User login
Drug approved for kids with sickle cell anemia
The US Food and Drug Administration (FDA) has approved a hydroxyurea product (Addmedica’s Siklos) for use in pediatric patients with sickle cell anemia.
Siklos is intended to reduce the frequency of painful crises and the need for blood transfusions in pediatric patients age 2 and older who have sickle cell anemia and recurrent moderate to severe painful crises.
The recommended dose of Siklos is 20 mg/kg once daily.
The FDA granted priority review and orphan drug designation to the application for Siklos.
The agency’s approval of Siklos was based on data from the ESCORT HU study (NCT02516579). The trial was an evaluation of Siklos in 405 patients, ages 2 to 18, with sickle cell disease (SCD).
Thirty-five percent of these patients (n=141) had not received hydroxyurea prior to study enrollment and were therefore evaluable for efficacy. The median follow-up was 23 months (range, 12 to 80 months).
The researchers found that Siklos prompted an increase in fetal hemoglobin. Median fetal hemoglobin percentages were 5.6% (range, 1.3 to 15.0) at baseline and 12.8% (range, 2.1 to 37.2) at around 6 months after Siklos initiation (the value closest to 6 months collected between 5 and 14 months).
In addition, the percentage of patients with at least 1 vaso-occlusive episode, 1 episode of acute chest syndrome, 1 hospitalization due to SCD, or 1 blood transfusion decreased after 12 months of Siklos treatment.
The proportion of patients with at least 1 vaso-occlusive episode was 69.2% at baseline and 42.5% at 12 months. The proportion with at least 1 episode of acute chest syndrome was 23.6% and 5.7%, respectively.
The proportion with at least 1 hospitalization due to SCD was 75.5% and 41.8%, respectively. And the proportion with at least 1 blood transfusion was 45.9% and 23.0%, respectively.
The most common adverse events (occurring in at least 10% of patients) were infections (39.8%), gastrointestinal disorders (13.1%), neutropenia (12.6%), nervous system disorders (11.1%), and metabolic and nutrition disorders (10.9%).
Full prescribing information for Siklos is available on the FDA website. ![]()
The US Food and Drug Administration (FDA) has approved a hydroxyurea product (Addmedica’s Siklos) for use in pediatric patients with sickle cell anemia.
Siklos is intended to reduce the frequency of painful crises and the need for blood transfusions in pediatric patients age 2 and older who have sickle cell anemia and recurrent moderate to severe painful crises.
The recommended dose of Siklos is 20 mg/kg once daily.
The FDA granted priority review and orphan drug designation to the application for Siklos.
The agency’s approval of Siklos was based on data from the ESCORT HU study (NCT02516579). The trial was an evaluation of Siklos in 405 patients, ages 2 to 18, with sickle cell disease (SCD).
Thirty-five percent of these patients (n=141) had not received hydroxyurea prior to study enrollment and were therefore evaluable for efficacy. The median follow-up was 23 months (range, 12 to 80 months).
The researchers found that Siklos prompted an increase in fetal hemoglobin. Median fetal hemoglobin percentages were 5.6% (range, 1.3 to 15.0) at baseline and 12.8% (range, 2.1 to 37.2) at around 6 months after Siklos initiation (the value closest to 6 months collected between 5 and 14 months).
In addition, the percentage of patients with at least 1 vaso-occlusive episode, 1 episode of acute chest syndrome, 1 hospitalization due to SCD, or 1 blood transfusion decreased after 12 months of Siklos treatment.
The proportion of patients with at least 1 vaso-occlusive episode was 69.2% at baseline and 42.5% at 12 months. The proportion with at least 1 episode of acute chest syndrome was 23.6% and 5.7%, respectively.
The proportion with at least 1 hospitalization due to SCD was 75.5% and 41.8%, respectively. And the proportion with at least 1 blood transfusion was 45.9% and 23.0%, respectively.
The most common adverse events (occurring in at least 10% of patients) were infections (39.8%), gastrointestinal disorders (13.1%), neutropenia (12.6%), nervous system disorders (11.1%), and metabolic and nutrition disorders (10.9%).
Full prescribing information for Siklos is available on the FDA website. ![]()
The US Food and Drug Administration (FDA) has approved a hydroxyurea product (Addmedica’s Siklos) for use in pediatric patients with sickle cell anemia.
Siklos is intended to reduce the frequency of painful crises and the need for blood transfusions in pediatric patients age 2 and older who have sickle cell anemia and recurrent moderate to severe painful crises.
The recommended dose of Siklos is 20 mg/kg once daily.
The FDA granted priority review and orphan drug designation to the application for Siklos.
The agency’s approval of Siklos was based on data from the ESCORT HU study (NCT02516579). The trial was an evaluation of Siklos in 405 patients, ages 2 to 18, with sickle cell disease (SCD).
Thirty-five percent of these patients (n=141) had not received hydroxyurea prior to study enrollment and were therefore evaluable for efficacy. The median follow-up was 23 months (range, 12 to 80 months).
The researchers found that Siklos prompted an increase in fetal hemoglobin. Median fetal hemoglobin percentages were 5.6% (range, 1.3 to 15.0) at baseline and 12.8% (range, 2.1 to 37.2) at around 6 months after Siklos initiation (the value closest to 6 months collected between 5 and 14 months).
In addition, the percentage of patients with at least 1 vaso-occlusive episode, 1 episode of acute chest syndrome, 1 hospitalization due to SCD, or 1 blood transfusion decreased after 12 months of Siklos treatment.
The proportion of patients with at least 1 vaso-occlusive episode was 69.2% at baseline and 42.5% at 12 months. The proportion with at least 1 episode of acute chest syndrome was 23.6% and 5.7%, respectively.
The proportion with at least 1 hospitalization due to SCD was 75.5% and 41.8%, respectively. And the proportion with at least 1 blood transfusion was 45.9% and 23.0%, respectively.
The most common adverse events (occurring in at least 10% of patients) were infections (39.8%), gastrointestinal disorders (13.1%), neutropenia (12.6%), nervous system disorders (11.1%), and metabolic and nutrition disorders (10.9%).
Full prescribing information for Siklos is available on the FDA website. ![]()
Nilotinib label updated with info on discontinuation
The US Food and Drug Administration (FDA) has approved an update to the product label for nilotinib (Tasigna) that includes information about how to discontinue the drug in certain patients.
Nilotinib, which was first approved by the FDA in 2007, is indicated for the treatment of patients with Philadelphia chromosome positive (Ph+) chronic myeloid leukemia (CML).
The updated prescribing information for the drug now outlines which of these patients may be eligible to stop receiving nilotinib.
Patients with chronic phase, Ph+ CML who have been taking nilotinib for 3 years or more (as first-line treatment or after failure with imatinib) and have achieved a sustained deep molecular response may be eligible to stop treatment.
Patients must have maintained a molecular response of at least MR4.0 for 1 year prior to discontinuation and achieved an MR4.5 at their last assessment.
Patients must have typical BCR-ABL transcripts (e13a2/b2a2 or e14a2/b3a2), no history of accelerated phase or blast crisis, and no past attempts at treatment discontinuation that resulted in relapse.
After discontinuation, patients must be monitored for possible loss of major molecular response (MMR). BCR-ABL transcript levels must be assessed and a complete blood count with differential performed monthly for 1 year, then every 6 weeks for the second year, and every 12 weeks thereafter.
BCR-ABL transcript levels should be measured using the MolecularMD MRDxTM BCR-ABL test, an FDA-authorized companion diagnostic validated to measure down to MR4.5.
If patients lose MMR, they must restart nilotinib within 4 weeks and receive the dose level they were receiving prior to discontinuation.
BCR-ABL transcript levels should be monitored every 2 weeks until they are lower than MMR for 4 consecutive measurements. Patients can then return to the original monitoring schedule.
The update of nilotinib’s label to include this information was based on results from 2 single-arm trials—ENESTfreedom and ENESTop.
ENESTfreedom
This phase 2 trial included 215 patients with Ph+, chronic phase CML. Researchers evaluated stopping treatment in 190 patients who had achieved a response of MR4.5 with nilotinib as first-line treatment. The patients had sustained deep molecular response for 1 year prior to treatment discontinuation.
Ninety-six weeks after stopping treatment, 48.9% of patients were still in MMR, also known as treatment-free remission (TFR).
Of the 88 patients who restarted nilotinib due to loss of MMR by the cut-off date, 98.9% were able to regain MMR (n=87). One patient discontinued the study at 7.1 weeks without regaining MMR after reinitiating treatment with nilotinib. Eighty-one patients (92.0%) regained MR4.5 by the cut-off date.
Common adverse events (AEs) in patients who discontinued nilotinib included musculoskeletal symptoms such as body aches, bone pain, and pain in extremities. However, these AEs decreased over time.
The incidence of musculoskeletal pain-related AEs decreased from 34.0% to 9.0% during the first and second 48 weeks of the TFR phase, respectively. In comparison, the incidence of such AEs was 17.0% during the treatment consolidation phase.
ENESTop
This phase 2 trial included 163 patients with Ph+, chronic phase CML. Researchers evaluated stopping treatment in 126 patients who had previously received imatinib, then switched to nilotinib and sustained a molecular response for 1 year prior to stopping nilotinib.
At 96 weeks, 53.2% of patients were still in TFR.
Fifty-six patients with confirmed loss of MR4.0 or loss of MMR restarted nilotinib by the cut-off date. Of these patients, 92.9% (n=52) regained both MR4.0 and MR4.5.
As in ENESTfreedom, patients who discontinued nilotinib had musculoskeletal symptoms that decreased over time.
The incidence of musculoskeletal pain-related AEs decreased from 47.9% to 15.1% during the first and second 48 weeks of the TFR phase, respectively. In comparison, the incidence of such AEs was 13.7% during the treatment consolidation phase.
Additional data from ENESTop and ENESTfreedom, as well as the recommendations for stopping nilotinib, are included in the updated prescribing information, which is available at https://www.us.tasigna.com/. ![]()
The US Food and Drug Administration (FDA) has approved an update to the product label for nilotinib (Tasigna) that includes information about how to discontinue the drug in certain patients.
Nilotinib, which was first approved by the FDA in 2007, is indicated for the treatment of patients with Philadelphia chromosome positive (Ph+) chronic myeloid leukemia (CML).
The updated prescribing information for the drug now outlines which of these patients may be eligible to stop receiving nilotinib.
Patients with chronic phase, Ph+ CML who have been taking nilotinib for 3 years or more (as first-line treatment or after failure with imatinib) and have achieved a sustained deep molecular response may be eligible to stop treatment.
Patients must have maintained a molecular response of at least MR4.0 for 1 year prior to discontinuation and achieved an MR4.5 at their last assessment.
Patients must have typical BCR-ABL transcripts (e13a2/b2a2 or e14a2/b3a2), no history of accelerated phase or blast crisis, and no past attempts at treatment discontinuation that resulted in relapse.
After discontinuation, patients must be monitored for possible loss of major molecular response (MMR). BCR-ABL transcript levels must be assessed and a complete blood count with differential performed monthly for 1 year, then every 6 weeks for the second year, and every 12 weeks thereafter.
BCR-ABL transcript levels should be measured using the MolecularMD MRDxTM BCR-ABL test, an FDA-authorized companion diagnostic validated to measure down to MR4.5.
If patients lose MMR, they must restart nilotinib within 4 weeks and receive the dose level they were receiving prior to discontinuation.
BCR-ABL transcript levels should be monitored every 2 weeks until they are lower than MMR for 4 consecutive measurements. Patients can then return to the original monitoring schedule.
The update of nilotinib’s label to include this information was based on results from 2 single-arm trials—ENESTfreedom and ENESTop.
ENESTfreedom
This phase 2 trial included 215 patients with Ph+, chronic phase CML. Researchers evaluated stopping treatment in 190 patients who had achieved a response of MR4.5 with nilotinib as first-line treatment. The patients had sustained deep molecular response for 1 year prior to treatment discontinuation.
Ninety-six weeks after stopping treatment, 48.9% of patients were still in MMR, also known as treatment-free remission (TFR).
Of the 88 patients who restarted nilotinib due to loss of MMR by the cut-off date, 98.9% were able to regain MMR (n=87). One patient discontinued the study at 7.1 weeks without regaining MMR after reinitiating treatment with nilotinib. Eighty-one patients (92.0%) regained MR4.5 by the cut-off date.
Common adverse events (AEs) in patients who discontinued nilotinib included musculoskeletal symptoms such as body aches, bone pain, and pain in extremities. However, these AEs decreased over time.
The incidence of musculoskeletal pain-related AEs decreased from 34.0% to 9.0% during the first and second 48 weeks of the TFR phase, respectively. In comparison, the incidence of such AEs was 17.0% during the treatment consolidation phase.
ENESTop
This phase 2 trial included 163 patients with Ph+, chronic phase CML. Researchers evaluated stopping treatment in 126 patients who had previously received imatinib, then switched to nilotinib and sustained a molecular response for 1 year prior to stopping nilotinib.
At 96 weeks, 53.2% of patients were still in TFR.
Fifty-six patients with confirmed loss of MR4.0 or loss of MMR restarted nilotinib by the cut-off date. Of these patients, 92.9% (n=52) regained both MR4.0 and MR4.5.
As in ENESTfreedom, patients who discontinued nilotinib had musculoskeletal symptoms that decreased over time.
The incidence of musculoskeletal pain-related AEs decreased from 47.9% to 15.1% during the first and second 48 weeks of the TFR phase, respectively. In comparison, the incidence of such AEs was 13.7% during the treatment consolidation phase.
Additional data from ENESTop and ENESTfreedom, as well as the recommendations for stopping nilotinib, are included in the updated prescribing information, which is available at https://www.us.tasigna.com/. ![]()
The US Food and Drug Administration (FDA) has approved an update to the product label for nilotinib (Tasigna) that includes information about how to discontinue the drug in certain patients.
Nilotinib, which was first approved by the FDA in 2007, is indicated for the treatment of patients with Philadelphia chromosome positive (Ph+) chronic myeloid leukemia (CML).
The updated prescribing information for the drug now outlines which of these patients may be eligible to stop receiving nilotinib.
Patients with chronic phase, Ph+ CML who have been taking nilotinib for 3 years or more (as first-line treatment or after failure with imatinib) and have achieved a sustained deep molecular response may be eligible to stop treatment.
Patients must have maintained a molecular response of at least MR4.0 for 1 year prior to discontinuation and achieved an MR4.5 at their last assessment.
Patients must have typical BCR-ABL transcripts (e13a2/b2a2 or e14a2/b3a2), no history of accelerated phase or blast crisis, and no past attempts at treatment discontinuation that resulted in relapse.
