User login
Risankizumab proves more effective in psoriasis than ustekinumab
, according to results of a pair of head-to-head trials published in the Lancet.
The replicate phase 3, randomized, double-blind, placebo- and active comparator–controlled trials, UltIMMa-1 (NCT02684370) and UltIMMa-2 (NCT02684375) altogether randomized 997 patients to risankizumab, ustekinumab, or placebo. The coprimary endpoints were the proportions of patients achieving 90% reduction in Psoriasis Area and Severity Index (PASI 90) at 16 weeks and a static Physician Global Assessment (sPGA) score of 0 or 1, and the 15 ranked secondary endpoints included proportions of those achieving PASI 100 or sPGA 0, both of which demonstrate total clearance of psoriasis, as well as measures of quality of life improvement.
Compared with those receiving either ustekinumab or placebo, a significantly higher proportion of patients receiving risankizumab achieved the coprimary endpoints, and all secondary endpoints were met. In UltIMMA-1, 75.3% of risankizumab patients achieved PASI 90, compared with 4.9% of placebo patients and 42% of ustekinumab patients (P less than .0001 when comparing it with both placebo and ustekinumab); sPGA of 0 or 1 was achieved by 87.8% of risankizumab patients and only 7.8% of placebo patients and 63% of ustekinumab patients (P less than .0001 when comparing it with both placebo and ustekinumab). Results were similar in UltIMMA-2: 74.8% of risankizumab patients achieved PASI 90, and 83.7% of them achieved sPGA 0 or 1 (P less than .0001 when comparing them with placebo and ustekinumab). According to results of the secondary endpoints, both studies also showed greater rates of clearance and improvements in quality of life among patients receiving risankizumab than among those receiving either placebo or ustekinumab.
The safety profiles across treatment groups were similar in both studies, with the most common adverse events including upper respiratory tract infection, headache, and diarrhea.
Risankizumab is a humanized IgG1 monoclonal antibody that targets the p19 subunit of only interleukin-23, unlike the studies’ active comparator, ustekinumab, which targets both interleukin-23 and interleukin-12. “Selectively blocking interleukin 23 with a p19 inhibitor appears to be one of the best ways to treat psoriasis,” commented Abigail Cline, MD, and Steven R. Feldman, MD, PhD, both of Wake Forest University, Winston-Salem, N.C., in an accompanying editorial (Lancet. 2018 Aug 7;392:616-71.).
The authors of the study reported relationships with various industry entities, including AbbVie, which sponsored the studies and developed risankizumab, and Boehringer Ingelheim, which collaborated in the studies. The authors of the editorial also disclosed relationships with entities, including AbbVie.
SOURCE: Gordon KB et al. Lancet. 2018 Aug 7;392:650-61.
, according to results of a pair of head-to-head trials published in the Lancet.
The replicate phase 3, randomized, double-blind, placebo- and active comparator–controlled trials, UltIMMa-1 (NCT02684370) and UltIMMa-2 (NCT02684375) altogether randomized 997 patients to risankizumab, ustekinumab, or placebo. The coprimary endpoints were the proportions of patients achieving 90% reduction in Psoriasis Area and Severity Index (PASI 90) at 16 weeks and a static Physician Global Assessment (sPGA) score of 0 or 1, and the 15 ranked secondary endpoints included proportions of those achieving PASI 100 or sPGA 0, both of which demonstrate total clearance of psoriasis, as well as measures of quality of life improvement.
Compared with those receiving either ustekinumab or placebo, a significantly higher proportion of patients receiving risankizumab achieved the coprimary endpoints, and all secondary endpoints were met. In UltIMMA-1, 75.3% of risankizumab patients achieved PASI 90, compared with 4.9% of placebo patients and 42% of ustekinumab patients (P less than .0001 when comparing it with both placebo and ustekinumab); sPGA of 0 or 1 was achieved by 87.8% of risankizumab patients and only 7.8% of placebo patients and 63% of ustekinumab patients (P less than .0001 when comparing it with both placebo and ustekinumab). Results were similar in UltIMMA-2: 74.8% of risankizumab patients achieved PASI 90, and 83.7% of them achieved sPGA 0 or 1 (P less than .0001 when comparing them with placebo and ustekinumab). According to results of the secondary endpoints, both studies also showed greater rates of clearance and improvements in quality of life among patients receiving risankizumab than among those receiving either placebo or ustekinumab.
The safety profiles across treatment groups were similar in both studies, with the most common adverse events including upper respiratory tract infection, headache, and diarrhea.
Risankizumab is a humanized IgG1 monoclonal antibody that targets the p19 subunit of only interleukin-23, unlike the studies’ active comparator, ustekinumab, which targets both interleukin-23 and interleukin-12. “Selectively blocking interleukin 23 with a p19 inhibitor appears to be one of the best ways to treat psoriasis,” commented Abigail Cline, MD, and Steven R. Feldman, MD, PhD, both of Wake Forest University, Winston-Salem, N.C., in an accompanying editorial (Lancet. 2018 Aug 7;392:616-71.).
The authors of the study reported relationships with various industry entities, including AbbVie, which sponsored the studies and developed risankizumab, and Boehringer Ingelheim, which collaborated in the studies. The authors of the editorial also disclosed relationships with entities, including AbbVie.
SOURCE: Gordon KB et al. Lancet. 2018 Aug 7;392:650-61.
, according to results of a pair of head-to-head trials published in the Lancet.
The replicate phase 3, randomized, double-blind, placebo- and active comparator–controlled trials, UltIMMa-1 (NCT02684370) and UltIMMa-2 (NCT02684375) altogether randomized 997 patients to risankizumab, ustekinumab, or placebo. The coprimary endpoints were the proportions of patients achieving 90% reduction in Psoriasis Area and Severity Index (PASI 90) at 16 weeks and a static Physician Global Assessment (sPGA) score of 0 or 1, and the 15 ranked secondary endpoints included proportions of those achieving PASI 100 or sPGA 0, both of which demonstrate total clearance of psoriasis, as well as measures of quality of life improvement.
Compared with those receiving either ustekinumab or placebo, a significantly higher proportion of patients receiving risankizumab achieved the coprimary endpoints, and all secondary endpoints were met. In UltIMMA-1, 75.3% of risankizumab patients achieved PASI 90, compared with 4.9% of placebo patients and 42% of ustekinumab patients (P less than .0001 when comparing it with both placebo and ustekinumab); sPGA of 0 or 1 was achieved by 87.8% of risankizumab patients and only 7.8% of placebo patients and 63% of ustekinumab patients (P less than .0001 when comparing it with both placebo and ustekinumab). Results were similar in UltIMMA-2: 74.8% of risankizumab patients achieved PASI 90, and 83.7% of them achieved sPGA 0 or 1 (P less than .0001 when comparing them with placebo and ustekinumab). According to results of the secondary endpoints, both studies also showed greater rates of clearance and improvements in quality of life among patients receiving risankizumab than among those receiving either placebo or ustekinumab.
The safety profiles across treatment groups were similar in both studies, with the most common adverse events including upper respiratory tract infection, headache, and diarrhea.
Risankizumab is a humanized IgG1 monoclonal antibody that targets the p19 subunit of only interleukin-23, unlike the studies’ active comparator, ustekinumab, which targets both interleukin-23 and interleukin-12. “Selectively blocking interleukin 23 with a p19 inhibitor appears to be one of the best ways to treat psoriasis,” commented Abigail Cline, MD, and Steven R. Feldman, MD, PhD, both of Wake Forest University, Winston-Salem, N.C., in an accompanying editorial (Lancet. 2018 Aug 7;392:616-71.).
The authors of the study reported relationships with various industry entities, including AbbVie, which sponsored the studies and developed risankizumab, and Boehringer Ingelheim, which collaborated in the studies. The authors of the editorial also disclosed relationships with entities, including AbbVie.
SOURCE: Gordon KB et al. Lancet. 2018 Aug 7;392:650-61.
FROM THE LANCET
Registration now open for the Crohn’s & Colitis Congress
Registration for the Crohn’s & Colitis Congress,® the premier conference on inflammatory bowel disease (IBD), is open. The Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association, will take place Feb. 7-9, 2019, at the Bellagio, in Las Vegas.
Led by committee chair Brent Polk, MD, AGAF, and co-chairs Maria T. Abreu, MD, AGAF, and David T. Rubin, MD, AGAF, invited faculty include IBD thought-leaders in the fields of GI, research investigation, surgery, pediatrics, advanced practice, IBD nursing, diet and nutrition, mental health, radiology, and pathology.
The 2019 Congress’ agenda includes main sessions that will emphasize case studies and panel discussions. There will also be parallel sessions on basic and translational science for senior and junior investigators.
In addition, several pre-Congress workshops, taking place Feb. 7, will be available for selection.
There will also be plenty of social events and plenty of time to enjoy Las Vegas; including a Friday night Welcome Reception that should not be missed. It’s a great opportunity to network and celebrate.
Abstract submissions for basic, translational, and clinical research will be accepted beginning Aug. 1 and ending Oct. 24.
To learn more and register, visit www.crohnscolitiscongress.org.
Registration for the Crohn’s & Colitis Congress,® the premier conference on inflammatory bowel disease (IBD), is open. The Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association, will take place Feb. 7-9, 2019, at the Bellagio, in Las Vegas.
Led by committee chair Brent Polk, MD, AGAF, and co-chairs Maria T. Abreu, MD, AGAF, and David T. Rubin, MD, AGAF, invited faculty include IBD thought-leaders in the fields of GI, research investigation, surgery, pediatrics, advanced practice, IBD nursing, diet and nutrition, mental health, radiology, and pathology.
The 2019 Congress’ agenda includes main sessions that will emphasize case studies and panel discussions. There will also be parallel sessions on basic and translational science for senior and junior investigators.
In addition, several pre-Congress workshops, taking place Feb. 7, will be available for selection.
There will also be plenty of social events and plenty of time to enjoy Las Vegas; including a Friday night Welcome Reception that should not be missed. It’s a great opportunity to network and celebrate.
Abstract submissions for basic, translational, and clinical research will be accepted beginning Aug. 1 and ending Oct. 24.
To learn more and register, visit www.crohnscolitiscongress.org.
Registration for the Crohn’s & Colitis Congress,® the premier conference on inflammatory bowel disease (IBD), is open. The Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association, will take place Feb. 7-9, 2019, at the Bellagio, in Las Vegas.
Led by committee chair Brent Polk, MD, AGAF, and co-chairs Maria T. Abreu, MD, AGAF, and David T. Rubin, MD, AGAF, invited faculty include IBD thought-leaders in the fields of GI, research investigation, surgery, pediatrics, advanced practice, IBD nursing, diet and nutrition, mental health, radiology, and pathology.
The 2019 Congress’ agenda includes main sessions that will emphasize case studies and panel discussions. There will also be parallel sessions on basic and translational science for senior and junior investigators.
In addition, several pre-Congress workshops, taking place Feb. 7, will be available for selection.
There will also be plenty of social events and plenty of time to enjoy Las Vegas; including a Friday night Welcome Reception that should not be missed. It’s a great opportunity to network and celebrate.
Abstract submissions for basic, translational, and clinical research will be accepted beginning Aug. 1 and ending Oct. 24.
To learn more and register, visit www.crohnscolitiscongress.org.
Hand hygiene linked to reduced ICU health care–associated infections
A hospital-wide infection control program (ICP) was found to be associated with reduced health care-associated severe sepsis/septic shock or death in the ICU, but it was not clear whether this decrease was a consequence of the ICP or because of a concomitant improvement in HAI case management, according to a the results of a prospective analysis.
In addition, there was no significant decrease in overall HAIs seen despite implementation of the program, according to the report published online in Clinical Microbiology and Infection (doi: 10.1016/j.cmi.2018.07.010), according to Stefan Hagel, MD, of the Institute for Infectious Diseases and Infection Control, Jena (Germany) University Hospital, and his colleagues.
They assessed two surveillance periods (September 2011 to August 2012 and May 2013 to August 2014). The ICP started in October 2012, and included hand-hygiene promotion and bundle implementation for common HAIs.
The data were analyzed by segmented mixed-effects Poisson regression and multi-state models and reported as adjusted incidence rate ratios (aIRR) and 50 adjusted hazard ratios (aHR) with 95% confidence intervals (CI).
In the first period, 62,154 patients were under surveillance, with 1,568 HAIs identified in 1,170 patients (4.3/100 admissions) and 2,336 HAIs identified in 1,711 patients (4.9/100 admissions) in the second surveillance period. No differences were found in the overall HAI incidence rates between the periods in the general wards and ICUs. There was only a slight decline in the incidence rate of HAIs in the ICUs (aIRR 0.98 [0.97, 1.00] per 1-week increment), compared with the general wards (aIRR 1.01 [1.00, 1.02]).
However, a reduction in severe HAIs (aIRR 0.13 [0.05, 0.32]) and a lower probability of HAI-associated in-hospital deaths (aHR 0.56 [0.31, 0.99]) were observed in the second period in the ICUs.
In attempting to explain the variance seen between the results for general wards and the ICU, an analysis of alcohol-based handrub solution consumption as a marker of hand-hygiene behavior indicated that a remarkable increase in consumption occurred in the ICUs while a less pronounced increase occurred in the general wards. “This finding might explain the observed decline in the HAI incidence after starting the campaign in the ICUs, which was not observed on the general wards.” Dr. Hagel and his colleagues suggested.
The authors discussed how several confounding factors that influenced the incidence of HAIs needed to be considered. As a consequence of the improvement in HAI management, the number of collected blood culture sets nearly doubled hospital-wide from 13,126 to 25,805 per year between 2011 and 2014, which likely undermined the study objective, they stated. The increase in cultures may have impacted the number of overall HAIs found.
“Although the primary aim of the study of reducing the overall incidence of HAIs was not achieved, the study demonstrated a decline of severe HAIs in patients in ICUs in the second surveillance period. Whether this result was a consequence of the ICP or a general improvement in HAI management remains unclear,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Hagel S et al. Clin Microbiol Infect. doi: 10.1016/j.cmi.2018.07.010].
A hospital-wide infection control program (ICP) was found to be associated with reduced health care-associated severe sepsis/septic shock or death in the ICU, but it was not clear whether this decrease was a consequence of the ICP or because of a concomitant improvement in HAI case management, according to a the results of a prospective analysis.
In addition, there was no significant decrease in overall HAIs seen despite implementation of the program, according to the report published online in Clinical Microbiology and Infection (doi: 10.1016/j.cmi.2018.07.010), according to Stefan Hagel, MD, of the Institute for Infectious Diseases and Infection Control, Jena (Germany) University Hospital, and his colleagues.
They assessed two surveillance periods (September 2011 to August 2012 and May 2013 to August 2014). The ICP started in October 2012, and included hand-hygiene promotion and bundle implementation for common HAIs.
The data were analyzed by segmented mixed-effects Poisson regression and multi-state models and reported as adjusted incidence rate ratios (aIRR) and 50 adjusted hazard ratios (aHR) with 95% confidence intervals (CI).
In the first period, 62,154 patients were under surveillance, with 1,568 HAIs identified in 1,170 patients (4.3/100 admissions) and 2,336 HAIs identified in 1,711 patients (4.9/100 admissions) in the second surveillance period. No differences were found in the overall HAI incidence rates between the periods in the general wards and ICUs. There was only a slight decline in the incidence rate of HAIs in the ICUs (aIRR 0.98 [0.97, 1.00] per 1-week increment), compared with the general wards (aIRR 1.01 [1.00, 1.02]).
However, a reduction in severe HAIs (aIRR 0.13 [0.05, 0.32]) and a lower probability of HAI-associated in-hospital deaths (aHR 0.56 [0.31, 0.99]) were observed in the second period in the ICUs.
In attempting to explain the variance seen between the results for general wards and the ICU, an analysis of alcohol-based handrub solution consumption as a marker of hand-hygiene behavior indicated that a remarkable increase in consumption occurred in the ICUs while a less pronounced increase occurred in the general wards. “This finding might explain the observed decline in the HAI incidence after starting the campaign in the ICUs, which was not observed on the general wards.” Dr. Hagel and his colleagues suggested.
The authors discussed how several confounding factors that influenced the incidence of HAIs needed to be considered. As a consequence of the improvement in HAI management, the number of collected blood culture sets nearly doubled hospital-wide from 13,126 to 25,805 per year between 2011 and 2014, which likely undermined the study objective, they stated. The increase in cultures may have impacted the number of overall HAIs found.
“Although the primary aim of the study of reducing the overall incidence of HAIs was not achieved, the study demonstrated a decline of severe HAIs in patients in ICUs in the second surveillance period. Whether this result was a consequence of the ICP or a general improvement in HAI management remains unclear,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Hagel S et al. Clin Microbiol Infect. doi: 10.1016/j.cmi.2018.07.010].
A hospital-wide infection control program (ICP) was found to be associated with reduced health care-associated severe sepsis/septic shock or death in the ICU, but it was not clear whether this decrease was a consequence of the ICP or because of a concomitant improvement in HAI case management, according to a the results of a prospective analysis.
In addition, there was no significant decrease in overall HAIs seen despite implementation of the program, according to the report published online in Clinical Microbiology and Infection (doi: 10.1016/j.cmi.2018.07.010), according to Stefan Hagel, MD, of the Institute for Infectious Diseases and Infection Control, Jena (Germany) University Hospital, and his colleagues.
They assessed two surveillance periods (September 2011 to August 2012 and May 2013 to August 2014). The ICP started in October 2012, and included hand-hygiene promotion and bundle implementation for common HAIs.
The data were analyzed by segmented mixed-effects Poisson regression and multi-state models and reported as adjusted incidence rate ratios (aIRR) and 50 adjusted hazard ratios (aHR) with 95% confidence intervals (CI).
In the first period, 62,154 patients were under surveillance, with 1,568 HAIs identified in 1,170 patients (4.3/100 admissions) and 2,336 HAIs identified in 1,711 patients (4.9/100 admissions) in the second surveillance period. No differences were found in the overall HAI incidence rates between the periods in the general wards and ICUs. There was only a slight decline in the incidence rate of HAIs in the ICUs (aIRR 0.98 [0.97, 1.00] per 1-week increment), compared with the general wards (aIRR 1.01 [1.00, 1.02]).
However, a reduction in severe HAIs (aIRR 0.13 [0.05, 0.32]) and a lower probability of HAI-associated in-hospital deaths (aHR 0.56 [0.31, 0.99]) were observed in the second period in the ICUs.
In attempting to explain the variance seen between the results for general wards and the ICU, an analysis of alcohol-based handrub solution consumption as a marker of hand-hygiene behavior indicated that a remarkable increase in consumption occurred in the ICUs while a less pronounced increase occurred in the general wards. “This finding might explain the observed decline in the HAI incidence after starting the campaign in the ICUs, which was not observed on the general wards.” Dr. Hagel and his colleagues suggested.
The authors discussed how several confounding factors that influenced the incidence of HAIs needed to be considered. As a consequence of the improvement in HAI management, the number of collected blood culture sets nearly doubled hospital-wide from 13,126 to 25,805 per year between 2011 and 2014, which likely undermined the study objective, they stated. The increase in cultures may have impacted the number of overall HAIs found.
