User login
Werewolf babies, blinding fries, and the gut library
Someone needs carrots, stat
Eat your veggies or you’ll … go blind? A U.K. teen took picky eating to a whole new level, literally losing his vision after a steady decade-long diet of strictly fries, Pringles, white bread, and ham.
Looks like Pringles needs to change their tagline a little bit: “Once you pop, the fun don’t stop – until you start losing hearing and vision!” We think it’s really catchy.
The teen first visited a doctor several years ago complaining of tiredness and was given B12 injections and sent on his merry way. Unfortunately, he quickly developed hearing and vision loss, and by age 17 years was diagnosed with nutritional optic neuropathy.
Somehow through all of this, he maintained a normal weight, proving once and for all the metabolism of teenage boys can withstand just about anything.
The chip-loving teen now joins the (very small) Nutritional Optic Neuropathy Hall of Fame of Developed Countries, previously only occupied by a man who pretty much drank vodka every day for breakfast, lunch, and dinner. Cheers!
Teen wolf? Try baby wolf
Every parent just wants their child to be happy, healthy, and covered in a thick layer of hair, right?
No?
Well, that’s too bad for dozens of parents in Spain, whose children developed hypertrichosis, aka “werewolf syndrome,” and suddenly sprouted full-body hair growth that Tom Selleck would be jealous of. After a brief investigation, they discovered the fast-paced hair growth was caused by an unfortunate medicine mix-up at the lab. Instead of receiving omeprazole for their gastric reflux, the children had been given minoxidil, a drug that treats alopecia.
Luckily for the children who don’t want to impersonate Michael J. Fox anymore, the hair will go away when they stop taking the drug.
No official statement yet on the mysterious sightings of wolf children roaming the Spanish countryside terrorizing locals and howling at the full moon.
Mouthwash in my veins
Let’s say you’re a person with hypertension. After years of your doctor badgering you to do more cardio exercise, you’ve finally committed to the morning jog. It’s a pain getting up that early in the morning, but the benefits will be worth it, right? You head back to your physician, eager to show off the new you. The doctor weighs you (down a few pounds, not bad), then takes a blood pressure reading, and ... it’s exactly the same.
What happened? Was all that work wasted?
Well, according to a study published in Free Radical Biology and Medicine, you may have an excuse: mouthwash usage.
It all has to do with nitric acid. Normally during cardio exercise, bacteria in the mouth convert nitrates into nitrites, and when these nitrites are swallowed, they are converted into nitric acid after being absorbed by the circulatory system. That widens the blood vessels and reduces blood pressure. Mouthwash changes all that. It inhibits those oral bacteria, and the whole process is stopped before it can begin.
The investigators found that, after 1 hour of exercise on a treadmill, study participants who received mouthwash beforehand saw their systolic blood pressure reduced by 2 mm Hg. And those who received the placebo (mint-flavored water)? They saw a 5.2-mm Hg reduction.
Bottom line to those with hypertension: You may have to start flossing. We know it’s annoying, but it’ll make your doctor happy, and it’ll make your dentist especially happy.
No books at this library
The human microbiome is a pretty hot scientific topic right now, but we here at LOTME are not scientists, or doctors, or experts of any kind, so we have a simple question: What’s in a gut?
Happily (yes, this is the sort of thing that makes us happy), researchers at MIT and the Broad Institute, both in Cambridge, Mass., have taken a very detailed look at the guts of about 90 people, with a dozen or so providing samples for up to 2 years, and can now tell us what’s in a gut: bacteria. Lots of bacteria … 7,758 different strains of bacteria.
According to a statement from MIT, the samples were obtained “through the OpenBiome organization, which collects stool samples for research and therapeutic purposes.” It also sounds like a fun place to work.
Those samples presented “a unique opportunity, and we thought that would be a great set of individuals to really try to dig down and characterize the microbial populations more thoroughly,” said Eric Alm, PhD, one of the investigators.
All of their data, along with samples of the bacteria strains they isolated, are available online at the Broad Institute–OpenBiome Microbiome Library. Which, if you think about it (and that is what we do here), makes it kind of like an Amazon for bacteria.
Hmmm … Alexa, order Turicibacter sanguinis. Uncle Leo’s birthday is coming up.
Someone needs carrots, stat
Eat your veggies or you’ll … go blind? A U.K. teen took picky eating to a whole new level, literally losing his vision after a steady decade-long diet of strictly fries, Pringles, white bread, and ham.
Looks like Pringles needs to change their tagline a little bit: “Once you pop, the fun don’t stop – until you start losing hearing and vision!” We think it’s really catchy.
The teen first visited a doctor several years ago complaining of tiredness and was given B12 injections and sent on his merry way. Unfortunately, he quickly developed hearing and vision loss, and by age 17 years was diagnosed with nutritional optic neuropathy.
Somehow through all of this, he maintained a normal weight, proving once and for all the metabolism of teenage boys can withstand just about anything.
The chip-loving teen now joins the (very small) Nutritional Optic Neuropathy Hall of Fame of Developed Countries, previously only occupied by a man who pretty much drank vodka every day for breakfast, lunch, and dinner. Cheers!
Teen wolf? Try baby wolf
Every parent just wants their child to be happy, healthy, and covered in a thick layer of hair, right?
No?
Well, that’s too bad for dozens of parents in Spain, whose children developed hypertrichosis, aka “werewolf syndrome,” and suddenly sprouted full-body hair growth that Tom Selleck would be jealous of. After a brief investigation, they discovered the fast-paced hair growth was caused by an unfortunate medicine mix-up at the lab. Instead of receiving omeprazole for their gastric reflux, the children had been given minoxidil, a drug that treats alopecia.
Luckily for the children who don’t want to impersonate Michael J. Fox anymore, the hair will go away when they stop taking the drug.
No official statement yet on the mysterious sightings of wolf children roaming the Spanish countryside terrorizing locals and howling at the full moon.
Mouthwash in my veins
Let’s say you’re a person with hypertension. After years of your doctor badgering you to do more cardio exercise, you’ve finally committed to the morning jog. It’s a pain getting up that early in the morning, but the benefits will be worth it, right? You head back to your physician, eager to show off the new you. The doctor weighs you (down a few pounds, not bad), then takes a blood pressure reading, and ... it’s exactly the same.
What happened? Was all that work wasted?
Well, according to a study published in Free Radical Biology and Medicine, you may have an excuse: mouthwash usage.
It all has to do with nitric acid. Normally during cardio exercise, bacteria in the mouth convert nitrates into nitrites, and when these nitrites are swallowed, they are converted into nitric acid after being absorbed by the circulatory system. That widens the blood vessels and reduces blood pressure. Mouthwash changes all that. It inhibits those oral bacteria, and the whole process is stopped before it can begin.
The investigators found that, after 1 hour of exercise on a treadmill, study participants who received mouthwash beforehand saw their systolic blood pressure reduced by 2 mm Hg. And those who received the placebo (mint-flavored water)? They saw a 5.2-mm Hg reduction.
Bottom line to those with hypertension: You may have to start flossing. We know it’s annoying, but it’ll make your doctor happy, and it’ll make your dentist especially happy.
No books at this library
The human microbiome is a pretty hot scientific topic right now, but we here at LOTME are not scientists, or doctors, or experts of any kind, so we have a simple question: What’s in a gut?
Happily (yes, this is the sort of thing that makes us happy), researchers at MIT and the Broad Institute, both in Cambridge, Mass., have taken a very detailed look at the guts of about 90 people, with a dozen or so providing samples for up to 2 years, and can now tell us what’s in a gut: bacteria. Lots of bacteria … 7,758 different strains of bacteria.
According to a statement from MIT, the samples were obtained “through the OpenBiome organization, which collects stool samples for research and therapeutic purposes.” It also sounds like a fun place to work.
Those samples presented “a unique opportunity, and we thought that would be a great set of individuals to really try to dig down and characterize the microbial populations more thoroughly,” said Eric Alm, PhD, one of the investigators.
All of their data, along with samples of the bacteria strains they isolated, are available online at the Broad Institute–OpenBiome Microbiome Library. Which, if you think about it (and that is what we do here), makes it kind of like an Amazon for bacteria.
Hmmm … Alexa, order Turicibacter sanguinis. Uncle Leo’s birthday is coming up.
Someone needs carrots, stat
Eat your veggies or you’ll … go blind? A U.K. teen took picky eating to a whole new level, literally losing his vision after a steady decade-long diet of strictly fries, Pringles, white bread, and ham.
Looks like Pringles needs to change their tagline a little bit: “Once you pop, the fun don’t stop – until you start losing hearing and vision!” We think it’s really catchy.
The teen first visited a doctor several years ago complaining of tiredness and was given B12 injections and sent on his merry way. Unfortunately, he quickly developed hearing and vision loss, and by age 17 years was diagnosed with nutritional optic neuropathy.
Somehow through all of this, he maintained a normal weight, proving once and for all the metabolism of teenage boys can withstand just about anything.
The chip-loving teen now joins the (very small) Nutritional Optic Neuropathy Hall of Fame of Developed Countries, previously only occupied by a man who pretty much drank vodka every day for breakfast, lunch, and dinner. Cheers!
Teen wolf? Try baby wolf
Every parent just wants their child to be happy, healthy, and covered in a thick layer of hair, right?
No?
Well, that’s too bad for dozens of parents in Spain, whose children developed hypertrichosis, aka “werewolf syndrome,” and suddenly sprouted full-body hair growth that Tom Selleck would be jealous of. After a brief investigation, they discovered the fast-paced hair growth was caused by an unfortunate medicine mix-up at the lab. Instead of receiving omeprazole for their gastric reflux, the children had been given minoxidil, a drug that treats alopecia.
Luckily for the children who don’t want to impersonate Michael J. Fox anymore, the hair will go away when they stop taking the drug.
No official statement yet on the mysterious sightings of wolf children roaming the Spanish countryside terrorizing locals and howling at the full moon.
Mouthwash in my veins
Let’s say you’re a person with hypertension. After years of your doctor badgering you to do more cardio exercise, you’ve finally committed to the morning jog. It’s a pain getting up that early in the morning, but the benefits will be worth it, right? You head back to your physician, eager to show off the new you. The doctor weighs you (down a few pounds, not bad), then takes a blood pressure reading, and ... it’s exactly the same.
What happened? Was all that work wasted?
Well, according to a study published in Free Radical Biology and Medicine, you may have an excuse: mouthwash usage.
It all has to do with nitric acid. Normally during cardio exercise, bacteria in the mouth convert nitrates into nitrites, and when these nitrites are swallowed, they are converted into nitric acid after being absorbed by the circulatory system. That widens the blood vessels and reduces blood pressure. Mouthwash changes all that. It inhibits those oral bacteria, and the whole process is stopped before it can begin.
The investigators found that, after 1 hour of exercise on a treadmill, study participants who received mouthwash beforehand saw their systolic blood pressure reduced by 2 mm Hg. And those who received the placebo (mint-flavored water)? They saw a 5.2-mm Hg reduction.
Bottom line to those with hypertension: You may have to start flossing. We know it’s annoying, but it’ll make your doctor happy, and it’ll make your dentist especially happy.
No books at this library
The human microbiome is a pretty hot scientific topic right now, but we here at LOTME are not scientists, or doctors, or experts of any kind, so we have a simple question: What’s in a gut?
Happily (yes, this is the sort of thing that makes us happy), researchers at MIT and the Broad Institute, both in Cambridge, Mass., have taken a very detailed look at the guts of about 90 people, with a dozen or so providing samples for up to 2 years, and can now tell us what’s in a gut: bacteria. Lots of bacteria … 7,758 different strains of bacteria.
According to a statement from MIT, the samples were obtained “through the OpenBiome organization, which collects stool samples for research and therapeutic purposes.” It also sounds like a fun place to work.
Those samples presented “a unique opportunity, and we thought that would be a great set of individuals to really try to dig down and characterize the microbial populations more thoroughly,” said Eric Alm, PhD, one of the investigators.
All of their data, along with samples of the bacteria strains they isolated, are available online at the Broad Institute–OpenBiome Microbiome Library. Which, if you think about it (and that is what we do here), makes it kind of like an Amazon for bacteria.
Hmmm … Alexa, order Turicibacter sanguinis. Uncle Leo’s birthday is coming up.
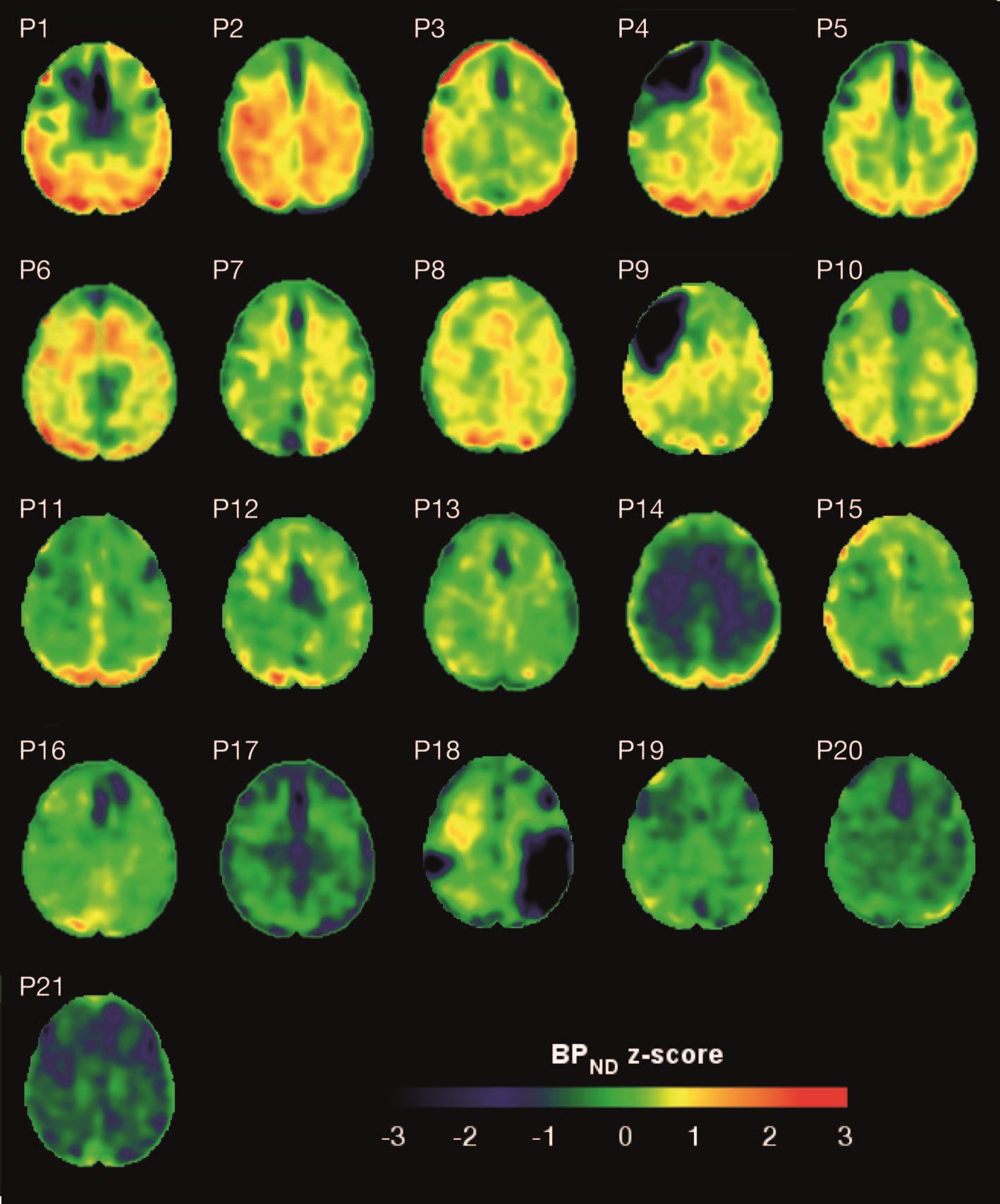
Hyperphosphorylated tau visible in TBI survivors decades after brain injury
Brain deposits of hyperphosphorylated tau are detectable in traumatic brain injury (TBI) patients 18-51 years after a single moderate to severe incident occurred, researchers reported Sept. 4 in Science Translational Medicine.
