User login
See Gastroenterology’s curated colorectal cancer research collection
Gastroenterology is proud to announce the release of a special collection of colorectal cancer articles. This curated collection includes some of the top colorectal cancer research published over the last 3 years with new research being added to the collection as it’s published.
View the special collection on Gastroenterology’s website, which is designed to help you quickly scan recent colorectal cancer research and easily navigate to studies of interest. Recent articles include:
- Use of Artificial Intelligence-Based Analytics From Live Colonoscopies to Optimize the Quality of the Colonoscopy Examination in Real Time: Proof of Concept
- Risk Factors for Early-Onset Colorectal Cancer
- Causes of Post-Colonoscopy Colorectal Cancers Based on World Endoscopy Organization System of Analysis
To view all of Gastroenterology’s curated article collections, please visit gastro.org/GastroCollections.
Gastroenterology is proud to announce the release of a special collection of colorectal cancer articles. This curated collection includes some of the top colorectal cancer research published over the last 3 years with new research being added to the collection as it’s published.
View the special collection on Gastroenterology’s website, which is designed to help you quickly scan recent colorectal cancer research and easily navigate to studies of interest. Recent articles include:
- Use of Artificial Intelligence-Based Analytics From Live Colonoscopies to Optimize the Quality of the Colonoscopy Examination in Real Time: Proof of Concept
- Risk Factors for Early-Onset Colorectal Cancer
- Causes of Post-Colonoscopy Colorectal Cancers Based on World Endoscopy Organization System of Analysis
To view all of Gastroenterology’s curated article collections, please visit gastro.org/GastroCollections.
Gastroenterology is proud to announce the release of a special collection of colorectal cancer articles. This curated collection includes some of the top colorectal cancer research published over the last 3 years with new research being added to the collection as it’s published.
View the special collection on Gastroenterology’s website, which is designed to help you quickly scan recent colorectal cancer research and easily navigate to studies of interest. Recent articles include:
- Use of Artificial Intelligence-Based Analytics From Live Colonoscopies to Optimize the Quality of the Colonoscopy Examination in Real Time: Proof of Concept
- Risk Factors for Early-Onset Colorectal Cancer
- Causes of Post-Colonoscopy Colorectal Cancers Based on World Endoscopy Organization System of Analysis
To view all of Gastroenterology’s curated article collections, please visit gastro.org/GastroCollections.
Social media and health information: Empowering or misleading?
The search engine giants, Dr. Google or Dr. Bing, are visited by most of our patients before seeking medical help. In 1976, medical student Tom Ferguson, MD, first coined the term e-Patient. It means a health consumer who uses the Internet to gather information about a medical condition for themselves or on behalf of family and friends and uses electronic communication tools to cope with medical conditions. Dr. Ferguson described e-Patients as “empowered medical consumers.”1
During the COVID-19 pandemic, social media and networking platforms – such as Facebook, Twitter, Instagram, Snapchat, YouTube, WhatsApp, online health support groups – are used increasingly by e-Patients to gather critical health information. Health care providers often take a conflicted stand on the use of social media. Though we want our patients to read about their illnesses and make informed choices, we often get frustrated by misdiagnoses, misinformation, and disinformation that comes with it.
According to a study investigating the differential diffusion of news stories distributed on Twitter from 2006 to 2017, fake news was considered more novel than true news, and people were more likely to share novel information.2 Bots accelerated the spread of true and fake news at the same rate, implying that fake news spreads more than the truth because humans, not robots, are more likely to spread it. Social media has promoted some of the best health campaigns, like public cancer awareness, the ALS Ice Bucket Challenge, World Heart Day, and others. At the same time, it has also provided a platform for antivaccination activists, dangerous and unproven alternative cancer therapies, weight loss pills, and nutrition plans.
According to a Pew Research Center survey, 72% of adult Internet users had searched online for information about a range of health issues of their own or for others in the past 12 months.3 A survey from 2019-2020 showed that those who relied on social media for news were among the least knowledgeable about key facts during the COVID-19 outbreak.4 About 74% of public posts about COVID-19 were linked to news organizations, while just 1% linked to health and science sites.5 While social media has emerged as one of the most significant health information sources, it famously has only a few safeguards in place against medical misinformation. Requiring responsibility and regulations for accurate or evidence-based information walks a thin line on infringing freedom of speech. Medical misinformation related to COVID-19 has become as contagious as the virus itself.
In February 2020, the World Health Organization warned that a massive ‘Infodemic’ had accompanied the COVID-19 outbreak, with an overabundance of information, some accurate and some not, making it difficult for people to find reliable sources and trustworthy information.6 The Black immunity myth, groups opposing vaccines, campaigns against 5G mobile phone networks, suggestions that SARS-CoV-2 was an engineered bioweapon, and online rumors leading to mob attacks in India and mass poisonings in Iran are some of the misleading health information that has circulated related to COVID-19.
In the Web 2.0 era, in which credible health information comes packaged with divisive and misleading information, social media’s full impact on health care, health outcomes, and mental health has yet to be explored. Social networks and media sharing networks have recently announced initiatives to stop misinformation and disinformation by fact-checking, flagging, issuing warnings, and deleting misinformation or misleading content. Providing links to more and correct information and partnering with health and science organizations can also encourage the spread of verifiable information.
While we have yet to see if social media safeguards are adequate, the medical community needs to proactively educate patients on the appropriate use of social media for health information, e-Health literacy, and media health literacy. Like health care providers evaluating scientific papers, we need to cultivate e-Patients’ ability to seek, evaluate, understand, and convey health information from electronic sources. Although the measurement and training tools for e-Health and media health literacy are still scarce, a good place to start could be to have simple conversations with patients. Encouraging patients to critically analyze online information, use credible social media sources, and recognizing the warnings, red flags, and links on unreliable information are some of the discussions worth considering. Equally important is to discourage patients from changing health behaviors or practices based on unverified social media resources and discussing the possible impact of medical misinformation.
A practical approach for e-Patients could be to ask the Five Ws, considered fundamental in information gathering: Who, What, Why, When, and Where.7,8
- Who runs the website? Examine the authors, sponsors, and sources. Federal agencies’ website addresses end in “.gov,” educational institutions maintain “.edu,” large professional or nonprofit organizations often use “.org,” and commercial websites use “.com.”
- What is offered, and What is the evidence? Does it provide unbelievable solutions or quick, miracle cures?
- Why was the site created? Is the mission or goal to inform, explain, or sell health or medical products? Check details on “About This Site” or “About Us.”
- When was the information written or the webpage last updated?
- Where are the privacy policies? Is your privacy protected?
The anonymity of sources, sponsors, financial interests, or the lack of medical credentials and reputable medical research, the use of testimonials as evidence, outdated or incomplete information, and emotional or exaggerated language should raise suspicion about the reliability of the information. Tools like the online tutorial and a checklist from the National Institute of Health’s National Library of Medicine can also be offered to e-Patients to learn how to evaluate health information online.9,10
Online health support groups widely used by patients can be an additional layer of support but can also be a source of misinformation. Since they have fewer gatekeepers than traditional face-to-face communication, keeping a check on the credibility of the information can be difficult. Support groups affiliated with local hospitals or national organizations, or those endorsed by well-known scientific societies, can be encouraged instead of less credible sources. Some online support groups, run by non–health care professionals but with experienced and reliable scientific panels, can be useful resources. However, patients must check for the credibility and reliability of the information.
Lastly, just as hospitalists take a social history of our patients, we could also ask for a “social media history” to understand patients’ sources of health information. We can then guide them toward more credible sources to make them truly empowered medical consumers.
Dr. Saigal is a hospitalist and clinical assistant professor of medicine in the division of hospital medicine at the Ohio State University Wexner Medical Center, Columbus.
References
1. Nelson R. Informatics: Empowering ePatients to drive health care reform - part I. Online J Issues Nurs. 2016 Sep 13;21(3):9.
2. Vosoughi S et al. The spread of true and false news online. Science. 2012;359(6380):1146-51.
3. Fox S. The social life of health information. Pew Research Center: Fact Tank. 2014 Jan 15. Accessed 2020 Jul 31.
4. Mitchel A, Jurkowitz M, Oliphant JB, Shearer E. Americans Who Mainly Get Their News on Social Media Are Less Engaged, Less Knowledgeable. Pew Research Center: Journalism & Media. 2020 Jul 30. Accessed 2020 Jul 31.
5. Stocking G, Matsa KE, Khuzam M. As COVID-19 Emerged in U.S., Facebook Posts About It Appeared in a Wide Range of Public Pages, Groups Pew Research Center: Journalism & Media. 2020 Jun 24. Accessed 2020 Jul 31.
6. Munich Security Conference. World Health Organization. 2020 Feb 15. Accessed 2020 Jul 31.
7. Levin-Zamir D, Bertschi I. Media health literacy, eHealth literacy, and the role of the social environment in context. Int J Environ Res Public Health. 2018 Aug 3;15(8):1643.
8. Online Health Information: Is It Reliable? National Institute on Aging, National Institutes of Health. 2018 Oct 31. Accessed 2020 Aug 10.
9. How To Evaluate Health Information on the Internet: Questions and Answers. Office of Dietary Supplements, National Institutes of Health. 2011 Jun 24. Accessed 2020 Aug 10.
10. Evaluating Internet Health Information: A Tutorial From the National Library of Medicine. Medline Plus. 2020 Mar 6. Accessed 2020 Aug 10.
The search engine giants, Dr. Google or Dr. Bing, are visited by most of our patients before seeking medical help. In 1976, medical student Tom Ferguson, MD, first coined the term e-Patient. It means a health consumer who uses the Internet to gather information about a medical condition for themselves or on behalf of family and friends and uses electronic communication tools to cope with medical conditions. Dr. Ferguson described e-Patients as “empowered medical consumers.”1
During the COVID-19 pandemic, social media and networking platforms – such as Facebook, Twitter, Instagram, Snapchat, YouTube, WhatsApp, online health support groups – are used increasingly by e-Patients to gather critical health information. Health care providers often take a conflicted stand on the use of social media. Though we want our patients to read about their illnesses and make informed choices, we often get frustrated by misdiagnoses, misinformation, and disinformation that comes with it.
According to a study investigating the differential diffusion of news stories distributed on Twitter from 2006 to 2017, fake news was considered more novel than true news, and people were more likely to share novel information.2 Bots accelerated the spread of true and fake news at the same rate, implying that fake news spreads more than the truth because humans, not robots, are more likely to spread it. Social media has promoted some of the best health campaigns, like public cancer awareness, the ALS Ice Bucket Challenge, World Heart Day, and others. At the same time, it has also provided a platform for antivaccination activists, dangerous and unproven alternative cancer therapies, weight loss pills, and nutrition plans.
According to a Pew Research Center survey, 72% of adult Internet users had searched online for information about a range of health issues of their own or for others in the past 12 months.3 A survey from 2019-2020 showed that those who relied on social media for news were among the least knowledgeable about key facts during the COVID-19 outbreak.4 About 74% of public posts about COVID-19 were linked to news organizations, while just 1% linked to health and science sites.5 While social media has emerged as one of the most significant health information sources, it famously has only a few safeguards in place against medical misinformation. Requiring responsibility and regulations for accurate or evidence-based information walks a thin line on infringing freedom of speech. Medical misinformation related to COVID-19 has become as contagious as the virus itself.
In February 2020, the World Health Organization warned that a massive ‘Infodemic’ had accompanied the COVID-19 outbreak, with an overabundance of information, some accurate and some not, making it difficult for people to find reliable sources and trustworthy information.6 The Black immunity myth, groups opposing vaccines, campaigns against 5G mobile phone networks, suggestions that SARS-CoV-2 was an engineered bioweapon, and online rumors leading to mob attacks in India and mass poisonings in Iran are some of the misleading health information that has circulated related to COVID-19.
In the Web 2.0 era, in which credible health information comes packaged with divisive and misleading information, social media’s full impact on health care, health outcomes, and mental health has yet to be explored. Social networks and media sharing networks have recently announced initiatives to stop misinformation and disinformation by fact-checking, flagging, issuing warnings, and deleting misinformation or misleading content. Providing links to more and correct information and partnering with health and science organizations can also encourage the spread of verifiable information.
While we have yet to see if social media safeguards are adequate, the medical community needs to proactively educate patients on the appropriate use of social media for health information, e-Health literacy, and media health literacy. Like health care providers evaluating scientific papers, we need to cultivate e-Patients’ ability to seek, evaluate, understand, and convey health information from electronic sources. Although the measurement and training tools for e-Health and media health literacy are still scarce, a good place to start could be to have simple conversations with patients. Encouraging patients to critically analyze online information, use credible social media sources, and recognizing the warnings, red flags, and links on unreliable information are some of the discussions worth considering. Equally important is to discourage patients from changing health behaviors or practices based on unverified social media resources and discussing the possible impact of medical misinformation.
A practical approach for e-Patients could be to ask the Five Ws, considered fundamental in information gathering: Who, What, Why, When, and Where.7,8
- Who runs the website? Examine the authors, sponsors, and sources. Federal agencies’ website addresses end in “.gov,” educational institutions maintain “.edu,” large professional or nonprofit organizations often use “.org,” and commercial websites use “.com.”
- What is offered, and What is the evidence? Does it provide unbelievable solutions or quick, miracle cures?
- Why was the site created? Is the mission or goal to inform, explain, or sell health or medical products? Check details on “About This Site” or “About Us.”
- When was the information written or the webpage last updated?
- Where are the privacy policies? Is your privacy protected?
The anonymity of sources, sponsors, financial interests, or the lack of medical credentials and reputable medical research, the use of testimonials as evidence, outdated or incomplete information, and emotional or exaggerated language should raise suspicion about the reliability of the information. Tools like the online tutorial and a checklist from the National Institute of Health’s National Library of Medicine can also be offered to e-Patients to learn how to evaluate health information online.9,10
Online health support groups widely used by patients can be an additional layer of support but can also be a source of misinformation. Since they have fewer gatekeepers than traditional face-to-face communication, keeping a check on the credibility of the information can be difficult. Support groups affiliated with local hospitals or national organizations, or those endorsed by well-known scientific societies, can be encouraged instead of less credible sources. Some online support groups, run by non–health care professionals but with experienced and reliable scientific panels, can be useful resources. However, patients must check for the credibility and reliability of the information.
Lastly, just as hospitalists take a social history of our patients, we could also ask for a “social media history” to understand patients’ sources of health information. We can then guide them toward more credible sources to make them truly empowered medical consumers.
Dr. Saigal is a hospitalist and clinical assistant professor of medicine in the division of hospital medicine at the Ohio State University Wexner Medical Center, Columbus.
References
1. Nelson R. Informatics: Empowering ePatients to drive health care reform - part I. Online J Issues Nurs. 2016 Sep 13;21(3):9.
2. Vosoughi S et al. The spread of true and false news online. Science. 2012;359(6380):1146-51.
3. Fox S. The social life of health information. Pew Research Center: Fact Tank. 2014 Jan 15. Accessed 2020 Jul 31.
4. Mitchel A, Jurkowitz M, Oliphant JB, Shearer E. Americans Who Mainly Get Their News on Social Media Are Less Engaged, Less Knowledgeable. Pew Research Center: Journalism & Media. 2020 Jul 30. Accessed 2020 Jul 31.
5. Stocking G, Matsa KE, Khuzam M. As COVID-19 Emerged in U.S., Facebook Posts About It Appeared in a Wide Range of Public Pages, Groups Pew Research Center: Journalism & Media. 2020 Jun 24. Accessed 2020 Jul 31.
6. Munich Security Conference. World Health Organization. 2020 Feb 15. Accessed 2020 Jul 31.
7. Levin-Zamir D, Bertschi I. Media health literacy, eHealth literacy, and the role of the social environment in context. Int J Environ Res Public Health. 2018 Aug 3;15(8):1643.
8. Online Health Information: Is It Reliable? National Institute on Aging, National Institutes of Health. 2018 Oct 31. Accessed 2020 Aug 10.
9. How To Evaluate Health Information on the Internet: Questions and Answers. Office of Dietary Supplements, National Institutes of Health. 2011 Jun 24. Accessed 2020 Aug 10.
10. Evaluating Internet Health Information: A Tutorial From the National Library of Medicine. Medline Plus. 2020 Mar 6. Accessed 2020 Aug 10.
The search engine giants, Dr. Google or Dr. Bing, are visited by most of our patients before seeking medical help. In 1976, medical student Tom Ferguson, MD, first coined the term e-Patient. It means a health consumer who uses the Internet to gather information about a medical condition for themselves or on behalf of family and friends and uses electronic communication tools to cope with medical conditions. Dr. Ferguson described e-Patients as “empowered medical consumers.”1
During the COVID-19 pandemic, social media and networking platforms – such as Facebook, Twitter, Instagram, Snapchat, YouTube, WhatsApp, online health support groups – are used increasingly by e-Patients to gather critical health information. Health care providers often take a conflicted stand on the use of social media. Though we want our patients to read about their illnesses and make informed choices, we often get frustrated by misdiagnoses, misinformation, and disinformation that comes with it.
According to a study investigating the differential diffusion of news stories distributed on Twitter from 2006 to 2017, fake news was considered more novel than true news, and people were more likely to share novel information.2 Bots accelerated the spread of true and fake news at the same rate, implying that fake news spreads more than the truth because humans, not robots, are more likely to spread it. Social media has promoted some of the best health campaigns, like public cancer awareness, the ALS Ice Bucket Challenge, World Heart Day, and others. At the same time, it has also provided a platform for antivaccination activists, dangerous and unproven alternative cancer therapies, weight loss pills, and nutrition plans.
According to a Pew Research Center survey, 72% of adult Internet users had searched online for information about a range of health issues of their own or for others in the past 12 months.3 A survey from 2019-2020 showed that those who relied on social media for news were among the least knowledgeable about key facts during the COVID-19 outbreak.4 About 74% of public posts about COVID-19 were linked to news organizations, while just 1% linked to health and science sites.5 While social media has emerged as one of the most significant health information sources, it famously has only a few safeguards in place against medical misinformation. Requiring responsibility and regulations for accurate or evidence-based information walks a thin line on infringing freedom of speech. Medical misinformation related to COVID-19 has become as contagious as the virus itself.
In February 2020, the World Health Organization warned that a massive ‘Infodemic’ had accompanied the COVID-19 outbreak, with an overabundance of information, some accurate and some not, making it difficult for people to find reliable sources and trustworthy information.6 The Black immunity myth, groups opposing vaccines, campaigns against 5G mobile phone networks, suggestions that SARS-CoV-2 was an engineered bioweapon, and online rumors leading to mob attacks in India and mass poisonings in Iran are some of the misleading health information that has circulated related to COVID-19.
In the Web 2.0 era, in which credible health information comes packaged with divisive and misleading information, social media’s full impact on health care, health outcomes, and mental health has yet to be explored. Social networks and media sharing networks have recently announced initiatives to stop misinformation and disinformation by fact-checking, flagging, issuing warnings, and deleting misinformation or misleading content. Providing links to more and correct information and partnering with health and science organizations can also encourage the spread of verifiable information.
While we have yet to see if social media safeguards are adequate, the medical community needs to proactively educate patients on the appropriate use of social media for health information, e-Health literacy, and media health literacy. Like health care providers evaluating scientific papers, we need to cultivate e-Patients’ ability to seek, evaluate, understand, and convey health information from electronic sources. Although the measurement and training tools for e-Health and media health literacy are still scarce, a good place to start could be to have simple conversations with patients. Encouraging patients to critically analyze online information, use credible social media sources, and recognizing the warnings, red flags, and links on unreliable information are some of the discussions worth considering. Equally important is to discourage patients from changing health behaviors or practices based on unverified social media resources and discussing the possible impact of medical misinformation.
A practical approach for e-Patients could be to ask the Five Ws, considered fundamental in information gathering: Who, What, Why, When, and Where.7,8
- Who runs the website? Examine the authors, sponsors, and sources. Federal agencies’ website addresses end in “.gov,” educational institutions maintain “.edu,” large professional or nonprofit organizations often use “.org,” and commercial websites use “.com.”
- What is offered, and What is the evidence? Does it provide unbelievable solutions or quick, miracle cures?
- Why was the site created? Is the mission or goal to inform, explain, or sell health or medical products? Check details on “About This Site” or “About Us.”
- When was the information written or the webpage last updated?
- Where are the privacy policies? Is your privacy protected?
The anonymity of sources, sponsors, financial interests, or the lack of medical credentials and reputable medical research, the use of testimonials as evidence, outdated or incomplete information, and emotional or exaggerated language should raise suspicion about the reliability of the information. Tools like the online tutorial and a checklist from the National Institute of Health’s National Library of Medicine can also be offered to e-Patients to learn how to evaluate health information online.9,10
Online health support groups widely used by patients can be an additional layer of support but can also be a source of misinformation. Since they have fewer gatekeepers than traditional face-to-face communication, keeping a check on the credibility of the information can be difficult. Support groups affiliated with local hospitals or national organizations, or those endorsed by well-known scientific societies, can be encouraged instead of less credible sources. Some online support groups, run by non–health care professionals but with experienced and reliable scientific panels, can be useful resources. However, patients must check for the credibility and reliability of the information.
Lastly, just as hospitalists take a social history of our patients, we could also ask for a “social media history” to understand patients’ sources of health information. We can then guide them toward more credible sources to make them truly empowered medical consumers.
Dr. Saigal is a hospitalist and clinical assistant professor of medicine in the division of hospital medicine at the Ohio State University Wexner Medical Center, Columbus.
References
1. Nelson R. Informatics: Empowering ePatients to drive health care reform - part I. Online J Issues Nurs. 2016 Sep 13;21(3):9.
2. Vosoughi S et al. The spread of true and false news online. Science. 2012;359(6380):1146-51.
3. Fox S. The social life of health information. Pew Research Center: Fact Tank. 2014 Jan 15. Accessed 2020 Jul 31.
4. Mitchel A, Jurkowitz M, Oliphant JB, Shearer E. Americans Who Mainly Get Their News on Social Media Are Less Engaged, Less Knowledgeable. Pew Research Center: Journalism & Media. 2020 Jul 30. Accessed 2020 Jul 31.
5. Stocking G, Matsa KE, Khuzam M. As COVID-19 Emerged in U.S., Facebook Posts About It Appeared in a Wide Range of Public Pages, Groups Pew Research Center: Journalism & Media. 2020 Jun 24. Accessed 2020 Jul 31.
6. Munich Security Conference. World Health Organization. 2020 Feb 15. Accessed 2020 Jul 31.
7. Levin-Zamir D, Bertschi I. Media health literacy, eHealth literacy, and the role of the social environment in context. Int J Environ Res Public Health. 2018 Aug 3;15(8):1643.
8. Online Health Information: Is It Reliable? National Institute on Aging, National Institutes of Health. 2018 Oct 31. Accessed 2020 Aug 10.
9. How To Evaluate Health Information on the Internet: Questions and Answers. Office of Dietary Supplements, National Institutes of Health. 2011 Jun 24. Accessed 2020 Aug 10.
10. Evaluating Internet Health Information: A Tutorial From the National Library of Medicine. Medline Plus. 2020 Mar 6. Accessed 2020 Aug 10.
Strategic approach mitigates impact of antidrug antibodies in patients with rheumatic diseases
Monitor antidrug antibodies for their impact on drug clearance to maximize treatment outcomes in rheumatology patients treated with biologics, Niels Vande Casteele, PharmD, PhD, said in a virtual presentation at the annual Perspectives in Rheumatic Diseases held by Global Academy for Medical Education.
Antidrug antibodies (ADAb) are associated with impaired drug efficacy and safety, he noted. Furthermore, he indicated that when ADAb bind to the drug, they can either block the activity of the drug directly and/or may cause the formation of complexes, leading to accelerated drug clearance and reduced drug exposure.
Dr. Vande Casteele, assistant professor in the department of medicine at the University of California, San Diego, outlined factors that contribute to immunogenicity, which occurs when the body reacts to neoantigens, or when there is a breakdown in immune tolerance, he said.
Genetics can play a key role in the risk for immunogenicity, as can the route of administration, dose, treatment duration, and concomitant diseases or medications, he explained.
In addition, product-related factors including sequence variation, glycosylation, host cells, contaminants and processing impurities, formulation, and handling and storage issues can impact immunogenicity, he noted.
For example, Dr. Vande Casteele cited a study in which the proportion of infliximab-treated patients with positive ADAbs was substantially higher among those receiving the drug intravenously, compared with those receiving it subcutaneously. As for treatment dosing, data on patients treated with infliximab have shown that maintenance therapy is associated with lower rates of immunogenicity, compared to episodic therapy, he said.
In terms of genetics, Dr. Vande Casteele cited a study published in January in Gastroenterology showing the presence of the HLA-DQA1*05 allele, carried by approximately 40% of the European population, significantly increased the rate of immunogenicity to infliximab and adalimumab in patients with Crohn’s disease (hazard ratio, 1.90).
Therapeutic drug monitoring and overcoming immunogenicity
Dr. Vande Casteele also reviewed how to measure ADAbs. “Antidrug antibody units and concentrations can differ across assays,” he said.
In clinical practice, “the majority of patients at the time of secondary loss of response will present with low drug exposure, and that is when you measure antidrug antibodies,” he said.
In rheumatology patients, the presence of ADAbs against anti–tumor necrosis factor monoclonal antibodies conveys a risk for treatment discontinuation, as well as “a risk of development of hypersensitivity reactions in all immune-mediated inflammatory diseases,” Dr. Vande Casteele said.
However, “the combined use of anti–tumor necrosis factor monoclonal antibodies and disease-modifying antirheumatic drugs reduces the development of antibodies and subsequent risks,” he noted.
For therapeutic drug monitoring in patients with a secondary loss of response, “first, look at the trough concentration,” Dr. Vande Casteele said. “If it is optimal, then ADAbs are probably inconsequential.” If the trough is low or undetectable, examine ADAbs, he added. To manage ADAbs, data support the use of drug dose escalation in some cases. However, “you may be able to overcome the antidrug antibodies in some patients with dose escalation, but this is not always a cost-effective strategy in the long term,” and some patients fail a drug despite adequate drug concentration, which may mean they are failing the mechanism, and not because of pharmacokinetic-related issues, he said.
Dr. Vande Casteele cited a post hoc analysis of the TAXIT trial, published in Gastroenterology. It was the first prospective study to look at proactive therapeutic drug monitoring in patients with inflammatory bowel diseases treated with maintenance infliximab. This post hoc analysis showed that ADAbs were overcome with dose escalation in nearly 50% of patients in the lowest two ADAb quartiles at the start of the trial, and although ADAb were masked by dose escalation in the highest two quartiles, measurement with a drug-sensitive assay showed that ADAb never disappeared, he said.
Another strategy to try to overcome immunogenicity is to add an immunomodulator, Dr. Vande Casteele said. He cited a recent study published in Rheumatology showing that the effect of methotrexate was mediated through immunogenicity for immunogenic compounds such as adalimumab.
Importantly, there is a risk for immunogenicity across agents, he noted. “Patients who are antibody positive to the prior anti-TNF are at a higher risk of developing antibodies to subsequent anti-TNFs.”
Dr. Vande Casteele reported receiving research grants from R-Biopharm; grants and personal fees from Takeda and UCB; and personal fees from Alimentiv (formerly Robarts Clinical Trials), Celltrion, and Prometheus. Global Academy for Medical Education and this news organization are owned by the same parent company.
Monitor antidrug antibodies for their impact on drug clearance to maximize treatment outcomes in rheumatology patients treated with biologics, Niels Vande Casteele, PharmD, PhD, said in a virtual presentation at the annual Perspectives in Rheumatic Diseases held by Global Academy for Medical Education.
Antidrug antibodies (ADAb) are associated with impaired drug efficacy and safety, he noted. Furthermore, he indicated that when ADAb bind to the drug, they can either block the activity of the drug directly and/or may cause the formation of complexes, leading to accelerated drug clearance and reduced drug exposure.
Dr. Vande Casteele, assistant professor in the department of medicine at the University of California, San Diego, outlined factors that contribute to immunogenicity, which occurs when the body reacts to neoantigens, or when there is a breakdown in immune tolerance, he said.
Genetics can play a key role in the risk for immunogenicity, as can the route of administration, dose, treatment duration, and concomitant diseases or medications, he explained.
In addition, product-related factors including sequence variation, glycosylation, host cells, contaminants and processing impurities, formulation, and handling and storage issues can impact immunogenicity, he noted.
For example, Dr. Vande Casteele cited a study in which the proportion of infliximab-treated patients with positive ADAbs was substantially higher among those receiving the drug intravenously, compared with those receiving it subcutaneously. As for treatment dosing, data on patients treated with infliximab have shown that maintenance therapy is associated with lower rates of immunogenicity, compared to episodic therapy, he said.
In terms of genetics, Dr. Vande Casteele cited a study published in January in Gastroenterology showing the presence of the HLA-DQA1*05 allele, carried by approximately 40% of the European population, significantly increased the rate of immunogenicity to infliximab and adalimumab in patients with Crohn’s disease (hazard ratio, 1.90).
Therapeutic drug monitoring and overcoming immunogenicity
Dr. Vande Casteele also reviewed how to measure ADAbs. “Antidrug antibody units and concentrations can differ across assays,” he said.
In clinical practice, “the majority of patients at the time of secondary loss of response will present with low drug exposure, and that is when you measure antidrug antibodies,” he said.
In rheumatology patients, the presence of ADAbs against anti–tumor necrosis factor monoclonal antibodies conveys a risk for treatment discontinuation, as well as “a risk of development of hypersensitivity reactions in all immune-mediated inflammatory diseases,” Dr. Vande Casteele said.
However, “the combined use of anti–tumor necrosis factor monoclonal antibodies and disease-modifying antirheumatic drugs reduces the development of antibodies and subsequent risks,” he noted.
For therapeutic drug monitoring in patients with a secondary loss of response, “first, look at the trough concentration,” Dr. Vande Casteele said. “If it is optimal, then ADAbs are probably inconsequential.” If the trough is low or undetectable, examine ADAbs, he added. To manage ADAbs, data support the use of drug dose escalation in some cases. However, “you may be able to overcome the antidrug antibodies in some patients with dose escalation, but this is not always a cost-effective strategy in the long term,” and some patients fail a drug despite adequate drug concentration, which may mean they are failing the mechanism, and not because of pharmacokinetic-related issues, he said.
Dr. Vande Casteele cited a post hoc analysis of the TAXIT trial, published in Gastroenterology. It was the first prospective study to look at proactive therapeutic drug monitoring in patients with inflammatory bowel diseases treated with maintenance infliximab. This post hoc analysis showed that ADAbs were overcome with dose escalation in nearly 50% of patients in the lowest two ADAb quartiles at the start of the trial, and although ADAb were masked by dose escalation in the highest two quartiles, measurement with a drug-sensitive assay showed that ADAb never disappeared, he said.
Another strategy to try to overcome immunogenicity is to add an immunomodulator, Dr. Vande Casteele said. He cited a recent study published in Rheumatology showing that the effect of methotrexate was mediated through immunogenicity for immunogenic compounds such as adalimumab.
Importantly, there is a risk for immunogenicity across agents, he noted. “Patients who are antibody positive to the prior anti-TNF are at a higher risk of developing antibodies to subsequent anti-TNFs.”
Dr. Vande Casteele reported receiving research grants from R-Biopharm; grants and personal fees from Takeda and UCB; and personal fees from Alimentiv (formerly Robarts Clinical Trials), Celltrion, and Prometheus. Global Academy for Medical Education and this news organization are owned by the same parent company.
Monitor antidrug antibodies for their impact on drug clearance to maximize treatment outcomes in rheumatology patients treated with biologics, Niels Vande Casteele, PharmD, PhD, said in a virtual presentation at the annual Perspectives in Rheumatic Diseases held by Global Academy for Medical Education.
Antidrug antibodies (ADAb) are associated with impaired drug efficacy and safety, he noted. Furthermore, he indicated that when ADAb bind to the drug, they can either block the activity of the drug directly and/or may cause the formation of complexes, leading to accelerated drug clearance and reduced drug exposure.
Dr. Vande Casteele, assistant professor in the department of medicine at the University of California, San Diego, outlined factors that contribute to immunogenicity, which occurs when the body reacts to neoantigens, or when there is a breakdown in immune tolerance, he said.
Genetics can play a key role in the risk for immunogenicity, as can the route of administration, dose, treatment duration, and concomitant diseases or medications, he explained.
In addition, product-related factors including sequence variation, glycosylation, host cells, contaminants and processing impurities, formulation, and handling and storage issues can impact immunogenicity, he noted.
For example, Dr. Vande Casteele cited a study in which the proportion of infliximab-treated patients with positive ADAbs was substantially higher among those receiving the drug intravenously, compared with those receiving it subcutaneously. As for treatment dosing, data on patients treated with infliximab have shown that maintenance therapy is associated with lower rates of immunogenicity, compared to episodic therapy, he said.
In terms of genetics, Dr. Vande Casteele cited a study published in January in Gastroenterology showing the presence of the HLA-DQA1*05 allele, carried by approximately 40% of the European population, significantly increased the rate of immunogenicity to infliximab and adalimumab in patients with Crohn’s disease (hazard ratio, 1.90).
Therapeutic drug monitoring and overcoming immunogenicity
Dr. Vande Casteele also reviewed how to measure ADAbs. “Antidrug antibody units and concentrations can differ across assays,” he said.
In clinical practice, “the majority of patients at the time of secondary loss of response will present with low drug exposure, and that is when you measure antidrug antibodies,” he said.
In rheumatology patients, the presence of ADAbs against anti–tumor necrosis factor monoclonal antibodies conveys a risk for treatment discontinuation, as well as “a risk of development of hypersensitivity reactions in all immune-mediated inflammatory diseases,” Dr. Vande Casteele said.
However, “the combined use of anti–tumor necrosis factor monoclonal antibodies and disease-modifying antirheumatic drugs reduces the development of antibodies and subsequent risks,” he noted.
For therapeutic drug monitoring in patients with a secondary loss of response, “first, look at the trough concentration,” Dr. Vande Casteele said. “If it is optimal, then ADAbs are probably inconsequential.” If the trough is low or undetectable, examine ADAbs, he added. To manage ADAbs, data support the use of drug dose escalation in some cases. However, “you may be able to overcome the antidrug antibodies in some patients with dose escalation, but this is not always a cost-effective strategy in the long term,” and some patients fail a drug despite adequate drug concentration, which may mean they are failing the mechanism, and not because of pharmacokinetic-related issues, he said.
Dr. Vande Casteele cited a post hoc analysis of the TAXIT trial, published in Gastroenterology. It was the first prospective study to look at proactive therapeutic drug monitoring in patients with inflammatory bowel diseases treated with maintenance infliximab. This post hoc analysis showed that ADAbs were overcome with dose escalation in nearly 50% of patients in the lowest two ADAb quartiles at the start of the trial, and although ADAb were masked by dose escalation in the highest two quartiles, measurement with a drug-sensitive assay showed that ADAb never disappeared, he said.
Another strategy to try to overcome immunogenicity is to add an immunomodulator, Dr. Vande Casteele said. He cited a recent study published in Rheumatology showing that the effect of methotrexate was mediated through immunogenicity for immunogenic compounds such as adalimumab.
Importantly, there is a risk for immunogenicity across agents, he noted. “Patients who are antibody positive to the prior anti-TNF are at a higher risk of developing antibodies to subsequent anti-TNFs.”
Dr. Vande Casteele reported receiving research grants from R-Biopharm; grants and personal fees from Takeda and UCB; and personal fees from Alimentiv (formerly Robarts Clinical Trials), Celltrion, and Prometheus. Global Academy for Medical Education and this news organization are owned by the same parent company.
FROM PRD 2020
Dermatologists play a key role in the transformation of transgender patients
, according to Doris Day, MD.
While clinical management of this patient population has historically been limited to experts in mental health, endocrinology, and select surgeons with experience in sex reassignment surgery, “what dermatologists provide on an aesthetic level through noninvasive or minimally invasive procedures can have a big impact in helping that transformation,” Dr. Day, of the department of dermatology at New York University Langone Health, said during the virtual annual Masters of Aesthetics Symposium. “But, we have to go through a transformation of sorts as well as we care for these patients, because we need to help them in the way that best matches their needs. We need to know about their mental health and the medicines they’re taking as well as their goals for their outcomes. If they’re working with surgeons for sex reassignment, we should have discussions with those clinicians as well.”
Gender-affirming hormone therapy is the primary medical intervention sought by transgender people, she said. This allows the acquisition of secondary sex characteristics more aligned with their gender identity. Feminizing hormone therapy affects the skin by reducing sebaceous gland activity, “which can lead to fewer acne breakouts and smaller pores but also cause drier skin,” Dr. Day said. “We can slow down the growth of body and facial hair and we can perform hair removal treatments. We see decreased male-pattern scalp hair loss, and we see smoother skin as the fat under the skin becomes thicker and the pores become smaller. We can also have increased pigment production, which is always a good thing.”
In a 2016 survey of 327 transgender individuals led by Dr. Day’s mentee, Brian A. Ginsberg, MD, and published in the Journal of the American Academy of Dermatology, most transgender women indicated that their face was most important to have changed, while for men it was the chest. Hair removal was the most common women’s facial procedure, followed by surgery then injectables, mostly performed by plastic surgeons.
Limitations of hormone therapy include the fact that it can take 2 or more years for associated changes to fully develop. “At least here in New York, patients want everything in a New York minute, so that’s always an issue,” she said. “We often recommend that patients wait at least 2 years after beginning hormone therapy before considering drastic feminization surgeries, but there are many options we have for them while they’re waiting for that. Even with hormone therapy, the bone structure of the face is unaffected, so we need to be artistic in creating a more feminized balance in order to help them physically match their gender to their identity.”
Noninvasive aesthetic procedures can compound the effects of hormone therapy, in addition to offering physical transformation beyond hormone therapy. She recalled assisting one of her patients transform from male to female. Over a period of 2 years, Dr. Day added Botox then Juvederm Voluma to the patient’s cheeks and chin, “and she started her transformation to a more feminized gender matching identity,” she said. Next came a hair transplant and the injection of more Voluma and fillers in the lips and cheeks on an as-needed basis.
“During one visit, I felt that we could still do more,” Dr. Day recalled. “She looked at me and said, ‘Actually, I feel so happy. This looks like me as I imagined I would look in my mind.’ I realized that my vision for her wasn’t the same as her vision for herself. She was thrilled with her transformation. I realized that as we see these patients, for all we learn about the science of gender transformation, the emotional aspects of our vision of what we can accomplish for our patients versus their vision of what their happiness level is may not entirely match. We have to be careful to help them celebrate their version of their femininity or masculinity, rather than trying to have our patients match what we think we can accomplish for them with our own sense of what femininity or masculinity is.”