“Although the primary aim of the study of reducing the overall incidence of HAIs was not achieved, the study demonstrated a decline of severe HAIs in patients in ICUs in the second surveillance period. Whether this result was a consequence of the ICP or a general improvement in HAI management remains unclear,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Hagel S et al. Clin Microbiol Infect. doi: 10.1016/j.cmi.2018.07.010].
FROM CLINICAL MICROBIOLOGY AND INFECTION
Key clinical point: Hand hygiene was the key factor associated with a decrease in severe HAIs.
Major finding: A reduction in severe HAIs (aIRR 0.13) and a lower probability of HAI-associated in-hospital deaths (aHR 0.56]) were observed.
Study details: A prospective database analysis of more nearly 65,000 hospitalized patients.
Disclosures: The authors reported that they had no conflicts of interest.
Source: Hagel S et al. Clin Microbiol Infect. doi: 10.1016/j.cmi.2018.07.010.
Learning Curves: Historical Trends of FDA-Reported Adverse Events for Dermal Fillers
Dermal fillers are considered Class III medical devices by the US Food and Drug Administration (FDA).1 Reports of adverse events (AEs) for medical devices are made public by the FDA to allow for transparent postmarketing surveillance.2The AE trends extracted from these historical data may help distinguish between expected learning curves of new dermal fillers versus unsafe products that may require FDA intervention. Considering that aesthetic treatments are not medically necessary, a low risk profile is paramount and determining what constitutes normal learning curves is important for impartial assessment of AEs as new fillers come on the market. The concept of a 3-year learning curve can be an important tool for safety monitoring going forward, creating a bar for quality that could trigger increased surveillance if a product fails to meet an expected arc of diminished AEs over time. This study serves to evaluate historical AE data and to establish learning curves for FDA-approved dermal fillers.
Methods
We searched the OpenFDA Device Adverse Event Report Browser (http://openfda.shinyapps.io/devicereports/) for reported AEs within the FDA product code LMH (Implant, Dermal, For Aesthetic Use) that were received from January 1, 1983, to December 31, 2017. For each reported AE, information related to the date of the reported event and the device brand name were recorded. Devices implicated in each AE were classified based on primary composition according to the following 5 categories: collagen, hyaluronic acid (HA), hydroxylapatite, poly-L-lactic acid (PLLA), and polymethyl methacrylate (PMMA). Inaccurate entries of reported AEs or those intended for nonaesthetic use were excluded from the study. A total of 8530 AEs were included in the study. To normalize the data, we obtained annual reports for the number of procedures performed by filler type from the American Society of Plastic Surgeons (ASPS) cosmetic procedure trends. 3 We calculated the annual AE rates for each approved filler by dividing the number of AEs by the number of procedures performed that year.
Results
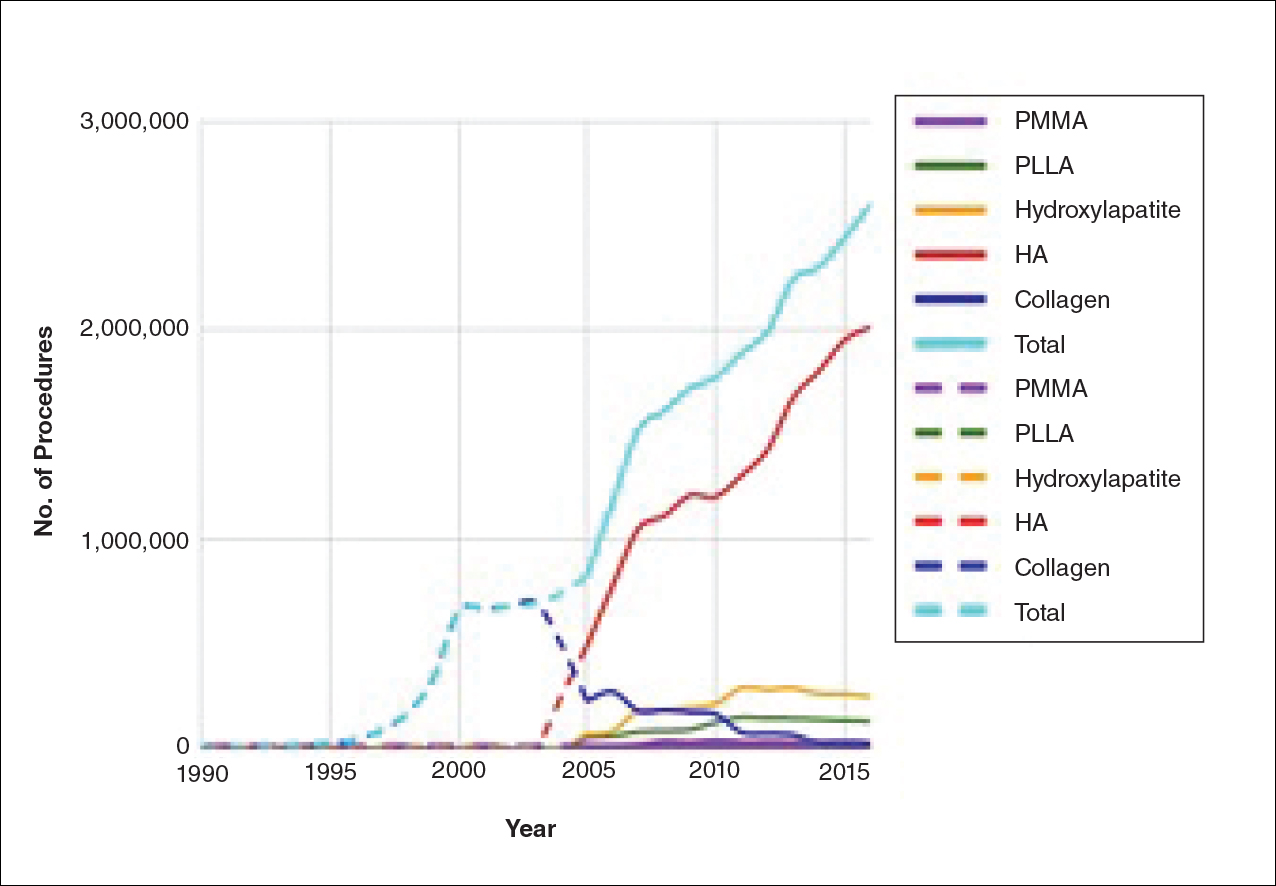
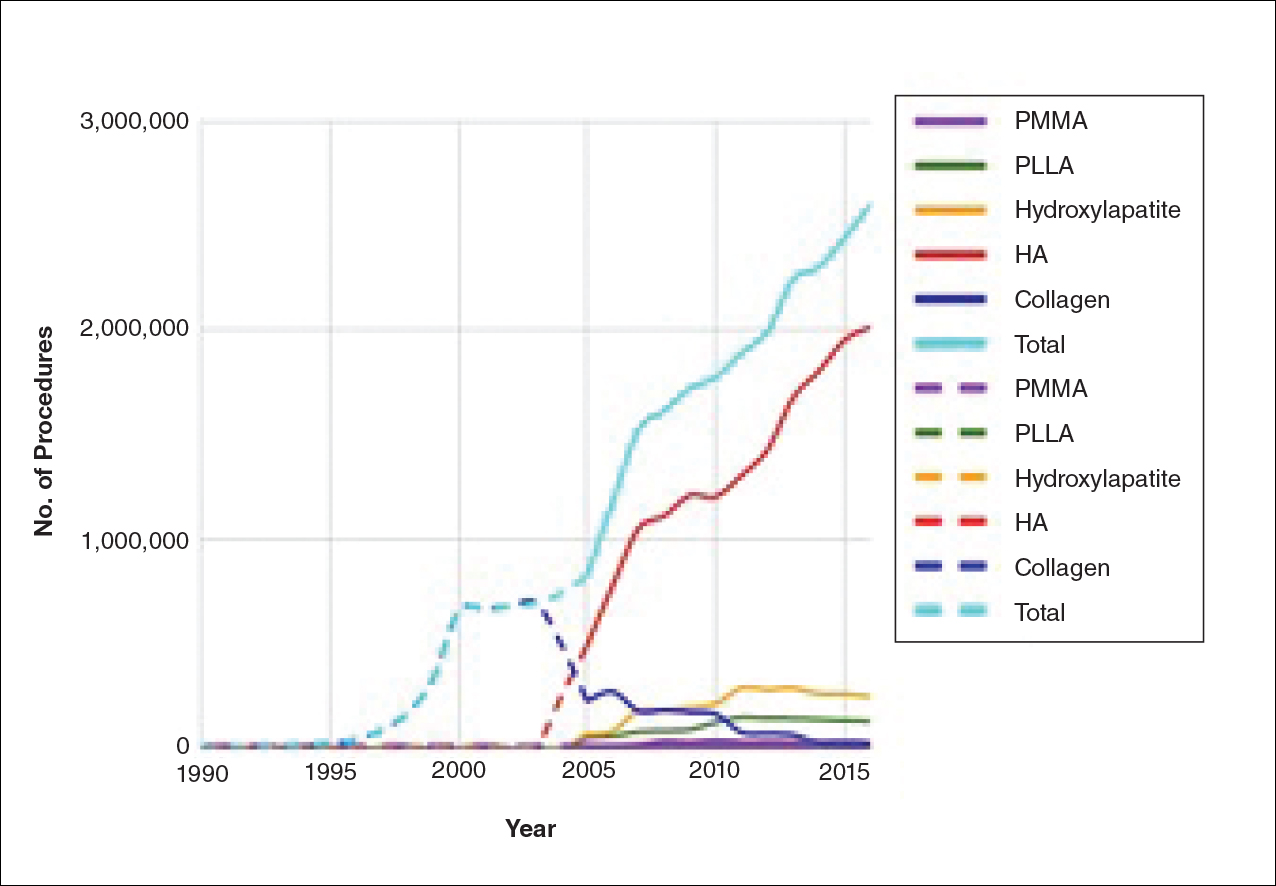
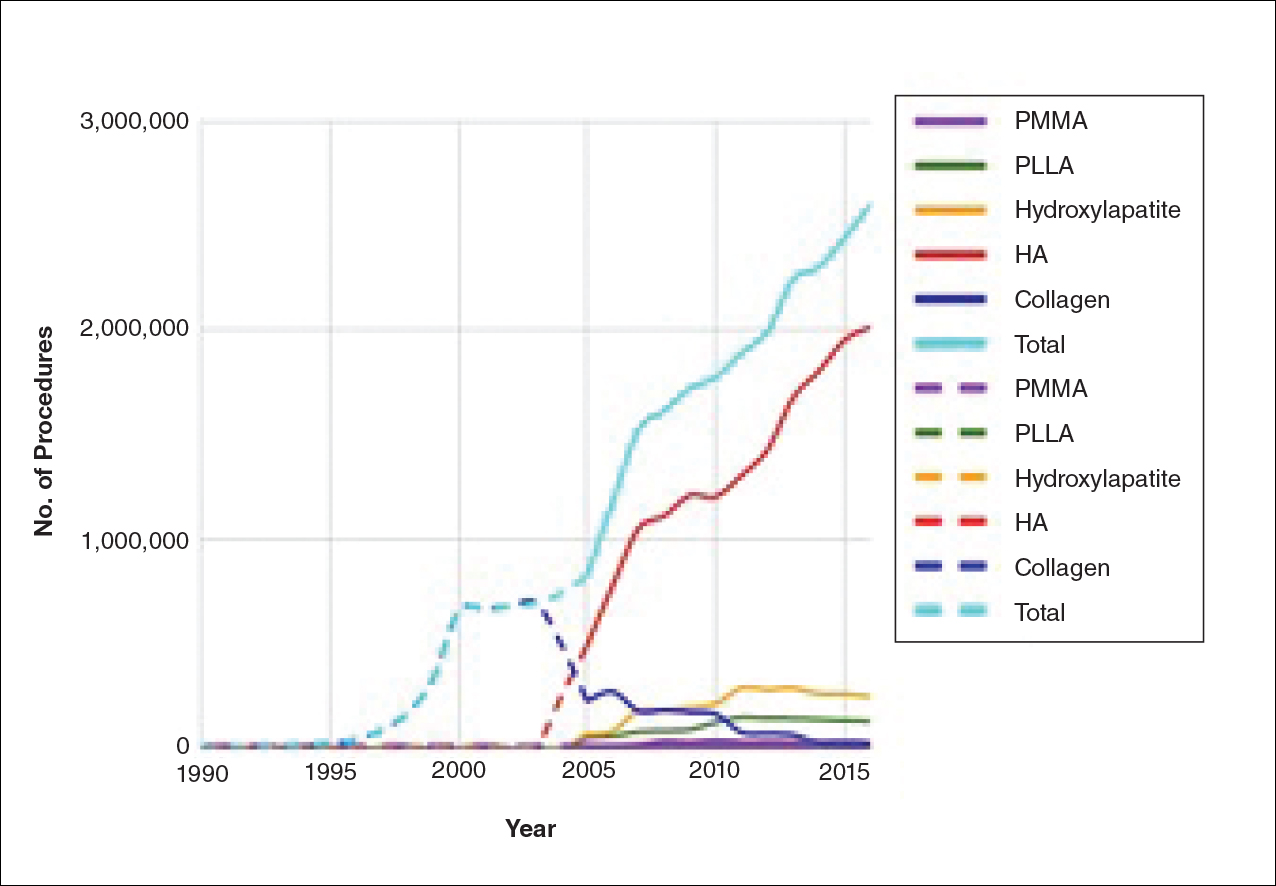
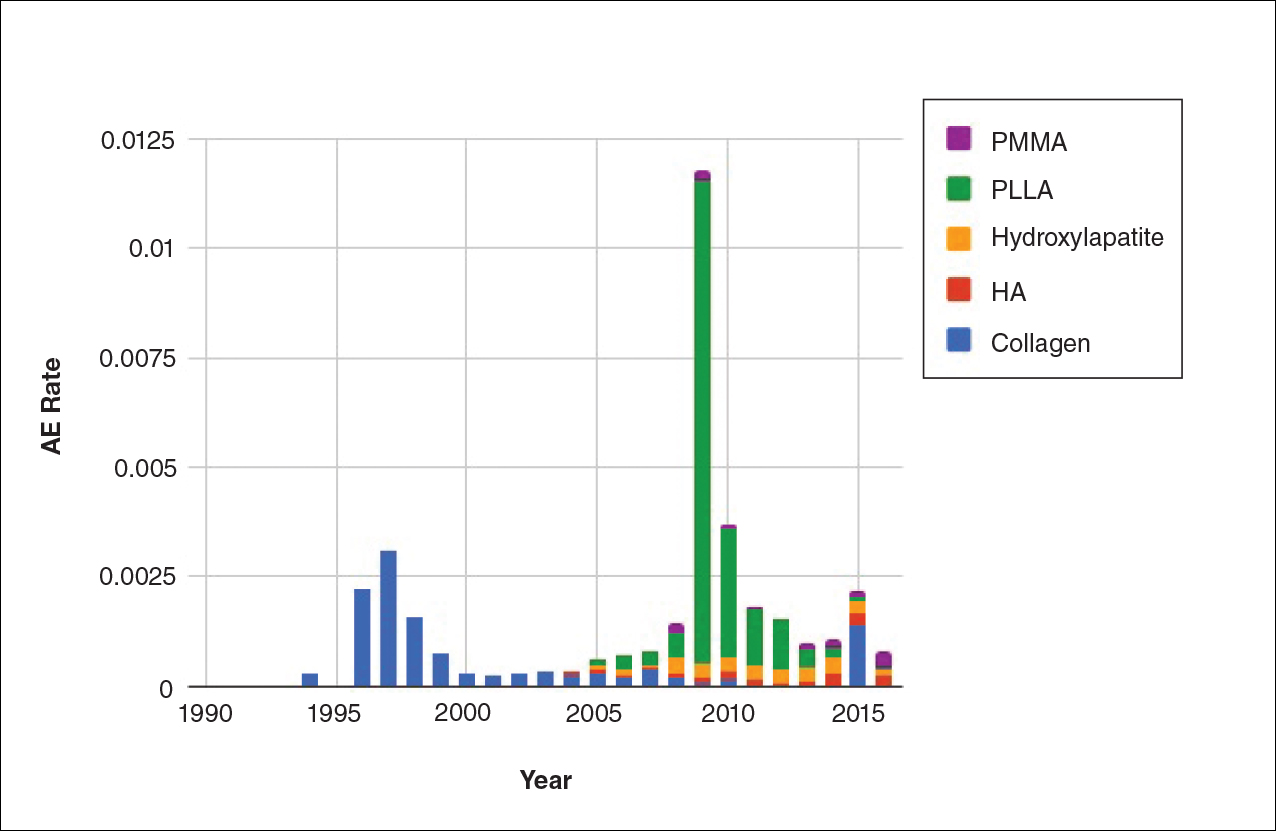
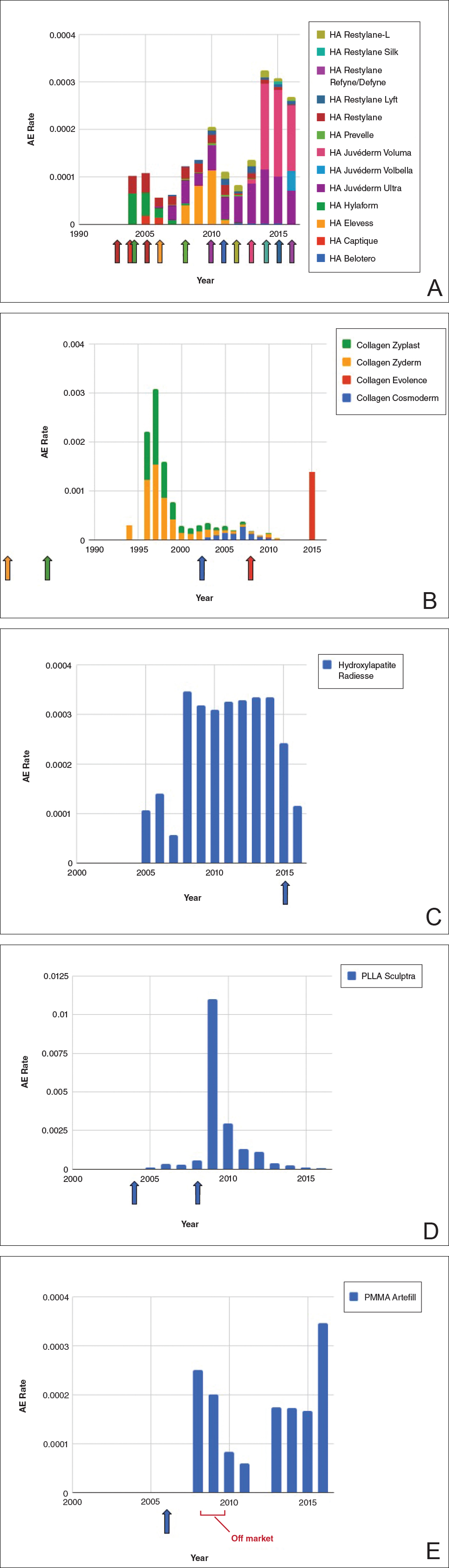
The trends of different filler types depicting the number of procedures performed over time are shown in Figure 1. Data from the ASPS dated back to 2005; therefore, the number of procedures performed prior to that were extrapolated with knowledge of products’ approval dates and market share, indicated by a dotted line. To determine AE rates for each year, we divided the number of AEs by the number of reported procedures for each filler type. The AE rates are displayed graphically in Figures 2 and 3 with superimposed FDA approval dates for each filler.4
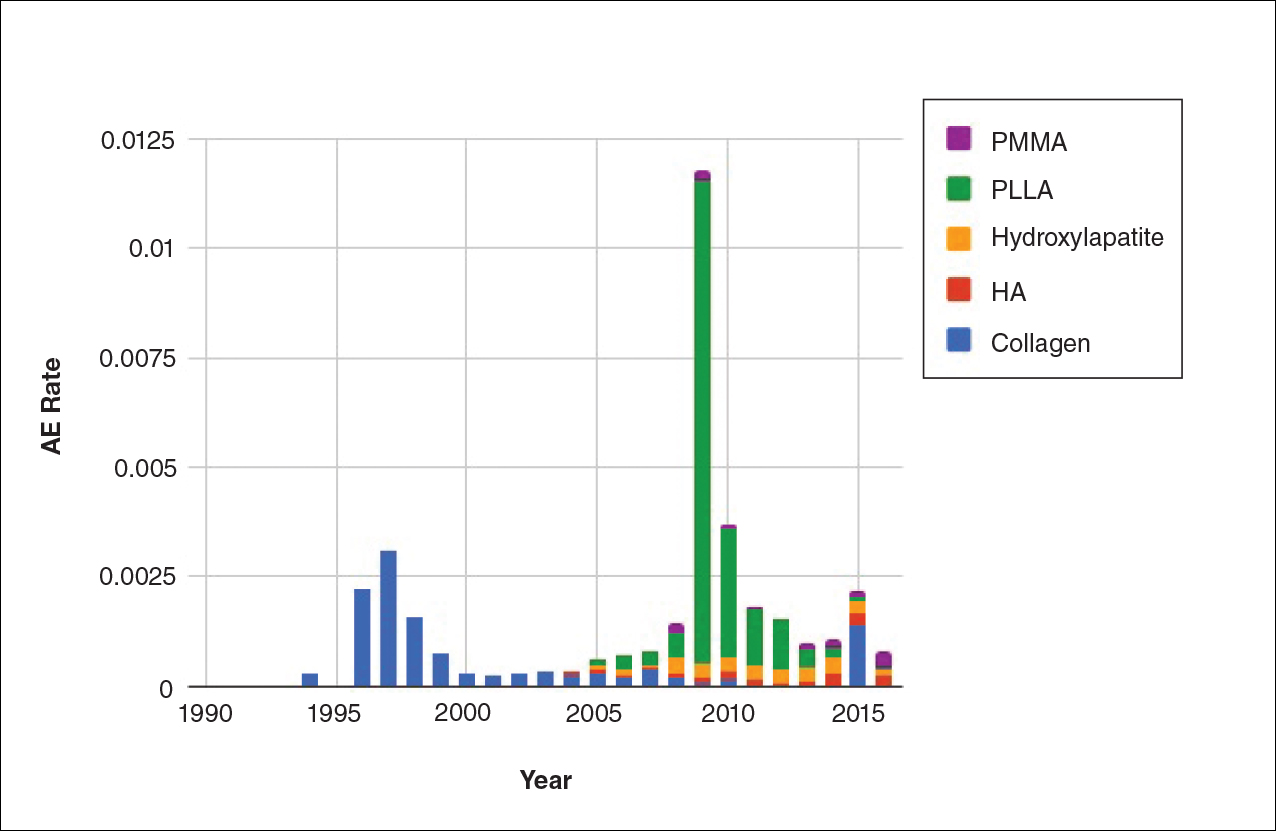
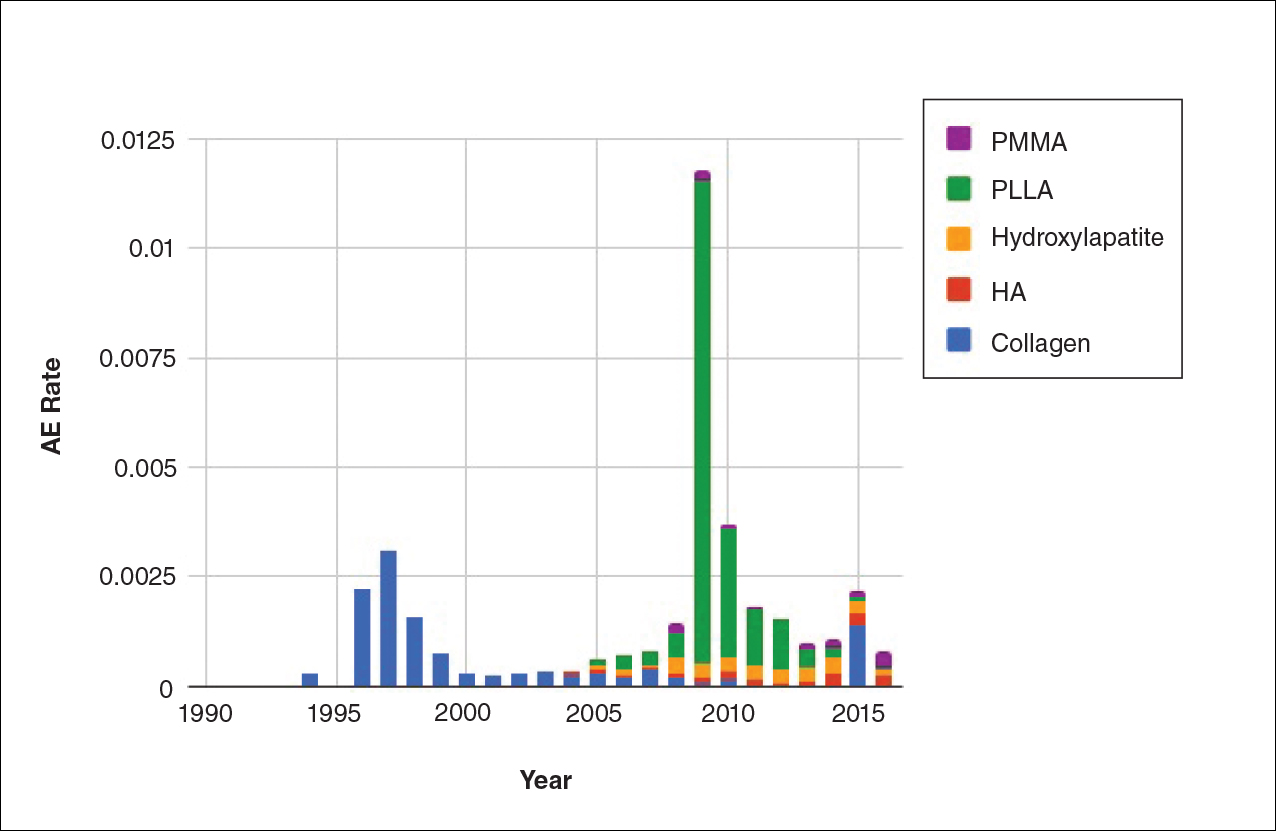
Two major peaks in reported AE rates for all fillers were noted in the late 1990s and late 2000s, mostly associated with collagen and PLLA fillers, respectively (Figure 2). Overall, there has been a low rate of AEs associated with HA fillers since their initial approval in the early 2000s.
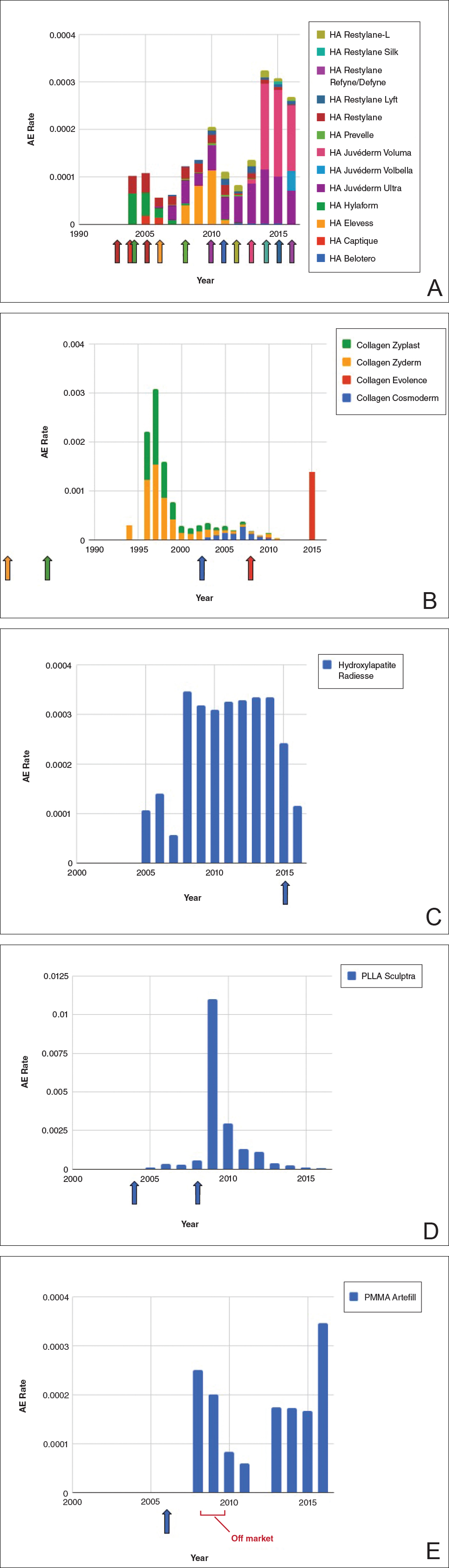
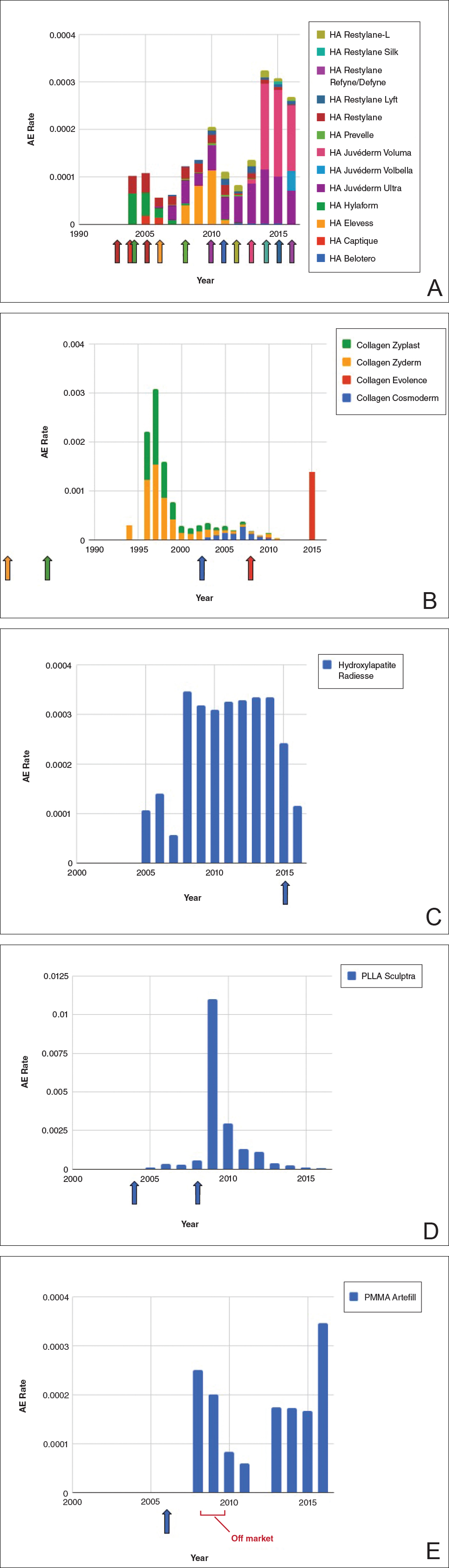
Individual filler AE rates also were analyzed. Hyaluronic acid fillers were associated with an extremely low rate of AEs, ranging from 1 to 4 AEs per 10,000 procedures (Figure 3A). This low AE rate profile underscores the safety of HA fillers, which has spurred their popularity. Adverseevent rates for collagen fillers spiked in the mid- to late 1990s and resolved over the course of the next 3 years (Figure 3B). Hydroxylapatite fillers had a rather uniform AE rate with an early indication of a drop-off after 2015 (Figure 3C). Poly-L-lactic acid fillers showed the steepest learning curve, with a peak of 1 AE per 100 procedures after they were approved in 2008 (Figure 3D); however, there is a comparable 3-year resolution of AE rates. Adverse events for PMMA fillers did not show specific resolution, meaning that they did not follow the 3-year arc that was seen for the other dermal fillers reported in the data set (Figure 3E).
Comment
Our study is unique in that it analyzes reported AE data over a 34-year period for injectable dermal fillers. To our knowledge, this novel method of calculating AE rates across dermal fillers and for individual products is the first of its kind that facilitates usage-normalized comparison of different filler types.
All OpenFDA data are self-reported and therefore have inherent limitations. Anyone can enter information on AEs in this system, including both patients and health care providers, so the quality of the input may be variable. However, this output is the only representation we have for nearly 35 years of AE history for this burgeoning category of popular aesthetic treatments. Another study limitation is that not everyone may know that reporting an AE in the OpenFDA is an option; therefore, we may be missing a portion of AEs due to underreporting. Underreporting may be especially at play in the years before the Internet was prevalent for residential use since access to the Internet would be required to report an AR on the website. However, examining the available data provides an important window into valuable information on complications that have occurred and have been reported for FDA-approved dermal fillers.
