User login
UK TAVI: Similar outcomes to surgery in real world
Transcatheter aortic valve replacement (TAVR) was not inferior to conventional surgery with respect to death from any cause at 1 year in a new real-world study in patients age 70 years or older with severe symptomatic aortic stenosis at increased operative risk due to age or comorbidity.
The UK TAVI study was presented March 29 at the “virtual” American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC).
The trial involved a broad group of patients who were treated at every medical center that performs the transcatheter procedure across the United Kingdom.
“The importance of this trial is that it confirms the effectiveness of the TAVR strategy in a real-world setting,” said lead author, William D. Toff, MD, professor of cardiology at the University of Leicester, United Kingdom.
Previous clinical trials have found TAVR to be noninferior or superior to open-heart surgery for various patient groups, but most trials have been limited to medical centers that perform a high volume of procedures or focus on the use of specific types of replacement valves, he noted.
“Our results are concordant with those from earlier trials in intermediate- and low-risk patients, but those earlier trials were performed in the best centers and had many exclusion criteria. We have replicated those results in populations more representative of the real world.”
“I think it is a very important message that supports the findings in earlier trials that were focused on showing whether TAVR can work under ideal conditions, while our trial shows that it does work in real-world clinical practice,” he added.
The UK TAVI trial enrolled 913 patients referred for treatment of severe aortic stenosis at 34 UK sites from 2014 to 2018. They were randomly assigned to receive TAVR or open-heart surgery.
Enrollment was limited to participants age 70 years or older (with additional risk factors) or age 80 years or older (with or without additional risk factors). The average age was 81 years.
Overall, participants were at intermediate to low risk from surgery, with a median Society of Thoracic Surgeons (STS) risk score of 2.6%. However, researchers did not specify a particular risk score cutoff for enrollment.
“This allowed the trial to evolve along with changes in guidelines and practice regarding TAVR over the course of the study and to reflect physicians’ nuanced, real-world approach to considering risk in decision-making rather than taking a formulaic approach,” Toff said.
At 1 year, the rate of death from any cause (the primary endpoint) was 4.6% in the TAVR group and 6.6% in the surgery group, a difference that met the trial’s prespecified threshold for noninferiority of TAVR.
Rates of death from cardiovascular disease or stroke were also similar between the two groups.
Patients who received TAVR had a significantly higher rate of vascular complications (4.8%) than those receiving surgery (1.3%).
TAVR patients were also more likely to have a pacemaker implanted. This occurred in 12.2% of TAVR patients and 6.6% of those undergoing surgery.
In addition, patients who underwent TAVR had a higher rate of aortic regurgitation. Mild aortic regurgitation occurred at 1 year in 38.3% of the TAVR group and 11.7% of the surgery group, whereas moderate regurgitation occurred in 2.3% of TAVR patients and 0.6% of surgery patients.
On the other hand, patients undergoing TAVR had a significantly lower rate of major bleeding complications, which occurred in 6.3% of patients having TAVR and 17.1% of those undergoing surgery.
TAVR was also associated with a shorter hospital stay, fewer days in intensive care, and a faster improvement in functional capacity and quality of life. Functional capacity and quality-of-life measures at 6 weeks after the procedure were better in the TAVR group but by 1 year they were similar in the two groups.
“Longer follow-up is required to confirm sustained clinical benefit and valve durability to inform clinical practice, particularly in younger patients,” Toff concluded.
“The results from our trial and others are encouraging, but patients need to be fully informed and know that the long-term durability of the TAVR valves and the long-term implications of the increased risk of aortic regurgitation are still uncertain,” he added.
The researchers plan to continue to track outcomes for a minimum of 5 years.
Discussant of the UK TAVI trial at an ACC press conference, Julia Grapsa, MD, Guys and St Thomas NHS Trust, London, United Kingdom, said it was a well-designed study.
“It was impressive to see so many UK sites and the age range of patients from 70 to 91 years, and the shorter hospital stays and functional recoveries as well as reduced major bleeding in the TAVR group,” Grapsa said.
“But something that was very striking to me was the increase in moderate aortic regurgitation in the TAVR arm, 2.3% versus 0.6% in the surgical arm, so it is very important to keep following these patients long term,” she added.
In answer to a question during the main session about using age alone as an inclusion criterion in those over 80 years old, Toff said, “We were more comfortable taking all comers over 80 years of age because of the uncertainty about TAVR is more in relation to its durability and the clinical significance of the aortic regurgitation, which may have consequences in the longer term. But the longer term for the over 80s is obviously less of a problem than for those in their 70s.”
This study was funded by the UK National Institute for Health Research Health Technology Assessment Programme. Toff reports no disclosures.
American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC). Abstract 20-LB-20410-ACC. Presented March 29, 2020.
This article first appeared on Medscape.com.
Transcatheter aortic valve replacement (TAVR) was not inferior to conventional surgery with respect to death from any cause at 1 year in a new real-world study in patients age 70 years or older with severe symptomatic aortic stenosis at increased operative risk due to age or comorbidity.
The UK TAVI study was presented March 29 at the “virtual” American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC).
The trial involved a broad group of patients who were treated at every medical center that performs the transcatheter procedure across the United Kingdom.
“The importance of this trial is that it confirms the effectiveness of the TAVR strategy in a real-world setting,” said lead author, William D. Toff, MD, professor of cardiology at the University of Leicester, United Kingdom.
Previous clinical trials have found TAVR to be noninferior or superior to open-heart surgery for various patient groups, but most trials have been limited to medical centers that perform a high volume of procedures or focus on the use of specific types of replacement valves, he noted.
“Our results are concordant with those from earlier trials in intermediate- and low-risk patients, but those earlier trials were performed in the best centers and had many exclusion criteria. We have replicated those results in populations more representative of the real world.”
“I think it is a very important message that supports the findings in earlier trials that were focused on showing whether TAVR can work under ideal conditions, while our trial shows that it does work in real-world clinical practice,” he added.
The UK TAVI trial enrolled 913 patients referred for treatment of severe aortic stenosis at 34 UK sites from 2014 to 2018. They were randomly assigned to receive TAVR or open-heart surgery.
Enrollment was limited to participants age 70 years or older (with additional risk factors) or age 80 years or older (with or without additional risk factors). The average age was 81 years.
Overall, participants were at intermediate to low risk from surgery, with a median Society of Thoracic Surgeons (STS) risk score of 2.6%. However, researchers did not specify a particular risk score cutoff for enrollment.
“This allowed the trial to evolve along with changes in guidelines and practice regarding TAVR over the course of the study and to reflect physicians’ nuanced, real-world approach to considering risk in decision-making rather than taking a formulaic approach,” Toff said.
At 1 year, the rate of death from any cause (the primary endpoint) was 4.6% in the TAVR group and 6.6% in the surgery group, a difference that met the trial’s prespecified threshold for noninferiority of TAVR.
Rates of death from cardiovascular disease or stroke were also similar between the two groups.
Patients who received TAVR had a significantly higher rate of vascular complications (4.8%) than those receiving surgery (1.3%).
TAVR patients were also more likely to have a pacemaker implanted. This occurred in 12.2% of TAVR patients and 6.6% of those undergoing surgery.
In addition, patients who underwent TAVR had a higher rate of aortic regurgitation. Mild aortic regurgitation occurred at 1 year in 38.3% of the TAVR group and 11.7% of the surgery group, whereas moderate regurgitation occurred in 2.3% of TAVR patients and 0.6% of surgery patients.
On the other hand, patients undergoing TAVR had a significantly lower rate of major bleeding complications, which occurred in 6.3% of patients having TAVR and 17.1% of those undergoing surgery.
TAVR was also associated with a shorter hospital stay, fewer days in intensive care, and a faster improvement in functional capacity and quality of life. Functional capacity and quality-of-life measures at 6 weeks after the procedure were better in the TAVR group but by 1 year they were similar in the two groups.
“Longer follow-up is required to confirm sustained clinical benefit and valve durability to inform clinical practice, particularly in younger patients,” Toff concluded.
“The results from our trial and others are encouraging, but patients need to be fully informed and know that the long-term durability of the TAVR valves and the long-term implications of the increased risk of aortic regurgitation are still uncertain,” he added.
The researchers plan to continue to track outcomes for a minimum of 5 years.
Discussant of the UK TAVI trial at an ACC press conference, Julia Grapsa, MD, Guys and St Thomas NHS Trust, London, United Kingdom, said it was a well-designed study.
“It was impressive to see so many UK sites and the age range of patients from 70 to 91 years, and the shorter hospital stays and functional recoveries as well as reduced major bleeding in the TAVR group,” Grapsa said.
“But something that was very striking to me was the increase in moderate aortic regurgitation in the TAVR arm, 2.3% versus 0.6% in the surgical arm, so it is very important to keep following these patients long term,” she added.
In answer to a question during the main session about using age alone as an inclusion criterion in those over 80 years old, Toff said, “We were more comfortable taking all comers over 80 years of age because of the uncertainty about TAVR is more in relation to its durability and the clinical significance of the aortic regurgitation, which may have consequences in the longer term. But the longer term for the over 80s is obviously less of a problem than for those in their 70s.”
This study was funded by the UK National Institute for Health Research Health Technology Assessment Programme. Toff reports no disclosures.
American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC). Abstract 20-LB-20410-ACC. Presented March 29, 2020.
This article first appeared on Medscape.com.
Transcatheter aortic valve replacement (TAVR) was not inferior to conventional surgery with respect to death from any cause at 1 year in a new real-world study in patients age 70 years or older with severe symptomatic aortic stenosis at increased operative risk due to age or comorbidity.
The UK TAVI study was presented March 29 at the “virtual” American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC).
The trial involved a broad group of patients who were treated at every medical center that performs the transcatheter procedure across the United Kingdom.
“The importance of this trial is that it confirms the effectiveness of the TAVR strategy in a real-world setting,” said lead author, William D. Toff, MD, professor of cardiology at the University of Leicester, United Kingdom.
Previous clinical trials have found TAVR to be noninferior or superior to open-heart surgery for various patient groups, but most trials have been limited to medical centers that perform a high volume of procedures or focus on the use of specific types of replacement valves, he noted.
“Our results are concordant with those from earlier trials in intermediate- and low-risk patients, but those earlier trials were performed in the best centers and had many exclusion criteria. We have replicated those results in populations more representative of the real world.”
“I think it is a very important message that supports the findings in earlier trials that were focused on showing whether TAVR can work under ideal conditions, while our trial shows that it does work in real-world clinical practice,” he added.
The UK TAVI trial enrolled 913 patients referred for treatment of severe aortic stenosis at 34 UK sites from 2014 to 2018. They were randomly assigned to receive TAVR or open-heart surgery.
Enrollment was limited to participants age 70 years or older (with additional risk factors) or age 80 years or older (with or without additional risk factors). The average age was 81 years.
Overall, participants were at intermediate to low risk from surgery, with a median Society of Thoracic Surgeons (STS) risk score of 2.6%. However, researchers did not specify a particular risk score cutoff for enrollment.
“This allowed the trial to evolve along with changes in guidelines and practice regarding TAVR over the course of the study and to reflect physicians’ nuanced, real-world approach to considering risk in decision-making rather than taking a formulaic approach,” Toff said.
At 1 year, the rate of death from any cause (the primary endpoint) was 4.6% in the TAVR group and 6.6% in the surgery group, a difference that met the trial’s prespecified threshold for noninferiority of TAVR.
Rates of death from cardiovascular disease or stroke were also similar between the two groups.
Patients who received TAVR had a significantly higher rate of vascular complications (4.8%) than those receiving surgery (1.3%).
TAVR patients were also more likely to have a pacemaker implanted. This occurred in 12.2% of TAVR patients and 6.6% of those undergoing surgery.
In addition, patients who underwent TAVR had a higher rate of aortic regurgitation. Mild aortic regurgitation occurred at 1 year in 38.3% of the TAVR group and 11.7% of the surgery group, whereas moderate regurgitation occurred in 2.3% of TAVR patients and 0.6% of surgery patients.
On the other hand, patients undergoing TAVR had a significantly lower rate of major bleeding complications, which occurred in 6.3% of patients having TAVR and 17.1% of those undergoing surgery.
TAVR was also associated with a shorter hospital stay, fewer days in intensive care, and a faster improvement in functional capacity and quality of life. Functional capacity and quality-of-life measures at 6 weeks after the procedure were better in the TAVR group but by 1 year they were similar in the two groups.
“Longer follow-up is required to confirm sustained clinical benefit and valve durability to inform clinical practice, particularly in younger patients,” Toff concluded.
“The results from our trial and others are encouraging, but patients need to be fully informed and know that the long-term durability of the TAVR valves and the long-term implications of the increased risk of aortic regurgitation are still uncertain,” he added.
The researchers plan to continue to track outcomes for a minimum of 5 years.
Discussant of the UK TAVI trial at an ACC press conference, Julia Grapsa, MD, Guys and St Thomas NHS Trust, London, United Kingdom, said it was a well-designed study.
“It was impressive to see so many UK sites and the age range of patients from 70 to 91 years, and the shorter hospital stays and functional recoveries as well as reduced major bleeding in the TAVR group,” Grapsa said.
“But something that was very striking to me was the increase in moderate aortic regurgitation in the TAVR arm, 2.3% versus 0.6% in the surgical arm, so it is very important to keep following these patients long term,” she added.
In answer to a question during the main session about using age alone as an inclusion criterion in those over 80 years old, Toff said, “We were more comfortable taking all comers over 80 years of age because of the uncertainty about TAVR is more in relation to its durability and the clinical significance of the aortic regurgitation, which may have consequences in the longer term. But the longer term for the over 80s is obviously less of a problem than for those in their 70s.”
This study was funded by the UK National Institute for Health Research Health Technology Assessment Programme. Toff reports no disclosures.
American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC). Abstract 20-LB-20410-ACC. Presented March 29, 2020.
This article first appeared on Medscape.com.
Vaginal artesunate quells CIN 2/3 lesions, clears HPV
In a small study, a self-administered vaginal insert containing the antimalarial agent artesunate resolved cervical intraepithelial neoplasia (CIN) 2/3 lesions in two-thirds of patients and cleared human papillomavirus (HPV) genotypes in nearly half of women whose lesions disappeared.
Among 28 women with biopsy-confirmed CIN 2/3 who used the inserts prior to a planned standard-of-care resection, histologic regression of lesions occurred in 19 patients. In 9 of the 19 women, there was clearance of baseline HPV genotypes.
These results were reported in an abstract that had been slated for presentation at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer. The meeting was canceled because of the COVID-19 pandemic. The study results were also published in Gynecologic Oncology.
An unexpected treatment
“The implications of having a safe, inexpensive, self-administered, shelf-stable, nonsurgical treatment for HPV intraepithelial disease, not only here in the U.S., but also extending to low-resource settings,” are self-evident, said study author Cornelia L. Trimble, MD, of Johns Hopkins University in Baltimore.
“This could change the entire landscape of care,” Dr. Trimble said in an interview. “Who’d have thunk that a freaking Chinese herbal medicine derived from the bark of a tree could have this effect?”
Artesunate is a derivative of artemisinin, an antimalarial isolated from the plant Artemisia annua, which is used in traditional Chinese medicine. According to the Centers for Disease Control and Prevention, intravenous artesunate is the first-line drug for treatment of severe malaria in the United States.
However, artesunate is neither approved by the Food and Drug Administration nor commercially available in the United States. The CDC provides artesunate to U.S. clinicians on an as-needed basis.
In addition to its antimalarial activity, artesunate has been shown to have a cytotoxic effect on squamous cells transformed by HPV in vitro. Dr. Trimble and colleagues are also testing a topical form of the drug for the treatment of vulvar intraepithelial neoplasia.
Patients, dosing, and efficacy
In the current study, Dr. Trimble and colleagues enrolled adult immunocompetent women with CIN 2/3, visible residual lesions, and detectable HPV. The patients were assigned sequentially to one of four treatment groups: one 5-day cycle of 50-mg inserts or one, two, or three 5-day cycles using 200-mg inserts.
The patients were instructed to place the inserts at bedtime using a vaginal applicator, followed by a tampon, and then remove the inserts in the morning.
In a modified intention-to-treat analysis including all women who received at least one dose of artesunate and who had endpoint data available, 19 of 28 (67.9%) had histologic regression of CIN lesions. Of the 19 patients, 9 (47.4%) had clearance of all HPV genotypes that had been present at baseline.
Asked how the investigators could distinguish between the treatment effect of the inserts and spontaneous clearance of lesions seen as part of the natural history of CIN in some patients, Dr. Trimble pointed to two observations suggesting an immunologic effect from treatment.
Specifically, although there was lesion regression to CIN 1 or less in all treatment groups, the patients who had only a single treatment cycle had a longer time to regression than those who received two or three cycles.
Additionally, among the nine patients who had viral clearance, three had clearance at the same study time point where histologic regression was observed. For the other six patients, the virus did not clear until several weeks following lesion regression.
These two observations suggest the therapeutic effect of artesunate is recognized by the immune system, which may stimulate a localized immune-mediated cytotoxic effect, Dr. Trimble said.
Safety and next steps
The safety analysis showed that side effects were generally mild and well tolerated. There were 161 adverse events among 29 women for whom safety data were available. The most frequently reported adverse events were vaginal itching (n = 13), vaginal pain (n = 12), vaginal discharge (n = 8), spotting (n = 6), uterine cramping (n = 6), vaginal dryness (n = 4), pelvic pain (n = 1), perineal pain (n = 1), and dyspareunia (n = 1).
Grade 2 adverse events included vaginal yeast infection (n = 6), bacterial vaginosis (n = 2), vaginal inflammation (n = 2), urinary tract infection (n = 2), and noninfective cystitis (n = 1). There were no grade 3 or 4 adverse events reported, and three women reported no noticeable side effects.
Dr. Trimble and colleagues are continuing to study immune responses in cervical tissues and are examining the composition and functions of the cervicovaginal metagenome, looking at bacterial, viral, and fungal components. The team has joined with collaborators at the University of Texas MD Anderson Cancer Center in Houston to look for immune markers in longitudinally collected, subject-matched cervical swabs.
Frantz Viral Therapeutics supplied the artesunate vaginal inserts and partial financial support for this study. Dr. Trimble disclosed relationships with a range of companies and organizations outside this work.
SOURCE: Trimble C L et al. SGO 2020, Abstract LBA 1.
In a small study, a self-administered vaginal insert containing the antimalarial agent artesunate resolved cervical intraepithelial neoplasia (CIN) 2/3 lesions in two-thirds of patients and cleared human papillomavirus (HPV) genotypes in nearly half of women whose lesions disappeared.
Among 28 women with biopsy-confirmed CIN 2/3 who used the inserts prior to a planned standard-of-care resection, histologic regression of lesions occurred in 19 patients. In 9 of the 19 women, there was clearance of baseline HPV genotypes.
These results were reported in an abstract that had been slated for presentation at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer. The meeting was canceled because of the COVID-19 pandemic. The study results were also published in Gynecologic Oncology.
An unexpected treatment
“The implications of having a safe, inexpensive, self-administered, shelf-stable, nonsurgical treatment for HPV intraepithelial disease, not only here in the U.S., but also extending to low-resource settings,” are self-evident, said study author Cornelia L. Trimble, MD, of Johns Hopkins University in Baltimore.
“This could change the entire landscape of care,” Dr. Trimble said in an interview. “Who’d have thunk that a freaking Chinese herbal medicine derived from the bark of a tree could have this effect?”
Artesunate is a derivative of artemisinin, an antimalarial isolated from the plant Artemisia annua, which is used in traditional Chinese medicine. According to the Centers for Disease Control and Prevention, intravenous artesunate is the first-line drug for treatment of severe malaria in the United States.
However, artesunate is neither approved by the Food and Drug Administration nor commercially available in the United States. The CDC provides artesunate to U.S. clinicians on an as-needed basis.
In addition to its antimalarial activity, artesunate has been shown to have a cytotoxic effect on squamous cells transformed by HPV in vitro. Dr. Trimble and colleagues are also testing a topical form of the drug for the treatment of vulvar intraepithelial neoplasia.
Patients, dosing, and efficacy
In the current study, Dr. Trimble and colleagues enrolled adult immunocompetent women with CIN 2/3, visible residual lesions, and detectable HPV. The patients were assigned sequentially to one of four treatment groups: one 5-day cycle of 50-mg inserts or one, two, or three 5-day cycles using 200-mg inserts.
The patients were instructed to place the inserts at bedtime using a vaginal applicator, followed by a tampon, and then remove the inserts in the morning.
In a modified intention-to-treat analysis including all women who received at least one dose of artesunate and who had endpoint data available, 19 of 28 (67.9%) had histologic regression of CIN lesions. Of the 19 patients, 9 (47.4%) had clearance of all HPV genotypes that had been present at baseline.
Asked how the investigators could distinguish between the treatment effect of the inserts and spontaneous clearance of lesions seen as part of the natural history of CIN in some patients, Dr. Trimble pointed to two observations suggesting an immunologic effect from treatment.
Specifically, although there was lesion regression to CIN 1 or less in all treatment groups, the patients who had only a single treatment cycle had a longer time to regression than those who received two or three cycles.
Additionally, among the nine patients who had viral clearance, three had clearance at the same study time point where histologic regression was observed. For the other six patients, the virus did not clear until several weeks following lesion regression.
These two observations suggest the therapeutic effect of artesunate is recognized by the immune system, which may stimulate a localized immune-mediated cytotoxic effect, Dr. Trimble said.
Safety and next steps
The safety analysis showed that side effects were generally mild and well tolerated. There were 161 adverse events among 29 women for whom safety data were available. The most frequently reported adverse events were vaginal itching (n = 13), vaginal pain (n = 12), vaginal discharge (n = 8), spotting (n = 6), uterine cramping (n = 6), vaginal dryness (n = 4), pelvic pain (n = 1), perineal pain (n = 1), and dyspareunia (n = 1).
Grade 2 adverse events included vaginal yeast infection (n = 6), bacterial vaginosis (n = 2), vaginal inflammation (n = 2), urinary tract infection (n = 2), and noninfective cystitis (n = 1). There were no grade 3 or 4 adverse events reported, and three women reported no noticeable side effects.
Dr. Trimble and colleagues are continuing to study immune responses in cervical tissues and are examining the composition and functions of the cervicovaginal metagenome, looking at bacterial, viral, and fungal components. The team has joined with collaborators at the University of Texas MD Anderson Cancer Center in Houston to look for immune markers in longitudinally collected, subject-matched cervical swabs.
Frantz Viral Therapeutics supplied the artesunate vaginal inserts and partial financial support for this study. Dr. Trimble disclosed relationships with a range of companies and organizations outside this work.
SOURCE: Trimble C L et al. SGO 2020, Abstract LBA 1.
In a small study, a self-administered vaginal insert containing the antimalarial agent artesunate resolved cervical intraepithelial neoplasia (CIN) 2/3 lesions in two-thirds of patients and cleared human papillomavirus (HPV) genotypes in nearly half of women whose lesions disappeared.
Among 28 women with biopsy-confirmed CIN 2/3 who used the inserts prior to a planned standard-of-care resection, histologic regression of lesions occurred in 19 patients. In 9 of the 19 women, there was clearance of baseline HPV genotypes.
These results were reported in an abstract that had been slated for presentation at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer. The meeting was canceled because of the COVID-19 pandemic. The study results were also published in Gynecologic Oncology.
An unexpected treatment
“The implications of having a safe, inexpensive, self-administered, shelf-stable, nonsurgical treatment for HPV intraepithelial disease, not only here in the U.S., but also extending to low-resource settings,” are self-evident, said study author Cornelia L. Trimble, MD, of Johns Hopkins University in Baltimore.
“This could change the entire landscape of care,” Dr. Trimble said in an interview. “Who’d have thunk that a freaking Chinese herbal medicine derived from the bark of a tree could have this effect?”
Artesunate is a derivative of artemisinin, an antimalarial isolated from the plant Artemisia annua, which is used in traditional Chinese medicine. According to the Centers for Disease Control and Prevention, intravenous artesunate is the first-line drug for treatment of severe malaria in the United States.
However, artesunate is neither approved by the Food and Drug Administration nor commercially available in the United States. The CDC provides artesunate to U.S. clinicians on an as-needed basis.
In addition to its antimalarial activity, artesunate has been shown to have a cytotoxic effect on squamous cells transformed by HPV in vitro. Dr. Trimble and colleagues are also testing a topical form of the drug for the treatment of vulvar intraepithelial neoplasia.
Patients, dosing, and efficacy
In the current study, Dr. Trimble and colleagues enrolled adult immunocompetent women with CIN 2/3, visible residual lesions, and detectable HPV. The patients were assigned sequentially to one of four treatment groups: one 5-day cycle of 50-mg inserts or one, two, or three 5-day cycles using 200-mg inserts.
The patients were instructed to place the inserts at bedtime using a vaginal applicator, followed by a tampon, and then remove the inserts in the morning.
In a modified intention-to-treat analysis including all women who received at least one dose of artesunate and who had endpoint data available, 19 of 28 (67.9%) had histologic regression of CIN lesions. Of the 19 patients, 9 (47.4%) had clearance of all HPV genotypes that had been present at baseline.
Asked how the investigators could distinguish between the treatment effect of the inserts and spontaneous clearance of lesions seen as part of the natural history of CIN in some patients, Dr. Trimble pointed to two observations suggesting an immunologic effect from treatment.
Specifically, although there was lesion regression to CIN 1 or less in all treatment groups, the patients who had only a single treatment cycle had a longer time to regression than those who received two or three cycles.
Additionally, among the nine patients who had viral clearance, three had clearance at the same study time point where histologic regression was observed. For the other six patients, the virus did not clear until several weeks following lesion regression.
These two observations suggest the therapeutic effect of artesunate is recognized by the immune system, which may stimulate a localized immune-mediated cytotoxic effect, Dr. Trimble said.
Safety and next steps
The safety analysis showed that side effects were generally mild and well tolerated. There were 161 adverse events among 29 women for whom safety data were available. The most frequently reported adverse events were vaginal itching (n = 13), vaginal pain (n = 12), vaginal discharge (n = 8), spotting (n = 6), uterine cramping (n = 6), vaginal dryness (n = 4), pelvic pain (n = 1), perineal pain (n = 1), and dyspareunia (n = 1).
Grade 2 adverse events included vaginal yeast infection (n = 6), bacterial vaginosis (n = 2), vaginal inflammation (n = 2), urinary tract infection (n = 2), and noninfective cystitis (n = 1). There were no grade 3 or 4 adverse events reported, and three women reported no noticeable side effects.
Dr. Trimble and colleagues are continuing to study immune responses in cervical tissues and are examining the composition and functions of the cervicovaginal metagenome, looking at bacterial, viral, and fungal components. The team has joined with collaborators at the University of Texas MD Anderson Cancer Center in Houston to look for immune markers in longitudinally collected, subject-matched cervical swabs.
