User login
Physical Activity Worsened Migraine Pain for Some
For a minority of women who are overweight or obese, physical activity consistently contributed to the worsening of migraine pain, according to a recent study. Furthermore, more frequent physical activity-related pain worsening was related to greater severity of other migraine symptoms and pain sensitivity. Participants included 132 women, aged 18 to 50 years, with neurologist-confirmed migraine and overweight/obesity seeking weight loss treatment in the Women’s Health and Migraine trial. Researchers found:
- Subjects reported 5.5 ± 2.8 (mean ± standard deviation) migraine attacks over 28 days.
- The intraclass correlation indicated high consistency in participants’ reports of activity-related pain worsening or not.
- On average, activity worsened pain in 34.8 ± 35.6% of attacks, had no effect on pain in 61.8 ± 34.6% of attacks, and improved pain in 3.4 ± 12.7% of attacks.
- Few participants (9.8%) reported activity-related pain worsening in all attacks.
- A higher percentage of attacks where physical activity worsened pain demonstrated small-sized correlations with more severe nausea, photophobia, phonophobia, and allodynia.
Pain worsening with physical activity during migraine attacks in women with overweight/obesity: A prospective evaluation of frequency, consistency, and correlates. [Published online ahead of print December 13, 2017]. Cephalalgia. doi:10.1177/0333102417747231.
For a minority of women who are overweight or obese, physical activity consistently contributed to the worsening of migraine pain, according to a recent study. Furthermore, more frequent physical activity-related pain worsening was related to greater severity of other migraine symptoms and pain sensitivity. Participants included 132 women, aged 18 to 50 years, with neurologist-confirmed migraine and overweight/obesity seeking weight loss treatment in the Women’s Health and Migraine trial. Researchers found:
- Subjects reported 5.5 ± 2.8 (mean ± standard deviation) migraine attacks over 28 days.
- The intraclass correlation indicated high consistency in participants’ reports of activity-related pain worsening or not.
- On average, activity worsened pain in 34.8 ± 35.6% of attacks, had no effect on pain in 61.8 ± 34.6% of attacks, and improved pain in 3.4 ± 12.7% of attacks.
- Few participants (9.8%) reported activity-related pain worsening in all attacks.
- A higher percentage of attacks where physical activity worsened pain demonstrated small-sized correlations with more severe nausea, photophobia, phonophobia, and allodynia.
Pain worsening with physical activity during migraine attacks in women with overweight/obesity: A prospective evaluation of frequency, consistency, and correlates. [Published online ahead of print December 13, 2017]. Cephalalgia. doi:10.1177/0333102417747231.
For a minority of women who are overweight or obese, physical activity consistently contributed to the worsening of migraine pain, according to a recent study. Furthermore, more frequent physical activity-related pain worsening was related to greater severity of other migraine symptoms and pain sensitivity. Participants included 132 women, aged 18 to 50 years, with neurologist-confirmed migraine and overweight/obesity seeking weight loss treatment in the Women’s Health and Migraine trial. Researchers found:
- Subjects reported 5.5 ± 2.8 (mean ± standard deviation) migraine attacks over 28 days.
- The intraclass correlation indicated high consistency in participants’ reports of activity-related pain worsening or not.
- On average, activity worsened pain in 34.8 ± 35.6% of attacks, had no effect on pain in 61.8 ± 34.6% of attacks, and improved pain in 3.4 ± 12.7% of attacks.
- Few participants (9.8%) reported activity-related pain worsening in all attacks.
- A higher percentage of attacks where physical activity worsened pain demonstrated small-sized correlations with more severe nausea, photophobia, phonophobia, and allodynia.
Pain worsening with physical activity during migraine attacks in women with overweight/obesity: A prospective evaluation of frequency, consistency, and correlates. [Published online ahead of print December 13, 2017]. Cephalalgia. doi:10.1177/0333102417747231.
Contaminated graft causes infection in ALL patient
, according to a letter to the editor published in Infection Control & Hospital Epidemiology.
Strains of Staphylococcus aureus found in isolates from the HSC graft and the patient were confirmed to be identical using pulsed-field gel electrophoresis, the authors, led by Zachary I. Willis, MD, MPH, of the department of pediatrics at the University of North Carolina at Chapel Hill, said.
“While multiple reports have found that low-grade bacterial contamination of HSC products is rarely consequential, our patient’s experience demonstrated that clinically significant infections may occur,” Dr. Willis and his colleagues wrote in the case report.
When less virulent organisms are found in HSC grafts, close observation may be warranted, the investigators said; however, a more aggressive approach might be considered when more virulent organisms are found.
“In such a case, we suggest obtaining blood cultures and considering preemptive antibiotics as guided by the identity and susceptibility of the contaminating organism,” the investigators wrote.
Dr. Willis and his colleagues reported the case of a 15-year-old boy with hypodiploid B-ALL who achieved complete remission after treatment and then underwent a 10/10 HLA allele–matched unrelated donor hematopoietic cell transplant.
The patient developed a fever of 38.3º C with tachycardia but no other sepsis signs approximately 24 hours after the transplant. Soon afterward, the care team was informed that there was a single colony each of Micrococcus and S. aureus in the culture of the HSC product. Methicillin susceptibility was later confirmed. Antibiotic treatment was changed accordingly, and as of 117 days post transplant, the patient was “doing well with no evidence of further infectious complications,” the investigators said.
Bacterial contamination of HSC grafts is relatively common, with reported rates ranging from 1% to 45%. However, the clinical significance of the contamination has been unclear. Moreover, contamination is not an absolute contraindication to infusion, as options for the patient are limited after a myeloablative preparative regimen.
There are some previous case reports also identifying infections caused by contaminated grafts, but in those cases, the evidence linking the graft to the infection was based solely on finding identical species, while in the present report, the graft and patient isolates were confirmed to be identical using pulsed-field gel electrophoresis.
The investigators reported having no outside funding and no financial disclosures.
SOURCE: Willis Z et al, Infect Control Hosp Epidemiol. 2018 Jan 23. doi: 10.1017/ice.2017.285.
, according to a letter to the editor published in Infection Control & Hospital Epidemiology.
Strains of Staphylococcus aureus found in isolates from the HSC graft and the patient were confirmed to be identical using pulsed-field gel electrophoresis, the authors, led by Zachary I. Willis, MD, MPH, of the department of pediatrics at the University of North Carolina at Chapel Hill, said.
“While multiple reports have found that low-grade bacterial contamination of HSC products is rarely consequential, our patient’s experience demonstrated that clinically significant infections may occur,” Dr. Willis and his colleagues wrote in the case report.
When less virulent organisms are found in HSC grafts, close observation may be warranted, the investigators said; however, a more aggressive approach might be considered when more virulent organisms are found.
“In such a case, we suggest obtaining blood cultures and considering preemptive antibiotics as guided by the identity and susceptibility of the contaminating organism,” the investigators wrote.
Dr. Willis and his colleagues reported the case of a 15-year-old boy with hypodiploid B-ALL who achieved complete remission after treatment and then underwent a 10/10 HLA allele–matched unrelated donor hematopoietic cell transplant.
The patient developed a fever of 38.3º C with tachycardia but no other sepsis signs approximately 24 hours after the transplant. Soon afterward, the care team was informed that there was a single colony each of Micrococcus and S. aureus in the culture of the HSC product. Methicillin susceptibility was later confirmed. Antibiotic treatment was changed accordingly, and as of 117 days post transplant, the patient was “doing well with no evidence of further infectious complications,” the investigators said.
Bacterial contamination of HSC grafts is relatively common, with reported rates ranging from 1% to 45%. However, the clinical significance of the contamination has been unclear. Moreover, contamination is not an absolute contraindication to infusion, as options for the patient are limited after a myeloablative preparative regimen.
There are some previous case reports also identifying infections caused by contaminated grafts, but in those cases, the evidence linking the graft to the infection was based solely on finding identical species, while in the present report, the graft and patient isolates were confirmed to be identical using pulsed-field gel electrophoresis.
The investigators reported having no outside funding and no financial disclosures.
SOURCE: Willis Z et al, Infect Control Hosp Epidemiol. 2018 Jan 23. doi: 10.1017/ice.2017.285.
, according to a letter to the editor published in Infection Control & Hospital Epidemiology.
Strains of Staphylococcus aureus found in isolates from the HSC graft and the patient were confirmed to be identical using pulsed-field gel electrophoresis, the authors, led by Zachary I. Willis, MD, MPH, of the department of pediatrics at the University of North Carolina at Chapel Hill, said.
“While multiple reports have found that low-grade bacterial contamination of HSC products is rarely consequential, our patient’s experience demonstrated that clinically significant infections may occur,” Dr. Willis and his colleagues wrote in the case report.
When less virulent organisms are found in HSC grafts, close observation may be warranted, the investigators said; however, a more aggressive approach might be considered when more virulent organisms are found.
“In such a case, we suggest obtaining blood cultures and considering preemptive antibiotics as guided by the identity and susceptibility of the contaminating organism,” the investigators wrote.
Dr. Willis and his colleagues reported the case of a 15-year-old boy with hypodiploid B-ALL who achieved complete remission after treatment and then underwent a 10/10 HLA allele–matched unrelated donor hematopoietic cell transplant.
The patient developed a fever of 38.3º C with tachycardia but no other sepsis signs approximately 24 hours after the transplant. Soon afterward, the care team was informed that there was a single colony each of Micrococcus and S. aureus in the culture of the HSC product. Methicillin susceptibility was later confirmed. Antibiotic treatment was changed accordingly, and as of 117 days post transplant, the patient was “doing well with no evidence of further infectious complications,” the investigators said.
Bacterial contamination of HSC grafts is relatively common, with reported rates ranging from 1% to 45%. However, the clinical significance of the contamination has been unclear. Moreover, contamination is not an absolute contraindication to infusion, as options for the patient are limited after a myeloablative preparative regimen.
There are some previous case reports also identifying infections caused by contaminated grafts, but in those cases, the evidence linking the graft to the infection was based solely on finding identical species, while in the present report, the graft and patient isolates were confirmed to be identical using pulsed-field gel electrophoresis.
