User login
Black Americans Are Younger, Sicker and at Higher Risk When Faced with Major Vascular Interventions
“BLACK PATIENTS PRESENT WITH MORE SEVERE VASCULAR DISEASE AND A GREATER BURDEN OF RISK FACTORS THAN WHITE PATIENTS AT TIME OF MAJOR VASCULAR INTERVENTION.” Journal of Vascular Surgery, February 2018.
African Americans come into the vascular operating room with significant co-morbidities that may explain their more severe level of disease and higher risk factors, report researchers who reviewed 76,000 vascular cases for their report in the February edition of the Journal of Vascular Surgery.
This study drills deeper into the severity of vascular disease in African Americans, adding more fuel to the discussion of health disparities between racial and ethnic groups explored by the American Medical Association, which found that minorities are less likely to receive routine medical care and face higher rates of morbidity and mortality than non-minorities.
Invited commentator Dr. William R. Flinn found the study so profound he stated, “It should be read by every vascular surgeon, in fact, by every physician.”
Researchers have observed similar outcomes in vascular surgical procedures, but determining the cause of these disparities is difficult, since databases do not provide detail on disease severity.
For this report, a multi-institutional team of vascular surgeons led by vascular surgeon Dr. Marc Schermerhorn from Beth Israel Deaconess Medical Center took direct aim at this problem. Using de-identified data from the Vascular Quality Initiative gathered between 2009 and 2014, they found that compared to white patients, black patients were:
- Younger
- More likely to smoke
- More often diagnosed with insulin-dependent diabetes, hypertension, congestive heart failure and end-stage renal disease
- Less often medicated with statins
- Less often insured
Black patients also were sicker at the time of surgery. Compared with whites, black patients had more severe:
- Carotid disease (36% versus 31% symptomatic lesions)
- AAA (27% versus 16% symptoms/rupture, and more iliac aneurysm)
- PAD (73% versus 62% critical limb ischemia)
Furthermore, black patients were less likely to be discharged on aspirin and statin therapy after treatment for AAA and PAD than whites.
The authors note that their study is limited by factors common to all database studies including missing data, variability in definitions, and no way to adjust for socio-economic factors, compliance, family support, hospital type and timing of referral.
“Even in hospitals invested in quality improvement – as evidenced by participation in the VQI – black patients present with more advanced disease and more comorbidities compared with whites, despite presenting at a younger age,” states first author Dr. Peter Soden. “And these disparities were uniform across the spectrum of vascular disease, including carotids, AAA and PAD.”
The increase in presenting risk factors, along with disparity in medical management, offers clues as to the well-reported worse outcomes for black patients after major vascular procedures.
“The majority of the disparities highlighted in this manuscript are not from biologic differences, but instead from social, economic and health care delivery factors,” noted Dr. Flinn. “What this most clearly suggests is that there are untold numbers of black [patients] throughout the country with undiagnosed and untreated carotid disease, abdominal aortic aneurysm and PAD (and hypertension, and diabetes, and chronic kidney disease) because they do not have equitable access to health care in the United States in the 21st century.
“The vascular community has a unique opportunity to contribute to the health care debate in this country,” he added. “I hope we have both the scientific rigor and the political courage to pursue it aggressively.”
To download the complete article (freely available Jan. 22 - March 31), click: vsweb.org/JVS-Severe.
“BLACK PATIENTS PRESENT WITH MORE SEVERE VASCULAR DISEASE AND A GREATER BURDEN OF RISK FACTORS THAN WHITE PATIENTS AT TIME OF MAJOR VASCULAR INTERVENTION.” Journal of Vascular Surgery, February 2018.
African Americans come into the vascular operating room with significant co-morbidities that may explain their more severe level of disease and higher risk factors, report researchers who reviewed 76,000 vascular cases for their report in the February edition of the Journal of Vascular Surgery.
This study drills deeper into the severity of vascular disease in African Americans, adding more fuel to the discussion of health disparities between racial and ethnic groups explored by the American Medical Association, which found that minorities are less likely to receive routine medical care and face higher rates of morbidity and mortality than non-minorities.
Invited commentator Dr. William R. Flinn found the study so profound he stated, “It should be read by every vascular surgeon, in fact, by every physician.”
Researchers have observed similar outcomes in vascular surgical procedures, but determining the cause of these disparities is difficult, since databases do not provide detail on disease severity.
For this report, a multi-institutional team of vascular surgeons led by vascular surgeon Dr. Marc Schermerhorn from Beth Israel Deaconess Medical Center took direct aim at this problem. Using de-identified data from the Vascular Quality Initiative gathered between 2009 and 2014, they found that compared to white patients, black patients were:
- Younger
- More likely to smoke
- More often diagnosed with insulin-dependent diabetes, hypertension, congestive heart failure and end-stage renal disease
- Less often medicated with statins
- Less often insured
Black patients also were sicker at the time of surgery. Compared with whites, black patients had more severe:
- Carotid disease (36% versus 31% symptomatic lesions)
- AAA (27% versus 16% symptoms/rupture, and more iliac aneurysm)
- PAD (73% versus 62% critical limb ischemia)
Furthermore, black patients were less likely to be discharged on aspirin and statin therapy after treatment for AAA and PAD than whites.
The authors note that their study is limited by factors common to all database studies including missing data, variability in definitions, and no way to adjust for socio-economic factors, compliance, family support, hospital type and timing of referral.
“Even in hospitals invested in quality improvement – as evidenced by participation in the VQI – black patients present with more advanced disease and more comorbidities compared with whites, despite presenting at a younger age,” states first author Dr. Peter Soden. “And these disparities were uniform across the spectrum of vascular disease, including carotids, AAA and PAD.”
The increase in presenting risk factors, along with disparity in medical management, offers clues as to the well-reported worse outcomes for black patients after major vascular procedures.
“The majority of the disparities highlighted in this manuscript are not from biologic differences, but instead from social, economic and health care delivery factors,” noted Dr. Flinn. “What this most clearly suggests is that there are untold numbers of black [patients] throughout the country with undiagnosed and untreated carotid disease, abdominal aortic aneurysm and PAD (and hypertension, and diabetes, and chronic kidney disease) because they do not have equitable access to health care in the United States in the 21st century.
“The vascular community has a unique opportunity to contribute to the health care debate in this country,” he added. “I hope we have both the scientific rigor and the political courage to pursue it aggressively.”
To download the complete article (freely available Jan. 22 - March 31), click: vsweb.org/JVS-Severe.
“BLACK PATIENTS PRESENT WITH MORE SEVERE VASCULAR DISEASE AND A GREATER BURDEN OF RISK FACTORS THAN WHITE PATIENTS AT TIME OF MAJOR VASCULAR INTERVENTION.” Journal of Vascular Surgery, February 2018.
African Americans come into the vascular operating room with significant co-morbidities that may explain their more severe level of disease and higher risk factors, report researchers who reviewed 76,000 vascular cases for their report in the February edition of the Journal of Vascular Surgery.
This study drills deeper into the severity of vascular disease in African Americans, adding more fuel to the discussion of health disparities between racial and ethnic groups explored by the American Medical Association, which found that minorities are less likely to receive routine medical care and face higher rates of morbidity and mortality than non-minorities.
Invited commentator Dr. William R. Flinn found the study so profound he stated, “It should be read by every vascular surgeon, in fact, by every physician.”
Researchers have observed similar outcomes in vascular surgical procedures, but determining the cause of these disparities is difficult, since databases do not provide detail on disease severity.
For this report, a multi-institutional team of vascular surgeons led by vascular surgeon Dr. Marc Schermerhorn from Beth Israel Deaconess Medical Center took direct aim at this problem. Using de-identified data from the Vascular Quality Initiative gathered between 2009 and 2014, they found that compared to white patients, black patients were:
- Younger
- More likely to smoke
- More often diagnosed with insulin-dependent diabetes, hypertension, congestive heart failure and end-stage renal disease
- Less often medicated with statins
- Less often insured
Black patients also were sicker at the time of surgery. Compared with whites, black patients had more severe:
- Carotid disease (36% versus 31% symptomatic lesions)
- AAA (27% versus 16% symptoms/rupture, and more iliac aneurysm)
- PAD (73% versus 62% critical limb ischemia)
Furthermore, black patients were less likely to be discharged on aspirin and statin therapy after treatment for AAA and PAD than whites.
The authors note that their study is limited by factors common to all database studies including missing data, variability in definitions, and no way to adjust for socio-economic factors, compliance, family support, hospital type and timing of referral.
“Even in hospitals invested in quality improvement – as evidenced by participation in the VQI – black patients present with more advanced disease and more comorbidities compared with whites, despite presenting at a younger age,” states first author Dr. Peter Soden. “And these disparities were uniform across the spectrum of vascular disease, including carotids, AAA and PAD.”
The increase in presenting risk factors, along with disparity in medical management, offers clues as to the well-reported worse outcomes for black patients after major vascular procedures.
“The majority of the disparities highlighted in this manuscript are not from biologic differences, but instead from social, economic and health care delivery factors,” noted Dr. Flinn. “What this most clearly suggests is that there are untold numbers of black [patients] throughout the country with undiagnosed and untreated carotid disease, abdominal aortic aneurysm and PAD (and hypertension, and diabetes, and chronic kidney disease) because they do not have equitable access to health care in the United States in the 21st century.
“The vascular community has a unique opportunity to contribute to the health care debate in this country,” he added. “I hope we have both the scientific rigor and the political courage to pursue it aggressively.”
To download the complete article (freely available Jan. 22 - March 31), click: vsweb.org/JVS-Severe.
Deadline Nearing for Wylie Scholar Award
Applications are due March 2 for the Wylie Scholar Award, co-sponsored by the SVS Foundation and Vascular Cures. The three-year, $150,000 grant is awarded to a promising vascular surgeon-scientist in North America and is designed to support outstanding surgeon-scientists conducting innovative academic research in the early stages of their careers.
Applications are due March 2 for the Wylie Scholar Award, co-sponsored by the SVS Foundation and Vascular Cures. The three-year, $150,000 grant is awarded to a promising vascular surgeon-scientist in North America and is designed to support outstanding surgeon-scientists conducting innovative academic research in the early stages of their careers.
Applications are due March 2 for the Wylie Scholar Award, co-sponsored by the SVS Foundation and Vascular Cures. The three-year, $150,000 grant is awarded to a promising vascular surgeon-scientist in North America and is designed to support outstanding surgeon-scientists conducting innovative academic research in the early stages of their careers.
Urge PAs to Get Involved in VAM Special Programming for Them
SVS members, please remind any vascular PAs with whom you work to consider submitting an abstract for the inaugural PA programming or be a speaker during our 2018 Vascular Annual Meeting. More information is here -- please forward to your PAs!
SVS members, please remind any vascular PAs with whom you work to consider submitting an abstract for the inaugural PA programming or be a speaker during our 2018 Vascular Annual Meeting. More information is here -- please forward to your PAs!
SVS members, please remind any vascular PAs with whom you work to consider submitting an abstract for the inaugural PA programming or be a speaker during our 2018 Vascular Annual Meeting. More information is here -- please forward to your PAs!
Postpartum Psychosis in a Young VA Patient: Diagnosis, Implications, and Treatment Recommendations
Postpartum psychosis is a psychiatric emergency that can endanger the life of the mother and the newborn child if untreated. About 1 to 2 mothers in 1,000 experiences postpartum psychosis after delivery.1 This rate is much higher among women with an established diagnosis of bipolar disorder before pregnancy.1
Expedient recognition, diagnosis, and referral to a high-level psychiatric facility (usually a locked inpatient unit) are critical for ensuring the safety of mother and infant. A diligent medical workup followed by thorough education for the patient and family are important steps in caring for patients with postpartum psychosis. Close mental health follow-up, pharmacologic interventions, informed decision making regarding breastfeeding, and preserving the sleep-wake cycle are critical for stabilization.2
The authors present the case of a patient admitted to VA Central California Health Care System (VACCHCS) with postpartum psychosis and a discussion on existing research on the prevalence of postpartum psychosis, relevant risk factors, the association with bipolar disorder, and treatment strategies.
Case Presentation
A 31-year-old active-duty female with no history of mental illness was admitted to the psychiatric unit because new-onset disorganized behavior was preventing her from functioning at her workplace. Two weeks after giving birth to her second child, the patient began exhibiting an uncharacteristic, debilitating labile mood and disorganized behavior. Her supervisors required her to present for medical attention about 3 months after the birth of her child. She was transferred to VACCHCS for higher level medical care on military orders. The patient’s husband initially attributed these psychiatric symptoms to vocational stress and taking care of 2 young children. He observed the patient exhibiting tearfulness about her job, which quickly alternated with euphoric episodes of singing and dancing at inappropriate times, such as when the children had quieted down and were being prepared to go to bed.
At the initial psychiatric evaluation after transfer to VACCHCS, the patient appeared well-kept and slightly overweight. In general her appearance was unremarkable. Throughout the examination she sang both subtly and loudly and at times was confrontational and irritable.
She related oddly and often was guarded and difficult to engage; she sang and played with her blanket in a childlike way. She smiled and laughed inappropriately, mumbled incoherently to herself, scanned the room suspiciously, and often made intense eye contact. Her affect was labile, both tearful and euphoric at several points in the examination. Her thought process was tangential, illogical, grandiose, difficult to redirect, and with loose associations. Her thought content consisted of delusions (“I’ve got the devil on my back”) and grandiosity (“I am everyone, I am you…the president, the mayor”), and she often stated that she planned to become a singer or performer.
The patient claimed she was neither suicidal nor had thoughts of infanticide. She reported having no visual and auditory hallucinations but often seemed to be responding to internal stimuli: She mumbled to herself and looked intensely at parts of the room. Cognitively, the patient was fully intact to recent and remote events but displayed a poor attention span. She did not exhibit any motor abnormalities, such as tremor, rigidity, weakness, sensory loss, or abnormal gait.
The patient’s workup included full chemistry, complete blood count, thyroid-stimulating hormone, antithyroid antibodies, calcium, rapid plasma reagin to rule out syphilis, toxicology, folate, vitamin B12, and vitamin D. All laboratory results were negative or within normal limits, although the urine drug screen was positive for cannabis. The patient’s husband noted that his wife never used cannabis except the weekend before her admission, when she impulsively went dancing, which was out of character for her. Her psychotic symptoms had been present weeks before the cannabis use; therefore, the her symptoms could not be attributed to a substance-induced psychotic disorder. A test for synthetic cannabis derivatives was negative. Newer synthetic compounds can cause more severe substance-induced psychotic symptoms than those of cannabis.3
The patient was diagnosed with postpartum psychosis and was started on the oral antipsychotic olanzapine 10 mg at bedtime. Additional doses were administered to control ongoing symptoms, which included a disorganized thought process; loose associations; euphoria; grandiosity; delusional content, such as “You are just a tool in place to help me;” reports of feeling as though she were in “outer space, outside in the galaxy;” decreased need for sleep; and irritability. The patient spent an entire interview with her eyes closed, stating that she could “hear” better because she was overstimulated if her eyes were open. She also described olfactory hallucinations of “strong perfume,” which the 2 providers present could not detect.
Olanzapine was not well tolerated because of sedation and was discontinued in favor of risperidone, 2 mg twice daily. Risperidone was more effective and better tolerated. Lithium was initiated the next day with target dosing at 300 mg in the morning and 600 mg at night. The patient became capable of linear, organized discussion and planning but remained euphoric with high energy; she exhibited grandiosity with frequent singing and dancing throughout her hospital stay. She often described her mood as “good, excellent, exuberant, exciting,” perseverating on the way words sounded and giggling in a childlike manner. She continued to have intrusive dreams of “hell and the devil” and that she was killed by gunshot.
The patient was continued on lithium and risperidone and transferred to a larger military hospital for further inpatient management, respecting military orders. Before discharge, a family conference was held with the patient and her husband to educate them on the importance of continued treatment, close follow-up, regular sleep patterns, and not breastfeeding while taking the prescribed medications. Although she was not back to her baseline at the time of transfer, the patient had stabilized significantly and gained sufficient insight into her condition.
Discussion
Postpartum psychosis can present with a prodromal phase consisting of fatigue, insomnia, restlessness, tearfulness, and emotional lability, making early identification difficult. Later, florid psychotic symptoms can include suspiciousness, confusion, incoherence, irrational statements, obsessive concern about the infant’s health, and delusions, including a belief that the baby is dead or defective. Some women might deny that the birth occurred or feel that they are unmarried, virginal, or persecuted.1 More concerning symptoms include auditory hallucinations commanding the mother to harm or kill the infant and/or herself. Symptoms often begin within days to weeks of birth, usually 2 to 3 weeks after delivery but can occur as long as 8 weeks postpartum.1 Several cases of infanticide and suicide have been documented.1 The risk of experiencing another psychotic episode in subsequent pregnancies can be as high as 50%.4-6 Regardless of symptom severity at onset, postpartum psychosis is a psychiatric emergency and must be treated as such.
Bipolar Disorder and Postpartum Psychosis
A close relationship exists between postpartum psychosis and development of bipolar disorder. A postpartum psychotic episode often is the harbinger of bipolar illness.7 About two-thirds of women who have an episode of postpartum psychosis will experience an underlying affective disorder within a year of childbirth.1,8 It is unclear what triggers the psychotic episode, but it has been theorized that major systemic shifts in hormone levelsor trauma of delivery could instigate development of symptoms.1,9
Risk factors include obstetric complications; perinatal infant mortality; previous episodes of bipolar disorder, psychosis, or postpartum psychosis; family history of bipolar disorder or postpartum psychosis; sleep deprivation; increased environmental stress; and lack of partner support.10 The strongest risk factor for developing postpartum psychosis is a personal or family history of bipolar disorder or a related psychotic disorder.11 This risk factor is identified in about 40% to 50% cases of postpartum psychosis.11
Treatment
Standard treatment for postpartum psychosis includes an antipsychotic and often lithium and benzodiazepines.1,7,10,11 This treatment approach differs slightly from treating a patient with a nonpostpartum psychotic illness, who generally would not receive mood stabilizers, such as lithium. Including a mood stabilizer for postpartum psychosis is warranted because of the association between postpartum psychosis and bipolar disorder, which is treated with a mood stabilizer.