Frantz Viral Therapeutics supplied the artesunate vaginal inserts and partial financial support for this study. Dr. Trimble disclosed relationships with a range of companies and organizations outside this work.
SOURCE: Trimble C L et al. SGO 2020, Abstract LBA 1.
FROM SGO 2020
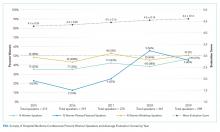
The Society of Hospital Medicine’s Commitment to Increasing Academic Representation for Women and Underrepresented Groups in Medicine: A Good Start
Documentation of gender-based disparities in medicine often focus on lower numbers of women in prominent positions as evidence of inequality and inequity; examples include lower proportion of women physicians as conference speakers,1 first and last authors of manuscripts,2 invited editorials,3 award recipients,4 grant recipients,5 medical society leadership,6 editorial boards,7 and presenters at grand rounds.8 Notably, these disparities are likely greater for intersectional physicians, who experience bias through multiple lenses of disadvantage.9 While the scarcity of women and marginalized populations in leadership roles in medicine provides convincing evidence that inequality exists, the underrepresentation of women and other marginalized physicians in prominent positions is also a cause of continued disparity. Fewer academic opportunities for women physicians and other underrepresented physician groups in medicine may perpetuate slower career advancement10 and contribute to less availability of mentors and sponsors.11 Less obviously, underrepresentation also unintentionally and explicitly signals to junior faculty from marginalized groups that they are not welcome and are unlikely to be successful.9,12
Improving representation of women in other fields has been demonstrated to reduce implicit and explicit sexism.13,14 Increasing diversity in academic leadership is likely to further improve diversity at all levels,9,15 which may in turn reduce gaps in health outcomes seen for marginalized patients.16-18 Measuring and eliminating bias that disadvantages underrepresented physicians in academic opportunities is a moral imperative for institutions and organizations. For this reason, the Society of Hospital Medicine (SHM) has been attempting to address this issue within its organizational structure, publications, and conference presenters.19
The first step for an organization that aims to increase representation of women and other marginalized groups in medicine is to assess the current representation of leadership and opportunities.20 If data are available, this review should include intersectional measurement of other axes of discrimination. Rapid analysis of large data sets of names is feasible using freely available computer algorithms, for example.21 Only once a baseline understanding of representation within an organization is established can identification of goals and areas of improvement and evaluation of efforts to increase representation begin. Reporting this data to the organization’s membership should be undertaken to increase the accountability of leadership to reduce gaps. This work is currently underway at the Journal of Hospital Medicine and within the Society of Hospital Medicine.19
This month’s issue of the Journal of Hospital Medicine includes an article written by Northcutt, et al that describes one such attempt, focusing on representation of conference speakers at SHM’s Annual Meeting. In this study, authors performed a pre- and postintervention analysis of an open call system for selecting didactic speakers for the SHM Annual Meeting. The open call system, implemented for the 2019 SHM Annual Meeting, invited all members to apply for a didactic session. The planning committee then utilized a standardized evaluation form to determine the final speaker list. In previous years, didactic speakers did not apply but were invited and were not formally evaluated. Northcutt et al report that this intervention was associated with a significant increase in the proportion of women conference speakers.22
The Northcutt article and the open call and evaluation system is one example of an intentional adjustment to the speaker selection process aimed at recruiting more diverse presenters. Other examples of intentional efforts to increase diversity within conferences include using curated lists designed to improve representation or contacting other national organizations for recommendations. 20 Efforts such as these are necessary because men in medicine are more likely to volunteer for prominent positions than women,23 meaning that any system of recruitment or allocation of academic opportunities that relies on self-promotion is likely to perpetuate underrepresentation. Using pre-existing speakers list or previous programs will also support ongoing disparities, because men have traditionally represented the majority of speakers.
Of course, conferences are an important and public representation of a society, but are only the starting point for working towards equity within a large organization such as SHM. Similar efforts must be directed towards authorship in SHM publications, representation on editorial boards, society leadership and employment opportunities. Once organizations have an established baseline around publications, leadership recruitment, and employment representation, a review of recruitment policies (for articles, speakers, leaders, and employees) should then be conducted, looking for areas that lead to bias.
Planning committees, editorial boards, and society leadership groups should also intentionally increase their own diversity, as increasing the proportion of women on a convening committee has been demonstrated to increase the number of invited women speakers.15,24 In addition, committees can adopt a mandate to increase diversity in invited speakers, editorials, and authorship; for example, direct instruction to avoid all-male panels led a conference planning committee to invite more women and increased the numbers of women speakers.25 A speaker, authorship, or editorial policy that emphasizes diversity and inclusion should be developed and made available to the organization’s membership.26
Finally, there is evidence that implicit bias training for editorial boards and conference planning committees may be effective.27 Implicit bias training emphasizes that judgements of merit and skill are often subjective and based on in-group membership rather than the quality of applicants.9 For example, underrepresentation of women at a neuroimmunology conference was not explained by quantity or impact of previous publications,28 and evaluation scores for the Society for Hospital Medicine’s Annual Meeting have increased as the proportion of women speakers has increased, suggesting that the presence of women presenters was associated with better presentations. To address concerns about how diversity and inclusion efforts may influence the quality of speakers and authors,29 objective criteria could be developed in advance of a selection process and candidates should be held to the same standard.30 The use of objective evaluation criteria in the selection of conference speakers has also been associated with increasing the proportion of women conference speakers. All in all, SHM’s efforts (and Northcutt’s work) should be lauded but also recognized as what they are: a good start. Continued vigilance focused on equity is the only way to ensure that the move towards greater representation continues.
1. Ruzycki SM, Fletcher S, Earp M, Bharwani A, Lithgow KC. Trends in the proportion of female speakers at medical conferences in the United States and in Canada, 2007 to 2017. JAMA Netw Open. 2019;2(4):e192103. https://doi.org/ 10.1001/jamanetworkopen.2019.2103.
2. Penn CA, Ebott JA, Larach DB, Hesson AM, Waljee JF, Larach MG. The gender authorship gap in gynecologic oncology research. Gynecol Oncol Rep. 2019;29:83-84. https://doi.org/10.1016/j.gore.2019.07.011.
3. Thomas EG, Jayabalasingham B, Collins T, Geertzen J, Bui C, Dominici F. Gender disparities in invited commentary authorship in 2459 medical journals. JAMA Netw Open. 2019;2(10):e1913682.https://doi.org/10.1001/jamanetworkopen.2019.13682.
4. Silver JK, Slocum CS, Bank AM, et al. Where are the women? The underrepresentation of women physicians among recognition award recipients from medical specialty societies. PM R. 2017;9(8):804-815. https://doi.org/ 10.1016/j.pmrj.2017.06.001.
5. Burns KEA, Straus SE, Liu K, Rizv, L, Guyatt G. Gender differences in grant and personnel award funding rates at the Canadian Institute of Health Research based on research content area: a retrospective analysis. PLoS Med. 2019;16(10):e1002935. https://doi.org/ 10.1371/journal.pmed.1002935.
6. Silver JK, Ghalib R, Poorman JA, Al-Assi D, Parangi S, Bhargava H, et al. Analysis of gender equity in leadership of physician-focused medical specialty societies, 2008-2017analysis of gender equity in leadership of physician-focused medical specialty societies, 2008-2017. JAMA Internal Medicine. 2019;179(3):433-435. https://doi.org/10.1001/jamainternmed.2018.5303.
7. Erren TC, Groß JV, Shaw DM, Selle B. Representation of women as authors, reviewers, editors in chief, and editorial board members at 6 general medical journals in 2010 and 2011. JAMA Intern Med. 2014;174(4):633-635. https://doi.org/ 10.1001/jamainternmed.2013.14760.
8. Files JA, Mayer AP, Ko MG, et al. Speaker introductions at internal medicine grand rounds: forms of address reveal gender bias. J Womens Health (Larchmt). 2017;26(5):413-419. https://doi.org/ 10.1089/jwh.2016.6044.
9. Price EG, Gozu A, Kern DE, et al. The role of cultural diversity climate in recruitment, promotion, and retention of faculty in academic medicine. J Gen Intern Med. 2005;20(7):565-571. https://doi.org/10.1111/j.1525-1497.2005.0127.x.
10. Carr PL, Gunn CM, Kaplan SA, Raj A, Freund KM. Inadequate progress for women in academic medicine: findings from the National Faculty Study. J Womens Health (Larchmt). 2015;24(3):190-199. https://doi.org/10.1089/jwh.2014.4848.
11. Farkas AH, Bonifacino E, Turner R, Tilstra SA, Corbelli JA. Mentorship of women in academic medicine: a systematic review. J Gen Intern Med. 2019;34(7):1322-1329. https://doi.org/10.1007/s11606-019-04955-2.
12. Pololi L, Cooper LA, Carr P. Race, disadvantage and faculty experiences in academic medicine. J Gen Intern Med. 2010;25(12):1363-1369. https://doi.org/10.1007/s11606-010-1478-7.
13. Beaman L CR, Duflo E, Pande R, Topalova P. Powerful women: does exposure reduce bias? Q J Econ. 2009;124(4):1497-1540.
14. Mansbridge J. Should Blacks represent Blacks and women represent women? A contingent “Yes”. J Polit. 1999;61(3):628-657. https://doi.org/ https://doi.org/10.2307/2647821.
15. Lithgow KC, Fletcher, S., Earp, M.E., Bharwani, A., Ruzycki, S.M. Association between the proprtion of women on a conference planning committee and the proportion of women conference speakers at medical conferences. JAMA Netw Open. 2020; In press.
16. Alsan M, Garrick, O., Graziani, G.C. Does diversity matter for health? Experimental evidence from Oakland. National Bureau of Economic Research. 2018.
17. Greenwood BN, Carnahan, S., Huang, L. Patient–physician gender concordance and increased mortality among female heart attack patients. Proc Natl Acad Sci USA. 2018;115(34):8569-8574. https://doi.org/10.1073/pnas.1800097115.
18. Silver JK, Bean AC, Slocum C, et al. Physician Workforce Disparities and Patient Care: A Narrative Review. Health Equity. 2019;3(1):360-777. https://doi.org/10.1089/heq.2019.0040.
19. Shah SS, Shaughnessy, E.E., Spector, N.D. Leading by example: How medical journals can improve representation in academic medicine. J Hos Med. 2019;14(7):393. https://doi.org/10.12788/jhm.3247.
20. Martin JL. Ten simple rules to achieve conference speaker gender balance. PLoS Comput Biol. 2014;10(11):e1003903. https://doi.org/ 10.1371/journal.pcbi.1003903.
21. Sumner J. The Gender Balance Assessment Tool (GBAT): a web-based tool for estimating gender balance in syllabi and bibliographies. Polit Sci Polit. 2018;2(51):396-400. https://doi.org/10.1017/S1049096517002074.
22. Northcutt N, Papp S, Keniston A, et al; on behalf of the Society of Hospital Medicine Diversity, Equity and Inclusion Special Interest Group. SPEAKers at the National Society of Hospital Medicine Meeting: A Follow-UP Study of Gender Equity for Conference Speakers from 2015 to 2019. The SPEAK Up Study. J Hosp Med. 2020;15(4):228-231. https://doi.org/10.12788/jhm.3401.
23. Wayne NL, Vermillion M, Uijtdehaage S. Gender differences in leadership amongst first-year medical students in the small-group setting. Acad Med. 2010;85(8):1276-1281. https://doi.org/10.1097/ACM.0b013e3181e5f2ce
24. Casadevall A, Handelsman J. The presence of female conveners correlates with a higher proportion of female speakers at scientific symposia. MBio. 2014;5(1):e00846-13. https://doi.org/10.1128/mBio.00846-13.25. Casadevall A. Achieving speaker gender equity at the American Society for Microbiology General Meeting. MBio. 2015;6(4):e01146. https://doi.org/10.1128/mBio.01146-15.
26. Health NIo. Guidelines for the inclusion of women, minorities, and persons with disabilities in NIH-supported conference grats 2003. https://grants.nih.gov/grants/guide/notice-files/NOT-OD-03-066.html. Accessed March 12, 2019.
27. Devine PG, Forscher PS, Cox WTL, Kaatz A, Sheridan J, Carnes M. A gender bias habit-breaking intervention led to increased hiring of female faculty in STEMM departments. J Exp Soc Psychol. 2017;73:211-215. https://doi.org/10.1016/j.jesp.2017.07.002.
28. Klein RS, Voskuhl, R, Segal BM, et al. Speaking out about gender imbalance in invited speakers improves diversity. Nat Immunol. 201;18(5):475-478. https://doi.org/10.1038/ni.3707.
29. Borrero-Mejias C, Starling AJ, Burch R, Loder E. Ten (Eleven) things not to say to your female colleagues. Headache. 2019;59(10):1846-1854. https://doi.org/10.1111/head.13647.
30. Bandiera G, Abrahams C, Ruetalo M, Hanson MD, Nickell L, Spadafora S. Identifying and promoting best practices in residency application and selection in a complex academic health network. Acad Med. 2015;90(12):1594-1601. https://doi.org/10.1097/ACM.0000000000000954.
Documentation of gender-based disparities in medicine often focus on lower numbers of women in prominent positions as evidence of inequality and inequity; examples include lower proportion of women physicians as conference speakers,1 first and last authors of manuscripts,2 invited editorials,3 award recipients,4 grant recipients,5 medical society leadership,6 editorial boards,7 and presenters at grand rounds.8 Notably, these disparities are likely greater for intersectional physicians, who experience bias through multiple lenses of disadvantage.9 While the scarcity of women and marginalized populations in leadership roles in medicine provides convincing evidence that inequality exists, the underrepresentation of women and other marginalized physicians in prominent positions is also a cause of continued disparity. Fewer academic opportunities for women physicians and other underrepresented physician groups in medicine may perpetuate slower career advancement10 and contribute to less availability of mentors and sponsors.11 Less obviously, underrepresentation also unintentionally and explicitly signals to junior faculty from marginalized groups that they are not welcome and are unlikely to be successful.9,12
Improving representation of women in other fields has been demonstrated to reduce implicit and explicit sexism.13,14 Increasing diversity in academic leadership is likely to further improve diversity at all levels,9,15 which may in turn reduce gaps in health outcomes seen for marginalized patients.16-18 Measuring and eliminating bias that disadvantages underrepresented physicians in academic opportunities is a moral imperative for institutions and organizations. For this reason, the Society of Hospital Medicine (SHM) has been attempting to address this issue within its organizational structure, publications, and conference presenters.19
The first step for an organization that aims to increase representation of women and other marginalized groups in medicine is to assess the current representation of leadership and opportunities.20 If data are available, this review should include intersectional measurement of other axes of discrimination. Rapid analysis of large data sets of names is feasible using freely available computer algorithms, for example.21 Only once a baseline understanding of representation within an organization is established can identification of goals and areas of improvement and evaluation of efforts to increase representation begin. Reporting this data to the organization’s membership should be undertaken to increase the accountability of leadership to reduce gaps. This work is currently underway at the Journal of Hospital Medicine and within the Society of Hospital Medicine.19
This month’s issue of the Journal of Hospital Medicine includes an article written by Northcutt, et al that describes one such attempt, focusing on representation of conference speakers at SHM’s Annual Meeting. In this study, authors performed a pre- and postintervention analysis of an open call system for selecting didactic speakers for the SHM Annual Meeting. The open call system, implemented for the 2019 SHM Annual Meeting, invited all members to apply for a didactic session. The planning committee then utilized a standardized evaluation form to determine the final speaker list. In previous years, didactic speakers did not apply but were invited and were not formally evaluated. Northcutt et al report that this intervention was associated with a significant increase in the proportion of women conference speakers.22
The Northcutt article and the open call and evaluation system is one example of an intentional adjustment to the speaker selection process aimed at recruiting more diverse presenters. Other examples of intentional efforts to increase diversity within conferences include using curated lists designed to improve representation or contacting other national organizations for recommendations. 20 Efforts such as these are necessary because men in medicine are more likely to volunteer for prominent positions than women,23 meaning that any system of recruitment or allocation of academic opportunities that relies on self-promotion is likely to perpetuate underrepresentation. Using pre-existing speakers list or previous programs will also support ongoing disparities, because men have traditionally represented the majority of speakers.
Of course, conferences are an important and public representation of a society, but are only the starting point for working towards equity within a large organization such as SHM. Similar efforts must be directed towards authorship in SHM publications, representation on editorial boards, society leadership and employment opportunities. Once organizations have an established baseline around publications, leadership recruitment, and employment representation, a review of recruitment policies (for articles, speakers, leaders, and employees) should then be conducted, looking for areas that lead to bias.
Planning committees, editorial boards, and society leadership groups should also intentionally increase their own diversity, as increasing the proportion of women on a convening committee has been demonstrated to increase the number of invited women speakers.15,24 In addition, committees can adopt a mandate to increase diversity in invited speakers, editorials, and authorship; for example, direct instruction to avoid all-male panels led a conference planning committee to invite more women and increased the numbers of women speakers.25 A speaker, authorship, or editorial policy that emphasizes diversity and inclusion should be developed and made available to the organization’s membership.26
Finally, there is evidence that implicit bias training for editorial boards and conference planning committees may be effective.27 Implicit bias training emphasizes that judgements of merit and skill are often subjective and based on in-group membership rather than the quality of applicants.9 For example, underrepresentation of women at a neuroimmunology conference was not explained by quantity or impact of previous publications,28 and evaluation scores for the Society for Hospital Medicine’s Annual Meeting have increased as the proportion of women speakers has increased, suggesting that the presence of women presenters was associated with better presentations. To address concerns about how diversity and inclusion efforts may influence the quality of speakers and authors,29 objective criteria could be developed in advance of a selection process and candidates should be held to the same standard.30 The use of objective evaluation criteria in the selection of conference speakers has also been associated with increasing the proportion of women conference speakers. All in all, SHM’s efforts (and Northcutt’s work) should be lauded but also recognized as what they are: a good start. Continued vigilance focused on equity is the only way to ensure that the move towards greater representation continues.
Documentation of gender-based disparities in medicine often focus on lower numbers of women in prominent positions as evidence of inequality and inequity; examples include lower proportion of women physicians as conference speakers,1 first and last authors of manuscripts,2 invited editorials,3 award recipients,4 grant recipients,5 medical society leadership,6 editorial boards,7 and presenters at grand rounds.8 Notably, these disparities are likely greater for intersectional physicians, who experience bias through multiple lenses of disadvantage.9 While the scarcity of women and marginalized populations in leadership roles in medicine provides convincing evidence that inequality exists, the underrepresentation of women and other marginalized physicians in prominent positions is also a cause of continued disparity. Fewer academic opportunities for women physicians and other underrepresented physician groups in medicine may perpetuate slower career advancement10 and contribute to less availability of mentors and sponsors.11 Less obviously, underrepresentation also unintentionally and explicitly signals to junior faculty from marginalized groups that they are not welcome and are unlikely to be successful.9,12
Improving representation of women in other fields has been demonstrated to reduce implicit and explicit sexism.13,14 Increasing diversity in academic leadership is likely to further improve diversity at all levels,9,15 which may in turn reduce gaps in health outcomes seen for marginalized patients.16-18 Measuring and eliminating bias that disadvantages underrepresented physicians in academic opportunities is a moral imperative for institutions and organizations. For this reason, the Society of Hospital Medicine (SHM) has been attempting to address this issue within its organizational structure, publications, and conference presenters.19
The first step for an organization that aims to increase representation of women and other marginalized groups in medicine is to assess the current representation of leadership and opportunities.20 If data are available, this review should include intersectional measurement of other axes of discrimination. Rapid analysis of large data sets of names is feasible using freely available computer algorithms, for example.21 Only once a baseline understanding of representation within an organization is established can identification of goals and areas of improvement and evaluation of efforts to increase representation begin. Reporting this data to the organization’s membership should be undertaken to increase the accountability of leadership to reduce gaps. This work is currently underway at the Journal of Hospital Medicine and within the Society of Hospital Medicine.19
This month’s issue of the Journal of Hospital Medicine includes an article written by Northcutt, et al that describes one such attempt, focusing on representation of conference speakers at SHM’s Annual Meeting. In this study, authors performed a pre- and postintervention analysis of an open call system for selecting didactic speakers for the SHM Annual Meeting. The open call system, implemented for the 2019 SHM Annual Meeting, invited all members to apply for a didactic session. The planning committee then utilized a standardized evaluation form to determine the final speaker list. In previous years, didactic speakers did not apply but were invited and were not formally evaluated. Northcutt et al report that this intervention was associated with a significant increase in the proportion of women conference speakers.22
The Northcutt article and the open call and evaluation system is one example of an intentional adjustment to the speaker selection process aimed at recruiting more diverse presenters. Other examples of intentional efforts to increase diversity within conferences include using curated lists designed to improve representation or contacting other national organizations for recommendations. 20 Efforts such as these are necessary because men in medicine are more likely to volunteer for prominent positions than women,23 meaning that any system of recruitment or allocation of academic opportunities that relies on self-promotion is likely to perpetuate underrepresentation. Using pre-existing speakers list or previous programs will also support ongoing disparities, because men have traditionally represented the majority of speakers.
Of course, conferences are an important and public representation of a society, but are only the starting point for working towards equity within a large organization such as SHM. Similar efforts must be directed towards authorship in SHM publications, representation on editorial boards, society leadership and employment opportunities. Once organizations have an established baseline around publications, leadership recruitment, and employment representation, a review of recruitment policies (for articles, speakers, leaders, and employees) should then be conducted, looking for areas that lead to bias.
Planning committees, editorial boards, and society leadership groups should also intentionally increase their own diversity, as increasing the proportion of women on a convening committee has been demonstrated to increase the number of invited women speakers.15,24 In addition, committees can adopt a mandate to increase diversity in invited speakers, editorials, and authorship; for example, direct instruction to avoid all-male panels led a conference planning committee to invite more women and increased the numbers of women speakers.25 A speaker, authorship, or editorial policy that emphasizes diversity and inclusion should be developed and made available to the organization’s membership.26
Finally, there is evidence that implicit bias training for editorial boards and conference planning committees may be effective.27 Implicit bias training emphasizes that judgements of merit and skill are often subjective and based on in-group membership rather than the quality of applicants.9 For example, underrepresentation of women at a neuroimmunology conference was not explained by quantity or impact of previous publications,28 and evaluation scores for the Society for Hospital Medicine’s Annual Meeting have increased as the proportion of women speakers has increased, suggesting that the presence of women presenters was associated with better presentations. To address concerns about how diversity and inclusion efforts may influence the quality of speakers and authors,29 objective criteria could be developed in advance of a selection process and candidates should be held to the same standard.30 The use of objective evaluation criteria in the selection of conference speakers has also been associated with increasing the proportion of women conference speakers. All in all, SHM’s efforts (and Northcutt’s work) should be lauded but also recognized as what they are: a good start. Continued vigilance focused on equity is the only way to ensure that the move towards greater representation continues.
1. Ruzycki SM, Fletcher S, Earp M, Bharwani A, Lithgow KC. Trends in the proportion of female speakers at medical conferences in the United States and in Canada, 2007 to 2017. JAMA Netw Open. 2019;2(4):e192103. https://doi.org/ 10.1001/jamanetworkopen.2019.2103.
2. Penn CA, Ebott JA, Larach DB, Hesson AM, Waljee JF, Larach MG. The gender authorship gap in gynecologic oncology research. Gynecol Oncol Rep. 2019;29:83-84. https://doi.org/10.1016/j.gore.2019.07.011.
3. Thomas EG, Jayabalasingham B, Collins T, Geertzen J, Bui C, Dominici F. Gender disparities in invited commentary authorship in 2459 medical journals. JAMA Netw Open. 2019;2(10):e1913682.https://doi.org/10.1001/jamanetworkopen.2019.13682.
4. Silver JK, Slocum CS, Bank AM, et al. Where are the women? The underrepresentation of women physicians among recognition award recipients from medical specialty societies. PM R. 2017;9(8):804-815. https://doi.org/ 10.1016/j.pmrj.2017.06.001.
5. Burns KEA, Straus SE, Liu K, Rizv, L, Guyatt G. Gender differences in grant and personnel award funding rates at the Canadian Institute of Health Research based on research content area: a retrospective analysis. PLoS Med. 2019;16(10):e1002935. https://doi.org/ 10.1371/journal.pmed.1002935.
6. Silver JK, Ghalib R, Poorman JA, Al-Assi D, Parangi S, Bhargava H, et al. Analysis of gender equity in leadership of physician-focused medical specialty societies, 2008-2017analysis of gender equity in leadership of physician-focused medical specialty societies, 2008-2017. JAMA Internal Medicine. 2019;179(3):433-435. https://doi.org/10.1001/jamainternmed.2018.5303.
7. Erren TC, Groß JV, Shaw DM, Selle B. Representation of women as authors, reviewers, editors in chief, and editorial board members at 6 general medical journals in 2010 and 2011. JAMA Intern Med. 2014;174(4):633-635. https://doi.org/ 10.1001/jamainternmed.2013.14760.
8. Files JA, Mayer AP, Ko MG, et al. Speaker introductions at internal medicine grand rounds: forms of address reveal gender bias. J Womens Health (Larchmt). 2017;26(5):413-419. https://doi.org/ 10.1089/jwh.2016.6044.
9. Price EG, Gozu A, Kern DE, et al. The role of cultural diversity climate in recruitment, promotion, and retention of faculty in academic medicine. J Gen Intern Med. 2005;20(7):565-571. https://doi.org/10.1111/j.1525-1497.2005.0127.x.
10. Carr PL, Gunn CM, Kaplan SA, Raj A, Freund KM. Inadequate progress for women in academic medicine: findings from the National Faculty Study. J Womens Health (Larchmt). 2015;24(3):190-199. https://doi.org/10.1089/jwh.2014.4848.
11. Farkas AH, Bonifacino E, Turner R, Tilstra SA, Corbelli JA. Mentorship of women in academic medicine: a systematic review. J Gen Intern Med. 2019;34(7):1322-1329. https://doi.org/10.1007/s11606-019-04955-2.
12. Pololi L, Cooper LA, Carr P. Race, disadvantage and faculty experiences in academic medicine. J Gen Intern Med. 2010;25(12):1363-1369. https://doi.org/10.1007/s11606-010-1478-7.
13. Beaman L CR, Duflo E, Pande R, Topalova P. Powerful women: does exposure reduce bias? Q J Econ. 2009;124(4):1497-1540.
14. Mansbridge J. Should Blacks represent Blacks and women represent women? A contingent “Yes”. J Polit. 1999;61(3):628-657. https://doi.org/ https://doi.org/10.2307/2647821.
15. Lithgow KC, Fletcher, S., Earp, M.E., Bharwani, A., Ruzycki, S.M. Association between the proprtion of women on a conference planning committee and the proportion of women conference speakers at medical conferences. JAMA Netw Open. 2020; In press.
16. Alsan M, Garrick, O., Graziani, G.C. Does diversity matter for health? Experimental evidence from Oakland. National Bureau of Economic Research. 2018.
17. Greenwood BN, Carnahan, S., Huang, L. Patient–physician gender concordance and increased mortality among female heart attack patients. Proc Natl Acad Sci USA. 2018;115(34):8569-8574. https://doi.org/10.1073/pnas.1800097115.
18. Silver JK, Bean AC, Slocum C, et al. Physician Workforce Disparities and Patient Care: A Narrative Review. Health Equity. 2019;3(1):360-777. https://doi.org/10.1089/heq.2019.0040.
19. Shah SS, Shaughnessy, E.E., Spector, N.D. Leading by example: How medical journals can improve representation in academic medicine. J Hos Med. 2019;14(7):393. https://doi.org/10.12788/jhm.3247.
20. Martin JL. Ten simple rules to achieve conference speaker gender balance. PLoS Comput Biol. 2014;10(11):e1003903. https://doi.org/ 10.1371/journal.pcbi.1003903.
21. Sumner J. The Gender Balance Assessment Tool (GBAT): a web-based tool for estimating gender balance in syllabi and bibliographies. Polit Sci Polit. 2018;2(51):396-400. https://doi.org/10.1017/S1049096517002074.
22. Northcutt N, Papp S, Keniston A, et al; on behalf of the Society of Hospital Medicine Diversity, Equity and Inclusion Special Interest Group. SPEAKers at the National Society of Hospital Medicine Meeting: A Follow-UP Study of Gender Equity for Conference Speakers from 2015 to 2019. The SPEAK Up Study. J Hosp Med. 2020;15(4):228-231. https://doi.org/10.12788/jhm.3401.
23. Wayne NL, Vermillion M, Uijtdehaage S. Gender differences in leadership amongst first-year medical students in the small-group setting. Acad Med. 2010;85(8):1276-1281. https://doi.org/10.1097/ACM.0b013e3181e5f2ce
24. Casadevall A, Handelsman J. The presence of female conveners correlates with a higher proportion of female speakers at scientific symposia. MBio. 2014;5(1):e00846-13. https://doi.org/10.1128/mBio.00846-13.25. Casadevall A. Achieving speaker gender equity at the American Society for Microbiology General Meeting. MBio. 2015;6(4):e01146. https://doi.org/10.1128/mBio.01146-15.
26. Health NIo. Guidelines for the inclusion of women, minorities, and persons with disabilities in NIH-supported conference grats 2003. https://grants.nih.gov/grants/guide/notice-files/NOT-OD-03-066.html. Accessed March 12, 2019.
27. Devine PG, Forscher PS, Cox WTL, Kaatz A, Sheridan J, Carnes M. A gender bias habit-breaking intervention led to increased hiring of female faculty in STEMM departments. J Exp Soc Psychol. 2017;73:211-215. https://doi.org/10.1016/j.jesp.2017.07.002.
28. Klein RS, Voskuhl, R, Segal BM, et al. Speaking out about gender imbalance in invited speakers improves diversity. Nat Immunol. 201;18(5):475-478. https://doi.org/10.1038/ni.3707.
29. Borrero-Mejias C, Starling AJ, Burch R, Loder E. Ten (Eleven) things not to say to your female colleagues. Headache. 2019;59(10):1846-1854. https://doi.org/10.1111/head.13647.
30. Bandiera G, Abrahams C, Ruetalo M, Hanson MD, Nickell L, Spadafora S. Identifying and promoting best practices in residency application and selection in a complex academic health network. Acad Med. 2015;90(12):1594-1601. https://doi.org/10.1097/ACM.0000000000000954.
1. Ruzycki SM, Fletcher S, Earp M, Bharwani A, Lithgow KC. Trends in the proportion of female speakers at medical conferences in the United States and in Canada, 2007 to 2017. JAMA Netw Open. 2019;2(4):e192103. https://doi.org/ 10.1001/jamanetworkopen.2019.2103.
2. Penn CA, Ebott JA, Larach DB, Hesson AM, Waljee JF, Larach MG. The gender authorship gap in gynecologic oncology research. Gynecol Oncol Rep. 2019;29:83-84. https://doi.org/10.1016/j.gore.2019.07.011.
3. Thomas EG, Jayabalasingham B, Collins T, Geertzen J, Bui C, Dominici F. Gender disparities in invited commentary authorship in 2459 medical journals. JAMA Netw Open. 2019;2(10):e1913682.https://doi.org/10.1001/jamanetworkopen.2019.13682.
4. Silver JK, Slocum CS, Bank AM, et al. Where are the women? The underrepresentation of women physicians among recognition award recipients from medical specialty societies. PM R. 2017;9(8):804-815. https://doi.org/ 10.1016/j.pmrj.2017.06.001.
5. Burns KEA, Straus SE, Liu K, Rizv, L, Guyatt G. Gender differences in grant and personnel award funding rates at the Canadian Institute of Health Research based on research content area: a retrospective analysis. PLoS Med. 2019;16(10):e1002935. https://doi.org/ 10.1371/journal.pmed.1002935.
6. Silver JK, Ghalib R, Poorman JA, Al-Assi D, Parangi S, Bhargava H, et al. Analysis of gender equity in leadership of physician-focused medical specialty societies, 2008-2017analysis of gender equity in leadership of physician-focused medical specialty societies, 2008-2017. JAMA Internal Medicine. 2019;179(3):433-435. https://doi.org/10.1001/jamainternmed.2018.5303.
7. Erren TC, Groß JV, Shaw DM, Selle B. Representation of women as authors, reviewers, editors in chief, and editorial board members at 6 general medical journals in 2010 and 2011. JAMA Intern Med. 2014;174(4):633-635. https://doi.org/ 10.1001/jamainternmed.2013.14760.
8. Files JA, Mayer AP, Ko MG, et al. Speaker introductions at internal medicine grand rounds: forms of address reveal gender bias. J Womens Health (Larchmt). 2017;26(5):413-419. https://doi.org/ 10.1089/jwh.2016.6044.
9. Price EG, Gozu A, Kern DE, et al. The role of cultural diversity climate in recruitment, promotion, and retention of faculty in academic medicine. J Gen Intern Med. 2005;20(7):565-571. https://doi.org/10.1111/j.1525-1497.2005.0127.x.
10. Carr PL, Gunn CM, Kaplan SA, Raj A, Freund KM. Inadequate progress for women in academic medicine: findings from the National Faculty Study. J Womens Health (Larchmt). 2015;24(3):190-199. https://doi.org/10.1089/jwh.2014.4848.
11. Farkas AH, Bonifacino E, Turner R, Tilstra SA, Corbelli JA. Mentorship of women in academic medicine: a systematic review. J Gen Intern Med. 2019;34(7):1322-1329. https://doi.org/10.1007/s11606-019-04955-2.
12. Pololi L, Cooper LA, Carr P. Race, disadvantage and faculty experiences in academic medicine. J Gen Intern Med. 2010;25(12):1363-1369. https://doi.org/10.1007/s11606-010-1478-7.
13. Beaman L CR, Duflo E, Pande R, Topalova P. Powerful women: does exposure reduce bias? Q J Econ. 2009;124(4):1497-1540.
14. Mansbridge J. Should Blacks represent Blacks and women represent women? A contingent “Yes”. J Polit. 1999;61(3):628-657. https://doi.org/ https://doi.org/10.2307/2647821.
15. Lithgow KC, Fletcher, S., Earp, M.E., Bharwani, A., Ruzycki, S.M. Association between the proprtion of women on a conference planning committee and the proportion of women conference speakers at medical conferences. JAMA Netw Open. 2020; In press.
16. Alsan M, Garrick, O., Graziani, G.C. Does diversity matter for health? Experimental evidence from Oakland. National Bureau of Economic Research. 2018.
17. Greenwood BN, Carnahan, S., Huang, L. Patient–physician gender concordance and increased mortality among female heart attack patients. Proc Natl Acad Sci USA. 2018;115(34):8569-8574. https://doi.org/10.1073/pnas.1800097115.
18. Silver JK, Bean AC, Slocum C, et al. Physician Workforce Disparities and Patient Care: A Narrative Review. Health Equity. 2019;3(1):360-777. https://doi.org/10.1089/heq.2019.0040.
19. Shah SS, Shaughnessy, E.E., Spector, N.D. Leading by example: How medical journals can improve representation in academic medicine. J Hos Med. 2019;14(7):393. https://doi.org/10.12788/jhm.3247.
20. Martin JL. Ten simple rules to achieve conference speaker gender balance. PLoS Comput Biol. 2014;10(11):e1003903. https://doi.org/ 10.1371/journal.pcbi.1003903.
21. Sumner J. The Gender Balance Assessment Tool (GBAT): a web-based tool for estimating gender balance in syllabi and bibliographies. Polit Sci Polit. 2018;2(51):396-400. https://doi.org/10.1017/S1049096517002074.
22. Northcutt N, Papp S, Keniston A, et al; on behalf of the Society of Hospital Medicine Diversity, Equity and Inclusion Special Interest Group. SPEAKers at the National Society of Hospital Medicine Meeting: A Follow-UP Study of Gender Equity for Conference Speakers from 2015 to 2019. The SPEAK Up Study. J Hosp Med. 2020;15(4):228-231. https://doi.org/10.12788/jhm.3401.
23. Wayne NL, Vermillion M, Uijtdehaage S. Gender differences in leadership amongst first-year medical students in the small-group setting. Acad Med. 2010;85(8):1276-1281. https://doi.org/10.1097/ACM.0b013e3181e5f2ce
24. Casadevall A, Handelsman J. The presence of female conveners correlates with a higher proportion of female speakers at scientific symposia. MBio. 2014;5(1):e00846-13. https://doi.org/10.1128/mBio.00846-13.25. Casadevall A. Achieving speaker gender equity at the American Society for Microbiology General Meeting. MBio. 2015;6(4):e01146. https://doi.org/10.1128/mBio.01146-15.
26. Health NIo. Guidelines for the inclusion of women, minorities, and persons with disabilities in NIH-supported conference grats 2003. https://grants.nih.gov/grants/guide/notice-files/NOT-OD-03-066.html. Accessed March 12, 2019.
27. Devine PG, Forscher PS, Cox WTL, Kaatz A, Sheridan J, Carnes M. A gender bias habit-breaking intervention led to increased hiring of female faculty in STEMM departments. J Exp Soc Psychol. 2017;73:211-215. https://doi.org/10.1016/j.jesp.2017.07.002.
28. Klein RS, Voskuhl, R, Segal BM, et al. Speaking out about gender imbalance in invited speakers improves diversity. Nat Immunol. 201;18(5):475-478. https://doi.org/10.1038/ni.3707.
29. Borrero-Mejias C, Starling AJ, Burch R, Loder E. Ten (Eleven) things not to say to your female colleagues. Headache. 2019;59(10):1846-1854. https://doi.org/10.1111/head.13647.
30. Bandiera G, Abrahams C, Ruetalo M, Hanson MD, Nickell L, Spadafora S. Identifying and promoting best practices in residency application and selection in a complex academic health network. Acad Med. 2015;90(12):1594-1601. https://doi.org/10.1097/ACM.0000000000000954.
© 2020 Society of Hospital Medicine
Leadership & Professional Development: Evidence-Based Strategies to Make Team Meetings More Effective
“Without meeting leadership skills, one joins the ranks of so many others who bear the responsibility for the meeting ‘problem’ and are the cause of so much frustration in the workplace.”1 Physicians, like so many others, often feel that team meetings are inefficient, a waste of time, and mentally draining. It does not have to be this way. There are evidence-based strategies that can make meetings truly work and actually enjoyable to attend.2 This is particularly important because eliminating meetings is a false solution. Hospitals need team meetings to promote coordination, collaboration, communication, and consensus decision-making. While no one individual can solve the meetings problem, each of us can find a meeting we lead and make it work better.
First, recognize that, as a leader, you are a steward of others’ time. As a steward, be intentional when designing meetings. Think carefully about who needs to be there, how much time to spend on the meeting, and how the meeting should be run. Dysfunction increases with meeting size, so invite attendees wisely; include only those essential to the meeting. For individuals not in the core group, offer them the opportunity to share their input premeeting if desired, share good meeting minutes with them, and welcome them to attend future meetings if desired. Consider “representative voices”—openly asking certain attendees to represent a group of stakeholders. Use a timed agenda to invite certain people for part, but not all, of the meeting.
Keep your meetings lean and deliberate. Avoid defaulting to one-hour meetings out of habit. Parkinson’s Law suggests that people will fill the time allotted to a particular task. If a meeting can be done in 30 minutes but is scheduled for 60 minutes, chances are that people will use the full hour. If a decision is reached faster than anticipated, end the meeting early. Refer back to your steward mindset and schedule meeting time with intention.
Meetings are often experienced psychologically like we experience interruptions. Thus, when attendees arrive at a meeting, express gratitude. Your job is to keep attendees active and engaged; therefore, facilitate the meeting actively and creatively. Try out different techniques such as devoting a few minutes to silent, written brainstorming. Leveraging silence gives attendees the opportunity to think on their own before contributing to the discussion and results in nearly twice the number of ideas.3 Perhaps members can be assigned explicit roles such as devil’s advocate, or each attendee can be assigned a specific agenda item, invoking responsibility and participation. If you always sit during meetings, try standing. If you have never tried a walking meeting, give it a go. Attendees appreciate mixing things up.
Lastly, remember to check-in with attendees to see how things are going. Never get too comfortable as a meeting leader, especially since meeting frustration abounds. Asking your team for feedback will carry over to other aspects of your role. You will be seen as a conscientious leader, open to exploration and professional development. This builds trust and creates a positive, collaborative work environment.
While you cannot control how others run their meetings, you do have the ability to make a meeting that you lead truly work. Be intentional with your role as a meeting facilitator and focus on the whole experience. Evaluate and learn from your team, show others that you care about your meetings so that they begin to care about theirs too.
1. Rogelberg SG. The Surprising Science of Meetings: How You Can Lead your Team to Peak Performance. Oxford University Press; 2019.
2. Rogelberg SG. Why your meetings stink–and what to do about it. Harvard Business Review. 2019;140-143. https://hbr.org/2019/01/why-your-meetings-stink-and-what-to-do-about-it. Accessed March 6, 2020.
3. Rogelberg SG, Kreamer L. The case for more silence in meetings. Harvard Business Review. https://hbr.org/2019/06/the-case-for-more-silence-in-meetings. Accessed August 2, 2019.
“Without meeting leadership skills, one joins the ranks of so many others who bear the responsibility for the meeting ‘problem’ and are the cause of so much frustration in the workplace.”1 Physicians, like so many others, often feel that team meetings are inefficient, a waste of time, and mentally draining. It does not have to be this way. There are evidence-based strategies that can make meetings truly work and actually enjoyable to attend.2 This is particularly important because eliminating meetings is a false solution. Hospitals need team meetings to promote coordination, collaboration, communication, and consensus decision-making. While no one individual can solve the meetings problem, each of us can find a meeting we lead and make it work better.
First, recognize that, as a leader, you are a steward of others’ time. As a steward, be intentional when designing meetings. Think carefully about who needs to be there, how much time to spend on the meeting, and how the meeting should be run. Dysfunction increases with meeting size, so invite attendees wisely; include only those essential to the meeting. For individuals not in the core group, offer them the opportunity to share their input premeeting if desired, share good meeting minutes with them, and welcome them to attend future meetings if desired. Consider “representative voices”—openly asking certain attendees to represent a group of stakeholders. Use a timed agenda to invite certain people for part, but not all, of the meeting.
Keep your meetings lean and deliberate. Avoid defaulting to one-hour meetings out of habit. Parkinson’s Law suggests that people will fill the time allotted to a particular task. If a meeting can be done in 30 minutes but is scheduled for 60 minutes, chances are that people will use the full hour. If a decision is reached faster than anticipated, end the meeting early. Refer back to your steward mindset and schedule meeting time with intention.
Meetings are often experienced psychologically like we experience interruptions. Thus, when attendees arrive at a meeting, express gratitude. Your job is to keep attendees active and engaged; therefore, facilitate the meeting actively and creatively. Try out different techniques such as devoting a few minutes to silent, written brainstorming. Leveraging silence gives attendees the opportunity to think on their own before contributing to the discussion and results in nearly twice the number of ideas.3 Perhaps members can be assigned explicit roles such as devil’s advocate, or each attendee can be assigned a specific agenda item, invoking responsibility and participation. If you always sit during meetings, try standing. If you have never tried a walking meeting, give it a go. Attendees appreciate mixing things up.
Lastly, remember to check-in with attendees to see how things are going. Never get too comfortable as a meeting leader, especially since meeting frustration abounds. Asking your team for feedback will carry over to other aspects of your role. You will be seen as a conscientious leader, open to exploration and professional development. This builds trust and creates a positive, collaborative work environment.
While you cannot control how others run their meetings, you do have the ability to make a meeting that you lead truly work. Be intentional with your role as a meeting facilitator and focus on the whole experience. Evaluate and learn from your team, show others that you care about your meetings so that they begin to care about theirs too.
“Without meeting leadership skills, one joins the ranks of so many others who bear the responsibility for the meeting ‘problem’ and are the cause of so much frustration in the workplace.”1 Physicians, like so many others, often feel that team meetings are inefficient, a waste of time, and mentally draining. It does not have to be this way. There are evidence-based strategies that can make meetings truly work and actually enjoyable to attend.2 This is particularly important because eliminating meetings is a false solution. Hospitals need team meetings to promote coordination, collaboration, communication, and consensus decision-making. While no one individual can solve the meetings problem, each of us can find a meeting we lead and make it work better.
First, recognize that, as a leader, you are a steward of others’ time. As a steward, be intentional when designing meetings. Think carefully about who needs to be there, how much time to spend on the meeting, and how the meeting should be run. Dysfunction increases with meeting size, so invite attendees wisely; include only those essential to the meeting. For individuals not in the core group, offer them the opportunity to share their input premeeting if desired, share good meeting minutes with them, and welcome them to attend future meetings if desired. Consider “representative voices”—openly asking certain attendees to represent a group of stakeholders. Use a timed agenda to invite certain people for part, but not all, of the meeting.
Keep your meetings lean and deliberate. Avoid defaulting to one-hour meetings out of habit. Parkinson’s Law suggests that people will fill the time allotted to a particular task. If a meeting can be done in 30 minutes but is scheduled for 60 minutes, chances are that people will use the full hour. If a decision is reached faster than anticipated, end the meeting early. Refer back to your steward mindset and schedule meeting time with intention.
Meetings are often experienced psychologically like we experience interruptions. Thus, when attendees arrive at a meeting, express gratitude. Your job is to keep attendees active and engaged; therefore, facilitate the meeting actively and creatively. Try out different techniques such as devoting a few minutes to silent, written brainstorming. Leveraging silence gives attendees the opportunity to think on their own before contributing to the discussion and results in nearly twice the number of ideas.3 Perhaps members can be assigned explicit roles such as devil’s advocate, or each attendee can be assigned a specific agenda item, invoking responsibility and participation. If you always sit during meetings, try standing. If you have never tried a walking meeting, give it a go. Attendees appreciate mixing things up.
Lastly, remember to check-in with attendees to see how things are going. Never get too comfortable as a meeting leader, especially since meeting frustration abounds. Asking your team for feedback will carry over to other aspects of your role. You will be seen as a conscientious leader, open to exploration and professional development. This builds trust and creates a positive, collaborative work environment.
While you cannot control how others run their meetings, you do have the ability to make a meeting that you lead truly work. Be intentional with your role as a meeting facilitator and focus on the whole experience. Evaluate and learn from your team, show others that you care about your meetings so that they begin to care about theirs too.
1. Rogelberg SG. The Surprising Science of Meetings: How You Can Lead your Team to Peak Performance. Oxford University Press; 2019.
2. Rogelberg SG. Why your meetings stink–and what to do about it. Harvard Business Review. 2019;140-143. https://hbr.org/2019/01/why-your-meetings-stink-and-what-to-do-about-it. Accessed March 6, 2020.
3. Rogelberg SG, Kreamer L. The case for more silence in meetings. Harvard Business Review. https://hbr.org/2019/06/the-case-for-more-silence-in-meetings. Accessed August 2, 2019.
1. Rogelberg SG. The Surprising Science of Meetings: How You Can Lead your Team to Peak Performance. Oxford University Press; 2019.
2. Rogelberg SG. Why your meetings stink–and what to do about it. Harvard Business Review. 2019;140-143. https://hbr.org/2019/01/why-your-meetings-stink-and-what-to-do-about-it. Accessed March 6, 2020.
3. Rogelberg SG, Kreamer L. The case for more silence in meetings. Harvard Business Review. https://hbr.org/2019/06/the-case-for-more-silence-in-meetings. Accessed August 2, 2019.
© 2020 Society of Hospital Medicine
SPEAKers at the National Society of Hospital Medicine Meeting: A Follow-UP Study of Gender Equity for Conference Speakers from 2015 to 2019. The SPEAK UP Study
Persistent gender disparities exist in pay,1,2 leadership opportunities,3,4 promotion,5 and speaking opportunities.6 While the gender distribution of the hospitalist workforce may be approaching parity,3,7,8 gender differences in leadership, speakership, and authorship have already been noted in hospital medicine.3 Between 2006 and 2012, women constituted less than a third (26%) of the presenters at the national conferences of the Society of Hospital Medicine (SHM) and the Society of General Internal Medicine (SGIM).3
The SHM Annual Meeting has historically had an “open call” peer review process for workshop presenters with the goal of increasing the diversity of presenters. In 2019, this process was expanded to include didactic speakers. Our aim in this study was to assess whether these open call procedures resulted in improved representation of women speakers and how the proportion of women speakers affects the overall evaluation scores of the conference. Our hypothesis was that the introduction of an open call process for the SHM conference didactic speakers would be associated with an increased proportion of women speakers, compared with the closed call processes, without a negative impact on conference scores.
METHODS
The study is a retrospective evaluation of data collected regarding speakers at the annual SHM conference from 2015 to 2019. The SHM national conference typically has two main types of offerings: workshops and didactics. Workshop presenters from 2015 to 2019 were selected via an open call process as defined below. Didactic speakers (except for plenary speakers) were selected using the open call process for 2019 only.
We aimed to compare (1) the number and proportion of women speakers, compared with men speakers, over time and (2) the proportion of women speakers when open call processes were utilized versus that seen with closed call processes. Open call included workshops for all years and didactics for 2019; closed call included didactics for 2015 to 2018 and plenary sessions 2015 to 2019 (Table). The speaker list for the conferences was obtained from conference pamphlets or agendas available via Internet searches or obtained through attendance at the conference.
Speaker Categories and Identification Process
We determined whether each individual was a featured speaker (one whose talk was unopposed by other sessions), plenary speaker (defined as such in the conference pamphlets), whether they spoke in a group format, and whether the speaking opportunity type was a workshop or a didactic session. Numbers of featured and plenary speakers were combined because of low numbers. SHM provided deidentified conference evaluation data for each year studied. For the purposes of this study, we analyzed all speakers which included physicians, advanced practice providers, and professionals such as nurses and other interdisciplinary team members. The same speaker could be included multiple times if they had multiple speaking opportunities.
Open Call Process
We defined the “open call process” (referred to as “open call” here forward) as the process utilized by SHM that includes the following two components: (1) advertisements to members of SHM and to the medical community at large through a variety of mechanisms including emails, websites, and social media outlets and (2) an online submission process that includes names of proposed speakers and their topic and, in the case of workshops, session objectives as well as an outline of the proposed workshop. SHM committees may also submit suggestions for topics and speakers. Annual Conference Committee members then review and rate submissions on the categories of topic, organization and clarity, objectives, and speaker qualifications (with a focus on institutional, geographic, and gender diversity). Scores are assigned from 1 to 5 (with 5 being the best score) for each category and a section for comments is available. All submissions are also evaluated by the course director.
After initial committee reviews, scores with marked reviewer discrepancies are rereviewed and discussed by the committee and course director. A cutoff score is then calculated with proposals falling below the cutoff threshold omitted from further consideration. Weekly calls are then focused on subcategories (ie tracks) with emphasis on clinical and educational content. Each of the tracks have a subcommittee with track leads to curate the best content first and then focus on final speaker selection. More recently, templates are shared with the track leads that include a location to call out gender and institutional diversity. Weekly calls are held to hone the content and determine the speakers.
For the purposes of this study, when the above process was not used, the authors refer to it as “closed call.” Closed call processes do not typically involve open invitations or a peer review process. (Table)
Gender
Gender was assigned based on the speaker’s self-identification by the pronouns used in their biography submitted to the conference or on their institutional website or other websites where the speaker was referenced. Persons using she/her/hers pronouns were noted as women and persons using he/him/his were noted as men. For the purposes of this study, we conceptualized gender as binary (ie woman/man) given the limited information we had from online sources.
ANALYSIS
REDCap, a secure, Web-based application for building and managing online survey and databases, was used to collect and manage all study data.9
All analyses were performed using SAS Enterprise Guide 8.1 (SAS Institute, Inc., Cary, North Carolina) using retrospectively collected data. A Cochran-Armitage test for trend was used to evaluate the proportion of women speakers from 2015 to 2019. A chi-square test was used to assess the proportion of women speakers for open call processes versus that seen with closed call. One-way analysis of variance (ANOVA) was used to evaluate annual conference evaluation scores from 2015 to 2019. Either numbers with proportions or means with standard deviations have been reported. Bonferroni’s correction for multiple comparisons was applied, with a P < .008 considered statistically significant.
RESULTS
Between 2015 and 2019, a total of 709 workshop and didactic presentations were given by 1,261 speakers at the annual Society of Hospital Medicine Conference. Of these, 505 (40%) were women; 756 (60%) were men. There were no missing data.
From 2015 to 2019, representation of women speakers increased from 35% of all speakers to 47% of all speakers (P = .0068). Women plenary speakers increased from 23% in 2015 to 45% in 2019 (P = .0396).
The proportion of women presenters for workshops (which have utilized an open call process throughout the study period), ranged from 43% to 53% from 2015 to 2019 with no statistically significant difference in gender distribution across years (Figure).
A greater proportion of speakers selected by an open call process were women compared to when speakers were selected by a closed call process (261 (47%) vs 244 (34%); P < .0001).
Of didactics or workshops given in a group format (N = 299), 82 (27%) were given by all-men groups and 38 (13%) were given by all-women groups. Women speakers participating in all-women group talks accounted for 21% of all women speakers; whereas men speakers participating in all-men group talks account for 26% of all men speakers (P = .02). We found that all-men group speaking opportunities did decrease from 41% of group talks in 2015 to 21% of group talks in 2019 (P = .0065).