Over time, Dr. Day said, the patient’s acne scars improved with fillers and microneedling treatments, and with the hormone therapy. “As we softened her appearance and as she made changes like the earrings that she wore and the hair style that she chose, she was in line with what her perception of her femininity was,” she said. “Little by little we’ve been watching her grow into her new self. It’s been a beautiful transformation. I was honored to be able to share in that journey with her.”
Dr. Day reported having no relevant financial disclosures.
, according to Doris Day, MD.
While clinical management of this patient population has historically been limited to experts in mental health, endocrinology, and select surgeons with experience in sex reassignment surgery, “what dermatologists provide on an aesthetic level through noninvasive or minimally invasive procedures can have a big impact in helping that transformation,” Dr. Day, of the department of dermatology at New York University Langone Health, said during the virtual annual Masters of Aesthetics Symposium. “But, we have to go through a transformation of sorts as well as we care for these patients, because we need to help them in the way that best matches their needs. We need to know about their mental health and the medicines they’re taking as well as their goals for their outcomes. If they’re working with surgeons for sex reassignment, we should have discussions with those clinicians as well.”
Gender-affirming hormone therapy is the primary medical intervention sought by transgender people, she said. This allows the acquisition of secondary sex characteristics more aligned with their gender identity. Feminizing hormone therapy affects the skin by reducing sebaceous gland activity, “which can lead to fewer acne breakouts and smaller pores but also cause drier skin,” Dr. Day said. “We can slow down the growth of body and facial hair and we can perform hair removal treatments. We see decreased male-pattern scalp hair loss, and we see smoother skin as the fat under the skin becomes thicker and the pores become smaller. We can also have increased pigment production, which is always a good thing.”
In a 2016 survey of 327 transgender individuals led by Dr. Day’s mentee, Brian A. Ginsberg, MD, and published in the Journal of the American Academy of Dermatology, most transgender women indicated that their face was most important to have changed, while for men it was the chest. Hair removal was the most common women’s facial procedure, followed by surgery then injectables, mostly performed by plastic surgeons.
Limitations of hormone therapy include the fact that it can take 2 or more years for associated changes to fully develop. “At least here in New York, patients want everything in a New York minute, so that’s always an issue,” she said. “We often recommend that patients wait at least 2 years after beginning hormone therapy before considering drastic feminization surgeries, but there are many options we have for them while they’re waiting for that. Even with hormone therapy, the bone structure of the face is unaffected, so we need to be artistic in creating a more feminized balance in order to help them physically match their gender to their identity.”
Noninvasive aesthetic procedures can compound the effects of hormone therapy, in addition to offering physical transformation beyond hormone therapy. She recalled assisting one of her patients transform from male to female. Over a period of 2 years, Dr. Day added Botox then Juvederm Voluma to the patient’s cheeks and chin, “and she started her transformation to a more feminized gender matching identity,” she said. Next came a hair transplant and the injection of more Voluma and fillers in the lips and cheeks on an as-needed basis.
“During one visit, I felt that we could still do more,” Dr. Day recalled. “She looked at me and said, ‘Actually, I feel so happy. This looks like me as I imagined I would look in my mind.’ I realized that my vision for her wasn’t the same as her vision for herself. She was thrilled with her transformation. I realized that as we see these patients, for all we learn about the science of gender transformation, the emotional aspects of our vision of what we can accomplish for our patients versus their vision of what their happiness level is may not entirely match. We have to be careful to help them celebrate their version of their femininity or masculinity, rather than trying to have our patients match what we think we can accomplish for them with our own sense of what femininity or masculinity is.”
Over time, Dr. Day said, the patient’s acne scars improved with fillers and microneedling treatments, and with the hormone therapy. “As we softened her appearance and as she made changes like the earrings that she wore and the hair style that she chose, she was in line with what her perception of her femininity was,” she said. “Little by little we’ve been watching her grow into her new self. It’s been a beautiful transformation. I was honored to be able to share in that journey with her.”
Dr. Day reported having no relevant financial disclosures.
, according to Doris Day, MD.
While clinical management of this patient population has historically been limited to experts in mental health, endocrinology, and select surgeons with experience in sex reassignment surgery, “what dermatologists provide on an aesthetic level through noninvasive or minimally invasive procedures can have a big impact in helping that transformation,” Dr. Day, of the department of dermatology at New York University Langone Health, said during the virtual annual Masters of Aesthetics Symposium. “But, we have to go through a transformation of sorts as well as we care for these patients, because we need to help them in the way that best matches their needs. We need to know about their mental health and the medicines they’re taking as well as their goals for their outcomes. If they’re working with surgeons for sex reassignment, we should have discussions with those clinicians as well.”
Gender-affirming hormone therapy is the primary medical intervention sought by transgender people, she said. This allows the acquisition of secondary sex characteristics more aligned with their gender identity. Feminizing hormone therapy affects the skin by reducing sebaceous gland activity, “which can lead to fewer acne breakouts and smaller pores but also cause drier skin,” Dr. Day said. “We can slow down the growth of body and facial hair and we can perform hair removal treatments. We see decreased male-pattern scalp hair loss, and we see smoother skin as the fat under the skin becomes thicker and the pores become smaller. We can also have increased pigment production, which is always a good thing.”
In a 2016 survey of 327 transgender individuals led by Dr. Day’s mentee, Brian A. Ginsberg, MD, and published in the Journal of the American Academy of Dermatology, most transgender women indicated that their face was most important to have changed, while for men it was the chest. Hair removal was the most common women’s facial procedure, followed by surgery then injectables, mostly performed by plastic surgeons.
Limitations of hormone therapy include the fact that it can take 2 or more years for associated changes to fully develop. “At least here in New York, patients want everything in a New York minute, so that’s always an issue,” she said. “We often recommend that patients wait at least 2 years after beginning hormone therapy before considering drastic feminization surgeries, but there are many options we have for them while they’re waiting for that. Even with hormone therapy, the bone structure of the face is unaffected, so we need to be artistic in creating a more feminized balance in order to help them physically match their gender to their identity.”
Noninvasive aesthetic procedures can compound the effects of hormone therapy, in addition to offering physical transformation beyond hormone therapy. She recalled assisting one of her patients transform from male to female. Over a period of 2 years, Dr. Day added Botox then Juvederm Voluma to the patient’s cheeks and chin, “and she started her transformation to a more feminized gender matching identity,” she said. Next came a hair transplant and the injection of more Voluma and fillers in the lips and cheeks on an as-needed basis.
“During one visit, I felt that we could still do more,” Dr. Day recalled. “She looked at me and said, ‘Actually, I feel so happy. This looks like me as I imagined I would look in my mind.’ I realized that my vision for her wasn’t the same as her vision for herself. She was thrilled with her transformation. I realized that as we see these patients, for all we learn about the science of gender transformation, the emotional aspects of our vision of what we can accomplish for our patients versus their vision of what their happiness level is may not entirely match. We have to be careful to help them celebrate their version of their femininity or masculinity, rather than trying to have our patients match what we think we can accomplish for them with our own sense of what femininity or masculinity is.”
Over time, Dr. Day said, the patient’s acne scars improved with fillers and microneedling treatments, and with the hormone therapy. “As we softened her appearance and as she made changes like the earrings that she wore and the hair style that she chose, she was in line with what her perception of her femininity was,” she said. “Little by little we’ve been watching her grow into her new self. It’s been a beautiful transformation. I was honored to be able to share in that journey with her.”
Dr. Day reported having no relevant financial disclosures.
FROM MOA 2020
Health Care Disparities Among Adolescents and Adults With Sickle Cell Disease: A Community-Based Needs Assessment to Inform Intervention Strategies
From the University of California San Francisco (Dr. Treadwell, Dr. Hessler, Yumei Chen, Swapandeep Mushiana, Dr. Potter, and Dr. Vichinsky), the University of California Los Angeles (Dr. Jacob), and the University of California Berkeley (Alex Chen).
Abstract
- Objective: Adolescents and adults with sickle cell disease (SCD) face pervasive disparities in health resources and outcomes. We explored barriers to and facilitators of care to identify opportunities to support implementation of evidence-based interventions aimed at improving care quality for patients with SCD.
- Methods: We engaged a representative sample of adolescents and adults with SCD (n = 58), health care providers (n = 51), and community stakeholders (health care administrators and community-based organization leads (n = 5) in Northern California in a community-based needs assessment. We conducted group interviews separately with participant groups to obtain in-depth perspectives. Adolescents and adults with SCD completed validated measures of pain interference, quality of care, self-efficacy, and barriers to care. Providers and community stakeholders completed surveys about barriers to SCD care.
- Results: We triangulated qualitative and quantitative data and found that participants with SCD (mean age, 31 ± 8.6 years), providers, and community stakeholders emphasized the social and emotional burden of SCD as barriers. Concrete barriers agreed upon included insurance and lack of resources for addressing pain impact. Adolescents and adults with SCD identified provider issues (lack of knowledge, implicit bias), transportation, and limited social support as barriers. Negative encounters with the health care system contributed to 84% of adolescents and adults with SCD reporting they chose to manage severe pain at home. Providers focused on structural barriers: lack of access to care guidelines, comfort level with and knowledge of SCD management, and poor care coordination.
- Conclusion: Strategies for improving access to compassionate, evidence-based quality care, as well as strategies for minimizing the burden of having SCD, are warranted for this medically complex population.
Keywords: barriers to care; quality of care; care access; care coordination.
Sickle cell disease (SCD), an inherited chronic medical condition, affects about 100,000 individuals in the United States, a population that is predominantly African American.1 These individuals experience multiple serious and life-threatening complications, most frequently recurrent vaso-occlusive pain episodes,2 and they require interactions with multidisciplinary specialists from childhood. Because of advances in treatments, the majority are reaching adulthood; however, there is a dearth of adult health care providers with the training and expertise to manage their complex medical needs.3 Other concrete barriers to adequate SCD care include insurance and distance to comprehensive SCD centers.4,5
Social, behavioral, and emotional factors may also contribute to challenges with SCD management. SCD may limit daily functional abilities and lead to diminished overall quality of life.6,7 Some adolescents and adults may require high doses of opioids, which contributes to health care providers’ perceptions that there is a high prevalence of drug addiction in the population.8,9 These providers express negative attitudes towards adults with SCD, and, consequently, delay medication administration when it is acutely needed and provide otherwise suboptimal treatment.8,10,11 Adult care providers may also be uncomfortable with prescribing and managing disease-modifying therapies (blood transfusion, hydroxyurea) that have established efficacy.12-17
As 1 of 8 programs funded by the National Heart, Lung, and Blood Institute’s (NHLBI) Sickle Cell Disease Implementation Consortium (SCDIC), we are using implementation science to reduce barriers to care and improve quality of care and health care outcomes in SCD.18,19 Given that adolescents and adults with SCD experience high mortality, severe pain, and progressive decline in their ability to function day to day, and also face lack of access to knowledgeable, compassionate providers in primary and emergency settings, the SCDIC focuses on individuals aged 15 to 45 years.6,8,9,11,12
Our regional SCDIC program, the Sickle Cell Care Coordination Initiative (SCCCI), brings together researchers, clinicians, adolescents, and adults with SCD and their families, dedicated community members, policy makers, and administrators to identify and address barriers to health care within 5 counties in Northern California. One of our first steps was to conduct a community-based needs assessment, designed to inform implementation of evidence-based interventions, accounting for unique contextual factors in our region.
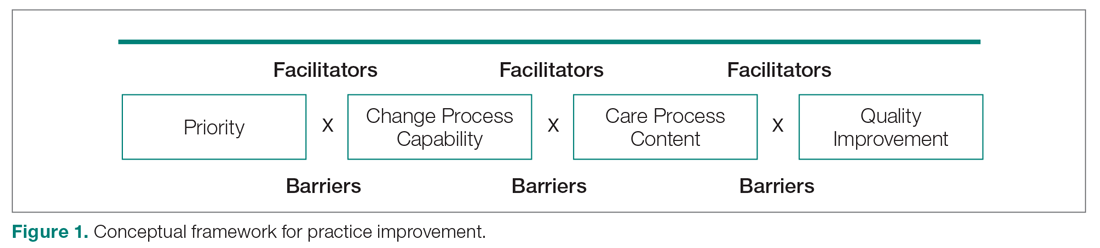
Conceptual Framework for Improving Medical Practice
Our needs assessment is guided by Solberg’s Conceptual Framework for Improving Medical Practice (Figure 1).20 Consistent with the overarching principles of the SCDIC, this conceptual framework focuses on the inadequate implementation of evidence-based guidelines, and on the need to first understand multifactorial facilitators and barriers to guideline implementation in order to effect change. The framework identifies 3 main elements that must be present to ensure improvements in quality-of-care processes and patient outcomes: priority, change process capability, and care process content. Priority refers to ample resource allocation for the specific change, as well as freedom from competing priorities for those implementing the change. Change process capability includes strong, effective leadership, adequate infrastructure for managing change (including resources and time), change management skills at all levels, and an established clinical information system. Care process content refers to context and systems-level changes, such as delivery system redesign as needed, support for self-management to lessen the impact of the disease, and decision support.21-23
The purpose of our community-based needs assessment was to evaluate barriers to care and quality of care in SCD, within Solberg’s conceptual model for improving medical practice. The specific aims were to evaluate access and barriers to care (eg, lack of provider expertise and training, health care system barriers such as poor care coordination and provider communication); evaluate quality of care; and assess patient needs related to pain, pain interference, self-efficacy, and self-management for adolescents and adults with SCD. We gathered the perspectives of a representative community of adolescents and adults with SCD, their providers, and community stakeholders in order to examine barriers, quality of life and care, and patient experiences in our region.
Methods
Design
In this cross-sectional study, adolescents and adults with SCD, their providers, and community stakeholders participated in group or individual qualitative interviews and completed surveys between October 2017 and March 2018.
Setting and Sample
Recruitment flyers were posted on a regional SCD-focused website, and clinical providers or a study coordinator introduced information about the needs assessment to potential participants with SCD during clinic visits at the participating centers. Participants with SCD were eligible if they had any diagnosis of SCD, were aged 15 to 48 years, and received health services within 5 Northern California counties (Alameda, Contra Costa, Sacramento, San Francisco, and Solano). They were excluded if they did not have a SCD diagnosis or had not received health services within the catchment area. As the project proceeded, participants were asked to refer other adolescents and adults with SCD for the interviews and surveys (snowball sampling). Our goal was to recruit 50 adolescents and adults with SCD into the study, aiming for 10 representatives from each county.
Providers and community stakeholders were recruited via emails, letters and informational flyers. We engaged our partner, the Sickle Cell Data Collection Program,2 to generate a list of providers and institutions that had seen patients with SCD in primary, emergency, or inpatient settings in the region. We contacted these institutions to describe the SCCCI and invite participation in the needs assessment. We also invited community-based organization leads and health care administrators who worked with SCD to participate. Providers accessed confidential surveys via a secure link on the study website or completed paper versions. Common data collected across providers included demographics and descriptions of practice settings.
Participants were eligible to be part of the study if they were health care providers (physicians and nurses) representing hematology, primary care, family medicine, internal medicine, or emergency medicine; ancillary staff (social work, psychology, child life); or leaders or administrators of clinical or sickle cell community-based organizations in Northern California (recruitment goal of n = 50). Providers were excluded if they practiced in specialties other than those noted or did not practice within the region.
Data Collection Procedures
After providing assent/consent, participating adolescents and adults with SCD took part in individual and group interviews and completed survey questionnaires. All procedures were conducted in a private space in the sickle cell center or community. Adolescents and adults with SCD completed the survey questionnaire on a tablet, with responses recorded directly in a REDCap (Research Electronic Data Capture) database,24 or on a paper version. Interviews lasted 60 (individual) to 90 (group) minutes, while survey completion time was 20 to 25 minutes. Each participant received a gift card upon completion as an expression of appreciation. All procedures were approved by the institutional review boards of the participating health care facilities.
Group and Individual Interviews
Participants with SCD and providers were invited to participate in a semi-structured qualitative interview prior to being presented with the surveys. Adolescents and adults with SCD were interviewed about barriers to care, quality of care, and pain-related experiences. Providers were asked about barriers to care and treatments. Interview guides were modified for community-based organization leaders and health care administrators who did not provide clinical services. Interview guides can be found in the Appendix. Interviews were conducted by research coordinators trained in qualitative research methods by the first author (MT). As appropriate with semi-structured interviews, the interviewers could word questions spontaneously, change the order of questions for ease of flow of conversation, and inform simultaneous coding of interviews with new themes as those might arise, as long as they touched on all topics within the interview guide.25 The interview guides were written, per qualitative research standards, based on the aims and purpose of the research,26 and were informed by existing literature on access and barriers to care in SCD, quality of care, and the needs of individuals with SCD, including in relation to impact of the disease, self-efficacy, and self-management.
Interviewees participated in either individual or group interviews, but not both. The decision for which type of interview an individual participated in was based on 2 factors: if there were not comparable participants for group interviews (eg, health care administrator and community-based organization lead), these interviews were done individually; and given that we were drawing participants from a 5-county area in Northern California, scheduling was challenging for individuals with SCD with regard to aligning schedules and traveling to a central location where the group interviews were conducted. Provider group interviews were easier to arrange because we could schedule them at the same time as regularly scheduled meetings at the participants’ health care institutions.
Interview Data Gathering and Analysis
Digital recordings of the interviews were cleaned of any participant identifying data and sent for transcription to an outside service. Transcripts were reviewed for completeness and imported into NVivo (www.qsrinternational.com), a qualitative data management program.
A thematic content analysis and deductive and inductive approaches were used to analyze the verbatim transcripts generated from the interviews. The research team was trained in the use of NVivo software to facilitate the coding process. A deductive coding scheme was initially used based on existing concepts in the literature regarding challenges to optimal SCD care, with new codes added as the thematic content analyses progressed. The initial coding, pattern coding, and use of displays to examine the relationships between different categories were conducted simultaneously.27,28 Using the constant comparative method, new concepts from participants with SCD and providers could be incorporated into subsequent interviews with other participants. For this study, the only additional concepts added were in relation to participant recruitment and retention in the SCDIC Registry. Research team members coded transcripts separately and came together weekly, constantly comparing codes and developing the consensus coding scheme. Where differences between coders existed, code meanings were discussed and clarified until consensus was reached.29
Quantitative data were analyzed using SPSS (v. 25, Chicago, IL). Descriptive statistics (means, standard deviations, frequencies, percentages) were used to summarize demographics (eg, age, gender, and race), economic status, and type of SCD. No systematic differences were detected from cases with missing values. Scale reliabilities (ie, Cronbach α) were evaluated for self-report measures.
Measurement
Adolescents and adults with SCD completed items from the PhenX Toolkit (consensus measures for Phenotypes and eXposures), assessing sociodemographics (age, sex, race, ethnicity, educational attainment, occupation, marital status, annual income, insurance), and clinical characteristics (sickle cell diagnosis and emergency department [ED] and hospital utilization for pain).30
Pain Interference Short Form (Patient-Reported Outcomes Measurement Information System [PROMIS]). The Pain Interference Form consists of 8 items that assess the degree to which pain interfered with day-to-day activities in the previous 7 days at home, including impacts on social, cognitive, emotional, and physical functioning; household chores and recreational activities; sleep; and enjoyment in life. Reliability and validity of the PROMIS Pain Interference Scale has been demonstrated, with strong negative correlations with Physical Function Scales (r = 0.717, P < 0.01), indicating that higher scores are associated with lower function (β = 0.707, P < 0.001).31 The Cronbach α estimate for the other items on the pain interference scale was 0.99. Validity analysis indicated strong correlations with pain-related domains: BPI Interference Subscale (rho = 0.90), SF-36 Bodily Pain Subscale (rho = –0.84), and 0–10 Numerical Rating of Pain Intensity (rho = 0.48).32
Adult Sickle Cell Quality of Life Measurement Information System (ASCQ-Me) Quality of Care (QOC). ASCQ-Me QOC consists of 27 items that measure the quality of care that adults with SCD have received from health care providers.33 There are 3 composites: provider communication (quality of patient and provider communication), ED care (quality of care in the ED), and access (to routine and emergency care). Internal consistency reliability for all 3 composites is greater than 0.70. Strong correlations of the provider communication composite with overall ratings of routine care (r = 0.65) and overall provider ratings (r = 0.83) provided evidence of construct validity. Similarly, the ED care composite was strongly correlated with overall ratings of QOC in the ED, and the access composite was highly correlated with overall evaluations of ED care (r = 0.70). Access, provider interaction, and ED care composites were reliable (Cronbach α, 0.70–0.83) and correlated with ratings of global care (r = 0.32–0.83), further indicating construct validity.33
Sickle Cell Self-Efficacy Scale (SCSES). The SCSES is a 9-item, self-administered questionnaire measuring perceptions of the ability to manage day-to-day issues resulting from SCD. SCSES items are scored on a 5-point scale ranging from Not sure at all (1) to Very sure (5). Individual item responses are summed to give an overall score, with higher scores indicating greater self-efficacy. The SCSES has acceptable reliability (r = 0.45, P < 0.001) and validity (α = 0.89).34,35
Sickle Cell Disease Barriers Checklist. This checklist consists of 53 items organized into 8 categories: insurance, transportation, accommodations and accessibility, provider knowledge and attitudes, social support, individual barriers such as forgetting or difficulties understanding instructions, emotional barriers (fear, anger), and disease-related barriers. Participants check applicable barriers, with a total score range of 0 to 53 and higher scores indicating more barriers to care. The SCD Barriers Checklist has demonstrated face validity and test-retest reliability (Pearson r = 0.74, P < 0.05).5
ED Provider Checklist. The ED provider survey is a checklist of 14 statements pertaining to issues regarding patient care, with which the provider rates level of agreement. Items representing the attitudes and beliefs of providers towards patients with SCD are rated on a Likert-type scale, with level of agreement indicated as 1 (strongly disagree) to 6 (strongly agree). The positive attitudes subscale consists of 4 items (Cronbach α= 0.85), and the negative attitudes subscale consists of 6 items (Cronbach α = 0.89). The Red-Flag Behaviors subscale includes 4 items that indicate behavior concerns about drug-seeking, such as requesting specific narcotics and changing behavior when the provider walks in.8,36,37
Sickle cell and primary care providers also completed a survey consisting of sets of items compiled from existing provider surveys; this survey consisted of a list of 16 barriers to using opioids, which the providers rated on a 5-point Likert-type scale (1, not a barrier; 5, complete barrier).13,16,38 Providers indicated their level of experience with caring for patients with SCD; care provided, such as routine health screenings; and comfort level with providing preventive care, managing comorbidities, and managing acute and chronic pain. Providers were asked what potential facilitators might improve care for patients with SCD, including higher reimbursement, case management services, access to pain management specialists, and access to clinical decision-support tools. Providers responded to specific questions about management with hydroxyurea (eg, criteria for, barriers to, and comfort level with prescribing).39 The surveys are included in the Appendix.
Triangulation
Data from the interviews and surveys were triangulated to enhance understanding of results generated from the different data sources.40 Convergence of findings, different facets of the same phenomenon, or new perspectives were examined.
Results
Qualitative Data
Adolescents and adults with SCD (n = 55) and health care providers and community stakeholders (n = 56) participated in group or individual interviews to help us gain an in-depth understanding of the needs and barriers related to SCD care in our 5-county region. Participants with SCD described their experiences, which included stigma, racism, labeling, and, consequently, stress. They also identified barriers such as lack of transportation, challenges with insurance, and lack of access to providers who were competent with pain management. They reported that having SCD in a health care system that was unable to meet their needs was burdensome.
Barriers to Care and Treatments. Adolescents and adults indicated that SCD and its sequelae posed significant barriers to health care. Feelings of tiredness and pain make it more difficult for them to seek care. The emotional burden of SCD (fear and anger) was a frequently cited barrier, which was fueled by previous negative encounters with the health care system. All adolescents and adults with SCD reported that they knew of stigma in relation to seeking pain management that was pervasive and long-standing, and the majority reported they had directly experienced stigma. They reported that being labeled as “drug-seekers” was typical when in the ED for pain management. Participants articulated unconscious bias or overt racism among providers: “people with sickle cell are Black ... and Black pain is never as valuable as White pain” (25-year-old male). Respondents with SCD described challenges to the credibility of their pain reports in the ED. They reported that ED providers expressed doubts regarding the existence and/or severity of their pain, consequently creating a feeling of disrespect for patients seeking pain relief. The issue of stigma was mentioned by only 2 of 56 providers during their interviews.
Lack of Access to Knowledgeable, Compassionate Providers. Lack of access to knowledgeable care providers was another prevalent theme expressed by adolescents and adults with SCD. Frustration occurred when providers did not have knowledge of SCD and its management, particularly pain assessment. Adolescents and adults with SCD noted the lack of compassion among providers: “I’ve been kicked out of the hospital because they felt like okay, well we gave you enough medication, you should be all right” (29-year-old female). Providers specifically mentioned lack of compassion and knowledge as barriers to SCD care much less often during their interviews compared with the adolescents and adults with SCD.
Health Care System Barriers. Patient participants often expressed concerns about concrete and structural aspects of care. Getting to their appointments was a challenge for half of the interviewees, as they either did not have access to a vehicle or could not afford to travel the needed distance to obtain quality care. Even when hospitals were accessible by public transportation, those with excruciating pain understandably preferred a more comfortable and private way to travel: “I would like to change that, something that will be much easier, convenient for sickle cell patients that do suffer with pain, that they don’t have to travel always to see the doctor” (30-year-old male).
Insurance and other financial barriers also played an important role in influencing decisions to seek health care services. Medical expenses were not covered, or co-pays were too high. The Medicaid managed care system could prevent access to knowledgeable providers who were not within network. Such a lack of access discouraged some adolescents and adults with SCD from seeking acute and preventive care.
Transition From Pediatric to Adult Care. Interviewees with SCD expressed distress about the gap between pediatric and adult care. They described how they had a long-standing relationship with their medical providers, who were familiar with their medical background and history from childhood. Adolescent interviewees reported an understanding of their own pain management as well as adherence to and satisfaction with their individualized pain plans. However, adults noted that satisfaction plummeted with increasing age due to the limited number of experienced adult SCD providers, which was compounded by negative experiences (stigma, racism, drug-seeking label).
One interviewee emphasized the difficulty of finding knowledgeable providers after transition: “When you’re a pediatric sickle cell [patient], you have the doctors there every step of the way, but not with adult sickle cell… I know when I first transitioned I never felt more alone in my life… you look at that ER doctor kind of with the same mindset as you would your hematologist who just hand walked you through everything. And adult care providers were a lot more blunt and cold and they’re like… ‘I don’t know; I’m not really educated in sickle cell.’” A sickle cell provider shared his insight about the problem of transitioning: “I think it’s particularly challenging because we, as a community, don’t really set them up for success. It’s different from other chronic conditions [in that] it’s much harder to find an adult sickle cell provider. There’s not a lot of adult hematologists that will take care of our adult patients, and so I know statistically, there’s like a drop-down in the overall outcomes of our kids after they age out of our pediatric program.”
Self-Management, Supporting Hydroxyurea Use. Interview participants with SCD reported using a variety of methods to manage pain at home and chose to go to the ED only when the pain became intolerable. Patients and providers expressed awareness of different resources for managing pain at home, yet they also indicated that these resources have not been consolidated in an accessible way for patients and families. Some resources cited included heat therapy, acupuncture, meditation, medical marijuana, virtual reality devices, and pain medications other than opioids.
Patients and providers expressed the need for increasing awareness and education about hydroxyurea. Many interview participants with SCD were concerned about side effects, multiple visits with a provider during dose titration, and ongoing laboratory monitoring. They also expressed difficulties with scheduling multiple appointments, depending on access to transportation and limited provider clinic hours. They were aware of strategies for improving adherence with hydroxyurea, including setting phone alarms, educating family members about hydroxyurea, and eliciting family support, but expressed needing help to consistently implement these strategies.
Safe Opioid Prescribing. Adult care providers expressed concerns about safe opioid prescribing for patients with SCD. They were reluctant to prescribe opioid doses needed to adequately control SCD pain. Providers expressed uncertainty and fear or concern about medical/legal liability or about their judgment about what’s safe and not safe for patients with chronic use/very high doses of opioids. “I know we’re in like this opiate epidemic here in this country but I feel like these patients don’t really fit under that umbrella that the problem is coming from so [I am] just trying to learn more about how to take care of them.”
Care Coordination and Provider Communication. Adolescents and adults with SCD reported having positive experiences—good communication, established trust, and compassionate care—with their usual providers. However, they perceived that ED physicians and nurses did not really care about them. Both interviewees with SCD and providers recognized the importance of good communication in all settings as the key to overcoming barriers to receiving quality care. All agreed on the importance of using individual pain plans so that all providers, especially ED providers, can be more at ease with treating adolescents and adults with SCD.
Quantitative Data: Adolescents and Adults With SCD
Fifty-eight adolescents and adults with SCD (aged 15 to 48 years) completed the survey. Three additional individuals who did not complete the interview completed the survey. Reasons for not completing the interview included scheduling challenges (n = 2) or a sickle cell pain episode (n = 1). The average age of participants was 31 years ± 8.6, more than half (57%) were female, and the majority (93%) were African American (Table 1). Most (71%) had never been married. Half (50%) had some college or an associate degree, and 40% were employed and reported an annual household income of less than $30,000. Insurance coverage was predominantly Medi-Cal (Medicaid, 69%). The majority of participants resided in Alameda (34.5%) or Contra Costa (21%) counties. The majority of sickle cell care was received in Alameda County, whether outpatient (52%), inpatient (40%), or ED care (41%). The majority (71%) had a diagnosis of SCD hemoglobin SS.
Pain. More than one-third of individuals with SCD reported 1 or 2 ED visits for pain in the previous 6 months (34%), and more than 3 hospitalizations (36%) related to pain in the previous year (Table 2). The majority (85%) reported having severe pain at home in the previous 6 months that they did not seek health care for, consistent with their reports in the qualitative interviews. More than half (59%) reported 4 or more of these severe pain episodes that led to inability to perform daily activities for 1 week or more. While pain interference on the PROMIS Pain Interference Short Form on average (T-score, 59.6 ± 8.6) was similar to that of the general population (T-score, 50 ± 10), a higher proportion of patients with SCD reported pain interference compared with the general population. The mean self-efficacy (confidence in ability to manage complications of SCD) score on the SCSES of 30.0 ± 7.3 (range, 9–45) was similar to that of other adults with SCD (mean, 32.2 ± 7.0). Twenty-five percent of the present sample had a low self-efficacy score (< 25).
Barriers to Care and Treatments. Consistent with the qualitative data, SCD-related symptoms such as tiredness (64%) and pain (62%) were reported most often as barriers to care (Table 3). Emotions (> 25%) such as worry/fear, frustration/anger, and lack of confidence were other important barriers to care. Provider knowledge and attitudes were cited next most often, with 38% of the sample indicating “Providers accuse me of drug-seeking” and “It is hard for me to find a provider who has enough experiences with or knowledge about SCD.” Participants expressed that they were not believed when in pain and “I am treated differently from other patients.” Almost half of respondents cited “I am not seen quickly enough when I am in pain” as a barrier to their care.
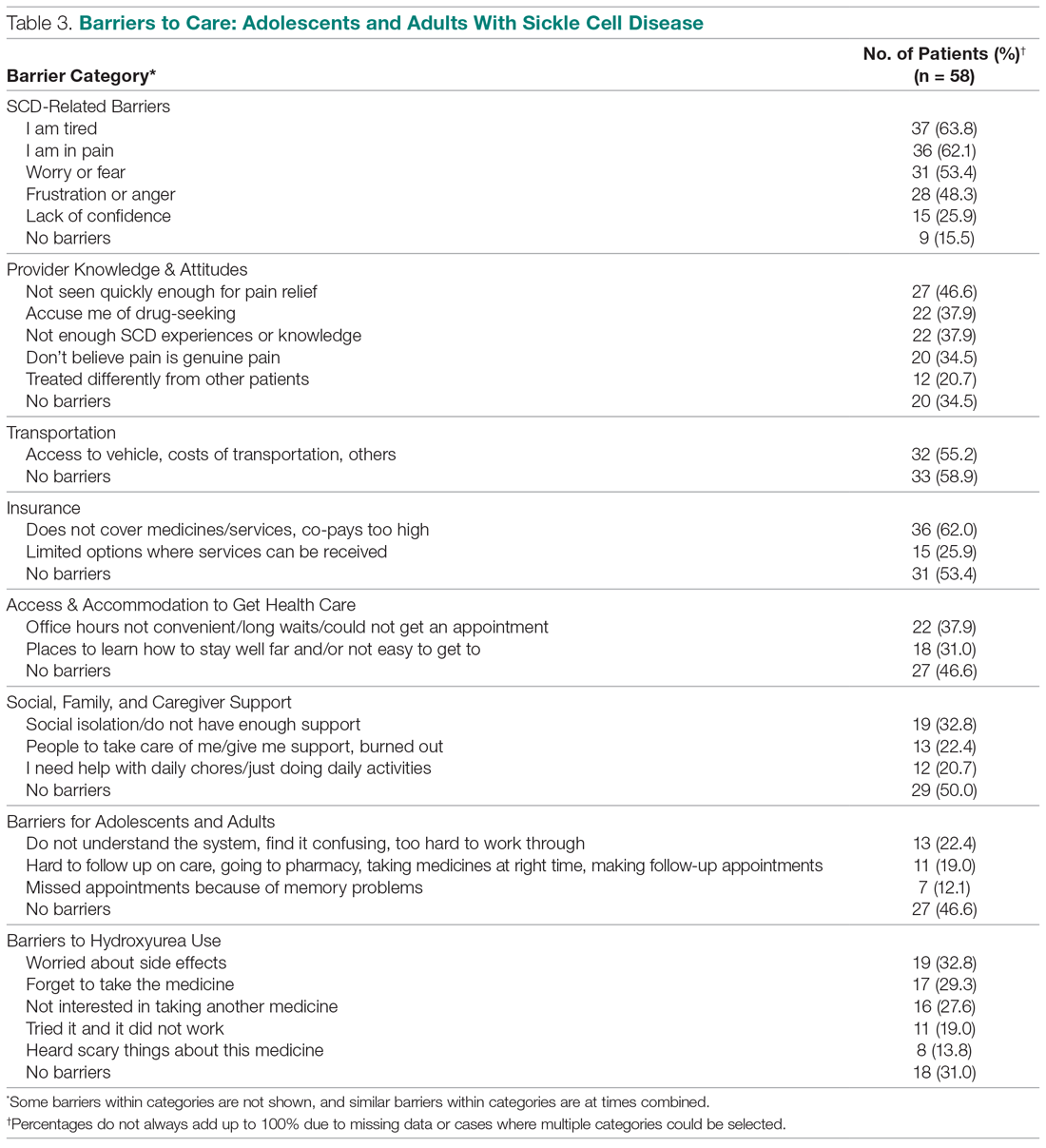
Consistent with the qualitative data, transportation barriers (not having a vehicle, costs of transportation, public transit not easy to get to) were cited by 55% of participants. About half of participants reported that insurance was an important barrier, with high co-pays and medications and other services not covered. In addition, gathering approvals was a long and fragmented process, particularly for consultations among providers (hematology, primary care provider, pain specialist). Furthermore, insurance provided limited choices about location for services.
Participants reported social support system burnout (22%), help needed with daily activities (21%), and social isolation or generally not having enough support (33%) as ongoing barriers. Difficulties were encountered with self-management (eg, taking medications on time or making follow-up appointments, 19%), with 22% of participants finding the health care system confusing or hard to understand. Thirty percent reported “Places for me to go to learn how to stay well are not close by or easy to get to.” ”Worry about side effects” (33%) was a common barrier to hydroxyurea use. Participants described “forgetting to take the medicine,” “tried before but it did not work,” “heard scary things” about hydroxyurea, and “not interested in taking another medicine” as barriers.
Quality of Care. More than half (51%) of the 53 participants who had accessed health care in the previous year rated their overall health care as poor on the ASCQ-Me QOC measure. This was significantly higher compared to the reports from more than 47,000 adults with Medicaid in 2017 (16%),41 and to the 2008-2009 report from 556 adults with SCD from across the United States (37%, Figure 2).33 The major contributor to these poor ratings for participants in our sample was low satisfaction with ED care.
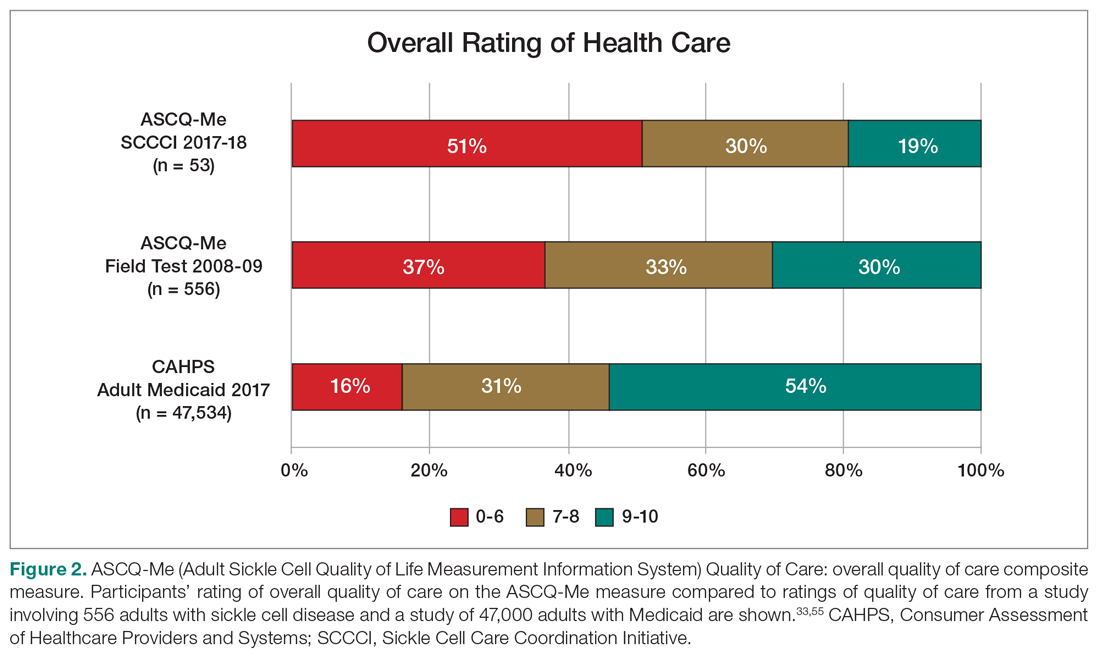
Sixty percent of the 42 participants who had accessed ED care in the past year indicated “never” or “sometimes” to the question “When you went to the ED for care, how often did you get it as soon as you wanted?” compared with only 16% of the 2017 adult Medicaid population responding (n = 25,789) (Figure 3). Forty-seven percent of those with an ED visit indicated that, in the previous 12 months, they had been made to wait “more than 2 hours before receiving treatment for acute pain in the ED.” However, in the previous 12 months, 39% reported that their wait time in the ED had been only “between five minutes and one hour.”
