User login
Fragmentation of sickle cell disease care starts in young adulthood
ORLANDO – While over time, results of a retrospective study suggest.
Nearly 60% of children between aged10-17 years were seen at just one facility over the course of 7 years in the analysis, which was based on analysis of data for nearly 7,000 patients seen in California during 1991-2016.
That contrasted sharply with young adults, aged 18-25 years, only about 20% of whom were admitted to one facility, said senior study author Anjlee Mahajan, MD, of the University of California, Davis, adding that another 20% were seen at five or more centers over a 7-year follow-up period.
Fragmentation of care didn’t increase the risk of death in this study, as investigators hypothesized it might. However, the outcomes and the quality of care among young adults with SCD who received inpatient care at multiple facilities nevertheless was likely to be affected, Dr. Mahajan said at the annual meeting of the American Society of Hematology.
“Imagine what that would be like to have a chronic, debilitating illness and to have to go to multiple different hospitals, during this vulnerable time period in your life, and being seen by different care providers who may not know you and may not have all of your records as well,” she said in a press conference at the meeting.
Providers and the health care system need to work harder to ensure young adults receive comprehensive and coordinated care, especially at a time when therapeutic advances are improving the treatment of this disease, according to the investigator.
“When you’re seen at one center, you can have a specific pain plan, and maybe when you are going into the emergency room and being admitted, your sickle cell care provider might come and visit you in the hospital or at least be in contact with your team,” Dr. Mahajan said in an interview. “That may not happen if you’re going to be seen at five different hospitals in 7 years.”
Encouraging the concept of “medical home” for SCD may be help ease transition from pediatric to adult care, thereby reducing fragmentation of care for young adults, according to Julie A. Panepinto, MD, professor of pediatric hematology and the director of the center for clinical effectiveness research at the Children’s Research Institute, Medical College of Wisconsin, Milwaukee.
“That 18- to 30-year-old age group historically and repeatedly over time is shown to be the age that relies on the emergency department and that has a higher mortality as they transition,” Dr. Panepinto said in an interview. “So ideally, you would have a pediatric program that’s comprehensive and that can transition an adult patient to a very similar setting with knowledgeable providers in SCD across the spectrum, from the emergency department to the hospital to the outpatient clinic.”
Dr. Mahajan reported no disclosures related to her group’s study. Coauthors provided disclosures related to Pfizer and Janssen.
SOURCE: Shatola A et al. ASH 2019. Abstract 4667.
ORLANDO – While over time, results of a retrospective study suggest.
Nearly 60% of children between aged10-17 years were seen at just one facility over the course of 7 years in the analysis, which was based on analysis of data for nearly 7,000 patients seen in California during 1991-2016.
That contrasted sharply with young adults, aged 18-25 years, only about 20% of whom were admitted to one facility, said senior study author Anjlee Mahajan, MD, of the University of California, Davis, adding that another 20% were seen at five or more centers over a 7-year follow-up period.
Fragmentation of care didn’t increase the risk of death in this study, as investigators hypothesized it might. However, the outcomes and the quality of care among young adults with SCD who received inpatient care at multiple facilities nevertheless was likely to be affected, Dr. Mahajan said at the annual meeting of the American Society of Hematology.
“Imagine what that would be like to have a chronic, debilitating illness and to have to go to multiple different hospitals, during this vulnerable time period in your life, and being seen by different care providers who may not know you and may not have all of your records as well,” she said in a press conference at the meeting.
Providers and the health care system need to work harder to ensure young adults receive comprehensive and coordinated care, especially at a time when therapeutic advances are improving the treatment of this disease, according to the investigator.
“When you’re seen at one center, you can have a specific pain plan, and maybe when you are going into the emergency room and being admitted, your sickle cell care provider might come and visit you in the hospital or at least be in contact with your team,” Dr. Mahajan said in an interview. “That may not happen if you’re going to be seen at five different hospitals in 7 years.”
Encouraging the concept of “medical home” for SCD may be help ease transition from pediatric to adult care, thereby reducing fragmentation of care for young adults, according to Julie A. Panepinto, MD, professor of pediatric hematology and the director of the center for clinical effectiveness research at the Children’s Research Institute, Medical College of Wisconsin, Milwaukee.
“That 18- to 30-year-old age group historically and repeatedly over time is shown to be the age that relies on the emergency department and that has a higher mortality as they transition,” Dr. Panepinto said in an interview. “So ideally, you would have a pediatric program that’s comprehensive and that can transition an adult patient to a very similar setting with knowledgeable providers in SCD across the spectrum, from the emergency department to the hospital to the outpatient clinic.”
Dr. Mahajan reported no disclosures related to her group’s study. Coauthors provided disclosures related to Pfizer and Janssen.
SOURCE: Shatola A et al. ASH 2019. Abstract 4667.
ORLANDO – While over time, results of a retrospective study suggest.
Nearly 60% of children between aged10-17 years were seen at just one facility over the course of 7 years in the analysis, which was based on analysis of data for nearly 7,000 patients seen in California during 1991-2016.
That contrasted sharply with young adults, aged 18-25 years, only about 20% of whom were admitted to one facility, said senior study author Anjlee Mahajan, MD, of the University of California, Davis, adding that another 20% were seen at five or more centers over a 7-year follow-up period.
Fragmentation of care didn’t increase the risk of death in this study, as investigators hypothesized it might. However, the outcomes and the quality of care among young adults with SCD who received inpatient care at multiple facilities nevertheless was likely to be affected, Dr. Mahajan said at the annual meeting of the American Society of Hematology.
“Imagine what that would be like to have a chronic, debilitating illness and to have to go to multiple different hospitals, during this vulnerable time period in your life, and being seen by different care providers who may not know you and may not have all of your records as well,” she said in a press conference at the meeting.
Providers and the health care system need to work harder to ensure young adults receive comprehensive and coordinated care, especially at a time when therapeutic advances are improving the treatment of this disease, according to the investigator.
“When you’re seen at one center, you can have a specific pain plan, and maybe when you are going into the emergency room and being admitted, your sickle cell care provider might come and visit you in the hospital or at least be in contact with your team,” Dr. Mahajan said in an interview. “That may not happen if you’re going to be seen at five different hospitals in 7 years.”
Encouraging the concept of “medical home” for SCD may be help ease transition from pediatric to adult care, thereby reducing fragmentation of care for young adults, according to Julie A. Panepinto, MD, professor of pediatric hematology and the director of the center for clinical effectiveness research at the Children’s Research Institute, Medical College of Wisconsin, Milwaukee.
“That 18- to 30-year-old age group historically and repeatedly over time is shown to be the age that relies on the emergency department and that has a higher mortality as they transition,” Dr. Panepinto said in an interview. “So ideally, you would have a pediatric program that’s comprehensive and that can transition an adult patient to a very similar setting with knowledgeable providers in SCD across the spectrum, from the emergency department to the hospital to the outpatient clinic.”
Dr. Mahajan reported no disclosures related to her group’s study. Coauthors provided disclosures related to Pfizer and Janssen.
SOURCE: Shatola A et al. ASH 2019. Abstract 4667.
REPORTING FROM ASH 2019
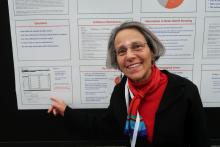
Researchers mine free-text diary entries for seizure cluster insights
BALTIMORE – Free-text diary entries by patients with epilepsy are a “largely untapped” source of information about the frequency and treatment of seizure clusters, researchers said at the annual meeting of the American Epilepsy Society. In addition, patients may describe other clinically relevant concerns such as tiredness, depression, head injury, or seizures while driving, researchers said.
To examine how seizure clusters are reflected in the electronic diaries of patients with epilepsy, Joyce A. Cramer, a clinical research consultant and colleagues examined data from EpiDiary, a set of mobile and Web-based apps designed to help patients with epilepsy manage their medications and record their symptoms. EpiDiary prompts patients to indicate whether they were seizure free, had a seizure, or had a seizure cluster on a given day. Patients also have the ability to enter free-text notes.
“This was the first-ever review of the unstructured, free-text notes,” Ms. Cramer said.
Investigators used lexical analysis to identify free-text comments that potentially were about seizure clusters, based on the use of words such as “lots,” “many,” or “repeat.” Researchers reviewed every flagged comment to confirm whether it pertained to a seizure cluster. They defined a cluster as two or more seizures on a calendar day.
An algorithm flagged 5,955 entries by 1,839 users. Clinician review confirmed that 2,645 of the flagged comments (44.4%) pertained to seizure clusters. Of the confirmed clusters, 512 (19.4%) were found only through the free-text notes and had not been documented through structured data elements such as seizure cluster check-boxes or seizure counts.
“Extra medicine was taken for clusters by 553 users on 3,818 days,” the researchers reported. “This was 30.1% of all users and 56.5% of those commenting on clusters.” In some instances, patients named specific medications, including lorazepam, clonazepam, midazolam, clobazam, rectal diazepam, other diazepam, and clorazepate.
Free-text diary entries could help researchers study various topics. The authors highlighted examples of entries that “contained other clinically relevant information,” including the following:
- Massive ongoing cluster with about 20% apneic events.
- My constant question seems to be: HOW can I function in life when just small outings bring about this incessant tiredness?
- Started feeling like I was having an aura and pulled over.
- Thought about suicide for the first time in a while.
Interpretations of the seizure cluster data are limited, the researchers noted. The algorithm might have missed some free-text comments that were about seizure clusters. And in some instances, researchers used words such as “puffs” to identify seizures when a connection to seizures was not entirely clear. In addition, patients may have used a definition of cluster that was different from the definition used by the investigators.
UCB Pharma and Irody, the company that owns EpiDiary, funded the study. Irody’s founder and president was a coauthor, and another author holds stock or options in Irody. Ms. Cramer consults for Irody, UCB, and other pharmaceutical companies.
SOURCE: Fisher RS et al. AES 2019. Abstract 1.424.
BALTIMORE – Free-text diary entries by patients with epilepsy are a “largely untapped” source of information about the frequency and treatment of seizure clusters, researchers said at the annual meeting of the American Epilepsy Society. In addition, patients may describe other clinically relevant concerns such as tiredness, depression, head injury, or seizures while driving, researchers said.
To examine how seizure clusters are reflected in the electronic diaries of patients with epilepsy, Joyce A. Cramer, a clinical research consultant and colleagues examined data from EpiDiary, a set of mobile and Web-based apps designed to help patients with epilepsy manage their medications and record their symptoms. EpiDiary prompts patients to indicate whether they were seizure free, had a seizure, or had a seizure cluster on a given day. Patients also have the ability to enter free-text notes.