Imaging with the tau-specific PET radioligand flortaucipir showed that the protein was most apparent in the right occipital cortex, and was associated with changes in cognitive scores, tau and beta amyloid in cerebrospinal fluid (CSF), and white matter density, Nikos Gorgoraptis, PhD, of Imperial College London and his colleagues wrote.
“The ability to detect tau pathology in vivo after TBI has major potential implications for diagnosis and prognostication of clinical outcomes after TBI,” the researchers explained. “It is also likely to assist in patient selection and stratification for future treatment trials targeting tau.”
The cohort study comprised 21 subjects (median age, 49 years) who had experienced a single moderate to severe TBI a median of 32 years (range, 18-51 years) before enrollment. A control group comprised 11 noninjured adults who were matched for age and other demographic factors. Everyone underwent a PET scan with flortaucipir, brain MRI, CSF sampling, apolipoprotein E genotyping, and neuropsychological testing.
TBI subjects were grouped according to recovery status: good and disabled. Overall, they showed impairments on multiple cognitive domains (processing speed, executive function, motivation, inhibition, and verbal and visual memory), compared with controls. These findings were largely driven by the disabled group.
Eight TBI subjects had elevated tau binding greater than 2,000 voxels above the threshold of detection (equivalent to 16 cm3 of brain volume), and seven had an increase of 249-1,999 voxels above threshold. Tau binding in the remainder was similar to that in controls. Recovery status didn’t correlate with the tau-binding strength.
Overall, the tau-binding signal appeared most strongly in the right lateral occipital cortex, regardless of functional recovery status.
In TBI subjects, CSF total tau correlated significantly with flortaucipir uptake in cortical gray matter, but not white matter. CSF phosphorylated tau correlated with uptake in white matter, but not gray matter.
The investigators also examined fractional anisotropy, a measure of fiber density, axonal diameter, and myelination in white matter. In TBI subjects, there was more flortaucipir uptake in areas of decreased fractional anisotropy, including association, commissural, and projection tracts.
“Correlations were observed in the genu and body of the corpus callosum, as well as in several association tracts within the ipsilateral (right) hemisphere, including the cingulum bundle, inferior longitudinal fasciculus, uncinate fasciculus, and anterior thalamic radiation, but not in the contralateral hemisphere. Higher cortical flortaucipir [signal] was associated with reduced tissue density in remote white matter regions including the corpus callosum and right prefrontal white matter. The same analysis for gray matter density did not show an association.”
The increased tau signal in TBI subjects “is in keeping with a causative role for traumatic axonal injury in the pathophysiology of posttraumatic tau pathology,” the authors said. “Mechanical forces exerted at the time of head injury are thought to disrupt axonal organization, producing damage to microtubule structure and associated axonal tau. This damage may lead to hyperphosphorylation of tau, misfolding, and neurofibrillary tangle formation, which eventually causes neurodegeneration. Mechanical forces are maximal in points of geometric inflection such as the base of cortical sulci, where tau pathology is seen in chronic traumatic encephalopathy.”
These patterns suggest that tau imaging could provide valuable diagnostic information about the type of posttraumatic neurodegeneration, they said.
The work was supported by the Medical Research Council and UK Dementia Research Institute. None of the authors declared having any competing interests related to the current study. Some authors reported financial ties to pharmaceutical companies.
SOURCE: Gorgoraptis N et al. Sci Transl Med. 2019;11:eaaw1993. doi: 10.1126/scitranslmed.aaw1993.
Brain deposits of hyperphosphorylated tau are detectable in traumatic brain injury (TBI) patients 18-51 years after a single moderate to severe incident occurred, researchers reported Sept. 4 in Science Translational Medicine.
Imaging with the tau-specific PET radioligand flortaucipir showed that the protein was most apparent in the right occipital cortex, and was associated with changes in cognitive scores, tau and beta amyloid in cerebrospinal fluid (CSF), and white matter density, Nikos Gorgoraptis, PhD, of Imperial College London and his colleagues wrote.
“The ability to detect tau pathology in vivo after TBI has major potential implications for diagnosis and prognostication of clinical outcomes after TBI,” the researchers explained. “It is also likely to assist in patient selection and stratification for future treatment trials targeting tau.”
The cohort study comprised 21 subjects (median age, 49 years) who had experienced a single moderate to severe TBI a median of 32 years (range, 18-51 years) before enrollment. A control group comprised 11 noninjured adults who were matched for age and other demographic factors. Everyone underwent a PET scan with flortaucipir, brain MRI, CSF sampling, apolipoprotein E genotyping, and neuropsychological testing.
TBI subjects were grouped according to recovery status: good and disabled. Overall, they showed impairments on multiple cognitive domains (processing speed, executive function, motivation, inhibition, and verbal and visual memory), compared with controls. These findings were largely driven by the disabled group.
Eight TBI subjects had elevated tau binding greater than 2,000 voxels above the threshold of detection (equivalent to 16 cm3 of brain volume), and seven had an increase of 249-1,999 voxels above threshold. Tau binding in the remainder was similar to that in controls. Recovery status didn’t correlate with the tau-binding strength.
Overall, the tau-binding signal appeared most strongly in the right lateral occipital cortex, regardless of functional recovery status.
In TBI subjects, CSF total tau correlated significantly with flortaucipir uptake in cortical gray matter, but not white matter. CSF phosphorylated tau correlated with uptake in white matter, but not gray matter.
The investigators also examined fractional anisotropy, a measure of fiber density, axonal diameter, and myelination in white matter. In TBI subjects, there was more flortaucipir uptake in areas of decreased fractional anisotropy, including association, commissural, and projection tracts.
“Correlations were observed in the genu and body of the corpus callosum, as well as in several association tracts within the ipsilateral (right) hemisphere, including the cingulum bundle, inferior longitudinal fasciculus, uncinate fasciculus, and anterior thalamic radiation, but not in the contralateral hemisphere. Higher cortical flortaucipir [signal] was associated with reduced tissue density in remote white matter regions including the corpus callosum and right prefrontal white matter. The same analysis for gray matter density did not show an association.”
The increased tau signal in TBI subjects “is in keeping with a causative role for traumatic axonal injury in the pathophysiology of posttraumatic tau pathology,” the authors said. “Mechanical forces exerted at the time of head injury are thought to disrupt axonal organization, producing damage to microtubule structure and associated axonal tau. This damage may lead to hyperphosphorylation of tau, misfolding, and neurofibrillary tangle formation, which eventually causes neurodegeneration. Mechanical forces are maximal in points of geometric inflection such as the base of cortical sulci, where tau pathology is seen in chronic traumatic encephalopathy.”
These patterns suggest that tau imaging could provide valuable diagnostic information about the type of posttraumatic neurodegeneration, they said.
The work was supported by the Medical Research Council and UK Dementia Research Institute. None of the authors declared having any competing interests related to the current study. Some authors reported financial ties to pharmaceutical companies.
SOURCE: Gorgoraptis N et al. Sci Transl Med. 2019;11:eaaw1993. doi: 10.1126/scitranslmed.aaw1993.
Brain deposits of hyperphosphorylated tau are detectable in traumatic brain injury (TBI) patients 18-51 years after a single moderate to severe incident occurred, researchers reported Sept. 4 in Science Translational Medicine.
Imaging with the tau-specific PET radioligand flortaucipir showed that the protein was most apparent in the right occipital cortex, and was associated with changes in cognitive scores, tau and beta amyloid in cerebrospinal fluid (CSF), and white matter density, Nikos Gorgoraptis, PhD, of Imperial College London and his colleagues wrote.
“The ability to detect tau pathology in vivo after TBI has major potential implications for diagnosis and prognostication of clinical outcomes after TBI,” the researchers explained. “It is also likely to assist in patient selection and stratification for future treatment trials targeting tau.”
The cohort study comprised 21 subjects (median age, 49 years) who had experienced a single moderate to severe TBI a median of 32 years (range, 18-51 years) before enrollment. A control group comprised 11 noninjured adults who were matched for age and other demographic factors. Everyone underwent a PET scan with flortaucipir, brain MRI, CSF sampling, apolipoprotein E genotyping, and neuropsychological testing.
TBI subjects were grouped according to recovery status: good and disabled. Overall, they showed impairments on multiple cognitive domains (processing speed, executive function, motivation, inhibition, and verbal and visual memory), compared with controls. These findings were largely driven by the disabled group.
Eight TBI subjects had elevated tau binding greater than 2,000 voxels above the threshold of detection (equivalent to 16 cm3 of brain volume), and seven had an increase of 249-1,999 voxels above threshold. Tau binding in the remainder was similar to that in controls. Recovery status didn’t correlate with the tau-binding strength.
Overall, the tau-binding signal appeared most strongly in the right lateral occipital cortex, regardless of functional recovery status.
In TBI subjects, CSF total tau correlated significantly with flortaucipir uptake in cortical gray matter, but not white matter. CSF phosphorylated tau correlated with uptake in white matter, but not gray matter.
The investigators also examined fractional anisotropy, a measure of fiber density, axonal diameter, and myelination in white matter. In TBI subjects, there was more flortaucipir uptake in areas of decreased fractional anisotropy, including association, commissural, and projection tracts.
“Correlations were observed in the genu and body of the corpus callosum, as well as in several association tracts within the ipsilateral (right) hemisphere, including the cingulum bundle, inferior longitudinal fasciculus, uncinate fasciculus, and anterior thalamic radiation, but not in the contralateral hemisphere. Higher cortical flortaucipir [signal] was associated with reduced tissue density in remote white matter regions including the corpus callosum and right prefrontal white matter. The same analysis for gray matter density did not show an association.”
The increased tau signal in TBI subjects “is in keeping with a causative role for traumatic axonal injury in the pathophysiology of posttraumatic tau pathology,” the authors said. “Mechanical forces exerted at the time of head injury are thought to disrupt axonal organization, producing damage to microtubule structure and associated axonal tau. This damage may lead to hyperphosphorylation of tau, misfolding, and neurofibrillary tangle formation, which eventually causes neurodegeneration. Mechanical forces are maximal in points of geometric inflection such as the base of cortical sulci, where tau pathology is seen in chronic traumatic encephalopathy.”
These patterns suggest that tau imaging could provide valuable diagnostic information about the type of posttraumatic neurodegeneration, they said.
The work was supported by the Medical Research Council and UK Dementia Research Institute. None of the authors declared having any competing interests related to the current study. Some authors reported financial ties to pharmaceutical companies.
SOURCE: Gorgoraptis N et al. Sci Transl Med. 2019;11:eaaw1993. doi: 10.1126/scitranslmed.aaw1993.
FROM SCIENCE TRANSLATIONAL MEDICINE
Type of renal dysfunction affects liver cirrhosis mortality risk
For non–status 1 patients with cirrhosis who are awaiting liver transplantation, type of renal dysfunction may be a key determinant of mortality risk, based on a retrospective analysis of more than 22,000 patients.
Risk of death was greatest for patients with acute on chronic kidney disease (AKI on CKD), followed by AKI alone, then CKD alone, reported lead author Giuseppe Cullaro, MD, of the University of California, San Francisco, and colleagues.
Although it is well known that renal dysfunction worsens outcomes among patients with liver cirrhosis, the impact of different types of kidney pathology on mortality risk has been minimally researched, the investigators wrote in Clinical Gastroenterology and Hepatology. “To date, studies evaluating the impact of renal dysfunction on prognosis in patients with cirrhosis have mostly focused on AKI.”
To learn more, the investigators performed a retrospective study involving acute, chronic, and acute on chronic kidney disease among patients with cirrhosis. They included data from 22,680 non–status 1 adults who were awaiting liver transplantation between 2007 and 2014, with at least 90 days on the wait list. Information was gathered from the Organ Procurement and Transplantation Network registry.
AKI was defined by fewer than 72 days of hemodialysis, or an increase in creatinine of at least 0.3 mg/dL or at least 50% in the last 7 days. CKD was identified by more than 72 days of hemodialysis, or an estimated glomerular filtration rate less than 60 mL/min/1.73 m2 for 90 days with a final rate of at least 30 mL/min/1.73 m2. Using these criteria, the researchers put patients into four possible categories: AKI on CKD, AKI, CKD, or normal renal function. The primary outcome was wait list mortality, which was defined as death, or removal from the wait list for illness. Follow-up started at the time of addition to the wait list and continued until transplant, removal from the wait list, or death.
Multivariate analysis, which accounted for final MELD-Na score and other confounders, showed that patients with AKI on CKD fared worst, with a 2.86-fold higher mortality risk (subhazard [SHR] ratio, 2.86) than that of patients with normal renal function. The mortality risk for acute on chronic kidney disease was followed closely by patients with AKI alone (SHR, 2.42), and more distantly by patients with CKD alone (SHR, 1.56). Further analysis showed that the disparity between mortality risks of each subgroup became more pronounced with increased MELD-Na score. In addition, evaluation of receiver operating characteristic curves for 6-month wait list mortality showed that the addition of renal function to MELD-Na score increased the accuracy of prognosis from an area under the curve of 0.71 to 0.80 (P less than .001).
“This suggests that incorporating the pattern of renal function could provide an opportunity to better prognosticate risk of mortality in the patients with cirrhosis who are the sickest,” the investigators concluded.
They also speculated about why outcomes may vary by type of kidney dysfunction.
“We suspect that those patients who experience AKI and AKI on CKD in our cohort likely had a triggering event – infection, bleeding, hypovolemia – that put these patients at greater risk for waitlist mortality,” the investigators wrote. “These events inherently carry more risk than stable nonliver-related elevations in serum creatinine that are seen in patients with CKD. Because of this heterogeneity of etiology in renal dysfunction in patients with cirrhosis, it is perhaps not surprising that unique renal function patterns variably impact mortality.”
The investigators noted that the findings from the study have “important implications for clinical practice,” and suggested that including type of renal dysfunction would have the most significant affect on accuracy of prognoses among patients at greatest risk of mortality.
The study was funded by a Paul B. Beeson Career Development Award and the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Verna disclosed relationships with Salix, Merck, and Gilead.
SOURCE: Cullaro et al. Clin Gastroenterol Hepatol. 2019 Feb 1. doi: 10.1016/j.cgh.2019.01.043.
Cirrhotic patients with renal failure have a sevenfold increase in mortality compared with those without renal failure. Acute kidney injury (AKI) is common in cirrhosis; increasingly, cirrhotic patients awaiting liver transplantation have or are also at risk for CKD. They are sicker, older, and have more comorbidities such as obesity and diabetes. In this study, the cumulative incidence of death on the wait list was much more pronounced for any form of AKI, with those with AKI on CKD having the highest cumulative incidence of wait list mortality compared with those with normal renal function. The study notably raises several important issues. First, AKI exerts a greater influence in risk of mortality on CKD than it does on those with normal renal function. This is relevant given the increasing prevalence of CKD in this population. Second, it emphasizes the need to effectively measure renal function. All serum creatinine-based equations overestimate glomerular filtration rate in the presence of renal dysfunction. Finally, the study highlights the importance of extrahepatic factors in determining mortality on the wait list. While in all comers, a mathematical model such as the MELDNa score may be able to predict mortality, for a specific patient the presence of comorbid conditions, malnutrition and sarcopenia, infections, critical illness, and now pattern of renal dysfunction, may all play a role.
