User login
Method may predict relapse at BCP-ALL diagnosis
Researchers say they have developed a technique that can help them determine, at diagnosis, whether children with B-cell precursor acute lymphoblastic leukemia (BCP-ALL) will relapse after treatment.
The method involves examining individual leukemia cells using mass cytometry.
In looking at the cells’ stage of development and signaling behavior, the researchers were able to identify a subset of malignant cells that predispose a patient to relapse.
The team described this method, which they termed “developmentally dependent predictor of relapse (DDPR),” in Nature Medicine.
Prior research suggested relapse may be driven by treatment-resistant cells that are present from the beginning of disease development.
“We wondered, can we identify those cells at the time the patient first presents to the clinic, and can we treat patients with a specific therapy to target them?” said study author Kara Davis, DO, of Stanford University in California.
Dr Davis and her colleagues used mass cytometry to analyze diagnostic bone marrow samples from 60 patients with BCP-ALL.
To pinpoint the problematic cells among the millions of cells in each patient’s sample, the researchers had to figure out how to organize the data.
“Every patient has vastly different features to their cancer,” Dr Davis said, “and we had to ask, ‘Is there any common thread between them?’”
The solution, the researchers found, was to match BCP-ALL cells and healthy B cells according to their developmental states, comparing the leukemic cells to the healthy cells.
The comparison revealed 6 features of leukemic cell populations that were associated with relapse.
Broadly, the features suggested that pro-BII cells with activated mTOR signaling were associated with relapse, as were pre-BI cells with activated and unresponsive pre-B-cell receptor signaling.
“We do not understand the mechanisms by which malignant cells from the pro-BII and pre-BI stages of development resist treatment,” Dr Davis noted.
However, she and her colleagues were able to show the leukemic cell features identified by DDPR could predict relapse in the BCP-ALL patients.
Of the 60 patients analyzed, there were 54 with at least 3 years of follow-up. The researchers divided these patients into a training cohort (n=44) and a validation cohort (n=10).
The team used an integrated cumulative/dynamic area under the curve (iAUC) and a C-statistic to assess DDPR performance in both cohorts.
In the training cohort, DDPR had an iAUC value of 0.92 and a C-statistic of 0.87. In the validation cohort, DDPR had an iAUC value of 0.85 and a C-statistic of 0.87.
The researchers also said DDPR “performed well” in predicting relapse-free survival in a retrospective analysis of both cohorts (P = 2.8 × 10−7).
Now, the researchers plan to validate DDPR in a larger number of patients and evaluate whether the same general approach could predict relapse in other cancers.
Researchers say they have developed a technique that can help them determine, at diagnosis, whether children with B-cell precursor acute lymphoblastic leukemia (BCP-ALL) will relapse after treatment.
The method involves examining individual leukemia cells using mass cytometry.
In looking at the cells’ stage of development and signaling behavior, the researchers were able to identify a subset of malignant cells that predispose a patient to relapse.
The team described this method, which they termed “developmentally dependent predictor of relapse (DDPR),” in Nature Medicine.
Prior research suggested relapse may be driven by treatment-resistant cells that are present from the beginning of disease development.
“We wondered, can we identify those cells at the time the patient first presents to the clinic, and can we treat patients with a specific therapy to target them?” said study author Kara Davis, DO, of Stanford University in California.
Dr Davis and her colleagues used mass cytometry to analyze diagnostic bone marrow samples from 60 patients with BCP-ALL.
To pinpoint the problematic cells among the millions of cells in each patient’s sample, the researchers had to figure out how to organize the data.
“Every patient has vastly different features to their cancer,” Dr Davis said, “and we had to ask, ‘Is there any common thread between them?’”
The solution, the researchers found, was to match BCP-ALL cells and healthy B cells according to their developmental states, comparing the leukemic cells to the healthy cells.
The comparison revealed 6 features of leukemic cell populations that were associated with relapse.
Broadly, the features suggested that pro-BII cells with activated mTOR signaling were associated with relapse, as were pre-BI cells with activated and unresponsive pre-B-cell receptor signaling.
“We do not understand the mechanisms by which malignant cells from the pro-BII and pre-BI stages of development resist treatment,” Dr Davis noted.
However, she and her colleagues were able to show the leukemic cell features identified by DDPR could predict relapse in the BCP-ALL patients.
Of the 60 patients analyzed, there were 54 with at least 3 years of follow-up. The researchers divided these patients into a training cohort (n=44) and a validation cohort (n=10).
The team used an integrated cumulative/dynamic area under the curve (iAUC) and a C-statistic to assess DDPR performance in both cohorts.
In the training cohort, DDPR had an iAUC value of 0.92 and a C-statistic of 0.87. In the validation cohort, DDPR had an iAUC value of 0.85 and a C-statistic of 0.87.
The researchers also said DDPR “performed well” in predicting relapse-free survival in a retrospective analysis of both cohorts (P = 2.8 × 10−7).
Now, the researchers plan to validate DDPR in a larger number of patients and evaluate whether the same general approach could predict relapse in other cancers.
Researchers say they have developed a technique that can help them determine, at diagnosis, whether children with B-cell precursor acute lymphoblastic leukemia (BCP-ALL) will relapse after treatment.
The method involves examining individual leukemia cells using mass cytometry.
In looking at the cells’ stage of development and signaling behavior, the researchers were able to identify a subset of malignant cells that predispose a patient to relapse.
The team described this method, which they termed “developmentally dependent predictor of relapse (DDPR),” in Nature Medicine.
Prior research suggested relapse may be driven by treatment-resistant cells that are present from the beginning of disease development.
“We wondered, can we identify those cells at the time the patient first presents to the clinic, and can we treat patients with a specific therapy to target them?” said study author Kara Davis, DO, of Stanford University in California.
Dr Davis and her colleagues used mass cytometry to analyze diagnostic bone marrow samples from 60 patients with BCP-ALL.
To pinpoint the problematic cells among the millions of cells in each patient’s sample, the researchers had to figure out how to organize the data.
“Every patient has vastly different features to their cancer,” Dr Davis said, “and we had to ask, ‘Is there any common thread between them?’”
The solution, the researchers found, was to match BCP-ALL cells and healthy B cells according to their developmental states, comparing the leukemic cells to the healthy cells.
The comparison revealed 6 features of leukemic cell populations that were associated with relapse.
Broadly, the features suggested that pro-BII cells with activated mTOR signaling were associated with relapse, as were pre-BI cells with activated and unresponsive pre-B-cell receptor signaling.
“We do not understand the mechanisms by which malignant cells from the pro-BII and pre-BI stages of development resist treatment,” Dr Davis noted.
However, she and her colleagues were able to show the leukemic cell features identified by DDPR could predict relapse in the BCP-ALL patients.
Of the 60 patients analyzed, there were 54 with at least 3 years of follow-up. The researchers divided these patients into a training cohort (n=44) and a validation cohort (n=10).
The team used an integrated cumulative/dynamic area under the curve (iAUC) and a C-statistic to assess DDPR performance in both cohorts.
In the training cohort, DDPR had an iAUC value of 0.92 and a C-statistic of 0.87. In the validation cohort, DDPR had an iAUC value of 0.85 and a C-statistic of 0.87.
The researchers also said DDPR “performed well” in predicting relapse-free survival in a retrospective analysis of both cohorts (P = 2.8 × 10−7).
Now, the researchers plan to validate DDPR in a larger number of patients and evaluate whether the same general approach could predict relapse in other cancers.
Outcomes appear similar with MAC and RIC
SALT LAKE CITY—New research suggests outcomes may be similar whether patients receive myeloablative conditioning (MAC) or reduced-intensity conditioning (RIC) prior to haploidentical peripheral blood stem cell transplant (haploPBSCT) with post-transplant cyclophosphamide (PTCy).
Results from 2 parallel, phase 2 trials showed that MAC-PTCy-haploPBSCT and RIC-PTCy-haploPBSCT produced comparable rates of engraftment, acute and chronic graft-versus host disease (GVHD), relapse, and non-relapse mortality (NRM).
Rates of overall survival (OS) and event-free survival (EFS) were significantly higher in the MAC group. However, the fact that some RIC recipients had received prior allogeneic transplants—and none of the MAC recipients had—appeared to play a role in survival outcomes.
Junichi Sugita, MD, PhD, of Hokkaido University in Sapporo, Japan, presented these results at the 2018 BMT Tandem Meetings (abstract 50*).
To compare MAC and RIC in the context of PTCy-haploPBSCT, Dr Sugita and his colleagues conducted 2 parallel studies—JSCT Haplo 14 MAC and JSCT Haplo 14 RIC.
Patients
There were 50 patients in the MAC trial and 77 in the RIC trial. They had median ages of 36 (range, 17 to 60) and 58 (range, 22 to 65), respectively (P<0.01). There was a greater percentage of male patients among MAC recipients (82% vs 62%, P=0.028).
Diagnoses were similar between the groups and included:
- Acute myeloid leukemia—23 MAC, 34 RIC
- Acute lymphoblastic leukemia—11 MAC, 14 RIC
- Myelodysplastic syndromes/myeloproliferative neoplasms—6 MAC, 12 RIC
- Lymphoma—6 MAC, 14 RIC
- “Other”—4 MAC, 3 RIC.
Forty-eight percent (n=24) of MAC recipients and 58% (n=45) of RIC recipients were not in remission at transplant (P=0.48). There were no significant differences in disease risk index (P=0.34).
Thirty-nine percent of RIC recipients (n=30) had a history of allogeneic transplant, but none of the MAC recipients did (P<0.01).
Conditioning and prophylaxis
There were 2 MAC regimens. One consisted of fludarabine (Flu, 30 mg/m2/day on days -6 to -4) plus total body irradiation (TBI, 12 Gy on days -3 to -1). The other consisted of Flu (30 mg/m2/day on days -6 to -2), busulfan (BU, 3.2 mg/kg/day on days -6 to -3), and TBI (4 Gy on day -1).
The RIC regimen consisted of Flu (30 mg/m2/day on days -6 to -2), BU (3.2 mg/kg/day on days -4 to -3), and TBI (4 Gy on day -1).
All patients received GVHD prophylaxis consisting of cyclophosphamide (50 mg/kg/day on days 3 and 4), tacrolimus (days 5 to 180), and mycophenolate mofetil (days 5 to 60).
Graft
Siblings were the most common donors for MAC recipients (50%, n=25), followed by parents (28%, n=14), children (16%, n=8), and “other” donors (6%, n=3).
Children were the most common donors for RIC recipients (60%, n=46), followed by siblings (33%, n=25), and parents (8%, n=6).
There was no significant difference between MAC and RIC recipients when it came to human leukocyte antigen matching, cytomegalovirus serostatus, or CD34 cell dose.
However, there was a significant difference in donor-recipient gender matching (P=0.033).
Fifty-two percent (n=26) of MAC recipients and 62% (n=48) of RIC recipients had a donor-recipient gender match. Forty-two percent (n=21) and 22% (n=17), respectively, had female donor to male recipient.
Engraftment and GVHD
“Hematopoietic recovery was similar between MAC and RIC,” Dr Sugita said.
The cumulative incidence of neutrophil engraftment was 98% in MAC recipients and 94% in RIC recipients. The median time to neutrophil engraftment was 17 days and 18 days, respectively (P=0.10).
The cumulative incidence of platelet engraftment was 84% in the MAC recipients and 74% in the RIC recipients. The median time to platelet engraftment was 31 days and 37 days, respectively (P=0.32).
“Complete chimerism was achieved in all engrafted patients,” Dr Sugita noted.
There was no significant difference between MAC and RIC recipients when it came to acute or chronic GVHD.
At day 100, the cumulative incidence of grade 2-4 acute GVHD was 18% in the MAC group and 14% in the RIC group (P=0.52). Grade 3-4 acute GVHD was 8% and 5%, respectively (P=0.52).
At 2 years, the cumulative incidence of all-grade chronic GVHD was 36% in the MAC group and 27% in the RIC group (P=0.24). Moderate to severe chronic GVHD was 20% in both groups (P=1.0).
Relapse and survival
There was no significant between-group difference in NRM or relapse.
The cumulative incidence of NRM at 2 years was 20% in the RIC group and 10% in the MAC group (P=0.15). The cumulative incidence of relapse at 2 years was 45% and 36%, respectively (P=0.32).
Survival was superior in the MAC recipients. The 2-year OS was 68% in the MAC group and 44% in the RIC group (P=0.02). The 2-year EFS was 54% and 35%, respectively (P=0.04).
However, survival appeared to be affected by history of allogeneic transplant.
“Patients with a history of prior allogenic SCT have significantly worse overall survival and event-free survival,” Dr Sugita said.
Two-year OS was 31% in RIC recipients with a history of transplant and 52% in RIC recipients without a history of transplant (P=0.04). The OS was 68% in MAC recipients, all of whom had no history of transplant.
Two-year EFS was 21%, 44%, and 54%, respectively (P=0.02 for difference between 2 RIC groups).
In a multivariate analysis, conditioning regimen was not a significant predictor of NRM. The hazard ratio (HR) for RIC was 1.13 (P=0.85).
Likewise, conditioning regimen was not a significant predictor of relapse (HR=0.81, P=0.53), OS (HR=0.85, P=0.66), or EFS (HR=0.73, P=0.34).
“Our results indicate that both MAC and RIC are valid options for PTCy-haplo,” Dr Sugita said in closing.
“Ideally, a more precise comparison of MAC and RIC should be studied further in the setting of, if possible, a randomized trial.”
*Data in the abstract differs from the presentation.
SALT LAKE CITY—New research suggests outcomes may be similar whether patients receive myeloablative conditioning (MAC) or reduced-intensity conditioning (RIC) prior to haploidentical peripheral blood stem cell transplant (haploPBSCT) with post-transplant cyclophosphamide (PTCy).
Results from 2 parallel, phase 2 trials showed that MAC-PTCy-haploPBSCT and RIC-PTCy-haploPBSCT produced comparable rates of engraftment, acute and chronic graft-versus host disease (GVHD), relapse, and non-relapse mortality (NRM).
Rates of overall survival (OS) and event-free survival (EFS) were significantly higher in the MAC group. However, the fact that some RIC recipients had received prior allogeneic transplants—and none of the MAC recipients had—appeared to play a role in survival outcomes.
Junichi Sugita, MD, PhD, of Hokkaido University in Sapporo, Japan, presented these results at the 2018 BMT Tandem Meetings (abstract 50*).
To compare MAC and RIC in the context of PTCy-haploPBSCT, Dr Sugita and his colleagues conducted 2 parallel studies—JSCT Haplo 14 MAC and JSCT Haplo 14 RIC.
Patients
There were 50 patients in the MAC trial and 77 in the RIC trial. They had median ages of 36 (range, 17 to 60) and 58 (range, 22 to 65), respectively (P<0.01). There was a greater percentage of male patients among MAC recipients (82% vs 62%, P=0.028).
Diagnoses were similar between the groups and included:
- Acute myeloid leukemia—23 MAC, 34 RIC
- Acute lymphoblastic leukemia—11 MAC, 14 RIC
- Myelodysplastic syndromes/myeloproliferative neoplasms—6 MAC, 12 RIC
- Lymphoma—6 MAC, 14 RIC
- “Other”—4 MAC, 3 RIC.
Forty-eight percent (n=24) of MAC recipients and 58% (n=45) of RIC recipients were not in remission at transplant (P=0.48). There were no significant differences in disease risk index (P=0.34).
Thirty-nine percent of RIC recipients (n=30) had a history of allogeneic transplant, but none of the MAC recipients did (P<0.01).
Conditioning and prophylaxis
There were 2 MAC regimens. One consisted of fludarabine (Flu, 30 mg/m2/day on days -6 to -4) plus total body irradiation (TBI, 12 Gy on days -3 to -1). The other consisted of Flu (30 mg/m2/day on days -6 to -2), busulfan (BU, 3.2 mg/kg/day on days -6 to -3), and TBI (4 Gy on day -1).
The RIC regimen consisted of Flu (30 mg/m2/day on days -6 to -2), BU (3.2 mg/kg/day on days -4 to -3), and TBI (4 Gy on day -1).
All patients received GVHD prophylaxis consisting of cyclophosphamide (50 mg/kg/day on days 3 and 4), tacrolimus (days 5 to 180), and mycophenolate mofetil (days 5 to 60).
Graft
Siblings were the most common donors for MAC recipients (50%, n=25), followed by parents (28%, n=14), children (16%, n=8), and “other” donors (6%, n=3).
Children were the most common donors for RIC recipients (60%, n=46), followed by siblings (33%, n=25), and parents (8%, n=6).
There was no significant difference between MAC and RIC recipients when it came to human leukocyte antigen matching, cytomegalovirus serostatus, or CD34 cell dose.
However, there was a significant difference in donor-recipient gender matching (P=0.033).
Fifty-two percent (n=26) of MAC recipients and 62% (n=48) of RIC recipients had a donor-recipient gender match. Forty-two percent (n=21) and 22% (n=17), respectively, had female donor to male recipient.
Engraftment and GVHD
“Hematopoietic recovery was similar between MAC and RIC,” Dr Sugita said.
The cumulative incidence of neutrophil engraftment was 98% in MAC recipients and 94% in RIC recipients. The median time to neutrophil engraftment was 17 days and 18 days, respectively (P=0.10).
The cumulative incidence of platelet engraftment was 84% in the MAC recipients and 74% in the RIC recipients. The median time to platelet engraftment was 31 days and 37 days, respectively (P=0.32).
“Complete chimerism was achieved in all engrafted patients,” Dr Sugita noted.
There was no significant difference between MAC and RIC recipients when it came to acute or chronic GVHD.
At day 100, the cumulative incidence of grade 2-4 acute GVHD was 18% in the MAC group and 14% in the RIC group (P=0.52). Grade 3-4 acute GVHD was 8% and 5%, respectively (P=0.52).
At 2 years, the cumulative incidence of all-grade chronic GVHD was 36% in the MAC group and 27% in the RIC group (P=0.24). Moderate to severe chronic GVHD was 20% in both groups (P=1.0).
Relapse and survival
There was no significant between-group difference in NRM or relapse.
The cumulative incidence of NRM at 2 years was 20% in the RIC group and 10% in the MAC group (P=0.15). The cumulative incidence of relapse at 2 years was 45% and 36%, respectively (P=0.32).
Survival was superior in the MAC recipients. The 2-year OS was 68% in the MAC group and 44% in the RIC group (P=0.02). The 2-year EFS was 54% and 35%, respectively (P=0.04).
However, survival appeared to be affected by history of allogeneic transplant.
“Patients with a history of prior allogenic SCT have significantly worse overall survival and event-free survival,” Dr Sugita said.
Two-year OS was 31% in RIC recipients with a history of transplant and 52% in RIC recipients without a history of transplant (P=0.04). The OS was 68% in MAC recipients, all of whom had no history of transplant.
Two-year EFS was 21%, 44%, and 54%, respectively (P=0.02 for difference between 2 RIC groups).
In a multivariate analysis, conditioning regimen was not a significant predictor of NRM. The hazard ratio (HR) for RIC was 1.13 (P=0.85).
Likewise, conditioning regimen was not a significant predictor of relapse (HR=0.81, P=0.53), OS (HR=0.85, P=0.66), or EFS (HR=0.73, P=0.34).
“Our results indicate that both MAC and RIC are valid options for PTCy-haplo,” Dr Sugita said in closing.
“Ideally, a more precise comparison of MAC and RIC should be studied further in the setting of, if possible, a randomized trial.”
*Data in the abstract differs from the presentation.
SALT LAKE CITY—New research suggests outcomes may be similar whether patients receive myeloablative conditioning (MAC) or reduced-intensity conditioning (RIC) prior to haploidentical peripheral blood stem cell transplant (haploPBSCT) with post-transplant cyclophosphamide (PTCy).
Results from 2 parallel, phase 2 trials showed that MAC-PTCy-haploPBSCT and RIC-PTCy-haploPBSCT produced comparable rates of engraftment, acute and chronic graft-versus host disease (GVHD), relapse, and non-relapse mortality (NRM).
Rates of overall survival (OS) and event-free survival (EFS) were significantly higher in the MAC group. However, the fact that some RIC recipients had received prior allogeneic transplants—and none of the MAC recipients had—appeared to play a role in survival outcomes.
Junichi Sugita, MD, PhD, of Hokkaido University in Sapporo, Japan, presented these results at the 2018 BMT Tandem Meetings (abstract 50*).
To compare MAC and RIC in the context of PTCy-haploPBSCT, Dr Sugita and his colleagues conducted 2 parallel studies—JSCT Haplo 14 MAC and JSCT Haplo 14 RIC.