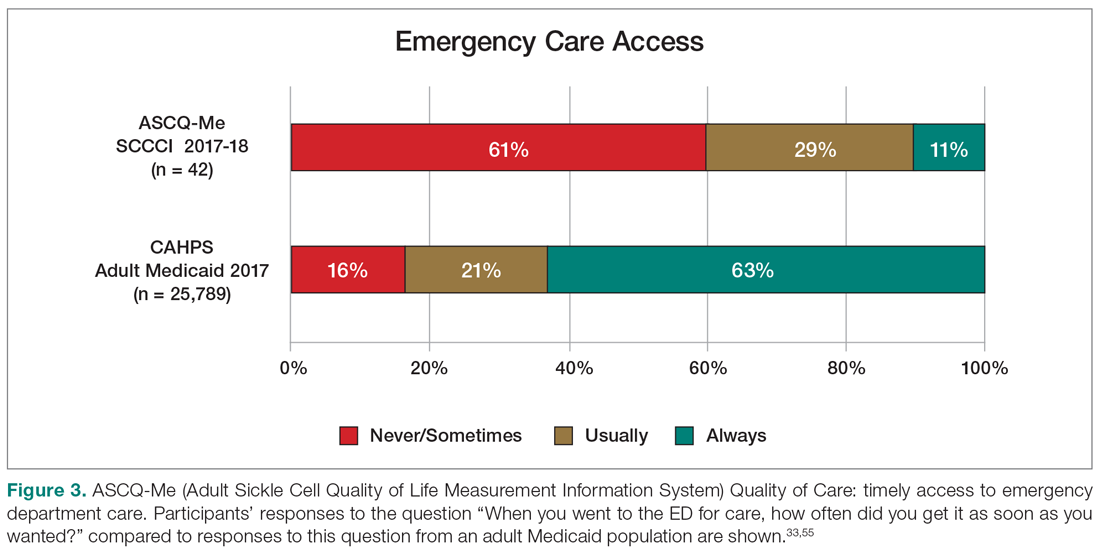
On the ASCQ-Me QOC Access to Care composite measure, 33% of 42 participants responding reported they were seen at a routine appointment as soon as they would have liked. This is significantly lower compared to 56% of the adult Medicaid population responding to the same question. Reports of provider communication (Provider Communication composite) for adolescents and adults with SCD were comparable to reports of adults with SCD from the ASCQ-Me field test,33 but adults with Medicaid reported higher ratings of quality communication behaviors (Figure 4).33,41 Nearly 60% of both groups with SCD reported that providers “always” performed quality communication behaviors—listened carefully, spent enough time, treated them with respect, and explained things well—compared with more than 70% of adults with Medicaid.
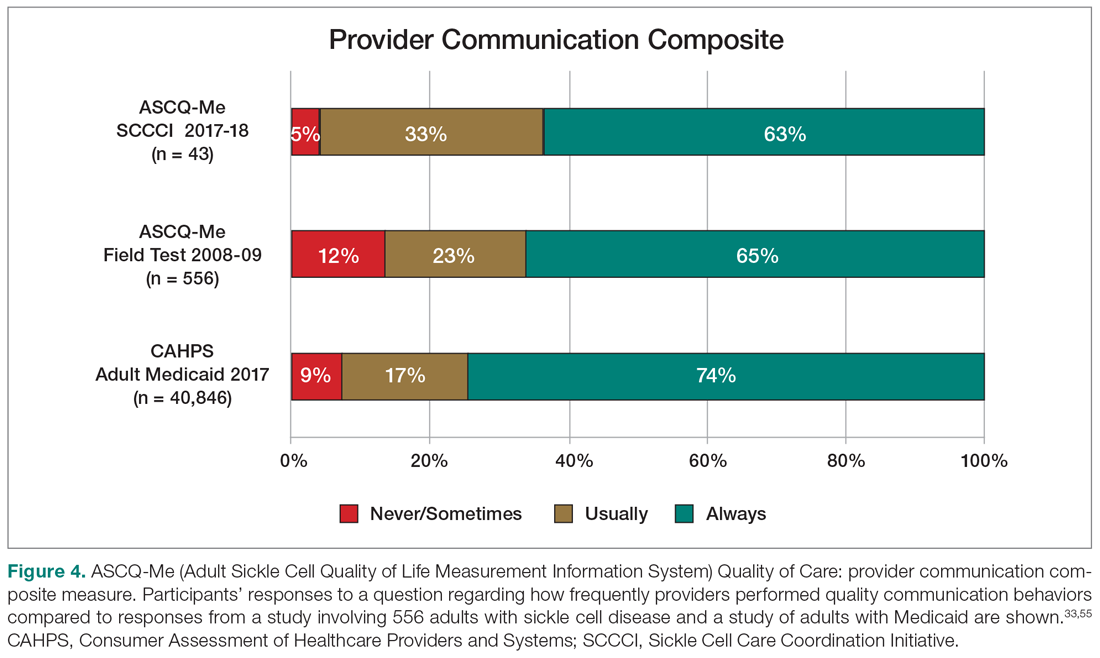
Participants from all counties reported the same number of barriers to care on average (3.3 ± 2.1). Adolescents and adults who reported more barriers to care also reported lower satisfaction with care (r = –0.47, P < 0.01) and less confidence in their ability to manage their SCD (self-efficacy, r = – 0.36, P < 0.05). Female participants reported more barriers to care on average compared with male participants (2.6 ± 2.4 vs 1.4 ± 2.0, P = 0.05). Participants with higher self-efficacy reported lower pain ratings (r = –0.47, P < 0.001).
Quantitative Data: Health Care Providers
Providers (n = 56) and community stakeholders (2 leaders of community-based organizations and 3 health care administrators) were interviewed, with 29 also completing the survey. The reason for not completing (n = 22) was not having the time once the interview was complete. A link to the survey was sent to any provider not completing at the time of the interview, with 2 follow-up reminders. The majority of providers were between the ages of 31 and 50 years (46.4%), female (71.4%), and white (66.1%) (Table 4). None were of Hispanic, Latinx, or Spanish origin. Thirty-six were physicians (64.3%), and 16 were allied health professionals (28.6%). Of the 56 providers, 32 indicated they had expertise caring for patients with SCD (57.1%), 14 were ED providers (25%), and 5 were primary care providers. Most of the providers practiced in an urban setting (91.1%).
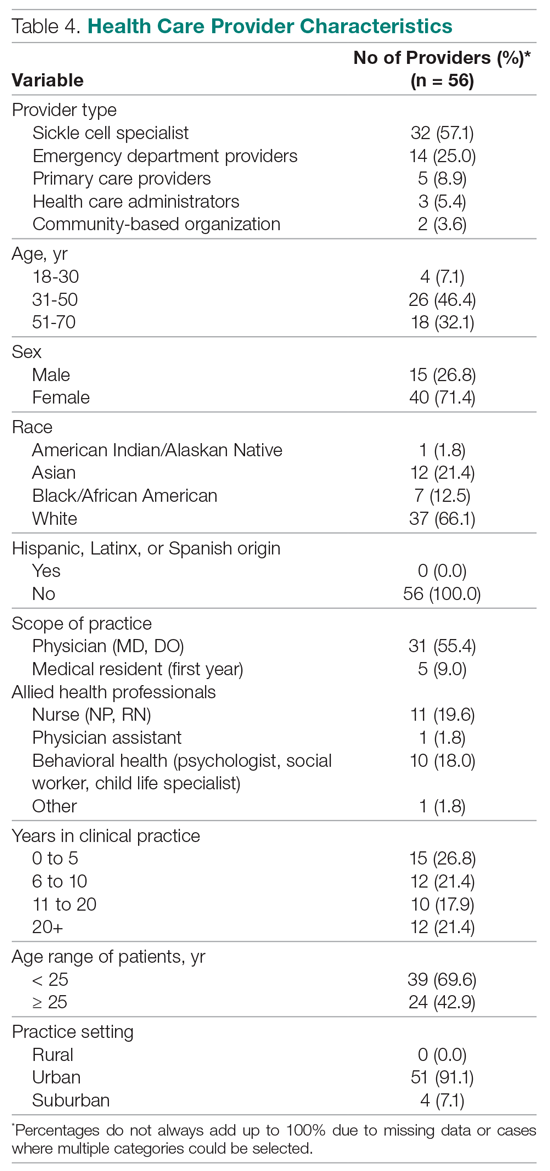
Barriers to Care: ED Provider Perspectives. Nine of 14 ED providers interviewed completed the survey on their perspectives regarding barriers to care in the ED, difficulty with follow-ups, ED training resources, and pain control for patients with SCD. ED providers (n = 8) indicated that “provider attitudes” were a barrier to care delivery in the ED for patients with SCD. Some providers (n = 7) indicated that “implicit bias,” “opioid epidemic,” “concern about addiction,” and “patient behavior” were barriers. Respondents indicated that “overcrowding” (n = 6) and “lack of care pathway/protocol” (n = 5) were barriers. When asked to express their level of agreement with statements about SCD care in the ED, respondents disagreed/strongly disagreed (n = 5) that they were “able to make a follow-up appointment” with a sickle cell specialist or primary care provider upon discharge from the ED, and others disagreed/strongly disagreed (n = 4) that they were able to make a “referral to a case management program.”
ED training and resources. Providers agreed/strongly agreed (n = 8) that they had the knowledge and training to care for patients with SCD, that they had access to needed medications, and that they had access to knowledgeable nursing staff with expertise in SCD care. All 9 ED providers indicated that they had sufficient physician/provider staffing to provide good pain management to persons with SCD in the ED.
Pain control in the ED. Seven ED providers indicated that their ED used individualized dosing protocols to treat sickle cell pain, and 5 respondents indicated their ED had a protocol for treating sickle cell pain. Surprisingly, only 3 indicated that they were aware of the NHLBI recommendations for the treatment of vaso-occlusive pain.
Barriers to Care: Primary Care Provider Perspectives. Twenty providers completed the SCD provider section of the survey, including 17 multidisciplinary SCD providers from 4 sickle cell special care centers and 3 community primary care providers. Of the 20, 12 were primary care providers for patients with SCD (Table 4).
Patient needs. Six primary care providers indicated that the medical needs of patients with SCD were being met, but none indicated that the behavioral health or mental health needs were being met.
Managing SCD comorbidities. Five primary care providers indicated they were very comfortable providing preventive ambulatory care to patients with SCD. Six indicated they were very comfortable managing acute pain episodes, but none were very comfortable managing comorbidities such as pulmonary hypertension, diabetes, or chronic pain.
Barriers to opioid use. Only 3 of 12 providers reviewing a list of 15 potential barriers to the use of opioids for SCD pain management indicated a perceived lack of efficacy of opioids, development of tolerance and dependence, and concerns about community perceptions as barriers. Two providers selected potential for diversion as a moderate barrier to opioid use.
Barriers to hydroxyurea use. Eight of 12 providers indicated that the common reasons that patients/families refuse hydroxyurea were “worry about side effects”; 7 chose “don’t want to take another medicine,” and 6 chose “worry about carcinogenic potential.” Others (n = 10) indicated that “patient/family adherence with hydroxyurea” and “patient/family adherence with required blood tests” were important barriers to hydroxyurea use. Eight of the 12 providers indicated that they were comfortable with managing hydroxyurea in patients with SCD.
Care redesign. Twenty SCD and primary care providers completed the Care Redesign section of the survey. Respondents (n = 11) indicated that they would see more patients with SCD if they had accessible case management services available without charge or if patient access to transportation to clinic was also available. Ten indicated that they would see more patients with SCD if they had an accessible community health worker (who understands patient’s/family’s social situation) and access to a pain management specialist on call to answer questions and who would manage chronic pain. All (n = 20) were willing to see more patients with SCD in their practices. Most reported that a clinical decision-support tool for SCD treatment (n = 13) and avoidance of complications (n = 12) would be useful.
Discussion
We evaluated access and barriers to care, quality of care, care coordination, and provider communication from the perspectives of adolescents and adults with SCD, their care providers, and community stakeholders, within the Solberg conceptual model for quality improvement. We found that barriers within the care process content domain (context and systems) were most salient for this population of adolescents and adults with SCD, with lack of provider knowledge and poor attitudes toward adolescents and adults with SCD, particularly in the ED, cited consistently by participant groups. Stigmatization and lack of provider compassion that affected the quality of care were particularly problematic. These findings are consistent with previous reports.42,43 Adult health care (particularly ED) provider biases and negative attitudes have been recognized as major barriers to optimal pain management in SCD.8,11,44,45 Interestingly, ED providers in our needs assessment indicated that they felt they had the training and resources to manage patients with SCD. However, only a few actually reported knowing about the NHLBI recommendations for the treatment of vaso-occlusive pain.
Within the care process content domain, we also found that SCD-related complications and associated emotions (fear, worry, anxiety), compounded by lack of access to knowledgeable and compassionate providers, pose a significant burden. Negative encounters with the health care system contributed to a striking 84% of patient participants choosing to manage severe pain at home, with pain seriously interfering with their ability to function on a daily basis. ED providers agreed that provider attitudes and implicit bias pose important barriers to care for adolescents and adults with SCD. Adolescents and adults with SCD wanted, and understood the need, to enhance self-management skills. Both they and their providers agreed that barriers to hydroxyurea uptake included worries about potential side effects, challenges with adherence to repeated laboratory testing, and support with remembering to take the medicine. However, providers uniformly expressed that access to behavioral and mental health services were, if not nonexistent, impossible to access.
Participants with SCD and their providers reported infrastructural challenges (change process capability), as manifested in limitations with accessing acute and preventive care due to transportation- and insurance- related issues. There were health system barriers that were particularly encountered during the transition from pediatric to adult care. These findings are consistent with previous reports that have found fewer interdisciplinary services available in the adult care settings compared with pediatrics.46,47 Furthermore, adult care providers were less willing to accept adults with SCD because of the complexity of their management, for which the providers did not have the necessary expertise.3,48-50 In addition, both adolescents and adults with SCD and primary care providers highlighted the inadequacies of the current system in addressing the chronic pain needs of this population. Linking back to the Solberg conceptual framework, our needs assessment results confirm the important role of establishing SCD care as a priority within a health care system—this requires leadership and vision. The vision and priorities must be implemented by effective health care teams. Multilevel approaches or interventions, when implemented, will lead to the desired outcomes.
Findings from our needs assessment within our 5-county region mirror needs assessment results from the broader consortium.51 The SCDIC has prioritized developing an intervention that addresses the challenges identified within the care process domain by directly enhancing provider access to patient individualized care plans in the electronic health record in the ED. Importantly, ED providers will be asked to view a short video that directly challenges bias and stigma in the ED. Previous studies have indeed found that attitudes can be improved by providers viewing short video segments of adults with SCD discussing their experiences.36,52 This ED protocol will be one of the interventions that we will roll out in Northern California, given the significance of negative ED encounters reported by needs assessment participants. An additional feature of the intervention is a script for adults with SCD that guides them through introducing their individualized pain plan to their ED providers, thereby enhancing their self-efficacy in a situation that has been so overwhelmingly challenging.
We will implement a second SCDIC intervention that utilizes a mobile app to support self-management on the part of the patient, by supporting motivation and adherence with hydroxyurea.53 A companion app supports hydroxyurea guideline adherence on the part of the provider, in keeping with one of our findings that providers are in need of decision-support tools. Elements of the intervention also align with our findings related to the importance of a support system in managing SCD, in that participants will identify a supportive partner who will play a specific role in supporting their adherence with hydroxyurea.
On our local level, we have, by necessity, partnered with leaders and community stakeholders throughout the region to ensure that these interventions to improve SCD care are prioritized. Grant funds provide initial resources for the SCDIC interventions, but our partnering health care administrators and medical directors must ensure that participating ED and hematology providers are free from competing priorities in order to implement the changes. We have partnered with a SCD community-based organization that is designing additional educational presentations for local emergency medicine providers, with the goal to bring to life very personal stories of bias and stigma within the EDs that directly contribute to decisions to avoid ED care despite severe symptoms.
Although we attempted to obtain samples of adolescents and adults with SCD and their providers that were representative across the 5-county region, the larger proportion of respondents were from 1 county. We did not assess concerns of age- and race-matched adults in our catchment area, so we cannot definitively say that our findings are unique to SCD. However, our results are consistent with findings from the national sample of adults with SCD who participated in the ASCQ-Me field test, and with results from the SCDIC needs assessment.33,51 Interviews and surveys are subject to self-report bias and, therefore, may or may not reflect the actual behaviors or thoughts of participants. Confidence is increased in our results given the triangulation of expressed concerns across participant groups and across data collection strategies. The majority of adolescents and adults with SCD (95%) completed both the interview and survey, while 64% of ED providers interviewed completed the survey, compared with 54% of SCD specialists and primary care providers. These response rates are more than acceptable within the realm of survey response rates.54,55
Although we encourage examining issues with care delivery within the conceptual framework for quality improvement presented, we recognize that grant funding allowed us to conduct an in-depth needs assessment that might not be feasible in other settings. Still, we would like readers to understand the importance of gathering data for improvement in a systematic manner across a range of participant groups, to ultimately inform the development of interventions and provide for evaluation of outcomes as a result of the interventions. This is particularly important for a disease, such as SCD, that is both medically and sociopolitically complex.
Conclusion
Our needs assessment brought into focus the multiple factors contributing to the disparities in health care experienced by adolescents and adults with SCD on our local level, and within the context of inequities in health resources and outcomes on the national level. We propose solutions that include specific interventions developed by a consortium of SCD and implementation science experts. We utilize a quality improvement framework to ensure that the elements of the interventions also address the barriers identified by our local providers and patients that are unique to our community. The pervasive challenges in SCD care, coupled with its medical complexities, may seem insurmountable, but our survey and qualitative results provide us with a road map for the way forward.
Acknowledgments: The authors thank the adolescents and adults with sickle cell disease, the providers, and the community stakeholders who completed the interviews and surveys. The authors also acknowledge the SCCCI co-investigators for their contributions to this project, including Michael Bell, MD, Ward Hagar, MD, Christine Hoehner, FNP, Kimberly Major, MSW, Anne Marsh, MD, Lynne Neumayr, MD, and Ted Wun, MD. We also thank Kamilah Bailey, Jameelah Hodge, Jennifer Kim, Michael Rowland, Adria Stauber, Amber Fearon, and Shanda Robertson, and the Sickle Cell Data Collection Program for their contributions.
Corresponding author: Marsha J. Treadwell, PhD, University of California San Francisco Benioff Children’s Hospital Oakland, 747 52nd St., Oakland, CA 94609; [email protected].
Financial disclosures: None.
Funding/support: This work was supported by grant # 1U01HL134007 from the National Heart, Lung, and Blood Institute to the University of California San Francisco Benioff Children’s Hospital Oakland.
1. Hassell KL. Population Estimates of sickle cell disease in the U.S. Am J Prev Med. 2010; 38:S512-S521.
2. Data & Statistics on Sickle Cell Disease. Centers for Disease Control and Prevention website. www.cdc.gov/ncbddd/sicklecell/data.html. Accessed March 25, 2020.
3. Inusa BPD, Stewart CE, Mathurin-Charles S, et al. Paediatric to adult transition care for patients with sickle cell disease: a global perspective. Lancet Haematol. 2020;7:e329-e341.
4. Smith SK, Johnston J, Rutherford C, et al. Identifying social-behavioral health needs of adults with sickle cell disease in the emergency department. J Emerg Nurs. 2017;43:444-450.
5. Treadwell MJ, Barreda F, Kaur K, et al. Emotional distress, barriers to care, and health-related quality of life in sickle cell disease. J Clin Outcomes Manag. 2015;22:8-17.
6. Treadwell MJ, Hassell K, Levine R, et al. Adult Sickle Cell Quality-of-Life Measurement Information System (ASCQ-Me): conceptual model based on review of the literature and formative research. Clin J Pain. 2014;30:902-914.
7. Rizio AA, Bhor M, Lin X, et al. The relationship between frequency and severity of vaso-occlusive crises and health-related quality of life and work productivity in adults with sickle cell disease. Qual Life Res. 2020;29:1533-1547.
8. Freiermuth CE, Haywood C, Silva S, et al. Attitudes toward patients with sickle cell disease in a multicenter sample of emergency department providers. Adv Emerg Nurs J. 2014;36:335-347.
9. Jenerette CM, Brewer C. Health-related stigma in young adults with sickle cell disease. J Natl Med Assoc. 2010;102:1050-1055.
10. Lazio MP, Costello HH, Courtney DM, et al. A comparison of analgesic management for emergency department patients with sickle cell disease and renal colic. Clin J Pain. 2010;26:199-205.
11. Haywood C, Tanabe P, Naik R, et al. The impact of race and disease on sickle cell patient wait times in the emergency department. Am J Emerg Med. 2013;31:651-656.
12. Haywood C, Beach MC, Lanzkron S, et al. A systematic review of barriers and interventions to improve appropriate use of therapies for sickle cell disease. J Natl Med Assoc. 2009;101:1022-1033.
13. Mainous AG, Tanner RJ, Harle CA, et al. Attitudes toward management of sickle cell disease and its complications: a national survey of academic family physicians. Anemia. 2015;2015:1-6.
14. Yawn BP, Buchanan GR, Afenyi-Annan AN, et al. Management of sickle cell disease: summary of the 2014 evidence-based report by expert panel members. JAMA. 2014;312:1033.
15. Lunyera J, Jonassaint C, Jonassaint J, et al. Attitudes of primary care physicians toward sickle cell disease care, guidelines, and comanaging hydroxyurea with a specialist. J Prim Care Community Health. 2017;8:37-40.
16. Whiteman LN, Haywood C, Lanzkron S, et al. Primary care providers’ comfort levels in caring for patients with sickle cell disease. South Med J. 2015;108:531-536.
17. Wong TE, Brandow AM, Lim W, Lottenberg R. Update on the use of hydroxyurea therapy in sickle cell disease. Blood. 2014;124:3850-4004.
18. DiMartino LD, Baumann AA, Hsu LL, et al. The sickle cell disease implementation consortium: Translating evidence-based guidelines into practice for sickle cell disease. Am J Hematol. 2018;93:E391-E395.
19. King AA, Baumann AA. Sickle cell disease and implementation science: A partnership to accelerate advances. Pediatr Blood Cancer. 2017;64:e26649.
20. Solberg LI. Improving medical practice: a conceptual framework. Ann Fam Med. 2007;5:251-256.
21. Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. J Am Med Assoc. 2002;288:5.
22. Bodenheimer T. Interventions to improve chronic illness care: evaluating their effectiveness. Dis Manag. 2003;6:63-71.
23. Tsai AC, Morton SC, Mangione CM, Keeler EB. A meta-analysis of interventions to improve care for chronic illnesses. Am J Manag Care. 2005;11:478-488.
24. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377-381.
25. Kallio H, Pietilä A-M, Johnson M, et al. Systematic methodological review: developing a framework for a qualitative semi-structured interview guide. J Adv Nurs. 2016;72:2954-2965.
26. Clarke V, Braun V. Successful Qualitative Research: A Practical Guide for Beginners. First. Thousand Oaks, CA: Sage; 2013.
27. Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277-1288.
28. Creswell JW, Hanson WE, Clark Plano VL, et al. Qualitative research designs: selection and implementation. Couns Psychol. 2007;35:236-264.
29. Miles MB, Huberman AM, Saldana J. Qualitative Data Analysis A Methods Sourcebook. 4th ed. Thousand Oaks, CA: Sage; 2019.
30. Eckman JR, Hassell KL, Huggins W, et al. Standard measures for sickle cell disease research: the PhenX Toolkit sickle cell disease collections. Blood Adv. 2017; 1: 2703-2711.
31. Kendall R, Wagner B, Brodke D, et al. The relationship of PROMIS pain interference and physical function scales. Pain Med. 2018;19:1720-1724.
32. Amtmann D, Cook KF, Jensen MP, et al. Development of a PROMIS item bank to measure pain interference. Pain. 2010;150:173-182.
33. Evensen CT, Treadwell MJ, Keller S, et al. Quality of care in sickle cell disease: Cross-sectional study and development of a measure for adults reporting on ambulatory and emergency department care. Medicine (Baltimore). 2016;95:e4528.
34. Edwards R, Telfair J, Cecil H, et al. Reliability and validity of a self-efficacy instrument specific to sickle cell disease. Behav Res Ther. 2000;38:951-963.
35. Edwards R, Telfair J, Cecil H, et al. Self-efficacy as a predictor of adult adjustment to sickle cell disease: one-year outcomes. Psychosom Med. 2001;63:850-858.
36. Puri Singh A, Haywood C, Beach MC, et al. Improving emergency providers’ attitudes toward sickle cell patients in pain. J Pain Symptom Manage. 2016;51:628-632.e3.
37. Glassberg JA, Tanabe P, Chow A, et al. Emergency provider analgesic practices and attitudes towards patients with sickle cell disease. Ann Emerg Med. 2013;62:293-302.e10.
38. Grahmann PH, Jackson KC 2nd, Lipman AG. Clinician beliefs about opioid use and barriers in chronic nonmalignant pain [published correction appears in J Pain Palliat Care Pharmacother. 2004;18:145-6]. J Pain Palliat Care Pharmacother. 2004;18:7-28.
39. Brandow AM, Panepinto JA. Hydroxyurea use in sickle cell disease: the battle with low prescription rates, poor patient compliance and fears of toxicities. Expert Rev Hematol. 2010;3:255-260.
40. Fielding N. Triangulation and mixed methods designs: data integration with new research technologies. J Mixed Meth Res. 2012;6:124-136.
41. 2017 CAHPS Health Plan Survey Chartbook. Agency for Healthcare Research and Quality website. www.ahrq.gov/cahps/cahps-database/comparative-data/2017-health-plan-chartbook/results-enrollee-population.html. Accessed September 8, 2020.
42. Bulgin D, Tanabe P, Jenerette C. Stigma of sickle cell disease: a systematic review. Issues Ment Health Nurs. 2018;1-11.
43. Wakefield EO, Zempsky WT, Puhl RM, et al. Conceptualizing pain-related stigma in adolescent chronic pain: a literature review and preliminary focus group findings. PAIN Rep. 2018;3:e679.
44. Nelson SC, Hackman HW. Race matters: Perceptions of race and racism in a sickle cell center. Pediatr Blood Cancer. 2013;60:451-454.
45. Dyal BW, Abudawood K, Schoppee TM, et al. Reflections of healthcare experiences of african americans with sickle cell disease or cancer: a qualitative study. Cancer Nurs. 2019;10.1097/NCC.0000000000000750.
46. Renedo A. Not being heard: barriers to high quality unplanned hospital care during young people’s transition to adult services - evidence from ‘this sickle cell life’ research. BMC Health Serv Res. 2019;19:876.
47. Ballas S, Vichinsky E. Is the medical home for adult patients with sickle cell disease a reality or an illusion? Hemoglobin. 2015;39:130-133.
48. Hankins JS, Osarogiagbon R, Adams-Graves P, et al. A transition pilot program for adolescents with sickle cell disease. J Pediatr Health Care. 2012;26 e45-e49.
49. Smith WR, Sisler IY, Johnson S, et al. Lessons learned from building a pediatric-to-adult sickle cell transition program. South Med J. 2019;112:190-197.
50. Lanzkron S, Sawicki GS, Hassell KL, et al. Transition to adulthood and adult health care for patients with sickle cell disease or cystic fibrosis: Current practices and research priorities. J Clin Transl Sci. 2018;2:334-342.
51. Kanter J, Gibson R, Lawrence RH, et al. Perceptions of US adolescents and adults with sickle cell disease on their quality of care. JAMA Netw Open. 2020;3:e206016.
52. Haywood C, Lanzkron S, Hughes MT, et al. A video-intervention to improve clinician attitudes toward patients with sickle cell disease: the results of a randomized experiment. J Gen Intern Med. 2011;26:518-523.
53. Hankins JS, Shah N, DiMartino L, et al. Integration of mobile health into sickle cell disease care to increase hydroxyurea utilization: protocol for an efficacy and implementation study. JMIR Res Protoc. 2020;9:e16319.
54. Fan W, Yan Z. Factors affecting response rates of the web survey: A systematic review. Comput Hum Behav. 2010;26:132-139.
55. Millar MM, Dillman DA. Improving response to web and mixed-mode surveys. Public Opin Q. 2011;75:249-269.
From the University of California San Francisco (Dr. Treadwell, Dr. Hessler, Yumei Chen, Swapandeep Mushiana, Dr. Potter, and Dr. Vichinsky), the University of California Los Angeles (Dr. Jacob), and the University of California Berkeley (Alex Chen).
Abstract
- Objective: Adolescents and adults with sickle cell disease (SCD) face pervasive disparities in health resources and outcomes. We explored barriers to and facilitators of care to identify opportunities to support implementation of evidence-based interventions aimed at improving care quality for patients with SCD.
- Methods: We engaged a representative sample of adolescents and adults with SCD (n = 58), health care providers (n = 51), and community stakeholders (health care administrators and community-based organization leads (n = 5) in Northern California in a community-based needs assessment. We conducted group interviews separately with participant groups to obtain in-depth perspectives. Adolescents and adults with SCD completed validated measures of pain interference, quality of care, self-efficacy, and barriers to care. Providers and community stakeholders completed surveys about barriers to SCD care.
- Results: We triangulated qualitative and quantitative data and found that participants with SCD (mean age, 31 ± 8.6 years), providers, and community stakeholders emphasized the social and emotional burden of SCD as barriers. Concrete barriers agreed upon included insurance and lack of resources for addressing pain impact. Adolescents and adults with SCD identified provider issues (lack of knowledge, implicit bias), transportation, and limited social support as barriers. Negative encounters with the health care system contributed to 84% of adolescents and adults with SCD reporting they chose to manage severe pain at home. Providers focused on structural barriers: lack of access to care guidelines, comfort level with and knowledge of SCD management, and poor care coordination.
- Conclusion: Strategies for improving access to compassionate, evidence-based quality care, as well as strategies for minimizing the burden of having SCD, are warranted for this medically complex population.
Keywords: barriers to care; quality of care; care access; care coordination.
Sickle cell disease (SCD), an inherited chronic medical condition, affects about 100,000 individuals in the United States, a population that is predominantly African American.1 These individuals experience multiple serious and life-threatening complications, most frequently recurrent vaso-occlusive pain episodes,2 and they require interactions with multidisciplinary specialists from childhood. Because of advances in treatments, the majority are reaching adulthood; however, there is a dearth of adult health care providers with the training and expertise to manage their complex medical needs.3 Other concrete barriers to adequate SCD care include insurance and distance to comprehensive SCD centers.4,5
Social, behavioral, and emotional factors may also contribute to challenges with SCD management. SCD may limit daily functional abilities and lead to diminished overall quality of life.6,7 Some adolescents and adults may require high doses of opioids, which contributes to health care providers’ perceptions that there is a high prevalence of drug addiction in the population.8,9 These providers express negative attitudes towards adults with SCD, and, consequently, delay medication administration when it is acutely needed and provide otherwise suboptimal treatment.8,10,11 Adult care providers may also be uncomfortable with prescribing and managing disease-modifying therapies (blood transfusion, hydroxyurea) that have established efficacy.12-17
As 1 of 8 programs funded by the National Heart, Lung, and Blood Institute’s (NHLBI) Sickle Cell Disease Implementation Consortium (SCDIC), we are using implementation science to reduce barriers to care and improve quality of care and health care outcomes in SCD.18,19 Given that adolescents and adults with SCD experience high mortality, severe pain, and progressive decline in their ability to function day to day, and also face lack of access to knowledgeable, compassionate providers in primary and emergency settings, the SCDIC focuses on individuals aged 15 to 45 years.6,8,9,11,12
Our regional SCDIC program, the Sickle Cell Care Coordination Initiative (SCCCI), brings together researchers, clinicians, adolescents, and adults with SCD and their families, dedicated community members, policy makers, and administrators to identify and address barriers to health care within 5 counties in Northern California. One of our first steps was to conduct a community-based needs assessment, designed to inform implementation of evidence-based interventions, accounting for unique contextual factors in our region.
Conceptual Framework for Improving Medical Practice
Our needs assessment is guided by Solberg’s Conceptual Framework for Improving Medical Practice (Figure 1).20 Consistent with the overarching principles of the SCDIC, this conceptual framework focuses on the inadequate implementation of evidence-based guidelines, and on the need to first understand multifactorial facilitators and barriers to guideline implementation in order to effect change. The framework identifies 3 main elements that must be present to ensure improvements in quality-of-care processes and patient outcomes: priority, change process capability, and care process content. Priority refers to ample resource allocation for the specific change, as well as freedom from competing priorities for those implementing the change. Change process capability includes strong, effective leadership, adequate infrastructure for managing change (including resources and time), change management skills at all levels, and an established clinical information system. Care process content refers to context and systems-level changes, such as delivery system redesign as needed, support for self-management to lessen the impact of the disease, and decision support.21-23
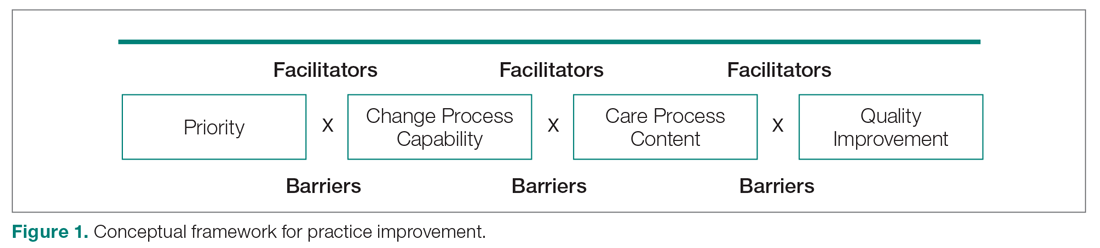
The purpose of our community-based needs assessment was to evaluate barriers to care and quality of care in SCD, within Solberg’s conceptual model for improving medical practice. The specific aims were to evaluate access and barriers to care (eg, lack of provider expertise and training, health care system barriers such as poor care coordination and provider communication); evaluate quality of care; and assess patient needs related to pain, pain interference, self-efficacy, and self-management for adolescents and adults with SCD. We gathered the perspectives of a representative community of adolescents and adults with SCD, their providers, and community stakeholders in order to examine barriers, quality of life and care, and patient experiences in our region.
Methods
Design
In this cross-sectional study, adolescents and adults with SCD, their providers, and community stakeholders participated in group or individual qualitative interviews and completed surveys between October 2017 and March 2018.
Setting and Sample
Recruitment flyers were posted on a regional SCD-focused website, and clinical providers or a study coordinator introduced information about the needs assessment to potential participants with SCD during clinic visits at the participating centers. Participants with SCD were eligible if they had any diagnosis of SCD, were aged 15 to 48 years, and received health services within 5 Northern California counties (Alameda, Contra Costa, Sacramento, San Francisco, and Solano). They were excluded if they did not have a SCD diagnosis or had not received health services within the catchment area. As the project proceeded, participants were asked to refer other adolescents and adults with SCD for the interviews and surveys (snowball sampling). Our goal was to recruit 50 adolescents and adults with SCD into the study, aiming for 10 representatives from each county.
Providers and community stakeholders were recruited via emails, letters and informational flyers. We engaged our partner, the Sickle Cell Data Collection Program,2 to generate a list of providers and institutions that had seen patients with SCD in primary, emergency, or inpatient settings in the region. We contacted these institutions to describe the SCCCI and invite participation in the needs assessment. We also invited community-based organization leads and health care administrators who worked with SCD to participate. Providers accessed confidential surveys via a secure link on the study website or completed paper versions. Common data collected across providers included demographics and descriptions of practice settings.
Participants were eligible to be part of the study if they were health care providers (physicians and nurses) representing hematology, primary care, family medicine, internal medicine, or emergency medicine; ancillary staff (social work, psychology, child life); or leaders or administrators of clinical or sickle cell community-based organizations in Northern California (recruitment goal of n = 50). Providers were excluded if they practiced in specialties other than those noted or did not practice within the region.
Data Collection Procedures
After providing assent/consent, participating adolescents and adults with SCD took part in individual and group interviews and completed survey questionnaires. All procedures were conducted in a private space in the sickle cell center or community. Adolescents and adults with SCD completed the survey questionnaire on a tablet, with responses recorded directly in a REDCap (Research Electronic Data Capture) database,24 or on a paper version. Interviews lasted 60 (individual) to 90 (group) minutes, while survey completion time was 20 to 25 minutes. Each participant received a gift card upon completion as an expression of appreciation. All procedures were approved by the institutional review boards of the participating health care facilities.
Group and Individual Interviews
Participants with SCD and providers were invited to participate in a semi-structured qualitative interview prior to being presented with the surveys. Adolescents and adults with SCD were interviewed about barriers to care, quality of care, and pain-related experiences. Providers were asked about barriers to care and treatments. Interview guides were modified for community-based organization leaders and health care administrators who did not provide clinical services. Interview guides can be found in the Appendix. Interviews were conducted by research coordinators trained in qualitative research methods by the first author (MT). As appropriate with semi-structured interviews, the interviewers could word questions spontaneously, change the order of questions for ease of flow of conversation, and inform simultaneous coding of interviews with new themes as those might arise, as long as they touched on all topics within the interview guide.25 The interview guides were written, per qualitative research standards, based on the aims and purpose of the research,26 and were informed by existing literature on access and barriers to care in SCD, quality of care, and the needs of individuals with SCD, including in relation to impact of the disease, self-efficacy, and self-management.
Interviewees participated in either individual or group interviews, but not both. The decision for which type of interview an individual participated in was based on 2 factors: if there were not comparable participants for group interviews (eg, health care administrator and community-based organization lead), these interviews were done individually; and given that we were drawing participants from a 5-county area in Northern California, scheduling was challenging for individuals with SCD with regard to aligning schedules and traveling to a central location where the group interviews were conducted. Provider group interviews were easier to arrange because we could schedule them at the same time as regularly scheduled meetings at the participants’ health care institutions.