Prevalence
Postpartum psychosis is identified in 1 to 2 per 1,000 childbirths. In women who have had an earlier episode of postpartum psychosis or have a diagnosis of bipolar disorder, the rate is up to 100 times higher.1 Kendell and colleagues found that psychiatric admissions occurred at a rate 7 times higher in the 30 days after birth than in the prepregnancy period, suggesting that metabolic factors might be involved in triggering postpartum psychotic symptoms.12 An abrupt hormonal loss occurs at childbirth; hormones peak 200-fold during gestation and decline rapidly within a day after birth.9 Despite the severity of symptoms in postpartum psychosis, these patients tend to have a better prognosis than that of women with psychotic episodes not related to pregnancy.4
Brockington and colleagues found that patients with postpartum psychosis had more mood lability, distractibility, and confusion than those with psychosis unrelated to pregnancy.15 Patients with postpartum psychosis were more likely to have impaired sensorium, bizarre quality of delusions, and memory loss. Psychosis with onset after childbirth included high levels of thought disorganization, delusions of reference, delusions of persecution, and greater levels of homicidal ideation and behavior.16 This study also reported symptoms such as visual, tactile, and olfactory hallucinations and a presentation similar to that of delirium.
Chandra and colleagues found that 53% of women with postpartum psychosis had delusions about the infant, including beliefs that someone would harm or kill the baby or that the baby would be harmed by their breast milk.17 Compared with women with bipolar disorder, Oostheuizen and colleagues found that women with postpartum psychosis had delusions of control, such as feeling under the influence of an overpowering force that controlled their actions.18 Infanticidal thoughts are common among patients with postpartum psychosis, and about 4% of women committed infanticide.1
Rapid stabilization and treatment are important because postpartum psychosis is considered a psychiatric emergency.7 Potential consequences of delayed diagnosis and treatment include harm or death of the infant by infanticide and death of the mother by suicide. A thorough physical examination is important to rule out metabolic or neuroendocrine causes of psychosis other than postpartum hormonal shifts. These could include causes of altered mental status: stroke, pulmonary embolism, amniotic fluid emboli, Sheehan syndrome, thyroid disorders, electrolyte abnormalities, acute hemorrhage, sepsis, and substance toxicity or withdrawal.10 A complete blood count, full chemistry, thyroid function tests, antithyroid antibody tests, calcium, vitamin B12, and folate should be measured.7,10
Initial treatment should include antipsychotics and often mood stabilizers such as lithium. Managing insomnia aggressively is also necessary for initial stabilization and to prevent a repeat manic episode if the patient develops bipolar disorder.2 Many experts argue that sleep loss in combination with other risk factors might be the final common pathway for development of postpartum psychosis in women predisposed to this disorder.19,20
Treating insomnia in an outpatient setting includes teaching sleep hygiene practices and relaxation techniques. Although these methods to regulate sleep could be encouraged during the emergent inpatient stabilization of a patient with postpartum psychosis, pharmacologic approaches are necessary for acute mania and psychosis. Concern about possible dependence on benzodiazepines and other sedating sleep aids are valid; however, the benefit of acute stabilization of psychotic symptoms outweighs the potential risk of dependence.
Typically, first-line treatment is an antipsychotic, and second-generation antipsychotics generally are preferred over first-generation antipsychotics because of their more benign adverse effect profile.21,22 There are no controlled trials that compare antipsychotics with placebo or other interventions for postpartum psychosis. Therefore, use of atypical antipsychotics is based on randomized trials demonstrating efficacy in reducing psychosis in bipolar disorder, depression with psychotic features, and schizoaffective disorder.23,24 Once the patient is treated with an antipsychotic, further use of psychotropic medications, such as lithium or other mood stabilizers, should be based on the patient’s clinical presentation. For example, the patient in this case study primarily had manic symptoms consistent with bipolar disorder, making lithium or another mood stabilizer an appropriate choice.
Bergink and colleagues demonstrated positive outcomes with a treatment algorithm involving sequential use of benzodiazepines to improve sleep, an antipsychotic to decrease acute manic symptoms, lithium to stabilize mood based on symptoms, and electroconvulsive therapy if other treatments were not successful.25 Case studies document that administering estrogen led to recovery from postpartum psychosis, although patients often relapsed when estrogen was stopped.26 Electroconvulsive therapy has shown promising results, especially in patients who do not respond to antipsychotic medications or lithium.27,28
Antipsychotic and Other Psychotropic Medications
Choice of an antipsychotic and other psychotropic medications to treat postpartum psychosis is based on the patient’s breastfeeding status. The benefits of treatment should be weighed against the risks of a breastfeeding infant’s exposure to the medication. Because postpartum psychosis is a psychiatric emergency, the benefits of the medication are considered to outweigh any potential adverse effect to the breastfeeding infant exposed to the medication. Risks of untreated postpartum psychosis to the infant include rejection of the infant, poor parental relationships, suicide, infanticide, long-term failure to bond with the child, delayed infant development, and failure to thrive.29 Also, many mothers—including the patient in this presentation—decide that the benefits of treatment outweigh those of breastfeeding and choose to feed their infant with formula. Even if the patient chooses to bottle-feed her infant, consider administering medications that are considered safer for breastfeeding because the patient may need to continue the psychotropic during later pregnancies to prevent future psychotic episodes.30 All psychotropic medications pass into breast milk.29 Studies on the long-term effect of these medications on the infant are limited, but experts tend to recommend olanzapine, quetiapine, and risperidone over aripiprazole and ziprasidone.21,31-33
Lithium often is used to treat postpartum psychosis. Studies examining risk to the infant after long-term exposure to lithium through breast milk have not been conducted, but the American Academy of Pediatrics discourages its use during breastfeeding because of concerns about toxicity in the infant.34-36
Sleep regulation is important to treat bipolar disorder and to prevent future episodes.2,20,21 To ensure safety of the infant and mother before discharge, family education is imperative to establish close follow-up, adequate sleep, and reduction of stressors.7,10 Separation from the infant might be necessary after discharge, and someone should monitor the infant at all times until the outpatient mental health provider confirms that all psychotic symptoms have resolved.7,10 Successful treatment of postpartum psychosis requires close communication among the mental health provider, the pediatrician, and the obstetrician or women’s health provider.10 Because a close-knit team approach after discharge from the acute psychiatric unit is necessary, the care of such a patient and her child provides an educational opportunity for individuals working in integrated care clinics.
Conclusion
Postpartum psychosis is a psychiatric emergency requiring immediate treatment to prevent dire outcomes such as suicide or infanticide. Treatment considerations include the cost-benefit analysis of breastfeeding and the toxicity of psychotropic medications when ingested by the infant via breast milk. A close relationship has been demonstrated between postpartum psychosis and bipolar disorder.
Preferred treatment regimens include lithium and an antipsychotic. Educate the family as a unit about the diagnosis and treatment, the importance of adequate sleep for treatment and prophylaxis, and the decision on whether to discontinue breastfeeding despite its well-known benefits for mother and infant. Stabilization is a multifaceted process and needs to be reinforced with a solid plan for support and follow-up appointments. Because of the higher risk of relapse, educate patients about prophylactic treatment during subsequent pregnancies and monitor for development of bipolar disorder in the future.
1. Sadock B, Sadock V, Ruiz P. Kaplan & Sadock’s Synopsis of Psychiatry. 11th ed. Philadelphia, PA: Wolters Kluwer; 2015.
2. Sharma V. Pharmacotherapy of postpartum psychosis. Expert Opin Pharmacother. 2003;4(10):1651-1658.
3. Bassir Nia A, Medrano B, Perkel C, Galynker I, Hurd YL. Psychiatric comorbidity associated with synthetic cannabinoid use compared to cannabis. J Psychopharmacol. 2016;30(12):1321-1330.
4. Rhohde A, Marneros A. Postpartum psychoses: onset and long-term course. Psychopathology. 1993;26(3-4):203-209.
5. Videbech P, Gouliaev G. First admission with puerperal psychosis: 7-14 years of follow-up. Acta Psychiatr Scand. 1995;91(3):167-173.
6. Terp IM, Engholm G, Møller H, Mortensen PB. A follow-up study of postpartum psychoses: prognosis and risk factors for readmission. Acta Psychiatr Scand. 1999;100(1):40-46.
7. Spinelli MG. Postpartum psychosis: detection of risk and management. Am J Psychiatry. 2009;166(4):405-408.
8. Blackmore ER, Rubinow DR, O’Connor TG, et al. Reproductive outcomes and risk of subsequent illness in women diagnosed with postpartum psychosis. Bipolar Disord. 2013;15(4):394-404.
9. Bloch M, Schmidt PJ, Danaceau M, Murphy J, Nieman L, Rubinow DR. Effects of gonadal steroids in women with a history of postpartum depression. Am J Psychiatry. 2000;157(6):924-930.
10. Monzon C, Lanza di Scalea T, Pearlstein T. Postpartum psychosis: updates and clinical issues. Psychiatric Times. 2014. http://www.psychiatrictimes.com/special-reports/postpartum -psychosis-updates-and-clinical-issues. Published January 15, 2014. Accessed December 14, 2017.
11. Davies W. Understanding the pathophysiology of postpartum psychosis: challenges and new approaches. World J Psychiatry. 2017;7(2):77-88.
12. Kendell RE, Chalmers JC, Platz C. Epidemiology of puerperal psychoses. Br J Psychiatry. 1987;150:662-673.
13. Leibenluft E. Women with bipolar illness: clinical and research issues. Am J Psychiatry. 1996;153(2):163-173.
14. Chaudron LH, Pies R. The relationship between postpartum psychosis and bipolar disorder: a review. J Clin Psychiatry. 2003;64(11):1284-1292.
15. Brockington IF, Cernik KF, Schofield EM, Downing AR, Francis AF, Keelan C. Puerperal psychosis: phenomena and diagnosis. Arch Gen Psychiatry. 1981;38(7):829-833.
16. Wisner KL, Peindl K, Hanusa BH. Symptomatology of affective and psychotic illnesses related to childbearing. J Affect Disord. 1994;30(2):77-87.
17. Chandra PS, Bhargavaraman RP, Raghunandan VN, Shaligram D. Delusions related to infant and their association with mother-infant interactions in postpartum psychotic disorders. Arch Womens Ment Health. 2006;9(5):285-288.
18. Oosthuizen P, Russouw H, Roberts M. Is puerperal psychosis bipolar mood disorder? A phenomenological comparison. Compr Psychiatry. 1995;36(1):77-81.
19. Sharma V, Mazmanian D. Sleep loss and postpartum psychosis. Bipolar Disord. 2003;5(2):98-105.
20 Bilszta JL, Meyer D, Buist AE. Bipolar affective disorder in the postnatal period: investigating the role of sleep. Bipolar Disord. 2010;12(5):568-578.
21. Doucet S, Jones I, Letourneau N, Dennis CL, Blackmore ER. Interventions for the prevention and treatment of postpartum psychosis: a systematic review. Arch Womens Ment Health. 2011;14(2):89-98.
22 Perlis RH, Welge JA, Vornik LA, Hirschfeld RM, Keck PE Jr. Atypical antipsychotics in the treatment of mania: a meta-analysis of randomized, placebo-controlled trials. J Clin Psychiatry. 2006;67(4):509-516.
23 Wijkstra J, Lijmer J, Balk FJ, Geddes JR, Nolen WA. Pharmacological treatment for unipolar psychotic depression: systematic review and meta-analysis. Br J Psychiatry. 2006;188:410-415.
24. Smith LA, Cornelius V, Warnock A, Tacchi MJ, Taylor D. Pharmacological interventions for acute bipolar mania: a systematic review of randomized placebo-controlled trials. Bipolar Disord. 2007;9(6):551-560.
25. Bergink V, Burgerhout KM, Koorengevel KM, et al. Treatment of psychosis and mania in the postpartum period. Am J Psychiatry. 2015;172(2):115-123.
26. Ahokas A, Aito M, Rimón R. Positive treatment effect of estradiol in postpartum psychosis: a pilot study. J Clin Psychiatry. 2000;61(3):166-169.
27. Reed P, Sermin N, Appleby L, Faragher B. A comparison of clinical response to electroconvulsive therapy in puerperal and non-puerperal psychoses. J Affect Disord. 1999;54(3):255-260.
28. Forray A, Ostroff RB. The use of electroconvulsive therapy in postpartum affective disorders. J ECT. 2007;23(3):188-193.
29. Robinson GE. Psychopharmacology in pregnancy and postpartum. Focus. 2012;10(1):3-14.
30. Wesseloo R, Kamperman AM, Munk-Olsen T, Pop VJ, Kushner SA, Bergink V. Risk of postpartum relapse in bipolar disorder and postpartum psychosis: a systematic review and meta-analysis. Am J Psychiatry. 2016;173(2):117-127.
31. Sharma V, Smith A, Mazmanian D. Olanzapine in the prevention of postpartum psychosis and mood episodes in bipolar disorder. Bipolar Disord. 2006;8(4):400-404.
32. Gobbi G. Quetiapine in postpartum psychosis. J Clin Psychopharmacol. 2014;34(6):744-745.
33. Uguz F. Second-generation antipsychotics during the lactation period: a comparative systematic review on infant safety. J Clin Psychopharmacol. 2016;36(3):244-252.
34. Sachs HC; Committee on Drugs. The transfer of drugs and therapeutics into human breast milk: an update on selected topics. Pediatrics. 2013;132(3):e796-e809.
35. Lithium [package insert]. Columbus, OH: Roxane Laboratories Inc; 2011.
36. Grandjean EM, Aubry JM. Lithium: updated human knowledge using an evidence-based approach: part III: clinical safety. CNS Drugs. 2009;23(5):397-418.
Postpartum psychosis is a psychiatric emergency that can endanger the life of the mother and the newborn child if untreated. About 1 to 2 mothers in 1,000 experiences postpartum psychosis after delivery.1 This rate is much higher among women with an established diagnosis of bipolar disorder before pregnancy.1
Expedient recognition, diagnosis, and referral to a high-level psychiatric facility (usually a locked inpatient unit) are critical for ensuring the safety of mother and infant. A diligent medical workup followed by thorough education for the patient and family are important steps in caring for patients with postpartum psychosis. Close mental health follow-up, pharmacologic interventions, informed decision making regarding breastfeeding, and preserving the sleep-wake cycle are critical for stabilization.2
The authors present the case of a patient admitted to VA Central California Health Care System (VACCHCS) with postpartum psychosis and a discussion on existing research on the prevalence of postpartum psychosis, relevant risk factors, the association with bipolar disorder, and treatment strategies.
Case Presentation
A 31-year-old active-duty female with no history of mental illness was admitted to the psychiatric unit because new-onset disorganized behavior was preventing her from functioning at her workplace. Two weeks after giving birth to her second child, the patient began exhibiting an uncharacteristic, debilitating labile mood and disorganized behavior. Her supervisors required her to present for medical attention about 3 months after the birth of her child. She was transferred to VACCHCS for higher level medical care on military orders. The patient’s husband initially attributed these psychiatric symptoms to vocational stress and taking care of 2 young children. He observed the patient exhibiting tearfulness about her job, which quickly alternated with euphoric episodes of singing and dancing at inappropriate times, such as when the children had quieted down and were being prepared to go to bed.
At the initial psychiatric evaluation after transfer to VACCHCS, the patient appeared well-kept and slightly overweight. In general her appearance was unremarkable. Throughout the examination she sang both subtly and loudly and at times was confrontational and irritable.
She related oddly and often was guarded and difficult to engage; she sang and played with her blanket in a childlike way. She smiled and laughed inappropriately, mumbled incoherently to herself, scanned the room suspiciously, and often made intense eye contact. Her affect was labile, both tearful and euphoric at several points in the examination. Her thought process was tangential, illogical, grandiose, difficult to redirect, and with loose associations. Her thought content consisted of delusions (“I’ve got the devil on my back”) and grandiosity (“I am everyone, I am you…the president, the mayor”), and she often stated that she planned to become a singer or performer.
The patient claimed she was neither suicidal nor had thoughts of infanticide. She reported having no visual and auditory hallucinations but often seemed to be responding to internal stimuli: She mumbled to herself and looked intensely at parts of the room. Cognitively, the patient was fully intact to recent and remote events but displayed a poor attention span. She did not exhibit any motor abnormalities, such as tremor, rigidity, weakness, sensory loss, or abnormal gait.
The patient’s workup included full chemistry, complete blood count, thyroid-stimulating hormone, antithyroid antibodies, calcium, rapid plasma reagin to rule out syphilis, toxicology, folate, vitamin B12, and vitamin D. All laboratory results were negative or within normal limits, although the urine drug screen was positive for cannabis. The patient’s husband noted that his wife never used cannabis except the weekend before her admission, when she impulsively went dancing, which was out of character for her. Her psychotic symptoms had been present weeks before the cannabis use; therefore, the her symptoms could not be attributed to a substance-induced psychotic disorder. A test for synthetic cannabis derivatives was negative. Newer synthetic compounds can cause more severe substance-induced psychotic symptoms than those of cannabis.3
The patient was diagnosed with postpartum psychosis and was started on the oral antipsychotic olanzapine 10 mg at bedtime. Additional doses were administered to control ongoing symptoms, which included a disorganized thought process; loose associations; euphoria; grandiosity; delusional content, such as “You are just a tool in place to help me;” reports of feeling as though she were in “outer space, outside in the galaxy;” decreased need for sleep; and irritability. The patient spent an entire interview with her eyes closed, stating that she could “hear” better because she was overstimulated if her eyes were open. She also described olfactory hallucinations of “strong perfume,” which the 2 providers present could not detect.
Olanzapine was not well tolerated because of sedation and was discontinued in favor of risperidone, 2 mg twice daily. Risperidone was more effective and better tolerated. Lithium was initiated the next day with target dosing at 300 mg in the morning and 600 mg at night. The patient became capable of linear, organized discussion and planning but remained euphoric with high energy; she exhibited grandiosity with frequent singing and dancing throughout her hospital stay. She often described her mood as “good, excellent, exuberant, exciting,” perseverating on the way words sounded and giggling in a childlike manner. She continued to have intrusive dreams of “hell and the devil” and that she was killed by gunshot.
The patient was continued on lithium and risperidone and transferred to a larger military hospital for further inpatient management, respecting military orders. Before discharge, a family conference was held with the patient and her husband to educate them on the importance of continued treatment, close follow-up, regular sleep patterns, and not breastfeeding while taking the prescribed medications. Although she was not back to her baseline at the time of transfer, the patient had stabilized significantly and gained sufficient insight into her condition.
Discussion
Postpartum psychosis can present with a prodromal phase consisting of fatigue, insomnia, restlessness, tearfulness, and emotional lability, making early identification difficult. Later, florid psychotic symptoms can include suspiciousness, confusion, incoherence, irrational statements, obsessive concern about the infant’s health, and delusions, including a belief that the baby is dead or defective. Some women might deny that the birth occurred or feel that they are unmarried, virginal, or persecuted.1 More concerning symptoms include auditory hallucinations commanding the mother to harm or kill the infant and/or herself. Symptoms often begin within days to weeks of birth, usually 2 to 3 weeks after delivery but can occur as long as 8 weeks postpartum.1 Several cases of infanticide and suicide have been documented.1 The risk of experiencing another psychotic episode in subsequent pregnancies can be as high as 50%.4-6 Regardless of symptom severity at onset, postpartum psychosis is a psychiatric emergency and must be treated as such.