Patients
There were 50 patients in the MAC trial and 77 in the RIC trial. They had median ages of 36 (range, 17 to 60) and 58 (range, 22 to 65), respectively (P<0.01). There was a greater percentage of male patients among MAC recipients (82% vs 62%, P=0.028).
Diagnoses were similar between the groups and included:
- Acute myeloid leukemia—23 MAC, 34 RIC
- Acute lymphoblastic leukemia—11 MAC, 14 RIC
- Myelodysplastic syndromes/myeloproliferative neoplasms—6 MAC, 12 RIC
- Lymphoma—6 MAC, 14 RIC
- “Other”—4 MAC, 3 RIC.
Forty-eight percent (n=24) of MAC recipients and 58% (n=45) of RIC recipients were not in remission at transplant (P=0.48). There were no significant differences in disease risk index (P=0.34).
Thirty-nine percent of RIC recipients (n=30) had a history of allogeneic transplant, but none of the MAC recipients did (P<0.01).
Conditioning and prophylaxis
There were 2 MAC regimens. One consisted of fludarabine (Flu, 30 mg/m2/day on days -6 to -4) plus total body irradiation (TBI, 12 Gy on days -3 to -1). The other consisted of Flu (30 mg/m2/day on days -6 to -2), busulfan (BU, 3.2 mg/kg/day on days -6 to -3), and TBI (4 Gy on day -1).
The RIC regimen consisted of Flu (30 mg/m2/day on days -6 to -2), BU (3.2 mg/kg/day on days -4 to -3), and TBI (4 Gy on day -1).
All patients received GVHD prophylaxis consisting of cyclophosphamide (50 mg/kg/day on days 3 and 4), tacrolimus (days 5 to 180), and mycophenolate mofetil (days 5 to 60).
Graft
Siblings were the most common donors for MAC recipients (50%, n=25), followed by parents (28%, n=14), children (16%, n=8), and “other” donors (6%, n=3).
Children were the most common donors for RIC recipients (60%, n=46), followed by siblings (33%, n=25), and parents (8%, n=6).
There was no significant difference between MAC and RIC recipients when it came to human leukocyte antigen matching, cytomegalovirus serostatus, or CD34 cell dose.
However, there was a significant difference in donor-recipient gender matching (P=0.033).
Fifty-two percent (n=26) of MAC recipients and 62% (n=48) of RIC recipients had a donor-recipient gender match. Forty-two percent (n=21) and 22% (n=17), respectively, had female donor to male recipient.
Engraftment and GVHD
“Hematopoietic recovery was similar between MAC and RIC,” Dr Sugita said.
The cumulative incidence of neutrophil engraftment was 98% in MAC recipients and 94% in RIC recipients. The median time to neutrophil engraftment was 17 days and 18 days, respectively (P=0.10).
The cumulative incidence of platelet engraftment was 84% in the MAC recipients and 74% in the RIC recipients. The median time to platelet engraftment was 31 days and 37 days, respectively (P=0.32).
“Complete chimerism was achieved in all engrafted patients,” Dr Sugita noted.
There was no significant difference between MAC and RIC recipients when it came to acute or chronic GVHD.
At day 100, the cumulative incidence of grade 2-4 acute GVHD was 18% in the MAC group and 14% in the RIC group (P=0.52). Grade 3-4 acute GVHD was 8% and 5%, respectively (P=0.52).
At 2 years, the cumulative incidence of all-grade chronic GVHD was 36% in the MAC group and 27% in the RIC group (P=0.24). Moderate to severe chronic GVHD was 20% in both groups (P=1.0).
Relapse and survival
There was no significant between-group difference in NRM or relapse.
The cumulative incidence of NRM at 2 years was 20% in the RIC group and 10% in the MAC group (P=0.15). The cumulative incidence of relapse at 2 years was 45% and 36%, respectively (P=0.32).
Survival was superior in the MAC recipients. The 2-year OS was 68% in the MAC group and 44% in the RIC group (P=0.02). The 2-year EFS was 54% and 35%, respectively (P=0.04).
However, survival appeared to be affected by history of allogeneic transplant.
“Patients with a history of prior allogenic SCT have significantly worse overall survival and event-free survival,” Dr Sugita said.
Two-year OS was 31% in RIC recipients with a history of transplant and 52% in RIC recipients without a history of transplant (P=0.04). The OS was 68% in MAC recipients, all of whom had no history of transplant.
Two-year EFS was 21%, 44%, and 54%, respectively (P=0.02 for difference between 2 RIC groups).
In a multivariate analysis, conditioning regimen was not a significant predictor of NRM. The hazard ratio (HR) for RIC was 1.13 (P=0.85).
Likewise, conditioning regimen was not a significant predictor of relapse (HR=0.81, P=0.53), OS (HR=0.85, P=0.66), or EFS (HR=0.73, P=0.34).
“Our results indicate that both MAC and RIC are valid options for PTCy-haplo,” Dr Sugita said in closing.
“Ideally, a more precise comparison of MAC and RIC should be studied further in the setting of, if possible, a randomized trial.”
*Data in the abstract differs from the presentation.
PK dosing software available in US
Pharmacokinetic (PK) dosing software intended for use in patients with hemophilia A is now available in the US.
This free, web-based, prescription software—myPKFiT for ADVATE—is intended to aid healthcare professionals in personalizing the dose and schedule of ADVATE, a full-length recombinant factor VIII product.
The software was cleared by the US Food and Drug Administration (FDA) for use in hemophilia A patients age 16 and older who weigh at least 45 kg and are receiving prophylaxis with ADVATE.
The myPKFiT software generates ADVATE dosage amount and frequency recommendations using a patient’s age and body weight information, as well as local laboratory factor VIII one-stage clotting activity measurements of sparse samples collected from the patient.
A minimum of 2 sparse sampling points are required at the recommended 3 to 4 hours (± 30 minutes) and at 24 to 32 hours (±1 hour) post-infusion.
The software output may be used to guide ADVATE use to maintain factor VIII activity levels at or above a user-specified minimum of 1% to 3% above natural baseline, in accordance with the FDA-approved dosing recommendations for ADVATE.
myPKFiT should only be used to evaluate prophylactic dosing regimens for hemophilia A patients treated with ADVATE.
The software should not be used for patients who have developed neutralizing antibodies to factor VIII products and is not indicated for use in patients with von Willebrand disease.
“A version of myPKFiT has already been widely adopted in Europe since 2014, and we’ve seen how important it has been in helping physicians develop personalized dosing regimens tailored to the specific needs of their patients,” said Andreas Busch, global head of research and development at Shire, the company behind myPKFiT for ADVATE.
“As part of our commitment to precision medicine, we are pleased to bring this innovative application to physicians and patients in the United States.”
More information on the myPKFiT software is available on the ADVATE website and the myPKFiT site.
Pharmacokinetic (PK) dosing software intended for use in patients with hemophilia A is now available in the US.
This free, web-based, prescription software—myPKFiT for ADVATE—is intended to aid healthcare professionals in personalizing the dose and schedule of ADVATE, a full-length recombinant factor VIII product.
The software was cleared by the US Food and Drug Administration (FDA) for use in hemophilia A patients age 16 and older who weigh at least 45 kg and are receiving prophylaxis with ADVATE.
The myPKFiT software generates ADVATE dosage amount and frequency recommendations using a patient’s age and body weight information, as well as local laboratory factor VIII one-stage clotting activity measurements of sparse samples collected from the patient.
A minimum of 2 sparse sampling points are required at the recommended 3 to 4 hours (± 30 minutes) and at 24 to 32 hours (±1 hour) post-infusion.
The software output may be used to guide ADVATE use to maintain factor VIII activity levels at or above a user-specified minimum of 1% to 3% above natural baseline, in accordance with the FDA-approved dosing recommendations for ADVATE.
myPKFiT should only be used to evaluate prophylactic dosing regimens for hemophilia A patients treated with ADVATE.
The software should not be used for patients who have developed neutralizing antibodies to factor VIII products and is not indicated for use in patients with von Willebrand disease.
“A version of myPKFiT has already been widely adopted in Europe since 2014, and we’ve seen how important it has been in helping physicians develop personalized dosing regimens tailored to the specific needs of their patients,” said Andreas Busch, global head of research and development at Shire, the company behind myPKFiT for ADVATE.
“As part of our commitment to precision medicine, we are pleased to bring this innovative application to physicians and patients in the United States.”
More information on the myPKFiT software is available on the ADVATE website and the myPKFiT site.
Pharmacokinetic (PK) dosing software intended for use in patients with hemophilia A is now available in the US.
This free, web-based, prescription software—myPKFiT for ADVATE—is intended to aid healthcare professionals in personalizing the dose and schedule of ADVATE, a full-length recombinant factor VIII product.
The software was cleared by the US Food and Drug Administration (FDA) for use in hemophilia A patients age 16 and older who weigh at least 45 kg and are receiving prophylaxis with ADVATE.
The myPKFiT software generates ADVATE dosage amount and frequency recommendations using a patient’s age and body weight information, as well as local laboratory factor VIII one-stage clotting activity measurements of sparse samples collected from the patient.
A minimum of 2 sparse sampling points are required at the recommended 3 to 4 hours (± 30 minutes) and at 24 to 32 hours (±1 hour) post-infusion.
The software output may be used to guide ADVATE use to maintain factor VIII activity levels at or above a user-specified minimum of 1% to 3% above natural baseline, in accordance with the FDA-approved dosing recommendations for ADVATE.
myPKFiT should only be used to evaluate prophylactic dosing regimens for hemophilia A patients treated with ADVATE.
The software should not be used for patients who have developed neutralizing antibodies to factor VIII products and is not indicated for use in patients with von Willebrand disease.
“A version of myPKFiT has already been widely adopted in Europe since 2014, and we’ve seen how important it has been in helping physicians develop personalized dosing regimens tailored to the specific needs of their patients,” said Andreas Busch, global head of research and development at Shire, the company behind myPKFiT for ADVATE.
“As part of our commitment to precision medicine, we are pleased to bring this innovative application to physicians and patients in the United States.”
More information on the myPKFiT software is available on the ADVATE website and the myPKFiT site.
One-month TB-prevention regimen effective in HIV+ individuals
BOSTON – A combination regimen of rifapentine plus isoniazid (1HP) can do in 1 month what it takes isoniazid monotherapy 9 months to accomplish: effectively prevent tuberculosis in persons with HIV infection, investigators in the randomized phase 3 BRIEF TB trial reported.
“Rates of tuberculosis or death in individuals on 1HP were essentially identical to the rates of tuberculosis or death in people who got the 9-months regimen,” said Richard Chaisson, MD, of Johns Hopkins University, Baltimore.
“People who got the 1-month regimen were more likely to complete it, had slightly less toxicity, and overall had very similar clinical outcomes,” he said at the annual Conference on Retroviruses & Opportunistic Infections.
Worldwide, more than 1,000 persons with HIV infection die from tuberculosis every day, he noted.
Although isoniazid preventive therapy (IPT) is highly effective, the rate of its use has been “appallingly poor,” Dr. Chaisson said.
“There’s a sense of futility amongst clinicians around the world, that they’re not going to even bother with giving TB-preventive therapy,” he commented.
Dr. Chaisson and coinvestigators conducted a randomized trial to test the hypothesis that 4 weeks of daily rifapentine and isoniazid would be noninferior to 9 months of isoniazid for TB prevention in person with HIV infection.
In a multicenter open-label trial, they enrolled 3,000 HIV-infected people aged 13 years and older from 45 sites in 10 countries. The patients had no evidence of active TB, but had either tuberculin skin test (TST) reactivity of 5 mm or greater and/or a positive interferon gamma release assay (IGRA), or lived in a high–TB burden area (prevalence of 60 or more cases per 100,000 population).
Patients were stratified by CD4+ cell count and antiretroviral therapy use at base line (yes or no). The median CD4 count was 470 cells/mm3, and 50% of patients were on ART. Only efavirenz-based or nevirapine-based ART was allowed during IPT therapy.
In the experimental arm, patients were randomized to 4 weeks of rifapentine 450 mg for those less than 45 kg, or 600 mg for those 45 kg or higher, plus 300 mg isoniazid daily, plus 25 mg vitamin B6, followed by 32 weeks of observation.
Patients in the control arm received isoniazid and vitamin B6 daily for 36 weeks.
A total of 1,498 patients assigned to standard-of-care isoniazid and 1,488 assigned to 1HP were available for the efficacy analysis.
Three years after the last patient had been enrolled, the primary endpoint – the incidence rate of first diagnosis of active TB, TB death, or death from an unknown cause – had occurred in 32 patients on the 1HP regimen, and 33 on 9-month isoniazid.
Events included confirmed active TB in 18 patients on 1HP and 14 on isoniazid, probable active TB in 11 and 10 patients, respectively, death related to TB in 2 patients on 9-month isoniazid (none in the 1HP group) and death from unknown causes in 3 and 7 patients, respectively.
The incidence of events per 100 person-years of follow-up was 0.65 for the 1HP regimen and 0.67 for 9 months of isoniazid, a difference that was not statistically significant.
There were two cases of isoniazid resistance and one of rifampin resistance in the 1HP arm vs. one each in the 9-month isoniazid arm. There were no cases of multidrug resistance in either arm.
The safety analysis showed that 83 patients on 1HP had at least one serious adverse event, compared with 108 patients on the 9-month regimen.
“This 1 HP regimen really could dramatically alter the landscape for preventing TB in people with HIV. It’s a simple regimen; it can be given to people with HIV, and the likelihood of them completing it is extremely high; and the likelihood of it working is extremely good,” Dr. Chaisson said at media briefing following his presentation of the data in session.
The study was funded by National Institute of Health grants. Sanofi supplied study medications. Dr. Chaisson disclosed serving as a consultant to Otsuka, and that his spouse is a Merck shareholder.
BOSTON – A combination regimen of rifapentine plus isoniazid (1HP) can do in 1 month what it takes isoniazid monotherapy 9 months to accomplish: effectively prevent tuberculosis in persons with HIV infection, investigators in the randomized phase 3 BRIEF TB trial reported.
“Rates of tuberculosis or death in individuals on 1HP were essentially identical to the rates of tuberculosis or death in people who got the 9-months regimen,” said Richard Chaisson, MD, of Johns Hopkins University, Baltimore.
“People who got the 1-month regimen were more likely to complete it, had slightly less toxicity, and overall had very similar clinical outcomes,” he said at the annual Conference on Retroviruses & Opportunistic Infections.
Worldwide, more than 1,000 persons with HIV infection die from tuberculosis every day, he noted.
Although isoniazid preventive therapy (IPT) is highly effective, the rate of its use has been “appallingly poor,” Dr. Chaisson said.
“There’s a sense of futility amongst clinicians around the world, that they’re not going to even bother with giving TB-preventive therapy,” he commented.
Dr. Chaisson and coinvestigators conducted a randomized trial to test the hypothesis that 4 weeks of daily rifapentine and isoniazid would be noninferior to 9 months of isoniazid for TB prevention in person with HIV infection.
In a multicenter open-label trial, they enrolled 3,000 HIV-infected people aged 13 years and older from 45 sites in 10 countries. The patients had no evidence of active TB, but had either tuberculin skin test (TST) reactivity of 5 mm or greater and/or a positive interferon gamma release assay (IGRA), or lived in a high–TB burden area (prevalence of 60 or more cases per 100,000 population).
Patients were stratified by CD4+ cell count and antiretroviral therapy use at base line (yes or no). The median CD4 count was 470 cells/mm3, and 50% of patients were on ART. Only efavirenz-based or nevirapine-based ART was allowed during IPT therapy.
In the experimental arm, patients were randomized to 4 weeks of rifapentine 450 mg for those less than 45 kg, or 600 mg for those 45 kg or higher, plus 300 mg isoniazid daily, plus 25 mg vitamin B6, followed by 32 weeks of observation.
Patients in the control arm received isoniazid and vitamin B6 daily for 36 weeks.
A total of 1,498 patients assigned to standard-of-care isoniazid and 1,488 assigned to 1HP were available for the efficacy analysis.
Three years after the last patient had been enrolled, the primary endpoint – the incidence rate of first diagnosis of active TB, TB death, or death from an unknown cause – had occurred in 32 patients on the 1HP regimen, and 33 on 9-month isoniazid.
Events included confirmed active TB in 18 patients on 1HP and 14 on isoniazid, probable active TB in 11 and 10 patients, respectively, death related to TB in 2 patients on 9-month isoniazid (none in the 1HP group) and death from unknown causes in 3 and 7 patients, respectively.
The incidence of events per 100 person-years of follow-up was 0.65 for the 1HP regimen and 0.67 for 9 months of isoniazid, a difference that was not statistically significant.
There were two cases of isoniazid resistance and one of rifampin resistance in the 1HP arm vs. one each in the 9-month isoniazid arm. There were no cases of multidrug resistance in either arm.
The safety analysis showed that 83 patients on 1HP had at least one serious adverse event, compared with 108 patients on the 9-month regimen.
“This 1 HP regimen really could dramatically alter the landscape for preventing TB in people with HIV. It’s a simple regimen; it can be given to people with HIV, and the likelihood of them completing it is extremely high; and the likelihood of it working is extremely good,” Dr. Chaisson said at media briefing following his presentation of the data in session.
The study was funded by National Institute of Health grants. Sanofi supplied study medications. Dr. Chaisson disclosed serving as a consultant to Otsuka, and that his spouse is a Merck shareholder.
BOSTON – A combination regimen of rifapentine plus isoniazid (1HP) can do in 1 month what it takes isoniazid monotherapy 9 months to accomplish: effectively prevent tuberculosis in persons with HIV infection, investigators in the randomized phase 3 BRIEF TB trial reported.
“Rates of tuberculosis or death in individuals on 1HP were essentially identical to the rates of tuberculosis or death in people who got the 9-months regimen,” said Richard Chaisson, MD, of Johns Hopkins University, Baltimore.
“People who got the 1-month regimen were more likely to complete it, had slightly less toxicity, and overall had very similar clinical outcomes,” he said at the annual Conference on Retroviruses & Opportunistic Infections.
Worldwide, more than 1,000 persons with HIV infection die from tuberculosis every day, he noted.
Although isoniazid preventive therapy (IPT) is highly effective, the rate of its use has been “appallingly poor,” Dr. Chaisson said.
“There’s a sense of futility amongst clinicians around the world, that they’re not going to even bother with giving TB-preventive therapy,” he commented.
Dr. Chaisson and coinvestigators conducted a randomized trial to test the hypothesis that 4 weeks of daily rifapentine and isoniazid would be noninferior to 9 months of isoniazid for TB prevention in person with HIV infection.
In a multicenter open-label trial, they enrolled 3,000 HIV-infected people aged 13 years and older from 45 sites in 10 countries. The patients had no evidence of active TB, but had either tuberculin skin test (TST) reactivity of 5 mm or greater and/or a positive interferon gamma release assay (IGRA), or lived in a high–TB burden area (prevalence of 60 or more cases per 100,000 population).
Patients were stratified by CD4+ cell count and antiretroviral therapy use at base line (yes or no). The median CD4 count was 470 cells/mm3, and 50% of patients were on ART. Only efavirenz-based or nevirapine-based ART was allowed during IPT therapy.
In the experimental arm, patients were randomized to 4 weeks of rifapentine 450 mg for those less than 45 kg, or 600 mg for those 45 kg or higher, plus 300 mg isoniazid daily, plus 25 mg vitamin B6, followed by 32 weeks of observation.
Patients in the control arm received isoniazid and vitamin B6 daily for 36 weeks.
A total of 1,498 patients assigned to standard-of-care isoniazid and 1,488 assigned to 1HP were available for the efficacy analysis.
Three years after the last patient had been enrolled, the primary endpoint – the incidence rate of first diagnosis of active TB, TB death, or death from an unknown cause – had occurred in 32 patients on the 1HP regimen, and 33 on 9-month isoniazid.
Events included confirmed active TB in 18 patients on 1HP and 14 on isoniazid, probable active TB in 11 and 10 patients, respectively, death related to TB in 2 patients on 9-month isoniazid (none in the 1HP group) and death from unknown causes in 3 and 7 patients, respectively.
The incidence of events per 100 person-years of follow-up was 0.65 for the 1HP regimen and 0.67 for 9 months of isoniazid, a difference that was not statistically significant.
There were two cases of isoniazid resistance and one of rifampin resistance in the 1HP arm vs. one each in the 9-month isoniazid arm. There were no cases of multidrug resistance in either arm.
The safety analysis showed that 83 patients on 1HP had at least one serious adverse event, compared with 108 patients on the 9-month regimen.
