User login
Comprehensive assessment of cancer survivors’ concerns to inform program development
Complex cancer treatments, limited personnel resources, and a growing number of cancer survivors are challenging cancer health care professionals’ abilities to provide comprehensive care. Cancer survivors have a range of needs that extend over the cancer care trajectory and that represent physical, psychological, social, and spiritual domains. Numerous studies have explored supportive care needs and recent systematic reviews have highlighted the supportive care needs related to cancer1 and to specific cancer types, including prostate cancer,2 breast cancer,3 gynecologic cancer,4 hematological cancer,5 and lung cancer.6 However, reviews are limited in that they do not always assess needs across the cancer trajectory or identify demographic or clinical variables that are associated with needs. These data are needed to focus survivorship program development in cancer centers in order to target populations most likely at risk for unmet needs, identify what salient concerns to address, and to appropriately schedule supportive care programs.
The importance of assessing the patient’s subjective view of his/her needs or concerns is well acknowledged as being fundamental to patient-centered care.7 Clinicians routinely assess needs in practice using a variety of screening tools. However, there needs to be a broader assessment of concerns and needs in a population of survivors with mixed cancer diagnoses, along with their appraisal of how well their needs were addressed by their health care team, to provide an overall identification of gaps in supportive care. The primary purpose of the present study was to prioritize survivors’ most salient physical, social, emotional, and spiritual concerns or needs; ascertain survivors’ perceived importance of those needs and the extent to which our institution, the University Hospitals Seidman Cancer Center, was attentive to those needs; and to identify who might be at risk for having greater concerns. The overall goal was to use the data to inform survivorship and supportive care program development.
Methods
Design, sample and setting
We used a cross-sectional design. Surveys were mailed once to a convenience sample of 2,750 adult patients who had been seen in follow-up during the previous 2 years (2010-2011) at all clinical sites of University Hospitals Seidman Cancer Center, a Midwestern National Cancer Institute-designated Comprehensive Cancer Center. Patients who had a noncancer diagnosis were excluded. The distribution list was screened for deceased individuals and those patients who had multiple visits during the time period. The project was reviewed and approved as nonresearch by the Case Western Reserve University Cancer Institutional Review Board.
Survey
An interdisciplinary team of clinicians, administrators, and researchers adapted the Mayo Clinic Cancer Center’s Cancer Survivors Survey of Needs8 to create a comprehensive survey for the cancer center. Input regarding the scope of the survey was sought from the Patient and Family Advisory Council of the cancer center. The survey, which was formatted for scanning purposes, consisted of 33 questions that were compiled into 4 sections. Sections 1 and 2 focused on demographic and treatment-related information, including use of community and hospital support services and preferences for follow-up care. In section 3, a quality-of-life framework was used to assess physical, social, emotional, and spiritual needs. Respondents were asked to rate their current level of concern for 19 physical effects, 10 social effects, 10 emotional effects, and 5 spiritual effects on a scale ranging from 0 (no concern) to 5 (extreme concern). In section 4, respondents were asked to indicate the importance of the cancer team addressing their physical, social, emotional, and spiritual needs. This was followed by their rating of the cancer team’s attention to their needs as Poor, Fair, Good, Excellent, or They did not ask about my needs. Respondents were asked about preferences for learning about physical, social, emotional, and spiritual effects. In addition to the 33 questions, there were 6 open-ended questions in which respondents were encouraged to share additional information about their needs, sources of support, and other concerns.
Procedures
Eligible respondents were mailed a cover letter explaining the survey from both the director and president of the cancer center, a survey, and a postage-paid return envelope. The option to respond to the survey by a telephone call to the director of the Office of Cancer Survivorship was offered in the cover letter.
Data analysis
Returned surveys were scanned into a Teleform database, verified, and exported into an SPSS data file. Data quality was checked by running frequency analyses and summarizing variables. Time-since-treatment responses were collapsed into 4 categories: on treatment, up to 2 years posttreatment, 2-5 years posttreatment, and more than 5 years posttreatment. Descriptive statistics were used to summarize demographic and medical characteristics of the respondents and to calculate the mean score for each concern for the total sample and then for each category of time since treatment. Because of the large number of respondents with breast cancer, the respondents were stratified into two groups, one of breast cancer the other of nonbreast cancer respondents. Then, the Mann-Whitney test was performed for each concern to examine differences between respondents with and without breast cancer.
To identify the most prevalent concerns, ratings for concerns were recoded into no concern (rated as 0), low concern (1 or 2), and moderate/high concern (3, 4, or 5). Since our interest was in the moderate and high concerns, the responses were dichotomized into moderate/high concerns and all other levels. Logistic regression models were then used to identify associations between a set of survivor characteristics or covariates (age, sex, living status, marital status, employment status, cancer type, and time since treatment) with the 12 most highly rated moderate/high concerns. All the analyses were performed using statistical software SPSS 20 and Stata 13.0
Results
Respondents
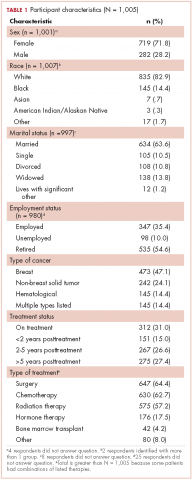
A total of 1,005 surveys were returned for a 37% response rate. Forty-two patients responded by telephone. The mean age of respondents was 64.9 years (range, 22-98; SD, 12.8). The typical respondent was female, white, and married (Table 1). Twenty-four percent of the respondents (n = 240) reported living alone. Although about 47% of respondents (n = 473) reported a breast cancer diagnosis, more than 17 cancers were identified, and 14% of respondents (n = 145) listed multiple diagnoses. About a third of respondents were receiving treatment when they completed the survey.
Just under half of the respondents (n = 498) reported using community resources for support and information about cancer, and 29.5% (n = 296) sought information on the internet during their cancer experience. The most commonly used community resources were The Gathering Place, a local organization offering free supportive programs and services to individuals with cancer and their families (n = 167), and the American Cancer Society (n = 138). Of the 496 respondents who reported accessing hospital resources, most (n = 322) said they used information that their health care team recommended. Other supportive options were used to a lesser degree: support groups (n = 92), chemotherapy and radiation therapy classes (n = 129), and supportive/educational programs offered by the cancer center (n = 27). Most of the respondents (n = 822, 88.6%) preferred to have their follow-up care remain with their cancer care team 1 year after treatments are completed. Almost two-thirds of respondents (n = 601, 64%) cited being seen at the cancer center for follow-up care as the most important factor in considering follow-up care.
Concerns In determining whether the large proportion of respondents with breast cancer skewed the study results, it was determined that median scores differed significantly in only four concerns. Compared with respondents without breast cancer, respondents with breast cancer were more likely to have significantly lower scores for concerns related to fatigue (P <.001) and sexual issues/intimacy (P = .001). Respondents with breast cancer were more likely to have significantly higher scores than respondents without breast cancer for concerns related to genetic counseling (P = .001) and fear of developing a new cancer (P = .010).
Fears of the cancer returning and developing a new cancer were the two most prevalent concerns, identified by 51% (n = 486) and 47.5% (n = 459), respectively (Table 2). Physical concerns, rated as moderate/high concerns by at least 25% of the sample, were fatigue (n = 336, 34.8%), changes in [the] body after cancer (n = 323, 33.7%), trouble sleeping (n = 302, 31.0%), sexual issues/intimacy (n = 263, 28.0%), memory and concentration (n = 261, 26.7%), and weight changes (n = 248, 25.5%). The most prevalent moderate/high social concerns were related to finances (n = 265, 27.5%) and debt from medical bills (n = 232, 25.1%). Managing stress (n = 279, 29.2%) and difficult emotions (n = 244, 25.1%) were prevalent moderate/high emotional concerns. Spiritual concerns were less often rated as moderate/high concerns. Having a breast cancer diagnosis was not significantly related to the number of reported moderate to high concerns (P = 1.00).
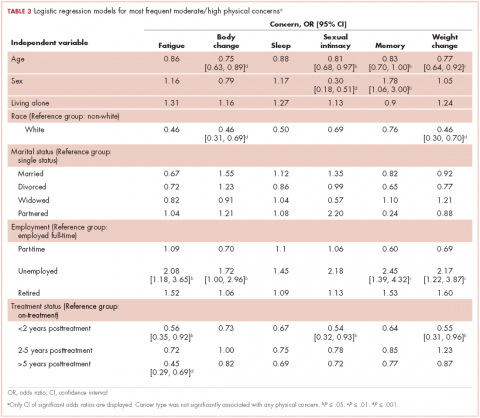
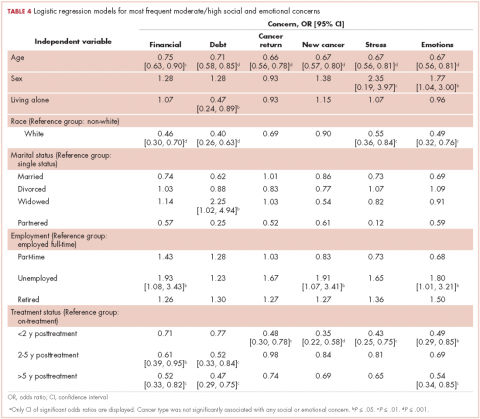
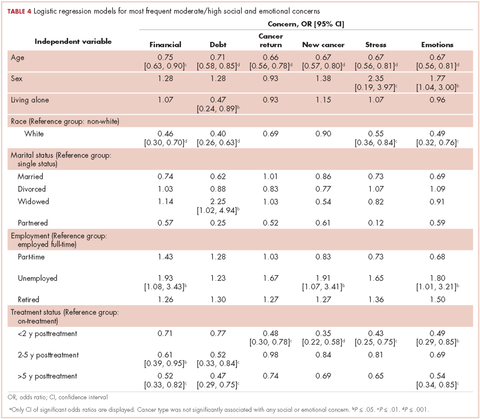
Variables associated with the 12 most frequent moderate/high concerns are shown in Tables 3 and 4. Age was associated with the most moderate/high concerns. With every decade of age, the odds of having the following moderate/high concerns decreased: bodily changes after cancer (odds ratio [OR], 0.75), sexual intimacy (OR, 0.81), memory and concentration (OR, 0.83), weight changes (OR, 0.77), financial (OR, 0.75), debt (OR, 0.71), cancer returning (OR, 0.66), developing a new cancer (OR, 0.67), managing stress (OR, 0.67), and managing difficult emotions (OR, 0.67).
Female sex was associated with lower odds of having a concern about sexual intimacy (OR, 0.30) and increased odds of having concerns related to memory and concentration (OR, 1.78), managing stress (OR, 2.35), and managing difficult emotions (OR, 1.77). Race was another demographic characteristic statistically associated with numerous moderate/high concerns. Survivors who identified white, were more likely than other people of other races to have fewer moderate/high concerns regarding bodily changes after cancer (OR, 0.46), weight change (OR, 0.46), finances (OR, 0.46), debt (OR, 0.40), managing stress (OR, 0.55), and managing difficult emotions (OR, 0.49). The odds of having a moderate/high concern regarding debt was 2.25 times higher given widowed marital status compared with those survivors who were single. Unemployment status, when compared with full-time employment, was significantly associated with increased odds of having moderate/high concerns related to fatigue (OR, 2.08), bodily changes after cancer (OR, 1.72), memory and concentration (OR, 2.45), weight changes (OR, 2.17), finances (OR, 1.93), developing a new cancer (OR, 1.91), and managing difficult emotions (OR, 1.80).
As expected, respondents who had completed treatment were less likely to have many of the moderate/high concerns as those still undergoing treatment. Survivors who were up to 2 years posttreatment were significantly more likely than those survivors receiving treatment to have fewer moderate/high concerns regarding fatigue (OR, 0.56), sexual intimacy (OR, 0.54), weight change (OR, 0.55), fears of the cancer returning (OR, 0.48), developing a new cancer (OR, 0.35), managing stress (OR, 0.43), and managing difficult emotions (OR, 0.49).
However, those improved odds were not sustained over the cancer trajectory. Compared with survivors who were receiving treatment, survivors who were between 2-5 years posttreatment did not have significantly reduced odds for moderate/high concerns related to fatigue, sleep, sexual intimacy, body changes, weight changes, memory, fears of the cancer returning, developing a new cancer, managing stress, and managing difficult emotions. They did have significantly reduced odds for having concerns only related to finances (OR, 0.61) and debt (OR, 0.52).
Long-term survivors, who were beyond 5 years posttreatment, had significantly reduced odds for having moderate/high concerns related to fatigue (OR, 0.45), finances (OR, 0.52), debt (OR, 0.47), and managing difficult emotions (OR, 0.54), compared with survivors receiving treatment. Moderate/high concerns related to sleep, sexual intimacy, body changes, weight changes, memory, fears of the cancer returning, developing a new cancer, managing stress did not have improved odds for these long-term survivors.
Attention to needs
The health care teams were rated highly for their attention to the patients’ physical needs. Most respondents (n = 845, 92.4%) viewed the health care team’s attention their physical needs as important and 763 (77.6%) survivors rated the team’s attention to these needs as excellent. The importance of addressing emotional needs was affirmed by 723 (78.5%) respondents, and although 454 (46.8%) viewed the team’s attention to these needs as excellent, 119 (12.3%) reported that the health care team did not ask about emotional needs. In addition, 566 respondents (60%) viewed having the health care team address their social needs as important, and most (n = 715, 74.2%) rated the team’s attention to social needs as good or excellent. Yet, 162 (16.8%) respondents reported that team did not ask about their social needs. The health care team’s addressing of spiritual needs was viewed as important by 346 (37.5%) respondents and ratings for how well the team attended to spiritual needs were: 148 (15.6%) poor or fair, 204 (21.5%) good, and 150 (15.8%) excellent. However, 448 (47.2%) respondents reported that the health care team did not ask about their spiritual needs.
Discussion
The primary purpose of this project was to prioritize survivors’ most salient physical, social, emotional, and spiritual concerns or needs and to assess the perceived importance of these needs and the extent to which the cancer center staff were attentive to those needs. The overall goal of this assessment was to inform the development of survivorship and supportive care programs by highlighting common concerns, demographic and medical factors associated with specific concerns, and timing of moderate/high level concerns along the cancer trajectory. There were 3 main findings.
First, the results support the need for enhancing supportive care services to meet emotional concerns of survivors beyond the treatment phase. Similar to other studies,8,9 emotional concerns ranked higher than all other concerns in this study with about 50% of the sample rating “fear the cancer will return” and “fear of developing a new cancer” as moderate/high concern. Although the odds of not having these emotional concerns improved up to 2 years posttreatment, these concerns are likely to resurface, as odds for survivors beyond 2 years were not significantly different from those receiving treatment. A recent systematic review reported that fear of cancer recurrence is experienced by about 73% of cancer survivors, with 49% reporting a moderate to high degree.10 It can have a chronic, stable trajectory for some survivors and is strongly associated with higher levels of anxiety, distress, and depression, and less global, emotional/mental, physical, role, social, and cognitive quality of life.10 In this sample, managing stress and difficult emotions were also rated as moderate/high concerns by at least 25% of the sample.
Second, the findings identified patients at risk for cancer-related concerns throughout the cancer trajectory. As demonstrated in other studies, younger age was associated with greater odds of having multiple greater moderate/high concerns.11-13 Unemployment was the second most common demographic factor associated with multiple moderate/high concerns related to physical symptoms, finances and emotions. Similarly, identifying as black, Asian, American Indian/Alaskan Native, or other was also associated with greater odds of having numerous physical, financial, and emotional concerns. Women had greater concerns related to memory, sexual intimacy, coping with difficult emotions, and stress.
Third, the results helped to identify gaps in supportive care at our cancer center. Although spiritual concerns were not prevalent as being moderate/high, they were still viewed by about a third of survivors as being an important area for the health care team to address. Yet, consistent with other need assessments, spiritual concerns in this study were least often addressed by staff.1 Assessment of spiritual care needs, screening for spiritual distress, and providing spiritual care are essential components of a clinician-patient relationship that supports healing.14 The importance of attending to spiritual care needs was underscored by a recent systematic review that found a positive association between overall spiritual well-being and quality of life in patients with cancer, with the meaning/peace factor consistently and positively associated with physical and mental health.15 Another identified gap was the health care team’s lack of attention to the patient’s social needs, which included concerns related to finances and debt from medical bills. In all, 46% of the respondents reported having financial concerns, with the odds of having moderate/high financial concerns being greatest during treatment to 2 years posttreatment. Attention to the financial burden of cancer patients is critical because the magnitude of cancer-related financial concerns is a significant, strong predictor of quality of life and adverse psychological issues such as depression, anxiety, and distress.16,17
There were several program implications based on the results. A periodic audit of the concerns of survivors and their views on how well their needs were being met was a relatively low cost endeavor. Although the findings were consistent with the literature, the results, when shared with administrators and clinicians, were instrumental in effecting change because they represented the concerns of survivors at the cancer center. Another program directive, based on the results, was to extend the routine screening of patients’ needs during treatment to posttreatment survivorship. Patients who are young, unemployed, do not identify as white, and female warrant more thorough assessment of needs and concerns along the cancer trajectory. Integral to these screenings is the need for patient-centered communication, with discussion of how cancer is affecting the different domains of quality of life within the context of the patient’s life. Lastly, the results clearly indicated the need for additional training of health care providers on how to assess and address spiritual well-being in cancer survivors.
There were limitations to this study, including use of a nonvalidated survey and cross-sectional approach that limited our ability to explore how concerns might change over the trajectory. Also, it was not possible to clarify medical information of the respondents, such as cancer stage. Although the response rate of this study was not high, we are confident in the results because of the large sample size and the finding that the large proportion of respondents with breast cancer was not influential. Despite these limitations, this needs assessment of cancer survivors over the trajectory of care provided insight into the scope of their concerns, identified vulnerable groups of survivors, and highlighted gaps in addressing those concerns. A quality- of-life framework for assessing needs assured a comprehensive focus and generated practice changes to strengthen holistic, comprehensive oncology care.
1. Harrison JD, Young JM, Price MA, Butow PN, Solomon MJ. What are the unmet supportive care needs of people with cancer? A systematic review. Support Care Cancer. 2009;17:1117-1128.
2. Paterson C, Robertson A, Smith A, Nabi G. Identifying the unmet supportive care needs of men living with and beyond prostate cancer: A systematic review. Eur J Oncol Nurs. 2015;19:405-418.
3. Fiszer C, Dolbeault S, Sultan S, Bredart A. Prevalence, intensity, and predictors of the supportive care needs of women diagnosed with breast cancer: A systematic review. Psychooncology. 2014;23:361-374.
4. Maguire R, Kotronoulas G, Simpson M, Paterson C. A systematic review of the supportive care needs of women living with and beyond cervical cancer. Gynecol Oncol. 2015;136:478-490.
5. Hall A, Lynagh M, Bryant J, Sanson-Fisher R. Supportive care needs of hematological cancer survivors: A critical review of the literature. Crit Rev Oncol Hematol. 2013;88:102-116.
6. Maguire R, Papadopoulou C, Kotronoulas G, Simpson MF, McPhelim J, Irvine L. A systematic review of supportive care needs of people living with lung cancer. Eur J Oncol Nurs. 2013;17:449-464.
7. Adler NE, Page EK. Cancer care for the whole patient: meeting psychosocial health needs. Washington, DC: National Academies Press; Institute of Medicine, 2008.
8. Ness S, Kokal J, Fee-Schroeder K, Novotny P, Satele D, Barton D. Concerns across the survivorship trajectory: results from a survey of cancer survivors. Oncol Nurs Forum. 2013;40:35-42.
9. Swash B, Hulbert-Williams N, Bramwell R. Unmet psychosocial needs in haematological cancer: A systematic review. Support Care Cancer. 2014;22:1131-1141.
10. Simard S, Thewes B, Humphris G, et al. Fear of cancer recurrence in adult cancer survivors: A systematic review of quantitative studies. J Cancer Surviv. 2013;7:300-322.
11. Choi KH, Park JH, Park JH, Park JS. Psychosocial needs of cancer patients and related factors: A multi-center, cross-sectional study in Korea. Psychooncology. 2013;22:1073-1080.
12. Pauwels EE, Charlier C, De Bourdeaudhuij I, Lechner L, Van Hoof E. Care needs after primary breast cancer treatment. Survivors’ associated sociodemographic and medical characteristics. Psychooncology. 2013;22:125-132.
13. Harrison JD, Young JM, Price MA, Butow PN, Solomon MJ. What are the unmet supportive care needs of people with cancer? A systematic review. Support Care Cancer. 2009;17:1117-1128.
14. Puchalski CM, Blatt B, Kogan M, Butler A. Spirituality and health: The development of a field. Academic Medicine. 2014;89:10-16.
15. Bai M, Lazenby M. A systematic review of associations between spiritual well-being and quality of life at the scale and factor levels in studies among patients with cancer. J Palliat Med. 2015;18:286-298.
16. Fenn KM, Evans SB, McCorkle R, et al. Impact of financial burden of cancer on survivors’ quality of life. J Oncol Pract. 2014;10:332-338.
17. Sharp L, Carsin AE, Timmons A. Associations between cancer-related financial stress and strain and psychological wellbeing among individuals living with cancer. Psychooncology. 2013;22:745-755.
Complex cancer treatments, limited personnel resources, and a growing number of cancer survivors are challenging cancer health care professionals’ abilities to provide comprehensive care. Cancer survivors have a range of needs that extend over the cancer care trajectory and that represent physical, psychological, social, and spiritual domains. Numerous studies have explored supportive care needs and recent systematic reviews have highlighted the supportive care needs related to cancer1 and to specific cancer types, including prostate cancer,2 breast cancer,3 gynecologic cancer,4 hematological cancer,5 and lung cancer.6 However, reviews are limited in that they do not always assess needs across the cancer trajectory or identify demographic or clinical variables that are associated with needs. These data are needed to focus survivorship program development in cancer centers in order to target populations most likely at risk for unmet needs, identify what salient concerns to address, and to appropriately schedule supportive care programs.