Bipolar Disorder and Postpartum Psychosis
A close relationship exists between postpartum psychosis and development of bipolar disorder. A postpartum psychotic episode often is the harbinger of bipolar illness.7 About two-thirds of women who have an episode of postpartum psychosis will experience an underlying affective disorder within a year of childbirth.1,8 It is unclear what triggers the psychotic episode, but it has been theorized that major systemic shifts in hormone levelsor trauma of delivery could instigate development of symptoms.1,9
Risk factors include obstetric complications; perinatal infant mortality; previous episodes of bipolar disorder, psychosis, or postpartum psychosis; family history of bipolar disorder or postpartum psychosis; sleep deprivation; increased environmental stress; and lack of partner support.10 The strongest risk factor for developing postpartum psychosis is a personal or family history of bipolar disorder or a related psychotic disorder.11 This risk factor is identified in about 40% to 50% cases of postpartum psychosis.11
Treatment
Standard treatment for postpartum psychosis includes an antipsychotic and often lithium and benzodiazepines.1,7,10,11 This treatment approach differs slightly from treating a patient with a nonpostpartum psychotic illness, who generally would not receive mood stabilizers, such as lithium. Including a mood stabilizer for postpartum psychosis is warranted because of the association between postpartum psychosis and bipolar disorder, which is treated with a mood stabilizer.
Prevalence
Postpartum psychosis is identified in 1 to 2 per 1,000 childbirths. In women who have had an earlier episode of postpartum psychosis or have a diagnosis of bipolar disorder, the rate is up to 100 times higher.1 Kendell and colleagues found that psychiatric admissions occurred at a rate 7 times higher in the 30 days after birth than in the prepregnancy period, suggesting that metabolic factors might be involved in triggering postpartum psychotic symptoms.12 An abrupt hormonal loss occurs at childbirth; hormones peak 200-fold during gestation and decline rapidly within a day after birth.9 Despite the severity of symptoms in postpartum psychosis, these patients tend to have a better prognosis than that of women with psychotic episodes not related to pregnancy.4
Brockington and colleagues found that patients with postpartum psychosis had more mood lability, distractibility, and confusion than those with psychosis unrelated to pregnancy.15 Patients with postpartum psychosis were more likely to have impaired sensorium, bizarre quality of delusions, and memory loss. Psychosis with onset after childbirth included high levels of thought disorganization, delusions of reference, delusions of persecution, and greater levels of homicidal ideation and behavior.16 This study also reported symptoms such as visual, tactile, and olfactory hallucinations and a presentation similar to that of delirium.
Chandra and colleagues found that 53% of women with postpartum psychosis had delusions about the infant, including beliefs that someone would harm or kill the baby or that the baby would be harmed by their breast milk.17 Compared with women with bipolar disorder, Oostheuizen and colleagues found that women with postpartum psychosis had delusions of control, such as feeling under the influence of an overpowering force that controlled their actions.18 Infanticidal thoughts are common among patients with postpartum psychosis, and about 4% of women committed infanticide.1
Rapid stabilization and treatment are important because postpartum psychosis is considered a psychiatric emergency.7 Potential consequences of delayed diagnosis and treatment include harm or death of the infant by infanticide and death of the mother by suicide. A thorough physical examination is important to rule out metabolic or neuroendocrine causes of psychosis other than postpartum hormonal shifts. These could include causes of altered mental status: stroke, pulmonary embolism, amniotic fluid emboli, Sheehan syndrome, thyroid disorders, electrolyte abnormalities, acute hemorrhage, sepsis, and substance toxicity or withdrawal.10 A complete blood count, full chemistry, thyroid function tests, antithyroid antibody tests, calcium, vitamin B12, and folate should be measured.7,10
Initial treatment should include antipsychotics and often mood stabilizers such as lithium. Managing insomnia aggressively is also necessary for initial stabilization and to prevent a repeat manic episode if the patient develops bipolar disorder.2 Many experts argue that sleep loss in combination with other risk factors might be the final common pathway for development of postpartum psychosis in women predisposed to this disorder.19,20
Treating insomnia in an outpatient setting includes teaching sleep hygiene practices and relaxation techniques. Although these methods to regulate sleep could be encouraged during the emergent inpatient stabilization of a patient with postpartum psychosis, pharmacologic approaches are necessary for acute mania and psychosis. Concern about possible dependence on benzodiazepines and other sedating sleep aids are valid; however, the benefit of acute stabilization of psychotic symptoms outweighs the potential risk of dependence.
Typically, first-line treatment is an antipsychotic, and second-generation antipsychotics generally are preferred over first-generation antipsychotics because of their more benign adverse effect profile.21,22 There are no controlled trials that compare antipsychotics with placebo or other interventions for postpartum psychosis. Therefore, use of atypical antipsychotics is based on randomized trials demonstrating efficacy in reducing psychosis in bipolar disorder, depression with psychotic features, and schizoaffective disorder.23,24 Once the patient is treated with an antipsychotic, further use of psychotropic medications, such as lithium or other mood stabilizers, should be based on the patient’s clinical presentation. For example, the patient in this case study primarily had manic symptoms consistent with bipolar disorder, making lithium or another mood stabilizer an appropriate choice.
Bergink and colleagues demonstrated positive outcomes with a treatment algorithm involving sequential use of benzodiazepines to improve sleep, an antipsychotic to decrease acute manic symptoms, lithium to stabilize mood based on symptoms, and electroconvulsive therapy if other treatments were not successful.25 Case studies document that administering estrogen led to recovery from postpartum psychosis, although patients often relapsed when estrogen was stopped.26 Electroconvulsive therapy has shown promising results, especially in patients who do not respond to antipsychotic medications or lithium.27,28
Antipsychotic and Other Psychotropic Medications
Choice of an antipsychotic and other psychotropic medications to treat postpartum psychosis is based on the patient’s breastfeeding status. The benefits of treatment should be weighed against the risks of a breastfeeding infant’s exposure to the medication. Because postpartum psychosis is a psychiatric emergency, the benefits of the medication are considered to outweigh any potential adverse effect to the breastfeeding infant exposed to the medication. Risks of untreated postpartum psychosis to the infant include rejection of the infant, poor parental relationships, suicide, infanticide, long-term failure to bond with the child, delayed infant development, and failure to thrive.29 Also, many mothers—including the patient in this presentation—decide that the benefits of treatment outweigh those of breastfeeding and choose to feed their infant with formula. Even if the patient chooses to bottle-feed her infant, consider administering medications that are considered safer for breastfeeding because the patient may need to continue the psychotropic during later pregnancies to prevent future psychotic episodes.30 All psychotropic medications pass into breast milk.29 Studies on the long-term effect of these medications on the infant are limited, but experts tend to recommend olanzapine, quetiapine, and risperidone over aripiprazole and ziprasidone.21,31-33
Lithium often is used to treat postpartum psychosis. Studies examining risk to the infant after long-term exposure to lithium through breast milk have not been conducted, but the American Academy of Pediatrics discourages its use during breastfeeding because of concerns about toxicity in the infant.34-36
Sleep regulation is important to treat bipolar disorder and to prevent future episodes.2,20,21 To ensure safety of the infant and mother before discharge, family education is imperative to establish close follow-up, adequate sleep, and reduction of stressors.7,10 Separation from the infant might be necessary after discharge, and someone should monitor the infant at all times until the outpatient mental health provider confirms that all psychotic symptoms have resolved.7,10 Successful treatment of postpartum psychosis requires close communication among the mental health provider, the pediatrician, and the obstetrician or women’s health provider.10 Because a close-knit team approach after discharge from the acute psychiatric unit is necessary, the care of such a patient and her child provides an educational opportunity for individuals working in integrated care clinics.
Conclusion
Postpartum psychosis is a psychiatric emergency requiring immediate treatment to prevent dire outcomes such as suicide or infanticide. Treatment considerations include the cost-benefit analysis of breastfeeding and the toxicity of psychotropic medications when ingested by the infant via breast milk. A close relationship has been demonstrated between postpartum psychosis and bipolar disorder.
Preferred treatment regimens include lithium and an antipsychotic. Educate the family as a unit about the diagnosis and treatment, the importance of adequate sleep for treatment and prophylaxis, and the decision on whether to discontinue breastfeeding despite its well-known benefits for mother and infant. Stabilization is a multifaceted process and needs to be reinforced with a solid plan for support and follow-up appointments. Because of the higher risk of relapse, educate patients about prophylactic treatment during subsequent pregnancies and monitor for development of bipolar disorder in the future.
Postpartum psychosis is a psychiatric emergency that can endanger the life of the mother and the newborn child if untreated. About 1 to 2 mothers in 1,000 experiences postpartum psychosis after delivery.1 This rate is much higher among women with an established diagnosis of bipolar disorder before pregnancy.1
Expedient recognition, diagnosis, and referral to a high-level psychiatric facility (usually a locked inpatient unit) are critical for ensuring the safety of mother and infant. A diligent medical workup followed by thorough education for the patient and family are important steps in caring for patients with postpartum psychosis. Close mental health follow-up, pharmacologic interventions, informed decision making regarding breastfeeding, and preserving the sleep-wake cycle are critical for stabilization.2
The authors present the case of a patient admitted to VA Central California Health Care System (VACCHCS) with postpartum psychosis and a discussion on existing research on the prevalence of postpartum psychosis, relevant risk factors, the association with bipolar disorder, and treatment strategies.
Case Presentation
A 31-year-old active-duty female with no history of mental illness was admitted to the psychiatric unit because new-onset disorganized behavior was preventing her from functioning at her workplace. Two weeks after giving birth to her second child, the patient began exhibiting an uncharacteristic, debilitating labile mood and disorganized behavior. Her supervisors required her to present for medical attention about 3 months after the birth of her child. She was transferred to VACCHCS for higher level medical care on military orders. The patient’s husband initially attributed these psychiatric symptoms to vocational stress and taking care of 2 young children. He observed the patient exhibiting tearfulness about her job, which quickly alternated with euphoric episodes of singing and dancing at inappropriate times, such as when the children had quieted down and were being prepared to go to bed.
At the initial psychiatric evaluation after transfer to VACCHCS, the patient appeared well-kept and slightly overweight. In general her appearance was unremarkable. Throughout the examination she sang both subtly and loudly and at times was confrontational and irritable.
She related oddly and often was guarded and difficult to engage; she sang and played with her blanket in a childlike way. She smiled and laughed inappropriately, mumbled incoherently to herself, scanned the room suspiciously, and often made intense eye contact. Her affect was labile, both tearful and euphoric at several points in the examination. Her thought process was tangential, illogical, grandiose, difficult to redirect, and with loose associations. Her thought content consisted of delusions (“I’ve got the devil on my back”) and grandiosity (“I am everyone, I am you…the president, the mayor”), and she often stated that she planned to become a singer or performer.
The patient claimed she was neither suicidal nor had thoughts of infanticide. She reported having no visual and auditory hallucinations but often seemed to be responding to internal stimuli: She mumbled to herself and looked intensely at parts of the room. Cognitively, the patient was fully intact to recent and remote events but displayed a poor attention span. She did not exhibit any motor abnormalities, such as tremor, rigidity, weakness, sensory loss, or abnormal gait.
The patient’s workup included full chemistry, complete blood count, thyroid-stimulating hormone, antithyroid antibodies, calcium, rapid plasma reagin to rule out syphilis, toxicology, folate, vitamin B12, and vitamin D. All laboratory results were negative or within normal limits, although the urine drug screen was positive for cannabis. The patient’s husband noted that his wife never used cannabis except the weekend before her admission, when she impulsively went dancing, which was out of character for her. Her psychotic symptoms had been present weeks before the cannabis use; therefore, the her symptoms could not be attributed to a substance-induced psychotic disorder. A test for synthetic cannabis derivatives was negative. Newer synthetic compounds can cause more severe substance-induced psychotic symptoms than those of cannabis.3
The patient was diagnosed with postpartum psychosis and was started on the oral antipsychotic olanzapine 10 mg at bedtime. Additional doses were administered to control ongoing symptoms, which included a disorganized thought process; loose associations; euphoria; grandiosity; delusional content, such as “You are just a tool in place to help me;” reports of feeling as though she were in “outer space, outside in the galaxy;” decreased need for sleep; and irritability. The patient spent an entire interview with her eyes closed, stating that she could “hear” better because she was overstimulated if her eyes were open. She also described olfactory hallucinations of “strong perfume,” which the 2 providers present could not detect.
Olanzapine was not well tolerated because of sedation and was discontinued in favor of risperidone, 2 mg twice daily. Risperidone was more effective and better tolerated. Lithium was initiated the next day with target dosing at 300 mg in the morning and 600 mg at night. The patient became capable of linear, organized discussion and planning but remained euphoric with high energy; she exhibited grandiosity with frequent singing and dancing throughout her hospital stay. She often described her mood as “good, excellent, exuberant, exciting,” perseverating on the way words sounded and giggling in a childlike manner. She continued to have intrusive dreams of “hell and the devil” and that she was killed by gunshot.
The patient was continued on lithium and risperidone and transferred to a larger military hospital for further inpatient management, respecting military orders. Before discharge, a family conference was held with the patient and her husband to educate them on the importance of continued treatment, close follow-up, regular sleep patterns, and not breastfeeding while taking the prescribed medications. Although she was not back to her baseline at the time of transfer, the patient had stabilized significantly and gained sufficient insight into her condition.
Discussion
Postpartum psychosis can present with a prodromal phase consisting of fatigue, insomnia, restlessness, tearfulness, and emotional lability, making early identification difficult. Later, florid psychotic symptoms can include suspiciousness, confusion, incoherence, irrational statements, obsessive concern about the infant’s health, and delusions, including a belief that the baby is dead or defective. Some women might deny that the birth occurred or feel that they are unmarried, virginal, or persecuted.1 More concerning symptoms include auditory hallucinations commanding the mother to harm or kill the infant and/or herself. Symptoms often begin within days to weeks of birth, usually 2 to 3 weeks after delivery but can occur as long as 8 weeks postpartum.1 Several cases of infanticide and suicide have been documented.1 The risk of experiencing another psychotic episode in subsequent pregnancies can be as high as 50%.4-6 Regardless of symptom severity at onset, postpartum psychosis is a psychiatric emergency and must be treated as such.
Bipolar Disorder and Postpartum Psychosis
A close relationship exists between postpartum psychosis and development of bipolar disorder. A postpartum psychotic episode often is the harbinger of bipolar illness.7 About two-thirds of women who have an episode of postpartum psychosis will experience an underlying affective disorder within a year of childbirth.1,8 It is unclear what triggers the psychotic episode, but it has been theorized that major systemic shifts in hormone levelsor trauma of delivery could instigate development of symptoms.1,9
Risk factors include obstetric complications; perinatal infant mortality; previous episodes of bipolar disorder, psychosis, or postpartum psychosis; family history of bipolar disorder or postpartum psychosis; sleep deprivation; increased environmental stress; and lack of partner support.10 The strongest risk factor for developing postpartum psychosis is a personal or family history of bipolar disorder or a related psychotic disorder.11 This risk factor is identified in about 40% to 50% cases of postpartum psychosis.11
Treatment
Standard treatment for postpartum psychosis includes an antipsychotic and often lithium and benzodiazepines.1,7,10,11 This treatment approach differs slightly from treating a patient with a nonpostpartum psychotic illness, who generally would not receive mood stabilizers, such as lithium. Including a mood stabilizer for postpartum psychosis is warranted because of the association between postpartum psychosis and bipolar disorder, which is treated with a mood stabilizer.
Prevalence
Postpartum psychosis is identified in 1 to 2 per 1,000 childbirths. In women who have had an earlier episode of postpartum psychosis or have a diagnosis of bipolar disorder, the rate is up to 100 times higher.1 Kendell and colleagues found that psychiatric admissions occurred at a rate 7 times higher in the 30 days after birth than in the prepregnancy period, suggesting that metabolic factors might be involved in triggering postpartum psychotic symptoms.12 An abrupt hormonal loss occurs at childbirth; hormones peak 200-fold during gestation and decline rapidly within a day after birth.9 Despite the severity of symptoms in postpartum psychosis, these patients tend to have a better prognosis than that of women with psychotic episodes not related to pregnancy.4
Brockington and colleagues found that patients with postpartum psychosis had more mood lability, distractibility, and confusion than those with psychosis unrelated to pregnancy.15 Patients with postpartum psychosis were more likely to have impaired sensorium, bizarre quality of delusions, and memory loss. Psychosis with onset after childbirth included high levels of thought disorganization, delusions of reference, delusions of persecution, and greater levels of homicidal ideation and behavior.16 This study also reported symptoms such as visual, tactile, and olfactory hallucinations and a presentation similar to that of delirium.
Chandra and colleagues found that 53% of women with postpartum psychosis had delusions about the infant, including beliefs that someone would harm or kill the baby or that the baby would be harmed by their breast milk.17 Compared with women with bipolar disorder, Oostheuizen and colleagues found that women with postpartum psychosis had delusions of control, such as feeling under the influence of an overpowering force that controlled their actions.18 Infanticidal thoughts are common among patients with postpartum psychosis, and about 4% of women committed infanticide.1
Rapid stabilization and treatment are important because postpartum psychosis is considered a psychiatric emergency.7 Potential consequences of delayed diagnosis and treatment include harm or death of the infant by infanticide and death of the mother by suicide. A thorough physical examination is important to rule out metabolic or neuroendocrine causes of psychosis other than postpartum hormonal shifts. These could include causes of altered mental status: stroke, pulmonary embolism, amniotic fluid emboli, Sheehan syndrome, thyroid disorders, electrolyte abnormalities, acute hemorrhage, sepsis, and substance toxicity or withdrawal.10 A complete blood count, full chemistry, thyroid function tests, antithyroid antibody tests, calcium, vitamin B12, and folate should be measured.7,10
Initial treatment should include antipsychotics and often mood stabilizers such as lithium. Managing insomnia aggressively is also necessary for initial stabilization and to prevent a repeat manic episode if the patient develops bipolar disorder.2 Many experts argue that sleep loss in combination with other risk factors might be the final common pathway for development of postpartum psychosis in women predisposed to this disorder.19,20
Treating insomnia in an outpatient setting includes teaching sleep hygiene practices and relaxation techniques. Although these methods to regulate sleep could be encouraged during the emergent inpatient stabilization of a patient with postpartum psychosis, pharmacologic approaches are necessary for acute mania and psychosis. Concern about possible dependence on benzodiazepines and other sedating sleep aids are valid; however, the benefit of acute stabilization of psychotic symptoms outweighs the potential risk of dependence.
