User login
The interesting history of dermatologist-developed skin care
Those of you who have visited my dermatology practice in Miami know that the art in my office is dedicated to the history of the skin care industry. I collect , and I have written this historical column in honor of the 50th anniversary of Dermatology News.
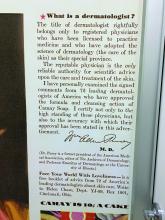
The first doctor to market his own cosmetic product, Erasmus Wilson, MD, faced scrutiny from his colleagues. Although he had contributed much to the field of dermatology, he was criticized by other dermatologists when he promoted a hair wash. The next doctor in my story, William Pusey, MD, was criticized for helping the company that manufactured Camay soap because he allowed his name to be used in Camay advertisements. The scrutiny that these two well-respected dermatologists endured from their colleagues deterred dermatologists from entering the skin care business for decades. The professional jealousy from dermatologic colleagues left the skin care field wide open for imposters, charlatans, and nondermatologists who had no concern for efficacy and patient outcomes to flourish. This is the story of a group of brilliant entrepreneurial dermatologists and one chiropractor who misrepresented himself as a dermatologist and how they influenced skin care as we know it.
Erasmus Wilson, MD1 (1809-1884): In 1840, Erasmus Wilson2 was a physician in London who chose to specialize in dermatology at a time when that specialization was frowned upon. He was a subeditor for The Lancet and wrote several books on dermatology including “Diseases of the Skin – A Practical and Theoretical Treatise,” “Portraits of the Diseases of the Skin,” and “Student’s Book on Diseases of the Skin.” He was the first professor of dermatology in the College of Surgeons and by 1869, was the leading English-speaking dermatologist in the world. He contributed much to dermatology, including his pioneering characterizations of Demodex mites, lichen planus, exfoliative dermatitis, neurotic excoriations, and roseola. Dr. Wilson was knighted in 1881 for his good works and notable generosity. (He was known for giving his poor patients money for food, endowing chairs in dermatology, and donating a famous obelisk in London).
In 1854, Dr. Wilson wrote a book for laypeople called “Healthy Skin: A Popular Treatise on the Skin and Hair, Their Preservation and Management,” in which he advocated cleanliness and bathing, which led to the popularity of Turkish baths and bathing resorts in Europe. Despite his undeniable contributions to dermatology, he was widely criticized by his colleagues for promoting a “Hair Wash” and a turtle oil soap. I cannot find any information about whether or not he developed the hair wash and turtle soap himself, but it seems that he earned income from sales of these two products, even though he was said to have donated it all to charities.
William A. Pusey MD (1865-1940): Dr. Pusey was the first chairman of dermatology at the University of Illinois College of Medicine, Chicago. He published several books, including “Care of the Skin and Hair,” “Syphilis as a Modern Problem,” “The Principles and Practices of Dermatology,” and “History of Dermatology” among others. He is best known for his work in developing the use of x-rays (roentgen rays) and phototherapy in dermatology, and in 1907, he was the first dermatologist to describe the use of solid carbon dioxide to treat skin lesions. He was president of the American Dermatological Association in 1910, president of the Chicago Medical Society in 1918, editor of the Archives of Dermatology in 1920, and president of the American Medical Association in 1924.
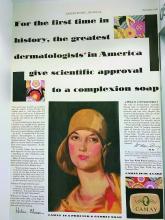
In the early 1920s, skin care companies were beginning to advertise their products using endorsements from celebrities and socialites, and were making misleading claims. Dr. Pusey wanted to work with these companies to help them perform evidence-based trials so they could make scientifically correct claims. Proctor & Gamble asked Dr. Pusey to advise them on how they could advertise honestly about their new soap, “Camay.” In Dr. Pusey’s words,3 “they (Proctor & Gamble) wanted to give the public authoritative advice about the use of soap and water. They suggested that I get a group of dermatologists of my selection to examine the soap and prepare instructions for bathing and the use of soap, and, if they found this soap was of high quality, to certify to that effect.” The research was performed as he suggested, and he allowed his name to be used in the Camay soap ads from 1926 to 1929. He said that he allowed them to use his name hoping to promote the need for evidence-based research, in contrast to the skin care products endorsed by socialites and celebrities that were flooding the market around that time.
Herbert Rattner, MD, at Northwestern University, Chicago, was his friend and one of the many dermatologists who criticized Dr. Pusey for allowing his name to be used in the Camay ads. Dr. Pusey’s reply to the criticism (according to Dr. Rattner) was that Proctor & Gamble was “proposing to do what the medical profession always is criticizing commercial concerns for not doing, namely, coming to physicians for information on medical matters. Could the profession hope to have any influence with business concerns if it was always eager to criticize bad commercial practices but never willing to support good ones?”3
While Dr. Pusey felt his reasons for adding his name to the Camay ads and research were justified, many of his friends stated that in hindsight, he regretted the action because of the negative response of his colleagues. It was years before dermatologists began providing input again into the skin care industry. During that time, radio, television and print ads were rampant with misleading claims – which led the way for a dermatologic imposter to make a fortune on skin care.
John Woodbury (1851-1909): John Woodbury, a chiropractor, never went to medical school, but that did not stop him from claiming he was a dermatologist and cosmetic surgeon. In 1889, he opened the John H. Woodbury Dermatological Institute in New York City, and over the next few years, opened Woodbury Dermatological Institutes in at least 5 states and employed 25 “physicians” who were not licensed to practice medicine. He came out with face soaps, tonics, and cold creams and spent a fortune on advertising these products and his institutes. In 1901, he sold his “Woodbury Soap” to the Andrew Jergens Company for $212,500 and 10% in royalties.
Multiple lawsuits occurred from 1898 to 1907 because he continued using the Woodbury name on his own products, despite having sold the “Woodbury” trademark to Jergens. He was sued for practicing medicine without a medical license and claiming to be a dermatologist when he was not. He lost most of these lawsuits, including one in 1907 in which the court ruled that corporations may not employ unlicensed professionals to practice medicine. In 1909, John Woodbury committed suicide. The Woodbury Soap company flourished in the 1930s and 1940s, as part of Jergens, until the brand was discontinued in 1970 when Jergens was acquired by American Brands.
The next dermatologists to come along did not make the same mistakes as those of their predecessors. They all made scientific discoveries through their basic science research in the laboratory, filed patents, formed skin care companies, perfected the formulations, and conducted research trials of the final product. Their marketing focused on science and efficacy and only rarely used their names and images in advertising, allowing them to maintain their reputations in the dermatology field.
Eugene Van Scott, MD (1922-present): Dermatologist Dr. Van Scott and dermatopharmacologist Ruey Yu, PhD, filed a method patent in the early 1970s on the effectiveness of alpha hydroxy acids to treat ichthyosis. They invented the abbreviation “AHA” and have continued their work on organic acids to this day. They now have more than 125 patents, which they have licensed to 60 companies in the cosmetics and pharmaceutical industries.
In 1988, 14 years after their initial publication, they founded the company they named Polystrata, which grew into today’s NeoStrata.4 Over the years, they had to defend their patents because many personal care companies used their technologies without licensing them. In 2007, they won a $41 million settlement in a patent infringement suit against Mary Kay filed in March 2005. They have both been very philanthropic in the dermatology world5 and are highly respected in the field. Among many other honors, Dr. Van Scott was named a Master Dermatologist by the American Academy of Dermatology in 1998 and received the Dermatology Foundation’s Distinguished Service Medallion in 2004.
Sheldon Pinnell, MD (1937-2013): After Dr. Pinnell completed his dermatology residency at Harvard Medical School, he spent 2 years studying collagen chemistry at the Max Planck Institute in Munich, Germany. In 1973, he returned to Duke University where he had earned his undergraduate degree before attending Yale University. He remained at Duke for the duration of his career and was professor and chief of dermatology there for many years. Early in his career, he focused on the role of vitamin C in collagen biosynthesis and discovered some of the mechanisms by which sun exposure causes photoaging. He described the use of the first (and most popular) topically applied L-ascorbic acid (vitamin C) to prevent and treat skin aging.
Dr. Pinnell’s many discoveries include showing that the addition of ascorbic acid to fibroblast cultures increases collagen production and that topically applied L-ascorbic acid penetrates into the skin best at a pH of 2-2.5. Dr. Pinnell changed the way the world uses topical antioxidants today; he was widely respected and was a member of the American Dermatological Association and an honorary member of the Society of Investigative Dermatology. He published more than 200 scientific articles and held 10 patents. He started the skin care company Skinceuticals, based on his antioxidant technologies. It was acquired by L’Oreal in 2005.
Richard Fitzpatrick, MD (1944-2014): The dermatologist affectionately known as “Fitz” is credited with being the first to use lasers for skin resurfacing. He went to medical school at Emory University and did his dermatology residency at the University of California, Los Angeles. He authored more than 130 publications and was one of the first doctors to specialize in cosmetic dermatology. He realized that fibroblast cell cultures used to produce the collagen filler CosmoPlast (no longer on the market) generated many growth factors that could rejuvenate the skin, and in 1999, he launched the skin care brand SkinMedica. In 2000, he received a patent for fibroblast-derived growth factors used topically for antiaging – a formula he called Tissue Nutrient Solution. In 2001, the popular product TNS Recovery Complex was launched based on the patented growth factor technology. It is still the most popular growth factor technology on the market.
What can we learn from these pioneers? I have had several interesting discussions about this topic with Leonard Hoenig, MD, section editor for Reflections on Dermatology: Past, Present, and Future, in Clinics in Dermatology. (Dr. Hoenig told me the interesting story that Listerine mouthwash was named in honor of Joseph Lister but accounts vary as to whether he gave permission to do so. This makes Dr. Lister the most famous physician to endorse a personal care product.) When Dr. Hoenig and I discussed the ethics of dermatologists creating a skin care line or retailing skin care in their medical practice, he stated my sentiments perfectly: “We should rely on professional, ethical, and legal guidelines to help us do what is right. Most importantly, we should have the best interests of our patients at heart when recommending any treatments.”
Dermatologists have unique knowledge, experience, and perspective on treating the skin with topical agents and have the true desire to improve skin health. If we do not discover, research, patent, and develop efficacious skin care products, someone else will do it – and I do not think they will do it as well as a dermatologist can.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks and a New York Times Best Sellers book for consumers. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., a company that independently tests skin care products and makes recommendations to physicians on which skin care technologies are best. Write to her at [email protected].
References
1. Everett MA. Int J Dermatol. 1978 May;17(4):345-52.
2. Moxon RK. N Engl J Med. 1976 Apr 1;294(14):762-4.
3. Rattner H. Arch Derm Syphilol. 1937;35(1):25-66.
4. Neostrata: More than Hope, by Elaine Strauss, U.S. 1 Newspaper, Feb. 24, 1999.
5. Two legends in the field of dermatology provide $1 million gift to Temple University school of medicine’s department of dermatology, Temple University, June 5, 2015.
Those of you who have visited my dermatology practice in Miami know that the art in my office is dedicated to the history of the skin care industry. I collect , and I have written this historical column in honor of the 50th anniversary of Dermatology News.
The first doctor to market his own cosmetic product, Erasmus Wilson, MD, faced scrutiny from his colleagues. Although he had contributed much to the field of dermatology, he was criticized by other dermatologists when he promoted a hair wash. The next doctor in my story, William Pusey, MD, was criticized for helping the company that manufactured Camay soap because he allowed his name to be used in Camay advertisements. The scrutiny that these two well-respected dermatologists endured from their colleagues deterred dermatologists from entering the skin care business for decades. The professional jealousy from dermatologic colleagues left the skin care field wide open for imposters, charlatans, and nondermatologists who had no concern for efficacy and patient outcomes to flourish. This is the story of a group of brilliant entrepreneurial dermatologists and one chiropractor who misrepresented himself as a dermatologist and how they influenced skin care as we know it.
Erasmus Wilson, MD1 (1809-1884): In 1840, Erasmus Wilson2 was a physician in London who chose to specialize in dermatology at a time when that specialization was frowned upon. He was a subeditor for The Lancet and wrote several books on dermatology including “Diseases of the Skin – A Practical and Theoretical Treatise,” “Portraits of the Diseases of the Skin,” and “Student’s Book on Diseases of the Skin.” He was the first professor of dermatology in the College of Surgeons and by 1869, was the leading English-speaking dermatologist in the world. He contributed much to dermatology, including his pioneering characterizations of Demodex mites, lichen planus, exfoliative dermatitis, neurotic excoriations, and roseola. Dr. Wilson was knighted in 1881 for his good works and notable generosity. (He was known for giving his poor patients money for food, endowing chairs in dermatology, and donating a famous obelisk in London).
In 1854, Dr. Wilson wrote a book for laypeople called “Healthy Skin: A Popular Treatise on the Skin and Hair, Their Preservation and Management,” in which he advocated cleanliness and bathing, which led to the popularity of Turkish baths and bathing resorts in Europe. Despite his undeniable contributions to dermatology, he was widely criticized by his colleagues for promoting a “Hair Wash” and a turtle oil soap. I cannot find any information about whether or not he developed the hair wash and turtle soap himself, but it seems that he earned income from sales of these two products, even though he was said to have donated it all to charities.
William A. Pusey MD (1865-1940): Dr. Pusey was the first chairman of dermatology at the University of Illinois College of Medicine, Chicago. He published several books, including “Care of the Skin and Hair,” “Syphilis as a Modern Problem,” “The Principles and Practices of Dermatology,” and “History of Dermatology” among others. He is best known for his work in developing the use of x-rays (roentgen rays) and phototherapy in dermatology, and in 1907, he was the first dermatologist to describe the use of solid carbon dioxide to treat skin lesions. He was president of the American Dermatological Association in 1910, president of the Chicago Medical Society in 1918, editor of the Archives of Dermatology in 1920, and president of the American Medical Association in 1924.
In the early 1920s, skin care companies were beginning to advertise their products using endorsements from celebrities and socialites, and were making misleading claims. Dr. Pusey wanted to work with these companies to help them perform evidence-based trials so they could make scientifically correct claims. Proctor & Gamble asked Dr. Pusey to advise them on how they could advertise honestly about their new soap, “Camay.” In Dr. Pusey’s words,3 “they (Proctor & Gamble) wanted to give the public authoritative advice about the use of soap and water. They suggested that I get a group of dermatologists of my selection to examine the soap and prepare instructions for bathing and the use of soap, and, if they found this soap was of high quality, to certify to that effect.” The research was performed as he suggested, and he allowed his name to be used in the Camay soap ads from 1926 to 1929. He said that he allowed them to use his name hoping to promote the need for evidence-based research, in contrast to the skin care products endorsed by socialites and celebrities that were flooding the market around that time.
Herbert Rattner, MD, at Northwestern University, Chicago, was his friend and one of the many dermatologists who criticized Dr. Pusey for allowing his name to be used in the Camay ads. Dr. Pusey’s reply to the criticism (according to Dr. Rattner) was that Proctor & Gamble was “proposing to do what the medical profession always is criticizing commercial concerns for not doing, namely, coming to physicians for information on medical matters. Could the profession hope to have any influence with business concerns if it was always eager to criticize bad commercial practices but never willing to support good ones?”3
While Dr. Pusey felt his reasons for adding his name to the Camay ads and research were justified, many of his friends stated that in hindsight, he regretted the action because of the negative response of his colleagues. It was years before dermatologists began providing input again into the skin care industry. During that time, radio, television and print ads were rampant with misleading claims – which led the way for a dermatologic imposter to make a fortune on skin care.
John Woodbury (1851-1909): John Woodbury, a chiropractor, never went to medical school, but that did not stop him from claiming he was a dermatologist and cosmetic surgeon. In 1889, he opened the John H. Woodbury Dermatological Institute in New York City, and over the next few years, opened Woodbury Dermatological Institutes in at least 5 states and employed 25 “physicians” who were not licensed to practice medicine. He came out with face soaps, tonics, and cold creams and spent a fortune on advertising these products and his institutes. In 1901, he sold his “Woodbury Soap” to the Andrew Jergens Company for $212,500 and 10% in royalties.
Multiple lawsuits occurred from 1898 to 1907 because he continued using the Woodbury name on his own products, despite having sold the “Woodbury” trademark to Jergens. He was sued for practicing medicine without a medical license and claiming to be a dermatologist when he was not. He lost most of these lawsuits, including one in 1907 in which the court ruled that corporations may not employ unlicensed professionals to practice medicine. In 1909, John Woodbury committed suicide. The Woodbury Soap company flourished in the 1930s and 1940s, as part of Jergens, until the brand was discontinued in 1970 when Jergens was acquired by American Brands.
The next dermatologists to come along did not make the same mistakes as those of their predecessors. They all made scientific discoveries through their basic science research in the laboratory, filed patents, formed skin care companies, perfected the formulations, and conducted research trials of the final product. Their marketing focused on science and efficacy and only rarely used their names and images in advertising, allowing them to maintain their reputations in the dermatology field.
Eugene Van Scott, MD (1922-present): Dermatologist Dr. Van Scott and dermatopharmacologist Ruey Yu, PhD, filed a method patent in the early 1970s on the effectiveness of alpha hydroxy acids to treat ichthyosis. They invented the abbreviation “AHA” and have continued their work on organic acids to this day. They now have more than 125 patents, which they have licensed to 60 companies in the cosmetics and pharmaceutical industries.
In 1988, 14 years after their initial publication, they founded the company they named Polystrata, which grew into today’s NeoStrata.4 Over the years, they had to defend their patents because many personal care companies used their technologies without licensing them. In 2007, they won a $41 million settlement in a patent infringement suit against Mary Kay filed in March 2005. They have both been very philanthropic in the dermatology world5 and are highly respected in the field. Among many other honors, Dr. Van Scott was named a Master Dermatologist by the American Academy of Dermatology in 1998 and received the Dermatology Foundation’s Distinguished Service Medallion in 2004.
Sheldon Pinnell, MD (1937-2013): After Dr. Pinnell completed his dermatology residency at Harvard Medical School, he spent 2 years studying collagen chemistry at the Max Planck Institute in Munich, Germany. In 1973, he returned to Duke University where he had earned his undergraduate degree before attending Yale University. He remained at Duke for the duration of his career and was professor and chief of dermatology there for many years. Early in his career, he focused on the role of vitamin C in collagen biosynthesis and discovered some of the mechanisms by which sun exposure causes photoaging. He described the use of the first (and most popular) topically applied L-ascorbic acid (vitamin C) to prevent and treat skin aging.
Dr. Pinnell’s many discoveries include showing that the addition of ascorbic acid to fibroblast cultures increases collagen production and that topically applied L-ascorbic acid penetrates into the skin best at a pH of 2-2.5. Dr. Pinnell changed the way the world uses topical antioxidants today; he was widely respected and was a member of the American Dermatological Association and an honorary member of the Society of Investigative Dermatology. He published more than 200 scientific articles and held 10 patents. He started the skin care company Skinceuticals, based on his antioxidant technologies. It was acquired by L’Oreal in 2005.
Richard Fitzpatrick, MD (1944-2014): The dermatologist affectionately known as “Fitz” is credited with being the first to use lasers for skin resurfacing. He went to medical school at Emory University and did his dermatology residency at the University of California, Los Angeles. He authored more than 130 publications and was one of the first doctors to specialize in cosmetic dermatology. He realized that fibroblast cell cultures used to produce the collagen filler CosmoPlast (no longer on the market) generated many growth factors that could rejuvenate the skin, and in 1999, he launched the skin care brand SkinMedica. In 2000, he received a patent for fibroblast-derived growth factors used topically for antiaging – a formula he called Tissue Nutrient Solution. In 2001, the popular product TNS Recovery Complex was launched based on the patented growth factor technology. It is still the most popular growth factor technology on the market.