The importance of assessing the patient’s subjective view of his/her needs or concerns is well acknowledged as being fundamental to patient-centered care.7 Clinicians routinely assess needs in practice using a variety of screening tools. However, there needs to be a broader assessment of concerns and needs in a population of survivors with mixed cancer diagnoses, along with their appraisal of how well their needs were addressed by their health care team, to provide an overall identification of gaps in supportive care. The primary purpose of the present study was to prioritize survivors’ most salient physical, social, emotional, and spiritual concerns or needs; ascertain survivors’ perceived importance of those needs and the extent to which our institution, the University Hospitals Seidman Cancer Center, was attentive to those needs; and to identify who might be at risk for having greater concerns. The overall goal was to use the data to inform survivorship and supportive care program development.
Methods
Design, sample and setting
We used a cross-sectional design. Surveys were mailed once to a convenience sample of 2,750 adult patients who had been seen in follow-up during the previous 2 years (2010-2011) at all clinical sites of University Hospitals Seidman Cancer Center, a Midwestern National Cancer Institute-designated Comprehensive Cancer Center. Patients who had a noncancer diagnosis were excluded. The distribution list was screened for deceased individuals and those patients who had multiple visits during the time period. The project was reviewed and approved as nonresearch by the Case Western Reserve University Cancer Institutional Review Board.
Survey
An interdisciplinary team of clinicians, administrators, and researchers adapted the Mayo Clinic Cancer Center’s Cancer Survivors Survey of Needs8 to create a comprehensive survey for the cancer center. Input regarding the scope of the survey was sought from the Patient and Family Advisory Council of the cancer center. The survey, which was formatted for scanning purposes, consisted of 33 questions that were compiled into 4 sections. Sections 1 and 2 focused on demographic and treatment-related information, including use of community and hospital support services and preferences for follow-up care. In section 3, a quality-of-life framework was used to assess physical, social, emotional, and spiritual needs. Respondents were asked to rate their current level of concern for 19 physical effects, 10 social effects, 10 emotional effects, and 5 spiritual effects on a scale ranging from 0 (no concern) to 5 (extreme concern). In section 4, respondents were asked to indicate the importance of the cancer team addressing their physical, social, emotional, and spiritual needs. This was followed by their rating of the cancer team’s attention to their needs as Poor, Fair, Good, Excellent, or They did not ask about my needs. Respondents were asked about preferences for learning about physical, social, emotional, and spiritual effects. In addition to the 33 questions, there were 6 open-ended questions in which respondents were encouraged to share additional information about their needs, sources of support, and other concerns.
Procedures
Eligible respondents were mailed a cover letter explaining the survey from both the director and president of the cancer center, a survey, and a postage-paid return envelope. The option to respond to the survey by a telephone call to the director of the Office of Cancer Survivorship was offered in the cover letter.
Data analysis
Returned surveys were scanned into a Teleform database, verified, and exported into an SPSS data file. Data quality was checked by running frequency analyses and summarizing variables. Time-since-treatment responses were collapsed into 4 categories: on treatment, up to 2 years posttreatment, 2-5 years posttreatment, and more than 5 years posttreatment. Descriptive statistics were used to summarize demographic and medical characteristics of the respondents and to calculate the mean score for each concern for the total sample and then for each category of time since treatment. Because of the large number of respondents with breast cancer, the respondents were stratified into two groups, one of breast cancer the other of nonbreast cancer respondents. Then, the Mann-Whitney test was performed for each concern to examine differences between respondents with and without breast cancer.
To identify the most prevalent concerns, ratings for concerns were recoded into no concern (rated as 0), low concern (1 or 2), and moderate/high concern (3, 4, or 5). Since our interest was in the moderate and high concerns, the responses were dichotomized into moderate/high concerns and all other levels. Logistic regression models were then used to identify associations between a set of survivor characteristics or covariates (age, sex, living status, marital status, employment status, cancer type, and time since treatment) with the 12 most highly rated moderate/high concerns. All the analyses were performed using statistical software SPSS 20 and Stata 13.0
Results
Respondents
A total of 1,005 surveys were returned for a 37% response rate. Forty-two patients responded by telephone. The mean age of respondents was 64.9 years (range, 22-98; SD, 12.8). The typical respondent was female, white, and married (Table 1). Twenty-four percent of the respondents (n = 240) reported living alone. Although about 47% of respondents (n = 473) reported a breast cancer diagnosis, more than 17 cancers were identified, and 14% of respondents (n = 145) listed multiple diagnoses. About a third of respondents were receiving treatment when they completed the survey.
Just under half of the respondents (n = 498) reported using community resources for support and information about cancer, and 29.5% (n = 296) sought information on the internet during their cancer experience. The most commonly used community resources were The Gathering Place, a local organization offering free supportive programs and services to individuals with cancer and their families (n = 167), and the American Cancer Society (n = 138). Of the 496 respondents who reported accessing hospital resources, most (n = 322) said they used information that their health care team recommended. Other supportive options were used to a lesser degree: support groups (n = 92), chemotherapy and radiation therapy classes (n = 129), and supportive/educational programs offered by the cancer center (n = 27). Most of the respondents (n = 822, 88.6%) preferred to have their follow-up care remain with their cancer care team 1 year after treatments are completed. Almost two-thirds of respondents (n = 601, 64%) cited being seen at the cancer center for follow-up care as the most important factor in considering follow-up care.
Concerns In determining whether the large proportion of respondents with breast cancer skewed the study results, it was determined that median scores differed significantly in only four concerns. Compared with respondents without breast cancer, respondents with breast cancer were more likely to have significantly lower scores for concerns related to fatigue (P <.001) and sexual issues/intimacy (P = .001). Respondents with breast cancer were more likely to have significantly higher scores than respondents without breast cancer for concerns related to genetic counseling (P = .001) and fear of developing a new cancer (P = .010).
Fears of the cancer returning and developing a new cancer were the two most prevalent concerns, identified by 51% (n = 486) and 47.5% (n = 459), respectively (Table 2). Physical concerns, rated as moderate/high concerns by at least 25% of the sample, were fatigue (n = 336, 34.8%), changes in [the] body after cancer (n = 323, 33.7%), trouble sleeping (n = 302, 31.0%), sexual issues/intimacy (n = 263, 28.0%), memory and concentration (n = 261, 26.7%), and weight changes (n = 248, 25.5%). The most prevalent moderate/high social concerns were related to finances (n = 265, 27.5%) and debt from medical bills (n = 232, 25.1%). Managing stress (n = 279, 29.2%) and difficult emotions (n = 244, 25.1%) were prevalent moderate/high emotional concerns. Spiritual concerns were less often rated as moderate/high concerns. Having a breast cancer diagnosis was not significantly related to the number of reported moderate to high concerns (P = 1.00).
Variables associated with the 12 most frequent moderate/high concerns are shown in Tables 3 and 4. Age was associated with the most moderate/high concerns. With every decade of age, the odds of having the following moderate/high concerns decreased: bodily changes after cancer (odds ratio [OR], 0.75), sexual intimacy (OR, 0.81), memory and concentration (OR, 0.83), weight changes (OR, 0.77), financial (OR, 0.75), debt (OR, 0.71), cancer returning (OR, 0.66), developing a new cancer (OR, 0.67), managing stress (OR, 0.67), and managing difficult emotions (OR, 0.67).
Female sex was associated with lower odds of having a concern about sexual intimacy (OR, 0.30) and increased odds of having concerns related to memory and concentration (OR, 1.78), managing stress (OR, 2.35), and managing difficult emotions (OR, 1.77). Race was another demographic characteristic statistically associated with numerous moderate/high concerns. Survivors who identified white, were more likely than other people of other races to have fewer moderate/high concerns regarding bodily changes after cancer (OR, 0.46), weight change (OR, 0.46), finances (OR, 0.46), debt (OR, 0.40), managing stress (OR, 0.55), and managing difficult emotions (OR, 0.49). The odds of having a moderate/high concern regarding debt was 2.25 times higher given widowed marital status compared with those survivors who were single. Unemployment status, when compared with full-time employment, was significantly associated with increased odds of having moderate/high concerns related to fatigue (OR, 2.08), bodily changes after cancer (OR, 1.72), memory and concentration (OR, 2.45), weight changes (OR, 2.17), finances (OR, 1.93), developing a new cancer (OR, 1.91), and managing difficult emotions (OR, 1.80).
As expected, respondents who had completed treatment were less likely to have many of the moderate/high concerns as those still undergoing treatment. Survivors who were up to 2 years posttreatment were significantly more likely than those survivors receiving treatment to have fewer moderate/high concerns regarding fatigue (OR, 0.56), sexual intimacy (OR, 0.54), weight change (OR, 0.55), fears of the cancer returning (OR, 0.48), developing a new cancer (OR, 0.35), managing stress (OR, 0.43), and managing difficult emotions (OR, 0.49).
However, those improved odds were not sustained over the cancer trajectory. Compared with survivors who were receiving treatment, survivors who were between 2-5 years posttreatment did not have significantly reduced odds for moderate/high concerns related to fatigue, sleep, sexual intimacy, body changes, weight changes, memory, fears of the cancer returning, developing a new cancer, managing stress, and managing difficult emotions. They did have significantly reduced odds for having concerns only related to finances (OR, 0.61) and debt (OR, 0.52).
Long-term survivors, who were beyond 5 years posttreatment, had significantly reduced odds for having moderate/high concerns related to fatigue (OR, 0.45), finances (OR, 0.52), debt (OR, 0.47), and managing difficult emotions (OR, 0.54), compared with survivors receiving treatment. Moderate/high concerns related to sleep, sexual intimacy, body changes, weight changes, memory, fears of the cancer returning, developing a new cancer, managing stress did not have improved odds for these long-term survivors.
Attention to needs
The health care teams were rated highly for their attention to the patients’ physical needs. Most respondents (n = 845, 92.4%) viewed the health care team’s attention their physical needs as important and 763 (77.6%) survivors rated the team’s attention to these needs as excellent. The importance of addressing emotional needs was affirmed by 723 (78.5%) respondents, and although 454 (46.8%) viewed the team’s attention to these needs as excellent, 119 (12.3%) reported that the health care team did not ask about emotional needs. In addition, 566 respondents (60%) viewed having the health care team address their social needs as important, and most (n = 715, 74.2%) rated the team’s attention to social needs as good or excellent. Yet, 162 (16.8%) respondents reported that team did not ask about their social needs. The health care team’s addressing of spiritual needs was viewed as important by 346 (37.5%) respondents and ratings for how well the team attended to spiritual needs were: 148 (15.6%) poor or fair, 204 (21.5%) good, and 150 (15.8%) excellent. However, 448 (47.2%) respondents reported that the health care team did not ask about their spiritual needs.
Discussion
The primary purpose of this project was to prioritize survivors’ most salient physical, social, emotional, and spiritual concerns or needs and to assess the perceived importance of these needs and the extent to which the cancer center staff were attentive to those needs. The overall goal of this assessment was to inform the development of survivorship and supportive care programs by highlighting common concerns, demographic and medical factors associated with specific concerns, and timing of moderate/high level concerns along the cancer trajectory. There were 3 main findings.
First, the results support the need for enhancing supportive care services to meet emotional concerns of survivors beyond the treatment phase. Similar to other studies,8,9 emotional concerns ranked higher than all other concerns in this study with about 50% of the sample rating “fear the cancer will return” and “fear of developing a new cancer” as moderate/high concern. Although the odds of not having these emotional concerns improved up to 2 years posttreatment, these concerns are likely to resurface, as odds for survivors beyond 2 years were not significantly different from those receiving treatment. A recent systematic review reported that fear of cancer recurrence is experienced by about 73% of cancer survivors, with 49% reporting a moderate to high degree.10 It can have a chronic, stable trajectory for some survivors and is strongly associated with higher levels of anxiety, distress, and depression, and less global, emotional/mental, physical, role, social, and cognitive quality of life.10 In this sample, managing stress and difficult emotions were also rated as moderate/high concerns by at least 25% of the sample.
Second, the findings identified patients at risk for cancer-related concerns throughout the cancer trajectory. As demonstrated in other studies, younger age was associated with greater odds of having multiple greater moderate/high concerns.11-13 Unemployment was the second most common demographic factor associated with multiple moderate/high concerns related to physical symptoms, finances and emotions. Similarly, identifying as black, Asian, American Indian/Alaskan Native, or other was also associated with greater odds of having numerous physical, financial, and emotional concerns. Women had greater concerns related to memory, sexual intimacy, coping with difficult emotions, and stress.
Third, the results helped to identify gaps in supportive care at our cancer center. Although spiritual concerns were not prevalent as being moderate/high, they were still viewed by about a third of survivors as being an important area for the health care team to address. Yet, consistent with other need assessments, spiritual concerns in this study were least often addressed by staff.1 Assessment of spiritual care needs, screening for spiritual distress, and providing spiritual care are essential components of a clinician-patient relationship that supports healing.14 The importance of attending to spiritual care needs was underscored by a recent systematic review that found a positive association between overall spiritual well-being and quality of life in patients with cancer, with the meaning/peace factor consistently and positively associated with physical and mental health.15 Another identified gap was the health care team’s lack of attention to the patient’s social needs, which included concerns related to finances and debt from medical bills. In all, 46% of the respondents reported having financial concerns, with the odds of having moderate/high financial concerns being greatest during treatment to 2 years posttreatment. Attention to the financial burden of cancer patients is critical because the magnitude of cancer-related financial concerns is a significant, strong predictor of quality of life and adverse psychological issues such as depression, anxiety, and distress.16,17
There were several program implications based on the results. A periodic audit of the concerns of survivors and their views on how well their needs were being met was a relatively low cost endeavor. Although the findings were consistent with the literature, the results, when shared with administrators and clinicians, were instrumental in effecting change because they represented the concerns of survivors at the cancer center. Another program directive, based on the results, was to extend the routine screening of patients’ needs during treatment to posttreatment survivorship. Patients who are young, unemployed, do not identify as white, and female warrant more thorough assessment of needs and concerns along the cancer trajectory. Integral to these screenings is the need for patient-centered communication, with discussion of how cancer is affecting the different domains of quality of life within the context of the patient’s life. Lastly, the results clearly indicated the need for additional training of health care providers on how to assess and address spiritual well-being in cancer survivors.
There were limitations to this study, including use of a nonvalidated survey and cross-sectional approach that limited our ability to explore how concerns might change over the trajectory. Also, it was not possible to clarify medical information of the respondents, such as cancer stage. Although the response rate of this study was not high, we are confident in the results because of the large sample size and the finding that the large proportion of respondents with breast cancer was not influential. Despite these limitations, this needs assessment of cancer survivors over the trajectory of care provided insight into the scope of their concerns, identified vulnerable groups of survivors, and highlighted gaps in addressing those concerns. A quality- of-life framework for assessing needs assured a comprehensive focus and generated practice changes to strengthen holistic, comprehensive oncology care.
Complex cancer treatments, limited personnel resources, and a growing number of cancer survivors are challenging cancer health care professionals’ abilities to provide comprehensive care. Cancer survivors have a range of needs that extend over the cancer care trajectory and that represent physical, psychological, social, and spiritual domains. Numerous studies have explored supportive care needs and recent systematic reviews have highlighted the supportive care needs related to cancer1 and to specific cancer types, including prostate cancer,2 breast cancer,3 gynecologic cancer,4 hematological cancer,5 and lung cancer.6 However, reviews are limited in that they do not always assess needs across the cancer trajectory or identify demographic or clinical variables that are associated with needs. These data are needed to focus survivorship program development in cancer centers in order to target populations most likely at risk for unmet needs, identify what salient concerns to address, and to appropriately schedule supportive care programs.
The importance of assessing the patient’s subjective view of his/her needs or concerns is well acknowledged as being fundamental to patient-centered care.7 Clinicians routinely assess needs in practice using a variety of screening tools. However, there needs to be a broader assessment of concerns and needs in a population of survivors with mixed cancer diagnoses, along with their appraisal of how well their needs were addressed by their health care team, to provide an overall identification of gaps in supportive care. The primary purpose of the present study was to prioritize survivors’ most salient physical, social, emotional, and spiritual concerns or needs; ascertain survivors’ perceived importance of those needs and the extent to which our institution, the University Hospitals Seidman Cancer Center, was attentive to those needs; and to identify who might be at risk for having greater concerns. The overall goal was to use the data to inform survivorship and supportive care program development.
Methods
Design, sample and setting
We used a cross-sectional design. Surveys were mailed once to a convenience sample of 2,750 adult patients who had been seen in follow-up during the previous 2 years (2010-2011) at all clinical sites of University Hospitals Seidman Cancer Center, a Midwestern National Cancer Institute-designated Comprehensive Cancer Center. Patients who had a noncancer diagnosis were excluded. The distribution list was screened for deceased individuals and those patients who had multiple visits during the time period. The project was reviewed and approved as nonresearch by the Case Western Reserve University Cancer Institutional Review Board.
Survey
An interdisciplinary team of clinicians, administrators, and researchers adapted the Mayo Clinic Cancer Center’s Cancer Survivors Survey of Needs8 to create a comprehensive survey for the cancer center. Input regarding the scope of the survey was sought from the Patient and Family Advisory Council of the cancer center. The survey, which was formatted for scanning purposes, consisted of 33 questions that were compiled into 4 sections. Sections 1 and 2 focused on demographic and treatment-related information, including use of community and hospital support services and preferences for follow-up care. In section 3, a quality-of-life framework was used to assess physical, social, emotional, and spiritual needs. Respondents were asked to rate their current level of concern for 19 physical effects, 10 social effects, 10 emotional effects, and 5 spiritual effects on a scale ranging from 0 (no concern) to 5 (extreme concern). In section 4, respondents were asked to indicate the importance of the cancer team addressing their physical, social, emotional, and spiritual needs. This was followed by their rating of the cancer team’s attention to their needs as Poor, Fair, Good, Excellent, or They did not ask about my needs. Respondents were asked about preferences for learning about physical, social, emotional, and spiritual effects. In addition to the 33 questions, there were 6 open-ended questions in which respondents were encouraged to share additional information about their needs, sources of support, and other concerns.
Procedures
Eligible respondents were mailed a cover letter explaining the survey from both the director and president of the cancer center, a survey, and a postage-paid return envelope. The option to respond to the survey by a telephone call to the director of the Office of Cancer Survivorship was offered in the cover letter.
Data analysis
Returned surveys were scanned into a Teleform database, verified, and exported into an SPSS data file. Data quality was checked by running frequency analyses and summarizing variables. Time-since-treatment responses were collapsed into 4 categories: on treatment, up to 2 years posttreatment, 2-5 years posttreatment, and more than 5 years posttreatment. Descriptive statistics were used to summarize demographic and medical characteristics of the respondents and to calculate the mean score for each concern for the total sample and then for each category of time since treatment. Because of the large number of respondents with breast cancer, the respondents were stratified into two groups, one of breast cancer the other of nonbreast cancer respondents. Then, the Mann-Whitney test was performed for each concern to examine differences between respondents with and without breast cancer.
To identify the most prevalent concerns, ratings for concerns were recoded into no concern (rated as 0), low concern (1 or 2), and moderate/high concern (3, 4, or 5). Since our interest was in the moderate and high concerns, the responses were dichotomized into moderate/high concerns and all other levels. Logistic regression models were then used to identify associations between a set of survivor characteristics or covariates (age, sex, living status, marital status, employment status, cancer type, and time since treatment) with the 12 most highly rated moderate/high concerns. All the analyses were performed using statistical software SPSS 20 and Stata 13.0
Results
Respondents
A total of 1,005 surveys were returned for a 37% response rate. Forty-two patients responded by telephone. The mean age of respondents was 64.9 years (range, 22-98; SD, 12.8). The typical respondent was female, white, and married (Table 1). Twenty-four percent of the respondents (n = 240) reported living alone. Although about 47% of respondents (n = 473) reported a breast cancer diagnosis, more than 17 cancers were identified, and 14% of respondents (n = 145) listed multiple diagnoses. About a third of respondents were receiving treatment when they completed the survey.
Just under half of the respondents (n = 498) reported using community resources for support and information about cancer, and 29.5% (n = 296) sought information on the internet during their cancer experience. The most commonly used community resources were The Gathering Place, a local organization offering free supportive programs and services to individuals with cancer and their families (n = 167), and the American Cancer Society (n = 138). Of the 496 respondents who reported accessing hospital resources, most (n = 322) said they used information that their health care team recommended. Other supportive options were used to a lesser degree: support groups (n = 92), chemotherapy and radiation therapy classes (n = 129), and supportive/educational programs offered by the cancer center (n = 27). Most of the respondents (n = 822, 88.6%) preferred to have their follow-up care remain with their cancer care team 1 year after treatments are completed. Almost two-thirds of respondents (n = 601, 64%) cited being seen at the cancer center for follow-up care as the most important factor in considering follow-up care.
Concerns In determining whether the large proportion of respondents with breast cancer skewed the study results, it was determined that median scores differed significantly in only four concerns. Compared with respondents without breast cancer, respondents with breast cancer were more likely to have significantly lower scores for concerns related to fatigue (P <.001) and sexual issues/intimacy (P = .001). Respondents with breast cancer were more likely to have significantly higher scores than respondents without breast cancer for concerns related to genetic counseling (P = .001) and fear of developing a new cancer (P = .010).
Fears of the cancer returning and developing a new cancer were the two most prevalent concerns, identified by 51% (n = 486) and 47.5% (n = 459), respectively (Table 2). Physical concerns, rated as moderate/high concerns by at least 25% of the sample, were fatigue (n = 336, 34.8%), changes in [the] body after cancer (n = 323, 33.7%), trouble sleeping (n = 302, 31.0%), sexual issues/intimacy (n = 263, 28.0%), memory and concentration (n = 261, 26.7%), and weight changes (n = 248, 25.5%). The most prevalent moderate/high social concerns were related to finances (n = 265, 27.5%) and debt from medical bills (n = 232, 25.1%). Managing stress (n = 279, 29.2%) and difficult emotions (n = 244, 25.1%) were prevalent moderate/high emotional concerns. Spiritual concerns were less often rated as moderate/high concerns. Having a breast cancer diagnosis was not significantly related to the number of reported moderate to high concerns (P = 1.00).
