User login
Management of race in psychotherapy and supervision
On the Friday evening after the public execution of George Floyd, we were painfully reminded of the urgency to address the inadequate management of race, racism, and anti-blackness in medical education, residency training, and postgraduate continuing medical education.
The reminder did not originate from the rioting that was occurring in some cities, though we could feel the ground shifting beneath our feet as civic protests that began in U.S. cities spread around the globe. Instead, it occurred during a webinar we were hosting for psychiatry residents focused on techniques for eliminating blind spots in the management of race in clinical psychotherapy supervision. (Dr. Jessica Isom chaired the webinar, Dr. Flavia DeSouza and Dr. Myra Mathis comoderated, and Dr. Ebony Dennis and Dr. Constance E. Dunlap served as discussants.)
Our panel had presented an ambitious agenda that included reviewing how the disavowal of bias, race, racism, and anti-blackness contributes to ineffective psychotherapy, undermines the quality of medical care, and perpetuates mental health disparities. We spent some time exploring how unacknowledged and unexamined conscious and unconscious racial stereotypes affect interpersonal relationships, the psychotherapeutic process, and the supervisory experience. Our presentation included a clinical vignette demonstrating how racism, colorism, and anti-blackness have global impact, influencing the self-esteem, identity formation, and identity consolidation of immigrants as they grapple with the unique form of racism that exists in America. Other clinical vignettes demonstrated blind spots that were retroactively identified though omitted in supervisory discussions. We also discussed alternative interventions and interpretations of the material presented.1-5
Because 21st-century trainees are generally psychologically astute and committed to social justice, we did two things. First, before the webinar, we provided them access to a prerecorded explanation of object relations theorist Melanie Klein’s paranoid-schizoid and depressive positions concepts, which were applied to theoretically explain the development of race, specifically the defenses used by early colonists that contributed to the development of “whiteness” and “blackness” as social constructs, and their influence on the development of the U.S. psyche. For example, as early colonists attempted to develop new and improved identities distinct from those they had in their homelands, they used enslaved black people (and other vulnerable groups) to “other.” What we mean here by othering is the process of using an other to project one’s badness into in order to relieve the self of uncomfortable aspects and feelings originating within the self. If this other accepts the projection (which is often the case with vulnerable parties), the self recognizes, that is, identifies (locates) the bad they just projected in the other, who is now experienced as a bad-other. This is projection in action. If the other accepts the projection and behaves accordingly, for example, in a manner that reflects badness, this becomes projective identification. Conversely, if the other does not accept these projections, the self (who projects) is left to cope with aspects of the self s/he might not have the capacity to manage. By capacity, we are speaking of the Bionian idea of the ability to experience an extreme emotion while also being able to think. Without the ego strength to cope with bad aspects of the self, the ego either collapses (and is unable to think) or further projection is attempted.6-8
We have seen this latter dynamic play out repeatedly when police officers fatally shoot black citizens and then claim that they feared for their lives; these same officers have been exonerated by juries by continuing to portray the deceased victims as threatening, dangerous objects not worthy of living. We are also seeing a global movement of black and nonblack people who are in touch with a justified rage that has motivated them to return these projections by collectively protesting, and in some cases, by rioting.
Back to the webinar
In anticipating the residents’ curiosity, impatience, and anger about the lack of progress, the second thing we did was to show a segment from the “Black Psychoanalysts Speak” trailer. In the clip played, senior psychoanalyst Kirkland C. Vaughans, PhD, shares: “The issue of race so prompts excessive anxiety that it blocks off our ability to think.”
We showed this clip to validate the trainees’ frustrations about the difficulty the broader establishment has had with addressing this serious, longstanding public health problem. We wanted these young psychiatrists to know that there are psychoanalysts, psychiatrists, psychologists, and social workers who have been committed to this work, even though the contributions of this diverse group have curiously been omitted from education and training curricula.9
So, what happened? What was the painful reminder? After the formal panel presentations, a black male psychiatry resident recounted his experience in a clinical supervision meeting that had occurred several days after the murder of George Floyd. In short, a patient had shared his reactions to yet another incident of fatal police use of force and paused to ask how the resident physician, Dr. A., was doing. The question was experienced as sincere concern about the psychiatrist’s mental well-being. The resident was not sure how to answer this question since it was a matter of self-disclosure, which was a reasonable and thoughtful consideration for a seasoned clinician and, certainly, for a novice therapist. The supervisor, Dr. B., seemingly eager to move on, to not think about this, responded to the resident by saying: “Now tell me about the patient.” In other words, what had just been shared by the resident – material that featured a patient’s reaction to another killing of a black man by police and the patient’s expressed concern for his black psychiatrist, and this resident physician appropriately seeking space in supervision to process and receive guidance about how to respond – all of this was considered separate (split off from) and extraneous to the patient’s treatment and the resident’s training. This is a problem. And, unfortunately, this problem or some variation of it is not rare.
Why is this still the state of affairs when we have identified racism as a major health concern and our patients and our trainees are asking for help?
Rethinking a metaphor
Despite calls to action over the last 50 years to encourage medicine to effectively address race and racism, deficits remain in didactic education, clinical rotations, and supervisory experiences of trainees learning how to do psychodynamic psychotherapy.8-10 Earlier that evening, we used the metaphor of a vehicular blind spot to capture what we believe occurs insupervision. Like drivers, supervisors generally have the ability to see. However, there are places (times) and positions (stances) that block their vision (awareness). Racism – whether institutionalized, interpersonally mediated, or internalized – also contributes to this blindness.
As is true of drivers managing a blind spot, what is required is for the drivers – the supervisors – to lean forward or reposition themselves so as to avoid collisions, maintain safety, and continue on course. We use this metaphor because it is understood that any clinician providing psychodynamic supervision to psychiatry residents, regardless of professional discipline, has the requisite skills and training.10-13
Until May 25, we thought eliminating blind spots would be effective. But, in the aftermath of the police killing of George Floyd, our eyes have been opened.
Hiding behind the blue wall of silence is an establishment that has looked the other way while black and brown women, men, and children have come to live in fear as a result of the state-sanctioned violence that repeatedly occurs across the nation. Excessive police use of force is a public health issue of crisis magnitude. However, the house of medicine, like many other established structures in society, has colluded with the societal constructs that have supported law enforcement by remaining willfully blind, often neutral, and by refusing to make the necessary adjustments, including connecting the dots between police violence and physical and mental health.
For example, racism has never been listed even in the index of the American Psychiatric Association’s (APA) Diagnostic and Statistical Manual of Mental Disorders.14 Being the victim of police use of force is not generally regarded as an adverse childhood experience, even though communities that are heavily policed experience harassment by law enforcement on a regular basis. The 12 causes of trauma listed on the website15 of the National Child Traumatic Stress Network – bullying, community violence, complex trauma, disasters, early childhood trauma, intimate partner violence, medical trauma, physical abuse, refugee trauma, sexual abuse, terrorism and violence, and traumatic grief – do not include maltreatment, abuse, or trauma resulting from interactions with members of law enforcement. Much of the adverse childhood experiences literature focuses on white, upper middle class children and on experiences within the home. When community level experiences, such as discrimination based on race or ethnicity, are included, as in the Philadelphia ACES study,16 as many as 40% reported ACE scores of greater than 4 for community level exposures.
As psychiatrists, we recognize the psychic underpinnings and parallels between the psychic projections onto black and brown people and the actual bullets pumped into the bodies of black and brown people; there is a lurid propensity to use these others as repositories. Those who have the privilege of being protected by law enforcement and the ability to avoid being used as containers for the psychic projections and bullets of some police officers also have the privilege of compartmentalizing and looking the other way when excessive acts of force – projections and projectiles – are used on other human beings. This partly explains why the injuries and deaths of black and brown people caused by police officers’ excessive use of force have continued even though these unjustified deaths are widely televised and disseminated via various social media platforms.
Prior to the death of George Floyd on May 25, other than the American Public Health Association, the National Medical Association (NMA) was the only major medical organization to issue a call to consider police use of force as a public health issue. In its July 2016 press release, provided in the aftermath of the death of Freddie Gray while in the custody of Baltimore police officers, the NMA summarized the scope of injuries citizens sustain during “the pre-custody (commission of a crime, during a fight, chase, and apprehension, during a siege or hostage situation, or during restraint or submission), custody (soon after being admitted to jail, during interrogation, during incarceration, or legal execution), and post-custody (revenge by police or rival criminals or after reentry into the community)” periods. It is noteworthy that the scope of these injuries is comparable to those encountered in a combat zone.17,18 According to the NMA:
“Injuries sustained by civilians at the hands of law enforcement include gunshot wounds, skull fractures, cervical spine injuries, facial fractures, broken legs, blunt trauma orbital floor fractures, laryngeal cartilage fractures, shoulder dislocations, cuts and bruises, concussions, hemorrhage, choking (positional or due to upper body holds), abdominal trauma, hemothorax, and pneumothorax. Complications of such injuries include posttraumatic brain swelling, infections following open fractures and lacerations, hydrocephalus due to blood or infection, as well as subdural and epidural hematomas and, in the most severe cases, death.”
In addition, there are multiple emotional and psychiatric sequelae of these injuries for the victims, families, upstanders, bystanders, and those viewing these images via various social media platforms. Increasingly, many are experiencing retraumatization each time a new death is reported. How do we explain that we are turning away from this as physicians and trainers of physicians? Seeing and not seeing – all of the methods used to avert one’s gaze and look the other way (to protect the psyches of nonmarginalized members of society from being disturbed and possibly traumatized) – these key defense mechanisms creep into consulting rooms and become fertile ground for the enactment described above.
Yet, there is reason to believe in change. It’s not simply because we are mental health professionals and that’s what we do. With the posting of position statements issued by major corporations and a growing number of medical organizations, many of us are experiencing a mixture of hope, anger, and sadness. Hope that widespread awareness will continue to tilt the axis of our country in a manner that opens eyes – and hearts – so that real work can be done; and anger and sadness because it has taken 400 years to receive even this level of validation.
In the meantime, we are encouraged by a joint position statement recently issued by the APA and the NMA, the first joint effort by these two medical organizations to partner and advocate for criminal justice reform. We mention this statement because the NMA has been committed to the needs of the black community since its inception in 1895, and the APA has as its mission a commitment to serve “the needs of evolving, diverse, underrepresented, and underserved patient populations” ... and the resources to do so. This is the kind of partnership that could transform words into meaningful action.19,20
Of course, resident psychiatrist Dr. A. had begun supervision with the discussion of his dyadic experience with his patient, which is set in the context of a global coronavirus pandemic that is disproportionately affecting black and brown people. And, while his peers are marching in protest, he and his fellow trainees deserve our support as they deal with their own psychic pain and prepare to steady themselves. For these psychiatrists will be called to provide care to those who will consult them once they begin to grapple with the experiences and, in some cases, traumas that have compelled them to take action and literally risk their safety and lives while protesting.
That evening, the residents were hungry for methods to fill the gaps in their training and supervision. In some cases, we provided scripts to be taken back to supervision. For example, the following is a potential scripted response for the supervisor in the enactment described above:
Resident speaking to supervisor: This is a black patient who, like many others, is affected by the chronic, repeated televised images of black men killed by police. I am also a black man.
I think what I have shared is pertinent to the patient’s care and my experience as a black male psychiatrist who will need to learn how to address this in my patients who are black and for other racialized groups, as well as with whites who might have rarely been cared for by a black man. Can we discuss this?
We also anticipated that some residents would need to exercise their right to request reassignment to another supervisor. And, until we do better at listening, seeing, and deepening our understanding, outside and inside the consulting room and in supervision, more residents might need to steer around those who have the potential to undermine training and adversely affect treatment. But, as a professional medical community in crisis, do we really want to proceed in such an ad hoc fashion?
Dr. Dunlap is a psychiatrist and psychoanalyst, and clinical professor of psychiatry and behavioral sciences at George Washington University. She is interested in the management of “difference” – race, gender, ethnicity, and intersectionality – in dyadic relationships and group dynamics; and the impact of racism on interpersonal relationships in institutional structures. Dr. Dunlap practices in Washington and has no disclosures.
Dr. Dennis is a clinical psychologist and psychoanalyst. Her interests are in gender and ethnic diversity, health equity, and supervision and training. Dr. Dennis practices in Washington and has no disclosures.
Dr. DeSouza is a PGY-4 psychiatry resident and public psychiatry fellow in the department of psychiatry at Yale University, New Haven, Conn. Her professional interests include health services development and delivery in low- and middle-income settings, as well as the intersection of mental health and spirituality. She has no disclosures.
Dr. Isom is a staff psychiatrist at the Codman Square Health Center in Dorchester, Mass., and Boston Medical Center. Her interests include racial mental health equity and population health approaches to community psychiatry. She has no disclosures.
Dr. Mathis is an addictions fellow in the department of psychiatry at Yale University and former programwide chief resident at Yale. Her interests include the intersection of racial justice and mental health, health equity, and spirituality. She has no disclosures.
References
1. Mental Health: Culture, Race, and Ethnicity. A Supplement to Mental Health: A Report of the Surgeon General. Rockville, Md.: Substance Abuse and Mental Health Services Administration, 2001.
2. Banaji MR and Greenwald AG. Blindspot: Hidden Biases of Good People. New York: Delacorte Press, 2013.
3. Anekwe ON. Voices in Bioethics. 2014.
4. Soute BJ. The American Psychoanalyst Magazine. 2017 Winter/Spring.
5. Powell DR. J Am Psychoanal Assoc. 2019 Jan 8. doi: 10.1177/000306511881847.
6. Allen TW. The Invention of the White Race. London: Verso, 1994.
7. Klein M. Int J Psychoanal. 1946;27(pt.3-4):99-100.
8. Bion WR. (1962b). Psychoanal Q. 2013 Apr;82(2):301-10.
9. Black Psychoanalysts Speak trailer.
10. Thomas A and Sillen S. Racism and Psychiatry. New York: Brunner/Mazel, 1972.
11. Jones BE et al. Am J Psychiatry. 1970 Dec;127(6):798-803.
12. Sabshin M et al. Am J Psychiatry. 1970 Dec;126(6):787-93.
13. Medlock M et al. Am J Psychiatry. 2017 May 9. doi: 10.1176/appi.ajp-rj.2016.110206.
14. Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5). Arlington, Va.: American Psychiatric Association, 2013.
15. “What is Child Trauma?” The National Child Traumatic Stress Network.
16. The Philadelphia Project. Philadelphia ACE Survey.
17. “Addressing law enforcement violence as a public health issue.” Washington: American Public Health Association. 2018 Nov 13. Policy# 20811.
18. National Medical Association position statement on police use of force. NMA 2016.
19. “APA and NMA jointly condemn systemic racism in America.” 2020 Jun 16.
20. APA Strategic Plan. 2015 Mar.
On the Friday evening after the public execution of George Floyd, we were painfully reminded of the urgency to address the inadequate management of race, racism, and anti-blackness in medical education, residency training, and postgraduate continuing medical education.
The reminder did not originate from the rioting that was occurring in some cities, though we could feel the ground shifting beneath our feet as civic protests that began in U.S. cities spread around the globe. Instead, it occurred during a webinar we were hosting for psychiatry residents focused on techniques for eliminating blind spots in the management of race in clinical psychotherapy supervision. (Dr. Jessica Isom chaired the webinar, Dr. Flavia DeSouza and Dr. Myra Mathis comoderated, and Dr. Ebony Dennis and Dr. Constance E. Dunlap served as discussants.)
Our panel had presented an ambitious agenda that included reviewing how the disavowal of bias, race, racism, and anti-blackness contributes to ineffective psychotherapy, undermines the quality of medical care, and perpetuates mental health disparities. We spent some time exploring how unacknowledged and unexamined conscious and unconscious racial stereotypes affect interpersonal relationships, the psychotherapeutic process, and the supervisory experience. Our presentation included a clinical vignette demonstrating how racism, colorism, and anti-blackness have global impact, influencing the self-esteem, identity formation, and identity consolidation of immigrants as they grapple with the unique form of racism that exists in America. Other clinical vignettes demonstrated blind spots that were retroactively identified though omitted in supervisory discussions. We also discussed alternative interventions and interpretations of the material presented.1-5
Because 21st-century trainees are generally psychologically astute and committed to social justice, we did two things. First, before the webinar, we provided them access to a prerecorded explanation of object relations theorist Melanie Klein’s paranoid-schizoid and depressive positions concepts, which were applied to theoretically explain the development of race, specifically the defenses used by early colonists that contributed to the development of “whiteness” and “blackness” as social constructs, and their influence on the development of the U.S. psyche. For example, as early colonists attempted to develop new and improved identities distinct from those they had in their homelands, they used enslaved black people (and other vulnerable groups) to “other.” What we mean here by othering is the process of using an other to project one’s badness into in order to relieve the self of uncomfortable aspects and feelings originating within the self. If this other accepts the projection (which is often the case with vulnerable parties), the self recognizes, that is, identifies (locates) the bad they just projected in the other, who is now experienced as a bad-other. This is projection in action. If the other accepts the projection and behaves accordingly, for example, in a manner that reflects badness, this becomes projective identification. Conversely, if the other does not accept these projections, the self (who projects) is left to cope with aspects of the self s/he might not have the capacity to manage. By capacity, we are speaking of the Bionian idea of the ability to experience an extreme emotion while also being able to think. Without the ego strength to cope with bad aspects of the self, the ego either collapses (and is unable to think) or further projection is attempted.6-8
We have seen this latter dynamic play out repeatedly when police officers fatally shoot black citizens and then claim that they feared for their lives; these same officers have been exonerated by juries by continuing to portray the deceased victims as threatening, dangerous objects not worthy of living. We are also seeing a global movement of black and nonblack people who are in touch with a justified rage that has motivated them to return these projections by collectively protesting, and in some cases, by rioting.
Back to the webinar
In anticipating the residents’ curiosity, impatience, and anger about the lack of progress, the second thing we did was to show a segment from the “Black Psychoanalysts Speak” trailer. In the clip played, senior psychoanalyst Kirkland C. Vaughans, PhD, shares: “The issue of race so prompts excessive anxiety that it blocks off our ability to think.”
We showed this clip to validate the trainees’ frustrations about the difficulty the broader establishment has had with addressing this serious, longstanding public health problem. We wanted these young psychiatrists to know that there are psychoanalysts, psychiatrists, psychologists, and social workers who have been committed to this work, even though the contributions of this diverse group have curiously been omitted from education and training curricula.9
So, what happened? What was the painful reminder? After the formal panel presentations, a black male psychiatry resident recounted his experience in a clinical supervision meeting that had occurred several days after the murder of George Floyd. In short, a patient had shared his reactions to yet another incident of fatal police use of force and paused to ask how the resident physician, Dr. A., was doing. The question was experienced as sincere concern about the psychiatrist’s mental well-being. The resident was not sure how to answer this question since it was a matter of self-disclosure, which was a reasonable and thoughtful consideration for a seasoned clinician and, certainly, for a novice therapist. The supervisor, Dr. B., seemingly eager to move on, to not think about this, responded to the resident by saying: “Now tell me about the patient.” In other words, what had just been shared by the resident – material that featured a patient’s reaction to another killing of a black man by police and the patient’s expressed concern for his black psychiatrist, and this resident physician appropriately seeking space in supervision to process and receive guidance about how to respond – all of this was considered separate (split off from) and extraneous to the patient’s treatment and the resident’s training. This is a problem. And, unfortunately, this problem or some variation of it is not rare.
Why is this still the state of affairs when we have identified racism as a major health concern and our patients and our trainees are asking for help?
Rethinking a metaphor
Despite calls to action over the last 50 years to encourage medicine to effectively address race and racism, deficits remain in didactic education, clinical rotations, and supervisory experiences of trainees learning how to do psychodynamic psychotherapy.8-10 Earlier that evening, we used the metaphor of a vehicular blind spot to capture what we believe occurs insupervision. Like drivers, supervisors generally have the ability to see. However, there are places (times) and positions (stances) that block their vision (awareness). Racism – whether institutionalized, interpersonally mediated, or internalized – also contributes to this blindness.
As is true of drivers managing a blind spot, what is required is for the drivers – the supervisors – to lean forward or reposition themselves so as to avoid collisions, maintain safety, and continue on course. We use this metaphor because it is understood that any clinician providing psychodynamic supervision to psychiatry residents, regardless of professional discipline, has the requisite skills and training.10-13
Until May 25, we thought eliminating blind spots would be effective. But, in the aftermath of the police killing of George Floyd, our eyes have been opened.
Hiding behind the blue wall of silence is an establishment that has looked the other way while black and brown women, men, and children have come to live in fear as a result of the state-sanctioned violence that repeatedly occurs across the nation. Excessive police use of force is a public health issue of crisis magnitude. However, the house of medicine, like many other established structures in society, has colluded with the societal constructs that have supported law enforcement by remaining willfully blind, often neutral, and by refusing to make the necessary adjustments, including connecting the dots between police violence and physical and mental health.
For example, racism has never been listed even in the index of the American Psychiatric Association’s (APA) Diagnostic and Statistical Manual of Mental Disorders.14 Being the victim of police use of force is not generally regarded as an adverse childhood experience, even though communities that are heavily policed experience harassment by law enforcement on a regular basis. The 12 causes of trauma listed on the website15 of the National Child Traumatic Stress Network – bullying, community violence, complex trauma, disasters, early childhood trauma, intimate partner violence, medical trauma, physical abuse, refugee trauma, sexual abuse, terrorism and violence, and traumatic grief – do not include maltreatment, abuse, or trauma resulting from interactions with members of law enforcement. Much of the adverse childhood experiences literature focuses on white, upper middle class children and on experiences within the home. When community level experiences, such as discrimination based on race or ethnicity, are included, as in the Philadelphia ACES study,16 as many as 40% reported ACE scores of greater than 4 for community level exposures.
As psychiatrists, we recognize the psychic underpinnings and parallels between the psychic projections onto black and brown people and the actual bullets pumped into the bodies of black and brown people; there is a lurid propensity to use these others as repositories. Those who have the privilege of being protected by law enforcement and the ability to avoid being used as containers for the psychic projections and bullets of some police officers also have the privilege of compartmentalizing and looking the other way when excessive acts of force – projections and projectiles – are used on other human beings. This partly explains why the injuries and deaths of black and brown people caused by police officers’ excessive use of force have continued even though these unjustified deaths are widely televised and disseminated via various social media platforms.