“This 1 HP regimen really could dramatically alter the landscape for preventing TB in people with HIV. It’s a simple regimen; it can be given to people with HIV, and the likelihood of them completing it is extremely high; and the likelihood of it working is extremely good,” Dr. Chaisson said at media briefing following his presentation of the data in session.
The study was funded by National Institute of Health grants. Sanofi supplied study medications. Dr. Chaisson disclosed serving as a consultant to Otsuka, and that his spouse is a Merck shareholder.
REPORTING FROM CROI
Key clinical point: A shorter tuberculosis-prevention regimen could improve adherence among persons infected with HIV.
Major finding: A 4-week regimen of rifapentine and isoniazid was noninferior to 9 months of isoniazid at preventing TB infections in person with HIV.
Data source: Randomized, controlled, open-label trial in 3000 HIV-positive persons aged 13 or older treated at 45 sites in 10 countries.
Disclosures: The study was funded by National Institutes of Health grants. Sanofi supplied study medications. Dr. Chaisson disclosed serving as a consultant to Otsuka, and that his spouse is a Merck shareholder.
Bloating. Flatulence. Think SIBO
MAUI, HAWAII – Recognition and effective treatment of small intestinal bowel overgrowth – aka, SIBO – is a highly practical skillset for nongastroenterologists to possess, Uma Mahadevan, MD, said at the 2018 Rheumatology Winter Clinical Symposium.
SIBO is a common accompaniment to a range of chronic diseases, especially as patients age. And it’s not a condition that warrants referral to a gastroenterologist, according to Dr. Mahadevan, professor of medicine and medical director of the Center for Colitis and Crohn’s Disease at the University of California, San Francisco.
“To diagnose SIBO properly you need to do a carbohydrate breath test. Those tests are notoriously inaccurate, and it’s not worth it. We just treat. If we think you have SIBO, you do a course of rifaximin. And you can do the same,” she told her audience of rheumatologists.
There is an alternative diagnostic test. It involves obtaining a jejunal aspirate culture that demonstrates a bacterial concentration of more than 1,000 colony-forming units/mL. That’s an invasive and expensive test. Given how common SIBO symptoms are in patients with various underlying chronic diseases and the highly favorable risk/benefit ratio of a course of rifaximin, it’s entirely reasonable to skip formal diagnostic testing and treat empirically when the clinical picture is consistent with SIBO, according to the gastroenterologist.
SIBO is a condition in which the small intestine becomes colonized with abnormally high counts of aerobic and anaerobic bacteria normally found in the colon. Bacteria commonly associated with SIBO include Escherichia coli as well as those from the genuses Lactobacillus, Bacteroides, and Streptococcus.
The etiology of SIBO involves diminished intestinal motility and altered mucosal defenses. With reduced GI motility, the small bowel can’t get cleared of debris efficiently. Colonic microbes grab a foothold and bloom. Conditions marked by diminished intestinal motility – and high rates of SIBO – include scleroderma, diabetes, irritable bowel syndrome, chronic pancreatitis, cirrhosis, common variable immunodeficiency, HIV infection, and radiation enteritis. Small bowel diverticula are a setup for SIBO. Long-term proton pump inhibitor–therapy fosters hypochlorydia, which promotes SIBO. Opioid therapy is another common cause of SIBO.
So is bariatric surgery. “Bariatric surgery has caused so much iatrogenic GI disease, it’s just amazing. There is bacterial overgrowth in that population, and it’s a lot more complex than basic SIBO,” Dr. Mahadevan said.
SIBO causes malabsorption across the intestinal microvillus membrane as a result of damage to enterocytes, as well as impaired digestion in the intestinal lumen.
The presenting hallmark symptoms of SIBO are bloating, flatulence, early satiety, abdominal discomfort, and in some cases chronic diarrhea.
“You get a lot of gas and bloating. Patients will say, ‘I eat a small amount and feel full; I look like I’m pregnant; I have a lot of gas. What’s wrong with me?’ Chances are they have SIBO,” Dr. Mahadevan said. “The older you get the more SIBO you have.”
First-line treatment, aimed at diminishing small bowel bacteria, is rifaximin at 550 mg three times per day for 10-14 days.
“This is a very low-risk antibiotic. And it’s very effective for SIBO, but patients may need multiple courses,” according to the gastroenterologist.
Indeed, 40% of patients will experience recurrent SIBO symptoms within 9 months after a round of rifaximin. Recurrences are more common in patients on chronic proton pump–inhibitor therapy, the elderly, and those who have undergone appendectomy. Such patients may need another course of rifaximin once or twice per year.
“If they need rifaximin every 6 months, fine. Patients will be so grateful to you for that course of rifaximin,” Dr. Mahadevan said.
Patients with methane-predominant bacterial overgrowth, as opposed to hydrogen-predominant overgrowth, often benefit from concomitant neomycin at 500 mg twice per day along with their 10-14 days of rifaximin.
“A lot of our cirrhotic patients are on both,” she noted.
Alternatives to rifaximin include amoxicillin/clavulanic acid in combination with metronidazole.
Two measures she routinely recommends to forestall recurrent SIBO are to have patients start probiotics after a course of rifaximin, and also to try the low-FODMAP (fermentable oligo-di-monosaccharides and polyols) diet. The evidence base in SIBO is weak, but the anecdotal experience has been strongly positive.
“These are two interventions you can provide to your patients with a lot of bloating and gas. It’ll make them feel much, much better,” the gastroenterologist said.
FODMAPs are short-chain carbohydrates, and the low-FODMAP diet is an elimination diet. The first 6 weeks are highly restrictive, then the foods on the high FODMAP list are reintroduced one at a time until the offenders are identified. The low-FODMAP diet hasn’t been conclusively proven effective for SIBO in a randomized clinical trial, but it does have a compelling evidence base for treatment of irritable bowel syndrome diarrhea (J Gastroenterol Hepatol. 2010 Feb;25[2]:252-8).
“Anecdotally, the use of a low-FODMAP diet in patients with bloating and gas is very effective as well. Patients have a good deal of success with it,” she said.
Audience members were eager to learn what particular specific probiotic microorganism Dr. Madahaven recommends.
“I think the more we understand the microbiome, the further away I’m going from specific probiotics because it’s just too complex for any one probiotic to be effective. I tell patients to try to get it from their diet: yogurt or kefir with live bacteria. That’s what I use now,” she replied.
MAUI, HAWAII – Recognition and effective treatment of small intestinal bowel overgrowth – aka, SIBO – is a highly practical skillset for nongastroenterologists to possess, Uma Mahadevan, MD, said at the 2018 Rheumatology Winter Clinical Symposium.
SIBO is a common accompaniment to a range of chronic diseases, especially as patients age. And it’s not a condition that warrants referral to a gastroenterologist, according to Dr. Mahadevan, professor of medicine and medical director of the Center for Colitis and Crohn’s Disease at the University of California, San Francisco.
“To diagnose SIBO properly you need to do a carbohydrate breath test. Those tests are notoriously inaccurate, and it’s not worth it. We just treat. If we think you have SIBO, you do a course of rifaximin. And you can do the same,” she told her audience of rheumatologists.
There is an alternative diagnostic test. It involves obtaining a jejunal aspirate culture that demonstrates a bacterial concentration of more than 1,000 colony-forming units/mL. That’s an invasive and expensive test. Given how common SIBO symptoms are in patients with various underlying chronic diseases and the highly favorable risk/benefit ratio of a course of rifaximin, it’s entirely reasonable to skip formal diagnostic testing and treat empirically when the clinical picture is consistent with SIBO, according to the gastroenterologist.
SIBO is a condition in which the small intestine becomes colonized with abnormally high counts of aerobic and anaerobic bacteria normally found in the colon. Bacteria commonly associated with SIBO include Escherichia coli as well as those from the genuses Lactobacillus, Bacteroides, and Streptococcus.
The etiology of SIBO involves diminished intestinal motility and altered mucosal defenses. With reduced GI motility, the small bowel can’t get cleared of debris efficiently. Colonic microbes grab a foothold and bloom. Conditions marked by diminished intestinal motility – and high rates of SIBO – include scleroderma, diabetes, irritable bowel syndrome, chronic pancreatitis, cirrhosis, common variable immunodeficiency, HIV infection, and radiation enteritis. Small bowel diverticula are a setup for SIBO. Long-term proton pump inhibitor–therapy fosters hypochlorydia, which promotes SIBO. Opioid therapy is another common cause of SIBO.
So is bariatric surgery. “Bariatric surgery has caused so much iatrogenic GI disease, it’s just amazing. There is bacterial overgrowth in that population, and it’s a lot more complex than basic SIBO,” Dr. Mahadevan said.
SIBO causes malabsorption across the intestinal microvillus membrane as a result of damage to enterocytes, as well as impaired digestion in the intestinal lumen.
The presenting hallmark symptoms of SIBO are bloating, flatulence, early satiety, abdominal discomfort, and in some cases chronic diarrhea.
“You get a lot of gas and bloating. Patients will say, ‘I eat a small amount and feel full; I look like I’m pregnant; I have a lot of gas. What’s wrong with me?’ Chances are they have SIBO,” Dr. Mahadevan said. “The older you get the more SIBO you have.”
First-line treatment, aimed at diminishing small bowel bacteria, is rifaximin at 550 mg three times per day for 10-14 days.
“This is a very low-risk antibiotic. And it’s very effective for SIBO, but patients may need multiple courses,” according to the gastroenterologist.
Indeed, 40% of patients will experience recurrent SIBO symptoms within 9 months after a round of rifaximin. Recurrences are more common in patients on chronic proton pump–inhibitor therapy, the elderly, and those who have undergone appendectomy. Such patients may need another course of rifaximin once or twice per year.
“If they need rifaximin every 6 months, fine. Patients will be so grateful to you for that course of rifaximin,” Dr. Mahadevan said.
Patients with methane-predominant bacterial overgrowth, as opposed to hydrogen-predominant overgrowth, often benefit from concomitant neomycin at 500 mg twice per day along with their 10-14 days of rifaximin.
“A lot of our cirrhotic patients are on both,” she noted.
Alternatives to rifaximin include amoxicillin/clavulanic acid in combination with metronidazole.
Two measures she routinely recommends to forestall recurrent SIBO are to have patients start probiotics after a course of rifaximin, and also to try the low-FODMAP (fermentable oligo-di-monosaccharides and polyols) diet. The evidence base in SIBO is weak, but the anecdotal experience has been strongly positive.
“These are two interventions you can provide to your patients with a lot of bloating and gas. It’ll make them feel much, much better,” the gastroenterologist said.
FODMAPs are short-chain carbohydrates, and the low-FODMAP diet is an elimination diet. The first 6 weeks are highly restrictive, then the foods on the high FODMAP list are reintroduced one at a time until the offenders are identified. The low-FODMAP diet hasn’t been conclusively proven effective for SIBO in a randomized clinical trial, but it does have a compelling evidence base for treatment of irritable bowel syndrome diarrhea (J Gastroenterol Hepatol. 2010 Feb;25[2]:252-8).
“Anecdotally, the use of a low-FODMAP diet in patients with bloating and gas is very effective as well. Patients have a good deal of success with it,” she said.
Audience members were eager to learn what particular specific probiotic microorganism Dr. Madahaven recommends.
“I think the more we understand the microbiome, the further away I’m going from specific probiotics because it’s just too complex for any one probiotic to be effective. I tell patients to try to get it from their diet: yogurt or kefir with live bacteria. That’s what I use now,” she replied.
MAUI, HAWAII – Recognition and effective treatment of small intestinal bowel overgrowth – aka, SIBO – is a highly practical skillset for nongastroenterologists to possess, Uma Mahadevan, MD, said at the 2018 Rheumatology Winter Clinical Symposium.
SIBO is a common accompaniment to a range of chronic diseases, especially as patients age. And it’s not a condition that warrants referral to a gastroenterologist, according to Dr. Mahadevan, professor of medicine and medical director of the Center for Colitis and Crohn’s Disease at the University of California, San Francisco.
“To diagnose SIBO properly you need to do a carbohydrate breath test. Those tests are notoriously inaccurate, and it’s not worth it. We just treat. If we think you have SIBO, you do a course of rifaximin. And you can do the same,” she told her audience of rheumatologists.
There is an alternative diagnostic test. It involves obtaining a jejunal aspirate culture that demonstrates a bacterial concentration of more than 1,000 colony-forming units/mL. That’s an invasive and expensive test. Given how common SIBO symptoms are in patients with various underlying chronic diseases and the highly favorable risk/benefit ratio of a course of rifaximin, it’s entirely reasonable to skip formal diagnostic testing and treat empirically when the clinical picture is consistent with SIBO, according to the gastroenterologist.
SIBO is a condition in which the small intestine becomes colonized with abnormally high counts of aerobic and anaerobic bacteria normally found in the colon. Bacteria commonly associated with SIBO include Escherichia coli as well as those from the genuses Lactobacillus, Bacteroides, and Streptococcus.
The etiology of SIBO involves diminished intestinal motility and altered mucosal defenses. With reduced GI motility, the small bowel can’t get cleared of debris efficiently. Colonic microbes grab a foothold and bloom. Conditions marked by diminished intestinal motility – and high rates of SIBO – include scleroderma, diabetes, irritable bowel syndrome, chronic pancreatitis, cirrhosis, common variable immunodeficiency, HIV infection, and radiation enteritis. Small bowel diverticula are a setup for SIBO. Long-term proton pump inhibitor–therapy fosters hypochlorydia, which promotes SIBO. Opioid therapy is another common cause of SIBO.
So is bariatric surgery. “Bariatric surgery has caused so much iatrogenic GI disease, it’s just amazing. There is bacterial overgrowth in that population, and it’s a lot more complex than basic SIBO,” Dr. Mahadevan said.
SIBO causes malabsorption across the intestinal microvillus membrane as a result of damage to enterocytes, as well as impaired digestion in the intestinal lumen.
The presenting hallmark symptoms of SIBO are bloating, flatulence, early satiety, abdominal discomfort, and in some cases chronic diarrhea.
“You get a lot of gas and bloating. Patients will say, ‘I eat a small amount and feel full; I look like I’m pregnant; I have a lot of gas. What’s wrong with me?’ Chances are they have SIBO,” Dr. Mahadevan said. “The older you get the more SIBO you have.”
First-line treatment, aimed at diminishing small bowel bacteria, is rifaximin at 550 mg three times per day for 10-14 days.
“This is a very low-risk antibiotic. And it’s very effective for SIBO, but patients may need multiple courses,” according to the gastroenterologist.
Indeed, 40% of patients will experience recurrent SIBO symptoms within 9 months after a round of rifaximin. Recurrences are more common in patients on chronic proton pump–inhibitor therapy, the elderly, and those who have undergone appendectomy. Such patients may need another course of rifaximin once or twice per year.
“If they need rifaximin every 6 months, fine. Patients will be so grateful to you for that course of rifaximin,” Dr. Mahadevan said.
Patients with methane-predominant bacterial overgrowth, as opposed to hydrogen-predominant overgrowth, often benefit from concomitant neomycin at 500 mg twice per day along with their 10-14 days of rifaximin.
“A lot of our cirrhotic patients are on both,” she noted.
Alternatives to rifaximin include amoxicillin/clavulanic acid in combination with metronidazole.
Two measures she routinely recommends to forestall recurrent SIBO are to have patients start probiotics after a course of rifaximin, and also to try the low-FODMAP (fermentable oligo-di-monosaccharides and polyols) diet. The evidence base in SIBO is weak, but the anecdotal experience has been strongly positive.
“These are two interventions you can provide to your patients with a lot of bloating and gas. It’ll make them feel much, much better,” the gastroenterologist said.
FODMAPs are short-chain carbohydrates, and the low-FODMAP diet is an elimination diet. The first 6 weeks are highly restrictive, then the foods on the high FODMAP list are reintroduced one at a time until the offenders are identified. The low-FODMAP diet hasn’t been conclusively proven effective for SIBO in a randomized clinical trial, but it does have a compelling evidence base for treatment of irritable bowel syndrome diarrhea (J Gastroenterol Hepatol. 2010 Feb;25[2]:252-8).
“Anecdotally, the use of a low-FODMAP diet in patients with bloating and gas is very effective as well. Patients have a good deal of success with it,” she said.
Audience members were eager to learn what particular specific probiotic microorganism Dr. Madahaven recommends.
“I think the more we understand the microbiome, the further away I’m going from specific probiotics because it’s just too complex for any one probiotic to be effective. I tell patients to try to get it from their diet: yogurt or kefir with live bacteria. That’s what I use now,” she replied.
EXPERT ANALYSIS FROM RWCS 2018
Do Psoriasis Patients Engage In Vigorous Physical Activity?
Psoriasis is a chronic inflammatory disease that affects approximately 2% to 3% of the US population.1 Patients with psoriasis are more likely to have cardiovascular risk factors (eg, obesity, metabolic syndrome) than individuals without psoriasis.2 In fact, recent evidence has suggested that a diagnosis of psoriasis is an independent risk factor for cardiometabolic diseases including diabetes, major adverse cardiovascular events, and obesity.3 Given the well-recognized health benefits of physical activity and the associated reduction in coronary heart disease risk,4 patients with psoriasis specifically may benefit from regular participation in physical activity. Thus, an enhanced understanding of the relationship between psoriasis and vigorous physical activity would help determine the role of initiating and recommending interventions that implement physical activity for patients with psoriasis. A review was conducted to determine the relationship between psoriasis and vigorous physical activity.
Methods
An English-language literature search of PubMed articles indexed for MEDLINE (January 1, 1946–October 15, 2017) as well as articles in the Embase database (January 1, 1947–October 15, 2017) and Cochrane Library (January 1, 1992–October 15, 2017) using the terms psoriasis and physical activity was performed. The search strategy was established based on a prior review of vigorous physical activity in eczema.5 The article titles and/or abstracts were reviewed, and the studies were excluded if they did not evaluate physical activity in patients with psoriasis. Studies without a control group also were excluded. Articles on patients with psoriatic arthritis and studies that involved modification of dietary intake also were excluded.
Two reviewers (M.A. and E.B.L.) independently extracted data from the studies and compiled the results. The following factors were included in the data extracted: study year, location, and design; method of diagnosis of psoriasis; total number of patients included in the study; and age, gender, and level of physical activity of the study patients. Level of physical activity was the exposure, and diagnosis of psoriasis was the dependent variable. Physical activity was defined differently across the studies that were evaluated. To determine study quality, we implemented the Newcastle–Ottawa Scale (NOS), a 9-star scoring system that includes items such as selection criteria, comparability, and study outcome.6 Studies with an NOS score of 7 or higher were included in the meta-analysis.
Results
The literature search generated 353 nonduplicate articles. A thorough review of the articles yielded 4 studies that were incorporated in the final analysis.7-10 We aimed to perform a meta-analysis; however, only 1 of the studies included in the final analysis had an NOS score of 7 or higher along with adequate data to be incorporated into our study.10 As a result, the meta-analysis was converted to a regular review.
The cross-sectional study we reviewed, which had an NOS score of 7, included males and females in the United States aged 20 to 59 years.10 Data were collected using the population-based National Health and Nutrition Examination Survey from 2003 to 2006. The survey measured the likelihood of participation in leisure-time moderate to vigorous physical activity (MVPA) and metabolic equivalent task (MET) minutes of MVPA in the past 30 days. Of 6549 participants, 385 were excluded from the analysis due to missing values for 1 or more of the study variables. Of the remaining 6164 participants, 84 (1.4%) reported having a diagnosis of psoriasis with few or no psoriasis patches at the time of the survey, and 71 (1.2%) reported having a diagnosis of psoriasis with few to extensive patches at the time of the survey.10
Participants with psoriasis were less likely to participate in MVPA in the previous 30 days compared to participants without psoriasis, but the association was not statistically significant.10 The study demonstrated that, on average, participants with psoriasis spent 31% (95% confidence interval [CI], −0.57 to −0.05) fewer MET minutes on leisure-time MVPA versus participants without psoriasis; however, this association was not statistically significant. It is important to note that the diagnosis of psoriasis was self-reported, and measures of disease duration or areas of involvement were not incorporated.
Comment
Our review revealed that vigorous physical activity may be reduced in patients with psoriasis compared to those without psoriasis. Initially, we aimed to perform a systematic review of the literature; however, only 1 study met the criteria for the systematic review, highlighting the need for more robust studies evaluating this subject.
Do et al10 demonstrated that psoriasis patients were less likely to participate in MVPA, but the findings were not statistically significant. Of those who participated in MVPA, MET minutes were fewer among patients with few to extensive skin lesions compared to those without psoriasis. The investigators suggested that psoriasis patients with more severe disease tend to exercise less and ultimately would benefit from regular vigorous physical activity.
