User login
Urgent/Emergency Management of Migraine Assessed
Emergency department (ED) visits for migraine are burdensome to patients and to the larger healthcare system and society, a recent study found. Furthermore, a substantial number of headache specialists are dissatisfied with the care their patients receive in the ED. Researchers
surveyed members of the American Headache Society (AHS) Emergency Department/Refractory/Inpatient (EDRI) Section to understand their practice regarding patients who call their office to be seen urgently, and to understand their communication with local EDs. There were 96 eligible AHS members, 50 of whom responded to questionnaires either by email or in person (52%).They found:
- Of total respondents, 59% reported giving rescue treatment to their patients to manage acute attacks.
- 54% reported using standard protocols for outpatients not responding to usual acute treatments.
- In the event of a request for urgent care, 12% of specialists reported bringing patients into the office most or all of the time, and 20% reported sending patients to the ED some or most of the time for headache management.
- 60% reported that their ED has a protocol for migraine management.
Minen MT, Ortega E, Lipton RB, Cowan R. American Headache Society survey about urgent and emergency management of headache patients. [Published online ahead of print September 12, 2018]. Headache. doi:10.1111/head.13387.
Emergency department (ED) visits for migraine are burdensome to patients and to the larger healthcare system and society, a recent study found. Furthermore, a substantial number of headache specialists are dissatisfied with the care their patients receive in the ED. Researchers
surveyed members of the American Headache Society (AHS) Emergency Department/Refractory/Inpatient (EDRI) Section to understand their practice regarding patients who call their office to be seen urgently, and to understand their communication with local EDs. There were 96 eligible AHS members, 50 of whom responded to questionnaires either by email or in person (52%).They found:
- Of total respondents, 59% reported giving rescue treatment to their patients to manage acute attacks.
- 54% reported using standard protocols for outpatients not responding to usual acute treatments.
- In the event of a request for urgent care, 12% of specialists reported bringing patients into the office most or all of the time, and 20% reported sending patients to the ED some or most of the time for headache management.
- 60% reported that their ED has a protocol for migraine management.
Minen MT, Ortega E, Lipton RB, Cowan R. American Headache Society survey about urgent and emergency management of headache patients. [Published online ahead of print September 12, 2018]. Headache. doi:10.1111/head.13387.
Emergency department (ED) visits for migraine are burdensome to patients and to the larger healthcare system and society, a recent study found. Furthermore, a substantial number of headache specialists are dissatisfied with the care their patients receive in the ED. Researchers
surveyed members of the American Headache Society (AHS) Emergency Department/Refractory/Inpatient (EDRI) Section to understand their practice regarding patients who call their office to be seen urgently, and to understand their communication with local EDs. There were 96 eligible AHS members, 50 of whom responded to questionnaires either by email or in person (52%).They found:
- Of total respondents, 59% reported giving rescue treatment to their patients to manage acute attacks.
- 54% reported using standard protocols for outpatients not responding to usual acute treatments.
- In the event of a request for urgent care, 12% of specialists reported bringing patients into the office most or all of the time, and 20% reported sending patients to the ED some or most of the time for headache management.
- 60% reported that their ED has a protocol for migraine management.
Minen MT, Ortega E, Lipton RB, Cowan R. American Headache Society survey about urgent and emergency management of headache patients. [Published online ahead of print September 12, 2018]. Headache. doi:10.1111/head.13387.
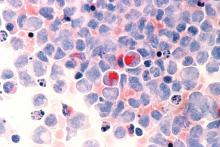
Venetoclax promising in unfit elderly AML patients
New York – For unfit elderly patients with acute myeloid leukemia (AML), venetoclax may be one of the most promising potential options that is emerging, according to an expert in the field.
The oral B-cell lymphoma 2 (BCL-2) inhibitor is the treatment that some in the AML community are “most excited about” for this population, Eunice S. Wang, MD, of Roswell Park Comprehensive Cancer Center in Buffalo, N.Y., said at the National Comprehensive Cancer Network (NCCN) Annual Congress: Hematologic Malignancies.
Venetoclax is currently approved by the Food and Drug Administration for previously treated chronic lymphocytic leukemia (CLL), alone or in combination with rituximab. It has been granted four Breakthrough Therapy designations from the FDA in AML. In July 2018, AbbVie submitted a Supplemental New Drug Application to the FDA for its use in combination with a hypomethylating agent (HMA) or in combination with low-dose cytarabine (LDAC) for the treatment of newly diagnosed AML patients who are ineligible for intensive chemotherapy.
“This agent doesn’t work on its own but had worked in the refractory setting and can be a great option upfront,” Dr. Wang said.
About half the patients were alive at 1 year following treatment with venetoclax plus low-dose chemotherapy, whether that was LDAC or an HMA, she said, commenting on recently reported results.
In a phase 1b trial, venetoclax was evaluated in combination with either azacitidine or decitabine. In recently reported preliminary results that included 57 patients aged 65 years or older who were ineligible for standard induction therapy, the combination was well tolerated and had promising activity (Lancet Oncol. 2018 Feb;19[2]:216-28).
Overall, 35 patients (61%) had complete remission (CR) or complete remission with incomplete marrow recovery (CRi).
In another report on this same trial, which included 33 patients from a single participating center who received venetoclax and azacytidine, the overall response rate was 91%, including 19 (58%) with CR and 9 (27%) with CRi (Blood. 2017 Dec;130 [Suppl 1]:181).
A separate phase 1/2 trial examined venetoclax plus LDAC in treatment-naive elderly patients unfit for intensive chemotherapy. In the 1-year outcomes that have been reported, the observed CR/CRi rate was 62%, median overall survival was an “encouraging” 11.4 months, and the observed 12-month overall survival was 46% in 61 patients treated at a venetoclax dose of 600 mg (Blood. 2017 Dec;130 [Suppl 1]:890).
In those 61 patients, treatment-related grade 3/4 adverse events included thrombocytopenia in 59%, neutropenia in 46%, febrile neutropenia in 36%, anemia in 28%, decreased white blood cell count in 26%, and one case of tumor lysis syndrome, according to the report.
Based on those findings in a cohort of patients with poor risk features, venetoclax 600 mg plus LDAC was carried forward to be evaluated in an ongoing phase 3 study, investigators noted at the time.
Dr. Wang reported financial relationships with AbbVie, Amgen, ImmunoGen, Incyte, Novartis, and Otsuka.
New York – For unfit elderly patients with acute myeloid leukemia (AML), venetoclax may be one of the most promising potential options that is emerging, according to an expert in the field.
The oral B-cell lymphoma 2 (BCL-2) inhibitor is the treatment that some in the AML community are “most excited about” for this population, Eunice S. Wang, MD, of Roswell Park Comprehensive Cancer Center in Buffalo, N.Y., said at the National Comprehensive Cancer Network (NCCN) Annual Congress: Hematologic Malignancies.
Venetoclax is currently approved by the Food and Drug Administration for previously treated chronic lymphocytic leukemia (CLL), alone or in combination with rituximab. It has been granted four Breakthrough Therapy designations from the FDA in AML. In July 2018, AbbVie submitted a Supplemental New Drug Application to the FDA for its use in combination with a hypomethylating agent (HMA) or in combination with low-dose cytarabine (LDAC) for the treatment of newly diagnosed AML patients who are ineligible for intensive chemotherapy.
“This agent doesn’t work on its own but had worked in the refractory setting and can be a great option upfront,” Dr. Wang said.
About half the patients were alive at 1 year following treatment with venetoclax plus low-dose chemotherapy, whether that was LDAC or an HMA, she said, commenting on recently reported results.
In a phase 1b trial, venetoclax was evaluated in combination with either azacitidine or decitabine. In recently reported preliminary results that included 57 patients aged 65 years or older who were ineligible for standard induction therapy, the combination was well tolerated and had promising activity (Lancet Oncol. 2018 Feb;19[2]:216-28).
Overall, 35 patients (61%) had complete remission (CR) or complete remission with incomplete marrow recovery (CRi).
In another report on this same trial, which included 33 patients from a single participating center who received venetoclax and azacytidine, the overall response rate was 91%, including 19 (58%) with CR and 9 (27%) with CRi (Blood. 2017 Dec;130 [Suppl 1]:181).
A separate phase 1/2 trial examined venetoclax plus LDAC in treatment-naive elderly patients unfit for intensive chemotherapy. In the 1-year outcomes that have been reported, the observed CR/CRi rate was 62%, median overall survival was an “encouraging” 11.4 months, and the observed 12-month overall survival was 46% in 61 patients treated at a venetoclax dose of 600 mg (Blood. 2017 Dec;130 [Suppl 1]:890).
In those 61 patients, treatment-related grade 3/4 adverse events included thrombocytopenia in 59%, neutropenia in 46%, febrile neutropenia in 36%, anemia in 28%, decreased white blood cell count in 26%, and one case of tumor lysis syndrome, according to the report.
Based on those findings in a cohort of patients with poor risk features, venetoclax 600 mg plus LDAC was carried forward to be evaluated in an ongoing phase 3 study, investigators noted at the time.
Dr. Wang reported financial relationships with AbbVie, Amgen, ImmunoGen, Incyte, Novartis, and Otsuka.
New York – For unfit elderly patients with acute myeloid leukemia (AML), venetoclax may be one of the most promising potential options that is emerging, according to an expert in the field.
The oral B-cell lymphoma 2 (BCL-2) inhibitor is the treatment that some in the AML community are “most excited about” for this population, Eunice S. Wang, MD, of Roswell Park Comprehensive Cancer Center in Buffalo, N.Y., said at the National Comprehensive Cancer Network (NCCN) Annual Congress: Hematologic Malignancies.