After discontinuation, patients must be monitored for possible loss of major molecular response (MMR). BCR-ABL transcript levels must be assessed and a complete blood count with differential performed monthly for 1 year, then every 6 weeks for the second year, and every 12 weeks thereafter.
BCR-ABL transcript levels should be measured using the MolecularMD MRDxTM BCR-ABL test, an FDA-authorized companion diagnostic validated to measure down to MR4.5.
If patients lose MMR, they must restart nilotinib within 4 weeks and receive the dose level they were receiving prior to discontinuation.
BCR-ABL transcript levels should be monitored every 2 weeks until they are lower than MMR for 4 consecutive measurements. Patients can then return to the original monitoring schedule.
The update of nilotinib’s label to include this information was based on results from 2 single-arm trials—ENESTfreedom and ENESTop.
ENESTfreedom
This phase 2 trial included 215 patients with Ph+, chronic phase CML. Researchers evaluated stopping treatment in 190 patients who had achieved a response of MR4.5 with nilotinib as first-line treatment. The patients had sustained deep molecular response for 1 year prior to treatment discontinuation.
Ninety-six weeks after stopping treatment, 48.9% of patients were still in MMR, also known as treatment-free remission (TFR).
Of the 88 patients who restarted nilotinib due to loss of MMR by the cut-off date, 98.9% were able to regain MMR (n=87). One patient discontinued the study at 7.1 weeks without regaining MMR after reinitiating treatment with nilotinib. Eighty-one patients (92.0%) regained MR4.5 by the cut-off date.
Common adverse events (AEs) in patients who discontinued nilotinib included musculoskeletal symptoms such as body aches, bone pain, and pain in extremities. However, these AEs decreased over time.
The incidence of musculoskeletal pain-related AEs decreased from 34.0% to 9.0% during the first and second 48 weeks of the TFR phase, respectively. In comparison, the incidence of such AEs was 17.0% during the treatment consolidation phase.
ENESTop
This phase 2 trial included 163 patients with Ph+, chronic phase CML. Researchers evaluated stopping treatment in 126 patients who had previously received imatinib, then switched to nilotinib and sustained a molecular response for 1 year prior to stopping nilotinib.
At 96 weeks, 53.2% of patients were still in TFR.
Fifty-six patients with confirmed loss of MR4.0 or loss of MMR restarted nilotinib by the cut-off date. Of these patients, 92.9% (n=52) regained both MR4.0 and MR4.5.
As in ENESTfreedom, patients who discontinued nilotinib had musculoskeletal symptoms that decreased over time.
The incidence of musculoskeletal pain-related AEs decreased from 47.9% to 15.1% during the first and second 48 weeks of the TFR phase, respectively. In comparison, the incidence of such AEs was 13.7% during the treatment consolidation phase.
Additional data from ENESTop and ENESTfreedom, as well as the recommendations for stopping nilotinib, are included in the updated prescribing information, which is available at https://www.us.tasigna.com/. ![]()
Isolation precautions are associated with higher costs, longer LOS
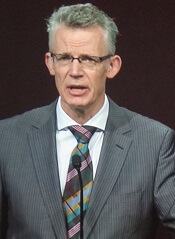
Clinical question: What are the effects of isolation precautions on hospital outcomes and cost of care?
Background: Previous studies have found that isolation precautions negatively affect various aspects of patient care, including frequency of contact with clinicians, adverse events in the hospital, measures of patient well-being, and patient experience scores. It is not known how isolation precautions affect other hospital-based metrics, such as 30-day readmissions, length of stay (LOS), in-hospital mortality, and cost of care.
Study design: Multisite, retrospective, propensity score–matched cohort study.
Setting: Three academic tertiary care hospitals in Toronto.
Synopsis: The authors used administrative databases and propensity-score modeling to match isolated patients and nonisolated controls. Researchers included 17,649 control patients, 737 patients isolated for methicillin-resistant Staphylococcus aureus (contact isolation), and 1,502 patients isolated for respiratory illnesses (contact and droplet isolation) in the study. Patients isolated for MRSA had a higher 30-day readmission rate than did controls (19% vs. 14.7%), a longer average length of stay (11.9 days vs. 9.1 days), and higher direct costs ($11,009 vs. $7,670). Patients isolated for respiratory illnesses had a longer average length of stay (8.5 days vs. 7.6 days) and higher direct costs ($7,194 vs. $6,294). No differences in adverse events rates or in-hospital mortality were observed between control patients and patients in either isolation group.
Some of the differences observed may be from illness severity rather than from the effects of isolation, especially in the MRSA group. There was no difference observed in rates of adverse outcomes, such as falls or medication errors, or in rates of formal patient complaints to the hospital. It is possible that propensity score modeling corrected for unidentified biases in prior studies that found differences in these types of outcomes.
Bottom line: Isolation precautions are associated with higher costs and longer LOS in hospitalized general medicine patients.
Citation: Tran K et al. The effect of hospital isolation precautions on patient outcomes and cost of care: A multisite, retrospective, propensity score-matched cohort study. J Gen Intern Med. 2017;32(3):262-8.
Dr. Wachter is an assistant professor of medicine at Duke University.
Clinical question: What are the effects of isolation precautions on hospital outcomes and cost of care?
Background: Previous studies have found that isolation precautions negatively affect various aspects of patient care, including frequency of contact with clinicians, adverse events in the hospital, measures of patient well-being, and patient experience scores. It is not known how isolation precautions affect other hospital-based metrics, such as 30-day readmissions, length of stay (LOS), in-hospital mortality, and cost of care.
Study design: Multisite, retrospective, propensity score–matched cohort study.
Setting: Three academic tertiary care hospitals in Toronto.
Synopsis: The authors used administrative databases and propensity-score modeling to match isolated patients and nonisolated controls. Researchers included 17,649 control patients, 737 patients isolated for methicillin-resistant Staphylococcus aureus (contact isolation), and 1,502 patients isolated for respiratory illnesses (contact and droplet isolation) in the study. Patients isolated for MRSA had a higher 30-day readmission rate than did controls (19% vs. 14.7%), a longer average length of stay (11.9 days vs. 9.1 days), and higher direct costs ($11,009 vs. $7,670). Patients isolated for respiratory illnesses had a longer average length of stay (8.5 days vs. 7.6 days) and higher direct costs ($7,194 vs. $6,294). No differences in adverse events rates or in-hospital mortality were observed between control patients and patients in either isolation group.
Some of the differences observed may be from illness severity rather than from the effects of isolation, especially in the MRSA group. There was no difference observed in rates of adverse outcomes, such as falls or medication errors, or in rates of formal patient complaints to the hospital. It is possible that propensity score modeling corrected for unidentified biases in prior studies that found differences in these types of outcomes.
Bottom line: Isolation precautions are associated with higher costs and longer LOS in hospitalized general medicine patients.
Citation: Tran K et al. The effect of hospital isolation precautions on patient outcomes and cost of care: A multisite, retrospective, propensity score-matched cohort study. J Gen Intern Med. 2017;32(3):262-8.
Dr. Wachter is an assistant professor of medicine at Duke University.
Clinical question: What are the effects of isolation precautions on hospital outcomes and cost of care?
Background: Previous studies have found that isolation precautions negatively affect various aspects of patient care, including frequency of contact with clinicians, adverse events in the hospital, measures of patient well-being, and patient experience scores. It is not known how isolation precautions affect other hospital-based metrics, such as 30-day readmissions, length of stay (LOS), in-hospital mortality, and cost of care.
Study design: Multisite, retrospective, propensity score–matched cohort study.
Setting: Three academic tertiary care hospitals in Toronto.
Synopsis: The authors used administrative databases and propensity-score modeling to match isolated patients and nonisolated controls. Researchers included 17,649 control patients, 737 patients isolated for methicillin-resistant Staphylococcus aureus (contact isolation), and 1,502 patients isolated for respiratory illnesses (contact and droplet isolation) in the study. Patients isolated for MRSA had a higher 30-day readmission rate than did controls (19% vs. 14.7%), a longer average length of stay (11.9 days vs. 9.1 days), and higher direct costs ($11,009 vs. $7,670). Patients isolated for respiratory illnesses had a longer average length of stay (8.5 days vs. 7.6 days) and higher direct costs ($7,194 vs. $6,294). No differences in adverse events rates or in-hospital mortality were observed between control patients and patients in either isolation group.
Some of the differences observed may be from illness severity rather than from the effects of isolation, especially in the MRSA group. There was no difference observed in rates of adverse outcomes, such as falls or medication errors, or in rates of formal patient complaints to the hospital. It is possible that propensity score modeling corrected for unidentified biases in prior studies that found differences in these types of outcomes.
Bottom line: Isolation precautions are associated with higher costs and longer LOS in hospitalized general medicine patients.
Citation: Tran K et al. The effect of hospital isolation precautions on patient outcomes and cost of care: A multisite, retrospective, propensity score-matched cohort study. J Gen Intern Med. 2017;32(3):262-8.
Dr. Wachter is an assistant professor of medicine at Duke University.
When cannabis use becomes another disorder
Despite the justified concern about rising opiate use in the United States, cannabis remains the most commonly used substance in the 12- to 17-year-old population.1 Cannabis use is widespread, particularly in states in which it has been decriminalized or legalized. While use of alcohol and nicotine has fallen among high school students from the years 2010 to 2015, marijuana use has remained relatively constant.2 In addition, the potency of cannabis with regard to tetrahydrocannabinol (THC) content has increased over the years. Despite the common belief among the public that cannabis use is benign, accumulating research is revealing a number of concerning consequences, especially in vulnerable populations and those who use cannabis regularly.
Case summary
Case discussion
Treatment for these adverse effects of cannabis is cessation of the drug. This can be accomplished through hard work with a counselor, who may recommend any of a number of treatments, including contingency management, cognitive behavioral therapy, systematic multidimensional family therapy, and motivational enhancement therapy, among others.5 While common lore is that it is impossible to stop cannabis use, the effect sizes of these treatments is in the moderate to large range. There are viable options to stop cannabis use, especially when it becomes problematic.
Dr. Althoff is associate professor of psychiatry, psychology, and pediatrics at the University of Vermont, Burlington. He is director of the division of behavioral genetics and conducts research on the development of self-regulation in children. Email him at [email protected].
References
1. “Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings,” Substance Abuse and Mental Health Services Administration Center for Behavioral Health Statistics and Quality, 2013.
2. “Monitoring the Future Survey, 2015,” National Institute on Drug Abuse.
3. Pharmaceuticals (Basel). 2012 Jul;5(7):719-26.
4. Nat Rev Neurosci. 2007 Nov;8(11):885-95.
5. Dtsch Arztebl Int. 2016 Sep;113(39): 653-9.
Despite the justified concern about rising opiate use in the United States, cannabis remains the most commonly used substance in the 12- to 17-year-old population.1 Cannabis use is widespread, particularly in states in which it has been decriminalized or legalized. While use of alcohol and nicotine has fallen among high school students from the years 2010 to 2015, marijuana use has remained relatively constant.2 In addition, the potency of cannabis with regard to tetrahydrocannabinol (THC) content has increased over the years. Despite the common belief among the public that cannabis use is benign, accumulating research is revealing a number of concerning consequences, especially in vulnerable populations and those who use cannabis regularly.
Case summary
Case discussion
Treatment for these adverse effects of cannabis is cessation of the drug. This can be accomplished through hard work with a counselor, who may recommend any of a number of treatments, including contingency management, cognitive behavioral therapy, systematic multidimensional family therapy, and motivational enhancement therapy, among others.5 While common lore is that it is impossible to stop cannabis use, the effect sizes of these treatments is in the moderate to large range. There are viable options to stop cannabis use, especially when it becomes problematic.
Dr. Althoff is associate professor of psychiatry, psychology, and pediatrics at the University of Vermont, Burlington. He is director of the division of behavioral genetics and conducts research on the development of self-regulation in children. Email him at [email protected].
References
1. “Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings,” Substance Abuse and Mental Health Services Administration Center for Behavioral Health Statistics and Quality, 2013.
2. “Monitoring the Future Survey, 2015,” National Institute on Drug Abuse.
3. Pharmaceuticals (Basel). 2012 Jul;5(7):719-26.
4. Nat Rev Neurosci. 2007 Nov;8(11):885-95.
5. Dtsch Arztebl Int. 2016 Sep;113(39): 653-9.
Despite the justified concern about rising opiate use in the United States, cannabis remains the most commonly used substance in the 12- to 17-year-old population.1 Cannabis use is widespread, particularly in states in which it has been decriminalized or legalized. While use of alcohol and nicotine has fallen among high school students from the years 2010 to 2015, marijuana use has remained relatively constant.2 In addition, the potency of cannabis with regard to tetrahydrocannabinol (THC) content has increased over the years. Despite the common belief among the public that cannabis use is benign, accumulating research is revealing a number of concerning consequences, especially in vulnerable populations and those who use cannabis regularly.
Case summary
Case discussion
Treatment for these adverse effects of cannabis is cessation of the drug. This can be accomplished through hard work with a counselor, who may recommend any of a number of treatments, including contingency management, cognitive behavioral therapy, systematic multidimensional family therapy, and motivational enhancement therapy, among others.5 While common lore is that it is impossible to stop cannabis use, the effect sizes of these treatments is in the moderate to large range. There are viable options to stop cannabis use, especially when it becomes problematic.
Dr. Althoff is associate professor of psychiatry, psychology, and pediatrics at the University of Vermont, Burlington. He is director of the division of behavioral genetics and conducts research on the development of self-regulation in children. Email him at [email protected].
References
1. “Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings,” Substance Abuse and Mental Health Services Administration Center for Behavioral Health Statistics and Quality, 2013.
2. “Monitoring the Future Survey, 2015,” National Institute on Drug Abuse.
3. Pharmaceuticals (Basel). 2012 Jul;5(7):719-26.
4. Nat Rev Neurosci. 2007 Nov;8(11):885-95.
5. Dtsch Arztebl Int. 2016 Sep;113(39): 653-9.
She’s Not My Mother: A 24-Year-Old Man With Capgras Delusion
Many patients admitted to inpatient psychiatric hospitals present with delusions; however, the Capgras delusion is a rare type that often appears as a sequela of certain medical and neurologic conditions.1 The Capgras delusion is a condition in which a person believes that either an individual or a group of people has been replaced by doubles or imposters.