Prior to the death of George Floyd on May 25, other than the American Public Health Association, the National Medical Association (NMA) was the only major medical organization to issue a call to consider police use of force as a public health issue. In its July 2016 press release, provided in the aftermath of the death of Freddie Gray while in the custody of Baltimore police officers, the NMA summarized the scope of injuries citizens sustain during “the pre-custody (commission of a crime, during a fight, chase, and apprehension, during a siege or hostage situation, or during restraint or submission), custody (soon after being admitted to jail, during interrogation, during incarceration, or legal execution), and post-custody (revenge by police or rival criminals or after reentry into the community)” periods. It is noteworthy that the scope of these injuries is comparable to those encountered in a combat zone.17,18 According to the NMA:
“Injuries sustained by civilians at the hands of law enforcement include gunshot wounds, skull fractures, cervical spine injuries, facial fractures, broken legs, blunt trauma orbital floor fractures, laryngeal cartilage fractures, shoulder dislocations, cuts and bruises, concussions, hemorrhage, choking (positional or due to upper body holds), abdominal trauma, hemothorax, and pneumothorax. Complications of such injuries include posttraumatic brain swelling, infections following open fractures and lacerations, hydrocephalus due to blood or infection, as well as subdural and epidural hematomas and, in the most severe cases, death.”
In addition, there are multiple emotional and psychiatric sequelae of these injuries for the victims, families, upstanders, bystanders, and those viewing these images via various social media platforms. Increasingly, many are experiencing retraumatization each time a new death is reported. How do we explain that we are turning away from this as physicians and trainers of physicians? Seeing and not seeing – all of the methods used to avert one’s gaze and look the other way (to protect the psyches of nonmarginalized members of society from being disturbed and possibly traumatized) – these key defense mechanisms creep into consulting rooms and become fertile ground for the enactment described above.
Yet, there is reason to believe in change. It’s not simply because we are mental health professionals and that’s what we do. With the posting of position statements issued by major corporations and a growing number of medical organizations, many of us are experiencing a mixture of hope, anger, and sadness. Hope that widespread awareness will continue to tilt the axis of our country in a manner that opens eyes – and hearts – so that real work can be done; and anger and sadness because it has taken 400 years to receive even this level of validation.
In the meantime, we are encouraged by a joint position statement recently issued by the APA and the NMA, the first joint effort by these two medical organizations to partner and advocate for criminal justice reform. We mention this statement because the NMA has been committed to the needs of the black community since its inception in 1895, and the APA has as its mission a commitment to serve “the needs of evolving, diverse, underrepresented, and underserved patient populations” ... and the resources to do so. This is the kind of partnership that could transform words into meaningful action.19,20
Of course, resident psychiatrist Dr. A. had begun supervision with the discussion of his dyadic experience with his patient, which is set in the context of a global coronavirus pandemic that is disproportionately affecting black and brown people. And, while his peers are marching in protest, he and his fellow trainees deserve our support as they deal with their own psychic pain and prepare to steady themselves. For these psychiatrists will be called to provide care to those who will consult them once they begin to grapple with the experiences and, in some cases, traumas that have compelled them to take action and literally risk their safety and lives while protesting.
That evening, the residents were hungry for methods to fill the gaps in their training and supervision. In some cases, we provided scripts to be taken back to supervision. For example, the following is a potential scripted response for the supervisor in the enactment described above:
Resident speaking to supervisor: This is a black patient who, like many others, is affected by the chronic, repeated televised images of black men killed by police. I am also a black man.
I think what I have shared is pertinent to the patient’s care and my experience as a black male psychiatrist who will need to learn how to address this in my patients who are black and for other racialized groups, as well as with whites who might have rarely been cared for by a black man. Can we discuss this?
We also anticipated that some residents would need to exercise their right to request reassignment to another supervisor. And, until we do better at listening, seeing, and deepening our understanding, outside and inside the consulting room and in supervision, more residents might need to steer around those who have the potential to undermine training and adversely affect treatment. But, as a professional medical community in crisis, do we really want to proceed in such an ad hoc fashion?
Dr. Dunlap is a psychiatrist and psychoanalyst, and clinical professor of psychiatry and behavioral sciences at George Washington University. She is interested in the management of “difference” – race, gender, ethnicity, and intersectionality – in dyadic relationships and group dynamics; and the impact of racism on interpersonal relationships in institutional structures. Dr. Dunlap practices in Washington and has no disclosures.
Dr. Dennis is a clinical psychologist and psychoanalyst. Her interests are in gender and ethnic diversity, health equity, and supervision and training. Dr. Dennis practices in Washington and has no disclosures.
Dr. DeSouza is a PGY-4 psychiatry resident and public psychiatry fellow in the department of psychiatry at Yale University, New Haven, Conn. Her professional interests include health services development and delivery in low- and middle-income settings, as well as the intersection of mental health and spirituality. She has no disclosures.
Dr. Isom is a staff psychiatrist at the Codman Square Health Center in Dorchester, Mass., and Boston Medical Center. Her interests include racial mental health equity and population health approaches to community psychiatry. She has no disclosures.
Dr. Mathis is an addictions fellow in the department of psychiatry at Yale University and former programwide chief resident at Yale. Her interests include the intersection of racial justice and mental health, health equity, and spirituality. She has no disclosures.
References
1. Mental Health: Culture, Race, and Ethnicity. A Supplement to Mental Health: A Report of the Surgeon General. Rockville, Md.: Substance Abuse and Mental Health Services Administration, 2001.
2. Banaji MR and Greenwald AG. Blindspot: Hidden Biases of Good People. New York: Delacorte Press, 2013.
3. Anekwe ON. Voices in Bioethics. 2014.
4. Soute BJ. The American Psychoanalyst Magazine. 2017 Winter/Spring.
5. Powell DR. J Am Psychoanal Assoc. 2019 Jan 8. doi: 10.1177/000306511881847.
6. Allen TW. The Invention of the White Race. London: Verso, 1994.
7. Klein M. Int J Psychoanal. 1946;27(pt.3-4):99-100.
8. Bion WR. (1962b). Psychoanal Q. 2013 Apr;82(2):301-10.
9. Black Psychoanalysts Speak trailer.
10. Thomas A and Sillen S. Racism and Psychiatry. New York: Brunner/Mazel, 1972.
11. Jones BE et al. Am J Psychiatry. 1970 Dec;127(6):798-803.
12. Sabshin M et al. Am J Psychiatry. 1970 Dec;126(6):787-93.
13. Medlock M et al. Am J Psychiatry. 2017 May 9. doi: 10.1176/appi.ajp-rj.2016.110206.
14. Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5). Arlington, Va.: American Psychiatric Association, 2013.
15. “What is Child Trauma?” The National Child Traumatic Stress Network.
16. The Philadelphia Project. Philadelphia ACE Survey.
17. “Addressing law enforcement violence as a public health issue.” Washington: American Public Health Association. 2018 Nov 13. Policy# 20811.
18. National Medical Association position statement on police use of force. NMA 2016.
19. “APA and NMA jointly condemn systemic racism in America.” 2020 Jun 16.
20. APA Strategic Plan. 2015 Mar.
On the Friday evening after the public execution of George Floyd, we were painfully reminded of the urgency to address the inadequate management of race, racism, and anti-blackness in medical education, residency training, and postgraduate continuing medical education.
The reminder did not originate from the rioting that was occurring in some cities, though we could feel the ground shifting beneath our feet as civic protests that began in U.S. cities spread around the globe. Instead, it occurred during a webinar we were hosting for psychiatry residents focused on techniques for eliminating blind spots in the management of race in clinical psychotherapy supervision. (Dr. Jessica Isom chaired the webinar, Dr. Flavia DeSouza and Dr. Myra Mathis comoderated, and Dr. Ebony Dennis and Dr. Constance E. Dunlap served as discussants.)
Our panel had presented an ambitious agenda that included reviewing how the disavowal of bias, race, racism, and anti-blackness contributes to ineffective psychotherapy, undermines the quality of medical care, and perpetuates mental health disparities. We spent some time exploring how unacknowledged and unexamined conscious and unconscious racial stereotypes affect interpersonal relationships, the psychotherapeutic process, and the supervisory experience. Our presentation included a clinical vignette demonstrating how racism, colorism, and anti-blackness have global impact, influencing the self-esteem, identity formation, and identity consolidation of immigrants as they grapple with the unique form of racism that exists in America. Other clinical vignettes demonstrated blind spots that were retroactively identified though omitted in supervisory discussions. We also discussed alternative interventions and interpretations of the material presented.1-5
Because 21st-century trainees are generally psychologically astute and committed to social justice, we did two things. First, before the webinar, we provided them access to a prerecorded explanation of object relations theorist Melanie Klein’s paranoid-schizoid and depressive positions concepts, which were applied to theoretically explain the development of race, specifically the defenses used by early colonists that contributed to the development of “whiteness” and “blackness” as social constructs, and their influence on the development of the U.S. psyche. For example, as early colonists attempted to develop new and improved identities distinct from those they had in their homelands, they used enslaved black people (and other vulnerable groups) to “other.” What we mean here by othering is the process of using an other to project one’s badness into in order to relieve the self of uncomfortable aspects and feelings originating within the self. If this other accepts the projection (which is often the case with vulnerable parties), the self recognizes, that is, identifies (locates) the bad they just projected in the other, who is now experienced as a bad-other. This is projection in action. If the other accepts the projection and behaves accordingly, for example, in a manner that reflects badness, this becomes projective identification. Conversely, if the other does not accept these projections, the self (who projects) is left to cope with aspects of the self s/he might not have the capacity to manage. By capacity, we are speaking of the Bionian idea of the ability to experience an extreme emotion while also being able to think. Without the ego strength to cope with bad aspects of the self, the ego either collapses (and is unable to think) or further projection is attempted.6-8
We have seen this latter dynamic play out repeatedly when police officers fatally shoot black citizens and then claim that they feared for their lives; these same officers have been exonerated by juries by continuing to portray the deceased victims as threatening, dangerous objects not worthy of living. We are also seeing a global movement of black and nonblack people who are in touch with a justified rage that has motivated them to return these projections by collectively protesting, and in some cases, by rioting.
Back to the webinar
In anticipating the residents’ curiosity, impatience, and anger about the lack of progress, the second thing we did was to show a segment from the “Black Psychoanalysts Speak” trailer. In the clip played, senior psychoanalyst Kirkland C. Vaughans, PhD, shares: “The issue of race so prompts excessive anxiety that it blocks off our ability to think.”
We showed this clip to validate the trainees’ frustrations about the difficulty the broader establishment has had with addressing this serious, longstanding public health problem. We wanted these young psychiatrists to know that there are psychoanalysts, psychiatrists, psychologists, and social workers who have been committed to this work, even though the contributions of this diverse group have curiously been omitted from education and training curricula.9
So, what happened? What was the painful reminder? After the formal panel presentations, a black male psychiatry resident recounted his experience in a clinical supervision meeting that had occurred several days after the murder of George Floyd. In short, a patient had shared his reactions to yet another incident of fatal police use of force and paused to ask how the resident physician, Dr. A., was doing. The question was experienced as sincere concern about the psychiatrist’s mental well-being. The resident was not sure how to answer this question since it was a matter of self-disclosure, which was a reasonable and thoughtful consideration for a seasoned clinician and, certainly, for a novice therapist. The supervisor, Dr. B., seemingly eager to move on, to not think about this, responded to the resident by saying: “Now tell me about the patient.” In other words, what had just been shared by the resident – material that featured a patient’s reaction to another killing of a black man by police and the patient’s expressed concern for his black psychiatrist, and this resident physician appropriately seeking space in supervision to process and receive guidance about how to respond – all of this was considered separate (split off from) and extraneous to the patient’s treatment and the resident’s training. This is a problem. And, unfortunately, this problem or some variation of it is not rare.
Why is this still the state of affairs when we have identified racism as a major health concern and our patients and our trainees are asking for help?
Rethinking a metaphor
Despite calls to action over the last 50 years to encourage medicine to effectively address race and racism, deficits remain in didactic education, clinical rotations, and supervisory experiences of trainees learning how to do psychodynamic psychotherapy.8-10 Earlier that evening, we used the metaphor of a vehicular blind spot to capture what we believe occurs insupervision. Like drivers, supervisors generally have the ability to see. However, there are places (times) and positions (stances) that block their vision (awareness). Racism – whether institutionalized, interpersonally mediated, or internalized – also contributes to this blindness.
As is true of drivers managing a blind spot, what is required is for the drivers – the supervisors – to lean forward or reposition themselves so as to avoid collisions, maintain safety, and continue on course. We use this metaphor because it is understood that any clinician providing psychodynamic supervision to psychiatry residents, regardless of professional discipline, has the requisite skills and training.10-13
Until May 25, we thought eliminating blind spots would be effective. But, in the aftermath of the police killing of George Floyd, our eyes have been opened.
Hiding behind the blue wall of silence is an establishment that has looked the other way while black and brown women, men, and children have come to live in fear as a result of the state-sanctioned violence that repeatedly occurs across the nation. Excessive police use of force is a public health issue of crisis magnitude. However, the house of medicine, like many other established structures in society, has colluded with the societal constructs that have supported law enforcement by remaining willfully blind, often neutral, and by refusing to make the necessary adjustments, including connecting the dots between police violence and physical and mental health.
For example, racism has never been listed even in the index of the American Psychiatric Association’s (APA) Diagnostic and Statistical Manual of Mental Disorders.14 Being the victim of police use of force is not generally regarded as an adverse childhood experience, even though communities that are heavily policed experience harassment by law enforcement on a regular basis. The 12 causes of trauma listed on the website15 of the National Child Traumatic Stress Network – bullying, community violence, complex trauma, disasters, early childhood trauma, intimate partner violence, medical trauma, physical abuse, refugee trauma, sexual abuse, terrorism and violence, and traumatic grief – do not include maltreatment, abuse, or trauma resulting from interactions with members of law enforcement. Much of the adverse childhood experiences literature focuses on white, upper middle class children and on experiences within the home. When community level experiences, such as discrimination based on race or ethnicity, are included, as in the Philadelphia ACES study,16 as many as 40% reported ACE scores of greater than 4 for community level exposures.
As psychiatrists, we recognize the psychic underpinnings and parallels between the psychic projections onto black and brown people and the actual bullets pumped into the bodies of black and brown people; there is a lurid propensity to use these others as repositories. Those who have the privilege of being protected by law enforcement and the ability to avoid being used as containers for the psychic projections and bullets of some police officers also have the privilege of compartmentalizing and looking the other way when excessive acts of force – projections and projectiles – are used on other human beings. This partly explains why the injuries and deaths of black and brown people caused by police officers’ excessive use of force have continued even though these unjustified deaths are widely televised and disseminated via various social media platforms.
Prior to the death of George Floyd on May 25, other than the American Public Health Association, the National Medical Association (NMA) was the only major medical organization to issue a call to consider police use of force as a public health issue. In its July 2016 press release, provided in the aftermath of the death of Freddie Gray while in the custody of Baltimore police officers, the NMA summarized the scope of injuries citizens sustain during “the pre-custody (commission of a crime, during a fight, chase, and apprehension, during a siege or hostage situation, or during restraint or submission), custody (soon after being admitted to jail, during interrogation, during incarceration, or legal execution), and post-custody (revenge by police or rival criminals or after reentry into the community)” periods. It is noteworthy that the scope of these injuries is comparable to those encountered in a combat zone.17,18 According to the NMA:
“Injuries sustained by civilians at the hands of law enforcement include gunshot wounds, skull fractures, cervical spine injuries, facial fractures, broken legs, blunt trauma orbital floor fractures, laryngeal cartilage fractures, shoulder dislocations, cuts and bruises, concussions, hemorrhage, choking (positional or due to upper body holds), abdominal trauma, hemothorax, and pneumothorax. Complications of such injuries include posttraumatic brain swelling, infections following open fractures and lacerations, hydrocephalus due to blood or infection, as well as subdural and epidural hematomas and, in the most severe cases, death.”
In addition, there are multiple emotional and psychiatric sequelae of these injuries for the victims, families, upstanders, bystanders, and those viewing these images via various social media platforms. Increasingly, many are experiencing retraumatization each time a new death is reported. How do we explain that we are turning away from this as physicians and trainers of physicians? Seeing and not seeing – all of the methods used to avert one’s gaze and look the other way (to protect the psyches of nonmarginalized members of society from being disturbed and possibly traumatized) – these key defense mechanisms creep into consulting rooms and become fertile ground for the enactment described above.
Yet, there is reason to believe in change. It’s not simply because we are mental health professionals and that’s what we do. With the posting of position statements issued by major corporations and a growing number of medical organizations, many of us are experiencing a mixture of hope, anger, and sadness. Hope that widespread awareness will continue to tilt the axis of our country in a manner that opens eyes – and hearts – so that real work can be done; and anger and sadness because it has taken 400 years to receive even this level of validation.
In the meantime, we are encouraged by a joint position statement recently issued by the APA and the NMA, the first joint effort by these two medical organizations to partner and advocate for criminal justice reform. We mention this statement because the NMA has been committed to the needs of the black community since its inception in 1895, and the APA has as its mission a commitment to serve “the needs of evolving, diverse, underrepresented, and underserved patient populations” ... and the resources to do so. This is the kind of partnership that could transform words into meaningful action.19,20
Of course, resident psychiatrist Dr. A. had begun supervision with the discussion of his dyadic experience with his patient, which is set in the context of a global coronavirus pandemic that is disproportionately affecting black and brown people. And, while his peers are marching in protest, he and his fellow trainees deserve our support as they deal with their own psychic pain and prepare to steady themselves. For these psychiatrists will be called to provide care to those who will consult them once they begin to grapple with the experiences and, in some cases, traumas that have compelled them to take action and literally risk their safety and lives while protesting.
That evening, the residents were hungry for methods to fill the gaps in their training and supervision. In some cases, we provided scripts to be taken back to supervision. For example, the following is a potential scripted response for the supervisor in the enactment described above:
Resident speaking to supervisor: This is a black patient who, like many others, is affected by the chronic, repeated televised images of black men killed by police. I am also a black man.
I think what I have shared is pertinent to the patient’s care and my experience as a black male psychiatrist who will need to learn how to address this in my patients who are black and for other racialized groups, as well as with whites who might have rarely been cared for by a black man. Can we discuss this?
We also anticipated that some residents would need to exercise their right to request reassignment to another supervisor. And, until we do better at listening, seeing, and deepening our understanding, outside and inside the consulting room and in supervision, more residents might need to steer around those who have the potential to undermine training and adversely affect treatment. But, as a professional medical community in crisis, do we really want to proceed in such an ad hoc fashion?
Dr. Dunlap is a psychiatrist and psychoanalyst, and clinical professor of psychiatry and behavioral sciences at George Washington University. She is interested in the management of “difference” – race, gender, ethnicity, and intersectionality – in dyadic relationships and group dynamics; and the impact of racism on interpersonal relationships in institutional structures. Dr. Dunlap practices in Washington and has no disclosures.
Dr. Dennis is a clinical psychologist and psychoanalyst. Her interests are in gender and ethnic diversity, health equity, and supervision and training. Dr. Dennis practices in Washington and has no disclosures.
Dr. DeSouza is a PGY-4 psychiatry resident and public psychiatry fellow in the department of psychiatry at Yale University, New Haven, Conn. Her professional interests include health services development and delivery in low- and middle-income settings, as well as the intersection of mental health and spirituality. She has no disclosures.
Dr. Isom is a staff psychiatrist at the Codman Square Health Center in Dorchester, Mass., and Boston Medical Center. Her interests include racial mental health equity and population health approaches to community psychiatry. She has no disclosures.
Dr. Mathis is an addictions fellow in the department of psychiatry at Yale University and former programwide chief resident at Yale. Her interests include the intersection of racial justice and mental health, health equity, and spirituality. She has no disclosures.
References
1. Mental Health: Culture, Race, and Ethnicity. A Supplement to Mental Health: A Report of the Surgeon General. Rockville, Md.: Substance Abuse and Mental Health Services Administration, 2001.
2. Banaji MR and Greenwald AG. Blindspot: Hidden Biases of Good People. New York: Delacorte Press, 2013.
3. Anekwe ON. Voices in Bioethics. 2014.
4. Soute BJ. The American Psychoanalyst Magazine. 2017 Winter/Spring.
5. Powell DR. J Am Psychoanal Assoc. 2019 Jan 8. doi: 10.1177/000306511881847.
6. Allen TW. The Invention of the White Race. London: Verso, 1994.
7. Klein M. Int J Psychoanal. 1946;27(pt.3-4):99-100.
8. Bion WR. (1962b). Psychoanal Q. 2013 Apr;82(2):301-10.
9. Black Psychoanalysts Speak trailer.
10. Thomas A and Sillen S. Racism and Psychiatry. New York: Brunner/Mazel, 1972.
11. Jones BE et al. Am J Psychiatry. 1970 Dec;127(6):798-803.
12. Sabshin M et al. Am J Psychiatry. 1970 Dec;126(6):787-93.
13. Medlock M et al. Am J Psychiatry. 2017 May 9. doi: 10.1176/appi.ajp-rj.2016.110206.
14. Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5). Arlington, Va.: American Psychiatric Association, 2013.
15. “What is Child Trauma?” The National Child Traumatic Stress Network.
16. The Philadelphia Project. Philadelphia ACE Survey.
17. “Addressing law enforcement violence as a public health issue.” Washington: American Public Health Association. 2018 Nov 13. Policy# 20811.
18. National Medical Association position statement on police use of force. NMA 2016.
19. “APA and NMA jointly condemn systemic racism in America.” 2020 Jun 16.
20. APA Strategic Plan. 2015 Mar.
Study evaluates number of needed to refer, biopsy for diagnosing a melanoma
At the same time, the number needed to refer to diagnose non-melanoma skin cancer was 4 and the number needed to biopsy was 1.5.
The findings come from a retrospective review of 707 patients referred to a tertiary medical center dermatology practice for suspicious lesions, presented in a poster session at the virtual annual meeting of the American Academy of Dermatology
“Multiple studies in the dermatology literature have looked at the number needed to treat (NNT) as a quality metric for dermatology clinics, where a lower number is ‘better,’” the study’s first author, Nikolai Klebanov, MD, said in an interview following the virtual meeting. “Our particular study is unique in that we estimated both the number needed to refer and number needed to biopsy to closely examine the process of referrals for suspicious lesions from primary care settings to specialists. We also looked closely at the underlying patient-centered characteristics, which could be used by all clinicians to streamline the referral process by reducing the volume of low-risk referrals.”
Dr. Klebanov, of the department of dermatology at Massachusetts General Hospital, Boston, and his associates reviewed 707 unique patient visits to the department during July 2015–February 2016. They calculated the number needed to refer and biopsy for melanoma as the ratio of biopsy-proven melanoma diagnoses among benign and dysplastic nevi and seborrheic keratoses. For nonmelanoma skin cancer, they used the ratio of basal and squamous cell carcinoma among actinic keratoses and seborrheic keratoses.