The investigators reported having no outside funding and no financial disclosures.
SOURCE: Willis Z et al, Infect Control Hosp Epidemiol. 2018 Jan 23. doi: 10.1017/ice.2017.285.
FROM INFECTION CONTROL & HOSPITAL EPIDEMIOLOGY
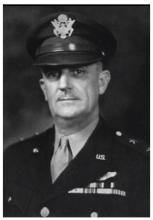
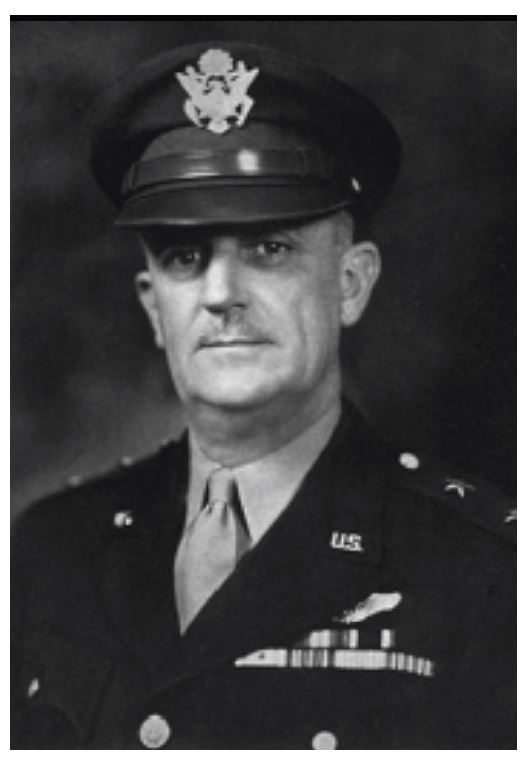
Major General David N.W. Grant: An Early Leader in Air Force Medicine
The U.S. Air Force Medical Center at Travis Air Force Base near Fairfield, California, is named in honor of Major General David Norvell Walker Grant, considered by many to be the father of the U.S. Air Force Medical Service. The first legacy organization of the U.S. Air Force was created within the U.S. Army in 1907 (Aeronautical Division, Signal Corps). Through a succession of evolutionary, organizational, and mission changes over 40 years, it became an independent service when the National Security Act of 1947 created the Department of the Air Force. Grant spent most of his career in the predecessor organizations, the U.S. Army Air Corps (1926-1941) and U.S. Army Air Forces (1941-1947).
A native Virginian, Grant graduated from the University of Virginia School of Medicine in 1915 and joined the Army Medical Corps in 1916. His service in World War I included assignments in Panama and within the continental U.S. From 1919 to 1922, he served in Germany in the Army of Occupation. Grant’s aviation medicine career began in 1931 when he attended the School of Aviation Medicine. After he completed the 6-month course, he was stationed at Randolph Field, Texas, for 5 years. In 1937, after more than a decade as a major, he was promoted to lieutenant colonel. He completed the Air Force Tactical School that same year.
In 1939, Grant became chief of the Medical Division, Office of the Chief of the Air Corps in Washington, DC. On creation of the U.S. Army Air Forces in 1941, he was appointed air surgeon and served in this capacity throughout World War II. He was promoted to colonel in 1941, brigadier general in 1942, and major general in 1943.
Early in preparations for war, Grant recognized that the medical needs of an air force differed significantly from those of large land armies. He and others were successful in their fight to establish a separate medical service for the air forces. During World War II, the U.S. Army Air Forces consisted of 2.4 million personnel and more than 80,000 aircraft. Today the U.S. Air Force has about 320,000 personnel who support and operate about 5,500 aircraft.
Grant was one of the first to understand the need for aeromedical evacuation and was responsible for its organization and operation in World War II. He also was instrumental in the establishment of the Convalescent Rehabilitation Program to help restore the wounded, ill, and injured to full capacity for further service or for their return to the civilian world.
The development and training of flight nurses were inherent in the aeromedical evacuation program. In 1943, the first class of flight nurses graduated from the U.S. Army Air Force School of Air Evacuations at Bowman Field, Kentucky. Second Lieutenant Geraldine Dishroon of Tulsa, Oklahoma, was the honor graduate in her class of 39 students. As she was to receive the first wings presented to a flight nurse, Grant removed his flight surgeon wings and pinned them on Lieutenant Dishroon as a sign of respect for her and the other new flight nurses. In 1944, Lieutenant Dishroon landed with the first air evacuation team on Omaha Beach after the D-Day invasion.
Under Grant’s leadership and guidance, aviation psychologists developed comprehensive mass testing procedures for selecting and classifying potential aircrew members, based on aptitude, personality, and interest. After 3 decades on active duty, Grant retired in 1946 and became medical director for the American Red Cross and national director of the Red Cross Blood Program.
In 1966, 2 years after Grant died, the 4167th Station Hospital at Travis Air Force Base was renamed the David Grant U.S. Air Force Medical Center in his honor.
About this column
This column provides biographical sketches of the namesakes of military and VA health care facilities. To learn more about the individual your facility was named for or to offer a topic suggestion, contact us at [email protected] or on Facebook.
The U.S. Air Force Medical Center at Travis Air Force Base near Fairfield, California, is named in honor of Major General David Norvell Walker Grant, considered by many to be the father of the U.S. Air Force Medical Service. The first legacy organization of the U.S. Air Force was created within the U.S. Army in 1907 (Aeronautical Division, Signal Corps). Through a succession of evolutionary, organizational, and mission changes over 40 years, it became an independent service when the National Security Act of 1947 created the Department of the Air Force. Grant spent most of his career in the predecessor organizations, the U.S. Army Air Corps (1926-1941) and U.S. Army Air Forces (1941-1947).
A native Virginian, Grant graduated from the University of Virginia School of Medicine in 1915 and joined the Army Medical Corps in 1916. His service in World War I included assignments in Panama and within the continental U.S. From 1919 to 1922, he served in Germany in the Army of Occupation. Grant’s aviation medicine career began in 1931 when he attended the School of Aviation Medicine. After he completed the 6-month course, he was stationed at Randolph Field, Texas, for 5 years. In 1937, after more than a decade as a major, he was promoted to lieutenant colonel. He completed the Air Force Tactical School that same year.
In 1939, Grant became chief of the Medical Division, Office of the Chief of the Air Corps in Washington, DC. On creation of the U.S. Army Air Forces in 1941, he was appointed air surgeon and served in this capacity throughout World War II. He was promoted to colonel in 1941, brigadier general in 1942, and major general in 1943.
Early in preparations for war, Grant recognized that the medical needs of an air force differed significantly from those of large land armies. He and others were successful in their fight to establish a separate medical service for the air forces. During World War II, the U.S. Army Air Forces consisted of 2.4 million personnel and more than 80,000 aircraft. Today the U.S. Air Force has about 320,000 personnel who support and operate about 5,500 aircraft.
Grant was one of the first to understand the need for aeromedical evacuation and was responsible for its organization and operation in World War II. He also was instrumental in the establishment of the Convalescent Rehabilitation Program to help restore the wounded, ill, and injured to full capacity for further service or for their return to the civilian world.
The development and training of flight nurses were inherent in the aeromedical evacuation program. In 1943, the first class of flight nurses graduated from the U.S. Army Air Force School of Air Evacuations at Bowman Field, Kentucky. Second Lieutenant Geraldine Dishroon of Tulsa, Oklahoma, was the honor graduate in her class of 39 students. As she was to receive the first wings presented to a flight nurse, Grant removed his flight surgeon wings and pinned them on Lieutenant Dishroon as a sign of respect for her and the other new flight nurses. In 1944, Lieutenant Dishroon landed with the first air evacuation team on Omaha Beach after the D-Day invasion.
Under Grant’s leadership and guidance, aviation psychologists developed comprehensive mass testing procedures for selecting and classifying potential aircrew members, based on aptitude, personality, and interest. After 3 decades on active duty, Grant retired in 1946 and became medical director for the American Red Cross and national director of the Red Cross Blood Program.
In 1966, 2 years after Grant died, the 4167th Station Hospital at Travis Air Force Base was renamed the David Grant U.S. Air Force Medical Center in his honor.
About this column
This column provides biographical sketches of the namesakes of military and VA health care facilities. To learn more about the individual your facility was named for or to offer a topic suggestion, contact us at [email protected] or on Facebook.
The U.S. Air Force Medical Center at Travis Air Force Base near Fairfield, California, is named in honor of Major General David Norvell Walker Grant, considered by many to be the father of the U.S. Air Force Medical Service. The first legacy organization of the U.S. Air Force was created within the U.S. Army in 1907 (Aeronautical Division, Signal Corps). Through a succession of evolutionary, organizational, and mission changes over 40 years, it became an independent service when the National Security Act of 1947 created the Department of the Air Force. Grant spent most of his career in the predecessor organizations, the U.S. Army Air Corps (1926-1941) and U.S. Army Air Forces (1941-1947).
A native Virginian, Grant graduated from the University of Virginia School of Medicine in 1915 and joined the Army Medical Corps in 1916. His service in World War I included assignments in Panama and within the continental U.S. From 1919 to 1922, he served in Germany in the Army of Occupation. Grant’s aviation medicine career began in 1931 when he attended the School of Aviation Medicine. After he completed the 6-month course, he was stationed at Randolph Field, Texas, for 5 years. In 1937, after more than a decade as a major, he was promoted to lieutenant colonel. He completed the Air Force Tactical School that same year.
In 1939, Grant became chief of the Medical Division, Office of the Chief of the Air Corps in Washington, DC. On creation of the U.S. Army Air Forces in 1941, he was appointed air surgeon and served in this capacity throughout World War II. He was promoted to colonel in 1941, brigadier general in 1942, and major general in 1943.
Early in preparations for war, Grant recognized that the medical needs of an air force differed significantly from those of large land armies. He and others were successful in their fight to establish a separate medical service for the air forces. During World War II, the U.S. Army Air Forces consisted of 2.4 million personnel and more than 80,000 aircraft. Today the U.S. Air Force has about 320,000 personnel who support and operate about 5,500 aircraft.
