allergy and skin tests during pregnancy pose a risk of anaphylaxis and thus should be avoided. Instead, the focus should be on obtaining a thorough medical history about exposures and eliminating specific asthma triggers. It is also inadvisable to start allergen immunotherapy during pregnancy because of the risk of anaphylaxis and the effect of treatment on the mother and fetus.18 However, maintenance doses of allergen immunotherapy can be continued during pregnancy.18
Patient education
Because of concern about the risks of taking medications during pregnancy, many women with asthma stop using their inhalers during pregnancy, thus compromising asthma control.8,13 The physician and multidisciplinary team must use every opportunity to emphasize the importance of good asthma control during pregnancy. Inhaler technique should also be reviewed and, if defective, corrected. Again, trigger avoidance and tobacco cessation should be addressed.
Drugs
The NAEPP recommendations state that asthma therapy should be continued during pregnancy, as it is safer both for mother and fetus to avoid exacerbations and uncontrolled asthma.12 Despite this, 25% of primary care physicians instruct their patients to decrease or discontinue their inhaled corticosteroid during pregnancy.19 As with asthma in general, treatment should involve using the lowest dose of drugs that achieves adequate control of symptoms.
In 2015, the US Food and Drug Administration (FDA) amended the labeling rule for medications used in pregnancy and lactation. The previous risk categories A (safest), B, C, D, and X (highest risk) are in the process of being removed from labels for all human prescription drugs and biologic products, to be replaced with a summary of the risks of taking the drug during pregnancy and lactation, a discussion of the data supporting the use, and relevant information to help healthcare providers make prescribing decisions and counsel women about the use of drugs during pregnancy and lactation (www.fda.gov/Drugs/DevelopmentApprovalProcess/DevelopmentResources/Labeling/ucm093307.htm).
ROLES OF CONTROLLER THERAPY AND RESCUE THERAPY
Inhaled corticosteroids
Inhaled corticosteroids are the mainstay of asthma controller therapy during pregnancy. A meta-analysis of 16 studies showed no increased risk of congenital malformations, cesarean delivery, or stillbirth among mothers who used these agents during pregnancy.20 Because there are more safety data for budesonide, it is currently the preferred inhaled corticosteroid during pregnancy.9 However, if a patient’s asthma is controlled with a different corticosteroid before pregnancy, that agent may be continued during pregnancy, especially if it is thought that switching formulations could adversely affect asthma control.12 This is mainly because current data do not prove that other inhaled corticosteroids are unsafe.
Inhaled beta-agonists
Inhaled beta-agonists, both short-acting and long-acting, are used for rescue therapy. Albuterol is the preferred short-acting agent for rescue therapy in pregnant women with asthma.12 Meta-analysis has shown no increased risk of major or minor congenital malformations in pregnant patients who use bronchodilators.20 Long-acting beta-agonists typically are used as add-on therapy when asthma cannot be controlled by an inhaled corticosteroid. They should not be used without a controller medication (ie, an inhaled corticosteroid).
Guidelines for rescue therapy are similar to those for nonpregnant asthmatic patients. Although data are limited as to the gestational effects of long-acting beta-agonists (ie, formoterol, salmeterol), it can be assumed that the toxicologic and pharmacologic profiles are similar to those of the short-acting bronchodilators. Thus, the safety of albuterol can be extended potentially to the long-acting beta-agonists.12
Combining controller and rescue therapy
When asthma is not adequately controlled on inhaled corticosteroids, a long-acting beta-agonist can be added or the dose of corticosteroid can be increased. The 2004 NAEPP guidelines stated that based on available literature, there was no clear advantage of one option over the other.12 A study that compared the 2 approaches found no difference in rates of congenital malformations.21
Leukotriene receptor antagonists
There is little in the literature regarding the use of leukotriene receptor antagonists during pregnancy. However, animal safety data are reassuring,12 and human studies have not found a higher risk of major congenital malformations.22,23 Thus, they are an alternative for patients whose asthma has been well controlled on these agents before pregnancy. Montelukast and zafirlukast are in former FDA pregnancy risk factor category B (probably safe) (Table 3). However, 5-lipoxygenase inhibitors such as zileuton are contraindicated based on animal studies showing teratogenicity.24
Omalizumab
Omalizumab, a recombinant anti-immunoglobulin E antibody, can be used for allergic asthma not controlled with inhaled corticosteroids (Table 3). An analysis of the omalizumab pregnancy registry25 found no significant increase in the rate of major congenital malformations, prematurity, or babies small for gestational age in asthmatic women taking omalizumab 8 weeks before conception or during pregnancy vs pregnant asthmatic women not taking omalizumab. However, this drug carries a risk of anaphylaxis and so should not be started during pregnancy.25
Theophylline
Because of potential toxicity, use of theophylline during pregnancy requires careful monitoring to ensure the serum concentration remains between 5 and 12 µg/mL.12 Drug interactions are also common: for example, alcohol may increase the serum concentration of theophylline, and theophylline may increase the toxic effect of formoterol.
Systemic corticosteroids
Pregnant women with asthma that is not well controlled despite the therapies described above may require a daily oral corticosteroid such as prednisone to achieve adequate control. Oral steroids are also a mainstay of treatment of asthma exacerbation.
Although use of corticosteroids in the first trimester was associated with orofacial cleft in infants,12 these studies did not include many women with asthma. In 2011, a nationwide cohort study from Denmark showed no increase in the risk of orofacial cleft with the use of corticosteroids during pregnancy.26
Preeclampsia, low birth weight, and preterm delivery have been described with corticosteroid use in pregnancy. It is not known whether these problems were a result of corticosteroid use or were due to the uncontrolled nature of the underlying condition that led to the steroid use. Since the risk of uncontrolled asthma to mother and fetus outweighs the risk of systemic corticosteroids, these drugs are recommended when indicated for management of maternal asthma.12
ACUTE EXACERBATIONS REQUIRE AGGRESSIVE MANAGEMENT
Based on a systematic review, 20% of pregnant women with asthma require some intervention for an asthma exacerbation during pregnancy, and 5.8% are admitted to the hospital for an exacerbation.11 Exacerbations were associated with a higher risk of low birth weight compared with rates in women without asthma.
Exacerbations are more common late in the second trimester and are unlikely to occur during labor and delivery.2 The incidence of exacerbations increases with the severity of asthma, from 8% in mild asthma, to 47% in moderate asthma, to 65% in severe asthma.27 Risk factors for exacerbations include poor prenatal care, obesity, and lack of appropriate treatment with inhaled corticosteroids.2 The main triggers are viral respiratory infections and noncompliance with inhaled corticosteroid therapy.11
Asthma exacerbations during pregnancy should be managed aggressively (Table 4),12 as the risk to the fetus of hypoxia far outweighs any risk from asthma medications. Close collaboration between the primary care physician and the obstetrician allows closer monitoring of mother and fetus.
The goal oxygen saturation must be above 95%.12 Signs of acute respiratory failure in a pregnant patient include a partial pressure of arterial oxygen less than 70 mm Hg or a partial pressure of carbon dioxide greater than 35 mm Hg.
In a multicenter study comparing nonpregnant and pregnant women visiting the emergency room for asthma exacerbations,28 pregnant women were less likely to be prescribed systemic corticosteroids either in the emergency room or at the time of hospital discharge, and they were also more likely to describe an ongoing exacerbation at 2-week follow-up. However, a recent study showed a significant increase in systemic corticosteroid treatment in the emergency room (51% to 78% across the time periods, odds ratio 3.11, 95% confidence interval 1.27–7.60, P = .01). There was also an increase in steroid treatment at discharge (42% to 63%, odds ratio 2.49, 95% confidence interval 0.97–6.37, P = .054), though the increase was not statistically significant.29 Although emergency room care for pregnant asthmatic women has improved, this group concluded that further improvement is still warranted, as 1 in 3 women is discharged without corticosteroid treatment.
- Kwon HL, Belanger K, Bracken MB. Asthma prevalence among pregnant and childbearing-aged women in the United States: estimates from national health surveys. Ann Epidemiol 2003; 13:317–324.
- Powell H, Murphy VE, Taylor DR, et al. Management of asthma in pregnancy guided by measurement of fraction of exhaled nitric oxide: a double-blind, randomised controlled trial. Lancet 2011; 378:983–990.
- Schatz M, Harden K, Forsythe A, et al. The course of asthma during pregnancy, post partum, and with successive pregnancies: a prospective analysis. J Allergy Clin Immunol 1988; 81:509–517.
- Gluck JC, Gluck PA. The effect of pregnancy on the course of asthma. Immunol Allergy Clin North Am 2006; 26:63–80.
- Beckmann CA. Peak flow values by gestation in women with asthma. Clin Nurs Res 2008; 17:174–181.
- Belanger K, Hellenbrand ME, Holford TR, Bracken M. Effect of pregnancy on maternal asthma symptoms and medication use. Obstet Gynecol 2010; 115:559–567.
- Lim AS, Stewart K, Abramson MJ, Ryan K, George J. Asthma during pregnancy: the experiences, concerns and views of pregnant women with asthma. J Asthma 2012; 49:474–479.
- Enriquez R, Wu P, Griffin MR, et al. Cessation of asthma medication in early pregnancy. Am J Obstet Gynecol 2006; 195:149–153.
- Bain E, Pierides KL, Clifton VL, et al. Interventions for managing asthma in pregnancy. Cochrane Database Syst Rev 2014; 10:CD010660.
- Murphy VE, Namazy JA, Powell H, et al. A meta-analysis of adverse perinatal outcomes in women with asthma. BJOG 2011; 118:1314–1323.
- Murphy VE, Clifton VL, Gibson PG. Asthma exacerbations during pregnancy: incidence and association with adverse pregnancy outcomes. Thorax 2006; 61:169–176.
- National Heart, Lung, and Blood Institute; National Asthma Education and Prevention Program Asthma and Pregnancy Working Group. NAEPP expert panel report. Managing asthma during pregnancy: recommendations for pharmacologic treatment—2004 update. J Allergy Clin Immunol 2005; 115:34–46.
- Lim AS, Stewart K, Abramson MJ, Walker SP, Smith CL, George J. Multidisciplinary Approach to Management of Maternal Asthma (MAMMA): a randomized controlled trial. Chest 2014; 145:1046–1054.
- Harding SM. Gastroesophageal reflux: a potential asthma trigger. Immunol Allergy Clin North Am 2005; 25:131–148.
- Ahmad S, Mokaddas E. Recent advances in the diagnosis and treatment of multidrug-resistant tuberculosis. Respir Med 2009; 103:1777–1790.
- van der Woude CJ, Metselaar HJ, Danese S. Management of gastrointestinal and liver diseases during pregnancy. Gut 2014; 63:1014–1023.
- Werler MM. Teratogen update: pseudoephedrine. Birth Defects Res A Clin Mol Teratol 2006; 76:445–452.
- Cox L, Nelson H, Lockey R, et al. Allergen immunotherapy: a practice parameter third update. J Allergy Clin Immunol 2011; 127(suppl 1):S1–S55.
- Lim AS, Stewart K, Abramson MJ, George J. Management of asthma in pregnant women by general practitioners: a cross sectional survey. BMC Fam Pract 2011; 12:121.
- Murphy VE, Wang G, Namazy JA, et al. The risk of congenital malformations, perinatal mortality and neonatal hospitalisation among pregnant women with asthma: a systematic review and meta-analysis. BJOG 2013; 120:812–822.
- Eltonsy S, Forget A, Beauchesne MF, Blais L. Risk of congenital malformations for asthmatic pregnant women using a long-acting beta2-agonist and inhaled corticosteroid combination versus higher-dose inhaled corticosteroid monotherapy. J Allergy Clin Immunol 2015; 135:123–130.
- Nelsen LM, Shields KE, Cunningham ML, et al. Congenital malformations among infants born to women receiving montelukast, inhaled corticosteroids, and other asthma medications. J Allergy Clin Immunol 2012; 129:251–254.e1–e6.
- Sarkar M, Koren G, Kalra S, et al. Montelukast use during pregnancy: a multicentre, prospective, comparative study of infant outcomes. Eur J Clin Pharmacol 2009; 65:1259–1264.
- Namazy JA, Schatz M. The safety of asthma medications during pregnancy: an update for clinicians. Ther Adv Respir Dis 2014; 8:103–110.
- Namazy J, Cabana MD, Scheuerle AE, et al. The Xolair Pregnancy Registry (EXPECT): the safety of omalizumab use during pregnancy. J Allergy Clin Immunol 2015; 135:407–412.
- Hviid A, Molgaard-Nielsen D. Corticosteroid use during pregnancy and risk of orofacial clefts. CMAJ 2011; 183:796–804.
- Murphy VE, Gibson P, Talbot PI, Clifton VL. Severe asthma exacerbations during pregnancy. Obstet Gynecol 2005; 106:1046–1054.
- Cydulka RK, Emerman CL, Schreiber D, Molander KH, Woodruff PG, Camargo CA Jr. Acute asthma among pregnant women presenting to the emergency department. Am J Respir Crit Care Med 1999; 160:887–892.
- Hasegawa K, Cydulka RK, Sullivan AF, et al. Improved management of acute asthma among pregnant women presenting to the ED. Chest 2015; 147:406–414.
- Kwon HL, Belanger K, Bracken MB. Asthma prevalence among pregnant and childbearing-aged women in the United States: estimates from national health surveys. Ann Epidemiol 2003; 13:317–324.
- Powell H, Murphy VE, Taylor DR, et al. Management of asthma in pregnancy guided by measurement of fraction of exhaled nitric oxide: a double-blind, randomised controlled trial. Lancet 2011; 378:983–990.
- Schatz M, Harden K, Forsythe A, et al. The course of asthma during pregnancy, post partum, and with successive pregnancies: a prospective analysis. J Allergy Clin Immunol 1988; 81:509–517.
- Gluck JC, Gluck PA. The effect of pregnancy on the course of asthma. Immunol Allergy Clin North Am 2006; 26:63–80.
- Beckmann CA. Peak flow values by gestation in women with asthma. Clin Nurs Res 2008; 17:174–181.
- Belanger K, Hellenbrand ME, Holford TR, Bracken M. Effect of pregnancy on maternal asthma symptoms and medication use. Obstet Gynecol 2010; 115:559–567.
- Lim AS, Stewart K, Abramson MJ, Ryan K, George J. Asthma during pregnancy: the experiences, concerns and views of pregnant women with asthma. J Asthma 2012; 49:474–479.
- Enriquez R, Wu P, Griffin MR, et al. Cessation of asthma medication in early pregnancy. Am J Obstet Gynecol 2006; 195:149–153.
- Bain E, Pierides KL, Clifton VL, et al. Interventions for managing asthma in pregnancy. Cochrane Database Syst Rev 2014; 10:CD010660.
- Murphy VE, Namazy JA, Powell H, et al. A meta-analysis of adverse perinatal outcomes in women with asthma. BJOG 2011; 118:1314–1323.
- Murphy VE, Clifton VL, Gibson PG. Asthma exacerbations during pregnancy: incidence and association with adverse pregnancy outcomes. Thorax 2006; 61:169–176.
- National Heart, Lung, and Blood Institute; National Asthma Education and Prevention Program Asthma and Pregnancy Working Group. NAEPP expert panel report. Managing asthma during pregnancy: recommendations for pharmacologic treatment—2004 update. J Allergy Clin Immunol 2005; 115:34–46.
- Lim AS, Stewart K, Abramson MJ, Walker SP, Smith CL, George J. Multidisciplinary Approach to Management of Maternal Asthma (MAMMA): a randomized controlled trial. Chest 2014; 145:1046–1054.
- Harding SM. Gastroesophageal reflux: a potential asthma trigger. Immunol Allergy Clin North Am 2005; 25:131–148.
- Ahmad S, Mokaddas E. Recent advances in the diagnosis and treatment of multidrug-resistant tuberculosis. Respir Med 2009; 103:1777–1790.
- van der Woude CJ, Metselaar HJ, Danese S. Management of gastrointestinal and liver diseases during pregnancy. Gut 2014; 63:1014–1023.
- Werler MM. Teratogen update: pseudoephedrine. Birth Defects Res A Clin Mol Teratol 2006; 76:445–452.
- Cox L, Nelson H, Lockey R, et al. Allergen immunotherapy: a practice parameter third update. J Allergy Clin Immunol 2011; 127(suppl 1):S1–S55.
- Lim AS, Stewart K, Abramson MJ, George J. Management of asthma in pregnant women by general practitioners: a cross sectional survey. BMC Fam Pract 2011; 12:121.
- Murphy VE, Wang G, Namazy JA, et al. The risk of congenital malformations, perinatal mortality and neonatal hospitalisation among pregnant women with asthma: a systematic review and meta-analysis. BJOG 2013; 120:812–822.
- Eltonsy S, Forget A, Beauchesne MF, Blais L. Risk of congenital malformations for asthmatic pregnant women using a long-acting beta2-agonist and inhaled corticosteroid combination versus higher-dose inhaled corticosteroid monotherapy. J Allergy Clin Immunol 2015; 135:123–130.
- Nelsen LM, Shields KE, Cunningham ML, et al. Congenital malformations among infants born to women receiving montelukast, inhaled corticosteroids, and other asthma medications. J Allergy Clin Immunol 2012; 129:251–254.e1–e6.
- Sarkar M, Koren G, Kalra S, et al. Montelukast use during pregnancy: a multicentre, prospective, comparative study of infant outcomes. Eur J Clin Pharmacol 2009; 65:1259–1264.
- Namazy JA, Schatz M. The safety of asthma medications during pregnancy: an update for clinicians. Ther Adv Respir Dis 2014; 8:103–110.
- Namazy J, Cabana MD, Scheuerle AE, et al. The Xolair Pregnancy Registry (EXPECT): the safety of omalizumab use during pregnancy. J Allergy Clin Immunol 2015; 135:407–412.
- Hviid A, Molgaard-Nielsen D. Corticosteroid use during pregnancy and risk of orofacial clefts. CMAJ 2011; 183:796–804.
- Murphy VE, Gibson P, Talbot PI, Clifton VL. Severe asthma exacerbations during pregnancy. Obstet Gynecol 2005; 106:1046–1054.
- Cydulka RK, Emerman CL, Schreiber D, Molander KH, Woodruff PG, Camargo CA Jr. Acute asthma among pregnant women presenting to the emergency department. Am J Respir Crit Care Med 1999; 160:887–892.
- Hasegawa K, Cydulka RK, Sullivan AF, et al. Improved management of acute asthma among pregnant women presenting to the ED. Chest 2015; 147:406–414.
KEY POINTS
- The benefits of good adherence to asthma regimens during pregnancy outweigh the risks associated with the medications used.
- For treatment of reflux disease in pregnant women with asthma, antacids (but not sodium bicarbonate, for fear of metabolic alkalosis) and sucralfate should be considered before a histamine 2 receptor antagonist such as ranitidine. Proton pump inhibitors should be considered only if reflux symptoms are refractory to other therapies.
- Uncontrolled maternal asthma contributes to poor maternal and fetal outcomes. Management by a multi-disciplinary team, including internist, obstetrician, pharmacist, nurse, allergist, and pulmonologist, improves care and outcomes.
Treating Helicobacter pylori effectively while minimizing misuse of antibiotics
Helicobacter pylori infection is an infectious disease and should be treated like one, with due consideration of antibiotic resistance and stewardship.1–4
This was the consensus of the 2015 Kyoto H pylori conference,2 and it signaled a fundamental shift in thinking. Up to now, H pylori treatment has not been based on infectious disease principles, leading to suboptimal results and antibiotic resistance. In addition, the conference recommended that H pylori infection be treated whenever it is found unless there are compelling reasons not to.
Here we review current and possible future regimens for eradicating H pylori that we hope will be more effective and will lead to less resistance than in the past.
H PYLORI AS AN INFECTIOUS DISEASE
Not until the late 1980s was H pylori recognized as the cause of peptic ulcer disease, which until then accounted for hundreds of thousands of hospitalizations and more than 100,000 surgical procedures each year.5 Now, peptic ulcer disease is routinely treated by eradicating H pylori. In addition, the World Health Organization has recommended considering H pylori eradication to reduce the risk of gastric cancer,6 which causes 738,000 deaths worldwide per year.7
The problems of how to diagnose and treat H pylori infection were taken on by gastroenterologists, and not by specialists in infectious disease.1 Even now, almost all the major reviews and consensus statements on H pylori come from gastroenterologists and are published in gastroenterology journals.2,8,9
But infectious diseases differ from most gastrointestinal diseases. In gastrointestinal problems such as constipation or inflammatory bowel disease,10 the causes are generally unknown, and there is a large placebo response to therapy. In contrast, in infectious diseases, the cause is generally known, there is no placebo response, and treatment success depends on susceptibility of the organism. Failure of proven regimens is generally due to resistant organisms, poor adherence, or, in the case of H pylori, poorly designed regimens in terms of doses, frequency of administration, or duration of therapy.
The differences extend to clinical trials of treatment.3 In other infectious diseases, treatment is based on susceptibility. The usual comparative approach in infectious diseases is a noninferiority trial in which the new treatment is compared with standard care, ie, a regimen that reliably achieves nearly 100% cure rates. Not so with H pylori. Most trials of H pylori therapy compared regimens in populations with high but unknown prevalences of resistance and therefore are of limited or no help to the clinician in choosing the best regimen for an individual patient.3
Many thousands of H pylori-infected patients participated in clinical trials in which the results would have been predictable if the researchers had assessed susceptibility before giving the drugs.11–13 Worse, many patients were also randomized to receive regimens that the investigators knew provided poor cure rates in the population being studied. This knowledge was generally not shared with the patients. This approach was used to demonstrate that a new regimen was superior to an old one, even though the new one was already known to be less affected by resistance to the key element in the comparator.
Clinicians generally do not test for susceptibility when treating H pylori, one reason being that such testing is often unavailable.3 However, almost every hospital, clinic, and major laboratory in the world provides susceptibility testing for other common local pathogens. H pylori is easy to grow, and laboratories could test for susceptibility if we asked them to.
Current H pylori recommendations may also contribute to the global increase in antimicrobal resistance.
As discussed below, all recent guidelines have recommended 4-drug non-bismuth-containing concomitant therapy as first-line therapy. An infectious disease colleague described it as a “hope therapy” because the prescriber hoped that the infection would be susceptible to either metronidazole or clarithromycin. All who receive this combination receive an antibiotic they do not need. This is an expedient rather than a medically rational choice resulting from failure to deal with H pylori as an infectious disease.
H PYLORI THERAPIES
Conceptually, treating infectious disease is straightforward: one should prescribe antimicrobial drugs to which the organism is susceptible3 (Table 1). However, clinical success lies in the details, which include the doses, frequency of doses, duration of therapy, timing of doses in relation to meals, and use of adjuvants such as antisecretory drugs, antacids, and probiotics. A number of regimens reliably yield high cure rates—95% or higher—if the organism is susceptible and the patients are adherent.
The effectiveness of any regimen may vary depending on the population it is used in, due to polymorphisms in drug-metabolizing enzymes such as CYP2C19.
Sequential therapy is obsolete
Sequential therapy for H pylori infection consisted of amoxicillin plus a proton pump inhibitor for 7 days, followed by clarithromycin, tinidazole, or metronidazole plus a proton pump inhibitor for a further 7 days. This regimen should not be used any more because concomitant therapy will always be superior (see below).
Need for 14 days of therapy
H pylori occupies a number of different niches in the body ranging from gastric mucus (which is technically outside the body) to inside gastric epithelial cells. As a general rule, 14-day therapy provides the best results, in part because the longer duration helps kill the organisms that persist in different niches.14,15
In addition, proton pump inhibitors, which are part of all the currently recommended regimens, require 3 or more days to reach their full antisecretory effectiveness, which further limits the effectiveness of short-duration therapies.
Shorter regimens should be used only if they are proved to be as good as 14-day regimens and if both achieve 95% or greater cure rates with susceptible infections.
How to choose a therapy
Since rational infectious-disease therapy is based on susceptibility, one should start by considering the susceptibility pattern in the local population and, therefore, the likely susceptibility in the patient in front of us.
Unfortunately, we do not yet have local or regional susceptibility data on H pylori for most locales. Until those data are available, we must use the indirect information that is available, such as the patient’s history of antibiotic use.
Triple therapy should not be used empirically
Triple therapy (Table 1) consists of the combination of:
- Clarithromycin or metronidazole or a fluoroquinolone
- Amoxicillin
- A proton pump inhibitor.
However, prior use of a macrolide (eg, erythromycin, clarithromycin, or azithromycin), metronidazole, or a fluoroquinolone (eg, ciprofloxacin, levofloxacin) almost guarantees resistance to those drugs. In the United States, resistance to clarithromycin, metronidazole, levofloxacin, and related drugs is already widespread, and none should be used empirically in triple therapies. In contrast, amoxicillin, tetracycline, and furazolidone can often be used again, as resistance to them is rare even with prior use.
For example, 14 days of clarithromycin triple therapy (clarithromycin, amoxicillin, and a proton pump inhibitor) can be expected to cure more than 95% of patients who have susceptible infections and about 20% of those with resistant infections.16 This 20% is due to the proton pump inhibitor and amoxicillin, as the contribution to the cure rate from clarithromycin is close to zero.
If the prevalence of resistance to clarithromycin is 25%, the cure rate in the entire population will be a little more than 75%—97% in the 75% of the population with susceptible infections and 20% in patients who previously received clarithromycin (Figure 1).
If we know that our patient has an infection that is susceptible to clarithromycin, metronidazole, or levofloxacin, good results could be achieved with triple therapy that includes a proton pump inhibitor, for 14 days. Fluoroquinolones have a number of black-box warnings from the US Food and Drug Administration (www.fda.gov/Drugs/DrugSafety/ucm500143.htm) and should always be a last choice. However, in the United States, lacking definite data about susceptibility to clarithromycin, metronidazole, and levofloxacin, we should assume resistance is present and use a 4-drug regimen (eg, concomitant therapy or bismuth quadruple therapy).
Concomitant therapy is preferred
Concomitant therapy is the combination of:
- Amoxicillin
- Metronidazole
- Clarithromycin
- A proton pump inhibitor.
Functionally, this is a combination of clarithromycin and metronidazole triple therapies, given simultaneously.17 The premise is that even though the prevalence of metronidazole resistance in the United States is high (20%–40%), and so is the prevalence of clarithromycin resistance (about 20%), the prevalence of resistance to both drugs at the same time is expected to be low (eg, 0.4 × 0.2 = 0.08, or 8%) unless the drugs had previously been used together, as in some older regimens that contained both. Thus, the metronidazole will kill the clarithromycin-resistant but metronidazole-susceptible strains, and the clarithromycin will kill the clarithromycin-susceptible, metronidazole-resistant strains. Only with dual resistant strains will this regimen fail (with a 20% cure rate due to the proton pump inhibitor and amoxicillin and a population cure rate of slightly more than 90%).
The downside of this highly recommended therapy is that all who receive it are getting an antibiotic that they don’t need, which is, in a global sense, inappropriate. In other words, all those who are cured by clarithromycin also receive metronidazole, which plays no role in treatment success, and those cured by metronidazole receive unneeded clarithromycin (Figure 2). Had susceptibility testing been available, those with susceptible strains would have received appropriate triple therapies, and those with dual resistance would not have received either antibiotic.
Thus, while we recommend concomitant therapy as an empiric regimen in populations that do not have high levels of resistance to metronidazole or clarithromycin (as those would also have a high prevalence of dual resistance), one must be aware of the “dirty little secret” of inappropriate antibiotic use that accompanies it and some other H pylori therapies (eg, vonoprazan triple therapy in Japan).18–20
Bismuth quadruple therapy is an alternative
Bismuth quadruple therapy (Table 1) consists of:
- Bismuth
- Tetracycline
- Metronidazole
- A proton pump inhibitor.
This was the first truly effective regimen for H pylori. Its advantage is that it can partially or completely overcome metronidazole resistance.21,22 As such, it is potentially ideal, as it should be effective despite resistance to clarithromycin, metronidazole, or levofloxacin, and it can be used in patients allergic to penicillin.
The major downside is a high frequency of side effects, particularly abdominal pain, nausea, and vomiting, often resulting in poor adherence. Most regimens that contain antibiotics have side effects, but adherence seems to be more of a problem with bismuth quadruple therapy, probably because of the combination of the high doses of metronidazole and tetracycline.22 In our experience, this regimen can be effective if the physician takes the time to explain to the patient that side effects are common but treatment success depends on completing the full course of 14 days.
Another problem is that tetracycline has become difficult to obtain in many areas, and doxycycline cannot be substituted in those with metronidazole resistance. To date, it has been difficult or impossible to obtain the same excellent results with doxycycline as can be obtained with tetracycline. It is not clear why.21
To use bismuth quadruple therapy one must often use a name-brand product, Pylera. Pylera is packaged as a 10-day course, which is effective against metronidazole-susceptible infections. However, 14 days are generally required to achieve a high cure rate with metronidazole-resistant infections, which are the main indication for use of this product. Moreover, Pylera does not include a proton pump inhibitor, which must be prescribed separately.
In the United States, Pylera is expensive, costing $740 to $790 with a coupon for a 10-day supply and proportionally more for the required 14-day supply (www.goodrx.com/pylera?drug-name=pylera), whereas in Europe it costs less than 70 Euros ($73).21 If generic tetracycline is available, the US cost for 14 days of generic bismuth quadruple therapy is less than $50.
An alternate and simpler approach is to substitute amoxicillin for tetracycline.23 This regimen has been used successfully in China and was shown to be noninferior to the tetracycline-containing regimen in a head-to-head comparison.24
Recent studies have confirmed earlier Italian studies suggesting that twice-a-day bismuth and tetracycline is effective, which would further simplify therapy and possibly reduce side effects.21,23,24 These variations on bismuth quadruple therapy have not yet been optimized to where one can reliably achieve 95% or greater cure rates, and further studies are needed.
Why include more than 1 antibiotic?
The H pylori load in the stomach is typically large, which increases the odds that a subpopulation of resistant organisms is present. Resistance may be due to a relatively high rate of mutation in certain bacterial genes.25 This is particularly a problem with clarithromycin, metronidazole, and fluoroquinolones and is reflected in a high rate of resistance among patients for whom single-drug regimens have failed. These drugs are always given with a second antimicrobial to which H pylori rarely becomes resistant, such as amoxicillin or tetracycline.