In 1923, French psychiatrist Joseph Capgras first described the delusion. He and Jean Reboul-Lachaux coauthored a paper on a 53-year-old woman. The patient was a paranoid megalomaniac who “transformed everyone in her entourage, even those closest to her, such as her husband and daughter, into various and numerous doubles.”2 She believed she was famous, wealthy, and of royal lineage. Although 3 of her children had died, she believed that they were abducted, and that her only surviving child was replaced by a look-alike.2,3 Although the prevalence of such delusions in the general population has not been fully studied, a psychiatric hospital in Turkey found a 1.3% prevalence (1.8% women and 0.9% men) in 920 admissions over 5 years.4
The Capgras delusion is one of many delusions related to the misidentification of people, places, or objects; these delusions collectively are known as delusional misidentification syndrome (DMS).5,6 The Fregoli delusion involves the belief that several different people are the same person in disguise. Intermetamorphosis is the belief that an individual has been transformed internally and externally to another person. Subjective doubles is the belief that a doppelganger of the afflicted person exists, living and functioning independently in the world. Reduplicative paramnesia is the belief that a person, place, or object has been duplicated. A rarer example of DMS is the Cotard delusion, which is the belief that the patient himself or herself is dead, putrefying, exsanguinating, or lacking internal organs.
The most common of the DMS is the Capgras delusion. One common presentation of Capgras delusion involves the spouse of the patient, who believes that an imposter of the same sex as their spouse has taken over his or her body. Rarer delusions are those in which a person misidentifies him or herself as the imposter.3,5,6
Case Presentation
This case involved a 24-year-old male veteran who had received a wide range of mental health diagnoses in the past, including major depressive disorder (MDD) with psychotic features, generalized anxiety disorder, cannabis use disorder, adjustment disorder, and borderline personality disorder. He also had a medical history related to a motor vehicle accident with subsequent intestinal rupture and colostomy placement that had occurred a year and a half prior to presentation. He had no history of brain trauma.
The patient voluntarily presented to the hospital for increased suicidal thoughts and was admitted voluntarily for stabilization and self-harm prevention. He stated that “I feel everything is unreal. I feel suicidal and guilt” and endorsed a plan to either walk into traffic or shoot himself in the head due to increasingly distressing thoughts and memories. According to the patient, he had reported to the police that he raped his ex-girlfriend a year previously, although she denied the claim to the police.
The patient further disclosed that he did not believe his mother was real. “Last year my sister told me it was not 2016, but it was 2022,” he said. “She told me that I have hurt my mother with a padlock—that you could no longer identify her face. I don’t remember having done this. I have lived with her since that time, so I don’t think it’s really [my mother].” He believed that his mother was replaced by “government employees” who were sent to elicit confessions for his behavior while in the military. He expressed guilt over several actions he had performed while in military service, such as punching a wall during boot camp, stealing “soak-up” pads, and napping during work hours. His mother was contacted by a staff psychiatrist in the inpatient unit and denied that any assault had taken place.
The patient’s psychiatric review of systems was positive for visual hallucinations (specifically “blurs” next to his bed in the morning that disappeared as he tried to touch them), depressed mood, anxiety, hopelessness, and insomnia. Pertinent negatives of the review of systems included a denial of manic symptoms and auditory hallucinations. For additional details of his past psychiatric history, the patient admitted that his motor vehicle accident, intestinal rupture, and colostomy were the result of his 1 suicide attempt a year and a half prior after a verbal dispute with the same ex-girlfriend that he believed he had raped. After undergoing extensive medical and surgical treatment, he began seeing an outpatient psychiatrist as well as attending substance use counseling to curtail his marijuana use. He was prescribed a combination of duloxetine and risperidone as an outpatient, which he was taking with intermittent adherence.
Regarding substance use, the patient admitted to using marijuana regularly in the past but quit completely 1 month prior and denied any other drug use or alcohol use. He reported a family history of a sister who was undergoing treatment for bipolar disorder. In his social history, the patient disclosed that he was raised by both parents and described a good childhood with a life absent of abuse in any form. He was single with no children. Although he was unemployed, he lived off the funds from an insurance settlement from his motor vehicle accident. He was living in a trailer with his brother and mother. He also denied having access to firearms.
The patient was overweight, neatly groomed, had good eye contact, and was calm and cooperative. He seemed anxious as evidenced by his continuous shaking of his feet; although speech was normal in rate and tone. He reported his mood as “depressed and anxious” with congruent and tearful affect. His thought process was concrete, although his thought content contained delusions, suicidal ideation, and paranoia. He denied any homicidal thoughts or thoughts of harming others. He did not present with any auditory or visual hallucinations. Insight and judgment were poor. The mental status examination revealed no notable deficits in cognition.
The patient’s differential diagnosis included schizophreniform disorder, exacerbation of MDD with psychotic features, and the psychotic component of cannabis use disorder. His outpatient risperidone and duloxetine were not restarted. Aripiprazole 15 mg daily was prescribed for his delusions, paranoia, and visual hallucinations. The patient also received a prescription for hydroxyzine 50 mg every 6 hours as needed for anxiety.
Because of the nature of his delusions, comorbid medical and neurologic conditions were considered. Neurology consultation recommended a noncontrast head computer tomography (CT) scan and an electroencephalogram (EEG). Laboratory workup included HIV antibody, thyroid panel, chemistry panel, complete blood count, hepatitis B serum antigen, urine drug screen, hepatitis C virus, and rapid plasma reagin. All laboratory results were benign and unremarkable, and the urine drug screen was negative. The noncontrast CT revealed no acute findings, and the EEG revealed no recorded epileptiform abnormalities or seizures.
Throughout his hospital course, the patient remained cooperative with treatment. Three days into the hospitalization, he stated that he believed the entire family had been replaced by imposters. He began to distrust members of his family and was reticent to communicate with them when they attempted to contact him. He also experienced fragmented sleep during his hospital stay, and trazodone 50 mg at bedtime was added.
After aripiprazole was increased to 20 mg daily on hospital day 2 and then to 30 mg daily on hospital day 3 due to the patient’s delusions, he began to doubt the validity of his beliefs. After showing gradual improvement over 6 days, the patient reported that he no longer believed that those memories were real. His sleep, depressed mood, anxiety, and paranoia had markedly improved toward the end of the hospitalization and suicidal ideation/intent resolved. The patient was discharged home to his mother and brother after 6 days of hospitalization with aripiprazole 30 mg daily and trazodone 50 mg at bedtime.
Discussion
The Capgras delusion can present in several different contexts. A psychiatric differential diagnosis includes disorders in the schizophrenia spectrum (brief psychotic disorder, schizophreniform disorder, and schizophrenia), schizoaffective disorder, delusional disorder, and substance-induced psychotic disorder. In addition to psychiatric disorders, the Capgras delusion has been shown to occur in several medical conditions, which include stroke, central nervous system tumors, subarachnoid hemorrhage, vitamin B12 deficiency, hepatic encephalopathy, hypothyroidism, hyperparathyroidism, epilepsy, and dementia.1,2,4,7
A 2007 retrospective study by Josephs examined 47 patients diagnosed with the Capgras delusion from several tertiary care centers. Of those patients, 38 (81%) had a neurodegenerative disease, most commonly Lewy body dementia (LBD).1 In his review of the Josephs study, Devinsky proposed that the loss of striatal D2 receptors in LBD may be implicated in the manifestation of Capgras delusions.2 The data suggest multiple brain regions may be involved, including the frontal lobes, right temporal lobe, right parietal lobe, parahippocampus, and amygdala.1,2 Most patients in the Josephs study demonstrated global atrophy on imaging studies. One hypothesis is that it is the disconnection of the frontal lobe to other brain regions that may be implicated.1,2,4 This results in intact recognition of facial features of familiar people, impaired emotional recognition, and impaired self-correction due to executive dysfunction.
Methamphetamine also has been implicated in a small number of cases of Capgras; the proposed mechanism involves dopaminergic neuronal impairment/loss.1,2 Additionally, Capgras delusions have been described in cases of patients treated with antimalarial medications, such as chloroquine.8 Younger patients with the Capgras delusion were more likely to have purely psychiatric comorbidities—such as schizophrenia, substance-induced psychosis, or schizoaffective disorder—as opposed to underlying medical conditions.1 In the case presented here, the Capgras delusion was thought to be due to a disorder in the schizophrenia spectrum, specifically schizophreniform disorder.
Because an increasing amount of evidence indicates that the Capgras delusion is associated with certain medical conditions, a workup should be performed to rule out underlying medical etiology. Of note, no official guidelines for the workup have been produced for the Capgras delusion. However, the workup may include brain imaging, such as magnetic resonance imaging and/or CT scan to rule out mass lesions, vascular malformations, stroke, or neuro-infectious processes; laboratory tests, such as vitamin B12, liver panel, HIV, rapid plasma reagin, hepatitis B and C viruses, parathyroid hormone levels, urine drug screen, and thyroid panel can be ordered to rule out other medical causes.1,2,6,7,9
Consultations with internal medicine and neurology departments may be beneficial. Although treatment of the underlying condition may lead to an improvement in the symptoms, full remission in all cases has not been consistently demonstrated in the current literature.5,7,9,10 Patients with the Capgras delusion are challenging to treat, because their delusions have been shown to be refractory to antipsychotic therapy. However, antipsychotics are currently the mainstay of treatment. Some case studies have shown efficacy with pimozide, tricyclic antidepressants, and mirtazapine.6,9
One case study in 2014 in India of a 45-year-old woman who believed her husband and son were replaced by imposters out to kill her, showed a 40% to 50% reduction of paranoia, irritability, and suspicious scanning behaviors with a combination of risperidone and trihexyphenidyl. Despite the improvements, the woman continued to have delusions.7
A notable feature associated with those experiencing the Capgras delusion is the increased risk of violent behaviors, often because of suspiciousness and paranoia. A 2004 review suggested the risk of violence and homicidality is much higher in male patients compared with that of female patients with the Capgras delusion.9 This is despite evidence suggesting that the prevalence of the Capgras delusion seems to be greater in women.6,9 Moreover, patients often demonstrated social withdrawal and self-isolation prior to violent acts. The victims often were family members or those who live with the patient, which is consistent with the evidence that those most familiar to patients are more likely to be misidentified.1,2,7,9,10
A 1989 case series that examined 8 cases of the Capgras delusion listed the following violent behaviors: shot and killed father, pointed knife at mother, held knife to mother’s throat, punched parents, threatened to stab husband with scissors, nonspecifically threatened physical harm to family, injured mother with axe, and threatened to stab son with knife and burn him. Seven of the 8 patients lived with the misidentified persons, and 5 of the 8 patients were treatment resistant. The study posited that chronicity of the delusion, content of the delusion, and accessibility of misidentified persons seemed to increase the risk of violent behaviors. These authors went on to suggest that despite the appearance of stability, patients may react violently to minute changes.10 Overall literature seems to suggest the importance of performing a violence and homicidality assessment with special attention to assessment for themes of hostility toward misidentified individuals.9,10
Conclusion
The Capgras delusion is an uncommon symptom associated with varied psychiatric, medical, iatrogenic, and neurologic conditions. Treatment of underlying medical conditions may improve or resolve the delusions. However, in this case, the patient did not seem to have any underlying medical conditions, and it was thought that he may have been experiencing a prodrome within the schizophrenia spectrum. This is consistent with the literature, which suggests that those with the delusions at younger ages may have a psychiatric etiology.
Although this patient was responsive to aripiprazole, the Capgras delusion has been known to be resistant to antipsychotic therapy. It is worth considering a medical and neurologic workup with the addition of a psychiatry referral. Further, while the patient in the presented case had the delusion that he had assaulted his mother, whom he misidentified as an imposter, the patient did not demonstrate any hostility and denied thoughts of harming her. However, given the increased risk of violence in patients with the Capgras delusion, a homicidality and violence assessment should be performed. While further recommendations are outside the scope of this article, the provider should be cognizant of local duty-to-warn and duty-to-protect laws regarding potentially homicidal patients.
1. Josephs KA. The Capgras delusion and its relationship to neurodegenerative disease. Arch Neurol. 2007;64(12):1762-1766.
2. Devinsky O. Behavioral neurology. The neurology of the Capgras delusion. Rev Neurol Dis. 2008;5(2):97-100.
3. Sadock BJ, Sadock VA. Kaplan & Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry. 10th ed. Philadelphia, PA: Wolters Kluwer; 2007.
4. Tamam L, Karatas G, Zeren T, Ozpyraz N. The prevalence of Capgras syndrome in a university hospital setting. Acta Neuropsychiatr. 2003;15(5):290-295.
5. Klein CA, Hirchan S. The masks of identities: who’s who? Delusional misidentification syndromes. J Am Acad Psychiatry Law. 2014;42(3):369-378.
6. Atta K. Forlenza N, Gujski M, Hashmi S, Isaac G. Delusional misidentification syndromes: separate disorders or unusual presentations of existing DSM-IV categories? Psychiatry (Edgemont). 2006;3(9):56-61.
7. Sathe H, Karia S, De Sousa A, Shah N. Capgras syndrome: a case report. Paripex Indian J Res. 2014;3(8):134-135. 8. Bhatia MS, Singhal PK, Agrawal P, Malik SC. Capgras’ syndrome in chloroquine induced psychosis. Indian J Psychiatry. 1988;30(3):311-313.
9. Bourget D, Whitehurst L. Capgras syndrome: a review of the neurophysiological correlates and presenting clinical features in cases involving physical violence. Can J Psychiatry. 2004;49(11):719-725.
10. Silva JA, Leong GB, Weinstock R, Boyer CL. Capgras syndrome and dangerousness. Bull Am Acad Psychiatry Law. 1989;17(1):5-14.
Many patients admitted to inpatient psychiatric hospitals present with delusions; however, the Capgras delusion is a rare type that often appears as a sequela of certain medical and neurologic conditions.1 The Capgras delusion is a condition in which a person believes that either an individual or a group of people has been replaced by doubles or imposters.
In 1923, French psychiatrist Joseph Capgras first described the delusion. He and Jean Reboul-Lachaux coauthored a paper on a 53-year-old woman. The patient was a paranoid megalomaniac who “transformed everyone in her entourage, even those closest to her, such as her husband and daughter, into various and numerous doubles.”2 She believed she was famous, wealthy, and of royal lineage. Although 3 of her children had died, she believed that they were abducted, and that her only surviving child was replaced by a look-alike.2,3 Although the prevalence of such delusions in the general population has not been fully studied, a psychiatric hospital in Turkey found a 1.3% prevalence (1.8% women and 0.9% men) in 920 admissions over 5 years.4
The Capgras delusion is one of many delusions related to the misidentification of people, places, or objects; these delusions collectively are known as delusional misidentification syndrome (DMS).5,6 The Fregoli delusion involves the belief that several different people are the same person in disguise. Intermetamorphosis is the belief that an individual has been transformed internally and externally to another person. Subjective doubles is the belief that a doppelganger of the afflicted person exists, living and functioning independently in the world. Reduplicative paramnesia is the belief that a person, place, or object has been duplicated. A rarer example of DMS is the Cotard delusion, which is the belief that the patient himself or herself is dead, putrefying, exsanguinating, or lacking internal organs.