Grant was one of the first to understand the need for aeromedical evacuation and was responsible for its organization and operation in World War II. He also was instrumental in the establishment of the Convalescent Rehabilitation Program to help restore the wounded, ill, and injured to full capacity for further service or for their return to the civilian world.
The development and training of flight nurses were inherent in the aeromedical evacuation program. In 1943, the first class of flight nurses graduated from the U.S. Army Air Force School of Air Evacuations at Bowman Field, Kentucky. Second Lieutenant Geraldine Dishroon of Tulsa, Oklahoma, was the honor graduate in her class of 39 students. As she was to receive the first wings presented to a flight nurse, Grant removed his flight surgeon wings and pinned them on Lieutenant Dishroon as a sign of respect for her and the other new flight nurses. In 1944, Lieutenant Dishroon landed with the first air evacuation team on Omaha Beach after the D-Day invasion.
Under Grant’s leadership and guidance, aviation psychologists developed comprehensive mass testing procedures for selecting and classifying potential aircrew members, based on aptitude, personality, and interest. After 3 decades on active duty, Grant retired in 1946 and became medical director for the American Red Cross and national director of the Red Cross Blood Program.
In 1966, 2 years after Grant died, the 4167th Station Hospital at Travis Air Force Base was renamed the David Grant U.S. Air Force Medical Center in his honor.
About this column
This column provides biographical sketches of the namesakes of military and VA health care facilities. To learn more about the individual your facility was named for or to offer a topic suggestion, contact us at [email protected] or on Facebook.
No need for structured PE assessment, team says
There is no need for a structured algorithm to rule out pulmonary embolism (PE) in patients who visit the emergency department (ED) for syncope, according to researchers.
The team analyzed data on nearly 1.7 million patients who presented to the ED for syncope in 4 different countries.
PE occurred in less than 1% of these patients and in less than 3% of patients who were hospitalized.
The researchers therefore concluded that PE should be considered in such patients, but a systematic protocol for ruling out PE is not necessary.
“Our results are saying that there is no need, so far, for using a structured clinical algorithm to assess pulmonary emboli in all the patients presenting [to the ED with syncope],” said Nicola Montano, MD, PhD, of the University of Milan in Italy.
Dr Montano and his colleagues described these results in JAMA Internal Medicine.
The team noted that, in the PESIT trial, researchers used a standardized algorithm to evaluate PE prevalence in patients hospitalized after a first syncope episode.
The algorithm was based on pretest clinical probability and results of the D-dimer assay. Any patient with positive D-dimer results or high pretest PE probability underwent computed tomography or ventilation perfusion lung scanning.
In this study, the prevalence of PE was 17.3%.
A subsequent study showed a much lower prevalence of PE and deep vein thrombosis in patients hospitalized for syncope. The prevalence of venous thromboembolism (VTE) in this study was 1.4%.
The differences between these studies and the fact that both studies included only hospitalized patients prompted Dr Montano and his colleagues to conduct the current study.
The team set out to determine PE/VTE prevalence in unselected patients with syncope presenting to the ED.
Results
The researchers analyzed administrative data from 5 databases in 4 countries—Canada, Denmark, Italy, and the US—collected from January 1, 2000, through September 30, 2016.
The data included 1,671,944 adults who presented to the ED for syncope. The prevalence of PE at ED or hospital discharge ranged from 0.06% to 0.55%. Among the hospitalized patients only, the prevalence of PE ranged from 0.15% to 2.10%.
At 90 days of follow-up, the prevalence of PE ranged from 0.14% to 0.83% for all patients and from 0.35% to 2.63% for hospitalized patients.
The prevalence of VTE at 90 days ranged from 0.30% to 1.37% for all patients and from 0.75% to 3.86% for hospitalized patients.
The researchers said the main limitation of this study is the use of administrative data because some patients with syncope, PE, or VTE may have been missed. ![]()
There is no need for a structured algorithm to rule out pulmonary embolism (PE) in patients who visit the emergency department (ED) for syncope, according to researchers.
The team analyzed data on nearly 1.7 million patients who presented to the ED for syncope in 4 different countries.
PE occurred in less than 1% of these patients and in less than 3% of patients who were hospitalized.
The researchers therefore concluded that PE should be considered in such patients, but a systematic protocol for ruling out PE is not necessary.
“Our results are saying that there is no need, so far, for using a structured clinical algorithm to assess pulmonary emboli in all the patients presenting [to the ED with syncope],” said Nicola Montano, MD, PhD, of the University of Milan in Italy.
Dr Montano and his colleagues described these results in JAMA Internal Medicine.
The team noted that, in the PESIT trial, researchers used a standardized algorithm to evaluate PE prevalence in patients hospitalized after a first syncope episode.
The algorithm was based on pretest clinical probability and results of the D-dimer assay. Any patient with positive D-dimer results or high pretest PE probability underwent computed tomography or ventilation perfusion lung scanning.
In this study, the prevalence of PE was 17.3%.
A subsequent study showed a much lower prevalence of PE and deep vein thrombosis in patients hospitalized for syncope. The prevalence of venous thromboembolism (VTE) in this study was 1.4%.
The differences between these studies and the fact that both studies included only hospitalized patients prompted Dr Montano and his colleagues to conduct the current study.
The team set out to determine PE/VTE prevalence in unselected patients with syncope presenting to the ED.
Results
The researchers analyzed administrative data from 5 databases in 4 countries—Canada, Denmark, Italy, and the US—collected from January 1, 2000, through September 30, 2016.
The data included 1,671,944 adults who presented to the ED for syncope. The prevalence of PE at ED or hospital discharge ranged from 0.06% to 0.55%. Among the hospitalized patients only, the prevalence of PE ranged from 0.15% to 2.10%.
At 90 days of follow-up, the prevalence of PE ranged from 0.14% to 0.83% for all patients and from 0.35% to 2.63% for hospitalized patients.
The prevalence of VTE at 90 days ranged from 0.30% to 1.37% for all patients and from 0.75% to 3.86% for hospitalized patients.
The researchers said the main limitation of this study is the use of administrative data because some patients with syncope, PE, or VTE may have been missed. ![]()
There is no need for a structured algorithm to rule out pulmonary embolism (PE) in patients who visit the emergency department (ED) for syncope, according to researchers.
The team analyzed data on nearly 1.7 million patients who presented to the ED for syncope in 4 different countries.
PE occurred in less than 1% of these patients and in less than 3% of patients who were hospitalized.
The researchers therefore concluded that PE should be considered in such patients, but a systematic protocol for ruling out PE is not necessary.
“Our results are saying that there is no need, so far, for using a structured clinical algorithm to assess pulmonary emboli in all the patients presenting [to the ED with syncope],” said Nicola Montano, MD, PhD, of the University of Milan in Italy.
Dr Montano and his colleagues described these results in JAMA Internal Medicine.
The team noted that, in the PESIT trial, researchers used a standardized algorithm to evaluate PE prevalence in patients hospitalized after a first syncope episode.
The algorithm was based on pretest clinical probability and results of the D-dimer assay. Any patient with positive D-dimer results or high pretest PE probability underwent computed tomography or ventilation perfusion lung scanning.
In this study, the prevalence of PE was 17.3%.
A subsequent study showed a much lower prevalence of PE and deep vein thrombosis in patients hospitalized for syncope. The prevalence of venous thromboembolism (VTE) in this study was 1.4%.
The differences between these studies and the fact that both studies included only hospitalized patients prompted Dr Montano and his colleagues to conduct the current study.
The team set out to determine PE/VTE prevalence in unselected patients with syncope presenting to the ED.
Results
The researchers analyzed administrative data from 5 databases in 4 countries—Canada, Denmark, Italy, and the US—collected from January 1, 2000, through September 30, 2016.
The data included 1,671,944 adults who presented to the ED for syncope. The prevalence of PE at ED or hospital discharge ranged from 0.06% to 0.55%. Among the hospitalized patients only, the prevalence of PE ranged from 0.15% to 2.10%.
At 90 days of follow-up, the prevalence of PE ranged from 0.14% to 0.83% for all patients and from 0.35% to 2.63% for hospitalized patients.
The prevalence of VTE at 90 days ranged from 0.30% to 1.37% for all patients and from 0.75% to 3.86% for hospitalized patients.
The researchers said the main limitation of this study is the use of administrative data because some patients with syncope, PE, or VTE may have been missed. ![]()
Phototherapeutic technology could fight MM, other cancers
Preclinical research suggests that light-triggered, chemotherapy-loaded nanoparticles could treat multiple myeloma (MM) and other malignancies.
Researchers showed that light emitted as part of traditional cancer-imaging techniques could also trigger a light-sensitive chemotherapy drug.
When this drug was packaged into nanoparticles that target lit-up cancer cells, the drug produced toxic free radicals that killed the cancer cells.
Researchers found this technique to be effective in mice with MM and aggressive, metastatic breast cancer.
“Our study shows that this phototherapeutic technology is particularly suited to attacking small tumors that spread to different parts of the body, including deep in the bone marrow,” said Samuel Achilefu, PhD, of Washington University in St. Louis, Missouri.
Dr Achilefu and his colleagues described the technology in Nature Communications.
The technology harnesses the chemotherapy drug titanocene. When used alone, titanocene did not work well in clinical trials, even at relatively high doses. However, when it is exposed to the radiation emitted by visible light, titanocene produces reactive particles that are toxic to cells, even at low doses.
Dr Achilefu and his colleagues packaged low doses of titanocene inside nanoparticles targeted to proteins on the surface of cancer cells. Specifically, the team used nanomicelles targeting VLA-4, “an attractive target for precision imaging and therapy” in MM, according to the researchers.
When these nanomicelles made contact with MM cells, their membranes fused together, releasing titanocene into the cells.