“This was the first-ever review of the unstructured, free-text notes,” Ms. Cramer said.
Investigators used lexical analysis to identify free-text comments that potentially were about seizure clusters, based on the use of words such as “lots,” “many,” or “repeat.” Researchers reviewed every flagged comment to confirm whether it pertained to a seizure cluster. They defined a cluster as two or more seizures on a calendar day.
An algorithm flagged 5,955 entries by 1,839 users. Clinician review confirmed that 2,645 of the flagged comments (44.4%) pertained to seizure clusters. Of the confirmed clusters, 512 (19.4%) were found only through the free-text notes and had not been documented through structured data elements such as seizure cluster check-boxes or seizure counts.
“Extra medicine was taken for clusters by 553 users on 3,818 days,” the researchers reported. “This was 30.1% of all users and 56.5% of those commenting on clusters.” In some instances, patients named specific medications, including lorazepam, clonazepam, midazolam, clobazam, rectal diazepam, other diazepam, and clorazepate.
Free-text diary entries could help researchers study various topics. The authors highlighted examples of entries that “contained other clinically relevant information,” including the following:
- Massive ongoing cluster with about 20% apneic events.
- My constant question seems to be: HOW can I function in life when just small outings bring about this incessant tiredness?
- Started feeling like I was having an aura and pulled over.
- Thought about suicide for the first time in a while.
Interpretations of the seizure cluster data are limited, the researchers noted. The algorithm might have missed some free-text comments that were about seizure clusters. And in some instances, researchers used words such as “puffs” to identify seizures when a connection to seizures was not entirely clear. In addition, patients may have used a definition of cluster that was different from the definition used by the investigators.
UCB Pharma and Irody, the company that owns EpiDiary, funded the study. Irody’s founder and president was a coauthor, and another author holds stock or options in Irody. Ms. Cramer consults for Irody, UCB, and other pharmaceutical companies.
SOURCE: Fisher RS et al. AES 2019. Abstract 1.424.
BALTIMORE – Free-text diary entries by patients with epilepsy are a “largely untapped” source of information about the frequency and treatment of seizure clusters, researchers said at the annual meeting of the American Epilepsy Society. In addition, patients may describe other clinically relevant concerns such as tiredness, depression, head injury, or seizures while driving, researchers said.
To examine how seizure clusters are reflected in the electronic diaries of patients with epilepsy, Joyce A. Cramer, a clinical research consultant and colleagues examined data from EpiDiary, a set of mobile and Web-based apps designed to help patients with epilepsy manage their medications and record their symptoms. EpiDiary prompts patients to indicate whether they were seizure free, had a seizure, or had a seizure cluster on a given day. Patients also have the ability to enter free-text notes.
“This was the first-ever review of the unstructured, free-text notes,” Ms. Cramer said.
Investigators used lexical analysis to identify free-text comments that potentially were about seizure clusters, based on the use of words such as “lots,” “many,” or “repeat.” Researchers reviewed every flagged comment to confirm whether it pertained to a seizure cluster. They defined a cluster as two or more seizures on a calendar day.
An algorithm flagged 5,955 entries by 1,839 users. Clinician review confirmed that 2,645 of the flagged comments (44.4%) pertained to seizure clusters. Of the confirmed clusters, 512 (19.4%) were found only through the free-text notes and had not been documented through structured data elements such as seizure cluster check-boxes or seizure counts.
“Extra medicine was taken for clusters by 553 users on 3,818 days,” the researchers reported. “This was 30.1% of all users and 56.5% of those commenting on clusters.” In some instances, patients named specific medications, including lorazepam, clonazepam, midazolam, clobazam, rectal diazepam, other diazepam, and clorazepate.
Free-text diary entries could help researchers study various topics. The authors highlighted examples of entries that “contained other clinically relevant information,” including the following:
- Massive ongoing cluster with about 20% apneic events.
- My constant question seems to be: HOW can I function in life when just small outings bring about this incessant tiredness?
- Started feeling like I was having an aura and pulled over.
- Thought about suicide for the first time in a while.
Interpretations of the seizure cluster data are limited, the researchers noted. The algorithm might have missed some free-text comments that were about seizure clusters. And in some instances, researchers used words such as “puffs” to identify seizures when a connection to seizures was not entirely clear. In addition, patients may have used a definition of cluster that was different from the definition used by the investigators.
UCB Pharma and Irody, the company that owns EpiDiary, funded the study. Irody’s founder and president was a coauthor, and another author holds stock or options in Irody. Ms. Cramer consults for Irody, UCB, and other pharmaceutical companies.
SOURCE: Fisher RS et al. AES 2019. Abstract 1.424.
REPORTING FROM AES 2019
Skip CTs for breakthrough seizures in chronic epilepsy
BALTIMORE – Head CTs for breakthrough seizures in chronic epilepsy are useful for known structural triggers such as brain tumors, but they don’t change management for most patients, according to a review from the SUNY Upstate Medical University, Syracuse, N.Y., emergency department.
“Nonselective use of ED neuroimaging in patients with no new neurological findings” and no known structural problem, is “very low yield, and increases the use of hospital resources and radiation exposure without impacting the immediate care,” concluded investigators led by Shahram Izadyar, MD, an epileptologist and associate professor of neurology at the university.
In short, CTs for breakthrough seizures – routine in many EDs – usually are a waste of time and money. Absent a known structural cause, “there really isn’t a reason to do imaging,” he said at the American Epilepsy Society annual meeting.
Dr. Izadyar wanted to look into the issue after noticing how common CTs were among his breakthrough patients. He and his team reviewed 90 adults with an established diagnosis of epilepsy and on at least one antiepileptic who presented to the university ED for breakthrough seizures during 2017-2018; 39 (43.3%) had head CTs, 51 (56.7%) did not.
CT changed management in three of the four patients (4.4%) who had a known brain tumor, leading, for instance, to steroids for increased tumor edema. The rest of the patients had nonfocal exams, and imaging had no impact on management.
There was no rhyme or reason why some people got CTs and others didn’t; it seemed to be dependent on the provider. Defensive medicine probably had something to do with it, as well as saving time by ordering a CT instead of doing a neurologic exam, Dr. Izadyar said.
People aren’t going to stop doing defensive medicine, but even a small reduction in unnecessary CTs would “be a positive change.” There’s the cost issue, but also the radiation exposure, which is considerable when people end up in the ED every few months for breakthrough seizures, he said.
There were no differences between the CT and no-CT groups in the suspected causes of breakthroughs (P = .93). About half the cases were probably because of noncompliance, about a quarter from sleep deprivation, and the rest from a change in seizure medication or some other issue.
Dr. Izadyar said the next step is taking the findings to his ED colleagues, and perhaps calculating how much money the university would save by skipping CTs in chronic epilepsy patients with no known structural problem.
There were slightly more men than women in the study, and the mean age was 38 years.
There was no industry funding, and the investigators didn’t have any relevant disclosures.
SOURCE: Ali S et al. AES 2019. Abstract 1.213.
BALTIMORE – Head CTs for breakthrough seizures in chronic epilepsy are useful for known structural triggers such as brain tumors, but they don’t change management for most patients, according to a review from the SUNY Upstate Medical University, Syracuse, N.Y., emergency department.
“Nonselective use of ED neuroimaging in patients with no new neurological findings” and no known structural problem, is “very low yield, and increases the use of hospital resources and radiation exposure without impacting the immediate care,” concluded investigators led by Shahram Izadyar, MD, an epileptologist and associate professor of neurology at the university.
In short, CTs for breakthrough seizures – routine in many EDs – usually are a waste of time and money. Absent a known structural cause, “there really isn’t a reason to do imaging,” he said at the American Epilepsy Society annual meeting.
Dr. Izadyar wanted to look into the issue after noticing how common CTs were among his breakthrough patients. He and his team reviewed 90 adults with an established diagnosis of epilepsy and on at least one antiepileptic who presented to the university ED for breakthrough seizures during 2017-2018; 39 (43.3%) had head CTs, 51 (56.7%) did not.
CT changed management in three of the four patients (4.4%) who had a known brain tumor, leading, for instance, to steroids for increased tumor edema. The rest of the patients had nonfocal exams, and imaging had no impact on management.
There was no rhyme or reason why some people got CTs and others didn’t; it seemed to be dependent on the provider. Defensive medicine probably had something to do with it, as well as saving time by ordering a CT instead of doing a neurologic exam, Dr. Izadyar said.
People aren’t going to stop doing defensive medicine, but even a small reduction in unnecessary CTs would “be a positive change.” There’s the cost issue, but also the radiation exposure, which is considerable when people end up in the ED every few months for breakthrough seizures, he said.
There were no differences between the CT and no-CT groups in the suspected causes of breakthroughs (P = .93). About half the cases were probably because of noncompliance, about a quarter from sleep deprivation, and the rest from a change in seizure medication or some other issue.
Dr. Izadyar said the next step is taking the findings to his ED colleagues, and perhaps calculating how much money the university would save by skipping CTs in chronic epilepsy patients with no known structural problem.
There were slightly more men than women in the study, and the mean age was 38 years.
There was no industry funding, and the investigators didn’t have any relevant disclosures.
SOURCE: Ali S et al. AES 2019. Abstract 1.213.
BALTIMORE – Head CTs for breakthrough seizures in chronic epilepsy are useful for known structural triggers such as brain tumors, but they don’t change management for most patients, according to a review from the SUNY Upstate Medical University, Syracuse, N.Y., emergency department.
“Nonselective use of ED neuroimaging in patients with no new neurological findings” and no known structural problem, is “very low yield, and increases the use of hospital resources and radiation exposure without impacting the immediate care,” concluded investigators led by Shahram Izadyar, MD, an epileptologist and associate professor of neurology at the university.
In short, CTs for breakthrough seizures – routine in many EDs – usually are a waste of time and money. Absent a known structural cause, “there really isn’t a reason to do imaging,” he said at the American Epilepsy Society annual meeting.
Dr. Izadyar wanted to look into the issue after noticing how common CTs were among his breakthrough patients. He and his team reviewed 90 adults with an established diagnosis of epilepsy and on at least one antiepileptic who presented to the university ED for breakthrough seizures during 2017-2018; 39 (43.3%) had head CTs, 51 (56.7%) did not.
CT changed management in three of the four patients (4.4%) who had a known brain tumor, leading, for instance, to steroids for increased tumor edema. The rest of the patients had nonfocal exams, and imaging had no impact on management.
There was no rhyme or reason why some people got CTs and others didn’t; it seemed to be dependent on the provider. Defensive medicine probably had something to do with it, as well as saving time by ordering a CT instead of doing a neurologic exam, Dr. Izadyar said.