What can we learn from these pioneers? I have had several interesting discussions about this topic with Leonard Hoenig, MD, section editor for Reflections on Dermatology: Past, Present, and Future, in Clinics in Dermatology. (Dr. Hoenig told me the interesting story that Listerine mouthwash was named in honor of Joseph Lister but accounts vary as to whether he gave permission to do so. This makes Dr. Lister the most famous physician to endorse a personal care product.) When Dr. Hoenig and I discussed the ethics of dermatologists creating a skin care line or retailing skin care in their medical practice, he stated my sentiments perfectly: “We should rely on professional, ethical, and legal guidelines to help us do what is right. Most importantly, we should have the best interests of our patients at heart when recommending any treatments.”
Dermatologists have unique knowledge, experience, and perspective on treating the skin with topical agents and have the true desire to improve skin health. If we do not discover, research, patent, and develop efficacious skin care products, someone else will do it – and I do not think they will do it as well as a dermatologist can.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks and a New York Times Best Sellers book for consumers. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., a company that independently tests skin care products and makes recommendations to physicians on which skin care technologies are best. Write to her at [email protected].
References
1. Everett MA. Int J Dermatol. 1978 May;17(4):345-52.
2. Moxon RK. N Engl J Med. 1976 Apr 1;294(14):762-4.
3. Rattner H. Arch Derm Syphilol. 1937;35(1):25-66.
4. Neostrata: More than Hope, by Elaine Strauss, U.S. 1 Newspaper, Feb. 24, 1999.
5. Two legends in the field of dermatology provide $1 million gift to Temple University school of medicine’s department of dermatology, Temple University, June 5, 2015.
Those of you who have visited my dermatology practice in Miami know that the art in my office is dedicated to the history of the skin care industry. I collect , and I have written this historical column in honor of the 50th anniversary of Dermatology News.
The first doctor to market his own cosmetic product, Erasmus Wilson, MD, faced scrutiny from his colleagues. Although he had contributed much to the field of dermatology, he was criticized by other dermatologists when he promoted a hair wash. The next doctor in my story, William Pusey, MD, was criticized for helping the company that manufactured Camay soap because he allowed his name to be used in Camay advertisements. The scrutiny that these two well-respected dermatologists endured from their colleagues deterred dermatologists from entering the skin care business for decades. The professional jealousy from dermatologic colleagues left the skin care field wide open for imposters, charlatans, and nondermatologists who had no concern for efficacy and patient outcomes to flourish. This is the story of a group of brilliant entrepreneurial dermatologists and one chiropractor who misrepresented himself as a dermatologist and how they influenced skin care as we know it.
Erasmus Wilson, MD1 (1809-1884): In 1840, Erasmus Wilson2 was a physician in London who chose to specialize in dermatology at a time when that specialization was frowned upon. He was a subeditor for The Lancet and wrote several books on dermatology including “Diseases of the Skin – A Practical and Theoretical Treatise,” “Portraits of the Diseases of the Skin,” and “Student’s Book on Diseases of the Skin.” He was the first professor of dermatology in the College of Surgeons and by 1869, was the leading English-speaking dermatologist in the world. He contributed much to dermatology, including his pioneering characterizations of Demodex mites, lichen planus, exfoliative dermatitis, neurotic excoriations, and roseola. Dr. Wilson was knighted in 1881 for his good works and notable generosity. (He was known for giving his poor patients money for food, endowing chairs in dermatology, and donating a famous obelisk in London).
In 1854, Dr. Wilson wrote a book for laypeople called “Healthy Skin: A Popular Treatise on the Skin and Hair, Their Preservation and Management,” in which he advocated cleanliness and bathing, which led to the popularity of Turkish baths and bathing resorts in Europe. Despite his undeniable contributions to dermatology, he was widely criticized by his colleagues for promoting a “Hair Wash” and a turtle oil soap. I cannot find any information about whether or not he developed the hair wash and turtle soap himself, but it seems that he earned income from sales of these two products, even though he was said to have donated it all to charities.
William A. Pusey MD (1865-1940): Dr. Pusey was the first chairman of dermatology at the University of Illinois College of Medicine, Chicago. He published several books, including “Care of the Skin and Hair,” “Syphilis as a Modern Problem,” “The Principles and Practices of Dermatology,” and “History of Dermatology” among others. He is best known for his work in developing the use of x-rays (roentgen rays) and phototherapy in dermatology, and in 1907, he was the first dermatologist to describe the use of solid carbon dioxide to treat skin lesions. He was president of the American Dermatological Association in 1910, president of the Chicago Medical Society in 1918, editor of the Archives of Dermatology in 1920, and president of the American Medical Association in 1924.
In the early 1920s, skin care companies were beginning to advertise their products using endorsements from celebrities and socialites, and were making misleading claims. Dr. Pusey wanted to work with these companies to help them perform evidence-based trials so they could make scientifically correct claims. Proctor & Gamble asked Dr. Pusey to advise them on how they could advertise honestly about their new soap, “Camay.” In Dr. Pusey’s words,3 “they (Proctor & Gamble) wanted to give the public authoritative advice about the use of soap and water. They suggested that I get a group of dermatologists of my selection to examine the soap and prepare instructions for bathing and the use of soap, and, if they found this soap was of high quality, to certify to that effect.” The research was performed as he suggested, and he allowed his name to be used in the Camay soap ads from 1926 to 1929. He said that he allowed them to use his name hoping to promote the need for evidence-based research, in contrast to the skin care products endorsed by socialites and celebrities that were flooding the market around that time.
Herbert Rattner, MD, at Northwestern University, Chicago, was his friend and one of the many dermatologists who criticized Dr. Pusey for allowing his name to be used in the Camay ads. Dr. Pusey’s reply to the criticism (according to Dr. Rattner) was that Proctor & Gamble was “proposing to do what the medical profession always is criticizing commercial concerns for not doing, namely, coming to physicians for information on medical matters. Could the profession hope to have any influence with business concerns if it was always eager to criticize bad commercial practices but never willing to support good ones?”3
While Dr. Pusey felt his reasons for adding his name to the Camay ads and research were justified, many of his friends stated that in hindsight, he regretted the action because of the negative response of his colleagues. It was years before dermatologists began providing input again into the skin care industry. During that time, radio, television and print ads were rampant with misleading claims – which led the way for a dermatologic imposter to make a fortune on skin care.
John Woodbury (1851-1909): John Woodbury, a chiropractor, never went to medical school, but that did not stop him from claiming he was a dermatologist and cosmetic surgeon. In 1889, he opened the John H. Woodbury Dermatological Institute in New York City, and over the next few years, opened Woodbury Dermatological Institutes in at least 5 states and employed 25 “physicians” who were not licensed to practice medicine. He came out with face soaps, tonics, and cold creams and spent a fortune on advertising these products and his institutes. In 1901, he sold his “Woodbury Soap” to the Andrew Jergens Company for $212,500 and 10% in royalties.
Multiple lawsuits occurred from 1898 to 1907 because he continued using the Woodbury name on his own products, despite having sold the “Woodbury” trademark to Jergens. He was sued for practicing medicine without a medical license and claiming to be a dermatologist when he was not. He lost most of these lawsuits, including one in 1907 in which the court ruled that corporations may not employ unlicensed professionals to practice medicine. In 1909, John Woodbury committed suicide. The Woodbury Soap company flourished in the 1930s and 1940s, as part of Jergens, until the brand was discontinued in 1970 when Jergens was acquired by American Brands.
The next dermatologists to come along did not make the same mistakes as those of their predecessors. They all made scientific discoveries through their basic science research in the laboratory, filed patents, formed skin care companies, perfected the formulations, and conducted research trials of the final product. Their marketing focused on science and efficacy and only rarely used their names and images in advertising, allowing them to maintain their reputations in the dermatology field.
Eugene Van Scott, MD (1922-present): Dermatologist Dr. Van Scott and dermatopharmacologist Ruey Yu, PhD, filed a method patent in the early 1970s on the effectiveness of alpha hydroxy acids to treat ichthyosis. They invented the abbreviation “AHA” and have continued their work on organic acids to this day. They now have more than 125 patents, which they have licensed to 60 companies in the cosmetics and pharmaceutical industries.
In 1988, 14 years after their initial publication, they founded the company they named Polystrata, which grew into today’s NeoStrata.4 Over the years, they had to defend their patents because many personal care companies used their technologies without licensing them. In 2007, they won a $41 million settlement in a patent infringement suit against Mary Kay filed in March 2005. They have both been very philanthropic in the dermatology world5 and are highly respected in the field. Among many other honors, Dr. Van Scott was named a Master Dermatologist by the American Academy of Dermatology in 1998 and received the Dermatology Foundation’s Distinguished Service Medallion in 2004.
Sheldon Pinnell, MD (1937-2013): After Dr. Pinnell completed his dermatology residency at Harvard Medical School, he spent 2 years studying collagen chemistry at the Max Planck Institute in Munich, Germany. In 1973, he returned to Duke University where he had earned his undergraduate degree before attending Yale University. He remained at Duke for the duration of his career and was professor and chief of dermatology there for many years. Early in his career, he focused on the role of vitamin C in collagen biosynthesis and discovered some of the mechanisms by which sun exposure causes photoaging. He described the use of the first (and most popular) topically applied L-ascorbic acid (vitamin C) to prevent and treat skin aging.
Dr. Pinnell’s many discoveries include showing that the addition of ascorbic acid to fibroblast cultures increases collagen production and that topically applied L-ascorbic acid penetrates into the skin best at a pH of 2-2.5. Dr. Pinnell changed the way the world uses topical antioxidants today; he was widely respected and was a member of the American Dermatological Association and an honorary member of the Society of Investigative Dermatology. He published more than 200 scientific articles and held 10 patents. He started the skin care company Skinceuticals, based on his antioxidant technologies. It was acquired by L’Oreal in 2005.
Richard Fitzpatrick, MD (1944-2014): The dermatologist affectionately known as “Fitz” is credited with being the first to use lasers for skin resurfacing. He went to medical school at Emory University and did his dermatology residency at the University of California, Los Angeles. He authored more than 130 publications and was one of the first doctors to specialize in cosmetic dermatology. He realized that fibroblast cell cultures used to produce the collagen filler CosmoPlast (no longer on the market) generated many growth factors that could rejuvenate the skin, and in 1999, he launched the skin care brand SkinMedica. In 2000, he received a patent for fibroblast-derived growth factors used topically for antiaging – a formula he called Tissue Nutrient Solution. In 2001, the popular product TNS Recovery Complex was launched based on the patented growth factor technology. It is still the most popular growth factor technology on the market.
What can we learn from these pioneers? I have had several interesting discussions about this topic with Leonard Hoenig, MD, section editor for Reflections on Dermatology: Past, Present, and Future, in Clinics in Dermatology. (Dr. Hoenig told me the interesting story that Listerine mouthwash was named in honor of Joseph Lister but accounts vary as to whether he gave permission to do so. This makes Dr. Lister the most famous physician to endorse a personal care product.) When Dr. Hoenig and I discussed the ethics of dermatologists creating a skin care line or retailing skin care in their medical practice, he stated my sentiments perfectly: “We should rely on professional, ethical, and legal guidelines to help us do what is right. Most importantly, we should have the best interests of our patients at heart when recommending any treatments.”
Dermatologists have unique knowledge, experience, and perspective on treating the skin with topical agents and have the true desire to improve skin health. If we do not discover, research, patent, and develop efficacious skin care products, someone else will do it – and I do not think they will do it as well as a dermatologist can.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks and a New York Times Best Sellers book for consumers. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., a company that independently tests skin care products and makes recommendations to physicians on which skin care technologies are best. Write to her at [email protected].
References
1. Everett MA. Int J Dermatol. 1978 May;17(4):345-52.
2. Moxon RK. N Engl J Med. 1976 Apr 1;294(14):762-4.
3. Rattner H. Arch Derm Syphilol. 1937;35(1):25-66.
4. Neostrata: More than Hope, by Elaine Strauss, U.S. 1 Newspaper, Feb. 24, 1999.
5. Two legends in the field of dermatology provide $1 million gift to Temple University school of medicine’s department of dermatology, Temple University, June 5, 2015.
Convalescent plasma actions spark trial recruitment concerns
The agency’s move took many investigators by surprise. The EUA was announced at the White House the day after President Donald J. Trump accused the FDA of delaying approval of therapeutics to hurt his re-election chances.
In a memo describing the decision, the FDA cited data from some controlled and uncontrolled studies and, primarily, data from an open-label expanded-access protocol overseen by the Mayo Clinic.
At the White House, FDA Commissioner Stephen Hahn, MD, said that plasma had been found to save the lives of 35 out of every 100 who were treated. That figure was later found to have been erroneous, and many experts pointed out that Hahn had conflated an absolute risk reduction with a relative reduction. After a firestorm of criticism, Hahn issued an apology.
“The criticism is entirely justified,” he tweeted. “What I should have said better is that the data show a relative risk reduction not an absolute risk reduction.”
About 15 randomized controlled trials – out of 54 total studies involving convalescent plasma – are underway in the United States, according to ClinicalTrials.gov. The FDA’s Aug. 23 emergency authorization gave clinicians wide leeway to employ convalescent plasma in patients hospitalized with COVID-19.
The agency noted, however, that “adequate and well-controlled randomized trials remain necessary for a definitive demonstration of COVID-19 convalescent plasma efficacy and to determine the optimal product attributes and appropriate patient populations for its use.”
But it’s not clear that people with COVID-19, especially those who are severely ill and hospitalized, will choose to enlist in a clinical trial – where they could receive a placebo – when they instead could get plasma.
“I’ve been asked repeatedly whether the EUA will affect our ability to recruit people into our hospitalized patient trial,” said Liise-anne Pirofski, MD, FIDSA, chief of the department of medicine, infectious diseases division at Albert Einstein College of Medicine and Montefiore Medical Center in the Bronx, New York. “I do not know,” she said, on a call with reporters organized by the Infectious Diseases Society of America.
“But,” she said, “I do know that the trial will continue and that we will discuss the evidence that we have with our patients and give them all that we can to help them weigh the evidence and make up their minds.”
Pirofski said the study being conducted at Montefiore and four other sites has since late April enrolled 190 patients out of a hoped-for 300.
When the study – which compares convalescent plasma to saline in hospitalized patients – was first designed, “there was not any funding for our trial and honestly not a whole lot of interest,” Pirofski told reporters. Individual donors helped support the initial rollout in late April and the trial quickly enrolled 150 patients as the pandemic peaked in the New York City area.
The National Institutes of Health has since given funding, which allowed the study to expand to New York University, Yale University, the University of Miami, and the University of Texas at Houston.
Hopeful, but a long way to go
Shmuel Shoham, MD, FIDSA, associate director of the transplant and oncology infectious diseases center at Johns Hopkins University School of Medicine in Baltimore, said that he’s hopeful that people will continue to enroll in his trial, which is seeking to determine if plasma can prevent COVID-19 in those who’ve been recently exposed.
“Volunteers joining the study is the only way that we’re going to get to know whether this stuff works for prevention and treatment,” Shoham said on the call. He urged physicians and other healthcare workers to talk with patients about considering trial participation.
Shoham’s study is being conducted at 30 US sites and one at the Navajo Nation. It has enrolled 25 out of a hoped-for 500 participants. “We have a long way to go,” said Shoham.
Another Hopkins study to determine whether plasma is helpful in shortening illness in nonhospitalized patients, which is being conducted at the same 31 sites, has enrolled 50 out of 600.
Shoham said recruiting patients with COVID for any study had proven to be difficult. “The vast majority of people that have coronavirus do not come to centers that do clinical trials or interventional trials,” he said, adding that, in addition, most of those “who have coronavirus don’t want to be in a trial. They just want to have coronavirus and get it over with.”
But it’s important to understand how to conduct trials in a pandemic – in part to get answers quickly, he said. Researchers have been looking at convalescent plasma for months, said Shoham. “Why don’t we have the randomized clinical trial data that we want?”
Pirofski noted that trials have also been hobbled in part by “the shifting areas of the pandemic.” Fewer cases make for fewer potential plasma donors.
Both Shoham and Pirofski also said that more needed to be done to encourage plasma donors to participate.
The US Department of Health & Human Services clarified in August that hospitals, physicians, health plans, and other health care workers could contact individuals who had recovered from COVID-19 without violating the HIPAA privacy rule.
Pirofski said she believes that trial investigators know it is legal to reach out to patients. But, she said, “it probably could be better known.”
This article first appeared on Medscape.com.
The agency’s move took many investigators by surprise. The EUA was announced at the White House the day after President Donald J. Trump accused the FDA of delaying approval of therapeutics to hurt his re-election chances.
In a memo describing the decision, the FDA cited data from some controlled and uncontrolled studies and, primarily, data from an open-label expanded-access protocol overseen by the Mayo Clinic.
At the White House, FDA Commissioner Stephen Hahn, MD, said that plasma had been found to save the lives of 35 out of every 100 who were treated. That figure was later found to have been erroneous, and many experts pointed out that Hahn had conflated an absolute risk reduction with a relative reduction. After a firestorm of criticism, Hahn issued an apology.
“The criticism is entirely justified,” he tweeted. “What I should have said better is that the data show a relative risk reduction not an absolute risk reduction.”
About 15 randomized controlled trials – out of 54 total studies involving convalescent plasma – are underway in the United States, according to ClinicalTrials.gov. The FDA’s Aug. 23 emergency authorization gave clinicians wide leeway to employ convalescent plasma in patients hospitalized with COVID-19.
The agency noted, however, that “adequate and well-controlled randomized trials remain necessary for a definitive demonstration of COVID-19 convalescent plasma efficacy and to determine the optimal product attributes and appropriate patient populations for its use.”
But it’s not clear that people with COVID-19, especially those who are severely ill and hospitalized, will choose to enlist in a clinical trial – where they could receive a placebo – when they instead could get plasma.
“I’ve been asked repeatedly whether the EUA will affect our ability to recruit people into our hospitalized patient trial,” said Liise-anne Pirofski, MD, FIDSA, chief of the department of medicine, infectious diseases division at Albert Einstein College of Medicine and Montefiore Medical Center in the Bronx, New York. “I do not know,” she said, on a call with reporters organized by the Infectious Diseases Society of America.
“But,” she said, “I do know that the trial will continue and that we will discuss the evidence that we have with our patients and give them all that we can to help them weigh the evidence and make up their minds.”
Pirofski said the study being conducted at Montefiore and four other sites has since late April enrolled 190 patients out of a hoped-for 300.
When the study – which compares convalescent plasma to saline in hospitalized patients – was first designed, “there was not any funding for our trial and honestly not a whole lot of interest,” Pirofski told reporters. Individual donors helped support the initial rollout in late April and the trial quickly enrolled 150 patients as the pandemic peaked in the New York City area.
The National Institutes of Health has since given funding, which allowed the study to expand to New York University, Yale University, the University of Miami, and the University of Texas at Houston.
Hopeful, but a long way to go
Shmuel Shoham, MD, FIDSA, associate director of the transplant and oncology infectious diseases center at Johns Hopkins University School of Medicine in Baltimore, said that he’s hopeful that people will continue to enroll in his trial, which is seeking to determine if plasma can prevent COVID-19 in those who’ve been recently exposed.
“Volunteers joining the study is the only way that we’re going to get to know whether this stuff works for prevention and treatment,” Shoham said on the call. He urged physicians and other healthcare workers to talk with patients about considering trial participation.
Shoham’s study is being conducted at 30 US sites and one at the Navajo Nation. It has enrolled 25 out of a hoped-for 500 participants. “We have a long way to go,” said Shoham.
Another Hopkins study to determine whether plasma is helpful in shortening illness in nonhospitalized patients, which is being conducted at the same 31 sites, has enrolled 50 out of 600.