Typically, first-line treatment is an antipsychotic, and second-generation antipsychotics generally are preferred over first-generation antipsychotics because of their more benign adverse effect profile.21,22 There are no controlled trials that compare antipsychotics with placebo or other interventions for postpartum psychosis. Therefore, use of atypical antipsychotics is based on randomized trials demonstrating efficacy in reducing psychosis in bipolar disorder, depression with psychotic features, and schizoaffective disorder.23,24 Once the patient is treated with an antipsychotic, further use of psychotropic medications, such as lithium or other mood stabilizers, should be based on the patient’s clinical presentation. For example, the patient in this case study primarily had manic symptoms consistent with bipolar disorder, making lithium or another mood stabilizer an appropriate choice.
Bergink and colleagues demonstrated positive outcomes with a treatment algorithm involving sequential use of benzodiazepines to improve sleep, an antipsychotic to decrease acute manic symptoms, lithium to stabilize mood based on symptoms, and electroconvulsive therapy if other treatments were not successful.25 Case studies document that administering estrogen led to recovery from postpartum psychosis, although patients often relapsed when estrogen was stopped.26 Electroconvulsive therapy has shown promising results, especially in patients who do not respond to antipsychotic medications or lithium.27,28
Antipsychotic and Other Psychotropic Medications
Choice of an antipsychotic and other psychotropic medications to treat postpartum psychosis is based on the patient’s breastfeeding status. The benefits of treatment should be weighed against the risks of a breastfeeding infant’s exposure to the medication. Because postpartum psychosis is a psychiatric emergency, the benefits of the medication are considered to outweigh any potential adverse effect to the breastfeeding infant exposed to the medication. Risks of untreated postpartum psychosis to the infant include rejection of the infant, poor parental relationships, suicide, infanticide, long-term failure to bond with the child, delayed infant development, and failure to thrive.29 Also, many mothers—including the patient in this presentation—decide that the benefits of treatment outweigh those of breastfeeding and choose to feed their infant with formula. Even if the patient chooses to bottle-feed her infant, consider administering medications that are considered safer for breastfeeding because the patient may need to continue the psychotropic during later pregnancies to prevent future psychotic episodes.30 All psychotropic medications pass into breast milk.29 Studies on the long-term effect of these medications on the infant are limited, but experts tend to recommend olanzapine, quetiapine, and risperidone over aripiprazole and ziprasidone.21,31-33
Lithium often is used to treat postpartum psychosis. Studies examining risk to the infant after long-term exposure to lithium through breast milk have not been conducted, but the American Academy of Pediatrics discourages its use during breastfeeding because of concerns about toxicity in the infant.34-36
Sleep regulation is important to treat bipolar disorder and to prevent future episodes.2,20,21 To ensure safety of the infant and mother before discharge, family education is imperative to establish close follow-up, adequate sleep, and reduction of stressors.7,10 Separation from the infant might be necessary after discharge, and someone should monitor the infant at all times until the outpatient mental health provider confirms that all psychotic symptoms have resolved.7,10 Successful treatment of postpartum psychosis requires close communication among the mental health provider, the pediatrician, and the obstetrician or women’s health provider.10 Because a close-knit team approach after discharge from the acute psychiatric unit is necessary, the care of such a patient and her child provides an educational opportunity for individuals working in integrated care clinics.
Conclusion
Postpartum psychosis is a psychiatric emergency requiring immediate treatment to prevent dire outcomes such as suicide or infanticide. Treatment considerations include the cost-benefit analysis of breastfeeding and the toxicity of psychotropic medications when ingested by the infant via breast milk. A close relationship has been demonstrated between postpartum psychosis and bipolar disorder.
Preferred treatment regimens include lithium and an antipsychotic. Educate the family as a unit about the diagnosis and treatment, the importance of adequate sleep for treatment and prophylaxis, and the decision on whether to discontinue breastfeeding despite its well-known benefits for mother and infant. Stabilization is a multifaceted process and needs to be reinforced with a solid plan for support and follow-up appointments. Because of the higher risk of relapse, educate patients about prophylactic treatment during subsequent pregnancies and monitor for development of bipolar disorder in the future.
1. Sadock B, Sadock V, Ruiz P. Kaplan & Sadock’s Synopsis of Psychiatry. 11th ed. Philadelphia, PA: Wolters Kluwer; 2015.
2. Sharma V. Pharmacotherapy of postpartum psychosis. Expert Opin Pharmacother. 2003;4(10):1651-1658.
3. Bassir Nia A, Medrano B, Perkel C, Galynker I, Hurd YL. Psychiatric comorbidity associated with synthetic cannabinoid use compared to cannabis. J Psychopharmacol. 2016;30(12):1321-1330.
4. Rhohde A, Marneros A. Postpartum psychoses: onset and long-term course. Psychopathology. 1993;26(3-4):203-209.
5. Videbech P, Gouliaev G. First admission with puerperal psychosis: 7-14 years of follow-up. Acta Psychiatr Scand. 1995;91(3):167-173.
6. Terp IM, Engholm G, Møller H, Mortensen PB. A follow-up study of postpartum psychoses: prognosis and risk factors for readmission. Acta Psychiatr Scand. 1999;100(1):40-46.
7. Spinelli MG. Postpartum psychosis: detection of risk and management. Am J Psychiatry. 2009;166(4):405-408.
8. Blackmore ER, Rubinow DR, O’Connor TG, et al. Reproductive outcomes and risk of subsequent illness in women diagnosed with postpartum psychosis. Bipolar Disord. 2013;15(4):394-404.
9. Bloch M, Schmidt PJ, Danaceau M, Murphy J, Nieman L, Rubinow DR. Effects of gonadal steroids in women with a history of postpartum depression. Am J Psychiatry. 2000;157(6):924-930.
10. Monzon C, Lanza di Scalea T, Pearlstein T. Postpartum psychosis: updates and clinical issues. Psychiatric Times. 2014. http://www.psychiatrictimes.com/special-reports/postpartum -psychosis-updates-and-clinical-issues. Published January 15, 2014. Accessed December 14, 2017.
11. Davies W. Understanding the pathophysiology of postpartum psychosis: challenges and new approaches. World J Psychiatry. 2017;7(2):77-88.
12. Kendell RE, Chalmers JC, Platz C. Epidemiology of puerperal psychoses. Br J Psychiatry. 1987;150:662-673.
13. Leibenluft E. Women with bipolar illness: clinical and research issues. Am J Psychiatry. 1996;153(2):163-173.
14. Chaudron LH, Pies R. The relationship between postpartum psychosis and bipolar disorder: a review. J Clin Psychiatry. 2003;64(11):1284-1292.
15. Brockington IF, Cernik KF, Schofield EM, Downing AR, Francis AF, Keelan C. Puerperal psychosis: phenomena and diagnosis. Arch Gen Psychiatry. 1981;38(7):829-833.
16. Wisner KL, Peindl K, Hanusa BH. Symptomatology of affective and psychotic illnesses related to childbearing. J Affect Disord. 1994;30(2):77-87.
17. Chandra PS, Bhargavaraman RP, Raghunandan VN, Shaligram D. Delusions related to infant and their association with mother-infant interactions in postpartum psychotic disorders. Arch Womens Ment Health. 2006;9(5):285-288.
18. Oosthuizen P, Russouw H, Roberts M. Is puerperal psychosis bipolar mood disorder? A phenomenological comparison. Compr Psychiatry. 1995;36(1):77-81.
19. Sharma V, Mazmanian D. Sleep loss and postpartum psychosis. Bipolar Disord. 2003;5(2):98-105.
20 Bilszta JL, Meyer D, Buist AE. Bipolar affective disorder in the postnatal period: investigating the role of sleep. Bipolar Disord. 2010;12(5):568-578.
21. Doucet S, Jones I, Letourneau N, Dennis CL, Blackmore ER. Interventions for the prevention and treatment of postpartum psychosis: a systematic review. Arch Womens Ment Health. 2011;14(2):89-98.
22 Perlis RH, Welge JA, Vornik LA, Hirschfeld RM, Keck PE Jr. Atypical antipsychotics in the treatment of mania: a meta-analysis of randomized, placebo-controlled trials. J Clin Psychiatry. 2006;67(4):509-516.
23 Wijkstra J, Lijmer J, Balk FJ, Geddes JR, Nolen WA. Pharmacological treatment for unipolar psychotic depression: systematic review and meta-analysis. Br J Psychiatry. 2006;188:410-415.
24. Smith LA, Cornelius V, Warnock A, Tacchi MJ, Taylor D. Pharmacological interventions for acute bipolar mania: a systematic review of randomized placebo-controlled trials. Bipolar Disord. 2007;9(6):551-560.
25. Bergink V, Burgerhout KM, Koorengevel KM, et al. Treatment of psychosis and mania in the postpartum period. Am J Psychiatry. 2015;172(2):115-123.
26. Ahokas A, Aito M, Rimón R. Positive treatment effect of estradiol in postpartum psychosis: a pilot study. J Clin Psychiatry. 2000;61(3):166-169.
27. Reed P, Sermin N, Appleby L, Faragher B. A comparison of clinical response to electroconvulsive therapy in puerperal and non-puerperal psychoses. J Affect Disord. 1999;54(3):255-260.
28. Forray A, Ostroff RB. The use of electroconvulsive therapy in postpartum affective disorders. J ECT. 2007;23(3):188-193.
29. Robinson GE. Psychopharmacology in pregnancy and postpartum. Focus. 2012;10(1):3-14.
30. Wesseloo R, Kamperman AM, Munk-Olsen T, Pop VJ, Kushner SA, Bergink V. Risk of postpartum relapse in bipolar disorder and postpartum psychosis: a systematic review and meta-analysis. Am J Psychiatry. 2016;173(2):117-127.
31. Sharma V, Smith A, Mazmanian D. Olanzapine in the prevention of postpartum psychosis and mood episodes in bipolar disorder. Bipolar Disord. 2006;8(4):400-404.
32. Gobbi G. Quetiapine in postpartum psychosis. J Clin Psychopharmacol. 2014;34(6):744-745.
33. Uguz F. Second-generation antipsychotics during the lactation period: a comparative systematic review on infant safety. J Clin Psychopharmacol. 2016;36(3):244-252.
34. Sachs HC; Committee on Drugs. The transfer of drugs and therapeutics into human breast milk: an update on selected topics. Pediatrics. 2013;132(3):e796-e809.
35. Lithium [package insert]. Columbus, OH: Roxane Laboratories Inc; 2011.
36. Grandjean EM, Aubry JM. Lithium: updated human knowledge using an evidence-based approach: part III: clinical safety. CNS Drugs. 2009;23(5):397-418.
1. Sadock B, Sadock V, Ruiz P. Kaplan & Sadock’s Synopsis of Psychiatry. 11th ed. Philadelphia, PA: Wolters Kluwer; 2015.
2. Sharma V. Pharmacotherapy of postpartum psychosis. Expert Opin Pharmacother. 2003;4(10):1651-1658.
3. Bassir Nia A, Medrano B, Perkel C, Galynker I, Hurd YL. Psychiatric comorbidity associated with synthetic cannabinoid use compared to cannabis. J Psychopharmacol. 2016;30(12):1321-1330.
4. Rhohde A, Marneros A. Postpartum psychoses: onset and long-term course. Psychopathology. 1993;26(3-4):203-209.
5. Videbech P, Gouliaev G. First admission with puerperal psychosis: 7-14 years of follow-up. Acta Psychiatr Scand. 1995;91(3):167-173.
6. Terp IM, Engholm G, Møller H, Mortensen PB. A follow-up study of postpartum psychoses: prognosis and risk factors for readmission. Acta Psychiatr Scand. 1999;100(1):40-46.
7. Spinelli MG. Postpartum psychosis: detection of risk and management. Am J Psychiatry. 2009;166(4):405-408.
8. Blackmore ER, Rubinow DR, O’Connor TG, et al. Reproductive outcomes and risk of subsequent illness in women diagnosed with postpartum psychosis. Bipolar Disord. 2013;15(4):394-404.
9. Bloch M, Schmidt PJ, Danaceau M, Murphy J, Nieman L, Rubinow DR. Effects of gonadal steroids in women with a history of postpartum depression. Am J Psychiatry. 2000;157(6):924-930.
10. Monzon C, Lanza di Scalea T, Pearlstein T. Postpartum psychosis: updates and clinical issues. Psychiatric Times. 2014. http://www.psychiatrictimes.com/special-reports/postpartum -psychosis-updates-and-clinical-issues. Published January 15, 2014. Accessed December 14, 2017.
11. Davies W. Understanding the pathophysiology of postpartum psychosis: challenges and new approaches. World J Psychiatry. 2017;7(2):77-88.
12. Kendell RE, Chalmers JC, Platz C. Epidemiology of puerperal psychoses. Br J Psychiatry. 1987;150:662-673.
13. Leibenluft E. Women with bipolar illness: clinical and research issues. Am J Psychiatry. 1996;153(2):163-173.
14. Chaudron LH, Pies R. The relationship between postpartum psychosis and bipolar disorder: a review. J Clin Psychiatry. 2003;64(11):1284-1292.
15. Brockington IF, Cernik KF, Schofield EM, Downing AR, Francis AF, Keelan C. Puerperal psychosis: phenomena and diagnosis. Arch Gen Psychiatry. 1981;38(7):829-833.
16. Wisner KL, Peindl K, Hanusa BH. Symptomatology of affective and psychotic illnesses related to childbearing. J Affect Disord. 1994;30(2):77-87.
17. Chandra PS, Bhargavaraman RP, Raghunandan VN, Shaligram D. Delusions related to infant and their association with mother-infant interactions in postpartum psychotic disorders. Arch Womens Ment Health. 2006;9(5):285-288.
18. Oosthuizen P, Russouw H, Roberts M. Is puerperal psychosis bipolar mood disorder? A phenomenological comparison. Compr Psychiatry. 1995;36(1):77-81.
19. Sharma V, Mazmanian D. Sleep loss and postpartum psychosis. Bipolar Disord. 2003;5(2):98-105.
20 Bilszta JL, Meyer D, Buist AE. Bipolar affective disorder in the postnatal period: investigating the role of sleep. Bipolar Disord. 2010;12(5):568-578.
21. Doucet S, Jones I, Letourneau N, Dennis CL, Blackmore ER. Interventions for the prevention and treatment of postpartum psychosis: a systematic review. Arch Womens Ment Health. 2011;14(2):89-98.
22 Perlis RH, Welge JA, Vornik LA, Hirschfeld RM, Keck PE Jr. Atypical antipsychotics in the treatment of mania: a meta-analysis of randomized, placebo-controlled trials. J Clin Psychiatry. 2006;67(4):509-516.
23 Wijkstra J, Lijmer J, Balk FJ, Geddes JR, Nolen WA. Pharmacological treatment for unipolar psychotic depression: systematic review and meta-analysis. Br J Psychiatry. 2006;188:410-415.
24. Smith LA, Cornelius V, Warnock A, Tacchi MJ, Taylor D. Pharmacological interventions for acute bipolar mania: a systematic review of randomized placebo-controlled trials. Bipolar Disord. 2007;9(6):551-560.
25. Bergink V, Burgerhout KM, Koorengevel KM, et al. Treatment of psychosis and mania in the postpartum period. Am J Psychiatry. 2015;172(2):115-123.
26. Ahokas A, Aito M, Rimón R. Positive treatment effect of estradiol in postpartum psychosis: a pilot study. J Clin Psychiatry. 2000;61(3):166-169.
27. Reed P, Sermin N, Appleby L, Faragher B. A comparison of clinical response to electroconvulsive therapy in puerperal and non-puerperal psychoses. J Affect Disord. 1999;54(3):255-260.
28. Forray A, Ostroff RB. The use of electroconvulsive therapy in postpartum affective disorders. J ECT. 2007;23(3):188-193.
29. Robinson GE. Psychopharmacology in pregnancy and postpartum. Focus. 2012;10(1):3-14.
30. Wesseloo R, Kamperman AM, Munk-Olsen T, Pop VJ, Kushner SA, Bergink V. Risk of postpartum relapse in bipolar disorder and postpartum psychosis: a systematic review and meta-analysis. Am J Psychiatry. 2016;173(2):117-127.
31. Sharma V, Smith A, Mazmanian D. Olanzapine in the prevention of postpartum psychosis and mood episodes in bipolar disorder. Bipolar Disord. 2006;8(4):400-404.
32. Gobbi G. Quetiapine in postpartum psychosis. J Clin Psychopharmacol. 2014;34(6):744-745.
33. Uguz F. Second-generation antipsychotics during the lactation period: a comparative systematic review on infant safety. J Clin Psychopharmacol. 2016;36(3):244-252.
34. Sachs HC; Committee on Drugs. The transfer of drugs and therapeutics into human breast milk: an update on selected topics. Pediatrics. 2013;132(3):e796-e809.
35. Lithium [package insert]. Columbus, OH: Roxane Laboratories Inc; 2011.
36. Grandjean EM, Aubry JM. Lithium: updated human knowledge using an evidence-based approach: part III: clinical safety. CNS Drugs. 2009;23(5):397-418.
Mogamulizumab is ‘valuable’ option for CTCL
LA JOLLA, CA—Mogamulizumab is a valuable new therapeutic option for patients with cutaneous T-cell lymphoma (CTCL), according to researchers.
Results of the phase 3 MAVORIC study indicated that mogamulizumab is more effective than vorinostat in previously treated patients with CTCL.
Mogamulizumab produced a better overall response rate (ORR) and prolonged progression-free survival (PFS) in these patients.
Infusion-related reactions and drug eruptions were more common in patients who received mogamulizumab.
Youn H. Kim, MD, of the Stanford Cancer Institute in Palo Alto, California, and her colleagues presented these results in a poster at the 10th Annual T-cell Lymphoma Forum. The study was funded by Kyowa Kirin Pharmaceutical Development, Inc.
MAVORIC enrolled 372 adults with histologically confirmed mycosis fungoides (MF) or Sézary syndrome (SS) who had failed at least 1 systemic therapy. They were randomized to receive mogamulizumab at 1.0 mg/kg (weekly for the first 4-week cycle and then every 2 weeks) or vorinostat at 400 mg daily.
Patients were treated until disease progression or unacceptable toxicity. Those receiving vorinostat could crossover to mogamulizumab if they progressed or experienced intolerable toxicity.
Baseline characteristics were similar between the treatment arms. The median age was 64 (range, 54-73) in the mogamulizumab arm and 65 (range, 56-72) in the vorinostat arm. Ninety-nine percent and 100% of patients, respectively, had an ECOG performance status of 0 to 1.
A little more than half of patients in each arm had MF—57% in the mogamulizumab arm and 53% in the vorinostat arm.