People aren’t going to stop doing defensive medicine, but even a small reduction in unnecessary CTs would “be a positive change.” There’s the cost issue, but also the radiation exposure, which is considerable when people end up in the ED every few months for breakthrough seizures, he said.
There were no differences between the CT and no-CT groups in the suspected causes of breakthroughs (P = .93). About half the cases were probably because of noncompliance, about a quarter from sleep deprivation, and the rest from a change in seizure medication or some other issue.
Dr. Izadyar said the next step is taking the findings to his ED colleagues, and perhaps calculating how much money the university would save by skipping CTs in chronic epilepsy patients with no known structural problem.
There were slightly more men than women in the study, and the mean age was 38 years.
There was no industry funding, and the investigators didn’t have any relevant disclosures.
SOURCE: Ali S et al. AES 2019. Abstract 1.213.
REPORTING FROM AES 2019
Care coordination, equity can eliminate disparities for nonwhite patients with DLBCL
ORLANDO – Patients with diffuse large B-cell lymphoma (DLBCL) who are members of an ethnic or racial minority do not have worse outcomes than whites when they receive appropriate treatment and institutional support, a study on disparities in cancer care shows.
Although previous studies have shown that minorities with DLBCL have worse outcomes than do whites, results of a study comparing outcomes from 155 patients of white heritage with those of 41 patients from black, Hispanic, or other minority backgrounds found no significant differences in either progression-free survival (PFS) or overall survival in 2 years over follow-up, reported Nilanjan Ghosh, MD, PhD, from the Levine Cancer Institute, Atrium Health, in Charlotte, N.C.
He attributes the results to his center’s robust nurse navigation program, equal access among all patients – regardless of ability to pay – to standard treatments, and to the availability of clinical trial participation and stem cell transplantation.
“I think a key message is that if you are able to offer the same treatment and clinical trials to people irrespective of their race or socioeconomic status and can provide support, you can get equal outcomes as long as the biology is the same in both groups,” he said at a briefing prior to presentation of data in an oral abstract session at the annual meeting of the American Society of Hematology.
Dr. Ghosh pointed to four separate studies that showed that minority populations with DLBCL have worse outcomes than did whites, and noted that both uninsured and Medicaid-insured patients have also been shown to have poorer results, suggesting a role of socioeconomic factors in determining who gets optimum care and who does not.
The investigators compared PFS and OS among white and nonwhite patients with DLBCL treated in their institution, which has a safety-net cancer center. They also looked at the frequencies of clinical trial participation and stem cell transplantation between the groups.
The study included all patients with de novo DLBCL who presented to their center during January 2016–January 2019. They used patient-reported descriptors of race/ethnicity to create one of two cohorts: either self-identified whites (155 patients) or nonwhites (41), a group that included black patients, Hispanic patients, Asian Americans, and Native Americans.
The authors collected data on demographics, disease characteristics (including revised International Prognostic Index and double-hit status), insurance data, treatment, trial enrollment, progression, and death.
They found that nonwhites were significantly younger at diagnosis (median 56 vs. 64 years; P = .007), with an even distribution between the sexes in each group.
Two-thirds of both white and nonwhite patients had government insurance (Medicare or Medicaid). Of the remaining patients, 33% of white had private insurance, compared with 27% of nonwhites. No whites were uninsured, but 3 of the 41 nonwhites (7%) had no insurance.
Of the 155 white patients, 121 (86%) received nurse navigation services, as did 33 of 41 (81%) of nonwhites. The services include lodging assistance for homeless patients, transportation services for patients without cars, and care coordination among primary care physicians, oncologists, and other specialists. The services are part of the center’s standard practice, with excess costs, if any, folded into the budget, Dr. Ghosh said.
Looking at disease characteristics and treatment, the investigators found that risk profiles were similar between the groups. A higher percentage of whites had double-hit lymphoma (11% vs. 7%), but this difference was not statistically significant.
The investigators also found that in their program race was not a barrier to optimum therapy, with 96% of whites and 98% of nonwhites receiving frontline therapy with an anthracycline and rituximab-based regimen, and 4% and 2%, respectively received a non–anthracycline based regimen.
In each group, 39% of patients had disease that either relapsed or was refractory to frontline therapy.
In all, 11% of whites and 12% of nonwhites enrolled in clinical trials, 11% and 19%, respectively, underwent stem cell transplantation.
For patients with relapsed/refractory disease, the 2-year PFS rates were 60% for whites, and 63% for nonwhites, and the 2-year OS rates were 74% and 81%, respectively.
Dr. Ghosh and colleagues concluded that “our safety net cancer center, with extensive nurse navigator support and access to standard treatments, stem cell transplants, and cutting-edge clinical trials may abrogate the inferior outcomes in minority populations that have been previously reported.”
The study was internally funded. Dr. Ghosh reported consulting fees, research funding, speakers bureau activity, and/or honoraria from multiple companies.
SOURCE: Hu B et al. ASH 2019. Abstract 425.
ORLANDO – Patients with diffuse large B-cell lymphoma (DLBCL) who are members of an ethnic or racial minority do not have worse outcomes than whites when they receive appropriate treatment and institutional support, a study on disparities in cancer care shows.
Although previous studies have shown that minorities with DLBCL have worse outcomes than do whites, results of a study comparing outcomes from 155 patients of white heritage with those of 41 patients from black, Hispanic, or other minority backgrounds found no significant differences in either progression-free survival (PFS) or overall survival in 2 years over follow-up, reported Nilanjan Ghosh, MD, PhD, from the Levine Cancer Institute, Atrium Health, in Charlotte, N.C.
He attributes the results to his center’s robust nurse navigation program, equal access among all patients – regardless of ability to pay – to standard treatments, and to the availability of clinical trial participation and stem cell transplantation.
“I think a key message is that if you are able to offer the same treatment and clinical trials to people irrespective of their race or socioeconomic status and can provide support, you can get equal outcomes as long as the biology is the same in both groups,” he said at a briefing prior to presentation of data in an oral abstract session at the annual meeting of the American Society of Hematology.
Dr. Ghosh pointed to four separate studies that showed that minority populations with DLBCL have worse outcomes than did whites, and noted that both uninsured and Medicaid-insured patients have also been shown to have poorer results, suggesting a role of socioeconomic factors in determining who gets optimum care and who does not.
The investigators compared PFS and OS among white and nonwhite patients with DLBCL treated in their institution, which has a safety-net cancer center. They also looked at the frequencies of clinical trial participation and stem cell transplantation between the groups.
The study included all patients with de novo DLBCL who presented to their center during January 2016–January 2019. They used patient-reported descriptors of race/ethnicity to create one of two cohorts: either self-identified whites (155 patients) or nonwhites (41), a group that included black patients, Hispanic patients, Asian Americans, and Native Americans.
The authors collected data on demographics, disease characteristics (including revised International Prognostic Index and double-hit status), insurance data, treatment, trial enrollment, progression, and death.
They found that nonwhites were significantly younger at diagnosis (median 56 vs. 64 years; P = .007), with an even distribution between the sexes in each group.
Two-thirds of both white and nonwhite patients had government insurance (Medicare or Medicaid). Of the remaining patients, 33% of white had private insurance, compared with 27% of nonwhites. No whites were uninsured, but 3 of the 41 nonwhites (7%) had no insurance.
Of the 155 white patients, 121 (86%) received nurse navigation services, as did 33 of 41 (81%) of nonwhites. The services include lodging assistance for homeless patients, transportation services for patients without cars, and care coordination among primary care physicians, oncologists, and other specialists. The services are part of the center’s standard practice, with excess costs, if any, folded into the budget, Dr. Ghosh said.
Looking at disease characteristics and treatment, the investigators found that risk profiles were similar between the groups. A higher percentage of whites had double-hit lymphoma (11% vs. 7%), but this difference was not statistically significant.
The investigators also found that in their program race was not a barrier to optimum therapy, with 96% of whites and 98% of nonwhites receiving frontline therapy with an anthracycline and rituximab-based regimen, and 4% and 2%, respectively received a non–anthracycline based regimen.
In each group, 39% of patients had disease that either relapsed or was refractory to frontline therapy.
In all, 11% of whites and 12% of nonwhites enrolled in clinical trials, 11% and 19%, respectively, underwent stem cell transplantation.
For patients with relapsed/refractory disease, the 2-year PFS rates were 60% for whites, and 63% for nonwhites, and the 2-year OS rates were 74% and 81%, respectively.
Dr. Ghosh and colleagues concluded that “our safety net cancer center, with extensive nurse navigator support and access to standard treatments, stem cell transplants, and cutting-edge clinical trials may abrogate the inferior outcomes in minority populations that have been previously reported.”
The study was internally funded. Dr. Ghosh reported consulting fees, research funding, speakers bureau activity, and/or honoraria from multiple companies.
SOURCE: Hu B et al. ASH 2019. Abstract 425.
ORLANDO – Patients with diffuse large B-cell lymphoma (DLBCL) who are members of an ethnic or racial minority do not have worse outcomes than whites when they receive appropriate treatment and institutional support, a study on disparities in cancer care shows.
Although previous studies have shown that minorities with DLBCL have worse outcomes than do whites, results of a study comparing outcomes from 155 patients of white heritage with those of 41 patients from black, Hispanic, or other minority backgrounds found no significant differences in either progression-free survival (PFS) or overall survival in 2 years over follow-up, reported Nilanjan Ghosh, MD, PhD, from the Levine Cancer Institute, Atrium Health, in Charlotte, N.C.
He attributes the results to his center’s robust nurse navigation program, equal access among all patients – regardless of ability to pay – to standard treatments, and to the availability of clinical trial participation and stem cell transplantation.
“I think a key message is that if you are able to offer the same treatment and clinical trials to people irrespective of their race or socioeconomic status and can provide support, you can get equal outcomes as long as the biology is the same in both groups,” he said at a briefing prior to presentation of data in an oral abstract session at the annual meeting of the American Society of Hematology.
Dr. Ghosh pointed to four separate studies that showed that minority populations with DLBCL have worse outcomes than did whites, and noted that both uninsured and Medicaid-insured patients have also been shown to have poorer results, suggesting a role of socioeconomic factors in determining who gets optimum care and who does not.
The investigators compared PFS and OS among white and nonwhite patients with DLBCL treated in their institution, which has a safety-net cancer center. They also looked at the frequencies of clinical trial participation and stem cell transplantation between the groups.
The study included all patients with de novo DLBCL who presented to their center during January 2016–January 2019. They used patient-reported descriptors of race/ethnicity to create one of two cohorts: either self-identified whites (155 patients) or nonwhites (41), a group that included black patients, Hispanic patients, Asian Americans, and Native Americans.