Frankel et al7 performed a prospective cohort study in US women to evaluate the role of physical activity in preventing psoriasis. The investigators reported that the most physically active quintile had a lower multivariate relative risk of psoriasis (0.72; 95% CI, 0.59–0.89; P<.001 for trend) compared to the least active quintile.7 Additionally, vigorous physical activity, which was defined as 6 or more MET minutes, was associated with a significantly lower risk of incident psoriasis (0.66; 95% CI, 0.54–0.81; P<.001 for trend), which maintained significance after adjusting for body mass index (BMI). The investigators suggested that, by decreasing chronic inflammation and lowering levels of proinflammatory cytokines, vigorous physical activity may reduce the risk of psoriasis development in women.7 It is plausible that vigorous physical activity modifies the state of chronic inflammation, which could subsequently reduce the risk of developing psoriasis; however, further long-term, randomized, prospective studies are needed to verify the relationship between physical activity and development of psoriasis.
Torres et al8 performed a cross-sectional questionnaire study to assess physical activity in patients with severe psoriasis (defined as >10% body surface area involvement and/or disease requiring systemic therapy or phototherapy) versus healthy controls. Physical activity level was measured using the International Physical Activity Questionnaire. The odds ratio of low-level physical activity compared to non–low-level physical activity among psoriasis patients versus controls was 3.42 (95% CI, 1.47–7.91; P=.002). Additionally, the average total MET minutes of psoriasis patients were significantly reduced compared to those of the healthy controls (P=.001). Thus, the investigators suggested that vigorous physical activity is less likely in psoriasis patients, which may contribute to the increased risk of cardiovascular disease in this population.8 Vigorous physical activity would benefit patients with psoriasis to help lower the chronic state of inflammation and cardiometabolic comorbidities.
Demirel et al9 performed a study to compare aerobic exercise capacity and daily physical activity level in psoriasis patients (n=30) compared to controls (n=30). Daily physical activity, measured with an accelerometer, was significantly higher in male patients with psoriasis compared to controls (P=.021). No significant difference was reported in maximal aerobic capacity in both male and female psoriasis patients versus controls. The investigators suggested that the level of daily physical activity is not limited in psoriasis patients, yet the small sample size may limit the generalizability of the study.
The ability to dissipate heat during exercise seems to be diminished in patients with psoriasis. Specifically, it has been suggested that psoriasis lesions interfere with normal perspiration.11 Moreover, joint involvement in patients with psoriatic arthritis may lead to physical functional disabilities that can interfere with the ability of these patients to participate in regular physical activity.12-14 For this reason, our review excluded articles that evaluated patients with psoriatic arthritis. Despite this exclusion, it is important to consider that comorbid psoriatic arthritis in clinical practice may impede patients with psoriasis from participating in physical activity. Additionally, various social aspects also may limit physical activity in psoriasis patients; for instance, psoriasis patients often avoid activities that involve increased exposure of the skin (eg, communal showers, wearing sports attire).15
Furthermore, obese psoriasis patients are less likely to exercise compared to obese individuals without psoriasis.16 In patients with higher BMI, the risk of psoriasis is increased.17 A systematic review suggested that weight loss may improve psoriasis severity.18 Bariatric surgery also may improve psoriasis.19 Moreover, obesity may interfere with response to biologic therapies for psoriasis. Specifically, higher BMI is linked with lower response to fixed-dose biologic therapies compared to weight-based biologic options (eg, infliximab).20,21
Conclusion
Given the increased risk of myocardial infarction in patients with psoriasis, it is important to recognize the barriers to physical activity that psoriasis patients face.22 Due to the considerable health benefits associated with regular physical activity, physicians should encourage patients with psoriasis to participate in physical activity as tolerated. Of note, the studies included in this review varied in their definitions of psoriasis disease severity and measures of physical activity level. Long-term, randomized, prospective studies are needed to clarify the relationship between psoriasis and physical activity. Evidence from these studies would help guide clinical recommendations regarding the role of physical activity for patients with psoriasis.
- Takeshita J, Gelfand JM, Li P, et al. Psoriasis in the US Medicare population: prevalence, treatment, and factors associated with biologic use. J Invest Dermatol. 2015;135:2955-2963.
- Prey S, Paul C, Bronsard V, et al. Cardiovascular risk factors in patients with plaque psoriasis: a systematic review of epidemiological studies. J Eur Acad Dermatol Venereol. 2010;24(suppl 2):23-30.
- Takeshita J, Grewal S, Langan SM, et al. Psoriasis and comorbid diseases: epidemiology. J Am Acad Dermatol. 2017;76:377-390.
- Leon AS. Biological mechanisms for the cardioprotective effects of aerobic exercise. Am J Lifestyle Med. 2009;3:32S-34S.
- Kim A, Silverberg JI. A systematic review of vigorous physical activity in eczema. Br J Dermatol. 2016;174:660-662.
- Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. The Ottawa Hospital Research Institute website. http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm. Accessed February 23, 2018.
- Frankel HC, Han J, Li T, et al. The association between physical activity and the risk of incident psoriasis. Arch Dermatol. 2012;148:918-924.
- Torres T, Alexandre JM, Mendonça D, et al. Levels of physical activity in patients with severe psoriasis: a cross-sectional questionnaire study. Am J Clin Dermatol. 2014;15:129-135.
- Demirel R, Genc A, Ucok K, et al. Do patients with mild to moderate psoriasis really have a sedentary lifestyle? Int J Dermatol. 2013;52:1129-1134.
- Do YK, Lakhani N, Malhotra R, et al. Association between psoriasis and leisure‐time physical activity: findings from the National Health and Nutrition Examination Survey. J Dermatol. 2015;42:148-153.
- Leibowitz E, Seidman DS, Laor A, et al. Are psoriatic patients at risk of heat intolerance? Br J Dermatol. 1991;124:439-442.
- Husted JA, Tom BD, Farewell VT, et al. Description and prediction of physical functional disability in psoriatic arthritis: a longitudinal analysis using a Markov model approach. Arthritis Rheum. 2005;53:404-409.
- Wilson FC, Icen M, Crowson CS, et al. Incidence and clinical predictors of psoriatic arthritis in patients with psoriasis: a population‐based study. Arthritis Rheum. 2009;61:233-239.
- Shih M, Hootman JM, Kruger J, et al. Physical activity in men and women with arthritis: National Health Interview Survey, 2002. Am J Prev Med. 2006;30:385-393.
- Ramsay B, O’Reagan M. A survey of the social and psychological effects of psoriasis. Br J Dermatol. 1988;118:195-201.
- Herron MD, Hinckley M, Hoffman MS, et al. Impact of obesity and smoking on psoriasis presentation and management. Arch Dermatol. 2005;141:1527-1534.
- Kumar S, Han J, Li T, et al. Obesity, waist circumference, weight change and the risk of psoriasis in US women. J Eur Acad Dermatol Venereol. 2013;27:1293-1298.
- Upala S, Sanguankeo A. Effect of lifestyle weight loss intervention on disease severity in patients with psoriasis: a systematic review and meta-analysis. Int J Obes (Lond). 2015;39:1197-1202.
- Sako EY, Famenini S, Wu JJ. Bariatric surgery and psoriasis. J Am Acad Dermatol. 2014;70:774-779.
- Clark L, Lebwohl M. The effect of weight on the efficacy of biologic therapy in patients with psoriasis. J Am Acad Dermatol. 2008;58:443-446.
- Puig L. Obesity and psoriasis: body weight and body mass index influence the response to biological treatment. J Eur Acad Dermatol Venereol. 2011;25:1007-1011.
- Wu JJ, Choi YM, Bebchuk JD. Risk of myocardial infarction in psoriasis patients: a retrospective cohort study. J Dermatolog Treat. 2015;26:230-234.
Psoriasis is a chronic inflammatory disease that affects approximately 2% to 3% of the US population.1 Patients with psoriasis are more likely to have cardiovascular risk factors (eg, obesity, metabolic syndrome) than individuals without psoriasis.2 In fact, recent evidence has suggested that a diagnosis of psoriasis is an independent risk factor for cardiometabolic diseases including diabetes, major adverse cardiovascular events, and obesity.3 Given the well-recognized health benefits of physical activity and the associated reduction in coronary heart disease risk,4 patients with psoriasis specifically may benefit from regular participation in physical activity. Thus, an enhanced understanding of the relationship between psoriasis and vigorous physical activity would help determine the role of initiating and recommending interventions that implement physical activity for patients with psoriasis. A review was conducted to determine the relationship between psoriasis and vigorous physical activity.
Methods
An English-language literature search of PubMed articles indexed for MEDLINE (January 1, 1946–October 15, 2017) as well as articles in the Embase database (January 1, 1947–October 15, 2017) and Cochrane Library (January 1, 1992–October 15, 2017) using the terms psoriasis and physical activity was performed. The search strategy was established based on a prior review of vigorous physical activity in eczema.5 The article titles and/or abstracts were reviewed, and the studies were excluded if they did not evaluate physical activity in patients with psoriasis. Studies without a control group also were excluded. Articles on patients with psoriatic arthritis and studies that involved modification of dietary intake also were excluded.
Two reviewers (M.A. and E.B.L.) independently extracted data from the studies and compiled the results. The following factors were included in the data extracted: study year, location, and design; method of diagnosis of psoriasis; total number of patients included in the study; and age, gender, and level of physical activity of the study patients. Level of physical activity was the exposure, and diagnosis of psoriasis was the dependent variable. Physical activity was defined differently across the studies that were evaluated. To determine study quality, we implemented the Newcastle–Ottawa Scale (NOS), a 9-star scoring system that includes items such as selection criteria, comparability, and study outcome.6 Studies with an NOS score of 7 or higher were included in the meta-analysis.
Results
The literature search generated 353 nonduplicate articles. A thorough review of the articles yielded 4 studies that were incorporated in the final analysis.7-10 We aimed to perform a meta-analysis; however, only 1 of the studies included in the final analysis had an NOS score of 7 or higher along with adequate data to be incorporated into our study.10 As a result, the meta-analysis was converted to a regular review.
The cross-sectional study we reviewed, which had an NOS score of 7, included males and females in the United States aged 20 to 59 years.10 Data were collected using the population-based National Health and Nutrition Examination Survey from 2003 to 2006. The survey measured the likelihood of participation in leisure-time moderate to vigorous physical activity (MVPA) and metabolic equivalent task (MET) minutes of MVPA in the past 30 days. Of 6549 participants, 385 were excluded from the analysis due to missing values for 1 or more of the study variables. Of the remaining 6164 participants, 84 (1.4%) reported having a diagnosis of psoriasis with few or no psoriasis patches at the time of the survey, and 71 (1.2%) reported having a diagnosis of psoriasis with few to extensive patches at the time of the survey.10
Participants with psoriasis were less likely to participate in MVPA in the previous 30 days compared to participants without psoriasis, but the association was not statistically significant.10 The study demonstrated that, on average, participants with psoriasis spent 31% (95% confidence interval [CI], −0.57 to −0.05) fewer MET minutes on leisure-time MVPA versus participants without psoriasis; however, this association was not statistically significant. It is important to note that the diagnosis of psoriasis was self-reported, and measures of disease duration or areas of involvement were not incorporated.
Comment
Our review revealed that vigorous physical activity may be reduced in patients with psoriasis compared to those without psoriasis. Initially, we aimed to perform a systematic review of the literature; however, only 1 study met the criteria for the systematic review, highlighting the need for more robust studies evaluating this subject.
Do et al10 demonstrated that psoriasis patients were less likely to participate in MVPA, but the findings were not statistically significant. Of those who participated in MVPA, MET minutes were fewer among patients with few to extensive skin lesions compared to those without psoriasis. The investigators suggested that psoriasis patients with more severe disease tend to exercise less and ultimately would benefit from regular vigorous physical activity.
Frankel et al7 performed a prospective cohort study in US women to evaluate the role of physical activity in preventing psoriasis. The investigators reported that the most physically active quintile had a lower multivariate relative risk of psoriasis (0.72; 95% CI, 0.59–0.89; P<.001 for trend) compared to the least active quintile.7 Additionally, vigorous physical activity, which was defined as 6 or more MET minutes, was associated with a significantly lower risk of incident psoriasis (0.66; 95% CI, 0.54–0.81; P<.001 for trend), which maintained significance after adjusting for body mass index (BMI). The investigators suggested that, by decreasing chronic inflammation and lowering levels of proinflammatory cytokines, vigorous physical activity may reduce the risk of psoriasis development in women.7 It is plausible that vigorous physical activity modifies the state of chronic inflammation, which could subsequently reduce the risk of developing psoriasis; however, further long-term, randomized, prospective studies are needed to verify the relationship between physical activity and development of psoriasis.
Torres et al8 performed a cross-sectional questionnaire study to assess physical activity in patients with severe psoriasis (defined as >10% body surface area involvement and/or disease requiring systemic therapy or phototherapy) versus healthy controls. Physical activity level was measured using the International Physical Activity Questionnaire. The odds ratio of low-level physical activity compared to non–low-level physical activity among psoriasis patients versus controls was 3.42 (95% CI, 1.47–7.91; P=.002). Additionally, the average total MET minutes of psoriasis patients were significantly reduced compared to those of the healthy controls (P=.001). Thus, the investigators suggested that vigorous physical activity is less likely in psoriasis patients, which may contribute to the increased risk of cardiovascular disease in this population.8 Vigorous physical activity would benefit patients with psoriasis to help lower the chronic state of inflammation and cardiometabolic comorbidities.
Demirel et al9 performed a study to compare aerobic exercise capacity and daily physical activity level in psoriasis patients (n=30) compared to controls (n=30). Daily physical activity, measured with an accelerometer, was significantly higher in male patients with psoriasis compared to controls (P=.021). No significant difference was reported in maximal aerobic capacity in both male and female psoriasis patients versus controls. The investigators suggested that the level of daily physical activity is not limited in psoriasis patients, yet the small sample size may limit the generalizability of the study.
The ability to dissipate heat during exercise seems to be diminished in patients with psoriasis. Specifically, it has been suggested that psoriasis lesions interfere with normal perspiration.11 Moreover, joint involvement in patients with psoriatic arthritis may lead to physical functional disabilities that can interfere with the ability of these patients to participate in regular physical activity.12-14 For this reason, our review excluded articles that evaluated patients with psoriatic arthritis. Despite this exclusion, it is important to consider that comorbid psoriatic arthritis in clinical practice may impede patients with psoriasis from participating in physical activity. Additionally, various social aspects also may limit physical activity in psoriasis patients; for instance, psoriasis patients often avoid activities that involve increased exposure of the skin (eg, communal showers, wearing sports attire).15
Furthermore, obese psoriasis patients are less likely to exercise compared to obese individuals without psoriasis.16 In patients with higher BMI, the risk of psoriasis is increased.17 A systematic review suggested that weight loss may improve psoriasis severity.18 Bariatric surgery also may improve psoriasis.19 Moreover, obesity may interfere with response to biologic therapies for psoriasis. Specifically, higher BMI is linked with lower response to fixed-dose biologic therapies compared to weight-based biologic options (eg, infliximab).20,21
Conclusion
Given the increased risk of myocardial infarction in patients with psoriasis, it is important to recognize the barriers to physical activity that psoriasis patients face.22 Due to the considerable health benefits associated with regular physical activity, physicians should encourage patients with psoriasis to participate in physical activity as tolerated. Of note, the studies included in this review varied in their definitions of psoriasis disease severity and measures of physical activity level. Long-term, randomized, prospective studies are needed to clarify the relationship between psoriasis and physical activity. Evidence from these studies would help guide clinical recommendations regarding the role of physical activity for patients with psoriasis.
Psoriasis is a chronic inflammatory disease that affects approximately 2% to 3% of the US population.1 Patients with psoriasis are more likely to have cardiovascular risk factors (eg, obesity, metabolic syndrome) than individuals without psoriasis.2 In fact, recent evidence has suggested that a diagnosis of psoriasis is an independent risk factor for cardiometabolic diseases including diabetes, major adverse cardiovascular events, and obesity.3 Given the well-recognized health benefits of physical activity and the associated reduction in coronary heart disease risk,4 patients with psoriasis specifically may benefit from regular participation in physical activity. Thus, an enhanced understanding of the relationship between psoriasis and vigorous physical activity would help determine the role of initiating and recommending interventions that implement physical activity for patients with psoriasis. A review was conducted to determine the relationship between psoriasis and vigorous physical activity.
Methods
An English-language literature search of PubMed articles indexed for MEDLINE (January 1, 1946–October 15, 2017) as well as articles in the Embase database (January 1, 1947–October 15, 2017) and Cochrane Library (January 1, 1992–October 15, 2017) using the terms psoriasis and physical activity was performed. The search strategy was established based on a prior review of vigorous physical activity in eczema.5 The article titles and/or abstracts were reviewed, and the studies were excluded if they did not evaluate physical activity in patients with psoriasis. Studies without a control group also were excluded. Articles on patients with psoriatic arthritis and studies that involved modification of dietary intake also were excluded.
Two reviewers (M.A. and E.B.L.) independently extracted data from the studies and compiled the results. The following factors were included in the data extracted: study year, location, and design; method of diagnosis of psoriasis; total number of patients included in the study; and age, gender, and level of physical activity of the study patients. Level of physical activity was the exposure, and diagnosis of psoriasis was the dependent variable. Physical activity was defined differently across the studies that were evaluated. To determine study quality, we implemented the Newcastle–Ottawa Scale (NOS), a 9-star scoring system that includes items such as selection criteria, comparability, and study outcome.6 Studies with an NOS score of 7 or higher were included in the meta-analysis.
Results
The literature search generated 353 nonduplicate articles. A thorough review of the articles yielded 4 studies that were incorporated in the final analysis.7-10 We aimed to perform a meta-analysis; however, only 1 of the studies included in the final analysis had an NOS score of 7 or higher along with adequate data to be incorporated into our study.10 As a result, the meta-analysis was converted to a regular review.
The cross-sectional study we reviewed, which had an NOS score of 7, included males and females in the United States aged 20 to 59 years.10 Data were collected using the population-based National Health and Nutrition Examination Survey from 2003 to 2006. The survey measured the likelihood of participation in leisure-time moderate to vigorous physical activity (MVPA) and metabolic equivalent task (MET) minutes of MVPA in the past 30 days. Of 6549 participants, 385 were excluded from the analysis due to missing values for 1 or more of the study variables. Of the remaining 6164 participants, 84 (1.4%) reported having a diagnosis of psoriasis with few or no psoriasis patches at the time of the survey, and 71 (1.2%) reported having a diagnosis of psoriasis with few to extensive patches at the time of the survey.10
Participants with psoriasis were less likely to participate in MVPA in the previous 30 days compared to participants without psoriasis, but the association was not statistically significant.10 The study demonstrated that, on average, participants with psoriasis spent 31% (95% confidence interval [CI], −0.57 to −0.05) fewer MET minutes on leisure-time MVPA versus participants without psoriasis; however, this association was not statistically significant. It is important to note that the diagnosis of psoriasis was self-reported, and measures of disease duration or areas of involvement were not incorporated.
Comment
Our review revealed that vigorous physical activity may be reduced in patients with psoriasis compared to those without psoriasis. Initially, we aimed to perform a systematic review of the literature; however, only 1 study met the criteria for the systematic review, highlighting the need for more robust studies evaluating this subject.
Do et al10 demonstrated that psoriasis patients were less likely to participate in MVPA, but the findings were not statistically significant. Of those who participated in MVPA, MET minutes were fewer among patients with few to extensive skin lesions compared to those without psoriasis. The investigators suggested that psoriasis patients with more severe disease tend to exercise less and ultimately would benefit from regular vigorous physical activity.
Frankel et al7 performed a prospective cohort study in US women to evaluate the role of physical activity in preventing psoriasis. The investigators reported that the most physically active quintile had a lower multivariate relative risk of psoriasis (0.72; 95% CI, 0.59–0.89; P<.001 for trend) compared to the least active quintile.7 Additionally, vigorous physical activity, which was defined as 6 or more MET minutes, was associated with a significantly lower risk of incident psoriasis (0.66; 95% CI, 0.54–0.81; P<.001 for trend), which maintained significance after adjusting for body mass index (BMI). The investigators suggested that, by decreasing chronic inflammation and lowering levels of proinflammatory cytokines, vigorous physical activity may reduce the risk of psoriasis development in women.7 It is plausible that vigorous physical activity modifies the state of chronic inflammation, which could subsequently reduce the risk of developing psoriasis; however, further long-term, randomized, prospective studies are needed to verify the relationship between physical activity and development of psoriasis.