Shoham said recruiting patients with COVID for any study had proven to be difficult. “The vast majority of people that have coronavirus do not come to centers that do clinical trials or interventional trials,” he said, adding that, in addition, most of those “who have coronavirus don’t want to be in a trial. They just want to have coronavirus and get it over with.”
But it’s important to understand how to conduct trials in a pandemic – in part to get answers quickly, he said. Researchers have been looking at convalescent plasma for months, said Shoham. “Why don’t we have the randomized clinical trial data that we want?”
Pirofski noted that trials have also been hobbled in part by “the shifting areas of the pandemic.” Fewer cases make for fewer potential plasma donors.
Both Shoham and Pirofski also said that more needed to be done to encourage plasma donors to participate.
The US Department of Health & Human Services clarified in August that hospitals, physicians, health plans, and other health care workers could contact individuals who had recovered from COVID-19 without violating the HIPAA privacy rule.
Pirofski said she believes that trial investigators know it is legal to reach out to patients. But, she said, “it probably could be better known.”
This article first appeared on Medscape.com.
The agency’s move took many investigators by surprise. The EUA was announced at the White House the day after President Donald J. Trump accused the FDA of delaying approval of therapeutics to hurt his re-election chances.
In a memo describing the decision, the FDA cited data from some controlled and uncontrolled studies and, primarily, data from an open-label expanded-access protocol overseen by the Mayo Clinic.
At the White House, FDA Commissioner Stephen Hahn, MD, said that plasma had been found to save the lives of 35 out of every 100 who were treated. That figure was later found to have been erroneous, and many experts pointed out that Hahn had conflated an absolute risk reduction with a relative reduction. After a firestorm of criticism, Hahn issued an apology.
“The criticism is entirely justified,” he tweeted. “What I should have said better is that the data show a relative risk reduction not an absolute risk reduction.”
About 15 randomized controlled trials – out of 54 total studies involving convalescent plasma – are underway in the United States, according to ClinicalTrials.gov. The FDA’s Aug. 23 emergency authorization gave clinicians wide leeway to employ convalescent plasma in patients hospitalized with COVID-19.
The agency noted, however, that “adequate and well-controlled randomized trials remain necessary for a definitive demonstration of COVID-19 convalescent plasma efficacy and to determine the optimal product attributes and appropriate patient populations for its use.”
But it’s not clear that people with COVID-19, especially those who are severely ill and hospitalized, will choose to enlist in a clinical trial – where they could receive a placebo – when they instead could get plasma.
“I’ve been asked repeatedly whether the EUA will affect our ability to recruit people into our hospitalized patient trial,” said Liise-anne Pirofski, MD, FIDSA, chief of the department of medicine, infectious diseases division at Albert Einstein College of Medicine and Montefiore Medical Center in the Bronx, New York. “I do not know,” she said, on a call with reporters organized by the Infectious Diseases Society of America.
“But,” she said, “I do know that the trial will continue and that we will discuss the evidence that we have with our patients and give them all that we can to help them weigh the evidence and make up their minds.”
Pirofski said the study being conducted at Montefiore and four other sites has since late April enrolled 190 patients out of a hoped-for 300.
When the study – which compares convalescent plasma to saline in hospitalized patients – was first designed, “there was not any funding for our trial and honestly not a whole lot of interest,” Pirofski told reporters. Individual donors helped support the initial rollout in late April and the trial quickly enrolled 150 patients as the pandemic peaked in the New York City area.
The National Institutes of Health has since given funding, which allowed the study to expand to New York University, Yale University, the University of Miami, and the University of Texas at Houston.
Hopeful, but a long way to go
Shmuel Shoham, MD, FIDSA, associate director of the transplant and oncology infectious diseases center at Johns Hopkins University School of Medicine in Baltimore, said that he’s hopeful that people will continue to enroll in his trial, which is seeking to determine if plasma can prevent COVID-19 in those who’ve been recently exposed.
“Volunteers joining the study is the only way that we’re going to get to know whether this stuff works for prevention and treatment,” Shoham said on the call. He urged physicians and other healthcare workers to talk with patients about considering trial participation.
Shoham’s study is being conducted at 30 US sites and one at the Navajo Nation. It has enrolled 25 out of a hoped-for 500 participants. “We have a long way to go,” said Shoham.
Another Hopkins study to determine whether plasma is helpful in shortening illness in nonhospitalized patients, which is being conducted at the same 31 sites, has enrolled 50 out of 600.
Shoham said recruiting patients with COVID for any study had proven to be difficult. “The vast majority of people that have coronavirus do not come to centers that do clinical trials or interventional trials,” he said, adding that, in addition, most of those “who have coronavirus don’t want to be in a trial. They just want to have coronavirus and get it over with.”
But it’s important to understand how to conduct trials in a pandemic – in part to get answers quickly, he said. Researchers have been looking at convalescent plasma for months, said Shoham. “Why don’t we have the randomized clinical trial data that we want?”
Pirofski noted that trials have also been hobbled in part by “the shifting areas of the pandemic.” Fewer cases make for fewer potential plasma donors.
Both Shoham and Pirofski also said that more needed to be done to encourage plasma donors to participate.
The US Department of Health & Human Services clarified in August that hospitals, physicians, health plans, and other health care workers could contact individuals who had recovered from COVID-19 without violating the HIPAA privacy rule.
Pirofski said she believes that trial investigators know it is legal to reach out to patients. But, she said, “it probably could be better known.”
This article first appeared on Medscape.com.
Nine antihypertensive drugs associated with reduced risk of depression
The risk of depression is elevated in patients with cardiovascular diseases, but several specific antihypertensive therapies are associated with a reduced risk, and none appear to increase the risk, according to a population-based study that evaluated 10 years of data in nearly 4 million subjects.
“As the first study on individual antihypertensives and risk of depression, we found a decreased risk of depression with nine drugs,” reported a collaborative group of investigators from multiple institutions in Denmark where the study was undertaken.
In a study period spanning from 2005 to 2015, risk of a diagnosis of depression was evaluated in patients taking any of 41 antihypertensive therapies in four major categories. These were identified as angiotensin agents (ACE inhibitors or angiotensin II receptor blockers), calcium antagonists, beta-blockers, and diuretics.
Within these groups, agents associated with a reduced risk of depression were: two angiotensin agents, enalapril and ramipril; three calcium antagonists, amlodipine, verapamil, and verapamil combinations; and four beta-blockers, propranolol, atenolol, bisoprolol, and carvedilol. The remaining drugs in these classes and diuretics were not associated with a reduced risk of depression. However, no antihypertensive agent was linked to an increased risk of depression.
All people living in Denmark are assigned a unique personal identification number that permits health information to be tracked across multiple registers. In this study, information was linked for several registries, including the Danish Medical Register on Vital Statistics, the Medicinal Product Statistics, and the Danish Psychiatric Central Register.
Data from a total of 3.75 million patients exposed to antihypertensive therapy during the study period were evaluated. Roughly 1 million of them were exposed to angiotensin drugs and slightly more than a million were exposed to diuretics. For calcium antagonists or beta-blockers, the numbers were approximately 835,000 and 775,000, respectively.
After adjustment for such factors as concomitant somatic diagnoses, sex, age, and employment status, the hazard ratios for depression among drugs associated with protection identified a risk reduction of 10%-25% in most cases when those who had been given 6-10 prescriptions or more than 10 prescriptions were compared with those who received 2 or fewer.
At the level of 10 or more prescriptions, for example, the risk reductions were 17% for ramipril (HR, 0.83; 95% CI, 0.78-0.89), 8% for enalapril (HR, 0.92; 95% CI, 0.88-0.96), 18% for amlodipine (HR, 0.82; 95% CI, 0.79-0.86), 15% for verapamil (HR, 0.85; 95% CI, 0.79-0.83), 28% for propranolol (HR, 0.72; 95% CI, 0.67-0.77), 20% for atenolol (HR, 0.80; 95% CI, 0.74-0.86), 25% for bisoprolol (HR, 0.75; 95% CI, 0.67-0.84), and 16% for carvedilol (HR, 0.84; 95% CI, 0.75-0.95).
For verapamil combinations, the risk reduction was 67% (HR, 0.33; 95% CI, 0.17-0.63), but the investigators cautioned that only 130 individuals were exposed to verapamil combinations, limiting the reliability of this analysis.
Interpreting the findings
A study hypothesis, the observed protective effect against depression, was expected for angiotensin drugs and calcium-channel blockers, but not for beta-blockers, according to the investigators.
“The renin-angiotensin systems is one of the pathways known to modulate inflammation in the central nervous system and seems involved in the regulation of the stress response. Angiotensin agents may also exert anti-inflammatory effects,” the investigators explained. “Dysregulation of intracellular calcium is evident in depression, including receptor-regulated calcium signaling.”
In contrast, beta-blockers have been associated with increased risk of depression in some but not all studies, according to the investigators. They maintained that some clinicians avoid these agents in patients with a history of mood disorders.
In attempting to account for the variability within drug classes regarding protection and lack of protection against depression, the investigators speculated that differences in pharmacologic properties, such as relative lipophilicity or anti-inflammatory effect, might be important.
Despite the large amount of data, William B. White, MD, professor emeritus at the Calhoun Cardiology Center, University of Connecticut, Farmington, is not convinced.
“In observational studies, even those with very large samples sizes, bias and confounding are hard to extricate with controls and propensity-score matching,” Dr. White said. From his perspective, the protective effects of some but not all drugs within a class “give one the impression that the findings are likely random.”
A member of the editorial board of the journal in which this study appeared, Dr. White said he was not involved in the review of the manuscript. Ultimately, he believed that the results are difficult to interpret.
“For example, there is no plausible rationale for why 2 of the 16 ACE inhibitors or angiotensin II receptor blockers or 4 of the 15 beta-blockers or 3 of the 10 calcium-channel blockers would reduce depression while the others in the class would have no effect,” he said.
Despite the investigators’ conclusion that these data should drive drug choice for patients at risk of depression, “I would say the results of this analysis would not lead me to alter clinical practice,” Dr. White added.
According to the principal investigator of the study, Lars Vedel Kessing, MD, DSc, professor of psychiatry at the University of Copenhagen, many variables affect choice of antihypertensive drug. However, the depression risk is elevated in patients with cardiovascular or cerebrovascular disease and hypertension.
When risk of a mood disorder is a concern, use of one of the nine drugs associated with protection from depression should be considered, “especially in patients at increased risk of developing depression, including patients with prior depression or anxiety and patients with a family history of depression,” he and his coinvestigators concluded.
However, Dr. Kessing said in an interview that the data do not help with individual treatment choices. “We do not compare different antihypertensives against each other due to the risk of confounding by indications, so, no, it is not reasonable to consider relative risk among specific agents.”
The authors reported no potential conflicts of interest involving this topic.
SOURCE: Kessing LV et al. Hypertension. 2020 Aug 24. doi: 10.1161/HYPERTENSIONAHA.120.15605.
The risk of depression is elevated in patients with cardiovascular diseases, but several specific antihypertensive therapies are associated with a reduced risk, and none appear to increase the risk, according to a population-based study that evaluated 10 years of data in nearly 4 million subjects.
“As the first study on individual antihypertensives and risk of depression, we found a decreased risk of depression with nine drugs,” reported a collaborative group of investigators from multiple institutions in Denmark where the study was undertaken.
In a study period spanning from 2005 to 2015, risk of a diagnosis of depression was evaluated in patients taking any of 41 antihypertensive therapies in four major categories. These were identified as angiotensin agents (ACE inhibitors or angiotensin II receptor blockers), calcium antagonists, beta-blockers, and diuretics.
Within these groups, agents associated with a reduced risk of depression were: two angiotensin agents, enalapril and ramipril; three calcium antagonists, amlodipine, verapamil, and verapamil combinations; and four beta-blockers, propranolol, atenolol, bisoprolol, and carvedilol. The remaining drugs in these classes and diuretics were not associated with a reduced risk of depression. However, no antihypertensive agent was linked to an increased risk of depression.
All people living in Denmark are assigned a unique personal identification number that permits health information to be tracked across multiple registers. In this study, information was linked for several registries, including the Danish Medical Register on Vital Statistics, the Medicinal Product Statistics, and the Danish Psychiatric Central Register.
Data from a total of 3.75 million patients exposed to antihypertensive therapy during the study period were evaluated. Roughly 1 million of them were exposed to angiotensin drugs and slightly more than a million were exposed to diuretics. For calcium antagonists or beta-blockers, the numbers were approximately 835,000 and 775,000, respectively.
After adjustment for such factors as concomitant somatic diagnoses, sex, age, and employment status, the hazard ratios for depression among drugs associated with protection identified a risk reduction of 10%-25% in most cases when those who had been given 6-10 prescriptions or more than 10 prescriptions were compared with those who received 2 or fewer.
At the level of 10 or more prescriptions, for example, the risk reductions were 17% for ramipril (HR, 0.83; 95% CI, 0.78-0.89), 8% for enalapril (HR, 0.92; 95% CI, 0.88-0.96), 18% for amlodipine (HR, 0.82; 95% CI, 0.79-0.86), 15% for verapamil (HR, 0.85; 95% CI, 0.79-0.83), 28% for propranolol (HR, 0.72; 95% CI, 0.67-0.77), 20% for atenolol (HR, 0.80; 95% CI, 0.74-0.86), 25% for bisoprolol (HR, 0.75; 95% CI, 0.67-0.84), and 16% for carvedilol (HR, 0.84; 95% CI, 0.75-0.95).
For verapamil combinations, the risk reduction was 67% (HR, 0.33; 95% CI, 0.17-0.63), but the investigators cautioned that only 130 individuals were exposed to verapamil combinations, limiting the reliability of this analysis.
Interpreting the findings
A study hypothesis, the observed protective effect against depression, was expected for angiotensin drugs and calcium-channel blockers, but not for beta-blockers, according to the investigators.
“The renin-angiotensin systems is one of the pathways known to modulate inflammation in the central nervous system and seems involved in the regulation of the stress response. Angiotensin agents may also exert anti-inflammatory effects,” the investigators explained. “Dysregulation of intracellular calcium is evident in depression, including receptor-regulated calcium signaling.”
In contrast, beta-blockers have been associated with increased risk of depression in some but not all studies, according to the investigators. They maintained that some clinicians avoid these agents in patients with a history of mood disorders.
In attempting to account for the variability within drug classes regarding protection and lack of protection against depression, the investigators speculated that differences in pharmacologic properties, such as relative lipophilicity or anti-inflammatory effect, might be important.
Despite the large amount of data, William B. White, MD, professor emeritus at the Calhoun Cardiology Center, University of Connecticut, Farmington, is not convinced.
“In observational studies, even those with very large samples sizes, bias and confounding are hard to extricate with controls and propensity-score matching,” Dr. White said. From his perspective, the protective effects of some but not all drugs within a class “give one the impression that the findings are likely random.”
A member of the editorial board of the journal in which this study appeared, Dr. White said he was not involved in the review of the manuscript. Ultimately, he believed that the results are difficult to interpret.
“For example, there is no plausible rationale for why 2 of the 16 ACE inhibitors or angiotensin II receptor blockers or 4 of the 15 beta-blockers or 3 of the 10 calcium-channel blockers would reduce depression while the others in the class would have no effect,” he said.
Despite the investigators’ conclusion that these data should drive drug choice for patients at risk of depression, “I would say the results of this analysis would not lead me to alter clinical practice,” Dr. White added.
According to the principal investigator of the study, Lars Vedel Kessing, MD, DSc, professor of psychiatry at the University of Copenhagen, many variables affect choice of antihypertensive drug. However, the depression risk is elevated in patients with cardiovascular or cerebrovascular disease and hypertension.
When risk of a mood disorder is a concern, use of one of the nine drugs associated with protection from depression should be considered, “especially in patients at increased risk of developing depression, including patients with prior depression or anxiety and patients with a family history of depression,” he and his coinvestigators concluded.
However, Dr. Kessing said in an interview that the data do not help with individual treatment choices. “We do not compare different antihypertensives against each other due to the risk of confounding by indications, so, no, it is not reasonable to consider relative risk among specific agents.”
The authors reported no potential conflicts of interest involving this topic.
SOURCE: Kessing LV et al. Hypertension. 2020 Aug 24. doi: 10.1161/HYPERTENSIONAHA.120.15605.
The risk of depression is elevated in patients with cardiovascular diseases, but several specific antihypertensive therapies are associated with a reduced risk, and none appear to increase the risk, according to a population-based study that evaluated 10 years of data in nearly 4 million subjects.
“As the first study on individual antihypertensives and risk of depression, we found a decreased risk of depression with nine drugs,” reported a collaborative group of investigators from multiple institutions in Denmark where the study was undertaken.
In a study period spanning from 2005 to 2015, risk of a diagnosis of depression was evaluated in patients taking any of 41 antihypertensive therapies in four major categories. These were identified as angiotensin agents (ACE inhibitors or angiotensin II receptor blockers), calcium antagonists, beta-blockers, and diuretics.
Within these groups, agents associated with a reduced risk of depression were: two angiotensin agents, enalapril and ramipril; three calcium antagonists, amlodipine, verapamil, and verapamil combinations; and four beta-blockers, propranolol, atenolol, bisoprolol, and carvedilol. The remaining drugs in these classes and diuretics were not associated with a reduced risk of depression. However, no antihypertensive agent was linked to an increased risk of depression.
All people living in Denmark are assigned a unique personal identification number that permits health information to be tracked across multiple registers. In this study, information was linked for several registries, including the Danish Medical Register on Vital Statistics, the Medicinal Product Statistics, and the Danish Psychiatric Central Register.
Data from a total of 3.75 million patients exposed to antihypertensive therapy during the study period were evaluated. Roughly 1 million of them were exposed to angiotensin drugs and slightly more than a million were exposed to diuretics. For calcium antagonists or beta-blockers, the numbers were approximately 835,000 and 775,000, respectively.
After adjustment for such factors as concomitant somatic diagnoses, sex, age, and employment status, the hazard ratios for depression among drugs associated with protection identified a risk reduction of 10%-25% in most cases when those who had been given 6-10 prescriptions or more than 10 prescriptions were compared with those who received 2 or fewer.
At the level of 10 or more prescriptions, for example, the risk reductions were 17% for ramipril (HR, 0.83; 95% CI, 0.78-0.89), 8% for enalapril (HR, 0.92; 95% CI, 0.88-0.96), 18% for amlodipine (HR, 0.82; 95% CI, 0.79-0.86), 15% for verapamil (HR, 0.85; 95% CI, 0.79-0.83), 28% for propranolol (HR, 0.72; 95% CI, 0.67-0.77), 20% for atenolol (HR, 0.80; 95% CI, 0.74-0.86), 25% for bisoprolol (HR, 0.75; 95% CI, 0.67-0.84), and 16% for carvedilol (HR, 0.84; 95% CI, 0.75-0.95).
For verapamil combinations, the risk reduction was 67% (HR, 0.33; 95% CI, 0.17-0.63), but the investigators cautioned that only 130 individuals were exposed to verapamil combinations, limiting the reliability of this analysis.
Interpreting the findings
A study hypothesis, the observed protective effect against depression, was expected for angiotensin drugs and calcium-channel blockers, but not for beta-blockers, according to the investigators.
“The renin-angiotensin systems is one of the pathways known to modulate inflammation in the central nervous system and seems involved in the regulation of the stress response. Angiotensin agents may also exert anti-inflammatory effects,” the investigators explained. “Dysregulation of intracellular calcium is evident in depression, including receptor-regulated calcium signaling.”
In contrast, beta-blockers have been associated with increased risk of depression in some but not all studies, according to the investigators. They maintained that some clinicians avoid these agents in patients with a history of mood disorders.