The researchers then delivered the imaging agent fluorodeoxyglucose (FDG). MM cells took up the FDG at high rates, causing the cells to glow in a positron emission tomography scan. This glow also triggered the titanocene, releasing free radicals and killing the MM cells.
This treatment strategy was used on mice with MM once a week for 4 weeks. In the weeks following, the treated mice had significantly smaller tumors and survived longer than control mice. Fifty percent of treated mice survived at least 90 days, and 50% of control mice survived 62 days.
This strategy also produced an anti-tumor effect in mice with breast cancer, although, in these experiments, the researchers used human serum albumin nanoparticles.
The effect in breast cancer was less pronounced than in MM. The researchers said this was likely due to the extreme aggressiveness of the breast cancer cell line used.
The team also found that certain MM cells were resistant to this treatment technique.
“This is an opportunity to learn because it’s similar to what is seen in patients—some of the cells become dormant but don’t die after treatment,” Dr Achilefu said. “When we looked closer at the cells that were resistant to our phototherapy, we saw that the surface protein we are targeting was not there.”
Specifically, the resistant cells had downregulated expression of CD49d, and the researchers believe this may have impaired the binding of nanomicelles to the MM cells.
“So next, we want to find out if we can pinpoint another surface protein to target and kill these resistant cells along with the myeloma cells that did respond to the original therapy, which could lead to complete remission,” Dr Achilefu said.
Furthermore, Dr Achilefu envisions that, one day, doctors might be able to use this technology to prevent cancer from recurring.
“We are interested in exploring whether this is something a patient in remission could take once a year for prevention,” Dr Achilefu said. “The toxicity appears to be low, so we imagine an outpatient procedure that could involve zapping any cancerous cells, making cancer a chronic condition that could be controlled long-term.”
Dr Achilefu and his colleagues believe this phototherapeutic technology is less toxic than standard radiation and chemotherapy because the titanocene and FDG are targeted to the same place at the same time only in cancer cells.
The body rids itself of titanocene through the liver, while FDG is cleared through the kidneys. The fact that these components are disposed of separately minimizes damage to other organs. When separated, the components are not toxic, according to the researchers. ![]()
Preclinical research suggests that light-triggered, chemotherapy-loaded nanoparticles could treat multiple myeloma (MM) and other malignancies.
Researchers showed that light emitted as part of traditional cancer-imaging techniques could also trigger a light-sensitive chemotherapy drug.
When this drug was packaged into nanoparticles that target lit-up cancer cells, the drug produced toxic free radicals that killed the cancer cells.
Researchers found this technique to be effective in mice with MM and aggressive, metastatic breast cancer.
“Our study shows that this phototherapeutic technology is particularly suited to attacking small tumors that spread to different parts of the body, including deep in the bone marrow,” said Samuel Achilefu, PhD, of Washington University in St. Louis, Missouri.
Dr Achilefu and his colleagues described the technology in Nature Communications.
The technology harnesses the chemotherapy drug titanocene. When used alone, titanocene did not work well in clinical trials, even at relatively high doses. However, when it is exposed to the radiation emitted by visible light, titanocene produces reactive particles that are toxic to cells, even at low doses.
Dr Achilefu and his colleagues packaged low doses of titanocene inside nanoparticles targeted to proteins on the surface of cancer cells. Specifically, the team used nanomicelles targeting VLA-4, “an attractive target for precision imaging and therapy” in MM, according to the researchers.
When these nanomicelles made contact with MM cells, their membranes fused together, releasing titanocene into the cells.
The researchers then delivered the imaging agent fluorodeoxyglucose (FDG). MM cells took up the FDG at high rates, causing the cells to glow in a positron emission tomography scan. This glow also triggered the titanocene, releasing free radicals and killing the MM cells.
This treatment strategy was used on mice with MM once a week for 4 weeks. In the weeks following, the treated mice had significantly smaller tumors and survived longer than control mice. Fifty percent of treated mice survived at least 90 days, and 50% of control mice survived 62 days.
This strategy also produced an anti-tumor effect in mice with breast cancer, although, in these experiments, the researchers used human serum albumin nanoparticles.
The effect in breast cancer was less pronounced than in MM. The researchers said this was likely due to the extreme aggressiveness of the breast cancer cell line used.
The team also found that certain MM cells were resistant to this treatment technique.
“This is an opportunity to learn because it’s similar to what is seen in patients—some of the cells become dormant but don’t die after treatment,” Dr Achilefu said. “When we looked closer at the cells that were resistant to our phototherapy, we saw that the surface protein we are targeting was not there.”
Specifically, the resistant cells had downregulated expression of CD49d, and the researchers believe this may have impaired the binding of nanomicelles to the MM cells.
“So next, we want to find out if we can pinpoint another surface protein to target and kill these resistant cells along with the myeloma cells that did respond to the original therapy, which could lead to complete remission,” Dr Achilefu said.
Furthermore, Dr Achilefu envisions that, one day, doctors might be able to use this technology to prevent cancer from recurring.
“We are interested in exploring whether this is something a patient in remission could take once a year for prevention,” Dr Achilefu said. “The toxicity appears to be low, so we imagine an outpatient procedure that could involve zapping any cancerous cells, making cancer a chronic condition that could be controlled long-term.”
Dr Achilefu and his colleagues believe this phototherapeutic technology is less toxic than standard radiation and chemotherapy because the titanocene and FDG are targeted to the same place at the same time only in cancer cells.
The body rids itself of titanocene through the liver, while FDG is cleared through the kidneys. The fact that these components are disposed of separately minimizes damage to other organs. When separated, the components are not toxic, according to the researchers. ![]()
Preclinical research suggests that light-triggered, chemotherapy-loaded nanoparticles could treat multiple myeloma (MM) and other malignancies.
Researchers showed that light emitted as part of traditional cancer-imaging techniques could also trigger a light-sensitive chemotherapy drug.
When this drug was packaged into nanoparticles that target lit-up cancer cells, the drug produced toxic free radicals that killed the cancer cells.
Researchers found this technique to be effective in mice with MM and aggressive, metastatic breast cancer.
“Our study shows that this phototherapeutic technology is particularly suited to attacking small tumors that spread to different parts of the body, including deep in the bone marrow,” said Samuel Achilefu, PhD, of Washington University in St. Louis, Missouri.
Dr Achilefu and his colleagues described the technology in Nature Communications.
The technology harnesses the chemotherapy drug titanocene. When used alone, titanocene did not work well in clinical trials, even at relatively high doses. However, when it is exposed to the radiation emitted by visible light, titanocene produces reactive particles that are toxic to cells, even at low doses.
Dr Achilefu and his colleagues packaged low doses of titanocene inside nanoparticles targeted to proteins on the surface of cancer cells. Specifically, the team used nanomicelles targeting VLA-4, “an attractive target for precision imaging and therapy” in MM, according to the researchers.
When these nanomicelles made contact with MM cells, their membranes fused together, releasing titanocene into the cells.
The researchers then delivered the imaging agent fluorodeoxyglucose (FDG). MM cells took up the FDG at high rates, causing the cells to glow in a positron emission tomography scan. This glow also triggered the titanocene, releasing free radicals and killing the MM cells.
This treatment strategy was used on mice with MM once a week for 4 weeks. In the weeks following, the treated mice had significantly smaller tumors and survived longer than control mice. Fifty percent of treated mice survived at least 90 days, and 50% of control mice survived 62 days.
This strategy also produced an anti-tumor effect in mice with breast cancer, although, in these experiments, the researchers used human serum albumin nanoparticles.
The effect in breast cancer was less pronounced than in MM. The researchers said this was likely due to the extreme aggressiveness of the breast cancer cell line used.
The team also found that certain MM cells were resistant to this treatment technique.
“This is an opportunity to learn because it’s similar to what is seen in patients—some of the cells become dormant but don’t die after treatment,” Dr Achilefu said. “When we looked closer at the cells that were resistant to our phototherapy, we saw that the surface protein we are targeting was not there.”
Specifically, the resistant cells had downregulated expression of CD49d, and the researchers believe this may have impaired the binding of nanomicelles to the MM cells.
“So next, we want to find out if we can pinpoint another surface protein to target and kill these resistant cells along with the myeloma cells that did respond to the original therapy, which could lead to complete remission,” Dr Achilefu said.
Furthermore, Dr Achilefu envisions that, one day, doctors might be able to use this technology to prevent cancer from recurring.
“We are interested in exploring whether this is something a patient in remission could take once a year for prevention,” Dr Achilefu said. “The toxicity appears to be low, so we imagine an outpatient procedure that could involve zapping any cancerous cells, making cancer a chronic condition that could be controlled long-term.”
Dr Achilefu and his colleagues believe this phototherapeutic technology is less toxic than standard radiation and chemotherapy because the titanocene and FDG are targeted to the same place at the same time only in cancer cells.
The body rids itself of titanocene through the liver, while FDG is cleared through the kidneys. The fact that these components are disposed of separately minimizes damage to other organs. When separated, the components are not toxic, according to the researchers. ![]()
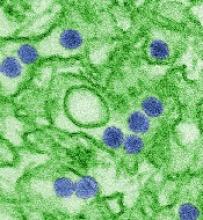
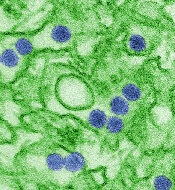
Zika vaccine candidate receives fast track designation
The US Food and Drug Administration (FDA) has granted fast track designation to TAK-426, a candidate vaccine for Zika virus.
TAK-426 is a purified, inactivated, alum-adjuvanted, whole Zika virus vaccine candidate being developed by Takeda Pharmaceutical Company Limited with the aid of federal funding.
TAK-426 is currently being studied in a phase 1 trial, ZIK-101 (NCT03343626).
This randomized, placebo-controlled, double-blind trial was designed to evaluate the safety and immunogenicity of TAK-426 in 240 male and female subjects between the ages of 18 and 49.
The trial is taking place in the continental US and US territories. It is being conducted under a US Investigational New Drug application.
Takeda says that, if initial data from ZIK-101 are supportive, the company will work to progress into phase 2 development as soon as possible.