The most common of the DMS is the Capgras delusion. One common presentation of Capgras delusion involves the spouse of the patient, who believes that an imposter of the same sex as their spouse has taken over his or her body. Rarer delusions are those in which a person misidentifies him or herself as the imposter.3,5,6
Case Presentation
This case involved a 24-year-old male veteran who had received a wide range of mental health diagnoses in the past, including major depressive disorder (MDD) with psychotic features, generalized anxiety disorder, cannabis use disorder, adjustment disorder, and borderline personality disorder. He also had a medical history related to a motor vehicle accident with subsequent intestinal rupture and colostomy placement that had occurred a year and a half prior to presentation. He had no history of brain trauma.
The patient voluntarily presented to the hospital for increased suicidal thoughts and was admitted voluntarily for stabilization and self-harm prevention. He stated that “I feel everything is unreal. I feel suicidal and guilt” and endorsed a plan to either walk into traffic or shoot himself in the head due to increasingly distressing thoughts and memories. According to the patient, he had reported to the police that he raped his ex-girlfriend a year previously, although she denied the claim to the police.
The patient further disclosed that he did not believe his mother was real. “Last year my sister told me it was not 2016, but it was 2022,” he said. “She told me that I have hurt my mother with a padlock—that you could no longer identify her face. I don’t remember having done this. I have lived with her since that time, so I don’t think it’s really [my mother].” He believed that his mother was replaced by “government employees” who were sent to elicit confessions for his behavior while in the military. He expressed guilt over several actions he had performed while in military service, such as punching a wall during boot camp, stealing “soak-up” pads, and napping during work hours. His mother was contacted by a staff psychiatrist in the inpatient unit and denied that any assault had taken place.
The patient’s psychiatric review of systems was positive for visual hallucinations (specifically “blurs” next to his bed in the morning that disappeared as he tried to touch them), depressed mood, anxiety, hopelessness, and insomnia. Pertinent negatives of the review of systems included a denial of manic symptoms and auditory hallucinations. For additional details of his past psychiatric history, the patient admitted that his motor vehicle accident, intestinal rupture, and colostomy were the result of his 1 suicide attempt a year and a half prior after a verbal dispute with the same ex-girlfriend that he believed he had raped. After undergoing extensive medical and surgical treatment, he began seeing an outpatient psychiatrist as well as attending substance use counseling to curtail his marijuana use. He was prescribed a combination of duloxetine and risperidone as an outpatient, which he was taking with intermittent adherence.
Regarding substance use, the patient admitted to using marijuana regularly in the past but quit completely 1 month prior and denied any other drug use or alcohol use. He reported a family history of a sister who was undergoing treatment for bipolar disorder. In his social history, the patient disclosed that he was raised by both parents and described a good childhood with a life absent of abuse in any form. He was single with no children. Although he was unemployed, he lived off the funds from an insurance settlement from his motor vehicle accident. He was living in a trailer with his brother and mother. He also denied having access to firearms.
The patient was overweight, neatly groomed, had good eye contact, and was calm and cooperative. He seemed anxious as evidenced by his continuous shaking of his feet; although speech was normal in rate and tone. He reported his mood as “depressed and anxious” with congruent and tearful affect. His thought process was concrete, although his thought content contained delusions, suicidal ideation, and paranoia. He denied any homicidal thoughts or thoughts of harming others. He did not present with any auditory or visual hallucinations. Insight and judgment were poor. The mental status examination revealed no notable deficits in cognition.
The patient’s differential diagnosis included schizophreniform disorder, exacerbation of MDD with psychotic features, and the psychotic component of cannabis use disorder. His outpatient risperidone and duloxetine were not restarted. Aripiprazole 15 mg daily was prescribed for his delusions, paranoia, and visual hallucinations. The patient also received a prescription for hydroxyzine 50 mg every 6 hours as needed for anxiety.
Because of the nature of his delusions, comorbid medical and neurologic conditions were considered. Neurology consultation recommended a noncontrast head computer tomography (CT) scan and an electroencephalogram (EEG). Laboratory workup included HIV antibody, thyroid panel, chemistry panel, complete blood count, hepatitis B serum antigen, urine drug screen, hepatitis C virus, and rapid plasma reagin. All laboratory results were benign and unremarkable, and the urine drug screen was negative. The noncontrast CT revealed no acute findings, and the EEG revealed no recorded epileptiform abnormalities or seizures.
Throughout his hospital course, the patient remained cooperative with treatment. Three days into the hospitalization, he stated that he believed the entire family had been replaced by imposters. He began to distrust members of his family and was reticent to communicate with them when they attempted to contact him. He also experienced fragmented sleep during his hospital stay, and trazodone 50 mg at bedtime was added.
After aripiprazole was increased to 20 mg daily on hospital day 2 and then to 30 mg daily on hospital day 3 due to the patient’s delusions, he began to doubt the validity of his beliefs. After showing gradual improvement over 6 days, the patient reported that he no longer believed that those memories were real. His sleep, depressed mood, anxiety, and paranoia had markedly improved toward the end of the hospitalization and suicidal ideation/intent resolved. The patient was discharged home to his mother and brother after 6 days of hospitalization with aripiprazole 30 mg daily and trazodone 50 mg at bedtime.
Discussion
The Capgras delusion can present in several different contexts. A psychiatric differential diagnosis includes disorders in the schizophrenia spectrum (brief psychotic disorder, schizophreniform disorder, and schizophrenia), schizoaffective disorder, delusional disorder, and substance-induced psychotic disorder. In addition to psychiatric disorders, the Capgras delusion has been shown to occur in several medical conditions, which include stroke, central nervous system tumors, subarachnoid hemorrhage, vitamin B12 deficiency, hepatic encephalopathy, hypothyroidism, hyperparathyroidism, epilepsy, and dementia.1,2,4,7
A 2007 retrospective study by Josephs examined 47 patients diagnosed with the Capgras delusion from several tertiary care centers. Of those patients, 38 (81%) had a neurodegenerative disease, most commonly Lewy body dementia (LBD).1 In his review of the Josephs study, Devinsky proposed that the loss of striatal D2 receptors in LBD may be implicated in the manifestation of Capgras delusions.2 The data suggest multiple brain regions may be involved, including the frontal lobes, right temporal lobe, right parietal lobe, parahippocampus, and amygdala.1,2 Most patients in the Josephs study demonstrated global atrophy on imaging studies. One hypothesis is that it is the disconnection of the frontal lobe to other brain regions that may be implicated.1,2,4 This results in intact recognition of facial features of familiar people, impaired emotional recognition, and impaired self-correction due to executive dysfunction.
Methamphetamine also has been implicated in a small number of cases of Capgras; the proposed mechanism involves dopaminergic neuronal impairment/loss.1,2 Additionally, Capgras delusions have been described in cases of patients treated with antimalarial medications, such as chloroquine.8 Younger patients with the Capgras delusion were more likely to have purely psychiatric comorbidities—such as schizophrenia, substance-induced psychosis, or schizoaffective disorder—as opposed to underlying medical conditions.1 In the case presented here, the Capgras delusion was thought to be due to a disorder in the schizophrenia spectrum, specifically schizophreniform disorder.
Because an increasing amount of evidence indicates that the Capgras delusion is associated with certain medical conditions, a workup should be performed to rule out underlying medical etiology. Of note, no official guidelines for the workup have been produced for the Capgras delusion. However, the workup may include brain imaging, such as magnetic resonance imaging and/or CT scan to rule out mass lesions, vascular malformations, stroke, or neuro-infectious processes; laboratory tests, such as vitamin B12, liver panel, HIV, rapid plasma reagin, hepatitis B and C viruses, parathyroid hormone levels, urine drug screen, and thyroid panel can be ordered to rule out other medical causes.1,2,6,7,9
Consultations with internal medicine and neurology departments may be beneficial. Although treatment of the underlying condition may lead to an improvement in the symptoms, full remission in all cases has not been consistently demonstrated in the current literature.5,7,9,10 Patients with the Capgras delusion are challenging to treat, because their delusions have been shown to be refractory to antipsychotic therapy. However, antipsychotics are currently the mainstay of treatment. Some case studies have shown efficacy with pimozide, tricyclic antidepressants, and mirtazapine.6,9
One case study in 2014 in India of a 45-year-old woman who believed her husband and son were replaced by imposters out to kill her, showed a 40% to 50% reduction of paranoia, irritability, and suspicious scanning behaviors with a combination of risperidone and trihexyphenidyl. Despite the improvements, the woman continued to have delusions.7
A notable feature associated with those experiencing the Capgras delusion is the increased risk of violent behaviors, often because of suspiciousness and paranoia. A 2004 review suggested the risk of violence and homicidality is much higher in male patients compared with that of female patients with the Capgras delusion.9 This is despite evidence suggesting that the prevalence of the Capgras delusion seems to be greater in women.6,9 Moreover, patients often demonstrated social withdrawal and self-isolation prior to violent acts. The victims often were family members or those who live with the patient, which is consistent with the evidence that those most familiar to patients are more likely to be misidentified.1,2,7,9,10
A 1989 case series that examined 8 cases of the Capgras delusion listed the following violent behaviors: shot and killed father, pointed knife at mother, held knife to mother’s throat, punched parents, threatened to stab husband with scissors, nonspecifically threatened physical harm to family, injured mother with axe, and threatened to stab son with knife and burn him. Seven of the 8 patients lived with the misidentified persons, and 5 of the 8 patients were treatment resistant. The study posited that chronicity of the delusion, content of the delusion, and accessibility of misidentified persons seemed to increase the risk of violent behaviors. These authors went on to suggest that despite the appearance of stability, patients may react violently to minute changes.10 Overall literature seems to suggest the importance of performing a violence and homicidality assessment with special attention to assessment for themes of hostility toward misidentified individuals.9,10
Conclusion
The Capgras delusion is an uncommon symptom associated with varied psychiatric, medical, iatrogenic, and neurologic conditions. Treatment of underlying medical conditions may improve or resolve the delusions. However, in this case, the patient did not seem to have any underlying medical conditions, and it was thought that he may have been experiencing a prodrome within the schizophrenia spectrum. This is consistent with the literature, which suggests that those with the delusions at younger ages may have a psychiatric etiology.
Although this patient was responsive to aripiprazole, the Capgras delusion has been known to be resistant to antipsychotic therapy. It is worth considering a medical and neurologic workup with the addition of a psychiatry referral. Further, while the patient in the presented case had the delusion that he had assaulted his mother, whom he misidentified as an imposter, the patient did not demonstrate any hostility and denied thoughts of harming her. However, given the increased risk of violence in patients with the Capgras delusion, a homicidality and violence assessment should be performed. While further recommendations are outside the scope of this article, the provider should be cognizant of local duty-to-warn and duty-to-protect laws regarding potentially homicidal patients.
Many patients admitted to inpatient psychiatric hospitals present with delusions; however, the Capgras delusion is a rare type that often appears as a sequela of certain medical and neurologic conditions.1 The Capgras delusion is a condition in which a person believes that either an individual or a group of people has been replaced by doubles or imposters.
In 1923, French psychiatrist Joseph Capgras first described the delusion. He and Jean Reboul-Lachaux coauthored a paper on a 53-year-old woman. The patient was a paranoid megalomaniac who “transformed everyone in her entourage, even those closest to her, such as her husband and daughter, into various and numerous doubles.”2 She believed she was famous, wealthy, and of royal lineage. Although 3 of her children had died, she believed that they were abducted, and that her only surviving child was replaced by a look-alike.2,3 Although the prevalence of such delusions in the general population has not been fully studied, a psychiatric hospital in Turkey found a 1.3% prevalence (1.8% women and 0.9% men) in 920 admissions over 5 years.4
The Capgras delusion is one of many delusions related to the misidentification of people, places, or objects; these delusions collectively are known as delusional misidentification syndrome (DMS).5,6 The Fregoli delusion involves the belief that several different people are the same person in disguise. Intermetamorphosis is the belief that an individual has been transformed internally and externally to another person. Subjective doubles is the belief that a doppelganger of the afflicted person exists, living and functioning independently in the world. Reduplicative paramnesia is the belief that a person, place, or object has been duplicated. A rarer example of DMS is the Cotard delusion, which is the belief that the patient himself or herself is dead, putrefying, exsanguinating, or lacking internal organs.
The most common of the DMS is the Capgras delusion. One common presentation of Capgras delusion involves the spouse of the patient, who believes that an imposter of the same sex as their spouse has taken over his or her body. Rarer delusions are those in which a person misidentifies him or herself as the imposter.3,5,6
Case Presentation
This case involved a 24-year-old male veteran who had received a wide range of mental health diagnoses in the past, including major depressive disorder (MDD) with psychotic features, generalized anxiety disorder, cannabis use disorder, adjustment disorder, and borderline personality disorder. He also had a medical history related to a motor vehicle accident with subsequent intestinal rupture and colostomy placement that had occurred a year and a half prior to presentation. He had no history of brain trauma.
The patient voluntarily presented to the hospital for increased suicidal thoughts and was admitted voluntarily for stabilization and self-harm prevention. He stated that “I feel everything is unreal. I feel suicidal and guilt” and endorsed a plan to either walk into traffic or shoot himself in the head due to increasingly distressing thoughts and memories. According to the patient, he had reported to the police that he raped his ex-girlfriend a year previously, although she denied the claim to the police.
The patient further disclosed that he did not believe his mother was real. “Last year my sister told me it was not 2016, but it was 2022,” he said. “She told me that I have hurt my mother with a padlock—that you could no longer identify her face. I don’t remember having done this. I have lived with her since that time, so I don’t think it’s really [my mother].” He believed that his mother was replaced by “government employees” who were sent to elicit confessions for his behavior while in the military. He expressed guilt over several actions he had performed while in military service, such as punching a wall during boot camp, stealing “soak-up” pads, and napping during work hours. His mother was contacted by a staff psychiatrist in the inpatient unit and denied that any assault had taken place.
The patient’s psychiatric review of systems was positive for visual hallucinations (specifically “blurs” next to his bed in the morning that disappeared as he tried to touch them), depressed mood, anxiety, hopelessness, and insomnia. Pertinent negatives of the review of systems included a denial of manic symptoms and auditory hallucinations. For additional details of his past psychiatric history, the patient admitted that his motor vehicle accident, intestinal rupture, and colostomy were the result of his 1 suicide attempt a year and a half prior after a verbal dispute with the same ex-girlfriend that he believed he had raped. After undergoing extensive medical and surgical treatment, he began seeing an outpatient psychiatrist as well as attending substance use counseling to curtail his marijuana use. He was prescribed a combination of duloxetine and risperidone as an outpatient, which he was taking with intermittent adherence.