Sumeet K. Asrani, MD, MSc, is a hepatologist affiliated with Baylor University Medical Center, Dallas. He has no conflicts of interest.
Cirrhotic patients with renal failure have a sevenfold increase in mortality compared with those without renal failure. Acute kidney injury (AKI) is common in cirrhosis; increasingly, cirrhotic patients awaiting liver transplantation have or are also at risk for CKD. They are sicker, older, and have more comorbidities such as obesity and diabetes. In this study, the cumulative incidence of death on the wait list was much more pronounced for any form of AKI, with those with AKI on CKD having the highest cumulative incidence of wait list mortality compared with those with normal renal function. The study notably raises several important issues. First, AKI exerts a greater influence in risk of mortality on CKD than it does on those with normal renal function. This is relevant given the increasing prevalence of CKD in this population. Second, it emphasizes the need to effectively measure renal function. All serum creatinine-based equations overestimate glomerular filtration rate in the presence of renal dysfunction. Finally, the study highlights the importance of extrahepatic factors in determining mortality on the wait list. While in all comers, a mathematical model such as the MELDNa score may be able to predict mortality, for a specific patient the presence of comorbid conditions, malnutrition and sarcopenia, infections, critical illness, and now pattern of renal dysfunction, may all play a role.
Sumeet K. Asrani, MD, MSc, is a hepatologist affiliated with Baylor University Medical Center, Dallas. He has no conflicts of interest.
Cirrhotic patients with renal failure have a sevenfold increase in mortality compared with those without renal failure. Acute kidney injury (AKI) is common in cirrhosis; increasingly, cirrhotic patients awaiting liver transplantation have or are also at risk for CKD. They are sicker, older, and have more comorbidities such as obesity and diabetes. In this study, the cumulative incidence of death on the wait list was much more pronounced for any form of AKI, with those with AKI on CKD having the highest cumulative incidence of wait list mortality compared with those with normal renal function. The study notably raises several important issues. First, AKI exerts a greater influence in risk of mortality on CKD than it does on those with normal renal function. This is relevant given the increasing prevalence of CKD in this population. Second, it emphasizes the need to effectively measure renal function. All serum creatinine-based equations overestimate glomerular filtration rate in the presence of renal dysfunction. Finally, the study highlights the importance of extrahepatic factors in determining mortality on the wait list. While in all comers, a mathematical model such as the MELDNa score may be able to predict mortality, for a specific patient the presence of comorbid conditions, malnutrition and sarcopenia, infections, critical illness, and now pattern of renal dysfunction, may all play a role.
Sumeet K. Asrani, MD, MSc, is a hepatologist affiliated with Baylor University Medical Center, Dallas. He has no conflicts of interest.
For non–status 1 patients with cirrhosis who are awaiting liver transplantation, type of renal dysfunction may be a key determinant of mortality risk, based on a retrospective analysis of more than 22,000 patients.
Risk of death was greatest for patients with acute on chronic kidney disease (AKI on CKD), followed by AKI alone, then CKD alone, reported lead author Giuseppe Cullaro, MD, of the University of California, San Francisco, and colleagues.
Although it is well known that renal dysfunction worsens outcomes among patients with liver cirrhosis, the impact of different types of kidney pathology on mortality risk has been minimally researched, the investigators wrote in Clinical Gastroenterology and Hepatology. “To date, studies evaluating the impact of renal dysfunction on prognosis in patients with cirrhosis have mostly focused on AKI.”
To learn more, the investigators performed a retrospective study involving acute, chronic, and acute on chronic kidney disease among patients with cirrhosis. They included data from 22,680 non–status 1 adults who were awaiting liver transplantation between 2007 and 2014, with at least 90 days on the wait list. Information was gathered from the Organ Procurement and Transplantation Network registry.
AKI was defined by fewer than 72 days of hemodialysis, or an increase in creatinine of at least 0.3 mg/dL or at least 50% in the last 7 days. CKD was identified by more than 72 days of hemodialysis, or an estimated glomerular filtration rate less than 60 mL/min/1.73 m2 for 90 days with a final rate of at least 30 mL/min/1.73 m2. Using these criteria, the researchers put patients into four possible categories: AKI on CKD, AKI, CKD, or normal renal function. The primary outcome was wait list mortality, which was defined as death, or removal from the wait list for illness. Follow-up started at the time of addition to the wait list and continued until transplant, removal from the wait list, or death.
Multivariate analysis, which accounted for final MELD-Na score and other confounders, showed that patients with AKI on CKD fared worst, with a 2.86-fold higher mortality risk (subhazard [SHR] ratio, 2.86) than that of patients with normal renal function. The mortality risk for acute on chronic kidney disease was followed closely by patients with AKI alone (SHR, 2.42), and more distantly by patients with CKD alone (SHR, 1.56). Further analysis showed that the disparity between mortality risks of each subgroup became more pronounced with increased MELD-Na score. In addition, evaluation of receiver operating characteristic curves for 6-month wait list mortality showed that the addition of renal function to MELD-Na score increased the accuracy of prognosis from an area under the curve of 0.71 to 0.80 (P less than .001).
“This suggests that incorporating the pattern of renal function could provide an opportunity to better prognosticate risk of mortality in the patients with cirrhosis who are the sickest,” the investigators concluded.
They also speculated about why outcomes may vary by type of kidney dysfunction.
“We suspect that those patients who experience AKI and AKI on CKD in our cohort likely had a triggering event – infection, bleeding, hypovolemia – that put these patients at greater risk for waitlist mortality,” the investigators wrote. “These events inherently carry more risk than stable nonliver-related elevations in serum creatinine that are seen in patients with CKD. Because of this heterogeneity of etiology in renal dysfunction in patients with cirrhosis, it is perhaps not surprising that unique renal function patterns variably impact mortality.”
The investigators noted that the findings from the study have “important implications for clinical practice,” and suggested that including type of renal dysfunction would have the most significant affect on accuracy of prognoses among patients at greatest risk of mortality.
The study was funded by a Paul B. Beeson Career Development Award and the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Verna disclosed relationships with Salix, Merck, and Gilead.
SOURCE: Cullaro et al. Clin Gastroenterol Hepatol. 2019 Feb 1. doi: 10.1016/j.cgh.2019.01.043.
For non–status 1 patients with cirrhosis who are awaiting liver transplantation, type of renal dysfunction may be a key determinant of mortality risk, based on a retrospective analysis of more than 22,000 patients.
Risk of death was greatest for patients with acute on chronic kidney disease (AKI on CKD), followed by AKI alone, then CKD alone, reported lead author Giuseppe Cullaro, MD, of the University of California, San Francisco, and colleagues.
Although it is well known that renal dysfunction worsens outcomes among patients with liver cirrhosis, the impact of different types of kidney pathology on mortality risk has been minimally researched, the investigators wrote in Clinical Gastroenterology and Hepatology. “To date, studies evaluating the impact of renal dysfunction on prognosis in patients with cirrhosis have mostly focused on AKI.”
To learn more, the investigators performed a retrospective study involving acute, chronic, and acute on chronic kidney disease among patients with cirrhosis. They included data from 22,680 non–status 1 adults who were awaiting liver transplantation between 2007 and 2014, with at least 90 days on the wait list. Information was gathered from the Organ Procurement and Transplantation Network registry.
AKI was defined by fewer than 72 days of hemodialysis, or an increase in creatinine of at least 0.3 mg/dL or at least 50% in the last 7 days. CKD was identified by more than 72 days of hemodialysis, or an estimated glomerular filtration rate less than 60 mL/min/1.73 m2 for 90 days with a final rate of at least 30 mL/min/1.73 m2. Using these criteria, the researchers put patients into four possible categories: AKI on CKD, AKI, CKD, or normal renal function. The primary outcome was wait list mortality, which was defined as death, or removal from the wait list for illness. Follow-up started at the time of addition to the wait list and continued until transplant, removal from the wait list, or death.
Multivariate analysis, which accounted for final MELD-Na score and other confounders, showed that patients with AKI on CKD fared worst, with a 2.86-fold higher mortality risk (subhazard [SHR] ratio, 2.86) than that of patients with normal renal function. The mortality risk for acute on chronic kidney disease was followed closely by patients with AKI alone (SHR, 2.42), and more distantly by patients with CKD alone (SHR, 1.56). Further analysis showed that the disparity between mortality risks of each subgroup became more pronounced with increased MELD-Na score. In addition, evaluation of receiver operating characteristic curves for 6-month wait list mortality showed that the addition of renal function to MELD-Na score increased the accuracy of prognosis from an area under the curve of 0.71 to 0.80 (P less than .001).
“This suggests that incorporating the pattern of renal function could provide an opportunity to better prognosticate risk of mortality in the patients with cirrhosis who are the sickest,” the investigators concluded.
They also speculated about why outcomes may vary by type of kidney dysfunction.
“We suspect that those patients who experience AKI and AKI on CKD in our cohort likely had a triggering event – infection, bleeding, hypovolemia – that put these patients at greater risk for waitlist mortality,” the investigators wrote. “These events inherently carry more risk than stable nonliver-related elevations in serum creatinine that are seen in patients with CKD. Because of this heterogeneity of etiology in renal dysfunction in patients with cirrhosis, it is perhaps not surprising that unique renal function patterns variably impact mortality.”
The investigators noted that the findings from the study have “important implications for clinical practice,” and suggested that including type of renal dysfunction would have the most significant affect on accuracy of prognoses among patients at greatest risk of mortality.
The study was funded by a Paul B. Beeson Career Development Award and the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Verna disclosed relationships with Salix, Merck, and Gilead.
SOURCE: Cullaro et al. Clin Gastroenterol Hepatol. 2019 Feb 1. doi: 10.1016/j.cgh.2019.01.043.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Part 1: Finding Your Inner Leader
Is it my imagination, or has there been a lot of discussion on leadership lately? In the past 3 years, all the meetings I have attended had at least 1 presentation on leadership or the traits of leaders. Sometimes—even in the oddest places—I have come across an article with “leadership” in the title. In fact, a serendipitous discovery of 2 publications is what inspired me to write this.
I spotted the first one in a reading basket when I was on vacation: It was an interview with Benjamin Zander, the conductor of the Boston Philharmonic Orchestra and the Boston Philharmonic Youth Orchestra.1 I was especially interested to read this because when I was in graduate school, Benjamin (the father of one of my classmates) visited our campus to give a presentation on talent and self-confidence. I can still hear him conducting us to emphatically believe in ourselves and others. This was echoed in his interview: “Never doubt the capacity of the people you lead to accomplish whatever you dream for them.” What a powerful concept: Believe in the possibilities of someone!
The second was an American Legion Auxiliary column, which emphasized that “leadership is not a title, but a responsibility.”2 This struck a chord with me because some prominent leaders don’t appear to ascribe to that assessment (although they should!).
After digesting these articles, I started thinking: What, exactly, is leadership? What do we even mean by leadership? How do we measure it? Is it measurable? How do we know when we see or experience good leadership? Can one learn to become a leader by simply reading a “how-to” article?
I think I can answer these questions with 2 principles that have guided me through my career as an NP: (1) Make use of another leader’s expertise to guide you, and (2) Continue to grow amid any setbacks.
For example, my transition from a full-time clinician to a Health Policy Coordinator or “policy wonk” did not have a distinct trajectory. Although my core set of clinical skills were essential, I knew early on that I had to expand by adapting specific organizational skills that would enable me to grow in my new role. But how was I to prioritize which skills to improve? More than a simple trial-and-error approach was required; I needed guidance. Fortunately, my new boss was willing to share her experience and the lessons she learned on the job. Key among them was to recognize the skills I already had—communicating and coordinating—and to develop those skills to be more effective in my new position.
Later in my career, I worked with colleagues to pursue legislation for NP prescriptive authority in Massachusetts. The political arena of Commonwealth’s health care laws was especially pivotal in changing how I saw setbacks. These weren’t to be accepted as a failure but as a challenge to figure out how to better succeed the next time. For several years, I was told “No” before we finally got a bill passed. But each round of my testimony was an opportunity to educate lawmakers and the public on the valuable role of NPs and the quality of care we provide. I try to share this story with new NPs as a good example of why they should persist through adversity.
Continue to: Over the next 3 weeks...
Over the next 3 weeks, join us on Thursdays as we continue to discuss what it means to be a leader—from the pitfalls to the victories. For those who are leaders or who work for one, please share your thoughts, experiences, and lessons learned. Maybe you can give a shoutout to someone who was a positive influence!
1. Labarre P. Leadership—Ben Zander. Fast Company website. www.fastcompany.com/35825/leadership-ben-zander. Published November 30, 1998. Accessed August 27, 2019.
2. Volunteer beyond the ALA: serve on boards, committees. American Legion Auxiliary. November 2018:29.
Is it my imagination, or has there been a lot of discussion on leadership lately? In the past 3 years, all the meetings I have attended had at least 1 presentation on leadership or the traits of leaders. Sometimes—even in the oddest places—I have come across an article with “leadership” in the title. In fact, a serendipitous discovery of 2 publications is what inspired me to write this.
I spotted the first one in a reading basket when I was on vacation: It was an interview with Benjamin Zander, the conductor of the Boston Philharmonic Orchestra and the Boston Philharmonic Youth Orchestra.1 I was especially interested to read this because when I was in graduate school, Benjamin (the father of one of my classmates) visited our campus to give a presentation on talent and self-confidence. I can still hear him conducting us to emphatically believe in ourselves and others. This was echoed in his interview: “Never doubt the capacity of the people you lead to accomplish whatever you dream for them.” What a powerful concept: Believe in the possibilities of someone!
The second was an American Legion Auxiliary column, which emphasized that “leadership is not a title, but a responsibility.”2 This struck a chord with me because some prominent leaders don’t appear to ascribe to that assessment (although they should!).
After digesting these articles, I started thinking: What, exactly, is leadership? What do we even mean by leadership? How do we measure it? Is it measurable? How do we know when we see or experience good leadership? Can one learn to become a leader by simply reading a “how-to” article?
I think I can answer these questions with 2 principles that have guided me through my career as an NP: (1) Make use of another leader’s expertise to guide you, and (2) Continue to grow amid any setbacks.
For example, my transition from a full-time clinician to a Health Policy Coordinator or “policy wonk” did not have a distinct trajectory. Although my core set of clinical skills were essential, I knew early on that I had to expand by adapting specific organizational skills that would enable me to grow in my new role. But how was I to prioritize which skills to improve? More than a simple trial-and-error approach was required; I needed guidance. Fortunately, my new boss was willing to share her experience and the lessons she learned on the job. Key among them was to recognize the skills I already had—communicating and coordinating—and to develop those skills to be more effective in my new position.
Later in my career, I worked with colleagues to pursue legislation for NP prescriptive authority in Massachusetts. The political arena of Commonwealth’s health care laws was especially pivotal in changing how I saw setbacks. These weren’t to be accepted as a failure but as a challenge to figure out how to better succeed the next time. For several years, I was told “No” before we finally got a bill passed. But each round of my testimony was an opportunity to educate lawmakers and the public on the valuable role of NPs and the quality of care we provide. I try to share this story with new NPs as a good example of why they should persist through adversity.
Continue to: Over the next 3 weeks...