In attempting to account for the variability within drug classes regarding protection and lack of protection against depression, the investigators speculated that differences in pharmacologic properties, such as relative lipophilicity or anti-inflammatory effect, might be important.
Despite the large amount of data, William B. White, MD, professor emeritus at the Calhoun Cardiology Center, University of Connecticut, Farmington, is not convinced.
“In observational studies, even those with very large samples sizes, bias and confounding are hard to extricate with controls and propensity-score matching,” Dr. White said. From his perspective, the protective effects of some but not all drugs within a class “give one the impression that the findings are likely random.”
A member of the editorial board of the journal in which this study appeared, Dr. White said he was not involved in the review of the manuscript. Ultimately, he believed that the results are difficult to interpret.
“For example, there is no plausible rationale for why 2 of the 16 ACE inhibitors or angiotensin II receptor blockers or 4 of the 15 beta-blockers or 3 of the 10 calcium-channel blockers would reduce depression while the others in the class would have no effect,” he said.
Despite the investigators’ conclusion that these data should drive drug choice for patients at risk of depression, “I would say the results of this analysis would not lead me to alter clinical practice,” Dr. White added.
According to the principal investigator of the study, Lars Vedel Kessing, MD, DSc, professor of psychiatry at the University of Copenhagen, many variables affect choice of antihypertensive drug. However, the depression risk is elevated in patients with cardiovascular or cerebrovascular disease and hypertension.
When risk of a mood disorder is a concern, use of one of the nine drugs associated with protection from depression should be considered, “especially in patients at increased risk of developing depression, including patients with prior depression or anxiety and patients with a family history of depression,” he and his coinvestigators concluded.
However, Dr. Kessing said in an interview that the data do not help with individual treatment choices. “We do not compare different antihypertensives against each other due to the risk of confounding by indications, so, no, it is not reasonable to consider relative risk among specific agents.”
The authors reported no potential conflicts of interest involving this topic.
SOURCE: Kessing LV et al. Hypertension. 2020 Aug 24. doi: 10.1161/HYPERTENSIONAHA.120.15605.
FROM HYPERTENSION
e-Interview With CHEST President-Elect Steven Q. Simpson, MD, FCCP
CHEST President-Elect Steven Q. Simpson, MD, FCCP, is Professor of Medicine in the Division of Pulmonary and Critical Care Medicine at the University of Kansas. He is also senior advisor to the Solving Sepsis initiative of the Biomedical Advanced Research and Development Authority (BARDA) of the US Department of Health and Human Services.
As we greet our new incoming CHEST President, we asked him for a few thoughts about his upcoming presidential year. He kindly offered these responses:
What would you like to accomplish as President of CHEST?
This is an interesting question, because a global pandemic and other developments in our world dictate that our organizational goals must adapt to a landscape that has shifted in recent months. My goals as President are somewhat different from what I stated when I ran for the office.
1. First, I will build on the efforts of my predecessors to ensure that CHEST is an inclusive and anti-racist organization. All CHEST members must have equal opportunities within our organization to advance their lives and their careers, regardless of race, ethnicity, sex, or gender. My goal is to examine our structures for participation and advancement to positions of leadership in the organization and to evaluate our educational and research offerings, all with the purpose of discovering and remedying places where we have been blind to our own systematic bias. Further, CHEST must advocate for and lead others to advocate for equality, for equal access to medical care, and for policies that promote them. We must be leaders in this arena, through both our voice and our actions.
2. We will build on CHEST’s new initiative to support the wellness of our members and to help us all perform at our best, day in and day out. I hope for our newly established Wellness Center to become a frequent stop for all CHEST members, myself included, to help us to sustain ourselves through the pandemic and beyond.
3. We must maintain both the quality and the feel of our educational and research offerings during this time when we cannot come together in person. My goal for us is that we use this time to embrace remote and nontemporally synchronous education, ie, web-based education, to make CHEST’s offerings the best anywhere. In the remainder of the 21st century, digital transformation of teaching and learning will advance tremendously, and our creative use of technology will become a norm. I hope that we never abandon in-person meetings, but using technology to improve information transfer and augmenting our members’ continuing education are clearly here to stay. My goal for us is that we maintain an atmosphere to both our in-person meetings and our remotely delivered meetings that makes generating new knowledge and learning what we generate enjoyable, even fun. I believe our digital transformation will make some interesting things possible over time.
4. My overall goal for CHEST in the coming year is not that we “make it through” the current pandemic, but that we emerge stronger, smarter, and better for the experience, and prepared for the next challenge(s).
Before COVID-19, I had goals for my presidency, and these issues have not disappeared. CHEST needs to be user- friendly for our members, from our website, to the ways in which we deliver education, to the type of research we develop and promote. On the research side, our members have long been interested in clinical research that informs and improves our patient care. My goal is to double down on promoting, supporting, and presenting research that serves exactly this purpose. We are growing our team-based education, and I have a special goal for CHEST to become the home for pulmonary, critical care, and sleep advanced practice providers. I care tremendously about our international members, and I will promote both international growth and catering of CHEST’s offerings to benefit our international members.
What do you consider to be the greatest strength of CHEST, and how will you build upon this during your Presidency?
There is zero doubt that CHEST’s greatest strength is the people who gravitate to our organization. From pure clinicians to academicians; from clinical researchers to clinical educators to outcomes mavens—all levels of the health-care team. At every level of this organization are members who all want to be better at what we do, who want to figure out the ways for doing that, who want to explore the boundaries of what that means, and who want to help others to do the same. That goes, as well, for the professional staff who support the members, and who have adopted the motto, “CRUSH lung disease,” because they share our mission and are here to help us do it better.
The absolutely most enjoyable thing about leadership is having the opportunity to survey the landscape and see who’s looking for opportunity, who’s a rising star, who’s looking for people to mentor, then matching those people with opportunities and with jobs to do. Good people who are motivated by the right principles rise to the occasion. My job as President is to help ensure that the organization via the CHEST Board of Regents is addressing the correct problems with the right vision, to identify the right talented and dedicated members for the jobs, and then to support and stay out of their way as they make the vision a reality.
What are some challenges facing CHEST, and how will you address these challenges?
The major immediate challenges facing CHEST are pandemic-related, in terms of helping to ensure the well-being of our members, and in helping them to address the inequities and disparities in care for our patients of color, who have been hardest hit by the emergence of SARS-CoV-2. I addressed these with my goals, above. To be more specific, though, our board will be using various techniques, including dialogue with our members of color, to understand and address our own implicit biases, so that we can achieve the correct vision and tone of inclusion for all of our members. Also addressed in my goals is the isolation from one another that we are all experiencing because of the pandemic. This situation makes it difficult for us to maintain the style and tone of live learning experiences that our CHEST members are accustomed to. The challenge is to develop materials that can be interactive at a distance, and this likely includes gamification of educational content and employing virtual reality. CHEST Innovations is already working in this arena, and it will be our job as member volunteers to support those efforts. The isolation affects our international members, as well, and our ability to travel to maintain relationships. The nice thing is that web conferencing works just as well for international meetings as for meetings in the US, although somebody often has to go to bed very late or get up very early in the morning to make them work! The efforts are worth our time. Again, we will be working in various arenas to maintain and grow our international relationships.
And finally, what is your charge to the members and new Fellows (FCCPs) of CHEST?
We do not yet see clearly whether to expect a massive winter surge of COVID-19 infections. However, it is a reasonably likely possibility. My charge to our members and our new Fellows is first to stay safe, yourself, and to take care of your mental and physical well-being, so that you can be present and functioning at peak levels for your patients. Make sure your family is, likewise, being safe. Secondly, keep doing what you do, which is excellent patient care, excellent teaching, excellent research to push the boundaries of our knowledge. And finally, you’ve seen my ideas of the challenges facing CHEST. I want you to survey, yourself, and tell me what you think our challenges, goals, and responsibilities should be. And if anything I’ve said resonates with you, volunteer to help us address our challenges and keep CHEST the professional home that you deserve and that you will never want to leave. CHEST wants you and needs you. We are so happy you are with us!
CHEST President-Elect Steven Q. Simpson, MD, FCCP, is Professor of Medicine in the Division of Pulmonary and Critical Care Medicine at the University of Kansas. He is also senior advisor to the Solving Sepsis initiative of the Biomedical Advanced Research and Development Authority (BARDA) of the US Department of Health and Human Services.
As we greet our new incoming CHEST President, we asked him for a few thoughts about his upcoming presidential year. He kindly offered these responses:
What would you like to accomplish as President of CHEST?
This is an interesting question, because a global pandemic and other developments in our world dictate that our organizational goals must adapt to a landscape that has shifted in recent months. My goals as President are somewhat different from what I stated when I ran for the office.
1. First, I will build on the efforts of my predecessors to ensure that CHEST is an inclusive and anti-racist organization. All CHEST members must have equal opportunities within our organization to advance their lives and their careers, regardless of race, ethnicity, sex, or gender. My goal is to examine our structures for participation and advancement to positions of leadership in the organization and to evaluate our educational and research offerings, all with the purpose of discovering and remedying places where we have been blind to our own systematic bias. Further, CHEST must advocate for and lead others to advocate for equality, for equal access to medical care, and for policies that promote them. We must be leaders in this arena, through both our voice and our actions.
2. We will build on CHEST’s new initiative to support the wellness of our members and to help us all perform at our best, day in and day out. I hope for our newly established Wellness Center to become a frequent stop for all CHEST members, myself included, to help us to sustain ourselves through the pandemic and beyond.
3. We must maintain both the quality and the feel of our educational and research offerings during this time when we cannot come together in person. My goal for us is that we use this time to embrace remote and nontemporally synchronous education, ie, web-based education, to make CHEST’s offerings the best anywhere. In the remainder of the 21st century, digital transformation of teaching and learning will advance tremendously, and our creative use of technology will become a norm. I hope that we never abandon in-person meetings, but using technology to improve information transfer and augmenting our members’ continuing education are clearly here to stay. My goal for us is that we maintain an atmosphere to both our in-person meetings and our remotely delivered meetings that makes generating new knowledge and learning what we generate enjoyable, even fun. I believe our digital transformation will make some interesting things possible over time.
4. My overall goal for CHEST in the coming year is not that we “make it through” the current pandemic, but that we emerge stronger, smarter, and better for the experience, and prepared for the next challenge(s).
Before COVID-19, I had goals for my presidency, and these issues have not disappeared. CHEST needs to be user- friendly for our members, from our website, to the ways in which we deliver education, to the type of research we develop and promote. On the research side, our members have long been interested in clinical research that informs and improves our patient care. My goal is to double down on promoting, supporting, and presenting research that serves exactly this purpose. We are growing our team-based education, and I have a special goal for CHEST to become the home for pulmonary, critical care, and sleep advanced practice providers. I care tremendously about our international members, and I will promote both international growth and catering of CHEST’s offerings to benefit our international members.
What do you consider to be the greatest strength of CHEST, and how will you build upon this during your Presidency?
There is zero doubt that CHEST’s greatest strength is the people who gravitate to our organization. From pure clinicians to academicians; from clinical researchers to clinical educators to outcomes mavens—all levels of the health-care team. At every level of this organization are members who all want to be better at what we do, who want to figure out the ways for doing that, who want to explore the boundaries of what that means, and who want to help others to do the same. That goes, as well, for the professional staff who support the members, and who have adopted the motto, “CRUSH lung disease,” because they share our mission and are here to help us do it better.
The absolutely most enjoyable thing about leadership is having the opportunity to survey the landscape and see who’s looking for opportunity, who’s a rising star, who’s looking for people to mentor, then matching those people with opportunities and with jobs to do. Good people who are motivated by the right principles rise to the occasion. My job as President is to help ensure that the organization via the CHEST Board of Regents is addressing the correct problems with the right vision, to identify the right talented and dedicated members for the jobs, and then to support and stay out of their way as they make the vision a reality.
What are some challenges facing CHEST, and how will you address these challenges?
The major immediate challenges facing CHEST are pandemic-related, in terms of helping to ensure the well-being of our members, and in helping them to address the inequities and disparities in care for our patients of color, who have been hardest hit by the emergence of SARS-CoV-2. I addressed these with my goals, above. To be more specific, though, our board will be using various techniques, including dialogue with our members of color, to understand and address our own implicit biases, so that we can achieve the correct vision and tone of inclusion for all of our members. Also addressed in my goals is the isolation from one another that we are all experiencing because of the pandemic. This situation makes it difficult for us to maintain the style and tone of live learning experiences that our CHEST members are accustomed to. The challenge is to develop materials that can be interactive at a distance, and this likely includes gamification of educational content and employing virtual reality. CHEST Innovations is already working in this arena, and it will be our job as member volunteers to support those efforts. The isolation affects our international members, as well, and our ability to travel to maintain relationships. The nice thing is that web conferencing works just as well for international meetings as for meetings in the US, although somebody often has to go to bed very late or get up very early in the morning to make them work! The efforts are worth our time. Again, we will be working in various arenas to maintain and grow our international relationships.
And finally, what is your charge to the members and new Fellows (FCCPs) of CHEST?
We do not yet see clearly whether to expect a massive winter surge of COVID-19 infections. However, it is a reasonably likely possibility. My charge to our members and our new Fellows is first to stay safe, yourself, and to take care of your mental and physical well-being, so that you can be present and functioning at peak levels for your patients. Make sure your family is, likewise, being safe. Secondly, keep doing what you do, which is excellent patient care, excellent teaching, excellent research to push the boundaries of our knowledge. And finally, you’ve seen my ideas of the challenges facing CHEST. I want you to survey, yourself, and tell me what you think our challenges, goals, and responsibilities should be. And if anything I’ve said resonates with you, volunteer to help us address our challenges and keep CHEST the professional home that you deserve and that you will never want to leave. CHEST wants you and needs you. We are so happy you are with us!
CHEST President-Elect Steven Q. Simpson, MD, FCCP, is Professor of Medicine in the Division of Pulmonary and Critical Care Medicine at the University of Kansas. He is also senior advisor to the Solving Sepsis initiative of the Biomedical Advanced Research and Development Authority (BARDA) of the US Department of Health and Human Services.
As we greet our new incoming CHEST President, we asked him for a few thoughts about his upcoming presidential year. He kindly offered these responses:
What would you like to accomplish as President of CHEST?
This is an interesting question, because a global pandemic and other developments in our world dictate that our organizational goals must adapt to a landscape that has shifted in recent months. My goals as President are somewhat different from what I stated when I ran for the office.
1. First, I will build on the efforts of my predecessors to ensure that CHEST is an inclusive and anti-racist organization. All CHEST members must have equal opportunities within our organization to advance their lives and their careers, regardless of race, ethnicity, sex, or gender. My goal is to examine our structures for participation and advancement to positions of leadership in the organization and to evaluate our educational and research offerings, all with the purpose of discovering and remedying places where we have been blind to our own systematic bias. Further, CHEST must advocate for and lead others to advocate for equality, for equal access to medical care, and for policies that promote them. We must be leaders in this arena, through both our voice and our actions.
2. We will build on CHEST’s new initiative to support the wellness of our members and to help us all perform at our best, day in and day out. I hope for our newly established Wellness Center to become a frequent stop for all CHEST members, myself included, to help us to sustain ourselves through the pandemic and beyond.
3. We must maintain both the quality and the feel of our educational and research offerings during this time when we cannot come together in person. My goal for us is that we use this time to embrace remote and nontemporally synchronous education, ie, web-based education, to make CHEST’s offerings the best anywhere. In the remainder of the 21st century, digital transformation of teaching and learning will advance tremendously, and our creative use of technology will become a norm. I hope that we never abandon in-person meetings, but using technology to improve information transfer and augmenting our members’ continuing education are clearly here to stay. My goal for us is that we maintain an atmosphere to both our in-person meetings and our remotely delivered meetings that makes generating new knowledge and learning what we generate enjoyable, even fun. I believe our digital transformation will make some interesting things possible over time.
4. My overall goal for CHEST in the coming year is not that we “make it through” the current pandemic, but that we emerge stronger, smarter, and better for the experience, and prepared for the next challenge(s).
Before COVID-19, I had goals for my presidency, and these issues have not disappeared. CHEST needs to be user- friendly for our members, from our website, to the ways in which we deliver education, to the type of research we develop and promote. On the research side, our members have long been interested in clinical research that informs and improves our patient care. My goal is to double down on promoting, supporting, and presenting research that serves exactly this purpose. We are growing our team-based education, and I have a special goal for CHEST to become the home for pulmonary, critical care, and sleep advanced practice providers. I care tremendously about our international members, and I will promote both international growth and catering of CHEST’s offerings to benefit our international members.
What do you consider to be the greatest strength of CHEST, and how will you build upon this during your Presidency?
There is zero doubt that CHEST’s greatest strength is the people who gravitate to our organization. From pure clinicians to academicians; from clinical researchers to clinical educators to outcomes mavens—all levels of the health-care team. At every level of this organization are members who all want to be better at what we do, who want to figure out the ways for doing that, who want to explore the boundaries of what that means, and who want to help others to do the same. That goes, as well, for the professional staff who support the members, and who have adopted the motto, “CRUSH lung disease,” because they share our mission and are here to help us do it better.
The absolutely most enjoyable thing about leadership is having the opportunity to survey the landscape and see who’s looking for opportunity, who’s a rising star, who’s looking for people to mentor, then matching those people with opportunities and with jobs to do. Good people who are motivated by the right principles rise to the occasion. My job as President is to help ensure that the organization via the CHEST Board of Regents is addressing the correct problems with the right vision, to identify the right talented and dedicated members for the jobs, and then to support and stay out of their way as they make the vision a reality.
What are some challenges facing CHEST, and how will you address these challenges?
The major immediate challenges facing CHEST are pandemic-related, in terms of helping to ensure the well-being of our members, and in helping them to address the inequities and disparities in care for our patients of color, who have been hardest hit by the emergence of SARS-CoV-2. I addressed these with my goals, above. To be more specific, though, our board will be using various techniques, including dialogue with our members of color, to understand and address our own implicit biases, so that we can achieve the correct vision and tone of inclusion for all of our members. Also addressed in my goals is the isolation from one another that we are all experiencing because of the pandemic. This situation makes it difficult for us to maintain the style and tone of live learning experiences that our CHEST members are accustomed to. The challenge is to develop materials that can be interactive at a distance, and this likely includes gamification of educational content and employing virtual reality. CHEST Innovations is already working in this arena, and it will be our job as member volunteers to support those efforts. The isolation affects our international members, as well, and our ability to travel to maintain relationships. The nice thing is that web conferencing works just as well for international meetings as for meetings in the US, although somebody often has to go to bed very late or get up very early in the morning to make them work! The efforts are worth our time. Again, we will be working in various arenas to maintain and grow our international relationships.
And finally, what is your charge to the members and new Fellows (FCCPs) of CHEST?
We do not yet see clearly whether to expect a massive winter surge of COVID-19 infections. However, it is a reasonably likely possibility. My charge to our members and our new Fellows is first to stay safe, yourself, and to take care of your mental and physical well-being, so that you can be present and functioning at peak levels for your patients. Make sure your family is, likewise, being safe. Secondly, keep doing what you do, which is excellent patient care, excellent teaching, excellent research to push the boundaries of our knowledge. And finally, you’ve seen my ideas of the challenges facing CHEST. I want you to survey, yourself, and tell me what you think our challenges, goals, and responsibilities should be. And if anything I’ve said resonates with you, volunteer to help us address our challenges and keep CHEST the professional home that you deserve and that you will never want to leave. CHEST wants you and needs you. We are so happy you are with us!