Torres et al8 performed a cross-sectional questionnaire study to assess physical activity in patients with severe psoriasis (defined as >10% body surface area involvement and/or disease requiring systemic therapy or phototherapy) versus healthy controls. Physical activity level was measured using the International Physical Activity Questionnaire. The odds ratio of low-level physical activity compared to non–low-level physical activity among psoriasis patients versus controls was 3.42 (95% CI, 1.47–7.91; P=.002). Additionally, the average total MET minutes of psoriasis patients were significantly reduced compared to those of the healthy controls (P=.001). Thus, the investigators suggested that vigorous physical activity is less likely in psoriasis patients, which may contribute to the increased risk of cardiovascular disease in this population.8 Vigorous physical activity would benefit patients with psoriasis to help lower the chronic state of inflammation and cardiometabolic comorbidities.
Demirel et al9 performed a study to compare aerobic exercise capacity and daily physical activity level in psoriasis patients (n=30) compared to controls (n=30). Daily physical activity, measured with an accelerometer, was significantly higher in male patients with psoriasis compared to controls (P=.021). No significant difference was reported in maximal aerobic capacity in both male and female psoriasis patients versus controls. The investigators suggested that the level of daily physical activity is not limited in psoriasis patients, yet the small sample size may limit the generalizability of the study.
The ability to dissipate heat during exercise seems to be diminished in patients with psoriasis. Specifically, it has been suggested that psoriasis lesions interfere with normal perspiration.11 Moreover, joint involvement in patients with psoriatic arthritis may lead to physical functional disabilities that can interfere with the ability of these patients to participate in regular physical activity.12-14 For this reason, our review excluded articles that evaluated patients with psoriatic arthritis. Despite this exclusion, it is important to consider that comorbid psoriatic arthritis in clinical practice may impede patients with psoriasis from participating in physical activity. Additionally, various social aspects also may limit physical activity in psoriasis patients; for instance, psoriasis patients often avoid activities that involve increased exposure of the skin (eg, communal showers, wearing sports attire).15
Furthermore, obese psoriasis patients are less likely to exercise compared to obese individuals without psoriasis.16 In patients with higher BMI, the risk of psoriasis is increased.17 A systematic review suggested that weight loss may improve psoriasis severity.18 Bariatric surgery also may improve psoriasis.19 Moreover, obesity may interfere with response to biologic therapies for psoriasis. Specifically, higher BMI is linked with lower response to fixed-dose biologic therapies compared to weight-based biologic options (eg, infliximab).20,21
Conclusion
Given the increased risk of myocardial infarction in patients with psoriasis, it is important to recognize the barriers to physical activity that psoriasis patients face.22 Due to the considerable health benefits associated with regular physical activity, physicians should encourage patients with psoriasis to participate in physical activity as tolerated. Of note, the studies included in this review varied in their definitions of psoriasis disease severity and measures of physical activity level. Long-term, randomized, prospective studies are needed to clarify the relationship between psoriasis and physical activity. Evidence from these studies would help guide clinical recommendations regarding the role of physical activity for patients with psoriasis.
- Takeshita J, Gelfand JM, Li P, et al. Psoriasis in the US Medicare population: prevalence, treatment, and factors associated with biologic use. J Invest Dermatol. 2015;135:2955-2963.
- Prey S, Paul C, Bronsard V, et al. Cardiovascular risk factors in patients with plaque psoriasis: a systematic review of epidemiological studies. J Eur Acad Dermatol Venereol. 2010;24(suppl 2):23-30.
- Takeshita J, Grewal S, Langan SM, et al. Psoriasis and comorbid diseases: epidemiology. J Am Acad Dermatol. 2017;76:377-390.
- Leon AS. Biological mechanisms for the cardioprotective effects of aerobic exercise. Am J Lifestyle Med. 2009;3:32S-34S.
- Kim A, Silverberg JI. A systematic review of vigorous physical activity in eczema. Br J Dermatol. 2016;174:660-662.
- Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. The Ottawa Hospital Research Institute website. http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm. Accessed February 23, 2018.
- Frankel HC, Han J, Li T, et al. The association between physical activity and the risk of incident psoriasis. Arch Dermatol. 2012;148:918-924.
- Torres T, Alexandre JM, Mendonça D, et al. Levels of physical activity in patients with severe psoriasis: a cross-sectional questionnaire study. Am J Clin Dermatol. 2014;15:129-135.
- Demirel R, Genc A, Ucok K, et al. Do patients with mild to moderate psoriasis really have a sedentary lifestyle? Int J Dermatol. 2013;52:1129-1134.
- Do YK, Lakhani N, Malhotra R, et al. Association between psoriasis and leisure‐time physical activity: findings from the National Health and Nutrition Examination Survey. J Dermatol. 2015;42:148-153.
- Leibowitz E, Seidman DS, Laor A, et al. Are psoriatic patients at risk of heat intolerance? Br J Dermatol. 1991;124:439-442.
- Husted JA, Tom BD, Farewell VT, et al. Description and prediction of physical functional disability in psoriatic arthritis: a longitudinal analysis using a Markov model approach. Arthritis Rheum. 2005;53:404-409.
- Wilson FC, Icen M, Crowson CS, et al. Incidence and clinical predictors of psoriatic arthritis in patients with psoriasis: a population‐based study. Arthritis Rheum. 2009;61:233-239.
- Shih M, Hootman JM, Kruger J, et al. Physical activity in men and women with arthritis: National Health Interview Survey, 2002. Am J Prev Med. 2006;30:385-393.
- Ramsay B, O’Reagan M. A survey of the social and psychological effects of psoriasis. Br J Dermatol. 1988;118:195-201.
- Herron MD, Hinckley M, Hoffman MS, et al. Impact of obesity and smoking on psoriasis presentation and management. Arch Dermatol. 2005;141:1527-1534.
- Kumar S, Han J, Li T, et al. Obesity, waist circumference, weight change and the risk of psoriasis in US women. J Eur Acad Dermatol Venereol. 2013;27:1293-1298.
- Upala S, Sanguankeo A. Effect of lifestyle weight loss intervention on disease severity in patients with psoriasis: a systematic review and meta-analysis. Int J Obes (Lond). 2015;39:1197-1202.
- Sako EY, Famenini S, Wu JJ. Bariatric surgery and psoriasis. J Am Acad Dermatol. 2014;70:774-779.
- Clark L, Lebwohl M. The effect of weight on the efficacy of biologic therapy in patients with psoriasis. J Am Acad Dermatol. 2008;58:443-446.
- Puig L. Obesity and psoriasis: body weight and body mass index influence the response to biological treatment. J Eur Acad Dermatol Venereol. 2011;25:1007-1011.
- Wu JJ, Choi YM, Bebchuk JD. Risk of myocardial infarction in psoriasis patients: a retrospective cohort study. J Dermatolog Treat. 2015;26:230-234.
- Takeshita J, Gelfand JM, Li P, et al. Psoriasis in the US Medicare population: prevalence, treatment, and factors associated with biologic use. J Invest Dermatol. 2015;135:2955-2963.
- Prey S, Paul C, Bronsard V, et al. Cardiovascular risk factors in patients with plaque psoriasis: a systematic review of epidemiological studies. J Eur Acad Dermatol Venereol. 2010;24(suppl 2):23-30.
- Takeshita J, Grewal S, Langan SM, et al. Psoriasis and comorbid diseases: epidemiology. J Am Acad Dermatol. 2017;76:377-390.
- Leon AS. Biological mechanisms for the cardioprotective effects of aerobic exercise. Am J Lifestyle Med. 2009;3:32S-34S.
- Kim A, Silverberg JI. A systematic review of vigorous physical activity in eczema. Br J Dermatol. 2016;174:660-662.
- Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. The Ottawa Hospital Research Institute website. http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm. Accessed February 23, 2018.
- Frankel HC, Han J, Li T, et al. The association between physical activity and the risk of incident psoriasis. Arch Dermatol. 2012;148:918-924.
- Torres T, Alexandre JM, Mendonça D, et al. Levels of physical activity in patients with severe psoriasis: a cross-sectional questionnaire study. Am J Clin Dermatol. 2014;15:129-135.
- Demirel R, Genc A, Ucok K, et al. Do patients with mild to moderate psoriasis really have a sedentary lifestyle? Int J Dermatol. 2013;52:1129-1134.
- Do YK, Lakhani N, Malhotra R, et al. Association between psoriasis and leisure‐time physical activity: findings from the National Health and Nutrition Examination Survey. J Dermatol. 2015;42:148-153.
- Leibowitz E, Seidman DS, Laor A, et al. Are psoriatic patients at risk of heat intolerance? Br J Dermatol. 1991;124:439-442.
- Husted JA, Tom BD, Farewell VT, et al. Description and prediction of physical functional disability in psoriatic arthritis: a longitudinal analysis using a Markov model approach. Arthritis Rheum. 2005;53:404-409.
- Wilson FC, Icen M, Crowson CS, et al. Incidence and clinical predictors of psoriatic arthritis in patients with psoriasis: a population‐based study. Arthritis Rheum. 2009;61:233-239.
- Shih M, Hootman JM, Kruger J, et al. Physical activity in men and women with arthritis: National Health Interview Survey, 2002. Am J Prev Med. 2006;30:385-393.
- Ramsay B, O’Reagan M. A survey of the social and psychological effects of psoriasis. Br J Dermatol. 1988;118:195-201.
- Herron MD, Hinckley M, Hoffman MS, et al. Impact of obesity and smoking on psoriasis presentation and management. Arch Dermatol. 2005;141:1527-1534.
- Kumar S, Han J, Li T, et al. Obesity, waist circumference, weight change and the risk of psoriasis in US women. J Eur Acad Dermatol Venereol. 2013;27:1293-1298.
- Upala S, Sanguankeo A. Effect of lifestyle weight loss intervention on disease severity in patients with psoriasis: a systematic review and meta-analysis. Int J Obes (Lond). 2015;39:1197-1202.
- Sako EY, Famenini S, Wu JJ. Bariatric surgery and psoriasis. J Am Acad Dermatol. 2014;70:774-779.
- Clark L, Lebwohl M. The effect of weight on the efficacy of biologic therapy in patients with psoriasis. J Am Acad Dermatol. 2008;58:443-446.
- Puig L. Obesity and psoriasis: body weight and body mass index influence the response to biological treatment. J Eur Acad Dermatol Venereol. 2011;25:1007-1011.
- Wu JJ, Choi YM, Bebchuk JD. Risk of myocardial infarction in psoriasis patients: a retrospective cohort study. J Dermatolog Treat. 2015;26:230-234.
Practice Points
- Psoriasis is associated with comorbid disease conditions, including cardiovascular disease.
- Regular physical activity is known to decrease the risk of developing cardiovascular disease.
- Patients with psoriasis would likely benefit from regular participation in vigorous physical activity to help reduce the risk of developing cardiovascular disease.
Mild cognitive impairment rises in heart patients with comorbidities
ANAHEIM, CALIF. – Across the spectrum of cardiovascular disease, the more comorbid conditions a patient has, the higher the likelihood of mild cognitive impairment, Jocasta Ball, PhD, reported at the American Heart Association scientific sessions.
Indeed, her cross-sectional analysis of baseline data on 2,161 participants in five randomized controlled trials of nurse-led chronic disease management in cardiovascular disease (CVD) showed that for every 1-unit increase in the age-adjusted Charlson Comorbidity Index, the likelihood of mild cognitive impairment (MCI) jumped by 19%.
This novel observation has important clinical implications: “MCI is becoming increasingly recognized as exerting a powerful and negative impact on the risk, management, and prognosis of CVD patients,” explained Dr. Ball of the Baker Heart and Diabetes Institute in Melbourne. “Because MCI undermines a patient’s ability to comply with medical treatment and adds to patient complexity, it is critical [to identify] higher-risk individuals who require closer surveillance and improved early intervention.”
She added that the findings open up a whole new field of research aimed at developing new interventions to help patients with CVD and MCI stay on track with their heart disease treatment program.
The 2,161 subjects, mean age 70 years and two-thirds male, ranged across the full spectrum of cardiovascular disease, from mild to severe. All were screened for MCI by completing the Montreal Cognitive Assessment, or MoCA. A MoCA score below 26 out of a possible 30 is defined as MCI.
Forty-seven percent of subjects had MCI. They were older, with a mean age of 73 years versus 67 years; were more likely to have a history of stroke, by a margin of 20% versus 12%; had a 52% prevalence of atrial fibrillation versus 44%; and had a 50% prevalence of heart failure versus 39% in subjects with normal cognition. In addition, 48% of the MCI group screened positive for depressive symptoms versus 37% of those without MCI, and 28% of patients with MCI had type 2 diabetes, compared with 22% of those without MCI. Renal disease was also significantly more prevalent in the MCI group, by a margin of 21% versus 14%.
In a multivariate regression analysis, the strongest predictors of MCI in patients across the spectrum of CVD were current smoking, with a 2.5-fold increased risk compared with that of nonsmokers, and atrial fibrillation, with a 1.3-fold increased risk.
Dr. Ball reported having no financial conflicts regarding her study.
SOURCE: Ball J. et al. AHA 2017, Abstract 16240.
ANAHEIM, CALIF. – Across the spectrum of cardiovascular disease, the more comorbid conditions a patient has, the higher the likelihood of mild cognitive impairment, Jocasta Ball, PhD, reported at the American Heart Association scientific sessions.
Indeed, her cross-sectional analysis of baseline data on 2,161 participants in five randomized controlled trials of nurse-led chronic disease management in cardiovascular disease (CVD) showed that for every 1-unit increase in the age-adjusted Charlson Comorbidity Index, the likelihood of mild cognitive impairment (MCI) jumped by 19%.
This novel observation has important clinical implications: “MCI is becoming increasingly recognized as exerting a powerful and negative impact on the risk, management, and prognosis of CVD patients,” explained Dr. Ball of the Baker Heart and Diabetes Institute in Melbourne. “Because MCI undermines a patient’s ability to comply with medical treatment and adds to patient complexity, it is critical [to identify] higher-risk individuals who require closer surveillance and improved early intervention.”
She added that the findings open up a whole new field of research aimed at developing new interventions to help patients with CVD and MCI stay on track with their heart disease treatment program.
The 2,161 subjects, mean age 70 years and two-thirds male, ranged across the full spectrum of cardiovascular disease, from mild to severe. All were screened for MCI by completing the Montreal Cognitive Assessment, or MoCA. A MoCA score below 26 out of a possible 30 is defined as MCI.
Forty-seven percent of subjects had MCI. They were older, with a mean age of 73 years versus 67 years; were more likely to have a history of stroke, by a margin of 20% versus 12%; had a 52% prevalence of atrial fibrillation versus 44%; and had a 50% prevalence of heart failure versus 39% in subjects with normal cognition. In addition, 48% of the MCI group screened positive for depressive symptoms versus 37% of those without MCI, and 28% of patients with MCI had type 2 diabetes, compared with 22% of those without MCI. Renal disease was also significantly more prevalent in the MCI group, by a margin of 21% versus 14%.
In a multivariate regression analysis, the strongest predictors of MCI in patients across the spectrum of CVD were current smoking, with a 2.5-fold increased risk compared with that of nonsmokers, and atrial fibrillation, with a 1.3-fold increased risk.
Dr. Ball reported having no financial conflicts regarding her study.
SOURCE: Ball J. et al. AHA 2017, Abstract 16240.
ANAHEIM, CALIF. – Across the spectrum of cardiovascular disease, the more comorbid conditions a patient has, the higher the likelihood of mild cognitive impairment, Jocasta Ball, PhD, reported at the American Heart Association scientific sessions.
Indeed, her cross-sectional analysis of baseline data on 2,161 participants in five randomized controlled trials of nurse-led chronic disease management in cardiovascular disease (CVD) showed that for every 1-unit increase in the age-adjusted Charlson Comorbidity Index, the likelihood of mild cognitive impairment (MCI) jumped by 19%.
This novel observation has important clinical implications: “MCI is becoming increasingly recognized as exerting a powerful and negative impact on the risk, management, and prognosis of CVD patients,” explained Dr. Ball of the Baker Heart and Diabetes Institute in Melbourne. “Because MCI undermines a patient’s ability to comply with medical treatment and adds to patient complexity, it is critical [to identify] higher-risk individuals who require closer surveillance and improved early intervention.”
She added that the findings open up a whole new field of research aimed at developing new interventions to help patients with CVD and MCI stay on track with their heart disease treatment program.
The 2,161 subjects, mean age 70 years and two-thirds male, ranged across the full spectrum of cardiovascular disease, from mild to severe. All were screened for MCI by completing the Montreal Cognitive Assessment, or MoCA. A MoCA score below 26 out of a possible 30 is defined as MCI.
Forty-seven percent of subjects had MCI. They were older, with a mean age of 73 years versus 67 years; were more likely to have a history of stroke, by a margin of 20% versus 12%; had a 52% prevalence of atrial fibrillation versus 44%; and had a 50% prevalence of heart failure versus 39% in subjects with normal cognition. In addition, 48% of the MCI group screened positive for depressive symptoms versus 37% of those without MCI, and 28% of patients with MCI had type 2 diabetes, compared with 22% of those without MCI. Renal disease was also significantly more prevalent in the MCI group, by a margin of 21% versus 14%.
In a multivariate regression analysis, the strongest predictors of MCI in patients across the spectrum of CVD were current smoking, with a 2.5-fold increased risk compared with that of nonsmokers, and atrial fibrillation, with a 1.3-fold increased risk.
Dr. Ball reported having no financial conflicts regarding her study.
SOURCE: Ball J. et al. AHA 2017, Abstract 16240.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point: The more comorbid conditions a patient with cardiovascular disease has, the greater the likelihood of mild cognitive impairment becomes.
Major finding: For each 1-unit increase in the Charlson Comorbidity Index, the likelihood of prevalent mild cognitive impairment rose by 19%.
Study details: This cross-sectional study assessed the association between mild cognitive impairment and Charlson Comorbidity Index score in 2,161 patients with cardiovascular disease of varied degrees of severity.
Disclosures: The presenter reported having no financial conflicts regarding her study.
Source: Ball J et al. AHA 2017, Abstract 16240
Enhanced recovery after surgery for the patient with chronic pain
CASE Chronic pelvic pain from endometriosis
A 40-year-old woman (G0) has a 20-year history of chronic pelvic pain. Stage III endometriosis is diagnosed on laparoscopic excision of endometriotic tissue. Postoperative pain symptoms include dysmenorrhea and deep dyspareunia, and the patient is feeling anxious. Physical examination reveals a retroverted uterus, right adnexal fullness and tenderness, and tenderness on palpation of the right levator ani and right obturator internus; rectovaginal examination findings are unremarkable. The patient, though now engaged in a pelvic floor physical therapy program, has yet to achieve the pain control she desires. After reviewing the treatment strategies for endometriosis with the patient, she elects definitive surgical management with minimally invasive hysterectomy and salpingo-oophorectomy. What pre-, intra-, and postoperative pain management plan do you devise for this patient?
Chronic pelvic pain presents a unique clinical challenge, as pain typically is multifactorial, and several peripheral pain generators may be involved. Although surgery can be performed to manage anatomically based disease processes, it does not address pain from musculoskeletal or neuropathic sources. A complete medical history and a physical examination are of utmost importance in developing a comprehensive multimodal management plan that may include surgery as treatment for the pain.
The standard of care for surgery is a minimally invasive approach (vaginal, laparoscopic, or robot-assisted laparoscopic), as it causes the least amount of trauma. Benefits of minimally invasive surgery include shorter hospitalization and faster recovery, likely owing to improved perioperative pain control, decreased blood loss, and fewer infections. Although this approach minimizes surgical trauma and thereby helps decrease the surgical stress response, the patient experience can be optimized with use of enhanced recovery pathways (ERPs), a multimodal approach to perioperative care.
ERPs were initially proposed as a means of reducing the degree of surgical injury and the subsequent physiologic stress response.1 This multimodal approach begins in the outpatient setting, includes preoperative and intraoperative modalities, and continues postoperatively. In patients with chronic pain, ERPs are even more important. Assigning “prehabilitation” and setting expectations for surgery goals are the first step in improving the patient experience. Intraoperative use of opioid-sparing anesthetics or regional anesthesia can improve recovery. After surgery, patients with chronic pain and/or opioid dependence receive medications on a schedule, along with short-interval follow-up. Ultimately, reducing acute postoperative pain may lower the risk of developing chronic pain.