Variables associated with the 12 most frequent moderate/high concerns are shown in Tables 3 and 4. Age was associated with the most moderate/high concerns. With every decade of age, the odds of having the following moderate/high concerns decreased: bodily changes after cancer (odds ratio [OR], 0.75), sexual intimacy (OR, 0.81), memory and concentration (OR, 0.83), weight changes (OR, 0.77), financial (OR, 0.75), debt (OR, 0.71), cancer returning (OR, 0.66), developing a new cancer (OR, 0.67), managing stress (OR, 0.67), and managing difficult emotions (OR, 0.67).
Female sex was associated with lower odds of having a concern about sexual intimacy (OR, 0.30) and increased odds of having concerns related to memory and concentration (OR, 1.78), managing stress (OR, 2.35), and managing difficult emotions (OR, 1.77). Race was another demographic characteristic statistically associated with numerous moderate/high concerns. Survivors who identified white, were more likely than other people of other races to have fewer moderate/high concerns regarding bodily changes after cancer (OR, 0.46), weight change (OR, 0.46), finances (OR, 0.46), debt (OR, 0.40), managing stress (OR, 0.55), and managing difficult emotions (OR, 0.49). The odds of having a moderate/high concern regarding debt was 2.25 times higher given widowed marital status compared with those survivors who were single. Unemployment status, when compared with full-time employment, was significantly associated with increased odds of having moderate/high concerns related to fatigue (OR, 2.08), bodily changes after cancer (OR, 1.72), memory and concentration (OR, 2.45), weight changes (OR, 2.17), finances (OR, 1.93), developing a new cancer (OR, 1.91), and managing difficult emotions (OR, 1.80).
As expected, respondents who had completed treatment were less likely to have many of the moderate/high concerns as those still undergoing treatment. Survivors who were up to 2 years posttreatment were significantly more likely than those survivors receiving treatment to have fewer moderate/high concerns regarding fatigue (OR, 0.56), sexual intimacy (OR, 0.54), weight change (OR, 0.55), fears of the cancer returning (OR, 0.48), developing a new cancer (OR, 0.35), managing stress (OR, 0.43), and managing difficult emotions (OR, 0.49).
However, those improved odds were not sustained over the cancer trajectory. Compared with survivors who were receiving treatment, survivors who were between 2-5 years posttreatment did not have significantly reduced odds for moderate/high concerns related to fatigue, sleep, sexual intimacy, body changes, weight changes, memory, fears of the cancer returning, developing a new cancer, managing stress, and managing difficult emotions. They did have significantly reduced odds for having concerns only related to finances (OR, 0.61) and debt (OR, 0.52).
Long-term survivors, who were beyond 5 years posttreatment, had significantly reduced odds for having moderate/high concerns related to fatigue (OR, 0.45), finances (OR, 0.52), debt (OR, 0.47), and managing difficult emotions (OR, 0.54), compared with survivors receiving treatment. Moderate/high concerns related to sleep, sexual intimacy, body changes, weight changes, memory, fears of the cancer returning, developing a new cancer, managing stress did not have improved odds for these long-term survivors.
Attention to needs
The health care teams were rated highly for their attention to the patients’ physical needs. Most respondents (n = 845, 92.4%) viewed the health care team’s attention their physical needs as important and 763 (77.6%) survivors rated the team’s attention to these needs as excellent. The importance of addressing emotional needs was affirmed by 723 (78.5%) respondents, and although 454 (46.8%) viewed the team’s attention to these needs as excellent, 119 (12.3%) reported that the health care team did not ask about emotional needs. In addition, 566 respondents (60%) viewed having the health care team address their social needs as important, and most (n = 715, 74.2%) rated the team’s attention to social needs as good or excellent. Yet, 162 (16.8%) respondents reported that team did not ask about their social needs. The health care team’s addressing of spiritual needs was viewed as important by 346 (37.5%) respondents and ratings for how well the team attended to spiritual needs were: 148 (15.6%) poor or fair, 204 (21.5%) good, and 150 (15.8%) excellent. However, 448 (47.2%) respondents reported that the health care team did not ask about their spiritual needs.
Discussion
The primary purpose of this project was to prioritize survivors’ most salient physical, social, emotional, and spiritual concerns or needs and to assess the perceived importance of these needs and the extent to which the cancer center staff were attentive to those needs. The overall goal of this assessment was to inform the development of survivorship and supportive care programs by highlighting common concerns, demographic and medical factors associated with specific concerns, and timing of moderate/high level concerns along the cancer trajectory. There were 3 main findings.
First, the results support the need for enhancing supportive care services to meet emotional concerns of survivors beyond the treatment phase. Similar to other studies,8,9 emotional concerns ranked higher than all other concerns in this study with about 50% of the sample rating “fear the cancer will return” and “fear of developing a new cancer” as moderate/high concern. Although the odds of not having these emotional concerns improved up to 2 years posttreatment, these concerns are likely to resurface, as odds for survivors beyond 2 years were not significantly different from those receiving treatment. A recent systematic review reported that fear of cancer recurrence is experienced by about 73% of cancer survivors, with 49% reporting a moderate to high degree.10 It can have a chronic, stable trajectory for some survivors and is strongly associated with higher levels of anxiety, distress, and depression, and less global, emotional/mental, physical, role, social, and cognitive quality of life.10 In this sample, managing stress and difficult emotions were also rated as moderate/high concerns by at least 25% of the sample.
Second, the findings identified patients at risk for cancer-related concerns throughout the cancer trajectory. As demonstrated in other studies, younger age was associated with greater odds of having multiple greater moderate/high concerns.11-13 Unemployment was the second most common demographic factor associated with multiple moderate/high concerns related to physical symptoms, finances and emotions. Similarly, identifying as black, Asian, American Indian/Alaskan Native, or other was also associated with greater odds of having numerous physical, financial, and emotional concerns. Women had greater concerns related to memory, sexual intimacy, coping with difficult emotions, and stress.
Third, the results helped to identify gaps in supportive care at our cancer center. Although spiritual concerns were not prevalent as being moderate/high, they were still viewed by about a third of survivors as being an important area for the health care team to address. Yet, consistent with other need assessments, spiritual concerns in this study were least often addressed by staff.1 Assessment of spiritual care needs, screening for spiritual distress, and providing spiritual care are essential components of a clinician-patient relationship that supports healing.14 The importance of attending to spiritual care needs was underscored by a recent systematic review that found a positive association between overall spiritual well-being and quality of life in patients with cancer, with the meaning/peace factor consistently and positively associated with physical and mental health.15 Another identified gap was the health care team’s lack of attention to the patient’s social needs, which included concerns related to finances and debt from medical bills. In all, 46% of the respondents reported having financial concerns, with the odds of having moderate/high financial concerns being greatest during treatment to 2 years posttreatment. Attention to the financial burden of cancer patients is critical because the magnitude of cancer-related financial concerns is a significant, strong predictor of quality of life and adverse psychological issues such as depression, anxiety, and distress.16,17
There were several program implications based on the results. A periodic audit of the concerns of survivors and their views on how well their needs were being met was a relatively low cost endeavor. Although the findings were consistent with the literature, the results, when shared with administrators and clinicians, were instrumental in effecting change because they represented the concerns of survivors at the cancer center. Another program directive, based on the results, was to extend the routine screening of patients’ needs during treatment to posttreatment survivorship. Patients who are young, unemployed, do not identify as white, and female warrant more thorough assessment of needs and concerns along the cancer trajectory. Integral to these screenings is the need for patient-centered communication, with discussion of how cancer is affecting the different domains of quality of life within the context of the patient’s life. Lastly, the results clearly indicated the need for additional training of health care providers on how to assess and address spiritual well-being in cancer survivors.
There were limitations to this study, including use of a nonvalidated survey and cross-sectional approach that limited our ability to explore how concerns might change over the trajectory. Also, it was not possible to clarify medical information of the respondents, such as cancer stage. Although the response rate of this study was not high, we are confident in the results because of the large sample size and the finding that the large proportion of respondents with breast cancer was not influential. Despite these limitations, this needs assessment of cancer survivors over the trajectory of care provided insight into the scope of their concerns, identified vulnerable groups of survivors, and highlighted gaps in addressing those concerns. A quality- of-life framework for assessing needs assured a comprehensive focus and generated practice changes to strengthen holistic, comprehensive oncology care.
1. Harrison JD, Young JM, Price MA, Butow PN, Solomon MJ. What are the unmet supportive care needs of people with cancer? A systematic review. Support Care Cancer. 2009;17:1117-1128.
2. Paterson C, Robertson A, Smith A, Nabi G. Identifying the unmet supportive care needs of men living with and beyond prostate cancer: A systematic review. Eur J Oncol Nurs. 2015;19:405-418.
3. Fiszer C, Dolbeault S, Sultan S, Bredart A. Prevalence, intensity, and predictors of the supportive care needs of women diagnosed with breast cancer: A systematic review. Psychooncology. 2014;23:361-374.
4. Maguire R, Kotronoulas G, Simpson M, Paterson C. A systematic review of the supportive care needs of women living with and beyond cervical cancer. Gynecol Oncol. 2015;136:478-490.
5. Hall A, Lynagh M, Bryant J, Sanson-Fisher R. Supportive care needs of hematological cancer survivors: A critical review of the literature. Crit Rev Oncol Hematol. 2013;88:102-116.
6. Maguire R, Papadopoulou C, Kotronoulas G, Simpson MF, McPhelim J, Irvine L. A systematic review of supportive care needs of people living with lung cancer. Eur J Oncol Nurs. 2013;17:449-464.
7. Adler NE, Page EK. Cancer care for the whole patient: meeting psychosocial health needs. Washington, DC: National Academies Press; Institute of Medicine, 2008.
8. Ness S, Kokal J, Fee-Schroeder K, Novotny P, Satele D, Barton D. Concerns across the survivorship trajectory: results from a survey of cancer survivors. Oncol Nurs Forum. 2013;40:35-42.
9. Swash B, Hulbert-Williams N, Bramwell R. Unmet psychosocial needs in haematological cancer: A systematic review. Support Care Cancer. 2014;22:1131-1141.
10. Simard S, Thewes B, Humphris G, et al. Fear of cancer recurrence in adult cancer survivors: A systematic review of quantitative studies. J Cancer Surviv. 2013;7:300-322.
11. Choi KH, Park JH, Park JH, Park JS. Psychosocial needs of cancer patients and related factors: A multi-center, cross-sectional study in Korea. Psychooncology. 2013;22:1073-1080.
12. Pauwels EE, Charlier C, De Bourdeaudhuij I, Lechner L, Van Hoof E. Care needs after primary breast cancer treatment. Survivors’ associated sociodemographic and medical characteristics. Psychooncology. 2013;22:125-132.
13. Harrison JD, Young JM, Price MA, Butow PN, Solomon MJ. What are the unmet supportive care needs of people with cancer? A systematic review. Support Care Cancer. 2009;17:1117-1128.
14. Puchalski CM, Blatt B, Kogan M, Butler A. Spirituality and health: The development of a field. Academic Medicine. 2014;89:10-16.
15. Bai M, Lazenby M. A systematic review of associations between spiritual well-being and quality of life at the scale and factor levels in studies among patients with cancer. J Palliat Med. 2015;18:286-298.
16. Fenn KM, Evans SB, McCorkle R, et al. Impact of financial burden of cancer on survivors’ quality of life. J Oncol Pract. 2014;10:332-338.
17. Sharp L, Carsin AE, Timmons A. Associations between cancer-related financial stress and strain and psychological wellbeing among individuals living with cancer. Psychooncology. 2013;22:745-755.
1. Harrison JD, Young JM, Price MA, Butow PN, Solomon MJ. What are the unmet supportive care needs of people with cancer? A systematic review. Support Care Cancer. 2009;17:1117-1128.
2. Paterson C, Robertson A, Smith A, Nabi G. Identifying the unmet supportive care needs of men living with and beyond prostate cancer: A systematic review. Eur J Oncol Nurs. 2015;19:405-418.
3. Fiszer C, Dolbeault S, Sultan S, Bredart A. Prevalence, intensity, and predictors of the supportive care needs of women diagnosed with breast cancer: A systematic review. Psychooncology. 2014;23:361-374.
4. Maguire R, Kotronoulas G, Simpson M, Paterson C. A systematic review of the supportive care needs of women living with and beyond cervical cancer. Gynecol Oncol. 2015;136:478-490.
5. Hall A, Lynagh M, Bryant J, Sanson-Fisher R. Supportive care needs of hematological cancer survivors: A critical review of the literature. Crit Rev Oncol Hematol. 2013;88:102-116.
6. Maguire R, Papadopoulou C, Kotronoulas G, Simpson MF, McPhelim J, Irvine L. A systematic review of supportive care needs of people living with lung cancer. Eur J Oncol Nurs. 2013;17:449-464.
7. Adler NE, Page EK. Cancer care for the whole patient: meeting psychosocial health needs. Washington, DC: National Academies Press; Institute of Medicine, 2008.
8. Ness S, Kokal J, Fee-Schroeder K, Novotny P, Satele D, Barton D. Concerns across the survivorship trajectory: results from a survey of cancer survivors. Oncol Nurs Forum. 2013;40:35-42.
9. Swash B, Hulbert-Williams N, Bramwell R. Unmet psychosocial needs in haematological cancer: A systematic review. Support Care Cancer. 2014;22:1131-1141.
10. Simard S, Thewes B, Humphris G, et al. Fear of cancer recurrence in adult cancer survivors: A systematic review of quantitative studies. J Cancer Surviv. 2013;7:300-322.
11. Choi KH, Park JH, Park JH, Park JS. Psychosocial needs of cancer patients and related factors: A multi-center, cross-sectional study in Korea. Psychooncology. 2013;22:1073-1080.
12. Pauwels EE, Charlier C, De Bourdeaudhuij I, Lechner L, Van Hoof E. Care needs after primary breast cancer treatment. Survivors’ associated sociodemographic and medical characteristics. Psychooncology. 2013;22:125-132.
13. Harrison JD, Young JM, Price MA, Butow PN, Solomon MJ. What are the unmet supportive care needs of people with cancer? A systematic review. Support Care Cancer. 2009;17:1117-1128.
14. Puchalski CM, Blatt B, Kogan M, Butler A. Spirituality and health: The development of a field. Academic Medicine. 2014;89:10-16.
15. Bai M, Lazenby M. A systematic review of associations between spiritual well-being and quality of life at the scale and factor levels in studies among patients with cancer. J Palliat Med. 2015;18:286-298.
16. Fenn KM, Evans SB, McCorkle R, et al. Impact of financial burden of cancer on survivors’ quality of life. J Oncol Pract. 2014;10:332-338.
17. Sharp L, Carsin AE, Timmons A. Associations between cancer-related financial stress and strain and psychological wellbeing among individuals living with cancer. Psychooncology. 2013;22:745-755.
Bilateral chylothorax in an AIDS patient with newly diagnosed Kaposi sarcoma
Kaposi sarcoma is an angioproliferative tumor that is associated with human herpes virus-8 (HHV-8). Mucocutaneous disease is the most common site for manifestation of AIDS-related Kaposi sarcoma, commonly affecting the lower extremities, oral mucosa, face, and genitalia. Pleural effusions can occur in 36%-60% of patients with Kaposi sarcoma, and it has been documented that chylothorax is a rare, but plausible presentation in patients with Kaposi sarcoma.1 We present here a case of bilateral chylothorax in a patient with AIDS-related Kaposi sarcoma.
Case presentation and summary
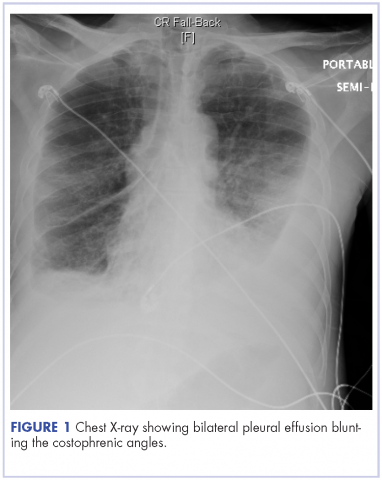
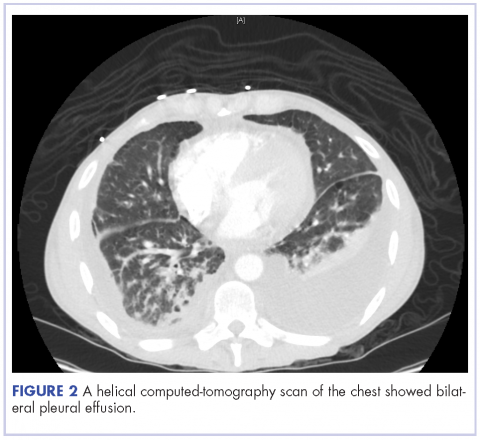
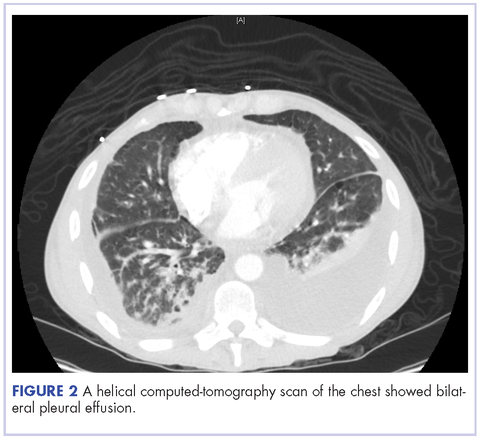
A 52-year-old MSM male with AIDS (CD4, <20 mm3; viral load, 58 copies/ml) presented to the emergency department with complaints of shortness of breath, productive cough, and diarrhea for 2 days prior to presentation. His medical history also included chronic obstructive pulmonary disease, coronary artery disease, and hyperlipidemia. The patient was not on HAART because of his history of noncompliance. The results of a chest X-ray and computed-tomography (CT) scan showed that the patient had bilateral pleural effusion and a spiculated 14-mm nodule in the left upper lobe.
The patient underwent ultrasound-guided placement of a 12-French left-sided chest catheter, and a milky white fluid was aspirated from the left pleural space. Laboratory analysis of the pleural fluid confirmed an exudate with an elevated triglyceride level of 120 mg/dL (chylous, >110 mg/dL) indicating chylothorax.
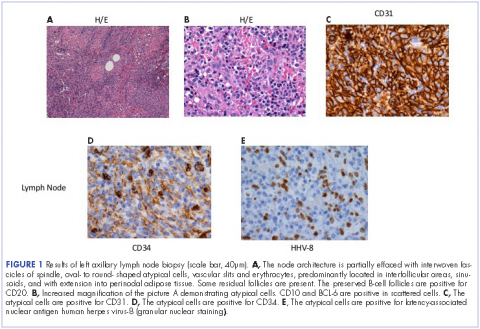
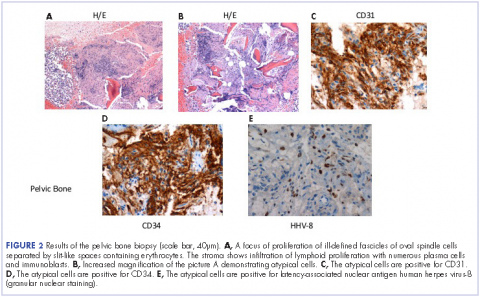
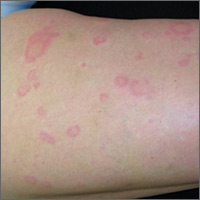
On close physical examination, the patient was found to have multiple irregular plaques on the back and lower extremities. As described by dermatology, there was a violaceous indurated plaque on the left axillae, violaceous indurated plaques with superficial scale grouped on the left midlateral back, and hyperpigmented lichenified plaques and papules on bilateral shins, with some with plate-like scale. Two punch biopsies were taken of the skin lesions, which confirmed Kaposi sarcoma, plaque stage from the lesion biopsied on the back, and patch stage from the lesion biopsied in the left axilla. Cytology of the pleural fluid was negative for malignant cells. On review by the radiologist of the CT scan of the chest, there was no indication of gross distention of the thoracic duct. Treatment options were offered to the patient, and the patient was considering options for chemotherapy and home hospice given his advanced disease state at the time of discharge.
Discussion
Chylothorax occurs with a thoracic duct obstruction, which results in leakage of lymphatic fluid into the pleural cavity. The two leading causes of chylothorax are trauma and malignancy, with lymphoma being the most common cause of chylothorax among those with malignancy.2 Chylothorax, however, is a rare but documented complication of Kaposi sarcoma. Marais and colleagues reported the case of a 3-year-old HIV-positive patient with newly diagnosed Kaposi sarcoma who was found to have tumor infiltration in the thoracic duct leading to bilateral chylothorax.3 Maradona and colleagues described a 40-year-old man with AIDS-related Kaposi sarcoma who was found to have pleural and pericardial Kaposi sarcoma with chylothorax.4 Priest and colleagues wrote about a 32-year-old patient with AIDS with biopsy-proven Kaposi sarcoma who required multiple therapeutic thoracenteses for rapidly recurrent left chylothorax effusions.5
There are two leading discussions as to the pathophysiology of chylothorax that is related to Kaposi sarcoma: chylothorax developing secondary to metastatic disease or the development of chylothorax secondary to primary Kaposi sarcoma arising from the pleural region.6 One case report examined pleural and lung biopsies in a 34-year-old patient with AIDS-related Kaposi sarcoma that showed immunohistochemical staining that was suggestive of early-stage Kaposi sarcoma of lymphatic endothelial origin. The authors were attempting to illustrate that Kaposi sarcoma may have a stem-cell origin which can differentiate into lymph cells. Kontantinopoulos and colleagues postulated that in situ Kaposi sarcoma can arise from the lymphatic system with a resultant clinical presentation of chylothorax.7 The more mainstream thought however, is that chylothorax has been found to develop secondary to metastatic disease. The present case, therefore, illustrates an unusual presentation of cytology negative chylothorax in a patient with AIDS-related Kaposi sarcoma.