Why include a proton pump inhibitor?
An antisecretory drug is needed to increase the gastric pH, which makes antimicrobial therapy more effective. It also decreases antibiotic washout from the stomach and likely protects and increases the gastric concentration of some antibiotics.
The activities of amoxicillin, fluoroquinolones, and to a lesser degree clarithromycin are pH-dependent. For example, keeping the gastric pH above 6.0 promotes H pylori replication,26,27 making it is more susceptible to amoxicillin (reviewed in detail by Dore et al21). A gastric pH of 6.0 or more is very difficult to achieve with proton pump inhibitors, and has been accomplished regularly only in people who metabolize these drugs slowly (“slow metabolizers”) who received both the proton pump inhibitor and amoxicillin every 6 hours for 14 days.21
With standard clarithromycin, metronidazole, or fluoroquinolone triple therapy, proton pump inhibitors appear to provide satisfactory cure rates when given for 14 days in standard doses. However, double doses (eg, 40 mg of omeprazole or an equivalent) may be slightly better, especially in the presence of resistance.
The cure rate reflects the sum of the 2 populations of organisms: the susceptible and the resistant. In triple therapy, increasing the gastric pH with a proton pump inhibitor makes the amoxicillin component of the regimen more effective against resistant organisms and thus increases the cure rate. For example, in Western countries, esomeprazole 40 mg (approximately equivalent to rabeprazole 40 mg, omeprazole or lansoprazole 60 mg, or pantoprazole 240 mg)28 given twice a day in a 14-day triple therapy regimen cures about 40% to 50% of resistant infections. This benefit will be evident in an improvement in cure rates in populations in which resistance has reduced the average cure rate. This is also why meta-analyses have shown better results with second-generation proton pump inhibitors and with longer duration of therapy.29,30
Generally, we recommend omeprazole 40 mg twice a day or an equivalent (Tables 1–3).
Would a potassium-competitive acid blocker be better than a proton pump inhibitor?
Vonoprazan is a potassium-competitive acid blocker. It does not require intermediate complex formation and is stable at low pH. It has a longer half-life than proton pump inhibitors, and its bioavailability is unaffected by food.31 It was recently approved in Japan for H pylori eradication in combination with clarithromycin or metronidazole plus amoxicillin.18
Vonoprazan is more effective than current proton pump inhibitors for keeping the gastric pH high. There are no published studies of vonoprazan dual therapy in Western countries, but given twice a day for 7 days along with twice-daily amoxicillin it cured only approximately 80% of clarithromycin-resistant strains. Further studies are needed to identify the optimum proton pump inhibitor or potassium-competitive acid blocker, dose, and duration.
Misuse of antibiotics
In triple therapy, the second antimicrobial drug (eg, amoxicillin) is given in part to prevent resistance from developing. It is not clear whether the combination is additive or synergistic, but until we can reliably maintain the intragastric pH above 6.0, which would increase the effectiveness of the amoxicillin component of the regimen, this practice cannot be considered as misuse of antibiotics.
In contrast, in the 4-drug nonbismuth combinations (concomitant, sequential, and hybrid therapies) and the new vonoprazan, clarithromycin, and metronidazole triple therapies, 1 of the antibiotics provides no benefit to some, often most, of the patients.18–20,32 This practice should end when susceptibility data become more widely available and when vonoprazan becomes available, so that we can deliver effective vonoprazan-amoxicillin dual therapy.
First-, second-, and third-line therapies
Many recommendations give advice in terms of first-, second-, and third-line therapies. In practice, a physician should have at least 2 first-line regimens (a first and a second choice). Both should be proven highly successful as empiric therapies in one’s patient population but differ in terms of primary antibiotics. This approach allows the clinician to tailor therapy depending on whether he or she suspects antibiotic resistance (eg, if the patient has taken clarithromycin before) or the patient is allergic or cannot take 1 or more drugs.
Two treatment failures with 2 different regimens known to be effective suggest poor compliance (a difficult patient) or a multiple-drug-resistant infection (a difficult infection). That patient would require salvage therapy (Table 2), which logically should be based on antimicrobial testing or, at a minimum, consultation with someone who frequently deals with this problem.
Test of cure
Monitoring the outcome of therapy (testing for cure) is essential, as it provides a reliable measure of the local effectiveness of particular therapies and also serves as an early warning of development of resistance in one’s patient population.14
Unless there are compelling reasons, testing for cure should use noninvasive testing with the urea breath test or stool antigen test. It is recommended that this be delayed at least 4 weeks to allow the organisms if still present to repopulate the stomach sufficiently for the tests to become positive. Because antibiotics, bismuth, and proton pump inhibitors reduce the bacterial load, they should be withheld at least 2 weeks before testing. Histamine-2 receptor antagonists can be substituted for proton pump inhibitors if antisecretory therapy is needed for symptoms, and continued up to the day before testing. The urea breath test should contain citric acid to overcome any residual pH effects. Physician groups should share their experience so as to alert the community about which therapies should likely be avoided.33
Salvage therapy
Salvage therapy is given after 2 or more treatment failures with different antibiotics. Ideally, the regimen should be based on the results of antimicrobial testing. Current regimens include rifabutin triple therapy, dual therapy (a protein pump inhibitor or vonoprazan and amoxicillin), or furazolidone quadruple therapy (Table 2).
Furazolidone is a synthetic nitrofuran derivative that is effective against many enteric organisms, including gram-negative bacteria and protozoa. It is not available in most Western countries but is available in many other parts of the world.34,35 It is also a monoamine oxidase inhibitor and thus interacts with many drugs and foods (eg, soy sauce, aged cheeses), leading to a relatively high rate of side effects such as fever, palpitations, and skin rash.
Rifabutin-containing regimens, generally, a proton pump inhibitor, amoxicillin 1 g, and rifabutin 150 mg, all twice a day (Table 3) provide average cure rates of less than 80% (typically in the mid-70% range).36 Borody et al37 reported greater than 95% success with a 12-day regimen consisting of rifabutin 150 mg once daily (half-dose), amoxicillin 1.5 g 3 times a day, and pantoprazole 80 mg (approximately equivalent to omeprazole 20 mg) 3 times a day. Ciccaglione et al,38 in a small study, used a 10-day quadruple regimen containing a proton pump inhibitor, amoxicillin, rifabutin, and bismuth (all twice a day), with high cure rates. The results of these studies are yet to be confirmed, and the optimal rifabutin-containing regimen remains to be determined.
PROBIOTICS
There is considerable interest in using probiotics to enhance the effectiveness of antimicrobial therapy for H pylori by increasing tolerability, reducing side effects, and therefore improving compliance.39,40
In a meta-analysis of 14 randomized trials (N = 1,671), when probiotics were added, pooled H pylori eradication rates were only slightly improved: 83.6% (95% CI 80.5%–86.7%) with probiotics and 74.8% (95% CI 71.1%–78.5%) without probiotics by intent-to-treat analysis.41
Another meta-analysis of probiotics suggested that those containing Saccharomyces boulardii, Lactobacillus, and Bifidobacterium significantly increased the eradication rate of triple therapy in populations with high rates of antimicrobial resistance and reduced the risk of overall H pylori therapy-related adverse effects, especially diarrhea.42,43
At present, we recommend that probiotics be considered only for patients who are likely not to comply with treatment (eg, those with irritable bowel syndrome or difficulty taking antibiotics), to try to take advantage of their ability to improve antibiotic tolerability.
- Graham DY. Helicobacter pylori update: gastric cancer, reliable therapy, and possible benefits. Gastroenterology 2015; 148:719–731.
- Sugano K, Tack J, Kuipers EJ, et al. Kyoto global consensus report on Helicobacter pylori gastritis. Gut 2015; 64:1353–1367.
- Graham DY, Dore MP. Helicobacter pylori therapy: a paradigm shift. Expert Rev Anti Infect Ther 2016; 14:577–585.
- Leja M, Axon A, Brenner H. Epidemiology of Helicobacter pylori infection. Helicobacter 2016; 21(suppl 1):3–7.
- Grossman MI. Closing remarks. Gastroenterology 1978; 74:487–488.
- Malfertheiner P, Megraud F, O’Morain CA, et al. Management of Helicobacter pylori infection—the Maastricht IV/ Florence Consensus Report. Gut 2012; 61:646–664.
- Fallone CA, Chiba N, van Zanten SV, et al. The Toronto consensus for the treatment of Helicobacter pylori infection in adults. Gastroenterology 2016; 151:51–69.
- IARC Helicobacter pylori Working Group. Volume 8. Helicobacter pylori eradication as a strategy for preventing gastric cancer. Lyon, France: International Agency for Research on Cancer, 2014.
- Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 2010; 127:2893–2917.
- Graham DY, Dore MP. Helicobacter pylori therapy demystified. Helicobacter 2011; 16:343–345.
- Gatta L, Vakil N, Leandro G, Di MF, Vaira D. Sequential therapy or triple therapy for Helicobacter pylori infection: systematic review and meta-analysis of randomized controlled trials in adults and children. Am J Gastroenterol 2009; 104:3069–3079.
- Graham DY, Fischbach L. Helicobacter pylori treatment in the era of increasing antibiotic resistance. Gut 2010; 59:1143–1153.
- Graham DY. Helicobacter pylori eradication therapy research: ethical issues and description of results. Clin Gastroenterol Hepatol 2010; 8:1032–1036.
- Graham DY, Shiotani A. New concepts of resistance in the treatment of Helicobacter pylori infections. Nat Clin Pract Gastroenterol Hepatol 2008; 5:321–331.
- Graham DY, Dore MP. Variability in the outcome of treatment of Helicobacter pylori infection: a critical analysis. In: Hunt RH, Tytgat GNJ, editors. Helicobacter pylori Basic Mechanisms to Clinical Cure 1998. Dordrecht, Netherlands: Kluwer Academic Publishers, 998:426–440.
- Graham DY. Hp-normogram (normo-graham) for assessing the outcome of H. pylori therapy: effect of resistance, duration, and CYP2C19 genotype. Helicobacter 2015; 21:85–90.
- Graham DY, Lee YC, Wu MS. Rational Helicobacter pylori therapy: evidence-based medicine rather than medicine-based evidence. Clin Gastroenterol Hepatol 2014; 12:177–186.
- Murakami K, Sakurai Y, Shiino M, Funao N, Nishmura A, Asaka M. Vonoprazan, a novel potassium-competitive acid blocker, as a component of first-line and second-line triple therapy for Helicobacter pylori eradication: a phase III, randomised, double-blind study. Gut 2016; 65:1439–1446.
- Graham DY. Vonoprazan Helicobacter pylori eradication therapy: ethical and interpretation issues. Gut 2016 Apr 7. pii: gutjnl-2016-311796. doi: 10.1136/gutjnl-2016-311796. [Epub ahead of print].
- Matsumoto H, Shiotani A, Katsumata R, et al. Helicobacter pylori eradication with proton pump inhibitors or potassium-competitive acid blockers: the effect of clarithromycin resistance. Dig Dis Sci 2016; 61:3215–3220.
- Dore MP, Lu H, Graham DY. Role of bismuth in improving Helicobacter pylori eradication with triple therapy. Gut 2016; 65:870–878.
- Graham DY, Lee SY. How to effectively use bismuth quadruple therapy: the good, the bad, and the ugly. Gastroenterol Clin North Am 2015; 44:537–563.
- Zhang W, Chen Q, Liang X, et al. Bismuth, lansoprazole, amoxicillin and metronidazole or clarithromycin as first-line Helicobacter pylori therapy. Gut 2015; 64:1715–1720.
- Chen Q, Zhang X, Fu Q, et al. Rescue therapy for Helicobacter pylori eradication: a randomized non-inferiority trial of amoxicillin or tetracycline for bismuth quadruple therapy. Am J Gastroenterol 2016; 111:1736–1742.
- Graham DY. Antibiotic resistance in Helicobacter pylori: implications for therapy. Gastroenterology 1998; 115:1272–1277.
- Marcus EA, Inatomi N, Nagami GT, et al. The effects of varying acidity on Helicobacter pylori growth and the bactericidal efficacy of ampicillin. Aliment Pharmacol Ther 2012; 36:972–979.
- Sachs G, Shin JM, Munson K, et al. Review article: the control of gastric acid and Helicobacter pylori eradication. Aliment Pharmacol Ther 2000; 14:1383–1401.
- Kirchheiner J, Glatt S, Fuhr U, et al. Relative potency of proton-pump inhibitors: comparison of effects on intragastric pH. Eur J Clin Pharmacol 2009; 65:19–31.
- Yuan Y, Ford AC, Khan KJ, et al. Optimum duration of regimens for Helicobacter pylori eradication. Cochrane Database Syst Rev 2013;12:CD008337.
- McNicholl AG, Linares PM, Nyssen OP, et al. Meta-analysis: esomeprazole or rabeprazole vs. first-generation pump inhibitors in the treatment of Helicobacter pylori infection. Aliment Pharmacol Ther 2012; 36:414–425.
- Sakurai Y, Nishimura A, Kennedy G, et al. Safety, tolerability, pharmacokinetics, and pharmacodynamics of single rising TAK-438 (vonoprazan) doses in healthy male Japanese/non-Japanese subjects. Clin Transl Gastroenterol 2015; 6:e94.
- Graham DY, Laine L. The Toronto Helicobacter pylori consensus in context. Gastroenterology 2016; 151:9–12.
- Uotani T, Graham DY. Diagnosis of Helicobacter pylori using the rapid urease test. Ann Transl Med 2015; 3:9.
- Lu H, Zhang W, Graham DY. Bismuth-containing quadruple therapy for Helicobacter pylori: lessons from China. Eur J Gastroenterol Hepatol 2013; 25:1134–1140.
- Graham DY, Lu H. Furazolidone in Helicobacter pylori therapy: misunderstood and often unfairly maligned drug told in a story of French bread. Saudi J Gastroenterol 2012; 8:1–2.
- Gisbert JP, Calvet X. Review article: rifabutin in the treatment of refractory Helicobacter pylori infection. Aliment Pharmacol Ther 2012; 35:209–221.
- Borody TJ, Pang G, Wettstein AR, et al. Efficacy and safety of rifabutin-containing ‘rescue therapy’ for resistant Helicobacter pylori infection. Aliment Pharmacol Ther 2006; 23:481–488.
- Ciccaglione AF, Tavani R, Grossi L, et al. Rifabutin containing triple therapy and rifabutin with bismuth containing quadruple therapy for third-line treatment of Helicobacter pylori infection: two pilot studies. Helicobacter 2016; 21:375–381.
- Homan M, Orel R. Are probiotics useful in Helicobacter pylori eradication? World J Gastroenterol 2015; 21:10644–10653.
- Zhang MM, Qian W, Qin YY, et al. Probiotics in Helicobacter pylori eradication therapy: a systematic review and meta-analysis. World J Gastroenterol 2015; 21:4345–4357.
- Tong JL, Ran ZH, Shen J, et al. Meta-analysis: the effect of supplementation with probiotics on eradication rates and adverse events during Helicobacter pylori eradication therapy. Aliment Pharmacol Ther 2007; 25:155–168.
- Szajewska H, Setty M, Mrukowicz J, et al. Probiotics in gastrointestinal diseases in children: hard and not-so-hard evidence of efficacy. J Pediatr Gastroenterol Nutr 2006; 42:454–475.
- Wang ZH, Gao QY, Fang JY. Meta-analysis of the efficacy and safety of Lactobacillus-containing and Bifidobacterium-containing probiotic compound preparation in Helicobacter pylori eradication therapy. J Clin Gastroenterol 2013; 47:25–32.
Helicobacter pylori infection is an infectious disease and should be treated like one, with due consideration of antibiotic resistance and stewardship.1–4
This was the consensus of the 2015 Kyoto H pylori conference,2 and it signaled a fundamental shift in thinking. Up to now, H pylori treatment has not been based on infectious disease principles, leading to suboptimal results and antibiotic resistance. In addition, the conference recommended that H pylori infection be treated whenever it is found unless there are compelling reasons not to.
Here we review current and possible future regimens for eradicating H pylori that we hope will be more effective and will lead to less resistance than in the past.
H PYLORI AS AN INFECTIOUS DISEASE
Not until the late 1980s was H pylori recognized as the cause of peptic ulcer disease, which until then accounted for hundreds of thousands of hospitalizations and more than 100,000 surgical procedures each year.5 Now, peptic ulcer disease is routinely treated by eradicating H pylori. In addition, the World Health Organization has recommended considering H pylori eradication to reduce the risk of gastric cancer,6 which causes 738,000 deaths worldwide per year.7
The problems of how to diagnose and treat H pylori infection were taken on by gastroenterologists, and not by specialists in infectious disease.1 Even now, almost all the major reviews and consensus statements on H pylori come from gastroenterologists and are published in gastroenterology journals.2,8,9
But infectious diseases differ from most gastrointestinal diseases. In gastrointestinal problems such as constipation or inflammatory bowel disease,10 the causes are generally unknown, and there is a large placebo response to therapy. In contrast, in infectious diseases, the cause is generally known, there is no placebo response, and treatment success depends on susceptibility of the organism. Failure of proven regimens is generally due to resistant organisms, poor adherence, or, in the case of H pylori, poorly designed regimens in terms of doses, frequency of administration, or duration of therapy.
The differences extend to clinical trials of treatment.3 In other infectious diseases, treatment is based on susceptibility. The usual comparative approach in infectious diseases is a noninferiority trial in which the new treatment is compared with standard care, ie, a regimen that reliably achieves nearly 100% cure rates. Not so with H pylori. Most trials of H pylori therapy compared regimens in populations with high but unknown prevalences of resistance and therefore are of limited or no help to the clinician in choosing the best regimen for an individual patient.3
Many thousands of H pylori-infected patients participated in clinical trials in which the results would have been predictable if the researchers had assessed susceptibility before giving the drugs.11–13 Worse, many patients were also randomized to receive regimens that the investigators knew provided poor cure rates in the population being studied. This knowledge was generally not shared with the patients. This approach was used to demonstrate that a new regimen was superior to an old one, even though the new one was already known to be less affected by resistance to the key element in the comparator.
Clinicians generally do not test for susceptibility when treating H pylori, one reason being that such testing is often unavailable.3 However, almost every hospital, clinic, and major laboratory in the world provides susceptibility testing for other common local pathogens. H pylori is easy to grow, and laboratories could test for susceptibility if we asked them to.
Current H pylori recommendations may also contribute to the global increase in antimicrobal resistance.
As discussed below, all recent guidelines have recommended 4-drug non-bismuth-containing concomitant therapy as first-line therapy. An infectious disease colleague described it as a “hope therapy” because the prescriber hoped that the infection would be susceptible to either metronidazole or clarithromycin. All who receive this combination receive an antibiotic they do not need. This is an expedient rather than a medically rational choice resulting from failure to deal with H pylori as an infectious disease.
H PYLORI THERAPIES
Conceptually, treating infectious disease is straightforward: one should prescribe antimicrobial drugs to which the organism is susceptible3 (Table 1). However, clinical success lies in the details, which include the doses, frequency of doses, duration of therapy, timing of doses in relation to meals, and use of adjuvants such as antisecretory drugs, antacids, and probiotics. A number of regimens reliably yield high cure rates—95% or higher—if the organism is susceptible and the patients are adherent.
The effectiveness of any regimen may vary depending on the population it is used in, due to polymorphisms in drug-metabolizing enzymes such as CYP2C19.
Sequential therapy is obsolete
Sequential therapy for H pylori infection consisted of amoxicillin plus a proton pump inhibitor for 7 days, followed by clarithromycin, tinidazole, or metronidazole plus a proton pump inhibitor for a further 7 days. This regimen should not be used any more because concomitant therapy will always be superior (see below).
Need for 14 days of therapy
H pylori occupies a number of different niches in the body ranging from gastric mucus (which is technically outside the body) to inside gastric epithelial cells. As a general rule, 14-day therapy provides the best results, in part because the longer duration helps kill the organisms that persist in different niches.14,15
In addition, proton pump inhibitors, which are part of all the currently recommended regimens, require 3 or more days to reach their full antisecretory effectiveness, which further limits the effectiveness of short-duration therapies.
Shorter regimens should be used only if they are proved to be as good as 14-day regimens and if both achieve 95% or greater cure rates with susceptible infections.
How to choose a therapy
Since rational infectious-disease therapy is based on susceptibility, one should start by considering the susceptibility pattern in the local population and, therefore, the likely susceptibility in the patient in front of us.
Unfortunately, we do not yet have local or regional susceptibility data on H pylori for most locales. Until those data are available, we must use the indirect information that is available, such as the patient’s history of antibiotic use.
Triple therapy should not be used empirically
Triple therapy (Table 1) consists of the combination of:
- Clarithromycin or metronidazole or a fluoroquinolone
- Amoxicillin
- A proton pump inhibitor.
However, prior use of a macrolide (eg, erythromycin, clarithromycin, or azithromycin), metronidazole, or a fluoroquinolone (eg, ciprofloxacin, levofloxacin) almost guarantees resistance to those drugs. In the United States, resistance to clarithromycin, metronidazole, levofloxacin, and related drugs is already widespread, and none should be used empirically in triple therapies. In contrast, amoxicillin, tetracycline, and furazolidone can often be used again, as resistance to them is rare even with prior use.
For example, 14 days of clarithromycin triple therapy (clarithromycin, amoxicillin, and a proton pump inhibitor) can be expected to cure more than 95% of patients who have susceptible infections and about 20% of those with resistant infections.16 This 20% is due to the proton pump inhibitor and amoxicillin, as the contribution to the cure rate from clarithromycin is close to zero.
If the prevalence of resistance to clarithromycin is 25%, the cure rate in the entire population will be a little more than 75%—97% in the 75% of the population with susceptible infections and 20% in patients who previously received clarithromycin (Figure 1).
If we know that our patient has an infection that is susceptible to clarithromycin, metronidazole, or levofloxacin, good results could be achieved with triple therapy that includes a proton pump inhibitor, for 14 days. Fluoroquinolones have a number of black-box warnings from the US Food and Drug Administration (www.fda.gov/Drugs/DrugSafety/ucm500143.htm) and should always be a last choice. However, in the United States, lacking definite data about susceptibility to clarithromycin, metronidazole, and levofloxacin, we should assume resistance is present and use a 4-drug regimen (eg, concomitant therapy or bismuth quadruple therapy).
Concomitant therapy is preferred
Concomitant therapy is the combination of:
- Amoxicillin
- Metronidazole
- Clarithromycin
- A proton pump inhibitor.
Functionally, this is a combination of clarithromycin and metronidazole triple therapies, given simultaneously.17 The premise is that even though the prevalence of metronidazole resistance in the United States is high (20%–40%), and so is the prevalence of clarithromycin resistance (about 20%), the prevalence of resistance to both drugs at the same time is expected to be low (eg, 0.4 × 0.2 = 0.08, or 8%) unless the drugs had previously been used together, as in some older regimens that contained both. Thus, the metronidazole will kill the clarithromycin-resistant but metronidazole-susceptible strains, and the clarithromycin will kill the clarithromycin-susceptible, metronidazole-resistant strains. Only with dual resistant strains will this regimen fail (with a 20% cure rate due to the proton pump inhibitor and amoxicillin and a population cure rate of slightly more than 90%).
The downside of this highly recommended therapy is that all who receive it are getting an antibiotic that they don’t need, which is, in a global sense, inappropriate. In other words, all those who are cured by clarithromycin also receive metronidazole, which plays no role in treatment success, and those cured by metronidazole receive unneeded clarithromycin (Figure 2). Had susceptibility testing been available, those with susceptible strains would have received appropriate triple therapies, and those with dual resistance would not have received either antibiotic.
Thus, while we recommend concomitant therapy as an empiric regimen in populations that do not have high levels of resistance to metronidazole or clarithromycin (as those would also have a high prevalence of dual resistance), one must be aware of the “dirty little secret” of inappropriate antibiotic use that accompanies it and some other H pylori therapies (eg, vonoprazan triple therapy in Japan).18–20
Bismuth quadruple therapy is an alternative
Bismuth quadruple therapy (Table 1) consists of:
- Bismuth
- Tetracycline
- Metronidazole
- A proton pump inhibitor.
This was the first truly effective regimen for H pylori. Its advantage is that it can partially or completely overcome metronidazole resistance.21,22 As such, it is potentially ideal, as it should be effective despite resistance to clarithromycin, metronidazole, or levofloxacin, and it can be used in patients allergic to penicillin.
The major downside is a high frequency of side effects, particularly abdominal pain, nausea, and vomiting, often resulting in poor adherence. Most regimens that contain antibiotics have side effects, but adherence seems to be more of a problem with bismuth quadruple therapy, probably because of the combination of the high doses of metronidazole and tetracycline.22 In our experience, this regimen can be effective if the physician takes the time to explain to the patient that side effects are common but treatment success depends on completing the full course of 14 days.
Another problem is that tetracycline has become difficult to obtain in many areas, and doxycycline cannot be substituted in those with metronidazole resistance. To date, it has been difficult or impossible to obtain the same excellent results with doxycycline as can be obtained with tetracycline. It is not clear why.21
To use bismuth quadruple therapy one must often use a name-brand product, Pylera. Pylera is packaged as a 10-day course, which is effective against metronidazole-susceptible infections. However, 14 days are generally required to achieve a high cure rate with metronidazole-resistant infections, which are the main indication for use of this product. Moreover, Pylera does not include a proton pump inhibitor, which must be prescribed separately.
In the United States, Pylera is expensive, costing $740 to $790 with a coupon for a 10-day supply and proportionally more for the required 14-day supply (www.goodrx.com/pylera?drug-name=pylera), whereas in Europe it costs less than 70 Euros ($73).21 If generic tetracycline is available, the US cost for 14 days of generic bismuth quadruple therapy is less than $50.
An alternate and simpler approach is to substitute amoxicillin for tetracycline.23 This regimen has been used successfully in China and was shown to be noninferior to the tetracycline-containing regimen in a head-to-head comparison.24
Recent studies have confirmed earlier Italian studies suggesting that twice-a-day bismuth and tetracycline is effective, which would further simplify therapy and possibly reduce side effects.21,23,24 These variations on bismuth quadruple therapy have not yet been optimized to where one can reliably achieve 95% or greater cure rates, and further studies are needed.
Why include more than 1 antibiotic?
The H pylori load in the stomach is typically large, which increases the odds that a subpopulation of resistant organisms is present. Resistance may be due to a relatively high rate of mutation in certain bacterial genes.25 This is particularly a problem with clarithromycin, metronidazole, and fluoroquinolones and is reflected in a high rate of resistance among patients for whom single-drug regimens have failed. These drugs are always given with a second antimicrobial to which H pylori rarely becomes resistant, such as amoxicillin or tetracycline.
Why include a proton pump inhibitor?
An antisecretory drug is needed to increase the gastric pH, which makes antimicrobial therapy more effective. It also decreases antibiotic washout from the stomach and likely protects and increases the gastric concentration of some antibiotics.
The activities of amoxicillin, fluoroquinolones, and to a lesser degree clarithromycin are pH-dependent. For example, keeping the gastric pH above 6.0 promotes H pylori replication,26,27 making it is more susceptible to amoxicillin (reviewed in detail by Dore et al21). A gastric pH of 6.0 or more is very difficult to achieve with proton pump inhibitors, and has been accomplished regularly only in people who metabolize these drugs slowly (“slow metabolizers”) who received both the proton pump inhibitor and amoxicillin every 6 hours for 14 days.21
With standard clarithromycin, metronidazole, or fluoroquinolone triple therapy, proton pump inhibitors appear to provide satisfactory cure rates when given for 14 days in standard doses. However, double doses (eg, 40 mg of omeprazole or an equivalent) may be slightly better, especially in the presence of resistance.
The cure rate reflects the sum of the 2 populations of organisms: the susceptible and the resistant. In triple therapy, increasing the gastric pH with a proton pump inhibitor makes the amoxicillin component of the regimen more effective against resistant organisms and thus increases the cure rate. For example, in Western countries, esomeprazole 40 mg (approximately equivalent to rabeprazole 40 mg, omeprazole or lansoprazole 60 mg, or pantoprazole 240 mg)28 given twice a day in a 14-day triple therapy regimen cures about 40% to 50% of resistant infections. This benefit will be evident in an improvement in cure rates in populations in which resistance has reduced the average cure rate. This is also why meta-analyses have shown better results with second-generation proton pump inhibitors and with longer duration of therapy.29,30
Generally, we recommend omeprazole 40 mg twice a day or an equivalent (Tables 1–3).
Would a potassium-competitive acid blocker be better than a proton pump inhibitor?
Vonoprazan is a potassium-competitive acid blocker. It does not require intermediate complex formation and is stable at low pH. It has a longer half-life than proton pump inhibitors, and its bioavailability is unaffected by food.31 It was recently approved in Japan for H pylori eradication in combination with clarithromycin or metronidazole plus amoxicillin.18
Vonoprazan is more effective than current proton pump inhibitors for keeping the gastric pH high. There are no published studies of vonoprazan dual therapy in Western countries, but given twice a day for 7 days along with twice-daily amoxicillin it cured only approximately 80% of clarithromycin-resistant strains. Further studies are needed to identify the optimum proton pump inhibitor or potassium-competitive acid blocker, dose, and duration.
Misuse of antibiotics
In triple therapy, the second antimicrobial drug (eg, amoxicillin) is given in part to prevent resistance from developing. It is not clear whether the combination is additive or synergistic, but until we can reliably maintain the intragastric pH above 6.0, which would increase the effectiveness of the amoxicillin component of the regimen, this practice cannot be considered as misuse of antibiotics.
In contrast, in the 4-drug nonbismuth combinations (concomitant, sequential, and hybrid therapies) and the new vonoprazan, clarithromycin, and metronidazole triple therapies, 1 of the antibiotics provides no benefit to some, often most, of the patients.18–20,32 This practice should end when susceptibility data become more widely available and when vonoprazan becomes available, so that we can deliver effective vonoprazan-amoxicillin dual therapy.
First-, second-, and third-line therapies
Many recommendations give advice in terms of first-, second-, and third-line therapies. In practice, a physician should have at least 2 first-line regimens (a first and a second choice). Both should be proven highly successful as empiric therapies in one’s patient population but differ in terms of primary antibiotics. This approach allows the clinician to tailor therapy depending on whether he or she suspects antibiotic resistance (eg, if the patient has taken clarithromycin before) or the patient is allergic or cannot take 1 or more drugs.