The authors collected data on demographics, disease characteristics (including revised International Prognostic Index and double-hit status), insurance data, treatment, trial enrollment, progression, and death.
They found that nonwhites were significantly younger at diagnosis (median 56 vs. 64 years; P = .007), with an even distribution between the sexes in each group.
Two-thirds of both white and nonwhite patients had government insurance (Medicare or Medicaid). Of the remaining patients, 33% of white had private insurance, compared with 27% of nonwhites. No whites were uninsured, but 3 of the 41 nonwhites (7%) had no insurance.
Of the 155 white patients, 121 (86%) received nurse navigation services, as did 33 of 41 (81%) of nonwhites. The services include lodging assistance for homeless patients, transportation services for patients without cars, and care coordination among primary care physicians, oncologists, and other specialists. The services are part of the center’s standard practice, with excess costs, if any, folded into the budget, Dr. Ghosh said.
Looking at disease characteristics and treatment, the investigators found that risk profiles were similar between the groups. A higher percentage of whites had double-hit lymphoma (11% vs. 7%), but this difference was not statistically significant.
The investigators also found that in their program race was not a barrier to optimum therapy, with 96% of whites and 98% of nonwhites receiving frontline therapy with an anthracycline and rituximab-based regimen, and 4% and 2%, respectively received a non–anthracycline based regimen.
In each group, 39% of patients had disease that either relapsed or was refractory to frontline therapy.
In all, 11% of whites and 12% of nonwhites enrolled in clinical trials, 11% and 19%, respectively, underwent stem cell transplantation.
For patients with relapsed/refractory disease, the 2-year PFS rates were 60% for whites, and 63% for nonwhites, and the 2-year OS rates were 74% and 81%, respectively.
Dr. Ghosh and colleagues concluded that “our safety net cancer center, with extensive nurse navigator support and access to standard treatments, stem cell transplants, and cutting-edge clinical trials may abrogate the inferior outcomes in minority populations that have been previously reported.”
The study was internally funded. Dr. Ghosh reported consulting fees, research funding, speakers bureau activity, and/or honoraria from multiple companies.
SOURCE: Hu B et al. ASH 2019. Abstract 425.
REPORTING FROM ASH 2019
Aspirin plus a DOAC may do more harm than good in some
ORLANDO – in a large registry-based cohort.
The study, which involved a cohort of 2,045 patients who were followed at 6 anticoagulation clinics in Michigan during January 2009–June 2019, also found no apparent improvement in thrombosis incidence with the addition of aspirin, Jordan K. Schaefer, MD, reported during a press briefing at the annual meeting of the American Society of Hematology.
Of the cohort patients, 639 adults who received a DOAC plus aspirin after VTE or for NVAF without a clear indication were compared with 639 propensity-matched controls. The bleeding event rate per 100 patient years was 39.50 vs. 32.32 at an average of 15.2 months of follow-up in the combination therapy and DOAC monotherapy groups, respectively, said Dr. Schaefer of the division of hematology/oncology, department of internal medicine, University of Michigan, Ann Arbor.
“This result was statistically significant for clinically relevant non-major bleeding, with an 18.7 rate per 100 patient years, compared with 13.5 for DOAC monotherapy,” (P = .02), he said. “We also saw a significant increase in non-major bleeding with combination therapy, compared with direct oral anticoagulant monotherapy” (rate, 32.82 vs. 25.88; P =.04).
No significant difference was seen overall (P =.07) or for other specific types of bleeding, he noted.
The observed rates of thrombosis in the groups, respectively, were 2.35 and 2.23 per 100 patient years (P =.95), he said, noting that patients on combination therapy also had more emergency department visits and hospitalizations, but those differences were not statistically significant.
“Direct-acting oral anticoagulants, which include apixaban, dabigatran, edoxaban, and rivaroxaban, are increasingly used in clinical practice for indications that include the prevention of strokes for patients with nonvalvular atrial fibrillation, and the treatment and secondary prevention of venous thromboembolic disease,” Dr. Schaefer said.
Aspirin is commonly used in clinical practice for various indications, including primary prevention of heart attacks, strokes, and colorectal cancer, as well as for thromboprophylaxis in patients with certain blood disorders or with certain cardiac devices, he added.
“Aspirin is used for the secondary prevention of thrombosis for patients with known coronary artery disease, peripheral artery disease, or carotid artery disease,” he said. “And while adding aspirin to a DOAC is often appropriate after acute coronary syndromes or percutaneous coronary intervention, many patients receive the combination therapy without a clear indication, he said, noting that increasing evidence in recent years, largely from patients treated with warfarin and aspirin, suggest that the approach may do more harm than good for certain patients.
Specifically, there’s a question of whether aspirin is increasing the rates of bleeding without protecting patients from adverse thrombotic outcomes.
“This has specifically been a concern for patients who are on full-dose anticoagulation,” he said.
In the current study, patient demographics, comorbidities, and concurrent medications were well balanced in the treatment and control groups after propensity score matching, he said, noting that patients with a history of heart valve replacement, recent MI, or less than 3 months of follow-up were excluded.
“These findings need to be confirmed in larger studies, but until such data [are] available, clinicians and patients should continue to balance the relative risks and benefits of adding aspirin to their direct oral anticoagulant therapy,” Dr. Schaefer said. “Further research needs to evaluate key subgroups to see if any particular population may benefit from combination therapy compared to DOAC therapy alone.”
Dr. Schaefer reported having no disclosures.
SOURCE: Schaeffer J et al. ASH 2019. Abstract 787.
ORLANDO – in a large registry-based cohort.
The study, which involved a cohort of 2,045 patients who were followed at 6 anticoagulation clinics in Michigan during January 2009–June 2019, also found no apparent improvement in thrombosis incidence with the addition of aspirin, Jordan K. Schaefer, MD, reported during a press briefing at the annual meeting of the American Society of Hematology.
Of the cohort patients, 639 adults who received a DOAC plus aspirin after VTE or for NVAF without a clear indication were compared with 639 propensity-matched controls. The bleeding event rate per 100 patient years was 39.50 vs. 32.32 at an average of 15.2 months of follow-up in the combination therapy and DOAC monotherapy groups, respectively, said Dr. Schaefer of the division of hematology/oncology, department of internal medicine, University of Michigan, Ann Arbor.
“This result was statistically significant for clinically relevant non-major bleeding, with an 18.7 rate per 100 patient years, compared with 13.5 for DOAC monotherapy,” (P = .02), he said. “We also saw a significant increase in non-major bleeding with combination therapy, compared with direct oral anticoagulant monotherapy” (rate, 32.82 vs. 25.88; P =.04).
No significant difference was seen overall (P =.07) or for other specific types of bleeding, he noted.
The observed rates of thrombosis in the groups, respectively, were 2.35 and 2.23 per 100 patient years (P =.95), he said, noting that patients on combination therapy also had more emergency department visits and hospitalizations, but those differences were not statistically significant.
“Direct-acting oral anticoagulants, which include apixaban, dabigatran, edoxaban, and rivaroxaban, are increasingly used in clinical practice for indications that include the prevention of strokes for patients with nonvalvular atrial fibrillation, and the treatment and secondary prevention of venous thromboembolic disease,” Dr. Schaefer said.
Aspirin is commonly used in clinical practice for various indications, including primary prevention of heart attacks, strokes, and colorectal cancer, as well as for thromboprophylaxis in patients with certain blood disorders or with certain cardiac devices, he added.
“Aspirin is used for the secondary prevention of thrombosis for patients with known coronary artery disease, peripheral artery disease, or carotid artery disease,” he said. “And while adding aspirin to a DOAC is often appropriate after acute coronary syndromes or percutaneous coronary intervention, many patients receive the combination therapy without a clear indication, he said, noting that increasing evidence in recent years, largely from patients treated with warfarin and aspirin, suggest that the approach may do more harm than good for certain patients.
Specifically, there’s a question of whether aspirin is increasing the rates of bleeding without protecting patients from adverse thrombotic outcomes.
“This has specifically been a concern for patients who are on full-dose anticoagulation,” he said.
In the current study, patient demographics, comorbidities, and concurrent medications were well balanced in the treatment and control groups after propensity score matching, he said, noting that patients with a history of heart valve replacement, recent MI, or less than 3 months of follow-up were excluded.
“These findings need to be confirmed in larger studies, but until such data [are] available, clinicians and patients should continue to balance the relative risks and benefits of adding aspirin to their direct oral anticoagulant therapy,” Dr. Schaefer said. “Further research needs to evaluate key subgroups to see if any particular population may benefit from combination therapy compared to DOAC therapy alone.”
Dr. Schaefer reported having no disclosures.
SOURCE: Schaeffer J et al. ASH 2019. Abstract 787.
ORLANDO – in a large registry-based cohort.
The study, which involved a cohort of 2,045 patients who were followed at 6 anticoagulation clinics in Michigan during January 2009–June 2019, also found no apparent improvement in thrombosis incidence with the addition of aspirin, Jordan K. Schaefer, MD, reported during a press briefing at the annual meeting of the American Society of Hematology.
Of the cohort patients, 639 adults who received a DOAC plus aspirin after VTE or for NVAF without a clear indication were compared with 639 propensity-matched controls. The bleeding event rate per 100 patient years was 39.50 vs. 32.32 at an average of 15.2 months of follow-up in the combination therapy and DOAC monotherapy groups, respectively, said Dr. Schaefer of the division of hematology/oncology, department of internal medicine, University of Michigan, Ann Arbor.
“This result was statistically significant for clinically relevant non-major bleeding, with an 18.7 rate per 100 patient years, compared with 13.5 for DOAC monotherapy,” (P = .02), he said. “We also saw a significant increase in non-major bleeding with combination therapy, compared with direct oral anticoagulant monotherapy” (rate, 32.82 vs. 25.88; P =.04).
No significant difference was seen overall (P =.07) or for other specific types of bleeding, he noted.
The observed rates of thrombosis in the groups, respectively, were 2.35 and 2.23 per 100 patient years (P =.95), he said, noting that patients on combination therapy also had more emergency department visits and hospitalizations, but those differences were not statistically significant.
“Direct-acting oral anticoagulants, which include apixaban, dabigatran, edoxaban, and rivaroxaban, are increasingly used in clinical practice for indications that include the prevention of strokes for patients with nonvalvular atrial fibrillation, and the treatment and secondary prevention of venous thromboembolic disease,” Dr. Schaefer said.
Aspirin is commonly used in clinical practice for various indications, including primary prevention of heart attacks, strokes, and colorectal cancer, as well as for thromboprophylaxis in patients with certain blood disorders or with certain cardiac devices, he added.