Regarding substance use, the patient admitted to using marijuana regularly in the past but quit completely 1 month prior and denied any other drug use or alcohol use. He reported a family history of a sister who was undergoing treatment for bipolar disorder. In his social history, the patient disclosed that he was raised by both parents and described a good childhood with a life absent of abuse in any form. He was single with no children. Although he was unemployed, he lived off the funds from an insurance settlement from his motor vehicle accident. He was living in a trailer with his brother and mother. He also denied having access to firearms.
The patient was overweight, neatly groomed, had good eye contact, and was calm and cooperative. He seemed anxious as evidenced by his continuous shaking of his feet; although speech was normal in rate and tone. He reported his mood as “depressed and anxious” with congruent and tearful affect. His thought process was concrete, although his thought content contained delusions, suicidal ideation, and paranoia. He denied any homicidal thoughts or thoughts of harming others. He did not present with any auditory or visual hallucinations. Insight and judgment were poor. The mental status examination revealed no notable deficits in cognition.
The patient’s differential diagnosis included schizophreniform disorder, exacerbation of MDD with psychotic features, and the psychotic component of cannabis use disorder. His outpatient risperidone and duloxetine were not restarted. Aripiprazole 15 mg daily was prescribed for his delusions, paranoia, and visual hallucinations. The patient also received a prescription for hydroxyzine 50 mg every 6 hours as needed for anxiety.
Because of the nature of his delusions, comorbid medical and neurologic conditions were considered. Neurology consultation recommended a noncontrast head computer tomography (CT) scan and an electroencephalogram (EEG). Laboratory workup included HIV antibody, thyroid panel, chemistry panel, complete blood count, hepatitis B serum antigen, urine drug screen, hepatitis C virus, and rapid plasma reagin. All laboratory results were benign and unremarkable, and the urine drug screen was negative. The noncontrast CT revealed no acute findings, and the EEG revealed no recorded epileptiform abnormalities or seizures.
Throughout his hospital course, the patient remained cooperative with treatment. Three days into the hospitalization, he stated that he believed the entire family had been replaced by imposters. He began to distrust members of his family and was reticent to communicate with them when they attempted to contact him. He also experienced fragmented sleep during his hospital stay, and trazodone 50 mg at bedtime was added.
After aripiprazole was increased to 20 mg daily on hospital day 2 and then to 30 mg daily on hospital day 3 due to the patient’s delusions, he began to doubt the validity of his beliefs. After showing gradual improvement over 6 days, the patient reported that he no longer believed that those memories were real. His sleep, depressed mood, anxiety, and paranoia had markedly improved toward the end of the hospitalization and suicidal ideation/intent resolved. The patient was discharged home to his mother and brother after 6 days of hospitalization with aripiprazole 30 mg daily and trazodone 50 mg at bedtime.
Discussion
The Capgras delusion can present in several different contexts. A psychiatric differential diagnosis includes disorders in the schizophrenia spectrum (brief psychotic disorder, schizophreniform disorder, and schizophrenia), schizoaffective disorder, delusional disorder, and substance-induced psychotic disorder. In addition to psychiatric disorders, the Capgras delusion has been shown to occur in several medical conditions, which include stroke, central nervous system tumors, subarachnoid hemorrhage, vitamin B12 deficiency, hepatic encephalopathy, hypothyroidism, hyperparathyroidism, epilepsy, and dementia.1,2,4,7
A 2007 retrospective study by Josephs examined 47 patients diagnosed with the Capgras delusion from several tertiary care centers. Of those patients, 38 (81%) had a neurodegenerative disease, most commonly Lewy body dementia (LBD).1 In his review of the Josephs study, Devinsky proposed that the loss of striatal D2 receptors in LBD may be implicated in the manifestation of Capgras delusions.2 The data suggest multiple brain regions may be involved, including the frontal lobes, right temporal lobe, right parietal lobe, parahippocampus, and amygdala.1,2 Most patients in the Josephs study demonstrated global atrophy on imaging studies. One hypothesis is that it is the disconnection of the frontal lobe to other brain regions that may be implicated.1,2,4 This results in intact recognition of facial features of familiar people, impaired emotional recognition, and impaired self-correction due to executive dysfunction.
Methamphetamine also has been implicated in a small number of cases of Capgras; the proposed mechanism involves dopaminergic neuronal impairment/loss.1,2 Additionally, Capgras delusions have been described in cases of patients treated with antimalarial medications, such as chloroquine.8 Younger patients with the Capgras delusion were more likely to have purely psychiatric comorbidities—such as schizophrenia, substance-induced psychosis, or schizoaffective disorder—as opposed to underlying medical conditions.1 In the case presented here, the Capgras delusion was thought to be due to a disorder in the schizophrenia spectrum, specifically schizophreniform disorder.
Because an increasing amount of evidence indicates that the Capgras delusion is associated with certain medical conditions, a workup should be performed to rule out underlying medical etiology. Of note, no official guidelines for the workup have been produced for the Capgras delusion. However, the workup may include brain imaging, such as magnetic resonance imaging and/or CT scan to rule out mass lesions, vascular malformations, stroke, or neuro-infectious processes; laboratory tests, such as vitamin B12, liver panel, HIV, rapid plasma reagin, hepatitis B and C viruses, parathyroid hormone levels, urine drug screen, and thyroid panel can be ordered to rule out other medical causes.1,2,6,7,9
Consultations with internal medicine and neurology departments may be beneficial. Although treatment of the underlying condition may lead to an improvement in the symptoms, full remission in all cases has not been consistently demonstrated in the current literature.5,7,9,10 Patients with the Capgras delusion are challenging to treat, because their delusions have been shown to be refractory to antipsychotic therapy. However, antipsychotics are currently the mainstay of treatment. Some case studies have shown efficacy with pimozide, tricyclic antidepressants, and mirtazapine.6,9
One case study in 2014 in India of a 45-year-old woman who believed her husband and son were replaced by imposters out to kill her, showed a 40% to 50% reduction of paranoia, irritability, and suspicious scanning behaviors with a combination of risperidone and trihexyphenidyl. Despite the improvements, the woman continued to have delusions.7
A notable feature associated with those experiencing the Capgras delusion is the increased risk of violent behaviors, often because of suspiciousness and paranoia. A 2004 review suggested the risk of violence and homicidality is much higher in male patients compared with that of female patients with the Capgras delusion.9 This is despite evidence suggesting that the prevalence of the Capgras delusion seems to be greater in women.6,9 Moreover, patients often demonstrated social withdrawal and self-isolation prior to violent acts. The victims often were family members or those who live with the patient, which is consistent with the evidence that those most familiar to patients are more likely to be misidentified.1,2,7,9,10
A 1989 case series that examined 8 cases of the Capgras delusion listed the following violent behaviors: shot and killed father, pointed knife at mother, held knife to mother’s throat, punched parents, threatened to stab husband with scissors, nonspecifically threatened physical harm to family, injured mother with axe, and threatened to stab son with knife and burn him. Seven of the 8 patients lived with the misidentified persons, and 5 of the 8 patients were treatment resistant. The study posited that chronicity of the delusion, content of the delusion, and accessibility of misidentified persons seemed to increase the risk of violent behaviors. These authors went on to suggest that despite the appearance of stability, patients may react violently to minute changes.10 Overall literature seems to suggest the importance of performing a violence and homicidality assessment with special attention to assessment for themes of hostility toward misidentified individuals.9,10
Conclusion
The Capgras delusion is an uncommon symptom associated with varied psychiatric, medical, iatrogenic, and neurologic conditions. Treatment of underlying medical conditions may improve or resolve the delusions. However, in this case, the patient did not seem to have any underlying medical conditions, and it was thought that he may have been experiencing a prodrome within the schizophrenia spectrum. This is consistent with the literature, which suggests that those with the delusions at younger ages may have a psychiatric etiology.
Although this patient was responsive to aripiprazole, the Capgras delusion has been known to be resistant to antipsychotic therapy. It is worth considering a medical and neurologic workup with the addition of a psychiatry referral. Further, while the patient in the presented case had the delusion that he had assaulted his mother, whom he misidentified as an imposter, the patient did not demonstrate any hostility and denied thoughts of harming her. However, given the increased risk of violence in patients with the Capgras delusion, a homicidality and violence assessment should be performed. While further recommendations are outside the scope of this article, the provider should be cognizant of local duty-to-warn and duty-to-protect laws regarding potentially homicidal patients.
1. Josephs KA. The Capgras delusion and its relationship to neurodegenerative disease. Arch Neurol. 2007;64(12):1762-1766.
2. Devinsky O. Behavioral neurology. The neurology of the Capgras delusion. Rev Neurol Dis. 2008;5(2):97-100.
3. Sadock BJ, Sadock VA. Kaplan & Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry. 10th ed. Philadelphia, PA: Wolters Kluwer; 2007.
4. Tamam L, Karatas G, Zeren T, Ozpyraz N. The prevalence of Capgras syndrome in a university hospital setting. Acta Neuropsychiatr. 2003;15(5):290-295.
5. Klein CA, Hirchan S. The masks of identities: who’s who? Delusional misidentification syndromes. J Am Acad Psychiatry Law. 2014;42(3):369-378.
6. Atta K. Forlenza N, Gujski M, Hashmi S, Isaac G. Delusional misidentification syndromes: separate disorders or unusual presentations of existing DSM-IV categories? Psychiatry (Edgemont). 2006;3(9):56-61.
7. Sathe H, Karia S, De Sousa A, Shah N. Capgras syndrome: a case report. Paripex Indian J Res. 2014;3(8):134-135. 8. Bhatia MS, Singhal PK, Agrawal P, Malik SC. Capgras’ syndrome in chloroquine induced psychosis. Indian J Psychiatry. 1988;30(3):311-313.
9. Bourget D, Whitehurst L. Capgras syndrome: a review of the neurophysiological correlates and presenting clinical features in cases involving physical violence. Can J Psychiatry. 2004;49(11):719-725.
10. Silva JA, Leong GB, Weinstock R, Boyer CL. Capgras syndrome and dangerousness. Bull Am Acad Psychiatry Law. 1989;17(1):5-14.
1. Josephs KA. The Capgras delusion and its relationship to neurodegenerative disease. Arch Neurol. 2007;64(12):1762-1766.
2. Devinsky O. Behavioral neurology. The neurology of the Capgras delusion. Rev Neurol Dis. 2008;5(2):97-100.
3. Sadock BJ, Sadock VA. Kaplan & Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry. 10th ed. Philadelphia, PA: Wolters Kluwer; 2007.
4. Tamam L, Karatas G, Zeren T, Ozpyraz N. The prevalence of Capgras syndrome in a university hospital setting. Acta Neuropsychiatr. 2003;15(5):290-295.
5. Klein CA, Hirchan S. The masks of identities: who’s who? Delusional misidentification syndromes. J Am Acad Psychiatry Law. 2014;42(3):369-378.
6. Atta K. Forlenza N, Gujski M, Hashmi S, Isaac G. Delusional misidentification syndromes: separate disorders or unusual presentations of existing DSM-IV categories? Psychiatry (Edgemont). 2006;3(9):56-61.
7. Sathe H, Karia S, De Sousa A, Shah N. Capgras syndrome: a case report. Paripex Indian J Res. 2014;3(8):134-135. 8. Bhatia MS, Singhal PK, Agrawal P, Malik SC. Capgras’ syndrome in chloroquine induced psychosis. Indian J Psychiatry. 1988;30(3):311-313.
9. Bourget D, Whitehurst L. Capgras syndrome: a review of the neurophysiological correlates and presenting clinical features in cases involving physical violence. Can J Psychiatry. 2004;49(11):719-725.
10. Silva JA, Leong GB, Weinstock R, Boyer CL. Capgras syndrome and dangerousness. Bull Am Acad Psychiatry Law. 1989;17(1):5-14.
Chemo-free combo should be option for rel/ref CLL, doc says
ATLANTA—The combination of venetoclax and rituximab (VR) should be a standard treatment option for adults with relapsed/refractory chronic lymphocytic leukemia (CLL), according to a speaker at the 2017 ASH Annual Meeting.
Data from the phase 3 MURANO study showed that patients with relapsed/refractory CLL who received VR had significantly longer progression-free survival (PFS) than those who received bendamustine and rituximab (BR).
In addition, “secondary endpoints were consistently in favor of venetoclax-rituximab,” said study investigator John F. Seymour, MBBS, PhD, of Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
Adverse events (AEs) were largely consistent with the known safety profiles of the drugs studied, but tumor lysis syndrome (TLS) was infrequent and occurred at a similar frequency in both treatment arms.
“Thus, overall, I believe venetoclax and rituximab should be considered as a suitable standard therapeutic option in patients with relapsed/refractory CLL,” Dr Seymour said.
It is important to note, however, that patients in the VR arm of this study could receive venetoclax for up to 2 years, whereas patients in the BR arm received study treatment for a maximum of six 28-day cycles.
Dr Seymour presented results from MURANO as a late-breaking abstract at ASH (LBA-2). The study was sponsored by Hoffman-La Roche and AbbVie.
MURANO enrolled 389 CLL patients who had received 1 to 3 prior therapies. Patients were randomized to receive VR (n=194) or BR (n=195). Baseline characteristics were similar between the treatment arms.
In both arms, patients received a single monthly dose of rituximab for 6 cycles. The first dose was 375 mg/m2, and all subsequent doses were 500 mg/m2.
In the VR arm, patients received a 4-week or 5-week dose ramp-up of venetoclax from 20 mg to 400 mg daily. This was intended to mitigate the risk of TLS, which has been observed in previous studies of venetoclax.
Patients in the VR arm continued with daily venetoclax at 400 mg for a maximum of 2 years or until disease progression or cessation due to toxicity. They started receiving rituximab after the ramp-up period (at week 6).
In the BR arm, patients received bendamustine at 70 mg/m2 on days 1 and 2 of each 28-day cycle for 6 cycles. Patients could proceed to subsequent therapy if they progressed.
The median follow-up was 23.8 months (range, 0-37.4 months).
Twenty-five percent of patients in the VR arm and 17% in the BR arm discontinued treatment ahead of schedule. Reasons for discontinuation (in the VR and BR arms, respectively) were disease progression (5% and 3%), AEs (12% and 6%), death (1% and 2%), and “other” (6% and 7%).