FDA pulls amputation boxed warning off canagliflozin label
The Food and Drug Administration has removed the boxed warning about the risk of leg and foot amputations for canagliflozin (Invokana, Invokamet, Janssen), a sodium-glucose cotransporter-2 (SGLT2) inhibitor for the treatment of type 2 diabetes, the agency announced Aug. 26.
As previously reported by Medscape Medical News, the FDA added the boxed warning to the canagliflozin label in May 2017, after an approximately doubled risk for lower-extremity amputations with the drug compared with placebo was seen during two trials.
The FDA said the decision to remove the boxed warning was made following a review of new data from three clinical trials, which demonstrated additional heart- and kidney-related benefits and led to additional approved uses for canagliflozin.
In 2018, canagliflozin was approved to reduce the risk of major adverse cardiovascular events in adults with type 2 diabetes who have established cardiovascular disease.
In 2019, canagliflozin was approved to reduce the risk of end-stage kidney disease, worsening of kidney function, cardiovascular death, and heart failure hospitalization, in adults with type 2 diabetes and diabetic kidney disease.
“Collectively, these newly identified effects of canagliflozin on heart and kidney disease show significantly enhanced benefit of this medicine,” the FDA said.
The safety information from these trials, the FDA said, suggests that the risk of amputation, “while still increased with canagliflozin, is lower than previously described, particularly when appropriately monitored.”
The agency added: “Based upon these considerations, FDA concluded that the boxed warning should be removed.”
The FDA announcement said clinicians and patients should continue to be aware of the importance of preventive foot care and to monitor for new pain, tenderness, sores, ulcers, and infections in the legs and feet. Risk factors that may predispose patients to amputation should be considered when choosing antidiabetic medicines.
Health care professionals are encouraged to report adverse reactions with canagliflozin to the FDA’s MedWatch program.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration has removed the boxed warning about the risk of leg and foot amputations for canagliflozin (Invokana, Invokamet, Janssen), a sodium-glucose cotransporter-2 (SGLT2) inhibitor for the treatment of type 2 diabetes, the agency announced Aug. 26.
As previously reported by Medscape Medical News, the FDA added the boxed warning to the canagliflozin label in May 2017, after an approximately doubled risk for lower-extremity amputations with the drug compared with placebo was seen during two trials.
The FDA said the decision to remove the boxed warning was made following a review of new data from three clinical trials, which demonstrated additional heart- and kidney-related benefits and led to additional approved uses for canagliflozin.
In 2018, canagliflozin was approved to reduce the risk of major adverse cardiovascular events in adults with type 2 diabetes who have established cardiovascular disease.
In 2019, canagliflozin was approved to reduce the risk of end-stage kidney disease, worsening of kidney function, cardiovascular death, and heart failure hospitalization, in adults with type 2 diabetes and diabetic kidney disease.
“Collectively, these newly identified effects of canagliflozin on heart and kidney disease show significantly enhanced benefit of this medicine,” the FDA said.
The safety information from these trials, the FDA said, suggests that the risk of amputation, “while still increased with canagliflozin, is lower than previously described, particularly when appropriately monitored.”
The agency added: “Based upon these considerations, FDA concluded that the boxed warning should be removed.”
The FDA announcement said clinicians and patients should continue to be aware of the importance of preventive foot care and to monitor for new pain, tenderness, sores, ulcers, and infections in the legs and feet. Risk factors that may predispose patients to amputation should be considered when choosing antidiabetic medicines.
Health care professionals are encouraged to report adverse reactions with canagliflozin to the FDA’s MedWatch program.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration has removed the boxed warning about the risk of leg and foot amputations for canagliflozin (Invokana, Invokamet, Janssen), a sodium-glucose cotransporter-2 (SGLT2) inhibitor for the treatment of type 2 diabetes, the agency announced Aug. 26.
As previously reported by Medscape Medical News, the FDA added the boxed warning to the canagliflozin label in May 2017, after an approximately doubled risk for lower-extremity amputations with the drug compared with placebo was seen during two trials.
The FDA said the decision to remove the boxed warning was made following a review of new data from three clinical trials, which demonstrated additional heart- and kidney-related benefits and led to additional approved uses for canagliflozin.
In 2018, canagliflozin was approved to reduce the risk of major adverse cardiovascular events in adults with type 2 diabetes who have established cardiovascular disease.
In 2019, canagliflozin was approved to reduce the risk of end-stage kidney disease, worsening of kidney function, cardiovascular death, and heart failure hospitalization, in adults with type 2 diabetes and diabetic kidney disease.
“Collectively, these newly identified effects of canagliflozin on heart and kidney disease show significantly enhanced benefit of this medicine,” the FDA said.
The safety information from these trials, the FDA said, suggests that the risk of amputation, “while still increased with canagliflozin, is lower than previously described, particularly when appropriately monitored.”
The agency added: “Based upon these considerations, FDA concluded that the boxed warning should be removed.”
The FDA announcement said clinicians and patients should continue to be aware of the importance of preventive foot care and to monitor for new pain, tenderness, sores, ulcers, and infections in the legs and feet. Risk factors that may predispose patients to amputation should be considered when choosing antidiabetic medicines.
Health care professionals are encouraged to report adverse reactions with canagliflozin to the FDA’s MedWatch program.
A version of this article originally appeared on Medscape.com.
Prognosis for rural hospitals worsens with pandemic
Jerome Antone said he is one of the lucky ones.
After becoming ill with COVID-19, Mr. Antone was hospitalized only 65 miles away from his small Alabama town. He is the mayor of Georgiana – population 1,700.
“It hit our rural community so rabid,” Mr. Antone said. The town’s hospital closed last year. If hospitals in nearby communities don’t have beds available, “you may have to go 4 or 5 hours away.”
Eighteen rural hospitals closed last year and the first 3 months of 2020 were “really big months,” said Mark Holmes, PhD, director of the Cecil G. Sheps Center for Health Services Research at the University of North Carolina at Chapel Hill. Many of the losses are in Southern states like Florida and Texas. More than 170 rural hospitals have closed nationwide since 2005, according to data collected by the Sheps Center.
It’s a dangerous scenario. “We know that a closure leads to higher mortality pretty quickly” among the populations served, said Dr. Holmes, who is also a professor at UNC Gillings School of Global Public Health. “That’s pretty clear.”
One 2019 study found that death rates in the surrounding communities increase nearly 6% after a rural hospital closes – and that’s when there’s not a pandemic.
Add to that what is known about the coronavirus: People who are obese or live with diabetes, hypertension, asthma, and other underlying health issues are more susceptible to COVID-19. Rural areas tend to have higher rates of these conditions. And rural residents are more likely to be older, sicker and poorer than those in urban areas. All this leaves rural communities particularly vulnerable to the coronavirus.
Congress approved billions in federal relief funds for health care providers. Initially, federal officials based what a hospital would get on its Medicare payments, but by late April they heeded criticism and carved out funds for rural hospitals and COVID-19 hot spots. Rural hospitals leapt at the chance to shore up already-negative budgets and prepare for the pandemic.
The funds “helped rural hospitals with the immediate storm,” said Don Williamson, MD, president of the Alabama Hospital Association. Nearly 80% of Alabama’s rural hospitals began the year with negative balance sheets and about 8 days’ worth of cash on hand.
Before the pandemic hit this year, hundreds of rural hospitals “were just trying to keep their doors open,” said Maggie Elehwany, vice president of government affairs with the National Rural Health Association. Then an estimated 70% of their income stopped as patients avoided the emergency room, doctor’s appointments, and elective surgeries.
“It was devastating,” Ms. Elehwany said.
Paul Taylor, chief executive of a 25-bed critical-access hospital and outpatient clinics in northwestern Arkansas, accepted millions in grants and loan money Congress approved this spring, largely through the CARES (Coronavirus Aid, Relief, and Economic Security) Act.
“For us, this was survival money and we spent it already,” Mr. Taylor said. With those funds, Ozarks Community Hospital increased surge capacity, expanding from 25 beds to 50 beds, adding negative pressure rooms and buying six ventilators. Taylor also ramped up COVID-19 testing at his hospital and clinics, located near some meat-processing plants.
Throughout June and July, Ozarks tested 1,000 patients a day and reported a 20% positive rate. The rate dropped to 16.9% in late July. But patients continue to avoid routine care.
Mr. Taylor said revenue is still constrained and he does not know how he will pay back $8 million that he borrowed from Medicare. The program allowed hospitals to borrow against future payments from the federal government, but stipulated that repayment would begin within 120 days.
For Mr. Taylor, this seems impossible. Medicare makes up 40% of Ozarks’ income. And he has to pay the loan back before he gets any more payments from Medicare. He’s hoping to refinance the hospital’s mortgage.
“If I get no relief and they take the money ... we won’t still be open,” Mr. Taylor said. Ozarks provides 625 jobs and serves an area with a population of about 75,000.
There are 1,300 small critical-access hospitals like Ozarks in rural America, and of those, 859 took advantage of the Medicare loans, sending about $3.1 billion into the local communities. But many rural communities have not yet experienced a surge in coronavirus cases – national leaders fear it will come as part of a new phase.
“There are pockets of rural America who say, ‘We haven’t seen a single COVID patient yet and we do not believe it’s real,’ ” Mr. Taylor said. “They will get hit sooner or later.”
Across the country, the reduced patient numbers and increased spending required to fight and prepare for the coronavirus was “like a knife cutting into a hospital’s blood supply,” said Ge Bai, PhD, associate professor of health policy and management at the Johns Hopkins Bloomberg School of Public Health in Baltimore.
Dr. Bai said the way the federal government reimbursed small rural hospitals through federal programs like Medicare before the pandemic was faulty and inefficient. “They are too weak to survive,” she said.
In rural Texas, about 2 hours from Dallas, Titus Regional Medical Center chief executive officer Terry Scoggin cut staff and furloughed workers even as his rural hospital faced down the pandemic. Titus Regional lost about $4 million last fiscal year and broke even each of the three years before that.
Mr. Scoggin said he did not cut from his clinical staff, though. Titus is now facing its second surge of the virus in the community. “The last 7 days, we’ve been testing 30% positive,” he said, including the case of his father, who contracted it at a nursing home and survived.
“It’s personal and this is real,” Mr. Scoggin said. “You know the people who are infected. You know the people who are passing away.”
Of his roughly 700 employees, 48 have tested positive for the virus and 1 has died. They are short on testing kits, medication, and supplies.
“Right now the staff is strained,” Mr. Scoggin said. “I’ve been blown away by their selflessness and unbelievable spirit. We’re resilient, we’re nimble, and we will make it. We don’t have a choice.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation, which is not affiliated with Kaiser Permanente.
Jerome Antone said he is one of the lucky ones.
After becoming ill with COVID-19, Mr. Antone was hospitalized only 65 miles away from his small Alabama town. He is the mayor of Georgiana – population 1,700.
“It hit our rural community so rabid,” Mr. Antone said. The town’s hospital closed last year. If hospitals in nearby communities don’t have beds available, “you may have to go 4 or 5 hours away.”
Eighteen rural hospitals closed last year and the first 3 months of 2020 were “really big months,” said Mark Holmes, PhD, director of the Cecil G. Sheps Center for Health Services Research at the University of North Carolina at Chapel Hill. Many of the losses are in Southern states like Florida and Texas. More than 170 rural hospitals have closed nationwide since 2005, according to data collected by the Sheps Center.
It’s a dangerous scenario. “We know that a closure leads to higher mortality pretty quickly” among the populations served, said Dr. Holmes, who is also a professor at UNC Gillings School of Global Public Health. “That’s pretty clear.”
One 2019 study found that death rates in the surrounding communities increase nearly 6% after a rural hospital closes – and that’s when there’s not a pandemic.
Add to that what is known about the coronavirus: People who are obese or live with diabetes, hypertension, asthma, and other underlying health issues are more susceptible to COVID-19. Rural areas tend to have higher rates of these conditions. And rural residents are more likely to be older, sicker and poorer than those in urban areas. All this leaves rural communities particularly vulnerable to the coronavirus.
Congress approved billions in federal relief funds for health care providers. Initially, federal officials based what a hospital would get on its Medicare payments, but by late April they heeded criticism and carved out funds for rural hospitals and COVID-19 hot spots. Rural hospitals leapt at the chance to shore up already-negative budgets and prepare for the pandemic.
The funds “helped rural hospitals with the immediate storm,” said Don Williamson, MD, president of the Alabama Hospital Association. Nearly 80% of Alabama’s rural hospitals began the year with negative balance sheets and about 8 days’ worth of cash on hand.
Before the pandemic hit this year, hundreds of rural hospitals “were just trying to keep their doors open,” said Maggie Elehwany, vice president of government affairs with the National Rural Health Association. Then an estimated 70% of their income stopped as patients avoided the emergency room, doctor’s appointments, and elective surgeries.
“It was devastating,” Ms. Elehwany said.
Paul Taylor, chief executive of a 25-bed critical-access hospital and outpatient clinics in northwestern Arkansas, accepted millions in grants and loan money Congress approved this spring, largely through the CARES (Coronavirus Aid, Relief, and Economic Security) Act.
“For us, this was survival money and we spent it already,” Mr. Taylor said. With those funds, Ozarks Community Hospital increased surge capacity, expanding from 25 beds to 50 beds, adding negative pressure rooms and buying six ventilators. Taylor also ramped up COVID-19 testing at his hospital and clinics, located near some meat-processing plants.
Throughout June and July, Ozarks tested 1,000 patients a day and reported a 20% positive rate. The rate dropped to 16.9% in late July. But patients continue to avoid routine care.
Mr. Taylor said revenue is still constrained and he does not know how he will pay back $8 million that he borrowed from Medicare. The program allowed hospitals to borrow against future payments from the federal government, but stipulated that repayment would begin within 120 days.
For Mr. Taylor, this seems impossible. Medicare makes up 40% of Ozarks’ income. And he has to pay the loan back before he gets any more payments from Medicare. He’s hoping to refinance the hospital’s mortgage.
“If I get no relief and they take the money ... we won’t still be open,” Mr. Taylor said. Ozarks provides 625 jobs and serves an area with a population of about 75,000.
There are 1,300 small critical-access hospitals like Ozarks in rural America, and of those, 859 took advantage of the Medicare loans, sending about $3.1 billion into the local communities. But many rural communities have not yet experienced a surge in coronavirus cases – national leaders fear it will come as part of a new phase.
“There are pockets of rural America who say, ‘We haven’t seen a single COVID patient yet and we do not believe it’s real,’ ” Mr. Taylor said. “They will get hit sooner or later.”
Across the country, the reduced patient numbers and increased spending required to fight and prepare for the coronavirus was “like a knife cutting into a hospital’s blood supply,” said Ge Bai, PhD, associate professor of health policy and management at the Johns Hopkins Bloomberg School of Public Health in Baltimore.
Dr. Bai said the way the federal government reimbursed small rural hospitals through federal programs like Medicare before the pandemic was faulty and inefficient. “They are too weak to survive,” she said.
In rural Texas, about 2 hours from Dallas, Titus Regional Medical Center chief executive officer Terry Scoggin cut staff and furloughed workers even as his rural hospital faced down the pandemic. Titus Regional lost about $4 million last fiscal year and broke even each of the three years before that.
Mr. Scoggin said he did not cut from his clinical staff, though. Titus is now facing its second surge of the virus in the community. “The last 7 days, we’ve been testing 30% positive,” he said, including the case of his father, who contracted it at a nursing home and survived.
“It’s personal and this is real,” Mr. Scoggin said. “You know the people who are infected. You know the people who are passing away.”
Of his roughly 700 employees, 48 have tested positive for the virus and 1 has died. They are short on testing kits, medication, and supplies.
“Right now the staff is strained,” Mr. Scoggin said. “I’ve been blown away by their selflessness and unbelievable spirit. We’re resilient, we’re nimble, and we will make it. We don’t have a choice.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation, which is not affiliated with Kaiser Permanente.
Jerome Antone said he is one of the lucky ones.
After becoming ill with COVID-19, Mr. Antone was hospitalized only 65 miles away from his small Alabama town. He is the mayor of Georgiana – population 1,700.
“It hit our rural community so rabid,” Mr. Antone said. The town’s hospital closed last year. If hospitals in nearby communities don’t have beds available, “you may have to go 4 or 5 hours away.”
Eighteen rural hospitals closed last year and the first 3 months of 2020 were “really big months,” said Mark Holmes, PhD, director of the Cecil G. Sheps Center for Health Services Research at the University of North Carolina at Chapel Hill. Many of the losses are in Southern states like Florida and Texas. More than 170 rural hospitals have closed nationwide since 2005, according to data collected by the Sheps Center.
It’s a dangerous scenario. “We know that a closure leads to higher mortality pretty quickly” among the populations served, said Dr. Holmes, who is also a professor at UNC Gillings School of Global Public Health. “That’s pretty clear.”
One 2019 study found that death rates in the surrounding communities increase nearly 6% after a rural hospital closes – and that’s when there’s not a pandemic.
Add to that what is known about the coronavirus: People who are obese or live with diabetes, hypertension, asthma, and other underlying health issues are more susceptible to COVID-19. Rural areas tend to have higher rates of these conditions. And rural residents are more likely to be older, sicker and poorer than those in urban areas. All this leaves rural communities particularly vulnerable to the coronavirus.
Congress approved billions in federal relief funds for health care providers. Initially, federal officials based what a hospital would get on its Medicare payments, but by late April they heeded criticism and carved out funds for rural hospitals and COVID-19 hot spots. Rural hospitals leapt at the chance to shore up already-negative budgets and prepare for the pandemic.
The funds “helped rural hospitals with the immediate storm,” said Don Williamson, MD, president of the Alabama Hospital Association. Nearly 80% of Alabama’s rural hospitals began the year with negative balance sheets and about 8 days’ worth of cash on hand.
Before the pandemic hit this year, hundreds of rural hospitals “were just trying to keep their doors open,” said Maggie Elehwany, vice president of government affairs with the National Rural Health Association. Then an estimated 70% of their income stopped as patients avoided the emergency room, doctor’s appointments, and elective surgeries.
“It was devastating,” Ms. Elehwany said.
Paul Taylor, chief executive of a 25-bed critical-access hospital and outpatient clinics in northwestern Arkansas, accepted millions in grants and loan money Congress approved this spring, largely through the CARES (Coronavirus Aid, Relief, and Economic Security) Act.
“For us, this was survival money and we spent it already,” Mr. Taylor said. With those funds, Ozarks Community Hospital increased surge capacity, expanding from 25 beds to 50 beds, adding negative pressure rooms and buying six ventilators. Taylor also ramped up COVID-19 testing at his hospital and clinics, located near some meat-processing plants.
Throughout June and July, Ozarks tested 1,000 patients a day and reported a 20% positive rate. The rate dropped to 16.9% in late July. But patients continue to avoid routine care.
Mr. Taylor said revenue is still constrained and he does not know how he will pay back $8 million that he borrowed from Medicare. The program allowed hospitals to borrow against future payments from the federal government, but stipulated that repayment would begin within 120 days.
For Mr. Taylor, this seems impossible. Medicare makes up 40% of Ozarks’ income. And he has to pay the loan back before he gets any more payments from Medicare. He’s hoping to refinance the hospital’s mortgage.
“If I get no relief and they take the money ... we won’t still be open,” Mr. Taylor said. Ozarks provides 625 jobs and serves an area with a population of about 75,000.
There are 1,300 small critical-access hospitals like Ozarks in rural America, and of those, 859 took advantage of the Medicare loans, sending about $3.1 billion into the local communities. But many rural communities have not yet experienced a surge in coronavirus cases – national leaders fear it will come as part of a new phase.
“There are pockets of rural America who say, ‘We haven’t seen a single COVID patient yet and we do not believe it’s real,’ ” Mr. Taylor said. “They will get hit sooner or later.”
