User login
Three-Step Algorithm for the Management of MS Relapse
Key clinical point: Management of multiple sclerosis relapse consists of three main steps: timely and careful evaluation; treatment, if necessary; and assessment of treatment response, according to an algorithm developed by MS clinicians.
Major finding: Between 3 and 5 weeks after the initial evaluation, the group recommends clinical reassessment using a tool such as the Assessing Relapse in Multiple Sclerosis (ARMS) Questionnaire.
Study details: A consensus statement developed by a work group of MS clinicians based on a literature review and clinical experience.
Disclosures: The work group did not receive funding. The authors disclosed financial ties with various pharmaceutical companies.
Citation: REPORTING FROM CMSC 2019
Key clinical point: Management of multiple sclerosis relapse consists of three main steps: timely and careful evaluation; treatment, if necessary; and assessment of treatment response, according to an algorithm developed by MS clinicians.
Major finding: Between 3 and 5 weeks after the initial evaluation, the group recommends clinical reassessment using a tool such as the Assessing Relapse in Multiple Sclerosis (ARMS) Questionnaire.
Study details: A consensus statement developed by a work group of MS clinicians based on a literature review and clinical experience.
Disclosures: The work group did not receive funding. The authors disclosed financial ties with various pharmaceutical companies.
Citation: REPORTING FROM CMSC 2019
Key clinical point: Management of multiple sclerosis relapse consists of three main steps: timely and careful evaluation; treatment, if necessary; and assessment of treatment response, according to an algorithm developed by MS clinicians.
Major finding: Between 3 and 5 weeks after the initial evaluation, the group recommends clinical reassessment using a tool such as the Assessing Relapse in Multiple Sclerosis (ARMS) Questionnaire.
Study details: A consensus statement developed by a work group of MS clinicians based on a literature review and clinical experience.
Disclosures: The work group did not receive funding. The authors disclosed financial ties with various pharmaceutical companies.
Citation: REPORTING FROM CMSC 2019
High-efficacy DMTs May Reduce Depressive Symptoms in MS
Key clinical point: Initial treatment with high-efficacy DMT is associated with a reduction in depressive symptoms, compared with an initial low-efficacy DMT.
Major finding: Initiation of high-efficacy DMT was associated with a reduction of 0.58 points/year in depression scores, compared with initiation of low-efficacy DMT.
Study details: An interim analysis of data for 1,501 participants in the ongoing MS PATHS study.
Disclosures: The study was not supported by outside funding. Ellen M. Mowry, MD, one of the investigators, reported having performed contracted research for Biogen, Genzyme, and Sun Pharma. Ms Youkyung and another two investigators reported disclosures or conflicts of interest.
Citation: REPORTING FROM CMSC 2019
Key clinical point: Initial treatment with high-efficacy DMT is associated with a reduction in depressive symptoms, compared with an initial low-efficacy DMT.
Major finding: Initiation of high-efficacy DMT was associated with a reduction of 0.58 points/year in depression scores, compared with initiation of low-efficacy DMT.
Study details: An interim analysis of data for 1,501 participants in the ongoing MS PATHS study.
Disclosures: The study was not supported by outside funding. Ellen M. Mowry, MD, one of the investigators, reported having performed contracted research for Biogen, Genzyme, and Sun Pharma. Ms Youkyung and another two investigators reported disclosures or conflicts of interest.
Citation: REPORTING FROM CMSC 2019
Key clinical point: Initial treatment with high-efficacy DMT is associated with a reduction in depressive symptoms, compared with an initial low-efficacy DMT.
Major finding: Initiation of high-efficacy DMT was associated with a reduction of 0.58 points/year in depression scores, compared with initiation of low-efficacy DMT.
Study details: An interim analysis of data for 1,501 participants in the ongoing MS PATHS study.
Disclosures: The study was not supported by outside funding. Ellen M. Mowry, MD, one of the investigators, reported having performed contracted research for Biogen, Genzyme, and Sun Pharma. Ms Youkyung and another two investigators reported disclosures or conflicts of interest.
Citation: REPORTING FROM CMSC 2019
Obesity tied to relapse in young patients with multiple sclerosis
, results of a recent large, single-center study show. The rate of switching to second-line disease-modifying therapy was consequently about 50% higher among the obese children in the study, which included a total of 453 pediatric patients.
The link between obesity and treatment response suggests that the management of these younger patients with MS could be improved through weight loss or body mass index (BMI)-adjusted dosing, according to Peter Huppke, MD, of Georg August University in Göttingen, Germany, and co-investigators.
“The findings do not indicate that obesity promotes greater disease activity, but pharmacokinetic factors are more likely associated with treatment response,” Dr. Huppke and co-authors said in a report on their study, which was published online ahead of print July 15 in JAMA Neurology.
This is believed to be the first-ever study to find an association between BMI and treatment response in pediatric patients with MS, according to the authors, who said they also confirmed a link between obesity and MS.
Specifically, obesity increased MS susceptibility by two-fold as compared with healthy controls, a finding that they said adds to a small but growing body of evidence that high BMI is associated with increased risk of the disease in these younger individuals.
This retrospective study included 453 pediatric patients with MS treated at the Center for MS in Childhood and Adolescence in Göttingen, Germany between 1990 and 2016. About two-thirds were female and the mean age at MS diagnosis was about 14 years.
Of those patients, 126 (27.8%) were classified as obese based on a BMI greater than the 90th percentile, according to the report.
Dr. Huppke and co-investigators found that high BMI was linked to a significantly increased odds of pediatric MS, with odds ratios of 2.19 (95% CI, 1.5-3.1; P < 0.001) in girls and 2.14 (95% CI, 1.3-3.5; P = 0.003) in boys.
A total of 277 of these pediatric patients received a first-line disease-modifying therapy for 6 months or longer, including 249 treated with interferon beta and 51 treated with glatiramer.
Relapses were more common in obese patients, according to the report. with an annualized relapse rate of 1.29, compared to just 0.72 for those who were not overweight (P < 0.001).
Consequently, likelihood of receiving a second-line treatment was about 1.5 times higher in the obese or extremely obese patients, investigators said.
“A healthy weight may potentially optimize treatment outcomes and reduce disease-related burden and health care costs,” they concluded in the report, adding that BMI-adjusted dosing may “increase the value” of first-line disease-modifying therapies.
Dr. Huppke reported disclosures related to Bayer Health Care, Merck Serono, and Novartis not associated with the current study.
SOURCE: Huppke B, et al. JAMA Neurol. 2019 Jul 15. doi: 10.1001/jamaneurol.2019.1997
, results of a recent large, single-center study show. The rate of switching to second-line disease-modifying therapy was consequently about 50% higher among the obese children in the study, which included a total of 453 pediatric patients.
The link between obesity and treatment response suggests that the management of these younger patients with MS could be improved through weight loss or body mass index (BMI)-adjusted dosing, according to Peter Huppke, MD, of Georg August University in Göttingen, Germany, and co-investigators.
“The findings do not indicate that obesity promotes greater disease activity, but pharmacokinetic factors are more likely associated with treatment response,” Dr. Huppke and co-authors said in a report on their study, which was published online ahead of print July 15 in JAMA Neurology.
This is believed to be the first-ever study to find an association between BMI and treatment response in pediatric patients with MS, according to the authors, who said they also confirmed a link between obesity and MS.
Specifically, obesity increased MS susceptibility by two-fold as compared with healthy controls, a finding that they said adds to a small but growing body of evidence that high BMI is associated with increased risk of the disease in these younger individuals.
This retrospective study included 453 pediatric patients with MS treated at the Center for MS in Childhood and Adolescence in Göttingen, Germany between 1990 and 2016. About two-thirds were female and the mean age at MS diagnosis was about 14 years.
Of those patients, 126 (27.8%) were classified as obese based on a BMI greater than the 90th percentile, according to the report.
Dr. Huppke and co-investigators found that high BMI was linked to a significantly increased odds of pediatric MS, with odds ratios of 2.19 (95% CI, 1.5-3.1; P < 0.001) in girls and 2.14 (95% CI, 1.3-3.5; P = 0.003) in boys.
A total of 277 of these pediatric patients received a first-line disease-modifying therapy for 6 months or longer, including 249 treated with interferon beta and 51 treated with glatiramer.
Relapses were more common in obese patients, according to the report. with an annualized relapse rate of 1.29, compared to just 0.72 for those who were not overweight (P < 0.001).
Consequently, likelihood of receiving a second-line treatment was about 1.5 times higher in the obese or extremely obese patients, investigators said.
“A healthy weight may potentially optimize treatment outcomes and reduce disease-related burden and health care costs,” they concluded in the report, adding that BMI-adjusted dosing may “increase the value” of first-line disease-modifying therapies.
Dr. Huppke reported disclosures related to Bayer Health Care, Merck Serono, and Novartis not associated with the current study.
SOURCE: Huppke B, et al. JAMA Neurol. 2019 Jul 15. doi: 10.1001/jamaneurol.2019.1997
, results of a recent large, single-center study show. The rate of switching to second-line disease-modifying therapy was consequently about 50% higher among the obese children in the study, which included a total of 453 pediatric patients.
The link between obesity and treatment response suggests that the management of these younger patients with MS could be improved through weight loss or body mass index (BMI)-adjusted dosing, according to Peter Huppke, MD, of Georg August University in Göttingen, Germany, and co-investigators.
“The findings do not indicate that obesity promotes greater disease activity, but pharmacokinetic factors are more likely associated with treatment response,” Dr. Huppke and co-authors said in a report on their study, which was published online ahead of print July 15 in JAMA Neurology.
This is believed to be the first-ever study to find an association between BMI and treatment response in pediatric patients with MS, according to the authors, who said they also confirmed a link between obesity and MS.
Specifically, obesity increased MS susceptibility by two-fold as compared with healthy controls, a finding that they said adds to a small but growing body of evidence that high BMI is associated with increased risk of the disease in these younger individuals.
This retrospective study included 453 pediatric patients with MS treated at the Center for MS in Childhood and Adolescence in Göttingen, Germany between 1990 and 2016. About two-thirds were female and the mean age at MS diagnosis was about 14 years.
Of those patients, 126 (27.8%) were classified as obese based on a BMI greater than the 90th percentile, according to the report.
Dr. Huppke and co-investigators found that high BMI was linked to a significantly increased odds of pediatric MS, with odds ratios of 2.19 (95% CI, 1.5-3.1; P < 0.001) in girls and 2.14 (95% CI, 1.3-3.5; P = 0.003) in boys.
A total of 277 of these pediatric patients received a first-line disease-modifying therapy for 6 months or longer, including 249 treated with interferon beta and 51 treated with glatiramer.
Relapses were more common in obese patients, according to the report. with an annualized relapse rate of 1.29, compared to just 0.72 for those who were not overweight (P < 0.001).
Consequently, likelihood of receiving a second-line treatment was about 1.5 times higher in the obese or extremely obese patients, investigators said.
“A healthy weight may potentially optimize treatment outcomes and reduce disease-related burden and health care costs,” they concluded in the report, adding that BMI-adjusted dosing may “increase the value” of first-line disease-modifying therapies.
Dr. Huppke reported disclosures related to Bayer Health Care, Merck Serono, and Novartis not associated with the current study.
SOURCE: Huppke B, et al. JAMA Neurol. 2019 Jul 15. doi: 10.1001/jamaneurol.2019.1997
FROM JAMA NEUROLOGY
Key clinical point: Obese children and adolescents with MS had about twice as many relapses on first-line treatment as compared with their non-obese counterparts.
Major finding: The annualized relapse rate was 1.29 for obese pediatric patients, compared to 0.72 for those who were not overweight (P < 0.001).
Study details: Retrospective study including 453 patients with pediatric MS treated at a center in Göttingen, Germany between 1990 and 2016.
Disclosures: The senior author reported disclosures related to Bayer Health Care, Merck Serono, and Novartis unrelated to the this study.
Source: Huppke B, et al. JAMA Neurol. 2019 Jul 15.
Register for the UCLA / SVS Symposium
Register today for the fourth annual UCLA / SVS Symposium. This year’s event, “A Comprehensive Review and Update of What’s New in Vascular and Endovascular Surgery,” will be held Aug. 24 to 26 at the Beverly Hilton in Beverly Hills, Calif. An internationally recognized faculty will present a comprehensive survey of generally accepted views. These will include basic science, pathogenesis, diagnosis and management of the broad spectrum of vascular disorders. Additionally, all speakers will address important new developments related to their topic that have taken place within the last year. Learn more and register today.
Register today for the fourth annual UCLA / SVS Symposium. This year’s event, “A Comprehensive Review and Update of What’s New in Vascular and Endovascular Surgery,” will be held Aug. 24 to 26 at the Beverly Hilton in Beverly Hills, Calif. An internationally recognized faculty will present a comprehensive survey of generally accepted views. These will include basic science, pathogenesis, diagnosis and management of the broad spectrum of vascular disorders. Additionally, all speakers will address important new developments related to their topic that have taken place within the last year. Learn more and register today.
Register today for the fourth annual UCLA / SVS Symposium. This year’s event, “A Comprehensive Review and Update of What’s New in Vascular and Endovascular Surgery,” will be held Aug. 24 to 26 at the Beverly Hilton in Beverly Hills, Calif. An internationally recognized faculty will present a comprehensive survey of generally accepted views. These will include basic science, pathogenesis, diagnosis and management of the broad spectrum of vascular disorders. Additionally, all speakers will address important new developments related to their topic that have taken place within the last year. Learn more and register today.
Crossword: Opioids in the News
New appointments at City of Hope, UA, and Fox Chase
The University of Arizona (UA) Cancer Center has a new interim director, two hematologists have earned new positions at City of Hope, and an assistant professor has joined Fox Chase Cancer Center.
William Cance, MD, has been appointed interim director of the UA Cancer Center. In this role, he will oversee clinical operations and research at the center’s primary locations in Tucson and Phoenix. He will also lead the UA Cancer Center’s efforts to renew its 5-year Cancer Center Support Grant from the National Cancer Institute (NCI).
In addition to his new role, Dr. Cance is a professor at the UA Colleges of Medicine and Pharmacy in Phoenix. He is board certified in general surgery and specializes in thyroid cancer, parathyroid disease, sarcoma, and gastrointestinal cancer. Dr. Cance has received funding from NCI, has served on the NCI Board of Scientific Counselors, and is a member of NCI Subcommittee F.
In other news, Larry Kwak, MD, PhD, has been appointed the deputy director of the Hematologic Malignancies and Stem Cell Transplantation Institute at City of Hope in Duarte, Calif. Dr. Kwak will work with the director of the Institute, Stephen J. Forman, MD, to oversee recruitment, clinical and laboratory research, and faculty development.
Dr. Kwak is also director of the Toni Stephenson Lymphoma Center, vice president and deputy director of the comprehensive cancer center, and the Dr. Michael Friedman Professor in Translational Medicine. Dr. Kwak was named one of TIME magazine’s “100 Most Influential People,” received the Chang-Yul Oh Memorial Award from the Korean Medical Association, and won the Ho-Am Prize in Medicine.
Also at City of Hope, Tanya Siddiqi, MD, has been appointed director of the chronic lymphocytic leukemia (CLL) program within the Toni Stephenson Lymphoma Center of the Hematologic Malignancies and Stem Cell Transplantation Institute. In this role, Dr. Siddiqi will oversee research efforts related to CLL. This includes maintaining the CLL tissue bank she developed, conducting translational studies and clinical trials, and investigating novel therapies for CLL.
Dr. Siddiqi is also an associate clinical professor in the department of hematology & hematopoietic cell transplantation, is the supervising physician of City of Hope’s anticoagulation clinic, and works in the Gehr Family Center for Leukemia Research. Dr. Siddiqi is a member of the National Comprehensive Cancer Network panels for CLL/SLL/hairy cell leukemia and venous thromboembolism.
Lastly, James M. Martin, MD, has been appointed assistant professor in the hematology and bone marrow transplant program within the department of hematology/oncology at Fox Chase Cancer Center in Philadelphia.
Dr. Martin received a medical degree from Ohio State University, Columbus, and completed an internship and residency at Rhode Island Hospital/Brown University, in Providence. He joined Fox Chase Cancer Center/Temple University in 2016 for a 3-year fellowship.
Movers in Medicine highlights career moves and personal achievements by hematologists and oncologists. Did you switch jobs, take on a new role, climb a mountain? Tell us all about it at [email protected], and you could be featured in Movers in Medicine.
The University of Arizona (UA) Cancer Center has a new interim director, two hematologists have earned new positions at City of Hope, and an assistant professor has joined Fox Chase Cancer Center.
William Cance, MD, has been appointed interim director of the UA Cancer Center. In this role, he will oversee clinical operations and research at the center’s primary locations in Tucson and Phoenix. He will also lead the UA Cancer Center’s efforts to renew its 5-year Cancer Center Support Grant from the National Cancer Institute (NCI).
In addition to his new role, Dr. Cance is a professor at the UA Colleges of Medicine and Pharmacy in Phoenix. He is board certified in general surgery and specializes in thyroid cancer, parathyroid disease, sarcoma, and gastrointestinal cancer. Dr. Cance has received funding from NCI, has served on the NCI Board of Scientific Counselors, and is a member of NCI Subcommittee F.
In other news, Larry Kwak, MD, PhD, has been appointed the deputy director of the Hematologic Malignancies and Stem Cell Transplantation Institute at City of Hope in Duarte, Calif. Dr. Kwak will work with the director of the Institute, Stephen J. Forman, MD, to oversee recruitment, clinical and laboratory research, and faculty development.
Dr. Kwak is also director of the Toni Stephenson Lymphoma Center, vice president and deputy director of the comprehensive cancer center, and the Dr. Michael Friedman Professor in Translational Medicine. Dr. Kwak was named one of TIME magazine’s “100 Most Influential People,” received the Chang-Yul Oh Memorial Award from the Korean Medical Association, and won the Ho-Am Prize in Medicine.
Also at City of Hope, Tanya Siddiqi, MD, has been appointed director of the chronic lymphocytic leukemia (CLL) program within the Toni Stephenson Lymphoma Center of the Hematologic Malignancies and Stem Cell Transplantation Institute. In this role, Dr. Siddiqi will oversee research efforts related to CLL. This includes maintaining the CLL tissue bank she developed, conducting translational studies and clinical trials, and investigating novel therapies for CLL.
Dr. Siddiqi is also an associate clinical professor in the department of hematology & hematopoietic cell transplantation, is the supervising physician of City of Hope’s anticoagulation clinic, and works in the Gehr Family Center for Leukemia Research. Dr. Siddiqi is a member of the National Comprehensive Cancer Network panels for CLL/SLL/hairy cell leukemia and venous thromboembolism.
Lastly, James M. Martin, MD, has been appointed assistant professor in the hematology and bone marrow transplant program within the department of hematology/oncology at Fox Chase Cancer Center in Philadelphia.
Dr. Martin received a medical degree from Ohio State University, Columbus, and completed an internship and residency at Rhode Island Hospital/Brown University, in Providence. He joined Fox Chase Cancer Center/Temple University in 2016 for a 3-year fellowship.
Movers in Medicine highlights career moves and personal achievements by hematologists and oncologists. Did you switch jobs, take on a new role, climb a mountain? Tell us all about it at [email protected], and you could be featured in Movers in Medicine.
The University of Arizona (UA) Cancer Center has a new interim director, two hematologists have earned new positions at City of Hope, and an assistant professor has joined Fox Chase Cancer Center.
William Cance, MD, has been appointed interim director of the UA Cancer Center. In this role, he will oversee clinical operations and research at the center’s primary locations in Tucson and Phoenix. He will also lead the UA Cancer Center’s efforts to renew its 5-year Cancer Center Support Grant from the National Cancer Institute (NCI).
In addition to his new role, Dr. Cance is a professor at the UA Colleges of Medicine and Pharmacy in Phoenix. He is board certified in general surgery and specializes in thyroid cancer, parathyroid disease, sarcoma, and gastrointestinal cancer. Dr. Cance has received funding from NCI, has served on the NCI Board of Scientific Counselors, and is a member of NCI Subcommittee F.
In other news, Larry Kwak, MD, PhD, has been appointed the deputy director of the Hematologic Malignancies and Stem Cell Transplantation Institute at City of Hope in Duarte, Calif. Dr. Kwak will work with the director of the Institute, Stephen J. Forman, MD, to oversee recruitment, clinical and laboratory research, and faculty development.
Dr. Kwak is also director of the Toni Stephenson Lymphoma Center, vice president and deputy director of the comprehensive cancer center, and the Dr. Michael Friedman Professor in Translational Medicine. Dr. Kwak was named one of TIME magazine’s “100 Most Influential People,” received the Chang-Yul Oh Memorial Award from the Korean Medical Association, and won the Ho-Am Prize in Medicine.
Also at City of Hope, Tanya Siddiqi, MD, has been appointed director of the chronic lymphocytic leukemia (CLL) program within the Toni Stephenson Lymphoma Center of the Hematologic Malignancies and Stem Cell Transplantation Institute. In this role, Dr. Siddiqi will oversee research efforts related to CLL. This includes maintaining the CLL tissue bank she developed, conducting translational studies and clinical trials, and investigating novel therapies for CLL.
Dr. Siddiqi is also an associate clinical professor in the department of hematology & hematopoietic cell transplantation, is the supervising physician of City of Hope’s anticoagulation clinic, and works in the Gehr Family Center for Leukemia Research. Dr. Siddiqi is a member of the National Comprehensive Cancer Network panels for CLL/SLL/hairy cell leukemia and venous thromboembolism.
Lastly, James M. Martin, MD, has been appointed assistant professor in the hematology and bone marrow transplant program within the department of hematology/oncology at Fox Chase Cancer Center in Philadelphia.
Dr. Martin received a medical degree from Ohio State University, Columbus, and completed an internship and residency at Rhode Island Hospital/Brown University, in Providence. He joined Fox Chase Cancer Center/Temple University in 2016 for a 3-year fellowship.
Movers in Medicine highlights career moves and personal achievements by hematologists and oncologists. Did you switch jobs, take on a new role, climb a mountain? Tell us all about it at [email protected], and you could be featured in Movers in Medicine.
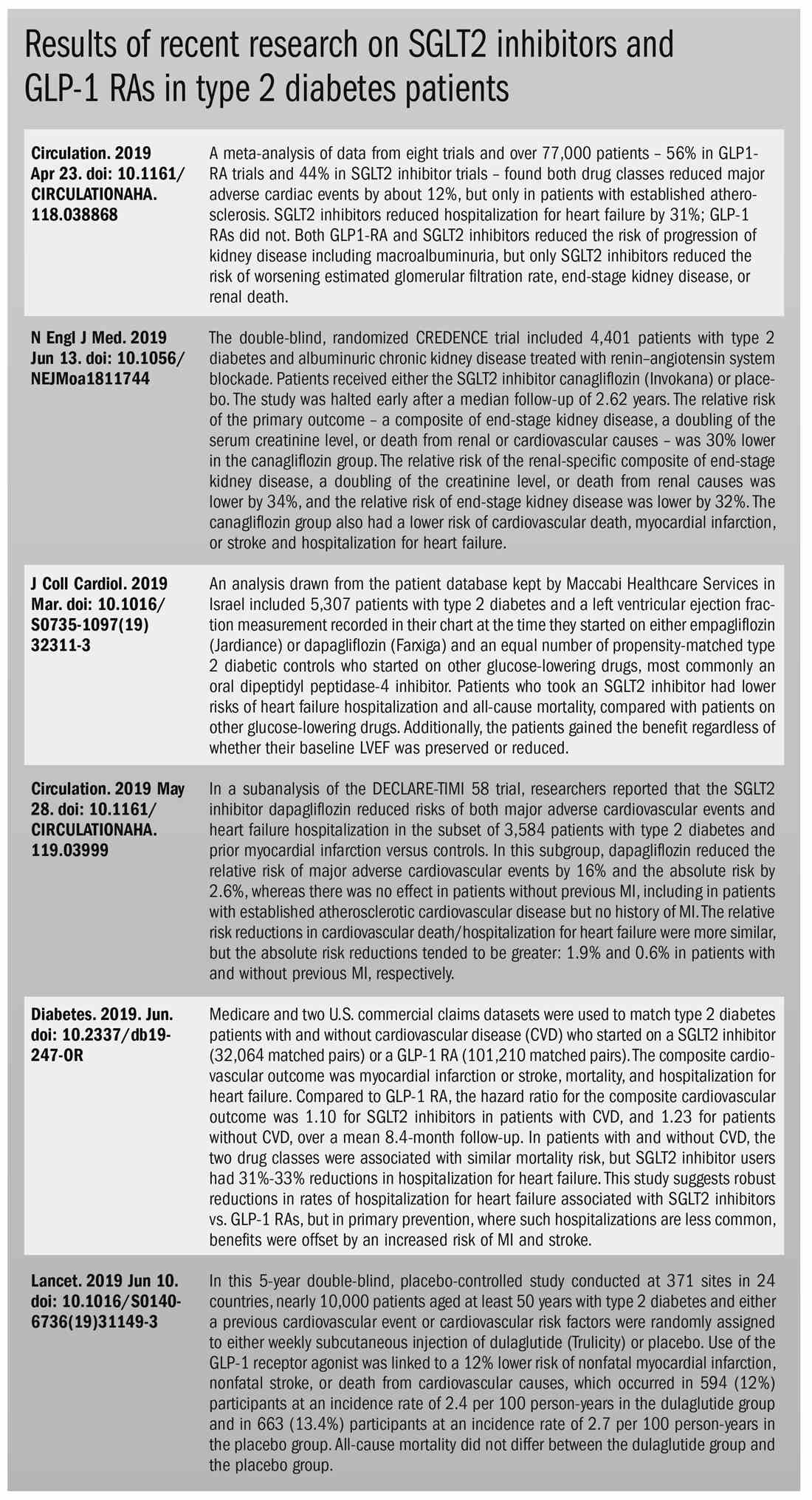
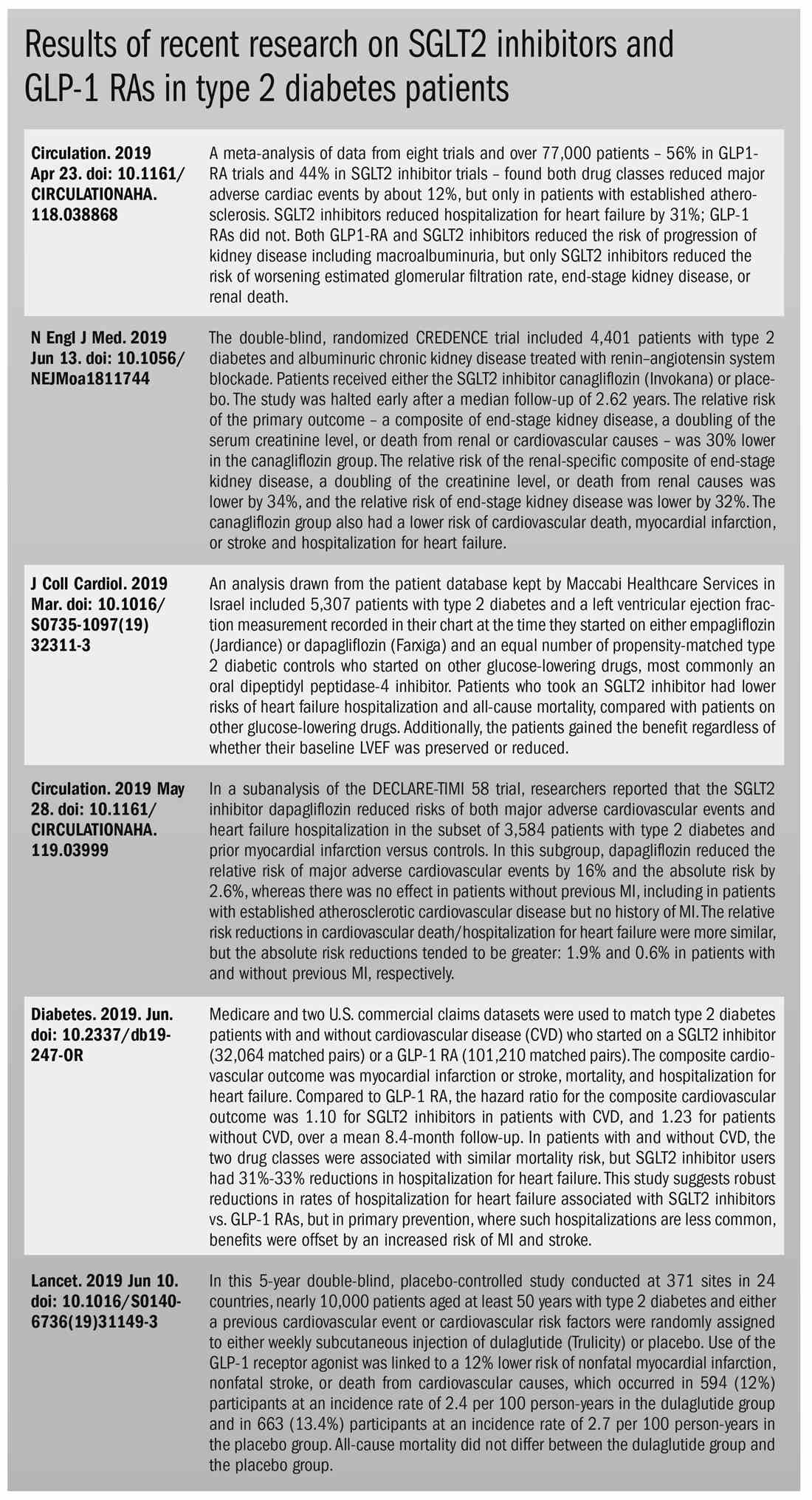
The costs and benefits of SGLT2 inhibitors & GLP-1 RAs
The options for treating type 2 diabetes without insulin have grown beyond metformin to include a long list of sodium-glucose cotransporter 2 (SGLT2) inhibitors and glucagonlike peptide–1 (GLP-1) receptor agonists that can be taken with or without metformin. These new drugs have cardiovascular and kidney benefits and help with weight loss, but they also carry risks and, according to some experts, their costs can be prohibitively expensive.
Given the medical community’s long-term experience with treating patients with metformin, and metformin’s lower cost, most of the physicians interviewed for this article advise using SGLT2 inhibitors and GLP-1 receptor agonists as second-line treatments. Others said that they would prefer to use the newer drugs as first-line therapies in select high-risk patients, but prior authorization hurdles created by insurance companies make that approach too burdensome.
“The economics of U.S. health care is stacked against many of our patients with diabetes in the current era,” Robert H. Hopkins Jr., MD, said in an interview.
Even when their insurance approves the drugs, patients still may not be able to afford the copay, explained Dr. Hopkins, professor of internal medicine and pediatrics and director of the division of general internal medicine at the University of Arkansas for Medical Sciences, Little Rock. “Sometimes patients can purchase drugs at a lower cost than the copay to purchase with the ‘drug coverage’ in their insurance plan – unfortunately, this is not the case with the newer diabetes medications we are discussing here.”
“SGLT2 inhibitors and GLP-1 agonists can cost several hundred dollars a month, and insurers often balk at paying for them. They’ll say, ‘Have you tried metformin?’ ” explained endocrinologist Victor Lawrence Roberts, MD, in a interview. “We have to work with insurance companies the best we can in a stepwise fashion.”
According to Dr. Roberts, 80% of his patients with diabetes struggle with the cost of medicine in general. “They’re either underinsured or not insured or their formulary is limited.
Douglas S. Paauw, MD, agreed in an interview that the newer drugs can be problematic on the insurance front.
“For some patients they aren’t affordable, especially for the uninsured if you can’t get them on an assistance program,” said Dr. Paauw, who is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the university.
Dr. Hopkins, who is on the Internal Medicine News board, noted that “unfortunately, the treatment of type 2 diabetes in patients who cannot achieve control with metformin, diet, weight control, and exercise is a story of the ‘haves’ and the ‘have nots.’ The ‘haves’ are those who have pharmacy benefits which make access to newer agents like SGLT2 inhibitors and GLP-1 agonists a possibility.”
“I have had very few of the ‘have nots’ who have been able to even consider these newer agents, which carry price tags of $600-$1,300 a month even with the availability of discounting coupons in the marketplace,” he added. “Most of these patients end up requiring a sulfonylurea or TZD [thiazolidinedione] as a second agent to achieve glycemic control. This makes it very difficult to achieve sufficient weight and metabolic control to avoid an eventual switch to insulin.”
Fatima Z. Syed, MD, an endocrine-trained general internist at DukeHealth in Durham, N.C., said she prescribes SGLT2 inhibitors and GLP-1 receptor agonists in combination with metformin. “I prescribe them frequently, but they are not first-line treatments,” she explained.
“Nothing replaces diet and exercise” as therapy for patients with type 2 diabetes, she added.
Neil S. Skolnik, MD, said that insurance companies were not preventing patients from using these drugs in his experience. He also provided an optimistic take on the accessibility of these drugs in the near future.
“Most insurance companies are now covering select SGLT2 inhibitors and GLP-1 receptor agonists for appropriate patients and those companies that currently do not will soon have to,” said Dr. Skolnik, who is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health.
“The outcomes [associated with use of the new drugs] are robust, the benefits are large, and are well worth the cost,” he added.
The side effects
While others praised these drugs for their beneficial effects, they also noted that the side effects of these drugs are serious and must be discussed with patients.
GLP-1 receptor agonists are linked to gastrointestinal symptoms, especially nausea, while SGLT2 inhibitors have been linked to kidney failure, ketoacidosis, and more. The Food and Drug Administration warned in 2018 that the SGLT2 inhibitors can cause a rare serious infection known as Fournier’s gangrene – necrotizing fasciitis of the perineum.
“We have to tell our patients to let us know right away if they get pain or swelling in the genital area,” Dr. Paauw, who is on the Internal Medicine News board, noted. “The chance that an infection could explode quickly is higher in those who take these drugs.”
Amputation risks also are associated with taking the SGLT2 inhibitor canagliflozin (Invokana). The FDA requires the manufacturer of this drug to include a black-box warning about the risk of “lower-limb amputations, most frequently of the toe and midfoot,” but also the leg. In approval trials, the risk doubled versus placebo.
These amputation risks “put a damper on some of the enthusiasm on behalf of physicians and patients ... for taking this drug,” noted Dr. Roberts, who is a professor of internal medicine at the University of Central Florida, Orlando.
While a manufacturer-funded study released last year found no link to amputations, the results weren’t powerful enough to rule out a moderately increased risk.
“[If] you are at high risk for having an amputation, we really have to take this risk very seriously,” said John B. Buse, MD, chief of the division of endocrinology at the University of North Carolina at Chapel Hill, in a presentation about the study at the 2018 annual scientific sessions of the American Diabetes Association.
The benefits
Despite these risks of adverse events, most interviewed agreed that the many benefits observed in those taking SGLT2 inhibitors or GLP-1 receptor agonists make them worth prescribing, at least to those who are able to afford them.
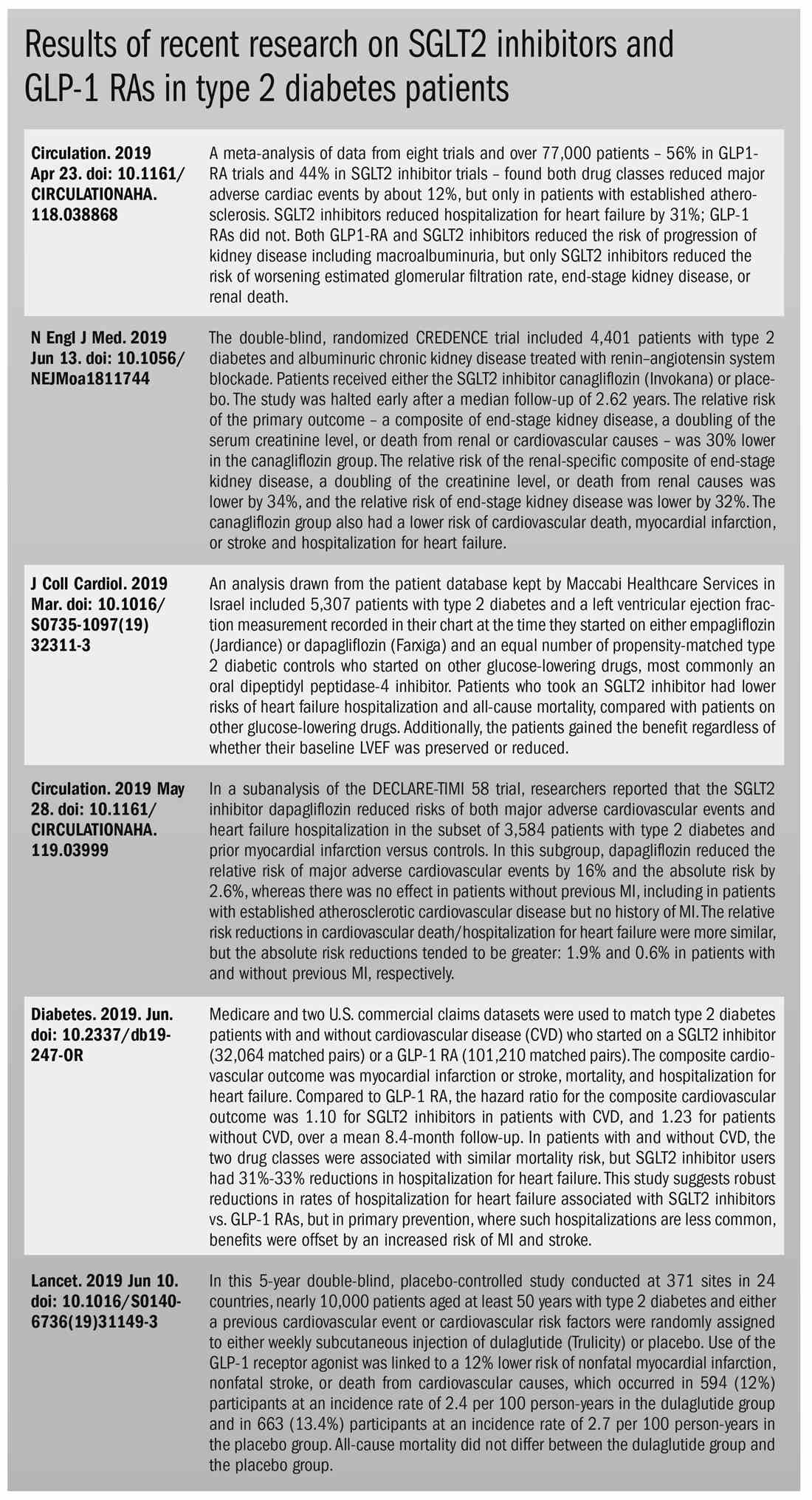
Both SGLT2 inhibitors and GLP-1 receptor agonists appear to have significant cardiovascular benefits. A 2019 meta-analysis and systematic review found that both drugs reduced major adverse cardiac events by about 12% (Circulation. 2019 Apr 23;139[17]:2022-31).
“They don’t cause hypoglycemia, they lower blood pressure, they don’t cause weight gain, and they might promote weight loss,” noted Dr. Paauw.
SGLT2 inhibitors also have shown signs of kidney benefits. The CREDENCE trial linked canagliflozin to a lowering of kidney disorders versus placebo (N Engl J Med. 2019 Jun 13;380[24]:2295-306). “The relative risk of the renal-specific composite of end-stage kidney disease, a doubling of the creatinine level, or death from renal causes was lower by 34% (hazard ratio, 0.66; 95% confidence interval, 0.53-0.81; P less than .001), and the relative risk of end-stage kidney disease was lower by 32% (HR, 0.68; 95% CI, 0.54-0.86; P = .002),” the trial investigators wrote.
“They showed very nicely that the drug improved the kidney function of those patients and reduced the kidney deterioration,” said Yehuda Handelsman, MD, an endocrinologist in Tarzana, Calif., who chaired the 2011 and 2015 American Association of Clinical Endocrinologists’ Comprehensive Diabetes Guidelines. The study was especially impressive, he added, because it included patients with low kidney function.
SGLT2 inhibitors’ “diuretic mechanism explains why there is a substantial reduction in heart failure hospitalizations in patients who take these drugs,” said cardiologist Marc E. Goldschmidt, MD, director of the Heart Success Program at Atlantic Health System’s Morristown (N.J.) Medical Center, in an interview. “Both the EMPA-REG Outcome and the CREDENCE trials demonstrated substantial benefit of this class of medications by showing a lower risk of cardiovascular death as well as death from any cause and a lower risk of hospitalization for heart failure."
Overall, the SGLT2 trial data have been very consistent with a benefit for cardiovascular risk reduction, particularly in regard to heart failure hospitalizations and even in potentially preventing heart failure in diabetics,” he added.
Dr. Skolnik, a columnist for Family Practice News, cited SGLT2 inhibitors and GLP-1 receptor agonists’ ability to slow renal disease progression, promote weight loss, and prevent poor cardiac outcomes.“These drugs should be used, in addition to metformin, in all patients with diabetes and vascular disease. These proven outcomes are far better than we ever were able to achieve previously and the strength of the evidence at this point is very strong,” said Dr. Skolnik. “In addition to the benefits of decreasing the development of cardiovascular disease, serious heart failure, and slowing progression of renal disease, these two classes of medication have additional benefits. Both classes help patients lose weight, which is very different from what was found with either sulfonylureas or insulin, which cause patients to gain weight. Also both the SGLT2 inhibitors and the GLP-1 RAs [receptor agonists] have a low incidence of hypoglycemia. For all these reasons, these have become important medications for us to use in primary care.”
Other recent trials offer “very powerful data” about SGLT2 inhibitors, Dr. Roberts said. That’s good news, since “our approach needs to be toward cardiovascular protection and preservation as well as managing blood sugar.”An Israeli trial, whose results were released in May 2019 at the annual meeting of the American College of Cardiology, found that, compared with other glucose-lowering drugs, taking an SGLT2 inhibitor was associated with lower risks of heart failure hospitalization and all-cause mortality (HR, 0.54; 95% CI, 0.44-0.65; P less than .001). This trial also offered a new detail: The patients gained the benefit regardless of whether their baseline left ventricular ejection fraction was preserved or reduced (J Coll Cardiol. 2019 Mar;73[9]:suppl 1). The SGLT2 inhibitors used in this trial included dapagliflozin (Farxiga) and empagliflozin (Jardiance).
In another study released this year, a subanalysis of the DECLARE-TIMI 58 trial, researchers reported that the SGLT2 inhibitor dapagliflozin reduced risks of both major adverse cardiovascular events and heart failure hospitalization in the subset of patients with type 2 diabetes and prior myocardial infarction versus controls (Circulation. 2019 May 28;139[22]:2516-27). The absolute risk reduction for major adverse cardiovascular events was 1.9% (HR, 0.81; 95% CI, 0.65-1.00; P = .046), while it was 0.6% for heart failure hospitalization (HR, 0.85; 95% CI, 0.72-1.00; P = .055).
These and other studies “speak volumes about the efficacy of managing blood sugar and addressing our biggest nemesis, which is cardiovascular disease,” Dr. Roberts said. “It’s irrefutable. The data [are] very good.”
Dr. Paauw said an SGLT2 inhibitor or GLP-1 receptor agonist is best reserved for use in select patients with cardiovascular risks and type 2 diabetes that need management beyond metformin.
For example, they might fit a 70-year-old with persistent hypertension who’s already taking a couple of blood pressure medications. “If they have another cardiovascular risk factor, the cardiovascular protection piece will be a bigger deal,” he said. Also, “it will probably help lower their blood pressure so they can avoid taking another blood pressure medicine.”
Trials of both GLP-1 receptor agonists and SGLT2 inhibitors have shown benefits “in improving [major adverse cardiac events], with the SGLT2 class showing substantial benefit in improving both heart failure and renal outcomes as well,” noted Dr. Skolnik. “It is in this context that one must address the question of whether the price of the medications are worthwhile. With such substantial benefit, there is no question in my mind that – for patients who have underlying cardiovascular illness, which includes patients with existent coronary disease, history of stroke, transient ischemic attack, or peripheral vascular disease – it is far and away worth it to prescribe these classes of medications.”
Indeed, the American Diabetes Association and the European Association for the Study of Diabetes’ most recent guidelines now call for a GLP-1 receptor agonist – instead of insulin – to be the first injectable used to treat type 2 diabetes (Diabetes Care 2018 Dec; 41[12]:2669-701).
“For the relatively small number of my patients who have been able to access and use these medications for months or longer, more have tolerated the GLP-1 agonists than SGLT2 inhibitors primarily due to urinary issues,” noted Dr. Hopkins.
Dipeptidyl peptidase–4 inhibitors are another option in patients with type 2 diabetes, but research suggests they may not be a top option for patients with cardiovascular risk. A 2018 review noted that cardiovascular outcome trials for alogliptin (Nesina), saxagliptin (Onglyza), and sitagliptin (Januvia) showed noninferiority but failed to demonstrate any superiority, compared with placebo in patients with type 2 diabetes mellitus and high cardiovascular risk (Circ Res. 2018 May 11;122[10]:1439-59).
The combination therapies
Many of the newer drugs are available as combinations with other types of diabetes drugs. In some cases, physicians create their own form of combination therapy by separately prescribing two or more diabetes drugs. Earlier this year, a study suggested the benefits of this kind of add-on therapy: Diabetes outcomes improved in patients who took the GLP-1 receptor agonist semaglutide and an SGLT2 inhibitor (Lancet Diabetes Endocrinol. 2019 Mar 1. doi: 10.1016/S2213-8587[19]30066-X).
Dr. Roberts suggested caution, however, when prescribing combination therapies. “My recommendation is always to begin with the individual medications to see if the patient tolerates the drugs and then decide which component needs to be titrated. It’s hard to titrate a combination drug, and it doesn’t leave a lot of flexibility. You never know which drug is doing what.
Dr. Handelsman said some patients may need to take three medications such as metformin, an SGLT2 inhibitor, and a GLP-1 receptor agonist.
“I don’t recommend using the combinations if you’re not familiar with the drugs ... These are relatively new pharmaceuticals, and most of us are on a learning curve as to how they fit into the armamentarium. If a drug is tolerated with a good response, you can certainly consider going to the combination tablets,” he added.
There is at least one drug that combines these three classes: The newly FDA-approved Qternmet XR, which combines dapagliflozin (an SGLT2 inhibitor), saxagliptin (a GLP-1 receptor agonist), and metformin. As of mid-June 2019, it was not yet available in the United States. Its sister drug Qtern, which combines dapagliflozin and saxagliptin, costs more than $500 a month with a free coupon, according to goodrx.com. In contrast, metformin is extremely inexpensive, costing just a few dollars a month for a common starting dose.
What about adding insulin?
“Both [SGLT2 inhibitors and GLP-1 receptor agonists] work very well with insulin,” Dr. Handelsman said. “There is a nice additive effect on the reduction of [hemoglobin] A1c. The only caution is that, although neither SGLT2 inhibitors nor GLP-1 receptor agonists cause hypoglycemia, in combination with insulin they do increase the risk of hypoglycemia. You may have to adjust the dose of insulin.”
Dr. Hopkins warned that cost becomes an even bigger issue when you add insulin into the mix.
“When insulin comes into the discussion, we are again stuck with astronomical costs which many struggle to afford,” he explained.
Indeed, the price tag on these drugs seems to be the biggest problem physicians have with them.
“The challenges in managing patients with diabetes aren’t the risks associated with the drugs. It’s dealing with their insurers,” noted Dr. Roberts.
Dr. Hopkins, Dr. Paauw, Dr. Roberts, and Dr. Syed reported no disclosures. Dr. Buse is an investigator for Johnson and Johnson. Dr. Goldschmidt is paid to speak by Novartis. Dr. Handelsman reported research grants, consulting work, and speaker honoraria from Amgen, Gilead, Lilly, Merck, Novo Nordisk, and others. Dr Skolnik reported nonfinancial support from AstraZeneca, Boehringer Ingelheim, Sanofi, and GlaxoSmithKline and personal fees from AstraZeneca, Boehringer Ingelheim, and Eli Lilly. He also serves on the advisory boards of AstraZeneca, Boehringer Ingelheim, Teva Pharmaceutical, Eli Lilly, Sanofi, Janssen Pharmaceuticals, Intarcia, Mylan, and GlaxoSmithKline.
Dr. Paauw and Dr. Skolnik are columnists for Family Practice News and Internal Medicine News.
M. Alexander Otto contributed to this report.
The options for treating type 2 diabetes without insulin have grown beyond metformin to include a long list of sodium-glucose cotransporter 2 (SGLT2) inhibitors and glucagonlike peptide–1 (GLP-1) receptor agonists that can be taken with or without metformin. These new drugs have cardiovascular and kidney benefits and help with weight loss, but they also carry risks and, according to some experts, their costs can be prohibitively expensive.
Given the medical community’s long-term experience with treating patients with metformin, and metformin’s lower cost, most of the physicians interviewed for this article advise using SGLT2 inhibitors and GLP-1 receptor agonists as second-line treatments. Others said that they would prefer to use the newer drugs as first-line therapies in select high-risk patients, but prior authorization hurdles created by insurance companies make that approach too burdensome.
“The economics of U.S. health care is stacked against many of our patients with diabetes in the current era,” Robert H. Hopkins Jr., MD, said in an interview.
Even when their insurance approves the drugs, patients still may not be able to afford the copay, explained Dr. Hopkins, professor of internal medicine and pediatrics and director of the division of general internal medicine at the University of Arkansas for Medical Sciences, Little Rock. “Sometimes patients can purchase drugs at a lower cost than the copay to purchase with the ‘drug coverage’ in their insurance plan – unfortunately, this is not the case with the newer diabetes medications we are discussing here.”
“SGLT2 inhibitors and GLP-1 agonists can cost several hundred dollars a month, and insurers often balk at paying for them. They’ll say, ‘Have you tried metformin?’ ” explained endocrinologist Victor Lawrence Roberts, MD, in a interview. “We have to work with insurance companies the best we can in a stepwise fashion.”
According to Dr. Roberts, 80% of his patients with diabetes struggle with the cost of medicine in general. “They’re either underinsured or not insured or their formulary is limited.
Douglas S. Paauw, MD, agreed in an interview that the newer drugs can be problematic on the insurance front.
“For some patients they aren’t affordable, especially for the uninsured if you can’t get them on an assistance program,” said Dr. Paauw, who is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the university.
Dr. Hopkins, who is on the Internal Medicine News board, noted that “unfortunately, the treatment of type 2 diabetes in patients who cannot achieve control with metformin, diet, weight control, and exercise is a story of the ‘haves’ and the ‘have nots.’ The ‘haves’ are those who have pharmacy benefits which make access to newer agents like SGLT2 inhibitors and GLP-1 agonists a possibility.”
“I have had very few of the ‘have nots’ who have been able to even consider these newer agents, which carry price tags of $600-$1,300 a month even with the availability of discounting coupons in the marketplace,” he added. “Most of these patients end up requiring a sulfonylurea or TZD [thiazolidinedione] as a second agent to achieve glycemic control. This makes it very difficult to achieve sufficient weight and metabolic control to avoid an eventual switch to insulin.”
Fatima Z. Syed, MD, an endocrine-trained general internist at DukeHealth in Durham, N.C., said she prescribes SGLT2 inhibitors and GLP-1 receptor agonists in combination with metformin. “I prescribe them frequently, but they are not first-line treatments,” she explained.
“Nothing replaces diet and exercise” as therapy for patients with type 2 diabetes, she added.
Neil S. Skolnik, MD, said that insurance companies were not preventing patients from using these drugs in his experience. He also provided an optimistic take on the accessibility of these drugs in the near future.
“Most insurance companies are now covering select SGLT2 inhibitors and GLP-1 receptor agonists for appropriate patients and those companies that currently do not will soon have to,” said Dr. Skolnik, who is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health.
“The outcomes [associated with use of the new drugs] are robust, the benefits are large, and are well worth the cost,” he added.
The side effects
While others praised these drugs for their beneficial effects, they also noted that the side effects of these drugs are serious and must be discussed with patients.
GLP-1 receptor agonists are linked to gastrointestinal symptoms, especially nausea, while SGLT2 inhibitors have been linked to kidney failure, ketoacidosis, and more. The Food and Drug Administration warned in 2018 that the SGLT2 inhibitors can cause a rare serious infection known as Fournier’s gangrene – necrotizing fasciitis of the perineum.
“We have to tell our patients to let us know right away if they get pain or swelling in the genital area,” Dr. Paauw, who is on the Internal Medicine News board, noted. “The chance that an infection could explode quickly is higher in those who take these drugs.”
Amputation risks also are associated with taking the SGLT2 inhibitor canagliflozin (Invokana). The FDA requires the manufacturer of this drug to include a black-box warning about the risk of “lower-limb amputations, most frequently of the toe and midfoot,” but also the leg. In approval trials, the risk doubled versus placebo.
These amputation risks “put a damper on some of the enthusiasm on behalf of physicians and patients ... for taking this drug,” noted Dr. Roberts, who is a professor of internal medicine at the University of Central Florida, Orlando.
While a manufacturer-funded study released last year found no link to amputations, the results weren’t powerful enough to rule out a moderately increased risk.
“[If] you are at high risk for having an amputation, we really have to take this risk very seriously,” said John B. Buse, MD, chief of the division of endocrinology at the University of North Carolina at Chapel Hill, in a presentation about the study at the 2018 annual scientific sessions of the American Diabetes Association.
The benefits
Despite these risks of adverse events, most interviewed agreed that the many benefits observed in those taking SGLT2 inhibitors or GLP-1 receptor agonists make them worth prescribing, at least to those who are able to afford them.
Both SGLT2 inhibitors and GLP-1 receptor agonists appear to have significant cardiovascular benefits. A 2019 meta-analysis and systematic review found that both drugs reduced major adverse cardiac events by about 12% (Circulation. 2019 Apr 23;139[17]:2022-31).
“They don’t cause hypoglycemia, they lower blood pressure, they don’t cause weight gain, and they might promote weight loss,” noted Dr. Paauw.
SGLT2 inhibitors also have shown signs of kidney benefits. The CREDENCE trial linked canagliflozin to a lowering of kidney disorders versus placebo (N Engl J Med. 2019 Jun 13;380[24]:2295-306). “The relative risk of the renal-specific composite of end-stage kidney disease, a doubling of the creatinine level, or death from renal causes was lower by 34% (hazard ratio, 0.66; 95% confidence interval, 0.53-0.81; P less than .001), and the relative risk of end-stage kidney disease was lower by 32% (HR, 0.68; 95% CI, 0.54-0.86; P = .002),” the trial investigators wrote.
“They showed very nicely that the drug improved the kidney function of those patients and reduced the kidney deterioration,” said Yehuda Handelsman, MD, an endocrinologist in Tarzana, Calif., who chaired the 2011 and 2015 American Association of Clinical Endocrinologists’ Comprehensive Diabetes Guidelines. The study was especially impressive, he added, because it included patients with low kidney function.
SGLT2 inhibitors’ “diuretic mechanism explains why there is a substantial reduction in heart failure hospitalizations in patients who take these drugs,” said cardiologist Marc E. Goldschmidt, MD, director of the Heart Success Program at Atlantic Health System’s Morristown (N.J.) Medical Center, in an interview. “Both the EMPA-REG Outcome and the CREDENCE trials demonstrated substantial benefit of this class of medications by showing a lower risk of cardiovascular death as well as death from any cause and a lower risk of hospitalization for heart failure."
Overall, the SGLT2 trial data have been very consistent with a benefit for cardiovascular risk reduction, particularly in regard to heart failure hospitalizations and even in potentially preventing heart failure in diabetics,” he added.
Dr. Skolnik, a columnist for Family Practice News, cited SGLT2 inhibitors and GLP-1 receptor agonists’ ability to slow renal disease progression, promote weight loss, and prevent poor cardiac outcomes.“These drugs should be used, in addition to metformin, in all patients with diabetes and vascular disease. These proven outcomes are far better than we ever were able to achieve previously and the strength of the evidence at this point is very strong,” said Dr. Skolnik. “In addition to the benefits of decreasing the development of cardiovascular disease, serious heart failure, and slowing progression of renal disease, these two classes of medication have additional benefits. Both classes help patients lose weight, which is very different from what was found with either sulfonylureas or insulin, which cause patients to gain weight. Also both the SGLT2 inhibitors and the GLP-1 RAs [receptor agonists] have a low incidence of hypoglycemia. For all these reasons, these have become important medications for us to use in primary care.”
Other recent trials offer “very powerful data” about SGLT2 inhibitors, Dr. Roberts said. That’s good news, since “our approach needs to be toward cardiovascular protection and preservation as well as managing blood sugar.”An Israeli trial, whose results were released in May 2019 at the annual meeting of the American College of Cardiology, found that, compared with other glucose-lowering drugs, taking an SGLT2 inhibitor was associated with lower risks of heart failure hospitalization and all-cause mortality (HR, 0.54; 95% CI, 0.44-0.65; P less than .001). This trial also offered a new detail: The patients gained the benefit regardless of whether their baseline left ventricular ejection fraction was preserved or reduced (J Coll Cardiol. 2019 Mar;73[9]:suppl 1). The SGLT2 inhibitors used in this trial included dapagliflozin (Farxiga) and empagliflozin (Jardiance).
In another study released this year, a subanalysis of the DECLARE-TIMI 58 trial, researchers reported that the SGLT2 inhibitor dapagliflozin reduced risks of both major adverse cardiovascular events and heart failure hospitalization in the subset of patients with type 2 diabetes and prior myocardial infarction versus controls (Circulation. 2019 May 28;139[22]:2516-27). The absolute risk reduction for major adverse cardiovascular events was 1.9% (HR, 0.81; 95% CI, 0.65-1.00; P = .046), while it was 0.6% for heart failure hospitalization (HR, 0.85; 95% CI, 0.72-1.00; P = .055).
These and other studies “speak volumes about the efficacy of managing blood sugar and addressing our biggest nemesis, which is cardiovascular disease,” Dr. Roberts said. “It’s irrefutable. The data [are] very good.”
Dr. Paauw said an SGLT2 inhibitor or GLP-1 receptor agonist is best reserved for use in select patients with cardiovascular risks and type 2 diabetes that need management beyond metformin.
For example, they might fit a 70-year-old with persistent hypertension who’s already taking a couple of blood pressure medications. “If they have another cardiovascular risk factor, the cardiovascular protection piece will be a bigger deal,” he said. Also, “it will probably help lower their blood pressure so they can avoid taking another blood pressure medicine.”
Trials of both GLP-1 receptor agonists and SGLT2 inhibitors have shown benefits “in improving [major adverse cardiac events], with the SGLT2 class showing substantial benefit in improving both heart failure and renal outcomes as well,” noted Dr. Skolnik. “It is in this context that one must address the question of whether the price of the medications are worthwhile. With such substantial benefit, there is no question in my mind that – for patients who have underlying cardiovascular illness, which includes patients with existent coronary disease, history of stroke, transient ischemic attack, or peripheral vascular disease – it is far and away worth it to prescribe these classes of medications.”
Indeed, the American Diabetes Association and the European Association for the Study of Diabetes’ most recent guidelines now call for a GLP-1 receptor agonist – instead of insulin – to be the first injectable used to treat type 2 diabetes (Diabetes Care 2018 Dec; 41[12]:2669-701).
“For the relatively small number of my patients who have been able to access and use these medications for months or longer, more have tolerated the GLP-1 agonists than SGLT2 inhibitors primarily due to urinary issues,” noted Dr. Hopkins.
Dipeptidyl peptidase–4 inhibitors are another option in patients with type 2 diabetes, but research suggests they may not be a top option for patients with cardiovascular risk. A 2018 review noted that cardiovascular outcome trials for alogliptin (Nesina), saxagliptin (Onglyza), and sitagliptin (Januvia) showed noninferiority but failed to demonstrate any superiority, compared with placebo in patients with type 2 diabetes mellitus and high cardiovascular risk (Circ Res. 2018 May 11;122[10]:1439-59).
The combination therapies
Many of the newer drugs are available as combinations with other types of diabetes drugs. In some cases, physicians create their own form of combination therapy by separately prescribing two or more diabetes drugs. Earlier this year, a study suggested the benefits of this kind of add-on therapy: Diabetes outcomes improved in patients who took the GLP-1 receptor agonist semaglutide and an SGLT2 inhibitor (Lancet Diabetes Endocrinol. 2019 Mar 1. doi: 10.1016/S2213-8587[19]30066-X).
Dr. Roberts suggested caution, however, when prescribing combination therapies. “My recommendation is always to begin with the individual medications to see if the patient tolerates the drugs and then decide which component needs to be titrated. It’s hard to titrate a combination drug, and it doesn’t leave a lot of flexibility. You never know which drug is doing what.
Dr. Handelsman said some patients may need to take three medications such as metformin, an SGLT2 inhibitor, and a GLP-1 receptor agonist.
“I don’t recommend using the combinations if you’re not familiar with the drugs ... These are relatively new pharmaceuticals, and most of us are on a learning curve as to how they fit into the armamentarium. If a drug is tolerated with a good response, you can certainly consider going to the combination tablets,” he added.
There is at least one drug that combines these three classes: The newly FDA-approved Qternmet XR, which combines dapagliflozin (an SGLT2 inhibitor), saxagliptin (a GLP-1 receptor agonist), and metformin. As of mid-June 2019, it was not yet available in the United States. Its sister drug Qtern, which combines dapagliflozin and saxagliptin, costs more than $500 a month with a free coupon, according to goodrx.com. In contrast, metformin is extremely inexpensive, costing just a few dollars a month for a common starting dose.
What about adding insulin?
“Both [SGLT2 inhibitors and GLP-1 receptor agonists] work very well with insulin,” Dr. Handelsman said. “There is a nice additive effect on the reduction of [hemoglobin] A1c. The only caution is that, although neither SGLT2 inhibitors nor GLP-1 receptor agonists cause hypoglycemia, in combination with insulin they do increase the risk of hypoglycemia. You may have to adjust the dose of insulin.”
Dr. Hopkins warned that cost becomes an even bigger issue when you add insulin into the mix.
“When insulin comes into the discussion, we are again stuck with astronomical costs which many struggle to afford,” he explained.
Indeed, the price tag on these drugs seems to be the biggest problem physicians have with them.
“The challenges in managing patients with diabetes aren’t the risks associated with the drugs. It’s dealing with their insurers,” noted Dr. Roberts.
Dr. Hopkins, Dr. Paauw, Dr. Roberts, and Dr. Syed reported no disclosures. Dr. Buse is an investigator for Johnson and Johnson. Dr. Goldschmidt is paid to speak by Novartis. Dr. Handelsman reported research grants, consulting work, and speaker honoraria from Amgen, Gilead, Lilly, Merck, Novo Nordisk, and others. Dr Skolnik reported nonfinancial support from AstraZeneca, Boehringer Ingelheim, Sanofi, and GlaxoSmithKline and personal fees from AstraZeneca, Boehringer Ingelheim, and Eli Lilly. He also serves on the advisory boards of AstraZeneca, Boehringer Ingelheim, Teva Pharmaceutical, Eli Lilly, Sanofi, Janssen Pharmaceuticals, Intarcia, Mylan, and GlaxoSmithKline.
Dr. Paauw and Dr. Skolnik are columnists for Family Practice News and Internal Medicine News.
M. Alexander Otto contributed to this report.
The options for treating type 2 diabetes without insulin have grown beyond metformin to include a long list of sodium-glucose cotransporter 2 (SGLT2) inhibitors and glucagonlike peptide–1 (GLP-1) receptor agonists that can be taken with or without metformin. These new drugs have cardiovascular and kidney benefits and help with weight loss, but they also carry risks and, according to some experts, their costs can be prohibitively expensive.
Given the medical community’s long-term experience with treating patients with metformin, and metformin’s lower cost, most of the physicians interviewed for this article advise using SGLT2 inhibitors and GLP-1 receptor agonists as second-line treatments. Others said that they would prefer to use the newer drugs as first-line therapies in select high-risk patients, but prior authorization hurdles created by insurance companies make that approach too burdensome.
“The economics of U.S. health care is stacked against many of our patients with diabetes in the current era,” Robert H. Hopkins Jr., MD, said in an interview.
Even when their insurance approves the drugs, patients still may not be able to afford the copay, explained Dr. Hopkins, professor of internal medicine and pediatrics and director of the division of general internal medicine at the University of Arkansas for Medical Sciences, Little Rock. “Sometimes patients can purchase drugs at a lower cost than the copay to purchase with the ‘drug coverage’ in their insurance plan – unfortunately, this is not the case with the newer diabetes medications we are discussing here.”
“SGLT2 inhibitors and GLP-1 agonists can cost several hundred dollars a month, and insurers often balk at paying for them. They’ll say, ‘Have you tried metformin?’ ” explained endocrinologist Victor Lawrence Roberts, MD, in a interview. “We have to work with insurance companies the best we can in a stepwise fashion.”
According to Dr. Roberts, 80% of his patients with diabetes struggle with the cost of medicine in general. “They’re either underinsured or not insured or their formulary is limited.
Douglas S. Paauw, MD, agreed in an interview that the newer drugs can be problematic on the insurance front.
“For some patients they aren’t affordable, especially for the uninsured if you can’t get them on an assistance program,” said Dr. Paauw, who is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the university.
Dr. Hopkins, who is on the Internal Medicine News board, noted that “unfortunately, the treatment of type 2 diabetes in patients who cannot achieve control with metformin, diet, weight control, and exercise is a story of the ‘haves’ and the ‘have nots.’ The ‘haves’ are those who have pharmacy benefits which make access to newer agents like SGLT2 inhibitors and GLP-1 agonists a possibility.”
“I have had very few of the ‘have nots’ who have been able to even consider these newer agents, which carry price tags of $600-$1,300 a month even with the availability of discounting coupons in the marketplace,” he added. “Most of these patients end up requiring a sulfonylurea or TZD [thiazolidinedione] as a second agent to achieve glycemic control. This makes it very difficult to achieve sufficient weight and metabolic control to avoid an eventual switch to insulin.”
Fatima Z. Syed, MD, an endocrine-trained general internist at DukeHealth in Durham, N.C., said she prescribes SGLT2 inhibitors and GLP-1 receptor agonists in combination with metformin. “I prescribe them frequently, but they are not first-line treatments,” she explained.
“Nothing replaces diet and exercise” as therapy for patients with type 2 diabetes, she added.
Neil S. Skolnik, MD, said that insurance companies were not preventing patients from using these drugs in his experience. He also provided an optimistic take on the accessibility of these drugs in the near future.
“Most insurance companies are now covering select SGLT2 inhibitors and GLP-1 receptor agonists for appropriate patients and those companies that currently do not will soon have to,” said Dr. Skolnik, who is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health.
“The outcomes [associated with use of the new drugs] are robust, the benefits are large, and are well worth the cost,” he added.
The side effects
While others praised these drugs for their beneficial effects, they also noted that the side effects of these drugs are serious and must be discussed with patients.
GLP-1 receptor agonists are linked to gastrointestinal symptoms, especially nausea, while SGLT2 inhibitors have been linked to kidney failure, ketoacidosis, and more. The Food and Drug Administration warned in 2018 that the SGLT2 inhibitors can cause a rare serious infection known as Fournier’s gangrene – necrotizing fasciitis of the perineum.
“We have to tell our patients to let us know right away if they get pain or swelling in the genital area,” Dr. Paauw, who is on the Internal Medicine News board, noted. “The chance that an infection could explode quickly is higher in those who take these drugs.”
Amputation risks also are associated with taking the SGLT2 inhibitor canagliflozin (Invokana). The FDA requires the manufacturer of this drug to include a black-box warning about the risk of “lower-limb amputations, most frequently of the toe and midfoot,” but also the leg. In approval trials, the risk doubled versus placebo.
These amputation risks “put a damper on some of the enthusiasm on behalf of physicians and patients ... for taking this drug,” noted Dr. Roberts, who is a professor of internal medicine at the University of Central Florida, Orlando.
While a manufacturer-funded study released last year found no link to amputations, the results weren’t powerful enough to rule out a moderately increased risk.
“[If] you are at high risk for having an amputation, we really have to take this risk very seriously,” said John B. Buse, MD, chief of the division of endocrinology at the University of North Carolina at Chapel Hill, in a presentation about the study at the 2018 annual scientific sessions of the American Diabetes Association.
The benefits
Despite these risks of adverse events, most interviewed agreed that the many benefits observed in those taking SGLT2 inhibitors or GLP-1 receptor agonists make them worth prescribing, at least to those who are able to afford them.
Both SGLT2 inhibitors and GLP-1 receptor agonists appear to have significant cardiovascular benefits. A 2019 meta-analysis and systematic review found that both drugs reduced major adverse cardiac events by about 12% (Circulation. 2019 Apr 23;139[17]:2022-31).
“They don’t cause hypoglycemia, they lower blood pressure, they don’t cause weight gain, and they might promote weight loss,” noted Dr. Paauw.
SGLT2 inhibitors also have shown signs of kidney benefits. The CREDENCE trial linked canagliflozin to a lowering of kidney disorders versus placebo (N Engl J Med. 2019 Jun 13;380[24]:2295-306). “The relative risk of the renal-specific composite of end-stage kidney disease, a doubling of the creatinine level, or death from renal causes was lower by 34% (hazard ratio, 0.66; 95% confidence interval, 0.53-0.81; P less than .001), and the relative risk of end-stage kidney disease was lower by 32% (HR, 0.68; 95% CI, 0.54-0.86; P = .002),” the trial investigators wrote.
“They showed very nicely that the drug improved the kidney function of those patients and reduced the kidney deterioration,” said Yehuda Handelsman, MD, an endocrinologist in Tarzana, Calif., who chaired the 2011 and 2015 American Association of Clinical Endocrinologists’ Comprehensive Diabetes Guidelines. The study was especially impressive, he added, because it included patients with low kidney function.
SGLT2 inhibitors’ “diuretic mechanism explains why there is a substantial reduction in heart failure hospitalizations in patients who take these drugs,” said cardiologist Marc E. Goldschmidt, MD, director of the Heart Success Program at Atlantic Health System’s Morristown (N.J.) Medical Center, in an interview. “Both the EMPA-REG Outcome and the CREDENCE trials demonstrated substantial benefit of this class of medications by showing a lower risk of cardiovascular death as well as death from any cause and a lower risk of hospitalization for heart failure."
Overall, the SGLT2 trial data have been very consistent with a benefit for cardiovascular risk reduction, particularly in regard to heart failure hospitalizations and even in potentially preventing heart failure in diabetics,” he added.
Dr. Skolnik, a columnist for Family Practice News, cited SGLT2 inhibitors and GLP-1 receptor agonists’ ability to slow renal disease progression, promote weight loss, and prevent poor cardiac outcomes.“These drugs should be used, in addition to metformin, in all patients with diabetes and vascular disease. These proven outcomes are far better than we ever were able to achieve previously and the strength of the evidence at this point is very strong,” said Dr. Skolnik. “In addition to the benefits of decreasing the development of cardiovascular disease, serious heart failure, and slowing progression of renal disease, these two classes of medication have additional benefits. Both classes help patients lose weight, which is very different from what was found with either sulfonylureas or insulin, which cause patients to gain weight. Also both the SGLT2 inhibitors and the GLP-1 RAs [receptor agonists] have a low incidence of hypoglycemia. For all these reasons, these have become important medications for us to use in primary care.”
Other recent trials offer “very powerful data” about SGLT2 inhibitors, Dr. Roberts said. That’s good news, since “our approach needs to be toward cardiovascular protection and preservation as well as managing blood sugar.”An Israeli trial, whose results were released in May 2019 at the annual meeting of the American College of Cardiology, found that, compared with other glucose-lowering drugs, taking an SGLT2 inhibitor was associated with lower risks of heart failure hospitalization and all-cause mortality (HR, 0.54; 95% CI, 0.44-0.65; P less than .001). This trial also offered a new detail: The patients gained the benefit regardless of whether their baseline left ventricular ejection fraction was preserved or reduced (J Coll Cardiol. 2019 Mar;73[9]:suppl 1). The SGLT2 inhibitors used in this trial included dapagliflozin (Farxiga) and empagliflozin (Jardiance).
In another study released this year, a subanalysis of the DECLARE-TIMI 58 trial, researchers reported that the SGLT2 inhibitor dapagliflozin reduced risks of both major adverse cardiovascular events and heart failure hospitalization in the subset of patients with type 2 diabetes and prior myocardial infarction versus controls (Circulation. 2019 May 28;139[22]:2516-27). The absolute risk reduction for major adverse cardiovascular events was 1.9% (HR, 0.81; 95% CI, 0.65-1.00; P = .046), while it was 0.6% for heart failure hospitalization (HR, 0.85; 95% CI, 0.72-1.00; P = .055).
These and other studies “speak volumes about the efficacy of managing blood sugar and addressing our biggest nemesis, which is cardiovascular disease,” Dr. Roberts said. “It’s irrefutable. The data [are] very good.”
Dr. Paauw said an SGLT2 inhibitor or GLP-1 receptor agonist is best reserved for use in select patients with cardiovascular risks and type 2 diabetes that need management beyond metformin.
For example, they might fit a 70-year-old with persistent hypertension who’s already taking a couple of blood pressure medications. “If they have another cardiovascular risk factor, the cardiovascular protection piece will be a bigger deal,” he said. Also, “it will probably help lower their blood pressure so they can avoid taking another blood pressure medicine.”
Trials of both GLP-1 receptor agonists and SGLT2 inhibitors have shown benefits “in improving [major adverse cardiac events], with the SGLT2 class showing substantial benefit in improving both heart failure and renal outcomes as well,” noted Dr. Skolnik. “It is in this context that one must address the question of whether the price of the medications are worthwhile. With such substantial benefit, there is no question in my mind that – for patients who have underlying cardiovascular illness, which includes patients with existent coronary disease, history of stroke, transient ischemic attack, or peripheral vascular disease – it is far and away worth it to prescribe these classes of medications.”
Indeed, the American Diabetes Association and the European Association for the Study of Diabetes’ most recent guidelines now call for a GLP-1 receptor agonist – instead of insulin – to be the first injectable used to treat type 2 diabetes (Diabetes Care 2018 Dec; 41[12]:2669-701).
“For the relatively small number of my patients who have been able to access and use these medications for months or longer, more have tolerated the GLP-1 agonists than SGLT2 inhibitors primarily due to urinary issues,” noted Dr. Hopkins.
Dipeptidyl peptidase–4 inhibitors are another option in patients with type 2 diabetes, but research suggests they may not be a top option for patients with cardiovascular risk. A 2018 review noted that cardiovascular outcome trials for alogliptin (Nesina), saxagliptin (Onglyza), and sitagliptin (Januvia) showed noninferiority but failed to demonstrate any superiority, compared with placebo in patients with type 2 diabetes mellitus and high cardiovascular risk (Circ Res. 2018 May 11;122[10]:1439-59).
The combination therapies
Many of the newer drugs are available as combinations with other types of diabetes drugs. In some cases, physicians create their own form of combination therapy by separately prescribing two or more diabetes drugs. Earlier this year, a study suggested the benefits of this kind of add-on therapy: Diabetes outcomes improved in patients who took the GLP-1 receptor agonist semaglutide and an SGLT2 inhibitor (Lancet Diabetes Endocrinol. 2019 Mar 1. doi: 10.1016/S2213-8587[19]30066-X).
Dr. Roberts suggested caution, however, when prescribing combination therapies. “My recommendation is always to begin with the individual medications to see if the patient tolerates the drugs and then decide which component needs to be titrated. It’s hard to titrate a combination drug, and it doesn’t leave a lot of flexibility. You never know which drug is doing what.
Dr. Handelsman said some patients may need to take three medications such as metformin, an SGLT2 inhibitor, and a GLP-1 receptor agonist.
“I don’t recommend using the combinations if you’re not familiar with the drugs ... These are relatively new pharmaceuticals, and most of us are on a learning curve as to how they fit into the armamentarium. If a drug is tolerated with a good response, you can certainly consider going to the combination tablets,” he added.
There is at least one drug that combines these three classes: The newly FDA-approved Qternmet XR, which combines dapagliflozin (an SGLT2 inhibitor), saxagliptin (a GLP-1 receptor agonist), and metformin. As of mid-June 2019, it was not yet available in the United States. Its sister drug Qtern, which combines dapagliflozin and saxagliptin, costs more than $500 a month with a free coupon, according to goodrx.com. In contrast, metformin is extremely inexpensive, costing just a few dollars a month for a common starting dose.
What about adding insulin?
“Both [SGLT2 inhibitors and GLP-1 receptor agonists] work very well with insulin,” Dr. Handelsman said. “There is a nice additive effect on the reduction of [hemoglobin] A1c. The only caution is that, although neither SGLT2 inhibitors nor GLP-1 receptor agonists cause hypoglycemia, in combination with insulin they do increase the risk of hypoglycemia. You may have to adjust the dose of insulin.”
Dr. Hopkins warned that cost becomes an even bigger issue when you add insulin into the mix.
“When insulin comes into the discussion, we are again stuck with astronomical costs which many struggle to afford,” he explained.
Indeed, the price tag on these drugs seems to be the biggest problem physicians have with them.
“The challenges in managing patients with diabetes aren’t the risks associated with the drugs. It’s dealing with their insurers,” noted Dr. Roberts.
Dr. Hopkins, Dr. Paauw, Dr. Roberts, and Dr. Syed reported no disclosures. Dr. Buse is an investigator for Johnson and Johnson. Dr. Goldschmidt is paid to speak by Novartis. Dr. Handelsman reported research grants, consulting work, and speaker honoraria from Amgen, Gilead, Lilly, Merck, Novo Nordisk, and others. Dr Skolnik reported nonfinancial support from AstraZeneca, Boehringer Ingelheim, Sanofi, and GlaxoSmithKline and personal fees from AstraZeneca, Boehringer Ingelheim, and Eli Lilly. He also serves on the advisory boards of AstraZeneca, Boehringer Ingelheim, Teva Pharmaceutical, Eli Lilly, Sanofi, Janssen Pharmaceuticals, Intarcia, Mylan, and GlaxoSmithKline.
Dr. Paauw and Dr. Skolnik are columnists for Family Practice News and Internal Medicine News.
M. Alexander Otto contributed to this report.
Which migraineurs seek care from a neurologist?
PHILADELPHIA – , said Alice R. Pressman, PhD at the annual meeting of the American Headache Society.
Dr. Pressman, executive director of research, development, and dissemination for Sutter Health, and her research colleagues analyzed data from primary care patients who sought care for migraine in the Sutter Health healthcare network in Northern California. They found that women were 10% more likely than men to consult a neurologist and that Asian patients had a longer time to a first neurology encounter for migraine, compared with Caucasian patients.
“Those who sought care from neurology had more severe migraine symptomology, disability, and comorbidities,” the researchers reported. Furthermore, patients with migraine seen by neurologists were more likely to receive prescriptions for acute and preventive migraine medications, compared with patients only seen by primary care physicians.
The study, known as the Migraine Signature Study, used electronic health records (EHR) and patient-reported questionnaire data to examine the clinical experiences and care of patients with migraine.
The primary care population consisted of 1.4 million adults with at least one office visit to primary care in 2013-2017. Using the validated Migraine Probability Algorithm, the researchers identified approximately 94,000 patients who sought care for migraine.
The investigators also invited 38,536 patients to complete an online survey about migraine criteria, symptomology, health resource utilization, and patient-reported outcomes such as disability, acute treatment optimization, cutaneous allodynia, depression, anxiety, and posttraumatic stress disorder (PTSD).
Of the patients who sought care for migraine, 72,624 patients did not receive migraine care from neurology, and 21,525 did.
Patients with migraine care from a neurologist were more likely to have at least one acute migraine medication order (89.4% vs. 80.6%), at least one preventive migraine medication order (78.6% vs. 49.1%), and any migraine medication order (95.3% vs. 85.9%). In addition, those with at least one medication order in the primary care setting had fewer orders per person per year, compared with those with at least one medication order in the neurology setting (1.1 vs. 1.6).
About one-third of the patients who sought care for migraine had no migraine encounters in the first 12 months of the study. Of the more than 33,000 patients with first migraine consults, approximately two-thirds did not receive a neurology consultation during the study and received their migraine diagnosis in the primary care setting.
Of the 31% of patients with first migraine consults in primary care who later had a neurology consult, two-thirds received a migraine diagnosis from neurology. “The high rate of initial migraine diagnosis within neurology was surprising among this sample with primary care encounters first,” the researchers said.
The investigators also examined patient-reported outcomes from 391 respondents who received migraine care from neurology and 399 respondents who received migraine care from primary care. “Patients who consulted a neurologist were likely to report moderate-to-severe disability, poor acute treatment optimization, and major depression,” they said. “Allodynia, anxiety, and PTSD did not differ by type of provider.”
Confounding may have influenced the results, and the researchers plan to assess factors such as headache frequency and severity using patient-reported survey data in future analyses.
The Migraine Signature Study was supported by Amgen, Inc.
PHILADELPHIA – , said Alice R. Pressman, PhD at the annual meeting of the American Headache Society.
Dr. Pressman, executive director of research, development, and dissemination for Sutter Health, and her research colleagues analyzed data from primary care patients who sought care for migraine in the Sutter Health healthcare network in Northern California. They found that women were 10% more likely than men to consult a neurologist and that Asian patients had a longer time to a first neurology encounter for migraine, compared with Caucasian patients.
“Those who sought care from neurology had more severe migraine symptomology, disability, and comorbidities,” the researchers reported. Furthermore, patients with migraine seen by neurologists were more likely to receive prescriptions for acute and preventive migraine medications, compared with patients only seen by primary care physicians.
The study, known as the Migraine Signature Study, used electronic health records (EHR) and patient-reported questionnaire data to examine the clinical experiences and care of patients with migraine.
The primary care population consisted of 1.4 million adults with at least one office visit to primary care in 2013-2017. Using the validated Migraine Probability Algorithm, the researchers identified approximately 94,000 patients who sought care for migraine.
The investigators also invited 38,536 patients to complete an online survey about migraine criteria, symptomology, health resource utilization, and patient-reported outcomes such as disability, acute treatment optimization, cutaneous allodynia, depression, anxiety, and posttraumatic stress disorder (PTSD).
Of the patients who sought care for migraine, 72,624 patients did not receive migraine care from neurology, and 21,525 did.
Patients with migraine care from a neurologist were more likely to have at least one acute migraine medication order (89.4% vs. 80.6%), at least one preventive migraine medication order (78.6% vs. 49.1%), and any migraine medication order (95.3% vs. 85.9%). In addition, those with at least one medication order in the primary care setting had fewer orders per person per year, compared with those with at least one medication order in the neurology setting (1.1 vs. 1.6).
About one-third of the patients who sought care for migraine had no migraine encounters in the first 12 months of the study. Of the more than 33,000 patients with first migraine consults, approximately two-thirds did not receive a neurology consultation during the study and received their migraine diagnosis in the primary care setting.
Of the 31% of patients with first migraine consults in primary care who later had a neurology consult, two-thirds received a migraine diagnosis from neurology. “The high rate of initial migraine diagnosis within neurology was surprising among this sample with primary care encounters first,” the researchers said.
The investigators also examined patient-reported outcomes from 391 respondents who received migraine care from neurology and 399 respondents who received migraine care from primary care. “Patients who consulted a neurologist were likely to report moderate-to-severe disability, poor acute treatment optimization, and major depression,” they said. “Allodynia, anxiety, and PTSD did not differ by type of provider.”
Confounding may have influenced the results, and the researchers plan to assess factors such as headache frequency and severity using patient-reported survey data in future analyses.
The Migraine Signature Study was supported by Amgen, Inc.
PHILADELPHIA – , said Alice R. Pressman, PhD at the annual meeting of the American Headache Society.
Dr. Pressman, executive director of research, development, and dissemination for Sutter Health, and her research colleagues analyzed data from primary care patients who sought care for migraine in the Sutter Health healthcare network in Northern California. They found that women were 10% more likely than men to consult a neurologist and that Asian patients had a longer time to a first neurology encounter for migraine, compared with Caucasian patients.
“Those who sought care from neurology had more severe migraine symptomology, disability, and comorbidities,” the researchers reported. Furthermore, patients with migraine seen by neurologists were more likely to receive prescriptions for acute and preventive migraine medications, compared with patients only seen by primary care physicians.
The study, known as the Migraine Signature Study, used electronic health records (EHR) and patient-reported questionnaire data to examine the clinical experiences and care of patients with migraine.
The primary care population consisted of 1.4 million adults with at least one office visit to primary care in 2013-2017. Using the validated Migraine Probability Algorithm, the researchers identified approximately 94,000 patients who sought care for migraine.
The investigators also invited 38,536 patients to complete an online survey about migraine criteria, symptomology, health resource utilization, and patient-reported outcomes such as disability, acute treatment optimization, cutaneous allodynia, depression, anxiety, and posttraumatic stress disorder (PTSD).
Of the patients who sought care for migraine, 72,624 patients did not receive migraine care from neurology, and 21,525 did.
Patients with migraine care from a neurologist were more likely to have at least one acute migraine medication order (89.4% vs. 80.6%), at least one preventive migraine medication order (78.6% vs. 49.1%), and any migraine medication order (95.3% vs. 85.9%). In addition, those with at least one medication order in the primary care setting had fewer orders per person per year, compared with those with at least one medication order in the neurology setting (1.1 vs. 1.6).
About one-third of the patients who sought care for migraine had no migraine encounters in the first 12 months of the study. Of the more than 33,000 patients with first migraine consults, approximately two-thirds did not receive a neurology consultation during the study and received their migraine diagnosis in the primary care setting.
Of the 31% of patients with first migraine consults in primary care who later had a neurology consult, two-thirds received a migraine diagnosis from neurology. “The high rate of initial migraine diagnosis within neurology was surprising among this sample with primary care encounters first,” the researchers said.
The investigators also examined patient-reported outcomes from 391 respondents who received migraine care from neurology and 399 respondents who received migraine care from primary care. “Patients who consulted a neurologist were likely to report moderate-to-severe disability, poor acute treatment optimization, and major depression,” they said. “Allodynia, anxiety, and PTSD did not differ by type of provider.”
Confounding may have influenced the results, and the researchers plan to assess factors such as headache frequency and severity using patient-reported survey data in future analyses.
The Migraine Signature Study was supported by Amgen, Inc.
EXPERT ANALYSIS FROM AHS 2019
In psoriasis, risankizumab outperforms adalimumab
Results of the IMMvent trial were published online ahead of print July 4 in the Lancet.
Risankizumab targets the p19 subunit of the cytokine IL-23. Selectivity for p19 has the potential to be safer than some other approaches that target the p40 subunit, because p19 is specific to IL-23, and many immune defense processes can function without IL-23. The p40 subunit is shared with IL-12, and blocking it can therefore lead to off-target effects.
Risankizumab was previously shown to have superior safety and efficacy over ustekinumab, which inhibits a subunit shared by IL-23 and IL-12 (Gordon KB et al. Lancet. 2018;392[10148]:650-61). Adalimumab is a TNF-alpha inhibitor that is frequently used to treat psoriasis, and which became available in biosimilar form in Europe in 2018.
The researchers randomized 605 adult patients from 66 sites in 11 countries to receive either risankizumab or adalimumab. The first phase (Part A) of the trial lasted up to 16 weeks, and tested the general superiority of risankizumab over adalimumab. The second phase (Part B), from week 16 to 44, evaluated the efficacy of risankizumab in participants who experienced an intermediate response, defined as Psoriasis Area and Severity Index (PASI) score of 50-90.
At the start of Part B, subjects initially receiving adalimumab who had at least a 90% improvement in PASI stayed on adalimumab (PASI 90), while those who had less than 50% improvement in PASI were switched to risankizumab. The remaining intermediate responders (PASI 50-90) were re-randomized to continue adalimumab or switch to risankizumab. All subjects initially randomized to risankizumab continued risankizumab during part B.
At the end of Part A, 72% of the risankizumab group achieved PASI 90, compared with 47% in the adalimumab group (p < 0.0001). A total of 84% in the risankizumab group had a static Physician’s Global Assessment (sPGA) score of 0 or 1 at the end of Part A, compared with 60% in the adalimumab group (p < 0.0001).
During Part B, among intermediate adalimumab responders, 66% of those switched to risankizumab achieved PASI 90, compared with 21% of continued on adalimumab (p < 0.0001).
In Part A, 56% of patients taking risankizumab experienced an adverse event, as did 57% of those taking adalimumab. Among adalimumab intermediate responders, 75% of those who switched to risankizumab during Part B had an adverse event, compared with 66% of those who continued adalimumab.
SOURCE: Reich K, et al. Lancet 2019, July 4 .
Until recently, TNF-alpha inhibitors have been the most commonly prescribed biologic agents for psoriasis. They are more targeted than small molecules like cyclosporine or methotrexate, but still are associated with immune side effects like infection and malignancy. Drugs that specifically target IL-23 home in on the pathogenicity of psoriasis, and they are not associated with infection and malignancy. The results of this study offer evidence that IL-23 inhibitors represent another effective and convenient option for the treatment of psoriasis. Physicians can select from IL-23 inhibitors, IL-17 inhibitors, and TNF-alpha inhibitors to determine the optimal treatment for patients based on patient weight, childbearing status, age, and comorbid conditions.
Mark Lebwohl, MD, is in the department of dermatology at Icahn School of Medicine at Mount Sinai, New York.
Until recently, TNF-alpha inhibitors have been the most commonly prescribed biologic agents for psoriasis. They are more targeted than small molecules like cyclosporine or methotrexate, but still are associated with immune side effects like infection and malignancy. Drugs that specifically target IL-23 home in on the pathogenicity of psoriasis, and they are not associated with infection and malignancy. The results of this study offer evidence that IL-23 inhibitors represent another effective and convenient option for the treatment of psoriasis. Physicians can select from IL-23 inhibitors, IL-17 inhibitors, and TNF-alpha inhibitors to determine the optimal treatment for patients based on patient weight, childbearing status, age, and comorbid conditions.
Mark Lebwohl, MD, is in the department of dermatology at Icahn School of Medicine at Mount Sinai, New York.
Until recently, TNF-alpha inhibitors have been the most commonly prescribed biologic agents for psoriasis. They are more targeted than small molecules like cyclosporine or methotrexate, but still are associated with immune side effects like infection and malignancy. Drugs that specifically target IL-23 home in on the pathogenicity of psoriasis, and they are not associated with infection and malignancy. The results of this study offer evidence that IL-23 inhibitors represent another effective and convenient option for the treatment of psoriasis. Physicians can select from IL-23 inhibitors, IL-17 inhibitors, and TNF-alpha inhibitors to determine the optimal treatment for patients based on patient weight, childbearing status, age, and comorbid conditions.
Mark Lebwohl, MD, is in the department of dermatology at Icahn School of Medicine at Mount Sinai, New York.
Results of the IMMvent trial were published online ahead of print July 4 in the Lancet.
Risankizumab targets the p19 subunit of the cytokine IL-23. Selectivity for p19 has the potential to be safer than some other approaches that target the p40 subunit, because p19 is specific to IL-23, and many immune defense processes can function without IL-23. The p40 subunit is shared with IL-12, and blocking it can therefore lead to off-target effects.
Risankizumab was previously shown to have superior safety and efficacy over ustekinumab, which inhibits a subunit shared by IL-23 and IL-12 (Gordon KB et al. Lancet. 2018;392[10148]:650-61). Adalimumab is a TNF-alpha inhibitor that is frequently used to treat psoriasis, and which became available in biosimilar form in Europe in 2018.
The researchers randomized 605 adult patients from 66 sites in 11 countries to receive either risankizumab or adalimumab. The first phase (Part A) of the trial lasted up to 16 weeks, and tested the general superiority of risankizumab over adalimumab. The second phase (Part B), from week 16 to 44, evaluated the efficacy of risankizumab in participants who experienced an intermediate response, defined as Psoriasis Area and Severity Index (PASI) score of 50-90.
At the start of Part B, subjects initially receiving adalimumab who had at least a 90% improvement in PASI stayed on adalimumab (PASI 90), while those who had less than 50% improvement in PASI were switched to risankizumab. The remaining intermediate responders (PASI 50-90) were re-randomized to continue adalimumab or switch to risankizumab. All subjects initially randomized to risankizumab continued risankizumab during part B.
At the end of Part A, 72% of the risankizumab group achieved PASI 90, compared with 47% in the adalimumab group (p < 0.0001). A total of 84% in the risankizumab group had a static Physician’s Global Assessment (sPGA) score of 0 or 1 at the end of Part A, compared with 60% in the adalimumab group (p < 0.0001).
During Part B, among intermediate adalimumab responders, 66% of those switched to risankizumab achieved PASI 90, compared with 21% of continued on adalimumab (p < 0.0001).
In Part A, 56% of patients taking risankizumab experienced an adverse event, as did 57% of those taking adalimumab. Among adalimumab intermediate responders, 75% of those who switched to risankizumab during Part B had an adverse event, compared with 66% of those who continued adalimumab.
SOURCE: Reich K, et al. Lancet 2019, July 4 .
Results of the IMMvent trial were published online ahead of print July 4 in the Lancet.
Risankizumab targets the p19 subunit of the cytokine IL-23. Selectivity for p19 has the potential to be safer than some other approaches that target the p40 subunit, because p19 is specific to IL-23, and many immune defense processes can function without IL-23. The p40 subunit is shared with IL-12, and blocking it can therefore lead to off-target effects.
Risankizumab was previously shown to have superior safety and efficacy over ustekinumab, which inhibits a subunit shared by IL-23 and IL-12 (Gordon KB et al. Lancet. 2018;392[10148]:650-61). Adalimumab is a TNF-alpha inhibitor that is frequently used to treat psoriasis, and which became available in biosimilar form in Europe in 2018.
The researchers randomized 605 adult patients from 66 sites in 11 countries to receive either risankizumab or adalimumab. The first phase (Part A) of the trial lasted up to 16 weeks, and tested the general superiority of risankizumab over adalimumab. The second phase (Part B), from week 16 to 44, evaluated the efficacy of risankizumab in participants who experienced an intermediate response, defined as Psoriasis Area and Severity Index (PASI) score of 50-90.
At the start of Part B, subjects initially receiving adalimumab who had at least a 90% improvement in PASI stayed on adalimumab (PASI 90), while those who had less than 50% improvement in PASI were switched to risankizumab. The remaining intermediate responders (PASI 50-90) were re-randomized to continue adalimumab or switch to risankizumab. All subjects initially randomized to risankizumab continued risankizumab during part B.
At the end of Part A, 72% of the risankizumab group achieved PASI 90, compared with 47% in the adalimumab group (p < 0.0001). A total of 84% in the risankizumab group had a static Physician’s Global Assessment (sPGA) score of 0 or 1 at the end of Part A, compared with 60% in the adalimumab group (p < 0.0001).
During Part B, among intermediate adalimumab responders, 66% of those switched to risankizumab achieved PASI 90, compared with 21% of continued on adalimumab (p < 0.0001).
In Part A, 56% of patients taking risankizumab experienced an adverse event, as did 57% of those taking adalimumab. Among adalimumab intermediate responders, 75% of those who switched to risankizumab during Part B had an adverse event, compared with 66% of those who continued adalimumab.
SOURCE: Reich K, et al. Lancet 2019, July 4 .
FROM THE LANCET
Can mindfulness-based cognitive therapy treat migraine?
PHILADELPHIA – , according to randomized clinical trial results.
“The fact that people can improve how they live their daily life even with the same amount of headache days and the same pain intensity is remarkable,” said study investigator Elizabeth K. Seng, PhD, associate professor of psychology at Yeshiva University and research associate professor of neurology at Albert Einstein College of Medicine, both in New York. “I think this gives us a little bit of a clue about when to use these kinds of treatments.”
Dr. Seng presented findings from the phase 2b pilot trial at the annual meeting of the American Headache Society.
To study the efficacy of mindfulness-based cognitive therapy for migraine, Dr. Seng and her research colleagues recruited participants with migraine in the New York City area between 2015 and 2018. In all, 60 patients were randomized to receive 8 weekly individual 75-minute mindfulness-based cognitive therapy for migraine sessions or 8 weeks on a wait list with treatment as usual.
Primary outcomes were Month 0 to Month 4 changes in perceived disability, measured using the Henry Ford Disability Inventory (HDI) and functional disability measured using the Migraine Disability Assessment Scale (MIDAS). Secondary outcomes included changes in headache days per 30 days and headache pain intensity.
Participants had a mean age of about 40 years, about 92% were women, and approximately half of the patients had chronic migraine. Participants had an average baseline HDI of 51.4, and 83.3% had MIDAS scores indicating severe disability. Patients averaged 10.4 headache attack days per month, and mean headache attack severity on a 0-10 scale was 6.2. Attrition did not significantly differ between the mindfulness-based cognitive therapy and control groups.
Patients who received mindfulness-based cognitive therapy for migraine experienced an approximately 15-point reduction on the HDI scale at 4 months, whereas wait-listed patients did not experience much of a change, Dr. Seng said. The difference between groups was statistically significant.
At 4 months, a smaller proportion of patients in the mindfulness-based cognitive therapy group had a MIDAS score of 21 or greater, but the difference between groups was not statistically significant. The data indicate a large effect that the study was underpowered to detect, Dr. Seng said.
A planned subgroup analysis found that mindfulness-based cognitive therapy produced changes in disability that were greater in patients with episodic migraine, compared with patients with chronic migraine. A reduction in MIDAS scores was statistically significant among patients with episodic migraine.
During the trial, one patient experienced increased headache frequency and intensity and changed their preventive treatment regimen, which investigators considered unrelated to mindfulness-based cognitive therapy. In addition, one patient experienced flooding – a vivid recollection of a traumatic event – which is an expected effect of meditation and relaxation therapy, Dr. Seng said. The patient completed the study and was satisfied with the mindfulness-based cognitive therapy training, she said.
“Preliminary evidence suggests that mindfulness-based cognitive therapy could be recommended to reduce headache-related disability in people with episodic migraine or people who have some kind of effective prevention on board, but they are still experiencing high levels of disability,” Dr. Seng said.
Although flooding may occur in patients with a trauma history who use meditation and relaxation, the techniques still may be useful, Dr. Seng said. “In the VA setting, we use meditation and relaxation all the time. But it helps to forewarn patients that they might experience distressful flooding and [to provide] techniques that they can use to reduce the impact of that.”
PHILADELPHIA – , according to randomized clinical trial results.
“The fact that people can improve how they live their daily life even with the same amount of headache days and the same pain intensity is remarkable,” said study investigator Elizabeth K. Seng, PhD, associate professor of psychology at Yeshiva University and research associate professor of neurology at Albert Einstein College of Medicine, both in New York. “I think this gives us a little bit of a clue about when to use these kinds of treatments.”
Dr. Seng presented findings from the phase 2b pilot trial at the annual meeting of the American Headache Society.
To study the efficacy of mindfulness-based cognitive therapy for migraine, Dr. Seng and her research colleagues recruited participants with migraine in the New York City area between 2015 and 2018. In all, 60 patients were randomized to receive 8 weekly individual 75-minute mindfulness-based cognitive therapy for migraine sessions or 8 weeks on a wait list with treatment as usual.
Primary outcomes were Month 0 to Month 4 changes in perceived disability, measured using the Henry Ford Disability Inventory (HDI) and functional disability measured using the Migraine Disability Assessment Scale (MIDAS). Secondary outcomes included changes in headache days per 30 days and headache pain intensity.
Participants had a mean age of about 40 years, about 92% were women, and approximately half of the patients had chronic migraine. Participants had an average baseline HDI of 51.4, and 83.3% had MIDAS scores indicating severe disability. Patients averaged 10.4 headache attack days per month, and mean headache attack severity on a 0-10 scale was 6.2. Attrition did not significantly differ between the mindfulness-based cognitive therapy and control groups.
Patients who received mindfulness-based cognitive therapy for migraine experienced an approximately 15-point reduction on the HDI scale at 4 months, whereas wait-listed patients did not experience much of a change, Dr. Seng said. The difference between groups was statistically significant.
At 4 months, a smaller proportion of patients in the mindfulness-based cognitive therapy group had a MIDAS score of 21 or greater, but the difference between groups was not statistically significant. The data indicate a large effect that the study was underpowered to detect, Dr. Seng said.
A planned subgroup analysis found that mindfulness-based cognitive therapy produced changes in disability that were greater in patients with episodic migraine, compared with patients with chronic migraine. A reduction in MIDAS scores was statistically significant among patients with episodic migraine.
During the trial, one patient experienced increased headache frequency and intensity and changed their preventive treatment regimen, which investigators considered unrelated to mindfulness-based cognitive therapy. In addition, one patient experienced flooding – a vivid recollection of a traumatic event – which is an expected effect of meditation and relaxation therapy, Dr. Seng said. The patient completed the study and was satisfied with the mindfulness-based cognitive therapy training, she said.
“Preliminary evidence suggests that mindfulness-based cognitive therapy could be recommended to reduce headache-related disability in people with episodic migraine or people who have some kind of effective prevention on board, but they are still experiencing high levels of disability,” Dr. Seng said.
Although flooding may occur in patients with a trauma history who use meditation and relaxation, the techniques still may be useful, Dr. Seng said. “In the VA setting, we use meditation and relaxation all the time. But it helps to forewarn patients that they might experience distressful flooding and [to provide] techniques that they can use to reduce the impact of that.”
PHILADELPHIA – , according to randomized clinical trial results.
“The fact that people can improve how they live their daily life even with the same amount of headache days and the same pain intensity is remarkable,” said study investigator Elizabeth K. Seng, PhD, associate professor of psychology at Yeshiva University and research associate professor of neurology at Albert Einstein College of Medicine, both in New York. “I think this gives us a little bit of a clue about when to use these kinds of treatments.”
Dr. Seng presented findings from the phase 2b pilot trial at the annual meeting of the American Headache Society.
To study the efficacy of mindfulness-based cognitive therapy for migraine, Dr. Seng and her research colleagues recruited participants with migraine in the New York City area between 2015 and 2018. In all, 60 patients were randomized to receive 8 weekly individual 75-minute mindfulness-based cognitive therapy for migraine sessions or 8 weeks on a wait list with treatment as usual.
Primary outcomes were Month 0 to Month 4 changes in perceived disability, measured using the Henry Ford Disability Inventory (HDI) and functional disability measured using the Migraine Disability Assessment Scale (MIDAS). Secondary outcomes included changes in headache days per 30 days and headache pain intensity.
Participants had a mean age of about 40 years, about 92% were women, and approximately half of the patients had chronic migraine. Participants had an average baseline HDI of 51.4, and 83.3% had MIDAS scores indicating severe disability. Patients averaged 10.4 headache attack days per month, and mean headache attack severity on a 0-10 scale was 6.2. Attrition did not significantly differ between the mindfulness-based cognitive therapy and control groups.
Patients who received mindfulness-based cognitive therapy for migraine experienced an approximately 15-point reduction on the HDI scale at 4 months, whereas wait-listed patients did not experience much of a change, Dr. Seng said. The difference between groups was statistically significant.
At 4 months, a smaller proportion of patients in the mindfulness-based cognitive therapy group had a MIDAS score of 21 or greater, but the difference between groups was not statistically significant. The data indicate a large effect that the study was underpowered to detect, Dr. Seng said.
A planned subgroup analysis found that mindfulness-based cognitive therapy produced changes in disability that were greater in patients with episodic migraine, compared with patients with chronic migraine. A reduction in MIDAS scores was statistically significant among patients with episodic migraine.
During the trial, one patient experienced increased headache frequency and intensity and changed their preventive treatment regimen, which investigators considered unrelated to mindfulness-based cognitive therapy. In addition, one patient experienced flooding – a vivid recollection of a traumatic event – which is an expected effect of meditation and relaxation therapy, Dr. Seng said. The patient completed the study and was satisfied with the mindfulness-based cognitive therapy training, she said.
“Preliminary evidence suggests that mindfulness-based cognitive therapy could be recommended to reduce headache-related disability in people with episodic migraine or people who have some kind of effective prevention on board, but they are still experiencing high levels of disability,” Dr. Seng said.
Although flooding may occur in patients with a trauma history who use meditation and relaxation, the techniques still may be useful, Dr. Seng said. “In the VA setting, we use meditation and relaxation all the time. But it helps to forewarn patients that they might experience distressful flooding and [to provide] techniques that they can use to reduce the impact of that.”
EXPERT ANALYSIS FROM AHS 2019