Interview Data Gathering and Analysis
Digital recordings of the interviews were cleaned of any participant identifying data and sent for transcription to an outside service. Transcripts were reviewed for completeness and imported into NVivo (www.qsrinternational.com), a qualitative data management program.
A thematic content analysis and deductive and inductive approaches were used to analyze the verbatim transcripts generated from the interviews. The research team was trained in the use of NVivo software to facilitate the coding process. A deductive coding scheme was initially used based on existing concepts in the literature regarding challenges to optimal SCD care, with new codes added as the thematic content analyses progressed. The initial coding, pattern coding, and use of displays to examine the relationships between different categories were conducted simultaneously.27,28 Using the constant comparative method, new concepts from participants with SCD and providers could be incorporated into subsequent interviews with other participants. For this study, the only additional concepts added were in relation to participant recruitment and retention in the SCDIC Registry. Research team members coded transcripts separately and came together weekly, constantly comparing codes and developing the consensus coding scheme. Where differences between coders existed, code meanings were discussed and clarified until consensus was reached.29
Quantitative data were analyzed using SPSS (v. 25, Chicago, IL). Descriptive statistics (means, standard deviations, frequencies, percentages) were used to summarize demographics (eg, age, gender, and race), economic status, and type of SCD. No systematic differences were detected from cases with missing values. Scale reliabilities (ie, Cronbach α) were evaluated for self-report measures.
Measurement
Adolescents and adults with SCD completed items from the PhenX Toolkit (consensus measures for Phenotypes and eXposures), assessing sociodemographics (age, sex, race, ethnicity, educational attainment, occupation, marital status, annual income, insurance), and clinical characteristics (sickle cell diagnosis and emergency department [ED] and hospital utilization for pain).30
Pain Interference Short Form (Patient-Reported Outcomes Measurement Information System [PROMIS]). The Pain Interference Form consists of 8 items that assess the degree to which pain interfered with day-to-day activities in the previous 7 days at home, including impacts on social, cognitive, emotional, and physical functioning; household chores and recreational activities; sleep; and enjoyment in life. Reliability and validity of the PROMIS Pain Interference Scale has been demonstrated, with strong negative correlations with Physical Function Scales (r = 0.717, P < 0.01), indicating that higher scores are associated with lower function (β = 0.707, P < 0.001).31 The Cronbach α estimate for the other items on the pain interference scale was 0.99. Validity analysis indicated strong correlations with pain-related domains: BPI Interference Subscale (rho = 0.90), SF-36 Bodily Pain Subscale (rho = –0.84), and 0–10 Numerical Rating of Pain Intensity (rho = 0.48).32
Adult Sickle Cell Quality of Life Measurement Information System (ASCQ-Me) Quality of Care (QOC). ASCQ-Me QOC consists of 27 items that measure the quality of care that adults with SCD have received from health care providers.33 There are 3 composites: provider communication (quality of patient and provider communication), ED care (quality of care in the ED), and access (to routine and emergency care). Internal consistency reliability for all 3 composites is greater than 0.70. Strong correlations of the provider communication composite with overall ratings of routine care (r = 0.65) and overall provider ratings (r = 0.83) provided evidence of construct validity. Similarly, the ED care composite was strongly correlated with overall ratings of QOC in the ED, and the access composite was highly correlated with overall evaluations of ED care (r = 0.70). Access, provider interaction, and ED care composites were reliable (Cronbach α, 0.70–0.83) and correlated with ratings of global care (r = 0.32–0.83), further indicating construct validity.33
Sickle Cell Self-Efficacy Scale (SCSES). The SCSES is a 9-item, self-administered questionnaire measuring perceptions of the ability to manage day-to-day issues resulting from SCD. SCSES items are scored on a 5-point scale ranging from Not sure at all (1) to Very sure (5). Individual item responses are summed to give an overall score, with higher scores indicating greater self-efficacy. The SCSES has acceptable reliability (r = 0.45, P < 0.001) and validity (α = 0.89).34,35
Sickle Cell Disease Barriers Checklist. This checklist consists of 53 items organized into 8 categories: insurance, transportation, accommodations and accessibility, provider knowledge and attitudes, social support, individual barriers such as forgetting or difficulties understanding instructions, emotional barriers (fear, anger), and disease-related barriers. Participants check applicable barriers, with a total score range of 0 to 53 and higher scores indicating more barriers to care. The SCD Barriers Checklist has demonstrated face validity and test-retest reliability (Pearson r = 0.74, P < 0.05).5
ED Provider Checklist. The ED provider survey is a checklist of 14 statements pertaining to issues regarding patient care, with which the provider rates level of agreement. Items representing the attitudes and beliefs of providers towards patients with SCD are rated on a Likert-type scale, with level of agreement indicated as 1 (strongly disagree) to 6 (strongly agree). The positive attitudes subscale consists of 4 items (Cronbach α= 0.85), and the negative attitudes subscale consists of 6 items (Cronbach α = 0.89). The Red-Flag Behaviors subscale includes 4 items that indicate behavior concerns about drug-seeking, such as requesting specific narcotics and changing behavior when the provider walks in.8,36,37
Sickle cell and primary care providers also completed a survey consisting of sets of items compiled from existing provider surveys; this survey consisted of a list of 16 barriers to using opioids, which the providers rated on a 5-point Likert-type scale (1, not a barrier; 5, complete barrier).13,16,38 Providers indicated their level of experience with caring for patients with SCD; care provided, such as routine health screenings; and comfort level with providing preventive care, managing comorbidities, and managing acute and chronic pain. Providers were asked what potential facilitators might improve care for patients with SCD, including higher reimbursement, case management services, access to pain management specialists, and access to clinical decision-support tools. Providers responded to specific questions about management with hydroxyurea (eg, criteria for, barriers to, and comfort level with prescribing).39 The surveys are included in the Appendix.
Triangulation
Data from the interviews and surveys were triangulated to enhance understanding of results generated from the different data sources.40 Convergence of findings, different facets of the same phenomenon, or new perspectives were examined.
Results
Qualitative Data
Adolescents and adults with SCD (n = 55) and health care providers and community stakeholders (n = 56) participated in group or individual interviews to help us gain an in-depth understanding of the needs and barriers related to SCD care in our 5-county region. Participants with SCD described their experiences, which included stigma, racism, labeling, and, consequently, stress. They also identified barriers such as lack of transportation, challenges with insurance, and lack of access to providers who were competent with pain management. They reported that having SCD in a health care system that was unable to meet their needs was burdensome.
Barriers to Care and Treatments. Adolescents and adults indicated that SCD and its sequelae posed significant barriers to health care. Feelings of tiredness and pain make it more difficult for them to seek care. The emotional burden of SCD (fear and anger) was a frequently cited barrier, which was fueled by previous negative encounters with the health care system. All adolescents and adults with SCD reported that they knew of stigma in relation to seeking pain management that was pervasive and long-standing, and the majority reported they had directly experienced stigma. They reported that being labeled as “drug-seekers” was typical when in the ED for pain management. Participants articulated unconscious bias or overt racism among providers: “people with sickle cell are Black ... and Black pain is never as valuable as White pain” (25-year-old male). Respondents with SCD described challenges to the credibility of their pain reports in the ED. They reported that ED providers expressed doubts regarding the existence and/or severity of their pain, consequently creating a feeling of disrespect for patients seeking pain relief. The issue of stigma was mentioned by only 2 of 56 providers during their interviews.
Lack of Access to Knowledgeable, Compassionate Providers. Lack of access to knowledgeable care providers was another prevalent theme expressed by adolescents and adults with SCD. Frustration occurred when providers did not have knowledge of SCD and its management, particularly pain assessment. Adolescents and adults with SCD noted the lack of compassion among providers: “I’ve been kicked out of the hospital because they felt like okay, well we gave you enough medication, you should be all right” (29-year-old female). Providers specifically mentioned lack of compassion and knowledge as barriers to SCD care much less often during their interviews compared with the adolescents and adults with SCD.
Health Care System Barriers. Patient participants often expressed concerns about concrete and structural aspects of care. Getting to their appointments was a challenge for half of the interviewees, as they either did not have access to a vehicle or could not afford to travel the needed distance to obtain quality care. Even when hospitals were accessible by public transportation, those with excruciating pain understandably preferred a more comfortable and private way to travel: “I would like to change that, something that will be much easier, convenient for sickle cell patients that do suffer with pain, that they don’t have to travel always to see the doctor” (30-year-old male).
Insurance and other financial barriers also played an important role in influencing decisions to seek health care services. Medical expenses were not covered, or co-pays were too high. The Medicaid managed care system could prevent access to knowledgeable providers who were not within network. Such a lack of access discouraged some adolescents and adults with SCD from seeking acute and preventive care.
Transition From Pediatric to Adult Care. Interviewees with SCD expressed distress about the gap between pediatric and adult care. They described how they had a long-standing relationship with their medical providers, who were familiar with their medical background and history from childhood. Adolescent interviewees reported an understanding of their own pain management as well as adherence to and satisfaction with their individualized pain plans. However, adults noted that satisfaction plummeted with increasing age due to the limited number of experienced adult SCD providers, which was compounded by negative experiences (stigma, racism, drug-seeking label).
One interviewee emphasized the difficulty of finding knowledgeable providers after transition: “When you’re a pediatric sickle cell [patient], you have the doctors there every step of the way, but not with adult sickle cell… I know when I first transitioned I never felt more alone in my life… you look at that ER doctor kind of with the same mindset as you would your hematologist who just hand walked you through everything. And adult care providers were a lot more blunt and cold and they’re like… ‘I don’t know; I’m not really educated in sickle cell.’” A sickle cell provider shared his insight about the problem of transitioning: “I think it’s particularly challenging because we, as a community, don’t really set them up for success. It’s different from other chronic conditions [in that] it’s much harder to find an adult sickle cell provider. There’s not a lot of adult hematologists that will take care of our adult patients, and so I know statistically, there’s like a drop-down in the overall outcomes of our kids after they age out of our pediatric program.”
Self-Management, Supporting Hydroxyurea Use. Interview participants with SCD reported using a variety of methods to manage pain at home and chose to go to the ED only when the pain became intolerable. Patients and providers expressed awareness of different resources for managing pain at home, yet they also indicated that these resources have not been consolidated in an accessible way for patients and families. Some resources cited included heat therapy, acupuncture, meditation, medical marijuana, virtual reality devices, and pain medications other than opioids.
Patients and providers expressed the need for increasing awareness and education about hydroxyurea. Many interview participants with SCD were concerned about side effects, multiple visits with a provider during dose titration, and ongoing laboratory monitoring. They also expressed difficulties with scheduling multiple appointments, depending on access to transportation and limited provider clinic hours. They were aware of strategies for improving adherence with hydroxyurea, including setting phone alarms, educating family members about hydroxyurea, and eliciting family support, but expressed needing help to consistently implement these strategies.
Safe Opioid Prescribing. Adult care providers expressed concerns about safe opioid prescribing for patients with SCD. They were reluctant to prescribe opioid doses needed to adequately control SCD pain. Providers expressed uncertainty and fear or concern about medical/legal liability or about their judgment about what’s safe and not safe for patients with chronic use/very high doses of opioids. “I know we’re in like this opiate epidemic here in this country but I feel like these patients don’t really fit under that umbrella that the problem is coming from so [I am] just trying to learn more about how to take care of them.”
Care Coordination and Provider Communication. Adolescents and adults with SCD reported having positive experiences—good communication, established trust, and compassionate care—with their usual providers. However, they perceived that ED physicians and nurses did not really care about them. Both interviewees with SCD and providers recognized the importance of good communication in all settings as the key to overcoming barriers to receiving quality care. All agreed on the importance of using individual pain plans so that all providers, especially ED providers, can be more at ease with treating adolescents and adults with SCD.
Quantitative Data: Adolescents and Adults With SCD
Fifty-eight adolescents and adults with SCD (aged 15 to 48 years) completed the survey. Three additional individuals who did not complete the interview completed the survey. Reasons for not completing the interview included scheduling challenges (n = 2) or a sickle cell pain episode (n = 1). The average age of participants was 31 years ± 8.6, more than half (57%) were female, and the majority (93%) were African American (Table 1). Most (71%) had never been married. Half (50%) had some college or an associate degree, and 40% were employed and reported an annual household income of less than $30,000. Insurance coverage was predominantly Medi-Cal (Medicaid, 69%). The majority of participants resided in Alameda (34.5%) or Contra Costa (21%) counties. The majority of sickle cell care was received in Alameda County, whether outpatient (52%), inpatient (40%), or ED care (41%). The majority (71%) had a diagnosis of SCD hemoglobin SS.
Pain. More than one-third of individuals with SCD reported 1 or 2 ED visits for pain in the previous 6 months (34%), and more than 3 hospitalizations (36%) related to pain in the previous year (Table 2). The majority (85%) reported having severe pain at home in the previous 6 months that they did not seek health care for, consistent with their reports in the qualitative interviews. More than half (59%) reported 4 or more of these severe pain episodes that led to inability to perform daily activities for 1 week or more. While pain interference on the PROMIS Pain Interference Short Form on average (T-score, 59.6 ± 8.6) was similar to that of the general population (T-score, 50 ± 10), a higher proportion of patients with SCD reported pain interference compared with the general population. The mean self-efficacy (confidence in ability to manage complications of SCD) score on the SCSES of 30.0 ± 7.3 (range, 9–45) was similar to that of other adults with SCD (mean, 32.2 ± 7.0). Twenty-five percent of the present sample had a low self-efficacy score (< 25).
Barriers to Care and Treatments. Consistent with the qualitative data, SCD-related symptoms such as tiredness (64%) and pain (62%) were reported most often as barriers to care (Table 3). Emotions (> 25%) such as worry/fear, frustration/anger, and lack of confidence were other important barriers to care. Provider knowledge and attitudes were cited next most often, with 38% of the sample indicating “Providers accuse me of drug-seeking” and “It is hard for me to find a provider who has enough experiences with or knowledge about SCD.” Participants expressed that they were not believed when in pain and “I am treated differently from other patients.” Almost half of respondents cited “I am not seen quickly enough when I am in pain” as a barrier to their care.
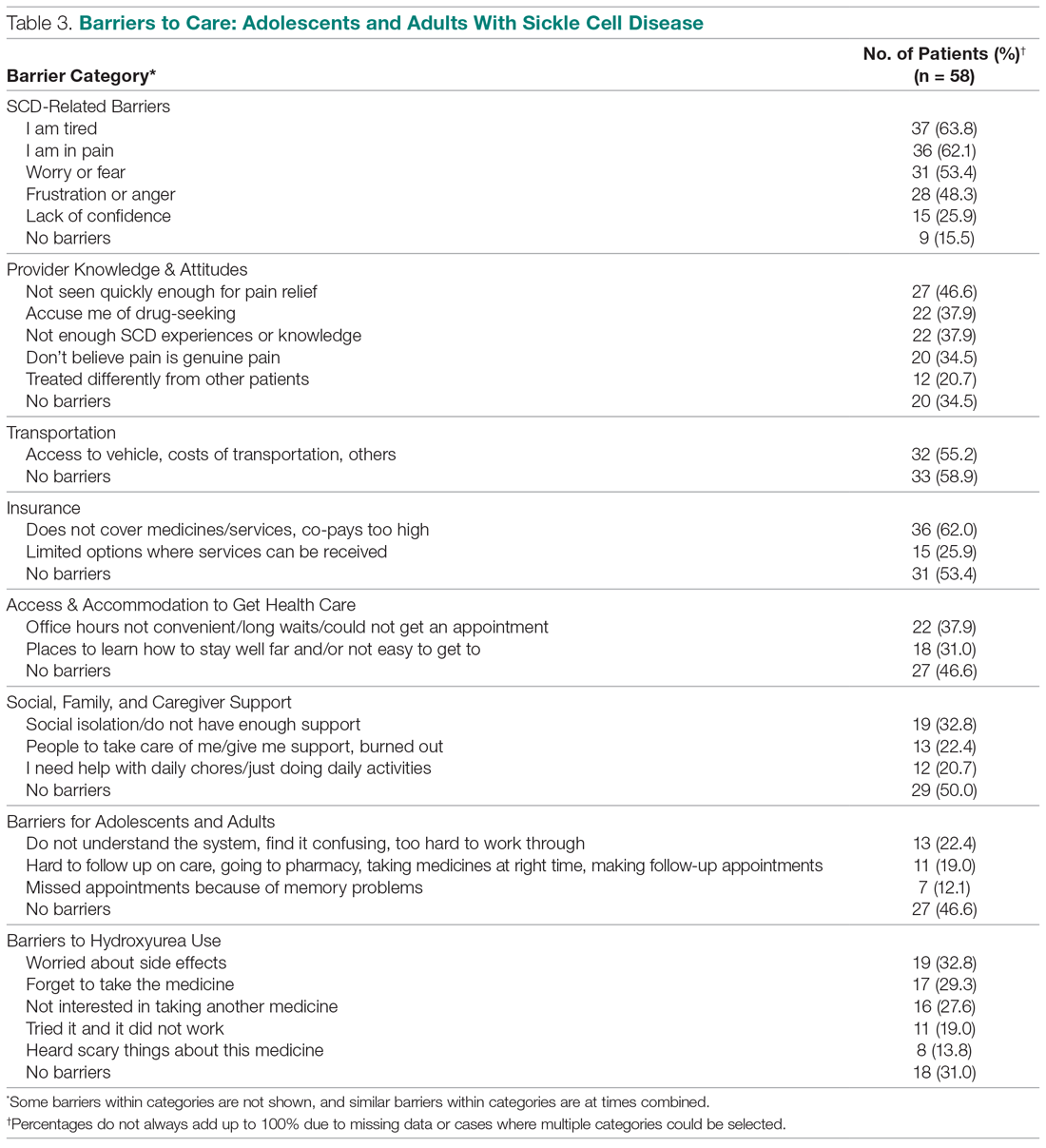
Consistent with the qualitative data, transportation barriers (not having a vehicle, costs of transportation, public transit not easy to get to) were cited by 55% of participants. About half of participants reported that insurance was an important barrier, with high co-pays and medications and other services not covered. In addition, gathering approvals was a long and fragmented process, particularly for consultations among providers (hematology, primary care provider, pain specialist). Furthermore, insurance provided limited choices about location for services.
Participants reported social support system burnout (22%), help needed with daily activities (21%), and social isolation or generally not having enough support (33%) as ongoing barriers. Difficulties were encountered with self-management (eg, taking medications on time or making follow-up appointments, 19%), with 22% of participants finding the health care system confusing or hard to understand. Thirty percent reported “Places for me to go to learn how to stay well are not close by or easy to get to.” ”Worry about side effects” (33%) was a common barrier to hydroxyurea use. Participants described “forgetting to take the medicine,” “tried before but it did not work,” “heard scary things” about hydroxyurea, and “not interested in taking another medicine” as barriers.
Quality of Care. More than half (51%) of the 53 participants who had accessed health care in the previous year rated their overall health care as poor on the ASCQ-Me QOC measure. This was significantly higher compared to the reports from more than 47,000 adults with Medicaid in 2017 (16%),41 and to the 2008-2009 report from 556 adults with SCD from across the United States (37%, Figure 2).33 The major contributor to these poor ratings for participants in our sample was low satisfaction with ED care.
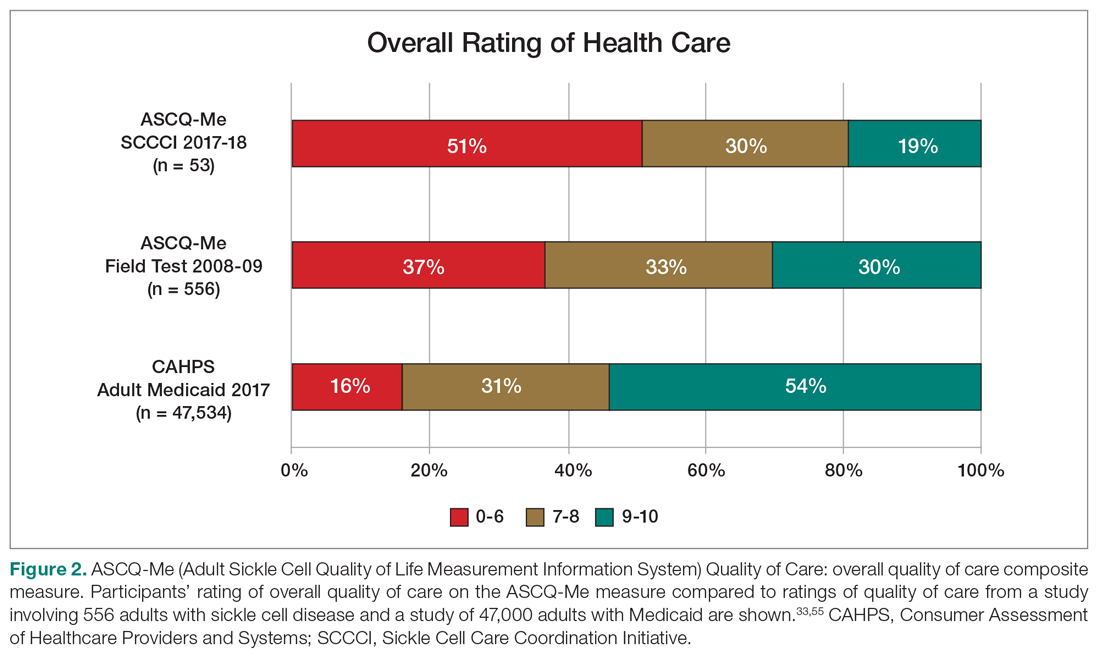
Sixty percent of the 42 participants who had accessed ED care in the past year indicated “never” or “sometimes” to the question “When you went to the ED for care, how often did you get it as soon as you wanted?” compared with only 16% of the 2017 adult Medicaid population responding (n = 25,789) (Figure 3). Forty-seven percent of those with an ED visit indicated that, in the previous 12 months, they had been made to wait “more than 2 hours before receiving treatment for acute pain in the ED.” However, in the previous 12 months, 39% reported that their wait time in the ED had been only “between five minutes and one hour.”
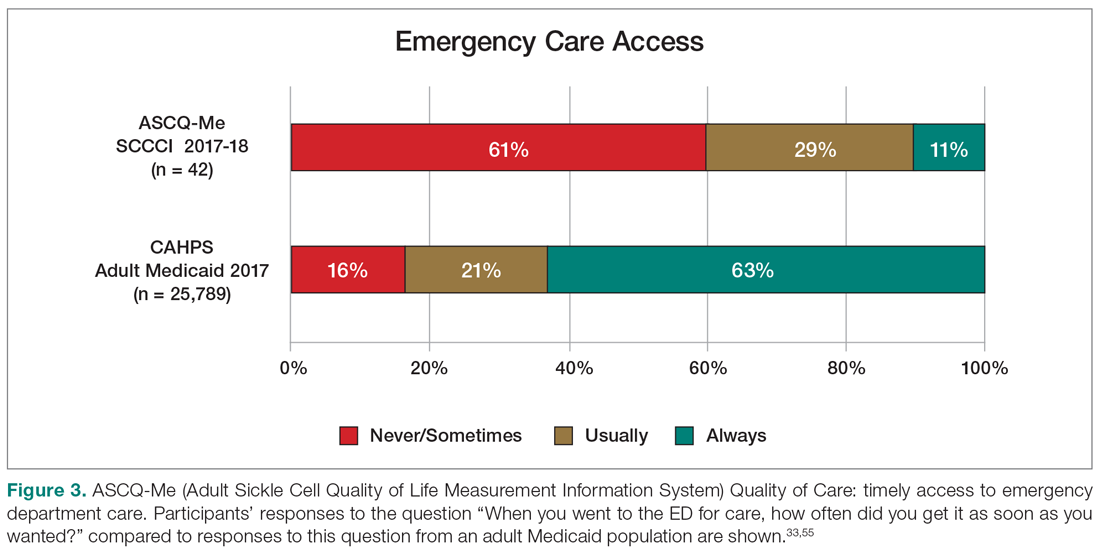
On the ASCQ-Me QOC Access to Care composite measure, 33% of 42 participants responding reported they were seen at a routine appointment as soon as they would have liked. This is significantly lower compared to 56% of the adult Medicaid population responding to the same question. Reports of provider communication (Provider Communication composite) for adolescents and adults with SCD were comparable to reports of adults with SCD from the ASCQ-Me field test,33 but adults with Medicaid reported higher ratings of quality communication behaviors (Figure 4).33,41 Nearly 60% of both groups with SCD reported that providers “always” performed quality communication behaviors—listened carefully, spent enough time, treated them with respect, and explained things well—compared with more than 70% of adults with Medicaid.
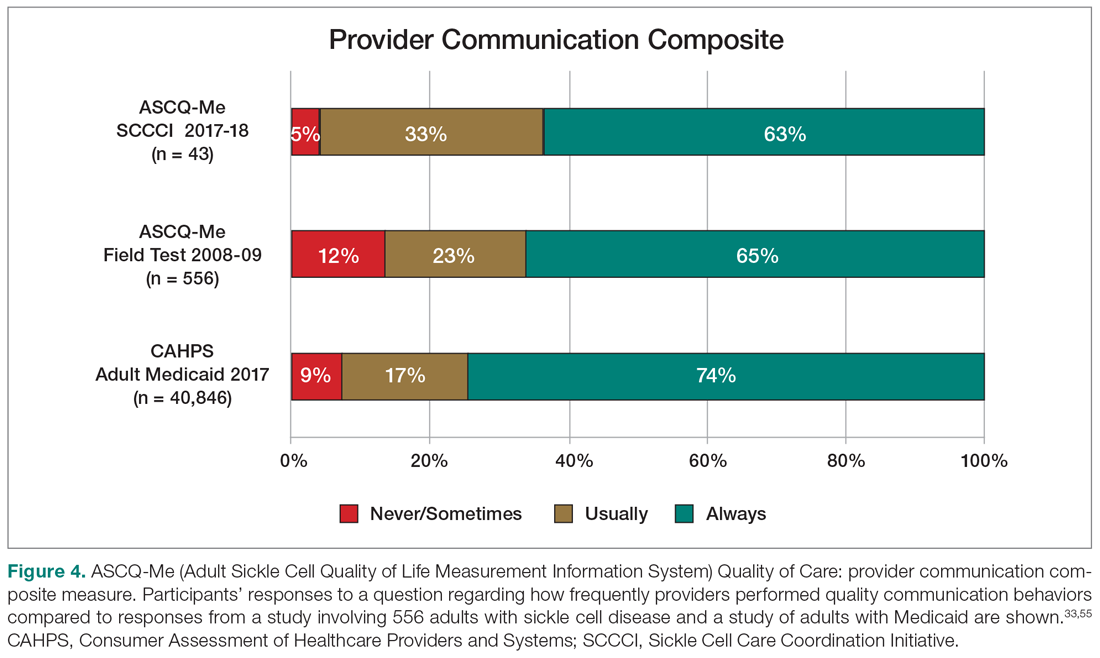
Participants from all counties reported the same number of barriers to care on average (3.3 ± 2.1). Adolescents and adults who reported more barriers to care also reported lower satisfaction with care (r = –0.47, P < 0.01) and less confidence in their ability to manage their SCD (self-efficacy, r = – 0.36, P < 0.05). Female participants reported more barriers to care on average compared with male participants (2.6 ± 2.4 vs 1.4 ± 2.0, P = 0.05). Participants with higher self-efficacy reported lower pain ratings (r = –0.47, P < 0.001).
Quantitative Data: Health Care Providers
Providers (n = 56) and community stakeholders (2 leaders of community-based organizations and 3 health care administrators) were interviewed, with 29 also completing the survey. The reason for not completing (n = 22) was not having the time once the interview was complete. A link to the survey was sent to any provider not completing at the time of the interview, with 2 follow-up reminders. The majority of providers were between the ages of 31 and 50 years (46.4%), female (71.4%), and white (66.1%) (Table 4). None were of Hispanic, Latinx, or Spanish origin. Thirty-six were physicians (64.3%), and 16 were allied health professionals (28.6%). Of the 56 providers, 32 indicated they had expertise caring for patients with SCD (57.1%), 14 were ED providers (25%), and 5 were primary care providers. Most of the providers practiced in an urban setting (91.1%).
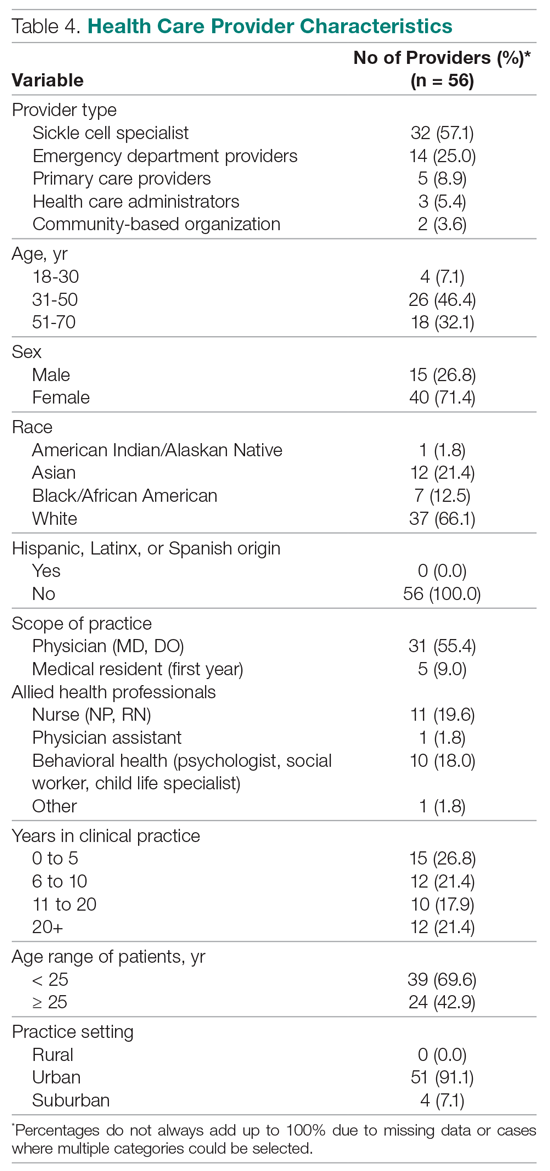
Barriers to Care: ED Provider Perspectives. Nine of 14 ED providers interviewed completed the survey on their perspectives regarding barriers to care in the ED, difficulty with follow-ups, ED training resources, and pain control for patients with SCD. ED providers (n = 8) indicated that “provider attitudes” were a barrier to care delivery in the ED for patients with SCD. Some providers (n = 7) indicated that “implicit bias,” “opioid epidemic,” “concern about addiction,” and “patient behavior” were barriers. Respondents indicated that “overcrowding” (n = 6) and “lack of care pathway/protocol” (n = 5) were barriers. When asked to express their level of agreement with statements about SCD care in the ED, respondents disagreed/strongly disagreed (n = 5) that they were “able to make a follow-up appointment” with a sickle cell specialist or primary care provider upon discharge from the ED, and others disagreed/strongly disagreed (n = 4) that they were able to make a “referral to a case management program.”
ED training and resources. Providers agreed/strongly agreed (n = 8) that they had the knowledge and training to care for patients with SCD, that they had access to needed medications, and that they had access to knowledgeable nursing staff with expertise in SCD care. All 9 ED providers indicated that they had sufficient physician/provider staffing to provide good pain management to persons with SCD in the ED.
Pain control in the ED. Seven ED providers indicated that their ED used individualized dosing protocols to treat sickle cell pain, and 5 respondents indicated their ED had a protocol for treating sickle cell pain. Surprisingly, only 3 indicated that they were aware of the NHLBI recommendations for the treatment of vaso-occlusive pain.
Barriers to Care: Primary Care Provider Perspectives. Twenty providers completed the SCD provider section of the survey, including 17 multidisciplinary SCD providers from 4 sickle cell special care centers and 3 community primary care providers. Of the 20, 12 were primary care providers for patients with SCD (Table 4).
Patient needs. Six primary care providers indicated that the medical needs of patients with SCD were being met, but none indicated that the behavioral health or mental health needs were being met.
Managing SCD comorbidities. Five primary care providers indicated they were very comfortable providing preventive ambulatory care to patients with SCD. Six indicated they were very comfortable managing acute pain episodes, but none were very comfortable managing comorbidities such as pulmonary hypertension, diabetes, or chronic pain.
Barriers to opioid use. Only 3 of 12 providers reviewing a list of 15 potential barriers to the use of opioids for SCD pain management indicated a perceived lack of efficacy of opioids, development of tolerance and dependence, and concerns about community perceptions as barriers. Two providers selected potential for diversion as a moderate barrier to opioid use.
Barriers to hydroxyurea use. Eight of 12 providers indicated that the common reasons that patients/families refuse hydroxyurea were “worry about side effects”; 7 chose “don’t want to take another medicine,” and 6 chose “worry about carcinogenic potential.” Others (n = 10) indicated that “patient/family adherence with hydroxyurea” and “patient/family adherence with required blood tests” were important barriers to hydroxyurea use. Eight of the 12 providers indicated that they were comfortable with managing hydroxyurea in patients with SCD.
Care redesign. Twenty SCD and primary care providers completed the Care Redesign section of the survey. Respondents (n = 11) indicated that they would see more patients with SCD if they had accessible case management services available without charge or if patient access to transportation to clinic was also available. Ten indicated that they would see more patients with SCD if they had an accessible community health worker (who understands patient’s/family’s social situation) and access to a pain management specialist on call to answer questions and who would manage chronic pain. All (n = 20) were willing to see more patients with SCD in their practices. Most reported that a clinical decision-support tool for SCD treatment (n = 13) and avoidance of complications (n = 12) would be useful.
Discussion
We evaluated access and barriers to care, quality of care, care coordination, and provider communication from the perspectives of adolescents and adults with SCD, their care providers, and community stakeholders, within the Solberg conceptual model for quality improvement. We found that barriers within the care process content domain (context and systems) were most salient for this population of adolescents and adults with SCD, with lack of provider knowledge and poor attitudes toward adolescents and adults with SCD, particularly in the ED, cited consistently by participant groups. Stigmatization and lack of provider compassion that affected the quality of care were particularly problematic. These findings are consistent with previous reports.42,43 Adult health care (particularly ED) provider biases and negative attitudes have been recognized as major barriers to optimal pain management in SCD.8,11,44,45 Interestingly, ED providers in our needs assessment indicated that they felt they had the training and resources to manage patients with SCD. However, only a few actually reported knowing about the NHLBI recommendations for the treatment of vaso-occlusive pain.
Within the care process content domain, we also found that SCD-related complications and associated emotions (fear, worry, anxiety), compounded by lack of access to knowledgeable and compassionate providers, pose a significant burden. Negative encounters with the health care system contributed to a striking 84% of patient participants choosing to manage severe pain at home, with pain seriously interfering with their ability to function on a daily basis. ED providers agreed that provider attitudes and implicit bias pose important barriers to care for adolescents and adults with SCD. Adolescents and adults with SCD wanted, and understood the need, to enhance self-management skills. Both they and their providers agreed that barriers to hydroxyurea uptake included worries about potential side effects, challenges with adherence to repeated laboratory testing, and support with remembering to take the medicine. However, providers uniformly expressed that access to behavioral and mental health services were, if not nonexistent, impossible to access.
Participants with SCD and their providers reported infrastructural challenges (change process capability), as manifested in limitations with accessing acute and preventive care due to transportation- and insurance- related issues. There were health system barriers that were particularly encountered during the transition from pediatric to adult care. These findings are consistent with previous reports that have found fewer interdisciplinary services available in the adult care settings compared with pediatrics.46,47 Furthermore, adult care providers were less willing to accept adults with SCD because of the complexity of their management, for which the providers did not have the necessary expertise.3,48-50 In addition, both adolescents and adults with SCD and primary care providers highlighted the inadequacies of the current system in addressing the chronic pain needs of this population. Linking back to the Solberg conceptual framework, our needs assessment results confirm the important role of establishing SCD care as a priority within a health care system—this requires leadership and vision. The vision and priorities must be implemented by effective health care teams. Multilevel approaches or interventions, when implemented, will lead to the desired outcomes.
Findings from our needs assessment within our 5-county region mirror needs assessment results from the broader consortium.51 The SCDIC has prioritized developing an intervention that addresses the challenges identified within the care process domain by directly enhancing provider access to patient individualized care plans in the electronic health record in the ED. Importantly, ED providers will be asked to view a short video that directly challenges bias and stigma in the ED. Previous studies have indeed found that attitudes can be improved by providers viewing short video segments of adults with SCD discussing their experiences.36,52 This ED protocol will be one of the interventions that we will roll out in Northern California, given the significance of negative ED encounters reported by needs assessment participants. An additional feature of the intervention is a script for adults with SCD that guides them through introducing their individualized pain plan to their ED providers, thereby enhancing their self-efficacy in a situation that has been so overwhelmingly challenging.
We will implement a second SCDIC intervention that utilizes a mobile app to support self-management on the part of the patient, by supporting motivation and adherence with hydroxyurea.53 A companion app supports hydroxyurea guideline adherence on the part of the provider, in keeping with one of our findings that providers are in need of decision-support tools. Elements of the intervention also align with our findings related to the importance of a support system in managing SCD, in that participants will identify a supportive partner who will play a specific role in supporting their adherence with hydroxyurea.
On our local level, we have, by necessity, partnered with leaders and community stakeholders throughout the region to ensure that these interventions to improve SCD care are prioritized. Grant funds provide initial resources for the SCDIC interventions, but our partnering health care administrators and medical directors must ensure that participating ED and hematology providers are free from competing priorities in order to implement the changes. We have partnered with a SCD community-based organization that is designing additional educational presentations for local emergency medicine providers, with the goal to bring to life very personal stories of bias and stigma within the EDs that directly contribute to decisions to avoid ED care despite severe symptoms.
Although we attempted to obtain samples of adolescents and adults with SCD and their providers that were representative across the 5-county region, the larger proportion of respondents were from 1 county. We did not assess concerns of age- and race-matched adults in our catchment area, so we cannot definitively say that our findings are unique to SCD. However, our results are consistent with findings from the national sample of adults with SCD who participated in the ASCQ-Me field test, and with results from the SCDIC needs assessment.33,51 Interviews and surveys are subject to self-report bias and, therefore, may or may not reflect the actual behaviors or thoughts of participants. Confidence is increased in our results given the triangulation of expressed concerns across participant groups and across data collection strategies. The majority of adolescents and adults with SCD (95%) completed both the interview and survey, while 64% of ED providers interviewed completed the survey, compared with 54% of SCD specialists and primary care providers. These response rates are more than acceptable within the realm of survey response rates.54,55
Although we encourage examining issues with care delivery within the conceptual framework for quality improvement presented, we recognize that grant funding allowed us to conduct an in-depth needs assessment that might not be feasible in other settings. Still, we would like readers to understand the importance of gathering data for improvement in a systematic manner across a range of participant groups, to ultimately inform the development of interventions and provide for evaluation of outcomes as a result of the interventions. This is particularly important for a disease, such as SCD, that is both medically and sociopolitically complex.