Across the country, the reduced patient numbers and increased spending required to fight and prepare for the coronavirus was “like a knife cutting into a hospital’s blood supply,” said Ge Bai, PhD, associate professor of health policy and management at the Johns Hopkins Bloomberg School of Public Health in Baltimore.
Dr. Bai said the way the federal government reimbursed small rural hospitals through federal programs like Medicare before the pandemic was faulty and inefficient. “They are too weak to survive,” she said.
In rural Texas, about 2 hours from Dallas, Titus Regional Medical Center chief executive officer Terry Scoggin cut staff and furloughed workers even as his rural hospital faced down the pandemic. Titus Regional lost about $4 million last fiscal year and broke even each of the three years before that.
Mr. Scoggin said he did not cut from his clinical staff, though. Titus is now facing its second surge of the virus in the community. “The last 7 days, we’ve been testing 30% positive,” he said, including the case of his father, who contracted it at a nursing home and survived.
“It’s personal and this is real,” Mr. Scoggin said. “You know the people who are infected. You know the people who are passing away.”
Of his roughly 700 employees, 48 have tested positive for the virus and 1 has died. They are short on testing kits, medication, and supplies.
“Right now the staff is strained,” Mr. Scoggin said. “I’ve been blown away by their selflessness and unbelievable spirit. We’re resilient, we’re nimble, and we will make it. We don’t have a choice.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation, which is not affiliated with Kaiser Permanente.
Reported COVID-19 symptoms by hospitalization status



Pregnancy can be ‘a vulnerable time’ for developing mental disorders
Pregnancy and the postpartum period are a “very vulnerable time for mental disorders,” according to Henry A. Nasrallah, MD.
“Those changes that are helping pregnancy can also have psychiatric and psychopathological implications,” Dr. Nasrallah said in a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
Numerous dramatic changes in physiology, immune functions, cognition, neuroplasticity, and behavior occur during pregnancy, noted Dr. Nasrallah of the University of Cincinnati. For example, the volume of the brain actually decreases during pregnancy, but brain size recovers over the 6 months after delivery. “Clearly, this is a transitional and a transient phenomenon,” he said. “The decrease in brain volume is associated with changes in brain metabolism and an increase in intracellular pH after delivery.”
But these changes can also carry risks for psychiatric disorders, Dr. Nasrallah explained. Changes in the hippocampus, which is “very plastic throughout adulthood,” have been linked to aging, cognition, pregnancy, and motherhood. “The hippocampus is the ‘Grand Central Station’ of memory in the brain, and the hippocampus is affected by neurodegenerative and psychiatric disorders, which disproportionately affect women,” he said at the meeting, presented by Global Academy for Medical Education.
Dr. Nasrallah said the hippocampus has particular susceptibility during pregnancy and in the postpartum period, or in women who have previously been pregnant.
Gender of the fetus can even affect the health of the mother, he added. In women who are pregnant with male fetuses, working memory and spatial ability are higher than in women who are pregnant with female fetuses, Dr. Nasrallah said. This is tied to higher numbers of proinflammatory cytokines present in male fetuses. In female fetuses, there are lower levels of interferon-gamma and interleukin (IL)-12 in the first trimester, and higher levels of IL-1 beta, tumor necrosis factor B, IL-5, and IL-10 in the second trimester.
In particular,
“Cytokine interleukin-10 and interleukin-6 are both increased during psychosis and during depression, so you can see the vulnerability for developing postpartum depression.” Some women “have other genes that make them susceptible for mood disorders, and the pregnancy can push them over the edge,” he said.
If women have bipolar disorder prior to delivery, “they have a very high risk of postpartum depression, possibly because of this immune dysregulation that serves the pregnancy, but unfortunately makes the woman vulnerable for postpartum psychiatric disorders,” Dr. Nasrallah said.
The effects of having children extend into middle age, Dr. Nasrallah said. Research has shown giving birth to more than one to two children can affect a woman’s risk for Alzheimer’s disease and risk for early-onset of the disease. Women who have three or fewer children later in life are also more likely to live longer, he said. In general, a longer reproductive period, duration of breastfeeding, and low number of pregnancies result in better cognition, while younger age at first pregnancy leads to worse cognition.
So-called pregnancy brain causes some cognitive functions to decline, and women may experience trouble concentrating and memory disturbance. “Other functions increase for the sake of the baby,” including a high reaction to threatening stimuli, absent-mindedness, motivation, reward, fear, executive functions, social cognition, salience, and attachment, Dr. Nasrallah said. In some cases, hormone-driven remodeling of the maternal brain can cause postpartum psychosis, which can reduce the anterior cingulate cortex, left parahippocampal gyrus volume, and left superior temporal gyrus volume.
Most changes in the brain, however, appear to be temporary, Dr. Nasrallah noted. Executive function improves 2-6 months after delivery, which includes goal and directed behavior, working memory, inhibitory function, and cognitive flexibility. In the postpartum period, “the gray matter increases in the first 3-4 months, especially in the brain areas that are involved in maternal behavior that includes amygdala, hypothalamus, and prefrontal cortex,” he added. “All of those changes correlate with positive maternal attachment, and so that makes it easier for the mother to bond with the baby.
“Don’t think of it as a negative,” he said. “The decline in brain volume is actually associated with better mothering and increased attachment between the mother and the baby, which is vital for survival of the baby.”
Global Academy and this news organization are owned by the same parent company. Dr. Nasrallah reports no relevant financial disclosures.
Pregnancy and the postpartum period are a “very vulnerable time for mental disorders,” according to Henry A. Nasrallah, MD.
“Those changes that are helping pregnancy can also have psychiatric and psychopathological implications,” Dr. Nasrallah said in a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
Numerous dramatic changes in physiology, immune functions, cognition, neuroplasticity, and behavior occur during pregnancy, noted Dr. Nasrallah of the University of Cincinnati. For example, the volume of the brain actually decreases during pregnancy, but brain size recovers over the 6 months after delivery. “Clearly, this is a transitional and a transient phenomenon,” he said. “The decrease in brain volume is associated with changes in brain metabolism and an increase in intracellular pH after delivery.”
But these changes can also carry risks for psychiatric disorders, Dr. Nasrallah explained. Changes in the hippocampus, which is “very plastic throughout adulthood,” have been linked to aging, cognition, pregnancy, and motherhood. “The hippocampus is the ‘Grand Central Station’ of memory in the brain, and the hippocampus is affected by neurodegenerative and psychiatric disorders, which disproportionately affect women,” he said at the meeting, presented by Global Academy for Medical Education.
Dr. Nasrallah said the hippocampus has particular susceptibility during pregnancy and in the postpartum period, or in women who have previously been pregnant.
Gender of the fetus can even affect the health of the mother, he added. In women who are pregnant with male fetuses, working memory and spatial ability are higher than in women who are pregnant with female fetuses, Dr. Nasrallah said. This is tied to higher numbers of proinflammatory cytokines present in male fetuses. In female fetuses, there are lower levels of interferon-gamma and interleukin (IL)-12 in the first trimester, and higher levels of IL-1 beta, tumor necrosis factor B, IL-5, and IL-10 in the second trimester.
In particular,
“Cytokine interleukin-10 and interleukin-6 are both increased during psychosis and during depression, so you can see the vulnerability for developing postpartum depression.” Some women “have other genes that make them susceptible for mood disorders, and the pregnancy can push them over the edge,” he said.
If women have bipolar disorder prior to delivery, “they have a very high risk of postpartum depression, possibly because of this immune dysregulation that serves the pregnancy, but unfortunately makes the woman vulnerable for postpartum psychiatric disorders,” Dr. Nasrallah said.
The effects of having children extend into middle age, Dr. Nasrallah said. Research has shown giving birth to more than one to two children can affect a woman’s risk for Alzheimer’s disease and risk for early-onset of the disease. Women who have three or fewer children later in life are also more likely to live longer, he said. In general, a longer reproductive period, duration of breastfeeding, and low number of pregnancies result in better cognition, while younger age at first pregnancy leads to worse cognition.
So-called pregnancy brain causes some cognitive functions to decline, and women may experience trouble concentrating and memory disturbance. “Other functions increase for the sake of the baby,” including a high reaction to threatening stimuli, absent-mindedness, motivation, reward, fear, executive functions, social cognition, salience, and attachment, Dr. Nasrallah said. In some cases, hormone-driven remodeling of the maternal brain can cause postpartum psychosis, which can reduce the anterior cingulate cortex, left parahippocampal gyrus volume, and left superior temporal gyrus volume.
Most changes in the brain, however, appear to be temporary, Dr. Nasrallah noted. Executive function improves 2-6 months after delivery, which includes goal and directed behavior, working memory, inhibitory function, and cognitive flexibility. In the postpartum period, “the gray matter increases in the first 3-4 months, especially in the brain areas that are involved in maternal behavior that includes amygdala, hypothalamus, and prefrontal cortex,” he added. “All of those changes correlate with positive maternal attachment, and so that makes it easier for the mother to bond with the baby.
“Don’t think of it as a negative,” he said. “The decline in brain volume is actually associated with better mothering and increased attachment between the mother and the baby, which is vital for survival of the baby.”
Global Academy and this news organization are owned by the same parent company. Dr. Nasrallah reports no relevant financial disclosures.
Pregnancy and the postpartum period are a “very vulnerable time for mental disorders,” according to Henry A. Nasrallah, MD.
“Those changes that are helping pregnancy can also have psychiatric and psychopathological implications,” Dr. Nasrallah said in a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
Numerous dramatic changes in physiology, immune functions, cognition, neuroplasticity, and behavior occur during pregnancy, noted Dr. Nasrallah of the University of Cincinnati. For example, the volume of the brain actually decreases during pregnancy, but brain size recovers over the 6 months after delivery. “Clearly, this is a transitional and a transient phenomenon,” he said. “The decrease in brain volume is associated with changes in brain metabolism and an increase in intracellular pH after delivery.”
But these changes can also carry risks for psychiatric disorders, Dr. Nasrallah explained. Changes in the hippocampus, which is “very plastic throughout adulthood,” have been linked to aging, cognition, pregnancy, and motherhood. “The hippocampus is the ‘Grand Central Station’ of memory in the brain, and the hippocampus is affected by neurodegenerative and psychiatric disorders, which disproportionately affect women,” he said at the meeting, presented by Global Academy for Medical Education.
Dr. Nasrallah said the hippocampus has particular susceptibility during pregnancy and in the postpartum period, or in women who have previously been pregnant.
Gender of the fetus can even affect the health of the mother, he added. In women who are pregnant with male fetuses, working memory and spatial ability are higher than in women who are pregnant with female fetuses, Dr. Nasrallah said. This is tied to higher numbers of proinflammatory cytokines present in male fetuses. In female fetuses, there are lower levels of interferon-gamma and interleukin (IL)-12 in the first trimester, and higher levels of IL-1 beta, tumor necrosis factor B, IL-5, and IL-10 in the second trimester.
In particular,
“Cytokine interleukin-10 and interleukin-6 are both increased during psychosis and during depression, so you can see the vulnerability for developing postpartum depression.” Some women “have other genes that make them susceptible for mood disorders, and the pregnancy can push them over the edge,” he said.
If women have bipolar disorder prior to delivery, “they have a very high risk of postpartum depression, possibly because of this immune dysregulation that serves the pregnancy, but unfortunately makes the woman vulnerable for postpartum psychiatric disorders,” Dr. Nasrallah said.
The effects of having children extend into middle age, Dr. Nasrallah said. Research has shown giving birth to more than one to two children can affect a woman’s risk for Alzheimer’s disease and risk for early-onset of the disease. Women who have three or fewer children later in life are also more likely to live longer, he said. In general, a longer reproductive period, duration of breastfeeding, and low number of pregnancies result in better cognition, while younger age at first pregnancy leads to worse cognition.
So-called pregnancy brain causes some cognitive functions to decline, and women may experience trouble concentrating and memory disturbance. “Other functions increase for the sake of the baby,” including a high reaction to threatening stimuli, absent-mindedness, motivation, reward, fear, executive functions, social cognition, salience, and attachment, Dr. Nasrallah said. In some cases, hormone-driven remodeling of the maternal brain can cause postpartum psychosis, which can reduce the anterior cingulate cortex, left parahippocampal gyrus volume, and left superior temporal gyrus volume.
Most changes in the brain, however, appear to be temporary, Dr. Nasrallah noted. Executive function improves 2-6 months after delivery, which includes goal and directed behavior, working memory, inhibitory function, and cognitive flexibility. In the postpartum period, “the gray matter increases in the first 3-4 months, especially in the brain areas that are involved in maternal behavior that includes amygdala, hypothalamus, and prefrontal cortex,” he added. “All of those changes correlate with positive maternal attachment, and so that makes it easier for the mother to bond with the baby.
“Don’t think of it as a negative,” he said. “The decline in brain volume is actually associated with better mothering and increased attachment between the mother and the baby, which is vital for survival of the baby.”
Global Academy and this news organization are owned by the same parent company. Dr. Nasrallah reports no relevant financial disclosures.
FROM FOCUS ON NEUROPSYCHIATRY 2020
Mapping melasma management
Melasma has such a high recurrence rate that, once the facial hyperpigmentation has been cleared, it’s best that treatment never entirely stops, Amit G. Pandya, MD, said at the virtual annual meeting of the American Academy of Dermatology.
He recommended alternating between a less-intensive maintenance therapy regimen in the winter months and an acute care regimen in the sunnier summer months. But . And that is largely a matter of location.
Location, location, location
Melasma has a distinctive symmetric bilateral distribution: “Melasma likes the central area of the forehead, whereas the lateral areas of the forehead are more involved in lichen planus pigmentosus. Melanoma likes the area above the eyebrow or under the eyebrow. However, it does not go below the superior orbital rim or above the inferior orbital rim,”said Dr. Pandya, a dermatologist at the Palo Alto Medical Foundation in Sunnyvale, Calif., who is also on the faculty at the University of Texas Southwestern Medical Center, Dallas.
Melasma is common on the bridge of the nose, but usually not along the nasolabial fold, where hyperpigmentation is much more likely to be due to seborrheic dermatitis or drug-induced hyperpigmentation. Melasma doesn’t affect the tip of the nose; that’s more likely a sign of sarcoidosis or drug-induced hyperpigmentation. Melasma is common on the zygomatic prominence, while acanthosis nigricans favors the concave area below the zygomatic prominence. And melasma stays above the mandible; pigmentation below the mandible is more suggestive of poikiloderma of Civatte. Lentigines are scattered broadly across sun-exposed areas of the face. They also tend to be less symmetrical than melasma, the dermatologist continued.
Acute treatment
Dr. Pandya’s acute treatment algorithm begins with topical 4% hydroquinone in patients who’ve never been on it before. A response to the drug, which blocks the tyrosine-to-melanin pathway, takes 4-6 weeks, with maximum effect not seen until 3-6 months or longer. Bluish-grey ochronosis is a rare side effect at the 4% concentration but becomes more common at higher concentrations or when the drug is used in combination therapy.
“Hydroquinone is a workhorse, the oldest and most effective depigmenting agent,” he said.
If the patient hasn’t responded positively by 3 months, Dr. Pandya moves on to daily use of the triple-drug combination of fluocinolone acetonide 0.01%/hydroquinone 4%/tretinoin 0.05% known as Tri-Luma, a kinder, gentler descendant of the 45-year-old Kligman-Willis compounded formula comprised of 0.1% dexamethasone, 5% hydroquinone, and 0.1% tretinoin.
If Tri-Luma also proves ineffective, Dr. Pandya turns to oral tranexamic acid. This is off-label therapy for the drug, a plasmin inhibitor, which is approved for the treatment of menorrhagia. But oral tranexamic acid is widely used for treatment of melasma in East Asia, and Dr. Pandya and others have evaluated it in placebo-controlled clinical trials. His conclusion is that oral tranexamic acid appears to be safe and effective for treatment of melasma.
“The drug is not approved for melasma, it’s approved for menorrhagia, so every doctor has to decide how much risk they want to take. The evidence suggests 500 mg per day is a good dose,” he said.
The collective clinical trials experience with oral tranexamic acid for melasma shows a side effect profile consisting of mild GI upset, headache, and myalgia. While increased thromboembolic risk is a theoretic concern, it hasn’t been an issue in the published studies, which typically exclude patients with a history of thromboembolic disease from enrollment. Patient satisfaction with the oral agent is high, according to Dr. Pandya.
In one randomized, open-label, 40-patient study, oral tranexamic acid plus a triple-combination cream featuring fluocinolone 0.01%, hydroquinone 2%, and tretinoin 0.05%, applied once a day, was significantly more effective and faster-acting than the topical therapy alone. At 8 weeks, the dual-therapy group averaged an 88% improvement in the Melasma Activity and Severity Index (MASI) scores, compared with 55% with the topical therapy alone (Indian J Dermatol. Sep-Oct 2015;60[5]:520).
Cysteamine 5% cream, which is available over the counter as Cyspera but is pricey, showed promising efficacy in a 40-patient, randomized, double-blind trial (J Dermatolog Treat. 2018 Mar;29[2]:182-9). Dr. Pandya said he’s looking forward to seeing further studies.
Chemical peels can be used, but multiple treatment sessions using a superficial peeling agent are required, and even then “the efficacy is usually not profound,” according to Dr. Pandya. Together with two colleagues he recently published a comprehensive systematic review of 113 published studies of all treatments for melasma in nearly 7,000 patients (Am J Clin Dermatol. 2020 Apr;21(2):173-225).
Newer lasers with various pulse lengths, fluences, wave lengths, and treatment frequency show “some promise,” but there have also been published reports of hypopigmentation and rebound hyperpigmentation. The optimal laser regimen remains elusive, he said.
Maintenance therapy
Dr. Pandya usually switches from hydroquinone to a different topical tyrosinase inhibitor for maintenance therapy, such as kojic acid, arbutin, or azelaic acid, all available OTC in many formulations. Alternatively, he might drop down to 2% hydroquinone for the winter months. Another option is triple-combination cream applied two or three times per week. A topical formulation of tranexamic acid is available, but studies of this agent in patients with melasma have yielded mixed results.
“I don’t think topical tranexamic acid is going to harm the patient, but I don’t think the efficacy is as good as with oral tranexamic acid,” he said.
Slap that melasma in irons
A comprehensive melasma management plan requires year-round frequent daily application of a broad spectrum sunscreen. And since it’s now evident that visible-wavelength light can worsen melasma through mechanisms similar to UVA and UVB, which are long recognized as the major drivers of the hyperpigmentation disorder, serious consideration should be given to the use of a tinted broad-spectrum sunscreen or makeup containing more than 3% iron oxide, which blocks visible light. In contrast, zinc oxide does not, Dr. Pandya noted.
In one influential study, aminolevulinic acid was applied on the arms of 20 patients; two sunscreens were applied on areas where the ALA was applied, and on one area, no sunscreen was applied. The minimal phototoxic dose of visible blue light was doubled with application of a broad-spectrum sunscreen containing titanium dioxide, zinc oxide, and 0.2% iron oxide, compared with no sunscreen, but increased 21-fold using a sunscreen containing titanium dioxide, zinc oxide, and 3.2% iron oxide (Dermatol Surg. 2008 Nov;34[11]:1469-76).
Moreover, in a double-blind, randomized trial including 61 patients with melasma, all on background 4% hydroquinone, those assigned to a broad-spectrum sunscreen containing iron oxide had a 78% improvement in MASI scores at 8 weeks, compared with a 62% improvement with a broad-spectrum UV-only sunscreen. Both sunscreens had a sun protection factor of at least 50 (Photodermatol Photoimmunol Photomed. 2014 Feb;30[1]:35-42).
Numerous sunscreen and makeup products containing more than 3% iron oxide are available OTC in various tints. It’s a matter of finding a color that matches the patient’s skin.
Concern has been raised that exposure to the visible blue light emitted by computer screens and cell phones could worsen melasma. Dr. Pandya noted that reassurance on that score was recently provided by French investigators. They measured the intensity of visible light at the wavelengths emitted by computer screens and laptops and determined that it was 100- to 1,000-fold less than sunlight in the same spectrum. They also conducted a prospective, randomized, split-face trial in 12 melasma patients. One side of the face was exposed to the visible blue light at the same wavelengths emitted by device screens, but at far greater intensity. Blinded evaluators found no split-face difference in modified MASI scores.
“These results suggest that at a 20-cm distance, a maximized use of a high-intensity computer screen for 8 hours per day during a 5-day period does not worsen melasma lesions. Although it is very unlikely that similar exposure during a longer period would start to affect melasma lesions, such a possibility cannot be ruled out,” according to the investigators (J Am Acad Dermatol. 2019 Dec 27;S0190-9622(19)33324-9. doi: 10.1016/j.jaad.2019.12.047).
Dr. Pandya reported serving as a consultant to Incyte, Pfizer, Viela Bio, and Villaris.
Melasma has such a high recurrence rate that, once the facial hyperpigmentation has been cleared, it’s best that treatment never entirely stops, Amit G. Pandya, MD, said at the virtual annual meeting of the American Academy of Dermatology.
He recommended alternating between a less-intensive maintenance therapy regimen in the winter months and an acute care regimen in the sunnier summer months. But . And that is largely a matter of location.
Location, location, location
Melasma has a distinctive symmetric bilateral distribution: “Melasma likes the central area of the forehead, whereas the lateral areas of the forehead are more involved in lichen planus pigmentosus. Melanoma likes the area above the eyebrow or under the eyebrow. However, it does not go below the superior orbital rim or above the inferior orbital rim,”said Dr. Pandya, a dermatologist at the Palo Alto Medical Foundation in Sunnyvale, Calif., who is also on the faculty at the University of Texas Southwestern Medical Center, Dallas.
Melasma is common on the bridge of the nose, but usually not along the nasolabial fold, where hyperpigmentation is much more likely to be due to seborrheic dermatitis or drug-induced hyperpigmentation. Melasma doesn’t affect the tip of the nose; that’s more likely a sign of sarcoidosis or drug-induced hyperpigmentation. Melasma is common on the zygomatic prominence, while acanthosis nigricans favors the concave area below the zygomatic prominence. And melasma stays above the mandible; pigmentation below the mandible is more suggestive of poikiloderma of Civatte. Lentigines are scattered broadly across sun-exposed areas of the face. They also tend to be less symmetrical than melasma, the dermatologist continued.
Acute treatment
Dr. Pandya’s acute treatment algorithm begins with topical 4% hydroquinone in patients who’ve never been on it before. A response to the drug, which blocks the tyrosine-to-melanin pathway, takes 4-6 weeks, with maximum effect not seen until 3-6 months or longer. Bluish-grey ochronosis is a rare side effect at the 4% concentration but becomes more common at higher concentrations or when the drug is used in combination therapy.
“Hydroquinone is a workhorse, the oldest and most effective depigmenting agent,” he said.
If the patient hasn’t responded positively by 3 months, Dr. Pandya moves on to daily use of the triple-drug combination of fluocinolone acetonide 0.01%/hydroquinone 4%/tretinoin 0.05% known as Tri-Luma, a kinder, gentler descendant of the 45-year-old Kligman-Willis compounded formula comprised of 0.1% dexamethasone, 5% hydroquinone, and 0.1% tretinoin.
If Tri-Luma also proves ineffective, Dr. Pandya turns to oral tranexamic acid. This is off-label therapy for the drug, a plasmin inhibitor, which is approved for the treatment of menorrhagia. But oral tranexamic acid is widely used for treatment of melasma in East Asia, and Dr. Pandya and others have evaluated it in placebo-controlled clinical trials. His conclusion is that oral tranexamic acid appears to be safe and effective for treatment of melasma.
“The drug is not approved for melasma, it’s approved for menorrhagia, so every doctor has to decide how much risk they want to take. The evidence suggests 500 mg per day is a good dose,” he said.
The collective clinical trials experience with oral tranexamic acid for melasma shows a side effect profile consisting of mild GI upset, headache, and myalgia. While increased thromboembolic risk is a theoretic concern, it hasn’t been an issue in the published studies, which typically exclude patients with a history of thromboembolic disease from enrollment. Patient satisfaction with the oral agent is high, according to Dr. Pandya.
In one randomized, open-label, 40-patient study, oral tranexamic acid plus a triple-combination cream featuring fluocinolone 0.01%, hydroquinone 2%, and tretinoin 0.05%, applied once a day, was significantly more effective and faster-acting than the topical therapy alone. At 8 weeks, the dual-therapy group averaged an 88% improvement in the Melasma Activity and Severity Index (MASI) scores, compared with 55% with the topical therapy alone (Indian J Dermatol. Sep-Oct 2015;60[5]:520).
Cysteamine 5% cream, which is available over the counter as Cyspera but is pricey, showed promising efficacy in a 40-patient, randomized, double-blind trial (J Dermatolog Treat. 2018 Mar;29[2]:182-9). Dr. Pandya said he’s looking forward to seeing further studies.
Chemical peels can be used, but multiple treatment sessions using a superficial peeling agent are required, and even then “the efficacy is usually not profound,” according to Dr. Pandya. Together with two colleagues he recently published a comprehensive systematic review of 113 published studies of all treatments for melasma in nearly 7,000 patients (Am J Clin Dermatol. 2020 Apr;21(2):173-225).
Newer lasers with various pulse lengths, fluences, wave lengths, and treatment frequency show “some promise,” but there have also been published reports of hypopigmentation and rebound hyperpigmentation. The optimal laser regimen remains elusive, he said.
Maintenance therapy
Dr. Pandya usually switches from hydroquinone to a different topical tyrosinase inhibitor for maintenance therapy, such as kojic acid, arbutin, or azelaic acid, all available OTC in many formulations. Alternatively, he might drop down to 2% hydroquinone for the winter months. Another option is triple-combination cream applied two or three times per week. A topical formulation of tranexamic acid is available, but studies of this agent in patients with melasma have yielded mixed results.
“I don’t think topical tranexamic acid is going to harm the patient, but I don’t think the efficacy is as good as with oral tranexamic acid,” he said.
Slap that melasma in irons
A comprehensive melasma management plan requires year-round frequent daily application of a broad spectrum sunscreen. And since it’s now evident that visible-wavelength light can worsen melasma through mechanisms similar to UVA and UVB, which are long recognized as the major drivers of the hyperpigmentation disorder, serious consideration should be given to the use of a tinted broad-spectrum sunscreen or makeup containing more than 3% iron oxide, which blocks visible light. In contrast, zinc oxide does not, Dr. Pandya noted.
In one influential study, aminolevulinic acid was applied on the arms of 20 patients; two sunscreens were applied on areas where the ALA was applied, and on one area, no sunscreen was applied. The minimal phototoxic dose of visible blue light was doubled with application of a broad-spectrum sunscreen containing titanium dioxide, zinc oxide, and 0.2% iron oxide, compared with no sunscreen, but increased 21-fold using a sunscreen containing titanium dioxide, zinc oxide, and 3.2% iron oxide (Dermatol Surg. 2008 Nov;34[11]:1469-76).
Moreover, in a double-blind, randomized trial including 61 patients with melasma, all on background 4% hydroquinone, those assigned to a broad-spectrum sunscreen containing iron oxide had a 78% improvement in MASI scores at 8 weeks, compared with a 62% improvement with a broad-spectrum UV-only sunscreen. Both sunscreens had a sun protection factor of at least 50 (Photodermatol Photoimmunol Photomed. 2014 Feb;30[1]:35-42).
Numerous sunscreen and makeup products containing more than 3% iron oxide are available OTC in various tints. It’s a matter of finding a color that matches the patient’s skin.
Concern has been raised that exposure to the visible blue light emitted by computer screens and cell phones could worsen melasma. Dr. Pandya noted that reassurance on that score was recently provided by French investigators. They measured the intensity of visible light at the wavelengths emitted by computer screens and laptops and determined that it was 100- to 1,000-fold less than sunlight in the same spectrum. They also conducted a prospective, randomized, split-face trial in 12 melasma patients. One side of the face was exposed to the visible blue light at the same wavelengths emitted by device screens, but at far greater intensity. Blinded evaluators found no split-face difference in modified MASI scores.
“These results suggest that at a 20-cm distance, a maximized use of a high-intensity computer screen for 8 hours per day during a 5-day period does not worsen melasma lesions. Although it is very unlikely that similar exposure during a longer period would start to affect melasma lesions, such a possibility cannot be ruled out,” according to the investigators (J Am Acad Dermatol. 2019 Dec 27;S0190-9622(19)33324-9. doi: 10.1016/j.jaad.2019.12.047).
Dr. Pandya reported serving as a consultant to Incyte, Pfizer, Viela Bio, and Villaris.
Melasma has such a high recurrence rate that, once the facial hyperpigmentation has been cleared, it’s best that treatment never entirely stops, Amit G. Pandya, MD, said at the virtual annual meeting of the American Academy of Dermatology.
He recommended alternating between a less-intensive maintenance therapy regimen in the winter months and an acute care regimen in the sunnier summer months. But . And that is largely a matter of location.
Location, location, location
Melasma has a distinctive symmetric bilateral distribution: “Melasma likes the central area of the forehead, whereas the lateral areas of the forehead are more involved in lichen planus pigmentosus. Melanoma likes the area above the eyebrow or under the eyebrow. However, it does not go below the superior orbital rim or above the inferior orbital rim,”said Dr. Pandya, a dermatologist at the Palo Alto Medical Foundation in Sunnyvale, Calif., who is also on the faculty at the University of Texas Southwestern Medical Center, Dallas.
Melasma is common on the bridge of the nose, but usually not along the nasolabial fold, where hyperpigmentation is much more likely to be due to seborrheic dermatitis or drug-induced hyperpigmentation. Melasma doesn’t affect the tip of the nose; that’s more likely a sign of sarcoidosis or drug-induced hyperpigmentation. Melasma is common on the zygomatic prominence, while acanthosis nigricans favors the concave area below the zygomatic prominence. And melasma stays above the mandible; pigmentation below the mandible is more suggestive of poikiloderma of Civatte. Lentigines are scattered broadly across sun-exposed areas of the face. They also tend to be less symmetrical than melasma, the dermatologist continued.
Acute treatment
Dr. Pandya’s acute treatment algorithm begins with topical 4% hydroquinone in patients who’ve never been on it before. A response to the drug, which blocks the tyrosine-to-melanin pathway, takes 4-6 weeks, with maximum effect not seen until 3-6 months or longer. Bluish-grey ochronosis is a rare side effect at the 4% concentration but becomes more common at higher concentrations or when the drug is used in combination therapy.
“Hydroquinone is a workhorse, the oldest and most effective depigmenting agent,” he said.
If the patient hasn’t responded positively by 3 months, Dr. Pandya moves on to daily use of the triple-drug combination of fluocinolone acetonide 0.01%/hydroquinone 4%/tretinoin 0.05% known as Tri-Luma, a kinder, gentler descendant of the 45-year-old Kligman-Willis compounded formula comprised of 0.1% dexamethasone, 5% hydroquinone, and 0.1% tretinoin.
If Tri-Luma also proves ineffective, Dr. Pandya turns to oral tranexamic acid. This is off-label therapy for the drug, a plasmin inhibitor, which is approved for the treatment of menorrhagia. But oral tranexamic acid is widely used for treatment of melasma in East Asia, and Dr. Pandya and others have evaluated it in placebo-controlled clinical trials. His conclusion is that oral tranexamic acid appears to be safe and effective for treatment of melasma.
“The drug is not approved for melasma, it’s approved for menorrhagia, so every doctor has to decide how much risk they want to take. The evidence suggests 500 mg per day is a good dose,” he said.
The collective clinical trials experience with oral tranexamic acid for melasma shows a side effect profile consisting of mild GI upset, headache, and myalgia. While increased thromboembolic risk is a theoretic concern, it hasn’t been an issue in the published studies, which typically exclude patients with a history of thromboembolic disease from enrollment. Patient satisfaction with the oral agent is high, according to Dr. Pandya.
In one randomized, open-label, 40-patient study, oral tranexamic acid plus a triple-combination cream featuring fluocinolone 0.01%, hydroquinone 2%, and tretinoin 0.05%, applied once a day, was significantly more effective and faster-acting than the topical therapy alone. At 8 weeks, the dual-therapy group averaged an 88% improvement in the Melasma Activity and Severity Index (MASI) scores, compared with 55% with the topical therapy alone (Indian J Dermatol. Sep-Oct 2015;60[5]:520).
Cysteamine 5% cream, which is available over the counter as Cyspera but is pricey, showed promising efficacy in a 40-patient, randomized, double-blind trial (J Dermatolog Treat. 2018 Mar;29[2]:182-9). Dr. Pandya said he’s looking forward to seeing further studies.
Chemical peels can be used, but multiple treatment sessions using a superficial peeling agent are required, and even then “the efficacy is usually not profound,” according to Dr. Pandya. Together with two colleagues he recently published a comprehensive systematic review of 113 published studies of all treatments for melasma in nearly 7,000 patients (Am J Clin Dermatol. 2020 Apr;21(2):173-225).
Newer lasers with various pulse lengths, fluences, wave lengths, and treatment frequency show “some promise,” but there have also been published reports of hypopigmentation and rebound hyperpigmentation. The optimal laser regimen remains elusive, he said.
Maintenance therapy
Dr. Pandya usually switches from hydroquinone to a different topical tyrosinase inhibitor for maintenance therapy, such as kojic acid, arbutin, or azelaic acid, all available OTC in many formulations. Alternatively, he might drop down to 2% hydroquinone for the winter months. Another option is triple-combination cream applied two or three times per week. A topical formulation of tranexamic acid is available, but studies of this agent in patients with melasma have yielded mixed results.
“I don’t think topical tranexamic acid is going to harm the patient, but I don’t think the efficacy is as good as with oral tranexamic acid,” he said.
Slap that melasma in irons
A comprehensive melasma management plan requires year-round frequent daily application of a broad spectrum sunscreen. And since it’s now evident that visible-wavelength light can worsen melasma through mechanisms similar to UVA and UVB, which are long recognized as the major drivers of the hyperpigmentation disorder, serious consideration should be given to the use of a tinted broad-spectrum sunscreen or makeup containing more than 3% iron oxide, which blocks visible light. In contrast, zinc oxide does not, Dr. Pandya noted.
In one influential study, aminolevulinic acid was applied on the arms of 20 patients; two sunscreens were applied on areas where the ALA was applied, and on one area, no sunscreen was applied. The minimal phototoxic dose of visible blue light was doubled with application of a broad-spectrum sunscreen containing titanium dioxide, zinc oxide, and 0.2% iron oxide, compared with no sunscreen, but increased 21-fold using a sunscreen containing titanium dioxide, zinc oxide, and 3.2% iron oxide (Dermatol Surg. 2008 Nov;34[11]:1469-76).
Moreover, in a double-blind, randomized trial including 61 patients with melasma, all on background 4% hydroquinone, those assigned to a broad-spectrum sunscreen containing iron oxide had a 78% improvement in MASI scores at 8 weeks, compared with a 62% improvement with a broad-spectrum UV-only sunscreen. Both sunscreens had a sun protection factor of at least 50 (Photodermatol Photoimmunol Photomed. 2014 Feb;30[1]:35-42).
Numerous sunscreen and makeup products containing more than 3% iron oxide are available OTC in various tints. It’s a matter of finding a color that matches the patient’s skin.
Concern has been raised that exposure to the visible blue light emitted by computer screens and cell phones could worsen melasma. Dr. Pandya noted that reassurance on that score was recently provided by French investigators. They measured the intensity of visible light at the wavelengths emitted by computer screens and laptops and determined that it was 100- to 1,000-fold less than sunlight in the same spectrum. They also conducted a prospective, randomized, split-face trial in 12 melasma patients. One side of the face was exposed to the visible blue light at the same wavelengths emitted by device screens, but at far greater intensity. Blinded evaluators found no split-face difference in modified MASI scores.
“These results suggest that at a 20-cm distance, a maximized use of a high-intensity computer screen for 8 hours per day during a 5-day period does not worsen melasma lesions. Although it is very unlikely that similar exposure during a longer period would start to affect melasma lesions, such a possibility cannot be ruled out,” according to the investigators (J Am Acad Dermatol. 2019 Dec 27;S0190-9622(19)33324-9. doi: 10.1016/j.jaad.2019.12.047).
Dr. Pandya reported serving as a consultant to Incyte, Pfizer, Viela Bio, and Villaris.
FROM AAD 20
Large study finds no link between TCI use, skin cancer in patients with AD
The results also suggest dose, frequency, and exposure duration to the topical calcineurin inhibitors (TCIs) tacrolimus and pimecrolimus are not associated with an increased risk of keratinocyte carcinomas (KCs), basal cell carcinomas (BCCs), and squamous cell carcinomas (SCCs) in patients with atopic dermatitis (AD), according to Maryam M. Asgari, MD, MPH, professor of dermatology, Harvard Medical School, Boston, and colleagues. In 2006, the Food and Drug Administration announced the addition of the boxed warning to the labeling of TCIs regarding a possible risk of cancer associated with use of pimecrolimus (Elidel) and with tacrolimus (Protopic), because of an increased risk of KCs associated with oral calcineurin inhibitors and reports of skin cancer in patients on TCIs.
“Controversy has surrounded the association between TCI exposure and KC risk since the black-box warning was issued by the FDA. A hypothesized mechanism of action for TCIs increasing KC risk includes a direct effect of calcineurin inhibition on DNA repair and apoptosis, which could influence keratinocyte carcinogenesis,” the authors of the study wrote in JAMA Dermatology. But, they added, there have been “conflicting results” in research exploring this association.
In the retrospective cohort study, Dr. Asgari and coauthors evaluated 93,746 adult patients with AD at Kaiser Permanente Northern California, diagnosed between January 2002 and December 2013, comparing skin cancer risk among 7,033 patients exposed to TCIs, 73,674 patients taking topical corticosteroids, and 46,141 patients who had not been exposed to TCIs or topical corticosteroids. Results were adjusted in a multivariate Cox regression analysis for age, gender, race/ethnicity, calendar year, number of dermatology visits per year, history of KCs, immunosuppression, prior systemic AD treatment, autoimmune disease, treatment with ultraviolet therapy, chemotherapy, and radiotherapy.
The researchers also examined how TCI dose, frequency and exposure duration impacted skin cancer risk. Patients were grouped by high-dose (0.1%) and low-dose (0.03%) formulations of tacrolimus; and the 1% formulation of pimecrolimus. Frequency of use was defined as low (once daily or less) or high (twice daily or more), and exposure duration was based on short- (less than 2 years), moderate- (2-4 years), and long-term (4 years or more) use. Patients were at least 40 years old (mean age, 58.5 years), 58.7% were women, 50.5% were White, 20.6% were Asian, 12.2% were Hispanic, and 7.9% were Black. They were followed for a mean of 7.70 years.
Compared with patients who were exposed to topical corticosteroids, there was no association between risk of KCs and exposure to TCIs in patients with AD (adjusted hazard ratio, 1.02; 95% confidence interval, 0.93-1.13). There were also no significant differences in risk of BCCs and TCI exposure (aHR, 1.01; 95% CI, 0.90-1.14) and risk of SCCs and TCI exposure (aHR, 0.94; 95% CI, 0.82-1.08), compared with patients exposed to topical corticosteroids.