Two treatment failures with 2 different regimens known to be effective suggest poor compliance (a difficult patient) or a multiple-drug-resistant infection (a difficult infection). That patient would require salvage therapy (Table 2), which logically should be based on antimicrobial testing or, at a minimum, consultation with someone who frequently deals with this problem.
Test of cure
Monitoring the outcome of therapy (testing for cure) is essential, as it provides a reliable measure of the local effectiveness of particular therapies and also serves as an early warning of development of resistance in one’s patient population.14
Unless there are compelling reasons, testing for cure should use noninvasive testing with the urea breath test or stool antigen test. It is recommended that this be delayed at least 4 weeks to allow the organisms if still present to repopulate the stomach sufficiently for the tests to become positive. Because antibiotics, bismuth, and proton pump inhibitors reduce the bacterial load, they should be withheld at least 2 weeks before testing. Histamine-2 receptor antagonists can be substituted for proton pump inhibitors if antisecretory therapy is needed for symptoms, and continued up to the day before testing. The urea breath test should contain citric acid to overcome any residual pH effects. Physician groups should share their experience so as to alert the community about which therapies should likely be avoided.33
Salvage therapy
Salvage therapy is given after 2 or more treatment failures with different antibiotics. Ideally, the regimen should be based on the results of antimicrobial testing. Current regimens include rifabutin triple therapy, dual therapy (a protein pump inhibitor or vonoprazan and amoxicillin), or furazolidone quadruple therapy (Table 2).
Furazolidone is a synthetic nitrofuran derivative that is effective against many enteric organisms, including gram-negative bacteria and protozoa. It is not available in most Western countries but is available in many other parts of the world.34,35 It is also a monoamine oxidase inhibitor and thus interacts with many drugs and foods (eg, soy sauce, aged cheeses), leading to a relatively high rate of side effects such as fever, palpitations, and skin rash.
Rifabutin-containing regimens, generally, a proton pump inhibitor, amoxicillin 1 g, and rifabutin 150 mg, all twice a day (Table 3) provide average cure rates of less than 80% (typically in the mid-70% range).36 Borody et al37 reported greater than 95% success with a 12-day regimen consisting of rifabutin 150 mg once daily (half-dose), amoxicillin 1.5 g 3 times a day, and pantoprazole 80 mg (approximately equivalent to omeprazole 20 mg) 3 times a day. Ciccaglione et al,38 in a small study, used a 10-day quadruple regimen containing a proton pump inhibitor, amoxicillin, rifabutin, and bismuth (all twice a day), with high cure rates. The results of these studies are yet to be confirmed, and the optimal rifabutin-containing regimen remains to be determined.
PROBIOTICS
There is considerable interest in using probiotics to enhance the effectiveness of antimicrobial therapy for H pylori by increasing tolerability, reducing side effects, and therefore improving compliance.39,40
In a meta-analysis of 14 randomized trials (N = 1,671), when probiotics were added, pooled H pylori eradication rates were only slightly improved: 83.6% (95% CI 80.5%–86.7%) with probiotics and 74.8% (95% CI 71.1%–78.5%) without probiotics by intent-to-treat analysis.41
Another meta-analysis of probiotics suggested that those containing Saccharomyces boulardii, Lactobacillus, and Bifidobacterium significantly increased the eradication rate of triple therapy in populations with high rates of antimicrobial resistance and reduced the risk of overall H pylori therapy-related adverse effects, especially diarrhea.42,43
At present, we recommend that probiotics be considered only for patients who are likely not to comply with treatment (eg, those with irritable bowel syndrome or difficulty taking antibiotics), to try to take advantage of their ability to improve antibiotic tolerability.
Helicobacter pylori infection is an infectious disease and should be treated like one, with due consideration of antibiotic resistance and stewardship.1–4
This was the consensus of the 2015 Kyoto H pylori conference,2 and it signaled a fundamental shift in thinking. Up to now, H pylori treatment has not been based on infectious disease principles, leading to suboptimal results and antibiotic resistance. In addition, the conference recommended that H pylori infection be treated whenever it is found unless there are compelling reasons not to.
Here we review current and possible future regimens for eradicating H pylori that we hope will be more effective and will lead to less resistance than in the past.
H PYLORI AS AN INFECTIOUS DISEASE
Not until the late 1980s was H pylori recognized as the cause of peptic ulcer disease, which until then accounted for hundreds of thousands of hospitalizations and more than 100,000 surgical procedures each year.5 Now, peptic ulcer disease is routinely treated by eradicating H pylori. In addition, the World Health Organization has recommended considering H pylori eradication to reduce the risk of gastric cancer,6 which causes 738,000 deaths worldwide per year.7
The problems of how to diagnose and treat H pylori infection were taken on by gastroenterologists, and not by specialists in infectious disease.1 Even now, almost all the major reviews and consensus statements on H pylori come from gastroenterologists and are published in gastroenterology journals.2,8,9
But infectious diseases differ from most gastrointestinal diseases. In gastrointestinal problems such as constipation or inflammatory bowel disease,10 the causes are generally unknown, and there is a large placebo response to therapy. In contrast, in infectious diseases, the cause is generally known, there is no placebo response, and treatment success depends on susceptibility of the organism. Failure of proven regimens is generally due to resistant organisms, poor adherence, or, in the case of H pylori, poorly designed regimens in terms of doses, frequency of administration, or duration of therapy.
The differences extend to clinical trials of treatment.3 In other infectious diseases, treatment is based on susceptibility. The usual comparative approach in infectious diseases is a noninferiority trial in which the new treatment is compared with standard care, ie, a regimen that reliably achieves nearly 100% cure rates. Not so with H pylori. Most trials of H pylori therapy compared regimens in populations with high but unknown prevalences of resistance and therefore are of limited or no help to the clinician in choosing the best regimen for an individual patient.3
Many thousands of H pylori-infected patients participated in clinical trials in which the results would have been predictable if the researchers had assessed susceptibility before giving the drugs.11–13 Worse, many patients were also randomized to receive regimens that the investigators knew provided poor cure rates in the population being studied. This knowledge was generally not shared with the patients. This approach was used to demonstrate that a new regimen was superior to an old one, even though the new one was already known to be less affected by resistance to the key element in the comparator.
Clinicians generally do not test for susceptibility when treating H pylori, one reason being that such testing is often unavailable.3 However, almost every hospital, clinic, and major laboratory in the world provides susceptibility testing for other common local pathogens. H pylori is easy to grow, and laboratories could test for susceptibility if we asked them to.
Current H pylori recommendations may also contribute to the global increase in antimicrobal resistance.
As discussed below, all recent guidelines have recommended 4-drug non-bismuth-containing concomitant therapy as first-line therapy. An infectious disease colleague described it as a “hope therapy” because the prescriber hoped that the infection would be susceptible to either metronidazole or clarithromycin. All who receive this combination receive an antibiotic they do not need. This is an expedient rather than a medically rational choice resulting from failure to deal with H pylori as an infectious disease.
H PYLORI THERAPIES
Conceptually, treating infectious disease is straightforward: one should prescribe antimicrobial drugs to which the organism is susceptible3 (Table 1). However, clinical success lies in the details, which include the doses, frequency of doses, duration of therapy, timing of doses in relation to meals, and use of adjuvants such as antisecretory drugs, antacids, and probiotics. A number of regimens reliably yield high cure rates—95% or higher—if the organism is susceptible and the patients are adherent.
The effectiveness of any regimen may vary depending on the population it is used in, due to polymorphisms in drug-metabolizing enzymes such as CYP2C19.
Sequential therapy is obsolete
Sequential therapy for H pylori infection consisted of amoxicillin plus a proton pump inhibitor for 7 days, followed by clarithromycin, tinidazole, or metronidazole plus a proton pump inhibitor for a further 7 days. This regimen should not be used any more because concomitant therapy will always be superior (see below).
Need for 14 days of therapy
H pylori occupies a number of different niches in the body ranging from gastric mucus (which is technically outside the body) to inside gastric epithelial cells. As a general rule, 14-day therapy provides the best results, in part because the longer duration helps kill the organisms that persist in different niches.14,15
In addition, proton pump inhibitors, which are part of all the currently recommended regimens, require 3 or more days to reach their full antisecretory effectiveness, which further limits the effectiveness of short-duration therapies.
Shorter regimens should be used only if they are proved to be as good as 14-day regimens and if both achieve 95% or greater cure rates with susceptible infections.
How to choose a therapy
Since rational infectious-disease therapy is based on susceptibility, one should start by considering the susceptibility pattern in the local population and, therefore, the likely susceptibility in the patient in front of us.
Unfortunately, we do not yet have local or regional susceptibility data on H pylori for most locales. Until those data are available, we must use the indirect information that is available, such as the patient’s history of antibiotic use.
Triple therapy should not be used empirically
Triple therapy (Table 1) consists of the combination of:
- Clarithromycin or metronidazole or a fluoroquinolone
- Amoxicillin
- A proton pump inhibitor.
However, prior use of a macrolide (eg, erythromycin, clarithromycin, or azithromycin), metronidazole, or a fluoroquinolone (eg, ciprofloxacin, levofloxacin) almost guarantees resistance to those drugs. In the United States, resistance to clarithromycin, metronidazole, levofloxacin, and related drugs is already widespread, and none should be used empirically in triple therapies. In contrast, amoxicillin, tetracycline, and furazolidone can often be used again, as resistance to them is rare even with prior use.
For example, 14 days of clarithromycin triple therapy (clarithromycin, amoxicillin, and a proton pump inhibitor) can be expected to cure more than 95% of patients who have susceptible infections and about 20% of those with resistant infections.16 This 20% is due to the proton pump inhibitor and amoxicillin, as the contribution to the cure rate from clarithromycin is close to zero.
If the prevalence of resistance to clarithromycin is 25%, the cure rate in the entire population will be a little more than 75%—97% in the 75% of the population with susceptible infections and 20% in patients who previously received clarithromycin (Figure 1).
If we know that our patient has an infection that is susceptible to clarithromycin, metronidazole, or levofloxacin, good results could be achieved with triple therapy that includes a proton pump inhibitor, for 14 days. Fluoroquinolones have a number of black-box warnings from the US Food and Drug Administration (www.fda.gov/Drugs/DrugSafety/ucm500143.htm) and should always be a last choice. However, in the United States, lacking definite data about susceptibility to clarithromycin, metronidazole, and levofloxacin, we should assume resistance is present and use a 4-drug regimen (eg, concomitant therapy or bismuth quadruple therapy).
Concomitant therapy is preferred
Concomitant therapy is the combination of:
- Amoxicillin
- Metronidazole
- Clarithromycin
- A proton pump inhibitor.
Functionally, this is a combination of clarithromycin and metronidazole triple therapies, given simultaneously.17 The premise is that even though the prevalence of metronidazole resistance in the United States is high (20%–40%), and so is the prevalence of clarithromycin resistance (about 20%), the prevalence of resistance to both drugs at the same time is expected to be low (eg, 0.4 × 0.2 = 0.08, or 8%) unless the drugs had previously been used together, as in some older regimens that contained both. Thus, the metronidazole will kill the clarithromycin-resistant but metronidazole-susceptible strains, and the clarithromycin will kill the clarithromycin-susceptible, metronidazole-resistant strains. Only with dual resistant strains will this regimen fail (with a 20% cure rate due to the proton pump inhibitor and amoxicillin and a population cure rate of slightly more than 90%).
The downside of this highly recommended therapy is that all who receive it are getting an antibiotic that they don’t need, which is, in a global sense, inappropriate. In other words, all those who are cured by clarithromycin also receive metronidazole, which plays no role in treatment success, and those cured by metronidazole receive unneeded clarithromycin (Figure 2). Had susceptibility testing been available, those with susceptible strains would have received appropriate triple therapies, and those with dual resistance would not have received either antibiotic.
Thus, while we recommend concomitant therapy as an empiric regimen in populations that do not have high levels of resistance to metronidazole or clarithromycin (as those would also have a high prevalence of dual resistance), one must be aware of the “dirty little secret” of inappropriate antibiotic use that accompanies it and some other H pylori therapies (eg, vonoprazan triple therapy in Japan).18–20
Bismuth quadruple therapy is an alternative
Bismuth quadruple therapy (Table 1) consists of:
- Bismuth
- Tetracycline
- Metronidazole
- A proton pump inhibitor.
This was the first truly effective regimen for H pylori. Its advantage is that it can partially or completely overcome metronidazole resistance.21,22 As such, it is potentially ideal, as it should be effective despite resistance to clarithromycin, metronidazole, or levofloxacin, and it can be used in patients allergic to penicillin.
The major downside is a high frequency of side effects, particularly abdominal pain, nausea, and vomiting, often resulting in poor adherence. Most regimens that contain antibiotics have side effects, but adherence seems to be more of a problem with bismuth quadruple therapy, probably because of the combination of the high doses of metronidazole and tetracycline.22 In our experience, this regimen can be effective if the physician takes the time to explain to the patient that side effects are common but treatment success depends on completing the full course of 14 days.
Another problem is that tetracycline has become difficult to obtain in many areas, and doxycycline cannot be substituted in those with metronidazole resistance. To date, it has been difficult or impossible to obtain the same excellent results with doxycycline as can be obtained with tetracycline. It is not clear why.21
To use bismuth quadruple therapy one must often use a name-brand product, Pylera. Pylera is packaged as a 10-day course, which is effective against metronidazole-susceptible infections. However, 14 days are generally required to achieve a high cure rate with metronidazole-resistant infections, which are the main indication for use of this product. Moreover, Pylera does not include a proton pump inhibitor, which must be prescribed separately.
In the United States, Pylera is expensive, costing $740 to $790 with a coupon for a 10-day supply and proportionally more for the required 14-day supply (www.goodrx.com/pylera?drug-name=pylera), whereas in Europe it costs less than 70 Euros ($73).21 If generic tetracycline is available, the US cost for 14 days of generic bismuth quadruple therapy is less than $50.
An alternate and simpler approach is to substitute amoxicillin for tetracycline.23 This regimen has been used successfully in China and was shown to be noninferior to the tetracycline-containing regimen in a head-to-head comparison.24
Recent studies have confirmed earlier Italian studies suggesting that twice-a-day bismuth and tetracycline is effective, which would further simplify therapy and possibly reduce side effects.21,23,24 These variations on bismuth quadruple therapy have not yet been optimized to where one can reliably achieve 95% or greater cure rates, and further studies are needed.
Why include more than 1 antibiotic?
The H pylori load in the stomach is typically large, which increases the odds that a subpopulation of resistant organisms is present. Resistance may be due to a relatively high rate of mutation in certain bacterial genes.25 This is particularly a problem with clarithromycin, metronidazole, and fluoroquinolones and is reflected in a high rate of resistance among patients for whom single-drug regimens have failed. These drugs are always given with a second antimicrobial to which H pylori rarely becomes resistant, such as amoxicillin or tetracycline.
Why include a proton pump inhibitor?
An antisecretory drug is needed to increase the gastric pH, which makes antimicrobial therapy more effective. It also decreases antibiotic washout from the stomach and likely protects and increases the gastric concentration of some antibiotics.
The activities of amoxicillin, fluoroquinolones, and to a lesser degree clarithromycin are pH-dependent. For example, keeping the gastric pH above 6.0 promotes H pylori replication,26,27 making it is more susceptible to amoxicillin (reviewed in detail by Dore et al21). A gastric pH of 6.0 or more is very difficult to achieve with proton pump inhibitors, and has been accomplished regularly only in people who metabolize these drugs slowly (“slow metabolizers”) who received both the proton pump inhibitor and amoxicillin every 6 hours for 14 days.21
With standard clarithromycin, metronidazole, or fluoroquinolone triple therapy, proton pump inhibitors appear to provide satisfactory cure rates when given for 14 days in standard doses. However, double doses (eg, 40 mg of omeprazole or an equivalent) may be slightly better, especially in the presence of resistance.
The cure rate reflects the sum of the 2 populations of organisms: the susceptible and the resistant. In triple therapy, increasing the gastric pH with a proton pump inhibitor makes the amoxicillin component of the regimen more effective against resistant organisms and thus increases the cure rate. For example, in Western countries, esomeprazole 40 mg (approximately equivalent to rabeprazole 40 mg, omeprazole or lansoprazole 60 mg, or pantoprazole 240 mg)28 given twice a day in a 14-day triple therapy regimen cures about 40% to 50% of resistant infections. This benefit will be evident in an improvement in cure rates in populations in which resistance has reduced the average cure rate. This is also why meta-analyses have shown better results with second-generation proton pump inhibitors and with longer duration of therapy.29,30
Generally, we recommend omeprazole 40 mg twice a day or an equivalent (Tables 1–3).
Would a potassium-competitive acid blocker be better than a proton pump inhibitor?
Vonoprazan is a potassium-competitive acid blocker. It does not require intermediate complex formation and is stable at low pH. It has a longer half-life than proton pump inhibitors, and its bioavailability is unaffected by food.31 It was recently approved in Japan for H pylori eradication in combination with clarithromycin or metronidazole plus amoxicillin.18
Vonoprazan is more effective than current proton pump inhibitors for keeping the gastric pH high. There are no published studies of vonoprazan dual therapy in Western countries, but given twice a day for 7 days along with twice-daily amoxicillin it cured only approximately 80% of clarithromycin-resistant strains. Further studies are needed to identify the optimum proton pump inhibitor or potassium-competitive acid blocker, dose, and duration.
Misuse of antibiotics
In triple therapy, the second antimicrobial drug (eg, amoxicillin) is given in part to prevent resistance from developing. It is not clear whether the combination is additive or synergistic, but until we can reliably maintain the intragastric pH above 6.0, which would increase the effectiveness of the amoxicillin component of the regimen, this practice cannot be considered as misuse of antibiotics.
In contrast, in the 4-drug nonbismuth combinations (concomitant, sequential, and hybrid therapies) and the new vonoprazan, clarithromycin, and metronidazole triple therapies, 1 of the antibiotics provides no benefit to some, often most, of the patients.18–20,32 This practice should end when susceptibility data become more widely available and when vonoprazan becomes available, so that we can deliver effective vonoprazan-amoxicillin dual therapy.
First-, second-, and third-line therapies
Many recommendations give advice in terms of first-, second-, and third-line therapies. In practice, a physician should have at least 2 first-line regimens (a first and a second choice). Both should be proven highly successful as empiric therapies in one’s patient population but differ in terms of primary antibiotics. This approach allows the clinician to tailor therapy depending on whether he or she suspects antibiotic resistance (eg, if the patient has taken clarithromycin before) or the patient is allergic or cannot take 1 or more drugs.
Two treatment failures with 2 different regimens known to be effective suggest poor compliance (a difficult patient) or a multiple-drug-resistant infection (a difficult infection). That patient would require salvage therapy (Table 2), which logically should be based on antimicrobial testing or, at a minimum, consultation with someone who frequently deals with this problem.
Test of cure
Monitoring the outcome of therapy (testing for cure) is essential, as it provides a reliable measure of the local effectiveness of particular therapies and also serves as an early warning of development of resistance in one’s patient population.14
Unless there are compelling reasons, testing for cure should use noninvasive testing with the urea breath test or stool antigen test. It is recommended that this be delayed at least 4 weeks to allow the organisms if still present to repopulate the stomach sufficiently for the tests to become positive. Because antibiotics, bismuth, and proton pump inhibitors reduce the bacterial load, they should be withheld at least 2 weeks before testing. Histamine-2 receptor antagonists can be substituted for proton pump inhibitors if antisecretory therapy is needed for symptoms, and continued up to the day before testing. The urea breath test should contain citric acid to overcome any residual pH effects. Physician groups should share their experience so as to alert the community about which therapies should likely be avoided.33
Salvage therapy
Salvage therapy is given after 2 or more treatment failures with different antibiotics. Ideally, the regimen should be based on the results of antimicrobial testing. Current regimens include rifabutin triple therapy, dual therapy (a protein pump inhibitor or vonoprazan and amoxicillin), or furazolidone quadruple therapy (Table 2).
Furazolidone is a synthetic nitrofuran derivative that is effective against many enteric organisms, including gram-negative bacteria and protozoa. It is not available in most Western countries but is available in many other parts of the world.34,35 It is also a monoamine oxidase inhibitor and thus interacts with many drugs and foods (eg, soy sauce, aged cheeses), leading to a relatively high rate of side effects such as fever, palpitations, and skin rash.
Rifabutin-containing regimens, generally, a proton pump inhibitor, amoxicillin 1 g, and rifabutin 150 mg, all twice a day (Table 3) provide average cure rates of less than 80% (typically in the mid-70% range).36 Borody et al37 reported greater than 95% success with a 12-day regimen consisting of rifabutin 150 mg once daily (half-dose), amoxicillin 1.5 g 3 times a day, and pantoprazole 80 mg (approximately equivalent to omeprazole 20 mg) 3 times a day. Ciccaglione et al,38 in a small study, used a 10-day quadruple regimen containing a proton pump inhibitor, amoxicillin, rifabutin, and bismuth (all twice a day), with high cure rates. The results of these studies are yet to be confirmed, and the optimal rifabutin-containing regimen remains to be determined.
PROBIOTICS
There is considerable interest in using probiotics to enhance the effectiveness of antimicrobial therapy for H pylori by increasing tolerability, reducing side effects, and therefore improving compliance.39,40
In a meta-analysis of 14 randomized trials (N = 1,671), when probiotics were added, pooled H pylori eradication rates were only slightly improved: 83.6% (95% CI 80.5%–86.7%) with probiotics and 74.8% (95% CI 71.1%–78.5%) without probiotics by intent-to-treat analysis.41
Another meta-analysis of probiotics suggested that those containing Saccharomyces boulardii, Lactobacillus, and Bifidobacterium significantly increased the eradication rate of triple therapy in populations with high rates of antimicrobial resistance and reduced the risk of overall H pylori therapy-related adverse effects, especially diarrhea.42,43
At present, we recommend that probiotics be considered only for patients who are likely not to comply with treatment (eg, those with irritable bowel syndrome or difficulty taking antibiotics), to try to take advantage of their ability to improve antibiotic tolerability.
- Graham DY. Helicobacter pylori update: gastric cancer, reliable therapy, and possible benefits. Gastroenterology 2015; 148:719–731.
- Sugano K, Tack J, Kuipers EJ, et al. Kyoto global consensus report on Helicobacter pylori gastritis. Gut 2015; 64:1353–1367.
- Graham DY, Dore MP. Helicobacter pylori therapy: a paradigm shift. Expert Rev Anti Infect Ther 2016; 14:577–585.
- Leja M, Axon A, Brenner H. Epidemiology of Helicobacter pylori infection. Helicobacter 2016; 21(suppl 1):3–7.
- Grossman MI. Closing remarks. Gastroenterology 1978; 74:487–488.
- Malfertheiner P, Megraud F, O’Morain CA, et al. Management of Helicobacter pylori infection—the Maastricht IV/ Florence Consensus Report. Gut 2012; 61:646–664.
- Fallone CA, Chiba N, van Zanten SV, et al. The Toronto consensus for the treatment of Helicobacter pylori infection in adults. Gastroenterology 2016; 151:51–69.
- IARC Helicobacter pylori Working Group. Volume 8. Helicobacter pylori eradication as a strategy for preventing gastric cancer. Lyon, France: International Agency for Research on Cancer, 2014.
- Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 2010; 127:2893–2917.
- Graham DY, Dore MP. Helicobacter pylori therapy demystified. Helicobacter 2011; 16:343–345.
- Gatta L, Vakil N, Leandro G, Di MF, Vaira D. Sequential therapy or triple therapy for Helicobacter pylori infection: systematic review and meta-analysis of randomized controlled trials in adults and children. Am J Gastroenterol 2009; 104:3069–3079.
- Graham DY, Fischbach L. Helicobacter pylori treatment in the era of increasing antibiotic resistance. Gut 2010; 59:1143–1153.
- Graham DY. Helicobacter pylori eradication therapy research: ethical issues and description of results. Clin Gastroenterol Hepatol 2010; 8:1032–1036.
- Graham DY, Shiotani A. New concepts of resistance in the treatment of Helicobacter pylori infections. Nat Clin Pract Gastroenterol Hepatol 2008; 5:321–331.
- Graham DY, Dore MP. Variability in the outcome of treatment of Helicobacter pylori infection: a critical analysis. In: Hunt RH, Tytgat GNJ, editors. Helicobacter pylori Basic Mechanisms to Clinical Cure 1998. Dordrecht, Netherlands: Kluwer Academic Publishers, 998:426–440.
- Graham DY. Hp-normogram (normo-graham) for assessing the outcome of H. pylori therapy: effect of resistance, duration, and CYP2C19 genotype. Helicobacter 2015; 21:85–90.
- Graham DY, Lee YC, Wu MS. Rational Helicobacter pylori therapy: evidence-based medicine rather than medicine-based evidence. Clin Gastroenterol Hepatol 2014; 12:177–186.
- Murakami K, Sakurai Y, Shiino M, Funao N, Nishmura A, Asaka M. Vonoprazan, a novel potassium-competitive acid blocker, as a component of first-line and second-line triple therapy for Helicobacter pylori eradication: a phase III, randomised, double-blind study. Gut 2016; 65:1439–1446.
- Graham DY. Vonoprazan Helicobacter pylori eradication therapy: ethical and interpretation issues. Gut 2016 Apr 7. pii: gutjnl-2016-311796. doi: 10.1136/gutjnl-2016-311796. [Epub ahead of print].
- Matsumoto H, Shiotani A, Katsumata R, et al. Helicobacter pylori eradication with proton pump inhibitors or potassium-competitive acid blockers: the effect of clarithromycin resistance. Dig Dis Sci 2016; 61:3215–3220.
- Dore MP, Lu H, Graham DY. Role of bismuth in improving Helicobacter pylori eradication with triple therapy. Gut 2016; 65:870–878.
- Graham DY, Lee SY. How to effectively use bismuth quadruple therapy: the good, the bad, and the ugly. Gastroenterol Clin North Am 2015; 44:537–563.
- Zhang W, Chen Q, Liang X, et al. Bismuth, lansoprazole, amoxicillin and metronidazole or clarithromycin as first-line Helicobacter pylori therapy. Gut 2015; 64:1715–1720.
- Chen Q, Zhang X, Fu Q, et al. Rescue therapy for Helicobacter pylori eradication: a randomized non-inferiority trial of amoxicillin or tetracycline for bismuth quadruple therapy. Am J Gastroenterol 2016; 111:1736–1742.
- Graham DY. Antibiotic resistance in Helicobacter pylori: implications for therapy. Gastroenterology 1998; 115:1272–1277.
- Marcus EA, Inatomi N, Nagami GT, et al. The effects of varying acidity on Helicobacter pylori growth and the bactericidal efficacy of ampicillin. Aliment Pharmacol Ther 2012; 36:972–979.
- Sachs G, Shin JM, Munson K, et al. Review article: the control of gastric acid and Helicobacter pylori eradication. Aliment Pharmacol Ther 2000; 14:1383–1401.
- Kirchheiner J, Glatt S, Fuhr U, et al. Relative potency of proton-pump inhibitors: comparison of effects on intragastric pH. Eur J Clin Pharmacol 2009; 65:19–31.
- Yuan Y, Ford AC, Khan KJ, et al. Optimum duration of regimens for Helicobacter pylori eradication. Cochrane Database Syst Rev 2013;12:CD008337.
- McNicholl AG, Linares PM, Nyssen OP, et al. Meta-analysis: esomeprazole or rabeprazole vs. first-generation pump inhibitors in the treatment of Helicobacter pylori infection. Aliment Pharmacol Ther 2012; 36:414–425.
- Sakurai Y, Nishimura A, Kennedy G, et al. Safety, tolerability, pharmacokinetics, and pharmacodynamics of single rising TAK-438 (vonoprazan) doses in healthy male Japanese/non-Japanese subjects. Clin Transl Gastroenterol 2015; 6:e94.
- Graham DY, Laine L. The Toronto Helicobacter pylori consensus in context. Gastroenterology 2016; 151:9–12.
- Uotani T, Graham DY. Diagnosis of Helicobacter pylori using the rapid urease test. Ann Transl Med 2015; 3:9.
- Lu H, Zhang W, Graham DY. Bismuth-containing quadruple therapy for Helicobacter pylori: lessons from China. Eur J Gastroenterol Hepatol 2013; 25:1134–1140.
- Graham DY, Lu H. Furazolidone in Helicobacter pylori therapy: misunderstood and often unfairly maligned drug told in a story of French bread. Saudi J Gastroenterol 2012; 8:1–2.
- Gisbert JP, Calvet X. Review article: rifabutin in the treatment of refractory Helicobacter pylori infection. Aliment Pharmacol Ther 2012; 35:209–221.
- Borody TJ, Pang G, Wettstein AR, et al. Efficacy and safety of rifabutin-containing ‘rescue therapy’ for resistant Helicobacter pylori infection. Aliment Pharmacol Ther 2006; 23:481–488.
- Ciccaglione AF, Tavani R, Grossi L, et al. Rifabutin containing triple therapy and rifabutin with bismuth containing quadruple therapy for third-line treatment of Helicobacter pylori infection: two pilot studies. Helicobacter 2016; 21:375–381.
- Homan M, Orel R. Are probiotics useful in Helicobacter pylori eradication? World J Gastroenterol 2015; 21:10644–10653.
- Zhang MM, Qian W, Qin YY, et al. Probiotics in Helicobacter pylori eradication therapy: a systematic review and meta-analysis. World J Gastroenterol 2015; 21:4345–4357.
- Tong JL, Ran ZH, Shen J, et al. Meta-analysis: the effect of supplementation with probiotics on eradication rates and adverse events during Helicobacter pylori eradication therapy. Aliment Pharmacol Ther 2007; 25:155–168.
- Szajewska H, Setty M, Mrukowicz J, et al. Probiotics in gastrointestinal diseases in children: hard and not-so-hard evidence of efficacy. J Pediatr Gastroenterol Nutr 2006; 42:454–475.
- Wang ZH, Gao QY, Fang JY. Meta-analysis of the efficacy and safety of Lactobacillus-containing and Bifidobacterium-containing probiotic compound preparation in Helicobacter pylori eradication therapy. J Clin Gastroenterol 2013; 47:25–32.