1. Sridar S, Garza EG, Cox J, Rumbak MJ. Serosanguineous pleural effusions in a patient with HIV and Kaposi sarcoma: pleuroscopic findings. J Bronchology Interv Pulmonol. 2011;18(4):337-339.
2. Light RW. Chylothorax and pseudochylothorax. In: Light RW, ed. Pleural diseases. 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2013:412-426.
3. Marais BJ, Pienaar J, Gie RP. Kaposi sarcoma with upper airway obstruction and bilateral chylothoraces. Pediatr Infect Dis J. 2003;22:926-928.
4. Maradona JA, Carton JA, Asensi V, Rodriguez-Guardado A. AIDS-related Kaposi sarcoma with chylothorax and pericardial involvement satisfactorily treated with liposomal doxorubicin. AIDS. 2002;16(5):806.
5. Priest ER, Weiss R. Chylothorax with Kaposi sarcoma. South Med J. 1991;84:806-807.
6. Pantanowitz L, Dezube BJ. Kaposi sarcoma in unusual locations. BMC Cancer. 2008;8:190.
7. Konstantinopoulos PA, Dezube BJ, Pantanowitz L. Morphologic and immunophenotypic evidence of in situ Kaposi sarcoma. BMC Clin Pathol. 2006;30:6:7.
Kaposi sarcoma is an angioproliferative tumor that is associated with human herpes virus-8 (HHV-8). Mucocutaneous disease is the most common site for manifestation of AIDS-related Kaposi sarcoma, commonly affecting the lower extremities, oral mucosa, face, and genitalia. Pleural effusions can occur in 36%-60% of patients with Kaposi sarcoma, and it has been documented that chylothorax is a rare, but plausible presentation in patients with Kaposi sarcoma.1 We present here a case of bilateral chylothorax in a patient with AIDS-related Kaposi sarcoma.
Case presentation and summary
A 52-year-old MSM male with AIDS (CD4, <20 mm3; viral load, 58 copies/ml) presented to the emergency department with complaints of shortness of breath, productive cough, and diarrhea for 2 days prior to presentation. His medical history also included chronic obstructive pulmonary disease, coronary artery disease, and hyperlipidemia. The patient was not on HAART because of his history of noncompliance. The results of a chest X-ray and computed-tomography (CT) scan showed that the patient had bilateral pleural effusion and a spiculated 14-mm nodule in the left upper lobe.
The patient underwent ultrasound-guided placement of a 12-French left-sided chest catheter, and a milky white fluid was aspirated from the left pleural space. Laboratory analysis of the pleural fluid confirmed an exudate with an elevated triglyceride level of 120 mg/dL (chylous, >110 mg/dL) indicating chylothorax.
On close physical examination, the patient was found to have multiple irregular plaques on the back and lower extremities. As described by dermatology, there was a violaceous indurated plaque on the left axillae, violaceous indurated plaques with superficial scale grouped on the left midlateral back, and hyperpigmented lichenified plaques and papules on bilateral shins, with some with plate-like scale. Two punch biopsies were taken of the skin lesions, which confirmed Kaposi sarcoma, plaque stage from the lesion biopsied on the back, and patch stage from the lesion biopsied in the left axilla. Cytology of the pleural fluid was negative for malignant cells. On review by the radiologist of the CT scan of the chest, there was no indication of gross distention of the thoracic duct. Treatment options were offered to the patient, and the patient was considering options for chemotherapy and home hospice given his advanced disease state at the time of discharge.
Discussion
Chylothorax occurs with a thoracic duct obstruction, which results in leakage of lymphatic fluid into the pleural cavity. The two leading causes of chylothorax are trauma and malignancy, with lymphoma being the most common cause of chylothorax among those with malignancy.2 Chylothorax, however, is a rare but documented complication of Kaposi sarcoma. Marais and colleagues reported the case of a 3-year-old HIV-positive patient with newly diagnosed Kaposi sarcoma who was found to have tumor infiltration in the thoracic duct leading to bilateral chylothorax.3 Maradona and colleagues described a 40-year-old man with AIDS-related Kaposi sarcoma who was found to have pleural and pericardial Kaposi sarcoma with chylothorax.4 Priest and colleagues wrote about a 32-year-old patient with AIDS with biopsy-proven Kaposi sarcoma who required multiple therapeutic thoracenteses for rapidly recurrent left chylothorax effusions.5
There are two leading discussions as to the pathophysiology of chylothorax that is related to Kaposi sarcoma: chylothorax developing secondary to metastatic disease or the development of chylothorax secondary to primary Kaposi sarcoma arising from the pleural region.6 One case report examined pleural and lung biopsies in a 34-year-old patient with AIDS-related Kaposi sarcoma that showed immunohistochemical staining that was suggestive of early-stage Kaposi sarcoma of lymphatic endothelial origin. The authors were attempting to illustrate that Kaposi sarcoma may have a stem-cell origin which can differentiate into lymph cells. Kontantinopoulos and colleagues postulated that in situ Kaposi sarcoma can arise from the lymphatic system with a resultant clinical presentation of chylothorax.7 The more mainstream thought however, is that chylothorax has been found to develop secondary to metastatic disease. The present case, therefore, illustrates an unusual presentation of cytology negative chylothorax in a patient with AIDS-related Kaposi sarcoma.
Kaposi sarcoma is an angioproliferative tumor that is associated with human herpes virus-8 (HHV-8). Mucocutaneous disease is the most common site for manifestation of AIDS-related Kaposi sarcoma, commonly affecting the lower extremities, oral mucosa, face, and genitalia. Pleural effusions can occur in 36%-60% of patients with Kaposi sarcoma, and it has been documented that chylothorax is a rare, but plausible presentation in patients with Kaposi sarcoma.1 We present here a case of bilateral chylothorax in a patient with AIDS-related Kaposi sarcoma.
Case presentation and summary
A 52-year-old MSM male with AIDS (CD4, <20 mm3; viral load, 58 copies/ml) presented to the emergency department with complaints of shortness of breath, productive cough, and diarrhea for 2 days prior to presentation. His medical history also included chronic obstructive pulmonary disease, coronary artery disease, and hyperlipidemia. The patient was not on HAART because of his history of noncompliance. The results of a chest X-ray and computed-tomography (CT) scan showed that the patient had bilateral pleural effusion and a spiculated 14-mm nodule in the left upper lobe.
The patient underwent ultrasound-guided placement of a 12-French left-sided chest catheter, and a milky white fluid was aspirated from the left pleural space. Laboratory analysis of the pleural fluid confirmed an exudate with an elevated triglyceride level of 120 mg/dL (chylous, >110 mg/dL) indicating chylothorax.
On close physical examination, the patient was found to have multiple irregular plaques on the back and lower extremities. As described by dermatology, there was a violaceous indurated plaque on the left axillae, violaceous indurated plaques with superficial scale grouped on the left midlateral back, and hyperpigmented lichenified plaques and papules on bilateral shins, with some with plate-like scale. Two punch biopsies were taken of the skin lesions, which confirmed Kaposi sarcoma, plaque stage from the lesion biopsied on the back, and patch stage from the lesion biopsied in the left axilla. Cytology of the pleural fluid was negative for malignant cells. On review by the radiologist of the CT scan of the chest, there was no indication of gross distention of the thoracic duct. Treatment options were offered to the patient, and the patient was considering options for chemotherapy and home hospice given his advanced disease state at the time of discharge.
Discussion
Chylothorax occurs with a thoracic duct obstruction, which results in leakage of lymphatic fluid into the pleural cavity. The two leading causes of chylothorax are trauma and malignancy, with lymphoma being the most common cause of chylothorax among those with malignancy.2 Chylothorax, however, is a rare but documented complication of Kaposi sarcoma. Marais and colleagues reported the case of a 3-year-old HIV-positive patient with newly diagnosed Kaposi sarcoma who was found to have tumor infiltration in the thoracic duct leading to bilateral chylothorax.3 Maradona and colleagues described a 40-year-old man with AIDS-related Kaposi sarcoma who was found to have pleural and pericardial Kaposi sarcoma with chylothorax.4 Priest and colleagues wrote about a 32-year-old patient with AIDS with biopsy-proven Kaposi sarcoma who required multiple therapeutic thoracenteses for rapidly recurrent left chylothorax effusions.5
There are two leading discussions as to the pathophysiology of chylothorax that is related to Kaposi sarcoma: chylothorax developing secondary to metastatic disease or the development of chylothorax secondary to primary Kaposi sarcoma arising from the pleural region.6 One case report examined pleural and lung biopsies in a 34-year-old patient with AIDS-related Kaposi sarcoma that showed immunohistochemical staining that was suggestive of early-stage Kaposi sarcoma of lymphatic endothelial origin. The authors were attempting to illustrate that Kaposi sarcoma may have a stem-cell origin which can differentiate into lymph cells. Kontantinopoulos and colleagues postulated that in situ Kaposi sarcoma can arise from the lymphatic system with a resultant clinical presentation of chylothorax.7 The more mainstream thought however, is that chylothorax has been found to develop secondary to metastatic disease. The present case, therefore, illustrates an unusual presentation of cytology negative chylothorax in a patient with AIDS-related Kaposi sarcoma.
1. Sridar S, Garza EG, Cox J, Rumbak MJ. Serosanguineous pleural effusions in a patient with HIV and Kaposi sarcoma: pleuroscopic findings. J Bronchology Interv Pulmonol. 2011;18(4):337-339.
2. Light RW. Chylothorax and pseudochylothorax. In: Light RW, ed. Pleural diseases. 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2013:412-426.
3. Marais BJ, Pienaar J, Gie RP. Kaposi sarcoma with upper airway obstruction and bilateral chylothoraces. Pediatr Infect Dis J. 2003;22:926-928.
4. Maradona JA, Carton JA, Asensi V, Rodriguez-Guardado A. AIDS-related Kaposi sarcoma with chylothorax and pericardial involvement satisfactorily treated with liposomal doxorubicin. AIDS. 2002;16(5):806.
5. Priest ER, Weiss R. Chylothorax with Kaposi sarcoma. South Med J. 1991;84:806-807.
6. Pantanowitz L, Dezube BJ. Kaposi sarcoma in unusual locations. BMC Cancer. 2008;8:190.
7. Konstantinopoulos PA, Dezube BJ, Pantanowitz L. Morphologic and immunophenotypic evidence of in situ Kaposi sarcoma. BMC Clin Pathol. 2006;30:6:7.
1. Sridar S, Garza EG, Cox J, Rumbak MJ. Serosanguineous pleural effusions in a patient with HIV and Kaposi sarcoma: pleuroscopic findings. J Bronchology Interv Pulmonol. 2011;18(4):337-339.
2. Light RW. Chylothorax and pseudochylothorax. In: Light RW, ed. Pleural diseases. 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2013:412-426.
3. Marais BJ, Pienaar J, Gie RP. Kaposi sarcoma with upper airway obstruction and bilateral chylothoraces. Pediatr Infect Dis J. 2003;22:926-928.
4. Maradona JA, Carton JA, Asensi V, Rodriguez-Guardado A. AIDS-related Kaposi sarcoma with chylothorax and pericardial involvement satisfactorily treated with liposomal doxorubicin. AIDS. 2002;16(5):806.
5. Priest ER, Weiss R. Chylothorax with Kaposi sarcoma. South Med J. 1991;84:806-807.
6. Pantanowitz L, Dezube BJ. Kaposi sarcoma in unusual locations. BMC Cancer. 2008;8:190.
7. Konstantinopoulos PA, Dezube BJ, Pantanowitz L. Morphologic and immunophenotypic evidence of in situ Kaposi sarcoma. BMC Clin Pathol. 2006;30:6:7.
The Princess and the Pea-sized Nodule
For years, this 33-year-old woman has had a firm, pea-sized nodule on her left upper back. It was never a problem until recently, when it suddenly enlarged and became red, swollen, and tender.
She was prescribed antibiotics (trimethoprim and sulfa) by a provider at her local urgent care center. Dubious of the diagnosis—carbuncle—she sought referral to dermatology.
The patient claims to be in otherwise excellent health, with no history of similar problems. She denies manual manipulation of the lesion.
EXAMINATION
The patient is afebrile and in no distress. On her upper left back is a round, cystic lesion measuring 3.5 cm. It appears swollen and red. The erythema, though impressive, is confined to
the area immediately around the margins. Palpation reveals increased warmth and modest tenderness. A central punctum can be seen in the center of the fluctuant lesion.

After a brief discussion of options, the lesion is incised and drained under sterile conditions with lidocaine and epinephrine. Cheesy, odoriferous material is expressed, effectively flattening the lesion.
What is the diagnosis?
DISCUSSION
Epidermal cysts are utterly common, especially in oil-rich areas such as the upper back. They are often mistakenly called sebaceous cysts; however, true sebaceous cysts are quite rare and contain only pure, clear oil.
When ruptured by trauma, epidermal cysts become inflamed and cheesy material leaks into deep tissues. This activates an immune response in which the body sends out white cells to clean up the leakage—what we call inflammation.
There are many types of cysts (eg, acne cysts, ganglion cysts, Bartholin gland cysts) but none resemble epidermal cysts. Providers often mistake epidermal cysts for carbuncles or boils and may prescribe oral or systemic antibiotics, or incise the cysts and pack the space. The truth is that inflamed epidermal cysts do not represent infection—hence the limited area of redness. By contrast, cellulitis or carbuncle would manifest with tenderness and blush of erythema over the entire area.
The fact that this lesion arose from a longstanding antecedent nodule is consistent with the diagnosis, as are the cheesy, odoriferous contents liberated by incision and drainage. Liberating the contents merely buys the patient relief from the pressure and pain, since the cyst wall is still present and will almost certainly fill up again. The ultimate solution is excision after the emptied cyst has had time to shrink back to its original size, which will minimize the scarring. There is no need to pack such cysts after incision and drainage, though they will continue to drain for a few days.
TAKE-HOME LEARNING POINTS
- Epidermal cysts are common, especially in oil-rich areas such as the face, back, chest, and neck.
- Epidermal cysts are often mistakenly called sebaceous cysts, but these are actually quite rare, containing clear sebum (oil) and no cheesy material.
- Even though such inflamed cysts are often mistaken for boils, carbuncles, and abscesses, they have nothing to do with bacteria or infection and therefore do not require antibiotics or packing after incision and drainage.
- For recurrent inflamed cysts, the treatment of choice is complete excision, done only after the cyst has shrunk to its smallest size.
For years, this 33-year-old woman has had a firm, pea-sized nodule on her left upper back. It was never a problem until recently, when it suddenly enlarged and became red, swollen, and tender.
She was prescribed antibiotics (trimethoprim and sulfa) by a provider at her local urgent care center. Dubious of the diagnosis—carbuncle—she sought referral to dermatology.
The patient claims to be in otherwise excellent health, with no history of similar problems. She denies manual manipulation of the lesion.
EXAMINATION
The patient is afebrile and in no distress. On her upper left back is a round, cystic lesion measuring 3.5 cm. It appears swollen and red. The erythema, though impressive, is confined to
the area immediately around the margins. Palpation reveals increased warmth and modest tenderness. A central punctum can be seen in the center of the fluctuant lesion.

After a brief discussion of options, the lesion is incised and drained under sterile conditions with lidocaine and epinephrine. Cheesy, odoriferous material is expressed, effectively flattening the lesion.
What is the diagnosis?
DISCUSSION
Epidermal cysts are utterly common, especially in oil-rich areas such as the upper back. They are often mistakenly called sebaceous cysts; however, true sebaceous cysts are quite rare and contain only pure, clear oil.
When ruptured by trauma, epidermal cysts become inflamed and cheesy material leaks into deep tissues. This activates an immune response in which the body sends out white cells to clean up the leakage—what we call inflammation.
There are many types of cysts (eg, acne cysts, ganglion cysts, Bartholin gland cysts) but none resemble epidermal cysts. Providers often mistake epidermal cysts for carbuncles or boils and may prescribe oral or systemic antibiotics, or incise the cysts and pack the space. The truth is that inflamed epidermal cysts do not represent infection—hence the limited area of redness. By contrast, cellulitis or carbuncle would manifest with tenderness and blush of erythema over the entire area.
The fact that this lesion arose from a longstanding antecedent nodule is consistent with the diagnosis, as are the cheesy, odoriferous contents liberated by incision and drainage. Liberating the contents merely buys the patient relief from the pressure and pain, since the cyst wall is still present and will almost certainly fill up again. The ultimate solution is excision after the emptied cyst has had time to shrink back to its original size, which will minimize the scarring. There is no need to pack such cysts after incision and drainage, though they will continue to drain for a few days.
TAKE-HOME LEARNING POINTS
- Epidermal cysts are common, especially in oil-rich areas such as the face, back, chest, and neck.
- Epidermal cysts are often mistakenly called sebaceous cysts, but these are actually quite rare, containing clear sebum (oil) and no cheesy material.
- Even though such inflamed cysts are often mistaken for boils, carbuncles, and abscesses, they have nothing to do with bacteria or infection and therefore do not require antibiotics or packing after incision and drainage.
- For recurrent inflamed cysts, the treatment of choice is complete excision, done only after the cyst has shrunk to its smallest size.
For years, this 33-year-old woman has had a firm, pea-sized nodule on her left upper back. It was never a problem until recently, when it suddenly enlarged and became red, swollen, and tender.
She was prescribed antibiotics (trimethoprim and sulfa) by a provider at her local urgent care center. Dubious of the diagnosis—carbuncle—she sought referral to dermatology.
The patient claims to be in otherwise excellent health, with no history of similar problems. She denies manual manipulation of the lesion.
EXAMINATION
The patient is afebrile and in no distress. On her upper left back is a round, cystic lesion measuring 3.5 cm. It appears swollen and red. The erythema, though impressive, is confined to
the area immediately around the margins. Palpation reveals increased warmth and modest tenderness. A central punctum can be seen in the center of the fluctuant lesion.

After a brief discussion of options, the lesion is incised and drained under sterile conditions with lidocaine and epinephrine. Cheesy, odoriferous material is expressed, effectively flattening the lesion.
What is the diagnosis?
DISCUSSION
Epidermal cysts are utterly common, especially in oil-rich areas such as the upper back. They are often mistakenly called sebaceous cysts; however, true sebaceous cysts are quite rare and contain only pure, clear oil.
When ruptured by trauma, epidermal cysts become inflamed and cheesy material leaks into deep tissues. This activates an immune response in which the body sends out white cells to clean up the leakage—what we call inflammation.
There are many types of cysts (eg, acne cysts, ganglion cysts, Bartholin gland cysts) but none resemble epidermal cysts. Providers often mistake epidermal cysts for carbuncles or boils and may prescribe oral or systemic antibiotics, or incise the cysts and pack the space. The truth is that inflamed epidermal cysts do not represent infection—hence the limited area of redness. By contrast, cellulitis or carbuncle would manifest with tenderness and blush of erythema over the entire area.
The fact that this lesion arose from a longstanding antecedent nodule is consistent with the diagnosis, as are the cheesy, odoriferous contents liberated by incision and drainage. Liberating the contents merely buys the patient relief from the pressure and pain, since the cyst wall is still present and will almost certainly fill up again. The ultimate solution is excision after the emptied cyst has had time to shrink back to its original size, which will minimize the scarring. There is no need to pack such cysts after incision and drainage, though they will continue to drain for a few days.
TAKE-HOME LEARNING POINTS
- Epidermal cysts are common, especially in oil-rich areas such as the face, back, chest, and neck.
- Epidermal cysts are often mistakenly called sebaceous cysts, but these are actually quite rare, containing clear sebum (oil) and no cheesy material.
- Even though such inflamed cysts are often mistaken for boils, carbuncles, and abscesses, they have nothing to do with bacteria or infection and therefore do not require antibiotics or packing after incision and drainage.
- For recurrent inflamed cysts, the treatment of choice is complete excision, done only after the cyst has shrunk to its smallest size.
Improving cancer care through modern portfolio theory
We struggle daily to improve cancer care – to improve our therapeutic outcomes in cancer – as individual physicians and as researchers. We work collectively to disseminate information and collaborate, and there are welcome calls for open data sharing to accelerate progress.1 We enroll patients on clinical trials, or we work in a basic science lab to discover mechanisms of carcinogenesis and potential therapeutic targets. We discuss “n of 1” trials and the “paradigm shift of precision oncology,” and we are optimistic about the future of cancer care.
Leaving the world of biology and clinical trials for a minute, we also can apply economic theory in our never-ending quest to improve cancer outcomes. One area of interest may be modern portfolio theory (MPT), which the economist Harry Markowitz introduced in an essay in 1952 and later won the Nobel Prize for his work.
At least 71 billionaires live in the San Francisco Bay Area, where I live, but 14,000 children (13%) in the area live below the poverty line.3 When there is a range of asset allocations in health care, results can vary not on the basis of the underlying disease state or the quality of the provider, but on access to care. As an example, most pediatric cancers are curable, yet a recent retrospective analysis of data in the SEER-Medicare registry showed that mortality within 1 month of diagnosis of childhood cancer related in part to socioeconomic factors – those patients with a lower socioeconomic status (which correlates with being an ethnic minority in the United States) were more likely to die within a month of diagnosis of their cancer than were patients with a higher socioeconomic status.3 Here is where MPT can transform the cancer outcomes landscape at no additional investment in basic science or costly precision medicine5: by triaging these patients according to their disease state rather than their ability to pay, they could be administered curative chemotherapy, placed on the appropriate clinical trial, and be cured of their cancer like other children of higher socioeconomic status.
My colleagues and I observed a similar trend when we looked at treatment of diffuse large-cell non-Hodgkin lymphoma in Medicare recipients.6 Although the cure rate is as high as 60%-80% with the use of CHOP (cyclophosphamide, doxorubicin, vincristine, prednisolone) or R (rituxin)-CHOP chemotherapy, we found that many patients had received suboptimal chemotherapy. Upon closer examination, we found that there were variations in care by socioeconomic status even in a single-payer system. Thus aspects of cultural literacy and additional efforts for triage need to be developed, but again, application of MPT could be instrumental in improving cancer cure rates by reducing disparities in care by allocating assets to solve access-to-care issues, and curing these patients of their non-Hodgkin lymphoma.
