User login
Child of The New Gastroenterologist
When Your First Job Isn’t Forever: Lessons from My Journey and What Early-Career GIs Need to Know
Introduction
For many of us in gastroenterology, landing that first attending job feels like the ultimate victory lap — the reward for all those years of training. We sign the contract, relocate, and imagine this will be our “forever job.” Reality often plays out differently.
In fact, 43% of physicians change jobs within five years, while 83% changed employers at least once in their careers.1 Even within our field — which is always in demand — turnover is high; 1 in 3 gastroenterologists are planning to leave their current role within two years.2 Why does this happen? More importantly, how do we navigate this transition with clarity and confidence as an early-career GI?
My Story: When I Dared to Change My “Forever Job”
When I signed my first attending contract, I didn’t negotiate a single thing. My priorities were simple: family in Toronto and visa requirements. After a decade of medical school, residency, and fellowship, everything else felt secondary. I was happy to be back home.
The job itself was good — reasonable hours, flexible colleagues, and ample opportunity to enhance my procedural skills. As I started carving out my niche in endobariatrics, the support I needed to grow further was not there. I kept telling myself that this job fulfilled my values and I needed to be patient: “this is my forever job. I am close to my family and that’s what matters.”
Then, during a suturing course at the American Society of Gastrointestinal Endoscopy, I had a casual chat with the course director (now my boss). It took me by surprise, but as the conversation continued, he offered me a job. It was tempting: the chance to build my own endobariatrics program with real institutional backing. The catch? It was in a city I had never been to, with no family or friends around. I politely said “no, thank you, I can’t.” He smiled, gave me his number, and said, “think about it.”
For the first time, I allowed myself to ask, “could I really leave my forever job?”
The Power of a Circle and a Spreadsheet
I leaned on my circle — a close group of fellowship friends who each took a turn being someone’s lifeline. We have monthly Zoom calls to talk about jobs, family, and career aspirations. When I shared my dilemma, I realized I wasn’t alone; one friend was also unhappy with her first job. Suddenly, we were asking one another, “can we really leave?”
I hired a career consultant familiar with physician visa issues — hands down, the best money I ever invested. The job search felt like dating: each interview was a first date; some needed a second or third date before I knew if it could be a match.
After every interview, I’d jump on Zoom with my circle. We’d screen-share my giant Excel spreadsheet — our decision matrix — with columns for everything I cared about:
- Institute
- Administrative Time
- Endobariatric support
- Director Title
- Salary
- On-call
- Vacation
- Proximity to airport
- Cost of living
- RVU percentage
- Endoscopy center buy-in
- Contract duration
- Support staff
- CME
We scored each job, line by line, and not a single job checked all the boxes. As I sat there in a state of decision paralysis, it became clear that this was not a simple decision.
The GI Community: A Small, Supportive World
The GI community is incredibly close-knit and kind-hearted. At every conference, I made a point to chat with as many colleagues as I could, to hear their perspectives on jobs and how they made tough career moves. Those conversations were real — no Google search or Excel sheet could offer the perspective and insight I gained by simply asking and leaning on the GI community.
Meanwhile, the person who had first offered me that job kept checking in, catching up at conferences, and bonding over our love for food and baking. With him, I never felt like I was being ‘interviewed’ — I felt valued. It did not feel like he was trying to fill a position with just anyone to improve the call pool. He genuinely wanted to understand what my goals were and how I envisioned my future. Through those conversations, he reminded me of my original passions, which were sidelined when so immersed in the daily routine.
I’ve learned that feeling valued doesn’t come from grand gestures in recruitment. It’s in the quiet signs of respect, trust, and being seen. He wasn’t looking for just anyone; he was looking for someone whose goals aligned with his group’s and someone in whom he wanted to invest. While others might chase the highest salary, the most flexible schedule, or the strongest ancillary support, I realized I valued something I did not realize that I was lacking until then: mentorship.
What I Learned: There is No Such Thing As “The Perfect Job”
After a full year of spreadsheets, Zoom calls, conference chats, and overthinking, I came to a big realization: there’s no perfect job — there’s no such thing as an ideal “forever job.” The only constant for humans is change. Our circumstances change, our priorities shift, our interests shuffle, and our finances evolve. The best job is simply the one that fits the stage of life you’re in at that given moment. For me, mentorship and growth became my top priorities, even if it meant moving away from family.
What Physicians Value Most in a Second Job
After their first job, early-career gastroenterologists often reevaluate what really matters. Recent surveys highlight four key priorities:
- Work-life balance:
In a 2022 CompHealth Group healthcare survey, 85% of physicians ranked work-life balance as their top job priority.3
- Mentorship and growth:
Nearly 1 in 3 physicians cited lack of mentorship or career advancement as their reason for leaving a first job, per the 2023 MGMA/Jackson Physician Search report.4
- Compensation:
While not always the main reason for leaving, 77% of physicians now list compensation as a top priority — a big jump from prior years.3
- Practice support:
Poor infrastructure, administrative overload, or understaffed teams are common dealbreakers. In the second job, physicians look for well-run practices with solid support staff and reduced burnout risk.5
Conclusion
Welcome the uncertainty, talk to your circle, lean on your community, and use a spreadsheet if you need to — but don’t forget to trust your gut. There’s no forever job or the perfect path, only the next move that feels most true to who you are in that moment.
Dr. Ismail (@mayyismail) is Assistant Professor of Clinical Medicine (Gastroenterology) at Temple University in Philadelphia, Pennsylvania. She declares no conflicts of interest.
References
1. CHG Healthcare. Survey: 62% of physicians made a career change in the last two years. CHG Healthcare blog. June 10, 2024. Accessed August 5, 2025.
2. Berg S. Physicians in these 10 specialties are less likely to quit. AMA News. Published June 24, 2025. Accessed July 2025.
3. Saley C. Survey: Work/life balance is #1 priority in physicians’ job search. CHG Healthcare Insights. March 10, 2022. Accessed August 2025.
4. Medical Group Management Association; Jackson Physician Search. Early‑Career Physician Recruiting & Retention Playbook. October 23, 2023. Accessed August 2025.
5. Von Rosenvinge EC, et al. A crisis in scope: Recruitment and retention challenges reported by VA gastroenterology section chiefs. Fed Pract. 2024 Aug. doi:10.12788/fp.0504.
Introduction
For many of us in gastroenterology, landing that first attending job feels like the ultimate victory lap — the reward for all those years of training. We sign the contract, relocate, and imagine this will be our “forever job.” Reality often plays out differently.
In fact, 43% of physicians change jobs within five years, while 83% changed employers at least once in their careers.1 Even within our field — which is always in demand — turnover is high; 1 in 3 gastroenterologists are planning to leave their current role within two years.2 Why does this happen? More importantly, how do we navigate this transition with clarity and confidence as an early-career GI?
My Story: When I Dared to Change My “Forever Job”
When I signed my first attending contract, I didn’t negotiate a single thing. My priorities were simple: family in Toronto and visa requirements. After a decade of medical school, residency, and fellowship, everything else felt secondary. I was happy to be back home.
The job itself was good — reasonable hours, flexible colleagues, and ample opportunity to enhance my procedural skills. As I started carving out my niche in endobariatrics, the support I needed to grow further was not there. I kept telling myself that this job fulfilled my values and I needed to be patient: “this is my forever job. I am close to my family and that’s what matters.”
Then, during a suturing course at the American Society of Gastrointestinal Endoscopy, I had a casual chat with the course director (now my boss). It took me by surprise, but as the conversation continued, he offered me a job. It was tempting: the chance to build my own endobariatrics program with real institutional backing. The catch? It was in a city I had never been to, with no family or friends around. I politely said “no, thank you, I can’t.” He smiled, gave me his number, and said, “think about it.”
For the first time, I allowed myself to ask, “could I really leave my forever job?”
The Power of a Circle and a Spreadsheet
I leaned on my circle — a close group of fellowship friends who each took a turn being someone’s lifeline. We have monthly Zoom calls to talk about jobs, family, and career aspirations. When I shared my dilemma, I realized I wasn’t alone; one friend was also unhappy with her first job. Suddenly, we were asking one another, “can we really leave?”
I hired a career consultant familiar with physician visa issues — hands down, the best money I ever invested. The job search felt like dating: each interview was a first date; some needed a second or third date before I knew if it could be a match.
After every interview, I’d jump on Zoom with my circle. We’d screen-share my giant Excel spreadsheet — our decision matrix — with columns for everything I cared about:
- Institute
- Administrative Time
- Endobariatric support
- Director Title
- Salary
- On-call
- Vacation
- Proximity to airport
- Cost of living
- RVU percentage
- Endoscopy center buy-in
- Contract duration
- Support staff
- CME
We scored each job, line by line, and not a single job checked all the boxes. As I sat there in a state of decision paralysis, it became clear that this was not a simple decision.
The GI Community: A Small, Supportive World
The GI community is incredibly close-knit and kind-hearted. At every conference, I made a point to chat with as many colleagues as I could, to hear their perspectives on jobs and how they made tough career moves. Those conversations were real — no Google search or Excel sheet could offer the perspective and insight I gained by simply asking and leaning on the GI community.
Meanwhile, the person who had first offered me that job kept checking in, catching up at conferences, and bonding over our love for food and baking. With him, I never felt like I was being ‘interviewed’ — I felt valued. It did not feel like he was trying to fill a position with just anyone to improve the call pool. He genuinely wanted to understand what my goals were and how I envisioned my future. Through those conversations, he reminded me of my original passions, which were sidelined when so immersed in the daily routine.
I’ve learned that feeling valued doesn’t come from grand gestures in recruitment. It’s in the quiet signs of respect, trust, and being seen. He wasn’t looking for just anyone; he was looking for someone whose goals aligned with his group’s and someone in whom he wanted to invest. While others might chase the highest salary, the most flexible schedule, or the strongest ancillary support, I realized I valued something I did not realize that I was lacking until then: mentorship.
What I Learned: There is No Such Thing As “The Perfect Job”
After a full year of spreadsheets, Zoom calls, conference chats, and overthinking, I came to a big realization: there’s no perfect job — there’s no such thing as an ideal “forever job.” The only constant for humans is change. Our circumstances change, our priorities shift, our interests shuffle, and our finances evolve. The best job is simply the one that fits the stage of life you’re in at that given moment. For me, mentorship and growth became my top priorities, even if it meant moving away from family.
What Physicians Value Most in a Second Job
After their first job, early-career gastroenterologists often reevaluate what really matters. Recent surveys highlight four key priorities:
- Work-life balance:
In a 2022 CompHealth Group healthcare survey, 85% of physicians ranked work-life balance as their top job priority.3
- Mentorship and growth:
Nearly 1 in 3 physicians cited lack of mentorship or career advancement as their reason for leaving a first job, per the 2023 MGMA/Jackson Physician Search report.4
- Compensation:
While not always the main reason for leaving, 77% of physicians now list compensation as a top priority — a big jump from prior years.3
- Practice support:
Poor infrastructure, administrative overload, or understaffed teams are common dealbreakers. In the second job, physicians look for well-run practices with solid support staff and reduced burnout risk.5
Conclusion
Welcome the uncertainty, talk to your circle, lean on your community, and use a spreadsheet if you need to — but don’t forget to trust your gut. There’s no forever job or the perfect path, only the next move that feels most true to who you are in that moment.
Dr. Ismail (@mayyismail) is Assistant Professor of Clinical Medicine (Gastroenterology) at Temple University in Philadelphia, Pennsylvania. She declares no conflicts of interest.
References
1. CHG Healthcare. Survey: 62% of physicians made a career change in the last two years. CHG Healthcare blog. June 10, 2024. Accessed August 5, 2025.
2. Berg S. Physicians in these 10 specialties are less likely to quit. AMA News. Published June 24, 2025. Accessed July 2025.
3. Saley C. Survey: Work/life balance is #1 priority in physicians’ job search. CHG Healthcare Insights. March 10, 2022. Accessed August 2025.
4. Medical Group Management Association; Jackson Physician Search. Early‑Career Physician Recruiting & Retention Playbook. October 23, 2023. Accessed August 2025.
5. Von Rosenvinge EC, et al. A crisis in scope: Recruitment and retention challenges reported by VA gastroenterology section chiefs. Fed Pract. 2024 Aug. doi:10.12788/fp.0504.
Introduction
For many of us in gastroenterology, landing that first attending job feels like the ultimate victory lap — the reward for all those years of training. We sign the contract, relocate, and imagine this will be our “forever job.” Reality often plays out differently.
In fact, 43% of physicians change jobs within five years, while 83% changed employers at least once in their careers.1 Even within our field — which is always in demand — turnover is high; 1 in 3 gastroenterologists are planning to leave their current role within two years.2 Why does this happen? More importantly, how do we navigate this transition with clarity and confidence as an early-career GI?
My Story: When I Dared to Change My “Forever Job”
When I signed my first attending contract, I didn’t negotiate a single thing. My priorities were simple: family in Toronto and visa requirements. After a decade of medical school, residency, and fellowship, everything else felt secondary. I was happy to be back home.
The job itself was good — reasonable hours, flexible colleagues, and ample opportunity to enhance my procedural skills. As I started carving out my niche in endobariatrics, the support I needed to grow further was not there. I kept telling myself that this job fulfilled my values and I needed to be patient: “this is my forever job. I am close to my family and that’s what matters.”
Then, during a suturing course at the American Society of Gastrointestinal Endoscopy, I had a casual chat with the course director (now my boss). It took me by surprise, but as the conversation continued, he offered me a job. It was tempting: the chance to build my own endobariatrics program with real institutional backing. The catch? It was in a city I had never been to, with no family or friends around. I politely said “no, thank you, I can’t.” He smiled, gave me his number, and said, “think about it.”
For the first time, I allowed myself to ask, “could I really leave my forever job?”
The Power of a Circle and a Spreadsheet
I leaned on my circle — a close group of fellowship friends who each took a turn being someone’s lifeline. We have monthly Zoom calls to talk about jobs, family, and career aspirations. When I shared my dilemma, I realized I wasn’t alone; one friend was also unhappy with her first job. Suddenly, we were asking one another, “can we really leave?”
I hired a career consultant familiar with physician visa issues — hands down, the best money I ever invested. The job search felt like dating: each interview was a first date; some needed a second or third date before I knew if it could be a match.
After every interview, I’d jump on Zoom with my circle. We’d screen-share my giant Excel spreadsheet — our decision matrix — with columns for everything I cared about:
- Institute
- Administrative Time
- Endobariatric support
- Director Title
- Salary
- On-call
- Vacation
- Proximity to airport
- Cost of living
- RVU percentage
- Endoscopy center buy-in
- Contract duration
- Support staff
- CME
We scored each job, line by line, and not a single job checked all the boxes. As I sat there in a state of decision paralysis, it became clear that this was not a simple decision.
The GI Community: A Small, Supportive World
The GI community is incredibly close-knit and kind-hearted. At every conference, I made a point to chat with as many colleagues as I could, to hear their perspectives on jobs and how they made tough career moves. Those conversations were real — no Google search or Excel sheet could offer the perspective and insight I gained by simply asking and leaning on the GI community.
Meanwhile, the person who had first offered me that job kept checking in, catching up at conferences, and bonding over our love for food and baking. With him, I never felt like I was being ‘interviewed’ — I felt valued. It did not feel like he was trying to fill a position with just anyone to improve the call pool. He genuinely wanted to understand what my goals were and how I envisioned my future. Through those conversations, he reminded me of my original passions, which were sidelined when so immersed in the daily routine.
I’ve learned that feeling valued doesn’t come from grand gestures in recruitment. It’s in the quiet signs of respect, trust, and being seen. He wasn’t looking for just anyone; he was looking for someone whose goals aligned with his group’s and someone in whom he wanted to invest. While others might chase the highest salary, the most flexible schedule, or the strongest ancillary support, I realized I valued something I did not realize that I was lacking until then: mentorship.
What I Learned: There is No Such Thing As “The Perfect Job”
After a full year of spreadsheets, Zoom calls, conference chats, and overthinking, I came to a big realization: there’s no perfect job — there’s no such thing as an ideal “forever job.” The only constant for humans is change. Our circumstances change, our priorities shift, our interests shuffle, and our finances evolve. The best job is simply the one that fits the stage of life you’re in at that given moment. For me, mentorship and growth became my top priorities, even if it meant moving away from family.
What Physicians Value Most in a Second Job
After their first job, early-career gastroenterologists often reevaluate what really matters. Recent surveys highlight four key priorities:
- Work-life balance:
In a 2022 CompHealth Group healthcare survey, 85% of physicians ranked work-life balance as their top job priority.3
- Mentorship and growth:
Nearly 1 in 3 physicians cited lack of mentorship or career advancement as their reason for leaving a first job, per the 2023 MGMA/Jackson Physician Search report.4
- Compensation:
While not always the main reason for leaving, 77% of physicians now list compensation as a top priority — a big jump from prior years.3
- Practice support:
Poor infrastructure, administrative overload, or understaffed teams are common dealbreakers. In the second job, physicians look for well-run practices with solid support staff and reduced burnout risk.5
Conclusion
Welcome the uncertainty, talk to your circle, lean on your community, and use a spreadsheet if you need to — but don’t forget to trust your gut. There’s no forever job or the perfect path, only the next move that feels most true to who you are in that moment.
Dr. Ismail (@mayyismail) is Assistant Professor of Clinical Medicine (Gastroenterology) at Temple University in Philadelphia, Pennsylvania. She declares no conflicts of interest.
References
1. CHG Healthcare. Survey: 62% of physicians made a career change in the last two years. CHG Healthcare blog. June 10, 2024. Accessed August 5, 2025.
2. Berg S. Physicians in these 10 specialties are less likely to quit. AMA News. Published June 24, 2025. Accessed July 2025.
3. Saley C. Survey: Work/life balance is #1 priority in physicians’ job search. CHG Healthcare Insights. March 10, 2022. Accessed August 2025.
4. Medical Group Management Association; Jackson Physician Search. Early‑Career Physician Recruiting & Retention Playbook. October 23, 2023. Accessed August 2025.
5. Von Rosenvinge EC, et al. A crisis in scope: Recruitment and retention challenges reported by VA gastroenterology section chiefs. Fed Pract. 2024 Aug. doi:10.12788/fp.0504.
Top 5 Tips for Becoming an Effective Gastroenterology Consultant
Gastroenterology (GI) subspecialty training is carefully designed to develop expertise in digestive diseases and gastrointestinal endoscopy, while facilitating the transition from generalist to subspecialty consultant. The concept of effective consultation extends far beyond clinical expertise and has been explored repeatedly, beginning with Goldman’s “Ten Commandments” in 1983.1,2 How should these best practices be specifically applied to GI? More importantly, what kind of experience would you want if you were the referring provider or the patient themselves?
Below are
1. Be Kind
Survey studies of medical/surgical residents and attending hospitalists have demonstrated that willingness to accept consultation requests was the single factor consistently rated as most important in determining the quality of the consultation interaction.3,4 Unfortunately, nearly 65% of respondents reported encountering pushback when requesting subspecialty consultation. It is critical to recognize that when you receive a GI consult request, the requester has already decided that it is needed. Whether that request comports with our individual notion of “necessary” or “important,” this is a colleague’s request for help. There are myriad reasons why a request may be made, but they are unified in this principle.
Effective teamwork in healthcare settings enhances clinical performance and patient safety. Positive relationships with colleagues and healthcare team members also mitigate the emotional basis for physician burnout.5 Be kind and courteous to those who seek your assistance. Move beyond the notion of the “bad” or “soft” consult and seek instead to understand how you can help.
A requesting physician may phrase the consult question vaguely or may know that the patient is having a GI-related issue, but simply lack the specific knowledge to know what is needed. In these instances, it is our role to listen and help guide them to the correct thought process to ensure the best care of the patient. These important interactions establish our reputation, create our referral bases, and directly affect our sense of personal satisfaction.
2. Be Timely
GI presents an appealing breadth of pathology, but this also corresponds to a wide variety of indications for consultation and, therefore, urgency of need. In a busy clinical practice, not all requests can be urgently prioritized. However, it is the consultant’s responsibility to identify patients that require urgent evaluation and intervention to avert a potential adverse outcome.
We are well-trained in the medical triage of consultations. There are explicit guidelines for assessing urgency for GI bleeding, foreign body ingestion, choledocholithiasis, and many other indications. However, there are often special contextual circumstances that will elevate the urgency of a seemingly non-urgent consult request. Does the patient have an upcoming surgery or treatment that will depend on your input? Are they facing an imminent loss of insurance coverage? Is their non-severe GI disease leading to more severe impact on non-GI organ systems? The referring provider knows the patient better than you – seek to understand the context of the consult request.
Timeliness also applies to our communication. Communicate recommendations directly to the consulting service as soon as the patient is seen. When a colleague reaches out with a concern about a patient, make sure to take that request seriously. If you are unable to address the concern immediately, at least provide acknowledgment and an estimated timeline for response. As the maxim states, the effectiveness of a consultant is just as dependent on availability as it is on ability.
3. Be Specific
The same survey studies indicate that the second most critical aspect of successful subspecialty consultation is delivering clear recommendations. Accordingly, I always urge my trainees to challenge me when we leave a consult interaction if they feel that our plan is vague or imprecise.
Specificity in consult recommendations is an essential way to demonstrate your expertise and provide value. Clear and definitive recommendations enhance others’ perception of your skill, reduce the need for additional clarifying communication, and lead to more efficient, higher quality care. Avoid vague language, such as asking the requester to “consider” a test or intervention. When recommending medication, specify the dose, frequency, duration, and expected timeline of effect. Rather than recommending “cross-sectional imaging,” specify what modality and protocol. Instead of recommending “adequate resuscitation,” specify your target endpoints. If you engage in multidisciplinary discussion, ensure you strive for a specific group consensus plan and communicate this to all members of the team.
Specificity also applies to the quality of your documentation. Ensure that your clinical notes outline your rationale for your recommended plan, specific contingencies based on results of recommended testing, and a plan for follow-up care. When referring for open-access endoscopy, specifically outline what to look for and which specimens or endoscopic interventions are needed. Be precise in your procedure documentation – avoid vague terms such as small/medium/large and instead quantify in terms of millimeter/centimeter measurement. If you do not adopt specific classification schemes (e.g. Prague classification, Paris classification, Eosinophilic Esophagitis Endoscopic Reference Score, etc.), ensure you provide enough descriptive language to convey an adequate understanding of the findings.
4. Be Helpful
A consultant’s primary directive is to be of service to the consulting provider and the patient. As an educational leader, I am often asked what attributes separate a high-performing trainee from an average one. My feeling is that the most critical attribute is a sense of ownership over patient care.
As a consultant, when others feel we are exhibiting engagement and ownership in a patient’s care, they perceive that we are working together as an effective healthcare team. Interestingly, survey studies of inpatient care show that primary services do not necessarily value assistance with orders or care coordination – they consider these as core aspects of their daily work. What they did value was ongoing daily progress notes/communication, regardless of patient acuity or consulting specialty. This is a potent signal that our continued engagement (both inpatient and outpatient) is perceived as helpful.
Helpfulness is further aided by ensuring mutual understanding. While survey data indicate that sharing specific literature citations may not always be perceived positively, explaining the consultant’s rationale for their recommendations is highly valued. Take the time to tactfully explain your assessment of the patient and why you arrived at your specific recommendations. If your recommendations differ from what the requester expected (e.g. a procedure was expected but is not offered), ensure you explain why and answer questions they may have. This fosters mutual respect and proactively averts conflict or discontent from misunderstanding.
Multidisciplinary collaboration is another important avenue for aiding our patients and colleagues. Studies across a wide range of disease processes (including GI bleeding, IBD, etc.) and medical settings have demonstrated that multidisciplinary collaboration unequivocally improves patient outcomes.6 The success of these collaborations relies on our willingness to fully engage in these conversations, despite the fact that they may often be logistically challenging.
We all know how difficult it can be to locate and organize multiple medical specialists with complex varying clinical schedules and busy personal lives. Choosing to do so demonstrates a dedication to providing the highest level of care and elevates both patient and physician satisfaction. Having chosen to cultivate several ongoing multidisciplinary conferences/collaborations, I can attest to the notion that the outcome is well worth the effort.
5. Be Honest
While we always strive to provide the answers for our patients and colleagues, we must also acknowledge our limitations. Be honest with yourself when you encounter a scenario that pushes beyond the boundaries of your knowledge and comfort. Be willing to admit when you yourself need to consult others or seek an outside referral to provide the care a patient needs. Aspiring physicians often espouse that a devotion to lifelong learning is a key driver of their desire to pursue a career in medicine. These scenarios provide a key opportunity to expand our knowledge while doing what is right for our patients.
Be equally honest about your comfort with “curbside” consultations. Studies show that subspecialists receive on average of 3-4 such requests per week.7 The perception of these interactions is starkly discrepant between the requester and recipient. While over 80% of surveyed primary nonsurgical services felt that curbside consultations were helpful in patient care, a similar proportion of subspecialists expressed concern that insufficient clinical information was provided, even leading to a fear of litigation. While straightforward, informal conversations on narrow, well-defined questions can be helpful and efficient, the consultant should always feel comfortable seeking an opportunity for formal consultation when the details are unclear or the case/question is complex.
Closing Thoughts
Being an effective GI consultant isn’t just about what you know—it’s about how you apply it, how you communicate it, and how you make others feel in the process.
The attributes outlined above are not ancillary traits—they are essential components of high-quality consultation. When consistently applied, they enhance collaboration, improve patient outcomes, and reinforce trust within the healthcare system. By committing to them, you establish your reputation of excellence and play a role in elevating the field of gastroenterology more broadly.
Dr. Kahn is based in the Division of Gastroenterology and Hepatology at Mayo Clinic, Scottsdale, Arizona. He reports no conflicts of interest in regard to this article.
References
1. Goldman L, et al. Ten commandments for effective consultations. Arch Intern Med. 1983 Sep.
2. Salerno SM, et al. Principles of effective consultation: an update for the 21st-century consultant. Arch Intern Med. 2007 Feb. doi: 10.1001/archinte.167.3.271.
3. Adams TN, et al. Hospitalist Perspective of Interactions with Medicine Subspecialty Consult Services. J Hosp Med. 2018 May. doi: 10.12788/jhm.2882.
4. Matsuo T, et al. Essential consultants’ skills and attitudes (Willing CONSULT): a cross-sectional survey. BMC Med Educ. 2021 Jul. doi: 10.1186/s12909-021-02810-9.
5. Welp A, Manser T. Integrating teamwork, clinician occupational well-being and patient safety - development of a conceptual framework based on a systematic review. BMC Health Serv Res. 2016 Jul. doi: 10.1186/s12913-016-1535-y.
6. Webster CS, et al. Interprofessional Learning in Multidisciplinary Healthcare Teams Is Associated With Reduced Patient Mortality: A Quantitative Systematic Review and Meta-analysis. J Patient Saf. 2024 Jan. doi: 10.1097/PTS.0000000000001170.
7. Lin M, et al. Curbside Consultations: The Good, the Bad, and the Ugly. Clin Gastroenterol Hepatol. 2016 Jan. doi: 10.1016/j.cgh.2015.09.026.
Gastroenterology (GI) subspecialty training is carefully designed to develop expertise in digestive diseases and gastrointestinal endoscopy, while facilitating the transition from generalist to subspecialty consultant. The concept of effective consultation extends far beyond clinical expertise and has been explored repeatedly, beginning with Goldman’s “Ten Commandments” in 1983.1,2 How should these best practices be specifically applied to GI? More importantly, what kind of experience would you want if you were the referring provider or the patient themselves?
Below are
1. Be Kind
Survey studies of medical/surgical residents and attending hospitalists have demonstrated that willingness to accept consultation requests was the single factor consistently rated as most important in determining the quality of the consultation interaction.3,4 Unfortunately, nearly 65% of respondents reported encountering pushback when requesting subspecialty consultation. It is critical to recognize that when you receive a GI consult request, the requester has already decided that it is needed. Whether that request comports with our individual notion of “necessary” or “important,” this is a colleague’s request for help. There are myriad reasons why a request may be made, but they are unified in this principle.
Effective teamwork in healthcare settings enhances clinical performance and patient safety. Positive relationships with colleagues and healthcare team members also mitigate the emotional basis for physician burnout.5 Be kind and courteous to those who seek your assistance. Move beyond the notion of the “bad” or “soft” consult and seek instead to understand how you can help.
A requesting physician may phrase the consult question vaguely or may know that the patient is having a GI-related issue, but simply lack the specific knowledge to know what is needed. In these instances, it is our role to listen and help guide them to the correct thought process to ensure the best care of the patient. These important interactions establish our reputation, create our referral bases, and directly affect our sense of personal satisfaction.
2. Be Timely
GI presents an appealing breadth of pathology, but this also corresponds to a wide variety of indications for consultation and, therefore, urgency of need. In a busy clinical practice, not all requests can be urgently prioritized. However, it is the consultant’s responsibility to identify patients that require urgent evaluation and intervention to avert a potential adverse outcome.
We are well-trained in the medical triage of consultations. There are explicit guidelines for assessing urgency for GI bleeding, foreign body ingestion, choledocholithiasis, and many other indications. However, there are often special contextual circumstances that will elevate the urgency of a seemingly non-urgent consult request. Does the patient have an upcoming surgery or treatment that will depend on your input? Are they facing an imminent loss of insurance coverage? Is their non-severe GI disease leading to more severe impact on non-GI organ systems? The referring provider knows the patient better than you – seek to understand the context of the consult request.
Timeliness also applies to our communication. Communicate recommendations directly to the consulting service as soon as the patient is seen. When a colleague reaches out with a concern about a patient, make sure to take that request seriously. If you are unable to address the concern immediately, at least provide acknowledgment and an estimated timeline for response. As the maxim states, the effectiveness of a consultant is just as dependent on availability as it is on ability.