An additional challenge in constructing this study was assessing the total number of injectable dermal filler treatments being performed annually across filler types for normalization of the data. Although the absolute numbers of filler use as captured by the ASPS are smaller than the true total filler use across all injectors, the relative use of different filler products will be similar across all specialties because it reflects product popularity. Annual surveys on aesthetic procedures also are conducted by the American Society for Dermatologic Surgery and the American Association for Facial Plastic and Reconstructive Surgery, but neither one captures the relative usage of different filler types. Because individual filler companies do not publish their annual sales numbers by product, the ASPS data give us the best gauge of relative use of fillers by product type given the available information. We conclude that the comparison of AE rates would remain the same even if we had data for total annual filler use across specialties.
Our graphical depiction of the data clearly demonstrates the low AE profile of HA fillers, which is in line with the general consensus of their safety that has contributed to their vast popularity; however, this study represents the first time usage-normalized AE rates are compared to other filler compositions. Hyaluronic acid fillers have the unique feature of being able to be dissolved with the hyaluronidase enzyme, which can limit adverse event potential as compared to other ingredient classes of filler types and may be reflected in their low overall AE profile. The AE rate spike and resolution for collagen fillers represent what we refer to as a “normal learning curve” based on our analysis of the data set as a whole, suggesting an appropriate time course of increased familiarity with the product without inherent issues with the product itself. Multiple sequential anatomic site indications were approved for hydroxylapatite fillers from 2006 through 2015, which may have yielded overlapping learning curves for each approval, resulting in a rather uniform AE rate. The early drop-off in AE rates after the 2015 anatomic site approval may represent the beginning of a normal learning curve, and continued surveillance of AE rates would be of value to confirm this trend. We saw a similar 3-year learning curve for PLLA fillers as the curve for collagen fillers, suggesting a normal learning curve and no out-of-line safety issues. Polymethylmethacrylate fillers were approved in 2006 and were taken off the market for a period in the late 2000s, explaining the drop-off. Once they were back on the market, we do not see a typical learning curve for PMMA, which may warrant surveillance for safety by both clinicians and the FDA.
Conclusion
Our study represents a novel method of evaluating the safety of medical devices, specifically aesthetic fillers. We showed that every AE rate curve for different filler types tells a story. Reactions to AEs for new fillers should be placed in the context of whether they seem to be following the established learning curve.
- Dermal fillers (soft tissue fillers). US Food and Drug Administration website. https://www.fda.gov/MedicalDevices/ucm2007470.htm. Updated May 31, 2018. Accessed June 29, 2018.
- Kass-Hout TA, Xu Z, Mohebbi M, et al. OpenFDA: an innovative platform providing access to a wealth of FDA’s publicly available data. J Am Med Inform Assoc. 2016;23:596-600.
- Plastic surgery statistics. American Society of Plastic Surgeons website. https://www.plasticsurgery.org/documents/News/Statistics/2017/plastic-surgery-statistics-full-report-2017.pdf. Accessed June 28, 2018.
- Dermal fillers approved by the Center for Devices and Radiological Health. US Food and Drug Administration website. https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/CosmeticDevices/WrinkleFillers/ucm227749.htm. Accessed June 28, 2018. Updated March 19, 2018.
Dermal fillers are considered Class III medical devices by the US Food and Drug Administration (FDA).1 Reports of adverse events (AEs) for medical devices are made public by the FDA to allow for transparent postmarketing surveillance.2The AE trends extracted from these historical data may help distinguish between expected learning curves of new dermal fillers versus unsafe products that may require FDA intervention. Considering that aesthetic treatments are not medically necessary, a low risk profile is paramount and determining what constitutes normal learning curves is important for impartial assessment of AEs as new fillers come on the market. The concept of a 3-year learning curve can be an important tool for safety monitoring going forward, creating a bar for quality that could trigger increased surveillance if a product fails to meet an expected arc of diminished AEs over time. This study serves to evaluate historical AE data and to establish learning curves for FDA-approved dermal fillers.
Methods
We searched the OpenFDA Device Adverse Event Report Browser (http://openfda.shinyapps.io/devicereports/) for reported AEs within the FDA product code LMH (Implant, Dermal, For Aesthetic Use) that were received from January 1, 1983, to December 31, 2017. For each reported AE, information related to the date of the reported event and the device brand name were recorded. Devices implicated in each AE were classified based on primary composition according to the following 5 categories: collagen, hyaluronic acid (HA), hydroxylapatite, poly-L-lactic acid (PLLA), and polymethyl methacrylate (PMMA). Inaccurate entries of reported AEs or those intended for nonaesthetic use were excluded from the study. A total of 8530 AEs were included in the study. To normalize the data, we obtained annual reports for the number of procedures performed by filler type from the American Society of Plastic Surgeons (ASPS) cosmetic procedure trends. 3 We calculated the annual AE rates for each approved filler by dividing the number of AEs by the number of procedures performed that year.
Results
The trends of different filler types depicting the number of procedures performed over time are shown in Figure 1. Data from the ASPS dated back to 2005; therefore, the number of procedures performed prior to that were extrapolated with knowledge of products’ approval dates and market share, indicated by a dotted line. To determine AE rates for each year, we divided the number of AEs by the number of reported procedures for each filler type. The AE rates are displayed graphically in Figures 2 and 3 with superimposed FDA approval dates for each filler.4
Two major peaks in reported AE rates for all fillers were noted in the late 1990s and late 2000s, mostly associated with collagen and PLLA fillers, respectively (Figure 2). Overall, there has been a low rate of AEs associated with HA fillers since their initial approval in the early 2000s.