A physician at a Bay Area health care system notes that the open slots in his schedule are triaged by his employer by the patient’s ability to pay – well-insured patients are seen within a few days, but there are very few slots for Medicaid patients, who have to wait weeks or longer to be seen. During this time, their malignancies have time to grow, and potentially metastasize. This may provide suboptimal outcomes for some patients in his community.
We solved this problem at a local hospital where all patients were on Medicaid or uninsured. We triaged patients according to severity of illness, with patients with rapidly growing cancers, particularly curable ones, were brought in as soon as possible and patients with stable benign hematologic conditions seen on a less urgent basis. A social worker and I saw patients together. She would find them resources such as transportation, food, copay assistance to help them through their treatment, and I would optimize their cancer care clinically. On a small scale, this application of MPT (or asset allocation) worked quite well. Perhaps it can be reproduced on a much larger scale. Return on investment relates largely to how you allocate your assets. What’s nice about these applications of MPT is that the return on investment – increasing the cure rate of cancer - is quite large for just a minimal change in asset allocation.
1. Bertagnolli M, Sartor O, Chabner BA, et al. Advantages of a truly open-access data-sharing model. N Engl J Med. 2017;376(12):1178-1181.
2. Baum M. Justice. In: The scepticaemic surgeon: how not to win friends and influence people. New York: Nova Science Pubkishers; November 30, 2014.
3. Glaeser E. Gentfrification and its discontents. Wall Street Journal. May 5, 2017.
4. Green AL, Furutani E, Riberio KB, Galindo CR. Death within 1 month of diagnosis in childhood cancer : analysis of risk factors and scope of the problem. J Clin Oncol. 2017;35(12):1320-1327.
5. McCartney M. Are we too captivated by precision medicine? http://www.bmj.com/content/356/bmj.j1168.long. Published March 9, 2017. Accessed May 12, 2017.
6. Griffiths R, Gleeson M, Knopf K, Danese M. Racial differences in treatment and survival in older patients with diffuse large B-cell lymphoma. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2995801/. Published November 12, 2010. Accessed May 12, 2017.
We struggle daily to improve cancer care – to improve our therapeutic outcomes in cancer – as individual physicians and as researchers. We work collectively to disseminate information and collaborate, and there are welcome calls for open data sharing to accelerate progress.1 We enroll patients on clinical trials, or we work in a basic science lab to discover mechanisms of carcinogenesis and potential therapeutic targets. We discuss “n of 1” trials and the “paradigm shift of precision oncology,” and we are optimistic about the future of cancer care.
Leaving the world of biology and clinical trials for a minute, we also can apply economic theory in our never-ending quest to improve cancer outcomes. One area of interest may be modern portfolio theory (MPT), which the economist Harry Markowitz introduced in an essay in 1952 and later won the Nobel Prize for his work.
At least 71 billionaires live in the San Francisco Bay Area, where I live, but 14,000 children (13%) in the area live below the poverty line.3 When there is a range of asset allocations in health care, results can vary not on the basis of the underlying disease state or the quality of the provider, but on access to care. As an example, most pediatric cancers are curable, yet a recent retrospective analysis of data in the SEER-Medicare registry showed that mortality within 1 month of diagnosis of childhood cancer related in part to socioeconomic factors – those patients with a lower socioeconomic status (which correlates with being an ethnic minority in the United States) were more likely to die within a month of diagnosis of their cancer than were patients with a higher socioeconomic status.3 Here is where MPT can transform the cancer outcomes landscape at no additional investment in basic science or costly precision medicine5: by triaging these patients according to their disease state rather than their ability to pay, they could be administered curative chemotherapy, placed on the appropriate clinical trial, and be cured of their cancer like other children of higher socioeconomic status.
My colleagues and I observed a similar trend when we looked at treatment of diffuse large-cell non-Hodgkin lymphoma in Medicare recipients.6 Although the cure rate is as high as 60%-80% with the use of CHOP (cyclophosphamide, doxorubicin, vincristine, prednisolone) or R (rituxin)-CHOP chemotherapy, we found that many patients had received suboptimal chemotherapy. Upon closer examination, we found that there were variations in care by socioeconomic status even in a single-payer system. Thus aspects of cultural literacy and additional efforts for triage need to be developed, but again, application of MPT could be instrumental in improving cancer cure rates by reducing disparities in care by allocating assets to solve access-to-care issues, and curing these patients of their non-Hodgkin lymphoma.
A physician at a Bay Area health care system notes that the open slots in his schedule are triaged by his employer by the patient’s ability to pay – well-insured patients are seen within a few days, but there are very few slots for Medicaid patients, who have to wait weeks or longer to be seen. During this time, their malignancies have time to grow, and potentially metastasize. This may provide suboptimal outcomes for some patients in his community.
We solved this problem at a local hospital where all patients were on Medicaid or uninsured. We triaged patients according to severity of illness, with patients with rapidly growing cancers, particularly curable ones, were brought in as soon as possible and patients with stable benign hematologic conditions seen on a less urgent basis. A social worker and I saw patients together. She would find them resources such as transportation, food, copay assistance to help them through their treatment, and I would optimize their cancer care clinically. On a small scale, this application of MPT (or asset allocation) worked quite well. Perhaps it can be reproduced on a much larger scale. Return on investment relates largely to how you allocate your assets. What’s nice about these applications of MPT is that the return on investment – increasing the cure rate of cancer - is quite large for just a minimal change in asset allocation.
We struggle daily to improve cancer care – to improve our therapeutic outcomes in cancer – as individual physicians and as researchers. We work collectively to disseminate information and collaborate, and there are welcome calls for open data sharing to accelerate progress.1 We enroll patients on clinical trials, or we work in a basic science lab to discover mechanisms of carcinogenesis and potential therapeutic targets. We discuss “n of 1” trials and the “paradigm shift of precision oncology,” and we are optimistic about the future of cancer care.
Leaving the world of biology and clinical trials for a minute, we also can apply economic theory in our never-ending quest to improve cancer outcomes. One area of interest may be modern portfolio theory (MPT), which the economist Harry Markowitz introduced in an essay in 1952 and later won the Nobel Prize for his work.
At least 71 billionaires live in the San Francisco Bay Area, where I live, but 14,000 children (13%) in the area live below the poverty line.3 When there is a range of asset allocations in health care, results can vary not on the basis of the underlying disease state or the quality of the provider, but on access to care. As an example, most pediatric cancers are curable, yet a recent retrospective analysis of data in the SEER-Medicare registry showed that mortality within 1 month of diagnosis of childhood cancer related in part to socioeconomic factors – those patients with a lower socioeconomic status (which correlates with being an ethnic minority in the United States) were more likely to die within a month of diagnosis of their cancer than were patients with a higher socioeconomic status.3 Here is where MPT can transform the cancer outcomes landscape at no additional investment in basic science or costly precision medicine5: by triaging these patients according to their disease state rather than their ability to pay, they could be administered curative chemotherapy, placed on the appropriate clinical trial, and be cured of their cancer like other children of higher socioeconomic status.
My colleagues and I observed a similar trend when we looked at treatment of diffuse large-cell non-Hodgkin lymphoma in Medicare recipients.6 Although the cure rate is as high as 60%-80% with the use of CHOP (cyclophosphamide, doxorubicin, vincristine, prednisolone) or R (rituxin)-CHOP chemotherapy, we found that many patients had received suboptimal chemotherapy. Upon closer examination, we found that there were variations in care by socioeconomic status even in a single-payer system. Thus aspects of cultural literacy and additional efforts for triage need to be developed, but again, application of MPT could be instrumental in improving cancer cure rates by reducing disparities in care by allocating assets to solve access-to-care issues, and curing these patients of their non-Hodgkin lymphoma.
A physician at a Bay Area health care system notes that the open slots in his schedule are triaged by his employer by the patient’s ability to pay – well-insured patients are seen within a few days, but there are very few slots for Medicaid patients, who have to wait weeks or longer to be seen. During this time, their malignancies have time to grow, and potentially metastasize. This may provide suboptimal outcomes for some patients in his community.
We solved this problem at a local hospital where all patients were on Medicaid or uninsured. We triaged patients according to severity of illness, with patients with rapidly growing cancers, particularly curable ones, were brought in as soon as possible and patients with stable benign hematologic conditions seen on a less urgent basis. A social worker and I saw patients together. She would find them resources such as transportation, food, copay assistance to help them through their treatment, and I would optimize their cancer care clinically. On a small scale, this application of MPT (or asset allocation) worked quite well. Perhaps it can be reproduced on a much larger scale. Return on investment relates largely to how you allocate your assets. What’s nice about these applications of MPT is that the return on investment – increasing the cure rate of cancer - is quite large for just a minimal change in asset allocation.
1. Bertagnolli M, Sartor O, Chabner BA, et al. Advantages of a truly open-access data-sharing model. N Engl J Med. 2017;376(12):1178-1181.
2. Baum M. Justice. In: The scepticaemic surgeon: how not to win friends and influence people. New York: Nova Science Pubkishers; November 30, 2014.
3. Glaeser E. Gentfrification and its discontents. Wall Street Journal. May 5, 2017.
4. Green AL, Furutani E, Riberio KB, Galindo CR. Death within 1 month of diagnosis in childhood cancer : analysis of risk factors and scope of the problem. J Clin Oncol. 2017;35(12):1320-1327.
5. McCartney M. Are we too captivated by precision medicine? http://www.bmj.com/content/356/bmj.j1168.long. Published March 9, 2017. Accessed May 12, 2017.
6. Griffiths R, Gleeson M, Knopf K, Danese M. Racial differences in treatment and survival in older patients with diffuse large B-cell lymphoma. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2995801/. Published November 12, 2010. Accessed May 12, 2017.
1. Bertagnolli M, Sartor O, Chabner BA, et al. Advantages of a truly open-access data-sharing model. N Engl J Med. 2017;376(12):1178-1181.
2. Baum M. Justice. In: The scepticaemic surgeon: how not to win friends and influence people. New York: Nova Science Pubkishers; November 30, 2014.
3. Glaeser E. Gentfrification and its discontents. Wall Street Journal. May 5, 2017.
4. Green AL, Furutani E, Riberio KB, Galindo CR. Death within 1 month of diagnosis in childhood cancer : analysis of risk factors and scope of the problem. J Clin Oncol. 2017;35(12):1320-1327.
5. McCartney M. Are we too captivated by precision medicine? http://www.bmj.com/content/356/bmj.j1168.long. Published March 9, 2017. Accessed May 12, 2017.
6. Griffiths R, Gleeson M, Knopf K, Danese M. Racial differences in treatment and survival in older patients with diffuse large B-cell lymphoma. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2995801/. Published November 12, 2010. Accessed May 12, 2017.
Metastatic Kaposi sarcoma with osseous involvement in a patient with AIDS
Kaposi sarcoma is an AIDS-defining illness associated with human herpes virus-8 (HHV-8) co-infection. It was described in 1872 by the Hungarian dermatologist Mortiz Kaposi, and was an isolated and sporadic occurrence before the emergence of HIV infection and AIDS.1 It was first affiliated as an AIDS-associated neoplasm in 1981.1 Kaposi sarcoma is a systemic disease that can present with cutaneous lesions with or without internal involvement. There are four subtypes: Classic, African endemic, AIDS-related (CD4 count, <200), and Kaposi sarcoma in iatrogenically immunosuppressed patients. The disease has the propensity to manifest in the skin and gastro-intestinal and respiratory tracts, and osseous involvement is rarely encountered. We present here the case of an AIDS-positive man with generalized bone pain as a result of metastasis from Kaposi sarcoma. Our discussion includes the epidemiological, clinical, pathological, and radiological facets of AIDS-related Kaposi sarcoma, and the anomaly of osseous involvement.
Case presentation and summary
He restarted his previous HAART regimen in March 2016, and was subsequently started on chemotherapy with liposomal doxorubicin (50 mg [20 mg/m2] in 250 ml D5W IV every 2 weeks) because of his extensive disease.2 He completed 6 cycles by June 2016. However, he returned in July 2016 with worsening back pain. A repeat CT scan revealed significant improvement in the disseminated lymphadenopathy, but worsening osseous metastatic disease was seen in the lumbar, thoracic, and pelvic regions. A pelvic lytic lesion biopsy revealed Kaposi sarcoma; pathology showed spindle cells positive for CD34, CD31, and HHV-8 (Figure 2). The patient received palliative radiation to the spine, aiding in pain management and ambulatory dysfunction. He continued with his noncompliance with all medications and outpatient follow-ups, and succumbed to his disease burden.
Discussion
Kaposi sarcoma is a low-grade mesenchymal tumor that involves the blood and lymphatic vessels.3 Its association with AIDS was revealed in the early 1980s at the start of the HIV epidemic in the United States. In 1994, Chang and colleagues discovered the association between Karposi sarcoma and HHV-8 by isolating DNA fragments of HHV in Kaposi sarcoma tumors from AIDS patients.4 The mode of transmission of HHV-8 has not been fully decoded. It has been presumed that adult homosexual contact continues to be an important route of transmission, inferring a common route of infection. In 1990, the overall risk of developing Kaposi sarcoma in AIDS patients was 20,000 times greater than it was in the general population, and 300 times greater than in other immunosuppressed patients.5 This suggests an increase in incidence, in direct relation, with a decrease in the CD4 count.
Kaposi sarcoma can present with a range of clinical features, from negligible cutaneous lesions to a hastily progressing neoplasm. Involvement in the musculoskeletal system is infrequent, but encountered increasingly in the AIDS-related subtype. Moreover, it is recurrently observed in the African population.6 In one of the largest reviews to date exploring Kaposi sarcoma involving the musculoskeletal system, Caponetti and colleagues observed the greatest osseous involvement distinctly in patients with CD4 and T-cell counts below 100 cells/mm3.6
Kaposi sarcoma musculoskeletal involvement, specifically bone, is atypical. If it does occur, it usually manifests as a result of contiguous invasion from an adjacent nonosseous lesion. Caponetti and colleagues that isolated osseous Kaposi sarcoma lesions (with no overlying skin lesion) were found to be more likely to be associated with AIDS in the review by Caponetti and colleagues.6 As in our patient, it is also typically a manifestation of more widely disseminated disease.7
Most of the osseous lytic lesions in AIDS patients are located in the axial skeleton. Radiological features of musculoskeletal Kaposi sarcoma are variable. As observed by Caponetti and colleagues, Kaposi sarcoma lesions can appear as a periosteal reaction, cortical erosions, osteolysis, or osseous destruction, with irregular-shaped cortical erosions being most typical.6 Despite their osteolytic features, Kaposi sarcoma lesions are often not visualized by conventional radiography.6 The preferred imaging for identification of lytic bone changes is CT (Figure 3). Magnetic resonance imaging can also help distinguish marrow abnormalities as well as adjacent soft tissues masses. Radiologically, Kaposi sarcoma osseous lesions have parallel features to bacillary angiomatosis, tuberculosis, or lymphoma.8 Therefore, biopsy of the lesion is essential in establishing the diagnosis of Kaposi sarcoma.
In theory, there should be clinical improvement in Kaposi sarcoma when immunity is restored. Cancers caused by the Epstein-Barr virus and Kaposi sarcoma-associated herpes virus may eventually also be preventable with vaccines.10
There is rarely bone involvement without the foreshadowing of a poor prognosis. Erroneous patient care may inevitably arise from Kaposi sarcoma in uncharacteristic sites. A differential of Kaposi sarcoma should be included if a patient with AIDS presents with osteolytic lesions on imaging. Biopsying the lesion cements the diagnosis and eliminates the possibility of mimicry conditions such as bacillary angiomatosis, benign vascular lesions, and angiosarcoma. As of today, a HAART regimen remains the standard initial care for patients with Kaposi sarcoma.
1. Radu O, Pantanowitz L. Kaposi sarcoma. Arch Pathol Lab Med. 2013;137:289-294.
2. Northfelt DW, Dezube BJ, Thommes JA, et al. Pegylated-liposomal doxorubicin versus doxorubicin, bleomycin, and vincristine in the treatment of AIDS-related Kaposi sarcoma: results of a randomized phase III clinical trial. J Clin Oncol. 1998;16(7):2445-2451.
3. Restrepo CS, Martinez S, Lemos JA, et al. Imaging manifestations of Kaposi sarcoma. RadioGraphics. 2006;26:1169-1185.
4. Chang Y, Cesarman E, Pessin MS, et al. Identification of herpes virus-like DNA sequences in AIDS-associated Kaposi sarcoma. Science. 1994;266:1865-1869.
5. Beral V, Peterman TA, Berkelman RL, Jaffe HW. Kaposi sarcoma among persons with AIDS: a sexually transmitted infection? Lancet. 1990;335:123-128.
6. Caponetti G, Dezube BJ, Restrepo CS, Pantanowitz I. Kaposi sarcoma of the musculoskeletal system: a review of 66 patients. Cancer. 2007;109(6):1040-1052.
7. Krishna G, Chitkara RK. Osseous Kaposi sarcoma. JAMA. 2003;286(9):1106.
8. Thanos L, Mylona S, Kalioras V, Pomoni M, Batakis N. Osseous Kaposi sarcoma in an HIV-positive patient. Skeletal Radiol. 2004;33(4):241-243.
9. Guiholt A, Dupin N, Marcelin AG, et al. Low T-cell response to human herpesvirus 8 in patients with AIDS-related and classic Kaposi sarcoma. J Infect Dis. 2006;194(8):1078-1088.
10. Gopal S, Achenbach CJ, Yanik EL, Dither DP, Eron JJ, Engels EA. Moving forward in HIV-associated cancer. J Clin Oncol. 2014;32(9):876-880.
Kaposi sarcoma is an AIDS-defining illness associated with human herpes virus-8 (HHV-8) co-infection. It was described in 1872 by the Hungarian dermatologist Mortiz Kaposi, and was an isolated and sporadic occurrence before the emergence of HIV infection and AIDS.1 It was first affiliated as an AIDS-associated neoplasm in 1981.1 Kaposi sarcoma is a systemic disease that can present with cutaneous lesions with or without internal involvement. There are four subtypes: Classic, African endemic, AIDS-related (CD4 count, <200), and Kaposi sarcoma in iatrogenically immunosuppressed patients. The disease has the propensity to manifest in the skin and gastro-intestinal and respiratory tracts, and osseous involvement is rarely encountered. We present here the case of an AIDS-positive man with generalized bone pain as a result of metastasis from Kaposi sarcoma. Our discussion includes the epidemiological, clinical, pathological, and radiological facets of AIDS-related Kaposi sarcoma, and the anomaly of osseous involvement.
Case presentation and summary
He restarted his previous HAART regimen in March 2016, and was subsequently started on chemotherapy with liposomal doxorubicin (50 mg [20 mg/m2] in 250 ml D5W IV every 2 weeks) because of his extensive disease.2 He completed 6 cycles by June 2016. However, he returned in July 2016 with worsening back pain. A repeat CT scan revealed significant improvement in the disseminated lymphadenopathy, but worsening osseous metastatic disease was seen in the lumbar, thoracic, and pelvic regions. A pelvic lytic lesion biopsy revealed Kaposi sarcoma; pathology showed spindle cells positive for CD34, CD31, and HHV-8 (Figure 2). The patient received palliative radiation to the spine, aiding in pain management and ambulatory dysfunction. He continued with his noncompliance with all medications and outpatient follow-ups, and succumbed to his disease burden.
Discussion
Kaposi sarcoma is a low-grade mesenchymal tumor that involves the blood and lymphatic vessels.3 Its association with AIDS was revealed in the early 1980s at the start of the HIV epidemic in the United States. In 1994, Chang and colleagues discovered the association between Karposi sarcoma and HHV-8 by isolating DNA fragments of HHV in Kaposi sarcoma tumors from AIDS patients.4 The mode of transmission of HHV-8 has not been fully decoded. It has been presumed that adult homosexual contact continues to be an important route of transmission, inferring a common route of infection. In 1990, the overall risk of developing Kaposi sarcoma in AIDS patients was 20,000 times greater than it was in the general population, and 300 times greater than in other immunosuppressed patients.5 This suggests an increase in incidence, in direct relation, with a decrease in the CD4 count.
Kaposi sarcoma can present with a range of clinical features, from negligible cutaneous lesions to a hastily progressing neoplasm. Involvement in the musculoskeletal system is infrequent, but encountered increasingly in the AIDS-related subtype. Moreover, it is recurrently observed in the African population.6 In one of the largest reviews to date exploring Kaposi sarcoma involving the musculoskeletal system, Caponetti and colleagues observed the greatest osseous involvement distinctly in patients with CD4 and T-cell counts below 100 cells/mm3.6
Kaposi sarcoma musculoskeletal involvement, specifically bone, is atypical. If it does occur, it usually manifests as a result of contiguous invasion from an adjacent nonosseous lesion. Caponetti and colleagues that isolated osseous Kaposi sarcoma lesions (with no overlying skin lesion) were found to be more likely to be associated with AIDS in the review by Caponetti and colleagues.6 As in our patient, it is also typically a manifestation of more widely disseminated disease.7
Most of the osseous lytic lesions in AIDS patients are located in the axial skeleton. Radiological features of musculoskeletal Kaposi sarcoma are variable. As observed by Caponetti and colleagues, Kaposi sarcoma lesions can appear as a periosteal reaction, cortical erosions, osteolysis, or osseous destruction, with irregular-shaped cortical erosions being most typical.6 Despite their osteolytic features, Kaposi sarcoma lesions are often not visualized by conventional radiography.6 The preferred imaging for identification of lytic bone changes is CT (Figure 3). Magnetic resonance imaging can also help distinguish marrow abnormalities as well as adjacent soft tissues masses. Radiologically, Kaposi sarcoma osseous lesions have parallel features to bacillary angiomatosis, tuberculosis, or lymphoma.8 Therefore, biopsy of the lesion is essential in establishing the diagnosis of Kaposi sarcoma.