- Graham DY. Helicobacter pylori update: gastric cancer, reliable therapy, and possible benefits. Gastroenterology 2015; 148:719–731.
- Sugano K, Tack J, Kuipers EJ, et al. Kyoto global consensus report on Helicobacter pylori gastritis. Gut 2015; 64:1353–1367.
- Graham DY, Dore MP. Helicobacter pylori therapy: a paradigm shift. Expert Rev Anti Infect Ther 2016; 14:577–585.
- Leja M, Axon A, Brenner H. Epidemiology of Helicobacter pylori infection. Helicobacter 2016; 21(suppl 1):3–7.
- Grossman MI. Closing remarks. Gastroenterology 1978; 74:487–488.
- Malfertheiner P, Megraud F, O’Morain CA, et al. Management of Helicobacter pylori infection—the Maastricht IV/ Florence Consensus Report. Gut 2012; 61:646–664.
- Fallone CA, Chiba N, van Zanten SV, et al. The Toronto consensus for the treatment of Helicobacter pylori infection in adults. Gastroenterology 2016; 151:51–69.
- IARC Helicobacter pylori Working Group. Volume 8. Helicobacter pylori eradication as a strategy for preventing gastric cancer. Lyon, France: International Agency for Research on Cancer, 2014.
- Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 2010; 127:2893–2917.
- Graham DY, Dore MP. Helicobacter pylori therapy demystified. Helicobacter 2011; 16:343–345.
- Gatta L, Vakil N, Leandro G, Di MF, Vaira D. Sequential therapy or triple therapy for Helicobacter pylori infection: systematic review and meta-analysis of randomized controlled trials in adults and children. Am J Gastroenterol 2009; 104:3069–3079.
- Graham DY, Fischbach L. Helicobacter pylori treatment in the era of increasing antibiotic resistance. Gut 2010; 59:1143–1153.
- Graham DY. Helicobacter pylori eradication therapy research: ethical issues and description of results. Clin Gastroenterol Hepatol 2010; 8:1032–1036.
- Graham DY, Shiotani A. New concepts of resistance in the treatment of Helicobacter pylori infections. Nat Clin Pract Gastroenterol Hepatol 2008; 5:321–331.
- Graham DY, Dore MP. Variability in the outcome of treatment of Helicobacter pylori infection: a critical analysis. In: Hunt RH, Tytgat GNJ, editors. Helicobacter pylori Basic Mechanisms to Clinical Cure 1998. Dordrecht, Netherlands: Kluwer Academic Publishers, 998:426–440.
- Graham DY. Hp-normogram (normo-graham) for assessing the outcome of H. pylori therapy: effect of resistance, duration, and CYP2C19 genotype. Helicobacter 2015; 21:85–90.
- Graham DY, Lee YC, Wu MS. Rational Helicobacter pylori therapy: evidence-based medicine rather than medicine-based evidence. Clin Gastroenterol Hepatol 2014; 12:177–186.
- Murakami K, Sakurai Y, Shiino M, Funao N, Nishmura A, Asaka M. Vonoprazan, a novel potassium-competitive acid blocker, as a component of first-line and second-line triple therapy for Helicobacter pylori eradication: a phase III, randomised, double-blind study. Gut 2016; 65:1439–1446.
- Graham DY. Vonoprazan Helicobacter pylori eradication therapy: ethical and interpretation issues. Gut 2016 Apr 7. pii: gutjnl-2016-311796. doi: 10.1136/gutjnl-2016-311796. [Epub ahead of print].
- Matsumoto H, Shiotani A, Katsumata R, et al. Helicobacter pylori eradication with proton pump inhibitors or potassium-competitive acid blockers: the effect of clarithromycin resistance. Dig Dis Sci 2016; 61:3215–3220.
- Dore MP, Lu H, Graham DY. Role of bismuth in improving Helicobacter pylori eradication with triple therapy. Gut 2016; 65:870–878.
- Graham DY, Lee SY. How to effectively use bismuth quadruple therapy: the good, the bad, and the ugly. Gastroenterol Clin North Am 2015; 44:537–563.
- Zhang W, Chen Q, Liang X, et al. Bismuth, lansoprazole, amoxicillin and metronidazole or clarithromycin as first-line Helicobacter pylori therapy. Gut 2015; 64:1715–1720.
- Chen Q, Zhang X, Fu Q, et al. Rescue therapy for Helicobacter pylori eradication: a randomized non-inferiority trial of amoxicillin or tetracycline for bismuth quadruple therapy. Am J Gastroenterol 2016; 111:1736–1742.
- Graham DY. Antibiotic resistance in Helicobacter pylori: implications for therapy. Gastroenterology 1998; 115:1272–1277.
- Marcus EA, Inatomi N, Nagami GT, et al. The effects of varying acidity on Helicobacter pylori growth and the bactericidal efficacy of ampicillin. Aliment Pharmacol Ther 2012; 36:972–979.
- Sachs G, Shin JM, Munson K, et al. Review article: the control of gastric acid and Helicobacter pylori eradication. Aliment Pharmacol Ther 2000; 14:1383–1401.
- Kirchheiner J, Glatt S, Fuhr U, et al. Relative potency of proton-pump inhibitors: comparison of effects on intragastric pH. Eur J Clin Pharmacol 2009; 65:19–31.
- Yuan Y, Ford AC, Khan KJ, et al. Optimum duration of regimens for Helicobacter pylori eradication. Cochrane Database Syst Rev 2013;12:CD008337.
- McNicholl AG, Linares PM, Nyssen OP, et al. Meta-analysis: esomeprazole or rabeprazole vs. first-generation pump inhibitors in the treatment of Helicobacter pylori infection. Aliment Pharmacol Ther 2012; 36:414–425.
- Sakurai Y, Nishimura A, Kennedy G, et al. Safety, tolerability, pharmacokinetics, and pharmacodynamics of single rising TAK-438 (vonoprazan) doses in healthy male Japanese/non-Japanese subjects. Clin Transl Gastroenterol 2015; 6:e94.
- Graham DY, Laine L. The Toronto Helicobacter pylori consensus in context. Gastroenterology 2016; 151:9–12.
- Uotani T, Graham DY. Diagnosis of Helicobacter pylori using the rapid urease test. Ann Transl Med 2015; 3:9.
- Lu H, Zhang W, Graham DY. Bismuth-containing quadruple therapy for Helicobacter pylori: lessons from China. Eur J Gastroenterol Hepatol 2013; 25:1134–1140.
- Graham DY, Lu H. Furazolidone in Helicobacter pylori therapy: misunderstood and often unfairly maligned drug told in a story of French bread. Saudi J Gastroenterol 2012; 8:1–2.
- Gisbert JP, Calvet X. Review article: rifabutin in the treatment of refractory Helicobacter pylori infection. Aliment Pharmacol Ther 2012; 35:209–221.
- Borody TJ, Pang G, Wettstein AR, et al. Efficacy and safety of rifabutin-containing ‘rescue therapy’ for resistant Helicobacter pylori infection. Aliment Pharmacol Ther 2006; 23:481–488.
- Ciccaglione AF, Tavani R, Grossi L, et al. Rifabutin containing triple therapy and rifabutin with bismuth containing quadruple therapy for third-line treatment of Helicobacter pylori infection: two pilot studies. Helicobacter 2016; 21:375–381.
- Homan M, Orel R. Are probiotics useful in Helicobacter pylori eradication? World J Gastroenterol 2015; 21:10644–10653.
- Zhang MM, Qian W, Qin YY, et al. Probiotics in Helicobacter pylori eradication therapy: a systematic review and meta-analysis. World J Gastroenterol 2015; 21:4345–4357.
- Tong JL, Ran ZH, Shen J, et al. Meta-analysis: the effect of supplementation with probiotics on eradication rates and adverse events during Helicobacter pylori eradication therapy. Aliment Pharmacol Ther 2007; 25:155–168.
- Szajewska H, Setty M, Mrukowicz J, et al. Probiotics in gastrointestinal diseases in children: hard and not-so-hard evidence of efficacy. J Pediatr Gastroenterol Nutr 2006; 42:454–475.
- Wang ZH, Gao QY, Fang JY. Meta-analysis of the efficacy and safety of Lactobacillus-containing and Bifidobacterium-containing probiotic compound preparation in Helicobacter pylori eradication therapy. J Clin Gastroenterol 2013; 47:25–32.
KEY POINTS
- We recommend clinicians have 2 first-line options to accommodate prior antibiotic use or drug allergy.
- We recommend 4-drug combinations as first-line treatments, ie, either concomitant therapy or bismuth-containing quadruple therapy, to be taken for 14 days.
- Concomitant therapy consists of the combination of amoxicillin, metronidazole, clarithromycin, and a proton pump inhibitor.
- Bismuth quadruple therapy consists of the combination of bismuth, tetracycline, metronidazole, and a proton pump inhibitor.
- After 2 treatments have failed, therapy with different regimens should be based on susceptibility testing.
Hypoglycemia after gastric bypass: An emerging complication
Bariatric surgery, though beneficial, is associated with complications, one of which is post-gastric bypass hypoglycemia (PGBH).1 The mean time from gastric bypass to documented hypoglycemia is about 28 months.2
PGBH is probably more common than initially thought. In older reports, the prevalence was only 0.1% to 0.36%.1,3 In contrast, in a mail survey in 2015,4 one-third of bariatric surgery patients reported symptoms that raised the suspicion of hypoglycemia. Those with suspicious symptoms were more likely to have undergone Roux-en-Y surgery, to have had no preoperative diabetes, to have had a longer interval since surgery, and to be female. Restricting the suspicion of postprandial hypoglycemia to those who reported more serious symptoms, including needing third-party assistance, the prevalence was 11.6%.
Kefurt et al5 followed Roux-en-Y patients who wore a continuous glucose monitor for 86 months after surgery and found that 38% had hypoglycemia; however, symptoms of hypoglycemia were not discussed.
Thus, the exact prevalence is currently unknown. But as time goes by and more procedures are performed, the incidence will likely rise.
OBESITY IS ON THE RISE, AND SO IS WEIGHT-LOSS SURGERY
Obesity is rampant, and its prevalence continues to rise. In 2011–2012, more than two-thirds of adults in the United States were reported as obese.6 Complications of obesity such as cardiac disease, diabetes, and cancer lead to increased mortality risk.7 Obesity is difficult to reverse, as many people fail to lose weight with diet, exercise, and pharmacotherapy.
Given the difficulty of losing weight and the complications that arise from obesity, bariatric surgery has become increasingly popular. Not only do patients lose significantly more weight with bariatric surgery than with conventional measures, but surgery also reduces and often cures conditions associated with obesity.8
Nguyen et al9 reported that 671,959 patients underwent gastric bypass procedures in the United States from 2003 to 2008. In a registry maintained by the American Society for Metabolic and Bariatric Surgery10 from June 2007 to May 2009, the most common bariatric procedure in the United States was Roux-en-Y gastric bypass, followed by sleeve gastrectomy.
DIFFERENTIAL DIAGNOSIS AND DEFINITIONS
The differential diagnosis for hyperinsulinemic hypoglycemia after gastric bypass surgery includes exogenous and endogenous causes (Table 1). Exogenous causes include abuse of insulin secretagogues such as sulfonylureas or meglitinides and abuse of insulin, which may occur in patients with Munchausen syndrome, Munchausen syndrome by proxy, or malingering. Endogenous causes include insulinoma, early and late dumping syndromes, and PGBH.
When differentiating endogenous from exogenous hypoglycemia, insulin and C-peptide levels are useful (Table 2). The pancreas produces proinsulin, which is broken down into insulin and C-peptide. Since exogenous insulin does not have a C-peptide component, people abusing insulin have elevated insulin levels with a low C-peptide level.11 Insulin secretagogues cause endogenous insulin secretion, resulting in elevated levels of both insulin and C-peptide. Thus, a screen for these medications is necessary to determine this as the cause.
Differentiating endogenous causes of hypoglycemia
Differentiating the endogenous causes (insulinoma, early or late dumping syndrome, and PGBH) can be challenging, as all 3 have similar biochemical profiles (Table 2).
Insulinoma is a tumor of pancreatic beta cells that produces excessive amounts of insulin. Unlike dumping syndrome, which only occurs postprandially, insulinoma primarily causes fasting hypoglycemia, although postprandial hypoglycemia can occur less commonly. Insulinoma after Roux-en-Y is rare. Only 7 cases have been reported.12
Dumping syndrome is classified as either early or late.
Early dumping syndrome usually occurs within 20 minutes of eating. The rapid transit of carbohydrates into the small intestine results in a fluid shift and a sympathetic response characterized by tachycardia, nausea, and diarrhea. Hypoglycemia is not present. Early dumping syndrome usually arises during the first few months after surgery.13
Late dumping syndrome usually occurs 1 to 4 hours after ingestion of a carbohydrate load, with symptoms of diaphoresis, dizziness, and fatigue caused by hypoglycemia from an excessive insulin release in response to the carbohydrates.13 It does not tend to cause neuroglycopenic symptoms.14 We define late dumping syndrome as postprandial hypoglycemic symptoms that occur after eating simple sugars and that resolve with dietary changes alone.
Differentiating late dumping syndrome from PGBH is difficult, as the line between the 2 processes is blurred.13
PGBH is defined as postprandial hypoglycemia (although it can be fasting in severe cases), often with neuroglycopenic symptoms, that occurs despite adherence to an acceptable bariatric diet (outlined in Table 3). We categorize PGBH as mild, moderate, or severe. Mild PGBH resolves with dietary changes with or without an alpha-glucosidase inhibitor. Moderate PGBH does not respond to an alpha-glucosidase inhibitor and dietary changes, and alternative or additional medication or medications are needed for resolution. Severe PGBH does not respond to dietary or medical interventions, and patients experience persistent episodes of neuroglycopenia.
THE EXACT MECHANISM IS UNCERTAIN
Patients with PGBH have a significant postprandial rise in glucose (often with levels > 200 mg/dL), leading to a robust insulin response and a subsequent drop in blood glucose.15
The exact mechanisms causing hypoglycemia are unknown, but excessive release of the incretin hormones glucagon-like peptide 1 (GLP-1) and gastric inhibitory polypeptide (GIP) are thought to contribute. GLP-1 is primarily secreted in the gut in response to nutrients, causing a glucose-dependent release of insulin and suppression of glucagon, as well as a delay in gastric emptying and motility. Salehi et al16 demonstrated excessive GLP-1 and insulin release after glucose administration in postbypass patients, with a more exaggerated response in those experiencing postprandial hypoglycemia.
Excessive incretin hormones may also contribute to pancreatic islet cell hyperplasia, leading to hyperinsulinism.17 Other proposed mechanisms of PGBH are the lack of a decrease in beta cell mass after gastric bypass, a postoperative increase in insulin sensitivity, a decrease in ghrelin (an insulin counterregulatory hormone), and an abnormal glucagon response.13,17
Pathologic changes vary widely
PGBH is a challenging diagnosis to make pathologically. On review of pancreatic tissue from 36 patients undergoing partial pancreatectomy for PGBH, the pancreatic islet cells of the PGBH group were larger and more irregular compared with controls.18,19 This histologic condition with islet-cell hypertrophy, hyperplasia, and other changes has been termed nesidioblastosis.11,14,20 However, the pancreatic tissue appears grossly normal. The histopathologic findings can vary greatly in individual cases and in one-third of cases the pancreatic changes can be minimal, so that “normal” and PGBH cells can be nearly impossible to distinguish from each other.21
DIAGNOSIS AND TREATMENT
We recommend a stepwise approach to evaluating and treating PGBH (Figures 1 and 2).
Step 1: Evaluate blood glucose and Whipple triad
The first step is a thorough history, including food consumption and timing of hypoglycemic symptoms. Give the patient a glucometer to take home, with instructions to check blood glucose levels when hypoglycemic symptoms occur. The patient should keep a log documenting time tested, food consumed, symptoms, and blood glucose data.
Hypoglycemic symptoms are categorized as autonomic and neuroglycopenic. Autonomic symptoms include anxiety, palpitations, tremulousness, and diaphoresis. Neuroglycopenic symptoms include confusion, falls, seizures, and loss of consciousness.12
There are degrees of hypoglycemia and hypoglycemic symptoms. Clinical hypoglycemia—a blood glucose level low enough to cause signs or symptoms—can be confirmed by the Whipple triad:
- Measured low blood glucose
- Symptoms of low blood glucose
- Relief of symptoms when low blood glucose is corrected.
Hypoglycemic symptoms can occur when the blood glucose level falls to less than 55 mg/dL in healthy people, but this cutoff can shift lower in someone who has recurrent hypoglycemia.
When the Whipple triad is documented, rule out nonhyperinsulinemic causes of hypoglycemia such as hypothyroidism, adrenal insufficiency, underlying organ dysfunction (ie, liver disease), and medications that cause hypoglycemia.
Step 2: Modify the diet
If postprandial hypoglycemia is occurring, the next step is dietary modification. Two studies showed that a low-carbohydrate diet prevented hypoglycemia; however, these diets contained nearly no carbohydrates (with meals consisting of eggs, sausage, cheese, and black coffee or tea).15,22
Instruct patients to never eat pure carbohydrates without fat or protein, as this can result in a more severe hypoglycemic response.22 In addition, foods with a high glycemic index (a measure of how a carbohydrate-containing food raises blood sugar) should be avoided, and a low glycemic index diet is recommended.23 High glycemic index foods include white bread, bagels, pretzels, and pineapple. Low glycemic index foods include 100% stone-ground whole wheat or pumpernickel bread, lima beans, butter beans, peas, legumes, lentils, and nonstarchy vegetables.
Our bariatric surgeons provide all postbariatric surgery patients with the dietary guidelines shown in Table 3.24 We also ask our patients with PGBH to limit carbohydrates to 15 to 30 g per meal and to limit added sugars to less than 4 g per meal, including regular and sugar alcohols (polyols). Snacks should contain only protein and fat. In severe cases, we further limit the diet to 15 g of carbohydrate per meal, with no added sugars.
The hypoglycemia occurring with PGBH is treated differently than the hypoglycemia that occurs in diabetic patients. Advise patients with PGBH to treat their hypoglycemic episodes with a simple sugar combined with a protein or fat (eg, a small handful of candy with a spoonful of peanut butter), as they will often have recurrent hypoglycemia if a simple sugar is used alone. If patients regain weight, ask them about frequent eating, which would be related to self-treatment of hypoglycemia.
Step 3: Start an alpha-glucosidase inhibitor
If postprandial hypoglycemia persists despite dietary modification, then start an alpha-glucosidase inhibitor such as acarbose. Acarbose inhibits carbohydrate absorption, resulting in a decreased insulin response; thus, it blunts the decline in postprandial blood glucose.
Unfortunately, gastrointestinal side effects such as flatulence, diarrhea, and abdominal pain occur in up to 20% of patients who take acarbose, often leading to its discontinuation.25 To minimize gastrointestinal side effects, we usually start with 25 mg of acarbose with 1 meal daily for 1 week, then increase the dosage weekly to 25 mg with the other 2 meals. If tolerated, acarbose can be increased to 50 to 100 mg with 3 meals daily.
Step 4: Obtain a mixed meal tolerance test or a provocation meal test
If dietary changes and an alpha-glucosidase inhibitor do not prevent postprandial hypoglycemia from recurring, then confirmation of PGBH is needed, using a mixed meal tolerance test or a provocation meal test.
In a mixed meal tolerance test, the meal consists of 55% carbohydrate, 30% fat, and 15% protein. Patients with hyperinsulinemic hypoglycemia have a rapid rise in blood glucose (> 200 mg/dL) with a robust insulin response that is often followed by hypoglycemia after ingesting a meal containing carbohydrates in this test. Insulin levels that remain elevated after the plasma glucose level falls to less than 55 mg/dL indicate hyperinsulinism.11
Nevertheless, a mixed meal tolerance test will not always induce hypoglycemia. In a study of 51 patients with PGBH, all wore a continuous glucose monitor, were instructed to follow their normal diet for 5 days, and then underwent a mixed meal tolerance test on day 6. The glucose monitor revealed hypoglycemia in 75% of patients, while the mixed meal tolerance test was positive in only 29%.5
Moreover, to date, there is no standardized mixed meal.5,15 This might also explain the difference in prevalence of hypoglycemia detected by this test.
Based on these conflicting findings, we recommend a provocation meal test—ie, the patient is given foods that have induced hypoglycemia earlier.
Of note, the Endocrine Society guidelines on hypoglycemia state that an oral glucose tolerance test should never be used to document postprandial hypoglycemia.26 Lev-Ran and Anderson27 found that an oral glucose tolerance test could be positive in at least 10% of normal people.
Step 5: Consider other pharmacotherapy
For moderate to severe PGBH in which dietary modification and acarbose have failed, additional medical therapy is the next step. Medical therapies include calcium channel blockers, somatostatin analogues (eg, octreotide), and diazoxide.
Calcium channel blockers inhibit insulin release from beta cells28 but at the risk of hypotension. Mordes and Alonso29 treated 6 PGBH patients with nifedipine or verapamil with or without acarbose, and symptoms resolved in 5 of the 6 patients.
When we treat PGBH, we often add a calcium channel blocker as the next step in therapy if the patient has hypertension or if the blood pressure can tolerate this. If the patient’s blood pressure is low, then avoiding calcium channel blocker therapy may be necessary. The next step would be octreotide and then diazoxide.
Somatostatin analogues such as octreotide inhibit GLP-1 and insulin release.30 The most common side effects of octreotide are diarrhea and abdominal pain. Bile stone formation can also occur, but this is not common.
Diazoxide opens adenosine triphosphate-sensitive potassium channels and reduces the opening of calcium channels, inhibiting insulin release and raising blood glucose. In a study of 6 Japanese patients with inoperable insulinoma, diazoxide was used to treat hypoglycemia.31 Unfortunately, the doses required to control the low blood sugars also led to adverse reactions, most of which involved edema secondary to volume overload and other heart failure symptoms. Diazoxide also commonly causes hypotension and hirsutism.
Step 6: 72-hour fast
A 72-hour fast is recommended in severe cases of PGBH in patients for whom dietary modification and the additional pharmacotherapy outlined in step 5 have failed. A 72-hour fast is always indicated in evaluating confirmed fasting hypoglycemia. People with insulinoma usually have fasting hypoglycemia, while patients with dumping syndrome do not. Patients with PGBH usually do not have fasting hypoglycemia, but they can in severe cases.11
For safety, this test should be done in the hospital. Baseline plasma levels of insulin, C-peptide, proinsulin, beta-hydroxybutyrate, and glucose should be obtained. The patient then fasts, consuming only noncaloric and noncaffeinated beverages for 72 hours. During this time, capillary glucose checks are performed every 6 hours. If the capillary glucose level falls below 55 mg/dL,11,26 then the baseline tests are redrawn along with a sulfonylurea screen. To reduce costs and unnecessary testing, the tests are not sent for laboratory processing unless the plasma glucose is less than 55 mg/dL.
When the plasma glucose is less than 55 mg/dL, insulin production should cease. Elevated insulin levels and insulin byproducts raise concern for hyperinsulinism. These values confirm hyperinsulinemic hypoglycemia26:
- Glucose < 55 mg/dL
- Insulin ≥ 3 µU/mL
- C-peptide ≥ 0.2 nmol/L
- Proinsulin ≥ 5.0 pmol/L.
After hypoglycemia is confirmed, 1 mg of glucagon is given intravenously, and plasma glucose levels are obtained at 10, 20, and 30 minutes.11,26 A rise in plasma glucose of at least 25 mg/dL after intravenous glucagon injection indicates hypoglycemia due to hyperinsulinemia. Two-thirds of patients with insulinoma experience hypoglycemia within the first 24 hours, and nearly all experience hypoglycemia within 48 hours.26
Step 7: Obtain pancreatic imaging
If fasting hypoglycemia is present and hyperinsulinemic hypoglycemia is confirmed during a 72-hour fast, then pancreatic imaging should be obtained to evaluate for an insulinoma. We also recommend pancreatic imaging to rule out insulinoma when severe PGBH has not responded to dietary modification or pharmacotherapy.
Imaging is not recommended in PGBH that has been successfully treated with dietary modification with or without pharmacotherapy.
Endoscopic ultrasonography alone has 80% to 92% sensitivity for localizing a pancreatic mass as small as 5 mm. However, when coupled with computed tomography or magnetic resonance imaging, the sensitivity increases to nearly 100%.12
Step 8: Selective arterial calcium stimulation test
If a patient is found to have hyperinsulinemic hypoglycemia during a 72-hour fast but pancreatic imaging is negative, then selective arterial calcium stimulation testing (SACST) and hepatic vein sampling should be performed. Also, for severe PGBH, in which hypoglycemia has persisted despite dietary modification and pharmacotherapy, SACST can be performed to evaluate for possible localization of hyperinsulinism in patients considering surgery. For mild and moderate cases of PGBH, in which the hypoglycemia has been successfully treated with dietary changes with or without pharmacotherapy, SACST is not necessary.
This test can localize the area of excess insulin production in the pancreas in patients with an insulinoma. Patients with severe PGBH usually have diffuse hyperinsulinism without localization on SACST.32,33
When SACST is performed, a sampling catheter is placed in the femoral vein. Calcium gluconate is injected into the major arteries of the pancreas (superior mesenteric, gastroduodenal, and splenic arteries). Calcium stimulates release of insulin from an insulinoma or hyperplastic beta cells. Resultant insulin levels are measured in the hepatic vein. If there is a greater than twofold increase in insulin release from 2 segments, then the test is considered positive.
Thompson et al34 documented that insulin release from insulinoma is almost 4 times higher than in diffuse nesidioblastosis. SACST has a sensitivity of 96% for detecting insulinomas.35
Step 9: Other alternatives and surgery
In patients with severe PGBH for whom dietary modification and all pharmacotherapy have failed and who continue to have debilitating neuroglycopenia, there are options before proceeding with surgery, the last resort in this condition.
Continuous glucose monitoring is helpful in many patients with severe PGBH. Many of them have hypoglycemia unawareness, and the monitor alerts them when their blood sugar is low. In addition, the monitor indicates when the blood sugar is dropping, so that intervention can occur before hypoglycemia occurs.
Unfortunately, insurance coverage for continuous monitors in this patient population is limited. We argue that insurance should cover the cost for these severe cases.
Pasireotide, a somatostatin analogue that is longer-acting than octreotide, is approved for use in Cushing disease and acromegaly and actually causes hyperglycemia. In a case report of a 50-year-old woman, pasireotide resulted in less hypoglycemia and higher glucagon levels then octreotide.36 Pasireotide is available from Novartis for compassionate use in patients with severe PGBH.
Glucocorticoids are another off-label option. However, in excess, they can lead to iatrogenic Cushing syndrome, which has its own complications. Prednisone and diazoxide have been used together to help prevent hypoglycemia in a patients with inoperable insulinoma.31
Tube feeding. Some researchers have studied altering nutrition access through surgical means. McLaughlin et al37 discussed a case of gastric tube insertion into the remnant stomach of a patient with PGBH, with resolution of hypoglycemic symptoms and hypoglycemia; however, this does not always provide complete resolution of symptoms.37,38 If gastric bypass reversal is being considered, a trial of solely remnant stomach tube feeds (with no oral intake) should be pursued first. If this ameliorates the hypoglycemia, then gastric bypass reversal may be of benefit.
Surgery is the last resort if all of the above treatments have failed and severe debilitating neuroglycopenia persists. However, surgery poses risks, and the success rate in correcting hypoglycemia is not ideal. Surgical options include Roux-en-Y reversal, gastric pouch resection, and pancreatic resection.
In a review by Mala,2 75 patients with documented PGBH underwent surgical therapy. Hypoglycemic symptoms resolved in 34 of 51 pancreatic resections, 13 of 17 Roux-en-Y reversals, and 9 of 11 gastric pouch resections. However, the follow-up period was short.
As noted above, we recommend calcium stimulation testing only for severe cases of PGBH when surgery is being considered to evaluate for possible localization of hyperinsulinism for which partial pancreatectomy would be of benefit. Since there is no localization in many PGBH cases and the success rates are slightly higher in gastric bypass reversal, bypass reversal is usually preferred over partial or complete pancreatectomy.2,32,33
POTENTIAL FUTURE THERAPIES
Given the elevated GLP-1 levels and robust insulin response to glucose observed in PGBH, blocking GLP-1 may provide clinical benefit. Salehi et al16 found that a GLP-1 antagonist prevented surges in GLP-1 and reduced hypoglycemic episodes in patients with PGBH. Unfortunately, the medication they used was given as a continuous infusion and is not currently available.
Conversely, a GLP-1 agonist showed benefit in a series of 5 cases of PGBH.39 In addition, an insulin receptor antibody is undergoing phase 2 trials and has been shown to reverse insulin-induced hypoglycemia in rodents and humans; it may be a novel therapy in the future for hyperinsulinemic hypoglycemia.40
MORE STUDY NEEDED
As the prevalence of obesity continues to rise and more people opt for bariatric surgery for weight loss, we will likely continue to see an increase in PGBH, since the onset of PGBH can be delayed for many years after surgery.28
Unfortunately, the disease process involved in PGBH is not well understood. For example, we do not know why GLP-1 elevations or a robust insulin response causing hypoglycemia occurs in some but not all gastric bypass patients. Study is needed to elucidate the pathophysiology to further understand why most patients have no hypoglycemia after gastric bypass, some have mild to moderate PGBH, and a small percentage have severe PGBH with debilitating neuroglycopenia unresponsive to dietary changes and medications.
- Sarwar H, Chapman WH 3rd, Pender JR, et al. Hypoglycemia after Roux-en-Y gastric bypass: the BOLD experience. Obes Surg 2014; 24:1120–1124.
- Mala T. Postprandial hyperinsulinemic hypoglycemia after gastric bypass surgical treatment. Surg Obes Relat Dis 2014; 10:1220–1225.
- Marsk R, Jonas E, Rasmussen F, Näslund E. Nationwide cohort study of post-gastric bypass hypoglycaemia including 5,040 patients undergoing surgery for obesity in 1986-2006 in Sweden. Diabetologia 2010; 53:2307–2311.
- Lee CJ, Clark JM, Schweitzer M, et al. Prevalence of and risk factors for hypoglycemic symptoms after gastric bypass and sleeve gastrectomy. Obesity (Silver Spring) 2015; 23:1079–1084.