In this article on patients with chronic pelvic pain, we highlight elements of ERPs within the framework of enhanced recovery after surgery. Many of the interventions proposed here also can be used to improve the surgical experience of patients without chronic pain.
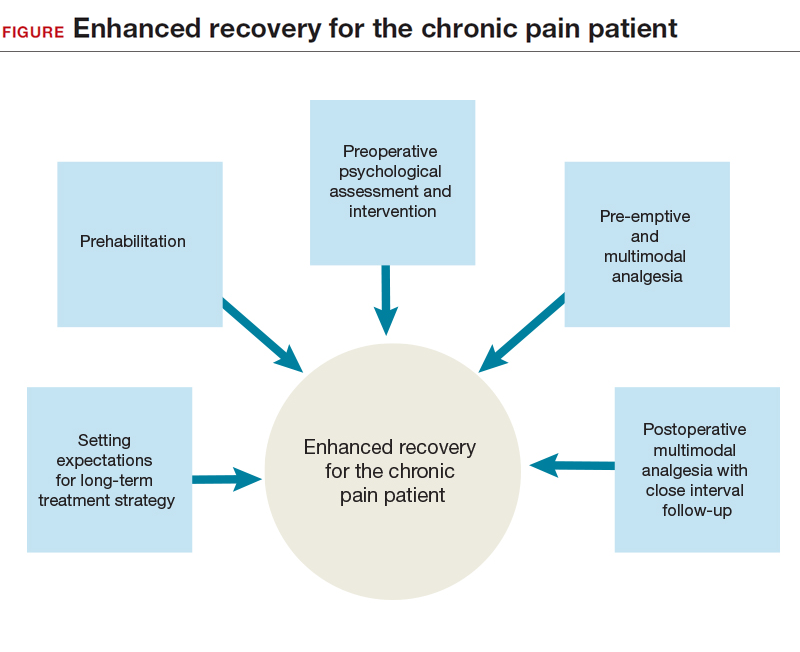
Preadmission education, expectations, and optimization
Preoperative counseling for elective procedures generally occurs in the outpatient setting. Although discussion traditionally has covered the type of procedure and its associated risks, benefits, and alternatives, new guidelines suggest a more mindful and comprehensive approach is warranted. Individualized patient-centered education programs have a positive impact on the perioperative course, effecting reductions in preoperative anxiety, opioid requirements, and hospital length of stay.2 From a pain management perspective, the clinician can take some time during preoperative counseling to inform the patient about the pain to be expected from surgery, the ways the pain will be managed intraoperatively and postoperatively, and the multimodal strategies that will be used throughout the patient’s stay2 and that may allow for early discharge. Although preadmission counseling still should address expectations for the surgery, it also presents an opportunity both to assess the patient’s ability to cope with the physical and psychological stress of surgery and to offer the patient appropriate need-based interventions, such as prehabilitation and cognitive-behavioral therapy (CBT).
Prehabilitation is the process of increasing functional capacity before surgery in order to mitigate the stress of the surgery. Prehabilitation may involve aerobic exercise, strength training, or functional task training. The gynecologic surgery literature lacks prehabilitation data, but data in the colorectal literature support use of a prehabilitation program for patients having a scheduled colectomy, with improved postoperative recovery.3 Although the colectomy cohort predominantly included older men, the principle that guides program implementation is the same: improve recovery after the stress of abdominal surgery. Indeed, a patient who opts for an elective surgery may have to wait several weeks before undergoing the procedure, and during this period behavioral interventions can take effect. With postoperative complications occurring more often in patients with reduced functional capacity, the data support using prehabilitation to decrease the incidence of postoperative complications, particularly among the most vulnerable patients.4 However, a definitive recommendation on use of pelvic floor exercises as an adjunct to prehabilitation cannot be made.4 Successful prehabilitation takes at least 4 weeks and should be part of a multimodal program that addresses other behavioral risk factors that may negatively affect recovery.5 For example, current tobacco users have compromised pulmonary status and wound healing immediately after surgery, and use more opioids.6 Conversely, smoking cessation for as little as 4 weeks before surgery is associated with fewer complications.7 In addition, given that alcohol abuse may compromise the surgical stress response and increase the risk of opioid misuse, addressing alcohol abuse preoperatively may improve postoperative recovery.8
Treating mood disorders that coexist with chronic pain disorders is an important part of outpatient multimodal management—psychological intervention is a useful adjunct to prehabilitation in reducing perioperative anxiety and improving postoperative functional capacity.9 For patients who have chronic pain and are undergoing surgery, it is important to address any anxiety, depression, or poor coping skills (eg, pain catastrophizing) to try to reduce the postoperative pain experience and decrease the risk of chronic postsurgical pain (CPSP).10,11
Before surgery, patients with chronic pain syndromes should be evaluated for emotional distress and pain coping ability. When possible, they should be referred to a pain psychologist, who can initiate CBT and other interventions. In addition, pain coping skills can be developed or reinforced to address preoperative anxiety and pain catastrophizing. These interventions, which may include use of visual imagery, breathing exercises, and other relaxation techniques, are applicable to the management of postoperative anxiety as well.
Read about preoperative multimodal analgesia and intra- and postoperative management.
Preoperative multimodal analgesia
Multimodal analgesia has several benefits. Simultaneous effects can be generated on multiple pain-related neurotransmitters, and a synergistic effect (eg, of acetaminophen and a nonsteroidal anti-inflammatory drug [NSAID]) can improve pain management. In addition, small doses of multiple medications can be given, instead of a large dose of a single medication. Of course, this strategy must be modified in elderly and patients with impaired renal function, who are at high risk for polypharmacy.
Preoperative administration of 3 medications—a selective cyclooxygenase 2 (COX-2) inhibitor, acetaminophen, and a gabapentinoid—is increasingly accepted as part of multimodal analgesia. The selective COX-2 inhibitor targets inflammatory prostaglandins and has anti-inflammatory and analgesic effects; acetaminophen, an effective analgesic with an unclear mechanism of action, can reduce postoperative opioid consumption12 and works synergistically with NSAIDs13; and the gabapentinoid gabapentin has an analgesic effect likely contributing to decreased movement-related pain and subsequent improved functional recovery (data are mixed on whether continuing gabapentin after surgery prevents CPSP).14−16
Although serotonin and norepinephrine reuptake inhibitors (SNRIs) are commonly used in outpatient management of chronic pelvic pain, data suggest that their role in perioperative pain management is evolving. As SNRIs may reduce central nervous system (CNS) sensitization,17 their analgesic effect is thought to result from increased descending inhibitory tone in the CNS, which makes this class of medication ideal for patients with chronic neuropathic pain.15
Limited data also suggest a role for SNRIs in decreasing immediate postoperative pain and CPSP in high-risk patients. Studies of duloxetine use in the immediate perioperative period have found reduced postoperative acute pain and opioid use.18,19 In addition, a short course of low-dose (37.5 mg) venlafaxine both before and after surgery has demonstrated a reduction in postoperative opioid use and a reduction in movement-related pain 6 months after surgery.20
Intraoperative management
The surgical and anesthesia teams share the goal of optimizing both pain control and postoperative recovery. Surgical team members, who want longer-acting anesthetics for infiltration of incision sites, discuss with the anesthesiologist the appropriateness of using peripheral nerve blocks or neuraxial anesthesia, given the patient’s history and planned procedure. Anesthesia team members can improve anesthesia and minimize intraoperative opioid use through several methods, including total intravenous anesthesia,21 dexamethasone,22 ketorolac,23 and intravenous ketamine. Ketamine, in particular, has a wide range of surgical applications and has been found to reduce postoperative pain, postoperative pain medication use, and the risk of CPSP.2
Incision sites should be infiltrated before and after surgery. Lidocaine traditionally is used for its rapid onset of action in reducing surgical site pain, but its short half-life may limit its applicability to postoperative pain. Recently, bupivacaine (half-life, 3.5 hours) and liposomal bupivacaine (24–34 hours) have gained more attention. Both of these medications appear to be as effective as lidocaine in reducing surgical site pain.24
Transversus abdominis plane (TAP) blocks have been used as an adjunct in pain management during abdominopelvic surgery. Although initial data on postoperative pain and opioid use reductions with TAP blocks were inconclusive,25 more recent data showed a role for TAP blocks in a multimodal approach for reducing opioid use during laparoscopic and open surgery.26,27 Given the small number of studies on using liposomal bupivacaine for peripheral nerve blocks (eg, TAP blocks) in postoperative pain management, current data are inconclusive.28
Postoperative management
The ERP approach calls for continuing multimodal analgesia after surgery—in most cases, scheduling early use of oral acetaminophen and ibuprofen, and providing short-acting, low-dose opioid analgesia as needed. All patients should be given a bowel regimen. Similar to undergoing prehabilitation for surgery, patients should prepare themselves for recovery. They should be encouraged to engage in early ambulation and oral intake and, when clinically appropriate, be given same-day discharge for minimally invasive surgical procedures.
Patients with chronic pain before surgery are at increased risk for suboptimal postoperative pain management, and those who are dependent on opioids require additional perioperative measures for adequate postoperative pain control. In these complicated cases, it is appropriate to enlist a pain specialist, potentially before surgery, to help plan perioperative and postoperative pain management.2 Postoperative pain management for opioid-dependent patients should include pharmacologic and nonpharmacologic interventions, such as use of nonopioid medications (eg, gabapentin) and continuation of CBT. Patients with chronic pain should be closely followed up for assessment of postoperative pain control and recovery.
CASE Resolved
Surgical management is one aspect of the longer term multimodal pain management strategy for this patient. After preoperative pelvic floor physical therapy, she is receptive to starting a trial of an SNRI for her pain and mood symptoms. Both interventions allow for optimization of her preoperative physical and psychological status. Expectations are set that she will be discharged the day of surgery and that the surgery is but one component of her multimodal treatment plan. In addition, before surgery, she takes oral acetaminophen, gabapentin, and celecoxib—previously having had no contraindications to these medications. During surgery, bupivacaine is used for infiltration of all incision sites, and the anesthesia team administers ketamine and a TAP block. After surgery, the patient is prepared for same-day discharge and given the NSAIDs and acetaminophen she is scheduled to take over the next 72 hours. She is also given a limited prescription for oxycodone for breakthrough pain. An office visit 1 to 2 weeks after surgery is scheduled.
ERP strategies for surgical management of endometriosis have not only improved this patient’s postoperative recovery but also reduced her surgical stress response and subsequent transition to chronic postoperative pain. Many of the strategies used in this case are applicable to patients without chronic pain.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997;78(5):606−617.
- Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17(2):131−157.
- Mayo NE, Feldman L, Scott S, et al. Impact of preoperative change in physical function on postoperative recovery: argument supporting prehabilitation for colorectal surgery. Surgery. 2011;150(3):505−514.
- Moran J, Guinan E, McCormick P, et al. The ability of prehabilitation to influence postoperative outcome after intra-abdominal operation: a systematic review and meta-analysis. Surgery. 2016;160(5):1189−1201.
- Tew GA, Ayyash R, Durrand J, Danjoux GR. Clinical guideline and recommendations on pre-operative exercise training in patients awaiting major non-cardiac surgery [published online ahead of print January 13, 2018]. Anaesthesia. doi:10.1111/anae.14177.
- Chiang HL, Chia YY, Lin HS, Chen CH. The implications of tobacco smoking on acute postoperative pain: a prospective observational study. Pain Res Manag. 2016;2016:9432493.
- Mastracci TM, Carli F, Finley RJ, Muccio S, Warner DO; Members of the Evidence-Based Reviews in Surgery Group. Effect of preoperative smoking cessation interventions on postoperative complications. J Am Coll Surg. 2011;212(6):1094−1096.
- Tonnesen H, Kehlet H. Preoperative alcoholism and postoperative morbidity. Br J Surg. 1999;86(7):869−874.
- Gillis C, Li C, Lee L, et al. Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology. 2014;121(5):937−947.
- Khan RS, Ahmed K, Blakeway E, et al. Catastrophizing: a predictive factor for postoperative pain. Am J Surg. 2011;201(1):122−131.
- Pinto PR, McIntyre T, Nogueira-Silva C, Almeida A, Araujo-Soares V. Risk factors for persistent postsurgical pain in women undergoing hysterectomy due to benign causes: a prospective predictive study. J Pain. 2012;13(11):1045−1057.
- Moon YE, Lee YK, Lee J, Moon DE. The effects of preoperative intravenous acetaminophen in patients undergoing abdominal hysterectomy. Arch Gynecol Obstet. 2011;284(6):1455−1460.
- Ong CK, Seymour RA, Lirk P, Merry AF. Combining paracetamol (acetaminophen) with nonsteroidal antiinflammatory drugs: a qualitative systematic review of analgesic efficacy for acute postoperative pain. Anesth Analg. 2010;110(4):1170−1179.
- Clarke H, Bonin RP, Orser BA, Englesakis M, Wijeysundera DN, Katz J. The prevention of chronic postsurgical pain using gabapentin and pregabalin: a combined systematic review and meta-analysis. Anesth Analg. 2012;115(2):428−442.
- Gilron I. Gabapentin and pregabalin for chronic neuropathic and early postsurgical pain: current evidence and future directions. Curr Opin Anaesthesiol. 2007;20(5):456−472.
- Chaparro LE, Smith SA, Moore RA, Wiffen PJ, Gilron I. Pharmacotherapy for the prevention of chronic pain after surgery in adults. Cochrane Database Syst Rev. 2013;(7):CD008307.
- Woolf CJ. Central sensitization: implications for the diagnosis and treatment of pain. Pain. 2011;152(3 suppl):S2−S15.
- Castro-Alves LJ, Oliveira de Medeiros AC, Neves SP, et al. Perioperative duloxetine to improve postoperative recovery after abdominal hysterectomy: a prospective, randomized, double-blinded, placebo-controlled study. Anesth Analg. 2016;122(1):98−104.
- Bedin A, Caldart Bedin RA, Vieira JE, Ashmawi HA. Duloxetine as an analgesic reduces opioid consumption after spine surgery: a randomized, double-blind, controlled study. Clin J Pain. 2017;33(10):865−869.
- Amr YM, Yousef AA. Evaluation of efficacy of the perioperative administration of venlafaxine or gabapentin on acute and chronic postmastectomy pain. Clin J Pain. 2010;26(5):381–385.
- Marret E, Rolin M, Beaussier M, Bonnet F. Meta-analysis of intravenous lidocaine and postoperative recovery after abdominal surgery. Br J Surg. 2008;95(11):1331–1338.
- De Oliveira GS Jr, Almeida MD, Benzon HT, McCarthy RJ. Perioperative single dose systemic dexamethasone for postoperative pain: a meta-analysis of randomized controlled trials. Anesthesiology. 2011;115(3):575–588.
- De Oliveira GS Jr, Agarwal D, Benzon HT. Perioperative single dose ketorolac to prevent postoperative pain: a meta-analysis of randomized trials. Anesth Analg. 2012;114(2):424–433.
- Hamilton TW, Athanassoglou V, Mellon S, et al. Liposomal bupivacaine infiltration at the surgical site for the management of postoperative pain. Cochrane Database Syst Rev. 2017;(2):CD011419.
- Charlton S, Cyna AM, Middleton P, Griffiths JD. Perioperative transversus abdominis plane (TAP) blocks for analgesia after abdominal surgery. Cochrane Database Syst Rev. 2010;(12):CD007705.
- Hain E, Maggiori L, Prost À la Denise J, Panis Y. Transversus abdominis plane (TAP) block in laparoscopic colorectal surgery improves postoperative pain management: a meta-analysis [published online ahead of print January 30, 2018]. Colorectal Dis. doi:10.1111/codi.14037.
- Staker JJ, Liu D, Church R, et al. A triple-blind, placebo-controlled randomised trial of the ilioinguinal-transversus abdominis plane (I-TAP) nerve block for elective caesarean section [published online ahead of print January 29, 2018]. Anaesthesia. doi:10.1111/anae.14222.
- Hamilton TW, Athanassoglou V, Trivella M, et al. Liposomal bupivacaine peripheral nerve block for the management of postoperative pain. Cochrane Database Syst Rev. 2016;(8):CD011476.
CASE Chronic pelvic pain from endometriosis
A 40-year-old woman (G0) has a 20-year history of chronic pelvic pain. Stage III endometriosis is diagnosed on laparoscopic excision of endometriotic tissue. Postoperative pain symptoms include dysmenorrhea and deep dyspareunia, and the patient is feeling anxious. Physical examination reveals a retroverted uterus, right adnexal fullness and tenderness, and tenderness on palpation of the right levator ani and right obturator internus; rectovaginal examination findings are unremarkable. The patient, though now engaged in a pelvic floor physical therapy program, has yet to achieve the pain control she desires. After reviewing the treatment strategies for endometriosis with the patient, she elects definitive surgical management with minimally invasive hysterectomy and salpingo-oophorectomy. What pre-, intra-, and postoperative pain management plan do you devise for this patient?
Chronic pelvic pain presents a unique clinical challenge, as pain typically is multifactorial, and several peripheral pain generators may be involved. Although surgery can be performed to manage anatomically based disease processes, it does not address pain from musculoskeletal or neuropathic sources. A complete medical history and a physical examination are of utmost importance in developing a comprehensive multimodal management plan that may include surgery as treatment for the pain.
The standard of care for surgery is a minimally invasive approach (vaginal, laparoscopic, or robot-assisted laparoscopic), as it causes the least amount of trauma. Benefits of minimally invasive surgery include shorter hospitalization and faster recovery, likely owing to improved perioperative pain control, decreased blood loss, and fewer infections. Although this approach minimizes surgical trauma and thereby helps decrease the surgical stress response, the patient experience can be optimized with use of enhanced recovery pathways (ERPs), a multimodal approach to perioperative care.
ERPs were initially proposed as a means of reducing the degree of surgical injury and the subsequent physiologic stress response.1 This multimodal approach begins in the outpatient setting, includes preoperative and intraoperative modalities, and continues postoperatively. In patients with chronic pain, ERPs are even more important. Assigning “prehabilitation” and setting expectations for surgery goals are the first step in improving the patient experience. Intraoperative use of opioid-sparing anesthetics or regional anesthesia can improve recovery. After surgery, patients with chronic pain and/or opioid dependence receive medications on a schedule, along with short-interval follow-up. Ultimately, reducing acute postoperative pain may lower the risk of developing chronic pain.
In this article on patients with chronic pelvic pain, we highlight elements of ERPs within the framework of enhanced recovery after surgery. Many of the interventions proposed here also can be used to improve the surgical experience of patients without chronic pain.
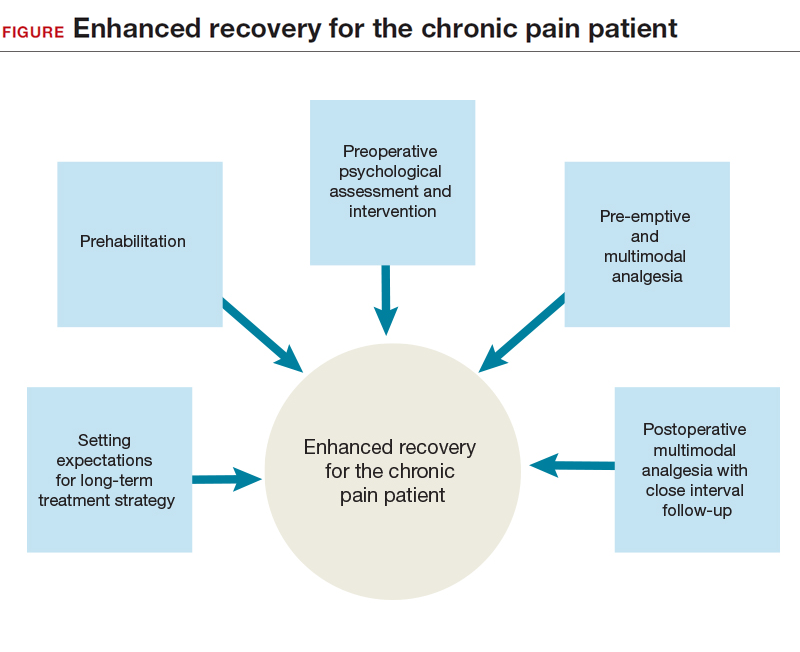
Preadmission education, expectations, and optimization
Preoperative counseling for elective procedures generally occurs in the outpatient setting. Although discussion traditionally has covered the type of procedure and its associated risks, benefits, and alternatives, new guidelines suggest a more mindful and comprehensive approach is warranted. Individualized patient-centered education programs have a positive impact on the perioperative course, effecting reductions in preoperative anxiety, opioid requirements, and hospital length of stay.2 From a pain management perspective, the clinician can take some time during preoperative counseling to inform the patient about the pain to be expected from surgery, the ways the pain will be managed intraoperatively and postoperatively, and the multimodal strategies that will be used throughout the patient’s stay2 and that may allow for early discharge. Although preadmission counseling still should address expectations for the surgery, it also presents an opportunity both to assess the patient’s ability to cope with the physical and psychological stress of surgery and to offer the patient appropriate need-based interventions, such as prehabilitation and cognitive-behavioral therapy (CBT).