3. Be Specific
The same survey studies indicate that the second most critical aspect of successful subspecialty consultation is delivering clear recommendations. Accordingly, I always urge my trainees to challenge me when we leave a consult interaction if they feel that our plan is vague or imprecise.
Specificity in consult recommendations is an essential way to demonstrate your expertise and provide value. Clear and definitive recommendations enhance others’ perception of your skill, reduce the need for additional clarifying communication, and lead to more efficient, higher quality care. Avoid vague language, such as asking the requester to “consider” a test or intervention. When recommending medication, specify the dose, frequency, duration, and expected timeline of effect. Rather than recommending “cross-sectional imaging,” specify what modality and protocol. Instead of recommending “adequate resuscitation,” specify your target endpoints. If you engage in multidisciplinary discussion, ensure you strive for a specific group consensus plan and communicate this to all members of the team.
Specificity also applies to the quality of your documentation. Ensure that your clinical notes outline your rationale for your recommended plan, specific contingencies based on results of recommended testing, and a plan for follow-up care. When referring for open-access endoscopy, specifically outline what to look for and which specimens or endoscopic interventions are needed. Be precise in your procedure documentation – avoid vague terms such as small/medium/large and instead quantify in terms of millimeter/centimeter measurement. If you do not adopt specific classification schemes (e.g. Prague classification, Paris classification, Eosinophilic Esophagitis Endoscopic Reference Score, etc.), ensure you provide enough descriptive language to convey an adequate understanding of the findings.
4. Be Helpful
A consultant’s primary directive is to be of service to the consulting provider and the patient. As an educational leader, I am often asked what attributes separate a high-performing trainee from an average one. My feeling is that the most critical attribute is a sense of ownership over patient care.
As a consultant, when others feel we are exhibiting engagement and ownership in a patient’s care, they perceive that we are working together as an effective healthcare team. Interestingly, survey studies of inpatient care show that primary services do not necessarily value assistance with orders or care coordination – they consider these as core aspects of their daily work. What they did value was ongoing daily progress notes/communication, regardless of patient acuity or consulting specialty. This is a potent signal that our continued engagement (both inpatient and outpatient) is perceived as helpful.
Helpfulness is further aided by ensuring mutual understanding. While survey data indicate that sharing specific literature citations may not always be perceived positively, explaining the consultant’s rationale for their recommendations is highly valued. Take the time to tactfully explain your assessment of the patient and why you arrived at your specific recommendations. If your recommendations differ from what the requester expected (e.g. a procedure was expected but is not offered), ensure you explain why and answer questions they may have. This fosters mutual respect and proactively averts conflict or discontent from misunderstanding.
Multidisciplinary collaboration is another important avenue for aiding our patients and colleagues. Studies across a wide range of disease processes (including GI bleeding, IBD, etc.) and medical settings have demonstrated that multidisciplinary collaboration unequivocally improves patient outcomes.6 The success of these collaborations relies on our willingness to fully engage in these conversations, despite the fact that they may often be logistically challenging.
We all know how difficult it can be to locate and organize multiple medical specialists with complex varying clinical schedules and busy personal lives. Choosing to do so demonstrates a dedication to providing the highest level of care and elevates both patient and physician satisfaction. Having chosen to cultivate several ongoing multidisciplinary conferences/collaborations, I can attest to the notion that the outcome is well worth the effort.
5. Be Honest
While we always strive to provide the answers for our patients and colleagues, we must also acknowledge our limitations. Be honest with yourself when you encounter a scenario that pushes beyond the boundaries of your knowledge and comfort. Be willing to admit when you yourself need to consult others or seek an outside referral to provide the care a patient needs. Aspiring physicians often espouse that a devotion to lifelong learning is a key driver of their desire to pursue a career in medicine. These scenarios provide a key opportunity to expand our knowledge while doing what is right for our patients.
Be equally honest about your comfort with “curbside” consultations. Studies show that subspecialists receive on average of 3-4 such requests per week.7 The perception of these interactions is starkly discrepant between the requester and recipient. While over 80% of surveyed primary nonsurgical services felt that curbside consultations were helpful in patient care, a similar proportion of subspecialists expressed concern that insufficient clinical information was provided, even leading to a fear of litigation. While straightforward, informal conversations on narrow, well-defined questions can be helpful and efficient, the consultant should always feel comfortable seeking an opportunity for formal consultation when the details are unclear or the case/question is complex.
Closing Thoughts
Being an effective GI consultant isn’t just about what you know—it’s about how you apply it, how you communicate it, and how you make others feel in the process.
The attributes outlined above are not ancillary traits—they are essential components of high-quality consultation. When consistently applied, they enhance collaboration, improve patient outcomes, and reinforce trust within the healthcare system. By committing to them, you establish your reputation of excellence and play a role in elevating the field of gastroenterology more broadly.
Dr. Kahn is based in the Division of Gastroenterology and Hepatology at Mayo Clinic, Scottsdale, Arizona. He reports no conflicts of interest in regard to this article.
References
1. Goldman L, et al. Ten commandments for effective consultations. Arch Intern Med. 1983 Sep.
2. Salerno SM, et al. Principles of effective consultation: an update for the 21st-century consultant. Arch Intern Med. 2007 Feb. doi: 10.1001/archinte.167.3.271.
3. Adams TN, et al. Hospitalist Perspective of Interactions with Medicine Subspecialty Consult Services. J Hosp Med. 2018 May. doi: 10.12788/jhm.2882.
4. Matsuo T, et al. Essential consultants’ skills and attitudes (Willing CONSULT): a cross-sectional survey. BMC Med Educ. 2021 Jul. doi: 10.1186/s12909-021-02810-9.
5. Welp A, Manser T. Integrating teamwork, clinician occupational well-being and patient safety - development of a conceptual framework based on a systematic review. BMC Health Serv Res. 2016 Jul. doi: 10.1186/s12913-016-1535-y.
6. Webster CS, et al. Interprofessional Learning in Multidisciplinary Healthcare Teams Is Associated With Reduced Patient Mortality: A Quantitative Systematic Review and Meta-analysis. J Patient Saf. 2024 Jan. doi: 10.1097/PTS.0000000000001170.
7. Lin M, et al. Curbside Consultations: The Good, the Bad, and the Ugly. Clin Gastroenterol Hepatol. 2016 Jan. doi: 10.1016/j.cgh.2015.09.026.
Gastroenterology (GI) subspecialty training is carefully designed to develop expertise in digestive diseases and gastrointestinal endoscopy, while facilitating the transition from generalist to subspecialty consultant. The concept of effective consultation extends far beyond clinical expertise and has been explored repeatedly, beginning with Goldman’s “Ten Commandments” in 1983.1,2 How should these best practices be specifically applied to GI? More importantly, what kind of experience would you want if you were the referring provider or the patient themselves?
Below are
1. Be Kind
Survey studies of medical/surgical residents and attending hospitalists have demonstrated that willingness to accept consultation requests was the single factor consistently rated as most important in determining the quality of the consultation interaction.3,4 Unfortunately, nearly 65% of respondents reported encountering pushback when requesting subspecialty consultation. It is critical to recognize that when you receive a GI consult request, the requester has already decided that it is needed. Whether that request comports with our individual notion of “necessary” or “important,” this is a colleague’s request for help. There are myriad reasons why a request may be made, but they are unified in this principle.
Effective teamwork in healthcare settings enhances clinical performance and patient safety. Positive relationships with colleagues and healthcare team members also mitigate the emotional basis for physician burnout.5 Be kind and courteous to those who seek your assistance. Move beyond the notion of the “bad” or “soft” consult and seek instead to understand how you can help.
A requesting physician may phrase the consult question vaguely or may know that the patient is having a GI-related issue, but simply lack the specific knowledge to know what is needed. In these instances, it is our role to listen and help guide them to the correct thought process to ensure the best care of the patient. These important interactions establish our reputation, create our referral bases, and directly affect our sense of personal satisfaction.
2. Be Timely
GI presents an appealing breadth of pathology, but this also corresponds to a wide variety of indications for consultation and, therefore, urgency of need. In a busy clinical practice, not all requests can be urgently prioritized. However, it is the consultant’s responsibility to identify patients that require urgent evaluation and intervention to avert a potential adverse outcome.
We are well-trained in the medical triage of consultations. There are explicit guidelines for assessing urgency for GI bleeding, foreign body ingestion, choledocholithiasis, and many other indications. However, there are often special contextual circumstances that will elevate the urgency of a seemingly non-urgent consult request. Does the patient have an upcoming surgery or treatment that will depend on your input? Are they facing an imminent loss of insurance coverage? Is their non-severe GI disease leading to more severe impact on non-GI organ systems? The referring provider knows the patient better than you – seek to understand the context of the consult request.
Timeliness also applies to our communication. Communicate recommendations directly to the consulting service as soon as the patient is seen. When a colleague reaches out with a concern about a patient, make sure to take that request seriously. If you are unable to address the concern immediately, at least provide acknowledgment and an estimated timeline for response. As the maxim states, the effectiveness of a consultant is just as dependent on availability as it is on ability.
3. Be Specific
The same survey studies indicate that the second most critical aspect of successful subspecialty consultation is delivering clear recommendations. Accordingly, I always urge my trainees to challenge me when we leave a consult interaction if they feel that our plan is vague or imprecise.
Specificity in consult recommendations is an essential way to demonstrate your expertise and provide value. Clear and definitive recommendations enhance others’ perception of your skill, reduce the need for additional clarifying communication, and lead to more efficient, higher quality care. Avoid vague language, such as asking the requester to “consider” a test or intervention. When recommending medication, specify the dose, frequency, duration, and expected timeline of effect. Rather than recommending “cross-sectional imaging,” specify what modality and protocol. Instead of recommending “adequate resuscitation,” specify your target endpoints. If you engage in multidisciplinary discussion, ensure you strive for a specific group consensus plan and communicate this to all members of the team.
Specificity also applies to the quality of your documentation. Ensure that your clinical notes outline your rationale for your recommended plan, specific contingencies based on results of recommended testing, and a plan for follow-up care. When referring for open-access endoscopy, specifically outline what to look for and which specimens or endoscopic interventions are needed. Be precise in your procedure documentation – avoid vague terms such as small/medium/large and instead quantify in terms of millimeter/centimeter measurement. If you do not adopt specific classification schemes (e.g. Prague classification, Paris classification, Eosinophilic Esophagitis Endoscopic Reference Score, etc.), ensure you provide enough descriptive language to convey an adequate understanding of the findings.
4. Be Helpful
A consultant’s primary directive is to be of service to the consulting provider and the patient. As an educational leader, I am often asked what attributes separate a high-performing trainee from an average one. My feeling is that the most critical attribute is a sense of ownership over patient care.
As a consultant, when others feel we are exhibiting engagement and ownership in a patient’s care, they perceive that we are working together as an effective healthcare team. Interestingly, survey studies of inpatient care show that primary services do not necessarily value assistance with orders or care coordination – they consider these as core aspects of their daily work. What they did value was ongoing daily progress notes/communication, regardless of patient acuity or consulting specialty. This is a potent signal that our continued engagement (both inpatient and outpatient) is perceived as helpful.
Helpfulness is further aided by ensuring mutual understanding. While survey data indicate that sharing specific literature citations may not always be perceived positively, explaining the consultant’s rationale for their recommendations is highly valued. Take the time to tactfully explain your assessment of the patient and why you arrived at your specific recommendations. If your recommendations differ from what the requester expected (e.g. a procedure was expected but is not offered), ensure you explain why and answer questions they may have. This fosters mutual respect and proactively averts conflict or discontent from misunderstanding.
Multidisciplinary collaboration is another important avenue for aiding our patients and colleagues. Studies across a wide range of disease processes (including GI bleeding, IBD, etc.) and medical settings have demonstrated that multidisciplinary collaboration unequivocally improves patient outcomes.6 The success of these collaborations relies on our willingness to fully engage in these conversations, despite the fact that they may often be logistically challenging.
We all know how difficult it can be to locate and organize multiple medical specialists with complex varying clinical schedules and busy personal lives. Choosing to do so demonstrates a dedication to providing the highest level of care and elevates both patient and physician satisfaction. Having chosen to cultivate several ongoing multidisciplinary conferences/collaborations, I can attest to the notion that the outcome is well worth the effort.
5. Be Honest
While we always strive to provide the answers for our patients and colleagues, we must also acknowledge our limitations. Be honest with yourself when you encounter a scenario that pushes beyond the boundaries of your knowledge and comfort. Be willing to admit when you yourself need to consult others or seek an outside referral to provide the care a patient needs. Aspiring physicians often espouse that a devotion to lifelong learning is a key driver of their desire to pursue a career in medicine. These scenarios provide a key opportunity to expand our knowledge while doing what is right for our patients.
Be equally honest about your comfort with “curbside” consultations. Studies show that subspecialists receive on average of 3-4 such requests per week.7 The perception of these interactions is starkly discrepant between the requester and recipient. While over 80% of surveyed primary nonsurgical services felt that curbside consultations were helpful in patient care, a similar proportion of subspecialists expressed concern that insufficient clinical information was provided, even leading to a fear of litigation. While straightforward, informal conversations on narrow, well-defined questions can be helpful and efficient, the consultant should always feel comfortable seeking an opportunity for formal consultation when the details are unclear or the case/question is complex.
Closing Thoughts
Being an effective GI consultant isn’t just about what you know—it’s about how you apply it, how you communicate it, and how you make others feel in the process.
The attributes outlined above are not ancillary traits—they are essential components of high-quality consultation. When consistently applied, they enhance collaboration, improve patient outcomes, and reinforce trust within the healthcare system. By committing to them, you establish your reputation of excellence and play a role in elevating the field of gastroenterology more broadly.
Dr. Kahn is based in the Division of Gastroenterology and Hepatology at Mayo Clinic, Scottsdale, Arizona. He reports no conflicts of interest in regard to this article.
References
1. Goldman L, et al. Ten commandments for effective consultations. Arch Intern Med. 1983 Sep.
2. Salerno SM, et al. Principles of effective consultation: an update for the 21st-century consultant. Arch Intern Med. 2007 Feb. doi: 10.1001/archinte.167.3.271.
3. Adams TN, et al. Hospitalist Perspective of Interactions with Medicine Subspecialty Consult Services. J Hosp Med. 2018 May. doi: 10.12788/jhm.2882.
4. Matsuo T, et al. Essential consultants’ skills and attitudes (Willing CONSULT): a cross-sectional survey. BMC Med Educ. 2021 Jul. doi: 10.1186/s12909-021-02810-9.
5. Welp A, Manser T. Integrating teamwork, clinician occupational well-being and patient safety - development of a conceptual framework based on a systematic review. BMC Health Serv Res. 2016 Jul. doi: 10.1186/s12913-016-1535-y.
6. Webster CS, et al. Interprofessional Learning in Multidisciplinary Healthcare Teams Is Associated With Reduced Patient Mortality: A Quantitative Systematic Review and Meta-analysis. J Patient Saf. 2024 Jan. doi: 10.1097/PTS.0000000000001170.
7. Lin M, et al. Curbside Consultations: The Good, the Bad, and the Ugly. Clin Gastroenterol Hepatol. 2016 Jan. doi: 10.1016/j.cgh.2015.09.026.
Practical Tips on Delivering Feedback to Trainees and Colleagues
Feedback is the purposeful practice of offering constructive, goal-directed input rooted in the power of observation and behavioral assessment. Healthcare inherently fosters a broad range of interactions among people with unique insights, and feedback can naturally emerge from this milieu. In medical training, feedback is an indispensable element that personalizes the learning process and drives the professional development of physicians through all career stages.
If delivered effectively, feedback can strengthen the relationship between the evaluator and recipient, promote self-reflection, and enhance motivation. As such, it has the potential to impact us and those we serve for a lifetime. Feedback has been invaluable to our growth as clinicians and has been embedded into our roles as educators. However, Here, we provide some “tried and true” practical tips on delivering feedback to trainees and co-workers and on navigating potential barriers based on lessons learned.
Barriers to Effective Feedback
- Time: Feedback is predicated on observation over time and consideration of repetitive processes rather than isolated events. Perhaps the most challenging factor faced by both parties is that of time constraints, leading to limited ability to engage and build rapport.
- Fear: Hesitancy by evaluators to provide feedback in fear of negative impacts on the recipient’s morale or rapport can lead them to shy away from personalized corrective feedback strategies and choose to rely on written evaluations or generic advice.
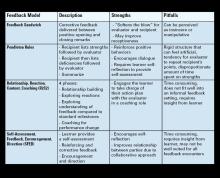
- Varying approaches: Feedback strategies have evolved from unidirectional, critique-based, hierarchical practices that emphasize the evaluator’s skills to models that prioritize the recipient’s goals and participation (see Table 1). Traditionally employed feedback models such as the “Feedback Sandwich” or the “Pendleton Rules” are criticized because of a lack of proven benefit on performance, recipient goal prioritization, and open communication.1,2 Studies showing incongruent perceptions of feedback adequacy between trainees and faculty further support the need for recipient-focused strategies.3 Recognition of the foundational role of the reciprocal learner-teacher alliance in feedback integration inspired newer feedback models, such as the “R2C2” and the “Self-Assessment, Feedback, Encouragement, Direction.”4,5
But which way is best? With increasing abundance and complexity of feedback frameworks, selecting an approach can feel overwhelming and impractical. A generic “one-size-fits-all” strategy or avoidance of feedback altogether can be detrimental. Structured feedback models can also lead to rigid, inauthentic interactions. Below, we suggest a more practical approach through our tips that unifies the common themes of various feedback models and embeds them into daily practice habits while leaving room for personalization.
Our Practical Feedback Tips
Tip 1: Set the scene: Create a positive feedback culture
Proactively creating a culture in which feedback is embedded and encouraged is perhaps the most important step. Priming both parties for feedback clarifies intent, increases receptiveness, and paves the way for growth and open communication. It also prevents the misinterpretation of unexpected feedback as an expression of disapproval. To do this, start by regularly stating your intentions at the start of every experience. Explicitly expressing your vision for mutual learning, bidirectional feedback, and growth in your respective roles attaches a positive intention to feedback. Providing a reminder that we are all works in progress and acknowledging this on a regular basis sets the stage for structured growth opportunities.
Scheduling future feedback encounters from the start maintains accountability and prevents feedback from being perceived as the consequence of a particular behavior. The number and timing of feedback sessions can be customized to the duration of the working relationship, generally allowing enough time for a second interaction (at the end of each week, halfway point, etc.).
Tip 2: Build rapport
Increasing clinical workloads and pressure to teach in time-constrained settings often results in insufficient time to engage in conversation and trust building. However, a foundational relationship is an essential precursor to meaningful feedback. Ramani et al. state that “relationships, not recipes, are more likely to promote feedback that has an impact on learner performance and ultimately patient care.”6 Building this rapport can begin by dedicating a few minutes (before/during rounds, between cases) to exchange information about career interests, hobbies, favorite restaurants, etc. This “small talk” is the beginning of a two-way exchange that ultimately develops into more meaningful exchanges.
In our experience, this simple step is impactful and fulfilling to both parties. This is also a good time for shared vulnerability by talking about what you are currently working on or have worked on at their stage to affirm that feedback is a continuous part of professional development and not a reflection of how far they are from competence at a given point in time.
Tip 3: Consider Timing, assess readiness, and preschedule sessions
Lack of attention to timing can hinder feedback acceptance. We suggest adhering to delivering positive feedback publicly and corrective feedback privately (“Praise in public, perfect in private”). This reinforces positive behaviors, increases motivation, and minimizes demoralization. Prolonged delays between the observed behavior and feedback can decrease its relevance. Conversely, delivering feedback too soon after an emotionally charged experience can be perceived as blame. Pre-designated times for feedback can minimize the guesswork and maintain your accountability for giving feedback without inadvertently linking it to one particular behavior. If the recipient does not appear to be in a state to receive feedback at the predesignated time, you can pivot to a “check-in” session to show support and strengthen rapport.
Tip 4: Customize to the learner and set shared goals
Diversity in backgrounds, perspectives, and personalities can impact how people perceive their own performances and experience feedback. Given the profound impact of sociocultural factors on feedback assimilation, maintaining the recipient and their goals at the core of performance evaluations is key to feedback acceptance.
A. Trainees
We suggest starting by introducing the idea of feedback as a partnership and something you feel privileged to do to help them achieve mutual goals. It helps to ask them to use the first day to get oriented with the experience, general expectations, challenges they expect to encounter, and their feedback goals. Tailoring your feedback to their goals creates a sense of shared purpose which increases motivation. Encouraging them to develop their own strategies allows them to play an active role in their growth. Giving them the opportunity to share their perceived strengths and deficiencies provides you with valuable information regarding their insight and ability to self-evaluate. This can help you predict their readiness for your feedback and to tailor your approach when there is a mismatch.
Examples:
- Medical student: Start with “What do you think you are doing well?” and “What do you think you need to work on?” Build on their response with encouragement and empathy. This helps make them more deliberate with what they work on because being a medical student can be overwhelming and can feel as though they have everything to work on.
- Resident/Fellow: By this point, trainees usually have an increased awareness of their strengths and deficiencies. Your questions can then be more specific, giving them autonomy over their learning, such as “What are some of the things you are working on that you want me to give you feedback on this week?” This makes them more aware, intentional, and receptive to your feedback because it is framed as something that they sought out.
B. Colleagues/Staff
Unlike the training environment in which feedback is built-in, giving feedback to co-workers requires you to establish a feedback-conducive environment and to develop a more in-depth understanding of coworkers’ personalities. Similar strategies can be applied, such as proactively setting the scene for open communication, scheduling check-ins, demonstrating receptiveness to feedback, and investing in trust-building.
Longer working relationships allow for strong foundational connections that make feedback less threatening. Personality assessment testing like Myers-Briggs Type Indicator or DiSC Assessment can aid in tailoring feedback to different individuals.7,8 An analytical thinker may appreciate direct, data-driven feedback. Relationship-oriented individuals might respond better to softer, encouragement-based approaches. Always maintain shared goals at the center of your interactions and consider collaborative opportunities such as quality improvement projects. This can improve your working relationship in a constructive way without casting blame.
Tip 5: Work on delivery: Bidirectional communication and body language
Non-verbal cues can have a profound impact on how your feedback is interpreted and on the recipient’s comfort to engage in conversation. Sitting down, making eye contact, nodding, and avoiding closed-off body posture can project support and feel less judgmental. Creating a safe and non-distracted environment with privacy can make them feel valued. Use motivating, respectful language focused on directly observed behaviors rather than personal attributes or second-hand reports.
Remember that focusing on repetitive patterns is likely more helpful than isolated incidents. Validate their hard work and give them a global idea of where they stand before diving into individual behaviors. Encourage their participation and empower them to suggest changes they plan to implement. Conclude by having them summarize their action plan to give them ownership and to verify that your feedback was interpreted as you intended. Thank them for being a part of the process, as it does take a partnership for feedback to be effective.
Tip 6: Be open to feedback
Demonstrating your willingness to accept and act on feedback reinforces a positive culture where feedback is normalized and valued. After an unintended outcome, initiate a two-way conversation and ask their input on anything they wish you would have done differently. This reaffirms your commitment to maintaining culture that does not revolve around one-sided critiques. Frequently soliciting feedback about your feedback skills can also guide you to adapt your approach and to recognize any ineffective feedback practices.
Tip 7: When things don’t go as planned
Receiving feedback, no matter how thoughtfully it is delivered, can be an emotionally-charged experience ending in hurt feelings. This happens because of misinterpretation of feedback as an indicator of inadequacy, heightened awareness of underlying insecurities, sociocultural or personal circumstances, frustration with oneself, needing additional guidance, or being caught off-guard by the assessment.
The evaluator should always acknowledge the recipient’s feelings, show compassion, and allow time for processing. When they are ready to talk, it is important to help reframe the recipients’ mindsets to recognize that feedback is not personal or defining and is not a “one and done” reflection of whether they have “made it.” Instead, it is a continual process that we benefit from through all career stages. Again, shared vulnerability can help to normalize feedback and maintain open dialogue. Setting an opportunity for a future check-in can reinforce support and lead to a more productive conversation after they have had time to process.
Conclusion
Effective feedback delivery is an invaluable skill that can result in meaningful goal-directed changes while strengthening professional relationships. Given the complexity of feedback interactions and the many factors that influence its acceptance, no single approach is suitable for all recipients and frequent adaptation of the approach is essential.
In our experience, adhering to these general overarching feedback principles (see Figure 1) has allowed us to have more successful interactions with trainees and colleagues.
Dr. Baliss is based in the Division of Gastroenterology, Washington University in St. Louis, Missouri. Dr. Hachem is director of the Division of Gastroenterology and Digestive Health at Intermountain Medical, Sandy, Utah. Both authors declare no conflicts of interest.
References
1. Parkes J, et al. Feedback sandwiches affect perceptions but not performance. Adv Health Sci Educ Theory Pract. 2013 Aug. doi:10.1007/s10459-012-9377-9.
2. van de Ridder JMM and Wijnen-Meijer M. Pendleton’s Rules: A Mini Review of a Feedback Method. Am J Biomed Sci & Res. 2023 May. doi: 10.34297/AJBSR.2023.19.002542.
3. Sender Liberman A, et al. Surgery residents and attending surgeons have different perceptions of feedback. Med Teach. 2005 Aug. doi: 10.1080/0142590500129183.
4. Sargeant J, et al. R2C2 in Action: Testing an Evidence-Based Model to Facilitate Feedback and Coaching in Residency. J Grad Med Educ. 2017 Apr. doi: 10.4300/JGME-D-16-00398.1.
5. Liakos W, et al. Frameworks for Effective Feedback in Health Professions Education. Acad Med. 2023 May. doi: 10.1097/ACM.0000000000004884.
6. Ramani S, et al. Feedback Redefined: Principles and Practice. J Gen Intern Med. 2019 May. doi: 10.1007/s11606-019-04874-2.
7. Woods RA and Hill PB. Myers-Briggs Type Indicator. StatPearls. StatPearls Publishing. 2022 Sept. https://www.ncbi.nlm.nih.gov/books/NBK554596/
8. Slowikowski MK. Using the DISC behavioral instrument to guide leadership and communication. AORN J. 2005 Nov. doi: 10.1016/s0001-2092(06)60276-7.
Feedback is the purposeful practice of offering constructive, goal-directed input rooted in the power of observation and behavioral assessment. Healthcare inherently fosters a broad range of interactions among people with unique insights, and feedback can naturally emerge from this milieu. In medical training, feedback is an indispensable element that personalizes the learning process and drives the professional development of physicians through all career stages.
If delivered effectively, feedback can strengthen the relationship between the evaluator and recipient, promote self-reflection, and enhance motivation. As such, it has the potential to impact us and those we serve for a lifetime. Feedback has been invaluable to our growth as clinicians and has been embedded into our roles as educators. However, Here, we provide some “tried and true” practical tips on delivering feedback to trainees and co-workers and on navigating potential barriers based on lessons learned.
Barriers to Effective Feedback
- Time: Feedback is predicated on observation over time and consideration of repetitive processes rather than isolated events. Perhaps the most challenging factor faced by both parties is that of time constraints, leading to limited ability to engage and build rapport.
- Fear: Hesitancy by evaluators to provide feedback in fear of negative impacts on the recipient’s morale or rapport can lead them to shy away from personalized corrective feedback strategies and choose to rely on written evaluations or generic advice.
- Varying approaches: Feedback strategies have evolved from unidirectional, critique-based, hierarchical practices that emphasize the evaluator’s skills to models that prioritize the recipient’s goals and participation (see Table 1). Traditionally employed feedback models such as the “Feedback Sandwich” or the “Pendleton Rules” are criticized because of a lack of proven benefit on performance, recipient goal prioritization, and open communication.1,2 Studies showing incongruent perceptions of feedback adequacy between trainees and faculty further support the need for recipient-focused strategies.3 Recognition of the foundational role of the reciprocal learner-teacher alliance in feedback integration inspired newer feedback models, such as the “R2C2” and the “Self-Assessment, Feedback, Encouragement, Direction.”4,5
But which way is best? With increasing abundance and complexity of feedback frameworks, selecting an approach can feel overwhelming and impractical. A generic “one-size-fits-all” strategy or avoidance of feedback altogether can be detrimental. Structured feedback models can also lead to rigid, inauthentic interactions. Below, we suggest a more practical approach through our tips that unifies the common themes of various feedback models and embeds them into daily practice habits while leaving room for personalization.
Our Practical Feedback Tips
Tip 1: Set the scene: Create a positive feedback culture
Proactively creating a culture in which feedback is embedded and encouraged is perhaps the most important step. Priming both parties for feedback clarifies intent, increases receptiveness, and paves the way for growth and open communication. It also prevents the misinterpretation of unexpected feedback as an expression of disapproval. To do this, start by regularly stating your intentions at the start of every experience. Explicitly expressing your vision for mutual learning, bidirectional feedback, and growth in your respective roles attaches a positive intention to feedback. Providing a reminder that we are all works in progress and acknowledging this on a regular basis sets the stage for structured growth opportunities.
Scheduling future feedback encounters from the start maintains accountability and prevents feedback from being perceived as the consequence of a particular behavior. The number and timing of feedback sessions can be customized to the duration of the working relationship, generally allowing enough time for a second interaction (at the end of each week, halfway point, etc.).
Tip 2: Build rapport
Increasing clinical workloads and pressure to teach in time-constrained settings often results in insufficient time to engage in conversation and trust building. However, a foundational relationship is an essential precursor to meaningful feedback. Ramani et al. state that “relationships, not recipes, are more likely to promote feedback that has an impact on learner performance and ultimately patient care.”6 Building this rapport can begin by dedicating a few minutes (before/during rounds, between cases) to exchange information about career interests, hobbies, favorite restaurants, etc. This “small talk” is the beginning of a two-way exchange that ultimately develops into more meaningful exchanges.