Conclusion
Our needs assessment brought into focus the multiple factors contributing to the disparities in health care experienced by adolescents and adults with SCD on our local level, and within the context of inequities in health resources and outcomes on the national level. We propose solutions that include specific interventions developed by a consortium of SCD and implementation science experts. We utilize a quality improvement framework to ensure that the elements of the interventions also address the barriers identified by our local providers and patients that are unique to our community. The pervasive challenges in SCD care, coupled with its medical complexities, may seem insurmountable, but our survey and qualitative results provide us with a road map for the way forward.
Acknowledgments: The authors thank the adolescents and adults with sickle cell disease, the providers, and the community stakeholders who completed the interviews and surveys. The authors also acknowledge the SCCCI co-investigators for their contributions to this project, including Michael Bell, MD, Ward Hagar, MD, Christine Hoehner, FNP, Kimberly Major, MSW, Anne Marsh, MD, Lynne Neumayr, MD, and Ted Wun, MD. We also thank Kamilah Bailey, Jameelah Hodge, Jennifer Kim, Michael Rowland, Adria Stauber, Amber Fearon, and Shanda Robertson, and the Sickle Cell Data Collection Program for their contributions.
Corresponding author: Marsha J. Treadwell, PhD, University of California San Francisco Benioff Children’s Hospital Oakland, 747 52nd St., Oakland, CA 94609; [email protected].
Financial disclosures: None.
Funding/support: This work was supported by grant # 1U01HL134007 from the National Heart, Lung, and Blood Institute to the University of California San Francisco Benioff Children’s Hospital Oakland.
From the University of California San Francisco (Dr. Treadwell, Dr. Hessler, Yumei Chen, Swapandeep Mushiana, Dr. Potter, and Dr. Vichinsky), the University of California Los Angeles (Dr. Jacob), and the University of California Berkeley (Alex Chen).
Abstract
- Objective: Adolescents and adults with sickle cell disease (SCD) face pervasive disparities in health resources and outcomes. We explored barriers to and facilitators of care to identify opportunities to support implementation of evidence-based interventions aimed at improving care quality for patients with SCD.
- Methods: We engaged a representative sample of adolescents and adults with SCD (n = 58), health care providers (n = 51), and community stakeholders (health care administrators and community-based organization leads (n = 5) in Northern California in a community-based needs assessment. We conducted group interviews separately with participant groups to obtain in-depth perspectives. Adolescents and adults with SCD completed validated measures of pain interference, quality of care, self-efficacy, and barriers to care. Providers and community stakeholders completed surveys about barriers to SCD care.
- Results: We triangulated qualitative and quantitative data and found that participants with SCD (mean age, 31 ± 8.6 years), providers, and community stakeholders emphasized the social and emotional burden of SCD as barriers. Concrete barriers agreed upon included insurance and lack of resources for addressing pain impact. Adolescents and adults with SCD identified provider issues (lack of knowledge, implicit bias), transportation, and limited social support as barriers. Negative encounters with the health care system contributed to 84% of adolescents and adults with SCD reporting they chose to manage severe pain at home. Providers focused on structural barriers: lack of access to care guidelines, comfort level with and knowledge of SCD management, and poor care coordination.
- Conclusion: Strategies for improving access to compassionate, evidence-based quality care, as well as strategies for minimizing the burden of having SCD, are warranted for this medically complex population.
Keywords: barriers to care; quality of care; care access; care coordination.
Sickle cell disease (SCD), an inherited chronic medical condition, affects about 100,000 individuals in the United States, a population that is predominantly African American.1 These individuals experience multiple serious and life-threatening complications, most frequently recurrent vaso-occlusive pain episodes,2 and they require interactions with multidisciplinary specialists from childhood. Because of advances in treatments, the majority are reaching adulthood; however, there is a dearth of adult health care providers with the training and expertise to manage their complex medical needs.3 Other concrete barriers to adequate SCD care include insurance and distance to comprehensive SCD centers.4,5
Social, behavioral, and emotional factors may also contribute to challenges with SCD management. SCD may limit daily functional abilities and lead to diminished overall quality of life.6,7 Some adolescents and adults may require high doses of opioids, which contributes to health care providers’ perceptions that there is a high prevalence of drug addiction in the population.8,9 These providers express negative attitudes towards adults with SCD, and, consequently, delay medication administration when it is acutely needed and provide otherwise suboptimal treatment.8,10,11 Adult care providers may also be uncomfortable with prescribing and managing disease-modifying therapies (blood transfusion, hydroxyurea) that have established efficacy.12-17
As 1 of 8 programs funded by the National Heart, Lung, and Blood Institute’s (NHLBI) Sickle Cell Disease Implementation Consortium (SCDIC), we are using implementation science to reduce barriers to care and improve quality of care and health care outcomes in SCD.18,19 Given that adolescents and adults with SCD experience high mortality, severe pain, and progressive decline in their ability to function day to day, and also face lack of access to knowledgeable, compassionate providers in primary and emergency settings, the SCDIC focuses on individuals aged 15 to 45 years.6,8,9,11,12
Our regional SCDIC program, the Sickle Cell Care Coordination Initiative (SCCCI), brings together researchers, clinicians, adolescents, and adults with SCD and their families, dedicated community members, policy makers, and administrators to identify and address barriers to health care within 5 counties in Northern California. One of our first steps was to conduct a community-based needs assessment, designed to inform implementation of evidence-based interventions, accounting for unique contextual factors in our region.
Conceptual Framework for Improving Medical Practice
Our needs assessment is guided by Solberg’s Conceptual Framework for Improving Medical Practice (Figure 1).20 Consistent with the overarching principles of the SCDIC, this conceptual framework focuses on the inadequate implementation of evidence-based guidelines, and on the need to first understand multifactorial facilitators and barriers to guideline implementation in order to effect change. The framework identifies 3 main elements that must be present to ensure improvements in quality-of-care processes and patient outcomes: priority, change process capability, and care process content. Priority refers to ample resource allocation for the specific change, as well as freedom from competing priorities for those implementing the change. Change process capability includes strong, effective leadership, adequate infrastructure for managing change (including resources and time), change management skills at all levels, and an established clinical information system. Care process content refers to context and systems-level changes, such as delivery system redesign as needed, support for self-management to lessen the impact of the disease, and decision support.21-23
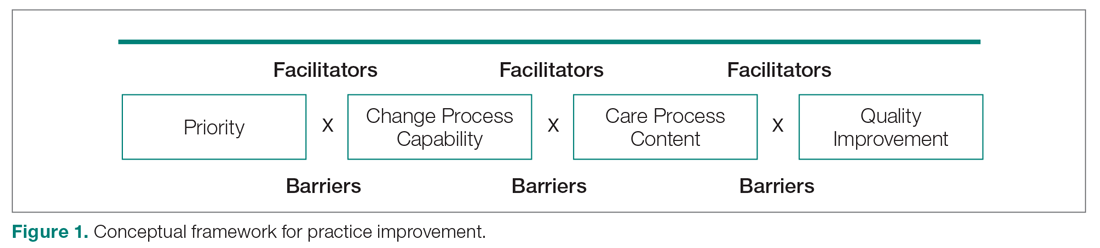
The purpose of our community-based needs assessment was to evaluate barriers to care and quality of care in SCD, within Solberg’s conceptual model for improving medical practice. The specific aims were to evaluate access and barriers to care (eg, lack of provider expertise and training, health care system barriers such as poor care coordination and provider communication); evaluate quality of care; and assess patient needs related to pain, pain interference, self-efficacy, and self-management for adolescents and adults with SCD. We gathered the perspectives of a representative community of adolescents and adults with SCD, their providers, and community stakeholders in order to examine barriers, quality of life and care, and patient experiences in our region.
Methods
Design
In this cross-sectional study, adolescents and adults with SCD, their providers, and community stakeholders participated in group or individual qualitative interviews and completed surveys between October 2017 and March 2018.
Setting and Sample
Recruitment flyers were posted on a regional SCD-focused website, and clinical providers or a study coordinator introduced information about the needs assessment to potential participants with SCD during clinic visits at the participating centers. Participants with SCD were eligible if they had any diagnosis of SCD, were aged 15 to 48 years, and received health services within 5 Northern California counties (Alameda, Contra Costa, Sacramento, San Francisco, and Solano). They were excluded if they did not have a SCD diagnosis or had not received health services within the catchment area. As the project proceeded, participants were asked to refer other adolescents and adults with SCD for the interviews and surveys (snowball sampling). Our goal was to recruit 50 adolescents and adults with SCD into the study, aiming for 10 representatives from each county.
Providers and community stakeholders were recruited via emails, letters and informational flyers. We engaged our partner, the Sickle Cell Data Collection Program,2 to generate a list of providers and institutions that had seen patients with SCD in primary, emergency, or inpatient settings in the region. We contacted these institutions to describe the SCCCI and invite participation in the needs assessment. We also invited community-based organization leads and health care administrators who worked with SCD to participate. Providers accessed confidential surveys via a secure link on the study website or completed paper versions. Common data collected across providers included demographics and descriptions of practice settings.
Participants were eligible to be part of the study if they were health care providers (physicians and nurses) representing hematology, primary care, family medicine, internal medicine, or emergency medicine; ancillary staff (social work, psychology, child life); or leaders or administrators of clinical or sickle cell community-based organizations in Northern California (recruitment goal of n = 50). Providers were excluded if they practiced in specialties other than those noted or did not practice within the region.
Data Collection Procedures
After providing assent/consent, participating adolescents and adults with SCD took part in individual and group interviews and completed survey questionnaires. All procedures were conducted in a private space in the sickle cell center or community. Adolescents and adults with SCD completed the survey questionnaire on a tablet, with responses recorded directly in a REDCap (Research Electronic Data Capture) database,24 or on a paper version. Interviews lasted 60 (individual) to 90 (group) minutes, while survey completion time was 20 to 25 minutes. Each participant received a gift card upon completion as an expression of appreciation. All procedures were approved by the institutional review boards of the participating health care facilities.
Group and Individual Interviews
Participants with SCD and providers were invited to participate in a semi-structured qualitative interview prior to being presented with the surveys. Adolescents and adults with SCD were interviewed about barriers to care, quality of care, and pain-related experiences. Providers were asked about barriers to care and treatments. Interview guides were modified for community-based organization leaders and health care administrators who did not provide clinical services. Interview guides can be found in the Appendix. Interviews were conducted by research coordinators trained in qualitative research methods by the first author (MT). As appropriate with semi-structured interviews, the interviewers could word questions spontaneously, change the order of questions for ease of flow of conversation, and inform simultaneous coding of interviews with new themes as those might arise, as long as they touched on all topics within the interview guide.25 The interview guides were written, per qualitative research standards, based on the aims and purpose of the research,26 and were informed by existing literature on access and barriers to care in SCD, quality of care, and the needs of individuals with SCD, including in relation to impact of the disease, self-efficacy, and self-management.
Interviewees participated in either individual or group interviews, but not both. The decision for which type of interview an individual participated in was based on 2 factors: if there were not comparable participants for group interviews (eg, health care administrator and community-based organization lead), these interviews were done individually; and given that we were drawing participants from a 5-county area in Northern California, scheduling was challenging for individuals with SCD with regard to aligning schedules and traveling to a central location where the group interviews were conducted. Provider group interviews were easier to arrange because we could schedule them at the same time as regularly scheduled meetings at the participants’ health care institutions.
Interview Data Gathering and Analysis
Digital recordings of the interviews were cleaned of any participant identifying data and sent for transcription to an outside service. Transcripts were reviewed for completeness and imported into NVivo (www.qsrinternational.com), a qualitative data management program.
A thematic content analysis and deductive and inductive approaches were used to analyze the verbatim transcripts generated from the interviews. The research team was trained in the use of NVivo software to facilitate the coding process. A deductive coding scheme was initially used based on existing concepts in the literature regarding challenges to optimal SCD care, with new codes added as the thematic content analyses progressed. The initial coding, pattern coding, and use of displays to examine the relationships between different categories were conducted simultaneously.27,28 Using the constant comparative method, new concepts from participants with SCD and providers could be incorporated into subsequent interviews with other participants. For this study, the only additional concepts added were in relation to participant recruitment and retention in the SCDIC Registry. Research team members coded transcripts separately and came together weekly, constantly comparing codes and developing the consensus coding scheme. Where differences between coders existed, code meanings were discussed and clarified until consensus was reached.29
Quantitative data were analyzed using SPSS (v. 25, Chicago, IL). Descriptive statistics (means, standard deviations, frequencies, percentages) were used to summarize demographics (eg, age, gender, and race), economic status, and type of SCD. No systematic differences were detected from cases with missing values. Scale reliabilities (ie, Cronbach α) were evaluated for self-report measures.
Measurement
Adolescents and adults with SCD completed items from the PhenX Toolkit (consensus measures for Phenotypes and eXposures), assessing sociodemographics (age, sex, race, ethnicity, educational attainment, occupation, marital status, annual income, insurance), and clinical characteristics (sickle cell diagnosis and emergency department [ED] and hospital utilization for pain).30
Pain Interference Short Form (Patient-Reported Outcomes Measurement Information System [PROMIS]). The Pain Interference Form consists of 8 items that assess the degree to which pain interfered with day-to-day activities in the previous 7 days at home, including impacts on social, cognitive, emotional, and physical functioning; household chores and recreational activities; sleep; and enjoyment in life. Reliability and validity of the PROMIS Pain Interference Scale has been demonstrated, with strong negative correlations with Physical Function Scales (r = 0.717, P < 0.01), indicating that higher scores are associated with lower function (β = 0.707, P < 0.001).31 The Cronbach α estimate for the other items on the pain interference scale was 0.99. Validity analysis indicated strong correlations with pain-related domains: BPI Interference Subscale (rho = 0.90), SF-36 Bodily Pain Subscale (rho = –0.84), and 0–10 Numerical Rating of Pain Intensity (rho = 0.48).32
Adult Sickle Cell Quality of Life Measurement Information System (ASCQ-Me) Quality of Care (QOC). ASCQ-Me QOC consists of 27 items that measure the quality of care that adults with SCD have received from health care providers.33 There are 3 composites: provider communication (quality of patient and provider communication), ED care (quality of care in the ED), and access (to routine and emergency care). Internal consistency reliability for all 3 composites is greater than 0.70. Strong correlations of the provider communication composite with overall ratings of routine care (r = 0.65) and overall provider ratings (r = 0.83) provided evidence of construct validity. Similarly, the ED care composite was strongly correlated with overall ratings of QOC in the ED, and the access composite was highly correlated with overall evaluations of ED care (r = 0.70). Access, provider interaction, and ED care composites were reliable (Cronbach α, 0.70–0.83) and correlated with ratings of global care (r = 0.32–0.83), further indicating construct validity.33
Sickle Cell Self-Efficacy Scale (SCSES). The SCSES is a 9-item, self-administered questionnaire measuring perceptions of the ability to manage day-to-day issues resulting from SCD. SCSES items are scored on a 5-point scale ranging from Not sure at all (1) to Very sure (5). Individual item responses are summed to give an overall score, with higher scores indicating greater self-efficacy. The SCSES has acceptable reliability (r = 0.45, P < 0.001) and validity (α = 0.89).34,35
Sickle Cell Disease Barriers Checklist. This checklist consists of 53 items organized into 8 categories: insurance, transportation, accommodations and accessibility, provider knowledge and attitudes, social support, individual barriers such as forgetting or difficulties understanding instructions, emotional barriers (fear, anger), and disease-related barriers. Participants check applicable barriers, with a total score range of 0 to 53 and higher scores indicating more barriers to care. The SCD Barriers Checklist has demonstrated face validity and test-retest reliability (Pearson r = 0.74, P < 0.05).5
ED Provider Checklist. The ED provider survey is a checklist of 14 statements pertaining to issues regarding patient care, with which the provider rates level of agreement. Items representing the attitudes and beliefs of providers towards patients with SCD are rated on a Likert-type scale, with level of agreement indicated as 1 (strongly disagree) to 6 (strongly agree). The positive attitudes subscale consists of 4 items (Cronbach α= 0.85), and the negative attitudes subscale consists of 6 items (Cronbach α = 0.89). The Red-Flag Behaviors subscale includes 4 items that indicate behavior concerns about drug-seeking, such as requesting specific narcotics and changing behavior when the provider walks in.8,36,37
Sickle cell and primary care providers also completed a survey consisting of sets of items compiled from existing provider surveys; this survey consisted of a list of 16 barriers to using opioids, which the providers rated on a 5-point Likert-type scale (1, not a barrier; 5, complete barrier).13,16,38 Providers indicated their level of experience with caring for patients with SCD; care provided, such as routine health screenings; and comfort level with providing preventive care, managing comorbidities, and managing acute and chronic pain. Providers were asked what potential facilitators might improve care for patients with SCD, including higher reimbursement, case management services, access to pain management specialists, and access to clinical decision-support tools. Providers responded to specific questions about management with hydroxyurea (eg, criteria for, barriers to, and comfort level with prescribing).39 The surveys are included in the Appendix.
Triangulation
Data from the interviews and surveys were triangulated to enhance understanding of results generated from the different data sources.40 Convergence of findings, different facets of the same phenomenon, or new perspectives were examined.
Results
Qualitative Data
Adolescents and adults with SCD (n = 55) and health care providers and community stakeholders (n = 56) participated in group or individual interviews to help us gain an in-depth understanding of the needs and barriers related to SCD care in our 5-county region. Participants with SCD described their experiences, which included stigma, racism, labeling, and, consequently, stress. They also identified barriers such as lack of transportation, challenges with insurance, and lack of access to providers who were competent with pain management. They reported that having SCD in a health care system that was unable to meet their needs was burdensome.
Barriers to Care and Treatments. Adolescents and adults indicated that SCD and its sequelae posed significant barriers to health care. Feelings of tiredness and pain make it more difficult for them to seek care. The emotional burden of SCD (fear and anger) was a frequently cited barrier, which was fueled by previous negative encounters with the health care system. All adolescents and adults with SCD reported that they knew of stigma in relation to seeking pain management that was pervasive and long-standing, and the majority reported they had directly experienced stigma. They reported that being labeled as “drug-seekers” was typical when in the ED for pain management. Participants articulated unconscious bias or overt racism among providers: “people with sickle cell are Black ... and Black pain is never as valuable as White pain” (25-year-old male). Respondents with SCD described challenges to the credibility of their pain reports in the ED. They reported that ED providers expressed doubts regarding the existence and/or severity of their pain, consequently creating a feeling of disrespect for patients seeking pain relief. The issue of stigma was mentioned by only 2 of 56 providers during their interviews.
Lack of Access to Knowledgeable, Compassionate Providers. Lack of access to knowledgeable care providers was another prevalent theme expressed by adolescents and adults with SCD. Frustration occurred when providers did not have knowledge of SCD and its management, particularly pain assessment. Adolescents and adults with SCD noted the lack of compassion among providers: “I’ve been kicked out of the hospital because they felt like okay, well we gave you enough medication, you should be all right” (29-year-old female). Providers specifically mentioned lack of compassion and knowledge as barriers to SCD care much less often during their interviews compared with the adolescents and adults with SCD.
Health Care System Barriers. Patient participants often expressed concerns about concrete and structural aspects of care. Getting to their appointments was a challenge for half of the interviewees, as they either did not have access to a vehicle or could not afford to travel the needed distance to obtain quality care. Even when hospitals were accessible by public transportation, those with excruciating pain understandably preferred a more comfortable and private way to travel: “I would like to change that, something that will be much easier, convenient for sickle cell patients that do suffer with pain, that they don’t have to travel always to see the doctor” (30-year-old male).
Insurance and other financial barriers also played an important role in influencing decisions to seek health care services. Medical expenses were not covered, or co-pays were too high. The Medicaid managed care system could prevent access to knowledgeable providers who were not within network. Such a lack of access discouraged some adolescents and adults with SCD from seeking acute and preventive care.
Transition From Pediatric to Adult Care. Interviewees with SCD expressed distress about the gap between pediatric and adult care. They described how they had a long-standing relationship with their medical providers, who were familiar with their medical background and history from childhood. Adolescent interviewees reported an understanding of their own pain management as well as adherence to and satisfaction with their individualized pain plans. However, adults noted that satisfaction plummeted with increasing age due to the limited number of experienced adult SCD providers, which was compounded by negative experiences (stigma, racism, drug-seeking label).
One interviewee emphasized the difficulty of finding knowledgeable providers after transition: “When you’re a pediatric sickle cell [patient], you have the doctors there every step of the way, but not with adult sickle cell… I know when I first transitioned I never felt more alone in my life… you look at that ER doctor kind of with the same mindset as you would your hematologist who just hand walked you through everything. And adult care providers were a lot more blunt and cold and they’re like… ‘I don’t know; I’m not really educated in sickle cell.’” A sickle cell provider shared his insight about the problem of transitioning: “I think it’s particularly challenging because we, as a community, don’t really set them up for success. It’s different from other chronic conditions [in that] it’s much harder to find an adult sickle cell provider. There’s not a lot of adult hematologists that will take care of our adult patients, and so I know statistically, there’s like a drop-down in the overall outcomes of our kids after they age out of our pediatric program.”
Self-Management, Supporting Hydroxyurea Use. Interview participants with SCD reported using a variety of methods to manage pain at home and chose to go to the ED only when the pain became intolerable. Patients and providers expressed awareness of different resources for managing pain at home, yet they also indicated that these resources have not been consolidated in an accessible way for patients and families. Some resources cited included heat therapy, acupuncture, meditation, medical marijuana, virtual reality devices, and pain medications other than opioids.
Patients and providers expressed the need for increasing awareness and education about hydroxyurea. Many interview participants with SCD were concerned about side effects, multiple visits with a provider during dose titration, and ongoing laboratory monitoring. They also expressed difficulties with scheduling multiple appointments, depending on access to transportation and limited provider clinic hours. They were aware of strategies for improving adherence with hydroxyurea, including setting phone alarms, educating family members about hydroxyurea, and eliciting family support, but expressed needing help to consistently implement these strategies.
Safe Opioid Prescribing. Adult care providers expressed concerns about safe opioid prescribing for patients with SCD. They were reluctant to prescribe opioid doses needed to adequately control SCD pain. Providers expressed uncertainty and fear or concern about medical/legal liability or about their judgment about what’s safe and not safe for patients with chronic use/very high doses of opioids. “I know we’re in like this opiate epidemic here in this country but I feel like these patients don’t really fit under that umbrella that the problem is coming from so [I am] just trying to learn more about how to take care of them.”
Care Coordination and Provider Communication. Adolescents and adults with SCD reported having positive experiences—good communication, established trust, and compassionate care—with their usual providers. However, they perceived that ED physicians and nurses did not really care about them. Both interviewees with SCD and providers recognized the importance of good communication in all settings as the key to overcoming barriers to receiving quality care. All agreed on the importance of using individual pain plans so that all providers, especially ED providers, can be more at ease with treating adolescents and adults with SCD.
Quantitative Data: Adolescents and Adults With SCD
Fifty-eight adolescents and adults with SCD (aged 15 to 48 years) completed the survey. Three additional individuals who did not complete the interview completed the survey. Reasons for not completing the interview included scheduling challenges (n = 2) or a sickle cell pain episode (n = 1). The average age of participants was 31 years ± 8.6, more than half (57%) were female, and the majority (93%) were African American (Table 1). Most (71%) had never been married. Half (50%) had some college or an associate degree, and 40% were employed and reported an annual household income of less than $30,000. Insurance coverage was predominantly Medi-Cal (Medicaid, 69%). The majority of participants resided in Alameda (34.5%) or Contra Costa (21%) counties. The majority of sickle cell care was received in Alameda County, whether outpatient (52%), inpatient (40%), or ED care (41%). The majority (71%) had a diagnosis of SCD hemoglobin SS.
Pain. More than one-third of individuals with SCD reported 1 or 2 ED visits for pain in the previous 6 months (34%), and more than 3 hospitalizations (36%) related to pain in the previous year (Table 2). The majority (85%) reported having severe pain at home in the previous 6 months that they did not seek health care for, consistent with their reports in the qualitative interviews. More than half (59%) reported 4 or more of these severe pain episodes that led to inability to perform daily activities for 1 week or more. While pain interference on the PROMIS Pain Interference Short Form on average (T-score, 59.6 ± 8.6) was similar to that of the general population (T-score, 50 ± 10), a higher proportion of patients with SCD reported pain interference compared with the general population. The mean self-efficacy (confidence in ability to manage complications of SCD) score on the SCSES of 30.0 ± 7.3 (range, 9–45) was similar to that of other adults with SCD (mean, 32.2 ± 7.0). Twenty-five percent of the present sample had a low self-efficacy score (< 25).
Barriers to Care and Treatments. Consistent with the qualitative data, SCD-related symptoms such as tiredness (64%) and pain (62%) were reported most often as barriers to care (Table 3). Emotions (> 25%) such as worry/fear, frustration/anger, and lack of confidence were other important barriers to care. Provider knowledge and attitudes were cited next most often, with 38% of the sample indicating “Providers accuse me of drug-seeking” and “It is hard for me to find a provider who has enough experiences with or knowledge about SCD.” Participants expressed that they were not believed when in pain and “I am treated differently from other patients.” Almost half of respondents cited “I am not seen quickly enough when I am in pain” as a barrier to their care.
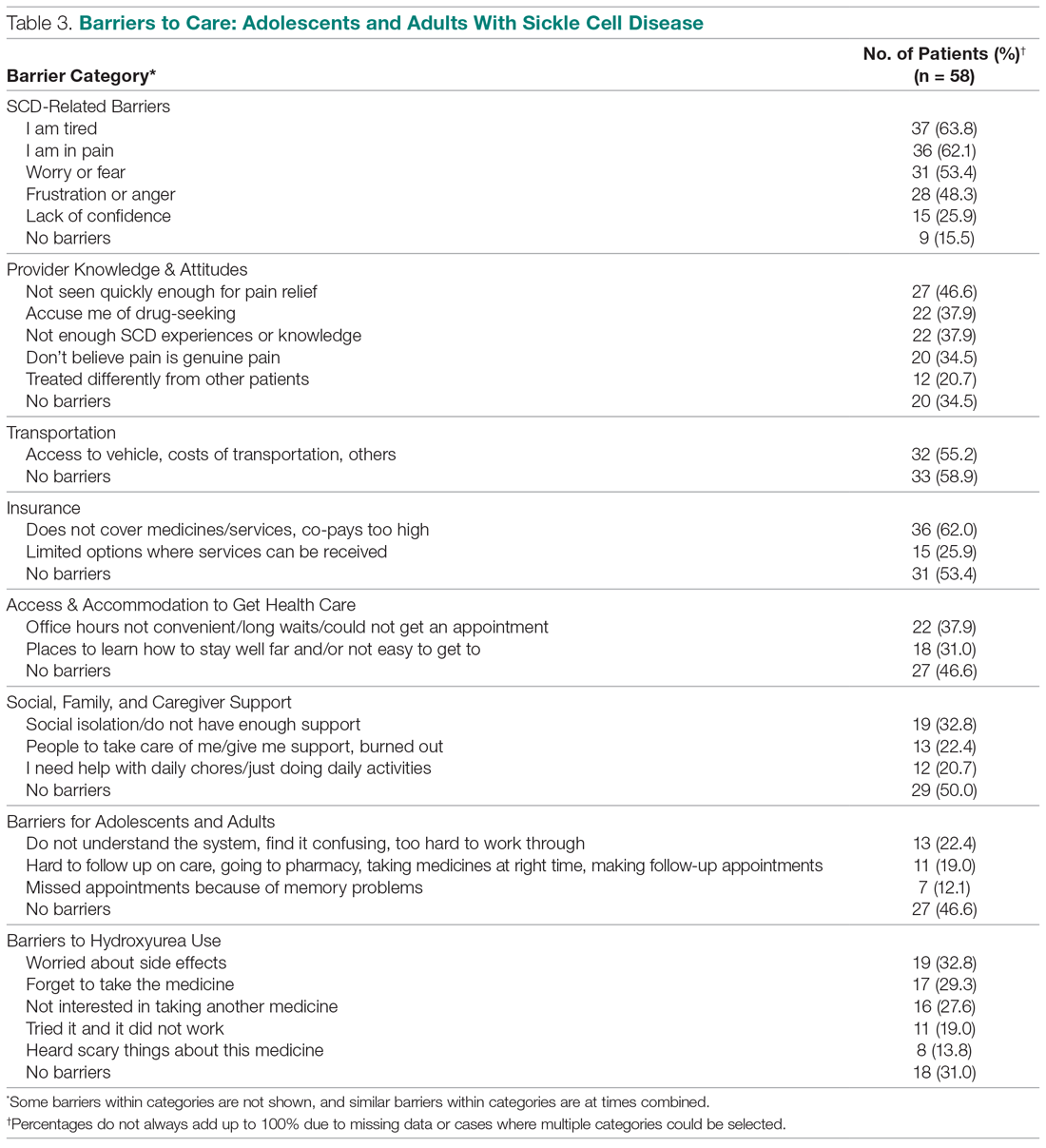
Consistent with the qualitative data, transportation barriers (not having a vehicle, costs of transportation, public transit not easy to get to) were cited by 55% of participants. About half of participants reported that insurance was an important barrier, with high co-pays and medications and other services not covered. In addition, gathering approvals was a long and fragmented process, particularly for consultations among providers (hematology, primary care provider, pain specialist). Furthermore, insurance provided limited choices about location for services.
Participants reported social support system burnout (22%), help needed with daily activities (21%), and social isolation or generally not having enough support (33%) as ongoing barriers. Difficulties were encountered with self-management (eg, taking medications on time or making follow-up appointments, 19%), with 22% of participants finding the health care system confusing or hard to understand. Thirty percent reported “Places for me to go to learn how to stay well are not close by or easy to get to.” ”Worry about side effects” (33%) was a common barrier to hydroxyurea use. Participants described “forgetting to take the medicine,” “tried before but it did not work,” “heard scary things” about hydroxyurea, and “not interested in taking another medicine” as barriers.
Quality of Care. More than half (51%) of the 53 participants who had accessed health care in the previous year rated their overall health care as poor on the ASCQ-Me QOC measure. This was significantly higher compared to the reports from more than 47,000 adults with Medicaid in 2017 (16%),41 and to the 2008-2009 report from 556 adults with SCD from across the United States (37%, Figure 2).33 The major contributor to these poor ratings for participants in our sample was low satisfaction with ED care.
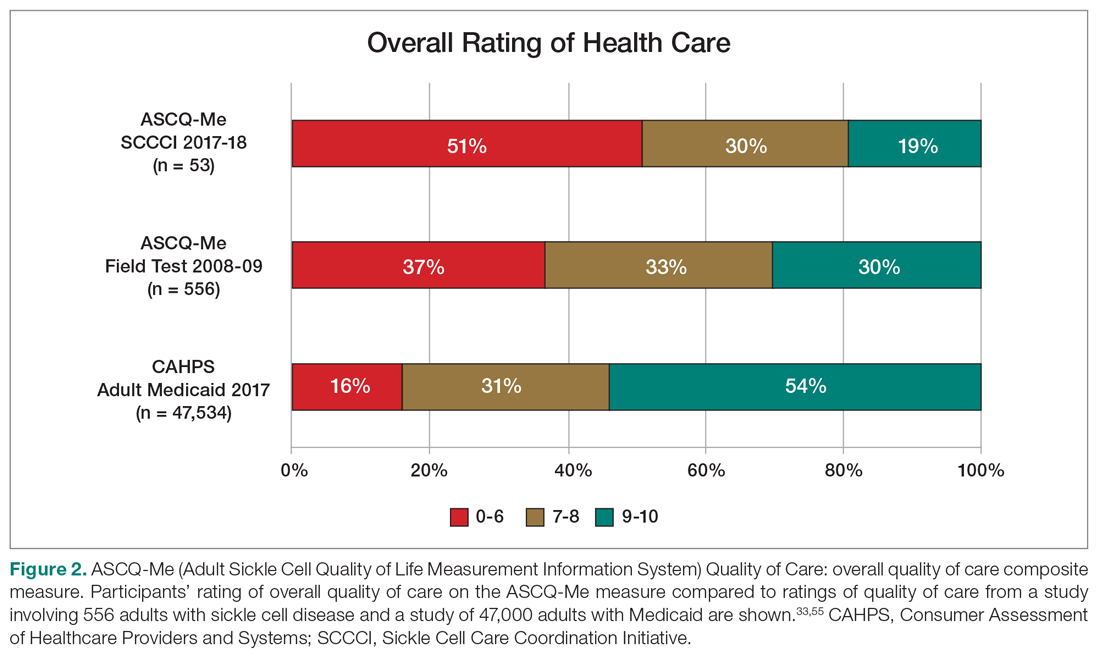
Sixty percent of the 42 participants who had accessed ED care in the past year indicated “never” or “sometimes” to the question “When you went to the ED for care, how often did you get it as soon as you wanted?” compared with only 16% of the 2017 adult Medicaid population responding (n = 25,789) (Figure 3). Forty-seven percent of those with an ED visit indicated that, in the previous 12 months, they had been made to wait “more than 2 hours before receiving treatment for acute pain in the ED.” However, in the previous 12 months, 39% reported that their wait time in the ED had been only “between five minutes and one hour.”
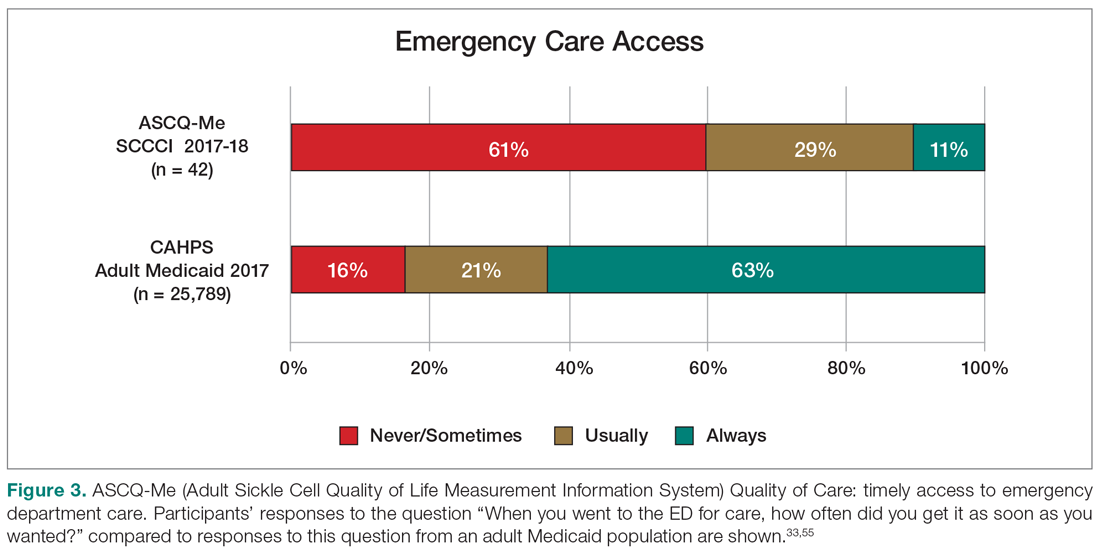
On the ASCQ-Me QOC Access to Care composite measure, 33% of 42 participants responding reported they were seen at a routine appointment as soon as they would have liked. This is significantly lower compared to 56% of the adult Medicaid population responding to the same question. Reports of provider communication (Provider Communication composite) for adolescents and adults with SCD were comparable to reports of adults with SCD from the ASCQ-Me field test,33 but adults with Medicaid reported higher ratings of quality communication behaviors (Figure 4).33,41 Nearly 60% of both groups with SCD reported that providers “always” performed quality communication behaviors—listened carefully, spent enough time, treated them with respect, and explained things well—compared with more than 70% of adults with Medicaid.
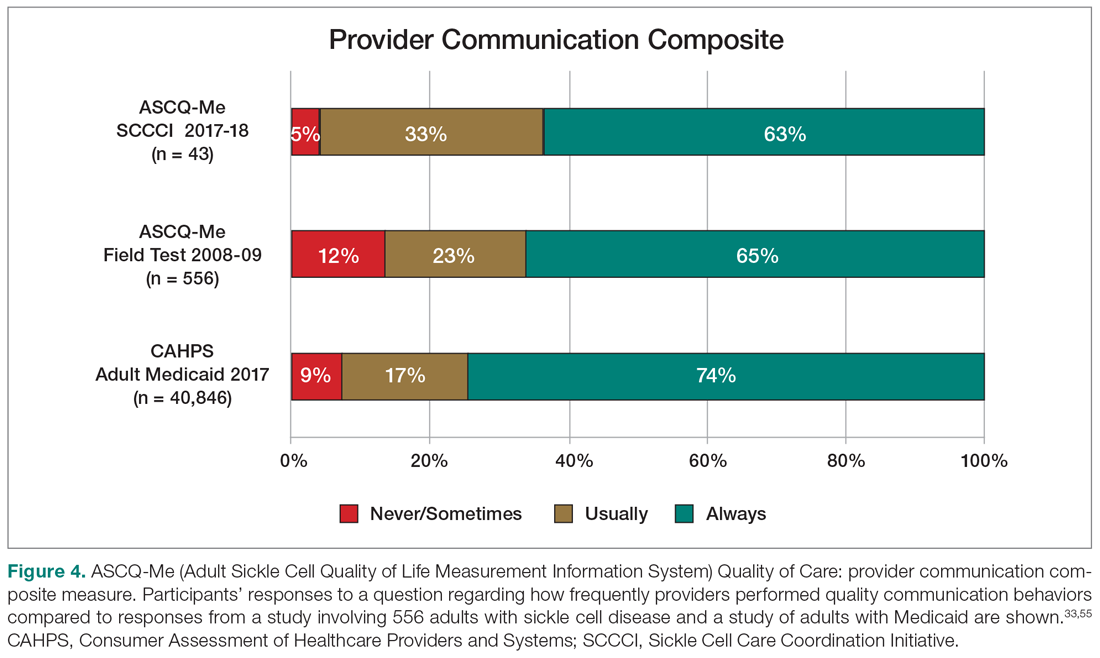
Participants from all counties reported the same number of barriers to care on average (3.3 ± 2.1). Adolescents and adults who reported more barriers to care also reported lower satisfaction with care (r = –0.47, P < 0.01) and less confidence in their ability to manage their SCD (self-efficacy, r = – 0.36, P < 0.05). Female participants reported more barriers to care on average compared with male participants (2.6 ± 2.4 vs 1.4 ± 2.0, P = 0.05). Participants with higher self-efficacy reported lower pain ratings (r = –0.47, P < 0.001).
Quantitative Data: Health Care Providers
Providers (n = 56) and community stakeholders (2 leaders of community-based organizations and 3 health care administrators) were interviewed, with 29 also completing the survey. The reason for not completing (n = 22) was not having the time once the interview was complete. A link to the survey was sent to any provider not completing at the time of the interview, with 2 follow-up reminders. The majority of providers were between the ages of 31 and 50 years (46.4%), female (71.4%), and white (66.1%) (Table 4). None were of Hispanic, Latinx, or Spanish origin. Thirty-six were physicians (64.3%), and 16 were allied health professionals (28.6%). Of the 56 providers, 32 indicated they had expertise caring for patients with SCD (57.1%), 14 were ED providers (25%), and 5 were primary care providers. Most of the providers practiced in an urban setting (91.1%).
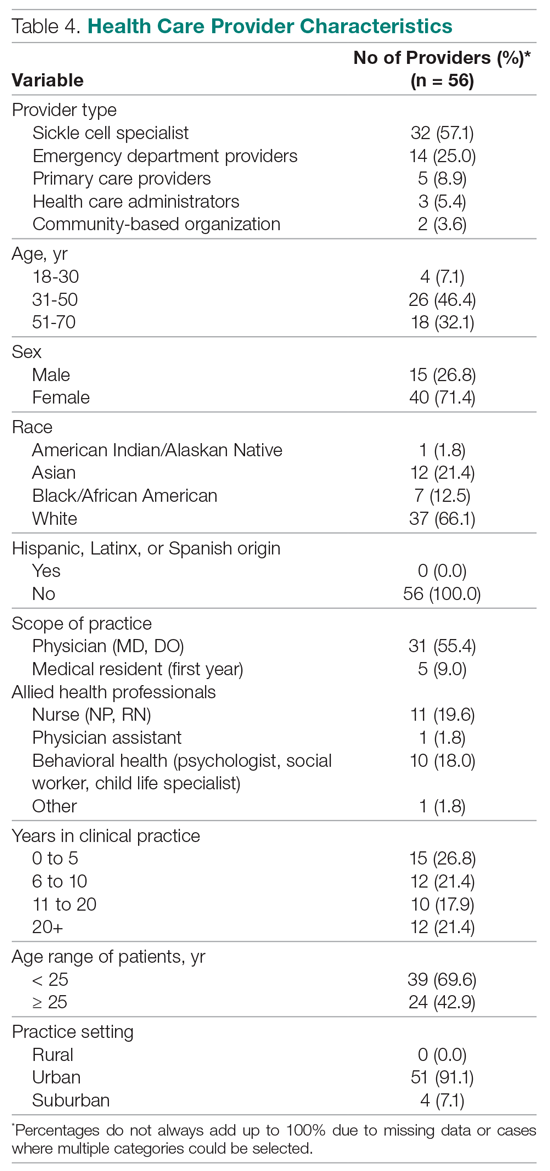
Barriers to Care: ED Provider Perspectives. Nine of 14 ED providers interviewed completed the survey on their perspectives regarding barriers to care in the ED, difficulty with follow-ups, ED training resources, and pain control for patients with SCD. ED providers (n = 8) indicated that “provider attitudes” were a barrier to care delivery in the ED for patients with SCD. Some providers (n = 7) indicated that “implicit bias,” “opioid epidemic,” “concern about addiction,” and “patient behavior” were barriers. Respondents indicated that “overcrowding” (n = 6) and “lack of care pathway/protocol” (n = 5) were barriers. When asked to express their level of agreement with statements about SCD care in the ED, respondents disagreed/strongly disagreed (n = 5) that they were “able to make a follow-up appointment” with a sickle cell specialist or primary care provider upon discharge from the ED, and others disagreed/strongly disagreed (n = 4) that they were able to make a “referral to a case management program.”
ED training and resources. Providers agreed/strongly agreed (n = 8) that they had the knowledge and training to care for patients with SCD, that they had access to needed medications, and that they had access to knowledgeable nursing staff with expertise in SCD care. All 9 ED providers indicated that they had sufficient physician/provider staffing to provide good pain management to persons with SCD in the ED.
Pain control in the ED. Seven ED providers indicated that their ED used individualized dosing protocols to treat sickle cell pain, and 5 respondents indicated their ED had a protocol for treating sickle cell pain. Surprisingly, only 3 indicated that they were aware of the NHLBI recommendations for the treatment of vaso-occlusive pain.
Barriers to Care: Primary Care Provider Perspectives. Twenty providers completed the SCD provider section of the survey, including 17 multidisciplinary SCD providers from 4 sickle cell special care centers and 3 community primary care providers. Of the 20, 12 were primary care providers for patients with SCD (Table 4).
Patient needs. Six primary care providers indicated that the medical needs of patients with SCD were being met, but none indicated that the behavioral health or mental health needs were being met.
Managing SCD comorbidities. Five primary care providers indicated they were very comfortable providing preventive ambulatory care to patients with SCD. Six indicated they were very comfortable managing acute pain episodes, but none were very comfortable managing comorbidities such as pulmonary hypertension, diabetes, or chronic pain.
Barriers to opioid use. Only 3 of 12 providers reviewing a list of 15 potential barriers to the use of opioids for SCD pain management indicated a perceived lack of efficacy of opioids, development of tolerance and dependence, and concerns about community perceptions as barriers. Two providers selected potential for diversion as a moderate barrier to opioid use.
Barriers to hydroxyurea use. Eight of 12 providers indicated that the common reasons that patients/families refuse hydroxyurea were “worry about side effects”; 7 chose “don’t want to take another medicine,” and 6 chose “worry about carcinogenic potential.” Others (n = 10) indicated that “patient/family adherence with hydroxyurea” and “patient/family adherence with required blood tests” were important barriers to hydroxyurea use. Eight of the 12 providers indicated that they were comfortable with managing hydroxyurea in patients with SCD.
Care redesign. Twenty SCD and primary care providers completed the Care Redesign section of the survey. Respondents (n = 11) indicated that they would see more patients with SCD if they had accessible case management services available without charge or if patient access to transportation to clinic was also available. Ten indicated that they would see more patients with SCD if they had an accessible community health worker (who understands patient’s/family’s social situation) and access to a pain management specialist on call to answer questions and who would manage chronic pain. All (n = 20) were willing to see more patients with SCD in their practices. Most reported that a clinical decision-support tool for SCD treatment (n = 13) and avoidance of complications (n = 12) would be useful.
Discussion
We evaluated access and barriers to care, quality of care, care coordination, and provider communication from the perspectives of adolescents and adults with SCD, their care providers, and community stakeholders, within the Solberg conceptual model for quality improvement. We found that barriers within the care process content domain (context and systems) were most salient for this population of adolescents and adults with SCD, with lack of provider knowledge and poor attitudes toward adolescents and adults with SCD, particularly in the ED, cited consistently by participant groups. Stigmatization and lack of provider compassion that affected the quality of care were particularly problematic. These findings are consistent with previous reports.42,43 Adult health care (particularly ED) provider biases and negative attitudes have been recognized as major barriers to optimal pain management in SCD.8,11,44,45 Interestingly, ED providers in our needs assessment indicated that they felt they had the training and resources to manage patients with SCD. However, only a few actually reported knowing about the NHLBI recommendations for the treatment of vaso-occlusive pain.
Within the care process content domain, we also found that SCD-related complications and associated emotions (fear, worry, anxiety), compounded by lack of access to knowledgeable and compassionate providers, pose a significant burden. Negative encounters with the health care system contributed to a striking 84% of patient participants choosing to manage severe pain at home, with pain seriously interfering with their ability to function on a daily basis. ED providers agreed that provider attitudes and implicit bias pose important barriers to care for adolescents and adults with SCD. Adolescents and adults with SCD wanted, and understood the need, to enhance self-management skills. Both they and their providers agreed that barriers to hydroxyurea uptake included worries about potential side effects, challenges with adherence to repeated laboratory testing, and support with remembering to take the medicine. However, providers uniformly expressed that access to behavioral and mental health services were, if not nonexistent, impossible to access.
Participants with SCD and their providers reported infrastructural challenges (change process capability), as manifested in limitations with accessing acute and preventive care due to transportation- and insurance- related issues. There were health system barriers that were particularly encountered during the transition from pediatric to adult care. These findings are consistent with previous reports that have found fewer interdisciplinary services available in the adult care settings compared with pediatrics.46,47 Furthermore, adult care providers were less willing to accept adults with SCD because of the complexity of their management, for which the providers did not have the necessary expertise.3,48-50 In addition, both adolescents and adults with SCD and primary care providers highlighted the inadequacies of the current system in addressing the chronic pain needs of this population. Linking back to the Solberg conceptual framework, our needs assessment results confirm the important role of establishing SCD care as a priority within a health care system—this requires leadership and vision. The vision and priorities must be implemented by effective health care teams. Multilevel approaches or interventions, when implemented, will lead to the desired outcomes.
Findings from our needs assessment within our 5-county region mirror needs assessment results from the broader consortium.51 The SCDIC has prioritized developing an intervention that addresses the challenges identified within the care process domain by directly enhancing provider access to patient individualized care plans in the electronic health record in the ED. Importantly, ED providers will be asked to view a short video that directly challenges bias and stigma in the ED. Previous studies have indeed found that attitudes can be improved by providers viewing short video segments of adults with SCD discussing their experiences.36,52 This ED protocol will be one of the interventions that we will roll out in Northern California, given the significance of negative ED encounters reported by needs assessment participants. An additional feature of the intervention is a script for adults with SCD that guides them through introducing their individualized pain plan to their ED providers, thereby enhancing their self-efficacy in a situation that has been so overwhelmingly challenging.
We will implement a second SCDIC intervention that utilizes a mobile app to support self-management on the part of the patient, by supporting motivation and adherence with hydroxyurea.53 A companion app supports hydroxyurea guideline adherence on the part of the provider, in keeping with one of our findings that providers are in need of decision-support tools. Elements of the intervention also align with our findings related to the importance of a support system in managing SCD, in that participants will identify a supportive partner who will play a specific role in supporting their adherence with hydroxyurea.
On our local level, we have, by necessity, partnered with leaders and community stakeholders throughout the region to ensure that these interventions to improve SCD care are prioritized. Grant funds provide initial resources for the SCDIC interventions, but our partnering health care administrators and medical directors must ensure that participating ED and hematology providers are free from competing priorities in order to implement the changes. We have partnered with a SCD community-based organization that is designing additional educational presentations for local emergency medicine providers, with the goal to bring to life very personal stories of bias and stigma within the EDs that directly contribute to decisions to avoid ED care despite severe symptoms.
Although we attempted to obtain samples of adolescents and adults with SCD and their providers that were representative across the 5-county region, the larger proportion of respondents were from 1 county. We did not assess concerns of age- and race-matched adults in our catchment area, so we cannot definitively say that our findings are unique to SCD. However, our results are consistent with findings from the national sample of adults with SCD who participated in the ASCQ-Me field test, and with results from the SCDIC needs assessment.33,51 Interviews and surveys are subject to self-report bias and, therefore, may or may not reflect the actual behaviors or thoughts of participants. Confidence is increased in our results given the triangulation of expressed concerns across participant groups and across data collection strategies. The majority of adolescents and adults with SCD (95%) completed both the interview and survey, while 64% of ED providers interviewed completed the survey, compared with 54% of SCD specialists and primary care providers. These response rates are more than acceptable within the realm of survey response rates.54,55
Although we encourage examining issues with care delivery within the conceptual framework for quality improvement presented, we recognize that grant funding allowed us to conduct an in-depth needs assessment that might not be feasible in other settings. Still, we would like readers to understand the importance of gathering data for improvement in a systematic manner across a range of participant groups, to ultimately inform the development of interventions and provide for evaluation of outcomes as a result of the interventions. This is particularly important for a disease, such as SCD, that is both medically and sociopolitically complex.
Conclusion
Our needs assessment brought into focus the multiple factors contributing to the disparities in health care experienced by adolescents and adults with SCD on our local level, and within the context of inequities in health resources and outcomes on the national level. We propose solutions that include specific interventions developed by a consortium of SCD and implementation science experts. We utilize a quality improvement framework to ensure that the elements of the interventions also address the barriers identified by our local providers and patients that are unique to our community. The pervasive challenges in SCD care, coupled with its medical complexities, may seem insurmountable, but our survey and qualitative results provide us with a road map for the way forward.
Acknowledgments: The authors thank the adolescents and adults with sickle cell disease, the providers, and the community stakeholders who completed the interviews and surveys. The authors also acknowledge the SCCCI co-investigators for their contributions to this project, including Michael Bell, MD, Ward Hagar, MD, Christine Hoehner, FNP, Kimberly Major, MSW, Anne Marsh, MD, Lynne Neumayr, MD, and Ted Wun, MD. We also thank Kamilah Bailey, Jameelah Hodge, Jennifer Kim, Michael Rowland, Adria Stauber, Amber Fearon, and Shanda Robertson, and the Sickle Cell Data Collection Program for their contributions.
Corresponding author: Marsha J. Treadwell, PhD, University of California San Francisco Benioff Children’s Hospital Oakland, 747 52nd St., Oakland, CA 94609; [email protected].
Financial disclosures: None.
Funding/support: This work was supported by grant # 1U01HL134007 from the National Heart, Lung, and Blood Institute to the University of California San Francisco Benioff Children’s Hospital Oakland.
1. Hassell KL. Population Estimates of sickle cell disease in the U.S. Am J Prev Med. 2010; 38:S512-S521.
2. Data & Statistics on Sickle Cell Disease. Centers for Disease Control and Prevention website. www.cdc.gov/ncbddd/sicklecell/data.html. Accessed March 25, 2020.
3. Inusa BPD, Stewart CE, Mathurin-Charles S, et al. Paediatric to adult transition care for patients with sickle cell disease: a global perspective. Lancet Haematol. 2020;7:e329-e341.
4. Smith SK, Johnston J, Rutherford C, et al. Identifying social-behavioral health needs of adults with sickle cell disease in the emergency department. J Emerg Nurs. 2017;43:444-450.
5. Treadwell MJ, Barreda F, Kaur K, et al. Emotional distress, barriers to care, and health-related quality of life in sickle cell disease. J Clin Outcomes Manag. 2015;22:8-17.
6. Treadwell MJ, Hassell K, Levine R, et al. Adult Sickle Cell Quality-of-Life Measurement Information System (ASCQ-Me): conceptual model based on review of the literature and formative research. Clin J Pain. 2014;30:902-914.
7. Rizio AA, Bhor M, Lin X, et al. The relationship between frequency and severity of vaso-occlusive crises and health-related quality of life and work productivity in adults with sickle cell disease. Qual Life Res. 2020;29:1533-1547.
8. Freiermuth CE, Haywood C, Silva S, et al. Attitudes toward patients with sickle cell disease in a multicenter sample of emergency department providers. Adv Emerg Nurs J. 2014;36:335-347.
9. Jenerette CM, Brewer C. Health-related stigma in young adults with sickle cell disease. J Natl Med Assoc. 2010;102:1050-1055.
10. Lazio MP, Costello HH, Courtney DM, et al. A comparison of analgesic management for emergency department patients with sickle cell disease and renal colic. Clin J Pain. 2010;26:199-205.
11. Haywood C, Tanabe P, Naik R, et al. The impact of race and disease on sickle cell patient wait times in the emergency department. Am J Emerg Med. 2013;31:651-656.
12. Haywood C, Beach MC, Lanzkron S, et al. A systematic review of barriers and interventions to improve appropriate use of therapies for sickle cell disease. J Natl Med Assoc. 2009;101:1022-1033.
13. Mainous AG, Tanner RJ, Harle CA, et al. Attitudes toward management of sickle cell disease and its complications: a national survey of academic family physicians. Anemia. 2015;2015:1-6.
14. Yawn BP, Buchanan GR, Afenyi-Annan AN, et al. Management of sickle cell disease: summary of the 2014 evidence-based report by expert panel members. JAMA. 2014;312:1033.
15. Lunyera J, Jonassaint C, Jonassaint J, et al. Attitudes of primary care physicians toward sickle cell disease care, guidelines, and comanaging hydroxyurea with a specialist. J Prim Care Community Health. 2017;8:37-40.
16. Whiteman LN, Haywood C, Lanzkron S, et al. Primary care providers’ comfort levels in caring for patients with sickle cell disease. South Med J. 2015;108:531-536.
17. Wong TE, Brandow AM, Lim W, Lottenberg R. Update on the use of hydroxyurea therapy in sickle cell disease. Blood. 2014;124:3850-4004.
18. DiMartino LD, Baumann AA, Hsu LL, et al. The sickle cell disease implementation consortium: Translating evidence-based guidelines into practice for sickle cell disease. Am J Hematol. 2018;93:E391-E395.
19. King AA, Baumann AA. Sickle cell disease and implementation science: A partnership to accelerate advances. Pediatr Blood Cancer. 2017;64:e26649.
20. Solberg LI. Improving medical practice: a conceptual framework. Ann Fam Med. 2007;5:251-256.
21. Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. J Am Med Assoc. 2002;288:5.
22. Bodenheimer T. Interventions to improve chronic illness care: evaluating their effectiveness. Dis Manag. 2003;6:63-71.
23. Tsai AC, Morton SC, Mangione CM, Keeler EB. A meta-analysis of interventions to improve care for chronic illnesses. Am J Manag Care. 2005;11:478-488.
24. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377-381.
25. Kallio H, Pietilä A-M, Johnson M, et al. Systematic methodological review: developing a framework for a qualitative semi-structured interview guide. J Adv Nurs. 2016;72:2954-2965.
26. Clarke V, Braun V. Successful Qualitative Research: A Practical Guide for Beginners. First. Thousand Oaks, CA: Sage; 2013.
27. Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277-1288.
28. Creswell JW, Hanson WE, Clark Plano VL, et al. Qualitative research designs: selection and implementation. Couns Psychol. 2007;35:236-264.
29. Miles MB, Huberman AM, Saldana J. Qualitative Data Analysis A Methods Sourcebook. 4th ed. Thousand Oaks, CA: Sage; 2019.
30. Eckman JR, Hassell KL, Huggins W, et al. Standard measures for sickle cell disease research: the PhenX Toolkit sickle cell disease collections. Blood Adv. 2017; 1: 2703-2711.
31. Kendall R, Wagner B, Brodke D, et al. The relationship of PROMIS pain interference and physical function scales. Pain Med. 2018;19:1720-1724.
32. Amtmann D, Cook KF, Jensen MP, et al. Development of a PROMIS item bank to measure pain interference. Pain. 2010;150:173-182.
33. Evensen CT, Treadwell MJ, Keller S, et al. Quality of care in sickle cell disease: Cross-sectional study and development of a measure for adults reporting on ambulatory and emergency department care. Medicine (Baltimore). 2016;95:e4528.
34. Edwards R, Telfair J, Cecil H, et al. Reliability and validity of a self-efficacy instrument specific to sickle cell disease. Behav Res Ther. 2000;38:951-963.
35. Edwards R, Telfair J, Cecil H, et al. Self-efficacy as a predictor of adult adjustment to sickle cell disease: one-year outcomes. Psychosom Med. 2001;63:850-858.
36. Puri Singh A, Haywood C, Beach MC, et al. Improving emergency providers’ attitudes toward sickle cell patients in pain. J Pain Symptom Manage. 2016;51:628-632.e3.
37. Glassberg JA, Tanabe P, Chow A, et al. Emergency provider analgesic practices and attitudes towards patients with sickle cell disease. Ann Emerg Med. 2013;62:293-302.e10.
38. Grahmann PH, Jackson KC 2nd, Lipman AG. Clinician beliefs about opioid use and barriers in chronic nonmalignant pain [published correction appears in J Pain Palliat Care Pharmacother. 2004;18:145-6]. J Pain Palliat Care Pharmacother. 2004;18:7-28.
39. Brandow AM, Panepinto JA. Hydroxyurea use in sickle cell disease: the battle with low prescription rates, poor patient compliance and fears of toxicities. Expert Rev Hematol. 2010;3:255-260.
40. Fielding N. Triangulation and mixed methods designs: data integration with new research technologies. J Mixed Meth Res. 2012;6:124-136.
41. 2017 CAHPS Health Plan Survey Chartbook. Agency for Healthcare Research and Quality website. www.ahrq.gov/cahps/cahps-database/comparative-data/2017-health-plan-chartbook/results-enrollee-population.html. Accessed September 8, 2020.
42. Bulgin D, Tanabe P, Jenerette C. Stigma of sickle cell disease: a systematic review. Issues Ment Health Nurs. 2018;1-11.
43. Wakefield EO, Zempsky WT, Puhl RM, et al. Conceptualizing pain-related stigma in adolescent chronic pain: a literature review and preliminary focus group findings. PAIN Rep. 2018;3:e679.
44. Nelson SC, Hackman HW. Race matters: Perceptions of race and racism in a sickle cell center. Pediatr Blood Cancer. 2013;60:451-454.
45. Dyal BW, Abudawood K, Schoppee TM, et al. Reflections of healthcare experiences of african americans with sickle cell disease or cancer: a qualitative study. Cancer Nurs. 2019;10.1097/NCC.0000000000000750.
46. Renedo A. Not being heard: barriers to high quality unplanned hospital care during young people’s transition to adult services - evidence from ‘this sickle cell life’ research. BMC Health Serv Res. 2019;19:876.
47. Ballas S, Vichinsky E. Is the medical home for adult patients with sickle cell disease a reality or an illusion? Hemoglobin. 2015;39:130-133.
48. Hankins JS, Osarogiagbon R, Adams-Graves P, et al. A transition pilot program for adolescents with sickle cell disease. J Pediatr Health Care. 2012;26 e45-e49.
49. Smith WR, Sisler IY, Johnson S, et al. Lessons learned from building a pediatric-to-adult sickle cell transition program. South Med J. 2019;112:190-197.
50. Lanzkron S, Sawicki GS, Hassell KL, et al. Transition to adulthood and adult health care for patients with sickle cell disease or cystic fibrosis: Current practices and research priorities. J Clin Transl Sci. 2018;2:334-342.
51. Kanter J, Gibson R, Lawrence RH, et al. Perceptions of US adolescents and adults with sickle cell disease on their quality of care. JAMA Netw Open. 2020;3:e206016.
52. Haywood C, Lanzkron S, Hughes MT, et al. A video-intervention to improve clinician attitudes toward patients with sickle cell disease: the results of a randomized experiment. J Gen Intern Med. 2011;26:518-523.
53. Hankins JS, Shah N, DiMartino L, et al. Integration of mobile health into sickle cell disease care to increase hydroxyurea utilization: protocol for an efficacy and implementation study. JMIR Res Protoc. 2020;9:e16319.
54. Fan W, Yan Z. Factors affecting response rates of the web survey: A systematic review. Comput Hum Behav. 2010;26:132-139.
55. Millar MM, Dillman DA. Improving response to web and mixed-mode surveys. Public Opin Q. 2011;75:249-269.
1. Hassell KL. Population Estimates of sickle cell disease in the U.S. Am J Prev Med. 2010; 38:S512-S521.
2. Data & Statistics on Sickle Cell Disease. Centers for Disease Control and Prevention website. www.cdc.gov/ncbddd/sicklecell/data.html. Accessed March 25, 2020.
3. Inusa BPD, Stewart CE, Mathurin-Charles S, et al. Paediatric to adult transition care for patients with sickle cell disease: a global perspective. Lancet Haematol. 2020;7:e329-e341.
4. Smith SK, Johnston J, Rutherford C, et al. Identifying social-behavioral health needs of adults with sickle cell disease in the emergency department. J Emerg Nurs. 2017;43:444-450.
5. Treadwell MJ, Barreda F, Kaur K, et al. Emotional distress, barriers to care, and health-related quality of life in sickle cell disease. J Clin Outcomes Manag. 2015;22:8-17.
6. Treadwell MJ, Hassell K, Levine R, et al. Adult Sickle Cell Quality-of-Life Measurement Information System (ASCQ-Me): conceptual model based on review of the literature and formative research. Clin J Pain. 2014;30:902-914.
7. Rizio AA, Bhor M, Lin X, et al. The relationship between frequency and severity of vaso-occlusive crises and health-related quality of life and work productivity in adults with sickle cell disease. Qual Life Res. 2020;29:1533-1547.
8. Freiermuth CE, Haywood C, Silva S, et al. Attitudes toward patients with sickle cell disease in a multicenter sample of emergency department providers. Adv Emerg Nurs J. 2014;36:335-347.
9. Jenerette CM, Brewer C. Health-related stigma in young adults with sickle cell disease. J Natl Med Assoc. 2010;102:1050-1055.
10. Lazio MP, Costello HH, Courtney DM, et al. A comparison of analgesic management for emergency department patients with sickle cell disease and renal colic. Clin J Pain. 2010;26:199-205.
11. Haywood C, Tanabe P, Naik R, et al. The impact of race and disease on sickle cell patient wait times in the emergency department. Am J Emerg Med. 2013;31:651-656.
12. Haywood C, Beach MC, Lanzkron S, et al. A systematic review of barriers and interventions to improve appropriate use of therapies for sickle cell disease. J Natl Med Assoc. 2009;101:1022-1033.
13. Mainous AG, Tanner RJ, Harle CA, et al. Attitudes toward management of sickle cell disease and its complications: a national survey of academic family physicians. Anemia. 2015;2015:1-6.
14. Yawn BP, Buchanan GR, Afenyi-Annan AN, et al. Management of sickle cell disease: summary of the 2014 evidence-based report by expert panel members. JAMA. 2014;312:1033.
15. Lunyera J, Jonassaint C, Jonassaint J, et al. Attitudes of primary care physicians toward sickle cell disease care, guidelines, and comanaging hydroxyurea with a specialist. J Prim Care Community Health. 2017;8:37-40.
16. Whiteman LN, Haywood C, Lanzkron S, et al. Primary care providers’ comfort levels in caring for patients with sickle cell disease. South Med J. 2015;108:531-536.
17. Wong TE, Brandow AM, Lim W, Lottenberg R. Update on the use of hydroxyurea therapy in sickle cell disease. Blood. 2014;124:3850-4004.
18. DiMartino LD, Baumann AA, Hsu LL, et al. The sickle cell disease implementation consortium: Translating evidence-based guidelines into practice for sickle cell disease. Am J Hematol. 2018;93:E391-E395.
19. King AA, Baumann AA. Sickle cell disease and implementation science: A partnership to accelerate advances. Pediatr Blood Cancer. 2017;64:e26649.
20. Solberg LI. Improving medical practice: a conceptual framework. Ann Fam Med. 2007;5:251-256.
21. Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. J Am Med Assoc. 2002;288:5.
22. Bodenheimer T. Interventions to improve chronic illness care: evaluating their effectiveness. Dis Manag. 2003;6:63-71.
23. Tsai AC, Morton SC, Mangione CM, Keeler EB. A meta-analysis of interventions to improve care for chronic illnesses. Am J Manag Care. 2005;11:478-488.
24. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377-381.
25. Kallio H, Pietilä A-M, Johnson M, et al. Systematic methodological review: developing a framework for a qualitative semi-structured interview guide. J Adv Nurs. 2016;72:2954-2965.
26. Clarke V, Braun V. Successful Qualitative Research: A Practical Guide for Beginners. First. Thousand Oaks, CA: Sage; 2013.
27. Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277-1288.
28. Creswell JW, Hanson WE, Clark Plano VL, et al. Qualitative research designs: selection and implementation. Couns Psychol. 2007;35:236-264.
29. Miles MB, Huberman AM, Saldana J. Qualitative Data Analysis A Methods Sourcebook. 4th ed. Thousand Oaks, CA: Sage; 2019.
30. Eckman JR, Hassell KL, Huggins W, et al. Standard measures for sickle cell disease research: the PhenX Toolkit sickle cell disease collections. Blood Adv. 2017; 1: 2703-2711.
31. Kendall R, Wagner B, Brodke D, et al. The relationship of PROMIS pain interference and physical function scales. Pain Med. 2018;19:1720-1724.
32. Amtmann D, Cook KF, Jensen MP, et al. Development of a PROMIS item bank to measure pain interference. Pain. 2010;150:173-182.
33. Evensen CT, Treadwell MJ, Keller S, et al. Quality of care in sickle cell disease: Cross-sectional study and development of a measure for adults reporting on ambulatory and emergency department care. Medicine (Baltimore). 2016;95:e4528.
34. Edwards R, Telfair J, Cecil H, et al. Reliability and validity of a self-efficacy instrument specific to sickle cell disease. Behav Res Ther. 2000;38:951-963.
35. Edwards R, Telfair J, Cecil H, et al. Self-efficacy as a predictor of adult adjustment to sickle cell disease: one-year outcomes. Psychosom Med. 2001;63:850-858.
36. Puri Singh A, Haywood C, Beach MC, et al. Improving emergency providers’ attitudes toward sickle cell patients in pain. J Pain Symptom Manage. 2016;51:628-632.e3.
37. Glassberg JA, Tanabe P, Chow A, et al. Emergency provider analgesic practices and attitudes towards patients with sickle cell disease. Ann Emerg Med. 2013;62:293-302.e10.
38. Grahmann PH, Jackson KC 2nd, Lipman AG. Clinician beliefs about opioid use and barriers in chronic nonmalignant pain [published correction appears in J Pain Palliat Care Pharmacother. 2004;18:145-6]. J Pain Palliat Care Pharmacother. 2004;18:7-28.
39. Brandow AM, Panepinto JA. Hydroxyurea use in sickle cell disease: the battle with low prescription rates, poor patient compliance and fears of toxicities. Expert Rev Hematol. 2010;3:255-260.
40. Fielding N. Triangulation and mixed methods designs: data integration with new research technologies. J Mixed Meth Res. 2012;6:124-136.
41. 2017 CAHPS Health Plan Survey Chartbook. Agency for Healthcare Research and Quality website. www.ahrq.gov/cahps/cahps-database/comparative-data/2017-health-plan-chartbook/results-enrollee-population.html. Accessed September 8, 2020.
42. Bulgin D, Tanabe P, Jenerette C. Stigma of sickle cell disease: a systematic review. Issues Ment Health Nurs. 2018;1-11.
43. Wakefield EO, Zempsky WT, Puhl RM, et al. Conceptualizing pain-related stigma in adolescent chronic pain: a literature review and preliminary focus group findings. PAIN Rep. 2018;3:e679.
44. Nelson SC, Hackman HW. Race matters: Perceptions of race and racism in a sickle cell center. Pediatr Blood Cancer. 2013;60:451-454.
45. Dyal BW, Abudawood K, Schoppee TM, et al. Reflections of healthcare experiences of african americans with sickle cell disease or cancer: a qualitative study. Cancer Nurs. 2019;10.1097/NCC.0000000000000750.
46. Renedo A. Not being heard: barriers to high quality unplanned hospital care during young people’s transition to adult services - evidence from ‘this sickle cell life’ research. BMC Health Serv Res. 2019;19:876.
47. Ballas S, Vichinsky E. Is the medical home for adult patients with sickle cell disease a reality or an illusion? Hemoglobin. 2015;39:130-133.
48. Hankins JS, Osarogiagbon R, Adams-Graves P, et al. A transition pilot program for adolescents with sickle cell disease. J Pediatr Health Care. 2012;26 e45-e49.
49. Smith WR, Sisler IY, Johnson S, et al. Lessons learned from building a pediatric-to-adult sickle cell transition program. South Med J. 2019;112:190-197.
50. Lanzkron S, Sawicki GS, Hassell KL, et al. Transition to adulthood and adult health care for patients with sickle cell disease or cystic fibrosis: Current practices and research priorities. J Clin Transl Sci. 2018;2:334-342.
51. Kanter J, Gibson R, Lawrence RH, et al. Perceptions of US adolescents and adults with sickle cell disease on their quality of care. JAMA Netw Open. 2020;3:e206016.
52. Haywood C, Lanzkron S, Hughes MT, et al. A video-intervention to improve clinician attitudes toward patients with sickle cell disease: the results of a randomized experiment. J Gen Intern Med. 2011;26:518-523.
53. Hankins JS, Shah N, DiMartino L, et al. Integration of mobile health into sickle cell disease care to increase hydroxyurea utilization: protocol for an efficacy and implementation study. JMIR Res Protoc. 2020;9:e16319.
54. Fan W, Yan Z. Factors affecting response rates of the web survey: A systematic review. Comput Hum Behav. 2010;26:132-139.
55. Millar MM, Dillman DA. Improving response to web and mixed-mode surveys. Public Opin Q. 2011;75:249-269.
Nationwide study questions routine long-term beta-blocker post MI
Current American and European guidelines recommending long-term beta-blocker therapy following an acute MI appear to be obsolete in the modern reperfusion era, suggests an analysis of Danish registry data.
Those guidelines are based on old randomized trials of beta-blocker therapy conducted prior to introduction of routine percutaneous coronary intervention and modern multidrug optimal medical therapy for acute MI. There have been no prospective controlled studies in the reperfusion era. And a new Danish national observational study strongly suggests it’s time to reexamine the beta-blocker recommendation, Anders Holt, MD, said at the virtual annual congress of the European Society of Cardiology.
“Stable, optimally treated MI patients do not seem to benefit from beta-blocker treatment exceeding 3 months post hospitalization – bearing in mind this doesn’t apply to patients with other indications for beta-blockers, like heart failure or atrial fibrillation,” said Dr. Holt of Copenhagen University Hospital.
His analysis of Danish national registry data on more than 30,000 patients hospitalized for acute MI during 2003-2018 earned him the annual ESC Young Investigator Award in Population Science.
“This was a crisp and clear presentation of a very creative use of observational epidemiology to try to understand the length of therapy that may or may not be appropriate,” commented award session cochair Paul M. Ridker, MD, director of the Center for Cardiovascular Disease Prevention at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School, both in Boston.
Dr. Holt reported on 30,177 patients optimally treated for a first MI in Danish hospitals during 2003-2018, none of whom had a prior indication or contraindication for beta-blocker therapy. “Optimally treated” meant they underwent percutaneous coronary revascularization and were discharged on a statin and aspirin. As a study requirement, all had to be stable 90 days post hospitalization, at which point 24,770 of the patients were on long-term beta-blocker therapy, and 5,407 (18%) were not. The two groups were comparable in terms of age, sex, comorbidities, and baseline medications. All patients were followed through the registries for a maximum of 3 years, the duration of beta-blocker therapy post MI recommended in American Heart Association/American College of Cardiology guidelines. (The Danish Society of Cardiology recommends 2 years.)
At 3 years post MI, there was no between-group difference in a composite outcome comprising cardiovascular death, recurrent MI, heart failure, stroke, angina, or a cardiac procedure, with a rate of 22.9% in the beta-blocker group and 21.6% in patients not on long-term beta-blocker therapy. The rate of recurrent MI was identical at 6.7% in both groups. Cardiovascular death occurred during 3 years of follow-up in 1.4% of patients on beta-blocker therapy and 1.7% who weren’t, a nonsignificant difference.
“We saw no evidence of any cardioprotective effect, but no increased risk of adverse events resulting in hospitalization, either,” Dr. Holt observed. “I would like to acknowledge that no evidence of effect does not necessarily equal evidence of no effect, but even if there was an effect we can with fair certainty say that it’s probably quite minimal.”
He noted that the Danish registry data indicates that each year since 2012 has shown a growing trend for Danish patients to dispense with long-term beta-blocker therapy after an acute MI.
“This might indicate we are nudging toward a change in practice, where more physicians are thinking that long-term beta-blocker therapy might not be indicated for all MI patients in the reperfusion era,” according to Dr. Holt.
Asked by the four-judge award panel about the possibility of unmeasured confounding in this observational study, Dr Holt responded: “I would be very cautious about asking patients to stop beta-blocker therapy after 3 months just based on this observational data. We can’t speak to causality in an observational study.” But he added that “well-designed observational studies provide valuable data regarding this topic and should not be ignored. They should possibly influence the guidelines and the designs for upcoming randomized trials.”
He conducted several supplementary analyses designed to address the possibility of unevenly distributed unmeasured confounding in the registry study. These analyses proved reassuring. A positive exposure control analysis compared 3-year outcomes in patients who remained on long-term statin therapy and those who didn’t. As expected, outcomes were significantly better in those who did: a 3-year composite outcome rate of 22.1%, compared with 32.1% in patients not on a statin; a cardiovascular death rate of 1.3% with and 2.1% without statin therapy; a recurrent MI rate of 6.6%, compared with 10.1% without a statin; and a 2.8% all-cause mortality with and 5.4% without statin therapy.
In contrast, all-cause mortality was unaffected by whether or not patients were on long-term beta-blocker therapy. And in a negative exposure outcome analysis, no association was found between beta-blocker therapy and the risk of hospitalization for pneumonia, as to be expected if the beta-blocker and no-beta-blocker groups were comparable in key respects.
Dr. Holt reported having no financial conflicts regarding his study.
Current American and European guidelines recommending long-term beta-blocker therapy following an acute MI appear to be obsolete in the modern reperfusion era, suggests an analysis of Danish registry data.
Those guidelines are based on old randomized trials of beta-blocker therapy conducted prior to introduction of routine percutaneous coronary intervention and modern multidrug optimal medical therapy for acute MI. There have been no prospective controlled studies in the reperfusion era. And a new Danish national observational study strongly suggests it’s time to reexamine the beta-blocker recommendation, Anders Holt, MD, said at the virtual annual congress of the European Society of Cardiology.
“Stable, optimally treated MI patients do not seem to benefit from beta-blocker treatment exceeding 3 months post hospitalization – bearing in mind this doesn’t apply to patients with other indications for beta-blockers, like heart failure or atrial fibrillation,” said Dr. Holt of Copenhagen University Hospital.
His analysis of Danish national registry data on more than 30,000 patients hospitalized for acute MI during 2003-2018 earned him the annual ESC Young Investigator Award in Population Science.
“This was a crisp and clear presentation of a very creative use of observational epidemiology to try to understand the length of therapy that may or may not be appropriate,” commented award session cochair Paul M. Ridker, MD, director of the Center for Cardiovascular Disease Prevention at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School, both in Boston.