Individual filler AE rates also were analyzed. Hyaluronic acid fillers were associated with an extremely low rate of AEs, ranging from 1 to 4 AEs per 10,000 procedures (Figure 3A). This low AE rate profile underscores the safety of HA fillers, which has spurred their popularity. Adverseevent rates for collagen fillers spiked in the mid- to late 1990s and resolved over the course of the next 3 years (Figure 3B). Hydroxylapatite fillers had a rather uniform AE rate with an early indication of a drop-off after 2015 (Figure 3C). Poly-L-lactic acid fillers showed the steepest learning curve, with a peak of 1 AE per 100 procedures after they were approved in 2008 (Figure 3D); however, there is a comparable 3-year resolution of AE rates. Adverse events for PMMA fillers did not show specific resolution, meaning that they did not follow the 3-year arc that was seen for the other dermal fillers reported in the data set (Figure 3E).
Comment
Our study is unique in that it analyzes reported AE data over a 34-year period for injectable dermal fillers. To our knowledge, this novel method of calculating AE rates across dermal fillers and for individual products is the first of its kind that facilitates usage-normalized comparison of different filler types.
All OpenFDA data are self-reported and therefore have inherent limitations. Anyone can enter information on AEs in this system, including both patients and health care providers, so the quality of the input may be variable. However, this output is the only representation we have for nearly 35 years of AE history for this burgeoning category of popular aesthetic treatments. Another study limitation is that not everyone may know that reporting an AE in the OpenFDA is an option; therefore, we may be missing a portion of AEs due to underreporting. Underreporting may be especially at play in the years before the Internet was prevalent for residential use since access to the Internet would be required to report an AR on the website. However, examining the available data provides an important window into valuable information on complications that have occurred and have been reported for FDA-approved dermal fillers.
An additional challenge in constructing this study was assessing the total number of injectable dermal filler treatments being performed annually across filler types for normalization of the data. Although the absolute numbers of filler use as captured by the ASPS are smaller than the true total filler use across all injectors, the relative use of different filler products will be similar across all specialties because it reflects product popularity. Annual surveys on aesthetic procedures also are conducted by the American Society for Dermatologic Surgery and the American Association for Facial Plastic and Reconstructive Surgery, but neither one captures the relative usage of different filler types. Because individual filler companies do not publish their annual sales numbers by product, the ASPS data give us the best gauge of relative use of fillers by product type given the available information. We conclude that the comparison of AE rates would remain the same even if we had data for total annual filler use across specialties.
Our graphical depiction of the data clearly demonstrates the low AE profile of HA fillers, which is in line with the general consensus of their safety that has contributed to their vast popularity; however, this study represents the first time usage-normalized AE rates are compared to other filler compositions. Hyaluronic acid fillers have the unique feature of being able to be dissolved with the hyaluronidase enzyme, which can limit adverse event potential as compared to other ingredient classes of filler types and may be reflected in their low overall AE profile. The AE rate spike and resolution for collagen fillers represent what we refer to as a “normal learning curve” based on our analysis of the data set as a whole, suggesting an appropriate time course of increased familiarity with the product without inherent issues with the product itself. Multiple sequential anatomic site indications were approved for hydroxylapatite fillers from 2006 through 2015, which may have yielded overlapping learning curves for each approval, resulting in a rather uniform AE rate. The early drop-off in AE rates after the 2015 anatomic site approval may represent the beginning of a normal learning curve, and continued surveillance of AE rates would be of value to confirm this trend. We saw a similar 3-year learning curve for PLLA fillers as the curve for collagen fillers, suggesting a normal learning curve and no out-of-line safety issues. Polymethylmethacrylate fillers were approved in 2006 and were taken off the market for a period in the late 2000s, explaining the drop-off. Once they were back on the market, we do not see a typical learning curve for PMMA, which may warrant surveillance for safety by both clinicians and the FDA.
Conclusion
Our study represents a novel method of evaluating the safety of medical devices, specifically aesthetic fillers. We showed that every AE rate curve for different filler types tells a story. Reactions to AEs for new fillers should be placed in the context of whether they seem to be following the established learning curve.
Dermal fillers are considered Class III medical devices by the US Food and Drug Administration (FDA).1 Reports of adverse events (AEs) for medical devices are made public by the FDA to allow for transparent postmarketing surveillance.2The AE trends extracted from these historical data may help distinguish between expected learning curves of new dermal fillers versus unsafe products that may require FDA intervention. Considering that aesthetic treatments are not medically necessary, a low risk profile is paramount and determining what constitutes normal learning curves is important for impartial assessment of AEs as new fillers come on the market. The concept of a 3-year learning curve can be an important tool for safety monitoring going forward, creating a bar for quality that could trigger increased surveillance if a product fails to meet an expected arc of diminished AEs over time. This study serves to evaluate historical AE data and to establish learning curves for FDA-approved dermal fillers.
Methods
We searched the OpenFDA Device Adverse Event Report Browser (http://openfda.shinyapps.io/devicereports/) for reported AEs within the FDA product code LMH (Implant, Dermal, For Aesthetic Use) that were received from January 1, 1983, to December 31, 2017. For each reported AE, information related to the date of the reported event and the device brand name were recorded. Devices implicated in each AE were classified based on primary composition according to the following 5 categories: collagen, hyaluronic acid (HA), hydroxylapatite, poly-L-lactic acid (PLLA), and polymethyl methacrylate (PMMA). Inaccurate entries of reported AEs or those intended for nonaesthetic use were excluded from the study. A total of 8530 AEs were included in the study. To normalize the data, we obtained annual reports for the number of procedures performed by filler type from the American Society of Plastic Surgeons (ASPS) cosmetic procedure trends. 3 We calculated the annual AE rates for each approved filler by dividing the number of AEs by the number of procedures performed that year.
Results
The trends of different filler types depicting the number of procedures performed over time are shown in Figure 1. Data from the ASPS dated back to 2005; therefore, the number of procedures performed prior to that were extrapolated with knowledge of products’ approval dates and market share, indicated by a dotted line. To determine AE rates for each year, we divided the number of AEs by the number of reported procedures for each filler type. The AE rates are displayed graphically in Figures 2 and 3 with superimposed FDA approval dates for each filler.4
Two major peaks in reported AE rates for all fillers were noted in the late 1990s and late 2000s, mostly associated with collagen and PLLA fillers, respectively (Figure 2). Overall, there has been a low rate of AEs associated with HA fillers since their initial approval in the early 2000s.
Individual filler AE rates also were analyzed. Hyaluronic acid fillers were associated with an extremely low rate of AEs, ranging from 1 to 4 AEs per 10,000 procedures (Figure 3A). This low AE rate profile underscores the safety of HA fillers, which has spurred their popularity. Adverseevent rates for collagen fillers spiked in the mid- to late 1990s and resolved over the course of the next 3 years (Figure 3B). Hydroxylapatite fillers had a rather uniform AE rate with an early indication of a drop-off after 2015 (Figure 3C). Poly-L-lactic acid fillers showed the steepest learning curve, with a peak of 1 AE per 100 procedures after they were approved in 2008 (Figure 3D); however, there is a comparable 3-year resolution of AE rates. Adverse events for PMMA fillers did not show specific resolution, meaning that they did not follow the 3-year arc that was seen for the other dermal fillers reported in the data set (Figure 3E).
Comment
Our study is unique in that it analyzes reported AE data over a 34-year period for injectable dermal fillers. To our knowledge, this novel method of calculating AE rates across dermal fillers and for individual products is the first of its kind that facilitates usage-normalized comparison of different filler types.