Survival
The study’s primary endpoint was investigator-assessed PFS. PFS according to an independent review committee (IRC) was a secondary endpoint.
According to investigators, the median PFS was not reached in the VR arm and was 17.0 months in the BR arm (hazard ratio [HR]=0.17, P<0.0001). According to the IRC, the median PFS was not reached in the VR arm and was 18.1 months in the BR arm (HR=0.17, P<0.0001).
According to investigators, the estimated PFS at 24 months was 84.9% in the VR arm and 36.3% in the BR arm. According to the IRC, the 24-month PFS was 82.8% and 37.4%, respectively.
The benefit with VR was consistent across subgroups. Patients had a PFS benefit regardless of their number of prior therapies, deletion 17p status, TP53 mutational status, baseline IGHV mutational status, and whether they had relapsed or refractory disease.
Dr Seymour acknowledged that the differences in treatment duration between the BR and VR arms may have affected the interpretation of these results.
“[T]he treatment duration differed, although, of course, the capacity to deliver more than 6 cycles of bendamustine-rituximab would have been problematic,” he said. “There is some data that antibody treatment may prolong progression-free survival. However, when this study was designed, in 2013, that data was certainly not available. And I believe, currently, maintenance antibody is not an accepted standard of treatment.”
The median overall survival (OS) was not reached in either treatment arm. The 1-year OS rate was 95.9% in the VR arm and 91.1% in the BR arm. The 2-year OS rate was 91.9% and 86.6%, respectively (HR=0.48, P=0.0186).
“[W]ith median follow-up of just on 2 years, there is already a clinically meaningful difference [in OS between the treatment arms],” Dr Seymour said.
“This is not attributable to any difference in availability of novel therapies. Of the 54 patients who received subsequent therapy after progression on the bendamustine-rituximab arm, 40 of those received novel targeted agents.”
Response and MRD
According to investigators, the overall response rate was 93.3% (181/194) in the VR arm and 67.7% (312/195) in the BR arm (P<0.0001). According to the IRC, the overall response rate was 92.3% (179/194) and 72.3% (141/195), respectively (P<0.0001).
According to investigators, the rate of complete response (CR) or CR with incomplete marrow recovery (CRi) was 26.8% (n=52) in the VR arm and 8.2% (n=16) in the BR arm. According to the IRC, the CR/CRi rate was 8.2% (n=16) and 3.6% (n=7), respectively.
Dr Seymour acknowledged the differences in CR/CRi between investigator and IRC assessments. He said 28 of the 42 discrepancies in the VR arm “were attributable to residual CT scan nodal abnormalities in the 16- to 30-mm size.” However, he also noted that 88% of these patients were negative for minimal residual disease (MRD) in the peripheral blood at that time point.
MRD was assessed every 3 months. Patients were counted as MRD-positive if they were positive by either allele-specific oligonucleotide polymerase chain reaction or multicolor flow cytometry. Patients were also counted as MRD-positive if there was a failure to collect a sample.
The proportion of patients who were MRD-negative in the VR and BR arms, respectively, was:
- 45% and 6% at 4 months
- 62% and 13% at 9 months
- 60% and 10% at 12 months
- 57% and 9% at 15 months
- 60% and 5% at 18 months.
Dr Seymour pointed out that 65 patients in the VR arm surpassed the maximum treatment duration for venetoclax (2 years) and therefore stopped receiving the drug, but only 12 of these patients have follow-up beyond 3 months.
“So information about the durability of response after cessation remains immature at the moment,” he said.
Safety
All patients in the VR arm and 98% in the BR arm had at least 1 AE. The rate of serious AEs was 46% and 43%, respectively. The rate of grade 3/4 AEs was 82% and 70%, respectively.
Grade 3/4 AEs with at least a 2% difference in incidence between the treatment arms (in the VR and BR arms, respectively) were neutropenia (58% and 39%), anemia (11% and 14%), thrombocytopenia (6% and 10%), febrile neutropenia (4% and 10%), pneumonia (5% and 8%), infusion-related reactions (2% and 5%), TLS (3% and 1%), hypotension (0% and 3%), hyperglycemia (2% and 0%), and hypogammaglobulinemia (2% and 0%).
The rate of grade 5 AEs was 5% in the VR arm and 6% in the BR arm.
Grade 5 AEs in the VR arm were pneumonia (n=3), sepsis (n=1), cardiac failure (n=1), myocardial infarction (n=1), sudden cardiac death (n=1), colorectal cancer (n=1), status epilepticus (n=1), and acute respiratory failure (n=1).
Grade 5 AEs in the BR arm included sepsis (n=2), lung cancer (n=2), Listeria sepsis (n=1), Scedosporium infection (n=1), lymphoma (n=1), hemorrhagic stroke (n=1), pulmonary embolism (n=1), acute myeloid leukemia (n=1), and sudden death (n=1). ![]()
ATLANTA—The combination of venetoclax and rituximab (VR) should be a standard treatment option for adults with relapsed/refractory chronic lymphocytic leukemia (CLL), according to a speaker at the 2017 ASH Annual Meeting.
Data from the phase 3 MURANO study showed that patients with relapsed/refractory CLL who received VR had significantly longer progression-free survival (PFS) than those who received bendamustine and rituximab (BR).
In addition, “secondary endpoints were consistently in favor of venetoclax-rituximab,” said study investigator John F. Seymour, MBBS, PhD, of Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
Adverse events (AEs) were largely consistent with the known safety profiles of the drugs studied, but tumor lysis syndrome (TLS) was infrequent and occurred at a similar frequency in both treatment arms.
“Thus, overall, I believe venetoclax and rituximab should be considered as a suitable standard therapeutic option in patients with relapsed/refractory CLL,” Dr Seymour said.
It is important to note, however, that patients in the VR arm of this study could receive venetoclax for up to 2 years, whereas patients in the BR arm received study treatment for a maximum of six 28-day cycles.
Dr Seymour presented results from MURANO as a late-breaking abstract at ASH (LBA-2). The study was sponsored by Hoffman-La Roche and AbbVie.
MURANO enrolled 389 CLL patients who had received 1 to 3 prior therapies. Patients were randomized to receive VR (n=194) or BR (n=195). Baseline characteristics were similar between the treatment arms.
In both arms, patients received a single monthly dose of rituximab for 6 cycles. The first dose was 375 mg/m2, and all subsequent doses were 500 mg/m2.
In the VR arm, patients received a 4-week or 5-week dose ramp-up of venetoclax from 20 mg to 400 mg daily. This was intended to mitigate the risk of TLS, which has been observed in previous studies of venetoclax.
Patients in the VR arm continued with daily venetoclax at 400 mg for a maximum of 2 years or until disease progression or cessation due to toxicity. They started receiving rituximab after the ramp-up period (at week 6).
In the BR arm, patients received bendamustine at 70 mg/m2 on days 1 and 2 of each 28-day cycle for 6 cycles. Patients could proceed to subsequent therapy if they progressed.
The median follow-up was 23.8 months (range, 0-37.4 months).
Twenty-five percent of patients in the VR arm and 17% in the BR arm discontinued treatment ahead of schedule. Reasons for discontinuation (in the VR and BR arms, respectively) were disease progression (5% and 3%), AEs (12% and 6%), death (1% and 2%), and “other” (6% and 7%).
Survival
The study’s primary endpoint was investigator-assessed PFS. PFS according to an independent review committee (IRC) was a secondary endpoint.
According to investigators, the median PFS was not reached in the VR arm and was 17.0 months in the BR arm (hazard ratio [HR]=0.17, P<0.0001). According to the IRC, the median PFS was not reached in the VR arm and was 18.1 months in the BR arm (HR=0.17, P<0.0001).
According to investigators, the estimated PFS at 24 months was 84.9% in the VR arm and 36.3% in the BR arm. According to the IRC, the 24-month PFS was 82.8% and 37.4%, respectively.
The benefit with VR was consistent across subgroups. Patients had a PFS benefit regardless of their number of prior therapies, deletion 17p status, TP53 mutational status, baseline IGHV mutational status, and whether they had relapsed or refractory disease.
Dr Seymour acknowledged that the differences in treatment duration between the BR and VR arms may have affected the interpretation of these results.
“[T]he treatment duration differed, although, of course, the capacity to deliver more than 6 cycles of bendamustine-rituximab would have been problematic,” he said. “There is some data that antibody treatment may prolong progression-free survival. However, when this study was designed, in 2013, that data was certainly not available. And I believe, currently, maintenance antibody is not an accepted standard of treatment.”
The median overall survival (OS) was not reached in either treatment arm. The 1-year OS rate was 95.9% in the VR arm and 91.1% in the BR arm. The 2-year OS rate was 91.9% and 86.6%, respectively (HR=0.48, P=0.0186).
“[W]ith median follow-up of just on 2 years, there is already a clinically meaningful difference [in OS between the treatment arms],” Dr Seymour said.
“This is not attributable to any difference in availability of novel therapies. Of the 54 patients who received subsequent therapy after progression on the bendamustine-rituximab arm, 40 of those received novel targeted agents.”
Response and MRD
According to investigators, the overall response rate was 93.3% (181/194) in the VR arm and 67.7% (312/195) in the BR arm (P<0.0001). According to the IRC, the overall response rate was 92.3% (179/194) and 72.3% (141/195), respectively (P<0.0001).
According to investigators, the rate of complete response (CR) or CR with incomplete marrow recovery (CRi) was 26.8% (n=52) in the VR arm and 8.2% (n=16) in the BR arm. According to the IRC, the CR/CRi rate was 8.2% (n=16) and 3.6% (n=7), respectively.
Dr Seymour acknowledged the differences in CR/CRi between investigator and IRC assessments. He said 28 of the 42 discrepancies in the VR arm “were attributable to residual CT scan nodal abnormalities in the 16- to 30-mm size.” However, he also noted that 88% of these patients were negative for minimal residual disease (MRD) in the peripheral blood at that time point.
MRD was assessed every 3 months. Patients were counted as MRD-positive if they were positive by either allele-specific oligonucleotide polymerase chain reaction or multicolor flow cytometry. Patients were also counted as MRD-positive if there was a failure to collect a sample.
The proportion of patients who were MRD-negative in the VR and BR arms, respectively, was:
- 45% and 6% at 4 months
- 62% and 13% at 9 months
- 60% and 10% at 12 months
- 57% and 9% at 15 months
- 60% and 5% at 18 months.
Dr Seymour pointed out that 65 patients in the VR arm surpassed the maximum treatment duration for venetoclax (2 years) and therefore stopped receiving the drug, but only 12 of these patients have follow-up beyond 3 months.
“So information about the durability of response after cessation remains immature at the moment,” he said.
Safety
All patients in the VR arm and 98% in the BR arm had at least 1 AE. The rate of serious AEs was 46% and 43%, respectively. The rate of grade 3/4 AEs was 82% and 70%, respectively.
Grade 3/4 AEs with at least a 2% difference in incidence between the treatment arms (in the VR and BR arms, respectively) were neutropenia (58% and 39%), anemia (11% and 14%), thrombocytopenia (6% and 10%), febrile neutropenia (4% and 10%), pneumonia (5% and 8%), infusion-related reactions (2% and 5%), TLS (3% and 1%), hypotension (0% and 3%), hyperglycemia (2% and 0%), and hypogammaglobulinemia (2% and 0%).
The rate of grade 5 AEs was 5% in the VR arm and 6% in the BR arm.
Grade 5 AEs in the VR arm were pneumonia (n=3), sepsis (n=1), cardiac failure (n=1), myocardial infarction (n=1), sudden cardiac death (n=1), colorectal cancer (n=1), status epilepticus (n=1), and acute respiratory failure (n=1).
Grade 5 AEs in the BR arm included sepsis (n=2), lung cancer (n=2), Listeria sepsis (n=1), Scedosporium infection (n=1), lymphoma (n=1), hemorrhagic stroke (n=1), pulmonary embolism (n=1), acute myeloid leukemia (n=1), and sudden death (n=1). ![]()
ATLANTA—The combination of venetoclax and rituximab (VR) should be a standard treatment option for adults with relapsed/refractory chronic lymphocytic leukemia (CLL), according to a speaker at the 2017 ASH Annual Meeting.
Data from the phase 3 MURANO study showed that patients with relapsed/refractory CLL who received VR had significantly longer progression-free survival (PFS) than those who received bendamustine and rituximab (BR).
In addition, “secondary endpoints were consistently in favor of venetoclax-rituximab,” said study investigator John F. Seymour, MBBS, PhD, of Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
Adverse events (AEs) were largely consistent with the known safety profiles of the drugs studied, but tumor lysis syndrome (TLS) was infrequent and occurred at a similar frequency in both treatment arms.
“Thus, overall, I believe venetoclax and rituximab should be considered as a suitable standard therapeutic option in patients with relapsed/refractory CLL,” Dr Seymour said.
It is important to note, however, that patients in the VR arm of this study could receive venetoclax for up to 2 years, whereas patients in the BR arm received study treatment for a maximum of six 28-day cycles.
Dr Seymour presented results from MURANO as a late-breaking abstract at ASH (LBA-2). The study was sponsored by Hoffman-La Roche and AbbVie.
MURANO enrolled 389 CLL patients who had received 1 to 3 prior therapies. Patients were randomized to receive VR (n=194) or BR (n=195). Baseline characteristics were similar between the treatment arms.
In both arms, patients received a single monthly dose of rituximab for 6 cycles. The first dose was 375 mg/m2, and all subsequent doses were 500 mg/m2.
In the VR arm, patients received a 4-week or 5-week dose ramp-up of venetoclax from 20 mg to 400 mg daily. This was intended to mitigate the risk of TLS, which has been observed in previous studies of venetoclax.
Patients in the VR arm continued with daily venetoclax at 400 mg for a maximum of 2 years or until disease progression or cessation due to toxicity. They started receiving rituximab after the ramp-up period (at week 6).
In the BR arm, patients received bendamustine at 70 mg/m2 on days 1 and 2 of each 28-day cycle for 6 cycles. Patients could proceed to subsequent therapy if they progressed.
The median follow-up was 23.8 months (range, 0-37.4 months).
Twenty-five percent of patients in the VR arm and 17% in the BR arm discontinued treatment ahead of schedule. Reasons for discontinuation (in the VR and BR arms, respectively) were disease progression (5% and 3%), AEs (12% and 6%), death (1% and 2%), and “other” (6% and 7%).
Survival
The study’s primary endpoint was investigator-assessed PFS. PFS according to an independent review committee (IRC) was a secondary endpoint.
According to investigators, the median PFS was not reached in the VR arm and was 17.0 months in the BR arm (hazard ratio [HR]=0.17, P<0.0001). According to the IRC, the median PFS was not reached in the VR arm and was 18.1 months in the BR arm (HR=0.17, P<0.0001).