We saw an average 3% annual increase in women speakers from 2015 to 2019, an 8% increase from 2018 to 2019 for all speakers, and an 11% increase in women speakers specific to didactic sessions. Overall conference ratings increased from a mean of 4.3 ± 0.24 in 2015 to a mean of 4.6 ± 0.14 in 2019 (n = 1,202; P < .0001; Figure).
DISCUSSION
The important findings of this study are that there has been an increase in women speakers over the last 5 years at the annual Society of Hospital Medicine Conference, that women had higher representation as speakers when open call processes were followed, and that conference scores continued to improve during the time frame studied. These findings suggest that a systematic open call process helps to support equitable speaking opportunities for men and women at a national hospital medicine conference without a negative impact on conference quality.
To recruit more diverse speakers, open call and peer review processes were used in addition to deliberate efforts at ensuring diversity in speakers. We found that over time, the proportion of women with speaking opportunities increased from 2015 to 2019. Interestingly, workshops, which had open call processes in place for the duration of the study period, had almost equal numbers of men and women presenting in all years. We also found that the number of all-men speaking groups decreased between 2015 and 2019.
A single process change can impact gender equity, but the target of true equity is expected to require additional measures such as assessment of committee structures and diversity, checklists, and reporting structures (data analysis and plans when goals not achieved).10-13 For instance, the American Society for Microbiology General Meeting was able to achieve gender equity in speakers by a multifold approach including ensuring the program committee was aware of gender statistics, increasing female representation among session convener teams, and direct instruction to try to avoid all-male sessions.11
It is important to acknowledge that these processes do require valuable resources including time. SHM has historically used committee volunteers to conduct the peer review process with each committee member reviewing 20 to 30 workshop submissions and 30 to 50 didactic sessions. While open processes with peer review seem to generate improved gender equity, ensuring processes are in place during the selection process is also key.
Several recent notable efforts to enhance gender equity and to increase diversity have been proposed. One such example of a process that may further improve gender equity was proposed by editors at the Journal of Hospital Medicine to assess current representation via demographics including gender, race, and ethnicity of authors with plans to assess patterns in the coming years.14 The American College of Physicians also published a position paper on achieving gender equity with a recommendation that organizational policies and procedures should be implemented that address implicit bias.15
Our study showed that, from 2015 to 2019, conference evaluations saw a significant increase in the score concurrently with the rise in proportion of women speakers. This finding suggests that quality does not seem to be affected by this new methodology for speaker selection and in fact this methodology may actually help improve the overall quality of the conference. To our knowledge, this is one of the first studies to concurrently evaluate speaker gender equity with conference quality.
Our study offers several strengths. This study took a pragmatic approach to understanding how processes can impact gender equity, and we were able to take advantage of the evolution of the open call system (ie workshops which have been an open call process for the duration of the study versus speaking opportunities that were not).
Our study also has several limitations. First, this study is retrospective in nature and thus other processes could have contributed to the improved gender equity, such as an organization’s priorities over time. During this study period, the SHM conference saw an average 3% increase annually in women speakers and an increase of 8% from 2018 to 2019 for all speakers compared to national trends of approximately 1%,6 which suggests that the open call processes in place could be contributing to the overall increases seen. Similarly, because of the retrospective nature of the study, we cannot be certain that the improvements in conference scores were directly the result of improved gender equity, although it does suggest that the improvements in gender equity did not have an adverse impact on the scores. We also did not assess how the composition of selection committee members for the meeting could have impacted the overall composition of the speakers. Our study looked at diversity only from the perspective of gender in a binary fashion, and thus additional studies are needed to assess how to improve diversity overall. It is unclear how this new open call for speakers affects race and ethnic diversity specifically. Identifying gender for the purposes of this study was facilitated by speakers providing their own biographies and the respective pronouns used in those biographies, and thus gender was easier to ascertain than race and ethnicity, which are not as readily available. For organizations to understand their diversity, equity, and inclusion efforts, enhancing the ability to fairly track and measure diversity will be key. Lastly, understanding of the exact composition of hospitalists from both a gender and race/ethnicity perspective is lacking. Studies have suggested that, based upon those surveyed or studied, there is a fairly equal balance of men and women albeit in academic groups.3
CONCLUSIONS
An open call approach to speakers at a national hospitalist conference seems to have contributed to improvements regarding gender equity in speaking opportunities with a concurrent improvement in overall rating of the conference. The open call system is a potential mechanism that other institutions and organizations could employ to enhance their diversity efforts.
Acknowledgments
Society of Hospital Medicine Diversity, Equity, Inclusion Special Interest Group
Work Group for SPEAK UP: Marisha Burden, MD, Daniel Cabrera, MD, Amira del Pino-Jones, MD, Areeba Kara, MD, Angela Keniston, MSPH, Keshav Khanijow, MD, Flora Kisuule, MD, Chiara Mandel, Benji Mathews, MD, David Paje, MD, Stephan Papp, MD, Snehal Patel, MD, Suchita Shah Sata, MD, Dustin Smith, MD, Kevin Vuernick
1. Weaver AC, Wetterneck TB, Whelan CT, Hinami K. A matter of priorities? Exploring the persistent gender pay gap in hospital medicine. J Hosp Med. 2015;10(8):486-490. https://doi.org/10.1002/jhm.2400.
2. Jena AB, Olenski AR, Blumenthal DM. Sex differences in physician salary in US public medical schools. JAMA Intern Med. 2016;176(9):1294-1304. https://doi.org/10.1001/jamainternmed.2016.3284.
3. Burden M, Frank MG, Keniston A, et al. Gender disparities in leadership and scholarly productivity of academic hospitalists. J Hosp Med. 2015;10(8):481-485. https://doi.org/10.1002/jhm.2340.
4. Silver JK, Ghalib R, Poorman JA, et al. Analysis of gender equity in leadership of physician-focused medical specialty societies, 2008-2017. JAMA Intern Med. 2019;179(3):433-435. https://doi.org/10.1001/jamainternmed.2018.5303.
5. Jena AB, Khullar D, Ho O, Olenski AR, Blumenthal DM. Sex differences in academic rank in US medical schools in 2014. JAMA. 2015;314(11):1149-1158. https://doi.org/10.1001/jama.2015.10680.
6. Ruzycki SM, Fletcher S, Earp M, Bharwani A, Lithgow KC. Trends in the Proportion of Female Speakers at Medical Conferences in the United States and in Canada, 2007 to 2017. JAMA Netw Open. 2019;2(4):e192103. https://doi.org/10.1001/jamanetworkopen.2019.2103
7. Reid MB, Misky GJ, Harrison RA, Sharpe B, Auerbach A, Glasheen JJ. Mentorship, productivity, and promotion among academic hospitalists. J Gen Intern Med. 2012;27(1):23-27. https://doi.org/10.1007/s11606-011-1892-5.
8. Today’s Hospitalist 2018 Compensation and Career Survey Results. https://www.todayshospitalist.com/salary-survey-results/. Accessed September 28, 2019.
9. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. https://doi.org/10.1016/j.jbi.2008.08.010.
10. Burden M, del Pino-Jones A, Shafer M, Sheth S, Rexrode K. Association of American Medical Colleagues (AAMC) Group on Women in Medicine and Science. Recruitment Toolkit: https://www.aamc.org/download/492864/data/equityinrecruitmenttoolkit.pdf. Accessed July 27, 2019.
11. Casadevall A. Achieving speaker gender equity at the american society for microbiology general meeting. MBio. 2015;6:e01146. https://doi.org/10.1128/mBio.01146-15.
12. Westring A, McDonald JM, Carr P, Grisso JA. An integrated framework for gender equity in academic medicine. Acad Med. 2016;91(8):1041-1044. https://doi.org/10.1097/ACM.0000000000001275.
13. Martin JL. Ten simple rules to achieve conference speaker gender balance. PLoS Comput Biol. 2014;10(11):e1003903. https://doi.org/10.1371/journal.pcbi.1003903.
14. Shah SS, Shaughnessy EE, Spector ND. Leading by example: how medical journals can improve representation in academic medicine. J Hosp Med. 2019;14(7):393. https://doi.org/10.12788/jhm.3247.
15. Butkus R, Serchen J, Moyer DV, et al. Achieving gender equity in physician compensation and career advancement: a position paper of the American College of Physicians. Ann Intern Med. 2018;168:721-723. https://doi.org/10.7326/M17-3438.
Persistent gender disparities exist in pay,1,2 leadership opportunities,3,4 promotion,5 and speaking opportunities.6 While the gender distribution of the hospitalist workforce may be approaching parity,3,7,8 gender differences in leadership, speakership, and authorship have already been noted in hospital medicine.3 Between 2006 and 2012, women constituted less than a third (26%) of the presenters at the national conferences of the Society of Hospital Medicine (SHM) and the Society of General Internal Medicine (SGIM).3
The SHM Annual Meeting has historically had an “open call” peer review process for workshop presenters with the goal of increasing the diversity of presenters. In 2019, this process was expanded to include didactic speakers. Our aim in this study was to assess whether these open call procedures resulted in improved representation of women speakers and how the proportion of women speakers affects the overall evaluation scores of the conference. Our hypothesis was that the introduction of an open call process for the SHM conference didactic speakers would be associated with an increased proportion of women speakers, compared with the closed call processes, without a negative impact on conference scores.
METHODS
The study is a retrospective evaluation of data collected regarding speakers at the annual SHM conference from 2015 to 2019. The SHM national conference typically has two main types of offerings: workshops and didactics. Workshop presenters from 2015 to 2019 were selected via an open call process as defined below. Didactic speakers (except for plenary speakers) were selected using the open call process for 2019 only.
We aimed to compare (1) the number and proportion of women speakers, compared with men speakers, over time and (2) the proportion of women speakers when open call processes were utilized versus that seen with closed call processes. Open call included workshops for all years and didactics for 2019; closed call included didactics for 2015 to 2018 and plenary sessions 2015 to 2019 (Table). The speaker list for the conferences was obtained from conference pamphlets or agendas available via Internet searches or obtained through attendance at the conference.
Speaker Categories and Identification Process
We determined whether each individual was a featured speaker (one whose talk was unopposed by other sessions), plenary speaker (defined as such in the conference pamphlets), whether they spoke in a group format, and whether the speaking opportunity type was a workshop or a didactic session. Numbers of featured and plenary speakers were combined because of low numbers. SHM provided deidentified conference evaluation data for each year studied. For the purposes of this study, we analyzed all speakers which included physicians, advanced practice providers, and professionals such as nurses and other interdisciplinary team members. The same speaker could be included multiple times if they had multiple speaking opportunities.
Open Call Process
We defined the “open call process” (referred to as “open call” here forward) as the process utilized by SHM that includes the following two components: (1) advertisements to members of SHM and to the medical community at large through a variety of mechanisms including emails, websites, and social media outlets and (2) an online submission process that includes names of proposed speakers and their topic and, in the case of workshops, session objectives as well as an outline of the proposed workshop. SHM committees may also submit suggestions for topics and speakers. Annual Conference Committee members then review and rate submissions on the categories of topic, organization and clarity, objectives, and speaker qualifications (with a focus on institutional, geographic, and gender diversity). Scores are assigned from 1 to 5 (with 5 being the best score) for each category and a section for comments is available. All submissions are also evaluated by the course director.
After initial committee reviews, scores with marked reviewer discrepancies are rereviewed and discussed by the committee and course director. A cutoff score is then calculated with proposals falling below the cutoff threshold omitted from further consideration. Weekly calls are then focused on subcategories (ie tracks) with emphasis on clinical and educational content. Each of the tracks have a subcommittee with track leads to curate the best content first and then focus on final speaker selection. More recently, templates are shared with the track leads that include a location to call out gender and institutional diversity. Weekly calls are held to hone the content and determine the speakers.
For the purposes of this study, when the above process was not used, the authors refer to it as “closed call.” Closed call processes do not typically involve open invitations or a peer review process. (Table)
Gender
Gender was assigned based on the speaker’s self-identification by the pronouns used in their biography submitted to the conference or on their institutional website or other websites where the speaker was referenced. Persons using she/her/hers pronouns were noted as women and persons using he/him/his were noted as men. For the purposes of this study, we conceptualized gender as binary (ie woman/man) given the limited information we had from online sources.
ANALYSIS
REDCap, a secure, Web-based application for building and managing online survey and databases, was used to collect and manage all study data.9
All analyses were performed using SAS Enterprise Guide 8.1 (SAS Institute, Inc., Cary, North Carolina) using retrospectively collected data. A Cochran-Armitage test for trend was used to evaluate the proportion of women speakers from 2015 to 2019. A chi-square test was used to assess the proportion of women speakers for open call processes versus that seen with closed call. One-way analysis of variance (ANOVA) was used to evaluate annual conference evaluation scores from 2015 to 2019. Either numbers with proportions or means with standard deviations have been reported. Bonferroni’s correction for multiple comparisons was applied, with a P < .008 considered statistically significant.
RESULTS
Between 2015 and 2019, a total of 709 workshop and didactic presentations were given by 1,261 speakers at the annual Society of Hospital Medicine Conference. Of these, 505 (40%) were women; 756 (60%) were men. There were no missing data.
From 2015 to 2019, representation of women speakers increased from 35% of all speakers to 47% of all speakers (P = .0068). Women plenary speakers increased from 23% in 2015 to 45% in 2019 (P = .0396).
The proportion of women presenters for workshops (which have utilized an open call process throughout the study period), ranged from 43% to 53% from 2015 to 2019 with no statistically significant difference in gender distribution across years (Figure).
A greater proportion of speakers selected by an open call process were women compared to when speakers were selected by a closed call process (261 (47%) vs 244 (34%); P < .0001).
Of didactics or workshops given in a group format (N = 299), 82 (27%) were given by all-men groups and 38 (13%) were given by all-women groups. Women speakers participating in all-women group talks accounted for 21% of all women speakers; whereas men speakers participating in all-men group talks account for 26% of all men speakers (P = .02). We found that all-men group speaking opportunities did decrease from 41% of group talks in 2015 to 21% of group talks in 2019 (P = .0065).
We saw an average 3% annual increase in women speakers from 2015 to 2019, an 8% increase from 2018 to 2019 for all speakers, and an 11% increase in women speakers specific to didactic sessions. Overall conference ratings increased from a mean of 4.3 ± 0.24 in 2015 to a mean of 4.6 ± 0.14 in 2019 (n = 1,202; P < .0001; Figure).
DISCUSSION
The important findings of this study are that there has been an increase in women speakers over the last 5 years at the annual Society of Hospital Medicine Conference, that women had higher representation as speakers when open call processes were followed, and that conference scores continued to improve during the time frame studied. These findings suggest that a systematic open call process helps to support equitable speaking opportunities for men and women at a national hospital medicine conference without a negative impact on conference quality.
To recruit more diverse speakers, open call and peer review processes were used in addition to deliberate efforts at ensuring diversity in speakers. We found that over time, the proportion of women with speaking opportunities increased from 2015 to 2019. Interestingly, workshops, which had open call processes in place for the duration of the study period, had almost equal numbers of men and women presenting in all years. We also found that the number of all-men speaking groups decreased between 2015 and 2019.
A single process change can impact gender equity, but the target of true equity is expected to require additional measures such as assessment of committee structures and diversity, checklists, and reporting structures (data analysis and plans when goals not achieved).10-13 For instance, the American Society for Microbiology General Meeting was able to achieve gender equity in speakers by a multifold approach including ensuring the program committee was aware of gender statistics, increasing female representation among session convener teams, and direct instruction to try to avoid all-male sessions.11
It is important to acknowledge that these processes do require valuable resources including time. SHM has historically used committee volunteers to conduct the peer review process with each committee member reviewing 20 to 30 workshop submissions and 30 to 50 didactic sessions. While open processes with peer review seem to generate improved gender equity, ensuring processes are in place during the selection process is also key.
Several recent notable efforts to enhance gender equity and to increase diversity have been proposed. One such example of a process that may further improve gender equity was proposed by editors at the Journal of Hospital Medicine to assess current representation via demographics including gender, race, and ethnicity of authors with plans to assess patterns in the coming years.14 The American College of Physicians also published a position paper on achieving gender equity with a recommendation that organizational policies and procedures should be implemented that address implicit bias.15
Our study showed that, from 2015 to 2019, conference evaluations saw a significant increase in the score concurrently with the rise in proportion of women speakers. This finding suggests that quality does not seem to be affected by this new methodology for speaker selection and in fact this methodology may actually help improve the overall quality of the conference. To our knowledge, this is one of the first studies to concurrently evaluate speaker gender equity with conference quality.
Our study offers several strengths. This study took a pragmatic approach to understanding how processes can impact gender equity, and we were able to take advantage of the evolution of the open call system (ie workshops which have been an open call process for the duration of the study versus speaking opportunities that were not).
Our study also has several limitations. First, this study is retrospective in nature and thus other processes could have contributed to the improved gender equity, such as an organization’s priorities over time. During this study period, the SHM conference saw an average 3% increase annually in women speakers and an increase of 8% from 2018 to 2019 for all speakers compared to national trends of approximately 1%,6 which suggests that the open call processes in place could be contributing to the overall increases seen. Similarly, because of the retrospective nature of the study, we cannot be certain that the improvements in conference scores were directly the result of improved gender equity, although it does suggest that the improvements in gender equity did not have an adverse impact on the scores. We also did not assess how the composition of selection committee members for the meeting could have impacted the overall composition of the speakers. Our study looked at diversity only from the perspective of gender in a binary fashion, and thus additional studies are needed to assess how to improve diversity overall. It is unclear how this new open call for speakers affects race and ethnic diversity specifically. Identifying gender for the purposes of this study was facilitated by speakers providing their own biographies and the respective pronouns used in those biographies, and thus gender was easier to ascertain than race and ethnicity, which are not as readily available. For organizations to understand their diversity, equity, and inclusion efforts, enhancing the ability to fairly track and measure diversity will be key. Lastly, understanding of the exact composition of hospitalists from both a gender and race/ethnicity perspective is lacking. Studies have suggested that, based upon those surveyed or studied, there is a fairly equal balance of men and women albeit in academic groups.3
CONCLUSIONS
An open call approach to speakers at a national hospitalist conference seems to have contributed to improvements regarding gender equity in speaking opportunities with a concurrent improvement in overall rating of the conference. The open call system is a potential mechanism that other institutions and organizations could employ to enhance their diversity efforts.
Acknowledgments
Society of Hospital Medicine Diversity, Equity, Inclusion Special Interest Group
Work Group for SPEAK UP: Marisha Burden, MD, Daniel Cabrera, MD, Amira del Pino-Jones, MD, Areeba Kara, MD, Angela Keniston, MSPH, Keshav Khanijow, MD, Flora Kisuule, MD, Chiara Mandel, Benji Mathews, MD, David Paje, MD, Stephan Papp, MD, Snehal Patel, MD, Suchita Shah Sata, MD, Dustin Smith, MD, Kevin Vuernick
Persistent gender disparities exist in pay,1,2 leadership opportunities,3,4 promotion,5 and speaking opportunities.6 While the gender distribution of the hospitalist workforce may be approaching parity,3,7,8 gender differences in leadership, speakership, and authorship have already been noted in hospital medicine.3 Between 2006 and 2012, women constituted less than a third (26%) of the presenters at the national conferences of the Society of Hospital Medicine (SHM) and the Society of General Internal Medicine (SGIM).3
The SHM Annual Meeting has historically had an “open call” peer review process for workshop presenters with the goal of increasing the diversity of presenters. In 2019, this process was expanded to include didactic speakers. Our aim in this study was to assess whether these open call procedures resulted in improved representation of women speakers and how the proportion of women speakers affects the overall evaluation scores of the conference. Our hypothesis was that the introduction of an open call process for the SHM conference didactic speakers would be associated with an increased proportion of women speakers, compared with the closed call processes, without a negative impact on conference scores.
METHODS
The study is a retrospective evaluation of data collected regarding speakers at the annual SHM conference from 2015 to 2019. The SHM national conference typically has two main types of offerings: workshops and didactics. Workshop presenters from 2015 to 2019 were selected via an open call process as defined below. Didactic speakers (except for plenary speakers) were selected using the open call process for 2019 only.
We aimed to compare (1) the number and proportion of women speakers, compared with men speakers, over time and (2) the proportion of women speakers when open call processes were utilized versus that seen with closed call processes. Open call included workshops for all years and didactics for 2019; closed call included didactics for 2015 to 2018 and plenary sessions 2015 to 2019 (Table). The speaker list for the conferences was obtained from conference pamphlets or agendas available via Internet searches or obtained through attendance at the conference.
Speaker Categories and Identification Process
We determined whether each individual was a featured speaker (one whose talk was unopposed by other sessions), plenary speaker (defined as such in the conference pamphlets), whether they spoke in a group format, and whether the speaking opportunity type was a workshop or a didactic session. Numbers of featured and plenary speakers were combined because of low numbers. SHM provided deidentified conference evaluation data for each year studied. For the purposes of this study, we analyzed all speakers which included physicians, advanced practice providers, and professionals such as nurses and other interdisciplinary team members. The same speaker could be included multiple times if they had multiple speaking opportunities.
Open Call Process
We defined the “open call process” (referred to as “open call” here forward) as the process utilized by SHM that includes the following two components: (1) advertisements to members of SHM and to the medical community at large through a variety of mechanisms including emails, websites, and social media outlets and (2) an online submission process that includes names of proposed speakers and their topic and, in the case of workshops, session objectives as well as an outline of the proposed workshop. SHM committees may also submit suggestions for topics and speakers. Annual Conference Committee members then review and rate submissions on the categories of topic, organization and clarity, objectives, and speaker qualifications (with a focus on institutional, geographic, and gender diversity). Scores are assigned from 1 to 5 (with 5 being the best score) for each category and a section for comments is available. All submissions are also evaluated by the course director.
After initial committee reviews, scores with marked reviewer discrepancies are rereviewed and discussed by the committee and course director. A cutoff score is then calculated with proposals falling below the cutoff threshold omitted from further consideration. Weekly calls are then focused on subcategories (ie tracks) with emphasis on clinical and educational content. Each of the tracks have a subcommittee with track leads to curate the best content first and then focus on final speaker selection. More recently, templates are shared with the track leads that include a location to call out gender and institutional diversity. Weekly calls are held to hone the content and determine the speakers.
For the purposes of this study, when the above process was not used, the authors refer to it as “closed call.” Closed call processes do not typically involve open invitations or a peer review process. (Table)
Gender
Gender was assigned based on the speaker’s self-identification by the pronouns used in their biography submitted to the conference or on their institutional website or other websites where the speaker was referenced. Persons using she/her/hers pronouns were noted as women and persons using he/him/his were noted as men. For the purposes of this study, we conceptualized gender as binary (ie woman/man) given the limited information we had from online sources.
ANALYSIS
REDCap, a secure, Web-based application for building and managing online survey and databases, was used to collect and manage all study data.9
All analyses were performed using SAS Enterprise Guide 8.1 (SAS Institute, Inc., Cary, North Carolina) using retrospectively collected data. A Cochran-Armitage test for trend was used to evaluate the proportion of women speakers from 2015 to 2019. A chi-square test was used to assess the proportion of women speakers for open call processes versus that seen with closed call. One-way analysis of variance (ANOVA) was used to evaluate annual conference evaluation scores from 2015 to 2019. Either numbers with proportions or means with standard deviations have been reported. Bonferroni’s correction for multiple comparisons was applied, with a P < .008 considered statistically significant.
RESULTS
Between 2015 and 2019, a total of 709 workshop and didactic presentations were given by 1,261 speakers at the annual Society of Hospital Medicine Conference. Of these, 505 (40%) were women; 756 (60%) were men. There were no missing data.
From 2015 to 2019, representation of women speakers increased from 35% of all speakers to 47% of all speakers (P = .0068). Women plenary speakers increased from 23% in 2015 to 45% in 2019 (P = .0396).
The proportion of women presenters for workshops (which have utilized an open call process throughout the study period), ranged from 43% to 53% from 2015 to 2019 with no statistically significant difference in gender distribution across years (Figure).
A greater proportion of speakers selected by an open call process were women compared to when speakers were selected by a closed call process (261 (47%) vs 244 (34%); P < .0001).
Of didactics or workshops given in a group format (N = 299), 82 (27%) were given by all-men groups and 38 (13%) were given by all-women groups. Women speakers participating in all-women group talks accounted for 21% of all women speakers; whereas men speakers participating in all-men group talks account for 26% of all men speakers (P = .02). We found that all-men group speaking opportunities did decrease from 41% of group talks in 2015 to 21% of group talks in 2019 (P = .0065).
We saw an average 3% annual increase in women speakers from 2015 to 2019, an 8% increase from 2018 to 2019 for all speakers, and an 11% increase in women speakers specific to didactic sessions. Overall conference ratings increased from a mean of 4.3 ± 0.24 in 2015 to a mean of 4.6 ± 0.14 in 2019 (n = 1,202; P < .0001; Figure).
DISCUSSION
The important findings of this study are that there has been an increase in women speakers over the last 5 years at the annual Society of Hospital Medicine Conference, that women had higher representation as speakers when open call processes were followed, and that conference scores continued to improve during the time frame studied. These findings suggest that a systematic open call process helps to support equitable speaking opportunities for men and women at a national hospital medicine conference without a negative impact on conference quality.
To recruit more diverse speakers, open call and peer review processes were used in addition to deliberate efforts at ensuring diversity in speakers. We found that over time, the proportion of women with speaking opportunities increased from 2015 to 2019. Interestingly, workshops, which had open call processes in place for the duration of the study period, had almost equal numbers of men and women presenting in all years. We also found that the number of all-men speaking groups decreased between 2015 and 2019.
A single process change can impact gender equity, but the target of true equity is expected to require additional measures such as assessment of committee structures and diversity, checklists, and reporting structures (data analysis and plans when goals not achieved).10-13 For instance, the American Society for Microbiology General Meeting was able to achieve gender equity in speakers by a multifold approach including ensuring the program committee was aware of gender statistics, increasing female representation among session convener teams, and direct instruction to try to avoid all-male sessions.11
It is important to acknowledge that these processes do require valuable resources including time. SHM has historically used committee volunteers to conduct the peer review process with each committee member reviewing 20 to 30 workshop submissions and 30 to 50 didactic sessions. While open processes with peer review seem to generate improved gender equity, ensuring processes are in place during the selection process is also key.