Prehabilitation is the process of increasing functional capacity before surgery in order to mitigate the stress of the surgery. Prehabilitation may involve aerobic exercise, strength training, or functional task training. The gynecologic surgery literature lacks prehabilitation data, but data in the colorectal literature support use of a prehabilitation program for patients having a scheduled colectomy, with improved postoperative recovery.3 Although the colectomy cohort predominantly included older men, the principle that guides program implementation is the same: improve recovery after the stress of abdominal surgery. Indeed, a patient who opts for an elective surgery may have to wait several weeks before undergoing the procedure, and during this period behavioral interventions can take effect. With postoperative complications occurring more often in patients with reduced functional capacity, the data support using prehabilitation to decrease the incidence of postoperative complications, particularly among the most vulnerable patients.4 However, a definitive recommendation on use of pelvic floor exercises as an adjunct to prehabilitation cannot be made.4 Successful prehabilitation takes at least 4 weeks and should be part of a multimodal program that addresses other behavioral risk factors that may negatively affect recovery.5 For example, current tobacco users have compromised pulmonary status and wound healing immediately after surgery, and use more opioids.6 Conversely, smoking cessation for as little as 4 weeks before surgery is associated with fewer complications.7 In addition, given that alcohol abuse may compromise the surgical stress response and increase the risk of opioid misuse, addressing alcohol abuse preoperatively may improve postoperative recovery.8
Treating mood disorders that coexist with chronic pain disorders is an important part of outpatient multimodal management—psychological intervention is a useful adjunct to prehabilitation in reducing perioperative anxiety and improving postoperative functional capacity.9 For patients who have chronic pain and are undergoing surgery, it is important to address any anxiety, depression, or poor coping skills (eg, pain catastrophizing) to try to reduce the postoperative pain experience and decrease the risk of chronic postsurgical pain (CPSP).10,11
Before surgery, patients with chronic pain syndromes should be evaluated for emotional distress and pain coping ability. When possible, they should be referred to a pain psychologist, who can initiate CBT and other interventions. In addition, pain coping skills can be developed or reinforced to address preoperative anxiety and pain catastrophizing. These interventions, which may include use of visual imagery, breathing exercises, and other relaxation techniques, are applicable to the management of postoperative anxiety as well.
Read about preoperative multimodal analgesia and intra- and postoperative management.
Preoperative multimodal analgesia
Multimodal analgesia has several benefits. Simultaneous effects can be generated on multiple pain-related neurotransmitters, and a synergistic effect (eg, of acetaminophen and a nonsteroidal anti-inflammatory drug [NSAID]) can improve pain management. In addition, small doses of multiple medications can be given, instead of a large dose of a single medication. Of course, this strategy must be modified in elderly and patients with impaired renal function, who are at high risk for polypharmacy.
Preoperative administration of 3 medications—a selective cyclooxygenase 2 (COX-2) inhibitor, acetaminophen, and a gabapentinoid—is increasingly accepted as part of multimodal analgesia. The selective COX-2 inhibitor targets inflammatory prostaglandins and has anti-inflammatory and analgesic effects; acetaminophen, an effective analgesic with an unclear mechanism of action, can reduce postoperative opioid consumption12 and works synergistically with NSAIDs13; and the gabapentinoid gabapentin has an analgesic effect likely contributing to decreased movement-related pain and subsequent improved functional recovery (data are mixed on whether continuing gabapentin after surgery prevents CPSP).14−16
Although serotonin and norepinephrine reuptake inhibitors (SNRIs) are commonly used in outpatient management of chronic pelvic pain, data suggest that their role in perioperative pain management is evolving. As SNRIs may reduce central nervous system (CNS) sensitization,17 their analgesic effect is thought to result from increased descending inhibitory tone in the CNS, which makes this class of medication ideal for patients with chronic neuropathic pain.15
Limited data also suggest a role for SNRIs in decreasing immediate postoperative pain and CPSP in high-risk patients. Studies of duloxetine use in the immediate perioperative period have found reduced postoperative acute pain and opioid use.18,19 In addition, a short course of low-dose (37.5 mg) venlafaxine both before and after surgery has demonstrated a reduction in postoperative opioid use and a reduction in movement-related pain 6 months after surgery.20
Intraoperative management
The surgical and anesthesia teams share the goal of optimizing both pain control and postoperative recovery. Surgical team members, who want longer-acting anesthetics for infiltration of incision sites, discuss with the anesthesiologist the appropriateness of using peripheral nerve blocks or neuraxial anesthesia, given the patient’s history and planned procedure. Anesthesia team members can improve anesthesia and minimize intraoperative opioid use through several methods, including total intravenous anesthesia,21 dexamethasone,22 ketorolac,23 and intravenous ketamine. Ketamine, in particular, has a wide range of surgical applications and has been found to reduce postoperative pain, postoperative pain medication use, and the risk of CPSP.2
Incision sites should be infiltrated before and after surgery. Lidocaine traditionally is used for its rapid onset of action in reducing surgical site pain, but its short half-life may limit its applicability to postoperative pain. Recently, bupivacaine (half-life, 3.5 hours) and liposomal bupivacaine (24–34 hours) have gained more attention. Both of these medications appear to be as effective as lidocaine in reducing surgical site pain.24
Transversus abdominis plane (TAP) blocks have been used as an adjunct in pain management during abdominopelvic surgery. Although initial data on postoperative pain and opioid use reductions with TAP blocks were inconclusive,25 more recent data showed a role for TAP blocks in a multimodal approach for reducing opioid use during laparoscopic and open surgery.26,27 Given the small number of studies on using liposomal bupivacaine for peripheral nerve blocks (eg, TAP blocks) in postoperative pain management, current data are inconclusive.28
Postoperative management
The ERP approach calls for continuing multimodal analgesia after surgery—in most cases, scheduling early use of oral acetaminophen and ibuprofen, and providing short-acting, low-dose opioid analgesia as needed. All patients should be given a bowel regimen. Similar to undergoing prehabilitation for surgery, patients should prepare themselves for recovery. They should be encouraged to engage in early ambulation and oral intake and, when clinically appropriate, be given same-day discharge for minimally invasive surgical procedures.
Patients with chronic pain before surgery are at increased risk for suboptimal postoperative pain management, and those who are dependent on opioids require additional perioperative measures for adequate postoperative pain control. In these complicated cases, it is appropriate to enlist a pain specialist, potentially before surgery, to help plan perioperative and postoperative pain management.2 Postoperative pain management for opioid-dependent patients should include pharmacologic and nonpharmacologic interventions, such as use of nonopioid medications (eg, gabapentin) and continuation of CBT. Patients with chronic pain should be closely followed up for assessment of postoperative pain control and recovery.
CASE Resolved
Surgical management is one aspect of the longer term multimodal pain management strategy for this patient. After preoperative pelvic floor physical therapy, she is receptive to starting a trial of an SNRI for her pain and mood symptoms. Both interventions allow for optimization of her preoperative physical and psychological status. Expectations are set that she will be discharged the day of surgery and that the surgery is but one component of her multimodal treatment plan. In addition, before surgery, she takes oral acetaminophen, gabapentin, and celecoxib—previously having had no contraindications to these medications. During surgery, bupivacaine is used for infiltration of all incision sites, and the anesthesia team administers ketamine and a TAP block. After surgery, the patient is prepared for same-day discharge and given the NSAIDs and acetaminophen she is scheduled to take over the next 72 hours. She is also given a limited prescription for oxycodone for breakthrough pain. An office visit 1 to 2 weeks after surgery is scheduled.
ERP strategies for surgical management of endometriosis have not only improved this patient’s postoperative recovery but also reduced her surgical stress response and subsequent transition to chronic postoperative pain. Many of the strategies used in this case are applicable to patients without chronic pain.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
CASE Chronic pelvic pain from endometriosis
A 40-year-old woman (G0) has a 20-year history of chronic pelvic pain. Stage III endometriosis is diagnosed on laparoscopic excision of endometriotic tissue. Postoperative pain symptoms include dysmenorrhea and deep dyspareunia, and the patient is feeling anxious. Physical examination reveals a retroverted uterus, right adnexal fullness and tenderness, and tenderness on palpation of the right levator ani and right obturator internus; rectovaginal examination findings are unremarkable. The patient, though now engaged in a pelvic floor physical therapy program, has yet to achieve the pain control she desires. After reviewing the treatment strategies for endometriosis with the patient, she elects definitive surgical management with minimally invasive hysterectomy and salpingo-oophorectomy. What pre-, intra-, and postoperative pain management plan do you devise for this patient?
Chronic pelvic pain presents a unique clinical challenge, as pain typically is multifactorial, and several peripheral pain generators may be involved. Although surgery can be performed to manage anatomically based disease processes, it does not address pain from musculoskeletal or neuropathic sources. A complete medical history and a physical examination are of utmost importance in developing a comprehensive multimodal management plan that may include surgery as treatment for the pain.
The standard of care for surgery is a minimally invasive approach (vaginal, laparoscopic, or robot-assisted laparoscopic), as it causes the least amount of trauma. Benefits of minimally invasive surgery include shorter hospitalization and faster recovery, likely owing to improved perioperative pain control, decreased blood loss, and fewer infections. Although this approach minimizes surgical trauma and thereby helps decrease the surgical stress response, the patient experience can be optimized with use of enhanced recovery pathways (ERPs), a multimodal approach to perioperative care.
ERPs were initially proposed as a means of reducing the degree of surgical injury and the subsequent physiologic stress response.1 This multimodal approach begins in the outpatient setting, includes preoperative and intraoperative modalities, and continues postoperatively. In patients with chronic pain, ERPs are even more important. Assigning “prehabilitation” and setting expectations for surgery goals are the first step in improving the patient experience. Intraoperative use of opioid-sparing anesthetics or regional anesthesia can improve recovery. After surgery, patients with chronic pain and/or opioid dependence receive medications on a schedule, along with short-interval follow-up. Ultimately, reducing acute postoperative pain may lower the risk of developing chronic pain.
In this article on patients with chronic pelvic pain, we highlight elements of ERPs within the framework of enhanced recovery after surgery. Many of the interventions proposed here also can be used to improve the surgical experience of patients without chronic pain.
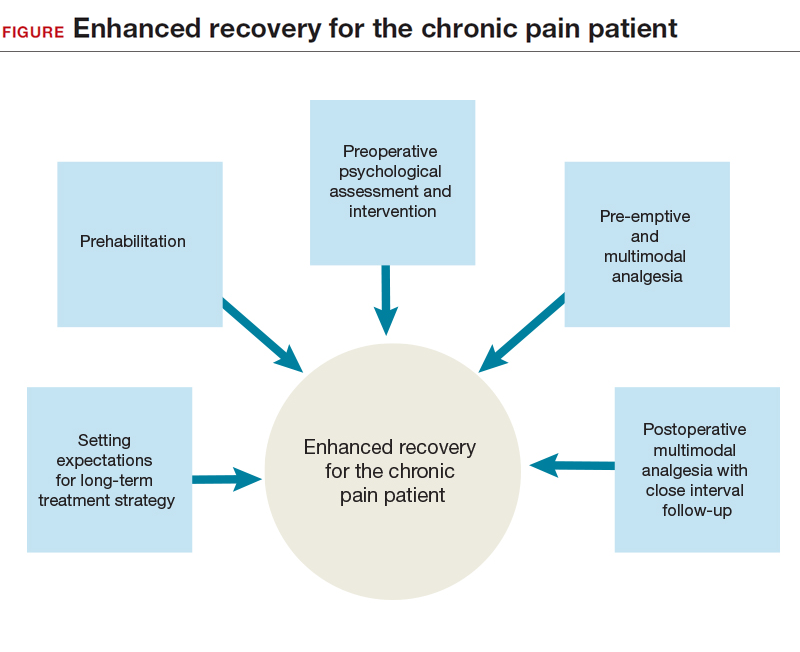
Preadmission education, expectations, and optimization
Preoperative counseling for elective procedures generally occurs in the outpatient setting. Although discussion traditionally has covered the type of procedure and its associated risks, benefits, and alternatives, new guidelines suggest a more mindful and comprehensive approach is warranted. Individualized patient-centered education programs have a positive impact on the perioperative course, effecting reductions in preoperative anxiety, opioid requirements, and hospital length of stay.2 From a pain management perspective, the clinician can take some time during preoperative counseling to inform the patient about the pain to be expected from surgery, the ways the pain will be managed intraoperatively and postoperatively, and the multimodal strategies that will be used throughout the patient’s stay2 and that may allow for early discharge. Although preadmission counseling still should address expectations for the surgery, it also presents an opportunity both to assess the patient’s ability to cope with the physical and psychological stress of surgery and to offer the patient appropriate need-based interventions, such as prehabilitation and cognitive-behavioral therapy (CBT).
Prehabilitation is the process of increasing functional capacity before surgery in order to mitigate the stress of the surgery. Prehabilitation may involve aerobic exercise, strength training, or functional task training. The gynecologic surgery literature lacks prehabilitation data, but data in the colorectal literature support use of a prehabilitation program for patients having a scheduled colectomy, with improved postoperative recovery.3 Although the colectomy cohort predominantly included older men, the principle that guides program implementation is the same: improve recovery after the stress of abdominal surgery. Indeed, a patient who opts for an elective surgery may have to wait several weeks before undergoing the procedure, and during this period behavioral interventions can take effect. With postoperative complications occurring more often in patients with reduced functional capacity, the data support using prehabilitation to decrease the incidence of postoperative complications, particularly among the most vulnerable patients.4 However, a definitive recommendation on use of pelvic floor exercises as an adjunct to prehabilitation cannot be made.4 Successful prehabilitation takes at least 4 weeks and should be part of a multimodal program that addresses other behavioral risk factors that may negatively affect recovery.5 For example, current tobacco users have compromised pulmonary status and wound healing immediately after surgery, and use more opioids.6 Conversely, smoking cessation for as little as 4 weeks before surgery is associated with fewer complications.7 In addition, given that alcohol abuse may compromise the surgical stress response and increase the risk of opioid misuse, addressing alcohol abuse preoperatively may improve postoperative recovery.8
Treating mood disorders that coexist with chronic pain disorders is an important part of outpatient multimodal management—psychological intervention is a useful adjunct to prehabilitation in reducing perioperative anxiety and improving postoperative functional capacity.9 For patients who have chronic pain and are undergoing surgery, it is important to address any anxiety, depression, or poor coping skills (eg, pain catastrophizing) to try to reduce the postoperative pain experience and decrease the risk of chronic postsurgical pain (CPSP).10,11
Before surgery, patients with chronic pain syndromes should be evaluated for emotional distress and pain coping ability. When possible, they should be referred to a pain psychologist, who can initiate CBT and other interventions. In addition, pain coping skills can be developed or reinforced to address preoperative anxiety and pain catastrophizing. These interventions, which may include use of visual imagery, breathing exercises, and other relaxation techniques, are applicable to the management of postoperative anxiety as well.
Read about preoperative multimodal analgesia and intra- and postoperative management.
Preoperative multimodal analgesia
Multimodal analgesia has several benefits. Simultaneous effects can be generated on multiple pain-related neurotransmitters, and a synergistic effect (eg, of acetaminophen and a nonsteroidal anti-inflammatory drug [NSAID]) can improve pain management. In addition, small doses of multiple medications can be given, instead of a large dose of a single medication. Of course, this strategy must be modified in elderly and patients with impaired renal function, who are at high risk for polypharmacy.
Preoperative administration of 3 medications—a selective cyclooxygenase 2 (COX-2) inhibitor, acetaminophen, and a gabapentinoid—is increasingly accepted as part of multimodal analgesia. The selective COX-2 inhibitor targets inflammatory prostaglandins and has anti-inflammatory and analgesic effects; acetaminophen, an effective analgesic with an unclear mechanism of action, can reduce postoperative opioid consumption12 and works synergistically with NSAIDs13; and the gabapentinoid gabapentin has an analgesic effect likely contributing to decreased movement-related pain and subsequent improved functional recovery (data are mixed on whether continuing gabapentin after surgery prevents CPSP).14−16
Although serotonin and norepinephrine reuptake inhibitors (SNRIs) are commonly used in outpatient management of chronic pelvic pain, data suggest that their role in perioperative pain management is evolving. As SNRIs may reduce central nervous system (CNS) sensitization,17 their analgesic effect is thought to result from increased descending inhibitory tone in the CNS, which makes this class of medication ideal for patients with chronic neuropathic pain.15
Limited data also suggest a role for SNRIs in decreasing immediate postoperative pain and CPSP in high-risk patients. Studies of duloxetine use in the immediate perioperative period have found reduced postoperative acute pain and opioid use.18,19 In addition, a short course of low-dose (37.5 mg) venlafaxine both before and after surgery has demonstrated a reduction in postoperative opioid use and a reduction in movement-related pain 6 months after surgery.20
Intraoperative management
The surgical and anesthesia teams share the goal of optimizing both pain control and postoperative recovery. Surgical team members, who want longer-acting anesthetics for infiltration of incision sites, discuss with the anesthesiologist the appropriateness of using peripheral nerve blocks or neuraxial anesthesia, given the patient’s history and planned procedure. Anesthesia team members can improve anesthesia and minimize intraoperative opioid use through several methods, including total intravenous anesthesia,21 dexamethasone,22 ketorolac,23 and intravenous ketamine. Ketamine, in particular, has a wide range of surgical applications and has been found to reduce postoperative pain, postoperative pain medication use, and the risk of CPSP.2
Incision sites should be infiltrated before and after surgery. Lidocaine traditionally is used for its rapid onset of action in reducing surgical site pain, but its short half-life may limit its applicability to postoperative pain. Recently, bupivacaine (half-life, 3.5 hours) and liposomal bupivacaine (24–34 hours) have gained more attention. Both of these medications appear to be as effective as lidocaine in reducing surgical site pain.24
Transversus abdominis plane (TAP) blocks have been used as an adjunct in pain management during abdominopelvic surgery. Although initial data on postoperative pain and opioid use reductions with TAP blocks were inconclusive,25 more recent data showed a role for TAP blocks in a multimodal approach for reducing opioid use during laparoscopic and open surgery.26,27 Given the small number of studies on using liposomal bupivacaine for peripheral nerve blocks (eg, TAP blocks) in postoperative pain management, current data are inconclusive.28
Postoperative management
The ERP approach calls for continuing multimodal analgesia after surgery—in most cases, scheduling early use of oral acetaminophen and ibuprofen, and providing short-acting, low-dose opioid analgesia as needed. All patients should be given a bowel regimen. Similar to undergoing prehabilitation for surgery, patients should prepare themselves for recovery. They should be encouraged to engage in early ambulation and oral intake and, when clinically appropriate, be given same-day discharge for minimally invasive surgical procedures.
Patients with chronic pain before surgery are at increased risk for suboptimal postoperative pain management, and those who are dependent on opioids require additional perioperative measures for adequate postoperative pain control. In these complicated cases, it is appropriate to enlist a pain specialist, potentially before surgery, to help plan perioperative and postoperative pain management.2 Postoperative pain management for opioid-dependent patients should include pharmacologic and nonpharmacologic interventions, such as use of nonopioid medications (eg, gabapentin) and continuation of CBT. Patients with chronic pain should be closely followed up for assessment of postoperative pain control and recovery.
CASE Resolved
Surgical management is one aspect of the longer term multimodal pain management strategy for this patient. After preoperative pelvic floor physical therapy, she is receptive to starting a trial of an SNRI for her pain and mood symptoms. Both interventions allow for optimization of her preoperative physical and psychological status. Expectations are set that she will be discharged the day of surgery and that the surgery is but one component of her multimodal treatment plan. In addition, before surgery, she takes oral acetaminophen, gabapentin, and celecoxib—previously having had no contraindications to these medications. During surgery, bupivacaine is used for infiltration of all incision sites, and the anesthesia team administers ketamine and a TAP block. After surgery, the patient is prepared for same-day discharge and given the NSAIDs and acetaminophen she is scheduled to take over the next 72 hours. She is also given a limited prescription for oxycodone for breakthrough pain. An office visit 1 to 2 weeks after surgery is scheduled.