“Aspirin is used for the secondary prevention of thrombosis for patients with known coronary artery disease, peripheral artery disease, or carotid artery disease,” he said. “And while adding aspirin to a DOAC is often appropriate after acute coronary syndromes or percutaneous coronary intervention, many patients receive the combination therapy without a clear indication, he said, noting that increasing evidence in recent years, largely from patients treated with warfarin and aspirin, suggest that the approach may do more harm than good for certain patients.
Specifically, there’s a question of whether aspirin is increasing the rates of bleeding without protecting patients from adverse thrombotic outcomes.
“This has specifically been a concern for patients who are on full-dose anticoagulation,” he said.
In the current study, patient demographics, comorbidities, and concurrent medications were well balanced in the treatment and control groups after propensity score matching, he said, noting that patients with a history of heart valve replacement, recent MI, or less than 3 months of follow-up were excluded.
“These findings need to be confirmed in larger studies, but until such data [are] available, clinicians and patients should continue to balance the relative risks and benefits of adding aspirin to their direct oral anticoagulant therapy,” Dr. Schaefer said. “Further research needs to evaluate key subgroups to see if any particular population may benefit from combination therapy compared to DOAC therapy alone.”
Dr. Schaefer reported having no disclosures.
SOURCE: Schaeffer J et al. ASH 2019. Abstract 787.
REPORTING FROM ASH 2019
Off-the-shelf cellular therapy shows promise in the lab
ORLANDO – A cellular therapy called FT596 is active against B-cell malignancies and, when combined with rituximab, can be more effective than traditional chimeric antigen receptor (CAR) T cells, preclinical research findings suggest.
FT596 is a universal, anti-CD19 CAR natural killer (NK) cell therapy derived from a master induced pluripotent stem cell (iPSC) line.
FT596 reduced tumor growth in mouse models of leukemia and lymphoma. When combined with rituximab, FT596 was able to overcome CD19 antigen escape.
Jode P. Goodridge, PhD, of Fate Therapeutics in San Diego, presented these results at the annual meeting of the American Society of Hematology.
Dr. Goodridge explained that FT596 begins with a source material, such as a fibroblast, that is reprogrammed into an iPSC progenitor cell. That cell is sorted and expanded into a renewable, homogeneous, pluripotent master iPSC line. The iPSCs are differentiated into CD34 cells, which are differentiated into NK cells. The iPSC-derived NK cells are then modified with the following:
- An anti-CD19 CAR that is optimized for NK-cell biology and contains an NKG2D transmembrane domain, a 2B4 costimulatory domain, and a CD3-zeta signaling domain.
- An interleukin-15 receptor fusion that promotes cell survival and reduces the need for cytokine support.
- A high-affinity 158V, noncleavable CD16 Fc receptor that enhances antibody-dependent cellular cytotoxicity when FT596 is combined with a monoclonal antibody such as rituximab.
Dr. Goodridge presented results with FT596, both alone and in combination with rituximab, in vitro and in vivo.
When compared with no treatment, three doses of FT596 monotherapy reduced tumor growth in a mouse model of leukemia (Nalm6). FT596 plus rituximab reduced tumor growth in a mouse model of lymphoma (Raji), when compared with no treatment or rituximab alone.
Three doses of FT596 proved more effective than a single dose of CD19 CAR T-cell therapy in a mouse model of lymphoma (Raji). FT596 both reduced tumor growth and prolonged survival in the mice.
Lastly, in vitro experiments in Raji cells showed that FT596 plus rituximab can produce deeper responses than primary CAR-T cells, and the combination can prevent antigen escape.
Dr. Goodridge said these results support the phase 1 study of FT596, given as monotherapy or in combination with rituximab or obinutuzumab, in patients with relapsed/refractory B-cell lymphomas or chronic lymphocytic leukemia.
Dr. Goodridge is employed by Fate Therapeutics, the company developing FT596.
SOURCE: Goodridge JP et al. ASH 2019. Abstract 301.
ORLANDO – A cellular therapy called FT596 is active against B-cell malignancies and, when combined with rituximab, can be more effective than traditional chimeric antigen receptor (CAR) T cells, preclinical research findings suggest.
FT596 is a universal, anti-CD19 CAR natural killer (NK) cell therapy derived from a master induced pluripotent stem cell (iPSC) line.
FT596 reduced tumor growth in mouse models of leukemia and lymphoma. When combined with rituximab, FT596 was able to overcome CD19 antigen escape.
Jode P. Goodridge, PhD, of Fate Therapeutics in San Diego, presented these results at the annual meeting of the American Society of Hematology.
Dr. Goodridge explained that FT596 begins with a source material, such as a fibroblast, that is reprogrammed into an iPSC progenitor cell. That cell is sorted and expanded into a renewable, homogeneous, pluripotent master iPSC line. The iPSCs are differentiated into CD34 cells, which are differentiated into NK cells. The iPSC-derived NK cells are then modified with the following:
- An anti-CD19 CAR that is optimized for NK-cell biology and contains an NKG2D transmembrane domain, a 2B4 costimulatory domain, and a CD3-zeta signaling domain.
- An interleukin-15 receptor fusion that promotes cell survival and reduces the need for cytokine support.
- A high-affinity 158V, noncleavable CD16 Fc receptor that enhances antibody-dependent cellular cytotoxicity when FT596 is combined with a monoclonal antibody such as rituximab.
Dr. Goodridge presented results with FT596, both alone and in combination with rituximab, in vitro and in vivo.
When compared with no treatment, three doses of FT596 monotherapy reduced tumor growth in a mouse model of leukemia (Nalm6). FT596 plus rituximab reduced tumor growth in a mouse model of lymphoma (Raji), when compared with no treatment or rituximab alone.
Three doses of FT596 proved more effective than a single dose of CD19 CAR T-cell therapy in a mouse model of lymphoma (Raji). FT596 both reduced tumor growth and prolonged survival in the mice.
Lastly, in vitro experiments in Raji cells showed that FT596 plus rituximab can produce deeper responses than primary CAR-T cells, and the combination can prevent antigen escape.
Dr. Goodridge said these results support the phase 1 study of FT596, given as monotherapy or in combination with rituximab or obinutuzumab, in patients with relapsed/refractory B-cell lymphomas or chronic lymphocytic leukemia.
Dr. Goodridge is employed by Fate Therapeutics, the company developing FT596.
SOURCE: Goodridge JP et al. ASH 2019. Abstract 301.
ORLANDO – A cellular therapy called FT596 is active against B-cell malignancies and, when combined with rituximab, can be more effective than traditional chimeric antigen receptor (CAR) T cells, preclinical research findings suggest.
FT596 is a universal, anti-CD19 CAR natural killer (NK) cell therapy derived from a master induced pluripotent stem cell (iPSC) line.
FT596 reduced tumor growth in mouse models of leukemia and lymphoma. When combined with rituximab, FT596 was able to overcome CD19 antigen escape.
Jode P. Goodridge, PhD, of Fate Therapeutics in San Diego, presented these results at the annual meeting of the American Society of Hematology.
Dr. Goodridge explained that FT596 begins with a source material, such as a fibroblast, that is reprogrammed into an iPSC progenitor cell. That cell is sorted and expanded into a renewable, homogeneous, pluripotent master iPSC line. The iPSCs are differentiated into CD34 cells, which are differentiated into NK cells. The iPSC-derived NK cells are then modified with the following:
- An anti-CD19 CAR that is optimized for NK-cell biology and contains an NKG2D transmembrane domain, a 2B4 costimulatory domain, and a CD3-zeta signaling domain.
- An interleukin-15 receptor fusion that promotes cell survival and reduces the need for cytokine support.
- A high-affinity 158V, noncleavable CD16 Fc receptor that enhances antibody-dependent cellular cytotoxicity when FT596 is combined with a monoclonal antibody such as rituximab.
Dr. Goodridge presented results with FT596, both alone and in combination with rituximab, in vitro and in vivo.
When compared with no treatment, three doses of FT596 monotherapy reduced tumor growth in a mouse model of leukemia (Nalm6). FT596 plus rituximab reduced tumor growth in a mouse model of lymphoma (Raji), when compared with no treatment or rituximab alone.
Three doses of FT596 proved more effective than a single dose of CD19 CAR T-cell therapy in a mouse model of lymphoma (Raji). FT596 both reduced tumor growth and prolonged survival in the mice.
Lastly, in vitro experiments in Raji cells showed that FT596 plus rituximab can produce deeper responses than primary CAR-T cells, and the combination can prevent antigen escape.
Dr. Goodridge said these results support the phase 1 study of FT596, given as monotherapy or in combination with rituximab or obinutuzumab, in patients with relapsed/refractory B-cell lymphomas or chronic lymphocytic leukemia.
Dr. Goodridge is employed by Fate Therapeutics, the company developing FT596.
SOURCE: Goodridge JP et al. ASH 2019. Abstract 301.
REPORTING FROM ASH 2019
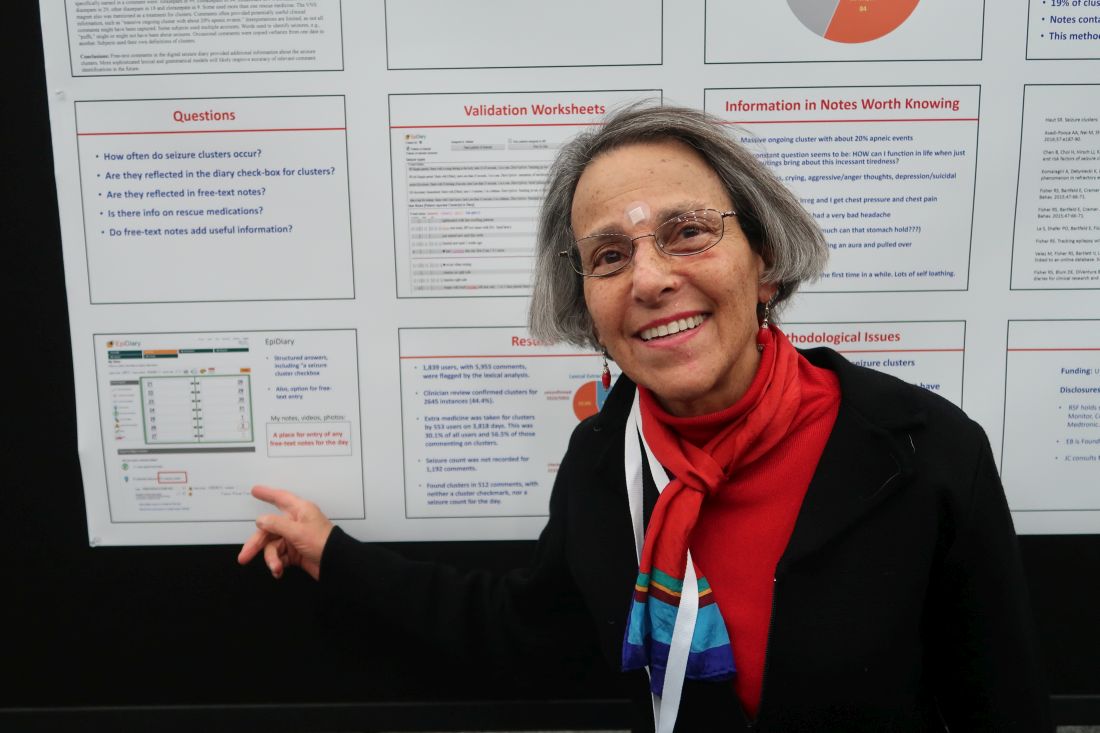
Kidney function in African American AML patients not linked to reduced survival compared with whites
ORLANDO – While African Americans with acute myeloid leukemia were more likely to have evidence of abnormal kidney function, the excess of this comorbidity didn’t affect overall survival, compared with whites, according to a study of more than 1,000 patients.