In theory, there should be clinical improvement in Kaposi sarcoma when immunity is restored. Cancers caused by the Epstein-Barr virus and Kaposi sarcoma-associated herpes virus may eventually also be preventable with vaccines.10
There is rarely bone involvement without the foreshadowing of a poor prognosis. Erroneous patient care may inevitably arise from Kaposi sarcoma in uncharacteristic sites. A differential of Kaposi sarcoma should be included if a patient with AIDS presents with osteolytic lesions on imaging. Biopsying the lesion cements the diagnosis and eliminates the possibility of mimicry conditions such as bacillary angiomatosis, benign vascular lesions, and angiosarcoma. As of today, a HAART regimen remains the standard initial care for patients with Kaposi sarcoma.
Kaposi sarcoma is an AIDS-defining illness associated with human herpes virus-8 (HHV-8) co-infection. It was described in 1872 by the Hungarian dermatologist Mortiz Kaposi, and was an isolated and sporadic occurrence before the emergence of HIV infection and AIDS.1 It was first affiliated as an AIDS-associated neoplasm in 1981.1 Kaposi sarcoma is a systemic disease that can present with cutaneous lesions with or without internal involvement. There are four subtypes: Classic, African endemic, AIDS-related (CD4 count, <200), and Kaposi sarcoma in iatrogenically immunosuppressed patients. The disease has the propensity to manifest in the skin and gastro-intestinal and respiratory tracts, and osseous involvement is rarely encountered. We present here the case of an AIDS-positive man with generalized bone pain as a result of metastasis from Kaposi sarcoma. Our discussion includes the epidemiological, clinical, pathological, and radiological facets of AIDS-related Kaposi sarcoma, and the anomaly of osseous involvement.
Case presentation and summary
He restarted his previous HAART regimen in March 2016, and was subsequently started on chemotherapy with liposomal doxorubicin (50 mg [20 mg/m2] in 250 ml D5W IV every 2 weeks) because of his extensive disease.2 He completed 6 cycles by June 2016. However, he returned in July 2016 with worsening back pain. A repeat CT scan revealed significant improvement in the disseminated lymphadenopathy, but worsening osseous metastatic disease was seen in the lumbar, thoracic, and pelvic regions. A pelvic lytic lesion biopsy revealed Kaposi sarcoma; pathology showed spindle cells positive for CD34, CD31, and HHV-8 (Figure 2). The patient received palliative radiation to the spine, aiding in pain management and ambulatory dysfunction. He continued with his noncompliance with all medications and outpatient follow-ups, and succumbed to his disease burden.
Discussion
Kaposi sarcoma is a low-grade mesenchymal tumor that involves the blood and lymphatic vessels.3 Its association with AIDS was revealed in the early 1980s at the start of the HIV epidemic in the United States. In 1994, Chang and colleagues discovered the association between Karposi sarcoma and HHV-8 by isolating DNA fragments of HHV in Kaposi sarcoma tumors from AIDS patients.4 The mode of transmission of HHV-8 has not been fully decoded. It has been presumed that adult homosexual contact continues to be an important route of transmission, inferring a common route of infection. In 1990, the overall risk of developing Kaposi sarcoma in AIDS patients was 20,000 times greater than it was in the general population, and 300 times greater than in other immunosuppressed patients.5 This suggests an increase in incidence, in direct relation, with a decrease in the CD4 count.
Kaposi sarcoma can present with a range of clinical features, from negligible cutaneous lesions to a hastily progressing neoplasm. Involvement in the musculoskeletal system is infrequent, but encountered increasingly in the AIDS-related subtype. Moreover, it is recurrently observed in the African population.6 In one of the largest reviews to date exploring Kaposi sarcoma involving the musculoskeletal system, Caponetti and colleagues observed the greatest osseous involvement distinctly in patients with CD4 and T-cell counts below 100 cells/mm3.6
Kaposi sarcoma musculoskeletal involvement, specifically bone, is atypical. If it does occur, it usually manifests as a result of contiguous invasion from an adjacent nonosseous lesion. Caponetti and colleagues that isolated osseous Kaposi sarcoma lesions (with no overlying skin lesion) were found to be more likely to be associated with AIDS in the review by Caponetti and colleagues.6 As in our patient, it is also typically a manifestation of more widely disseminated disease.7
Most of the osseous lytic lesions in AIDS patients are located in the axial skeleton. Radiological features of musculoskeletal Kaposi sarcoma are variable. As observed by Caponetti and colleagues, Kaposi sarcoma lesions can appear as a periosteal reaction, cortical erosions, osteolysis, or osseous destruction, with irregular-shaped cortical erosions being most typical.6 Despite their osteolytic features, Kaposi sarcoma lesions are often not visualized by conventional radiography.6 The preferred imaging for identification of lytic bone changes is CT (Figure 3). Magnetic resonance imaging can also help distinguish marrow abnormalities as well as adjacent soft tissues masses. Radiologically, Kaposi sarcoma osseous lesions have parallel features to bacillary angiomatosis, tuberculosis, or lymphoma.8 Therefore, biopsy of the lesion is essential in establishing the diagnosis of Kaposi sarcoma.
In theory, there should be clinical improvement in Kaposi sarcoma when immunity is restored. Cancers caused by the Epstein-Barr virus and Kaposi sarcoma-associated herpes virus may eventually also be preventable with vaccines.10
There is rarely bone involvement without the foreshadowing of a poor prognosis. Erroneous patient care may inevitably arise from Kaposi sarcoma in uncharacteristic sites. A differential of Kaposi sarcoma should be included if a patient with AIDS presents with osteolytic lesions on imaging. Biopsying the lesion cements the diagnosis and eliminates the possibility of mimicry conditions such as bacillary angiomatosis, benign vascular lesions, and angiosarcoma. As of today, a HAART regimen remains the standard initial care for patients with Kaposi sarcoma.
1. Radu O, Pantanowitz L. Kaposi sarcoma. Arch Pathol Lab Med. 2013;137:289-294.
2. Northfelt DW, Dezube BJ, Thommes JA, et al. Pegylated-liposomal doxorubicin versus doxorubicin, bleomycin, and vincristine in the treatment of AIDS-related Kaposi sarcoma: results of a randomized phase III clinical trial. J Clin Oncol. 1998;16(7):2445-2451.
3. Restrepo CS, Martinez S, Lemos JA, et al. Imaging manifestations of Kaposi sarcoma. RadioGraphics. 2006;26:1169-1185.
4. Chang Y, Cesarman E, Pessin MS, et al. Identification of herpes virus-like DNA sequences in AIDS-associated Kaposi sarcoma. Science. 1994;266:1865-1869.
5. Beral V, Peterman TA, Berkelman RL, Jaffe HW. Kaposi sarcoma among persons with AIDS: a sexually transmitted infection? Lancet. 1990;335:123-128.
6. Caponetti G, Dezube BJ, Restrepo CS, Pantanowitz I. Kaposi sarcoma of the musculoskeletal system: a review of 66 patients. Cancer. 2007;109(6):1040-1052.
7. Krishna G, Chitkara RK. Osseous Kaposi sarcoma. JAMA. 2003;286(9):1106.
8. Thanos L, Mylona S, Kalioras V, Pomoni M, Batakis N. Osseous Kaposi sarcoma in an HIV-positive patient. Skeletal Radiol. 2004;33(4):241-243.
9. Guiholt A, Dupin N, Marcelin AG, et al. Low T-cell response to human herpesvirus 8 in patients with AIDS-related and classic Kaposi sarcoma. J Infect Dis. 2006;194(8):1078-1088.
10. Gopal S, Achenbach CJ, Yanik EL, Dither DP, Eron JJ, Engels EA. Moving forward in HIV-associated cancer. J Clin Oncol. 2014;32(9):876-880.
1. Radu O, Pantanowitz L. Kaposi sarcoma. Arch Pathol Lab Med. 2013;137:289-294.
2. Northfelt DW, Dezube BJ, Thommes JA, et al. Pegylated-liposomal doxorubicin versus doxorubicin, bleomycin, and vincristine in the treatment of AIDS-related Kaposi sarcoma: results of a randomized phase III clinical trial. J Clin Oncol. 1998;16(7):2445-2451.
3. Restrepo CS, Martinez S, Lemos JA, et al. Imaging manifestations of Kaposi sarcoma. RadioGraphics. 2006;26:1169-1185.
4. Chang Y, Cesarman E, Pessin MS, et al. Identification of herpes virus-like DNA sequences in AIDS-associated Kaposi sarcoma. Science. 1994;266:1865-1869.
5. Beral V, Peterman TA, Berkelman RL, Jaffe HW. Kaposi sarcoma among persons with AIDS: a sexually transmitted infection? Lancet. 1990;335:123-128.
6. Caponetti G, Dezube BJ, Restrepo CS, Pantanowitz I. Kaposi sarcoma of the musculoskeletal system: a review of 66 patients. Cancer. 2007;109(6):1040-1052.
7. Krishna G, Chitkara RK. Osseous Kaposi sarcoma. JAMA. 2003;286(9):1106.
8. Thanos L, Mylona S, Kalioras V, Pomoni M, Batakis N. Osseous Kaposi sarcoma in an HIV-positive patient. Skeletal Radiol. 2004;33(4):241-243.
9. Guiholt A, Dupin N, Marcelin AG, et al. Low T-cell response to human herpesvirus 8 in patients with AIDS-related and classic Kaposi sarcoma. J Infect Dis. 2006;194(8):1078-1088.
10. Gopal S, Achenbach CJ, Yanik EL, Dither DP, Eron JJ, Engels EA. Moving forward in HIV-associated cancer. J Clin Oncol. 2014;32(9):876-880.
T-cell product improves outcomes of haplo-HSCT
MADRID—Updated results of a phase 1/2 study suggest the T-cell product BPX-501 lowers the risks associated with haploidentical hematopoietic stem cell transplant (haplo-HSCT).
In this ongoing study, researchers are testing BPX-501 in pediatric patients undergoing haplo-HSCT to treat a range of hematologic disorders.
Patients treated thus far have experienced rapid engraftment and early hospital discharge, a low rate of acute graft-versus-host disease (GHVD), no extensive chronic GVHD, and a low rate of transplant-related mortality at 180 days.
“The combination of haploidentical transplantation and BPX-501 infusion is an effective strategy for children in need of an allograft lacking a compatible donor,” said study investigator Mattia Algeri, MD, of Ospedale Pediatrico Bambino Gesù in Rome, Italy.
Dr Algeri presented these results during the Presidential Symposium at the 22nd Congress of the European Hematology Association (EHA) as abstract S146.
The research was sponsored by Bellicum Pharmaceuticals, Inc., the company developing BPX-501.
About BPX-501
BPX-501 consists of genetically modified donor T cells incorporating the CaspaCIDe safety switch, which is designed to eliminate the T cells in the event of toxicity.
Rimiducid is used to activate the CaspaCIDe safety switch, which consists of the CID-binding domain coupled to the signaling domain of caspase-9, an enzyme that is part of the apoptotic pathway.
The goal of this therapy is to allow physicians to more safely perform haplo-HSCTs.
Patients
Dr Algeri and his colleagues have tested BPX-501 in 98 pediatric patients treated at centers in Europe and the US.
Fifty-nine patients had non-malignant conditions, including primary immune deficiency (n=26), thalassemia major (n=8), sickle cell disease (n=5), Diamond-Blackfan anemia (n=2), Swachman-Diamond syndrome (n=1), Fanconi anemia (n=9), hemophagocytic lymphohistiocytosis (n=6), aplastic anemia (n=1), and osteoporosis (n=1).
Thirty-nine patients had malignant conditions, including acute lymphoblastic leukemia (ALL, n=21), acute myeloid leukemia (AML, n=14), myelodysplastic syndromes (MDS, n=3), and non-Hodgkin lymphoma (NHL, n=1).
The patients received BPX-501 after an alpha/beta T-cell-depleted haplo-HSCT. All patients had at least 6 months of follow-up.
Overall results
Ninety-five percent of the patients engrafted (93/98), and the researchers said they observed rapid recovery of T cells, B cells, and immunoglobulins.
At 180 days, the incidence of transplant-related mortality was 5%, and there were no cases of post-transplant lymphoproliferative disorder.
The cumulative incidence of grade 2-4 acute GVHD was 14%. For patients with at least 1 year of follow-up, the cumulative incidence of chronic GVHD at 1 year was 3%.
Eleven patients received rimiducid—10 who had uncontrollable acute GVHD and 1 who developed late acute GVHD. In all of these patients, GVHD resolved and has not recurred.
There were no adverse events associated with BPX-501 or rimiducid.
European cohort
Dr Algeri presented more detailed data on the 61 patients treated at centers in Europe.
Fifteen of these patients had ALL, 10 had AML, 16 had primary immune deficiency, 7 had thalassemia major, 1 had sickle cell disease, 2 had Diamond-Blackfan anemia, 5 had Fanconi anemia, 4 had hemophagocytic lymphohistiocytosis, and 1 had osteoporosis.
Their median age was 4.8 (range, 0.25-17), and 56% were male. The patients received busulfan-based conditioning (41%), total body irradiation (36%), treosulfan-based conditioning (18%), and other conditioning (5%).
Ninety-five percent of the patients had a parent donor, and the other 5% had a sibling donor. The median donor age was 36 (range, 19-50).
The patients’ median time to neutrophil recovery was 15 days (range, 9-75), and their median time to platelet recovery was 10 days (range, 4-64). Their median time to discharge was 25 days (range, 14-122).
The cumulative incidence of acute grade 2-4 GVHD was 9.9%, and the cumulative incidence of acute grade 3-4 GVHD was 3.3%.
There were no cases of transplant-related mortality at 180 days and no cases of extensive chronic GVHD.
“These preliminary data compare favorably to previously published data on matched, unrelated donor transplantation,” Dr Algeri said. “And for this reason, an observational matched, unrelated donor study is being initiated to enable comparison of the safety and efficacy of haploidentical transplantation and BPX-501 infusion to the standard of care for patients without a matched sibling donor.” ![]()
MADRID—Updated results of a phase 1/2 study suggest the T-cell product BPX-501 lowers the risks associated with haploidentical hematopoietic stem cell transplant (haplo-HSCT).
In this ongoing study, researchers are testing BPX-501 in pediatric patients undergoing haplo-HSCT to treat a range of hematologic disorders.
Patients treated thus far have experienced rapid engraftment and early hospital discharge, a low rate of acute graft-versus-host disease (GHVD), no extensive chronic GVHD, and a low rate of transplant-related mortality at 180 days.
“The combination of haploidentical transplantation and BPX-501 infusion is an effective strategy for children in need of an allograft lacking a compatible donor,” said study investigator Mattia Algeri, MD, of Ospedale Pediatrico Bambino Gesù in Rome, Italy.
Dr Algeri presented these results during the Presidential Symposium at the 22nd Congress of the European Hematology Association (EHA) as abstract S146.
The research was sponsored by Bellicum Pharmaceuticals, Inc., the company developing BPX-501.
About BPX-501
BPX-501 consists of genetically modified donor T cells incorporating the CaspaCIDe safety switch, which is designed to eliminate the T cells in the event of toxicity.
Rimiducid is used to activate the CaspaCIDe safety switch, which consists of the CID-binding domain coupled to the signaling domain of caspase-9, an enzyme that is part of the apoptotic pathway.
The goal of this therapy is to allow physicians to more safely perform haplo-HSCTs.
Patients
Dr Algeri and his colleagues have tested BPX-501 in 98 pediatric patients treated at centers in Europe and the US.
Fifty-nine patients had non-malignant conditions, including primary immune deficiency (n=26), thalassemia major (n=8), sickle cell disease (n=5), Diamond-Blackfan anemia (n=2), Swachman-Diamond syndrome (n=1), Fanconi anemia (n=9), hemophagocytic lymphohistiocytosis (n=6), aplastic anemia (n=1), and osteoporosis (n=1).
Thirty-nine patients had malignant conditions, including acute lymphoblastic leukemia (ALL, n=21), acute myeloid leukemia (AML, n=14), myelodysplastic syndromes (MDS, n=3), and non-Hodgkin lymphoma (NHL, n=1).
The patients received BPX-501 after an alpha/beta T-cell-depleted haplo-HSCT. All patients had at least 6 months of follow-up.
Overall results
Ninety-five percent of the patients engrafted (93/98), and the researchers said they observed rapid recovery of T cells, B cells, and immunoglobulins.
At 180 days, the incidence of transplant-related mortality was 5%, and there were no cases of post-transplant lymphoproliferative disorder.
The cumulative incidence of grade 2-4 acute GVHD was 14%. For patients with at least 1 year of follow-up, the cumulative incidence of chronic GVHD at 1 year was 3%.
Eleven patients received rimiducid—10 who had uncontrollable acute GVHD and 1 who developed late acute GVHD. In all of these patients, GVHD resolved and has not recurred.
There were no adverse events associated with BPX-501 or rimiducid.
European cohort
Dr Algeri presented more detailed data on the 61 patients treated at centers in Europe.
Fifteen of these patients had ALL, 10 had AML, 16 had primary immune deficiency, 7 had thalassemia major, 1 had sickle cell disease, 2 had Diamond-Blackfan anemia, 5 had Fanconi anemia, 4 had hemophagocytic lymphohistiocytosis, and 1 had osteoporosis.
Their median age was 4.8 (range, 0.25-17), and 56% were male. The patients received busulfan-based conditioning (41%), total body irradiation (36%), treosulfan-based conditioning (18%), and other conditioning (5%).
Ninety-five percent of the patients had a parent donor, and the other 5% had a sibling donor. The median donor age was 36 (range, 19-50).
The patients’ median time to neutrophil recovery was 15 days (range, 9-75), and their median time to platelet recovery was 10 days (range, 4-64). Their median time to discharge was 25 days (range, 14-122).
The cumulative incidence of acute grade 2-4 GVHD was 9.9%, and the cumulative incidence of acute grade 3-4 GVHD was 3.3%.
There were no cases of transplant-related mortality at 180 days and no cases of extensive chronic GVHD.
“These preliminary data compare favorably to previously published data on matched, unrelated donor transplantation,” Dr Algeri said. “And for this reason, an observational matched, unrelated donor study is being initiated to enable comparison of the safety and efficacy of haploidentical transplantation and BPX-501 infusion to the standard of care for patients without a matched sibling donor.” ![]()
MADRID—Updated results of a phase 1/2 study suggest the T-cell product BPX-501 lowers the risks associated with haploidentical hematopoietic stem cell transplant (haplo-HSCT).
In this ongoing study, researchers are testing BPX-501 in pediatric patients undergoing haplo-HSCT to treat a range of hematologic disorders.
Patients treated thus far have experienced rapid engraftment and early hospital discharge, a low rate of acute graft-versus-host disease (GHVD), no extensive chronic GVHD, and a low rate of transplant-related mortality at 180 days.
“The combination of haploidentical transplantation and BPX-501 infusion is an effective strategy for children in need of an allograft lacking a compatible donor,” said study investigator Mattia Algeri, MD, of Ospedale Pediatrico Bambino Gesù in Rome, Italy.
Dr Algeri presented these results during the Presidential Symposium at the 22nd Congress of the European Hematology Association (EHA) as abstract S146.
The research was sponsored by Bellicum Pharmaceuticals, Inc., the company developing BPX-501.
About BPX-501
BPX-501 consists of genetically modified donor T cells incorporating the CaspaCIDe safety switch, which is designed to eliminate the T cells in the event of toxicity.
Rimiducid is used to activate the CaspaCIDe safety switch, which consists of the CID-binding domain coupled to the signaling domain of caspase-9, an enzyme that is part of the apoptotic pathway.
The goal of this therapy is to allow physicians to more safely perform haplo-HSCTs.
Patients
Dr Algeri and his colleagues have tested BPX-501 in 98 pediatric patients treated at centers in Europe and the US.
Fifty-nine patients had non-malignant conditions, including primary immune deficiency (n=26), thalassemia major (n=8), sickle cell disease (n=5), Diamond-Blackfan anemia (n=2), Swachman-Diamond syndrome (n=1), Fanconi anemia (n=9), hemophagocytic lymphohistiocytosis (n=6), aplastic anemia (n=1), and osteoporosis (n=1).
Thirty-nine patients had malignant conditions, including acute lymphoblastic leukemia (ALL, n=21), acute myeloid leukemia (AML, n=14), myelodysplastic syndromes (MDS, n=3), and non-Hodgkin lymphoma (NHL, n=1).
The patients received BPX-501 after an alpha/beta T-cell-depleted haplo-HSCT. All patients had at least 6 months of follow-up.
Overall results
Ninety-five percent of the patients engrafted (93/98), and the researchers said they observed rapid recovery of T cells, B cells, and immunoglobulins.
At 180 days, the incidence of transplant-related mortality was 5%, and there were no cases of post-transplant lymphoproliferative disorder.
The cumulative incidence of grade 2-4 acute GVHD was 14%. For patients with at least 1 year of follow-up, the cumulative incidence of chronic GVHD at 1 year was 3%.
Eleven patients received rimiducid—10 who had uncontrollable acute GVHD and 1 who developed late acute GVHD. In all of these patients, GVHD resolved and has not recurred.
There were no adverse events associated with BPX-501 or rimiducid.
European cohort
Dr Algeri presented more detailed data on the 61 patients treated at centers in Europe.
Fifteen of these patients had ALL, 10 had AML, 16 had primary immune deficiency, 7 had thalassemia major, 1 had sickle cell disease, 2 had Diamond-Blackfan anemia, 5 had Fanconi anemia, 4 had hemophagocytic lymphohistiocytosis, and 1 had osteoporosis.
Their median age was 4.8 (range, 0.25-17), and 56% were male. The patients received busulfan-based conditioning (41%), total body irradiation (36%), treosulfan-based conditioning (18%), and other conditioning (5%).
Ninety-five percent of the patients had a parent donor, and the other 5% had a sibling donor. The median donor age was 36 (range, 19-50).
The patients’ median time to neutrophil recovery was 15 days (range, 9-75), and their median time to platelet recovery was 10 days (range, 4-64). Their median time to discharge was 25 days (range, 14-122).
The cumulative incidence of acute grade 2-4 GVHD was 9.9%, and the cumulative incidence of acute grade 3-4 GVHD was 3.3%.
There were no cases of transplant-related mortality at 180 days and no cases of extensive chronic GVHD.
“These preliminary data compare favorably to previously published data on matched, unrelated donor transplantation,” Dr Algeri said. “And for this reason, an observational matched, unrelated donor study is being initiated to enable comparison of the safety and efficacy of haploidentical transplantation and BPX-501 infusion to the standard of care for patients without a matched sibling donor.” ![]()
Single-dose NEPA found non-inferior to aprepitant/granisetron
WASHINGTON, DC—In a head-to-head study comparing a single-dose oral antiemetic to a 3-day oral regimen, the single dose has shown itself to be non-inferior to the multi-day regimen in preventing chemotherapy-induced nausea and vomiting (CINV).
The investigators evaluated netupitant/palonosetron (NEPA) against aprepitant/granisetron (APR/GRAN) in patients on highly emetogenic chemotherapy.
They found the data suggest “that NEPA, in a single dose, had equivalent efficacy to a 3-day oral aprepitant/granisetron regimen,” according to the lead investigator and abstract presenter.
Li Zhang, MD, of Sun Yat-sen University Cancer Center in Guangzhou, China, presented the data at the Multinational Association of Supportive Care in Cancer/International Society of Oral Oncology (MASCC/ISOO) Congress (abstract PS049, pp S55 – S56).
NEPA is a combination of the selective NK1RA netupitant (300 mg) and the clinically and pharmacologically active 5-HT3RA, palonosetron (0.5 mg) for the prevention of CINV.
Oral palonosetron prevents nausea and vomiting during the acute phase of treatment.
Netupitant prevents nausea and vomiting during both the acute and delayed phase after cancer chemotherapy.
It is formulated into a single oral capsule.
Study design
The study was a phase 3 randomized, double-blind, double-dummy study conducted in 828 chemotherapy-naïve Asian patients receiving cisplatin-based highly emetogenic chemotherapy (HEC) agents.
Patients received a single oral dose of NEPA on day 1 or a 3-day oral APR/GRAN regimen (days 1-3).
All patients received oral dexamethasone on days 1-4.
The primary efficacy endpoint was complete response (CR), defined as no emesis or rescue medication needed during the overall (0-120 hour) phase.
The investigators defined non-inferiority to be the lower limit of the two-sided 95% confidence interval greater than the non-inferiority margin set at ̶ 10%.
Secondary endpoints included no emesis, no rescue medication, and no significant nausea (NSN), defined as <25 mm on 100 mm visual analog scale (VAS).
Results
The baseline demographics were comparable between the NEPA (n=413) and APR/GRAN (n=416) arms: 71% of the patients were male, a mean age of 55 years, and a little more than half were ECOG performance status 1.
The most common cancer types were lung and head and neck cancer.
Patients had received a median cisplatin dose of 73 and 72 mg/m2 in the NEPA and APR/GRAN arms, respectively.
Within the first 24 hours (acute phase), NEPA was non-inferior to APR/GRAN. NEPA had a CR rate of 84.5% and APR/GRAN had a CR rate of 87.0%. The risk difference between the 2 agents was -2.5% (range, -7.2%, 2.3%).
In the delayed phase (25-120 hours), NEPA had a CR rate of 77.9% and APR/GRAN, 74.3%. The risk difference was 3.7% (range, -2.1%, 9.5%).
Overall, for both phases, the CR rate was 73.8% for NEPA and 72.4% for APR/GRAN. The risk difference was 1.5% (range, -4.5%, 7.5%).
Dr Zhang pointed out that although the overall CR rates were similar, the daily rates of patients experiencing CINV remained in the range of 13% - 15% for patients in the APR/GRAN arm.
However, daily rates of CINV for patients receiving NEPA declined from 16% to 8% over the 5 days. The investigators believe this suggests a benefit for delayed CINV.
Regarding secondary endpoints, significantly more patients receiving NEPA did not require rescue medication in the delayed phase and overall than patients in the APR/GRAN arm.
Treatment-emergent adverse events (TEAEs) were comparable between the arms—58.1% in the NEPA arm and 57.5% in the APR/GRAN arm, as were serious TEAS, at 4.5% and 4.6% for NEPA and APR/GRAN, respectively. And the no emesis and no significant nausea rates favored NEPA.
The most common treatment-emergent adverse events occurring in 2% or more of the patients in both arms were constipation and hiccups.
Two serious treatment-related adverse events occurred in each arm, 1 leading to discontinuation in the NEPA arm.
The investigators concluded that NEPA, as a convenient capsule administered once per cycle, is at least as effective as the 3-day regimen of APR/GRAN in patients receiving HEC.
NEPA (Akynzeo®) is approved by the US Food and Drug Administration and marketed globally by Helsinn, Lugano, Switzerland, the sponsor of the trial.
For the full US prescribing information, see the package insert.
WASHINGTON, DC—In a head-to-head study comparing a single-dose oral antiemetic to a 3-day oral regimen, the single dose has shown itself to be non-inferior to the multi-day regimen in preventing chemotherapy-induced nausea and vomiting (CINV).
The investigators evaluated netupitant/palonosetron (NEPA) against aprepitant/granisetron (APR/GRAN) in patients on highly emetogenic chemotherapy.
They found the data suggest “that NEPA, in a single dose, had equivalent efficacy to a 3-day oral aprepitant/granisetron regimen,” according to the lead investigator and abstract presenter.
Li Zhang, MD, of Sun Yat-sen University Cancer Center in Guangzhou, China, presented the data at the Multinational Association of Supportive Care in Cancer/International Society of Oral Oncology (MASCC/ISOO) Congress (abstract PS049, pp S55 – S56).
NEPA is a combination of the selective NK1RA netupitant (300 mg) and the clinically and pharmacologically active 5-HT3RA, palonosetron (0.5 mg) for the prevention of CINV.
Oral palonosetron prevents nausea and vomiting during the acute phase of treatment.
Netupitant prevents nausea and vomiting during both the acute and delayed phase after cancer chemotherapy.
It is formulated into a single oral capsule.
Study design
The study was a phase 3 randomized, double-blind, double-dummy study conducted in 828 chemotherapy-naïve Asian patients receiving cisplatin-based highly emetogenic chemotherapy (HEC) agents.
Patients received a single oral dose of NEPA on day 1 or a 3-day oral APR/GRAN regimen (days 1-3).
All patients received oral dexamethasone on days 1-4.
The primary efficacy endpoint was complete response (CR), defined as no emesis or rescue medication needed during the overall (0-120 hour) phase.
The investigators defined non-inferiority to be the lower limit of the two-sided 95% confidence interval greater than the non-inferiority margin set at ̶ 10%.
Secondary endpoints included no emesis, no rescue medication, and no significant nausea (NSN), defined as <25 mm on 100 mm visual analog scale (VAS).
Results
The baseline demographics were comparable between the NEPA (n=413) and APR/GRAN (n=416) arms: 71% of the patients were male, a mean age of 55 years, and a little more than half were ECOG performance status 1.
The most common cancer types were lung and head and neck cancer.
Patients had received a median cisplatin dose of 73 and 72 mg/m2 in the NEPA and APR/GRAN arms, respectively.
Within the first 24 hours (acute phase), NEPA was non-inferior to APR/GRAN. NEPA had a CR rate of 84.5% and APR/GRAN had a CR rate of 87.0%. The risk difference between the 2 agents was -2.5% (range, -7.2%, 2.3%).
In the delayed phase (25-120 hours), NEPA had a CR rate of 77.9% and APR/GRAN, 74.3%. The risk difference was 3.7% (range, -2.1%, 9.5%).
Overall, for both phases, the CR rate was 73.8% for NEPA and 72.4% for APR/GRAN. The risk difference was 1.5% (range, -4.5%, 7.5%).
Dr Zhang pointed out that although the overall CR rates were similar, the daily rates of patients experiencing CINV remained in the range of 13% - 15% for patients in the APR/GRAN arm.
However, daily rates of CINV for patients receiving NEPA declined from 16% to 8% over the 5 days. The investigators believe this suggests a benefit for delayed CINV.
Regarding secondary endpoints, significantly more patients receiving NEPA did not require rescue medication in the delayed phase and overall than patients in the APR/GRAN arm.
Treatment-emergent adverse events (TEAEs) were comparable between the arms—58.1% in the NEPA arm and 57.5% in the APR/GRAN arm, as were serious TEAS, at 4.5% and 4.6% for NEPA and APR/GRAN, respectively. And the no emesis and no significant nausea rates favored NEPA.
The most common treatment-emergent adverse events occurring in 2% or more of the patients in both arms were constipation and hiccups.
Two serious treatment-related adverse events occurred in each arm, 1 leading to discontinuation in the NEPA arm.
The investigators concluded that NEPA, as a convenient capsule administered once per cycle, is at least as effective as the 3-day regimen of APR/GRAN in patients receiving HEC.
NEPA (Akynzeo®) is approved by the US Food and Drug Administration and marketed globally by Helsinn, Lugano, Switzerland, the sponsor of the trial.
For the full US prescribing information, see the package insert.
WASHINGTON, DC—In a head-to-head study comparing a single-dose oral antiemetic to a 3-day oral regimen, the single dose has shown itself to be non-inferior to the multi-day regimen in preventing chemotherapy-induced nausea and vomiting (CINV).
The investigators evaluated netupitant/palonosetron (NEPA) against aprepitant/granisetron (APR/GRAN) in patients on highly emetogenic chemotherapy.
They found the data suggest “that NEPA, in a single dose, had equivalent efficacy to a 3-day oral aprepitant/granisetron regimen,” according to the lead investigator and abstract presenter.
Li Zhang, MD, of Sun Yat-sen University Cancer Center in Guangzhou, China, presented the data at the Multinational Association of Supportive Care in Cancer/International Society of Oral Oncology (MASCC/ISOO) Congress (abstract PS049, pp S55 – S56).
NEPA is a combination of the selective NK1RA netupitant (300 mg) and the clinically and pharmacologically active 5-HT3RA, palonosetron (0.5 mg) for the prevention of CINV.
Oral palonosetron prevents nausea and vomiting during the acute phase of treatment.
Netupitant prevents nausea and vomiting during both the acute and delayed phase after cancer chemotherapy.
It is formulated into a single oral capsule.
Study design
The study was a phase 3 randomized, double-blind, double-dummy study conducted in 828 chemotherapy-naïve Asian patients receiving cisplatin-based highly emetogenic chemotherapy (HEC) agents.
Patients received a single oral dose of NEPA on day 1 or a 3-day oral APR/GRAN regimen (days 1-3).
All patients received oral dexamethasone on days 1-4.
The primary efficacy endpoint was complete response (CR), defined as no emesis or rescue medication needed during the overall (0-120 hour) phase.
The investigators defined non-inferiority to be the lower limit of the two-sided 95% confidence interval greater than the non-inferiority margin set at ̶ 10%.
Secondary endpoints included no emesis, no rescue medication, and no significant nausea (NSN), defined as <25 mm on 100 mm visual analog scale (VAS).
Results
The baseline demographics were comparable between the NEPA (n=413) and APR/GRAN (n=416) arms: 71% of the patients were male, a mean age of 55 years, and a little more than half were ECOG performance status 1.
The most common cancer types were lung and head and neck cancer.
Patients had received a median cisplatin dose of 73 and 72 mg/m2 in the NEPA and APR/GRAN arms, respectively.
Within the first 24 hours (acute phase), NEPA was non-inferior to APR/GRAN. NEPA had a CR rate of 84.5% and APR/GRAN had a CR rate of 87.0%. The risk difference between the 2 agents was -2.5% (range, -7.2%, 2.3%).
In the delayed phase (25-120 hours), NEPA had a CR rate of 77.9% and APR/GRAN, 74.3%. The risk difference was 3.7% (range, -2.1%, 9.5%).
Overall, for both phases, the CR rate was 73.8% for NEPA and 72.4% for APR/GRAN. The risk difference was 1.5% (range, -4.5%, 7.5%).
Dr Zhang pointed out that although the overall CR rates were similar, the daily rates of patients experiencing CINV remained in the range of 13% - 15% for patients in the APR/GRAN arm.
However, daily rates of CINV for patients receiving NEPA declined from 16% to 8% over the 5 days. The investigators believe this suggests a benefit for delayed CINV.
Regarding secondary endpoints, significantly more patients receiving NEPA did not require rescue medication in the delayed phase and overall than patients in the APR/GRAN arm.
Treatment-emergent adverse events (TEAEs) were comparable between the arms—58.1% in the NEPA arm and 57.5% in the APR/GRAN arm, as were serious TEAS, at 4.5% and 4.6% for NEPA and APR/GRAN, respectively. And the no emesis and no significant nausea rates favored NEPA.
The most common treatment-emergent adverse events occurring in 2% or more of the patients in both arms were constipation and hiccups.
Two serious treatment-related adverse events occurred in each arm, 1 leading to discontinuation in the NEPA arm.
The investigators concluded that NEPA, as a convenient capsule administered once per cycle, is at least as effective as the 3-day regimen of APR/GRAN in patients receiving HEC.
NEPA (Akynzeo®) is approved by the US Food and Drug Administration and marketed globally by Helsinn, Lugano, Switzerland, the sponsor of the trial.
For the full US prescribing information, see the package insert.
Lower dose of rivaroxaban receives priority review
The US Food and Drug Administration (FDA) has accepted for priority review a supplemental new drug application (sNDA) for rivaroxaban (XARELTO®).
The sNDA is for a 10 mg once-daily dose of rivaroxaban to reduce the risk of venous thromboembolism (VTE) in patients who have received at least 6 months of standard anticoagulant therapy.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA plans to make a decision on the rivaroxaban sNDA by October 28, 2017.
The sNDA is supported by data from the EINSTEIN CHOICE study. Patients enrolled in this study had confirmed VTE and were treated initially with standard anticoagulant therapy for 6 to 12 months.
During EINSTEIN CHOICE, 3365 patients received rivaroxaban at 10 mg, rivaroxaban at 20 mg, or aspirin at 100 mg once daily for up to 12 months of extended treatment.
Both rivaroxaban doses were superior to aspirin in preventing fatal or non-fatal recurrent VTE, the study’s primary efficacy endpoint.
The rate of recurrent VTE was 1.2% in the 10 mg rivaroxaban arm (hazard ratio [HR]=0.26; 95% CI, 0.14 to 0.47; P<0.001), 1.5% in the 20 mg rivaroxaban arm (HR=0.34; 95% CI, 0.20 to 0.59; P<0.001), and 4.4% in the aspirin arm. Fatal VTE occurred in 0%, 0.2%, and 0.2% of patients, respectively.
The primary safety endpoint was major bleeding as defined by the International Society on Thrombosis and Haemostasis.
The rate of major bleeding was 0.4% for the 10 mg rivaroxaban group (HR=1.64; 95% CI, 0.39 to 6.84; P=0.50), 0.5% for the 20 mg rivaroxaban group (HR=2.01; 95% CI, 0.50 to 8.04; P=0.32), and 0.3% for the aspirin group. ![]()
The US Food and Drug Administration (FDA) has accepted for priority review a supplemental new drug application (sNDA) for rivaroxaban (XARELTO®).
The sNDA is for a 10 mg once-daily dose of rivaroxaban to reduce the risk of venous thromboembolism (VTE) in patients who have received at least 6 months of standard anticoagulant therapy.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA plans to make a decision on the rivaroxaban sNDA by October 28, 2017.
The sNDA is supported by data from the EINSTEIN CHOICE study. Patients enrolled in this study had confirmed VTE and were treated initially with standard anticoagulant therapy for 6 to 12 months.
During EINSTEIN CHOICE, 3365 patients received rivaroxaban at 10 mg, rivaroxaban at 20 mg, or aspirin at 100 mg once daily for up to 12 months of extended treatment.
Both rivaroxaban doses were superior to aspirin in preventing fatal or non-fatal recurrent VTE, the study’s primary efficacy endpoint.
The rate of recurrent VTE was 1.2% in the 10 mg rivaroxaban arm (hazard ratio [HR]=0.26; 95% CI, 0.14 to 0.47; P<0.001), 1.5% in the 20 mg rivaroxaban arm (HR=0.34; 95% CI, 0.20 to 0.59; P<0.001), and 4.4% in the aspirin arm. Fatal VTE occurred in 0%, 0.2%, and 0.2% of patients, respectively.
The primary safety endpoint was major bleeding as defined by the International Society on Thrombosis and Haemostasis.
The rate of major bleeding was 0.4% for the 10 mg rivaroxaban group (HR=1.64; 95% CI, 0.39 to 6.84; P=0.50), 0.5% for the 20 mg rivaroxaban group (HR=2.01; 95% CI, 0.50 to 8.04; P=0.32), and 0.3% for the aspirin group. ![]()
The US Food and Drug Administration (FDA) has accepted for priority review a supplemental new drug application (sNDA) for rivaroxaban (XARELTO®).
The sNDA is for a 10 mg once-daily dose of rivaroxaban to reduce the risk of venous thromboembolism (VTE) in patients who have received at least 6 months of standard anticoagulant therapy.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA plans to make a decision on the rivaroxaban sNDA by October 28, 2017.
The sNDA is supported by data from the EINSTEIN CHOICE study. Patients enrolled in this study had confirmed VTE and were treated initially with standard anticoagulant therapy for 6 to 12 months.
During EINSTEIN CHOICE, 3365 patients received rivaroxaban at 10 mg, rivaroxaban at 20 mg, or aspirin at 100 mg once daily for up to 12 months of extended treatment.
Both rivaroxaban doses were superior to aspirin in preventing fatal or non-fatal recurrent VTE, the study’s primary efficacy endpoint.
The rate of recurrent VTE was 1.2% in the 10 mg rivaroxaban arm (hazard ratio [HR]=0.26; 95% CI, 0.14 to 0.47; P<0.001), 1.5% in the 20 mg rivaroxaban arm (HR=0.34; 95% CI, 0.20 to 0.59; P<0.001), and 4.4% in the aspirin arm. Fatal VTE occurred in 0%, 0.2%, and 0.2% of patients, respectively.
The primary safety endpoint was major bleeding as defined by the International Society on Thrombosis and Haemostasis.
The rate of major bleeding was 0.4% for the 10 mg rivaroxaban group (HR=1.64; 95% CI, 0.39 to 6.84; P=0.50), 0.5% for the 20 mg rivaroxaban group (HR=2.01; 95% CI, 0.50 to 8.04; P=0.32), and 0.3% for the aspirin group. ![]()
Persistent rash on extremities

Given the history that the rash persisted for longer than 3 months, the FP made the diagnosis of chronic urticaria. The cause of chronic urticaria (>6 weeks duration) is determined in less than 20% of cases. Because no cause was found in this case, the patient’s urticaria was determined to be chronic idiopathic urticaria.
Chronic urticaria is twice as common in women than in men. Urticaria is a dynamic process in which new wheals evolve as old ones resolve. The wheals result from localized capillary vasodilation, followed by transudation of protein-rich fluid into the surrounding skin. The wheals resolve when the fluid is slowly reabsorbed. Patients may benefit from avoiding potential urticarial precipitants such as aspirin, nonsteroidal anti-inflammatory drugs, opiates, and alcohol.
Second-generation H1 antihistamines, such as cetirizine, should be prescribed as first-line treatment for chronic urticaria. Increasing the dose of cetirizine from 10 mg/d to 20 mg/d produces a significant improvement in the severity of wheals and itching in urticaria refractory to the standard doses of antihistamines. The National Institute for Health and Care Excellence (NICE) notes in its 2014 evidence summary that international guidelines suggest that non-sedating antihistamines may be used at up to quadruple the manufacturers’ recommended dosages before changing to an alternative therapy. NICE recommends waiting up to 4 weeks to allow full effectiveness of the antihistamines before considering referral to a specialist.
The patient in this case was started on cetirizine 10 mg twice daily with written instructions to gradually increase up to 20 mg twice daily if the lower doses were not working. With cetirizine 20 mg twice daily, the chronic urticaria subsided and the patient was satisfied with the results.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Usatine R. Urticaria and angioedema. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 863-870.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com

Given the history that the rash persisted for longer than 3 months, the FP made the diagnosis of chronic urticaria. The cause of chronic urticaria (>6 weeks duration) is determined in less than 20% of cases. Because no cause was found in this case, the patient’s urticaria was determined to be chronic idiopathic urticaria.
Chronic urticaria is twice as common in women than in men. Urticaria is a dynamic process in which new wheals evolve as old ones resolve. The wheals result from localized capillary vasodilation, followed by transudation of protein-rich fluid into the surrounding skin. The wheals resolve when the fluid is slowly reabsorbed. Patients may benefit from avoiding potential urticarial precipitants such as aspirin, nonsteroidal anti-inflammatory drugs, opiates, and alcohol.
Second-generation H1 antihistamines, such as cetirizine, should be prescribed as first-line treatment for chronic urticaria. Increasing the dose of cetirizine from 10 mg/d to 20 mg/d produces a significant improvement in the severity of wheals and itching in urticaria refractory to the standard doses of antihistamines. The National Institute for Health and Care Excellence (NICE) notes in its 2014 evidence summary that international guidelines suggest that non-sedating antihistamines may be used at up to quadruple the manufacturers’ recommended dosages before changing to an alternative therapy. NICE recommends waiting up to 4 weeks to allow full effectiveness of the antihistamines before considering referral to a specialist.
The patient in this case was started on cetirizine 10 mg twice daily with written instructions to gradually increase up to 20 mg twice daily if the lower doses were not working. With cetirizine 20 mg twice daily, the chronic urticaria subsided and the patient was satisfied with the results.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Usatine R. Urticaria and angioedema. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 863-870.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com

Given the history that the rash persisted for longer than 3 months, the FP made the diagnosis of chronic urticaria. The cause of chronic urticaria (>6 weeks duration) is determined in less than 20% of cases. Because no cause was found in this case, the patient’s urticaria was determined to be chronic idiopathic urticaria.