Dr. Holt reported on 30,177 patients optimally treated for a first MI in Danish hospitals during 2003-2018, none of whom had a prior indication or contraindication for beta-blocker therapy. “Optimally treated” meant they underwent percutaneous coronary revascularization and were discharged on a statin and aspirin. As a study requirement, all had to be stable 90 days post hospitalization, at which point 24,770 of the patients were on long-term beta-blocker therapy, and 5,407 (18%) were not. The two groups were comparable in terms of age, sex, comorbidities, and baseline medications. All patients were followed through the registries for a maximum of 3 years, the duration of beta-blocker therapy post MI recommended in American Heart Association/American College of Cardiology guidelines. (The Danish Society of Cardiology recommends 2 years.)
At 3 years post MI, there was no between-group difference in a composite outcome comprising cardiovascular death, recurrent MI, heart failure, stroke, angina, or a cardiac procedure, with a rate of 22.9% in the beta-blocker group and 21.6% in patients not on long-term beta-blocker therapy. The rate of recurrent MI was identical at 6.7% in both groups. Cardiovascular death occurred during 3 years of follow-up in 1.4% of patients on beta-blocker therapy and 1.7% who weren’t, a nonsignificant difference.
“We saw no evidence of any cardioprotective effect, but no increased risk of adverse events resulting in hospitalization, either,” Dr. Holt observed. “I would like to acknowledge that no evidence of effect does not necessarily equal evidence of no effect, but even if there was an effect we can with fair certainty say that it’s probably quite minimal.”
He noted that the Danish registry data indicates that each year since 2012 has shown a growing trend for Danish patients to dispense with long-term beta-blocker therapy after an acute MI.
“This might indicate we are nudging toward a change in practice, where more physicians are thinking that long-term beta-blocker therapy might not be indicated for all MI patients in the reperfusion era,” according to Dr. Holt.
Asked by the four-judge award panel about the possibility of unmeasured confounding in this observational study, Dr Holt responded: “I would be very cautious about asking patients to stop beta-blocker therapy after 3 months just based on this observational data. We can’t speak to causality in an observational study.” But he added that “well-designed observational studies provide valuable data regarding this topic and should not be ignored. They should possibly influence the guidelines and the designs for upcoming randomized trials.”
He conducted several supplementary analyses designed to address the possibility of unevenly distributed unmeasured confounding in the registry study. These analyses proved reassuring. A positive exposure control analysis compared 3-year outcomes in patients who remained on long-term statin therapy and those who didn’t. As expected, outcomes were significantly better in those who did: a 3-year composite outcome rate of 22.1%, compared with 32.1% in patients not on a statin; a cardiovascular death rate of 1.3% with and 2.1% without statin therapy; a recurrent MI rate of 6.6%, compared with 10.1% without a statin; and a 2.8% all-cause mortality with and 5.4% without statin therapy.
In contrast, all-cause mortality was unaffected by whether or not patients were on long-term beta-blocker therapy. And in a negative exposure outcome analysis, no association was found between beta-blocker therapy and the risk of hospitalization for pneumonia, as to be expected if the beta-blocker and no-beta-blocker groups were comparable in key respects.
Dr. Holt reported having no financial conflicts regarding his study.
Current American and European guidelines recommending long-term beta-blocker therapy following an acute MI appear to be obsolete in the modern reperfusion era, suggests an analysis of Danish registry data.
Those guidelines are based on old randomized trials of beta-blocker therapy conducted prior to introduction of routine percutaneous coronary intervention and modern multidrug optimal medical therapy for acute MI. There have been no prospective controlled studies in the reperfusion era. And a new Danish national observational study strongly suggests it’s time to reexamine the beta-blocker recommendation, Anders Holt, MD, said at the virtual annual congress of the European Society of Cardiology.
“Stable, optimally treated MI patients do not seem to benefit from beta-blocker treatment exceeding 3 months post hospitalization – bearing in mind this doesn’t apply to patients with other indications for beta-blockers, like heart failure or atrial fibrillation,” said Dr. Holt of Copenhagen University Hospital.
His analysis of Danish national registry data on more than 30,000 patients hospitalized for acute MI during 2003-2018 earned him the annual ESC Young Investigator Award in Population Science.
“This was a crisp and clear presentation of a very creative use of observational epidemiology to try to understand the length of therapy that may or may not be appropriate,” commented award session cochair Paul M. Ridker, MD, director of the Center for Cardiovascular Disease Prevention at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School, both in Boston.
Dr. Holt reported on 30,177 patients optimally treated for a first MI in Danish hospitals during 2003-2018, none of whom had a prior indication or contraindication for beta-blocker therapy. “Optimally treated” meant they underwent percutaneous coronary revascularization and were discharged on a statin and aspirin. As a study requirement, all had to be stable 90 days post hospitalization, at which point 24,770 of the patients were on long-term beta-blocker therapy, and 5,407 (18%) were not. The two groups were comparable in terms of age, sex, comorbidities, and baseline medications. All patients were followed through the registries for a maximum of 3 years, the duration of beta-blocker therapy post MI recommended in American Heart Association/American College of Cardiology guidelines. (The Danish Society of Cardiology recommends 2 years.)
At 3 years post MI, there was no between-group difference in a composite outcome comprising cardiovascular death, recurrent MI, heart failure, stroke, angina, or a cardiac procedure, with a rate of 22.9% in the beta-blocker group and 21.6% in patients not on long-term beta-blocker therapy. The rate of recurrent MI was identical at 6.7% in both groups. Cardiovascular death occurred during 3 years of follow-up in 1.4% of patients on beta-blocker therapy and 1.7% who weren’t, a nonsignificant difference.
“We saw no evidence of any cardioprotective effect, but no increased risk of adverse events resulting in hospitalization, either,” Dr. Holt observed. “I would like to acknowledge that no evidence of effect does not necessarily equal evidence of no effect, but even if there was an effect we can with fair certainty say that it’s probably quite minimal.”
He noted that the Danish registry data indicates that each year since 2012 has shown a growing trend for Danish patients to dispense with long-term beta-blocker therapy after an acute MI.
“This might indicate we are nudging toward a change in practice, where more physicians are thinking that long-term beta-blocker therapy might not be indicated for all MI patients in the reperfusion era,” according to Dr. Holt.
Asked by the four-judge award panel about the possibility of unmeasured confounding in this observational study, Dr Holt responded: “I would be very cautious about asking patients to stop beta-blocker therapy after 3 months just based on this observational data. We can’t speak to causality in an observational study.” But he added that “well-designed observational studies provide valuable data regarding this topic and should not be ignored. They should possibly influence the guidelines and the designs for upcoming randomized trials.”
He conducted several supplementary analyses designed to address the possibility of unevenly distributed unmeasured confounding in the registry study. These analyses proved reassuring. A positive exposure control analysis compared 3-year outcomes in patients who remained on long-term statin therapy and those who didn’t. As expected, outcomes were significantly better in those who did: a 3-year composite outcome rate of 22.1%, compared with 32.1% in patients not on a statin; a cardiovascular death rate of 1.3% with and 2.1% without statin therapy; a recurrent MI rate of 6.6%, compared with 10.1% without a statin; and a 2.8% all-cause mortality with and 5.4% without statin therapy.
In contrast, all-cause mortality was unaffected by whether or not patients were on long-term beta-blocker therapy. And in a negative exposure outcome analysis, no association was found between beta-blocker therapy and the risk of hospitalization for pneumonia, as to be expected if the beta-blocker and no-beta-blocker groups were comparable in key respects.
Dr. Holt reported having no financial conflicts regarding his study.
FROM ESC CONGRESS 2020
Breaking the glass ceiling in interventional endoscopy: Practical considerations for women
Subspecialty training in advanced endoscopy has become increasingly appealing to GI fellows. The allure of an ever-evolving and innovative field is demonstrated by a substantial increase in the number of training programs over the last 2 decades, from 10 in the year 2000 to over 100 currently.1 Despite its increasing popularity, women interventionalists have been a glaring absence in this phenomenon.
For the 2018-2019 academic year, women represented only 12% of incoming advanced endoscopy fellows who matched through the American Society for Gastrointestinal Endoscopy (ASGE) match program. Perhaps more concerning, studies have found that the percentage of female trainees interested in advanced endoscopy diminishes as general GI fellowship progresses.2
Several potential contributors have been cited that elucidate this disparity including work-life balance, radiation exposure, and lack of mentorship.2 Implicit bias also undoubtedly plays a role.
Choosing a career path: Academia vs. private practice
The decision to pursue academia versus private practice in the field of advanced endoscopy is not always straightforward. For a relatively saturated subspecialty, geographic constraints and availability of positions may limit one path or another. Although an interventional practice is best supported by a tertiary care center, there is a known opportunity conflict between the number of advanced endoscopy trainees and the availability of academic positions.3
Although private practice may offer more autonomy in scheduling and fewer nonclinical responsibilities, there may be increased pressure to retain high clinical volumes with direct financial consequences, as well as limitations in overall career advancement. Pursuing an academic path, however, may lead to less flexibility in scheduling, more travel involved with speaking engagements, and teaching and/or research responsibilities disrupting a favorable work-life balance.3 Regardless of career path, the best environment to thrive as an advanced endoscopist and a mother is one in which there is recognition and support of the challenging early family years.
Family planning
Given the long and arduous training, along with the pressures of the early faculty/clinical years, there is no perfect time for a pregnancy. Even when a pregnancy is planned, there is no certainty it will follow the intended course. The challenges specific to a career in advanced endoscopy are not well described.
Considerations during a pregnancy
When to divulge
For female interventionalists, determining when to divulge a pregnancy and the duration of maternity leave can be elusive. There is a fine balance between revealing prematurely given the risk of miscarriage and waiting so long that appropriate precautions are forsaken. One might consider disclosing the pregnancy to a few key personnel in the endoscopy unit and/or a radiation safety officer to optimize early measures to prevent occupational hazards.
Maternity leave
Every institution and practice differ in the details of maternity leave policies. These details should be reviewed and negotiated in advance. At a minimum, they are guided by the federal Family and Medical Leave Act, which entitles employees to 12 weeks of unpaid, job-protected leave.4 Each pregnancy, delivery, and postpartum period is unique and unpredictable. While early planning and consideration of coverage are crucial, it is imperative to be realistic and fluid about the postpartum journey. The unpredictable need for an extended leave has the potential to lead to career stagnancy. It is important to remember that this is a small fraction of time in the context of an entire career.
Fluoroscopy exposure
The exposure to fluoroscopy and potential adverse effects on a pregnancy has been cited frequently by women as a barrier to pursuing advanced endoscopy.2 Given the paucity of women in this field, there has yet to be definitive data on the management of fluoroscopy risk while pregnant. The ASGE Quality Assurance Endoscopy Committee has acknowledged the importance of such data and is currently preparing guidelines for radiation safety that will address the risks for pregnant endoscopists and strategies to minimize fetal exposure. The use of a fetal monitor and an early discussion with the institution’s radiation safety officer are essential to minimize fetal exposure.
Optimizing ergonomics
There have been several publications demonstrating the deleterious musculoskeletal impacts of poor ergonomics while performing endoscopy, with women being at greater risk.5The New Gastroenterologist has also published a primer on this topic. In addition to inadequate education on biomechanics and inconsistent implementation of preventative safeguards, poor endoscope design has been shown to contribute. This can be accentuated for women in advanced endoscopy who perform complex procedures with therapeutic endoscopes equipped with suboptimal handle size and dial placement.
The potential for musculoskeletal injury increases during pregnancy. The standard measures to optimize biomechanics include screen at eye level, bed at hip height, a cushioned mat, and an athletic stance.6 In addition, back injury during pregnancy in advanced endoscopy is not uncommon. Several considerations should be entertained including use of double lead versus standard two-piece 0.5-mm lead with shielding curtains and walls, sitting during procedures when possible, and incorporating short breaks in the endoscopy schedule. Furthermore, more focus and innovation are required from endoscope manufacturers to tailor toward female hand anatomy. Until then, these small but meaningful measures may help to ensure optimal biomechanics to prevent injury.
Breastfeeding/pumping
Breastfeeding in the field of advanced endoscopy has traditionally been challenging. Navigating the collection and storage of breast milk during a busy day of interventional cases can be overwhelming. The previously stagnant industry of electric breast pumps has recently been revolutionized by the innovation of wearable breast pumps. Women are no longer required to find private space to connect to a loud, wired, contraption at least 30 minutes at a time, several times a day. In the context of a busy endoscopy schedule, this antiquated ritual is nearly incompatible with the continuation of breast feeding after returning to work. With relatively silent, wearable breast pumps, it is now possible to continue patient care whether in the clinic or in the endoscopy suite with minimal disruption to a productive day.
Resources
Although there continues to be a void for dedicated mentorship for female interventionalists, there have been many organizational initiatives to unite female gastroenterologists and promote the advancement of women. Several specific initiatives have been particularly effective. Women in Endoscopy (WIE) is a global organization that champions the advancement of women in GI through education, professional growth, and leadership development. In collaboration with the American Gastroenterological Association, they have recently held a virtual event focused on career advancement in the context of unique challenges for women, “Cross Your T’s to Success: How to Deliver a Great Talk, Get Your New Title and Seize Your Next Career Twist.” WIE has also recently launched a webinar series, “Women in Advanced Endoscopy: Fellows Educational Series,” that highlights practicing female interventionalists and illuminating the path to entering the field for trainees. In addition, the ASGE Leadership Education and Development (LEAD) Program has had longstanding success in providing young female gastroenterologists an opportunity to enhance their career advancement skills and facilitate the path to leadership positions. The popularity and success of the LEAD program has led the ASGE to create a special interest group known as ASGE Women in Endoscopy (AWE) with a mission to develop resources for career development during the first 5 years after fellowship. The American College of Gastroenterology also has a unique networking platform for women known as the Women in GI Circle. Furthermore, social media platforms such as Facebook’s Physician Moms Group (PMG) and Ladies of the Gut (LOG; group accessible by invitation only) have proved powerful in connecting female endoscopists and providing a great resource for quick guidance, encouragement, and commiseration. There are also multiple Facebook groups for breastfeeding physicians including Dr. Milk and other pump-specific groups. These online communities have facilitated the dissemination of high-quality resources for troubleshooting and general camaraderie.
Conclusion
Women remain a minority in GI, and especially in advanced endoscopy. Compared with surgical subspecialties that have witnessed substantial progress in the recruitment of women over the past decade, advanced endoscopy seems to be lagging far behind. Recent studies have shown that unified efforts from the surgical societies, such as establishing mentorship programs for trainees, have managed to increase the rates of women in general surgery programs from 14% in 2001 to 40% in 2017.7,8 As the barriers for women entering advanced endoscopy are further understood, the underlying concern of reconciling a challenging field and motherhood has emerged as a common thread. While the practical information presented here cannot overcome the cultural constructs and implicit biases in which women practice advanced endoscopy, the hope is to provide a pragmatic approach to the perceived barriers and promote dialogue among women so that they, too, can pursue and thrive in the field of advanced endoscopy.
References
1. Trindade AJ et al. Characteristics, goals, and motivations of applicants pursuing a fourth-year advanced endoscopy fellowship. Gastrointest Endosc. 2012;76(5):939-44.
2. Pollack MJ et al. Gender disparities and gastroenterology trainee attitudes toward advanced endoscopic training. Gastrointest Endosc. 2010;72(5):1111.
3. Granato CM et al. Career prospects and professional landscape after advanced endoscopy fellowship training: a survey assessing graduates from 2009 to 2013. Gastrointest Endosc. 2016;84(2):266-71.
4. Family and Medical Leave Act. US Department of Labor. Accessed May 15, 2020. https://www.dol.gov/agencies/whd/fmla.
5. Pedrosa MC et al. Minimizing occupational hazards in endoscopy: Personal protective equipment, radiation safety, and ergonomics. Gastrointest Endosc. 2010;72(2):227-35.
6. Singla M et al. Training the endo-athlete: An update in ergonomics in endoscopy. Clin Gastro Hepatol. 2018;16(7):1003-6.
7. Aziz HB et al. 2018 ACS Governors Survey: Gender inequality and harassment remain a challenge in surgery. Bulletin of the American College of Surgeons. Accessed August 22, 2020. https://bulletin.facs.org/2019/09/2018-acs-governors-survey-gender-inequality-and-harassment-remain-a-challenge-in-surgery/
8. Abelson JS et al. The climb to break the glass ceiling in surgery: trends in women progressing from medical school to surgical training and academic leadership from 1994 to 2015. Am J Surg. 2016;212(4):566-72.e1.
Dr. Hasan is director of interventional endoscopy, department of gastroenterology and hepatology, NorthBay Healthcare Group; Dr. Schulman is an assistant professor, director of bariatric endoscopy, division of gastroenterology and hepatology, University of Michigan, Ann Arbor.
Subspecialty training in advanced endoscopy has become increasingly appealing to GI fellows. The allure of an ever-evolving and innovative field is demonstrated by a substantial increase in the number of training programs over the last 2 decades, from 10 in the year 2000 to over 100 currently.1 Despite its increasing popularity, women interventionalists have been a glaring absence in this phenomenon.
For the 2018-2019 academic year, women represented only 12% of incoming advanced endoscopy fellows who matched through the American Society for Gastrointestinal Endoscopy (ASGE) match program. Perhaps more concerning, studies have found that the percentage of female trainees interested in advanced endoscopy diminishes as general GI fellowship progresses.2
Several potential contributors have been cited that elucidate this disparity including work-life balance, radiation exposure, and lack of mentorship.2 Implicit bias also undoubtedly plays a role.
Choosing a career path: Academia vs. private practice
The decision to pursue academia versus private practice in the field of advanced endoscopy is not always straightforward. For a relatively saturated subspecialty, geographic constraints and availability of positions may limit one path or another. Although an interventional practice is best supported by a tertiary care center, there is a known opportunity conflict between the number of advanced endoscopy trainees and the availability of academic positions.3
Although private practice may offer more autonomy in scheduling and fewer nonclinical responsibilities, there may be increased pressure to retain high clinical volumes with direct financial consequences, as well as limitations in overall career advancement. Pursuing an academic path, however, may lead to less flexibility in scheduling, more travel involved with speaking engagements, and teaching and/or research responsibilities disrupting a favorable work-life balance.3 Regardless of career path, the best environment to thrive as an advanced endoscopist and a mother is one in which there is recognition and support of the challenging early family years.
Family planning
Given the long and arduous training, along with the pressures of the early faculty/clinical years, there is no perfect time for a pregnancy. Even when a pregnancy is planned, there is no certainty it will follow the intended course. The challenges specific to a career in advanced endoscopy are not well described.
Considerations during a pregnancy
When to divulge
For female interventionalists, determining when to divulge a pregnancy and the duration of maternity leave can be elusive. There is a fine balance between revealing prematurely given the risk of miscarriage and waiting so long that appropriate precautions are forsaken. One might consider disclosing the pregnancy to a few key personnel in the endoscopy unit and/or a radiation safety officer to optimize early measures to prevent occupational hazards.
Maternity leave
Every institution and practice differ in the details of maternity leave policies. These details should be reviewed and negotiated in advance. At a minimum, they are guided by the federal Family and Medical Leave Act, which entitles employees to 12 weeks of unpaid, job-protected leave.4 Each pregnancy, delivery, and postpartum period is unique and unpredictable. While early planning and consideration of coverage are crucial, it is imperative to be realistic and fluid about the postpartum journey. The unpredictable need for an extended leave has the potential to lead to career stagnancy. It is important to remember that this is a small fraction of time in the context of an entire career.
Fluoroscopy exposure
The exposure to fluoroscopy and potential adverse effects on a pregnancy has been cited frequently by women as a barrier to pursuing advanced endoscopy.2 Given the paucity of women in this field, there has yet to be definitive data on the management of fluoroscopy risk while pregnant. The ASGE Quality Assurance Endoscopy Committee has acknowledged the importance of such data and is currently preparing guidelines for radiation safety that will address the risks for pregnant endoscopists and strategies to minimize fetal exposure. The use of a fetal monitor and an early discussion with the institution’s radiation safety officer are essential to minimize fetal exposure.
Optimizing ergonomics
There have been several publications demonstrating the deleterious musculoskeletal impacts of poor ergonomics while performing endoscopy, with women being at greater risk.5The New Gastroenterologist has also published a primer on this topic. In addition to inadequate education on biomechanics and inconsistent implementation of preventative safeguards, poor endoscope design has been shown to contribute. This can be accentuated for women in advanced endoscopy who perform complex procedures with therapeutic endoscopes equipped with suboptimal handle size and dial placement.
The potential for musculoskeletal injury increases during pregnancy. The standard measures to optimize biomechanics include screen at eye level, bed at hip height, a cushioned mat, and an athletic stance.6 In addition, back injury during pregnancy in advanced endoscopy is not uncommon. Several considerations should be entertained including use of double lead versus standard two-piece 0.5-mm lead with shielding curtains and walls, sitting during procedures when possible, and incorporating short breaks in the endoscopy schedule. Furthermore, more focus and innovation are required from endoscope manufacturers to tailor toward female hand anatomy. Until then, these small but meaningful measures may help to ensure optimal biomechanics to prevent injury.
Breastfeeding/pumping
Breastfeeding in the field of advanced endoscopy has traditionally been challenging. Navigating the collection and storage of breast milk during a busy day of interventional cases can be overwhelming. The previously stagnant industry of electric breast pumps has recently been revolutionized by the innovation of wearable breast pumps. Women are no longer required to find private space to connect to a loud, wired, contraption at least 30 minutes at a time, several times a day. In the context of a busy endoscopy schedule, this antiquated ritual is nearly incompatible with the continuation of breast feeding after returning to work. With relatively silent, wearable breast pumps, it is now possible to continue patient care whether in the clinic or in the endoscopy suite with minimal disruption to a productive day.
Resources
Although there continues to be a void for dedicated mentorship for female interventionalists, there have been many organizational initiatives to unite female gastroenterologists and promote the advancement of women. Several specific initiatives have been particularly effective. Women in Endoscopy (WIE) is a global organization that champions the advancement of women in GI through education, professional growth, and leadership development. In collaboration with the American Gastroenterological Association, they have recently held a virtual event focused on career advancement in the context of unique challenges for women, “Cross Your T’s to Success: How to Deliver a Great Talk, Get Your New Title and Seize Your Next Career Twist.” WIE has also recently launched a webinar series, “Women in Advanced Endoscopy: Fellows Educational Series,” that highlights practicing female interventionalists and illuminating the path to entering the field for trainees. In addition, the ASGE Leadership Education and Development (LEAD) Program has had longstanding success in providing young female gastroenterologists an opportunity to enhance their career advancement skills and facilitate the path to leadership positions. The popularity and success of the LEAD program has led the ASGE to create a special interest group known as ASGE Women in Endoscopy (AWE) with a mission to develop resources for career development during the first 5 years after fellowship. The American College of Gastroenterology also has a unique networking platform for women known as the Women in GI Circle. Furthermore, social media platforms such as Facebook’s Physician Moms Group (PMG) and Ladies of the Gut (LOG; group accessible by invitation only) have proved powerful in connecting female endoscopists and providing a great resource for quick guidance, encouragement, and commiseration. There are also multiple Facebook groups for breastfeeding physicians including Dr. Milk and other pump-specific groups. These online communities have facilitated the dissemination of high-quality resources for troubleshooting and general camaraderie.
Conclusion
Women remain a minority in GI, and especially in advanced endoscopy. Compared with surgical subspecialties that have witnessed substantial progress in the recruitment of women over the past decade, advanced endoscopy seems to be lagging far behind. Recent studies have shown that unified efforts from the surgical societies, such as establishing mentorship programs for trainees, have managed to increase the rates of women in general surgery programs from 14% in 2001 to 40% in 2017.7,8 As the barriers for women entering advanced endoscopy are further understood, the underlying concern of reconciling a challenging field and motherhood has emerged as a common thread. While the practical information presented here cannot overcome the cultural constructs and implicit biases in which women practice advanced endoscopy, the hope is to provide a pragmatic approach to the perceived barriers and promote dialogue among women so that they, too, can pursue and thrive in the field of advanced endoscopy.
References
1. Trindade AJ et al. Characteristics, goals, and motivations of applicants pursuing a fourth-year advanced endoscopy fellowship. Gastrointest Endosc. 2012;76(5):939-44.
2. Pollack MJ et al. Gender disparities and gastroenterology trainee attitudes toward advanced endoscopic training. Gastrointest Endosc. 2010;72(5):1111.
3. Granato CM et al. Career prospects and professional landscape after advanced endoscopy fellowship training: a survey assessing graduates from 2009 to 2013. Gastrointest Endosc. 2016;84(2):266-71.
4. Family and Medical Leave Act. US Department of Labor. Accessed May 15, 2020. https://www.dol.gov/agencies/whd/fmla.
5. Pedrosa MC et al. Minimizing occupational hazards in endoscopy: Personal protective equipment, radiation safety, and ergonomics. Gastrointest Endosc. 2010;72(2):227-35.
6. Singla M et al. Training the endo-athlete: An update in ergonomics in endoscopy. Clin Gastro Hepatol. 2018;16(7):1003-6.
7. Aziz HB et al. 2018 ACS Governors Survey: Gender inequality and harassment remain a challenge in surgery. Bulletin of the American College of Surgeons. Accessed August 22, 2020. https://bulletin.facs.org/2019/09/2018-acs-governors-survey-gender-inequality-and-harassment-remain-a-challenge-in-surgery/
8. Abelson JS et al. The climb to break the glass ceiling in surgery: trends in women progressing from medical school to surgical training and academic leadership from 1994 to 2015. Am J Surg. 2016;212(4):566-72.e1.
Dr. Hasan is director of interventional endoscopy, department of gastroenterology and hepatology, NorthBay Healthcare Group; Dr. Schulman is an assistant professor, director of bariatric endoscopy, division of gastroenterology and hepatology, University of Michigan, Ann Arbor.
Subspecialty training in advanced endoscopy has become increasingly appealing to GI fellows. The allure of an ever-evolving and innovative field is demonstrated by a substantial increase in the number of training programs over the last 2 decades, from 10 in the year 2000 to over 100 currently.1 Despite its increasing popularity, women interventionalists have been a glaring absence in this phenomenon.
For the 2018-2019 academic year, women represented only 12% of incoming advanced endoscopy fellows who matched through the American Society for Gastrointestinal Endoscopy (ASGE) match program. Perhaps more concerning, studies have found that the percentage of female trainees interested in advanced endoscopy diminishes as general GI fellowship progresses.2
Several potential contributors have been cited that elucidate this disparity including work-life balance, radiation exposure, and lack of mentorship.2 Implicit bias also undoubtedly plays a role.
Choosing a career path: Academia vs. private practice
The decision to pursue academia versus private practice in the field of advanced endoscopy is not always straightforward. For a relatively saturated subspecialty, geographic constraints and availability of positions may limit one path or another. Although an interventional practice is best supported by a tertiary care center, there is a known opportunity conflict between the number of advanced endoscopy trainees and the availability of academic positions.3
Although private practice may offer more autonomy in scheduling and fewer nonclinical responsibilities, there may be increased pressure to retain high clinical volumes with direct financial consequences, as well as limitations in overall career advancement. Pursuing an academic path, however, may lead to less flexibility in scheduling, more travel involved with speaking engagements, and teaching and/or research responsibilities disrupting a favorable work-life balance.3 Regardless of career path, the best environment to thrive as an advanced endoscopist and a mother is one in which there is recognition and support of the challenging early family years.
Family planning
Given the long and arduous training, along with the pressures of the early faculty/clinical years, there is no perfect time for a pregnancy. Even when a pregnancy is planned, there is no certainty it will follow the intended course. The challenges specific to a career in advanced endoscopy are not well described.
Considerations during a pregnancy
When to divulge
For female interventionalists, determining when to divulge a pregnancy and the duration of maternity leave can be elusive. There is a fine balance between revealing prematurely given the risk of miscarriage and waiting so long that appropriate precautions are forsaken. One might consider disclosing the pregnancy to a few key personnel in the endoscopy unit and/or a radiation safety officer to optimize early measures to prevent occupational hazards.
Maternity leave
Every institution and practice differ in the details of maternity leave policies. These details should be reviewed and negotiated in advance. At a minimum, they are guided by the federal Family and Medical Leave Act, which entitles employees to 12 weeks of unpaid, job-protected leave.4 Each pregnancy, delivery, and postpartum period is unique and unpredictable. While early planning and consideration of coverage are crucial, it is imperative to be realistic and fluid about the postpartum journey. The unpredictable need for an extended leave has the potential to lead to career stagnancy. It is important to remember that this is a small fraction of time in the context of an entire career.
Fluoroscopy exposure
The exposure to fluoroscopy and potential adverse effects on a pregnancy has been cited frequently by women as a barrier to pursuing advanced endoscopy.2 Given the paucity of women in this field, there has yet to be definitive data on the management of fluoroscopy risk while pregnant. The ASGE Quality Assurance Endoscopy Committee has acknowledged the importance of such data and is currently preparing guidelines for radiation safety that will address the risks for pregnant endoscopists and strategies to minimize fetal exposure. The use of a fetal monitor and an early discussion with the institution’s radiation safety officer are essential to minimize fetal exposure.
Optimizing ergonomics
There have been several publications demonstrating the deleterious musculoskeletal impacts of poor ergonomics while performing endoscopy, with women being at greater risk.5The New Gastroenterologist has also published a primer on this topic. In addition to inadequate education on biomechanics and inconsistent implementation of preventative safeguards, poor endoscope design has been shown to contribute. This can be accentuated for women in advanced endoscopy who perform complex procedures with therapeutic endoscopes equipped with suboptimal handle size and dial placement.
The potential for musculoskeletal injury increases during pregnancy. The standard measures to optimize biomechanics include screen at eye level, bed at hip height, a cushioned mat, and an athletic stance.6 In addition, back injury during pregnancy in advanced endoscopy is not uncommon. Several considerations should be entertained including use of double lead versus standard two-piece 0.5-mm lead with shielding curtains and walls, sitting during procedures when possible, and incorporating short breaks in the endoscopy schedule. Furthermore, more focus and innovation are required from endoscope manufacturers to tailor toward female hand anatomy. Until then, these small but meaningful measures may help to ensure optimal biomechanics to prevent injury.
Breastfeeding/pumping
Breastfeeding in the field of advanced endoscopy has traditionally been challenging. Navigating the collection and storage of breast milk during a busy day of interventional cases can be overwhelming. The previously stagnant industry of electric breast pumps has recently been revolutionized by the innovation of wearable breast pumps. Women are no longer required to find private space to connect to a loud, wired, contraption at least 30 minutes at a time, several times a day. In the context of a busy endoscopy schedule, this antiquated ritual is nearly incompatible with the continuation of breast feeding after returning to work. With relatively silent, wearable breast pumps, it is now possible to continue patient care whether in the clinic or in the endoscopy suite with minimal disruption to a productive day.
Resources
Although there continues to be a void for dedicated mentorship for female interventionalists, there have been many organizational initiatives to unite female gastroenterologists and promote the advancement of women. Several specific initiatives have been particularly effective. Women in Endoscopy (WIE) is a global organization that champions the advancement of women in GI through education, professional growth, and leadership development. In collaboration with the American Gastroenterological Association, they have recently held a virtual event focused on career advancement in the context of unique challenges for women, “Cross Your T’s to Success: How to Deliver a Great Talk, Get Your New Title and Seize Your Next Career Twist.” WIE has also recently launched a webinar series, “Women in Advanced Endoscopy: Fellows Educational Series,” that highlights practicing female interventionalists and illuminating the path to entering the field for trainees. In addition, the ASGE Leadership Education and Development (LEAD) Program has had longstanding success in providing young female gastroenterologists an opportunity to enhance their career advancement skills and facilitate the path to leadership positions. The popularity and success of the LEAD program has led the ASGE to create a special interest group known as ASGE Women in Endoscopy (AWE) with a mission to develop resources for career development during the first 5 years after fellowship. The American College of Gastroenterology also has a unique networking platform for women known as the Women in GI Circle. Furthermore, social media platforms such as Facebook’s Physician Moms Group (PMG) and Ladies of the Gut (LOG; group accessible by invitation only) have proved powerful in connecting female endoscopists and providing a great resource for quick guidance, encouragement, and commiseration. There are also multiple Facebook groups for breastfeeding physicians including Dr. Milk and other pump-specific groups. These online communities have facilitated the dissemination of high-quality resources for troubleshooting and general camaraderie.
Conclusion
Women remain a minority in GI, and especially in advanced endoscopy. Compared with surgical subspecialties that have witnessed substantial progress in the recruitment of women over the past decade, advanced endoscopy seems to be lagging far behind. Recent studies have shown that unified efforts from the surgical societies, such as establishing mentorship programs for trainees, have managed to increase the rates of women in general surgery programs from 14% in 2001 to 40% in 2017.7,8 As the barriers for women entering advanced endoscopy are further understood, the underlying concern of reconciling a challenging field and motherhood has emerged as a common thread. While the practical information presented here cannot overcome the cultural constructs and implicit biases in which women practice advanced endoscopy, the hope is to provide a pragmatic approach to the perceived barriers and promote dialogue among women so that they, too, can pursue and thrive in the field of advanced endoscopy.
References
1. Trindade AJ et al. Characteristics, goals, and motivations of applicants pursuing a fourth-year advanced endoscopy fellowship. Gastrointest Endosc. 2012;76(5):939-44.
2. Pollack MJ et al. Gender disparities and gastroenterology trainee attitudes toward advanced endoscopic training. Gastrointest Endosc. 2010;72(5):1111.
3. Granato CM et al. Career prospects and professional landscape after advanced endoscopy fellowship training: a survey assessing graduates from 2009 to 2013. Gastrointest Endosc. 2016;84(2):266-71.
4. Family and Medical Leave Act. US Department of Labor. Accessed May 15, 2020. https://www.dol.gov/agencies/whd/fmla.
5. Pedrosa MC et al. Minimizing occupational hazards in endoscopy: Personal protective equipment, radiation safety, and ergonomics. Gastrointest Endosc. 2010;72(2):227-35.
6. Singla M et al. Training the endo-athlete: An update in ergonomics in endoscopy. Clin Gastro Hepatol. 2018;16(7):1003-6.
7. Aziz HB et al. 2018 ACS Governors Survey: Gender inequality and harassment remain a challenge in surgery. Bulletin of the American College of Surgeons. Accessed August 22, 2020. https://bulletin.facs.org/2019/09/2018-acs-governors-survey-gender-inequality-and-harassment-remain-a-challenge-in-surgery/
8. Abelson JS et al. The climb to break the glass ceiling in surgery: trends in women progressing from medical school to surgical training and academic leadership from 1994 to 2015. Am J Surg. 2016;212(4):566-72.e1.
Dr. Hasan is director of interventional endoscopy, department of gastroenterology and hepatology, NorthBay Healthcare Group; Dr. Schulman is an assistant professor, director of bariatric endoscopy, division of gastroenterology and hepatology, University of Michigan, Ann Arbor.
Promising Trends Seen in AIDS-Associated NHL
Prognoses for patients with AIDS-associated, non-Hodgkin lymphomas (AIDS-NHLs) have improved dramatically as HIV/AIDS has become easier to treat, and “we’re actually seeing patients with long-term remissions that are translating to cure,” a hematologist told colleagues at the virtual 2020 annual meeting of the Association of VA Hematology/Oncology (AVAHO).
“Even those with low CD4 counts initially have more chance of survival compared to the historic patients in the pre-HAART [highly active antiretroviral therapy] era,” explained Erin Reid, MD, MS, of the University of California at San Diego Moores Cancer Center. “They’re seeing complete-response rates and overall-survival rates that are nearly matching what we’re seeing in the non-HIV lymphoma cases. And aggressive infection prophylaxis has seemed to mitigate some of the infectious complications.”
Still, Reid said, a severe form of AIDS-NHL continues to have very poor outcomes, although specific regimens appear to be brightening the picture somewhat.
According to Dr. Reid, AIDS-NHLs are the most common malignancy in the HIV-positive population, and patients with these cancers are more likely to have aggressive lymphomas. These patients are also more likely to have lymphomas associated with Epstein-Barr virus—40 to 80%, depending on the subtype of lymphoma—and Kaposi sarcoma-associated herpesvirus (also known as human herpesvirus-8, or HHV8).
“These viruses are driving these cancers, and it begs the question of whether there’s something we can do to target these viruses within these cancer cells in a way that’s therapeutic,” she said.
Compared with the non-HIV population, patients with AIDS-NHL “are much more likely to present with advanced stage, extranodal disease and central nervous system involvement,” she said.
HAART Benefits
It’s become clear that HIV control via HAART has benefits in terms of higher tolerance of chemotherapy doses—“we’re able to use more full or traditional dose regimens”—and perhaps cancer suppression too, she said. A 2013 meta-analysis “favored concurrent therapy with chemotherapy [and HAART]. This has become our recommended standard of care for virtually all cases, except the very rare ones where you cannot find a regimen that is compatible from a PK [pharmacokinetics] standpoint.”
Reid also noted that the HAART era has changed the role of CD4 counts in AIDS-NHLs. “While CD4 count still has some predictive value, its impact on mortality appears attenuated,” she said.
EPOCH Treatment
With regard to treatment, she emphasized the importance of HAART: “We would recommend concurrent HAART whenever possible with chemotherapy, or start it immediately afterward.”
Aggressive infection prophylaxis also is recommended through granulocyte colony-stimulating factor and agents to target threats from pneumocystis jiroveci pneumonia, gram negative rods, and varicella-zoster virus. “I’ve moved away from fungal prophylaxis over the years, only dealing with it if there’s a known fungal infection,” she said.
As for treatment of AIDS-NHL, Reid Suggested that research supports the EPOCH regimen --etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin. However, “we still need strategies for refractory and relapsed disease,” she said.
Reid noted that she has started to see more plasmablastic cases, although her experience is anecdotal. Plasmablastic lymphoma is much more common in the HIV-positive setting, she said.
Lifespans are poor for these patients, with many failing to live for a year. But research hints that the prognosis in AIDS-NHL patients on HAART may actually be better than in the non-HIV population, she said.
A trial published in September 2020, in fact, reports that 87% of 15 patients with AIDS-associated plasmablastic lymphoma survived for at least one year on the EPOCH regimen. Overall, the study found that “people with a collection of HIV-associated lymphomas were doing well overall with the EPOCH backbone,” Reid explained.
Reid reported no relevant disclosures.
Prognoses for patients with AIDS-associated, non-Hodgkin lymphomas (AIDS-NHLs) have improved dramatically as HIV/AIDS has become easier to treat, and “we’re actually seeing patients with long-term remissions that are translating to cure,” a hematologist told colleagues at the virtual 2020 annual meeting of the Association of VA Hematology/Oncology (AVAHO).