A total of 63% of African Americans with acute myeloid leukemia (AML) presented with a renal function abnormality that could have excluded them from a clinical trial, compared with 56% in the overall cohort; however, analysis of outcomes data suggested that renal function abnormalities were not associated with decreased survival in African Americans versus whites, said Abby Statler, PhD, MPH, of the Cleveland Clinic.
The findings may have implications for the design of clinical trials that might exclude patients on the basis of comorbidities that don’t actually affect survival, according to Dr. Statler.
“If we’re able to liberalize renal function eligibility criteria ... this may reduce racial disparities in clinical trial enrollment, which might be a major step in improving the diversity of cancer patient populations,” Dr. Statler said in a press conference at the annual meeting of the American Society of Hematology.
Overly restrictive criteria could be a significant barrier to clinical trial enrollment among minority patient populations, according to Dr. Statler.
Eligibility criteria are generally biased toward “fit” patient populations, which means they may discriminate against less-fit groups, such as African Americans who, compared with whites, have higher rates of comorbidities and report poorer overall health, according to Dr. Statler.
Laura Michaelis, MD, who chaired the press conference, said these findings suggest current clinical trial designs may be “too restrictive.”
“Once it’s published and validated, [these] data should definitely make us think twice about when you limit a patient’s enrollment in a trial,” Dr. Michaelis said in an interview.
Restrictive eligibility criteria may not only limit access to minority populations, but also may slow clinical trial accrual and completion, and make it harder to generalize clinical trial findings to the overall population, said Dr. Michaelis, associate professor of medicine in the division of hematology and oncology, Medical College of Wisconsin, Milwaukee.
The study by Dr. Statler and colleagues included 1,040 AML patients who received chemotherapy at Cleveland Clinic between 2003 and 2019. About 10% of the patients in the analysis were African American and 90% were white.
Median overall survival was not significantly different by race, at 13.7 months for African Americans and 14.9 months for whites (P = 0.89), according to results published in the study abstract.
Mild creatinine elevation did not appear to affect survival in this study, according to the investigator. Survival was not significantly different between patients with normal creatinine and those with creatinine up to 1.5 times the upper limit of normal. However, higher levels of creatinine were significantly associated with worse survival, Dr. Statler said.
Further analyses showed that these survival findings by creatinine level held up specifically in the African American subgroup as well, Dr. Statler said in the press conference.
Dr. Statler provided no disclosures related to the presentation. Study coauthors described disclosures related to Amgen, SimulStat, Bristol-Myers Squibb, Takeda, Pfizer, Novartis, Celgene Corporation, Abbvie, and Incyte, among others.
SOURCE: Statler A et al. ASH 2019, Abstract 381.
ORLANDO – While African Americans with acute myeloid leukemia were more likely to have evidence of abnormal kidney function, the excess of this comorbidity didn’t affect overall survival, compared with whites, according to a study of more than 1,000 patients.
A total of 63% of African Americans with acute myeloid leukemia (AML) presented with a renal function abnormality that could have excluded them from a clinical trial, compared with 56% in the overall cohort; however, analysis of outcomes data suggested that renal function abnormalities were not associated with decreased survival in African Americans versus whites, said Abby Statler, PhD, MPH, of the Cleveland Clinic.
The findings may have implications for the design of clinical trials that might exclude patients on the basis of comorbidities that don’t actually affect survival, according to Dr. Statler.
“If we’re able to liberalize renal function eligibility criteria ... this may reduce racial disparities in clinical trial enrollment, which might be a major step in improving the diversity of cancer patient populations,” Dr. Statler said in a press conference at the annual meeting of the American Society of Hematology.
Overly restrictive criteria could be a significant barrier to clinical trial enrollment among minority patient populations, according to Dr. Statler.
Eligibility criteria are generally biased toward “fit” patient populations, which means they may discriminate against less-fit groups, such as African Americans who, compared with whites, have higher rates of comorbidities and report poorer overall health, according to Dr. Statler.
Laura Michaelis, MD, who chaired the press conference, said these findings suggest current clinical trial designs may be “too restrictive.”
“Once it’s published and validated, [these] data should definitely make us think twice about when you limit a patient’s enrollment in a trial,” Dr. Michaelis said in an interview.
Restrictive eligibility criteria may not only limit access to minority populations, but also may slow clinical trial accrual and completion, and make it harder to generalize clinical trial findings to the overall population, said Dr. Michaelis, associate professor of medicine in the division of hematology and oncology, Medical College of Wisconsin, Milwaukee.
The study by Dr. Statler and colleagues included 1,040 AML patients who received chemotherapy at Cleveland Clinic between 2003 and 2019. About 10% of the patients in the analysis were African American and 90% were white.
Median overall survival was not significantly different by race, at 13.7 months for African Americans and 14.9 months for whites (P = 0.89), according to results published in the study abstract.
Mild creatinine elevation did not appear to affect survival in this study, according to the investigator. Survival was not significantly different between patients with normal creatinine and those with creatinine up to 1.5 times the upper limit of normal. However, higher levels of creatinine were significantly associated with worse survival, Dr. Statler said.
Further analyses showed that these survival findings by creatinine level held up specifically in the African American subgroup as well, Dr. Statler said in the press conference.
Dr. Statler provided no disclosures related to the presentation. Study coauthors described disclosures related to Amgen, SimulStat, Bristol-Myers Squibb, Takeda, Pfizer, Novartis, Celgene Corporation, Abbvie, and Incyte, among others.
SOURCE: Statler A et al. ASH 2019, Abstract 381.
ORLANDO – While African Americans with acute myeloid leukemia were more likely to have evidence of abnormal kidney function, the excess of this comorbidity didn’t affect overall survival, compared with whites, according to a study of more than 1,000 patients.
A total of 63% of African Americans with acute myeloid leukemia (AML) presented with a renal function abnormality that could have excluded them from a clinical trial, compared with 56% in the overall cohort; however, analysis of outcomes data suggested that renal function abnormalities were not associated with decreased survival in African Americans versus whites, said Abby Statler, PhD, MPH, of the Cleveland Clinic.
The findings may have implications for the design of clinical trials that might exclude patients on the basis of comorbidities that don’t actually affect survival, according to Dr. Statler.
“If we’re able to liberalize renal function eligibility criteria ... this may reduce racial disparities in clinical trial enrollment, which might be a major step in improving the diversity of cancer patient populations,” Dr. Statler said in a press conference at the annual meeting of the American Society of Hematology.
Overly restrictive criteria could be a significant barrier to clinical trial enrollment among minority patient populations, according to Dr. Statler.
Eligibility criteria are generally biased toward “fit” patient populations, which means they may discriminate against less-fit groups, such as African Americans who, compared with whites, have higher rates of comorbidities and report poorer overall health, according to Dr. Statler.
Laura Michaelis, MD, who chaired the press conference, said these findings suggest current clinical trial designs may be “too restrictive.”
“Once it’s published and validated, [these] data should definitely make us think twice about when you limit a patient’s enrollment in a trial,” Dr. Michaelis said in an interview.
Restrictive eligibility criteria may not only limit access to minority populations, but also may slow clinical trial accrual and completion, and make it harder to generalize clinical trial findings to the overall population, said Dr. Michaelis, associate professor of medicine in the division of hematology and oncology, Medical College of Wisconsin, Milwaukee.
The study by Dr. Statler and colleagues included 1,040 AML patients who received chemotherapy at Cleveland Clinic between 2003 and 2019. About 10% of the patients in the analysis were African American and 90% were white.
Median overall survival was not significantly different by race, at 13.7 months for African Americans and 14.9 months for whites (P = 0.89), according to results published in the study abstract.
Mild creatinine elevation did not appear to affect survival in this study, according to the investigator. Survival was not significantly different between patients with normal creatinine and those with creatinine up to 1.5 times the upper limit of normal. However, higher levels of creatinine were significantly associated with worse survival, Dr. Statler said.
Further analyses showed that these survival findings by creatinine level held up specifically in the African American subgroup as well, Dr. Statler said in the press conference.
Dr. Statler provided no disclosures related to the presentation. Study coauthors described disclosures related to Amgen, SimulStat, Bristol-Myers Squibb, Takeda, Pfizer, Novartis, Celgene Corporation, Abbvie, and Incyte, among others.
SOURCE: Statler A et al. ASH 2019, Abstract 381.
REPORTING FROM ASH 2019
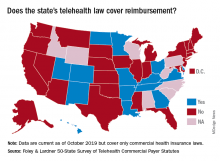
More states pushing plans to pay for telehealth care
More states are enacting laws that require private plans to cover telehealth services, but fair payment remains a challenge for providers, a new analysis finds.
In 2019, 42 states and the District of Columbia had commercial payer telehealth laws, according to a December report by Foley & Lardner LLP, an international law firm. In contrast, about 30 states had such laws in 2015, according to a 2015 report by the National Conference of State Legislatures. Telehealth coverage laws generally require private plans to cover services provided via telehealth to the extent they cover in-person services of the same nature. The measures also frequently protect patients from cost-shifting, in which an insurer imposes higher deductibles or copays for telehealth services.
Private coverage for asynchronous telehealth and remote patient monitoring (RPM) is also growing. Twenty-four states mandate coverage for store and forward asynchronous telehealth, while 13 states require commercial health plans to cover RPM services, the analysis found. In addition, most telehealth coverage laws do not limit where a patient can receive telehealth services. However, some states, such as Arizona, Tennessee, and Washington, still require that patients be located in a particular clinical setting at the time of the telehealth consultation.