Several recent notable efforts to enhance gender equity and to increase diversity have been proposed. One such example of a process that may further improve gender equity was proposed by editors at the Journal of Hospital Medicine to assess current representation via demographics including gender, race, and ethnicity of authors with plans to assess patterns in the coming years.14 The American College of Physicians also published a position paper on achieving gender equity with a recommendation that organizational policies and procedures should be implemented that address implicit bias.15
Our study showed that, from 2015 to 2019, conference evaluations saw a significant increase in the score concurrently with the rise in proportion of women speakers. This finding suggests that quality does not seem to be affected by this new methodology for speaker selection and in fact this methodology may actually help improve the overall quality of the conference. To our knowledge, this is one of the first studies to concurrently evaluate speaker gender equity with conference quality.
Our study offers several strengths. This study took a pragmatic approach to understanding how processes can impact gender equity, and we were able to take advantage of the evolution of the open call system (ie workshops which have been an open call process for the duration of the study versus speaking opportunities that were not).
Our study also has several limitations. First, this study is retrospective in nature and thus other processes could have contributed to the improved gender equity, such as an organization’s priorities over time. During this study period, the SHM conference saw an average 3% increase annually in women speakers and an increase of 8% from 2018 to 2019 for all speakers compared to national trends of approximately 1%,6 which suggests that the open call processes in place could be contributing to the overall increases seen. Similarly, because of the retrospective nature of the study, we cannot be certain that the improvements in conference scores were directly the result of improved gender equity, although it does suggest that the improvements in gender equity did not have an adverse impact on the scores. We also did not assess how the composition of selection committee members for the meeting could have impacted the overall composition of the speakers. Our study looked at diversity only from the perspective of gender in a binary fashion, and thus additional studies are needed to assess how to improve diversity overall. It is unclear how this new open call for speakers affects race and ethnic diversity specifically. Identifying gender for the purposes of this study was facilitated by speakers providing their own biographies and the respective pronouns used in those biographies, and thus gender was easier to ascertain than race and ethnicity, which are not as readily available. For organizations to understand their diversity, equity, and inclusion efforts, enhancing the ability to fairly track and measure diversity will be key. Lastly, understanding of the exact composition of hospitalists from both a gender and race/ethnicity perspective is lacking. Studies have suggested that, based upon those surveyed or studied, there is a fairly equal balance of men and women albeit in academic groups.3
CONCLUSIONS
An open call approach to speakers at a national hospitalist conference seems to have contributed to improvements regarding gender equity in speaking opportunities with a concurrent improvement in overall rating of the conference. The open call system is a potential mechanism that other institutions and organizations could employ to enhance their diversity efforts.
Acknowledgments
Society of Hospital Medicine Diversity, Equity, Inclusion Special Interest Group
Work Group for SPEAK UP: Marisha Burden, MD, Daniel Cabrera, MD, Amira del Pino-Jones, MD, Areeba Kara, MD, Angela Keniston, MSPH, Keshav Khanijow, MD, Flora Kisuule, MD, Chiara Mandel, Benji Mathews, MD, David Paje, MD, Stephan Papp, MD, Snehal Patel, MD, Suchita Shah Sata, MD, Dustin Smith, MD, Kevin Vuernick
1. Weaver AC, Wetterneck TB, Whelan CT, Hinami K. A matter of priorities? Exploring the persistent gender pay gap in hospital medicine. J Hosp Med. 2015;10(8):486-490. https://doi.org/10.1002/jhm.2400.
2. Jena AB, Olenski AR, Blumenthal DM. Sex differences in physician salary in US public medical schools. JAMA Intern Med. 2016;176(9):1294-1304. https://doi.org/10.1001/jamainternmed.2016.3284.
3. Burden M, Frank MG, Keniston A, et al. Gender disparities in leadership and scholarly productivity of academic hospitalists. J Hosp Med. 2015;10(8):481-485. https://doi.org/10.1002/jhm.2340.
4. Silver JK, Ghalib R, Poorman JA, et al. Analysis of gender equity in leadership of physician-focused medical specialty societies, 2008-2017. JAMA Intern Med. 2019;179(3):433-435. https://doi.org/10.1001/jamainternmed.2018.5303.
5. Jena AB, Khullar D, Ho O, Olenski AR, Blumenthal DM. Sex differences in academic rank in US medical schools in 2014. JAMA. 2015;314(11):1149-1158. https://doi.org/10.1001/jama.2015.10680.
6. Ruzycki SM, Fletcher S, Earp M, Bharwani A, Lithgow KC. Trends in the Proportion of Female Speakers at Medical Conferences in the United States and in Canada, 2007 to 2017. JAMA Netw Open. 2019;2(4):e192103. https://doi.org/10.1001/jamanetworkopen.2019.2103
7. Reid MB, Misky GJ, Harrison RA, Sharpe B, Auerbach A, Glasheen JJ. Mentorship, productivity, and promotion among academic hospitalists. J Gen Intern Med. 2012;27(1):23-27. https://doi.org/10.1007/s11606-011-1892-5.
8. Today’s Hospitalist 2018 Compensation and Career Survey Results. https://www.todayshospitalist.com/salary-survey-results/. Accessed September 28, 2019.
9. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. https://doi.org/10.1016/j.jbi.2008.08.010.
10. Burden M, del Pino-Jones A, Shafer M, Sheth S, Rexrode K. Association of American Medical Colleagues (AAMC) Group on Women in Medicine and Science. Recruitment Toolkit: https://www.aamc.org/download/492864/data/equityinrecruitmenttoolkit.pdf. Accessed July 27, 2019.
11. Casadevall A. Achieving speaker gender equity at the american society for microbiology general meeting. MBio. 2015;6:e01146. https://doi.org/10.1128/mBio.01146-15.
12. Westring A, McDonald JM, Carr P, Grisso JA. An integrated framework for gender equity in academic medicine. Acad Med. 2016;91(8):1041-1044. https://doi.org/10.1097/ACM.0000000000001275.
13. Martin JL. Ten simple rules to achieve conference speaker gender balance. PLoS Comput Biol. 2014;10(11):e1003903. https://doi.org/10.1371/journal.pcbi.1003903.
14. Shah SS, Shaughnessy EE, Spector ND. Leading by example: how medical journals can improve representation in academic medicine. J Hosp Med. 2019;14(7):393. https://doi.org/10.12788/jhm.3247.
15. Butkus R, Serchen J, Moyer DV, et al. Achieving gender equity in physician compensation and career advancement: a position paper of the American College of Physicians. Ann Intern Med. 2018;168:721-723. https://doi.org/10.7326/M17-3438.
1. Weaver AC, Wetterneck TB, Whelan CT, Hinami K. A matter of priorities? Exploring the persistent gender pay gap in hospital medicine. J Hosp Med. 2015;10(8):486-490. https://doi.org/10.1002/jhm.2400.
2. Jena AB, Olenski AR, Blumenthal DM. Sex differences in physician salary in US public medical schools. JAMA Intern Med. 2016;176(9):1294-1304. https://doi.org/10.1001/jamainternmed.2016.3284.
3. Burden M, Frank MG, Keniston A, et al. Gender disparities in leadership and scholarly productivity of academic hospitalists. J Hosp Med. 2015;10(8):481-485. https://doi.org/10.1002/jhm.2340.
4. Silver JK, Ghalib R, Poorman JA, et al. Analysis of gender equity in leadership of physician-focused medical specialty societies, 2008-2017. JAMA Intern Med. 2019;179(3):433-435. https://doi.org/10.1001/jamainternmed.2018.5303.
5. Jena AB, Khullar D, Ho O, Olenski AR, Blumenthal DM. Sex differences in academic rank in US medical schools in 2014. JAMA. 2015;314(11):1149-1158. https://doi.org/10.1001/jama.2015.10680.
6. Ruzycki SM, Fletcher S, Earp M, Bharwani A, Lithgow KC. Trends in the Proportion of Female Speakers at Medical Conferences in the United States and in Canada, 2007 to 2017. JAMA Netw Open. 2019;2(4):e192103. https://doi.org/10.1001/jamanetworkopen.2019.2103
7. Reid MB, Misky GJ, Harrison RA, Sharpe B, Auerbach A, Glasheen JJ. Mentorship, productivity, and promotion among academic hospitalists. J Gen Intern Med. 2012;27(1):23-27. https://doi.org/10.1007/s11606-011-1892-5.
8. Today’s Hospitalist 2018 Compensation and Career Survey Results. https://www.todayshospitalist.com/salary-survey-results/. Accessed September 28, 2019.
9. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. https://doi.org/10.1016/j.jbi.2008.08.010.
10. Burden M, del Pino-Jones A, Shafer M, Sheth S, Rexrode K. Association of American Medical Colleagues (AAMC) Group on Women in Medicine and Science. Recruitment Toolkit: https://www.aamc.org/download/492864/data/equityinrecruitmenttoolkit.pdf. Accessed July 27, 2019.
11. Casadevall A. Achieving speaker gender equity at the american society for microbiology general meeting. MBio. 2015;6:e01146. https://doi.org/10.1128/mBio.01146-15.
12. Westring A, McDonald JM, Carr P, Grisso JA. An integrated framework for gender equity in academic medicine. Acad Med. 2016;91(8):1041-1044. https://doi.org/10.1097/ACM.0000000000001275.
13. Martin JL. Ten simple rules to achieve conference speaker gender balance. PLoS Comput Biol. 2014;10(11):e1003903. https://doi.org/10.1371/journal.pcbi.1003903.
14. Shah SS, Shaughnessy EE, Spector ND. Leading by example: how medical journals can improve representation in academic medicine. J Hosp Med. 2019;14(7):393. https://doi.org/10.12788/jhm.3247.
15. Butkus R, Serchen J, Moyer DV, et al. Achieving gender equity in physician compensation and career advancement: a position paper of the American College of Physicians. Ann Intern Med. 2018;168:721-723. https://doi.org/10.7326/M17-3438.
© 2020 Society of Hospital Medicine
VICTORIA: Vericiguat seen as novel success in tough-to-treat, high-risk heart failure
Not too many years ago, clinicians who treat patients with heart failure, especially those at high risk for decompensation, lamented what seemed a dearth of new drug therapy options.
Now, with the toolbox brimming with new guideline-supported alternatives, .
Importantly, it entered an especially high-risk population with heart failure and reduced ejection fraction (HFrEF); everyone in the trial had experienced a prior, usually quite recent, heart failure exacerbation.
In such patients, the addition of vericiguat (Merck/Bayer) to standard drug and device therapies was followed by a moderately but significantly reduced relative risk for the trial’s primary clinical endpoint over about 11 months.
Recipients benefited with a 10% drop in adjusted risk (P = .019) for cardiovascular (CV) death or first heart failure hospitalization compared to a placebo control group.
But researchers leading the 5050-patient Vericiguat Global Study in Subjects with Heart Failure with Reduced Ejection Fraction (VICTORIA), as well as unaffiliated experts who have studied the trial, say that in this case, risk reduction in absolute numbers is a more telling outcome.
“Remember who we’re talking about here in terms of the patients who have this degree of morbidity and mortality,” VICTORIA study chair Paul W. Armstrong, MD, University of Alberta, Edmonton, Canada, told theheart.org | Medscape Cardiology, pointing to the “incredible placebo-group event rate and relatively modest follow-up of 10.8 months.”
The control group’s primary-endpoint event rate was 37.8 per 100 patient-years, 4.2 points higher than the rate for patients who received vericiguat. “And from there you get a number needed to treat of 24 to prevent one event, which is low,” Armstrong said.
“Think about the hundreds of thousands of people with this disease and what that means at the public health level.” About one in four patients with heart failure experience such exacerbations each year, he said.
Armstrong is lead author on the 42-country trial’s publication today in the New England Journal of Medicine, timed to coincide with his online presentation for the American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC). The annual session was conducted virtually this year following the traditional live meeting’s cancelation due to the COVID-19 pandemic.
The VICTORIA presentation and publication flesh out the cursory top-line primary results that Merck unveiled in November 2019, which had not included the magnitude of the vericiguat relative benefit for the primary endpoint.
The trial represents “another win” for the treatment of heart failure, Clyde W. Yancy, MD, Northwestern University, Chicago, Illinois, said as an invited discussant following Armstrong’s presentation.
“Hospitalization for heart failure generates a major inflection point in the natural history of this condition, with a marked change in the risk for re-hospitalization and death. Up until now, no prior therapies have attenuated this risk, except for more intensive processes and care improvement strategies,” he said.
“Now we have a therapy that may be the first one to change that natural history after a person with heart failure has had a worsening event.”
Interestingly, the primary-endpoint reduction was driven by a significant drop in heart failure hospitalizations, even within a fairly short follow-up time.
“What was fascinating is that the requisite number of events were accrued in less than 12 months — meaning that inexplicably, this is one of the few times we’ve had a trial where the event rate realized was higher than the event rate predicted,” Yancy observed for theheart.org | Medscape Cardiology.
Although the effect size was similar to what was observed for dapagliflozin (Farxiga, AstraZeneca) in DAPA-HF and sacubitril/valsartan (Entresto, Novartis) in PARADIGM-HF, he said, VICTORIA’s population was much sicker and had an “astonishingly high” event rate even while receiving aggressive background heart failure therapy.
It included “triple therapy with renin-angiotensin system inhibitors, β-blockers, and mineralocorticoid receptor antagonists in 60% of patients, and at least double therapy in 90% of patients.” Also, Yancy said, 30% of the population had implantable devices, such as defibrillators and biventricular pacemakers.
Such patients with advanced, late-stage disease are common as the latest therapies for heart failure prolong their survival, notes Lynne W. Stevenson, MD, Vanderbilt University, Nashville, Tennessee, also as an invited discussant after Armstrong’s presentation.
“It’s a unique population with longer disease duration, more severe disease, and narrow options,” one in which personalized approaches are needed. Yet VICTORIA-like patients “have been actively excluded from all the trials that have shown benefit,” she said.
“VICTORIA finally addresses this population of decompensated patients,” she said, and seems to show that vericiguat may help some of them.
At the University of Glasgow, United Kingdom, John J.V. McMurray, MBChB, MD, agreed that the relative risk reduction was “small but significant,” but also that the control group’s event rate was “very high, reflecting the inclusion and exclusion criteria.”
As a result, McMurray told theheart.org | Medscape Cardiology, there was “quite a large absolute risk reduction and small number needed to treat. Also on the positive side: no significant excess of the adverse effects we might have been concerned about,” for example, hypotension.
Vericiguat, if ultimately approved in heart failure, “isn’t going to be first-line or widely used, but it is an additional asset,” he said. “Anything that helps in heart failure is valuable. There are always patients who can’t tolerate treatments, and always people who need more done.”
It’s appealing that the drug works by a long but unfruitfully explored mechanism that has little to do directly with the renin-angiotensin-aldosterone system.
Vericiguat is a soluble guanylate cyclase stimulator that boosts cyclic guanosine monophosphate activity along several pathways, potentiating the salutary pulmonary artery–vasodilating effects of nitric oxide. It improved natriuretic peptide levels in the preceding phase 2 SOCRATES-REDUCED study.
“This is not a me-too drug. It’s a new avenue for heart failure patients,” Armstrong said in an interview. It’s taken once daily, “was relatively easy to titrate up to the target dose, pretty well tolerated, and very safe. And remarkably, you don’t need to measure renal function.”
However, because the drug’s mechanism resides in the same neighborhood of biochemical pathways affected by chronic nitrates and by phosphodiesterase type 5 inhibitors, such as sildenafil and tadalafil, patients taking those drugs were excluded from VICTORIA. Acute nitrates were allowed, however.
“Hospitalization for heart failure generates a major inflection point in the natural history of this condition, with a marked change in the risk for re-hospitalization and death. Up until now, no prior therapies have attenuated this risk, except for more intensive processes and care improvement strategies,” he said.
“Now we have a therapy that may be the first one to change that natural history after a person with heart failure has had a worsening event.”
Interestingly, the primary-endpoint reduction was driven by a significant drop in heart failure hospitalizations, even within a fairly short follow-up time.
“What was fascinating is that the requisite number of events were accrued in less than 12 months — meaning that inexplicably, this is one of the few times we’ve had a trial where the event rate realized was higher than the event rate predicted,” Yancy observed for theheart.org | Medscape Cardiology.
Although the effect size was similar to what was observed for dapagliflozin (Farxiga, AstraZeneca) in DAPA-HF and sacubitril/valsartan (Entresto, Novartis) in PARADIGM-HF, he said, VICTORIA’s population was much sicker and had an “astonishingly high” event rate even while receiving aggressive background heart failure therapy.
It included “triple therapy with renin-angiotensin system inhibitors, β-blockers, and mineralocorticoid receptor antagonists in 60% of patients, and at least double therapy in 90% of patients.” Also, Yancy said, 30% of the population had implantable devices, such as defibrillators and biventricular pacemakers.
Such patients with advanced, late-stage disease are common as the latest therapies for heart failure prolong their survival, notes Lynne W. Stevenson, MD, Vanderbilt University, Nashville, Tennessee, also as an invited discussant after Armstrong’s presentation.
“It’s a unique population with longer disease duration, more severe disease, and narrow options,” one in which personalized approaches are needed. Yet VICTORIA-like patients “have been actively excluded from all the trials that have shown benefit,” she said.
“VICTORIA finally addresses this population of decompensated patients,” she said, and seems to show that vericiguat may help some of them.
At the University of Glasgow, United Kingdom, John J.V. McMurray, MBChB, MD, agreed that the relative risk reduction was “small but significant,” but also that the control group’s event rate was “very high, reflecting the inclusion and exclusion criteria.”
As a result, McMurray told theheart.org | Medscape Cardiology, there was “quite a large absolute risk reduction and small number needed to treat. Also on the positive side: no significant excess of the adverse effects we might have been concerned about,” for example, hypotension.
Vericiguat, if ultimately approved in heart failure, “isn’t going to be first-line or widely used, but it is an additional asset,” he said. “Anything that helps in heart failure is valuable. There are always patients who can’t tolerate treatments, and always people who need more done.”
It’s appealing that the drug works by a long but unfruitfully explored mechanism that has little to do directly with the renin-angiotensin-aldosterone system.
Vericiguat is a soluble guanylate cyclase stimulator that boosts cyclic guanosine monophosphate activity along several pathways, potentiating the salutary pulmonary artery–vasodilating effects of nitric oxide. It improved natriuretic peptide levels in the preceding phase 2 SOCRATES-REDUCED study.
“This is not a me-too drug. It’s a new avenue for heart failure patients,” Armstrong said in an interview. It’s taken once daily, “was relatively easy to titrate up to the target dose, pretty well tolerated, and very safe. And remarkably, you don’t need to measure renal function.”
However, because the drug’s mechanism resides in the same neighborhood of biochemical pathways affected by chronic nitrates and by phosphodiesterase type 5 inhibitors, such as sildenafil and tadalafil, patients taking those drugs were excluded from VICTORIA. Acute nitrates were allowed, however.
Symptomatic hypotension occurred in less than 10% and syncope in 4% or less of both groups; neither difference between the two groups was significant. Anemia developed more often in patients receiving vericiguat (7.6%) than in the control group (5.7%).
“We think that on balance, vericiguat is a useful alternative option for patients. But certainly the only thing we can say at this point is it works in the high-risk population that we studied,” Armstrong said. “Whether it works in lower-risk populations and how it compares is speculation, of course.”
The drug’s cost, whatever it might be if approved, is another factor affecting how it would be used, noted several observers.
“We don’t know what the cost-effectiveness will be. It should be reasonable because the benefit was on hospitalization. That’s a costly outcome,” Yancy said.
McMurray was also hopeful. “If the treatment is well tolerated and reasonably priced, it may still be a valuable asset for at least a subset of patients.”
VICTORIA was supported by Merck Sharp & Dohme Corp and Bayer AG. Armstrong discloses receiving research grants from Merck, Bayer AG, Sanofi-Aventis, Boehringer Ingelheim, and CSL Ltd and consulting fees from Merck, Bayer AG, AstraZeneca, and Novartis. Y ancy has previously disclosed no relevant financial relationships. Stevenson has previously disclosed receiving research grants from Novartis, consulting or serving on an advisory board for Abbott and travel expenses or meals from Novartis and St Jude Medical. McMurray has previously disclosed nonfinancial support or other support from AstraZeneca, Bayer, Cardiorentis, Amgen, Oxford University/Bayer, Theracos, AbbVie, DalCor, Pfizer, Merck, Novartis, GlaxoSmithKline, Bristol-Myers Squibb, and Vifor-Fresenius.
American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC). Presented March 28, 2020. Session 402-08.
N Engl J Med. Published online March 28, 2020. Full text; Circulation. Published online March 28, 2020. Full text.
This article first appeared on Medscape.com.
Not too many years ago, clinicians who treat patients with heart failure, especially those at high risk for decompensation, lamented what seemed a dearth of new drug therapy options.
Now, with the toolbox brimming with new guideline-supported alternatives, .
Importantly, it entered an especially high-risk population with heart failure and reduced ejection fraction (HFrEF); everyone in the trial had experienced a prior, usually quite recent, heart failure exacerbation.
In such patients, the addition of vericiguat (Merck/Bayer) to standard drug and device therapies was followed by a moderately but significantly reduced relative risk for the trial’s primary clinical endpoint over about 11 months.
Recipients benefited with a 10% drop in adjusted risk (P = .019) for cardiovascular (CV) death or first heart failure hospitalization compared to a placebo control group.
But researchers leading the 5050-patient Vericiguat Global Study in Subjects with Heart Failure with Reduced Ejection Fraction (VICTORIA), as well as unaffiliated experts who have studied the trial, say that in this case, risk reduction in absolute numbers is a more telling outcome.
“Remember who we’re talking about here in terms of the patients who have this degree of morbidity and mortality,” VICTORIA study chair Paul W. Armstrong, MD, University of Alberta, Edmonton, Canada, told theheart.org | Medscape Cardiology, pointing to the “incredible placebo-group event rate and relatively modest follow-up of 10.8 months.”
The control group’s primary-endpoint event rate was 37.8 per 100 patient-years, 4.2 points higher than the rate for patients who received vericiguat. “And from there you get a number needed to treat of 24 to prevent one event, which is low,” Armstrong said.
“Think about the hundreds of thousands of people with this disease and what that means at the public health level.” About one in four patients with heart failure experience such exacerbations each year, he said.
Armstrong is lead author on the 42-country trial’s publication today in the New England Journal of Medicine, timed to coincide with his online presentation for the American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC). The annual session was conducted virtually this year following the traditional live meeting’s cancelation due to the COVID-19 pandemic.
The VICTORIA presentation and publication flesh out the cursory top-line primary results that Merck unveiled in November 2019, which had not included the magnitude of the vericiguat relative benefit for the primary endpoint.
The trial represents “another win” for the treatment of heart failure, Clyde W. Yancy, MD, Northwestern University, Chicago, Illinois, said as an invited discussant following Armstrong’s presentation.
“Hospitalization for heart failure generates a major inflection point in the natural history of this condition, with a marked change in the risk for re-hospitalization and death. Up until now, no prior therapies have attenuated this risk, except for more intensive processes and care improvement strategies,” he said.
“Now we have a therapy that may be the first one to change that natural history after a person with heart failure has had a worsening event.”
Interestingly, the primary-endpoint reduction was driven by a significant drop in heart failure hospitalizations, even within a fairly short follow-up time.
“What was fascinating is that the requisite number of events were accrued in less than 12 months — meaning that inexplicably, this is one of the few times we’ve had a trial where the event rate realized was higher than the event rate predicted,” Yancy observed for theheart.org | Medscape Cardiology.
Although the effect size was similar to what was observed for dapagliflozin (Farxiga, AstraZeneca) in DAPA-HF and sacubitril/valsartan (Entresto, Novartis) in PARADIGM-HF, he said, VICTORIA’s population was much sicker and had an “astonishingly high” event rate even while receiving aggressive background heart failure therapy.
It included “triple therapy with renin-angiotensin system inhibitors, β-blockers, and mineralocorticoid receptor antagonists in 60% of patients, and at least double therapy in 90% of patients.” Also, Yancy said, 30% of the population had implantable devices, such as defibrillators and biventricular pacemakers.
Such patients with advanced, late-stage disease are common as the latest therapies for heart failure prolong their survival, notes Lynne W. Stevenson, MD, Vanderbilt University, Nashville, Tennessee, also as an invited discussant after Armstrong’s presentation.
“It’s a unique population with longer disease duration, more severe disease, and narrow options,” one in which personalized approaches are needed. Yet VICTORIA-like patients “have been actively excluded from all the trials that have shown benefit,” she said.
“VICTORIA finally addresses this population of decompensated patients,” she said, and seems to show that vericiguat may help some of them.
At the University of Glasgow, United Kingdom, John J.V. McMurray, MBChB, MD, agreed that the relative risk reduction was “small but significant,” but also that the control group’s event rate was “very high, reflecting the inclusion and exclusion criteria.”
As a result, McMurray told theheart.org | Medscape Cardiology, there was “quite a large absolute risk reduction and small number needed to treat. Also on the positive side: no significant excess of the adverse effects we might have been concerned about,” for example, hypotension.
Vericiguat, if ultimately approved in heart failure, “isn’t going to be first-line or widely used, but it is an additional asset,” he said. “Anything that helps in heart failure is valuable. There are always patients who can’t tolerate treatments, and always people who need more done.”
It’s appealing that the drug works by a long but unfruitfully explored mechanism that has little to do directly with the renin-angiotensin-aldosterone system.
Vericiguat is a soluble guanylate cyclase stimulator that boosts cyclic guanosine monophosphate activity along several pathways, potentiating the salutary pulmonary artery–vasodilating effects of nitric oxide. It improved natriuretic peptide levels in the preceding phase 2 SOCRATES-REDUCED study.
“This is not a me-too drug. It’s a new avenue for heart failure patients,” Armstrong said in an interview. It’s taken once daily, “was relatively easy to titrate up to the target dose, pretty well tolerated, and very safe. And remarkably, you don’t need to measure renal function.”
However, because the drug’s mechanism resides in the same neighborhood of biochemical pathways affected by chronic nitrates and by phosphodiesterase type 5 inhibitors, such as sildenafil and tadalafil, patients taking those drugs were excluded from VICTORIA. Acute nitrates were allowed, however.
“Hospitalization for heart failure generates a major inflection point in the natural history of this condition, with a marked change in the risk for re-hospitalization and death. Up until now, no prior therapies have attenuated this risk, except for more intensive processes and care improvement strategies,” he said.
“Now we have a therapy that may be the first one to change that natural history after a person with heart failure has had a worsening event.”
Interestingly, the primary-endpoint reduction was driven by a significant drop in heart failure hospitalizations, even within a fairly short follow-up time.
“What was fascinating is that the requisite number of events were accrued in less than 12 months — meaning that inexplicably, this is one of the few times we’ve had a trial where the event rate realized was higher than the event rate predicted,” Yancy observed for theheart.org | Medscape Cardiology.
Although the effect size was similar to what was observed for dapagliflozin (Farxiga, AstraZeneca) in DAPA-HF and sacubitril/valsartan (Entresto, Novartis) in PARADIGM-HF, he said, VICTORIA’s population was much sicker and had an “astonishingly high” event rate even while receiving aggressive background heart failure therapy.
It included “triple therapy with renin-angiotensin system inhibitors, β-blockers, and mineralocorticoid receptor antagonists in 60% of patients, and at least double therapy in 90% of patients.” Also, Yancy said, 30% of the population had implantable devices, such as defibrillators and biventricular pacemakers.
Such patients with advanced, late-stage disease are common as the latest therapies for heart failure prolong their survival, notes Lynne W. Stevenson, MD, Vanderbilt University, Nashville, Tennessee, also as an invited discussant after Armstrong’s presentation.
“It’s a unique population with longer disease duration, more severe disease, and narrow options,” one in which personalized approaches are needed. Yet VICTORIA-like patients “have been actively excluded from all the trials that have shown benefit,” she said.
“VICTORIA finally addresses this population of decompensated patients,” she said, and seems to show that vericiguat may help some of them.
At the University of Glasgow, United Kingdom, John J.V. McMurray, MBChB, MD, agreed that the relative risk reduction was “small but significant,” but also that the control group’s event rate was “very high, reflecting the inclusion and exclusion criteria.”
As a result, McMurray told theheart.org | Medscape Cardiology, there was “quite a large absolute risk reduction and small number needed to treat. Also on the positive side: no significant excess of the adverse effects we might have been concerned about,” for example, hypotension.
Vericiguat, if ultimately approved in heart failure, “isn’t going to be first-line or widely used, but it is an additional asset,” he said. “Anything that helps in heart failure is valuable. There are always patients who can’t tolerate treatments, and always people who need more done.”
It’s appealing that the drug works by a long but unfruitfully explored mechanism that has little to do directly with the renin-angiotensin-aldosterone system.
Vericiguat is a soluble guanylate cyclase stimulator that boosts cyclic guanosine monophosphate activity along several pathways, potentiating the salutary pulmonary artery–vasodilating effects of nitric oxide. It improved natriuretic peptide levels in the preceding phase 2 SOCRATES-REDUCED study.
“This is not a me-too drug. It’s a new avenue for heart failure patients,” Armstrong said in an interview. It’s taken once daily, “was relatively easy to titrate up to the target dose, pretty well tolerated, and very safe. And remarkably, you don’t need to measure renal function.”
However, because the drug’s mechanism resides in the same neighborhood of biochemical pathways affected by chronic nitrates and by phosphodiesterase type 5 inhibitors, such as sildenafil and tadalafil, patients taking those drugs were excluded from VICTORIA. Acute nitrates were allowed, however.
Symptomatic hypotension occurred in less than 10% and syncope in 4% or less of both groups; neither difference between the two groups was significant. Anemia developed more often in patients receiving vericiguat (7.6%) than in the control group (5.7%).
“We think that on balance, vericiguat is a useful alternative option for patients. But certainly the only thing we can say at this point is it works in the high-risk population that we studied,” Armstrong said. “Whether it works in lower-risk populations and how it compares is speculation, of course.”
The drug’s cost, whatever it might be if approved, is another factor affecting how it would be used, noted several observers.
“We don’t know what the cost-effectiveness will be. It should be reasonable because the benefit was on hospitalization. That’s a costly outcome,” Yancy said.
McMurray was also hopeful. “If the treatment is well tolerated and reasonably priced, it may still be a valuable asset for at least a subset of patients.”
VICTORIA was supported by Merck Sharp & Dohme Corp and Bayer AG. Armstrong discloses receiving research grants from Merck, Bayer AG, Sanofi-Aventis, Boehringer Ingelheim, and CSL Ltd and consulting fees from Merck, Bayer AG, AstraZeneca, and Novartis. Y ancy has previously disclosed no relevant financial relationships. Stevenson has previously disclosed receiving research grants from Novartis, consulting or serving on an advisory board for Abbott and travel expenses or meals from Novartis and St Jude Medical. McMurray has previously disclosed nonfinancial support or other support from AstraZeneca, Bayer, Cardiorentis, Amgen, Oxford University/Bayer, Theracos, AbbVie, DalCor, Pfizer, Merck, Novartis, GlaxoSmithKline, Bristol-Myers Squibb, and Vifor-Fresenius.
American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC). Presented March 28, 2020. Session 402-08.
N Engl J Med. Published online March 28, 2020. Full text; Circulation. Published online March 28, 2020. Full text.
This article first appeared on Medscape.com.
Not too many years ago, clinicians who treat patients with heart failure, especially those at high risk for decompensation, lamented what seemed a dearth of new drug therapy options.
Now, with the toolbox brimming with new guideline-supported alternatives, .
Importantly, it entered an especially high-risk population with heart failure and reduced ejection fraction (HFrEF); everyone in the trial had experienced a prior, usually quite recent, heart failure exacerbation.
In such patients, the addition of vericiguat (Merck/Bayer) to standard drug and device therapies was followed by a moderately but significantly reduced relative risk for the trial’s primary clinical endpoint over about 11 months.
Recipients benefited with a 10% drop in adjusted risk (P = .019) for cardiovascular (CV) death or first heart failure hospitalization compared to a placebo control group.
But researchers leading the 5050-patient Vericiguat Global Study in Subjects with Heart Failure with Reduced Ejection Fraction (VICTORIA), as well as unaffiliated experts who have studied the trial, say that in this case, risk reduction in absolute numbers is a more telling outcome.
“Remember who we’re talking about here in terms of the patients who have this degree of morbidity and mortality,” VICTORIA study chair Paul W. Armstrong, MD, University of Alberta, Edmonton, Canada, told theheart.org | Medscape Cardiology, pointing to the “incredible placebo-group event rate and relatively modest follow-up of 10.8 months.”
The control group’s primary-endpoint event rate was 37.8 per 100 patient-years, 4.2 points higher than the rate for patients who received vericiguat. “And from there you get a number needed to treat of 24 to prevent one event, which is low,” Armstrong said.
“Think about the hundreds of thousands of people with this disease and what that means at the public health level.” About one in four patients with heart failure experience such exacerbations each year, he said.
Armstrong is lead author on the 42-country trial’s publication today in the New England Journal of Medicine, timed to coincide with his online presentation for the American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC). The annual session was conducted virtually this year following the traditional live meeting’s cancelation due to the COVID-19 pandemic.
The VICTORIA presentation and publication flesh out the cursory top-line primary results that Merck unveiled in November 2019, which had not included the magnitude of the vericiguat relative benefit for the primary endpoint.
The trial represents “another win” for the treatment of heart failure, Clyde W. Yancy, MD, Northwestern University, Chicago, Illinois, said as an invited discussant following Armstrong’s presentation.
“Hospitalization for heart failure generates a major inflection point in the natural history of this condition, with a marked change in the risk for re-hospitalization and death. Up until now, no prior therapies have attenuated this risk, except for more intensive processes and care improvement strategies,” he said.
“Now we have a therapy that may be the first one to change that natural history after a person with heart failure has had a worsening event.”
Interestingly, the primary-endpoint reduction was driven by a significant drop in heart failure hospitalizations, even within a fairly short follow-up time.
“What was fascinating is that the requisite number of events were accrued in less than 12 months — meaning that inexplicably, this is one of the few times we’ve had a trial where the event rate realized was higher than the event rate predicted,” Yancy observed for theheart.org | Medscape Cardiology.
Although the effect size was similar to what was observed for dapagliflozin (Farxiga, AstraZeneca) in DAPA-HF and sacubitril/valsartan (Entresto, Novartis) in PARADIGM-HF, he said, VICTORIA’s population was much sicker and had an “astonishingly high” event rate even while receiving aggressive background heart failure therapy.
It included “triple therapy with renin-angiotensin system inhibitors, β-blockers, and mineralocorticoid receptor antagonists in 60% of patients, and at least double therapy in 90% of patients.” Also, Yancy said, 30% of the population had implantable devices, such as defibrillators and biventricular pacemakers.
Such patients with advanced, late-stage disease are common as the latest therapies for heart failure prolong their survival, notes Lynne W. Stevenson, MD, Vanderbilt University, Nashville, Tennessee, also as an invited discussant after Armstrong’s presentation.
“It’s a unique population with longer disease duration, more severe disease, and narrow options,” one in which personalized approaches are needed. Yet VICTORIA-like patients “have been actively excluded from all the trials that have shown benefit,” she said.
“VICTORIA finally addresses this population of decompensated patients,” she said, and seems to show that vericiguat may help some of them.
At the University of Glasgow, United Kingdom, John J.V. McMurray, MBChB, MD, agreed that the relative risk reduction was “small but significant,” but also that the control group’s event rate was “very high, reflecting the inclusion and exclusion criteria.”
As a result, McMurray told theheart.org | Medscape Cardiology, there was “quite a large absolute risk reduction and small number needed to treat. Also on the positive side: no significant excess of the adverse effects we might have been concerned about,” for example, hypotension.
Vericiguat, if ultimately approved in heart failure, “isn’t going to be first-line or widely used, but it is an additional asset,” he said. “Anything that helps in heart failure is valuable. There are always patients who can’t tolerate treatments, and always people who need more done.”
It’s appealing that the drug works by a long but unfruitfully explored mechanism that has little to do directly with the renin-angiotensin-aldosterone system.
Vericiguat is a soluble guanylate cyclase stimulator that boosts cyclic guanosine monophosphate activity along several pathways, potentiating the salutary pulmonary artery–vasodilating effects of nitric oxide. It improved natriuretic peptide levels in the preceding phase 2 SOCRATES-REDUCED study.
“This is not a me-too drug. It’s a new avenue for heart failure patients,” Armstrong said in an interview. It’s taken once daily, “was relatively easy to titrate up to the target dose, pretty well tolerated, and very safe. And remarkably, you don’t need to measure renal function.”
However, because the drug’s mechanism resides in the same neighborhood of biochemical pathways affected by chronic nitrates and by phosphodiesterase type 5 inhibitors, such as sildenafil and tadalafil, patients taking those drugs were excluded from VICTORIA. Acute nitrates were allowed, however.
“Hospitalization for heart failure generates a major inflection point in the natural history of this condition, with a marked change in the risk for re-hospitalization and death. Up until now, no prior therapies have attenuated this risk, except for more intensive processes and care improvement strategies,” he said.
“Now we have a therapy that may be the first one to change that natural history after a person with heart failure has had a worsening event.”
Interestingly, the primary-endpoint reduction was driven by a significant drop in heart failure hospitalizations, even within a fairly short follow-up time.
“What was fascinating is that the requisite number of events were accrued in less than 12 months — meaning that inexplicably, this is one of the few times we’ve had a trial where the event rate realized was higher than the event rate predicted,” Yancy observed for theheart.org | Medscape Cardiology.
Although the effect size was similar to what was observed for dapagliflozin (Farxiga, AstraZeneca) in DAPA-HF and sacubitril/valsartan (Entresto, Novartis) in PARADIGM-HF, he said, VICTORIA’s population was much sicker and had an “astonishingly high” event rate even while receiving aggressive background heart failure therapy.
It included “triple therapy with renin-angiotensin system inhibitors, β-blockers, and mineralocorticoid receptor antagonists in 60% of patients, and at least double therapy in 90% of patients.” Also, Yancy said, 30% of the population had implantable devices, such as defibrillators and biventricular pacemakers.
Such patients with advanced, late-stage disease are common as the latest therapies for heart failure prolong their survival, notes Lynne W. Stevenson, MD, Vanderbilt University, Nashville, Tennessee, also as an invited discussant after Armstrong’s presentation.
“It’s a unique population with longer disease duration, more severe disease, and narrow options,” one in which personalized approaches are needed. Yet VICTORIA-like patients “have been actively excluded from all the trials that have shown benefit,” she said.
“VICTORIA finally addresses this population of decompensated patients,” she said, and seems to show that vericiguat may help some of them.
At the University of Glasgow, United Kingdom, John J.V. McMurray, MBChB, MD, agreed that the relative risk reduction was “small but significant,” but also that the control group’s event rate was “very high, reflecting the inclusion and exclusion criteria.”
As a result, McMurray told theheart.org | Medscape Cardiology, there was “quite a large absolute risk reduction and small number needed to treat. Also on the positive side: no significant excess of the adverse effects we might have been concerned about,” for example, hypotension.
Vericiguat, if ultimately approved in heart failure, “isn’t going to be first-line or widely used, but it is an additional asset,” he said. “Anything that helps in heart failure is valuable. There are always patients who can’t tolerate treatments, and always people who need more done.”
It’s appealing that the drug works by a long but unfruitfully explored mechanism that has little to do directly with the renin-angiotensin-aldosterone system.
Vericiguat is a soluble guanylate cyclase stimulator that boosts cyclic guanosine monophosphate activity along several pathways, potentiating the salutary pulmonary artery–vasodilating effects of nitric oxide. It improved natriuretic peptide levels in the preceding phase 2 SOCRATES-REDUCED study.
“This is not a me-too drug. It’s a new avenue for heart failure patients,” Armstrong said in an interview. It’s taken once daily, “was relatively easy to titrate up to the target dose, pretty well tolerated, and very safe. And remarkably, you don’t need to measure renal function.”
However, because the drug’s mechanism resides in the same neighborhood of biochemical pathways affected by chronic nitrates and by phosphodiesterase type 5 inhibitors, such as sildenafil and tadalafil, patients taking those drugs were excluded from VICTORIA. Acute nitrates were allowed, however.
Symptomatic hypotension occurred in less than 10% and syncope in 4% or less of both groups; neither difference between the two groups was significant. Anemia developed more often in patients receiving vericiguat (7.6%) than in the control group (5.7%).
“We think that on balance, vericiguat is a useful alternative option for patients. But certainly the only thing we can say at this point is it works in the high-risk population that we studied,” Armstrong said. “Whether it works in lower-risk populations and how it compares is speculation, of course.”
The drug’s cost, whatever it might be if approved, is another factor affecting how it would be used, noted several observers.
“We don’t know what the cost-effectiveness will be. It should be reasonable because the benefit was on hospitalization. That’s a costly outcome,” Yancy said.
McMurray was also hopeful. “If the treatment is well tolerated and reasonably priced, it may still be a valuable asset for at least a subset of patients.”
VICTORIA was supported by Merck Sharp & Dohme Corp and Bayer AG. Armstrong discloses receiving research grants from Merck, Bayer AG, Sanofi-Aventis, Boehringer Ingelheim, and CSL Ltd and consulting fees from Merck, Bayer AG, AstraZeneca, and Novartis. Y ancy has previously disclosed no relevant financial relationships. Stevenson has previously disclosed receiving research grants from Novartis, consulting or serving on an advisory board for Abbott and travel expenses or meals from Novartis and St Jude Medical. McMurray has previously disclosed nonfinancial support or other support from AstraZeneca, Bayer, Cardiorentis, Amgen, Oxford University/Bayer, Theracos, AbbVie, DalCor, Pfizer, Merck, Novartis, GlaxoSmithKline, Bristol-Myers Squibb, and Vifor-Fresenius.
American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC). Presented March 28, 2020. Session 402-08.
N Engl J Med. Published online March 28, 2020. Full text; Circulation. Published online March 28, 2020. Full text.
This article first appeared on Medscape.com.
TAILOR-PCI: Clopidogrel genotyping trial narrowly misses endpoint
The largest trial to date investigating the clinical utility of using genetic testing to detect clopidogrel loss-of-function genotype to guide antiplatelet therapy in patients undergoing percutaneous coronary intervention (PCI) missed its primary endpoint of a 50% reduction in cardiovascular events at 1 year.
However, the TAILOR-PCI trial did show a 34% reduction in such events at 1 year, as well as a statistically significant 40% reduction in the total number of events per patient receiving genetically guided treatment compared with patients who received standard treatment.
In addition, a post hoc analysis found a significant 79% reduction in the rate of adverse events in the first 3 months of treatment among patients who received genetically guided therapy compared with those who did not.
The study was presented March 28 during the “virtual” American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology.
“Although these results fell short of the effect size that we predicted, they nevertheless provide a signal that offers support for the benefit of genetically guided therapy, with approximately one-third fewer adverse events in the patients who received genetically guided treatment compared with those who did not,” concluded Naveen L. Pereira, MD, professor of medicine at the Mayo Clinic in Rochester, Minnesota, and co-principal investigator of the study.
Pereira said the post hoc analysis of the first 3 months of treatment was particularly interesting. “This period immediately after PCI is when patients are at the highest risk for adverse events. We now know that antiplatelet drug therapy is critical during the first 3 months after PCI. Our findings suggest that the lion’s share of the benefit of genetically guided therapy may occur during this high-risk period,” he noted.
However, he added, “Because this wasn’t a preplanned analysis, we can’t draw firm conclusions from it, but it merits further study.”
Asked during an ACC virtual press conference how these results may influence clinical practice, Pereira said he hopes it changes practice toward genotyping.
“We set a very high standard in trying to achieve a 50% reduction in events, but we did see a 34% reduction. I think the probability of the results being true is very high,” he said. “I hope people pay attention to that. I’m not sure what the guidelines will do, but I believe if clopidogrel genetic information is made available to the physician, not changing therapy in a patient who has the loss-of-function gene will now be very difficult.”
Discussant of the trial, Roxana Mehran, MD, Mount Sinai Hospital, New York City, said she thought the results were good enough clinically to justify using genotyping to guide therapy.
“The trial showed an absolute 1.8% reduction and a relative 34% reduction in cardiovascular events, which did not quite meet the P value for significance, and they are supported by a significant reduction in multiple events, and a large difference at 3 months, although these are not primary analyses. So, for me this trial has shown that tailoring antiplatelet therapy by genetic testing is beneficial,” she said.
Another outside commentator, Patrick O’Gara, MD, Brigham and Women’s Hospital, Boston, Massachusetts, described TAILOR-PCI as a “terrific study.”
“Together with the study presented last year showing genotype-guided clopidogrel treatment was noninferior to ticagrelor/prasugrel in STEMI [non-ST-segment elevation myocardial infarction] patients, it chips away at the biologic appropriateness of targeting therapies based on genetic risk,” he said.
“I would hate people to focus on the fact the primary endpoint was missed by one hundredth of a percentage point but hope they would rather consider the bigger picture of making this genotype test more available and accessible to inform clinical decision making,” O’Gara added. “It just makes too much sense to ignore this potential.”
The TAILOR-PCI trial enrolled 5302 patients from 40 centers in the United States, Canada, Mexico, and South Korea who had undergone PCI with stenting. They were randomly assigned to genetic testing for the clopidogrel loss-of-function variant or a group that received standard treatment (clopidogrel) without genetic testing.
In the genetic testing group, 35% of patients were found to have the clopidogrel loss-of-function variant and were therefore prescribed ticagrelor, whereas those without the loss-of-function variant received clopidogrel.
After 1 year, the primary endpoint, a composite of cardiovascular death, MI, stroke, definite or probable stent thrombosis, and severe recurrent ischemia, occurred in 35 patients (4%) of the group that received genetically guided treatment, compared with 54 (5.9%) in the conventionally treated group (adjusted hazard ratio [HR], 0.66; 95% confidence interval [CI], 0.43 - 1.02; P = .56).
A prespecified analysis of total events (rather than just analysis of first event per patient) showed a 40% reduction in the genotyped group (HR, 0.60; 95% CI, 0.41 - 0.89; P = .011).
“Multiple adverse events represent a higher burden on the patient, so it is encouraging to see a significant reduction in cumulative events with genetically guided therapy,” Pereira said.
There was no difference in the safety endpoint of TIMI major bleeding or minor bleeding between the two groups: 1.9% in the genetically guided group vs 1.6% in the conventional treatment group.
The results did not differ between various subgroups in the trial, including race or ethnicity. Although Asian patients have a higher occurrence of the clopidogrel loss-of-function gene, the event risk reductions were similar in Asian and white patients in the study.
Pereira said the study may have been underpowered because of recent improvements in care. When the TAILOR-PCI trial was designed in 2012, around 10% to 12% of patients who received a stent could be expected to have a major adverse event, but during the trial, greater use of drug-coated stents and other treatments significantly reduced the expected rate of adverse events and made it more difficult for the trial to reach its goal of a 50% reduction in adverse events with the number of patients enrolled, he explained.
As part of the discussion, Mehran pointed out that more than 80% of the patients in the trial had acute coronary syndrome (ACS) and yet were being sent home on clopidogrel, which she said she found “daunting.”
“This begs the question of whether they were lower-risk patients and not really the hot unstable ACS patients with large thrombus burden where we see higher event rates,” Mehran commented. She also noted the results must be considered in the new era of platelet monotherapy, where aspirin is being withdrawn, and asked whether clopidogrel monotherapy would be considered safe without aspirin on board.
The researchers are planning a cost-effectiveness analysis of genetically guided therapy based on these data, and they are also continuing to follow patients over the longer term.
The TAILOR-PCI study was funded by the Mayo Clinic in collaboration with the National Heart, Lung, and Blood Institute. Spartan Bioscience Inc supplied the genetic tests used. Pereira reports no relevant disclosures.
American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology. Abstract 20-LB-20309-ACC. Presented March 28, 2020.
This article first appeared on Medscape.com.
The largest trial to date investigating the clinical utility of using genetic testing to detect clopidogrel loss-of-function genotype to guide antiplatelet therapy in patients undergoing percutaneous coronary intervention (PCI) missed its primary endpoint of a 50% reduction in cardiovascular events at 1 year.
However, the TAILOR-PCI trial did show a 34% reduction in such events at 1 year, as well as a statistically significant 40% reduction in the total number of events per patient receiving genetically guided treatment compared with patients who received standard treatment.
In addition, a post hoc analysis found a significant 79% reduction in the rate of adverse events in the first 3 months of treatment among patients who received genetically guided therapy compared with those who did not.
The study was presented March 28 during the “virtual” American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology.
“Although these results fell short of the effect size that we predicted, they nevertheless provide a signal that offers support for the benefit of genetically guided therapy, with approximately one-third fewer adverse events in the patients who received genetically guided treatment compared with those who did not,” concluded Naveen L. Pereira, MD, professor of medicine at the Mayo Clinic in Rochester, Minnesota, and co-principal investigator of the study.
Pereira said the post hoc analysis of the first 3 months of treatment was particularly interesting. “This period immediately after PCI is when patients are at the highest risk for adverse events. We now know that antiplatelet drug therapy is critical during the first 3 months after PCI. Our findings suggest that the lion’s share of the benefit of genetically guided therapy may occur during this high-risk period,” he noted.
However, he added, “Because this wasn’t a preplanned analysis, we can’t draw firm conclusions from it, but it merits further study.”
Asked during an ACC virtual press conference how these results may influence clinical practice, Pereira said he hopes it changes practice toward genotyping.
“We set a very high standard in trying to achieve a 50% reduction in events, but we did see a 34% reduction. I think the probability of the results being true is very high,” he said. “I hope people pay attention to that. I’m not sure what the guidelines will do, but I believe if clopidogrel genetic information is made available to the physician, not changing therapy in a patient who has the loss-of-function gene will now be very difficult.”
Discussant of the trial, Roxana Mehran, MD, Mount Sinai Hospital, New York City, said she thought the results were good enough clinically to justify using genotyping to guide therapy.
“The trial showed an absolute 1.8% reduction and a relative 34% reduction in cardiovascular events, which did not quite meet the P value for significance, and they are supported by a significant reduction in multiple events, and a large difference at 3 months, although these are not primary analyses. So, for me this trial has shown that tailoring antiplatelet therapy by genetic testing is beneficial,” she said.
Another outside commentator, Patrick O’Gara, MD, Brigham and Women’s Hospital, Boston, Massachusetts, described TAILOR-PCI as a “terrific study.”
“Together with the study presented last year showing genotype-guided clopidogrel treatment was noninferior to ticagrelor/prasugrel in STEMI [non-ST-segment elevation myocardial infarction] patients, it chips away at the biologic appropriateness of targeting therapies based on genetic risk,” he said.
“I would hate people to focus on the fact the primary endpoint was missed by one hundredth of a percentage point but hope they would rather consider the bigger picture of making this genotype test more available and accessible to inform clinical decision making,” O’Gara added. “It just makes too much sense to ignore this potential.”
The TAILOR-PCI trial enrolled 5302 patients from 40 centers in the United States, Canada, Mexico, and South Korea who had undergone PCI with stenting. They were randomly assigned to genetic testing for the clopidogrel loss-of-function variant or a group that received standard treatment (clopidogrel) without genetic testing.
In the genetic testing group, 35% of patients were found to have the clopidogrel loss-of-function variant and were therefore prescribed ticagrelor, whereas those without the loss-of-function variant received clopidogrel.
After 1 year, the primary endpoint, a composite of cardiovascular death, MI, stroke, definite or probable stent thrombosis, and severe recurrent ischemia, occurred in 35 patients (4%) of the group that received genetically guided treatment, compared with 54 (5.9%) in the conventionally treated group (adjusted hazard ratio [HR], 0.66; 95% confidence interval [CI], 0.43 - 1.02; P = .56).
A prespecified analysis of total events (rather than just analysis of first event per patient) showed a 40% reduction in the genotyped group (HR, 0.60; 95% CI, 0.41 - 0.89; P = .011).
“Multiple adverse events represent a higher burden on the patient, so it is encouraging to see a significant reduction in cumulative events with genetically guided therapy,” Pereira said.
There was no difference in the safety endpoint of TIMI major bleeding or minor bleeding between the two groups: 1.9% in the genetically guided group vs 1.6% in the conventional treatment group.
The results did not differ between various subgroups in the trial, including race or ethnicity. Although Asian patients have a higher occurrence of the clopidogrel loss-of-function gene, the event risk reductions were similar in Asian and white patients in the study.
Pereira said the study may have been underpowered because of recent improvements in care. When the TAILOR-PCI trial was designed in 2012, around 10% to 12% of patients who received a stent could be expected to have a major adverse event, but during the trial, greater use of drug-coated stents and other treatments significantly reduced the expected rate of adverse events and made it more difficult for the trial to reach its goal of a 50% reduction in adverse events with the number of patients enrolled, he explained.
As part of the discussion, Mehran pointed out that more than 80% of the patients in the trial had acute coronary syndrome (ACS) and yet were being sent home on clopidogrel, which she said she found “daunting.”
“This begs the question of whether they were lower-risk patients and not really the hot unstable ACS patients with large thrombus burden where we see higher event rates,” Mehran commented. She also noted the results must be considered in the new era of platelet monotherapy, where aspirin is being withdrawn, and asked whether clopidogrel monotherapy would be considered safe without aspirin on board.
The researchers are planning a cost-effectiveness analysis of genetically guided therapy based on these data, and they are also continuing to follow patients over the longer term.
The TAILOR-PCI study was funded by the Mayo Clinic in collaboration with the National Heart, Lung, and Blood Institute. Spartan Bioscience Inc supplied the genetic tests used. Pereira reports no relevant disclosures.
American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology. Abstract 20-LB-20309-ACC. Presented March 28, 2020.
This article first appeared on Medscape.com.
The largest trial to date investigating the clinical utility of using genetic testing to detect clopidogrel loss-of-function genotype to guide antiplatelet therapy in patients undergoing percutaneous coronary intervention (PCI) missed its primary endpoint of a 50% reduction in cardiovascular events at 1 year.
However, the TAILOR-PCI trial did show a 34% reduction in such events at 1 year, as well as a statistically significant 40% reduction in the total number of events per patient receiving genetically guided treatment compared with patients who received standard treatment.
In addition, a post hoc analysis found a significant 79% reduction in the rate of adverse events in the first 3 months of treatment among patients who received genetically guided therapy compared with those who did not.
The study was presented March 28 during the “virtual” American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology.
“Although these results fell short of the effect size that we predicted, they nevertheless provide a signal that offers support for the benefit of genetically guided therapy, with approximately one-third fewer adverse events in the patients who received genetically guided treatment compared with those who did not,” concluded Naveen L. Pereira, MD, professor of medicine at the Mayo Clinic in Rochester, Minnesota, and co-principal investigator of the study.
Pereira said the post hoc analysis of the first 3 months of treatment was particularly interesting. “This period immediately after PCI is when patients are at the highest risk for adverse events. We now know that antiplatelet drug therapy is critical during the first 3 months after PCI. Our findings suggest that the lion’s share of the benefit of genetically guided therapy may occur during this high-risk period,” he noted.
However, he added, “Because this wasn’t a preplanned analysis, we can’t draw firm conclusions from it, but it merits further study.”
Asked during an ACC virtual press conference how these results may influence clinical practice, Pereira said he hopes it changes practice toward genotyping.
“We set a very high standard in trying to achieve a 50% reduction in events, but we did see a 34% reduction. I think the probability of the results being true is very high,” he said. “I hope people pay attention to that. I’m not sure what the guidelines will do, but I believe if clopidogrel genetic information is made available to the physician, not changing therapy in a patient who has the loss-of-function gene will now be very difficult.”
Discussant of the trial, Roxana Mehran, MD, Mount Sinai Hospital, New York City, said she thought the results were good enough clinically to justify using genotyping to guide therapy.
“The trial showed an absolute 1.8% reduction and a relative 34% reduction in cardiovascular events, which did not quite meet the P value for significance, and they are supported by a significant reduction in multiple events, and a large difference at 3 months, although these are not primary analyses. So, for me this trial has shown that tailoring antiplatelet therapy by genetic testing is beneficial,” she said.
Another outside commentator, Patrick O’Gara, MD, Brigham and Women’s Hospital, Boston, Massachusetts, described TAILOR-PCI as a “terrific study.”
“Together with the study presented last year showing genotype-guided clopidogrel treatment was noninferior to ticagrelor/prasugrel in STEMI [non-ST-segment elevation myocardial infarction] patients, it chips away at the biologic appropriateness of targeting therapies based on genetic risk,” he said.
“I would hate people to focus on the fact the primary endpoint was missed by one hundredth of a percentage point but hope they would rather consider the bigger picture of making this genotype test more available and accessible to inform clinical decision making,” O’Gara added. “It just makes too much sense to ignore this potential.”
The TAILOR-PCI trial enrolled 5302 patients from 40 centers in the United States, Canada, Mexico, and South Korea who had undergone PCI with stenting. They were randomly assigned to genetic testing for the clopidogrel loss-of-function variant or a group that received standard treatment (clopidogrel) without genetic testing.
In the genetic testing group, 35% of patients were found to have the clopidogrel loss-of-function variant and were therefore prescribed ticagrelor, whereas those without the loss-of-function variant received clopidogrel.
After 1 year, the primary endpoint, a composite of cardiovascular death, MI, stroke, definite or probable stent thrombosis, and severe recurrent ischemia, occurred in 35 patients (4%) of the group that received genetically guided treatment, compared with 54 (5.9%) in the conventionally treated group (adjusted hazard ratio [HR], 0.66; 95% confidence interval [CI], 0.43 - 1.02; P = .56).
A prespecified analysis of total events (rather than just analysis of first event per patient) showed a 40% reduction in the genotyped group (HR, 0.60; 95% CI, 0.41 - 0.89; P = .011).
“Multiple adverse events represent a higher burden on the patient, so it is encouraging to see a significant reduction in cumulative events with genetically guided therapy,” Pereira said.
There was no difference in the safety endpoint of TIMI major bleeding or minor bleeding between the two groups: 1.9% in the genetically guided group vs 1.6% in the conventional treatment group.
The results did not differ between various subgroups in the trial, including race or ethnicity. Although Asian patients have a higher occurrence of the clopidogrel loss-of-function gene, the event risk reductions were similar in Asian and white patients in the study.
Pereira said the study may have been underpowered because of recent improvements in care. When the TAILOR-PCI trial was designed in 2012, around 10% to 12% of patients who received a stent could be expected to have a major adverse event, but during the trial, greater use of drug-coated stents and other treatments significantly reduced the expected rate of adverse events and made it more difficult for the trial to reach its goal of a 50% reduction in adverse events with the number of patients enrolled, he explained.
As part of the discussion, Mehran pointed out that more than 80% of the patients in the trial had acute coronary syndrome (ACS) and yet were being sent home on clopidogrel, which she said she found “daunting.”
“This begs the question of whether they were lower-risk patients and not really the hot unstable ACS patients with large thrombus burden where we see higher event rates,” Mehran commented. She also noted the results must be considered in the new era of platelet monotherapy, where aspirin is being withdrawn, and asked whether clopidogrel monotherapy would be considered safe without aspirin on board.
The researchers are planning a cost-effectiveness analysis of genetically guided therapy based on these data, and they are also continuing to follow patients over the longer term.
The TAILOR-PCI study was funded by the Mayo Clinic in collaboration with the National Heart, Lung, and Blood Institute. Spartan Bioscience Inc supplied the genetic tests used. Pereira reports no relevant disclosures.
American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology. Abstract 20-LB-20309-ACC. Presented March 28, 2020.
This article first appeared on Medscape.com.
More than one in three cardiologists burned out, many ready to bolt
Even before the COVID-19 pandemic, , a new survey shows.
“It is important to recognize the personal and professional repercussions of physician burnout,” lead author Laxmi Mehta, MD, director of preventive cardiology and women’s cardiovascular health at Ohio State University, Columbus, said during an online session of the American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC).
The new ACC 2019 Well Being Survey was sent to 19,348 ACC members in the fall of 2019 and sought to take a deeper dive into the issue of burnout after the ACC’s most recent Professional Life Survey revealed that one in four U.S. cardiologists were burned out in 2015.
While the number of cardiologists who reported feeling stressed fell from 49.5% in 2015 to 43.9% in 2019, the number of cardiologists who reported being burned out increased by 32% from 26.8% to 35.4%, Mehta said.
Among those currently feeling burned out, 23.9% reported having one or more symptoms of burnout, 9.9% had chronic burnout and work frustrations, and 1.6% were “completely burned out” and at the point where they may need to seek help.
Burned-out cardiologists were more likely than those who felt stressed or no burnout to say they may have made a major medical error in the past 3 months (58.3% vs 33.1% and 8.6%; P ≤ .001).
The Usual Suspects
As previously observed, burnout was highest among mid-career cardiologists with 8 to 21 years in practice vs early-career and late-career cardiologists (45.3% vs 35.4% and 31.5%; P ≤ .001) and in women vs men (45.3% vs 33.5%; P ≤ .001). Of the 2025 ACC members who responded, 362 were women.
Several initiatives are underway by the ACC to increase the diversity of cardiology as a specialty, but attention is also needed for mid-career cardiologists, who may not see the “light at the end of the tunnel,” as they take on more clinical demands and more administrative roles, Mehta observed.
Not surprising, clocking 60 or more hours per week increased the risk for burnout, compared with working 40 to 59 hours per week or fewer than 40 hours per week (41.5% vs 29.5% and 17.9%; P ≤ .001).
Burned-out cardiologists were also more likely than those who felt stressed or no burnout to report working in a hectic work environment (59.5% vs 32.3% and 14.6%; P ≤ .001) and to have plans to leave their current practice setting (58.1% vs 27.9% and 14.0%; P ≤ .001).
Factors that played a significant role in those plans were the desire to spend more time with family, on-call time, excessive work or relative value unit (RVU) targets, electronic health records, and the pressure to maintain high patient satisfaction scores, Mehta noted.
“Is any of this relatable to decreasing numbers of cardiologists in the U.S., or is there work to try and relate actual work force availability to burnout?” asked session moderator B. Hadley Wilson, MD, executive vice chair of the Sanger Heart & Vascular Institute in Charlotte, North Carolina, and a member of ACC’s Board of Trustees, following the presentation.
“It’s hard to decipher all of those exact details, but we do know that the cardiology work force tends to be older, so the mid-careers are going to be pulling on a lot more weight in the next few years, so that is a concern,” Mehta replied.
A big factor, however, is the excessive work hours put in by all cardiologists, especially the increasing amount of time spent with electronic medical records and administrative tasks, which is “taking away the fun we had in cardiology,” she added.
Limitations of the survey include the potential for bias; burnout was self-reported and may vary over time; and the 14% response rate was less than ideal, although the results are consistent with other national surveys, Mehta said.
In the recent Medscape Cardiologist Lifestyle, Happiness & Burnout Report 2020, 29% of respondents reported feeling burnout, 2% depressed, and 15% both burned out and depressed.
The Elephant in the Room
The new findings are “certainly a call to action, but it’s hard to avoid the elephant in the room, which is COVID-19,” said panelist Sandra Lewis, MD, Legacy Good Samaritan Hospital & Medical Center, Portland, Oregon.
“The implications of burnout are really front-and-center with our colleagues, who are working long hours, have hectic work environments, lack of control, and, more than that, a lack of safety of the work situations that we have worked so hard to achieve, as we run out of protective gear, we don’t have masks, as we see our colleagues falling victim to this.”
During her presentation, Mehta highlighted the ACC Clinician Well Being Portal and its COVID-19 Hub, but also several self-care strategies to employ, such as relinquishing control during these uncharted waters, revisiting personal strengths and abilities leveraged in other times of uncertainty, and giving yourself a “brain break” by challenging yourself to chat with a colleague for 30 minutes on topics unrelated to COVID-19 and other workplace stressors.
Wilson said the global pandemic only heightens concerns about burnout among cardiologists, which he likened to a “runaway train.”
“These are not great signals, I think they’re shocking, quite frankly,” Wilson told theheart.org | Medscape Cardiology.
“ACC is setting up a task force from the board of trustees to get to work right away and see about ways we can turn this around as quickly as possible and be a voice for the clinicians,” he said. “It’s not only cardiologists, it’s everybody on our cardiovascular care team, including nurses, physician assistants, nurse practitioners, and even pharmacists. Everybody’s burning out.”
The authors and Wilson report no relevant conflicts of interest.
American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC). Abstract 403.08. Presented March 28, 2020.
This article first appeared on Medscape.com.
Even before the COVID-19 pandemic, , a new survey shows.
“It is important to recognize the personal and professional repercussions of physician burnout,” lead author Laxmi Mehta, MD, director of preventive cardiology and women’s cardiovascular health at Ohio State University, Columbus, said during an online session of the American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC).
The new ACC 2019 Well Being Survey was sent to 19,348 ACC members in the fall of 2019 and sought to take a deeper dive into the issue of burnout after the ACC’s most recent Professional Life Survey revealed that one in four U.S. cardiologists were burned out in 2015.
While the number of cardiologists who reported feeling stressed fell from 49.5% in 2015 to 43.9% in 2019, the number of cardiologists who reported being burned out increased by 32% from 26.8% to 35.4%, Mehta said.
Among those currently feeling burned out, 23.9% reported having one or more symptoms of burnout, 9.9% had chronic burnout and work frustrations, and 1.6% were “completely burned out” and at the point where they may need to seek help.
Burned-out cardiologists were more likely than those who felt stressed or no burnout to say they may have made a major medical error in the past 3 months (58.3% vs 33.1% and 8.6%; P ≤ .001).
The Usual Suspects
As previously observed, burnout was highest among mid-career cardiologists with 8 to 21 years in practice vs early-career and late-career cardiologists (45.3% vs 35.4% and 31.5%; P ≤ .001) and in women vs men (45.3% vs 33.5%; P ≤ .001). Of the 2025 ACC members who responded, 362 were women.
Several initiatives are underway by the ACC to increase the diversity of cardiology as a specialty, but attention is also needed for mid-career cardiologists, who may not see the “light at the end of the tunnel,” as they take on more clinical demands and more administrative roles, Mehta observed.
Not surprising, clocking 60 or more hours per week increased the risk for burnout, compared with working 40 to 59 hours per week or fewer than 40 hours per week (41.5% vs 29.5% and 17.9%; P ≤ .001).
Burned-out cardiologists were also more likely than those who felt stressed or no burnout to report working in a hectic work environment (59.5% vs 32.3% and 14.6%; P ≤ .001) and to have plans to leave their current practice setting (58.1% vs 27.9% and 14.0%; P ≤ .001).
Factors that played a significant role in those plans were the desire to spend more time with family, on-call time, excessive work or relative value unit (RVU) targets, electronic health records, and the pressure to maintain high patient satisfaction scores, Mehta noted.
“Is any of this relatable to decreasing numbers of cardiologists in the U.S., or is there work to try and relate actual work force availability to burnout?” asked session moderator B. Hadley Wilson, MD, executive vice chair of the Sanger Heart & Vascular Institute in Charlotte, North Carolina, and a member of ACC’s Board of Trustees, following the presentation.
“It’s hard to decipher all of those exact details, but we do know that the cardiology work force tends to be older, so the mid-careers are going to be pulling on a lot more weight in the next few years, so that is a concern,” Mehta replied.
A big factor, however, is the excessive work hours put in by all cardiologists, especially the increasing amount of time spent with electronic medical records and administrative tasks, which is “taking away the fun we had in cardiology,” she added.
Limitations of the survey include the potential for bias; burnout was self-reported and may vary over time; and the 14% response rate was less than ideal, although the results are consistent with other national surveys, Mehta said.
In the recent Medscape Cardiologist Lifestyle, Happiness & Burnout Report 2020, 29% of respondents reported feeling burnout, 2% depressed, and 15% both burned out and depressed.
The Elephant in the Room
The new findings are “certainly a call to action, but it’s hard to avoid the elephant in the room, which is COVID-19,” said panelist Sandra Lewis, MD, Legacy Good Samaritan Hospital & Medical Center, Portland, Oregon.
“The implications of burnout are really front-and-center with our colleagues, who are working long hours, have hectic work environments, lack of control, and, more than that, a lack of safety of the work situations that we have worked so hard to achieve, as we run out of protective gear, we don’t have masks, as we see our colleagues falling victim to this.”
During her presentation, Mehta highlighted the ACC Clinician Well Being Portal and its COVID-19 Hub, but also several self-care strategies to employ, such as relinquishing control during these uncharted waters, revisiting personal strengths and abilities leveraged in other times of uncertainty, and giving yourself a “brain break” by challenging yourself to chat with a colleague for 30 minutes on topics unrelated to COVID-19 and other workplace stressors.
Wilson said the global pandemic only heightens concerns about burnout among cardiologists, which he likened to a “runaway train.”
“These are not great signals, I think they’re shocking, quite frankly,” Wilson told theheart.org | Medscape Cardiology.
“ACC is setting up a task force from the board of trustees to get to work right away and see about ways we can turn this around as quickly as possible and be a voice for the clinicians,” he said. “It’s not only cardiologists, it’s everybody on our cardiovascular care team, including nurses, physician assistants, nurse practitioners, and even pharmacists. Everybody’s burning out.”
The authors and Wilson report no relevant conflicts of interest.
American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC). Abstract 403.08. Presented March 28, 2020.
This article first appeared on Medscape.com.
Even before the COVID-19 pandemic, , a new survey shows.
“It is important to recognize the personal and professional repercussions of physician burnout,” lead author Laxmi Mehta, MD, director of preventive cardiology and women’s cardiovascular health at Ohio State University, Columbus, said during an online session of the American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC).
The new ACC 2019 Well Being Survey was sent to 19,348 ACC members in the fall of 2019 and sought to take a deeper dive into the issue of burnout after the ACC’s most recent Professional Life Survey revealed that one in four U.S. cardiologists were burned out in 2015.
While the number of cardiologists who reported feeling stressed fell from 49.5% in 2015 to 43.9% in 2019, the number of cardiologists who reported being burned out increased by 32% from 26.8% to 35.4%, Mehta said.
Among those currently feeling burned out, 23.9% reported having one or more symptoms of burnout, 9.9% had chronic burnout and work frustrations, and 1.6% were “completely burned out” and at the point where they may need to seek help.
Burned-out cardiologists were more likely than those who felt stressed or no burnout to say they may have made a major medical error in the past 3 months (58.3% vs 33.1% and 8.6%; P ≤ .001).
The Usual Suspects
As previously observed, burnout was highest among mid-career cardiologists with 8 to 21 years in practice vs early-career and late-career cardiologists (45.3% vs 35.4% and 31.5%; P ≤ .001) and in women vs men (45.3% vs 33.5%; P ≤ .001). Of the 2025 ACC members who responded, 362 were women.
Several initiatives are underway by the ACC to increase the diversity of cardiology as a specialty, but attention is also needed for mid-career cardiologists, who may not see the “light at the end of the tunnel,” as they take on more clinical demands and more administrative roles, Mehta observed.
Not surprising, clocking 60 or more hours per week increased the risk for burnout, compared with working 40 to 59 hours per week or fewer than 40 hours per week (41.5% vs 29.5% and 17.9%; P ≤ .001).
Burned-out cardiologists were also more likely than those who felt stressed or no burnout to report working in a hectic work environment (59.5% vs 32.3% and 14.6%; P ≤ .001) and to have plans to leave their current practice setting (58.1% vs 27.9% and 14.0%; P ≤ .001).
Factors that played a significant role in those plans were the desire to spend more time with family, on-call time, excessive work or relative value unit (RVU) targets, electronic health records, and the pressure to maintain high patient satisfaction scores, Mehta noted.
“Is any of this relatable to decreasing numbers of cardiologists in the U.S., or is there work to try and relate actual work force availability to burnout?” asked session moderator B. Hadley Wilson, MD, executive vice chair of the Sanger Heart & Vascular Institute in Charlotte, North Carolina, and a member of ACC’s Board of Trustees, following the presentation.
“It’s hard to decipher all of those exact details, but we do know that the cardiology work force tends to be older, so the mid-careers are going to be pulling on a lot more weight in the next few years, so that is a concern,” Mehta replied.
A big factor, however, is the excessive work hours put in by all cardiologists, especially the increasing amount of time spent with electronic medical records and administrative tasks, which is “taking away the fun we had in cardiology,” she added.
Limitations of the survey include the potential for bias; burnout was self-reported and may vary over time; and the 14% response rate was less than ideal, although the results are consistent with other national surveys, Mehta said.
In the recent Medscape Cardiologist Lifestyle, Happiness & Burnout Report 2020, 29% of respondents reported feeling burnout, 2% depressed, and 15% both burned out and depressed.
The Elephant in the Room
The new findings are “certainly a call to action, but it’s hard to avoid the elephant in the room, which is COVID-19,” said panelist Sandra Lewis, MD, Legacy Good Samaritan Hospital & Medical Center, Portland, Oregon.
“The implications of burnout are really front-and-center with our colleagues, who are working long hours, have hectic work environments, lack of control, and, more than that, a lack of safety of the work situations that we have worked so hard to achieve, as we run out of protective gear, we don’t have masks, as we see our colleagues falling victim to this.”
During her presentation, Mehta highlighted the ACC Clinician Well Being Portal and its COVID-19 Hub, but also several self-care strategies to employ, such as relinquishing control during these uncharted waters, revisiting personal strengths and abilities leveraged in other times of uncertainty, and giving yourself a “brain break” by challenging yourself to chat with a colleague for 30 minutes on topics unrelated to COVID-19 and other workplace stressors.
Wilson said the global pandemic only heightens concerns about burnout among cardiologists, which he likened to a “runaway train.”
“These are not great signals, I think they’re shocking, quite frankly,” Wilson told theheart.org | Medscape Cardiology.
“ACC is setting up a task force from the board of trustees to get to work right away and see about ways we can turn this around as quickly as possible and be a voice for the clinicians,” he said. “It’s not only cardiologists, it’s everybody on our cardiovascular care team, including nurses, physician assistants, nurse practitioners, and even pharmacists. Everybody’s burning out.”
The authors and Wilson report no relevant conflicts of interest.
American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC). Abstract 403.08. Presented March 28, 2020.
This article first appeared on Medscape.com.
Primordial cardiovascular prevention draws closer
A powerful genetic predisposition to cardiovascular disease was overcome by low lifetime exposure to LDL cholesterol and systolic blood pressure in a naturalistic study conducted in nearly half a million people, Brian A. Ference, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
This novel finding potentially opens the door to primordial cardiovascular prevention, the earliest possible form of primary prevention, in which cardiovascular risk factors are curtailed before they can become established.
“It’s important to note that the trajectories of lifetime risk for cardiovascular disease predicted by a PGS [polygenic risk score] are not fixed. At the same level of a PGS for coronary artery disease, participants with lower lifetime exposure to LDL and systolic blood pressure had a lower trajectory of risk for cardiovascular disease. This finding implies that the trajectory of cardiovascular risk predicted by a PGS can be reduced by lowering LDL and blood pressure,” observed Dr. Ference, professor of translational therapeutics and executive director of the Center for Naturally Randomised Trials at the University of Cambridge (England).
Together with an international team of coinvestigators, he analyzed lifetime cardiovascular risk as predicted by a PGS derived by genomic testing in relation to lifetime LDL and systolic blood pressure levels in 445,566 participants in the UK Biobank. Subjects had a mean age of 57.2 years at enrollment and 65.2 years at last follow-up. The primary study outcome, a first major coronary event (MCE) as defined by a fatal or nonfatal MI or coronary revascularization, occurred in 23,032 subjects.
The investigators found a stepwise increase in MCE risk across increasing quintiles of genetic risk as reflected in the PGS, such that participants in the top PGS quintile were at 2.8-fold greater risk of an MCE than those in the first quintile. The risk was essentially the same in men and women.
A key finding was that, at any level of lifetime MCE risk as defined by PGS, the actual event rate varied 10-fold depending upon lifetime exposure to LDL cholesterol and systolic blood pressure (SBP). For example, men in the top PGS quintile with high lifetime SBP and LDL cholesterol had a 93% lifetime MCE risk, but that MCE risk plummeted to 8% in those in the top quintile but with low lifetime SBP and LDL cholesterol.
Small differences in those two cardiovascular risk factors over the course of many decades had a big impact. For example, it took only a 10-mg/dL lower lifetime exposure to LDL cholesterol and a 2–mm Hg lower SBP to blunt the trajectory of lifetime risk for MCE in individuals in the middle quintile of PGS to the more favorable trajectory of those in the lowest PGS quintile. Conversely, with a 10-mg/dL increase in LDL cholesterol and 2–mm Hg greater SBP over the course of a lifetime, the trajectory of risk for people in the middle quintile of PGS became essentially superimposable upon the trajectory associated with the highest PGS quintile, the cardiologist explained.
“Participants with low lifetime exposure to LDL and blood pressure had a low lifetime risk of cardiovascular disease at all levels of PGS for coronary disease. This implies that LDL and blood pressure, which are modifiable, may be more powerful determinants of lifetime risk than polygenic predisposition,” Dr. Ference declared.
Discussant Vera Bittner, MD, professor of medicine at the University of Alabama, Birmingham, said that for her this study carried a heartening take-home message: “The polygenic risk score can stratify the population into different risk groups and, at the same time, lifetime exposure to LDL and blood pressure significantly modifies the risk, suggesting that genetics is not destiny, and we may be able to intervene.”
“To be able to know what your cardiovascular risk is from an early age and to plan therapies to prevent cardiovascular disease would be incredible,” agreed session chair B. Hadley Wilson, MD, of the Sanger Heart and Vascular Institute in Charlotte, N.C.
Sekar Kathiresan, MD, said the study introduces the PGS as a new risk factor for coronary artery disease. Focusing efforts to achieve lifelong low exposure to LDL cholesterol and blood pressure in those individuals in the top 10%-20% in PGS should provide a great absolute reduction in MCE risk.
“It potentially can give you a 30- or 40-year head start in understanding who’s at risk because the factor can be measured as early as birth,” observed Dr. Kathiresan, a cardiologist who is director of the Center for Genomic Medicine at Massachusetts General Hospital, Boston.
“It’s also very inexpensive: You get the information once, bank it, and use it throughout life,” noted Paul M. Ridker, MD, director of the Center for Cardiovascular Disease Prevention and professor of medicine at Harvard Medical School, Boston.
“A genome-wide scan will give us information not just on cardiovascular risk, but on cancer risk, on risk of kidney disease, and on the risk of a host of other issues. It’s a very different way of thinking about risk presentation across a whole variety of endpoints,” Dr. Ridker added.
Dr. Ference reported receiving fees and/or research grants from Merck, Amgen, Regeneron, Sanofi, Novartis, Pfizer, Eli Lilly, NovoNordisk, The Medicines Company, Mylan, Daiichi Sankyo, Silence Therapeutics, Ionis Pharmaceuticals, dalCOR, CiVi Pharma, KrKa Pharmaceuticals, Medtronic, and Celera.
A powerful genetic predisposition to cardiovascular disease was overcome by low lifetime exposure to LDL cholesterol and systolic blood pressure in a naturalistic study conducted in nearly half a million people, Brian A. Ference, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
This novel finding potentially opens the door to primordial cardiovascular prevention, the earliest possible form of primary prevention, in which cardiovascular risk factors are curtailed before they can become established.
“It’s important to note that the trajectories of lifetime risk for cardiovascular disease predicted by a PGS [polygenic risk score] are not fixed. At the same level of a PGS for coronary artery disease, participants with lower lifetime exposure to LDL and systolic blood pressure had a lower trajectory of risk for cardiovascular disease. This finding implies that the trajectory of cardiovascular risk predicted by a PGS can be reduced by lowering LDL and blood pressure,” observed Dr. Ference, professor of translational therapeutics and executive director of the Center for Naturally Randomised Trials at the University of Cambridge (England).
Together with an international team of coinvestigators, he analyzed lifetime cardiovascular risk as predicted by a PGS derived by genomic testing in relation to lifetime LDL and systolic blood pressure levels in 445,566 participants in the UK Biobank. Subjects had a mean age of 57.2 years at enrollment and 65.2 years at last follow-up. The primary study outcome, a first major coronary event (MCE) as defined by a fatal or nonfatal MI or coronary revascularization, occurred in 23,032 subjects.
The investigators found a stepwise increase in MCE risk across increasing quintiles of genetic risk as reflected in the PGS, such that participants in the top PGS quintile were at 2.8-fold greater risk of an MCE than those in the first quintile. The risk was essentially the same in men and women.
A key finding was that, at any level of lifetime MCE risk as defined by PGS, the actual event rate varied 10-fold depending upon lifetime exposure to LDL cholesterol and systolic blood pressure (SBP). For example, men in the top PGS quintile with high lifetime SBP and LDL cholesterol had a 93% lifetime MCE risk, but that MCE risk plummeted to 8% in those in the top quintile but with low lifetime SBP and LDL cholesterol.
Small differences in those two cardiovascular risk factors over the course of many decades had a big impact. For example, it took only a 10-mg/dL lower lifetime exposure to LDL cholesterol and a 2–mm Hg lower SBP to blunt the trajectory of lifetime risk for MCE in individuals in the middle quintile of PGS to the more favorable trajectory of those in the lowest PGS quintile. Conversely, with a 10-mg/dL increase in LDL cholesterol and 2–mm Hg greater SBP over the course of a lifetime, the trajectory of risk for people in the middle quintile of PGS became essentially superimposable upon the trajectory associated with the highest PGS quintile, the cardiologist explained.
“Participants with low lifetime exposure to LDL and blood pressure had a low lifetime risk of cardiovascular disease at all levels of PGS for coronary disease. This implies that LDL and blood pressure, which are modifiable, may be more powerful determinants of lifetime risk than polygenic predisposition,” Dr. Ference declared.
Discussant Vera Bittner, MD, professor of medicine at the University of Alabama, Birmingham, said that for her this study carried a heartening take-home message: “The polygenic risk score can stratify the population into different risk groups and, at the same time, lifetime exposure to LDL and blood pressure significantly modifies the risk, suggesting that genetics is not destiny, and we may be able to intervene.”
“To be able to know what your cardiovascular risk is from an early age and to plan therapies to prevent cardiovascular disease would be incredible,” agreed session chair B. Hadley Wilson, MD, of the Sanger Heart and Vascular Institute in Charlotte, N.C.
Sekar Kathiresan, MD, said the study introduces the PGS as a new risk factor for coronary artery disease. Focusing efforts to achieve lifelong low exposure to LDL cholesterol and blood pressure in those individuals in the top 10%-20% in PGS should provide a great absolute reduction in MCE risk.
“It potentially can give you a 30- or 40-year head start in understanding who’s at risk because the factor can be measured as early as birth,” observed Dr. Kathiresan, a cardiologist who is director of the Center for Genomic Medicine at Massachusetts General Hospital, Boston.
“It’s also very inexpensive: You get the information once, bank it, and use it throughout life,” noted Paul M. Ridker, MD, director of the Center for Cardiovascular Disease Prevention and professor of medicine at Harvard Medical School, Boston.
“A genome-wide scan will give us information not just on cardiovascular risk, but on cancer risk, on risk of kidney disease, and on the risk of a host of other issues. It’s a very different way of thinking about risk presentation across a whole variety of endpoints,” Dr. Ridker added.
Dr. Ference reported receiving fees and/or research grants from Merck, Amgen, Regeneron, Sanofi, Novartis, Pfizer, Eli Lilly, NovoNordisk, The Medicines Company, Mylan, Daiichi Sankyo, Silence Therapeutics, Ionis Pharmaceuticals, dalCOR, CiVi Pharma, KrKa Pharmaceuticals, Medtronic, and Celera.
A powerful genetic predisposition to cardiovascular disease was overcome by low lifetime exposure to LDL cholesterol and systolic blood pressure in a naturalistic study conducted in nearly half a million people, Brian A. Ference, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
This novel finding potentially opens the door to primordial cardiovascular prevention, the earliest possible form of primary prevention, in which cardiovascular risk factors are curtailed before they can become established.
“It’s important to note that the trajectories of lifetime risk for cardiovascular disease predicted by a PGS [polygenic risk score] are not fixed. At the same level of a PGS for coronary artery disease, participants with lower lifetime exposure to LDL and systolic blood pressure had a lower trajectory of risk for cardiovascular disease. This finding implies that the trajectory of cardiovascular risk predicted by a PGS can be reduced by lowering LDL and blood pressure,” observed Dr. Ference, professor of translational therapeutics and executive director of the Center for Naturally Randomised Trials at the University of Cambridge (England).
Together with an international team of coinvestigators, he analyzed lifetime cardiovascular risk as predicted by a PGS derived by genomic testing in relation to lifetime LDL and systolic blood pressure levels in 445,566 participants in the UK Biobank. Subjects had a mean age of 57.2 years at enrollment and 65.2 years at last follow-up. The primary study outcome, a first major coronary event (MCE) as defined by a fatal or nonfatal MI or coronary revascularization, occurred in 23,032 subjects.
The investigators found a stepwise increase in MCE risk across increasing quintiles of genetic risk as reflected in the PGS, such that participants in the top PGS quintile were at 2.8-fold greater risk of an MCE than those in the first quintile. The risk was essentially the same in men and women.
A key finding was that, at any level of lifetime MCE risk as defined by PGS, the actual event rate varied 10-fold depending upon lifetime exposure to LDL cholesterol and systolic blood pressure (SBP). For example, men in the top PGS quintile with high lifetime SBP and LDL cholesterol had a 93% lifetime MCE risk, but that MCE risk plummeted to 8% in those in the top quintile but with low lifetime SBP and LDL cholesterol.
Small differences in those two cardiovascular risk factors over the course of many decades had a big impact. For example, it took only a 10-mg/dL lower lifetime exposure to LDL cholesterol and a 2–mm Hg lower SBP to blunt the trajectory of lifetime risk for MCE in individuals in the middle quintile of PGS to the more favorable trajectory of those in the lowest PGS quintile. Conversely, with a 10-mg/dL increase in LDL cholesterol and 2–mm Hg greater SBP over the course of a lifetime, the trajectory of risk for people in the middle quintile of PGS became essentially superimposable upon the trajectory associated with the highest PGS quintile, the cardiologist explained.
“Participants with low lifetime exposure to LDL and blood pressure had a low lifetime risk of cardiovascular disease at all levels of PGS for coronary disease. This implies that LDL and blood pressure, which are modifiable, may be more powerful determinants of lifetime risk than polygenic predisposition,” Dr. Ference declared.
Discussant Vera Bittner, MD, professor of medicine at the University of Alabama, Birmingham, said that for her this study carried a heartening take-home message: “The polygenic risk score can stratify the population into different risk groups and, at the same time, lifetime exposure to LDL and blood pressure significantly modifies the risk, suggesting that genetics is not destiny, and we may be able to intervene.”
“To be able to know what your cardiovascular risk is from an early age and to plan therapies to prevent cardiovascular disease would be incredible,” agreed session chair B. Hadley Wilson, MD, of the Sanger Heart and Vascular Institute in Charlotte, N.C.
Sekar Kathiresan, MD, said the study introduces the PGS as a new risk factor for coronary artery disease. Focusing efforts to achieve lifelong low exposure to LDL cholesterol and blood pressure in those individuals in the top 10%-20% in PGS should provide a great absolute reduction in MCE risk.
“It potentially can give you a 30- or 40-year head start in understanding who’s at risk because the factor can be measured as early as birth,” observed Dr. Kathiresan, a cardiologist who is director of the Center for Genomic Medicine at Massachusetts General Hospital, Boston.
“It’s also very inexpensive: You get the information once, bank it, and use it throughout life,” noted Paul M. Ridker, MD, director of the Center for Cardiovascular Disease Prevention and professor of medicine at Harvard Medical School, Boston.
“A genome-wide scan will give us information not just on cardiovascular risk, but on cancer risk, on risk of kidney disease, and on the risk of a host of other issues. It’s a very different way of thinking about risk presentation across a whole variety of endpoints,” Dr. Ridker added.
Dr. Ference reported receiving fees and/or research grants from Merck, Amgen, Regeneron, Sanofi, Novartis, Pfizer, Eli Lilly, NovoNordisk, The Medicines Company, Mylan, Daiichi Sankyo, Silence Therapeutics, Ionis Pharmaceuticals, dalCOR, CiVi Pharma, KrKa Pharmaceuticals, Medtronic, and Celera.
REPORTING FROM ACC 20
Rivaroxaban plus aspirin safely benefits PAD patients after limb revascularization
A combined antithrombotic regimen of rivaroxaban plus aspirin was safe and effective for reducing ischemic events in patients with symptomatic peripheral artery disease who had just undergone peripheral artery revascularization in VOYAGER PAD, a multicenter randomized trial with nearly 6,600 patients.
The study and its results were a groundbreaking advance for this patient population, who until now have had no evidence-based treatment available, Mark P. Bonaca, MD, said on March 28 at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
The study design excluded a small percentage of patients (about 2%) because of their very high bleeding-risk history. Among the treated patients, in those who received a combination of 2.5 mg rivaroxaban twice daily plus 100 mg of aspirin daily, bleeding events were more common, compared with control patients who received aspirin alone. But the patients who received both drugs showed no excess of fatal bleeds or intracranial hemorrhages, and the rate of ischemic events prevented by rivaroxaban plus aspirin exceeded the excess rate of bleeds by three- to sixfold, depending on how bleeding episodes were defined, noted Dr. Bonaca, executive director of CPC Clinical Research and CPC Community Health, an academic research organization affiliated with the University of Colorado at Denver in Aurora.
“This was a much anticipated and important trial. Those of us who treat patients with lower-limb peripheral artery disease have not had much evidence on how to treat these patients, particularly those who have just undergone revascularization. This trial gives us the evidence,” commented Mark A. Creager, MD, professor of medicine and director of the Heart and Vascular Center at Dartmouth-Hitchcock Medical Center in Lebanon, N.H. “The bleeding risk [from adding rivaroxaban treatment] was substantially less than the benefit from preventing major adverse limb events and major adverse cardiovascular events,” producing a “favorable balance” of benefit, compared with risk, Dr. Creager said in an interview. “In the right patients, the benefit greatly outweighed the risk.”
“This was an incredible trial that will advance care,” commented Joshua A. Beckman, MD, professor of medicine and director of Vascular Medicine at Vanderbilt University in Nashville, Tenn. “The treatment was beneficial for patients across a range of symptom severity, from claudication to critical limb ischemia,” and the results expand the range of patients proven to benefit from the rivaroxaban plus aspirin combination from the types of patients with peripheral artery disease (PAD) enrolled in the COMPASS trial. That pivotal trial showed similar benefit from the dual-antithrombotic regimen, but in patients who had both coronary artery disease as well as atherosclerotic disease in at least one additional vascular bed, such as lower-limb arteries (N Engl J Med. 2017 Oct 5;377[14]:1319-30). In addition to “bringing acute limb ischemia to the cardiovascular community,” the results also identified a very useful time point in the clinical presentation of these patients for starting a combined rivaroxaban plus aspirin regimen: when patients are hospitalized for their revascularization procedure, said Dr. Beckman, a designated discussant for the report.
Among the 6,564 patients randomized in the study, about two-thirds underwent endovascular revascularization within 10 days before starting their study treatment, and the remaining third had undergone surgical revascularization. The study focused on patients “with symptomatic PAD but without known coronary artery disease,” noted Dr. Bonaca.
VOYAGER PAD trial
The VOYAGER PAD (Vascular Outcomes Study of Acetylsalicylic Acid Along With Rivaroxaban in Endovascular Or Surgical Limb Revascularization for Peripheral Artery Disease) trial enrolled patients during 2015-2018 at 534 sites in 34 countries. The study’s primary endpoint was a composite of acute limb ischemia, major amputation for vascular causes, myocardial infarction, ischemic stroke, or death from cardiovascular causes, and was reduced during a median follow-up of 28 months from 19.9% with aspirin alone to 17.3% on the combined regimen, a 2.6% absolute difference and a 15% relative risk reduction that was statistically significant, an endpoint primarily driven by a reduction in acute limb ischemia. The primary safety endpoint was the rate of TIMI (Thrombolysis in Myocardial Infarction) major bleeds, which was 0.8% higher in the patients who received the anticoagulant, a 43% relative increase that just missed statistical significance. But that result demonstrated the small but important increased risk for bleeding events that the dual regimen produced in these patients, Dr. Bonaca said. Simultaneously with his report the findings also appeared in an article published online (N Engl J Med. 2020 Mar 28. doi: 10.1056/NEJMoa2000052).
Dr. Bonaca cautioned that one limitation of his report on the primary outcome of VOYAGER PAD is that the results of an important subgroup analysis won’t be known until a second report during the ACC online sessions on March 29, which will examine the impact that treatment with the antiplatelet drug clopidogrel had on both the efficacy and safety outcomes. Half of the enrolled patients received clopidogrel at the discretion of their treating physicians; addition or exclusion of concurrent clopidogrel treatment was outside of the study’s design. “Is efficacy the same with or without clopidogrel, and what is the bleeding cost,” especially in patients who receive three antithrombotic drugs? “It will be very important to understand,” Dr. Bonaca said.
“Until now, we had no idea of what was the best antithrombotic strategy for patients after a successful peripheral vascular intervention.” VOYAGER PAD was “an unprecedented vascular study that addressed an unmet patient need,” commented Roxana Mehran, MD, a designated discussant for the study and professor of medicine and director of Interventional Cardiovascular Research at Mount Sinai Medical Center in New York.
VOYAGER PAD was sponsored by Bayer and Janssen, the companies that market rivaroxaban (Xarelto). The institution that Dr. Bonaca directs has received research funding from Bayer and Janssen, and also from Amgen, Aralez, AstraZeneca, Merck, Novo Nordisk, Pfizer, and Sanofi. Dr. Creager had no disclosures. Dr. Beckman has served as a data safety monitor for Bayer and for Novartis, and has been a consultant to Amgen, AstraZeneca, JanOne and Sanofi. Dr. Mehran has received research funding from Bayer and has been a consultant to Janssen, and she has also received research funding or been a consultant to several other companies.
SOURCE: Bonaca MP et al. ACC 20, Abstract 402-10.
A combined antithrombotic regimen of rivaroxaban plus aspirin was safe and effective for reducing ischemic events in patients with symptomatic peripheral artery disease who had just undergone peripheral artery revascularization in VOYAGER PAD, a multicenter randomized trial with nearly 6,600 patients.
The study and its results were a groundbreaking advance for this patient population, who until now have had no evidence-based treatment available, Mark P. Bonaca, MD, said on March 28 at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
The study design excluded a small percentage of patients (about 2%) because of their very high bleeding-risk history. Among the treated patients, in those who received a combination of 2.5 mg rivaroxaban twice daily plus 100 mg of aspirin daily, bleeding events were more common, compared with control patients who received aspirin alone. But the patients who received both drugs showed no excess of fatal bleeds or intracranial hemorrhages, and the rate of ischemic events prevented by rivaroxaban plus aspirin exceeded the excess rate of bleeds by three- to sixfold, depending on how bleeding episodes were defined, noted Dr. Bonaca, executive director of CPC Clinical Research and CPC Community Health, an academic research organization affiliated with the University of Colorado at Denver in Aurora.
“This was a much anticipated and important trial. Those of us who treat patients with lower-limb peripheral artery disease have not had much evidence on how to treat these patients, particularly those who have just undergone revascularization. This trial gives us the evidence,” commented Mark A. Creager, MD, professor of medicine and director of the Heart and Vascular Center at Dartmouth-Hitchcock Medical Center in Lebanon, N.H. “The bleeding risk [from adding rivaroxaban treatment] was substantially less than the benefit from preventing major adverse limb events and major adverse cardiovascular events,” producing a “favorable balance” of benefit, compared with risk, Dr. Creager said in an interview. “In the right patients, the benefit greatly outweighed the risk.”
“This was an incredible trial that will advance care,” commented Joshua A. Beckman, MD, professor of medicine and director of Vascular Medicine at Vanderbilt University in Nashville, Tenn. “The treatment was beneficial for patients across a range of symptom severity, from claudication to critical limb ischemia,” and the results expand the range of patients proven to benefit from the rivaroxaban plus aspirin combination from the types of patients with peripheral artery disease (PAD) enrolled in the COMPASS trial. That pivotal trial showed similar benefit from the dual-antithrombotic regimen, but in patients who had both coronary artery disease as well as atherosclerotic disease in at least one additional vascular bed, such as lower-limb arteries (N Engl J Med. 2017 Oct 5;377[14]:1319-30). In addition to “bringing acute limb ischemia to the cardiovascular community,” the results also identified a very useful time point in the clinical presentation of these patients for starting a combined rivaroxaban plus aspirin regimen: when patients are hospitalized for their revascularization procedure, said Dr. Beckman, a designated discussant for the report.
Among the 6,564 patients randomized in the study, about two-thirds underwent endovascular revascularization within 10 days before starting their study treatment, and the remaining third had undergone surgical revascularization. The study focused on patients “with symptomatic PAD but without known coronary artery disease,” noted Dr. Bonaca.
VOYAGER PAD trial
The VOYAGER PAD (Vascular Outcomes Study of Acetylsalicylic Acid Along With Rivaroxaban in Endovascular Or Surgical Limb Revascularization for Peripheral Artery Disease) trial enrolled patients during 2015-2018 at 534 sites in 34 countries. The study’s primary endpoint was a composite of acute limb ischemia, major amputation for vascular causes, myocardial infarction, ischemic stroke, or death from cardiovascular causes, and was reduced during a median follow-up of 28 months from 19.9% with aspirin alone to 17.3% on the combined regimen, a 2.6% absolute difference and a 15% relative risk reduction that was statistically significant, an endpoint primarily driven by a reduction in acute limb ischemia. The primary safety endpoint was the rate of TIMI (Thrombolysis in Myocardial Infarction) major bleeds, which was 0.8% higher in the patients who received the anticoagulant, a 43% relative increase that just missed statistical significance. But that result demonstrated the small but important increased risk for bleeding events that the dual regimen produced in these patients, Dr. Bonaca said. Simultaneously with his report the findings also appeared in an article published online (N Engl J Med. 2020 Mar 28. doi: 10.1056/NEJMoa2000052).
Dr. Bonaca cautioned that one limitation of his report on the primary outcome of VOYAGER PAD is that the results of an important subgroup analysis won’t be known until a second report during the ACC online sessions on March 29, which will examine the impact that treatment with the antiplatelet drug clopidogrel had on both the efficacy and safety outcomes. Half of the enrolled patients received clopidogrel at the discretion of their treating physicians; addition or exclusion of concurrent clopidogrel treatment was outside of the study’s design. “Is efficacy the same with or without clopidogrel, and what is the bleeding cost,” especially in patients who receive three antithrombotic drugs? “It will be very important to understand,” Dr. Bonaca said.
“Until now, we had no idea of what was the best antithrombotic strategy for patients after a successful peripheral vascular intervention.” VOYAGER PAD was “an unprecedented vascular study that addressed an unmet patient need,” commented Roxana Mehran, MD, a designated discussant for the study and professor of medicine and director of Interventional Cardiovascular Research at Mount Sinai Medical Center in New York.
VOYAGER PAD was sponsored by Bayer and Janssen, the companies that market rivaroxaban (Xarelto). The institution that Dr. Bonaca directs has received research funding from Bayer and Janssen, and also from Amgen, Aralez, AstraZeneca, Merck, Novo Nordisk, Pfizer, and Sanofi. Dr. Creager had no disclosures. Dr. Beckman has served as a data safety monitor for Bayer and for Novartis, and has been a consultant to Amgen, AstraZeneca, JanOne and Sanofi. Dr. Mehran has received research funding from Bayer and has been a consultant to Janssen, and she has also received research funding or been a consultant to several other companies.
SOURCE: Bonaca MP et al. ACC 20, Abstract 402-10.
A combined antithrombotic regimen of rivaroxaban plus aspirin was safe and effective for reducing ischemic events in patients with symptomatic peripheral artery disease who had just undergone peripheral artery revascularization in VOYAGER PAD, a multicenter randomized trial with nearly 6,600 patients.
The study and its results were a groundbreaking advance for this patient population, who until now have had no evidence-based treatment available, Mark P. Bonaca, MD, said on March 28 at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
The study design excluded a small percentage of patients (about 2%) because of their very high bleeding-risk history. Among the treated patients, in those who received a combination of 2.5 mg rivaroxaban twice daily plus 100 mg of aspirin daily, bleeding events were more common, compared with control patients who received aspirin alone. But the patients who received both drugs showed no excess of fatal bleeds or intracranial hemorrhages, and the rate of ischemic events prevented by rivaroxaban plus aspirin exceeded the excess rate of bleeds by three- to sixfold, depending on how bleeding episodes were defined, noted Dr. Bonaca, executive director of CPC Clinical Research and CPC Community Health, an academic research organization affiliated with the University of Colorado at Denver in Aurora.
“This was a much anticipated and important trial. Those of us who treat patients with lower-limb peripheral artery disease have not had much evidence on how to treat these patients, particularly those who have just undergone revascularization. This trial gives us the evidence,” commented Mark A. Creager, MD, professor of medicine and director of the Heart and Vascular Center at Dartmouth-Hitchcock Medical Center in Lebanon, N.H. “The bleeding risk [from adding rivaroxaban treatment] was substantially less than the benefit from preventing major adverse limb events and major adverse cardiovascular events,” producing a “favorable balance” of benefit, compared with risk, Dr. Creager said in an interview. “In the right patients, the benefit greatly outweighed the risk.”
“This was an incredible trial that will advance care,” commented Joshua A. Beckman, MD, professor of medicine and director of Vascular Medicine at Vanderbilt University in Nashville, Tenn. “The treatment was beneficial for patients across a range of symptom severity, from claudication to critical limb ischemia,” and the results expand the range of patients proven to benefit from the rivaroxaban plus aspirin combination from the types of patients with peripheral artery disease (PAD) enrolled in the COMPASS trial. That pivotal trial showed similar benefit from the dual-antithrombotic regimen, but in patients who had both coronary artery disease as well as atherosclerotic disease in at least one additional vascular bed, such as lower-limb arteries (N Engl J Med. 2017 Oct 5;377[14]:1319-30). In addition to “bringing acute limb ischemia to the cardiovascular community,” the results also identified a very useful time point in the clinical presentation of these patients for starting a combined rivaroxaban plus aspirin regimen: when patients are hospitalized for their revascularization procedure, said Dr. Beckman, a designated discussant for the report.
Among the 6,564 patients randomized in the study, about two-thirds underwent endovascular revascularization within 10 days before starting their study treatment, and the remaining third had undergone surgical revascularization. The study focused on patients “with symptomatic PAD but without known coronary artery disease,” noted Dr. Bonaca.
VOYAGER PAD trial
The VOYAGER PAD (Vascular Outcomes Study of Acetylsalicylic Acid Along With Rivaroxaban in Endovascular Or Surgical Limb Revascularization for Peripheral Artery Disease) trial enrolled patients during 2015-2018 at 534 sites in 34 countries. The study’s primary endpoint was a composite of acute limb ischemia, major amputation for vascular causes, myocardial infarction, ischemic stroke, or death from cardiovascular causes, and was reduced during a median follow-up of 28 months from 19.9% with aspirin alone to 17.3% on the combined regimen, a 2.6% absolute difference and a 15% relative risk reduction that was statistically significant, an endpoint primarily driven by a reduction in acute limb ischemia. The primary safety endpoint was the rate of TIMI (Thrombolysis in Myocardial Infarction) major bleeds, which was 0.8% higher in the patients who received the anticoagulant, a 43% relative increase that just missed statistical significance. But that result demonstrated the small but important increased risk for bleeding events that the dual regimen produced in these patients, Dr. Bonaca said. Simultaneously with his report the findings also appeared in an article published online (N Engl J Med. 2020 Mar 28. doi: 10.1056/NEJMoa2000052).
Dr. Bonaca cautioned that one limitation of his report on the primary outcome of VOYAGER PAD is that the results of an important subgroup analysis won’t be known until a second report during the ACC online sessions on March 29, which will examine the impact that treatment with the antiplatelet drug clopidogrel had on both the efficacy and safety outcomes. Half of the enrolled patients received clopidogrel at the discretion of their treating physicians; addition or exclusion of concurrent clopidogrel treatment was outside of the study’s design. “Is efficacy the same with or without clopidogrel, and what is the bleeding cost,” especially in patients who receive three antithrombotic drugs? “It will be very important to understand,” Dr. Bonaca said.
“Until now, we had no idea of what was the best antithrombotic strategy for patients after a successful peripheral vascular intervention.” VOYAGER PAD was “an unprecedented vascular study that addressed an unmet patient need,” commented Roxana Mehran, MD, a designated discussant for the study and professor of medicine and director of Interventional Cardiovascular Research at Mount Sinai Medical Center in New York.
VOYAGER PAD was sponsored by Bayer and Janssen, the companies that market rivaroxaban (Xarelto). The institution that Dr. Bonaca directs has received research funding from Bayer and Janssen, and also from Amgen, Aralez, AstraZeneca, Merck, Novo Nordisk, Pfizer, and Sanofi. Dr. Creager had no disclosures. Dr. Beckman has served as a data safety monitor for Bayer and for Novartis, and has been a consultant to Amgen, AstraZeneca, JanOne and Sanofi. Dr. Mehran has received research funding from Bayer and has been a consultant to Janssen, and she has also received research funding or been a consultant to several other companies.
SOURCE: Bonaca MP et al. ACC 20, Abstract 402-10.
REPORTING FROM ACC 20
Key clinical point: Combined treatment with rivaroxaban plus aspirin safely reduced a composite measure of adverse ischemic events in PAD patients following lower-limb revascularization.
Major finding: The primary event outcome occurred in 17.3% of patients on rivaroxaban plus aspirin, and in 19.9% on aspirin alone.
Study details: VOYAGER PAD, a multicenter, international randomized trial with 6,564 patients.
Disclosures: VOYAGER PAD was sponsored by Bayer and Janssen, the companies that market rivaroxaban (Xarelto). The institution that Dr. Bonaca directs has received research funding from Bayer and Janssen, and also from Amgen, Aralez, AstraZeneca, Merck, Novo Nordisk, Pfizer, and Sanofi. Dr. Creager had no disclosures. Dr. Beckman has served as a data safety monitor for Bayer and for Novartis, and has been a consultant to Amgen, AstraZeneca, JanOne and Sanofi. Dr. Mehran has received research funding from Bayer and has been a consultant to Janssen, and she has also received research funding or been a consultant to several other companies.
Source: Bonaca MP. ACC 20, Abstract 402-10.