Over the next 3 weeks, join us on Thursdays as we continue to discuss what it means to be a leader—from the pitfalls to the victories. For those who are leaders or who work for one, please share your thoughts, experiences, and lessons learned. Maybe you can give a shoutout to someone who was a positive influence!
Is it my imagination, or has there been a lot of discussion on leadership lately? In the past 3 years, all the meetings I have attended had at least 1 presentation on leadership or the traits of leaders. Sometimes—even in the oddest places—I have come across an article with “leadership” in the title. In fact, a serendipitous discovery of 2 publications is what inspired me to write this.
I spotted the first one in a reading basket when I was on vacation: It was an interview with Benjamin Zander, the conductor of the Boston Philharmonic Orchestra and the Boston Philharmonic Youth Orchestra.1 I was especially interested to read this because when I was in graduate school, Benjamin (the father of one of my classmates) visited our campus to give a presentation on talent and self-confidence. I can still hear him conducting us to emphatically believe in ourselves and others. This was echoed in his interview: “Never doubt the capacity of the people you lead to accomplish whatever you dream for them.” What a powerful concept: Believe in the possibilities of someone!
The second was an American Legion Auxiliary column, which emphasized that “leadership is not a title, but a responsibility.”2 This struck a chord with me because some prominent leaders don’t appear to ascribe to that assessment (although they should!).
After digesting these articles, I started thinking: What, exactly, is leadership? What do we even mean by leadership? How do we measure it? Is it measurable? How do we know when we see or experience good leadership? Can one learn to become a leader by simply reading a “how-to” article?
I think I can answer these questions with 2 principles that have guided me through my career as an NP: (1) Make use of another leader’s expertise to guide you, and (2) Continue to grow amid any setbacks.
For example, my transition from a full-time clinician to a Health Policy Coordinator or “policy wonk” did not have a distinct trajectory. Although my core set of clinical skills were essential, I knew early on that I had to expand by adapting specific organizational skills that would enable me to grow in my new role. But how was I to prioritize which skills to improve? More than a simple trial-and-error approach was required; I needed guidance. Fortunately, my new boss was willing to share her experience and the lessons she learned on the job. Key among them was to recognize the skills I already had—communicating and coordinating—and to develop those skills to be more effective in my new position.
Later in my career, I worked with colleagues to pursue legislation for NP prescriptive authority in Massachusetts. The political arena of Commonwealth’s health care laws was especially pivotal in changing how I saw setbacks. These weren’t to be accepted as a failure but as a challenge to figure out how to better succeed the next time. For several years, I was told “No” before we finally got a bill passed. But each round of my testimony was an opportunity to educate lawmakers and the public on the valuable role of NPs and the quality of care we provide. I try to share this story with new NPs as a good example of why they should persist through adversity.
Continue to: Over the next 3 weeks...
Over the next 3 weeks, join us on Thursdays as we continue to discuss what it means to be a leader—from the pitfalls to the victories. For those who are leaders or who work for one, please share your thoughts, experiences, and lessons learned. Maybe you can give a shoutout to someone who was a positive influence!
1. Labarre P. Leadership—Ben Zander. Fast Company website. www.fastcompany.com/35825/leadership-ben-zander. Published November 30, 1998. Accessed August 27, 2019.
2. Volunteer beyond the ALA: serve on boards, committees. American Legion Auxiliary. November 2018:29.
1. Labarre P. Leadership—Ben Zander. Fast Company website. www.fastcompany.com/35825/leadership-ben-zander. Published November 30, 1998. Accessed August 27, 2019.
2. Volunteer beyond the ALA: serve on boards, committees. American Legion Auxiliary. November 2018:29.
VA Pathologist Indicted for Patient Deaths Due to Misdiagnoses
Levy was chief pathologist at Veterans Health Care System of the Ozarks in Fayetteville, Arkansas. During his 12-year tenure at the US Department of Veterans Affairs (VA), he read almost 34,000 pathology slides. However, at the same time, he was working under the influence of alcohol and 2-methyl-2-butanol (2M2B)—a substance that intoxicates but cannot be detected in routine tests.
The VA fired Levy last year, and the VA Office of the Inspector General (OIG) began an investigation of his actions and of agency lapses in overseeing him. The 18-month review found that 8.9% of Levy’s diagnoses involved clinical errors—the normal misdiagnosis rate for pathologists is 0.7%. Hundreds of Levy’s misdiagnoses were not serious, but ≥ 15 may have led to deaths and harmful illness in 15 other patients. Some patients were not diagnosed when they should have been. Some were told they were sick when they were not and suffered unnecessary invasive treatment.
Levy knowingly falsified diagnoses for 3 veterans. One patient was diagnosed with diffuse large B-cell lymphoma—a type of cancer he did not have. He received the wrong treatment and died. Levy diagnosed another patient, also wrongly, with small cell carcinoma; that patient died of squamous cell carcinoma that spread. The third patient was given a benign test result for prostate cancer. Untreated, he died after the cancer spread.
One patient was given antibiotics instead of treatment for what was later diagnosed as late-stage neck and throat cancer. In an interview with the Washington Post he said, “I went from ‘Your earache isn’t anything’ to stage 4.”
How was Levy able to wreak such havoc? One reason was that despite concerns and complaints from colleagues, he looked good on paper. He falsified records to indicate that his deputy concurred with his diagnoses in mandated peer reviews. He also appeared “clean” in inspections through using 2M2B.
Levy was fired not for his work performance but for being arrested for driving while intoxicated. He had been a “star hire” with an medical degree from the University of Chicago, who had completed a pathology residency at the University of California at San Francisco and a fellowship at Duke University focusing on disease of the blood. But he also had a 1996 arrest for a driving under the influence (DUI) on his record when he joined the VA in 2005.
In 2015, a fact-finding panel interviewed Levy about reports that he was under the influence while on duty. He denied the allegations. In 2016, Levy arrived at the radiology department to assist with a biopsy with a blood alcohol level of nearly 0.4. He was suspended, his alcohol impairment was reported to the state medical boards, and his medical privileges were revoked. He entered a VA treatment program in 2016, then returned to work. Levy, who also sat on oversight boards and medical committees, seemed drowsy and was speaking “nonsense” at an October 2017 meeting of the hospital’s tumor board, according to meeting minutes provided to The Post.
He was suspended again in 2017 for being under the influence but allowed to continue with nonclinical work until he was again arrested for DUI in 2018, when the police toxicology test detected 2M2B. He was finally dismissed in April 2018. Nonetheless, even after he had arrived impaired at the laboratory twice, the VA had awarded him 2 performance bonuses, based on the supposedly low clinical error rate and 42 urine and blood samples that turned up negative for alcohol and drugs.
In addition to 3 counts of involuntary manslaughter, the indictment charges that Levy devised a scheme to defraud the VA and to obtain money and property from the VA in the form of salary, benefits, and performance awards. He is charged with 12 counts of wire fraud, 12 counts of mail fraud, and 4 counts of making false statements related to 12 occasions between 2017 and 2018, when Levy was reportedly buying 2M2B over the Internet while he was contractually obligated to submit to random drug and alcohol screens.
After being fired, Levy moved to a small island in the Dutch Caribbean and found a position teaching pathology at a local medical school. At the time of his VA hiring, Levy held a medical license issued by Mississippi. His active medical licenses in California and Florida were revoked only this spring. The VA did not notify the3 states where Levy was licensed that he could no longer practice until June 2018.
The Office of Inspector General (OIG) has identified other VA physicians who continued to practice even after they were found to have compromised patient care, and the Government Accountability Office found “weak systems” for ensuring that problems are addressed in a timely fashion. A VA spokesperson, however, quoted in The Washington Post, said the Levy case was “an isolated incident,” and that the agency has “strengthened internal controls” to ensure that errors are more quickly identified and addressed. The Fayetteville Medical Center also has increased monitoring of its clinical laboratory, according to a Washington Post report. VA officials also said they have added oversight of small specialty staffs across the system to ensure “independent and objective oversight.”
The VA has contacted the families in the 30 most serious cases to advise them of their legal and treatment options, according to the Washington Post.
“The arrest of Dr. Levy was accomplished as a result of the strong leadership of the US Attorney’s Office and the extensive work of special agents of the VA OIG, supported by the medical expertise of the OIG’s health care inspection professionals,” said Michael Missal, the VA’s inspector general, in a press release issued by the US Attorney’s Office in the Western District of Arkansas. “These charges send a clear signal that anyone entrusted with the care of veterans will be held accountable for placing them at risk by working while impaired or through other misconduct.”
Levy is in jail in Fayetteville. The trial date for his case is set for October 7.
Levy was chief pathologist at Veterans Health Care System of the Ozarks in Fayetteville, Arkansas. During his 12-year tenure at the US Department of Veterans Affairs (VA), he read almost 34,000 pathology slides. However, at the same time, he was working under the influence of alcohol and 2-methyl-2-butanol (2M2B)—a substance that intoxicates but cannot be detected in routine tests.
The VA fired Levy last year, and the VA Office of the Inspector General (OIG) began an investigation of his actions and of agency lapses in overseeing him. The 18-month review found that 8.9% of Levy’s diagnoses involved clinical errors—the normal misdiagnosis rate for pathologists is 0.7%. Hundreds of Levy’s misdiagnoses were not serious, but ≥ 15 may have led to deaths and harmful illness in 15 other patients. Some patients were not diagnosed when they should have been. Some were told they were sick when they were not and suffered unnecessary invasive treatment.
Levy knowingly falsified diagnoses for 3 veterans. One patient was diagnosed with diffuse large B-cell lymphoma—a type of cancer he did not have. He received the wrong treatment and died. Levy diagnosed another patient, also wrongly, with small cell carcinoma; that patient died of squamous cell carcinoma that spread. The third patient was given a benign test result for prostate cancer. Untreated, he died after the cancer spread.
One patient was given antibiotics instead of treatment for what was later diagnosed as late-stage neck and throat cancer. In an interview with the Washington Post he said, “I went from ‘Your earache isn’t anything’ to stage 4.”
How was Levy able to wreak such havoc? One reason was that despite concerns and complaints from colleagues, he looked good on paper. He falsified records to indicate that his deputy concurred with his diagnoses in mandated peer reviews. He also appeared “clean” in inspections through using 2M2B.
Levy was fired not for his work performance but for being arrested for driving while intoxicated. He had been a “star hire” with an medical degree from the University of Chicago, who had completed a pathology residency at the University of California at San Francisco and a fellowship at Duke University focusing on disease of the blood. But he also had a 1996 arrest for a driving under the influence (DUI) on his record when he joined the VA in 2005.
In 2015, a fact-finding panel interviewed Levy about reports that he was under the influence while on duty. He denied the allegations. In 2016, Levy arrived at the radiology department to assist with a biopsy with a blood alcohol level of nearly 0.4. He was suspended, his alcohol impairment was reported to the state medical boards, and his medical privileges were revoked. He entered a VA treatment program in 2016, then returned to work. Levy, who also sat on oversight boards and medical committees, seemed drowsy and was speaking “nonsense” at an October 2017 meeting of the hospital’s tumor board, according to meeting minutes provided to The Post.
He was suspended again in 2017 for being under the influence but allowed to continue with nonclinical work until he was again arrested for DUI in 2018, when the police toxicology test detected 2M2B. He was finally dismissed in April 2018. Nonetheless, even after he had arrived impaired at the laboratory twice, the VA had awarded him 2 performance bonuses, based on the supposedly low clinical error rate and 42 urine and blood samples that turned up negative for alcohol and drugs.
In addition to 3 counts of involuntary manslaughter, the indictment charges that Levy devised a scheme to defraud the VA and to obtain money and property from the VA in the form of salary, benefits, and performance awards. He is charged with 12 counts of wire fraud, 12 counts of mail fraud, and 4 counts of making false statements related to 12 occasions between 2017 and 2018, when Levy was reportedly buying 2M2B over the Internet while he was contractually obligated to submit to random drug and alcohol screens.
After being fired, Levy moved to a small island in the Dutch Caribbean and found a position teaching pathology at a local medical school. At the time of his VA hiring, Levy held a medical license issued by Mississippi. His active medical licenses in California and Florida were revoked only this spring. The VA did not notify the3 states where Levy was licensed that he could no longer practice until June 2018.
The Office of Inspector General (OIG) has identified other VA physicians who continued to practice even after they were found to have compromised patient care, and the Government Accountability Office found “weak systems” for ensuring that problems are addressed in a timely fashion. A VA spokesperson, however, quoted in The Washington Post, said the Levy case was “an isolated incident,” and that the agency has “strengthened internal controls” to ensure that errors are more quickly identified and addressed. The Fayetteville Medical Center also has increased monitoring of its clinical laboratory, according to a Washington Post report. VA officials also said they have added oversight of small specialty staffs across the system to ensure “independent and objective oversight.”
The VA has contacted the families in the 30 most serious cases to advise them of their legal and treatment options, according to the Washington Post.
“The arrest of Dr. Levy was accomplished as a result of the strong leadership of the US Attorney’s Office and the extensive work of special agents of the VA OIG, supported by the medical expertise of the OIG’s health care inspection professionals,” said Michael Missal, the VA’s inspector general, in a press release issued by the US Attorney’s Office in the Western District of Arkansas. “These charges send a clear signal that anyone entrusted with the care of veterans will be held accountable for placing them at risk by working while impaired or through other misconduct.”
Levy is in jail in Fayetteville. The trial date for his case is set for October 7.
Levy was chief pathologist at Veterans Health Care System of the Ozarks in Fayetteville, Arkansas. During his 12-year tenure at the US Department of Veterans Affairs (VA), he read almost 34,000 pathology slides. However, at the same time, he was working under the influence of alcohol and 2-methyl-2-butanol (2M2B)—a substance that intoxicates but cannot be detected in routine tests.
The VA fired Levy last year, and the VA Office of the Inspector General (OIG) began an investigation of his actions and of agency lapses in overseeing him. The 18-month review found that 8.9% of Levy’s diagnoses involved clinical errors—the normal misdiagnosis rate for pathologists is 0.7%. Hundreds of Levy’s misdiagnoses were not serious, but ≥ 15 may have led to deaths and harmful illness in 15 other patients. Some patients were not diagnosed when they should have been. Some were told they were sick when they were not and suffered unnecessary invasive treatment.
Levy knowingly falsified diagnoses for 3 veterans. One patient was diagnosed with diffuse large B-cell lymphoma—a type of cancer he did not have. He received the wrong treatment and died. Levy diagnosed another patient, also wrongly, with small cell carcinoma; that patient died of squamous cell carcinoma that spread. The third patient was given a benign test result for prostate cancer. Untreated, he died after the cancer spread.
One patient was given antibiotics instead of treatment for what was later diagnosed as late-stage neck and throat cancer. In an interview with the Washington Post he said, “I went from ‘Your earache isn’t anything’ to stage 4.”
How was Levy able to wreak such havoc? One reason was that despite concerns and complaints from colleagues, he looked good on paper. He falsified records to indicate that his deputy concurred with his diagnoses in mandated peer reviews. He also appeared “clean” in inspections through using 2M2B.
Levy was fired not for his work performance but for being arrested for driving while intoxicated. He had been a “star hire” with an medical degree from the University of Chicago, who had completed a pathology residency at the University of California at San Francisco and a fellowship at Duke University focusing on disease of the blood. But he also had a 1996 arrest for a driving under the influence (DUI) on his record when he joined the VA in 2005.