ERP strategies for surgical management of endometriosis have not only improved this patient’s postoperative recovery but also reduced her surgical stress response and subsequent transition to chronic postoperative pain. Many of the strategies used in this case are applicable to patients without chronic pain.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997;78(5):606−617.
- Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17(2):131−157.
- Mayo NE, Feldman L, Scott S, et al. Impact of preoperative change in physical function on postoperative recovery: argument supporting prehabilitation for colorectal surgery. Surgery. 2011;150(3):505−514.
- Moran J, Guinan E, McCormick P, et al. The ability of prehabilitation to influence postoperative outcome after intra-abdominal operation: a systematic review and meta-analysis. Surgery. 2016;160(5):1189−1201.
- Tew GA, Ayyash R, Durrand J, Danjoux GR. Clinical guideline and recommendations on pre-operative exercise training in patients awaiting major non-cardiac surgery [published online ahead of print January 13, 2018]. Anaesthesia. doi:10.1111/anae.14177.
- Chiang HL, Chia YY, Lin HS, Chen CH. The implications of tobacco smoking on acute postoperative pain: a prospective observational study. Pain Res Manag. 2016;2016:9432493.
- Mastracci TM, Carli F, Finley RJ, Muccio S, Warner DO; Members of the Evidence-Based Reviews in Surgery Group. Effect of preoperative smoking cessation interventions on postoperative complications. J Am Coll Surg. 2011;212(6):1094−1096.
- Tonnesen H, Kehlet H. Preoperative alcoholism and postoperative morbidity. Br J Surg. 1999;86(7):869−874.
- Gillis C, Li C, Lee L, et al. Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology. 2014;121(5):937−947.
- Khan RS, Ahmed K, Blakeway E, et al. Catastrophizing: a predictive factor for postoperative pain. Am J Surg. 2011;201(1):122−131.
- Pinto PR, McIntyre T, Nogueira-Silva C, Almeida A, Araujo-Soares V. Risk factors for persistent postsurgical pain in women undergoing hysterectomy due to benign causes: a prospective predictive study. J Pain. 2012;13(11):1045−1057.
- Moon YE, Lee YK, Lee J, Moon DE. The effects of preoperative intravenous acetaminophen in patients undergoing abdominal hysterectomy. Arch Gynecol Obstet. 2011;284(6):1455−1460.
- Ong CK, Seymour RA, Lirk P, Merry AF. Combining paracetamol (acetaminophen) with nonsteroidal antiinflammatory drugs: a qualitative systematic review of analgesic efficacy for acute postoperative pain. Anesth Analg. 2010;110(4):1170−1179.
- Clarke H, Bonin RP, Orser BA, Englesakis M, Wijeysundera DN, Katz J. The prevention of chronic postsurgical pain using gabapentin and pregabalin: a combined systematic review and meta-analysis. Anesth Analg. 2012;115(2):428−442.
- Gilron I. Gabapentin and pregabalin for chronic neuropathic and early postsurgical pain: current evidence and future directions. Curr Opin Anaesthesiol. 2007;20(5):456−472.
- Chaparro LE, Smith SA, Moore RA, Wiffen PJ, Gilron I. Pharmacotherapy for the prevention of chronic pain after surgery in adults. Cochrane Database Syst Rev. 2013;(7):CD008307.
- Woolf CJ. Central sensitization: implications for the diagnosis and treatment of pain. Pain. 2011;152(3 suppl):S2−S15.
- Castro-Alves LJ, Oliveira de Medeiros AC, Neves SP, et al. Perioperative duloxetine to improve postoperative recovery after abdominal hysterectomy: a prospective, randomized, double-blinded, placebo-controlled study. Anesth Analg. 2016;122(1):98−104.
- Bedin A, Caldart Bedin RA, Vieira JE, Ashmawi HA. Duloxetine as an analgesic reduces opioid consumption after spine surgery: a randomized, double-blind, controlled study. Clin J Pain. 2017;33(10):865−869.
- Amr YM, Yousef AA. Evaluation of efficacy of the perioperative administration of venlafaxine or gabapentin on acute and chronic postmastectomy pain. Clin J Pain. 2010;26(5):381–385.
- Marret E, Rolin M, Beaussier M, Bonnet F. Meta-analysis of intravenous lidocaine and postoperative recovery after abdominal surgery. Br J Surg. 2008;95(11):1331–1338.
- De Oliveira GS Jr, Almeida MD, Benzon HT, McCarthy RJ. Perioperative single dose systemic dexamethasone for postoperative pain: a meta-analysis of randomized controlled trials. Anesthesiology. 2011;115(3):575–588.
- De Oliveira GS Jr, Agarwal D, Benzon HT. Perioperative single dose ketorolac to prevent postoperative pain: a meta-analysis of randomized trials. Anesth Analg. 2012;114(2):424–433.
- Hamilton TW, Athanassoglou V, Mellon S, et al. Liposomal bupivacaine infiltration at the surgical site for the management of postoperative pain. Cochrane Database Syst Rev. 2017;(2):CD011419.
- Charlton S, Cyna AM, Middleton P, Griffiths JD. Perioperative transversus abdominis plane (TAP) blocks for analgesia after abdominal surgery. Cochrane Database Syst Rev. 2010;(12):CD007705.
- Hain E, Maggiori L, Prost À la Denise J, Panis Y. Transversus abdominis plane (TAP) block in laparoscopic colorectal surgery improves postoperative pain management: a meta-analysis [published online ahead of print January 30, 2018]. Colorectal Dis. doi:10.1111/codi.14037.
- Staker JJ, Liu D, Church R, et al. A triple-blind, placebo-controlled randomised trial of the ilioinguinal-transversus abdominis plane (I-TAP) nerve block for elective caesarean section [published online ahead of print January 29, 2018]. Anaesthesia. doi:10.1111/anae.14222.
- Hamilton TW, Athanassoglou V, Trivella M, et al. Liposomal bupivacaine peripheral nerve block for the management of postoperative pain. Cochrane Database Syst Rev. 2016;(8):CD011476.
- Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997;78(5):606−617.
- Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17(2):131−157.
- Mayo NE, Feldman L, Scott S, et al. Impact of preoperative change in physical function on postoperative recovery: argument supporting prehabilitation for colorectal surgery. Surgery. 2011;150(3):505−514.
- Moran J, Guinan E, McCormick P, et al. The ability of prehabilitation to influence postoperative outcome after intra-abdominal operation: a systematic review and meta-analysis. Surgery. 2016;160(5):1189−1201.
- Tew GA, Ayyash R, Durrand J, Danjoux GR. Clinical guideline and recommendations on pre-operative exercise training in patients awaiting major non-cardiac surgery [published online ahead of print January 13, 2018]. Anaesthesia. doi:10.1111/anae.14177.
- Chiang HL, Chia YY, Lin HS, Chen CH. The implications of tobacco smoking on acute postoperative pain: a prospective observational study. Pain Res Manag. 2016;2016:9432493.
- Mastracci TM, Carli F, Finley RJ, Muccio S, Warner DO; Members of the Evidence-Based Reviews in Surgery Group. Effect of preoperative smoking cessation interventions on postoperative complications. J Am Coll Surg. 2011;212(6):1094−1096.
- Tonnesen H, Kehlet H. Preoperative alcoholism and postoperative morbidity. Br J Surg. 1999;86(7):869−874.
- Gillis C, Li C, Lee L, et al. Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology. 2014;121(5):937−947.
- Khan RS, Ahmed K, Blakeway E, et al. Catastrophizing: a predictive factor for postoperative pain. Am J Surg. 2011;201(1):122−131.
- Pinto PR, McIntyre T, Nogueira-Silva C, Almeida A, Araujo-Soares V. Risk factors for persistent postsurgical pain in women undergoing hysterectomy due to benign causes: a prospective predictive study. J Pain. 2012;13(11):1045−1057.
- Moon YE, Lee YK, Lee J, Moon DE. The effects of preoperative intravenous acetaminophen in patients undergoing abdominal hysterectomy. Arch Gynecol Obstet. 2011;284(6):1455−1460.
- Ong CK, Seymour RA, Lirk P, Merry AF. Combining paracetamol (acetaminophen) with nonsteroidal antiinflammatory drugs: a qualitative systematic review of analgesic efficacy for acute postoperative pain. Anesth Analg. 2010;110(4):1170−1179.
- Clarke H, Bonin RP, Orser BA, Englesakis M, Wijeysundera DN, Katz J. The prevention of chronic postsurgical pain using gabapentin and pregabalin: a combined systematic review and meta-analysis. Anesth Analg. 2012;115(2):428−442.
- Gilron I. Gabapentin and pregabalin for chronic neuropathic and early postsurgical pain: current evidence and future directions. Curr Opin Anaesthesiol. 2007;20(5):456−472.
- Chaparro LE, Smith SA, Moore RA, Wiffen PJ, Gilron I. Pharmacotherapy for the prevention of chronic pain after surgery in adults. Cochrane Database Syst Rev. 2013;(7):CD008307.
- Woolf CJ. Central sensitization: implications for the diagnosis and treatment of pain. Pain. 2011;152(3 suppl):S2−S15.
- Castro-Alves LJ, Oliveira de Medeiros AC, Neves SP, et al. Perioperative duloxetine to improve postoperative recovery after abdominal hysterectomy: a prospective, randomized, double-blinded, placebo-controlled study. Anesth Analg. 2016;122(1):98−104.
- Bedin A, Caldart Bedin RA, Vieira JE, Ashmawi HA. Duloxetine as an analgesic reduces opioid consumption after spine surgery: a randomized, double-blind, controlled study. Clin J Pain. 2017;33(10):865−869.
- Amr YM, Yousef AA. Evaluation of efficacy of the perioperative administration of venlafaxine or gabapentin on acute and chronic postmastectomy pain. Clin J Pain. 2010;26(5):381–385.
- Marret E, Rolin M, Beaussier M, Bonnet F. Meta-analysis of intravenous lidocaine and postoperative recovery after abdominal surgery. Br J Surg. 2008;95(11):1331–1338.
- De Oliveira GS Jr, Almeida MD, Benzon HT, McCarthy RJ. Perioperative single dose systemic dexamethasone for postoperative pain: a meta-analysis of randomized controlled trials. Anesthesiology. 2011;115(3):575–588.
- De Oliveira GS Jr, Agarwal D, Benzon HT. Perioperative single dose ketorolac to prevent postoperative pain: a meta-analysis of randomized trials. Anesth Analg. 2012;114(2):424–433.
- Hamilton TW, Athanassoglou V, Mellon S, et al. Liposomal bupivacaine infiltration at the surgical site for the management of postoperative pain. Cochrane Database Syst Rev. 2017;(2):CD011419.
- Charlton S, Cyna AM, Middleton P, Griffiths JD. Perioperative transversus abdominis plane (TAP) blocks for analgesia after abdominal surgery. Cochrane Database Syst Rev. 2010;(12):CD007705.
- Hain E, Maggiori L, Prost À la Denise J, Panis Y. Transversus abdominis plane (TAP) block in laparoscopic colorectal surgery improves postoperative pain management: a meta-analysis [published online ahead of print January 30, 2018]. Colorectal Dis. doi:10.1111/codi.14037.
- Staker JJ, Liu D, Church R, et al. A triple-blind, placebo-controlled randomised trial of the ilioinguinal-transversus abdominis plane (I-TAP) nerve block for elective caesarean section [published online ahead of print January 29, 2018]. Anaesthesia. doi:10.1111/anae.14222.
- Hamilton TW, Athanassoglou V, Trivella M, et al. Liposomal bupivacaine peripheral nerve block for the management of postoperative pain. Cochrane Database Syst Rev. 2016;(8):CD011476.
Migraine: More Than Just a Headache
Data paint mixed picture on e-cigarettes
ORLANDO – E-cigarettes are likely safer than traditional cigarettes but it depends on the user, the voltage used, and the kind of liquid, according to a panel of experts at the joint congress of the American Academy of Allergy, Asthma and Immunology and the World Asthma Organization.
Thomas Casale, MD, professor of medicine at the University of South Florida, Tampa, said studies have found that in some ways, e-cigarettes seem safer. For example, the levels of carcinogens such as formaldehyde and heavy metals are found at levels that are 9-450 times higher in combustible cigarette smoke than e-cigarette vapor, he said. And toxic compounds have been found to be significantly lower in the urine of e-cigarette users compared to traditional cigarette smokers.
But it’s not so simple. While e-cigarettes typically cause lower exposure to formaldehyde, when heated at a higher voltage, exposure to formaldehyde hemiacetal, a formaldehyde precursor, is about seven times higher for someone smoking 3 mL of e-cigarette fluid a day – similar to a pack a day – than the formaldehyde exposure of someone smoking the same quantity of combustible cigarettes.
Dr. Casale added that experienced e-cigarette users typically take longer puffs than traditional smokers and that the unregulated e-cigarette industry is rife with mislabeling on things such as how much nicotine is in a given fluid.
“It’s dependent upon the device, the battery, how much it heats up and what’s in the liquid,” he said. “So in general, are they safer? Probably. But not exactly.”
There are also no long-term data on e-cigarettes, he added.
The evidence on how e-cigarettes affects traditional smoking habits is also mixed.
Some studies have indicated that e-cigarettes use can be helpful in kicking a traditional cigarette habit, said Jill Poole, MD, of the University of Nebraska, Omaha.
A survey by the U.S. Census Bureau found that, in the 2014-2015 data collection year, about 60% of smokers of combustible cigarettes who also smoked e-cigarettes tried to quit smoking combustibles, compared to 40% of those who didn’t smoke e-cigarettes. And 8% of e-cigarette users were successful over 3 months, compared to 4% of nonusers.
But data reveals risks for kids who’ve never smoked and then start using e-cigarettes.
“Does noncigarette tobacco use among never smoking youth determine subsequent smoking initiation?” she said. “The answer is yes.”
Dr. Poole added that a study published this year found that youths who’d never smoked traditional cigarettes were 87% more likely to start if they had first tried e-cigarettes (JAMA Pediatr. 2018;172(2):181-187).
And more children are using e-cigarettes frequently. The National Youth Tobacco Survey found that 16% of high schoolers in 2016 had used e-cigarettes in the past 30 days, way up from 1.5% in 2011, even as traditional cigarette use has declined from 15.8% to 9.3% among those children over that time.
Loretta Que, MD, associate professor of medicine at Duke University, Durham, N.C., noted how advertising for e-cigarettes is similar to the old ads for traditional cigarettes, attempting to convey coolness. With their wide array of colors and thousands of flavors, there is no doubt that e-cigarette pens have caught on among children, she said.
“They’re becoming something akin to an iPhone case or a handbag.”
ORLANDO – E-cigarettes are likely safer than traditional cigarettes but it depends on the user, the voltage used, and the kind of liquid, according to a panel of experts at the joint congress of the American Academy of Allergy, Asthma and Immunology and the World Asthma Organization.
Thomas Casale, MD, professor of medicine at the University of South Florida, Tampa, said studies have found that in some ways, e-cigarettes seem safer. For example, the levels of carcinogens such as formaldehyde and heavy metals are found at levels that are 9-450 times higher in combustible cigarette smoke than e-cigarette vapor, he said. And toxic compounds have been found to be significantly lower in the urine of e-cigarette users compared to traditional cigarette smokers.
But it’s not so simple. While e-cigarettes typically cause lower exposure to formaldehyde, when heated at a higher voltage, exposure to formaldehyde hemiacetal, a formaldehyde precursor, is about seven times higher for someone smoking 3 mL of e-cigarette fluid a day – similar to a pack a day – than the formaldehyde exposure of someone smoking the same quantity of combustible cigarettes.
Dr. Casale added that experienced e-cigarette users typically take longer puffs than traditional smokers and that the unregulated e-cigarette industry is rife with mislabeling on things such as how much nicotine is in a given fluid.
“It’s dependent upon the device, the battery, how much it heats up and what’s in the liquid,” he said. “So in general, are they safer? Probably. But not exactly.”
There are also no long-term data on e-cigarettes, he added.
The evidence on how e-cigarettes affects traditional smoking habits is also mixed.
Some studies have indicated that e-cigarettes use can be helpful in kicking a traditional cigarette habit, said Jill Poole, MD, of the University of Nebraska, Omaha.
A survey by the U.S. Census Bureau found that, in the 2014-2015 data collection year, about 60% of smokers of combustible cigarettes who also smoked e-cigarettes tried to quit smoking combustibles, compared to 40% of those who didn’t smoke e-cigarettes. And 8% of e-cigarette users were successful over 3 months, compared to 4% of nonusers.
But data reveals risks for kids who’ve never smoked and then start using e-cigarettes.
“Does noncigarette tobacco use among never smoking youth determine subsequent smoking initiation?” she said. “The answer is yes.”
Dr. Poole added that a study published this year found that youths who’d never smoked traditional cigarettes were 87% more likely to start if they had first tried e-cigarettes (JAMA Pediatr. 2018;172(2):181-187).
And more children are using e-cigarettes frequently. The National Youth Tobacco Survey found that 16% of high schoolers in 2016 had used e-cigarettes in the past 30 days, way up from 1.5% in 2011, even as traditional cigarette use has declined from 15.8% to 9.3% among those children over that time.
Loretta Que, MD, associate professor of medicine at Duke University, Durham, N.C., noted how advertising for e-cigarettes is similar to the old ads for traditional cigarettes, attempting to convey coolness. With their wide array of colors and thousands of flavors, there is no doubt that e-cigarette pens have caught on among children, she said.
“They’re becoming something akin to an iPhone case or a handbag.”
ORLANDO – E-cigarettes are likely safer than traditional cigarettes but it depends on the user, the voltage used, and the kind of liquid, according to a panel of experts at the joint congress of the American Academy of Allergy, Asthma and Immunology and the World Asthma Organization.
Thomas Casale, MD, professor of medicine at the University of South Florida, Tampa, said studies have found that in some ways, e-cigarettes seem safer. For example, the levels of carcinogens such as formaldehyde and heavy metals are found at levels that are 9-450 times higher in combustible cigarette smoke than e-cigarette vapor, he said. And toxic compounds have been found to be significantly lower in the urine of e-cigarette users compared to traditional cigarette smokers.
But it’s not so simple. While e-cigarettes typically cause lower exposure to formaldehyde, when heated at a higher voltage, exposure to formaldehyde hemiacetal, a formaldehyde precursor, is about seven times higher for someone smoking 3 mL of e-cigarette fluid a day – similar to a pack a day – than the formaldehyde exposure of someone smoking the same quantity of combustible cigarettes.
Dr. Casale added that experienced e-cigarette users typically take longer puffs than traditional smokers and that the unregulated e-cigarette industry is rife with mislabeling on things such as how much nicotine is in a given fluid.
“It’s dependent upon the device, the battery, how much it heats up and what’s in the liquid,” he said. “So in general, are they safer? Probably. But not exactly.”
There are also no long-term data on e-cigarettes, he added.
The evidence on how e-cigarettes affects traditional smoking habits is also mixed.
Some studies have indicated that e-cigarettes use can be helpful in kicking a traditional cigarette habit, said Jill Poole, MD, of the University of Nebraska, Omaha.
A survey by the U.S. Census Bureau found that, in the 2014-2015 data collection year, about 60% of smokers of combustible cigarettes who also smoked e-cigarettes tried to quit smoking combustibles, compared to 40% of those who didn’t smoke e-cigarettes. And 8% of e-cigarette users were successful over 3 months, compared to 4% of nonusers.
But data reveals risks for kids who’ve never smoked and then start using e-cigarettes.
“Does noncigarette tobacco use among never smoking youth determine subsequent smoking initiation?” she said. “The answer is yes.”
Dr. Poole added that a study published this year found that youths who’d never smoked traditional cigarettes were 87% more likely to start if they had first tried e-cigarettes (JAMA Pediatr. 2018;172(2):181-187).
And more children are using e-cigarettes frequently. The National Youth Tobacco Survey found that 16% of high schoolers in 2016 had used e-cigarettes in the past 30 days, way up from 1.5% in 2011, even as traditional cigarette use has declined from 15.8% to 9.3% among those children over that time.
Loretta Que, MD, associate professor of medicine at Duke University, Durham, N.C., noted how advertising for e-cigarettes is similar to the old ads for traditional cigarettes, attempting to convey coolness. With their wide array of colors and thousands of flavors, there is no doubt that e-cigarette pens have caught on among children, she said.
“They’re becoming something akin to an iPhone case or a handbag.”
EXPERT ANALYSIS FROM THE AAAAI/WAO JOINT CONGRESS



