Venetoclax is currently approved by the Food and Drug Administration for previously treated chronic lymphocytic leukemia (CLL), alone or in combination with rituximab. It has been granted four Breakthrough Therapy designations from the FDA in AML. In July 2018, AbbVie submitted a Supplemental New Drug Application to the FDA for its use in combination with a hypomethylating agent (HMA) or in combination with low-dose cytarabine (LDAC) for the treatment of newly diagnosed AML patients who are ineligible for intensive chemotherapy.
“This agent doesn’t work on its own but had worked in the refractory setting and can be a great option upfront,” Dr. Wang said.
About half the patients were alive at 1 year following treatment with venetoclax plus low-dose chemotherapy, whether that was LDAC or an HMA, she said, commenting on recently reported results.
In a phase 1b trial, venetoclax was evaluated in combination with either azacitidine or decitabine. In recently reported preliminary results that included 57 patients aged 65 years or older who were ineligible for standard induction therapy, the combination was well tolerated and had promising activity (Lancet Oncol. 2018 Feb;19[2]:216-28).
Overall, 35 patients (61%) had complete remission (CR) or complete remission with incomplete marrow recovery (CRi).
In another report on this same trial, which included 33 patients from a single participating center who received venetoclax and azacytidine, the overall response rate was 91%, including 19 (58%) with CR and 9 (27%) with CRi (Blood. 2017 Dec;130 [Suppl 1]:181).
A separate phase 1/2 trial examined venetoclax plus LDAC in treatment-naive elderly patients unfit for intensive chemotherapy. In the 1-year outcomes that have been reported, the observed CR/CRi rate was 62%, median overall survival was an “encouraging” 11.4 months, and the observed 12-month overall survival was 46% in 61 patients treated at a venetoclax dose of 600 mg (Blood. 2017 Dec;130 [Suppl 1]:890).
In those 61 patients, treatment-related grade 3/4 adverse events included thrombocytopenia in 59%, neutropenia in 46%, febrile neutropenia in 36%, anemia in 28%, decreased white blood cell count in 26%, and one case of tumor lysis syndrome, according to the report.
Based on those findings in a cohort of patients with poor risk features, venetoclax 600 mg plus LDAC was carried forward to be evaluated in an ongoing phase 3 study, investigators noted at the time.
Dr. Wang reported financial relationships with AbbVie, Amgen, ImmunoGen, Incyte, Novartis, and Otsuka.
EXPERT ANALYSIS FROM THE NCCN ANNUAL CONGRESS: HEMATOLOGIC MALIGNANCIES
Female Gender and Daily Stress Linked with Migraine
Researchers discovered 10.7% prevalence of migraines and synergism between female gender and stress on risk of migraine in a recent study, suggesting health interventions targeting women under stress may be beneficial. This analysis was based on data from 42,282 persons aged ≥12 years who participated in a 2013–2014 community health survey. A multivariate log-binomial model was used to calculate adjusted prevalence ratios for migraines associated with individual and joint exposures of female gender and stress. Researchers used relative excess risk due to interaction (RERI), attributable proportion (AP), and synergy index (S index) to measure additive interaction. They found:
- The adjusted prevalence ratios were 2.37 for female vs male, 1.63 for persons with high vs low levels of stress, and 3.38 for women with high stress vs men with low stress.
- The RERI estimate was 0.38, the AP estimate was 0.11, and the S index was 1.19.
Slatculescu AM, Chen Y. Synergism between female gender and high levels of daily stress associated with migraine headaches in Ontario, Canada. [Published online ahead of print August 28, 2018]. Neuroepidemiol. doi:10.1159/000492503.
Researchers discovered 10.7% prevalence of migraines and synergism between female gender and stress on risk of migraine in a recent study, suggesting health interventions targeting women under stress may be beneficial. This analysis was based on data from 42,282 persons aged ≥12 years who participated in a 2013–2014 community health survey. A multivariate log-binomial model was used to calculate adjusted prevalence ratios for migraines associated with individual and joint exposures of female gender and stress. Researchers used relative excess risk due to interaction (RERI), attributable proportion (AP), and synergy index (S index) to measure additive interaction. They found:
- The adjusted prevalence ratios were 2.37 for female vs male, 1.63 for persons with high vs low levels of stress, and 3.38 for women with high stress vs men with low stress.
- The RERI estimate was 0.38, the AP estimate was 0.11, and the S index was 1.19.
Slatculescu AM, Chen Y. Synergism between female gender and high levels of daily stress associated with migraine headaches in Ontario, Canada. [Published online ahead of print August 28, 2018]. Neuroepidemiol. doi:10.1159/000492503.
Researchers discovered 10.7% prevalence of migraines and synergism between female gender and stress on risk of migraine in a recent study, suggesting health interventions targeting women under stress may be beneficial. This analysis was based on data from 42,282 persons aged ≥12 years who participated in a 2013–2014 community health survey. A multivariate log-binomial model was used to calculate adjusted prevalence ratios for migraines associated with individual and joint exposures of female gender and stress. Researchers used relative excess risk due to interaction (RERI), attributable proportion (AP), and synergy index (S index) to measure additive interaction. They found:
- The adjusted prevalence ratios were 2.37 for female vs male, 1.63 for persons with high vs low levels of stress, and 3.38 for women with high stress vs men with low stress.
- The RERI estimate was 0.38, the AP estimate was 0.11, and the S index was 1.19.
Slatculescu AM, Chen Y. Synergism between female gender and high levels of daily stress associated with migraine headaches in Ontario, Canada. [Published online ahead of print August 28, 2018]. Neuroepidemiol. doi:10.1159/000492503.
Two immunologists receive Nobel Prize in medicine
Two immunologists have been awarded the Nobel Prize in Physiology or Medicine for discoveries that represent a “paradigmatic shift in the fight against cancer,” the Nobel committee said.
James P. Allison, PhD, of MD Anderson Cancer Center, and Tasuku Honjo, MD, PhD, of Kyoto University, shared the prize for their discovery of cancer therapies that work by inhibiting negative immune regulation.
Dr. Allison studied the protein CTLA-4 found on T cells, which acts as a T-cell brake, and Dr. Honjo discovered a protein on immune cells called PD-1 that also acts as a T-cell brake.
In addition to sharing the honor, the scientists will split the 9 million Swedish kronor ($1.01 million) that comes with the prize.
Drs. Allison and Honjo, working in parallel, pursued different strategies for inhibiting the brakes on the immune system. Both strategies produced effective checkpoint inhibitors in the treatment of cancer.
James P. Allison
Dr. Allison was one of several scientists during the 1990s who noticed that CTLA-4 functions as a brake on T cells. Unlike other scientists, however, he set out to investigate whether blocking CTLA-4 with an antibody he had already developed could release the brake on the immune system.
The antibody had “spectacular” effects in curing mice with cancer. Despite little interest from the pharmaceutical industry, Dr. Allison continued efforts to develop the antibody therapy for humans.
The antibody turned out to be ipilimumab, which was approved in 2011 by the U.S. Food and Drug Administration (FDA) for the treatment of advanced melanoma.
Tasuko Honjo
A few years prior to Dr. Allison’s finding, Dr. Honjo discovered PD-1 and set out to determine its function. PD-1 also operates as a T-cell brake, but it uses a different mechanism than does CTLA-4.
Dr. Honjo and others demonstrated in animal experiments that PD-1 blockade could be an effective anticancer therapy. Over the years he demonstrated the efficacy of targeting PD-1 in different types of human cancers.
The first two PD-1 checkpoint inhibitors—pembrolizumab and nivolumab—were approved by the FDA in 2014 for the treatment of melanoma.
Nivolumab is also approved to treat classical Hodgkin lymphoma (HL), non-small cell lung cancer (NSCLC), small cell lung cancer, squamous cell carcinoma of the head and neck, colorectal cancer, hepatocellular carcinoma, renal cell carcinoma, urothelial carcinoma, and microsatellite instability-high or mismatch repair deficient colorectal cancer.
Pembrolizumab is also approved to treat primary mediastinal large B-cell lymphoma, advanced NSCLC, classical HL, advanced gastric cancer, advanced cervical cancer, head and neck squamous cell cancer, advanced urothelial bladder cancer, and microsatellite instability-high cancer.
And targeting both CTLA-4 and PD-1 in combination therapy together may prove to be even more effective in eliminating cancer cells than either strategy alone, as is being demonstrated in patients with melanoma.
The Nobel organization wrote in a press release, “Checkpoint therapy has now revolutionized cancer treatment and has fundamentally changed the way we view how cancer can be managed.”
Two immunologists have been awarded the Nobel Prize in Physiology or Medicine for discoveries that represent a “paradigmatic shift in the fight against cancer,” the Nobel committee said.
James P. Allison, PhD, of MD Anderson Cancer Center, and Tasuku Honjo, MD, PhD, of Kyoto University, shared the prize for their discovery of cancer therapies that work by inhibiting negative immune regulation.
Dr. Allison studied the protein CTLA-4 found on T cells, which acts as a T-cell brake, and Dr. Honjo discovered a protein on immune cells called PD-1 that also acts as a T-cell brake.
In addition to sharing the honor, the scientists will split the 9 million Swedish kronor ($1.01 million) that comes with the prize.
Drs. Allison and Honjo, working in parallel, pursued different strategies for inhibiting the brakes on the immune system. Both strategies produced effective checkpoint inhibitors in the treatment of cancer.
James P. Allison
Dr. Allison was one of several scientists during the 1990s who noticed that CTLA-4 functions as a brake on T cells. Unlike other scientists, however, he set out to investigate whether blocking CTLA-4 with an antibody he had already developed could release the brake on the immune system.
The antibody had “spectacular” effects in curing mice with cancer. Despite little interest from the pharmaceutical industry, Dr. Allison continued efforts to develop the antibody therapy for humans.
The antibody turned out to be ipilimumab, which was approved in 2011 by the U.S. Food and Drug Administration (FDA) for the treatment of advanced melanoma.
Tasuko Honjo
A few years prior to Dr. Allison’s finding, Dr. Honjo discovered PD-1 and set out to determine its function. PD-1 also operates as a T-cell brake, but it uses a different mechanism than does CTLA-4.
Dr. Honjo and others demonstrated in animal experiments that PD-1 blockade could be an effective anticancer therapy. Over the years he demonstrated the efficacy of targeting PD-1 in different types of human cancers.
The first two PD-1 checkpoint inhibitors—pembrolizumab and nivolumab—were approved by the FDA in 2014 for the treatment of melanoma.
Nivolumab is also approved to treat classical Hodgkin lymphoma (HL), non-small cell lung cancer (NSCLC), small cell lung cancer, squamous cell carcinoma of the head and neck, colorectal cancer, hepatocellular carcinoma, renal cell carcinoma, urothelial carcinoma, and microsatellite instability-high or mismatch repair deficient colorectal cancer.
Pembrolizumab is also approved to treat primary mediastinal large B-cell lymphoma, advanced NSCLC, classical HL, advanced gastric cancer, advanced cervical cancer, head and neck squamous cell cancer, advanced urothelial bladder cancer, and microsatellite instability-high cancer.
And targeting both CTLA-4 and PD-1 in combination therapy together may prove to be even more effective in eliminating cancer cells than either strategy alone, as is being demonstrated in patients with melanoma.
The Nobel organization wrote in a press release, “Checkpoint therapy has now revolutionized cancer treatment and has fundamentally changed the way we view how cancer can be managed.”
Two immunologists have been awarded the Nobel Prize in Physiology or Medicine for discoveries that represent a “paradigmatic shift in the fight against cancer,” the Nobel committee said.
James P. Allison, PhD, of MD Anderson Cancer Center, and Tasuku Honjo, MD, PhD, of Kyoto University, shared the prize for their discovery of cancer therapies that work by inhibiting negative immune regulation.
Dr. Allison studied the protein CTLA-4 found on T cells, which acts as a T-cell brake, and Dr. Honjo discovered a protein on immune cells called PD-1 that also acts as a T-cell brake.
In addition to sharing the honor, the scientists will split the 9 million Swedish kronor ($1.01 million) that comes with the prize.
Drs. Allison and Honjo, working in parallel, pursued different strategies for inhibiting the brakes on the immune system. Both strategies produced effective checkpoint inhibitors in the treatment of cancer.
James P. Allison
Dr. Allison was one of several scientists during the 1990s who noticed that CTLA-4 functions as a brake on T cells. Unlike other scientists, however, he set out to investigate whether blocking CTLA-4 with an antibody he had already developed could release the brake on the immune system.
The antibody had “spectacular” effects in curing mice with cancer. Despite little interest from the pharmaceutical industry, Dr. Allison continued efforts to develop the antibody therapy for humans.
The antibody turned out to be ipilimumab, which was approved in 2011 by the U.S. Food and Drug Administration (FDA) for the treatment of advanced melanoma.
Tasuko Honjo
A few years prior to Dr. Allison’s finding, Dr. Honjo discovered PD-1 and set out to determine its function. PD-1 also operates as a T-cell brake, but it uses a different mechanism than does CTLA-4.
Dr. Honjo and others demonstrated in animal experiments that PD-1 blockade could be an effective anticancer therapy. Over the years he demonstrated the efficacy of targeting PD-1 in different types of human cancers.
The first two PD-1 checkpoint inhibitors—pembrolizumab and nivolumab—were approved by the FDA in 2014 for the treatment of melanoma.
Nivolumab is also approved to treat classical Hodgkin lymphoma (HL), non-small cell lung cancer (NSCLC), small cell lung cancer, squamous cell carcinoma of the head and neck, colorectal cancer, hepatocellular carcinoma, renal cell carcinoma, urothelial carcinoma, and microsatellite instability-high or mismatch repair deficient colorectal cancer.
Pembrolizumab is also approved to treat primary mediastinal large B-cell lymphoma, advanced NSCLC, classical HL, advanced gastric cancer, advanced cervical cancer, head and neck squamous cell cancer, advanced urothelial bladder cancer, and microsatellite instability-high cancer.
And targeting both CTLA-4 and PD-1 in combination therapy together may prove to be even more effective in eliminating cancer cells than either strategy alone, as is being demonstrated in patients with melanoma.
The Nobel organization wrote in a press release, “Checkpoint therapy has now revolutionized cancer treatment and has fundamentally changed the way we view how cancer can be managed.”
Concurrent ‘never event’ prescribing may worsen dementia in Parkinson’s
Nearly half of Medicare beneficiaries with Parkinson’s disease were concurrently prescribed a high-potency anticholinergic medication and an acetylcholinesterase inhibitor, with higher rates of potential prescribing errors seen among women and Hispanic patients, according to a cross-sectional analysis of Centers for Medicare & Medicaid Services data published in JAMA Neurology.
“Coadministration of a drug with high anticholinergic activity and an [acetylcholinesterase inhibitor] represents a frank prescribing error because these drugs have opposing pharmacologic effects,” wrote Sneha Mantri, MD, of the Parkinson’s Disease Research, Education, and Clinical Center at the Philadelphia VA Medical Center, and her colleagues. “In patients with Parkinson disease, who bear additional risks of cognitive impairment and vulnerability to anticholinergic activity, coprescribing of an [acetylcholinesterase inhibitor] and a high-potency anticholinergic medication can be considered a never event because it is a medication error likely to contribute to disability.”
Dr. Mantri and her colleagues analyzed the inpatient, outpatient, and prescription data of 268,407 Medicare beneficiaries with Parkinson’s, of whom 73,093 patients (27.2%) were prescribed a minimum of one antidementia medication fill. Patients were mean 78.9 years old, and the demographics of the Medicare beneficiaries were 50.1% male, 86.7% white, 5.5% black, 2.7% Hispanic, 2.7% Asian, and 0.7% Native American. The most common antidementia prescriptions were donepezil hydrochloride (63.0%), memantine hydrochloride (41.8%), and rivastigmine tartrate (26.4%). The researchers measured medications in cases of coprescription with potential anticholinergic (ACH) activity using the Anticholinergic Cognitive Burden Scale.
They found antidementia medication use was associated with patients who were black (adjusted odds ratio, 1.33; 95% confidence interval, 1.28-1.38) and Hispanic (aOR, 1.28; 95% CI, 1.22-1.35). Meanwhile, a negative association was found between Native American patients and antidementia medication use (aOR, 0.62; 95% CI, 0.51-0.74) compared with white patients and women (aOR, 0.85; 95% CI, 0.84-0.87) compared with men. The researchers noted that 28,495 patients (44.5%) were prescribed concurrently one high-potency anticholinergic and acetylcholinesterase inhibitors, with higher rates of prescribing seen for Hispanic (aOR, 1.11; 95% CI, 1.00-1.23) and women (aOR, 1.30; 95% CI, 1.25-1.35). High prevalence clusters of this type of prescribing were statistically high in the Southern and Midwestern states, they added.
Limitations included the study of a single year of data and the absence of conclusive data of dementia prevalence among Parkinson’s patients based on antidementia medication use alone and potential off-label use of antidementia medication analyzed in the study, the researchers said.
“In determining whether anticholinergic drug exposure has a causal role in clinical dementia in Parkinson disease, future studies may take a clinical trial approach, in which high-potency anticholinergic medications are replaced with lower-potency alternatives, and the change in cognitive testing and cognitive trajectory are measured,” Dr. Mantri and her colleagues wrote. “Such an approach will allow the calculation of anticholinergic drug safety in terms that are easily understood, such as number needed to harm.”
This study was funded by a grant from the National Institute of Neurological Diseases and Stroke of the National Institutes of Health. The authors report no relevant conflicts of interest.
SOURCE: Mantri S et al. JAMA Neurol. 2018 Oct 1. doi: 10.1001/jamaneurol.2018.2820.
Describing the prescribing patterns of antidementia medication for patients with Parkinson’s disease is useful, particularly with regard to black and Hispanic patients, but the analysis by Sneha Mantri, MD, and her colleagues has methodological issues that limit its impact, wrote Christopher W. Hess, MD, Michael S. Okun, MD, and Adolfo Ramirez-Zamora, MD, wrote in an editorial.
While the researchers used the Anticholinergic Cognitive Burden (ACB) Scale and graded acetylcholinesterase inhibitor and high anticholinergic (ACH) activity medication combinations with the highest ACB score (3 on a scale of 0 to 3) and labeled them as a prescribing error, the ACB scale score alone should not be the sole determination of whether a prescription combination is deemed an error, the authors said.
“A problem, however, arises in defining the coadministration of an antidementia drug and a medication with high ACH activity as a prescribing error or a never event in all clinical circumstances,” the authors wrote. “Across the literature in this area, the most important principle repeatedly emphasized was that these resources are intended to identify potentially inappropriate medication (not inappropriate medications), and the recommendations and ratings provided cannot replace patient-specific clinical judgment.”
Further, medications such as clozapine and quetiapine fumarate are often prescribed for patients with Parkinson’s disease–related psychosis as a standard of care; those medications also have an ACB score of 3, which would label them as prescribing errors and never events under the study by Mantri et al., the authors continued.
“Variability in ACH activity scoring methods is an additional concern, as no criterion standard exists for ranking relative ACH activity and the scores for medications to treat Parkinson disease (such as quetiapine for Parkinson disease psychosis) can markedly differ between the scales commonly used (such as the ACB Scale),” they wrote.
Christopher W. Hess, MD, Michael S. Okun, MD, and Adolfo Ramirez-Zamora, MD, are affiliated with the Fixel Center for Neurological Diseases in the department of neurology at the University of Florida in Gainesville. These comments summarize their editorial (JAMA Neurol. 2018 Oct 1 doi: 10.1001/jamaneurol.2018.2826).They reported no relevant conflicts of interest.
Describing the prescribing patterns of antidementia medication for patients with Parkinson’s disease is useful, particularly with regard to black and Hispanic patients, but the analysis by Sneha Mantri, MD, and her colleagues has methodological issues that limit its impact, wrote Christopher W. Hess, MD, Michael S. Okun, MD, and Adolfo Ramirez-Zamora, MD, wrote in an editorial.
While the researchers used the Anticholinergic Cognitive Burden (ACB) Scale and graded acetylcholinesterase inhibitor and high anticholinergic (ACH) activity medication combinations with the highest ACB score (3 on a scale of 0 to 3) and labeled them as a prescribing error, the ACB scale score alone should not be the sole determination of whether a prescription combination is deemed an error, the authors said.
“A problem, however, arises in defining the coadministration of an antidementia drug and a medication with high ACH activity as a prescribing error or a never event in all clinical circumstances,” the authors wrote. “Across the literature in this area, the most important principle repeatedly emphasized was that these resources are intended to identify potentially inappropriate medication (not inappropriate medications), and the recommendations and ratings provided cannot replace patient-specific clinical judgment.”
Further, medications such as clozapine and quetiapine fumarate are often prescribed for patients with Parkinson’s disease–related psychosis as a standard of care; those medications also have an ACB score of 3, which would label them as prescribing errors and never events under the study by Mantri et al., the authors continued.
“Variability in ACH activity scoring methods is an additional concern, as no criterion standard exists for ranking relative ACH activity and the scores for medications to treat Parkinson disease (such as quetiapine for Parkinson disease psychosis) can markedly differ between the scales commonly used (such as the ACB Scale),” they wrote.
Christopher W. Hess, MD, Michael S. Okun, MD, and Adolfo Ramirez-Zamora, MD, are affiliated with the Fixel Center for Neurological Diseases in the department of neurology at the University of Florida in Gainesville. These comments summarize their editorial (JAMA Neurol. 2018 Oct 1 doi: 10.1001/jamaneurol.2018.2826).They reported no relevant conflicts of interest.
Describing the prescribing patterns of antidementia medication for patients with Parkinson’s disease is useful, particularly with regard to black and Hispanic patients, but the analysis by Sneha Mantri, MD, and her colleagues has methodological issues that limit its impact, wrote Christopher W. Hess, MD, Michael S. Okun, MD, and Adolfo Ramirez-Zamora, MD, wrote in an editorial.
While the researchers used the Anticholinergic Cognitive Burden (ACB) Scale and graded acetylcholinesterase inhibitor and high anticholinergic (ACH) activity medication combinations with the highest ACB score (3 on a scale of 0 to 3) and labeled them as a prescribing error, the ACB scale score alone should not be the sole determination of whether a prescription combination is deemed an error, the authors said.
“A problem, however, arises in defining the coadministration of an antidementia drug and a medication with high ACH activity as a prescribing error or a never event in all clinical circumstances,” the authors wrote. “Across the literature in this area, the most important principle repeatedly emphasized was that these resources are intended to identify potentially inappropriate medication (not inappropriate medications), and the recommendations and ratings provided cannot replace patient-specific clinical judgment.”
Further, medications such as clozapine and quetiapine fumarate are often prescribed for patients with Parkinson’s disease–related psychosis as a standard of care; those medications also have an ACB score of 3, which would label them as prescribing errors and never events under the study by Mantri et al., the authors continued.
“Variability in ACH activity scoring methods is an additional concern, as no criterion standard exists for ranking relative ACH activity and the scores for medications to treat Parkinson disease (such as quetiapine for Parkinson disease psychosis) can markedly differ between the scales commonly used (such as the ACB Scale),” they wrote.
Christopher W. Hess, MD, Michael S. Okun, MD, and Adolfo Ramirez-Zamora, MD, are affiliated with the Fixel Center for Neurological Diseases in the department of neurology at the University of Florida in Gainesville. These comments summarize their editorial (JAMA Neurol. 2018 Oct 1 doi: 10.1001/jamaneurol.2018.2826).They reported no relevant conflicts of interest.
Nearly half of Medicare beneficiaries with Parkinson’s disease were concurrently prescribed a high-potency anticholinergic medication and an acetylcholinesterase inhibitor, with higher rates of potential prescribing errors seen among women and Hispanic patients, according to a cross-sectional analysis of Centers for Medicare & Medicaid Services data published in JAMA Neurology.
“Coadministration of a drug with high anticholinergic activity and an [acetylcholinesterase inhibitor] represents a frank prescribing error because these drugs have opposing pharmacologic effects,” wrote Sneha Mantri, MD, of the Parkinson’s Disease Research, Education, and Clinical Center at the Philadelphia VA Medical Center, and her colleagues. “In patients with Parkinson disease, who bear additional risks of cognitive impairment and vulnerability to anticholinergic activity, coprescribing of an [acetylcholinesterase inhibitor] and a high-potency anticholinergic medication can be considered a never event because it is a medication error likely to contribute to disability.”
Dr. Mantri and her colleagues analyzed the inpatient, outpatient, and prescription data of 268,407 Medicare beneficiaries with Parkinson’s, of whom 73,093 patients (27.2%) were prescribed a minimum of one antidementia medication fill. Patients were mean 78.9 years old, and the demographics of the Medicare beneficiaries were 50.1% male, 86.7% white, 5.5% black, 2.7% Hispanic, 2.7% Asian, and 0.7% Native American. The most common antidementia prescriptions were donepezil hydrochloride (63.0%), memantine hydrochloride (41.8%), and rivastigmine tartrate (26.4%). The researchers measured medications in cases of coprescription with potential anticholinergic (ACH) activity using the Anticholinergic Cognitive Burden Scale.
They found antidementia medication use was associated with patients who were black (adjusted odds ratio, 1.33; 95% confidence interval, 1.28-1.38) and Hispanic (aOR, 1.28; 95% CI, 1.22-1.35). Meanwhile, a negative association was found between Native American patients and antidementia medication use (aOR, 0.62; 95% CI, 0.51-0.74) compared with white patients and women (aOR, 0.85; 95% CI, 0.84-0.87) compared with men. The researchers noted that 28,495 patients (44.5%) were prescribed concurrently one high-potency anticholinergic and acetylcholinesterase inhibitors, with higher rates of prescribing seen for Hispanic (aOR, 1.11; 95% CI, 1.00-1.23) and women (aOR, 1.30; 95% CI, 1.25-1.35). High prevalence clusters of this type of prescribing were statistically high in the Southern and Midwestern states, they added.
Limitations included the study of a single year of data and the absence of conclusive data of dementia prevalence among Parkinson’s patients based on antidementia medication use alone and potential off-label use of antidementia medication analyzed in the study, the researchers said.
“In determining whether anticholinergic drug exposure has a causal role in clinical dementia in Parkinson disease, future studies may take a clinical trial approach, in which high-potency anticholinergic medications are replaced with lower-potency alternatives, and the change in cognitive testing and cognitive trajectory are measured,” Dr. Mantri and her colleagues wrote. “Such an approach will allow the calculation of anticholinergic drug safety in terms that are easily understood, such as number needed to harm.”
This study was funded by a grant from the National Institute of Neurological Diseases and Stroke of the National Institutes of Health. The authors report no relevant conflicts of interest.
SOURCE: Mantri S et al. JAMA Neurol. 2018 Oct 1. doi: 10.1001/jamaneurol.2018.2820.
Nearly half of Medicare beneficiaries with Parkinson’s disease were concurrently prescribed a high-potency anticholinergic medication and an acetylcholinesterase inhibitor, with higher rates of potential prescribing errors seen among women and Hispanic patients, according to a cross-sectional analysis of Centers for Medicare & Medicaid Services data published in JAMA Neurology.
“Coadministration of a drug with high anticholinergic activity and an [acetylcholinesterase inhibitor] represents a frank prescribing error because these drugs have opposing pharmacologic effects,” wrote Sneha Mantri, MD, of the Parkinson’s Disease Research, Education, and Clinical Center at the Philadelphia VA Medical Center, and her colleagues. “In patients with Parkinson disease, who bear additional risks of cognitive impairment and vulnerability to anticholinergic activity, coprescribing of an [acetylcholinesterase inhibitor] and a high-potency anticholinergic medication can be considered a never event because it is a medication error likely to contribute to disability.”
Dr. Mantri and her colleagues analyzed the inpatient, outpatient, and prescription data of 268,407 Medicare beneficiaries with Parkinson’s, of whom 73,093 patients (27.2%) were prescribed a minimum of one antidementia medication fill. Patients were mean 78.9 years old, and the demographics of the Medicare beneficiaries were 50.1% male, 86.7% white, 5.5% black, 2.7% Hispanic, 2.7% Asian, and 0.7% Native American. The most common antidementia prescriptions were donepezil hydrochloride (63.0%), memantine hydrochloride (41.8%), and rivastigmine tartrate (26.4%). The researchers measured medications in cases of coprescription with potential anticholinergic (ACH) activity using the Anticholinergic Cognitive Burden Scale.
They found antidementia medication use was associated with patients who were black (adjusted odds ratio, 1.33; 95% confidence interval, 1.28-1.38) and Hispanic (aOR, 1.28; 95% CI, 1.22-1.35). Meanwhile, a negative association was found between Native American patients and antidementia medication use (aOR, 0.62; 95% CI, 0.51-0.74) compared with white patients and women (aOR, 0.85; 95% CI, 0.84-0.87) compared with men. The researchers noted that 28,495 patients (44.5%) were prescribed concurrently one high-potency anticholinergic and acetylcholinesterase inhibitors, with higher rates of prescribing seen for Hispanic (aOR, 1.11; 95% CI, 1.00-1.23) and women (aOR, 1.30; 95% CI, 1.25-1.35). High prevalence clusters of this type of prescribing were statistically high in the Southern and Midwestern states, they added.
Limitations included the study of a single year of data and the absence of conclusive data of dementia prevalence among Parkinson’s patients based on antidementia medication use alone and potential off-label use of antidementia medication analyzed in the study, the researchers said.
“In determining whether anticholinergic drug exposure has a causal role in clinical dementia in Parkinson disease, future studies may take a clinical trial approach, in which high-potency anticholinergic medications are replaced with lower-potency alternatives, and the change in cognitive testing and cognitive trajectory are measured,” Dr. Mantri and her colleagues wrote. “Such an approach will allow the calculation of anticholinergic drug safety in terms that are easily understood, such as number needed to harm.”
This study was funded by a grant from the National Institute of Neurological Diseases and Stroke of the National Institutes of Health. The authors report no relevant conflicts of interest.
SOURCE: Mantri S et al. JAMA Neurol. 2018 Oct 1. doi: 10.1001/jamaneurol.2018.2820.
FROM JAMA NEUROLOGY
Key clinical point: Medicare beneficiaries with Parkinson’s disease often are concurrently prescribed a high-potency anticholinergic medication and an acetylcholinesterase inhibitor.
Major finding: More than 44% of patients experienced at least one never event, with higher rates of potential prescribing errors seen in Hispanic patients (adjusted OR, 1.11) and women (adjusted OR, 1.30).
Study details: An analysis of inpatient, outpatient, and prescription data for 268,407 Medicare beneficiaries with Parkinson’s disease over 12 months.
Disclosures: This study was funded by a grant from the National Institute of Neurological Diseases and Stroke of the National Institutes of Health. The authors reported no relevant conflicts of interest.
Source: Mantri S et al. JAMA Neurol. 2018 Oct 1. doi: 10.1001/jamaneurol.2018.2820.
Low-dose ketamine controls pain from severe chest injury, while sparing opioid consumption
SAN DIEGO – while reducing opioid consumption.
The anesthetic didn’t make much difference in pain control or opioid use overall in a randomized study of 93 patients with thoracic injury Nathan Kugler, MD, said at the annual meeting of the American Association for the Surgery of Trauma. But among severely injured patients, it cut the opioid mean equivalency dose by about 164 mg over the 48-hour infusion and by 328 mg over a mean hospital stay while maintaining pain control, said Dr. Kugler, a surgical resident at the Medical College of Wisconsin, Milwaukee.
“With increasing focus on multimodal pain strategies, opioid-based regimens continue to be the backbone of pain control,” he said. “We have used ketamine effectively for failure of maximum therapy and demonstrated an opioid-sparing effect.” This new research shows that the drug can be an effective adjunct for acute pain control for severely injured patients in the emergency setting.
The study recruited 93 patients with thoracic injury; they had a mean of six broken ribs, mostly caused by motor vehicle accidents. Most of the patients were male (75%), and their mean age was 46 years. The mean Injury Severity Score was about 15; about 30% had flail chest.
All patients received a standardized acute pain medication regime comprising acetaminophen, nonsteroidal anti-inflammatories, methocarbamol (Robaxin), and intravenous opioids. Regional therapies included rib block with an epidural catheter. In addition, they were randomized to placebo infusions or to 48 hours of IV ketamine at 2.5 mcg/kg per minute. “To put this in perspective, for a 70-kg patient, that is a mean of 10.5 mg/hour,” Dr. Kugler said.
The primary endpoint was a reduction of at least 2 points on an 11-point pain scale. Secondary endpoints included opioid use in oral morphine equivalents (OME); respiratory complications; and psychoactive events. The primary outcome was assessed with an area under the curve model.
In the overall group, there was no significant between-group difference in pain score. Nor were there differences in the total OME at 12-24 hours (184 mg ketamine vs. 230 mg placebo), or at 48 hours (86 vs. 113 mg).
Dr. Kugler also looked at these outcomes in patients who had only rib fractures independent of other chest injury. He saw no significant differences in pain scores or OME at 24 or 48 hours.
However, significant differences did emerge in the group of severely injured patients with an Injury Severity Score of more than 15. There were no differences in pain scores at either time point. However, ketamine allowed patients to achieve the same level of pain control with significantly less opioid medication. The OME at 12-24 hours was 50.5 mg vs 94 mg. At 24-48 hours, it was 87 mg vs. 64 mg.
This worked out to a mean OME savings of 148 mg over a patient’s entire hospitalization.
“We saw a very nice separation of opioid consumption that began early and continued to separate over the 48-hour infusion and even after it was discontinued,” Dr. Kugler said.
This benefit was achieved without any additional adverse events, he added. There were no significant differences in confusion; epidural placement; length of stay; respiratory event, sedation, hallucinations, delusions or disturbing dreams; or unplanned transfers to the ICU.
Dr. Kugler disclosed that he and primary investigator Thomas Carver, MD, also of the Medical College of Wisconsin, Milwaukee, are both paid consultants for InnoVital Systems.
SAN DIEGO – while reducing opioid consumption.
The anesthetic didn’t make much difference in pain control or opioid use overall in a randomized study of 93 patients with thoracic injury Nathan Kugler, MD, said at the annual meeting of the American Association for the Surgery of Trauma. But among severely injured patients, it cut the opioid mean equivalency dose by about 164 mg over the 48-hour infusion and by 328 mg over a mean hospital stay while maintaining pain control, said Dr. Kugler, a surgical resident at the Medical College of Wisconsin, Milwaukee.
“With increasing focus on multimodal pain strategies, opioid-based regimens continue to be the backbone of pain control,” he said. “We have used ketamine effectively for failure of maximum therapy and demonstrated an opioid-sparing effect.” This new research shows that the drug can be an effective adjunct for acute pain control for severely injured patients in the emergency setting.
The study recruited 93 patients with thoracic injury; they had a mean of six broken ribs, mostly caused by motor vehicle accidents. Most of the patients were male (75%), and their mean age was 46 years. The mean Injury Severity Score was about 15; about 30% had flail chest.
All patients received a standardized acute pain medication regime comprising acetaminophen, nonsteroidal anti-inflammatories, methocarbamol (Robaxin), and intravenous opioids. Regional therapies included rib block with an epidural catheter. In addition, they were randomized to placebo infusions or to 48 hours of IV ketamine at 2.5 mcg/kg per minute. “To put this in perspective, for a 70-kg patient, that is a mean of 10.5 mg/hour,” Dr. Kugler said.
The primary endpoint was a reduction of at least 2 points on an 11-point pain scale. Secondary endpoints included opioid use in oral morphine equivalents (OME); respiratory complications; and psychoactive events. The primary outcome was assessed with an area under the curve model.
In the overall group, there was no significant between-group difference in pain score. Nor were there differences in the total OME at 12-24 hours (184 mg ketamine vs. 230 mg placebo), or at 48 hours (86 vs. 113 mg).
Dr. Kugler also looked at these outcomes in patients who had only rib fractures independent of other chest injury. He saw no significant differences in pain scores or OME at 24 or 48 hours.
However, significant differences did emerge in the group of severely injured patients with an Injury Severity Score of more than 15. There were no differences in pain scores at either time point. However, ketamine allowed patients to achieve the same level of pain control with significantly less opioid medication. The OME at 12-24 hours was 50.5 mg vs 94 mg. At 24-48 hours, it was 87 mg vs. 64 mg.
This worked out to a mean OME savings of 148 mg over a patient’s entire hospitalization.
“We saw a very nice separation of opioid consumption that began early and continued to separate over the 48-hour infusion and even after it was discontinued,” Dr. Kugler said.
This benefit was achieved without any additional adverse events, he added. There were no significant differences in confusion; epidural placement; length of stay; respiratory event, sedation, hallucinations, delusions or disturbing dreams; or unplanned transfers to the ICU.
Dr. Kugler disclosed that he and primary investigator Thomas Carver, MD, also of the Medical College of Wisconsin, Milwaukee, are both paid consultants for InnoVital Systems.
SAN DIEGO – while reducing opioid consumption.
The anesthetic didn’t make much difference in pain control or opioid use overall in a randomized study of 93 patients with thoracic injury Nathan Kugler, MD, said at the annual meeting of the American Association for the Surgery of Trauma. But among severely injured patients, it cut the opioid mean equivalency dose by about 164 mg over the 48-hour infusion and by 328 mg over a mean hospital stay while maintaining pain control, said Dr. Kugler, a surgical resident at the Medical College of Wisconsin, Milwaukee.
“With increasing focus on multimodal pain strategies, opioid-based regimens continue to be the backbone of pain control,” he said. “We have used ketamine effectively for failure of maximum therapy and demonstrated an opioid-sparing effect.” This new research shows that the drug can be an effective adjunct for acute pain control for severely injured patients in the emergency setting.
The study recruited 93 patients with thoracic injury; they had a mean of six broken ribs, mostly caused by motor vehicle accidents. Most of the patients were male (75%), and their mean age was 46 years. The mean Injury Severity Score was about 15; about 30% had flail chest.
All patients received a standardized acute pain medication regime comprising acetaminophen, nonsteroidal anti-inflammatories, methocarbamol (Robaxin), and intravenous opioids. Regional therapies included rib block with an epidural catheter. In addition, they were randomized to placebo infusions or to 48 hours of IV ketamine at 2.5 mcg/kg per minute. “To put this in perspective, for a 70-kg patient, that is a mean of 10.5 mg/hour,” Dr. Kugler said.
The primary endpoint was a reduction of at least 2 points on an 11-point pain scale. Secondary endpoints included opioid use in oral morphine equivalents (OME); respiratory complications; and psychoactive events. The primary outcome was assessed with an area under the curve model.
In the overall group, there was no significant between-group difference in pain score. Nor were there differences in the total OME at 12-24 hours (184 mg ketamine vs. 230 mg placebo), or at 48 hours (86 vs. 113 mg).
Dr. Kugler also looked at these outcomes in patients who had only rib fractures independent of other chest injury. He saw no significant differences in pain scores or OME at 24 or 48 hours.
However, significant differences did emerge in the group of severely injured patients with an Injury Severity Score of more than 15. There were no differences in pain scores at either time point. However, ketamine allowed patients to achieve the same level of pain control with significantly less opioid medication. The OME at 12-24 hours was 50.5 mg vs 94 mg. At 24-48 hours, it was 87 mg vs. 64 mg.
This worked out to a mean OME savings of 148 mg over a patient’s entire hospitalization.
“We saw a very nice separation of opioid consumption that began early and continued to separate over the 48-hour infusion and even after it was discontinued,” Dr. Kugler said.
This benefit was achieved without any additional adverse events, he added. There were no significant differences in confusion; epidural placement; length of stay; respiratory event, sedation, hallucinations, delusions or disturbing dreams; or unplanned transfers to the ICU.
Dr. Kugler disclosed that he and primary investigator Thomas Carver, MD, also of the Medical College of Wisconsin, Milwaukee, are both paid consultants for InnoVital Systems.
REPORTING FROM THE AAST ANNUAL MEETING
Key clinical point: Low-dose ketamine controlled pain while reducing opioid use among patients with severe thoracic injury.
Major finding: Compared with placebo, ketamine reduced opioids conferred OME savings of 148 mg over a patient’s entire hospitalization.
Study details: The randomized study comprised 93 patients with thoracic injury.
Disclosures: Dr. Kugler disclosed that he and primary investigator Thomas Carver, MD, are both paid consultants for InnoVital Systems.
Source: Carver T et al. AAST 2018, Oral abstract 2
October 2018 Question 2
Correct Answer: B
Rationale
This patient has large varices, which should be treated. In patients with cirrhosis and medium/large varices that have never bled, nonselective beta-blockers reduce the risk of first variceal hemorrhage by 50%. In high-quality randomized-controlled trials, endoscopic variceal ligation (EVL) is as effective as nonselective beta-blockers in preventing first variceal hemorrhage. Therefore, either of these therapies should be used for the prevention of first variceal bleeding. In this case, propranolol is not the best choice in the setting of diabetes, asthma as well as a blood pressure and pulse that are low already. Endoscopic variceal band ligation would be preferred in this patient. It is also more effective than sclerotherapy and is associated with fewer side effects. TIPS would be effective, but more invasive and not first-line for treatment of nonbleeding varices and comes with increased risk of hepatic encephalopathy and potentially mortality. The combination of nadolol and endoscopic variceal band ligation may have more side effects without a further reduction in the risk of first variceal hemorrhage beyond either therapy alone.
References
1. Gluud L.L., Klingenberg S., Nikolova D., Gluud C. Banding ligation versus beta-blockers as primary prophylaxis in esophageal varices: systematic review of randomized trials. Am J Gastroenterol. 2007;102(12):2842-8.
2. Gluud L.L., Krag A. Banding ligation versus betablockers for primary prevention in oesophageal varices in adults. Cochrane Database Syst Rev. 2012;8:CD004544. doi: 10.1002/14651858. CD004544.
3. Villanueva C., Piqueras M., Aracil C., et al. A randomized controlled trial comparing ligation and sclerotherapy as emergency endoscopic treatment added to somatostatin in acute variceal bleeding. J Hepatol. 2006;45(4):560-7.
Correct Answer: B
Rationale
This patient has large varices, which should be treated. In patients with cirrhosis and medium/large varices that have never bled, nonselective beta-blockers reduce the risk of first variceal hemorrhage by 50%. In high-quality randomized-controlled trials, endoscopic variceal ligation (EVL) is as effective as nonselective beta-blockers in preventing first variceal hemorrhage. Therefore, either of these therapies should be used for the prevention of first variceal bleeding. In this case, propranolol is not the best choice in the setting of diabetes, asthma as well as a blood pressure and pulse that are low already. Endoscopic variceal band ligation would be preferred in this patient. It is also more effective than sclerotherapy and is associated with fewer side effects. TIPS would be effective, but more invasive and not first-line for treatment of nonbleeding varices and comes with increased risk of hepatic encephalopathy and potentially mortality. The combination of nadolol and endoscopic variceal band ligation may have more side effects without a further reduction in the risk of first variceal hemorrhage beyond either therapy alone.
References
1. Gluud L.L., Klingenberg S., Nikolova D., Gluud C. Banding ligation versus beta-blockers as primary prophylaxis in esophageal varices: systematic review of randomized trials. Am J Gastroenterol. 2007;102(12):2842-8.
2. Gluud L.L., Krag A. Banding ligation versus betablockers for primary prevention in oesophageal varices in adults. Cochrane Database Syst Rev. 2012;8:CD004544. doi: 10.1002/14651858. CD004544.
3. Villanueva C., Piqueras M., Aracil C., et al. A randomized controlled trial comparing ligation and sclerotherapy as emergency endoscopic treatment added to somatostatin in acute variceal bleeding. J Hepatol. 2006;45(4):560-7.
Correct Answer: B
Rationale
This patient has large varices, which should be treated. In patients with cirrhosis and medium/large varices that have never bled, nonselective beta-blockers reduce the risk of first variceal hemorrhage by 50%. In high-quality randomized-controlled trials, endoscopic variceal ligation (EVL) is as effective as nonselective beta-blockers in preventing first variceal hemorrhage. Therefore, either of these therapies should be used for the prevention of first variceal bleeding. In this case, propranolol is not the best choice in the setting of diabetes, asthma as well as a blood pressure and pulse that are low already. Endoscopic variceal band ligation would be preferred in this patient. It is also more effective than sclerotherapy and is associated with fewer side effects. TIPS would be effective, but more invasive and not first-line for treatment of nonbleeding varices and comes with increased risk of hepatic encephalopathy and potentially mortality. The combination of nadolol and endoscopic variceal band ligation may have more side effects without a further reduction in the risk of first variceal hemorrhage beyond either therapy alone.
References
1. Gluud L.L., Klingenberg S., Nikolova D., Gluud C. Banding ligation versus beta-blockers as primary prophylaxis in esophageal varices: systematic review of randomized trials. Am J Gastroenterol. 2007;102(12):2842-8.
2. Gluud L.L., Krag A. Banding ligation versus betablockers for primary prevention in oesophageal varices in adults. Cochrane Database Syst Rev. 2012;8:CD004544. doi: 10.1002/14651858. CD004544.
3. Villanueva C., Piqueras M., Aracil C., et al. A randomized controlled trial comparing ligation and sclerotherapy as emergency endoscopic treatment added to somatostatin in acute variceal bleeding. J Hepatol. 2006;45(4):560-7.
A 59-year-old woman with a history of cirrhosis due to nonalcoholic steatohepatitis presents for endoscopic evaluation of varices. Her past medical history includes obesity, diabetes, hypertension, and mild asthma. She appears well and has no signs of decompensation. Her vitals are: temperature, 98.6 ºF; blood pressure, 90/51 mm Hg; heart rate, 58 beats/minute; O2 saturation, 98% on room air. Her endoscopy reveals mild portal hypertensive gastropathy, large esophageal varices, and no gastric varices.
Which is the best approach in the management of this patient?
October 2018 Question 1
Correct Answer: A
Rationale
This patient has an idiopathic, nonNSAID, non-H. pylori-associated ulcer and should be on daily PPI indefinitely. These patients have a high rate of recurrent bleeding (42%) and mortality when followed prospectively without being on antisecretory therapy. Although no randomized trials have assessed the benefit of medical cotherapy in this population, antiulcer therapy seems to reduce recurrent idiopathic ulcers.
References
1. Wong G.L.H., Wong V.W.S., Chan Y., et al. High incidence of mortality and recurrent bleeding in patients with Helicobacter pylori-negative idiopathic bleeding ulcers. Gastroenterology. 2009;137:525-31.
2. Laine L., Jensen D.M. Management of patients with ulcer bleeding. Am J Gastroenterol. 2012;107(3):345-60.
Correct Answer: A
Rationale
This patient has an idiopathic, nonNSAID, non-H. pylori-associated ulcer and should be on daily PPI indefinitely. These patients have a high rate of recurrent bleeding (42%) and mortality when followed prospectively without being on antisecretory therapy. Although no randomized trials have assessed the benefit of medical cotherapy in this population, antiulcer therapy seems to reduce recurrent idiopathic ulcers.
References
1. Wong G.L.H., Wong V.W.S., Chan Y., et al. High incidence of mortality and recurrent bleeding in patients with Helicobacter pylori-negative idiopathic bleeding ulcers. Gastroenterology. 2009;137:525-31.
2. Laine L., Jensen D.M. Management of patients with ulcer bleeding. Am J Gastroenterol. 2012;107(3):345-60.
Correct Answer: A
Rationale
This patient has an idiopathic, nonNSAID, non-H. pylori-associated ulcer and should be on daily PPI indefinitely. These patients have a high rate of recurrent bleeding (42%) and mortality when followed prospectively without being on antisecretory therapy. Although no randomized trials have assessed the benefit of medical cotherapy in this population, antiulcer therapy seems to reduce recurrent idiopathic ulcers.
References
1. Wong G.L.H., Wong V.W.S., Chan Y., et al. High incidence of mortality and recurrent bleeding in patients with Helicobacter pylori-negative idiopathic bleeding ulcers. Gastroenterology. 2009;137:525-31.
2. Laine L., Jensen D.M. Management of patients with ulcer bleeding. Am J Gastroenterol. 2012;107(3):345-60.
A 60-year-old woman is admitted to the hospital with an upper GI bleed and found to have a gastric ulcer. Biopsies from the ulcer show no malignancy. Gastric biopsies reveal no Helicobacter pylori and stool antigen for H. pylori is also negative. The patient denies any NSAID use. She is discharged home on twice-daily PPI. Two months later, she returns for a follow-up endoscopy, and the ulcer has healed.
What is your recommendation for this patient?
Palliative care consultations reduce hospital costs
Background: Health care costs are on the rise, and previous studies have found that PCC can reduce hospital costs. Timing of consultation and allocation of palliative care intervention to a certain population of patients may reveal a more significant cost reduction.
Study design: Meta-analysis.
Setting: English peer reviewed articles.
Synopsis: A systematic search was performed for articles that provided economic evaluation of PCC for adult inpatients in acute care hospitals. Patients were included if they had least one of seven conditions: cancer, heart failure, liver failure, kidney failure, chronic obstructive pulmonary disease, AIDS/HIV, or neurodegenerative conditions. Six data sets were reviewed, which included 133,118 patients altogether. There was a significant reduction in costs with PCC within 3 days of admission, regardless of the diagnosis (–$3,237; 95% confidence interval, –$3,581 to –$2,893). In the stratified analysis, the pooled meta-analysis suggested a statistically significant reduction in costs for both cancer (–$4,251; 95% CI, –$4,664 to –$3,837; P less than .001) and noncancer (–$2,105; 95% CI, –$2,698 to –$1,511; P less than .001) subsamples. In patients with cancer, the treatment effect was greater for patients with four or more comorbidities than it was for those with two or fewer.
Only six samples were evaluated, and causation could not be established because all samples had observational designs. There also was potential interpretation bias because the private investigator for each of the samples contributed to interpretation of the data and participated as an author. Overall evaluation of the economic value of PCC in this study was limited because analysis was focused to a single index hospital admission rather than including additional hospitalizations and outpatient costs.
Bottom line: Acute care hospitals might reduce hospital costs by increasing resources to allow palliative care consultations in patients with serious illnesses.
Citation: May P et al. Economics of palliative care for hospitalized adults with serious illness. JAMA Intern Med. 2018;178(6):820-9.
Dr. Libot is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
Background: Health care costs are on the rise, and previous studies have found that PCC can reduce hospital costs. Timing of consultation and allocation of palliative care intervention to a certain population of patients may reveal a more significant cost reduction.
Study design: Meta-analysis.
Setting: English peer reviewed articles.
Synopsis: A systematic search was performed for articles that provided economic evaluation of PCC for adult inpatients in acute care hospitals. Patients were included if they had least one of seven conditions: cancer, heart failure, liver failure, kidney failure, chronic obstructive pulmonary disease, AIDS/HIV, or neurodegenerative conditions. Six data sets were reviewed, which included 133,118 patients altogether. There was a significant reduction in costs with PCC within 3 days of admission, regardless of the diagnosis (–$3,237; 95% confidence interval, –$3,581 to –$2,893). In the stratified analysis, the pooled meta-analysis suggested a statistically significant reduction in costs for both cancer (–$4,251; 95% CI, –$4,664 to –$3,837; P less than .001) and noncancer (–$2,105; 95% CI, –$2,698 to –$1,511; P less than .001) subsamples. In patients with cancer, the treatment effect was greater for patients with four or more comorbidities than it was for those with two or fewer.
Only six samples were evaluated, and causation could not be established because all samples had observational designs. There also was potential interpretation bias because the private investigator for each of the samples contributed to interpretation of the data and participated as an author. Overall evaluation of the economic value of PCC in this study was limited because analysis was focused to a single index hospital admission rather than including additional hospitalizations and outpatient costs.
Bottom line: Acute care hospitals might reduce hospital costs by increasing resources to allow palliative care consultations in patients with serious illnesses.
Citation: May P et al. Economics of palliative care for hospitalized adults with serious illness. JAMA Intern Med. 2018;178(6):820-9.
Dr. Libot is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
Background: Health care costs are on the rise, and previous studies have found that PCC can reduce hospital costs. Timing of consultation and allocation of palliative care intervention to a certain population of patients may reveal a more significant cost reduction.
Study design: Meta-analysis.
Setting: English peer reviewed articles.
Synopsis: A systematic search was performed for articles that provided economic evaluation of PCC for adult inpatients in acute care hospitals. Patients were included if they had least one of seven conditions: cancer, heart failure, liver failure, kidney failure, chronic obstructive pulmonary disease, AIDS/HIV, or neurodegenerative conditions. Six data sets were reviewed, which included 133,118 patients altogether. There was a significant reduction in costs with PCC within 3 days of admission, regardless of the diagnosis (–$3,237; 95% confidence interval, –$3,581 to –$2,893). In the stratified analysis, the pooled meta-analysis suggested a statistically significant reduction in costs for both cancer (–$4,251; 95% CI, –$4,664 to –$3,837; P less than .001) and noncancer (–$2,105; 95% CI, –$2,698 to –$1,511; P less than .001) subsamples. In patients with cancer, the treatment effect was greater for patients with four or more comorbidities than it was for those with two or fewer.
Only six samples were evaluated, and causation could not be established because all samples had observational designs. There also was potential interpretation bias because the private investigator for each of the samples contributed to interpretation of the data and participated as an author. Overall evaluation of the economic value of PCC in this study was limited because analysis was focused to a single index hospital admission rather than including additional hospitalizations and outpatient costs.
Bottom line: Acute care hospitals might reduce hospital costs by increasing resources to allow palliative care consultations in patients with serious illnesses.
Citation: May P et al. Economics of palliative care for hospitalized adults with serious illness. JAMA Intern Med. 2018;178(6):820-9.
Dr. Libot is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
ALEX: Alectinib showed superior CNS efficacy in ALK+ NSCLC
For patients with treatment-naive anaplastic lymphoma kinase–positive (ALK+) non–small cell lung cancer (NSCLC), twice-daily oral treatment with alectinib (600 mg) was associated with significantly greater activity in the CNS and significantly delayed CNS progression, compared with crizotinib (200 mg), based on secondary analyses from the pivotal phase 3 ALEX trial.
Time to CNS progression was significantly longer with alectinib versus crizotinib (hazard ratio, 0.18; 95% confidence interval, 0.09-0.36) regardless of whether patients had asymptomatic baseline CNS metastases or a prior history of radiotherapy. For patients with baseline asymptomatic CNS metastases, the 12-month cumulative incidence of CNS progression was 16% with alectinib versus 58.3% with crizotinib. Among patients without asymptomatic CNS metastases at baseline, these rates were 4.6% versus 31.5%, respectively.
The findings “consolidate alectinib as the standard of care for untreated, advanced ALK+ NSCLC, irrespective of the presence or absence of baseline CNS metastases,” Shirish M. Gadgeel, MD, of the University of Michigan, Ann Arbor, and his associates wrote in Annals of Oncology.
ALEX was the first study of an ALK inhibitor to include a prospective, standardized intention-to-treat analysis of CNS lesions, regardless of whether patients had these lesions at baseline. All patients underwent brain imaging at baseline and every 8 weeks thereafter. In the primary analysis of 303 patients, alectinib significantly improved progression-free survival in patients with and without baseline CNS disease and showed a significantly higher intracranial overall response rate, irrespective of whether patients had previously received radiotherapy.
Based on these results, National Comprehensive Cancer Network guidelines were updated to include a category 1 recommendation for the first-line use of alectinib in patients with ALK+ NSCLC.
The current analysis focused on CNS efficacy. In all, 122 patients had CNS metastases at baseline. Progression-free survival was similar regardless of whether patients had these lesions (HR, 0.40; 95% CI, 0.25-0.64) or not (HR, 0.51; 95% CI, 0.33-0.80; P = .36). History of radiotherapy also did not significantly affect overall CNS response or progression-free survival.
“Our data are in agreement with a pooled analysis of alectinib phase 2 trials, which demonstrated that central nervous system efficacy of alectinib is maintained regardless of radiotherapy history in crizotinib-pretreated patients,” the investigators wrote.
Because ALEX excluded patients with symptomatic CNS disease, its effects in this population remain unclear, they noted. “ALEX data strongly suggest that in asymptomatic patients, treating CNS metastases with alectinib alone may result in a reduced or delayed need for local CNS treatment.”
F. Hoffman-La Roche funded the study. Dr. Gadgeel reported honoraria and consultancy fees from Roche/Genentech, ARIAD Pharmaceuticals, AstraZeneca, Bristol-Myers Squibb, and Pfizer.
SOURCE: Gadgeel SM et al. Ann Oncol. 2018 Sep 12. doi: 10.1093/annonc/mdy405.
The results of the phase 3 ALEX trial provide strong rationale for the first-line use of alectinib in patients with non–small cell lung cancer (NSCLC) harboring anaplastic lymphoma kinase (ALK) gene rearrangements.
Alectinib showed robust evidence of intracranial and extracranial efficacy, not only eliciting responses in existing brain metastases but also helping prevent new ones. These results likely translate into significant improvements in quality of life, function, and survival for patients, and reduce the well-documented health economic burden associated with the development of CNS metastases.
Newer-generation ALK inhibitors, such as brigatinib and lorlatinib, also show CNS activity and are currently in phase 3 trials. It will be important to assess their effects on brain metastases to help determine their role in managing patients with ALK-positive NSCLC.
Alesha A. Thai, MD, is with the Peter MacCallum Cancer Centre in Melbourne and Benjamin J. Solomon, MD, is with the University of Melbourne. Dr. Thai disclosed no conflicts of interest. Dr. Solomon disclosed advisory board relationships with Roche-Genentech, Pfizer, Novartis, AstraZeneca, Merck, and Bristol-Myers Squibb. These comments are from their editorial (Ann Oncol. 2018 Sep 18. doi: 10.1093/annonc/mdy415).
The results of the phase 3 ALEX trial provide strong rationale for the first-line use of alectinib in patients with non–small cell lung cancer (NSCLC) harboring anaplastic lymphoma kinase (ALK) gene rearrangements.
Alectinib showed robust evidence of intracranial and extracranial efficacy, not only eliciting responses in existing brain metastases but also helping prevent new ones. These results likely translate into significant improvements in quality of life, function, and survival for patients, and reduce the well-documented health economic burden associated with the development of CNS metastases.
Newer-generation ALK inhibitors, such as brigatinib and lorlatinib, also show CNS activity and are currently in phase 3 trials. It will be important to assess their effects on brain metastases to help determine their role in managing patients with ALK-positive NSCLC.
Alesha A. Thai, MD, is with the Peter MacCallum Cancer Centre in Melbourne and Benjamin J. Solomon, MD, is with the University of Melbourne. Dr. Thai disclosed no conflicts of interest. Dr. Solomon disclosed advisory board relationships with Roche-Genentech, Pfizer, Novartis, AstraZeneca, Merck, and Bristol-Myers Squibb. These comments are from their editorial (Ann Oncol. 2018 Sep 18. doi: 10.1093/annonc/mdy415).
The results of the phase 3 ALEX trial provide strong rationale for the first-line use of alectinib in patients with non–small cell lung cancer (NSCLC) harboring anaplastic lymphoma kinase (ALK) gene rearrangements.
Alectinib showed robust evidence of intracranial and extracranial efficacy, not only eliciting responses in existing brain metastases but also helping prevent new ones. These results likely translate into significant improvements in quality of life, function, and survival for patients, and reduce the well-documented health economic burden associated with the development of CNS metastases.
Newer-generation ALK inhibitors, such as brigatinib and lorlatinib, also show CNS activity and are currently in phase 3 trials. It will be important to assess their effects on brain metastases to help determine their role in managing patients with ALK-positive NSCLC.
Alesha A. Thai, MD, is with the Peter MacCallum Cancer Centre in Melbourne and Benjamin J. Solomon, MD, is with the University of Melbourne. Dr. Thai disclosed no conflicts of interest. Dr. Solomon disclosed advisory board relationships with Roche-Genentech, Pfizer, Novartis, AstraZeneca, Merck, and Bristol-Myers Squibb. These comments are from their editorial (Ann Oncol. 2018 Sep 18. doi: 10.1093/annonc/mdy415).
For patients with treatment-naive anaplastic lymphoma kinase–positive (ALK+) non–small cell lung cancer (NSCLC), twice-daily oral treatment with alectinib (600 mg) was associated with significantly greater activity in the CNS and significantly delayed CNS progression, compared with crizotinib (200 mg), based on secondary analyses from the pivotal phase 3 ALEX trial.
Time to CNS progression was significantly longer with alectinib versus crizotinib (hazard ratio, 0.18; 95% confidence interval, 0.09-0.36) regardless of whether patients had asymptomatic baseline CNS metastases or a prior history of radiotherapy. For patients with baseline asymptomatic CNS metastases, the 12-month cumulative incidence of CNS progression was 16% with alectinib versus 58.3% with crizotinib. Among patients without asymptomatic CNS metastases at baseline, these rates were 4.6% versus 31.5%, respectively.
The findings “consolidate alectinib as the standard of care for untreated, advanced ALK+ NSCLC, irrespective of the presence or absence of baseline CNS metastases,” Shirish M. Gadgeel, MD, of the University of Michigan, Ann Arbor, and his associates wrote in Annals of Oncology.
ALEX was the first study of an ALK inhibitor to include a prospective, standardized intention-to-treat analysis of CNS lesions, regardless of whether patients had these lesions at baseline. All patients underwent brain imaging at baseline and every 8 weeks thereafter. In the primary analysis of 303 patients, alectinib significantly improved progression-free survival in patients with and without baseline CNS disease and showed a significantly higher intracranial overall response rate, irrespective of whether patients had previously received radiotherapy.
Based on these results, National Comprehensive Cancer Network guidelines were updated to include a category 1 recommendation for the first-line use of alectinib in patients with ALK+ NSCLC.
The current analysis focused on CNS efficacy. In all, 122 patients had CNS metastases at baseline. Progression-free survival was similar regardless of whether patients had these lesions (HR, 0.40; 95% CI, 0.25-0.64) or not (HR, 0.51; 95% CI, 0.33-0.80; P = .36). History of radiotherapy also did not significantly affect overall CNS response or progression-free survival.
“Our data are in agreement with a pooled analysis of alectinib phase 2 trials, which demonstrated that central nervous system efficacy of alectinib is maintained regardless of radiotherapy history in crizotinib-pretreated patients,” the investigators wrote.
Because ALEX excluded patients with symptomatic CNS disease, its effects in this population remain unclear, they noted. “ALEX data strongly suggest that in asymptomatic patients, treating CNS metastases with alectinib alone may result in a reduced or delayed need for local CNS treatment.”
F. Hoffman-La Roche funded the study. Dr. Gadgeel reported honoraria and consultancy fees from Roche/Genentech, ARIAD Pharmaceuticals, AstraZeneca, Bristol-Myers Squibb, and Pfizer.
SOURCE: Gadgeel SM et al. Ann Oncol. 2018 Sep 12. doi: 10.1093/annonc/mdy405.
For patients with treatment-naive anaplastic lymphoma kinase–positive (ALK+) non–small cell lung cancer (NSCLC), twice-daily oral treatment with alectinib (600 mg) was associated with significantly greater activity in the CNS and significantly delayed CNS progression, compared with crizotinib (200 mg), based on secondary analyses from the pivotal phase 3 ALEX trial.
Time to CNS progression was significantly longer with alectinib versus crizotinib (hazard ratio, 0.18; 95% confidence interval, 0.09-0.36) regardless of whether patients had asymptomatic baseline CNS metastases or a prior history of radiotherapy. For patients with baseline asymptomatic CNS metastases, the 12-month cumulative incidence of CNS progression was 16% with alectinib versus 58.3% with crizotinib. Among patients without asymptomatic CNS metastases at baseline, these rates were 4.6% versus 31.5%, respectively.
The findings “consolidate alectinib as the standard of care for untreated, advanced ALK+ NSCLC, irrespective of the presence or absence of baseline CNS metastases,” Shirish M. Gadgeel, MD, of the University of Michigan, Ann Arbor, and his associates wrote in Annals of Oncology.
ALEX was the first study of an ALK inhibitor to include a prospective, standardized intention-to-treat analysis of CNS lesions, regardless of whether patients had these lesions at baseline. All patients underwent brain imaging at baseline and every 8 weeks thereafter. In the primary analysis of 303 patients, alectinib significantly improved progression-free survival in patients with and without baseline CNS disease and showed a significantly higher intracranial overall response rate, irrespective of whether patients had previously received radiotherapy.
Based on these results, National Comprehensive Cancer Network guidelines were updated to include a category 1 recommendation for the first-line use of alectinib in patients with ALK+ NSCLC.
The current analysis focused on CNS efficacy. In all, 122 patients had CNS metastases at baseline. Progression-free survival was similar regardless of whether patients had these lesions (HR, 0.40; 95% CI, 0.25-0.64) or not (HR, 0.51; 95% CI, 0.33-0.80; P = .36). History of radiotherapy also did not significantly affect overall CNS response or progression-free survival.
“Our data are in agreement with a pooled analysis of alectinib phase 2 trials, which demonstrated that central nervous system efficacy of alectinib is maintained regardless of radiotherapy history in crizotinib-pretreated patients,” the investigators wrote.
Because ALEX excluded patients with symptomatic CNS disease, its effects in this population remain unclear, they noted. “ALEX data strongly suggest that in asymptomatic patients, treating CNS metastases with alectinib alone may result in a reduced or delayed need for local CNS treatment.”
F. Hoffman-La Roche funded the study. Dr. Gadgeel reported honoraria and consultancy fees from Roche/Genentech, ARIAD Pharmaceuticals, AstraZeneca, Bristol-Myers Squibb, and Pfizer.
SOURCE: Gadgeel SM et al. Ann Oncol. 2018 Sep 12. doi: 10.1093/annonc/mdy405.
FROM ANNALS OF ONCOLOGY
Key clinical point: Alectinib showed superior CNS activity and significantly delayed CNS progression over crizotinib in patients with treatment-naive anaplastic lymphoma kinase–positive non–small cell lung cancer.
Major finding: Time to CNS progression was significantly longer with alectinib versus crizotinib (hazard ratio, 0.18; 95% confidence interval, 0.09-0.36) and was comparable among patients with and without baseline CNS metastases or prior radiotherapy.
Study details: A phase 3 trial of 303 patients receiving alectinib (600 mg) or crizotinib (250 mg) twice daily.
Disclosures: F. Hoffman-La Roche funded the study. Dr. Gadgeel disclosed honoraria and consultancy fees from Roche/Genentech, ARIAD Pharmaceuticals, AstraZeneca, Bristol-Myers Squibb, and Pfizer.
Source: Gadgeel SM et al. Ann Oncol. 2018 Sep 12. doi: 10.1093/annonc/mdy405.