In 2015, a fact-finding panel interviewed Levy about reports that he was under the influence while on duty. He denied the allegations. In 2016, Levy arrived at the radiology department to assist with a biopsy with a blood alcohol level of nearly 0.4. He was suspended, his alcohol impairment was reported to the state medical boards, and his medical privileges were revoked. He entered a VA treatment program in 2016, then returned to work. Levy, who also sat on oversight boards and medical committees, seemed drowsy and was speaking “nonsense” at an October 2017 meeting of the hospital’s tumor board, according to meeting minutes provided to The Post.
He was suspended again in 2017 for being under the influence but allowed to continue with nonclinical work until he was again arrested for DUI in 2018, when the police toxicology test detected 2M2B. He was finally dismissed in April 2018. Nonetheless, even after he had arrived impaired at the laboratory twice, the VA had awarded him 2 performance bonuses, based on the supposedly low clinical error rate and 42 urine and blood samples that turned up negative for alcohol and drugs.
In addition to 3 counts of involuntary manslaughter, the indictment charges that Levy devised a scheme to defraud the VA and to obtain money and property from the VA in the form of salary, benefits, and performance awards. He is charged with 12 counts of wire fraud, 12 counts of mail fraud, and 4 counts of making false statements related to 12 occasions between 2017 and 2018, when Levy was reportedly buying 2M2B over the Internet while he was contractually obligated to submit to random drug and alcohol screens.
After being fired, Levy moved to a small island in the Dutch Caribbean and found a position teaching pathology at a local medical school. At the time of his VA hiring, Levy held a medical license issued by Mississippi. His active medical licenses in California and Florida were revoked only this spring. The VA did not notify the3 states where Levy was licensed that he could no longer practice until June 2018.
The Office of Inspector General (OIG) has identified other VA physicians who continued to practice even after they were found to have compromised patient care, and the Government Accountability Office found “weak systems” for ensuring that problems are addressed in a timely fashion. A VA spokesperson, however, quoted in The Washington Post, said the Levy case was “an isolated incident,” and that the agency has “strengthened internal controls” to ensure that errors are more quickly identified and addressed. The Fayetteville Medical Center also has increased monitoring of its clinical laboratory, according to a Washington Post report. VA officials also said they have added oversight of small specialty staffs across the system to ensure “independent and objective oversight.”
The VA has contacted the families in the 30 most serious cases to advise them of their legal and treatment options, according to the Washington Post.
“The arrest of Dr. Levy was accomplished as a result of the strong leadership of the US Attorney’s Office and the extensive work of special agents of the VA OIG, supported by the medical expertise of the OIG’s health care inspection professionals,” said Michael Missal, the VA’s inspector general, in a press release issued by the US Attorney’s Office in the Western District of Arkansas. “These charges send a clear signal that anyone entrusted with the care of veterans will be held accountable for placing them at risk by working while impaired or through other misconduct.”
Levy is in jail in Fayetteville. The trial date for his case is set for October 7.
Clinical trial enrollment linked to lower death rate in lung cancer patients
ALEXANDRIA, VA. – Patients with metastatic non–small cell lung cancer (NSCLC) who enrolled in clinical trials had a near 50% lower risk of death versus patients who received treatment outside a clinical trial, according to results of a single-center, retrospective medical record review.
Median survival was almost doubled for those patients with NSCLC enrolled in therapeutic drug trials, according to lead author Christina Merkhofer, MD, a hematology-oncology fellow at the University of Washington and Fred Hutchinson Cancer Center, both in Seattle.
The findings suggest that clinical trials, beyond supporting drug development, provide a direct benefit to NSCLC patients through provision of promising agents, enhanced supportive care, or both, according to Dr. Merkhofer and coauthors, who will present their findings in a poster at the Quality Care Symposium, sponsored by the American Society of Clinical Oncology.
The retrospective study included a total of 371 patients diagnosed with metastatic NSCLC between 2001 and 2015, of whom 118 (32%) enrolled in at least one clinical trial, Dr. Merkhofer reported at a press briefing ahead of the symposium.
Median survival was 838 days for the clinical trial enrollees versus 454 days for nonenrollees, according to the investigators. The risk of death was 47% lower (hazard ratio, 0.53; 95% confidence interval, 0.13-0.92; P = .002) for enrollees relative to nonenrollees after adjustment for variables including sex, performance status, smoking history, histology, presence of brain metastases, and EGFR/ALK status.
Based on this study by Dr. Merkhofer and colleagues, participating in therapeutic drug trials appears to improve survival in patients with advanced lung cancer, ASCO expert Merry-Jennifer Markham, MD, said in a statement.
Oncologists have a “duty” to enroll patients in clinical trials as appropriate, said Dr. Markham, chair of the Quality Care Symposium’s news planning team.
“We must work to better understand factors associated with enrollment so that the prospective benefits can be made accessible to all who are eligible,” she said.
The research is part of a larger investigation looking at “areas of uncertainty” in clinical trial participation, such as whether specific trial design characteristics are linked to survival benefit, according to Dr. Merkhofer.
“The study can support research evaluating health care policies or research that looks at incentives for patient participation in trials, such as financing transportation or lodging, [and] can help with research that addresses some of these important barriers to trial participation,” Dr. Merkhofer said in an ASCO press release.
Dr. Merkhofer had no disclosures related to the study. Her coauthors reported disclosures related to numerous pharmaceutical companies.
SOURCE: Merkhofer C et al. QCS2019, Abstract 137.
ALEXANDRIA, VA. – Patients with metastatic non–small cell lung cancer (NSCLC) who enrolled in clinical trials had a near 50% lower risk of death versus patients who received treatment outside a clinical trial, according to results of a single-center, retrospective medical record review.
Median survival was almost doubled for those patients with NSCLC enrolled in therapeutic drug trials, according to lead author Christina Merkhofer, MD, a hematology-oncology fellow at the University of Washington and Fred Hutchinson Cancer Center, both in Seattle.
The findings suggest that clinical trials, beyond supporting drug development, provide a direct benefit to NSCLC patients through provision of promising agents, enhanced supportive care, or both, according to Dr. Merkhofer and coauthors, who will present their findings in a poster at the Quality Care Symposium, sponsored by the American Society of Clinical Oncology.
The retrospective study included a total of 371 patients diagnosed with metastatic NSCLC between 2001 and 2015, of whom 118 (32%) enrolled in at least one clinical trial, Dr. Merkhofer reported at a press briefing ahead of the symposium.
Median survival was 838 days for the clinical trial enrollees versus 454 days for nonenrollees, according to the investigators. The risk of death was 47% lower (hazard ratio, 0.53; 95% confidence interval, 0.13-0.92; P = .002) for enrollees relative to nonenrollees after adjustment for variables including sex, performance status, smoking history, histology, presence of brain metastases, and EGFR/ALK status.
Based on this study by Dr. Merkhofer and colleagues, participating in therapeutic drug trials appears to improve survival in patients with advanced lung cancer, ASCO expert Merry-Jennifer Markham, MD, said in a statement.
Oncologists have a “duty” to enroll patients in clinical trials as appropriate, said Dr. Markham, chair of the Quality Care Symposium’s news planning team.
“We must work to better understand factors associated with enrollment so that the prospective benefits can be made accessible to all who are eligible,” she said.
The research is part of a larger investigation looking at “areas of uncertainty” in clinical trial participation, such as whether specific trial design characteristics are linked to survival benefit, according to Dr. Merkhofer.
“The study can support research evaluating health care policies or research that looks at incentives for patient participation in trials, such as financing transportation or lodging, [and] can help with research that addresses some of these important barriers to trial participation,” Dr. Merkhofer said in an ASCO press release.
Dr. Merkhofer had no disclosures related to the study. Her coauthors reported disclosures related to numerous pharmaceutical companies.
SOURCE: Merkhofer C et al. QCS2019, Abstract 137.
ALEXANDRIA, VA. – Patients with metastatic non–small cell lung cancer (NSCLC) who enrolled in clinical trials had a near 50% lower risk of death versus patients who received treatment outside a clinical trial, according to results of a single-center, retrospective medical record review.
Median survival was almost doubled for those patients with NSCLC enrolled in therapeutic drug trials, according to lead author Christina Merkhofer, MD, a hematology-oncology fellow at the University of Washington and Fred Hutchinson Cancer Center, both in Seattle.
The findings suggest that clinical trials, beyond supporting drug development, provide a direct benefit to NSCLC patients through provision of promising agents, enhanced supportive care, or both, according to Dr. Merkhofer and coauthors, who will present their findings in a poster at the Quality Care Symposium, sponsored by the American Society of Clinical Oncology.
The retrospective study included a total of 371 patients diagnosed with metastatic NSCLC between 2001 and 2015, of whom 118 (32%) enrolled in at least one clinical trial, Dr. Merkhofer reported at a press briefing ahead of the symposium.
Median survival was 838 days for the clinical trial enrollees versus 454 days for nonenrollees, according to the investigators. The risk of death was 47% lower (hazard ratio, 0.53; 95% confidence interval, 0.13-0.92; P = .002) for enrollees relative to nonenrollees after adjustment for variables including sex, performance status, smoking history, histology, presence of brain metastases, and EGFR/ALK status.
Based on this study by Dr. Merkhofer and colleagues, participating in therapeutic drug trials appears to improve survival in patients with advanced lung cancer, ASCO expert Merry-Jennifer Markham, MD, said in a statement.
Oncologists have a “duty” to enroll patients in clinical trials as appropriate, said Dr. Markham, chair of the Quality Care Symposium’s news planning team.
“We must work to better understand factors associated with enrollment so that the prospective benefits can be made accessible to all who are eligible,” she said.
The research is part of a larger investigation looking at “areas of uncertainty” in clinical trial participation, such as whether specific trial design characteristics are linked to survival benefit, according to Dr. Merkhofer.
“The study can support research evaluating health care policies or research that looks at incentives for patient participation in trials, such as financing transportation or lodging, [and] can help with research that addresses some of these important barriers to trial participation,” Dr. Merkhofer said in an ASCO press release.
Dr. Merkhofer had no disclosures related to the study. Her coauthors reported disclosures related to numerous pharmaceutical companies.
SOURCE: Merkhofer C et al. QCS2019, Abstract 137.
REPORTING FROM QCS 2019
Predicted risk of cardiac complications varies among risk calculators
Background: A critical juncture in the American Heart Association/American College of Cardiology 2014 perioperative guidelines relies on clinicians categorizing patients undergoing noncardiac surgery as either low risk (less than 1%) or elevated risk (greater than or equal to 1%) for a MACE. The purpose of this study is to determine whether there is variability between the three risk calculators endorsed by the ACC/AHA guidelines as prediction tools to make this risk stratification.
Study design: Retrospective observational study.
Setting: National Surgical Quality Improvement Program database.
Synopsis: The NSQIP database was used to identify 10,000 patients who had undergone noncardiac surgery. The risk of MACE for each patient was then calculated using the Revised Cardiac Risk Index, the American College of Surgeons National Surgical Quality Improvement Program Surgical Risk Calculator, and the National Surgical Quality Improvement Program Myocardial Infarction or Cardiac Arrest calculator. Data were analyzed using the intraclass correlation coefficient and kappa analysis. Results demonstrated that 29% of the time the three calculators disagreed on which patients were classified as low risk. This suggests that, when following the ACC/AHA perioperative guidelines, a recommendation for further preoperative cardiac testing may depend on which risk prediction tool is used to calculate the risk of MACE.
Bottom line: Nearly one-third of the time, the three risk calculators recommended in the ACC/AHA 2014 perioperative guidelines do not agree on which patients are classified as low risk; this may affect clinical decision making for some patients.
Citation: Glance LG et al. Impact of the choice of risk model for identifying low-risk patients using the 2014 American College of Cardiology/American Heart Association perioperative guidelines. Anesthesiology. 2018;129(5):889-900.
Dr. Bordin-Wosk is an assistant clinical professor in the division of hospital medicine at the University of California, San Diego.
Background: A critical juncture in the American Heart Association/American College of Cardiology 2014 perioperative guidelines relies on clinicians categorizing patients undergoing noncardiac surgery as either low risk (less than 1%) or elevated risk (greater than or equal to 1%) for a MACE. The purpose of this study is to determine whether there is variability between the three risk calculators endorsed by the ACC/AHA guidelines as prediction tools to make this risk stratification.
Study design: Retrospective observational study.
Setting: National Surgical Quality Improvement Program database.
Synopsis: The NSQIP database was used to identify 10,000 patients who had undergone noncardiac surgery. The risk of MACE for each patient was then calculated using the Revised Cardiac Risk Index, the American College of Surgeons National Surgical Quality Improvement Program Surgical Risk Calculator, and the National Surgical Quality Improvement Program Myocardial Infarction or Cardiac Arrest calculator. Data were analyzed using the intraclass correlation coefficient and kappa analysis. Results demonstrated that 29% of the time the three calculators disagreed on which patients were classified as low risk. This suggests that, when following the ACC/AHA perioperative guidelines, a recommendation for further preoperative cardiac testing may depend on which risk prediction tool is used to calculate the risk of MACE.
Bottom line: Nearly one-third of the time, the three risk calculators recommended in the ACC/AHA 2014 perioperative guidelines do not agree on which patients are classified as low risk; this may affect clinical decision making for some patients.
Citation: Glance LG et al. Impact of the choice of risk model for identifying low-risk patients using the 2014 American College of Cardiology/American Heart Association perioperative guidelines. Anesthesiology. 2018;129(5):889-900.
Dr. Bordin-Wosk is an assistant clinical professor in the division of hospital medicine at the University of California, San Diego.
Background: A critical juncture in the American Heart Association/American College of Cardiology 2014 perioperative guidelines relies on clinicians categorizing patients undergoing noncardiac surgery as either low risk (less than 1%) or elevated risk (greater than or equal to 1%) for a MACE. The purpose of this study is to determine whether there is variability between the three risk calculators endorsed by the ACC/AHA guidelines as prediction tools to make this risk stratification.
Study design: Retrospective observational study.
Setting: National Surgical Quality Improvement Program database.
Synopsis: The NSQIP database was used to identify 10,000 patients who had undergone noncardiac surgery. The risk of MACE for each patient was then calculated using the Revised Cardiac Risk Index, the American College of Surgeons National Surgical Quality Improvement Program Surgical Risk Calculator, and the National Surgical Quality Improvement Program Myocardial Infarction or Cardiac Arrest calculator. Data were analyzed using the intraclass correlation coefficient and kappa analysis. Results demonstrated that 29% of the time the three calculators disagreed on which patients were classified as low risk. This suggests that, when following the ACC/AHA perioperative guidelines, a recommendation for further preoperative cardiac testing may depend on which risk prediction tool is used to calculate the risk of MACE.
Bottom line: Nearly one-third of the time, the three risk calculators recommended in the ACC/AHA 2014 perioperative guidelines do not agree on which patients are classified as low risk; this may affect clinical decision making for some patients.
Citation: Glance LG et al. Impact of the choice of risk model for identifying low-risk patients using the 2014 American College of Cardiology/American Heart Association perioperative guidelines. Anesthesiology. 2018;129(5):889-900.
Dr. Bordin-Wosk is an assistant clinical professor in the division of hospital medicine at the University of California, San Diego.
Diagnosis and management of gastroparesis and functional dyspepsia pose challenges
CHICAGO – Because gastroparesis and functional dyspepsia share several symptoms (e.g., upper abdominal pain, fullness, and bloating) and pathophysiological abnormalities (e.g., delayed gastric emptying, impaired gastric accommodation, and visceral hypersensitivity), it can be hard to distinguish the two conditions, according to a lecture presented at Freston Conference 2019, sponsored by the American Gastroenterological Association. Additional research into the role of diet in these conditions will improve the treatment of these patients, said Linda Nguyen, MD, director of neurogastroenterology and motility at Stanford (Calif.) University.
Distinguishing the disorders
The accepted definition of gastroparesis is abnormal gastric emptying in the absence of a mechanical obstruction. The condition’s symptoms include nausea, vomiting, bloating, early satiety, abdominal pain, and weight loss. A previous consensus held that if a patient had abdominal pain, he or she did not have gastroparesis. Yet studies indicate that up to 80% of patients with gastroparesis have pain.
Functional dyspepsia is defined as bothersome postprandial fullness, early satiety, and epigastric pain or burning in the absence of structural abnormality. The disorder can be subdivided into postprandial distress (i.e., meal-related symptomatology) and epigastric pain syndrome (i.e., pain or burning that may or may not be related to meals). Either of these alternatives may entail nausea and vomiting.
Comparing the pathophysiologies of gastroparesis and functional dyspepsia helps to distinguish these disorders from each other. A 2019 review described rapid gastric emptying and duodenal eosinophilia in patients with functional dyspepsia, but not in patients with gastroparesis. Patients with epigastric pain syndrome had sensitivity to acid, bile, and fats. Patients with idiopathic gastroparesis, which is the most common type, had a weak antral pump and abnormal duodenal feedback, but patients with functional dyspepsia did not have these characteristics (J Neurogastroenterol Motil. 2019;25[1]:27-35).
Examining symptoms and severity
One examination of patients with gastroparesis found that approximately 46% of them had a body mass index of 25 or greater. About 26% of patients had a BMI greater than 30. Yet these patients were eating less than 60% of their recommended daily allowances, based on their age, height, weight, and sex (Clin Gastroenterol Hepatol. 2011;9[12]:1056-64).
Accelerating gastric emptying may not relieve symptoms completely in a patient with gastroparesis, said Dr. Nguyen. A 2007 study of patients with gastroparesis found that 43% had impaired accommodation, and 29% had visceral hypersensitivity (Gut. 2007;56[1]:29-36). The same data indicated that gastric emptying time was not correlated with symptom severity. Impaired accommodation, however, was associated with early satiety and weight loss. Visceral hypersensitivity was associated with pain, early satiety, and weight loss. These data suggest that accommodation and visceral hypersensitivity may influence symptom severity in gastroparesis, said Dr. Nguyen.
Other researchers compared mild, moderate, and severe symptoms of early satiety in patients with gastroparesis. They found that patients with severe symptoms of early satiety have more delayed gastric emptying than do patients with mild or moderate symptoms of early satiety (Neurogastroenterol Motil. 2017;29[4].).
Dr. Nguyen and colleagues examined normal gastric emptying, compared with severely delayed gastric emptying, which they defined as greater than 35% retention at 4 hours. They found that severely delayed gastric emptying was associated with more severe symptoms, particularly nausea and vomiting, as measured by Gastroparesis Cardinal Symptom Index (GCSI). Extreme symptoms may help differentiate between gastroparesis and functional dyspepsia, said Dr. Nguyen.
Dietary and pharmacologic treatment
Although clinicians might consider recommending dietary modifications to treat gastroparesis or functional dyspepsia, the literature contains little evidence about their efficacy in these indications, said Dr. Nguyen. Based on a study by Tack and colleagues, some clinicians recommend small, frequent meals that are low in fat and low in fiber to patients with gastroparesis. Such a diet could be harmful, however, to patients with comorbid diabetes, irritable bowel syndrome, or renal failure.
Common dietary recommendations for functional dyspepsia include small, frequent meals; decreased fat consumption; and avoidance of citrus and spicy foods. These recommendations are based on small studies in which patients reported which foods tended to cause their symptoms. Trials of dietary modifications in functional dyspepsia, however, are lacking.
Nevertheless, the literature can guide the selection of pharmacotherapy for these disorders. Talley et al. examined the effects of neuromodulators such as amitriptyline, a tricyclic antidepressant, and escitalopram in functional dyspepsia. About 70% of the sample had postprandial distress syndrome, and 20% met criteria for idiopathic gastroparesis. Amitriptyline provided greater symptomatic relief to these patients than did placebo, but escitalopram did not. Patients who met criteria for idiopathic gastroparesis did not respond well to tricyclic antidepressants, but patients with epigastric pain syndrome did. Furthermore, compared with patients with normal gastric emptying, those with delayed emptying did not respond to tricyclic antidepressants. A separate study found that the tricyclic antidepressant nortriptyline did not improve symptoms of gastroparesis (JAMA. 2013;310[24]:2640-9).
Promotility agents may be beneficial for certain patients. A study published this year suggests that, compared with placebo, prucalopride is effective for nausea, vomiting, fullness, bloating, and gastric emptying in patients with idiopathic gastroparesis (Am J Gastroenterol. 2019;114[8]:1265-74.). A 2017 meta-analysis, however, found that proton pump inhibitors were more effective than promotility agents in patients with functional dyspepsia (Am J Gastroenterol. 2017;112[7]:988-1013.).
Pyloric dysfunction may accompany gastroparesis in some patients. Increased severity of gastric emptying delay is associated with increased pylorospasm. Endoscopists have gained experience in performing pyloric myotomy, and this treatment has become more popular. Uncontrolled studies indicate that the proportion of patients with decreased symptom severity after this procedure is higher than 70% and can be as high as 86% (Gastrointest Endosc. 2017;85[1]:123-8). The predictors of a good response include idiopathic etiology, male sex, moderate symptom severity, and greater delay in gastric emptying.
Functional dyspepsia should perhaps be understood as normal gastric emptying and symptoms of epigastric pain syndrome, said Dr. Nguyen. Those patients may respond to neuromodulators, she added. Idiopathic gastroparesis appears to be characterized by severe delay in gastric emptying, postprandial symptoms, nausea, and vomiting. “In the middle is the gray zone, where you have these patients with postprandial distress with or without delayed gastric emptying,” said Dr. Nguyen. Functional dyspepsia and gastroparesis could be two ends of a spectrum, and the best management for patients with symptoms that occur in both disorders is unclear.
CHICAGO – Because gastroparesis and functional dyspepsia share several symptoms (e.g., upper abdominal pain, fullness, and bloating) and pathophysiological abnormalities (e.g., delayed gastric emptying, impaired gastric accommodation, and visceral hypersensitivity), it can be hard to distinguish the two conditions, according to a lecture presented at Freston Conference 2019, sponsored by the American Gastroenterological Association. Additional research into the role of diet in these conditions will improve the treatment of these patients, said Linda Nguyen, MD, director of neurogastroenterology and motility at Stanford (Calif.) University.
Distinguishing the disorders
The accepted definition of gastroparesis is abnormal gastric emptying in the absence of a mechanical obstruction. The condition’s symptoms include nausea, vomiting, bloating, early satiety, abdominal pain, and weight loss. A previous consensus held that if a patient had abdominal pain, he or she did not have gastroparesis. Yet studies indicate that up to 80% of patients with gastroparesis have pain.
Functional dyspepsia is defined as bothersome postprandial fullness, early satiety, and epigastric pain or burning in the absence of structural abnormality. The disorder can be subdivided into postprandial distress (i.e., meal-related symptomatology) and epigastric pain syndrome (i.e., pain or burning that may or may not be related to meals). Either of these alternatives may entail nausea and vomiting.
Comparing the pathophysiologies of gastroparesis and functional dyspepsia helps to distinguish these disorders from each other. A 2019 review described rapid gastric emptying and duodenal eosinophilia in patients with functional dyspepsia, but not in patients with gastroparesis. Patients with epigastric pain syndrome had sensitivity to acid, bile, and fats. Patients with idiopathic gastroparesis, which is the most common type, had a weak antral pump and abnormal duodenal feedback, but patients with functional dyspepsia did not have these characteristics (J Neurogastroenterol Motil. 2019;25[1]:27-35).
Examining symptoms and severity
One examination of patients with gastroparesis found that approximately 46% of them had a body mass index of 25 or greater. About 26% of patients had a BMI greater than 30. Yet these patients were eating less than 60% of their recommended daily allowances, based on their age, height, weight, and sex (Clin Gastroenterol Hepatol. 2011;9[12]:1056-64).
Accelerating gastric emptying may not relieve symptoms completely in a patient with gastroparesis, said Dr. Nguyen. A 2007 study of patients with gastroparesis found that 43% had impaired accommodation, and 29% had visceral hypersensitivity (Gut. 2007;56[1]:29-36). The same data indicated that gastric emptying time was not correlated with symptom severity. Impaired accommodation, however, was associated with early satiety and weight loss. Visceral hypersensitivity was associated with pain, early satiety, and weight loss. These data suggest that accommodation and visceral hypersensitivity may influence symptom severity in gastroparesis, said Dr. Nguyen.
Other researchers compared mild, moderate, and severe symptoms of early satiety in patients with gastroparesis. They found that patients with severe symptoms of early satiety have more delayed gastric emptying than do patients with mild or moderate symptoms of early satiety (Neurogastroenterol Motil. 2017;29[4].).
Dr. Nguyen and colleagues examined normal gastric emptying, compared with severely delayed gastric emptying, which they defined as greater than 35% retention at 4 hours. They found that severely delayed gastric emptying was associated with more severe symptoms, particularly nausea and vomiting, as measured by Gastroparesis Cardinal Symptom Index (GCSI). Extreme symptoms may help differentiate between gastroparesis and functional dyspepsia, said Dr. Nguyen.
Dietary and pharmacologic treatment
Although clinicians might consider recommending dietary modifications to treat gastroparesis or functional dyspepsia, the literature contains little evidence about their efficacy in these indications, said Dr. Nguyen. Based on a study by Tack and colleagues, some clinicians recommend small, frequent meals that are low in fat and low in fiber to patients with gastroparesis. Such a diet could be harmful, however, to patients with comorbid diabetes, irritable bowel syndrome, or renal failure.
Common dietary recommendations for functional dyspepsia include small, frequent meals; decreased fat consumption; and avoidance of citrus and spicy foods. These recommendations are based on small studies in which patients reported which foods tended to cause their symptoms. Trials of dietary modifications in functional dyspepsia, however, are lacking.
Nevertheless, the literature can guide the selection of pharmacotherapy for these disorders. Talley et al. examined the effects of neuromodulators such as amitriptyline, a tricyclic antidepressant, and escitalopram in functional dyspepsia. About 70% of the sample had postprandial distress syndrome, and 20% met criteria for idiopathic gastroparesis. Amitriptyline provided greater symptomatic relief to these patients than did placebo, but escitalopram did not. Patients who met criteria for idiopathic gastroparesis did not respond well to tricyclic antidepressants, but patients with epigastric pain syndrome did. Furthermore, compared with patients with normal gastric emptying, those with delayed emptying did not respond to tricyclic antidepressants. A separate study found that the tricyclic antidepressant nortriptyline did not improve symptoms of gastroparesis (JAMA. 2013;310[24]:2640-9).
Promotility agents may be beneficial for certain patients. A study published this year suggests that, compared with placebo, prucalopride is effective for nausea, vomiting, fullness, bloating, and gastric emptying in patients with idiopathic gastroparesis (Am J Gastroenterol. 2019;114[8]:1265-74.). A 2017 meta-analysis, however, found that proton pump inhibitors were more effective than promotility agents in patients with functional dyspepsia (Am J Gastroenterol. 2017;112[7]:988-1013.).
Pyloric dysfunction may accompany gastroparesis in some patients. Increased severity of gastric emptying delay is associated with increased pylorospasm. Endoscopists have gained experience in performing pyloric myotomy, and this treatment has become more popular. Uncontrolled studies indicate that the proportion of patients with decreased symptom severity after this procedure is higher than 70% and can be as high as 86% (Gastrointest Endosc. 2017;85[1]:123-8). The predictors of a good response include idiopathic etiology, male sex, moderate symptom severity, and greater delay in gastric emptying.
Functional dyspepsia should perhaps be understood as normal gastric emptying and symptoms of epigastric pain syndrome, said Dr. Nguyen. Those patients may respond to neuromodulators, she added. Idiopathic gastroparesis appears to be characterized by severe delay in gastric emptying, postprandial symptoms, nausea, and vomiting. “In the middle is the gray zone, where you have these patients with postprandial distress with or without delayed gastric emptying,” said Dr. Nguyen. Functional dyspepsia and gastroparesis could be two ends of a spectrum, and the best management for patients with symptoms that occur in both disorders is unclear.
CHICAGO – Because gastroparesis and functional dyspepsia share several symptoms (e.g., upper abdominal pain, fullness, and bloating) and pathophysiological abnormalities (e.g., delayed gastric emptying, impaired gastric accommodation, and visceral hypersensitivity), it can be hard to distinguish the two conditions, according to a lecture presented at Freston Conference 2019, sponsored by the American Gastroenterological Association. Additional research into the role of diet in these conditions will improve the treatment of these patients, said Linda Nguyen, MD, director of neurogastroenterology and motility at Stanford (Calif.) University.
Distinguishing the disorders
The accepted definition of gastroparesis is abnormal gastric emptying in the absence of a mechanical obstruction. The condition’s symptoms include nausea, vomiting, bloating, early satiety, abdominal pain, and weight loss. A previous consensus held that if a patient had abdominal pain, he or she did not have gastroparesis. Yet studies indicate that up to 80% of patients with gastroparesis have pain.
Functional dyspepsia is defined as bothersome postprandial fullness, early satiety, and epigastric pain or burning in the absence of structural abnormality. The disorder can be subdivided into postprandial distress (i.e., meal-related symptomatology) and epigastric pain syndrome (i.e., pain or burning that may or may not be related to meals). Either of these alternatives may entail nausea and vomiting.
Comparing the pathophysiologies of gastroparesis and functional dyspepsia helps to distinguish these disorders from each other. A 2019 review described rapid gastric emptying and duodenal eosinophilia in patients with functional dyspepsia, but not in patients with gastroparesis. Patients with epigastric pain syndrome had sensitivity to acid, bile, and fats. Patients with idiopathic gastroparesis, which is the most common type, had a weak antral pump and abnormal duodenal feedback, but patients with functional dyspepsia did not have these characteristics (J Neurogastroenterol Motil. 2019;25[1]:27-35).
Examining symptoms and severity
One examination of patients with gastroparesis found that approximately 46% of them had a body mass index of 25 or greater. About 26% of patients had a BMI greater than 30. Yet these patients were eating less than 60% of their recommended daily allowances, based on their age, height, weight, and sex (Clin Gastroenterol Hepatol. 2011;9[12]:1056-64).
Accelerating gastric emptying may not relieve symptoms completely in a patient with gastroparesis, said Dr. Nguyen. A 2007 study of patients with gastroparesis found that 43% had impaired accommodation, and 29% had visceral hypersensitivity (Gut. 2007;56[1]:29-36). The same data indicated that gastric emptying time was not correlated with symptom severity. Impaired accommodation, however, was associated with early satiety and weight loss. Visceral hypersensitivity was associated with pain, early satiety, and weight loss. These data suggest that accommodation and visceral hypersensitivity may influence symptom severity in gastroparesis, said Dr. Nguyen.
Other researchers compared mild, moderate, and severe symptoms of early satiety in patients with gastroparesis. They found that patients with severe symptoms of early satiety have more delayed gastric emptying than do patients with mild or moderate symptoms of early satiety (Neurogastroenterol Motil. 2017;29[4].).
Dr. Nguyen and colleagues examined normal gastric emptying, compared with severely delayed gastric emptying, which they defined as greater than 35% retention at 4 hours. They found that severely delayed gastric emptying was associated with more severe symptoms, particularly nausea and vomiting, as measured by Gastroparesis Cardinal Symptom Index (GCSI). Extreme symptoms may help differentiate between gastroparesis and functional dyspepsia, said Dr. Nguyen.
Dietary and pharmacologic treatment
Although clinicians might consider recommending dietary modifications to treat gastroparesis or functional dyspepsia, the literature contains little evidence about their efficacy in these indications, said Dr. Nguyen. Based on a study by Tack and colleagues, some clinicians recommend small, frequent meals that are low in fat and low in fiber to patients with gastroparesis. Such a diet could be harmful, however, to patients with comorbid diabetes, irritable bowel syndrome, or renal failure.
Common dietary recommendations for functional dyspepsia include small, frequent meals; decreased fat consumption; and avoidance of citrus and spicy foods. These recommendations are based on small studies in which patients reported which foods tended to cause their symptoms. Trials of dietary modifications in functional dyspepsia, however, are lacking.
Nevertheless, the literature can guide the selection of pharmacotherapy for these disorders. Talley et al. examined the effects of neuromodulators such as amitriptyline, a tricyclic antidepressant, and escitalopram in functional dyspepsia. About 70% of the sample had postprandial distress syndrome, and 20% met criteria for idiopathic gastroparesis. Amitriptyline provided greater symptomatic relief to these patients than did placebo, but escitalopram did not. Patients who met criteria for idiopathic gastroparesis did not respond well to tricyclic antidepressants, but patients with epigastric pain syndrome did. Furthermore, compared with patients with normal gastric emptying, those with delayed emptying did not respond to tricyclic antidepressants. A separate study found that the tricyclic antidepressant nortriptyline did not improve symptoms of gastroparesis (JAMA. 2013;310[24]:2640-9).
Promotility agents may be beneficial for certain patients. A study published this year suggests that, compared with placebo, prucalopride is effective for nausea, vomiting, fullness, bloating, and gastric emptying in patients with idiopathic gastroparesis (Am J Gastroenterol. 2019;114[8]:1265-74.). A 2017 meta-analysis, however, found that proton pump inhibitors were more effective than promotility agents in patients with functional dyspepsia (Am J Gastroenterol. 2017;112[7]:988-1013.).
Pyloric dysfunction may accompany gastroparesis in some patients. Increased severity of gastric emptying delay is associated with increased pylorospasm. Endoscopists have gained experience in performing pyloric myotomy, and this treatment has become more popular. Uncontrolled studies indicate that the proportion of patients with decreased symptom severity after this procedure is higher than 70% and can be as high as 86% (Gastrointest Endosc. 2017;85[1]:123-8). The predictors of a good response include idiopathic etiology, male sex, moderate symptom severity, and greater delay in gastric emptying.
Functional dyspepsia should perhaps be understood as normal gastric emptying and symptoms of epigastric pain syndrome, said Dr. Nguyen. Those patients may respond to neuromodulators, she added. Idiopathic gastroparesis appears to be characterized by severe delay in gastric emptying, postprandial symptoms, nausea, and vomiting. “In the middle is the gray zone, where you have these patients with postprandial distress with or without delayed gastric emptying,” said Dr. Nguyen. Functional dyspepsia and gastroparesis could be two ends of a spectrum, and the best management for patients with symptoms that occur in both disorders is unclear.
EXPERT ANALYSIS FROM FRESTON CONFERENCE 2019
Out-of-pocket cost of oral TKIs linked to poor lung cancer survival
ALEXANDRIA, VA. – Higher out-of-pocket costs for oral tyrosine kinase inhibitors (TKIs) were linked to inferior survival in patients with advanced, biomarker-positive lung cancers in an analysis of state-level registry data, an investigator reported at a press conference ahead of the Quality Care Symposium, sponsored by the American Society of Clinical Oncology.
Higher out-of-pocket cost burden was also linked to lower numbers of TKI prescriptions and shorter duration of TKI therapy in the study, which included patients diagnosed with EGFR- and ALK-positive non–small cell lung cancer (NSCLC) between 2010 and 2016.
The findings would suggest a need for a review of coverage for these effective medications, according to Bernardo H. L. Goulart, MD, a thoracic oncologist and health services researcher at the University of Washington and Fred Hutchinson Cancer Research Center, both in Seattle.
“Making sure that the cost to the patients is affordable could mitigate this financial toxicity, and hopefully help patients stay on therapy and derive the survival benefit that these medications are supposed to offer,” Dr. Goulart said in an interview.
The study included data on 106 patients with EGFR- and ALK-positive stage IV NSCLC in the Washington Surveillance, Epidemiology, and End Results registry who had at least one oral TKI prescription. Investigators linked that registry data with commercial and Medicare claims, then divided this patient cohort into quartiles based on out-of-pocket costs.
In the top quartile, the median monthly out-of-pocket cost for TKI treatment was $2,888, compared with just $1,431 in the other three quartiles – essentially half the cost, Dr. Goulart said.
Median survival in the patients in the top out-of-pocket cost quartile was just 9 months, compared with 22 months in the lower three quartiles, he added.
“That difference is remarkable,” Dr. Goulart said, adding that the survival in the top-cost quartile reflects a survival that might be expected with conventional, nontargeted chemotherapy, while survival in the remaining patients mirrored what might be expected based on clinical trials of TKIs in this setting.
Patients in the high-cost quartile were 2.31 times as likely to die as patients in the lower quartiles, according to results of a multivariable analysis that adjusted for patient, disease-specific, and financial characteristics including qualification for low-income subsidies.
The mean medication possession ratio, a measure of medication adherence, was lower in the high-cost quartile (1.06 vs. 1.20 for the lower three quartiles; P = .02), and median duration of therapy was likewise lower in the high-cost quartile (4 vs. 8 months; P less than .01), according to data reported in the study abstract.
While multiple previous studies have linked out-of-pocket costs to decreased adherence and duration of therapy, the present study is one of the few to evaluate the link between cost of oral cancer medications and survival, according to Dr. Goulart.
In one other recent study showing a relationship between financial toxicity and survival, researchers at Fred Hutch showing that Washington cancer patients who filed for bankruptcy were more likely to die, compared with cancer patients not filing for bankruptcy, even after adjustment for a variety of patient characteristics.
The present study results raise a “serious concern” that some patients are unable to afford their medications, which is having a detrimental effect on survival, Dr. Goulart said. Alternatively, the out-of-pocket costs may not have an effect on survival; rather, they may be a “marker of very poor insurance coverage” that reflects higher costs for multiple other aspects of their care.
“The out-of-pocket cost for these drugs can be pretty astronomical, and we have at least a plausible hypothesis that they are taking a toll on patient’s survival,” he added.
If the findings of this study are confirmed in more and larger studies, there could be important implications for health policy and oncology practice, according to Dr. Goulart.
“The biggest action would be to involve patient advocates and physician groups such as ASCO, and advocate for changes in policy for coverage and out-of-pocket costs for these oral TKIs, at least for the patients that have the mutations,” he explained.
Another action, according to Dr. Goulart, would be to try to equip oncology clinics everywhere with patient financial-assistance programs to link patients to entities that can help them afford the cost of TKIs.
“Patients who attend small, remote cancer clinics might not have access to a financial specialist who can help them navigate these costs,” he said.
Funding for the study came from the National Institutes of Health. Dr. Goulart reported disclosures related to Flatiron Health (travel, accommodations, and expenses).
SOURCE: Goulart BHL et al. SCS 2019, Abstract 3.
ALEXANDRIA, VA. – Higher out-of-pocket costs for oral tyrosine kinase inhibitors (TKIs) were linked to inferior survival in patients with advanced, biomarker-positive lung cancers in an analysis of state-level registry data, an investigator reported at a press conference ahead of the Quality Care Symposium, sponsored by the American Society of Clinical Oncology.
Higher out-of-pocket cost burden was also linked to lower numbers of TKI prescriptions and shorter duration of TKI therapy in the study, which included patients diagnosed with EGFR- and ALK-positive non–small cell lung cancer (NSCLC) between 2010 and 2016.
The findings would suggest a need for a review of coverage for these effective medications, according to Bernardo H. L. Goulart, MD, a thoracic oncologist and health services researcher at the University of Washington and Fred Hutchinson Cancer Research Center, both in Seattle.
“Making sure that the cost to the patients is affordable could mitigate this financial toxicity, and hopefully help patients stay on therapy and derive the survival benefit that these medications are supposed to offer,” Dr. Goulart said in an interview.
The study included data on 106 patients with EGFR- and ALK-positive stage IV NSCLC in the Washington Surveillance, Epidemiology, and End Results registry who had at least one oral TKI prescription. Investigators linked that registry data with commercial and Medicare claims, then divided this patient cohort into quartiles based on out-of-pocket costs.
In the top quartile, the median monthly out-of-pocket cost for TKI treatment was $2,888, compared with just $1,431 in the other three quartiles – essentially half the cost, Dr. Goulart said.
Median survival in the patients in the top out-of-pocket cost quartile was just 9 months, compared with 22 months in the lower three quartiles, he added.
“That difference is remarkable,” Dr. Goulart said, adding that the survival in the top-cost quartile reflects a survival that might be expected with conventional, nontargeted chemotherapy, while survival in the remaining patients mirrored what might be expected based on clinical trials of TKIs in this setting.
Patients in the high-cost quartile were 2.31 times as likely to die as patients in the lower quartiles, according to results of a multivariable analysis that adjusted for patient, disease-specific, and financial characteristics including qualification for low-income subsidies.
The mean medication possession ratio, a measure of medication adherence, was lower in the high-cost quartile (1.06 vs. 1.20 for the lower three quartiles; P = .02), and median duration of therapy was likewise lower in the high-cost quartile (4 vs. 8 months; P less than .01), according to data reported in the study abstract.
While multiple previous studies have linked out-of-pocket costs to decreased adherence and duration of therapy, the present study is one of the few to evaluate the link between cost of oral cancer medications and survival, according to Dr. Goulart.
In one other recent study showing a relationship between financial toxicity and survival, researchers at Fred Hutch showing that Washington cancer patients who filed for bankruptcy were more likely to die, compared with cancer patients not filing for bankruptcy, even after adjustment for a variety of patient characteristics.
The present study results raise a “serious concern” that some patients are unable to afford their medications, which is having a detrimental effect on survival, Dr. Goulart said. Alternatively, the out-of-pocket costs may not have an effect on survival; rather, they may be a “marker of very poor insurance coverage” that reflects higher costs for multiple other aspects of their care.
“The out-of-pocket cost for these drugs can be pretty astronomical, and we have at least a plausible hypothesis that they are taking a toll on patient’s survival,” he added.
If the findings of this study are confirmed in more and larger studies, there could be important implications for health policy and oncology practice, according to Dr. Goulart.
“The biggest action would be to involve patient advocates and physician groups such as ASCO, and advocate for changes in policy for coverage and out-of-pocket costs for these oral TKIs, at least for the patients that have the mutations,” he explained.
Another action, according to Dr. Goulart, would be to try to equip oncology clinics everywhere with patient financial-assistance programs to link patients to entities that can help them afford the cost of TKIs.
“Patients who attend small, remote cancer clinics might not have access to a financial specialist who can help them navigate these costs,” he said.
Funding for the study came from the National Institutes of Health. Dr. Goulart reported disclosures related to Flatiron Health (travel, accommodations, and expenses).
SOURCE: Goulart BHL et al. SCS 2019, Abstract 3.
ALEXANDRIA, VA. – Higher out-of-pocket costs for oral tyrosine kinase inhibitors (TKIs) were linked to inferior survival in patients with advanced, biomarker-positive lung cancers in an analysis of state-level registry data, an investigator reported at a press conference ahead of the Quality Care Symposium, sponsored by the American Society of Clinical Oncology.
Higher out-of-pocket cost burden was also linked to lower numbers of TKI prescriptions and shorter duration of TKI therapy in the study, which included patients diagnosed with EGFR- and ALK-positive non–small cell lung cancer (NSCLC) between 2010 and 2016.
The findings would suggest a need for a review of coverage for these effective medications, according to Bernardo H. L. Goulart, MD, a thoracic oncologist and health services researcher at the University of Washington and Fred Hutchinson Cancer Research Center, both in Seattle.
“Making sure that the cost to the patients is affordable could mitigate this financial toxicity, and hopefully help patients stay on therapy and derive the survival benefit that these medications are supposed to offer,” Dr. Goulart said in an interview.
The study included data on 106 patients with EGFR- and ALK-positive stage IV NSCLC in the Washington Surveillance, Epidemiology, and End Results registry who had at least one oral TKI prescription. Investigators linked that registry data with commercial and Medicare claims, then divided this patient cohort into quartiles based on out-of-pocket costs.
In the top quartile, the median monthly out-of-pocket cost for TKI treatment was $2,888, compared with just $1,431 in the other three quartiles – essentially half the cost, Dr. Goulart said.
Median survival in the patients in the top out-of-pocket cost quartile was just 9 months, compared with 22 months in the lower three quartiles, he added.
“That difference is remarkable,” Dr. Goulart said, adding that the survival in the top-cost quartile reflects a survival that might be expected with conventional, nontargeted chemotherapy, while survival in the remaining patients mirrored what might be expected based on clinical trials of TKIs in this setting.
Patients in the high-cost quartile were 2.31 times as likely to die as patients in the lower quartiles, according to results of a multivariable analysis that adjusted for patient, disease-specific, and financial characteristics including qualification for low-income subsidies.
The mean medication possession ratio, a measure of medication adherence, was lower in the high-cost quartile (1.06 vs. 1.20 for the lower three quartiles; P = .02), and median duration of therapy was likewise lower in the high-cost quartile (4 vs. 8 months; P less than .01), according to data reported in the study abstract.
While multiple previous studies have linked out-of-pocket costs to decreased adherence and duration of therapy, the present study is one of the few to evaluate the link between cost of oral cancer medications and survival, according to Dr. Goulart.
In one other recent study showing a relationship between financial toxicity and survival, researchers at Fred Hutch showing that Washington cancer patients who filed for bankruptcy were more likely to die, compared with cancer patients not filing for bankruptcy, even after adjustment for a variety of patient characteristics.
The present study results raise a “serious concern” that some patients are unable to afford their medications, which is having a detrimental effect on survival, Dr. Goulart said. Alternatively, the out-of-pocket costs may not have an effect on survival; rather, they may be a “marker of very poor insurance coverage” that reflects higher costs for multiple other aspects of their care.
“The out-of-pocket cost for these drugs can be pretty astronomical, and we have at least a plausible hypothesis that they are taking a toll on patient’s survival,” he added.
If the findings of this study are confirmed in more and larger studies, there could be important implications for health policy and oncology practice, according to Dr. Goulart.
“The biggest action would be to involve patient advocates and physician groups such as ASCO, and advocate for changes in policy for coverage and out-of-pocket costs for these oral TKIs, at least for the patients that have the mutations,” he explained.
Another action, according to Dr. Goulart, would be to try to equip oncology clinics everywhere with patient financial-assistance programs to link patients to entities that can help them afford the cost of TKIs.
“Patients who attend small, remote cancer clinics might not have access to a financial specialist who can help them navigate these costs,” he said.
Funding for the study came from the National Institutes of Health. Dr. Goulart reported disclosures related to Flatiron Health (travel, accommodations, and expenses).
SOURCE: Goulart BHL et al. SCS 2019, Abstract 3.
REPORTING FROM QCS 2019
siRNA drug safely halved LDL cholesterol in phase 3 ORION-11
PARIS – A small interfering RNA drug, inclisiran, safely halved LDL cholesterol levels in more than 800 patients in a phase 3, multicenter study, in a big step toward this drug coming onto the market and offering an alternative way to harness the potent cholesterol-lowering power of PCSK9 inhibition.