Takeda’s Zika program is supported by federal funds from the Biomedical Advanced Research and Development Authority (BARDA) within the Office of the Assistant Secretary for Preparedness and Response in the US Department of Health and Human Services (contract No. HHSO100201600015C).
“We recognize the public health threat posed by the Zika virus,” said Laurence De Moerlooze, PhD, lead of the global Zika program at Takeda.
“As soon as Takeda received funding from BARDA, we mobilized a team and prioritized development of this vaccine candidate, initiating a phase 1 trial within 15 months of contract signature. With fast track designation, the ongoing support of BARDA, and the abilities of our organization, we are confident that we will continue to make expedient progress.”
About fast track designation
The FDA’s fast track designation is a process designed to facilitate the development and expedite the review of drugs and vaccines with the potential to treat serious or life-threatening conditions and address unmet medical needs.
The fast track process allows for more frequent interactions with the FDA, rolling reviews of a product application, and eligibility for priority review if relevant criteria are met. The FDA’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months. ![]()
The US Food and Drug Administration (FDA) has granted fast track designation to TAK-426, a candidate vaccine for Zika virus.
TAK-426 is a purified, inactivated, alum-adjuvanted, whole Zika virus vaccine candidate being developed by Takeda Pharmaceutical Company Limited with the aid of federal funding.
TAK-426 is currently being studied in a phase 1 trial, ZIK-101 (NCT03343626).
This randomized, placebo-controlled, double-blind trial was designed to evaluate the safety and immunogenicity of TAK-426 in 240 male and female subjects between the ages of 18 and 49.
The trial is taking place in the continental US and US territories. It is being conducted under a US Investigational New Drug application.
Takeda says that, if initial data from ZIK-101 are supportive, the company will work to progress into phase 2 development as soon as possible.
Takeda’s Zika program is supported by federal funds from the Biomedical Advanced Research and Development Authority (BARDA) within the Office of the Assistant Secretary for Preparedness and Response in the US Department of Health and Human Services (contract No. HHSO100201600015C).
“We recognize the public health threat posed by the Zika virus,” said Laurence De Moerlooze, PhD, lead of the global Zika program at Takeda.
“As soon as Takeda received funding from BARDA, we mobilized a team and prioritized development of this vaccine candidate, initiating a phase 1 trial within 15 months of contract signature. With fast track designation, the ongoing support of BARDA, and the abilities of our organization, we are confident that we will continue to make expedient progress.”
About fast track designation
The FDA’s fast track designation is a process designed to facilitate the development and expedite the review of drugs and vaccines with the potential to treat serious or life-threatening conditions and address unmet medical needs.
The fast track process allows for more frequent interactions with the FDA, rolling reviews of a product application, and eligibility for priority review if relevant criteria are met. The FDA’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months. ![]()
The US Food and Drug Administration (FDA) has granted fast track designation to TAK-426, a candidate vaccine for Zika virus.
TAK-426 is a purified, inactivated, alum-adjuvanted, whole Zika virus vaccine candidate being developed by Takeda Pharmaceutical Company Limited with the aid of federal funding.
TAK-426 is currently being studied in a phase 1 trial, ZIK-101 (NCT03343626).
This randomized, placebo-controlled, double-blind trial was designed to evaluate the safety and immunogenicity of TAK-426 in 240 male and female subjects between the ages of 18 and 49.
The trial is taking place in the continental US and US territories. It is being conducted under a US Investigational New Drug application.
Takeda says that, if initial data from ZIK-101 are supportive, the company will work to progress into phase 2 development as soon as possible.
Takeda’s Zika program is supported by federal funds from the Biomedical Advanced Research and Development Authority (BARDA) within the Office of the Assistant Secretary for Preparedness and Response in the US Department of Health and Human Services (contract No. HHSO100201600015C).
“We recognize the public health threat posed by the Zika virus,” said Laurence De Moerlooze, PhD, lead of the global Zika program at Takeda.
“As soon as Takeda received funding from BARDA, we mobilized a team and prioritized development of this vaccine candidate, initiating a phase 1 trial within 15 months of contract signature. With fast track designation, the ongoing support of BARDA, and the abilities of our organization, we are confident that we will continue to make expedient progress.”
About fast track designation
The FDA’s fast track designation is a process designed to facilitate the development and expedite the review of drugs and vaccines with the potential to treat serious or life-threatening conditions and address unmet medical needs.
The fast track process allows for more frequent interactions with the FDA, rolling reviews of a product application, and eligibility for priority review if relevant criteria are met. The FDA’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months. ![]()
MDedge Daily News: The flu vaccine flop’s Cold War connection
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
APOE4 may determine memory loss in Alzheimer’s, a recent flu vaccine flop may have a Cold War connection, treating women’s urinary incontinence could have a restful side effect, and why the 3 months after a heart attack are particularly perilous.
Listen to the MDedge Daily News podcast for all the details on today’s top news.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
APOE4 may determine memory loss in Alzheimer’s, a recent flu vaccine flop may have a Cold War connection, treating women’s urinary incontinence could have a restful side effect, and why the 3 months after a heart attack are particularly perilous.
Listen to the MDedge Daily News podcast for all the details on today’s top news.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
APOE4 may determine memory loss in Alzheimer’s, a recent flu vaccine flop may have a Cold War connection, treating women’s urinary incontinence could have a restful side effect, and why the 3 months after a heart attack are particularly perilous.
Listen to the MDedge Daily News podcast for all the details on today’s top news.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Letrozole promising as maintenance treatment for high-grade serous ovarian cancer
Maintenance therapy with an aromatase inhibitor may improve progression-free survival in women with estrogen receptor (ER)–positive, high-grade serous ovarian cancers, results of a non-randomized, single-center study suggest.
Patients who received compared with patients who declined the treatment, investigators reported in Gynecologic Oncology.
The benefit of letrozole maintenance treatment was also apparent in women with residual disease who received bevacizumab maintenance treatment, wrote first author Viola Heinzelmann-Schwarz, MD, of the Gynecological Cancer Center, University of Basel, Switzerland, and her coauthors.
The results “strongly suggest that endocrine maintenance therapy has more advantage than disadvantage for use in ovarian cancer patients and seems clearly justified,” when considered alongside other data regarding the potential benefit of letrozole in other treatment settings, Dr. Heinzelmann-Schwarz and her colleagues said.
“In contrast to available expensive maintenance medications like antiangiogenic [drugs] and PARP inhibitors, antihormonal drugs have a favorable safety profile, low cost, easy intake regimen with one tablet daily and an established prognostic target,” they added.
While the role of aromatase inhibitor maintenance therapy in high-grade serous ovarian cancer is unclear, previous studies have shown that patients with low-grade serous ovarian cancer may benefit from endocrine therapy.
Those studies in low-grade serous ovarian cancer include several small case series, and one retrospective analysis showing improved progression-free survival among women treated with endocrine therapy versus women who received observation only (J Clin Oncol. 2017 Apr. doi: 10.1200/JCO.2016.71.0632).
The more recent report by Dr. Heinzelmann-Schwarz and her colleagues included 50 women with ER-positive, FIGO (Fédération Internationale de Gynécologie et d’Obstétrique) stage III/IV high-grade serous ovarian cancer who were offered off-label letrozole treatment after debulking surgery and platinum-based chemotherapy. Twenty-three received letrozole maintenance treatment, and 27 declined.
In the group of women who received letrozole maintenance treatment, 60% were recurrence free at 24 months, compared with 38.5% of patients in the observation group (P = .035).
“This positive effect could particularly be seen when the treatment was initiated within 3 months after the end of adjuvant chemotherapy,” Dr. Heinzelmann-Schwarz and her coauthors wrote.
Among women with residual disease who received maintenance bevacizumab in addition to letrozole, 87.5% were recurrence free at 12 months, compared with 20.8% of patients who received bevacizumab only, the investigators said.
Minor side effects such as hot flushes, fatigue, and bone pain led to discontinuation in two patients (6.4%), and no serious adverse effects were seen during treatment, according to investigators.
Almost half of all high-grade serous ovarian cancers express ER, according to results of separate retrospective analyses also described by Dr. Heinzelmann-Schwarz and her colleagues in Gynecologic Oncology. They found that ER expression was similar regardless of drug resistance status (platinum sensitive versus platinum resistant) or treatment setting (primary or recurrent).
Dr. Heinzelmann-Schwarz and colleagues declared no conflicts of interest.
SOURCE: Heinzelmann-Schwarz V et al. Gyn Oncol. 2018 Jan. doi: 10.1016/j.ygyno.2017.10.036.
Maintenance therapy with an aromatase inhibitor may improve progression-free survival in women with estrogen receptor (ER)–positive, high-grade serous ovarian cancers, results of a non-randomized, single-center study suggest.
Patients who received compared with patients who declined the treatment, investigators reported in Gynecologic Oncology.
The benefit of letrozole maintenance treatment was also apparent in women with residual disease who received bevacizumab maintenance treatment, wrote first author Viola Heinzelmann-Schwarz, MD, of the Gynecological Cancer Center, University of Basel, Switzerland, and her coauthors.
The results “strongly suggest that endocrine maintenance therapy has more advantage than disadvantage for use in ovarian cancer patients and seems clearly justified,” when considered alongside other data regarding the potential benefit of letrozole in other treatment settings, Dr. Heinzelmann-Schwarz and her colleagues said.
“In contrast to available expensive maintenance medications like antiangiogenic [drugs] and PARP inhibitors, antihormonal drugs have a favorable safety profile, low cost, easy intake regimen with one tablet daily and an established prognostic target,” they added.
While the role of aromatase inhibitor maintenance therapy in high-grade serous ovarian cancer is unclear, previous studies have shown that patients with low-grade serous ovarian cancer may benefit from endocrine therapy.
Those studies in low-grade serous ovarian cancer include several small case series, and one retrospective analysis showing improved progression-free survival among women treated with endocrine therapy versus women who received observation only (J Clin Oncol. 2017 Apr. doi: 10.1200/JCO.2016.71.0632).