All OpenFDA data are self-reported and therefore have inherent limitations. Anyone can enter information on AEs in this system, including both patients and health care providers, so the quality of the input may be variable. However, this output is the only representation we have for nearly 35 years of AE history for this burgeoning category of popular aesthetic treatments. Another study limitation is that not everyone may know that reporting an AE in the OpenFDA is an option; therefore, we may be missing a portion of AEs due to underreporting. Underreporting may be especially at play in the years before the Internet was prevalent for residential use since access to the Internet would be required to report an AR on the website. However, examining the available data provides an important window into valuable information on complications that have occurred and have been reported for FDA-approved dermal fillers.
An additional challenge in constructing this study was assessing the total number of injectable dermal filler treatments being performed annually across filler types for normalization of the data. Although the absolute numbers of filler use as captured by the ASPS are smaller than the true total filler use across all injectors, the relative use of different filler products will be similar across all specialties because it reflects product popularity. Annual surveys on aesthetic procedures also are conducted by the American Society for Dermatologic Surgery and the American Association for Facial Plastic and Reconstructive Surgery, but neither one captures the relative usage of different filler types. Because individual filler companies do not publish their annual sales numbers by product, the ASPS data give us the best gauge of relative use of fillers by product type given the available information. We conclude that the comparison of AE rates would remain the same even if we had data for total annual filler use across specialties.
Our graphical depiction of the data clearly demonstrates the low AE profile of HA fillers, which is in line with the general consensus of their safety that has contributed to their vast popularity; however, this study represents the first time usage-normalized AE rates are compared to other filler compositions. Hyaluronic acid fillers have the unique feature of being able to be dissolved with the hyaluronidase enzyme, which can limit adverse event potential as compared to other ingredient classes of filler types and may be reflected in their low overall AE profile. The AE rate spike and resolution for collagen fillers represent what we refer to as a “normal learning curve” based on our analysis of the data set as a whole, suggesting an appropriate time course of increased familiarity with the product without inherent issues with the product itself. Multiple sequential anatomic site indications were approved for hydroxylapatite fillers from 2006 through 2015, which may have yielded overlapping learning curves for each approval, resulting in a rather uniform AE rate. The early drop-off in AE rates after the 2015 anatomic site approval may represent the beginning of a normal learning curve, and continued surveillance of AE rates would be of value to confirm this trend. We saw a similar 3-year learning curve for PLLA fillers as the curve for collagen fillers, suggesting a normal learning curve and no out-of-line safety issues. Polymethylmethacrylate fillers were approved in 2006 and were taken off the market for a period in the late 2000s, explaining the drop-off. Once they were back on the market, we do not see a typical learning curve for PMMA, which may warrant surveillance for safety by both clinicians and the FDA.
Conclusion
Our study represents a novel method of evaluating the safety of medical devices, specifically aesthetic fillers. We showed that every AE rate curve for different filler types tells a story. Reactions to AEs for new fillers should be placed in the context of whether they seem to be following the established learning curve.
- Dermal fillers (soft tissue fillers). US Food and Drug Administration website. https://www.fda.gov/MedicalDevices/ucm2007470.htm. Updated May 31, 2018. Accessed June 29, 2018.
- Kass-Hout TA, Xu Z, Mohebbi M, et al. OpenFDA: an innovative platform providing access to a wealth of FDA’s publicly available data. J Am Med Inform Assoc. 2016;23:596-600.
- Plastic surgery statistics. American Society of Plastic Surgeons website. https://www.plasticsurgery.org/documents/News/Statistics/2017/plastic-surgery-statistics-full-report-2017.pdf. Accessed June 28, 2018.
- Dermal fillers approved by the Center for Devices and Radiological Health. US Food and Drug Administration website. https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/CosmeticDevices/WrinkleFillers/ucm227749.htm. Accessed June 28, 2018. Updated March 19, 2018.
- Dermal fillers (soft tissue fillers). US Food and Drug Administration website. https://www.fda.gov/MedicalDevices/ucm2007470.htm. Updated May 31, 2018. Accessed June 29, 2018.
- Kass-Hout TA, Xu Z, Mohebbi M, et al. OpenFDA: an innovative platform providing access to a wealth of FDA’s publicly available data. J Am Med Inform Assoc. 2016;23:596-600.
- Plastic surgery statistics. American Society of Plastic Surgeons website. https://www.plasticsurgery.org/documents/News/Statistics/2017/plastic-surgery-statistics-full-report-2017.pdf. Accessed June 28, 2018.
- Dermal fillers approved by the Center for Devices and Radiological Health. US Food and Drug Administration website. https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/CosmeticDevices/WrinkleFillers/ucm227749.htm. Accessed June 28, 2018. Updated March 19, 2018.
Resident Pearl
- The US Food and Drug Administration’s (FDA) adverse event database, OpenFDA, provides extensive information regarding safety for a variety of cosmetic devices. Injectable dermal fillers are classified as a medical device by the FDA; therefore, safety studies can be performed using this publicly available database.
Brown Papules on the Penis
The Diagnosis: Bowenoid Papulosis
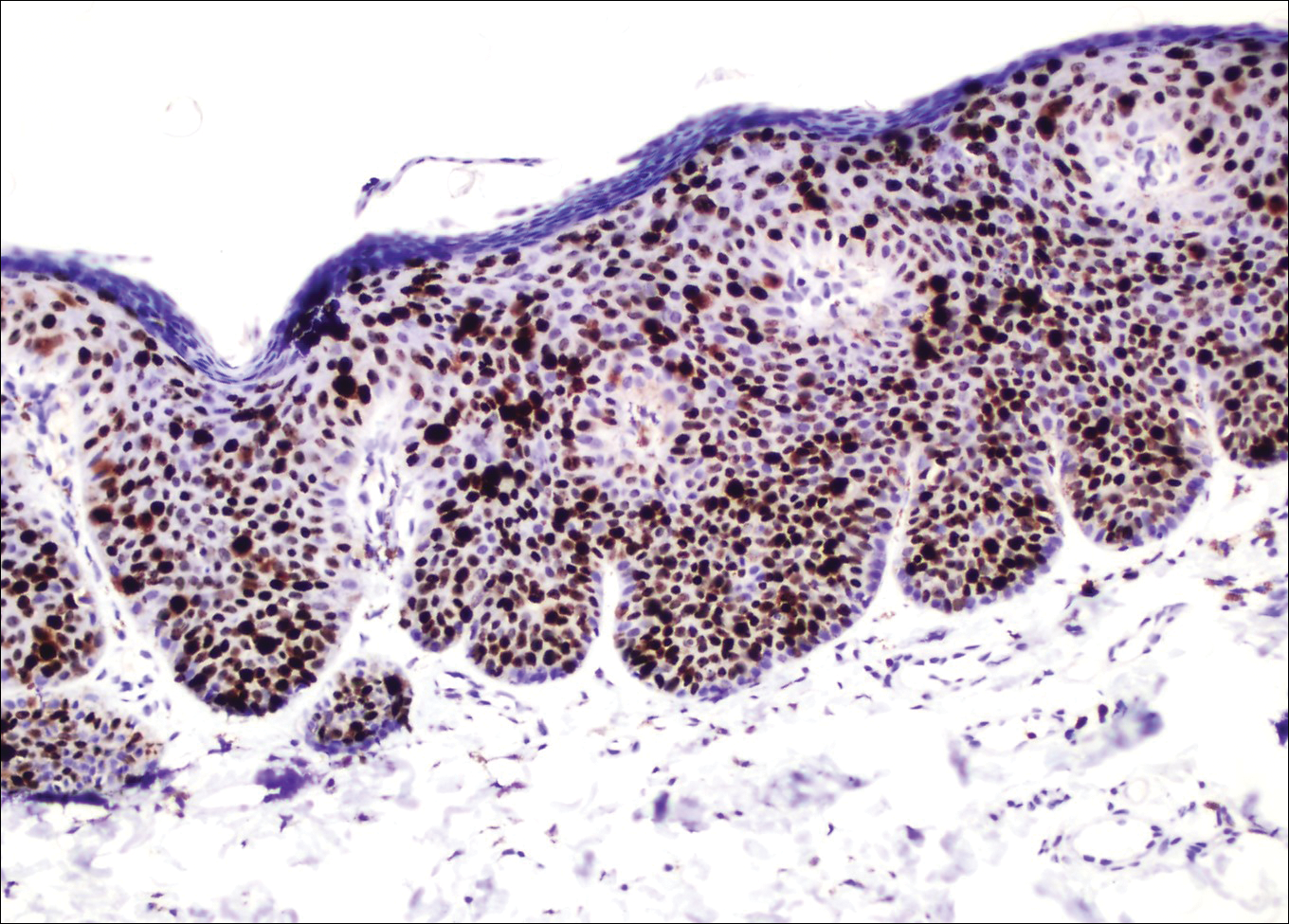
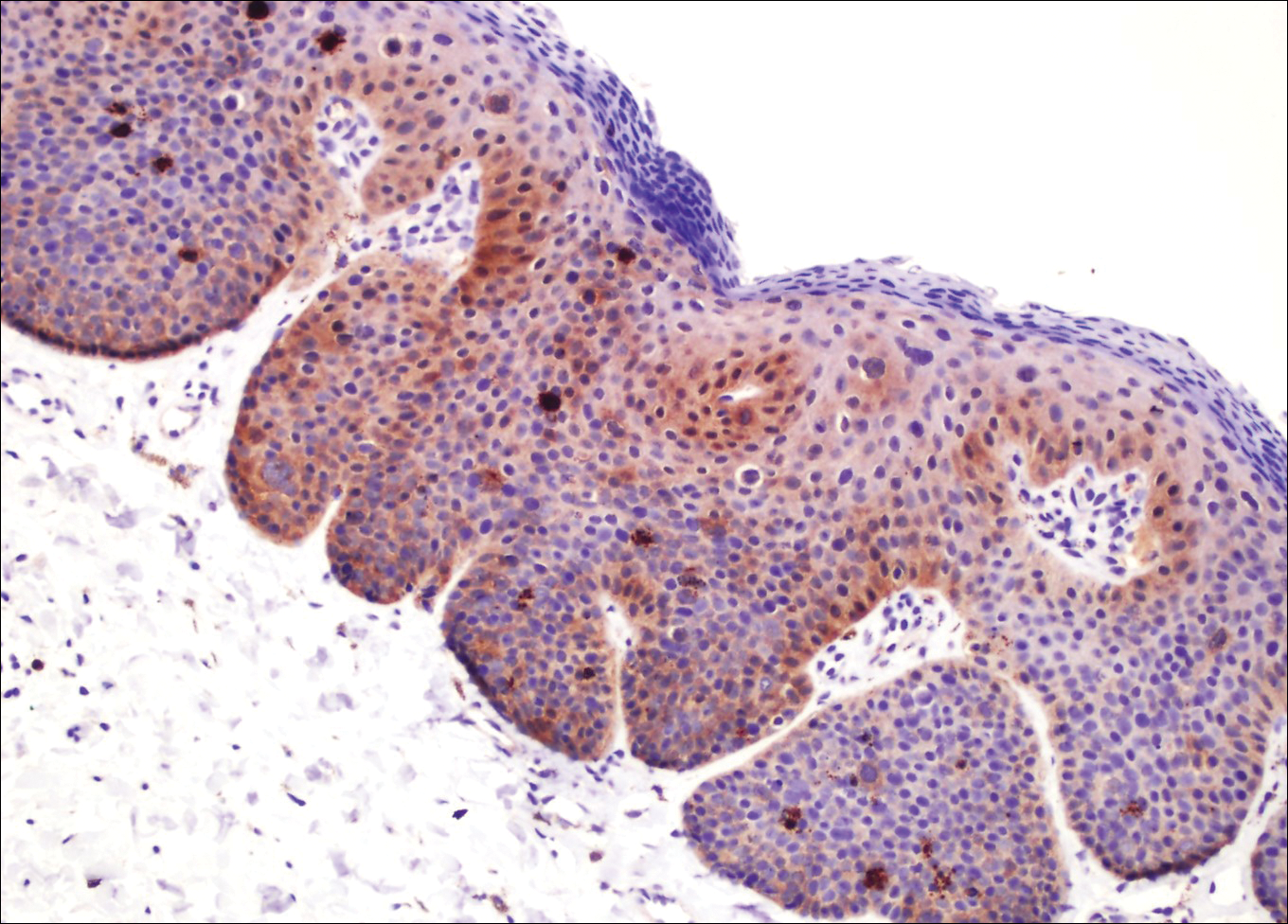
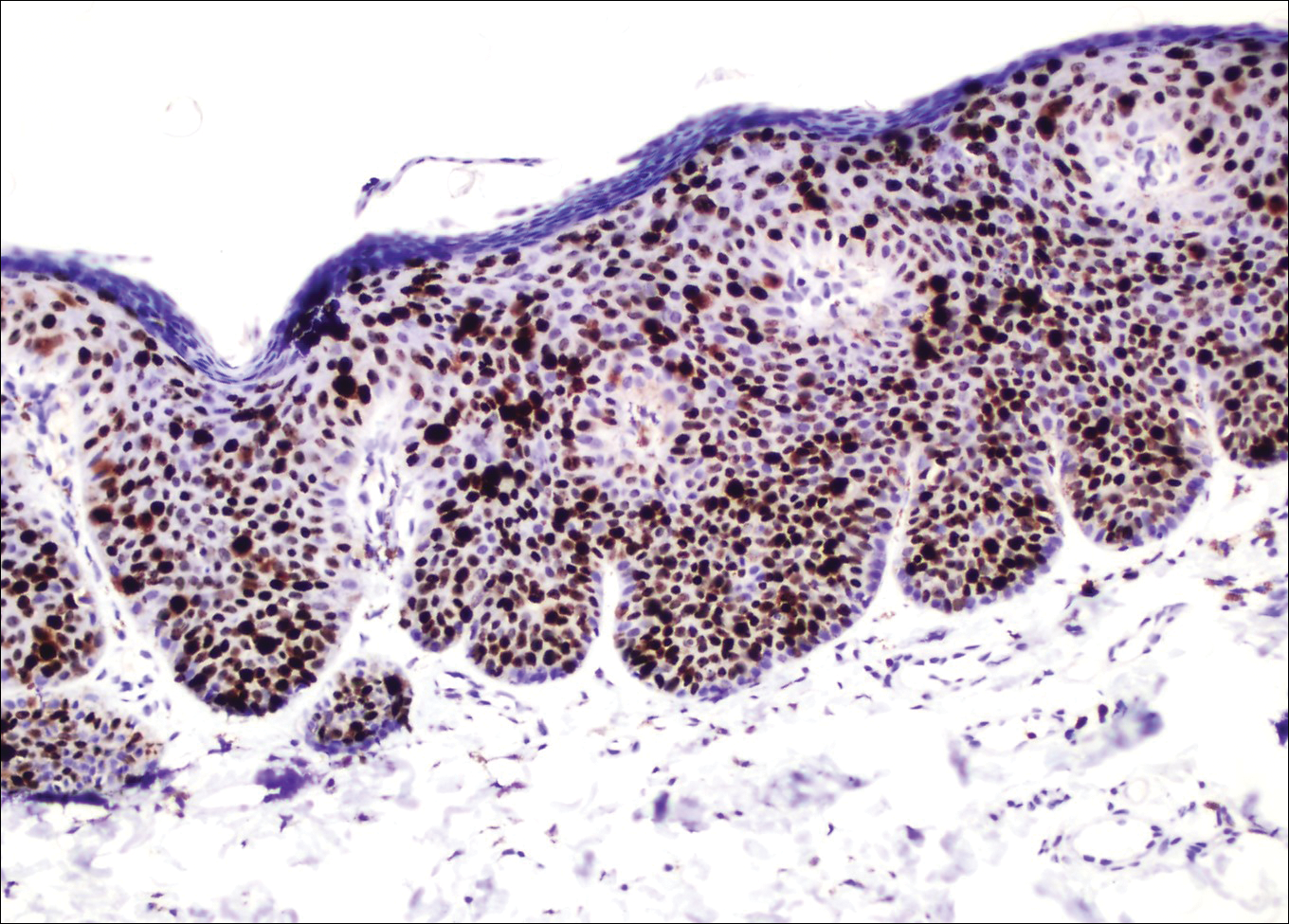
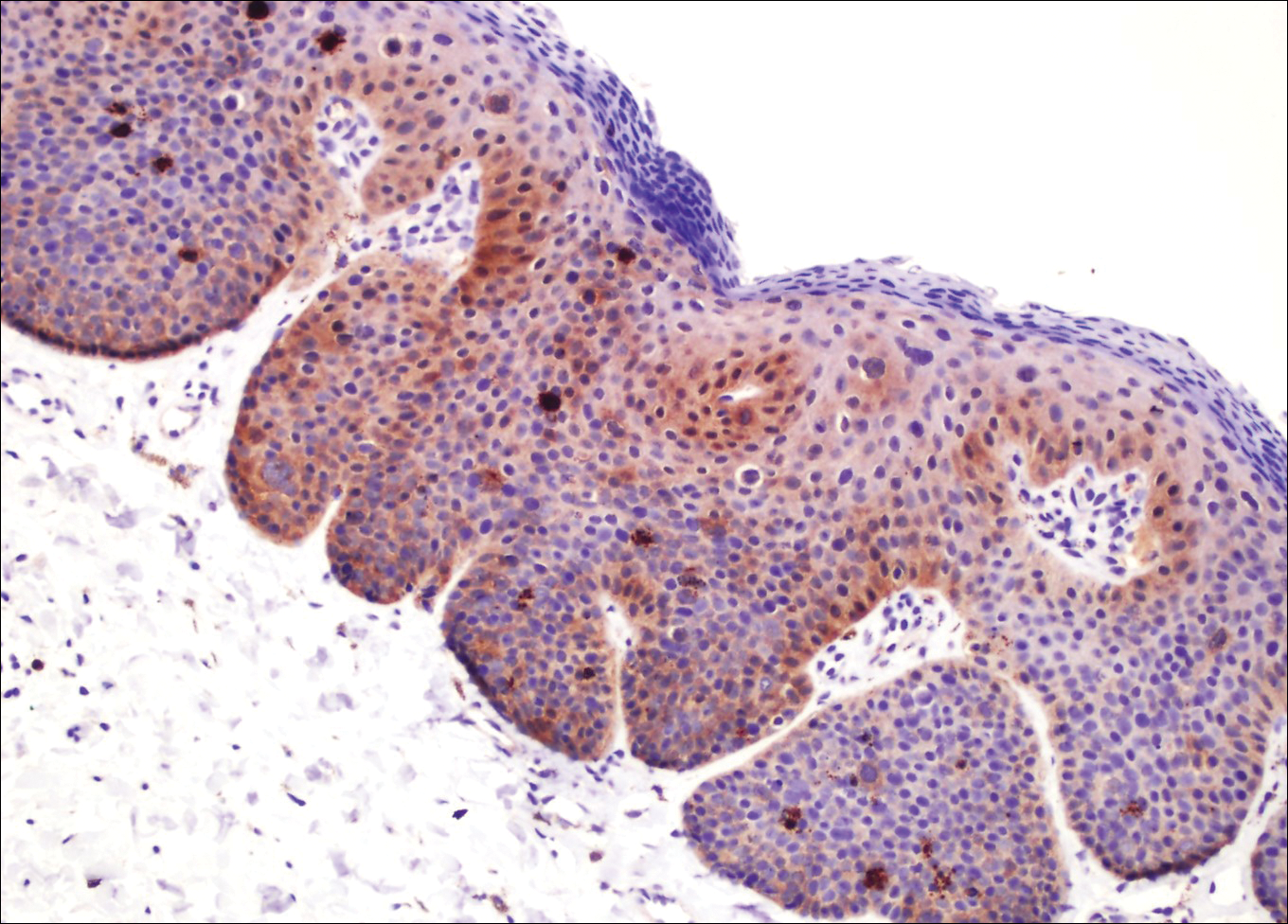
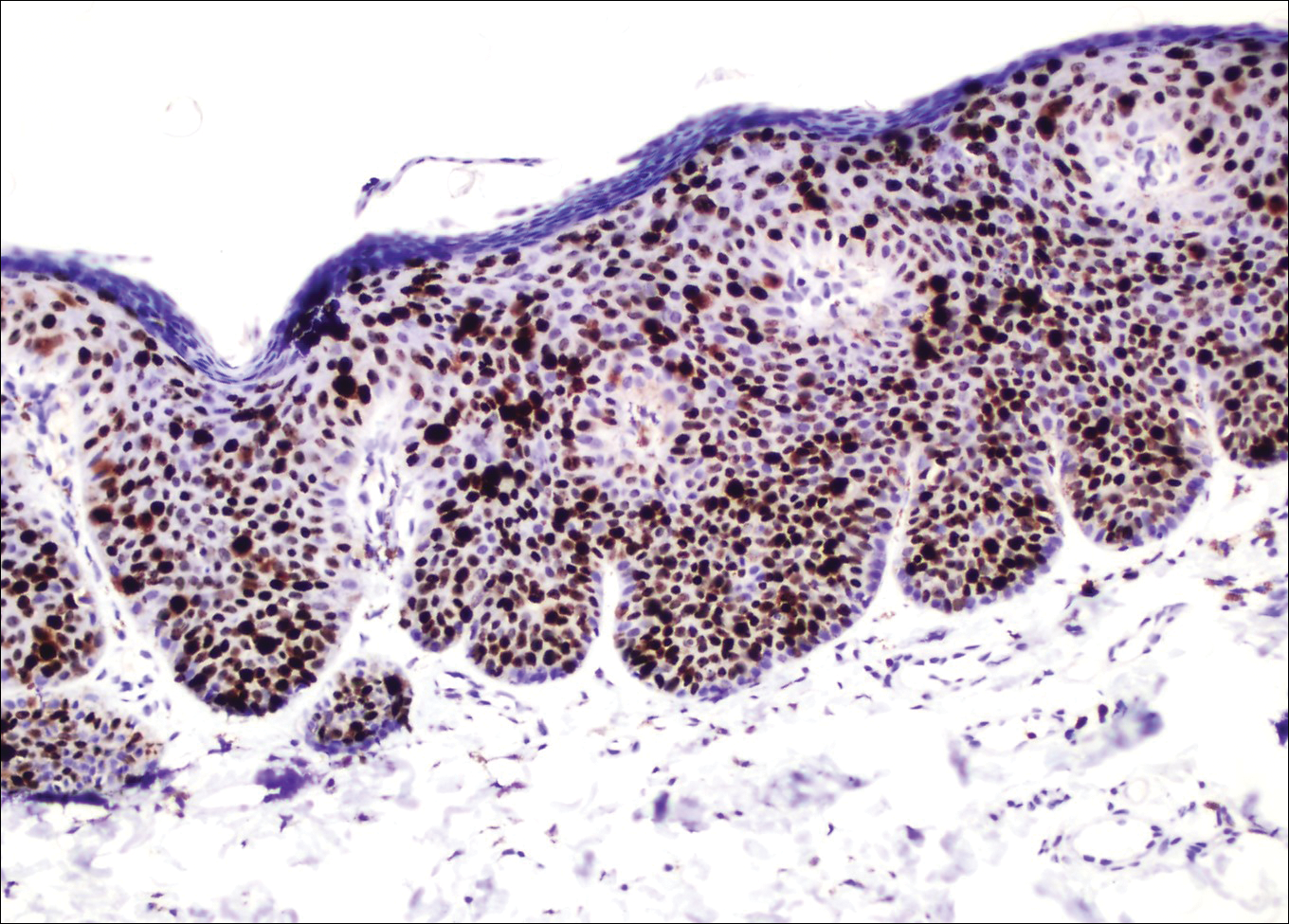
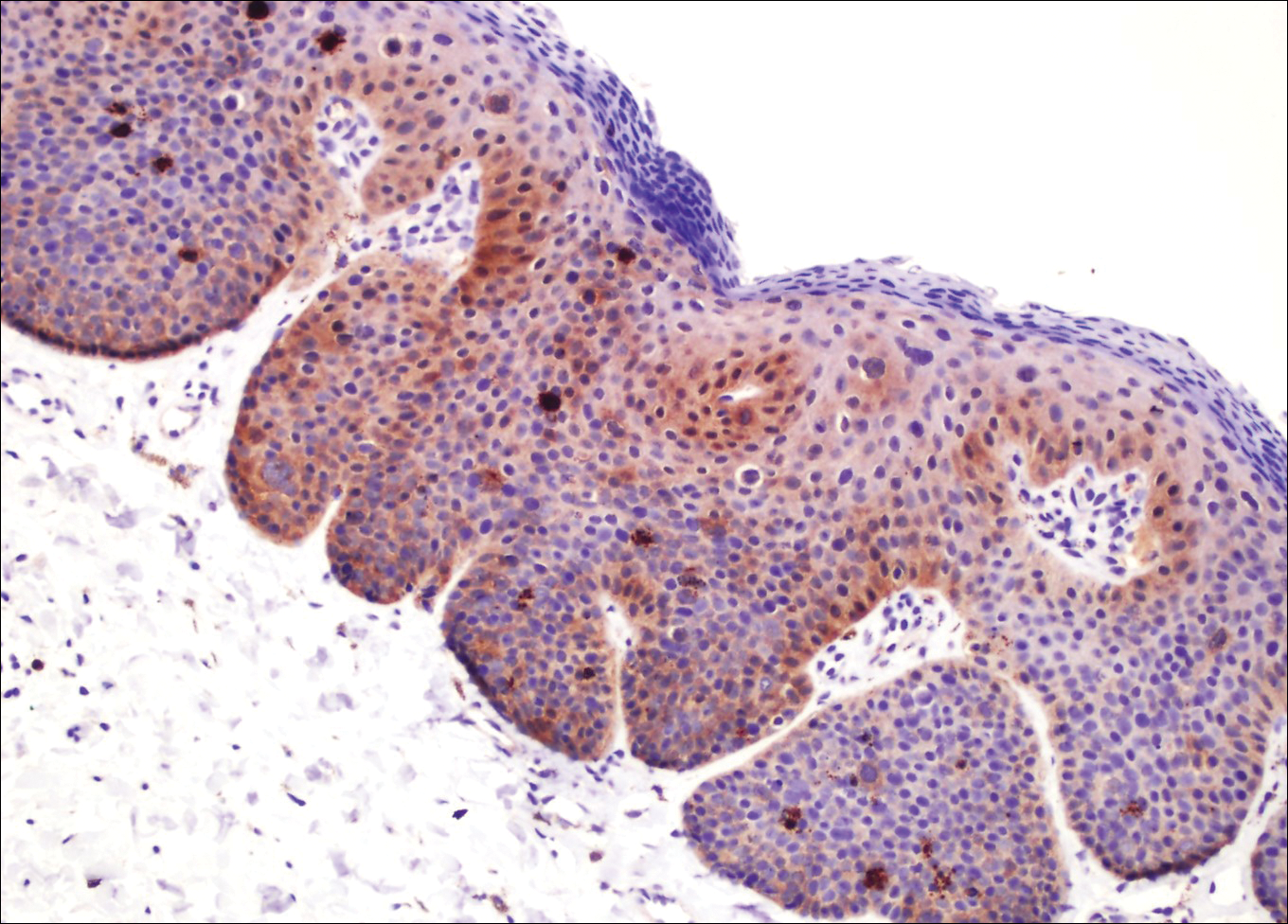
A 4-mm punch biopsy was performed from the active border of brown plaques on the dorsal penis. Histopathology revealed parakeratotic hyperkeratosis, acanthosis, loss of maturation in epithelium, and full-size atypia (Figure 1). Ki-67 index was 90% positive in the epidermis (Figure 2). Staining for p16 and human papillomavirus (HPV) screening was positive for HPV type 16 (Figure 3). Serologic tests for other sexually transmitted infections were negative. A diagnosis of penile bowenoid papulosis (BP) with grade 3 penile intraepithelial neoplasia was made, and treatment with topical 5-fluorouracil (5-FU) was initiated. Almost total regression was appreciated at 1-month follow-up (Figure 4), and he also was recurrence free at 1-year follow-up.


Penile intraepithelial neoplasia (PIN), or penile squamous cell carcinoma in situ, is a rare disease with high morbidity and mortality rates. Clinically, PIN is comprised of a clinical spectrum including 3 different entities: erythroplasia of Queyrat, Bowen disease, and BP.1 Histologically, PIN also is classified into 3 subtypes according to histological depth of epidermal atypia.1
Bowenoid papulosis usually is characterized by multiple red-brown or flesh-colored papules that most commonly appear on the shaft or glans of the penis. Bowenoid papulosis frequently is associated with high-risk types of HPV, such as HPV type 16, and is sometimes difficult to differentiate clinically from pigmented condyloma acuminatum. The clinical lesions of BP usually are less papillomatous, smoother topped, more polymorphic, and more coalescent compared to common genital viral condyloma acuminatum.2 Bowenoid papulosis usually is seen in young (<30 years of age) sexually active men, unlike the patches or plaques of erythroplasia of Queyrat or Bowen disease, which are seen in older men aged 45 to 75 years. Bowenoid papulosis also has a lower malignancy potential than erythroplasia of Queyrat and Bowen disease.2
Penile melanosis, penile lentigo, and seborrheic keratosis comprise the differential diagnosis of dark spots on the penis and also should be kept in mind. Penile melanosis is the most common cause of dark spots on the penis. When the dark spots have irregular borders and change in color, they may be misdiagnosed as malignant lesions such as melanoma.3 In most cases, biopsy is indicated. Histologically, penile melanosis is characterized by hyperpigmentation of the basal cell layer with no melanocytic hyperplasia. Treatment is unnecessary in most cases.
Penile lentigo presents as small flat pigmented spots on the penile skin with clearly defined margins surrounded by normal-appearing skin. Histologically, it is characterized by hyperplasia of melanocytes above the basement membrane of the epidermis.3
Penile pigmented seborrheic keratosis is a rare clinical entity that can be easily misinterpreted as condyloma acuminatum. Histologically, it is characterized by basal cell hyperplasia with cystic formation in the thickened epidermis. Excisional biopsy may be the only way to rule out malignant disease.
Treatment options for PIN include cryotherapy, CO2 or Nd:YAG lasers, photodynamic therapy, topical 5-FU or imiquimod therapy, and surgical excision such as Mohs micrographic surgery.4-9 Although these therapeutic modalities usually are effective, recurrence is common.6 The patients' discomfort and poor cosmetic and functional outcomes from the surgical removal of lesions also present a challenge in treatment planning.
In our patient, we quickly achieved a good result with topical 5-FU, though the disease was in local advanced stage. It is important for clinicians to consider 5-FU as an effective treatment option for PIN before planning surgery.
- Deen K, Burdon-Jones D. Imiquimod in the treatment of penile intraepithelial neoplasia: an update. Australas J Dermatol. 2017;58:86-92.