The median number of prior systemic therapies was 3 in both arms (range, 1-18 in the mogamulizumab arm and 0-14 in the vorinostat arm).
Efficacy
The primary endpoint was PFS, and mogamulizumab provided a significant improvement there. The median PFS was 7.7 months with mogamulizumab and 3.1 months with vorinostat (hazard ratio=0.53, P<0.0001).
The researchers also observed a significant improvement in global ORR with mogamulizumab. It was 28% (52/189) in that arm and 5% (9/186) in the vorinostat arm (P<0.0001).
For patients with MF, the ORR was 21% with mogamulizumab and 7% with vorinostat. For SS patients, the ORR was 37% and 2%, respectively.
Responses by disease compartment were superior with mogamulizumab as well.
“Especially in the blood compartment, mogamulizumab had very striking activity over vorinostat,” Dr Kim said.
The blood ORR was 68% with mogamulizumab and 19% with vorinostat. The skin ORR was 42% and 16%, respectively. The lymph node ORR was 17% and 4%, respectively. The viscera ORR was 0% in both arms.
After crossover, the ORR in the mogamulizumab arm was 30% (41/136).
The median duration of response (DOR) was 14 months in the mogamulizumab arm and 9 months in the vorinostat arm.
For MF patients, the median DOR was 13 months with mogamulizumab and 9 months with vorinostat. For SS patients, the median DOR was 17 months and 7 months, respectively.
Safety
“Side effects [of mogamulizumab] were very well tolerable,” Dr Kim said. “Most significant is rash and infusion reactions, but, in terms of severe adverse events, [they] were very minimal.”
The most common treatment-emergent adverse events (AEs), occurring in at least 20% of patients in either arm (mogamulizumab and vorinostat, respectively), were:
- Infusion-related reactions (33.2% vs 0.5%)
- Drug eruptions (23.9% vs 0.5%)
- Diarrhea (23.4% vs 61.8%)
- Nausea (15.2% vs 42.5%)
- Thrombocytopenia (11.4% vs 30.6%)
- Dysgeusia (3.3% vs 28.0%)
- Increased blood creatinine (3.3% vs 28.0%)
- Decreased appetite (7.6% vs 24.7%).
There were no grade 4 AEs in the mogamulizumab arm and 2 cases of grade 4 thrombocytopenia in the vorinostat arm.
Grade 3 AEs in the mogamulizumab arm included drug eruptions (n=8), infusion-related reactions (n=3), fatigue (n=3), decreased appetite (n=2), nausea (n=1), pyrexia (n=1), and diarrhea (n=1).
Grade 3 AEs in the vorinostat arm included thrombocytopenia (n=11), fatigue (n=11), diarrhea (n=9), nausea (n=3), decreased appetite (n=2), and dysgeusia (n=1).
“So the results are, overall, positive,” Dr Kim said. “The data is submitted to the [US Food and Drug Administration]. We are really hoping that [mogamulizumab] will be approved so that we would have a new, exciting treatment for our patients with mycosis fungoides and Sézary syndrome.” ![]()
LA JOLLA, CA—Mogamulizumab is a valuable new therapeutic option for patients with cutaneous T-cell lymphoma (CTCL), according to researchers.
Results of the phase 3 MAVORIC study indicated that mogamulizumab is more effective than vorinostat in previously treated patients with CTCL.
Mogamulizumab produced a better overall response rate (ORR) and prolonged progression-free survival (PFS) in these patients.
Infusion-related reactions and drug eruptions were more common in patients who received mogamulizumab.
Youn H. Kim, MD, of the Stanford Cancer Institute in Palo Alto, California, and her colleagues presented these results in a poster at the 10th Annual T-cell Lymphoma Forum. The study was funded by Kyowa Kirin Pharmaceutical Development, Inc.
MAVORIC enrolled 372 adults with histologically confirmed mycosis fungoides (MF) or Sézary syndrome (SS) who had failed at least 1 systemic therapy. They were randomized to receive mogamulizumab at 1.0 mg/kg (weekly for the first 4-week cycle and then every 2 weeks) or vorinostat at 400 mg daily.
Patients were treated until disease progression or unacceptable toxicity. Those receiving vorinostat could crossover to mogamulizumab if they progressed or experienced intolerable toxicity.
Baseline characteristics were similar between the treatment arms. The median age was 64 (range, 54-73) in the mogamulizumab arm and 65 (range, 56-72) in the vorinostat arm. Ninety-nine percent and 100% of patients, respectively, had an ECOG performance status of 0 to 1.
A little more than half of patients in each arm had MF—57% in the mogamulizumab arm and 53% in the vorinostat arm.
The median number of prior systemic therapies was 3 in both arms (range, 1-18 in the mogamulizumab arm and 0-14 in the vorinostat arm).
Efficacy
The primary endpoint was PFS, and mogamulizumab provided a significant improvement there. The median PFS was 7.7 months with mogamulizumab and 3.1 months with vorinostat (hazard ratio=0.53, P<0.0001).
The researchers also observed a significant improvement in global ORR with mogamulizumab. It was 28% (52/189) in that arm and 5% (9/186) in the vorinostat arm (P<0.0001).
For patients with MF, the ORR was 21% with mogamulizumab and 7% with vorinostat. For SS patients, the ORR was 37% and 2%, respectively.
Responses by disease compartment were superior with mogamulizumab as well.
“Especially in the blood compartment, mogamulizumab had very striking activity over vorinostat,” Dr Kim said.
The blood ORR was 68% with mogamulizumab and 19% with vorinostat. The skin ORR was 42% and 16%, respectively. The lymph node ORR was 17% and 4%, respectively. The viscera ORR was 0% in both arms.
After crossover, the ORR in the mogamulizumab arm was 30% (41/136).
The median duration of response (DOR) was 14 months in the mogamulizumab arm and 9 months in the vorinostat arm.
For MF patients, the median DOR was 13 months with mogamulizumab and 9 months with vorinostat. For SS patients, the median DOR was 17 months and 7 months, respectively.
Safety
“Side effects [of mogamulizumab] were very well tolerable,” Dr Kim said. “Most significant is rash and infusion reactions, but, in terms of severe adverse events, [they] were very minimal.”
The most common treatment-emergent adverse events (AEs), occurring in at least 20% of patients in either arm (mogamulizumab and vorinostat, respectively), were:
- Infusion-related reactions (33.2% vs 0.5%)
- Drug eruptions (23.9% vs 0.5%)
- Diarrhea (23.4% vs 61.8%)
- Nausea (15.2% vs 42.5%)
- Thrombocytopenia (11.4% vs 30.6%)
- Dysgeusia (3.3% vs 28.0%)
- Increased blood creatinine (3.3% vs 28.0%)
- Decreased appetite (7.6% vs 24.7%).
There were no grade 4 AEs in the mogamulizumab arm and 2 cases of grade 4 thrombocytopenia in the vorinostat arm.
Grade 3 AEs in the mogamulizumab arm included drug eruptions (n=8), infusion-related reactions (n=3), fatigue (n=3), decreased appetite (n=2), nausea (n=1), pyrexia (n=1), and diarrhea (n=1).
Grade 3 AEs in the vorinostat arm included thrombocytopenia (n=11), fatigue (n=11), diarrhea (n=9), nausea (n=3), decreased appetite (n=2), and dysgeusia (n=1).
“So the results are, overall, positive,” Dr Kim said. “The data is submitted to the [US Food and Drug Administration]. We are really hoping that [mogamulizumab] will be approved so that we would have a new, exciting treatment for our patients with mycosis fungoides and Sézary syndrome.” ![]()
LA JOLLA, CA—Mogamulizumab is a valuable new therapeutic option for patients with cutaneous T-cell lymphoma (CTCL), according to researchers.
Results of the phase 3 MAVORIC study indicated that mogamulizumab is more effective than vorinostat in previously treated patients with CTCL.
Mogamulizumab produced a better overall response rate (ORR) and prolonged progression-free survival (PFS) in these patients.
Infusion-related reactions and drug eruptions were more common in patients who received mogamulizumab.
Youn H. Kim, MD, of the Stanford Cancer Institute in Palo Alto, California, and her colleagues presented these results in a poster at the 10th Annual T-cell Lymphoma Forum. The study was funded by Kyowa Kirin Pharmaceutical Development, Inc.
MAVORIC enrolled 372 adults with histologically confirmed mycosis fungoides (MF) or Sézary syndrome (SS) who had failed at least 1 systemic therapy. They were randomized to receive mogamulizumab at 1.0 mg/kg (weekly for the first 4-week cycle and then every 2 weeks) or vorinostat at 400 mg daily.
Patients were treated until disease progression or unacceptable toxicity. Those receiving vorinostat could crossover to mogamulizumab if they progressed or experienced intolerable toxicity.
Baseline characteristics were similar between the treatment arms. The median age was 64 (range, 54-73) in the mogamulizumab arm and 65 (range, 56-72) in the vorinostat arm. Ninety-nine percent and 100% of patients, respectively, had an ECOG performance status of 0 to 1.
A little more than half of patients in each arm had MF—57% in the mogamulizumab arm and 53% in the vorinostat arm.
The median number of prior systemic therapies was 3 in both arms (range, 1-18 in the mogamulizumab arm and 0-14 in the vorinostat arm).
Efficacy
The primary endpoint was PFS, and mogamulizumab provided a significant improvement there. The median PFS was 7.7 months with mogamulizumab and 3.1 months with vorinostat (hazard ratio=0.53, P<0.0001).
The researchers also observed a significant improvement in global ORR with mogamulizumab. It was 28% (52/189) in that arm and 5% (9/186) in the vorinostat arm (P<0.0001).
For patients with MF, the ORR was 21% with mogamulizumab and 7% with vorinostat. For SS patients, the ORR was 37% and 2%, respectively.
Responses by disease compartment were superior with mogamulizumab as well.
“Especially in the blood compartment, mogamulizumab had very striking activity over vorinostat,” Dr Kim said.
The blood ORR was 68% with mogamulizumab and 19% with vorinostat. The skin ORR was 42% and 16%, respectively. The lymph node ORR was 17% and 4%, respectively. The viscera ORR was 0% in both arms.
After crossover, the ORR in the mogamulizumab arm was 30% (41/136).
The median duration of response (DOR) was 14 months in the mogamulizumab arm and 9 months in the vorinostat arm.
For MF patients, the median DOR was 13 months with mogamulizumab and 9 months with vorinostat. For SS patients, the median DOR was 17 months and 7 months, respectively.
Safety
“Side effects [of mogamulizumab] were very well tolerable,” Dr Kim said. “Most significant is rash and infusion reactions, but, in terms of severe adverse events, [they] were very minimal.”
The most common treatment-emergent adverse events (AEs), occurring in at least 20% of patients in either arm (mogamulizumab and vorinostat, respectively), were:
- Infusion-related reactions (33.2% vs 0.5%)
- Drug eruptions (23.9% vs 0.5%)
- Diarrhea (23.4% vs 61.8%)
- Nausea (15.2% vs 42.5%)
- Thrombocytopenia (11.4% vs 30.6%)
- Dysgeusia (3.3% vs 28.0%)
- Increased blood creatinine (3.3% vs 28.0%)
- Decreased appetite (7.6% vs 24.7%).
There were no grade 4 AEs in the mogamulizumab arm and 2 cases of grade 4 thrombocytopenia in the vorinostat arm.
Grade 3 AEs in the mogamulizumab arm included drug eruptions (n=8), infusion-related reactions (n=3), fatigue (n=3), decreased appetite (n=2), nausea (n=1), pyrexia (n=1), and diarrhea (n=1).
Grade 3 AEs in the vorinostat arm included thrombocytopenia (n=11), fatigue (n=11), diarrhea (n=9), nausea (n=3), decreased appetite (n=2), and dysgeusia (n=1).
“So the results are, overall, positive,” Dr Kim said. “The data is submitted to the [US Food and Drug Administration]. We are really hoping that [mogamulizumab] will be approved so that we would have a new, exciting treatment for our patients with mycosis fungoides and Sézary syndrome.” ![]()
Children with sickle cell anemia fall short on antibiotic adherence
Despite the increased risk for invasive pneumococcal disease, prophylactic antibiotics are underused in children with sickle cell anemia, according to data from more than 2,000 children in six states.
Less than one-fifth (18%) of young children (aged 3 months to 5 years) with sickle cell anemia (SCA) receive at least 300 days of prophylactic antibiotics to reduce their risk of pneumococcal infections, the analysis found.
“Although the effectiveness of daily penicillin prophylaxis has been known for decades, limited evidence indicates low rates of compliance among children,” wrote Sarah L. Reeves, PhD, of the University of Michigan, Ann Arbor, and her colleagues. The report was published in Pediatrics.
The researchers reviewed Medicaid claims for 2,821 children with SCA from the period of 2005-2012 for a total of 5,014 person-years. The data were taken from six states: Florida, Illinois, Louisiana, Michigan, South Carolina, and Texas. Antibiotic prophylaxis was defined as four different treatment protocols: oral penicillin; oral penicillin or erythromycin; oral penicillin, erythromycin, or amoxicillin; or any antibiotic that could protect against Streptococcus pneumoniae.
Overall, the children in the study averaged 1.7 sickle cell disease–related inpatient hospitalizations annually, as well as 13.2 sickle cell disease–related outpatient visits and 3.8 emergency department visits per year.
The proportion of children who received 300 days or more of prophylactic antibiotics varied by state, by year, and by type of treatment. “In this multistate analysis, receipt of antibiotic prophylaxis among children with SCA was persistently low, irrespective of year or state,” the researchers noted.
The odds that a child received 300 days or more of prophylactic antibiotics increased with each outpatient visit, including well child visits and sickle cell disease–related visits (odds ratios 1.08 and 1.01, respectively).
A child in the third quartile of sickle cell disease–related outpatient visits (defined as 17 annual visits) was 15% more likely than was a child in the first quartile (defined as six annual visits) to receive at least 300 days of antibiotics.
The study findings were limited by several factors including potential overestimation of how many children received medication, the researchers said. However, the results suggest the need for practical and effective intervention that targets barriers to treatment adherence, they said.
“Provider-focused strategies to increase adherence could capitalize on the numerous annual outpatient encounters with the health care system that children with SCA are already experiencing,” they wrote.
The study was supported by a grant from the Agency for Healthcare Research and Quality and the Centers for Medicare and Medicaid Services. The researchers reported having no financial disclosures.
SOURCE: Reeves S et al. Pediatrics. 2018;141(3):e20172182. doi: 10.1542/peds.2017-2182.
Despite the increased risk for invasive pneumococcal disease, prophylactic antibiotics are underused in children with sickle cell anemia, according to data from more than 2,000 children in six states.
Less than one-fifth (18%) of young children (aged 3 months to 5 years) with sickle cell anemia (SCA) receive at least 300 days of prophylactic antibiotics to reduce their risk of pneumococcal infections, the analysis found.
“Although the effectiveness of daily penicillin prophylaxis has been known for decades, limited evidence indicates low rates of compliance among children,” wrote Sarah L. Reeves, PhD, of the University of Michigan, Ann Arbor, and her colleagues. The report was published in Pediatrics.
The researchers reviewed Medicaid claims for 2,821 children with SCA from the period of 2005-2012 for a total of 5,014 person-years. The data were taken from six states: Florida, Illinois, Louisiana, Michigan, South Carolina, and Texas. Antibiotic prophylaxis was defined as four different treatment protocols: oral penicillin; oral penicillin or erythromycin; oral penicillin, erythromycin, or amoxicillin; or any antibiotic that could protect against Streptococcus pneumoniae.
Overall, the children in the study averaged 1.7 sickle cell disease–related inpatient hospitalizations annually, as well as 13.2 sickle cell disease–related outpatient visits and 3.8 emergency department visits per year.
The proportion of children who received 300 days or more of prophylactic antibiotics varied by state, by year, and by type of treatment. “In this multistate analysis, receipt of antibiotic prophylaxis among children with SCA was persistently low, irrespective of year or state,” the researchers noted.
The odds that a child received 300 days or more of prophylactic antibiotics increased with each outpatient visit, including well child visits and sickle cell disease–related visits (odds ratios 1.08 and 1.01, respectively).
A child in the third quartile of sickle cell disease–related outpatient visits (defined as 17 annual visits) was 15% more likely than was a child in the first quartile (defined as six annual visits) to receive at least 300 days of antibiotics.
The study findings were limited by several factors including potential overestimation of how many children received medication, the researchers said. However, the results suggest the need for practical and effective intervention that targets barriers to treatment adherence, they said.
“Provider-focused strategies to increase adherence could capitalize on the numerous annual outpatient encounters with the health care system that children with SCA are already experiencing,” they wrote.
The study was supported by a grant from the Agency for Healthcare Research and Quality and the Centers for Medicare and Medicaid Services. The researchers reported having no financial disclosures.
SOURCE: Reeves S et al. Pediatrics. 2018;141(3):e20172182. doi: 10.1542/peds.2017-2182.
Despite the increased risk for invasive pneumococcal disease, prophylactic antibiotics are underused in children with sickle cell anemia, according to data from more than 2,000 children in six states.
Less than one-fifth (18%) of young children (aged 3 months to 5 years) with sickle cell anemia (SCA) receive at least 300 days of prophylactic antibiotics to reduce their risk of pneumococcal infections, the analysis found.
“Although the effectiveness of daily penicillin prophylaxis has been known for decades, limited evidence indicates low rates of compliance among children,” wrote Sarah L. Reeves, PhD, of the University of Michigan, Ann Arbor, and her colleagues. The report was published in Pediatrics.
The researchers reviewed Medicaid claims for 2,821 children with SCA from the period of 2005-2012 for a total of 5,014 person-years. The data were taken from six states: Florida, Illinois, Louisiana, Michigan, South Carolina, and Texas. Antibiotic prophylaxis was defined as four different treatment protocols: oral penicillin; oral penicillin or erythromycin; oral penicillin, erythromycin, or amoxicillin; or any antibiotic that could protect against Streptococcus pneumoniae.
Overall, the children in the study averaged 1.7 sickle cell disease–related inpatient hospitalizations annually, as well as 13.2 sickle cell disease–related outpatient visits and 3.8 emergency department visits per year.
The proportion of children who received 300 days or more of prophylactic antibiotics varied by state, by year, and by type of treatment. “In this multistate analysis, receipt of antibiotic prophylaxis among children with SCA was persistently low, irrespective of year or state,” the researchers noted.
The odds that a child received 300 days or more of prophylactic antibiotics increased with each outpatient visit, including well child visits and sickle cell disease–related visits (odds ratios 1.08 and 1.01, respectively).
A child in the third quartile of sickle cell disease–related outpatient visits (defined as 17 annual visits) was 15% more likely than was a child in the first quartile (defined as six annual visits) to receive at least 300 days of antibiotics.