Of the 707 patients, 54% were female, and males were slightly older than females (a mean of 58 vs. 54 years, respectively). The researchers found that lesions were more commonly benign among all age groups, while the frequency of premalignant and malignant lesions such as actinic keratoses, nonmelanoma skin cancer, and melanoma was highest for males and increased with age. Nevi were the most common benign diagnosis among patients 39 years of age and younger, while seborrheic keratoses were more common among patients aged 40 years and older.
The researchers found that the number needed to treat for melanoma was 31.5 and the number needed to biopsy was 7.5, which represents a 4.2-fold difference. Meanwhile, the number needed to refer for nonmelanoma skin cancer was 4, and the number needed to biopsy was 1.5, which represents a 2.7-fold difference. Despite variable rates of skin cancer between demographics, the biopsy rate ranged between 18% and 30%, for a mean of 23.4%.
“We found that most young patients referred for a ‘suspicious lesion’ on clinical prebiopsy assessment by the dermatologist were determined to actually have a benign nevus, and that older patients were most likely to have a seborrheic keratosis as the underlying lesion,” Dr. Klebanov said. “Among the minority of patients in each demographic group who were selected for biopsy, those lesions which were found to be benign were also largely nevi and keratoses. Even by being mindful of just the patient’s age, primary care providers can follow patients clinically with a tailored differential diagnosis in mind before referral, and dermatologists can reduce the number of biopsies they perform on patients who are being referred.”
He added that he and his colleagues were surprised that despite very low rates of skin cancer in young patients, and thus different pretest probabilities of cancer, biopsy rates across demographics were consistently around 20%. “We also found a disproportionate number of female patients younger than age 40 who were referred for suspicious lesions, while in the older age groups, the ratio of males to females was approximately equal.”
Dr. Klebanov acknowledged certain limitations of the study, including its single-center, retrospective design, and that information was not collected on patients’ family history of skin cancer, Fitzpatrick skin type, nor the clinical course of the lesion while it was followed by the primary care office. “The nuanced differences in these factors may certainly play a role in decisions for individual patients,” he said.
The study’s principal investigator was Hensin Tsao MD, PhD, clinical director of the MGH Melanoma & Pigmented Lesion Center The work was supported by the Alpha Omega Alpha Carolyn Kuckein Research Fellowship. The researchers reported having no financial disclosures.
SOURCE: Klebanov N et al. AAD 20. Abstract 15881.
At the same time, the number needed to refer to diagnose non-melanoma skin cancer was 4 and the number needed to biopsy was 1.5.
The findings come from a retrospective review of 707 patients referred to a tertiary medical center dermatology practice for suspicious lesions, presented in a poster session at the virtual annual meeting of the American Academy of Dermatology
“Multiple studies in the dermatology literature have looked at the number needed to treat (NNT) as a quality metric for dermatology clinics, where a lower number is ‘better,’” the study’s first author, Nikolai Klebanov, MD, said in an interview following the virtual meeting. “Our particular study is unique in that we estimated both the number needed to refer and number needed to biopsy to closely examine the process of referrals for suspicious lesions from primary care settings to specialists. We also looked closely at the underlying patient-centered characteristics, which could be used by all clinicians to streamline the referral process by reducing the volume of low-risk referrals.”
Dr. Klebanov, of the department of dermatology at Massachusetts General Hospital, Boston, and his associates reviewed 707 unique patient visits to the department during July 2015–February 2016. They calculated the number needed to refer and biopsy for melanoma as the ratio of biopsy-proven melanoma diagnoses among benign and dysplastic nevi and seborrheic keratoses. For nonmelanoma skin cancer, they used the ratio of basal and squamous cell carcinoma among actinic keratoses and seborrheic keratoses.
Of the 707 patients, 54% were female, and males were slightly older than females (a mean of 58 vs. 54 years, respectively). The researchers found that lesions were more commonly benign among all age groups, while the frequency of premalignant and malignant lesions such as actinic keratoses, nonmelanoma skin cancer, and melanoma was highest for males and increased with age. Nevi were the most common benign diagnosis among patients 39 years of age and younger, while seborrheic keratoses were more common among patients aged 40 years and older.
The researchers found that the number needed to treat for melanoma was 31.5 and the number needed to biopsy was 7.5, which represents a 4.2-fold difference. Meanwhile, the number needed to refer for nonmelanoma skin cancer was 4, and the number needed to biopsy was 1.5, which represents a 2.7-fold difference. Despite variable rates of skin cancer between demographics, the biopsy rate ranged between 18% and 30%, for a mean of 23.4%.
“We found that most young patients referred for a ‘suspicious lesion’ on clinical prebiopsy assessment by the dermatologist were determined to actually have a benign nevus, and that older patients were most likely to have a seborrheic keratosis as the underlying lesion,” Dr. Klebanov said. “Among the minority of patients in each demographic group who were selected for biopsy, those lesions which were found to be benign were also largely nevi and keratoses. Even by being mindful of just the patient’s age, primary care providers can follow patients clinically with a tailored differential diagnosis in mind before referral, and dermatologists can reduce the number of biopsies they perform on patients who are being referred.”
He added that he and his colleagues were surprised that despite very low rates of skin cancer in young patients, and thus different pretest probabilities of cancer, biopsy rates across demographics were consistently around 20%. “We also found a disproportionate number of female patients younger than age 40 who were referred for suspicious lesions, while in the older age groups, the ratio of males to females was approximately equal.”
Dr. Klebanov acknowledged certain limitations of the study, including its single-center, retrospective design, and that information was not collected on patients’ family history of skin cancer, Fitzpatrick skin type, nor the clinical course of the lesion while it was followed by the primary care office. “The nuanced differences in these factors may certainly play a role in decisions for individual patients,” he said.
The study’s principal investigator was Hensin Tsao MD, PhD, clinical director of the MGH Melanoma & Pigmented Lesion Center The work was supported by the Alpha Omega Alpha Carolyn Kuckein Research Fellowship. The researchers reported having no financial disclosures.
SOURCE: Klebanov N et al. AAD 20. Abstract 15881.
At the same time, the number needed to refer to diagnose non-melanoma skin cancer was 4 and the number needed to biopsy was 1.5.
The findings come from a retrospective review of 707 patients referred to a tertiary medical center dermatology practice for suspicious lesions, presented in a poster session at the virtual annual meeting of the American Academy of Dermatology
“Multiple studies in the dermatology literature have looked at the number needed to treat (NNT) as a quality metric for dermatology clinics, where a lower number is ‘better,’” the study’s first author, Nikolai Klebanov, MD, said in an interview following the virtual meeting. “Our particular study is unique in that we estimated both the number needed to refer and number needed to biopsy to closely examine the process of referrals for suspicious lesions from primary care settings to specialists. We also looked closely at the underlying patient-centered characteristics, which could be used by all clinicians to streamline the referral process by reducing the volume of low-risk referrals.”
Dr. Klebanov, of the department of dermatology at Massachusetts General Hospital, Boston, and his associates reviewed 707 unique patient visits to the department during July 2015–February 2016. They calculated the number needed to refer and biopsy for melanoma as the ratio of biopsy-proven melanoma diagnoses among benign and dysplastic nevi and seborrheic keratoses. For nonmelanoma skin cancer, they used the ratio of basal and squamous cell carcinoma among actinic keratoses and seborrheic keratoses.
Of the 707 patients, 54% were female, and males were slightly older than females (a mean of 58 vs. 54 years, respectively). The researchers found that lesions were more commonly benign among all age groups, while the frequency of premalignant and malignant lesions such as actinic keratoses, nonmelanoma skin cancer, and melanoma was highest for males and increased with age. Nevi were the most common benign diagnosis among patients 39 years of age and younger, while seborrheic keratoses were more common among patients aged 40 years and older.
The researchers found that the number needed to treat for melanoma was 31.5 and the number needed to biopsy was 7.5, which represents a 4.2-fold difference. Meanwhile, the number needed to refer for nonmelanoma skin cancer was 4, and the number needed to biopsy was 1.5, which represents a 2.7-fold difference. Despite variable rates of skin cancer between demographics, the biopsy rate ranged between 18% and 30%, for a mean of 23.4%.
“We found that most young patients referred for a ‘suspicious lesion’ on clinical prebiopsy assessment by the dermatologist were determined to actually have a benign nevus, and that older patients were most likely to have a seborrheic keratosis as the underlying lesion,” Dr. Klebanov said. “Among the minority of patients in each demographic group who were selected for biopsy, those lesions which were found to be benign were also largely nevi and keratoses. Even by being mindful of just the patient’s age, primary care providers can follow patients clinically with a tailored differential diagnosis in mind before referral, and dermatologists can reduce the number of biopsies they perform on patients who are being referred.”
He added that he and his colleagues were surprised that despite very low rates of skin cancer in young patients, and thus different pretest probabilities of cancer, biopsy rates across demographics were consistently around 20%. “We also found a disproportionate number of female patients younger than age 40 who were referred for suspicious lesions, while in the older age groups, the ratio of males to females was approximately equal.”
Dr. Klebanov acknowledged certain limitations of the study, including its single-center, retrospective design, and that information was not collected on patients’ family history of skin cancer, Fitzpatrick skin type, nor the clinical course of the lesion while it was followed by the primary care office. “The nuanced differences in these factors may certainly play a role in decisions for individual patients,” he said.
The study’s principal investigator was Hensin Tsao MD, PhD, clinical director of the MGH Melanoma & Pigmented Lesion Center The work was supported by the Alpha Omega Alpha Carolyn Kuckein Research Fellowship. The researchers reported having no financial disclosures.
SOURCE: Klebanov N et al. AAD 20. Abstract 15881.
FROM AAD 20
LAA Closure noninferior to DOACs to prevent AF-related events
Left atrial appendage closure was noninferior to use of direct oral anticoagulants for the prevention of atrial fibrillation (AFib)–related events in high-risk patients, based on data from 402 adults.
Given the limitations of vitamin K antagonists for preventing stroke in AFib, “a novel site-specific therapeutic alternative, mechanical left atrial appendage occlusion [LAAO], entered clinical practice,” but has not been compared with current safe and effective oral anticoagulants, wrote Pavel Osmancik, MD, of University Hospital Kralovske Vinohrady, Prague, and colleagues.
In a study published in the Journal of the American College of Cardiology, the researchers randomized 201 moderate- or high-risk adults with nonvalvular AFib to LAAO and another 201 to direct oral anticoagulants (DOAC).
Patients in the LAAO group underwent transesophageal echocardiography to exclude left atrial thrombi and underwent implantation with Boston Scientific’s Watchman, Watchman-FLX, or Abbott’s Amulet devices. Patients in the DOAC group received rivaroxaban, apixaban, or dabigatran at the manufacturer-recommended dose.
The primary outcome was a composite of complications related to procedures or devices, thromboembolic events (including stroke), and clinically significant bleeding. After an average of 20 months follow-up, 35 patients in the LAAO group and 41 in the DOAC group met the primary outcome (11% per 100 patient-years vs. 13% per 100 patient-years).
In addition, no differences appeared between the groups for the endpoint components of all-stroke/transient ischemic attack event (subdistribution hazard ratio, 1.00), clinically significantly bleeding (sHR, 0.81), or cardiovascular death (sHR, 0.75).
Nine patients experienced major complications related to LAAO, including clinically significant bleeding (sHR, 0.81; 95% CI, 0.44-1.52) and cardiovascular death (sHR, 0.75; 95% CI, 0.34-1.62). Major LAAO-related complications occurred in nine (4.5%) patients, with a short-term (up to 7 days or hospital discharge) complication rate of 2.1% and a 2.7% late complication rate. The late complications included three pericardial effusions, one of which resulted in death, the researchers wrote.
The study findings were limited by several factors, including the inability to assess the differences among the components of the composite primary endpoint. For example, “Regarding the primary endpoint, stroke reduction may be more important than bleeding reduction,” the investigators wrote.
The results were strengthened, however, by the enrollment of a high-risk AF population and is the first known randomized trial to compare percutaneous LAAO and DOACs for stroke prevention in this group. But the late complication rate of 2.7% is “suboptimal” and safety issues reinforce the need for refinement of operator technique and device technology with LAAO, they concluded.
‘Important step forward,’ with caveats
“How LAAO might stack up against DOAC therapy has remained an open question: Compared with warfarin, DOACs are easier to use and are associated with a reduction in mortality, driven by a substantially lower risk of intracranial hemorrhage and fatal bleeding,” wrote Matthew J. Price, MD, of the Scripps Clinic in La Jolla, Calif., and Jacqueline Saw, MD, of Vancouver General Hospital, in an accompanying editorial.
Previous studies of LAAO have shown a reduced risk of gastrointestinal bleeding, but procedure hazards interfered with long-term benefits, they said. The current study findings of similar rates of stroke and lower bleeding rates with LAAO, compared with DOAC, “are provocative given the clinical consensus that DOACs are safer, well tolerated, and generally better than warfarin, which was an easy target for transcatheter LAAO, given warfarin’s extensive limitations,” the editorialists wrote. Although the findings lend support to the use of LAAO, clinicians should consider several caveats such as the inclusion of patients who were “not optimal candidates for long-term OAC but were selected because they were at high risk for bleeding or because OAC treatment had already failed.”
However, “despite its imperfections, PRAGUE-17 is an important step forward and reinforces the role of transcatheter LAAO as a stroke-prevention strategy for patients with [AFib] at high risk of bleeding or medical treatment failure, even in the modern era of the DOACs,” they concluded. “Going forward, successful enrollment in ongoing and planned clinical trials while avoiding off-label procedures will be critical to define the appropriate use of transcatheter LAAO in expanded patient populations.”
The study was supported by the Ministry of Health of the Czech Republic. Dr. Osmancik disclosed speaking honoraria from Bayer and Abbot. Dr. Price’s financial disclosures included honoraria, speaker bureau fees, and/or research grants from Abbott Vascular, AstraZeneca, Boston Scientific, Chiesi USA, Daiichi Sankyo, and Medtronic. Dr. Saw disclosed receiving unrestricted research grant support several Canadian research institutes and fees and honoraria from AstraZeneca, Abbott Vascular, Boston Scientific, and Servier, among other drug companies.
SOURCES: Osmancik P et al. J Am Coll Cardiol. 2020;75:3122-35; Price MJ, Saw J. J Am Coll Cardiol. 2020;75:3136-9.
Left atrial appendage closure was noninferior to use of direct oral anticoagulants for the prevention of atrial fibrillation (AFib)–related events in high-risk patients, based on data from 402 adults.
Given the limitations of vitamin K antagonists for preventing stroke in AFib, “a novel site-specific therapeutic alternative, mechanical left atrial appendage occlusion [LAAO], entered clinical practice,” but has not been compared with current safe and effective oral anticoagulants, wrote Pavel Osmancik, MD, of University Hospital Kralovske Vinohrady, Prague, and colleagues.
In a study published in the Journal of the American College of Cardiology, the researchers randomized 201 moderate- or high-risk adults with nonvalvular AFib to LAAO and another 201 to direct oral anticoagulants (DOAC).
Patients in the LAAO group underwent transesophageal echocardiography to exclude left atrial thrombi and underwent implantation with Boston Scientific’s Watchman, Watchman-FLX, or Abbott’s Amulet devices. Patients in the DOAC group received rivaroxaban, apixaban, or dabigatran at the manufacturer-recommended dose.
The primary outcome was a composite of complications related to procedures or devices, thromboembolic events (including stroke), and clinically significant bleeding. After an average of 20 months follow-up, 35 patients in the LAAO group and 41 in the DOAC group met the primary outcome (11% per 100 patient-years vs. 13% per 100 patient-years).
In addition, no differences appeared between the groups for the endpoint components of all-stroke/transient ischemic attack event (subdistribution hazard ratio, 1.00), clinically significantly bleeding (sHR, 0.81), or cardiovascular death (sHR, 0.75).
Nine patients experienced major complications related to LAAO, including clinically significant bleeding (sHR, 0.81; 95% CI, 0.44-1.52) and cardiovascular death (sHR, 0.75; 95% CI, 0.34-1.62). Major LAAO-related complications occurred in nine (4.5%) patients, with a short-term (up to 7 days or hospital discharge) complication rate of 2.1% and a 2.7% late complication rate. The late complications included three pericardial effusions, one of which resulted in death, the researchers wrote.
The study findings were limited by several factors, including the inability to assess the differences among the components of the composite primary endpoint. For example, “Regarding the primary endpoint, stroke reduction may be more important than bleeding reduction,” the investigators wrote.
The results were strengthened, however, by the enrollment of a high-risk AF population and is the first known randomized trial to compare percutaneous LAAO and DOACs for stroke prevention in this group. But the late complication rate of 2.7% is “suboptimal” and safety issues reinforce the need for refinement of operator technique and device technology with LAAO, they concluded.
‘Important step forward,’ with caveats
“How LAAO might stack up against DOAC therapy has remained an open question: Compared with warfarin, DOACs are easier to use and are associated with a reduction in mortality, driven by a substantially lower risk of intracranial hemorrhage and fatal bleeding,” wrote Matthew J. Price, MD, of the Scripps Clinic in La Jolla, Calif., and Jacqueline Saw, MD, of Vancouver General Hospital, in an accompanying editorial.
Previous studies of LAAO have shown a reduced risk of gastrointestinal bleeding, but procedure hazards interfered with long-term benefits, they said. The current study findings of similar rates of stroke and lower bleeding rates with LAAO, compared with DOAC, “are provocative given the clinical consensus that DOACs are safer, well tolerated, and generally better than warfarin, which was an easy target for transcatheter LAAO, given warfarin’s extensive limitations,” the editorialists wrote. Although the findings lend support to the use of LAAO, clinicians should consider several caveats such as the inclusion of patients who were “not optimal candidates for long-term OAC but were selected because they were at high risk for bleeding or because OAC treatment had already failed.”
However, “despite its imperfections, PRAGUE-17 is an important step forward and reinforces the role of transcatheter LAAO as a stroke-prevention strategy for patients with [AFib] at high risk of bleeding or medical treatment failure, even in the modern era of the DOACs,” they concluded. “Going forward, successful enrollment in ongoing and planned clinical trials while avoiding off-label procedures will be critical to define the appropriate use of transcatheter LAAO in expanded patient populations.”
The study was supported by the Ministry of Health of the Czech Republic. Dr. Osmancik disclosed speaking honoraria from Bayer and Abbot. Dr. Price’s financial disclosures included honoraria, speaker bureau fees, and/or research grants from Abbott Vascular, AstraZeneca, Boston Scientific, Chiesi USA, Daiichi Sankyo, and Medtronic. Dr. Saw disclosed receiving unrestricted research grant support several Canadian research institutes and fees and honoraria from AstraZeneca, Abbott Vascular, Boston Scientific, and Servier, among other drug companies.
SOURCES: Osmancik P et al. J Am Coll Cardiol. 2020;75:3122-35; Price MJ, Saw J. J Am Coll Cardiol. 2020;75:3136-9.
Left atrial appendage closure was noninferior to use of direct oral anticoagulants for the prevention of atrial fibrillation (AFib)–related events in high-risk patients, based on data from 402 adults.
Given the limitations of vitamin K antagonists for preventing stroke in AFib, “a novel site-specific therapeutic alternative, mechanical left atrial appendage occlusion [LAAO], entered clinical practice,” but has not been compared with current safe and effective oral anticoagulants, wrote Pavel Osmancik, MD, of University Hospital Kralovske Vinohrady, Prague, and colleagues.
In a study published in the Journal of the American College of Cardiology, the researchers randomized 201 moderate- or high-risk adults with nonvalvular AFib to LAAO and another 201 to direct oral anticoagulants (DOAC).
Patients in the LAAO group underwent transesophageal echocardiography to exclude left atrial thrombi and underwent implantation with Boston Scientific’s Watchman, Watchman-FLX, or Abbott’s Amulet devices. Patients in the DOAC group received rivaroxaban, apixaban, or dabigatran at the manufacturer-recommended dose.
The primary outcome was a composite of complications related to procedures or devices, thromboembolic events (including stroke), and clinically significant bleeding. After an average of 20 months follow-up, 35 patients in the LAAO group and 41 in the DOAC group met the primary outcome (11% per 100 patient-years vs. 13% per 100 patient-years).
In addition, no differences appeared between the groups for the endpoint components of all-stroke/transient ischemic attack event (subdistribution hazard ratio, 1.00), clinically significantly bleeding (sHR, 0.81), or cardiovascular death (sHR, 0.75).
Nine patients experienced major complications related to LAAO, including clinically significant bleeding (sHR, 0.81; 95% CI, 0.44-1.52) and cardiovascular death (sHR, 0.75; 95% CI, 0.34-1.62). Major LAAO-related complications occurred in nine (4.5%) patients, with a short-term (up to 7 days or hospital discharge) complication rate of 2.1% and a 2.7% late complication rate. The late complications included three pericardial effusions, one of which resulted in death, the researchers wrote.
The study findings were limited by several factors, including the inability to assess the differences among the components of the composite primary endpoint. For example, “Regarding the primary endpoint, stroke reduction may be more important than bleeding reduction,” the investigators wrote.
The results were strengthened, however, by the enrollment of a high-risk AF population and is the first known randomized trial to compare percutaneous LAAO and DOACs for stroke prevention in this group. But the late complication rate of 2.7% is “suboptimal” and safety issues reinforce the need for refinement of operator technique and device technology with LAAO, they concluded.
‘Important step forward,’ with caveats
“How LAAO might stack up against DOAC therapy has remained an open question: Compared with warfarin, DOACs are easier to use and are associated with a reduction in mortality, driven by a substantially lower risk of intracranial hemorrhage and fatal bleeding,” wrote Matthew J. Price, MD, of the Scripps Clinic in La Jolla, Calif., and Jacqueline Saw, MD, of Vancouver General Hospital, in an accompanying editorial.
Previous studies of LAAO have shown a reduced risk of gastrointestinal bleeding, but procedure hazards interfered with long-term benefits, they said. The current study findings of similar rates of stroke and lower bleeding rates with LAAO, compared with DOAC, “are provocative given the clinical consensus that DOACs are safer, well tolerated, and generally better than warfarin, which was an easy target for transcatheter LAAO, given warfarin’s extensive limitations,” the editorialists wrote. Although the findings lend support to the use of LAAO, clinicians should consider several caveats such as the inclusion of patients who were “not optimal candidates for long-term OAC but were selected because they were at high risk for bleeding or because OAC treatment had already failed.”
However, “despite its imperfections, PRAGUE-17 is an important step forward and reinforces the role of transcatheter LAAO as a stroke-prevention strategy for patients with [AFib] at high risk of bleeding or medical treatment failure, even in the modern era of the DOACs,” they concluded. “Going forward, successful enrollment in ongoing and planned clinical trials while avoiding off-label procedures will be critical to define the appropriate use of transcatheter LAAO in expanded patient populations.”