The more recent report by Dr. Heinzelmann-Schwarz and her colleagues included 50 women with ER-positive, FIGO (Fédération Internationale de Gynécologie et d’Obstétrique) stage III/IV high-grade serous ovarian cancer who were offered off-label letrozole treatment after debulking surgery and platinum-based chemotherapy. Twenty-three received letrozole maintenance treatment, and 27 declined.
In the group of women who received letrozole maintenance treatment, 60% were recurrence free at 24 months, compared with 38.5% of patients in the observation group (P = .035).
“This positive effect could particularly be seen when the treatment was initiated within 3 months after the end of adjuvant chemotherapy,” Dr. Heinzelmann-Schwarz and her coauthors wrote.
Among women with residual disease who received maintenance bevacizumab in addition to letrozole, 87.5% were recurrence free at 12 months, compared with 20.8% of patients who received bevacizumab only, the investigators said.
Minor side effects such as hot flushes, fatigue, and bone pain led to discontinuation in two patients (6.4%), and no serious adverse effects were seen during treatment, according to investigators.
Almost half of all high-grade serous ovarian cancers express ER, according to results of separate retrospective analyses also described by Dr. Heinzelmann-Schwarz and her colleagues in Gynecologic Oncology. They found that ER expression was similar regardless of drug resistance status (platinum sensitive versus platinum resistant) or treatment setting (primary or recurrent).
Dr. Heinzelmann-Schwarz and colleagues declared no conflicts of interest.
SOURCE: Heinzelmann-Schwarz V et al. Gyn Oncol. 2018 Jan. doi: 10.1016/j.ygyno.2017.10.036.
Maintenance therapy with an aromatase inhibitor may improve progression-free survival in women with estrogen receptor (ER)–positive, high-grade serous ovarian cancers, results of a non-randomized, single-center study suggest.
Patients who received compared with patients who declined the treatment, investigators reported in Gynecologic Oncology.
The benefit of letrozole maintenance treatment was also apparent in women with residual disease who received bevacizumab maintenance treatment, wrote first author Viola Heinzelmann-Schwarz, MD, of the Gynecological Cancer Center, University of Basel, Switzerland, and her coauthors.
The results “strongly suggest that endocrine maintenance therapy has more advantage than disadvantage for use in ovarian cancer patients and seems clearly justified,” when considered alongside other data regarding the potential benefit of letrozole in other treatment settings, Dr. Heinzelmann-Schwarz and her colleagues said.
“In contrast to available expensive maintenance medications like antiangiogenic [drugs] and PARP inhibitors, antihormonal drugs have a favorable safety profile, low cost, easy intake regimen with one tablet daily and an established prognostic target,” they added.
While the role of aromatase inhibitor maintenance therapy in high-grade serous ovarian cancer is unclear, previous studies have shown that patients with low-grade serous ovarian cancer may benefit from endocrine therapy.
Those studies in low-grade serous ovarian cancer include several small case series, and one retrospective analysis showing improved progression-free survival among women treated with endocrine therapy versus women who received observation only (J Clin Oncol. 2017 Apr. doi: 10.1200/JCO.2016.71.0632).
The more recent report by Dr. Heinzelmann-Schwarz and her colleagues included 50 women with ER-positive, FIGO (Fédération Internationale de Gynécologie et d’Obstétrique) stage III/IV high-grade serous ovarian cancer who were offered off-label letrozole treatment after debulking surgery and platinum-based chemotherapy. Twenty-three received letrozole maintenance treatment, and 27 declined.
In the group of women who received letrozole maintenance treatment, 60% were recurrence free at 24 months, compared with 38.5% of patients in the observation group (P = .035).
“This positive effect could particularly be seen when the treatment was initiated within 3 months after the end of adjuvant chemotherapy,” Dr. Heinzelmann-Schwarz and her coauthors wrote.
Among women with residual disease who received maintenance bevacizumab in addition to letrozole, 87.5% were recurrence free at 12 months, compared with 20.8% of patients who received bevacizumab only, the investigators said.
Minor side effects such as hot flushes, fatigue, and bone pain led to discontinuation in two patients (6.4%), and no serious adverse effects were seen during treatment, according to investigators.
Almost half of all high-grade serous ovarian cancers express ER, according to results of separate retrospective analyses also described by Dr. Heinzelmann-Schwarz and her colleagues in Gynecologic Oncology. They found that ER expression was similar regardless of drug resistance status (platinum sensitive versus platinum resistant) or treatment setting (primary or recurrent).
Dr. Heinzelmann-Schwarz and colleagues declared no conflicts of interest.
SOURCE: Heinzelmann-Schwarz V et al. Gyn Oncol. 2018 Jan. doi: 10.1016/j.ygyno.2017.10.036.
FROM GYNECOLOGIC ONCOLOGY
Key clinical point: Endocrine therapy may have a role in maintenance treatment for patients with estrogen receptor (ER)–positive high-grade serous ovarian cancer (HGSOC) after debulking surgery and platinum-based chemotherapy.
Major finding: Recurrence-free survival at 24 months was 60% for patients receiving the aromatase inhibitor letrozole as maintenance therapy, compared with 38.5% for patients who declined treatment (P = .035).
Data source: A prospective, single-center, nonrandomized study including 50 patients with newly diagnosed FIGO stage III/IV HGSOC and positive estrogen receptor expression.
Disclosures: The authors declared no conflicts of interest.
Source: Heinzelmann-Schwarz V et al. Gyn Oncol. 2018 Jan. doi: 10.1016/j.ygyno.2017.10.036.
Frontline brentuximab vedotin improved Hodgkin lymphoma outcomes
Replacing bleomycin with brentuximab vedotin in the classic ABVD regimen improved a measure of progression-free survival and reduced pulmonary toxicity in patients with previously untreated Hodgkin lymphoma, findings from a randomized, phase 3 trial suggest.
Patients receiving brentuximab plus chemotherapy had a “statistically significant and clinically meaningful improvement” in the rate of modified progression-free survival, according to results published in the New England Journal of Medicine.
Pulmonary toxicity also occurred at a lower rate with the regimen containing brentuximab, an anti-CD30 antibody–drug conjugate, wrote Joseph M. Connors, MD, of the British Columbia Cancer Agency, Vancouver, and his coauthors.
Taken together, these findings suggest brentuximab vedotin and chemotherapy had “substantially less pulmonary toxicity and appears to be more effective for frontline treatment of advanced-stage classic Hodgkin lymphoma,” the researchers wrote.
Bleomycin is often omitted from later cycles of chemotherapy for patients with Hodgkin lymphoma due to pulmonary symptoms, and is sometimes associated with unpredictable or even fatal pulmonary toxicity, the researchers noted.
The brentuximab vedotin arm of the trial did have more neurotoxicity, which was largely reversible, and more myelotoxicity, though that “can be ameliorated with prophylactic granulocyte colony-stimulating factor (G-CSF),” the researchers wrote.
The study by Dr. Connors and colleagues, known as ECHELON-1, was an open-label, multicenter, randomized phase 3 trial including patients with previously untreated stage III or IV classic Hodgkin lymphoma. Among enrolled patients, 664 received brentuximab vedotin plus doxorubicin, vinblastine, and dacarbazine (AVD), and 670 received standard doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD).
The study used a primary endpoint of progression-free survival augmented to include not only time to disease progression or death, but also “modified progression,” which the researchers defined as evidence of noncomplete response at the end of frontline chemotherapy.
It is accepted practice to give more chemotherapy or radiotherapy in Hodgkin lymphoma patients who have a positive PET scan at the end of frontline therapy, since metabolically detectable residual disease reliably predicts imminent progression, Dr. Connors and coauthors wrote.
“In this context, the conventional endpoint of progression-free survival does not accurately assess the curative intent of frontline chemotherapy,” they wrote.
With a median 24.9-month follow-up, modified 2-year progression-free survival in the trial was 82.1% for patients receiving brentuximab plus AVD, versus 77.2% for ABVD (P = .03), a 23% risk reduction.
Pulmonary toxicity of grade 3 or higher occurred in less than 1% of patients in the brentuximab vedotin plus AVD arm of the trial and in 3% of the ABVD arm.
Neutropenia was reported in 58% and 45% in the brentuximab vedotin plus AVD and ABVD arms, respectively, while febrile neutropenia was reported in 19% and 8%, respectively.
In the brentuximab plus AVD group, the rate of febrile neutropenia was 11% for those patients who received primary prophylaxis with G-CSF, and 21% for patients who did not, the researchers noted.
Peripheral neuropathy was seen in 67% and 43% of the brentuximab vedotin plus AVD and ABVD arms, respectively, and about two-thirds of the patients in the brentuximab vedotin plus AVD arm had improvement or resolution at the final follow-up visit.
The study was supported by Millennium Pharmaceuticals and Seattle Genetics. Researchers reported ties to Millennium Pharmaceuticals, Takeda Pharmaceuticals, Seattle Genetics, and other companies.
SOURCE: Connors JM et al. N Engl J Med. 2018;378:331-44.
The incorporation of the CD30 immunotoxin brentuximab vedotin into frontline therapy for Hodgkin lymphoma “has been eagerly anticipated, and the wait is over,” Dan L. Longo, MD, and Vincent T. DeVita Jr., MD, wrote in an editorial.
Results of the randomized phase 3 trial by Dr. Connors and colleagues suggest that, with a relatively short follow-up, adding brentuximab vedotin to AVD combination chemotherapy “merits consideration” as a first-line treatment, according to Dr. Longo and Dr. DeVita.
“Although it is too early to rule out unanticipated late side effects … brentuximab vedotin + AVD appears to be more effective than ABVD (and is unlikely to be less effective) and is associated with fewer, more treatable toxicities,” they wrote.
Adverse effects of ABVD are generally modest, but the bleomycin in the regimen can result in serious pulmonary toxicity. While the rate of serious pulmonary toxicity is low, “clinicians have the impression that it is unpredictable,” the authors noted.
Beyond a significant improvement in modified progression-free survival with a follow-up of 25 months, brentuximab vedotin plus AVD was associated with lower pulmonary toxicity, they noted.