Overall, the landscape for reimbursement of telehealth services by commercial payers has improved, said Jacqueline Acosta, a health care attorney with Foley & Lardner and a coauthor of the report.
“[Foley& Lardner’s] 2017 report really noted that implementation [of telehealth] had really picked up both from providers and patients asking for telemedicine, but reimbursement still lagged behind,” Ms. Acosta said in an interview. “This one shows real progress on that front.”
However, the survey notes that payment parity for telehealth services remains lacking. Payment parity refers to insurers paying for telehealth services at the same or an equivalent rate as those delivered in-person. In 2019, 16 states had laws that specifically addressed reimbursement of telehealth services, but only 10 offer true payment parity, according to the Foley analysis. The 10 states with payment parity laws are Arkansas, Delaware, Georgia, Hawaii, Kentucky, Minnesota, Missouri, New Mexico, Utah, and Virginia. Other telehealth reimbursement measures often include ambiguity or allow room for payment negotiation, Ms. Acosta said.
She predicts that more payment parity laws and improved telehealth coverage laws are on the horizon for 2020 and beyond. California, for example, recently revised its telehealth law to require both coverage and payment parity for telehealth services. Mississippi meanwhile, recently expanded its law to include RPM coverage.
That states are revising existing laws and expanding their statutes shows an optimistic trend toward telehealth acceptance and coverage growth, Ms. Acosta said.
More states are enacting laws that require private plans to cover telehealth services, but fair payment remains a challenge for providers, a new analysis finds.
In 2019, 42 states and the District of Columbia had commercial payer telehealth laws, according to a December report by Foley & Lardner LLP, an international law firm. In contrast, about 30 states had such laws in 2015, according to a 2015 report by the National Conference of State Legislatures. Telehealth coverage laws generally require private plans to cover services provided via telehealth to the extent they cover in-person services of the same nature. The measures also frequently protect patients from cost-shifting, in which an insurer imposes higher deductibles or copays for telehealth services.
Private coverage for asynchronous telehealth and remote patient monitoring (RPM) is also growing. Twenty-four states mandate coverage for store and forward asynchronous telehealth, while 13 states require commercial health plans to cover RPM services, the analysis found. In addition, most telehealth coverage laws do not limit where a patient can receive telehealth services. However, some states, such as Arizona, Tennessee, and Washington, still require that patients be located in a particular clinical setting at the time of the telehealth consultation.
Overall, the landscape for reimbursement of telehealth services by commercial payers has improved, said Jacqueline Acosta, a health care attorney with Foley & Lardner and a coauthor of the report.
“[Foley& Lardner’s] 2017 report really noted that implementation [of telehealth] had really picked up both from providers and patients asking for telemedicine, but reimbursement still lagged behind,” Ms. Acosta said in an interview. “This one shows real progress on that front.”
However, the survey notes that payment parity for telehealth services remains lacking. Payment parity refers to insurers paying for telehealth services at the same or an equivalent rate as those delivered in-person. In 2019, 16 states had laws that specifically addressed reimbursement of telehealth services, but only 10 offer true payment parity, according to the Foley analysis. The 10 states with payment parity laws are Arkansas, Delaware, Georgia, Hawaii, Kentucky, Minnesota, Missouri, New Mexico, Utah, and Virginia. Other telehealth reimbursement measures often include ambiguity or allow room for payment negotiation, Ms. Acosta said.
She predicts that more payment parity laws and improved telehealth coverage laws are on the horizon for 2020 and beyond. California, for example, recently revised its telehealth law to require both coverage and payment parity for telehealth services. Mississippi meanwhile, recently expanded its law to include RPM coverage.
That states are revising existing laws and expanding their statutes shows an optimistic trend toward telehealth acceptance and coverage growth, Ms. Acosta said.
More states are enacting laws that require private plans to cover telehealth services, but fair payment remains a challenge for providers, a new analysis finds.
In 2019, 42 states and the District of Columbia had commercial payer telehealth laws, according to a December report by Foley & Lardner LLP, an international law firm. In contrast, about 30 states had such laws in 2015, according to a 2015 report by the National Conference of State Legislatures. Telehealth coverage laws generally require private plans to cover services provided via telehealth to the extent they cover in-person services of the same nature. The measures also frequently protect patients from cost-shifting, in which an insurer imposes higher deductibles or copays for telehealth services.
Private coverage for asynchronous telehealth and remote patient monitoring (RPM) is also growing. Twenty-four states mandate coverage for store and forward asynchronous telehealth, while 13 states require commercial health plans to cover RPM services, the analysis found. In addition, most telehealth coverage laws do not limit where a patient can receive telehealth services. However, some states, such as Arizona, Tennessee, and Washington, still require that patients be located in a particular clinical setting at the time of the telehealth consultation.
Overall, the landscape for reimbursement of telehealth services by commercial payers has improved, said Jacqueline Acosta, a health care attorney with Foley & Lardner and a coauthor of the report.
“[Foley& Lardner’s] 2017 report really noted that implementation [of telehealth] had really picked up both from providers and patients asking for telemedicine, but reimbursement still lagged behind,” Ms. Acosta said in an interview. “This one shows real progress on that front.”
However, the survey notes that payment parity for telehealth services remains lacking. Payment parity refers to insurers paying for telehealth services at the same or an equivalent rate as those delivered in-person. In 2019, 16 states had laws that specifically addressed reimbursement of telehealth services, but only 10 offer true payment parity, according to the Foley analysis. The 10 states with payment parity laws are Arkansas, Delaware, Georgia, Hawaii, Kentucky, Minnesota, Missouri, New Mexico, Utah, and Virginia. Other telehealth reimbursement measures often include ambiguity or allow room for payment negotiation, Ms. Acosta said.
She predicts that more payment parity laws and improved telehealth coverage laws are on the horizon for 2020 and beyond. California, for example, recently revised its telehealth law to require both coverage and payment parity for telehealth services. Mississippi meanwhile, recently expanded its law to include RPM coverage.
That states are revising existing laws and expanding their statutes shows an optimistic trend toward telehealth acceptance and coverage growth, Ms. Acosta said.
Newly identified genetic changes contribute to transformation of follicular lymphoma
A molecular analysis of a patient with follicular lymphoma (FL) that became B-lymphoblastic leukemia/lymphoma (B-ALL/LBL) uncovered genetic changes that may improve understanding of this transformation.
“The study provides new insights into the pathogenesis of FL-B-ALL/LBL transformation and suggests novel, disease biology–based therapeutic approaches to this aggressive and currently incurable disease,” wrote Jonathan Belman, MD, PhD, of the Hospital of the University of Pennsylvania, Philadelphia, and coauthors. Their findings were published in Cold Spring Harbor Molecular Case Studies.
To further understand the rare occasions when FL transforms into a more aggressive form of lymphoma, the researchers investigated a 36-year-old man with low-grade FL that became B-ALL/LBL roughly 1 year after diagnosis. Their analysis included immunoglobulin (Ig) gene rearrangement studies, cytogenetic analysis, and whole exome sequencing of the patient’s FL, B-ALL/LBL, and normal cells.
Next generation sequencing of Ig rearrangements from normal, FL, and B-ALL/LBL specimens revealed considerable somatic hypermutation (SHM) in a single neoplastic clone – IgHV4-34_JH6 – in the FL cells. By comparison, though no dominant clone was found in the B-ALL/LBL specimen, there was even more extensive SHM, along with clones that could be traced to the FL lineage.
In addition, fluorescence in situ hybridization (FISH) studies on the FL specimen were positive for rearrangements of BCL2 and BCL6 genes; a rearrangement of BCL6 is associated with clinical aggressiveness. Those same two rearrangements were found in the B-ALL/LBL specimen, along with a MYC gene rearrangement unseen in the FL.
“MYC translocations are well known to contribute to high aggressiveness of lymphomas, and are hallmark of FL-B-ALL/LBL transformation,” the researchers wrote.
Finally, comparative whole exome sequencing of normal tissue plus the cancerous specimens identified 751 single nucleotide variants. The normal tissue contained 111 of those mutations, while the FL specimens contained 116 mutations – 11 of which were shared solely with B-ALL/LBL – and the B-ALL/LBL specimens contained a striking 575 unique mutations. Notably, a nonsense mutation in the KMT2D gene that was shared by FL and B-ALL/LBL may have contributed to lymphomagenesis.
The study was funded by a grant from the National Institutes of Health, the Abramson Cancer Center Translational Center in Lymphoma, the Daniel B. Allanoff Foundation, and a Hematopathology Divisional Training grant.
SOURCE: Belman JP et al. Cold Spring Harb Mol Case Stud. 2019 Nov 27. doi: 10.1101/mcs.a004614.
A molecular analysis of a patient with follicular lymphoma (FL) that became B-lymphoblastic leukemia/lymphoma (B-ALL/LBL) uncovered genetic changes that may improve understanding of this transformation.
“The study provides new insights into the pathogenesis of FL-B-ALL/LBL transformation and suggests novel, disease biology–based therapeutic approaches to this aggressive and currently incurable disease,” wrote Jonathan Belman, MD, PhD, of the Hospital of the University of Pennsylvania, Philadelphia, and coauthors. Their findings were published in Cold Spring Harbor Molecular Case Studies.
To further understand the rare occasions when FL transforms into a more aggressive form of lymphoma, the researchers investigated a 36-year-old man with low-grade FL that became B-ALL/LBL roughly 1 year after diagnosis. Their analysis included immunoglobulin (Ig) gene rearrangement studies, cytogenetic analysis, and whole exome sequencing of the patient’s FL, B-ALL/LBL, and normal cells.
Next generation sequencing of Ig rearrangements from normal, FL, and B-ALL/LBL specimens revealed considerable somatic hypermutation (SHM) in a single neoplastic clone – IgHV4-34_JH6 – in the FL cells. By comparison, though no dominant clone was found in the B-ALL/LBL specimen, there was even more extensive SHM, along with clones that could be traced to the FL lineage.
In addition, fluorescence in situ hybridization (FISH) studies on the FL specimen were positive for rearrangements of BCL2 and BCL6 genes; a rearrangement of BCL6 is associated with clinical aggressiveness. Those same two rearrangements were found in the B-ALL/LBL specimen, along with a MYC gene rearrangement unseen in the FL.
“MYC translocations are well known to contribute to high aggressiveness of lymphomas, and are hallmark of FL-B-ALL/LBL transformation,” the researchers wrote.