According to investigators, the estimated PFS at 24 months was 84.9% in the VR arm and 36.3% in the BR arm. According to the IRC, the 24-month PFS was 82.8% and 37.4%, respectively.
The benefit with VR was consistent across subgroups. Patients had a PFS benefit regardless of their number of prior therapies, deletion 17p status, TP53 mutational status, baseline IGHV mutational status, and whether they had relapsed or refractory disease.
Dr Seymour acknowledged that the differences in treatment duration between the BR and VR arms may have affected the interpretation of these results.
“[T]he treatment duration differed, although, of course, the capacity to deliver more than 6 cycles of bendamustine-rituximab would have been problematic,” he said. “There is some data that antibody treatment may prolong progression-free survival. However, when this study was designed, in 2013, that data was certainly not available. And I believe, currently, maintenance antibody is not an accepted standard of treatment.”
The median overall survival (OS) was not reached in either treatment arm. The 1-year OS rate was 95.9% in the VR arm and 91.1% in the BR arm. The 2-year OS rate was 91.9% and 86.6%, respectively (HR=0.48, P=0.0186).
“[W]ith median follow-up of just on 2 years, there is already a clinically meaningful difference [in OS between the treatment arms],” Dr Seymour said.
“This is not attributable to any difference in availability of novel therapies. Of the 54 patients who received subsequent therapy after progression on the bendamustine-rituximab arm, 40 of those received novel targeted agents.”
Response and MRD
According to investigators, the overall response rate was 93.3% (181/194) in the VR arm and 67.7% (312/195) in the BR arm (P<0.0001). According to the IRC, the overall response rate was 92.3% (179/194) and 72.3% (141/195), respectively (P<0.0001).
According to investigators, the rate of complete response (CR) or CR with incomplete marrow recovery (CRi) was 26.8% (n=52) in the VR arm and 8.2% (n=16) in the BR arm. According to the IRC, the CR/CRi rate was 8.2% (n=16) and 3.6% (n=7), respectively.
Dr Seymour acknowledged the differences in CR/CRi between investigator and IRC assessments. He said 28 of the 42 discrepancies in the VR arm “were attributable to residual CT scan nodal abnormalities in the 16- to 30-mm size.” However, he also noted that 88% of these patients were negative for minimal residual disease (MRD) in the peripheral blood at that time point.
MRD was assessed every 3 months. Patients were counted as MRD-positive if they were positive by either allele-specific oligonucleotide polymerase chain reaction or multicolor flow cytometry. Patients were also counted as MRD-positive if there was a failure to collect a sample.
The proportion of patients who were MRD-negative in the VR and BR arms, respectively, was:
- 45% and 6% at 4 months
- 62% and 13% at 9 months
- 60% and 10% at 12 months
- 57% and 9% at 15 months
- 60% and 5% at 18 months.
Dr Seymour pointed out that 65 patients in the VR arm surpassed the maximum treatment duration for venetoclax (2 years) and therefore stopped receiving the drug, but only 12 of these patients have follow-up beyond 3 months.
“So information about the durability of response after cessation remains immature at the moment,” he said.
Safety
All patients in the VR arm and 98% in the BR arm had at least 1 AE. The rate of serious AEs was 46% and 43%, respectively. The rate of grade 3/4 AEs was 82% and 70%, respectively.
Grade 3/4 AEs with at least a 2% difference in incidence between the treatment arms (in the VR and BR arms, respectively) were neutropenia (58% and 39%), anemia (11% and 14%), thrombocytopenia (6% and 10%), febrile neutropenia (4% and 10%), pneumonia (5% and 8%), infusion-related reactions (2% and 5%), TLS (3% and 1%), hypotension (0% and 3%), hyperglycemia (2% and 0%), and hypogammaglobulinemia (2% and 0%).
The rate of grade 5 AEs was 5% in the VR arm and 6% in the BR arm.
Grade 5 AEs in the VR arm were pneumonia (n=3), sepsis (n=1), cardiac failure (n=1), myocardial infarction (n=1), sudden cardiac death (n=1), colorectal cancer (n=1), status epilepticus (n=1), and acute respiratory failure (n=1).
Grade 5 AEs in the BR arm included sepsis (n=2), lung cancer (n=2), Listeria sepsis (n=1), Scedosporium infection (n=1), lymphoma (n=1), hemorrhagic stroke (n=1), pulmonary embolism (n=1), acute myeloid leukemia (n=1), and sudden death (n=1). ![]()
More Medicaid pay leads to more pediatric participation
If you provide better Medicaid payment, pediatricians will participate.
“Office-based primary care pediatricians, who had historically been more resistant to [Medicaid] participation than either their subspecialist or safety net and institution-based peers, increased their participation in the Medicaid program nationally from before to after the 2013 to 2014 Medicaid payment increase,” noted Suk-fong S. Tang, PhD, research analyst at American Academy of Pediatrics, and colleagues.
“That we found participation increases in 4 of 5 indicators nationally and by different measures in the majority of studied states speaks to the robustness of our conclusions,” they wrote.
The researchers looked at office-based primary care pediatricians’ participation in Medicaid between 2011 to 2012 and 2015 to 2016 (prior to and following the temporary Medicaid pay increases provided by the Affordable Care Act) across 27 states and found that those accepting at least some new patients insured by Medicaid increased by 3% to 77%. Pediatricians accepting all new patients insured by Medicaid increased by 6% to 43% and those accepting these patients at least as often as new privately insured patients increased by 6% to 56%. The average percentage of patients insured by Medicaid per provider panel increased by 6% to 31%.
“In light of such findings, the cost and benefits of recruiting new participants versus incentivizing existing participants to increase their Medicaid capacity merit further investigation and the potential for both strategies to improve access should be considered,” the authors wrote.
The AAP Friends of Children Fund supported the study. The researchers reported no relevant financial conflicts of interest.
SOURCE: Tang S et al. Pediatrics 2018 Jan. doi: 10.1542/peds.2017-2570.
There are a number of ways to use payments as the carrot to increase pediatrician participation in Medicaid: raising rates for preventive care as with private insurance, fully covering the cost of vaccines, paying for developmental screening, and providing incentives for up-to-date immunization rates and meeting targets for developmental and lead screening.
Payments should be done as a per-member-per-month care coordination payment and claims should be simplified so they can be paid in a timely manner.
Stephen Berman, MD, of the University of Colorado, expressed his views in a commentary accompanying Dr. Suk-fong’s study (Pediatrics 2018 Jan. doi: 10.1542/peds.2017-3241 ).
There are a number of ways to use payments as the carrot to increase pediatrician participation in Medicaid: raising rates for preventive care as with private insurance, fully covering the cost of vaccines, paying for developmental screening, and providing incentives for up-to-date immunization rates and meeting targets for developmental and lead screening.
Payments should be done as a per-member-per-month care coordination payment and claims should be simplified so they can be paid in a timely manner.
Stephen Berman, MD, of the University of Colorado, expressed his views in a commentary accompanying Dr. Suk-fong’s study (Pediatrics 2018 Jan. doi: 10.1542/peds.2017-3241 ).
There are a number of ways to use payments as the carrot to increase pediatrician participation in Medicaid: raising rates for preventive care as with private insurance, fully covering the cost of vaccines, paying for developmental screening, and providing incentives for up-to-date immunization rates and meeting targets for developmental and lead screening.
Payments should be done as a per-member-per-month care coordination payment and claims should be simplified so they can be paid in a timely manner.
Stephen Berman, MD, of the University of Colorado, expressed his views in a commentary accompanying Dr. Suk-fong’s study (Pediatrics 2018 Jan. doi: 10.1542/peds.2017-3241 ).
If you provide better Medicaid payment, pediatricians will participate.
“Office-based primary care pediatricians, who had historically been more resistant to [Medicaid] participation than either their subspecialist or safety net and institution-based peers, increased their participation in the Medicaid program nationally from before to after the 2013 to 2014 Medicaid payment increase,” noted Suk-fong S. Tang, PhD, research analyst at American Academy of Pediatrics, and colleagues.
“That we found participation increases in 4 of 5 indicators nationally and by different measures in the majority of studied states speaks to the robustness of our conclusions,” they wrote.
The researchers looked at office-based primary care pediatricians’ participation in Medicaid between 2011 to 2012 and 2015 to 2016 (prior to and following the temporary Medicaid pay increases provided by the Affordable Care Act) across 27 states and found that those accepting at least some new patients insured by Medicaid increased by 3% to 77%. Pediatricians accepting all new patients insured by Medicaid increased by 6% to 43% and those accepting these patients at least as often as new privately insured patients increased by 6% to 56%. The average percentage of patients insured by Medicaid per provider panel increased by 6% to 31%.
“In light of such findings, the cost and benefits of recruiting new participants versus incentivizing existing participants to increase their Medicaid capacity merit further investigation and the potential for both strategies to improve access should be considered,” the authors wrote.
The AAP Friends of Children Fund supported the study. The researchers reported no relevant financial conflicts of interest.
SOURCE: Tang S et al. Pediatrics 2018 Jan. doi: 10.1542/peds.2017-2570.
If you provide better Medicaid payment, pediatricians will participate.
“Office-based primary care pediatricians, who had historically been more resistant to [Medicaid] participation than either their subspecialist or safety net and institution-based peers, increased their participation in the Medicaid program nationally from before to after the 2013 to 2014 Medicaid payment increase,” noted Suk-fong S. Tang, PhD, research analyst at American Academy of Pediatrics, and colleagues.
“That we found participation increases in 4 of 5 indicators nationally and by different measures in the majority of studied states speaks to the robustness of our conclusions,” they wrote.
The researchers looked at office-based primary care pediatricians’ participation in Medicaid between 2011 to 2012 and 2015 to 2016 (prior to and following the temporary Medicaid pay increases provided by the Affordable Care Act) across 27 states and found that those accepting at least some new patients insured by Medicaid increased by 3% to 77%. Pediatricians accepting all new patients insured by Medicaid increased by 6% to 43% and those accepting these patients at least as often as new privately insured patients increased by 6% to 56%. The average percentage of patients insured by Medicaid per provider panel increased by 6% to 31%.
“In light of such findings, the cost and benefits of recruiting new participants versus incentivizing existing participants to increase their Medicaid capacity merit further investigation and the potential for both strategies to improve access should be considered,” the authors wrote.
The AAP Friends of Children Fund supported the study. The researchers reported no relevant financial conflicts of interest.
SOURCE: Tang S et al. Pediatrics 2018 Jan. doi: 10.1542/peds.2017-2570.
FROM PEDIATRICS
Key clinical point: Better Medicaid pay increases physician participation in the program.
Major finding: Percentage of pediatricians accepting some Medicaid patients increased from 3% to 77% during the temporary increase.
Study details: A study of office-based primary care pediatricians’ participation in Medicaid between the periods of 2011-2012 and 2015-2016 in 27 states, before and after temporary Medicaid pay increases provided by the ACA.
Disclosures: The AAP Friends of Children Fund supported the study. The researchers reported no relevant financial conflicts of interest.
Source: Tang S et al. Pediatrics 2018 Jan. doi:10.1542/peds.2017-2570.
Ertugliflozin gets FDA thumbs-up for glucose control
The Food and Drug Administration has approved ertugliflozin for use both as monotherapy and in combination with sitagliptin or metformin to control blood glucose in patients with type 2 diabetes.
The FDA approval covers ertugliflozin monotherapy (Steglatro, Merck and Pfizer) and ertugliflozin plus sitagliptin, a dipeptidyl peptidase–4 (DPP-4) inhibitor, as a fixed-dose combination (Steglujan, Merck) and ertugliflozin plus metformin (Segluromet, Merck).
Ertugliflozin is the third sodium glucose cotransporter 2 (SGLT2) inhibitor to win FDA approval. Another such agent, empagliflozin, recently won a second indication for lowering the risk for cardiovascular death in adults with type 2 diabetes and established heart disease.
The American Diabetes Association recognized the value of SGLT2 inhibitors in patients with type 2 diabetes in its 2018 Standards of Care in Diabetes, now recommending that clinicians consider adding agents proved to reduce major cardiovascular events and cardiovascular death – such as the SGLT2 inhibitor empagliflozin or the glucagonlike peptide–1 agonist liraglutide – to the regimens of patients with diabetes and atherosclerotic cardiovascular disease (Diabetes Care 2018;41(Suppl. 1):S86-S104. doi: 10.2337/dc18-S009).
The Food and Drug Administration has approved ertugliflozin for use both as monotherapy and in combination with sitagliptin or metformin to control blood glucose in patients with type 2 diabetes.
The FDA approval covers ertugliflozin monotherapy (Steglatro, Merck and Pfizer) and ertugliflozin plus sitagliptin, a dipeptidyl peptidase–4 (DPP-4) inhibitor, as a fixed-dose combination (Steglujan, Merck) and ertugliflozin plus metformin (Segluromet, Merck).
Ertugliflozin is the third sodium glucose cotransporter 2 (SGLT2) inhibitor to win FDA approval. Another such agent, empagliflozin, recently won a second indication for lowering the risk for cardiovascular death in adults with type 2 diabetes and established heart disease.
The American Diabetes Association recognized the value of SGLT2 inhibitors in patients with type 2 diabetes in its 2018 Standards of Care in Diabetes, now recommending that clinicians consider adding agents proved to reduce major cardiovascular events and cardiovascular death – such as the SGLT2 inhibitor empagliflozin or the glucagonlike peptide–1 agonist liraglutide – to the regimens of patients with diabetes and atherosclerotic cardiovascular disease (Diabetes Care 2018;41(Suppl. 1):S86-S104. doi: 10.2337/dc18-S009).
The Food and Drug Administration has approved ertugliflozin for use both as monotherapy and in combination with sitagliptin or metformin to control blood glucose in patients with type 2 diabetes.
The FDA approval covers ertugliflozin monotherapy (Steglatro, Merck and Pfizer) and ertugliflozin plus sitagliptin, a dipeptidyl peptidase–4 (DPP-4) inhibitor, as a fixed-dose combination (Steglujan, Merck) and ertugliflozin plus metformin (Segluromet, Merck).
Ertugliflozin is the third sodium glucose cotransporter 2 (SGLT2) inhibitor to win FDA approval. Another such agent, empagliflozin, recently won a second indication for lowering the risk for cardiovascular death in adults with type 2 diabetes and established heart disease.