- Porter WM, Francis N, Hawkins D, et al. Penile intraepithelial neoplasia: clinical spectrum and treatment of 35 cases. Br J Dermatol. 2002;147:1159-1165.
- Fahmy M. Dermatological disease of the penis. In: Fahmy M. Congenital Anomalies of the Penis. Cham, Switzerland: Springer; 2017:257-264.
- Shimizu A, Kato M, Ishikawa O. Bowenoid papulosis successfully treated with imiquimod 5% cream. J Dermatol. 2014;41:545-546.
- Lucky M, Murthy KV, Rogers B, et al. The treatment of penile carcinoma in situ (CIS) within a UK supra-regional network [published online December 15, 2014]. BJU Int. 2015;115:595-598.
- Alnajjar HM, Lam W, Bolgeri M, et al. Treatment of carcinoma in situ of the glans penis with topical chemotherapy agents. Eur Urol. 2012;62:923-928.
- Wang XL, Wang HW, Guo MX, et al. Combination of immunotherapy and photodynamic therapy in the treatment of bowenoid papulosis. Photodiagnosis Photodyn Ther. 2007;4:88-93.
- Zreik A, Rewhorn M, Vint R, et al. Carbon dioxide laser treatment of penile intraepithelial neoplasia [published online December 7, 2016]. Surgeon. 2017;15:321-324.
- Machan M, Brodland D, Zitelli J. Penile squamous cell carcinoma: penis-preserving treatment with Mohs micrographic surgery. Dermatol Surg. 2016;42:936-944.
The Diagnosis: Bowenoid Papulosis
A 4-mm punch biopsy was performed from the active border of brown plaques on the dorsal penis. Histopathology revealed parakeratotic hyperkeratosis, acanthosis, loss of maturation in epithelium, and full-size atypia (Figure 1). Ki-67 index was 90% positive in the epidermis (Figure 2). Staining for p16 and human papillomavirus (HPV) screening was positive for HPV type 16 (Figure 3). Serologic tests for other sexually transmitted infections were negative. A diagnosis of penile bowenoid papulosis (BP) with grade 3 penile intraepithelial neoplasia was made, and treatment with topical 5-fluorouracil (5-FU) was initiated. Almost total regression was appreciated at 1-month follow-up (Figure 4), and he also was recurrence free at 1-year follow-up.


Penile intraepithelial neoplasia (PIN), or penile squamous cell carcinoma in situ, is a rare disease with high morbidity and mortality rates. Clinically, PIN is comprised of a clinical spectrum including 3 different entities: erythroplasia of Queyrat, Bowen disease, and BP.1 Histologically, PIN also is classified into 3 subtypes according to histological depth of epidermal atypia.1
Bowenoid papulosis usually is characterized by multiple red-brown or flesh-colored papules that most commonly appear on the shaft or glans of the penis. Bowenoid papulosis frequently is associated with high-risk types of HPV, such as HPV type 16, and is sometimes difficult to differentiate clinically from pigmented condyloma acuminatum. The clinical lesions of BP usually are less papillomatous, smoother topped, more polymorphic, and more coalescent compared to common genital viral condyloma acuminatum.2 Bowenoid papulosis usually is seen in young (<30 years of age) sexually active men, unlike the patches or plaques of erythroplasia of Queyrat or Bowen disease, which are seen in older men aged 45 to 75 years. Bowenoid papulosis also has a lower malignancy potential than erythroplasia of Queyrat and Bowen disease.2
Penile melanosis, penile lentigo, and seborrheic keratosis comprise the differential diagnosis of dark spots on the penis and also should be kept in mind. Penile melanosis is the most common cause of dark spots on the penis. When the dark spots have irregular borders and change in color, they may be misdiagnosed as malignant lesions such as melanoma.3 In most cases, biopsy is indicated. Histologically, penile melanosis is characterized by hyperpigmentation of the basal cell layer with no melanocytic hyperplasia. Treatment is unnecessary in most cases.
Penile lentigo presents as small flat pigmented spots on the penile skin with clearly defined margins surrounded by normal-appearing skin. Histologically, it is characterized by hyperplasia of melanocytes above the basement membrane of the epidermis.3
Penile pigmented seborrheic keratosis is a rare clinical entity that can be easily misinterpreted as condyloma acuminatum. Histologically, it is characterized by basal cell hyperplasia with cystic formation in the thickened epidermis. Excisional biopsy may be the only way to rule out malignant disease.
Treatment options for PIN include cryotherapy, CO2 or Nd:YAG lasers, photodynamic therapy, topical 5-FU or imiquimod therapy, and surgical excision such as Mohs micrographic surgery.4-9 Although these therapeutic modalities usually are effective, recurrence is common.6 The patients' discomfort and poor cosmetic and functional outcomes from the surgical removal of lesions also present a challenge in treatment planning.
In our patient, we quickly achieved a good result with topical 5-FU, though the disease was in local advanced stage. It is important for clinicians to consider 5-FU as an effective treatment option for PIN before planning surgery.
The Diagnosis: Bowenoid Papulosis
A 4-mm punch biopsy was performed from the active border of brown plaques on the dorsal penis. Histopathology revealed parakeratotic hyperkeratosis, acanthosis, loss of maturation in epithelium, and full-size atypia (Figure 1). Ki-67 index was 90% positive in the epidermis (Figure 2). Staining for p16 and human papillomavirus (HPV) screening was positive for HPV type 16 (Figure 3). Serologic tests for other sexually transmitted infections were negative. A diagnosis of penile bowenoid papulosis (BP) with grade 3 penile intraepithelial neoplasia was made, and treatment with topical 5-fluorouracil (5-FU) was initiated. Almost total regression was appreciated at 1-month follow-up (Figure 4), and he also was recurrence free at 1-year follow-up.


Penile intraepithelial neoplasia (PIN), or penile squamous cell carcinoma in situ, is a rare disease with high morbidity and mortality rates. Clinically, PIN is comprised of a clinical spectrum including 3 different entities: erythroplasia of Queyrat, Bowen disease, and BP.1 Histologically, PIN also is classified into 3 subtypes according to histological depth of epidermal atypia.1
Bowenoid papulosis usually is characterized by multiple red-brown or flesh-colored papules that most commonly appear on the shaft or glans of the penis. Bowenoid papulosis frequently is associated with high-risk types of HPV, such as HPV type 16, and is sometimes difficult to differentiate clinically from pigmented condyloma acuminatum. The clinical lesions of BP usually are less papillomatous, smoother topped, more polymorphic, and more coalescent compared to common genital viral condyloma acuminatum.2 Bowenoid papulosis usually is seen in young (<30 years of age) sexually active men, unlike the patches or plaques of erythroplasia of Queyrat or Bowen disease, which are seen in older men aged 45 to 75 years. Bowenoid papulosis also has a lower malignancy potential than erythroplasia of Queyrat and Bowen disease.2
Penile melanosis, penile lentigo, and seborrheic keratosis comprise the differential diagnosis of dark spots on the penis and also should be kept in mind. Penile melanosis is the most common cause of dark spots on the penis. When the dark spots have irregular borders and change in color, they may be misdiagnosed as malignant lesions such as melanoma.3 In most cases, biopsy is indicated. Histologically, penile melanosis is characterized by hyperpigmentation of the basal cell layer with no melanocytic hyperplasia. Treatment is unnecessary in most cases.
Penile lentigo presents as small flat pigmented spots on the penile skin with clearly defined margins surrounded by normal-appearing skin. Histologically, it is characterized by hyperplasia of melanocytes above the basement membrane of the epidermis.3
Penile pigmented seborrheic keratosis is a rare clinical entity that can be easily misinterpreted as condyloma acuminatum. Histologically, it is characterized by basal cell hyperplasia with cystic formation in the thickened epidermis. Excisional biopsy may be the only way to rule out malignant disease.
Treatment options for PIN include cryotherapy, CO2 or Nd:YAG lasers, photodynamic therapy, topical 5-FU or imiquimod therapy, and surgical excision such as Mohs micrographic surgery.4-9 Although these therapeutic modalities usually are effective, recurrence is common.6 The patients' discomfort and poor cosmetic and functional outcomes from the surgical removal of lesions also present a challenge in treatment planning.
In our patient, we quickly achieved a good result with topical 5-FU, though the disease was in local advanced stage. It is important for clinicians to consider 5-FU as an effective treatment option for PIN before planning surgery.
- Deen K, Burdon-Jones D. Imiquimod in the treatment of penile intraepithelial neoplasia: an update. Australas J Dermatol. 2017;58:86-92.
- Porter WM, Francis N, Hawkins D, et al. Penile intraepithelial neoplasia: clinical spectrum and treatment of 35 cases. Br J Dermatol. 2002;147:1159-1165.
- Fahmy M. Dermatological disease of the penis. In: Fahmy M. Congenital Anomalies of the Penis. Cham, Switzerland: Springer; 2017:257-264.
- Shimizu A, Kato M, Ishikawa O. Bowenoid papulosis successfully treated with imiquimod 5% cream. J Dermatol. 2014;41:545-546.
- Lucky M, Murthy KV, Rogers B, et al. The treatment of penile carcinoma in situ (CIS) within a UK supra-regional network [published online December 15, 2014]. BJU Int. 2015;115:595-598.
- Alnajjar HM, Lam W, Bolgeri M, et al. Treatment of carcinoma in situ of the glans penis with topical chemotherapy agents. Eur Urol. 2012;62:923-928.
- Wang XL, Wang HW, Guo MX, et al. Combination of immunotherapy and photodynamic therapy in the treatment of bowenoid papulosis. Photodiagnosis Photodyn Ther. 2007;4:88-93.
- Zreik A, Rewhorn M, Vint R, et al. Carbon dioxide laser treatment of penile intraepithelial neoplasia [published online December 7, 2016]. Surgeon. 2017;15:321-324.
- Machan M, Brodland D, Zitelli J. Penile squamous cell carcinoma: penis-preserving treatment with Mohs micrographic surgery. Dermatol Surg. 2016;42:936-944.
- Deen K, Burdon-Jones D. Imiquimod in the treatment of penile intraepithelial neoplasia: an update. Australas J Dermatol. 2017;58:86-92.
- Porter WM, Francis N, Hawkins D, et al. Penile intraepithelial neoplasia: clinical spectrum and treatment of 35 cases. Br J Dermatol. 2002;147:1159-1165.
- Fahmy M. Dermatological disease of the penis. In: Fahmy M. Congenital Anomalies of the Penis. Cham, Switzerland: Springer; 2017:257-264.
- Shimizu A, Kato M, Ishikawa O. Bowenoid papulosis successfully treated with imiquimod 5% cream. J Dermatol. 2014;41:545-546.
- Lucky M, Murthy KV, Rogers B, et al. The treatment of penile carcinoma in situ (CIS) within a UK supra-regional network [published online December 15, 2014]. BJU Int. 2015;115:595-598.
- Alnajjar HM, Lam W, Bolgeri M, et al. Treatment of carcinoma in situ of the glans penis with topical chemotherapy agents. Eur Urol. 2012;62:923-928.
- Wang XL, Wang HW, Guo MX, et al. Combination of immunotherapy and photodynamic therapy in the treatment of bowenoid papulosis. Photodiagnosis Photodyn Ther. 2007;4:88-93.
- Zreik A, Rewhorn M, Vint R, et al. Carbon dioxide laser treatment of penile intraepithelial neoplasia [published online December 7, 2016]. Surgeon. 2017;15:321-324.
- Machan M, Brodland D, Zitelli J. Penile squamous cell carcinoma: penis-preserving treatment with Mohs micrographic surgery. Dermatol Surg. 2016;42:936-944.

A 32-year-old man presented to the outpatient clinic with reddish brown lesions on the penis of 5 months' duration. Dermatologic examination revealed multiple mildly infiltrated, bright reddish brown papules and plaques on the dorsal penis.
Excision of a Bartholin gland cyst
Bartholin gland cysts comprise up to 2% of all outpatient gynecology visits each year1 and are a common consult for trainees in obstetrics and gynecology. Although excision of a Bartholin gland cyst is a procedure performed infrequently, knowledge of its anatomy and physiology is important for ObGyn trainees and practicing gynecologists, especially when attempts at conservative management have been exhausted.
Before proceeding with surgical excision, it is important to understand the basics of Bartholin gland anatomy, pathologies, and treatment options. This video demonstrates the excisional technique for a 46-year-old woman with a recurrent, symptomatic Bartholin gland cyst who failed prior conservative management. I hope that you will find this video from my colleagues beneficial to your clinical practice.

- Marzano DA, Haefner HK. The bartholin gland cyst: past, present, and future. J Low Genit Tract Dis. 2004;8(3):195–204.
Bartholin gland cysts comprise up to 2% of all outpatient gynecology visits each year1 and are a common consult for trainees in obstetrics and gynecology. Although excision of a Bartholin gland cyst is a procedure performed infrequently, knowledge of its anatomy and physiology is important for ObGyn trainees and practicing gynecologists, especially when attempts at conservative management have been exhausted.
Before proceeding with surgical excision, it is important to understand the basics of Bartholin gland anatomy, pathologies, and treatment options. This video demonstrates the excisional technique for a 46-year-old woman with a recurrent, symptomatic Bartholin gland cyst who failed prior conservative management. I hope that you will find this video from my colleagues beneficial to your clinical practice.

Bartholin gland cysts comprise up to 2% of all outpatient gynecology visits each year1 and are a common consult for trainees in obstetrics and gynecology. Although excision of a Bartholin gland cyst is a procedure performed infrequently, knowledge of its anatomy and physiology is important for ObGyn trainees and practicing gynecologists, especially when attempts at conservative management have been exhausted.
Before proceeding with surgical excision, it is important to understand the basics of Bartholin gland anatomy, pathologies, and treatment options. This video demonstrates the excisional technique for a 46-year-old woman with a recurrent, symptomatic Bartholin gland cyst who failed prior conservative management. I hope that you will find this video from my colleagues beneficial to your clinical practice.

- Marzano DA, Haefner HK. The bartholin gland cyst: past, present, and future. J Low Genit Tract Dis. 2004;8(3):195–204.
- Marzano DA, Haefner HK. The bartholin gland cyst: past, present, and future. J Low Genit Tract Dis. 2004;8(3):195–204.
Itraconazole for BCC: Does it work?
CHICAGO – Justin J. Leitenberger, MD, declared at the annual meeting of the American College of Mohs Surgery.
The oral antifungal inhibits the hedgehog signaling pathway, a key driver of BCC. And while itraconazole is not as potent an inhibitor of hedgehog pathway expression as, say vismodegib (Erivedge), the antifungal acts at a separate site on the pathway, making it an attractive candidate for combination therapy, explained Dr. Leitenberger of Oregon Health & Science University, Portland.
Dermatologists at Stanford University have led the way in exploring oral itraconazole as a treatment for BCC. Among a series of 29 patients with one or more large but nonadvanced BCCs, 19 were treated using oral itraconazole at 200 mg b.i.d. for 1 month or 100 mg b.i.d. for an average of 2.3 months. Hedgehog pathway expression was reduced by 65% in the itraconazole-treated patients, as compared with the 90% reduction which is achieved with vismodegib.
Of more direct clinical relevance, however, itraconazole also reduced tumor area by 24%. Four of eight patients with 57 tumors achieved a partial response, and the other four had stable disease (J Clin Oncol. 2014 Mar 10;32[8]:745-51).
The Stanford group has also shown that combination therapy with oral itraconazole and intravenous arsenic trioxide reduces hedgehog pathway expression by 75%, up by an absolute 10% from itraconazole alone. The two agents inhibit the pathway at different sites.
Five patients with metastatic BCC who relapsed after treatment with vismodegib received intravenous arsenic trioxide for the first 5 days of every month, followed by oral itraconazole at 200 mg b.i.d. on days 6-28. Three patients completed three such cycles, while two discontinued early because of progressive disease or adverse events including a grade 3 infection and grade 2 transaminitis. All three patients who completed three treatment cycles achieved stable disease. The Stanford investigators speculated that concurrent continuous dosing might be required to obtain tumor shrinkage (JAMA Dermatol. 2016 Apr;152[4]:452-6).
Lots more work remains to be done in order to optimize combination therapy utilizing oral itraconazole for advanced BCC. Different dosing regimens and combinations of hedgehog pathway inhibitors need to be studied. Another important question is how effective itraconazole-based combinations will be in vismodegib-naive as compared with vismodegib-resistant patients, Dr. Leitenberger observed.
He reported having no financial conflicts regarding his presentation.
CHICAGO – Justin J. Leitenberger, MD, declared at the annual meeting of the American College of Mohs Surgery.
The oral antifungal inhibits the hedgehog signaling pathway, a key driver of BCC. And while itraconazole is not as potent an inhibitor of hedgehog pathway expression as, say vismodegib (Erivedge), the antifungal acts at a separate site on the pathway, making it an attractive candidate for combination therapy, explained Dr. Leitenberger of Oregon Health & Science University, Portland.
Dermatologists at Stanford University have led the way in exploring oral itraconazole as a treatment for BCC. Among a series of 29 patients with one or more large but nonadvanced BCCs, 19 were treated using oral itraconazole at 200 mg b.i.d. for 1 month or 100 mg b.i.d. for an average of 2.3 months. Hedgehog pathway expression was reduced by 65% in the itraconazole-treated patients, as compared with the 90% reduction which is achieved with vismodegib.
Of more direct clinical relevance, however, itraconazole also reduced tumor area by 24%. Four of eight patients with 57 tumors achieved a partial response, and the other four had stable disease (J Clin Oncol. 2014 Mar 10;32[8]:745-51).
The Stanford group has also shown that combination therapy with oral itraconazole and intravenous arsenic trioxide reduces hedgehog pathway expression by 75%, up by an absolute 10% from itraconazole alone. The two agents inhibit the pathway at different sites.
Five patients with metastatic BCC who relapsed after treatment with vismodegib received intravenous arsenic trioxide for the first 5 days of every month, followed by oral itraconazole at 200 mg b.i.d. on days 6-28. Three patients completed three such cycles, while two discontinued early because of progressive disease or adverse events including a grade 3 infection and grade 2 transaminitis. All three patients who completed three treatment cycles achieved stable disease. The Stanford investigators speculated that concurrent continuous dosing might be required to obtain tumor shrinkage (JAMA Dermatol. 2016 Apr;152[4]:452-6).
Lots more work remains to be done in order to optimize combination therapy utilizing oral itraconazole for advanced BCC. Different dosing regimens and combinations of hedgehog pathway inhibitors need to be studied. Another important question is how effective itraconazole-based combinations will be in vismodegib-naive as compared with vismodegib-resistant patients, Dr. Leitenberger observed.
He reported having no financial conflicts regarding his presentation.
CHICAGO – Justin J. Leitenberger, MD, declared at the annual meeting of the American College of Mohs Surgery.
The oral antifungal inhibits the hedgehog signaling pathway, a key driver of BCC. And while itraconazole is not as potent an inhibitor of hedgehog pathway expression as, say vismodegib (Erivedge), the antifungal acts at a separate site on the pathway, making it an attractive candidate for combination therapy, explained Dr. Leitenberger of Oregon Health & Science University, Portland.
Dermatologists at Stanford University have led the way in exploring oral itraconazole as a treatment for BCC. Among a series of 29 patients with one or more large but nonadvanced BCCs, 19 were treated using oral itraconazole at 200 mg b.i.d. for 1 month or 100 mg b.i.d. for an average of 2.3 months. Hedgehog pathway expression was reduced by 65% in the itraconazole-treated patients, as compared with the 90% reduction which is achieved with vismodegib.
Of more direct clinical relevance, however, itraconazole also reduced tumor area by 24%. Four of eight patients with 57 tumors achieved a partial response, and the other four had stable disease (J Clin Oncol. 2014 Mar 10;32[8]:745-51).
The Stanford group has also shown that combination therapy with oral itraconazole and intravenous arsenic trioxide reduces hedgehog pathway expression by 75%, up by an absolute 10% from itraconazole alone. The two agents inhibit the pathway at different sites.
Five patients with metastatic BCC who relapsed after treatment with vismodegib received intravenous arsenic trioxide for the first 5 days of every month, followed by oral itraconazole at 200 mg b.i.d. on days 6-28. Three patients completed three such cycles, while two discontinued early because of progressive disease or adverse events including a grade 3 infection and grade 2 transaminitis. All three patients who completed three treatment cycles achieved stable disease. The Stanford investigators speculated that concurrent continuous dosing might be required to obtain tumor shrinkage (JAMA Dermatol. 2016 Apr;152[4]:452-6).
Lots more work remains to be done in order to optimize combination therapy utilizing oral itraconazole for advanced BCC. Different dosing regimens and combinations of hedgehog pathway inhibitors need to be studied. Another important question is how effective itraconazole-based combinations will be in vismodegib-naive as compared with vismodegib-resistant patients, Dr. Leitenberger observed.
He reported having no financial conflicts regarding his presentation.
EXPERT ANALYSIS FROM THE ACMS ANNUAL MEETING
Speaking the unspeakable: Talking to children about parental mental illness
You probably think you know how to talk with a child about death. But somehow talking about a parent’s mental illness may seem more difficult. Even medical professionals, as most people, can find themselves feeling more judgmental or uneasy talking about mental illness than about physical problems. But with a prevalence of about one in four people having mental disorders, we need to be prepared for this discussion.
Sometimes family members, or even parents themselves, have asked me to tell a child about a parent’s mental illness or substance use. They know the child is confused and scared but don’t know what to say about this still-hushed issue. Other times, children’s behaviors show that they are struggling – by their aggression, depression, decline in school performance, anger, anxiety, or running away – and I find out only by asking that they are experiencing life with a mentally ill parent.
Both are times to get more information about the nature of the parent’s symptoms, what is being done about it; what the child has seen, heard, or experienced; the child’s safety; and what intrinsic or cultural attitudes the family has about the problem. It is best if the affected parents themselves are able to talk realistically about the illness with the child. Sometimes we, as pediatric professionals, can help get the conversation started or may need to step in.
Teens can understand the nature of mental illness as a brain disorder, but often have acquired misinformation from peers, the other parent who is hurt and angry, or the Internet that needs to be respectfully corrected. They may be less willing to have such a discussion than would younger children, as they may have experienced verbal or physical aggression from the parent, embarrassment in front of peers, or teasing by classmates. They may have developed coping strategies of writing off the parent, defiance, aggressive responses, or denial.
It is important to find a relaxed moment and begin by saying, “May I ask what you have noticed about your parent’s behavior?” and “What did you make of it?” If they do not answer, you could add, “You know, like acting different or strange.” It is very valuable to be able to name it, if you know the diagnosis, to make the illness more objective. Teens are typically egocentric and wonder if they are prone to develop a similar condition, as well as anxious about who will be there for them if the parent does not get better; both are good questions to address.
Both adolescents and school-aged children are very attuned to when things in life are “unfair,” and having an ill parent certainly qualifies. It is important for whoever has this discussion to empathize, and to acknowledge that it is unfair and that feeling angry, sad, or confused is natural – without giving them permission for misbehavior. It may be easier for some children to have a journal in which to write questions to have an adult answer later. Any child can be given hope by knowing that the parent is getting help (or that you will work on this), especially if the parents themselves say they are trying to get better. The children need to know that although mental illness tends to get better and worse at unexpected times, mental health can be improved. It is essential that children of school age and older have a clear plan for what to do if the parent loses control or is in danger. This might include getting out of the house and calling the parent’s partner, a trusted neighbor, or 911.
While teens may feel guilty about their anger or things they might have said or done in reaction to the ill parent, school-aged and preschool children are more likely to feel guilty that they somehow contributed to the parent’s condition through misbehavior or some imagined influence. Eliciting these thoughts may simply require asking, “What thoughts have you had about why this happened?” or having another family member prompting them by saying, “I have been wondering if there is something I should have done. Have you wondered about that, too?”
What is harder to explain is the impression children may get that their depressed or psychotic or drug-abusing parents no longer love them; and the parents may have said hurtful things to them. School-aged children can be told and can understand an illness of “the feelings and thinking parts of the brain” as being similar to other physical illnesses, such as the flu, that “make people act tired or grouchy or say things they do not mean.” Children of all ages need to be reassured that, inside, their parents still love them, and “it is the illness talking” if they act or speak otherwise. In the case of substance abuse disorders, which might seem more of a choice by the parent than would other mental illnesses, it can be helpful to point out that “drugs and alcohol can be stronger than people and can take over their brains.” The National Alliance on Mental Illness (www.nami.org) offers support programs that may be helpful for older children.
Sometimes families may resist telling a child about parental mental illness because of personal beliefs, cultural stigma, or privacy concerns. I try to emphasize that by being honest in giving children an understanding of their parents’ mental illness, one is helping them trust the adults in their lives. They need the truth and also to practice formulating things to say to counter those who have incorrect ideas, or who insult or make fun of them. They need the truth about mental illness to make sense of their experiences so they can feel lovable and hopeful about their own futures and can recognize illness symptoms in themselves. Giving them words, ensuring their safety and support, and strengthening their coping can help buffer the impact of this common adverse childhood experience to help prevent long-term negative effects.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
You probably think you know how to talk with a child about death. But somehow talking about a parent’s mental illness may seem more difficult. Even medical professionals, as most people, can find themselves feeling more judgmental or uneasy talking about mental illness than about physical problems. But with a prevalence of about one in four people having mental disorders, we need to be prepared for this discussion.
Sometimes family members, or even parents themselves, have asked me to tell a child about a parent’s mental illness or substance use. They know the child is confused and scared but don’t know what to say about this still-hushed issue. Other times, children’s behaviors show that they are struggling – by their aggression, depression, decline in school performance, anger, anxiety, or running away – and I find out only by asking that they are experiencing life with a mentally ill parent.
Both are times to get more information about the nature of the parent’s symptoms, what is being done about it; what the child has seen, heard, or experienced; the child’s safety; and what intrinsic or cultural attitudes the family has about the problem. It is best if the affected parents themselves are able to talk realistically about the illness with the child. Sometimes we, as pediatric professionals, can help get the conversation started or may need to step in.
Teens can understand the nature of mental illness as a brain disorder, but often have acquired misinformation from peers, the other parent who is hurt and angry, or the Internet that needs to be respectfully corrected. They may be less willing to have such a discussion than would younger children, as they may have experienced verbal or physical aggression from the parent, embarrassment in front of peers, or teasing by classmates. They may have developed coping strategies of writing off the parent, defiance, aggressive responses, or denial.
It is important to find a relaxed moment and begin by saying, “May I ask what you have noticed about your parent’s behavior?” and “What did you make of it?” If they do not answer, you could add, “You know, like acting different or strange.” It is very valuable to be able to name it, if you know the diagnosis, to make the illness more objective. Teens are typically egocentric and wonder if they are prone to develop a similar condition, as well as anxious about who will be there for them if the parent does not get better; both are good questions to address.
Both adolescents and school-aged children are very attuned to when things in life are “unfair,” and having an ill parent certainly qualifies. It is important for whoever has this discussion to empathize, and to acknowledge that it is unfair and that feeling angry, sad, or confused is natural – without giving them permission for misbehavior. It may be easier for some children to have a journal in which to write questions to have an adult answer later. Any child can be given hope by knowing that the parent is getting help (or that you will work on this), especially if the parents themselves say they are trying to get better. The children need to know that although mental illness tends to get better and worse at unexpected times, mental health can be improved. It is essential that children of school age and older have a clear plan for what to do if the parent loses control or is in danger. This might include getting out of the house and calling the parent’s partner, a trusted neighbor, or 911.
While teens may feel guilty about their anger or things they might have said or done in reaction to the ill parent, school-aged and preschool children are more likely to feel guilty that they somehow contributed to the parent’s condition through misbehavior or some imagined influence. Eliciting these thoughts may simply require asking, “What thoughts have you had about why this happened?” or having another family member prompting them by saying, “I have been wondering if there is something I should have done. Have you wondered about that, too?”
What is harder to explain is the impression children may get that their depressed or psychotic or drug-abusing parents no longer love them; and the parents may have said hurtful things to them. School-aged children can be told and can understand an illness of “the feelings and thinking parts of the brain” as being similar to other physical illnesses, such as the flu, that “make people act tired or grouchy or say things they do not mean.” Children of all ages need to be reassured that, inside, their parents still love them, and “it is the illness talking” if they act or speak otherwise. In the case of substance abuse disorders, which might seem more of a choice by the parent than would other mental illnesses, it can be helpful to point out that “drugs and alcohol can be stronger than people and can take over their brains.” The National Alliance on Mental Illness (www.nami.org) offers support programs that may be helpful for older children.
Sometimes families may resist telling a child about parental mental illness because of personal beliefs, cultural stigma, or privacy concerns. I try to emphasize that by being honest in giving children an understanding of their parents’ mental illness, one is helping them trust the adults in their lives. They need the truth and also to practice formulating things to say to counter those who have incorrect ideas, or who insult or make fun of them. They need the truth about mental illness to make sense of their experiences so they can feel lovable and hopeful about their own futures and can recognize illness symptoms in themselves. Giving them words, ensuring their safety and support, and strengthening their coping can help buffer the impact of this common adverse childhood experience to help prevent long-term negative effects.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
You probably think you know how to talk with a child about death. But somehow talking about a parent’s mental illness may seem more difficult. Even medical professionals, as most people, can find themselves feeling more judgmental or uneasy talking about mental illness than about physical problems. But with a prevalence of about one in four people having mental disorders, we need to be prepared for this discussion.
Sometimes family members, or even parents themselves, have asked me to tell a child about a parent’s mental illness or substance use. They know the child is confused and scared but don’t know what to say about this still-hushed issue. Other times, children’s behaviors show that they are struggling – by their aggression, depression, decline in school performance, anger, anxiety, or running away – and I find out only by asking that they are experiencing life with a mentally ill parent.
Both are times to get more information about the nature of the parent’s symptoms, what is being done about it; what the child has seen, heard, or experienced; the child’s safety; and what intrinsic or cultural attitudes the family has about the problem. It is best if the affected parents themselves are able to talk realistically about the illness with the child. Sometimes we, as pediatric professionals, can help get the conversation started or may need to step in.
Teens can understand the nature of mental illness as a brain disorder, but often have acquired misinformation from peers, the other parent who is hurt and angry, or the Internet that needs to be respectfully corrected. They may be less willing to have such a discussion than would younger children, as they may have experienced verbal or physical aggression from the parent, embarrassment in front of peers, or teasing by classmates. They may have developed coping strategies of writing off the parent, defiance, aggressive responses, or denial.
It is important to find a relaxed moment and begin by saying, “May I ask what you have noticed about your parent’s behavior?” and “What did you make of it?” If they do not answer, you could add, “You know, like acting different or strange.” It is very valuable to be able to name it, if you know the diagnosis, to make the illness more objective. Teens are typically egocentric and wonder if they are prone to develop a similar condition, as well as anxious about who will be there for them if the parent does not get better; both are good questions to address.
Both adolescents and school-aged children are very attuned to when things in life are “unfair,” and having an ill parent certainly qualifies. It is important for whoever has this discussion to empathize, and to acknowledge that it is unfair and that feeling angry, sad, or confused is natural – without giving them permission for misbehavior. It may be easier for some children to have a journal in which to write questions to have an adult answer later. Any child can be given hope by knowing that the parent is getting help (or that you will work on this), especially if the parents themselves say they are trying to get better. The children need to know that although mental illness tends to get better and worse at unexpected times, mental health can be improved. It is essential that children of school age and older have a clear plan for what to do if the parent loses control or is in danger. This might include getting out of the house and calling the parent’s partner, a trusted neighbor, or 911.
While teens may feel guilty about their anger or things they might have said or done in reaction to the ill parent, school-aged and preschool children are more likely to feel guilty that they somehow contributed to the parent’s condition through misbehavior or some imagined influence. Eliciting these thoughts may simply require asking, “What thoughts have you had about why this happened?” or having another family member prompting them by saying, “I have been wondering if there is something I should have done. Have you wondered about that, too?”
What is harder to explain is the impression children may get that their depressed or psychotic or drug-abusing parents no longer love them; and the parents may have said hurtful things to them. School-aged children can be told and can understand an illness of “the feelings and thinking parts of the brain” as being similar to other physical illnesses, such as the flu, that “make people act tired or grouchy or say things they do not mean.” Children of all ages need to be reassured that, inside, their parents still love them, and “it is the illness talking” if they act or speak otherwise. In the case of substance abuse disorders, which might seem more of a choice by the parent than would other mental illnesses, it can be helpful to point out that “drugs and alcohol can be stronger than people and can take over their brains.” The National Alliance on Mental Illness (www.nami.org) offers support programs that may be helpful for older children.
Sometimes families may resist telling a child about parental mental illness because of personal beliefs, cultural stigma, or privacy concerns. I try to emphasize that by being honest in giving children an understanding of their parents’ mental illness, one is helping them trust the adults in their lives. They need the truth and also to practice formulating things to say to counter those who have incorrect ideas, or who insult or make fun of them. They need the truth about mental illness to make sense of their experiences so they can feel lovable and hopeful about their own futures and can recognize illness symptoms in themselves. Giving them words, ensuring their safety and support, and strengthening their coping can help buffer the impact of this common adverse childhood experience to help prevent long-term negative effects.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
Declining lung function linked to heart failure, stroke
Rapid declines in spirometric measures of lung function were associated with higher risks of cardiovascular disease, according to a recent analysis of a large, prospective cohort study.
Rapid declines in forced expiratory volume in 1 second (FEV1) were associated with increased incidence of heart failure, stroke, and death in the analysis of the ARIC (Atherosclerosis Risk in Communities) study.
The risk of incident heart failure among FEV1 rapid decliners was particularly high, with a fourfold increase within 12 months. That suggests clinicians should carefully consider incipient heart failure in patients with rapid changes in FEV1, investigators reported in the Journal of the American College of Cardiology.
Rapid declines in forced vital capacity (FVC) were also associated with higher incidences of heart failure and death in the analysis by Odilson M. Silvestre, MD, of the division of cardiovascular medicine at Brigham and Women’s Hospital, Boston, and colleagues.
The analysis included a total of 10,351 ARIC participants with a mean follow-up of 17 years. All had undergone spirometry at the first study visit between 1987 and 1989, and on the second visit between 1990 and 1992.
One-quarter of participants were classified as FEV1 rapid decliners, defined by an FEV1 decrease of at least 1.9% per year. Likewise, one-quarter of participants were classified as FVC rapid decliners, based on an FVC decrease of at least 2.1%.
Rapid decline in FEV1 was associated with a higher risk of incident heart failure (hazard ratio, 1.17; 95% confidence interval, 1.04-1.33; P = .010), and was most prognostic in the first year of follow-up (HR, 4.22; 95% CI, 1.34-13.26; P = .01), investigators said.
Rapid decline in FVC was likewise associated with a greater heart failure risk (HR, 1.27; 95% CI, 1.12-1.44; P less than .001).
Increased heart failure risk persisted after excluding patients with incident coronary heart disease in both the FEV1 and FVC rapid decliners, the investigators said.
A rapid decline in FEV1 was also associated with a higher stroke risk (HR, 1.25; 95% CI, 1.04-1.50; P = .015).
FEV1 rapid decliners had a higher overall rate of incident cardiovascular disease than those without rapid decline, even after adjustment for baseline variables such as age, sex, race, body mass index, and heart rate (HR, 1.15; 95% CI, 1.04-1.26; P = .004), and FVC rapid decliners likewise had a 19% greater risk of the composite endpoint (HR, 1.19; 95% CI, 1.08-1.32; P less than .001).
The National Heart, Lung, and Blood Institute, the American Heart Association, and other sources supported the study. Dr. Silvestre reported having no relevant conflicts.
SOURCE: Silvestre OM et al. J Am Coll Cardiol. 2018 Sep 4;72(10):1109-22.
Cardiologists and pulmonologists should closely collaborate to better identify the relationship between lung function decline and early cardiovascular disease detection, said the authors of an editorial accompanying the study.
Improved collaboration would help manage these conditions, stopping early disease progression and preventing overt cardiovascular disease, wrote Daniel A. Duprez, MD, PhD, and David R. Jacobs Jr., PhD.
“The resulting symptomatic and prognostic benefits outweigh those attainable by treating either condition alone,” noted Dr. Duprez and Dr. Jacobs.
The study by Dr. Silvestre and coauthors showed that rapid declines in forced expiratory volume in one second (FEV1) and forced vital capacity (FVC) among participants in the ARIC (Atherosclerosis Risk in Communities) study were associated with a higher incidence of composite cardiovascular disease, heart failure, and total death.
The association between FEV1 and new heart failure was substantially impacted by 22 heart failure events occurring in the first year, with a hazard ratio of 4.22 for predicting those cases, the editorial authors noted.
“We suggest that this association with early cases could be the result of reversed causality, reflecting heart failure undiagnosed at the second spirometry test,” they explained (J Am Coll Cardiol. 2018 Sep 4;72[10]:1123-5).
Dr. Duprez is with the cardiovascular division of the University of Minnesota, Minneapolis, and Dr. Jacobs is with the division of epidemiology and community health at the University of Minnesota, Minneapolis. Dr. Duprez and Dr. Jacobs reported they had no relevant disclosures.
Cardiologists and pulmonologists should closely collaborate to better identify the relationship between lung function decline and early cardiovascular disease detection, said the authors of an editorial accompanying the study.
Improved collaboration would help manage these conditions, stopping early disease progression and preventing overt cardiovascular disease, wrote Daniel A. Duprez, MD, PhD, and David R. Jacobs Jr., PhD.
“The resulting symptomatic and prognostic benefits outweigh those attainable by treating either condition alone,” noted Dr. Duprez and Dr. Jacobs.
The study by Dr. Silvestre and coauthors showed that rapid declines in forced expiratory volume in one second (FEV1) and forced vital capacity (FVC) among participants in the ARIC (Atherosclerosis Risk in Communities) study were associated with a higher incidence of composite cardiovascular disease, heart failure, and total death.
The association between FEV1 and new heart failure was substantially impacted by 22 heart failure events occurring in the first year, with a hazard ratio of 4.22 for predicting those cases, the editorial authors noted.
“We suggest that this association with early cases could be the result of reversed causality, reflecting heart failure undiagnosed at the second spirometry test,” they explained (J Am Coll Cardiol. 2018 Sep 4;72[10]:1123-5).
Dr. Duprez is with the cardiovascular division of the University of Minnesota, Minneapolis, and Dr. Jacobs is with the division of epidemiology and community health at the University of Minnesota, Minneapolis. Dr. Duprez and Dr. Jacobs reported they had no relevant disclosures.
Cardiologists and pulmonologists should closely collaborate to better identify the relationship between lung function decline and early cardiovascular disease detection, said the authors of an editorial accompanying the study.
Improved collaboration would help manage these conditions, stopping early disease progression and preventing overt cardiovascular disease, wrote Daniel A. Duprez, MD, PhD, and David R. Jacobs Jr., PhD.
“The resulting symptomatic and prognostic benefits outweigh those attainable by treating either condition alone,” noted Dr. Duprez and Dr. Jacobs.
The study by Dr. Silvestre and coauthors showed that rapid declines in forced expiratory volume in one second (FEV1) and forced vital capacity (FVC) among participants in the ARIC (Atherosclerosis Risk in Communities) study were associated with a higher incidence of composite cardiovascular disease, heart failure, and total death.
The association between FEV1 and new heart failure was substantially impacted by 22 heart failure events occurring in the first year, with a hazard ratio of 4.22 for predicting those cases, the editorial authors noted.
“We suggest that this association with early cases could be the result of reversed causality, reflecting heart failure undiagnosed at the second spirometry test,” they explained (J Am Coll Cardiol. 2018 Sep 4;72[10]:1123-5).
Dr. Duprez is with the cardiovascular division of the University of Minnesota, Minneapolis, and Dr. Jacobs is with the division of epidemiology and community health at the University of Minnesota, Minneapolis. Dr. Duprez and Dr. Jacobs reported they had no relevant disclosures.
Rapid declines in spirometric measures of lung function were associated with higher risks of cardiovascular disease, according to a recent analysis of a large, prospective cohort study.
Rapid declines in forced expiratory volume in 1 second (FEV1) were associated with increased incidence of heart failure, stroke, and death in the analysis of the ARIC (Atherosclerosis Risk in Communities) study.
The risk of incident heart failure among FEV1 rapid decliners was particularly high, with a fourfold increase within 12 months. That suggests clinicians should carefully consider incipient heart failure in patients with rapid changes in FEV1, investigators reported in the Journal of the American College of Cardiology.
Rapid declines in forced vital capacity (FVC) were also associated with higher incidences of heart failure and death in the analysis by Odilson M. Silvestre, MD, of the division of cardiovascular medicine at Brigham and Women’s Hospital, Boston, and colleagues.
The analysis included a total of 10,351 ARIC participants with a mean follow-up of 17 years. All had undergone spirometry at the first study visit between 1987 and 1989, and on the second visit between 1990 and 1992.
One-quarter of participants were classified as FEV1 rapid decliners, defined by an FEV1 decrease of at least 1.9% per year. Likewise, one-quarter of participants were classified as FVC rapid decliners, based on an FVC decrease of at least 2.1%.
Rapid decline in FEV1 was associated with a higher risk of incident heart failure (hazard ratio, 1.17; 95% confidence interval, 1.04-1.33; P = .010), and was most prognostic in the first year of follow-up (HR, 4.22; 95% CI, 1.34-13.26; P = .01), investigators said.
Rapid decline in FVC was likewise associated with a greater heart failure risk (HR, 1.27; 95% CI, 1.12-1.44; P less than .001).
Increased heart failure risk persisted after excluding patients with incident coronary heart disease in both the FEV1 and FVC rapid decliners, the investigators said.
A rapid decline in FEV1 was also associated with a higher stroke risk (HR, 1.25; 95% CI, 1.04-1.50; P = .015).
FEV1 rapid decliners had a higher overall rate of incident cardiovascular disease than those without rapid decline, even after adjustment for baseline variables such as age, sex, race, body mass index, and heart rate (HR, 1.15; 95% CI, 1.04-1.26; P = .004), and FVC rapid decliners likewise had a 19% greater risk of the composite endpoint (HR, 1.19; 95% CI, 1.08-1.32; P less than .001).
The National Heart, Lung, and Blood Institute, the American Heart Association, and other sources supported the study. Dr. Silvestre reported having no relevant conflicts.
SOURCE: Silvestre OM et al. J Am Coll Cardiol. 2018 Sep 4;72(10):1109-22.
Rapid declines in spirometric measures of lung function were associated with higher risks of cardiovascular disease, according to a recent analysis of a large, prospective cohort study.
Rapid declines in forced expiratory volume in 1 second (FEV1) were associated with increased incidence of heart failure, stroke, and death in the analysis of the ARIC (Atherosclerosis Risk in Communities) study.
The risk of incident heart failure among FEV1 rapid decliners was particularly high, with a fourfold increase within 12 months. That suggests clinicians should carefully consider incipient heart failure in patients with rapid changes in FEV1, investigators reported in the Journal of the American College of Cardiology.
Rapid declines in forced vital capacity (FVC) were also associated with higher incidences of heart failure and death in the analysis by Odilson M. Silvestre, MD, of the division of cardiovascular medicine at Brigham and Women’s Hospital, Boston, and colleagues.
The analysis included a total of 10,351 ARIC participants with a mean follow-up of 17 years. All had undergone spirometry at the first study visit between 1987 and 1989, and on the second visit between 1990 and 1992.
One-quarter of participants were classified as FEV1 rapid decliners, defined by an FEV1 decrease of at least 1.9% per year. Likewise, one-quarter of participants were classified as FVC rapid decliners, based on an FVC decrease of at least 2.1%.
Rapid decline in FEV1 was associated with a higher risk of incident heart failure (hazard ratio, 1.17; 95% confidence interval, 1.04-1.33; P = .010), and was most prognostic in the first year of follow-up (HR, 4.22; 95% CI, 1.34-13.26; P = .01), investigators said.
Rapid decline in FVC was likewise associated with a greater heart failure risk (HR, 1.27; 95% CI, 1.12-1.44; P less than .001).
Increased heart failure risk persisted after excluding patients with incident coronary heart disease in both the FEV1 and FVC rapid decliners, the investigators said.
A rapid decline in FEV1 was also associated with a higher stroke risk (HR, 1.25; 95% CI, 1.04-1.50; P = .015).
FEV1 rapid decliners had a higher overall rate of incident cardiovascular disease than those without rapid decline, even after adjustment for baseline variables such as age, sex, race, body mass index, and heart rate (HR, 1.15; 95% CI, 1.04-1.26; P = .004), and FVC rapid decliners likewise had a 19% greater risk of the composite endpoint (HR, 1.19; 95% CI, 1.08-1.32; P less than .001).
The National Heart, Lung, and Blood Institute, the American Heart Association, and other sources supported the study. Dr. Silvestre reported having no relevant conflicts.
SOURCE: Silvestre OM et al. J Am Coll Cardiol. 2018 Sep 4;72(10):1109-22.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Key clinical point: Rapid declines in spirometric measures of lung function were associated with higher risks of heart failure, among other adverse cardiovascular outcomes.
Major finding: Rapid decline in forced expiratory volume in 1 second was associated with higher risk of incident heart failure (HR, 1.17; 95% CI, 1.04-1.33; P = .010), and was most prognostic in the first year of follow-up (HR, 4.22; 95% CI, 1.34-13.26; P = .01).
Study details: An analysis including a total of 10,351 participants in a large, prospective cohort study with a mean follow-up of 17 years.
Disclosures: The National Heart, Lung, and Blood Institute, the American Heart Association, and other sources supported the study. Dr. Silvestre reported having no relevant conflicts.
Source: Silvestre OM et al. J Am Coll Cardiol. 2018 Sep 4;72(10):1109-22.
Children and teens are at risk for drug-drug interactions
“During 2013-2014, one-fifth of children and adolescents used at least one prescription medication and [about] 1 in 10 concurrently used two [or more] prescription medications,” Dima M. Qato, PharmD, MPH, PhD, of the University of Illinois at Chicago, and her colleagues wrote in Pediatrics. “Among children and adolescents concurrently using two [or more] prescription medications, 1 in 12 was at risk for a major DDI.”
The researchers used data from the six most recent cycles of the National Health and Nutrition Examination Survey conducted by the National Center for Health Statistics, beginning with the 2003-2004 cycle through the 2013-2014 cycle, yielding a sample of 23,152 participants aged 0-19 years across the 10-year period. The survey differentiated between prescriptions for acute use (used for 30 days or less) or for chronic use. Concurrent use was defined as using two or more prescription drugs within the 30 days prior to taking the survey. The Micromedex was used to determine the possibility of having a DDI.
The investigators noted a “notable” decrease in the use of acute drug treatments from 11% at the beginning to 7% at the end of the 10-year cycle (P less than .01). This was “driven largely by a decrease in the use of antibiotics.”
They identified the most commonly used prescription drugs, including respiratory agents, especially bronchodilators (the most common type was albuterol); psychotherapeutic agents, especially CNS stimulants (most commonly methylphenidate); and antidepressants (most commonly fluoxetine).
“Among concurrent users of prescription medications, combinations that involved respiratory agents, such as bronchodilators and leukotriene modifiers, and psychotropic medications, including antidepressants, atypical antipsychotics, and CNS stimulants, were the most prevalent,” Dr. Qato and her colleagues wrote. Of the 301 concurrent users in the 2013-2014 survey cycle, 156 unique drugs were used.
Of the children and adolescents who were concurrently using prescription medications, 8% were at risk for major DDIs, the researchers noted. “Nearly half of interacting regimens used involved psychotropic agents, primarily antidepressants, the most common adverse interaction effect being QT prolongation.” About 68% of these regimens included use of at least one acute medication.
They also found that “prescription medications associated with an increased risk of suicidality are commonly used in children and adolescents and are often used together. For example, more than half of adolescent girls taking antidepressants concurrently use at least two additional psychotropic medications or hormonal contraceptives. Although there is some evidence that the combined use of these drugs may increase the onset and severity of suicidal thoughts and behavior, we found no cases of DDIs associated with suicidality.”
Dr. Qato and her colleagues noted some limitations to their study, including using the potential for DDI rather than actual adverse events, survey data being limited to prescription medications and not over-the-counter treatments, and the possible misclassification of chronic medications as acute medications depending on when treatments were initiated.
That being said, the investigators concluded that treatment “and prevention efforts to reduce the burden of adverse drug events in younger populations should be used to consider the role of interacting drug combinations, especially among these individuals.”
Funding for the study was provided by the Robert Woods Johnson Foundation. No relevant financial disclosures were reported.
SOURCE: Qato DM et al. Pediatrics. 2018 Aug 27. doi: 10.1542/peds.2018-1042.
Technology could play a key role in preventing adverse events from drug-drug interactions (DDI) in pediatric patients.
There are apps that can be embedded within EHRs, but there are risks of alert fatigue, which could cause DDI warnings to be ignored altogether, as well as not enough alerts, especially if EHRs are not communicating between doctors, leading to missed DDI avoidance opportunities. The solution is to select alerts that strike the balance between the two.
Stephen Downs, MD , of the University of Indiana, Indianapolis, chairs the advisory board for the American Academy of Pediatrics Child Health Informatics Center. These comments are summarized from a commentary accompanying the article by Qato et al (Pediatrics. 2018 Aug 27. doi: 10.1542/ peds.2018-2023 ).
Technology could play a key role in preventing adverse events from drug-drug interactions (DDI) in pediatric patients.
There are apps that can be embedded within EHRs, but there are risks of alert fatigue, which could cause DDI warnings to be ignored altogether, as well as not enough alerts, especially if EHRs are not communicating between doctors, leading to missed DDI avoidance opportunities. The solution is to select alerts that strike the balance between the two.
Stephen Downs, MD , of the University of Indiana, Indianapolis, chairs the advisory board for the American Academy of Pediatrics Child Health Informatics Center. These comments are summarized from a commentary accompanying the article by Qato et al (Pediatrics. 2018 Aug 27. doi: 10.1542/ peds.2018-2023 ).
Technology could play a key role in preventing adverse events from drug-drug interactions (DDI) in pediatric patients.
There are apps that can be embedded within EHRs, but there are risks of alert fatigue, which could cause DDI warnings to be ignored altogether, as well as not enough alerts, especially if EHRs are not communicating between doctors, leading to missed DDI avoidance opportunities. The solution is to select alerts that strike the balance between the two.
Stephen Downs, MD , of the University of Indiana, Indianapolis, chairs the advisory board for the American Academy of Pediatrics Child Health Informatics Center. These comments are summarized from a commentary accompanying the article by Qato et al (Pediatrics. 2018 Aug 27. doi: 10.1542/ peds.2018-2023 ).
“During 2013-2014, one-fifth of children and adolescents used at least one prescription medication and [about] 1 in 10 concurrently used two [or more] prescription medications,” Dima M. Qato, PharmD, MPH, PhD, of the University of Illinois at Chicago, and her colleagues wrote in Pediatrics. “Among children and adolescents concurrently using two [or more] prescription medications, 1 in 12 was at risk for a major DDI.”
The researchers used data from the six most recent cycles of the National Health and Nutrition Examination Survey conducted by the National Center for Health Statistics, beginning with the 2003-2004 cycle through the 2013-2014 cycle, yielding a sample of 23,152 participants aged 0-19 years across the 10-year period. The survey differentiated between prescriptions for acute use (used for 30 days or less) or for chronic use. Concurrent use was defined as using two or more prescription drugs within the 30 days prior to taking the survey. The Micromedex was used to determine the possibility of having a DDI.
The investigators noted a “notable” decrease in the use of acute drug treatments from 11% at the beginning to 7% at the end of the 10-year cycle (P less than .01). This was “driven largely by a decrease in the use of antibiotics.”
They identified the most commonly used prescription drugs, including respiratory agents, especially bronchodilators (the most common type was albuterol); psychotherapeutic agents, especially CNS stimulants (most commonly methylphenidate); and antidepressants (most commonly fluoxetine).
“Among concurrent users of prescription medications, combinations that involved respiratory agents, such as bronchodilators and leukotriene modifiers, and psychotropic medications, including antidepressants, atypical antipsychotics, and CNS stimulants, were the most prevalent,” Dr. Qato and her colleagues wrote. Of the 301 concurrent users in the 2013-2014 survey cycle, 156 unique drugs were used.
Of the children and adolescents who were concurrently using prescription medications, 8% were at risk for major DDIs, the researchers noted. “Nearly half of interacting regimens used involved psychotropic agents, primarily antidepressants, the most common adverse interaction effect being QT prolongation.” About 68% of these regimens included use of at least one acute medication.
They also found that “prescription medications associated with an increased risk of suicidality are commonly used in children and adolescents and are often used together. For example, more than half of adolescent girls taking antidepressants concurrently use at least two additional psychotropic medications or hormonal contraceptives. Although there is some evidence that the combined use of these drugs may increase the onset and severity of suicidal thoughts and behavior, we found no cases of DDIs associated with suicidality.”
Dr. Qato and her colleagues noted some limitations to their study, including using the potential for DDI rather than actual adverse events, survey data being limited to prescription medications and not over-the-counter treatments, and the possible misclassification of chronic medications as acute medications depending on when treatments were initiated.
That being said, the investigators concluded that treatment “and prevention efforts to reduce the burden of adverse drug events in younger populations should be used to consider the role of interacting drug combinations, especially among these individuals.”
Funding for the study was provided by the Robert Woods Johnson Foundation. No relevant financial disclosures were reported.
SOURCE: Qato DM et al. Pediatrics. 2018 Aug 27. doi: 10.1542/peds.2018-1042.
“During 2013-2014, one-fifth of children and adolescents used at least one prescription medication and [about] 1 in 10 concurrently used two [or more] prescription medications,” Dima M. Qato, PharmD, MPH, PhD, of the University of Illinois at Chicago, and her colleagues wrote in Pediatrics. “Among children and adolescents concurrently using two [or more] prescription medications, 1 in 12 was at risk for a major DDI.”
The researchers used data from the six most recent cycles of the National Health and Nutrition Examination Survey conducted by the National Center for Health Statistics, beginning with the 2003-2004 cycle through the 2013-2014 cycle, yielding a sample of 23,152 participants aged 0-19 years across the 10-year period. The survey differentiated between prescriptions for acute use (used for 30 days or less) or for chronic use. Concurrent use was defined as using two or more prescription drugs within the 30 days prior to taking the survey. The Micromedex was used to determine the possibility of having a DDI.
The investigators noted a “notable” decrease in the use of acute drug treatments from 11% at the beginning to 7% at the end of the 10-year cycle (P less than .01). This was “driven largely by a decrease in the use of antibiotics.”
They identified the most commonly used prescription drugs, including respiratory agents, especially bronchodilators (the most common type was albuterol); psychotherapeutic agents, especially CNS stimulants (most commonly methylphenidate); and antidepressants (most commonly fluoxetine).
“Among concurrent users of prescription medications, combinations that involved respiratory agents, such as bronchodilators and leukotriene modifiers, and psychotropic medications, including antidepressants, atypical antipsychotics, and CNS stimulants, were the most prevalent,” Dr. Qato and her colleagues wrote. Of the 301 concurrent users in the 2013-2014 survey cycle, 156 unique drugs were used.
Of the children and adolescents who were concurrently using prescription medications, 8% were at risk for major DDIs, the researchers noted. “Nearly half of interacting regimens used involved psychotropic agents, primarily antidepressants, the most common adverse interaction effect being QT prolongation.” About 68% of these regimens included use of at least one acute medication.
They also found that “prescription medications associated with an increased risk of suicidality are commonly used in children and adolescents and are often used together. For example, more than half of adolescent girls taking antidepressants concurrently use at least two additional psychotropic medications or hormonal contraceptives. Although there is some evidence that the combined use of these drugs may increase the onset and severity of suicidal thoughts and behavior, we found no cases of DDIs associated with suicidality.”
Dr. Qato and her colleagues noted some limitations to their study, including using the potential for DDI rather than actual adverse events, survey data being limited to prescription medications and not over-the-counter treatments, and the possible misclassification of chronic medications as acute medications depending on when treatments were initiated.
That being said, the investigators concluded that treatment “and prevention efforts to reduce the burden of adverse drug events in younger populations should be used to consider the role of interacting drug combinations, especially among these individuals.”
Funding for the study was provided by the Robert Woods Johnson Foundation. No relevant financial disclosures were reported.
SOURCE: Qato DM et al. Pediatrics. 2018 Aug 27. doi: 10.1542/peds.2018-1042.
FROM PEDIATRICS
Key clinical point: Children are at risk for drug-drug interactions from concurrent use of two or more medications.
Major finding: Of adolescents using two or more drugs, 1 in 12 are at risk for a major drug-drug interaction.
Study details: Researchers used data from the six most recent cycles of the National Health and Nutrition Examination Survey conducted by the National Center for Health Statistics, yielding a sample of 23,152 participants aged 0-19 years across the 10-year period.
Disclosures: Funding for the study was provided by the Robert Woods Johnson Foundation. No relevant financial disclosures were reported.
Source: Qato DM et al. Pediatrics. 2018 Aug 27. doi: 10.1542/peds.2018-1042.