- Kefurt R, Langer FB, Schindler K, Shakeri-Leidenmühler S, Ludvik B, Prager G. Hypoglycemia after Roux-En-Y gastric bypass: detection rates of continuous glucose monitoring (CGM) versus mixed meal test. Surg Obes Relat Dis 2015; 11:564–569.
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA 2014; 311:806–814.
- Bray GA, Frühbeck G, Ryan DH, Wilding JPH. Management of obesity. Lancet 2016; 387:1947–1956.
- Hunter Mehaffey J, Turrentine FE, Miller MS, Schirmer BD, Hallowell PT. Roux-en-Y gastric bypass 10-year follow-up: the found population. Surg Obes Relat Dis 2016; 12:778–782.
- Nguyen NT, Masoomi H, Magno CP, Nguyen XM, Laugenour K, Lane J. Trends in use of bariatric surgery, 2003-2008. J Am Coll Surg 2011; 213:261–266.
- DeMaria EJ, Pate V, Warthen M, Winegar DA. Baseline data from American Society for Metabolic and Bariatric Surgery-designated Bariatric Surgery Centers of Excellence using the Bariatric Outcomes Longitudinal Database. Surg Obes Relat Dis 2010; 6:347–355.
- Service FJ. Hypoglycemic disorders. N Engl J Med 1995; 332:1144–1152.
- Mulla CM, Storino A, Yee EU, et al. Insulinoma after bariatric surgery: diagnostic dilemma and therapeutic approaches. Obes Surg 2016; 26:874–881.
- Malik S, Mitchell JE, Steffen K, et al. Recognition and management of hyperinsulinemic hypoglycemia after bariatric surgery. Obes Res Clin Pract 2016; 10:1–14.
- Service GJ, Thompson GB, Service FJ, Andrews JC, Collazo-Clavell ML, Lloyd RV. Hyperinsulinemic hypoglycemia with nesidioblastosis after gastric-bypass surgery. N Engl J Med 2005; 353:249–254.
- Kellogg TA, Bantle JP, Leslie DB, et al. Postgastric bypass hyperinsulinemic hypoglycemia syndrome: characterization and response to a modified diet. Surg Obes Relat Dis 2008; 4:492–499.
- Salehi M, Gastaldelli A, D’Alessio DA. Blockade of glucagon-like peptide 1 receptor corrects postprandial hypoglycemia after gastric bypass. Gastroenterology 2014; 146:669–680.e2.
- Cummings DE. Gastric bypass and nesidioblastosis—too much of a good thing for islets? N Engl J Med 2005; 353:300–302.
- Rumilla KM, Erickson LA, Service FJ, et al. Hyperinsulinemic hypoglycemia with nesidioblastosis: histologic features and growth factor expression. Mod Pathol 2009; 22:239–245.
- Anlauf M, Wieben D, Perren A, et al. Persistent hyperinsulinemic hypoglycemia in 15 adults with diffuse nesidioblastosis: diagnostic criteria, incidence, and characterization of beta-cell changes. Am J Surg Pathol 2005; 29:524–533.
- Zumkeller W. Nesidioblastosis. Endocr Relat Cancer 1999; 6:421–428.
- Klöppel G, Anlauf M, Raffel A, Perren A, Knoefel WT. Adult diffuse nesidioblastosis: genetically or environmentally induced? Hum Pathol 2008; 39:3–8.
- Bantle JP, Ikramuddin S, Kellogg TA, Buchwald H. Hyperinsulinemic hypoglycemia developing late after gastric bypass. Obes Surg 2007; 17:592–594.
- Hirose S, Iwahashi Y, Seo A, Sumiyoshi M, Takahashi T, Tamori Y. Concurrent therapy with a low-carbohydrate diet and miglitol remarkably improved the postprandial blood glucose and insulin levels in a patient with reactive hypoglycemia due to late dumping syndrome. Intern Med 2016; 55:1137–1142.
- Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Surg Obes Relat Dis 2013; 9:159–191.
- Tack J, Arts J, Caenepeel P, De Wulf D, Bisschops R. Pathophysiology, diagnosis and management of postoperative dumping syndrome. Nat Rev Gastroenterol Hepatol 2009; 6:583–590.
- Cryer PE, Axelrod L, Grossman AB, et al. Evaluation and management of adult hypoglycemic disorders: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2009; 94:709–728.
- Lev-Ran A, Anderson RW. The diagnosis of postprandial hypoglycemia. Diabetes 1981; 30:996–999.
- Szollosi A, Nenquin M, Henquin JC. Pharmacological stimulation and inhibition of insulin secretion in mouse islets lacking ATP-sensitive K+ channels. Br J Pharmacol 2010; 159:669–677.
- Mordes JP, Alonso LC. Evaluation, medical therapy, and course of adult persistent hyperinsulinemic hypoglycemia after Roux-en-Y gastric bypass surgery: a case series. Endocr Pract 2015; 21:237–246.
- Myint KS, Greenfield JR, Farooqi IS, Henning E, Holst JJ, Finer N. Prolonged successful therapy for hyperinsulinaemic hypoglycaemia after gastric bypass: the pathophysiological role of GLP1 and its response to a somatostatin analogue. Eur J Endocrinol 2012; 166:951–955.
- Komatsu Y, Nakamura A, Takihata M, et al. Safety and tolerability of diazoxide in Japanese patients with hyperinsulinemic hypoglycemia. Endocr J 2016; 63:311–314.
- Z’graggen K, Guweidhi A, Steffen R, et al. Severe recurrent hypoglycemia after gastric bypass surgery. Obes Surg 2008; 18:981–988.
- Mathavan VK, Arregui M, Davis C, Singh K, Patel A, Meacham J. Management of postgastric bypass noninsulinoma pancreatogenous hypoglycemia. Surg Endosc 2010; 24:2547–2555.
- Thompson SM, Vella A, Thompson GB, et al. Selective arterial calcium stimulation with hepatic venous sampling differentiates insulinoma from nesidioblastosis. J Clin Endocrinol Metab 2015; 100:4189–4197.
- Wiesli P, Brändle M, Schmid C, et al. Selective arterial calcium stimulation and hepatic venous sampling in the evaluation of hyperinsulinemic hypoglycemia: potential and limitations. J Vasc Interv Radiol 2004; 15:1251–1256.
- de Heide LJ, Laskewitz AJ, Apers JA. Treatment of severe postRYGB hyperinsulinemic hypoglycemia with pasireotide: a comparison with octreotide on insulin, glucagon, and GLP-1. Surg Obes Relat Dis 2014; 10:e31–e33.
- McLaughlin T, Peck M, Holst J, Deacon C. Reversible hyperinsulinemic hypoglycemia after gastric bypass: a consequence of altered nutrient delivery. J Clin Endocrinol Metab 2010; 95:1851–1855.
- Rao BB, Click B, Eid G, Codario RA. Management of refractory noninsulinoma pancreatogenous hypoglycemia syndrome with gastric bypass reversal: a case report and review of the literature. Case Rep Endocrinol 2015; 2015:384526.
- Abrahamsson N, Engström BE, Sundbom M, Karlsson FA. GLP1 analogs as treatment of postprandial hypoglycemia following gastric bypass surgery: a potential new indication? Eur J Endocrinol 2013; 169:885–889.
- Corbin JA, Bhaskar B, Goldfine ID, et al. Inhibition of insulin receptor function by a human, allosteric monoclonal antibody: a potential new approach for the treatment of hyperinsulinemic hypoglycemia. MAbs 2014; 6:262–272.
Bariatric surgery, though beneficial, is associated with complications, one of which is post-gastric bypass hypoglycemia (PGBH).1 The mean time from gastric bypass to documented hypoglycemia is about 28 months.2
PGBH is probably more common than initially thought. In older reports, the prevalence was only 0.1% to 0.36%.1,3 In contrast, in a mail survey in 2015,4 one-third of bariatric surgery patients reported symptoms that raised the suspicion of hypoglycemia. Those with suspicious symptoms were more likely to have undergone Roux-en-Y surgery, to have had no preoperative diabetes, to have had a longer interval since surgery, and to be female. Restricting the suspicion of postprandial hypoglycemia to those who reported more serious symptoms, including needing third-party assistance, the prevalence was 11.6%.
Kefurt et al5 followed Roux-en-Y patients who wore a continuous glucose monitor for 86 months after surgery and found that 38% had hypoglycemia; however, symptoms of hypoglycemia were not discussed.
Thus, the exact prevalence is currently unknown. But as time goes by and more procedures are performed, the incidence will likely rise.
OBESITY IS ON THE RISE, AND SO IS WEIGHT-LOSS SURGERY
Obesity is rampant, and its prevalence continues to rise. In 2011–2012, more than two-thirds of adults in the United States were reported as obese.6 Complications of obesity such as cardiac disease, diabetes, and cancer lead to increased mortality risk.7 Obesity is difficult to reverse, as many people fail to lose weight with diet, exercise, and pharmacotherapy.
Given the difficulty of losing weight and the complications that arise from obesity, bariatric surgery has become increasingly popular. Not only do patients lose significantly more weight with bariatric surgery than with conventional measures, but surgery also reduces and often cures conditions associated with obesity.8
Nguyen et al9 reported that 671,959 patients underwent gastric bypass procedures in the United States from 2003 to 2008. In a registry maintained by the American Society for Metabolic and Bariatric Surgery10 from June 2007 to May 2009, the most common bariatric procedure in the United States was Roux-en-Y gastric bypass, followed by sleeve gastrectomy.
DIFFERENTIAL DIAGNOSIS AND DEFINITIONS
The differential diagnosis for hyperinsulinemic hypoglycemia after gastric bypass surgery includes exogenous and endogenous causes (Table 1). Exogenous causes include abuse of insulin secretagogues such as sulfonylureas or meglitinides and abuse of insulin, which may occur in patients with Munchausen syndrome, Munchausen syndrome by proxy, or malingering. Endogenous causes include insulinoma, early and late dumping syndromes, and PGBH.
When differentiating endogenous from exogenous hypoglycemia, insulin and C-peptide levels are useful (Table 2). The pancreas produces proinsulin, which is broken down into insulin and C-peptide. Since exogenous insulin does not have a C-peptide component, people abusing insulin have elevated insulin levels with a low C-peptide level.11 Insulin secretagogues cause endogenous insulin secretion, resulting in elevated levels of both insulin and C-peptide. Thus, a screen for these medications is necessary to determine this as the cause.
Differentiating endogenous causes of hypoglycemia
Differentiating the endogenous causes (insulinoma, early or late dumping syndrome, and PGBH) can be challenging, as all 3 have similar biochemical profiles (Table 2).
Insulinoma is a tumor of pancreatic beta cells that produces excessive amounts of insulin. Unlike dumping syndrome, which only occurs postprandially, insulinoma primarily causes fasting hypoglycemia, although postprandial hypoglycemia can occur less commonly. Insulinoma after Roux-en-Y is rare. Only 7 cases have been reported.12
Dumping syndrome is classified as either early or late.
Early dumping syndrome usually occurs within 20 minutes of eating. The rapid transit of carbohydrates into the small intestine results in a fluid shift and a sympathetic response characterized by tachycardia, nausea, and diarrhea. Hypoglycemia is not present. Early dumping syndrome usually arises during the first few months after surgery.13
Late dumping syndrome usually occurs 1 to 4 hours after ingestion of a carbohydrate load, with symptoms of diaphoresis, dizziness, and fatigue caused by hypoglycemia from an excessive insulin release in response to the carbohydrates.13 It does not tend to cause neuroglycopenic symptoms.14 We define late dumping syndrome as postprandial hypoglycemic symptoms that occur after eating simple sugars and that resolve with dietary changes alone.
Differentiating late dumping syndrome from PGBH is difficult, as the line between the 2 processes is blurred.13
PGBH is defined as postprandial hypoglycemia (although it can be fasting in severe cases), often with neuroglycopenic symptoms, that occurs despite adherence to an acceptable bariatric diet (outlined in Table 3). We categorize PGBH as mild, moderate, or severe. Mild PGBH resolves with dietary changes with or without an alpha-glucosidase inhibitor. Moderate PGBH does not respond to an alpha-glucosidase inhibitor and dietary changes, and alternative or additional medication or medications are needed for resolution. Severe PGBH does not respond to dietary or medical interventions, and patients experience persistent episodes of neuroglycopenia.
THE EXACT MECHANISM IS UNCERTAIN
Patients with PGBH have a significant postprandial rise in glucose (often with levels > 200 mg/dL), leading to a robust insulin response and a subsequent drop in blood glucose.15
The exact mechanisms causing hypoglycemia are unknown, but excessive release of the incretin hormones glucagon-like peptide 1 (GLP-1) and gastric inhibitory polypeptide (GIP) are thought to contribute. GLP-1 is primarily secreted in the gut in response to nutrients, causing a glucose-dependent release of insulin and suppression of glucagon, as well as a delay in gastric emptying and motility. Salehi et al16 demonstrated excessive GLP-1 and insulin release after glucose administration in postbypass patients, with a more exaggerated response in those experiencing postprandial hypoglycemia.
Excessive incretin hormones may also contribute to pancreatic islet cell hyperplasia, leading to hyperinsulinism.17 Other proposed mechanisms of PGBH are the lack of a decrease in beta cell mass after gastric bypass, a postoperative increase in insulin sensitivity, a decrease in ghrelin (an insulin counterregulatory hormone), and an abnormal glucagon response.13,17
Pathologic changes vary widely
PGBH is a challenging diagnosis to make pathologically. On review of pancreatic tissue from 36 patients undergoing partial pancreatectomy for PGBH, the pancreatic islet cells of the PGBH group were larger and more irregular compared with controls.18,19 This histologic condition with islet-cell hypertrophy, hyperplasia, and other changes has been termed nesidioblastosis.11,14,20 However, the pancreatic tissue appears grossly normal. The histopathologic findings can vary greatly in individual cases and in one-third of cases the pancreatic changes can be minimal, so that “normal” and PGBH cells can be nearly impossible to distinguish from each other.21
DIAGNOSIS AND TREATMENT
We recommend a stepwise approach to evaluating and treating PGBH (Figures 1 and 2).
Step 1: Evaluate blood glucose and Whipple triad
The first step is a thorough history, including food consumption and timing of hypoglycemic symptoms. Give the patient a glucometer to take home, with instructions to check blood glucose levels when hypoglycemic symptoms occur. The patient should keep a log documenting time tested, food consumed, symptoms, and blood glucose data.
Hypoglycemic symptoms are categorized as autonomic and neuroglycopenic. Autonomic symptoms include anxiety, palpitations, tremulousness, and diaphoresis. Neuroglycopenic symptoms include confusion, falls, seizures, and loss of consciousness.12
There are degrees of hypoglycemia and hypoglycemic symptoms. Clinical hypoglycemia—a blood glucose level low enough to cause signs or symptoms—can be confirmed by the Whipple triad:
- Measured low blood glucose
- Symptoms of low blood glucose
- Relief of symptoms when low blood glucose is corrected.
Hypoglycemic symptoms can occur when the blood glucose level falls to less than 55 mg/dL in healthy people, but this cutoff can shift lower in someone who has recurrent hypoglycemia.
When the Whipple triad is documented, rule out nonhyperinsulinemic causes of hypoglycemia such as hypothyroidism, adrenal insufficiency, underlying organ dysfunction (ie, liver disease), and medications that cause hypoglycemia.
Step 2: Modify the diet
If postprandial hypoglycemia is occurring, the next step is dietary modification. Two studies showed that a low-carbohydrate diet prevented hypoglycemia; however, these diets contained nearly no carbohydrates (with meals consisting of eggs, sausage, cheese, and black coffee or tea).15,22
Instruct patients to never eat pure carbohydrates without fat or protein, as this can result in a more severe hypoglycemic response.22 In addition, foods with a high glycemic index (a measure of how a carbohydrate-containing food raises blood sugar) should be avoided, and a low glycemic index diet is recommended.23 High glycemic index foods include white bread, bagels, pretzels, and pineapple. Low glycemic index foods include 100% stone-ground whole wheat or pumpernickel bread, lima beans, butter beans, peas, legumes, lentils, and nonstarchy vegetables.
Our bariatric surgeons provide all postbariatric surgery patients with the dietary guidelines shown in Table 3.24 We also ask our patients with PGBH to limit carbohydrates to 15 to 30 g per meal and to limit added sugars to less than 4 g per meal, including regular and sugar alcohols (polyols). Snacks should contain only protein and fat. In severe cases, we further limit the diet to 15 g of carbohydrate per meal, with no added sugars.
The hypoglycemia occurring with PGBH is treated differently than the hypoglycemia that occurs in diabetic patients. Advise patients with PGBH to treat their hypoglycemic episodes with a simple sugar combined with a protein or fat (eg, a small handful of candy with a spoonful of peanut butter), as they will often have recurrent hypoglycemia if a simple sugar is used alone. If patients regain weight, ask them about frequent eating, which would be related to self-treatment of hypoglycemia.
Step 3: Start an alpha-glucosidase inhibitor
If postprandial hypoglycemia persists despite dietary modification, then start an alpha-glucosidase inhibitor such as acarbose. Acarbose inhibits carbohydrate absorption, resulting in a decreased insulin response; thus, it blunts the decline in postprandial blood glucose.
Unfortunately, gastrointestinal side effects such as flatulence, diarrhea, and abdominal pain occur in up to 20% of patients who take acarbose, often leading to its discontinuation.25 To minimize gastrointestinal side effects, we usually start with 25 mg of acarbose with 1 meal daily for 1 week, then increase the dosage weekly to 25 mg with the other 2 meals. If tolerated, acarbose can be increased to 50 to 100 mg with 3 meals daily.
Step 4: Obtain a mixed meal tolerance test or a provocation meal test
If dietary changes and an alpha-glucosidase inhibitor do not prevent postprandial hypoglycemia from recurring, then confirmation of PGBH is needed, using a mixed meal tolerance test or a provocation meal test.
In a mixed meal tolerance test, the meal consists of 55% carbohydrate, 30% fat, and 15% protein. Patients with hyperinsulinemic hypoglycemia have a rapid rise in blood glucose (> 200 mg/dL) with a robust insulin response that is often followed by hypoglycemia after ingesting a meal containing carbohydrates in this test. Insulin levels that remain elevated after the plasma glucose level falls to less than 55 mg/dL indicate hyperinsulinism.11
Nevertheless, a mixed meal tolerance test will not always induce hypoglycemia. In a study of 51 patients with PGBH, all wore a continuous glucose monitor, were instructed to follow their normal diet for 5 days, and then underwent a mixed meal tolerance test on day 6. The glucose monitor revealed hypoglycemia in 75% of patients, while the mixed meal tolerance test was positive in only 29%.5
Moreover, to date, there is no standardized mixed meal.5,15 This might also explain the difference in prevalence of hypoglycemia detected by this test.
Based on these conflicting findings, we recommend a provocation meal test—ie, the patient is given foods that have induced hypoglycemia earlier.
Of note, the Endocrine Society guidelines on hypoglycemia state that an oral glucose tolerance test should never be used to document postprandial hypoglycemia.26 Lev-Ran and Anderson27 found that an oral glucose tolerance test could be positive in at least 10% of normal people.
Step 5: Consider other pharmacotherapy
For moderate to severe PGBH in which dietary modification and acarbose have failed, additional medical therapy is the next step. Medical therapies include calcium channel blockers, somatostatin analogues (eg, octreotide), and diazoxide.
Calcium channel blockers inhibit insulin release from beta cells28 but at the risk of hypotension. Mordes and Alonso29 treated 6 PGBH patients with nifedipine or verapamil with or without acarbose, and symptoms resolved in 5 of the 6 patients.
When we treat PGBH, we often add a calcium channel blocker as the next step in therapy if the patient has hypertension or if the blood pressure can tolerate this. If the patient’s blood pressure is low, then avoiding calcium channel blocker therapy may be necessary. The next step would be octreotide and then diazoxide.
Somatostatin analogues such as octreotide inhibit GLP-1 and insulin release.30 The most common side effects of octreotide are diarrhea and abdominal pain. Bile stone formation can also occur, but this is not common.
Diazoxide opens adenosine triphosphate-sensitive potassium channels and reduces the opening of calcium channels, inhibiting insulin release and raising blood glucose. In a study of 6 Japanese patients with inoperable insulinoma, diazoxide was used to treat hypoglycemia.31 Unfortunately, the doses required to control the low blood sugars also led to adverse reactions, most of which involved edema secondary to volume overload and other heart failure symptoms. Diazoxide also commonly causes hypotension and hirsutism.
Step 6: 72-hour fast
A 72-hour fast is recommended in severe cases of PGBH in patients for whom dietary modification and the additional pharmacotherapy outlined in step 5 have failed. A 72-hour fast is always indicated in evaluating confirmed fasting hypoglycemia. People with insulinoma usually have fasting hypoglycemia, while patients with dumping syndrome do not. Patients with PGBH usually do not have fasting hypoglycemia, but they can in severe cases.11
For safety, this test should be done in the hospital. Baseline plasma levels of insulin, C-peptide, proinsulin, beta-hydroxybutyrate, and glucose should be obtained. The patient then fasts, consuming only noncaloric and noncaffeinated beverages for 72 hours. During this time, capillary glucose checks are performed every 6 hours. If the capillary glucose level falls below 55 mg/dL,11,26 then the baseline tests are redrawn along with a sulfonylurea screen. To reduce costs and unnecessary testing, the tests are not sent for laboratory processing unless the plasma glucose is less than 55 mg/dL.
When the plasma glucose is less than 55 mg/dL, insulin production should cease. Elevated insulin levels and insulin byproducts raise concern for hyperinsulinism. These values confirm hyperinsulinemic hypoglycemia26:
- Glucose < 55 mg/dL
- Insulin ≥ 3 µU/mL
- C-peptide ≥ 0.2 nmol/L
- Proinsulin ≥ 5.0 pmol/L.
After hypoglycemia is confirmed, 1 mg of glucagon is given intravenously, and plasma glucose levels are obtained at 10, 20, and 30 minutes.11,26 A rise in plasma glucose of at least 25 mg/dL after intravenous glucagon injection indicates hypoglycemia due to hyperinsulinemia. Two-thirds of patients with insulinoma experience hypoglycemia within the first 24 hours, and nearly all experience hypoglycemia within 48 hours.26
Step 7: Obtain pancreatic imaging
If fasting hypoglycemia is present and hyperinsulinemic hypoglycemia is confirmed during a 72-hour fast, then pancreatic imaging should be obtained to evaluate for an insulinoma. We also recommend pancreatic imaging to rule out insulinoma when severe PGBH has not responded to dietary modification or pharmacotherapy.
Imaging is not recommended in PGBH that has been successfully treated with dietary modification with or without pharmacotherapy.
Endoscopic ultrasonography alone has 80% to 92% sensitivity for localizing a pancreatic mass as small as 5 mm. However, when coupled with computed tomography or magnetic resonance imaging, the sensitivity increases to nearly 100%.12
Step 8: Selective arterial calcium stimulation test
If a patient is found to have hyperinsulinemic hypoglycemia during a 72-hour fast but pancreatic imaging is negative, then selective arterial calcium stimulation testing (SACST) and hepatic vein sampling should be performed. Also, for severe PGBH, in which hypoglycemia has persisted despite dietary modification and pharmacotherapy, SACST can be performed to evaluate for possible localization of hyperinsulinism in patients considering surgery. For mild and moderate cases of PGBH, in which the hypoglycemia has been successfully treated with dietary changes with or without pharmacotherapy, SACST is not necessary.
This test can localize the area of excess insulin production in the pancreas in patients with an insulinoma. Patients with severe PGBH usually have diffuse hyperinsulinism without localization on SACST.32,33
When SACST is performed, a sampling catheter is placed in the femoral vein. Calcium gluconate is injected into the major arteries of the pancreas (superior mesenteric, gastroduodenal, and splenic arteries). Calcium stimulates release of insulin from an insulinoma or hyperplastic beta cells. Resultant insulin levels are measured in the hepatic vein. If there is a greater than twofold increase in insulin release from 2 segments, then the test is considered positive.
Thompson et al34 documented that insulin release from insulinoma is almost 4 times higher than in diffuse nesidioblastosis. SACST has a sensitivity of 96% for detecting insulinomas.35
Step 9: Other alternatives and surgery
In patients with severe PGBH for whom dietary modification and all pharmacotherapy have failed and who continue to have debilitating neuroglycopenia, there are options before proceeding with surgery, the last resort in this condition.
Continuous glucose monitoring is helpful in many patients with severe PGBH. Many of them have hypoglycemia unawareness, and the monitor alerts them when their blood sugar is low. In addition, the monitor indicates when the blood sugar is dropping, so that intervention can occur before hypoglycemia occurs.
Unfortunately, insurance coverage for continuous monitors in this patient population is limited. We argue that insurance should cover the cost for these severe cases.
Pasireotide, a somatostatin analogue that is longer-acting than octreotide, is approved for use in Cushing disease and acromegaly and actually causes hyperglycemia. In a case report of a 50-year-old woman, pasireotide resulted in less hypoglycemia and higher glucagon levels then octreotide.36 Pasireotide is available from Novartis for compassionate use in patients with severe PGBH.
Glucocorticoids are another off-label option. However, in excess, they can lead to iatrogenic Cushing syndrome, which has its own complications. Prednisone and diazoxide have been used together to help prevent hypoglycemia in a patients with inoperable insulinoma.31
Tube feeding. Some researchers have studied altering nutrition access through surgical means. McLaughlin et al37 discussed a case of gastric tube insertion into the remnant stomach of a patient with PGBH, with resolution of hypoglycemic symptoms and hypoglycemia; however, this does not always provide complete resolution of symptoms.37,38 If gastric bypass reversal is being considered, a trial of solely remnant stomach tube feeds (with no oral intake) should be pursued first. If this ameliorates the hypoglycemia, then gastric bypass reversal may be of benefit.
Surgery is the last resort if all of the above treatments have failed and severe debilitating neuroglycopenia persists. However, surgery poses risks, and the success rate in correcting hypoglycemia is not ideal. Surgical options include Roux-en-Y reversal, gastric pouch resection, and pancreatic resection.
In a review by Mala,2 75 patients with documented PGBH underwent surgical therapy. Hypoglycemic symptoms resolved in 34 of 51 pancreatic resections, 13 of 17 Roux-en-Y reversals, and 9 of 11 gastric pouch resections. However, the follow-up period was short.
As noted above, we recommend calcium stimulation testing only for severe cases of PGBH when surgery is being considered to evaluate for possible localization of hyperinsulinism for which partial pancreatectomy would be of benefit. Since there is no localization in many PGBH cases and the success rates are slightly higher in gastric bypass reversal, bypass reversal is usually preferred over partial or complete pancreatectomy.2,32,33
POTENTIAL FUTURE THERAPIES
Given the elevated GLP-1 levels and robust insulin response to glucose observed in PGBH, blocking GLP-1 may provide clinical benefit. Salehi et al16 found that a GLP-1 antagonist prevented surges in GLP-1 and reduced hypoglycemic episodes in patients with PGBH. Unfortunately, the medication they used was given as a continuous infusion and is not currently available.
Conversely, a GLP-1 agonist showed benefit in a series of 5 cases of PGBH.39 In addition, an insulin receptor antibody is undergoing phase 2 trials and has been shown to reverse insulin-induced hypoglycemia in rodents and humans; it may be a novel therapy in the future for hyperinsulinemic hypoglycemia.40
MORE STUDY NEEDED
As the prevalence of obesity continues to rise and more people opt for bariatric surgery for weight loss, we will likely continue to see an increase in PGBH, since the onset of PGBH can be delayed for many years after surgery.28
Unfortunately, the disease process involved in PGBH is not well understood. For example, we do not know why GLP-1 elevations or a robust insulin response causing hypoglycemia occurs in some but not all gastric bypass patients. Study is needed to elucidate the pathophysiology to further understand why most patients have no hypoglycemia after gastric bypass, some have mild to moderate PGBH, and a small percentage have severe PGBH with debilitating neuroglycopenia unresponsive to dietary changes and medications.
Bariatric surgery, though beneficial, is associated with complications, one of which is post-gastric bypass hypoglycemia (PGBH).1 The mean time from gastric bypass to documented hypoglycemia is about 28 months.2
PGBH is probably more common than initially thought. In older reports, the prevalence was only 0.1% to 0.36%.1,3 In contrast, in a mail survey in 2015,4 one-third of bariatric surgery patients reported symptoms that raised the suspicion of hypoglycemia. Those with suspicious symptoms were more likely to have undergone Roux-en-Y surgery, to have had no preoperative diabetes, to have had a longer interval since surgery, and to be female. Restricting the suspicion of postprandial hypoglycemia to those who reported more serious symptoms, including needing third-party assistance, the prevalence was 11.6%.
Kefurt et al5 followed Roux-en-Y patients who wore a continuous glucose monitor for 86 months after surgery and found that 38% had hypoglycemia; however, symptoms of hypoglycemia were not discussed.
Thus, the exact prevalence is currently unknown. But as time goes by and more procedures are performed, the incidence will likely rise.
OBESITY IS ON THE RISE, AND SO IS WEIGHT-LOSS SURGERY
Obesity is rampant, and its prevalence continues to rise. In 2011–2012, more than two-thirds of adults in the United States were reported as obese.6 Complications of obesity such as cardiac disease, diabetes, and cancer lead to increased mortality risk.7 Obesity is difficult to reverse, as many people fail to lose weight with diet, exercise, and pharmacotherapy.
Given the difficulty of losing weight and the complications that arise from obesity, bariatric surgery has become increasingly popular. Not only do patients lose significantly more weight with bariatric surgery than with conventional measures, but surgery also reduces and often cures conditions associated with obesity.8
Nguyen et al9 reported that 671,959 patients underwent gastric bypass procedures in the United States from 2003 to 2008. In a registry maintained by the American Society for Metabolic and Bariatric Surgery10 from June 2007 to May 2009, the most common bariatric procedure in the United States was Roux-en-Y gastric bypass, followed by sleeve gastrectomy.
DIFFERENTIAL DIAGNOSIS AND DEFINITIONS
The differential diagnosis for hyperinsulinemic hypoglycemia after gastric bypass surgery includes exogenous and endogenous causes (Table 1). Exogenous causes include abuse of insulin secretagogues such as sulfonylureas or meglitinides and abuse of insulin, which may occur in patients with Munchausen syndrome, Munchausen syndrome by proxy, or malingering. Endogenous causes include insulinoma, early and late dumping syndromes, and PGBH.