The study findings were limited by several factors including potential overestimation of how many children received medication, the researchers said. However, the results suggest the need for practical and effective intervention that targets barriers to treatment adherence, they said.
“Provider-focused strategies to increase adherence could capitalize on the numerous annual outpatient encounters with the health care system that children with SCA are already experiencing,” they wrote.
The study was supported by a grant from the Agency for Healthcare Research and Quality and the Centers for Medicare and Medicaid Services. The researchers reported having no financial disclosures.
SOURCE: Reeves S et al. Pediatrics. 2018;141(3):e20172182. doi: 10.1542/peds.2017-2182.
FROM PEDIATRICS
Key clinical point:
Major finding: A total of 18% of children with sickle cell anemia in Florida, Illinois, Louisiana, Michigan, South Carolina, and Texas received 300 days or more of prophylactic antibiotics.
Study details: A review of 2,821 children aged 3 months to 5 years with sickle cell anemia.
Disclosures: The study was supported by a grant from the Agency for Healthcare Research and Quality and the Centers for Medicare and Medicaid Services. The researchers reported having no financial disclosures.
Source: Reeves S et al. Pediatrics. 2018;141(3):e20172182. doi: 10.1542/peds.2017-2182.
Silent No More: Harassment in the Workplace
Sexual harassment is one of the most insidious and caustic evils in the US workplace—and it knows no bounds, judging by the rampant allegations throughout 2017 and into 2018. While sexual harassment affects both sexes, the majority of cases target women.
In a recent survey, the New York Times asked 615 men about objectionable behavior toward colleagues, including whether they have made uninvited attempts to stroke, fondle, or kiss a coworker. Twenty-five percent admitted to telling crude jokes or sharing inappropriate videos. Two percent said they had pressured people into sexual acts by offering rewards or threatening retaliation—that means 12 men admitted to this.1
Sadly, the health care industry is not immune from this corruption. In fact, sexual harassment is a major problem in health care—one that is particularly prevalent in nursing, according to Fiedler and Hamby.2 More than 50% of female nurses, physicians, and students report experiencing sexual harassment.3 And even that, I believe, is an underreported percentage.
Sexual harassment in the workplace includes any situation in which there is a demand for sexual favors in exchange for a job benefit or where an unwanted condition on any person’s employment is imposed because of that person’s sex. Since 1964, Title VII of the Civil Rights Act (42 USC Sec.2000e-2[a]) has prohibited discrimination in places of employment based on an individual’s sex.4 In 1976, it was acknowledged that this also prohibits sexual harassment as a form of sex discrimination. In 1991, amendments (42 USC Sec.1981 [a][1]) authorized compensatory and punitive damages as well as jury trials.5
The Equal Employment Opportunity Commission (EEOC), the federal agency that enforces Title VII, stipulates that
- Harassment can include unwelcome sexual advances, requests for sexual favors, and other verbal or physical harassment—but it does not have to be sexual in nature (eg, making offensive comments about women in general).
- Both women and men can be victims and harassers—and the victim and harasser can be the same sex.
- Harassment is illegal when it is so frequent or severe that it creates a hostile or offensive work environment, or when it results in an adverse employment decision (eg, the victim being fired or demoted).6
Although the EEOC guidelines are not law, they do guide the judicial interpretation of what constitutes sexual harassment. Sexual harassment is an increasing source of workplace lawsuits that often result in large judgments against employers. Clinicians can file class-action suits against hospitals and other institutions, and juries may render verdicts on harassment complaints to the tune of millions of dollars.
Unfortunately, it is common for workplace harassment to go unreported. According to the EEOC, standard responses to workplace sexual harassment include avoiding the harasser, denying or downplaying the gravity of the situation, or attempting to ignore, forget, or endure the behavior. The least common response is to take formal action—either by reporting it internally or filing a legal complaint. Further, roughly three of four individuals who experience harassment in the workplace never tell a supervisor, manager, or union representative due to fear of disbelief, inaction, blame, or social or professional retaliation.7
How can we, as clinicians, protect ourselves and others from this type of harassment? Establishing a strong zero-tolerance policy on sexual harassment and reporting unacceptable behavior is the only answer. I realize this is no easy issue, but we must be firm in our resolve. Although 2017 was a watershed year with “Silence Breaker” or “#MeToo,” there are still many voices not being heard.8
So, here is my request: If you have been directly affected by, or have observed, objectionable behavior that violates your organization’s policy or code of conduct (or your personal sense of decency), document the incident and report it. You may be hesitant; maybe you think the behavior is an isolated act, or maybe the offender is a well-liked colleague who usually acts professionally. But your role is not to decide whether this behavior is acute or chronic—the human resources department will determine that. Maybe you are reluctant to report harassment because you fear reprisal. This is understandable, but remember that intimidation allows the behavior to persist. If the incident was upsetting and objectionable, it needs to be reported—no matter what.
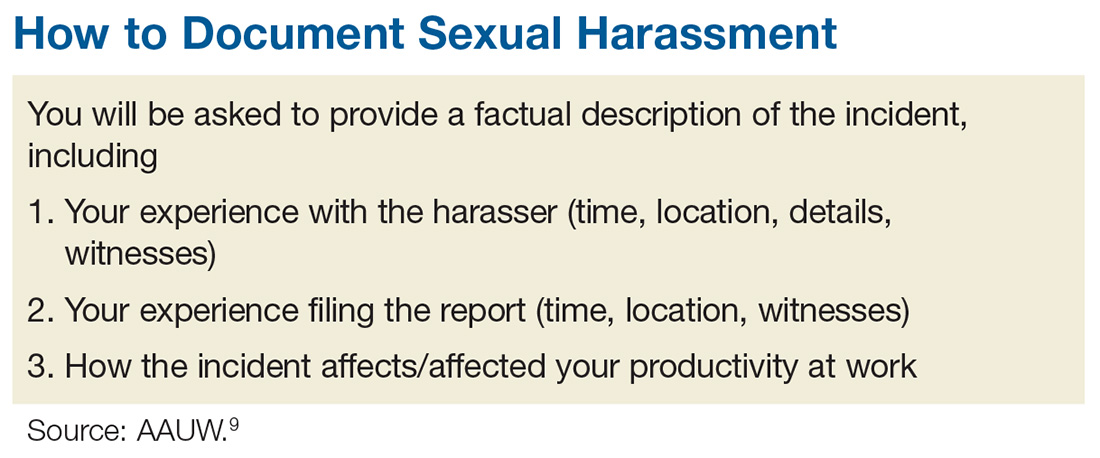
The process of documenting and reporting varies depending on your institution’s policy but typically involves writing a factual description of the incident, including the time, place, and a list of any witnesses (including patients). Make sure your report is objective, and include any effect the behavior has had on patient care. Document any verbal exchanges verbatim, if possible. File the report as soon as possible, and remember to document everything. Nothing is trivial when it comes to building a case against sexual harassment. After you document and report the incident, continue to act professionally.9
If you are unable to resolve a harassment-related issue through your employer’s internal procedure, you may need to pursue the matter via the EEOC or your state’s human rights or civil rights enforcement agency.10 But know that any time and effort you put into reporting this is worthwhile; predatory behavior often crosses the workplace to other social realms. The other people being affected will be grateful that you came forward.
Some of you may be reading this and thinking, “Easy for you to say, Randy. You are not the one being harassed!” I know. This is not an easy topic for anyone. I have been shocked and appalled by the level and prevalence of sexual harassment in the workplace. I was always taught (by my grandmother—thank you!) to respect women. My hope is that by introducing this sensitive topic, we can open the discussion and encourage everyone to speak up. Please share your thoughts, comments, and ideas with me at [email protected]—let’s start a conversation.
1. Patel JK, Griggs T, Cain Miller C. The UpShot: We asked 615 men about how they conduct themselves at work. The New York Times. December 28, 2017. www.nytimes.com/interactive/2017/12/28/upshot/sexual-harassment-survey-600-men.html. Accessed January 16, 2018.
2. Fiedler A, Hamby E. Sexual harassment in the workplace: nurses’ perceptions. J Nurs Adm. 2000;30(10):497-503.
3. Lockwood W. Sexual harassment in healthcare. www.rn.org/courses/coursematerial-236.pdf. Accessed January 16, 2018.
4. Legal Information Institute. 42 U.S. Code § 2000e–2 - Unlawful employment practices. www.law.cornell.edu/uscode/text/42/2000e-2. Accessed January 16, 2018.
5. US Equal Employment Opportunity Commission (EEOC). The Civil Rights Act of 1991. www.eeoc.gov/laws/statutes/cra-1991.cfm. Accessed January 16, 2018.
6. US EEOC. Sexual harassment. www.eeoc.gov/laws/types/sexual_harassment.cfm. Accessed January 16, 2018.
7. US EEOC. Select task force on the study of harassment in the workplace. June 2016. www.eeoc.gov/eeoc/task_force/harassment/report.cfm. Accessed January 16, 2018.
8. O’Brien SA, Carpenter J. 2017 was the year of (certain) women’s voices. December 28, 2017. www.ozarksfirst.com/news/business/2017-was-the-year-of-certain-womens-voices/889901636. Accessed January 16, 2018.
9. AAUW. Know your rights at work. www.aauw.org/what-we-do/legal-resources/know-your-rights-at-work/workplace-sexual-harassment/. Accessed January 16, 2018.
10. EEOC’s Charge Processing Procedures. http://employment.findlaw.com/employment-discrimination/eeoc-s-charge-processing-procedures.html. Accessed January 16, 2018.
Sexual harassment is one of the most insidious and caustic evils in the US workplace—and it knows no bounds, judging by the rampant allegations throughout 2017 and into 2018. While sexual harassment affects both sexes, the majority of cases target women.
In a recent survey, the New York Times asked 615 men about objectionable behavior toward colleagues, including whether they have made uninvited attempts to stroke, fondle, or kiss a coworker. Twenty-five percent admitted to telling crude jokes or sharing inappropriate videos. Two percent said they had pressured people into sexual acts by offering rewards or threatening retaliation—that means 12 men admitted to this.1
Sadly, the health care industry is not immune from this corruption. In fact, sexual harassment is a major problem in health care—one that is particularly prevalent in nursing, according to Fiedler and Hamby.2 More than 50% of female nurses, physicians, and students report experiencing sexual harassment.3 And even that, I believe, is an underreported percentage.
Sexual harassment in the workplace includes any situation in which there is a demand for sexual favors in exchange for a job benefit or where an unwanted condition on any person’s employment is imposed because of that person’s sex. Since 1964, Title VII of the Civil Rights Act (42 USC Sec.2000e-2[a]) has prohibited discrimination in places of employment based on an individual’s sex.4 In 1976, it was acknowledged that this also prohibits sexual harassment as a form of sex discrimination. In 1991, amendments (42 USC Sec.1981 [a][1]) authorized compensatory and punitive damages as well as jury trials.5
The Equal Employment Opportunity Commission (EEOC), the federal agency that enforces Title VII, stipulates that
- Harassment can include unwelcome sexual advances, requests for sexual favors, and other verbal or physical harassment—but it does not have to be sexual in nature (eg, making offensive comments about women in general).
- Both women and men can be victims and harassers—and the victim and harasser can be the same sex.
- Harassment is illegal when it is so frequent or severe that it creates a hostile or offensive work environment, or when it results in an adverse employment decision (eg, the victim being fired or demoted).6
Although the EEOC guidelines are not law, they do guide the judicial interpretation of what constitutes sexual harassment. Sexual harassment is an increasing source of workplace lawsuits that often result in large judgments against employers. Clinicians can file class-action suits against hospitals and other institutions, and juries may render verdicts on harassment complaints to the tune of millions of dollars.
Unfortunately, it is common for workplace harassment to go unreported. According to the EEOC, standard responses to workplace sexual harassment include avoiding the harasser, denying or downplaying the gravity of the situation, or attempting to ignore, forget, or endure the behavior. The least common response is to take formal action—either by reporting it internally or filing a legal complaint. Further, roughly three of four individuals who experience harassment in the workplace never tell a supervisor, manager, or union representative due to fear of disbelief, inaction, blame, or social or professional retaliation.7
How can we, as clinicians, protect ourselves and others from this type of harassment? Establishing a strong zero-tolerance policy on sexual harassment and reporting unacceptable behavior is the only answer. I realize this is no easy issue, but we must be firm in our resolve. Although 2017 was a watershed year with “Silence Breaker” or “#MeToo,” there are still many voices not being heard.8
So, here is my request: If you have been directly affected by, or have observed, objectionable behavior that violates your organization’s policy or code of conduct (or your personal sense of decency), document the incident and report it. You may be hesitant; maybe you think the behavior is an isolated act, or maybe the offender is a well-liked colleague who usually acts professionally. But your role is not to decide whether this behavior is acute or chronic—the human resources department will determine that. Maybe you are reluctant to report harassment because you fear reprisal. This is understandable, but remember that intimidation allows the behavior to persist. If the incident was upsetting and objectionable, it needs to be reported—no matter what.
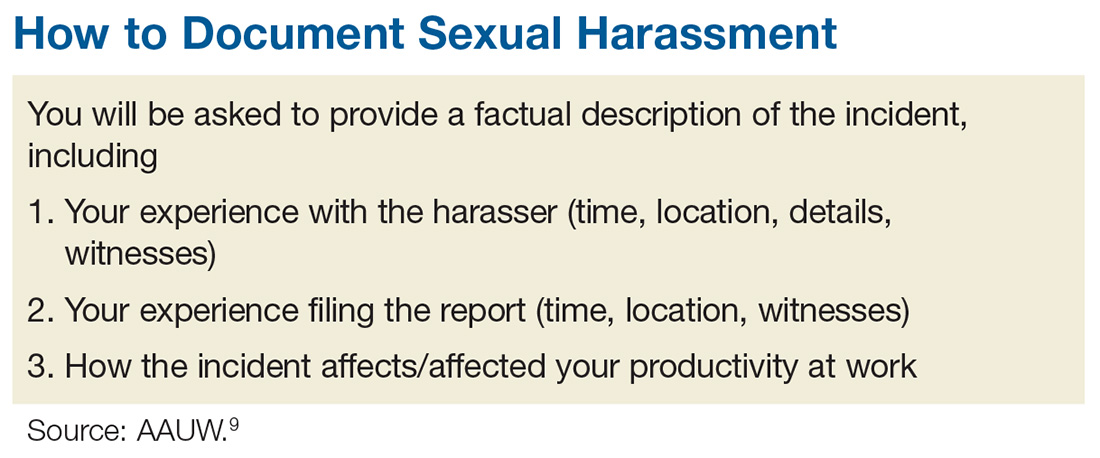
The process of documenting and reporting varies depending on your institution’s policy but typically involves writing a factual description of the incident, including the time, place, and a list of any witnesses (including patients). Make sure your report is objective, and include any effect the behavior has had on patient care. Document any verbal exchanges verbatim, if possible. File the report as soon as possible, and remember to document everything. Nothing is trivial when it comes to building a case against sexual harassment. After you document and report the incident, continue to act professionally.9
If you are unable to resolve a harassment-related issue through your employer’s internal procedure, you may need to pursue the matter via the EEOC or your state’s human rights or civil rights enforcement agency.10 But know that any time and effort you put into reporting this is worthwhile; predatory behavior often crosses the workplace to other social realms. The other people being affected will be grateful that you came forward.
Some of you may be reading this and thinking, “Easy for you to say, Randy. You are not the one being harassed!” I know. This is not an easy topic for anyone. I have been shocked and appalled by the level and prevalence of sexual harassment in the workplace. I was always taught (by my grandmother—thank you!) to respect women. My hope is that by introducing this sensitive topic, we can open the discussion and encourage everyone to speak up. Please share your thoughts, comments, and ideas with me at [email protected]—let’s start a conversation.
Sexual harassment is one of the most insidious and caustic evils in the US workplace—and it knows no bounds, judging by the rampant allegations throughout 2017 and into 2018. While sexual harassment affects both sexes, the majority of cases target women.
In a recent survey, the New York Times asked 615 men about objectionable behavior toward colleagues, including whether they have made uninvited attempts to stroke, fondle, or kiss a coworker. Twenty-five percent admitted to telling crude jokes or sharing inappropriate videos. Two percent said they had pressured people into sexual acts by offering rewards or threatening retaliation—that means 12 men admitted to this.1
Sadly, the health care industry is not immune from this corruption. In fact, sexual harassment is a major problem in health care—one that is particularly prevalent in nursing, according to Fiedler and Hamby.2 More than 50% of female nurses, physicians, and students report experiencing sexual harassment.3 And even that, I believe, is an underreported percentage.
Sexual harassment in the workplace includes any situation in which there is a demand for sexual favors in exchange for a job benefit or where an unwanted condition on any person’s employment is imposed because of that person’s sex. Since 1964, Title VII of the Civil Rights Act (42 USC Sec.2000e-2[a]) has prohibited discrimination in places of employment based on an individual’s sex.4 In 1976, it was acknowledged that this also prohibits sexual harassment as a form of sex discrimination. In 1991, amendments (42 USC Sec.1981 [a][1]) authorized compensatory and punitive damages as well as jury trials.5
The Equal Employment Opportunity Commission (EEOC), the federal agency that enforces Title VII, stipulates that
- Harassment can include unwelcome sexual advances, requests for sexual favors, and other verbal or physical harassment—but it does not have to be sexual in nature (eg, making offensive comments about women in general).
- Both women and men can be victims and harassers—and the victim and harasser can be the same sex.
- Harassment is illegal when it is so frequent or severe that it creates a hostile or offensive work environment, or when it results in an adverse employment decision (eg, the victim being fired or demoted).6
Although the EEOC guidelines are not law, they do guide the judicial interpretation of what constitutes sexual harassment. Sexual harassment is an increasing source of workplace lawsuits that often result in large judgments against employers. Clinicians can file class-action suits against hospitals and other institutions, and juries may render verdicts on harassment complaints to the tune of millions of dollars.
Unfortunately, it is common for workplace harassment to go unreported. According to the EEOC, standard responses to workplace sexual harassment include avoiding the harasser, denying or downplaying the gravity of the situation, or attempting to ignore, forget, or endure the behavior. The least common response is to take formal action—either by reporting it internally or filing a legal complaint. Further, roughly three of four individuals who experience harassment in the workplace never tell a supervisor, manager, or union representative due to fear of disbelief, inaction, blame, or social or professional retaliation.7
How can we, as clinicians, protect ourselves and others from this type of harassment? Establishing a strong zero-tolerance policy on sexual harassment and reporting unacceptable behavior is the only answer. I realize this is no easy issue, but we must be firm in our resolve. Although 2017 was a watershed year with “Silence Breaker” or “#MeToo,” there are still many voices not being heard.8
So, here is my request: If you have been directly affected by, or have observed, objectionable behavior that violates your organization’s policy or code of conduct (or your personal sense of decency), document the incident and report it. You may be hesitant; maybe you think the behavior is an isolated act, or maybe the offender is a well-liked colleague who usually acts professionally. But your role is not to decide whether this behavior is acute or chronic—the human resources department will determine that. Maybe you are reluctant to report harassment because you fear reprisal. This is understandable, but remember that intimidation allows the behavior to persist. If the incident was upsetting and objectionable, it needs to be reported—no matter what.