In our experience, this simple step is impactful and fulfilling to both parties. This is also a good time for shared vulnerability by talking about what you are currently working on or have worked on at their stage to affirm that feedback is a continuous part of professional development and not a reflection of how far they are from competence at a given point in time.
Tip 3: Consider Timing, assess readiness, and preschedule sessions
Lack of attention to timing can hinder feedback acceptance. We suggest adhering to delivering positive feedback publicly and corrective feedback privately (“Praise in public, perfect in private”). This reinforces positive behaviors, increases motivation, and minimizes demoralization. Prolonged delays between the observed behavior and feedback can decrease its relevance. Conversely, delivering feedback too soon after an emotionally charged experience can be perceived as blame. Pre-designated times for feedback can minimize the guesswork and maintain your accountability for giving feedback without inadvertently linking it to one particular behavior. If the recipient does not appear to be in a state to receive feedback at the predesignated time, you can pivot to a “check-in” session to show support and strengthen rapport.
Tip 4: Customize to the learner and set shared goals
Diversity in backgrounds, perspectives, and personalities can impact how people perceive their own performances and experience feedback. Given the profound impact of sociocultural factors on feedback assimilation, maintaining the recipient and their goals at the core of performance evaluations is key to feedback acceptance.
A. Trainees
We suggest starting by introducing the idea of feedback as a partnership and something you feel privileged to do to help them achieve mutual goals. It helps to ask them to use the first day to get oriented with the experience, general expectations, challenges they expect to encounter, and their feedback goals. Tailoring your feedback to their goals creates a sense of shared purpose which increases motivation. Encouraging them to develop their own strategies allows them to play an active role in their growth. Giving them the opportunity to share their perceived strengths and deficiencies provides you with valuable information regarding their insight and ability to self-evaluate. This can help you predict their readiness for your feedback and to tailor your approach when there is a mismatch.
Examples:
- Medical student: Start with “What do you think you are doing well?” and “What do you think you need to work on?” Build on their response with encouragement and empathy. This helps make them more deliberate with what they work on because being a medical student can be overwhelming and can feel as though they have everything to work on.
- Resident/Fellow: By this point, trainees usually have an increased awareness of their strengths and deficiencies. Your questions can then be more specific, giving them autonomy over their learning, such as “What are some of the things you are working on that you want me to give you feedback on this week?” This makes them more aware, intentional, and receptive to your feedback because it is framed as something that they sought out.
B. Colleagues/Staff
Unlike the training environment in which feedback is built-in, giving feedback to co-workers requires you to establish a feedback-conducive environment and to develop a more in-depth understanding of coworkers’ personalities. Similar strategies can be applied, such as proactively setting the scene for open communication, scheduling check-ins, demonstrating receptiveness to feedback, and investing in trust-building.
Longer working relationships allow for strong foundational connections that make feedback less threatening. Personality assessment testing like Myers-Briggs Type Indicator or DiSC Assessment can aid in tailoring feedback to different individuals.7,8 An analytical thinker may appreciate direct, data-driven feedback. Relationship-oriented individuals might respond better to softer, encouragement-based approaches. Always maintain shared goals at the center of your interactions and consider collaborative opportunities such as quality improvement projects. This can improve your working relationship in a constructive way without casting blame.
Tip 5: Work on delivery: Bidirectional communication and body language
Non-verbal cues can have a profound impact on how your feedback is interpreted and on the recipient’s comfort to engage in conversation. Sitting down, making eye contact, nodding, and avoiding closed-off body posture can project support and feel less judgmental. Creating a safe and non-distracted environment with privacy can make them feel valued. Use motivating, respectful language focused on directly observed behaviors rather than personal attributes or second-hand reports.
Remember that focusing on repetitive patterns is likely more helpful than isolated incidents. Validate their hard work and give them a global idea of where they stand before diving into individual behaviors. Encourage their participation and empower them to suggest changes they plan to implement. Conclude by having them summarize their action plan to give them ownership and to verify that your feedback was interpreted as you intended. Thank them for being a part of the process, as it does take a partnership for feedback to be effective.
Tip 6: Be open to feedback
Demonstrating your willingness to accept and act on feedback reinforces a positive culture where feedback is normalized and valued. After an unintended outcome, initiate a two-way conversation and ask their input on anything they wish you would have done differently. This reaffirms your commitment to maintaining culture that does not revolve around one-sided critiques. Frequently soliciting feedback about your feedback skills can also guide you to adapt your approach and to recognize any ineffective feedback practices.
Tip 7: When things don’t go as planned
Receiving feedback, no matter how thoughtfully it is delivered, can be an emotionally-charged experience ending in hurt feelings. This happens because of misinterpretation of feedback as an indicator of inadequacy, heightened awareness of underlying insecurities, sociocultural or personal circumstances, frustration with oneself, needing additional guidance, or being caught off-guard by the assessment.
The evaluator should always acknowledge the recipient’s feelings, show compassion, and allow time for processing. When they are ready to talk, it is important to help reframe the recipients’ mindsets to recognize that feedback is not personal or defining and is not a “one and done” reflection of whether they have “made it.” Instead, it is a continual process that we benefit from through all career stages. Again, shared vulnerability can help to normalize feedback and maintain open dialogue. Setting an opportunity for a future check-in can reinforce support and lead to a more productive conversation after they have had time to process.
Conclusion
Effective feedback delivery is an invaluable skill that can result in meaningful goal-directed changes while strengthening professional relationships. Given the complexity of feedback interactions and the many factors that influence its acceptance, no single approach is suitable for all recipients and frequent adaptation of the approach is essential.
In our experience, adhering to these general overarching feedback principles (see Figure 1) has allowed us to have more successful interactions with trainees and colleagues.
Dr. Baliss is based in the Division of Gastroenterology, Washington University in St. Louis, Missouri. Dr. Hachem is director of the Division of Gastroenterology and Digestive Health at Intermountain Medical, Sandy, Utah. Both authors declare no conflicts of interest.
References
1. Parkes J, et al. Feedback sandwiches affect perceptions but not performance. Adv Health Sci Educ Theory Pract. 2013 Aug. doi:10.1007/s10459-012-9377-9.
2. van de Ridder JMM and Wijnen-Meijer M. Pendleton’s Rules: A Mini Review of a Feedback Method. Am J Biomed Sci & Res. 2023 May. doi: 10.34297/AJBSR.2023.19.002542.
3. Sender Liberman A, et al. Surgery residents and attending surgeons have different perceptions of feedback. Med Teach. 2005 Aug. doi: 10.1080/0142590500129183.
4. Sargeant J, et al. R2C2 in Action: Testing an Evidence-Based Model to Facilitate Feedback and Coaching in Residency. J Grad Med Educ. 2017 Apr. doi: 10.4300/JGME-D-16-00398.1.
5. Liakos W, et al. Frameworks for Effective Feedback in Health Professions Education. Acad Med. 2023 May. doi: 10.1097/ACM.0000000000004884.
6. Ramani S, et al. Feedback Redefined: Principles and Practice. J Gen Intern Med. 2019 May. doi: 10.1007/s11606-019-04874-2.
7. Woods RA and Hill PB. Myers-Briggs Type Indicator. StatPearls. StatPearls Publishing. 2022 Sept. https://www.ncbi.nlm.nih.gov/books/NBK554596/
8. Slowikowski MK. Using the DISC behavioral instrument to guide leadership and communication. AORN J. 2005 Nov. doi: 10.1016/s0001-2092(06)60276-7.
Feedback is the purposeful practice of offering constructive, goal-directed input rooted in the power of observation and behavioral assessment. Healthcare inherently fosters a broad range of interactions among people with unique insights, and feedback can naturally emerge from this milieu. In medical training, feedback is an indispensable element that personalizes the learning process and drives the professional development of physicians through all career stages.
If delivered effectively, feedback can strengthen the relationship between the evaluator and recipient, promote self-reflection, and enhance motivation. As such, it has the potential to impact us and those we serve for a lifetime. Feedback has been invaluable to our growth as clinicians and has been embedded into our roles as educators. However, Here, we provide some “tried and true” practical tips on delivering feedback to trainees and co-workers and on navigating potential barriers based on lessons learned.
Barriers to Effective Feedback
- Time: Feedback is predicated on observation over time and consideration of repetitive processes rather than isolated events. Perhaps the most challenging factor faced by both parties is that of time constraints, leading to limited ability to engage and build rapport.
- Fear: Hesitancy by evaluators to provide feedback in fear of negative impacts on the recipient’s morale or rapport can lead them to shy away from personalized corrective feedback strategies and choose to rely on written evaluations or generic advice.
- Varying approaches: Feedback strategies have evolved from unidirectional, critique-based, hierarchical practices that emphasize the evaluator’s skills to models that prioritize the recipient’s goals and participation (see Table 1). Traditionally employed feedback models such as the “Feedback Sandwich” or the “Pendleton Rules” are criticized because of a lack of proven benefit on performance, recipient goal prioritization, and open communication.1,2 Studies showing incongruent perceptions of feedback adequacy between trainees and faculty further support the need for recipient-focused strategies.3 Recognition of the foundational role of the reciprocal learner-teacher alliance in feedback integration inspired newer feedback models, such as the “R2C2” and the “Self-Assessment, Feedback, Encouragement, Direction.”4,5
But which way is best? With increasing abundance and complexity of feedback frameworks, selecting an approach can feel overwhelming and impractical. A generic “one-size-fits-all” strategy or avoidance of feedback altogether can be detrimental. Structured feedback models can also lead to rigid, inauthentic interactions. Below, we suggest a more practical approach through our tips that unifies the common themes of various feedback models and embeds them into daily practice habits while leaving room for personalization.
Our Practical Feedback Tips
Tip 1: Set the scene: Create a positive feedback culture
Proactively creating a culture in which feedback is embedded and encouraged is perhaps the most important step. Priming both parties for feedback clarifies intent, increases receptiveness, and paves the way for growth and open communication. It also prevents the misinterpretation of unexpected feedback as an expression of disapproval. To do this, start by regularly stating your intentions at the start of every experience. Explicitly expressing your vision for mutual learning, bidirectional feedback, and growth in your respective roles attaches a positive intention to feedback. Providing a reminder that we are all works in progress and acknowledging this on a regular basis sets the stage for structured growth opportunities.
Scheduling future feedback encounters from the start maintains accountability and prevents feedback from being perceived as the consequence of a particular behavior. The number and timing of feedback sessions can be customized to the duration of the working relationship, generally allowing enough time for a second interaction (at the end of each week, halfway point, etc.).
Tip 2: Build rapport
Increasing clinical workloads and pressure to teach in time-constrained settings often results in insufficient time to engage in conversation and trust building. However, a foundational relationship is an essential precursor to meaningful feedback. Ramani et al. state that “relationships, not recipes, are more likely to promote feedback that has an impact on learner performance and ultimately patient care.”6 Building this rapport can begin by dedicating a few minutes (before/during rounds, between cases) to exchange information about career interests, hobbies, favorite restaurants, etc. This “small talk” is the beginning of a two-way exchange that ultimately develops into more meaningful exchanges.
In our experience, this simple step is impactful and fulfilling to both parties. This is also a good time for shared vulnerability by talking about what you are currently working on or have worked on at their stage to affirm that feedback is a continuous part of professional development and not a reflection of how far they are from competence at a given point in time.
Tip 3: Consider Timing, assess readiness, and preschedule sessions
Lack of attention to timing can hinder feedback acceptance. We suggest adhering to delivering positive feedback publicly and corrective feedback privately (“Praise in public, perfect in private”). This reinforces positive behaviors, increases motivation, and minimizes demoralization. Prolonged delays between the observed behavior and feedback can decrease its relevance. Conversely, delivering feedback too soon after an emotionally charged experience can be perceived as blame. Pre-designated times for feedback can minimize the guesswork and maintain your accountability for giving feedback without inadvertently linking it to one particular behavior. If the recipient does not appear to be in a state to receive feedback at the predesignated time, you can pivot to a “check-in” session to show support and strengthen rapport.
Tip 4: Customize to the learner and set shared goals
Diversity in backgrounds, perspectives, and personalities can impact how people perceive their own performances and experience feedback. Given the profound impact of sociocultural factors on feedback assimilation, maintaining the recipient and their goals at the core of performance evaluations is key to feedback acceptance.
A. Trainees
We suggest starting by introducing the idea of feedback as a partnership and something you feel privileged to do to help them achieve mutual goals. It helps to ask them to use the first day to get oriented with the experience, general expectations, challenges they expect to encounter, and their feedback goals. Tailoring your feedback to their goals creates a sense of shared purpose which increases motivation. Encouraging them to develop their own strategies allows them to play an active role in their growth. Giving them the opportunity to share their perceived strengths and deficiencies provides you with valuable information regarding their insight and ability to self-evaluate. This can help you predict their readiness for your feedback and to tailor your approach when there is a mismatch.
Examples:
- Medical student: Start with “What do you think you are doing well?” and “What do you think you need to work on?” Build on their response with encouragement and empathy. This helps make them more deliberate with what they work on because being a medical student can be overwhelming and can feel as though they have everything to work on.
- Resident/Fellow: By this point, trainees usually have an increased awareness of their strengths and deficiencies. Your questions can then be more specific, giving them autonomy over their learning, such as “What are some of the things you are working on that you want me to give you feedback on this week?” This makes them more aware, intentional, and receptive to your feedback because it is framed as something that they sought out.
B. Colleagues/Staff
Unlike the training environment in which feedback is built-in, giving feedback to co-workers requires you to establish a feedback-conducive environment and to develop a more in-depth understanding of coworkers’ personalities. Similar strategies can be applied, such as proactively setting the scene for open communication, scheduling check-ins, demonstrating receptiveness to feedback, and investing in trust-building.
Longer working relationships allow for strong foundational connections that make feedback less threatening. Personality assessment testing like Myers-Briggs Type Indicator or DiSC Assessment can aid in tailoring feedback to different individuals.7,8 An analytical thinker may appreciate direct, data-driven feedback. Relationship-oriented individuals might respond better to softer, encouragement-based approaches. Always maintain shared goals at the center of your interactions and consider collaborative opportunities such as quality improvement projects. This can improve your working relationship in a constructive way without casting blame.
Tip 5: Work on delivery: Bidirectional communication and body language
Non-verbal cues can have a profound impact on how your feedback is interpreted and on the recipient’s comfort to engage in conversation. Sitting down, making eye contact, nodding, and avoiding closed-off body posture can project support and feel less judgmental. Creating a safe and non-distracted environment with privacy can make them feel valued. Use motivating, respectful language focused on directly observed behaviors rather than personal attributes or second-hand reports.
Remember that focusing on repetitive patterns is likely more helpful than isolated incidents. Validate their hard work and give them a global idea of where they stand before diving into individual behaviors. Encourage their participation and empower them to suggest changes they plan to implement. Conclude by having them summarize their action plan to give them ownership and to verify that your feedback was interpreted as you intended. Thank them for being a part of the process, as it does take a partnership for feedback to be effective.
Tip 6: Be open to feedback
Demonstrating your willingness to accept and act on feedback reinforces a positive culture where feedback is normalized and valued. After an unintended outcome, initiate a two-way conversation and ask their input on anything they wish you would have done differently. This reaffirms your commitment to maintaining culture that does not revolve around one-sided critiques. Frequently soliciting feedback about your feedback skills can also guide you to adapt your approach and to recognize any ineffective feedback practices.
Tip 7: When things don’t go as planned
Receiving feedback, no matter how thoughtfully it is delivered, can be an emotionally-charged experience ending in hurt feelings. This happens because of misinterpretation of feedback as an indicator of inadequacy, heightened awareness of underlying insecurities, sociocultural or personal circumstances, frustration with oneself, needing additional guidance, or being caught off-guard by the assessment.
The evaluator should always acknowledge the recipient’s feelings, show compassion, and allow time for processing. When they are ready to talk, it is important to help reframe the recipients’ mindsets to recognize that feedback is not personal or defining and is not a “one and done” reflection of whether they have “made it.” Instead, it is a continual process that we benefit from through all career stages. Again, shared vulnerability can help to normalize feedback and maintain open dialogue. Setting an opportunity for a future check-in can reinforce support and lead to a more productive conversation after they have had time to process.
Conclusion
Effective feedback delivery is an invaluable skill that can result in meaningful goal-directed changes while strengthening professional relationships. Given the complexity of feedback interactions and the many factors that influence its acceptance, no single approach is suitable for all recipients and frequent adaptation of the approach is essential.
In our experience, adhering to these general overarching feedback principles (see Figure 1) has allowed us to have more successful interactions with trainees and colleagues.
Dr. Baliss is based in the Division of Gastroenterology, Washington University in St. Louis, Missouri. Dr. Hachem is director of the Division of Gastroenterology and Digestive Health at Intermountain Medical, Sandy, Utah. Both authors declare no conflicts of interest.
References
1. Parkes J, et al. Feedback sandwiches affect perceptions but not performance. Adv Health Sci Educ Theory Pract. 2013 Aug. doi:10.1007/s10459-012-9377-9.
2. van de Ridder JMM and Wijnen-Meijer M. Pendleton’s Rules: A Mini Review of a Feedback Method. Am J Biomed Sci & Res. 2023 May. doi: 10.34297/AJBSR.2023.19.002542.
3. Sender Liberman A, et al. Surgery residents and attending surgeons have different perceptions of feedback. Med Teach. 2005 Aug. doi: 10.1080/0142590500129183.
4. Sargeant J, et al. R2C2 in Action: Testing an Evidence-Based Model to Facilitate Feedback and Coaching in Residency. J Grad Med Educ. 2017 Apr. doi: 10.4300/JGME-D-16-00398.1.
5. Liakos W, et al. Frameworks for Effective Feedback in Health Professions Education. Acad Med. 2023 May. doi: 10.1097/ACM.0000000000004884.
6. Ramani S, et al. Feedback Redefined: Principles and Practice. J Gen Intern Med. 2019 May. doi: 10.1007/s11606-019-04874-2.
7. Woods RA and Hill PB. Myers-Briggs Type Indicator. StatPearls. StatPearls Publishing. 2022 Sept. https://www.ncbi.nlm.nih.gov/books/NBK554596/
8. Slowikowski MK. Using the DISC behavioral instrument to guide leadership and communication. AORN J. 2005 Nov. doi: 10.1016/s0001-2092(06)60276-7.
Clinical Research in Early Career Academic Medicine
Conducting clinical research as an early career gastroenterologist can take on many forms and has varying definitions of success. This article focuses on key factors to consider and should be supplemented with mentorship tailored to personal interests, goals, and institutional criteria for success. In this article, we will discuss selected high-yield topics that assist in early-career research. We will briefly discuss 1. Defining your niche, 2. Collaboration, 3. Visibility, 4. Time management, 5. Funding, 6. Receiving mentorship, and 7. Providing mentorship. We will conclude with discussing several authors’ experience in the research lab of the first author (FELD Lab – Fostering Equity in Liver and Digestive disease).
Defining Your Niche
Defining your niche is an essential component of an early career, as when academicians must transition from a trainee, who is supporting the research of an established mentor, to defining their own subspeciality area of investigation. Early-career academics should build on their prior work, but should also explore their own passions and skill set to define what will be unique about their research program and contributions to the field. Of course, positioning oneself at the intersection of two or more seemingly unrelated fields opens much opportunity for large impact but comes at a cost of identifying mentorship and justifying the niche to funders.
Collaboration
Fostering a collaborative environment is essential for early-career physician-researchers. One effective approach is to establish collaboration circles with other early career academics. Expanding research endeavors beyond a single institution to a multi-center framework enriches both scope and impact. This collaborative approach not only amplifies the depth of research but also facilitates peer mentorship and sponsorship. Participation in such networks can significantly enhance scholarly output and broaden professional reach during this critical phase of academic progression. Furthermore, prioritizing the promotion of colleagues within these networks is crucial. Proactive sponsorship opportunities, such as inviting peers to present at institutional seminars, strengthen both individual and collective academic visibility.
Collaboration is also essential to foster between trainees involved in early-career investigators’ work. An interconnected lab environment ensures that trainees remain informed about concurrent projects, thereby fostering a culture of shared knowledge and optimized productivity. Encouraging trainees to spearhead research aligned with their interests, under mentor guidance, nurtures independent inquiry and leadership. By establishing explicit roles, responsibilities, and authorship agreements at the outset of collaborative projects, early career mentors can avoid future conflicts and preserve a collaborative culture within the lab. This structured approach cultivates a supportive ecosystem, advancing both individual and collective research achievements.
Visibility
Establishing visibility and developing name recognition are crucial components of career advancement for early-career academic physicians. By clearly defining their areas of expertise, faculty can position themselves as leaders within their discipline. Active participation in professional societies, both at the local and national level, engagement with interest groups, and frequent contributions to educational events can be effective strategies for gaining recognition. Leveraging social media platforms can be helpful in enhancing visibility by facilitating connections and promoting research to a broader audience.
Moreover, research visibility plays a vital role in academic promotion. A strong publication record, reflected by an increasing h-index, demonstrates the impact and relevance of one’s research. Self-citation, when appropriate, can reinforce the continuity and progression of scholarly contributions. While publishing in high-impact journals is desirable, adaptability in resubmitting to other journals following rejections ensures that research remains visible and accessible. It also clearly establishes by whom the work was first done, before someone else investigates the line of inquiry. Through a combination of strategic engagement and publication efforts, early-career physicians can effectively build their professional reputation and advance their academic careers.
Time Management
Time management is essential for any research, and particularly in early career when efficiency in clinical care duties is still being gained. Securing protected time for research is essential to develop a niche, build connections (both institutionally and beyond their institutions), and demonstrate productivity that can be utilized to support future grant efforts.
Similarly, using protected time efficiently is required. Without organization and planning, research time can be spent with scattered meetings and responding to various tasks that do not directly support your research. It is helpful to be introspective about the time of the day you are most productive in your research efforts and blocking off that time to focus on research tasks and minimizing distractions. Blocking monthly time for larger scale thinking and planning is also important. Weekly lab and individual one-on-one meetings also support time management for trainees and lab members, to ensure efficiency and progress. Additionally, robust clinical support is essential to ensure that research time remains protected and patient care moves forward. When negotiating for positions, and in regular meetings thereafter, it is important to advocate for sufficient clinical staffing such that non-physician tasks can be appropriately delegated to another member of the care team.
Funding
Securing adequate funding poses a significant challenge for all early-career physician-scientists, particularly because of the discrepancy between National Institutes of Health salary caps and the higher average salaries in academic gastroenterology. This financial gap can deter physicians from pursuing research-intensive careers altogether and can derail early investigators who do not obtain funding rapidly. To overcome this, early-career investigators may need to adopt flexible strategies, such as accepting a lower salary that aligns with grant funding limits or funneling incentive or bonus pay to research accounts. Alternatively, they can advocate for institutional support to bridge the salary gap, ensuring their research efforts remain financially viable.
Institutions committed to fostering research excellence may offer supplemental funding or bridge programs to retain talented physician-scientists, thereby mitigating the financial strain and encouraging long-term engagement in research. Regular meetings to review salary and support sources, including philanthropy, foundation grants, and other streams, should be undertaken with leadership to align the researcher’s timeline and available funding. If career development funding appears untenable, consideration of multi–principal investigator R01s or equivalent with senior established investigators can be a promising path.
Receiving Mentorship
Effective mentorship for early-career physician-scientists should be approached through a team-based model that leverages both internal and external mentors. Internal mentors, familiar with the specific culture, expectations, and advancement pathways of the institution, can provide invaluable guidance on navigating institutional metrics for success, such as promotion criteria, grant acquisition, and clinical-research balance. External mentors, on the other hand, bring a broader perspective by offering innovative career development strategies and solutions derived from experiences at their home institutions. This multimodal mentorship model ensures a well-rounded approach to professional growth.
All national gastroenterology societies, including the American Gastroenterological Association, the American College of Gastroenterology, and the American Society for Gastrointestinal Endoscopy, and American Association for the Study of Liver Disease, offer structured early-career mentorship programs designed to connect emerging researchers with experienced leaders in the field (see below). These programs typically require a formal application process and are highly regarded for their exceptional quality and impact. Participation in such initiatives can significantly enhance career development by expanding networks, fostering interdisciplinary collaboration, and providing tailored guidance that complements institutional support. Integrating both internal and external mentorship opportunities ensures a robust and dynamic foundation for long-term success in academic medicine.
- AGA Career Compass (https://gastro.org/fellows-and-early-career/mentoring/)
- ACG Early Career Leadership Program (https://gi.org/acg-institute/early-career-leadership-program/)
- AGA-AASLD Academic Skills Workshop (https://gastro.org/news/applications-now-being-accepted-for-the-2024-aga-aasld-academic-skills-workshop/)
- AASLD Women’s Initiative Committee Leadership Program (https://www.aasld.org/promoting-leadership-potential-women-hepatology)
- Scrubs n Heels Mentorship Matrix (https://scrubsandheels.com/matrix/)
Providing Mentorship
The trainee authors on this manuscript describe in this section what has been helpful for them as mentees in the FELD research lab.
Student doctor Nguyen describes her experience as a lab member and things she finds most helpful as a medical student in the lab:
- Upon joining the team, a one-to-one meeting to discuss trainee’s personal and professional goals, and availability, was crucial to building the mentor-mentee relationship. Establishing this meaningful mentorship early on clarified expectations on both sides, built trust, and increased motivation. As a trainee, it is essential for me to see how my work aligns with a long-term goal and to receive ample guidance throughout the process.
- One of the most impactful experiences has been joining informal lunch sessions where trainees discussed data collection protocols and exchanged insights. In doing so, Dr. Feld has cultivated a lab culture that encourages curiosity, constructive feedback, and collaborative learning.
- To increase productivity, our team of trainees created a useful group message thread where we coordinated more sessions to collaborate. This coordination formed stronger relationships between team members and fostered a sense of shared purpose.
Dr. Cooper, a third year internal medicine resident, describes her experience as both a research mentee and a mentor to the junior trainees: “As a resident pursuing a career in academic gastroenterology and hepatology, I have found three key elements to be most helpful: intentional mentorship, structured meetings, and leadership development.”
- Intentional mentorship: Prior to joining the lab, I met with Dr. Feld to discuss my research experience and my goals. She took the time to understand these within the context of my training timeline and tailored project opportunities that aligned with my interests and were both feasible and impactful for my next steps. This intentional approach not only fostered a productive research experience but also established a mentor-mentee relationship built on genuine care for my growth and development.
- Regular meetings: Frequent lab meetings promote accountability, teamwork, and shared problem-solving skills. The open exchange of ideas fosters collaboration and joint problem solving to elevate the quality of our research. They are also an opportunity to observe key decision-making points during the research process and have been a great way to learn more about solid methodology.
- Supervised leadership: I have had ample time to lead discussions and coordinate projects among the junior trainees. These monitored leadership experiences promote project management skills, mentorship, and team dynamic awareness while maintaining the safety net of senior guidance. This model helped me transition from a trainee supporting others’ research to a more independent role, contributing to multi-disciplinary projects while mentoring junior members.
Conclusion
In conclusion, many exciting opportunities and notable barriers exist to establishing a clinical research laboratory in the early career. While excellence in each of the areas outlined may evolve, some aspects will come easier than others and with time, persistence, and a bit of luck, the research world will be a better place because of your contributions!
Dr. Feld is assistant professor of gastroenterology and hepatology and physician executive of Diversity, Equity, Inclusion and Belonging for the department of medicine at the University of Massachusetts (UMass) Chan Medical School, Worcester. Ms. Nguyen is a medical student at UMass Chan Medical School. Dr. Cooper is a resident physician at UMass Chan Medical School. Dr. Rabinowitz is an attending physician in the Inflammatory Bowel Disease Center at Beth Israel Deaconess Medical Center, Boston, Mass. Dr. Uchida is codirector of the Multidisciplinary Eosinophilic Gastrointestinal Disease Clinic at the University of Utah School of Medicine, Salt Lake City.
Conducting clinical research as an early career gastroenterologist can take on many forms and has varying definitions of success. This article focuses on key factors to consider and should be supplemented with mentorship tailored to personal interests, goals, and institutional criteria for success. In this article, we will discuss selected high-yield topics that assist in early-career research. We will briefly discuss 1. Defining your niche, 2. Collaboration, 3. Visibility, 4. Time management, 5. Funding, 6. Receiving mentorship, and 7. Providing mentorship. We will conclude with discussing several authors’ experience in the research lab of the first author (FELD Lab – Fostering Equity in Liver and Digestive disease).
Defining Your Niche
Defining your niche is an essential component of an early career, as when academicians must transition from a trainee, who is supporting the research of an established mentor, to defining their own subspeciality area of investigation. Early-career academics should build on their prior work, but should also explore their own passions and skill set to define what will be unique about their research program and contributions to the field. Of course, positioning oneself at the intersection of two or more seemingly unrelated fields opens much opportunity for large impact but comes at a cost of identifying mentorship and justifying the niche to funders.
Collaboration
Fostering a collaborative environment is essential for early-career physician-researchers. One effective approach is to establish collaboration circles with other early career academics. Expanding research endeavors beyond a single institution to a multi-center framework enriches both scope and impact. This collaborative approach not only amplifies the depth of research but also facilitates peer mentorship and sponsorship. Participation in such networks can significantly enhance scholarly output and broaden professional reach during this critical phase of academic progression. Furthermore, prioritizing the promotion of colleagues within these networks is crucial. Proactive sponsorship opportunities, such as inviting peers to present at institutional seminars, strengthen both individual and collective academic visibility.
Collaboration is also essential to foster between trainees involved in early-career investigators’ work. An interconnected lab environment ensures that trainees remain informed about concurrent projects, thereby fostering a culture of shared knowledge and optimized productivity. Encouraging trainees to spearhead research aligned with their interests, under mentor guidance, nurtures independent inquiry and leadership. By establishing explicit roles, responsibilities, and authorship agreements at the outset of collaborative projects, early career mentors can avoid future conflicts and preserve a collaborative culture within the lab. This structured approach cultivates a supportive ecosystem, advancing both individual and collective research achievements.
Visibility
Establishing visibility and developing name recognition are crucial components of career advancement for early-career academic physicians. By clearly defining their areas of expertise, faculty can position themselves as leaders within their discipline. Active participation in professional societies, both at the local and national level, engagement with interest groups, and frequent contributions to educational events can be effective strategies for gaining recognition. Leveraging social media platforms can be helpful in enhancing visibility by facilitating connections and promoting research to a broader audience.
Moreover, research visibility plays a vital role in academic promotion. A strong publication record, reflected by an increasing h-index, demonstrates the impact and relevance of one’s research. Self-citation, when appropriate, can reinforce the continuity and progression of scholarly contributions. While publishing in high-impact journals is desirable, adaptability in resubmitting to other journals following rejections ensures that research remains visible and accessible. It also clearly establishes by whom the work was first done, before someone else investigates the line of inquiry. Through a combination of strategic engagement and publication efforts, early-career physicians can effectively build their professional reputation and advance their academic careers.
Time Management
Time management is essential for any research, and particularly in early career when efficiency in clinical care duties is still being gained. Securing protected time for research is essential to develop a niche, build connections (both institutionally and beyond their institutions), and demonstrate productivity that can be utilized to support future grant efforts.
Similarly, using protected time efficiently is required. Without organization and planning, research time can be spent with scattered meetings and responding to various tasks that do not directly support your research. It is helpful to be introspective about the time of the day you are most productive in your research efforts and blocking off that time to focus on research tasks and minimizing distractions. Blocking monthly time for larger scale thinking and planning is also important. Weekly lab and individual one-on-one meetings also support time management for trainees and lab members, to ensure efficiency and progress. Additionally, robust clinical support is essential to ensure that research time remains protected and patient care moves forward. When negotiating for positions, and in regular meetings thereafter, it is important to advocate for sufficient clinical staffing such that non-physician tasks can be appropriately delegated to another member of the care team.
Funding
Securing adequate funding poses a significant challenge for all early-career physician-scientists, particularly because of the discrepancy between National Institutes of Health salary caps and the higher average salaries in academic gastroenterology. This financial gap can deter physicians from pursuing research-intensive careers altogether and can derail early investigators who do not obtain funding rapidly. To overcome this, early-career investigators may need to adopt flexible strategies, such as accepting a lower salary that aligns with grant funding limits or funneling incentive or bonus pay to research accounts. Alternatively, they can advocate for institutional support to bridge the salary gap, ensuring their research efforts remain financially viable.
Institutions committed to fostering research excellence may offer supplemental funding or bridge programs to retain talented physician-scientists, thereby mitigating the financial strain and encouraging long-term engagement in research. Regular meetings to review salary and support sources, including philanthropy, foundation grants, and other streams, should be undertaken with leadership to align the researcher’s timeline and available funding. If career development funding appears untenable, consideration of multi–principal investigator R01s or equivalent with senior established investigators can be a promising path.
Receiving Mentorship
Effective mentorship for early-career physician-scientists should be approached through a team-based model that leverages both internal and external mentors. Internal mentors, familiar with the specific culture, expectations, and advancement pathways of the institution, can provide invaluable guidance on navigating institutional metrics for success, such as promotion criteria, grant acquisition, and clinical-research balance. External mentors, on the other hand, bring a broader perspective by offering innovative career development strategies and solutions derived from experiences at their home institutions. This multimodal mentorship model ensures a well-rounded approach to professional growth.
All national gastroenterology societies, including the American Gastroenterological Association, the American College of Gastroenterology, and the American Society for Gastrointestinal Endoscopy, and American Association for the Study of Liver Disease, offer structured early-career mentorship programs designed to connect emerging researchers with experienced leaders in the field (see below). These programs typically require a formal application process and are highly regarded for their exceptional quality and impact. Participation in such initiatives can significantly enhance career development by expanding networks, fostering interdisciplinary collaboration, and providing tailored guidance that complements institutional support. Integrating both internal and external mentorship opportunities ensures a robust and dynamic foundation for long-term success in academic medicine.
- AGA Career Compass (https://gastro.org/fellows-and-early-career/mentoring/)
- ACG Early Career Leadership Program (https://gi.org/acg-institute/early-career-leadership-program/)
- AGA-AASLD Academic Skills Workshop (https://gastro.org/news/applications-now-being-accepted-for-the-2024-aga-aasld-academic-skills-workshop/)
- AASLD Women’s Initiative Committee Leadership Program (https://www.aasld.org/promoting-leadership-potential-women-hepatology)
- Scrubs n Heels Mentorship Matrix (https://scrubsandheels.com/matrix/)
Providing Mentorship
The trainee authors on this manuscript describe in this section what has been helpful for them as mentees in the FELD research lab.
Student doctor Nguyen describes her experience as a lab member and things she finds most helpful as a medical student in the lab:
- Upon joining the team, a one-to-one meeting to discuss trainee’s personal and professional goals, and availability, was crucial to building the mentor-mentee relationship. Establishing this meaningful mentorship early on clarified expectations on both sides, built trust, and increased motivation. As a trainee, it is essential for me to see how my work aligns with a long-term goal and to receive ample guidance throughout the process.
- One of the most impactful experiences has been joining informal lunch sessions where trainees discussed data collection protocols and exchanged insights. In doing so, Dr. Feld has cultivated a lab culture that encourages curiosity, constructive feedback, and collaborative learning.
- To increase productivity, our team of trainees created a useful group message thread where we coordinated more sessions to collaborate. This coordination formed stronger relationships between team members and fostered a sense of shared purpose.
Dr. Cooper, a third year internal medicine resident, describes her experience as both a research mentee and a mentor to the junior trainees: “As a resident pursuing a career in academic gastroenterology and hepatology, I have found three key elements to be most helpful: intentional mentorship, structured meetings, and leadership development.”
- Intentional mentorship: Prior to joining the lab, I met with Dr. Feld to discuss my research experience and my goals. She took the time to understand these within the context of my training timeline and tailored project opportunities that aligned with my interests and were both feasible and impactful for my next steps. This intentional approach not only fostered a productive research experience but also established a mentor-mentee relationship built on genuine care for my growth and development.
- Regular meetings: Frequent lab meetings promote accountability, teamwork, and shared problem-solving skills. The open exchange of ideas fosters collaboration and joint problem solving to elevate the quality of our research. They are also an opportunity to observe key decision-making points during the research process and have been a great way to learn more about solid methodology.
- Supervised leadership: I have had ample time to lead discussions and coordinate projects among the junior trainees. These monitored leadership experiences promote project management skills, mentorship, and team dynamic awareness while maintaining the safety net of senior guidance. This model helped me transition from a trainee supporting others’ research to a more independent role, contributing to multi-disciplinary projects while mentoring junior members.
Conclusion
In conclusion, many exciting opportunities and notable barriers exist to establishing a clinical research laboratory in the early career. While excellence in each of the areas outlined may evolve, some aspects will come easier than others and with time, persistence, and a bit of luck, the research world will be a better place because of your contributions!
Dr. Feld is assistant professor of gastroenterology and hepatology and physician executive of Diversity, Equity, Inclusion and Belonging for the department of medicine at the University of Massachusetts (UMass) Chan Medical School, Worcester. Ms. Nguyen is a medical student at UMass Chan Medical School. Dr. Cooper is a resident physician at UMass Chan Medical School. Dr. Rabinowitz is an attending physician in the Inflammatory Bowel Disease Center at Beth Israel Deaconess Medical Center, Boston, Mass. Dr. Uchida is codirector of the Multidisciplinary Eosinophilic Gastrointestinal Disease Clinic at the University of Utah School of Medicine, Salt Lake City.
Conducting clinical research as an early career gastroenterologist can take on many forms and has varying definitions of success. This article focuses on key factors to consider and should be supplemented with mentorship tailored to personal interests, goals, and institutional criteria for success. In this article, we will discuss selected high-yield topics that assist in early-career research. We will briefly discuss 1. Defining your niche, 2. Collaboration, 3. Visibility, 4. Time management, 5. Funding, 6. Receiving mentorship, and 7. Providing mentorship. We will conclude with discussing several authors’ experience in the research lab of the first author (FELD Lab – Fostering Equity in Liver and Digestive disease).
Defining Your Niche
Defining your niche is an essential component of an early career, as when academicians must transition from a trainee, who is supporting the research of an established mentor, to defining their own subspeciality area of investigation. Early-career academics should build on their prior work, but should also explore their own passions and skill set to define what will be unique about their research program and contributions to the field. Of course, positioning oneself at the intersection of two or more seemingly unrelated fields opens much opportunity for large impact but comes at a cost of identifying mentorship and justifying the niche to funders.
Collaboration
Fostering a collaborative environment is essential for early-career physician-researchers. One effective approach is to establish collaboration circles with other early career academics. Expanding research endeavors beyond a single institution to a multi-center framework enriches both scope and impact. This collaborative approach not only amplifies the depth of research but also facilitates peer mentorship and sponsorship. Participation in such networks can significantly enhance scholarly output and broaden professional reach during this critical phase of academic progression. Furthermore, prioritizing the promotion of colleagues within these networks is crucial. Proactive sponsorship opportunities, such as inviting peers to present at institutional seminars, strengthen both individual and collective academic visibility.
Collaboration is also essential to foster between trainees involved in early-career investigators’ work. An interconnected lab environment ensures that trainees remain informed about concurrent projects, thereby fostering a culture of shared knowledge and optimized productivity. Encouraging trainees to spearhead research aligned with their interests, under mentor guidance, nurtures independent inquiry and leadership. By establishing explicit roles, responsibilities, and authorship agreements at the outset of collaborative projects, early career mentors can avoid future conflicts and preserve a collaborative culture within the lab. This structured approach cultivates a supportive ecosystem, advancing both individual and collective research achievements.
Visibility
Establishing visibility and developing name recognition are crucial components of career advancement for early-career academic physicians. By clearly defining their areas of expertise, faculty can position themselves as leaders within their discipline. Active participation in professional societies, both at the local and national level, engagement with interest groups, and frequent contributions to educational events can be effective strategies for gaining recognition. Leveraging social media platforms can be helpful in enhancing visibility by facilitating connections and promoting research to a broader audience.
Moreover, research visibility plays a vital role in academic promotion. A strong publication record, reflected by an increasing h-index, demonstrates the impact and relevance of one’s research. Self-citation, when appropriate, can reinforce the continuity and progression of scholarly contributions. While publishing in high-impact journals is desirable, adaptability in resubmitting to other journals following rejections ensures that research remains visible and accessible. It also clearly establishes by whom the work was first done, before someone else investigates the line of inquiry. Through a combination of strategic engagement and publication efforts, early-career physicians can effectively build their professional reputation and advance their academic careers.
Time Management
Time management is essential for any research, and particularly in early career when efficiency in clinical care duties is still being gained. Securing protected time for research is essential to develop a niche, build connections (both institutionally and beyond their institutions), and demonstrate productivity that can be utilized to support future grant efforts.
Similarly, using protected time efficiently is required. Without organization and planning, research time can be spent with scattered meetings and responding to various tasks that do not directly support your research. It is helpful to be introspective about the time of the day you are most productive in your research efforts and blocking off that time to focus on research tasks and minimizing distractions. Blocking monthly time for larger scale thinking and planning is also important. Weekly lab and individual one-on-one meetings also support time management for trainees and lab members, to ensure efficiency and progress. Additionally, robust clinical support is essential to ensure that research time remains protected and patient care moves forward. When negotiating for positions, and in regular meetings thereafter, it is important to advocate for sufficient clinical staffing such that non-physician tasks can be appropriately delegated to another member of the care team.
Funding
Securing adequate funding poses a significant challenge for all early-career physician-scientists, particularly because of the discrepancy between National Institutes of Health salary caps and the higher average salaries in academic gastroenterology. This financial gap can deter physicians from pursuing research-intensive careers altogether and can derail early investigators who do not obtain funding rapidly. To overcome this, early-career investigators may need to adopt flexible strategies, such as accepting a lower salary that aligns with grant funding limits or funneling incentive or bonus pay to research accounts. Alternatively, they can advocate for institutional support to bridge the salary gap, ensuring their research efforts remain financially viable.
Institutions committed to fostering research excellence may offer supplemental funding or bridge programs to retain talented physician-scientists, thereby mitigating the financial strain and encouraging long-term engagement in research. Regular meetings to review salary and support sources, including philanthropy, foundation grants, and other streams, should be undertaken with leadership to align the researcher’s timeline and available funding. If career development funding appears untenable, consideration of multi–principal investigator R01s or equivalent with senior established investigators can be a promising path.
Receiving Mentorship
Effective mentorship for early-career physician-scientists should be approached through a team-based model that leverages both internal and external mentors. Internal mentors, familiar with the specific culture, expectations, and advancement pathways of the institution, can provide invaluable guidance on navigating institutional metrics for success, such as promotion criteria, grant acquisition, and clinical-research balance. External mentors, on the other hand, bring a broader perspective by offering innovative career development strategies and solutions derived from experiences at their home institutions. This multimodal mentorship model ensures a well-rounded approach to professional growth.
All national gastroenterology societies, including the American Gastroenterological Association, the American College of Gastroenterology, and the American Society for Gastrointestinal Endoscopy, and American Association for the Study of Liver Disease, offer structured early-career mentorship programs designed to connect emerging researchers with experienced leaders in the field (see below). These programs typically require a formal application process and are highly regarded for their exceptional quality and impact. Participation in such initiatives can significantly enhance career development by expanding networks, fostering interdisciplinary collaboration, and providing tailored guidance that complements institutional support. Integrating both internal and external mentorship opportunities ensures a robust and dynamic foundation for long-term success in academic medicine.
- AGA Career Compass (https://gastro.org/fellows-and-early-career/mentoring/)
- ACG Early Career Leadership Program (https://gi.org/acg-institute/early-career-leadership-program/)
- AGA-AASLD Academic Skills Workshop (https://gastro.org/news/applications-now-being-accepted-for-the-2024-aga-aasld-academic-skills-workshop/)
- AASLD Women’s Initiative Committee Leadership Program (https://www.aasld.org/promoting-leadership-potential-women-hepatology)
- Scrubs n Heels Mentorship Matrix (https://scrubsandheels.com/matrix/)
Providing Mentorship
The trainee authors on this manuscript describe in this section what has been helpful for them as mentees in the FELD research lab.
Student doctor Nguyen describes her experience as a lab member and things she finds most helpful as a medical student in the lab:
- Upon joining the team, a one-to-one meeting to discuss trainee’s personal and professional goals, and availability, was crucial to building the mentor-mentee relationship. Establishing this meaningful mentorship early on clarified expectations on both sides, built trust, and increased motivation. As a trainee, it is essential for me to see how my work aligns with a long-term goal and to receive ample guidance throughout the process.
- One of the most impactful experiences has been joining informal lunch sessions where trainees discussed data collection protocols and exchanged insights. In doing so, Dr. Feld has cultivated a lab culture that encourages curiosity, constructive feedback, and collaborative learning.
- To increase productivity, our team of trainees created a useful group message thread where we coordinated more sessions to collaborate. This coordination formed stronger relationships between team members and fostered a sense of shared purpose.
Dr. Cooper, a third year internal medicine resident, describes her experience as both a research mentee and a mentor to the junior trainees: “As a resident pursuing a career in academic gastroenterology and hepatology, I have found three key elements to be most helpful: intentional mentorship, structured meetings, and leadership development.”
- Intentional mentorship: Prior to joining the lab, I met with Dr. Feld to discuss my research experience and my goals. She took the time to understand these within the context of my training timeline and tailored project opportunities that aligned with my interests and were both feasible and impactful for my next steps. This intentional approach not only fostered a productive research experience but also established a mentor-mentee relationship built on genuine care for my growth and development.
- Regular meetings: Frequent lab meetings promote accountability, teamwork, and shared problem-solving skills. The open exchange of ideas fosters collaboration and joint problem solving to elevate the quality of our research. They are also an opportunity to observe key decision-making points during the research process and have been a great way to learn more about solid methodology.
- Supervised leadership: I have had ample time to lead discussions and coordinate projects among the junior trainees. These monitored leadership experiences promote project management skills, mentorship, and team dynamic awareness while maintaining the safety net of senior guidance. This model helped me transition from a trainee supporting others’ research to a more independent role, contributing to multi-disciplinary projects while mentoring junior members.
Conclusion
In conclusion, many exciting opportunities and notable barriers exist to establishing a clinical research laboratory in the early career. While excellence in each of the areas outlined may evolve, some aspects will come easier than others and with time, persistence, and a bit of luck, the research world will be a better place because of your contributions!
Dr. Feld is assistant professor of gastroenterology and hepatology and physician executive of Diversity, Equity, Inclusion and Belonging for the department of medicine at the University of Massachusetts (UMass) Chan Medical School, Worcester. Ms. Nguyen is a medical student at UMass Chan Medical School. Dr. Cooper is a resident physician at UMass Chan Medical School. Dr. Rabinowitz is an attending physician in the Inflammatory Bowel Disease Center at Beth Israel Deaconess Medical Center, Boston, Mass. Dr. Uchida is codirector of the Multidisciplinary Eosinophilic Gastrointestinal Disease Clinic at the University of Utah School of Medicine, Salt Lake City.
Transitioning from Employment in Academia to Private Practice
After more than 10 years of serving in a large academic medical center in Chicago, Illinois, that was part of a national health care system, the decision to transition into private practice wasn’t one I made lightly.
Having built a rewarding career and spent over a quarter of my life in an academic medical center and a national health system, the move to starting an independent practice from scratch was both exciting and daunting. The notion of leaving behind the structure, resources, and safety of the large health system was unsettling. However, as the landscape of health care continues to evolve, with worsening large structural problems within the U.S. health care system, I realized that starting an independent gastroenterology practice — focused on trying to fix some of these large-scale problems from the start — would not only align with my professional goals but also provide the personal satisfaction I had failed to find.
As I reflect on my journey, there are a few key lessons I learned from making this leap — lessons that helped me transition from a highly structured employed physician environment to leading a thriving independent practice focused on redesigning gastroenterology care from scratch.
Lesson 1: Autonomy Opens the Door to Innovation
One of the primary reasons I left the employed physician setting was to gain greater control over my clinical practice and decision-making processes.
In a national health care system, the goal of standardization often dictates not only clinical care, but many “back end” aspects of the entire health care experience. We often see the things that are more visible, such as what supplies/equipment you use, how your patient appointments are scheduled, how many support staff members are assigned to help your practice, what electronic health record system you use, and how shared resources (like GI lab block time or anesthesia teams) are allocated.
However, this also impacts things we don’t usually see, such as what fees are billed for care you are providing (like facility fees), communication systems that your patients need to navigate for help, human resource systems you use, and retirement/health benefits you and your other team members receive.
Standardization has two adverse consequences: 1) it does not allow for personalization and as a result, 2) it suppresses innovation. Standard protocols can streamline processes, but they sometimes fail to account for the nuanced differences between patients, such as genetic factors, unique medical histories, or responses/failures to prior treatments. This rigidity can stifle innovation, as physicians are often bound by guidelines that may not reflect the latest advancements or allow for creative, individualized approaches to care. In the long term, an overemphasis on standardization risks turning health care into a one-size-fits-all model, undermining the potential for breakthroughs.
The transition was challenging at first, as we needed to engage our entire new practice with a different mindset now that many of us had autonomy for the first time. Instead of everyone just practicing health care the way they had done before, we took a page from Elon Musk and challenged every member of the team to ask three questions about everything they do on a daily basis:
- Is what I am doing helping a patient get healthy? (Question every requirement)
- If not, do I still need to do this? (Delete any part of the process you can)
- If so, how can I make this easier, faster, or automated? (Simplify and optimize, accelerate cycle time, and automate)
The freedom to innovate is a hallmark of independent practice. Embracing innovation in every aspect of the practice has been the most critical lesson of this journey.
Lesson 2: Financial Stewardship is Critical for Sustainability
Running an independent practice is not just about medicine — it’s also about managing a business.
This was a stark shift from the large academic health systems, where financial decisions were handled by the “administration.” In my new role as a business owner, understanding the financial aspects of health care was crucial for success. The cost of what patients pay for health care in the United States (either directly in deductibles and coinsurance or indirectly through insurance premiums) is unsustainably high. However, inflation continues to cause substantial increases in almost all the costs of delivering care: medical supplies, salaries, benefits, IT costs, etc. It was critical to develop a financial plan that accounted for these two macro-economic trends, and ideally helped solve for both. In our case, delivering high quality care with a lower cost to patients and payers.
We started by reevaluating our relationship with payers. Whereas being part of a large academic health system, we are often taught to look at payers as the adversary; as an independent practice looking to redesign the health care experience, it was critical for us to look to the payers as a partner in this journey. Understanding payer expectations and structuring contracts that aligned with shared goals of reducing total health care costs for patients was one of the foundations of our financial plan.
Offering office-based endoscopy was one innovation we implemented to significantly impact both patient affordability and practice revenue. By performing procedures like colonoscopies and upper endoscopies in an office setting rather than a hospital or ambulatory surgery center, we eliminated facility fees, which are often a significant part of the total cost of care. This directly lowers out-of-pocket expenses for patients and reduces the overall financial burden on insurance companies. At the same time, it allows the practice to capture more of the revenue from these procedures, without the overhead costs associated with larger facilities. This model creates a win-win situation: patients save money while receiving the same quality of care, and the practice experiences an increase in profitability and autonomy in managing its services.
Lesson 3: Collaborative Care and Multidisciplinary Teams Can Exist Anywhere
One aspect I deeply valued in academia was the collaborative environment — having specialists across disciplines work together on challenging cases. In private practice, I was concerned that I would lose this collegial atmosphere. However, I quickly learned that building a robust network of multidisciplinary collaborators was achievable in independent practice, just like it was in a large health system.
In our practice, we established close relationships with primary care physicians, surgeons, advanced practice providers, dietitians, behavioral health specialists, and others. These partnerships were not just referral networks but integrated care teams where communication and shared decision-making were prioritized. By fostering collaboration, we could offer patients comprehensive care that addressed their physical, psychological, and nutritional needs.
For example, managing patients with chronic conditions like inflammatory bowel disease, cirrhosis, or obesity requires more than just prescribing medications. It involves regular monitoring, dietary adjustments, psychological support, and in some cases, surgical intervention. In an academic setting, coordinating this level of care can be cumbersome due to institutional barriers and siloed departments. In our practice, some of these relationships are achieved through partnerships with other like-minded practices. In other situations, team members of other disciplines are employed directly by our practice. Being in an independent practice allowed us the flexibility to prioritize working with the right team members first, and then structuring the relationship model second.
Lesson 4: Technology Is a Vital Tool in Redesigning Health Care
When I worked in a large academic health system, technology was often seen as an administrative burden rather than a clinical asset. Electronic health records (EHR) and a lot of the other IT systems that health care workers and patients interacted with on a regular basis were viewed as a barrier to care or a cause of time burdens instead of as tools to make health care easier. As we built our new practice from scratch, it was critical that we had an IT infrastructure that aligned with our core goals: simplify and automate the health care experience for everyone.
For our practice, we didn’t try to re-invent the wheel. Instead we copied from other industries who had already figured out a great solution for a problem we had. We wanted our patients to have a great customer service experience when interacting with our practice for scheduling, questions, refills, etc. So we implemented a unified communication system that some Fortune 100 companies, with perennial high scores for customer service, used. We wanted a great human resource system that would streamline the administrative time it would take to handle all HR needs for our practice. So we implemented an HR information system that had the best ratings for automation and integration with other business systems. At every point in the process, we reminded ourselves to focus on simplification and automation for every user of the system.
Conclusion: A Rewarding Transition
The lessons I’ve learned along the way — embracing autonomy, understanding financial stewardship, fostering collaboration, and leveraging technology — have helped me work toward a better total health care experience for the community.
This journey has also been deeply fulfilling on a personal level. It has allowed me to build stronger relationships with my patients, focus on long-term health outcomes, and create a practice where innovation and quality truly matter. While the challenges of running a private practice are real, the rewards — both for me and my patients — are immeasurable. If I had to do it all over again, I wouldn’t hesitate for a moment. If anything, I should have done it earlier.
Dr. Gupta is Managing Partner at Midwest Digestive Health & Nutrition, in Des Plaines, Illinois. He has reported no conflicts of interest in relation to this article.
After more than 10 years of serving in a large academic medical center in Chicago, Illinois, that was part of a national health care system, the decision to transition into private practice wasn’t one I made lightly.
Having built a rewarding career and spent over a quarter of my life in an academic medical center and a national health system, the move to starting an independent practice from scratch was both exciting and daunting. The notion of leaving behind the structure, resources, and safety of the large health system was unsettling. However, as the landscape of health care continues to evolve, with worsening large structural problems within the U.S. health care system, I realized that starting an independent gastroenterology practice — focused on trying to fix some of these large-scale problems from the start — would not only align with my professional goals but also provide the personal satisfaction I had failed to find.
As I reflect on my journey, there are a few key lessons I learned from making this leap — lessons that helped me transition from a highly structured employed physician environment to leading a thriving independent practice focused on redesigning gastroenterology care from scratch.
Lesson 1: Autonomy Opens the Door to Innovation
One of the primary reasons I left the employed physician setting was to gain greater control over my clinical practice and decision-making processes.
In a national health care system, the goal of standardization often dictates not only clinical care, but many “back end” aspects of the entire health care experience. We often see the things that are more visible, such as what supplies/equipment you use, how your patient appointments are scheduled, how many support staff members are assigned to help your practice, what electronic health record system you use, and how shared resources (like GI lab block time or anesthesia teams) are allocated.
However, this also impacts things we don’t usually see, such as what fees are billed for care you are providing (like facility fees), communication systems that your patients need to navigate for help, human resource systems you use, and retirement/health benefits you and your other team members receive.
Standardization has two adverse consequences: 1) it does not allow for personalization and as a result, 2) it suppresses innovation. Standard protocols can streamline processes, but they sometimes fail to account for the nuanced differences between patients, such as genetic factors, unique medical histories, or responses/failures to prior treatments. This rigidity can stifle innovation, as physicians are often bound by guidelines that may not reflect the latest advancements or allow for creative, individualized approaches to care. In the long term, an overemphasis on standardization risks turning health care into a one-size-fits-all model, undermining the potential for breakthroughs.
The transition was challenging at first, as we needed to engage our entire new practice with a different mindset now that many of us had autonomy for the first time. Instead of everyone just practicing health care the way they had done before, we took a page from Elon Musk and challenged every member of the team to ask three questions about everything they do on a daily basis:
- Is what I am doing helping a patient get healthy? (Question every requirement)
- If not, do I still need to do this? (Delete any part of the process you can)
- If so, how can I make this easier, faster, or automated? (Simplify and optimize, accelerate cycle time, and automate)
The freedom to innovate is a hallmark of independent practice. Embracing innovation in every aspect of the practice has been the most critical lesson of this journey.
Lesson 2: Financial Stewardship is Critical for Sustainability
Running an independent practice is not just about medicine — it’s also about managing a business.
This was a stark shift from the large academic health systems, where financial decisions were handled by the “administration.” In my new role as a business owner, understanding the financial aspects of health care was crucial for success. The cost of what patients pay for health care in the United States (either directly in deductibles and coinsurance or indirectly through insurance premiums) is unsustainably high. However, inflation continues to cause substantial increases in almost all the costs of delivering care: medical supplies, salaries, benefits, IT costs, etc. It was critical to develop a financial plan that accounted for these two macro-economic trends, and ideally helped solve for both. In our case, delivering high quality care with a lower cost to patients and payers.
We started by reevaluating our relationship with payers. Whereas being part of a large academic health system, we are often taught to look at payers as the adversary; as an independent practice looking to redesign the health care experience, it was critical for us to look to the payers as a partner in this journey. Understanding payer expectations and structuring contracts that aligned with shared goals of reducing total health care costs for patients was one of the foundations of our financial plan.
Offering office-based endoscopy was one innovation we implemented to significantly impact both patient affordability and practice revenue. By performing procedures like colonoscopies and upper endoscopies in an office setting rather than a hospital or ambulatory surgery center, we eliminated facility fees, which are often a significant part of the total cost of care. This directly lowers out-of-pocket expenses for patients and reduces the overall financial burden on insurance companies. At the same time, it allows the practice to capture more of the revenue from these procedures, without the overhead costs associated with larger facilities. This model creates a win-win situation: patients save money while receiving the same quality of care, and the practice experiences an increase in profitability and autonomy in managing its services.
Lesson 3: Collaborative Care and Multidisciplinary Teams Can Exist Anywhere
One aspect I deeply valued in academia was the collaborative environment — having specialists across disciplines work together on challenging cases. In private practice, I was concerned that I would lose this collegial atmosphere. However, I quickly learned that building a robust network of multidisciplinary collaborators was achievable in independent practice, just like it was in a large health system.
In our practice, we established close relationships with primary care physicians, surgeons, advanced practice providers, dietitians, behavioral health specialists, and others. These partnerships were not just referral networks but integrated care teams where communication and shared decision-making were prioritized. By fostering collaboration, we could offer patients comprehensive care that addressed their physical, psychological, and nutritional needs.
For example, managing patients with chronic conditions like inflammatory bowel disease, cirrhosis, or obesity requires more than just prescribing medications. It involves regular monitoring, dietary adjustments, psychological support, and in some cases, surgical intervention. In an academic setting, coordinating this level of care can be cumbersome due to institutional barriers and siloed departments. In our practice, some of these relationships are achieved through partnerships with other like-minded practices. In other situations, team members of other disciplines are employed directly by our practice. Being in an independent practice allowed us the flexibility to prioritize working with the right team members first, and then structuring the relationship model second.
Lesson 4: Technology Is a Vital Tool in Redesigning Health Care
When I worked in a large academic health system, technology was often seen as an administrative burden rather than a clinical asset. Electronic health records (EHR) and a lot of the other IT systems that health care workers and patients interacted with on a regular basis were viewed as a barrier to care or a cause of time burdens instead of as tools to make health care easier. As we built our new practice from scratch, it was critical that we had an IT infrastructure that aligned with our core goals: simplify and automate the health care experience for everyone.
For our practice, we didn’t try to re-invent the wheel. Instead we copied from other industries who had already figured out a great solution for a problem we had. We wanted our patients to have a great customer service experience when interacting with our practice for scheduling, questions, refills, etc. So we implemented a unified communication system that some Fortune 100 companies, with perennial high scores for customer service, used. We wanted a great human resource system that would streamline the administrative time it would take to handle all HR needs for our practice. So we implemented an HR information system that had the best ratings for automation and integration with other business systems. At every point in the process, we reminded ourselves to focus on simplification and automation for every user of the system.
Conclusion: A Rewarding Transition
The lessons I’ve learned along the way — embracing autonomy, understanding financial stewardship, fostering collaboration, and leveraging technology — have helped me work toward a better total health care experience for the community.
This journey has also been deeply fulfilling on a personal level. It has allowed me to build stronger relationships with my patients, focus on long-term health outcomes, and create a practice where innovation and quality truly matter. While the challenges of running a private practice are real, the rewards — both for me and my patients — are immeasurable. If I had to do it all over again, I wouldn’t hesitate for a moment. If anything, I should have done it earlier.
Dr. Gupta is Managing Partner at Midwest Digestive Health & Nutrition, in Des Plaines, Illinois. He has reported no conflicts of interest in relation to this article.
After more than 10 years of serving in a large academic medical center in Chicago, Illinois, that was part of a national health care system, the decision to transition into private practice wasn’t one I made lightly.
Having built a rewarding career and spent over a quarter of my life in an academic medical center and a national health system, the move to starting an independent practice from scratch was both exciting and daunting. The notion of leaving behind the structure, resources, and safety of the large health system was unsettling. However, as the landscape of health care continues to evolve, with worsening large structural problems within the U.S. health care system, I realized that starting an independent gastroenterology practice — focused on trying to fix some of these large-scale problems from the start — would not only align with my professional goals but also provide the personal satisfaction I had failed to find.
As I reflect on my journey, there are a few key lessons I learned from making this leap — lessons that helped me transition from a highly structured employed physician environment to leading a thriving independent practice focused on redesigning gastroenterology care from scratch.
Lesson 1: Autonomy Opens the Door to Innovation
One of the primary reasons I left the employed physician setting was to gain greater control over my clinical practice and decision-making processes.
In a national health care system, the goal of standardization often dictates not only clinical care, but many “back end” aspects of the entire health care experience. We often see the things that are more visible, such as what supplies/equipment you use, how your patient appointments are scheduled, how many support staff members are assigned to help your practice, what electronic health record system you use, and how shared resources (like GI lab block time or anesthesia teams) are allocated.
However, this also impacts things we don’t usually see, such as what fees are billed for care you are providing (like facility fees), communication systems that your patients need to navigate for help, human resource systems you use, and retirement/health benefits you and your other team members receive.
Standardization has two adverse consequences: 1) it does not allow for personalization and as a result, 2) it suppresses innovation. Standard protocols can streamline processes, but they sometimes fail to account for the nuanced differences between patients, such as genetic factors, unique medical histories, or responses/failures to prior treatments. This rigidity can stifle innovation, as physicians are often bound by guidelines that may not reflect the latest advancements or allow for creative, individualized approaches to care. In the long term, an overemphasis on standardization risks turning health care into a one-size-fits-all model, undermining the potential for breakthroughs.
The transition was challenging at first, as we needed to engage our entire new practice with a different mindset now that many of us had autonomy for the first time. Instead of everyone just practicing health care the way they had done before, we took a page from Elon Musk and challenged every member of the team to ask three questions about everything they do on a daily basis:
- Is what I am doing helping a patient get healthy? (Question every requirement)
- If not, do I still need to do this? (Delete any part of the process you can)
- If so, how can I make this easier, faster, or automated? (Simplify and optimize, accelerate cycle time, and automate)
The freedom to innovate is a hallmark of independent practice. Embracing innovation in every aspect of the practice has been the most critical lesson of this journey.
Lesson 2: Financial Stewardship is Critical for Sustainability
Running an independent practice is not just about medicine — it’s also about managing a business.
This was a stark shift from the large academic health systems, where financial decisions were handled by the “administration.” In my new role as a business owner, understanding the financial aspects of health care was crucial for success. The cost of what patients pay for health care in the United States (either directly in deductibles and coinsurance or indirectly through insurance premiums) is unsustainably high. However, inflation continues to cause substantial increases in almost all the costs of delivering care: medical supplies, salaries, benefits, IT costs, etc. It was critical to develop a financial plan that accounted for these two macro-economic trends, and ideally helped solve for both. In our case, delivering high quality care with a lower cost to patients and payers.
We started by reevaluating our relationship with payers. Whereas being part of a large academic health system, we are often taught to look at payers as the adversary; as an independent practice looking to redesign the health care experience, it was critical for us to look to the payers as a partner in this journey. Understanding payer expectations and structuring contracts that aligned with shared goals of reducing total health care costs for patients was one of the foundations of our financial plan.
Offering office-based endoscopy was one innovation we implemented to significantly impact both patient affordability and practice revenue. By performing procedures like colonoscopies and upper endoscopies in an office setting rather than a hospital or ambulatory surgery center, we eliminated facility fees, which are often a significant part of the total cost of care. This directly lowers out-of-pocket expenses for patients and reduces the overall financial burden on insurance companies. At the same time, it allows the practice to capture more of the revenue from these procedures, without the overhead costs associated with larger facilities. This model creates a win-win situation: patients save money while receiving the same quality of care, and the practice experiences an increase in profitability and autonomy in managing its services.
Lesson 3: Collaborative Care and Multidisciplinary Teams Can Exist Anywhere
One aspect I deeply valued in academia was the collaborative environment — having specialists across disciplines work together on challenging cases. In private practice, I was concerned that I would lose this collegial atmosphere. However, I quickly learned that building a robust network of multidisciplinary collaborators was achievable in independent practice, just like it was in a large health system.
In our practice, we established close relationships with primary care physicians, surgeons, advanced practice providers, dietitians, behavioral health specialists, and others. These partnerships were not just referral networks but integrated care teams where communication and shared decision-making were prioritized. By fostering collaboration, we could offer patients comprehensive care that addressed their physical, psychological, and nutritional needs.
For example, managing patients with chronic conditions like inflammatory bowel disease, cirrhosis, or obesity requires more than just prescribing medications. It involves regular monitoring, dietary adjustments, psychological support, and in some cases, surgical intervention. In an academic setting, coordinating this level of care can be cumbersome due to institutional barriers and siloed departments. In our practice, some of these relationships are achieved through partnerships with other like-minded practices. In other situations, team members of other disciplines are employed directly by our practice. Being in an independent practice allowed us the flexibility to prioritize working with the right team members first, and then structuring the relationship model second.
Lesson 4: Technology Is a Vital Tool in Redesigning Health Care
When I worked in a large academic health system, technology was often seen as an administrative burden rather than a clinical asset. Electronic health records (EHR) and a lot of the other IT systems that health care workers and patients interacted with on a regular basis were viewed as a barrier to care or a cause of time burdens instead of as tools to make health care easier. As we built our new practice from scratch, it was critical that we had an IT infrastructure that aligned with our core goals: simplify and automate the health care experience for everyone.
For our practice, we didn’t try to re-invent the wheel. Instead we copied from other industries who had already figured out a great solution for a problem we had. We wanted our patients to have a great customer service experience when interacting with our practice for scheduling, questions, refills, etc. So we implemented a unified communication system that some Fortune 100 companies, with perennial high scores for customer service, used. We wanted a great human resource system that would streamline the administrative time it would take to handle all HR needs for our practice. So we implemented an HR information system that had the best ratings for automation and integration with other business systems. At every point in the process, we reminded ourselves to focus on simplification and automation for every user of the system.
Conclusion: A Rewarding Transition
The lessons I’ve learned along the way — embracing autonomy, understanding financial stewardship, fostering collaboration, and leveraging technology — have helped me work toward a better total health care experience for the community.
This journey has also been deeply fulfilling on a personal level. It has allowed me to build stronger relationships with my patients, focus on long-term health outcomes, and create a practice where innovation and quality truly matter. While the challenges of running a private practice are real, the rewards — both for me and my patients — are immeasurable. If I had to do it all over again, I wouldn’t hesitate for a moment. If anything, I should have done it earlier.
Dr. Gupta is Managing Partner at Midwest Digestive Health & Nutrition, in Des Plaines, Illinois. He has reported no conflicts of interest in relation to this article.
Navigating as a GI Locum: My Path and Guide to This Alternative Practice Model
My successful career in academic gastroenterology makes me a natural proponent of the academic model of practice. However, in my current role as a locum tenens, I have witnessed the versatility that locum assignments offer gastroenterologists, particularly when flexibility in their professional lives is paramount.
The locum tenens industry is a growing feature of the healthcare staffing landscape. My perspective is unique, transitioning from professor of medicine and chief of gastroenterology at an academic medical center to a self-employed locum gastroenterologist.
As chief, I hired locums to offer additional coverage to the faculty staffing as our division, inclusive of GI fellowship and endoscopy volume, expanded. I recruited, supervised, and assigned responsibilities to the locums. Not only were these physicians professional and competent, but they also contributed to my division’s forward evolution. Based on this experience, I was confident that I could successfully perform as a locum gastroenterologist myself.
My work as a locum these past 5 years has been a positive professional transition for me. I have enjoyed meeting and working with new colleagues, including international locums who travel to work in the United States. I have also witnessed how early-career and mid-career gastroenterologists have taken advantage of this flexible and well-remunerated work.
What It Entails to Be a Locum Tenens
I suspect you have been on the receiving end of emails and postcards from locum tenens companies recruiting for potential assignments and have wondered about the specifics. Essentially, a locum physician functions as an independent contractor who accepts a temporary position at a healthcare organization to provide clinical staffing support during periods of staffing disruption.
Assignments vary in geographic location, facility work site (outpatient vs inpatient), hours, required skills, cadence of assignment, and expected length of staffing need. The locum physician has complete control over selecting the assignment location, the intensity of responsibilities, and the time they wish to commit to the position. Temporal flexibility offers locums the opportunity to commit from a few weeks per year to a full-time commitment. Locums can also combine multiple assignments in different regions or states to match the targeted number of weeks they wish to commit to and the financial goal they have set.
I have met physicians working a few weeks a year during time off from their permanent jobs to supplement their incomes, as well as fully employed physicians leveraging locum placements to explore locations or practices that they have an interest in. Gastroenterologists facing planned or unplanned life events may find the role enticing as locum opportunities offer an elevated level of flexibility and autonomy.
The Role of the Locum Tenens Company
Locum tenens companies have arrangements with healthcare facilities to provide temporary staffing. They aim to recruit prospective physicians, establish a collaborative relationship, and align these physicians with a locum assignment that benefits all parties.
Once the physician has completed the company’s credentialing packet, the company facilitates credentialing for new state medical licensures and the specific healthcare facility. The company conducts all negotiations, communications, and financial arrangements between the locum physician and the facility. Locum physicians do not communicate directly with the facility, at least not initially. The company also provides medical malpractice coverage through an established insurance broker. The company arranges travel (flights, car rentals, and hotels) for the assignment, and the healthcare facility reimburses the company.
Lastly, the company arranges a phone interview between the locum physician and the facility’s gastroenterologist or medical director for a more detailed description of expected responsibilities and level of staffing for endoscopy before the locum physician decides whether the job is a “good fit” for their skills and objectives. It is critical at this point that the locum physician does their due diligence, asking thoughtful questions to ensure a comprehensive understanding of the role before committing.
What Does It Mean to Be an Independent Contractor
An independent contractor is contracted to perform work but is not an employee of an organization (ie, self-employed). This is an important distinction when it comes to the IRS, tax obligations, and allowable deductions.
Initially, this may seem confusing, but some websites review the specifics of these significant taxation differences. Because you are an independent contractor, your paycheck depicts your compensation without any deductions taken. At year’s end, you receive form 1099 rather than the more familiar W-2. The most critical difference is that as a W-2 employed person, you and the employer each contribute half of the obligated Social Security and Medicare taxes owed, but as an independent contractor you are required to pay the entire obligated Social Security and Medicare taxes.
Also important to consider is that although the locum tenens company facilitates necessary documentation, travel, and work schedules, you will be responsible for tracking your work-related finances, and maintaining your CME. This is not difficult but requires attention throughout the year and is manageable with a bit of organizing. A simple example is that meals are deductible on your taxes and can be easily tallied by the government’s per diem rate found at www.gsa.gov — so it is not necessary to save receipts. While it is important to become familiar with these financial nuances as they will affect your net income, they are not as intimidating or complex as you may initially believe.
Primary Benefits of Locum Tenens Assignments
In my experience, the benefits of working as a locum gastroenterologist include the opportunity to remain engaged in a gratifying career while having enhanced autonomy and flexibility. You can construct a schedule in a location most pleasing to you that fits your financial needs. You may work just a few weeks per year to full-time. You can uniquely plan for your desired personal time and alternative professional ambitions. If you choose to transition back to traditional full-time employment, the pivot remains feasible because you have demonstrated attractive professional attributes such as adaptability in different settings, maintenance of necessary skill sets, and collaboration with medical staffing of various complexities.
Quick Points to Consider
- Review the tax obligations and deductions before signing on to your first assignment.
- Healthcare benefits are not provided. If you must purchase healthcare, your healthcare premiums are 100% deductible.
- Malpractice insurance is provided through the locum tenens company.
- The points on flights, hotels, and car rentals remain in your accounts and can be used by you for personal travel in the future.
- You may be able to negotiate hourly rates and terms of responsibilities in certain instances. There’s no harm in requesting.
- Before accepting an assignment, review the website and location of the facility, accessibility to airports, frequency of flights, the physician directory, and services available.
- If your plans change and you are unable to complete a scheduled assignment previously confirmed, you must notify the locum tenens company within a specified window from the start date (usually 30 days) to avoid penalty.
Institutions utilizing locum physicians generally are doing so because their staffing is not optimal; for example, there may have been a transition in leadership or the facility may be located in a rural area. Self-awareness is key; recognize that you are essentially a guest who may need to adapt to the prevailing culture and make do with the resources at hand. You are not there to step in, innovate, or institute changes. Most often the office staff, nurses, and other physicians are very grateful that you are present and a part of the team.
Dr. Bartholomew is a gastroenterologist based in Sarasota, Florida. She has no conflicts to declare in relation to this article.
My successful career in academic gastroenterology makes me a natural proponent of the academic model of practice. However, in my current role as a locum tenens, I have witnessed the versatility that locum assignments offer gastroenterologists, particularly when flexibility in their professional lives is paramount.
The locum tenens industry is a growing feature of the healthcare staffing landscape. My perspective is unique, transitioning from professor of medicine and chief of gastroenterology at an academic medical center to a self-employed locum gastroenterologist.
As chief, I hired locums to offer additional coverage to the faculty staffing as our division, inclusive of GI fellowship and endoscopy volume, expanded. I recruited, supervised, and assigned responsibilities to the locums. Not only were these physicians professional and competent, but they also contributed to my division’s forward evolution. Based on this experience, I was confident that I could successfully perform as a locum gastroenterologist myself.
My work as a locum these past 5 years has been a positive professional transition for me. I have enjoyed meeting and working with new colleagues, including international locums who travel to work in the United States. I have also witnessed how early-career and mid-career gastroenterologists have taken advantage of this flexible and well-remunerated work.
What It Entails to Be a Locum Tenens
I suspect you have been on the receiving end of emails and postcards from locum tenens companies recruiting for potential assignments and have wondered about the specifics. Essentially, a locum physician functions as an independent contractor who accepts a temporary position at a healthcare organization to provide clinical staffing support during periods of staffing disruption.
Assignments vary in geographic location, facility work site (outpatient vs inpatient), hours, required skills, cadence of assignment, and expected length of staffing need. The locum physician has complete control over selecting the assignment location, the intensity of responsibilities, and the time they wish to commit to the position. Temporal flexibility offers locums the opportunity to commit from a few weeks per year to a full-time commitment. Locums can also combine multiple assignments in different regions or states to match the targeted number of weeks they wish to commit to and the financial goal they have set.
I have met physicians working a few weeks a year during time off from their permanent jobs to supplement their incomes, as well as fully employed physicians leveraging locum placements to explore locations or practices that they have an interest in. Gastroenterologists facing planned or unplanned life events may find the role enticing as locum opportunities offer an elevated level of flexibility and autonomy.
The Role of the Locum Tenens Company
Locum tenens companies have arrangements with healthcare facilities to provide temporary staffing. They aim to recruit prospective physicians, establish a collaborative relationship, and align these physicians with a locum assignment that benefits all parties.
Once the physician has completed the company’s credentialing packet, the company facilitates credentialing for new state medical licensures and the specific healthcare facility. The company conducts all negotiations, communications, and financial arrangements between the locum physician and the facility. Locum physicians do not communicate directly with the facility, at least not initially. The company also provides medical malpractice coverage through an established insurance broker. The company arranges travel (flights, car rentals, and hotels) for the assignment, and the healthcare facility reimburses the company.
Lastly, the company arranges a phone interview between the locum physician and the facility’s gastroenterologist or medical director for a more detailed description of expected responsibilities and level of staffing for endoscopy before the locum physician decides whether the job is a “good fit” for their skills and objectives. It is critical at this point that the locum physician does their due diligence, asking thoughtful questions to ensure a comprehensive understanding of the role before committing.
What Does It Mean to Be an Independent Contractor
An independent contractor is contracted to perform work but is not an employee of an organization (ie, self-employed). This is an important distinction when it comes to the IRS, tax obligations, and allowable deductions.
Initially, this may seem confusing, but some websites review the specifics of these significant taxation differences. Because you are an independent contractor, your paycheck depicts your compensation without any deductions taken. At year’s end, you receive form 1099 rather than the more familiar W-2. The most critical difference is that as a W-2 employed person, you and the employer each contribute half of the obligated Social Security and Medicare taxes owed, but as an independent contractor you are required to pay the entire obligated Social Security and Medicare taxes.
Also important to consider is that although the locum tenens company facilitates necessary documentation, travel, and work schedules, you will be responsible for tracking your work-related finances, and maintaining your CME. This is not difficult but requires attention throughout the year and is manageable with a bit of organizing. A simple example is that meals are deductible on your taxes and can be easily tallied by the government’s per diem rate found at www.gsa.gov — so it is not necessary to save receipts. While it is important to become familiar with these financial nuances as they will affect your net income, they are not as intimidating or complex as you may initially believe.
Primary Benefits of Locum Tenens Assignments
In my experience, the benefits of working as a locum gastroenterologist include the opportunity to remain engaged in a gratifying career while having enhanced autonomy and flexibility. You can construct a schedule in a location most pleasing to you that fits your financial needs. You may work just a few weeks per year to full-time. You can uniquely plan for your desired personal time and alternative professional ambitions. If you choose to transition back to traditional full-time employment, the pivot remains feasible because you have demonstrated attractive professional attributes such as adaptability in different settings, maintenance of necessary skill sets, and collaboration with medical staffing of various complexities.
Quick Points to Consider
- Review the tax obligations and deductions before signing on to your first assignment.
- Healthcare benefits are not provided. If you must purchase healthcare, your healthcare premiums are 100% deductible.
- Malpractice insurance is provided through the locum tenens company.
- The points on flights, hotels, and car rentals remain in your accounts and can be used by you for personal travel in the future.
- You may be able to negotiate hourly rates and terms of responsibilities in certain instances. There’s no harm in requesting.
- Before accepting an assignment, review the website and location of the facility, accessibility to airports, frequency of flights, the physician directory, and services available.
- If your plans change and you are unable to complete a scheduled assignment previously confirmed, you must notify the locum tenens company within a specified window from the start date (usually 30 days) to avoid penalty.
Institutions utilizing locum physicians generally are doing so because their staffing is not optimal; for example, there may have been a transition in leadership or the facility may be located in a rural area. Self-awareness is key; recognize that you are essentially a guest who may need to adapt to the prevailing culture and make do with the resources at hand. You are not there to step in, innovate, or institute changes. Most often the office staff, nurses, and other physicians are very grateful that you are present and a part of the team.
Dr. Bartholomew is a gastroenterologist based in Sarasota, Florida. She has no conflicts to declare in relation to this article.
My successful career in academic gastroenterology makes me a natural proponent of the academic model of practice. However, in my current role as a locum tenens, I have witnessed the versatility that locum assignments offer gastroenterologists, particularly when flexibility in their professional lives is paramount.
The locum tenens industry is a growing feature of the healthcare staffing landscape. My perspective is unique, transitioning from professor of medicine and chief of gastroenterology at an academic medical center to a self-employed locum gastroenterologist.
As chief, I hired locums to offer additional coverage to the faculty staffing as our division, inclusive of GI fellowship and endoscopy volume, expanded. I recruited, supervised, and assigned responsibilities to the locums. Not only were these physicians professional and competent, but they also contributed to my division’s forward evolution. Based on this experience, I was confident that I could successfully perform as a locum gastroenterologist myself.
My work as a locum these past 5 years has been a positive professional transition for me. I have enjoyed meeting and working with new colleagues, including international locums who travel to work in the United States. I have also witnessed how early-career and mid-career gastroenterologists have taken advantage of this flexible and well-remunerated work.
What It Entails to Be a Locum Tenens
I suspect you have been on the receiving end of emails and postcards from locum tenens companies recruiting for potential assignments and have wondered about the specifics. Essentially, a locum physician functions as an independent contractor who accepts a temporary position at a healthcare organization to provide clinical staffing support during periods of staffing disruption.
Assignments vary in geographic location, facility work site (outpatient vs inpatient), hours, required skills, cadence of assignment, and expected length of staffing need. The locum physician has complete control over selecting the assignment location, the intensity of responsibilities, and the time they wish to commit to the position. Temporal flexibility offers locums the opportunity to commit from a few weeks per year to a full-time commitment. Locums can also combine multiple assignments in different regions or states to match the targeted number of weeks they wish to commit to and the financial goal they have set.
I have met physicians working a few weeks a year during time off from their permanent jobs to supplement their incomes, as well as fully employed physicians leveraging locum placements to explore locations or practices that they have an interest in. Gastroenterologists facing planned or unplanned life events may find the role enticing as locum opportunities offer an elevated level of flexibility and autonomy.
The Role of the Locum Tenens Company
Locum tenens companies have arrangements with healthcare facilities to provide temporary staffing. They aim to recruit prospective physicians, establish a collaborative relationship, and align these physicians with a locum assignment that benefits all parties.
Once the physician has completed the company’s credentialing packet, the company facilitates credentialing for new state medical licensures and the specific healthcare facility. The company conducts all negotiations, communications, and financial arrangements between the locum physician and the facility. Locum physicians do not communicate directly with the facility, at least not initially. The company also provides medical malpractice coverage through an established insurance broker. The company arranges travel (flights, car rentals, and hotels) for the assignment, and the healthcare facility reimburses the company.
Lastly, the company arranges a phone interview between the locum physician and the facility’s gastroenterologist or medical director for a more detailed description of expected responsibilities and level of staffing for endoscopy before the locum physician decides whether the job is a “good fit” for their skills and objectives. It is critical at this point that the locum physician does their due diligence, asking thoughtful questions to ensure a comprehensive understanding of the role before committing.
What Does It Mean to Be an Independent Contractor
An independent contractor is contracted to perform work but is not an employee of an organization (ie, self-employed). This is an important distinction when it comes to the IRS, tax obligations, and allowable deductions.
Initially, this may seem confusing, but some websites review the specifics of these significant taxation differences. Because you are an independent contractor, your paycheck depicts your compensation without any deductions taken. At year’s end, you receive form 1099 rather than the more familiar W-2. The most critical difference is that as a W-2 employed person, you and the employer each contribute half of the obligated Social Security and Medicare taxes owed, but as an independent contractor you are required to pay the entire obligated Social Security and Medicare taxes.
Also important to consider is that although the locum tenens company facilitates necessary documentation, travel, and work schedules, you will be responsible for tracking your work-related finances, and maintaining your CME. This is not difficult but requires attention throughout the year and is manageable with a bit of organizing. A simple example is that meals are deductible on your taxes and can be easily tallied by the government’s per diem rate found at www.gsa.gov — so it is not necessary to save receipts. While it is important to become familiar with these financial nuances as they will affect your net income, they are not as intimidating or complex as you may initially believe.
Primary Benefits of Locum Tenens Assignments
In my experience, the benefits of working as a locum gastroenterologist include the opportunity to remain engaged in a gratifying career while having enhanced autonomy and flexibility. You can construct a schedule in a location most pleasing to you that fits your financial needs. You may work just a few weeks per year to full-time. You can uniquely plan for your desired personal time and alternative professional ambitions. If you choose to transition back to traditional full-time employment, the pivot remains feasible because you have demonstrated attractive professional attributes such as adaptability in different settings, maintenance of necessary skill sets, and collaboration with medical staffing of various complexities.
Quick Points to Consider
- Review the tax obligations and deductions before signing on to your first assignment.
- Healthcare benefits are not provided. If you must purchase healthcare, your healthcare premiums are 100% deductible.
- Malpractice insurance is provided through the locum tenens company.
- The points on flights, hotels, and car rentals remain in your accounts and can be used by you for personal travel in the future.
- You may be able to negotiate hourly rates and terms of responsibilities in certain instances. There’s no harm in requesting.
- Before accepting an assignment, review the website and location of the facility, accessibility to airports, frequency of flights, the physician directory, and services available.
- If your plans change and you are unable to complete a scheduled assignment previously confirmed, you must notify the locum tenens company within a specified window from the start date (usually 30 days) to avoid penalty.
Institutions utilizing locum physicians generally are doing so because their staffing is not optimal; for example, there may have been a transition in leadership or the facility may be located in a rural area. Self-awareness is key; recognize that you are essentially a guest who may need to adapt to the prevailing culture and make do with the resources at hand. You are not there to step in, innovate, or institute changes. Most often the office staff, nurses, and other physicians are very grateful that you are present and a part of the team.
Dr. Bartholomew is a gastroenterologist based in Sarasota, Florida. She has no conflicts to declare in relation to this article.
Navigating and Negotiating Maternity/Paternity Leave in Private Practice
Marybeth Spanarkel, MD, a Duke University School of Medicine alumna (1979), completed her internal medicine and gastroenterology training at the University of Pennsylvania, National Institutes of Health, and Johns Hopkins. Initially groomed for an academic role, she chose a clinical position in private practice at Duke Regional Hospital in Durham, North Carolina, where she worked for 25 years.
At age 59, Dr. Spanarkel suffered a neck injury leading to permanent C5-6 radiculopathy, which abruptly ended her career as a clinical gastroenterologist. Since then, she has been a passionate advocate for ergonomic reform in endoscopy. Currently, she is the senior medical adviser and cofounder of ColoWrap, a device designed to improve colonoscopy procedures and reduce ergonomic risk.

Dr. Spanarkel spoke with GI & Hepatology News about the issues that gastroenterologists should consider when negotiating maternity/paternity leave in private practice.
Would you share with the readers your experience with maternity leave in private practice?
As a mother of four, I had two children during my GI fellowship, and received my full salary each time for a 3-month maternity leave. My third child arrived in the time period between leaving my academic position and starting in private practice. My fourth child was born after 2 years in private practice, and I took 3 weeks off. Fortunately, I was not asked to pay upfront overhead fees in my 15-person practice. However, my reduced productivity during that time was factored into my salary calculations, leading to a decreased income for the following 6 months.
How does pregnancy affect your performance and productivity as a GI physician?
“We” may be having a baby, but “You” are pregnant. While some may experience few symptoms, most pregnant doctors deal with problems such as nausea and extreme fatigue, especially in the first trimester. The third trimester may result in reduced physical agility, particularly when performing procedures. Even in uncomplicated pregnancies, balancing the physiologic changes with the demands of a full-time GI role can be strenuous. And this doesn’t even take into account potential infertility issues, pregnancy complications, or newborn concerns that physicians may encounter.
And after childbirth?
Post childbirth, despite a supportive partner, the primary responsibilities such as feeding, nursing support, and bonding often fall on the biological mother. These duties are superimposed on the doctor’s own recovery and postpartum changes. While the United States commonly recognizes 3 months as a standard maternity leave, some European countries advocate for up to 12 months, demonstrating again that this is not an “overnight” transition.
In the past, GI doctors were mostly male, but now there’s a growing number of females in the field. Despite this shift, studies still highlight continued gender disparities in salaries and leadership opportunities, and support for pregnancy-related issues has been largely under-addressed.1,2,3
How do academic centers manage maternity leave?
In academic centers or large healthcare settings, maternity leave policies are more standardized compared with private practice. Doctors are salaried depending on their level of training and experience and then they are assigned a mix of clinical, research, teaching, and/or administrative duties.
Typically, maternity leave in these centers is a standard 3-month period, often combining paid time off (PTO) with unpaid or paid leave. In some cases, short- or long-term disability payments are available, especially for complications. But, the financial impact of a doctor’s maternity leave on the overall unit is usually minimal due to the number of participants in the system. The extra workload is diffused over a larger number of doctors, so the new schedule is generally manageable.4 And since the salary of the employee/physician includes a portion of nonclinical time (administrative, teaching, research), the actual decrease in revenue isn’t that dramatic.
How about maternity leave in private practice?
Maternity leave in private practice, especially if there is only a small number of partners, is handled entirely differently. Think of a household budget (rent, utilities, salaries, benefits, insurance) that is shared by “roommates,” the other partners in the group. To understand how maternity leave affects a private practice, you have to understand how your private practice operates.
Typically, newly hired private practice physicians receive a set salary, with the expectation that their patient revenue will eventually cover both their share of overhead and their salary. The practice might set a monthly quota, offering a bonus for exceeding it, or they may retain the extra revenue until the physician becomes a full partner.
Income in private practice is almost entirely generated by seeing patients and performing procedures, as opposed to non-reimbursable activities such as committee meetings or lectures. Physicians learn to be highly efficient with their time, a standard also expected of their employees. They have more control over their schedules, vacation time, and patient/procedure load. Since income is affected only after overhead costs are covered, each doctor’s approach to workload and pace doesn’t typically concern the other partners. Some physicians may be highly aggressive and efficient (and thus increase their salaries), while others may prefer a slower pace due to external responsibilities.
This arrangement is often seen as fair because the established practice helps you get started by providing the environment for you to generate revenue. This includes patient referrals, office space, and staff. In return, the practice not only hopes you will achieve its goals/quotas but may expect a return on its investment in you.
Additionally, access to shared passive revenue streams, such as a pathology lab, clinical research trials, or facility fees from an endoscopy center, may only be available once a certain level of productivity or full partnership is reached.
The initial years in private practice can be seen as a trial period. Your professional reputation, liability, and patient population are more directly in your own hands. Decision-making, patient management, and potential complications are more wholly your responsibility, which can feel isolating. However, providing excellent care can build your reputation, as satisfied patients will seek you out and generate more referrals. During this time, you need to demonstrate to your prospective partners your commitment to delivering high-quality patient care and to meeting certain minimum standards of volume. If clinical medicine is your passion, the right private practice role can be a fulfilling platform where you do what you love to do and simultaneously are well compensated for it.
How does taking maternity affect shared overhead?
Any physician requiring “leave” will affect the overall revenue of a practice. Issues regarding maternity leave in private practice can also be applied to adoption, paternity, surrogacy, foster care, or medical leave. For instance, if the cumulative overhead is $100k per month in a practice with five doctors, each doctor contributes $20k monthly, totaling $240k each annually.
For example, Dr. “Jones” generates $480k in charges/collections, so after paying his share of overhead, his salary is $240k for the year. In contrast, Dr. “Smith” works more intensely, doubling the patients and procedures of Dr. “Jones,” and generates $960k. After deducting the overhead, his salary is $720k, more than twice his partner’s salary.
Let’s say the practice is considering hiring a new doctor who is 2 months pregnant. If he/she generates $380k in charges in the first year but owes $240k in shared overhead, his/her salary would be $140k, which is not very attractive as a “starting salary” for a highly competent, well-trained GI physician. In extreme cases, with high overhead and low productivity, there might be no revenue for salary once the overhead is paid.
In private practice, is there hesitancy hiring a pregnant person?
While it’s illegal to inquire about pregnancy during employment interviews, partners in private practice might still hesitate to hire a pregnant person. Concerns include sharing overhead costs, handling extra calls or emergencies, and wanting new physicians to contribute equally.
However, this viewpoint can be shortsighted. , as older partners might also face personal or medical needs. Adopting a flexible, empathetic approach toward partners can foster goodwill, potentially enhancing revenue, teamwork, and patient care over a long-term career. The value of empathy should not be underestimated.
What should you consider when you are applying for a new private practice job?
When applying for a private practice position, here are some key points to consider:
- If possible, have your children while employed by a large healthcare system with an established leave policy.
- In a private practice job, ensure the employment contract clearly outlines the terms of medical leave (maternity, paternity, adoption, illness), including details on overhead, benefits, salary, call schedule, and the path to full partnership. Consider having a lawyer review the contract.
- Inquire about how other types of leave, like sabbatical, personal, family, military, or medical, are managed. Understand the implications for salary and overhead, for example, in cases of a partner needing extended leave for surgery or rehabilitation.
- Review the requirements for becoming a full partner, particularly if this includes potential future passive income sources. Does maternity leave (or other types of leave) alter this path?
- Examine the entire benefit package, with a focus on long-term disability policies, considering the statistics on both temporary and permanent disability among GI doctors.5
- Negotiate terms for overhead during leave. Options might include a long term or interest-free loan to cover the 3-month sum, a 50% reduction in overhead charges, or “overhead protection insurance” where a designated policy covers overhead for partners on medical leave.
Remember, a brief leave in a 30-year career is relatively minor. Prioritize taking enough time for yourself and your child. Concentrate on long term fairness when engaged in salary negotiations. Don’t rush back; there will be time later to compensate for a temporary decrease in salary, but limited opportunities to spend age-specific time with your young child.
References
1. Butkus R, et al. Achieving Gender Equity in Physician Compensation and Career Advancement: A Position Paper of the American College of Physicians. Ann Intern Med. 2018 May 15. doi: 10.7326/M17-3438.
2. American Medical Association. Advancing Gender Equity in Medicine: Resources for physicians. 2024 Feb 28.
3. Devi J, et al. Fixing the leaky pipeline: gender imbalance in gastroenterology in Asia-Pacific region. J Gastroenterol Hepatol. 2023 Sept. doi: 10.1111/jgh.16353.
4. Mahadevan U, et al. Closing the gender gap: building a successful career and leadership in research as a female gastroenterologist. Lancet Gastroenterol Hepatol. 2022 Jun. doi: 10.1016/S2468-1253(22)00135-2.
5. Murphy R. Know your maternity leave options. 2024 Apr 4.
Marybeth Spanarkel, MD, a Duke University School of Medicine alumna (1979), completed her internal medicine and gastroenterology training at the University of Pennsylvania, National Institutes of Health, and Johns Hopkins. Initially groomed for an academic role, she chose a clinical position in private practice at Duke Regional Hospital in Durham, North Carolina, where she worked for 25 years.
At age 59, Dr. Spanarkel suffered a neck injury leading to permanent C5-6 radiculopathy, which abruptly ended her career as a clinical gastroenterologist. Since then, she has been a passionate advocate for ergonomic reform in endoscopy. Currently, she is the senior medical adviser and cofounder of ColoWrap, a device designed to improve colonoscopy procedures and reduce ergonomic risk.

Dr. Spanarkel spoke with GI & Hepatology News about the issues that gastroenterologists should consider when negotiating maternity/paternity leave in private practice.
Would you share with the readers your experience with maternity leave in private practice?
As a mother of four, I had two children during my GI fellowship, and received my full salary each time for a 3-month maternity leave. My third child arrived in the time period between leaving my academic position and starting in private practice. My fourth child was born after 2 years in private practice, and I took 3 weeks off. Fortunately, I was not asked to pay upfront overhead fees in my 15-person practice. However, my reduced productivity during that time was factored into my salary calculations, leading to a decreased income for the following 6 months.
How does pregnancy affect your performance and productivity as a GI physician?
“We” may be having a baby, but “You” are pregnant. While some may experience few symptoms, most pregnant doctors deal with problems such as nausea and extreme fatigue, especially in the first trimester. The third trimester may result in reduced physical agility, particularly when performing procedures. Even in uncomplicated pregnancies, balancing the physiologic changes with the demands of a full-time GI role can be strenuous. And this doesn’t even take into account potential infertility issues, pregnancy complications, or newborn concerns that physicians may encounter.
And after childbirth?
Post childbirth, despite a supportive partner, the primary responsibilities such as feeding, nursing support, and bonding often fall on the biological mother. These duties are superimposed on the doctor’s own recovery and postpartum changes. While the United States commonly recognizes 3 months as a standard maternity leave, some European countries advocate for up to 12 months, demonstrating again that this is not an “overnight” transition.
In the past, GI doctors were mostly male, but now there’s a growing number of females in the field. Despite this shift, studies still highlight continued gender disparities in salaries and leadership opportunities, and support for pregnancy-related issues has been largely under-addressed.1,2,3
How do academic centers manage maternity leave?
In academic centers or large healthcare settings, maternity leave policies are more standardized compared with private practice. Doctors are salaried depending on their level of training and experience and then they are assigned a mix of clinical, research, teaching, and/or administrative duties.
Typically, maternity leave in these centers is a standard 3-month period, often combining paid time off (PTO) with unpaid or paid leave. In some cases, short- or long-term disability payments are available, especially for complications. But, the financial impact of a doctor’s maternity leave on the overall unit is usually minimal due to the number of participants in the system. The extra workload is diffused over a larger number of doctors, so the new schedule is generally manageable.4 And since the salary of the employee/physician includes a portion of nonclinical time (administrative, teaching, research), the actual decrease in revenue isn’t that dramatic.
How about maternity leave in private practice?
Maternity leave in private practice, especially if there is only a small number of partners, is handled entirely differently. Think of a household budget (rent, utilities, salaries, benefits, insurance) that is shared by “roommates,” the other partners in the group. To understand how maternity leave affects a private practice, you have to understand how your private practice operates.
Typically, newly hired private practice physicians receive a set salary, with the expectation that their patient revenue will eventually cover both their share of overhead and their salary. The practice might set a monthly quota, offering a bonus for exceeding it, or they may retain the extra revenue until the physician becomes a full partner.
Income in private practice is almost entirely generated by seeing patients and performing procedures, as opposed to non-reimbursable activities such as committee meetings or lectures. Physicians learn to be highly efficient with their time, a standard also expected of their employees. They have more control over their schedules, vacation time, and patient/procedure load. Since income is affected only after overhead costs are covered, each doctor’s approach to workload and pace doesn’t typically concern the other partners. Some physicians may be highly aggressive and efficient (and thus increase their salaries), while others may prefer a slower pace due to external responsibilities.
This arrangement is often seen as fair because the established practice helps you get started by providing the environment for you to generate revenue. This includes patient referrals, office space, and staff. In return, the practice not only hopes you will achieve its goals/quotas but may expect a return on its investment in you.
Additionally, access to shared passive revenue streams, such as a pathology lab, clinical research trials, or facility fees from an endoscopy center, may only be available once a certain level of productivity or full partnership is reached.
The initial years in private practice can be seen as a trial period. Your professional reputation, liability, and patient population are more directly in your own hands. Decision-making, patient management, and potential complications are more wholly your responsibility, which can feel isolating. However, providing excellent care can build your reputation, as satisfied patients will seek you out and generate more referrals. During this time, you need to demonstrate to your prospective partners your commitment to delivering high-quality patient care and to meeting certain minimum standards of volume. If clinical medicine is your passion, the right private practice role can be a fulfilling platform where you do what you love to do and simultaneously are well compensated for it.
How does taking maternity affect shared overhead?
Any physician requiring “leave” will affect the overall revenue of a practice. Issues regarding maternity leave in private practice can also be applied to adoption, paternity, surrogacy, foster care, or medical leave. For instance, if the cumulative overhead is $100k per month in a practice with five doctors, each doctor contributes $20k monthly, totaling $240k each annually.
For example, Dr. “Jones” generates $480k in charges/collections, so after paying his share of overhead, his salary is $240k for the year. In contrast, Dr. “Smith” works more intensely, doubling the patients and procedures of Dr. “Jones,” and generates $960k. After deducting the overhead, his salary is $720k, more than twice his partner’s salary.
Let’s say the practice is considering hiring a new doctor who is 2 months pregnant. If he/she generates $380k in charges in the first year but owes $240k in shared overhead, his/her salary would be $140k, which is not very attractive as a “starting salary” for a highly competent, well-trained GI physician. In extreme cases, with high overhead and low productivity, there might be no revenue for salary once the overhead is paid.
In private practice, is there hesitancy hiring a pregnant person?
While it’s illegal to inquire about pregnancy during employment interviews, partners in private practice might still hesitate to hire a pregnant person. Concerns include sharing overhead costs, handling extra calls or emergencies, and wanting new physicians to contribute equally.
However, this viewpoint can be shortsighted. , as older partners might also face personal or medical needs. Adopting a flexible, empathetic approach toward partners can foster goodwill, potentially enhancing revenue, teamwork, and patient care over a long-term career. The value of empathy should not be underestimated.
What should you consider when you are applying for a new private practice job?
When applying for a private practice position, here are some key points to consider:
- If possible, have your children while employed by a large healthcare system with an established leave policy.
- In a private practice job, ensure the employment contract clearly outlines the terms of medical leave (maternity, paternity, adoption, illness), including details on overhead, benefits, salary, call schedule, and the path to full partnership. Consider having a lawyer review the contract.
- Inquire about how other types of leave, like sabbatical, personal, family, military, or medical, are managed. Understand the implications for salary and overhead, for example, in cases of a partner needing extended leave for surgery or rehabilitation.
- Review the requirements for becoming a full partner, particularly if this includes potential future passive income sources. Does maternity leave (or other types of leave) alter this path?
- Examine the entire benefit package, with a focus on long-term disability policies, considering the statistics on both temporary and permanent disability among GI doctors.5
- Negotiate terms for overhead during leave. Options might include a long term or interest-free loan to cover the 3-month sum, a 50% reduction in overhead charges, or “overhead protection insurance” where a designated policy covers overhead for partners on medical leave.
Remember, a brief leave in a 30-year career is relatively minor. Prioritize taking enough time for yourself and your child. Concentrate on long term fairness when engaged in salary negotiations. Don’t rush back; there will be time later to compensate for a temporary decrease in salary, but limited opportunities to spend age-specific time with your young child.
References
1. Butkus R, et al. Achieving Gender Equity in Physician Compensation and Career Advancement: A Position Paper of the American College of Physicians. Ann Intern Med. 2018 May 15. doi: 10.7326/M17-3438.
2. American Medical Association. Advancing Gender Equity in Medicine: Resources for physicians. 2024 Feb 28.
3. Devi J, et al. Fixing the leaky pipeline: gender imbalance in gastroenterology in Asia-Pacific region. J Gastroenterol Hepatol. 2023 Sept. doi: 10.1111/jgh.16353.
4. Mahadevan U, et al. Closing the gender gap: building a successful career and leadership in research as a female gastroenterologist. Lancet Gastroenterol Hepatol. 2022 Jun. doi: 10.1016/S2468-1253(22)00135-2.
5. Murphy R. Know your maternity leave options. 2024 Apr 4.
Marybeth Spanarkel, MD, a Duke University School of Medicine alumna (1979), completed her internal medicine and gastroenterology training at the University of Pennsylvania, National Institutes of Health, and Johns Hopkins. Initially groomed for an academic role, she chose a clinical position in private practice at Duke Regional Hospital in Durham, North Carolina, where she worked for 25 years.
At age 59, Dr. Spanarkel suffered a neck injury leading to permanent C5-6 radiculopathy, which abruptly ended her career as a clinical gastroenterologist. Since then, she has been a passionate advocate for ergonomic reform in endoscopy. Currently, she is the senior medical adviser and cofounder of ColoWrap, a device designed to improve colonoscopy procedures and reduce ergonomic risk.

Dr. Spanarkel spoke with GI & Hepatology News about the issues that gastroenterologists should consider when negotiating maternity/paternity leave in private practice.
Would you share with the readers your experience with maternity leave in private practice?
As a mother of four, I had two children during my GI fellowship, and received my full salary each time for a 3-month maternity leave. My third child arrived in the time period between leaving my academic position and starting in private practice. My fourth child was born after 2 years in private practice, and I took 3 weeks off. Fortunately, I was not asked to pay upfront overhead fees in my 15-person practice. However, my reduced productivity during that time was factored into my salary calculations, leading to a decreased income for the following 6 months.
How does pregnancy affect your performance and productivity as a GI physician?
“We” may be having a baby, but “You” are pregnant. While some may experience few symptoms, most pregnant doctors deal with problems such as nausea and extreme fatigue, especially in the first trimester. The third trimester may result in reduced physical agility, particularly when performing procedures. Even in uncomplicated pregnancies, balancing the physiologic changes with the demands of a full-time GI role can be strenuous. And this doesn’t even take into account potential infertility issues, pregnancy complications, or newborn concerns that physicians may encounter.
And after childbirth?
Post childbirth, despite a supportive partner, the primary responsibilities such as feeding, nursing support, and bonding often fall on the biological mother. These duties are superimposed on the doctor’s own recovery and postpartum changes. While the United States commonly recognizes 3 months as a standard maternity leave, some European countries advocate for up to 12 months, demonstrating again that this is not an “overnight” transition.
In the past, GI doctors were mostly male, but now there’s a growing number of females in the field. Despite this shift, studies still highlight continued gender disparities in salaries and leadership opportunities, and support for pregnancy-related issues has been largely under-addressed.1,2,3
How do academic centers manage maternity leave?
In academic centers or large healthcare settings, maternity leave policies are more standardized compared with private practice. Doctors are salaried depending on their level of training and experience and then they are assigned a mix of clinical, research, teaching, and/or administrative duties.
Typically, maternity leave in these centers is a standard 3-month period, often combining paid time off (PTO) with unpaid or paid leave. In some cases, short- or long-term disability payments are available, especially for complications. But, the financial impact of a doctor’s maternity leave on the overall unit is usually minimal due to the number of participants in the system. The extra workload is diffused over a larger number of doctors, so the new schedule is generally manageable.4 And since the salary of the employee/physician includes a portion of nonclinical time (administrative, teaching, research), the actual decrease in revenue isn’t that dramatic.
How about maternity leave in private practice?
Maternity leave in private practice, especially if there is only a small number of partners, is handled entirely differently. Think of a household budget (rent, utilities, salaries, benefits, insurance) that is shared by “roommates,” the other partners in the group. To understand how maternity leave affects a private practice, you have to understand how your private practice operates.
Typically, newly hired private practice physicians receive a set salary, with the expectation that their patient revenue will eventually cover both their share of overhead and their salary. The practice might set a monthly quota, offering a bonus for exceeding it, or they may retain the extra revenue until the physician becomes a full partner.
Income in private practice is almost entirely generated by seeing patients and performing procedures, as opposed to non-reimbursable activities such as committee meetings or lectures. Physicians learn to be highly efficient with their time, a standard also expected of their employees. They have more control over their schedules, vacation time, and patient/procedure load. Since income is affected only after overhead costs are covered, each doctor’s approach to workload and pace doesn’t typically concern the other partners. Some physicians may be highly aggressive and efficient (and thus increase their salaries), while others may prefer a slower pace due to external responsibilities.
This arrangement is often seen as fair because the established practice helps you get started by providing the environment for you to generate revenue. This includes patient referrals, office space, and staff. In return, the practice not only hopes you will achieve its goals/quotas but may expect a return on its investment in you.
Additionally, access to shared passive revenue streams, such as a pathology lab, clinical research trials, or facility fees from an endoscopy center, may only be available once a certain level of productivity or full partnership is reached.
The initial years in private practice can be seen as a trial period. Your professional reputation, liability, and patient population are more directly in your own hands. Decision-making, patient management, and potential complications are more wholly your responsibility, which can feel isolating. However, providing excellent care can build your reputation, as satisfied patients will seek you out and generate more referrals. During this time, you need to demonstrate to your prospective partners your commitment to delivering high-quality patient care and to meeting certain minimum standards of volume. If clinical medicine is your passion, the right private practice role can be a fulfilling platform where you do what you love to do and simultaneously are well compensated for it.
How does taking maternity affect shared overhead?
Any physician requiring “leave” will affect the overall revenue of a practice. Issues regarding maternity leave in private practice can also be applied to adoption, paternity, surrogacy, foster care, or medical leave. For instance, if the cumulative overhead is $100k per month in a practice with five doctors, each doctor contributes $20k monthly, totaling $240k each annually.
For example, Dr. “Jones” generates $480k in charges/collections, so after paying his share of overhead, his salary is $240k for the year. In contrast, Dr. “Smith” works more intensely, doubling the patients and procedures of Dr. “Jones,” and generates $960k. After deducting the overhead, his salary is $720k, more than twice his partner’s salary.
Let’s say the practice is considering hiring a new doctor who is 2 months pregnant. If he/she generates $380k in charges in the first year but owes $240k in shared overhead, his/her salary would be $140k, which is not very attractive as a “starting salary” for a highly competent, well-trained GI physician. In extreme cases, with high overhead and low productivity, there might be no revenue for salary once the overhead is paid.
In private practice, is there hesitancy hiring a pregnant person?
While it’s illegal to inquire about pregnancy during employment interviews, partners in private practice might still hesitate to hire a pregnant person. Concerns include sharing overhead costs, handling extra calls or emergencies, and wanting new physicians to contribute equally.
However, this viewpoint can be shortsighted. , as older partners might also face personal or medical needs. Adopting a flexible, empathetic approach toward partners can foster goodwill, potentially enhancing revenue, teamwork, and patient care over a long-term career. The value of empathy should not be underestimated.
What should you consider when you are applying for a new private practice job?
When applying for a private practice position, here are some key points to consider:
- If possible, have your children while employed by a large healthcare system with an established leave policy.
- In a private practice job, ensure the employment contract clearly outlines the terms of medical leave (maternity, paternity, adoption, illness), including details on overhead, benefits, salary, call schedule, and the path to full partnership. Consider having a lawyer review the contract.
- Inquire about how other types of leave, like sabbatical, personal, family, military, or medical, are managed. Understand the implications for salary and overhead, for example, in cases of a partner needing extended leave for surgery or rehabilitation.
- Review the requirements for becoming a full partner, particularly if this includes potential future passive income sources. Does maternity leave (or other types of leave) alter this path?
- Examine the entire benefit package, with a focus on long-term disability policies, considering the statistics on both temporary and permanent disability among GI doctors.5
- Negotiate terms for overhead during leave. Options might include a long term or interest-free loan to cover the 3-month sum, a 50% reduction in overhead charges, or “overhead protection insurance” where a designated policy covers overhead for partners on medical leave.
Remember, a brief leave in a 30-year career is relatively minor. Prioritize taking enough time for yourself and your child. Concentrate on long term fairness when engaged in salary negotiations. Don’t rush back; there will be time later to compensate for a temporary decrease in salary, but limited opportunities to spend age-specific time with your young child.
References
1. Butkus R, et al. Achieving Gender Equity in Physician Compensation and Career Advancement: A Position Paper of the American College of Physicians. Ann Intern Med. 2018 May 15. doi: 10.7326/M17-3438.
2. American Medical Association. Advancing Gender Equity in Medicine: Resources for physicians. 2024 Feb 28.
3. Devi J, et al. Fixing the leaky pipeline: gender imbalance in gastroenterology in Asia-Pacific region. J Gastroenterol Hepatol. 2023 Sept. doi: 10.1111/jgh.16353.
4. Mahadevan U, et al. Closing the gender gap: building a successful career and leadership in research as a female gastroenterologist. Lancet Gastroenterol Hepatol. 2022 Jun. doi: 10.1016/S2468-1253(22)00135-2.
5. Murphy R. Know your maternity leave options. 2024 Apr 4.
Achieving Promotion for Junior Faculty in Academic Medicine: An Interview With Experts
Academic medicine plays a crucial role at the crossroads of medical practice, education, and research, influencing the future landscape of healthcare. Many physicians aspire to pursue and sustain a career in academic medicine to contribute to the advancement of medical knowledge, enhance patient care, and influence the trajectory of the medical field. Opting for a career in academic medicine can offer benefits such as increased autonomy and scheduling flexibility, which can significantly improve the quality of life. In addition, engagement in scholarly activities and working in a dynamic environment with continuous learning opportunities can help mitigate burnout.
However, embarking on an academic career can be daunting for junior faculty members who face the challenge of providing clinical care while excelling in research and dedicating time to mentorship and teaching trainees. According to a report by the Association of American Medical Colleges, 38% of physicians leave academic medicine within a decade of obtaining a faculty position. Barriers to promotion and retention within academic medicine include ineffective mentorship, unclear or inconsistent promotion criteria, and disparities in gender/ethnic representation.
In this article, we interview two accomplished physicians in academic medicine who have attained the rank of professors.
Interview with Sophie Balzora, MD
Dr. Balzora is a professor of medicine at NYU Grossman School of Medicine and a practicing gastroenterologist specializing in the care of patients with inflammatory bowel disease at NYU Langone Health. She serves as the American College of Gastroenterology’s Diversity, Equity, and Inclusion Committee Chair, on the Advisory Board of ACG’s Leadership, Ethics, and Equity (LE&E) Center, and is president and cofounder of the Association of Black Gastroenterologists and Hepatologists (ABGH). Dr. Balzora was promoted to full professor 11 years after graduating from fellowship.
What would you identify as some of the most important factors that led to your success in achieving a promotion to professor of medicine?
Surround yourself with individuals whose professional and personal priorities align with yours. To achieve this, it is essential to gain an understanding of what is important to you, what you envision your success to look like, and establish a timeline to achieve it. The concept of personal success and how to best achieve it will absolutely change as you grow, and that is okay and expected. Connecting with those outside of your clinical interests, at other institutions, and even outside of the medical field, can help you achieve these goals and better shape how you see your career unfolding and how you want it to look.
Historically, the proportion of physicians who achieve professorship is lower among women compared with men. What do you believe are some of the barriers involved in this, and how would you counsel women who are interested in pursuing the rank of professor?
Systemic gender bias and discrimination, over-mentorship and under-sponsorship, inconsistent parental leave, and delayed parenthood are a few of the factors that contribute to the observed disparities in academic rank. Predictably, for women from underrepresented backgrounds in medicine, the chasm grows.
What has helped me most is to keep my eyes on the prize, and to recognize that the prize is different for everyone. It’s important not to make direct comparisons to any other individual, because they are not you. Harness what makes you different and drown out the naysayers — the “we’ve never seen this done before” camp, the “it’s too soon [for someone like you] to go up for promotion” folks. While these voices are sometimes well intentioned, they can distract you from your goals and ambitions because they are rooted in bias and adherence to traditional expectations. To do something new, and to change the game, requires going against the grain and utilizing your skills and talents to achieve what you want to achieve in a way that works for you.
What are some practical tips you have for junior gastroenterologists to track their promotion in academia?
- Keep your curriculum vitae (CV) up to date and formatted to your institutional guidelines. Ensure that you document your academic activities, even if it doesn’t seem important in the moment. When it’s time to submit that promotion portfolio, you want to be ready and organized.
- Remember: “No” is a full sentence, and saying it takes practice and time and confidence. It is a skill I still struggle to adopt at times, but it’s important to recognize the power of no, for it opens opportunities to say yes to other things.
- Lift as you climb — a critical part of changing the status quo is fostering the future of those underrepresented in medicine. A professional goal of mine that keeps me steady and passionate is to create supporting and enriching systemic and institutional changes that work to dismantle the obstacles perpetuating disparities in academic rank for women and those underrepresented in medicine. Discovering your “why” is a complex, difficult, and rewarding journey.
Interview with Mark Schattner, MD, AGAF
Dr. Schattner is a professor of clinical medicine at Weill Cornell College of Medicine and chief of the gastroenterology, hepatology, and nutrition service at Memorial Sloan Kettering Cancer Center, both in New York. He is a former president of the New York Society for Gastrointestinal Endoscopy and a fellow of the AGA and ASGE.
In your role as chief, you serve as a mentor for early career gastroenterologists for pursuing career promotion. What advice do you have for achieving this?
Promoting junior faculty is one of the prime responsibilities of a service chief. Generally, the early steps of promotion are straightforward, with criteria becoming more stringent as you progress. I think it is critical to understand the criteria used by promotion committees and to be aware of the various available tracks. I believe every meeting a junior faculty member has with their service chief should include, at the least, a brief check-in on where they are in the promotion process and plans (both short term and long term) to move forward. Successful promotion is facilitated when done upon a solid foundation of production and accomplishment. It is very challenging or even impossible when trying to piece together a package from discordant activities.
Most institutions require or encourage academic involvement at both national and international levels for career promotion. Do you have advice for junior faculty about how to achieve this type of recognition or experience?
The easiest place to start is with regional professional societies. Active involvement in these local societies fosters valuable networking and lays the groundwork for involvement at the national or international level. I would strongly encourage junior faculty to seek opportunities for a leadership position at any level in these societies and move up the ladder as their career matures. This is also a very good avenue to network and get invited to join collaborative research projects, which can be a fruitful means to enhance your academic productivity.
In your opinion, what factors are likely to hinder or delay an individual’s promotion?
I think it is crucial to consider the career track you are on. If you are very clinically productive and love to teach, that is completely appropriate, and most institutions will recognize the value of that and promote you along a clinical-educator tract. On the other hand, if you have a passion for research and can successfully lead research and compete for grants, then you would move along a traditional tenure track. It is also critical to think ahead, know the criteria on which you will be judged, and incorporate that into your practice early. Trying to scramble to enhance your CV in a short time just for promotion will likely prove ineffective.
Do you have advice for junior faculty who have families about how to manage career goals but also prioritize time with family?
There is no one-size-fits-all approach to this. I think this requires a lot of shared decision-making with your family. Compromise will undoubtedly be required. For example, I always chose to live in close proximity to my workplace, eliminating any commuting time. This choice really allowed me spend time with my family.
In conclusion, a career in academic medicine presents both opportunities and challenges. A successful academic career, and achieving promotion to the rank of professor of medicine, requires a combination of factors including understanding institution-specific criteria for promotion, proactive engagement at the regional and national level, and envisioning your career goals and creating a timeline to achieve them. There are challenges to promotion, including navigating systemic biases and balancing career goals with family commitments, which also requires consideration and open communication. Ultimately, we hope these insights provide valuable guidance and advice for junior faculty who are navigating this complex environment of academic medicine and are motivated toward achieving professional fulfillment and satisfaction in their careers.
Dr. Rolston is based in the Department of Gastroenterology, Hepatology, and Nutrition, Memorial Sloan Kettering Cancer Center, New York. She reports no conflicts in relation this article. Dr. Balzora and Dr. Schattner are based in the Division of Gastroenterology and Hepatology, New York University Langone Health, New York. Dr. Schattner is a consultant for Boston Scientific and Novo Nordisk. Dr. Balzora reports no conflicts in relation to this article.
References
Campbell KM. Mitigating the isolation of minoritized faculty in academic medicine. J Gen Intern Med. 2023 May. doi: 10.1007/s11606-022-07982-8.
Howard-Anderson JR et al. Strategies for developing a successful career in academic medicine. Am J Med Sci. 2024 Apr. doi: 10.1016/j.amjms.2023.12.010.
Murphy M et al. Women’s experiences of promotion and tenure in academic medicine and potential implications for gender disparities in career advancement: A qualitative analysis. JAMA Netw Open. 2021 Sep 1. doi: 10.1001/jamanetworkopen.2021.25843.
Sambunjak D et al. Mentoring in academic medicine: A systematic review. JAMA. 2006 Sep 6. doi: 10.1001/jama.296.9.1103.
Shen MR et al. Impact of mentoring on academic career success for women in medicine: A systematic review. Acad Med. 2022 Mar 1. doi: 10.1097/ACM.0000000000004563.
Academic medicine plays a crucial role at the crossroads of medical practice, education, and research, influencing the future landscape of healthcare. Many physicians aspire to pursue and sustain a career in academic medicine to contribute to the advancement of medical knowledge, enhance patient care, and influence the trajectory of the medical field. Opting for a career in academic medicine can offer benefits such as increased autonomy and scheduling flexibility, which can significantly improve the quality of life. In addition, engagement in scholarly activities and working in a dynamic environment with continuous learning opportunities can help mitigate burnout.
However, embarking on an academic career can be daunting for junior faculty members who face the challenge of providing clinical care while excelling in research and dedicating time to mentorship and teaching trainees. According to a report by the Association of American Medical Colleges, 38% of physicians leave academic medicine within a decade of obtaining a faculty position. Barriers to promotion and retention within academic medicine include ineffective mentorship, unclear or inconsistent promotion criteria, and disparities in gender/ethnic representation.
In this article, we interview two accomplished physicians in academic medicine who have attained the rank of professors.
Interview with Sophie Balzora, MD
Dr. Balzora is a professor of medicine at NYU Grossman School of Medicine and a practicing gastroenterologist specializing in the care of patients with inflammatory bowel disease at NYU Langone Health. She serves as the American College of Gastroenterology’s Diversity, Equity, and Inclusion Committee Chair, on the Advisory Board of ACG’s Leadership, Ethics, and Equity (LE&E) Center, and is president and cofounder of the Association of Black Gastroenterologists and Hepatologists (ABGH). Dr. Balzora was promoted to full professor 11 years after graduating from fellowship.
What would you identify as some of the most important factors that led to your success in achieving a promotion to professor of medicine?
Surround yourself with individuals whose professional and personal priorities align with yours. To achieve this, it is essential to gain an understanding of what is important to you, what you envision your success to look like, and establish a timeline to achieve it. The concept of personal success and how to best achieve it will absolutely change as you grow, and that is okay and expected. Connecting with those outside of your clinical interests, at other institutions, and even outside of the medical field, can help you achieve these goals and better shape how you see your career unfolding and how you want it to look.
Historically, the proportion of physicians who achieve professorship is lower among women compared with men. What do you believe are some of the barriers involved in this, and how would you counsel women who are interested in pursuing the rank of professor?
Systemic gender bias and discrimination, over-mentorship and under-sponsorship, inconsistent parental leave, and delayed parenthood are a few of the factors that contribute to the observed disparities in academic rank. Predictably, for women from underrepresented backgrounds in medicine, the chasm grows.
What has helped me most is to keep my eyes on the prize, and to recognize that the prize is different for everyone. It’s important not to make direct comparisons to any other individual, because they are not you. Harness what makes you different and drown out the naysayers — the “we’ve never seen this done before” camp, the “it’s too soon [for someone like you] to go up for promotion” folks. While these voices are sometimes well intentioned, they can distract you from your goals and ambitions because they are rooted in bias and adherence to traditional expectations. To do something new, and to change the game, requires going against the grain and utilizing your skills and talents to achieve what you want to achieve in a way that works for you.
What are some practical tips you have for junior gastroenterologists to track their promotion in academia?
- Keep your curriculum vitae (CV) up to date and formatted to your institutional guidelines. Ensure that you document your academic activities, even if it doesn’t seem important in the moment. When it’s time to submit that promotion portfolio, you want to be ready and organized.
- Remember: “No” is a full sentence, and saying it takes practice and time and confidence. It is a skill I still struggle to adopt at times, but it’s important to recognize the power of no, for it opens opportunities to say yes to other things.
- Lift as you climb — a critical part of changing the status quo is fostering the future of those underrepresented in medicine. A professional goal of mine that keeps me steady and passionate is to create supporting and enriching systemic and institutional changes that work to dismantle the obstacles perpetuating disparities in academic rank for women and those underrepresented in medicine. Discovering your “why” is a complex, difficult, and rewarding journey.
Interview with Mark Schattner, MD, AGAF
Dr. Schattner is a professor of clinical medicine at Weill Cornell College of Medicine and chief of the gastroenterology, hepatology, and nutrition service at Memorial Sloan Kettering Cancer Center, both in New York. He is a former president of the New York Society for Gastrointestinal Endoscopy and a fellow of the AGA and ASGE.
In your role as chief, you serve as a mentor for early career gastroenterologists for pursuing career promotion. What advice do you have for achieving this?
Promoting junior faculty is one of the prime responsibilities of a service chief. Generally, the early steps of promotion are straightforward, with criteria becoming more stringent as you progress. I think it is critical to understand the criteria used by promotion committees and to be aware of the various available tracks. I believe every meeting a junior faculty member has with their service chief should include, at the least, a brief check-in on where they are in the promotion process and plans (both short term and long term) to move forward. Successful promotion is facilitated when done upon a solid foundation of production and accomplishment. It is very challenging or even impossible when trying to piece together a package from discordant activities.
Most institutions require or encourage academic involvement at both national and international levels for career promotion. Do you have advice for junior faculty about how to achieve this type of recognition or experience?
The easiest place to start is with regional professional societies. Active involvement in these local societies fosters valuable networking and lays the groundwork for involvement at the national or international level. I would strongly encourage junior faculty to seek opportunities for a leadership position at any level in these societies and move up the ladder as their career matures. This is also a very good avenue to network and get invited to join collaborative research projects, which can be a fruitful means to enhance your academic productivity.
In your opinion, what factors are likely to hinder or delay an individual’s promotion?
I think it is crucial to consider the career track you are on. If you are very clinically productive and love to teach, that is completely appropriate, and most institutions will recognize the value of that and promote you along a clinical-educator tract. On the other hand, if you have a passion for research and can successfully lead research and compete for grants, then you would move along a traditional tenure track. It is also critical to think ahead, know the criteria on which you will be judged, and incorporate that into your practice early. Trying to scramble to enhance your CV in a short time just for promotion will likely prove ineffective.
Do you have advice for junior faculty who have families about how to manage career goals but also prioritize time with family?
There is no one-size-fits-all approach to this. I think this requires a lot of shared decision-making with your family. Compromise will undoubtedly be required. For example, I always chose to live in close proximity to my workplace, eliminating any commuting time. This choice really allowed me spend time with my family.
In conclusion, a career in academic medicine presents both opportunities and challenges. A successful academic career, and achieving promotion to the rank of professor of medicine, requires a combination of factors including understanding institution-specific criteria for promotion, proactive engagement at the regional and national level, and envisioning your career goals and creating a timeline to achieve them. There are challenges to promotion, including navigating systemic biases and balancing career goals with family commitments, which also requires consideration and open communication. Ultimately, we hope these insights provide valuable guidance and advice for junior faculty who are navigating this complex environment of academic medicine and are motivated toward achieving professional fulfillment and satisfaction in their careers.
Dr. Rolston is based in the Department of Gastroenterology, Hepatology, and Nutrition, Memorial Sloan Kettering Cancer Center, New York. She reports no conflicts in relation this article. Dr. Balzora and Dr. Schattner are based in the Division of Gastroenterology and Hepatology, New York University Langone Health, New York. Dr. Schattner is a consultant for Boston Scientific and Novo Nordisk. Dr. Balzora reports no conflicts in relation to this article.
References
Campbell KM. Mitigating the isolation of minoritized faculty in academic medicine. J Gen Intern Med. 2023 May. doi: 10.1007/s11606-022-07982-8.
Howard-Anderson JR et al. Strategies for developing a successful career in academic medicine. Am J Med Sci. 2024 Apr. doi: 10.1016/j.amjms.2023.12.010.
Murphy M et al. Women’s experiences of promotion and tenure in academic medicine and potential implications for gender disparities in career advancement: A qualitative analysis. JAMA Netw Open. 2021 Sep 1. doi: 10.1001/jamanetworkopen.2021.25843.
Sambunjak D et al. Mentoring in academic medicine: A systematic review. JAMA. 2006 Sep 6. doi: 10.1001/jama.296.9.1103.
Shen MR et al. Impact of mentoring on academic career success for women in medicine: A systematic review. Acad Med. 2022 Mar 1. doi: 10.1097/ACM.0000000000004563.
Academic medicine plays a crucial role at the crossroads of medical practice, education, and research, influencing the future landscape of healthcare. Many physicians aspire to pursue and sustain a career in academic medicine to contribute to the advancement of medical knowledge, enhance patient care, and influence the trajectory of the medical field. Opting for a career in academic medicine can offer benefits such as increased autonomy and scheduling flexibility, which can significantly improve the quality of life. In addition, engagement in scholarly activities and working in a dynamic environment with continuous learning opportunities can help mitigate burnout.
However, embarking on an academic career can be daunting for junior faculty members who face the challenge of providing clinical care while excelling in research and dedicating time to mentorship and teaching trainees. According to a report by the Association of American Medical Colleges, 38% of physicians leave academic medicine within a decade of obtaining a faculty position. Barriers to promotion and retention within academic medicine include ineffective mentorship, unclear or inconsistent promotion criteria, and disparities in gender/ethnic representation.
In this article, we interview two accomplished physicians in academic medicine who have attained the rank of professors.
Interview with Sophie Balzora, MD
Dr. Balzora is a professor of medicine at NYU Grossman School of Medicine and a practicing gastroenterologist specializing in the care of patients with inflammatory bowel disease at NYU Langone Health. She serves as the American College of Gastroenterology’s Diversity, Equity, and Inclusion Committee Chair, on the Advisory Board of ACG’s Leadership, Ethics, and Equity (LE&E) Center, and is president and cofounder of the Association of Black Gastroenterologists and Hepatologists (ABGH). Dr. Balzora was promoted to full professor 11 years after graduating from fellowship.
What would you identify as some of the most important factors that led to your success in achieving a promotion to professor of medicine?
Surround yourself with individuals whose professional and personal priorities align with yours. To achieve this, it is essential to gain an understanding of what is important to you, what you envision your success to look like, and establish a timeline to achieve it. The concept of personal success and how to best achieve it will absolutely change as you grow, and that is okay and expected. Connecting with those outside of your clinical interests, at other institutions, and even outside of the medical field, can help you achieve these goals and better shape how you see your career unfolding and how you want it to look.
Historically, the proportion of physicians who achieve professorship is lower among women compared with men. What do you believe are some of the barriers involved in this, and how would you counsel women who are interested in pursuing the rank of professor?
Systemic gender bias and discrimination, over-mentorship and under-sponsorship, inconsistent parental leave, and delayed parenthood are a few of the factors that contribute to the observed disparities in academic rank. Predictably, for women from underrepresented backgrounds in medicine, the chasm grows.
What has helped me most is to keep my eyes on the prize, and to recognize that the prize is different for everyone. It’s important not to make direct comparisons to any other individual, because they are not you. Harness what makes you different and drown out the naysayers — the “we’ve never seen this done before” camp, the “it’s too soon [for someone like you] to go up for promotion” folks. While these voices are sometimes well intentioned, they can distract you from your goals and ambitions because they are rooted in bias and adherence to traditional expectations. To do something new, and to change the game, requires going against the grain and utilizing your skills and talents to achieve what you want to achieve in a way that works for you.
What are some practical tips you have for junior gastroenterologists to track their promotion in academia?
- Keep your curriculum vitae (CV) up to date and formatted to your institutional guidelines. Ensure that you document your academic activities, even if it doesn’t seem important in the moment. When it’s time to submit that promotion portfolio, you want to be ready and organized.
- Remember: “No” is a full sentence, and saying it takes practice and time and confidence. It is a skill I still struggle to adopt at times, but it’s important to recognize the power of no, for it opens opportunities to say yes to other things.
- Lift as you climb — a critical part of changing the status quo is fostering the future of those underrepresented in medicine. A professional goal of mine that keeps me steady and passionate is to create supporting and enriching systemic and institutional changes that work to dismantle the obstacles perpetuating disparities in academic rank for women and those underrepresented in medicine. Discovering your “why” is a complex, difficult, and rewarding journey.
Interview with Mark Schattner, MD, AGAF
Dr. Schattner is a professor of clinical medicine at Weill Cornell College of Medicine and chief of the gastroenterology, hepatology, and nutrition service at Memorial Sloan Kettering Cancer Center, both in New York. He is a former president of the New York Society for Gastrointestinal Endoscopy and a fellow of the AGA and ASGE.
In your role as chief, you serve as a mentor for early career gastroenterologists for pursuing career promotion. What advice do you have for achieving this?
Promoting junior faculty is one of the prime responsibilities of a service chief. Generally, the early steps of promotion are straightforward, with criteria becoming more stringent as you progress. I think it is critical to understand the criteria used by promotion committees and to be aware of the various available tracks. I believe every meeting a junior faculty member has with their service chief should include, at the least, a brief check-in on where they are in the promotion process and plans (both short term and long term) to move forward. Successful promotion is facilitated when done upon a solid foundation of production and accomplishment. It is very challenging or even impossible when trying to piece together a package from discordant activities.
Most institutions require or encourage academic involvement at both national and international levels for career promotion. Do you have advice for junior faculty about how to achieve this type of recognition or experience?
The easiest place to start is with regional professional societies. Active involvement in these local societies fosters valuable networking and lays the groundwork for involvement at the national or international level. I would strongly encourage junior faculty to seek opportunities for a leadership position at any level in these societies and move up the ladder as their career matures. This is also a very good avenue to network and get invited to join collaborative research projects, which can be a fruitful means to enhance your academic productivity.
In your opinion, what factors are likely to hinder or delay an individual’s promotion?
I think it is crucial to consider the career track you are on. If you are very clinically productive and love to teach, that is completely appropriate, and most institutions will recognize the value of that and promote you along a clinical-educator tract. On the other hand, if you have a passion for research and can successfully lead research and compete for grants, then you would move along a traditional tenure track. It is also critical to think ahead, know the criteria on which you will be judged, and incorporate that into your practice early. Trying to scramble to enhance your CV in a short time just for promotion will likely prove ineffective.
Do you have advice for junior faculty who have families about how to manage career goals but also prioritize time with family?
There is no one-size-fits-all approach to this. I think this requires a lot of shared decision-making with your family. Compromise will undoubtedly be required. For example, I always chose to live in close proximity to my workplace, eliminating any commuting time. This choice really allowed me spend time with my family.
In conclusion, a career in academic medicine presents both opportunities and challenges. A successful academic career, and achieving promotion to the rank of professor of medicine, requires a combination of factors including understanding institution-specific criteria for promotion, proactive engagement at the regional and national level, and envisioning your career goals and creating a timeline to achieve them. There are challenges to promotion, including navigating systemic biases and balancing career goals with family commitments, which also requires consideration and open communication. Ultimately, we hope these insights provide valuable guidance and advice for junior faculty who are navigating this complex environment of academic medicine and are motivated toward achieving professional fulfillment and satisfaction in their careers.
Dr. Rolston is based in the Department of Gastroenterology, Hepatology, and Nutrition, Memorial Sloan Kettering Cancer Center, New York. She reports no conflicts in relation this article. Dr. Balzora and Dr. Schattner are based in the Division of Gastroenterology and Hepatology, New York University Langone Health, New York. Dr. Schattner is a consultant for Boston Scientific and Novo Nordisk. Dr. Balzora reports no conflicts in relation to this article.
References
Campbell KM. Mitigating the isolation of minoritized faculty in academic medicine. J Gen Intern Med. 2023 May. doi: 10.1007/s11606-022-07982-8.
Howard-Anderson JR et al. Strategies for developing a successful career in academic medicine. Am J Med Sci. 2024 Apr. doi: 10.1016/j.amjms.2023.12.010.
Murphy M et al. Women’s experiences of promotion and tenure in academic medicine and potential implications for gender disparities in career advancement: A qualitative analysis. JAMA Netw Open. 2021 Sep 1. doi: 10.1001/jamanetworkopen.2021.25843.
Sambunjak D et al. Mentoring in academic medicine: A systematic review. JAMA. 2006 Sep 6. doi: 10.1001/jama.296.9.1103.
Shen MR et al. Impact of mentoring on academic career success for women in medicine: A systematic review. Acad Med. 2022 Mar 1. doi: 10.1097/ACM.0000000000004563.
From Mentee to Mentor
Mentoring is universally recognized as a key contributor to a successful career in academic medicine. Most of those who recently transitioned from fellow to faculty got to their current positions with the help of one or more mentors. While many will still need mentoring, coaching, and sponsoring, many are also eager to give back and wonder when and how to make that transition from mentee to mentor.
Dr. Lok: Senior Mentor’s Perspective
I (ASL) completed my hepatology fellowship training in London under Professor Dame Sheila Sherlock. I did not realize how fortunate I was until Dame Sheila’s retirement celebration (2 months before the end of my fellowship) when more than 200 former mentees flew in from all over the world to express their appreciation. Dame Sheila had always embraced all of us as part of the Sherlock family. I benefited tremendously not only from clinical and research training with Dame Sheila and her motherly love that continued well after I completed my fellowship but also the connections and support from my “siblings” who were the Who’s Who in Hepatology.
My transition from mentee to mentor occurred insidiously after my return to Hong Kong, coaching and collaborating with residents, fellows, and early career faculty in their research projects. A key tip I shared with them was the importance of establishing a robust database and sample repository — a vital element to success as a clinical investigator. Working in a busy clinical environment with no protected time and limited resources, we began by identifying clinical dilemmas that we faced in clinics each day and determined which ones were “solvable” if we dove deep. Through keen observations, protocolized clinical care, and robust data recording, we published in Gastroenterology one of the first prospective studies of hepatitis B reactivation in patients receiving chemotherapy, and it continues to be cited. Many principles in mentoring apply universally. Indeed, one of my most accomplished mentees in Hong Kong is a nephrologist with whom I continue to coauthor topics in UpToDate. This is an example of how mentee-mentor relationship can evolve and last, and how each can learn from the other to provide guidance on multi-disciplinary care of complex medical problems.
I became more involved in mentoring after I moved to the United States. I was first hired as Hepatology Program Director at Tulane University and then at the University of Michigan. These roles gave me a sense of responsibility not just to mentor one resident, fellow, or faculty on a research project but to have a holistic approach, providing the necessary guidance and support to help mentees make the best of their potentials and build successful careers, which in turn allows me to build a world-class program.
Over the years, I have mentored more than 60 trainees from all over the world, some of whom have now become division chiefs, department chairs, and chief medical officers of hospitals. Every mentor has a different style, and I had been criticized for being a “Tiger Mom.” I have mellowed over the years, and I hope I am no longer perceived as a “tiger,” though tough love is crucial in mentoring. I hope I am still considered a “mom,” because I see the role of a mentor as that of a parent, providing unconditional love and support with the only expectation that the mentees try to do their best to maximize their potentials and reach their goals. Mentoring is a time investment. It can be exhausting, frustrating, and heart-breaking. It is rarely recognized, and the time and effort rarely compensated. Thus, one should take on mentoring as a calling, a desire to pay it forward, and an understanding that problems can be solved only when generations of physicians and researchers continue to work on them.
A mentor, just like a parent, helps mentees recognize their potentials — passion, strengths, and weaknesses — and to set ambitious yet realistic goals. A very important role of a mentor is to help mentees determine their short- and long-term goals by guiding them to leverage their strengths and passion toward areas and niches that are important and attainable.
Each goal must be accompanied by a plan on how to get there based on resources available. Here is where tough love comes into play. Because there are so many distractions in life, mentees can veer off and be lost. Research projects (and life) never go exactly as planned, and it is difficult to keep going when projects hit a roadblock and papers and grants are rejected. A mentor must help mentees accept and learn from failures and persevere with renewed commitment or find an alternative path (when it is clear the original path is doomed). The most important role of the mentor is to continue to believe in the mentee. Project failure must not be equated to mentee failure though there are times when it is clear some mentees have their interests and talents in other areas. Helping mentees find an alternative path to success and fulfillment can be a blessing. Indeed, two of my mentees who were successful researchers during their early careers have now become successful chief medical officers of major hospitals. They are happy, and I am very proud of them. Times have changed, so my coauthor, who has been faculty for 3.5 years, will share his journey from mentee to mentor.
Dr. Chen: Early Mentor’s Perspective
I (VLC) completed training in 2020 and have mentored only people who are early in their careers, i.e., medical students, residents, and fellows. My transition from mentee to mentor was primarily motivated by gratitude to my past mentors. Watching my own former trainees move on to the next stages of their careers has been hugely fulfilling. It is important that mentee-mentor relationships are mutually beneficial, and I offer a few points to junior faculty considering taking on trainees as mentees.
Taking on a mentee is a commitment. Take it seriously. While a mentee’s success is ultimately their responsibility, mentors are implicitly agreeing to give them opportunities commensurate to their skills and motivation. If you are not in a position to offer such opportunities, do not accept mentees.
Mentorship takes time. Explaining and reviewing research protocols, reading abstract or manuscript drafts, and meeting with mentees to plan for next steps take more time than one might expect.
Understand what potential mentees want. Most trainees are looking for help making it to the next stage of their career (college to medical school, residency to fellowship, etc.) and need abstracts and/or publications to get there. When I work with residents applying to GI fellowship, the goal is that by the time fellowship applications are submitted (early in third year of residency), they have at a minimum presented an abstract at Digestive Diseases Week (DDW) in their second year and submitted an abstract to the American College of Gastroenterology and/or American Association for the Study of Liver Diseases meetings in their third year. This requires planning to ensure they start working early enough to meet conference abstract deadlines. In my opinion, it is reasonable to give the trainee a less ambitious project or a piece of a larger project (i.e., middle authorship on a paper).
By contrast, for trainees who are seriously interested in a research career, the goal is not superfluous abstracts. Rather it is crucial to ensure that the trainee leads a meaningful project that will be a steppingstone to their future career and/or provide preliminary data to support grant applications. Similarly, training in research methodology should be more rigorous for these mentees.
Recognize the limitations of your circumstances. Early-stage faculty often operate on a shoestring budget and little protected time. Even those with 50% or more protected research time and excellent nursing support will find that the time they spend on patient care extends far beyond the time spent in endoscopy units and clinics. Time management and discipline — including not getting bogged down on low-impact research studies — are essential skills.
Be (slightly) selfish. Make sure that you get something out of the mentee as well. Ask yourself:
Do I have work they can help me with? Avoid creating projects simply to give a trainee something to do. It is much better to have them work on a project that you want to do anyway.
How do the trainee’s skills fit in with the type of work that I do? A trainee with no background in statistics may not be able to conduct analyses but may be able to do chart reviews.
Consider “testing” a potential mentee by assigning a limited, straightforward task. If the mentee completes this quickly and to a high standard, then move on to progressively more important or high-stakes projects.
Set concrete and realistic expectations, keeping in mind that trainees have other commitments such as classes and clinical rotations.
Serving as a mentor to the next generation of gastroenterologists is a privilege that junior faculty should not take lightly, and an opportunity for a symbiotic relationship.
Dr. Chen and Dr. Lok are with the Division of Gastroenterology and Hepatology, University of Michigan, Ann Arbor, Michigan. They have no financial conflicts related to this article.
Mentoring is universally recognized as a key contributor to a successful career in academic medicine. Most of those who recently transitioned from fellow to faculty got to their current positions with the help of one or more mentors. While many will still need mentoring, coaching, and sponsoring, many are also eager to give back and wonder when and how to make that transition from mentee to mentor.
Dr. Lok: Senior Mentor’s Perspective
I (ASL) completed my hepatology fellowship training in London under Professor Dame Sheila Sherlock. I did not realize how fortunate I was until Dame Sheila’s retirement celebration (2 months before the end of my fellowship) when more than 200 former mentees flew in from all over the world to express their appreciation. Dame Sheila had always embraced all of us as part of the Sherlock family. I benefited tremendously not only from clinical and research training with Dame Sheila and her motherly love that continued well after I completed my fellowship but also the connections and support from my “siblings” who were the Who’s Who in Hepatology.
My transition from mentee to mentor occurred insidiously after my return to Hong Kong, coaching and collaborating with residents, fellows, and early career faculty in their research projects. A key tip I shared with them was the importance of establishing a robust database and sample repository — a vital element to success as a clinical investigator. Working in a busy clinical environment with no protected time and limited resources, we began by identifying clinical dilemmas that we faced in clinics each day and determined which ones were “solvable” if we dove deep. Through keen observations, protocolized clinical care, and robust data recording, we published in Gastroenterology one of the first prospective studies of hepatitis B reactivation in patients receiving chemotherapy, and it continues to be cited. Many principles in mentoring apply universally. Indeed, one of my most accomplished mentees in Hong Kong is a nephrologist with whom I continue to coauthor topics in UpToDate. This is an example of how mentee-mentor relationship can evolve and last, and how each can learn from the other to provide guidance on multi-disciplinary care of complex medical problems.
I became more involved in mentoring after I moved to the United States. I was first hired as Hepatology Program Director at Tulane University and then at the University of Michigan. These roles gave me a sense of responsibility not just to mentor one resident, fellow, or faculty on a research project but to have a holistic approach, providing the necessary guidance and support to help mentees make the best of their potentials and build successful careers, which in turn allows me to build a world-class program.
Over the years, I have mentored more than 60 trainees from all over the world, some of whom have now become division chiefs, department chairs, and chief medical officers of hospitals. Every mentor has a different style, and I had been criticized for being a “Tiger Mom.” I have mellowed over the years, and I hope I am no longer perceived as a “tiger,” though tough love is crucial in mentoring. I hope I am still considered a “mom,” because I see the role of a mentor as that of a parent, providing unconditional love and support with the only expectation that the mentees try to do their best to maximize their potentials and reach their goals. Mentoring is a time investment. It can be exhausting, frustrating, and heart-breaking. It is rarely recognized, and the time and effort rarely compensated. Thus, one should take on mentoring as a calling, a desire to pay it forward, and an understanding that problems can be solved only when generations of physicians and researchers continue to work on them.
A mentor, just like a parent, helps mentees recognize their potentials — passion, strengths, and weaknesses — and to set ambitious yet realistic goals. A very important role of a mentor is to help mentees determine their short- and long-term goals by guiding them to leverage their strengths and passion toward areas and niches that are important and attainable.
Each goal must be accompanied by a plan on how to get there based on resources available. Here is where tough love comes into play. Because there are so many distractions in life, mentees can veer off and be lost. Research projects (and life) never go exactly as planned, and it is difficult to keep going when projects hit a roadblock and papers and grants are rejected. A mentor must help mentees accept and learn from failures and persevere with renewed commitment or find an alternative path (when it is clear the original path is doomed). The most important role of the mentor is to continue to believe in the mentee. Project failure must not be equated to mentee failure though there are times when it is clear some mentees have their interests and talents in other areas. Helping mentees find an alternative path to success and fulfillment can be a blessing. Indeed, two of my mentees who were successful researchers during their early careers have now become successful chief medical officers of major hospitals. They are happy, and I am very proud of them. Times have changed, so my coauthor, who has been faculty for 3.5 years, will share his journey from mentee to mentor.
Dr. Chen: Early Mentor’s Perspective
I (VLC) completed training in 2020 and have mentored only people who are early in their careers, i.e., medical students, residents, and fellows. My transition from mentee to mentor was primarily motivated by gratitude to my past mentors. Watching my own former trainees move on to the next stages of their careers has been hugely fulfilling. It is important that mentee-mentor relationships are mutually beneficial, and I offer a few points to junior faculty considering taking on trainees as mentees.
Taking on a mentee is a commitment. Take it seriously. While a mentee’s success is ultimately their responsibility, mentors are implicitly agreeing to give them opportunities commensurate to their skills and motivation. If you are not in a position to offer such opportunities, do not accept mentees.
Mentorship takes time. Explaining and reviewing research protocols, reading abstract or manuscript drafts, and meeting with mentees to plan for next steps take more time than one might expect.
Understand what potential mentees want. Most trainees are looking for help making it to the next stage of their career (college to medical school, residency to fellowship, etc.) and need abstracts and/or publications to get there. When I work with residents applying to GI fellowship, the goal is that by the time fellowship applications are submitted (early in third year of residency), they have at a minimum presented an abstract at Digestive Diseases Week (DDW) in their second year and submitted an abstract to the American College of Gastroenterology and/or American Association for the Study of Liver Diseases meetings in their third year. This requires planning to ensure they start working early enough to meet conference abstract deadlines. In my opinion, it is reasonable to give the trainee a less ambitious project or a piece of a larger project (i.e., middle authorship on a paper).
By contrast, for trainees who are seriously interested in a research career, the goal is not superfluous abstracts. Rather it is crucial to ensure that the trainee leads a meaningful project that will be a steppingstone to their future career and/or provide preliminary data to support grant applications. Similarly, training in research methodology should be more rigorous for these mentees.
Recognize the limitations of your circumstances. Early-stage faculty often operate on a shoestring budget and little protected time. Even those with 50% or more protected research time and excellent nursing support will find that the time they spend on patient care extends far beyond the time spent in endoscopy units and clinics. Time management and discipline — including not getting bogged down on low-impact research studies — are essential skills.
Be (slightly) selfish. Make sure that you get something out of the mentee as well. Ask yourself:
Do I have work they can help me with? Avoid creating projects simply to give a trainee something to do. It is much better to have them work on a project that you want to do anyway.
How do the trainee’s skills fit in with the type of work that I do? A trainee with no background in statistics may not be able to conduct analyses but may be able to do chart reviews.
Consider “testing” a potential mentee by assigning a limited, straightforward task. If the mentee completes this quickly and to a high standard, then move on to progressively more important or high-stakes projects.
Set concrete and realistic expectations, keeping in mind that trainees have other commitments such as classes and clinical rotations.
Serving as a mentor to the next generation of gastroenterologists is a privilege that junior faculty should not take lightly, and an opportunity for a symbiotic relationship.
Dr. Chen and Dr. Lok are with the Division of Gastroenterology and Hepatology, University of Michigan, Ann Arbor, Michigan. They have no financial conflicts related to this article.
Mentoring is universally recognized as a key contributor to a successful career in academic medicine. Most of those who recently transitioned from fellow to faculty got to their current positions with the help of one or more mentors. While many will still need mentoring, coaching, and sponsoring, many are also eager to give back and wonder when and how to make that transition from mentee to mentor.
Dr. Lok: Senior Mentor’s Perspective
I (ASL) completed my hepatology fellowship training in London under Professor Dame Sheila Sherlock. I did not realize how fortunate I was until Dame Sheila’s retirement celebration (2 months before the end of my fellowship) when more than 200 former mentees flew in from all over the world to express their appreciation. Dame Sheila had always embraced all of us as part of the Sherlock family. I benefited tremendously not only from clinical and research training with Dame Sheila and her motherly love that continued well after I completed my fellowship but also the connections and support from my “siblings” who were the Who’s Who in Hepatology.
My transition from mentee to mentor occurred insidiously after my return to Hong Kong, coaching and collaborating with residents, fellows, and early career faculty in their research projects. A key tip I shared with them was the importance of establishing a robust database and sample repository — a vital element to success as a clinical investigator. Working in a busy clinical environment with no protected time and limited resources, we began by identifying clinical dilemmas that we faced in clinics each day and determined which ones were “solvable” if we dove deep. Through keen observations, protocolized clinical care, and robust data recording, we published in Gastroenterology one of the first prospective studies of hepatitis B reactivation in patients receiving chemotherapy, and it continues to be cited. Many principles in mentoring apply universally. Indeed, one of my most accomplished mentees in Hong Kong is a nephrologist with whom I continue to coauthor topics in UpToDate. This is an example of how mentee-mentor relationship can evolve and last, and how each can learn from the other to provide guidance on multi-disciplinary care of complex medical problems.
I became more involved in mentoring after I moved to the United States. I was first hired as Hepatology Program Director at Tulane University and then at the University of Michigan. These roles gave me a sense of responsibility not just to mentor one resident, fellow, or faculty on a research project but to have a holistic approach, providing the necessary guidance and support to help mentees make the best of their potentials and build successful careers, which in turn allows me to build a world-class program.
Over the years, I have mentored more than 60 trainees from all over the world, some of whom have now become division chiefs, department chairs, and chief medical officers of hospitals. Every mentor has a different style, and I had been criticized for being a “Tiger Mom.” I have mellowed over the years, and I hope I am no longer perceived as a “tiger,” though tough love is crucial in mentoring. I hope I am still considered a “mom,” because I see the role of a mentor as that of a parent, providing unconditional love and support with the only expectation that the mentees try to do their best to maximize their potentials and reach their goals. Mentoring is a time investment. It can be exhausting, frustrating, and heart-breaking. It is rarely recognized, and the time and effort rarely compensated. Thus, one should take on mentoring as a calling, a desire to pay it forward, and an understanding that problems can be solved only when generations of physicians and researchers continue to work on them.
A mentor, just like a parent, helps mentees recognize their potentials — passion, strengths, and weaknesses — and to set ambitious yet realistic goals. A very important role of a mentor is to help mentees determine their short- and long-term goals by guiding them to leverage their strengths and passion toward areas and niches that are important and attainable.
Each goal must be accompanied by a plan on how to get there based on resources available. Here is where tough love comes into play. Because there are so many distractions in life, mentees can veer off and be lost. Research projects (and life) never go exactly as planned, and it is difficult to keep going when projects hit a roadblock and papers and grants are rejected. A mentor must help mentees accept and learn from failures and persevere with renewed commitment or find an alternative path (when it is clear the original path is doomed). The most important role of the mentor is to continue to believe in the mentee. Project failure must not be equated to mentee failure though there are times when it is clear some mentees have their interests and talents in other areas. Helping mentees find an alternative path to success and fulfillment can be a blessing. Indeed, two of my mentees who were successful researchers during their early careers have now become successful chief medical officers of major hospitals. They are happy, and I am very proud of them. Times have changed, so my coauthor, who has been faculty for 3.5 years, will share his journey from mentee to mentor.
Dr. Chen: Early Mentor’s Perspective
I (VLC) completed training in 2020 and have mentored only people who are early in their careers, i.e., medical students, residents, and fellows. My transition from mentee to mentor was primarily motivated by gratitude to my past mentors. Watching my own former trainees move on to the next stages of their careers has been hugely fulfilling. It is important that mentee-mentor relationships are mutually beneficial, and I offer a few points to junior faculty considering taking on trainees as mentees.
Taking on a mentee is a commitment. Take it seriously. While a mentee’s success is ultimately their responsibility, mentors are implicitly agreeing to give them opportunities commensurate to their skills and motivation. If you are not in a position to offer such opportunities, do not accept mentees.
Mentorship takes time. Explaining and reviewing research protocols, reading abstract or manuscript drafts, and meeting with mentees to plan for next steps take more time than one might expect.
Understand what potential mentees want. Most trainees are looking for help making it to the next stage of their career (college to medical school, residency to fellowship, etc.) and need abstracts and/or publications to get there. When I work with residents applying to GI fellowship, the goal is that by the time fellowship applications are submitted (early in third year of residency), they have at a minimum presented an abstract at Digestive Diseases Week (DDW) in their second year and submitted an abstract to the American College of Gastroenterology and/or American Association for the Study of Liver Diseases meetings in their third year. This requires planning to ensure they start working early enough to meet conference abstract deadlines. In my opinion, it is reasonable to give the trainee a less ambitious project or a piece of a larger project (i.e., middle authorship on a paper).
By contrast, for trainees who are seriously interested in a research career, the goal is not superfluous abstracts. Rather it is crucial to ensure that the trainee leads a meaningful project that will be a steppingstone to their future career and/or provide preliminary data to support grant applications. Similarly, training in research methodology should be more rigorous for these mentees.
Recognize the limitations of your circumstances. Early-stage faculty often operate on a shoestring budget and little protected time. Even those with 50% or more protected research time and excellent nursing support will find that the time they spend on patient care extends far beyond the time spent in endoscopy units and clinics. Time management and discipline — including not getting bogged down on low-impact research studies — are essential skills.
Be (slightly) selfish. Make sure that you get something out of the mentee as well. Ask yourself:
Do I have work they can help me with? Avoid creating projects simply to give a trainee something to do. It is much better to have them work on a project that you want to do anyway.
How do the trainee’s skills fit in with the type of work that I do? A trainee with no background in statistics may not be able to conduct analyses but may be able to do chart reviews.
Consider “testing” a potential mentee by assigning a limited, straightforward task. If the mentee completes this quickly and to a high standard, then move on to progressively more important or high-stakes projects.
Set concrete and realistic expectations, keeping in mind that trainees have other commitments such as classes and clinical rotations.
Serving as a mentor to the next generation of gastroenterologists is a privilege that junior faculty should not take lightly, and an opportunity for a symbiotic relationship.
Dr. Chen and Dr. Lok are with the Division of Gastroenterology and Hepatology, University of Michigan, Ann Arbor, Michigan. They have no financial conflicts related to this article.
Early career considerations for gastroenterologists interested in diversity, equity, and inclusion roles

Highlighting the importance of DEI across all aspects of medicine is long overdue, and the field of gastroenterology is no exception. Diversity in the gastroenterology workforce still has significant room for improvement with only 12% of all gastroenterology fellows in 2018 identifying as Black, Latino/a/x, American Indian or Alaskan Native, or Native Hawaiian or Pacific Islander.1 Moreover, only 4.4% of practicing gastroenterologists identify as Black, 6.7% identify as Latino/a/x, 0.1% as American Indian or Alaskan Native, and 0.003% as Native Hawaiian or Pacific Islander.2
The intensified focus on diversity in GI is welcomed, but increasing physician workforce diversity is only one of the necessary steps. If our ultimate goal is to improve health outcomes and achieve health equity for historically marginalized racial, ethnic, and socioeconomically disadvantaged communities, we must critically evaluate the path beyond just enhancing workforce diversity.
Black and Latino/a/x physicians are more likely to care for historically marginalized communities,3 which has been shown to improve all-cause mortality and reduce racial disparities.4 Additionally, diverse work teams are more innovative and productive.5 Therefore, expanding diversity must include 1) providing equitable policies and access to opportunities and promotions; 2) building inclusive environments in our institutions and practices; and 3) providing space for all people to feel like they can belong, feel respected at work, and genuinely have their opinions and ideas valued. What diversity, equity, inclusion, and belonging provide for us and our patients are avenues to thrive, solve complex problems, and tackle prominent issues within our institutions, workplaces, and communities.
To this end, many academic centers, hospitals, and private practice entities have produced a flurry of new DEI initiatives coupled with titles and roles. Some of these roles have thankfully brought recognition and economic compensation to the people doing this work. Still, as an early career gastroenterologist, you may be offered or are considering taking on a DEI role during your early career. As two underrepresented minority women in medicine who took on DEI roles with their first jobs, we wanted to highlight a few aspects to think about during your early career:
Does the DEI role come with resources?
Historically, DEI efforts were treated as “extra work,” or an activity that was done using one’s own personal time. In addition, this work called upon the small number of physicians underrepresented in medicine, largely uncompensated and with an exorbitant minority tax during a critical moment in establishing their early careers. DEI should no longer be seen as an extracurricular activity but as a vital component of an institution’s success.
If you are considering a DEI role, the first question to ask is, “Does this role come with extra compensation or protected time?” We highly recommend not taking on the role if the answer is no. If your institution or employer is only offering increased minority tax, you are being set up to either fail, burn out, or both. Your employer or institution does not appear to value your time or effort in DEI, and you should interpret their lack of compensation or protected time as such.
If the answer is yes, then here are a few other things to consider: Is there institutional support for you to be successful in your new role? As DEI work challenges you to come up with solutions to combat years of historic marginalization for racial and ethnic minorities, this work can sometimes feel overwhelming and isolating. The importance of the DEI community and mentorship within and outside your institution is critical. You should consider joining DEI working groups or committees through GI national societies, the Association of American Medical Colleges, or the Accreditation Council for Graduate Medical Education. You can also connect with a fantastic network of people engaged in this work via social media and lean on friends and colleagues leading similar initiatives across the country.
Other critical logistical questions are if your role will come with administrative support, whether there is a budget for programs or events, and whether your institution/employer will support you in seeking continued professional development for your DEI role.6
Make sure to understand the “ask” from your division, department, or company.
Before confirming you are willing to take on this role, get a clear vision of what you are being asked to accomplish. There are so many opportunities to improve the DEI landscape. Therefore, knowing what you are specifically being asked to do will be critical to your success.
Are you being asked to work on diversity?
Does your institution want you to focus on and improve the recruitment and retention of trainees, physicians, or staff underrepresented in medicine? If so, you will need to have access to all the prior work and statistics. Capture the landscape before your interventions (% underrepresented in medicine [URiM] trainees, % URiM faculty at each level, % of URiM trainees retained as faculty, % of URiM faculty being promoted each year, etc.) This will allow you to determine the outcomes of your proposed improvements or programs.
Is your employer focused on equity?
Are you being asked to think about ways to operationalize improved patient health equity, or are you being asked to build equitable opportunities/programs for career advancement for URiMs at your institution? For either equity issue, you first need to understand the scope of the problem to ask for the necessary resources for a potential solution. Discuss timeline expectations, as equity work is a marathon and may take years to move the needle on any particular issue. This timeline is also critical for your employer to be aware of and support, as unrealistic timelines and expectations will also set you up for failure.
Or, are you being asked to concentrate on inclusion?
Does your institution need an assessment of how inclusive the climate is for trainees, staff, or physicians? Does this assessment align with your division or department’s impression, and how do you plan to work toward potential solutions for improvement?
Although diversity, equity, and inclusion are interconnected entities, they all have distinct objectives and solutions. It is essential to understand your vision and your employer’s vision for this role. If they are not aligned, having early and in-depth conversations about aligning your visions will set you on a path to success in your early career.
Know your why or more importantly, your who?
Early career physicians who are considering taking on DEI work do so for a reason. Being passionate about this type of work is usually born from a personal experience or your deep-rooted values. For us, experiencing and witnessing health disparities for our family members and people who look like us are what initially fueled our passion for this work. Additional experiences with trainees and patients keep us invigorated to continue highlighting the importance of DEI and encourage others to be passionate about DEI’s huge value added. As DEI work can come with challenges, remembering and re-centering on why you are passionate about this work or who you are engaging in this work for can keep you going.
There are several aspects to consider before taking on a DEI role, but overall, the work is rewarding and can be a great addition to the building blocks of your early career. In the short term, you build a DEI community network of peers, mentors, colleagues, and friends beyond your immediate institution and specialty. You also can demonstrate your leadership skills and potential early on in your career. In the long-term, engaging in these types of roles helps build a climate and culture that is conducive to enacting change for our patients and communities, including advancing healthcare equity and working toward recruitment, retention, and expansion efforts for our trainees and faculty. Overall, we think this type of work in your early career can be an integral part of your personal and professional development, while also having an impact that ripples beyond the walls of the endoscopy suite.
Dr. Fritz is an assistant professor of medicine in the division of gastroenterology at Washington University School of Medicine, St. Louis. Dr. Rodriguez is a gastroenterologist with Brigham and Women’s Hospital in Boston. Neither Dr. Rodriguez nor Dr. Fritz disclosed no conflicts of interest.
References
1. Santhosh L,Babik JM. Trends in racial and ethnic diversity in internal medicine subspecialty fellowships from 2006 to 2018. JAMA Network Open 2020;3:e1920482-e1920482.
2. Colleges AoAM. Physician Specialty Data Report/Active physicians who identified as Black or African-American, 2021. 2022.
3. Komaromy M et al. The role of black and Hispanic physicians in providing health care for underserved populations. New England Journal of Medicine 1996;334:1305-10.
4. Snyder JE et al. Black representation in the primary care physician workforce and its association with population life expectancy and mortality rates in the US. JAMA Network Open 2023;6:e236687-e236687.
5. Page S. Diversity bonuses and the business case. The Diversity Bonus: Princeton University Press, 2017:184-208.
6. Vela MB et al. Diversity, equity, and inclusion officer position available: Proceed with caution. Journal of Graduate Medical Education 2021;13:771-3.
Helpful resources
Diversity and Inclusion Toolkit Resources, AAMC
Blackinggastro.org, The Association of Black Gastroenterologists and Hepatologists (ABGH)
Podcast: Clinical Problem Solvers: Anti-Racism in Medicine

Highlighting the importance of DEI across all aspects of medicine is long overdue, and the field of gastroenterology is no exception. Diversity in the gastroenterology workforce still has significant room for improvement with only 12% of all gastroenterology fellows in 2018 identifying as Black, Latino/a/x, American Indian or Alaskan Native, or Native Hawaiian or Pacific Islander.1 Moreover, only 4.4% of practicing gastroenterologists identify as Black, 6.7% identify as Latino/a/x, 0.1% as American Indian or Alaskan Native, and 0.003% as Native Hawaiian or Pacific Islander.2
The intensified focus on diversity in GI is welcomed, but increasing physician workforce diversity is only one of the necessary steps. If our ultimate goal is to improve health outcomes and achieve health equity for historically marginalized racial, ethnic, and socioeconomically disadvantaged communities, we must critically evaluate the path beyond just enhancing workforce diversity.
Black and Latino/a/x physicians are more likely to care for historically marginalized communities,3 which has been shown to improve all-cause mortality and reduce racial disparities.4 Additionally, diverse work teams are more innovative and productive.5 Therefore, expanding diversity must include 1) providing equitable policies and access to opportunities and promotions; 2) building inclusive environments in our institutions and practices; and 3) providing space for all people to feel like they can belong, feel respected at work, and genuinely have their opinions and ideas valued. What diversity, equity, inclusion, and belonging provide for us and our patients are avenues to thrive, solve complex problems, and tackle prominent issues within our institutions, workplaces, and communities.
To this end, many academic centers, hospitals, and private practice entities have produced a flurry of new DEI initiatives coupled with titles and roles. Some of these roles have thankfully brought recognition and economic compensation to the people doing this work. Still, as an early career gastroenterologist, you may be offered or are considering taking on a DEI role during your early career. As two underrepresented minority women in medicine who took on DEI roles with their first jobs, we wanted to highlight a few aspects to think about during your early career:
Does the DEI role come with resources?
Historically, DEI efforts were treated as “extra work,” or an activity that was done using one’s own personal time. In addition, this work called upon the small number of physicians underrepresented in medicine, largely uncompensated and with an exorbitant minority tax during a critical moment in establishing their early careers. DEI should no longer be seen as an extracurricular activity but as a vital component of an institution’s success.
If you are considering a DEI role, the first question to ask is, “Does this role come with extra compensation or protected time?” We highly recommend not taking on the role if the answer is no. If your institution or employer is only offering increased minority tax, you are being set up to either fail, burn out, or both. Your employer or institution does not appear to value your time or effort in DEI, and you should interpret their lack of compensation or protected time as such.
If the answer is yes, then here are a few other things to consider: Is there institutional support for you to be successful in your new role? As DEI work challenges you to come up with solutions to combat years of historic marginalization for racial and ethnic minorities, this work can sometimes feel overwhelming and isolating. The importance of the DEI community and mentorship within and outside your institution is critical. You should consider joining DEI working groups or committees through GI national societies, the Association of American Medical Colleges, or the Accreditation Council for Graduate Medical Education. You can also connect with a fantastic network of people engaged in this work via social media and lean on friends and colleagues leading similar initiatives across the country.
Other critical logistical questions are if your role will come with administrative support, whether there is a budget for programs or events, and whether your institution/employer will support you in seeking continued professional development for your DEI role.6
Make sure to understand the “ask” from your division, department, or company.
Before confirming you are willing to take on this role, get a clear vision of what you are being asked to accomplish. There are so many opportunities to improve the DEI landscape. Therefore, knowing what you are specifically being asked to do will be critical to your success.
Are you being asked to work on diversity?
Does your institution want you to focus on and improve the recruitment and retention of trainees, physicians, or staff underrepresented in medicine? If so, you will need to have access to all the prior work and statistics. Capture the landscape before your interventions (% underrepresented in medicine [URiM] trainees, % URiM faculty at each level, % of URiM trainees retained as faculty, % of URiM faculty being promoted each year, etc.) This will allow you to determine the outcomes of your proposed improvements or programs.
Is your employer focused on equity?
Are you being asked to think about ways to operationalize improved patient health equity, or are you being asked to build equitable opportunities/programs for career advancement for URiMs at your institution? For either equity issue, you first need to understand the scope of the problem to ask for the necessary resources for a potential solution. Discuss timeline expectations, as equity work is a marathon and may take years to move the needle on any particular issue. This timeline is also critical for your employer to be aware of and support, as unrealistic timelines and expectations will also set you up for failure.
Or, are you being asked to concentrate on inclusion?
Does your institution need an assessment of how inclusive the climate is for trainees, staff, or physicians? Does this assessment align with your division or department’s impression, and how do you plan to work toward potential solutions for improvement?
Although diversity, equity, and inclusion are interconnected entities, they all have distinct objectives and solutions. It is essential to understand your vision and your employer’s vision for this role. If they are not aligned, having early and in-depth conversations about aligning your visions will set you on a path to success in your early career.
Know your why or more importantly, your who?
Early career physicians who are considering taking on DEI work do so for a reason. Being passionate about this type of work is usually born from a personal experience or your deep-rooted values. For us, experiencing and witnessing health disparities for our family members and people who look like us are what initially fueled our passion for this work. Additional experiences with trainees and patients keep us invigorated to continue highlighting the importance of DEI and encourage others to be passionate about DEI’s huge value added. As DEI work can come with challenges, remembering and re-centering on why you are passionate about this work or who you are engaging in this work for can keep you going.
There are several aspects to consider before taking on a DEI role, but overall, the work is rewarding and can be a great addition to the building blocks of your early career. In the short term, you build a DEI community network of peers, mentors, colleagues, and friends beyond your immediate institution and specialty. You also can demonstrate your leadership skills and potential early on in your career. In the long-term, engaging in these types of roles helps build a climate and culture that is conducive to enacting change for our patients and communities, including advancing healthcare equity and working toward recruitment, retention, and expansion efforts for our trainees and faculty. Overall, we think this type of work in your early career can be an integral part of your personal and professional development, while also having an impact that ripples beyond the walls of the endoscopy suite.
Dr. Fritz is an assistant professor of medicine in the division of gastroenterology at Washington University School of Medicine, St. Louis. Dr. Rodriguez is a gastroenterologist with Brigham and Women’s Hospital in Boston. Neither Dr. Rodriguez nor Dr. Fritz disclosed no conflicts of interest.
References
1. Santhosh L,Babik JM. Trends in racial and ethnic diversity in internal medicine subspecialty fellowships from 2006 to 2018. JAMA Network Open 2020;3:e1920482-e1920482.
2. Colleges AoAM. Physician Specialty Data Report/Active physicians who identified as Black or African-American, 2021. 2022.
3. Komaromy M et al. The role of black and Hispanic physicians in providing health care for underserved populations. New England Journal of Medicine 1996;334:1305-10.
4. Snyder JE et al. Black representation in the primary care physician workforce and its association with population life expectancy and mortality rates in the US. JAMA Network Open 2023;6:e236687-e236687.
5. Page S. Diversity bonuses and the business case. The Diversity Bonus: Princeton University Press, 2017:184-208.
6. Vela MB et al. Diversity, equity, and inclusion officer position available: Proceed with caution. Journal of Graduate Medical Education 2021;13:771-3.
Helpful resources
Diversity and Inclusion Toolkit Resources, AAMC
Blackinggastro.org, The Association of Black Gastroenterologists and Hepatologists (ABGH)
Podcast: Clinical Problem Solvers: Anti-Racism in Medicine

Highlighting the importance of DEI across all aspects of medicine is long overdue, and the field of gastroenterology is no exception. Diversity in the gastroenterology workforce still has significant room for improvement with only 12% of all gastroenterology fellows in 2018 identifying as Black, Latino/a/x, American Indian or Alaskan Native, or Native Hawaiian or Pacific Islander.1 Moreover, only 4.4% of practicing gastroenterologists identify as Black, 6.7% identify as Latino/a/x, 0.1% as American Indian or Alaskan Native, and 0.003% as Native Hawaiian or Pacific Islander.2
The intensified focus on diversity in GI is welcomed, but increasing physician workforce diversity is only one of the necessary steps. If our ultimate goal is to improve health outcomes and achieve health equity for historically marginalized racial, ethnic, and socioeconomically disadvantaged communities, we must critically evaluate the path beyond just enhancing workforce diversity.
Black and Latino/a/x physicians are more likely to care for historically marginalized communities,3 which has been shown to improve all-cause mortality and reduce racial disparities.4 Additionally, diverse work teams are more innovative and productive.5 Therefore, expanding diversity must include 1) providing equitable policies and access to opportunities and promotions; 2) building inclusive environments in our institutions and practices; and 3) providing space for all people to feel like they can belong, feel respected at work, and genuinely have their opinions and ideas valued. What diversity, equity, inclusion, and belonging provide for us and our patients are avenues to thrive, solve complex problems, and tackle prominent issues within our institutions, workplaces, and communities.
To this end, many academic centers, hospitals, and private practice entities have produced a flurry of new DEI initiatives coupled with titles and roles. Some of these roles have thankfully brought recognition and economic compensation to the people doing this work. Still, as an early career gastroenterologist, you may be offered or are considering taking on a DEI role during your early career. As two underrepresented minority women in medicine who took on DEI roles with their first jobs, we wanted to highlight a few aspects to think about during your early career:
Does the DEI role come with resources?
Historically, DEI efforts were treated as “extra work,” or an activity that was done using one’s own personal time. In addition, this work called upon the small number of physicians underrepresented in medicine, largely uncompensated and with an exorbitant minority tax during a critical moment in establishing their early careers. DEI should no longer be seen as an extracurricular activity but as a vital component of an institution’s success.
If you are considering a DEI role, the first question to ask is, “Does this role come with extra compensation or protected time?” We highly recommend not taking on the role if the answer is no. If your institution or employer is only offering increased minority tax, you are being set up to either fail, burn out, or both. Your employer or institution does not appear to value your time or effort in DEI, and you should interpret their lack of compensation or protected time as such.
If the answer is yes, then here are a few other things to consider: Is there institutional support for you to be successful in your new role? As DEI work challenges you to come up with solutions to combat years of historic marginalization for racial and ethnic minorities, this work can sometimes feel overwhelming and isolating. The importance of the DEI community and mentorship within and outside your institution is critical. You should consider joining DEI working groups or committees through GI national societies, the Association of American Medical Colleges, or the Accreditation Council for Graduate Medical Education. You can also connect with a fantastic network of people engaged in this work via social media and lean on friends and colleagues leading similar initiatives across the country.
Other critical logistical questions are if your role will come with administrative support, whether there is a budget for programs or events, and whether your institution/employer will support you in seeking continued professional development for your DEI role.6
Make sure to understand the “ask” from your division, department, or company.
Before confirming you are willing to take on this role, get a clear vision of what you are being asked to accomplish. There are so many opportunities to improve the DEI landscape. Therefore, knowing what you are specifically being asked to do will be critical to your success.
Are you being asked to work on diversity?
Does your institution want you to focus on and improve the recruitment and retention of trainees, physicians, or staff underrepresented in medicine? If so, you will need to have access to all the prior work and statistics. Capture the landscape before your interventions (% underrepresented in medicine [URiM] trainees, % URiM faculty at each level, % of URiM trainees retained as faculty, % of URiM faculty being promoted each year, etc.) This will allow you to determine the outcomes of your proposed improvements or programs.
Is your employer focused on equity?
Are you being asked to think about ways to operationalize improved patient health equity, or are you being asked to build equitable opportunities/programs for career advancement for URiMs at your institution? For either equity issue, you first need to understand the scope of the problem to ask for the necessary resources for a potential solution. Discuss timeline expectations, as equity work is a marathon and may take years to move the needle on any particular issue. This timeline is also critical for your employer to be aware of and support, as unrealistic timelines and expectations will also set you up for failure.
Or, are you being asked to concentrate on inclusion?
Does your institution need an assessment of how inclusive the climate is for trainees, staff, or physicians? Does this assessment align with your division or department’s impression, and how do you plan to work toward potential solutions for improvement?
Although diversity, equity, and inclusion are interconnected entities, they all have distinct objectives and solutions. It is essential to understand your vision and your employer’s vision for this role. If they are not aligned, having early and in-depth conversations about aligning your visions will set you on a path to success in your early career.
Know your why or more importantly, your who?
Early career physicians who are considering taking on DEI work do so for a reason. Being passionate about this type of work is usually born from a personal experience or your deep-rooted values. For us, experiencing and witnessing health disparities for our family members and people who look like us are what initially fueled our passion for this work. Additional experiences with trainees and patients keep us invigorated to continue highlighting the importance of DEI and encourage others to be passionate about DEI’s huge value added. As DEI work can come with challenges, remembering and re-centering on why you are passionate about this work or who you are engaging in this work for can keep you going.
There are several aspects to consider before taking on a DEI role, but overall, the work is rewarding and can be a great addition to the building blocks of your early career. In the short term, you build a DEI community network of peers, mentors, colleagues, and friends beyond your immediate institution and specialty. You also can demonstrate your leadership skills and potential early on in your career. In the long-term, engaging in these types of roles helps build a climate and culture that is conducive to enacting change for our patients and communities, including advancing healthcare equity and working toward recruitment, retention, and expansion efforts for our trainees and faculty. Overall, we think this type of work in your early career can be an integral part of your personal and professional development, while also having an impact that ripples beyond the walls of the endoscopy suite.
Dr. Fritz is an assistant professor of medicine in the division of gastroenterology at Washington University School of Medicine, St. Louis. Dr. Rodriguez is a gastroenterologist with Brigham and Women’s Hospital in Boston. Neither Dr. Rodriguez nor Dr. Fritz disclosed no conflicts of interest.
References
1. Santhosh L,Babik JM. Trends in racial and ethnic diversity in internal medicine subspecialty fellowships from 2006 to 2018. JAMA Network Open 2020;3:e1920482-e1920482.
2. Colleges AoAM. Physician Specialty Data Report/Active physicians who identified as Black or African-American, 2021. 2022.
3. Komaromy M et al. The role of black and Hispanic physicians in providing health care for underserved populations. New England Journal of Medicine 1996;334:1305-10.
4. Snyder JE et al. Black representation in the primary care physician workforce and its association with population life expectancy and mortality rates in the US. JAMA Network Open 2023;6:e236687-e236687.
5. Page S. Diversity bonuses and the business case. The Diversity Bonus: Princeton University Press, 2017:184-208.
6. Vela MB et al. Diversity, equity, and inclusion officer position available: Proceed with caution. Journal of Graduate Medical Education 2021;13:771-3.
Helpful resources
Diversity and Inclusion Toolkit Resources, AAMC
Blackinggastro.org, The Association of Black Gastroenterologists and Hepatologists (ABGH)
Podcast: Clinical Problem Solvers: Anti-Racism in Medicine