The study was supported by the Ministry of Health of the Czech Republic. Dr. Osmancik disclosed speaking honoraria from Bayer and Abbot. Dr. Price’s financial disclosures included honoraria, speaker bureau fees, and/or research grants from Abbott Vascular, AstraZeneca, Boston Scientific, Chiesi USA, Daiichi Sankyo, and Medtronic. Dr. Saw disclosed receiving unrestricted research grant support several Canadian research institutes and fees and honoraria from AstraZeneca, Abbott Vascular, Boston Scientific, and Servier, among other drug companies.
SOURCES: Osmancik P et al. J Am Coll Cardiol. 2020;75:3122-35; Price MJ, Saw J. J Am Coll Cardiol. 2020;75:3136-9.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Key clinical point:
Major finding: A composite primary outcome including stroke and death was not significantly different in high-risk patients randomized to left atrial appendage occlusion or direct oral anticoagulants at roughly 20 months’ follow-up (11% vs. 13%, respectively).
Study details: The data come from the PRAGUE-17 study, a randomized trial of 402 adults at increased risk for atrial fibrillation.
Disclosures: The study was supported by the Ministry of Health of the Czech Republic. Dr. Osmancik disclosed speaking honoraria from Bayer and Abbot.
Sources: Osmancik P et al. J Am Coll Cardiol. 2020;75:3122-35; Price MJ, Saw J. J Am Coll Cardiol. 2020;75:3136-9.
Highlights in Ovarian Cancer From ASCO 2020
The DESKTOP III trial, whose results were eagerly awaited, compared surgery followed by chemotherapy versus chemotherapy only in recurrent platinum-sensitive ovarian cancer. Dr. Maurie Markman, from Cancer Treatment Centers of America in Philadelphia, reports that the DESKTOP results, initially announced in 2017, continue to show an improvement in progression-free survival in favor of surgery plus chemotherapy.
Dr. Markman next comments on the SOLO-2 study assessing maintenance olaparib in patients with platinum-sensitive relapsed ovarian cancer and a BRCA mutation, which showed significantly improved overall survival for patients receiving olaparib.
Among other olaparib trials, the phase 3 PAOLA-1 study looked at olaparib plus bevacizumab in platinum-sensitive recurrent ovarian cancer. The study explored the efficacy of this combination in treating tumors with BRCA1/BRCA2 mutations and found that all patients benefited.
Finally, Dr. Markman reports on noteworthy abstracts, including studies examining the adequacy of genetic testing and real-world data in management of patients with ovarian cancer.
Maurie Markman, MD
Maurie Markman, MD, Clinical Professor of Medicine, Drexel University College of Medicine; President, Medicine & Science, Cancer Treatment Centers of America, Philadelphia, Pennsylvania. Maurie Markman, MD, has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: Merck, Inc. Serve(d) as a speaker or a member of a speakers bureau for: Genentech, Inc; Clovis; Tesaro; AstraZeneca Pharmaceuticals, LP
The DESKTOP III trial, whose results were eagerly awaited, compared surgery followed by chemotherapy versus chemotherapy only in recurrent platinum-sensitive ovarian cancer. Dr. Maurie Markman, from Cancer Treatment Centers of America in Philadelphia, reports that the DESKTOP results, initially announced in 2017, continue to show an improvement in progression-free survival in favor of surgery plus chemotherapy.
Dr. Markman next comments on the SOLO-2 study assessing maintenance olaparib in patients with platinum-sensitive relapsed ovarian cancer and a BRCA mutation, which showed significantly improved overall survival for patients receiving olaparib.
Among other olaparib trials, the phase 3 PAOLA-1 study looked at olaparib plus bevacizumab in platinum-sensitive recurrent ovarian cancer. The study explored the efficacy of this combination in treating tumors with BRCA1/BRCA2 mutations and found that all patients benefited.
Finally, Dr. Markman reports on noteworthy abstracts, including studies examining the adequacy of genetic testing and real-world data in management of patients with ovarian cancer.
Maurie Markman, MD
Maurie Markman, MD, Clinical Professor of Medicine, Drexel University College of Medicine; President, Medicine & Science, Cancer Treatment Centers of America, Philadelphia, Pennsylvania. Maurie Markman, MD, has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: Merck, Inc. Serve(d) as a speaker or a member of a speakers bureau for: Genentech, Inc; Clovis; Tesaro; AstraZeneca Pharmaceuticals, LP
The DESKTOP III trial, whose results were eagerly awaited, compared surgery followed by chemotherapy versus chemotherapy only in recurrent platinum-sensitive ovarian cancer. Dr. Maurie Markman, from Cancer Treatment Centers of America in Philadelphia, reports that the DESKTOP results, initially announced in 2017, continue to show an improvement in progression-free survival in favor of surgery plus chemotherapy.
Dr. Markman next comments on the SOLO-2 study assessing maintenance olaparib in patients with platinum-sensitive relapsed ovarian cancer and a BRCA mutation, which showed significantly improved overall survival for patients receiving olaparib.
Among other olaparib trials, the phase 3 PAOLA-1 study looked at olaparib plus bevacizumab in platinum-sensitive recurrent ovarian cancer. The study explored the efficacy of this combination in treating tumors with BRCA1/BRCA2 mutations and found that all patients benefited.
Finally, Dr. Markman reports on noteworthy abstracts, including studies examining the adequacy of genetic testing and real-world data in management of patients with ovarian cancer.
Maurie Markman, MD
Maurie Markman, MD, Clinical Professor of Medicine, Drexel University College of Medicine; President, Medicine & Science, Cancer Treatment Centers of America, Philadelphia, Pennsylvania. Maurie Markman, MD, has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: Merck, Inc. Serve(d) as a speaker or a member of a speakers bureau for: Genentech, Inc; Clovis; Tesaro; AstraZeneca Pharmaceuticals, LP

Hashtag medicine: #ShareTheMicNowMed highlights Black female physicians on social media
Prominent female physicians are handing over their social media platforms today to black female physicians as part of a campaign called #ShareTheMicNowMed.
The social media event, which will play out on both Twitter and Instagram, is an offshoot of #ShareTheMicNow, held earlier this month. For that event, more than 90 women, including A-list celebrities like Ellen DeGeneres, Julia Roberts, and Senator Elizabeth Warren, swapped accounts with women of color, such as “I’m Still Here” author Austin Channing Brown, Olympic fencer Ibtihaj Muhammad, and #MeToo founder Tarana Burke.
The physician event will feature 10 teams of two, with one physician handing over her account to her black female counterpart for the day. The takeover will allow the black physician to share her thoughts about the successes and challenges she faces as a woman of color in medicine.
“It was such an honor to be contacted by Arghavan Salles, MD, PhD, to participate in an event that has a goal of connecting like-minded women from various backgrounds to share a diverse perspective with a different audience,” Minnesota family medicine physician Jay-Sheree Allen, MD, told Medscape Medical News. “This event is not only incredibly important but timely.”
Only about 5% of all active physicians in 2018 identified as Black or African American, according to a report by the Association of American Medical Colleges. And of those, just over a third are female, the report found.
“I think that as we hear those small numbers we often celebrate the success of those people without looking back and understanding where all of the barriers are that are limiting talented black women from entering medicine at every stage,” another campaign participant, Chicago pediatrician Rebekah Fenton, MD, told Medscape Medical News.
Allen says that, amid continuing worldwide protests over racial injustice, prompted by the death of George Floyd while in Minneapolis police custody last month, the online event is very timely and an important way to advocate for black lives and engage in a productive conversation.
“I believe that with the #ShareTheMicNowMed movement we will start to show people how they can become allies. I always say that a candle loses nothing by lighting another candle, and sharing that stage is one of the many ways you can support the Black Lives Matters movement by amplifying black voices,” she said.
Allen went on to add that women in medicine have many of the same experiences as any other doctor but do face some unique challenges. This is especially true for female physicians of color, she noted.
To join the conversation follow the hashtag #ShareTheMicNowMed all day on Monday, June 22, 2020.
This article originally appeared on Medscape.com.
Prominent female physicians are handing over their social media platforms today to black female physicians as part of a campaign called #ShareTheMicNowMed.
The social media event, which will play out on both Twitter and Instagram, is an offshoot of #ShareTheMicNow, held earlier this month. For that event, more than 90 women, including A-list celebrities like Ellen DeGeneres, Julia Roberts, and Senator Elizabeth Warren, swapped accounts with women of color, such as “I’m Still Here” author Austin Channing Brown, Olympic fencer Ibtihaj Muhammad, and #MeToo founder Tarana Burke.
The physician event will feature 10 teams of two, with one physician handing over her account to her black female counterpart for the day. The takeover will allow the black physician to share her thoughts about the successes and challenges she faces as a woman of color in medicine.
“It was such an honor to be contacted by Arghavan Salles, MD, PhD, to participate in an event that has a goal of connecting like-minded women from various backgrounds to share a diverse perspective with a different audience,” Minnesota family medicine physician Jay-Sheree Allen, MD, told Medscape Medical News. “This event is not only incredibly important but timely.”
Only about 5% of all active physicians in 2018 identified as Black or African American, according to a report by the Association of American Medical Colleges. And of those, just over a third are female, the report found.
“I think that as we hear those small numbers we often celebrate the success of those people without looking back and understanding where all of the barriers are that are limiting talented black women from entering medicine at every stage,” another campaign participant, Chicago pediatrician Rebekah Fenton, MD, told Medscape Medical News.
Allen says that, amid continuing worldwide protests over racial injustice, prompted by the death of George Floyd while in Minneapolis police custody last month, the online event is very timely and an important way to advocate for black lives and engage in a productive conversation.
“I believe that with the #ShareTheMicNowMed movement we will start to show people how they can become allies. I always say that a candle loses nothing by lighting another candle, and sharing that stage is one of the many ways you can support the Black Lives Matters movement by amplifying black voices,” she said.
Allen went on to add that women in medicine have many of the same experiences as any other doctor but do face some unique challenges. This is especially true for female physicians of color, she noted.
To join the conversation follow the hashtag #ShareTheMicNowMed all day on Monday, June 22, 2020.
This article originally appeared on Medscape.com.
Prominent female physicians are handing over their social media platforms today to black female physicians as part of a campaign called #ShareTheMicNowMed.
The social media event, which will play out on both Twitter and Instagram, is an offshoot of #ShareTheMicNow, held earlier this month. For that event, more than 90 women, including A-list celebrities like Ellen DeGeneres, Julia Roberts, and Senator Elizabeth Warren, swapped accounts with women of color, such as “I’m Still Here” author Austin Channing Brown, Olympic fencer Ibtihaj Muhammad, and #MeToo founder Tarana Burke.
The physician event will feature 10 teams of two, with one physician handing over her account to her black female counterpart for the day. The takeover will allow the black physician to share her thoughts about the successes and challenges she faces as a woman of color in medicine.
“It was such an honor to be contacted by Arghavan Salles, MD, PhD, to participate in an event that has a goal of connecting like-minded women from various backgrounds to share a diverse perspective with a different audience,” Minnesota family medicine physician Jay-Sheree Allen, MD, told Medscape Medical News. “This event is not only incredibly important but timely.”
Only about 5% of all active physicians in 2018 identified as Black or African American, according to a report by the Association of American Medical Colleges. And of those, just over a third are female, the report found.
“I think that as we hear those small numbers we often celebrate the success of those people without looking back and understanding where all of the barriers are that are limiting talented black women from entering medicine at every stage,” another campaign participant, Chicago pediatrician Rebekah Fenton, MD, told Medscape Medical News.
Allen says that, amid continuing worldwide protests over racial injustice, prompted by the death of George Floyd while in Minneapolis police custody last month, the online event is very timely and an important way to advocate for black lives and engage in a productive conversation.
“I believe that with the #ShareTheMicNowMed movement we will start to show people how they can become allies. I always say that a candle loses nothing by lighting another candle, and sharing that stage is one of the many ways you can support the Black Lives Matters movement by amplifying black voices,” she said.
Allen went on to add that women in medicine have many of the same experiences as any other doctor but do face some unique challenges. This is especially true for female physicians of color, she noted.
To join the conversation follow the hashtag #ShareTheMicNowMed all day on Monday, June 22, 2020.
This article originally appeared on Medscape.com.
Daily Recap: Headache as COVID evolution predictor; psoriasis drug treats canker sores
Here are the stories our MDedge editors across specialties think you need to know about today:
Headache may predict clinical evolution of COVID-19
Headache may be a key symptom of COVID-19 that predicts the disease’s clinical evolution, new research suggests. An observational study of more than 100 patients showed that headache onset could occur during the presymptomatic or symptomatic phase of COVID-19.
Headache itself was associated with a shorter symptomatic period, while headache and anosmia were associated with a shorter hospitalization period.
It seems that those patients who start early on, during the asymptomatic or early symptomatic period of COVID-19, with headache have a more localized inflammatory response that may reflect the ability of the body to better control and respond to the infection,” lead investigator Patricia Pozo-Rosich, MD, PhD, said at the virtual annual meeting of the American Headache Society. Read more.
More tops news from the AHS meeting is available on our website.
Pilot study shows apremilast effective for severe recurrent canker sores
Apremilast was highly effective in treating patients with severe recurrent aphthous stomatitis, with rapid response and an excellent safety profile, results from a small pilot study showed.
Apremilast is approved by the FDA for psoriasis and was shown in a recent phase 2 trial to be effective for Behçet’s disease aphthosis.
Dr. Alison Bruce and colleagues found that, within 4 weeks of therapy, complete clearance of RAS lesions occurred in all patients except one in whom ulcers were reported to be less severe. Remission in all patients was sustained during 16 weeks of treatment, Dr. Bruce noted at the virtual annual meeting of the American Academy of Dermatology. Read more.
For more top news from the AAD virtual conference, visit our website.
Where does dexamethasone fit in with diabetic ketoacidosis in COVID-19?
A new article in the Journal of Clinical Endocrinology & Metabolism (JCEM) addresses unique concerns and considerations regarding diabetic ketoacidosis (DKA) in the setting of COVID-19.
“Hospitals and clinicians need to be able to quickly identify and manage DKA in COVID patients to save lives. This involves determining the options for management, including when less intensive subcutaneous insulin is indicated, and understanding how to guide patients on avoiding this serious complication,” corresponding author Marie E. McDonnell, MD, said in an Endocrine Society statement.
The new article briefly touches on the fact that upward adjustments to intensive intravenous insulin therapy for DKA may be necessary in patients with COVID-19 who are receiving concomitant corticosteroids or vasopressors. But it was written prior to the June 16 announcement of the “RECOVERY” trial results with dexamethasone. The UK National Health Service immediately approved the drug’s use in the COVID-19 setting, despite the fact that there has been no published article on the findings yet.
“The peer review will be critical. It looks as if it only benefits people who need respiratory support, but I want to understand that in much more detail,” said Dr. McDonnell. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Headache may predict clinical evolution of COVID-19
Headache may be a key symptom of COVID-19 that predicts the disease’s clinical evolution, new research suggests. An observational study of more than 100 patients showed that headache onset could occur during the presymptomatic or symptomatic phase of COVID-19.
Headache itself was associated with a shorter symptomatic period, while headache and anosmia were associated with a shorter hospitalization period.
It seems that those patients who start early on, during the asymptomatic or early symptomatic period of COVID-19, with headache have a more localized inflammatory response that may reflect the ability of the body to better control and respond to the infection,” lead investigator Patricia Pozo-Rosich, MD, PhD, said at the virtual annual meeting of the American Headache Society. Read more.
More tops news from the AHS meeting is available on our website.
Pilot study shows apremilast effective for severe recurrent canker sores
Apremilast was highly effective in treating patients with severe recurrent aphthous stomatitis, with rapid response and an excellent safety profile, results from a small pilot study showed.
Apremilast is approved by the FDA for psoriasis and was shown in a recent phase 2 trial to be effective for Behçet’s disease aphthosis.
Dr. Alison Bruce and colleagues found that, within 4 weeks of therapy, complete clearance of RAS lesions occurred in all patients except one in whom ulcers were reported to be less severe. Remission in all patients was sustained during 16 weeks of treatment, Dr. Bruce noted at the virtual annual meeting of the American Academy of Dermatology. Read more.
For more top news from the AAD virtual conference, visit our website.
Where does dexamethasone fit in with diabetic ketoacidosis in COVID-19?
A new article in the Journal of Clinical Endocrinology & Metabolism (JCEM) addresses unique concerns and considerations regarding diabetic ketoacidosis (DKA) in the setting of COVID-19.
“Hospitals and clinicians need to be able to quickly identify and manage DKA in COVID patients to save lives. This involves determining the options for management, including when less intensive subcutaneous insulin is indicated, and understanding how to guide patients on avoiding this serious complication,” corresponding author Marie E. McDonnell, MD, said in an Endocrine Society statement.
The new article briefly touches on the fact that upward adjustments to intensive intravenous insulin therapy for DKA may be necessary in patients with COVID-19 who are receiving concomitant corticosteroids or vasopressors. But it was written prior to the June 16 announcement of the “RECOVERY” trial results with dexamethasone. The UK National Health Service immediately approved the drug’s use in the COVID-19 setting, despite the fact that there has been no published article on the findings yet.
“The peer review will be critical. It looks as if it only benefits people who need respiratory support, but I want to understand that in much more detail,” said Dr. McDonnell. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Headache may predict clinical evolution of COVID-19
Headache may be a key symptom of COVID-19 that predicts the disease’s clinical evolution, new research suggests. An observational study of more than 100 patients showed that headache onset could occur during the presymptomatic or symptomatic phase of COVID-19.
Headache itself was associated with a shorter symptomatic period, while headache and anosmia were associated with a shorter hospitalization period.
It seems that those patients who start early on, during the asymptomatic or early symptomatic period of COVID-19, with headache have a more localized inflammatory response that may reflect the ability of the body to better control and respond to the infection,” lead investigator Patricia Pozo-Rosich, MD, PhD, said at the virtual annual meeting of the American Headache Society. Read more.
More tops news from the AHS meeting is available on our website.
Pilot study shows apremilast effective for severe recurrent canker sores
Apremilast was highly effective in treating patients with severe recurrent aphthous stomatitis, with rapid response and an excellent safety profile, results from a small pilot study showed.
Apremilast is approved by the FDA for psoriasis and was shown in a recent phase 2 trial to be effective for Behçet’s disease aphthosis.
Dr. Alison Bruce and colleagues found that, within 4 weeks of therapy, complete clearance of RAS lesions occurred in all patients except one in whom ulcers were reported to be less severe. Remission in all patients was sustained during 16 weeks of treatment, Dr. Bruce noted at the virtual annual meeting of the American Academy of Dermatology. Read more.
For more top news from the AAD virtual conference, visit our website.
Where does dexamethasone fit in with diabetic ketoacidosis in COVID-19?
A new article in the Journal of Clinical Endocrinology & Metabolism (JCEM) addresses unique concerns and considerations regarding diabetic ketoacidosis (DKA) in the setting of COVID-19.
“Hospitals and clinicians need to be able to quickly identify and manage DKA in COVID patients to save lives. This involves determining the options for management, including when less intensive subcutaneous insulin is indicated, and understanding how to guide patients on avoiding this serious complication,” corresponding author Marie E. McDonnell, MD, said in an Endocrine Society statement.
The new article briefly touches on the fact that upward adjustments to intensive intravenous insulin therapy for DKA may be necessary in patients with COVID-19 who are receiving concomitant corticosteroids or vasopressors. But it was written prior to the June 16 announcement of the “RECOVERY” trial results with dexamethasone. The UK National Health Service immediately approved the drug’s use in the COVID-19 setting, despite the fact that there has been no published article on the findings yet.
“The peer review will be critical. It looks as if it only benefits people who need respiratory support, but I want to understand that in much more detail,” said Dr. McDonnell. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Mycosis Fungoides Manifesting as a Morbilliform Eruption Mimicking a Viral Exanthem
To the Editor:
Mycosis fungoides (MF) is the most common type of primary cutaneous lymphoma, occurring in approximately 4 of 1 million individuals per year in the United States.1 It classically occurs in patch, plaque, and tumor stages with lesions preferentially occurring on regions of the body spared from sun exposure2; however, MF is known to have variable presentations and has been reported to imitate at least 25 other dermatoses.3 This case describes MF as a morbilliform eruption mimicking a viral exanthem.
A 30-year-old man with a 12-year history of nodular sclerosing Hodgkin lymphoma (HL) presented with a widespread rash of 2 weeks’ duration. At the time of diagnosis of HL, the patient had several slightly enlarged, hyperdense, bilateral inguinal lymph nodes seen on positron emission tomography–computed tomography. He achieved complete remission 11 years prior after 6 cycles of ABVD (doxorubicin-bleomycin-vinblastine-dacarbazine) chemotherapy. He initially presented to us prior to starting chemotherapy for evaluation of what he described as eczema on the bilateral arms and legs that had been present for 10 years. Findings from a skin biopsy of an erythematous scaling patch on the left lateral thigh were consistent with MF. One year later, new lesions on the left lateral thigh were clinically and histologically consistent with lymphomatoid papulosis (LyP).
At the current presentation, the patient denied any changes in medications, which consisted of topical clobetasol, triamcinolone, and mupirocin; however, he reported that his young child had recently been diagnosed with bronchitis and impetigo. Physical examination revealed pink-orange macules and papules on the anterior and posterior trunk, medial upper arms, and bilateral legs involving 18% of the body surface area. A complete blood cell count showed no leukocytosis or left shift. A respiratory viral panel was positive for human metapneumovirus. Two weeks later, the patient noted improvement of the rash with use of topical triamcinolone.
Four months later, the rash still had not completely resolved and now involved 50% of the body surface area. A punch biopsy of the left lower abdomen demonstrated an atypical lymphoid infiltrate with focal epidermotropism and predominance of CD4 over CD8 cells (approximately 4:1 ratio), and CD30 labeled rare cells. Polymerase chain reaction analysis of the biopsy revealed monoclonal T-cell receptor gamma chain gene rearrangement. Taken together, the findings were consistent with MF. The patient started narrowband UVB phototherapy and completed a total of 25 treatments, reaching a maximum 4-minute dose, with minimal improvement.
Three months later, the patient had 90% body surface area involvement and started treatment with intramuscular interferon alfa-2b at 1 million units 3 times weekly. He noticed improvement within the first week of treatment and reported that his skin was clear until 5 months later when he woke up one morning with a morbilliform eruption on the anterior trunk, thighs, and upper arms (Figure 1). Biopsy from the right thigh showed an infiltrate of CD3+ lymphocytes with a predominance of CD4 over CD8 cells (approximately 6:1 ratio), both in the dermis and epidermis (Figure 2). CD30 highlighted approximately 10% of cells (Figure 3). Findings again were consistent with MF. Flow cytometry was negative for peripheral blood involvement.