While the brentuximab vedotin had more neutropenia and neuropathy, neutropenia could be addressed with G-CSF between doses, and neuropathy was mainly low grade and completely resolved most of the time, the authors said.
Brentuximab had promising single-agent activity in previous Hodgkin lymphoma studies, so substituting it for bleomycin “had the potential to improve on ABVD. And it did,” Dr. Longo and Dr. DeVita wrote.
Dr. Longo is with Dana-Farber Cancer Institute, Boston, and Dr. DeVita is with the Yale Cancer Center, New Haven, Conn. These comments are based on their editorial appearing in the New England Journal of Medicine (2018 Jan 24. doi: 10.1056/NEJMe1715141). Dr. DeVita reported no disclosures, and Dr. Longo reported employment as Deputy Editor with the New England Journal of Medicine.
The incorporation of the CD30 immunotoxin brentuximab vedotin into frontline therapy for Hodgkin lymphoma “has been eagerly anticipated, and the wait is over,” Dan L. Longo, MD, and Vincent T. DeVita Jr., MD, wrote in an editorial.
Results of the randomized phase 3 trial by Dr. Connors and colleagues suggest that, with a relatively short follow-up, adding brentuximab vedotin to AVD combination chemotherapy “merits consideration” as a first-line treatment, according to Dr. Longo and Dr. DeVita.
“Although it is too early to rule out unanticipated late side effects … brentuximab vedotin + AVD appears to be more effective than ABVD (and is unlikely to be less effective) and is associated with fewer, more treatable toxicities,” they wrote.
Adverse effects of ABVD are generally modest, but the bleomycin in the regimen can result in serious pulmonary toxicity. While the rate of serious pulmonary toxicity is low, “clinicians have the impression that it is unpredictable,” the authors noted.
Beyond a significant improvement in modified progression-free survival with a follow-up of 25 months, brentuximab vedotin plus AVD was associated with lower pulmonary toxicity, they noted.
While the brentuximab vedotin had more neutropenia and neuropathy, neutropenia could be addressed with G-CSF between doses, and neuropathy was mainly low grade and completely resolved most of the time, the authors said.
Brentuximab had promising single-agent activity in previous Hodgkin lymphoma studies, so substituting it for bleomycin “had the potential to improve on ABVD. And it did,” Dr. Longo and Dr. DeVita wrote.
Dr. Longo is with Dana-Farber Cancer Institute, Boston, and Dr. DeVita is with the Yale Cancer Center, New Haven, Conn. These comments are based on their editorial appearing in the New England Journal of Medicine (2018 Jan 24. doi: 10.1056/NEJMe1715141). Dr. DeVita reported no disclosures, and Dr. Longo reported employment as Deputy Editor with the New England Journal of Medicine.
The incorporation of the CD30 immunotoxin brentuximab vedotin into frontline therapy for Hodgkin lymphoma “has been eagerly anticipated, and the wait is over,” Dan L. Longo, MD, and Vincent T. DeVita Jr., MD, wrote in an editorial.
Results of the randomized phase 3 trial by Dr. Connors and colleagues suggest that, with a relatively short follow-up, adding brentuximab vedotin to AVD combination chemotherapy “merits consideration” as a first-line treatment, according to Dr. Longo and Dr. DeVita.
“Although it is too early to rule out unanticipated late side effects … brentuximab vedotin + AVD appears to be more effective than ABVD (and is unlikely to be less effective) and is associated with fewer, more treatable toxicities,” they wrote.
Adverse effects of ABVD are generally modest, but the bleomycin in the regimen can result in serious pulmonary toxicity. While the rate of serious pulmonary toxicity is low, “clinicians have the impression that it is unpredictable,” the authors noted.
Beyond a significant improvement in modified progression-free survival with a follow-up of 25 months, brentuximab vedotin plus AVD was associated with lower pulmonary toxicity, they noted.
While the brentuximab vedotin had more neutropenia and neuropathy, neutropenia could be addressed with G-CSF between doses, and neuropathy was mainly low grade and completely resolved most of the time, the authors said.
Brentuximab had promising single-agent activity in previous Hodgkin lymphoma studies, so substituting it for bleomycin “had the potential to improve on ABVD. And it did,” Dr. Longo and Dr. DeVita wrote.
Dr. Longo is with Dana-Farber Cancer Institute, Boston, and Dr. DeVita is with the Yale Cancer Center, New Haven, Conn. These comments are based on their editorial appearing in the New England Journal of Medicine (2018 Jan 24. doi: 10.1056/NEJMe1715141). Dr. DeVita reported no disclosures, and Dr. Longo reported employment as Deputy Editor with the New England Journal of Medicine.
Replacing bleomycin with brentuximab vedotin in the classic ABVD regimen improved a measure of progression-free survival and reduced pulmonary toxicity in patients with previously untreated Hodgkin lymphoma, findings from a randomized, phase 3 trial suggest.
Patients receiving brentuximab plus chemotherapy had a “statistically significant and clinically meaningful improvement” in the rate of modified progression-free survival, according to results published in the New England Journal of Medicine.
Pulmonary toxicity also occurred at a lower rate with the regimen containing brentuximab, an anti-CD30 antibody–drug conjugate, wrote Joseph M. Connors, MD, of the British Columbia Cancer Agency, Vancouver, and his coauthors.
Taken together, these findings suggest brentuximab vedotin and chemotherapy had “substantially less pulmonary toxicity and appears to be more effective for frontline treatment of advanced-stage classic Hodgkin lymphoma,” the researchers wrote.
Bleomycin is often omitted from later cycles of chemotherapy for patients with Hodgkin lymphoma due to pulmonary symptoms, and is sometimes associated with unpredictable or even fatal pulmonary toxicity, the researchers noted.
The brentuximab vedotin arm of the trial did have more neurotoxicity, which was largely reversible, and more myelotoxicity, though that “can be ameliorated with prophylactic granulocyte colony-stimulating factor (G-CSF),” the researchers wrote.
The study by Dr. Connors and colleagues, known as ECHELON-1, was an open-label, multicenter, randomized phase 3 trial including patients with previously untreated stage III or IV classic Hodgkin lymphoma. Among enrolled patients, 664 received brentuximab vedotin plus doxorubicin, vinblastine, and dacarbazine (AVD), and 670 received standard doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD).
The study used a primary endpoint of progression-free survival augmented to include not only time to disease progression or death, but also “modified progression,” which the researchers defined as evidence of noncomplete response at the end of frontline chemotherapy.
It is accepted practice to give more chemotherapy or radiotherapy in Hodgkin lymphoma patients who have a positive PET scan at the end of frontline therapy, since metabolically detectable residual disease reliably predicts imminent progression, Dr. Connors and coauthors wrote.
“In this context, the conventional endpoint of progression-free survival does not accurately assess the curative intent of frontline chemotherapy,” they wrote.
With a median 24.9-month follow-up, modified 2-year progression-free survival in the trial was 82.1% for patients receiving brentuximab plus AVD, versus 77.2% for ABVD (P = .03), a 23% risk reduction.
Pulmonary toxicity of grade 3 or higher occurred in less than 1% of patients in the brentuximab vedotin plus AVD arm of the trial and in 3% of the ABVD arm.
Neutropenia was reported in 58% and 45% in the brentuximab vedotin plus AVD and ABVD arms, respectively, while febrile neutropenia was reported in 19% and 8%, respectively.
In the brentuximab plus AVD group, the rate of febrile neutropenia was 11% for those patients who received primary prophylaxis with G-CSF, and 21% for patients who did not, the researchers noted.
Peripheral neuropathy was seen in 67% and 43% of the brentuximab vedotin plus AVD and ABVD arms, respectively, and about two-thirds of the patients in the brentuximab vedotin plus AVD arm had improvement or resolution at the final follow-up visit.
The study was supported by Millennium Pharmaceuticals and Seattle Genetics. Researchers reported ties to Millennium Pharmaceuticals, Takeda Pharmaceuticals, Seattle Genetics, and other companies.
SOURCE: Connors JM et al. N Engl J Med. 2018;378:331-44.
Replacing bleomycin with brentuximab vedotin in the classic ABVD regimen improved a measure of progression-free survival and reduced pulmonary toxicity in patients with previously untreated Hodgkin lymphoma, findings from a randomized, phase 3 trial suggest.
Patients receiving brentuximab plus chemotherapy had a “statistically significant and clinically meaningful improvement” in the rate of modified progression-free survival, according to results published in the New England Journal of Medicine.
Pulmonary toxicity also occurred at a lower rate with the regimen containing brentuximab, an anti-CD30 antibody–drug conjugate, wrote Joseph M. Connors, MD, of the British Columbia Cancer Agency, Vancouver, and his coauthors.
Taken together, these findings suggest brentuximab vedotin and chemotherapy had “substantially less pulmonary toxicity and appears to be more effective for frontline treatment of advanced-stage classic Hodgkin lymphoma,” the researchers wrote.
Bleomycin is often omitted from later cycles of chemotherapy for patients with Hodgkin lymphoma due to pulmonary symptoms, and is sometimes associated with unpredictable or even fatal pulmonary toxicity, the researchers noted.
The brentuximab vedotin arm of the trial did have more neurotoxicity, which was largely reversible, and more myelotoxicity, though that “can be ameliorated with prophylactic granulocyte colony-stimulating factor (G-CSF),” the researchers wrote.
The study by Dr. Connors and colleagues, known as ECHELON-1, was an open-label, multicenter, randomized phase 3 trial including patients with previously untreated stage III or IV classic Hodgkin lymphoma. Among enrolled patients, 664 received brentuximab vedotin plus doxorubicin, vinblastine, and dacarbazine (AVD), and 670 received standard doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD).
The study used a primary endpoint of progression-free survival augmented to include not only time to disease progression or death, but also “modified progression,” which the researchers defined as evidence of noncomplete response at the end of frontline chemotherapy.
It is accepted practice to give more chemotherapy or radiotherapy in Hodgkin lymphoma patients who have a positive PET scan at the end of frontline therapy, since metabolically detectable residual disease reliably predicts imminent progression, Dr. Connors and coauthors wrote.