When differentiating endogenous from exogenous hypoglycemia, insulin and C-peptide levels are useful (Table 2). The pancreas produces proinsulin, which is broken down into insulin and C-peptide. Since exogenous insulin does not have a C-peptide component, people abusing insulin have elevated insulin levels with a low C-peptide level.11 Insulin secretagogues cause endogenous insulin secretion, resulting in elevated levels of both insulin and C-peptide. Thus, a screen for these medications is necessary to determine this as the cause.
Differentiating endogenous causes of hypoglycemia
Differentiating the endogenous causes (insulinoma, early or late dumping syndrome, and PGBH) can be challenging, as all 3 have similar biochemical profiles (Table 2).
Insulinoma is a tumor of pancreatic beta cells that produces excessive amounts of insulin. Unlike dumping syndrome, which only occurs postprandially, insulinoma primarily causes fasting hypoglycemia, although postprandial hypoglycemia can occur less commonly. Insulinoma after Roux-en-Y is rare. Only 7 cases have been reported.12
Dumping syndrome is classified as either early or late.
Early dumping syndrome usually occurs within 20 minutes of eating. The rapid transit of carbohydrates into the small intestine results in a fluid shift and a sympathetic response characterized by tachycardia, nausea, and diarrhea. Hypoglycemia is not present. Early dumping syndrome usually arises during the first few months after surgery.13
Late dumping syndrome usually occurs 1 to 4 hours after ingestion of a carbohydrate load, with symptoms of diaphoresis, dizziness, and fatigue caused by hypoglycemia from an excessive insulin release in response to the carbohydrates.13 It does not tend to cause neuroglycopenic symptoms.14 We define late dumping syndrome as postprandial hypoglycemic symptoms that occur after eating simple sugars and that resolve with dietary changes alone.
Differentiating late dumping syndrome from PGBH is difficult, as the line between the 2 processes is blurred.13
PGBH is defined as postprandial hypoglycemia (although it can be fasting in severe cases), often with neuroglycopenic symptoms, that occurs despite adherence to an acceptable bariatric diet (outlined in Table 3). We categorize PGBH as mild, moderate, or severe. Mild PGBH resolves with dietary changes with or without an alpha-glucosidase inhibitor. Moderate PGBH does not respond to an alpha-glucosidase inhibitor and dietary changes, and alternative or additional medication or medications are needed for resolution. Severe PGBH does not respond to dietary or medical interventions, and patients experience persistent episodes of neuroglycopenia.
THE EXACT MECHANISM IS UNCERTAIN
Patients with PGBH have a significant postprandial rise in glucose (often with levels > 200 mg/dL), leading to a robust insulin response and a subsequent drop in blood glucose.15
The exact mechanisms causing hypoglycemia are unknown, but excessive release of the incretin hormones glucagon-like peptide 1 (GLP-1) and gastric inhibitory polypeptide (GIP) are thought to contribute. GLP-1 is primarily secreted in the gut in response to nutrients, causing a glucose-dependent release of insulin and suppression of glucagon, as well as a delay in gastric emptying and motility. Salehi et al16 demonstrated excessive GLP-1 and insulin release after glucose administration in postbypass patients, with a more exaggerated response in those experiencing postprandial hypoglycemia.
Excessive incretin hormones may also contribute to pancreatic islet cell hyperplasia, leading to hyperinsulinism.17 Other proposed mechanisms of PGBH are the lack of a decrease in beta cell mass after gastric bypass, a postoperative increase in insulin sensitivity, a decrease in ghrelin (an insulin counterregulatory hormone), and an abnormal glucagon response.13,17
Pathologic changes vary widely
PGBH is a challenging diagnosis to make pathologically. On review of pancreatic tissue from 36 patients undergoing partial pancreatectomy for PGBH, the pancreatic islet cells of the PGBH group were larger and more irregular compared with controls.18,19 This histologic condition with islet-cell hypertrophy, hyperplasia, and other changes has been termed nesidioblastosis.11,14,20 However, the pancreatic tissue appears grossly normal. The histopathologic findings can vary greatly in individual cases and in one-third of cases the pancreatic changes can be minimal, so that “normal” and PGBH cells can be nearly impossible to distinguish from each other.21
DIAGNOSIS AND TREATMENT
We recommend a stepwise approach to evaluating and treating PGBH (Figures 1 and 2).
Step 1: Evaluate blood glucose and Whipple triad
The first step is a thorough history, including food consumption and timing of hypoglycemic symptoms. Give the patient a glucometer to take home, with instructions to check blood glucose levels when hypoglycemic symptoms occur. The patient should keep a log documenting time tested, food consumed, symptoms, and blood glucose data.
Hypoglycemic symptoms are categorized as autonomic and neuroglycopenic. Autonomic symptoms include anxiety, palpitations, tremulousness, and diaphoresis. Neuroglycopenic symptoms include confusion, falls, seizures, and loss of consciousness.12
There are degrees of hypoglycemia and hypoglycemic symptoms. Clinical hypoglycemia—a blood glucose level low enough to cause signs or symptoms—can be confirmed by the Whipple triad:
- Measured low blood glucose
- Symptoms of low blood glucose
- Relief of symptoms when low blood glucose is corrected.
Hypoglycemic symptoms can occur when the blood glucose level falls to less than 55 mg/dL in healthy people, but this cutoff can shift lower in someone who has recurrent hypoglycemia.
When the Whipple triad is documented, rule out nonhyperinsulinemic causes of hypoglycemia such as hypothyroidism, adrenal insufficiency, underlying organ dysfunction (ie, liver disease), and medications that cause hypoglycemia.
Step 2: Modify the diet
If postprandial hypoglycemia is occurring, the next step is dietary modification. Two studies showed that a low-carbohydrate diet prevented hypoglycemia; however, these diets contained nearly no carbohydrates (with meals consisting of eggs, sausage, cheese, and black coffee or tea).15,22
Instruct patients to never eat pure carbohydrates without fat or protein, as this can result in a more severe hypoglycemic response.22 In addition, foods with a high glycemic index (a measure of how a carbohydrate-containing food raises blood sugar) should be avoided, and a low glycemic index diet is recommended.23 High glycemic index foods include white bread, bagels, pretzels, and pineapple. Low glycemic index foods include 100% stone-ground whole wheat or pumpernickel bread, lima beans, butter beans, peas, legumes, lentils, and nonstarchy vegetables.
Our bariatric surgeons provide all postbariatric surgery patients with the dietary guidelines shown in Table 3.24 We also ask our patients with PGBH to limit carbohydrates to 15 to 30 g per meal and to limit added sugars to less than 4 g per meal, including regular and sugar alcohols (polyols). Snacks should contain only protein and fat. In severe cases, we further limit the diet to 15 g of carbohydrate per meal, with no added sugars.
The hypoglycemia occurring with PGBH is treated differently than the hypoglycemia that occurs in diabetic patients. Advise patients with PGBH to treat their hypoglycemic episodes with a simple sugar combined with a protein or fat (eg, a small handful of candy with a spoonful of peanut butter), as they will often have recurrent hypoglycemia if a simple sugar is used alone. If patients regain weight, ask them about frequent eating, which would be related to self-treatment of hypoglycemia.
Step 3: Start an alpha-glucosidase inhibitor
If postprandial hypoglycemia persists despite dietary modification, then start an alpha-glucosidase inhibitor such as acarbose. Acarbose inhibits carbohydrate absorption, resulting in a decreased insulin response; thus, it blunts the decline in postprandial blood glucose.
Unfortunately, gastrointestinal side effects such as flatulence, diarrhea, and abdominal pain occur in up to 20% of patients who take acarbose, often leading to its discontinuation.25 To minimize gastrointestinal side effects, we usually start with 25 mg of acarbose with 1 meal daily for 1 week, then increase the dosage weekly to 25 mg with the other 2 meals. If tolerated, acarbose can be increased to 50 to 100 mg with 3 meals daily.
Step 4: Obtain a mixed meal tolerance test or a provocation meal test
If dietary changes and an alpha-glucosidase inhibitor do not prevent postprandial hypoglycemia from recurring, then confirmation of PGBH is needed, using a mixed meal tolerance test or a provocation meal test.
In a mixed meal tolerance test, the meal consists of 55% carbohydrate, 30% fat, and 15% protein. Patients with hyperinsulinemic hypoglycemia have a rapid rise in blood glucose (> 200 mg/dL) with a robust insulin response that is often followed by hypoglycemia after ingesting a meal containing carbohydrates in this test. Insulin levels that remain elevated after the plasma glucose level falls to less than 55 mg/dL indicate hyperinsulinism.11
Nevertheless, a mixed meal tolerance test will not always induce hypoglycemia. In a study of 51 patients with PGBH, all wore a continuous glucose monitor, were instructed to follow their normal diet for 5 days, and then underwent a mixed meal tolerance test on day 6. The glucose monitor revealed hypoglycemia in 75% of patients, while the mixed meal tolerance test was positive in only 29%.5
Moreover, to date, there is no standardized mixed meal.5,15 This might also explain the difference in prevalence of hypoglycemia detected by this test.
Based on these conflicting findings, we recommend a provocation meal test—ie, the patient is given foods that have induced hypoglycemia earlier.
Of note, the Endocrine Society guidelines on hypoglycemia state that an oral glucose tolerance test should never be used to document postprandial hypoglycemia.26 Lev-Ran and Anderson27 found that an oral glucose tolerance test could be positive in at least 10% of normal people.
Step 5: Consider other pharmacotherapy
For moderate to severe PGBH in which dietary modification and acarbose have failed, additional medical therapy is the next step. Medical therapies include calcium channel blockers, somatostatin analogues (eg, octreotide), and diazoxide.
Calcium channel blockers inhibit insulin release from beta cells28 but at the risk of hypotension. Mordes and Alonso29 treated 6 PGBH patients with nifedipine or verapamil with or without acarbose, and symptoms resolved in 5 of the 6 patients.
When we treat PGBH, we often add a calcium channel blocker as the next step in therapy if the patient has hypertension or if the blood pressure can tolerate this. If the patient’s blood pressure is low, then avoiding calcium channel blocker therapy may be necessary. The next step would be octreotide and then diazoxide.
Somatostatin analogues such as octreotide inhibit GLP-1 and insulin release.30 The most common side effects of octreotide are diarrhea and abdominal pain. Bile stone formation can also occur, but this is not common.
Diazoxide opens adenosine triphosphate-sensitive potassium channels and reduces the opening of calcium channels, inhibiting insulin release and raising blood glucose. In a study of 6 Japanese patients with inoperable insulinoma, diazoxide was used to treat hypoglycemia.31 Unfortunately, the doses required to control the low blood sugars also led to adverse reactions, most of which involved edema secondary to volume overload and other heart failure symptoms. Diazoxide also commonly causes hypotension and hirsutism.
Step 6: 72-hour fast
A 72-hour fast is recommended in severe cases of PGBH in patients for whom dietary modification and the additional pharmacotherapy outlined in step 5 have failed. A 72-hour fast is always indicated in evaluating confirmed fasting hypoglycemia. People with insulinoma usually have fasting hypoglycemia, while patients with dumping syndrome do not. Patients with PGBH usually do not have fasting hypoglycemia, but they can in severe cases.11
For safety, this test should be done in the hospital. Baseline plasma levels of insulin, C-peptide, proinsulin, beta-hydroxybutyrate, and glucose should be obtained. The patient then fasts, consuming only noncaloric and noncaffeinated beverages for 72 hours. During this time, capillary glucose checks are performed every 6 hours. If the capillary glucose level falls below 55 mg/dL,11,26 then the baseline tests are redrawn along with a sulfonylurea screen. To reduce costs and unnecessary testing, the tests are not sent for laboratory processing unless the plasma glucose is less than 55 mg/dL.
When the plasma glucose is less than 55 mg/dL, insulin production should cease. Elevated insulin levels and insulin byproducts raise concern for hyperinsulinism. These values confirm hyperinsulinemic hypoglycemia26:
- Glucose < 55 mg/dL
- Insulin ≥ 3 µU/mL
- C-peptide ≥ 0.2 nmol/L
- Proinsulin ≥ 5.0 pmol/L.
After hypoglycemia is confirmed, 1 mg of glucagon is given intravenously, and plasma glucose levels are obtained at 10, 20, and 30 minutes.11,26 A rise in plasma glucose of at least 25 mg/dL after intravenous glucagon injection indicates hypoglycemia due to hyperinsulinemia. Two-thirds of patients with insulinoma experience hypoglycemia within the first 24 hours, and nearly all experience hypoglycemia within 48 hours.26
Step 7: Obtain pancreatic imaging
If fasting hypoglycemia is present and hyperinsulinemic hypoglycemia is confirmed during a 72-hour fast, then pancreatic imaging should be obtained to evaluate for an insulinoma. We also recommend pancreatic imaging to rule out insulinoma when severe PGBH has not responded to dietary modification or pharmacotherapy.
Imaging is not recommended in PGBH that has been successfully treated with dietary modification with or without pharmacotherapy.
Endoscopic ultrasonography alone has 80% to 92% sensitivity for localizing a pancreatic mass as small as 5 mm. However, when coupled with computed tomography or magnetic resonance imaging, the sensitivity increases to nearly 100%.12
Step 8: Selective arterial calcium stimulation test
If a patient is found to have hyperinsulinemic hypoglycemia during a 72-hour fast but pancreatic imaging is negative, then selective arterial calcium stimulation testing (SACST) and hepatic vein sampling should be performed. Also, for severe PGBH, in which hypoglycemia has persisted despite dietary modification and pharmacotherapy, SACST can be performed to evaluate for possible localization of hyperinsulinism in patients considering surgery. For mild and moderate cases of PGBH, in which the hypoglycemia has been successfully treated with dietary changes with or without pharmacotherapy, SACST is not necessary.
This test can localize the area of excess insulin production in the pancreas in patients with an insulinoma. Patients with severe PGBH usually have diffuse hyperinsulinism without localization on SACST.32,33
When SACST is performed, a sampling catheter is placed in the femoral vein. Calcium gluconate is injected into the major arteries of the pancreas (superior mesenteric, gastroduodenal, and splenic arteries). Calcium stimulates release of insulin from an insulinoma or hyperplastic beta cells. Resultant insulin levels are measured in the hepatic vein. If there is a greater than twofold increase in insulin release from 2 segments, then the test is considered positive.
Thompson et al34 documented that insulin release from insulinoma is almost 4 times higher than in diffuse nesidioblastosis. SACST has a sensitivity of 96% for detecting insulinomas.35
Step 9: Other alternatives and surgery
In patients with severe PGBH for whom dietary modification and all pharmacotherapy have failed and who continue to have debilitating neuroglycopenia, there are options before proceeding with surgery, the last resort in this condition.
Continuous glucose monitoring is helpful in many patients with severe PGBH. Many of them have hypoglycemia unawareness, and the monitor alerts them when their blood sugar is low. In addition, the monitor indicates when the blood sugar is dropping, so that intervention can occur before hypoglycemia occurs.
Unfortunately, insurance coverage for continuous monitors in this patient population is limited. We argue that insurance should cover the cost for these severe cases.
Pasireotide, a somatostatin analogue that is longer-acting than octreotide, is approved for use in Cushing disease and acromegaly and actually causes hyperglycemia. In a case report of a 50-year-old woman, pasireotide resulted in less hypoglycemia and higher glucagon levels then octreotide.36 Pasireotide is available from Novartis for compassionate use in patients with severe PGBH.
Glucocorticoids are another off-label option. However, in excess, they can lead to iatrogenic Cushing syndrome, which has its own complications. Prednisone and diazoxide have been used together to help prevent hypoglycemia in a patients with inoperable insulinoma.31
Tube feeding. Some researchers have studied altering nutrition access through surgical means. McLaughlin et al37 discussed a case of gastric tube insertion into the remnant stomach of a patient with PGBH, with resolution of hypoglycemic symptoms and hypoglycemia; however, this does not always provide complete resolution of symptoms.37,38 If gastric bypass reversal is being considered, a trial of solely remnant stomach tube feeds (with no oral intake) should be pursued first. If this ameliorates the hypoglycemia, then gastric bypass reversal may be of benefit.
Surgery is the last resort if all of the above treatments have failed and severe debilitating neuroglycopenia persists. However, surgery poses risks, and the success rate in correcting hypoglycemia is not ideal. Surgical options include Roux-en-Y reversal, gastric pouch resection, and pancreatic resection.
In a review by Mala,2 75 patients with documented PGBH underwent surgical therapy. Hypoglycemic symptoms resolved in 34 of 51 pancreatic resections, 13 of 17 Roux-en-Y reversals, and 9 of 11 gastric pouch resections. However, the follow-up period was short.
As noted above, we recommend calcium stimulation testing only for severe cases of PGBH when surgery is being considered to evaluate for possible localization of hyperinsulinism for which partial pancreatectomy would be of benefit. Since there is no localization in many PGBH cases and the success rates are slightly higher in gastric bypass reversal, bypass reversal is usually preferred over partial or complete pancreatectomy.2,32,33
POTENTIAL FUTURE THERAPIES
Given the elevated GLP-1 levels and robust insulin response to glucose observed in PGBH, blocking GLP-1 may provide clinical benefit. Salehi et al16 found that a GLP-1 antagonist prevented surges in GLP-1 and reduced hypoglycemic episodes in patients with PGBH. Unfortunately, the medication they used was given as a continuous infusion and is not currently available.
Conversely, a GLP-1 agonist showed benefit in a series of 5 cases of PGBH.39 In addition, an insulin receptor antibody is undergoing phase 2 trials and has been shown to reverse insulin-induced hypoglycemia in rodents and humans; it may be a novel therapy in the future for hyperinsulinemic hypoglycemia.40
MORE STUDY NEEDED
As the prevalence of obesity continues to rise and more people opt for bariatric surgery for weight loss, we will likely continue to see an increase in PGBH, since the onset of PGBH can be delayed for many years after surgery.28
Unfortunately, the disease process involved in PGBH is not well understood. For example, we do not know why GLP-1 elevations or a robust insulin response causing hypoglycemia occurs in some but not all gastric bypass patients. Study is needed to elucidate the pathophysiology to further understand why most patients have no hypoglycemia after gastric bypass, some have mild to moderate PGBH, and a small percentage have severe PGBH with debilitating neuroglycopenia unresponsive to dietary changes and medications.
- Sarwar H, Chapman WH 3rd, Pender JR, et al. Hypoglycemia after Roux-en-Y gastric bypass: the BOLD experience. Obes Surg 2014; 24:1120–1124.
- Mala T. Postprandial hyperinsulinemic hypoglycemia after gastric bypass surgical treatment. Surg Obes Relat Dis 2014; 10:1220–1225.
- Marsk R, Jonas E, Rasmussen F, Näslund E. Nationwide cohort study of post-gastric bypass hypoglycaemia including 5,040 patients undergoing surgery for obesity in 1986-2006 in Sweden. Diabetologia 2010; 53:2307–2311.
- Lee CJ, Clark JM, Schweitzer M, et al. Prevalence of and risk factors for hypoglycemic symptoms after gastric bypass and sleeve gastrectomy. Obesity (Silver Spring) 2015; 23:1079–1084.
- Kefurt R, Langer FB, Schindler K, Shakeri-Leidenmühler S, Ludvik B, Prager G. Hypoglycemia after Roux-En-Y gastric bypass: detection rates of continuous glucose monitoring (CGM) versus mixed meal test. Surg Obes Relat Dis 2015; 11:564–569.
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA 2014; 311:806–814.
- Bray GA, Frühbeck G, Ryan DH, Wilding JPH. Management of obesity. Lancet 2016; 387:1947–1956.
- Hunter Mehaffey J, Turrentine FE, Miller MS, Schirmer BD, Hallowell PT. Roux-en-Y gastric bypass 10-year follow-up: the found population. Surg Obes Relat Dis 2016; 12:778–782.
- Nguyen NT, Masoomi H, Magno CP, Nguyen XM, Laugenour K, Lane J. Trends in use of bariatric surgery, 2003-2008. J Am Coll Surg 2011; 213:261–266.
- DeMaria EJ, Pate V, Warthen M, Winegar DA. Baseline data from American Society for Metabolic and Bariatric Surgery-designated Bariatric Surgery Centers of Excellence using the Bariatric Outcomes Longitudinal Database. Surg Obes Relat Dis 2010; 6:347–355.
- Service FJ. Hypoglycemic disorders. N Engl J Med 1995; 332:1144–1152.
- Mulla CM, Storino A, Yee EU, et al. Insulinoma after bariatric surgery: diagnostic dilemma and therapeutic approaches. Obes Surg 2016; 26:874–881.
- Malik S, Mitchell JE, Steffen K, et al. Recognition and management of hyperinsulinemic hypoglycemia after bariatric surgery. Obes Res Clin Pract 2016; 10:1–14.
- Service GJ, Thompson GB, Service FJ, Andrews JC, Collazo-Clavell ML, Lloyd RV. Hyperinsulinemic hypoglycemia with nesidioblastosis after gastric-bypass surgery. N Engl J Med 2005; 353:249–254.
- Kellogg TA, Bantle JP, Leslie DB, et al. Postgastric bypass hyperinsulinemic hypoglycemia syndrome: characterization and response to a modified diet. Surg Obes Relat Dis 2008; 4:492–499.
- Salehi M, Gastaldelli A, D’Alessio DA. Blockade of glucagon-like peptide 1 receptor corrects postprandial hypoglycemia after gastric bypass. Gastroenterology 2014; 146:669–680.e2.
- Cummings DE. Gastric bypass and nesidioblastosis—too much of a good thing for islets? N Engl J Med 2005; 353:300–302.
- Rumilla KM, Erickson LA, Service FJ, et al. Hyperinsulinemic hypoglycemia with nesidioblastosis: histologic features and growth factor expression. Mod Pathol 2009; 22:239–245.
- Anlauf M, Wieben D, Perren A, et al. Persistent hyperinsulinemic hypoglycemia in 15 adults with diffuse nesidioblastosis: diagnostic criteria, incidence, and characterization of beta-cell changes. Am J Surg Pathol 2005; 29:524–533.
- Zumkeller W. Nesidioblastosis. Endocr Relat Cancer 1999; 6:421–428.
- Klöppel G, Anlauf M, Raffel A, Perren A, Knoefel WT. Adult diffuse nesidioblastosis: genetically or environmentally induced? Hum Pathol 2008; 39:3–8.
- Bantle JP, Ikramuddin S, Kellogg TA, Buchwald H. Hyperinsulinemic hypoglycemia developing late after gastric bypass. Obes Surg 2007; 17:592–594.
- Hirose S, Iwahashi Y, Seo A, Sumiyoshi M, Takahashi T, Tamori Y. Concurrent therapy with a low-carbohydrate diet and miglitol remarkably improved the postprandial blood glucose and insulin levels in a patient with reactive hypoglycemia due to late dumping syndrome. Intern Med 2016; 55:1137–1142.
- Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Surg Obes Relat Dis 2013; 9:159–191.
- Tack J, Arts J, Caenepeel P, De Wulf D, Bisschops R. Pathophysiology, diagnosis and management of postoperative dumping syndrome. Nat Rev Gastroenterol Hepatol 2009; 6:583–590.
- Cryer PE, Axelrod L, Grossman AB, et al. Evaluation and management of adult hypoglycemic disorders: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2009; 94:709–728.
- Lev-Ran A, Anderson RW. The diagnosis of postprandial hypoglycemia. Diabetes 1981; 30:996–999.
- Szollosi A, Nenquin M, Henquin JC. Pharmacological stimulation and inhibition of insulin secretion in mouse islets lacking ATP-sensitive K+ channels. Br J Pharmacol 2010; 159:669–677.
- Mordes JP, Alonso LC. Evaluation, medical therapy, and course of adult persistent hyperinsulinemic hypoglycemia after Roux-en-Y gastric bypass surgery: a case series. Endocr Pract 2015; 21:237–246.
- Myint KS, Greenfield JR, Farooqi IS, Henning E, Holst JJ, Finer N. Prolonged successful therapy for hyperinsulinaemic hypoglycaemia after gastric bypass: the pathophysiological role of GLP1 and its response to a somatostatin analogue. Eur J Endocrinol 2012; 166:951–955.
- Komatsu Y, Nakamura A, Takihata M, et al. Safety and tolerability of diazoxide in Japanese patients with hyperinsulinemic hypoglycemia. Endocr J 2016; 63:311–314.
- Z’graggen K, Guweidhi A, Steffen R, et al. Severe recurrent hypoglycemia after gastric bypass surgery. Obes Surg 2008; 18:981–988.
- Mathavan VK, Arregui M, Davis C, Singh K, Patel A, Meacham J. Management of postgastric bypass noninsulinoma pancreatogenous hypoglycemia. Surg Endosc 2010; 24:2547–2555.
- Thompson SM, Vella A, Thompson GB, et al. Selective arterial calcium stimulation with hepatic venous sampling differentiates insulinoma from nesidioblastosis. J Clin Endocrinol Metab 2015; 100:4189–4197.
- Wiesli P, Brändle M, Schmid C, et al. Selective arterial calcium stimulation and hepatic venous sampling in the evaluation of hyperinsulinemic hypoglycemia: potential and limitations. J Vasc Interv Radiol 2004; 15:1251–1256.
- de Heide LJ, Laskewitz AJ, Apers JA. Treatment of severe postRYGB hyperinsulinemic hypoglycemia with pasireotide: a comparison with octreotide on insulin, glucagon, and GLP-1. Surg Obes Relat Dis 2014; 10:e31–e33.
- McLaughlin T, Peck M, Holst J, Deacon C. Reversible hyperinsulinemic hypoglycemia after gastric bypass: a consequence of altered nutrient delivery. J Clin Endocrinol Metab 2010; 95:1851–1855.
- Rao BB, Click B, Eid G, Codario RA. Management of refractory noninsulinoma pancreatogenous hypoglycemia syndrome with gastric bypass reversal: a case report and review of the literature. Case Rep Endocrinol 2015; 2015:384526.
- Abrahamsson N, Engström BE, Sundbom M, Karlsson FA. GLP1 analogs as treatment of postprandial hypoglycemia following gastric bypass surgery: a potential new indication? Eur J Endocrinol 2013; 169:885–889.
- Corbin JA, Bhaskar B, Goldfine ID, et al. Inhibition of insulin receptor function by a human, allosteric monoclonal antibody: a potential new approach for the treatment of hyperinsulinemic hypoglycemia. MAbs 2014; 6:262–272.
- Sarwar H, Chapman WH 3rd, Pender JR, et al. Hypoglycemia after Roux-en-Y gastric bypass: the BOLD experience. Obes Surg 2014; 24:1120–1124.
- Mala T. Postprandial hyperinsulinemic hypoglycemia after gastric bypass surgical treatment. Surg Obes Relat Dis 2014; 10:1220–1225.
- Marsk R, Jonas E, Rasmussen F, Näslund E. Nationwide cohort study of post-gastric bypass hypoglycaemia including 5,040 patients undergoing surgery for obesity in 1986-2006 in Sweden. Diabetologia 2010; 53:2307–2311.
- Lee CJ, Clark JM, Schweitzer M, et al. Prevalence of and risk factors for hypoglycemic symptoms after gastric bypass and sleeve gastrectomy. Obesity (Silver Spring) 2015; 23:1079–1084.
- Kefurt R, Langer FB, Schindler K, Shakeri-Leidenmühler S, Ludvik B, Prager G. Hypoglycemia after Roux-En-Y gastric bypass: detection rates of continuous glucose monitoring (CGM) versus mixed meal test. Surg Obes Relat Dis 2015; 11:564–569.
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA 2014; 311:806–814.
- Bray GA, Frühbeck G, Ryan DH, Wilding JPH. Management of obesity. Lancet 2016; 387:1947–1956.
- Hunter Mehaffey J, Turrentine FE, Miller MS, Schirmer BD, Hallowell PT. Roux-en-Y gastric bypass 10-year follow-up: the found population. Surg Obes Relat Dis 2016; 12:778–782.
- Nguyen NT, Masoomi H, Magno CP, Nguyen XM, Laugenour K, Lane J. Trends in use of bariatric surgery, 2003-2008. J Am Coll Surg 2011; 213:261–266.
- DeMaria EJ, Pate V, Warthen M, Winegar DA. Baseline data from American Society for Metabolic and Bariatric Surgery-designated Bariatric Surgery Centers of Excellence using the Bariatric Outcomes Longitudinal Database. Surg Obes Relat Dis 2010; 6:347–355.
- Service FJ. Hypoglycemic disorders. N Engl J Med 1995; 332:1144–1152.
- Mulla CM, Storino A, Yee EU, et al. Insulinoma after bariatric surgery: diagnostic dilemma and therapeutic approaches. Obes Surg 2016; 26:874–881.
- Malik S, Mitchell JE, Steffen K, et al. Recognition and management of hyperinsulinemic hypoglycemia after bariatric surgery. Obes Res Clin Pract 2016; 10:1–14.
- Service GJ, Thompson GB, Service FJ, Andrews JC, Collazo-Clavell ML, Lloyd RV. Hyperinsulinemic hypoglycemia with nesidioblastosis after gastric-bypass surgery. N Engl J Med 2005; 353:249–254.
- Kellogg TA, Bantle JP, Leslie DB, et al. Postgastric bypass hyperinsulinemic hypoglycemia syndrome: characterization and response to a modified diet. Surg Obes Relat Dis 2008; 4:492–499.
- Salehi M, Gastaldelli A, D’Alessio DA. Blockade of glucagon-like peptide 1 receptor corrects postprandial hypoglycemia after gastric bypass. Gastroenterology 2014; 146:669–680.e2.
- Cummings DE. Gastric bypass and nesidioblastosis—too much of a good thing for islets? N Engl J Med 2005; 353:300–302.
- Rumilla KM, Erickson LA, Service FJ, et al. Hyperinsulinemic hypoglycemia with nesidioblastosis: histologic features and growth factor expression. Mod Pathol 2009; 22:239–245.
- Anlauf M, Wieben D, Perren A, et al. Persistent hyperinsulinemic hypoglycemia in 15 adults with diffuse nesidioblastosis: diagnostic criteria, incidence, and characterization of beta-cell changes. Am J Surg Pathol 2005; 29:524–533.