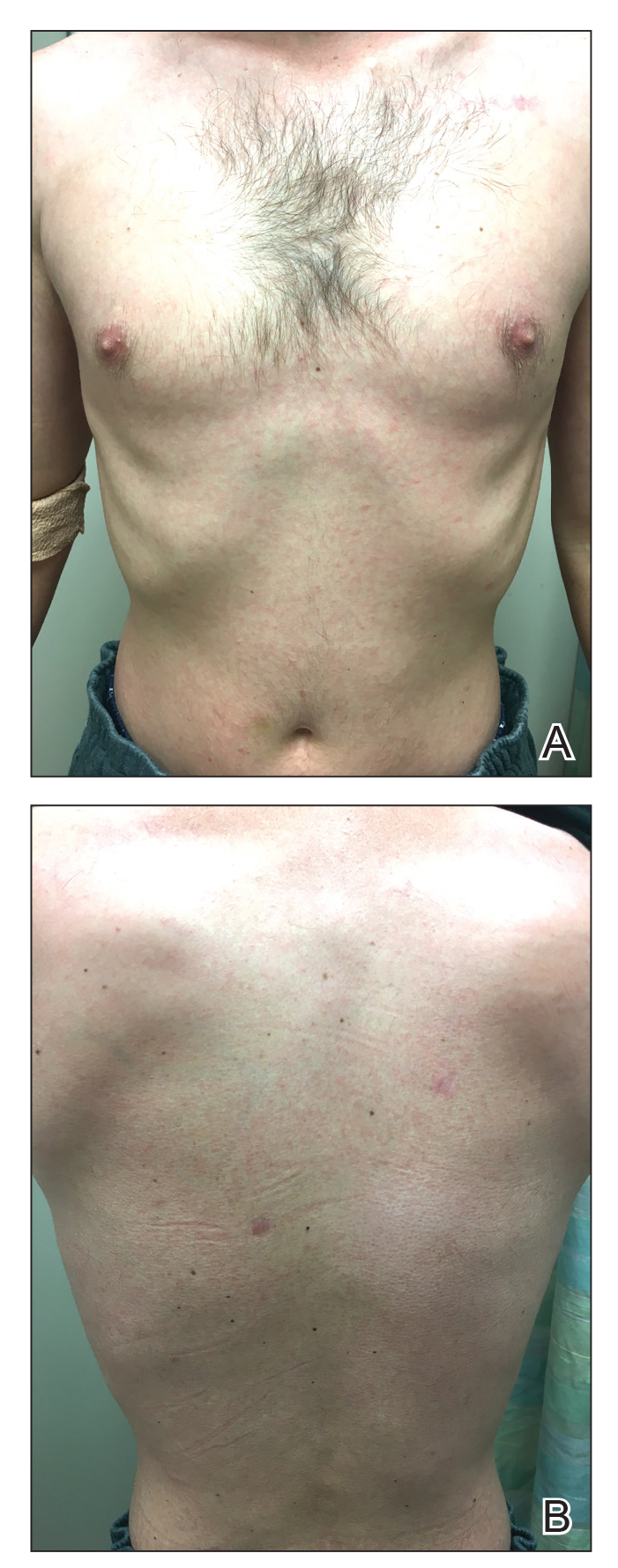
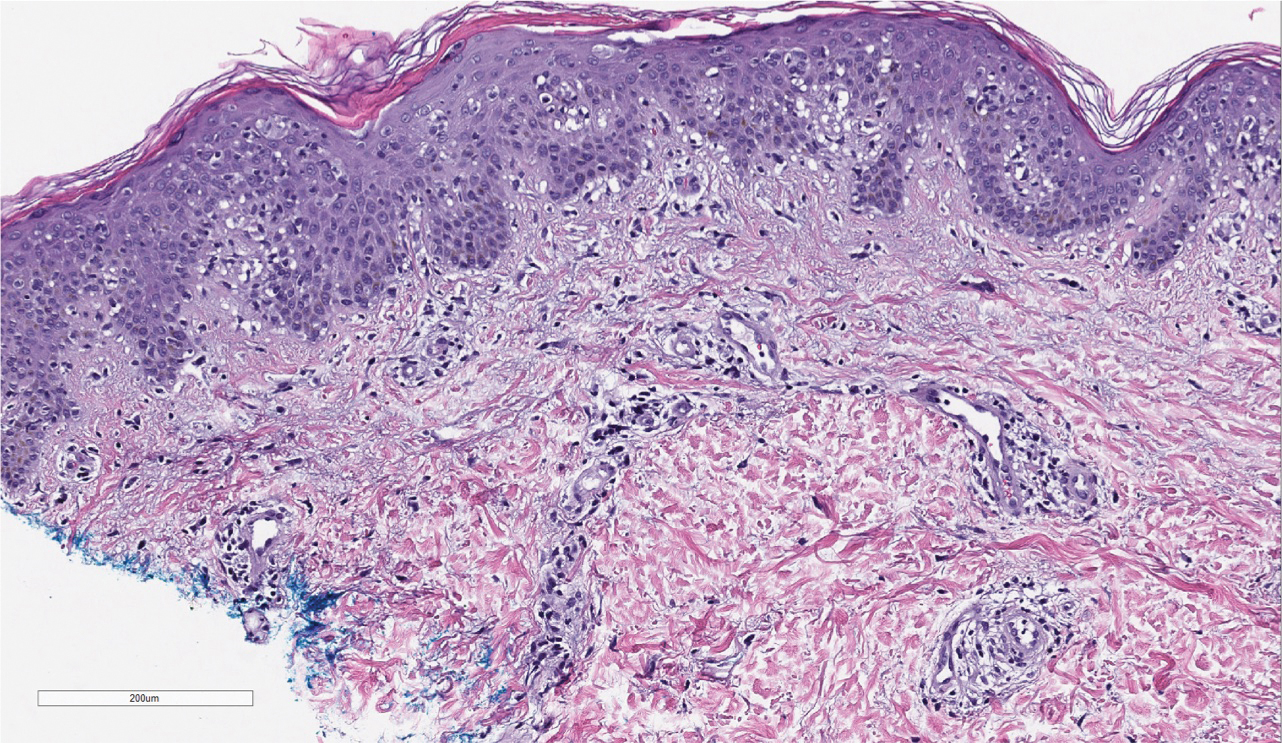
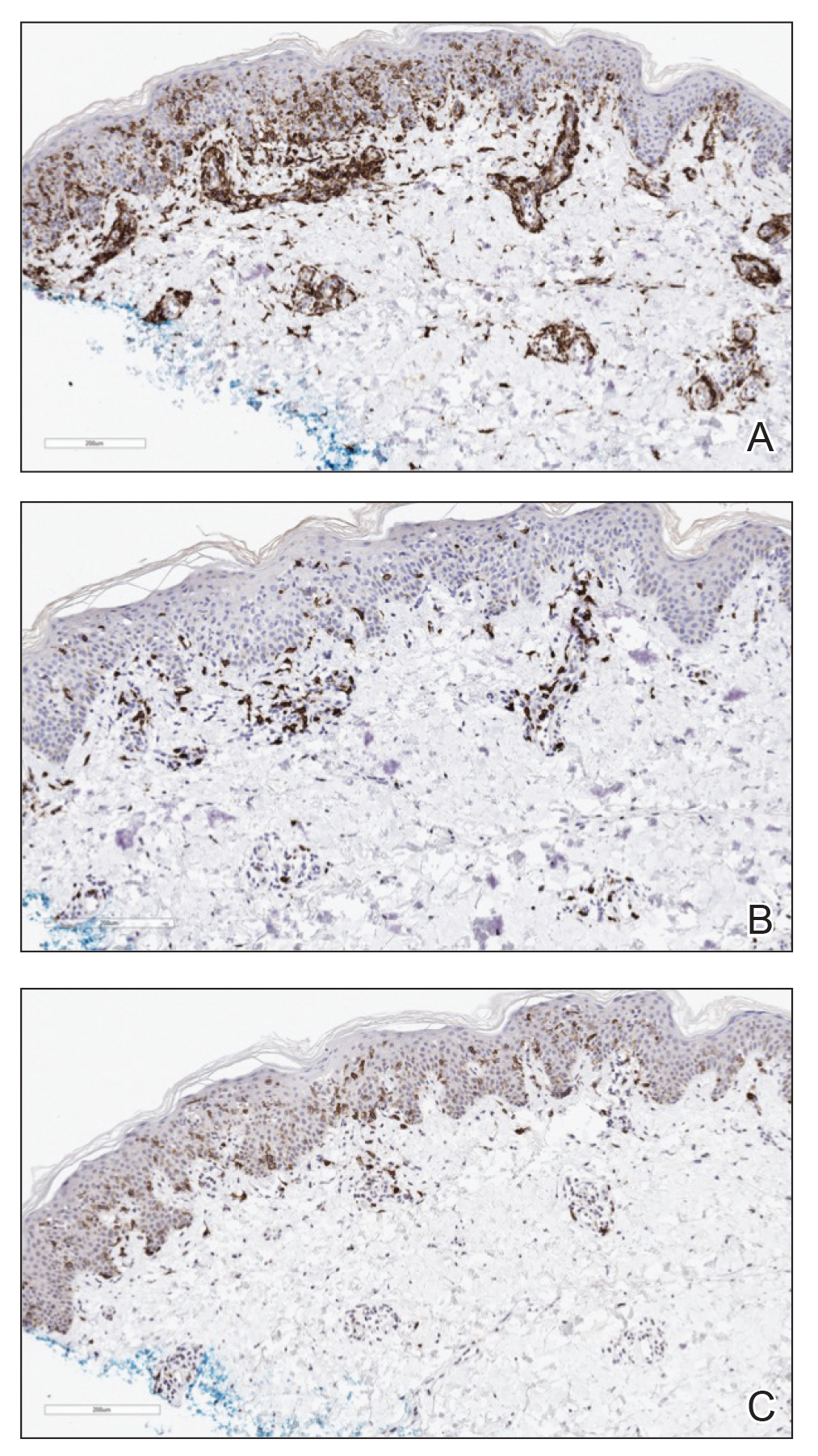
Three months later, the patient reported enlargement of several left inguinal nodes. Fine needle aspiration of 1 node demonstrated an atypical lymphoid proliferation consistent with MF. Positron emission tomography–computed tomography showed several mildly enlarged inguinal lymph nodes, which were unchanged from the initial diagnosis of HL. There were no hypermetabolic lesions. One month later, the patient started extracorporeal electrophoresis in addition to interferon alfa-2b with notable improvement of the rash. The rash later recurred after completion of these treatments and continues to have a waxing and waning course. It is currently managed with triamcinolone cream only.
At the time of the initial diagnosis of MF, the patient’s lesions appeared as eczematous patches on the face, abdomen, buttocks, and legs. Based on the history of a sick child at home, viral panel positive for human metapneumovirus, and clinical appearance, a viral exanthem was considered to be a likely explanation for the patient’s new-onset morbilliform eruption rash occurring 12 years later. A drug reaction also was considered in the differential based on the appearance of the rash; however, it was deemed less likely because the patient reported no changes in his medications at the time of rash onset. Persistence of the eruption for many months was less consistent with a reactive condition. A biopsy demonstrated the rash to be histologically consistent with MF. This patient was a rare case of MF manifesting as a morbilliform eruption mimicking a viral exanthem.
Various inflammatory conditions, including drug eruptions and lichen sclerosus et atrophicus, may mimic MF, not only based on their histophenotypic findings but also occasionally clonal proliferation by molecular study.4,5 In our patient, one consideration was the possibility of a viral infection mimicking MF; however, biopsies showed both definite histophenotypic features of MF and clonality. More importantly, subsequent biopsy also revealed similar findings by morphology, immunohistochemical study, and T-cell gene rearrangement study, confirming the diagnosis of MF.
Another interesting feature of our case was the occurrence of HL, LyP, and MF in the same patient. Lymphomatoid papulosis is a chronic condition characterized by self-healing lesions and histologic features suggestive of malignancy that lies within a spectrum of primary cutaneous CD30+ lymphoproliferative disorders. There is a known association between LyP and an increased incidence of lymphomas, including MF and HL.1 In a 2016 study, lymphomas occurred in 52% of patients with LyP (N=180), with MF being the most frequently associated lymphoma.6 Notably, biopsies consistent with both HL and MF, respectively, in our patient were positive for the CD30 marker. Patients with HL also are at increased risk for developing other malignancies, with the risk of leukemias and non-HLs greater than that of solid tumors.5 There have been multiple reported cases of HL and MF occurring in the same patient and at least one prior reported case of LyP, HL, and MF occurring in the same patient.6,7
This case highlights the myriad presentations of MF and describes an unusual case of MF manifesting as a morbilliform eruption mimicking a viral exanthem.
- de la Garza Bravo MM, Patel KP, Loghavi S, et al. Shared clonality in distinctive lesions of lymphomatoid papulosis and mycosis fungoides occurring in the same patients suggests a common origin [published online December 31, 2014]. Hum Pathol. 2015;46:558-569.
- Howard MS, Smoller BR. Mycosis fungoides: classic disease and variant presentations. Semin Cutan Med Surg. 2000;19:91-99.
- Zackheim HS, Mccalmont TH. Mycosis fungoides: the great imitator. J Am Acad Dermatol. 2002;47:914-918.
- Suchak R, Verdolini R, Robson A, et al. Extragenital lichen sclerosus et atrophicus mimicking cutaneous T-cell lymphoma: report of a case. J Cutan Pathol. 2010;37:982-986.
- Sarantopoulos GP, Palla B, Said J, et al. Mimics of cutaneous lymphoma: report of the 2011 Society for Hematopathology/European Association for Haematopathology workshop. Am J Clin Pathol. 2013;139:536-551.
- Wieser I, Oh CW, Talpur R, et al. Lymphomatoid papulosis: treatment response and associated lymphomas in a study of 180 patients. J Am Acad Dermatol. 2016;74:59-67.
- Sont JK, van Stiphout WA, Noordijk EM, et al. Increased risk of second cancers in managing Hodgkins disease: the 20-year Leiden experience. Ann Hematol. 1992;65:213-218.
To the Editor:
Mycosis fungoides (MF) is the most common type of primary cutaneous lymphoma, occurring in approximately 4 of 1 million individuals per year in the United States.1 It classically occurs in patch, plaque, and tumor stages with lesions preferentially occurring on regions of the body spared from sun exposure2; however, MF is known to have variable presentations and has been reported to imitate at least 25 other dermatoses.3 This case describes MF as a morbilliform eruption mimicking a viral exanthem.
A 30-year-old man with a 12-year history of nodular sclerosing Hodgkin lymphoma (HL) presented with a widespread rash of 2 weeks’ duration. At the time of diagnosis of HL, the patient had several slightly enlarged, hyperdense, bilateral inguinal lymph nodes seen on positron emission tomography–computed tomography. He achieved complete remission 11 years prior after 6 cycles of ABVD (doxorubicin-bleomycin-vinblastine-dacarbazine) chemotherapy. He initially presented to us prior to starting chemotherapy for evaluation of what he described as eczema on the bilateral arms and legs that had been present for 10 years. Findings from a skin biopsy of an erythematous scaling patch on the left lateral thigh were consistent with MF. One year later, new lesions on the left lateral thigh were clinically and histologically consistent with lymphomatoid papulosis (LyP).
At the current presentation, the patient denied any changes in medications, which consisted of topical clobetasol, triamcinolone, and mupirocin; however, he reported that his young child had recently been diagnosed with bronchitis and impetigo. Physical examination revealed pink-orange macules and papules on the anterior and posterior trunk, medial upper arms, and bilateral legs involving 18% of the body surface area. A complete blood cell count showed no leukocytosis or left shift. A respiratory viral panel was positive for human metapneumovirus. Two weeks later, the patient noted improvement of the rash with use of topical triamcinolone.
Four months later, the rash still had not completely resolved and now involved 50% of the body surface area. A punch biopsy of the left lower abdomen demonstrated an atypical lymphoid infiltrate with focal epidermotropism and predominance of CD4 over CD8 cells (approximately 4:1 ratio), and CD30 labeled rare cells. Polymerase chain reaction analysis of the biopsy revealed monoclonal T-cell receptor gamma chain gene rearrangement. Taken together, the findings were consistent with MF. The patient started narrowband UVB phototherapy and completed a total of 25 treatments, reaching a maximum 4-minute dose, with minimal improvement.
Three months later, the patient had 90% body surface area involvement and started treatment with intramuscular interferon alfa-2b at 1 million units 3 times weekly. He noticed improvement within the first week of treatment and reported that his skin was clear until 5 months later when he woke up one morning with a morbilliform eruption on the anterior trunk, thighs, and upper arms (Figure 1). Biopsy from the right thigh showed an infiltrate of CD3+ lymphocytes with a predominance of CD4 over CD8 cells (approximately 6:1 ratio), both in the dermis and epidermis (Figure 2). CD30 highlighted approximately 10% of cells (Figure 3). Findings again were consistent with MF. Flow cytometry was negative for peripheral blood involvement.
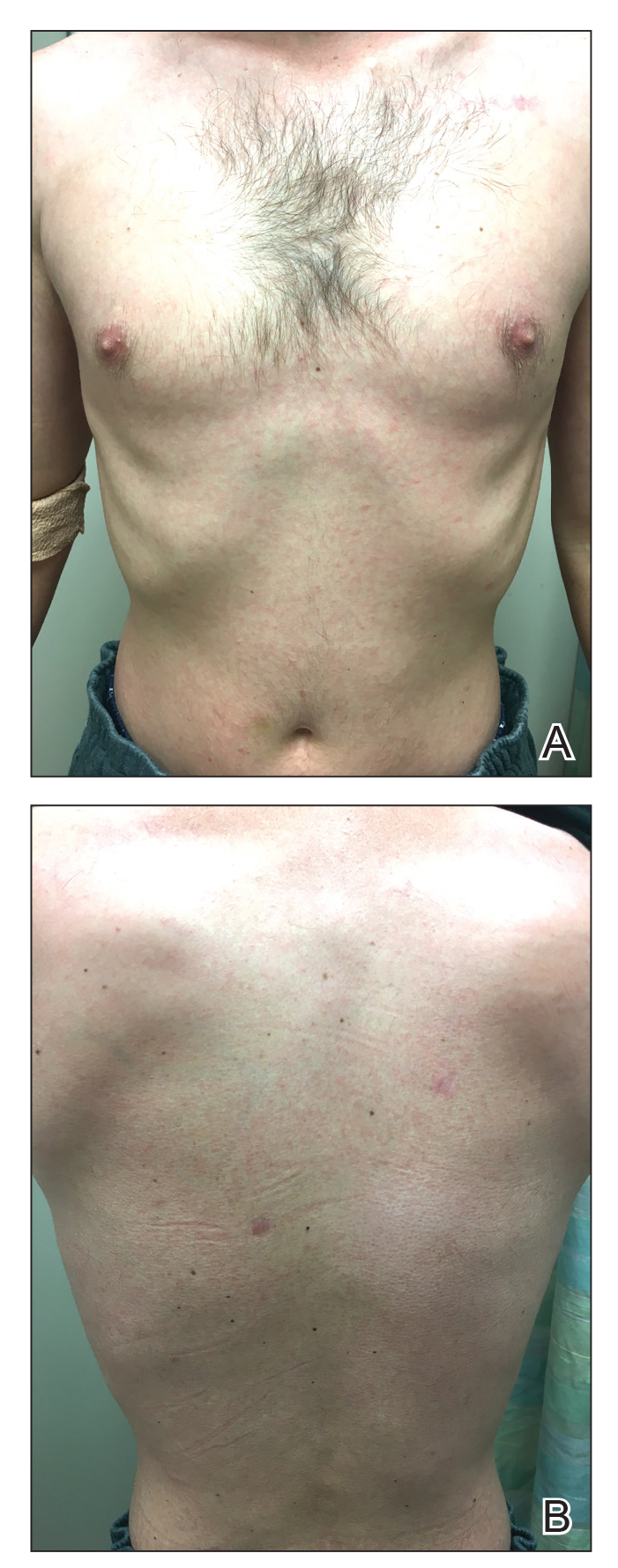
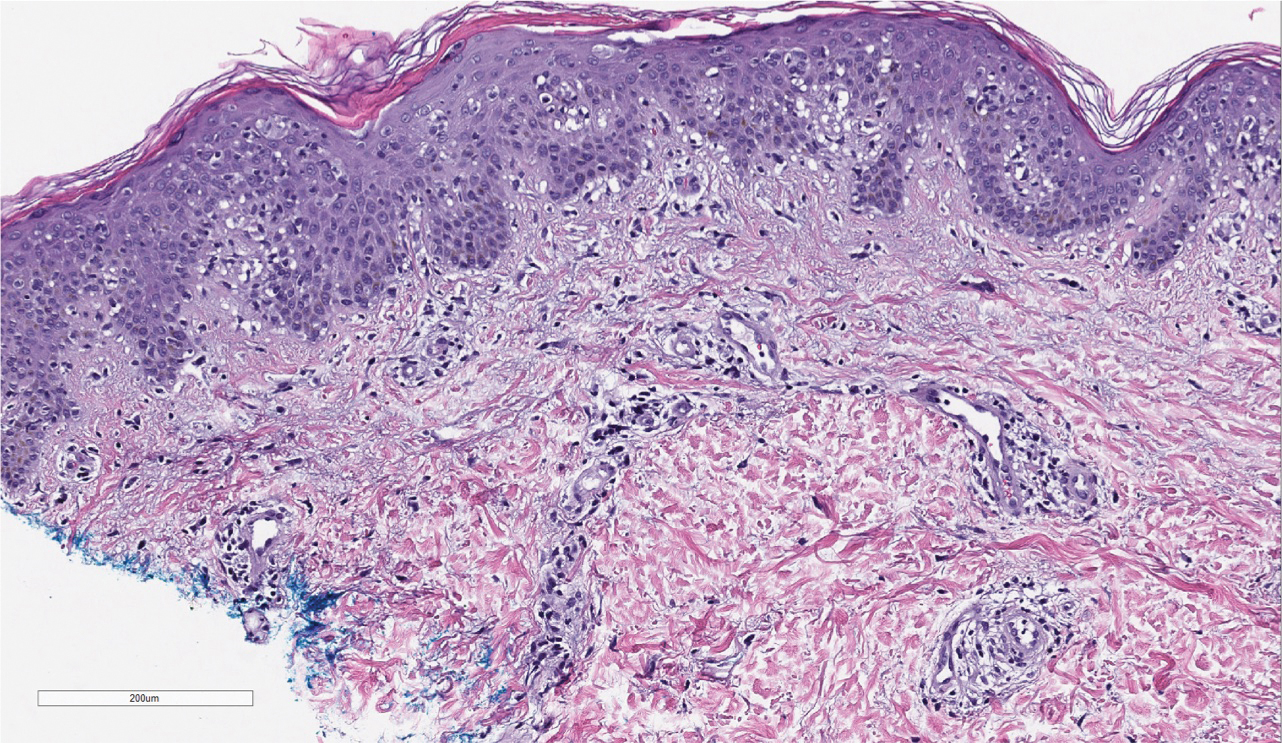
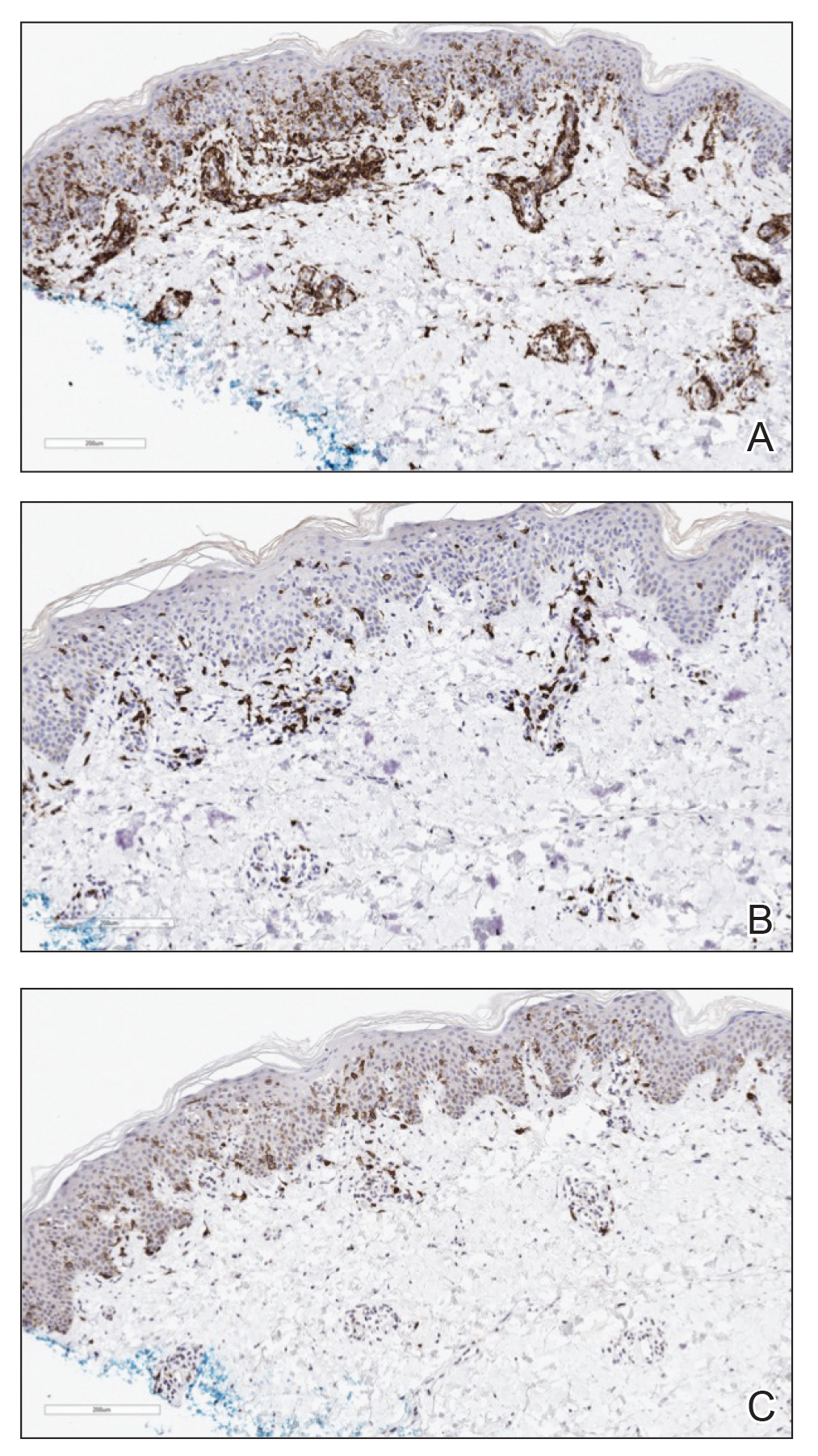
Three months later, the patient reported enlargement of several left inguinal nodes. Fine needle aspiration of 1 node demonstrated an atypical lymphoid proliferation consistent with MF. Positron emission tomography–computed tomography showed several mildly enlarged inguinal lymph nodes, which were unchanged from the initial diagnosis of HL. There were no hypermetabolic lesions. One month later, the patient started extracorporeal electrophoresis in addition to interferon alfa-2b with notable improvement of the rash. The rash later recurred after completion of these treatments and continues to have a waxing and waning course. It is currently managed with triamcinolone cream only.