“In this context, the conventional endpoint of progression-free survival does not accurately assess the curative intent of frontline chemotherapy,” they wrote.
With a median 24.9-month follow-up, modified 2-year progression-free survival in the trial was 82.1% for patients receiving brentuximab plus AVD, versus 77.2% for ABVD (P = .03), a 23% risk reduction.
Pulmonary toxicity of grade 3 or higher occurred in less than 1% of patients in the brentuximab vedotin plus AVD arm of the trial and in 3% of the ABVD arm.
Neutropenia was reported in 58% and 45% in the brentuximab vedotin plus AVD and ABVD arms, respectively, while febrile neutropenia was reported in 19% and 8%, respectively.
In the brentuximab plus AVD group, the rate of febrile neutropenia was 11% for those patients who received primary prophylaxis with G-CSF, and 21% for patients who did not, the researchers noted.
Peripheral neuropathy was seen in 67% and 43% of the brentuximab vedotin plus AVD and ABVD arms, respectively, and about two-thirds of the patients in the brentuximab vedotin plus AVD arm had improvement or resolution at the final follow-up visit.
The study was supported by Millennium Pharmaceuticals and Seattle Genetics. Researchers reported ties to Millennium Pharmaceuticals, Takeda Pharmaceuticals, Seattle Genetics, and other companies.
SOURCE: Connors JM et al. N Engl J Med. 2018;378:331-44.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point:
Major finding: Modified 2-year progression-free survival was 82.1% with the brentuximab vedotin–containing regimen versus 77.2% for ABVD (P = .03).
Study details: An open-label, multicenter, randomized phase 3 trial including 1,334 patients with previously untreated stage III or IV classic Hodgkin lymphoma.
Disclosures: The study was supported by Millennium Pharmaceuticals and Seattle Genetics. Researchers reported ties to Millennium Pharmaceuticals, Takeda Pharmaceuticals, Seattle Genetics, and other companies.
Source: Connors JM et al. N Engl J Med. 2018;378:331-44.
Integrate brief CBT interventions into medication management visits
Patients who are treated with psychotropics may experience better recovery from their symptoms and improved quality of life when they receive targeted treatment with cognitive-behavioral therapy (CBT). Clinicians can use certain CBT techniques to “jump-start” recovery in patients before prescribed medications produce their intended therapeutic effects. When practitioners are familiar with their use, techniques such as behavioral activation and tools that enhance adherence can be employed during a brief medication management (“med check”) visit.
Take these steps to implement brief CBT interventions into your patient’s routine visits:
- develop a clear, formulation-driven treatment target
- design an intervention that can be explained during a brief visit
- have handouts and worksheets available for patients to use
- provide written explanations and reminders for patients to use in out-of-session practice.
We present a case report that illustrates incorporating brief CBT interventions in a patient with major depressive disorder (MDD).
CASE REPORT
Using CBT to help a patient with MDD
Mr. L, age 52, presents with moderate MDD, and is started on fluoxetine, 20 mg/d. Mr. L has significant anhedonia and poor energy, and has been avoiding going to work and seeing friends. The psychiatrist explains to him how individuals with depression often want to refrain from activity and “shut down,” but that doing so will not improve his quality of life, and his mood will worsen.
The psychiatrist asks Mr. L to identify a pleasurable or important activity to complete before his next appointment. Mr. L decides that he would like to call a friend, because he has been isolated and his friends have been calling him. The psychiatrist encourages him to call one of his golf buddies. She instructs Mr. L to set reminders, such as cell phone alarms and notes on the refrigerator, to prompt him to “Call Phil Saturday at 10
To increase the likelihood that Mr. L will make this call, he and his psychiatrist discuss anticipated obstacles and potential facilitators of this behavior.
The psychiatrist also encourages Mr. L to complete a Behavioral Activation Worksheet (for examples, see http://www.cci.health.wa.gov.au/docs/ACF3B92.pdf or https://www.therapistaid.com/worksheets/behavioral-activation.pdf) to track his depression, pleasure, and sense of achievement before and after completing this activity.
As illustrated by this case, collaborating with the patient is critical to developing a realistic treatment plan that incorporates CBT techniques. With your help and encouragement, patients can use these tools to reach their goals and target the symptoms of their illnesses.
1. Wright JH, McCray LW. Restoring energy and enjoying life. In: Wright JH, McCray LW. Breaking free from depression: pathways to wellness. New York, NY: The Guilford Press; 2012:97-129.
2. Wright JH, Basco MR, Thase ME. Working with automatic thoughts. In: Wright JH, Basco MR, Thase ME. Learning cognitive-behavior therapy: an illustrated guide. Arlington, VA: American Psychiatric Publishing, Inc.; 2005:118-121.
Patients who are treated with psychotropics may experience better recovery from their symptoms and improved quality of life when they receive targeted treatment with cognitive-behavioral therapy (CBT). Clinicians can use certain CBT techniques to “jump-start” recovery in patients before prescribed medications produce their intended therapeutic effects. When practitioners are familiar with their use, techniques such as behavioral activation and tools that enhance adherence can be employed during a brief medication management (“med check”) visit.
Take these steps to implement brief CBT interventions into your patient’s routine visits:
- develop a clear, formulation-driven treatment target
- design an intervention that can be explained during a brief visit
- have handouts and worksheets available for patients to use
- provide written explanations and reminders for patients to use in out-of-session practice.
We present a case report that illustrates incorporating brief CBT interventions in a patient with major depressive disorder (MDD).
CASE REPORT
Using CBT to help a patient with MDD
Mr. L, age 52, presents with moderate MDD, and is started on fluoxetine, 20 mg/d. Mr. L has significant anhedonia and poor energy, and has been avoiding going to work and seeing friends. The psychiatrist explains to him how individuals with depression often want to refrain from activity and “shut down,” but that doing so will not improve his quality of life, and his mood will worsen.
The psychiatrist asks Mr. L to identify a pleasurable or important activity to complete before his next appointment. Mr. L decides that he would like to call a friend, because he has been isolated and his friends have been calling him. The psychiatrist encourages him to call one of his golf buddies. She instructs Mr. L to set reminders, such as cell phone alarms and notes on the refrigerator, to prompt him to “Call Phil Saturday at 10
To increase the likelihood that Mr. L will make this call, he and his psychiatrist discuss anticipated obstacles and potential facilitators of this behavior.
The psychiatrist also encourages Mr. L to complete a Behavioral Activation Worksheet (for examples, see http://www.cci.health.wa.gov.au/docs/ACF3B92.pdf or https://www.therapistaid.com/worksheets/behavioral-activation.pdf) to track his depression, pleasure, and sense of achievement before and after completing this activity.
As illustrated by this case, collaborating with the patient is critical to developing a realistic treatment plan that incorporates CBT techniques. With your help and encouragement, patients can use these tools to reach their goals and target the symptoms of their illnesses.
Patients who are treated with psychotropics may experience better recovery from their symptoms and improved quality of life when they receive targeted treatment with cognitive-behavioral therapy (CBT). Clinicians can use certain CBT techniques to “jump-start” recovery in patients before prescribed medications produce their intended therapeutic effects. When practitioners are familiar with their use, techniques such as behavioral activation and tools that enhance adherence can be employed during a brief medication management (“med check”) visit.
Take these steps to implement brief CBT interventions into your patient’s routine visits:
- develop a clear, formulation-driven treatment target
- design an intervention that can be explained during a brief visit
- have handouts and worksheets available for patients to use
- provide written explanations and reminders for patients to use in out-of-session practice.
We present a case report that illustrates incorporating brief CBT interventions in a patient with major depressive disorder (MDD).
CASE REPORT
Using CBT to help a patient with MDD
Mr. L, age 52, presents with moderate MDD, and is started on fluoxetine, 20 mg/d. Mr. L has significant anhedonia and poor energy, and has been avoiding going to work and seeing friends. The psychiatrist explains to him how individuals with depression often want to refrain from activity and “shut down,” but that doing so will not improve his quality of life, and his mood will worsen.
The psychiatrist asks Mr. L to identify a pleasurable or important activity to complete before his next appointment. Mr. L decides that he would like to call a friend, because he has been isolated and his friends have been calling him. The psychiatrist encourages him to call one of his golf buddies. She instructs Mr. L to set reminders, such as cell phone alarms and notes on the refrigerator, to prompt him to “Call Phil Saturday at 10
To increase the likelihood that Mr. L will make this call, he and his psychiatrist discuss anticipated obstacles and potential facilitators of this behavior.
The psychiatrist also encourages Mr. L to complete a Behavioral Activation Worksheet (for examples, see http://www.cci.health.wa.gov.au/docs/ACF3B92.pdf or https://www.therapistaid.com/worksheets/behavioral-activation.pdf) to track his depression, pleasure, and sense of achievement before and after completing this activity.
As illustrated by this case, collaborating with the patient is critical to developing a realistic treatment plan that incorporates CBT techniques. With your help and encouragement, patients can use these tools to reach their goals and target the symptoms of their illnesses.
1. Wright JH, McCray LW. Restoring energy and enjoying life. In: Wright JH, McCray LW. Breaking free from depression: pathways to wellness. New York, NY: The Guilford Press; 2012:97-129.
2. Wright JH, Basco MR, Thase ME. Working with automatic thoughts. In: Wright JH, Basco MR, Thase ME. Learning cognitive-behavior therapy: an illustrated guide. Arlington, VA: American Psychiatric Publishing, Inc.; 2005:118-121.
1. Wright JH, McCray LW. Restoring energy and enjoying life. In: Wright JH, McCray LW. Breaking free from depression: pathways to wellness. New York, NY: The Guilford Press; 2012:97-129.
2. Wright JH, Basco MR, Thase ME. Working with automatic thoughts. In: Wright JH, Basco MR, Thase ME. Learning cognitive-behavior therapy: an illustrated guide. Arlington, VA: American Psychiatric Publishing, Inc.; 2005:118-121.