Results were similar for risk of KCs (aHR, 1.03; 95% CI, 0.92-1.14), BCCs (aHR, 1.04; 95% CI, 0.91-1.19), and SCCs (aHR, 0.91; 95% CI, 0.78-1.06) when patients exposed to TCIs were compared with those with AD who were unexposed to any medication. In secondary analyses, Dr. Asgari and coauthors found no association with overall risk of KCs, or risk of BCCs or SCCs, and the dose, frequency, or exposure duration to TCIs.
“Our findings appear to support those of smaller postmarketing surveillance studies of TCI and KC risk and may provide some reassurance about the safety profile of this class of topical agents in the treatment of AD,” they concluded.
In an interview, Jonathan Silverberg, MD, PhD, MPH, associate professor of dermatology, George Washington University, Washington, said initial concerns surrounding TCIs were based on high doses potentially increasing the risk of malignancy, and off-label use of TCIs for inflammatory skin diseases other than AD.
“However, the FDA’s concerns may not have been justified,” he said. The manufacturers of pimecrolimus and tacrolimus have published results of 10-year observational registries that assess cancer risk, which “found no evidence of any associations between TCIs and malignancy,” noted Dr. Silverberg, who is also director of clinical research and contact dermatitis at George Washington University.
Elizabeth Hughes, MD, a dermatologist in private practice in San Antonio, said in an interview that initial enthusiasm was “huge” for use of TCIs like tacrolimus in patients with AD when they first became available, especially in the pediatric population, for whom clinicians are hesitant to use long-term strong topical steroids. However, parents of children taking the medication soon became concerned about potential side effects.
“The TCIs can be absorbed to a small extent through body surface area, so it was not a big leap to become concerned that infants and small children could absorb enough ... into the bloodstream to give a similar side effect profile as oral tacrolimus,” she said.
The addition of the boxed warning in 2006 was frustrating for dermatologists “because a medication we needed very much for a young population now was ‘labeled’ and parents were scared to use it,” Dr. Hughes explained.
Dr. Silverberg noted that, while the results of the new study are unlikely to change clinical practice, they are reassuring, and provide real-world data and “further confirmation of previous studies showing no associations between AD and malignancy.”
“Since AD and skin cancer are both commonly managed by dermatologists, there is potential for increased surveillance and detection of skin cancers in AD patients. So, the greatest chance of seeing a false-positive signal for malignancy would likely occur with skin cancers,” he pointed out. “Yet, even in the case of skin cancers, there were no demonstrable signals.”
Based on the results, “I think it is definitely reasonable to reconsider” the TCI boxed warning, but there isn’t much precedent for boxed warnings to be removed from labeling, Dr. Silverberg commented. “Unfortunately, the black-box warning may persist despite a lot of reassuring data.”
In a related editorial, Aaron M. Drucker, MD, ScM, and Mina Tadrous, PharmD, PhD, of the University of Toronto, said the boxed warning “had the intent of helping patients and clinicians understand possible risks,” but also carried the “potential for harm” if patients discontinued or did not adhere to treatment. “Safety warnings on topical medications could lead to undertreatment of atopic dermatitis, reduced quality of life and, potentially, increased use of more toxic systemic medications.”
Long-term studies of medications and cancer risk are challenging to perform, having to account for dose-response relationships, confounding by indication, and time bias, among other factors, and this study “recognizes and attempts to address many of these challenges,” Dr. Drucker and Dr. Tadrous wrote.
These results are similar to previous studies that have “consistently reported no or minimal association between TCI use and skin cancer,” they noted, adding that, “if an association exists, it is likely very small, meaning that skin cancer attributable to TCI use is rare. Clinicians can use this evidence to counsel and reassure patients for whom the benefits of ongoing treatment with TCIs may outweigh the harms.”
This study was funded by a grant from Valeant Pharmaceuticals. Dr. Asgari reported receiving grants from Valeant during the study, and from Pfizer not related to the study. The other authors reported no relevant conflicts of interest. Dr. Drucker reported relationships with the Canadian Agency for Drugs and Technology in Health, CME Outfitters, Eczema Society of Canada, Sanofi, Regeneron, and RTI Health Solutions in the form of paid fees, consultancies, honoraria, educational grants, and other compensation paid to him and/or his institution. Dr. Tadrous reported no relevant disclosures. Dr. Silverberg reported receiving honoraria for advisory board, speaker, and consultant services from numerous pharmaceutical manufacturers, and research grants for investigator services from GlaxoSmithKline and Galderma. Dr. Hughes Tichy reported no relevant financial disclosures. Dr. Silverberg is a member of the Dermatology News editorial advisory board.
SOURCE: Asgari MM et al. JAMA Dermatol. 2020 Aug 12. doi: 10.1001/jamadermatol.2020.2240.
The results also suggest dose, frequency, and exposure duration to the topical calcineurin inhibitors (TCIs) tacrolimus and pimecrolimus are not associated with an increased risk of keratinocyte carcinomas (KCs), basal cell carcinomas (BCCs), and squamous cell carcinomas (SCCs) in patients with atopic dermatitis (AD), according to Maryam M. Asgari, MD, MPH, professor of dermatology, Harvard Medical School, Boston, and colleagues. In 2006, the Food and Drug Administration announced the addition of the boxed warning to the labeling of TCIs regarding a possible risk of cancer associated with use of pimecrolimus (Elidel) and with tacrolimus (Protopic), because of an increased risk of KCs associated with oral calcineurin inhibitors and reports of skin cancer in patients on TCIs.
“Controversy has surrounded the association between TCI exposure and KC risk since the black-box warning was issued by the FDA. A hypothesized mechanism of action for TCIs increasing KC risk includes a direct effect of calcineurin inhibition on DNA repair and apoptosis, which could influence keratinocyte carcinogenesis,” the authors of the study wrote in JAMA Dermatology. But, they added, there have been “conflicting results” in research exploring this association.
In the retrospective cohort study, Dr. Asgari and coauthors evaluated 93,746 adult patients with AD at Kaiser Permanente Northern California, diagnosed between January 2002 and December 2013, comparing skin cancer risk among 7,033 patients exposed to TCIs, 73,674 patients taking topical corticosteroids, and 46,141 patients who had not been exposed to TCIs or topical corticosteroids. Results were adjusted in a multivariate Cox regression analysis for age, gender, race/ethnicity, calendar year, number of dermatology visits per year, history of KCs, immunosuppression, prior systemic AD treatment, autoimmune disease, treatment with ultraviolet therapy, chemotherapy, and radiotherapy.
The researchers also examined how TCI dose, frequency and exposure duration impacted skin cancer risk. Patients were grouped by high-dose (0.1%) and low-dose (0.03%) formulations of tacrolimus; and the 1% formulation of pimecrolimus. Frequency of use was defined as low (once daily or less) or high (twice daily or more), and exposure duration was based on short- (less than 2 years), moderate- (2-4 years), and long-term (4 years or more) use. Patients were at least 40 years old (mean age, 58.5 years), 58.7% were women, 50.5% were White, 20.6% were Asian, 12.2% were Hispanic, and 7.9% were Black. They were followed for a mean of 7.70 years.
Compared with patients who were exposed to topical corticosteroids, there was no association between risk of KCs and exposure to TCIs in patients with AD (adjusted hazard ratio, 1.02; 95% confidence interval, 0.93-1.13). There were also no significant differences in risk of BCCs and TCI exposure (aHR, 1.01; 95% CI, 0.90-1.14) and risk of SCCs and TCI exposure (aHR, 0.94; 95% CI, 0.82-1.08), compared with patients exposed to topical corticosteroids.
Results were similar for risk of KCs (aHR, 1.03; 95% CI, 0.92-1.14), BCCs (aHR, 1.04; 95% CI, 0.91-1.19), and SCCs (aHR, 0.91; 95% CI, 0.78-1.06) when patients exposed to TCIs were compared with those with AD who were unexposed to any medication. In secondary analyses, Dr. Asgari and coauthors found no association with overall risk of KCs, or risk of BCCs or SCCs, and the dose, frequency, or exposure duration to TCIs.
“Our findings appear to support those of smaller postmarketing surveillance studies of TCI and KC risk and may provide some reassurance about the safety profile of this class of topical agents in the treatment of AD,” they concluded.
In an interview, Jonathan Silverberg, MD, PhD, MPH, associate professor of dermatology, George Washington University, Washington, said initial concerns surrounding TCIs were based on high doses potentially increasing the risk of malignancy, and off-label use of TCIs for inflammatory skin diseases other than AD.
“However, the FDA’s concerns may not have been justified,” he said. The manufacturers of pimecrolimus and tacrolimus have published results of 10-year observational registries that assess cancer risk, which “found no evidence of any associations between TCIs and malignancy,” noted Dr. Silverberg, who is also director of clinical research and contact dermatitis at George Washington University.
Elizabeth Hughes, MD, a dermatologist in private practice in San Antonio, said in an interview that initial enthusiasm was “huge” for use of TCIs like tacrolimus in patients with AD when they first became available, especially in the pediatric population, for whom clinicians are hesitant to use long-term strong topical steroids. However, parents of children taking the medication soon became concerned about potential side effects.
“The TCIs can be absorbed to a small extent through body surface area, so it was not a big leap to become concerned that infants and small children could absorb enough ... into the bloodstream to give a similar side effect profile as oral tacrolimus,” she said.
The addition of the boxed warning in 2006 was frustrating for dermatologists “because a medication we needed very much for a young population now was ‘labeled’ and parents were scared to use it,” Dr. Hughes explained.
Dr. Silverberg noted that, while the results of the new study are unlikely to change clinical practice, they are reassuring, and provide real-world data and “further confirmation of previous studies showing no associations between AD and malignancy.”
“Since AD and skin cancer are both commonly managed by dermatologists, there is potential for increased surveillance and detection of skin cancers in AD patients. So, the greatest chance of seeing a false-positive signal for malignancy would likely occur with skin cancers,” he pointed out. “Yet, even in the case of skin cancers, there were no demonstrable signals.”
Based on the results, “I think it is definitely reasonable to reconsider” the TCI boxed warning, but there isn’t much precedent for boxed warnings to be removed from labeling, Dr. Silverberg commented. “Unfortunately, the black-box warning may persist despite a lot of reassuring data.”
In a related editorial, Aaron M. Drucker, MD, ScM, and Mina Tadrous, PharmD, PhD, of the University of Toronto, said the boxed warning “had the intent of helping patients and clinicians understand possible risks,” but also carried the “potential for harm” if patients discontinued or did not adhere to treatment. “Safety warnings on topical medications could lead to undertreatment of atopic dermatitis, reduced quality of life and, potentially, increased use of more toxic systemic medications.”
Long-term studies of medications and cancer risk are challenging to perform, having to account for dose-response relationships, confounding by indication, and time bias, among other factors, and this study “recognizes and attempts to address many of these challenges,” Dr. Drucker and Dr. Tadrous wrote.
These results are similar to previous studies that have “consistently reported no or minimal association between TCI use and skin cancer,” they noted, adding that, “if an association exists, it is likely very small, meaning that skin cancer attributable to TCI use is rare. Clinicians can use this evidence to counsel and reassure patients for whom the benefits of ongoing treatment with TCIs may outweigh the harms.”
This study was funded by a grant from Valeant Pharmaceuticals. Dr. Asgari reported receiving grants from Valeant during the study, and from Pfizer not related to the study. The other authors reported no relevant conflicts of interest. Dr. Drucker reported relationships with the Canadian Agency for Drugs and Technology in Health, CME Outfitters, Eczema Society of Canada, Sanofi, Regeneron, and RTI Health Solutions in the form of paid fees, consultancies, honoraria, educational grants, and other compensation paid to him and/or his institution. Dr. Tadrous reported no relevant disclosures. Dr. Silverberg reported receiving honoraria for advisory board, speaker, and consultant services from numerous pharmaceutical manufacturers, and research grants for investigator services from GlaxoSmithKline and Galderma. Dr. Hughes Tichy reported no relevant financial disclosures. Dr. Silverberg is a member of the Dermatology News editorial advisory board.
SOURCE: Asgari MM et al. JAMA Dermatol. 2020 Aug 12. doi: 10.1001/jamadermatol.2020.2240.
The results also suggest dose, frequency, and exposure duration to the topical calcineurin inhibitors (TCIs) tacrolimus and pimecrolimus are not associated with an increased risk of keratinocyte carcinomas (KCs), basal cell carcinomas (BCCs), and squamous cell carcinomas (SCCs) in patients with atopic dermatitis (AD), according to Maryam M. Asgari, MD, MPH, professor of dermatology, Harvard Medical School, Boston, and colleagues. In 2006, the Food and Drug Administration announced the addition of the boxed warning to the labeling of TCIs regarding a possible risk of cancer associated with use of pimecrolimus (Elidel) and with tacrolimus (Protopic), because of an increased risk of KCs associated with oral calcineurin inhibitors and reports of skin cancer in patients on TCIs.
“Controversy has surrounded the association between TCI exposure and KC risk since the black-box warning was issued by the FDA. A hypothesized mechanism of action for TCIs increasing KC risk includes a direct effect of calcineurin inhibition on DNA repair and apoptosis, which could influence keratinocyte carcinogenesis,” the authors of the study wrote in JAMA Dermatology. But, they added, there have been “conflicting results” in research exploring this association.
In the retrospective cohort study, Dr. Asgari and coauthors evaluated 93,746 adult patients with AD at Kaiser Permanente Northern California, diagnosed between January 2002 and December 2013, comparing skin cancer risk among 7,033 patients exposed to TCIs, 73,674 patients taking topical corticosteroids, and 46,141 patients who had not been exposed to TCIs or topical corticosteroids. Results were adjusted in a multivariate Cox regression analysis for age, gender, race/ethnicity, calendar year, number of dermatology visits per year, history of KCs, immunosuppression, prior systemic AD treatment, autoimmune disease, treatment with ultraviolet therapy, chemotherapy, and radiotherapy.
The researchers also examined how TCI dose, frequency and exposure duration impacted skin cancer risk. Patients were grouped by high-dose (0.1%) and low-dose (0.03%) formulations of tacrolimus; and the 1% formulation of pimecrolimus. Frequency of use was defined as low (once daily or less) or high (twice daily or more), and exposure duration was based on short- (less than 2 years), moderate- (2-4 years), and long-term (4 years or more) use. Patients were at least 40 years old (mean age, 58.5 years), 58.7% were women, 50.5% were White, 20.6% were Asian, 12.2% were Hispanic, and 7.9% were Black. They were followed for a mean of 7.70 years.
Compared with patients who were exposed to topical corticosteroids, there was no association between risk of KCs and exposure to TCIs in patients with AD (adjusted hazard ratio, 1.02; 95% confidence interval, 0.93-1.13). There were also no significant differences in risk of BCCs and TCI exposure (aHR, 1.01; 95% CI, 0.90-1.14) and risk of SCCs and TCI exposure (aHR, 0.94; 95% CI, 0.82-1.08), compared with patients exposed to topical corticosteroids.
Results were similar for risk of KCs (aHR, 1.03; 95% CI, 0.92-1.14), BCCs (aHR, 1.04; 95% CI, 0.91-1.19), and SCCs (aHR, 0.91; 95% CI, 0.78-1.06) when patients exposed to TCIs were compared with those with AD who were unexposed to any medication. In secondary analyses, Dr. Asgari and coauthors found no association with overall risk of KCs, or risk of BCCs or SCCs, and the dose, frequency, or exposure duration to TCIs.
“Our findings appear to support those of smaller postmarketing surveillance studies of TCI and KC risk and may provide some reassurance about the safety profile of this class of topical agents in the treatment of AD,” they concluded.
In an interview, Jonathan Silverberg, MD, PhD, MPH, associate professor of dermatology, George Washington University, Washington, said initial concerns surrounding TCIs were based on high doses potentially increasing the risk of malignancy, and off-label use of TCIs for inflammatory skin diseases other than AD.
“However, the FDA’s concerns may not have been justified,” he said. The manufacturers of pimecrolimus and tacrolimus have published results of 10-year observational registries that assess cancer risk, which “found no evidence of any associations between TCIs and malignancy,” noted Dr. Silverberg, who is also director of clinical research and contact dermatitis at George Washington University.
Elizabeth Hughes, MD, a dermatologist in private practice in San Antonio, said in an interview that initial enthusiasm was “huge” for use of TCIs like tacrolimus in patients with AD when they first became available, especially in the pediatric population, for whom clinicians are hesitant to use long-term strong topical steroids. However, parents of children taking the medication soon became concerned about potential side effects.
“The TCIs can be absorbed to a small extent through body surface area, so it was not a big leap to become concerned that infants and small children could absorb enough ... into the bloodstream to give a similar side effect profile as oral tacrolimus,” she said.
The addition of the boxed warning in 2006 was frustrating for dermatologists “because a medication we needed very much for a young population now was ‘labeled’ and parents were scared to use it,” Dr. Hughes explained.
Dr. Silverberg noted that, while the results of the new study are unlikely to change clinical practice, they are reassuring, and provide real-world data and “further confirmation of previous studies showing no associations between AD and malignancy.”
“Since AD and skin cancer are both commonly managed by dermatologists, there is potential for increased surveillance and detection of skin cancers in AD patients. So, the greatest chance of seeing a false-positive signal for malignancy would likely occur with skin cancers,” he pointed out. “Yet, even in the case of skin cancers, there were no demonstrable signals.”
Based on the results, “I think it is definitely reasonable to reconsider” the TCI boxed warning, but there isn’t much precedent for boxed warnings to be removed from labeling, Dr. Silverberg commented. “Unfortunately, the black-box warning may persist despite a lot of reassuring data.”
In a related editorial, Aaron M. Drucker, MD, ScM, and Mina Tadrous, PharmD, PhD, of the University of Toronto, said the boxed warning “had the intent of helping patients and clinicians understand possible risks,” but also carried the “potential for harm” if patients discontinued or did not adhere to treatment. “Safety warnings on topical medications could lead to undertreatment of atopic dermatitis, reduced quality of life and, potentially, increased use of more toxic systemic medications.”
Long-term studies of medications and cancer risk are challenging to perform, having to account for dose-response relationships, confounding by indication, and time bias, among other factors, and this study “recognizes and attempts to address many of these challenges,” Dr. Drucker and Dr. Tadrous wrote.
These results are similar to previous studies that have “consistently reported no or minimal association between TCI use and skin cancer,” they noted, adding that, “if an association exists, it is likely very small, meaning that skin cancer attributable to TCI use is rare. Clinicians can use this evidence to counsel and reassure patients for whom the benefits of ongoing treatment with TCIs may outweigh the harms.”
This study was funded by a grant from Valeant Pharmaceuticals. Dr. Asgari reported receiving grants from Valeant during the study, and from Pfizer not related to the study. The other authors reported no relevant conflicts of interest. Dr. Drucker reported relationships with the Canadian Agency for Drugs and Technology in Health, CME Outfitters, Eczema Society of Canada, Sanofi, Regeneron, and RTI Health Solutions in the form of paid fees, consultancies, honoraria, educational grants, and other compensation paid to him and/or his institution. Dr. Tadrous reported no relevant disclosures. Dr. Silverberg reported receiving honoraria for advisory board, speaker, and consultant services from numerous pharmaceutical manufacturers, and research grants for investigator services from GlaxoSmithKline and Galderma. Dr. Hughes Tichy reported no relevant financial disclosures. Dr. Silverberg is a member of the Dermatology News editorial advisory board.
SOURCE: Asgari MM et al. JAMA Dermatol. 2020 Aug 12. doi: 10.1001/jamadermatol.2020.2240.
FROM JAMA DERMATOLOGY