Finally, comparative whole exome sequencing of normal tissue plus the cancerous specimens identified 751 single nucleotide variants. The normal tissue contained 111 of those mutations, while the FL specimens contained 116 mutations – 11 of which were shared solely with B-ALL/LBL – and the B-ALL/LBL specimens contained a striking 575 unique mutations. Notably, a nonsense mutation in the KMT2D gene that was shared by FL and B-ALL/LBL may have contributed to lymphomagenesis.
The study was funded by a grant from the National Institutes of Health, the Abramson Cancer Center Translational Center in Lymphoma, the Daniel B. Allanoff Foundation, and a Hematopathology Divisional Training grant.
SOURCE: Belman JP et al. Cold Spring Harb Mol Case Stud. 2019 Nov 27. doi: 10.1101/mcs.a004614.
A molecular analysis of a patient with follicular lymphoma (FL) that became B-lymphoblastic leukemia/lymphoma (B-ALL/LBL) uncovered genetic changes that may improve understanding of this transformation.
“The study provides new insights into the pathogenesis of FL-B-ALL/LBL transformation and suggests novel, disease biology–based therapeutic approaches to this aggressive and currently incurable disease,” wrote Jonathan Belman, MD, PhD, of the Hospital of the University of Pennsylvania, Philadelphia, and coauthors. Their findings were published in Cold Spring Harbor Molecular Case Studies.
To further understand the rare occasions when FL transforms into a more aggressive form of lymphoma, the researchers investigated a 36-year-old man with low-grade FL that became B-ALL/LBL roughly 1 year after diagnosis. Their analysis included immunoglobulin (Ig) gene rearrangement studies, cytogenetic analysis, and whole exome sequencing of the patient’s FL, B-ALL/LBL, and normal cells.
Next generation sequencing of Ig rearrangements from normal, FL, and B-ALL/LBL specimens revealed considerable somatic hypermutation (SHM) in a single neoplastic clone – IgHV4-34_JH6 – in the FL cells. By comparison, though no dominant clone was found in the B-ALL/LBL specimen, there was even more extensive SHM, along with clones that could be traced to the FL lineage.
In addition, fluorescence in situ hybridization (FISH) studies on the FL specimen were positive for rearrangements of BCL2 and BCL6 genes; a rearrangement of BCL6 is associated with clinical aggressiveness. Those same two rearrangements were found in the B-ALL/LBL specimen, along with a MYC gene rearrangement unseen in the FL.
“MYC translocations are well known to contribute to high aggressiveness of lymphomas, and are hallmark of FL-B-ALL/LBL transformation,” the researchers wrote.
Finally, comparative whole exome sequencing of normal tissue plus the cancerous specimens identified 751 single nucleotide variants. The normal tissue contained 111 of those mutations, while the FL specimens contained 116 mutations – 11 of which were shared solely with B-ALL/LBL – and the B-ALL/LBL specimens contained a striking 575 unique mutations. Notably, a nonsense mutation in the KMT2D gene that was shared by FL and B-ALL/LBL may have contributed to lymphomagenesis.
The study was funded by a grant from the National Institutes of Health, the Abramson Cancer Center Translational Center in Lymphoma, the Daniel B. Allanoff Foundation, and a Hematopathology Divisional Training grant.
SOURCE: Belman JP et al. Cold Spring Harb Mol Case Stud. 2019 Nov 27. doi: 10.1101/mcs.a004614.
FROM COLD SPRING HARBOR MOLECULAR CASE STUDIES
Myeloma patients over age 70 can benefit from auto-HC transplant
ORLANDO – Age 70 may be the new 60, at least when it comes to outcomes following autologous hematopoietic cell transplantation (auto-HCT) in multiple myeloma.
A large-scale study looking at transplant outcomes across age groups in multiple myeloma patients found similar rates of nonrelapse mortality, relapse/progression, progression-free survival, and overall survival between patients who were aged 70 years and older and those who were aged 60-69 years.
“Age has no implication in terms of the antimyeloma effect of transplant,” Anita D’Souza, MD, of the Medical College of Wisconsin, Milwaukee, said at the annual meeting of the American Society of Hematology.
The study analyzed outcomes from 15,999 multiple myeloma patients aged 20 years or older in the United States who received a single auto-HCT with melphalan conditioning within 12 months of diagnosis between 2013 and 2017. Within that dataset, the researchers compared outcomes from 7,032 patients aged 60-69 years and 2,092 patients aged 70 years and older.
This is the largest study of auto-HCT in older adults with multiple myeloma, the researchers said, and provides important data about the benefit of transplant at any age.
Univariate analysis showed that 100-day nonrelapse mortality was higher in patients aged 70 years and older – at 1% – compared with younger patients (P less than .01). Also, 2-year overall survival was lower in older adults – at 86% – compared with 60- to 69-year-olds (P less than .01).
However, on multivariate analysis with 60- to 69-year-olds as the reference group, patients older than age 70 years had similar nonrelapse mortality (hazard ratio [HR] 1.3, 95% confidence interval [CI] 1, 1.7, P = .06). The same trends were seen for relapse/progression (HR 1.0, 95% CI, 0.9-1, P = .6), progression-free survival (HR 1.1, 95% CI 1-1.2, P = .2), and overall survival (HR 1.2, 95% CI 1-1.4, P = .03). Given the large sample size, a P value of .01 was considered statistically significant.
Over the course of the study period, the percentage of patients aged 70 and older who received a transplant grew each year, rising to 28% by 2017. But Dr. D’Souza said that number is still too low given the safety and efficacy of auto-HCT in these patients.
“Every patient with myeloma should be referred to a transplant center,” she said.
Dr. D’Souza reported financial disclosures related to EDO-Mundapharma, Merck, Prothena, Sanofi, TeneoBio, Prothena, Pfizer, Imbrium, and Akcea. Other study authors reported financial relationships with multiple companies including Celgene, Takeda, BMS, and Janssen.
SOURCE: Munshi PN et al. ASH 2019, Abstract 782.
ORLANDO – Age 70 may be the new 60, at least when it comes to outcomes following autologous hematopoietic cell transplantation (auto-HCT) in multiple myeloma.
A large-scale study looking at transplant outcomes across age groups in multiple myeloma patients found similar rates of nonrelapse mortality, relapse/progression, progression-free survival, and overall survival between patients who were aged 70 years and older and those who were aged 60-69 years.
“Age has no implication in terms of the antimyeloma effect of transplant,” Anita D’Souza, MD, of the Medical College of Wisconsin, Milwaukee, said at the annual meeting of the American Society of Hematology.
The study analyzed outcomes from 15,999 multiple myeloma patients aged 20 years or older in the United States who received a single auto-HCT with melphalan conditioning within 12 months of diagnosis between 2013 and 2017. Within that dataset, the researchers compared outcomes from 7,032 patients aged 60-69 years and 2,092 patients aged 70 years and older.
This is the largest study of auto-HCT in older adults with multiple myeloma, the researchers said, and provides important data about the benefit of transplant at any age.
Univariate analysis showed that 100-day nonrelapse mortality was higher in patients aged 70 years and older – at 1% – compared with younger patients (P less than .01). Also, 2-year overall survival was lower in older adults – at 86% – compared with 60- to 69-year-olds (P less than .01).
However, on multivariate analysis with 60- to 69-year-olds as the reference group, patients older than age 70 years had similar nonrelapse mortality (hazard ratio [HR] 1.3, 95% confidence interval [CI] 1, 1.7, P = .06). The same trends were seen for relapse/progression (HR 1.0, 95% CI, 0.9-1, P = .6), progression-free survival (HR 1.1, 95% CI 1-1.2, P = .2), and overall survival (HR 1.2, 95% CI 1-1.4, P = .03). Given the large sample size, a P value of .01 was considered statistically significant.
Over the course of the study period, the percentage of patients aged 70 and older who received a transplant grew each year, rising to 28% by 2017. But Dr. D’Souza said that number is still too low given the safety and efficacy of auto-HCT in these patients.
“Every patient with myeloma should be referred to a transplant center,” she said.
Dr. D’Souza reported financial disclosures related to EDO-Mundapharma, Merck, Prothena, Sanofi, TeneoBio, Prothena, Pfizer, Imbrium, and Akcea. Other study authors reported financial relationships with multiple companies including Celgene, Takeda, BMS, and Janssen.
SOURCE: Munshi PN et al. ASH 2019, Abstract 782.
ORLANDO – Age 70 may be the new 60, at least when it comes to outcomes following autologous hematopoietic cell transplantation (auto-HCT) in multiple myeloma.
A large-scale study looking at transplant outcomes across age groups in multiple myeloma patients found similar rates of nonrelapse mortality, relapse/progression, progression-free survival, and overall survival between patients who were aged 70 years and older and those who were aged 60-69 years.
“Age has no implication in terms of the antimyeloma effect of transplant,” Anita D’Souza, MD, of the Medical College of Wisconsin, Milwaukee, said at the annual meeting of the American Society of Hematology.
The study analyzed outcomes from 15,999 multiple myeloma patients aged 20 years or older in the United States who received a single auto-HCT with melphalan conditioning within 12 months of diagnosis between 2013 and 2017. Within that dataset, the researchers compared outcomes from 7,032 patients aged 60-69 years and 2,092 patients aged 70 years and older.
This is the largest study of auto-HCT in older adults with multiple myeloma, the researchers said, and provides important data about the benefit of transplant at any age.
Univariate analysis showed that 100-day nonrelapse mortality was higher in patients aged 70 years and older – at 1% – compared with younger patients (P less than .01). Also, 2-year overall survival was lower in older adults – at 86% – compared with 60- to 69-year-olds (P less than .01).
However, on multivariate analysis with 60- to 69-year-olds as the reference group, patients older than age 70 years had similar nonrelapse mortality (hazard ratio [HR] 1.3, 95% confidence interval [CI] 1, 1.7, P = .06). The same trends were seen for relapse/progression (HR 1.0, 95% CI, 0.9-1, P = .6), progression-free survival (HR 1.1, 95% CI 1-1.2, P = .2), and overall survival (HR 1.2, 95% CI 1-1.4, P = .03). Given the large sample size, a P value of .01 was considered statistically significant.
Over the course of the study period, the percentage of patients aged 70 and older who received a transplant grew each year, rising to 28% by 2017. But Dr. D’Souza said that number is still too low given the safety and efficacy of auto-HCT in these patients.
“Every patient with myeloma should be referred to a transplant center,” she said.
Dr. D’Souza reported financial disclosures related to EDO-Mundapharma, Merck, Prothena, Sanofi, TeneoBio, Prothena, Pfizer, Imbrium, and Akcea. Other study authors reported financial relationships with multiple companies including Celgene, Takeda, BMS, and Janssen.
SOURCE: Munshi PN et al. ASH 2019, Abstract 782.
REPORTING FROM ASH 2019