“Even those with low CD4 counts initially have more chance of survival compared to the historic patients in the pre-HAART [highly active antiretroviral therapy] era,” explained Erin Reid, MD, MS, of the University of California at San Diego Moores Cancer Center. “They’re seeing complete-response rates and overall-survival rates that are nearly matching what we’re seeing in the non-HIV lymphoma cases. And aggressive infection prophylaxis has seemed to mitigate some of the infectious complications.”
Still, Reid said, a severe form of AIDS-NHL continues to have very poor outcomes, although specific regimens appear to be brightening the picture somewhat.
According to Dr. Reid, AIDS-NHLs are the most common malignancy in the HIV-positive population, and patients with these cancers are more likely to have aggressive lymphomas. These patients are also more likely to have lymphomas associated with Epstein-Barr virus—40 to 80%, depending on the subtype of lymphoma—and Kaposi sarcoma-associated herpesvirus (also known as human herpesvirus-8, or HHV8).
“These viruses are driving these cancers, and it begs the question of whether there’s something we can do to target these viruses within these cancer cells in a way that’s therapeutic,” she said.
Compared with the non-HIV population, patients with AIDS-NHL “are much more likely to present with advanced stage, extranodal disease and central nervous system involvement,” she said.
HAART Benefits
It’s become clear that HIV control via HAART has benefits in terms of higher tolerance of chemotherapy doses—“we’re able to use more full or traditional dose regimens”—and perhaps cancer suppression too, she said. A 2013 meta-analysis “favored concurrent therapy with chemotherapy [and HAART]. This has become our recommended standard of care for virtually all cases, except the very rare ones where you cannot find a regimen that is compatible from a PK [pharmacokinetics] standpoint.”
Reid also noted that the HAART era has changed the role of CD4 counts in AIDS-NHLs. “While CD4 count still has some predictive value, its impact on mortality appears attenuated,” she said.
EPOCH Treatment
With regard to treatment, she emphasized the importance of HAART: “We would recommend concurrent HAART whenever possible with chemotherapy, or start it immediately afterward.”
Aggressive infection prophylaxis also is recommended through granulocyte colony-stimulating factor and agents to target threats from pneumocystis jiroveci pneumonia, gram negative rods, and varicella-zoster virus. “I’ve moved away from fungal prophylaxis over the years, only dealing with it if there’s a known fungal infection,” she said.
As for treatment of AIDS-NHL, Reid Suggested that research supports the EPOCH regimen --etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin. However, “we still need strategies for refractory and relapsed disease,” she said.
Reid noted that she has started to see more plasmablastic cases, although her experience is anecdotal. Plasmablastic lymphoma is much more common in the HIV-positive setting, she said.
Lifespans are poor for these patients, with many failing to live for a year. But research hints that the prognosis in AIDS-NHL patients on HAART may actually be better than in the non-HIV population, she said.
A trial published in September 2020, in fact, reports that 87% of 15 patients with AIDS-associated plasmablastic lymphoma survived for at least one year on the EPOCH regimen. Overall, the study found that “people with a collection of HIV-associated lymphomas were doing well overall with the EPOCH backbone,” Reid explained.
Reid reported no relevant disclosures.
Prognoses for patients with AIDS-associated, non-Hodgkin lymphomas (AIDS-NHLs) have improved dramatically as HIV/AIDS has become easier to treat, and “we’re actually seeing patients with long-term remissions that are translating to cure,” a hematologist told colleagues at the virtual 2020 annual meeting of the Association of VA Hematology/Oncology (AVAHO).
“Even those with low CD4 counts initially have more chance of survival compared to the historic patients in the pre-HAART [highly active antiretroviral therapy] era,” explained Erin Reid, MD, MS, of the University of California at San Diego Moores Cancer Center. “They’re seeing complete-response rates and overall-survival rates that are nearly matching what we’re seeing in the non-HIV lymphoma cases. And aggressive infection prophylaxis has seemed to mitigate some of the infectious complications.”
Still, Reid said, a severe form of AIDS-NHL continues to have very poor outcomes, although specific regimens appear to be brightening the picture somewhat.
According to Dr. Reid, AIDS-NHLs are the most common malignancy in the HIV-positive population, and patients with these cancers are more likely to have aggressive lymphomas. These patients are also more likely to have lymphomas associated with Epstein-Barr virus—40 to 80%, depending on the subtype of lymphoma—and Kaposi sarcoma-associated herpesvirus (also known as human herpesvirus-8, or HHV8).
“These viruses are driving these cancers, and it begs the question of whether there’s something we can do to target these viruses within these cancer cells in a way that’s therapeutic,” she said.
Compared with the non-HIV population, patients with AIDS-NHL “are much more likely to present with advanced stage, extranodal disease and central nervous system involvement,” she said.
HAART Benefits
It’s become clear that HIV control via HAART has benefits in terms of higher tolerance of chemotherapy doses—“we’re able to use more full or traditional dose regimens”—and perhaps cancer suppression too, she said. A 2013 meta-analysis “favored concurrent therapy with chemotherapy [and HAART]. This has become our recommended standard of care for virtually all cases, except the very rare ones where you cannot find a regimen that is compatible from a PK [pharmacokinetics] standpoint.”
Reid also noted that the HAART era has changed the role of CD4 counts in AIDS-NHLs. “While CD4 count still has some predictive value, its impact on mortality appears attenuated,” she said.
EPOCH Treatment
With regard to treatment, she emphasized the importance of HAART: “We would recommend concurrent HAART whenever possible with chemotherapy, or start it immediately afterward.”
Aggressive infection prophylaxis also is recommended through granulocyte colony-stimulating factor and agents to target threats from pneumocystis jiroveci pneumonia, gram negative rods, and varicella-zoster virus. “I’ve moved away from fungal prophylaxis over the years, only dealing with it if there’s a known fungal infection,” she said.
As for treatment of AIDS-NHL, Reid Suggested that research supports the EPOCH regimen --etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin. However, “we still need strategies for refractory and relapsed disease,” she said.
Reid noted that she has started to see more plasmablastic cases, although her experience is anecdotal. Plasmablastic lymphoma is much more common in the HIV-positive setting, she said.
Lifespans are poor for these patients, with many failing to live for a year. But research hints that the prognosis in AIDS-NHL patients on HAART may actually be better than in the non-HIV population, she said.
A trial published in September 2020, in fact, reports that 87% of 15 patients with AIDS-associated plasmablastic lymphoma survived for at least one year on the EPOCH regimen. Overall, the study found that “people with a collection of HIV-associated lymphomas were doing well overall with the EPOCH backbone,” Reid explained.
Reid reported no relevant disclosures.
Bleed Disorders Are Possible in VA Population
Although it may seem that veterans would have a very low risk of bleeding disorders since they were medically cleared for military service, a hematologist/oncologist cautioned that veterans might indeed suffer from both inherited and noninherited forms of these conditions. At the virtual 2020 annual meeting of the Association of VA Hematology/Oncology (AVAHO) Bethany Samuelson Bannow, MD, of Oregon Health & Science University’s Knight Cancer Institute urged colleagues to understand the diagnosis and treatment of bleeding disorders.
“Most importantly, even though these are patients you probably don’t see on a regular basis, you are never alone,” since colleagues are available to help, she said. Samuelson Bannow treats patients at US Department of Veterans Affairs (VA) Portland Health Care System and used her presentation to focus on 4 types of bleeding disorders. A summary of her perspective and recommendations follows.
Acquired hemophilia: Watch for Infections
Acquired hemophilia affects only an estimated 1.3 to 1.5 in 1 million people, but VA physicians may see it more often since it affects an older population (median age is 78 years), Samuelson Bannow said. “I’ve seen about 4 cases in the last 2 years,” she said. “I’m not sure if we’re a magnet, but it does come up.”
The diagnosis is based on laboratory findings, and a lack of personal or family history of coagulopathy is key, she said. Twenty percent or more of patients older than 65 years die from the disorder, but bleeding usually isn’t the cause. Instead, patients tend to die from infections, she said.
Initial treatment must focus on stopping the bleeding, she said. The new drug porcine antihemophilic factor (recombinant)—Obizur—“is very helpful” and is Samuelson Bannow’s first choice, but it may not widely available at all VA medical centers. Recombinant FVIIa (NovoSeven) and activated prothrombin complex concentrate (Feiba) also are options.
“The goal is to overpower the clotting cascade and get that burst of thrombin generation that you need to get the bleeding under control. Titrate to the amount of bleeding the patient is having, and make sure you’re doing local control as well,” Samuelson Bannow said. She added that the 2 agents may not work depending on the patient. Neither is preferred and both may be appropriate. “There’s no real reason to pick one over the other beyond convenience and availability.”
There’s another “equally important component of management,” she said: Inhibitor eradication. “The only way to do this is with immune suppression. You’re going to have to suppress the immune system to get rid of the inhibitor. That’s why we see such high rates of death because we have to use heavy-hitter immunosuppressants.”
Treatment options include steroids and cyclophosphamide (a common first-line option), rituximab, calcineurin inhibitors, and mycophenolate mofetil. “Just be aware that there is an increased risk of infection with these agents,” she said. “You want to see a decrease in the titer of your inhibitor. This can take 3 or more weeks, and it can take longer for it to disappear entirely. Look for normalized factor VIII level and absent inhibitor.”
She added: “I tend to do a slow taper, one agent at a time, over the course of weeks. If you see a return of the inhibitor, you can ramp back up as needed. Continue to monitor for a year or more since patients are at high risk of recurrence.”
Acquired von Willebrand Syndrome: Fix the Associated Conditions
Acquired von Willebrand Syndrome is another rare bleeding disorder that may appear in veterans “since it’s associated with a lot of conditions that we see in the VA,” such as heart disorders, solid tumors, vascular malformations, and lymphoproliferative and myeloproliferative disorders, Samuelson Bannow said.
As with acquired hemophilia, the key is to focus on controlling the bleeding, she said. Then, she advised, focus on the associated condition: “Correct the underlying disorder: Treat the malignancy, address the [cardiac] shear stress, correct hypothyroidism, correct the cardiac defects.”
Inherited Hemophilia: Don’t Rule It Out
It’s possible to “sneak through” military medical screening with undiagnosed inherited bleeding disorders, Dr. Samuelson Bannow said. That’s because service members may have never had an injury that triggered abnormal bleeding, she said. “You can see how someone could slip into the military with a [low clotting factor level]. The classic presentation is going to be joint bleeds and abnormalities. These can be traumatic and spontaneous without any kind of an injury,” she said.
A general rule for these patients is to “replace what’s missing, and 100% is always normal.” The 100% refers to clotting factor level. She recommended reviewing 2013 guidelines for the treatment of the disorder.
Inherited von Willebrand Syndrome: Ask About Tonsillectomies
Inherited von Willebrand Syndrome is more common in women than it is in men. Bleeding “will primarily be mucocutaneous and trauma-induced,” said. Samuelson Bannow. She recommended asking patients if they have had a tonsillectomy and, if so, did they suffer from unusual bleeding. “If they did not have excessive bleeding, it’s a pretty good sign their hemostasis is good.”
She recommends a nasal spray drug called desmopressin (DDAVP, Stimate) for management. “It’s critical to know that you must test for efficacy first,” she said. “One of the most common mistakes that people make is that they may give patients DDAVP before surgery without knowing if it works or not. It doesn’t work for every patient.” She typically avoids this drug in patients aged > 65 years, or even > 60 years, due to increased thrombosis risk.
Recombinant von Willebrand factor (Vonvendi) is a “very helpful drug at patients at increased risk of thrombosis,” she said. However, she noted that the drug, at last check, is not on the VA’s formulary.
At the end of her presentation, Samuelson Bannow urged colleagues to contact specialized Hemophilia Treatment Centers (HTCs) near them: “Follow this link, find an HTC [Hemophilia Treatment Center] near you, and create a partnership.”
Samuelson Bannow reported no relevant disclosures.
Although it may seem that veterans would have a very low risk of bleeding disorders since they were medically cleared for military service, a hematologist/oncologist cautioned that veterans might indeed suffer from both inherited and noninherited forms of these conditions. At the virtual 2020 annual meeting of the Association of VA Hematology/Oncology (AVAHO) Bethany Samuelson Bannow, MD, of Oregon Health & Science University’s Knight Cancer Institute urged colleagues to understand the diagnosis and treatment of bleeding disorders.
“Most importantly, even though these are patients you probably don’t see on a regular basis, you are never alone,” since colleagues are available to help, she said. Samuelson Bannow treats patients at US Department of Veterans Affairs (VA) Portland Health Care System and used her presentation to focus on 4 types of bleeding disorders. A summary of her perspective and recommendations follows.
Acquired hemophilia: Watch for Infections
Acquired hemophilia affects only an estimated 1.3 to 1.5 in 1 million people, but VA physicians may see it more often since it affects an older population (median age is 78 years), Samuelson Bannow said. “I’ve seen about 4 cases in the last 2 years,” she said. “I’m not sure if we’re a magnet, but it does come up.”
The diagnosis is based on laboratory findings, and a lack of personal or family history of coagulopathy is key, she said. Twenty percent or more of patients older than 65 years die from the disorder, but bleeding usually isn’t the cause. Instead, patients tend to die from infections, she said.
Initial treatment must focus on stopping the bleeding, she said. The new drug porcine antihemophilic factor (recombinant)—Obizur—“is very helpful” and is Samuelson Bannow’s first choice, but it may not widely available at all VA medical centers. Recombinant FVIIa (NovoSeven) and activated prothrombin complex concentrate (Feiba) also are options.
“The goal is to overpower the clotting cascade and get that burst of thrombin generation that you need to get the bleeding under control. Titrate to the amount of bleeding the patient is having, and make sure you’re doing local control as well,” Samuelson Bannow said. She added that the 2 agents may not work depending on the patient. Neither is preferred and both may be appropriate. “There’s no real reason to pick one over the other beyond convenience and availability.”
There’s another “equally important component of management,” she said: Inhibitor eradication. “The only way to do this is with immune suppression. You’re going to have to suppress the immune system to get rid of the inhibitor. That’s why we see such high rates of death because we have to use heavy-hitter immunosuppressants.”
Treatment options include steroids and cyclophosphamide (a common first-line option), rituximab, calcineurin inhibitors, and mycophenolate mofetil. “Just be aware that there is an increased risk of infection with these agents,” she said. “You want to see a decrease in the titer of your inhibitor. This can take 3 or more weeks, and it can take longer for it to disappear entirely. Look for normalized factor VIII level and absent inhibitor.”
She added: “I tend to do a slow taper, one agent at a time, over the course of weeks. If you see a return of the inhibitor, you can ramp back up as needed. Continue to monitor for a year or more since patients are at high risk of recurrence.”
Acquired von Willebrand Syndrome: Fix the Associated Conditions
Acquired von Willebrand Syndrome is another rare bleeding disorder that may appear in veterans “since it’s associated with a lot of conditions that we see in the VA,” such as heart disorders, solid tumors, vascular malformations, and lymphoproliferative and myeloproliferative disorders, Samuelson Bannow said.
As with acquired hemophilia, the key is to focus on controlling the bleeding, she said. Then, she advised, focus on the associated condition: “Correct the underlying disorder: Treat the malignancy, address the [cardiac] shear stress, correct hypothyroidism, correct the cardiac defects.”
Inherited Hemophilia: Don’t Rule It Out
It’s possible to “sneak through” military medical screening with undiagnosed inherited bleeding disorders, Dr. Samuelson Bannow said. That’s because service members may have never had an injury that triggered abnormal bleeding, she said. “You can see how someone could slip into the military with a [low clotting factor level]. The classic presentation is going to be joint bleeds and abnormalities. These can be traumatic and spontaneous without any kind of an injury,” she said.
A general rule for these patients is to “replace what’s missing, and 100% is always normal.” The 100% refers to clotting factor level. She recommended reviewing 2013 guidelines for the treatment of the disorder.
Inherited von Willebrand Syndrome: Ask About Tonsillectomies
Inherited von Willebrand Syndrome is more common in women than it is in men. Bleeding “will primarily be mucocutaneous and trauma-induced,” said. Samuelson Bannow. She recommended asking patients if they have had a tonsillectomy and, if so, did they suffer from unusual bleeding. “If they did not have excessive bleeding, it’s a pretty good sign their hemostasis is good.”
She recommends a nasal spray drug called desmopressin (DDAVP, Stimate) for management. “It’s critical to know that you must test for efficacy first,” she said. “One of the most common mistakes that people make is that they may give patients DDAVP before surgery without knowing if it works or not. It doesn’t work for every patient.” She typically avoids this drug in patients aged > 65 years, or even > 60 years, due to increased thrombosis risk.
Recombinant von Willebrand factor (Vonvendi) is a “very helpful drug at patients at increased risk of thrombosis,” she said. However, she noted that the drug, at last check, is not on the VA’s formulary.
At the end of her presentation, Samuelson Bannow urged colleagues to contact specialized Hemophilia Treatment Centers (HTCs) near them: “Follow this link, find an HTC [Hemophilia Treatment Center] near you, and create a partnership.”
Samuelson Bannow reported no relevant disclosures.
Although it may seem that veterans would have a very low risk of bleeding disorders since they were medically cleared for military service, a hematologist/oncologist cautioned that veterans might indeed suffer from both inherited and noninherited forms of these conditions. At the virtual 2020 annual meeting of the Association of VA Hematology/Oncology (AVAHO) Bethany Samuelson Bannow, MD, of Oregon Health & Science University’s Knight Cancer Institute urged colleagues to understand the diagnosis and treatment of bleeding disorders.
“Most importantly, even though these are patients you probably don’t see on a regular basis, you are never alone,” since colleagues are available to help, she said. Samuelson Bannow treats patients at US Department of Veterans Affairs (VA) Portland Health Care System and used her presentation to focus on 4 types of bleeding disorders. A summary of her perspective and recommendations follows.
Acquired hemophilia: Watch for Infections
Acquired hemophilia affects only an estimated 1.3 to 1.5 in 1 million people, but VA physicians may see it more often since it affects an older population (median age is 78 years), Samuelson Bannow said. “I’ve seen about 4 cases in the last 2 years,” she said. “I’m not sure if we’re a magnet, but it does come up.”
The diagnosis is based on laboratory findings, and a lack of personal or family history of coagulopathy is key, she said. Twenty percent or more of patients older than 65 years die from the disorder, but bleeding usually isn’t the cause. Instead, patients tend to die from infections, she said.
Initial treatment must focus on stopping the bleeding, she said. The new drug porcine antihemophilic factor (recombinant)—Obizur—“is very helpful” and is Samuelson Bannow’s first choice, but it may not widely available at all VA medical centers. Recombinant FVIIa (NovoSeven) and activated prothrombin complex concentrate (Feiba) also are options.
“The goal is to overpower the clotting cascade and get that burst of thrombin generation that you need to get the bleeding under control. Titrate to the amount of bleeding the patient is having, and make sure you’re doing local control as well,” Samuelson Bannow said. She added that the 2 agents may not work depending on the patient. Neither is preferred and both may be appropriate. “There’s no real reason to pick one over the other beyond convenience and availability.”
There’s another “equally important component of management,” she said: Inhibitor eradication. “The only way to do this is with immune suppression. You’re going to have to suppress the immune system to get rid of the inhibitor. That’s why we see such high rates of death because we have to use heavy-hitter immunosuppressants.”
Treatment options include steroids and cyclophosphamide (a common first-line option), rituximab, calcineurin inhibitors, and mycophenolate mofetil. “Just be aware that there is an increased risk of infection with these agents,” she said. “You want to see a decrease in the titer of your inhibitor. This can take 3 or more weeks, and it can take longer for it to disappear entirely. Look for normalized factor VIII level and absent inhibitor.”
She added: “I tend to do a slow taper, one agent at a time, over the course of weeks. If you see a return of the inhibitor, you can ramp back up as needed. Continue to monitor for a year or more since patients are at high risk of recurrence.”
Acquired von Willebrand Syndrome: Fix the Associated Conditions
Acquired von Willebrand Syndrome is another rare bleeding disorder that may appear in veterans “since it’s associated with a lot of conditions that we see in the VA,” such as heart disorders, solid tumors, vascular malformations, and lymphoproliferative and myeloproliferative disorders, Samuelson Bannow said.
As with acquired hemophilia, the key is to focus on controlling the bleeding, she said. Then, she advised, focus on the associated condition: “Correct the underlying disorder: Treat the malignancy, address the [cardiac] shear stress, correct hypothyroidism, correct the cardiac defects.”
Inherited Hemophilia: Don’t Rule It Out
It’s possible to “sneak through” military medical screening with undiagnosed inherited bleeding disorders, Dr. Samuelson Bannow said. That’s because service members may have never had an injury that triggered abnormal bleeding, she said. “You can see how someone could slip into the military with a [low clotting factor level]. The classic presentation is going to be joint bleeds and abnormalities. These can be traumatic and spontaneous without any kind of an injury,” she said.
A general rule for these patients is to “replace what’s missing, and 100% is always normal.” The 100% refers to clotting factor level. She recommended reviewing 2013 guidelines for the treatment of the disorder.
Inherited von Willebrand Syndrome: Ask About Tonsillectomies
Inherited von Willebrand Syndrome is more common in women than it is in men. Bleeding “will primarily be mucocutaneous and trauma-induced,” said. Samuelson Bannow. She recommended asking patients if they have had a tonsillectomy and, if so, did they suffer from unusual bleeding. “If they did not have excessive bleeding, it’s a pretty good sign their hemostasis is good.”
She recommends a nasal spray drug called desmopressin (DDAVP, Stimate) for management. “It’s critical to know that you must test for efficacy first,” she said. “One of the most common mistakes that people make is that they may give patients DDAVP before surgery without knowing if it works or not. It doesn’t work for every patient.” She typically avoids this drug in patients aged > 65 years, or even > 60 years, due to increased thrombosis risk.
Recombinant von Willebrand factor (Vonvendi) is a “very helpful drug at patients at increased risk of thrombosis,” she said. However, she noted that the drug, at last check, is not on the VA’s formulary.
At the end of her presentation, Samuelson Bannow urged colleagues to contact specialized Hemophilia Treatment Centers (HTCs) near them: “Follow this link, find an HTC [Hemophilia Treatment Center] near you, and create a partnership.”
Samuelson Bannow reported no relevant disclosures.
Valvular AFib heightens risk in TAVR
Atrial fibrillation has been known to confer an increased risk for poor outcomes after transcatheter aortic valve replacement, but there’s been no evidence of how the etiology of AFib can influence post-TAVR outcomes.
Now, a group of researchers from Bern (Switzerland) University are reporting that valvular AFib almost triples the risk of death or debilitating stroke, compared with patients with no AFib, and significantly increases the risk over nonvalvular AFib.*
“The present findings may have implications for risk stratification in patients undergoing TAVR,” wrote Taishi Okuno, MD, and colleagues in what they said is the first study “to appreciate the combined effect” of AFib and mitral stenosis in TAVR. “The identification of valvular AFib may refine the estimated risk for adverse clinical outcomes in patients undergoing TAVR,” they wrote in JACC: Cardiovascular Interventions.
“The fact that valvular AFib seems to confer a higher risk is an interesting finding,” Fred Welt, MD, professor of cardiology at the University of Utah, Salt Lake City, said in an interview. “I think it helps to a certain extent in prognostication because we can say to patients who have concomitant mitral valve disease that they are at higher risk.” Dr. Welt is also chair of the American College of Cardiology Interventional Council.
The analysis included 1,472 patients with aortic stenosis who had TAVR at Bern University Hospital between August 2007 and June 2018, 32% of whom (465) had atrial fibrillation, subcategorized as nonvalvular (26%, 376) and valvular (6%, 89). The primary endpoint, a composite of cardiovascular death or disabling stroke 1 year after TAVR, occurred in 9.3% of patients with no AFib, 14.5% of those with nonvalvular AFib and 24.2% of patients with valvular AFib.
In terms of hazard ratios, patients with nonvalvular AFib had a 57% greater risk of poor outcomes (P = .009) and those with valvular AFib had a 275% greater risk (P < .001), compared with patients with no AFib. Patients with valvular AFib had a 77% higher rate of cardiovascular death or stroke than those with nonvalvular AFib (P = .027).**
In their analysis, Dr. Okuno and colleagues acknowledged that the definition of valvular AFib used in guidelines and clinical trials isn’t uniform. Valvular atrial fibrillation was defined as AFib with mitral stenosis or a mitral valve prosthesis.
To account for the varying definitions of valvular and nonvalvular AFib, the researchers performed a sensitivity analysis of AFib patients with significant valve disease other than mitral stenosis; 42% of patients in the nonvalvular group fit this definition. Patients with AFib and valvular disease other than mitral stenosis had almost twice the risk of cardiovascular death or disabling stroke at 1 year, compared with patients who had AFib but no significant disease of any valve (20.1% vs. 10.9%, P = .03).
Furthermore, when they excluded patients with mild mitral stenosis from the valvular AFib group, “the effect of an increased risk for cardiovascular death or disabling stroke was no longer statistically significant.”
When the researchers separated out the two elements of the composite endpoint, they found valvular AFib carried a significantly higher risk of cardiovascular death – 21.1% (P < .002) vs. 7% for no AFib and 12.3% (P = .003) for nonvalvular AFib. However, the incidence of cardiovascular events – disabling stroke, nondisabling stroke and transient ischemic attack – showed no significant difference across the three groups, Dr. Okuno and colleagues noted. Specifically, the rates of disabling stroke were 3.8%, 3.7% and 5.7% in the no-AFib, nonvalvular-AFib, and valvular-AFib groups, respectively
In an invited editorial, Bernard Iung, MD, and Vincent Algalarrondo, MD, PhD, noted the problems with the definitions for valvular and nonvalvular AFib. “The term valvular AFib now frequently refers to patients with AFib associated with moderate or severe mitral stenosis or a mechanical heart valve,” they wrote. The definition is justified, they noted, because there’s little evidence on the use of non–vitamin K antagonist oral anticoagulants (NOACs) in patients with mitral stenosis.
They noted the term nonvalvular is “ambiguous” because it doesn’t exclude valvular disease but rather only a subset defined by the restrictive use of a class of anticoagulants. Hence, the definition of valvular AFib “is subject to criticisms and remains not standardized.”
“The individualization of valvular AFib in patients undergoing TAVR is debatable, and the definition used in the present study also included mild mitral stenosis and bioprostheses, thereby highlighting again the lack of a clear and uniform definition of the concept of valvular AFib,” they wrote.
While Dr. Welt said the findings may help in stratifying risk in patients with valvular AFib, he’s not certain how that would influence treatment decisions. “In most cases when we’re considering TAVR in these patients it’s because they have severe symptomatic aortic stenosis,” he said.
Surgery as an alternative is fraught with consequences, he said. “Would it be because you would want to repair the mitral valve as well?” he said. “And once you get into that territory, you’re talking about double-valve surgery, which is a much riskier operation than isolated aortic valve replacement.”
The study raises important questions about patients with valvular AFib, Dr. Welt added. “Why are these patients dying at higher rate? Is it some other arrhythmia or some other hemodynamic problem? Are there other things we can learn about these patients that would help us to better treat patients?”
But exploring these findings further with a randomized clinical trial may not be practical, he added. “The number of patients in whom this is an issue is in the scheme of things rather low: 6%,” he said.
Dr. Okuno has no relevant financial disclosures. Dr. Iung is a consultant for Edwards Lifesciences. Dr. Algalarrondo has been a consultant for Pfizer and Alnylam. Dr. Welt disclosed a relationship with Medtronic.
SOURCE: Okuno T et al. JACC Cardiovasc Interv. 2020 Sep 21. doi: 10.1016/j.jcin.2020.05.049.
Corrections, 9/29/20: An earlier version of this article misstated the increase in risk of (*) death or debilitating stroke and of (**) a poor outcome in those with valvular Afib.
Atrial fibrillation has been known to confer an increased risk for poor outcomes after transcatheter aortic valve replacement, but there’s been no evidence of how the etiology of AFib can influence post-TAVR outcomes.
Now, a group of researchers from Bern (Switzerland) University are reporting that valvular AFib almost triples the risk of death or debilitating stroke, compared with patients with no AFib, and significantly increases the risk over nonvalvular AFib.*
“The present findings may have implications for risk stratification in patients undergoing TAVR,” wrote Taishi Okuno, MD, and colleagues in what they said is the first study “to appreciate the combined effect” of AFib and mitral stenosis in TAVR. “The identification of valvular AFib may refine the estimated risk for adverse clinical outcomes in patients undergoing TAVR,” they wrote in JACC: Cardiovascular Interventions.
“The fact that valvular AFib seems to confer a higher risk is an interesting finding,” Fred Welt, MD, professor of cardiology at the University of Utah, Salt Lake City, said in an interview. “I think it helps to a certain extent in prognostication because we can say to patients who have concomitant mitral valve disease that they are at higher risk.” Dr. Welt is also chair of the American College of Cardiology Interventional Council.
The analysis included 1,472 patients with aortic stenosis who had TAVR at Bern University Hospital between August 2007 and June 2018, 32% of whom (465) had atrial fibrillation, subcategorized as nonvalvular (26%, 376) and valvular (6%, 89). The primary endpoint, a composite of cardiovascular death or disabling stroke 1 year after TAVR, occurred in 9.3% of patients with no AFib, 14.5% of those with nonvalvular AFib and 24.2% of patients with valvular AFib.
In terms of hazard ratios, patients with nonvalvular AFib had a 57% greater risk of poor outcomes (P = .009) and those with valvular AFib had a 275% greater risk (P < .001), compared with patients with no AFib. Patients with valvular AFib had a 77% higher rate of cardiovascular death or stroke than those with nonvalvular AFib (P = .027).**
In their analysis, Dr. Okuno and colleagues acknowledged that the definition of valvular AFib used in guidelines and clinical trials isn’t uniform. Valvular atrial fibrillation was defined as AFib with mitral stenosis or a mitral valve prosthesis.
To account for the varying definitions of valvular and nonvalvular AFib, the researchers performed a sensitivity analysis of AFib patients with significant valve disease other than mitral stenosis; 42% of patients in the nonvalvular group fit this definition. Patients with AFib and valvular disease other than mitral stenosis had almost twice the risk of cardiovascular death or disabling stroke at 1 year, compared with patients who had AFib but no significant disease of any valve (20.1% vs. 10.9%, P = .03).
Furthermore, when they excluded patients with mild mitral stenosis from the valvular AFib group, “the effect of an increased risk for cardiovascular death or disabling stroke was no longer statistically significant.”
When the researchers separated out the two elements of the composite endpoint, they found valvular AFib carried a significantly higher risk of cardiovascular death – 21.1% (P < .002) vs. 7% for no AFib and 12.3% (P = .003) for nonvalvular AFib. However, the incidence of cardiovascular events – disabling stroke, nondisabling stroke and transient ischemic attack – showed no significant difference across the three groups, Dr. Okuno and colleagues noted. Specifically, the rates of disabling stroke were 3.8%, 3.7% and 5.7% in the no-AFib, nonvalvular-AFib, and valvular-AFib groups, respectively
In an invited editorial, Bernard Iung, MD, and Vincent Algalarrondo, MD, PhD, noted the problems with the definitions for valvular and nonvalvular AFib. “The term valvular AFib now frequently refers to patients with AFib associated with moderate or severe mitral stenosis or a mechanical heart valve,” they wrote. The definition is justified, they noted, because there’s little evidence on the use of non–vitamin K antagonist oral anticoagulants (NOACs) in patients with mitral stenosis.
They noted the term nonvalvular is “ambiguous” because it doesn’t exclude valvular disease but rather only a subset defined by the restrictive use of a class of anticoagulants. Hence, the definition of valvular AFib “is subject to criticisms and remains not standardized.”
“The individualization of valvular AFib in patients undergoing TAVR is debatable, and the definition used in the present study also included mild mitral stenosis and bioprostheses, thereby highlighting again the lack of a clear and uniform definition of the concept of valvular AFib,” they wrote.
While Dr. Welt said the findings may help in stratifying risk in patients with valvular AFib, he’s not certain how that would influence treatment decisions. “In most cases when we’re considering TAVR in these patients it’s because they have severe symptomatic aortic stenosis,” he said.
Surgery as an alternative is fraught with consequences, he said. “Would it be because you would want to repair the mitral valve as well?” he said. “And once you get into that territory, you’re talking about double-valve surgery, which is a much riskier operation than isolated aortic valve replacement.”
The study raises important questions about patients with valvular AFib, Dr. Welt added. “Why are these patients dying at higher rate? Is it some other arrhythmia or some other hemodynamic problem? Are there other things we can learn about these patients that would help us to better treat patients?”
But exploring these findings further with a randomized clinical trial may not be practical, he added. “The number of patients in whom this is an issue is in the scheme of things rather low: 6%,” he said.
Dr. Okuno has no relevant financial disclosures. Dr. Iung is a consultant for Edwards Lifesciences. Dr. Algalarrondo has been a consultant for Pfizer and Alnylam. Dr. Welt disclosed a relationship with Medtronic.
SOURCE: Okuno T et al. JACC Cardiovasc Interv. 2020 Sep 21. doi: 10.1016/j.jcin.2020.05.049.
Corrections, 9/29/20: An earlier version of this article misstated the increase in risk of (*) death or debilitating stroke and of (**) a poor outcome in those with valvular Afib.
Atrial fibrillation has been known to confer an increased risk for poor outcomes after transcatheter aortic valve replacement, but there’s been no evidence of how the etiology of AFib can influence post-TAVR outcomes.
Now, a group of researchers from Bern (Switzerland) University are reporting that valvular AFib almost triples the risk of death or debilitating stroke, compared with patients with no AFib, and significantly increases the risk over nonvalvular AFib.*
“The present findings may have implications for risk stratification in patients undergoing TAVR,” wrote Taishi Okuno, MD, and colleagues in what they said is the first study “to appreciate the combined effect” of AFib and mitral stenosis in TAVR. “The identification of valvular AFib may refine the estimated risk for adverse clinical outcomes in patients undergoing TAVR,” they wrote in JACC: Cardiovascular Interventions.
“The fact that valvular AFib seems to confer a higher risk is an interesting finding,” Fred Welt, MD, professor of cardiology at the University of Utah, Salt Lake City, said in an interview. “I think it helps to a certain extent in prognostication because we can say to patients who have concomitant mitral valve disease that they are at higher risk.” Dr. Welt is also chair of the American College of Cardiology Interventional Council.
The analysis included 1,472 patients with aortic stenosis who had TAVR at Bern University Hospital between August 2007 and June 2018, 32% of whom (465) had atrial fibrillation, subcategorized as nonvalvular (26%, 376) and valvular (6%, 89). The primary endpoint, a composite of cardiovascular death or disabling stroke 1 year after TAVR, occurred in 9.3% of patients with no AFib, 14.5% of those with nonvalvular AFib and 24.2% of patients with valvular AFib.
In terms of hazard ratios, patients with nonvalvular AFib had a 57% greater risk of poor outcomes (P = .009) and those with valvular AFib had a 275% greater risk (P < .001), compared with patients with no AFib. Patients with valvular AFib had a 77% higher rate of cardiovascular death or stroke than those with nonvalvular AFib (P = .027).**
In their analysis, Dr. Okuno and colleagues acknowledged that the definition of valvular AFib used in guidelines and clinical trials isn’t uniform. Valvular atrial fibrillation was defined as AFib with mitral stenosis or a mitral valve prosthesis.
To account for the varying definitions of valvular and nonvalvular AFib, the researchers performed a sensitivity analysis of AFib patients with significant valve disease other than mitral stenosis; 42% of patients in the nonvalvular group fit this definition. Patients with AFib and valvular disease other than mitral stenosis had almost twice the risk of cardiovascular death or disabling stroke at 1 year, compared with patients who had AFib but no significant disease of any valve (20.1% vs. 10.9%, P = .03).
Furthermore, when they excluded patients with mild mitral stenosis from the valvular AFib group, “the effect of an increased risk for cardiovascular death or disabling stroke was no longer statistically significant.”
When the researchers separated out the two elements of the composite endpoint, they found valvular AFib carried a significantly higher risk of cardiovascular death – 21.1% (P < .002) vs. 7% for no AFib and 12.3% (P = .003) for nonvalvular AFib. However, the incidence of cardiovascular events – disabling stroke, nondisabling stroke and transient ischemic attack – showed no significant difference across the three groups, Dr. Okuno and colleagues noted. Specifically, the rates of disabling stroke were 3.8%, 3.7% and 5.7% in the no-AFib, nonvalvular-AFib, and valvular-AFib groups, respectively
In an invited editorial, Bernard Iung, MD, and Vincent Algalarrondo, MD, PhD, noted the problems with the definitions for valvular and nonvalvular AFib. “The term valvular AFib now frequently refers to patients with AFib associated with moderate or severe mitral stenosis or a mechanical heart valve,” they wrote. The definition is justified, they noted, because there’s little evidence on the use of non–vitamin K antagonist oral anticoagulants (NOACs) in patients with mitral stenosis.
They noted the term nonvalvular is “ambiguous” because it doesn’t exclude valvular disease but rather only a subset defined by the restrictive use of a class of anticoagulants. Hence, the definition of valvular AFib “is subject to criticisms and remains not standardized.”
“The individualization of valvular AFib in patients undergoing TAVR is debatable, and the definition used in the present study also included mild mitral stenosis and bioprostheses, thereby highlighting again the lack of a clear and uniform definition of the concept of valvular AFib,” they wrote.
While Dr. Welt said the findings may help in stratifying risk in patients with valvular AFib, he’s not certain how that would influence treatment decisions. “In most cases when we’re considering TAVR in these patients it’s because they have severe symptomatic aortic stenosis,” he said.
Surgery as an alternative is fraught with consequences, he said. “Would it be because you would want to repair the mitral valve as well?” he said. “And once you get into that territory, you’re talking about double-valve surgery, which is a much riskier operation than isolated aortic valve replacement.”
The study raises important questions about patients with valvular AFib, Dr. Welt added. “Why are these patients dying at higher rate? Is it some other arrhythmia or some other hemodynamic problem? Are there other things we can learn about these patients that would help us to better treat patients?”
But exploring these findings further with a randomized clinical trial may not be practical, he added. “The number of patients in whom this is an issue is in the scheme of things rather low: 6%,” he said.
Dr. Okuno has no relevant financial disclosures. Dr. Iung is a consultant for Edwards Lifesciences. Dr. Algalarrondo has been a consultant for Pfizer and Alnylam. Dr. Welt disclosed a relationship with Medtronic.
SOURCE: Okuno T et al. JACC Cardiovasc Interv. 2020 Sep 21. doi: 10.1016/j.jcin.2020.05.049.
Corrections, 9/29/20: An earlier version of this article misstated the increase in risk of (*) death or debilitating stroke and of (**) a poor outcome in those with valvular Afib.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY