User login
Tips to improve immunization rates in your office
In October 2018 the US Food and Drug Administration expanded the approved use of the human papillomavirus (HPV) vaccine (Gardasil 9) to adults aged 27 through 45.1 In June 2019, the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP) voted to extend catch-up HPV vaccination to include all individuals through age 26 and to catch-up HPV vaccination, based on shared clinical decision making, for all adults aged 27 through 45.2 HPV viruses are associated with cervical cancer, as well as several other forms of cancer that affect both women and men. Approval for the expanded use of the HPV vaccine was based on data of the vaccine’s use in women.1,3
Unfortunately, adult immunization rates, including among pregnant women, do not equal the higher rates in childhood vaccine uptake, according to Kevin A. Ault, MD, and colleagues. Less than half of women (46.6%) receive influenza vaccination prior to and during pregnancy, for instance.4 Dr. Ault has identified the need for an “immunization champion”—someone who can manage one-on-one conversations with patients in the office setting to enhance the acceptance and uptake of adult and maternal vaccines.
OBG Management:
Dr. Kevin A. Ault, MD: The main thing a practice needs to do is to identify someone who is interested, and this person does not have to be a physician. In fact, he or she can frequently be a member of your nursing staff or office staff. And the word “champion” involves a lot of nuts and bolts: such details as how do you store the vaccine, how do you keep track of it, where are the vaccine information statements filed, where can the provider get more information if there is a question about contraindications? One person should organize all these details. The mechanics of vaccine administration are important as well, as the research shows that the more automated the process is, the better and more smoothly it is carried out. There is certainly a role for “standing orders” for adult vaccines.
OBG Management: What communication approach do you take with patients to enhance vaccination acceptance and uptake?
Dr. Ault: There are multiple research studies that show that provider recommendation is the most important way to get both nonpregnant and pregnant adults to receive vaccinations. Take the pertussis vaccine (the whooping cough booster) as an example. It is a relatively new vaccine recommendation during pregnancy. Your approach is relatively straightforward when explaining it to pregnant women. Make the point that we do not want your newborn to have whooping cough in those first few months of life before the newborn or infant vaccine becomes effective. Most people know they had a whooping cough, or pertussis, vaccine when they were younger, and the concept of the booster is well-known to patients. You should explain that the maternal antibodies pass through the placenta to the fetus, and they provide benefit for the first few months of life after birth.
The pertussis vaccine does not have all the “baggage” of the influenza vaccine. Talking with patients about the flu vaccine may present more challenges. Typically, each fall there is a popular press publication that explains “the 10, or 20, most common myths about influenza vaccine.” Every fall I try to find one of those articles, print it out, and even carry it in my jacket pocket and talk about all the myths. For example, there is a myth that “I always get sick when I get the flu shot.” Obstetricians should be giving patients an inactivated vaccine that does not contain any live flu virus. We should be able to explain to patients, your arm will be sore, and you may have some muscle aches, but you will not have the flu from your flu vaccine.
I think another reason that pregnant women do not always take the flu vaccine is that we do not yet have normalized influenza vaccination in the adult population. Women in their twenties and thirties are generally very healthy and have other concerns when they are pregnant, and they perhaps do not realize that they are more vulnerable to devastating effects of influenza while pregnant. Additionally, maternal influenza vaccination does protect the newborn from flu for the first few months. It is vital that those patients who are due during the dark winter months, when the flu is in season, get vaccinated.
Combat the myths and tell your patients the reasons for flu vaccination. Also tell them that you got your flu shot, like most health care professionals do every fall. You should be prepared to talk about safety. There are wonderful safety data, even some published in 2017 and 2018, about pertussis vaccine safety during pregnancy, and it is very reassuring to patients. For flu, the idea of vaccinating women against influenza has been around for decades, and so we have reliable information about that as well. Certainly, the risks are very minor, and the benefits are potentially huge for the pregnant woman and for the newborn.
OBG Management: When do you recommend that ObGyns administer the flu vaccine for pregnant women?
Dr. Ault: There are 2 issues to this question: when throughout the year and when during the pregnancy to administer the vaccine. First, you want to give the flu vaccine during the usual influenza season during the fall. As soon as the vaccine is available, you will recommend that pregnant women, even in their late pregnancy, get vaccinated so that their newborns who are 3 and 4 months old in the peak flu season are protected. The patients who deliver over the summer, who are coming in for their postpartum visit during the fall, should be getting vaccinated as well, because they are still vulnerable to influenza and pneumonia for several months postpartum.
If you have patients that come in for preconception visits, you could say: “Let’s get this out of the way. You could be pregnant by the time flu season really gets cranked up.”
Because we see patients 10 or 12 times during pregnancy, we certainly have plenty of opportunities to educate patients about and administer the flu vaccine. There are older data that demonstrate if patients do not get the flu vaccine done during early pregnancy, the opportunity may be lost. It is different now because there is more emphasis on vaccinating all adults. Your patients certainly can get their vaccine at the pharmacy or at their primary care doctor; however, delaying until later pregnancy usually means not getting the vaccine.
I would like to address one recent study from Donahue and colleagues that showed a potentially increased risk of miscarriage with flu vaccination.5 That study was an anomaly, as there are many other studies into the issue. Yes, there are not a lot of first trimester data, but there are other studies, including studies by the same authors, that did not find this to be the case.6-10
The 2017 study by Donahue and colleagues was an anomaly because the group of women they were vaccinating were already at high risk for miscarriage. The women were older, had diabetes, or a history of miscarriages. There is selection bias in the study because the pregnant women who were vaccinated were already at higher risk for miscarriage. The Centers for Disease Control and Prevention and the American College of Obstetricians and Gynecologists are not going to change any of their recommendations based on a single study that is different than our previous data.11
Current recommended adult (anyone over 18 years old) immunization schedule
ACOG Immunization Champions (ACOG members who have demonstrated exceptional progress in increasing immunization rates among adults and pregnant women in their communities through leadership, innovation, collaboration, and educational activities aimed at following ACOG and CDC guidance.)
Summary of Maternal Immunization Recommendations is a provider resource from ACOG and the Centers for Disease Control and Prevention.
Maternal Immunization Toolkit contains materials, including the Vaccines During Pregnancy Poster, to support ObGyns on recommending the influenza vaccine and the Tdap vaccine to all pregnant patients.
Influenza Immunization During Pregnancy Toolkit
CDC vaccine schedules app for health care providers
CDC Vaccine Information Statements (available for clinician or patient download)
- FDA approves expanded use of Gardasil 9 to include individuals 27 through 45 years old [press release]. Washington, DC: Food and Drug Administration; October 5, 2018.
- Color/Blue2. Splete H. ACIP extends HPV vaccine coverage. June 27, 2019. https://www.mdedge.com/obgyn/article/203656/vaccines/acip-extends-hpv-vaccine-coverage. Accessed July 5, 2019.
- Levy BS, Downs Jr L. The HPV vaccine is now recommended for adults aged 27–45: Counseling implications. OBG Manag. 2019;31(1):9-11.
- Frew PM, Randall LA, Malik F, et al. Clinician perspectives on strategies to improve patient maternal immunization acceptability in obstetrics and gynecology practice settings. Hum Vaccin Immunother. 2018;14(7):1548–1557.
- Donahue JG, Kieke BA, King JP, et al. Association of spontaneous abortion with receipt of inactivated influenza vaccine containing H1N1pdm09 in 2010-11 and 2011-12. Vaccine. 2017;35(40):5314-5322.
- Moro PL, Broder K, Zheteyeva Y, et al. Adverse events in pregnant women following administration of trivalent inactivated influenza vaccine and live attenuated influenza vaccine in the Vaccine Adverse Event Reporting System, 1990-2009. Am J Obstet Gynecol. 2011;204:146.e1-146.e7.
- Irving SA, Kieke BA, Donahue JG, et al; Vaccine Safety Datalink. Trivalent inactivated influenza vaccine and spontaneous abortion. 2013;121:159-165.
- Kharbanda EO, Vazquez-Benitez G, Lipkind H, et al; Vaccine Safety Datalink Team. Inactivated influenza vaccine during pregnancy and risks for adverse obstetric events. Obstet Gynecol. 2013;122:659-667.
- Nordin JD, Kharbanda EO, Vazquez-Benitez G, et al; Vaccine Safety Datalink. Maternal Influenza vaccine and risks for preterm or small for gestational age birth. J Pediatrics. 2014;164:1051-1057.e2.
- Kharbanda EO, Vazquez-Benitez G, Romitti PA, et al; Vaccine Safety Datalink. First trimester influenza vaccination and risks for major structural birth defects in offspring. 2017;187:234-239.e4.
- Flu vaccination and possible safety signal. CDC website. https://www.cdc.gov/flu/professionals/vaccination/vaccination-possible-safety-signal.html. Last reviewed September 13, 2017. Accessed May 15, 2019.
In October 2018 the US Food and Drug Administration expanded the approved use of the human papillomavirus (HPV) vaccine (Gardasil 9) to adults aged 27 through 45.1 In June 2019, the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP) voted to extend catch-up HPV vaccination to include all individuals through age 26 and to catch-up HPV vaccination, based on shared clinical decision making, for all adults aged 27 through 45.2 HPV viruses are associated with cervical cancer, as well as several other forms of cancer that affect both women and men. Approval for the expanded use of the HPV vaccine was based on data of the vaccine’s use in women.1,3
Unfortunately, adult immunization rates, including among pregnant women, do not equal the higher rates in childhood vaccine uptake, according to Kevin A. Ault, MD, and colleagues. Less than half of women (46.6%) receive influenza vaccination prior to and during pregnancy, for instance.4 Dr. Ault has identified the need for an “immunization champion”—someone who can manage one-on-one conversations with patients in the office setting to enhance the acceptance and uptake of adult and maternal vaccines.
OBG Management:
Dr. Kevin A. Ault, MD: The main thing a practice needs to do is to identify someone who is interested, and this person does not have to be a physician. In fact, he or she can frequently be a member of your nursing staff or office staff. And the word “champion” involves a lot of nuts and bolts: such details as how do you store the vaccine, how do you keep track of it, where are the vaccine information statements filed, where can the provider get more information if there is a question about contraindications? One person should organize all these details. The mechanics of vaccine administration are important as well, as the research shows that the more automated the process is, the better and more smoothly it is carried out. There is certainly a role for “standing orders” for adult vaccines.
OBG Management: What communication approach do you take with patients to enhance vaccination acceptance and uptake?
Dr. Ault: There are multiple research studies that show that provider recommendation is the most important way to get both nonpregnant and pregnant adults to receive vaccinations. Take the pertussis vaccine (the whooping cough booster) as an example. It is a relatively new vaccine recommendation during pregnancy. Your approach is relatively straightforward when explaining it to pregnant women. Make the point that we do not want your newborn to have whooping cough in those first few months of life before the newborn or infant vaccine becomes effective. Most people know they had a whooping cough, or pertussis, vaccine when they were younger, and the concept of the booster is well-known to patients. You should explain that the maternal antibodies pass through the placenta to the fetus, and they provide benefit for the first few months of life after birth.
The pertussis vaccine does not have all the “baggage” of the influenza vaccine. Talking with patients about the flu vaccine may present more challenges. Typically, each fall there is a popular press publication that explains “the 10, or 20, most common myths about influenza vaccine.” Every fall I try to find one of those articles, print it out, and even carry it in my jacket pocket and talk about all the myths. For example, there is a myth that “I always get sick when I get the flu shot.” Obstetricians should be giving patients an inactivated vaccine that does not contain any live flu virus. We should be able to explain to patients, your arm will be sore, and you may have some muscle aches, but you will not have the flu from your flu vaccine.
I think another reason that pregnant women do not always take the flu vaccine is that we do not yet have normalized influenza vaccination in the adult population. Women in their twenties and thirties are generally very healthy and have other concerns when they are pregnant, and they perhaps do not realize that they are more vulnerable to devastating effects of influenza while pregnant. Additionally, maternal influenza vaccination does protect the newborn from flu for the first few months. It is vital that those patients who are due during the dark winter months, when the flu is in season, get vaccinated.
Combat the myths and tell your patients the reasons for flu vaccination. Also tell them that you got your flu shot, like most health care professionals do every fall. You should be prepared to talk about safety. There are wonderful safety data, even some published in 2017 and 2018, about pertussis vaccine safety during pregnancy, and it is very reassuring to patients. For flu, the idea of vaccinating women against influenza has been around for decades, and so we have reliable information about that as well. Certainly, the risks are very minor, and the benefits are potentially huge for the pregnant woman and for the newborn.
OBG Management: When do you recommend that ObGyns administer the flu vaccine for pregnant women?
Dr. Ault: There are 2 issues to this question: when throughout the year and when during the pregnancy to administer the vaccine. First, you want to give the flu vaccine during the usual influenza season during the fall. As soon as the vaccine is available, you will recommend that pregnant women, even in their late pregnancy, get vaccinated so that their newborns who are 3 and 4 months old in the peak flu season are protected. The patients who deliver over the summer, who are coming in for their postpartum visit during the fall, should be getting vaccinated as well, because they are still vulnerable to influenza and pneumonia for several months postpartum.
If you have patients that come in for preconception visits, you could say: “Let’s get this out of the way. You could be pregnant by the time flu season really gets cranked up.”
Because we see patients 10 or 12 times during pregnancy, we certainly have plenty of opportunities to educate patients about and administer the flu vaccine. There are older data that demonstrate if patients do not get the flu vaccine done during early pregnancy, the opportunity may be lost. It is different now because there is more emphasis on vaccinating all adults. Your patients certainly can get their vaccine at the pharmacy or at their primary care doctor; however, delaying until later pregnancy usually means not getting the vaccine.
I would like to address one recent study from Donahue and colleagues that showed a potentially increased risk of miscarriage with flu vaccination.5 That study was an anomaly, as there are many other studies into the issue. Yes, there are not a lot of first trimester data, but there are other studies, including studies by the same authors, that did not find this to be the case.6-10
The 2017 study by Donahue and colleagues was an anomaly because the group of women they were vaccinating were already at high risk for miscarriage. The women were older, had diabetes, or a history of miscarriages. There is selection bias in the study because the pregnant women who were vaccinated were already at higher risk for miscarriage. The Centers for Disease Control and Prevention and the American College of Obstetricians and Gynecologists are not going to change any of their recommendations based on a single study that is different than our previous data.11
Current recommended adult (anyone over 18 years old) immunization schedule
ACOG Immunization Champions (ACOG members who have demonstrated exceptional progress in increasing immunization rates among adults and pregnant women in their communities through leadership, innovation, collaboration, and educational activities aimed at following ACOG and CDC guidance.)
Summary of Maternal Immunization Recommendations is a provider resource from ACOG and the Centers for Disease Control and Prevention.
Maternal Immunization Toolkit contains materials, including the Vaccines During Pregnancy Poster, to support ObGyns on recommending the influenza vaccine and the Tdap vaccine to all pregnant patients.
Influenza Immunization During Pregnancy Toolkit
CDC vaccine schedules app for health care providers
CDC Vaccine Information Statements (available for clinician or patient download)
In October 2018 the US Food and Drug Administration expanded the approved use of the human papillomavirus (HPV) vaccine (Gardasil 9) to adults aged 27 through 45.1 In June 2019, the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP) voted to extend catch-up HPV vaccination to include all individuals through age 26 and to catch-up HPV vaccination, based on shared clinical decision making, for all adults aged 27 through 45.2 HPV viruses are associated with cervical cancer, as well as several other forms of cancer that affect both women and men. Approval for the expanded use of the HPV vaccine was based on data of the vaccine’s use in women.1,3
Unfortunately, adult immunization rates, including among pregnant women, do not equal the higher rates in childhood vaccine uptake, according to Kevin A. Ault, MD, and colleagues. Less than half of women (46.6%) receive influenza vaccination prior to and during pregnancy, for instance.4 Dr. Ault has identified the need for an “immunization champion”—someone who can manage one-on-one conversations with patients in the office setting to enhance the acceptance and uptake of adult and maternal vaccines.
OBG Management:
Dr. Kevin A. Ault, MD: The main thing a practice needs to do is to identify someone who is interested, and this person does not have to be a physician. In fact, he or she can frequently be a member of your nursing staff or office staff. And the word “champion” involves a lot of nuts and bolts: such details as how do you store the vaccine, how do you keep track of it, where are the vaccine information statements filed, where can the provider get more information if there is a question about contraindications? One person should organize all these details. The mechanics of vaccine administration are important as well, as the research shows that the more automated the process is, the better and more smoothly it is carried out. There is certainly a role for “standing orders” for adult vaccines.
OBG Management: What communication approach do you take with patients to enhance vaccination acceptance and uptake?
Dr. Ault: There are multiple research studies that show that provider recommendation is the most important way to get both nonpregnant and pregnant adults to receive vaccinations. Take the pertussis vaccine (the whooping cough booster) as an example. It is a relatively new vaccine recommendation during pregnancy. Your approach is relatively straightforward when explaining it to pregnant women. Make the point that we do not want your newborn to have whooping cough in those first few months of life before the newborn or infant vaccine becomes effective. Most people know they had a whooping cough, or pertussis, vaccine when they were younger, and the concept of the booster is well-known to patients. You should explain that the maternal antibodies pass through the placenta to the fetus, and they provide benefit for the first few months of life after birth.
The pertussis vaccine does not have all the “baggage” of the influenza vaccine. Talking with patients about the flu vaccine may present more challenges. Typically, each fall there is a popular press publication that explains “the 10, or 20, most common myths about influenza vaccine.” Every fall I try to find one of those articles, print it out, and even carry it in my jacket pocket and talk about all the myths. For example, there is a myth that “I always get sick when I get the flu shot.” Obstetricians should be giving patients an inactivated vaccine that does not contain any live flu virus. We should be able to explain to patients, your arm will be sore, and you may have some muscle aches, but you will not have the flu from your flu vaccine.
I think another reason that pregnant women do not always take the flu vaccine is that we do not yet have normalized influenza vaccination in the adult population. Women in their twenties and thirties are generally very healthy and have other concerns when they are pregnant, and they perhaps do not realize that they are more vulnerable to devastating effects of influenza while pregnant. Additionally, maternal influenza vaccination does protect the newborn from flu for the first few months. It is vital that those patients who are due during the dark winter months, when the flu is in season, get vaccinated.
Combat the myths and tell your patients the reasons for flu vaccination. Also tell them that you got your flu shot, like most health care professionals do every fall. You should be prepared to talk about safety. There are wonderful safety data, even some published in 2017 and 2018, about pertussis vaccine safety during pregnancy, and it is very reassuring to patients. For flu, the idea of vaccinating women against influenza has been around for decades, and so we have reliable information about that as well. Certainly, the risks are very minor, and the benefits are potentially huge for the pregnant woman and for the newborn.
OBG Management: When do you recommend that ObGyns administer the flu vaccine for pregnant women?
Dr. Ault: There are 2 issues to this question: when throughout the year and when during the pregnancy to administer the vaccine. First, you want to give the flu vaccine during the usual influenza season during the fall. As soon as the vaccine is available, you will recommend that pregnant women, even in their late pregnancy, get vaccinated so that their newborns who are 3 and 4 months old in the peak flu season are protected. The patients who deliver over the summer, who are coming in for their postpartum visit during the fall, should be getting vaccinated as well, because they are still vulnerable to influenza and pneumonia for several months postpartum.
If you have patients that come in for preconception visits, you could say: “Let’s get this out of the way. You could be pregnant by the time flu season really gets cranked up.”
Because we see patients 10 or 12 times during pregnancy, we certainly have plenty of opportunities to educate patients about and administer the flu vaccine. There are older data that demonstrate if patients do not get the flu vaccine done during early pregnancy, the opportunity may be lost. It is different now because there is more emphasis on vaccinating all adults. Your patients certainly can get their vaccine at the pharmacy or at their primary care doctor; however, delaying until later pregnancy usually means not getting the vaccine.
I would like to address one recent study from Donahue and colleagues that showed a potentially increased risk of miscarriage with flu vaccination.5 That study was an anomaly, as there are many other studies into the issue. Yes, there are not a lot of first trimester data, but there are other studies, including studies by the same authors, that did not find this to be the case.6-10
The 2017 study by Donahue and colleagues was an anomaly because the group of women they were vaccinating were already at high risk for miscarriage. The women were older, had diabetes, or a history of miscarriages. There is selection bias in the study because the pregnant women who were vaccinated were already at higher risk for miscarriage. The Centers for Disease Control and Prevention and the American College of Obstetricians and Gynecologists are not going to change any of their recommendations based on a single study that is different than our previous data.11
Current recommended adult (anyone over 18 years old) immunization schedule
ACOG Immunization Champions (ACOG members who have demonstrated exceptional progress in increasing immunization rates among adults and pregnant women in their communities through leadership, innovation, collaboration, and educational activities aimed at following ACOG and CDC guidance.)
Summary of Maternal Immunization Recommendations is a provider resource from ACOG and the Centers for Disease Control and Prevention.
Maternal Immunization Toolkit contains materials, including the Vaccines During Pregnancy Poster, to support ObGyns on recommending the influenza vaccine and the Tdap vaccine to all pregnant patients.
Influenza Immunization During Pregnancy Toolkit
CDC vaccine schedules app for health care providers
CDC Vaccine Information Statements (available for clinician or patient download)
- FDA approves expanded use of Gardasil 9 to include individuals 27 through 45 years old [press release]. Washington, DC: Food and Drug Administration; October 5, 2018.
- Color/Blue2. Splete H. ACIP extends HPV vaccine coverage. June 27, 2019. https://www.mdedge.com/obgyn/article/203656/vaccines/acip-extends-hpv-vaccine-coverage. Accessed July 5, 2019.
- Levy BS, Downs Jr L. The HPV vaccine is now recommended for adults aged 27–45: Counseling implications. OBG Manag. 2019;31(1):9-11.
- Frew PM, Randall LA, Malik F, et al. Clinician perspectives on strategies to improve patient maternal immunization acceptability in obstetrics and gynecology practice settings. Hum Vaccin Immunother. 2018;14(7):1548–1557.
- Donahue JG, Kieke BA, King JP, et al. Association of spontaneous abortion with receipt of inactivated influenza vaccine containing H1N1pdm09 in 2010-11 and 2011-12. Vaccine. 2017;35(40):5314-5322.
- Moro PL, Broder K, Zheteyeva Y, et al. Adverse events in pregnant women following administration of trivalent inactivated influenza vaccine and live attenuated influenza vaccine in the Vaccine Adverse Event Reporting System, 1990-2009. Am J Obstet Gynecol. 2011;204:146.e1-146.e7.
- Irving SA, Kieke BA, Donahue JG, et al; Vaccine Safety Datalink. Trivalent inactivated influenza vaccine and spontaneous abortion. 2013;121:159-165.
- Kharbanda EO, Vazquez-Benitez G, Lipkind H, et al; Vaccine Safety Datalink Team. Inactivated influenza vaccine during pregnancy and risks for adverse obstetric events. Obstet Gynecol. 2013;122:659-667.
- Nordin JD, Kharbanda EO, Vazquez-Benitez G, et al; Vaccine Safety Datalink. Maternal Influenza vaccine and risks for preterm or small for gestational age birth. J Pediatrics. 2014;164:1051-1057.e2.
- Kharbanda EO, Vazquez-Benitez G, Romitti PA, et al; Vaccine Safety Datalink. First trimester influenza vaccination and risks for major structural birth defects in offspring. 2017;187:234-239.e4.
- Flu vaccination and possible safety signal. CDC website. https://www.cdc.gov/flu/professionals/vaccination/vaccination-possible-safety-signal.html. Last reviewed September 13, 2017. Accessed May 15, 2019.
- FDA approves expanded use of Gardasil 9 to include individuals 27 through 45 years old [press release]. Washington, DC: Food and Drug Administration; October 5, 2018.
- Color/Blue2. Splete H. ACIP extends HPV vaccine coverage. June 27, 2019. https://www.mdedge.com/obgyn/article/203656/vaccines/acip-extends-hpv-vaccine-coverage. Accessed July 5, 2019.
- Levy BS, Downs Jr L. The HPV vaccine is now recommended for adults aged 27–45: Counseling implications. OBG Manag. 2019;31(1):9-11.
- Frew PM, Randall LA, Malik F, et al. Clinician perspectives on strategies to improve patient maternal immunization acceptability in obstetrics and gynecology practice settings. Hum Vaccin Immunother. 2018;14(7):1548–1557.
- Donahue JG, Kieke BA, King JP, et al. Association of spontaneous abortion with receipt of inactivated influenza vaccine containing H1N1pdm09 in 2010-11 and 2011-12. Vaccine. 2017;35(40):5314-5322.
- Moro PL, Broder K, Zheteyeva Y, et al. Adverse events in pregnant women following administration of trivalent inactivated influenza vaccine and live attenuated influenza vaccine in the Vaccine Adverse Event Reporting System, 1990-2009. Am J Obstet Gynecol. 2011;204:146.e1-146.e7.
- Irving SA, Kieke BA, Donahue JG, et al; Vaccine Safety Datalink. Trivalent inactivated influenza vaccine and spontaneous abortion. 2013;121:159-165.
- Kharbanda EO, Vazquez-Benitez G, Lipkind H, et al; Vaccine Safety Datalink Team. Inactivated influenza vaccine during pregnancy and risks for adverse obstetric events. Obstet Gynecol. 2013;122:659-667.
- Nordin JD, Kharbanda EO, Vazquez-Benitez G, et al; Vaccine Safety Datalink. Maternal Influenza vaccine and risks for preterm or small for gestational age birth. J Pediatrics. 2014;164:1051-1057.e2.
- Kharbanda EO, Vazquez-Benitez G, Romitti PA, et al; Vaccine Safety Datalink. First trimester influenza vaccination and risks for major structural birth defects in offspring. 2017;187:234-239.e4.
- Flu vaccination and possible safety signal. CDC website. https://www.cdc.gov/flu/professionals/vaccination/vaccination-possible-safety-signal.html. Last reviewed September 13, 2017. Accessed May 15, 2019.
Sensitive gray matters in treating teen depression
Carla is an otherwise-healthy 14-year-old female followed by her pediatrician for symptoms of depression and anxiety that have worsened over the past 8 months. Anhedonia, irritability, poor concentration, fatigue, hypersomnolence, and significant weight gain have increasingly led to further dysphoria, social isolation, and obsessive rumination, all of which now contribute to more dysfunction in both her home and school life. Based on Carla’s apprehension over “taking pills,” she was referred for outpatient therapy 5 months ago but because of difficulty maintaining weekly appointments, she stopped attending after 6 weeks, citing difficulty aligning with her therapist.
Carla was seen in an urgent, unscheduled follow-up appointment 2 months prior to address increased thoughts of wishing to be dead. She had neither a plan nor a desire to act on these ideations. During an interview, she was distant with poor eye contact, and her affect was notably blunted. Her mother, who had accompanied her in the waiting room, expressed frustration to the nurse about discovering that Carla was using cannabis, that she often appeared aloof and unmotivated to do much of anything but “sit in her room and play on her phone for hours on end.” She compared Carla with her ex-husband, who had similar mood swings that often led to erratic and violent outbursts towards Carla and her mother, behaviors that ultimately led them to leave him when Carla was 6 years old.
After a discussion over the risks and benefits of various treatment options, Carla was started on low-dose fluoxetine with a plan to titrate the medication after 2 weeks. A referral for outpatient substance use treatment also was initiated. Carla’s mother telephoned 10 days later in an update that things have drastically improved in Carla’s mood and activity. The following week her mother called back again with concerns that Carla is no longer sleeping, appears restless, impulsive, and disinhibited.
Discussion
Carla’s initial presentation is common to primary care settings. Based on her earliest reported symptoms, she would qualify for a diagnosis of major depression. Decisions regarding initial treatment for children and adolescents must take into account the severity of symptoms, risks, autonomy of the patient and family, as well as available evidence. Her response to outpatient therapy is not an anomaly. With an ever-increasing demand on mental health services, the availability of consistent, quality outpatient therapy for this population is not always easy to secure.1,2 Combining targeted therapy with pharmacologic interventions for major depression appear to have the most effective outcomes.3
Carla’s progression also illustrates the challenges and potential pitfalls of attempting to understand and address her symptoms according to a single nosology. Depression is a like a fever. It can be caused by a myriad of factors and, left to linger, may lead to further residual complications. Focusing attention to her symptoms also may lead to a differential including adjustment problems, social anxiety, effects of trauma, surreptitious substance use, or even bipolar depression.
To begin with, a clear delineation of Carla’s historic symptoms and any possible medical contributions to her presentation are necessary to investigate. Specific inquiries into past episodes of activation including hyperarousal, impulsivity, restlessness, and insomnia should be elucidated prior to consideration of medication selection.4 Considering Carla’s age and the known association between antidepressant-induced manic conversion among children aged 10-14 years,5 any pharmacologic intervention will benefit from the maxim “start low and go slow.” Her symptoms of activation arise within the setting of titration of an antidepressant. This may raise considerations to her specific metabolism and physiological concentrations of the medication as well as cumulative day exposure.
Complementary to Carla’s own history is that of family members. Often obtaining a reliable family psychiatric history is an exercise fraught with bias, vagueness, and generalizations.6 However, given the known heritability of bipolar disorders and the implications for treating depression in such individuals, compared with unipolar depressive symptoms, clarifying the nature of family illness may elucidate potential susceptibilities previously unconsidered.7 In this case, descriptions of Carla’s father’s behavior raise concerns for underlying bipolar disorder, as do the accounts of traumatic stress exposure and their compounded preponderance for increased suicide risk.8
Unfortunately, Carla’s current environmental cues and maladaptive behaviors may be perpetuating her symptoms and possibly placing her on a trajectory for further illness. Exploration of her relationship with her caregivers regarding the interpretation of her symptoms, and need for treatment should be undertaken so as to expand supportive roles. Education regarding cannabis use among adolescents and age-specific risks for later depression, anxiety, and suicide is warranted in a climate when accessibility is on the rise.9 Whether or not cannabis use itself leads to amotivation is the subject of current debate.10 A growing body of evidence is clearly illustrating that Carla’s sedentary behaviors and perceived loneliness likely exacerbate her mental well-being. Such patterns indicate the need for environmental intervention to change such cycles.
Finally, Carla’s progression through treatment speak to the need for open and honest discussions regarding realistic benefits as well potential risks. Progressive symptoms of depression left untreated can be life-threatening themselves, just as effects of activation as described in the vignette above can easily and quickly progress into situations that pose safety concerns. Amidst such periods of intervention, close communication and follow up with patients and their supports ameliorate potential adverse events and lead to better outcomes.
Outcome
Carla’s mother was advised to discontinue the medication, closely monitor Carla’s behavior and sleep, and schedule an emergent follow-up appointment for the next day. A safety plan indicating circumstances in which Carla would require closer medical supervision for safety was reviewed with her mother. Carla was later initiated on lamotrigine and restarted interpersonal therapy.
References
1. N Engl J Med. 2015 May 21;372(21):2029-38.
2. J Pediatr. 2010 Nov;157(5):848-51.
3. Arch Gen Psychiatry. 2007 Oct;64(10):1132-43.
4. Curr Probl Pediatr Adolesc Health Care. 2018 Feb;48(2):50-62.
5. Arch Pediatr Adolesc Med. 2004 Aug;158(8):773-80.
6. Can J Psychiatry. 1993 Nov;38(9):590-4.
7. Appl Clin Genet. 2014 Feb 12;7:33-42.
8. J Am Acad Child Adolesc Psychiatry. 2017 Dec;56(12):1073-1080.
9. JAMA Psychiatry. 2019;76(4):426-34.
10. Subst Use Misuse. 2018 Jun 7;53(7):1158-69.
Carla is an otherwise-healthy 14-year-old female followed by her pediatrician for symptoms of depression and anxiety that have worsened over the past 8 months. Anhedonia, irritability, poor concentration, fatigue, hypersomnolence, and significant weight gain have increasingly led to further dysphoria, social isolation, and obsessive rumination, all of which now contribute to more dysfunction in both her home and school life. Based on Carla’s apprehension over “taking pills,” she was referred for outpatient therapy 5 months ago but because of difficulty maintaining weekly appointments, she stopped attending after 6 weeks, citing difficulty aligning with her therapist.
Carla was seen in an urgent, unscheduled follow-up appointment 2 months prior to address increased thoughts of wishing to be dead. She had neither a plan nor a desire to act on these ideations. During an interview, she was distant with poor eye contact, and her affect was notably blunted. Her mother, who had accompanied her in the waiting room, expressed frustration to the nurse about discovering that Carla was using cannabis, that she often appeared aloof and unmotivated to do much of anything but “sit in her room and play on her phone for hours on end.” She compared Carla with her ex-husband, who had similar mood swings that often led to erratic and violent outbursts towards Carla and her mother, behaviors that ultimately led them to leave him when Carla was 6 years old.
After a discussion over the risks and benefits of various treatment options, Carla was started on low-dose fluoxetine with a plan to titrate the medication after 2 weeks. A referral for outpatient substance use treatment also was initiated. Carla’s mother telephoned 10 days later in an update that things have drastically improved in Carla’s mood and activity. The following week her mother called back again with concerns that Carla is no longer sleeping, appears restless, impulsive, and disinhibited.
Discussion
Carla’s initial presentation is common to primary care settings. Based on her earliest reported symptoms, she would qualify for a diagnosis of major depression. Decisions regarding initial treatment for children and adolescents must take into account the severity of symptoms, risks, autonomy of the patient and family, as well as available evidence. Her response to outpatient therapy is not an anomaly. With an ever-increasing demand on mental health services, the availability of consistent, quality outpatient therapy for this population is not always easy to secure.1,2 Combining targeted therapy with pharmacologic interventions for major depression appear to have the most effective outcomes.3
Carla’s progression also illustrates the challenges and potential pitfalls of attempting to understand and address her symptoms according to a single nosology. Depression is a like a fever. It can be caused by a myriad of factors and, left to linger, may lead to further residual complications. Focusing attention to her symptoms also may lead to a differential including adjustment problems, social anxiety, effects of trauma, surreptitious substance use, or even bipolar depression.
To begin with, a clear delineation of Carla’s historic symptoms and any possible medical contributions to her presentation are necessary to investigate. Specific inquiries into past episodes of activation including hyperarousal, impulsivity, restlessness, and insomnia should be elucidated prior to consideration of medication selection.4 Considering Carla’s age and the known association between antidepressant-induced manic conversion among children aged 10-14 years,5 any pharmacologic intervention will benefit from the maxim “start low and go slow.” Her symptoms of activation arise within the setting of titration of an antidepressant. This may raise considerations to her specific metabolism and physiological concentrations of the medication as well as cumulative day exposure.
Complementary to Carla’s own history is that of family members. Often obtaining a reliable family psychiatric history is an exercise fraught with bias, vagueness, and generalizations.6 However, given the known heritability of bipolar disorders and the implications for treating depression in such individuals, compared with unipolar depressive symptoms, clarifying the nature of family illness may elucidate potential susceptibilities previously unconsidered.7 In this case, descriptions of Carla’s father’s behavior raise concerns for underlying bipolar disorder, as do the accounts of traumatic stress exposure and their compounded preponderance for increased suicide risk.8
Unfortunately, Carla’s current environmental cues and maladaptive behaviors may be perpetuating her symptoms and possibly placing her on a trajectory for further illness. Exploration of her relationship with her caregivers regarding the interpretation of her symptoms, and need for treatment should be undertaken so as to expand supportive roles. Education regarding cannabis use among adolescents and age-specific risks for later depression, anxiety, and suicide is warranted in a climate when accessibility is on the rise.9 Whether or not cannabis use itself leads to amotivation is the subject of current debate.10 A growing body of evidence is clearly illustrating that Carla’s sedentary behaviors and perceived loneliness likely exacerbate her mental well-being. Such patterns indicate the need for environmental intervention to change such cycles.
Finally, Carla’s progression through treatment speak to the need for open and honest discussions regarding realistic benefits as well potential risks. Progressive symptoms of depression left untreated can be life-threatening themselves, just as effects of activation as described in the vignette above can easily and quickly progress into situations that pose safety concerns. Amidst such periods of intervention, close communication and follow up with patients and their supports ameliorate potential adverse events and lead to better outcomes.
Outcome
Carla’s mother was advised to discontinue the medication, closely monitor Carla’s behavior and sleep, and schedule an emergent follow-up appointment for the next day. A safety plan indicating circumstances in which Carla would require closer medical supervision for safety was reviewed with her mother. Carla was later initiated on lamotrigine and restarted interpersonal therapy.
References
1. N Engl J Med. 2015 May 21;372(21):2029-38.
2. J Pediatr. 2010 Nov;157(5):848-51.
3. Arch Gen Psychiatry. 2007 Oct;64(10):1132-43.
4. Curr Probl Pediatr Adolesc Health Care. 2018 Feb;48(2):50-62.
5. Arch Pediatr Adolesc Med. 2004 Aug;158(8):773-80.
6. Can J Psychiatry. 1993 Nov;38(9):590-4.
7. Appl Clin Genet. 2014 Feb 12;7:33-42.
8. J Am Acad Child Adolesc Psychiatry. 2017 Dec;56(12):1073-1080.
9. JAMA Psychiatry. 2019;76(4):426-34.
10. Subst Use Misuse. 2018 Jun 7;53(7):1158-69.
Carla is an otherwise-healthy 14-year-old female followed by her pediatrician for symptoms of depression and anxiety that have worsened over the past 8 months. Anhedonia, irritability, poor concentration, fatigue, hypersomnolence, and significant weight gain have increasingly led to further dysphoria, social isolation, and obsessive rumination, all of which now contribute to more dysfunction in both her home and school life. Based on Carla’s apprehension over “taking pills,” she was referred for outpatient therapy 5 months ago but because of difficulty maintaining weekly appointments, she stopped attending after 6 weeks, citing difficulty aligning with her therapist.
Carla was seen in an urgent, unscheduled follow-up appointment 2 months prior to address increased thoughts of wishing to be dead. She had neither a plan nor a desire to act on these ideations. During an interview, she was distant with poor eye contact, and her affect was notably blunted. Her mother, who had accompanied her in the waiting room, expressed frustration to the nurse about discovering that Carla was using cannabis, that she often appeared aloof and unmotivated to do much of anything but “sit in her room and play on her phone for hours on end.” She compared Carla with her ex-husband, who had similar mood swings that often led to erratic and violent outbursts towards Carla and her mother, behaviors that ultimately led them to leave him when Carla was 6 years old.
After a discussion over the risks and benefits of various treatment options, Carla was started on low-dose fluoxetine with a plan to titrate the medication after 2 weeks. A referral for outpatient substance use treatment also was initiated. Carla’s mother telephoned 10 days later in an update that things have drastically improved in Carla’s mood and activity. The following week her mother called back again with concerns that Carla is no longer sleeping, appears restless, impulsive, and disinhibited.
Discussion
Carla’s initial presentation is common to primary care settings. Based on her earliest reported symptoms, she would qualify for a diagnosis of major depression. Decisions regarding initial treatment for children and adolescents must take into account the severity of symptoms, risks, autonomy of the patient and family, as well as available evidence. Her response to outpatient therapy is not an anomaly. With an ever-increasing demand on mental health services, the availability of consistent, quality outpatient therapy for this population is not always easy to secure.1,2 Combining targeted therapy with pharmacologic interventions for major depression appear to have the most effective outcomes.3
Carla’s progression also illustrates the challenges and potential pitfalls of attempting to understand and address her symptoms according to a single nosology. Depression is a like a fever. It can be caused by a myriad of factors and, left to linger, may lead to further residual complications. Focusing attention to her symptoms also may lead to a differential including adjustment problems, social anxiety, effects of trauma, surreptitious substance use, or even bipolar depression.
To begin with, a clear delineation of Carla’s historic symptoms and any possible medical contributions to her presentation are necessary to investigate. Specific inquiries into past episodes of activation including hyperarousal, impulsivity, restlessness, and insomnia should be elucidated prior to consideration of medication selection.4 Considering Carla’s age and the known association between antidepressant-induced manic conversion among children aged 10-14 years,5 any pharmacologic intervention will benefit from the maxim “start low and go slow.” Her symptoms of activation arise within the setting of titration of an antidepressant. This may raise considerations to her specific metabolism and physiological concentrations of the medication as well as cumulative day exposure.
Complementary to Carla’s own history is that of family members. Often obtaining a reliable family psychiatric history is an exercise fraught with bias, vagueness, and generalizations.6 However, given the known heritability of bipolar disorders and the implications for treating depression in such individuals, compared with unipolar depressive symptoms, clarifying the nature of family illness may elucidate potential susceptibilities previously unconsidered.7 In this case, descriptions of Carla’s father’s behavior raise concerns for underlying bipolar disorder, as do the accounts of traumatic stress exposure and their compounded preponderance for increased suicide risk.8
Unfortunately, Carla’s current environmental cues and maladaptive behaviors may be perpetuating her symptoms and possibly placing her on a trajectory for further illness. Exploration of her relationship with her caregivers regarding the interpretation of her symptoms, and need for treatment should be undertaken so as to expand supportive roles. Education regarding cannabis use among adolescents and age-specific risks for later depression, anxiety, and suicide is warranted in a climate when accessibility is on the rise.9 Whether or not cannabis use itself leads to amotivation is the subject of current debate.10 A growing body of evidence is clearly illustrating that Carla’s sedentary behaviors and perceived loneliness likely exacerbate her mental well-being. Such patterns indicate the need for environmental intervention to change such cycles.
Finally, Carla’s progression through treatment speak to the need for open and honest discussions regarding realistic benefits as well potential risks. Progressive symptoms of depression left untreated can be life-threatening themselves, just as effects of activation as described in the vignette above can easily and quickly progress into situations that pose safety concerns. Amidst such periods of intervention, close communication and follow up with patients and their supports ameliorate potential adverse events and lead to better outcomes.
Outcome
Carla’s mother was advised to discontinue the medication, closely monitor Carla’s behavior and sleep, and schedule an emergent follow-up appointment for the next day. A safety plan indicating circumstances in which Carla would require closer medical supervision for safety was reviewed with her mother. Carla was later initiated on lamotrigine and restarted interpersonal therapy.
References
1. N Engl J Med. 2015 May 21;372(21):2029-38.
2. J Pediatr. 2010 Nov;157(5):848-51.
3. Arch Gen Psychiatry. 2007 Oct;64(10):1132-43.
4. Curr Probl Pediatr Adolesc Health Care. 2018 Feb;48(2):50-62.
5. Arch Pediatr Adolesc Med. 2004 Aug;158(8):773-80.
6. Can J Psychiatry. 1993 Nov;38(9):590-4.
7. Appl Clin Genet. 2014 Feb 12;7:33-42.
8. J Am Acad Child Adolesc Psychiatry. 2017 Dec;56(12):1073-1080.
9. JAMA Psychiatry. 2019;76(4):426-34.
10. Subst Use Misuse. 2018 Jun 7;53(7):1158-69.
Little association found between in utero H1N1 vaccine and 5-year health outcomes
according to Laura K. Walsh of the University of Ottawa and associates.
The investigators conducted a population-based retrospective cohort study from November 2009 to October 2010 of all live births within the province of Ontario. Of the 104,249 eligible live births reported to the Ontario birth registry, 31,295 were exposed to the H1N1 vaccine in utero. After adjustment, there were no significant differences in the women who did and did not receive vaccines during pregnancy, according to the study, published in the BMJ.
After a median follow-up of 5 years, 14% of children received an asthma diagnosis, with a median age at diagnosis of 1.8 years. Children were more likely to receive an asthma diagnosis if their mothers had a preexisting condition or if they were born preterm. At follow-up, 34% of children had at least one upper respiratory tract infection. Sensory disorder, neoplasm, and pediatric complex chronic condition were rare, each occurring in less than 1% of the study cohort (BMJ. 2019 Jul 10. doi: 10.1136/bmj.l4151).
No significant association was found between prenatal exposure to the H1N1 vaccine and upper or lower respiratory infections, otitis media, all infections, neoplasms, sensory disorders, rates of urgent and inpatient health services use, pediatric complex chronic conditions, or mortality. A weak but significant association was observed for asthma (adjusted hazard ratio, 1.05; 95% confidence interval, 1.02-1.09), and a weak inverse association was found for gastrointestinal infections (adjusted incidence rate ratio, 0.94; 95% CI, 0.91-0.98).
“Although we observed a small, but statistically significant, increase in pediatric asthma and a reduction in gastrointestinal infections, we are not aware of any biologic mechanisms to explain these findings. Future studies in different settings and with different influenza vaccine formulations will be important for developing the evidence base on longer-term pediatric outcomes following influenza vaccination during pregnancy,” the investigators concluded.
The study was funded by grants from the Canadian Institutes of Health Research and the Institute for Clinical Evaluative Sciences.
according to Laura K. Walsh of the University of Ottawa and associates.
The investigators conducted a population-based retrospective cohort study from November 2009 to October 2010 of all live births within the province of Ontario. Of the 104,249 eligible live births reported to the Ontario birth registry, 31,295 were exposed to the H1N1 vaccine in utero. After adjustment, there were no significant differences in the women who did and did not receive vaccines during pregnancy, according to the study, published in the BMJ.
After a median follow-up of 5 years, 14% of children received an asthma diagnosis, with a median age at diagnosis of 1.8 years. Children were more likely to receive an asthma diagnosis if their mothers had a preexisting condition or if they were born preterm. At follow-up, 34% of children had at least one upper respiratory tract infection. Sensory disorder, neoplasm, and pediatric complex chronic condition were rare, each occurring in less than 1% of the study cohort (BMJ. 2019 Jul 10. doi: 10.1136/bmj.l4151).
No significant association was found between prenatal exposure to the H1N1 vaccine and upper or lower respiratory infections, otitis media, all infections, neoplasms, sensory disorders, rates of urgent and inpatient health services use, pediatric complex chronic conditions, or mortality. A weak but significant association was observed for asthma (adjusted hazard ratio, 1.05; 95% confidence interval, 1.02-1.09), and a weak inverse association was found for gastrointestinal infections (adjusted incidence rate ratio, 0.94; 95% CI, 0.91-0.98).
“Although we observed a small, but statistically significant, increase in pediatric asthma and a reduction in gastrointestinal infections, we are not aware of any biologic mechanisms to explain these findings. Future studies in different settings and with different influenza vaccine formulations will be important for developing the evidence base on longer-term pediatric outcomes following influenza vaccination during pregnancy,” the investigators concluded.
The study was funded by grants from the Canadian Institutes of Health Research and the Institute for Clinical Evaluative Sciences.
according to Laura K. Walsh of the University of Ottawa and associates.
The investigators conducted a population-based retrospective cohort study from November 2009 to October 2010 of all live births within the province of Ontario. Of the 104,249 eligible live births reported to the Ontario birth registry, 31,295 were exposed to the H1N1 vaccine in utero. After adjustment, there were no significant differences in the women who did and did not receive vaccines during pregnancy, according to the study, published in the BMJ.
After a median follow-up of 5 years, 14% of children received an asthma diagnosis, with a median age at diagnosis of 1.8 years. Children were more likely to receive an asthma diagnosis if their mothers had a preexisting condition or if they were born preterm. At follow-up, 34% of children had at least one upper respiratory tract infection. Sensory disorder, neoplasm, and pediatric complex chronic condition were rare, each occurring in less than 1% of the study cohort (BMJ. 2019 Jul 10. doi: 10.1136/bmj.l4151).
No significant association was found between prenatal exposure to the H1N1 vaccine and upper or lower respiratory infections, otitis media, all infections, neoplasms, sensory disorders, rates of urgent and inpatient health services use, pediatric complex chronic conditions, or mortality. A weak but significant association was observed for asthma (adjusted hazard ratio, 1.05; 95% confidence interval, 1.02-1.09), and a weak inverse association was found for gastrointestinal infections (adjusted incidence rate ratio, 0.94; 95% CI, 0.91-0.98).
“Although we observed a small, but statistically significant, increase in pediatric asthma and a reduction in gastrointestinal infections, we are not aware of any biologic mechanisms to explain these findings. Future studies in different settings and with different influenza vaccine formulations will be important for developing the evidence base on longer-term pediatric outcomes following influenza vaccination during pregnancy,” the investigators concluded.
The study was funded by grants from the Canadian Institutes of Health Research and the Institute for Clinical Evaluative Sciences.
FROM THE BMJ
Most authors of endoscopy practice guidelines have undisclosed financial conflicts
SAN DIEGO – Authors of endoscopy clinical practice guidelines (CPGs) received many more payments from industry than they disclosed, according to a new review of publicly available data.
Additionally, many of the payments came from pharmaceutical companies or medical device manufacturers whose products were directly related to the practice guideline topic at hand, said Amir Rumann, MD, and coauthors, who presented their findings in a poster session at the annual Digestive Disease Week®.
The researchers found that, of 581 authors listed in 38 CPGs, 127 had initially disclosed payments when the guidelines were published. A search of the federal Open Payments database, however, found that 452 of these authors had payments that they did not disclose in the CPG publication process.
For authors with undisclosed payments, the median value of the total undisclosed amounts was $2,445, from a median of 2.5 unique companies, according to records maintained by the Centers for Medicare & Medicaid Services. The interquartile range for payments was $167-$10,380.
“There is a high burden of undisclosed payments by pharmaceutical and medical device manufacturers to authors of endoscopy guidelines in the United States,” wrote Dr. Rumman and coauthors at the University of Toronto, where Dr. Rumann is a gastroenterology resident.
Of the authors who disclosed payments, 20 (16%) disclosed payments from sources directly related to the CPG in the publication. But the Open Payments database search yielded 314 (54%) disclosed payments that were judged directly related to the CPG topic at hand.
Of the 38 CPGs included in the analysis, 24 were from the American Society for Gastrointestinal Endoscopy (ASGE), and 4 were from the American Gastroenterological Association (AGA). According to the analysis performed by Dr. Rumman and his coauthors, 23 of these guidelines adhered to standards proposed by the National Academy of Medicine for development of “trustworthy” CPGs.
“The prevalence of conflicts of interest in the form of industry payments among physicians is well described in academic literature. A number of studies, including several from our group, have found there is a high burden of these payments among authors and chairs of CPGs in various therapeutic areas,” commented senior author Samir Grover, MD, a gastroenterologist at the University of Toronto. “Additionally, the existing literature has shown that many of these payments go undisclosed in the CPG themselves. This is concerning. Although the presence of these payments doesn’t necessarily indicate any obvious wrongdoing on the part of the recipients, it can undermine public and professional trust in guidelines.”
In its 2011 report, the National Academy of Medicine outlined three criteria for trustworthy guidelines. These include ensuring that committee chairs do not have financial conflicts of interest (COIs), limiting authors who do have financial COIs to less than half of the guideline drafting panel, and disclosing financially motivated relationships between individual health care providers and members of industry. “To our surprise, our findings demonstrated that none of the CPGs we identified met all of these criteria,” noted Dr. Grover, adding that “this finding highlights the importance of accountability at both the contributor level (to ensure conflicts are appropriately declared) and at the level of the sponsoring society (to ensure that guideline committee members and chairs are selected a priori for reasons that include impact of conflicts).”
Dr. Rumann and his colleagues conducted a cross-sectional study, including all endoscopy-related CPGs from AGA and ASGE published from 2014 through 2017. They performed a manual reconciliation between financial COIs disclosed in CPG documents and those reported in the Open Payments database maintained by CMS, which includes data from August 2013 to December 2017. “We decided to focus on CPGs of relevance to endoscopy, as the majority of the work to date has revolved around pharma and not devices, a potentially significant other source for industry payments to physicians,” explained Dr. Grover.
In the Open Payments database, payment types are recorded as general payments, research payments, or ownerships or investments. For each payment transaction, the type, amount, and date of payment are recorded, as is the payer.
In all, 91 individuals appeared as authors 581 times. The median number of CPGs per author was 2 with a range of 1-26.
About 80% of authors had payments reported in the Open Payments database. Though Dr. Grover acknowledged that reporting errors may exist in the Open Payments database, this fact, he said, “highlights the need for greater involvement of physicians in correct declaration of their payments.”
Among the guideline authors, 119 (20.5%) had originally disclosed general payments. However, more than three times that many authors had undisclosed records of general payments that showed up in the Open Payments database query. In all, 399 authors (68.6%) had received general payments, according to the database.
Though all 12 of the ownership or investment payments seen on Open Payments were disclosed, just 40 of 74 research payments were disclosed, said Dr. Rumann and coauthors.
“Given the potential impact of these undisclosed payments on CPGs, stricter policies on conflict of interest disclosures are needed,” they wrote.
When asked whether he would expect change to come from the findings, Dr. Grover replied, “First and foremost, we want to increase the awareness of the issue, among both the health professions and the public. While we believe that more research into COI in general is required, our study, along with similar papers in the field, show that CPGs authors need to be more cognizant of declaration of potential conflicts. In addition to being hopeful that readers of the article will be prompted to exert more diligence in tracking and declaring any payments they have received, we are hopeful that sponsoring societies self-regulate the membership of CPG committees and the choice of chairs in accordance with established criteria to mitigate conflicts.”
Dr. Rumann and other coauthors reported no conflicts of interest. Senior author Samir Grover, MD, reported financial relationships with several pharmaceutical companies.
SOURCE: Rumann A et al. DDW 2019, poster Sa1004.
SAN DIEGO – Authors of endoscopy clinical practice guidelines (CPGs) received many more payments from industry than they disclosed, according to a new review of publicly available data.
Additionally, many of the payments came from pharmaceutical companies or medical device manufacturers whose products were directly related to the practice guideline topic at hand, said Amir Rumann, MD, and coauthors, who presented their findings in a poster session at the annual Digestive Disease Week®.
The researchers found that, of 581 authors listed in 38 CPGs, 127 had initially disclosed payments when the guidelines were published. A search of the federal Open Payments database, however, found that 452 of these authors had payments that they did not disclose in the CPG publication process.
For authors with undisclosed payments, the median value of the total undisclosed amounts was $2,445, from a median of 2.5 unique companies, according to records maintained by the Centers for Medicare & Medicaid Services. The interquartile range for payments was $167-$10,380.
“There is a high burden of undisclosed payments by pharmaceutical and medical device manufacturers to authors of endoscopy guidelines in the United States,” wrote Dr. Rumman and coauthors at the University of Toronto, where Dr. Rumann is a gastroenterology resident.
Of the authors who disclosed payments, 20 (16%) disclosed payments from sources directly related to the CPG in the publication. But the Open Payments database search yielded 314 (54%) disclosed payments that were judged directly related to the CPG topic at hand.
Of the 38 CPGs included in the analysis, 24 were from the American Society for Gastrointestinal Endoscopy (ASGE), and 4 were from the American Gastroenterological Association (AGA). According to the analysis performed by Dr. Rumman and his coauthors, 23 of these guidelines adhered to standards proposed by the National Academy of Medicine for development of “trustworthy” CPGs.
“The prevalence of conflicts of interest in the form of industry payments among physicians is well described in academic literature. A number of studies, including several from our group, have found there is a high burden of these payments among authors and chairs of CPGs in various therapeutic areas,” commented senior author Samir Grover, MD, a gastroenterologist at the University of Toronto. “Additionally, the existing literature has shown that many of these payments go undisclosed in the CPG themselves. This is concerning. Although the presence of these payments doesn’t necessarily indicate any obvious wrongdoing on the part of the recipients, it can undermine public and professional trust in guidelines.”
In its 2011 report, the National Academy of Medicine outlined three criteria for trustworthy guidelines. These include ensuring that committee chairs do not have financial conflicts of interest (COIs), limiting authors who do have financial COIs to less than half of the guideline drafting panel, and disclosing financially motivated relationships between individual health care providers and members of industry. “To our surprise, our findings demonstrated that none of the CPGs we identified met all of these criteria,” noted Dr. Grover, adding that “this finding highlights the importance of accountability at both the contributor level (to ensure conflicts are appropriately declared) and at the level of the sponsoring society (to ensure that guideline committee members and chairs are selected a priori for reasons that include impact of conflicts).”
Dr. Rumann and his colleagues conducted a cross-sectional study, including all endoscopy-related CPGs from AGA and ASGE published from 2014 through 2017. They performed a manual reconciliation between financial COIs disclosed in CPG documents and those reported in the Open Payments database maintained by CMS, which includes data from August 2013 to December 2017. “We decided to focus on CPGs of relevance to endoscopy, as the majority of the work to date has revolved around pharma and not devices, a potentially significant other source for industry payments to physicians,” explained Dr. Grover.
In the Open Payments database, payment types are recorded as general payments, research payments, or ownerships or investments. For each payment transaction, the type, amount, and date of payment are recorded, as is the payer.
In all, 91 individuals appeared as authors 581 times. The median number of CPGs per author was 2 with a range of 1-26.
About 80% of authors had payments reported in the Open Payments database. Though Dr. Grover acknowledged that reporting errors may exist in the Open Payments database, this fact, he said, “highlights the need for greater involvement of physicians in correct declaration of their payments.”
Among the guideline authors, 119 (20.5%) had originally disclosed general payments. However, more than three times that many authors had undisclosed records of general payments that showed up in the Open Payments database query. In all, 399 authors (68.6%) had received general payments, according to the database.
Though all 12 of the ownership or investment payments seen on Open Payments were disclosed, just 40 of 74 research payments were disclosed, said Dr. Rumann and coauthors.
“Given the potential impact of these undisclosed payments on CPGs, stricter policies on conflict of interest disclosures are needed,” they wrote.
When asked whether he would expect change to come from the findings, Dr. Grover replied, “First and foremost, we want to increase the awareness of the issue, among both the health professions and the public. While we believe that more research into COI in general is required, our study, along with similar papers in the field, show that CPGs authors need to be more cognizant of declaration of potential conflicts. In addition to being hopeful that readers of the article will be prompted to exert more diligence in tracking and declaring any payments they have received, we are hopeful that sponsoring societies self-regulate the membership of CPG committees and the choice of chairs in accordance with established criteria to mitigate conflicts.”
Dr. Rumann and other coauthors reported no conflicts of interest. Senior author Samir Grover, MD, reported financial relationships with several pharmaceutical companies.
SOURCE: Rumann A et al. DDW 2019, poster Sa1004.
SAN DIEGO – Authors of endoscopy clinical practice guidelines (CPGs) received many more payments from industry than they disclosed, according to a new review of publicly available data.
Additionally, many of the payments came from pharmaceutical companies or medical device manufacturers whose products were directly related to the practice guideline topic at hand, said Amir Rumann, MD, and coauthors, who presented their findings in a poster session at the annual Digestive Disease Week®.
The researchers found that, of 581 authors listed in 38 CPGs, 127 had initially disclosed payments when the guidelines were published. A search of the federal Open Payments database, however, found that 452 of these authors had payments that they did not disclose in the CPG publication process.
For authors with undisclosed payments, the median value of the total undisclosed amounts was $2,445, from a median of 2.5 unique companies, according to records maintained by the Centers for Medicare & Medicaid Services. The interquartile range for payments was $167-$10,380.
“There is a high burden of undisclosed payments by pharmaceutical and medical device manufacturers to authors of endoscopy guidelines in the United States,” wrote Dr. Rumman and coauthors at the University of Toronto, where Dr. Rumann is a gastroenterology resident.
Of the authors who disclosed payments, 20 (16%) disclosed payments from sources directly related to the CPG in the publication. But the Open Payments database search yielded 314 (54%) disclosed payments that were judged directly related to the CPG topic at hand.
Of the 38 CPGs included in the analysis, 24 were from the American Society for Gastrointestinal Endoscopy (ASGE), and 4 were from the American Gastroenterological Association (AGA). According to the analysis performed by Dr. Rumman and his coauthors, 23 of these guidelines adhered to standards proposed by the National Academy of Medicine for development of “trustworthy” CPGs.
“The prevalence of conflicts of interest in the form of industry payments among physicians is well described in academic literature. A number of studies, including several from our group, have found there is a high burden of these payments among authors and chairs of CPGs in various therapeutic areas,” commented senior author Samir Grover, MD, a gastroenterologist at the University of Toronto. “Additionally, the existing literature has shown that many of these payments go undisclosed in the CPG themselves. This is concerning. Although the presence of these payments doesn’t necessarily indicate any obvious wrongdoing on the part of the recipients, it can undermine public and professional trust in guidelines.”
In its 2011 report, the National Academy of Medicine outlined three criteria for trustworthy guidelines. These include ensuring that committee chairs do not have financial conflicts of interest (COIs), limiting authors who do have financial COIs to less than half of the guideline drafting panel, and disclosing financially motivated relationships between individual health care providers and members of industry. “To our surprise, our findings demonstrated that none of the CPGs we identified met all of these criteria,” noted Dr. Grover, adding that “this finding highlights the importance of accountability at both the contributor level (to ensure conflicts are appropriately declared) and at the level of the sponsoring society (to ensure that guideline committee members and chairs are selected a priori for reasons that include impact of conflicts).”
Dr. Rumann and his colleagues conducted a cross-sectional study, including all endoscopy-related CPGs from AGA and ASGE published from 2014 through 2017. They performed a manual reconciliation between financial COIs disclosed in CPG documents and those reported in the Open Payments database maintained by CMS, which includes data from August 2013 to December 2017. “We decided to focus on CPGs of relevance to endoscopy, as the majority of the work to date has revolved around pharma and not devices, a potentially significant other source for industry payments to physicians,” explained Dr. Grover.
In the Open Payments database, payment types are recorded as general payments, research payments, or ownerships or investments. For each payment transaction, the type, amount, and date of payment are recorded, as is the payer.
In all, 91 individuals appeared as authors 581 times. The median number of CPGs per author was 2 with a range of 1-26.
About 80% of authors had payments reported in the Open Payments database. Though Dr. Grover acknowledged that reporting errors may exist in the Open Payments database, this fact, he said, “highlights the need for greater involvement of physicians in correct declaration of their payments.”
Among the guideline authors, 119 (20.5%) had originally disclosed general payments. However, more than three times that many authors had undisclosed records of general payments that showed up in the Open Payments database query. In all, 399 authors (68.6%) had received general payments, according to the database.
Though all 12 of the ownership or investment payments seen on Open Payments were disclosed, just 40 of 74 research payments were disclosed, said Dr. Rumann and coauthors.
“Given the potential impact of these undisclosed payments on CPGs, stricter policies on conflict of interest disclosures are needed,” they wrote.
When asked whether he would expect change to come from the findings, Dr. Grover replied, “First and foremost, we want to increase the awareness of the issue, among both the health professions and the public. While we believe that more research into COI in general is required, our study, along with similar papers in the field, show that CPGs authors need to be more cognizant of declaration of potential conflicts. In addition to being hopeful that readers of the article will be prompted to exert more diligence in tracking and declaring any payments they have received, we are hopeful that sponsoring societies self-regulate the membership of CPG committees and the choice of chairs in accordance with established criteria to mitigate conflicts.”
Dr. Rumann and other coauthors reported no conflicts of interest. Senior author Samir Grover, MD, reported financial relationships with several pharmaceutical companies.
SOURCE: Rumann A et al. DDW 2019, poster Sa1004.
REPORTING FROM DDW 2019
Universal adolescent education on healthy relationships needed
Sexually active adolescent girls face reproductive coercion (RC) and adolescent relationship abuse (ARA), but there seems to be no statistically significant demographic factors, so education should be universally provided, wrote Amber L. Hill, MSPH, and colleagues in Obstetrics & Gynecology.
Ms. Hill of the University of Pittsburgh and colleagues conducted a secondary analysis of data from a cross-sectional baseline survey that had been used in a cluster-randomized trial. The SHARP (School Health Center Healthy Adolescent Relationship Program) trial, investigated an educational intervention regarding healthy relationships. Their analysis included survey data for 550 sexually active girls aged 14-19 years who’d received services from any of eight student health centers across Northern California during the 2012-2013 school year.
The investigators explained that ARA includes physical, sexual, and emotional abuse among adolescents in a romantic relationship; they further described RC as a form of ARA that increases risks of unintended pregnancy, such as contraceptive sabotage, condom manipulation, and pregnancy coercion. RC was defined as a positive response on a 10-item validated measure, and ARA was defined by positive response to at least one of three items that had been derived from Conflict Tactics Scale 2 and the Sexual Experiences Survey.
Among all females in the analysis, 12% reported reproductive coercion, and 17% reported relationship abuse . Black and Hispanic girls were the most likely to report RC, each at 15%; white girls were the most likely to report ARA at 22%. However, none of the demographic differences evaluated in this analysis, including these, were statistically significant, the authors cautioned.
One of the limitations of this study is that its sample was limited to school health centers in Northern California so it may not be generalizable. Furthermore, its cross-sectional design limits causal inference.
“By highlighting the relevance of reproductive coercion in adolescence, this study substantiates the urgent need for developmentally appropriate interventions,” Ms. Hill and associates concluded.
The authors did not report any potential conflicts of interest. Grants from the National Institute of Justice, Office of Justice Programs, U.S. Department of Justice and the National Center for Advancing Translational Sciences of the National Institutes of Health supported the study.
SOURCE: Hill AL et al. Obstet Gynecol. 2019;134(2):351-9.
Sexually active adolescent girls face reproductive coercion (RC) and adolescent relationship abuse (ARA), but there seems to be no statistically significant demographic factors, so education should be universally provided, wrote Amber L. Hill, MSPH, and colleagues in Obstetrics & Gynecology.
Ms. Hill of the University of Pittsburgh and colleagues conducted a secondary analysis of data from a cross-sectional baseline survey that had been used in a cluster-randomized trial. The SHARP (School Health Center Healthy Adolescent Relationship Program) trial, investigated an educational intervention regarding healthy relationships. Their analysis included survey data for 550 sexually active girls aged 14-19 years who’d received services from any of eight student health centers across Northern California during the 2012-2013 school year.
The investigators explained that ARA includes physical, sexual, and emotional abuse among adolescents in a romantic relationship; they further described RC as a form of ARA that increases risks of unintended pregnancy, such as contraceptive sabotage, condom manipulation, and pregnancy coercion. RC was defined as a positive response on a 10-item validated measure, and ARA was defined by positive response to at least one of three items that had been derived from Conflict Tactics Scale 2 and the Sexual Experiences Survey.
Among all females in the analysis, 12% reported reproductive coercion, and 17% reported relationship abuse . Black and Hispanic girls were the most likely to report RC, each at 15%; white girls were the most likely to report ARA at 22%. However, none of the demographic differences evaluated in this analysis, including these, were statistically significant, the authors cautioned.
One of the limitations of this study is that its sample was limited to school health centers in Northern California so it may not be generalizable. Furthermore, its cross-sectional design limits causal inference.
“By highlighting the relevance of reproductive coercion in adolescence, this study substantiates the urgent need for developmentally appropriate interventions,” Ms. Hill and associates concluded.
The authors did not report any potential conflicts of interest. Grants from the National Institute of Justice, Office of Justice Programs, U.S. Department of Justice and the National Center for Advancing Translational Sciences of the National Institutes of Health supported the study.
SOURCE: Hill AL et al. Obstet Gynecol. 2019;134(2):351-9.
Sexually active adolescent girls face reproductive coercion (RC) and adolescent relationship abuse (ARA), but there seems to be no statistically significant demographic factors, so education should be universally provided, wrote Amber L. Hill, MSPH, and colleagues in Obstetrics & Gynecology.
Ms. Hill of the University of Pittsburgh and colleagues conducted a secondary analysis of data from a cross-sectional baseline survey that had been used in a cluster-randomized trial. The SHARP (School Health Center Healthy Adolescent Relationship Program) trial, investigated an educational intervention regarding healthy relationships. Their analysis included survey data for 550 sexually active girls aged 14-19 years who’d received services from any of eight student health centers across Northern California during the 2012-2013 school year.
The investigators explained that ARA includes physical, sexual, and emotional abuse among adolescents in a romantic relationship; they further described RC as a form of ARA that increases risks of unintended pregnancy, such as contraceptive sabotage, condom manipulation, and pregnancy coercion. RC was defined as a positive response on a 10-item validated measure, and ARA was defined by positive response to at least one of three items that had been derived from Conflict Tactics Scale 2 and the Sexual Experiences Survey.
Among all females in the analysis, 12% reported reproductive coercion, and 17% reported relationship abuse . Black and Hispanic girls were the most likely to report RC, each at 15%; white girls were the most likely to report ARA at 22%. However, none of the demographic differences evaluated in this analysis, including these, were statistically significant, the authors cautioned.
One of the limitations of this study is that its sample was limited to school health centers in Northern California so it may not be generalizable. Furthermore, its cross-sectional design limits causal inference.
“By highlighting the relevance of reproductive coercion in adolescence, this study substantiates the urgent need for developmentally appropriate interventions,” Ms. Hill and associates concluded.
The authors did not report any potential conflicts of interest. Grants from the National Institute of Justice, Office of Justice Programs, U.S. Department of Justice and the National Center for Advancing Translational Sciences of the National Institutes of Health supported the study.
SOURCE: Hill AL et al. Obstet Gynecol. 2019;134(2):351-9.
FROM OBSTETRICS & GYNECOLOGY
Discovery of peer review and patient safety reports
Question: A patient died unexpectedly during hospitalization for a diabetic foot infection. The autopsy revealed the presence of a large saddle pulmonary embolus. The hospital’s peer review committee met to determine if care was suboptimal and whether prophylactic anticoagulation should have been used. When the attending doctor was subsequently sued for malpractice, the plaintiff’s attorney sought to subpoena all of the medical records, including the minutes of the peer review committee. Given this hypothetical scenario, which of the following can occur?
A. “Discovery” is the legal term given to the process during the pretrial phase for amassing relevant documents and other information.
B. A subpoena duces tecum, which is a court order for the production of relevant documents and one that should normally be obeyed, may be issued.
C. The hospital declines to hand over certain types of hospital records, such as peer review minutes, which in this case are statutorily protected from discovery.
D. The plaintiff attorney goes to the judge for an order to compel production and may or may not be successful.
E. All are correct.
Answer: E. Physicians and other participants regularly meet, under strict confidential conditions, to discuss adverse events that occur in their institution. Such records are protected from “discovery,” which is a pretrial procedure for collecting evidence in preparation for trial. The rationale for keeping these records beyond the reach of the discovery process is to encourage participants to engage in candid and free-rein analysis of adverse medical events so as to avoid future mishaps. If the content and nature of these discussions were freely available to parties in litigation, there would be a natural reluctance to express one’s viewpoints in a forthright manner.
Any given state’s statute on discovery requires careful reading because it could differ from another state’s directive – with important legal consequences. As an example, Hawaii’s statute1 contains several inclusions and exclusions and reads in part: “... the information and data protected shall include proceedings and records of a peer review committee, hospital quality assurance committee, or health care review organization that include recordings, transcripts, minutes, and summaries of meetings, conversations, notes, materials, or reports created for, by, or at the direction of a peer review committee, quality assurance committee, or a health care review organization when related to a medical error reporting system. ... Information and data protected from discovery shall not include incident reports, occurrence reports, statements, or similar reports that state facts concerning a specific situation and shall not include records made in the regular course of business by a hospital ... including patient medical records. Original sources of information ... shall not be construed as being immune from discovery ... merely because they were reviewed ... or were in fact submitted to, a health care review organization.”
Predictably, plaintiff attorneys in a medical malpractice lawsuit will attempt to discover information regarding adverse events, hoping to learn about potential errors and judgment lapses, and thus gain an advantage over the defendant doctor and/or hospital. Several recent court cases highlight the contentious nature regarding whether a particular hospital report is to be deemed discoverable. Organized medicine, led by the American Medical Association, has mounted a vigorous response in arguing against the release of peer review and patient safety documents.
The AMA2 recently weighed in on the case of Daley v. Teruel and Ingalls Memorial Hospital. In 2013, a renal failure patient died in an Illinois hospital from injuries that arose from prolonged hypoglycemia. She had received insulin, but when her blood glucose dropped to 16 mg/dl, the treatment team was not alerted and she was later found unresponsive with irreversible brain damage. The issue was whether incident reports from the case that were submitted to a certified PSO (patient safety organization) could be discovered. The Federal Patient Safety and Quality Improvement Act (PSQIA) had created PSOs to aggregate data from multiple sources to reduce adverse events and errors and improve medication safety.
An Illinois lower court ruled that, as part of the discovery process, the hospital had to turn over the report. However, the Illinois Appellate Court ruled in favor of the hospital, holding that the PSQIA protects the report because it is a “patient safety work product.”3 The AMA amicus brief had emphasized that Congress created a safeguarded patient safety process under the PSQIA to encourage hospitals to submit patient safety outcomes without fear of increased liability risk and that “these voluntarily created materials should be used for their intended purpose, not as a roadmap for litigation.”
New Jersey has also ruled against the discovery of a hospital’s self-critical report of a patient’s care, prepared in accordance with New Jersey’s Patient Safety Act.4 The plaintiff alleged that, when she reported to the emergency room at Chilton Medical Center complaining of persistent abdominal pain, fever, body aches, weakness, and a phlegmatic cough, she was incorrectly diagnosed as having pneumonia. In fact, she had appendicitis and a pelvic abscess. The New Jersey Supreme Court affirmed the panel’s order shielding the redacted document from discovery, but it reversed the judgment to the extent it ended the defendants’ discovery obligation with respect to this dispute, requiring instead that the lower court address, through current discovery rules, the proper balancing of interests between requesting and responding parties.
In a recent Michigan case,5 the trial court had earlier ruled that peer review documents at issue were in fact discoverable. Like similar statutes elsewhere, Michigan’s peer review privileges serve to encourage participation to improve on patient morbidity and mortality. The case centered on a court order compelling a Michigan hospital to release a physician’s credentialing file in a medical liability lawsuit on the narrow basis that the nondiscoverability privilege applied only to peer review deliberations and was inapplicable in the case. The trial judge had opined that, if all materials viewed by peer review committees were deemed undiscoverable, a hospital could never be held accountable for any negligent act within the purview of the committee. In its amicus brief in support of the hospital, the AMA argued that Michigan’s peer review privilege has historically spanned the bounds of the actual peer review process, and it countered that hospitals can be held liable – and are regularly held liable – without opening up these documents and that plaintiffs can use the same discovery mechanisms generally available to plaintiffs in other lawsuits.6 The case is currently under appeal.
In contrast, at least two state supreme courts have ruled to limit protections from discovery. The Florida Supreme Court has held that the federal law was intended to improve overall health care rather than to act as a shield to providers. In a case of alleged malpractice with severe neurological injuries, the court took a restrictive interpretation of the PSQIA as it relates to Florida’s risk-management and discovery laws, holding that patient safety work and related reports, when required by state law, do not come under the definition of patient safety work product and were therefore discoverable.7
The Pennsylvania Supreme Court has likewise ruled that documents generated by a hospital’s outside contractor are not protected from discovery under the state’s Peer Review Protection Act. It agreed with a lower-court ruling that Monongahela Valley Hospital could not claim privilege for a performance file on an emergency department physician employed by the hospital’s contractor University of Pittsburgh Medical Center Emergency Medicine.8 The case alleged that the plaintiff’s chest and back pain was misdiagnosed as reflux disease when in fact it was a myocardial infarct.
Dr. Tan is professor of medicine and former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
References
1. Hawaii Revised Statutes §624-25.5 (2012).
2. AMA fights to protect patient-safety work from legal discovery. AMA Morning Rounds. 2018 Aug 1.
3. Daley v. Teruel and Ingalls Memorial Hospital, 2018 Ill. App. LEXIS 440 (Ill. App. Ct. 2018).
4. Brugaletta v. Garcia, 190 A.3d 419 (NJ. 2018).
5. Dwyer v. Ascension Crittenton Hospital. Michigan Supreme Court SC: 158668, 919 N.W.2d 407 (Mi. 2018).
6. Appellate court case puts peer-review protections in danger. AMA Morning Rounds. 2019 Mar 29.
7. Charles v. Southern Baptist Hospital of Florida, Inc., 2017 Fla. LEXIS 231 (Fla. Jan. 31, 2017).
8. Reginelli v. Boggs, 2018 Pa. LEXIS 1503 (Pa. 2018).
Question: A patient died unexpectedly during hospitalization for a diabetic foot infection. The autopsy revealed the presence of a large saddle pulmonary embolus. The hospital’s peer review committee met to determine if care was suboptimal and whether prophylactic anticoagulation should have been used. When the attending doctor was subsequently sued for malpractice, the plaintiff’s attorney sought to subpoena all of the medical records, including the minutes of the peer review committee. Given this hypothetical scenario, which of the following can occur?
A. “Discovery” is the legal term given to the process during the pretrial phase for amassing relevant documents and other information.
B. A subpoena duces tecum, which is a court order for the production of relevant documents and one that should normally be obeyed, may be issued.
C. The hospital declines to hand over certain types of hospital records, such as peer review minutes, which in this case are statutorily protected from discovery.
D. The plaintiff attorney goes to the judge for an order to compel production and may or may not be successful.
E. All are correct.
Answer: E. Physicians and other participants regularly meet, under strict confidential conditions, to discuss adverse events that occur in their institution. Such records are protected from “discovery,” which is a pretrial procedure for collecting evidence in preparation for trial. The rationale for keeping these records beyond the reach of the discovery process is to encourage participants to engage in candid and free-rein analysis of adverse medical events so as to avoid future mishaps. If the content and nature of these discussions were freely available to parties in litigation, there would be a natural reluctance to express one’s viewpoints in a forthright manner.
Any given state’s statute on discovery requires careful reading because it could differ from another state’s directive – with important legal consequences. As an example, Hawaii’s statute1 contains several inclusions and exclusions and reads in part: “... the information and data protected shall include proceedings and records of a peer review committee, hospital quality assurance committee, or health care review organization that include recordings, transcripts, minutes, and summaries of meetings, conversations, notes, materials, or reports created for, by, or at the direction of a peer review committee, quality assurance committee, or a health care review organization when related to a medical error reporting system. ... Information and data protected from discovery shall not include incident reports, occurrence reports, statements, or similar reports that state facts concerning a specific situation and shall not include records made in the regular course of business by a hospital ... including patient medical records. Original sources of information ... shall not be construed as being immune from discovery ... merely because they were reviewed ... or were in fact submitted to, a health care review organization.”
Predictably, plaintiff attorneys in a medical malpractice lawsuit will attempt to discover information regarding adverse events, hoping to learn about potential errors and judgment lapses, and thus gain an advantage over the defendant doctor and/or hospital. Several recent court cases highlight the contentious nature regarding whether a particular hospital report is to be deemed discoverable. Organized medicine, led by the American Medical Association, has mounted a vigorous response in arguing against the release of peer review and patient safety documents.
The AMA2 recently weighed in on the case of Daley v. Teruel and Ingalls Memorial Hospital. In 2013, a renal failure patient died in an Illinois hospital from injuries that arose from prolonged hypoglycemia. She had received insulin, but when her blood glucose dropped to 16 mg/dl, the treatment team was not alerted and she was later found unresponsive with irreversible brain damage. The issue was whether incident reports from the case that were submitted to a certified PSO (patient safety organization) could be discovered. The Federal Patient Safety and Quality Improvement Act (PSQIA) had created PSOs to aggregate data from multiple sources to reduce adverse events and errors and improve medication safety.
An Illinois lower court ruled that, as part of the discovery process, the hospital had to turn over the report. However, the Illinois Appellate Court ruled in favor of the hospital, holding that the PSQIA protects the report because it is a “patient safety work product.”3 The AMA amicus brief had emphasized that Congress created a safeguarded patient safety process under the PSQIA to encourage hospitals to submit patient safety outcomes without fear of increased liability risk and that “these voluntarily created materials should be used for their intended purpose, not as a roadmap for litigation.”
New Jersey has also ruled against the discovery of a hospital’s self-critical report of a patient’s care, prepared in accordance with New Jersey’s Patient Safety Act.4 The plaintiff alleged that, when she reported to the emergency room at Chilton Medical Center complaining of persistent abdominal pain, fever, body aches, weakness, and a phlegmatic cough, she was incorrectly diagnosed as having pneumonia. In fact, she had appendicitis and a pelvic abscess. The New Jersey Supreme Court affirmed the panel’s order shielding the redacted document from discovery, but it reversed the judgment to the extent it ended the defendants’ discovery obligation with respect to this dispute, requiring instead that the lower court address, through current discovery rules, the proper balancing of interests between requesting and responding parties.
In a recent Michigan case,5 the trial court had earlier ruled that peer review documents at issue were in fact discoverable. Like similar statutes elsewhere, Michigan’s peer review privileges serve to encourage participation to improve on patient morbidity and mortality. The case centered on a court order compelling a Michigan hospital to release a physician’s credentialing file in a medical liability lawsuit on the narrow basis that the nondiscoverability privilege applied only to peer review deliberations and was inapplicable in the case. The trial judge had opined that, if all materials viewed by peer review committees were deemed undiscoverable, a hospital could never be held accountable for any negligent act within the purview of the committee. In its amicus brief in support of the hospital, the AMA argued that Michigan’s peer review privilege has historically spanned the bounds of the actual peer review process, and it countered that hospitals can be held liable – and are regularly held liable – without opening up these documents and that plaintiffs can use the same discovery mechanisms generally available to plaintiffs in other lawsuits.6 The case is currently under appeal.
In contrast, at least two state supreme courts have ruled to limit protections from discovery. The Florida Supreme Court has held that the federal law was intended to improve overall health care rather than to act as a shield to providers. In a case of alleged malpractice with severe neurological injuries, the court took a restrictive interpretation of the PSQIA as it relates to Florida’s risk-management and discovery laws, holding that patient safety work and related reports, when required by state law, do not come under the definition of patient safety work product and were therefore discoverable.7
The Pennsylvania Supreme Court has likewise ruled that documents generated by a hospital’s outside contractor are not protected from discovery under the state’s Peer Review Protection Act. It agreed with a lower-court ruling that Monongahela Valley Hospital could not claim privilege for a performance file on an emergency department physician employed by the hospital’s contractor University of Pittsburgh Medical Center Emergency Medicine.8 The case alleged that the plaintiff’s chest and back pain was misdiagnosed as reflux disease when in fact it was a myocardial infarct.
Dr. Tan is professor of medicine and former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
References
1. Hawaii Revised Statutes §624-25.5 (2012).
2. AMA fights to protect patient-safety work from legal discovery. AMA Morning Rounds. 2018 Aug 1.
3. Daley v. Teruel and Ingalls Memorial Hospital, 2018 Ill. App. LEXIS 440 (Ill. App. Ct. 2018).
4. Brugaletta v. Garcia, 190 A.3d 419 (NJ. 2018).
5. Dwyer v. Ascension Crittenton Hospital. Michigan Supreme Court SC: 158668, 919 N.W.2d 407 (Mi. 2018).
6. Appellate court case puts peer-review protections in danger. AMA Morning Rounds. 2019 Mar 29.
7. Charles v. Southern Baptist Hospital of Florida, Inc., 2017 Fla. LEXIS 231 (Fla. Jan. 31, 2017).
8. Reginelli v. Boggs, 2018 Pa. LEXIS 1503 (Pa. 2018).
Question: A patient died unexpectedly during hospitalization for a diabetic foot infection. The autopsy revealed the presence of a large saddle pulmonary embolus. The hospital’s peer review committee met to determine if care was suboptimal and whether prophylactic anticoagulation should have been used. When the attending doctor was subsequently sued for malpractice, the plaintiff’s attorney sought to subpoena all of the medical records, including the minutes of the peer review committee. Given this hypothetical scenario, which of the following can occur?
A. “Discovery” is the legal term given to the process during the pretrial phase for amassing relevant documents and other information.
B. A subpoena duces tecum, which is a court order for the production of relevant documents and one that should normally be obeyed, may be issued.
C. The hospital declines to hand over certain types of hospital records, such as peer review minutes, which in this case are statutorily protected from discovery.
D. The plaintiff attorney goes to the judge for an order to compel production and may or may not be successful.
E. All are correct.
Answer: E. Physicians and other participants regularly meet, under strict confidential conditions, to discuss adverse events that occur in their institution. Such records are protected from “discovery,” which is a pretrial procedure for collecting evidence in preparation for trial. The rationale for keeping these records beyond the reach of the discovery process is to encourage participants to engage in candid and free-rein analysis of adverse medical events so as to avoid future mishaps. If the content and nature of these discussions were freely available to parties in litigation, there would be a natural reluctance to express one’s viewpoints in a forthright manner.
Any given state’s statute on discovery requires careful reading because it could differ from another state’s directive – with important legal consequences. As an example, Hawaii’s statute1 contains several inclusions and exclusions and reads in part: “... the information and data protected shall include proceedings and records of a peer review committee, hospital quality assurance committee, or health care review organization that include recordings, transcripts, minutes, and summaries of meetings, conversations, notes, materials, or reports created for, by, or at the direction of a peer review committee, quality assurance committee, or a health care review organization when related to a medical error reporting system. ... Information and data protected from discovery shall not include incident reports, occurrence reports, statements, or similar reports that state facts concerning a specific situation and shall not include records made in the regular course of business by a hospital ... including patient medical records. Original sources of information ... shall not be construed as being immune from discovery ... merely because they were reviewed ... or were in fact submitted to, a health care review organization.”
Predictably, plaintiff attorneys in a medical malpractice lawsuit will attempt to discover information regarding adverse events, hoping to learn about potential errors and judgment lapses, and thus gain an advantage over the defendant doctor and/or hospital. Several recent court cases highlight the contentious nature regarding whether a particular hospital report is to be deemed discoverable. Organized medicine, led by the American Medical Association, has mounted a vigorous response in arguing against the release of peer review and patient safety documents.
The AMA2 recently weighed in on the case of Daley v. Teruel and Ingalls Memorial Hospital. In 2013, a renal failure patient died in an Illinois hospital from injuries that arose from prolonged hypoglycemia. She had received insulin, but when her blood glucose dropped to 16 mg/dl, the treatment team was not alerted and she was later found unresponsive with irreversible brain damage. The issue was whether incident reports from the case that were submitted to a certified PSO (patient safety organization) could be discovered. The Federal Patient Safety and Quality Improvement Act (PSQIA) had created PSOs to aggregate data from multiple sources to reduce adverse events and errors and improve medication safety.
An Illinois lower court ruled that, as part of the discovery process, the hospital had to turn over the report. However, the Illinois Appellate Court ruled in favor of the hospital, holding that the PSQIA protects the report because it is a “patient safety work product.”3 The AMA amicus brief had emphasized that Congress created a safeguarded patient safety process under the PSQIA to encourage hospitals to submit patient safety outcomes without fear of increased liability risk and that “these voluntarily created materials should be used for their intended purpose, not as a roadmap for litigation.”
New Jersey has also ruled against the discovery of a hospital’s self-critical report of a patient’s care, prepared in accordance with New Jersey’s Patient Safety Act.4 The plaintiff alleged that, when she reported to the emergency room at Chilton Medical Center complaining of persistent abdominal pain, fever, body aches, weakness, and a phlegmatic cough, she was incorrectly diagnosed as having pneumonia. In fact, she had appendicitis and a pelvic abscess. The New Jersey Supreme Court affirmed the panel’s order shielding the redacted document from discovery, but it reversed the judgment to the extent it ended the defendants’ discovery obligation with respect to this dispute, requiring instead that the lower court address, through current discovery rules, the proper balancing of interests between requesting and responding parties.
In a recent Michigan case,5 the trial court had earlier ruled that peer review documents at issue were in fact discoverable. Like similar statutes elsewhere, Michigan’s peer review privileges serve to encourage participation to improve on patient morbidity and mortality. The case centered on a court order compelling a Michigan hospital to release a physician’s credentialing file in a medical liability lawsuit on the narrow basis that the nondiscoverability privilege applied only to peer review deliberations and was inapplicable in the case. The trial judge had opined that, if all materials viewed by peer review committees were deemed undiscoverable, a hospital could never be held accountable for any negligent act within the purview of the committee. In its amicus brief in support of the hospital, the AMA argued that Michigan’s peer review privilege has historically spanned the bounds of the actual peer review process, and it countered that hospitals can be held liable – and are regularly held liable – without opening up these documents and that plaintiffs can use the same discovery mechanisms generally available to plaintiffs in other lawsuits.6 The case is currently under appeal.
In contrast, at least two state supreme courts have ruled to limit protections from discovery. The Florida Supreme Court has held that the federal law was intended to improve overall health care rather than to act as a shield to providers. In a case of alleged malpractice with severe neurological injuries, the court took a restrictive interpretation of the PSQIA as it relates to Florida’s risk-management and discovery laws, holding that patient safety work and related reports, when required by state law, do not come under the definition of patient safety work product and were therefore discoverable.7
The Pennsylvania Supreme Court has likewise ruled that documents generated by a hospital’s outside contractor are not protected from discovery under the state’s Peer Review Protection Act. It agreed with a lower-court ruling that Monongahela Valley Hospital could not claim privilege for a performance file on an emergency department physician employed by the hospital’s contractor University of Pittsburgh Medical Center Emergency Medicine.8 The case alleged that the plaintiff’s chest and back pain was misdiagnosed as reflux disease when in fact it was a myocardial infarct.
Dr. Tan is professor of medicine and former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
References
1. Hawaii Revised Statutes §624-25.5 (2012).
2. AMA fights to protect patient-safety work from legal discovery. AMA Morning Rounds. 2018 Aug 1.
3. Daley v. Teruel and Ingalls Memorial Hospital, 2018 Ill. App. LEXIS 440 (Ill. App. Ct. 2018).
4. Brugaletta v. Garcia, 190 A.3d 419 (NJ. 2018).
5. Dwyer v. Ascension Crittenton Hospital. Michigan Supreme Court SC: 158668, 919 N.W.2d 407 (Mi. 2018).
6. Appellate court case puts peer-review protections in danger. AMA Morning Rounds. 2019 Mar 29.
7. Charles v. Southern Baptist Hospital of Florida, Inc., 2017 Fla. LEXIS 231 (Fla. Jan. 31, 2017).
8. Reginelli v. Boggs, 2018 Pa. LEXIS 1503 (Pa. 2018).
Gynecologic surgeries linked with persistent opioid use
– showing that persistent opioid use can follow such surgeries.
For a study published in Obstetrics & Gynecology, Jason D. Wright, MD, of Columbia University, New York, and colleagues looked at insurance claims data from 729,625 opioid-naive women, median age 44 years, who had undergone a myomectomy; a minimally invasive, vaginal, or abdominal hysterectomy; an open or laparoscopic oophorectomy; endometrial ablation; tubal ligation; or dilation and curettage. The vast majority of subjects, 93%, had commercial health insurance, with the rest enrolled in Medicaid. Women undergoing multiple surgical procedures, with serious comorbidities, or who underwent another surgery within 6 months of the initial one, were excluded from the analysis.
Dr. Wright and colleagues found that 60% of patients in the cohort received an initial opioid prescription in the perioperative period. Additional opioids were then prescribed to 6.8% (P less than .001) of those women between 90 and 180 days after surgery. The rate of additional prescriptions varied by year across the study period, from 2009 to 2016, and declined to 6% by the final year of the study. The rate of further opioid prescriptions varied according to procedure: 4.8% for myomectomy, 6.6% for minimally invasive hysterectomy, 6.7% for abdominal hysterectomy, 6.3% for endometrial ablation, 7% for tubal ligation, and 7.2% for dilation and curettage (P less than .001).
Factors significantly increasing likelihood of a new prescription included younger age and a history of depression, anxiety, or a substance abuse disorder. Also, a higher total dose of opioids initially prescribed, and a greater number of days supplied, were associated with increased risk for an additional prescription.
“These data demonstrate that the rate of new persistent opioid use after common gynecologic procedures is substantial,” Dr. Wright and colleagues wrote in their analysis, noting that prior studies across a wide range of surgeries have shown rates of new persistent opioid use to be between 3% and 8%. “Careful risk assessment of patients preoperatively may be useful to mitigate opioid misuse in high risk populations,” the investigators wrote. “Women with underlying psychosocial disorders, medical comorbidities, or a history of substance use disorder are at particular risk for persistent opioid use and should be prescribed opioids with extra caution.”
Dr. Wright and colleagues’ study “provides powerful data that should cause gynecological surgeons to pause when writing an opioid prescription,” David M. Jaspan, DO, chairman of obstetrics and gynecology at Einstein Medical Center, Philadelphia, said in an interview. “Is an opioid the best first line medication for this patient? Would an NSAID work better? Is multimodal medication an option? What are the patient characteristics that may be associated with persistent use?”
Dr. Wright and colleagues noted among the study’s limitations the fact that actual opioid use could not be measured, nor could use of nonopioid painkillers.
Dr. Wright has served as a consultant for Tesaro and Clovis Oncology. Dr. Alfred I. Neugut disclosed relationships with various pharmaceutical firms. Dr. Dawn L. Hershman received a grant from the Breast Cancer Research Foundation/Conquer Cancer Foundation. The remaining coauthors had no relevant financial disclosures.
SOURCE: Wright JD et al. Obstet Gynecol. 2019. doi: 10.1097/AOG.0000000000003358.
– showing that persistent opioid use can follow such surgeries.
For a study published in Obstetrics & Gynecology, Jason D. Wright, MD, of Columbia University, New York, and colleagues looked at insurance claims data from 729,625 opioid-naive women, median age 44 years, who had undergone a myomectomy; a minimally invasive, vaginal, or abdominal hysterectomy; an open or laparoscopic oophorectomy; endometrial ablation; tubal ligation; or dilation and curettage. The vast majority of subjects, 93%, had commercial health insurance, with the rest enrolled in Medicaid. Women undergoing multiple surgical procedures, with serious comorbidities, or who underwent another surgery within 6 months of the initial one, were excluded from the analysis.
Dr. Wright and colleagues found that 60% of patients in the cohort received an initial opioid prescription in the perioperative period. Additional opioids were then prescribed to 6.8% (P less than .001) of those women between 90 and 180 days after surgery. The rate of additional prescriptions varied by year across the study period, from 2009 to 2016, and declined to 6% by the final year of the study. The rate of further opioid prescriptions varied according to procedure: 4.8% for myomectomy, 6.6% for minimally invasive hysterectomy, 6.7% for abdominal hysterectomy, 6.3% for endometrial ablation, 7% for tubal ligation, and 7.2% for dilation and curettage (P less than .001).
Factors significantly increasing likelihood of a new prescription included younger age and a history of depression, anxiety, or a substance abuse disorder. Also, a higher total dose of opioids initially prescribed, and a greater number of days supplied, were associated with increased risk for an additional prescription.
“These data demonstrate that the rate of new persistent opioid use after common gynecologic procedures is substantial,” Dr. Wright and colleagues wrote in their analysis, noting that prior studies across a wide range of surgeries have shown rates of new persistent opioid use to be between 3% and 8%. “Careful risk assessment of patients preoperatively may be useful to mitigate opioid misuse in high risk populations,” the investigators wrote. “Women with underlying psychosocial disorders, medical comorbidities, or a history of substance use disorder are at particular risk for persistent opioid use and should be prescribed opioids with extra caution.”
Dr. Wright and colleagues’ study “provides powerful data that should cause gynecological surgeons to pause when writing an opioid prescription,” David M. Jaspan, DO, chairman of obstetrics and gynecology at Einstein Medical Center, Philadelphia, said in an interview. “Is an opioid the best first line medication for this patient? Would an NSAID work better? Is multimodal medication an option? What are the patient characteristics that may be associated with persistent use?”
Dr. Wright and colleagues noted among the study’s limitations the fact that actual opioid use could not be measured, nor could use of nonopioid painkillers.
Dr. Wright has served as a consultant for Tesaro and Clovis Oncology. Dr. Alfred I. Neugut disclosed relationships with various pharmaceutical firms. Dr. Dawn L. Hershman received a grant from the Breast Cancer Research Foundation/Conquer Cancer Foundation. The remaining coauthors had no relevant financial disclosures.
SOURCE: Wright JD et al. Obstet Gynecol. 2019. doi: 10.1097/AOG.0000000000003358.
– showing that persistent opioid use can follow such surgeries.
For a study published in Obstetrics & Gynecology, Jason D. Wright, MD, of Columbia University, New York, and colleagues looked at insurance claims data from 729,625 opioid-naive women, median age 44 years, who had undergone a myomectomy; a minimally invasive, vaginal, or abdominal hysterectomy; an open or laparoscopic oophorectomy; endometrial ablation; tubal ligation; or dilation and curettage. The vast majority of subjects, 93%, had commercial health insurance, with the rest enrolled in Medicaid. Women undergoing multiple surgical procedures, with serious comorbidities, or who underwent another surgery within 6 months of the initial one, were excluded from the analysis.
Dr. Wright and colleagues found that 60% of patients in the cohort received an initial opioid prescription in the perioperative period. Additional opioids were then prescribed to 6.8% (P less than .001) of those women between 90 and 180 days after surgery. The rate of additional prescriptions varied by year across the study period, from 2009 to 2016, and declined to 6% by the final year of the study. The rate of further opioid prescriptions varied according to procedure: 4.8% for myomectomy, 6.6% for minimally invasive hysterectomy, 6.7% for abdominal hysterectomy, 6.3% for endometrial ablation, 7% for tubal ligation, and 7.2% for dilation and curettage (P less than .001).
Factors significantly increasing likelihood of a new prescription included younger age and a history of depression, anxiety, or a substance abuse disorder. Also, a higher total dose of opioids initially prescribed, and a greater number of days supplied, were associated with increased risk for an additional prescription.
“These data demonstrate that the rate of new persistent opioid use after common gynecologic procedures is substantial,” Dr. Wright and colleagues wrote in their analysis, noting that prior studies across a wide range of surgeries have shown rates of new persistent opioid use to be between 3% and 8%. “Careful risk assessment of patients preoperatively may be useful to mitigate opioid misuse in high risk populations,” the investigators wrote. “Women with underlying psychosocial disorders, medical comorbidities, or a history of substance use disorder are at particular risk for persistent opioid use and should be prescribed opioids with extra caution.”
Dr. Wright and colleagues’ study “provides powerful data that should cause gynecological surgeons to pause when writing an opioid prescription,” David M. Jaspan, DO, chairman of obstetrics and gynecology at Einstein Medical Center, Philadelphia, said in an interview. “Is an opioid the best first line medication for this patient? Would an NSAID work better? Is multimodal medication an option? What are the patient characteristics that may be associated with persistent use?”
Dr. Wright and colleagues noted among the study’s limitations the fact that actual opioid use could not be measured, nor could use of nonopioid painkillers.
Dr. Wright has served as a consultant for Tesaro and Clovis Oncology. Dr. Alfred I. Neugut disclosed relationships with various pharmaceutical firms. Dr. Dawn L. Hershman received a grant from the Breast Cancer Research Foundation/Conquer Cancer Foundation. The remaining coauthors had no relevant financial disclosures.
SOURCE: Wright JD et al. Obstet Gynecol. 2019. doi: 10.1097/AOG.0000000000003358.
FROM OBSTETRICS & GYNECOLOGY
Acne before puberty: When to treat, when to worry
NEWPORT BEACH, CALIF. – according to Sheila Fallon Friedlander, MD.
“This is something you are going to see in your practice,” said Dr. Friedlander, a pediatric dermatologists at Rady Children’s Hospital–San Diego. It’s important to know when it’s time to be concerned and when another condition may be masquerading as acne, she said at the at Skin Disease Education Foundation’s Women’s & Pediatric Dermatology Seminar.
Dr. Friedlander, who is professor of dermatology and pediatrics at the University of California, San Diego, talked about treating acne in the following prepubertal age groups:
Neonatal acne (ages birth to 4 weeks)
Acne appears in this population up to 20% of the time, according to research, and it is much more common in males than in females, at a ratio of five to one.
The cause is “most likely the relationship between placental androgens and the baby’s adrenal glands,” Dr. Friedlander said. However, something more serious could be going on. “Look at the child and see if he’s sick. If he looks sick, then we need to worry.”
Hormonal abnormalities also could be a cause, she said. Refer a baby to a specialist if there are other signs of hyperandrogenism. However, “the likelihood is very low,” and she’s never needed to refer a neonate with acne for evaluation.
As for treatment, she said, “Mainly, I’m using tincture of time.” However, “many of my mothers have told me that topical yogurt application will work.” Why yogurt? It’s possible that its bacteria could play a role in combating acne, she said.
Masquerader alert! Beware of neonatal cephalic pustulosis, Dr. Friedlander cautioned, which may be an inflammatory response to yeast. Ketoconazole cream may be helpful.
Infantile acne (ages 0-12 months)
This form of acne is more common in males and may hint at the future development of severe adolescent acne. It does resolve but it may take months or years, Dr. Friedlander said.
In general, this acne isn’t a sign of something more serious. “You do not need to go crazy with the work-up,” she said. “With mild to moderate disease, with nothing else suspicious, I don’t do a big work-up.”
However, do consider whether the child is undergoing precocious puberty, Dr. Friedlander said. Signs include axillary hair, pubic hair, and body odor.
As for treatment of infantile acne, “start out topically” and consider options such as Bactrim (sulfamethoxazole/trimethoprim) and erythromycin.
Masquerader alert! Idiopathic facial aseptic granuloma can be mistaken for acne and abscess, and ultrasound is helpful to confirm it. “It’s not so easy to treat,” she said. “Ivermectin may be helpful. Sometimes you do cultures and make sure something else isn’t going on.”
Midchildhood (ages 1-7 years)
“It’s not as common to have acne develop in this age group, but when it develops you need to be concerned,” Dr. Friedlander said. “This is the age period when there is more often something really wrong.”
Be on the lookout for a family history of hormonal abnormalities, and check if the child is on medication. “You need to look carefully,” she said, adding that it’s important to check for signs of premature puberty such as giant spikes in growth, abnormally large hands and feet, genital changes, and body odor. Check blood pressure if you’re worried about an adrenal tumor.
It’s possible for children to develop precocious puberty – with acne – because of exposure to testosterone gel used by a father. Dehydroepiandrosterone (DHEA) creams also may cause the condition. “The more creams out there with androgenic effects, the more we may see it,” Dr. Friedlander said. “This is something to ask about because families may not be forthcoming.”
Masquerader alert! Perioral dermatitis may look like acne, and it may be linked to inhaled or topical steroids, she said.
Other masqueraders include demodex folliculitis, angiofibromas (think tuberous sclerosis), and keratosis pilaris (the most common type of bump on a children aged 1-7 years). The latter condition “is not the end of the world,” said Dr. Friedlander, who added that “I’ve never cured anyone of it.”
Prepubertal acne (ages 7 years to puberty)
Acne in this group is generally not worrisome, Dr. Friedlander said, but investigate further if there’s significant inflammation and signs of early sexual development or virilization.
Benzoyl peroxide wash may be enough to help the condition initially, and consider topical clindamycin or a combination product. “Start out slow,” she said. Twice a week to start might be appropriate. Moisturizers can be helpful, as can topical adapalene.
Also, keep in mind that even mild acne can be emotionally devastating to a child in this age group and worthy of treatment. “Your assessment may be very different than hers,” she said. It’s possible that “she has a few lesions, but she feels like an outcast.”
Dr. Friedlander reported no relevant financial disclosures. SDEF and this news organization are owned by the same parent company.
NEWPORT BEACH, CALIF. – according to Sheila Fallon Friedlander, MD.
“This is something you are going to see in your practice,” said Dr. Friedlander, a pediatric dermatologists at Rady Children’s Hospital–San Diego. It’s important to know when it’s time to be concerned and when another condition may be masquerading as acne, she said at the at Skin Disease Education Foundation’s Women’s & Pediatric Dermatology Seminar.
Dr. Friedlander, who is professor of dermatology and pediatrics at the University of California, San Diego, talked about treating acne in the following prepubertal age groups:
Neonatal acne (ages birth to 4 weeks)
Acne appears in this population up to 20% of the time, according to research, and it is much more common in males than in females, at a ratio of five to one.
The cause is “most likely the relationship between placental androgens and the baby’s adrenal glands,” Dr. Friedlander said. However, something more serious could be going on. “Look at the child and see if he’s sick. If he looks sick, then we need to worry.”
Hormonal abnormalities also could be a cause, she said. Refer a baby to a specialist if there are other signs of hyperandrogenism. However, “the likelihood is very low,” and she’s never needed to refer a neonate with acne for evaluation.
As for treatment, she said, “Mainly, I’m using tincture of time.” However, “many of my mothers have told me that topical yogurt application will work.” Why yogurt? It’s possible that its bacteria could play a role in combating acne, she said.
Masquerader alert! Beware of neonatal cephalic pustulosis, Dr. Friedlander cautioned, which may be an inflammatory response to yeast. Ketoconazole cream may be helpful.
Infantile acne (ages 0-12 months)
This form of acne is more common in males and may hint at the future development of severe adolescent acne. It does resolve but it may take months or years, Dr. Friedlander said.
In general, this acne isn’t a sign of something more serious. “You do not need to go crazy with the work-up,” she said. “With mild to moderate disease, with nothing else suspicious, I don’t do a big work-up.”
However, do consider whether the child is undergoing precocious puberty, Dr. Friedlander said. Signs include axillary hair, pubic hair, and body odor.
As for treatment of infantile acne, “start out topically” and consider options such as Bactrim (sulfamethoxazole/trimethoprim) and erythromycin.
Masquerader alert! Idiopathic facial aseptic granuloma can be mistaken for acne and abscess, and ultrasound is helpful to confirm it. “It’s not so easy to treat,” she said. “Ivermectin may be helpful. Sometimes you do cultures and make sure something else isn’t going on.”
Midchildhood (ages 1-7 years)
“It’s not as common to have acne develop in this age group, but when it develops you need to be concerned,” Dr. Friedlander said. “This is the age period when there is more often something really wrong.”
Be on the lookout for a family history of hormonal abnormalities, and check if the child is on medication. “You need to look carefully,” she said, adding that it’s important to check for signs of premature puberty such as giant spikes in growth, abnormally large hands and feet, genital changes, and body odor. Check blood pressure if you’re worried about an adrenal tumor.
It’s possible for children to develop precocious puberty – with acne – because of exposure to testosterone gel used by a father. Dehydroepiandrosterone (DHEA) creams also may cause the condition. “The more creams out there with androgenic effects, the more we may see it,” Dr. Friedlander said. “This is something to ask about because families may not be forthcoming.”
Masquerader alert! Perioral dermatitis may look like acne, and it may be linked to inhaled or topical steroids, she said.
Other masqueraders include demodex folliculitis, angiofibromas (think tuberous sclerosis), and keratosis pilaris (the most common type of bump on a children aged 1-7 years). The latter condition “is not the end of the world,” said Dr. Friedlander, who added that “I’ve never cured anyone of it.”
Prepubertal acne (ages 7 years to puberty)
Acne in this group is generally not worrisome, Dr. Friedlander said, but investigate further if there’s significant inflammation and signs of early sexual development or virilization.
Benzoyl peroxide wash may be enough to help the condition initially, and consider topical clindamycin or a combination product. “Start out slow,” she said. Twice a week to start might be appropriate. Moisturizers can be helpful, as can topical adapalene.
Also, keep in mind that even mild acne can be emotionally devastating to a child in this age group and worthy of treatment. “Your assessment may be very different than hers,” she said. It’s possible that “she has a few lesions, but she feels like an outcast.”
Dr. Friedlander reported no relevant financial disclosures. SDEF and this news organization are owned by the same parent company.
NEWPORT BEACH, CALIF. – according to Sheila Fallon Friedlander, MD.
“This is something you are going to see in your practice,” said Dr. Friedlander, a pediatric dermatologists at Rady Children’s Hospital–San Diego. It’s important to know when it’s time to be concerned and when another condition may be masquerading as acne, she said at the at Skin Disease Education Foundation’s Women’s & Pediatric Dermatology Seminar.
Dr. Friedlander, who is professor of dermatology and pediatrics at the University of California, San Diego, talked about treating acne in the following prepubertal age groups:
Neonatal acne (ages birth to 4 weeks)
Acne appears in this population up to 20% of the time, according to research, and it is much more common in males than in females, at a ratio of five to one.
The cause is “most likely the relationship between placental androgens and the baby’s adrenal glands,” Dr. Friedlander said. However, something more serious could be going on. “Look at the child and see if he’s sick. If he looks sick, then we need to worry.”
Hormonal abnormalities also could be a cause, she said. Refer a baby to a specialist if there are other signs of hyperandrogenism. However, “the likelihood is very low,” and she’s never needed to refer a neonate with acne for evaluation.
As for treatment, she said, “Mainly, I’m using tincture of time.” However, “many of my mothers have told me that topical yogurt application will work.” Why yogurt? It’s possible that its bacteria could play a role in combating acne, she said.
Masquerader alert! Beware of neonatal cephalic pustulosis, Dr. Friedlander cautioned, which may be an inflammatory response to yeast. Ketoconazole cream may be helpful.
Infantile acne (ages 0-12 months)
This form of acne is more common in males and may hint at the future development of severe adolescent acne. It does resolve but it may take months or years, Dr. Friedlander said.
In general, this acne isn’t a sign of something more serious. “You do not need to go crazy with the work-up,” she said. “With mild to moderate disease, with nothing else suspicious, I don’t do a big work-up.”
However, do consider whether the child is undergoing precocious puberty, Dr. Friedlander said. Signs include axillary hair, pubic hair, and body odor.
As for treatment of infantile acne, “start out topically” and consider options such as Bactrim (sulfamethoxazole/trimethoprim) and erythromycin.
Masquerader alert! Idiopathic facial aseptic granuloma can be mistaken for acne and abscess, and ultrasound is helpful to confirm it. “It’s not so easy to treat,” she said. “Ivermectin may be helpful. Sometimes you do cultures and make sure something else isn’t going on.”
Midchildhood (ages 1-7 years)
“It’s not as common to have acne develop in this age group, but when it develops you need to be concerned,” Dr. Friedlander said. “This is the age period when there is more often something really wrong.”
Be on the lookout for a family history of hormonal abnormalities, and check if the child is on medication. “You need to look carefully,” she said, adding that it’s important to check for signs of premature puberty such as giant spikes in growth, abnormally large hands and feet, genital changes, and body odor. Check blood pressure if you’re worried about an adrenal tumor.
It’s possible for children to develop precocious puberty – with acne – because of exposure to testosterone gel used by a father. Dehydroepiandrosterone (DHEA) creams also may cause the condition. “The more creams out there with androgenic effects, the more we may see it,” Dr. Friedlander said. “This is something to ask about because families may not be forthcoming.”
Masquerader alert! Perioral dermatitis may look like acne, and it may be linked to inhaled or topical steroids, she said.
Other masqueraders include demodex folliculitis, angiofibromas (think tuberous sclerosis), and keratosis pilaris (the most common type of bump on a children aged 1-7 years). The latter condition “is not the end of the world,” said Dr. Friedlander, who added that “I’ve never cured anyone of it.”
Prepubertal acne (ages 7 years to puberty)
Acne in this group is generally not worrisome, Dr. Friedlander said, but investigate further if there’s significant inflammation and signs of early sexual development or virilization.
Benzoyl peroxide wash may be enough to help the condition initially, and consider topical clindamycin or a combination product. “Start out slow,” she said. Twice a week to start might be appropriate. Moisturizers can be helpful, as can topical adapalene.
Also, keep in mind that even mild acne can be emotionally devastating to a child in this age group and worthy of treatment. “Your assessment may be very different than hers,” she said. It’s possible that “she has a few lesions, but she feels like an outcast.”
Dr. Friedlander reported no relevant financial disclosures. SDEF and this news organization are owned by the same parent company.
REPORTING FROM SDEF WOMEN’S & PEDIATRIC DERMATOLOGY SEMINAR
Alopecia areata: Study finds racial disparities
, according to a new study involving registry data for more than 11,000 individuals.
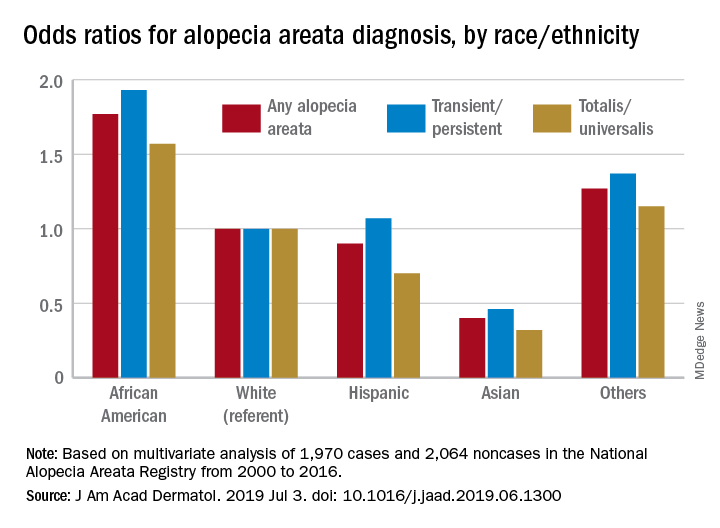
These new findings “raise a different perspective from the conventional view that AA does not differ by race/ethnicity,” said Hemin Lee, MD, MPH, of the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital, Boston, and associates.
Multivariate-adjusted odds ratios for ever-diagnosis of AA were 1.77 for African Americans and 0.4 for Asians when whites were the referent group. Hispanics/Latinos were similar to whites, with an odds ratio of 0.9, and the group of other races/ethnicities (including American Indians and Pacific Islanders) was higher at 1.27, the investigators noted. The report is in the Journal of the American Academy of Dermatology.
The odds played out in a similar fashion when broken down by AA subtype. With whites as the referent at 1.0, blacks were most likely to have been diagnosed with AA transient/persistent at 1.93 and Asians were lowest at 0.46. For AA totalis/universalis, odds ratios were 1.57 for blacks and 0.32 for Asians, they said, based on 2000-2016 data from the National Alopecia Areata Registry.
“An intricate interplay between genetic and environmental factors may account for the racial differences. Pathogenesis of AA is at times linked with autoimmunity by its strong association with HLA class II alleles,” Dr. Lee and associates wrote.
The study involved 11,404 participants from the registry: 9,340 had reported at least one episode of AA and 2,064 had no history of lifetime alopecia. The multivariate analysis was based on the same group of noncases but a subgroup of 1,970 AA patients who had been enrolled in the registry “through academic institutions after dermatologist-confirmed diagnosis,” they said.
There was no funding source to report. One of Dr. Lee’s associates has received honoraria from Abbvie, Amgen, the Centers for Disease Control and Prevention, Janssen, Merck, Novartis, Pfizer, and Amgen, which have been donated to charity, and is an investigator for Sanofi/Regeneron with no financial compensation. All other authors have no conflicts of interest.
SOURCE: Lee H et al. J Am Acad Dermatol. 2019 Jul 3. doi: 10.1016/j.jaad.2019.06.1300.
, according to a new study involving registry data for more than 11,000 individuals.
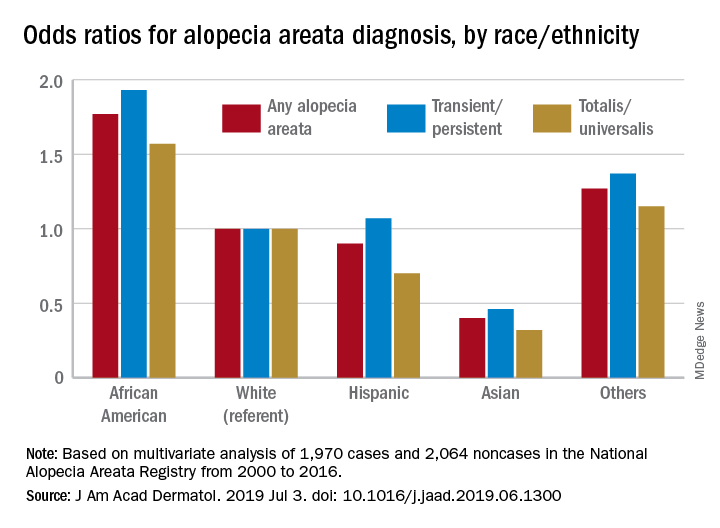
These new findings “raise a different perspective from the conventional view that AA does not differ by race/ethnicity,” said Hemin Lee, MD, MPH, of the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital, Boston, and associates.
Multivariate-adjusted odds ratios for ever-diagnosis of AA were 1.77 for African Americans and 0.4 for Asians when whites were the referent group. Hispanics/Latinos were similar to whites, with an odds ratio of 0.9, and the group of other races/ethnicities (including American Indians and Pacific Islanders) was higher at 1.27, the investigators noted. The report is in the Journal of the American Academy of Dermatology.
The odds played out in a similar fashion when broken down by AA subtype. With whites as the referent at 1.0, blacks were most likely to have been diagnosed with AA transient/persistent at 1.93 and Asians were lowest at 0.46. For AA totalis/universalis, odds ratios were 1.57 for blacks and 0.32 for Asians, they said, based on 2000-2016 data from the National Alopecia Areata Registry.
“An intricate interplay between genetic and environmental factors may account for the racial differences. Pathogenesis of AA is at times linked with autoimmunity by its strong association with HLA class II alleles,” Dr. Lee and associates wrote.
The study involved 11,404 participants from the registry: 9,340 had reported at least one episode of AA and 2,064 had no history of lifetime alopecia. The multivariate analysis was based on the same group of noncases but a subgroup of 1,970 AA patients who had been enrolled in the registry “through academic institutions after dermatologist-confirmed diagnosis,” they said.
There was no funding source to report. One of Dr. Lee’s associates has received honoraria from Abbvie, Amgen, the Centers for Disease Control and Prevention, Janssen, Merck, Novartis, Pfizer, and Amgen, which have been donated to charity, and is an investigator for Sanofi/Regeneron with no financial compensation. All other authors have no conflicts of interest.
SOURCE: Lee H et al. J Am Acad Dermatol. 2019 Jul 3. doi: 10.1016/j.jaad.2019.06.1300.
, according to a new study involving registry data for more than 11,000 individuals.
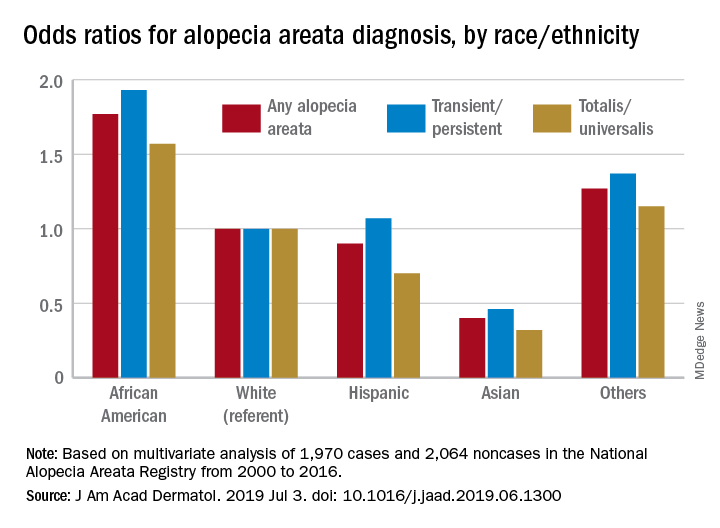
These new findings “raise a different perspective from the conventional view that AA does not differ by race/ethnicity,” said Hemin Lee, MD, MPH, of the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital, Boston, and associates.
Multivariate-adjusted odds ratios for ever-diagnosis of AA were 1.77 for African Americans and 0.4 for Asians when whites were the referent group. Hispanics/Latinos were similar to whites, with an odds ratio of 0.9, and the group of other races/ethnicities (including American Indians and Pacific Islanders) was higher at 1.27, the investigators noted. The report is in the Journal of the American Academy of Dermatology.
The odds played out in a similar fashion when broken down by AA subtype. With whites as the referent at 1.0, blacks were most likely to have been diagnosed with AA transient/persistent at 1.93 and Asians were lowest at 0.46. For AA totalis/universalis, odds ratios were 1.57 for blacks and 0.32 for Asians, they said, based on 2000-2016 data from the National Alopecia Areata Registry.
“An intricate interplay between genetic and environmental factors may account for the racial differences. Pathogenesis of AA is at times linked with autoimmunity by its strong association with HLA class II alleles,” Dr. Lee and associates wrote.
The study involved 11,404 participants from the registry: 9,340 had reported at least one episode of AA and 2,064 had no history of lifetime alopecia. The multivariate analysis was based on the same group of noncases but a subgroup of 1,970 AA patients who had been enrolled in the registry “through academic institutions after dermatologist-confirmed diagnosis,” they said.
There was no funding source to report. One of Dr. Lee’s associates has received honoraria from Abbvie, Amgen, the Centers for Disease Control and Prevention, Janssen, Merck, Novartis, Pfizer, and Amgen, which have been donated to charity, and is an investigator for Sanofi/Regeneron with no financial compensation. All other authors have no conflicts of interest.
SOURCE: Lee H et al. J Am Acad Dermatol. 2019 Jul 3. doi: 10.1016/j.jaad.2019.06.1300.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Hypertension, white matter hyperintensities, and dementia: What’s the link?
LOS ANGELES – While uncontrolled hypertension is an established risk factor for dementias including Alzheimer’s disease, the pathways by which it might lead to dementia remain poorly understood.
In research presented at the Alzheimer’s Association International Conference, Jérémie Lespinasse, PharmD, an investigator with the University of Bordeaux and INSERM U1219 in Bordeaux, France, presented data showing that hypertension-linked increases in the brain’s load of white matter hyperintensities – an imaging biomarker linked to small-vessel disease – was associated with cognitive decline independent of amyloid cascade biomarkers.
“We know that hypertension is related to cognitive decline and dementia, including Alzheimer’s dementia,” Carole Dufouil, PhD, the study’s last author and the research director at INSERM U1219, said in an interview. “But we didn’t know the pathway. It could go through what’s more typical of vascular pathology or it could go through what’s more typical of AD – and that’s what we wanted to test.”
The researchers found that the impact of hypertension on cognition doesn’t “go through amyloid,” Dr. Dufouil said, but rather a typically vascular pathway of white matter hyperintensities and neurodegeneration. “This is a big difference from other brain markers for which you know they exist, but you don’t know how to treat them,” she said. “This one is treatable.”
For their research, Dr. Lespinasse, Dr. Dufouil, and colleagues used a cross-sectional sample of data from the MEMENTO study, a 5-year observational cohort of 2,323 patients recruited at 26 memory centers in France between 2011 and 2014. Of the patients in MEMENTO, 62% were women, and the mean age was 71. All patients were deemed free of dementia and had isolated cognitive complaints or mild cognitive impairment at baseline. A total of 60% had hypertension, and 17% had uncontrolled hypertension defined as above 140/90 mm Hg despite treatment. Cognitive testing and MRI was conducted on all patients, while 60% also had 18F-fluorodeoxyglucose PET scanning and a minority, 18%, had cerebrospinal fluid samples.
The investigators found in using a structural equation model that the uncontrolled hypertension subjects had significantly lower cognition when compared against those without (P = .001). About half of the harmful effect of uncontrolled hypertension on brain functions was mediated by white matter hyperintensities load (P = .021) and neurodegeneration (P = .024) but not by cerebrospinal fluid biomarkers for amyloid-beta 42/40 ratio or tau.
The study’s main limitation was its use of cross-sectional data, the investigators said, while its strength was in a multifactorial model that allowed for a more integrative look at the relationships among hypertension, Alzheimer’s biomarkers, white matter hyperintensities, and cognition.
The investigators stressed the importance of controlling hypertension generally – and for all clinicians to be more aware of its cognitive impacts. Dr. Dufouil said that memory clinics should make blood pressure monitoring a key part of their workups, and should ensure that people are well controlled. “Up until recently it hasn’t been obvious” that control of hypertension has a key role in dementia prevention.
“It’s now obvious,” she said.
Dr. Lespinasse and Dr. Dufouil disclosed no industry relationships.
LOS ANGELES – While uncontrolled hypertension is an established risk factor for dementias including Alzheimer’s disease, the pathways by which it might lead to dementia remain poorly understood.
In research presented at the Alzheimer’s Association International Conference, Jérémie Lespinasse, PharmD, an investigator with the University of Bordeaux and INSERM U1219 in Bordeaux, France, presented data showing that hypertension-linked increases in the brain’s load of white matter hyperintensities – an imaging biomarker linked to small-vessel disease – was associated with cognitive decline independent of amyloid cascade biomarkers.
“We know that hypertension is related to cognitive decline and dementia, including Alzheimer’s dementia,” Carole Dufouil, PhD, the study’s last author and the research director at INSERM U1219, said in an interview. “But we didn’t know the pathway. It could go through what’s more typical of vascular pathology or it could go through what’s more typical of AD – and that’s what we wanted to test.”
The researchers found that the impact of hypertension on cognition doesn’t “go through amyloid,” Dr. Dufouil said, but rather a typically vascular pathway of white matter hyperintensities and neurodegeneration. “This is a big difference from other brain markers for which you know they exist, but you don’t know how to treat them,” she said. “This one is treatable.”
For their research, Dr. Lespinasse, Dr. Dufouil, and colleagues used a cross-sectional sample of data from the MEMENTO study, a 5-year observational cohort of 2,323 patients recruited at 26 memory centers in France between 2011 and 2014. Of the patients in MEMENTO, 62% were women, and the mean age was 71. All patients were deemed free of dementia and had isolated cognitive complaints or mild cognitive impairment at baseline. A total of 60% had hypertension, and 17% had uncontrolled hypertension defined as above 140/90 mm Hg despite treatment. Cognitive testing and MRI was conducted on all patients, while 60% also had 18F-fluorodeoxyglucose PET scanning and a minority, 18%, had cerebrospinal fluid samples.
The investigators found in using a structural equation model that the uncontrolled hypertension subjects had significantly lower cognition when compared against those without (P = .001). About half of the harmful effect of uncontrolled hypertension on brain functions was mediated by white matter hyperintensities load (P = .021) and neurodegeneration (P = .024) but not by cerebrospinal fluid biomarkers for amyloid-beta 42/40 ratio or tau.
The study’s main limitation was its use of cross-sectional data, the investigators said, while its strength was in a multifactorial model that allowed for a more integrative look at the relationships among hypertension, Alzheimer’s biomarkers, white matter hyperintensities, and cognition.
The investigators stressed the importance of controlling hypertension generally – and for all clinicians to be more aware of its cognitive impacts. Dr. Dufouil said that memory clinics should make blood pressure monitoring a key part of their workups, and should ensure that people are well controlled. “Up until recently it hasn’t been obvious” that control of hypertension has a key role in dementia prevention.
“It’s now obvious,” she said.
Dr. Lespinasse and Dr. Dufouil disclosed no industry relationships.
LOS ANGELES – While uncontrolled hypertension is an established risk factor for dementias including Alzheimer’s disease, the pathways by which it might lead to dementia remain poorly understood.
In research presented at the Alzheimer’s Association International Conference, Jérémie Lespinasse, PharmD, an investigator with the University of Bordeaux and INSERM U1219 in Bordeaux, France, presented data showing that hypertension-linked increases in the brain’s load of white matter hyperintensities – an imaging biomarker linked to small-vessel disease – was associated with cognitive decline independent of amyloid cascade biomarkers.
“We know that hypertension is related to cognitive decline and dementia, including Alzheimer’s dementia,” Carole Dufouil, PhD, the study’s last author and the research director at INSERM U1219, said in an interview. “But we didn’t know the pathway. It could go through what’s more typical of vascular pathology or it could go through what’s more typical of AD – and that’s what we wanted to test.”
The researchers found that the impact of hypertension on cognition doesn’t “go through amyloid,” Dr. Dufouil said, but rather a typically vascular pathway of white matter hyperintensities and neurodegeneration. “This is a big difference from other brain markers for which you know they exist, but you don’t know how to treat them,” she said. “This one is treatable.”
For their research, Dr. Lespinasse, Dr. Dufouil, and colleagues used a cross-sectional sample of data from the MEMENTO study, a 5-year observational cohort of 2,323 patients recruited at 26 memory centers in France between 2011 and 2014. Of the patients in MEMENTO, 62% were women, and the mean age was 71. All patients were deemed free of dementia and had isolated cognitive complaints or mild cognitive impairment at baseline. A total of 60% had hypertension, and 17% had uncontrolled hypertension defined as above 140/90 mm Hg despite treatment. Cognitive testing and MRI was conducted on all patients, while 60% also had 18F-fluorodeoxyglucose PET scanning and a minority, 18%, had cerebrospinal fluid samples.
The investigators found in using a structural equation model that the uncontrolled hypertension subjects had significantly lower cognition when compared against those without (P = .001). About half of the harmful effect of uncontrolled hypertension on brain functions was mediated by white matter hyperintensities load (P = .021) and neurodegeneration (P = .024) but not by cerebrospinal fluid biomarkers for amyloid-beta 42/40 ratio or tau.
The study’s main limitation was its use of cross-sectional data, the investigators said, while its strength was in a multifactorial model that allowed for a more integrative look at the relationships among hypertension, Alzheimer’s biomarkers, white matter hyperintensities, and cognition.
The investigators stressed the importance of controlling hypertension generally – and for all clinicians to be more aware of its cognitive impacts. Dr. Dufouil said that memory clinics should make blood pressure monitoring a key part of their workups, and should ensure that people are well controlled. “Up until recently it hasn’t been obvious” that control of hypertension has a key role in dementia prevention.
“It’s now obvious,” she said.
Dr. Lespinasse and Dr. Dufouil disclosed no industry relationships.
REPORTING FROM AAIC 2019