The American Diabetes Association recognized the value of SGLT2 inhibitors in patients with type 2 diabetes in its 2018 Standards of Care in Diabetes, now recommending that clinicians consider adding agents proved to reduce major cardiovascular events and cardiovascular death – such as the SGLT2 inhibitor empagliflozin or the glucagonlike peptide–1 agonist liraglutide – to the regimens of patients with diabetes and atherosclerotic cardiovascular disease (Diabetes Care 2018;41(Suppl. 1):S86-S104. doi: 10.2337/dc18-S009).
Loneliness is common, and not just in the elderly
MONTREAL – Loneliness is associated with poorer health, but isn’t necessarily more common among older adults; one in five adults in a primary care population reported being lonely, a number higher than previously reported, a study showed.
In a survey of 940 adults seeking care in primary care clinics, 193 (21%) reported loneliness, with women more likely than men to say they were lonely. “Respondents identifying as having poorer health classifications were more likely to report high loneliness scores,” said Rebecca Mullen, MD, and her colleagues in a poster presented at the annual meeting of the North American Primary Care Research Group.
Those who said they were lonely also had a higher level of health care utilization, and reported they had a lower number of healthy days than the respondents who didn’t report loneliness.
The study was conducted in outpatient practice-based research networks in both urban and rural settings in the states of Virginia and Colorado. Participants were adult, English-speaking primary care patients who were given the UCLA Three-Item Loneliness Scale. The scale asks how often respondents feel a lack of companionship, feel left out, and feel isolated from others; responses are “hardly ever,” “sometimes,” and “often.”
The investigators sought to determine whether high loneliness scores on this scale – the primary outcome – were correlated with health care utilization, the number of healthy days reported by patients, and demographic information. These associations were the study’s secondary outcomes.
After statistical analysis, several variables emerged as being significantly associated with high loneliness scores. These included the number of reported days with poor physical or mental health (odds ratio, 1.06), the number of primary care office visits (OR, 1.06), the number of hospitalizations (OR, 1.16), the number of emergency department or urgent care visits (OR ,1.27), and gender.
When compared with male respondents, females had an OR of 1.56 for reporting loneliness.
Race and ethnicity were not associated with a greater risk of loneliness; neither were disability or employment status, or whether the respondent was in a relationship.
And despite other studies indicating an increased prevalence of loneliness among the elderly, “our findings suggest loneliness is not age related,” wrote Dr. Mullen and her colleagues.
The investigators said they plan to examine their data further, to see if factors such as living in a rural or urban environment are associated with differences in loneliness. Going into still more detail, they plan to use demographic data to plot out respondents’ residences, and then look for spatial associations and links to other comorbidities. Integrating the questionnaire with data from the electronic record will allow Dr. Mullen and her colleagues to search for further associations as well, they said.
Finally, the investigators plan to build partnerships with the community, public health agencies, and those involved in health policy to build interventions against loneliness targeted at both the individual and the community. Some of these interventions, they said, could begin in the clinic: “[T]he primary care health care setting may be an appropriate context to consider intervention delivery.”
Dr. Mullen reported no relevant financial conflicts of interest.
SOURCE: Mullen R et al. Abstract P196.
MONTREAL – Loneliness is associated with poorer health, but isn’t necessarily more common among older adults; one in five adults in a primary care population reported being lonely, a number higher than previously reported, a study showed.
In a survey of 940 adults seeking care in primary care clinics, 193 (21%) reported loneliness, with women more likely than men to say they were lonely. “Respondents identifying as having poorer health classifications were more likely to report high loneliness scores,” said Rebecca Mullen, MD, and her colleagues in a poster presented at the annual meeting of the North American Primary Care Research Group.
Those who said they were lonely also had a higher level of health care utilization, and reported they had a lower number of healthy days than the respondents who didn’t report loneliness.
The study was conducted in outpatient practice-based research networks in both urban and rural settings in the states of Virginia and Colorado. Participants were adult, English-speaking primary care patients who were given the UCLA Three-Item Loneliness Scale. The scale asks how often respondents feel a lack of companionship, feel left out, and feel isolated from others; responses are “hardly ever,” “sometimes,” and “often.”
The investigators sought to determine whether high loneliness scores on this scale – the primary outcome – were correlated with health care utilization, the number of healthy days reported by patients, and demographic information. These associations were the study’s secondary outcomes.
After statistical analysis, several variables emerged as being significantly associated with high loneliness scores. These included the number of reported days with poor physical or mental health (odds ratio, 1.06), the number of primary care office visits (OR, 1.06), the number of hospitalizations (OR, 1.16), the number of emergency department or urgent care visits (OR ,1.27), and gender.
When compared with male respondents, females had an OR of 1.56 for reporting loneliness.
Race and ethnicity were not associated with a greater risk of loneliness; neither were disability or employment status, or whether the respondent was in a relationship.
And despite other studies indicating an increased prevalence of loneliness among the elderly, “our findings suggest loneliness is not age related,” wrote Dr. Mullen and her colleagues.
The investigators said they plan to examine their data further, to see if factors such as living in a rural or urban environment are associated with differences in loneliness. Going into still more detail, they plan to use demographic data to plot out respondents’ residences, and then look for spatial associations and links to other comorbidities. Integrating the questionnaire with data from the electronic record will allow Dr. Mullen and her colleagues to search for further associations as well, they said.
Finally, the investigators plan to build partnerships with the community, public health agencies, and those involved in health policy to build interventions against loneliness targeted at both the individual and the community. Some of these interventions, they said, could begin in the clinic: “[T]he primary care health care setting may be an appropriate context to consider intervention delivery.”
Dr. Mullen reported no relevant financial conflicts of interest.
SOURCE: Mullen R et al. Abstract P196.
MONTREAL – Loneliness is associated with poorer health, but isn’t necessarily more common among older adults; one in five adults in a primary care population reported being lonely, a number higher than previously reported, a study showed.
In a survey of 940 adults seeking care in primary care clinics, 193 (21%) reported loneliness, with women more likely than men to say they were lonely. “Respondents identifying as having poorer health classifications were more likely to report high loneliness scores,” said Rebecca Mullen, MD, and her colleagues in a poster presented at the annual meeting of the North American Primary Care Research Group.
Those who said they were lonely also had a higher level of health care utilization, and reported they had a lower number of healthy days than the respondents who didn’t report loneliness.
The study was conducted in outpatient practice-based research networks in both urban and rural settings in the states of Virginia and Colorado. Participants were adult, English-speaking primary care patients who were given the UCLA Three-Item Loneliness Scale. The scale asks how often respondents feel a lack of companionship, feel left out, and feel isolated from others; responses are “hardly ever,” “sometimes,” and “often.”
The investigators sought to determine whether high loneliness scores on this scale – the primary outcome – were correlated with health care utilization, the number of healthy days reported by patients, and demographic information. These associations were the study’s secondary outcomes.
After statistical analysis, several variables emerged as being significantly associated with high loneliness scores. These included the number of reported days with poor physical or mental health (odds ratio, 1.06), the number of primary care office visits (OR, 1.06), the number of hospitalizations (OR, 1.16), the number of emergency department or urgent care visits (OR ,1.27), and gender.
When compared with male respondents, females had an OR of 1.56 for reporting loneliness.
Race and ethnicity were not associated with a greater risk of loneliness; neither were disability or employment status, or whether the respondent was in a relationship.
And despite other studies indicating an increased prevalence of loneliness among the elderly, “our findings suggest loneliness is not age related,” wrote Dr. Mullen and her colleagues.
The investigators said they plan to examine their data further, to see if factors such as living in a rural or urban environment are associated with differences in loneliness. Going into still more detail, they plan to use demographic data to plot out respondents’ residences, and then look for spatial associations and links to other comorbidities. Integrating the questionnaire with data from the electronic record will allow Dr. Mullen and her colleagues to search for further associations as well, they said.
Finally, the investigators plan to build partnerships with the community, public health agencies, and those involved in health policy to build interventions against loneliness targeted at both the individual and the community. Some of these interventions, they said, could begin in the clinic: “[T]he primary care health care setting may be an appropriate context to consider intervention delivery.”
Dr. Mullen reported no relevant financial conflicts of interest.
SOURCE: Mullen R et al. Abstract P196.
REPORTING FROM NAPCRG 2017
Key clinical point: One in five adults – and more women than men – reported loneliness.
Major finding: Of 940 adults surveyed, 193 (21%) reported being lonely.
Study details: A prospective survey of 940 adults seeking care in primary care clinics.
Disclosures: Dr. Mullen reported no relevant financial conflicts of interest.
Urgent endoscopy is associated with lower mortality in high-risk patients with acute nonvariceal GI bleeding
Clinical question: Is urgent endoscopy (less than 6 hours after ED presentation) better than elective endoscopy (6-48 hours after presentation) to decrease mortality and rebleeding in high-risk patients with acute nonvariceal upper GI bleeding (ANVGIB)?
Background: High-risk ANVGIB patients (Glasgow-Blatchford score greater than 7) are recommended to undergo early endoscopy, within 24 hours of presentation. The impact of urgent endoscopy (less than 6 hours) on patient outcomes is not clear.
Study design: Retrospective observation study.
Setting: Single tertiary referral center in South Korea.
Synopsis: Investigators retrospectively reviewed 961 high-risk ANVGIB patients, 571 patients underwent urgent endoscopy and 390 patients had elective endoscopy (6-48 hours), to compare clinical features and outcomes. The urgent group was slightly older, had a higher Rockall score, lower blood pressure, and higher incidence of shock on admission.
Urgent endoscopy was associated with significantly lower 28-day mortality (1.6% vs 3.8%). Urgent endoscopy also was associated with higher packed red blood cell transfusion volume (2.6 U vs. 2.3 U) and greater need for endoscopic intervention (69.5% vs. 53.5%) and embolization (2.8% vs. 0.5%). There was no significant difference in rebleeding rates, need for ICU admission, vasopressor use, and length of hospital stay between the urgent and elective endoscopy groups. The authors conclude that urgent endoscopy was associated with lower mortality rate but not rebleeding in high-risk patients with ANVGIB.
Despite differences between these two groups, based on this retrospective data, it is reasonable to suggest that urgent endoscopy may be beneficial for reducing mortality in high-risk patients with ANVGIB.
Bottom line: Urgent endoscopy may be beneficial in reducing mortality in high-risk patients with acute nonvariceal gastrointestinal bleeding.
Citation: Cho SH et al. Outcomes and role of urgent endoscopy in high-risk patients with acute nonvariceal gastrointestinal bleeding. Clin Gastroenterol Hepatol. 2017 Jun 19. pii: S1542-3565(17)30736-X.
Dr. Patel is a hospitalist and an assistant professor of medicine, Duke University Health System.
Clinical question: Is urgent endoscopy (less than 6 hours after ED presentation) better than elective endoscopy (6-48 hours after presentation) to decrease mortality and rebleeding in high-risk patients with acute nonvariceal upper GI bleeding (ANVGIB)?
Background: High-risk ANVGIB patients (Glasgow-Blatchford score greater than 7) are recommended to undergo early endoscopy, within 24 hours of presentation. The impact of urgent endoscopy (less than 6 hours) on patient outcomes is not clear.
Study design: Retrospective observation study.
Setting: Single tertiary referral center in South Korea.
Synopsis: Investigators retrospectively reviewed 961 high-risk ANVGIB patients, 571 patients underwent urgent endoscopy and 390 patients had elective endoscopy (6-48 hours), to compare clinical features and outcomes. The urgent group was slightly older, had a higher Rockall score, lower blood pressure, and higher incidence of shock on admission.
Urgent endoscopy was associated with significantly lower 28-day mortality (1.6% vs 3.8%). Urgent endoscopy also was associated with higher packed red blood cell transfusion volume (2.6 U vs. 2.3 U) and greater need for endoscopic intervention (69.5% vs. 53.5%) and embolization (2.8% vs. 0.5%). There was no significant difference in rebleeding rates, need for ICU admission, vasopressor use, and length of hospital stay between the urgent and elective endoscopy groups. The authors conclude that urgent endoscopy was associated with lower mortality rate but not rebleeding in high-risk patients with ANVGIB.
Despite differences between these two groups, based on this retrospective data, it is reasonable to suggest that urgent endoscopy may be beneficial for reducing mortality in high-risk patients with ANVGIB.
Bottom line: Urgent endoscopy may be beneficial in reducing mortality in high-risk patients with acute nonvariceal gastrointestinal bleeding.
Citation: Cho SH et al. Outcomes and role of urgent endoscopy in high-risk patients with acute nonvariceal gastrointestinal bleeding. Clin Gastroenterol Hepatol. 2017 Jun 19. pii: S1542-3565(17)30736-X.
Dr. Patel is a hospitalist and an assistant professor of medicine, Duke University Health System.
Clinical question: Is urgent endoscopy (less than 6 hours after ED presentation) better than elective endoscopy (6-48 hours after presentation) to decrease mortality and rebleeding in high-risk patients with acute nonvariceal upper GI bleeding (ANVGIB)?
Background: High-risk ANVGIB patients (Glasgow-Blatchford score greater than 7) are recommended to undergo early endoscopy, within 24 hours of presentation. The impact of urgent endoscopy (less than 6 hours) on patient outcomes is not clear.
Study design: Retrospective observation study.
Setting: Single tertiary referral center in South Korea.
Synopsis: Investigators retrospectively reviewed 961 high-risk ANVGIB patients, 571 patients underwent urgent endoscopy and 390 patients had elective endoscopy (6-48 hours), to compare clinical features and outcomes. The urgent group was slightly older, had a higher Rockall score, lower blood pressure, and higher incidence of shock on admission.
Urgent endoscopy was associated with significantly lower 28-day mortality (1.6% vs 3.8%). Urgent endoscopy also was associated with higher packed red blood cell transfusion volume (2.6 U vs. 2.3 U) and greater need for endoscopic intervention (69.5% vs. 53.5%) and embolization (2.8% vs. 0.5%). There was no significant difference in rebleeding rates, need for ICU admission, vasopressor use, and length of hospital stay between the urgent and elective endoscopy groups. The authors conclude that urgent endoscopy was associated with lower mortality rate but not rebleeding in high-risk patients with ANVGIB.
Despite differences between these two groups, based on this retrospective data, it is reasonable to suggest that urgent endoscopy may be beneficial for reducing mortality in high-risk patients with ANVGIB.
Bottom line: Urgent endoscopy may be beneficial in reducing mortality in high-risk patients with acute nonvariceal gastrointestinal bleeding.
Citation: Cho SH et al. Outcomes and role of urgent endoscopy in high-risk patients with acute nonvariceal gastrointestinal bleeding. Clin Gastroenterol Hepatol. 2017 Jun 19. pii: S1542-3565(17)30736-X.
Dr. Patel is a hospitalist and an assistant professor of medicine, Duke University Health System.