- Zumkeller W. Nesidioblastosis. Endocr Relat Cancer 1999; 6:421–428.
- Klöppel G, Anlauf M, Raffel A, Perren A, Knoefel WT. Adult diffuse nesidioblastosis: genetically or environmentally induced? Hum Pathol 2008; 39:3–8.
- Bantle JP, Ikramuddin S, Kellogg TA, Buchwald H. Hyperinsulinemic hypoglycemia developing late after gastric bypass. Obes Surg 2007; 17:592–594.
- Hirose S, Iwahashi Y, Seo A, Sumiyoshi M, Takahashi T, Tamori Y. Concurrent therapy with a low-carbohydrate diet and miglitol remarkably improved the postprandial blood glucose and insulin levels in a patient with reactive hypoglycemia due to late dumping syndrome. Intern Med 2016; 55:1137–1142.
- Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Surg Obes Relat Dis 2013; 9:159–191.
- Tack J, Arts J, Caenepeel P, De Wulf D, Bisschops R. Pathophysiology, diagnosis and management of postoperative dumping syndrome. Nat Rev Gastroenterol Hepatol 2009; 6:583–590.
- Cryer PE, Axelrod L, Grossman AB, et al. Evaluation and management of adult hypoglycemic disorders: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2009; 94:709–728.
- Lev-Ran A, Anderson RW. The diagnosis of postprandial hypoglycemia. Diabetes 1981; 30:996–999.
- Szollosi A, Nenquin M, Henquin JC. Pharmacological stimulation and inhibition of insulin secretion in mouse islets lacking ATP-sensitive K+ channels. Br J Pharmacol 2010; 159:669–677.
- Mordes JP, Alonso LC. Evaluation, medical therapy, and course of adult persistent hyperinsulinemic hypoglycemia after Roux-en-Y gastric bypass surgery: a case series. Endocr Pract 2015; 21:237–246.
- Myint KS, Greenfield JR, Farooqi IS, Henning E, Holst JJ, Finer N. Prolonged successful therapy for hyperinsulinaemic hypoglycaemia after gastric bypass: the pathophysiological role of GLP1 and its response to a somatostatin analogue. Eur J Endocrinol 2012; 166:951–955.
- Komatsu Y, Nakamura A, Takihata M, et al. Safety and tolerability of diazoxide in Japanese patients with hyperinsulinemic hypoglycemia. Endocr J 2016; 63:311–314.
- Z’graggen K, Guweidhi A, Steffen R, et al. Severe recurrent hypoglycemia after gastric bypass surgery. Obes Surg 2008; 18:981–988.
- Mathavan VK, Arregui M, Davis C, Singh K, Patel A, Meacham J. Management of postgastric bypass noninsulinoma pancreatogenous hypoglycemia. Surg Endosc 2010; 24:2547–2555.
- Thompson SM, Vella A, Thompson GB, et al. Selective arterial calcium stimulation with hepatic venous sampling differentiates insulinoma from nesidioblastosis. J Clin Endocrinol Metab 2015; 100:4189–4197.
- Wiesli P, Brändle M, Schmid C, et al. Selective arterial calcium stimulation and hepatic venous sampling in the evaluation of hyperinsulinemic hypoglycemia: potential and limitations. J Vasc Interv Radiol 2004; 15:1251–1256.
- de Heide LJ, Laskewitz AJ, Apers JA. Treatment of severe postRYGB hyperinsulinemic hypoglycemia with pasireotide: a comparison with octreotide on insulin, glucagon, and GLP-1. Surg Obes Relat Dis 2014; 10:e31–e33.
- McLaughlin T, Peck M, Holst J, Deacon C. Reversible hyperinsulinemic hypoglycemia after gastric bypass: a consequence of altered nutrient delivery. J Clin Endocrinol Metab 2010; 95:1851–1855.
- Rao BB, Click B, Eid G, Codario RA. Management of refractory noninsulinoma pancreatogenous hypoglycemia syndrome with gastric bypass reversal: a case report and review of the literature. Case Rep Endocrinol 2015; 2015:384526.
- Abrahamsson N, Engström BE, Sundbom M, Karlsson FA. GLP1 analogs as treatment of postprandial hypoglycemia following gastric bypass surgery: a potential new indication? Eur J Endocrinol 2013; 169:885–889.
- Corbin JA, Bhaskar B, Goldfine ID, et al. Inhibition of insulin receptor function by a human, allosteric monoclonal antibody: a potential new approach for the treatment of hyperinsulinemic hypoglycemia. MAbs 2014; 6:262–272.
KEY POINTS
- The differential diagnosis for endogenous causes of hyperinsulinemic hypoglycemia after gastric bypass surgery includes insulinoma, late dumping syndrome, and post-gastric bypass hypoglycemia (PGBH).
- The Whipple triad consists of measured low blood glucose, symptoms of low blood glucose, and reversal of symptoms when low blood glucose is corrected. If the triad is not present, then hypoglycemia is not causing the patient’s symptoms.
- PGBH should initially be treated with a high-protein, high-fiber, low-carbohydrate diet and then, if hypoglycemia persists, by medication (initially acarbose, then a calcium channel blocker and octreotide or diazoxide or both).
- PGBH ranges from mild, in which neuroglycopenia resolves with dietary changes with or without acarbose, to severe, in which neuroglycopenia persists despite dietary changes and multiple drugs.
- Gastric bypass reversal and pancreatic surgery are a last resort for patients with debilitating neuroglycopenia when dietary modification and drug therapy fail.
Hypertrophic osteoarthropathy: Uncommon presentation of lung cancer
A 43-year-old woman presented to the clinic complaining of bilateral ankle joint pain for 2 months. She denied a history of fever, weight loss, addictions, cough, or trauma. On physical examinatio, she had swelling of the ankle and wrist joints and digital clubbing (Figure 1). Active movement of the ankles and wrists was restricted due to pain. The examination was otherwise unremarkable.
Radiography of both ankles showed a lamellar type periosteal reaction suggestive of periostitis (Figure 2). Computed tomography of the chest revealed a spiculated mass over the right lower lobe. Biopsy study of the mass was positive for squamous cell carcinoma. She was referred to the oncology center for further management.
FEATURES OF HYPERTROPHIC OSTEOARTHROPATHY
Digital clubbing is one of the oldest signs in clinical medicine. It is characterized by bulbous enlargement of the terminal segments of the fingers and toes due to proliferation of subungual connective tissue. It usually appears as a painless finger deformity and is clinically appreciated as a loss of the normal angle between the nail bed and proximal nail fold.
Hypertrophic osteoarthropathy is a symptomatic form of clubbing associated with proliferative periostosis of the distal end of long tubular bones, commonly those adjacent to the wrist and ankle joints.1 The laminated appearance of these bones on radiography is due to the excess connective tissue secondary to new osteoid material deposited under the periosteum.
There is evidence to suggest that clubbing and hypertrophic osteoarthropathy represent different stages of the same disease process.2 In most cases, finger deformity is the first manifestation; as the disease progresses, periostosis becomes evident.
Hypertrophic osteoarthropathy can be classified as primary or secondary. The primary form, also known as primary pachydermoperiostosis, is rare and constitutes only 3% of all cases.3 The exact cause is not yet known; it occurs as a hereditary disease with autosomal dominant inheritance with variable penetrance. Congenital clubbing without periostosis is of no clinical significance.4
CONDITIONS ASSOCIATED WITH CLUBBING
Primary bronchogenic carcinoma is the most common cause of clubbing and hypertrophic osteoarthropathy. In one retrospective series, 4.5% of patients with lung cancer had radiologic evidence of hypertrophic osteoarthropathy.5 Other malignancies associated with this condition are mesothelioma, hepatocellular carcinoma, and certain types of gastrointestinal adenocarcinoma.
Other conditions associated with clubbing include:
- Cardiovascular disease such as congenital cyanotic heart disease and infective endocarditis
- Gastrointestinal conditions such as cirrhosis, primary sclerosing cholangitis, Crohn disease, and ulcerative colitis
- Infections such as lung abscess and empyema.
Clubbing is generally bilaterally symmetrical. Asymmetric clubbing is rare and usually indicates impaired regional blood flow due to vascular disease. Unilateral clubbing or hypertrophic osteoarthropathy restricted to 1 upper limb can result from an anomaly of the aortic arch or from a subclavian or brachial artery aneurysm. Clubbing affecting predominantly the lower limbs has been reported in coarctation of aorta and patent ductus arteriosus.6 Rare cases of unidigital clubbing are reported in sarcoidosis.7
The importance of recognizing hypertrophic osteoarthropathy cannot be overemphasized. If any of the manifestations of the syndrome become evident in a previously healthy person, a thorough evaluation for an underlying disease should be done.
Clubbing should be differentiated from pseudoclubbing, which is seen in conditions such as hyperparathyroidism and scleroderma. The central mechanism for nail deformity in pseudoclubbing is acro-osteolysis with the resulting collapse of the subungual soft tissues. The important features differentiating it from true clubbing are preservation of the angle between the nail bed and proximal nail fold and asymmetric finger involvement.8
MANAGEMENT
The management of primary hypertrophic osteoarthropathy focuses on relieving the symptoms of periosteitis. Secondary forms require a detailed evaluation to rule out the underlying disease. In refractory cases, a bone-modifying agent (eg, zoledronic acid),9 octreotide,10 nonsteroidal anti-inflammatory drugs, or vagotomy11 may help.
- Martínez-Lavín M, Matucci-Cerinic M, Jajic I, Pineda C. Hypertrophic osteoarthropathy: consensus on its definition, classification, assessment and diagnostic criteria. J Rheumatol 1993; 20:1386–1387.
- Martínez-Lavín M. Digital clubbing and hypertrophic osteoarthropathy: a unifying hypothesis. J Rheumatol 1987; 14:6–8.
- Jajic Z, Jajic I, Nemcic T. Primary hypertrophic osteoarthropathy: clinical, radiologic, and scintigraphic characteristics. Arch Med Res 2001; 32:136–142.
- Walker HK, Hall WD, Hurst JW, eds. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd ed. Boston, MA: Butterworths; 1990.
- Izumi M, Takayama K, Yabuuchi H, Abe K, Nakanishi Y. Incidence of hypertrophic pulmonary osteoarthropathy associated with primary lung cancer. Respirology 2010; 15:809–812.
- Anoop TM, George KC. Images in clinical medicine. Differential clubbing and cyanosis. N Engl J Med 2011; 364:666.
- Singh A. Unidigital clubbing. Am J Med 2008; 121:e15.
- Santiago MB, Lima I, Feitosa AC, Braz Ade S, Miranda LG. Pseudoclubbing: is it different from clubbing? Semin Arthritis Rheum 2009; 38:452–457.
- Tachibana I, Gehi D, Rubin CD. Treatment of hypertrophic osteoarthropathy with underlying pulmonary adenocarcinoma using zoledronic acid. J Clin Rheumatol 2015; 21:333–334.
- Birch E, Jenkins D, Noble S. Treatment of painful hypertrophic osteoarthropathy associated with non-small cell lung cancer with octreotide: a case report and review of the literature. BMJ Support Palliat Care 2011; 1:189–192.
- Nguyen S, Hojjati M. Review of current therapies for secondary hypertrophic pulmonary osteoarthropathy. Clin Rheumatol 2011; 30:7–13.
A 43-year-old woman presented to the clinic complaining of bilateral ankle joint pain for 2 months. She denied a history of fever, weight loss, addictions, cough, or trauma. On physical examinatio, she had swelling of the ankle and wrist joints and digital clubbing (Figure 1). Active movement of the ankles and wrists was restricted due to pain. The examination was otherwise unremarkable.
Radiography of both ankles showed a lamellar type periosteal reaction suggestive of periostitis (Figure 2). Computed tomography of the chest revealed a spiculated mass over the right lower lobe. Biopsy study of the mass was positive for squamous cell carcinoma. She was referred to the oncology center for further management.
FEATURES OF HYPERTROPHIC OSTEOARTHROPATHY
Digital clubbing is one of the oldest signs in clinical medicine. It is characterized by bulbous enlargement of the terminal segments of the fingers and toes due to proliferation of subungual connective tissue. It usually appears as a painless finger deformity and is clinically appreciated as a loss of the normal angle between the nail bed and proximal nail fold.
Hypertrophic osteoarthropathy is a symptomatic form of clubbing associated with proliferative periostosis of the distal end of long tubular bones, commonly those adjacent to the wrist and ankle joints.1 The laminated appearance of these bones on radiography is due to the excess connective tissue secondary to new osteoid material deposited under the periosteum.
There is evidence to suggest that clubbing and hypertrophic osteoarthropathy represent different stages of the same disease process.2 In most cases, finger deformity is the first manifestation; as the disease progresses, periostosis becomes evident.
Hypertrophic osteoarthropathy can be classified as primary or secondary. The primary form, also known as primary pachydermoperiostosis, is rare and constitutes only 3% of all cases.3 The exact cause is not yet known; it occurs as a hereditary disease with autosomal dominant inheritance with variable penetrance. Congenital clubbing without periostosis is of no clinical significance.4
CONDITIONS ASSOCIATED WITH CLUBBING
Primary bronchogenic carcinoma is the most common cause of clubbing and hypertrophic osteoarthropathy. In one retrospective series, 4.5% of patients with lung cancer had radiologic evidence of hypertrophic osteoarthropathy.5 Other malignancies associated with this condition are mesothelioma, hepatocellular carcinoma, and certain types of gastrointestinal adenocarcinoma.
Other conditions associated with clubbing include:
- Cardiovascular disease such as congenital cyanotic heart disease and infective endocarditis
- Gastrointestinal conditions such as cirrhosis, primary sclerosing cholangitis, Crohn disease, and ulcerative colitis
- Infections such as lung abscess and empyema.
Clubbing is generally bilaterally symmetrical. Asymmetric clubbing is rare and usually indicates impaired regional blood flow due to vascular disease. Unilateral clubbing or hypertrophic osteoarthropathy restricted to 1 upper limb can result from an anomaly of the aortic arch or from a subclavian or brachial artery aneurysm. Clubbing affecting predominantly the lower limbs has been reported in coarctation of aorta and patent ductus arteriosus.6 Rare cases of unidigital clubbing are reported in sarcoidosis.7
The importance of recognizing hypertrophic osteoarthropathy cannot be overemphasized. If any of the manifestations of the syndrome become evident in a previously healthy person, a thorough evaluation for an underlying disease should be done.
Clubbing should be differentiated from pseudoclubbing, which is seen in conditions such as hyperparathyroidism and scleroderma. The central mechanism for nail deformity in pseudoclubbing is acro-osteolysis with the resulting collapse of the subungual soft tissues. The important features differentiating it from true clubbing are preservation of the angle between the nail bed and proximal nail fold and asymmetric finger involvement.8
MANAGEMENT
The management of primary hypertrophic osteoarthropathy focuses on relieving the symptoms of periosteitis. Secondary forms require a detailed evaluation to rule out the underlying disease. In refractory cases, a bone-modifying agent (eg, zoledronic acid),9 octreotide,10 nonsteroidal anti-inflammatory drugs, or vagotomy11 may help.
A 43-year-old woman presented to the clinic complaining of bilateral ankle joint pain for 2 months. She denied a history of fever, weight loss, addictions, cough, or trauma. On physical examinatio, she had swelling of the ankle and wrist joints and digital clubbing (Figure 1). Active movement of the ankles and wrists was restricted due to pain. The examination was otherwise unremarkable.
Radiography of both ankles showed a lamellar type periosteal reaction suggestive of periostitis (Figure 2). Computed tomography of the chest revealed a spiculated mass over the right lower lobe. Biopsy study of the mass was positive for squamous cell carcinoma. She was referred to the oncology center for further management.
FEATURES OF HYPERTROPHIC OSTEOARTHROPATHY
Digital clubbing is one of the oldest signs in clinical medicine. It is characterized by bulbous enlargement of the terminal segments of the fingers and toes due to proliferation of subungual connective tissue. It usually appears as a painless finger deformity and is clinically appreciated as a loss of the normal angle between the nail bed and proximal nail fold.
Hypertrophic osteoarthropathy is a symptomatic form of clubbing associated with proliferative periostosis of the distal end of long tubular bones, commonly those adjacent to the wrist and ankle joints.1 The laminated appearance of these bones on radiography is due to the excess connective tissue secondary to new osteoid material deposited under the periosteum.
There is evidence to suggest that clubbing and hypertrophic osteoarthropathy represent different stages of the same disease process.2 In most cases, finger deformity is the first manifestation; as the disease progresses, periostosis becomes evident.
Hypertrophic osteoarthropathy can be classified as primary or secondary. The primary form, also known as primary pachydermoperiostosis, is rare and constitutes only 3% of all cases.3 The exact cause is not yet known; it occurs as a hereditary disease with autosomal dominant inheritance with variable penetrance. Congenital clubbing without periostosis is of no clinical significance.4
CONDITIONS ASSOCIATED WITH CLUBBING
Primary bronchogenic carcinoma is the most common cause of clubbing and hypertrophic osteoarthropathy. In one retrospective series, 4.5% of patients with lung cancer had radiologic evidence of hypertrophic osteoarthropathy.5 Other malignancies associated with this condition are mesothelioma, hepatocellular carcinoma, and certain types of gastrointestinal adenocarcinoma.
Other conditions associated with clubbing include:
- Cardiovascular disease such as congenital cyanotic heart disease and infective endocarditis
- Gastrointestinal conditions such as cirrhosis, primary sclerosing cholangitis, Crohn disease, and ulcerative colitis
- Infections such as lung abscess and empyema.
Clubbing is generally bilaterally symmetrical. Asymmetric clubbing is rare and usually indicates impaired regional blood flow due to vascular disease. Unilateral clubbing or hypertrophic osteoarthropathy restricted to 1 upper limb can result from an anomaly of the aortic arch or from a subclavian or brachial artery aneurysm. Clubbing affecting predominantly the lower limbs has been reported in coarctation of aorta and patent ductus arteriosus.6 Rare cases of unidigital clubbing are reported in sarcoidosis.7
The importance of recognizing hypertrophic osteoarthropathy cannot be overemphasized. If any of the manifestations of the syndrome become evident in a previously healthy person, a thorough evaluation for an underlying disease should be done.
Clubbing should be differentiated from pseudoclubbing, which is seen in conditions such as hyperparathyroidism and scleroderma. The central mechanism for nail deformity in pseudoclubbing is acro-osteolysis with the resulting collapse of the subungual soft tissues. The important features differentiating it from true clubbing are preservation of the angle between the nail bed and proximal nail fold and asymmetric finger involvement.8
MANAGEMENT
The management of primary hypertrophic osteoarthropathy focuses on relieving the symptoms of periosteitis. Secondary forms require a detailed evaluation to rule out the underlying disease. In refractory cases, a bone-modifying agent (eg, zoledronic acid),9 octreotide,10 nonsteroidal anti-inflammatory drugs, or vagotomy11 may help.
- Martínez-Lavín M, Matucci-Cerinic M, Jajic I, Pineda C. Hypertrophic osteoarthropathy: consensus on its definition, classification, assessment and diagnostic criteria. J Rheumatol 1993; 20:1386–1387.
- Martínez-Lavín M. Digital clubbing and hypertrophic osteoarthropathy: a unifying hypothesis. J Rheumatol 1987; 14:6–8.
- Jajic Z, Jajic I, Nemcic T. Primary hypertrophic osteoarthropathy: clinical, radiologic, and scintigraphic characteristics. Arch Med Res 2001; 32:136–142.
- Walker HK, Hall WD, Hurst JW, eds. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd ed. Boston, MA: Butterworths; 1990.
- Izumi M, Takayama K, Yabuuchi H, Abe K, Nakanishi Y. Incidence of hypertrophic pulmonary osteoarthropathy associated with primary lung cancer. Respirology 2010; 15:809–812.
- Anoop TM, George KC. Images in clinical medicine. Differential clubbing and cyanosis. N Engl J Med 2011; 364:666.
- Singh A. Unidigital clubbing. Am J Med 2008; 121:e15.
- Santiago MB, Lima I, Feitosa AC, Braz Ade S, Miranda LG. Pseudoclubbing: is it different from clubbing? Semin Arthritis Rheum 2009; 38:452–457.
- Tachibana I, Gehi D, Rubin CD. Treatment of hypertrophic osteoarthropathy with underlying pulmonary adenocarcinoma using zoledronic acid. J Clin Rheumatol 2015; 21:333–334.
- Birch E, Jenkins D, Noble S. Treatment of painful hypertrophic osteoarthropathy associated with non-small cell lung cancer with octreotide: a case report and review of the literature. BMJ Support Palliat Care 2011; 1:189–192.
- Nguyen S, Hojjati M. Review of current therapies for secondary hypertrophic pulmonary osteoarthropathy. Clin Rheumatol 2011; 30:7–13.
- Martínez-Lavín M, Matucci-Cerinic M, Jajic I, Pineda C. Hypertrophic osteoarthropathy: consensus on its definition, classification, assessment and diagnostic criteria. J Rheumatol 1993; 20:1386–1387.
- Martínez-Lavín M. Digital clubbing and hypertrophic osteoarthropathy: a unifying hypothesis. J Rheumatol 1987; 14:6–8.
- Jajic Z, Jajic I, Nemcic T. Primary hypertrophic osteoarthropathy: clinical, radiologic, and scintigraphic characteristics. Arch Med Res 2001; 32:136–142.
- Walker HK, Hall WD, Hurst JW, eds. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd ed. Boston, MA: Butterworths; 1990.
- Izumi M, Takayama K, Yabuuchi H, Abe K, Nakanishi Y. Incidence of hypertrophic pulmonary osteoarthropathy associated with primary lung cancer. Respirology 2010; 15:809–812.
- Anoop TM, George KC. Images in clinical medicine. Differential clubbing and cyanosis. N Engl J Med 2011; 364:666.
- Singh A. Unidigital clubbing. Am J Med 2008; 121:e15.
- Santiago MB, Lima I, Feitosa AC, Braz Ade S, Miranda LG. Pseudoclubbing: is it different from clubbing? Semin Arthritis Rheum 2009; 38:452–457.
- Tachibana I, Gehi D, Rubin CD. Treatment of hypertrophic osteoarthropathy with underlying pulmonary adenocarcinoma using zoledronic acid. J Clin Rheumatol 2015; 21:333–334.
- Birch E, Jenkins D, Noble S. Treatment of painful hypertrophic osteoarthropathy associated with non-small cell lung cancer with octreotide: a case report and review of the literature. BMJ Support Palliat Care 2011; 1:189–192.
- Nguyen S, Hojjati M. Review of current therapies for secondary hypertrophic pulmonary osteoarthropathy. Clin Rheumatol 2011; 30:7–13.
Peer-reviewers for 2016
We thank those who reviewed manuscripts submitted to the Cleveland Clinic Journal of Medicine in the year ending December 31, 2016. Reviewing papers for scientific journals is an arduous task and involves considerable time and effort. We are grateful to these reviewers for contributing their expertise this past year.
—Brian F. Mandell, MD, PhD, Editor in Chief
We thank those who reviewed manuscripts submitted to the Cleveland Clinic Journal of Medicine in the year ending December 31, 2016. Reviewing papers for scientific journals is an arduous task and involves considerable time and effort. We are grateful to these reviewers for contributing their expertise this past year.
—Brian F. Mandell, MD, PhD, Editor in Chief
We thank those who reviewed manuscripts submitted to the Cleveland Clinic Journal of Medicine in the year ending December 31, 2016. Reviewing papers for scientific journals is an arduous task and involves considerable time and effort. We are grateful to these reviewers for contributing their expertise this past year.
—Brian F. Mandell, MD, PhD, Editor in Chief
Risk for obstetric complications when treating cervical dysplasia
Cervical dysplasia is a condition commonly encountered by the gynecologist. It is either treated (with excision or ablation) or monitored, depending on the lesion grade, cytologic history, medical history, and reproductive goals. Cervical dysplasia commonly arises in women of reproductive age. Therefore, consider reproductive effects when deciding whether to treat or monitor, as well as when choosing the treatment modality.
Background
Approximately two-thirds of human papillomavirus infections resolve within a year, and more than 90% resolve within 2 years. Similarly, low-grade cervical intraepithelial neoplasia (CIN 1) lesions frequently resolve. High-grade (CIN 2 and CIN 3) lesions regress less commonly, with 5% and 12%-40% progressing to invasive cancer, respectively. Therefore, treatment is typically recommended.
Obstetric implications
Potential obstetric risks of treatment for CIN include infertility, spontaneous abortion, preterm premature rupture of membranes (PPROM), preterm delivery, and perinatal/neonatal mortality. These risks are discussed individually below. Mechanisms that have been suggested for such complications include decreased cervical mucous, cervical scarring impeding conception or dilation, loss of cervical volume, collagen breakdown, and immunologic processes due to decreased physical defenses or microbiome shifts.
Fertility
Studies have shown that treatment does not appear to impede conception. The overall pregnancy rate is higher among treated women than untreated women. Pregnancy rates are not different among women intending to conceive or among women attempting conception for more than 12 months, with the caveat being that these studies are heterogenous.2,3
Miscarriage
No difference has been observed in total (less than 24 weeks) miscarriage rate or first trimester (less than 12 weeks) miscarriage rate among treated and untreated women. However, the second trimester miscarriage rate is significantly higher among treated women (risk ratio, 2.60).2 This risk is most notable following laser conization or LEEP.4 There may also be an association between ablation and pregnancy loss.
Preterm birth and PPROM
Several studies and meta-analyses show an association between preterm birth and treatment for CIN using LEEP or CKC. There is an increased risk of severe preterm delivery (relative risk, 2.78), extreme preterm delivery (relative risk, 5.33), and low birth weight (relative risk, 2.86) with CKC.5 LEEP is associated with the same outcomes, albeit the risk is lower than with CKC.6 The risk of preterm birth is even lower for ablation.7
The risk of PPROM is approximately two times higher among those treated with LEEP, and PPROM rates are higher among those treated with CKC, compared with LEEP.9,10
Other complications
Ectopic pregnancy and termination rates may be higher in treated women, compared with untreated women.2 However, there does not appear to be an increased risk for perinatal/neonatal mortality, cesarean section, or neonatal intensive care unit admission among women treated with excisional procedures.6
Pointers for practice
- Due to the potential for adverse obstetric complications following excisional procedures for cervical dysplasia, gynecologists should closely adhere to the American Society for Colposcopy and Cervical Pathology guidelines when determining the appropriateness of dysplasia interventions. The decision to treat, versus monitor, dysplasia in a woman who plans future childbearing should be made with the patient after thorough discussion of the risks and benefits of each path.
- Women younger than age 30 years should not be screened for high-risk human papillomavirus because of both its high incidence and its high rate of spontaneous resolution.
- For reproductive-aged women with CIN 2 and adequate colposcopy, the American Society for Colposcopy and Cervical Pathology supports either monitoring with cytology and colposcopy every 6 months for a year or excisional treatment. However, women with CIN 3, inadequate colposcopy, prior cervical cancer, diethylstilbestrol exposure, or decreased immunity should undergo excisional treatment.
- When selecting an excisional method (LEEP or CKC), surgeons should choose the most appropriate technique for the patient’s pathology but should acknowledge the observed higher rates of PPROM, preterm birth, and low-birth-weight infants among those receiving CKC, and tailor the size of the excision to the specific lesion.
- Consider recommending a 12-month interval between treatment and pregnancy to ensure resolution of high-grade dysplasia. Furthermore, obstetric risk may be increased within 12 months following treatment.
Dr. Robbins is a resident in the department of obstetrics and gynecology at the University of North Carolina, Chapel Hill. Dr. Rossi is an assistant professor in the division of gynecologic oncology at UNC, Chapel Hill. They reported having no relevant financial disclosures.
References
1. Am J Obstet Gynecol. 2011 Jul;205(1):19-27.
2. Cochrane Database Syst Rev. 2015 Sep 29;(9):CD008478.
3. BMJ. 2014 Oct 28;349:g6192.
4. Obstet Gynecol. 2016 Dec;128(6):1265-73.
5. BMJ. 2008 Sep 18;337:a1284.
6. Arch Gynecol Obstet. 2014 Jan;289(1):85-99.
7. BJOG. 2011 Aug;118(9):1031-41.
8. Obstet Gynecol. 2013 May;121(5):1063-8.
9. Lancet. 2006 Feb 11;367(9509):489-98.
10. Gynecol Obstet Invest. 2014;77(4):240-4.
Cervical dysplasia is a condition commonly encountered by the gynecologist. It is either treated (with excision or ablation) or monitored, depending on the lesion grade, cytologic history, medical history, and reproductive goals. Cervical dysplasia commonly arises in women of reproductive age. Therefore, consider reproductive effects when deciding whether to treat or monitor, as well as when choosing the treatment modality.
Background
Approximately two-thirds of human papillomavirus infections resolve within a year, and more than 90% resolve within 2 years. Similarly, low-grade cervical intraepithelial neoplasia (CIN 1) lesions frequently resolve. High-grade (CIN 2 and CIN 3) lesions regress less commonly, with 5% and 12%-40% progressing to invasive cancer, respectively. Therefore, treatment is typically recommended.
Obstetric implications
Potential obstetric risks of treatment for CIN include infertility, spontaneous abortion, preterm premature rupture of membranes (PPROM), preterm delivery, and perinatal/neonatal mortality. These risks are discussed individually below. Mechanisms that have been suggested for such complications include decreased cervical mucous, cervical scarring impeding conception or dilation, loss of cervical volume, collagen breakdown, and immunologic processes due to decreased physical defenses or microbiome shifts.
Fertility
Studies have shown that treatment does not appear to impede conception. The overall pregnancy rate is higher among treated women than untreated women. Pregnancy rates are not different among women intending to conceive or among women attempting conception for more than 12 months, with the caveat being that these studies are heterogenous.2,3
Miscarriage
No difference has been observed in total (less than 24 weeks) miscarriage rate or first trimester (less than 12 weeks) miscarriage rate among treated and untreated women. However, the second trimester miscarriage rate is significantly higher among treated women (risk ratio, 2.60).2 This risk is most notable following laser conization or LEEP.4 There may also be an association between ablation and pregnancy loss.
Preterm birth and PPROM
Several studies and meta-analyses show an association between preterm birth and treatment for CIN using LEEP or CKC. There is an increased risk of severe preterm delivery (relative risk, 2.78), extreme preterm delivery (relative risk, 5.33), and low birth weight (relative risk, 2.86) with CKC.5 LEEP is associated with the same outcomes, albeit the risk is lower than with CKC.6 The risk of preterm birth is even lower for ablation.7
The risk of PPROM is approximately two times higher among those treated with LEEP, and PPROM rates are higher among those treated with CKC, compared with LEEP.9,10
Other complications
Ectopic pregnancy and termination rates may be higher in treated women, compared with untreated women.2 However, there does not appear to be an increased risk for perinatal/neonatal mortality, cesarean section, or neonatal intensive care unit admission among women treated with excisional procedures.6
Pointers for practice
- Due to the potential for adverse obstetric complications following excisional procedures for cervical dysplasia, gynecologists should closely adhere to the American Society for Colposcopy and Cervical Pathology guidelines when determining the appropriateness of dysplasia interventions. The decision to treat, versus monitor, dysplasia in a woman who plans future childbearing should be made with the patient after thorough discussion of the risks and benefits of each path.
- Women younger than age 30 years should not be screened for high-risk human papillomavirus because of both its high incidence and its high rate of spontaneous resolution.
- For reproductive-aged women with CIN 2 and adequate colposcopy, the American Society for Colposcopy and Cervical Pathology supports either monitoring with cytology and colposcopy every 6 months for a year or excisional treatment. However, women with CIN 3, inadequate colposcopy, prior cervical cancer, diethylstilbestrol exposure, or decreased immunity should undergo excisional treatment.
- When selecting an excisional method (LEEP or CKC), surgeons should choose the most appropriate technique for the patient’s pathology but should acknowledge the observed higher rates of PPROM, preterm birth, and low-birth-weight infants among those receiving CKC, and tailor the size of the excision to the specific lesion.
- Consider recommending a 12-month interval between treatment and pregnancy to ensure resolution of high-grade dysplasia. Furthermore, obstetric risk may be increased within 12 months following treatment.
Dr. Robbins is a resident in the department of obstetrics and gynecology at the University of North Carolina, Chapel Hill. Dr. Rossi is an assistant professor in the division of gynecologic oncology at UNC, Chapel Hill. They reported having no relevant financial disclosures.
References
1. Am J Obstet Gynecol. 2011 Jul;205(1):19-27.
2. Cochrane Database Syst Rev. 2015 Sep 29;(9):CD008478.
3. BMJ. 2014 Oct 28;349:g6192.
4. Obstet Gynecol. 2016 Dec;128(6):1265-73.
5. BMJ. 2008 Sep 18;337:a1284.
6. Arch Gynecol Obstet. 2014 Jan;289(1):85-99.
7. BJOG. 2011 Aug;118(9):1031-41.
8. Obstet Gynecol. 2013 May;121(5):1063-8.
9. Lancet. 2006 Feb 11;367(9509):489-98.
10. Gynecol Obstet Invest. 2014;77(4):240-4.
Cervical dysplasia is a condition commonly encountered by the gynecologist. It is either treated (with excision or ablation) or monitored, depending on the lesion grade, cytologic history, medical history, and reproductive goals. Cervical dysplasia commonly arises in women of reproductive age. Therefore, consider reproductive effects when deciding whether to treat or monitor, as well as when choosing the treatment modality.
Background
Approximately two-thirds of human papillomavirus infections resolve within a year, and more than 90% resolve within 2 years. Similarly, low-grade cervical intraepithelial neoplasia (CIN 1) lesions frequently resolve. High-grade (CIN 2 and CIN 3) lesions regress less commonly, with 5% and 12%-40% progressing to invasive cancer, respectively. Therefore, treatment is typically recommended.
Obstetric implications
Potential obstetric risks of treatment for CIN include infertility, spontaneous abortion, preterm premature rupture of membranes (PPROM), preterm delivery, and perinatal/neonatal mortality. These risks are discussed individually below. Mechanisms that have been suggested for such complications include decreased cervical mucous, cervical scarring impeding conception or dilation, loss of cervical volume, collagen breakdown, and immunologic processes due to decreased physical defenses or microbiome shifts.
Fertility
Studies have shown that treatment does not appear to impede conception. The overall pregnancy rate is higher among treated women than untreated women. Pregnancy rates are not different among women intending to conceive or among women attempting conception for more than 12 months, with the caveat being that these studies are heterogenous.2,3
Miscarriage
No difference has been observed in total (less than 24 weeks) miscarriage rate or first trimester (less than 12 weeks) miscarriage rate among treated and untreated women. However, the second trimester miscarriage rate is significantly higher among treated women (risk ratio, 2.60).2 This risk is most notable following laser conization or LEEP.4 There may also be an association between ablation and pregnancy loss.
Preterm birth and PPROM
Several studies and meta-analyses show an association between preterm birth and treatment for CIN using LEEP or CKC. There is an increased risk of severe preterm delivery (relative risk, 2.78), extreme preterm delivery (relative risk, 5.33), and low birth weight (relative risk, 2.86) with CKC.5 LEEP is associated with the same outcomes, albeit the risk is lower than with CKC.6 The risk of preterm birth is even lower for ablation.7
The risk of PPROM is approximately two times higher among those treated with LEEP, and PPROM rates are higher among those treated with CKC, compared with LEEP.9,10
Other complications
Ectopic pregnancy and termination rates may be higher in treated women, compared with untreated women.2 However, there does not appear to be an increased risk for perinatal/neonatal mortality, cesarean section, or neonatal intensive care unit admission among women treated with excisional procedures.6
Pointers for practice
- Due to the potential for adverse obstetric complications following excisional procedures for cervical dysplasia, gynecologists should closely adhere to the American Society for Colposcopy and Cervical Pathology guidelines when determining the appropriateness of dysplasia interventions. The decision to treat, versus monitor, dysplasia in a woman who plans future childbearing should be made with the patient after thorough discussion of the risks and benefits of each path.
- Women younger than age 30 years should not be screened for high-risk human papillomavirus because of both its high incidence and its high rate of spontaneous resolution.
- For reproductive-aged women with CIN 2 and adequate colposcopy, the American Society for Colposcopy and Cervical Pathology supports either monitoring with cytology and colposcopy every 6 months for a year or excisional treatment. However, women with CIN 3, inadequate colposcopy, prior cervical cancer, diethylstilbestrol exposure, or decreased immunity should undergo excisional treatment.
- When selecting an excisional method (LEEP or CKC), surgeons should choose the most appropriate technique for the patient’s pathology but should acknowledge the observed higher rates of PPROM, preterm birth, and low-birth-weight infants among those receiving CKC, and tailor the size of the excision to the specific lesion.
- Consider recommending a 12-month interval between treatment and pregnancy to ensure resolution of high-grade dysplasia. Furthermore, obstetric risk may be increased within 12 months following treatment.
Dr. Robbins is a resident in the department of obstetrics and gynecology at the University of North Carolina, Chapel Hill. Dr. Rossi is an assistant professor in the division of gynecologic oncology at UNC, Chapel Hill. They reported having no relevant financial disclosures.
References
1. Am J Obstet Gynecol. 2011 Jul;205(1):19-27.
2. Cochrane Database Syst Rev. 2015 Sep 29;(9):CD008478.
3. BMJ. 2014 Oct 28;349:g6192.
4. Obstet Gynecol. 2016 Dec;128(6):1265-73.
5. BMJ. 2008 Sep 18;337:a1284.
6. Arch Gynecol Obstet. 2014 Jan;289(1):85-99.
7. BJOG. 2011 Aug;118(9):1031-41.
8. Obstet Gynecol. 2013 May;121(5):1063-8.
9. Lancet. 2006 Feb 11;367(9509):489-98.
10. Gynecol Obstet Invest. 2014;77(4):240-4.
Refining the use of electronic fetal monitoring
Electronic fetal monitoring (EFM) is the most commonly used instrument in obstetrics and is the perceived standard of care. However, the U.S. Preventive Services Task Force recommended against its use in low-risk women in 1996 (a “D” rating) – signifying the lack of evidence for benefit and the potential for harm – and said there was insufficient evidence to recommend for or against its use in high-risk women (a “C” rating).
Today, available data still suggest that EFM does not reduce overall perinatal mortality or the risk of cerebral palsy. Moreover, its use is associated with increased operative vaginal deliveries and cesarean deliveries.
Given the near-zero positive predictive value of EFM for stillbirth or cerebral palsy, some have called EFM “useless” and a “failure.” However, I see potential in the technology. I believe that we are beginning to see evidence emerge that – if confirmed and expanded – will enable us to quantify and interpret indeterminate EFM patterns in new ways that positively impact clinical outcomes.
Despite EFM’s routine use and our specialty’s well-ingrained clinical habits, we should critically and meaningfully examine new science and new data on category II fetal heart rate tracings as they come to light. In the meantime, there is more we can do to resolve concerning elements of these tracings – without using supplemental oxygen – or to provide reassurance of fetal well-being so that cesarean deliveries are not unnecessarily performed.
Emerging research
An abnormal or indeterminate fetal heart rate tracing is the second most common indication for primary cesarean, after labor arrest, according to a study published in 2011 of more than 32,000 live births. Given the rarity of category III tracings (“abnormal”), it is likely that category II tracings (“indeterminate”) account for most of the cesarean deliveries performed out of concern for fetal acidemia (Obstet Gynecol. 2011 Jul;118[1]:29-38).
Until recently, we’ve known very little about the patterns contained within category II of our current three-tier system for categorizing fetal heart rate patterns. The system was defined by the 2008 consensus workshop sponsored by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), the American College of Obstetricians and Gynecologists, and the Society for Maternal-Fetal Medicine (Obstet Gynecol. 2008 Sep;112[3]:661-6).
We have reasonable data to know that the vast majority of patients with category I fetal heart rate tracings will have a normal pH. We also have reasonable data showing us that patients with category III tracings have a high risk of acidemia and morbidity. However, the majority of tracings we see during labor at term fall into category II, with no clear indication of risk and characterized most often by the presence of decelerations.
As we’ve delved more deeply into the highly variable and complex category II tracings defined in 2008, we’ve begun to demonstrate that tracings can have different meanings for different patients, and that particular clinical factors can make EFM patterns more informative and predictive. In other words, EFM patterns may require different interpretations based on a priori risk and clinical factors.
One of these factors may be the presence of meconium. In a prospective cohort of more than 3,000 women with category II tracings, the presence of meconium – especially thick meconium – was associated with a higher risk of acidemia and neonatal morbidity than when meconium was absent. Interestingly, the negative predictive value was higher than the overall predictive ability in this cohort, which suggests that the absence of meconium in the setting of a category II tracing can be considered a reassuring feature (Am J Obstet Gynecol. 2014;211:644.e1-8).
We have also found through retrospective cohort studies that magnesium sulfate can impact fetal heart rate tracings, causing a transient decrease in variability (Obstet Gynecol. 2012 Jun;119[6]:1129-36 and Am J Perinatol. 2014 Nov;31[10]:869-74). In addition, intrauterine growth restricted fetuses have a higher risk of decelerations without a commensurate higher risk of morbidity (Am J Perinatol. 2015 Jul;32[9]:873-8).
Such findings need to be reproduced, expanded, and further analyzed to show us how the risk of acidemia can be better predicted. For now, just as we increasingly appreciate that tracings have a transient nature and should be considered with two lenses – one looking back in time and one looking forward – we have a growing sense that EFM should not be interpreted without consideration of clinical factors.
Research at our institution and others has shown that acidemia is more significantly associated with non-NICHD measures of fetal heart rate deceleration than with each of the main deceleration types defined by the 2008 NICHD system (i.e., repetitive variable, repetitive late, and repetitive prolonged).
For instance, Emily Hamilton, MD, and her colleagues at PeriGen, a perinatal software company, found that only prolonged decelerations, in addition to the variability within the deceleration and a depth below 60 beats per minute for more than 60 seconds, could discriminate between cases of metabolic acidosis and those with normal umbilical artery gases (J Matern Fetal Neonatal Med. 2012 Jun;25[6]:648-53).
In a 4-year retrospective cohort study of nearly 5,340 consecutive singleton, term, nonanomalous gestations, we found acidemia was most significantly associated with a calculation of the “total deceleration area” – the sum of the estimates of area within all the decelerations. This measure accounted for the frequency, depth, and duration of all decelerations in the final 30 minutes of EFM.
Each of the NICHD deceleration types was associated in our study with acidemia after adjustment for fever, obesity, prolonged first stage, and nulliparity. However, total deceleration area had superior predictive ability. After the same adjustments were made, an abnormal total deceleration area (greater than the 95th percentile) was significantly associated with an increased risk for acidemia (odds ratio, 3.79) (Am J Obstet Gynecol. 2012 Sep;207[3]:206.e1-8).
Pathophysiologically, it seems logical that the total area is most predictive, as it captures both the temporal and dose effect of decelerations. At this point, however, we can only apply this concept crudely at the bedside. There is more work to do to translate such findings into software-driven bedside tools.
Gaining reassurance
Although efforts to manage intrapartum fetal heart rate tracings focus largely on attempting to better predict who is at greatest risk for acidemia, it is important and worthwhile that we also attempt to determine whether a fetus with a category II tracing is not acidotic.
Research has consistently shown that the presence of accelerations, whether spontaneous or stimulated, is a highly reliable indicator of normal neonatal umbilical cord pH. It is therefore reasonable, when faced with indeterminate tracings (e.g., minimal variability), to consider scalp stimulation to elicit fetal heart rate acceleration. Scalp stimulation is the easiest noninvasive tool to employ to quickly secure clinical reassurance – within a couple of minutes – that the fetus is not acidotic.
For guidance on managing repetitive variable decelerations, amnioinfusion with normal saline is similarly worthy of consideration. It has been demonstrated (Level A evidence) to resolve variable fetal heart rate decelerations and reduce the incidence of cesarean delivery for nonreassuring fetal heart rate patterns. Both amnioinfusion and scalp stimulation are recommended in the 2014 ACOG/SMFM consensus statement on “Safe Prevention of the Primary Cesarean Delivery” (Obstet Gynecol. 2014 Mar;123[3]:693-711).
Oxygen administration, on the other hand, is ingrained in practice and is included in the American College of Obstetricians and Gynecologists’ practice bulletin on managing intrapartum fetal rate tracings. It is listed as a possible resuscitative measure for category II or III tracings, despite the fact that there are extremely limited data for its effectiveness or safety in labor.
Maureen S. Hamel, MD, and her colleagues at the Warren Albert Medical School at Brown University reviewed the literature and concluded that the only two randomized trials investigating the use of maternal oxygen supplementation in laboring women do not support the idea that supplementation may benefit the fetus. Moreover, they contended that oxygen supplementation may even be harmful (Am J Obstet Gynecol. 2014 Aug;211[2]:124-7).
If supplemental oxygen were a medication, we would want to know the dose, as well as the length and duration of administration before fetal heart rate tracing improved. We don’t know the answers to these questions.
There is research ongoing, both observational studies and at least one registered randomized clinical trial, that should provide more information and guidance on the impact of supplemental oxygen in the setting of category II fetal heart rate patterns. I do not expect these findings to resolve all the questions. We’re going to need a thorough body of work to provide us with definitive answers.
Dr. Cahill is the chief of the division of maternal-fetal medicine at Washington University in St. Louis. She reported having no financial disclosures relevant to this Master Class.
Electronic fetal monitoring (EFM) is the most commonly used instrument in obstetrics and is the perceived standard of care. However, the U.S. Preventive Services Task Force recommended against its use in low-risk women in 1996 (a “D” rating) – signifying the lack of evidence for benefit and the potential for harm – and said there was insufficient evidence to recommend for or against its use in high-risk women (a “C” rating).
Today, available data still suggest that EFM does not reduce overall perinatal mortality or the risk of cerebral palsy. Moreover, its use is associated with increased operative vaginal deliveries and cesarean deliveries.
Given the near-zero positive predictive value of EFM for stillbirth or cerebral palsy, some have called EFM “useless” and a “failure.” However, I see potential in the technology. I believe that we are beginning to see evidence emerge that – if confirmed and expanded – will enable us to quantify and interpret indeterminate EFM patterns in new ways that positively impact clinical outcomes.
Despite EFM’s routine use and our specialty’s well-ingrained clinical habits, we should critically and meaningfully examine new science and new data on category II fetal heart rate tracings as they come to light. In the meantime, there is more we can do to resolve concerning elements of these tracings – without using supplemental oxygen – or to provide reassurance of fetal well-being so that cesarean deliveries are not unnecessarily performed.
Emerging research
An abnormal or indeterminate fetal heart rate tracing is the second most common indication for primary cesarean, after labor arrest, according to a study published in 2011 of more than 32,000 live births. Given the rarity of category III tracings (“abnormal”), it is likely that category II tracings (“indeterminate”) account for most of the cesarean deliveries performed out of concern for fetal acidemia (Obstet Gynecol. 2011 Jul;118[1]:29-38).
Until recently, we’ve known very little about the patterns contained within category II of our current three-tier system for categorizing fetal heart rate patterns. The system was defined by the 2008 consensus workshop sponsored by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), the American College of Obstetricians and Gynecologists, and the Society for Maternal-Fetal Medicine (Obstet Gynecol. 2008 Sep;112[3]:661-6).
We have reasonable data to know that the vast majority of patients with category I fetal heart rate tracings will have a normal pH. We also have reasonable data showing us that patients with category III tracings have a high risk of acidemia and morbidity. However, the majority of tracings we see during labor at term fall into category II, with no clear indication of risk and characterized most often by the presence of decelerations.
As we’ve delved more deeply into the highly variable and complex category II tracings defined in 2008, we’ve begun to demonstrate that tracings can have different meanings for different patients, and that particular clinical factors can make EFM patterns more informative and predictive. In other words, EFM patterns may require different interpretations based on a priori risk and clinical factors.
One of these factors may be the presence of meconium. In a prospective cohort of more than 3,000 women with category II tracings, the presence of meconium – especially thick meconium – was associated with a higher risk of acidemia and neonatal morbidity than when meconium was absent. Interestingly, the negative predictive value was higher than the overall predictive ability in this cohort, which suggests that the absence of meconium in the setting of a category II tracing can be considered a reassuring feature (Am J Obstet Gynecol. 2014;211:644.e1-8).
We have also found through retrospective cohort studies that magnesium sulfate can impact fetal heart rate tracings, causing a transient decrease in variability (Obstet Gynecol. 2012 Jun;119[6]:1129-36 and Am J Perinatol. 2014 Nov;31[10]:869-74). In addition, intrauterine growth restricted fetuses have a higher risk of decelerations without a commensurate higher risk of morbidity (Am J Perinatol. 2015 Jul;32[9]:873-8).
Such findings need to be reproduced, expanded, and further analyzed to show us how the risk of acidemia can be better predicted. For now, just as we increasingly appreciate that tracings have a transient nature and should be considered with two lenses – one looking back in time and one looking forward – we have a growing sense that EFM should not be interpreted without consideration of clinical factors.
Research at our institution and others has shown that acidemia is more significantly associated with non-NICHD measures of fetal heart rate deceleration than with each of the main deceleration types defined by the 2008 NICHD system (i.e., repetitive variable, repetitive late, and repetitive prolonged).
For instance, Emily Hamilton, MD, and her colleagues at PeriGen, a perinatal software company, found that only prolonged decelerations, in addition to the variability within the deceleration and a depth below 60 beats per minute for more than 60 seconds, could discriminate between cases of metabolic acidosis and those with normal umbilical artery gases (J Matern Fetal Neonatal Med. 2012 Jun;25[6]:648-53).
In a 4-year retrospective cohort study of nearly 5,340 consecutive singleton, term, nonanomalous gestations, we found acidemia was most significantly associated with a calculation of the “total deceleration area” – the sum of the estimates of area within all the decelerations. This measure accounted for the frequency, depth, and duration of all decelerations in the final 30 minutes of EFM.
Each of the NICHD deceleration types was associated in our study with acidemia after adjustment for fever, obesity, prolonged first stage, and nulliparity. However, total deceleration area had superior predictive ability. After the same adjustments were made, an abnormal total deceleration area (greater than the 95th percentile) was significantly associated with an increased risk for acidemia (odds ratio, 3.79) (Am J Obstet Gynecol. 2012 Sep;207[3]:206.e1-8).
Pathophysiologically, it seems logical that the total area is most predictive, as it captures both the temporal and dose effect of decelerations. At this point, however, we can only apply this concept crudely at the bedside. There is more work to do to translate such findings into software-driven bedside tools.
Gaining reassurance
Although efforts to manage intrapartum fetal heart rate tracings focus largely on attempting to better predict who is at greatest risk for acidemia, it is important and worthwhile that we also attempt to determine whether a fetus with a category II tracing is not acidotic.
Research has consistently shown that the presence of accelerations, whether spontaneous or stimulated, is a highly reliable indicator of normal neonatal umbilical cord pH. It is therefore reasonable, when faced with indeterminate tracings (e.g., minimal variability), to consider scalp stimulation to elicit fetal heart rate acceleration. Scalp stimulation is the easiest noninvasive tool to employ to quickly secure clinical reassurance – within a couple of minutes – that the fetus is not acidotic.
For guidance on managing repetitive variable decelerations, amnioinfusion with normal saline is similarly worthy of consideration. It has been demonstrated (Level A evidence) to resolve variable fetal heart rate decelerations and reduce the incidence of cesarean delivery for nonreassuring fetal heart rate patterns. Both amnioinfusion and scalp stimulation are recommended in the 2014 ACOG/SMFM consensus statement on “Safe Prevention of the Primary Cesarean Delivery” (Obstet Gynecol. 2014 Mar;123[3]:693-711).
Oxygen administration, on the other hand, is ingrained in practice and is included in the American College of Obstetricians and Gynecologists’ practice bulletin on managing intrapartum fetal rate tracings. It is listed as a possible resuscitative measure for category II or III tracings, despite the fact that there are extremely limited data for its effectiveness or safety in labor.
Maureen S. Hamel, MD, and her colleagues at the Warren Albert Medical School at Brown University reviewed the literature and concluded that the only two randomized trials investigating the use of maternal oxygen supplementation in laboring women do not support the idea that supplementation may benefit the fetus. Moreover, they contended that oxygen supplementation may even be harmful (Am J Obstet Gynecol. 2014 Aug;211[2]:124-7).
If supplemental oxygen were a medication, we would want to know the dose, as well as the length and duration of administration before fetal heart rate tracing improved. We don’t know the answers to these questions.
There is research ongoing, both observational studies and at least one registered randomized clinical trial, that should provide more information and guidance on the impact of supplemental oxygen in the setting of category II fetal heart rate patterns. I do not expect these findings to resolve all the questions. We’re going to need a thorough body of work to provide us with definitive answers.
Dr. Cahill is the chief of the division of maternal-fetal medicine at Washington University in St. Louis. She reported having no financial disclosures relevant to this Master Class.
Electronic fetal monitoring (EFM) is the most commonly used instrument in obstetrics and is the perceived standard of care. However, the U.S. Preventive Services Task Force recommended against its use in low-risk women in 1996 (a “D” rating) – signifying the lack of evidence for benefit and the potential for harm – and said there was insufficient evidence to recommend for or against its use in high-risk women (a “C” rating).
Today, available data still suggest that EFM does not reduce overall perinatal mortality or the risk of cerebral palsy. Moreover, its use is associated with increased operative vaginal deliveries and cesarean deliveries.
Given the near-zero positive predictive value of EFM for stillbirth or cerebral palsy, some have called EFM “useless” and a “failure.” However, I see potential in the technology. I believe that we are beginning to see evidence emerge that – if confirmed and expanded – will enable us to quantify and interpret indeterminate EFM patterns in new ways that positively impact clinical outcomes.
Despite EFM’s routine use and our specialty’s well-ingrained clinical habits, we should critically and meaningfully examine new science and new data on category II fetal heart rate tracings as they come to light. In the meantime, there is more we can do to resolve concerning elements of these tracings – without using supplemental oxygen – or to provide reassurance of fetal well-being so that cesarean deliveries are not unnecessarily performed.
Emerging research
An abnormal or indeterminate fetal heart rate tracing is the second most common indication for primary cesarean, after labor arrest, according to a study published in 2011 of more than 32,000 live births. Given the rarity of category III tracings (“abnormal”), it is likely that category II tracings (“indeterminate”) account for most of the cesarean deliveries performed out of concern for fetal acidemia (Obstet Gynecol. 2011 Jul;118[1]:29-38).
Until recently, we’ve known very little about the patterns contained within category II of our current three-tier system for categorizing fetal heart rate patterns. The system was defined by the 2008 consensus workshop sponsored by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), the American College of Obstetricians and Gynecologists, and the Society for Maternal-Fetal Medicine (Obstet Gynecol. 2008 Sep;112[3]:661-6).
We have reasonable data to know that the vast majority of patients with category I fetal heart rate tracings will have a normal pH. We also have reasonable data showing us that patients with category III tracings have a high risk of acidemia and morbidity. However, the majority of tracings we see during labor at term fall into category II, with no clear indication of risk and characterized most often by the presence of decelerations.
As we’ve delved more deeply into the highly variable and complex category II tracings defined in 2008, we’ve begun to demonstrate that tracings can have different meanings for different patients, and that particular clinical factors can make EFM patterns more informative and predictive. In other words, EFM patterns may require different interpretations based on a priori risk and clinical factors.
One of these factors may be the presence of meconium. In a prospective cohort of more than 3,000 women with category II tracings, the presence of meconium – especially thick meconium – was associated with a higher risk of acidemia and neonatal morbidity than when meconium was absent. Interestingly, the negative predictive value was higher than the overall predictive ability in this cohort, which suggests that the absence of meconium in the setting of a category II tracing can be considered a reassuring feature (Am J Obstet Gynecol. 2014;211:644.e1-8).
We have also found through retrospective cohort studies that magnesium sulfate can impact fetal heart rate tracings, causing a transient decrease in variability (Obstet Gynecol. 2012 Jun;119[6]:1129-36 and Am J Perinatol. 2014 Nov;31[10]:869-74). In addition, intrauterine growth restricted fetuses have a higher risk of decelerations without a commensurate higher risk of morbidity (Am J Perinatol. 2015 Jul;32[9]:873-8).
Such findings need to be reproduced, expanded, and further analyzed to show us how the risk of acidemia can be better predicted. For now, just as we increasingly appreciate that tracings have a transient nature and should be considered with two lenses – one looking back in time and one looking forward – we have a growing sense that EFM should not be interpreted without consideration of clinical factors.
Research at our institution and others has shown that acidemia is more significantly associated with non-NICHD measures of fetal heart rate deceleration than with each of the main deceleration types defined by the 2008 NICHD system (i.e., repetitive variable, repetitive late, and repetitive prolonged).
For instance, Emily Hamilton, MD, and her colleagues at PeriGen, a perinatal software company, found that only prolonged decelerations, in addition to the variability within the deceleration and a depth below 60 beats per minute for more than 60 seconds, could discriminate between cases of metabolic acidosis and those with normal umbilical artery gases (J Matern Fetal Neonatal Med. 2012 Jun;25[6]:648-53).
In a 4-year retrospective cohort study of nearly 5,340 consecutive singleton, term, nonanomalous gestations, we found acidemia was most significantly associated with a calculation of the “total deceleration area” – the sum of the estimates of area within all the decelerations. This measure accounted for the frequency, depth, and duration of all decelerations in the final 30 minutes of EFM.
Each of the NICHD deceleration types was associated in our study with acidemia after adjustment for fever, obesity, prolonged first stage, and nulliparity. However, total deceleration area had superior predictive ability. After the same adjustments were made, an abnormal total deceleration area (greater than the 95th percentile) was significantly associated with an increased risk for acidemia (odds ratio, 3.79) (Am J Obstet Gynecol. 2012 Sep;207[3]:206.e1-8).
Pathophysiologically, it seems logical that the total area is most predictive, as it captures both the temporal and dose effect of decelerations. At this point, however, we can only apply this concept crudely at the bedside. There is more work to do to translate such findings into software-driven bedside tools.
Gaining reassurance
Although efforts to manage intrapartum fetal heart rate tracings focus largely on attempting to better predict who is at greatest risk for acidemia, it is important and worthwhile that we also attempt to determine whether a fetus with a category II tracing is not acidotic.
Research has consistently shown that the presence of accelerations, whether spontaneous or stimulated, is a highly reliable indicator of normal neonatal umbilical cord pH. It is therefore reasonable, when faced with indeterminate tracings (e.g., minimal variability), to consider scalp stimulation to elicit fetal heart rate acceleration. Scalp stimulation is the easiest noninvasive tool to employ to quickly secure clinical reassurance – within a couple of minutes – that the fetus is not acidotic.
For guidance on managing repetitive variable decelerations, amnioinfusion with normal saline is similarly worthy of consideration. It has been demonstrated (Level A evidence) to resolve variable fetal heart rate decelerations and reduce the incidence of cesarean delivery for nonreassuring fetal heart rate patterns. Both amnioinfusion and scalp stimulation are recommended in the 2014 ACOG/SMFM consensus statement on “Safe Prevention of the Primary Cesarean Delivery” (Obstet Gynecol. 2014 Mar;123[3]:693-711).
Oxygen administration, on the other hand, is ingrained in practice and is included in the American College of Obstetricians and Gynecologists’ practice bulletin on managing intrapartum fetal rate tracings. It is listed as a possible resuscitative measure for category II or III tracings, despite the fact that there are extremely limited data for its effectiveness or safety in labor.
Maureen S. Hamel, MD, and her colleagues at the Warren Albert Medical School at Brown University reviewed the literature and concluded that the only two randomized trials investigating the use of maternal oxygen supplementation in laboring women do not support the idea that supplementation may benefit the fetus. Moreover, they contended that oxygen supplementation may even be harmful (Am J Obstet Gynecol. 2014 Aug;211[2]:124-7).
If supplemental oxygen were a medication, we would want to know the dose, as well as the length and duration of administration before fetal heart rate tracing improved. We don’t know the answers to these questions.
There is research ongoing, both observational studies and at least one registered randomized clinical trial, that should provide more information and guidance on the impact of supplemental oxygen in the setting of category II fetal heart rate patterns. I do not expect these findings to resolve all the questions. We’re going to need a thorough body of work to provide us with definitive answers.
Dr. Cahill is the chief of the division of maternal-fetal medicine at Washington University in St. Louis. She reported having no financial disclosures relevant to this Master Class.