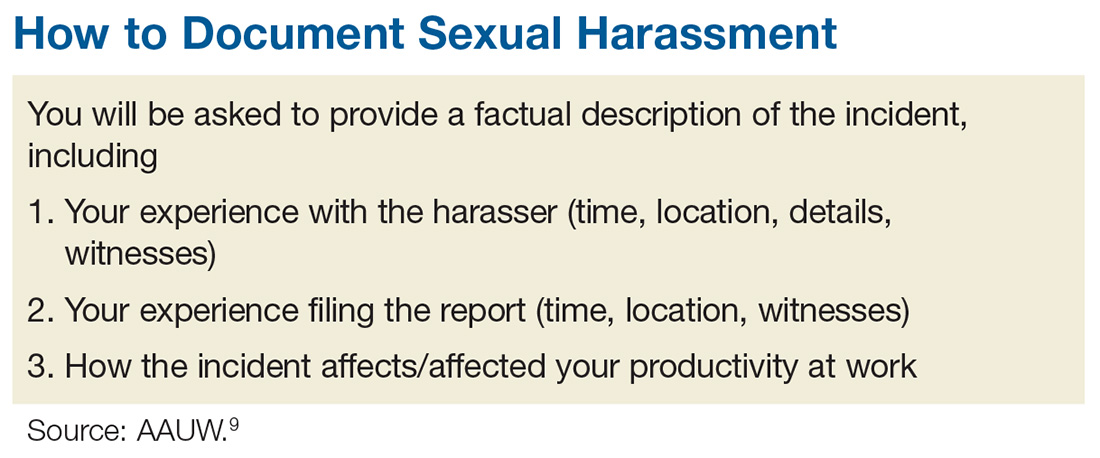
The process of documenting and reporting varies depending on your institution’s policy but typically involves writing a factual description of the incident, including the time, place, and a list of any witnesses (including patients). Make sure your report is objective, and include any effect the behavior has had on patient care. Document any verbal exchanges verbatim, if possible. File the report as soon as possible, and remember to document everything. Nothing is trivial when it comes to building a case against sexual harassment. After you document and report the incident, continue to act professionally.9
If you are unable to resolve a harassment-related issue through your employer’s internal procedure, you may need to pursue the matter via the EEOC or your state’s human rights or civil rights enforcement agency.10 But know that any time and effort you put into reporting this is worthwhile; predatory behavior often crosses the workplace to other social realms. The other people being affected will be grateful that you came forward.
Some of you may be reading this and thinking, “Easy for you to say, Randy. You are not the one being harassed!” I know. This is not an easy topic for anyone. I have been shocked and appalled by the level and prevalence of sexual harassment in the workplace. I was always taught (by my grandmother—thank you!) to respect women. My hope is that by introducing this sensitive topic, we can open the discussion and encourage everyone to speak up. Please share your thoughts, comments, and ideas with me at [email protected]—let’s start a conversation.
1. Patel JK, Griggs T, Cain Miller C. The UpShot: We asked 615 men about how they conduct themselves at work. The New York Times. December 28, 2017. www.nytimes.com/interactive/2017/12/28/upshot/sexual-harassment-survey-600-men.html. Accessed January 16, 2018.
2. Fiedler A, Hamby E. Sexual harassment in the workplace: nurses’ perceptions. J Nurs Adm. 2000;30(10):497-503.
3. Lockwood W. Sexual harassment in healthcare. www.rn.org/courses/coursematerial-236.pdf. Accessed January 16, 2018.
4. Legal Information Institute. 42 U.S. Code § 2000e–2 - Unlawful employment practices. www.law.cornell.edu/uscode/text/42/2000e-2. Accessed January 16, 2018.
5. US Equal Employment Opportunity Commission (EEOC). The Civil Rights Act of 1991. www.eeoc.gov/laws/statutes/cra-1991.cfm. Accessed January 16, 2018.
6. US EEOC. Sexual harassment. www.eeoc.gov/laws/types/sexual_harassment.cfm. Accessed January 16, 2018.
7. US EEOC. Select task force on the study of harassment in the workplace. June 2016. www.eeoc.gov/eeoc/task_force/harassment/report.cfm. Accessed January 16, 2018.
8. O’Brien SA, Carpenter J. 2017 was the year of (certain) women’s voices. December 28, 2017. www.ozarksfirst.com/news/business/2017-was-the-year-of-certain-womens-voices/889901636. Accessed January 16, 2018.
9. AAUW. Know your rights at work. www.aauw.org/what-we-do/legal-resources/know-your-rights-at-work/workplace-sexual-harassment/. Accessed January 16, 2018.
10. EEOC’s Charge Processing Procedures. http://employment.findlaw.com/employment-discrimination/eeoc-s-charge-processing-procedures.html. Accessed January 16, 2018.
1. Patel JK, Griggs T, Cain Miller C. The UpShot: We asked 615 men about how they conduct themselves at work. The New York Times. December 28, 2017. www.nytimes.com/interactive/2017/12/28/upshot/sexual-harassment-survey-600-men.html. Accessed January 16, 2018.
2. Fiedler A, Hamby E. Sexual harassment in the workplace: nurses’ perceptions. J Nurs Adm. 2000;30(10):497-503.
3. Lockwood W. Sexual harassment in healthcare. www.rn.org/courses/coursematerial-236.pdf. Accessed January 16, 2018.
4. Legal Information Institute. 42 U.S. Code § 2000e–2 - Unlawful employment practices. www.law.cornell.edu/uscode/text/42/2000e-2. Accessed January 16, 2018.
5. US Equal Employment Opportunity Commission (EEOC). The Civil Rights Act of 1991. www.eeoc.gov/laws/statutes/cra-1991.cfm. Accessed January 16, 2018.
6. US EEOC. Sexual harassment. www.eeoc.gov/laws/types/sexual_harassment.cfm. Accessed January 16, 2018.
7. US EEOC. Select task force on the study of harassment in the workplace. June 2016. www.eeoc.gov/eeoc/task_force/harassment/report.cfm. Accessed January 16, 2018.
8. O’Brien SA, Carpenter J. 2017 was the year of (certain) women’s voices. December 28, 2017. www.ozarksfirst.com/news/business/2017-was-the-year-of-certain-womens-voices/889901636. Accessed January 16, 2018.
9. AAUW. Know your rights at work. www.aauw.org/what-we-do/legal-resources/know-your-rights-at-work/workplace-sexual-harassment/. Accessed January 16, 2018.
10. EEOC’s Charge Processing Procedures. http://employment.findlaw.com/employment-discrimination/eeoc-s-charge-processing-procedures.html. Accessed January 16, 2018.
Myth Buster: Adrenal “Fatigue”
This video was filmed at Metabolic & Endocrine Disease Summit (MEDS). Click here to learn more.
This video was filmed at Metabolic & Endocrine Disease Summit (MEDS). Click here to learn more.
This video was filmed at Metabolic & Endocrine Disease Summit (MEDS). Click here to learn more.
'This has to change': Surgeon pain, disability on the rise
The evidence has been accumulating for decades: Practicing surgery can exact a toll on surgeons’ physical well-being in ways that can shorten careers and contribute to professional dissatisfaction.
“Ergonomists have described the surgeon’s work environment and working conditions as equal to, if not at times harsher than, those of certain industrial workers,” wrote Sherise Epstein, MPH, and the coauthors of the systematic review and meta-analysis of studies addressing the issue. Ms. Epstein, currently a 4th-year medical student at the University of California, San Diego, and her team found a high prevalence of work-related musculoskeletal disorders and pain among surgeons and interventionalists, with pooled prevalence estimates for pain among these physicians ranging from 35% to 60% of all respondents. Cervical spine disease, rotator cuff pathology, and degenerative lumbar spine disease were each reported by nearly one in five respondents in the pooled analyses, with increasing prevalence over the duration of the study period (JAMA Surg. 2017 Dec 27. doi:10.1001/jamasurg.2017.49).
These findings, called “worrisome” by the study’s authors, come at a time when the demand for surgeons and interventionalists is expected soon to outstrip supply, and point to a major stressor for a profession already plagued by high rates of burnout and depression.
The results of the study are in line with previous work that finds a high – and increasing – rate of pain and disability among at-risk physicians, who endure long work hours, awkward positioning, and few opportunities for breaks.
The study also suggested a possible linkage between work-related pain and other factors, such as burnout and depression, that lead to attrition in the surgical profession.
Adrian Park, MD, FACS, a general surgeon who has long studied the issue of work-related musculoskeletal disorders (MSDs) among surgeons and interventionalists, was not surprised by the study’s findings. “This just goes to further the narrative, which is a consistent one: These aren’t just sporadic instances of individual surgeons having a tough time; this is an increasingly broadly recognized problem. ... These are the consequences of surgeons simply getting up and going to work each week,” Dr. Park said in an interview.
To take a long view of the published data on work-related injury and pain for at-risk physicians, Ms. Epstein and her collaborators identified 126 articles reporting physician work-related MSDs that met quality standards; the studies spanned 1974 to 2016, and 23 countries were represented.
A total of 21 articles were eventually included in the meta-analysis, which included responses from 5,828 physicians. Most of the respondents were male (78.5%), with a mean age of 46 years and a mean 12.8 years in practice. The mean number of hours spent in procedures per week was 14.4.
Sixteen cross-sectional studies included in the meta-analysis examined injury prevalence, with 14 studies eventually meeting eligibility criteria for quantitative synthesis. A total of 4,245 physicians were included in this portion of the analysis; 1,232 were orthopedic surgeons, 1,118 were interventional cardiologists, and 582 were general surgeons (a variety of other subspecialties made up the remainder).
The career prevalence of degenerative lumbar spine disease was estimated at 19%, with prevalence increasing over time in a series of surveys of interventional cardiologists, said Ms. Epstein and her colleagues. Among this group, the prevalence climbed from 6.5% in 1997 to 24.7% in 2015, an increase in prevalence of over 18%, they said. The investigators’ estimate of lumbar spine disease prevalence from their own data also showed an increase, to 21%, for studies published within the past decade.
Rotator cuff pathology during the study period was estimated at 18% overall, and carpal tunnel syndrome at 9% overall; carpal tunnel syndrome also appears to be increasing in prevalence, estimated at 12% within the last decade.
Musculoskeletal pain that was judged to be work related was common, as reported in 18 cross-sectional studies. Taken together, the studies used a total of five validated tools that measured both pain prevalence and related disability. Twelve of the studies met criteria for inclusion in the quantitative synthesis.
Neck, back, and shoulder pain were all common in this group of surgeons and interventionalists. Neck pain had a 60% estimated 12-month prevalence, and shoulder pain was almost as common, with a 52% prevalence; back pain was reported for about half (49%) of respondents.
Just 10 of the included studies addressed disability burden, said Ms. Epstein and her colleagues. Overall, 12% of physicians responding in this subset of studies reported that they required work modification, leave of absence, or early retirement because of work-related MSDs.
In a separate arm of the analysis, Ms. Epstein and her collaborators looked at studies that discussed ergonomic assessments and interventions, using a qualitative approach. A total of 101 studies, 50 of them in the United States, were included. None of the studies, they said, “included long-term surveillance for work-related MSDs”; rather, they focused on short-term outcomes and, in some cases, on real-time electromyographic data.
Of the 101 studies looking at ergonomics, about a third (n = 38) looked primarily at ergonomically designed devices or technology, while another third (n = 37) focused on educational or behavioral interventions and modifications. These were the studies included in the investigators’ analysis.
A lack of awareness of ergonomic recommendations on the part of the surgeons themselves was identified in several studies. Several specialties, publishing in a total of eight countries, have put forward “at least one article describing a need for ergonomics education during medical training.” And, said the investigators, “A few studies have found that ergonomics education during medical training appears feasible, accepted, and effective at changing behaviors and reducing symptoms.”
In addition to the usual limitations inherent to the meta-analysis research design (selection bias, self-reported data, small samples of individual studies), the study was limited by the elusive nature of the topic. Work-related pain and disability among surgeons remains underreported and underestimated, according to both Dr. Park and the study investigators. Further research is needed, and the investigators wrote: “Ultimately, this work should be integrated with research on preventing surgeon burnout and attrition given shared risk factors.”
Micro breaks can help
What’s the solution? Dr. Park says that some fixes are low tech, and can be put in place immediately. He and his team implemented a series of brief breaks, taken every half hour during a procedure, that they dubbed “targeted stretching micro breaks.” These are 45- to 50-second breaks during which a series of exercise physiologist–designed brief stretches are undertaken that do not require breaking scrub.
In a study of 66 surgeons and operating room staff, Dr. Park, chair of the department of surgery at Anne Arundel Medical Center, Annapolis, Md., and his collaborators found that surgeons reported less pain and fatigue, and improved mental focus, when they took micro breaks during a procedure. When surgeons took micro breaks, operative time was no longer than when they didn’t take the breaks (Ann Surg. 2017 Feb;265[2]:340-6).
“We do this all the time in our operating room now,” said Dr. Park. “And it makes a difference in terms of pain, in terms of alertness, in terms of stamina. And it costs nothing.”
Major redesign of tools and workspace
Other targets for technological improvement include offering better-designed handles for laparoscopic instruments. “We’ve had one size fits all forever. Why has it taken us so long to recognize that there’s not one size of surgical hand?” asked Dr. Park. He made the point that the influx of women – whose hands are smaller on average than men’s – into the surgical professions makes this a particularly pressing issue.
“The high-tech piece is going to be a better understanding of the operative work flow,” said Dr. Park, calling for “a meaningful revisiting of the surgeon-device interface and the surgeon-patient interface.”
A fundamental redesign of the operating room will eventually be in order, he said, contrasting the surgeon’s environments with that of an airline pilot. In the cockpit, the pilot sees a “heads-up” display of a limited amount of data, with an eye to controlling the cognitive workload for the operator. By contrast, said Dr. Park, in the OR, there are “lights flashing, and things pinging,” and pieces of equipment don’t “talk” to each other, presenting sometimes overwhelming sensory input that just potentiates the stress of the environment. Operating room design, he said, should move toward an ergonomically improved and stimulus-controlled environment.
As the leader of the surgical team, and as a physician whose foremost concern is the patient on the table, the surgeon may inadvertently have fallen into a role where his or her well-being is neglected.
Dr. Park suggested that, in the surgical profession, “it has never felt safe or appropriate to talk about ourselves.” But for the good of the profession, and ultimately for patient care, “this has to change.”
Ms. Epstein and her coauthors reported no conflicts of interest. .
We rarely think of surgeons as athletes and certainly we sometimes don’t look like athletes, but surgery is a performance sport that includes strength and grace. Many surgeons are also very active outside the OR. So, not only OR activity but all the other activities are stacked upon our bodies. Posture, strength training, and ergonomics need to be part of our training just as it would for a pitcher for the Kansas City Royals. You wouldn’t expect the pitcher’s arm to last long without coaching and training physically. That player’s career would be shortened. Why would we expect surgeons to be different? Our game is 90% mental, but the other half is physical (with respect to Yogi Berra).
We rarely think of surgeons as athletes and certainly we sometimes don’t look like athletes, but surgery is a performance sport that includes strength and grace. Many surgeons are also very active outside the OR. So, not only OR activity but all the other activities are stacked upon our bodies. Posture, strength training, and ergonomics need to be part of our training just as it would for a pitcher for the Kansas City Royals. You wouldn’t expect the pitcher’s arm to last long without coaching and training physically. That player’s career would be shortened. Why would we expect surgeons to be different? Our game is 90% mental, but the other half is physical (with respect to Yogi Berra).
We rarely think of surgeons as athletes and certainly we sometimes don’t look like athletes, but surgery is a performance sport that includes strength and grace. Many surgeons are also very active outside the OR. So, not only OR activity but all the other activities are stacked upon our bodies. Posture, strength training, and ergonomics need to be part of our training just as it would for a pitcher for the Kansas City Royals. You wouldn’t expect the pitcher’s arm to last long without coaching and training physically. That player’s career would be shortened. Why would we expect surgeons to be different? Our game is 90% mental, but the other half is physical (with respect to Yogi Berra).
The evidence has been accumulating for decades: Practicing surgery can exact a toll on surgeons’ physical well-being in ways that can shorten careers and contribute to professional dissatisfaction.
“Ergonomists have described the surgeon’s work environment and working conditions as equal to, if not at times harsher than, those of certain industrial workers,” wrote Sherise Epstein, MPH, and the coauthors of the systematic review and meta-analysis of studies addressing the issue. Ms. Epstein, currently a 4th-year medical student at the University of California, San Diego, and her team found a high prevalence of work-related musculoskeletal disorders and pain among surgeons and interventionalists, with pooled prevalence estimates for pain among these physicians ranging from 35% to 60% of all respondents. Cervical spine disease, rotator cuff pathology, and degenerative lumbar spine disease were each reported by nearly one in five respondents in the pooled analyses, with increasing prevalence over the duration of the study period (JAMA Surg. 2017 Dec 27. doi:10.1001/jamasurg.2017.49).
These findings, called “worrisome” by the study’s authors, come at a time when the demand for surgeons and interventionalists is expected soon to outstrip supply, and point to a major stressor for a profession already plagued by high rates of burnout and depression.
The results of the study are in line with previous work that finds a high – and increasing – rate of pain and disability among at-risk physicians, who endure long work hours, awkward positioning, and few opportunities for breaks.
The study also suggested a possible linkage between work-related pain and other factors, such as burnout and depression, that lead to attrition in the surgical profession.
Adrian Park, MD, FACS, a general surgeon who has long studied the issue of work-related musculoskeletal disorders (MSDs) among surgeons and interventionalists, was not surprised by the study’s findings. “This just goes to further the narrative, which is a consistent one: These aren’t just sporadic instances of individual surgeons having a tough time; this is an increasingly broadly recognized problem. ... These are the consequences of surgeons simply getting up and going to work each week,” Dr. Park said in an interview.
To take a long view of the published data on work-related injury and pain for at-risk physicians, Ms. Epstein and her collaborators identified 126 articles reporting physician work-related MSDs that met quality standards; the studies spanned 1974 to 2016, and 23 countries were represented.
A total of 21 articles were eventually included in the meta-analysis, which included responses from 5,828 physicians. Most of the respondents were male (78.5%), with a mean age of 46 years and a mean 12.8 years in practice. The mean number of hours spent in procedures per week was 14.4.
Sixteen cross-sectional studies included in the meta-analysis examined injury prevalence, with 14 studies eventually meeting eligibility criteria for quantitative synthesis. A total of 4,245 physicians were included in this portion of the analysis; 1,232 were orthopedic surgeons, 1,118 were interventional cardiologists, and 582 were general surgeons (a variety of other subspecialties made up the remainder).
The career prevalence of degenerative lumbar spine disease was estimated at 19%, with prevalence increasing over time in a series of surveys of interventional cardiologists, said Ms. Epstein and her colleagues. Among this group, the prevalence climbed from 6.5% in 1997 to 24.7% in 2015, an increase in prevalence of over 18%, they said. The investigators’ estimate of lumbar spine disease prevalence from their own data also showed an increase, to 21%, for studies published within the past decade.
Rotator cuff pathology during the study period was estimated at 18% overall, and carpal tunnel syndrome at 9% overall; carpal tunnel syndrome also appears to be increasing in prevalence, estimated at 12% within the last decade.
Musculoskeletal pain that was judged to be work related was common, as reported in 18 cross-sectional studies. Taken together, the studies used a total of five validated tools that measured both pain prevalence and related disability. Twelve of the studies met criteria for inclusion in the quantitative synthesis.
Neck, back, and shoulder pain were all common in this group of surgeons and interventionalists. Neck pain had a 60% estimated 12-month prevalence, and shoulder pain was almost as common, with a 52% prevalence; back pain was reported for about half (49%) of respondents.
Just 10 of the included studies addressed disability burden, said Ms. Epstein and her colleagues. Overall, 12% of physicians responding in this subset of studies reported that they required work modification, leave of absence, or early retirement because of work-related MSDs.
In a separate arm of the analysis, Ms. Epstein and her collaborators looked at studies that discussed ergonomic assessments and interventions, using a qualitative approach. A total of 101 studies, 50 of them in the United States, were included. None of the studies, they said, “included long-term surveillance for work-related MSDs”; rather, they focused on short-term outcomes and, in some cases, on real-time electromyographic data.
Of the 101 studies looking at ergonomics, about a third (n = 38) looked primarily at ergonomically designed devices or technology, while another third (n = 37) focused on educational or behavioral interventions and modifications. These were the studies included in the investigators’ analysis.
A lack of awareness of ergonomic recommendations on the part of the surgeons themselves was identified in several studies. Several specialties, publishing in a total of eight countries, have put forward “at least one article describing a need for ergonomics education during medical training.” And, said the investigators, “A few studies have found that ergonomics education during medical training appears feasible, accepted, and effective at changing behaviors and reducing symptoms.”
In addition to the usual limitations inherent to the meta-analysis research design (selection bias, self-reported data, small samples of individual studies), the study was limited by the elusive nature of the topic. Work-related pain and disability among surgeons remains underreported and underestimated, according to both Dr. Park and the study investigators. Further research is needed, and the investigators wrote: “Ultimately, this work should be integrated with research on preventing surgeon burnout and attrition given shared risk factors.”
Micro breaks can help
What’s the solution? Dr. Park says that some fixes are low tech, and can be put in place immediately. He and his team implemented a series of brief breaks, taken every half hour during a procedure, that they dubbed “targeted stretching micro breaks.” These are 45- to 50-second breaks during which a series of exercise physiologist–designed brief stretches are undertaken that do not require breaking scrub.
In a study of 66 surgeons and operating room staff, Dr. Park, chair of the department of surgery at Anne Arundel Medical Center, Annapolis, Md., and his collaborators found that surgeons reported less pain and fatigue, and improved mental focus, when they took micro breaks during a procedure. When surgeons took micro breaks, operative time was no longer than when they didn’t take the breaks (Ann Surg. 2017 Feb;265[2]:340-6).
“We do this all the time in our operating room now,” said Dr. Park. “And it makes a difference in terms of pain, in terms of alertness, in terms of stamina. And it costs nothing.”
Major redesign of tools and workspace
Other targets for technological improvement include offering better-designed handles for laparoscopic instruments. “We’ve had one size fits all forever. Why has it taken us so long to recognize that there’s not one size of surgical hand?” asked Dr. Park. He made the point that the influx of women – whose hands are smaller on average than men’s – into the surgical professions makes this a particularly pressing issue.
“The high-tech piece is going to be a better understanding of the operative work flow,” said Dr. Park, calling for “a meaningful revisiting of the surgeon-device interface and the surgeon-patient interface.”
A fundamental redesign of the operating room will eventually be in order, he said, contrasting the surgeon’s environments with that of an airline pilot. In the cockpit, the pilot sees a “heads-up” display of a limited amount of data, with an eye to controlling the cognitive workload for the operator. By contrast, said Dr. Park, in the OR, there are “lights flashing, and things pinging,” and pieces of equipment don’t “talk” to each other, presenting sometimes overwhelming sensory input that just potentiates the stress of the environment. Operating room design, he said, should move toward an ergonomically improved and stimulus-controlled environment.
As the leader of the surgical team, and as a physician whose foremost concern is the patient on the table, the surgeon may inadvertently have fallen into a role where his or her well-being is neglected.
Dr. Park suggested that, in the surgical profession, “it has never felt safe or appropriate to talk about ourselves.” But for the good of the profession, and ultimately for patient care, “this has to change.”
Ms. Epstein and her coauthors reported no conflicts of interest. .
The evidence has been accumulating for decades: Practicing surgery can exact a toll on surgeons’ physical well-being in ways that can shorten careers and contribute to professional dissatisfaction.
“Ergonomists have described the surgeon’s work environment and working conditions as equal to, if not at times harsher than, those of certain industrial workers,” wrote Sherise Epstein, MPH, and the coauthors of the systematic review and meta-analysis of studies addressing the issue. Ms. Epstein, currently a 4th-year medical student at the University of California, San Diego, and her team found a high prevalence of work-related musculoskeletal disorders and pain among surgeons and interventionalists, with pooled prevalence estimates for pain among these physicians ranging from 35% to 60% of all respondents. Cervical spine disease, rotator cuff pathology, and degenerative lumbar spine disease were each reported by nearly one in five respondents in the pooled analyses, with increasing prevalence over the duration of the study period (JAMA Surg. 2017 Dec 27. doi:10.1001/jamasurg.2017.49).
These findings, called “worrisome” by the study’s authors, come at a time when the demand for surgeons and interventionalists is expected soon to outstrip supply, and point to a major stressor for a profession already plagued by high rates of burnout and depression.
The results of the study are in line with previous work that finds a high – and increasing – rate of pain and disability among at-risk physicians, who endure long work hours, awkward positioning, and few opportunities for breaks.
The study also suggested a possible linkage between work-related pain and other factors, such as burnout and depression, that lead to attrition in the surgical profession.
Adrian Park, MD, FACS, a general surgeon who has long studied the issue of work-related musculoskeletal disorders (MSDs) among surgeons and interventionalists, was not surprised by the study’s findings. “This just goes to further the narrative, which is a consistent one: These aren’t just sporadic instances of individual surgeons having a tough time; this is an increasingly broadly recognized problem. ... These are the consequences of surgeons simply getting up and going to work each week,” Dr. Park said in an interview.
To take a long view of the published data on work-related injury and pain for at-risk physicians, Ms. Epstein and her collaborators identified 126 articles reporting physician work-related MSDs that met quality standards; the studies spanned 1974 to 2016, and 23 countries were represented.
A total of 21 articles were eventually included in the meta-analysis, which included responses from 5,828 physicians. Most of the respondents were male (78.5%), with a mean age of 46 years and a mean 12.8 years in practice. The mean number of hours spent in procedures per week was 14.4.
Sixteen cross-sectional studies included in the meta-analysis examined injury prevalence, with 14 studies eventually meeting eligibility criteria for quantitative synthesis. A total of 4,245 physicians were included in this portion of the analysis; 1,232 were orthopedic surgeons, 1,118 were interventional cardiologists, and 582 were general surgeons (a variety of other subspecialties made up the remainder).
The career prevalence of degenerative lumbar spine disease was estimated at 19%, with prevalence increasing over time in a series of surveys of interventional cardiologists, said Ms. Epstein and her colleagues. Among this group, the prevalence climbed from 6.5% in 1997 to 24.7% in 2015, an increase in prevalence of over 18%, they said. The investigators’ estimate of lumbar spine disease prevalence from their own data also showed an increase, to 21%, for studies published within the past decade.
Rotator cuff pathology during the study period was estimated at 18% overall, and carpal tunnel syndrome at 9% overall; carpal tunnel syndrome also appears to be increasing in prevalence, estimated at 12% within the last decade.
Musculoskeletal pain that was judged to be work related was common, as reported in 18 cross-sectional studies. Taken together, the studies used a total of five validated tools that measured both pain prevalence and related disability. Twelve of the studies met criteria for inclusion in the quantitative synthesis.
Neck, back, and shoulder pain were all common in this group of surgeons and interventionalists. Neck pain had a 60% estimated 12-month prevalence, and shoulder pain was almost as common, with a 52% prevalence; back pain was reported for about half (49%) of respondents.
Just 10 of the included studies addressed disability burden, said Ms. Epstein and her colleagues. Overall, 12% of physicians responding in this subset of studies reported that they required work modification, leave of absence, or early retirement because of work-related MSDs.
In a separate arm of the analysis, Ms. Epstein and her collaborators looked at studies that discussed ergonomic assessments and interventions, using a qualitative approach. A total of 101 studies, 50 of them in the United States, were included. None of the studies, they said, “included long-term surveillance for work-related MSDs”; rather, they focused on short-term outcomes and, in some cases, on real-time electromyographic data.
Of the 101 studies looking at ergonomics, about a third (n = 38) looked primarily at ergonomically designed devices or technology, while another third (n = 37) focused on educational or behavioral interventions and modifications. These were the studies included in the investigators’ analysis.
A lack of awareness of ergonomic recommendations on the part of the surgeons themselves was identified in several studies. Several specialties, publishing in a total of eight countries, have put forward “at least one article describing a need for ergonomics education during medical training.” And, said the investigators, “A few studies have found that ergonomics education during medical training appears feasible, accepted, and effective at changing behaviors and reducing symptoms.”
In addition to the usual limitations inherent to the meta-analysis research design (selection bias, self-reported data, small samples of individual studies), the study was limited by the elusive nature of the topic. Work-related pain and disability among surgeons remains underreported and underestimated, according to both Dr. Park and the study investigators. Further research is needed, and the investigators wrote: “Ultimately, this work should be integrated with research on preventing surgeon burnout and attrition given shared risk factors.”
Micro breaks can help
What’s the solution? Dr. Park says that some fixes are low tech, and can be put in place immediately. He and his team implemented a series of brief breaks, taken every half hour during a procedure, that they dubbed “targeted stretching micro breaks.” These are 45- to 50-second breaks during which a series of exercise physiologist–designed brief stretches are undertaken that do not require breaking scrub.
In a study of 66 surgeons and operating room staff, Dr. Park, chair of the department of surgery at Anne Arundel Medical Center, Annapolis, Md., and his collaborators found that surgeons reported less pain and fatigue, and improved mental focus, when they took micro breaks during a procedure. When surgeons took micro breaks, operative time was no longer than when they didn’t take the breaks (Ann Surg. 2017 Feb;265[2]:340-6).
“We do this all the time in our operating room now,” said Dr. Park. “And it makes a difference in terms of pain, in terms of alertness, in terms of stamina. And it costs nothing.”
Major redesign of tools and workspace
Other targets for technological improvement include offering better-designed handles for laparoscopic instruments. “We’ve had one size fits all forever. Why has it taken us so long to recognize that there’s not one size of surgical hand?” asked Dr. Park. He made the point that the influx of women – whose hands are smaller on average than men’s – into the surgical professions makes this a particularly pressing issue.
“The high-tech piece is going to be a better understanding of the operative work flow,” said Dr. Park, calling for “a meaningful revisiting of the surgeon-device interface and the surgeon-patient interface.”
A fundamental redesign of the operating room will eventually be in order, he said, contrasting the surgeon’s environments with that of an airline pilot. In the cockpit, the pilot sees a “heads-up” display of a limited amount of data, with an eye to controlling the cognitive workload for the operator. By contrast, said Dr. Park, in the OR, there are “lights flashing, and things pinging,” and pieces of equipment don’t “talk” to each other, presenting sometimes overwhelming sensory input that just potentiates the stress of the environment. Operating room design, he said, should move toward an ergonomically improved and stimulus-controlled environment.
As the leader of the surgical team, and as a physician whose foremost concern is the patient on the table, the surgeon may inadvertently have fallen into a role where his or her well-being is neglected.
Dr. Park suggested that, in the surgical profession, “it has never felt safe or appropriate to talk about ourselves.” But for the good of the profession, and ultimately for patient care, “this has to change.”
Ms. Epstein and her coauthors reported no conflicts of interest. .
Satisfaction is high for cantharidin in molluscum contagiosum
said Marla N. Jahnke, MD, of the Henry Ford Health System, Detroit, and her associates.
It is important to be careful when applying or handling cantharidin near the eyes, they noted. Also, parents must be counseled about possible side effects such as painful blistering, dyspigmentation, scarring, and itching, and that multiple treatment sessions may be needed.
The researchers did a retrospective chart review on patients under age 18 years treated with a cantharidin 0.7% solution between March 2013 and March 2014 at their institution, and performed a telephone survey to collect treatment outcomes from caregivers. Of the 62 caregivers contacted, the pediatric patients’ median age was 5 years (range 1.7-13), and 45% of the patients were white, 26% were black, 20% were Middle Eastern, 6% were Latino, and 3% were Asian, Pacific Islander, or Indian.
After cantharidin treatment, the caregivers most often described temporary discoloration (18%), severe blistering (10%), and pain that was excessive or greater than the caregiver expected (10%). Other outcomes described included itching (8%), scarring (6%), irritation (5%), bleeding (3%), and spreading of lesions (2%).
“Two patients returned to the office within 1 week of treatment because of excessive localized blistering that healed without long-term complications when topical emollients were used. ... Caregivers often could not confirm that they had washed off the cantharidin as recommended (1.5-2 hours after in-office application),” Dr. Jahnke and her associates noted in a research letter, which was published in the Journal of the American Academy of Dermatology.
Treatment satisfaction was high, with 94% of caregivers saying they would request cantharidin again if molluscum contagiosum were to recur on the child’s face, and 92% saying they would recommend it to others whose children had facial molluscum contagiosum. On a scale of 1 to 10, the average treatment satisfaction score was 8.7. The caregivers said that cantharidin was well tolerated by their children because it was painless when applied. The need for multiple office visits was the biggest complaint, the researchers revealed.
SOURCE: J Am Acad Dermatol. 2018 Jan. doi: 10.1016/j.jaad.2017.09.006.
said Marla N. Jahnke, MD, of the Henry Ford Health System, Detroit, and her associates.
It is important to be careful when applying or handling cantharidin near the eyes, they noted. Also, parents must be counseled about possible side effects such as painful blistering, dyspigmentation, scarring, and itching, and that multiple treatment sessions may be needed.
The researchers did a retrospective chart review on patients under age 18 years treated with a cantharidin 0.7% solution between March 2013 and March 2014 at their institution, and performed a telephone survey to collect treatment outcomes from caregivers. Of the 62 caregivers contacted, the pediatric patients’ median age was 5 years (range 1.7-13), and 45% of the patients were white, 26% were black, 20% were Middle Eastern, 6% were Latino, and 3% were Asian, Pacific Islander, or Indian.
After cantharidin treatment, the caregivers most often described temporary discoloration (18%), severe blistering (10%), and pain that was excessive or greater than the caregiver expected (10%). Other outcomes described included itching (8%), scarring (6%), irritation (5%), bleeding (3%), and spreading of lesions (2%).
“Two patients returned to the office within 1 week of treatment because of excessive localized blistering that healed without long-term complications when topical emollients were used. ... Caregivers often could not confirm that they had washed off the cantharidin as recommended (1.5-2 hours after in-office application),” Dr. Jahnke and her associates noted in a research letter, which was published in the Journal of the American Academy of Dermatology.
Treatment satisfaction was high, with 94% of caregivers saying they would request cantharidin again if molluscum contagiosum were to recur on the child’s face, and 92% saying they would recommend it to others whose children had facial molluscum contagiosum. On a scale of 1 to 10, the average treatment satisfaction score was 8.7. The caregivers said that cantharidin was well tolerated by their children because it was painless when applied. The need for multiple office visits was the biggest complaint, the researchers revealed.
SOURCE: J Am Acad Dermatol. 2018 Jan. doi: 10.1016/j.jaad.2017.09.006.
said Marla N. Jahnke, MD, of the Henry Ford Health System, Detroit, and her associates.
It is important to be careful when applying or handling cantharidin near the eyes, they noted. Also, parents must be counseled about possible side effects such as painful blistering, dyspigmentation, scarring, and itching, and that multiple treatment sessions may be needed.
The researchers did a retrospective chart review on patients under age 18 years treated with a cantharidin 0.7% solution between March 2013 and March 2014 at their institution, and performed a telephone survey to collect treatment outcomes from caregivers. Of the 62 caregivers contacted, the pediatric patients’ median age was 5 years (range 1.7-13), and 45% of the patients were white, 26% were black, 20% were Middle Eastern, 6% were Latino, and 3% were Asian, Pacific Islander, or Indian.
After cantharidin treatment, the caregivers most often described temporary discoloration (18%), severe blistering (10%), and pain that was excessive or greater than the caregiver expected (10%). Other outcomes described included itching (8%), scarring (6%), irritation (5%), bleeding (3%), and spreading of lesions (2%).
“Two patients returned to the office within 1 week of treatment because of excessive localized blistering that healed without long-term complications when topical emollients were used. ... Caregivers often could not confirm that they had washed off the cantharidin as recommended (1.5-2 hours after in-office application),” Dr. Jahnke and her associates noted in a research letter, which was published in the Journal of the American Academy of Dermatology.
Treatment satisfaction was high, with 94% of caregivers saying they would request cantharidin again if molluscum contagiosum were to recur on the child’s face, and 92% saying they would recommend it to others whose children had facial molluscum contagiosum. On a scale of 1 to 10, the average treatment satisfaction score was 8.7. The caregivers said that cantharidin was well tolerated by their children because it was painless when applied. The need for multiple office visits was the biggest complaint, the researchers revealed.
SOURCE: J Am Acad Dermatol. 2018 Jan. doi: 10.1016/j.jaad.2017.09.006.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY






