User login
AUGUSTUS: Dual surpasses triple therapy when AFib patients have PCI or ACS
NEW ORLEANS – For patients with atrial fibrillation and either a recent acute coronary syndrome or percutaneous coronary intervention, combined treatment for 6 months with the anticoagulant apixaban and a P2Y12 inhibitor antiplatelet drug, but without aspirin, was safer than and as effective as a regimen that either also included aspirin or that substituted a vitamin K antagonist, such as warfarin, for the direct-acting oral anticoagulant, based on results from a multicenter, randomized trial with more than 4,600 patients.
The apixaban plus P2Y12 inhibitor (typically, clopidogrel) combination “resulted in less bleeding and fewer hospitalizations without significant differences in ischemic events than regimens that included a vitamin K antagonist, aspirin, or both,” Renato D. Lopes, MD, said at the annual meeting of the American College of Cardiology. Concurrently, his report of the results also appeared in an online article.
This finding in the AUGUSTUS trial gives clinicians more guidance for the long-standing dilemma of how to best prevent arterial thrombus formation in patients with atrial fibrillation (AFib). To prevent a stroke, these patients routinely receive treatment with an anticoagulant when they have an acute coronary syndrome (ACS) event or undergo percutaneous coronary intervention (PCI). Typically, they receive several months of dual antiplatelet therapy with aspirin plus a P2Y12 inhibitor to prevent a clot from forming in the stented or unstable region of a coronary artery.
These patients are not uncommon; this circumstance occurs for about 20% of all AFib patients, and poses the question of what is the safest and most effective way to treat them. Should they get triple therapy with an anticoagulant, aspirin, and a P2Y12 inhibitor, an option that could cause excess bleeding; or should one of the three drugs drop out with the potential for an increased rate of ischemic events? The AUGUSTUS findings suggest that one solution is treatment with a combination of the direct-acting oral anticoagulant apixaban (Eliquis) and the P2Y12 inhibitor clopidogrel (Plavix) but without aspirin.
For the majority of patients like the ones enrolled, “less is more.” By dropping aspirin from the treatment mix, patients did better, said Dr. Lopes, a professor of medicine at Duke University in Durham, N.C.
Dr. Lopes and his associates designed AUGUSTUS (A Study of Apixaban in Patients With Atrial Fibrillation, Not Caused by a Heart Valve Problem, Who Are at Risk for Thrombosis [Blood Clots] Due to Having Had a Recent Coronary Event, Such as a Heart Attack or a Procedure to Open the Vessels of the Heart) as a two-by-two factorial study to address two different questions: During 6 months of treatment, how did apixaban compare with a vitamin K antagonist (usually warfarin) in these patients for safety and efficacy, and how did aspirin compare with placebo in this setting for the same endpoints?
The trial enrolled 4,614 patients at 492 sites in 33 countries. All patients in the study received a P2Y12 inhibitor, with 93% treated with clopidogrel. The study had roughly as many patients as the combined total of patients enrolled in two smaller, prior studies that had looked at roughly the same questions in similar patients.
“The aspirin part is the more interesting, and probably more unique and important finding,” John H. Alexander, MD, a coinvestigator on the study, said in a video interview. Regardless of the anticoagulant used, patients who received aspirin had a 16% rate of major bleeds or clinically relevant non-major bleeds, compared with a 9% rate among those on placebo, a statistically significant result that underscored the bleeding risk posed by adding aspirin to an anticoagulant and a P2Y12 inhibitor.
The results also showed no statistically significant difference in any efficacy measure with or without aspirin, including the rate of death or hospitalization, or of any individual ischemic endpoint. However the results showed a signal of a small increase in the rates of each of three types of ischemic events – stent thrombosis, MI, and need for urgent revascularization, each of which showed a numerical increase when aspirin was dropped. But the increase was small.
Dr. Lopes calculated that, for example, to prevent one episode of stent thrombosis by treating with aspirin also would cause 15 major or clinically relevant non-major bleeds, which makes inclusion of aspirin something of a judgment call for each patient, said Dr. Alexander, a professor of medicine at Duke. An AFib patient with a high risk for thrombosis but a low risk for bleeding following PCI or an ACS event might be a reasonable patient to treat with aspirin along with apixaban and a P2Y12 inhibitor, he explained.
The rate of major or clinically relevant bleeds was 11% with apixaban and 15% with a vitamin K antagonist, a statistically significant difference. Patients treated with apixaban also had a significantly reduced rate of death or hospitalization, 24%, compared with 27% among those on the vitamin K antagonist, as well as a significantly lower rate of stroke.
Overall the lowest bleeding rate was in patients on apixaban but no aspirin, a 7% rate, while the highest rate was in patients on a vitamin K antagonist plus aspirin, a 19% rate.
Dr. Alexander said that it would be an overreach to extrapolate these findings to other direct-acting oral anticoagulants, compared with a vitamin K antagonist, but he believed that the findings the study generated about aspirin were probably relevant regardless of the anticoagulant used.
[email protected]
On Twitter @mitchelzoler
It’s very reassuring to see that you can use a direct-acting oral anticoagulant like apixaban along with a P2Y12 inhibitor, but with no aspirin, and have no statistically significant increase in ischemic events. This is a fantastic finding. The finding shows once again that warfarin is a problematic drug. As the cost for direct-acting oral anticoagulants has decreased, their use has increased.
These results were not unexpected and also are probably the final nail in the coffin for using a combination of warfarin and aspirin. Prior findings from the PIONEER AF-PCI study that used rivaroxaban (N Engl J Med. 2016 Dec 22;375[25]:2423-34) and from the RE-DUAL PCI study that used dabigatran (N Engl J Med. 2017 Oct 19;377[16]:1513-24) also showed the advantages of using a direct-acting oral anticoagulant when compared with a vitamin K antagonist in this setting, The AUGUSTUS trial, with just over 4,600 patients, had nearly as many patients as the roughly 4,850 enrolled in these two prior studies put together.
Dhanunjaya Lakkireddy, MD , is medical director of the Kansas City Heart Rhythm Institute in Overland Park. He had no disclosures. He made these comments as the designated discussant during a press briefing.
It’s very reassuring to see that you can use a direct-acting oral anticoagulant like apixaban along with a P2Y12 inhibitor, but with no aspirin, and have no statistically significant increase in ischemic events. This is a fantastic finding. The finding shows once again that warfarin is a problematic drug. As the cost for direct-acting oral anticoagulants has decreased, their use has increased.
These results were not unexpected and also are probably the final nail in the coffin for using a combination of warfarin and aspirin. Prior findings from the PIONEER AF-PCI study that used rivaroxaban (N Engl J Med. 2016 Dec 22;375[25]:2423-34) and from the RE-DUAL PCI study that used dabigatran (N Engl J Med. 2017 Oct 19;377[16]:1513-24) also showed the advantages of using a direct-acting oral anticoagulant when compared with a vitamin K antagonist in this setting, The AUGUSTUS trial, with just over 4,600 patients, had nearly as many patients as the roughly 4,850 enrolled in these two prior studies put together.
Dhanunjaya Lakkireddy, MD , is medical director of the Kansas City Heart Rhythm Institute in Overland Park. He had no disclosures. He made these comments as the designated discussant during a press briefing.
It’s very reassuring to see that you can use a direct-acting oral anticoagulant like apixaban along with a P2Y12 inhibitor, but with no aspirin, and have no statistically significant increase in ischemic events. This is a fantastic finding. The finding shows once again that warfarin is a problematic drug. As the cost for direct-acting oral anticoagulants has decreased, their use has increased.
These results were not unexpected and also are probably the final nail in the coffin for using a combination of warfarin and aspirin. Prior findings from the PIONEER AF-PCI study that used rivaroxaban (N Engl J Med. 2016 Dec 22;375[25]:2423-34) and from the RE-DUAL PCI study that used dabigatran (N Engl J Med. 2017 Oct 19;377[16]:1513-24) also showed the advantages of using a direct-acting oral anticoagulant when compared with a vitamin K antagonist in this setting, The AUGUSTUS trial, with just over 4,600 patients, had nearly as many patients as the roughly 4,850 enrolled in these two prior studies put together.
Dhanunjaya Lakkireddy, MD , is medical director of the Kansas City Heart Rhythm Institute in Overland Park. He had no disclosures. He made these comments as the designated discussant during a press briefing.
NEW ORLEANS – For patients with atrial fibrillation and either a recent acute coronary syndrome or percutaneous coronary intervention, combined treatment for 6 months with the anticoagulant apixaban and a P2Y12 inhibitor antiplatelet drug, but without aspirin, was safer than and as effective as a regimen that either also included aspirin or that substituted a vitamin K antagonist, such as warfarin, for the direct-acting oral anticoagulant, based on results from a multicenter, randomized trial with more than 4,600 patients.
The apixaban plus P2Y12 inhibitor (typically, clopidogrel) combination “resulted in less bleeding and fewer hospitalizations without significant differences in ischemic events than regimens that included a vitamin K antagonist, aspirin, or both,” Renato D. Lopes, MD, said at the annual meeting of the American College of Cardiology. Concurrently, his report of the results also appeared in an online article.
This finding in the AUGUSTUS trial gives clinicians more guidance for the long-standing dilemma of how to best prevent arterial thrombus formation in patients with atrial fibrillation (AFib). To prevent a stroke, these patients routinely receive treatment with an anticoagulant when they have an acute coronary syndrome (ACS) event or undergo percutaneous coronary intervention (PCI). Typically, they receive several months of dual antiplatelet therapy with aspirin plus a P2Y12 inhibitor to prevent a clot from forming in the stented or unstable region of a coronary artery.
These patients are not uncommon; this circumstance occurs for about 20% of all AFib patients, and poses the question of what is the safest and most effective way to treat them. Should they get triple therapy with an anticoagulant, aspirin, and a P2Y12 inhibitor, an option that could cause excess bleeding; or should one of the three drugs drop out with the potential for an increased rate of ischemic events? The AUGUSTUS findings suggest that one solution is treatment with a combination of the direct-acting oral anticoagulant apixaban (Eliquis) and the P2Y12 inhibitor clopidogrel (Plavix) but without aspirin.
For the majority of patients like the ones enrolled, “less is more.” By dropping aspirin from the treatment mix, patients did better, said Dr. Lopes, a professor of medicine at Duke University in Durham, N.C.
Dr. Lopes and his associates designed AUGUSTUS (A Study of Apixaban in Patients With Atrial Fibrillation, Not Caused by a Heart Valve Problem, Who Are at Risk for Thrombosis [Blood Clots] Due to Having Had a Recent Coronary Event, Such as a Heart Attack or a Procedure to Open the Vessels of the Heart) as a two-by-two factorial study to address two different questions: During 6 months of treatment, how did apixaban compare with a vitamin K antagonist (usually warfarin) in these patients for safety and efficacy, and how did aspirin compare with placebo in this setting for the same endpoints?
The trial enrolled 4,614 patients at 492 sites in 33 countries. All patients in the study received a P2Y12 inhibitor, with 93% treated with clopidogrel. The study had roughly as many patients as the combined total of patients enrolled in two smaller, prior studies that had looked at roughly the same questions in similar patients.
“The aspirin part is the more interesting, and probably more unique and important finding,” John H. Alexander, MD, a coinvestigator on the study, said in a video interview. Regardless of the anticoagulant used, patients who received aspirin had a 16% rate of major bleeds or clinically relevant non-major bleeds, compared with a 9% rate among those on placebo, a statistically significant result that underscored the bleeding risk posed by adding aspirin to an anticoagulant and a P2Y12 inhibitor.
The results also showed no statistically significant difference in any efficacy measure with or without aspirin, including the rate of death or hospitalization, or of any individual ischemic endpoint. However the results showed a signal of a small increase in the rates of each of three types of ischemic events – stent thrombosis, MI, and need for urgent revascularization, each of which showed a numerical increase when aspirin was dropped. But the increase was small.
Dr. Lopes calculated that, for example, to prevent one episode of stent thrombosis by treating with aspirin also would cause 15 major or clinically relevant non-major bleeds, which makes inclusion of aspirin something of a judgment call for each patient, said Dr. Alexander, a professor of medicine at Duke. An AFib patient with a high risk for thrombosis but a low risk for bleeding following PCI or an ACS event might be a reasonable patient to treat with aspirin along with apixaban and a P2Y12 inhibitor, he explained.
The rate of major or clinically relevant bleeds was 11% with apixaban and 15% with a vitamin K antagonist, a statistically significant difference. Patients treated with apixaban also had a significantly reduced rate of death or hospitalization, 24%, compared with 27% among those on the vitamin K antagonist, as well as a significantly lower rate of stroke.
Overall the lowest bleeding rate was in patients on apixaban but no aspirin, a 7% rate, while the highest rate was in patients on a vitamin K antagonist plus aspirin, a 19% rate.
Dr. Alexander said that it would be an overreach to extrapolate these findings to other direct-acting oral anticoagulants, compared with a vitamin K antagonist, but he believed that the findings the study generated about aspirin were probably relevant regardless of the anticoagulant used.
[email protected]
On Twitter @mitchelzoler
NEW ORLEANS – For patients with atrial fibrillation and either a recent acute coronary syndrome or percutaneous coronary intervention, combined treatment for 6 months with the anticoagulant apixaban and a P2Y12 inhibitor antiplatelet drug, but without aspirin, was safer than and as effective as a regimen that either also included aspirin or that substituted a vitamin K antagonist, such as warfarin, for the direct-acting oral anticoagulant, based on results from a multicenter, randomized trial with more than 4,600 patients.
The apixaban plus P2Y12 inhibitor (typically, clopidogrel) combination “resulted in less bleeding and fewer hospitalizations without significant differences in ischemic events than regimens that included a vitamin K antagonist, aspirin, or both,” Renato D. Lopes, MD, said at the annual meeting of the American College of Cardiology. Concurrently, his report of the results also appeared in an online article.
This finding in the AUGUSTUS trial gives clinicians more guidance for the long-standing dilemma of how to best prevent arterial thrombus formation in patients with atrial fibrillation (AFib). To prevent a stroke, these patients routinely receive treatment with an anticoagulant when they have an acute coronary syndrome (ACS) event or undergo percutaneous coronary intervention (PCI). Typically, they receive several months of dual antiplatelet therapy with aspirin plus a P2Y12 inhibitor to prevent a clot from forming in the stented or unstable region of a coronary artery.
These patients are not uncommon; this circumstance occurs for about 20% of all AFib patients, and poses the question of what is the safest and most effective way to treat them. Should they get triple therapy with an anticoagulant, aspirin, and a P2Y12 inhibitor, an option that could cause excess bleeding; or should one of the three drugs drop out with the potential for an increased rate of ischemic events? The AUGUSTUS findings suggest that one solution is treatment with a combination of the direct-acting oral anticoagulant apixaban (Eliquis) and the P2Y12 inhibitor clopidogrel (Plavix) but without aspirin.
For the majority of patients like the ones enrolled, “less is more.” By dropping aspirin from the treatment mix, patients did better, said Dr. Lopes, a professor of medicine at Duke University in Durham, N.C.
Dr. Lopes and his associates designed AUGUSTUS (A Study of Apixaban in Patients With Atrial Fibrillation, Not Caused by a Heart Valve Problem, Who Are at Risk for Thrombosis [Blood Clots] Due to Having Had a Recent Coronary Event, Such as a Heart Attack or a Procedure to Open the Vessels of the Heart) as a two-by-two factorial study to address two different questions: During 6 months of treatment, how did apixaban compare with a vitamin K antagonist (usually warfarin) in these patients for safety and efficacy, and how did aspirin compare with placebo in this setting for the same endpoints?
The trial enrolled 4,614 patients at 492 sites in 33 countries. All patients in the study received a P2Y12 inhibitor, with 93% treated with clopidogrel. The study had roughly as many patients as the combined total of patients enrolled in two smaller, prior studies that had looked at roughly the same questions in similar patients.
“The aspirin part is the more interesting, and probably more unique and important finding,” John H. Alexander, MD, a coinvestigator on the study, said in a video interview. Regardless of the anticoagulant used, patients who received aspirin had a 16% rate of major bleeds or clinically relevant non-major bleeds, compared with a 9% rate among those on placebo, a statistically significant result that underscored the bleeding risk posed by adding aspirin to an anticoagulant and a P2Y12 inhibitor.
The results also showed no statistically significant difference in any efficacy measure with or without aspirin, including the rate of death or hospitalization, or of any individual ischemic endpoint. However the results showed a signal of a small increase in the rates of each of three types of ischemic events – stent thrombosis, MI, and need for urgent revascularization, each of which showed a numerical increase when aspirin was dropped. But the increase was small.
Dr. Lopes calculated that, for example, to prevent one episode of stent thrombosis by treating with aspirin also would cause 15 major or clinically relevant non-major bleeds, which makes inclusion of aspirin something of a judgment call for each patient, said Dr. Alexander, a professor of medicine at Duke. An AFib patient with a high risk for thrombosis but a low risk for bleeding following PCI or an ACS event might be a reasonable patient to treat with aspirin along with apixaban and a P2Y12 inhibitor, he explained.
The rate of major or clinically relevant bleeds was 11% with apixaban and 15% with a vitamin K antagonist, a statistically significant difference. Patients treated with apixaban also had a significantly reduced rate of death or hospitalization, 24%, compared with 27% among those on the vitamin K antagonist, as well as a significantly lower rate of stroke.
Overall the lowest bleeding rate was in patients on apixaban but no aspirin, a 7% rate, while the highest rate was in patients on a vitamin K antagonist plus aspirin, a 19% rate.
Dr. Alexander said that it would be an overreach to extrapolate these findings to other direct-acting oral anticoagulants, compared with a vitamin K antagonist, but he believed that the findings the study generated about aspirin were probably relevant regardless of the anticoagulant used.
[email protected]
On Twitter @mitchelzoler
REPORTING FROM ACC 19
Improving research dissemination among hospitalists
Social media a great platform
Medical journals and societies are trying to figure out ways to use social media to connect with hospitalists and others interested in their subject matter, says Charlie Wray, DO, MS, lead author of a paper proposing a way they can do that: implementing a journal-sponsored club on Twitter.
“At the Journal of Hospital Medicine (JHM), we noticed that there was a large community of hospitalists on Twitter who were looking for a community to engage in hospital medicine topics,” Dr. Wray said. “We created #JHMChat to bring the hospital medicine community together on a regular basis to talk about pertinent research, medical education philosophies, and value-based care interventions. Our ultimate goal was to increase engagement, networking, and communication among this community, while highlighting the work that is being published in JHM.”
A study of #JHMChat showed that social media is a great platform for large organizations to reach out, connect, and create a community around, he added. “We were very surprised by both the Twitter metrics (i.e., number of participants and overall impressions), which showed very large dissemination numbers, in addition to the external dissemination metrics (i.e., page views and altmetrics scores), which showed that each chat basically corresponded to a release of a new issue. This could be informative to other journals as they look for ways to increase their web traffic or disseminate their work to their respective audiences.”
Dr. Wray hopes the study alerts hospitalists to the fact that there is a large and ever-growing community available within social media.
“Second, we know that careers in hospital medicine can be tough, regardless of whether you’re at a community hospital or a large academic center. Knowing that there is a community with which you can connect to is both comforting and reassuring.”
Reference
Wray C et al. The adoption of an online journal club to improve research dissemination and social media engagement among hospitalists. J Hosp Med. 2018 Nov;13(11):764-9.
Social media a great platform
Social media a great platform
Medical journals and societies are trying to figure out ways to use social media to connect with hospitalists and others interested in their subject matter, says Charlie Wray, DO, MS, lead author of a paper proposing a way they can do that: implementing a journal-sponsored club on Twitter.
“At the Journal of Hospital Medicine (JHM), we noticed that there was a large community of hospitalists on Twitter who were looking for a community to engage in hospital medicine topics,” Dr. Wray said. “We created #JHMChat to bring the hospital medicine community together on a regular basis to talk about pertinent research, medical education philosophies, and value-based care interventions. Our ultimate goal was to increase engagement, networking, and communication among this community, while highlighting the work that is being published in JHM.”
A study of #JHMChat showed that social media is a great platform for large organizations to reach out, connect, and create a community around, he added. “We were very surprised by both the Twitter metrics (i.e., number of participants and overall impressions), which showed very large dissemination numbers, in addition to the external dissemination metrics (i.e., page views and altmetrics scores), which showed that each chat basically corresponded to a release of a new issue. This could be informative to other journals as they look for ways to increase their web traffic or disseminate their work to their respective audiences.”
Dr. Wray hopes the study alerts hospitalists to the fact that there is a large and ever-growing community available within social media.
“Second, we know that careers in hospital medicine can be tough, regardless of whether you’re at a community hospital or a large academic center. Knowing that there is a community with which you can connect to is both comforting and reassuring.”
Reference
Wray C et al. The adoption of an online journal club to improve research dissemination and social media engagement among hospitalists. J Hosp Med. 2018 Nov;13(11):764-9.
Medical journals and societies are trying to figure out ways to use social media to connect with hospitalists and others interested in their subject matter, says Charlie Wray, DO, MS, lead author of a paper proposing a way they can do that: implementing a journal-sponsored club on Twitter.
“At the Journal of Hospital Medicine (JHM), we noticed that there was a large community of hospitalists on Twitter who were looking for a community to engage in hospital medicine topics,” Dr. Wray said. “We created #JHMChat to bring the hospital medicine community together on a regular basis to talk about pertinent research, medical education philosophies, and value-based care interventions. Our ultimate goal was to increase engagement, networking, and communication among this community, while highlighting the work that is being published in JHM.”
A study of #JHMChat showed that social media is a great platform for large organizations to reach out, connect, and create a community around, he added. “We were very surprised by both the Twitter metrics (i.e., number of participants and overall impressions), which showed very large dissemination numbers, in addition to the external dissemination metrics (i.e., page views and altmetrics scores), which showed that each chat basically corresponded to a release of a new issue. This could be informative to other journals as they look for ways to increase their web traffic or disseminate their work to their respective audiences.”
Dr. Wray hopes the study alerts hospitalists to the fact that there is a large and ever-growing community available within social media.
“Second, we know that careers in hospital medicine can be tough, regardless of whether you’re at a community hospital or a large academic center. Knowing that there is a community with which you can connect to is both comforting and reassuring.”
Reference
Wray C et al. The adoption of an online journal club to improve research dissemination and social media engagement among hospitalists. J Hosp Med. 2018 Nov;13(11):764-9.
Triplet appears safe, effective for gynecologic cancers
HONOLULU – Pembrolizumab plus bevacizumab and oral metronomic cyclophosphamide can be effective in patients with recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer, a phase 2 trial suggests.
The tumor response rate observed with the three-drug regimen (40%) was better than response rates previously reported for pembrolizumab monotherapy (8%) and bevacizumab plus cyclophosphamide (24%), according to Emese Zsiros, MD, PhD, of Roswell Park Comprehensive Cancer Center in Buffalo, N.Y.
The combination proved “very safe” and was associated with “excellent quality of life,” she said at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer.
Dr. Zsiros and her colleagues enrolled 40 patients on a phase 2 trial (NCT02853318) of pembrolizumab, bevacizumab, and oral cyclophosphamide in recurrent, advanced-stage epithelial ovarian, fallopian tube, or primary peritoneal cancer. The trial had a safety lead-in cohort of five patients.
At baseline, the mean patient age was 62.2 years (range, 44.9-88.7 years). Most patients (82.5%, n = 33) had high-grade serous histology. The patients had received a mean of 3.2 (range, 1-12) prior lines of chemotherapy. Most patients (75%, n = 30) were platinum resistant, but 10 patients (25%) were platinum sensitive and declined platinum-based therapy.
Study treatment consisted of IV pembrolizumab at 200 mg plus IV bevacizumab at 15 mg/kg every 3 weeks and oral cyclophosphamide at 50 mg every day. Patients were treated until disease progression or unacceptable toxicity.
Results
“The triple regimen was, overall, really well tolerated,” Dr. Zsiros said.
The most common grade 1/2 treatment-related adverse events (AEs) were fatigue (n = 14), diarrhea (n = 13), nausea (n = 9), hypertension (n =7), white blood cell decrease (n = 6), and arthralgia (n = 6).
Grade 3 related AEs included hypertension (n = 5), lymphocyte count decrease (n = 3), and white blood cell decrease (n = 1). There was one grade 4 drug-related AE of decreased lymphocyte count.
The overall response rate was 40%, with all 16 responders having a partial response. The rate of stable disease was 55% (n = 22).
“Only 2 patients out of the 40 progressed after initiation of the treatment, and I would like to point out that both of these patients had a very large disease burden,” Dr. Zsiros said.
She also noted that more than 77% of patients had a decrease in tumor size from baseline.
The disease control rate (partial response plus stable disease) was 95.0% (n = 38) initially and 62.5% (n = 25) at 6 months. However, three patients had not yet reached 6 months follow-up at the data cutoff.
“I would like to point out that 30% of the patients [n = 12] derived an especially long-term clinical benefit over 12 months and 12 cycles of treatment,” Dr. Zsiros said.
She added that quality of life assessment revealed “high physical, emotional, cognitive, and social functioning throughout the clinical trial.” The researchers also observed significantly improved body image from baseline (P less than .002).
Dr. Zsiros reported relationships with Iovance Biotherapeutics and AstraZeneca. The trial was sponsored by Roswell Park Cancer Institute in collaboration with the National Cancer Institute.
SOURCE: Zsiros E et al. SGO 2019, Abstract LBA4.
HONOLULU – Pembrolizumab plus bevacizumab and oral metronomic cyclophosphamide can be effective in patients with recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer, a phase 2 trial suggests.
The tumor response rate observed with the three-drug regimen (40%) was better than response rates previously reported for pembrolizumab monotherapy (8%) and bevacizumab plus cyclophosphamide (24%), according to Emese Zsiros, MD, PhD, of Roswell Park Comprehensive Cancer Center in Buffalo, N.Y.
The combination proved “very safe” and was associated with “excellent quality of life,” she said at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer.
Dr. Zsiros and her colleagues enrolled 40 patients on a phase 2 trial (NCT02853318) of pembrolizumab, bevacizumab, and oral cyclophosphamide in recurrent, advanced-stage epithelial ovarian, fallopian tube, or primary peritoneal cancer. The trial had a safety lead-in cohort of five patients.
At baseline, the mean patient age was 62.2 years (range, 44.9-88.7 years). Most patients (82.5%, n = 33) had high-grade serous histology. The patients had received a mean of 3.2 (range, 1-12) prior lines of chemotherapy. Most patients (75%, n = 30) were platinum resistant, but 10 patients (25%) were platinum sensitive and declined platinum-based therapy.
Study treatment consisted of IV pembrolizumab at 200 mg plus IV bevacizumab at 15 mg/kg every 3 weeks and oral cyclophosphamide at 50 mg every day. Patients were treated until disease progression or unacceptable toxicity.
Results
“The triple regimen was, overall, really well tolerated,” Dr. Zsiros said.
The most common grade 1/2 treatment-related adverse events (AEs) were fatigue (n = 14), diarrhea (n = 13), nausea (n = 9), hypertension (n =7), white blood cell decrease (n = 6), and arthralgia (n = 6).
Grade 3 related AEs included hypertension (n = 5), lymphocyte count decrease (n = 3), and white blood cell decrease (n = 1). There was one grade 4 drug-related AE of decreased lymphocyte count.
The overall response rate was 40%, with all 16 responders having a partial response. The rate of stable disease was 55% (n = 22).
“Only 2 patients out of the 40 progressed after initiation of the treatment, and I would like to point out that both of these patients had a very large disease burden,” Dr. Zsiros said.
She also noted that more than 77% of patients had a decrease in tumor size from baseline.
The disease control rate (partial response plus stable disease) was 95.0% (n = 38) initially and 62.5% (n = 25) at 6 months. However, three patients had not yet reached 6 months follow-up at the data cutoff.
“I would like to point out that 30% of the patients [n = 12] derived an especially long-term clinical benefit over 12 months and 12 cycles of treatment,” Dr. Zsiros said.
She added that quality of life assessment revealed “high physical, emotional, cognitive, and social functioning throughout the clinical trial.” The researchers also observed significantly improved body image from baseline (P less than .002).
Dr. Zsiros reported relationships with Iovance Biotherapeutics and AstraZeneca. The trial was sponsored by Roswell Park Cancer Institute in collaboration with the National Cancer Institute.
SOURCE: Zsiros E et al. SGO 2019, Abstract LBA4.
HONOLULU – Pembrolizumab plus bevacizumab and oral metronomic cyclophosphamide can be effective in patients with recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer, a phase 2 trial suggests.
The tumor response rate observed with the three-drug regimen (40%) was better than response rates previously reported for pembrolizumab monotherapy (8%) and bevacizumab plus cyclophosphamide (24%), according to Emese Zsiros, MD, PhD, of Roswell Park Comprehensive Cancer Center in Buffalo, N.Y.
The combination proved “very safe” and was associated with “excellent quality of life,” she said at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer.
Dr. Zsiros and her colleagues enrolled 40 patients on a phase 2 trial (NCT02853318) of pembrolizumab, bevacizumab, and oral cyclophosphamide in recurrent, advanced-stage epithelial ovarian, fallopian tube, or primary peritoneal cancer. The trial had a safety lead-in cohort of five patients.
At baseline, the mean patient age was 62.2 years (range, 44.9-88.7 years). Most patients (82.5%, n = 33) had high-grade serous histology. The patients had received a mean of 3.2 (range, 1-12) prior lines of chemotherapy. Most patients (75%, n = 30) were platinum resistant, but 10 patients (25%) were platinum sensitive and declined platinum-based therapy.
Study treatment consisted of IV pembrolizumab at 200 mg plus IV bevacizumab at 15 mg/kg every 3 weeks and oral cyclophosphamide at 50 mg every day. Patients were treated until disease progression or unacceptable toxicity.
Results
“The triple regimen was, overall, really well tolerated,” Dr. Zsiros said.
The most common grade 1/2 treatment-related adverse events (AEs) were fatigue (n = 14), diarrhea (n = 13), nausea (n = 9), hypertension (n =7), white blood cell decrease (n = 6), and arthralgia (n = 6).
Grade 3 related AEs included hypertension (n = 5), lymphocyte count decrease (n = 3), and white blood cell decrease (n = 1). There was one grade 4 drug-related AE of decreased lymphocyte count.
The overall response rate was 40%, with all 16 responders having a partial response. The rate of stable disease was 55% (n = 22).
“Only 2 patients out of the 40 progressed after initiation of the treatment, and I would like to point out that both of these patients had a very large disease burden,” Dr. Zsiros said.
She also noted that more than 77% of patients had a decrease in tumor size from baseline.
The disease control rate (partial response plus stable disease) was 95.0% (n = 38) initially and 62.5% (n = 25) at 6 months. However, three patients had not yet reached 6 months follow-up at the data cutoff.
“I would like to point out that 30% of the patients [n = 12] derived an especially long-term clinical benefit over 12 months and 12 cycles of treatment,” Dr. Zsiros said.
She added that quality of life assessment revealed “high physical, emotional, cognitive, and social functioning throughout the clinical trial.” The researchers also observed significantly improved body image from baseline (P less than .002).
Dr. Zsiros reported relationships with Iovance Biotherapeutics and AstraZeneca. The trial was sponsored by Roswell Park Cancer Institute in collaboration with the National Cancer Institute.
SOURCE: Zsiros E et al. SGO 2019, Abstract LBA4.
REPORTING FROM SGO 2019
Long-term metformin offsets diabetes in patients with higher glucose/HbA1c, history of gestational diabetes
Metformin is especially effective in diabetes prevention among persons with higher baseline fasting glucose, higher hemoglobin A1c (HbA1c), or a history of gestational diabetes, based on 15-year follow-up results from the Diabetes Prevention Program and the Diabetes Prevention Program Outcomes Study.
Beyond those subgroups, metformin remained effective regardless of how diabetes was diagnosed, with a risk reduction of up to 36%, according to a report published in Diabetes Care.
“These results should help to prioritize those groups at high risk of developing diabetes who will benefit most from being treated with metformin,” said the report’s writing committee, chaired by David M. Nathan, MD, professor of medicine at Harvard Medical School, Boston.
However, the link between higher HbA1c and better efficacy of metformin should be “considered carefully,” according to Dr. Nathan and his cocommittee members, who noted that the original criteria for the Diabetes Prevention Program study were based on glucose level, rather than HbA1c level.
Initial results of the Diabetes Prevention Program study indicated a particular benefit of metformin after an average of 2.8 years of follow-up in individuals with higher baseline fasting glucose levels and in women with a self-reported history of gestational diabetes (N Engl J Med. 2002 Feb 7;346[6]:393-403).
Those results prompted the American Diabetes Association and others to recommend consideration of metformin for diabetes prevention in individuals considered to be at high risk, Dr. Nathan and his colleagues noted. “This recommendation is further supported by the demonstrated cost savings of metformin in diabetes prevention.”
The Diabetes Prevention Program study originally included 3,234 high-risk participants enrolled between 1996 and 1999 and randomized to masked metformin, placebo, or intensive lifestyle intervention. The 15-year follow-up analysis considered the 2,155 individuals randomized to the metformin or placebo groups, of whom 1,861 (86%) chose to continue in the Diabetes Prevention Program Outcomes Study, in which they continued to receive metformin unmasked.
Over the 15 years, the incidence of diabetes development based on fasting or 2-hour glucose results was 17% lower in the metformin group, compared with the placebo group (hazard ratio, 0.83; or –1.25 cases per 100 person-years), according to Dr. Nathan and his colleagues.
For diabetes development based on HbA1c level, metformin was linked to a 36% reduction in risk, compared with placebo, or –1.67 cases per 100 person-years.
Higher baseline fasting plasma glucose (110-125 mg/dL vs. 95-109 mg/dL) was associated with a greater effect of metformin in reducing diabetes development over 15 years (P = .0004).
Metformin’s effect in reducing diabetes development was “nearly identical” in participants with an HbA1c of 6.0%-6.4%, compared with less than 6.0%, with HRs of 0.63 and 0.61, respectively; however, looking at rate differences, there was “substantial heterogeneity” between the groups, at –3.88 and –1.03 cases per 100 person-years, respectively, the investigators wrote.
For women with a history of gestational diabetes, metformin was linked to a 41% reduction in diabetes development, compared with placebo (P = .03); in women without gestational diabetes, the difference was a nonsignificant 6% reduction, compared with placebo. In terms of risk differences, this translated into a reduction of 4.57 cases per 100 person-years in women with gestational diabetes, compared with a reduction of just 0.38 cases in women without such a history. The authors noted that it is “complicated” to determine whether greater credence be given to the results based on glucose or those based on HbA1c.
On the one hand, the generalizability of the HbA1c analyses is adversely affected because the analyses were performed post hoc on a set of participants who had initially been selected for the study based on prediabetes defined by glucose. On the other, the HbA1c results may be more clinically relevant because “in many countries, oral glucose tolerance tests are not used routinely for the identification of persons at high risk for diabetes or with diabetes,” the authors wrote.
Continued follow-up of these patients will provide additional data on the potential long-term benefits of metformin use, such as the incidence of cardiovascular disease, cancer, and microvascular disease, the investigators concluded.
The National Institute of Diabetes and Digestive and Kidney Diseases and Department of Veterans Affairs, among others, funded the Diabetes Prevention Program and subsequent outcomes study. Lipha provided medication and LifeScan donated materials during the studies. Additional funding to the Diabetes Prevention Program was provided by Bristol-Myers Squibb and Parke-Davis.
SOURCE: Nathan DM et al. Diabetes Care. 2019 Mar 15. doi: 10.2337/dc18-1970.
Metformin is especially effective in diabetes prevention among persons with higher baseline fasting glucose, higher hemoglobin A1c (HbA1c), or a history of gestational diabetes, based on 15-year follow-up results from the Diabetes Prevention Program and the Diabetes Prevention Program Outcomes Study.
Beyond those subgroups, metformin remained effective regardless of how diabetes was diagnosed, with a risk reduction of up to 36%, according to a report published in Diabetes Care.
“These results should help to prioritize those groups at high risk of developing diabetes who will benefit most from being treated with metformin,” said the report’s writing committee, chaired by David M. Nathan, MD, professor of medicine at Harvard Medical School, Boston.
However, the link between higher HbA1c and better efficacy of metformin should be “considered carefully,” according to Dr. Nathan and his cocommittee members, who noted that the original criteria for the Diabetes Prevention Program study were based on glucose level, rather than HbA1c level.
Initial results of the Diabetes Prevention Program study indicated a particular benefit of metformin after an average of 2.8 years of follow-up in individuals with higher baseline fasting glucose levels and in women with a self-reported history of gestational diabetes (N Engl J Med. 2002 Feb 7;346[6]:393-403).
Those results prompted the American Diabetes Association and others to recommend consideration of metformin for diabetes prevention in individuals considered to be at high risk, Dr. Nathan and his colleagues noted. “This recommendation is further supported by the demonstrated cost savings of metformin in diabetes prevention.”
The Diabetes Prevention Program study originally included 3,234 high-risk participants enrolled between 1996 and 1999 and randomized to masked metformin, placebo, or intensive lifestyle intervention. The 15-year follow-up analysis considered the 2,155 individuals randomized to the metformin or placebo groups, of whom 1,861 (86%) chose to continue in the Diabetes Prevention Program Outcomes Study, in which they continued to receive metformin unmasked.
Over the 15 years, the incidence of diabetes development based on fasting or 2-hour glucose results was 17% lower in the metformin group, compared with the placebo group (hazard ratio, 0.83; or –1.25 cases per 100 person-years), according to Dr. Nathan and his colleagues.
For diabetes development based on HbA1c level, metformin was linked to a 36% reduction in risk, compared with placebo, or –1.67 cases per 100 person-years.
Higher baseline fasting plasma glucose (110-125 mg/dL vs. 95-109 mg/dL) was associated with a greater effect of metformin in reducing diabetes development over 15 years (P = .0004).
Metformin’s effect in reducing diabetes development was “nearly identical” in participants with an HbA1c of 6.0%-6.4%, compared with less than 6.0%, with HRs of 0.63 and 0.61, respectively; however, looking at rate differences, there was “substantial heterogeneity” between the groups, at –3.88 and –1.03 cases per 100 person-years, respectively, the investigators wrote.
For women with a history of gestational diabetes, metformin was linked to a 41% reduction in diabetes development, compared with placebo (P = .03); in women without gestational diabetes, the difference was a nonsignificant 6% reduction, compared with placebo. In terms of risk differences, this translated into a reduction of 4.57 cases per 100 person-years in women with gestational diabetes, compared with a reduction of just 0.38 cases in women without such a history. The authors noted that it is “complicated” to determine whether greater credence be given to the results based on glucose or those based on HbA1c.
On the one hand, the generalizability of the HbA1c analyses is adversely affected because the analyses were performed post hoc on a set of participants who had initially been selected for the study based on prediabetes defined by glucose. On the other, the HbA1c results may be more clinically relevant because “in many countries, oral glucose tolerance tests are not used routinely for the identification of persons at high risk for diabetes or with diabetes,” the authors wrote.
Continued follow-up of these patients will provide additional data on the potential long-term benefits of metformin use, such as the incidence of cardiovascular disease, cancer, and microvascular disease, the investigators concluded.
The National Institute of Diabetes and Digestive and Kidney Diseases and Department of Veterans Affairs, among others, funded the Diabetes Prevention Program and subsequent outcomes study. Lipha provided medication and LifeScan donated materials during the studies. Additional funding to the Diabetes Prevention Program was provided by Bristol-Myers Squibb and Parke-Davis.
SOURCE: Nathan DM et al. Diabetes Care. 2019 Mar 15. doi: 10.2337/dc18-1970.
Metformin is especially effective in diabetes prevention among persons with higher baseline fasting glucose, higher hemoglobin A1c (HbA1c), or a history of gestational diabetes, based on 15-year follow-up results from the Diabetes Prevention Program and the Diabetes Prevention Program Outcomes Study.
Beyond those subgroups, metformin remained effective regardless of how diabetes was diagnosed, with a risk reduction of up to 36%, according to a report published in Diabetes Care.
“These results should help to prioritize those groups at high risk of developing diabetes who will benefit most from being treated with metformin,” said the report’s writing committee, chaired by David M. Nathan, MD, professor of medicine at Harvard Medical School, Boston.
However, the link between higher HbA1c and better efficacy of metformin should be “considered carefully,” according to Dr. Nathan and his cocommittee members, who noted that the original criteria for the Diabetes Prevention Program study were based on glucose level, rather than HbA1c level.
Initial results of the Diabetes Prevention Program study indicated a particular benefit of metformin after an average of 2.8 years of follow-up in individuals with higher baseline fasting glucose levels and in women with a self-reported history of gestational diabetes (N Engl J Med. 2002 Feb 7;346[6]:393-403).
Those results prompted the American Diabetes Association and others to recommend consideration of metformin for diabetes prevention in individuals considered to be at high risk, Dr. Nathan and his colleagues noted. “This recommendation is further supported by the demonstrated cost savings of metformin in diabetes prevention.”
The Diabetes Prevention Program study originally included 3,234 high-risk participants enrolled between 1996 and 1999 and randomized to masked metformin, placebo, or intensive lifestyle intervention. The 15-year follow-up analysis considered the 2,155 individuals randomized to the metformin or placebo groups, of whom 1,861 (86%) chose to continue in the Diabetes Prevention Program Outcomes Study, in which they continued to receive metformin unmasked.
Over the 15 years, the incidence of diabetes development based on fasting or 2-hour glucose results was 17% lower in the metformin group, compared with the placebo group (hazard ratio, 0.83; or –1.25 cases per 100 person-years), according to Dr. Nathan and his colleagues.
For diabetes development based on HbA1c level, metformin was linked to a 36% reduction in risk, compared with placebo, or –1.67 cases per 100 person-years.
Higher baseline fasting plasma glucose (110-125 mg/dL vs. 95-109 mg/dL) was associated with a greater effect of metformin in reducing diabetes development over 15 years (P = .0004).
Metformin’s effect in reducing diabetes development was “nearly identical” in participants with an HbA1c of 6.0%-6.4%, compared with less than 6.0%, with HRs of 0.63 and 0.61, respectively; however, looking at rate differences, there was “substantial heterogeneity” between the groups, at –3.88 and –1.03 cases per 100 person-years, respectively, the investigators wrote.
For women with a history of gestational diabetes, metformin was linked to a 41% reduction in diabetes development, compared with placebo (P = .03); in women without gestational diabetes, the difference was a nonsignificant 6% reduction, compared with placebo. In terms of risk differences, this translated into a reduction of 4.57 cases per 100 person-years in women with gestational diabetes, compared with a reduction of just 0.38 cases in women without such a history. The authors noted that it is “complicated” to determine whether greater credence be given to the results based on glucose or those based on HbA1c.
On the one hand, the generalizability of the HbA1c analyses is adversely affected because the analyses were performed post hoc on a set of participants who had initially been selected for the study based on prediabetes defined by glucose. On the other, the HbA1c results may be more clinically relevant because “in many countries, oral glucose tolerance tests are not used routinely for the identification of persons at high risk for diabetes or with diabetes,” the authors wrote.
Continued follow-up of these patients will provide additional data on the potential long-term benefits of metformin use, such as the incidence of cardiovascular disease, cancer, and microvascular disease, the investigators concluded.
The National Institute of Diabetes and Digestive and Kidney Diseases and Department of Veterans Affairs, among others, funded the Diabetes Prevention Program and subsequent outcomes study. Lipha provided medication and LifeScan donated materials during the studies. Additional funding to the Diabetes Prevention Program was provided by Bristol-Myers Squibb and Parke-Davis.
SOURCE: Nathan DM et al. Diabetes Care. 2019 Mar 15. doi: 10.2337/dc18-1970.
FROM DIABETES CARE
TAVR tops surgery in low-risk patients
NEW ORLEANS – Patients with severely symptomatic aortic stenosis at low surgical risk had significantly better key outcomes with transcatheter aortic valve replacement than with surgical valve replacement through 1 year of follow-up in the landmark PARTNER 3 and Evolut Low Risk randomized trials presented at the annual meeting of the American College of Cardiology.
As the two study presenters stepped down from the stage after sharing their results, the packed audience in the meeting’s main arena rose to shower them with a prolonged standing ovation.
“This is a historic moment, and all of us here should recognize it as such,” thundered discussant Eugene Braunwald, MD, professor of medicine at Harvard Medical School, Boston. “We’re going to remember it. We’re going to tell our grandchildren and great grandchildren that we were there at the time these incredible advances in the care of patients with aortic stenosis were presented.”
This was in fact the day that transcatheter aortic valve replacement (TAVR), a relatively young, rapidly evolving nonsurgical technique, finally overtook surgical aortic valve replacement (SAVR), a mature operation first successfully performed back in 1962. Previous large, randomized trials had established that TAVR was superior to SAVR in extreme-risk patients and noninferior to surgery in high- and intermediate-risk patients, yet with the advantage of much quicker recovery. The only remaining question was how TAVR would stack up in low-risk patients, who comprise 80% of those who currently undergo SAVR for aortic stenosis.
“Two separate groups using two separate valves have come to very similar conclusions. This doesn’t double the acceptability, it quadruples it,” Dr. Braunwald said.
PARTNER 3
Martin B. Leon, MD, presented the findings of the PARTNER 3 (Placement of Aortic Transcatheter Valves) trial, in which 1,000 low-risk patients at 71 centers were randomized to TAVR with transfemoral placement of the balloon-expandable Edwards Lifesciences Sapien 3 bioprosthetic valve or to SAVR. The mean age of the patients was 73 years, with a mean Society of Thoracic Surgeons risk score of 1.9%. Operators had to have more than 1 year of experience using the Sapien 3 valve in order to participate in the trial.
At 1 year post procedure, the rate of the primary composite endpoint comprising death, stroke, or cardiovascular rehospitalization was 8.5% in the TAVR group and 15.1% with SAVR, for a highly significant 46% relative risk reduction. All three components of the primary endpoint occurred significantly less often in the TAVR group. And the rate of the key endpoint of death or disabling stroke was 1.0% with TAVR, compared with 2.9% with SAVR, reported Dr. Leon, coprincipal investigator in PARTNER 3 and professor of medicine at Columbia University, New York.
TAVR also outperformed SAVR on all six prespecified major secondary endpoints. These included new-onset atrial fibrillation within 30 days, at 5.0% with TAVR and 39.5% with SAVR; length of index hospitalization at 3 versus 7 days; all stroke at 30 days at 0.6% versus 2.4%; and death or a significant deterioration in quality of life at 30 days as measured by the Kansas City Cardiomyopathy Questionnaire at 3.9% versus 30.6%. There was significantly less life-threatening or major bleeding within 30 days in the TAVR group, by a margin of 3.6% versus 24.5%, and similarly low rates of new pacemaker implantation at 6.5% versus 4.0%. There was, however, a higher 30-day incidence of new left bundle branch block with TAVR, by a margin of 22% versus 8%, which may eventually translate into need for a pacemaker.
“Based upon these findings, TAVR, through 1 year, should be considered the preferred therapy in low-surgical-risk aortic stenosis patients. The PARTNER randomized trials over the past 12 years clearly indicate that the relative value of TAVR, compared with surgery, is independent of surgical risk profiles,” Dr. Leon declared.
Evolut Low Risk
Michael J. Reardon, MD, coprincipal investigator for the Evolut Low Risk study and professor of cardiovascular surgery at Houston Methodist Hospital, reported on 1,468 patients randomized to TAVR with a Medtronic self-expanding, supra-annular bioprosthetic valve or to SAVR. Of them, 22% of patients got the most recent version of the valve, known as the Evolut PRO, 74% got the Evolut R, and the remainder received the first-generation CoreValve.
The primary endpoint – death or disabling stroke – was slightly different from that in PARTNER 3. At 1 year, the rate was 2.9% in the TAVR arm and 4.6% with SAVR, a statistically significant difference, while at 2 years the rate was 5.3% with TAVR and 6.7% with SAVR, a difference that was not significant. Impressively, the rate of the composite of death, disabling stroke, or heart failure hospitalizations through 1 year was 5.6% with TAVR versus 10.2% with SAVR.
“We’ve shown that, with TAVR, you’re more likely to be alive, without a stroke, and outside the hospital. This is exactly what my patients tell me they want when we sit down for shared decision-making and talk about their expectations,” Dr. Reardon said.
Noting the striking similarity of across-the-board outcomes in the two trials, Dr. Reardon concluded, “I think what we’re seeing here is a class effect of TAVR, and we have to recognize it as such.”
Dr. Leon agreed, with a caveat. “I think the class effect for these two versions of TAVR systems is very real. I wouldn’t presume to think that every TAVR device will perform the same way, so I think we need a lot more data on the newer devices that are being introduced.”
The reaction
During the question-and-answer session, the two investigators were asked about stroke rates, which were significantly lower in the TAVR patients even though in the early randomized trials in high-risk patients the stroke rates were twice as high with TAVR than SAVR. The explanation probably lies in a mix of device refinements over time, better techniques, standardized procedures, and careful patient selection, they said.
“If you look at stroke in the TAVR arm in both these trials, we’re almost approaching the background stroke rate in a group of 74-year-olds sitting around in a room,” Dr. Reardon observed.
Both trials will continue to assess participants both clinically and by echocardiography through 10 years, in part to assess TAVR valve durability, but also to evaluate the durability of surgical valves, which isn’t nearly as well established as most people think, according to the investigators.
“There is a myth of surgical bioprosthetic valve immortality. It’s based upon relatively few numbers of patients, largely sponsor-based studies, with numbers at risk at 15-20 years that are extremely low,” Dr. Leon asserted. “The majority of surgical valves being used today and touted as being durable are backed by only 2-4 years of data.”
In contrast, he added, “We have 5-year TAVR data which is absolutely definitive of no early structural valve deterioration.”
Discussant Mayra E. Guerrero, MD, of the Mayo Clinic in Rochester, Minn., expressed concern that “this paradigm shift to ‘TAVR for all’ ” could break the bank for many institutions because the cost of TAVR valves is far greater than for SAVR valves. But she was heartened by the fresh PARTNER 3 and Evolut Low Risk data showing TAVR patients had fewer ICU days, shorter hospital stays, fewer strokes, more frequent discharge home, and a lower rehospitalization rate.
Dr. Reardon was reassuring on this score.
“I am 100% convinced that when we do the financials for these two trials, TAVR is going to be a cost saver and a huge winner,” the surgeon said.
He reported serving as a consultant to Medtronic and receiving research grants from Medtronic and Boston Scientific. Dr. Leon reported receiving research grants from Edwards Lifesciences and St. Jude Medical and acting as a consultant to several medical device companies.
The two trials have been published online by the New England Journal of Medicine.
SOURCES: Leon MB et al. N Engl J Med. 2019 Mar 16. doi: 10.1056/NEJMoa1814052; Reardon MJ et al. N Engl J Med. 2019 Mar 16. doi: 10.1056/NEJMoa1816885.
NEW ORLEANS – Patients with severely symptomatic aortic stenosis at low surgical risk had significantly better key outcomes with transcatheter aortic valve replacement than with surgical valve replacement through 1 year of follow-up in the landmark PARTNER 3 and Evolut Low Risk randomized trials presented at the annual meeting of the American College of Cardiology.
As the two study presenters stepped down from the stage after sharing their results, the packed audience in the meeting’s main arena rose to shower them with a prolonged standing ovation.
“This is a historic moment, and all of us here should recognize it as such,” thundered discussant Eugene Braunwald, MD, professor of medicine at Harvard Medical School, Boston. “We’re going to remember it. We’re going to tell our grandchildren and great grandchildren that we were there at the time these incredible advances in the care of patients with aortic stenosis were presented.”
This was in fact the day that transcatheter aortic valve replacement (TAVR), a relatively young, rapidly evolving nonsurgical technique, finally overtook surgical aortic valve replacement (SAVR), a mature operation first successfully performed back in 1962. Previous large, randomized trials had established that TAVR was superior to SAVR in extreme-risk patients and noninferior to surgery in high- and intermediate-risk patients, yet with the advantage of much quicker recovery. The only remaining question was how TAVR would stack up in low-risk patients, who comprise 80% of those who currently undergo SAVR for aortic stenosis.
“Two separate groups using two separate valves have come to very similar conclusions. This doesn’t double the acceptability, it quadruples it,” Dr. Braunwald said.
PARTNER 3
Martin B. Leon, MD, presented the findings of the PARTNER 3 (Placement of Aortic Transcatheter Valves) trial, in which 1,000 low-risk patients at 71 centers were randomized to TAVR with transfemoral placement of the balloon-expandable Edwards Lifesciences Sapien 3 bioprosthetic valve or to SAVR. The mean age of the patients was 73 years, with a mean Society of Thoracic Surgeons risk score of 1.9%. Operators had to have more than 1 year of experience using the Sapien 3 valve in order to participate in the trial.
At 1 year post procedure, the rate of the primary composite endpoint comprising death, stroke, or cardiovascular rehospitalization was 8.5% in the TAVR group and 15.1% with SAVR, for a highly significant 46% relative risk reduction. All three components of the primary endpoint occurred significantly less often in the TAVR group. And the rate of the key endpoint of death or disabling stroke was 1.0% with TAVR, compared with 2.9% with SAVR, reported Dr. Leon, coprincipal investigator in PARTNER 3 and professor of medicine at Columbia University, New York.
TAVR also outperformed SAVR on all six prespecified major secondary endpoints. These included new-onset atrial fibrillation within 30 days, at 5.0% with TAVR and 39.5% with SAVR; length of index hospitalization at 3 versus 7 days; all stroke at 30 days at 0.6% versus 2.4%; and death or a significant deterioration in quality of life at 30 days as measured by the Kansas City Cardiomyopathy Questionnaire at 3.9% versus 30.6%. There was significantly less life-threatening or major bleeding within 30 days in the TAVR group, by a margin of 3.6% versus 24.5%, and similarly low rates of new pacemaker implantation at 6.5% versus 4.0%. There was, however, a higher 30-day incidence of new left bundle branch block with TAVR, by a margin of 22% versus 8%, which may eventually translate into need for a pacemaker.
“Based upon these findings, TAVR, through 1 year, should be considered the preferred therapy in low-surgical-risk aortic stenosis patients. The PARTNER randomized trials over the past 12 years clearly indicate that the relative value of TAVR, compared with surgery, is independent of surgical risk profiles,” Dr. Leon declared.
Evolut Low Risk
Michael J. Reardon, MD, coprincipal investigator for the Evolut Low Risk study and professor of cardiovascular surgery at Houston Methodist Hospital, reported on 1,468 patients randomized to TAVR with a Medtronic self-expanding, supra-annular bioprosthetic valve or to SAVR. Of them, 22% of patients got the most recent version of the valve, known as the Evolut PRO, 74% got the Evolut R, and the remainder received the first-generation CoreValve.
The primary endpoint – death or disabling stroke – was slightly different from that in PARTNER 3. At 1 year, the rate was 2.9% in the TAVR arm and 4.6% with SAVR, a statistically significant difference, while at 2 years the rate was 5.3% with TAVR and 6.7% with SAVR, a difference that was not significant. Impressively, the rate of the composite of death, disabling stroke, or heart failure hospitalizations through 1 year was 5.6% with TAVR versus 10.2% with SAVR.
“We’ve shown that, with TAVR, you’re more likely to be alive, without a stroke, and outside the hospital. This is exactly what my patients tell me they want when we sit down for shared decision-making and talk about their expectations,” Dr. Reardon said.
Noting the striking similarity of across-the-board outcomes in the two trials, Dr. Reardon concluded, “I think what we’re seeing here is a class effect of TAVR, and we have to recognize it as such.”
Dr. Leon agreed, with a caveat. “I think the class effect for these two versions of TAVR systems is very real. I wouldn’t presume to think that every TAVR device will perform the same way, so I think we need a lot more data on the newer devices that are being introduced.”
The reaction
During the question-and-answer session, the two investigators were asked about stroke rates, which were significantly lower in the TAVR patients even though in the early randomized trials in high-risk patients the stroke rates were twice as high with TAVR than SAVR. The explanation probably lies in a mix of device refinements over time, better techniques, standardized procedures, and careful patient selection, they said.
“If you look at stroke in the TAVR arm in both these trials, we’re almost approaching the background stroke rate in a group of 74-year-olds sitting around in a room,” Dr. Reardon observed.
Both trials will continue to assess participants both clinically and by echocardiography through 10 years, in part to assess TAVR valve durability, but also to evaluate the durability of surgical valves, which isn’t nearly as well established as most people think, according to the investigators.
“There is a myth of surgical bioprosthetic valve immortality. It’s based upon relatively few numbers of patients, largely sponsor-based studies, with numbers at risk at 15-20 years that are extremely low,” Dr. Leon asserted. “The majority of surgical valves being used today and touted as being durable are backed by only 2-4 years of data.”
In contrast, he added, “We have 5-year TAVR data which is absolutely definitive of no early structural valve deterioration.”
Discussant Mayra E. Guerrero, MD, of the Mayo Clinic in Rochester, Minn., expressed concern that “this paradigm shift to ‘TAVR for all’ ” could break the bank for many institutions because the cost of TAVR valves is far greater than for SAVR valves. But she was heartened by the fresh PARTNER 3 and Evolut Low Risk data showing TAVR patients had fewer ICU days, shorter hospital stays, fewer strokes, more frequent discharge home, and a lower rehospitalization rate.
Dr. Reardon was reassuring on this score.
“I am 100% convinced that when we do the financials for these two trials, TAVR is going to be a cost saver and a huge winner,” the surgeon said.
He reported serving as a consultant to Medtronic and receiving research grants from Medtronic and Boston Scientific. Dr. Leon reported receiving research grants from Edwards Lifesciences and St. Jude Medical and acting as a consultant to several medical device companies.
The two trials have been published online by the New England Journal of Medicine.
SOURCES: Leon MB et al. N Engl J Med. 2019 Mar 16. doi: 10.1056/NEJMoa1814052; Reardon MJ et al. N Engl J Med. 2019 Mar 16. doi: 10.1056/NEJMoa1816885.
NEW ORLEANS – Patients with severely symptomatic aortic stenosis at low surgical risk had significantly better key outcomes with transcatheter aortic valve replacement than with surgical valve replacement through 1 year of follow-up in the landmark PARTNER 3 and Evolut Low Risk randomized trials presented at the annual meeting of the American College of Cardiology.
As the two study presenters stepped down from the stage after sharing their results, the packed audience in the meeting’s main arena rose to shower them with a prolonged standing ovation.
“This is a historic moment, and all of us here should recognize it as such,” thundered discussant Eugene Braunwald, MD, professor of medicine at Harvard Medical School, Boston. “We’re going to remember it. We’re going to tell our grandchildren and great grandchildren that we were there at the time these incredible advances in the care of patients with aortic stenosis were presented.”
This was in fact the day that transcatheter aortic valve replacement (TAVR), a relatively young, rapidly evolving nonsurgical technique, finally overtook surgical aortic valve replacement (SAVR), a mature operation first successfully performed back in 1962. Previous large, randomized trials had established that TAVR was superior to SAVR in extreme-risk patients and noninferior to surgery in high- and intermediate-risk patients, yet with the advantage of much quicker recovery. The only remaining question was how TAVR would stack up in low-risk patients, who comprise 80% of those who currently undergo SAVR for aortic stenosis.
“Two separate groups using two separate valves have come to very similar conclusions. This doesn’t double the acceptability, it quadruples it,” Dr. Braunwald said.
PARTNER 3
Martin B. Leon, MD, presented the findings of the PARTNER 3 (Placement of Aortic Transcatheter Valves) trial, in which 1,000 low-risk patients at 71 centers were randomized to TAVR with transfemoral placement of the balloon-expandable Edwards Lifesciences Sapien 3 bioprosthetic valve or to SAVR. The mean age of the patients was 73 years, with a mean Society of Thoracic Surgeons risk score of 1.9%. Operators had to have more than 1 year of experience using the Sapien 3 valve in order to participate in the trial.
At 1 year post procedure, the rate of the primary composite endpoint comprising death, stroke, or cardiovascular rehospitalization was 8.5% in the TAVR group and 15.1% with SAVR, for a highly significant 46% relative risk reduction. All three components of the primary endpoint occurred significantly less often in the TAVR group. And the rate of the key endpoint of death or disabling stroke was 1.0% with TAVR, compared with 2.9% with SAVR, reported Dr. Leon, coprincipal investigator in PARTNER 3 and professor of medicine at Columbia University, New York.
TAVR also outperformed SAVR on all six prespecified major secondary endpoints. These included new-onset atrial fibrillation within 30 days, at 5.0% with TAVR and 39.5% with SAVR; length of index hospitalization at 3 versus 7 days; all stroke at 30 days at 0.6% versus 2.4%; and death or a significant deterioration in quality of life at 30 days as measured by the Kansas City Cardiomyopathy Questionnaire at 3.9% versus 30.6%. There was significantly less life-threatening or major bleeding within 30 days in the TAVR group, by a margin of 3.6% versus 24.5%, and similarly low rates of new pacemaker implantation at 6.5% versus 4.0%. There was, however, a higher 30-day incidence of new left bundle branch block with TAVR, by a margin of 22% versus 8%, which may eventually translate into need for a pacemaker.
“Based upon these findings, TAVR, through 1 year, should be considered the preferred therapy in low-surgical-risk aortic stenosis patients. The PARTNER randomized trials over the past 12 years clearly indicate that the relative value of TAVR, compared with surgery, is independent of surgical risk profiles,” Dr. Leon declared.
Evolut Low Risk
Michael J. Reardon, MD, coprincipal investigator for the Evolut Low Risk study and professor of cardiovascular surgery at Houston Methodist Hospital, reported on 1,468 patients randomized to TAVR with a Medtronic self-expanding, supra-annular bioprosthetic valve or to SAVR. Of them, 22% of patients got the most recent version of the valve, known as the Evolut PRO, 74% got the Evolut R, and the remainder received the first-generation CoreValve.
The primary endpoint – death or disabling stroke – was slightly different from that in PARTNER 3. At 1 year, the rate was 2.9% in the TAVR arm and 4.6% with SAVR, a statistically significant difference, while at 2 years the rate was 5.3% with TAVR and 6.7% with SAVR, a difference that was not significant. Impressively, the rate of the composite of death, disabling stroke, or heart failure hospitalizations through 1 year was 5.6% with TAVR versus 10.2% with SAVR.
“We’ve shown that, with TAVR, you’re more likely to be alive, without a stroke, and outside the hospital. This is exactly what my patients tell me they want when we sit down for shared decision-making and talk about their expectations,” Dr. Reardon said.
Noting the striking similarity of across-the-board outcomes in the two trials, Dr. Reardon concluded, “I think what we’re seeing here is a class effect of TAVR, and we have to recognize it as such.”
Dr. Leon agreed, with a caveat. “I think the class effect for these two versions of TAVR systems is very real. I wouldn’t presume to think that every TAVR device will perform the same way, so I think we need a lot more data on the newer devices that are being introduced.”
The reaction
During the question-and-answer session, the two investigators were asked about stroke rates, which were significantly lower in the TAVR patients even though in the early randomized trials in high-risk patients the stroke rates were twice as high with TAVR than SAVR. The explanation probably lies in a mix of device refinements over time, better techniques, standardized procedures, and careful patient selection, they said.
“If you look at stroke in the TAVR arm in both these trials, we’re almost approaching the background stroke rate in a group of 74-year-olds sitting around in a room,” Dr. Reardon observed.
Both trials will continue to assess participants both clinically and by echocardiography through 10 years, in part to assess TAVR valve durability, but also to evaluate the durability of surgical valves, which isn’t nearly as well established as most people think, according to the investigators.
“There is a myth of surgical bioprosthetic valve immortality. It’s based upon relatively few numbers of patients, largely sponsor-based studies, with numbers at risk at 15-20 years that are extremely low,” Dr. Leon asserted. “The majority of surgical valves being used today and touted as being durable are backed by only 2-4 years of data.”
In contrast, he added, “We have 5-year TAVR data which is absolutely definitive of no early structural valve deterioration.”
Discussant Mayra E. Guerrero, MD, of the Mayo Clinic in Rochester, Minn., expressed concern that “this paradigm shift to ‘TAVR for all’ ” could break the bank for many institutions because the cost of TAVR valves is far greater than for SAVR valves. But she was heartened by the fresh PARTNER 3 and Evolut Low Risk data showing TAVR patients had fewer ICU days, shorter hospital stays, fewer strokes, more frequent discharge home, and a lower rehospitalization rate.
Dr. Reardon was reassuring on this score.
“I am 100% convinced that when we do the financials for these two trials, TAVR is going to be a cost saver and a huge winner,” the surgeon said.
He reported serving as a consultant to Medtronic and receiving research grants from Medtronic and Boston Scientific. Dr. Leon reported receiving research grants from Edwards Lifesciences and St. Jude Medical and acting as a consultant to several medical device companies.
The two trials have been published online by the New England Journal of Medicine.
SOURCES: Leon MB et al. N Engl J Med. 2019 Mar 16. doi: 10.1056/NEJMoa1814052; Reardon MJ et al. N Engl J Med. 2019 Mar 16. doi: 10.1056/NEJMoa1816885.
REPORTING FROM ACC 19
After a Need for Speed, a Spine Entwined?
ANSWER
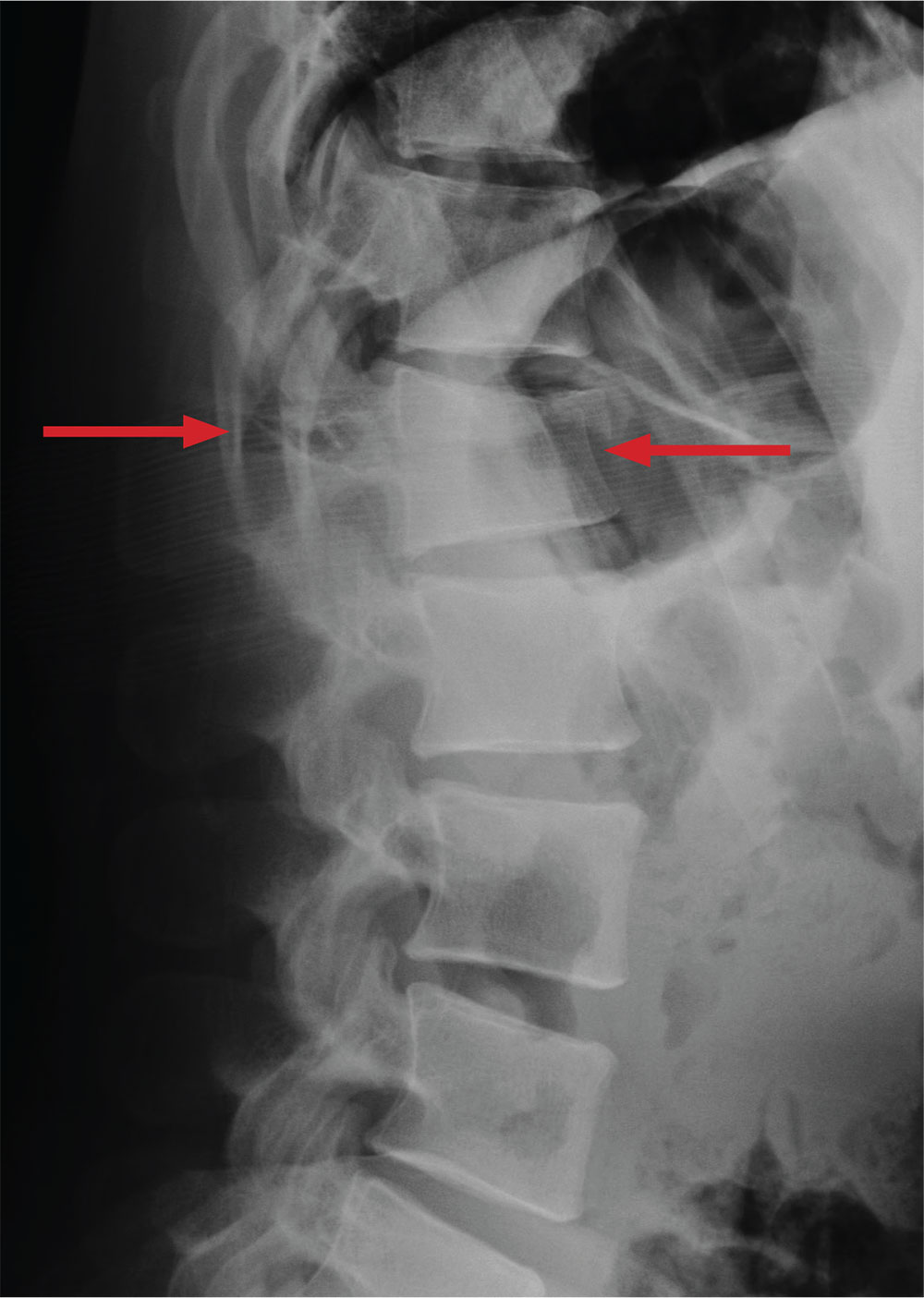
The radiograph demonstrates a comminuted fracture of the superior end plate of L1. There is a loss of height of about 20% to 25%.
Of note, there is a lucency that appears to extend horizontally through the pedicles and into the spinous process. If this observation is accurate, then the patient would have a three-column injury. Such fractures are known as Chance fractures, and they are typically unstable and require operative intervention for stabilization.
Chance fractures are better visualized on CT. Subsequent testing
ANSWER
The radiograph demonstrates a comminuted fracture of the superior end plate of L1. There is a loss of height of about 20% to 25%.
Of note, there is a lucency that appears to extend horizontally through the pedicles and into the spinous process. If this observation is accurate, then the patient would have a three-column injury. Such fractures are known as Chance fractures, and they are typically unstable and require operative intervention for stabilization.
Chance fractures are better visualized on CT. Subsequent testing
ANSWER
The radiograph demonstrates a comminuted fracture of the superior end plate of L1. There is a loss of height of about 20% to 25%.
Of note, there is a lucency that appears to extend horizontally through the pedicles and into the spinous process. If this observation is accurate, then the patient would have a three-column injury. Such fractures are known as Chance fractures, and they are typically unstable and require operative intervention for stabilization.
Chance fractures are better visualized on CT. Subsequent testing
A 28-year-old man is brought to your emergency department via ambulance after a motor vehicle accident. The patient was a restrained driver who was driving too fast, lost control, and ended up in a ditch. His vehicle then rolled over several times. He reportedly self-extricated and was ambulatory at the scene.
His primary complaints include left shoulder, chest wall, and back pain. He denies any significant medical history.
On physical examination, you note a man with normal vital signs who, although slightly anxious, is in no obvious distress. He has moderate tenderness over the left shoulder and sternum and at the thoracolumbar juncture. No step-offs are appreciated. He is able to move all extremities and is neurovascularly intact.
As you await lab results, you obtain a lateral radiograph of the lumbar spine (shown). What is your impression?
First primary prevention CVD guidelines form ACC, AHA
Also today, a new coronary artery calcium score threshold may identify patients at particular risk, how to reduce the risk of drowning in pediatric patients, and an algorithm in smartwatches proves effective at detecting atrial fibrillation.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, a new coronary artery calcium score threshold may identify patients at particular risk, how to reduce the risk of drowning in pediatric patients, and an algorithm in smartwatches proves effective at detecting atrial fibrillation.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, a new coronary artery calcium score threshold may identify patients at particular risk, how to reduce the risk of drowning in pediatric patients, and an algorithm in smartwatches proves effective at detecting atrial fibrillation.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
CDC exhorts more testing and treatment of HIV
Approximately 80% of HIV infections in the United States in 2016 were spread by almost 40% of infected individuals who did not know their status or were not receiving care, according to data from the Centers for Disease Control and Prevention.
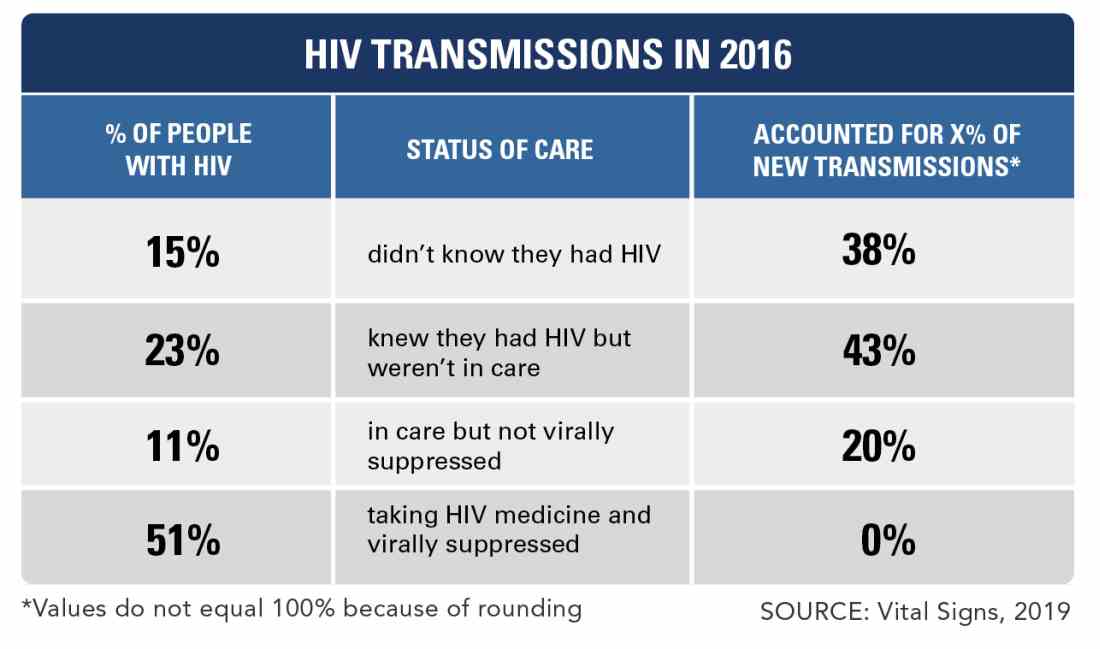
However, leadership at the Department of Health & Human Services has developed a “bold but completely achievable” plan to reduce HIV infections within the next decade, Vice Adm. Jerome M. Adams, MD, the U.S. surgeon general, said in a teleconference to announce the results of a new Vital Signs report on the impact of undiagnosed and untreated HIV.
In the early release Vital Signs from Morbidity and Mortality Weekly Report, Li Zihao, PhD, and his colleagues at the CDC used a model to estimate rates of HIV transmission in 2016 based on data from the National HIV Behavioral Surveillance on needle-sharing behavior and sexual behaviors. The overall transmission rate was 3.5/100,000 person-years. Of these transmissions, 73.0% were from men who have sex with men, 9.7% from intravenous drug users, and 12% from heterosexuals.
The percentages of transmissions for those who were acutely ill with HIV but unaware, not acutely ill but unaware, aware of HIV infection but not treated, receiving care but not virally suppressed, and receiving care and virally suppressed were 4.0%, 33.6%, 42.6%, 19.8%, and 0%, respectively, the researchers said.
The study “emphasizes the impact that HIV resources could have,” by showing the importance of identifying infected individuals early and using the tools now available to treat them before they can transmit the disease, Jonathan Mermin, MD, director of the CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, said during the conference.
“Today’s treatment regimens are simpler than those prescribed in the past, sometimes requiring only single-tablet formulations, with fewer side effects; most persons with HIV infection can achieve viral suppression within 6 months of initiating treatment,” the researchers wrote.
In the wake of the findings and at the start of the CDC’s 2019 National HIV Prevention Conference, the CDC proposed a federal initiative, “Ending the HIV Epidemic: A Plan for America.”
The goal is to reduce the incidence of new HIV infections by at least 90% over the next decade, starting with a focus on parts of the country with the highest disease burden, according to the CDC.
“Today’s Vital Signs report illustrates how a goal that once seemed impossible is now within our reach.” Robert R. Redfield, MD, director of the Centers for Disease Control and Prevention, said during the conference. “If we increase access to testing and treatment for people with HIV, we could prevent a lion’s share of infections,” he said.
The plan involves working to identify individuals at risk, treating those who test positive as quickly as possible, and keeping them in care. Updated information on the CDC website provides more details for clinicians on how to have conversations about HIV with patients, the latest information about antiretroviral therapy, and details about prevention for partners including post- and pre-exposure prophylaxis (PEP and PreP), and condoms.
Eugene McCray, MD, director of the CDC’s Division of HIV/AIDS Prevention, emphasized that the CDC recommends HIV testing for all individuals aged 13-64 years at least once in their lives. He added that everyone who tests positive should seek medical care, that everyone with HIV deserves support to combat stigma, and that those at risk should be empowered to take advantage of proven effective prevention strategies.
Clinicians can access the updated CDC page on caring for HIV patients here.
SOURCE: Li Z et al. MMWR Morb Mortal Wkly Rep. 2019 March 18. doi: org/10.15585/mmwr.mm6811e1.
Approximately 80% of HIV infections in the United States in 2016 were spread by almost 40% of infected individuals who did not know their status or were not receiving care, according to data from the Centers for Disease Control and Prevention.
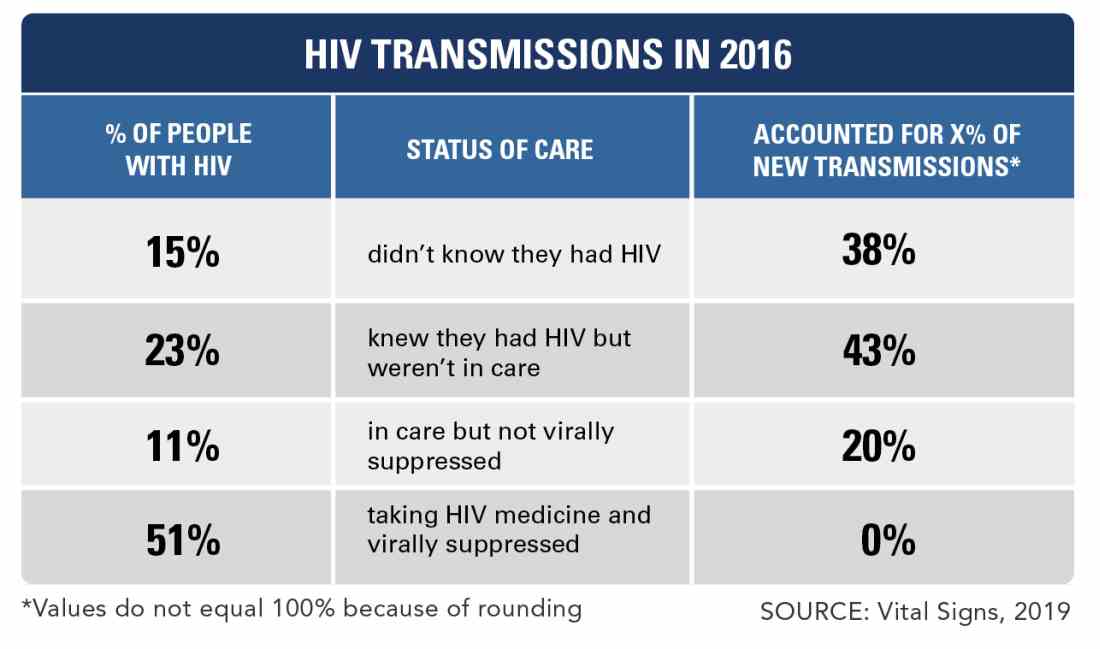
However, leadership at the Department of Health & Human Services has developed a “bold but completely achievable” plan to reduce HIV infections within the next decade, Vice Adm. Jerome M. Adams, MD, the U.S. surgeon general, said in a teleconference to announce the results of a new Vital Signs report on the impact of undiagnosed and untreated HIV.
In the early release Vital Signs from Morbidity and Mortality Weekly Report, Li Zihao, PhD, and his colleagues at the CDC used a model to estimate rates of HIV transmission in 2016 based on data from the National HIV Behavioral Surveillance on needle-sharing behavior and sexual behaviors. The overall transmission rate was 3.5/100,000 person-years. Of these transmissions, 73.0% were from men who have sex with men, 9.7% from intravenous drug users, and 12% from heterosexuals.
The percentages of transmissions for those who were acutely ill with HIV but unaware, not acutely ill but unaware, aware of HIV infection but not treated, receiving care but not virally suppressed, and receiving care and virally suppressed were 4.0%, 33.6%, 42.6%, 19.8%, and 0%, respectively, the researchers said.
The study “emphasizes the impact that HIV resources could have,” by showing the importance of identifying infected individuals early and using the tools now available to treat them before they can transmit the disease, Jonathan Mermin, MD, director of the CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, said during the conference.
“Today’s treatment regimens are simpler than those prescribed in the past, sometimes requiring only single-tablet formulations, with fewer side effects; most persons with HIV infection can achieve viral suppression within 6 months of initiating treatment,” the researchers wrote.
In the wake of the findings and at the start of the CDC’s 2019 National HIV Prevention Conference, the CDC proposed a federal initiative, “Ending the HIV Epidemic: A Plan for America.”
The goal is to reduce the incidence of new HIV infections by at least 90% over the next decade, starting with a focus on parts of the country with the highest disease burden, according to the CDC.
“Today’s Vital Signs report illustrates how a goal that once seemed impossible is now within our reach.” Robert R. Redfield, MD, director of the Centers for Disease Control and Prevention, said during the conference. “If we increase access to testing and treatment for people with HIV, we could prevent a lion’s share of infections,” he said.
The plan involves working to identify individuals at risk, treating those who test positive as quickly as possible, and keeping them in care. Updated information on the CDC website provides more details for clinicians on how to have conversations about HIV with patients, the latest information about antiretroviral therapy, and details about prevention for partners including post- and pre-exposure prophylaxis (PEP and PreP), and condoms.
Eugene McCray, MD, director of the CDC’s Division of HIV/AIDS Prevention, emphasized that the CDC recommends HIV testing for all individuals aged 13-64 years at least once in their lives. He added that everyone who tests positive should seek medical care, that everyone with HIV deserves support to combat stigma, and that those at risk should be empowered to take advantage of proven effective prevention strategies.
Clinicians can access the updated CDC page on caring for HIV patients here.
SOURCE: Li Z et al. MMWR Morb Mortal Wkly Rep. 2019 March 18. doi: org/10.15585/mmwr.mm6811e1.
Approximately 80% of HIV infections in the United States in 2016 were spread by almost 40% of infected individuals who did not know their status or were not receiving care, according to data from the Centers for Disease Control and Prevention.
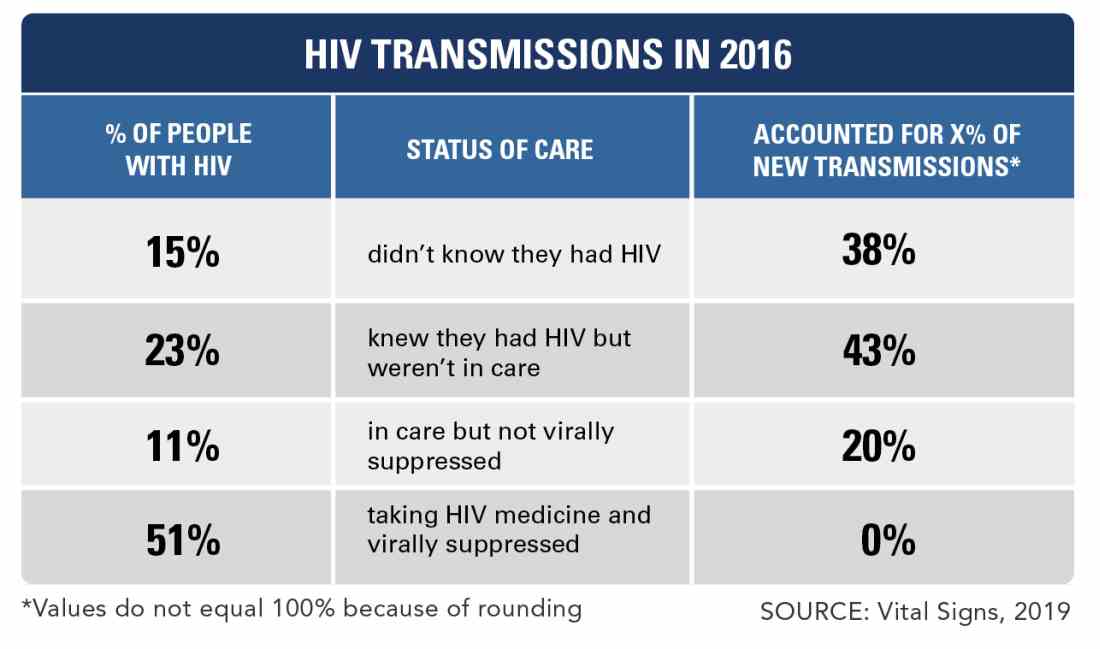
However, leadership at the Department of Health & Human Services has developed a “bold but completely achievable” plan to reduce HIV infections within the next decade, Vice Adm. Jerome M. Adams, MD, the U.S. surgeon general, said in a teleconference to announce the results of a new Vital Signs report on the impact of undiagnosed and untreated HIV.
In the early release Vital Signs from Morbidity and Mortality Weekly Report, Li Zihao, PhD, and his colleagues at the CDC used a model to estimate rates of HIV transmission in 2016 based on data from the National HIV Behavioral Surveillance on needle-sharing behavior and sexual behaviors. The overall transmission rate was 3.5/100,000 person-years. Of these transmissions, 73.0% were from men who have sex with men, 9.7% from intravenous drug users, and 12% from heterosexuals.
The percentages of transmissions for those who were acutely ill with HIV but unaware, not acutely ill but unaware, aware of HIV infection but not treated, receiving care but not virally suppressed, and receiving care and virally suppressed were 4.0%, 33.6%, 42.6%, 19.8%, and 0%, respectively, the researchers said.
The study “emphasizes the impact that HIV resources could have,” by showing the importance of identifying infected individuals early and using the tools now available to treat them before they can transmit the disease, Jonathan Mermin, MD, director of the CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, said during the conference.
“Today’s treatment regimens are simpler than those prescribed in the past, sometimes requiring only single-tablet formulations, with fewer side effects; most persons with HIV infection can achieve viral suppression within 6 months of initiating treatment,” the researchers wrote.
In the wake of the findings and at the start of the CDC’s 2019 National HIV Prevention Conference, the CDC proposed a federal initiative, “Ending the HIV Epidemic: A Plan for America.”
The goal is to reduce the incidence of new HIV infections by at least 90% over the next decade, starting with a focus on parts of the country with the highest disease burden, according to the CDC.
“Today’s Vital Signs report illustrates how a goal that once seemed impossible is now within our reach.” Robert R. Redfield, MD, director of the Centers for Disease Control and Prevention, said during the conference. “If we increase access to testing and treatment for people with HIV, we could prevent a lion’s share of infections,” he said.
The plan involves working to identify individuals at risk, treating those who test positive as quickly as possible, and keeping them in care. Updated information on the CDC website provides more details for clinicians on how to have conversations about HIV with patients, the latest information about antiretroviral therapy, and details about prevention for partners including post- and pre-exposure prophylaxis (PEP and PreP), and condoms.
Eugene McCray, MD, director of the CDC’s Division of HIV/AIDS Prevention, emphasized that the CDC recommends HIV testing for all individuals aged 13-64 years at least once in their lives. He added that everyone who tests positive should seek medical care, that everyone with HIV deserves support to combat stigma, and that those at risk should be empowered to take advantage of proven effective prevention strategies.
Clinicians can access the updated CDC page on caring for HIV patients here.
SOURCE: Li Z et al. MMWR Morb Mortal Wkly Rep. 2019 March 18. doi: org/10.15585/mmwr.mm6811e1.
FROM THE CDC
Measles cases confirmed in three more states
Forty more cases and three more states were added to the measles count in the last week, bringing the U.S. total to 268 cases in 15 states so far in 2019, according to the Centers for Disease Control and Prevention.
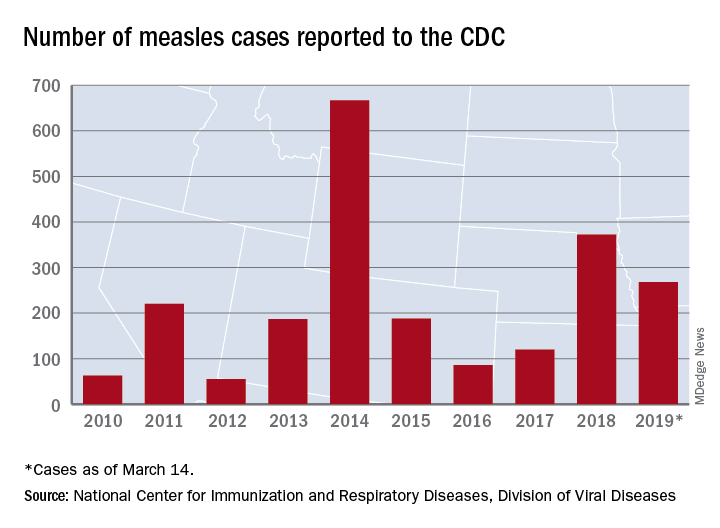
Arizona, Michigan, and Missouri reported their first confirmed cases of the year, joining California (one outbreak), Colorado, Connecticut, Georgia, Illinois (one outbreak), Kentucky, New Hampshire, New Jersey, New York (two outbreaks), Oregon, Texas (one outbreak), and Washington (one outbreak), the CDC reported March 18.
Brooklyn, N.Y., has become the epicenter of measles activity since mid-February, and with 25 of the 40 new cases occurring there, the borough has now led the nation for four consecutive weeks. There have been 157 confirmed cases in Brooklyn and one in Queens since the outbreak began in October of 2018, the New York City Department of Health and Mental Hygiene reported.
Michigan’s first case of measles is travel related and involved an individual visiting from Israel following a stay in New York, the Michigan Department of Health and Human Services and Oakland County Health Division announced March 13.
In Arizona, the state department of health services and the Pima County Public Health Department announced that a 12-month-old infant from Pima County has been diagnosed with measles after traveling to Asia.
A single case of measles, contracted while the person was traveling out of state, has been reported in Jefferson County, Mo., and is being managed by the county health department, according to St. Louis Public Radio.
Forty more cases and three more states were added to the measles count in the last week, bringing the U.S. total to 268 cases in 15 states so far in 2019, according to the Centers for Disease Control and Prevention.
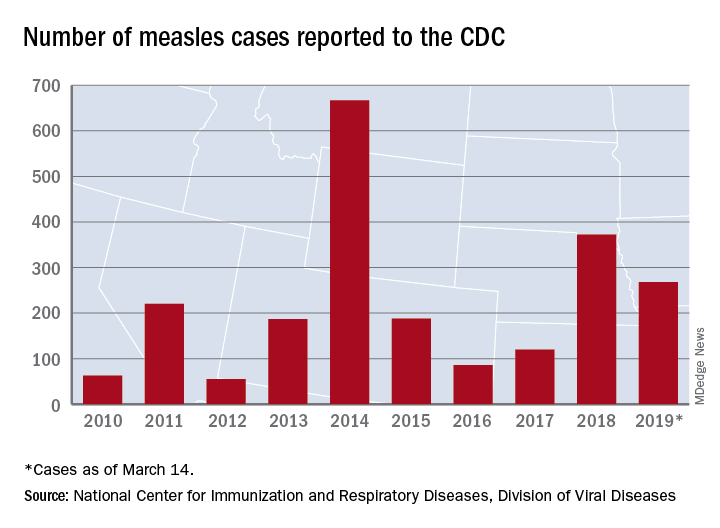
Arizona, Michigan, and Missouri reported their first confirmed cases of the year, joining California (one outbreak), Colorado, Connecticut, Georgia, Illinois (one outbreak), Kentucky, New Hampshire, New Jersey, New York (two outbreaks), Oregon, Texas (one outbreak), and Washington (one outbreak), the CDC reported March 18.
Brooklyn, N.Y., has become the epicenter of measles activity since mid-February, and with 25 of the 40 new cases occurring there, the borough has now led the nation for four consecutive weeks. There have been 157 confirmed cases in Brooklyn and one in Queens since the outbreak began in October of 2018, the New York City Department of Health and Mental Hygiene reported.
Michigan’s first case of measles is travel related and involved an individual visiting from Israel following a stay in New York, the Michigan Department of Health and Human Services and Oakland County Health Division announced March 13.
In Arizona, the state department of health services and the Pima County Public Health Department announced that a 12-month-old infant from Pima County has been diagnosed with measles after traveling to Asia.
A single case of measles, contracted while the person was traveling out of state, has been reported in Jefferson County, Mo., and is being managed by the county health department, according to St. Louis Public Radio.
Forty more cases and three more states were added to the measles count in the last week, bringing the U.S. total to 268 cases in 15 states so far in 2019, according to the Centers for Disease Control and Prevention.
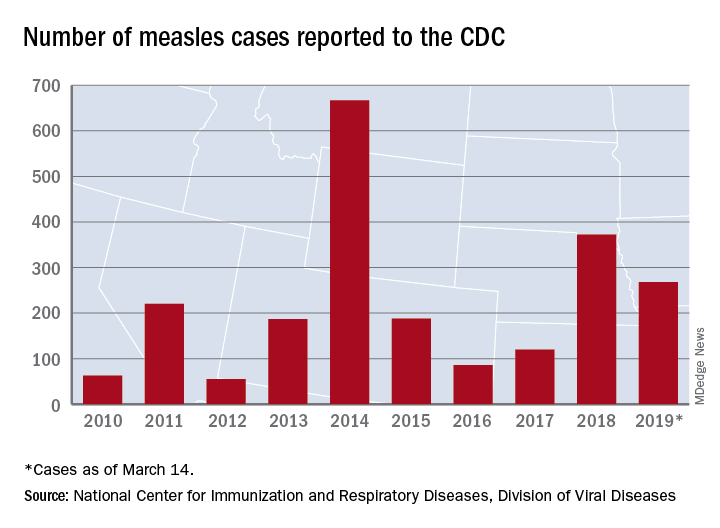
Arizona, Michigan, and Missouri reported their first confirmed cases of the year, joining California (one outbreak), Colorado, Connecticut, Georgia, Illinois (one outbreak), Kentucky, New Hampshire, New Jersey, New York (two outbreaks), Oregon, Texas (one outbreak), and Washington (one outbreak), the CDC reported March 18.
Brooklyn, N.Y., has become the epicenter of measles activity since mid-February, and with 25 of the 40 new cases occurring there, the borough has now led the nation for four consecutive weeks. There have been 157 confirmed cases in Brooklyn and one in Queens since the outbreak began in October of 2018, the New York City Department of Health and Mental Hygiene reported.
Michigan’s first case of measles is travel related and involved an individual visiting from Israel following a stay in New York, the Michigan Department of Health and Human Services and Oakland County Health Division announced March 13.
In Arizona, the state department of health services and the Pima County Public Health Department announced that a 12-month-old infant from Pima County has been diagnosed with measles after traveling to Asia.
A single case of measles, contracted while the person was traveling out of state, has been reported in Jefferson County, Mo., and is being managed by the county health department, according to St. Louis Public Radio.
The New Gastroenterologist seeks its next editor-in-chief
AGA’s cutting-edge, trainee and early-career focused e-newsletter The New Gastroenterologist (TNG) is seeking applications for the position of editor-in-chief (EIC). The role will facilitate the communication of the latest clinical advances among peers and build strong leadership skills managing editorial responsibilities as well as working with reviewers and fellow editors at AGA’s journals.
The term is from Oct. 1, 2019 – Sept. 30, 2022, with a transition period starting July 2019.

About TNG
TNG content covers highly relevant clinical topics, such as endoscopic management of obesity and quality metrics on colonoscopy. Also included in each issue are articles that focus on career pathways, financial and legal matters, perspectives from private practice, and other topics that are relevant to early-career GIs.
Honorarium
The EIC will receive an annual honorarium of $5,000.
Qualifications
• AGA member, between second year of fellowship and five years post-fellowship.
• Experience identifying and promoting newsworthy content that is relevant to the trainee and early-career GI community, as well as excellent judgment that expands the outstanding reputation of TNG and AGA.
• Experience in medical, scientific or news-related publishing is preferred, but not required.
• Familiarity with AGA and its priorities, activities and stances on important issues is ideal, preferably via past volunteer member experience with the association.
• The EIC must be able to devote sufficient time to TNG matters and may not accept editorial appointments to competing publications during their tenure as EIC.
For more information or to apply view the full request for application.
If you have questions, please contact Ryan Farrell, managing editor, The New Gastroenterologist, at [email protected].
AGA’s cutting-edge, trainee and early-career focused e-newsletter The New Gastroenterologist (TNG) is seeking applications for the position of editor-in-chief (EIC). The role will facilitate the communication of the latest clinical advances among peers and build strong leadership skills managing editorial responsibilities as well as working with reviewers and fellow editors at AGA’s journals.
The term is from Oct. 1, 2019 – Sept. 30, 2022, with a transition period starting July 2019.

About TNG
TNG content covers highly relevant clinical topics, such as endoscopic management of obesity and quality metrics on colonoscopy. Also included in each issue are articles that focus on career pathways, financial and legal matters, perspectives from private practice, and other topics that are relevant to early-career GIs.
Honorarium
The EIC will receive an annual honorarium of $5,000.
Qualifications
• AGA member, between second year of fellowship and five years post-fellowship.
• Experience identifying and promoting newsworthy content that is relevant to the trainee and early-career GI community, as well as excellent judgment that expands the outstanding reputation of TNG and AGA.
• Experience in medical, scientific or news-related publishing is preferred, but not required.
• Familiarity with AGA and its priorities, activities and stances on important issues is ideal, preferably via past volunteer member experience with the association.
• The EIC must be able to devote sufficient time to TNG matters and may not accept editorial appointments to competing publications during their tenure as EIC.
For more information or to apply view the full request for application.
If you have questions, please contact Ryan Farrell, managing editor, The New Gastroenterologist, at [email protected].
AGA’s cutting-edge, trainee and early-career focused e-newsletter The New Gastroenterologist (TNG) is seeking applications for the position of editor-in-chief (EIC). The role will facilitate the communication of the latest clinical advances among peers and build strong leadership skills managing editorial responsibilities as well as working with reviewers and fellow editors at AGA’s journals.
The term is from Oct. 1, 2019 – Sept. 30, 2022, with a transition period starting July 2019.

About TNG
TNG content covers highly relevant clinical topics, such as endoscopic management of obesity and quality metrics on colonoscopy. Also included in each issue are articles that focus on career pathways, financial and legal matters, perspectives from private practice, and other topics that are relevant to early-career GIs.
Honorarium
The EIC will receive an annual honorarium of $5,000.
Qualifications
• AGA member, between second year of fellowship and five years post-fellowship.
• Experience identifying and promoting newsworthy content that is relevant to the trainee and early-career GI community, as well as excellent judgment that expands the outstanding reputation of TNG and AGA.
• Experience in medical, scientific or news-related publishing is preferred, but not required.
• Familiarity with AGA and its priorities, activities and stances on important issues is ideal, preferably via past volunteer member experience with the association.
• The EIC must be able to devote sufficient time to TNG matters and may not accept editorial appointments to competing publications during their tenure as EIC.
For more information or to apply view the full request for application.
If you have questions, please contact Ryan Farrell, managing editor, The New Gastroenterologist, at [email protected].