At the time of the initial diagnosis of MF, the patient’s lesions appeared as eczematous patches on the face, abdomen, buttocks, and legs. Based on the history of a sick child at home, viral panel positive for human metapneumovirus, and clinical appearance, a viral exanthem was considered to be a likely explanation for the patient’s new-onset morbilliform eruption rash occurring 12 years later. A drug reaction also was considered in the differential based on the appearance of the rash; however, it was deemed less likely because the patient reported no changes in his medications at the time of rash onset. Persistence of the eruption for many months was less consistent with a reactive condition. A biopsy demonstrated the rash to be histologically consistent with MF. This patient was a rare case of MF manifesting as a morbilliform eruption mimicking a viral exanthem.
Various inflammatory conditions, including drug eruptions and lichen sclerosus et atrophicus, may mimic MF, not only based on their histophenotypic findings but also occasionally clonal proliferation by molecular study.4,5 In our patient, one consideration was the possibility of a viral infection mimicking MF; however, biopsies showed both definite histophenotypic features of MF and clonality. More importantly, subsequent biopsy also revealed similar findings by morphology, immunohistochemical study, and T-cell gene rearrangement study, confirming the diagnosis of MF.
Another interesting feature of our case was the occurrence of HL, LyP, and MF in the same patient. Lymphomatoid papulosis is a chronic condition characterized by self-healing lesions and histologic features suggestive of malignancy that lies within a spectrum of primary cutaneous CD30+ lymphoproliferative disorders. There is a known association between LyP and an increased incidence of lymphomas, including MF and HL.1 In a 2016 study, lymphomas occurred in 52% of patients with LyP (N=180), with MF being the most frequently associated lymphoma.6 Notably, biopsies consistent with both HL and MF, respectively, in our patient were positive for the CD30 marker. Patients with HL also are at increased risk for developing other malignancies, with the risk of leukemias and non-HLs greater than that of solid tumors.5 There have been multiple reported cases of HL and MF occurring in the same patient and at least one prior reported case of LyP, HL, and MF occurring in the same patient.6,7
This case highlights the myriad presentations of MF and describes an unusual case of MF manifesting as a morbilliform eruption mimicking a viral exanthem.
To the Editor:
Mycosis fungoides (MF) is the most common type of primary cutaneous lymphoma, occurring in approximately 4 of 1 million individuals per year in the United States.1 It classically occurs in patch, plaque, and tumor stages with lesions preferentially occurring on regions of the body spared from sun exposure2; however, MF is known to have variable presentations and has been reported to imitate at least 25 other dermatoses.3 This case describes MF as a morbilliform eruption mimicking a viral exanthem.
A 30-year-old man with a 12-year history of nodular sclerosing Hodgkin lymphoma (HL) presented with a widespread rash of 2 weeks’ duration. At the time of diagnosis of HL, the patient had several slightly enlarged, hyperdense, bilateral inguinal lymph nodes seen on positron emission tomography–computed tomography. He achieved complete remission 11 years prior after 6 cycles of ABVD (doxorubicin-bleomycin-vinblastine-dacarbazine) chemotherapy. He initially presented to us prior to starting chemotherapy for evaluation of what he described as eczema on the bilateral arms and legs that had been present for 10 years. Findings from a skin biopsy of an erythematous scaling patch on the left lateral thigh were consistent with MF. One year later, new lesions on the left lateral thigh were clinically and histologically consistent with lymphomatoid papulosis (LyP).
At the current presentation, the patient denied any changes in medications, which consisted of topical clobetasol, triamcinolone, and mupirocin; however, he reported that his young child had recently been diagnosed with bronchitis and impetigo. Physical examination revealed pink-orange macules and papules on the anterior and posterior trunk, medial upper arms, and bilateral legs involving 18% of the body surface area. A complete blood cell count showed no leukocytosis or left shift. A respiratory viral panel was positive for human metapneumovirus. Two weeks later, the patient noted improvement of the rash with use of topical triamcinolone.
Four months later, the rash still had not completely resolved and now involved 50% of the body surface area. A punch biopsy of the left lower abdomen demonstrated an atypical lymphoid infiltrate with focal epidermotropism and predominance of CD4 over CD8 cells (approximately 4:1 ratio), and CD30 labeled rare cells. Polymerase chain reaction analysis of the biopsy revealed monoclonal T-cell receptor gamma chain gene rearrangement. Taken together, the findings were consistent with MF. The patient started narrowband UVB phototherapy and completed a total of 25 treatments, reaching a maximum 4-minute dose, with minimal improvement.
Three months later, the patient had 90% body surface area involvement and started treatment with intramuscular interferon alfa-2b at 1 million units 3 times weekly. He noticed improvement within the first week of treatment and reported that his skin was clear until 5 months later when he woke up one morning with a morbilliform eruption on the anterior trunk, thighs, and upper arms (Figure 1). Biopsy from the right thigh showed an infiltrate of CD3+ lymphocytes with a predominance of CD4 over CD8 cells (approximately 6:1 ratio), both in the dermis and epidermis (Figure 2). CD30 highlighted approximately 10% of cells (Figure 3). Findings again were consistent with MF. Flow cytometry was negative for peripheral blood involvement.
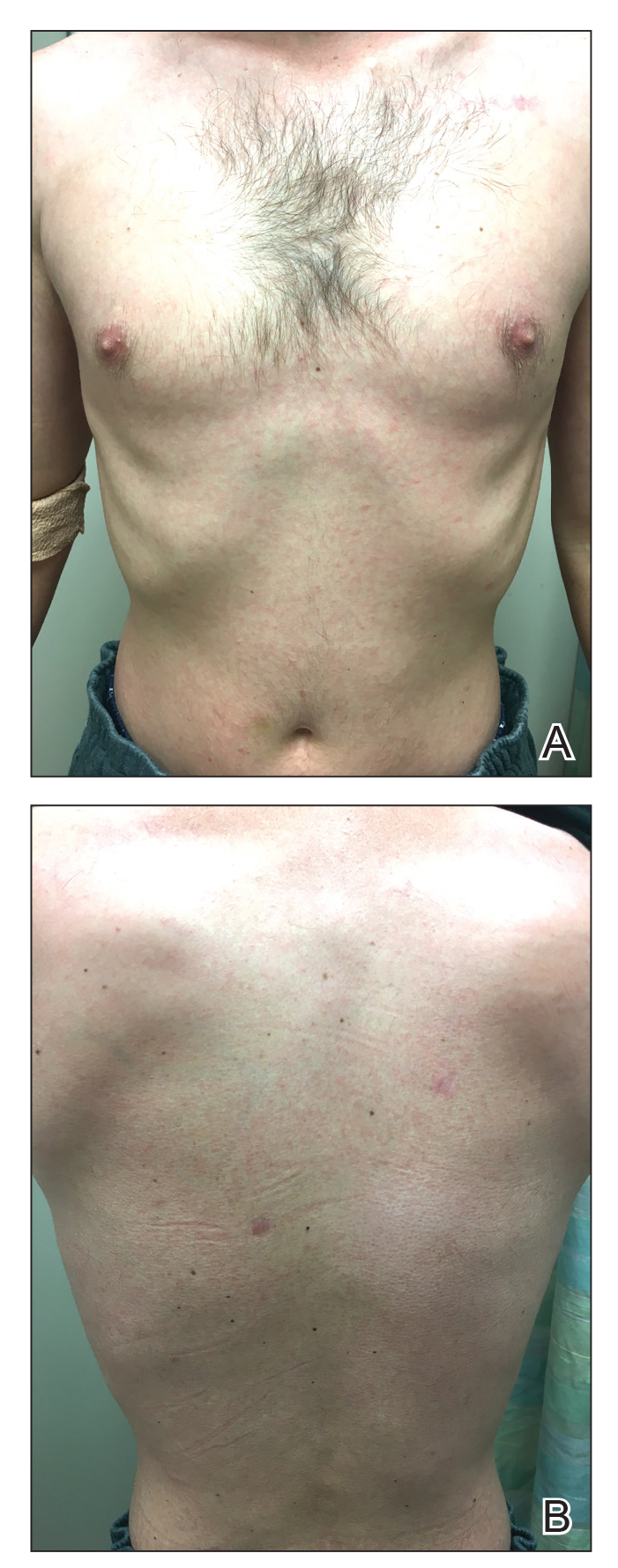
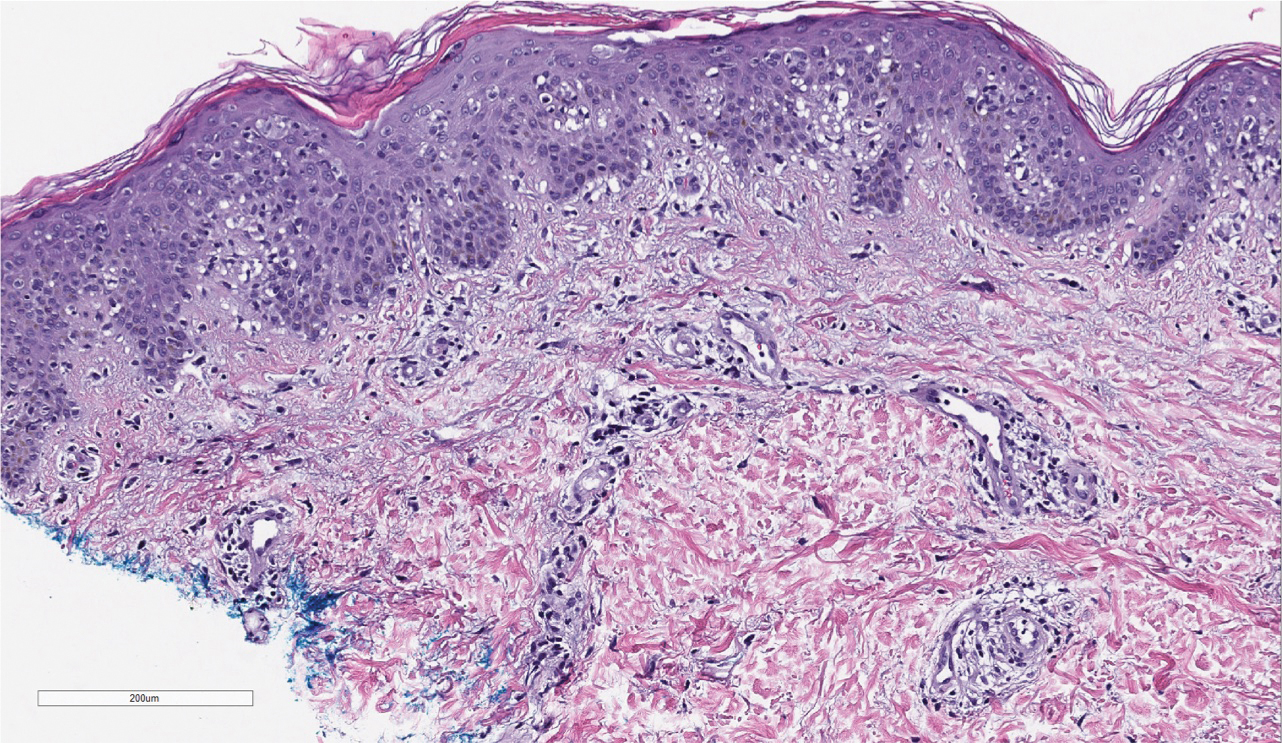
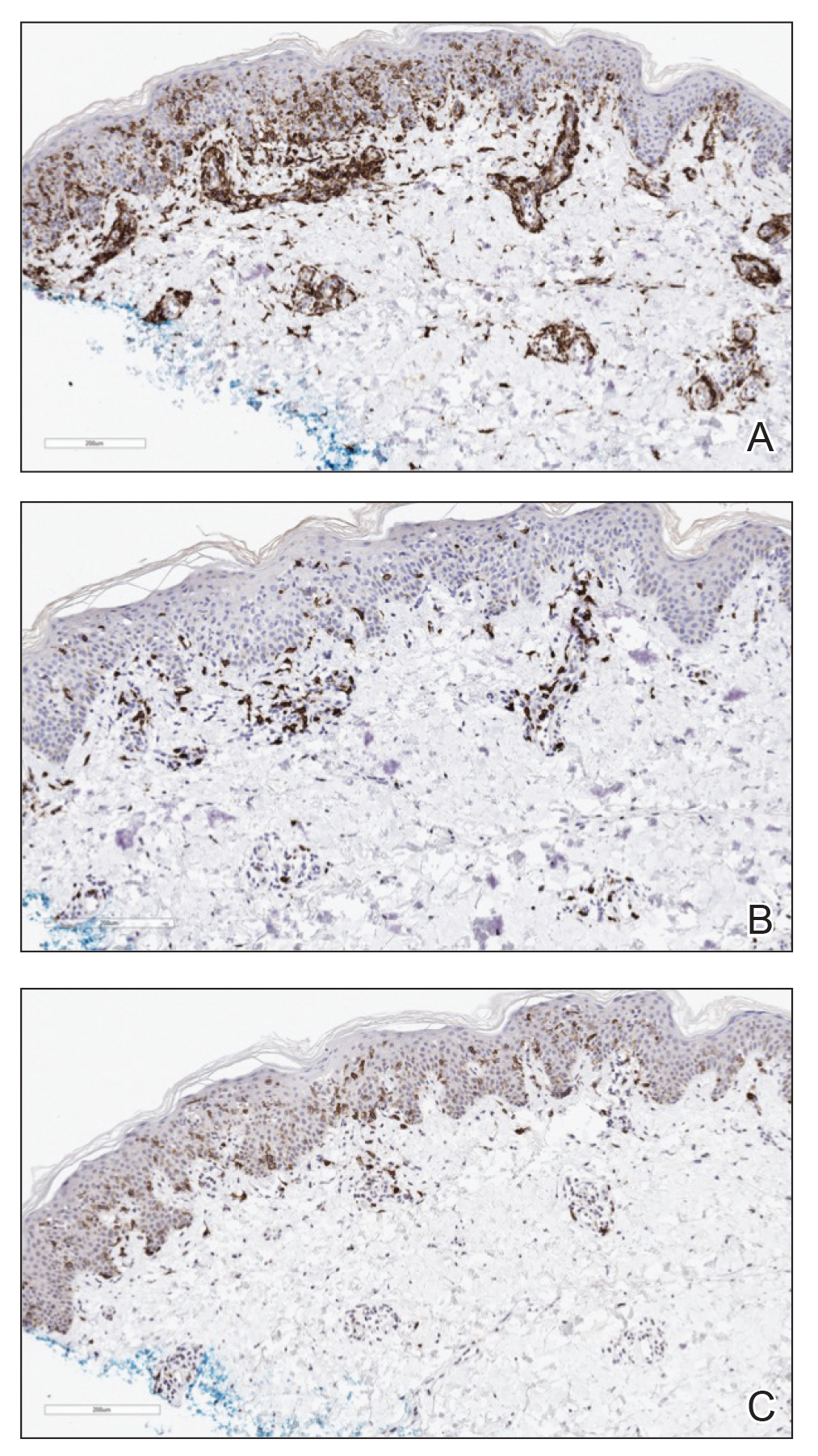
Three months later, the patient reported enlargement of several left inguinal nodes. Fine needle aspiration of 1 node demonstrated an atypical lymphoid proliferation consistent with MF. Positron emission tomography–computed tomography showed several mildly enlarged inguinal lymph nodes, which were unchanged from the initial diagnosis of HL. There were no hypermetabolic lesions. One month later, the patient started extracorporeal electrophoresis in addition to interferon alfa-2b with notable improvement of the rash. The rash later recurred after completion of these treatments and continues to have a waxing and waning course. It is currently managed with triamcinolone cream only.
At the time of the initial diagnosis of MF, the patient’s lesions appeared as eczematous patches on the face, abdomen, buttocks, and legs. Based on the history of a sick child at home, viral panel positive for human metapneumovirus, and clinical appearance, a viral exanthem was considered to be a likely explanation for the patient’s new-onset morbilliform eruption rash occurring 12 years later. A drug reaction also was considered in the differential based on the appearance of the rash; however, it was deemed less likely because the patient reported no changes in his medications at the time of rash onset. Persistence of the eruption for many months was less consistent with a reactive condition. A biopsy demonstrated the rash to be histologically consistent with MF. This patient was a rare case of MF manifesting as a morbilliform eruption mimicking a viral exanthem.
Various inflammatory conditions, including drug eruptions and lichen sclerosus et atrophicus, may mimic MF, not only based on their histophenotypic findings but also occasionally clonal proliferation by molecular study.4,5 In our patient, one consideration was the possibility of a viral infection mimicking MF; however, biopsies showed both definite histophenotypic features of MF and clonality. More importantly, subsequent biopsy also revealed similar findings by morphology, immunohistochemical study, and T-cell gene rearrangement study, confirming the diagnosis of MF.
Another interesting feature of our case was the occurrence of HL, LyP, and MF in the same patient. Lymphomatoid papulosis is a chronic condition characterized by self-healing lesions and histologic features suggestive of malignancy that lies within a spectrum of primary cutaneous CD30+ lymphoproliferative disorders. There is a known association between LyP and an increased incidence of lymphomas, including MF and HL.1 In a 2016 study, lymphomas occurred in 52% of patients with LyP (N=180), with MF being the most frequently associated lymphoma.6 Notably, biopsies consistent with both HL and MF, respectively, in our patient were positive for the CD30 marker. Patients with HL also are at increased risk for developing other malignancies, with the risk of leukemias and non-HLs greater than that of solid tumors.5 There have been multiple reported cases of HL and MF occurring in the same patient and at least one prior reported case of LyP, HL, and MF occurring in the same patient.6,7
This case highlights the myriad presentations of MF and describes an unusual case of MF manifesting as a morbilliform eruption mimicking a viral exanthem.
- de la Garza Bravo MM, Patel KP, Loghavi S, et al. Shared clonality in distinctive lesions of lymphomatoid papulosis and mycosis fungoides occurring in the same patients suggests a common origin [published online December 31, 2014]. Hum Pathol. 2015;46:558-569.
- Howard MS, Smoller BR. Mycosis fungoides: classic disease and variant presentations. Semin Cutan Med Surg. 2000;19:91-99.
- Zackheim HS, Mccalmont TH. Mycosis fungoides: the great imitator. J Am Acad Dermatol. 2002;47:914-918.
- Suchak R, Verdolini R, Robson A, et al. Extragenital lichen sclerosus et atrophicus mimicking cutaneous T-cell lymphoma: report of a case. J Cutan Pathol. 2010;37:982-986.
- Sarantopoulos GP, Palla B, Said J, et al. Mimics of cutaneous lymphoma: report of the 2011 Society for Hematopathology/European Association for Haematopathology workshop. Am J Clin Pathol. 2013;139:536-551.
- Wieser I, Oh CW, Talpur R, et al. Lymphomatoid papulosis: treatment response and associated lymphomas in a study of 180 patients. J Am Acad Dermatol. 2016;74:59-67.
- Sont JK, van Stiphout WA, Noordijk EM, et al. Increased risk of second cancers in managing Hodgkins disease: the 20-year Leiden experience. Ann Hematol. 1992;65:213-218.
- de la Garza Bravo MM, Patel KP, Loghavi S, et al. Shared clonality in distinctive lesions of lymphomatoid papulosis and mycosis fungoides occurring in the same patients suggests a common origin [published online December 31, 2014]. Hum Pathol. 2015;46:558-569.
- Howard MS, Smoller BR. Mycosis fungoides: classic disease and variant presentations. Semin Cutan Med Surg. 2000;19:91-99.
- Zackheim HS, Mccalmont TH. Mycosis fungoides: the great imitator. J Am Acad Dermatol. 2002;47:914-918.
- Suchak R, Verdolini R, Robson A, et al. Extragenital lichen sclerosus et atrophicus mimicking cutaneous T-cell lymphoma: report of a case. J Cutan Pathol. 2010;37:982-986.
- Sarantopoulos GP, Palla B, Said J, et al. Mimics of cutaneous lymphoma: report of the 2011 Society for Hematopathology/European Association for Haematopathology workshop. Am J Clin Pathol. 2013;139:536-551.
- Wieser I, Oh CW, Talpur R, et al. Lymphomatoid papulosis: treatment response and associated lymphomas in a study of 180 patients. J Am Acad Dermatol. 2016;74:59-67.
- Sont JK, van Stiphout WA, Noordijk EM, et al. Increased risk of second cancers in managing Hodgkins disease: the 20-year Leiden experience. Ann Hematol. 1992;65:213-218.
Practice Points
- Mycosis fungoides classically occurs in patch, plaque, and tumor stages, with lesions preferentially occurring on regions of the body spared from sun exposure; however, the condition may present atypically, mimicking a variety of other conditions.
- Lymphomatoid papulosis exists within a spectrum of primary cutaneous CD30+ lymphoproliferative disorders and is associated with increased incidence of lymphomas.
‘COVID-sorting’: How we decide whom to get close to and whom to avoid
I was recently interviewed, as a gay psychiatrist treating gay patients who lived through the AIDS epidemic, about my perspectives on living through a COVID pandemic: Were there parallels and contrasts between the two? A month later, listening to patients remotely via teletherapy, I’m experiencing an unsettling similarity to serosorting, a phenomenon that emerged during the AIDS epidemic.
Serosorting is the practice of choosing a sexual partner based on their HIV serostatus. Sorting out who was positive from who was negative allowed people to give themselves permission to have unprotected sex without risk of getting HIV. However, it was not uncommon to make those decisions without really knowing a potential partner’s actual serostatus. In fact, a lot of people serosorted by guessing.
Why not just ask a potential partner, “What’s your serostatus?” Apparently, for some, introducing the subject of HIV was deemed a sexual buzzkill. Instead, assumptions were made based on outer appearances.
Did someone look healthy? Were they well built? Were they overweight, meaning not emaciated from AIDS? If so, they were presumed negative and safe to have risky, unprotected sex with them.
Some imagined age correlated with serostatus. Since anyone older than some arbitrary age – like 30, to pull a number out of a hat – was expected to be more likely to have HIV than someone under 30, they would use that guideline in choosing sexual partners. However, these decisions were made without factual knowledge, like a blood test, but using some internal reasoning process.
Which brings us to what might be called “COVID-sorting.”
Some of my patients believe they had COVID-19, although they’d not been tested to either confirm or disprove that belief. Others had positive COVID-19 antibody tests, which they believe provides immunity. Among that group, some had symptoms, others did not.
Yet regardless of what they actually know or don’t know, patients are making calculations about managing physical distancing using their own internal formulas. They make risk calculations having little to do with actual knowledge of public health precautions on preventing COVID’s spread.
For example, one patient was planning a Memorial Day weekend in a shared Fire Island house with five friends and acquaintances. All six live alone and, as far as he knows, all are physically distancing. Consequently, my patient doesn’t think house-sharing is anything to worry about, even though he doesn’t know how scrupulously others have followed distancing guidelines.
Another patient, recovering at home after being ill with COVID-19, felt safe inviting someone over for sex who had also been ill and recovered. He didn’t think they could infect each other, presuming, not altogether unreasonably, they were both immune.
Finally, there are those who don’t know whether they had COVID-19, but think they did because they experienced influenza-like symptoms. They are giving themselves permission to meet up with others who feel the same.
Yet a Mount Sinai study, which has not yet been peer-reviewed, raises fascinating issues about immunity. The study included 719 people who suspected they had COVID-19 based on some respiratory symptoms. The majority, 62%, had no antibodies. Researchers believe they mistook influenza, another viral infection, or allergies for COVID-19 (medRxiv. 2020 May 5. doi: 10.1101/2020.04.04.2008516).
The study also included 624 people who tested positive for the virus and recovered. All but three developed antibodies. Many assume those who are antibody-positive are now immune. They may be right. However, we don’t know definitively that they are, and if they are, we do not yet know how long immunity may last. Further, as reported in the New York Times, just because you test positive for antibodies, doesn’t mean you have them.
It should be underscored that COVID-sorting is not limited to gay men or psychiatric patients. And as many states have begun opening up restrictions on social gatherings, we are seeing an all-too-human psychological mindset with wider implications – rising numbers of cases. As we move forward, all of us will have to decide for ourselves, and not only in sexual situations, how to get on with our lives in a post–COVID-19 era.
Given how much is still unknown, it is likely each of us will come up with our own algorithm of risk assessment. It is likely that the formulas used will not necessarily be based on scientific facts, although that would be ideal. If past epidemic and recent pandemic behaviors are any indicators, people’s actions will reflect some combination of their own needs and desires, their own comfort level with risk-taking, and their relative understanding of complex subjects like virology, immunology, epidemiology, and public health. The challenge faced by public health officials today is to translate complex scientific and medical issues into messages average people can understand.
What exactly can be done? I’m not exactly sure, but I hope that improved education and communication can help. In the first 2 decades of the AIDS epidemic, efforts were made to change and tailor HIV-prevention messages to specific, at-risk demographic groups. Today, public health messages aimed at preventing COVID-19’s spread that resonate with older people can fall on a younger person’s deaf ears. One message size does not fit all. Hopefully, public health officials and government leaders will act on this sooner rather than later.
Dr. Drescher, a psychoanalyst, is clinical professor of psychiatry at Columbia University, and training and supervising analyst at the William A. White Institute, both in New York. He also is emeritus editor of the Journal of Gay & Lesbian Mental Health. Dr. Drescher has no other disclosures.
I was recently interviewed, as a gay psychiatrist treating gay patients who lived through the AIDS epidemic, about my perspectives on living through a COVID pandemic: Were there parallels and contrasts between the two? A month later, listening to patients remotely via teletherapy, I’m experiencing an unsettling similarity to serosorting, a phenomenon that emerged during the AIDS epidemic.
Serosorting is the practice of choosing a sexual partner based on their HIV serostatus. Sorting out who was positive from who was negative allowed people to give themselves permission to have unprotected sex without risk of getting HIV. However, it was not uncommon to make those decisions without really knowing a potential partner’s actual serostatus. In fact, a lot of people serosorted by guessing.
Why not just ask a potential partner, “What’s your serostatus?” Apparently, for some, introducing the subject of HIV was deemed a sexual buzzkill. Instead, assumptions were made based on outer appearances.
Did someone look healthy? Were they well built? Were they overweight, meaning not emaciated from AIDS? If so, they were presumed negative and safe to have risky, unprotected sex with them.
Some imagined age correlated with serostatus. Since anyone older than some arbitrary age – like 30, to pull a number out of a hat – was expected to be more likely to have HIV than someone under 30, they would use that guideline in choosing sexual partners. However, these decisions were made without factual knowledge, like a blood test, but using some internal reasoning process.
Which brings us to what might be called “COVID-sorting.”
Some of my patients believe they had COVID-19, although they’d not been tested to either confirm or disprove that belief. Others had positive COVID-19 antibody tests, which they believe provides immunity. Among that group, some had symptoms, others did not.
Yet regardless of what they actually know or don’t know, patients are making calculations about managing physical distancing using their own internal formulas. They make risk calculations having little to do with actual knowledge of public health precautions on preventing COVID’s spread.
For example, one patient was planning a Memorial Day weekend in a shared Fire Island house with five friends and acquaintances. All six live alone and, as far as he knows, all are physically distancing. Consequently, my patient doesn’t think house-sharing is anything to worry about, even though he doesn’t know how scrupulously others have followed distancing guidelines.
Another patient, recovering at home after being ill with COVID-19, felt safe inviting someone over for sex who had also been ill and recovered. He didn’t think they could infect each other, presuming, not altogether unreasonably, they were both immune.
Finally, there are those who don’t know whether they had COVID-19, but think they did because they experienced influenza-like symptoms. They are giving themselves permission to meet up with others who feel the same.
Yet a Mount Sinai study, which has not yet been peer-reviewed, raises fascinating issues about immunity. The study included 719 people who suspected they had COVID-19 based on some respiratory symptoms. The majority, 62%, had no antibodies. Researchers believe they mistook influenza, another viral infection, or allergies for COVID-19 (medRxiv. 2020 May 5. doi: 10.1101/2020.04.04.2008516).
The study also included 624 people who tested positive for the virus and recovered. All but three developed antibodies. Many assume those who are antibody-positive are now immune. They may be right. However, we don’t know definitively that they are, and if they are, we do not yet know how long immunity may last. Further, as reported in the New York Times, just because you test positive for antibodies, doesn’t mean you have them.
It should be underscored that COVID-sorting is not limited to gay men or psychiatric patients. And as many states have begun opening up restrictions on social gatherings, we are seeing an all-too-human psychological mindset with wider implications – rising numbers of cases. As we move forward, all of us will have to decide for ourselves, and not only in sexual situations, how to get on with our lives in a post–COVID-19 era.
Given how much is still unknown, it is likely each of us will come up with our own algorithm of risk assessment. It is likely that the formulas used will not necessarily be based on scientific facts, although that would be ideal. If past epidemic and recent pandemic behaviors are any indicators, people’s actions will reflect some combination of their own needs and desires, their own comfort level with risk-taking, and their relative understanding of complex subjects like virology, immunology, epidemiology, and public health. The challenge faced by public health officials today is to translate complex scientific and medical issues into messages average people can understand.
What exactly can be done? I’m not exactly sure, but I hope that improved education and communication can help. In the first 2 decades of the AIDS epidemic, efforts were made to change and tailor HIV-prevention messages to specific, at-risk demographic groups. Today, public health messages aimed at preventing COVID-19’s spread that resonate with older people can fall on a younger person’s deaf ears. One message size does not fit all. Hopefully, public health officials and government leaders will act on this sooner rather than later.
Dr. Drescher, a psychoanalyst, is clinical professor of psychiatry at Columbia University, and training and supervising analyst at the William A. White Institute, both in New York. He also is emeritus editor of the Journal of Gay & Lesbian Mental Health. Dr. Drescher has no other disclosures.
I was recently interviewed, as a gay psychiatrist treating gay patients who lived through the AIDS epidemic, about my perspectives on living through a COVID pandemic: Were there parallels and contrasts between the two? A month later, listening to patients remotely via teletherapy, I’m experiencing an unsettling similarity to serosorting, a phenomenon that emerged during the AIDS epidemic.
Serosorting is the practice of choosing a sexual partner based on their HIV serostatus. Sorting out who was positive from who was negative allowed people to give themselves permission to have unprotected sex without risk of getting HIV. However, it was not uncommon to make those decisions without really knowing a potential partner’s actual serostatus. In fact, a lot of people serosorted by guessing.
Why not just ask a potential partner, “What’s your serostatus?” Apparently, for some, introducing the subject of HIV was deemed a sexual buzzkill. Instead, assumptions were made based on outer appearances.
Did someone look healthy? Were they well built? Were they overweight, meaning not emaciated from AIDS? If so, they were presumed negative and safe to have risky, unprotected sex with them.
Some imagined age correlated with serostatus. Since anyone older than some arbitrary age – like 30, to pull a number out of a hat – was expected to be more likely to have HIV than someone under 30, they would use that guideline in choosing sexual partners. However, these decisions were made without factual knowledge, like a blood test, but using some internal reasoning process.
Which brings us to what might be called “COVID-sorting.”
Some of my patients believe they had COVID-19, although they’d not been tested to either confirm or disprove that belief. Others had positive COVID-19 antibody tests, which they believe provides immunity. Among that group, some had symptoms, others did not.
Yet regardless of what they actually know or don’t know, patients are making calculations about managing physical distancing using their own internal formulas. They make risk calculations having little to do with actual knowledge of public health precautions on preventing COVID’s spread.
For example, one patient was planning a Memorial Day weekend in a shared Fire Island house with five friends and acquaintances. All six live alone and, as far as he knows, all are physically distancing. Consequently, my patient doesn’t think house-sharing is anything to worry about, even though he doesn’t know how scrupulously others have followed distancing guidelines.
Another patient, recovering at home after being ill with COVID-19, felt safe inviting someone over for sex who had also been ill and recovered. He didn’t think they could infect each other, presuming, not altogether unreasonably, they were both immune.
Finally, there are those who don’t know whether they had COVID-19, but think they did because they experienced influenza-like symptoms. They are giving themselves permission to meet up with others who feel the same.
Yet a Mount Sinai study, which has not yet been peer-reviewed, raises fascinating issues about immunity. The study included 719 people who suspected they had COVID-19 based on some respiratory symptoms. The majority, 62%, had no antibodies. Researchers believe they mistook influenza, another viral infection, or allergies for COVID-19 (medRxiv. 2020 May 5. doi: 10.1101/2020.04.04.2008516).
The study also included 624 people who tested positive for the virus and recovered. All but three developed antibodies. Many assume those who are antibody-positive are now immune. They may be right. However, we don’t know definitively that they are, and if they are, we do not yet know how long immunity may last. Further, as reported in the New York Times, just because you test positive for antibodies, doesn’t mean you have them.
It should be underscored that COVID-sorting is not limited to gay men or psychiatric patients. And as many states have begun opening up restrictions on social gatherings, we are seeing an all-too-human psychological mindset with wider implications – rising numbers of cases. As we move forward, all of us will have to decide for ourselves, and not only in sexual situations, how to get on with our lives in a post–COVID-19 era.
Given how much is still unknown, it is likely each of us will come up with our own algorithm of risk assessment. It is likely that the formulas used will not necessarily be based on scientific facts, although that would be ideal. If past epidemic and recent pandemic behaviors are any indicators, people’s actions will reflect some combination of their own needs and desires, their own comfort level with risk-taking, and their relative understanding of complex subjects like virology, immunology, epidemiology, and public health. The challenge faced by public health officials today is to translate complex scientific and medical issues into messages average people can understand.
What exactly can be done? I’m not exactly sure, but I hope that improved education and communication can help. In the first 2 decades of the AIDS epidemic, efforts were made to change and tailor HIV-prevention messages to specific, at-risk demographic groups. Today, public health messages aimed at preventing COVID-19’s spread that resonate with older people can fall on a younger person’s deaf ears. One message size does not fit all. Hopefully, public health officials and government leaders will act on this sooner rather than later.
Dr. Drescher, a psychoanalyst, is clinical professor of psychiatry at Columbia University, and training and supervising analyst at the William A. White Institute, both in New York. He also is emeritus editor of the Journal of Gay & Lesbian Mental Health. Dr. Drescher has no other disclosures.
‘Collateral damage’: COVID-19 threatens patients with COPD
according to a commentary published in CHEST (2020 May 28. doi: 10.1016/j.chest.2020.05.549) by a group of physicians who study COPD.
Not only is COPD among the most prevalent underlying diseases among hospitalized COVID-19 patients (Clin Microbiol Infect. 2020 Jun 8. doi: 10.1016/j.cmi.2020.05.041), but other unanticipated factors of treatment put these patients at extra risk. Valerie Press, MD, assistant professor of medicine and pediatrics at the University of Chicago, and colleagues aimed to alert physicians to be aware of potential negative effects, or collateral damage, that the pandemic can have on their patients with COPD, even those without a COVID-19 diagnosis.
These concerns include that patients may delay presenting to the ED with acute exacerbations of COPD and once they present they may be at later stages of the exacerbation. Further, evaluation for COVID-19 as a possible trigger of acute exacerbations of COPD (AECOPD) is essential; however, implementing proven AECOPD therapies remains challenging. For instance, routine therapy with corticosteroids for AECOPD may be delayed due to diagnostic uncertainty and hesitation to treat COVID-19 with steroids while COVID-19 testing is pending,” Dr. Press and her colleagues stated.
Shortages and scarcity of medications such as albuterol inhalers to treat COPD have been reported. In addition, patients with COPD are currently less likely to access their health care providers because of fear of COVID-19 infection. This barrier to care and the current higher threshold for presenting to the hospital may to lead to more cases of AECOPD and worsening health in these patients, according to the authors.
Dr. Press said in an interview: “Access to medications delivered through inhalers is challenging even without the pandemic due to high cost of medications. Generic medications are key to improving access for patients with chronic lung disease, so once the generic albuterol becomes available, this should help with access. In the meantime, some companies help provide medications at reduced cost, but usually only on a short time basis. In addition, some pharmacies have lower-cost albuterol inhalers, but these are often not supplied with a full month of dosing.”
In addition to all these concerns is the economic toll this pandemic is taking on patients. The association between COPD and socioeconomic status has been studied in depth (Am J Respir Crit Care Med. 2019; 199[8]:961-69) and would indicate that low-income patients with COPD would face an increased burden during an economic downturn. The authors noted, “Historic rapid job loss and unemployment in the U.S., coupled with a health system of employment-integrated health insurance coverage, makes it more likely that people with COPD will not be able to afford their medication.”
Dr. Press stressed that the COVID pandemic has highlighted critically important disparities in access to health care and disparities in health. “Many of the recommendations regarding stay-at-home and other safety mechanisms to prevent contracting and spreading COVID-19 have not been feasible for all sub-populations in the United States. Those that were essential workers did not have the ability to stay home. Further, those that rely on public transportation had less opportunities to social distance. Finally, while telemedicine opportunities have advanced for clinical care, not all patients have equal access to these capabilities and health disparities could widen in this regard as well. Clinicians have a responsibility to identify social determinants of health that increase risks to our patients’ health and limit their safety.”*
The authors offer some concrete suggestions of how physicians can address some of these concerns, including the following:
- Be alert to potential barriers to accessing medication and be aware of generic albuterol inhaler recently approved by the FDA in response to COVID-19–related shortages.
- Use telemedicine to monitor patients and improvement of home self-management. Clinicians should help patients “seek care with worsening symptoms and have clear management guidelines regarding seeking phone/video visits; implementing therapy with corticosteroids, antibiotics, or inhalers and nebulizers; COVID-19 testing recommendations; and thresholds for seeking emergent, urgent, or outpatient care in person,” Dr. Press added, “Building on the work of nurse advice lines and case management and other support services for high-risk patients with COPD may continue via telehealth and telephone visits.”
- Ensure that untried therapy for COVID-19 “does not displace proven and necessary treatments for patients with COPD, hence placing them at increased risk for poor outcomes.”
Dr. Press is also concerned about the post–COVID-19 period for patients with COPD. “It is too early to know if there are specific after effects of the COVID infection on patients with COPD, but given the damage the virus does to even healthy lungs, there is reason to have concern that COVID could cause worsening damage to the lungs of individuals with COPD.”
She noted, “Post-ICU [PICU] syndrome has been recognized in patients with ARDS generally, and patients who recover from critical illness may have long-lasting (and permanent) effects on strength, cognition, disability, and pulmonary function. Whether the PICU syndrome in patients with ARDS due to COVID-19 specifically is different from the PICU syndrome due to other causes remains unknown. But clinicians whose patients with COPD survive COVID-19 may expect long-lasting effects and slow recovery in cases where COVID-19 led to severe ARDS and a prolonged ICU stay. Assessment of overall patient recovery and functional capacity (beyond lung function and dyspnea symptoms) including deconditioning, anxiety, PTSD, weakness, and malnutrition will need to be addressed. Additionally, clinicians may help patients and their families understand the expected recovery and help facilitate family conversations about residual effects of COVID-19.”
The authors had no disclosures.
SOURCE: Press V et al. Chest. 2020 May 28. doi:10.1016/j.chest.2020.05.549.
CORRECTION: *This story was updated with further comments and clarifications from Dr. Press. 6/23/2020
according to a commentary published in CHEST (2020 May 28. doi: 10.1016/j.chest.2020.05.549) by a group of physicians who study COPD.
Not only is COPD among the most prevalent underlying diseases among hospitalized COVID-19 patients (Clin Microbiol Infect. 2020 Jun 8. doi: 10.1016/j.cmi.2020.05.041), but other unanticipated factors of treatment put these patients at extra risk. Valerie Press, MD, assistant professor of medicine and pediatrics at the University of Chicago, and colleagues aimed to alert physicians to be aware of potential negative effects, or collateral damage, that the pandemic can have on their patients with COPD, even those without a COVID-19 diagnosis.
These concerns include that patients may delay presenting to the ED with acute exacerbations of COPD and once they present they may be at later stages of the exacerbation. Further, evaluation for COVID-19 as a possible trigger of acute exacerbations of COPD (AECOPD) is essential; however, implementing proven AECOPD therapies remains challenging. For instance, routine therapy with corticosteroids for AECOPD may be delayed due to diagnostic uncertainty and hesitation to treat COVID-19 with steroids while COVID-19 testing is pending,” Dr. Press and her colleagues stated.
Shortages and scarcity of medications such as albuterol inhalers to treat COPD have been reported. In addition, patients with COPD are currently less likely to access their health care providers because of fear of COVID-19 infection. This barrier to care and the current higher threshold for presenting to the hospital may to lead to more cases of AECOPD and worsening health in these patients, according to the authors.
Dr. Press said in an interview: “Access to medications delivered through inhalers is challenging even without the pandemic due to high cost of medications. Generic medications are key to improving access for patients with chronic lung disease, so once the generic albuterol becomes available, this should help with access. In the meantime, some companies help provide medications at reduced cost, but usually only on a short time basis. In addition, some pharmacies have lower-cost albuterol inhalers, but these are often not supplied with a full month of dosing.”