In the reported study – which enrolled patients with established cardiovascular disease, familial hypercholesterolemia, type 2 diabetes, or a high Framingham Risk Score – participants received inclisiran as a semiannual subcutaneous injection. The safe efficacy this produced showed the viability of a new way to deliver lipid-lowering therapy that guarantees compliance and is convenient for patients.
The prospect of lowering cholesterol with about the same potency as the monoclonal antibodies that block PCSK9 (proprotein convertase subtilisin/kexin type 9) activity but administered as a biannual injection “enables provider control over medication adherence, and may offer patients a meaningful new choice that is safe and convenient and has assured results,” Kausik K. Ray, MD, said at the annual congress of the European Society of Cardiology. The durable effect of the small interfering RNA (siRNA) agent “offers a huge advantage,” and “opens the field,” said Dr. Ray, a cardiologist and professor of public health at Imperial College, London.
He also highlighted the “excellent” safety profile seen in the 811 patients treated with inclisiran, compared with 804 patients in the study who received placebo. After four total injections of inclisiran spaced out over 450 days (about 15 months), the rate of treatment-emergent adverse events and serious events was virtually the same in the two treatment arms, and with no signal of inclisiran causing liver effects, renal or muscle injury, damage to blood components, or malignancy. The serial treatment with inclisiran that patients received – at baseline, 90, 270, and 450 days – produced no severe injection-site reactions, and transient mild or moderate injection-site reactions in just under 5% of patients.
Safety issues, such as more-severe injection-site reactions, thrombocytopenia, hepatotoxicity, and flu-like symptoms, plagued siRNA drugs during their earlier days of development, but more recently next-generation siRNA drugs with modified structures have produced much better safety performance, noted Richard C. Becker, MD, professor of medicine and director of the Heart, Lung, & Vascular Institute at the University of Cincinnati. The new-generation siRNAs such as inclisiran are “very well tolerated,” he said in an interview.
The Food and Drug Administration approved the first siRNA drug in August 2018, and in the year since then a few others have also come onto the U.S. market, Dr. Becker said.
Like other siRNA drugs, the activity of inclisiran comes from a short RNA segment that is antisense to a particular messenger RNA (mRNA) target. In the case of inclisiran, the target is the mRNA for the PCSK9 enzyme produced in hepatocytes, and that decreases the number of LDL cholesterol receptors on the cell’s surface. When the antisense RNA molecule encounters a PCSK9 mRNA, the two bind and the mRNA is then degraded by a normal cell process. This cuts the cell’s production of the PCSK9 protein, resulting in more LDL cholesterol receptors on the cell’s surface that pull more LDL cholesterol from the blood. The blocking of PCSK9 activity by inclisiran is roughly equivalent to the action of the PCSK9 monoclonal antibodies that have now been on the U.S. market for a few years. Also like other siRNA drugs, the RNA of inclisiran is packaged so that, once injected into a patient, the RNA molecules travel to the liver and enter hepatocytes, where they exert their activity.
“No one has concerns about inclisiran being able to lower LDL [cholesterol], and there have been no safety signals. The data we have seen so far look very reassuring, and in particular has been very safe for the liver,” commented Marc S. Sabatine, MD, professor of medicine at Harvard Medical School, Boston, who has led several studies involving PCSK9-targeted drugs and is helping to run ORION-4, a 15,000-patient study of inclisiran designed to assess the drug’s effect on clinical events. Results from ORION-4 are not expected until about 2024.
“The PCSK9 inhibitors in general have been a huge advance for patients, and the more kinds of drugs we have to target PCSK9, the better,” he said in an interview.
The study reported by Dr. Ray, ORION-11, enrolled 1,617 patients with high atherosclerotic disease risk at 70 sites in six European countries and South Africa. The study’s primary efficacy endpoint was reduction from baseline in LDL cholesterol both at 510 days (about 17 months) after the first dose and also throughout the 15-month period that started 3 months after the first dose. The average reduction seen after 510 days was 54%, compared with baseline, and the time-averaged reduction during the 15-month window examined was 50%, Dr. Ray said. The results also showed a consistent reduction in LDL cholesterol in virtually every patient treated with inclisiran.
Two other phase 3 studies of inclisiran with similar design have been completed, and the results will come out before the end of 2019, according to a statement from the Medicines Company, which is developing the drug. The statement also said that the company plans to file their data with the FDA for marketing approval for inclisiran before the end of 2019. In the recent past, the FDA has approved drugs for the indication of lowering LDL cholesterol before evidence is available to prove that the agent has benefits for reducing clinical events.
Future studies of inclisiran will explore the efficacy of a single annual injection of the drug as an approach to primary prevention of cardiovascular disease, Dr. Ray said.
ORION-11 was sponsored by the Medicines Company. Dr. Ray is a consultant to it and to several other companies. Dr. Becker had no relevant disclosures. Dr. Sabatine has received research support from the Medicines Company and several other companies, and has received personal fees from Anthos Therapeutics, Bristol-Myers Squibb, CVS Caremark, Daiichi Sankyo, DalCor Pharmaceuticals, Dyrnamix, and Ionis.
PARIS – A small interfering RNA drug, inclisiran, safely halved LDL cholesterol levels in more than 800 patients in a phase 3, multicenter study, in a big step toward this drug coming onto the market and offering an alternative way to harness the potent cholesterol-lowering power of PCSK9 inhibition.
In the reported study – which enrolled patients with established cardiovascular disease, familial hypercholesterolemia, type 2 diabetes, or a high Framingham Risk Score – participants received inclisiran as a semiannual subcutaneous injection. The safe efficacy this produced showed the viability of a new way to deliver lipid-lowering therapy that guarantees compliance and is convenient for patients.
The prospect of lowering cholesterol with about the same potency as the monoclonal antibodies that block PCSK9 (proprotein convertase subtilisin/kexin type 9) activity but administered as a biannual injection “enables provider control over medication adherence, and may offer patients a meaningful new choice that is safe and convenient and has assured results,” Kausik K. Ray, MD, said at the annual congress of the European Society of Cardiology. The durable effect of the small interfering RNA (siRNA) agent “offers a huge advantage,” and “opens the field,” said Dr. Ray, a cardiologist and professor of public health at Imperial College, London.
He also highlighted the “excellent” safety profile seen in the 811 patients treated with inclisiran, compared with 804 patients in the study who received placebo. After four total injections of inclisiran spaced out over 450 days (about 15 months), the rate of treatment-emergent adverse events and serious events was virtually the same in the two treatment arms, and with no signal of inclisiran causing liver effects, renal or muscle injury, damage to blood components, or malignancy. The serial treatment with inclisiran that patients received – at baseline, 90, 270, and 450 days – produced no severe injection-site reactions, and transient mild or moderate injection-site reactions in just under 5% of patients.
Safety issues, such as more-severe injection-site reactions, thrombocytopenia, hepatotoxicity, and flu-like symptoms, plagued siRNA drugs during their earlier days of development, but more recently next-generation siRNA drugs with modified structures have produced much better safety performance, noted Richard C. Becker, MD, professor of medicine and director of the Heart, Lung, & Vascular Institute at the University of Cincinnati. The new-generation siRNAs such as inclisiran are “very well tolerated,” he said in an interview.
The Food and Drug Administration approved the first siRNA drug in August 2018, and in the year since then a few others have also come onto the U.S. market, Dr. Becker said.
Like other siRNA drugs, the activity of inclisiran comes from a short RNA segment that is antisense to a particular messenger RNA (mRNA) target. In the case of inclisiran, the target is the mRNA for the PCSK9 enzyme produced in hepatocytes, and that decreases the number of LDL cholesterol receptors on the cell’s surface. When the antisense RNA molecule encounters a PCSK9 mRNA, the two bind and the mRNA is then degraded by a normal cell process. This cuts the cell’s production of the PCSK9 protein, resulting in more LDL cholesterol receptors on the cell’s surface that pull more LDL cholesterol from the blood. The blocking of PCSK9 activity by inclisiran is roughly equivalent to the action of the PCSK9 monoclonal antibodies that have now been on the U.S. market for a few years. Also like other siRNA drugs, the RNA of inclisiran is packaged so that, once injected into a patient, the RNA molecules travel to the liver and enter hepatocytes, where they exert their activity.
“No one has concerns about inclisiran being able to lower LDL [cholesterol], and there have been no safety signals. The data we have seen so far look very reassuring, and in particular has been very safe for the liver,” commented Marc S. Sabatine, MD, professor of medicine at Harvard Medical School, Boston, who has led several studies involving PCSK9-targeted drugs and is helping to run ORION-4, a 15,000-patient study of inclisiran designed to assess the drug’s effect on clinical events. Results from ORION-4 are not expected until about 2024.
“The PCSK9 inhibitors in general have been a huge advance for patients, and the more kinds of drugs we have to target PCSK9, the better,” he said in an interview.
The study reported by Dr. Ray, ORION-11, enrolled 1,617 patients with high atherosclerotic disease risk at 70 sites in six European countries and South Africa. The study’s primary efficacy endpoint was reduction from baseline in LDL cholesterol both at 510 days (about 17 months) after the first dose and also throughout the 15-month period that started 3 months after the first dose. The average reduction seen after 510 days was 54%, compared with baseline, and the time-averaged reduction during the 15-month window examined was 50%, Dr. Ray said. The results also showed a consistent reduction in LDL cholesterol in virtually every patient treated with inclisiran.
Two other phase 3 studies of inclisiran with similar design have been completed, and the results will come out before the end of 2019, according to a statement from the Medicines Company, which is developing the drug. The statement also said that the company plans to file their data with the FDA for marketing approval for inclisiran before the end of 2019. In the recent past, the FDA has approved drugs for the indication of lowering LDL cholesterol before evidence is available to prove that the agent has benefits for reducing clinical events.
Future studies of inclisiran will explore the efficacy of a single annual injection of the drug as an approach to primary prevention of cardiovascular disease, Dr. Ray said.
ORION-11 was sponsored by the Medicines Company. Dr. Ray is a consultant to it and to several other companies. Dr. Becker had no relevant disclosures. Dr. Sabatine has received research support from the Medicines Company and several other companies, and has received personal fees from Anthos Therapeutics, Bristol-Myers Squibb, CVS Caremark, Daiichi Sankyo, DalCor Pharmaceuticals, Dyrnamix, and Ionis.
PARIS – A small interfering RNA drug, inclisiran, safely halved LDL cholesterol levels in more than 800 patients in a phase 3, multicenter study, in a big step toward this drug coming onto the market and offering an alternative way to harness the potent cholesterol-lowering power of PCSK9 inhibition.
In the reported study – which enrolled patients with established cardiovascular disease, familial hypercholesterolemia, type 2 diabetes, or a high Framingham Risk Score – participants received inclisiran as a semiannual subcutaneous injection. The safe efficacy this produced showed the viability of a new way to deliver lipid-lowering therapy that guarantees compliance and is convenient for patients.
The prospect of lowering cholesterol with about the same potency as the monoclonal antibodies that block PCSK9 (proprotein convertase subtilisin/kexin type 9) activity but administered as a biannual injection “enables provider control over medication adherence, and may offer patients a meaningful new choice that is safe and convenient and has assured results,” Kausik K. Ray, MD, said at the annual congress of the European Society of Cardiology. The durable effect of the small interfering RNA (siRNA) agent “offers a huge advantage,” and “opens the field,” said Dr. Ray, a cardiologist and professor of public health at Imperial College, London.
He also highlighted the “excellent” safety profile seen in the 811 patients treated with inclisiran, compared with 804 patients in the study who received placebo. After four total injections of inclisiran spaced out over 450 days (about 15 months), the rate of treatment-emergent adverse events and serious events was virtually the same in the two treatment arms, and with no signal of inclisiran causing liver effects, renal or muscle injury, damage to blood components, or malignancy. The serial treatment with inclisiran that patients received – at baseline, 90, 270, and 450 days – produced no severe injection-site reactions, and transient mild or moderate injection-site reactions in just under 5% of patients.
Safety issues, such as more-severe injection-site reactions, thrombocytopenia, hepatotoxicity, and flu-like symptoms, plagued siRNA drugs during their earlier days of development, but more recently next-generation siRNA drugs with modified structures have produced much better safety performance, noted Richard C. Becker, MD, professor of medicine and director of the Heart, Lung, & Vascular Institute at the University of Cincinnati. The new-generation siRNAs such as inclisiran are “very well tolerated,” he said in an interview.
The Food and Drug Administration approved the first siRNA drug in August 2018, and in the year since then a few others have also come onto the U.S. market, Dr. Becker said.
Like other siRNA drugs, the activity of inclisiran comes from a short RNA segment that is antisense to a particular messenger RNA (mRNA) target. In the case of inclisiran, the target is the mRNA for the PCSK9 enzyme produced in hepatocytes, and that decreases the number of LDL cholesterol receptors on the cell’s surface. When the antisense RNA molecule encounters a PCSK9 mRNA, the two bind and the mRNA is then degraded by a normal cell process. This cuts the cell’s production of the PCSK9 protein, resulting in more LDL cholesterol receptors on the cell’s surface that pull more LDL cholesterol from the blood. The blocking of PCSK9 activity by inclisiran is roughly equivalent to the action of the PCSK9 monoclonal antibodies that have now been on the U.S. market for a few years. Also like other siRNA drugs, the RNA of inclisiran is packaged so that, once injected into a patient, the RNA molecules travel to the liver and enter hepatocytes, where they exert their activity.
“No one has concerns about inclisiran being able to lower LDL [cholesterol], and there have been no safety signals. The data we have seen so far look very reassuring, and in particular has been very safe for the liver,” commented Marc S. Sabatine, MD, professor of medicine at Harvard Medical School, Boston, who has led several studies involving PCSK9-targeted drugs and is helping to run ORION-4, a 15,000-patient study of inclisiran designed to assess the drug’s effect on clinical events. Results from ORION-4 are not expected until about 2024.
“The PCSK9 inhibitors in general have been a huge advance for patients, and the more kinds of drugs we have to target PCSK9, the better,” he said in an interview.
The study reported by Dr. Ray, ORION-11, enrolled 1,617 patients with high atherosclerotic disease risk at 70 sites in six European countries and South Africa. The study’s primary efficacy endpoint was reduction from baseline in LDL cholesterol both at 510 days (about 17 months) after the first dose and also throughout the 15-month period that started 3 months after the first dose. The average reduction seen after 510 days was 54%, compared with baseline, and the time-averaged reduction during the 15-month window examined was 50%, Dr. Ray said. The results also showed a consistent reduction in LDL cholesterol in virtually every patient treated with inclisiran.
Two other phase 3 studies of inclisiran with similar design have been completed, and the results will come out before the end of 2019, according to a statement from the Medicines Company, which is developing the drug. The statement also said that the company plans to file their data with the FDA for marketing approval for inclisiran before the end of 2019. In the recent past, the FDA has approved drugs for the indication of lowering LDL cholesterol before evidence is available to prove that the agent has benefits for reducing clinical events.
Future studies of inclisiran will explore the efficacy of a single annual injection of the drug as an approach to primary prevention of cardiovascular disease, Dr. Ray said.
ORION-11 was sponsored by the Medicines Company. Dr. Ray is a consultant to it and to several other companies. Dr. Becker had no relevant disclosures. Dr. Sabatine has received research support from the Medicines Company and several other companies, and has received personal fees from Anthos Therapeutics, Bristol-Myers Squibb, CVS Caremark, Daiichi Sankyo, DalCor Pharmaceuticals, Dyrnamix, and Ionis.
REPORTING FROM THE ESC CONGRESS 2019