Chronic urticaria is twice as common in women than in men. Urticaria is a dynamic process in which new wheals evolve as old ones resolve. The wheals result from localized capillary vasodilation, followed by transudation of protein-rich fluid into the surrounding skin. The wheals resolve when the fluid is slowly reabsorbed. Patients may benefit from avoiding potential urticarial precipitants such as aspirin, nonsteroidal anti-inflammatory drugs, opiates, and alcohol.
Second-generation H1 antihistamines, such as cetirizine, should be prescribed as first-line treatment for chronic urticaria. Increasing the dose of cetirizine from 10 mg/d to 20 mg/d produces a significant improvement in the severity of wheals and itching in urticaria refractory to the standard doses of antihistamines. The National Institute for Health and Care Excellence (NICE) notes in its 2014 evidence summary that international guidelines suggest that non-sedating antihistamines may be used at up to quadruple the manufacturers’ recommended dosages before changing to an alternative therapy. NICE recommends waiting up to 4 weeks to allow full effectiveness of the antihistamines before considering referral to a specialist.
The patient in this case was started on cetirizine 10 mg twice daily with written instructions to gradually increase up to 20 mg twice daily if the lower doses were not working. With cetirizine 20 mg twice daily, the chronic urticaria subsided and the patient was satisfied with the results.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Usatine R. Urticaria and angioedema. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 863-870.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
A rare case of hypoglycemia induced by a classic gastrointestinal stromal tumor
Hypoglycemia, a frequently encountered medical emergency, is usually seen in patients with diabetes, most commonly as a result of iatrogenesis. However, it can also be encountered in nondiabetic patients. Various causes, such as pancreatic islet cell tumors producing insulin, primary or secondary adrenal insufficiency, advanced liver disease, pheochromocytoma and hypothyroidism, have been found to contribute to the condition in the nondiabetic population.1 In rare cases, an excessive production of insulin-like growth factor (IGF-2) – a condition known as nonislet cell tumor-induced hypoglycemia (NICTH) – has also been found to cause hypoglycemia. Hypoinsulinemic hypoglycemia, with low IGF-1 levels and an IGF-2-IgF1 ratio of greater than 10, is found to be suggestive of NICTH.
Case presentation and summary
An 81-year-old man with a history of diabetes mellitus, systolic heart failure, chronic kidney disease, and metastatic classical gastrointestinal spindle cell sarcoma presented to the emergency department with an acute change in mental status resulting from a new onset hypoglycemia. He was admitted, and during his hospital stay, he experienced severe hypoglycemic episodes with symptomatic presentations of diaphoresis on multiple occasions. A detailed history revealed that for diabetes, the patient had been on insulin for the first 12 years after his diagnosis, after which he was switched to metformin 500 mg twice daily for about 2 years, and as a satisfactory glycemic control was attained, eventually metformin had also been stopped 3 years prior to the current presentation.
The patient’s past medical records were obtained from the hospital at which he had been diagnosed gastrointestinal spindle cell sarcoma. Patient had not received treatment for the cancer as the disease was too widespread to be treated. The gastrointestinal spindle cell sarcoma, which had initially been surgically resected 7 years before the current presentation, had a recurrence 3 years later with abdominal and pulmonary metastasis, but no liver metastasis. No further intervention was carried out because the widely metastasized disease would not have benefited from any more surgical intervention and chemotherapy was not initiated because of the patient’s comorbid illnesses.
A blood sample drawn from the patient at the time of one hypoglycemic event, revealed low serum insulin <0.1 U/ml (normal, 2-19.6 U/ml); low C-peptide level, 0.59 ng/ml (0.8-3.85 ng/ml); low IGF-1, 16 ng/ml (5-4 ng/ml); and IGF-3, 0.9 ng/ml (2.2-4.5 ng/ml). IGF-2 levels were found to be markedly elevated at 945 ng/ml (47-350 ng/ml). The calculated IGF-2-IGF-1 ratio was 59.06 (normal, <10), suggesting NICTH as the etiology for the patient’s hypoglycemia.
The hypoglycemic episodes were initially treated with a continuous dextrose infusion followed by diazoxide treatment. However, diazoxide did not prevent his hypoglycemic episodes, so dexamethasone was considered as an alternative for his condition. The dexamethasone treatment resulted in the normalization of the patient’s serum glucose levels and resolution of his symptoms. The patient was discharged in a satisfactory state few days later and followed up thereafter. No recurrence of hypoglycemic episodes was found, and he was continued on dexamethasone therapy.
Discussion
Hypoglycemia due to NICTH is rare, with a prevalence of four times less than that of insulinoma.3 In most cases, NICTH occurs in patients with solid tumors of mesenchymal and epithelial origins such as hepatocellular carcinoma, gastric carcinoma or mesothelioma.4 In NICTH, the serum levels of insulin, C-peptide, and IGF-1 are usually decreased or undetectable. However, the circulating levels of total IGF2 may be increased, decreased, or normal. Concurrent normal to high morning cortisol and normal response to cosyntropin stimulation can rule out adrenal insufficiency and suggest NICTH. An IGF-2: IGF-1 ratio of >10 is considered to be clinically significant and highly suggestive of NICTH.5 Hypoglycemia in NICTH can be managed by administration of oral glucose, intravenous dextrose or glucagon. In some cases, diazoxide, a potent inhibitor of insulin secretion, has been found to be useful.6 Diazoxide directly inhibits the release of insulin through stimulation of adrenergic receptors and also has an extra pancreatic hyperglycemic effect, probably by inhibiting cyclic adenosine monophosphate phosphodiesterase, resulting in higher plasma levels of cyclic AMP and enhanced glycogenolysis.
Glucocorticoid therapy has been shown to suppress IGF-2 in a dose dependent manner and also by increasing gluconeogenesis.7 Surgical resection of the tumor whenever possible is the treatment of choice followed by radiotherapy and chemotherapy for inoperable disease and if successful, usually results in resolution of hypoglycemia. Imatinib, is the chemotherapeutic drug of choice for metastatic GIST, but many case reports have suggested worsening of hypoglycemia in advanced GIST with the use of the drug.8 The patient described in our report was not on any chemotherapy, hence hypoglycemia could not be attributed to it. On the basis of findings among 24 patients with GIST, Rikhof and colleagues have recommended monitoring plasma levels of pro-IGF-IIE to identify patients at high risk for developing hypoglycemia, especially those with progressive disease.9 Furthermore, over expression of IGF-2 as a predictor of potential relapse may be an area for potential research and further study.10
1. Marks V, Teale JD. Tumours producing hypoglycaemia. Diabetes Metab Rev. 1991;7:79-91.
2. Dutta P, Aggarwal A, Gogate Y, Nahar U, Shah VN, Singla M. Non-islet cell tumor-induced hypoglycemia: a report of five cases and brief review of the literature. Endocrinol Diabetes Metab Case Rep. 2013;2013:130046
3. de Groot JW, Rikhof B, van Doorn J, et al. Non-islet cell tumour-induced hypoglycaemia: a review of the literature including two new cases. Endocr Relat Cancer. 2007;14:979-93.
4. Fukuda I, Hizuka N, Ishikawa Y, et al. Clinical features of insulin-like growth factor II producing non-islet-cell tumor hypoglycemia
5. Marks V, Teale JD: Tumours producing hypoglycaemia. Endocr Relat Cancer. 1998;5:111-129.
6. Le Roith D. Tumor-induced hypoglycemia. N Engl J Med. 1999;341:757-758.
7. Teale JD, Marks V. Glucocorticoid therapy suppresses abnormal secretion of big IGF-II by non-islet cell tumours inducing hypoglycaemia (NICTH). Clin Endocrinol .1998;49:491-498.
8. Hamberg P, De Jong FA, Boonstra JG, et al. Non-islet-cell tumor induced hypoglycemia in patients with advanced gastrointestinal stromal tumor possibly worsened by imatinib. J Clin Oncol. 2006;24:e30-e31.
9. Rikhof B, van Doorn J, Suurmeijer AJ, et al. Insulin-like growth factors and insulin-like growth factor-binding proteins in relation to disease status and incidence of hypoglycaemia in patients with a gastrointestinal stromal tumour. Ann Oncol. 2009;20:1582-1588.
10. Braconi C, Bracci R, Bearzi I, et al. Insulin-like growth factor (IGF) 1 and 2 help to predict disease outcome in GIST patients. Ann Oncol. 2008;19:1293-1298.
Hypoglycemia, a frequently encountered medical emergency, is usually seen in patients with diabetes, most commonly as a result of iatrogenesis. However, it can also be encountered in nondiabetic patients. Various causes, such as pancreatic islet cell tumors producing insulin, primary or secondary adrenal insufficiency, advanced liver disease, pheochromocytoma and hypothyroidism, have been found to contribute to the condition in the nondiabetic population.1 In rare cases, an excessive production of insulin-like growth factor (IGF-2) – a condition known as nonislet cell tumor-induced hypoglycemia (NICTH) – has also been found to cause hypoglycemia. Hypoinsulinemic hypoglycemia, with low IGF-1 levels and an IGF-2-IgF1 ratio of greater than 10, is found to be suggestive of NICTH.
Case presentation and summary
An 81-year-old man with a history of diabetes mellitus, systolic heart failure, chronic kidney disease, and metastatic classical gastrointestinal spindle cell sarcoma presented to the emergency department with an acute change in mental status resulting from a new onset hypoglycemia. He was admitted, and during his hospital stay, he experienced severe hypoglycemic episodes with symptomatic presentations of diaphoresis on multiple occasions. A detailed history revealed that for diabetes, the patient had been on insulin for the first 12 years after his diagnosis, after which he was switched to metformin 500 mg twice daily for about 2 years, and as a satisfactory glycemic control was attained, eventually metformin had also been stopped 3 years prior to the current presentation.
The patient’s past medical records were obtained from the hospital at which he had been diagnosed gastrointestinal spindle cell sarcoma. Patient had not received treatment for the cancer as the disease was too widespread to be treated. The gastrointestinal spindle cell sarcoma, which had initially been surgically resected 7 years before the current presentation, had a recurrence 3 years later with abdominal and pulmonary metastasis, but no liver metastasis. No further intervention was carried out because the widely metastasized disease would not have benefited from any more surgical intervention and chemotherapy was not initiated because of the patient’s comorbid illnesses.
A blood sample drawn from the patient at the time of one hypoglycemic event, revealed low serum insulin <0.1 U/ml (normal, 2-19.6 U/ml); low C-peptide level, 0.59 ng/ml (0.8-3.85 ng/ml); low IGF-1, 16 ng/ml (5-4 ng/ml); and IGF-3, 0.9 ng/ml (2.2-4.5 ng/ml). IGF-2 levels were found to be markedly elevated at 945 ng/ml (47-350 ng/ml). The calculated IGF-2-IGF-1 ratio was 59.06 (normal, <10), suggesting NICTH as the etiology for the patient’s hypoglycemia.
The hypoglycemic episodes were initially treated with a continuous dextrose infusion followed by diazoxide treatment. However, diazoxide did not prevent his hypoglycemic episodes, so dexamethasone was considered as an alternative for his condition. The dexamethasone treatment resulted in the normalization of the patient’s serum glucose levels and resolution of his symptoms. The patient was discharged in a satisfactory state few days later and followed up thereafter. No recurrence of hypoglycemic episodes was found, and he was continued on dexamethasone therapy.
Discussion
Hypoglycemia due to NICTH is rare, with a prevalence of four times less than that of insulinoma.3 In most cases, NICTH occurs in patients with solid tumors of mesenchymal and epithelial origins such as hepatocellular carcinoma, gastric carcinoma or mesothelioma.4 In NICTH, the serum levels of insulin, C-peptide, and IGF-1 are usually decreased or undetectable. However, the circulating levels of total IGF2 may be increased, decreased, or normal. Concurrent normal to high morning cortisol and normal response to cosyntropin stimulation can rule out adrenal insufficiency and suggest NICTH. An IGF-2: IGF-1 ratio of >10 is considered to be clinically significant and highly suggestive of NICTH.5 Hypoglycemia in NICTH can be managed by administration of oral glucose, intravenous dextrose or glucagon. In some cases, diazoxide, a potent inhibitor of insulin secretion, has been found to be useful.6 Diazoxide directly inhibits the release of insulin through stimulation of adrenergic receptors and also has an extra pancreatic hyperglycemic effect, probably by inhibiting cyclic adenosine monophosphate phosphodiesterase, resulting in higher plasma levels of cyclic AMP and enhanced glycogenolysis.
Glucocorticoid therapy has been shown to suppress IGF-2 in a dose dependent manner and also by increasing gluconeogenesis.7 Surgical resection of the tumor whenever possible is the treatment of choice followed by radiotherapy and chemotherapy for inoperable disease and if successful, usually results in resolution of hypoglycemia. Imatinib, is the chemotherapeutic drug of choice for metastatic GIST, but many case reports have suggested worsening of hypoglycemia in advanced GIST with the use of the drug.8 The patient described in our report was not on any chemotherapy, hence hypoglycemia could not be attributed to it. On the basis of findings among 24 patients with GIST, Rikhof and colleagues have recommended monitoring plasma levels of pro-IGF-IIE to identify patients at high risk for developing hypoglycemia, especially those with progressive disease.9 Furthermore, over expression of IGF-2 as a predictor of potential relapse may be an area for potential research and further study.10
Hypoglycemia, a frequently encountered medical emergency, is usually seen in patients with diabetes, most commonly as a result of iatrogenesis. However, it can also be encountered in nondiabetic patients. Various causes, such as pancreatic islet cell tumors producing insulin, primary or secondary adrenal insufficiency, advanced liver disease, pheochromocytoma and hypothyroidism, have been found to contribute to the condition in the nondiabetic population.1 In rare cases, an excessive production of insulin-like growth factor (IGF-2) – a condition known as nonislet cell tumor-induced hypoglycemia (NICTH) – has also been found to cause hypoglycemia. Hypoinsulinemic hypoglycemia, with low IGF-1 levels and an IGF-2-IgF1 ratio of greater than 10, is found to be suggestive of NICTH.
Case presentation and summary
An 81-year-old man with a history of diabetes mellitus, systolic heart failure, chronic kidney disease, and metastatic classical gastrointestinal spindle cell sarcoma presented to the emergency department with an acute change in mental status resulting from a new onset hypoglycemia. He was admitted, and during his hospital stay, he experienced severe hypoglycemic episodes with symptomatic presentations of diaphoresis on multiple occasions. A detailed history revealed that for diabetes, the patient had been on insulin for the first 12 years after his diagnosis, after which he was switched to metformin 500 mg twice daily for about 2 years, and as a satisfactory glycemic control was attained, eventually metformin had also been stopped 3 years prior to the current presentation.
The patient’s past medical records were obtained from the hospital at which he had been diagnosed gastrointestinal spindle cell sarcoma. Patient had not received treatment for the cancer as the disease was too widespread to be treated. The gastrointestinal spindle cell sarcoma, which had initially been surgically resected 7 years before the current presentation, had a recurrence 3 years later with abdominal and pulmonary metastasis, but no liver metastasis. No further intervention was carried out because the widely metastasized disease would not have benefited from any more surgical intervention and chemotherapy was not initiated because of the patient’s comorbid illnesses.
A blood sample drawn from the patient at the time of one hypoglycemic event, revealed low serum insulin <0.1 U/ml (normal, 2-19.6 U/ml); low C-peptide level, 0.59 ng/ml (0.8-3.85 ng/ml); low IGF-1, 16 ng/ml (5-4 ng/ml); and IGF-3, 0.9 ng/ml (2.2-4.5 ng/ml). IGF-2 levels were found to be markedly elevated at 945 ng/ml (47-350 ng/ml). The calculated IGF-2-IGF-1 ratio was 59.06 (normal, <10), suggesting NICTH as the etiology for the patient’s hypoglycemia.
The hypoglycemic episodes were initially treated with a continuous dextrose infusion followed by diazoxide treatment. However, diazoxide did not prevent his hypoglycemic episodes, so dexamethasone was considered as an alternative for his condition. The dexamethasone treatment resulted in the normalization of the patient’s serum glucose levels and resolution of his symptoms. The patient was discharged in a satisfactory state few days later and followed up thereafter. No recurrence of hypoglycemic episodes was found, and he was continued on dexamethasone therapy.
Discussion
Hypoglycemia due to NICTH is rare, with a prevalence of four times less than that of insulinoma.3 In most cases, NICTH occurs in patients with solid tumors of mesenchymal and epithelial origins such as hepatocellular carcinoma, gastric carcinoma or mesothelioma.4 In NICTH, the serum levels of insulin, C-peptide, and IGF-1 are usually decreased or undetectable. However, the circulating levels of total IGF2 may be increased, decreased, or normal. Concurrent normal to high morning cortisol and normal response to cosyntropin stimulation can rule out adrenal insufficiency and suggest NICTH. An IGF-2: IGF-1 ratio of >10 is considered to be clinically significant and highly suggestive of NICTH.5 Hypoglycemia in NICTH can be managed by administration of oral glucose, intravenous dextrose or glucagon. In some cases, diazoxide, a potent inhibitor of insulin secretion, has been found to be useful.6 Diazoxide directly inhibits the release of insulin through stimulation of adrenergic receptors and also has an extra pancreatic hyperglycemic effect, probably by inhibiting cyclic adenosine monophosphate phosphodiesterase, resulting in higher plasma levels of cyclic AMP and enhanced glycogenolysis.
Glucocorticoid therapy has been shown to suppress IGF-2 in a dose dependent manner and also by increasing gluconeogenesis.7 Surgical resection of the tumor whenever possible is the treatment of choice followed by radiotherapy and chemotherapy for inoperable disease and if successful, usually results in resolution of hypoglycemia. Imatinib, is the chemotherapeutic drug of choice for metastatic GIST, but many case reports have suggested worsening of hypoglycemia in advanced GIST with the use of the drug.8 The patient described in our report was not on any chemotherapy, hence hypoglycemia could not be attributed to it. On the basis of findings among 24 patients with GIST, Rikhof and colleagues have recommended monitoring plasma levels of pro-IGF-IIE to identify patients at high risk for developing hypoglycemia, especially those with progressive disease.9 Furthermore, over expression of IGF-2 as a predictor of potential relapse may be an area for potential research and further study.10
1. Marks V, Teale JD. Tumours producing hypoglycaemia. Diabetes Metab Rev. 1991;7:79-91.
2. Dutta P, Aggarwal A, Gogate Y, Nahar U, Shah VN, Singla M. Non-islet cell tumor-induced hypoglycemia: a report of five cases and brief review of the literature. Endocrinol Diabetes Metab Case Rep. 2013;2013:130046
3. de Groot JW, Rikhof B, van Doorn J, et al. Non-islet cell tumour-induced hypoglycaemia: a review of the literature including two new cases. Endocr Relat Cancer. 2007;14:979-93.
4. Fukuda I, Hizuka N, Ishikawa Y, et al. Clinical features of insulin-like growth factor II producing non-islet-cell tumor hypoglycemia
5. Marks V, Teale JD: Tumours producing hypoglycaemia. Endocr Relat Cancer. 1998;5:111-129.
6. Le Roith D. Tumor-induced hypoglycemia. N Engl J Med. 1999;341:757-758.
7. Teale JD, Marks V. Glucocorticoid therapy suppresses abnormal secretion of big IGF-II by non-islet cell tumours inducing hypoglycaemia (NICTH). Clin Endocrinol .1998;49:491-498.
8. Hamberg P, De Jong FA, Boonstra JG, et al. Non-islet-cell tumor induced hypoglycemia in patients with advanced gastrointestinal stromal tumor possibly worsened by imatinib. J Clin Oncol. 2006;24:e30-e31.
9. Rikhof B, van Doorn J, Suurmeijer AJ, et al. Insulin-like growth factors and insulin-like growth factor-binding proteins in relation to disease status and incidence of hypoglycaemia in patients with a gastrointestinal stromal tumour. Ann Oncol. 2009;20:1582-1588.
10. Braconi C, Bracci R, Bearzi I, et al. Insulin-like growth factor (IGF) 1 and 2 help to predict disease outcome in GIST patients. Ann Oncol. 2008;19:1293-1298.
1. Marks V, Teale JD. Tumours producing hypoglycaemia. Diabetes Metab Rev. 1991;7:79-91.
2. Dutta P, Aggarwal A, Gogate Y, Nahar U, Shah VN, Singla M. Non-islet cell tumor-induced hypoglycemia: a report of five cases and brief review of the literature. Endocrinol Diabetes Metab Case Rep. 2013;2013:130046
3. de Groot JW, Rikhof B, van Doorn J, et al. Non-islet cell tumour-induced hypoglycaemia: a review of the literature including two new cases. Endocr Relat Cancer. 2007;14:979-93.
4. Fukuda I, Hizuka N, Ishikawa Y, et al. Clinical features of insulin-like growth factor II producing non-islet-cell tumor hypoglycemia
5. Marks V, Teale JD: Tumours producing hypoglycaemia. Endocr Relat Cancer. 1998;5:111-129.
6. Le Roith D. Tumor-induced hypoglycemia. N Engl J Med. 1999;341:757-758.
7. Teale JD, Marks V. Glucocorticoid therapy suppresses abnormal secretion of big IGF-II by non-islet cell tumours inducing hypoglycaemia (NICTH). Clin Endocrinol .1998;49:491-498.
8. Hamberg P, De Jong FA, Boonstra JG, et al. Non-islet-cell tumor induced hypoglycemia in patients with advanced gastrointestinal stromal tumor possibly worsened by imatinib. J Clin Oncol. 2006;24:e30-e31.
9. Rikhof B, van Doorn J, Suurmeijer AJ, et al. Insulin-like growth factors and insulin-like growth factor-binding proteins in relation to disease status and incidence of hypoglycaemia in patients with a gastrointestinal stromal tumour. Ann Oncol. 2009;20:1582-1588.
10. Braconi C, Bracci R, Bearzi I, et al. Insulin-like growth factor (IGF) 1 and 2 help to predict disease outcome in GIST patients. Ann Oncol. 2008;19:1293-1298.