In addition to all these concerns is the economic toll this pandemic is taking on patients. The association between COPD and socioeconomic status has been studied in depth (Am J Respir Crit Care Med. 2019; 199[8]:961-69) and would indicate that low-income patients with COPD would face an increased burden during an economic downturn. The authors noted, “Historic rapid job loss and unemployment in the U.S., coupled with a health system of employment-integrated health insurance coverage, makes it more likely that people with COPD will not be able to afford their medication.”
Dr. Press stressed that the COVID pandemic has highlighted critically important disparities in access to health care and disparities in health. “Many of the recommendations regarding stay-at-home and other safety mechanisms to prevent contracting and spreading COVID-19 have not been feasible for all sub-populations in the United States. Those that were essential workers did not have the ability to stay home. Further, those that rely on public transportation had less opportunities to social distance. Finally, while telemedicine opportunities have advanced for clinical care, not all patients have equal access to these capabilities and health disparities could widen in this regard as well. Clinicians have a responsibility to identify social determinants of health that increase risks to our patients’ health and limit their safety.”*
The authors offer some concrete suggestions of how physicians can address some of these concerns, including the following:
- Be alert to potential barriers to accessing medication and be aware of generic albuterol inhaler recently approved by the FDA in response to COVID-19–related shortages.
- Use telemedicine to monitor patients and improvement of home self-management. Clinicians should help patients “seek care with worsening symptoms and have clear management guidelines regarding seeking phone/video visits; implementing therapy with corticosteroids, antibiotics, or inhalers and nebulizers; COVID-19 testing recommendations; and thresholds for seeking emergent, urgent, or outpatient care in person,” Dr. Press added, “Building on the work of nurse advice lines and case management and other support services for high-risk patients with COPD may continue via telehealth and telephone visits.”
- Ensure that untried therapy for COVID-19 “does not displace proven and necessary treatments for patients with COPD, hence placing them at increased risk for poor outcomes.”
Dr. Press is also concerned about the post–COVID-19 period for patients with COPD. “It is too early to know if there are specific after effects of the COVID infection on patients with COPD, but given the damage the virus does to even healthy lungs, there is reason to have concern that COVID could cause worsening damage to the lungs of individuals with COPD.”
She noted, “Post-ICU [PICU] syndrome has been recognized in patients with ARDS generally, and patients who recover from critical illness may have long-lasting (and permanent) effects on strength, cognition, disability, and pulmonary function. Whether the PICU syndrome in patients with ARDS due to COVID-19 specifically is different from the PICU syndrome due to other causes remains unknown. But clinicians whose patients with COPD survive COVID-19 may expect long-lasting effects and slow recovery in cases where COVID-19 led to severe ARDS and a prolonged ICU stay. Assessment of overall patient recovery and functional capacity (beyond lung function and dyspnea symptoms) including deconditioning, anxiety, PTSD, weakness, and malnutrition will need to be addressed. Additionally, clinicians may help patients and their families understand the expected recovery and help facilitate family conversations about residual effects of COVID-19.”
The authors had no disclosures.
SOURCE: Press V et al. Chest. 2020 May 28. doi:10.1016/j.chest.2020.05.549.
CORRECTION: *This story was updated with further comments and clarifications from Dr. Press. 6/23/2020
according to a commentary published in CHEST (2020 May 28. doi: 10.1016/j.chest.2020.05.549) by a group of physicians who study COPD.
Not only is COPD among the most prevalent underlying diseases among hospitalized COVID-19 patients (Clin Microbiol Infect. 2020 Jun 8. doi: 10.1016/j.cmi.2020.05.041), but other unanticipated factors of treatment put these patients at extra risk. Valerie Press, MD, assistant professor of medicine and pediatrics at the University of Chicago, and colleagues aimed to alert physicians to be aware of potential negative effects, or collateral damage, that the pandemic can have on their patients with COPD, even those without a COVID-19 diagnosis.
These concerns include that patients may delay presenting to the ED with acute exacerbations of COPD and once they present they may be at later stages of the exacerbation. Further, evaluation for COVID-19 as a possible trigger of acute exacerbations of COPD (AECOPD) is essential; however, implementing proven AECOPD therapies remains challenging. For instance, routine therapy with corticosteroids for AECOPD may be delayed due to diagnostic uncertainty and hesitation to treat COVID-19 with steroids while COVID-19 testing is pending,” Dr. Press and her colleagues stated.
Shortages and scarcity of medications such as albuterol inhalers to treat COPD have been reported. In addition, patients with COPD are currently less likely to access their health care providers because of fear of COVID-19 infection. This barrier to care and the current higher threshold for presenting to the hospital may to lead to more cases of AECOPD and worsening health in these patients, according to the authors.
Dr. Press said in an interview: “Access to medications delivered through inhalers is challenging even without the pandemic due to high cost of medications. Generic medications are key to improving access for patients with chronic lung disease, so once the generic albuterol becomes available, this should help with access. In the meantime, some companies help provide medications at reduced cost, but usually only on a short time basis. In addition, some pharmacies have lower-cost albuterol inhalers, but these are often not supplied with a full month of dosing.”
In addition to all these concerns is the economic toll this pandemic is taking on patients. The association between COPD and socioeconomic status has been studied in depth (Am J Respir Crit Care Med. 2019; 199[8]:961-69) and would indicate that low-income patients with COPD would face an increased burden during an economic downturn. The authors noted, “Historic rapid job loss and unemployment in the U.S., coupled with a health system of employment-integrated health insurance coverage, makes it more likely that people with COPD will not be able to afford their medication.”
Dr. Press stressed that the COVID pandemic has highlighted critically important disparities in access to health care and disparities in health. “Many of the recommendations regarding stay-at-home and other safety mechanisms to prevent contracting and spreading COVID-19 have not been feasible for all sub-populations in the United States. Those that were essential workers did not have the ability to stay home. Further, those that rely on public transportation had less opportunities to social distance. Finally, while telemedicine opportunities have advanced for clinical care, not all patients have equal access to these capabilities and health disparities could widen in this regard as well. Clinicians have a responsibility to identify social determinants of health that increase risks to our patients’ health and limit their safety.”*
The authors offer some concrete suggestions of how physicians can address some of these concerns, including the following:
- Be alert to potential barriers to accessing medication and be aware of generic albuterol inhaler recently approved by the FDA in response to COVID-19–related shortages.
- Use telemedicine to monitor patients and improvement of home self-management. Clinicians should help patients “seek care with worsening symptoms and have clear management guidelines regarding seeking phone/video visits; implementing therapy with corticosteroids, antibiotics, or inhalers and nebulizers; COVID-19 testing recommendations; and thresholds for seeking emergent, urgent, or outpatient care in person,” Dr. Press added, “Building on the work of nurse advice lines and case management and other support services for high-risk patients with COPD may continue via telehealth and telephone visits.”
- Ensure that untried therapy for COVID-19 “does not displace proven and necessary treatments for patients with COPD, hence placing them at increased risk for poor outcomes.”
Dr. Press is also concerned about the post–COVID-19 period for patients with COPD. “It is too early to know if there are specific after effects of the COVID infection on patients with COPD, but given the damage the virus does to even healthy lungs, there is reason to have concern that COVID could cause worsening damage to the lungs of individuals with COPD.”
She noted, “Post-ICU [PICU] syndrome has been recognized in patients with ARDS generally, and patients who recover from critical illness may have long-lasting (and permanent) effects on strength, cognition, disability, and pulmonary function. Whether the PICU syndrome in patients with ARDS due to COVID-19 specifically is different from the PICU syndrome due to other causes remains unknown. But clinicians whose patients with COPD survive COVID-19 may expect long-lasting effects and slow recovery in cases where COVID-19 led to severe ARDS and a prolonged ICU stay. Assessment of overall patient recovery and functional capacity (beyond lung function and dyspnea symptoms) including deconditioning, anxiety, PTSD, weakness, and malnutrition will need to be addressed. Additionally, clinicians may help patients and their families understand the expected recovery and help facilitate family conversations about residual effects of COVID-19.”
The authors had no disclosures.
SOURCE: Press V et al. Chest. 2020 May 28. doi:10.1016/j.chest.2020.05.549.
CORRECTION: *This story was updated with further comments and clarifications from Dr. Press. 6/23/2020
FROM CHEST
Headache may predict clinical evolution of COVID-19
new research suggests. An observational study of more than 100 patients showed that headache onset could occur during the presymptomatic or symptomatic phase of COVID-19 and could resemble tension-type or migraine headache.
Headache itself was associated with a shorter symptomatic period, while headache and anosmia were associated with a shorter hospitalization period. In a subgroup of participants, headache persisted even after the symptoms of COVID-19 had been resolved.
Investigators noted that understanding the pathophysiology of headache in COVID-19 could improve understanding of migraine and other headache disorders. “It seems that those patients who start early on, during the asymptomatic or early symptomatic period of COVID-19, with headache have a more localized inflammatory response that may reflect the ability of the body to better control and respond to the infection by SARS-CoV-2,” lead investigator Patricia Pozo-Rosich, MD, PhD, head of the headache and craniofacial pain unit at Vall d’Hebron University Hospital, Barcelona, said in an interview.
She presented the findings at the virtual annual meeting of the American Headache Society.
Systemic inflammation
Headache is one of the main symptoms of COVID-19. A recent study of 214 patients with COVID-19 showed that approximately 13% of the participants had headache and 5% had anosmia.
SARS-CoV-2 penetrates the cells through the ACE2 receptor, which is present throughout the body. “SARS-CoV-2 enters the body through the nasal cavity and it probably penetrates the nervous system in the periphery through afferent branches of the olfactory and trigeminal nerve,” Dr. Pozo-Rosich said. It travels to the lungs and, later, the bloodstream. This generates systemic inflammation that may turn into a cytokine storm. Evidence has identified cortical hyperintensities and olfactory bulb hyperintensities in patients with COVID-19, suggesting that the virus directly infects the CNS.
Interleukin-6, one of the main inflammatory molecules, has been proven to be related to COVID-19 and has become a therapeutic target. Levels of IL-6 may be lower and tend to be more stable in patients with both COVID-19 and headache than in patients with COVID-19 only.
The researchers observed 130 patients (51% women; mean age, 54 years) with COVID-19 who were attended by neurologists at Vall d’Hebron. In this group, 74.4% had headache. Patients with headache tended to be younger than those without headache (mean age, 50 years vs. 63 years, respectively) and tended to be women (58.6% vs. 29.4%).
Approximately one-third of patients with headache had a history of migraine. Most reported mild to moderate pain that resembled tension-type headache. In participants with severe pain and migraine-like features, headache more often began during the asymptomatic phase of COVID-19.
Disease evolution predictor?
The investigators followed up on 100 of the 130 patients with COVID-19, of whom 74 had headache. About 38% of these patients had ongoing headache after 6 weeks, which suggests that some patients may develop a new daily persistent headache once a 3-month period has elapsed. Half of this group had no previous headache history. Headache had been the prodromal symptom of COVID-19 for 21.4% of these patients.
Results showed that headache predicted the clinical evolution of COVID-19. The symptomatic phase of COVID-19 was 7 days shorter for patients with headache than for those without headache. In addition, the period of hospitalization was 7 days shorter for patients with headache and anosmia, compared with patients who had neither headache nor anosmia.
Most therapies, including ibuprofen, candesartan, and anti–calcitonin gene–related peptide (CGRP) monoclonal antibodies, are safe for treating headache in COVID-19, the investigators noted. “We should just try to initially avoid steroids to avoid interference with the body’s reaction to SARS-CoV-2,” Dr. Pozo-Rosich said.
Researchers at Sidney Kimmel Medical College, Philadelphia, are currently studying intranasal vazegepant, an anti-CGRP therapy, as a way to potentially blunt the severe inflammatory response in the lungs of patients with COVID-19, she noted, adding that this peptide may have a future role not only in headache, but also in COVID-19.
Historical link to viral infections
Commenting on the study, Matthew S. Robbins, MD, associate professor of neurology at Weill Cornell Medicine, New York, said the findings associating headache with a shorter symptomatic phase of COVID-19 were “interesting.”
“Headache is common with mild viral infections. More severe viral infections may simply feature more overwhelming respiratory symptoms and fever that lead to underreporting or underascertainment of headache,” said Dr. Robbins, who was not involved with the research.
He noted that the finding showing an association of headache and COVID-19 with a younger age and in women “may be related to a higher prevalence of migraine biology in such patients, and being triggered by the virus or the psychological stress associated with it.”
Dr. Robbins added that viral illnesses have long been associated with new daily persistent headache, “dating back to the early 1980s,” when it was first described in association with Epstein-Barr virus. These infections have also been implicated in the progression of migraine to chronic migraine in adolescents.
“In my view, treatment should be aimed at the symptomatic headache type for which new daily persistent headache resembles, regardless of the potential inciting factor,” Dr. Robbins said.
Dr. Pozo-Rosich has received consulting fees from Allergan, Amgen, Almirall, Biohaven, Chiesi, Eli Lilly, Medscape, Novartis, and Teva Pharmaceuticals. Dr. Robbins has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research suggests. An observational study of more than 100 patients showed that headache onset could occur during the presymptomatic or symptomatic phase of COVID-19 and could resemble tension-type or migraine headache.
Headache itself was associated with a shorter symptomatic period, while headache and anosmia were associated with a shorter hospitalization period. In a subgroup of participants, headache persisted even after the symptoms of COVID-19 had been resolved.
Investigators noted that understanding the pathophysiology of headache in COVID-19 could improve understanding of migraine and other headache disorders. “It seems that those patients who start early on, during the asymptomatic or early symptomatic period of COVID-19, with headache have a more localized inflammatory response that may reflect the ability of the body to better control and respond to the infection by SARS-CoV-2,” lead investigator Patricia Pozo-Rosich, MD, PhD, head of the headache and craniofacial pain unit at Vall d’Hebron University Hospital, Barcelona, said in an interview.
She presented the findings at the virtual annual meeting of the American Headache Society.
Systemic inflammation
Headache is one of the main symptoms of COVID-19. A recent study of 214 patients with COVID-19 showed that approximately 13% of the participants had headache and 5% had anosmia.
SARS-CoV-2 penetrates the cells through the ACE2 receptor, which is present throughout the body. “SARS-CoV-2 enters the body through the nasal cavity and it probably penetrates the nervous system in the periphery through afferent branches of the olfactory and trigeminal nerve,” Dr. Pozo-Rosich said. It travels to the lungs and, later, the bloodstream. This generates systemic inflammation that may turn into a cytokine storm. Evidence has identified cortical hyperintensities and olfactory bulb hyperintensities in patients with COVID-19, suggesting that the virus directly infects the CNS.
Interleukin-6, one of the main inflammatory molecules, has been proven to be related to COVID-19 and has become a therapeutic target. Levels of IL-6 may be lower and tend to be more stable in patients with both COVID-19 and headache than in patients with COVID-19 only.
The researchers observed 130 patients (51% women; mean age, 54 years) with COVID-19 who were attended by neurologists at Vall d’Hebron. In this group, 74.4% had headache. Patients with headache tended to be younger than those without headache (mean age, 50 years vs. 63 years, respectively) and tended to be women (58.6% vs. 29.4%).
Approximately one-third of patients with headache had a history of migraine. Most reported mild to moderate pain that resembled tension-type headache. In participants with severe pain and migraine-like features, headache more often began during the asymptomatic phase of COVID-19.
Disease evolution predictor?
The investigators followed up on 100 of the 130 patients with COVID-19, of whom 74 had headache. About 38% of these patients had ongoing headache after 6 weeks, which suggests that some patients may develop a new daily persistent headache once a 3-month period has elapsed. Half of this group had no previous headache history. Headache had been the prodromal symptom of COVID-19 for 21.4% of these patients.
Results showed that headache predicted the clinical evolution of COVID-19. The symptomatic phase of COVID-19 was 7 days shorter for patients with headache than for those without headache. In addition, the period of hospitalization was 7 days shorter for patients with headache and anosmia, compared with patients who had neither headache nor anosmia.
Most therapies, including ibuprofen, candesartan, and anti–calcitonin gene–related peptide (CGRP) monoclonal antibodies, are safe for treating headache in COVID-19, the investigators noted. “We should just try to initially avoid steroids to avoid interference with the body’s reaction to SARS-CoV-2,” Dr. Pozo-Rosich said.
Researchers at Sidney Kimmel Medical College, Philadelphia, are currently studying intranasal vazegepant, an anti-CGRP therapy, as a way to potentially blunt the severe inflammatory response in the lungs of patients with COVID-19, she noted, adding that this peptide may have a future role not only in headache, but also in COVID-19.
Historical link to viral infections
Commenting on the study, Matthew S. Robbins, MD, associate professor of neurology at Weill Cornell Medicine, New York, said the findings associating headache with a shorter symptomatic phase of COVID-19 were “interesting.”
“Headache is common with mild viral infections. More severe viral infections may simply feature more overwhelming respiratory symptoms and fever that lead to underreporting or underascertainment of headache,” said Dr. Robbins, who was not involved with the research.
He noted that the finding showing an association of headache and COVID-19 with a younger age and in women “may be related to a higher prevalence of migraine biology in such patients, and being triggered by the virus or the psychological stress associated with it.”
Dr. Robbins added that viral illnesses have long been associated with new daily persistent headache, “dating back to the early 1980s,” when it was first described in association with Epstein-Barr virus. These infections have also been implicated in the progression of migraine to chronic migraine in adolescents.
“In my view, treatment should be aimed at the symptomatic headache type for which new daily persistent headache resembles, regardless of the potential inciting factor,” Dr. Robbins said.
Dr. Pozo-Rosich has received consulting fees from Allergan, Amgen, Almirall, Biohaven, Chiesi, Eli Lilly, Medscape, Novartis, and Teva Pharmaceuticals. Dr. Robbins has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research suggests. An observational study of more than 100 patients showed that headache onset could occur during the presymptomatic or symptomatic phase of COVID-19 and could resemble tension-type or migraine headache.
Headache itself was associated with a shorter symptomatic period, while headache and anosmia were associated with a shorter hospitalization period. In a subgroup of participants, headache persisted even after the symptoms of COVID-19 had been resolved.
Investigators noted that understanding the pathophysiology of headache in COVID-19 could improve understanding of migraine and other headache disorders. “It seems that those patients who start early on, during the asymptomatic or early symptomatic period of COVID-19, with headache have a more localized inflammatory response that may reflect the ability of the body to better control and respond to the infection by SARS-CoV-2,” lead investigator Patricia Pozo-Rosich, MD, PhD, head of the headache and craniofacial pain unit at Vall d’Hebron University Hospital, Barcelona, said in an interview.
She presented the findings at the virtual annual meeting of the American Headache Society.
Systemic inflammation
Headache is one of the main symptoms of COVID-19. A recent study of 214 patients with COVID-19 showed that approximately 13% of the participants had headache and 5% had anosmia.
SARS-CoV-2 penetrates the cells through the ACE2 receptor, which is present throughout the body. “SARS-CoV-2 enters the body through the nasal cavity and it probably penetrates the nervous system in the periphery through afferent branches of the olfactory and trigeminal nerve,” Dr. Pozo-Rosich said. It travels to the lungs and, later, the bloodstream. This generates systemic inflammation that may turn into a cytokine storm. Evidence has identified cortical hyperintensities and olfactory bulb hyperintensities in patients with COVID-19, suggesting that the virus directly infects the CNS.
Interleukin-6, one of the main inflammatory molecules, has been proven to be related to COVID-19 and has become a therapeutic target. Levels of IL-6 may be lower and tend to be more stable in patients with both COVID-19 and headache than in patients with COVID-19 only.
The researchers observed 130 patients (51% women; mean age, 54 years) with COVID-19 who were attended by neurologists at Vall d’Hebron. In this group, 74.4% had headache. Patients with headache tended to be younger than those without headache (mean age, 50 years vs. 63 years, respectively) and tended to be women (58.6% vs. 29.4%).
Approximately one-third of patients with headache had a history of migraine. Most reported mild to moderate pain that resembled tension-type headache. In participants with severe pain and migraine-like features, headache more often began during the asymptomatic phase of COVID-19.
Disease evolution predictor?
The investigators followed up on 100 of the 130 patients with COVID-19, of whom 74 had headache. About 38% of these patients had ongoing headache after 6 weeks, which suggests that some patients may develop a new daily persistent headache once a 3-month period has elapsed. Half of this group had no previous headache history. Headache had been the prodromal symptom of COVID-19 for 21.4% of these patients.
Results showed that headache predicted the clinical evolution of COVID-19. The symptomatic phase of COVID-19 was 7 days shorter for patients with headache than for those without headache. In addition, the period of hospitalization was 7 days shorter for patients with headache and anosmia, compared with patients who had neither headache nor anosmia.
Most therapies, including ibuprofen, candesartan, and anti–calcitonin gene–related peptide (CGRP) monoclonal antibodies, are safe for treating headache in COVID-19, the investigators noted. “We should just try to initially avoid steroids to avoid interference with the body’s reaction to SARS-CoV-2,” Dr. Pozo-Rosich said.
Researchers at Sidney Kimmel Medical College, Philadelphia, are currently studying intranasal vazegepant, an anti-CGRP therapy, as a way to potentially blunt the severe inflammatory response in the lungs of patients with COVID-19, she noted, adding that this peptide may have a future role not only in headache, but also in COVID-19.
Historical link to viral infections
Commenting on the study, Matthew S. Robbins, MD, associate professor of neurology at Weill Cornell Medicine, New York, said the findings associating headache with a shorter symptomatic phase of COVID-19 were “interesting.”
“Headache is common with mild viral infections. More severe viral infections may simply feature more overwhelming respiratory symptoms and fever that lead to underreporting or underascertainment of headache,” said Dr. Robbins, who was not involved with the research.
He noted that the finding showing an association of headache and COVID-19 with a younger age and in women “may be related to a higher prevalence of migraine biology in such patients, and being triggered by the virus or the psychological stress associated with it.”
Dr. Robbins added that viral illnesses have long been associated with new daily persistent headache, “dating back to the early 1980s,” when it was first described in association with Epstein-Barr virus. These infections have also been implicated in the progression of migraine to chronic migraine in adolescents.
“In my view, treatment should be aimed at the symptomatic headache type for which new daily persistent headache resembles, regardless of the potential inciting factor,” Dr. Robbins said.
Dr. Pozo-Rosich has received consulting fees from Allergan, Amgen, Almirall, Biohaven, Chiesi, Eli Lilly, Medscape, Novartis, and Teva Pharmaceuticals. Dr. Robbins has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM AHS 2020














